Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 16/53/12. The contractual start date was in November 2017. The final report began editorial review in May 2019 and was accepted for publication in September 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Mark Pearson is a member of Health Services and Delivery Research Funding Committee (2019–present). Geoff Wong is Joint Deputy Chairperson of the National Institute for Health Research Health Technology Assessment Prioritisation Committee: Integrated Community Health and Social Care (A) (2015–present).
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Carrieri et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Parts of this report have been reproduced from Carrieri et al. 1 © The Author(s). 2020 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
To restore balance and achieve physician well-being, we must first acknowledge that no one person or institution is to blame for the physician burnout epidemic. It is the unintended net result of multiple, highly disruptive changes in society at large; the medical profession; and the healthcare system.
Rothernberger2
The growing incidence of mental ill-health in health professionals, including doctors, across specialties and throughout careers3 is a major issue in many countries. 4–9 We use ‘mental ill-health’ as a broad term to encompass a variety of conditions, including psychological distress, stress, burnout, depression, addiction and suicide (see also Chapter 3, Terminology). A study conducted by American Medical Association and Mayo Clinic researchers in 2014 reported that 54% of physicians in the USA are experiencing professional burnout. 10 Suicide rates among doctors are also higher than in the general population. A review in the Journal of the American Medical Association of four decades of studies on physician suicide estimated that the chances of dying by suicide are 70% higher for male physicians and 250–400% higher for female physicians. 11 In the UK, the mental health of the NHS workforce, including that of doctors, is of great concern. 12–16 In 2015, the Head of Thought Leadership at The King’s Fund declared that stress levels among NHS staff are ‘astonishingly high’ and need to be treated as ‘public health problem’. 17 In the 2018 NHS staff survey, 39.8% of respondents indicated that they had been unwell in the previous 12 months because of work-related stress. This appears to be the worst result in 5 years. 18,19 In the UK, the key outcomes associated with mental ill-health in doctors include presenteeism (doctors working despite being unwell),20–22 absenteeism (doctors taking sickness leave frequently, which could result in gaps in the service)23 and workforce retention issues (doctors leaving the NHS either temporarily or permanently). 24–27 There is growing interest among different organisations and journals in understanding and addressing the issue of mental ill-health in doctors. This spans from the British Medical Journal collection on doctors’ well-being28 to the Health Education England’s NHS Staff and Learner’s Mental Wellbeing Commission. 29 Such initiatives mirror calls for internationally co-ordinated research efforts to develop evidence-based strategies to tackle the high incidence of mental ill-health among health-care professionals at a global level. 30,31
Current interventions and initiatives to tackle doctors’ mental ill-health seem to have limited effect. 18 One of the main reasons we have undertaken this research project is to better understand what is more likely to work and why (i.e. to develop evidence-based recommendations on how ‘the physician mental ill-health epidemic’2 can be addressed). The well-being of the health workforce, including doctors, not only is an important value in itself, but can significantly impact workforce planning, cost, health-care quality and patient outcomes. 32–34 Although mental ill-health is prevalent among all groups of health-care professionals working in the NHS, our research focuses on doctors across specialties and career stages. This focus reflects the current recruitment and workforce retention issues (e.g. doctors in training, general practice and emergency medicine), the significant potential for sick doctors to inadvertently cause harm to patients and the financial implications of doctors’ mental ill-health. 5,15
Why are doctors at risk of mental ill-health?
A considerable number of individual, occupational and broader sociocultural causative risk factors lead to mental ill-health. 2,24,35 Peer-reviewed and grey literature suggests that these factors include the emotionally demanding nature of the profession;23,36 the increasing workload resulting from attempting to provide more, and higher-quality, care on shrinking budgets;37 systems of clinical governance that lead to loss of autonomy and erosion of professional values;38 rigid organisational structures and inflexible working hours;39 and highly bureaucratic professional regulatory systems (e.g. appraisals, revalidation, Care Quality Commission visits). 40 Doctors are also at higher risk than the general population of developing addiction and substance misuse because of their knowledge of and access to drugs and potential for them to self-medicate. 12 Moreover, all of these factors may be aggravated by doctors’ tendency to avoid seeking help and support when unwell or under pressure41,42 and by a perceived stigma among doctors about mental illness. 7,43
The factors associated with mental ill-health and decisions to leave the medical profession include heavy workload, long working hours, high levels of regulation and scrutiny, perceived reduced autonomy, and fear of complaints and negligence claims. 24,25 Doctors’ presenteeism may be underpinned by collective norms to be present, fear of career repercussions, fear of letting down colleagues and patients, difficulties arranging cover, difficulties prioritising their own health needs and recognising their own vulnerability to illness, and work-related stress. 16,44
Current interventions and gaps
There is a large body of literature on interventions that offer support, advice and/or treatment to doctors experiencing mental health difficulties, and that address the associated impacts, such as presenteeism, absenteeism and workforce retention. 2,26 This literature tends to be restricted to specific disciplines and to be undertaken in silos. It also tends to focus on workplace interventions aimed at increasing doctors’ ‘productivity’ and ‘resilience’, placing responsibility for good mental health with doctors themselves. We found evidence of this from both systematic reviews and commentaries. 15,45–47 Our awareness of this tendency to focus on the individual, which also mirrors broader sociopolitical strategies and discourses,48,49 compounded by the realisation of its limitations, was one of the reasons that led us to undertake this study [see also a graphic report of the initial Care Under Pressure (CUP) symposium in 201550]. An important limit of this tendency is the lack of consideration of the organisational and structural contexts that may have a detrimental effect on doctors’ well-being. There are, however, commentators who have criticised this narrow view of resilience, for example arguing that interventions should also focus on organisational support and systemic factors contributing to mental ill-health, rather than on individual doctors,8,16,51 and advocating for a shift from ‘individual’ to ‘organisational resilience’. 46
The culture of the medical profession can also play an important role. As the ‘culture of medicine’ starts early in undergraduate medical programmes, doctors in training are affected both directly (e.g. by becoming ill themselves) and indirectly (e.g. through their colleagues being ill) by mental ill-health. Therefore, systemic strategies need also to start early in a doctor’s career, with medical training emphasising pathways to help and increasing awareness – and destigmatisation – of mental illness in doctors. 52 Interventions and initiatives that offer support, advice and/or treatment to doctors experiencing mental ill-health have not been synthesised in a way that takes into account the heterogeneity of these interventions and the many dimensions (e.g. individual, organisational, cultural, social) of the problem. Currently, it is not clear which components within these interventions matter more (or less) than others, for whom they matter and in what contexts. 53 For example, a given intervention might work well for some doctors and not others (which might be influenced by personal factors such as age, gender, seniority), and in some contexts and not others (as it might be influenced by organisational factors, such as the degree of organisational change, or societal factors, such as recent media portrayal). Therefore, there is a need for research approaches that are sensitive to the complexities of the problem of mental ill-health in doctors.
Methods
Project aim
This research aims to improve understanding of how, why and in what contexts mental health services and support interventions can be designed to minimise the incidence of doctors’ mental ill-health.
Project objectives
-
To conduct a realist review of interventions to tackle doctors’ mental ill-health and its impact on the clinical workforce and patient care, drawing on diverse literature sources and engaging iteratively with diverse stakeholder perspectives to produce actionable theory.
-
To produce recommendations that support the tailoring, implementation, monitoring and evaluation of contextually sensitive strategies to tackle mental ill-health and its impacts.
Review questions
-
What are the processes by which mental ill-health in doctors develop and lead to its negative impacts, and where are the gaps that interventions do not address currently?
-
What are the mechanisms, acting at individual, group, profession and organisational levels, by which interventions to reduce doctors’ mental ill-health at the different stages are believed to result in their intended outcomes?
-
What are the important contexts which determine whether or not the different mechanisms produce the intended outcomes?
-
What changes are needed to existing and/or future interventions to make them more effective?
Chapter 2 Review methods
Research plan
We followed a similar methodology to that used in a previous National Institute for Health Research Health Services and Delivery Research programme project54 that was conducted by many of the same research team members. 54,55 Any evidence synthesis that seeks to make sense of interventions aiming to improve doctors’ mental ill-health must take into account the contexts in which these interventions are situated. This generates an in-depth understanding of which components within these interventions matter more (or less) than others, for whom they matter and in what ways. A realist review can synthesise relevant data found within qualitative, quantitative and mixed-methods research. By following an interpretive, theory-driven approach to analysing data from such diverse literature sources, realist reviews move beyond description, to provide findings that coherently and transferably explain how and why contexts can influence outcomes. This is particularly relevant to complex programmes characterised by significant levels of heterogeneity. The plan of investigation followed a detailed protocol based on Pawson et al. ’s56 five iterative stages for realist reviews: (1) locating existing theories, (2) searching for evidence, (3) selecting articles, (4) extracting and organising data and (5) synthesising the evidence and drawing conclusions. The reporting is consistent with the Realist And Meta-narrative Evidence Syntheses: Evolving Standards (RAMESES) quality and publication standards for realist reviews. 57 The project ran for 18 months from November 2017 to April 2019. Regular project team meetings and stakeholder meetings throughout the lifecycle of the project ensured that multiple perspectives and interpretations were brought to bear on the research.
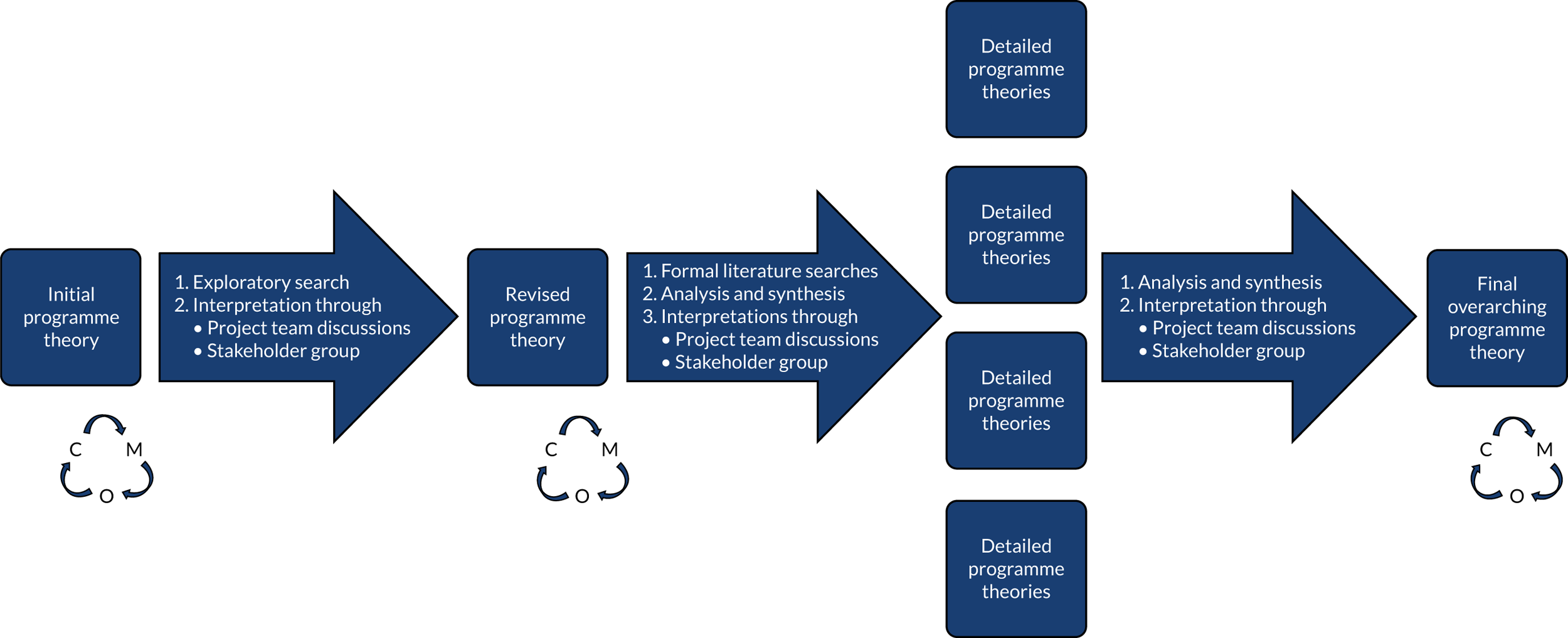
The protocol has been published in BMJ Open58 and the review has been registered with PROSPERO (CRD42017069870). The review design and methodology is explained in more detail in the sections below and illustrated in Figure 1.
FIGURE 1.
Flow diagram of the project. Note that dashed arrows indicate iteration where necessary. Reproduced from Wong et al. 54 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original text.

Stakeholder group
A stakeholder group was recruited for the CUP review to provide content expertise, feedback on and refinement of our programme theory and to coproduce non-academic outputs. The stakeholder group did not provide us with data, but feedback and advice based on their expertise and experience. A total of 22 people were involved in the stakeholder group during the review, including patient representatives, clinicians, doctors in training, medical educators and academics. Consultations with stakeholder group members took place as part of 2-hour meetings at regular intervals throughout the project and e-mail exchange. Additional ‘satellite’ face-to-face meetings were also arranged with some stakeholders who could not attend the main meetings, as well as Skype™ (Microsoft Corporation, Redmond, WA, USA) and telephone conversations. Table 1 provides a list of the face-to-face meetings, including the number of participants and key topics discussed.
| Date | Stakeholder group members | Key topics discussed | Examples of stakeholders’ contribution |
|---|---|---|---|
| 30 January 2018 | Four patient representatives, four clinicians and three academics | Discussed inconsistencies in current support for doctors in the NHS and the complexity of embedding intervention, particularly in the current overworked context of doctors |
|
| 21 February 2018 (satellite meeting) | Two medical educators, one of whom was a clinician, and one trainee | Discussed the support available to medical students across the UK and the impact of medical school on doctoring culture |
|
| 13 March 2018 | Three patient representatives, four clinicians and one academic | Discussed initial findings from the literature review and explored how these reflected stakeholders’ experiences |
|
| 21 May 2018 | Three clinicians and academics | Discussed initial findings for the literature review and explored how these reflected stakeholder’s experiences |
|
| 11 September 2018 | Three patient representatives, two academics, one representative from relevant medical organisation and two clinicians | Continued the discussion of emerging findings from the review. Assessed stakeholder’s views on who is responsible for doctors’ well-being at work, and if and how they would like to be involved with the production and dissemination of the project findings |
|
| 8 October 2018 (satellite meeting) | One medical educator and clinician, and one clinician and comics artist | Discussed initial findings from the literature review, explored how these reflected stakeholders’ experiences and discussed their willingness to be involved in co-production of dissemination output |
|
| 27 February 2019 | One clinician, one clinician and academic, one medical educator and three academics | Discussed the findings, how to convey them in an accessible way and the non-academic outputs |
|
| 12 March 2019 | Two medical educators and clinicians, one medical educator, one clinician, two patient representatives and one researcher | Discussed the findings, the dissemination strategy for the non-academic outputs and the stakeholders’ willingness to continue to collaborate in the production of these outputs |
|
Stakeholder group meetings took place at the University of Exeter or in London. To leave more time for discussion, we circulated any relevant preparatory material [e.g. summaries of previous meeting(s)], ahead of meetings when necessary. The meetings usually started with a brief slide presentation by our project team to introduce stakeholders to the topic under discussion and realist methods, and to provide a quick update on progress with the review. We presented high-level programme theory to the group in the form of statements and visual prompts to obtain their feedback. Discussions were designed to be more open ended in the early stages of the review, but focused on particular aspects of the programme theory as the project progressed. Later stakeholder groups focused on actionable findings and dissemination of the study. We used a framework called the evidence integration triangle (EIT)59 to ensure that discussions focused on the real-world impact of our study. The three components of the EIT (practical evidence-based interventions; pragmatic, longitudinal measures of progress; and participatory implementation processes) were used to structure discussions at the stakeholder group meetings and the workshop with policy-makers at the end of the project. Of the three components, the pragmatic longitudinal measures of progress proved by far the most challenging (see Chapter 5, Strengths and limitations of this review). Facilitation of the meetings ensured that everyone was able to contribute and voice their opinion, whether in agreement or disagreement. Notes from these meetings were used to set direction for the review and to refine programme theory, rather than as primary data for analysis, and the report does not include any verbatim data excerpts from these meetings.
Discussions with stakeholders helped ground the review in the practical reality experienced by participants and the challenges they faced in their respective roles. The sharing of these experiences re-enforced our decisions at times (e.g. to critically question the focus on ‘resilience’ in doctors) and prompted us to pay close attention to aspects that we had missed at others (e.g. the taboo around doctors expressing vulnerability). Stakeholders’ questions and contributions also prompted us to look more broadly in the literature for substantive explanatory theory, for example leading us to identify social cure theory and an emerging body of work on vulnerability that we drew on to shape our thinking and interpretation (for more information about the substantive theories used see Chapter 3, Summary of the 19 CMOcs in four main groupings). Our engagement with the stakeholder group and policy-makers also ensured that data were ‘translated’ and interpreted in ways relevant to the UK context.
In running the stakeholder group we took care to express realist review terms in everyday language so as to avoid methodological jargon, while still adequately conveying the nuances of the review findings. Stakeholder involvement also contributed significantly to the development of actionable findings in a form that would be usable and engaging. More details on actionable findings emerging from the review are presented in the Discussion.
The stakeholder group included strong patient and public involvement throughout the project. DC led the patient and public involvement component of the review following MP’s guidance. DC organised a briefing session with the patient representatives (n = 4 in total) before the first stakeholder meeting, to set the ground rules and to discuss the terms of their involvement and any key issues that needed to be addressed to facilitate meaningful participation. 60 In the stakeholder meetings, patients and members of the public provided significant input to programme theory development, often highlighting aspects and questioning assumptions that the rest of the group were taking for granted (e.g. the relational, financial, psychosocial complexity of the sickness absence pathway in the NHS, the importance of safe spaces in the workplace for doctors, and the complexities of making patients and the public aware that doctors are human and can become ill).
Steering Group
We set up a separate Steering Group to oversee the governance of the project and to provide high-level advice on dissemination strategies and conceptual aspects of the project. The group comprised one academic and clinician, one local NHS transformation manager and one patient representative. The range of expertise of the group included mental health services; nursing and complex intervention research methods; occupational stress in banking; stress involved in ‘fast-moving’ decision-making contexts, such as weather forecasting; and workforce management and resilience at both individual- and system-wide levels in the NHS.
Step 1: locating existing theories
In this first step of the review we identified theories that helped to understand (1) the processes leading to mental ill-health in doctors; and (2) how interventions aiming to support doctors experiencing mental ill-health are supposed to work (and for whom), when they work, when they do not, why they are not effective and why they are not being used. The rationale for this step is that interventions are ‘theories incarnate’ (i.e. interventions are underpinned by assumptions about why certain components are required). Such assumptions usually include a mix of scientific and experiential knowledge, including tacit assumptions that do not always become articulated (e.g. tacit knowledge). 61 Interventions are designed in a certain way based on assumptions about what is needed to achieve desired outcome(s). 62
To locate these assumptions, we iteratively drew on (1) discussions between DC and the clinical team of therapists working at the NHS Practitioner Health Programme; (2) informal discussions, advice and feedback from key content experts, representing multidisciplinary perspectives in our Stakeholder Group; and (3) an exploratory search of relevant literature.
Building the initial programme theory required iterative discussions (either at our regular face-to-face project team meetings or by e-mail) within the project team to make sense of and synthesise the different theories.
Step 2: searching for evidence
Main search
We developed a search strategy to identify examples of relevant programme theory in the published literature using MEDLINE via Ovid. Searching was designed, piloted and conducted by an information specialist (SB) in consultation with the review team. Search terms were derived from the titles, abstracts and indexing terms of relevant studies already known to the review team from background reading and consultation with stakeholders. These ‘empirically derived’ search terms were supplemented with relevant synonyms selected in consultation with the review team. Several versions of the search strategy were tested in MEDLINE via Ovid by checking that the relevant pre-identified studies were returned and by refining the search terms to optimise the sensitivity and specificity of the search (i.e. maximising the retrieval of known relevant studies while minimising the retrieval of irrelevant studies). In the process of testing and refining the search, we identified additional relevant studies which we also made sure were retrieved in subsequent iterations of the search.
The final search strategy consisted of the three components of the PICo (population, phenomenon of interest, context) question formulation tool:63
-
doctors and medical trainees (the population)
-
effects of mental ill-health in the workplace, such as presenteeism, absenteeism or burn out (the phenomenon of interest)
-
mental ill-health and workplace causes of mental ill-health, such as patient demand or work pressure (the context).
Each of the three components (population, phenomenon of interest, context) comprised relevant search terms combined using the OR Boolean operator. The three components were combined together using the AND Boolean operator. We found that this approach was the most effective way to retrieve our pre-identified set of papers and additional papers identified during the development of the search. Search terms included free-text terms (i.e. terms in the title and abstracts of bibliographic records) and indexing terms (e.g. medical subject headings in MEDLINE). We did not limit the search results by study type, date or language.
In December 2017 the final search strategy was translated and run in a selection of medical and psychology bibliographic databases, including MEDLINE, MEDLINE In-Process and Other Non-indexed Citations and PsycINFO (all via Ovid); and Applied Social Sciences Index and Abstracts (ASSIA) (via ProQuest). The MEDLINE search strategy is reproduced in Appendix 1. Search results were exported to EndNote (X8, Clarivate Analytics, Philadelphia, PA, USA) and de-duplicated using the automated deduplication feature and manual checking.
As our review was particularly focused on the UK context, we supplemented the bibliographic database searches described above (which were conducted in databases that index international literature) with searches that aimed to retrieve UK-based studies. We did this by conducting author, forwards and backwards citation searching on UK-based studies and first authors of studies identified by the bibliographic database searches. UK-based source studies and authors were identified by searching the EndNote library of bibliographic database results for terms such as UK, England, Wales, Ireland and Scotland, in the title and abstract fields. Forwards and author citation searches were conducted on relevant studies thus identified using Scopus and Web of Science. (We first searched for the source study or author and associated citations in Web of Science and if Web of Science did not index the item of interest we repeated the process in Scopus.) Backwards citation searching was conducted manually by inspecting the reference lists of UK-based studies. We also hand-searched journals with a UK focus via the relevant journal websites, including the British Medical Journal and BMC Medicine.
Step 3: selecting articles
The review was limited to English-language literature. We applied the following inclusion criteria:
-
Mental ill-health and its impacts (e.g. presenteeism, absenteeism and workforce retention) – all studies that focused on one or more of these aspects. Note that generic occupational health services targeting whole populations of doctors, rather than doctors experiencing mental ill-health, were not included. Studies about improving clinical practice (and the indirect effect this may have on doctors’ well-being) were labelled as not included/minor relevance.
-
Study design – all study designs.
-
Types of settings – all health-care settings.
-
Types of participants – all studies that included medical doctors.
-
Types of intervention – interventions or resources that focus on improving mental ill-health and minimising its impact.
-
Outcome measures – all mental health outcomes and measures relevant to its impacts (e.g. absenteeism, presenteeism and workforce retention).
Using EndNote, DC screened the titles and abstracts of all articles resulting from the main and supplementary searches (forward citation tracking and author citation tracking). A random 10% sample of the three sets of results were also screened independently for consistency of application of the inclusion criteria by CP (the second reviewer). Small inconsistencies were identified that were resolved through discussion. DC then screened the full texts of the papers resulting from the first round of screening and classified them in categories based on their potential to contribute to programme theory.
We had initially planned to sort included studies into those which could make ‘major’ or ‘minor’ contributions to our programme theory. 62 By doing this we intended to prioritise studies from the UK, but also to include studies from other countries that provided useful insights for the UK. Our criteria for classifying studies as ‘major’ or ‘minor’ were as follows (see also Carrieri et al. 58).
Major
-
Studies that contributed to the research questions and were conducted in an NHS context.
-
Studies that contributed to the research questions and were conducted in contexts (e.g. publicly and universal-funded health-care systems) with similarities to the NHS.
-
Studies that contributed to the research questions and could clearly help to identify mechanisms which could plausibly operate in the context of the NHS.
Minor
-
Studies conducted in health-care systems that were markedly different from the NHS (e.g. fee for service and private insurance scheme systems), but where the mechanisms could plausibly operate in the context of doctors working in the NHS.
However, as the analysis progressed, we noted that even those documents that we had assumed would make a minor contribution still contained important and relevant data for our study, and hence we extracted and analysed data from all included documents.
The full text of a 10% sample of documents from the main search and a separate 10% sample of full texts from the supplementary searches were assessed and discussed between DC and CP to ensure that decisions for final inclusion and classification into categories have been made consistently. Small inconsistencies were identified that were resolved through discussion.
Step 4: extracting and organising data
Once article selection was finalised, DC analysed the full text of the included studies, using NVivo 12 Pro (QSR International, Warrington, UK) to manage the data. Initial coding followed both an inductive mode (codes emerging from the analysis of the literature) and a deductive mode (codes created in advance informed by the initial programme theory, stakeholder group discussions and exploratory literature searching). The coding framework resulting from the analysis of the richest papers (mostly UK policy documents, systematic reviews and qualitative research) was applied to the rest of the studies and refined as the analysis progressed. To ensure consistency in conceptual coding, CP assessed a random 10% sample of coded articles.
The analysis was driven by a realist logic. We sought to interpret and explain mechanisms causing mental ill-health in doctors and medical students (with a particular focus on presenteeism, absenteeism and workforce retention), and to identify relevant contexts or circumstances when these mechanisms were likely to be ‘triggered’. These contexts and mechanisms became our ‘causative factors’ codes. Examples of preliminary ‘causative codes’ included organisation and training levels, doctors’ profession and identity. We simultaneously sought to identify ‘guiding principles’ and features underpinning the interventions and recommendations discussed mostly in policy document, reviews and commentaries. The juxtaposition of these ‘guiding principles’ (underpinning interventions and recommendations) with the ‘causative factors’, allowed us to identify particular configurations of mechanisms and contexts that were more likely to reduce or prevent mental ill-health in doctors, as well as important limits and barriers to the access and effectiveness of such interventions. An obvious example was the link between the ‘coherence’ guiding principle code and the ‘lack of trust towards employer and loss of control’ causative factors code. This link highlighted the importance for doctors to have confidence in an intervention, whereas included studies reported instances in which there was lack of coherence between an intervention and the context in which it was implemented (e.g. the employer or leadership level failing to properly communicate such intervention and/or to making it accessible to the workforce).
We compared and contrasted these configurations of context-mechanism-outcome configurations (CMOcs) with the evolving programme theory, so as to understand the place of and relationships between each CMOc within the programme theory. As the review progressed we iteratively refined the programme theory driven by interpretations of the data included in the literature, and by feedback received by our stakeholders (Figure 2).
FIGURE 2.
Programme theory development process. Reproduced from Papoutsi et al. 55 Contains information licensed under the Non-Commercial Government Licence v2.0.
We also coded articles for more descriptive categories, such as relevant background information, study characteristics and recommendations provided. The characteristics of the documents were summarised in Table 2 (see Appendices 2–4).
| Authors | Year | Country | Publication type | Method | Intervention level | Prevention | Screening | Therapy | Target | Career stage |
|---|---|---|---|---|---|---|---|---|---|---|
| Allen et al.64 | 2017 | Australia | A | Quantitative | Structural | ✗ | ✗ | Obstetrics, gynaecology | C, T | |
| Bakker et al.65 | 2000 | The Netherlands | B | Quantitative | Mixed | ✗ | GPs | C, T | ||
| Barbosa et al.66 | 2013 | USA | A | Quantitative | Structural | ✗ | Medical students | U | ||
| Bar-Sela et al.67 | 2012 | Israel | A | Quantitative | Structural | ✗ | Oncologists | T, C | ||
| Beckman68 | 2015 | USA | Com | Mixed | ✗ | ✗ | Primary care | T, C, U | ||
| Benson and Magraith69 | 2005 | Australia | Com | Mixed | ✗ | GP | C | |||
| Bitonte and DeSanto70 | 2014 | USA | Com | Mixed | ✗ | Medical students | U | |||
| Blais et al.71 | 2010 | Canada | B | Quantitative | Mixed | ✗ | Physicians | T, C | ||
| Boorman72 | 2009 | UK | D | Mixed | ✗ | ✗ | ✗ | NHS workforce | C, T | |
| Bragard et al.73 | 2006 | Belgium | Com | Mixed | ✗ | Oncologists | T, C | |||
| Brazeau74 | 2010 | USA | Com | Structural | ✗ | Medical students | U | |||
| Bugaj et al.75 | 2016 | Germany | A | Quantitative | Structural | ✗ | Medical students | U | ||
| Bugaj et al.76 | 2016 | Germany | B | Review | Mixed | ✗ | ✗ | Medical students | U | |
| Bughi et al.77 | 2017 | USA | A | Quantitative | Individual | ✗ | First-year medical students | U | ||
| Peile and Carter et al.78 | 2005 | UK | Com | Mixed | ✗ | ✗ | Medical students | U | ||
| Carvour et al.79 | 2016 | USA | B | Review | Structural | ✗ | Medical trainees | T | ||
| Chambers et al.80 | 2017 | New Zealand | B | Mixed | Structural | ✗ | Doctors and dentists | C | ||
| Chang et al.81 | 2013 | USA | B | Quantitative | Individual | ✗ | Medical students | U | ||
| Chaukos et al.82 | 2018 | USA | B | Quantitative | Mixed | ✗ | Residents | T, C | ||
| Clarke et al.83 | 2014 | UK | B | Qualitative | Mixed | Doctors | C, T | |||
| Clough et al.84 | 2017 | Australia | B | Systematic review | Mixed | ✗ | ✗ | Doctors | C, T | |
| Cockerell85,86 | 2016 Part I; 2017 Part II | USA | Com | Individual | ✗ | ✗ | Physicians | T, C | ||
| Cornelius et al.87 | 2017 | USA | A | Quantitative | Structural | ✗ | Emergency medicine residents | T, C | ||
| Cornwell and Fitzsimons88 | 2017 | UK | D | Mixed | NHS staff | C, T | ||||
| Davies et al.89 | 2016 | UK | A | Quantitative | Individual | ✗ | Doctors | C, T | ||
| de Vibe et al.90 | 2013 | Norway | A | RCT | Individual | ✗ | Medical and psychology students | U | ||
| Deng et al.91 | 2016 | China | B | Quantitative | Individual | ✗ | Oncology doctors and nurses | C, T | ||
| Department of Health and Social Care40 | 2008 | UK | D | Review | Mixed | ✗ | ✗ | ✗ | NHS doctors | C, T, U |
| Department of Health and Social Care92 | 2009 | UK | D | Mixed | ✗ | ✗ | ✗ | NHS workforce | C, T | |
| Devi93 | 2011 | USA | B | Review | Mixed | ✗ | Doctors and medical students | C, T, U | ||
| Dobkin and Hutchinson94 | 2013 | Canada | B | Literature review | Mixed | ✗ | Medical students | U | ||
| Doran et al.24 | 2016 | UK | B | Mixed | Structural | ✗ | GP | C | ||
| Downs et al.95 | 2014 | USA | B | Quantitative | Mixed | ✗ | ✗ | ✗ | Medical students | U |
| Dunn et al.96 | 2007 | USA | A | Quantitative | Mixed | ✗ | ✗ | ✗ | Physicians | C, T |
| Dyer97 | 2018 | UK | Com | Structural | ✗ | Doctors | T | |||
| Dyrbye et al.98 | 2016 | USA | A | RCT | Individual | ✗ | Physicians | T, C | ||
| Dyrbye et al.99 | 2017 | USA | B | Quantitative | Individual | ✗ | Medical students | U | ||
| Dyrbye et al.100 | 2017 | USA | B | Quantitative | Structural | ✗ | First-year medical students | U | ||
| Eisenstein101 | 2018 | USA | Com | Mixed | ✗ | Doctors | C, T, U | |||
| Epstein and Krasner102 | 2013 | USA | Com | Mixed | Physicians – other HCPs | T, C | ||||
| Ey et al.103 | 2013 | USA | B | Quantitative | Structural | ✗ | ✗ | Residents | T | |
| Ey et al.104 | 2016 | USA | A | Quantitative | Mixed | ✗ | ✗ | ✗ | Medical trainees and faculty | U, T, C |
| Feld and Heyse-Moore105 | 2006 | UK | A | Quantitative | Structural | ✗ | ✗ | Palliative care | T, C | |
| Firth-Cozens106 | 2007 | UK | B | Review | Mixed | ✗ | Psychiatrists (and doctors) | C, T | ||
| Flowers107 | 2005 | USA/UK | B | Review | Mixed | ✗ | Medical students | U | ||
| Foster et al.108 | 2012 | USA | A | Quantitative | Mixed | ✗ | Residents | T, C | ||
| Fothergill et al.109 | 2004 | UK | B | Systematic review | Mixed | ✗ | ✗ | Physiatrists | T, C | |
| Gardiner et al.110 | 2015 | USA | B | Quantitative | Mixed | ✗ | ✗ | ✗ | Family medicine residents | T, C |
| Gardiner et al.111 | 2013 | Australia | A | Quasi-experimental | Mixed | ✗ | GPs | C | ||
| Garelick et al.112 | 2007 | UK | B | Quantitative | Individual | ✗ | Doctors | T, C | ||
| Garside113 | 1993 | Canada | B | Review | Structural | ✗ | ✗ | Physicians (mostly primary health care) | T, C | |
| Gazelle et al.114 | 2015 | USA | Com | Individual | ✗ | ✗ | Physicians | T, C | ||
| Geller et al.115 | 2008 | USA | A | Mixed | Individual | ✗ | Clinical genetics | T, C | ||
| George et al.116 | 2012 | USA | A | Qualitative | Structural | ✗ | Year 1 medical students | U | ||
| Gerada117 | 2018 | UK | Com | Mixed | ✗ | Doctors | C, T | |||
| Goldhagen et al.118 | 2015 | USA | A | Quantitative | Individual | ✗ | Resident physicians | T, C | ||
| Goodman and Schorling119 | 2012 | USA | A | Quantitative | Mixed | ✗ | Physicians | T, C | ||
| Graham et al.120 | 2000 | UK | B | Quantitative | Structural | ✗ | Doctors | C | ||
| Gregory and Menser121 | 2015 | USA | A | Quantitative | Structural | ✗ | ✗ | Primary care | T, C | |
| Gulen et al.122 | 2016 | Turkey | B | Quantitative | Structural | ✗ | Emergency medicine residents | T, C | ||
| Gunasingam et al.123 | 2015 | Australia | A | RCT | Structural | ✗ | ✗ | Junior doctors | T, C | |
| Haizlip et al.124 | 2012 | USA | Com | Mixed | ✗ | Physicians and trainees | T, C | |||
| Hamader and Noehammer125 | 2013 | Austria | B | Qualitative | Mixed | ✗ | Medical students, occupational health and psychology | U, T, C | ||
| Haramati et al.4 | 2017 | USA | Com | Mixed | ✗ | ✗ | ✗ | Doctors and medical students | T, C, U | |
| Harrison et al.126 | 2014 | UK | B | Qualitative | Mixed | ✗ | ✗ | Doctors | C | |
| Haward et al.127 | 2003 | UK | B | Quantitative | Structural | ✗ | Cancer teams | C, T | ||
| Hegenbarth128 | 2011 | Switzerland | Com | Structural | ✗ | Doctors | T, C, U | |||
| Hill et al.129 | 2016 | UK | B | Systematic review | Mixed | ✗ | ✗ | Palliative care staff | T, C | |
| Hill and Smith130 | 2009 | USA | B | Quantitative | Mixed | ✗ | Residents in academic otolaryngology | T, C | ||
| Hlubocky et al.131 | 2016 | USA | Com | Mixed | ✗ | ✗ | ✗ | Oncology | C | |
| Hochberg et al.132 | 2013 | USA | A | Quantitative | Structural | ✗ | ✗ | Resident surgeons | T, C | |
| Holoshitz and Wann133 | 2017 | USA | Com | Individual | ✗ | ✗ | Physicians | C | ||
| Horsfall134 | 2014 | UK | D | Mixed | ✗ | ✗ | Doctors under investigation | C, T | ||
| Hotchkiss135 | 2008 | USA | B | Quantitative | Mixed | ✗ | Physicians | T, C | ||
| Howlett et al.136 | 2015 | Canada | A | Quantitative | Mixed | ✗ | Emergency medicine staff | |||
| Ireland et al.137 | 2017 | Australia | A | RCT | Individual | ✗ | ✗ | Doctors | T, C | |
| Isaksson Rø et al.138 | 2010 | Norway | B | Quantitative | Individual | ✗ | Physicians | T, C | ||
| Isaksson Rø et al.139 | 2012 | Norway | B | Quantitative | Mixed | ✗ | ✗ | Doctors | T, C | |
| Kemper and Khirallah140 | 2015 | USA | A | Quantitative | Individual | ✗ | Doctors and other health workers | C, T | ||
| Kjeldmand and Holmström141 | 2008 | Sweden | B | Qualitative | Structural | ✗ | GPs | C | ||
| Kötter et al.142 | 2015 | Germany | B | Qualitative | Structural | ✗ | ✗ | Medical students | U | |
| Krasner et al.143 | 2009 | USA | A | Quantitative | Individual | ✗ | Primary care | C | ||
| Kumar144 | 2011 | New Zealand | C | Structural | ✗ | Psychiatrists | CT | |||
| Kushnir et al.145 | 1994 | Israel | A | Quantitative | Individual | ✗ | Occupational health | C, T | ||
| Lapa et al.146 | 2016 | Portugal | B | Quantitative | Mixed | ✗ | Anaesthesia | T, C | ||
| Lederer et al.147 | 2008 | Austria | B | Quantitative | Structural | ✗ | Intensive care physicians/nurses | C, T | ||
| Lee et al.148 | 2016 | Taiwan | B | Quantitative | Mixed | ✗ | Hospital staff | C | ||
| Lefebvre149 | 2012 | Canada | Com | Mixed | ✗ | ✗ | ✗ | Residents/physicians | T, C | |
| Leff et al.150 | 2017 | USA | Com | Structural | ✗ | ✗ | End-of-life care physicians and social workers | T, C | ||
| Lim and Pinto151 | 2009 | New Zealand | B | Quantitative | Structural | ✗ | Radiologists | C, T | ||
| Linzer et al.152 | 2015 | USA | A | RCT | Structural | ✗ | ✗ | Primary care physicians | C | |
| Linzer et al.153 | 2001 | USA and the Netherlands | B | Quantitative | Mixed | ✗ | Physicians | T, C | ||
| Luthar et al.154 | 2017 | USA | A | RCT | Structural | ✗ | ✗ | Physicians | C, T | |
| Lyons and Dolezal155 | 2017 | UK and Ireland | Com | Mixed | ✗ | ✗ | C, T, U | |||
| Mache et al.156 | 2017 | Germany | A | Quasi-experimental | Mixed | ✗ | Oncology | C, T | ||
| Maslach and Leiter157 | 2017 | USA | B | Review | Mixed | ✗ | ✗ | C, T, U | ||
| McCartney158 | 2018 | UK | Com | Structural | ✗ | C, T | ||||
| McClafferty and Brown159 | 2014 | USA | B | Review | Mixed | Physicians/paediatricians | T, C | |||
| McCray et al.160 | 2008 | USA | B | Review | Mixed | ✗ | ✗ | ✗ | Students-doctors, HCPs | U, T, C |
| McCue and Sachs161 | 1991 | USA | A | Quantitative | Mixed | ✗ | ✗ | Paediatrics residents | T, C | |
| McKenna et al.162 | 2016 | USA | Com | Structural | ✗ | Medical students | U | |||
| McKevitt and Morgan163 | 1997 | UK | B | Qualitative | Structural | ✗ | ✗ | ✗ | Doctors | C, T, U |
| McKinley et al.164 | 2017 | USA | B | Review | Mixed | ✗ | ✗ | ✗ | Paediatric residency | T |
| McManus et al.165 | 2011 | UK | B | Quantitative | Individual | ✗ | Doctors | T, C | ||
| McNeill et al.166 | 2014 | Australia | B | Quantitative | Structural | ✗ | Medical students | U | ||
| Mechaber et al.167 | 2008 | USA | B | Quantitative | Structural | ✗ | ✗ | Generalist physicians | C | |
| Merteen et al.168 | 2014 | UK | B | Quantitative | Individual | ✗ | ✗ | ✗ | Doctors | T, C |
| Mehta et al.169 | 2016 | USA | A | Quantitative | Structural | ✗ | Palliative care team | T, C | ||
| Milstein et al.170 | 2009 | USA | A | Mixed | Individual | ✗ | ✗ | Paediatric house officers | T | |
| Montgomery et al.171 | 2011 | Greece/UK | B | Review | Mixed | ✗ | Hospital staff | T, C | ||
| Moutier et al.172 | 2012 | USA | B | Quantitative | Structural | ✗ | ✗ | Medical students, residents, faculty | U, T, C | |
| Murdoch and Eagles173 | 2007 | UK | A | Quantitative | Structural | ✗ | ✗ | Psychiatrists | C | |
| Myszkowski et al.174 | 2017 | France | B | Quantitative | Individual | ✗ | Internal medicine | T, C | ||
| NHS England175 | 2016 | UK | D | Mixed | ✗ | ✗ | ✗ | NHS workforce | ||
| Nielsen and Tulinius176 | 2009 | Denmark | B | Qualitative | Structural | ✗ | Nine GPs | T, C | ||
| Nomura et al.177 | 2016 | Japan | B | Mixed | Structural | ✗ | Paediatric residents | T, C | ||
| Oczkowski178 | 2015 | Canada | Com | Mixed | ✗ | Medical students/physicians | U, T, C | |||
| Oman et al.179 | 2006 | USA | A | RCT | Individual | ✗ | ✗ | Doctros/HCPs | C, T | |
| Paice et al.180 | 2004 | UK | B | Quantitative | Structural | ✗ | Doctors in training | T | ||
| Paice et al.181 | 2002 | UK | B | Quantitative | Mixed | ✗ | ✗ | ✗ | Doctors | C |
| Panagioti et al.47 | 2017 | UK | B | Systematic review and meta-analysis | Mixed | ✗ | ✗ | Physicians | C, T | |
| Penfold182 | 2018 | UK | Com | Structural | ✗ | Trainees | T | |||
| Pereira et al.183 | 2015 | Brazil | B | Qualitative | Individual | ✗ | Medical students | U | ||
| Prins et al.184 | 2007 | The Netherlands | B | Quantitative | Structural | ✗ | ✗ | Residents | T, C | |
| Rabin et al.185 | 2005 | Israel | Com | Mixed | ✗ | ✗ | ✗ | Doctors, mostly GP | T, C | |
| Raj186 | 2016 | USA | B | Systematic review | Mixed | ✗ | ✗ | ✗ | Physicians/residents | T, C |
| Ramirez et al.187 | 1996 | UK | B | Quantitative | Structural | ✗ | Gastroenterologists, surgeons, radiologists oncologists | C, T | ||
| Isaksson Rø et al.188 | 2016 | Norway | B | Qualitative | Structural | ✗ | Peer counsellors | C, T | ||
| Regehr et al.189 | 2014 | Canada | B | Review | Individual | ✗ | ✗ | ✗ | Physicians | T, C |
| Riley et al.190 | 2018a | UK | B | Qualitative | Mixed | ✗ | Mostly GPs | T, C | ||
| Riley et al.191 | 2018b | UK | B | Qualitative | Mixed | ✗ | ✗ | Mostly GPs | T, C | |
| Ringrose et al.192 | 2009 | The Netherlands | A | Mixed | Structural | ✗ | ✗ | Medical residents | T | |
| Ripp et al.193 | 2016 | USA | A | Quantitative | Structural | ✗ | ✗ | Residents | T, C | |
| Ripp et al.194 | 2017 | USA | C | Mixed | ✗ | ✗ | ✗ | Medical students | U | |
| Ripp et al.195 | 2015 | USA | B | Quantitative | Structural | ✗ | Internal medicine residents | T, C | ||
| Rippstein-Leuenberger et al.196 | 2017 | Switzerland | B | Quantitative | Individual | ✗ | Intensive care unit HCPs | C, T | ||
| Isaksson Rø et al.197 | 2008 | Norway | A | Quantitative | Mixed | ✗ | Doctors | C | ||
| Roberts et al.198 | 2002 | UK | C | Structural | ✗ | ✗ | ✗ | Psychiatrists | C, T, U | |
| Robertson and Cooper199 | 2010 | UK | D | Mixed | ✗ | ✗ | ✗ | NHS workforce | ||
| Rohland et al.200 | 2004 | USA | A | Quantitative | Individual | ✗ | Physicians | T, C | ||
| Rothenberger2 | 2017 | USA | B | Systematic review | Mixed | ✗ | ✗ | Physicians, medical students, trainees | C, T, U | |
| Runyan et al.201 | 2016 | USA | B | Quantitative | Structural | ✗ | Family medicine residents | T | ||
| Sallon et al.202 | 2017 | Israel | A | Quantitative | Mixed (mostly individual) | ✗ | ✗ | Hospital staff | C, T | |
| Sanchez et al.203 | 2016 | USA | B | Mixed | Structural | ✗ | Physicians | T, C | ||
| Schapira et al.204 | 2017 | Australia | Com | Mixed | ✗ | Oncology | T, C | |||
| Schattner205 | 2017 | Israel | Com | Structural | ✗ | Physicians | T, C | |||
| Schmitz et al.206 | 2012 | USA | Com | Structural | ✗ | Emergency medicine residents | T, C | |||
| Schneider et al.207 | 2014 | USA | B | Qualitative | Mixed | ✗ | ✗ | Physicians | T, C | |
| Scholz et al.208 | 2016 | Germany | A | Quantitative | Individual | ✗ | Medical students | U | ||
| Seoane et al.209 | 2016 | USA | B | Quantitative | Structural | ✗ | Medical students | U | ||
| Shanafelt et al.210 | 2012 | USA | B | Quantitative | Individual | ✗ | Surgeons | C | ||
| Shanafelt et al.211 | 2014 | USA | A | Quantitative | Individual | ✗ | ✗ | Surgeons | C | |
| Shapiro et al.212 | 2011 | USA | B | Review | Individual | ✗ | Physicians | C | ||
| Shapiro and Galowitz213 | 2016 | USA | Com | Structural | ✗ | ✗ | Doctors | T, C | ||
| Sharifi214 | 2012 | USA | B | Individual | ✗ | ✗ | Mental health care providers | C | ||
| Shiralkar et al.215 | 2013 | USA | B | Systematic review | Mixed | ✗ | ✗ | Medical students | U | |
| Siedsma and Emlet216 | 2015 | USA | A | RCT | Mixed | ✗ | ✗ | ✗ | Physicians | T, C |
| Sigsbee and Bernat217 | 2014 | USA | B | Review | Mixed | ✗ | ✗ | Physicians | T, C | |
| Slavin and Chibnall218 | 2016 | USA | Com | Mixed | ✗ | ✗ | ✗ | Medical students, residents, physicians | U, T, C | |
| Slavin et al.219 | 2011 | USA | Com | Mixed | ✗ | Medical students/practising physicians | U, T | |||
| Smith220 | 2016 | USA | A | Action research | Structural | ✗ | ✗ | Medical students | U | |
| Squiers et al.221 | 2017 | USA | B | Review | Mixed | Physicians | T, C | |||
| Talisman et al.222 | 2015 | USA | B | Mixed | Individual | ✗ | Physicians, health-care faculty | T, C | ||
| Tucker et al.223 | 2017 | Canada | A | Quantitative | Mixed | ✗ | Third year medical trainees | U, T | ||
| van Vliet et al.224 | 2017 | The Netherlands | A | Quantitative | Mixed | ✗ | Medical and nursing students | U | ||
| Verweij et al.225 | 2016 | The Netherlands | A | Mixed | Individual | ✗ | ✗ | GPs | C | |
| Waddimba et al.226 | 2016 | USA | B | Quantitative | Individual | ✗ | Physicians | T, C | ||
| Wald et al.227 | 2016 | USA/Israel | A | Mixed | Mixed | ✗ | Medical, nursing faculty and medical students | U, T | ||
| Warde et al.228 | 2014 | USA | B | Quantitative | Mixed | ✗ | Medical students | U | ||
| West et al.53 | 2014 | USA | A | RCT | Structural | ✗ | ✗ | Physicians | T, C | |
| West et al.229 | 2016 | USA | B | Systematic review and meta-analysis | Mixed | ✗ | ✗ | ✗ | Physicians | T, C |
| Wild et al.230 | 2014 | Germany | B | Quantitative | Mixed | ✗ | Medical and psychology students | U | ||
| Wilkie and Raffaelli231 | 2005 | UK | Com | Structural | ✗ | ✗ | C, T | |||
| Williams et al.232 | 1998 | UK | D | Systematic literature review and interviews | Mixed | ✗ | ✗ | ✗ | C, T | |
| Winefield et al.233 | 1998 | Australia | A | Quantitative | Individual | ✗ | GPs | T, C | ||
| Wolf234 | 1994 | USA | B | Review | ✗ | Medical students | U | |||
| Zhang et al.235 | 2017 | Canada | A | Quantitative | Structural | ✗ | ✗ | ✗ | Trainee surgeons | C, T |
| Zwack and Schweitzer236 | 2013 | Germany | B | Qualitative | Mixed | ✗ | ✗ | Physicians | C, T |
The aim of the analysis was to reach theoretical saturation, in that sufficient information has been captured to portray and explain the processes leading to mental ill-health and the mechanisms that can remedy this situation. Excerpts coded under specific concepts in NVivo were then exported into a Microsoft Word document (Microsoft Corporation, Redmond, WA, USA). Drawing on the analysis of the literature done in NVivo, Word documents were used as coding reports, to provide a more flexible space to test the viability of different CMOcs and build the narrative of the synthesis. This included adding explanatory text through abductive and retroductive analysis (see Step 5: synthesising the evidence and drawing conclusions).
Step 5: synthesising the evidence and drawing conclusions
We used a realist logic of analysis to analyse and synthesise the data. We used the coding of the included studies conducted on NVivo to draw relationships between contexts, mechanisms and outcomes, and to develop our initial programme theory. To develop and refine the CMOcs, and the programme theory, we made judgements about the relevance and rigour of content within included articles following a series of questions that are commonly used in realist reviews (see also Papoutsi et al. 54).
Relevance
-
Are the contents of a section of text within an included document referring to data that might be relevant to programme theory development?
Judgements about trustworthiness and rigour
-
Are the data sufficiently trustworthy to warrant making changes (if needed) to the programme theory?
Interpretation of meaning
-
If the section of text is relevant and trustworthy enough, do its contents provide data that may be interpreted as functioning as context, mechanism or outcome?
Interpretations and judgements about CMOcs
-
What is the CMOc (partial or complete) for the data?
-
Are there data to inform CMOcs contained within this document or other included documents? If so, which other documents?
-
How does this CMOc relate to CMOcs that have already been developed?
Interpretations and judgements about programme theory
-
How does this (full or partial) CMOc relate to the programme theory?
-
Within this same document are there data which inform how the CMOc relates to the programme theory? If not, are there data in other documents? Which ones?
-
In light of this CMOc and any supporting data, does the programme theory need to be changed?
We used abductive and/or retroductive reasoning (see Glossary), particularly to infer and elaborate on mechanisms (which often remained hidden or were not articulated adequately). This means that we followed a process of constantly moving from data to theory, in order to refine explanations about why certain behaviours are occurring, and tried to frame these explanations at a level of abstraction that could cover a range of phenomena or patterns of behaviour.
We sought relationships between contexts, mechanisms and outcomes both within the same included study and across different sources (e.g. mechanisms inferred from one study could help explain how contexts influenced outcomes in a different study). Therefore, we often synthesised data from different sources to compile CMOcs, as not all parts of the CMOcs were always articulated in the same source.
In summary, the process of evidence synthesis was achieved by the following analytic processes. 237
-
Juxtaposition of data sources: comparing and contrasting between data presented in different articles. For example, when data about mental ill-health in doctors in an in-depth qualitative source enabled insights into how outcomes are achieved, as described in a quantitative study.
-
Reconciling ‘contradictory’ or disconfirming data: when outcomes differ in apparently similar circumstances, further investigation is necessary to find explanations for why these different results occurred. This involved a closer consideration of context and what counts as context for different types of ‘problems’, in order to understand how the mechanisms triggered can explain differences in outcomes.
-
Consolidation of sources of evidence: when there are similarities between findings presented in different sources, a judgement needs to be made about whether these similarities are adequate to form patterns in the development of CMOcs and programme theory, or whether there are nuances that need to be highlighted, and to what end.
Chapter 3 Results
Results of the review
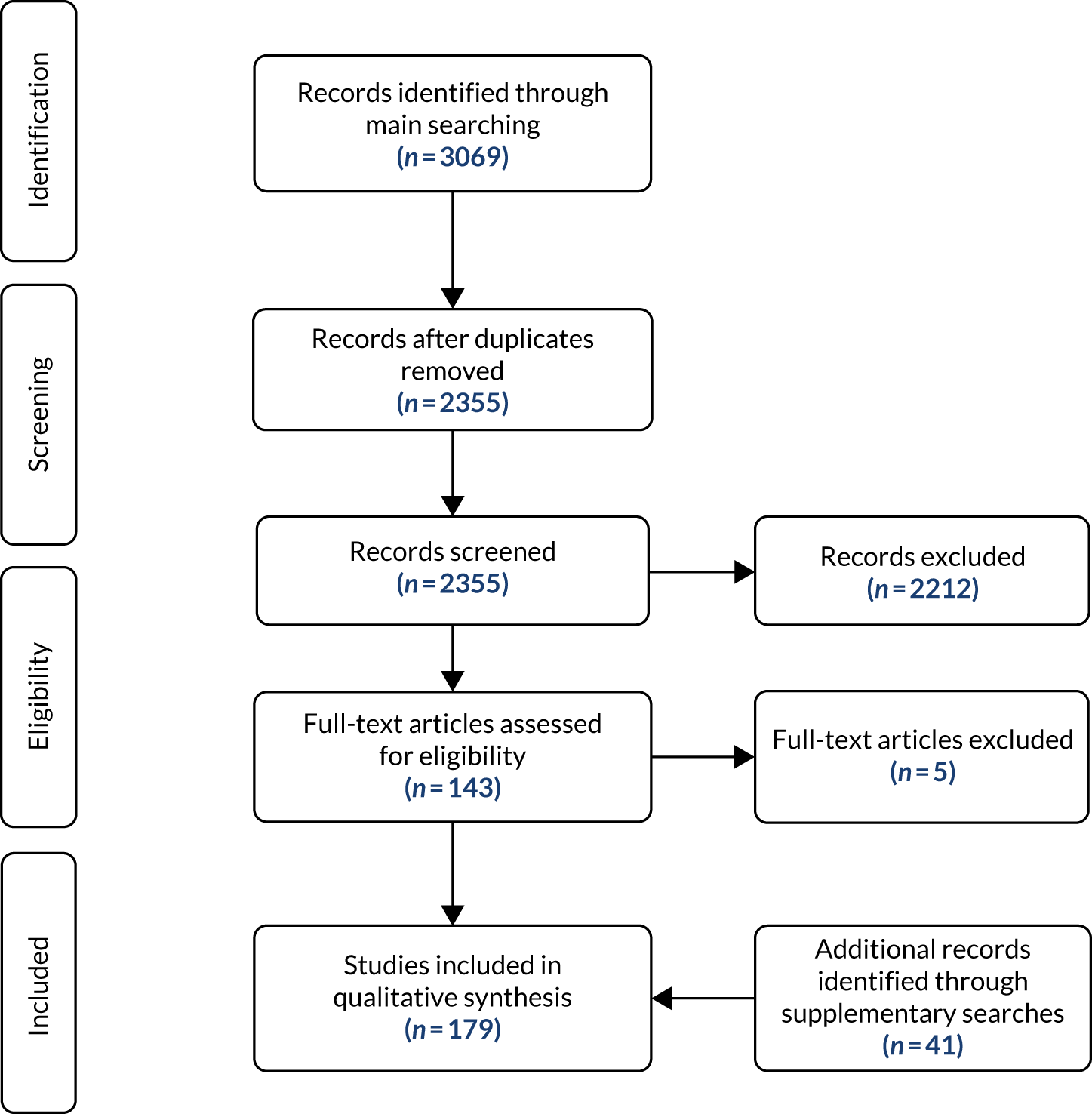
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram (Figure 3) reports the number of studies identified, included and excluded. Table 2 provides a description of the included studies. Of the 3069 records identified by the main searches, 179 articles met the inclusion criteria and were included in the study.
FIGURE 3.
The PRISMA flow diagram.
Characteristics of included studies
The country most represented in the included studies is the USA (45% of the included studies are published by authors working in the USA; 22.3% are from the UK). The majority of the included studies (74%) have been published in the 2010s. The most common study type is empirical research (which were not specific interventions, but included reviews, qualitative and quantitative studies that explored the issue of doctor’s mental ill-heath) (48%), followed by intervention studies (any empirical study based on an intervention) (27%), commentaries (20%) and policy documents (5%). In Realist synthesis findings, we use the term ‘grey literature’ to refer to both commentaries and policy documents. The most common level of intervention discussed in the included studies is mixed (46%), followed by structural (33%) and individual (21%). The majority of the interventions discussed are preventative, followed by treatment and screening. Most studies refer to doctors or physicians in general, rather than to specific specialties or career stages. Table 2 provides an overview of the studies included.
For a more in-depth description of these studies, see Appendices 2–4.
Cost information within included papers
As stated in the review protocol, our expectation was that the reporting of cost information in economic evaluations or other sources would make it unlikely to be able to link cost data directly to the context–mechanism–outcome configurations identified in the review. This expectation was proven to be founded, so consistent with the protocol we identified any source that made a reference to costs, including general estimates of financial losses due to mental ill-health and related problems, and the specific costs of interventions. This is presented in Appendices 2–4 in the last column of the tables with the heading ‘£’. When economic considerations were found in an included study, they were categorised into quantitative information (when figures are provided) or qualitative information (when no figures are provided). An example of quantitative information would be:
Together these factors have a serious impact on healthcare, contributing to an overall fall in provision of services with costs for absenteeism and high turnover for nurses alone estimated at $91,000–$98,000.17.
Sallon et al. 202
An example of qualitative information would be:
Thirty minutes allotted at least three times per week, built into students’ schedules, is more cost effective than eventual counseling, and more pragmatic as it attempts to prevent mental health issues.
Bitonte and DeSanto70
The majority of sources in which reference was made to costs contained unquantified claims of cost saving as a result of interventions (e.g. Bitonte and DeSanto70 and Ireland et al. 137), unquantified claims of increased direct and indirect costs as a result of burnout,2,84,194 or unquantified references to the ‘low costs’ of interventions. 123,154,172
One source quantified the direct costs of providing a ‘National Support Service’ for doctors134 and other sources contained summary statements of approximate costs of training that are ‘lost’ when health professionals leave their profession. 24,72,175 Two sources72,84 identified one or more studies in which the costs of an intervention were quantified. Inclusion of these cited sources was outside the scope of our review, but we note the observation in Clough et al. ’s 2017 systematic review84 that, even when cost information was reported, there was a lack of detail.
Less than one-quarter of included sources provided cost information [35/179 (19%)]. Of these, costs in five (3%) sources were quantified, 24 (13%) sources contained unquantified narrative claims and six (3%) sources contained a mix of quantified costs and unquantified narrative claims.
A minority of included sources quantified costs and there was a lack of methodological detail about how estimates of direct or indirect costs had been calculated. There was a paucity of detail about direct, indirect, or total costs that we could meaningfully extract. No included sources reported a health economic analysis (either cost–consequence modelling or prospective comparative evaluation), but it should be noted that our search strategy was not explicitly designed to locate such studies.
Realist synthesis findings
The presentation of the main findings from the analysis and synthesis of the literature reviewed is structured in five sections. Processes leading to mental ill-health in doctors focuses primarily on the processes leading to mental ill-health in doctors; Reducing mental ill-health: groups, belonging and relationality and Reducing mental ill-health: balance and timeliness focus on the factors which can reduce mental ill-health in doctors; whereas Implementation methods: engendering trust explores implementation methods (i.e. ideas on how to improve current interventions or the implementation of new ones). In Summary of the 19 CMOcs in four main groupings we provide an indication on how we have drawn on substantive theory.
These first four sections are organised as follows:
-
‘Overall narrative’ to introduce each CMOc or relevant group of CMOcs.
-
‘Realist analysis’: exposition of CMOcs.
-
‘Relevant extracts from papers included in the review’: illustrative quotations from the included literature that we have used to make our interpretations and inferences for each CMOc. Each of these quotation is contextualised, that is we provide a brief description of the type of source, country of origin, target population, career stage and year of publication. Some of these data consist of quotations presented in relevant included studies, other data come from interpretations drawn by the authors of these studies (e.g. in the discussion section). The full list of quotations extracted from the literature is available from the author on request.
The CMOcs collectively have been developed drawing on all sources included in this review: empirical studies and grey literature. After each specific CMOc, we provide an indication of the specific subset of resources which support it, for example to highlight that the supporting literature comes from a particular country or publication type.
Overview of all CMOcs
Box 1 provides an overview of all CMOs.
CMOc 1: underdeveloped workforce planning.
CMOc 2: normalisation of high workload.
CMOc 3: loss of autonomy.
CMOc 4: stigma towards vulnerability.
CMOc 5: hiding vulnerability.
CMOc 6: isolation.
Reducing mental ill-health: groups, belonging and relationalityCMOc 7: positive and meaningful workplace relations.
CMOc 8: functional working groups.
CMOc 9: balancing quality and quantity of time at work.
CMOc 10: limits of groups.
CMOc 11: ‘organic’ spaces to connect.
Reducing mental ill-health: balance and timelinessCMOc 12: recognising both positive and negative performance.
CMOc 13: balancing prevention of mental ill-health with promotion of well-being.
CMOc 14: acknowledging the positive and negative aspects of the profession.
CMOc 15: timely support.
Implementation methods: engendering trustCMOc 16: endorsement.
CMOc 17: expertise.
CMOc 18: engagement.
CMOc 19: evaluation.
Terminology
When it comes to stress, burnout and mental health in general, there is a plethora of different labels, mainstreamed and contested diagnoses, and unclear definitions – and their number continues to grow. 238 We have adopted the term ‘mental ill-health’ as an umbrella term to try to encompass this large variety of conditions and changeable labels. However, drawing on our analysis, we became aware that the term mental ill-health risks clouding important aspects of the issue we are investigating. Therefore, we have also adopted the term ‘vulnerability’ as a key term, which came up in the conceptual analysis. Vulnerability is a less clinical term and its meaning extends beyond mental ill-health, as it also allows us to focus on doctors’ suffering in general and on relevant contextual causative factors which may lead to a mental ill-health diagnosis. For example, vulnerability allows us to reflect on feelings of shame or fear that doctors who are facing psychological and emotional difficulties may experience due to external or internalised stigma (e.g. see CMOcs 4 and 5). Vulnerability lends itself to consider individual, organisational and wider sociocultural dimensions of the problem we are investigating. We discuss this idea further in How does existing substantive theory link with our findings?. For an in-depth recent reflection on the importance of the idea of vulnerability in medical education and clinical practice, we refer the reader to Piemonte. 239
Processes leading to mental ill-health in doctors
The studies included depict a complex picture of the different processes leading to mental ill-health in doctors, which mirrors the dimensions (individual biographical, organisational, professional and sociocultural) described in Chapter 1. However, the realist approach allowed us to uncover significant links between, or aspects of, these dimensions.
Alongside resources and workload, our analysis shows that there are other intertwined key organisational aspects that need to be considered to better understand and address the problem of mental ill-health in doctors: work structure, workforce planning and governance (see in particular Underdeveloped workforce planning and normalisation of high workload and Loss of autonomy).
Another important causative factor mentioned in the included studies is the medical culture and identity, and in particular the ideas of invulnerability, perfectionism, and the stigma around mental ill-health within the medical profession (see Stigma towards vulnerability).
Considerations of biographical aspects (i.e. related to individual doctors’ psychological predisposition to mental ill-health, personal contexts and/or traumatic events outside work) were often strongly intertwined with the dimensions described above. Therefore, we do not dedicate a specific CMOc to biographical factors alone.
Underdeveloped workforce planning and normalisation of high workload
A significant part of the included literature47,121 recognises that organisational aspects are associated with mental ill-health and can also represent a barrier to the access of interventions (if such interventions are available and accessible). Many studies suggest that both the individual doctors and the organisation have a role to play to address the issue of mental ill-health. 2,4,121,240 This argument is made also in relation to the organisation of medical schools. 142 We provide here two examples from a commentary and a research study respectively:
We are unlikely to ‘resilience our way out’ of this [the Mental Health of Medical Students, Residents, and Physicians] problem. Instead, multipronged interventions are needed that not only help individuals but also reduce the toxicity of the educational and clinical environments.
Slavin and Chibnall, commentary, USA, medical students, trainees, consultants, 2016218
. . . there is a general tendency to blame the person, rather than the job, for burnout. This [ . . . ] prevents a more realistic ‘both-and’ approach, which recognizes that both the person and the organization have a role to play in improving the workplace and people’s performance within it.
Maslach and Leiter, research, USA, doctors, consultants, trainees, medical students, 2017157
Among the organisational causes of mental ill-health in doctors, the included studies highlight the risks of ineffective workforce planning, alongside the lack of support for doctors experiencing work-related pressure. The studies which support this CMOc comprise research, commentaries and policy documents. Examples of underdeveloped work planning include demanding and rigid rotas, weak or absent ‘well-being’ services and weak or absent treatment support services. Examples of intervention include organisational measures to support workforce planning and well-being, and both the organisation and doctors recognising a shared responsibility for doctors’ well-being and patient outcomes.
CMOc 1: underdeveloped workforce planning
In a workplace in which basic support structures to enable doctors to do their job are not in place (context), doctors may feel that they must make up for the deficiencies of the organisation for patients and colleagues (mechanism). This may contribute to a toxic working culture in which overwork and its negative consequences are normalised (outcome).
Relevant extracts from papers included in the review
There were inconsistencies in the range of services offered by different NHS Trusts, and many services suffered from staff shortages and inadequate resourcing, with funding often historically based rather than related to current needs.
Boorman, policy document UK, NHS workforce, 2009. © Crown copyright72
Trainees [ . . . ] reported [ . . . ] seniors in a working culture ‘institutionally opposed’ to hearing complaints; doctors [ . . . ] emotionally blackmailed or bullied into reporting only timetabled hours, [ . . . ] individuals made to feel that working excessive hours was a personal failure of time management rather than the consequence of a systemic mismatch of workload.
Clarke et al. , research, UK, doctors, trainee, consultant, 201483
Physicians, it seems, have become quite skilled at sacrificing personal and family time in service to patients and the increasing demands of practice.
Beckman, commentary, USA, primary care, trainees, consultants, medical students, 201568
If burnout is a problem of whole health care systems, it is less likely to be effectively minimized by solely intervening at the individual level. It requires an organization-embedded approach. 47
Panagioti et al. , research, UK, physicians, consultants, trainees, 201747
The analysis also shows a link between inadequate workforce planning and support at the organisational level (which, as described by CMOc 1, can result in a toxic culture of normalisation of overwork) and doctors’ presenteeism, and/or their decision to leave the profession. This link is made explicit by CMOc 2. The studies which support CMOc 2 comprise research, commentaries and policy documents. As some quotations show, we did find some suggestions in the literature that women and trainees may feel extra pressure to work when ill. However, we do not have sufficient data to further stratify this CMOc.
Normalisation of high workload
CMOc 2: normalisation of high workload
When high workload and its negative consequences (e.g. distress, burnout) are normalised (context), overworked or sick doctors may feel they are letting down their colleagues and patients (mechanism). This can contribute to presenteeism (outcome) and associated negative consequences on mental health (outcome 1) and workforce retention (outcome 2).
Relevant extracts from papers included in the review
Importantly, presenteeism is unlikely to decrease if individuals are operating in environments where working through illness is viewed as ‘normal’ or, at worst, ‘necessary’ behaviour.
Chambers et al. , research, New Zealand, doctors and dentists, consultant, 201780
All doctors referred to the ‘burden’ which their absence placed on colleagues, who would be expected to assume their duties.
McKevitt and Morgan, research, UK, doctors, trainees, consultants, medical students, 1997163
Loss of autonomy
Another significant organisational factor that emerged strongly from the analysis of the included studies is the paradox that doctors increasingly have more responsibilities and tasks, but less control over their work. Doctors are trained to deal with complex issues and to be able to make difficult decisions. This requires a certain degree of work autonomy and control. However, the practice of medicine is increasingly subjected to stringent regulations and external control, and is becoming more clerical, leaving less space for clinical judgement and less time for working clinically with colleagues and patient-facing work (see also The relational nature of health, well-being and health care). The analysis shows that this loss of control can be linked to doctors perceiving a tension between their expectations and the reality of what their job entails. This CMOc is linked to the previous two CMOcs, as the increasing bureaucratisation of clinical work can also be perceived as signalling lack of appreciation of doctors and their job at an organisational level. Some studies also mention that technological innovation (e.g. electronic medical records may also play a role in the increasing bureaucratisation of clinical work72). The issue of electronic medical records is mostly present in US literature and is linked to billing practices. 221 However, lack of control and autonomy are also described in UK literature. 182 Crucially, the feeling of lack of autonomy and control is a potential cause of stress in itself, irrespective of other variables such as workload.
CMOc 3: loss of autonomy
When doctors experience lack of autonomy over their work (context 1) and when they feel that some aspects of their work are less meaningful (context 2), they may feel dissatisfied with their job (e.g. because they are unable to do the job they were trained for) (mechanism). This can make doctors more vulnerable to stress and mental ill-health, irrespective of workload (outcome).
Examples of contexts in which doctors feel more control include meaningful working relationship with colleagues and a sense of connectedness to the workplace and profession. These are discussed in Reducing mental ill-health: groups, belonging and relationality.
Relevant extracts from papers included in the review
Although most efforts at preventing physician burnout are focused on improving individual physician resilience, health care organizations are failing to change the system that is increasingly asking doctors to perform tasks, largely administrative in nature, for which they have no passion.
Squiers et al. , research, USA, physicians, trainees, consultants, 2017221
You spent more time ticking boxes than you did talking to the patients sometimes [ . . . ] that put more stress on me and I felt it affected my rapport with the patients.
Doran et al. , research, UK, general practitioners, consultants, 201624
This study confirms that autonomy and feeling well managed and resourced make a substantial contribution to overall job satisfaction. [ . . . ], the transfer of various responsibilities from clinicians to managers may undermine professional morale, as may the practice of establishing standards against which doctors’ performance is judged, without their involvement.
Ramirez et al. , research, UK, gastroenterologists, surgeons, radiologists oncologists, consultants, trainees, 1996187
Stigma towards vulnerability
The analysis identified a central taboo within the medical culture: the difficulty of managing the status of being a doctor, more specifically a too rigid demarcation between ‘being a doctor’ and ‘being a patient’. This demarcation appears to be endemic in the medical profession, but it can also be influenced by wider societal factors, including the fact that some patients may expect doctors to never be ill, or may find it counterintuitive and uncanny for a doctor to occupy simultaneously the role of doctor and of patient, and members of the medical profession may assume that patients have such expectations. Drawing on the analysis of the included studies, it is plausible to argue that most of the ideas of invulnerability of doctors and the stigma towards mental ill-health stem from a clear-cut distinction and separation between the role of doctors and that of patients. This distinction is coupled by an unrealistic expectation that doctors cannot/should not be patients (or that, if they become patients, their status of doctor is seriously under threat). Vulnerability, including emotional and psychological aspects of self-care for doctors, tends to be considered by other doctors as unprofessional. Although the focus of our research is mental health, it is important to highlight that, overall in the included studies, the culture of invincibility can refer to both physical and mental conditions.
Significant implications of this key element of medical culture include doctors’ lack of self-care skills; their reluctance to seek help, or their tendency to do so when it is ‘too late’ (often when the problems become so serious that it is no longer possible for doctors to hide them); and doctors’ difficulty in providing support to colleagues who are unwell. Moreover, in a similar vein to CMOc 3, this CMOc highlights that such medical culture, and the unrealistic strains and expectations that it puts on doctors from the medical school years, can be a potential cause of stress in itself, irrespective of other variables such as workload.
Context-mechanism-outcome configuration 4 has also strong links to the idea that preventative measures – from training in medical schools onwards – can counterbalance such dangerous medical culture. We will attempt to focus specifically on preventative measures in Reducing mental ill-health: balance and timeliness (see in particular CMOc 14: acknowledging the positive and negative aspects of the profession).
Context-mechanism-outcome configuration 4 focuses predominantly on the aspects of medical culture which may cause doctors to hide their difficulties (i.e. ‘being vulnerable is not professional for doctors’). CMOc 5 describes the same phenomenon, but it places the emphasis on the organisational stigma towards doctors’ vulnerability, which can explain further why doctors may tend to hide their difficulties and not seek support if available (e.g. they may be afraid to undergo severe sanctions and ultimately lose their job).
CMOc 4: stigma towards vulnerability
In a professional culture in which mental ill-health and vulnerability may be seen as unprofessional (context), doctors (and medical students) may feel ashamed (mechanism 1) or afraid (mechanism 2) of not living up to their professional identity if they experience mental ill-health (or other difficulties at work). This can lead doctors (and medical students) to adopt strategies which involve hiding their difficulties from themselves and colleagues (outcome).
Relevant extracts from papers included in the review
Illness doesn’t belong to us. It belongs to them, the patients. Doctors need to be taught to be ill. We need permission to be ill and to acknowledge that we are not superhuman.
McKevitt and Morgan, research, UK, doctors, trainee, consultant, medical student, 1997163
Perhaps symptomatic of the stigma attached to mental illness and the culture of invulnerability within medicine, some GP [general practitioner] participants described how they felt ashamed, embarrassed, humiliated and a sense of having failed, due to their perceived lack of resilience and inability to cope.
Riley et al. , research, UK, general practitioners, trainees, consultants, 2018191
. . . there is a cultural expectation within medicine that doctors do not expect themselves or their colleagues to be sick, with only one-third of junior UK doctors registered with a general practitioner [ . . . ],worries about confidentiality can lead doctors to take responsibility for their own care.
Montgomery et al. , research, UK/Greece, hospital staff, trainees, consultants, 2011171
Medical training emphasizes perfectionism, denial of personal vulnerability, and delayed gratification. Traits such as compulsiveness, guilt, and self-denial may facilitate success in medical education and training; however, in a long-term career, these same traits can fuel feelings of inadequacy. [ . . . ] these factors contribute to burnout.
Gazelle et al. , commentary, USA, physicians, trainees, consultants, 2015114
Medical students often avoid seeking help because they believe it might affect their future career plans or fear that they will be seen as ‘weak’ by others.
Shiralkar et al. , research, USA, medical students, 2013215
CMOc 5: hiding vulnerability
When there is mental health support available for doctors (context 1), doctors who understand the system and that confidentiality is difficult to achieve (context 2) may fear that seeking support could jeopardise their career (mechanism) and so they may hide their distress rather than seek support (outcome).
Relevant extracts from papers included in the review
. . . this study reported that only 1 in 4 of these at-risk surgeons sought professional help. Those who did not seek help said their reticence to do so (among other reasons) stemmed from the requirement of some state-licensing boards to report their personal psychiatric/psychological care.
Hochberg et al. , intervention, USA, surgeons, trainees, consultants, 2013132
. . . evidence suggests that providers experiencing suicidal thoughts may be less likely to seek mental health care because of concerns about their medical licensure. (The same providers are, however, more likely to self-prescribe antidepressants).
Carvour et al. , research, USA, medical trainees, 201679
[Doctors] do not ask for treatment early, if at all. The system [ . . . ] may militate against their being able to do this easily. There are too many worries about confidentiality and potential impact on career and colleagues for many doctors to do what they would tell their patients to do.
Department of Health and Social Care, policy, UK, doctors, trainees, consultants, medical students, 2008. 40 © Crown copyright
Isolation
This last CMOc of Processes leading to mental ill-health in doctors links, and makes more explicit, significant patterns in the previous five CMOcs. Taken together, CMOcs 1–5 may point to a risk of isolation among doctors (which may be the outcome of organisational, professional culture, sociocultural and individual dimensions). Linking to CMOcs 1–2, doctors may feel isolated as a result of deciding to take sickness absence, and experiencing fear and guilt for letting down colleagues, managers and patients, even if their sickness absence may also depend on other factors (e.g. lack of work planning measures and lack of support). CMOc 3 highlights how governance and regulatory practices can challenge doctors’ autonomy, increase clerical work and also increase dissatisfaction. One of the consequences of this management regimen can be a feeling of being isolated or disconnected from the essence of their job. Finally, CMOcs 4 and 5 show that doctors inhabit a professional and organisational milieu of stigma (external and internalised), whereby challenges and vulnerabilities (including, but not limited to, CMOcs 1–3) can be experienced as a potential threat to their identity as doctors. In this case, the isolation may occur because doctors may fear losing their status, and their job if they seek support, or try to talk about such challenges, or admit to themselves that they are experiencing these challenges. This multifaceted isolation can also lead to a lack of trust towards co-workers in the work environment (e.g. colleagues, managers, regulations, support). Included studies highlight not only a lack of support for doctors (see CMOc 1: underdeveloped workforce planning), but also that doctors may not seek support even if they are aware of its existence because of lack of trust [e.g. they may see this support as an additional, potentially also punitive or individual-blaming, form of control and management (CMOc 5)]. 191 Isolation can also contribute to explaining why interventions that target the individual level only (e.g. individual resilience training; see also Chapter 1) seem less successful than expected. By targeting and placing the emphasis on the individual and their own skill set, such interventions may feed doctors’ feelings of isolation.
CMOc 6: isolation
When doctors work in physical and emotional isolation (context) they are likely to feel less supported by their colleagues and/or their employing organisation (mechanism 1) and/or mistrust of these groups (mechanism 2). This can make doctors more vulnerable to work-related pressure and mental ill-health (outcome).
Relevant extracts from papers included in the review
Physicians are increasingly isolated – physically because they work in diverse settings or emotionally because there is little time for learning about each other’s stresses, discussing challenging professional situations, and developing personal connections. This sense of isolation may be exacerbated as [ . . . ]electronic documentation is rapidly replacing collegial face-to-face communication. [ . . . ].
Epstein and Krasner, commentary, USA, doctors and other health-care professionals, 2013102
[ . . . ] disconnection is the single greatest threat to our efforts to foster resilience and to promote wellness in medical education.
McKenna et al. , commentary, USA, medical students, 2016162
Medicine is a collective venture (Kivimaki et al. , 2001) and when working relationships become impaired the ability to manage one’s tasks as a doctor in a complex working environment becomes almost impossible.
Davies et al. , intervention, UK, doctors, consultants, trainees, 201689
Reducing mental ill-health: groups, belonging and relationality
The relational nature of health, well-being and health care
As discussed in Processes leading to mental ill-health in doctors, the included literature suggests that a work environment which encourages or indirectly leads to isolation may make doctors more vulnerable and stressed, and it can therefore represent an important causative or aggravating factor of work-related pressures. Moreover, cultural and professional identity aspects (e.g. the medical culture of invincibility and perfectionism) can contribute to this isolating environment.
In this section, we move from the causes to the factors which can reduce mental ill-health in doctors. The analysis of the included studies suggests that a work environment characterised by a strong sense of connectedness, collegiality and community can reduce the incidence and the intensity of doctors’ mental ill-health. Collegiality can occur at different levels (e.g. with colleagues from the same specialty, from different specialties and from different professional groups). 185 Although resilience training for individual doctors – and other approaches which target only the individual – may work in certain circumstances (see Limits of groups), the analysis shows that resilience is more a relational than an individual feature. This argument is supported by different types of studies: empirical research,176,202 reviews2 and commentaries. 162
Based on our analysis, we can highlight the functions of groups and connectedness (from specific support groups to general relationship and connectedness in the workplace), that is why and how groups and relationality can reduce the incidence and intensity of doctors’ mental ill-health, and/or contribute to ‘genuine’ resilience of the workforce. Group support and a relational work environment have the following interrelated functions:
-
Foster a sense of belonging in doctors to their teams/colleagues, and to the profession (belonging and connectedness are prerequisites to individual self-fulfilment and are foundational to individual resilience). 162
-
Foster a sense of meaning in work (which can counterbalance the challenges identified in CMOcs 1–3).
-
Contribute to alleviate the stigma towards mental health and vulnerability in the medical culture. Groups can normalise, rather than stigmatise, mental ill-health issues. They allow doctors experiencing such challenges to be listened to and be understood by peers, and they offer the opportunity to the whole group to recognise that such challenges are not unusual, but tend to be shared (see CMOcs 4 and 5).
-
Protect individuals and groups from work-related pressure by fostering mutual support and ‘mutual care’ (e.g. doctors can recognise sign of stress in their colleagues and support them) (see CMOcs 4 and 5). 131
-
Offer more opportunities for improvement of care provided to patients (e.g. doctors can share challenging/meaningful experiences increasing professional confidence) and mutual learning.
It is important to clarify that our analysis refers to groups which function well. Dysfunctional groups will not necessarily provide the possible benefits we have listed in the bullet points above. It is beyond the scope of this review to provide exact details of what is needed for a group to function well. However, we do provide some references and points to consider in How does existing substantive theory link with our findings?, particularly in relation to the social identity approach (see Summary of the 19 CMOcs in four main groupings).
CMOc 7: positive and meaningful workplace relations
Positive and meaningful workplace relations (context) can foster a sense of belonging between colleagues and towards the medical profession (mechanism). This can lead to an increased capacity to work under pressure (outcome).
Relevant extracts from papers included in the review
In medicine, group membership, or ‘being part of the club,’ can serve as a much-needed safety net when adversity overwhelms a learner’s individual resilience.
McKenna et al. , commentary, USA, medical students, 2016162
According to qualitative studies, being part of a Balint group helped GPs [general practitioners] recognize their professional identity and rediscover the joy of being a physician [ . . . ] participation in a Balint group reduced burnout levels and sensitivity to stress among GPs.
Bar-Sela et al. , intervention, Israel, oncologists, trainees, consultants, 201267
Debriefing programmes are low cost, easily coordinated and potentially have the capacity to offer institutional support throughout the course of an internship. The availability of personnel trained in debriefing would be a valuable asset to any unit supervising training junior doctors.
Gunasingam et al. , intervention, Australia, doctors, trainees, 2015123
Efforts to improve collegiality can provide better resident and staff well-being and also improve health care provider outcomes.
McKinley et al. , research, USA, paediatric residents, 2017164
Success of the palliative care service is contingent on the cohesion and wellbeing of the team members, especially as caseloads and job demands have increased.
Mehta et al. , intervention, USA, palliative care team, trainees, consultants, 2016169
Medical residency is undoubtedly stressful, and it has been compared to surviving a dysfunctional family. Negative relational experiences have been shown to affect both current learning and future patient care.
Foster et al. , intervention, USA, doctors, trainees, consultants, 2012108
CMOc 8: functional working groups
Working in functional groups (context) can make doctors feel more supported (mechanism 1) and more at ease with vulnerability (mechanism 2). This can normalise vulnerability (outcome 1) and reduce the stigma around mental ill-health (outcome 2).
Relevant extracts from papers included in the review
Once individuals felt safe in the group, they would share more personal matters such as fear of overload when faced with a run of deaths or profound feelings of loss at the death of a patient they knew well and sadness for the family’s grief.
Feld and Heyse-Moore, intervention, UK, palliative care, trainees, consultants, 2006105
[ . . . ] in a Balint group, the doctor can learn to recognise personal reactions, develop an awareness of the early signals of distress, and internalise what is learnt from the interaction with other participants. [ . . . ]debrief, ‘normalise’ emotional reactions, reduce stress by sharing experiences, reinforce the value of their work, and reformulate boundaries.
Benson and Magraith, commentary, Australia, general practitioner, consultants, 200569
Team working was beneficial to the mental health of its members, allowing problems and pressures to be shared, and individuals to be supported by colleagues.
Haward et al. , research, UK, cancer teams, consultants, trainees, 2003127
Seeing my own struggles/thoughts amongst the topics discussed – makes you feel less alone.
Tucket et al. , intervention, Canada, medical trainees, 2017223
Balancing quality and quantity of time at work
Reducing doctors’ working hours would appear to be a reasonable way to address work-related stress and burnout, but some included studies, mostly research53 and commentaries,162 suggest that reduced hours may increase a sense of disconnection from work, which can in turn exacerbate working pressure and mental ill-health outcomes (see Isolation). Moreover, discussion with stakeholder groups suggested that approaches based solely on a quantitative reduction of working time may foster a competition between ‘life’ and ‘work’, whereby the former may be experienced to be better than the latter (or the latter to become a ‘problem to be avoided or escaped’). Therefore, focusing also on quality of work (i.e. making work a functional and meaningful part of doctors’ lives and fostering a sense of meaning within, rather than outside work) appears to be a stronger strategy to tackle work pressures and mental ill-health. A relational work environment (discussed in The relational nature of health, well-being and health care) can help to increase job satisfaction and meaning. The relational nature of medicine extends also beyond colleagues and the health-care workforce. For many doctors, spending time with patients can represent another key relational factor,190 which creates meaning within work (see Loss of autonomy and The relational nature of health, well-being and health care).
Thus, resilience and other ‘wellness’ interventions in medical education and clinical practice, which focus less on the competition between work and life, and more on making work a functional and enjoyable part of doctors’ lives, may be more likely to achieve their intended outcomes of reducing stress and mental ill-health. Examples of interventions include reduction of working hours or similar ‘work–life balance’ interventions and participation in mentoring networks; or reduction of working hours and more time with patients (i.e. patient-centred care, if this is part of the deontology/ethos of the specialty).
CMOc 9: balancing quality and quantity of time at work
When doctors (for different reasons) have less connectedness and meaning at work (context), they may feel they can find fulfilment only outside work (mechanism), making it less likely that their condition will improve (outcome).
Relevant extracts from papers included in the review
Although receiving unstructured protected time offered some benefits by itself, the advantages of the small-group curriculum were greater and persisted after the intervention concluded, particularly for meaning and the closely associated interpersonal aspects of burnout.
West et al. intervention, USA, physicians, trainees, consultants, 201453
[ . . . ] despite good intentions, duty hours limitations have produced little concrete benefit and have created many unintended negative consequences. Like many things in medicine, duty hours must be carefully titrated to strike a balance between resident wellness, patient safety, and quality education.
Lefebvre, commentary, Canada, physicians, trainees, consultants, 2012149
A straightforward practical implication is that to prevent burnout, GPs [general practitioners] should be provided with the opportunity to restore the balance in the doctor-patient relationship.
Bakkar et al. , research, the Netherlands, general practitioners, consultant, trainees, 200065
Limits of groups
In realist reviews, ‘knowing how social programmes work involves tracing the limits on when and where they work’. 62 As illustrated in The relational nature of health, well-being and health care, belonging and relationality appear to be key to a healthy work environment and to the success of interventions aiming to address mental ill-health. However, the literature – mostly research studies – also suggests that in certain delicate circumstances individual one-to-one support may be more appropriate than group support approaches, particularly in cases of peer (same specialty) and immediate colleague group support. These circumstances include significant confidentiality issues; doctors being investigated; doctors facing litigation; and doctors experiencing death of patient or colleague. However, concerning the experience of death, we also found empirical evidence that functioning group support could also work, for example (taken from evidence for CMOc 9):
Once individuals felt safe in the group, they would share more personal matters such as fear of overload when faced with a run of deaths or profound feelings of loss at the death of a patient they knew well and sadness for the family’s grief.
Feld and Heyse-Moore, intervention, UK, palliative care, trainees, consultants, 2006105
Highlighting the limit of group interventions is important in the light of the medical culture discussed earlier (see CMOc 4: stigma towards vulnerability and CMOc 5: hiding vulnerability), in which vulnerability is deemed to be unprofessional and stigmatised. Arguably, such medical culture represents an additional factor which may complicate group (support) dynamics, particularly when there are confidentiality issues and delicate distressing situations. Moreover, broadly speaking, certain forms of individual one-to-one support could also work as a proxy to promote or improve connectedness in a work environment, as the person offering support could help the individual doctors receiving it to develop more connectedness and relationship in the workplace, for example:
[ . . . ] tailored mentorship programs for individual residents would allow not only monitoring of stress tolerance and workload imbalance but also development of resident–faculty interactions that might help to bridge existing generation gaps.
Nomura et al. , commentary, USA, primary care, medical students, trainees, consultants, 2016177
CMOc 10: limits of groups
Sick doctors (and medical students) with particularly delicate circumstances (context) may not feel safe to share their problems (mechanism 1) and/or may not identify with the other group members (mechanism 2). This can result in a dysfunctional group (outcome 1) and intensification of mental ill-health in doctors (outcome 2).
Relevant extracts from papers included in the review
[ . . . ] there are situations where a particular clinician has been at the ‘sharp end of an error,’ and such a circumstance is not conducive to group peer support.
Shapiro and Galowitz, commentary, USA, doctors, trainees, consultants, 2016213
I felt that my feelings were somewhat minimized. Because I was not yet having severe behavioral problems? Because I was still functional, had a good job and got along great with my staff? Experiencing death and grief – heavy loads of responsibility were not enough.
Sanchez et al. , research, USA, physicians, trainees, consultants, 2016203
[ . . . ] the experts interviewed pointed out the importance of intervention options at the first signs of psychological problems to avoid stigmatization and sanctions, to provide a quick anonymous psychological counselling outside of the clinic as well as to improve social acceptance of psychosocial problems.
Hamader and Noehammer, research, Austria, medical students, occupational health and psychology, 2013125
Focus group evaluation demonstrated that students greatly valued the Facebook [Facebook, Inc., Menlo Park, CA, USA; www.facebook.com] group, particularly the YouTube [YouTube, LLC, San Bruno, CA, USA; www.youtube.com] testimonials containing advice from older students. [ . . . ] The Facebook platform prompted peer-to-peer discussions about stress and engendered friendships amongst students, while also offering the benefit of anonymity.
George et al. , intervention, USA, medical students, 2012116
‘Organic’ spaces to connect
Some research studies and commentaries provide insight on how organisations could foster relationality. These studies cover both the medical school and the clinical work environments. The overarching point made is that functioning groups are more likely to occur if they are not enforced. Initiatives to foster relationality and belonging are more likely to be successful if relationships between colleagues are not externally imposed through mandatory activities. The literature suggests steps that can be made in this direction. For example, programmes and institutions can create – or protect – psychologically safe spaces, formal and informal opportunities that encourage medical students and doctors to communicate (e.g. share work experiences, difficult cases), without fear of being judged, and to develop collegiality and connectedness, and to learn from each other. This will probably allow doctors and other colleagues to share each other’s experiences, ways of working and values, leading to the emergence of spontaneous connections. More specific examples of promoting connectedness include spaces such as doctors’ mess; newsletters and other opportunities for doctors to share stories; and virtuous humour. Overall, we did not find a significant number of studies to support this idea. Given the limited number of data informing this CMOc, we are not able to draw conclusions around the circumstances in which protected times and psychologically safe spaces are more likely to trigger positive responses. It could be hypothesised that positive relationships between colleagues may need to be in place for protected times and spaces to work towards intended outcomes. However, this idea (alongside CMOc 10) can also serve as a reminder that it takes time and commitment (individual and organisational) to build relationships, and one intervention might not make a difference. For example, as a general practitioner (GP) interviewed in one of the included studies pointed out:
I work in a fantastic team. I love all my partners. I love the team I work with. And that’s something that we have created over, over that, all those years. [ . . . ] it’s not just something I parachuted into; it’s been carefully created by me and my partners over that time.
Riley et al. , research, UK, GPs, trainees, consultants, 2018190
Data also show that certain specialties such as palliative care tend to have more standard support groups105 and debriefing. 150 Chapter 4 will present some key methodological principles that can guide the implementation of interventions, including those that foster connectedness.
CMOc 11: ‘organic’ spaces to connect
If there are protected times and psychologically safe spaces for students/doctors to congregate within the confines of the work environment (context), students/doctors are likely to bond over whatever is most important to them at that time (mechanism). This may improve connectedness (outcome).
Relevant extracts from papers included in the review
Medical schools often facilitate group identification of their students by setting up activities in which students cooperate to work towards a common goal. However, the competitive nature of medical school may undermine a shared group identity [ . . . ]. Strategies such as utilising a pass/fail [ . . . ] may reduce this competitive atmosphere.
Research, Australia, medical students, 2014166
Sharing a laugh is a simple pleasure and a shared experience which brings people together. In a place where life and death hang in the balance, it is easy to become self-important, arrogant, or closed-minded. By poking fun at ourselves, humor can keep us humble, and [ . . . ] together.
Oczkowski, commentary, Canada, physicians, trainees, medical students, 2015178
Writing about our experiences as oncologists can help us understand them with greater clarity. [ . . . ] Reading and writing narratives in oncology may strengthen us emotionally, allowing us to be more fully present for our patients and our loved ones.
Schapira et al. , commentary, Australia, oncologists, trainees, consultants, 2017204
Reducing mental ill-health: balance and timeliness
Balancing negative with positive
In the NHS, and other health-care services, it is common to report mistakes made by health-care staff or anything else that harms, or comes close to harming, patients. This practice mirrors cultural trends and norms to place more emphasis on identifying and examining failures and mistakes than on recognising and reflecting on positive practice and outcomes. Such ‘negativity bias’ (which often starts to be cultivated in medical schools124) can help to improve patient outcomes, but it also contributes to pressing concerns about workplace cultures of blame, stress and burnout. This negativity bias may also be reinforced by the bureaucratisation of medical work described in Loss of autonomy (i.e. the governance and regulation of clinical work may encourage more focus on mistakes than on positive performance). It can also be linked to the medical culture of invincibility described in Stigma towards vulnerability.
On the other hand, positive feedback can improve learning, morale and sometimes performance in health-care environments. In a similar vein, actively promoting and focusing on the well-being – including the ‘mental health’ (as opposed to mental ill-health) – of doctors is equally important as developing measures to deal with mental ill-health.
A focus on the ‘positive’ can inform preventative measures, which may reduce the incidence and intensity of mental ill-health in doctors. For example, promoting health and well-being may result in the development of measures to tackle underdeveloped work planning and normalisation of overwork described in CMOc 1: underdeveloped workforce planning and CMOc 2: normalisation of high workload.
CMOc 12: recognising both positive and negative performance
When supervision and feedback recognise both positive and negative performance and promote doctors’ (and students’) learning from both of these (context), doctors (and students) may feel more fairly treated (mechanism 1) and more inclined to value their colleagues and employing organisation (mechanism 2), potentially leading to more connectedness and engagement at work (outcome 1) and a more supportive work culture (outcome 2).
CMOc 13: balancing prevention of mental ill-health with promotion of well-being
In a work environment that actively demonstrates the importance of the balance between health and well-being with dealing with stress and mental ill-health (context), doctors (and students) are more likely to feel that caring about their own well-being is legitimate (mechanism 1) and less afraid to acknowledge vulnerability (mechanism 2). This can contribute to a de-stigmatisation of mental ill-health and vulnerability (outcome).
Relevant extracts from included studies
We must continue to improve our care of patients through evaluation of error and flawed judgment. But [ . . . ] we can balance their effects by making a conscious effort also to notice the positive. Following the lead of appreciative inquiry, we can recognize successes and seek to learn how they are achieved.
Hazlip et al. , commentary, USA, consultants, trainees, 2012124
The term ‘mental health’ has come to imply mental illness, not health, and the study of pathology has far outstripped any exploration of disease prevention and health promotion in psychiatry.
Flowers, research, USA/UK, medical students, 2005107
We recommend the following changes to the medical education system to promote students’ well-being and flourishing: [ . . . ]
Encourage and celebrate achievement [ . . . ]
Promote positive emotions [ . . . ]
Slavin et al. , commentary, USA, medical students, trainees, 2011219
We must allow doctors to become patients without the fear of sanctions or blame, and afford them the same compassion as they are expected to give to their own patients.
Gerada, commentary, UK, consultants, trainees, 2018117
Acknowledging the positive and negative aspects of the profession
The integration in the medical curriculum, and in further professional development training, of open discussions about the stress and difficulties doctors will probably encounter in their career, the difficult decisions they may make and the possibility of making mistakes can better prepare doctors to practise their work.
Data from included studies show that doctors may encounter difficulties transitioning from medical education to clinical work, particularly76,170,209 the emotionally demanding nature of the work, which includes long working hours and complicated rotas that frequently change at short notice;168 being exposed to complex biopsychosocial situations, including seeing patients with symptoms that are not part of a recognised disease entity; 67,147 being exposed to death and dying;67,91,169,176 being exposed to aggressive interactions with patients;106,241 and doctors suffering from substance abuse206 and financial concerns. 79,190
Our analysis shows that developing such awareness is portrayed as a constructive way to train doctors to deal with difficulties. Our analysis shows that developing awareness of the challenges doctors face in the workplace can be an important first step in preventing mental ill-health. The risk of developing, and consequences of, mental ill-health can increase where the relationship between workplace stressors and the development of mental ill-health is unacknowledged or silenced (see Stigma towards vulnerability and Isolation). It is therefore important to acknowledge this problem, with the provision of training being one way of doing so. This awareness and preparedness can, in turn, contribute to fostering a culture of acceptance towards work pressure and mental ill-health, improve relationships with colleagues and decrease stigma. CMOc 14 is a reformulation of the concepts in CMOc 4 (about the danger of a professional culture of invincibility) from a preventative point of view (i.e. it suggests what can be done to prevent stigma towards mental ill-health in medicine). The idea of introducing more awareness about the difficulties of the medical profession is intended to be complementary to Stigma towards vulnerability, rather than in contradiction. In the light of CMOcs 12 and 13, it is plausible to argue that anticipatory training that seeks to balance the positive and negative aspects of a career in medicine may put present and future doctors in a better position to navigate their career, and to be potentially more equipped to deal with work-related pressures and vulnerability.
CMOc 14: acknowledging the positive and negative aspects of the profession
When both the positive and negative aspects of a medical career are recognised (context), doctors (and medical students) may feel less inadequate and helpless when they or their colleagues experience stress or mental ill-health (mechanism). This may lead to increased capacity to deal with work pressure (outcome 1) and to recognition and acceptance of vulnerability (outcome 2).
Examples of interventions
-
Role models.
Relevant extracts from included studies
From medical school onwards, doctors need to be enabled to understand the nature of the stress that a career in medicine can bring, and the possible impact on their health, their relationships and their work. [ . . . ] [and] acquire skills that help deal with stressors without resorting to counterproductive ways of coping.
Barbosa et al. , intervention, USA, medical students, 201366
[ . . . ] doctors [ . . . ] find that their training has not prepared them for the demands of a health service that is becoming increasingly complex and less cohesive with [ . . . ] less autonomy and increased accountability. [ . . . ] The answer is not to be found within individuals but between individuals and the culture they find themselves in.
Davies et al. , intervention, UK, doctors, trainees, consultants, 201689
Educating medical students about the complexity and challenges of medicine, emphasizing the normality of feelings of vulnerability and stress, the acceptability of acknowledging difficulty as the first step in managing it and that seeking support is adaptive rather than a sign of weakness.
Meerten et al. , research, UK, doctors, trainees, consultants, 2014168
It is advantageous to obtain a clear understanding and have realistic expectations about what it takes to become a doctor and the road that has to be travelled prior even to entering medical school.
Wolf, research, USA, medical students, 1994234
[ . . . ] realistic expectations of a modern career in medicine underpin contentedness in the medical workplace. Medical schools must work closely with postgraduate deans responsible for junior doctors to ensure that undergraduate education encompasses [ . . . ] also the appropriate processes to prepare doctors for the rapidly changing environment of medical practice.
Peile and Carter, commentary, UK, medical students, 200578
A culture in which trainees and faculty speak openly about the challenges of training and its anticipated impact will serve to promote wellness and destigmatize stress-related concerns.
Ripp et al. , commentary, USA, medical students, 2017194
Timely support
The timeliness of support can make a significant impact on its success and the health of doctors. This appears to be particularly the case in certain contexts when doctors may be particularly vulnerable (e.g. when doctors experience traumatic events, such as the death of a colleague, sickness absence, when doctors attempt suicide or during the training period). This CMOc is particularly linked with CMOc 10. Some included studies (policy reports mostly72,92) argue that the value of timeliness can also be financial (i.e. in the long term, intervening early may be a more cost-effective strategy than dealing with worse outcomes or even the death of a doctor).
CMOc 15: timely support
Timely support when doctors (and students) are particularly vulnerable (e.g. after a suicide attempt, death of a colleague, addiction) (context) may represent their only source of hope (mechanism) and reduce the intensity of mental ill-health and its related outcomes, including suicide (outcome).
Relevant extracts from included studies
Approximately 20% of survivors of unsuccessful suicide attempts will attempt harm within a year and as a group they are twice as likely to succeed in committing suicide compared with those who have never attempted to take their own life.
Horsfall, policy, UK, doctors under investigations, 2014. © General Medical Council134
Strategies to address substance abuse problems include encouraging confidential self-reporting, increasing access to treatment programs and local resources, and allowing protected feedback from co-workers to help identify problems early on.
Schmitz et al. , commentary, USA, emergency medicine, trainees, consultants, 2012206
During orientation, trainees are encouraged by RFWP [Resident and Faculty Wellness Program] staff and program leadership to not wait for a crisis to access counseling.
Ey et al. , intervention, USA, medical trainees and faculty, 2016104
[ . . . ] provide extra support for all doctors during life events, complaints and disciplinary actions, and for psychiatrists when a patient dies by suicide – all factors known to precede the onset of depression in doctors [ . . . ] the inadequacy of the help provided for mental health problems may contribute to tragic consequences.
Firth-Cozens et al. , research, UK, doctors and psychiatrists, consultants, trainees, 2007106
Implementation methods: engendering trust
Reducing mental ill-health: groups, belonging and relationality illustrated why interventions which aim to foster a sense of belonging and relationality in the workplace may be more effective. Reducing mental ill-health: balance and timeliness presented key preventative measures which can increase connectedness, and reduce stigma on mental ill-health and vulnerability. However, in our quest to provide realist causal explanations, the literature analysed also suggests that the content of interventions is an important, but not sufficient, ingredient in its success. How interventions are delivered is equally important. Thus, while Reducing mental ill-health: groups, belonging and relationality and Reducing mental ill-health: balance and timeliness focused mainly on the ‘agenda’ of interventions, this section is geared towards action (i.e. towards implementation methods).
The implementation-guiding principles distilled from the literature are the following: endorsement, expertise, engagement and evaluation. These interrelated general principles can guide the design and implementation of new interventions/initiatives, as well as modifications to existing interventions/initiatives, and/or the contexts they are embedded in. They are also in line with knowledge mobilisation and implementation literature. We present each of them in more detail below.
Endorsement
Interventions are more likely to work if they are endorsed by senior levels of the organisation involved. Signs of such involvement include that the organisation openly acknowledges that the profession of the doctor can be demanding and stressing71 (see also CMOc 14: acknowledging the positive and negative aspects of the profession); makes efforts to help doctors to navigate the services and support available; and establishes clear lines of accountability, roles and responsibilities to deliver an intervention. A crucial reason for this principle is that the problem (causes and effects) of mental ill-health in doctors involves different agents and stakeholders (see Underdeveloped workforce planning and normalisation of high workload and Chapter 1).
CMOc 16: endorsement
Doctors are less likely to engage with an intervention (outcome) if it is not endorsed by the employing organisation and senior leadership (context) because they may then lack trust in it (mechanism 1) and may also feel frustrated (mechanism 2) if they cannot access it because of work constraints.
Example of intervention strategies
-
Publicise interventions.
-
Strong endorsement message at leadership level.
-
Allow protected time for doctors to access interventions.
-
Develop clear care pathway for doctors at national and local level.
Relevant extracts from papers included in the review
These explanations are reflected by the respondents’ suggestions about the need for the medical profession to acknowledge that physicians can have problems and for the QPHP [Quebec Physicians Health Program] services to be better known by the profession.
Blais et al. , research, Canada, physicians, trainees, consultants, 201071
Programs that aim to improve resident wellness can only be effective if residents’ time is truly protected and the curriculum is not just another time demand.
Chaukos et al. , research, USA, doctors, trainees, consultants, 201882
Chief and senior residents became a significant source of referrals to the RWP [Residents Wellness Programme] with residents reporting, ‘If my chief said it helped her and urged me to come, I decided it must be okay’.
Ey et al. , research, USA, doctors, trainees, 2013103
The dean himself sent a strong, consistent message to medical students, residents, fellows, and faculty emphasizing that no stigma should be attached to mental illness and encouraging everyone, sick or well, to participate in the program.
Moutier et al. , research, USA, medical students, trainees, consultants, 2012172
The drive to deliver an effective staff health and well-being service requires board commitment, clearly identified top management leadership and staff engagement. Without this, initiatives, however well intentioned, are likely to be less than fully effective.
Department of Health and Social Care, policy, UK, NHS workforce, 2009. 92 © Crown copyright
Expertise
The analysis shows that interventions are more likely to be successful if they are managed and delivered by competent individuals/teams who are able to understand the specific contexts, culture and needs. The need for confidentiality, and the potentially challenging roles of the doctor and patient, are frequently mentioned in the data; these and some other needs, culture and contexts have been discussed in Processes leading to mental ill-health in doctors and Reducing mental ill-health: groups, belonging and relationality. It is important to highlight that such expertise can require specific and regular training for non-medical staff in charge of such interventions, and for doctors (or other allied health-care professionals) who are involved in the delivery of interventions. To a certain extent, the idea of balanced training, discussed in Acknowledging the positive and negative aspects of the profession, could represent a further justification of the importance of such training.
This CMOc about expertise is linked to previous CMOcs in Processes leading to mental ill-health in doctors and Reducing mental ill-health: balance and timeliness. In clinical practice, expertise may be hindered by over-regulation (see Loss of autonomy) and by an excessive focus on fighting negative performance (see Balancing negative with positive). Excessive and ‘negative’ regulations and management of clinical work may decrease doctors’ satisfaction, and make them more vulnerable to stress. However, this CMOc also shows that overemphasis on regulation and on recognising and fighting negative performance can not only become a trigger of mental ill-health in itself, but also hinder the assessment and often delicate care received by doctors experiencing mental ill-health (for an example see Dyer97 and Loss of autonomy and Balancing negative with positive).
CMOc 17: expertise
If those delivering interventions do not have specific training to address the needs of sick doctors (context), the recipients may be less likely to trust the intervention (mechanism) and the intervention may be ineffective (outcome 1), and/or harmful (outcome 2) or not accessed at all (outcome 3).
Examples of intervention strategies and of needed training include
-
Develop strict safeguards and rules on confidentiality and communicate them explicitly to doctors.
-
Encourage doctors to be registered with a GP outside their own practice.
-
Make training in health and well-being an integral part of management training and leadership development at local, regional and national levels, and of annual performance assessment and personal development planning processes.
Relevant extracts from papers included in the review
Employing coaches who understand the culture and system of medicine is one important step towards supporting physicians in a process that prioritizes self-care.
Schneider et al. , research, USA, physicians, trainees, consultants, 2014207
Attention not only should be given to the medical residents, but also to their supervisors in developing supportive skills as well as improving their present relationship with residents.
Prins et al. , research, the Netherlands, doctors, trainees, consultants, 2007184
The aspirations of the National Service Framework and the NHS Plan will come to nothing if there are not sufficient trained and experienced staff to implement them, and senior staff are increasingly looking forward to early retirement rather than the continued satisfactions of working within the NHS.
Roberts et al. , commentary, UK, psychiatrists, medical students, trainees, consultants, 2002198
Why did Julien die and what could have been done to save him? His father has used his own medical training and experience and spent thousands of hours searching for answers. [ . . . ] and describes the way clinician addiction is handled in the NHS as ‘amateurish’.
Dyer, commentary, UK, trainees, 201897
Line management training [ . . . ] focuses on educating managers to be more aware of psychologically healthy and supportive work environments. [ . . . ] coaching them to spot signs of poor mental health and learning tips on how their own behaviours towards staff can positively or negatively influence the psychological wellbeing of their staff.
NHS England, policy, UK, NHS workforce, 2016. Contains public sector information licensed under the Open Government Licence v3.0175
Engagement
Engaging doctors and other stakeholders in the design, implementation, monitoring and improvement of interventions can contribute to their effectiveness.
The importance of engagement is discussed in the literature in relation to doctors, medical workforce in general and medical students. From the analysis of the data we can distill several positive aspects of engagement: it can help to tailor interventions to the needs and context of the target audience (this is also linked to the idea of expertise discussed in Acknowledging the positive and negative aspects of the profession); it can help to build trust in the intervention and a sense of control in the target audience, who may feel the need to be listened to; and it could also be a faster way to lead to changes than top-down approaches. Drawing on the idea of the importance of groups and relatedness discussed in Reducing mental ill-health: groups, belonging and relationality, we could also argue that engagement activities, if effective, may also contribute to increase relatedness in the workplace.
Giving more control (space for input) to doctors can also have a ‘therapeutic’ value, particularly in contexts in which doctors feel that regulations and changes are often imposed on them in a ‘top-down’ fashion (‘work control’ is also a dimension of burnout)157 (see also Loss of autonomy).
CMOc 18: engagement
If doctors (and students) are involved in the development and implementation of interventions (context), the recipients are more likely to trust (mechanism 1) and feel ownership (mechanism 2) of the intervention. As a result, it is more likely to be used (outcome 1) and to be effective (outcome 2).
Examples of intervention strategies include
-
Encourage doctors and managers to co-produce strategies to give trainees greater autonomy over their working patterns, tasks and environments.
-
Involve staff and staff representatives to develop health and well-being strategies.
Relevant extracts from papers included in the review
Doctors and managers should work together locally to formulate strategies to give trainees greater autonomy over their working patterns, tasks, and environments. We have a duty to empower emerging medical professionals so that they can continue to shape the future of one of our proudest institutions – the NHS.
Penfold, commentary, UK, doctors, trainees, 2018182
[ . . . ] the focus should lie on giving students more scope for the individual organization of their studies. Especially, as the university environment and the reduction of study pressures have been proven to contribute to the reduction of health problems.
Bugaj et al. , research, Germany, medical students, 201676
[ . . . ] collaborative action planning [ . . . ] gives physicians the opportunity to provide input and share their ideas regarding decisions affecting their work and helps physicians and practice leaders work in partnership toward a shared goal.
Hlubocky et al. , commentary, USA, oncology. Consultants, 2016131
Evaluation
A final important implementation point made in the literature is that the effectiveness of an intervention over time is underpinned by a regular review of its effects on the targeted population. We do not have a lot of data to support this CMOc (all the main references are reported below). However, drawing on these data and the previous CMOcs, we can hypothesise that a process of regular review can help to identify any needed adjustments to improve the effectiveness of the intervention and to ensure it remains tailored to the needs of its users. Alongside regular monitoring it may also help if organisations regularly survey the workforce to identify any risk factors, increasing the likelihood of intervening in a timely manner (see Acknowledging the positive and negative aspects of the profession). Both the evaluation of interventions and the monitoring of the workforce may also be part of workforce engagement activities (see Engagement). Regular review, if it is conducted in a transparent way and if it informs change in the workplace (see Chapter 4, Summary of key findings), can be seen by the workforce as a tangible sign that the organisation values its workforce; therefore, it can in itself increase trust in the organisation. This could also create further opportunities to discuss stress and vulnerability, to create a shared language across different levels of the organisation, thereby potentially contributing to destigmatisation of vulnerability (see Processes leading to mental ill-health in doctors) and connectedness in the workplace (see Reducing mental ill-health: groups, belonging and relationality). Sharing the evaluation results with the workforce may also ‘provide useful information both to those who are doing well (affirmation and reassurance) and encourage behavioural change to those who are struggling’,211 as it may at the same time contribute to normalise vulnerability and convey the positive message that doctors can experience and overcome difficulties.
We can also hypothesise that this monitoring and evaluation exercise may also have negative repercussions. For example, it may be met with criticism or cynicism (it could be seen as an additional form of bureaucracy and surveillance see Stigma towards vulnerability and Balancing negative with positive); however, this risk may be reduced if the evaluation follows the ideas of engagement and endorsement in previous CMOcs (CMOc 18 and CMOc 16, respectively).
CMOc 19: evaluation
If the outcomes of interventions and the well-being of the workforce are regularly reviewed and monitored (context 1), and commitment to act on the outcome of these regular review exercises is shown (context 2 and CMOc 16), then doctors may feel more supported (mechanism) and engage with efforts to tailor these interventions (outcome 1). This may also lead to greater awareness about vulnerability and well-being in the workplace (outcome 2).
Examples of intervention strategies include:
-
Establish longitudinal surveys of staff health and well-being.
-
Carry out anonymous regular monitoring of well-being and morale of physicians, and consider such monitoring in organisation decision-making processes and priorities setting.
Relevant extracts from papers included in the review
[ . . . ] a regular iterative process of inquiry and feedback from physicians can identify issues that negatively affect well-being and barriers to improvement. [ . . . ] assessment of well-being using reliable and valid instruments further establishes the value and creates a common language that can help physicians and the organization address well-being issues.
Dunn et al. , intervention, USA, physicians, trainees, consultants, 200796
Assessing levels of stress among residents may [ . . . ] contribute to a form of intervention. Moreover, the very use of well-being measures among residents could increase their self-awareness and activate helpful and cathartic discussions on stress, coping strategies and vulnerabilities, consequently partly preventing stress symptoms (Levey, 2001).
Myszkowski et al. , research, France, internal medicine, trainees, consultant, 2017174
Knight et al. 10 have been the only group to conduct formal surveys of PHP [Practitioner Health Programme] participants. They found correlations between satisfaction and successful recovery that echoed classic findings in the addictions literature, and underscored the importance of surveying participants as part of the effort to assess treatment engagement and successful completion.
Sanchez et al. , research, USA, doctors, trainees, consultants 2016203
Collectively, these findings suggest that periodic assessment and feedback may have relatively universal benefit for physicians because it seems to provide useful information both to those who are doing well (affirmation and reassurance) and to encourage behavioral change to those who are struggling.
Shanafelt et al. , intervention, USA, surgeons, 2014211
Summary of the 19 CMOcs in four main groupings
Table 3 provides a summary of the 19 CMOcs identified through our research in their four main clusters. These constitute our final programme theory. This overview is also presented graphically in Appendix 5.
| CMOc | Summary |
|---|---|
| Processes leading to mental ill-health in doctors | |
| CMOc 1: underdeveloped workforce planning | In a workplace in which basic support structures to enable doctors to do their job are not in place (context), doctors may feel that they must make up for the deficiencies of the organisation for patients and colleagues (mechanism). This may contribute to a toxic working culture in which overwork and its negative consequences are normalised (outcome) |
| CMOc 2: normalisation of high workload | When high workload and its negative consequences (e.g. distress, burnout) are normalised (context), overworked or sick doctors may feel that they are letting down their colleagues and patients (mechanism). This can contribute to presenteeism (outcome) and associated negative consequences on mental health (outcome 1) and workforce retention (outcome 2) |
| CMOc 3: loss of autonomy | When doctors experience lack of autonomy over their work (context 1) and some aspects of their work as less meaningful (context 2), they may feel dissatisfied with their job (e.g. because they are unable to do the job they were trained for) (mechanism). This can make doctors more vulnerable to stress and mental ill-health, irrespective of workload (outcome) |
| CMOc 4: stigma towards vulnerability | In a professional culture in which mental ill-health and vulnerability may be seen as unprofessional (context), doctors (and medical students) may feel ashamed (mechanism 1) or afraid (mechanism 2) of not living up to their professional identity if they experience mental ill-health (or other difficulties at work). This can lead doctors (and medical students) to adopt strategies which involve hiding their difficulties from themselves and colleagues (outcome) |
| CMOc 5: hiding vulnerability | When there is mental health support available for doctors (context 1), doctors who understand the system and that confidentiality is difficult to achieve (context 2) may fear that seeking support could jeopardise their career (mechanism) and so they may hide their distress rather than seek support (outcome) |
| CMOc 6: isolation | When doctors work in physical and emotional isolation (context), they are likely to feel less supported by their colleagues and/or their employing organisation (mechanism 1) and/or to mistrust these groups (mechanism 2). This can make doctors more vulnerable to work-related pressure and mental ill-health (outcome) |
| Reducing mental ill-health: groups, belonging and relationality | |
| CMOc 7: positive and meaningful workplace relations | Positive and meaningful workplace relations (context) can foster a sense of belonging between colleagues and towards the medical profession (mechanism). This can lead to an increased capacity to work under pressure (outcome) |
| CMOc 8: functional working groups | Working in functional groups (context) can make doctors feel more supported (mechanism 1) and more at ease with vulnerability (mechanism 2). This can normalise vulnerability (outcome 1) and reduce the stigma around mental ill-health (outcome 2) |
| CMOc 9: balancing quality and quantity of time at work | When doctors (for different reasons) have less connectedness and meaning at work (context), they may feel they can find fulfilment only outside work (mechanism), making it less likely that their condition will improve (outcome) |
| CMOc 10: limits of groups | Sick doctors (and medical students) with particularly delicate circumstances (context) may not feel safe to share their problems (mechanism 1) and/or may not identify with the other group members (mechanism 2). This can result in a dysfunctional group (outcome 1) and intensification of mental ill-health in doctors (outcome 2) |
| CMOc 11: ‘organic’ spaces to connect | If there are protected times and psychologically safe spaces for students/doctors to congregate within the confines of the work environment (context), students/doctors are likely to bond over whatever is most important to them at that time (mechanism). This may improve connectedness (outcome) |
| Reducing mental ill-health: balance and timeliness | |
| CMOc 12: recognising both positive and negative performance | When supervision and feedback recognise both positive and negative performance and promote doctors’ (and students’) learning from both of these (context), doctors (and students) may feel more fairly treated (mechanism 1) and more inclined to value their colleagues and employing organisation (mechanism 2), potentially leading to more connectedness and engagement at work (outcome 1), and a more supportive work culture (outcome 2) |
| CMOc 13: balancing prevention of mental ill-health with promotion of well-being | In a work environment that actively demonstrates the importance of the balance between health and well-being with dealing with stress and mental ill-health (context), doctors (and students) are more likely to feel that caring about their own well-being is legitimate (mechanism 1) and less afraid to acknowledge vulnerability (mechanism 2). This can contribute to a destigmatisation of mental ill-health and vulnerability (outcome) |
| CMOc 14: acknowledging the positive and negative aspects of the profession | When both the positive and negative aspects of a medical career are recognised (context), doctors (and medical students) may feel less inadequate and helpless when they or their colleagues experience stress or mental ill-health (mechanism). This may lead to increased capacity to deal with work pressure (outcome 1) and to recognition and acceptance of vulnerability (outcome 2) |
| CMOc 15: timely support | Timely support when doctors (and students) are particularly vulnerable (e.g. after a suicide attempt, death of a colleague, addiction) (context) may represent their only source of hope (mechanism) and reduce the intensity of mental ill-health and its related outcomes, including suicide (outcome) |
| Implementation methods: engendering trust | |
| CMOc 16: endorsement | Doctors are less likely to engage with an intervention (outcome) if it is not endorsed by the employing organisation and senior leadership (context), as they may then lack trust in it (mechanism 1) and may also feel frustrated (mechanism 2) if they cannot access it because of work constraints |
| CMOc 17: expertise | If those delivering interventions do not have specific training to address the needs of sick doctors (context), the recipients may be less likely to trust the intervention (mechanism) and the intervention may be ineffective (outcome 1) and/or harmful (outcome 2) or not accessed at all (outcome 3) |
| CMOc 18: engagement | If doctors (and students) are involved in the development and implementation of interventions (context), the recipients are more likely to trust (mechanism 1) and feel ownership (mechanism 2) of the intervention. As a result, it is more likely to be used (outcome 1) and to be effective (outcome 2) |
| CMOc 19: evaluation | If the outcomes of interventions and the well-being of the workforce are regularly reviewed and monitored (context 1), and commitment to action the outcome of these regular review exercises is shown (context 2, and CMOc 16), then doctors may feel more supported (mechanism) and engage with efforts to tailor these interventions (outcome 1). This may also lead to greater awareness about vulnerability and well-being in the workplace (outcome 2) |
How does existing substantive theory link with our findings?
Our analysis and synthesis of the literature was guided by a number of theoretical perspectives. These helped us develop our thinking in the process of interpreting data from the literature, articulating the assumptions underlying some of these interpretations and establishing the relevance of our work with a wider body of theoretical literature beyond the articles reviewed. We identified relevant theories by iterative reading of our data, alongside theoretical literature in the fields of social psychology, ethics, professional identities in health care and medical humanities, and through discussions with content experts. By identifying analogy or correspondence of our CMOcs with substantive theories, we were able to gain confidence in proposing causal explanations. 242
Social cure framework
Social psychology approaches to health and well-being strongly resonated with our analysis (e.g. social identity theory243 and the integrated social identity model of stress244,245). These approaches have recently been synthesised into the ‘social cure’ framework, which proposes that there is a positive impact on health when individuals identify themselves as members of groups that provide them with a positive sense of identity. 243 Social identity is defined as the basis for meaningful group life; group life in turn is seen as central to our human nature and a key source of meaning and purpose. Therefore, social identity is central to good and bad health. 243 This emphasis on group membership foregrounds that humans are relational beings (i.e. in the sense that their life experiences are shaped in relation to their environment and other people). This also frames concepts of autonomy – and arguably resilience – as underpinned by sociocultural and environmental processes, rather than purely within the control of individuals acting independently. In using the ‘social cure’ lens to develop and substantiate our CMOcs, we situate our work within broader research emphasising the relational nature of health,246–248 relational autonomy,249 care ethics, feminist work and other critiques of modern liberal political philosophy. 250
The ‘social cure’ framework has a strong evidence base243 and social identity approaches have been used widely in the study of interprofessional relationships in health care. 251 In our review, we used the ‘social cure’ framework to provide theoretical substantiation and to bring together our key findings on:
-
isolation as an important process or aggravating factor leading to mental ill-health in doctors (see Processes leading to mental ill-health in doctors)
-
groups, connectedness and belonging as key from preventative, mitigating and therapeutic points of view (see Reducing mental ill-health: groups, belonging and relationality)
-
balancing positive and negative aspects of professional identity and performance (see Reducing mental ill-health: balance and timeliness)
-
principles necessary to engender trust in interventions (see Implementation methods: engendering trust).
To complement the ‘social cure’ framework, our analysis has also been informed by theoretical work on professional identities in health care. In ways that extend (rather than contradict) our approach to social identity, we viewed professional identities as relational and negotiated in practice through intra- and interprofessional working. 252,253 In doing this, we also aimed to highlight the relevance of professions as self-organising entities in the health-care service and their structural role in influencing power and control dynamics, including conditions of clinicians’ self-identification with the medical profession. Instead of commonplace narratives of professional dominance and stable professional identities, our analysis emphasised ‘the incoherence, self-doubt, insecurity, antagonism or fragility evident in those moments of reflexivity when the actor interrogates rather than secures or glorifies the self’. 254 Professional legitimacy and role relationships are seen not as given and static, but as constantly constructed and reproduced at the intersection of organisational contexts and internalised professional imperatives. 253
Box 2 outlines key tenets of social cure that are relevant to the CMOcs identified in our study. Unless otherwise specified, these tenets are drawn from a recent volume on social cure. 243
Individuals’ internalised group memberships (i.e. their social identity) can be an essential source of psychological robustness and resilience, as long as individuals perceive such group memberships to be important and compatible with each other. Group membership can foster:
-
connection and positive orientation towards others
-
a sense of meaning, purpose and worth
-
effective social support
-
feelings of control, efficiency and power
Social identification (the identification of an individual with a group) can provide an important basis for members of stigmatised groups to come together and challenge their stigma in ways that are beneficial to their health.
Social cure tenet related to CMOcs 12–15: balancing positive with negativeTraumatic events often have the capacity to undermine one’s sense of meaningful connections to others (they can represent a social identity threat). Groups (and individuals within them) experience traumas and tell stories to help them make sense of these experiences. When such stories cannot be told or told with shame only, they can be devastating. If they can be told with pride they can become a source of individual and group enrichment. The motivation and well-being of a workforce are enhanced when managers take steps to foster (rather than undermine) workers’ shared identities (see also research with hospital workers255). Arguably, a work culture that balances ‘positives’ with ‘negatives’ can help to foster such sharing of stories.
Social cure tenet related to CMOcs 16–19: endorsement, expertise, engagement, evaluationOften the most important and difficult part of any support attempt is convincing the recipient that the source of support has their interest at heart. Training is more effective if it consolidates team-based social identifications. Treatment for traumatic stress is more effective when administered by an ‘insider’.
Vulnerability
Our analysis has also been informed by scholarly perspectives that criticise reductionist approaches to clinical care provision and recognise the importance of human vulnerability alongside clinical detachment – in both medical practice and education. 239,256 As Piemonte suggests:
[ . . . ] the culture of contemporary medicine is entrenched so deeply in calculative understanding of clinical care that the affective experience of practicing clinicians and the personal development of future clinicians are largely ignored.
Piemonte, p. 98239
A large number of articles included in the review referred to how vulnerability and distress experienced by medical doctors is seen as something that needs to be hidden or something one needs to be ashamed of. Emotional responses in the context of clinical practice are dismissed as unprofessional and clashing with the ideal of medical detachment. This has been illustrated in detail as part of CMOcs 4 and 5.
Although detachment has an important role to play in clinical practice, medicine exposes both doctors and patients to challenging and delicate decisions and experiences, which can encompass biomedical and psychosocial aspects, and which are ultimately linked to illness, mortality and vulnerability. Therefore, approaches in medical education and practice that bring together the biopsychosocial elements of medicine have the potential to contribute to improved patient outcomes, clinical skills and doctors’ well-being. This fits with a view of medicine in our analysis that is not ‘an applied science but rather an engaged praxis, an amalgamation of theoretical, technical and practical knowledge’. 239
Chapter 4 Discussion
Summary of key findings
Our aim in this review was to improve understanding of how, why and in what contexts mental health services and support interventions can be designed in order to minimise the incidence of doctors’ mental ill-health. We summarise our main findings here, in relation to the four research questions. Findings for research questions 2 and 3 are presented together in view of the close interactions between the identified mechanisms and contexts. A summary of the four main clusters of CMOcs has been presented in Chapter 3, Summary of the 19 CMOcs in four main groupings (see Table 3).
Research question 1
What are the processes by which mental ill-health in doctors develops and leads to its negative impacts and where are the gaps that interventions do not address currently?
Our findings suggest that the development of mental ill-health in doctors results from the interaction of a significant and complex workload, organisational management and the professional culture of medicine. Doctors experiencing heavy workloads, together with a diminished level of control over their work, are unlikely to be able to perform at the high standards that they expect of themselves and their profession. In a professional culture which doctors experience as discouraging the sharing of vulnerabilities, in which professional regulation is perceived by doctors as likely to judge mental ill-health as potentially making a doctor unfit to practise, and in an organisational environment that promotes individual rather than collegial responsibility, doctors are unlikely to take steps that could prevent the development of mental ill-health. Although interventions that target individual doctors (e.g. to prevent doctors’ mental ill-health or ameliorate it once established) may address parts of these processes, the way in which individuals and the wider context interact suggests that interventions that address multiple organisational and professional issues simultaneously are more likely to be successful. In other words, the gaps in intervention targets tended to be more associated with ‘level’ (e.g. individual and/or team and/or employer), rather than ‘stage’ of the process.
Research questions 2 and 3
What are the mechanisms, acting at individual, group, profession and organisational levels, by which interventions to reduce doctors’ mental ill-health at the different stages are believed to result in their intended outcomes?
What are the important contexts which determine whether the different mechanisms produce the intended outcomes?
Our second and third research questions focused on the mechanisms, which may operate differently in different contexts, by which it is believed that interventions reduce doctors’ mental ill-health. We interpreted ‘reducing mental ill-health’ as either preventing the development of mental ill-health or ameliorating mental ill-health once it is established, and identified how professional and organisational culture could shape the operation of mechanisms.
We found that doctors’ working relationships, with other doctors and health-care staff as well as with the organisation in which they work, explained a key part of how mental ill-health could be prevented and reduced. Although not operating in a linear fashion, facilitative contexts, such as meaningful workplace relations and functional working groups, enabled the protective mechanisms of a sense of belonging and an ease with vulnerability to function. These mechanisms could interact with (or provide the context for) other protective mechanisms to operate, such as identifying with colleagues and finding meaning in work. Relationality, recognising the importance of meaningful human relationships in the workplace, provides an overarching explanatory concept here.
We also found that the tone set by organisations about a medical career could have important implications for mental ill-health. Constructive workplace feedback on performance, as well as an organisation’s demonstrable valuing of employees’ health and well-being, could provide the context for doctors to contribute to and benefit from an upwards cycle of interacting mechanisms, such as legitimating their own well-being, acknowledging vulnerability and valuing colleagues. A professional culture that recognises both the positive and negative aspects of a medical career could play a role by preventing feelings of inadequacy and helplessness in doctors. Finally, when doctors are affected negatively by significant life events, the provision of timely support in the workplace is crucial for hope to play a role in recovery.
In relation to costs, limitations in reporting meant that we were unable to link cost data to CMOcs. Even when this cost information was reported, there was a lack of methodological detail about how costs had been calculated. A minority of included sources quantified costs and there was a lack of methodological detail about how estimates of direct or indirect costs had been reached and a paucity of detail about direct, indirect or total costs that we could meaningfully extract. No included sources reported a health economic analysis (either cost–consequence modelling or prospective comparative evaluation), but it should be noted that our search strategy was not explicitly designed to locate such studies.
Research question 4
What changes are needed to existing and/or future interventions to make them more effective?
This review has identified how social identity, group membership and the ‘humanising’ of doctors’ work (in contrast to a reductionist view of clinical encounters) can play an important role in the prevention and reduction of mental ill-health in doctors. We noted earlier in this report (see How does existing substantive theory link with our findings?) how approaches drawing on aspects of theories of biopsychosocial health and well-being (the social identity approach243) can be used in tandem with our more specific CMOcs to underpin the refinement of strategies to reduce mental ill-health in doctors. Taken together, this has enabled us to articulate recommendations about strategy development for different audiences (Table 4). We also worked iteratively with the stakeholder group, experts and policy-makers to develop and refine the recommendations (consistent with our protocol; see also Chapter 2, Stakeholder group). Although these recommendations are presented separately to aid comprehension, the interdependency of these levels should be acknowledged in intervention design (e.g. doctors prioritising relationships at work may not be feasible if there are no organisational structures to support this at the level of team leaders and senior management). We have also developed 10 CUP principles to refine interventions, for those who deliver interventions, which draw out the interdependence of the different levels (Box 3).
| Audience | Key recommendations and principles for refining/designing strategies to reduce mental ill-health in doctors |
|---|---|
| Policy-makers | Policies that aim to secure the future of the NHS workforce must foster a supportive work culture in which individuals can thrive. Policies and interventions that target the individual in the absence of a supportive work culture are unlikely to succeed (CMOcs 1–3, 7–9, 12–14, 16 and 19) |
| Employers | Ensure influential nominated board-level responsibility for the well-being of staff. This should include regular immersion in practice settings, as well as regular reports on progress against key performance indicators (e.g. absenteeism might be detected by sickness absence, rota gaps and vacant posts; presenteeism might be detected by complaints and errors; workforce retention might be detected by staff turnover; general staff well-being might be detected via annual staff surveys, markers of overwork and occupational health referrals) (CMOcs 12–13, 16–19) |
| Team leaders | Actively look out for behaviours that may be potentially stigmatising and encourage help-seeking. In performance reviews, emphasise the positive as well as the negative, and ensure that doctors know that their hard work in often challenging circumstances is valued. Make clear that prioritising own health is important for patient care (CMOcs 12–15) |
| Doctors | Recognise when you are working under pressure and, even when your workload is high, prioritise your relationships at work (CMOcs 7–11) |
| Other health-care team members | Recognise that the whole team may, at times, be providing care under pressure. Try to normalise discussions of struggle in the context of challenging work (CMOcs 7, 8, 11–13) |
| Patients | Know that doctors and other health professionals are usually doing the best job they can in difficult circumstances. A thank you when things go well will always be appreciated! (CMOCs 4, 5, 7 and 12) |
| Researchers | Use research syntheses and stakeholder involvement to target your research to the areas of greatest need. Research of all kinds will be needed to develop theory and interventions, and design appropriate outcome measures, approaches to evaluation and implementation, in relation to doctors’ mental ill-health (CMOcs 1–19) |
| Those refining/designing interventions | Adopt our 10 CUP principles (see Box 3) (CMOcs 1–19) |
-
Be clear about who the intervention is for (given the continuum from full health, to ‘under pressure’, to mental ill-health).
-
Give options by signposting to a range of interventions (e.g. a ‘one-stop shop’ of local, regional and national resources).
-
Ensure that information about the intervention is readily and rapidly available.
-
Ensure that interventions are accessible to someone who works long and inflexible hours.
-
At the initial enquiry stage, invest time in building trust and normalising stigma and struggle.
-
Provide interventions in groups, whenever possible, to prioritise connectedness, relationships and belonging.
-
Ensure that interventions for individuals are endorsed by or embedded in the workplace, where possible.
-
Encourage and empower individuals to tackle low-level everyday hassles at work, to free up capacity to deal with bigger issues.
-
Emphasise that prioritising and investing in physical and mental health is essential for optimal patient care.
-
Evaluate and improve the intervention regularly, using data such as numbers and types of attendee, programme adherence and user perceptions.
Please note that the research evidence indicates that system-wide approaches are more likely to succeed in tackling mental ill-health in doctors.
Chapter 5 Conclusions and recommendations
In summary, the distinct contribution of this review to knowledge is that:
-
Doctors are more likely to experience mental ill-health when they feel isolated, when they feel unable to do the job they were trained for, and when they fear the repercussions of seeking help and support (CMOcs 1–6).
-
Interventions that emphasise relationships and belonging (e.g. to a health-care team or to the profession) are more likely to promote well-being and improve workplace cultures (CMOcs 7–11).
-
The health and well-being of staff is important in itself, and is a necessary precondition to excellent patient care. Interventions that create a people-focused working culture that recognises this important link between doctors’ and patients’ health and well-being, that balances positive and negative performance and promotes doctors’ learning from both and that acknowledges the positive and negative aspects of a medical career are likely to help doctors to thrive at work and deal with work pressures (CMOcs 12–15).
-
Doctors need to have confidence in an intervention, and those delivering it, for the intervention to be effective, and this trust seems to be easily lost (CMOcs 16–19).
The implication of these findings is that evaluating and improving existing interventions is likely to be more effective than developing new ones. There is no shortage of interventions described in the peer-reviewed and grey literature, but many fall short of meeting the 10 CUP principles that we have developed through this research (see Box 3). The role of undergraduate medical education in forming doctors’ professional culture is important for the way it can develop healthy or unhealthy attitudes and behaviour in relation to coping and disclosure. If supportive working cultures can be created, medical schools could provide an opportunity to emphasise the importance of looking after one’s own health, to normalise discussions of struggle in the context of challenging work, to recognise the positive and negative aspects of medical careers, and to understand how and when to seek help.
It is also clear that complex problems require complex solutions, and so many interventions to tackle doctors’ mental ill-health are likely to be multidimensional and multilevel. It is important to carefully identify and map out the stakeholders involved in the wider context of interventions, as they may not always be obvious and can include (but are not limited to) doctors, managers, administrative staff, employers, the profession of medicine, professional bodies, regulators, patients and educators. These stakeholders would ideally be aware of each other’s involvement, clearly acknowledge their responsibility in the well-being of doctors, and clarify/agree together their roles in relation to the design and/or communication and/or embedding of interventions. Involvement of key stakeholders and end users in the design and implementation of interventions is likely to help to ensure that it fits with local priorities and working routines, although the involvement process must be carefully managed to avoid unintended consequences, such as could arise from unhelpful power dynamics within the process.
It is important to develop efficient, tailored systems not only to communicate to doctors and other relevant stakeholders the existence of an intervention, but also to show that there are clear lines of responsibilities across the different levels of the organisation. For example, endorsement from leadership and/or other relevant levels of the organisation will probably increase the success rate of an intervention. Given the likely range and complexity of strategies available to doctors at different stages of mental ill-health, which may be tailored for different contexts, doctors may need a guide through the system. This may be a person who guides them (similar to the care co-ordinator role provided for some patients) or a web resource that signposts them to the range of interventions available to them.
Strengths and limitations of this review
There are many strengths of this research, as well as some limitations. By undertaking a realist review, we have been able to find, analyse and synthesise data from across disciplinary silos and ‘sense check’ our findings against feedback from various perspectives. The multidisciplinary research team worked closely with a large, diverse group of individuals in the stakeholder group and sense-making groups, and ‘translated’ the findings through these interactions. This was in contrast to much of the research into doctors’ mental ill-health identified through our review, which tended to be limited to quite specific perspectives occurring in disciplinary silos. We undertook a comprehensive, rigorous process throughout the research, following the RAMESES quality standards for realist synthesis,57 as well as good practice standards for working collaboratively with stakeholders. This allowed us to successfully analyse and synthesise a large and diverse literature into ‘actionable theory’ that will be relevant to a range of audiences. Use of the EIT within the stakeholder discussions helped us to achieve this focus on actionable theory and think how we would demonstrate the impact of any positive change through tangible outcome measures. However, this reflected only one of the three elements of the EIT framework, and we found the other two elements (intervention programme/policy, and participatory implementation process) less helpful as a reflection tool, perhaps as the ideas they reflected were already embedded within our research process, although they might be helpful for other teams or projects. The explanatory theories that we have produced through the realist review process, to address our research questions, have considerable consilience. That is, they are able to provide explanatory accounts for many of our data and have analogy with substantive theories. In addition, we have been able to reflect critically on a wider literature, engage with stakeholders and thereby identify the importance of other aspects (meaningful work, relatedness, humanity), despite the preponderance of studies using ‘objective’ measures. The key limitation of our research, as is common to all literature-based research methods, is that the findings are only as good as the literature available to synthesise. In this study, only literature published in the English language was included, and most of the literature came from the USA, with a smaller component from the UK, which made the interpretation of the relevance of the data from included documents to the UK health-care setting more challenging. Inevitably, the included literature was also variable in its quality and, given the scale, breadth and diversity of literature, we did not undertake further rounds of searching, as is typical of many realist reviews. In addition, one researcher led the bulk of the data extraction, although the close working within the project team, involving biweekly meetings and circulation of key papers and drafts by e-mail and telephone discussions, as well as the iterative stakeholder meetings and sense-making meetings throughout the project, helped to ensure that the findings were not unduly influenced by a single researcher. We were greatly assisted through these methodological challenges, interpretations and explorations of the transferability of ideas within the data by our stakeholder group and sense-making meetings.
Non-academic outputs
Our non-academic outputs include:
-
comic strips to illustrate our CMOcs (drafts available at Graphic Medicine;50 see Appendix 6)
-
an animation to illustrate our CMOcs (under development; see Appendix 6)
-
a short film in which we asked patients to answer the question ‘why is the health of your doctor important to you?’ [URL: https://sites.exeter.ac.uk/cup/ (accessed 22 November 2019)]
-
a National Institute for Health Research blog, Care Under Pressure: Going Beyond Individual-Level Interventions to Improve Doctors’ Mental Health [URL: www.dc.nihr.ac.uk/blog/care-under-pressure-going-beyond-individual-level-interventions-to-improve-doctors-mental-health/8656 (accessed 6 November 2019)]
-
BMJ Opinion article ‘“Care Under Pressure”: How Can We Achieve Wellbeing at Work for Doctors?’ [URL: https://blogs.bmj.com/bmj/2019/02/01/care-under-pressure-how-can-we-achieve-wellbeing-at-work-for-doctors/ (accessed 6 November 2019)].
We provide in Appendix 6 a reflective piece written by Matilda Tristram (animator, illustrator and writer) and Ian Williams (GP and comics artist), the artists who have worked with us to produce the comic strips and animation. This piece offers an insight into the process of developing creative research outputs from the perspective of the artist collaborators. Apart from being an interesting piece of work in itself, we thought that a few lessons could be drawn out for future research with regard to incorporating artistic outputs:
-
When possible, try to engage artists who are already invested in the topic area.
-
Start the dialogue as early as possible in the project and allow appropriate time for the collaboration and creative ideas to develop.
-
Make sure it is appropriately budgeted for.
Future research
Future research can build on the work presented here to evaluate and refine interventional strategies that have been already implemented, or design, implement and evaluate new interventional strategies. This might use a realist evaluation approach or a complex intervention trial approach. The use of the EIT in this research helpfully focused attention on pragmatic, longitudinal measures of progress. In reality, however, the consideration of outcome measures within the included literature was relatively unsophisticated, with a tendency to focus on outcomes that were easy to measure (such as self-reported measures of burnout), rather than those that reflected the complexity of multifaceted, multilevel problems. This should be a priority for future research. Once high-quality, theoretically informed interventions have been developed and evaluated in small studies, they will need to be assessed at scale. Similarly, our review identified very few studies that offer a formal health economic analysis, either of the problem of doctors’ mental ill-health or of interventions. Future research will also need to explore the role that medical education can play to provide crucial preventative anticipatory training (e.g. in relation to self-reflective skills to understand vulnerability to mental ill-health and group working skills).
Acknowledgements
We would like to express our sincere gratitude to the members of our stakeholder group, those who took part in the policy workshop and others who offered their perspective through individual meetings, for their significant contributions to the programme theory and actionable findings emerging from the review. These included (alphabetically by first name) Alex Aylward, Alex Blohm, Andrew Tressider, Andy Grant, Clare Gerada, Daisy Robinson, Derek Gallen, Diana Frost, Fady Awad, Ian Fussell, Jackye Hayden, Jill Maben, Jodie Blackadder, Julie Harvey, Katrina Wyatt, Kirsten Leslie, Laura Hill, Linda Gask, Luna Dolezal, Lynn Monrouxe, Lynn Tatnell, Mark Tarrant, Nadine Dyar, Nicola Brennan, Paul Dieppe, Peta Foxall, Richard Jones, Robert Lewis, Ruth Riley, Sarah Huline-Dickens, Theresa Hewitt-Moran and Vik Mohan. We would also like to thank the members of our Study Steering Group (alphabetically by first name), Barbara Jones, Dave Richards (chairperson) and Nigel Reed, for their excellent advice and guidance throughout. Finally, we would like to thank Marilyn Evans for her administrative support.
Contributions of authors
Dr Daniele Carrieri (https://orcid.org/0000-0002-3143-8430) (Research Fellow) carried out the exploratory literature search for the review, contributed to the formal search strategies, screened the resulting references, carried out the coding, applied a realist logic of analysis to the data, developed and refined the programme theory and CMOcs for the review, identified the theoretical ideas underpinning this analysis, facilitated the stakeholder meetings and drafted and revised the final report.
Dr Mark Pearson (https://orcid.org/0000-0001-7628-7421) (Senior Lecturer, Implementation Science) developed the research project, contributed to the formal search strategies and to the development and refinement of programme theory and CMOcs, provided methodological support and input, developed and facilitated patient and public involvement in the stakeholder group and revised the final report.
Professor Karen Mattick (https://orcid.org/0000-0003-1800-773X) (Professor, Medical Education) developed the research project, contributed to the formal search strategies and to the development and refinement of programme theory and CMOcs, provided relevant content and theoretical literature and revised the final report.
Dr Chrysanthi Papoutsi (https://orcid.org/0000-0003-1189-7100) (Health Service Researcher) developed the research project, carried out consistency checks on the literature retrieved from the formal searches, as well as consistency checks on the screening and coding process, applied a realist logic of analysis to the data, developed and refined the programme theory and CMOcs for the review, contributed theoretical ideas underpinning this analysis and revised this report.
Mr Simon Briscoe (https://orcid.org/0000-0002-6982-4521) (Information Specialist) developed and conducted the main and additional search strategies, and contributed to writing the literature search sections for the final report.
Dr Geoff Wong (https://orcid.org/0000-0002-5384-4157) (General Practitioner, Clinical Research Fellow, Realist Approaches) developed the research project, applied a realist logic of analysis to the data, developed and refined the programme theory and CMOcs for the review, contributed theoretical ideas underpinning this analysis and revised this report.
Professor Mark Jackson (https://orcid.org/0000-0002-3248-2636) (Professor of the History of Medicine) developed the project and contributed to the theoretical ideas underpinning the analysis of the report.
Publications
Carrieri D, Briscoe S, Jackson M, Mattick K, Papoutsi C, Pearson M, Wong G. ‘Care Under Pressure’: a realist review of interventions to tackle doctors’ mental ill-health and its impacts on the clinical workforce and patient care. BMJ Open 2018;8:e021273.
Carrieri D, Mattick K, Pearson M, Papoutsi C, Briscoe S, Wong G, Jackson M. Optimising strategies to address mental ill-health in doctors and medical students: ‘Care Under Pressure’ realist review and implementation guidance. BMC Med 2020;18:76.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Carrieri D, Mattick K, Pearson M, Papoutsi C, Briscoe S, Wong G, et al. Optimising strategies to address mental ill-health in doctors and medical students: ‘Care Under Pressure’ realist review and implementation guidance. BMC Med 2020;18. https://doi.org/10.1186/s12916-020-01532-x.
- Rothenberger DA. Physician burnout and well-being: a systematic review and framework for action. Dis Colon Rectum 2017;60:567-76. https://doi.org/10.1097/DCR.0000000000000844.
- Maben J, Taylor C, Dawson J, Leamy M, McCarthy I, Reynolds E, et al. A Realist Informed Mixed-Methods Evaluation of Schwartz Center Rounds® in England. Health Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06370.
- Haramati A, Cotton S, Padmore JS, Wald HS, Weissinger PA. Strategies to promote resilience, empathy and well-being in the health professions: insights from the 2015 CENTILE Conference. Med Teach 2017;39:118-19. https://doi.org/10.1080/0142159X.2017.1279278.
- Anonymous . The future of the NHS. Lancet 2017;389. https://doi.org/10.1016/S0140-6736(17)30994-7.
- Shanafelt TD, Hasan O, Dyrbye LN, Sinsky C, Satele D, Sloan J, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc 2015;90:1600-13. https://doi.org/10.1016/j.mayocp.2015.08.023.
- Hayes B, Prihodova L, Walsh G, Doyle F, Doherty S. What’s up doc? A national cross-sectional study of psychological wellbeing of hospital doctors in Ireland. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-018023.
- Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet 2009;374:1714-21. https://doi.org/10.1016/S0140-6736(09)61424-0.
- Dyrbye LN, Wittlin NM, Hardeman RR, Yeazel M, Herrin J, Dovidio JF, et al. A prognostic index to identify the risk of developing depression symptoms among U.S. medical students derived from a national, four-year longitudinal study. Acad Med 2019;94:217-26. https://doi.org/10.1097/ACM.0000000000002437.
- Shanafelt TD, Gorringe G, Menaker R, Storz KA, Reeves D, Buskirk SJ, et al. Impact of organizational leadership on physician burnout and satisfaction. Mayo Clin Proc 2015;90:432-40. https://doi.org/10.1016/j.mayocp.2015.01.012.
- Hampton T. Experts address risk of physician suicide. JAMA 2005;294:1189-91. https://doi.org/10.1001/jama.294.10.1189.
- Marshall EJ. Doctors’ health and fitness to practise: treating addicted doctors. Occup Med 2008;58:334-40. https://doi.org/10.1093/occmed/kqn081.
- Brooks SK, Gerada C, Chalder T. The specific needs of doctors with mental health problems: qualitative analysis of doctor-patients’ experiences with the Practitioner Health Programme. J Ment Health 2017;26:161-6. https://doi.org/10.1080/09638237.2016.1244712.
- Braquehais MD, Eiroa-Orosa FJ, Holmes KM, Lusilla P, Bravo M, Mozo X, et al. Differences in physicians’ and nurses’ recent suicide attempts: an exploratory study. Arch Suicide Res 2016;20:273-9. https://doi.org/10.1080/13811118.2014.996693.
- Wilkinson E. UK NHS staff: stressed, exhausted, burnt out. Lancet 2015;385:841-2. https://doi.org/10.1016/S0140-6736(15)60470-6.
- Spiers J, Buszewicz M, Chew-Graham CA, Gerada C, Kessler D, Leggett N, et al. Barriers, facilitators, and survival strategies for GPs seeking treatment for distress: a qualitative study. Br J Gen Pract 2017;67:e700-e708. https://doi.org/10.3399/bjgp17X692573.
- Limb M. Stress levels of NHS staff are ‘astonishingly high’ and need treating as a public health problem, says King’s Fund. BMJ Careers 2015;351. https://doi.org/10.1136/bmj.h6003.
- Rimmer A. Staff stress levels reflect rising pressure on NHS, says NHS leaders. BMJ 2018;360. https://doi.org/10.1136/bmj.k1074.
- Thornton J. NHS staff survey: just 29% of organisations take health and wellbeing seriously. BMJ 2019;364. https://doi.org/10.1136/bmj.l924.
- Oxtoby K. Why doctors don’t take sick leave. BMJ 2015. https://doi.org/10.1136/bmj.h6272.
- Oxtoby K. Why doctors need to resist’ presenteeism’. BMJ 2015. https://doi.org/10.1136/bmj.h6607.
- Davies M. Medicolegal aspects of working while unwell. BMJ 2015;351. https://doi.org/10.1136/bmj.h6721.
- Weinberg A, Creed F. Stress and psychiatric disorder in healthcare professionals and hospital staff. Lancet 2000;355:533-7. https://doi.org/10.1016/S0140-6736(99)07366-3.
- Doran N, Fox F, Rodham K, Taylor G, Harris M. Lost to the NHS: a mixed methods study of why GPs leave practice early in England. Br J Gen Pract 2016;66:e128-35. https://doi.org/10.3399/bjgp16X683425.
- Smith F, Lachish S, Goldacre MJ, Lambert TW. Factors influencing the decisions of senior UK doctors to retire or remain in medicine: national surveys of the UK-trained medical graduates of 1974 and 1977. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-017650.
- Silver MP, Hamilton AD, Biswas A, Warrick NI. A systematic review of physician retirement planning. Hum Resour Health 2016;14. https://doi.org/10.1186/s12960-016-0166-z.
- Lambert TW, Smith F, Goldacre MJ. Why doctors consider leaving UK medicine: qualitative analysis of comments from questionnaire surveys three years after graduation. J R Soc Med 2017;111:18-30. https://doi.org/10.1177/0141076817738502.
- The BMJ . Wellbeing Campaign n.d. www.bmj.com/wellbeing (accessed 4 November 2019).
- Health Education England . NHS Staff and Learners’ Mental Wellbeing Commission 2019.
- Dyrbye LN, Trockel M, Frank E, Olson K, Linzer M, Lemaire J, et al. Development of a research agenda to identify evidence-based strategies to improve physician wellness and reduce burnout. Ann Intern Med 2017;166:743-4. https://doi.org/10.7326/M16-2956.
- Lemaire JB, Wallace JE. Burnout among doctors. BMJ 2017;358. https://doi.org/10.1136/bmj.j3360.
- Kreitzer MJ, Klatt M. Educational innovations to foster resilience in the health professions. Med Teach 2017;39:153-9. https://doi.org/10.1080/0142159X.2016.1248917.
- Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff 2008;27:759-69. https://doi.org/10.1377/hlthaff.27.3.759.
- Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med 2014;12:573-6. https://doi.org/10.1370/afm.1713.
- Brooks SK, Gerada C, Chalder T. Review of literature on the mental health of doctors: are specialist services needed?. J Ment Health 2011;20:146-56. https://doi.org/10.3109/09638237.2010.541300.
- Riley R, Weiss MC. A qualitative thematic review: emotional labour in healthcare settings. J Adv Nurs 2016;72:6-17. https://doi.org/10.1111/jan.12738.
- Jones MC, Wells M, Gao C, Cassidy B, Davie J. Work stress and well-being in oncology settings: a multidisciplinary study of health care professionals. Psychooncology 2013;22:46-53. https://doi.org/10.1002/pon.2055.
- Freidson E. Doctoring Together: A Study of Professional Social Control. Amsterdam: Elsevier; 1975.
- Leape L, Berwick D, Clancy C, Conway J, Gluck P, Guest J, et al. Transforming healthcare: a safety imperative. Qual Saf Health Care 2009;18:424-8. https://doi.org/10.1136/qshc.2009.036954.
- Department of Health and Social Care (DHSC) . Mental Health and Ill Health in Doctors 2008.
- Garelick AI. Doctors’ Health: Stigma and the Professional Discomfort in Seeking Help. London: Royal College of Physicians; 2012.
- Kay M, Mitchell G, Clavarino A, Doust J. Doctors as patients: a systematic review of doctors’ health access and the barriers they experience. Br J Gen Pract 2008;58:501-8. https://doi.org/10.3399/bjgp08X319486.
- Stanton J, Randal P. Developing a psychiatrist-patient relationship when both people are doctors: a qualitative study. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010216.
- McKevitt C, Morgan M, Dundas R, Holland W. Sickness absence and working through illness: a comparison of two professional groups. J Pub Health 1999;19:295-300. https://doi.org/10.1093/oxfordjournals.pubmed.a024633.
- Balme E, Gerada C, Page L. Doctors need to be supported, not trained in resilience. BMJ Careers 2015;15. https://doi.org/10.1136/bmj.h4709.
- Cheshire A, Ridge D, Hughes J, Peters D, Panagioti M, Simon C, et al. Influences on GP coping and resilience: a qualitative study in primary care. Br J Gen Pract 2017;67:e428-e436. https://doi.org/10.3399/bjgp17X690893.
- Panagioti M, Panagopoulou E, Bower P, Lewith G, Kontopantelis E, Chew-Graham C, et al. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis. JAMA Intern Med 2017;177:195-20. https://doi.org/10.1001/jamainternmed.2016.7674.
- Petersen A, Lupton D. The New Public Health. Discourses, Knowledges, Strategies. Thousand Oaks, CA: SAGE Publications Ltd; 1997.
- Jackson M. The Age of Stress: Science and the Search for Stability. Oxford: Oxford University Press; 2013.
- Graphic Medicine . Care Under Pressure n.d. www.graphicmedicine.org/care-under-pressure/ (accessed 4 November 2019).
- Gerada C. Clare Gerada: dissecting resilience. BMJ 2018;363. https://doi.org/10.1136/bmj.k4974.
- Meyers MF. Why Physicians Die by Suicide: Lessons Learned from their Families and Others Who Cared. Gorham, ME: Myers Publisher; 2017.
- West CP, Dyrbye LN, Rabatin JT, Call TG, Davidson JH, Multari A, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med 2014;174:527-33. https://doi.org/10.1001/jamainternmed.2013.14387.
- Wong G, Brennan N, Mattick K, Pearson M, Briscoe S, Papoutsi C. Interventions to improve antimicrobial prescribing of doctors in training: the IMPACT (IMProving Antimicrobial presCribing of doctors in Training) realist review. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-009059.
- Papoutsi C, Mattick K, Pearson M, Brennan N, Briscoe S, Wong G. Interventions to improve antimicrobial prescribing of doctors in training (IMPACT): a realist review. Health Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06100.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist Synthesis: An Introduction. ESRC Research Methods Programme. Manchester: University of Manchester; 2004.
- Wong G, Westhorp G, Manzano A, Greenhalgh J, Jagosh J, Greenhalgh T. RAMESES II reporting standards for realist evaluations. BMC Med 2016;14. https://doi.org/10.1186/s12916-016-0643-1.
- Carrieri D, Briscoe S, Jackson M, Mattick K, Papoutsi C, Pearson M, et al. ‘Care Under Pressure’: a realist review of interventions to tackle doctors’ mental ill-health and its impacts on the clinical workforce and patient care. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-021273.
- Glasgow RE, Green LW, Taylor MV, Stange KC. An evidence integration triangle for aligning science with policy and practice. Am J Prev Med 2012;42:646-54. https://doi.org/10.1016/j.amepre.2012.02.016.
- Gibson A, Britten N, Lynch J. Theoretical directions for an emancipatory concept of patient and public involvement. Health 2012;16:531-47. https://doi.org/10.1177/1363459312438563.
- Polanyi M. Personal Knowledge. London: Routledge; 2012.
- Pawson R. Evidence-based Policy: A Realist Perspective. Thousand Oaks, CA: SAGE Publications Ltd; 2006.
- Stern C, Jordan Z, McArthur A. Developing the review question and inclusion criteria. Am J Nurs 2014;114:53-6. https://doi.org/10.1097/01.NAJ.0000445689.67800.86.
- Allen R, Watt F, Jansen B, Coghlan E, Nathan EA. Minimising compassion fatigue in obstetrics/gynaecology doctors: exploring an intervention for an occupational hazard. Australas Psychiatry 2017;25:403-6. https://doi.org/10.1177/1039856217700776.
- Bakker AB, Schaufeli WB, Sixma HJ, Bosveld W, van Dierendonck D. Patient demands, lack of reciprocity, and burnout: a five-year longitudinal study among general practitioners. J Organ Behav 2000;21:425-41.
- Barbosa P, Raymond G, Zlotnick C, Wilk J, Toomey R, Mitchell J. Mindfulness-based stress reduction training is associated with greater empathy and reduced anxiety for graduate healthcare students. Educ Health (Abingdon) 2013;26:9-14. https://doi.org/10.4103/1357-6283.112794.
- Bar-Sela G, Lulav-Grinwald D, Mitnik I. ‘Balint group’ meetings for oncology residents as a tool to improve therapeutic communication skills and reduce burnout level. J Cancer Educ 2012;27:786-9. https://doi.org/10.1007/s13187-012-0407-3.
- Beckman H. The role of medical culture in the journey to resilience. Acad Med 2015;90:710-12. https://doi.org/10.1097/ACM.0000000000000711.
- Benson J, Magraith K. Compassion fatigue and burnout: the role of Balint groups. Aust Fam Physician 2005;34:497-8.
- Bitonte RA, DeSanto DJ. Mandatory physical exercise for the prevention of mental illness in medical students. Ment Illn 2014;6. https://doi.org/10.4081/mi.2014.5549.
- Blais R, Safianyk C, Magnan A, Lapierre A. Physician, heal thyself: survey of users of the Quebec Physicians Health Program. Can Fam Physician 2010;56:e383-9.
- Boorman S. The Final Report of the Independent NHS Health and Well-Being Review (2009) 2009.
- Bragard I, Razavi D, Marchal S, Merckaert I, Delvaux N, Libert Y, et al. Teaching communication and stress management skills to junior physicians dealing with cancer patients: a Belgian Interuniversity Curriculum. Support Care Cancer 2006;14:454-61. https://doi.org/10.1007/s00520-005-0008-3.
- Brazeau CM. The surest way to prevent burnout in medical school and beyond. Acad Med 2010;85:569-70. https://doi.org/10.1097/ACM.0b013e3181d2d643.
- Bugaj TJ, Mücksch C, Schmid C, Junne F, Erschens R, Herzog W, et al. Peer-led stress prevention seminars in the first year of medical school – a project report. GMS J Med Educ 2016;33. https://doi.org/10.3205/zma001002.
- Bugaj T, Cranz A, Junne F, Erschens R, Herzog W, Nikendei C. Psychosocial burden in medical students and specific prevention strategies. Ment Health Prev 2016;4:24-30. https://doi.org/10.1016/j.mhp.2015.12.003.
- Bughi SA, Lie DA, Zia SK, Rosenthal J. Using a personality inventory to identify risk of distress and burnout among early stage medical students. Educ Health 2017;30:26-30. https://doi.org/10.4103/1357-6283.210499.
- Peile E, Carter Y. Selecting and supporting contented doctors. BMJ 2005;330:269-70. https://doi.org/10.1136/bmj.330.7486.269.
- Carvour ML, Ayyar BK, Chien KS, Ramirez NC, Yamamoto H. A patient-centered approach to postgraduate trainee health and wellness: an applied review and health care delivery model. Acad Med 2016;91:1205-10. https://doi.org/10.1097/ACM.0000000000001301.
- Chambers C, Frampton C, Barclay M. Presenteeism in the New Zealand senior medical workforce – a mixed-methods analysis. N Z Med J 2017;130:10-21.
- Chang E, Eddins-Folensbee F, Porter B, Coverdale J. Utilization of counseling services at one medical school. South Med J 2013;106:449-53. https://doi.org/10.1097/SMJ.0b013e3182a05994.
- Chaukos D, Chad-Friedman E, Mehta DH, Byerly L, Celik A, McCoy TH, et al. SMART-R: A Prospective Cohort Study of a Resilience Curriculum for Residents by Residents. Acad Psychiatry 2018;42:78-83. https://doi.org/10.1007/s40596-017-0808-z.
- Clarke RT, Pitcher A, Lambert TW, Goldacre MJ. UK doctors’ views on the implementation of the European Working Time Directive as applied to medical practice: a qualitative analysis. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2013-004390.
- Clough BA, March S, Chan RJ, Casey LM, Phillips R, Ireland MJ. Psychosocial interventions for managing occupational stress and burnout among medical doctors: a systematic review. Syst Rev 2017;6. https://doi.org/10.1186/s13643-017-0526-3.
- Cockerell CJ. Pressure and disenchantment in physicians – Part I: developing an approach to reconnect with what is noble about medicine. Clin Dermatol 2016;34:650-3. https://doi.org/10.1016/j.clindermatol.2016.04.004.
- Cockerell CJ. Pressure and disenchantment in physicians – Part II: lessons for physicians from the Tao Te Ching. Clin Dermatol 2017;35:100-4. https://doi.org/10.1016/j.clindermatol.2016.04.005.
- Cornelius A, Cornelius BG, Edens MA. Increasing resident wellness through a novel retreat curriculum. Cureus 2017;9. https://doi.org/10.7759/cureus.1524.
- Cornwell J, Fitzsimons B. Behind Closed Doors. Can We Expect NHS Staff to be the Shock Absorbers of a System Under Pressure?. London: The Point of Care Foundation; 2017.
- Davies SR, Meerton M, Rost F, Garelick AI. A sea change for sick doctors – how do doctors fare after presenting to a specialist psychotherapy service?. J Ment Health 2016;25:238-44. https://doi.org/10.3109/09638237.2015.1124386.
- de Vibe M, Solhaug I, Tyssen R, Friborg O, Rosenvinge JH, Sørlie T, et al. Mindfulness training for stress management: a randomised controlled study of medical and psychology students. BMC Med Educ 2013;13. https://doi.org/10.1186/1472-6920-13-107.
- Deng YT, Liu J, Zhang J, Huang BY, Yi TW, Wang YQ, et al. A multicenter study on the validation of the Burnout Battery: a new visual analog scale to screen job burnout in oncology professionals. Psychooncology 2017;26:1120-5. https://doi.org/10.1002/pon.4291.
- Department of Health and Social Care . NHS Health and Wellbeing Review: Interim Report 2009.
- Devi S. Doctors in distress. Lancet 2011;377:454-5. https://doi.org/10.1016/S0140-6736(11)60145-1.
- Dobkin PL, Hutchinson TA. Teaching mindfulness in medical school: where are we now and where are we going?. Med Educ 2013;47:768-79. https://doi.org/10.1111/medu.12200.
- Downs N, Feng W, Kirby B, McGuire T, Moutier C, Norcross W, et al. Listening to depression and suicide risk in medical students: the Healer Education Assessment and Referral (HEAR) program. Acad Psychiatry 2014;38:547-53. https://doi.org/10.1007/s40596-014-0115-x.
- Dunn PM, Arnetz BB, Christensen JF, Homer L. Meeting the imperative to improve physician well-being: assessment of an innovative program. J Gen Intern Med 2007;22:1544-52. https://doi.org/10.1007/s11606-007-0363-5.
- Dyer C. Julien Warshafsky: how this doctor died and what it tells us about the system that failed him. BMJ 2018;361. https://doi.org/10.1136/bmj.k2564.
- Dyrbye LN, West CP, Richards ML, Ross HJ, Satele D, Shanafelt TD. A randomized, controlled study of an online intervention to promote job satisfaction and well-being among physicians. Burn Res 2016;3:69-75. https://doi.org/10.1016/j.burn.2016.06.002.
- Dyrbye LN, Satele D, Shanafelt TD. Healthy exercise habits are associated with lower risk of burnout and higher quality of life among U.S. medical students. Acad Med 2017;92:1006-11. https://doi.org/10.1097/ACM.0000000000001540.
- Dyrbye LN, Shanafelt TD, Werner L, Sood A, Satele D, Wolanskyj AP. The impact of a required longitudinal stress management and resilience training course for first-year medical students. J Gen Intern Med 2017;32:1309-14. https://doi.org/10.1007/s11606-017-4171-2.
- Eisenstein L. To fight burnout, organize. N Engl J Med 2018;379:509-11. https://doi.org/10.1056/NEJMp1803771.
- Epstein RM, Krasner MS. Physician resilience: what it means, why it matters, and how to promote it. Acad Med 2013;88:301-3. https://doi.org/10.1097/ACM.0b013e318280cff0.
- Ey S, Moffit M, Kinzie JM, Choi D, Girard DE. ‘If you build it, they will come’: attitudes of medical residents and fellows about seeking services in a resident wellness program. J Grad Med Educ 2013;5:486-92. https://doi.org/10.4300/JGME-D-12-00048.1.
- Ey S, Moffit M, Kinzie JM, Brunett PH. Feasibility of a comprehensive wellness and suicide prevention program: a decade of caring for physicians in training and practice. J Grad Med Educ 2016;8:747-53. https://doi.org/10.4300/JGME-D-16-00034.1.
- Feld J, Heyse-Moore L. An evaluation of a support group for junior doctors working in palliative medicine. Am J Hosp Palliat Care 2006;23:287-96. https://doi.org/10.1177/1049909106290717.
- Firth-Cozens J. Improving the health of psychiatrists. Adv Psychiatr Treat 2007;13:161-8. https://doi.org/10.1192/apt.bp.106.003277.
- Flowers LK. The missing curriculum: experience with emotional competence education and training for premedical and medical students. J Natl Med Assoc 2005;97:1280-7.
- Foster E, Biery N, Dostal J, Larson D. RAFT (Resident Assessment Facilitation Team): supporting resident well-being through an integrated advising and assessment process. Fam Med 2012;44:731-4.
- Fothergill A, Edwards D, Burnard P. Stress, burnout, coping and stress management in psychiatrists: findings from a systematic review. Int J Soc Psychiatry 2004;50:54-65. https://doi.org/10.1177/0020764004040953.
- Gardiner P, Filippelli AC, Lebensohn P, Bonakdar R. The incorporation of stress management programming into family medicine residencies – results of a national survey of residency directors: a CERA study. Fam Med 2015;47:272-8.
- Gardiner M, Kearns H, Tiggemann M. Effectiveness of cognitive behavioural coaching in improving the well-being and retention of rural general practitioners. Aust J Rural Health 2013;21:183-9. https://doi.org/10.1111/ajr.12033.
- Garelick AI, Gross SR, Richardson I, von der Tann M, Bland J, Hale R. Which doctors and with what problems contact a specialist service for doctors? A cross sectional investigation. BMC Med 2007;5. https://doi.org/10.1186/1741-7015-5-26.
- Garside B. Physicians mutual aid group: a response to AIDS-related burnout. Health Soc Work 1993;18:259-67. https://doi.org/10.1093/hsw/18.4.259.
- Gazelle G, Liebschutz JM, Riess H. Physician burnout: coaching a way out. J Gen Intern Med 2015;30:508-13. https://doi.org/10.1007/s11606-014-3144-y.
- Geller G, Bernhardt BA, Carrese J, Rushton CH, Kolodner K. What do clinicians derive from partnering with their patients? A reliable and valid measure of ‘personal meaning in patient care’. Patient Educ Couns 2008;72:293-300. https://doi.org/10.1016/j.pec.2008.03.025.
- George DR, Dellasega C, Whitehead M. Facebook stress management group for Year 1 medical students. Med Educ 2012;46. https://doi.org/10.1111/medu.12034.
- Gerada C. For doctors with mental illness, ‘help me’ can be the hardest words. The Guardian 2018. www.theguardian.com/commentisfree/2018/jun/06/doctors-mental-health-problems-taboo (accessed 20 August 2019).
- Goldhagen BE, Kingsolver K, Stinnett SS, Rosdahl JA. Stress and burnout in residents: impact of mindfulness-based resilience training. Adv Med Educ Pract 2015;6:525-32. https://doi.org/10.2147/AMEP.S88580.
- Goodman MJ, Schorling JB. A mindfulness course decreases burnout and improves well-being among healthcare providers. Int J Psychiatry Med 2012;43:119-28. https://doi.org/10.2190/PM.43.2.b.
- Graham J, Ramirez AJ, Field S, Richards MA. Job stress and satisfaction among clinical radiologists. Clin Radiol 2000;55:182-5. https://doi.org/10.1053/crad.1999.0379.
- Gregory ST, Menser T. Burnout among primary care physicians: a test of the areas of worklife model. J Healthc Manage 2015;60:133-48. https://doi.org/10.1097/00115514-201503000-00009.
- Gulen B, Serinken M, Eken C, Karcıoglu Ö, Kucukdagli OT, Kilic E, et al. Serum S100B as a surrogate biomarker in the diagnoses of burnout and depression in emergency medicine residents. Acad Emerg Med 2016;23:786-9. https://doi.org/10.1111/acem.12973.
- Gunasingam N, Burns K, Edwards J, Dinh M, Walton M. Reducing stress and burnout in junior doctors: the impact of debriefing sessions. Postgrad Med J 2015;91:182-7. https://doi.org/10.1136/postgradmedj-2014-132847.
- Haizlip J, May N, Schorling J, Williams A, Plews-Ogan M. Perspective: the negativity bias, medical education, and the culture of academic medicine: why culture change is hard. Acad Med 2012;87:1205-9. https://doi.org/10.1097/ACM.0b013e3182628f03.
- Hamader G, Noehammer E, Noehammer E. Psychology of Well-being: Theory, Perspectives and Practice. Hauppauge, NY: Nova Science Publishers; 2013.
- Harrison R, Anderson J, Laloë PA, Santillo M, Lawton R, Wright J. Mentorship for newly appointed consultants: what makes it work?. Postgrad Med J 2014;90:439-45. https://doi.org/10.1136/postgradmedj-2013-132333.
- Haward R, Amir Z, Borrill C, Dawson J, Scully J, West M, et al. Breast cancer teams: the impact of constitution, new cancer workload, and methods of operation on their effectiveness. Br J Cancer 2003;89:15-22. https://doi.org/10.1038/sj.bjc.6601073.
- Hegenbarth C. Rescuing doctors in distress. CMAJ 2011;183:E153-4. https://doi.org/10.1503/cmaj.109-3760.
- Hill RC, Dempster M, Donnelly M, McCorry NK. Improving the wellbeing of staff who work in palliative care settings: a systematic review of psychosocial interventions. Palliat Med 2016;30:825-33. https://doi.org/10.1177/0269216316637237.
- Hill JD, Smith RJ. Monitoring stress levels in postgraduate medical training. Laryngoscope 2009;119:75-8. https://doi.org/10.1002/lary.20013.
- Hlubocky FJ, Back AL, Shanafelt TD. Addressing burnout in oncology: why cancer care clinicians are at risk, what individuals can do, and how organizations can respond. Am Soc Clin Oncol Educ Book 2016;35:271-9. https://doi.org/10.14694/EDBK_156120.
- Hochberg MS, Berman RS, Kalet AL, Zabar SR, Gillespie C, Pachter HL. The stress of residency: recognizing the signs of depression and suicide in you and your fellow residents. Am J Surg 2013;205:141-6. https://doi.org/10.1016/j.amjsurg.2012.08.003.
- Holoshitz N, Wann S. Burnout – there’s an app for that: helping physicians deal with job-related stress. JAMA Cardiol 2017;2:1185-6. https://doi.org/10.1001/jamacardio.2017.1758.
- Horsfall S. Doctors Who Commit Suicide While Under GMC Fitness to Practice Investigation. London: General Medical Council; 2014.
- Hotchkiss NF. Predictors of reactivation and gender differences at a physician health program by age, marital status, primary presenting problem, referral source, and referral status. Diss Abstr Int 2008;69.
- Howlett M, Doody K, Murray J, LeBlanc-Duchin D, Fraser J, Atkinson PR. Burnout in emergency department healthcare professionals is associated with coping style: a cross-sectional survey. Emerg Med J 2015;32:722-7. https://doi.org/10.1136/emermed-2014-203750.
- Ireland MJ, Clough B, Gill K, Langan F, O’Connor A, Spencer L. A randomized controlled trial of mindfulness to reduce stress and burnout among intern medical practitioners. Med Teach 2017;39:409-14. https://doi.org/10.1080/0142159X.2017.1294749.
- Isaksson Rø KE, Tyssen R, Hoffart A, Sexton H, Aasland OG, Gude T. A three-year cohort study of the relationships between coping, job stress and burnout after a counselling intervention for help-seeking physicians. BMC Public Health 2010;10. https://doi.org/10.1186/1471-2458-10-213.
- Isaksson Rø KE, Tyssen R, Gude T, Aasland OG. Will sick leave after a counselling intervention prevent later burnout? A 3-year follow-up study of Norwegian doctors. Scand J Public Health 2012;40:278-85. https://doi.org/10.1177/1403494812443607.
- Kemper KJ, Khirallah M. Acute effects of online mind-body skills training on resilience, mindfulness, and empathy. J Evid Based Complementary Altern Med 2015;20:247-53. https://doi.org/10.1177/2156587215575816.
- Kjeldmand D, Holmström I. Balint groups as a means to increase job satisfaction and prevent burnout among general practitioners. Ann Fam Med 2008;6:138-45. https://doi.org/10.1370/afm.813.
- Kötter T, Pohontsch NJ, Voltmer E. Stressors and starting points for health-promoting interventions in medical school from the students’ perspective: a qualitative study. Perspect Med Educ 2015;4:128-35. https://doi.org/10.1007/s40037-015-0189-5.
- Krasner MS, Epstein RM, Beckman H, Suchman AL, Chapman B, Mooney CJ, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA 2009;302:1284-93. https://doi.org/10.1001/jama.2009.1384.
- Kumar S. Burnout in psychiatrists. World Psychiatry 2007;6:186-9.
- Kushnir T, Malkinson R, Ribak J. Teaching stress management skills to occupational and environmental health physicians and practitioners. A graduate-level practicum. J Occup Med 1994;36:1335-40. https://doi.org/10.1097/00043764-199412000-00016.
- Lapa TA, Carvalho SA, Viana JS, Ferreira PL, Pinto-Gouveia J. Stressors in anaesthesiology: development and validation of a new questionnaire: a cross-sectional study of Portuguese anaesthesiologists. Eur J Anaesthesiol 2016;33:807-15. https://doi.org/10.1097/EJA.0000000000000518.
- Lederer W, Kinzl JF, Traweger C, Dosch J, Sumann G. Fully developed burnout and burnout risk in intensive care personnel at a university hospital. Anaesth Intensive Care 2008;36:208-13. https://doi.org/10.1177/0310057X0803600211.
- Lee YC, Huang SC, Huang CH, Wu HH. A new approach to identify high burnout medical staffs by Kernel K-means cluster analysis in a regional teaching hospital in Taiwan. Inquiry 2016;53. https://doi.org/10.1177/0046958016679306.
- Lefebvre DC. Perspective: resident physician wellness: a new hope. Acad Med 2012;87:598-602. https://doi.org/10.1097/ACM.0b013e31824d47ff.
- Leff V, Klement A, Galanos A. A successful debrief program for house staff. J Soc Work End Life Palliat Care 2017;13:87-90. https://doi.org/10.1080/15524256.2017.1314234.
- Lim RC, Pinto C. Work stress, satisfaction and burnout in New Zealand radiologists: comparison of public hospital and private practice in New Zealand. J Med Imaging Radiat Oncol 2009;53:194-9. https://doi.org/10.1111/j.1754-9485.2009.02063.x.
- Linzer M, Poplau S, Grossman E, Varkey A, Yale S, Williams E, et al. A cluster randomized trial of interventions to improve work conditions and clinician burnout in primary care: results from the Healthy Work Place (HWP) study. J Gen Intern Med 2015;30:1105-11. https://doi.org/10.1007/s11606-015-3235-4.
- Linzer M, Visser MR, Oort FJ, Smets EM, McMurray JE, de Haes HC. Society of General Internal Medicine (SGIM) Career Satisfaction Study Group (CSSG) . Predicting and preventing physician burnout: results from the United States and the Netherlands. Am J Med 2001;111:170-5. https://doi.org/10.1016/S0002-9343(01)00814-2.
- Luthar SS, Curlee A, Tye SJ, Engelman JC, Stonnington CM. Fostering resilience among mothers under stress: ‘authentic connections groups’ for medical professionals. Womens Health Issues 2017;27:382-90. https://doi.org/10.1016/j.whi.2017.02.007.
- Lyons B, Dolezal L. Shame, stigma and medicine. Med Humanit 2017;43:208-10. https://doi.org/10.1136/medhum-2017-011392.
- Mache S, Vitzthum K, Hauschild I, Groneberg D. A pilot study evaluation of psychosocial competency training for junior physicians working in oncology and hematology. Psychooncology 2017;26:1894-900. https://doi.org/10.1002/pon.4403.
- Maslach C, Leiter MP. New insights into burnout and health care: strategies for improving civility and alleviating burnout. Med Teach 2017;39:160-3. https://doi.org/10.1080/0142159X.2016.1248918.
- McCartney M. Margaret McCartney: we should stop fuelling anxiety. BMJ 2018;361. https://doi.org/10.1136/bmj.k2399.
- McClafferty H, Brown OW. Section on integrative medicine. Physician health and wellness. Pediatrics 2014;134:830-5. https://doi.org/10.1542/peds.2014-2278.
- McCray LW, Cronholm PF, Bogner HR, Gallo JJ, Neill RA. Resident physician burnout: is there hope?. Fam Med 2008;40:626-32.
- McCue JD, Sachs CL. A stress management workshop improves residents’ coping skills. Arch Intern Med 1991;151:2273-7. https://doi.org/10.1001/archinte.1991.00400110117023.
- McKenna KM, Hashimoto DA, Maguire MS, Bynum WE. The missing link: connection is the key to resilience in medical education. Acad Med 2016;91:1197-9. https://doi.org/10.1097/ACM.0000000000001311.
- McKevitt C, Morgan M. Illness doesn’t belong to us. J R Soc Med 1997;90:491-5. https://doi.org/10.1177/014107689709000907.
- McKinley TF, Boland KA, Mahan JD. Burnout and interventions in pediatric residency: a literature review. Burn Res 2017;6:9-17. https://doi.org/10.1016/j.burn.2017.02.003.
- McManus IC, Jonvik H, Richards P, Paice E. Vocation and avocation: leisure activities correlate with professional engagement, but not burnout, in a cross-sectional survey of UK doctors. BMC Med 2011;9. https://doi.org/10.1186/1741-7015-9-100.
- McNeill KG, Kerr A, Mavor KI. Identity and norms: the role of group membership in medical student wellbeing. Perspect Med Educ 2014;3:101-12. https://doi.org/10.1007/s40037-013-0102-z.
- Mechaber HF, Levine RB, Manwell LB, Mundt MP, Linzer M, Schwartz M, et al. Part-time physicians . . . prevalent, connected, and satisfied. J Gen Intern Med 2008;23:300-3. https://doi.org/10.1007/s11606-008-0514-3.
- Meerten M, Rost F, Bland J, Garelick AI. Self-referrals to a doctors’ mental health service over 10 years. Occup Med 2014;64:172-6. https://doi.org/10.1093/occmed/kqt177.
- Mehta DH, Perez GK, Traeger L, Park ER, Goldman RE, Haime V, et al. Building resiliency in a palliative care team: a pilot study. J Pain Symptom Manage 2016;51:604-8. https://doi.org/10.1016/j.jpainsymman.2015.10.013.
- Milstein JM, Raingruber BJ, Bennett SH, Kon AA, Winn CA, Paterniti DA. Burnout assessment in house officers: evaluation of an intervention to reduce stress. Med Teach 2009;31:338-41. https://doi.org/10.1080/01421590802208552.
- Montgomery A, Panagopoulou E, Kehoe I, Valkanos E. Connecting organisational culture and quality of care in the hospital: is job burnout the missing link?. J Health Organ Manag 2011;25:108-23. https://doi.org/10.1108/14777261111116851.
- Moutier C, Norcross W, Jong P, Norman M, Kirby B, McGuire T, et al. The suicide prevention and depression awareness program at the University of California, San Diego School of Medicine. Acad Med 2012;87:320-6. https://doi.org/10.1097/ACM.0b013e31824451ad.
- Murdoch JM, Eagles JM. ‘Stress-busting’ groups for consultant psychiatrists. Psychiatr Bull 2007;31:128-31. https://doi.org/10.1192/pb.bp.106.010934.
- Myszkowski N, Villoing B, Zenasni F, Jaury P, Boujut E. Monitoring stress among internal medicine residents: an experience-driven, practical and short measure. Psychol Health Med 2017;22:719-26. https://doi.org/10.1080/13548506.2016.1220599.
- NHS England . NHS Staff Health and Wellbeing: CQUIN Supplementary Guidance 2016. www.england.nhs.uk/wp-content/uploads/2016/03/HWB-CQUIN-Guidance.pdf.
- Nielsen HG, Tulinius C. Preventing burnout among general practitioners: is there a possible route?. Educ Prim Care 2009;20:353-9. https://doi.org/10.1080/14739879.2009.11493817.
- Nomura O, Mishina H, Kobayashi Y, Ishiguro A, Sakai H, Kato H. Limitation of duty hour regulations for pediatric resident wellness: a mixed methods study in Japan. Medicine 2016;95. https://doi.org/10.1097/MD.0000000000004867.
- Oczkowski S. Virtuous laughter: we should teach medical learners the art of humor. Crit Care 2015;19. https://doi.org/10.1186/s13054-015-0927-4.
- Oman D, Hedberg J, Thoresen CE. Passage meditation reduces perceived stress in health professionals: a randomized, controlled trial. J Consult Clin Psychol 2006;74:714-19. https://doi.org/10.1037/0022-006X.74.4.714.
- Paice E, Aitken M, Houghton A, Firth-Cozens J. Bullying among doctors in training: cross sectional questionnaire survey. BMJ 2004;329:658-9. https://doi.org/10.1136/bmj.38133.502569.AE.
- Paice E, Rutter H, Wetherell M, Winder B, McManus IC. Stressful incidents, stress and coping strategies in the pre-registration house officer year. Med Educ 2002;36:56-65. https://doi.org/10.1046/j.1365-2923.2002.01101.x.
- Penfold R. Why junior doctors need more autonomy. BMJ 2018;363. https://doi.org/10.1136/bmj.k4525.
- Pereira MA, Barbosa MA, de Rezende JC, Damiano RF. Medical student stress: an elective course as a possibility of help. BMC Res Notes 2015;8. https://doi.org/10.1186/s13104-015-1399-y.
- Prins JT, Hoekstra-Weebers JE, Gazendam-Donofrio SM, Van De Wiel HB, Sprangers F, Jaspers FC, et al. The role of social support in burnout among Dutch medical residents. Psychol Health Med 2007;12:1-6. https://doi.org/10.1080/13548500600782214.
- Rabin S, Matalon A, Maoz B, Shiber A. Keeping doctors healthy: a salutogenic perspective. Fam Syst Health 2005;23:94-102. https://doi.org/10.1037/1091-7527.23.1.94.
- Raj KS. Well-being in residency: a systematic review. J Grad Med Educ 2016;8:674-84. https://doi.org/10.4300/JGME-D-15-00764.1.
- Ramirez AJ, Graham J, Richards MA, Cull A, Gregory WM. Mental health of hospital consultants: the effects of stress and satisfaction at work. Lancet 1996;347:724-8. https://doi.org/10.1016/S0140-6736(96)90077-X.
- Isaksson Rø K, Veggeland F, Aasland OG. Peer counselling for doctors in Norway: a qualitative study of the relationship between support and surveillance. Soc Sci Med 2016;162:193-200. https://doi.org/10.1016/j.socscimed.2016.06.037.
- Regehr C, Glancy D, Pitts A, LeBlanc VR. Interventions to reduce the consequences of stress in physicians: a review and meta-analysis. J Nerv Ment Dis 2014;202:353-9. https://doi.org/10.1097/NMD.0000000000000130.
- Riley R, Spiers J, Buszewicz M, Taylor AK, Thornton G, Chew-Graham CA. What are the sources of stress and distress for general practitioners working in England? A qualitative study. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-017361.
- Riley R, Spiers J, Chew-Graham CA, Taylor AK, Thornton GA, Buszewicz M. ‘Treading water but drowning slowly’: what are GPs’ experiences of living and working with mental illness and distress in England? A qualitative study. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-018620.
- Ringrose R, Houterman S, Koops W, Oei G. Burnout in medical residents: a questionnaire and interview study. Psychol Health Med 2009;14:476-86. https://doi.org/10.1080/13548500903012822.
- Ripp JA, Fallar R, Korenstein D. A randomized controlled trial to decrease job burnout in first-year internal medicine residents using a facilitated discussion group intervention. J Grad Med Educ 2016;8:256-9. https://doi.org/10.4300/JGME-D-15-00120.1.
- Ripp JA, Privitera MR, West CP, Leiter R, Logio L, Shapiro J, et al. Well-being in graduate medical education: a call for action. Acad Med 2017;92:914-17. https://doi.org/10.1097/ACM.0000000000001735.
- Ripp JA, Bellini L, Fallar R, Bazari H, Katz JT, Korenstein D. The impact of duty hours restrictions on job burnout in internal medicine residents: a three-institution comparison study. Acad Med 2015;90:494-9. https://doi.org/10.1097/ACM.0000000000000641.
- Rippstein-Leuenberger K, Mauthner O, Bryan Sexton J, Schwendimann R. A qualitative analysis of the Three Good Things intervention in healthcare workers. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-015826.
- Isaksson Rø KE, Gude T, Tyssen R, Aasland OG. Counselling for burnout in Norwegian doctors: one year cohort study. BMJ 2008;337. https://doi.org/10.1136/bmj.a2004.
- Roberts G, Moore B, Coles C. Mentoring for newly appointed consultant psychiatrists. Psychiatr Bull 2002;26:106-9. https://doi.org/10.1192/pb.26.3.106.
- Robertson I, Cooper C. The Boorman Report on the Health and Well-Being of NHS Staff: Practical Advice for Implementing Its Recommendations 2010.
- Rohland BM, Kruse GR, Rohrer JE. Validation of a single-item measure of burnout against the Maslach Burnout Inventory among physicians. Stress Health 2004;20:75-9. https://doi.org/10.1002/smi.1002.
- Runyan C, Savageau JA, Potts S, Weinreb L. Impact of a family medicine resident wellness curriculum: a feasibility study. Med Educ Online 2016;21. https://doi.org/10.3402/meo.v21.30648.
- Sallon S, Katz-Eisner D, Yaffe H, Bdolah-Abram T. Caring for the caregivers: results of an extended, five-component stress-reduction intervention for hospital staff. Behav Med 2017;43:47-60. https://doi.org/10.1080/08964289.2015.1053426.
- Sanchez LT, Candilis PJ, Arnstein F, Eaton J, Barnes Blood D, Chinman GA, et al. Effectiveness of a unique support group for physicians in a physician health program. J Psychiatr Pract 2016;22:56-63. https://doi.org/10.1097/PRA.0000000000000121.
- Schapira L, Meisel JL, Srivastava R. For our patients, for ourselves: the value of personal reflection in oncology. Am Soc Clin Oncol Educ Book 2017;37:765-70. https://doi.org/10.14694/EDBK_175520.
- Schattner A. Residents’ responsibilities: adopting a wider view. Med Teach 2017;39:1286-9. https://doi.org/10.1080/0142159X.2017.1319916.
- Schmitz GR, Clark M, Heron S, Sanson T, Kuhn G, Bourne C, et al. Strategies for coping with stress in emergency medicine: early education is vital. J Emerg Trauma Shock 2012;5:64-9. https://doi.org/10.4103/0974-2700.93117.
- Schneider S, Kingsolver K, Rosdahl J. Physician coaching to enhance well-being: a qualitative analysis of a pilot intervention. Explore 2014;10:372-9. https://doi.org/10.1016/j.explore.2014.08.007.
- Scholz M, Neumann C, Wild K, Garreis F, Hammer CM, Ropohl A, et al. Teaching to relax: development of a program to potentiate stress – results of a feasibility study with medical undergraduate students. Appl Psychophysiol Biofeedback 2016;41:275-81. https://doi.org/10.1007/s10484-015-9327-4.
- Seoane L, Tompkins LM, De Conciliis A, Boysen PG. Virtues education in medical school: the foundation for professional formation. Ochsner J 2016;16:50-5.
- Shanafelt TD, Oreskovich MR, Dyrbye LN, Satele DV, Hanks JB, Sloan JA, et al. Avoiding burnout: the personal health habits and wellness practices of US surgeons. Ann Surg 2012;255:625-33. https://doi.org/10.1097/SLA.0b013e31824b2fa0.
- Shanafelt TD, Kaups KL, Nelson H, Satele DV, Sloan JA, Oreskovich MR, et al. An interactive individualized intervention to promote behavioral change to increase personal well-being in US surgeons. Ann Surg 2014;259:82-8. https://doi.org/10.1097/SLA.0b013e3182a58fa4.
- Shapiro J, Astin J, Shapiro SL, Robitshek D, Shapiro DH. Coping with loss of control in the practice of medicine. Fam Syst Health 2011;29:15-28. https://doi.org/10.1037/a0022921.
- Shapiro J, Galowitz P. Peer support for clinicians: a programmatic approach. Acad Med 2016;91:1200-4. https://doi.org/10.1097/ACM.0000000000001297.
- Sharifi PS. Fostering self-care and mindfulness in mental health care providers. Diss Abstr Int 2012;73.
- Shiralkar MT, Harris TB, Eddins-Folensbee FF, Coverdale JH. A systematic review of stress-management programs for medical students. Acad Psychiatry 2013;37:158-64. https://doi.org/10.1176/appi.ap.12010003.
- Siedsma M, Emlet L. Physician burnout: can we make a difference together?. Crit Care 2015;19. https://doi.org/10.1186/s13054-015-0990-x.
- Sigsbee B, Bernat JL. Physician burnout: a neurologic crisis. Neurology 2014;83:2302-6. https://doi.org/10.1212/WNL.0000000000001077.
- Slavin SJ, Chibnall JT. Finding the why, changing the how: improving the mental health of medical students, residents, and physicians. Acad Med 2016;91:1194-6. https://doi.org/10.1097/ACM.0000000000001226.
- Slavin SJ, Hatchett L, Chibnall JT, Schindler D, Fendell G. Helping medical students and residents flourish: a path to transform medical education. Acad Med 2011;86. https://doi.org/10.1097/ACM.0b013e3182316558.
- Smith S. Breaking down the barriers of stigma: Understanding and fostering help-seeking behaviors in medical students. Diss Abstr Int 2016;77.
- Squiers JJ, Lobdell KW, Fann JI, DiMaio JM. Physician burnout: are we treating the symptoms instead of the disease?. Ann Thorac Surg 2017;104:1117-22. https://doi.org/10.1016/j.athoracsur.2017.08.009.
- Talisman N, Harazduk N, Rush C, Graves K, Haramati A. The impact of mind-body medicine facilitation on affirming and enhancing professional identity in health care professions faculty. Acad Med 2015;90:780-4. https://doi.org/10.1097/ACM.0000000000000720.
- Tucker T, Bouvette M, Daly S, Grassau P. Finding the sweet spot: developing, implementing and evaluating a burn out and compassion fatigue intervention for third year medical trainees. Eval Program Plann 2017;65:106-12. https://doi.org/10.1016/j.evalprogplan.2017.07.006.
- van Vliet M, Jong M, Jong MC. Long-term benefits by a mind-body medicine skills course on perceived stress and empathy among medical and nursing students. Med Teach 2017;39:710-19. https://doi.org/10.1080/0142159X.2017.1309374.
- Verweij H, Waumans RC, Smeijers D, Lucassen PL, Donders AR, van der Horst HE, et al. Mindfulness-based stress reduction for GPs: results of a controlled mixed methods pilot study in Dutch primary care. Br J Gen Pract 2016;66:e99-105. https://doi.org/10.3399/bjgp16X683497.
- Waddimba AC, Scribani M, Nieves MA, Krupa N, May JJ, Jenkins P. Validation of single-item screening measures for provider burnout in a rural health care network. Eval Health Prof 2016;39:215-25. https://doi.org/10.1177/0163278715573866.
- Wald HS, Haramati A, Bachner YG, Urkin J. Promoting resiliency for interprofessional faculty and senior medical students: outcomes of a workshop using mind-body medicine and interactive reflective writing. Med Teach 2016;38:525-8. https://doi.org/10.3109/0142159X.2016.1150980.
- Warde CM, Vermillion M, Uijtdehaage S. A medical student leadership course led to teamwork, advocacy, and mindfulness. Fam Med 2014;46:459-62.
- West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet 2016;388:2272-81. https://doi.org/10.1016/S0140-6736(16)31279-X.
- Wild K, Scholz M, Ropohl A, Bräuer L, Paulsen F, Burger PH. Strategies against burnout and anxiety in medical education – implementation and evaluation of a new course on relaxation techniques (Relacs) for medical students. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0114967.
- Wilkie G, Raffaelli D. In at the deep end: making the transition from SpR to consultant. Adv Psychiatr Treat 2005;11:107-14. https://doi.org/10.1192/apt.11.2.107.
- Williams S, Michie S, Pattani S. Improving the Health of the NHS Workforce: Report of the Partnership on the Health of the NHS Workforce 1998.
- Winefield H, Farmer E, Denson L. Work stress management for women general practitioners: an evaluation. Psychol Health Med 1998;3:163-70. https://doi.org/10.1080/13548509808402232.
- Wolf TM. Stress, coping and health: enhancing well-being during medical school. Med Educ 1994;28:8-17. https://doi.org/10.1111/j.1365-2923.1994.tb02679.x.
- Zhang H, Isaac A, Wright ED, Alrajhi Y, Seikaly H. Formal mentorship in a surgical residency training program: a prospective interventional study. J Otolaryngol Head Neck Surg 2017;46. https://doi.org/10.1186/s40463-017-0186-2.
- Zwack J, Schweitzer J. If every fifth physician is affected by burnout, what about the other four? Resilience strategies of experienced physicians. Acad Med 2013;88:382-9. https://doi.org/10.1097/ACM.0b013e318281696b.
- Pawson R. The Science of Evaluation: A Realist Manifesto. London: SAGE Publications Ltd; 2013.
- Jutel AG, Conrad P. Putting a Name to it: Diagnosis in Contemporary Society. Baltimore, MD: JHU Press; 2014.
- Piemonte NM. Afflicted: How Vulnerability Can Heal Medical Education and Practice. Cambridge, MA: MIT Press; 2018.
- Kumar S, Hatcher S, Dutu G, Fischer J, Ma’u E. Stresses experienced by psychiatrists and their role in burnout: a national follow-up study. Int J Soc Psychiatry 2011;57:166-79. https://doi.org/10.1177/0020764009341211.
- Kumar S. Burnout and psychiatrists: what do we know and where to from here?. Epidemiol Psychiatr Sci 2011;20:295-301. https://doi.org/10.1017/S204579601100059X.
- Wong G, Emmel N. Doing Realist Research. London: Sage; 2018.
- Haslam C, Jetten J, Cruwys T, Dingle G, Haslam A. The New Psychology of Health: Unlocking the Social Cure. Abingdon: Routledge; 2018.
- Haslam SA, Reicher S. Stressing the group: social identity and the unfolding dynamics of responses to stress. J Appl Psychol 2006;91:1037-52. https://doi.org/10.1037/0021-9010.91.5.1037.
- Jetten J, Haslam C, Alexander SH. The Social Cure: Identity, Health and Well-being. Hove: Psychology Press; 2012.
- Engel GL. The need for a new medical model: a challenge for biomedicine. Science 1977;196:129-36. https://doi.org/10.1126/science.847460.
- Wilkinson R, Pickett K. The Spirit Level. Why Equality Is Better For Everyone. UK: Penguin; 2010.
- Frank AW. Letting Stories Breathe: a Socio-Narratology. Chicago, IL: University of Chicago Press; 2010.
- Prainsack B, Buyx A. Solidarity in Biomedicine and Beyond. Vol. 33. Cambridge: Cambridge University Press; 2017.
- Prainsack B. The ‘we’ in the ‘me’: solidarity and health care in the era of personalized medicine. Sci Technol Human Values 2018;43:21-44. https://doi.org/10.1177/0162243917736139.
- Kreindler SA, Dowd DA, Dana Star N, Gottschalk T. Silos and social identity: the social identity approach as a framework for understanding and overcoming divisions in health care. Milbank Q 2012;90:347-74. https://doi.org/10.1111/j.1468-0009.2012.00666.x.
- Sluss DM, Ashforth BE. Relational identity and identification: defining ourselves through work relationships. Acad Manage Rev 2007;32:9-32. https://doi.org/10.5465/amr.2007.23463672.
- Currie G, Finn R, Martin G. Role transition and the interaction of relational and social identity: new nursing roles in the English NHS. Organ Stud 2010;31:941-61. https://doi.org/10.1177/0170840610373199.
- Ybema S, Keenoy T, Oswick C, Beverungen A, Ellis N, Sabelis I. Articulating identities. Hum Relat 2009;62:299-322. https://doi.org/10.1177/0018726708101904.
- Haslam SA, Steffens NK, Peters K, Boyce RA, Mallett CJ, Fransen K. A social identity approach to leadership development: the 5R program. Pers Psychol 2017;16. https://doi.org/10.1027/1866-5888/a000176.
- Sweeney KG. The information paradox. Occas Pap R Coll Gen Pract 1998;76:17-25. https://doi.org/10.1016/S0921-8009(98)00022-6.
Appendix 1 First search report
Interventions to reduce mental ill-health
Database: MEDLINE
Host: Ovid.
Data range searched: 1946 to November week 4 2017.
Date searched: 6 December 2017.
Searcher: SB.
Hits: 1517.
Search strategy
-
(doctor* or medic or medics or “medical trainee*” or “medical student*” or physician*).tw.
-
exp *Physicians/
-
*Students, Medical/
-
or/1-3
-
(“mental health” or “mental ill health” or stress* or distress* or anxiety or anxious or depression or depressed or “well being” or wellbeing or resilienc*).tw.
-
(pressure* adj3 (work* or "patient* demand*")).tw.
-
*Mental Health/
-
Stress, Psychological/
-
*Depression/
-
*Anxiety/
-
or/5-10
-
(retention or presenteeism or absenteeism or “leaving medicine” or “sick leave” or burnout or “burn* out").tw.
-
Presenteeism/
-
*Absenteeism/
-
*Sick Leave/
-
or/12-15
-
4 and 11 and 16
Database: MEDLINE In-Process & Other Non-Indexed Citations
Host: Ovid.
Data parameters: 1946 to 6 December 2017.
Date searched: 6 December 2017.
Searcher: SB.
Hits: 267.
Search strategy
-
(doctor* or medic or medics or “medical trainee*” or “medical student*” or physician*).tw.
-
(“mental health” or “mental ill health” or stress* or distress* or anxiety or anxious or depression or depressed or “well being” or wellbeing or resilienc*).tw.
-
(pressure* adj3 (work* or “patient* demand*”)).tw.
-
2 or 3
-
(retention or presenteeism or absenteeism or “leaving medicine” or “sick leave" or burnout or “burn* out”).tw.
-
1 and 4 and 5
Database: PsycINFO
Host: Ovid.
Data range searched: 1806 to November week 2 2017.
Date searched: 6 December 2017.
Searcher: SB.
Hits: 1025.
Search strategy
-
(doctor* or medic or medics or “medical trainee*” or “medical student*” or physician*).tw.
-
exp *physicians/
-
*medical students/
-
or/1-3
-
(“mental health” or “mental ill health” or stress* or distress* or anxiety or anxious or depression or depressed or “well being” or wellbeing or resilienc*).tw.
-
(pressure* adj3 (work* or “patient* demand*”)).tw.
-
*mental health/
-
psychological stress/
-
*major depression/
-
*anxiety/
-
or/5-10
-
(retention or presenteeism or absenteeism or “leaving medicine” or “sick leave” or burnout or “burn* out”).tw.
-
*employee absenteeism/
-
*employee leave benefits/
-
or/12-14
-
4 and 11 and 15
Database: Applied Social Sciences Index and Abstracts
Host: ProQuest.
Data range searched: 1987 to 6 December 2017.
Date Searched: 6 December 2017.
Searcher: SB.
Hits: 260.
Search strategy
-
(ti,ab(doctor* OR medic or medics OR “medical trainee*” OR “medical student*” OR physician*) OR MAINSUBJECT.EXACT.EXPLODE(“Doctors”) OR MAINSUBJECT.EXACT(“Medical students”))
-
(ti,ab(“mental health” OR “mental ill health” OR stress* OR distress* OR anxiety or anxious OR depression OR depressed OR “well being” OR wellbeing OR resilienc*) OR (pressure* n/2 (work* OR “patient* demand*”)) OR MAINSUBJECT.EXACT(“Mental health”) OR MAINSUBJECT.EXACT.EXPLODE(“Stress”) OR MAINSUBJECT.EXACT(“Depression”) OR MAINSUBJECT.EXACT(“Anxiety”) OR MAINSUBJECT.EXACT(“Anxiety-Depression”))
-
(ti,ab(retention OR presenteeism OR absenteeism OR “leaving medicine” OR “sick leave” OR burnout OR “burn* out”) OR MAINSUBJECT.EXACT(“Absenteeism”) OR MAINSUBJECT.EXACT.EXPLODE(“Sick leave”))
-
1 AND 2 AND 3
Number of results per bibliographic database and in total
| Database | Number of results |
|---|---|
| MEDLINE | 1517 |
| MEDLINE In-Process & Other Non-Indexed Citations | 267 |
| PyscINFO | 1025 |
| ASSIA | 260 |
| Total number of results | 3069 |
| Duplicate results | 634 |
| Total number of unique results | 2435 |
Appendix 2 Characteristics of all included studies
| Reference | Year | Country | Type of paper | Study design/methods | Level and type of interventions | Sample/setting | Prevention | Screening | Therapy | Objectives | Findings/outcome measures | £ | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Allen et al.64 | 2017 | Australia | Research (intervention study) | Questionnaires (pre/post intervention) | Structural: monthly psychiatric-led Balint style discussion groups | 25 obstetrics and gynaecology | C, T | ✗ | ✗ | Explore the indicators of occupational stress in a group of obstetrics and gynaecology doctors and to investigate the impact of work-focused discussion groups over a 6-month period | Intervention was associated with improved rates of, burnout and compassion satisfaction. It is unclear what particular aspects of the group process led to an improvement, raising questions about whether it was social connectedness, being heard in a confidential space or learning coping skills from peers | N | |
| Barbosa et al.66 | 2013 | USA | Research (intervention study) | Quasi-experimental trial, questionnaires | As above | Medical students | U | ✗ | Examine the impact of MBSR training on students from five health-care graduate programmes | The results provide supportive evidence of MBSR as a behavioural intervention to reduce anxiety and increase empathy among graduate health-care students, but does not diminish burnout | N | ||
| Bar-Sela et al.67 | 2012 | Israel | Research (intervention study) | Maslach Burnout Inventory and an expectations questionnaire |
Structural: Balint groups inspired case group discussions Duration: 1.5 hours Frequency: monthly |
17 oncologists in hospital setting | T, C | ✗ | Examine the impact of Balint-type case discussion groups on burnout, communication skills and self-awareness | Burnout parameter seems to have decreased (but difficult to measure) | N | ||
| Beckman68 | 2015 | USA | Commentary | Mixed, individual and cultural changes (medical culture, conceptual intervention from medical education) | Primary care | T, C, U | ✗ | ✗ | List of recommendations (individual and structural) about what medical schools, primary care practices and the medical community could do to positively influence the culture of medicine | Make student, practitioner and staff wellness a dashboard metric of success for medical schools, primary care practices and health-care systems; increase availability of Balint or reflection groups | N | ||
| Bakker et al.65 | 2000 | The Netherlands | Research | Longitudinal study, questionnaires | Mixed: highlights the importance of perceptions of reciprocity in the burnout process and provides several guidelines for interventions aimed at reducing or preventing burnout among GPs | 567 GPs | C, T | ✗ | Test a process model for burnout. Examine the consequences of dealing with demanding patient behaviours from the perspectives of equity theory and social exchange theory | To prevent burnout, GPs should be provided with the opportunity to restore the balance in the doctor–patient relationship (including opportunity to terminate the relationship). This can be achieved by teaching medical students and practising doctors to develop an attitude of ‘detached concern’ | N | ||
| Benson and Magraith69 | 2005 | Australia | Commentary | n/a | Mixed: mostly structural Balint groups, but also individual (relaxation, exercise, etc.) and other structural. Minimise organisational issues (e.g. administration) | GP | C | ✗ | Discussing the impact of Balint groups on burnout and compassion fatigue in GPs | Balint groups can protect GP from compassion fatigue and burnout | N | ||
| Bitonte and DeSanto70 | 2014 | USA | Commentary | Mixed: mandatory physical exercise | Medical students | U | ✗ | Propose 30 minutes a day, three to five times per week of exercise; more cost-effective than counselling, but it also reduces the chances that they will experience burnout | Time for exercise implemented into the curriculum will assist in preventing mental illness, but it will also improve the general health of the medical student population, which is important for them but also for the health and well-being of the general population | Y qual | |||
| Blais et al.71 | 2010 | Canada | Research | Questionnaires | Mixed; individual; physician health programme Quebec; but call for structural solutions | 92 physicians | T, C | ✗ | Document the opinions of the users of the Quebec Physicians Health Program about the services that they received | Burnout is not only a personal problem, but also a collective problem. Actions are needed to prevent this problem. Family physicians are likely to be the first ones consulted by sick physician patients; they play a key role in referring those colleagues to the appropriate help programmes when needed | N | ||
| Bragard et al.73 | 2006 | Belgium | Commentary | Mixed: stress management and communication skills with cancer patients training (40 hours) | Oncologists | T, C | ✗ | Describe a Belgian interuniversity curriculum theoretical roots, principles and techniques developed for junior physicians dealing with cancer patients | This course could lead not only to communication skills improvements, but also to burnout prevention | N | |||
| Brazeau74 | 2010 | USA | Commentary | Structural: add burnout prevention skills to the mainstream medical curriculum | Medical students | U | ✗ | Suggest how to prevent burnout in medical school and beyond | We need systemic administrative changes in medical schools and teaching institutions nationwide to develop and support a culture of well-being at all stages of medical education and beyond | N | |||
| Bugaj et al.75 | 2016 | Germany | Research (intervention study) | Questionnaires | Structural: PAL-led stress prevention seminars | 75 medical students | U | ✗ | Showcase the seminar concept and evaluate first-year medical student’s acceptance of the intervention programme after 1 year of implementation | The concept of PAL seems to be suitable for the field of stress prevention. Accordingly, student participants evaluated the seminars and student tutors very positively | N | ||
| Bugaj et al.76 | 2016 | Germany | Research | Review | Mixed: individual coping styles and mental health promotion and interventions in medical school | Medical students | U | ✗ | ✗ | Review of causes of distress and psychosocial burden, as well as of relevant prevention strategies for medical students | Twofold consideration of prevention strategies for medical students: specific interventions promoting medical students’ mental health, and sound medical education and training, with an emphasis on clinical teaching | N | |
| Bughi et al.77 | 2017 | USA | Research (intervention study) | Cross-sectional survey | Individual: use Myers–Briggs personality inventory to identify risk of distress and burnout | 185 medical first-year students | U | ✗ | Examine the purported link between MB preferences, distress and burnout scores | Use of a personality inventory may help identify students at risk of burnout and allow appropriate early stress management | N | ||
| Carvour et al.79 | 2016 | USA | Research | Review | Structural: patient-centred medical home perspective; care co-ordination and referral support; confidential care without perceived conflicts of interest in the training environment; co-location of medical and mental health care; and accommodations for schedule constraints | Postgraduate medical trainees | T | ✗ | Review the literature on health-care needs of postgraduate trainees; describe practical interventions to improve access to care; explore the role of the medical home in developing and supporting institutional efforts to promote wellness | This proposed model upholds the idea that one important step towards improving health and wellness is to apply the relevant, evidence-based and patient-centred principles of the field to the care of those who train within it | N | ||
| Chambers et al.80 | 2017 | New Zealand | Research | Mixed: cross-sectional online survey qualitative and quantitative | Structural: organisational prevention campaign to create environment that foster work–life balance, culture of self-care and fights macho culture | 1806 senior doctors and dentists | C | ✗ | Estimate rates of presenteeism in the New Zealand senior medical workforce and identify reasons why this workforce feels pressured to work through illness | More than half of the sample reported coming to work unwell often and sometimes in a 24-month period. Reasons for presenteeism included difficulties accessing short-term sickness cover and concern for the impact of sick leave on patients, as well as sociocultural norms | Y qual | ||
| Chang et al.81 | 2013 | USA | Research | Survey | Individual: counselling | Medical students | U | ✗ | Assess the usage of mental health counselling services by medical students | Medical schools may benefit from efforts to identify and diminish barriers to accessing mental health counselling services | N | ||
| Chaukos et al.82 | 2018 | USA | Research | Surveys and wearable health-tracking device to assess feasibility of wearables for studying resident health behaviours | Mixed: SMART-R – a 6-hour group-based curriculum that teaches meditation, behavioural skills and positive perspective-taking strategies (with programme leadership support) | Medicine and psychiatry residents | T, C | ✗ | Determine the feasibility of a resident-led resiliency curriculum developed by residents, for residents | The problem of physician burnout requires a multipronged solution. Resident-led initiatives, such as the SMART-R programme, will not fix the burnout problem, but they can generate awareness and emphasise the importance of well-being early in residency and beyond | N | ||
| Clough et al.84 | 2017 | Australia | Research | Systematic review | Mixed: individual (based on cognitive and behavioural principles, relaxation); structural (support group intervention) | Doctors | C, T | ✗ | ✗ | Review psychosocial interventions aimed at reducing occupational stress and burnout in doctors | The quality of research examining the benefits of interventions for occupational stress and burnout in medical doctors remains low. Interventions focused on cognitive and behavioural principles appear to show promise | Y qual | |
| Cockerell85,86 | 2016 part I; 2017 part II | USA | Commentary | Individual: exploration of meditation and a Chinese spiritual text (the Tao Te Ching) as a tool physicians can use to reduce stress | Physicians (particularly dermatologists) | T, C | ✗ | ✗ | Show some extracts from the Chinese text | Thoughts can be directed to things that are positive and soothing | N | ||
| Cornelius et al.87 | 2017 | USA | Research (intervention study) | Survey (after retreat) | Structural: ‘amazing race’ residency retreat to promote well-being, which incorporates team-building, resident bonding and faculty–resident bonding | 25 emergency medicine residents | T, C | ✗ | Assess the satisfaction regarding the retreat curriculum, which emphasises team building between residents and faculty (reducing isolation, depression, suicide) | This retreat proved to be a low-cost and easily implemented activity with which the residents expressed high levels of satisfaction | N | ||
| de Vibe et al.90 | 2013 | Norway | Research (intervention study) | Randomised controlled study | Individual: 7-week MBSR | 288 medical and psychology students (randomly allocated to intervention and control group) | U | ✗ | Examine the effect of a 7-week MBSR on mental distress, study stress, burnout, subjective well-being and mindfulness of medical and psychology students | The intervention had no statistically significant effect on student burnout. Only female students showed a significant intervention effect on mental distress, study stress and well-being. There is a need for more research on mindfulness-based interventions that includes gender as a variable | N | ||
| Deng et al.91 | 2017 | China | Research | Self-administered questionnaires: cross-sectional study | Individual: Burnout Battery (screening burnout among oncologists) | 538 oncology doctors and nurses | C, T | ✗ | Develop a novel tool – the Burnout Battery – for briefly screening burnout among oncology professionals in China and assessing its validity | Chinese oncology professionals exhibit high levels of burnout. Working long hours and perceiving clinical work as the most stressful part of the job were the main factors associated with burnout. The Burnout Battery appears to be a simple and useful tool for screening burnout | N | ||
| Devi93 | 2011 | USA | Research | Review/report | Mixed: mandatory counselling; improve training to reduce stigma and bullying | Doctors and medical students | C, T, U | ✗ | Review of US research into the effect of studying and practising medicine has on the mental health of young doctors and surgeons | We have to change the environment in which we are teaching future physicians | N | ||
| Dobkin and Hutchinson94 | 2013 | Canada | Research | Literature review | Mixed: lectures, integration of mindfulness in curricula | Medical students | U | ✗ | Examine the literature and related websites to determine the extent to which mindfulness teaching is carried out with medical students and residents | Evidence points to the usefulness of teaching mindful practices, but various issues remain (when?, how?, for whom it works better?) | N | ||
| Doran et al.24 | 2016 | UK | Research | Mixed method: online survey and interviews | Structural: reduce administration work, increase time spent with patients | GP (143 survey; 21 interview) | C | ✗ | Explore the reasons why GPs leave general practice early | To improve retention of young GPs, the pace of administrative change needs to be minimised and the time spent by GPs on work that is not face-to-face patient care reduced | Y quant | ||
| Downs et al.95 | 2014 | USA | Research | Survey | Mixed: HEAR programme, an interactive screening programme (survey, electronic correspondence with counsellor) designed to increase mental health services utilisation and decrease suicide risk | Medical students | U | ✗ | ✗ | ✗ | Describe a 4-year trial of the HEAR programme. The goals of the HEAR programme are to educate, destigmatise, identify, refer and treat individuals with depression, particularly those with increased suicide risk | This interventional programme was effective in detecting several medical students with suicidal ideation who were not in treatment and engaging them in mental health treatment | N |
| Dunn et al.96 | 2007 | USA | Research (intervention study) | Questionnaires | Mixed: three components – (1) leadership valuing physician well-being equal to quality of care and financial stewardship; (2) physicians identifying factors that influenced well-being, followed by plans for improvement with accountability; and (3) measuring the well-being of physicians regularly using validated instruments | 22–32 physicians. From 2000 to 2005 | C, T | ✗ | ✗ | ✗ | Determine whether or not data-guided interventions and a systematic improvement process to enhance physician work–life balance and organisational efficacy can improve physician and organisational well-being | Establishing physician well-being as an essential value of the organisation helps create the intended culture. A regular iterative process of inquiry and feedback from physicians can identify issues that negatively affect well-being and barriers to improvement | N |
| Dyrbye et al.98 | 2016 | USA | Research (intervention study) | Randomised trial | Individual: 10-week online intervention to promote well-being and satisfaction | 290 physicians (half intervention, half control group) | T, C | ✗ | Test intervention | Although participants found the micro-tasks in the intervention arm worthwhile, they did not result in measurable improvements in well-being or professional satisfaction when compared with the control group. These results highlight the critical importance of an appropriate control group in studies evaluating interventions to address physician burnout and distress | Y qual | ||
| Dyrbye et al.99 | 2017 | USA | Research | Mann–Whitney tests, Fisher’s exact tests and multivariate logistic regression | Individual: healthy exercise habits | 4402 medical students | U | ✗ | Explore relationships between burnout, quality of life and compliance with Centers for Disease Control and Prevention physical exercise recommendations, to inform students about individual strategies | Students whose aerobic exercise and/or strength training habits are consistent with Centers for Disease Control and Prevention guidelines appear less likely to experience burnout and to have higher quality of life. Schools should consider encouraging fitness among students as part of their approach to reducing burnout and promoting wellness | N | ||
| Dyrbye et al.100 | 2017 | USA | Research | Survey (before/after) | Structural: stress management and resilience course | First-year medical students | U | ✗ | Determine if a required longitudinal stress management and resilience course improves well-being | The course did not lead to measurable improvements. Medical schools should consider offering a variety of effective options so that students can select activities they want to engage in | N | ||
| Epstein and Krasner102 | 2013 | USA | Commentary | Mixed: methods for enhancing resilience – (1) self-awareness and self-monitoring, (2) self-regulation and resilience, and (3) public accountability, communities of care and health-care institutions | Physicians and other health-care professionals | T, C | ✗ | Offer thoughts about strategies and recommendations for developing and maintaining physician resilience | We need creative, forward-looking intervention research to identify the essential elements and the optimal timing and dose of such approaches | N | |||
| Ey et al.103 | 2013 | USA | Research | Electronic e-mail survey | Structural: educational outreach efforts to promote, and lower access barriers to, resident wellness programme – a counselling/coaching services | 450 residents | T | ✗ | ✗ | Evaluate whether or not educational outreach efforts and development of a resident-specific counselling programme were viewed as accessible and valued resources for physicians in training | The programme reduced access barriers, but time (to access service) remained the biggest obstacle. More research is needed to address sex and ethnic differences, and the influence of attitude, in the use of services to address personal care needs | N | |
| Ey et al.104 | 2016 | USA | Research (intervention study) | Client satisfaction questionnaire | Mixed: on-site resident and faculty wellness programme, comprehensive suicide and depression prevention programme (e.g. individual counselling, monthly group support, workshops) | Medical trainees and faculty | U, T, C | ✗ | ✗ | ✗ | Report on the feasibility and utilisation of a wellness and suicide prevention programme for residents, fellows and faculty in an academic health centre | Increased utilisation over 10 years, high satisfaction and consistent institutional support suggest that this comprehensive model of care is feasible and valued (can also overcome traditional access barriers) | N |
| Feld and Heyes-Moore105 | 2006 | UK | Research | Questionnaire | Structural: support group | Palliative care | T, C | ✗ | ✗ | Evaluate a support group for junior doctors working in palliative medicine | Doctors in palliative medicine experience stress and find support groups useful. Whether or not they take the form of support group, interventions are needed and should involve expert psychologically trained practitioners | N | |
| Flowers107 | 2005 | USA and UK | Research | Review | Mixed: emotional competence training – ‘psychonormality’ course (self-awareness/development/responsibility/reflection; relationships) | Medical students | U | ✗ | Outline a five-step course designed to train students for emotionally competent medical practice | Medical schools and residencies should evaluate incorporating this training into their curricula and faculty development. Benefits include improved doctor–patient relationships, higher retention of competent, professional, satisfied and healthier physicians, particularly under-represented minorities | N | ||
| Foster et al.108 | 2012 | USA | Research (intervention study) | Survey, pilot study | Mixed: RAFT to support residents’ well-being. RAFT: feedback process utilising small-group dialogue that replaces the traditional semi-annual, faculty-wide review of resident performance | Residents | T, C | ✗ | Report on a pilot study conducted with cohorts of residents with different levels of exposure to the RAFT innovation | It cannot be claimed that RAFT is solely responsible for the residency’s capacity to maintain resident well-being | N | ||
| Fothergill et al.109 | 2004 | UK | Research | Systematic review | Mixed: support from colleagues and outside interests | Psychiatrists | T, C | ✗ | ✗ | Review the current evidence for the effectiveness of stress management interventions for those working in the psychiatric profession | The personal stresses associated with patient suicide needs to be addressed to avoid the real psychological problems experienced by psychiatrists trying to cope with this difficult situation | N | |
| Gardiner et al.110 | 2015 | USA | Research | Survey | Mixed: Balint groups, stress management lectures/workshops, retreats, etc. | 212 family medicine residents | T, C | ✗ | ✗ | ✗ | Review the current state of implementation of stress management services and programming in family medicine residency | It is necessary to evaluate whether or not residency programmes are providing appropriate stress management skills for residents that will improve physician wellness and patient outcomes | N |
| Gardiner et al.111 | 2013 | Australia | Research (intervention study) | Quasi-experimental study with an intervention group and deidentified data for a baseline group and a control group | Mixed: a 9-hour cognitive–behavioural group and individual coaching programme | GPs intervention group (n = 69), baseline group (n = 205) and control group (n = 312) | C | ✗ | To determine the relationship between cognitive–behavioural coaching, the well-being of rural GPs, their intentions to leave and actual leaving | Cognitive–behavioural coaching reduced the stress levels of rural GPs who self-identified the need for managing stress and reduced their intention to leave rural general practice. More GPs from the coaching group remained in rural general practice | Y qual | ||
| Garelick et al.112 | 2007 | UK | Research | Questionnaire | Individual: MedNet – a self-referral, face-to-face, psychotherapeutic service for doctors | 121 self-referred doctors presenting in 2002–4 | T, C | ✗ | Delineate characteristic of doctors utilising MedNet service, determine effectiveness of service | MedNet clients represent both ends of the spectrum of severity, enabling early clinical engagement is of importance both in terms of personal health and protecting patient care | N | ||
| Garside113 | 1993 | Canada | Research | Review | Structural: physicians mutual aid group as a response to caring for patients with AIDS-related burnout | Physicians (mostly primary healthcare) | T, C | ✗ | ✗ | Offer suggestions to overcoming resistance physicians might have to participating in such groups and reviews modalities to facilitate participants to share emotional stresses within the group | With appropriate facilitation, physicians under stress from providing care to people with AIDS can benefit from the experience of mutual aid | N | |
| Gazelle et al.114 | 2015 | USA | Commentary | Case example | Individual: professional coaching | Physician | T, C | ✗ | ✗ | Demonstrate the potential of professional coaching to address physician burnout | Hospitals, medical schools, insurers and practices could consider coaching to improve physician quality of life | N | |
| Geller et al.115 | 2008 | USA | Research (intervention study) | Mixed qualitative focus groups, and survey | Individual: scale to measure ‘personal meaning in patient care’ how doctors connect with patients, which could be useful to identify providers at risk of burnout | Clinical genetics professional physicians, nurses, counsellors | T, C | ✗ | Develop and validate a measure of ‘personal meaning’ that practitioners derive from patient care | The scale could be useful in identifying providers at risk of burnout, in evaluating interventions, enhance meaning and improve communication with providers and patients | N | ||
| George et al.116 | 2012 | USA | Research (intervention study) | Focus group evaluation of intervention | Structural: Facebook/YouTube stress management group | First-year medical students | U | ✗ | Evaluate the effectiveness of Facebook stress management platform | Social media as a delivery system (offers both ‘group’ and ‘anonymity’ advantages) is effective as tool to manage stress. Older students should develop content. These social networks can be important components of a support system for medical students, and can also offer advantages over learning platforms | N | ||
| Goldhagen et al.118 | 2015 | USA | Research (intervention study) | Survey | Individual: mindfulness based resilience training | Resident physicians | T, C | ✗ | Tests whether or not intervention would decrease stress and burnout in residents | There was no significant short-term change in stress and burnout after the intervention | N | ||
| Goodman and Schorling119 | 2012 | USA | Research (intervention study) | Survey | Mixed: continuing education course based on mindfulness-based stress reduction. 2.5 hours per week for 8 weeks plus a 7-hour retreat. The classes included training in formal mindfulness practices and discussion focusing on the application of mindfulness at work | 93 physicians from multiple specialties, nurses and psychologists, in university and community | T, C | ✗ | Determine if a continuing education course based on mindfulness-based stress reduction could decrease burnout and improve mental well-being among health-care providers, from different professions | This course based on mindfulness-based stress reduction was associated with significant improvements in burnout scores and mental well-being for a broad range of health-care providers | N | ||
| Gregory and Menser121 | 2015 | USA | Research (intervention study) | Longitudinal electronic survey | Structural: AWS aetiological model which focuses on workplace conditions as causes of burnout | 153 primary care physicians | T, C | ✗ | ✗ | Determine the applicability of the AWS to measure burnout and help to develop interventions | The AWS model provides key insights into the domains of work that cause stress and burnout, and can guide interventions | N | |
| Gulen et al.122 | 2016 | Turkey | Research | Prospective observational study | Structural: biomarker to screen emergency medicine residents for high risk for depression and burnout | 53 emergency medicine residents | T, C | ✗ | Investigate the relationship of the glial marker S100B in sera of emergency physicians with burnout syndrome and depression | S100B levels correlate with depression scores and emotional exhaustion in burnout syndrome. S100B can be used as a marker to screen emergency medicine residents and detect individuals with high risk for depression and burnout syndrome | N | ||
| Gunasingam et al.123 | 2015 | Australia | Research (intervention study) | Prospective randomised controlled study | Structural: debriefing sessions (to reduce stress and burnout) | Junior doctors (postgraduate Year 1) | T, C | ✗ | ✗ | Examine the prevalence of burnout in a cohort of junior doctors and whether or not debriefing sessions reduced levels of burnout | Burnout is prevalent among postgraduate Year 1 doctors. Debriefing sessions, although considered a valuable support mechanism, did not improve burnout scores using the Maslach Burnout Inventory | Y qual | |
| Haizlip et al.124 | 2012 | USA | Commentary | Mixed: positive psychology (culture change) | Physicians and trainees | T, C | ✗ | Discuss the challenges to change culture in medical education | Practices rooted in positive psychology are powerful tools to counteract the negativity bias and aid in achieving desired culture change | N | |||
| Hamader and Noehammer125 | 2013 | Austria | Research (chapter in book) | Qualitative study: interviews | Mixed (e.g. training, counselling) | Medical students, residency training, occupational health and psychology | U, T, C | ✗ | Investigate experts’ opinion, medical students’ and young doctors’ point of view on prevention of anxiety depression burnout | During medical studies, well-being can be promoted by teaching how to develop a balanced life and learning style and a realistic preparation for the job. During residency, more institutional support is required, such as providing stress management training, mentoring programmes and career counselling | N | ||
| Haramati et al.4 | 2017 | USA | Commentary | Mixed: special issue of medical teacher on physician burnout | Doctors and medical students | T, C, U | ✗ | ✗ | ✗ | Report from CENTILE conference 2015 | Burnout is a job environment problem (not individual) | N | |
| Hegenbarth128 | 2011 | Switzerland | Commentary | Structural: ReMed (rete medicorum) a support network that helps doctors in crisis under extreme pressure to get help from their medical colleagues | Doctors | T, C, U | ✗ | N | |||||
| Hill and Smith130 | 2009 | USA | Research | Survey | Mixed: MBI-HSS as tool to monitor stress | Residents in academic otolaryngology | T, C | ✗ | Describe the use of the MBI-HSS as a method of monitoring stress levels in an academic otolaryngology residency training programme and introduce this survey as a tool for wider use in meeting ACGME requirements | The MBI-HSS is an established and validated tool for identifying burnout in resident physicians. Residency programme directors may find it useful to monitor resident well-being and stress | N | ||
| Hlubocky et al.131 | 2016 | USA | Position paper | Discussion of fictional exemplary case | Mixed: individual (e.g. mindful self-compassion) and organisational (e.g. improve work environment) interventions | Oncology | C | ✗ | ✗ | ✗ | Argue for the need to incorporate systematically in oncology care clinician-tailored and organisational-based interventions to prevent and tackle burnout | Prevent and target burnout using wellness strategies and interventions at the individual and organisational level, incorporated into routine oncology care | Y qual |
| Hochberg et al.132 | 2013 | USA | Research (intervention study) | Survey | Structural: interactive seminar (facilitated by surgeon) training to recognise sign of stress, depression, suicide in themselves and colleagues | 21 resident Surgeons | T, C | ✗ | ✗ | Suggests that the symptoms, causes and treatment of stress among surgeons can be taught effectively to surgical resident learners | As a group, highly selected and highly trained residents are poor at identifying the signs of depression, stress and potential suicide among fellow residents | N | |
| Holoshitz and Wann133 | 2017 | USA | Commentary | n/a | Individual: mindfulness [with elements of structural (org) changes] | Physicians | C | ✗ | ✗ | Argue for effectiveness of mindfulness to reduce burnout | Mindfulness, cognitive–behavioural therapy, relaxation and schedule changes are best techniques for reducing and preventing burnout | N | |
| Hotchkiss135 | 2008 | USA | Research (dissertation) | Statistical analyses of archived demographic data | Mixed: CPHP | 1239 physicians who used the service from 1997 to 2007 | T, C | ✗ | Examine the degree to which the prediction of CPHP physician reactivation (going back to service) is related to selected demographic factors (e.g. gender, age group). Provide information about predispositions of continued physician stress and CPHP reactivation |
Older physicians with physical problems had a higher risk of reactivation. More women came to CPHP for psychiatric, family and stress problems than men. More women were self-referred than men More men were referred to CPHP than women by the Board of Medical Examiners |
N | ||
| Howlett et al.136 | 2015 | Canada | Research (intervention study) | Survey | Mixed: training staff to adopt more task-oriented and less emotion-oriented coping styles, and a staff coping style assessment (for managers) | 616 staff at emergency department in seven hospitals | ✗ | Examine the relationship between coping styles and burnout in emergency physicians, and other health-care practitioners at seven emergency departments | Interventions to increase the use of more effective task-oriented coping styles maybe protective against burnout and improve staff well-being along with patient outcomes | N | |||
| Ireland et al.137 | 2017 | Australia | Research (intervention study) | Randomised controlled trial (the control condition constituted extra break time, which was equivalent to the mindfulness training time) | Individual: 10-week mindfulness training programme | 44 intern doctors | T, C | ✗ | ✗ | Examine the effectiveness of a mindfulness training intervention in reducing stress and burnout among medical practitioners | Participants undergoing the training reported greater improvements in stress and burnout relative to participants in the control condition. Doctors would benefit from the inclusion of this training to general medical education | Y qual | |
| Isaksson Røet al.138 | 2010 | Norway | Research | Survey: 3-year follow-up self-report assessment | Individual: counselling and focus on doctors’ coping strategies | 184 physicians | T, C | ✗ | Investigate the roles of coping strategies, job stress and personality traits in burnout reduction after a counselling intervention for distressed physicians | Coping strategies and job stress could be important foci in intervention programmes that aim to reduce or prevent burnout in help-seeking physicians | N | ||
| Isaksson Rø et al.139 | 2012 | Norway | Research | Self-report assessment | Mixed: sick leave after counselling intervention (to prevent doctors burnout) | 184 doctors | T, C | ✗ | ✗ | Examine whether or not a spell of sickness absence after a counselling intervention could predict reduction in emotional exhaustion among doctors at work 3 years later | The number of weeks of sickness absence after a counselling intervention for burnout had a positive predictive effect on reduction in emotional exhaustion among doctors at work 3 years later | Y qual | |
| Kemper and Khirallah140 | 2015 | USA | Research (intervention study) | Prospective cohort questionnaire study | Individual: 1-hour online elective mind–body skill training for resilience, effectiveness and mindfulness | 513 mixed doctors and other health workers | C, T | ✗ | Evaluate the effects of this training for health professionals on mindfulness, resilience, and empathy | This training is attractive to diverse health professionals with high levels of stress and burnout, and can improve empathy and mindfulness | N | ||
| Kjeldmand and Holmström141 | 2008 | Sweden | Research | Qualitative study (interviews) | Structural: Balint groups | 9 GPs | C | ✗ | Explore GPs’ experience of participating in Balint groups and its influence on their work life | Balint groups might help GPs handle a demanding work life and prevent burnout. These groups might not suit all GPs, and additional ways to reduce stress and increase job satisfaction should be offered | Y qual | ||
| Kötter et al.142 | 2015 | Germany | Research | Qualitative focus groups | Structural: peer groups and mentoring programmes | 16 medical students | U | ✗ | ✗ | Identify stressors and possible starting points for health-promoting interventions from the perspective of the students themselves | Problems and solutions were more at the organisational level. The curriculum should enhance students’ health, peer groups and mentoring programmes were perceived as helpful | N | |
| Krasner et al.143 | 2009 | USA | Research (intervention study) | Quantitative study: self-administered surveys, ‘before-and-after study’ | Individual: training in: mindfulness, self-awareness exercises, meaningful clinical experiences narratives, appreciative interviews, didactic material and discussion. 8-week intensive phase (2.5 hours/week, 7-hour retreat), followed by a 10-month maintenance phase (2.5 hours/month), but mentions ideal model of individual intervention supported at organisational level | 70 primary care physicians | C | ✗ | Determine the impact of an intensive educational programme in mindfulness, communication and self-awareness on primary care physicians’ well-being, psychological distress, burnout and capacity for relating to patients | Participation in a mindful communication programme was associated with short-term and sustained improvements in well-being and patient-centred care | N | ||
| Kumar144 | 2007 | New Zealand | Commentary | Structural: explore positive aspects of the profession and develop preventative strategies and effective treatment programmes against burnout | Psychiatrists | C, T | ✗ | Review of interventions to address burnout in psychiatrists | Factors related to the work environment appear to play a stronger role in causing burnout in psychiatrists than personal factors | N | |||
| Kushnir et al.145 | 1994 | Israel | Research (intervention study) | Questionnaires | Individual: stress management skills training | Second-/third-year students, master occupational health | C, T | ✗ | Evaluate the training | This training may benefit practitioners and patients alike | N | ||
| Lapa et al.146 | 2016 | Portugal | Research | Questionnaire-based cross-sectional, correlational, observational study | Mixed: SQA | Anaesthesia | T, C | x | Validate the SQA | SQA is a well-adjusted measure for assessing stressors in anaesthesia physicians and includes clinical, organisational and team stress factors | N | ||
| Lederer et al.147 | 2008 | Austria | Research | Survey | Structural: supervision with facilitator to prevent FdBO | 33 physicians, 150 nurses, intensive care | C, T | ✗ | Evaluate the prevalence of FdBO in intensive care personnel; determine whether or not factors related to employment and work are associated with FdBO | Results indicate that support provided by a facilitator can help prevent precursor symptoms of burnout and ultimately burnout | N | ||
| Lee et al.148 | 2016 | Taiwan | Research | Survey | Mixed: kernel k-means cluster analysis to identify staff with high burnout (and provide timely assistance, e.g. mindfulness, positivity currency) | Hospital staff | C | ✗ | Use kernel k-means cluster analysis to identify medical staffs with high burnout, such that the hospital management can take actions to improve the resilience, further reduce the potential medical errors and, eventually, enhance the patient safety | The hospital management needs to keep track of medical staffs’ fatigue conditions and provide timely assistance for burnout, through assistance programmes, mindfulness-based stress reduction programmes, positivity currency build-up and forming appreciative inquiry groups | N | ||
| Lefebvre149 | 2012 | Canada | Commentary | Mixed: implementation of resident wellness programmes into residency training | Residents/physicians | T, C | ✗ | ✗ | ✗ | Advocate for utility of resident wellness programme | Existing programmes are well attended, efficacious and free from debate; however, further research is needed to clearly establish their benefit | N | |
| Leff et al.150 | 2017 | USA | Commentary | Structural: monthly debrief programme in end of life care lead by physicians and clinical social workers | End of life care physicians and social workers | T, C | ✗ | ✗ | Discuss utility of intervention | Debriefing provides opportunities for residency physicians to reflect on the affective side of their work and helps promote resiliency | N | ||
| Lim and Pinto151 | 2009 | New Zealand | Research | Questionnaires | N/A points towards structural | 136 radiologists | C, T | ✗ | Identify differences in radiologists’ work stress, job satisfaction and professional burnout between public hospital and private practice work environments | There is a trend towards a higher rate of psychiatric morbidity among radiologists who practice in public hospitals. Clinical autonomy and having the financial resources to be able to perform their work properly are important to radiologists’ job satisfaction | N | ||
| Linzer et al.152 | 2015 | USA | Research (intervention study) | Cluster randomised control trial | Structural: improving work conditions (time pressure, workplace chaos) | 166 primary care physicians in 34 clinics | C | ✗ | ✗ | Assess if better work conditions reduce clinician stress and burnout | Organisations may be able to improve burnout, dissatisfaction and retention by addressing communication and workflow, and initiating quality improvement projects | N | |
| Linzer et al.153 | 2001 | USA and the Netherlands | Research | Surveys | Mixed: predictive (and preventative) model of physician burnout | > 3000 physicians | T, C | ✗ | Compare data from two large physician surveys (Dutch and USA) to better understand the interplay of the predictors of physician burnout and to develop strategies for prevention | Work control needs to be explicitly addressed; the organisation should commit to understanding and addressing work home interference | N | ||
| Luthar et al.154 | 2017 | USA | Research (intervention study) | Randomised controlled intervention (participants assessed at baseline, after the intervention, and 3 months follow-up on multiple psychological measures plus plasma cortisol) | Structural: facilitated colleague support groups –ACGs based on the structured relational psychotherapy mothers’ groups | 40 women and mothers: physicians, PhD clinicians, physician assistants and nurses practitioners | C, T | ✗ | ✗ | Report on effects of ACG to foster resilience among professional women at high risk for stress and burnout | There is a critical need for interventions sensitive to the needs of health-care providers who are women. Facilitated colleague support groups could be a viable, low-cost, preventative intervention to mitigate burnout and distress for mothers in high-stress professional settings, such as hospitals | Y quant | |
| Mache et al.156 | 2017 | Germany | Research (intervention study) | Quasi-experimental study | Mixed: training content included work-related self-care strategies, problem-solving techniques solution-focused counselling (developing support system among colleagues) | 80 oncology doctors | C, T | ✗ | Evaluate a work-related self-care psychosocial competency training in oncology and haematology medicine for junior physicians | Intervention group reached a decrease in perceived job stress and emotional exhaustion | N | ||
| McClafferty and Brown159 | 2014 | USA | Research | Review | Mixed | Physicians/paediatricians | T, C | ✗ | Overview of physician burnout, preventative physician health and wellness, and discussion of emerging initiatives to promote health at all levels of paediatric training | A primary purpose of this clinical report is to shift the focus from burnout treatment to preventative physician health and wellness | N | ||
| McCray et al.160 | 2008 | USA | Research | Review | Mixed: self-care interventions, support groups | Students, doctors, health-care professionals | U, T, C | ✗ | ✗ | ✗ | Despite the serious personal and professional consequences of burnout, few interventions exist to combat this problem | Prospective, controlled studies are needed to examine the effect of interventions to manage burnout among resident physicians | N |
| McCue and Sachs161 | 1991 | USA | Research (intervention study) | Survey | MIxed: stress management workshop (half day) – individual and relational skills | Physicians (medicine, paediatrics) residents | T, C | ✗ | ✗ | Test stress management workshop to improve residents’ coping skills | Such workshops were received positively and can lead to significant short-term improvement in burnout scores | Y quant | |
| McKenna et al.162 | 2016 | USA | Commentary | Structural: encouraging (personal, professional) sense of belonging at work | Medical students | U | ✗ | Propose that the connection to colleagues, patients and profession is fundamental to medical learners’ resilience, highlighting ‘social resilience’ as a key factor in overall well-being | Resilience/wellness programme should focus on fostering connection. They should focus less on the competition between work and life and more on making work a functional and enjoyable part of lives | N | |||
| McKinley et al.164 | 2017 | USA | Research | Literature review | Mixed: individual (training), structural (work hours) | Paediatric residency (and related disciplines) | T | ✗ | ✗ | ✗ | Detail the present research on paediatric resident burnout in context with related disciplines (family and internal medicine) | Perhaps the most striking finding from the literature is the dissonance between causes of burnout in residents and evidence of few reported specific interventions | N |
| McManus et al.165 | 2011 | UK | Research | Questionnaire | Individual: avocation/leisure activities as key element for job satisfaction and reduction of burnout | 2845 doctors | T, C | ✗ | Explore the link between vocation (job satisfaction and lack of burnout) and avocation | Doctors with greater avocation/leisure activities have a greater sense of vocation/engagement. Being burned out did not relate to avocation/leisure activities | N | ||
| McNeill et al.166 | 2014 | Australia | Research | Questionnaire | Structural: role of group membership in well-being | 92 medical students | U | ✗ | Explore the link between group identification and well-being in medical students | Activities that promote co-operation and shared experiences among medical students will be helpful for their well-being (e.g. student representative to deliver positive messages, utilising pass/fail rather than grading system to reduce competitive atmosphere) | N | ||
| Mechaber et al.167 | 2008 | USA | Research | Survey | Structural: part-time work | Generalist physicians and their patients | C | ✗ | ✗ | Determine the impact of part-time status on (1) physician stress, burnout, satisfaction, work control and intent to leave; (2) patient satisfaction and trust; and (3) perceptions of organisational culture | Part time is a successful practice style for physicians and their patients. If favourable outcomes influence career choice, an increased demand for part-time practice is likely to occur | N | |
| Merteen et al.168 | 2014 | UK | Research | Questionnaires | Individual: doctors’ mental health service | 916 doctors who attended MedNet: a mental health service (closed in 2015, now DocHealth) | T, C | ✗ | ✗ | ✗ | Investigate the change in self-referral rates to MedNet and associated morbidity over 10 years | Doctors may be more willing to seek help than a decade ago. More research is needed to confirm the reasons for this. More resource is needed to meet the increase in demand | N |
| Mehta et al.169 | 2016 | USA | Research (intervention study) | Survey | Structural: team-based resiliency intervention (RRRP) | Multidisciplinary team of palliative care team (physicians, nurse practitioners, nurses and social workers) | T, C | ✗ | Test the RRRP for palliative care clinicians, to decrease stress and increase resiliency | RRRP may help promote resiliency and protect against the negative consequences of stress for PCCs | N | ||
| Milstein et al.170 | 2009 | USA | Research (intervention study) | Quasi-experimental study. Questionnaire and qualitative interviews | Individual: self-administered psychotherapeutic tool | Paediatric house officers (seven in control group, eight in study group) | T | ✗ | ✗ | Measure burnout in house officers and establish whether or not utilisation of a psychotherapeutic tool individually by physicians reduces symptoms of burnout | Methods identifying individuals at risk for burnout and interventions to cope with stress may be valuable to training | N | |
| Montgomery et al.171 | 2011 | Greece/UK | Research | Literature review | Mixed: improving quality of care through changes in organisation of hospital and hospital culture, involving doctors and other stakeholders | Hospital staff | T, C | ✗ | Use physician burnout as an important link between organisational culture and quality of care | A more real approach to promote quality of care is to recognise that its success is embedded in the organisational culture of the hospital and whether physicians experience burnout | N | ||
| Moutier et al.172 | 2012 | USA | Research | Survey | Structural: suicide prevention and awareness programme based on (1) screening, assessment and referral, and (2) education (grand rounds) | Medical students, residents, faculty physicians | U, T, C | ✗ | ✗ | Document the process of developing and implementing the programme | The programme was well received in its first year | Y qual | |
| Myszkowski et al.174 | 2017 | France | Research | Questionnaires | Individual: the IMRSS (monitoring purpose) | 259 internal medicine | T, C | ✗ | Evaluate the effectiveness of IMRSS | Because of its short length and robust psychometric qualities, the use of the IMRSS is recommended to quickly and frequently assess and monitor stress among internal medicine residents | N | ||
| Nielsen and Tulinius176 | 2009 | Denmark | Research | Qualitative interviews and participant observation | Structural: supervision group (including training on reflective practice and preventing burnout) | 9 GPs | T, C | ✗ | Report a case study of a supervision group | Longitudinal prospective studies on how supervision groups may contribute to the prevention of burnout deserve to be further researched | N | ||
| Nomura et al.177 | 2016 | Japan | Research | Mixed method (qualitative/quantitive) | Structural: duty hour regulation – overnight call shift system | Paediatric residents (41 survey, 4 focus group interview) | T, C | ✗ | Elucidate the prevalence of depressive symptoms after implementing an overnight call shift system and the factors associated with burnout or depression among residents | The overnight call shift system was effective in reducing working hours, but its effectiveness in managing mental health issues among paediatric residents remains unclear. Protective factors against burnout included the presence of peer support among residents, supervision by attending physicians | N | ||
| Oczkowski178 | 2015 | Canada | Commentary | Mixed: effective and virtuous use of humour | Medical students/physicians | U, T, C | ✗ | Argue that humour can relieve stress and create community | It is time we make a serious effort to teach medical students and residents the art of virtuous humour | N | |||
| Oman et al.179 | 2006 | USA | Research (intervention study) | Randomised controlled trial | Individual: spiritual intervention, 8 weeks, 2 hours per week comprehensive meditation training using non-sectarian, spiritually based self-management tools based on passage meditation | Physicians, nurses, chaplains and other health professionals | C, T | ✗ | ✗ | Evaluate the training | Results appear most likely to generalise to other populations that are similarly self-selected, such as health professionals who enrol in continuing professional education courses that use similar promotional materials | N | |
| Pereira et al.183 | 2015 | Brazil | Research | Qualitative case study | Individual: elective course ‘Strategies of Coping with Professional Stress’ mixed approach – progressive relaxation, diaphragmatic breathing, cognitive restructuring and social skills training (e.g. assertiveness), physician identity, medical vocation, ego defence mechanisms, work psychodynamics | 76 medical students | U | ✗ | Show the result of the course | The course produced benefits to the students, representing theoretical and practical learning, and an opportunity for reflection and self-knowledge, which caused psychological, behavioural and lifestyle changes | N | ||
| Prins et al.184 | 2007 | The Netherlands | Research | Questionnaires | Structural: social support (received from supervisors, fellow medical residents, nurses, patients) | Residents | T, C | ✗ | ✗ | (1) Explore medical residents’ satisfaction with emotional, appreciative and informative support received from supervisors, fellow medical residents, nurses and patients; (2) the correlation between levels of satisfaction and burnout | Medical residents appeared to be least satisfied with the social support they received from their supervisors compared with the other potential support-givers. The best predictor of burnout was dissatisfaction. Attention should be given to the also to supervisors in developing supportive skills | N | |
| Rabin et al.185 | 2005 | Israel | Commentary | Mixed: salutogenic model (including education, training, supervision and support groups) | Doctors, mostly GPs | T, C | ✗ | ✗ | ✗ | Offer a salutogenic perspective as a way of preventing doctors’ burnout | Salutogenesis is a theoretical reference to examine the resources necessary for physicians to cope with their professional stress to enable them to treat themselves and their patients in the most appropriate and coherent manner | N | |
| Raj186 | 2016 | USA | Research | Systematic review | Mixed: autonomy, competence building, strong social connection | Physicians/residents | T, C | ✗ | ✗ | ✗ | Review the research on resident well-being, identify factors associated with well-being, summarise well-being promotion interventions and provide a framework for future research | Future research should focus on cross-sectional studies, including sleep, coping mechanisms, resident autonomy, building competence and enhanced social relatedness | N |
| Ramirez et al.187 | 1996 | UK | Research | Questionnaire based survey | Structural: maintaining and enhancing job satisfaction, providing training in communication and management skills | 882 consultants (gastroenterologists, surgeons, radiologists and oncologists) | C, T | ✗ | Estimate burnout and psychiatric morbidity in consultants via questionnaire | Consultants’ mental health can be protected by maintaining or enhancing job satisfaction, and providing training in communication and management skills | N | ||
| Isaksson Rø et al.188 | 2016 | Norway | Research | Qualitative focus group interviews | Structural: peer support | 61 peer counsellors | C, T | ✗ | Understand how the framework of organised peer support can negotiate potentially conflicting considerations (e.g. whether emphasis is put on elements such as formalised rules, incentives and sanctions, or on informal elements such as dialogue, collegiality and voluntariness) | How the peer support programme is designed, such as the degree of formalisation and the balance between ‘hard’ and ‘soft’ ways to regulate the interaction between peer counsellors and doctors, is key for the ability to achieve the stated objectives of the service | N | ||
| Regehr et al.189 | 2014 | Canada | Research | Review and meta-analysis | Individual: cognitive, behavioural and mindfulness interventions | Physicians | T, C | ✗ | ✗ | ✗ | Examine the effectiveness of interventions aimed at addressing stress, anxiety and burnout in physicians and medical trainees | Cognitive, behavioural and mindfulness-based approaches are effective in reducing stress in medical students and practising physicians, and contribute to lower levels of burnout | N |
| Ringrose et al.192 | 2009 | The Netherlands | Research (intervention study) | Questionnaire and in-depth interviews | Structural: regular monitoring (questionnaire, interview) | Medical residents (58 questionnaire, 10 interviews) | T | ✗ | ✗ | Assess the burnout rates and potential determinants of burnout in a sample of medical residents | Regular burnout screenings recommended in order to efficiently identify residents at risk. This allows improved monitoring facilitating prevention of escalating burnout symptom | N | |
| Ripp et al.193 | 2016 | USA | Research (intervention study) | Surveys | Structural: facilitated discussion group | 39 first-year residents | T, C | ✗ | ✗ | Test the effectiveness of this intervention | The intervention did not decrease burnout in resident physicians. Future discussion-based interventions for reducing resident burnout should be voluntary and effectively free participants from clinical duties | N | |
| Ripp et al.194 | 2017 | USA | Commentary | Mixed: recommendations on how to improve medical students well-being (from a collaborative of medical educators, academic leaders and researchers) | Medical students | U | ✗ | ✗ | ✗ | Argue for the importance of developing a ‘menu’ of wellness options to reach a variety of learners and standardise the effort to ameliorate burnout | These multilevel changes will promote a culture in which trainees can learn in settings that will sustain them over the course of their careers | Y qual | |
| Ripp et al.195 | 2015 | USA | Research | Survey | Structural: duty hours restriction | 239 internal medicine residents | T, C | ✗ | Measure the impact of decreased work hours on developing burnout in internal medicine residents | Job burnout and self-reported sleepiness in internal medicine resident physicians were unchanged. The persistently high rates of resident burnout probably reflect the multifactorial nature of job stress in doctors in training | N | ||
| Rippstein-Leuenberger et al.196 | 2017 | Switzerland | Research | Questionnaire (short list of questions) | Individual: daily ‘Three Good Things’ intervention survey (resilience, positive psychology) | 32 intensive care unit health-care professionals | C, T | ✗ | Explore the content of the ‘good things’ reported by health-care workers participating in the ‘Three Good Things’ intervention | The findings show the personal and professional relevance of supportive relationships strengthened by clear communication and common activities that foster positive emotions | Y qual | ||
| Isaksson Rø et al.197 | 2008 | Norway | Research (intervention study) | Cohort study followed by self-reported assessment at 1 year | Mixed: counselling [1 day (individual) or 1 week (group based)] aimed at motivating reflection on and acknowledgement of the doctors’ situation and personal needs | 227 doctors | C | ✗ | Investigate levels and predictors of change in dimensions of burnout after this intervention | Counselling intervention could be conducive to reduction of doctors’ burnout. Considering doctors’ reluctance to seek help, it is important to offer interventions that facilitate access and that can enhance motivation to reconsider personal and professional priorities | N | ||
| Roberts et al.198 | 2002 | UK | Research/commentary | n/a | Structural: mentoring system from medical school throughout career practice | Psychiatrists | C, T, U | ✗ | ✗ | ✗ | Advocate for the importance of mentoring to fight isolation, blame and error culture, demotivated staff, retention, early retirement | Mentoring from medical school through medical practice can contribute to staff morale, motivation, and performance | N |
| Rohland et al.200 | 2004 | USA | Research (intervention study) | Survey | Individual: single-item measure of burnout | 307 physicians | T, C | ✗ | Validate a single-item measure of burnout against Maslach Burnout Inventory | In surveys in which emotional exhaustion is the primary subscale of interest, a single-item measure of burnout may be used in order to increase response rates | N | ||
| Rothenberger2 | 2017 | USA | Research | Systematic review | Mixed, including aligning personal and organisational values and enabling physicians to devote 20% of their work activities to the part of their medical practice that is especially meaningful to them | Physicians, medical students, trainees | C, T, U | ✗ | ✗ | Provide summary of knowledge about physician burnout; develop a framework to reverse its negative impact, decrease its prevalence, and implement effective organisational and personal interventions | Aligning personal and organisational values and enabling physicians to devote 20% of their work activities to the part of their medical practice that is especially meaningful to them are two effective strategies | Y quant, qual | |
| Runyan et al.201 | 2016 | USA | Research | Survey (before/after) | Structural: introduce a 1-month wellness curriculum | 12 second-year family medicine residents | T | ✗ | Evaluate the impact of the wellness curriculum on burnout, empathy, stress and self-compassion | Encouraging resiliency skills during residency may be more effective than trying to undo patterns of thinking and behaving among practising physicians when patterns are more concretised | N | ||
| Sallon et al.202 | 2017 | Israel | Research (intervention study) | Questionnaire (pre/post intervention) |
Mixed (mostly individual): CCG Multimodal: cognitive (mindfulness), somatic (relaxation), dynamic (dance, the only group element), emotive (drawing) and hands on (acupressure, shiatzu) |
Hospital staff: 118 participants, 97 control (majority nurses) | C, T | ✗ | ✗ | Assess effectiveness of CCG intervention on hospital staff | Multiple and flexible techniques (like CCG) may be more successful in reducing stress and burnout | Y quant | |
| Sanchez et al.203 | 2016 | USA | Research | Survey (combined quant and qual) | Structural: physician health programme peer support group | 85 physicians | T, C | ✗ | Survey physician attitudes to a physician health programme support group that goes beyond classic addiction model | This is a successful treatment intervention that can be replicated | N | ||
| Schapira et al.204 | 2017 | Australia | Commentary | Mixed: use of narratives in oncology (reading/writing) to achieve self-awareness and sense of community, reducing burnout | Oncology | T, C | ✗ | Discuss the role of narratives to build social support among oncologists | Reading, reflecting and sharing stories serve an important role in the professional development of oncologists | N | |||
| Schattner205 | 2017 | Israel | Commentary | Structural: Accreditation Council for Graduate Medical Education Regulation to limit residents’ continuous and weekly hours | Physicians (mostly residents) | T, C | ✗ | Discuss the link between residents’ well-being and patient-centered care | Future internal medicine training programs may need to be redesigned to meet these goals | N | |||
| Schmitz et al.206 | 2012 | USA | Commentary | Structural: curriculum for wellness and cultural changes | Emergency medicine residents | T, C | ✗ | Advocate for preventative approaches (resilience/well-being) and for cultural change | A change in culture and focus on resiliency, rather than burnout, in wellness education is needed to adequately address and optimise physician self-care | N | |||
| Schneider et al.207 | 2014 | USA | Research | Qualitative semistructured interviews | Mixed (mostly individual): physician well-being coaching to build self-awareness, self-care, coping and stress-reduction strategies that allow for greater resilience (but suggesting also to implement coaching programmes at organisational level) | 11 physicians | T, C | ✗ | ✗ | Evaluate the perceived impact of physician well-being coaching on physician stress and resiliency | Devaluing self-care while prioritising the care of others may be a significant source of burnout for physicians. Coaching can help physicians alter this pattern through skill development and increased self-awareness | Y qual | |
| Scholz et al.208 | 2016 | Germany | Research (intervention study) | Survey to collect psychometric data | Individual: elective course on relaxation techniques and autogenic training | 42 medical students | U | ✗ | Pilot effectiveness of intervention | We postulate the integration of courses on relaxation strategies in the medical curriculum | N | ||
| Seoane et al.209 | 2016 | USA | Research | Questionnaire | Structural: virtues education course that focuses on the development of virtues and character strengths necessary in the practice of medicine | 30 medical students | U | ✗ | Describe and evaluate course | After completing the course, students self-reported improved understanding of the virtues and their importance to the practice of medicine | N | ||
| Shanafelt et al.210 | 2012 | USA | Research | Cross-sectional survey | Individual: personal wellness practices of surgeons (body and mind) | 7197 Surgeons | C | ✗ | Evaluate personal health habits, routine medical care practices, and personal wellness strategies of surgeons and explore associations with burnout and quality of life | Flexibility (certain personal strategies to avoid burnout may be effective for all surgeons) and all specialties. Hospitals should consider how they can help surgeons maintain resilience by developing interventions that are flexible to surgeons and that promote meaning in work | N | ||
| Shanafelt et al.211 | 2014 | USA | Research (intervention study) | Survey (before/after) | Individual: computer-based intervention to promote well-being | 1150 surgeons | C | ✗ | ✗ | Evaluate the utility of a computer-based, interactive and individualised intervention for promoting well-being in US surgeons | US surgeons do not reliably calibrate their level of distress. After self-assessment and individualised feedback, half of participating surgeons reported that they were contemplating behavioural changes to improve personal well-being | N | |
| Shapiro et al.212 | 2011 | USA | Research | Review of literature | Individual: strategies for physicians to cope with loss of control and reduce stress/burnout | Physicians | C | ✗ | Explore professional areas in which physicians may experience lack of control, maladaptive ways of coping and burnout. Discuss an empirically validated model of optimal strategies to regain sense of control | Focusing on issues of psychological control in doctors (from training) is paramount for improving well-being of doctors and clinical practice | N | ||
| Shapiro and Galowitz213 | 2016 | USA, 25 national and international programmes | Commentary | Structural: peer support programme | Doctors | T, C | ✗ | ✗ | Suggest stategies to help doctors coping with loss of control | Creating a peer support programme is one way forward, away from a culture of invulnerability, isolation, and shame, and towards a culture that truly values a sense of shared organisational responsibility for clinician well-being and patient safety | N | ||
| Sharifi214 | 2012 | USA | Dissertation | Presentation on mindfulness given to mental health-care providers | Individual: mindfulness-based stress reduction programme | 7 mental health-care providers | C | ✗ | ✗ | Share information about and advocate for the use of mindfulness-based stress reduction programme practice | This mindfulness practice offers a promising approach to therapist self-care and helping to prevent burnout, compassion fatigue and therapist incompetence | N | |
| Shiralkar et al.215 | 2013 | USA | Research | Systematic review | Mixed: self-hypnosis, meditation, changes in the length and type of curriculum, and changes in the grading system | Medical students | U | ✗ | ✗ | Identify all controlled trials of stress management interventions and determine the efficacy of those interventions | Opportunities to advance research exist by developing high-quality studies with attention to randomisation and standard outcome measures | N | |
| Siedsma and Emlet216 | 2015 | USA | Research (intervention study) | Randomised clinical trial | Mixed: facilitated physician small-group curriculum (incorporating elements of mindfulness, reflection, shared experience and small-group learning for 9 months). Protected time (1 hour of paid time every other week) for participants was provided by the institution | 74 physicians, 350 non-trial participants | T, C | ✗ | ✗ | ✗ | Test the hypothesis that an intervention involving a facilitated physician small-group curriculum would result in improvement in well-being | An intervention for physicians based on a facilitated small-group curriculum improved meaning and engagement in work and reduced depersonalisation, with sustained results 12 months after the study | N |
| Sigsbee and Bernat217 | 2014 | USA | Research | Review | Mixed | Physicians | T, C | ✗ | ✗ | Review the causes of burnout in neurologists and suggest interventions | The rapid ongoing changes in the health-care delivery system provide an opportunity for a proactive and thoughtful effort to accomplish these goals | N | |
| Slavin and Chibnall 218 | 2016 | USA | Commentary | Mixed: multipronged strategy based on changes to the medical curriculum (e.g. mindfulness, change to pass/fail grading, confidential option for tracking depression so that ‘positive‘ students are contacted by mental health provider) | Medical students, residents, physicians | U, T, C | ✗ | ✗ | ✗ | Discuss strategies to improve the mental health of medical students, residents and doctors | Leaders of residency programmes, medical schools and hospitals need to have the courage to measure mental health outcomes | N | |
| Slavin et al.219 | 2011 | USA | Commentary | Mixed: changes in education system (promoting positive emotions, facilitating engagement, etc.) | Medical students with references to practising physicians | U, T | ✗ | Provide recommendations to help medical students to flourish | Five recommendations to medical education based on Seligman’s elements for individuals to flourish: positive emotion, engagement, relationships, meaning, achievement | N | |||
| Smith220 | 2016 | USA | Research (intervention study) | PhD dissertation action research | Structural: antistigma campaign | Medical students | U | ✗ | ✗ | Explore whether or not a help-seeking, antistigma campaign improved help-seeking behaviours | Students more likely to seek help from personal resources (close family and friends), but need prompting for college or formal resources. Students’ beliefs and attitudes influenced by those closest to them. First-year students more likely to seek help than their second-year classmates | N | |
| Squiers et al.221 | 2017 | USA | Research | Review | Mixed | Physicians | T, C | ✗ | ✗ | Evaluate potential solutions for physician burnout, both on the individual level and organisational scale | Call for a shift in the focus of interventions towards one proposed root cause of burnout | N | |
| Talisman et al.222 | 2015 | USA | Research | Mixed methods (qual/quant) | Individual: 11-week elective course ‘mind-body medicine’ to offer tools to reduce stress and increase self-awareness | 62 course facilitators (physicians, health-care faculty) | T, C | ✗ | Explore if ‘mind-body medicine’ facilitation is associated with changes in professional identity, self-awareness and/or perceived stress | Such teaching experiences may significantly contribute to attenuating potential burnout by supporting healthy personal and professional formation and increasing professional satisfaction among faculty and staff within academic health centres | N | ||
| Tucker et al.223 | 2017 | Canada | Research (intervention study) | Questionnaires before/after training | Mixed: one workshop on self-reflection to recognise/prevent compassion fatigue and burnout, individual and group activities, followed by Facebook page administered by research team for ongoing resources support (as part of third-year training) | 165 third-year medical trainees | U, T | ✗ | Evaluate this intervention | Educators have important responsibility to integrate compassion fatigue and burnout programmes into ‘the sweet spot’ that third-year offers, as trainees shift from theoretical to experiential practice as future clinicians | N | ||
| van Vliet et al.224 | 2017 | The Netherlands | Research (intervention study) | Survey (post intervention at 6- and 12-month follow-up) | Mixed: mind–body medicine course – experimental sessions of mind–body techniques and group reflection | Dutch medical (second-year) and Swedish nursing students | U | ✗ | Investigate whether a mind–body medicine course could reduce perceived stress and increase empathy and self-reflection in medical and nursing students | This study demonstrated long-term beneficial effects of the mind–body medicine course on perceived stress and empathy in medical and nursing students | N | ||
| Verweij et al.225 | 2016 | The Netherlands | Research (intervention study) | Mixed-methods pilot study, including questionnaires and qualitative interviews | Individual: training mindfulness-based stress reduction | 50 GPs | C | ✗ | ✗ | Gain insight into the feasibility and effectiveness of mindfulness-based stress reduction on burnout, empathy and (work-related) well-being in GPs | When offered as part of the regular CPD programme, mindfulness-based stress reduction appeared to be feasible and acceptable for GPs. GPs became more aware and could recognise and change maladaptive patterns, such as perfectionism. GPs possibly found intervention acceptable because non-directive | N | |
| Waddimba et al.226 | 2016 | USA | Research | Questionnaire | Individual: training mindfulness-based stress reduction | Physicians | T, C | ✗ | Validate single-item screening measures for provider burnout in a rural health-care network | The three single-item measures tested varied in effectiveness as a screening tool for dimensions of burnout | N | ||
| Wald et al.227 | 2016 | USA/Israel | Research (intervention study) | Mixed methods | Mixed: workshop using mind–body medicine and interactive reflective writing to promote resilience | Medical, nursing faculty and senior medical students | UT | ✗ | Participants reported better understanding of professional burnout/resiliency and felt better prepared to use meditation and reflective writing as coping tools | Successful implementation of this intervention provides good rationale for studying its impact over a longer period of time | N | ||
| Warde et al.228 | 2014 | USA | Research | Survey | Mixed: the UCLA-PRIME programme (leadership, mindfulness, self-care, advocacy, resiliency course); 3-week relationship-centred leadership course. To build medical students’ resilience/capacity to persist in working with underserved groups and experience the sustaining satisfaction of caring for those who need it the most | 20 UCLA-PRIMA medical students | U | ✗ | Assess students’ reactions to the programme | The programme promoted qualities in students that characterise effective and resilient physician leaders; students were more mindful, related to each other effectively and co-ordinated their activities well with one another | N | ||
| West et al.53 | 2014 | USA | Research (intervention study) | Randomised clinical trial | Structural: 19 biweekly facilitated physician discussion groups incorporating elements of mindfulness, reflection, shared experience and small-group learning for 9 months. Protected time (1 hour of paid time every other week) for participants was provided by the institution | 74 physicians, 350 non-trial participants (physicians receiving only protected time) | T, C | ✗ | ✗ | To test the hypothesis that an intervention involving a facilitated physician small-group curriculum would result in improvement in well-being | An intervention for physicians based on a facilitated small-group curriculum improved meaning and engagement in work and reduced depersonalisation, with sustained results at 12 months after the study | N | |
| West et al.229 | 2016 | USA | Research | Systematic review and meta-analysis | Mixed: individual and structural and blend | Physicians | T, C | ✗ | ✗ | ✗ | Undertake a systematic review and meta-analysis of studies to prevent and reduce physicians’ burnout | Individual, focused and structural strategies can result in reductions in burnout among physicians. Further research is needed to establish which interventions are most effective in specific populations, as well as how individual and organisational solutions might be combined | N |
| Wild et al.230 | 2014 | Germany | Research | Survey | Mixed: elective course for learning relaxation techniques (autogenic training and progressive muscle relaxation) | 42 medical and psychology students | U | ✗ | Evaluate the intervention | Mandatory inclusion of relaxation techniques in an existing curriculum cannot be advocated based on the study results alone | N | ||
| Winefield et al.233 | 1998 | Australia | Research (intervention study) | Surveys | Individual: stress management seminars (3 hours) | 20 GPs (women) | T, C | ✗ | Evaluate effect of seminars | Significant reduction of both psychological distress and emotional exhaustion was achieved, a sufficiently promising result to encourage further research | Y qual | ||
| Wolf234 | 1994 | USA | Research | Review | Medical students | U | ✗ | Review the literature on stress, coping and health during undergraduate medical education | It is essential to incorporate the principles of health promotion and disease prevention throughout medical education in order to minimise and prevent later burnout and impairment | N | |||
| Zhang et al.235 | 2017 | Canada | Research (intervention study) | Survey | Structural: formal mentorship programme | 8 postgraduate trainees surgeons | C, T | ✗ | ✗ | ✗ | Determine the effects of a formal mentorship programme on the well-being of otolaryngology head and neck surgery resident physicians | The formal mentorship programme can potentially alleviate high levels of stress and burnout within a surgical residency programme and achieve higher levels of personal satisfaction, as well as overall quality of life | N |
| Zwack et al.236 | 2013 | Germany | Research | Qualitative interviews | Mixed: conservation of resource theory-inspired approach to promote resilience. Invest personal resources in a way that initiates positive resource spirals in spite of stressful working conditions | 200 physicians of different ages, disciplines and hierarchical status | C, T | ✗ | ✗ | Identify health-promoting strategies employed by experienced physicians, to define prototypical resilience processes and key aspects of resilience fostering preventative actions | Interventions should sensitise doctors to defensive negative spirals resulting from strain, retreat and shrinking resource pool. Enriching traditional stress management approaches (e.g. relaxation) with this diversified pool of social resources and fields of interest, together with realistic expectancies and good self-knowledge, will support sustainable coping | N | |
Appendix 3 Characteristics of studies from supplementary searches (all UK)
| Reference | Year | Type of paper | Study design | Type of intervention | Sample/setting | Prevention | Screening | Therapy | Objectives | Findings/outcome measures | £ | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Boorman72 | 2009 | Policy review | Mixed: review, survey, consultation | Mixed | NHS workforce | C, T | ✗ | ✗ | ✗ | Provide recommendations on how to promote health and well-being of NHS staff; examples of case studies | Improve organisational behaviour, performance and NHS staff well-being. Reduce sick leave, stress, burnout, mental health and muscle skeletal conditions | Y quant |
| Cornwell et al.88 | 2017 | Policy briefing | Mixed | NHS staff | C, T | ✗ | ✗ | ✗ | Draw attention to the importance of NHS staff experience, the risks to patients when staff are stressed and burned out and the consequences for NHS services | Recommendations at individual, organisational and national level to improve staff well-being. Highlight a duty of care to staff | Y quant/qual | |
| Davies et al.89 | 2016 | Research (intervention study) | Comparison of service monitoring data | Individual: MedNet is a psychodynamically informed confidential self-referral service for doctors | 124 doctors | C, T | ✗ | Examine the health and work trajectory of MedNet clients between 2002 and 2007, followed up in 2010 | Doctors show improvements and continue to progress in their careers after a psychotherapeutically orientated intervention | Y qual | ||
| Department of Health and Social Care40 | 2008 | Policy research | Review | Mixed (mostly structural) | NHS doctors | C, T, U | ✗ | ✗ | ✗ | Assessment of causes leading doctors to experience mental ill-health, barriers to help-seeking and recommendations to address the problem | Principles to guide local and national clinical care of doctors (e.g. treat doctor as patients, confidentiality); training for managers/employers; more self-awareness in doctors | Y qual |
| Department of Health and Social Care92 | 2009 | Policy review | Mixed: review, survey, stakeholder engagement | Mixed | NHS workforce survey (11,000 responses), focus groups, quantitative models | C, T | ✗ | ✗ | ✗ | Provide recommendations with clear roles and responsibilities on how to promote health and well-being of NHS staff (and business case for investing in this); examples of case studies | Reduce and prevent (mental) health problems and consequences (e.g. absence); improve quality of care; financial savings; strengthen NHS ‘brand’ | Y qual/quant |
| Devi93 | 2011 | Research | Review/report | Mixed: mandatory counselling; improve training to reduce stigma and bullying | Doctors and medical students | C, T, U | ✗ | Review of US research into the effect studying and practising medicine has on the mental health of young doctors and surgeons | We have to change the environment in which we are teaching future physicians | N | ||
| Firth-Cozens106 | 2007 | Research | Review | Mixed: individual (career counselling) and organisational (lifelong training, good system for recognising and reporting doctors’ difficulties) | Psychiatrists (and other doctors) | C, T | ✗ | Explores the individual and organisational causes of mental ill-health in doctors, particularly psychiatrists, and suggests a variety of interventions | Psychiatrists need to play a key role in demonstrating the importance of dealing with the mental health problems of doctors and in delivering appropriate training | Y qual | ||
| Graham et al.120 | 2000 | Research | Questionnaire | Structural: points to the need for more communication training for radiologists (as consultants who feel insufficiently trained are at greater risk of burnout) | 882 doctors | C | ✗ | Examine sources of stress and satisfaction for radiologists and hospital consultants in other specialties, in order to understand this difference | A greater proportion of radiologists than other specialists felt insufficiently trained in communication skills | N | ||
| Harrison et al.126 | 2014 | Research | Qualitative interviews | Mixed: mentorship (enhanced job satisfaction and well-being) | 30 doctors, including registrars, those newly appointed to consultant grade, senior doctors and medical leaders from nine hospitals in the north of England | C | ✗ | ✗ | To explore perceptions of mentorship, the extent to which UK doctors appear to value mentorship and factors that may contribute to its successful use | An organisational culture in which mentorship is the norm may enable ‘social network’ approaches (doctors have the opportunity to engage with a range of mentors through informal and naturally occurring relationships) | Y qual | |
| Haward et al.127 | 2003 | Research | Questionnaire | Structural: multidisciplinary cancer team | Random sample of 72 breast cancer teams in England | C, T | ✗ | Evaluate the effectiveness (quality of care, workforce conditions) of multidisciplinary cancer teams | The multidisciplinary cancer teams reported lower levels of mental ill-health than NHS workforce and population as a whole | Y qual | ||
| Hill et al.129 | 2016 | Research | Systematic review | Mixed: relaxation, education, support, cognitive training, targeted stress, fatigue, burnout, depression | Palliative care staff | T, C | ✗ | ✗ | Investigate quantitative studies exploring the effectiveness of psychosocial interventions to improve psychological well-being of palliative care staff | It is impossible at this time to recommend or promote any specific psychosocial intervention. There is an urgent need to address the lack of intervention development work and high-quality research in this area | N | |
| Horsfall134 | 2014 | Policy review | Case review of doctors who committed suicide while going through General Medical Council investigation; General Medical Council processes. Interviews with General Medical Council staff, and stakeholders (BMA, PHP, RCGP) | Mixed | NHS doctors under investigation | C, T | ✗ | ✗ | Establish if the General Medical Council’s processes could be improved to reduce the impact of investigations on vulnerable doctors | Recommendations to reduce doctors’ suicide include improve the General Medical Council’s investigation processes; offer anticipatory resilience training from medical school; ensure that General Medical Council staff spend more time in clinical setting and are more trained to deal with doctors; establish a national support service for doctors | Y qual, quant | |
| Lyons and Dolezal155 | 2017 | Research | Commentary | Mixed: importance of exploring shame and stigma in medicine | C, T, U | ✗ | ✗ | Overview on shame in medicine | Shame has a fundamental and overlooked relationship, with damaging and well-documented phenomena in health care, including moral distress, ethical erosion, compassion fatigue, burnout, stress and ill-health | N | ||
| McKevitt and Morgan163 | 1997 | Research | Qualitative interviews | Structural: change doctors attitude to their own health from university training ‘permission to be ill’; reduce organisational barriers (e.g. difficulty to take sick leave) | 64 doctors interviewed face-to-face or by telephone | C, T, U | ✗ | ✗ | Gain insight of experiences of doctors who are ill (physically/psychologically) | Doctors expressed that illness is inappropriate for them. This is reinforced by the organisation of medical work which discourages doctors from seeking and obtaining help | N | |
| Murdoch and Eagles173 | 2007 | Research (intervention study) | Questionnaires | Structural: mutual support groups | 25 psychiatrists | C | ✗ | ✗ | Describe the function of ‘stress-busting’ groups and report a survey on work-related stress among a small cohort of consultant psychiatrists | ‘Stress-busting’ groups may constitute a helpful approach to work-related stress and a utilisation of the skills of psychiatrists to our mutual benefit | N | |
| NHS England175 | 2016 | Policy guidance review | Review and case studies | Mixed | NHS workforce | ✗ | ✗ | ✗ | Provide rationale for focusing on staff health and well-being, and information on best practice examples | Recommendations include make support for NHS workforce’s mental health part of the NHS organisational culture; provide more support at local level (e.g. talking therapies, yoga, mindfulness) | Y qual, quant | |
| Paice et al.181 | 2002 | Research | Questionnaire | Mixed: better supervision, more time to talk with and about patients, less workload, sleep deprivation and bullying | A cohort of 2456 doctors followed from the time of their application to medical school, studied towards the end of their pre-registration year, from 336 UK hospitals | C | ✗ | ✗ | ✗ | To gain a deeper understanding of the causes of stress in newly qualified doctors, how they cope and what interventions might make the year less traumatic | Centrality of relationship between doctor in training and supervising consultant. More supervision for new doctors and surgeons, less public humiliation and bullying. Change tradition of house officers covering ward at night | N |
| Paice et al.180 | 2004 | Research | Cross-sectional questionnaire survey | Structural: train trainers, give staff access to safe means of complaining | 2730 doctors in training | T | ✗ | Investigate how commonly doctors in training experienced persistent and serious bullying, who were the sources of this behaviour and what action was taken to deal with it | Most of the negative behaviours were perpetrated by other doctors, in a pecking order of seniority. An educational rather than a punitive approach is needed to help trainers develop effective ways of encouraging better performance without becoming a source of distress to junior colleague | N | ||
| Panagioti et al.47 | 2017 | Research | Systematic review and meta-analysis | Mixed | Randomised clinical trials and controlled before–after studies of interventions targeting burnout in physicians | C, T | ✗ | ✗ | Evaluate effectiveness of interventions to reduce burnout and if different types of interventions (physician- or organisation-directed interventions), physician characteristics (length of experience) and health-care setting (primary or secondary care) were associated with improved effects | Physicians could gain important benefits from interventions to reduce burnout, especially from organisation-directed intervention | Y qual | |
| Robertson and Cooper199 | 2010 | Policy implementation guidance | n/a | Mixed | NHS workforce | ✗ | ✗ | ✗ | Practical advice on implementing Boorman report72 | Same as Boorman report72 | Y qual | |
| Wilkie and Raffaelli231 | 2005 | Research/commentary | n/a | Structural: transition group for newly appointed consultants | West of Scotland | C, T | ✗ | ✗ | Advocate for structural transition groups to provide peer support during this transitional process | Transition to consultant level can be one of the most stressful part of career. Transition groups can provide support and help developing professional identity | N | |
| Williams et al.232 | 1998 | Policy review and research | Systematic literature review and interviews | Mixed | 462 papers and other sources. Interviews with 25 key individuals | C, T | ✗ | ✗ | ✗ | Recommendations on how to promote health and well-being of NHS staff | Programme of action which aims to improve physical and psychological health, work attendance, organisational efficiency and long-term financial savings | Y qual/quant |
Appendix 4 Characteristics of studies suggested by stakeholders
| Reference | Year | Country | Type of paper | Study design/methods | Level and type of interventions | Sample/setting | Prevention | Screening | Therapy | Objectives | Findings/outcome measures | £ | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Clarke et al.83 | 2014 | UK | Research | Qualitative methods/survey open responses | Mixed: role of working hour regulation | 2459 respondents | C, T | ✗ | Report on doctors’ views (at very different levels of seniority), about their concerns about the European Working Time Directive and its implementation in the NHS | Frequent dissociation between rotas and actual hours worked, adverse effects on training opportunities and quality, concerns about patient safety, lowering of morale and job satisfaction, and attempts reportedly made in some hospitals to persuade junior doctors to collude in the inaccurate reporting of compliance | N | ||
| Dyer97 | 2018 | UK | Commentary | n/a | Structural: governance systems to deal with ill doctors (particularly with addiction) | T | ✗ | Reflect on the death of a doctors with addiction, and what can be learned | Need to rethink fitness to practice and systems to deal with doctors’ health problems | N | |||
| Eisenstein101 | 2018 | USA | Commentary | n/a | Mixed: role of collective action to drive positive change | C, T, U | ✗ | Discuss the importance of collective action from medical school onwards, to tackle causes of burnout | The social determinants of health – and physicians’ sense of powerlessness in the face of them – seem crucially missing from the discussion of burnout | N | |||
| Gerada117 | 2018 | UK | Commentary | n/a | Mixed: individual and structural processes aggravating mental ill-health in doctors and reducing access to support | C, T | ✗ | Discuss the taboo within medicine and society in general of mental ill-health in doctors | We must allow doctors to become patients without the fear of sanctions or blame, and afford them the same compassion as they are expected to give to their own patients | N | |||
| Maslach and Leiter157 | 2017 | USA | Research | Review | Mixed: (1) get educated about what burnout is, and what to do about it; (2) enhance team perspective; (3) build a culture of appreciation; and (4) realistic strategies and support for restoring energy | n/a | C, T, U | ✗ | ✗ | Overview on current research on burnout and implications for health-care practitioners and medical students | Giving a greater emphasis to the social dynamics of health-care teams can help new physicians in avoiding potential pitfalls and recover from unavoidable strains | Y qual | |
| McCartney158 | 2018 | UK | Commentary | Structural: reflections on the potentially anxiogenic tone of health-care language and systems of governance | C, T | ✗ | Before release, health promotion materials and guidelines (which should say what reasonably should not be done, as well as what should) should be assessed for accuracy and potential anxiety by an independent body and citizen reviewers | ||||||
| Penfold182 | 2018 | UK | Commentary | Structural: loss of control over work in doctors (especially trainees) | Trainees | T | ✗ | Discuss why giving more autonomy to trainees can help in tackling low morale | Doctors should have opportunities to influence how care is delivered in hospitals, general practices and the wider health-care system. | N | |||
| Riley et al.190 | 2018 | UK | Research | Qualitative study | Mixed: support and cultural change (reduce stigma) | Mostly GPs | T, C | ✗ | Report the sources of stress and distress experienced by GPs | Culture change and access to informal and formal support is therefore crucial in enabling GPs to do their job effectively and to stay well | Y qual | ||
| Riley et al.191 | 2018 | UK | Research | Qualitative study | Mixed: support and cultural change (reduce stigma) | Mostly GPs | ✗ | ✗ | Provide an in-depth account of GPs experiences of living and working with mental illness and distress | There is a considerable degree of mental ill-health and reduced well-being among GPs. The solutions are complex and lie in prevention and provision | N | ||
Appendix 5 Graphic overview of programme theory
Appendix 6 Reflective piece about producing non-academic outputs of artist collaborators
Drawing on all results
I was first involved in Care Under Pressure when I was invited to take part in a one day symposium. In the run up to meeting Daniele Carrieri, who organised the event, said he couldn’t resist asking if I would do some drawing during the event. He liked my Guardian work. We agreed payment for the drawing and I proposed to make a short comic strip about the proceedings.
Daniele invited me to take part in the project because my work fitted, to some extent, with the theme of the proposed research. The Bad Doctor (Myriad Editions 2014) was a graphic novel about a stressed GP dealing with his own history of mental health problems and the strips I drew for The Guardian often had a slightly downbeat or despairing tone. The theme of Care Under Pressure certainly resonates with my experience of working in healthcare. I feel that pastoral care for both medical students and young doctors was virtually non-existent when I was in training, where owning up to mental or physical illness was seen as evidence of weakness, or ones being ‘unfit’ to be a doctor. Over the years I have made use of counselling services provided for healthcare staff, and I feel that these services should be expanded. The use of supportive structures should be normalized in healthcare.
It was nice to see Ian Fussell at the symposium. We had met several times before and I had done a workshop for him in Truro. The meeting was interesting, but I found that, while drawing I couldn’t speak or contribute to the debate. Drawing switches off the verbal areas of the brain. Daniele and I have kept in touch since the meeting, and he has updated me periodically over the course of the project. He has always made it plain that he wanted to use cartoons and other visual media as part of the final report.

I have been very busy over the past couple of years, finishing The Lady Doctor (Myriad Editions 2019) and bringing up a toddler while working two days a week as a GP. I have said ‘no’ to virtually all projects suggested to me, and have been very wary of over-committing myself, but when Daniele suggested commissioning me to do some comic strips for the final report it came at a time when I seemed to have a period of relatively free time coming up. Daniele was keen for me to consider doing some animation alongside the comics. I had no experience of this, but wondered whether I could get Matilda Tristram interested in taking part in the project. Matilda and I have taught a couple of workshops together. I love her work and, as I currently seem to watch CBeebies, for whom she writes several of the animated programmes, far more than any other TV channel, hers is the first name that sprang to mind when Daniele mentioned animation. I thought it might be a fun collaboration and push me into doing something of which I had no previous experience.
I asked Matilda and she, too, had a period of relative quiet on the horizon although It didn’t actually turn out like that for either of us.

We pencilled in a week at the end of March when we could meet up and do some work. Matilda came down to Brighton and we spent a whole day brainstorming a story for a three part, three-minute animation. We also talked through how we would go about the technical aspects of putting the animation together, as well as first principles in animation (I hadn’t heard the term ‘rolling boil’ before, at least not outside cooking) and tips for making things as straightforward as possible. What I hadn’t quite realized was just how much drawing is involved with even the simplest of stop-motion animation. I spent the next two days drawing hundreds of frames and hadn’t even finished the first vignette.
The comic strips I started to make responded to the bullet points in the condensed results document. I found it much easier to respond to/portray the negative findings rather than the more positive ones. This may be because I feel that comics, having a history of subversion, seems suited to irony and ridicule, whereas portraying positive messages risks, to my mind, becoming earnest and schmaltzy, like those inspirational posters one might see, in a clip-frame, on the office wall of a down-market financial advisor. I obviously feel more comfortable poking fun rather than offering easy maxims or lifestyle tips. After tackling the negative material first, I tried to relay positive messages within slightly downbeat strips and was told that the result was strangely moving.
When I have discussed Care Under Pressure with colleagues and academics, they have generally expressed interest and suggested that this is a very important area of study. They look forward to reading the results and recommendations. I, too, look forward to the publication and to the reception. I am glad to be involved and look forward to future collaboration.
Ian Williams
May 2019
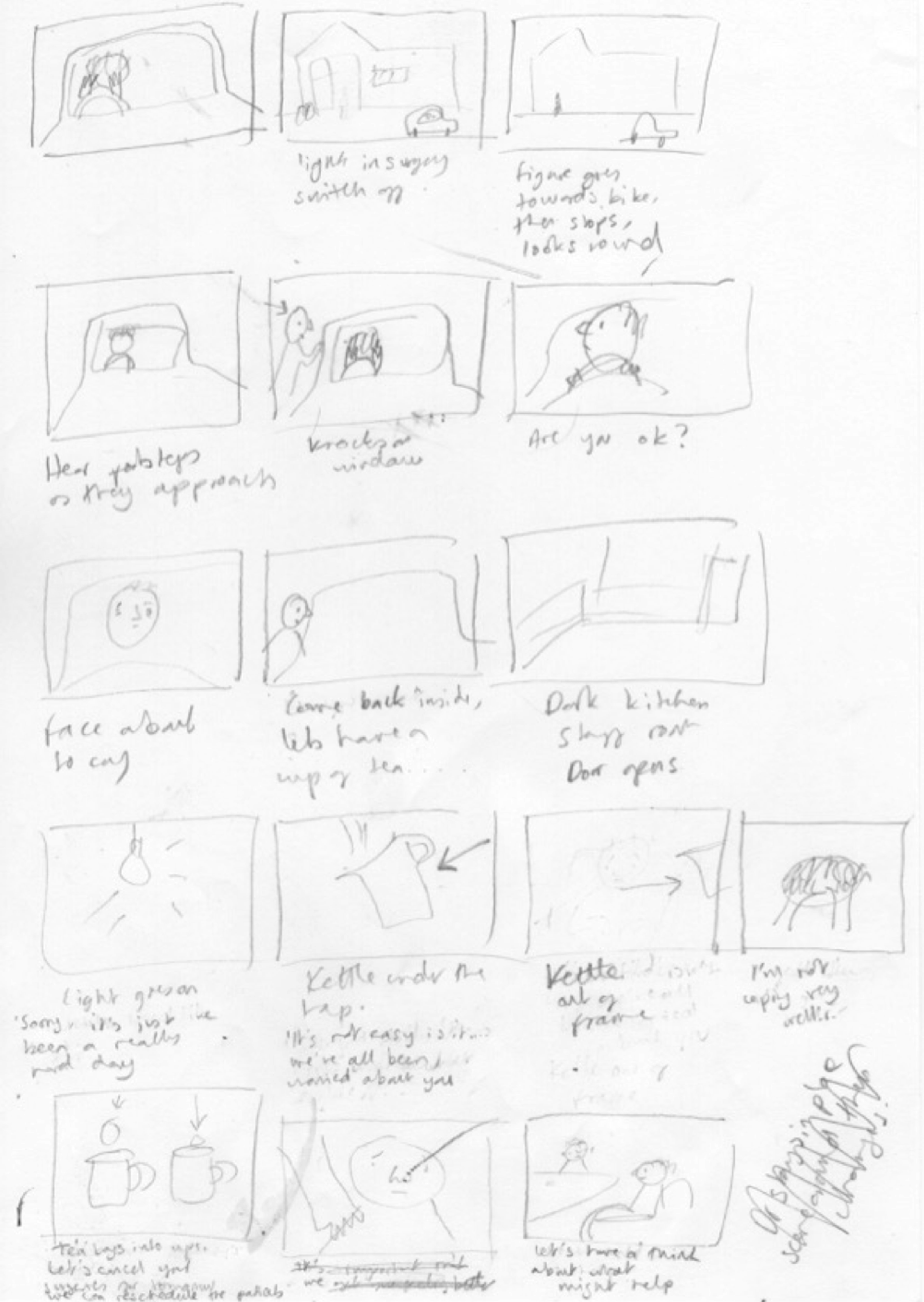
Storyboarding from our brainstorming session
I first met Ian five years ago, I’d been writing a diary comic about having bowel cancer during my first pregnancy. Ian was very supportive; through him, I found out about Graphic Medicine, and got to know the work of many different brilliant authors who write comics about various medical experiences. I love Ian’s work, and really admire both of his books, so I was more than happy to be involved when he suggested that I help with Care Under Pressure.
My experience of healthcare is as a patient, and during my time in hospital I was always interested to know about my doctors as people, and really appreciated it when they seemed to care about me as an individual. I used to Google all my surgical consultants, anaesthetists, oncologists, to try to find out about them. It seemed odd that they knew so much about me, about my life, the difficult choices I had to make, even the inside of my body (a space that I had no mental picture of at all) – while I knew so little about them.
Several dangerous mistakes were made that led to a delay in my own diagnosis. My symptoms weren’t recognised as bowel cancer symptoms (they were confused with pregnancy symptoms) and, after two visits to A and E, I had to refuse to leave the hospital until I’d had an MRI scan, which would eventually diagnose a tumour causing total blockage of my colon. It was clear that the ‘pressure’ we are describing, too many patients, not enough time, younger doctors not feeling able to contradict more senior doctors (one of whom suggested I have an abortion so I could be given an X-Ray), had a very definite negative impact on patient safety, as well as on the wellbeing of the doctors who were caring for me.
So I feel strongly that CUP is a vital project!
Ian and I had a great day brainstorming ideas, and coming up with stories and scenarios that could work. Although I trained as an animator, I’ve been working for ten years as a writer for animated kids’ TV. For this job, I think of the stories, write the scripts, and do a bit of storyboarding. My role in the CUP project has been to condense our ideas into short scripts, and to produce animatics for Ian to use as a reference when he is animating. An animatic is a storyboard that has been added to a video timeline. The point of it is to give a feel for the timing of the whole thing before it has been animated.
With a project like this, although we are using simplified dialogue and images, and the odd archetype, it’s important that it feels emotionally ‘real’. I think we have managed to do this. It has been a very enjoyable project so far, and I’m looking forward to putting all Ian’s drawings together, for the final animation.
Matilda Tristram
May 2019
Glossary
- Abductive/retroductive analysis
- An analytical process based on identifying hidden causal processes that lie beneath identified patterns or changes in those patterns.
- Context–mechanism–outcome configurations
- Relationships between the building blocks of realist analysis (i.e. how mechanisms are triggered under specific contexts to cause particular outcomes).
- Contexts
- Settings, structures, environments, conditions or circumstances that trigger behavioural and emotional responses (i.e. mechanisms) in those affected.
- Mechanisms
- The way in which individuals and groups respond to and reason about the resources, opportunities or challenges offered by a particular programme, intervention or process. Mechanisms are triggered in specific contexts and lead to changes in behaviour.
- Outcomes
- Impacts or behaviours resulting from the interaction between mechanisms and contexts.
- Practitioner Health Programme
- A confidential service for doctors and dentists with psychological issues and addiction problems. This London-based service, founded in 2008, has become one of the largest non-regulatory confidential programmes for sick doctors in Europe.
- Programme theory
- A set of theoretical explanations or assumptions about how a particular programme, process or interventions is expected to work.
List of abbreviations
- CMOc
- context–mechanism–outcome configuration
- CUP
- Care Under Pressure
- EIT
- evidence integration triangle
- GP
- general practitioner
- RAMESES
- Realist And Meta-narrative Evidence Syntheses: Evolving Standards
