Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/136/70. The contractual start date was in January 2014. The final report began editorial review in October 2018 and was accepted for publication in April 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
All authors report grants from the Department for Children, Schools and Families (now the Department for Education), grants from the Department of Health and Social Care, non-financial support from the Youth Justice Board for England and Wales, grants and non-financial support from the National Institute for Health Research (NIHR) Clinical Research Network, during the conduct of the study. David Cottrell reports being the chairperson of the NIHR Clinician Scientist Fellowship panel during the conduct of the study. Ian M Goodyer reports personal fees from Lundbeck (Copenhagen, Denmark), outside the submitted work, and was a member of Efficacy and Mechanism Evaluation Prioritisation Group during the conduct of the study.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Fonagy et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Conduct disorder (CD) is the most common behavioural disorder in childhood and adolescence. 1 It is characterised by antisocial behaviour, or violation of acceptable social norms, such as aggression, destructive behaviour or habitual deception. 2 The prevalence of the disorder is approximately 8% of boys and 5% of girls aged 11–16 years. 1 However, among looked-after children aged 11–15 years, the prevalence of CD was found to be 40.5%. 3 As of 2014, there were a total of 1,240,000 known cases of CD in England. 1
The main risk factors for developing CD include poor or erratic parenting, impulsiveness, and growing up in a low-income household or a high-crime area. 4 The disorder is associated with increased risk of criminal behaviour, substance abuse, and poor academic achievement and employment going into adulthood. 5,6 These risks are associated with significant financial, societal and interpersonal costs. 7 The average potential savings from early intervention have been estimated at £9300 per child. 8 Without intervention, about 50% of adolescents with CD will develop antisocial personality disorder, and those who do not will still go on to have long-term psychological and behavioural problems. 9
Multisystemic therapy (MST) has previously been identified by the National Institute for Health and Care Excellence (NICE) as a promising intervention for reducing recidivism in delinquent young people and improving individual and family pathology. MST is an intensive, family-focused programme, combining aspects of cognitive–behavioural and family therapy. 10 In the USA, there has been some evidence that MST can reduce criminal activity11 and recidivism,12 and improve antisocial behaviour13 and family cohesion14 compared with management as usual (MAU). However, other studies, outside the USA, have found no differences between MST and MAU on measures of antisocial behaviour15 and criminal conviction. 16 This heterogeneity in results can be explained in a number of ways, including differences in fidelity of treatment implementation, variable quality of standard MAU services, differences in sentencing policies between national justice systems (specifically alternatives to incarceration), and the quality of integration of MST with other services.
The Systemic Therapy for At Risk Teens (START) trial is a national randomised evaluation of MST in the context of the UK, developed to inform policy-makers, service commissioners and professionals about the value of MST in the management of antisocial behaviour compared with standard management practices. Results from the first phase of the trial (from baseline to 18-months’ follow-up) have been reported in The Lancet Psychiatry. 17 A total of 684 families took part in the pragmatic, individually randomised, single-blind, controlled superiority trial conducted across nine community-based MST services in England. Young people aged 11–17 years were randomly allocated to receive either MST (n = 342) or MAU (n = 342). The primary outcome for the first phase of the trial was proportion of out-of-home placements. Secondary outcomes included offending data [collected via the Police National Computer (PNC), a centralised database], substance misuse, individual and family well-being, and a range of behavioural and cognitive outcomes. Data were collected at baseline, and at 6-month intervals until 18 months. An economic evaluation to assess the cost-effectiveness of MST compared with MAU was also conducted.
Overall, there were no significant differences between the groups in the proportion of out-of-home placements [odds ratio (OR) 1.25, 95% confidence interval (CI) 0.77 to 2.05; p = 0.37] or time to first offence [hazard ratio (HR) 1.06, 95% CI 0.84 to 1.33; p = 0.64]. However, the total number of offences at 18 months was greater in the MST group (average 0.65 offences, 95% CI 0.28 to 1.02 offences; p = 0.00067). Improvements in CD diagnoses (> 40% reduction) were notable in both groups, but no group differences were found. Longitudinal models consistently supported short-term reductions in self-reported depression and parent-reported delinquency in the MST group compared with MAU, but these differences were not sustained in the long term. There was no evidence of MST’s superiority with regard to secondary outcomes, with the exception of parental well-being and self-reported callous and unemotional traits. The mean total service costs were not found to be significantly different (MST £28,687 vs. MAU £30,928; adjusted difference –£1623, 95% CI –£7684 to £4438; p = 0.60).
Overall, the results from the first phase of the trial suggest that, although MST followed by MAU led to behavioural and emotional improvements, there was no evidence to suggest its superiority to MAU alone among a population of adolescents with moderate to severe antisocial behaviour problems.
Objectives
The second phase of the START trial extended the follow-up period to 4 years for secondary outcomes and to 5 years for the primary outcome. The aim was to evaluate the medium- to long-term effectiveness and cost-effectiveness of MST compared with MAU in the UK. Extending the follow-up period enables stakeholders to make informed, evidence-based decisions about the role of MST in treating CD.
The primary objective was to compare MST with MAU in terms of the proportion of young people who had criminal convictions by 5 years post intervention. This was evaluated using data from the PNC, a centralised database of offending data across the UK. Secondary outcomes included measures of psychiatric problems and outcomes in areas where CD can result in poor outcomes: educational attainment, work adjustment, social relationships, pregnancy and physical health.
In addition, the cost-effectiveness of MST compared with MAU was explored at the 4-year follow-up in terms of quality-adjusted life-years (QALYs) and offending. Two qualitative substudies were also designed for a subsample of the families to better understand the subjective experiences of young people and their parents or carers and to better characterise the life circumstances and quality of young people’s lives post intervention. Qualitative Study 1 was carried out approximately 18 months post randomisation. Qualitative Study 2 took place around the 48-month follow-up visit.
Chapter 2 Methods
The first phase of the START trial involved a follow-up period of 18 months. The present report concerns the second phase, which followed families from 18 months to 4 years for self-report data and to 5 years for objective offending data. In this section we describe the trial as it was designed at the outset, including recruitment, randomisation, data collection procedures, and descriptions of the MST and MAU interventions. This is followed by methodology specific to the second phase of the trial, including the approaches to statistical and health economic analyses, and descriptions of the methodologies used for the two qualitative studies. The full description of the trial design and study methodology used in the first phase of the trial can be found in the protocol paper. 18
Trial design
The trial was a pragmatic, individually randomised, multicentre superiority study. Allocation was carried out by minimisation, controlling for the number of past convictions, gender and age at onset of criminal behaviour. Treatment centre was also included in the minimisation stratification to control for differences between centres.
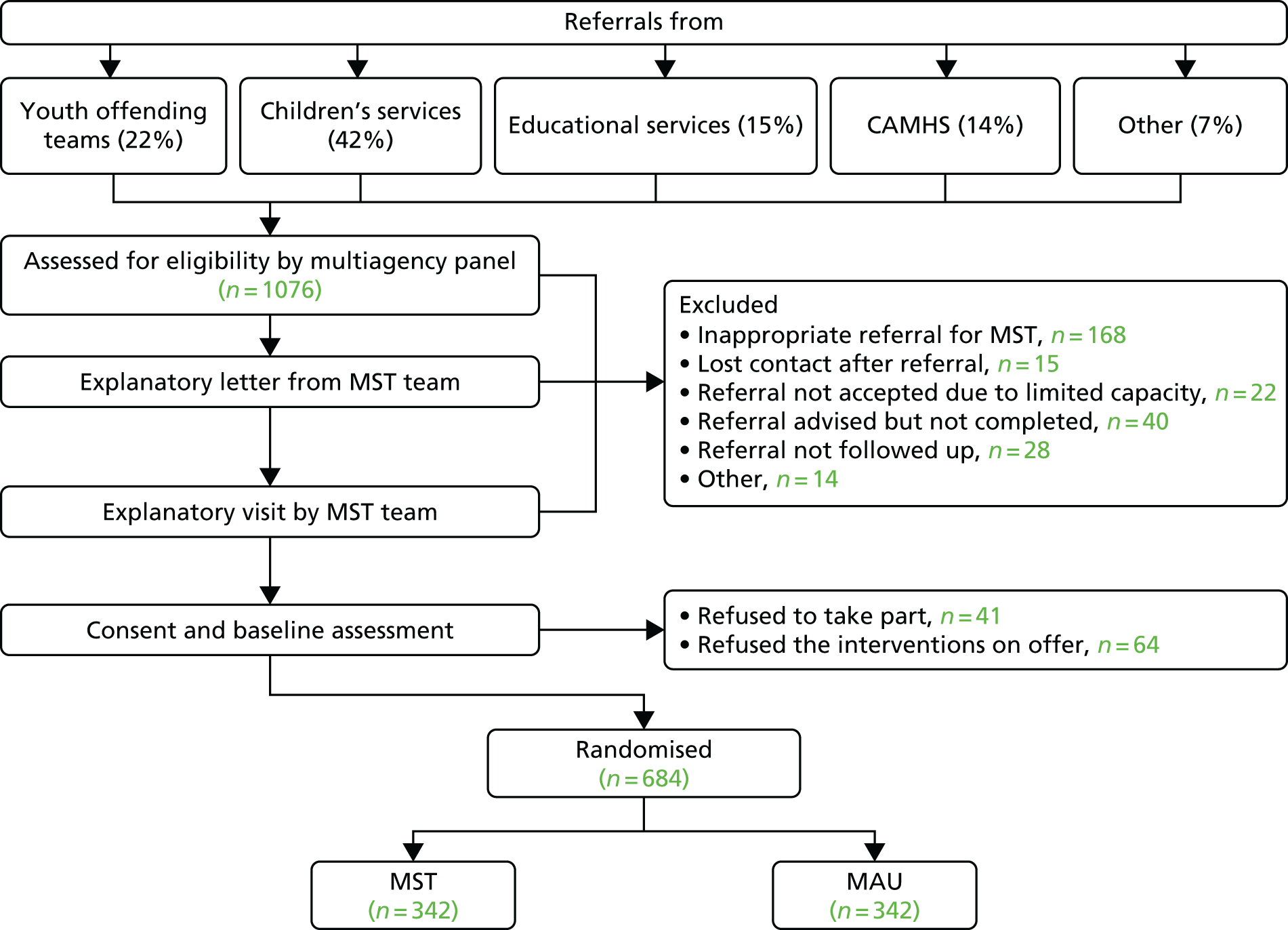
Figure 1 illustrates participant referral flow. Participants were referred to the trial by youth offending teams, children’s services, educational services, child and adolescent mental health services (CAMHS) and other referrers. Referred participants were screened for eligibility by a multiagency panel at each site. Those who met the inclusion criteria were considered eligible, and were sent a plain-English letter explaining the study and consent procedures and inviting them to take part. After a brief period (1–2 weeks), the families were contacted by a member of the MST team to arrange an explanatory meeting in person. This meeting was used to explain to the family what participation in the trial entailed and give them the opportunity to ask questions, but also to identify any potential exclusion criteria (e.g. risk of injury to worker, severe substance dependence). Unless the family decided at this stage to not take part, a member of the research team contacted them telephone, no longer than 3 days later, to arrange a second meeting. The second meeting entailed reviewing and completing consent forms, and completing pre-randomisation questionnaires and measures of the secondary outcomes in the study. Both information sheets and consent forms were written with input from families who had previously completed MST, and ensured to be appropriate and accessible in terms of language and age. Following the second meeting, if the family agreed to take part and no contraindications were identified, a member of the research team contacted the MST site to obtain allocation (1 : 1 ratio).
FIGURE 1.
Referral flow.
Assessments for secondary outcomes were conducted at baseline, and at 6, 12, 18, 24, 36 and 48 months post randomisation. Measures were typically completed in the family home. A member of the research team telephoned in advance to arrange the visit at a convenient time for the family. The questionnaire pack required approximately 2 hours to complete for both the young person and the parent or carer. After each visit, the family received £25 to thank them for their time.
Research assistants were carefully supervised on an ongoing daily basis by the trial co-ordinator, and had additional supervision meetings once every 2 weeks with the project co-ordinator, who had substantial experience in clinical and research activities with young people, including in MST.
The study protocol was approved by the London South-East Research Ethics Committee (reference number 09/H1102/55). The trial was overseen by the Trial Steering Committee and the Data Monitoring and Ethics Committee. Both committees were independently chaired and reviewed trial progress throughout the study. Progress reports were submitted to the funder every 6 months. One serious adverse event was recorded: a participant in the MAU group had died. This participant had been seen by the research team at the 12-month follow-up, and news of their death was reported to the research team at 36 months. The sponsor and the ethics committee reviewed the case and agreed that the death was not related to the intervention or the trial.
Eligibility criteria for participants
The aim of the trial was to increase generalisability by using the minimum number of entry criteria. Young people were considered to be eligible for the trial if they met the following inclusion criteria:
-
were aged 11–17 years
-
had sufficient family involvement for MST to be applied, excluding adolescents already in local authority care or foster accommodation
-
had no existing agency involvement (e.g. the family were already engaged with a therapist) that would interfere with MST
-
met one of the following criteria indicating their suitability for MST:
-
– persistent (weekly) and enduring (≥ 6 months) violent and aggressive interpersonal behaviour OR
-
– a significant risk of harm to self or to others OR
-
– at least one conviction and three warnings, reprimands or convictions in the last 18 months OR
-
– current diagnosis of externalising disorder and a record of unsuccessful outpatient treatment OR
-
– permanent school exclusion.
-
Additional referral criteria were developed to reflect the different referral routes into the trial, including Youth Offending Services, Social Services, CAMHS and education services. As a result, eligible candidates could be referred if they met three of the following features indicative of ‘risk status’:
-
excluded or at significant risk of school exclusion
-
high levels of non-attendance at school
-
an offending history or at significant risk of offending
-
previous episodes on the Child Protection Register
-
previous episodes of being looked after
-
previous referral to family group conference to prevent young person from becoming looked after
-
history of siblings being looked after.
Exclusion criteria included:
-
history or current diagnosis of psychosis
-
generalised learning problems (clinical diagnosis) as indicated by intelligence quotient (IQ) below 65
-
risk of injury or harm to a worker
-
presenting issues for which MST has not been empirically validated, in particular substance abuse in the absence of criminal conduct or sex offending as the sole presenting issue. 18
Settings and locations in which the data were collected
Nine MST pilot sites across England participated in the trial: Peterborough, Leeds, Trafford, Barnsley, Sheffield, Reading, Hackney, Greenwich, and Merton and Kingston. Data were typically collected in the family home, or, in rare cases where this was not possible, at another safe, private and convenient location, such as a meeting room in a local authority building.
Chapter 3 Interventions
Key elements of the interventions are described below, but additional information can be found in Appendix 5. It should be noted that MST is a multifaceted programme and the MST intervention as described below is related specifically to MST implementation for young people with CD. Other MST adaptations exist for young people with substance misuse problems, problem sexual behaviour and psychiatric emergencies, and for family reunification for young people in care.
Multisystemic therapy
Multisystemic therapy is a manualised, licensed programme for young people exhibiting antisocial behaviour and their families. The programme uses a social-ecological approach with the aim of simultaneously affecting the multiple systems around the young person, including home life, school, peer relationships and the wider community. The techniques used in MST draw from cognitive–behavioural therapy, behavioural therapy, strategic family therapy and structural family therapy.
The MST therapist works intensively with the family, focusing primarily on the young person’s caregiver(s) to improve their parenting skills and the parent–child relationship, improve communication problems, foster support from social networks, encourage the young person’s participation in education and reduce any associations with delinquent peers. The intervention lasts between 3 and 5 months, depending on the family’s needs. Average treatment duration in this trial was 139 days. The therapists have a small caseload (four to six cases), meet with the family three times a week in the family home, and are available to be contacted 24 hours a day. The content of the programme is individualised to the specific needs of each family.
All nine trial sites were licensed by MST services to deliver the programme. Each MST team consists of at least three specially trained clinicians supervised by an accredited MST supervisor. Each team is offered weekly 1-hour conference calls for consultation with a staff member of MST services. Clinical teams additionally benefit from input and collaboration with local mental health-care professionals with postgraduate qualifications in the field of psychology, counselling or social work.
Treatment fidelity is maintained through (1) manualised weekly group supervision with a MST expert from MST services, (2) a well-developed quality assurance system and twice-yearly implementation reviews, and (3) the Therapist Adherence Measure – Revised (TAM-R). The TAM-R assessment is evaluated using a rating scale completed by a research assistant by speaking with the parents or carers. These assessments were carried out by an independent research group to maintain research separation and prevent possible researcher bias. Results from the first phase of the trial (baseline to 18 months) found good levels of treatment adherence, with an average TAM-R score of 0.698 (standard error 0.012, range 0.610–0.806) across all sites; the cut-off point for satisfactory adherence is 0.61.
After completing the MST programme, participants in the MST group received MAU.
Management as usual
Because this was a pragmatic trial involving several collaborating services across nine different sites, it was never possible to prespecify MAU content. As a result, MAU consisted of the standard care offered to young people and families who met eligibility criteria for the trial. There was a significant amount of variability in the MAU group in the type of care offered, the duration and intensity of care, and practitioners’ theoretical approaches. However, it was expected that all treatment approaches were designed in line with current community practice and treatment guidelines issued by the Social Care Institute for Excellence and NICE. Families in the MAU group were offered services specific to their particular needs (e.g. intervention for substance misuse or support for re-engaging with education). A range of professionals was involved in MAU care, including social workers, probation officers and specialist therapists.
Service use was monitored using a version of the Child and Adolescent Service Use Schedule (CA-SUS) designed specifically for the trial. The CA-SUS recorded contact with all health, social care and criminal justice sector services, including the number and duration of contacts. Results suggest that MAU programmes were multicomponent, no less resource-intensive than MST, and consistent with the complex needs and difficulties of this population. The use of MAU services in both the MST and the MAU groups, including mean number of contacts, total duration of all contacts and percentage of young people making use of each service, can be found in Table 1. At 12 months’ follow-up, the MST group had slightly briefer contacts with all services combined [t(484) = 2.03; p = 0.0429], but these differences were no longer observed at 18 months.
| Follow-up time point | Group | |||||
|---|---|---|---|---|---|---|
| MAU | MST | |||||
| Number (SD) of contacts | Duration (SD) of contacts (minutes) | Number (%) used | Number (SD) of contacts | Duration (SD) of contacts (minutes) | Number (%) used | |
| Baseline | ||||||
| CAMHS | 1.42 (3.9) | 75.61 (222.9) | 72 (25.3) | 2.47 (9.7) | 128.79 (495.1) | 72 (24.7) |
| Social care | 4.74 (10.7) | 252.33 (815.5) | 122 (42.9) | 5.45 (12.4) | 344.77 (949.7) | 123 (42.2) |
| YOT | 6.12 (14.2) | 290.6 (715.9) | 87 (30.6) | 5.17 (11.8) | 321.96 (1644.6) | 82 (28.1) |
| 6-month follow-up | ||||||
| CAMHS | 1.5 (6.0) | 94.41 (417.3) | 53 (19.9) | 2.13 (8.4) | 267.95 (2443.8) | 56 (22.3) |
| Social care | 5.82 (16.2) | 286.28 (711.2) | 102 (38.3) | 4.42 (11.5) | 250.05 (821.4) | 91 (36.2) |
| YOT | 4.47 (10.8) | 222.07 (613.2) | 67 (25.1) | 4.93 (11.3) | 240.7 (600.3) | 70 (27.8) |
| 12-month follow-up | ||||||
| CAMHS | 4.02 (19.1) | 547.04 (4050.1) | 50 (20.4) | 1.66 (7.3) | 77.03 (270.6) | 57 (23.8) |
| Social care | 5.44 (15.4) | 318.85 (1179) | 92 (37.5) | 4.52 (9.8) | 256.24 (679.3) | 91 (38) |
| YOT | 5.07 (13.7) | 228 (587) | 57 (23.2) | 4.59 (14.7) | 194.18 (554.9) | 55 (23) |
| 18-month follow-up | ||||||
| CAMHS | 6.84 (21.3) | 729.19 (4250) | 89 (40) | 6.27 (19.9) | 486.35 (3066.3) | 89 (42.5) |
| Social care | 13.93 (27) | 716.67 (1553.1) | 138 (62.1) | 12.43 (22.4) | 722.71 (1576.8) | 122 (58.3) |
| YOT | 14.21 (29.9) | 640.53 (1415.9) | 87 (39.1) | 12.92 (24) | 584.38 (1175.1) | 92 (44) |
Chapter 4 Outcomes
The primary outcome [i.e. the proportion of young people with criminal conviction(s) in the MST group compared with MAU at 5-year follow-up] was assessed using objective data from the PNC. The police database export includes offence date, offence type, offence outcome (e.g. conviction, caution) and disposal category (e.g. immediate custody, community service, caution). Offence outcomes are classified as violent, non-violent or breach for the purposes of the analysis.
Table 2 contains a summary of the secondary measures and time points at which data were collected. Appendix 1, Table 20, contains additional data on internal consistency of the measures used (where applicable).
| Measure name | Measure construct(s) | Collected at (time point) | Completed by | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 6 months | 12 months | 18 months | 24 months | 36 months | 48 months | Parent | Young person | Teacher | ||
| Family Information Form | Demographic information | ✗ | (If necessary) | ✗ | ✗ | ||||||
| SDQ20 | Antisocial behavioural problems and beliefs, and young people’s and parental well-being | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| ICUT21 | Callous and unemotional traits | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| SRD22 | Conduct problems | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| ABAS23 | Antisocial behaviour and attitudes | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| Youth Materialism Scale24 | Materialistic values | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| Conners Comprehensive Behavior Rating Scale (ADHD and Learning & Language subscales)25 | ADHD symptoms | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| APQ26 | Parenting controls, and skills for monitoring and supervision | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| Loeber Caregiver Questionnaire27 | Family functioning (parental supervision and involvement) | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| FACES-IV28 | Family functioning (family adaptability and cohesion) | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| LEE29 | Family functioning (levels of expressed emotions) | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| CTS230 | Degree of conflict in the parental relationship | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| SMF31 | Well-being and adjustment | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| GHQ32 | Screen for minor psychiatric disorders | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| DAWBA33 | Psychiatric disorders | ✗ | ✗ | ✗ | ✗ | ||||||
| WASI-II34 | Child IQ | ✗ | ✗ | ||||||||
| Expectancies Questionnaire | Nature of delivery of interventions in MST and MAU groups | ✗ | ✗ | ✗ | ✗ | ||||||
| CPAS35 | Nature of delivery of interventions in MST and MAU groups | ✗ | ✗ | ✗ | ✗ | ||||||
| RTC | Nature of delivery of interventions in MST and MAU groups | ✗ | ✗ | ✗ | ✗ | ||||||
| CA-SUS | Data on use of all services and other resource use | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| EQ-5D-3L measure of health-related quality of life36 | QALYs | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| CLES-A37 | Significant life events | ✗ | ✗ | ✗ | ✗ | ||||||
| SF-3638 | Quality of life | ✗ | ✗ | ✗ | ✗ | ||||||
| ARQ39 | Psychological resilience | ✗ | ✗ | ✗ | ✗ | ||||||
| K-SADS40 | Screening for affective disorders and schizophrenia | ✗ | ✗a | ||||||||
| ASR41 | Behavioural and emotional problems | ✗ | ✗ | ✗ | ✗ | ||||||
| ABCL41 | Behavioural and emotional problems | ✗ | ✗ | ✗ | ✗ | ||||||
| Adult Materialism Scale42 | Materialistic values | ✗ | ✗ | ✗ | ✗a | ||||||
| SCID40 | Screening for personality disorders | ✗ | ✗a | ||||||||
| National Pupil Database | Educational participation (attendance and exclusions) | ✗ | ✗ | ✗ | |||||||
Changes to trial outcomes
Educational attainment (number of absences and exclusions) was initially intended to be collected from the National Pupil Database. However, it became apparent during the first phase of the trial that the data available from the database are collected over rigid time periods tied to school term dates. As a result, the data could not be reliably matched to the data collection points for the participants in the study, and therefore were not collected during the second phase. Data on whether participants were in full- or part-time education or employment were still collected as part of the Adult Self-Report measure and the Work and Relationships questionnaire.
The trial initially included an intention to carry out a characterisation of the MST and MAU services using the Children and Young People – Resources, Evaluation and Systems Schedule (CYPRESS) measure. This was unfortunately not possible during the second phase of the trial. Most of the MST sites had closed by 24-month follow-up and it was not possible to contact the practitioners associated with the MAU services delivered in the first phase of the trial, who had frequently left their posts or were no longer delivering the relevant service. As a result, a meaningful CYPRESS evaluation was not possible. However, we include a report on the CYPRESS evaluation carried out during the first phase of the trial in Appendix 6.
The Child Attachment Interview was trialled, but was determined to be not acceptable to the young people within the sample, and was therefore discontinued in favour of retaining the collaboration of the participants.
Sample size
Annual recruitment into MST was estimated at 140 families per year. Of these, approximately 30% were estimated to meet the criteria and agree to randomisation. By this calculation, each site was estimated to be able to recruit and treat about 70 families over 1.5 years, for a total of 700 participants (350 in each group). On the assumption that 30% of the MAU group would have out-of-home placements, this sample size would give 86% power to detect a 10% difference in out-of-home placements (a reduction from 30% to 20%).
Randomisation
Participants who met the criteria and screening procedures were randomised on a 1 : 1 basis by an assistant from University College London’s Trials Unit who was independent of the trial team.
Randomisation was initiated by the research assistant using a secure telephone randomisation service that ensured both allocation and concealment. A computer-generated algorithm incorporating a random element generated the allocation using the following stratification factors: treatment centre, gender, age (11–14, 15–17 years), age at onset of severe conduct problems (2–11, ≥ 11 years) and number of past convictions (≤ 2/≥ 3). These strata were selected because previous research has shown that younger age at onset and more previous convictions are associated with poorer prognosis. Minimisation ensured an even distribution of participants across both treatment groups.
Investigators and RAs were blind to treatment allocation. Allocation data were kept physically inaccessible to investigators and RAs to avoid leakage of the information. All coding, data entry and data cleaning were conducted by research team members blind to allocation. Treatment fidelity was assessed by a geographically separate research group who did not have access to outcomes.
Patient and public involvement
Each MST site had its own dedicated patient and public involvement group, which met regularly to advocate for patients and liaise with the clinical team. These groups were independent of the trial and provided an extra layer of oversight to service delivery. The trial itself had patient involvement at both the planning and the delivery stages. During study design, a meeting was organised by Music and Change UK, a mental health charity that advocates for young people. The purpose of the meeting was to receive feedback from young advisors on the study methodology and content. During the course of the study, a Trial Steering Committee met regularly to discuss the study progress and resolve arising issues. The committee included a patient-public liaison member: this was a parent of a young person with similar mental health and behavioural problems to those of the young people who took part in the study. The parent was able to advise the committee and the research team on conducting the research in a mindful way and keeping family perspectives in mind.
Chapter 5 Statistical methods
All analyses, except where specified, were prespecified in a statistical analysis plan agreed with the Data Monitoring and Ethics Committee.
Missing data
All analyses were performed with statistical methods that handle missing outcome data that are missing at random. That is, the probability of an observation being missing depends only on observed variables that are accounted for in the model.
As an additional analysis, we used multiple imputation on a data set with all baseline and outcome variables. Twenty complete data sets were imputed using predictive mean matching. Pooled analyses were performed using Rubin’s rules. 43 This analysis should be treated as exploratory, as it will be using postbaseline data in the imputation, meaning that comparisons between groups cannot be treated as causal.
Primary outcome
The primary outcome was analysed using a mixed-effects logistic regression model with a fixed effect for treatment group allocation. The model was adjusted for number of convictions prior to randomisation, gender, age at onset of criminal behaviour (early or late) as fixed effects, and site as a random effect. The model was fitted in R (The R Foundation for Statistical Computing, Vienna, Austria) using the glmer function in the library lme4.
The primary analysis estimated the effect of group (i.e. the OR between MAU and MST) from the model, along with the CI and p-value, calculated from the Wald test, for whether or not the difference is significant.
Secondary outcomes
Secondary outcomes were analysed according to whether they were time-to-event, count data or continuous data.
The time-to-event outcome (time to first offence) was analysed using a Cox proportional hazards model adjusted for the same fixed effects as the primary outcome.
The count data outcomes (number of offences, and delinquency volume and variety outcomes) were analysed using Poisson mixed models adjusted for the same fixed and random effects as the primary outcome. An additional baseline effect was included for the delinquency outcomes representing the measurement at the baseline.
The continuous outcomes (all questionnaire outcomes) were analysed with a linear mixed-effects model adjusted for the same fixed effects as the primary outcome. In addition, a random intercept and slope for each individual were included.
For both the count and the continuous outcomes, separate treatment effects for each follow-up time were included. The estimated treatment effect for each time, together with the CI and p-value, was extracted directly from the model.
For young person outcomes that are measured only in participants aged ≥ 18 years, we treated observations not taken because of age as missing.
Subgroup analyses
The primary outcome and time to first offence outcome were tested for subgroup effects, with the following moderators considered:
-
gender
-
age
-
onset of CD (≤ 11 years vs. > 11 years old)
-
baseline Inventory of Callous-Unemotional Traits (ICUT) score*
-
baseline peer delinquency score*
-
baseline Antisocial Beliefs and Attitudes Scale score*
-
previous offence or no previous offence at baseline
-
diagnosis of CD or attention deficit hyperactivity disorder at baseline
-
diagnosis of CD, depression or anxiety at baseline
-
referral path.
Variables marked with * were treated as continuous variables, and the others were treated as binary.
For the primary analysis results, two-sided p-values < 0.05 were considered significant. For secondary outcomes, there was a considerable multiple testing burden. We applied a procedure called Benjamini–Hochberg44 to control the false-discovery rate at 5%. The false-discovery rate is the proportion of rejected null hypotheses that are in fact true (i.e. the proportion of positive findings that are in fact false positives). Thus, we do not control the probability of making any type I error, but control the proportion of significant results that are type I errors to be < 5%. This procedure was applied separately to the non-imputed and imputed analyses.
Chapter 6 Economic evaluation
Please note that in this chapter some material has been reproduced from the protocol paper (Fonagy et al. 18). This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. The text below includes minor additions and formatting changes to the original text.
The economic evaluation took a wide-ranging perspective and included all health, social care and education-based services, plus costs falling on the criminal justice sector, costs resulting from crimes committed and out-of-pocket expenses for trial participants. 17 Although a NHS/Personal Social Services perspective is preferred for submissions to NICE,45 this perspective is likely to be too narrow to capture all of the relevant costs associated with this population.
The primary economic evaluation, a cost–utility analysis, was undertaken, using QALYs as the measure of effect. A secondary analysis explored cost-effectiveness in terms of the primary outcome, namely the proportion of the sample with criminal convictions over the follow-up period. Both analyses were carried out at the 48-month follow-up point.
Resource use and costs
Resource use was recorded in interviews with young people and their families using CA-SUS. 46,47 For this medium- to long-term follow-up of the original trial, the CA-SUS was completed at 30 months, for the period since the end of the trial (24 months), and at the 36-, 42- and 48-month follow-ups, covering service use for the period since the previous assessment of these data.
Resource use data were collected in the following domains:
-
delivery of the MST intervention
-
use of accommodation services – foster care, residential care, staffed accommodation
-
use of education services – mainstream school, specialist school, residential school, hospital school, pupil referral unit, home tuition, further education
-
use of NHS secondary care services – inpatient stays (mental health and all medical specialties), outpatient appointments (mental health and all medical specialties), accident and emergency attendances (including use of ambulance services)
-
use of community-based services – counsellor, family therapist, social worker, family support worker, education welfare officer, mentor, advice service
-
use of prescribed psychotropic medication – antidepressants, medication for attention deficit hyperactivity disorder, benzodiazepines, medication for sleep disturbance, antipsychotics, antiepileptics
-
criminal justice system resource use – police custody, youth custody, probation officer, youth offending team, solicitor, court appearance. 17
Nationally applicable unit costs were applied to each item of service use reported in the CA-SUS to calculate the total costs for each trial participant. Unit costs for education services were taken from national statistics of school income and expenditure for local authority maintained schools in England for 2011–12 and 2012–13. 48 Unit costs for hospital services were taken from the national schedule of NHS Reference Costs 2012 to 2013. 49 Costs contained in the 2013 Unit Costs of Health and Social Care were used to calculate costs of accommodation and of community-based health, social and voluntary sector services. 50 The cost of medication was calculated based on averages listed in the British National Formulary51 for the generic drug and using daily dose information collected using the CA-SUS. Unit costs for the criminal justice sector were taken from the 2013 Unit Costs in Criminal Justice52 and reports from the Home Office on the cost of criminal justice. 53
The cost of the MST intervention was calculated using a standard microcosting approach54 and utilised data on salaries of therapists as well as employer on-costs (National Insurance and superannuation), and appropriate managerial, administrative and capital overheads and conditions of service. 50 Costs of MST training, provision of MST supervision and the MST licence were also incorporated into the total cost of the intervention. 17 A detailed costing schema of the MST intervention has been published previously. 17 All unit costs are reported in UK pounds sterling for the 2012–13 financial year and inflated where necessary. Costs and outcomes were discounted at a rate of 3.5% annually, as recommended by NICE. 45
Effectiveness
The primary outcome of the economic evaluation was QALYs, calculated from health states derived from the EuroQol-5 Dimensions, three-level version (EQ-5D-3L), measure of health-related quality-of-life instrument and using the area under the curve approach. 55 The EQ-5D-3L was completed at 30, 36, 42 and 48 months’ follow-ups.
Economic analysis
Service use was reported descriptively using means and standard deviations (SDs). No statistical comparisons were made in order to avoid problems with multiple significance testing.
Differences in costs and outcomes between trial groups were compared using random-effects linear regression. The total costs, as well as the costs per sector, over the 48-month follow-up period in each trial group were summarised using the mean and SD for two data sets: the observed data and the multiply imputed data. Analyses compared mean costs, despite the skewed nature of cost data, to enable inferences to be made about the arithmetic mean, which is the most meaningful summary statistic for cost. 56 The validity of the results was confirmed by examining CIs from bias-corrected accelerated non-parametric bootstrap. Differences in QALYs were compared using the mean and SD for three data sets: observed data, mean imputation of baseline data and multiply imputed data. Differences in proportion with criminal convictions were compared using the mean and SD for two data sets: observed data and multiply imputed data. In all cases, multiple imputation followed the approach described in Missing data.
Cost-effectiveness of MST compared with MAU at 48 months’ follow-up was assessed by calculating incremental cost-effectiveness ratios (ICERs): the additional cost of one intervention compared with another divided by the additional effect. 17,57 ICERs are calculated from four sample means and are therefore subject to statistical uncertainty. Cost-effectiveness planes were generated using 1000 bootstrapped resamples from regression models of total cost and outcome by trial group. These were then used to calculate the probability that MST is the optimal choice for different values a decision-maker is willing to pay for a unit improvement in outcome (the ceiling ratio, λ). Cost-effectiveness acceptability curves are presented by plotting these probabilities for a range of possible values of λ to explore the uncertainty that exists around estimates of mean costs and effects, and to show the probability that MST is cost-effective compared with MAU. 17,58
In line with the clinical analyses, all economic analyses were controlled for treatment centre, number of previous convictions, gender and age at onset of criminal behaviour, plus the baseline measurement of the variables of interest.
As a result of an administrative error, the EQ-5D-5L was excluded from the outcome packs in the early stages of the original study, which resulted in extensive missing EQ-5D-3L data [68% (n = 462) at baseline, 49% (n = 336) at 6 months, 37% (n = 251) at 12 months, and 33% (n = 223) at 18 months], and economic analyses using QALYs were abandoned in the original economic evaluation. 17 Given that the data were missing completely at random, we have attempted to impute these missing values to generate a complete sample for economic analyses in the present study. The impact of missing data is explored in sensitivity analyses by employing different means of imputing these data, including multiple imputation, mean imputation and identification of an appropriate imputation value from the current literature.
Chapter 7 Qualitative study 1
Key aspects of the qualitative study design, methodology and outcomes are summarised in the main body of this report. Supplementary documents (interview schedules and coding frameworks) are available in Appendix 7, Tables 46–51.
Recruitment
Families taking part in the START trial were invited to take part in an optional qualitative interview about their experiences of MST following the completion of the 18-month follow-up period (i.e. approximately 1 year after finishing MST). Families who had completed their 18-month follow-up measures were approached to take part in the study. In total, 14 young people and 13 of their parents or carers agreed to be interviewed. Of the five families who did not take part, two initially agreed but an appointment could not be scheduled successfully, and three more did not respond to the letter and could not be reached by telephone.
Following the initial letter and information sheet inviting families to take part, families were contacted by telephone to arrange for the interview to take place. All interviews took place in the family home. Informed written consent procedures were completed immediately prior to the interview.
Participants
Of the young people who took part in the study, eight (57%) were male. The mean participant age at the time of interview was 16 years. Six were white British (43%), five were of mixed ethnicity (36%), two were black British (14%) and one participant was Asian (7%).
Procedure
Parents or carers and young people were interviewed separately using semistructured interview schedules. Questions were open-ended, with suggested prompts and follow-up questions. The interview schedules covered topics including participants’ experience of MST, changes (or lack thereof) during and after MST, and the ways in which participants believed MST helped (or did not help) them. The purpose of the interview and the interview schedule was to encourage participants to describe their experiences with MST from their own perspective and in their own words. Interviews were audio-recorded and lasted for an average of around 45 minutes for young people and 70 minutes for parents or carers.
Analysis
Audio-recordings of the qualitative interviews were transcribed verbatim. Transcripts were analysed using a framework analysis. 59 The method is a systematic analysis designed to facilitate analysis of large numbers of qualitative data. A thematic coding framework is developed first, which is then used to code occurrences of each thematic category within the entire data set. The process is dynamic, with both the coding framework and the coding patterns continuously revised throughout.
Chapter 8 Qualitative study 2
Similar to the first qualitative study, the main aspects of the methodology and results are summarised below, but supplementary material is available in Appendix 8.
Recruitment
The purpose of the second qualitative study was to evaluate the long-term impact of MST as young people began their transition into adulthood and how this affected their maturity levels, their relationships and their outlook on the future. Families who took part in the START trial were invited to take part in this study 4 years after baseline evaluation. In total, 32 young people agreed to take part in the study; 16 had been allocated to the MST group, and 16 had been allocated to the MAU group.
Participants
Participants were matched on the basis of age, gender and region where possible. Sixteen participants were male, with a mean age of 18.3 years (SD 1.25 years, range 17–21 years); the other 16 participants were female, with a mean age of 17.7 years (SD 1.01 years, range 16–19 years). Participants in the MST group were found to be significantly younger (mean age 17.4 years, SD 0.81 years) than those who received MAU [mean age 18.6 years, SD 1.21 years, t(30) 3.09; p < 0.01].
Procedure
Participants were approached following the completion of their 48-month follow-up measures. All interviews were conducted in the participants’ homes. The semistructured interviews lasted an average of 57 minutes (range 19−117 minutes). The interview schedule focused on recent events in the young person’s life (e.g. ‘how have things been going over the last month or so?’), on important life relationships (e.g. ‘how would you describe your relationship with your parents?’) and on the future (‘how do you feel about your future?’). MST-related questions began with a prompt (e.g. ‘do you remember working with [insert name] during [insert rough date]?’) and continued with a general question (‘what can you tell me about that?’).
Analysis
Interviews were audio-recorded, transcribed verbatim and anonymised. Each transcript was analysed individually using interpretative phenomenological analysis. 60 A key organising construct emerged from this process: considering participant material in terms of how far it demonstrated a participant being forward-looking and hopeful in outlook (‘mature’) or static and frustrated (‘stuck’). Material illustrating this construct within each of four life domains (family relationships, peer relationships, child–adult transition and work-related experiences) was recorded in a table for each of the first 16 participants. Each entry in the tables was codified in terms of presence or lack of maturity and this coding system was then applied to the other 16 cases. The aim was to see whether or not there was a difference in the degree of maturity displayed between MST and MAU groups. The researcher ratings were then checked against an independent rater, blinded to condition.
Chapter 9 Results
This section will outline the baseline characteristics of the sample, including participant flow and attrition, demographic variables at baseline and diagnostic summary. We begin by focusing on the primary outcomes (offending), followed by the secondary; these are the results from self-report data pertaining to psychological and emotional well-being, social adjustment, family functioning, and behaviour, as reported by both the young person and their parent or carer. This is followed by the results of the economic analysis and the relative costs and cost-effectiveness of the interventions. The results of the qualitative studies presented here are not exhaustive; we aimed to emphasise the key findings and give some sense of the subjective lived experiences of the young people and their families who took part in the trial. However, we were conscious of not rendering the section inaccessible because of excessive length.
Participant flow
Although 684 participants were initially randomised, one participant asked to be entirely removed from the trial during the second phase (i.e. from the 24-month follow-up point onwards). As a result, the total number of participants in the second phase was 683.
Figure 2 illustrates participant flow at each follow-up point. Table 3 outlines the different reasons why data were not collected. Every effort was made to ensure that data were collected. The research team offered flexible appointments to the families in order to accommodate other commitments, in terms of both time and location. Communication was carried out by telephone calls, text messages, e-mails and letters, according to family preference or to minimise the loss of contact. Other professionals involved with the families also helped with engagement and sometimes facilitated data collection meetings. In Table 3, ‘dropped out’ refers to a participant who explicitly requested to no longer participate in the trial and to not be contacted. Data for each time point had a set time window within which they could be collected; if it was not possible to collect the data within that window, they were classed as ‘overdue’.
FIGURE 2.
Participant flow.

| Reason | Follow-up time point (n) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 24 months | 36 months | 48 months | |||||||
| MST | MAU | Both | MST | MAU | Both | MST | MAU | Both | |
| Data collected | 239 | 239 | 478 | 225 | 208 | 433 | 183 | 166 | 349 |
| Refused | 4 | 10 | 14 | 6 | 8 | 14 | 9 | 9 | 18 |
| Lost contact | 8 | 14 | 22 | 23 | 24 | 47 | 37 | 49 | 86 |
| Moved abroad | 3 | 1 | 4 | 1 | 1 | 2 | 5 | 3 | 8 |
| Failed attempts | 13 | 12 | 25 | 7 | 13 | 20 | 19 | 13 | 32 |
| Overdue | 11 | 17 | 28 | 10 | 25 | 35 | 11 | 24 | 35 |
| Unknown | 0 | 4 | 4 | 2 | 0 | 2 | 1 | 0 | 1 |
| Other | 6 | 4 | 10 | 0 | 2 | 2 | 1 | 1 | 2 |
| Dropped out | 58 | 40 | 98 | 68 | 60 | 128 | 76 | 76 | 152 |
| Total | 342 | 341 | 683 | 342 | 341 | 683 | 342 | 341 | 683 |
Follow-up measures took place between August 2011 (earliest 18-month follow-up point) and September 2016 (latest 48-month follow-up point). Offending data were additionally collected up to September 2017.
Baseline data
Tables 4 and 5 outline the demographic and diagnostic characteristics of the young people in the sample at baseline. Appendix 2, Table 21, contains data on the routine care received by young people in each group at baseline.
| Characteristic | Group | |
|---|---|---|
| MST (N = 342) | MAU (N = 342) | |
| Age (years), mean (SD) | 13.7 (1.4) | 13.9 (1.4) |
| Sex, n (%) | ||
| Female | 126 (37) | 124 (36) |
| Male | 216 (63) | 218 (64) |
| Socioeconomic status (range 1–6), mean (SD) | 3.0 (1.4) | 2.9 (1.3) |
| Proportion on state benefits or earning < £20,000 each year, n (%) | 258 (75) | 267 (78) |
| Ethnicity, n (%) | ||
| White British/European | 261 (76) | 274 (80) |
| Black African/Afro-Caribbean | 38 (11) | 33 (10) |
| Asian | 6 (2) | 10 (3) |
| Mixed/other | 34 (10) | 17 (5) |
| Marital status of parent(s) or carer(s), n (%) | ||
| Single or widowed | 142 (42) | 131 (38) |
| Separated or divorced | 77 (23) | 59 (17) |
| Married or cohabiting | 123 (36) | 147 (43) |
| Average number of siblings,a mean (SD) | 2.5 (1.3) | 2.5 (1.4) |
| Number with siblings offending, n (%) | 118 (35) | 126 (37) |
| Offences in the year before referral | ||
| Non-offender on referral, n (%) | 124 (36) | 111 (32) |
| Total number of offences, mean (SD) | 1.1 (2.2) | 1.2 (2.5) |
| Violent offences, mean (SD) | 0.4 (1.0) | 0.4 (0.9) |
| Non-violent offences, mean (SD) | 0.5 (1.2) | 0.6 (1.3) |
| Number with custodial sentences, n (%) | 4 (1) | 6 (2) |
| Diagnosis | Group, n (%) | |
|---|---|---|
| MST (N = 342) | MAU (N = 342) | |
| CD | 262 (77) | 270 (79) |
| Oppositional defiant disorder | 14 (4) | 14 (4) |
| Any CD | 274 (80) | 280 (82) |
| Social phobia | 12 (4) | 9 (3) |
| Obsessive–compulsive disorder | 1 (< 1) | 2 (1) |
| Post-traumatic stress disorder | 25 (7) | 26 (8) |
| Separation anxiety disorder | 7 (2) | 15 (4) |
| Specific phobia | 6 (2) | 13 (4) |
| Generalised anxiety disorder | 6 (2) | 9 (3) |
| Panic disorder | 5 (1) | 3 (1) |
| ADHD combined | 113 (33) | 91 (27) |
| ADHD hyperactive-impulsive | 8 (2) | 3 (1) |
| ADHD inattentive | 13 (4) | 12 (4) |
| Pervasive developmental disorder or autism | 3 (1) | 4 (1) |
| Eating disorders | 2 (1) | 2 (1) |
| Tic disorder | 7 (2) | 4 (1) |
| Major depression | 30 (9) | 42 (12) |
| Any emotional disorder | 73 (22) | 90 (26) |
| Mixed anxiety and CD | 46 (13) | 56 (16) |
| Number without diagnosis | 50 (15) | 50 (15) |
| Number of Axis I diagnoses, mean (SD) | 1.5 (1.0) | 1.5 (1.1) |
| Onset of CD | 148 (43) | 149 (44) |
| ICUT score, mean (SD) | 33.5 (9.7) | 32.7 (9.6) |
| Peer delinquency score (SRDM), mean (SD) | 5.0 (4.7) | 4.9 (4.7) |
Outcomes and estimation
Primary outcome
There were no significant differences between the MST and MAU groups in the proportion of young people with a recorded criminal conviction at the 60-month follow-up. In the MST group, 55% (188 out of 342) had a criminal conviction at this end point, compared with 53% (180 out of 341) of those in the MAU group (OR 1.13, 95% CI 0.82 to 1.56; p = 0.44).
Interaction tests were carried out for prespecified subgroups. Of these, only baseline peer delinquency score was found to be significant (p = 0.015). The effects of gender, age, onset of CD, baseline ICUT score, baseline Antisocial Beliefs and Attitudes Scale score, offender status at baseline, diagnosis of CD or attention deficit hyperactivity disorder at baseline, and diagnosis of CD, depression or anxiety at baseline were not significant; all p-values can be found in Table 6.
| Variable | Interaction p-value |
|---|---|
| Sex | 0.077 |
| Age | 0.46 |
| Onset of CD | 0.81 |
| Baseline ICUT score | 0.46 |
| Baseline peer delinquency score | 0.015 |
| Baseline ABAS score | 0.21 |
| Offender status at baseline | 0.67 |
| Diagnosis of CD or ADHD at baseline | 0.82 |
| Diagnosis of CD, depression or anxiety at baseline | 0.87 |
| Referrer path | N/Aa |
Secondary offending outcomes
No group differences were found in median time to first offence; median value was 36 months post baseline for the MST group, and 48 months for the MAU group (HR 1.03, 95% CI 0.84 to 1.26; p = 0.78). There was a significant interaction of baseline peer delinquency scores (p = 0.015), but not of any of the other prespecified subgroups (p > 0.05). Figure 3 illustrates the proportion of non-offenders over the follow-up period.
FIGURE 3.
Kaplan–Meier plot of time to first offence. Reprinted from The Lancet Psychiatry, volume 7, Fonagy et al. , Multisystemic therapy versus management as usual in the treatment of adolescent antisocial behaviour (START): 5-year follow-up of a pragmatic, randomised controlled, superiority trial, pp. 420–30,19 copyright (2020), with permission from Elsevier.
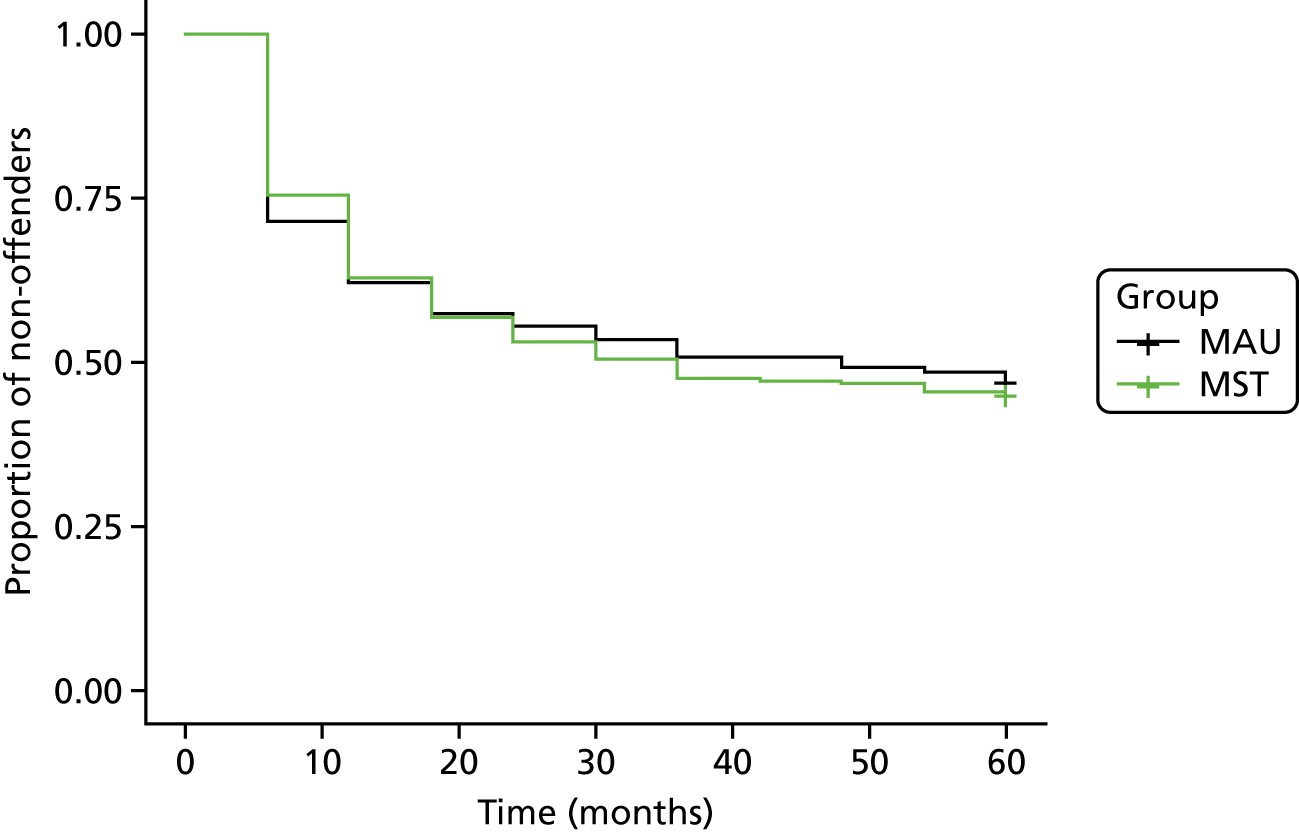
There were significantly more overall offences in the MST group than in the MAU group at 24, 36 and 48 months’ follow-up. The mean number of offences in the MST group at 24 months was 0.75 compared with 0.41 in the MAU group (adjusted mean difference 0.37 offences, 95% CI 0.05 to 0.69 offences; p = 0.024). At 36 months, young people in the MST group had an average of 0.45 offences, compared with 0.37 in the MAU group (adjusted mean difference 0.38, 95% CI 0 to 0.69; p = 0.048). At 48 months, those in the MST group had an average of 0.39 offences compared with 0.38 in the MAU group (adjusted mean difference 0.38 offences, 95% CI 0.03 to 0.72 offences, p = 0.033). However, these differences were no longer present at the 60-month follow-up. There were also no significant group differences when the numbers of violent and non-violent offences were analysed separately. Tables 7–9 contain a summary of secondary offending outcomes.
| Follow-up time point | Group, mean number | Difference (95% CI) | p-value | |
|---|---|---|---|---|
| MST | MAU | |||
| 24 months | 0.75 | 0.41 | 0.35 (0.03 to 0.67) | 0.031 |
| 36 months | 0.45 | 0.37 | 0.33 (–0.02 to 0.67) | 0.063 |
| 48 months | 0.39 | 0.38 | 0.35 (0 to 0.69) | 0.049 |
| 60 months | 0.30 | 0.28 | –0.08 (–0.46 to 0.31) | 0.700 |
| Follow-up time point | Group, mean number | Difference (95% CI) | p-value | |
|---|---|---|---|---|
| MST | MAU | |||
| 24 months | 0.22 | 0.12 | 0.15 (–0.26 to 0.57) | 0.78 |
| 36 months | 0.12 | 0.11 | –0.01 (–0.49 to 0.47) | 0.96 |
| 48 months | 0.11 | 0.14 | 0.11 (–0.37 to 0.58) | 0.66 |
| 60 months | 0.08 | 0.08 | –0.29 (–0.85 to 0.28) | 0.32 |
| Follow-up time point | Group, mean number | Difference (95% CI) | p-value | |
|---|---|---|---|---|
| MST | MAU | |||
| 24 months | 0.32 | 0.18 | 0.34 (–0.03 to 0.71) | 0.075 |
| 36 months | 0.20 | 0.17 | 0.34 (–0.08 to 0.75) | 0.110 |
| 48 months | 0.17 | 0.15 | 0.38 (–0.04 to 0.8) | 0.078 |
| 60 months | 0.10 | 0.11 | –0.15 (–0.67 to 0.37) | 0.560 |
Young person-rated secondary end points
After correcting for multiple testing, there were no significant group differences on any of the self-report measures completed by young people between the 24- and 48-month follow-ups.
The full results of the secondary outcomes completed by young people can be found in Appendix 3, Tables 22–35.
Analyses of employment and education did not yield significant group differences. At the 48-month follow-up, 70% of young people in the MST group were in education or employment, compared with 82% of those in the MAU group (OR 0.53, 95% CI 0.27 to 1.03; p = 0.062).
There were also no differences in pregnancy (becoming pregnant or fathering a pregnancy), with 17% of young people reporting a pregnancy over the course of the follow-up period in the MST group, compared with 22% in the MAU group (OR 0.72, 95% CI 0.46 to 1.13; p = 0.16).
Parent-rated secondary end points
Parents in the MAU group (mean 8.22) reported higher scores on the Inconsistent Discipline subscale of the Alabama Parenting Questionnaire than those in the MST group (mean 7.74) at the 24-month follow-up (95% CI –1.05 to –0.24; p = 0.0023). The differences were no longer significant at the 36- and 48-month follow-ups.
No other group differences were statistically significant after correcting for multiple testing. The full results of the parent-rated secondary outcomes can be found in Appendix 4, Tables 36–45.
Economic evaluation
Data completeness
Service-use data were available for 313 (92%) participants in the MST group and 298 (87%) participants in the MAU group. Three participants in the MST group and two in the MAU group were identified as influential outliers,61 that is, with total costs in the 99th percentile, and were removed from the analysis. As noted in Chapter 2, because of an administrative error, the EQ-5D-3L measure was excluded from the outcome pack at the beginning of the trial, so complete health-related quality of life data were available for only 95 (27%) participants in the MST group and 72 (21%) participants in the MAU group. The availability of EQ-5D-3L data at each time point is summarised in Table 10.
| Follow-up time point | Group, n (%) | |
|---|---|---|
| MST | MAU | |
| Baseline | 111 (32) | 110 (32) |
| 6 months | 190 (55) | 158 (46) |
| 12 months | 223 (65) | 210 (62) |
| 18 months | 244 (71) | 218 (64) |
| 24 months | 240 (70) | 217 (64) |
| 36 months | 213 (62) | 184 (54) |
| 48 months | 167 (49) | 141 (41) |
| Complete | 95 (27) | 72 (21) |
Resource use over follow-up
The use of services over the period from study entry to 48 months’ follow-up was broadly similar across the two groups and is detailed in Table 11. Accident and emergency was the most commonly used secondary health-care service in both groups (accessed by 53% of MST and 56% of MAU participants), whereas general practitioner (GP) contacts in a GP surgery were the most commonly used primary-care service (used by 70% in MST and 73% in MAU), and around 50% in both groups had contact with a social worker. Criminal justice system services were also commonly used across both groups, with a high proportion of participants reporting contacts with police (61% in MST and 64% in MAU) and stays in police custody (28% in MST and 30% in MAU). Time spent in foster and residential care was longer in the MST group (total 29 days on average in MST, 18 days in MAU), but use of staffed accommodation was higher in the MAU group (14 days MST, 18 days MAU). The majority of young people were registered in mainstream education at some point over the follow-up period (58% MST, 57% MAU), but a relatively large proportion were registered in specialist schools (26% in both groups) or pupil referral units (29% MST, 26% MAU).
| Service | Group | |||||
|---|---|---|---|---|---|---|
| MST (n = 310) | MAU (n = 296) | |||||
| Mean (SD) | Range | % using | Mean (SD) | Range | % using | |
| MST (hours of direct contact) | 35.65 (24.49) | 0–114 | 75 | 0 | 0 | 0 |
| Accommodation | ||||||
| Foster care (days) | 11.77 (64.03) | 0–746 | 7 | 7.64 (40.79) | 0–418 | 7 |
| Residential care (days) | 17.06 (79.28) | 0–556 | 6 | 10.36 (68.03) | 0–953 | 5 |
| Staffed accommodation (days) | 14.45 (56.34) | 0–365 | 11 | 18.26 (72.38) | 0–641 | 11 |
| Other (days) | 3.77 (21.90) | 0–207 | 5 | 5.26 (35.59) | 0–378 | 5 |
| Education | ||||||
| Mainstream school (hours) | 1124.56 (1453.50) | 0–6020 | 58 | 958.43 (1323.47) | 0–9360 | 57 |
| Specialist school (hours) | 293.78 (729.36) | 0–5629 | 26 | 301.94 (874.59) | 0–10,355 | 26 |
| Residential school (hours) | 21.46 (163.25) | 0–2063 | 3 | 26.38 (214.87) | 0–3120 | < 1 |
| Hospital school (hours) | 0 | 0 | 0 | 3.70 (37.47) | 0–488 | < 1 |
| Pupil referral unit (hours) | 198.00 (423.63) | 0–2290 | 29 | 168.00 (370.49) | 0–2275 | 26 |
| Home tuition (hours) | 22.95 (135.40) | 0–1430 | 7 | 10.84 (64.31) | 0–780 | 6 |
| Further education (hours) | 421.61 (635.50) | 0–3120 | 50 | 422.47 (664.70) | 0–3868 | 50 |
| Secondary health care | ||||||
| Inpatient stay (nights) | 0.71 (3.23) | 0–44 | 15 | 3.48 (26.99) | 0–365 | 21 |
| Outpatient appointments (contacts) | 1.99 (5.20) | 0–40 | 35 | 2.37 (9.15) | 0–143 | 39 |
| Accident and emergency (contacts) | 1.40 (2.93) | 0–20 | 53 | 2.03 (4.83) | 0–62 | 56 |
| Community based | ||||||
| GP: home (contacts) | 0.21 (0.84) | 0–7 | 9 | 0.29 (1.87) | 0–28 | 8 |
| GP: surgery (contacts) | 5.64 (10.75) | 0–137 | 70 | 6.07 (9.38) | 0–76 | 73 |
| GP: telephone (contacts) | 0.45 (1.74) | 0–20 | 12 | 0.29 (1.83) | 0–28 | 8 |
| Practice nurse (contacts) | 0.82 (2.62) | 0–25 | 26 | 1.06 (4.97) | 0–76 | 26 |
| District nurse, health visitor, midwife or school/college nurse (contacts) | 2.16 (8.70) | 0–86 | 18 | 2.31 (8.92) | 0–100 | 22 |
| Community paediatrician (contacts) | 0.05 (0.28) | 0–3 | 4 | 0.07 (0.49) | 0–6 | 3 |
| Care co-ordinator, case manager, key worker (contacts) | 5.25 (28.37) | 0–312 | 12 | 4.88 (21.77) | 0–198 | 15 |
| Psychiatrist (contacts) | 0.66 (2.81) | 0–35 | 13 | 1.34 (5.76) | 0–55 | 15 |
| Clinical psychologist (contacts) | 0.56 (2.69) | 0–30 | 12 | 1.75 (9.02) | 0–83 | 14 |
| CAMHS worker (contacts) | 2.32 (8.39) | 0–89 | 25 | 3.61 (9.77) | 0–75 | 32 |
| Community psychiatric nurse (contacts) | 0.25 (1.97) | 0–27 | 4 | 0.48 (4.37) | 0–53 | 4 |
| Counsellor (contacts) | 1.71 (7.18) | 0–73 | 12 | 2.74 (10.25) | 0–104 | 17 |
| Family therapist (contacts) | 0.54 (4.19) | 0–50 | 4 | 0.93 (3.96) | 0–39 | 10 |
| Art/drama/music/occupational therapy (contacts) | 0.16 (1.57) | 0–26 | 3 | 0.31 (2.28) | 0–26 | 4 |
| Social worker (contacts) | 11.55 (24.12) | 0–214 | 47 | 11.73 (20.29) | 0–117 | 54 |
| Family support worker (contacts) | 4.97 (17.56) | 0–160 | 22 | 7.19 (22.12) | 0–176 | 26 |
| Social services youth worker (contacts) | 1.91 (11.12) | 0–156 | 8 | 1.98 (10.16) | 0–113 | 11 |
| Accommodation key worker (contacts) | 4.70 (24.26) | 0–232 | 12 | 1.52 (9.76) | 0–135 | 7 |
| Educational psychologist (contacts) | 0.53 (3.80) | 0–52 | 7 | 0.33 (2.26) | 0–28 | 6 |
| Education welfare officer (contacts) | 2.67 (11.71) | 0–113 | 17 | 0.61 (2.78) | 0–26 | 13 |
| Connexions worker (contacts) | 3.21 (9.84) | 0–100 | 37 | 4.44 (11.80) | 0–80 | 36 |
| Mentor (contacts) | 6.92 (27.53) | 0–228 | 18 | 5.86 (22.37) | 0–214 | 19 |
| Drug/alcohol support worker (contacts) | 2.42 (8.70) | 0–65 | 15 | 2.10 (8.27) | 0–77 | 15 |
| Advice service, e.g. Citizens Advice, housing association, careers advice (contacts) | 1.02 (4.70) | 0–52 | 13 | 0.84 (4.33) | 0–52 | 12 |
| Helpline (contacts) | 0.52 (8.52) | 0–150 | 3 | 0.03 (0.22) | 0–2 | 2 |
| Complementary therapist (contacts) | 0.07 (0.79) | 0–12 | 1 | 0.32 (5.23) | 0–90 | 1 |
| Criminal justice system | ||||||
| Police custody (days) | 3.93 (28.35) | 0–364 | 28 | 1.20 (4.08) | 0–44 | 30 |
| Youth custody (days) | 3.32 (20.53) | 0–180 | 5 | 5.08 (28.31) | 0–231 | 6 |
| Probation officer (contacts) | 2.27 (14.57) | 0–180 | 6 | 2.09 (10.60) | 0–120 | 9 |
| Youth offending team worker (contacts) | 16.64 (43.73) | 0–396 | 37 | 17.25 (38.48) | 0–264 | 39 |
| Police (contacts) | 11.49 (29.50) | 0–305 | 61 | 14.61 (58.70) | 0–675 | 64 |
| Solicitor (contacts) | 2.15 (6.04) | 0–63 | 36 | 1.96 (4.66) | 0–46 | 34 |
| Court appearance as victim (number) | 0.07 (0.48) | 0–5 | 4 | 0.04 (0.24) | 0–3 | 3 |
| Court appearance as defendant (number) | 1.31 (4.48) | 0–63 | 29 | 1.28 (4.23) | 0–46 | 29 |
The use of services over the long-term follow-up period only, between the 24-month and 48-month follow-up, is detailed in Table 12. Again, service use was broadly similar across the two groups during this period and the patterns of use differed little. Accident and emergency remained the most commonly used secondary health-care service in both groups (accessed by 36% in MST and 40% in MAU), and GP contacts in a GP surgery remained the most commonly used primary health-care service (accessed by 60% in MST and 62% in MAU). Police contacts were higher in the MST group (45% in MST vs. 36% in MAU), but there was little difference between the groups in terms of other criminal justice sector resources. In terms of education, as would be expected given the age of the population, a smaller proportion of young people were registered to attend mainstream school over the 24- to 48-month follow-up period, and a larger proportion were in further education.
| Service | Group | |||||
|---|---|---|---|---|---|---|
| MST (n = 300) | MAU (n = 286) | |||||
| Mean (SD) | Range | % using | Mean (SD) | Range | % using | |
| Accommodation | ||||||
| Foster care (days) | 9.27 (50.94) | 0–646 | 6 | 6.51 (38.69) | 0–358 | 4 |
| Residential care (days) | 16.75 (76.79) | 0–540 | 6 | 8.20 (54.64) | 0–720 | 4 |
| Staffed accommodation (days) | 14.83 (57.09) | 0–365 | 11 | 18.35 (73.14) | 0–641 | 10 |
| Other (days) | 3.06 (21.09) | 0–207 | 3 | 3.60 (31.29) | 0–360 | 3 |
| Education | ||||||
| Mainstream school (hours) | 339.70 (735.60) | 0–5577 | 28 | 257.06 (757.88) | 0–9360 | 25 |
| Specialist school (hours) | 126.81 (413.96) | 0–3120 | 15 | 149.42 (706.76) | 0–10,205 | 22 |
| Residential school (hours) | 17.71 (159.46) | 0–2062 | 2 | 23.45 (206.58) | 0–3120 | 4 |
| Hospital school (hours) | – | – | – | 1.71 (28.86) | 0–488 | < 1 |
| Pupil referral unit (hours) | 56.68 (221.74) | 0–1980 | 11 | 73.63 (246.04) | 0–2275 | 13 |
| Home tuition (hours) | 10.59 (100.80) | 0–1320 | 3 | 1.06 (8.86) | 0–102 | 2 |
| Further education (hours) | 316.51 (513.90) | 0–3120 | 45 | 309.91 (547.07) | 0–3560 | 44 |
| Secondary health care | ||||||
| Inpatient stay (nights) | 0.41 (1.89) | 0–16 | 9 | 2.87 (24.13) | 0–365 | 14 |
| Outpatient appointments (contacts) | 1.19 (3.94) | 0–40 | 24 | 1.70 (8.75) | 0–140 | 28 |
| Accident and emergency (contacts) | 0.70 (1.30) | 0–9 | 36 | 0.89 (1.67) | 0–11 | 40 |
| Community based | ||||||
| GP: home (contacts) | 0.13 (0.64) | 0–7 | 6 | 0.26 (1.88) | 0–28 | 6 |
| GP: surgery (contacts) | 3.75 (9.05) | 0–130 | 60 | 4.06 (7.49) | 0–53 | 62 |
| GP: telephone (contacts) | 0.31 (1.17) | 0–10 | 1 | 0.24 (1.76) | 0–28 | 8 |
| Practice nurse (contacts) | 0.70 (2.64) | 0–25 | 18 | 0.75 (3.39) | 0–46 | 18 |
| District nurse, health visitor, midwife or school/college nurse (contacts) | 1.73 (8.39) | 0–86 | 13 | 1.41 (5.54) | 0–53 | 15 |
| Community paediatrician (contacts) | 0.03 (0.24) | 0–3 | 2 | 0.02 (0.22) | 0–3 | 1 |
| Care co-ordinator, case manager, key worker (contacts) | 3.83 (20.49) | 0–217 | 11 | 2.67 (17.09) | 0–198 | 10 |
| Psychiatrist (contacts) | 0.44 (2.52) | 0–33 | 8 | 0.87 (4.69) | 0–52 | 9 |
| Clinical psychologist (contacts) | 0.32 (2.12) | 0–30 | 7 | 0.72 (4.88) | 0–52 | 7 |
| CAMHS worker (contacts) | 1.47 (6.21) | 0–59 | 15 | 1.86 (7.10) | 0–60 | 19 |
| Community psychiatric nurse (contacts) | 0.14 (1.26) | 0–16 | 2 | 0.34 (3.49) | 0–52 | 2 |
| Counsellor (contacts) | 0.86 (3.59) | 0–26 | 9 | 1.72 (8.98) | 0–104 | 9 |
| Family therapist (contacts) | 0.17 (2.34) | 0–40 | 2 | 0.30 (2.43) | 0–29 | 3 |
| Art/drama/music/occupational therapy (contacts) | 0.13 (1.54) | 0–26 | 2 | 0.15 (1.63) | 0–26 | 2 |
| Social worker (contacts) | 6.74 (15.79) | 0–116 | 36 | 6.34 (14.09) | 0–100 | 36 |
| Family support worker (contacts) | 3.14 (14.10) | 0–160 | 16 | 3.73 (16.43) | 0–169 | 15 |
| Social services youth worker (contacts) | 1.69 (11.11) | 0–156 | 6 | 1.26 (8.49) | 0–100 | 6 |
| Accommodation key worker (contacts) | 4.31 (23.06) | 0–232 | 10 | 1.26 (8.38) | 0–105 | 6 |
| Educational psychologist (contacts) | 0.25 (3.07) | 0–52 | 3 | 0.05 (0.28) | 0–2 | 3 |
| Education welfare officer (contacts) | 1.24 (7.54) | 0–100 | 8 | 0.21 (1.69) | 0–26 | 5 |
| Connexions worker (contacts) | 2.05 (7.98) | 0–100 | 27 | 2.54 (8.21) | 0–61 | 27 |
| Mentor (contacts) | 1.77 (7.64) | 0–65 | 8 | 1.97 (12.05) | 0–176 | 9 |
| Drug/alcohol support worker (contacts) | 1.40 (6.75) | 0–65 | 10 | 1.16 (5.58) | 0–49 | 9 |
| Advice service, e.g. Citizens Advice, housing association, careers advice (contacts) | 0.99 (4.75) | 0–52 | 12 | 0.85 (4.40) | 0–52 | 12 |
| Helpline (contacts) | 0.53 (8.66) | 0–150 | 2 | 0.03 (0.22) | 0–2 | 2 |
| Complementary therapist (contacts) | 0.07 (0.77) | 0–12 | 1 | 0.01 (0.18) | 0–3 | < 1 |
| Criminal justice system | ||||||
| Police custody (days) | 3.67 (28.68) | 0–363 | 19 | 0.58 (2.65) | 0–37 | 17 |
| Youth custody (days) | 1.40 (14.24) | 0–180 | 1 | 3.31 (23.40) | 0–210 | 2 |
| Probation officer (contacts) | 2.31 (14.78) | 0–180 | 5 | 1.32 (7.52) | 0–72 | 6 |
| Youth offending team worker (contacts) | 9.53 (38.53) | 0–396 | 22 | 8.14 (23.72) | 0–192 | 23 |
| Police (contacts) | 5.42 (20.07) | 0–200 | 45 | 6.52 (35.55) | 0–481 | 36 |
| Solicitor (contacts) | 1.40 (4.75) | 0–60 | 25 | 0.93 (2.51) | 0–20 | 24 |
| Court appearance as victim (number) | 0.04 (0.39) | 0–5 | 2 | 0.02 (0.21) | 0–3 | 2 |
| Court appearance as defendant (number) | 1.13 (4.41) | 0–62 | 24 | 1.01 (3.94) | 0–45 | 23 |
The use of prescribed psychotropic medication is summarised in Table 13. Antidepressants were most frequently prescribed in both groups (used by 12% of participants), and a slightly greater proportion in the MAU group used medication than in the MST group.
| Medication type | Group, % prescribed | |
|---|---|---|
| MST (n = 310) | MAU (n = 296) | |
| Antidepressants | 12 | 12 |
| ADHD | 11 | 11 |
| Benzodiazepines | 0 | < 1 |
| Sleep disturbance | 4 | 5 |
| Antipsychotics | 1 | 3 |
| Antiepileptics | < 1 | 2 |
Costs over follow-up
The total costs per participant over the 48-month follow-up period for observed and multiply imputed data are summarised in Table 14. For observed data, total mean costs of services used were slightly higher for the MST group (£52,846.46) than for the MAU group (£51,582.36). However, this difference was not statistically significant (adjusted mean difference £481.51, 95% CI –£10,374.50 to £11,337.51; p = 0.931). The total costs were also higher, by a greater magnitude, in the MST group than in the MAU group for multiply imputed data (£62,579.80 for MST and £55,983.17 for MAU). However, this difference was also not statistically significant (adjusted mean difference £5629.48, 95% CI –£11,163.70 to £22,422.67; p = 0.511). The majority of the total costs comprised criminal justice services costs and community services costs, both of which were higher in the MST group, but these differences were very small and not statistically significant (adjusted mean difference of £58.09 for community services and £200.92 for criminal justice services).
| Service | Group, mean (SD) | Difference | 95% CI | p-value | ||
|---|---|---|---|---|---|---|
| MST | MAU | Mean (MST – MAU) | Adjusted mean (MST – MAU) | |||
| Observed | (n = 310) | (n = 296) | ||||
| Intervention | 2132.57 (1810.46) | 2132.57 | 2128.86 | 1888.29 to 2369.42 | < 0.0001 | |
| Accommodation | 3972.15 (12,554.36) | 4133.77 (17,615.73) | –161.62 | –304.00 | –2745.36 to 2137.36 | 0.807 |
| Education | 9465.69 (15,968.87) | 8736.11 (18,457.71) | 729.58 | 1013.44 | –1645.85 to 3672.72 | 0.454 |
| Secondary health care | 805.74 (2064.53) | 2503.71 (15,617.96) | –1697.97 | –1650.53 | –3404.31 to 103.25 | 0.065 |
| Community services | 15,479.16 (34,953.72) | 15,369.85 (27,817.58) | 109.31 | 58.09 | –4980.52 to 5096.70 | 0.982 |
| Medication | 194.92 (1871.70) | 188.58 (1592.41) | 6.33 | 4.29 | –276.05 to 284.64 | 0.976 |
| Criminal justice | 21,353.46 (42,097.75) | 20,920.34 (38,634.21) | 433.12 | 200.92 | –6105.67 to 6507.51 | 0.950 |
| Total | 52,846.46 (69,254.61) | 51,852.36 (67,148.76) | 994.10 | 481.51 | –10,374.50 to 11,337.51 | 0.931 |
| Multiply imputed | (n = 342) | (n = 341) | ||||
| Total | 62,579.80 (6817.81) | 55,983.17 (5189.48) | 6596.63 | 5629.48 | –11,163.70 to 22,422.67 | 0.511 |
Outcomes over follow-up period
Table 15 summarises EQ-5D-3L utility scores over the follow-up period. Utility scores were higher in the MAU group than in the MST group at both baseline and 48 months’ follow-up. The mean utility scores decreased over the trial period in both groups (from 0.885 to 0.767 for MST and from 0.912 to 0.833 for MAU).
| Follow-up time point | Group | |||
|---|---|---|---|---|
| MST | MAU | |||
| n | Mean score (SD) | n | Mean score (SD) | |
| Baseline | 100 | 0.885 (0.194) | 98 | 0.912 (0.139) |
| 6 months | 184 | 0.882 (0.188) | 151 | 0.906 (0.153) |
| 12 months | 216 | 0.889 (0.189) | 199 | 0.874 (0.205) |
| 18 months | 237 | 0.882 (0.196) | 214 | 0.885 (0.174) |
| 24 months | 236 | 0.885 (0.197) | 215 | 0.887 (0.182) |
| 36 months | 209 | 0.869 (0.225) | 183 | 0.862 (0.197) |
| 48 months | 163 | 0.767 (0.308) | 140 | 0.833 (0.243) |
Table 16 summarises QALYs over follow-up for three data sets: observed data, mean imputation of baseline data and multiply imputed data. In all cases, QALYs were slightly lower in the MST group than in the MAU group, but none of these differences was significant. In the observed data, mean QALYs were 3.219 in the MST group compared with 3.360 in the MAU group (adjusted mean difference –0.123 QALYs, 95% CI –0.289 to 0.042 QALYs; p = 0.142). Using mean imputation of missing baseline results, a recommended approach for dealing with missing baseline data,62 QALYs were 3.172 in the MST group compared with 3.300 in the MAU group (adjusted mean difference –0.091 QALYs, 95% CI –0.247 to 0.064 QALYs; p = 0.246). Multiple imputation of missing data resulted in much smaller differences (adjusted mean difference –0.025 QALYs, 95% CI –0.131 to 0.081 QALYs; p = 0.643). No suitable imputation value was identified from current literature, so this analysis was not undertaken.
| Data set | Group | Difference | 95% CI | p-value | ||||
|---|---|---|---|---|---|---|---|---|
| MST | MAU | |||||||
| n | Mean (SD) | n | Mean (SD) | Mean (MST – MAU) | Adjusted mean (MST – MAU) | |||
| Observed data | 95 | 3.219 (0.611) | 72 | 3.360 (0.437) | –0.142 | –0.123 | –0.289 to 0.042 | 0.142 |
| Mean imputation of baseline data | 163 | 3.172 (0.613) | 140 | 3.300 (0.460) | –0.128 | –0.091 | –0.247 to 0.064 | 0.246 |
| Multiply imputed data | 342 | 3.328 (0.793) | 341 | 3.596 (0.939) | –0.031 | –0.025 | –0.131 to 0.081 | 0.643 |
Table 17 summarises the primary outcome, namely the proportion of the sample with criminal convictions. At baseline a greater proportion in the MAU group had criminal convictions (adjusted mean difference –0.02), whereas at 48 months a greater proportion in the MST group had criminal convictions for both observed (adjusted mean difference 0.02) and multiply imputed (adjusted mean difference 0.03) data sets. However, these differences were not statistically significant.
| Follow-up time point | Group | Difference | 95% CI | p-value | ||||
|---|---|---|---|---|---|---|---|---|
| MST | MAU | |||||||
| n | Mean (SD) | n | Mean (SD) | Mean (MST – MAU) | Adjusted mean (MST – MAU) | |||
| Baseline | 310 | 0.41 (0.42) | 296 | 0.45 (0.50) | –0.03 | –0.02 | –0.08 to 0.04 | 0.536 |
| 48 months (observed data) | 308 | 0.54 (0.50) | 294 | 0.52 (0.50) | 0.02 | 0.02 | –0.06 to 0.09 | 0.663 |
| 48 months (multiply imputed data) | 342 | 0.53 (0.50) | 341 | 0.51 (0.50) | 0.02 | 0.03 | –0.04 to 0.10 | 0.400 |
Cost-effectiveness analysis using multiply imputed data
Multiply imputed total costs and outcomes per participant at 48 months are summarised in Table 18. Costs are higher in the MST group (adjusted mean difference £5629.48), and outcomes, both QALYs and proportion with convictions, are poorer in the MST group (adjusted mean difference –0.025 and 0.03, respectively).
| Total cost/outcomes | Group, mean | Adjusted mean difference | |
|---|---|---|---|
| MST (n = 342) | MAU (n = 341) | ||
| Total cost | 62579.80 | 55983.17 | 5629.48 |
| QALYs | 3.328 | 3.596 | –0.025 |
| Proportion with convictions | 0.53 | 0.51 | 0.03 |
Figure 4 shows the scatterplot of bootstrapped mean differences in costs and QALYs at 48 months and indicates that MST is dominated by MAU. The y-axis indicates the difference in costs between trial groups (MST – MAU), whereas the x-axis indicates the difference in QALYs (MST – MAU). Points lying above the x-axis indicate that MST is more costly than MAU, whereas points lying below the x-axis indicate that MST is less costly than MAU. Points lying to the right of the y-axis indicate that MST is more effective than MAU, whereas points lying to the left of the y-axis indicate that MST is less effective than MAU. The majority of scatter points lie in the north-west quadrant (51%), where MST is less effective and more costly than MAU. Very few points (7%) lie in the south-east quadrant, where MST is more effective and less costly than MAU. The remaining scatter points lie in the north-east (24%; MST more effective and more costly) and south-west (18%; MST less effective and less costly) quadrants.
FIGURE 4.
Bootstrapped mean differences in costs and effects of MST compared with MAU at the 48-month follow-up. Reprinted from The Lancet Psychiatry, volume 7, Fonagy et al. , Multisystemic therapy versus management as usual in the treatment of adolescent antisocial behaviour (START): 5-year follow-up of a pragmatic, randomised controlled, superiority trial, pp. 420–30,19 copyright (2020), with permission from Elsevier.
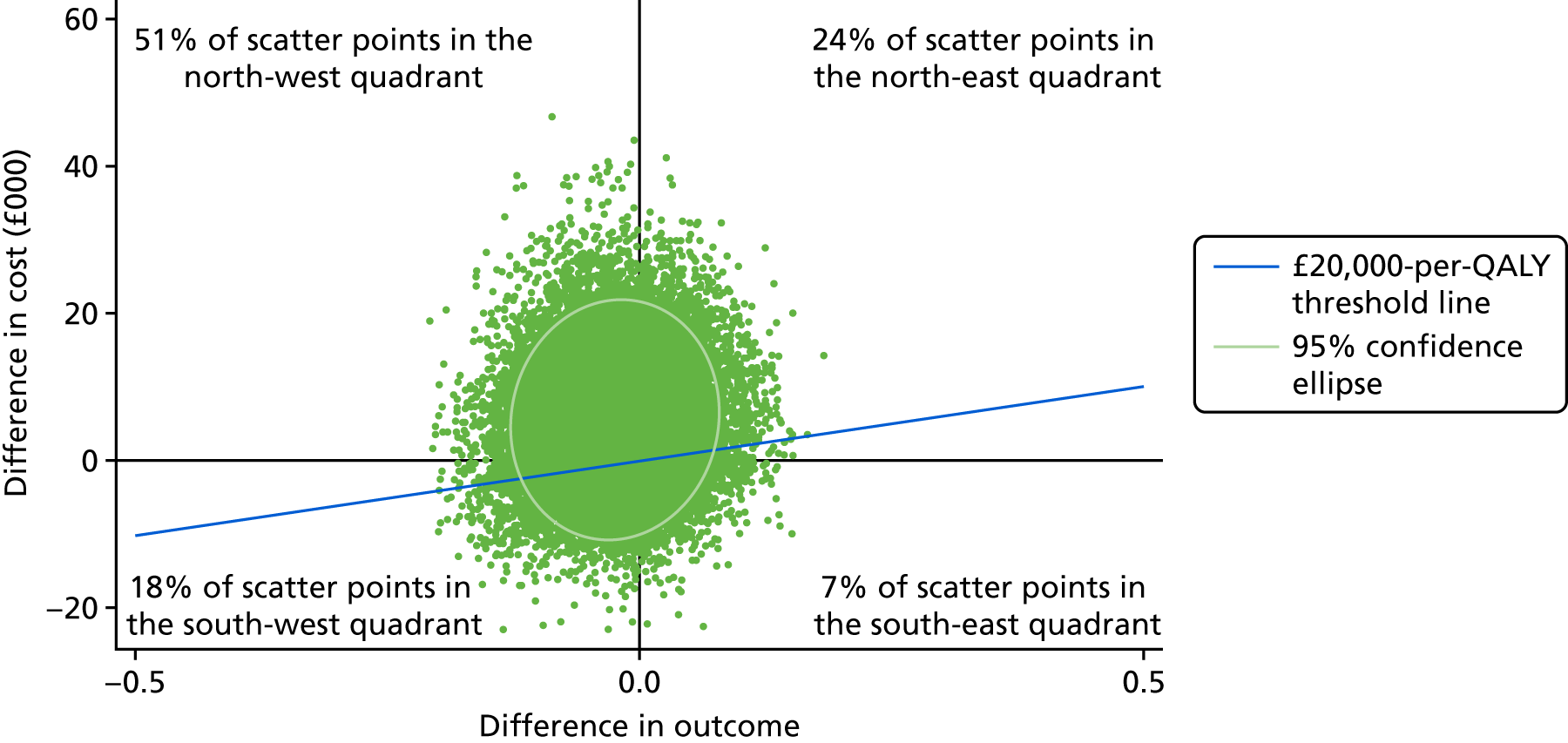
The cost-effectiveness acceptability curve using QALYs as the outcome (Figure 5) shows the probability that MST is cost-effective compared with MAU, and suggests that MST is not cost-effective compared with MAU at 48 months at the NICE willingness-to-pay threshold of £20,000 per QALY, as the probability of this is < 50%. The probability of MST being cost-effective compared with MAU ranges from 19% to 25% for a willingness-to-pay threshold ranging from £0 to £250,000 per QALY. Cost-effectiveness analyses were repeated for mean imputation of QALYs, and the results remained the same, with no evidence of MST being cost-effective compared with MAU for the full range of values of willingness to pay for QALYs.
FIGURE 5.
Cost-effectiveness acceptability curve showing the probability that MST is cost-effective compared with MAU for different willingness-to-pay thresholds for a unit improvement in QALYs at 48 months’ follow-up. Reprinted from The Lancet Psychiatry, volume 7, Fonagy et al. , Multisystemic therapy versus management as usual in the treatment of adolescent antisocial behaviour (START): 5-year follow-up of a pragmatic, randomised controlled, superiority trial, pp. 420–30,19 copyright (2020), with permission from Elsevier.
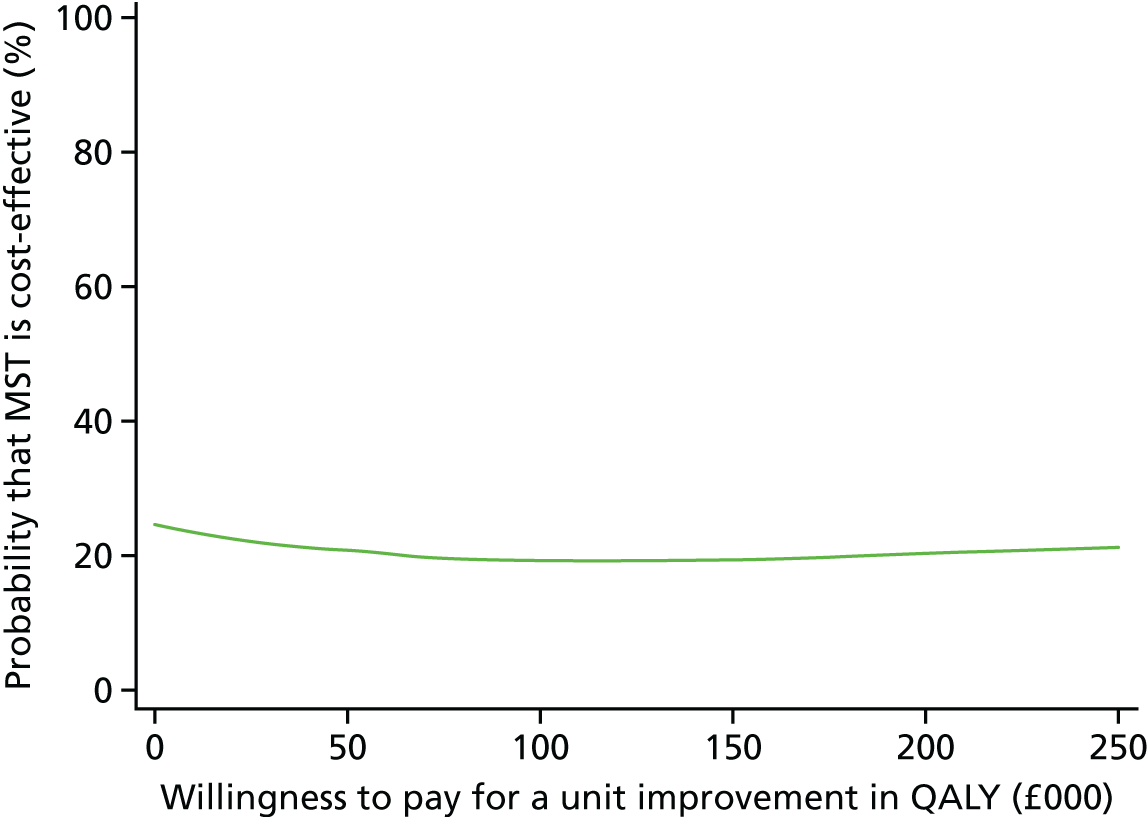
Figure 6 shows the scatterplot of bootstrapped mean differences in costs and proportion of sample with convictions. The majority of scatter points lie in the north-west quadrant (62%), where MST is less effective and more costly than MAU. Very few points (6%) lie in the south-east quadrant, where MST is more effective and less costly than MAU. The remaining scatter points lie in the north-east (13%; MST more effective and more costly) and south-west (18%; MST less effective and less costly) quadrants.
FIGURE 6.
Bootstrapped mean differences in costs and effects (proportion with convictions) of MST compared with MAU at 48 months’ follow-up. Reprinted from The Lancet Psychiatry, volume 7, Fonagy et al. , Multisystemic therapy versus management as usual in the treatment of adolescent antisocial behaviour (START): 5-year follow-up of a pragmatic, randomised controlled, superiority trial, pp. 420–30,19 copyright (2020), with permission from Elsevier.
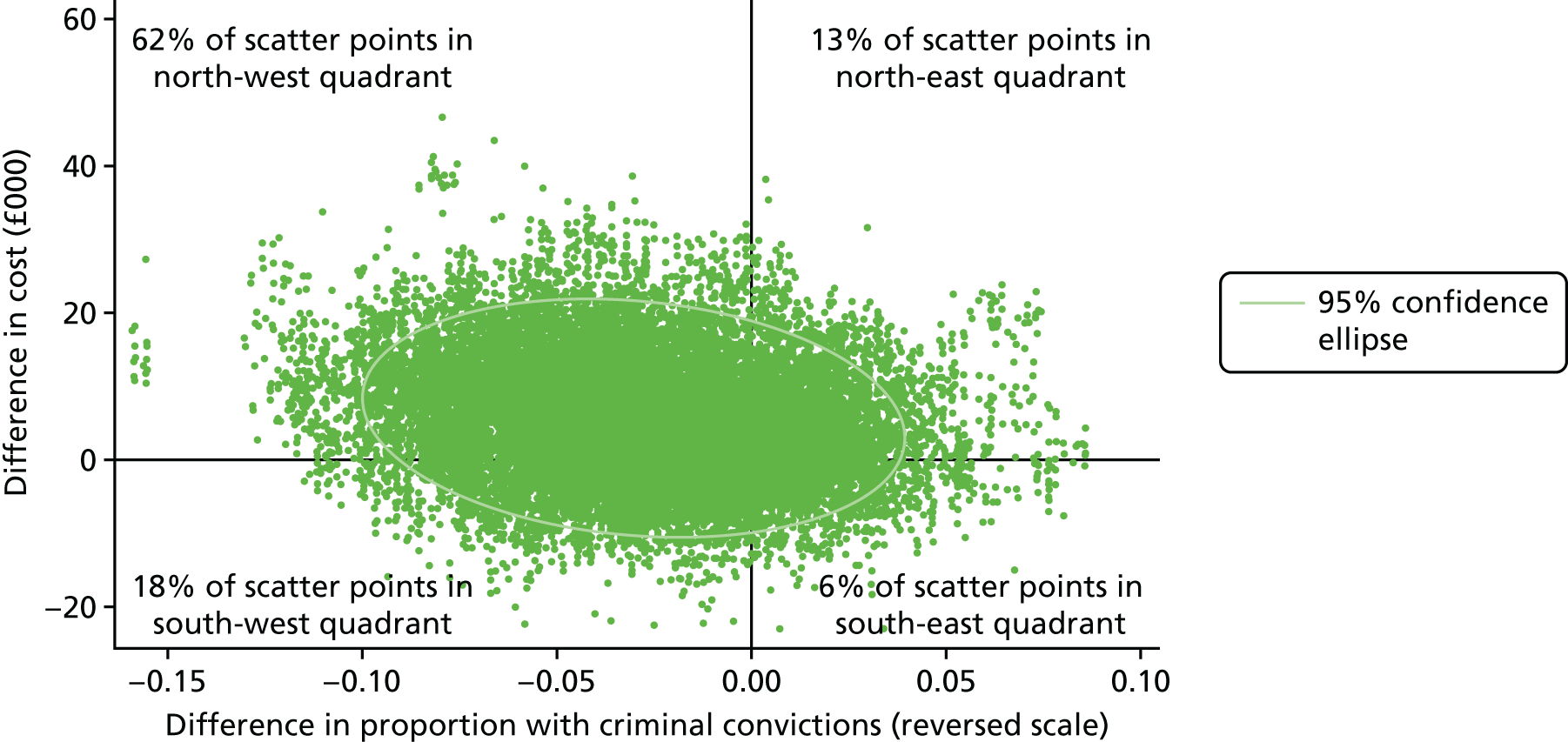
The cost-effectiveness acceptability curve using criminal convictions as the outcome (Figure 7) suggests that the probability of MST being cost-effective compared with MAU remains < 25% for a range of willingness-to-pay thresholds for a percentage point reduction in criminal convictions.
FIGURE 7.
Cost-effectiveness acceptability curve showing the probability that MST is cost-effective compared with MAU for different willingness-to-pay thresholds for a percentage point reduction in criminal convictions at 48 months’ follow-up. Reprinted from The Lancet Psychiatry, volume 7, Fonagy et al. , Multisystemic therapy versus management as usual in the treatment of adolescent antisocial behaviour (START): 5-year follow-up of a pragmatic, randomised controlled, superiority trial, pp. 420–30,19 copyright (2020), with permission from Elsevier.
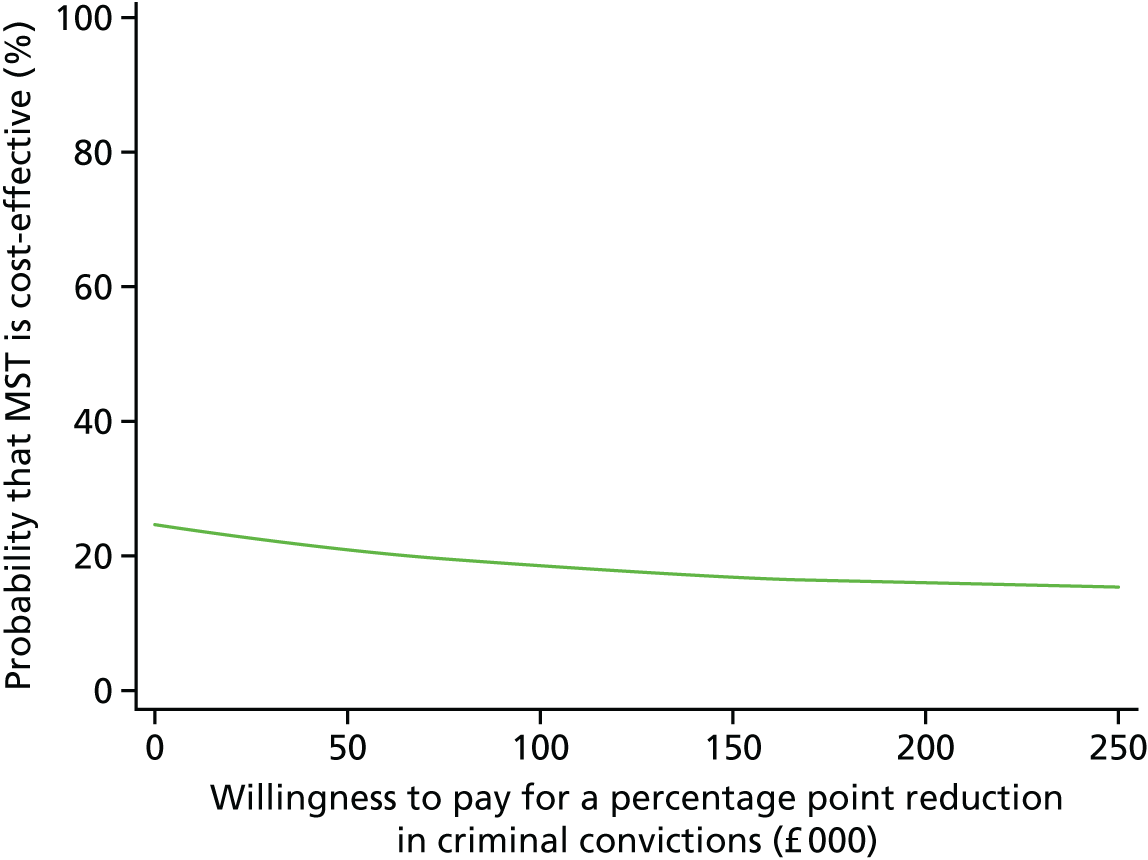
Qualitative study 1
The analysis generated 15 themes that were grouped under four domains; these are summarised in Table 19. The first domain related to how families described their change trajectory (or lack thereof) after taking part in MST. The second and third domains related to how families attributed initial and sustained change to aspects of MST. The fourth and final domain related to families’ descriptions of factors unrelated to MST that affected change.
| Domain | Prevalencea (n) | |
|---|---|---|
| Parents (N = 13) | Young people (N = 14) | |
| 1. Trajectories of change | 5 | 9 |
| 2. Attributions of initial change | 13 | 11 |
| 3. Attributions of sustained change | 12 | 9 |
| 4. Change attributed to extratherapeutic factors | 12 | 12 |
Domain 1: trajectories of change
The trajectories of change described by parents or carers and young people were complex, and different trajectories were described for different problems. Important areas of improvement included family relationships and effective communication. Secondary areas included family atmosphere, relationship between the young person and other members of the family, and effective conflict management. Families explained that often things got worse before they got better, and improvements continued to be ‘up and down’. Four types of trajectories were identified.
Type 1: continuing improvements
Four parents felt that positive changes had begun during MST and continued to improve in the year that followed.
Type 2: maintained improvements
Five parents said that they had seen positive changes during MST, and that these had been sustained in the year that followed. One young person succinctly articulated seeing these changes in their parent:
So like, even after MST like stopped coming, like we’d still follow that agreement [behavioural contract], so we never like end up arguing again and going back to where we was.
Young person, MST
These changes were gradual and, despite occasional difficulties (e.g. the young person dropping out of school), they could still see the positive outcomes of the programme.
Type 3: some changes, struggle to maintain
Three parents described that they saw some positive changes as a result of MST, but found them hard to maintain. Some parents felt that the changes were sporadic or small, or did not generalise outside the family home (e.g. to the school environment).
Type 4: no change/worse
One parent and three young people felt that MST had not led to positive changes, or that things had deteriorated during or after the programme. The young people in this group felt annoyed that MST had not been able to help them, and several described their relationship with a support worker to be more helpful:
All the people that had tried to talk to me and all of that, I found it difficult so I didn’t really give much away . . . I think they probably did everything right but it was just me as a person that didn’t want to engage with them.
Young person, MST
Domain 2: attributions of initial change
Regarding which aspects of MST had helped to bring about positive changes, families spoke about motivation to change, the therapeutic alliance, techniques they had learned as a result of MST, and better understanding and communication between the parent and the young person.
Parents or carers often described entering the programme with feelings of desperation, and sometimes hopelessness. Young people had more mixed feelings, including feeling ‘nagged’ or ‘bored’, but some felt that the involvement of a therapist helped them understand the gravity of their situation.
Many families had positive feelings about their therapist, including the fact that they were non-judgemental and collaborative and offered practical support. Parents or carers valued the role of the therapist as a mediator and ‘someone to talk to’. However, young people sometimes felt that the therapist was taking their parent’s ‘side’.
Some of the techniques that parents or carers found valuable included behavioural parenting techniques, conflict management (e.g. the importance of being able to calm down and walk away during an argument), recognising dysfunctional behavioural patterns (e.g. action contributing to a reaction) and learning to think before acting:
. . . before I didn’t know that quite a lot of the things I was doing was making the situation worse even though I was trying to stop it, I was making it 10 times worse.
Parent, MST
Families also emphasised the importance of seeing the results from engaging in MST, including improved communication (listening and understanding rather than arguing) and being able to test new approaches and seeing them work. Seeing results also had a positive effect on parents’ or carers’ self-esteem.
Domain 3: families’ attributions of sustained change
Families who felt that they had sustained or improved on the positive changes they saw as a result of MST spoke about the reasons for this. Continuing to use the techniques and strategies that they learned was important, and this prevented the family from sliding into old patterns. Parents in particular spoke about the importance of generalisability, or being able to use MST principles in new contexts or situations, including with their other children. Families who thought that they had not sustained the changes felt that they needed more support to maintain them.
Positive changes contributed to understanding each other better, ‘bonding’, doing more things together, enjoying each other’s company, and having more mutual trust and respect between the young person and their parent(s) or carer(s). Many families spoke about rough patches during and following the programme; however, families felt that it was important to persevere in spite of these ups and down and to keep using the strategies they learned:
I mean every problem that you come across in life you can apply the things you’ve learnt, and instead of losing your temper and acting irrationally, thinking through and finding strategies for dealing with the problem, yeah it’s useful in every situation.
Parent, MST
Young people felt that they had more motivation and more aspirations for the future, which kept them out of trouble and in education. However, families who felt less able to sustain positive changes felt that they lacked support, and also felt frustrated at their inability to get the additional support they needed.
Domain 4: change attributed to extratherapeutic factors
All families spoke about factors besides MST that promoted or hindered positive change. Examples of these factors include individual factors for the parent or young person, such as mental and physical health, and the young person’s maturity. Environmental factors, such as extended family, school, peers and community, also had an influence. These include safety within the community, the stress associated with lack of money, changing schools (which may have had a positive or a negative impact), involvement with antisocial peers, or parents’ relationships with current partners or ex-partners.
Qualitative study 2
The coding revealed good inter-rater agreement for male data (92.7% agreement, κ = 0.73) and for female data (87.5% agreement, κ = 0.76). We examined evidence of an effect of therapy group (MST or MAU) on maturity score (mature vs. stuck). Among male participants, a Mann–Whitney U-test that indicated significantly greater maturity was associated with having received MST (median = 1) instead of MAU (median = 0.25), U = 12; p = 023. Among female participants, differences in maturity were not significantly associated with receiving MST (median = 1) relative to receiving MAU (median = 0.88), U = 21; p = 16. Illustrative examples of how maturity was apparent are presented below. This is summarised below.
Male young people
Domain 1: growth and the child–adult transition
Growth was a key theme distinguishing MST and MAU among the young men who took part in the study. The more mature accounts suggested that the therapeutic process had enabled them to become more empathetic when engaging with others:
When you’re younger you don’t have the experience of dealing with certain situations . . . As you get older you learn different ways . . . I help people in America who self-harm . . . it’s over Skype [Microsoft Corporation, Redmond, WA, USA] . . . Everything I’ve learnt through counselling and therapy . . . I just say to them ‘look you should speak to a cop or a doctor or whoever or a teacher about how you’re feeling and know that you’re not alone’.
MST, mature
What is impressive here is partly the participant’s apparently altruistic activities that are evoked in parallel with his own experiences of the therapy process, and the acquired skills that distinguish his current self from his former self.
Participants in the MST group emphasised the shift between being a child and being an adult, and having to ‘face the real world’. By contrast, those who had received MAU felt relatively constrained, in the sense of feeling less prepared for the future or the perception of having significant/insurmountable obstacles:
I just can’t like see how my life’s gonna go . . . I can’t . . . vision that right now . . . I don’t really think in front. I’m not an in front person . . . I’ll wait till that point comes and I probably won’t be ready for that point, but I’ll just wait for that point to come.
MAU, stuck
Domain 2: work and occupations
Positive experiences of working were seen as having a positive impact on the ‘mature’ participants’ lives. Meaningful personal occupations, such as being involved in creative activities (e.g. making music), had also had a similar effect.
Among the less mature participants, work was seen as a way of keeping out of trouble. The young men who were rated as more ‘stuck’ in their narratives were more indifferent to the value of work and their accounts suggested relatively limited personal power in securing employment.
Domain 3: relationships with peers
There were stark differences between MST and MAU participants within this domain. Young men who had received MAU felt considerably more ‘stuck’ in this area than those who had received MST. Some in the MST group were able to develop close platonic relationships, whereas others spoke about being able to achieve intimacy in a romantic context. In the MAU group, there was more difficulty in finding a constructive, valued role for other people in their life; for them, relationships were at best unsatisfactory and at worst destructive, having a negative impact on their self-esteem.
Domain 4: family relationships
Group differences were least pronounced in the domain of family relationships. Most participants spoke about improved relationships with their family members since adolescence. A lot of the time, current family relationships were described as mundane but calm, in contrast with more turbulent relationships in the past.
Female young people
Domain 1: growth and the child–adult transition
Among the young women who took part in the study, there were different factors involved in ‘turning things around’. Participants appeared to believe that MST may have helped them successfully meet challenges and transition to the beginnings of an adult life. A prominent theme in both groups was the ability to let go of the adversity they had faced in the past and to be able to transcend it going forward:
Everyone used to kind of [say] you’re not going to do anything . . . not going to be able to get a good job . . . not going to pass your exams . . . So that was . . . kind of drilled into me that I was going to . . . be a failure in life . . . that controlled the way I was. But . . . realising that I actually can do something and . . . [finding] something that I really enjoy . . . [makes me] want to prove that what they made me believe isn’t . . . the truth . . . so I [can] prove them wrong and . . . prove myself wrong.
MST, mature
When I had [my daughter] I’ve had social services move us straight onto a child protection plan . . . they thought I’d neglect [my daughter] obviously not having been parented right myself . . . you knuckle down a bit more ‘cos you know you’ve got people watching over you. . . . [with] a risk of you losing that child . . . you work more hard to keep them . . . It proves it’s worth it though ‘cos she’s off child protection now . . . came off it yesterday at the child protection review.
MAU, mature
However, participants also felt that their personal or social opportunities had been restricted, and that potential sources of support had been cut off.
Domain 2: work and occupations
As with young men, work was an important feature in the young women’s accounts of their current lives. They recognised the opportunities and challenges of working relationships, but also held aspirations for future work that was more rewarding. Work provided challenges with both co-workers and customers, but also gave the young women a foundation of confidence. The young women’s accounts were noticeably more reflective than the men’s, but there was little difference between those in the MST group and those who received MAU.
Domain 3: relationships with peers
Learning to identify unfulfilling, negative relationships was seen as an important aspect of personal growth by the participants. Emphasis was placed on loyalty and protectiveness, and quality or quantity of relationships.
Domain 4: family relationships
Participants acknowledged the role that MST played in improving their family relationships. However, among those who had received MAU, similar sentiments were expressed in reference to growth and maturity. The young women were able to recognise their own shortcomings in their approach to relating to their parents or carers. Across diverse family circumstances, the young women were able to reframe family relationships in a positive way. However, some still described parental relationships that were destructive and filled with conflict.
Results summary
The overall results of the second phase of the START trial indicated that there were few differences between MST and MAU. There were no differences in the primary outcome between the treatment arms; the proportion of young people with a criminal conviction in the 5-year follow-up to randomisation was not significantly different between MST and MAU. The predicted moderators were also found not to be significant, with the exception of the baseline peer delinquency score. Analysis of the secondary offending outcomes suggests that young people in the MST group had a greater mean number of offences over the follow-up period, but these differences disappeared by 60 months. Almost none of the secondary end points, based on self-report data from young people and their families, showed any significant differences between the groups (with the exception being parents’ perceptions of inconsistent discipline at 24 months only). The economic evaluation suffered from partially missing baseline data for the measure of health status, but this affected only one aspect of the analysis. The results suggest that service use was similar in the MST and MAU groups, with the MST group reporting a somewhat greater number of police contacts. Service costs for MST were found to be higher than those for MAU and unlikely to be more cost-effective. The first qualitative study, conducted around 18 months after randomisation, suggested that families had different trajectories following the MST intervention, with some continuing to improve and others struggling. Parents or carers and young people spoke about the different factors to which they attributed change, including the specific techniques and approach of MST, as well as external factors. The second qualitative study was conducted later to address the transition from childhood to adulthood. In male (but not in female) participants, receiving MST was associated with significantly higher maturity levels. Participants spoke about different aspects of the transition to adulthood, including work and relationships.
Chapter 10 Discussion
Interpretation
The results of the second phase of the START trial, as reported here, continued follow-up to 48 months for secondary outcomes and to 60 months for primary outcomes. The outcomes of the first phase17 did not find any evidence that MST was superior to MAU in reducing out-of-home placements or criminal convictions. The secondary outcomes in the first phase suggested that antisocial behaviour, as based on parents’ or carers’ reports, improved more rapidly in the MAU condition, although these group differences were not sustained in the long term (i.e. at 18 months’ follow-up).
The results of the 60-month follow-up are consistent with those reported in the first phase; there is no evidence of MST being superior to MAU in reducing criminal convictions among this population. Although young people in the MST group had more criminal convictions on average at the 24-, 36- and 48-month follow-up points, these differences were not sustained to the 60-month follow-up.
Secondary outcomes reported by young people, including antisocial behaviour, psychiatric problems, and emotional and physical well-being, did not yield any significant group differences, which suggests that MST did not benefit young people in terms of these domains beyond the provisions of MAU. The results also indicate that MST did not contribute to improved employment or education rates, or to differences in pregnancy rates.
Significant group differences in parent-rated perceptions of inconsistent discipline were found at 24 months, but none of the outcomes consistently favoured one group over the other in the long term. This is in contrast to the outcomes of the first phase of the trial, which suggested that, according to parents or carers, the intervention brought about more rapid change to young people’s antisocial behaviour in the MST group than in the MAU group. Data from the present longer-term follow-up suggest that there is no consistent pattern to the differences in behavioural change beyond 18 months.
The results from the economic analysis, in line with the results from the first phase of the trial, do not indicate any economic benefit for MST, with evidence instead to suggest there is a higher probability of MAU being cost-effective as a result of lower costs and slightly better outcomes in the MAU group. Although EQ-5D-3L scores were very similar in the two groups at all time points, it is interesting to note that scores fell over time, suggesting a reduction in health-related quality of life over time for the sample as a whole. It is hard to know exactly what is driving this reduction, but it may relate to the transition from young person to adulthood, as young people move away from home, their families and the services they are familiar with, and move out of education and into employment or unemployment.
It is unclear why the results of the present trial are at odds with previous US-based research that found MST to be beneficial compared with MAU. 11–14 One possibility is the difference between the juvenile criminal justice systems of the USA and the UK. The criminal justice system in the USA has a stronger punitive emphasis than that in the UK, where the emphasis is on rehabilitation. 63 The MST approach may have more common ground with MAU services in the UK than with those in the USA; previous studies have found larger effects when MST was compared with non-multimodal treatment. 64 Alternatively, young people in the USA may have more of an incentive to engage with MST.
In addition, it is also possible that MAU was able to effectively address the wide range of individual needs that contributed to the young person’s antisocial behaviour problems. MST is essentially a social learning-based model that strongly targets parenting skills and contingent interactions between young people and their parents or carers to reduce behavioural problems. The evidence base for MST suggests that it is less effective when antisocial behaviour is accompanied by comorbid conditions, especially serious emotional disturbance. In this respect, parental qualitative interviews from an earlier small randomised controlled trial evaluation of MST in the UK revealed that, in some cases, parents or carers believed that MST was not a good match for their children’s emotional needs (e.g. when their children had symptoms of depression and post-traumatic stress disorder as a result of maltreatment).
Young people in our sample were not typically referred to court, and we are likely to have randomised a more diverse group of antisocial young people in our trial than in previous MST evaluations. MST may not have been able to better address the diverse needs of our sample of antisocial young people than MAU. It is noteworthy that all young people in the trial were subject to multiagency review and treatment planning prior to randomisation in an effort to define their mental health needs and to provide a credible MAU based on these.
Although this is a potential explanation for the absence of group differences, it is curious that the results of our qualitative study suggest that, at least for some of our participants, MST conferred a benefit, especially males, where as MAU did not. Young people who were interviewed from the MST group showed greater evidence of having become more mature post intervention than those in MAU group.
How do we explain these findings? First, as can occur with a mixed-methods design, the qualitative group threw up inductively something that we did not quantitatively measure – the multifaceted construct of maturity – so we are unable to look at the whole sample in relation to this construct. Second, and speculatively, it may be that the maturity and well-being of young people benefited from the coherent delivery of an integrated intervention by one professional (MST) in a way that is not captured by symptom-reduction measures. For example, from the professional viewpoint, MST is an intervention designed to reduce antisocial behaviour by targeting parenting skills and family interactions. It may be that, for young people and parents or carers, receiving MST was seen as a chance to turn the young person’s life around. In this respect, the intense involvement of a committed professional, coming to their house numerous times a week, may have validated young people and sent a message about parental investment and concern that was not captured in the quantitative measures.
This idea is consistent with the qualitative findings, suggesting that the intervention helped young people better understand the impact of their behaviour on their parents’ or carers’ lives, and that, when young people were involved in sessions, the therapist allowed them to imagine a better future. These data suggest growth in the young person and changes that may be thought of from the vantage point of ‘maturity’. These changes were perhaps driven by renewed investment, concern and commitment on the part of parents or carers that was not skill based. In turn, the young person felt validated, and began to work on changing their lives in ways commensurate with their own goals, which was aided by the modelling and support of the MST therapist.
The implication is that a by-product of MST is growth towards greater maturity, which is related to the young person’s intrinsic motivation and goals (as opposed to reducing antisocial behaviour), which may reflect more extrinsic goals. Although speculative, the qualitative findings open up potentially exciting and beneficial avenues for future MST trials.
Generalisability
The present outcomes represent what is to our knowledge the largest trial, with longest follow-up, of MST in the UK to date. Although the recruitment criteria limited the population sample, the results do not support MST as superior to MAU for young people with CD for reducing offending rates, or for psychological, emotional or physical well-being.
The sample for this study may be broadly considered to be representative of the general UK population. Young people were recruited into the trial using a careful and thorough process, with 87% of the eligible families approached agreeing to take part. It is somewhat less clear how representative the sample is of the population of young people with antisocial behaviour problems, although the two groups were matched on a range of demographic parameters, and moderator analyses did not yield significant differences in outcomes.
It is possible that the outcome of the trial would have been different had it been compared with different MAU services, or had young people with more severe behavioural difficulties been included, but further research would be required to evaluate this.
Limitations
There are a number of limitations to this study. These include some failures arising from practical barriers or human error, others stemming from the pragmatic nature of the trial, and still others that can be attributed to the inherent nature of conducting randomised controlled trials with human participants. We outline these below.
The study failed to deliver on three elements of the intended data collection: objective education data, the CYPRESS evaluation and the proportion of missing EQ-5D-3L data at baseline. It was intended that objective education data (attendance, suspensions and exclusions) would be collected from the National Pupil Database. Although it was possible to obtain the data, it would not have been possible to match them to the study’s follow-up points, as they are collected and stored based on school term dates. Efforts to obtain this information from schools directly were also unsuccessful. The absence of comprehensive data on school adjustment is disappointing, but unfortunately consistent with other randomised controlled trials of MST, none of which were able to deliver education data post intervention. On a similar note, although we were able to obtain objective offending data from the PNC, we understand that it is not a perfect repository of information. The first issue is that the information it contains is supplied by police staff, and therefore is prone to human error and delays. 65 Second, not all committed crimes will be detected by police,66 although we supplemented the offending data in our sample with self-reported data. The barriers that come with database reliance should be taken into consideration in subsequent evaluations that have outcomes based in education or offending.
The CYPRESS measure is designed to define service characteristics; this was another measure for which we were not able to collect data. At this stage of the follow-up period, most of the MST sites that had taken part in the intervention were no longer being funded and had closed, with the clinical staff moving on to other posts. This was, of course, not possible to anticipate in the planning stages. However, the CYPRESS evaluations that were carried out during the first phase of the trial still give us some meaningful insight into the service delivery frameworks of both MST and MAU.
The economic evaluation was limited by a substantial number of missing EQ-5D-3L data as a result of an administrative error that was identified and rectified during the trial. Health-related quality of life was recorded for some time points, and a number of different approaches were taken to impute these missing data to make best use of the available information. The method selected made no difference to the results reported, and similar results were found when outcomes were measured in terms of offending, thus giving greater confidence in the validity of the results. Perhaps more importantly, the EQ-5D-3L may not have been the most appropriate measure for this particular population. Although NICE recommends the use of the EQ-5D-3L in all health economic evaluations to allow comparison across groups and interventions, the current population is defined less by their health status and more by their behaviour. As a result, a health-related measure of quality of life may have not have been sensitive enough to changes in the broader quality of these young people’s lives. In terms of the cost data, in common with most clinical trials, use of services was self-reported by young people and their parents or carers, which will inevitably have limited accuracy. However, there is no reason to assume any bias in accuracy between the two groups, and the pattern of costs and effects remained consistent over a long period of time, with little difference in service use or costs between the two groups, and little difference in outcomes, giving us greater confidence in the conclusion that there is no evidence to suggest that MST is cost-effective compared with MAU.
It is possible that selective attrition had an impact on the results of the study. Although the percentage of participants who were followed up was substantial for a study of this size and duration, dropouts may have been self-selecting. As a result, the findings represent a sample of participants who chose to continue taking part in the study. However, data for the primary outcome were objective and were collected from a national database, which minimised the self-selection bias. It is also worth noting that some measures were not collected despite participants’ willingness, because in some cases parents had lost touch with their children and therefore could not meaningfully report on their behaviour or well-being. Certain measures were also designed for young people aged ≥ 18 year, which reduced the pool of available participants.
Another limitation is the lack of clarity about whether or not the services received by those in the MAU group were representative of reality. The services provided to those in the MAU group were deliberately not standardised; the aim of the trial was to contrast MST services with whatever provision was typically awarded to young people with CD. Because services made proactive bids to participate in the trial, it is possible that the MAU services associated with the trial were of a higher standard or entailed a higher level of involvement than may typically be expected. However, these findings do suggest that MST is not superior to MAU when MAU is delivered to a high standard.
Finally, there are certain methodological limitations that necessarily affect all randomised controlled trials evaluating psychological intervention. First, unlike pharmacological interventions, it is impossible for a psychological intervention to be double-blind. The research assistants who collected the data were blinded to treatment condition, but it would not have been possible for the service users to be blinded to their own treatment. Second, some psychosocial problems can be self-correcting over time, in which case these effects would be indistinguishable from the effects of the intervention. Although this is true, the projected long-term outcomes for young people with CD are generally poor, and evidence from this and other trials evaluating organised treatment approaches suggests that interventions of this type can improve young people’s mental health and well-being and have a positive effect on family functioning. Finally, as discussed earlier, it was not possible to maintain perfect separation between MST and MAU delivery, as practitioners involved in MST may have influenced the teams delivering MAU. These are all methodological problems that can, and probably did, influence this trial, and therefore should be considered when interpreting the outcomes.
Implications for practice
The outcomes of the trial suggest that MST is well accepted and tolerated by service users. Families who engaged with MST spoke positively about the impact it had on them. This was particularly true for parents, who noticed improvements in young people’s behaviour before the young person noticed it themselves, and reported improvements in their own mental health and their perceived family functioning. 17 This is also evident in the results from the first qualitative study, in which young people and parents or carers spoke positively about the intervention and its effects on their well-being and their family. This was also corroborated by the relatively few dropouts from the intervention; most families completed the 4-month programme. This is something that young people and parents or carers may want to consider when deciding which treatment pathway is right for them.
Nevertheless, we were unable to demonstrate an objective superiority of MST to MAU in terms of reducing criminal behaviour at the 5-year follow-up. This is a finding that may be especially pertinent to professionals who need to make decisions about service commission or referrals. Although MST does lead to positive outcomes for young people and their families, other alternatives may be more suitable, depending on service availability and considerations around funding. The economic analysis does not suggest that MST is more cost-effective, and the service costs are higher than those for MAU. This finding may also factor in decisions made by commissioners or clinicians. The outcomes of the second qualitative study also suggest that MST was helpful for changing young people’s attitudes to and capacity for employment, and their outlook on their future work prospects. These findings may be beneficial for programmes focused on workforce development, which may want to incorporate aspects of MST principles into work with young people with CD.
The research team is aware that the teams that implemented MST could not have maintained a perfect separation between the delivery of MST and MAU. As a result, some aspects of MST delivery may have influenced the delivery of MAU. Monitoring this was not an aim of the trial, so we are unable to comment on the extent and outcomes of this officially, but it was something that we noticed informally and should be a consideration both for service delivery and for similar future trials.
In broader terms of treating young people with CD, the present study contributes to a wealth of existing literature that suggests that organised treatment holds substantial benefits for young people who experience these problems, as well as for their families. Young people with behavioural problems often receive inadequate support, if they receive support at all. This can have serious, long-term consequences for the young person’s well-being. Both service users and practitioners need to be aware of the value and benefits of organised interventions, which includes MST, the services that constituted the MAU group, and other types of programmes and therapeutic approaches available to young people with these types of problems. Moreover, the findings from the second phase of the trial, as described here, suggest that the positive outcomes observed in the first phase (up to 18 months’ follow-up) are maintained in the long term.
Future research
To our knowledge, the present study has yielded the largest data set related to young people with CD to date. There is significant potential to expand the scope of these findings beyond what has been reported here. It is the intention of the research team to carry out multiple follow-up analyses before making the data set publicly accessible via an open access policy. Initial follow-up analyses will include causal modelling of the outcomes in order to identify predictors of outcomes, moderators and/or mediators. This will be done using sophisticated data analysis approaches, including multilevel modelling and bi-factor analysis. The results of one of these analyses, focusing on using a bi-factor model for distinguishing between general and specific therapeutic changes, have already been published. 67
Future research may focus on identifying individuals who particularly benefited from MST. Earlier in this report we have discussed the potential of MST being more beneficial to young people whose CD problems are on the more severe end of the spectrum; however, this has not yet been tested empirically. Identifying specific moderators could help to deliver a more personalised treatment approach as well as interventions that are better tailored to the specific needs of young people with behavioural problems. This is particularly in the light of the fact that none of the moderators used in this study, despite being selected on the basis of previous research, yielded a significant result (with the exception of baseline peer delinquency). Assumptions can be tested in small-scale studies, and then evaluated in larger samples.
As discussed in Limitations, this trial had its share of barriers and drawbacks. Future trials with a similar design should take these into account at the planning stage and make efforts to mitigate or eliminate the effects. This may mean taking into account the limitations of education and criminal-offending databases and either consulting multiple sources (where possible) or supplementing with self-reported data. We have also noted that delivering MST at a specific site may have influenced MAU delivery. Although a solution to this was not possible in this case because of the limited number of sites that were funded for MST, other trials may consider a cluster randomised trial instead, which could help reduce this.
Finally, there are broader questions about the structure of mental health disorders in adolescents, and their diagnosis and treatment, which future research must ultimately address. The research team hopes to combine the data set resulting from this study with the work done on the RESTART (Researching cognitive and brain functioning in Typically-developing and At-Risk Teens) trial to begin formulating research to address these overarching issues.
Chapter 11 Conclusions
Although there is strong support for the principles of MST, the outcomes of the present trial indicate no evidence that their systemic application has led to long-term improvements superior to those from MAU. There were no significant differences between the arms in the proportion of young people with a criminal conviction by the final 60-month follow-up point. Some differences were found at 36 and 48 months’ follow-up, with young people in the MST group having had a slightly greater mean number of offences. However, these differences were not consistent, and the evidence does not suggest that there is a risk associated with this finding.
The outcomes for young people in the MAU group were good, relative to the expectations in the literature for this cohort of young people; ultimately, improvements in antisocial behaviour, emotional well-being, mental health and family functioning were not different between the group. The economic analysis indicated that MST may be more costly than MAU, but this can be managed on a local level, with decisions about implementation being weighed against the costs within the specific service or local authority. This is particularly true in the light of the likelihood that MST delivery had some influence on MAU delivery within the same site.
The qualitative studies indicate that MST was well received by the families, and most felt that positive relationships with the therapist and the techniques learned as part of the programme had helped them enact and sustain changes. Even years after completing MST, young people felt that it had helped them foster better relationships, participate in the workforce and have a more optimistic outlook on life. A more mature approach to these areas was found to be associated with MST in young men. This trial did not include an evaluation of clinicians’ experiences, but future trials may want to consider this.
There is some indication from the current trial that MST may be more beneficial to young people with more severe criminal behaviour and mental health difficulties, although there was insufficient power to explore this empirically. This may be an avenue to explore in further studies, and may have implications for practice, as more severe behavioural symptoms tend to be associated with additional costs, such as custodial sentences or out-of-home placements. Similarly, the outcomes of the qualitative studies suggest that elements of MST were found to be beneficial by both young people and their parents or carers, even in the absence of severe difficulties. It may be possible for some services to explore a more pragmatic, scaled-down implementation of specific MST principles where this is necessary and cost-effective. However, further research into this approach would be necessary.
One of the challenges of the present trial was the difficulty in integrating some of the objective data available in national databases to inform the methodology. More resources may be dedicated to establishing how existing data sets can be made more readily available for research within this population.
The principles of MST are ultimately based on evidence-based therapeutic approaches, and the outcomes of the present trial suggest that MST leads to outcomes comparable to those of MAU. The intensive nature of MST may positively contribute to improved monitoring and identification of young people’s needs and risk factors. Therefore, elements of the MST framework may be adapted by services if these are deemed beneficial and cost-effective at the local level.
Acknowledgements
Protocol
The protocol can be accessed at www.ncbi.nlm.nih.gov/pubmed/23962220.
Thank you
The trial team would like to thank the research assistants, administrative assistants and interns who assisted with data collection and management over the course of the START trial: Anna Abramowski, Gemma Antoniak, Ifkar Arifin, Chloe Austerberry, Helen Baldwin, Jakki Birtwistle, Isobel Brunton, Matthew Bury, Angeline Dharmaindra, Jessie Greisbach, Karolina Kaminska, Ulrike Klossek, Nikki Knight, Nicolas Lorenzini, Pauline Martin, Christina Maurice, Melissa McRae, Lauren Mountain, Jennifer O’Connell, Rebecca Packer, Lauren Pae, Emma Percy, Rebecca Ramsden, Alix Smith, Samantha Tipping, Kasturi Torchia, David Turgoose, Kate Watchorn and April Wiltshire.
Thank you to Hannah Guzinska and Dominic Conroy for carrying out qualitative study 1 and 2, respectively. Thank you to Cressida Gaffney for her work on CYPRESS during the first phase of the trial.
Thank you to Nicole Hickey (Imperial College London), who prepared the youth offending data from the PNC records.
Thank you to Eric Taylor and the members of the Trial Steering Committee that he chaired, and to Philip Graham and the members of the Data Management and Ethics Committee that he chaired, for their counsel.
Thank you to Cathy James (National Multisystemic Therapy Programme Lead) and Kathryn Harney (Associate Director of Research, Greater Manchester Mental Health NHS Foundation Trust) for their support, co-operation and guidance.
Thank you to the young people, parents and carers who took the time and effort to make this research happen, and without whom it would not have been possible.
Contributions of authors
Professor Peter Fonagy conducted the design, delivery, data analysis and write-up of the research.
Dr Stephen Butler advised on the day-to-day running of the trial and liaised with the clinical sites.
Professor David Cottrell advised on the effectiveness and management of the interventions in CAMHS.
Professor Stephen Scott advised on running randomised controlled trials with antisocial young people.
Professor Stephen Pilling developed the trial method, including the assessment of therapist competence, treatment fidelity and parallel process evaluation.
Professor Ivan Eisler advised on the implementation of systemic interventions.
Dr Peter Fuggle was the senior co-investigator responsible for the clinical validity of the research.
Dr Abdullah Kraam provided the psychiatric coverage for the trial and the establishment of diagnostic categories.
Professor Sarah Byford conducted the economic evaluation of the intervention.
Professor James Wason carried out the statistical data analysis.
Professor Jonathan A Smith was responsible for the qualitative research.
Dr Alisa Anokhina was the trial co-ordinator responsible for trial closure, preparation of data for analysis, and consolidation of the final report.
Ms Rachel Ellison was the trial co-ordinator responsible for the day-to-day running of the trial and management of the research assistants.
Ms Elizabeth Simes was the trial co-ordinator responsible for the day-to-day running of the trial and management of the research assistants.
Ms Poushali Ganguli conducted the economic evaluation of the intervention.
Dr Elizabeth Allison advised on the conceptualisation and application of the design and the interpretation of data, and supervised the research staff.
Professor Ian M Goodyer was the senior co-investigator with joint responsibility for design, delivery, analysis and write-up of the research.
Publications
Fonagy P, Butler S, Cottrell D, Scott S, Pilling S, Eisler I, et al. Multisystemic therapy versus management as usual in the treatment of adolescent antisocial behaviour (START): a pragmatic, randomised controlled, superiority trial. Lancet Psychiatry 2018;5:119–33.
Fonagy P, Butler S, Cottrell D, Scott S, Pilling S, Eiser I, et al. Multisystemic therapy versus management as usual in the treatment of adolescent antisocial behaviour (START): 5-year follow-up of a pragmatic, randomised controlled, superiority trial. Lancet Psychiatry 2020;7:420–30.
Data-sharing statement
Requests for data access should be addressed to the corresponding author.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- National Institute for Health and Care Excellence . Antisocial Behaviour and Conduct Disorders in Children and Young People: Recognition and Management 2017. www.nice.org.uk/guidance/cg158/chapter/introduction (accessed 29 October 2018).
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders (DSM-5®) 2013. https://doi.org/10.1176/appi.books.9780890425596.
- Ford T, Goodman R, Meltzer H. The British Child and Adolescent Mental Health Survey 1999: the prevalence of DSM-IV disorders. J Am Acad Child Adolesc Psychiatry 2003;42:1203-11. https://doi.org/10.1097/00004583-200310000-00011.
- Murray J, Farrington DP. Risk factors for conduct disorder and delinquency: key findings from longitudinal studies. Can J Psychiatry 2010;55:633-42. https://doi.org/10.1177/070674371005501003.
- Frick PJ, Ray JV, Thornton LC, Kahn RE. Can callous-unemotional traits enhance the understanding, diagnosis, and treatment of serious conduct problems in children and adolescents? A comprehensive review. Psychol Bull 2014;140:1-57. https://doi.org/10.1037/a0033076.
- Erskine HE, Norman RE, Ferrari AJ, Chan GC, Copeland WE, Whiteford HA, et al. Long-term outcomes of attention-deficit/hyperactivity disorder and conduct disorder: a systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry 2016;55:841-50. https://doi.org/10.1016/j.jaac.2016.06.016.
- Scott S, Knapp M, Henderson J, Maughan B. Financial cost of social exclusion: follow up study of antisocial children into adulthood. BMJ 2001;323. https://doi.org/10.1136/bmj.323.7306.191.
- Knapp M, McDaid D, Parsonage M. Mental Health Promotion and Mental Illness Prevention: The Economic Case. London: Department of Health and Social Care; 2011.
- Blair RJR, Leibenluft E, Pine DS. Conduct disorder and callous–unemotional traits in youth. N Engl J Med 2014;371:2207-16. https://doi.org/10.1056/NEJMra1315612.
- Henggeler SW. Multisystemic therapy: an overview of clinical procedures, outcomes, and policy implications. Child Psychol Psychiatry Rev 1999;4:2-10. https://doi.org/10.1017/S1360641798001786.
- Henggeler SW, Clingempeel WG, Brondino MJ, Pickrel SG. Four-year follow-up of multisystemic therapy with substance-abusing and substance-dependent juvenile offenders. J Am Acad Child Adolesc Psychiatry 2002;41:868-74. https://doi.org/10.1097/00004583-200207000-00021.
- Schaeffer CM, Borduin CM. Long-term follow-up to a randomized clinical trial of multisystemic therapy with serious and violent juvenile offenders. J Consult Clin Psychol 2005;73:445-53. https://doi.org/10.1037/0022-006X.73.3.445.
- Borduin CM, Mann BJ, Cone LT, Henggeler SW, Fucci BR, Blaske DM, et al. Multisystemic treatment of serious juvenile offenders: long-term prevention of criminality and violence. J Consult Clin Psychol 1995;63:569-78. https://doi.org/10.1037/0022-006X.63.4.569.
- Henggeler SW, Melton GB, Smith LA. Family preservation using multisystemic therapy: an effective alternative to incarcerating serious juvenile offenders. J Consult Clin Psychol 1992;60:953-61. https://doi.org/10.1037/0022-006X.60.6.953.
- Sundell K, Hansson K, Löfholm CA, Olsson T, Gustle LH, Kadesjö C. The transportability of multisystemic therapy to Sweden: short-term results from a randomized trial of conduct-disordered youths. J Fam Psychol 2008;22:550-60. https://doi.org/10.1037/a0012790.
- Leschied AW, Cunningham A. Seeking Effective Interventions for Serious Young Offenders: Interim Results of a Four-year Randomized Study of Multisystemic Therapy in Ontario, Canada. London, ON: Centre for Children and Families in the Justice System (London Family Court Clinic Incorporated); 2002.
- Fonagy P, Butler S, Cottrell D, Scott S, Pilling S, Eisler I, et al. Multisystemic therapy versus management as usual in the treatment of adolescent antisocial behaviour (START): a pragmatic, randomised controlled, superiority trial. Lancet Psychiatry 2018;5:119-33. https://doi.org/10.1016/S2215-0366(18)30001-4.
- Fonagy P, Butler S, Goodyer I, Cottrell D, Scott S, Pilling S, et al. Evaluation of multisystemic therapy pilot services in the Systemic Therapy for At Risk Teens (START) trial: study protocol for a randomised controlled trial. Trials 2013;14. https://doi.org/10.1186/1745-6215-14-265.
- Fonagy P, Butler S, Cottrell D, Scott S, Pilling S, Eiser I, et al. Multisystemic therapy versus management as usual in the treatment of adolescent antisocial behaviour (START): 5-year follow-up of a pragmatic, randomised controlled, superiority trial. Lancet Psychiatry 2020;7:420-30. https://doi.org/10.1016/S2215-0366(20)30131-0.
- Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry 2001;40:1337-45. https://doi.org/10.1097/00004583-200111000-00015.
- Kimonis ER, Frick PJ, Skeem JL, Marsee MA, Cruise K, Munoz LC, et al. Assessing callous-unemotional traits in adolescent offenders: validation of the Inventory of Callous-Unemotional Traits. Int J Law Psychiatry 2008;31:241-52. https://doi.org/10.1016/j.ijlp.2008.04.002.
- Elliott DS, Canter RJ, Knowles BA. The Epidemiology of Delinquent Behavior and Drug Use Among American Adolescents, 1976–1978. Boulder, CO: Behavioral Research Institute; 1981.
- Butler SM, Leschied AW, Fearon P. Antisocial beliefs and attitudes in pre-adolescent and adolescent youth: the development of the antisocial beliefs and attitudes scales (ABAS). J Youth Adolesc 2007;36:1058-71. https://doi.org/10.1007/s10964-007-9178-2.
- Goldberg ME, Gorn GJ, Peracchio LA, Bamossy G. Understanding materialism among youth. J Consum Psychol 2003;13:278-88. https://doi.org/10.1207/S15327663JCP1303_09.
- Conners CK, Sitarenios G, Parker JD, Epstein JN. The revised Conners’ Parent Rating Scale (CPRS-R): factor structure, reliability, and criterion validity. J Abnorm Child Psychol 1998;26:257-68. https://doi.org/10.1023/A:1022602400621.
- Essau CA, Sasagawa S, Frick PJ. Psychometric properties of the Alabama parenting questionnaire. J Child Fam Stud 2006;15:595-614. https://doi.org/10.1007/s10826-006-9036-y.
- Farrington DP. Serious and Violent Juvenile Offenders: Risk Factors and Successful Interventions. Thousand Oaks, CA: Sage Publications Ltd; 1999.
- Olson DH, Bell R, Portner J. Family Adaptability and Cohesion Evaluation Scales, FACES-II. Minneapolis, MN: Family Inventories Manual Life Innovations; 1992.
- Gerlsma C, Hale WW. Predictive power and construct validity of the Level of Expressed Emotion (LEE) scale. Depressed out-patients and couples from the general community. Br J Psychiatry 1997;170:520-5. https://doi.org/10.1192/bjp.170.6.520.
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised conflict tactics scales (CTS2) development and preliminary psychometric data. J Fam Issues 1996;17:283-316. https://doi.org/10.1177/019251396017003001.
- Sharp C, Goodyer IM, Croudace TJ. The Short Mood and Feelings Questionnaire (SMFQ): a unidimensional item response theory and categorical data factor analysis of self-report ratings from a community sample of 7-through 11-year-old children. J Abnorm Child Psychol 2006;34:379-91. https://doi.org/10.1007/s10802-006-9027-x.
- Goldberg D. Manual of the General Health Questionnaire. Windsor: National Foundation for Educational Research; 1978.
- Goodman R, Ford T, Richards H, Gatward R, Meltzer H. The Development and Well-Being Assessment: description and initial validation of an integrated assessment of child and adolescent psychopathology. J Child Psychol Psychiatry 2000;41:645-55. https://doi.org/10.1111/j.1469-7610.2000.tb02345.x.
- McCrimmon AW, Smith AD. Review of the Wechsler Abbreviated Scale of Intelligence (WASI-II). Los Angeles, CA: Sage Publications Ltd; 2013.
- Gaston L, Marmar CR, Horvath AO, Greenberg LS. The Working Alliance: Theory, Research, and Practice. New York, NY: John Wiley & Sons Inc.; 1994.
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. https://doi.org/10.1007/s11136-011-9903-x.
- Coddington RD. The significance of life events as etiologic factors in the diseases of children: I—A survey of professional workers. J Psychosom Res 1972;16:7-18. https://doi.org/10.1016/0022-3999(72)90018-9.
- Ware JE. SF-36 health survey update. Spine 2000;25:3130-9. https://doi.org/10.1097/00007632-200012150-00008.
- Gartland D, Bond L, Olsson CA, Buzwell S, Sawyer SM. Development of a multi-dimensional measure of resilience in adolescents: the Adolescent Resilience Questionnaire. BMC Med Res Methodol 2011;11. https://doi.org/10.1186/1471-2288-11-134.
- First MB, Spitzer RL, Williams JBW, Benjamin LS. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II). Washington, DC: American Psychiatric Press Inc.; 1997.
- Achenbach TM, Rescorla LA, Maruish ME. The Use of Psychological Testing for Treatment Planning and Outcomes Assessment: Instruments for Children and Adolescents. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; 2004.
- Richins ML, Dawson S. A consumer values orientation for materialism and its measurement: scale development and validation. J Consum Res 1992;19:303-16. https://doi.org/10.1086/209304.
- Carpenter J, Kenward M. Multiple Imputation and its Application. Chichester: John Wiley & Sons; 2012.
- Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Series B Stat Methodol 1995:289-300. https://doi.org/10.1111/j.2517-6161.1995.tb02031.x.
- National Institute for Health and Care Excellence . Guide to the Methods of Technology Appraisal 2013 2013.
- Barrett B, Byford S, Chitsabesan P, Kenning C. Mental health provision for young offenders: service use and cost. Br J Psychiatry 2006;188:541-6. https://doi.org/10.1192/bjp.bp.105.010108.
- Byford S, Barrett B, Roberts C, Clark A, Edwards V, Smethurst N, et al. Economic evaluation of a randomised controlled trial for anorexia nervosa in adolescents. Br J Psychiatry 2007;191:436-40. https://doi.org/10.1192/bjp.bp.107.036806.
- Department for Education . Statistics: Local Authority and School Finance 2013 n.d. www.gov.uk/government/collections/statistics-local-authority-school-finance-data (accessed 1 March 2019).
- Department of Health and Social Care . NHS Reference Costs 2012 to 2013 2013. www.gov.uk/government/publications/nhs-reference-costs-2012-to-2013 (accessed 26 February 2019).
- Curtis LA. Unit Costs of Health and Social Care 2013. Canterbury: Personal Social Services Research Unit, University of Kent; 2013.
- Royal Pharmaceutical Society (RPS) . British National Formulary 2016. www.medicinescomplete.com/mc/bnf/current/ (accessed 28 January 2019).
- Brookes N, Barrett B, Netten A, Knapp E. Unit Costs in Criminal Justice (UCCJ) 2013. Canterbury: Personal Social Services Research Unit, University of Kent; 2013.
- Harries R. The Cost of Criminal Justice, Home Office Research Findings No. 103. London: Home Office Research, Development, and Statistics Directorate; 1999.
- Beecham J, Knapp M, Thornicroft G. Measuring Mental Health Needs. London: Royal College of Psychiatrists; 2001.
- Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ 2005;14:487-96. https://doi.org/10.1002/hec.944.
- Barber JA, Thompson SG. Analysis of cost data in randomized trials: an application of the non-parametric bootstrap. Stat Med 2000;19:3219-36. https://doi.org/10.1002/1097-0258(20001215)19:23<3219::AID-SIM623>3.0.CO;2-P.
- Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2015.
- Fenwick E, Byford S. A guide to cost-effectiveness acceptability curves. Br J Psychiatry 2005;187:106-8. https://doi.org/10.1192/bjp.187.2.106.
- Ritchie J, Spencer L, Burgess RG, Bryman A. Analyzing Qualitative Data. London: Routledge; 1994.
- Smith JA, Flowers, P, Larkin M. Interpretative Phenomenological Analysis: Theory, Method, Research. London: Sage Publications Ltd; 2009.
- Weichle T, Hynes DM, Durazo-Arvizu R, Tarlov E, Zhang Q. Impact of alternative approaches to assess outlying and influential observations on health care costs. SpringerPlus 2013;2. https://doi.org/10.1186/2193-1801-2-614.
- White IR, Thompson SG. Adjusting for partially missing baseline measurements in randomized trials. Stat Med 2005;24:993-1007. https://doi.org/10.1002/sim.1981.
- Muncie J. The ‘punitive turn’ in juvenile justice: Cultures of control and rights compliance in Western Europe and the USA. Youth Justice 2008;8:107-21. https://doi.org/10.1177/1473225408091372.
- van der Stouwe T, Asscher JJ, Stams GJ, Deković M, van der Laan PH. The effectiveness of Multisystemic Therapy (MST): a meta-analysis. Clin Psychol Rev 2014;34:468-81. https://doi.org/10.1016/j.cpr.2014.06.006.
- Francis B, Soothill K, Humphreys L. Development of a Reoffending Measure Using the Police National Computer Database. Lancaster: Lancaster University; 2007.
- Farrington DP, Auty KM, Coid JW, Turner RE. Self-reported and official offending from age 10 to age 56. Eur J Crim Pol Res 2013;19:135-51. https://doi.org/10.1007/s10610-012-9195-x.
- Constantinou MP, Goodyer IM, Eisler I, Butler S, Kraam A, Scott S, et al. Changes in general and specific psychopathology factors over a psychosocial intervention [published online ahead of print January 14 2019]. J Am Acad Child Adolesc Psychiatry 2019. https://doi.org/10.1016/j.jaac.2018.11.011.
- Clark LA, Watson D. Constructing validity: basic issues in objective scale development. Psychol Assess 1995;7:309-19. https://doi.org/10.1037/1040-3590.7.3.309.
Appendix 1 Internal consistency of secondary outcome measures based on START I (up to the 18-month follow-up)
| Assessment | Time point | Cronbach’s α (reliability coefficient) | Mean inter-item correlationa | |||
|---|---|---|---|---|---|---|
| Baseline (T1) | 6 months (T2) | 12 months (T3) | 18 months (T4) | |||
| Parent questionnaires | ||||||
| GHQ | ✗ | ✗ | ✗ | ✗ | 0.95 | 0.41 |
| CBRS – Parent form (CBRS) | ✗ | ✗ | ✗ | ✗ | 0.89 | 0.26 |
| ICUT | ✗ | ✗ | ✗ | ✗ | 0.85 | 0.20 |
| SDQ | ✗ | ✗ | ✗ | ✗ | 0.72 | 0.06 |
| CTS2S | ✗ | ✗ | ✗ | ✗ | 0.83 | 0.20 |
| APQ | ✗ | ✗ | ✗ | ✗ | 0.62 | 0.07 |
| FACES-IV | ✗ | ✗ | ✗ | ✗ | 0.73 | 0.08 |
| Loeber Caregiver Questionnaire | ✗ | ✗ | ✗ | ✗ | 0.76 | 0.15 |
| Young person questionnaires | ||||||
| MFQ | ✗ | ✗ | ✗ | ✗ | 0.89 | 0.58 |
| ICUT | ✗ | ✗ | ✗ | ✗ | 0.78 | 0.13 |
| SRDM | ✗ | ✗ | ✗ | ✗ | 0.92 | 0.19 |
| LEE | ✗ | ✗ | ✗ | ✗ | 0.98 | 0.08 |
| ABAS | ✗ | ✗ | ✗ | ✗ | 0.93 | 0.17 |
| SDQ | ✗ | ✗ | ✗ | ✗ | 0.70 | 0.08 |
| APQ | ✗ | ✗ | ✗ | ✗ | 0.61 | 0.10 |
| Youth Materialism Scale | ✗ | ✗ | ✗ | ✗ | 0.84 | 0.27 |
| Education data | ||||||
| CBRS – Teacher form | ✗ | ✗ | ✗ | ✗ | 0.89 | 0.26 |
Appendix 2 Routine care received by the two groups at baseline
| Type of care | Group | |||||
|---|---|---|---|---|---|---|
| MAU (N = 284) | MST (N = 291) | |||||
| Mean (SD) number of contacts | Mean (SD) duration (hours) | Number (%) used | Mean (SD) number of contacts | Mean (SD) duration (hours) | Number (%) used | |
| Care co-ordinator | 0.15 (1.8) | 6.89 (77.9) | 4 (1.4) | 1.1 (8.1) | 46.63 (372.4) | 9 (3) |
| Psychiatrist | 0.21 (0.9) | 10.49 (50.6) | 18 (6.3) | 0.13 (0.8) | 7.15 (44.1) | 12 (4.1) |
| Clinical psychologist | 0.34 (2.1) | 19.26 (127.5) | 16 (5.6) | 0.48 (4) | 30.73 (248.6) | 13 (4.4) |
| CAMHS worker | 0.67 (2.5) | 36.53 (145.8) | 45 (15.8) | 0.68 (3.4) | 39.84 (208.1) | 43 (14.7) |
| Community psychiatric nurse | 0.04 (0.3) | 2.43 (21.6) | 4 (1.4) | 0.07 (1.2) | 4.43 (73.8) | 2 (0.6) |
| Total routine CAMHS | 1.42 (3.9) | 75.61 (222.9) | 72 (25.3) | 2.47 (9.7) | 128.79 (495.1) | 72 (24.7) |
| Social worker | 3.07 (7.7) | 159.62 (633.1) | 100 (35.2) | 3.37 (7.5) | 221.74 (687.7) | 100 (34.3) |
| Family support worker | 1.18 (5.8) | 58.25 (293.6) | 23 (8) | 1.91 (9.2) | 113.24 (598.3) | 29 (9.9) |
| Social services youth worker | 0.49 (3.8) | 34.46 (382.4) | 12 (4.2) | 0.17 (1.1) | 9.83 (58.9) | 11 (3.7) |
| Total routine social care | 4.74 (10.7) | 252.33 (815.5) | 122 (42.9) | 5.45 (12.4) | 344.77 (949.7) | 123 (42.2) |
| Total routine YOT | 6.12 (14.2) | 290.6 (715.9) | 87 (30.6) | 5.17 (11.8) | 321.96 (1644.6) | 82 (28.1) |
| Total | 12.28 (18) | 618.55 (1136) | 199 (70) | 13.09 (19.9) | 795.53 (2032.2) | 190 (65.2) |
Appendix 3 Young person-rated secondary end points
| Variable | ARQ end point | ||||
|---|---|---|---|---|---|
| Self | Family | School | Friends | Area | |
| 24 months | |||||
| MST | 112.60 | 34.86 | 46.40 | 45.58 | 15.21 |
| MAU | 102.06 | 35.11 | 43.20 | 44.42 | 14.40 |
| Difference (95% CI); p-value | 8.41 (–4.52 to 21.35); p = 0.21 | 1.56 (–2.40 to 5.52); p = 0.45 | 0.11 (–7.43 to 7.65); p = 0.98 | –0.53 (–5.30 to 4.24); p = 0.83 | 0.85 (–1.86 to 3.57); p = 0.54 |
| 36 months | |||||
| MST | 92.08 | 34.28 | 45.35 | 43.84 | 13.73 |
| MAU | 104.01 | 33.59 | 43.16 | 43.66 | 14.41 |
| Difference (95% CI); p-value | –7.52 (–15.67 to 0.63); p = 0.075 | 0.50 (–2.05 to 3.05); p = 0.7 | –0.92 (–5.43 to 3.60); p = 0.69 | –0.59 (–3.02 to 1.84); p = 0.64 | –1.08 (–2.56 to 0.40); p = 0.16 |
| 48 months | |||||
| MST | 116.39 | 35.70 | 45.82 | 46.46 | 15.63 |
| MAU | 115.92 | 34.57 | 45.60 | 46.29 | 16.16 |
| Difference (95% CI); p-value | 2.52 (–4.73 to 9.76); p = 0.5 | 0.78 (–1.90 to 3.47); p = 0.57 | 4.26 (–1.69 to 10.21); p = 0.17 | 1.56 (–0.89 to 4.01); p = 0.21 | 0.65 (–1.13 to 2.44); p = 0.48 |
| Variable | APQ end point | ||||
|---|---|---|---|---|---|
| Corporal punishment | Inconsistent discipline score | Positive parenting score | Problems of monitoring and supervision | Parental involvement | |
| 24 months | |||||
| MST | 3.48 | 7.28 | 11.22 | 7.27 | 8.39 |
| MAU | 3.46 | 7.36 | 11.20 | 6.93 | 8.35 |
| Difference (95% CI); p-value | –0.06 (–0.30 to 0.19); p = 0.66 | –0.05 (–0.52 to 0.43); p = 0.84 | 0.35 (–0.15 to 0.85); p = 0.17 | 0.26 (–0.20 to 0.73); p = 0.27 | 0.25 (–0.23 to 0.74); p = 0.3 |
| 36 months | |||||
| MST | 3.58 | 7.80 | 11.38 | 7.30 | 8.22 |
| MAU | 3.47 | 7.45 | 11.33 | 6.98 | 8.44 |
| Difference (95% CI); p-value | –0.06 (–0.35 to 0.22); p = 0.67 | 0.01 (–0.63 to 0.66); p = 0.97 | 0.20 (–0.33 to 0.74); p = 0.46 | 0.15 (–0.48 to 0.79); p = 0.64 | 0.04 (–0.59 to 0.68); p = 0.9 |
| 48 months | |||||
| MST | 3.71 | 7.35 | 10.80 | 6.93 | 7.20 |
| MAU | 3.46 | 7.48 | 11.26 | 6.68 | 8.23 |
| Difference (95% CI); p-value | –0.01 (–0.36 to 0.34); p = 0.96 | 0.32 (–0.49 to 1.14); p = 0.44 | 0.37 (–0.36 to 1.10); p = 0.32 | 0.18 (–0.58 to 0.94); p = 0.65 | –0.13 (–1.01 to 0.76); p = 0.78 |
| Variable | Scale/score end point | ||||
|---|---|---|---|---|---|
| Antisocial Beliefs and Attitudes Scales total score | Young person ICUT | LEE | Youth Materialism Scale | Short Mood and Feelings Questionnaire | |
| 24 months | |||||
| MST | 49.93 | 27.43 | 77.16 | 35.74 | 6.47 |
| MAU | 50.68 | 28.08 | 77.70 | 37.16 | 5.63 |
| Difference (95% CI); p-value | –0.06 (–3.01 to 2.89); p = 0.97 | –0.92 (–2.19 to 0.35); p = 0.15 | –1.31 (–3.81 to 1.19); p = 0.3 | –0.81 (–2.07 to 0.45); p = 0.21 | 0.26 (–0.54 to 1.06); p = 0.53 |
| 36 months | |||||
| MST | 48.93 | 27.30 | 77.01 | 36.25 | 5.79 |
| MAU | 48.93 | 26.98 | 78.23 | 36.88 | 5.88 |
| Difference (95% CI); p-value | 0.46 (–3.28 to 2.36); p = 0.75 | –0.66 (–2.11 to 0.79); p = 0.37 | 0.04 (–2.60 to 2.67); p = 0.98 | –0.45 (–2.15 to 1.24); p = 0.6 | 0.00 (–1.05 to 1.05); p = 0.99 |
| 48 months | |||||
| MST | 48.87 | 26.07 | 78.77 | 35.29 | 7.37 |
| MAU | 49.11 | 26.00 | 76.29 | 37.19 | 5.37 |
| Difference (95% CI); p-value | –0.07 (–4.47 to 4.34); p = 0.98 | –0.32 (–2.04 to 1.41); p = 0.72 | –0.02 (–3.42 to 3.37); p = 0.99 | –0.59 (–3.11 to 1.94); p = 0.65 | 2.17 (0.76 to 3.57); p = 0.0044 |
| Variable | Delivery measure end point | |||||
|---|---|---|---|---|---|---|
| Delinquency variety | Delinquency volume | Variety of substance misuse | Volume of substance misuse | Peer delinquency score | Peer substance misuse | |
| 24 months | ||||||
| MST | 1.93 | 1.49 | 0.67 | 1.49 | 2.73 | 3.37 |
| MAU | 2.06 | 1.53 | 0.65 | 1.53 | 2.92 | 3.49 |
| Difference (95% CI); p-value | 0.03 (–0.39 to 0.45); p = 0.9 | –0.04 (–0.27 to 0.18); p = 0.7 | –0.09 (–0.32 to 0.14); p = 0.44 | –0.04 (–0.27 to 0.18); p = 0.7 | –0.67 (–1.36 to 0.02); p = 0.061 | –0.09 (–0.39 to 0.21); p = 0.54 |
| 36 months | ||||||
| MST | 1.60 | 1.58 | 0.71 | 1.58 | 2.44 | 3.58 |
| MAU | 1.60 | 1.37 | 0.59 | 1.37 | 2.42 | 3.64 |
| Difference (95% CI); p-value | –0.05 (–0.48 to 0.39); p = 0.84 | 0.07 (–0.15 to 0.30); p = 0.54 | 0.06 (–0.17 to 0.29); p = 0.61 | 0.07 (–0.15 to 0.30); p = 0.54 | –0.39 (–1.05 to 0.27); p = 0.25 | 0.06 (–0.27 to 0.40); p = 0.71 |
| 48 months | ||||||
| MST | 2.15 | 1.79 | 0.81 | 1.79 | 2.96 | 4.01 |
| MAU | 1.14 | 1.35 | 0.56 | 1.35 | 2.20 | 3.65 |
| Difference (95% CI); p-value | 0.67 (0.08 to 1.26); p = 0.03 | 0.10 (–0.18 to 0.39); p = 0.48 | 0.09 (–0.21 to 0.39); p = 0.57 | 0.10 (–0.18 to 0.39); p = 0.48 | 0.89 (–0.08 to 1.86); p = 0.077 | 0.42 (–0.06 to 0.90); p = 0.098 |
| Variable | SF-36 domain end point | |||||||
|---|---|---|---|---|---|---|---|---|
| SF-36 emotional well-being | SF-36 energy or fatigue | SF-36 general health | SF-36 limitations due to emotional problems | SF-36 limitations due to physical health | SF-36 pain | SF-36 average physical functioning | SF-36 social functioning | |
| 24 months | ||||||||
| MST | 71.61 | 59.52 | 68.51 | 82.26 | 88.21 | 81.23 | 83.25 | 80.12 |
| MAU | 66.70 | 60.79 | 62.29 | 80.65 | 81.96 | 83.83 | 85.14 | 75.88 |
| Difference (95% CI); p-value | 1.71 (–3.36 to 6.79); p = 0.51 | –1.94 (–5.95 to 2.06); p = 0.34 | 4.79 (–0.53 to 10.11); p = 0.084 | 3.18 (–5.12 to 11.47); p = 0.46 | 4.78 (–2.96 to 12.53); p = 0.23 | –0.02 (–4.79 to 4.74); p = 0.99 | –1.95 (–8.06 to 4.16); p = 0.53 | 4.26 (–1.85 to 10.37); p = 0.18 |
| 36 months | ||||||||
| MST | 72.28 | 62.48 | 63.29 | 84.21 | 86.04 | 81.88 | 87.35 | 80.23 |
| MAU | 67.81 | 60.72 | 64.22 | 79.28 | 83.77 | 80.78 | 82.35 | 76.91 |
| Difference (95% CI); p-value | 3.88 (0.15 to 7.61); p = 0.044 | 1.88 (–2.26 to 6.01); p = 0.38 | 0.74 (–3.86 to 5.34); p = 0.75 | 4.01 (–3.17 to 11.19); p = 0.28 | 2.89 (–2.72 to 8.51); p = 0.31 | 1.69 (–3.11 to 6.49); p = 0.49 | 3.09 (–2.10 to 8.28); p = 0.25 | 3.91 (–1.36 to 9.19); p = 0.15 |
| 48 months | ||||||||
| MST | 64.85 | 54.90 | 59.39 | 74.46 | 83.99 | 80.56 | 79.19 | 72.92 |
| MAU | 70.53 | 60.48 | 63.58 | 79.52 | 86.17 | 77.29 | 77.93 | 74.56 |
| Difference (95% CI); p-value | –3.49 (–8.17 to 1.19); p = 0.15 | –3.74 (–7.99 to 0.52); p = 0.09 | –2.21 (–6.87 to 2.45); p = 0.36 | 0.25 (–8.71 to 9.20); p = 0.96 | –1.54 (–8.18 to 5.11); p = 0.65 | 0.51 (–4.77 to 5.79); p = 0.85 | 3.44 (–1.71 to 8.59); p = 0.19 | –0.55 (–6.43 to 5.33); p = 0.85 |
| Variable | SDQ end point | |||||
|---|---|---|---|---|---|---|
| Conduct problems | Emotional problems | Hyperactivity | Impact | Prosocial | Total difficulties score | |
| 24 months | ||||||
| MST | 3.54 | 3.61 | 5.42 | 1.66 | 7.02 | 15.67 |
| MAU | 3.62 | 3.75 | 5.39 | 1.72 | 7.11 | 15.94 |
| Difference (95% CI); p-value | 0.09 (–0.21 to 0.38); p = 0.57 | –0.18 (–0.53 to 0.16); p = 0.29 | 0.11 (–0.22 to 0.44); p = 0.52 | 0.02 (–0.38 to 0.41); p = 0.94 | –0.07 (–0.39 to 0.26); p = 0.69 | –0.09 (–0.92 to 0.74); p = 0.83 |
| 36 months | ||||||
| MST | 3.22 | 3.57 | 5.38 | 2.16 | 6.96 | 15.16 |
| MAU | 3.20 | 3.86 | 5.18 | 1.78 | 7.16 | 15.32 |
| Difference (95% CI); p-value | –0.07 (–0.43 to 0.28); p = 0.69 | –0.38 (–0.80 to 0.05); p = 0.085 | 0.03 (–0.36 to 0.41); p = 0.9 | 0.16 (–0.44 to 0.76); p = 0.6 | –0.21 (–0.58 to 0.16); p = 0.27 | –0.61 (–1.46 to 0.23); p = 0.16 |
| 48 months | ||||||
| MST | 3.58 | 3.40 | 5.63 | 2.37 | 6.95 | 16.30 |
| MAU | 3.10 | 4.15 | 5.54 | 1.71 | 7.32 | 16.27 |
| Difference (95% CI); p-value | 0.36 (–0.14 to 0.87); p = 0.16 | –0.53 (–1.06 to –0.01); p = 0.053 | 0.32 (–0.39 to 1.02); p = 0.39 | 0.91 (0.39 to 1.42); p = 0.0013 | –0.10 (–0.63 to 0.44); p = 0.72 | 0.15 (–1.24 to 1.53); p = 0.84 |
| Variable | Adult Materialism Scale total |
|---|---|
| 24 months | |
| MST | 71.97 |
| MAU | 77.46 |
| Difference (95% CI); p-value | –0.57 (–11.19 to 10.05); p = 0.92 |
| 36 months | |
| MST | 72.82 |
| MAU | 73.17 |
| Difference (95% CI); p-value | –0.60 (–5.23 to 4.03); p = 0.8 |
| 48 months | |
| MST | 68.84 |
| MAU | 73.10 |
| Difference (95% CI); p-value | –0.96 (–6.59 to 4.67); p = 0.74 |
| Variable | ASR end point | |||||
|---|---|---|---|---|---|---|
| Friends | Spouse/partner | Family | Job | Education | Mean adaptive | |
| 24 months | ||||||
| MST | 43.39 | 45.58 | 45.00 | 49.14 | 46.62 | 42.96 |
| MAU | 46.87 | 44.17 | 48.88 | 50.03 | 44.59 | 47.07 |
| Difference (95% CI); p-value | –0.54 (–5.01 to 3.92); p = 0.81 | 0.21 (–7.34 to 7.75); p = 0.96 | –2.49 (–6.27 to 1.29); p = 0.21 | –0.85 (–5.42 to 3.72); p = 0.72 | 0.43 (–5.51 to 6.37); p = 0.89 | –1.26 (–4.63 to 2.12); p = 0.47 |
| 36 months | ||||||
| MST | 47.29 | 44.02 | 47.01 | 48.61 | 48.33 | 46.71 |
| MAU | 47.58 | 44.95 | 48.84 | 49.09 | 45.20 | 46.84 |
| Difference (95% CI); p-value | 0.79 (–1.67 to 3.25); p = 0.53 | –0.05 (–6.22 to 6.11); p = 0.99 | –1.77 (–3.95 to 0.41); p = 0.12 | –0.58 (–2.82 to 1.65); p = 0.61 | 0.85 (–2.79 to 4.50); p = 0.65 | –0.01 (–1.84 to 1.82); p = 0.99 |
| 48 months | ||||||
| MST | 46.62 | 48.33 | 48.80 | 49.29 | 43.82 | 46.21 |
| MAU | 47.96 | 45.22 | 48.54 | 48.41 | 45.68 | 47.09 |
| Difference (95% CI); p-value | 0.04 (–2.47 to 2.55); p = 0.97 | 0.69 (–4.66 to 6.04); p = 0.8 | –0.73 (–2.97 to 1.50); p = 0.52 | –0.58 (–3.82 to 2.66); p = 0.73 | –0.95 (–5.73 to 3.84); p = 0.7 | –0.23 (–2.34 to 1.87); p = 0.83 |
| Variable | ASR end point | ||||
|---|---|---|---|---|---|
| Personal strengths | Anxious/depressed | Withdrawn | Somatic complaints | Thought problems | |
| 24 months | |||||
| MST | 39.67 | 54.22 | 56.92 | 54.87 | 57.58 |
| MAU | 46.35 | 53.91 | 58.05 | 55.15 | 57.69 |
| Difference (95% CI); p-value | –2.95 (–8.44 to 2.53); p = 0.3 | –0.40 (–2.56 to 1.75); p = 0.72 | –0.32 (–2.56 to 1.93); p = 0.78 | –0.25 (–2.20 to 1.70); p = 0.8 | 1.02 (–1.21 to 3.26); p = 0.38 |
| 36 months | |||||
| MST | 42.31 | 53.58 | 56.30 | 55.98 | 57.11 |
| MAU | 43.28 | 53.98 | 57.62 | 55.71 | 57.94 |
| Difference (95% CI); p-value | –0.08 (–3.19 to 3.03); p = 0.96 | –0.87 (–2.65 to 0.92); p = 0.35 | –0.82 (–2.84 to 1.20); p = 0.43 | –0.13 (–1.68 to 1.42); p = 0.87 | –0.14 (–2.42 to 2.14); p = 0.91 |
| 48 months | |||||
| MST | 41.76 | 54.77 | 57.00 | 56.82 | 57.60 |
| MAU | 42.11 | 54.23 | 56.94 | 56.21 | 57.85 |
| Difference (95% CI); p-value | 0.19 (–3.11 to 3.49); p = 0.91 | 0.07 (–1.32 to 1.46); p = 0.92 | –0.04 (–1.74 to 1.66); p = 0.97 | –0.19 (–1.60 to 1.23); p = 0.8 | –1.05 (–2.88 to 0.77); p = 0.26 |
| Variable | ASR end point | ||||
|---|---|---|---|---|---|
| Attention problems | Aggressive behaviour | Rule breaking behaviour | Intrusive | Internalising problems | |
| 24 months | |||||
| MST | 54.88 | 58.35 | 56.47 | 53.77 | 51.83 |
| MAU | 55.08 | 57.52 | 58.23 | 53.55 | 52.36 |
| Difference (95% CI); p-value | –1.00 (–3.39 to 1.38); p = 0.42 | –0.04 (–2.95 to 2.87); p = 0.98 | –1.47 (–4.27 to 1.32); p = 0.31 | 0.05 (–2.35 to 2.44); p = 0.97 | 0.86 (–2.22 to 3.94); p = 0.59 |
| 36 months | |||||
| MST | 56.07 | 57.74 | 58.31 | 53.13 | 50.31 |
| MAU | 55.51 | 57.66 | 57.90 | 53.98 | 51.83 |
| Difference (95% CI); p-value | –1.30 (–3.61 to 1.02); p = 0.28 | –0.62 (–2.67 to 1.43); p = 0.56 | –0.07 (–2.16 to 2.03); p = 0.95 | –0.33 (–1.70 to 1.03); p = 0.64 | –0.41 (–3.20 to 2.39); p = 0.78 |
| 48 months | |||||
| MST | 55.61 | 57.63 | 58.60 | 53.27 | 52.36 |
| MAU | 56.11 | 57.68 | 58.09 | 53.75 | 52.16 |
| Difference (95% CI); p-value | –0.06 (–1.77 to 1.65); p = 0.95 | –0.66 (–2.46 to 1.15); p = 0.48 | 0.55 (–1.51 to 2.61); p = 0.61 | 0.36 (–1.35 to 2.07); p = 0.68 | 0.26 (–1.99 to 2.52); p = 0.82 |
| Variable | ASR end point | ||||
|---|---|---|---|---|---|
| Externalising problems | Total problems | Critical items | Tobacco per day | Alcohol days drunk | |
| 24 months | |||||
| MST | 54.18 | 52.03 | 60.27 | 56.13 | 57.32 |
| MAU | 55.90 | 54.45 | 58.68 | 55.15 | 60.80 |
| Difference (95% CI); p-value | –1.16 (–4.26 to 1.94); p = 0.47 | –0.49 (–3.43 to 2.44); p = 0.74 | 0.80 (–2.16 to 3.76); p = 0.6 | 1.84 (–0.56 to 4.24); p = 0.15 | –1.41 (–4.99 to 2.17); p = 0.45 |
| 36 months | |||||
| MST | 54.92 | 52.41 | 58.13 | 56.87 | 57.19 |
| MAU | 56.62 | 54.66 | 59.24 | 56.38 | 60.28 |
| Difference (95% CI); p-value | –0.72 (–2.99 to 1.54); p = 0.54 | –0.59 (–2.89 to 1.71); p = 0.62 | –0.79 (–2.82 to 1.24); p = 0.45 | 0.95 (–0.99 to 2.89); p = 0.35 | –0.61 (–3.21 to 1.99); p = 0.65 |
| 48 months | |||||
| MST | 55.36 | 53.43 | 59.57 | 57.91 | 58.49 |
| MAU | 56.53 | 54.36 | 59.39 | 57.07 | 58.77 |
| Difference (95% CI); p-value | –0.17 (–2.88 to 2.53); p = 0.9 | –0.41 (–2.67 to 1.85); p = 0.72 | –0.74 (–2.66 to 1.19); p = 0.46 | 0.80 (–1.23 to 2.83); p = 0.45 | 1.12 (–0.85 to 3.08); p = 0.27 |
| Variable | ASR end point | ||||
|---|---|---|---|---|---|
| Drug days used | Mean substance use | Depressive problems | Anxiety problems | Somatic problems | |
| 24 months | |||||
| MST | 62.83 | 60.58 | 55.61 | 53.15 | 54.50 |
| MAU | 62.45 | 61.39 | 55.48 | 53.33 | 54.22 |
| Difference (95% CI); p-value | –2.88 (–9.66 to 3.89); p = 0.41 | –0.88 (–3.89 to 2.14); p = 0.57 | –0.44 (–3.00 to 2.11); p = 0.74 | –0.32 (–2.58 to 1.95); p = 0.79 | 0.45 (–1.61 to 2.52); p = 0.67 |
| 36 months | |||||
| MST | 63.58 | 60.75 | 56.16 | 52.26 | 55.37 |
| MAU | 62.85 | 61.61 | 55.57 | 53.07 | 54.90 |
| Difference (95% CI); p-value | 0.87 (–3.37 to 5.11); p = 0.69 | 0.79 (–1.43 to 3.00); p = 0.49 | 0.15 (–1.65 to 1.95); p = 0.87 | –1.08 (–2.46 to 0.29); p = 0.13 | 0.26 (–1.48 to 2.00); p = 0.77 |
| 48 months | |||||
| MST | 60.76 | 60.93 | 57.96 | 53.41 | 55.37 |
| MAU | 62.73 | 61.19 | 55.87 | 53.18 | 55.31 |
| Difference (95% CI); p-value | –0.52 (–4.73 to 3.69); p = 0.81 | 0.73 (–1.14 to 2.60); p = 0.45 | 1.42 (0.19 to 2.65); p = 0.025 | 0.15 (–1.13 to 1.42); p = 0.82 | –0.51 (–1.95 to 0.93); p = 0.49 |
| Variable | ASR end point | ||||
|---|---|---|---|---|---|
| Avoidant personality | ADHD problems | Antisocial personality | Sluggish cognitive tempo | Obsessive–compulsive problems | |
| 24 months | |||||
| MST | 55.94 | 57.76 | 55.71 | 55.54 | 55.47 |
| MAU | 57.26 | 56.79 | 57.06 | 56.43 | 54.57 |
| Difference (95% CI); p-value | –0.70 (–2.52 to 1.12); p = 0.46 | –1.12 (–5.19 to 2.95); p = 0.59 | –0.97 (–3.22 to 1.28); p = 0.4 | –0.09 (–2.04 to 1.86); p = 0.93 | 0.33 (–1.54 to 2.20); p = 0.73 |
| 36 months | |||||
| MST | 55.31 | 58.44 | 57.25 | 55.04 | 53.92 |
| MAU | 56.75 | 57.62 | 56.95 | 56.07 | 54.04 |
| Difference (95% CI); p-value | –0.98 (–2.57 to 0.60); p = 0.23 | –0.84 (–3.04 to 1.37); p = 0.46 | –0.03 (–1.81 to 1.76); p = 0.97 | –0.74 (–2.61 to 1.14); p = 0.45 | –0.14 (–1.90 to 1.63); p = 0.88 |
| 48 months | |||||
| MST | 55.49 | 57.81 | 57.59 | 55.47 | 53.95 |
| MAU | 55.77 | 57.81 | 56.99 | 55.43 | 54.09 |
| Difference (95% CI); p-value | –0.20 (–1.70 to 1.29); p = 0.79 | –0.29 (–2.88 to 2.30); p = 0.83 | –0.11 (–1.97 to 1.74); p = 0.91 | –0.71 (–2.18 to 0.76); p = 0.35 | –0.40 (–1.92 to 1.12); p = 0.61 |
| Variable | CLES-A end point | |||
|---|---|---|---|---|
| 0–3 months | 0–6 months | 0–9 months | 0–12 months | |
| 24 months | ||||
| MST | 173.91 | 254.77 | 290.19 | 314.63 |
| MAU | 188.12 | 274.06 | 307.12 | 327.84 |
| Difference (95% CI); p-value | –5.71 (–34.27 to 22.85); p = 0.7 | –15.75 (–56.08 to 24.57); p = 0.44 | –15.42 (–62.30 to 31.47); p = 0.52 | –16.43 (–65.82 to 32.97); p = 0.52 |
| 36 months | ||||
| MST | 164.94 | 244.81 | 283.86 | 303.40 |
| MAU | 178.49 | 255.25 | 287.94 | 307.94 |
| Difference (95% CI); p-value | –7.39 (–37.95 to 23.16); p = 0.64 | –8.80 (–51.87 to 34.28); p = 0.69 | –3.79 (–53.95 to 46.37); p = 0.88 | –3.75 (–54.79 to 47.28); p = 0.89 |
| 48 months | ||||
| MST | 173.25 | 254.35 | 295.30 | 316.21 |
| MAU | 177.12 | 251.91 | 291.39 | 316.00 |
| Difference (95% CI); p-value | 5.46 (–25.67 to 36.58); p = 0.73 | 14.01 (–32.62 to 60.64); p = 0.56 | 12.88 (–39.48 to 65.24); p = 0.63 | 13.70 (–42.62 to 70.02); p = 0.63 |
Appendix 4 Parent-rated secondary outcomes
| Variable | APQ end point | ||||
|---|---|---|---|---|---|
| Corporal punishment | Inconsistent discipline score | Positive parenting score | Problems of monitoring and supervision | Parental involvement | |
| 24 months | |||||
| MST | 3.32 | 7.74 | 12.65 | 6.20 | 9.73 |
| MAU | 3.33 | 8.22 | 12.85 | 6.46 | 9.91 |
| Difference (95% CI); p-value | –0.01 (–0.14 to 0.13); p = 0.92 | –0.64 (–1.05 to –0.24); p = 0.0023 | 0.07 (–0.31 to 0.45); p = 0.72 | –0.53 (–1.00 to –0.06); p = 0.028 | –0.25 (–0.63 to 0.13); p = 0.2 |
| 36 months | |||||
| MST | 3.31 | 8.07 | 13.03 | 6.82 | 10.35 |
| MAU | 3.31 | 8.66 | 12.77 | 6.67 | 9.65 |
| Difference (95% CI); p-value | –0.03 (–0.19 to 0.13); p = 0.69 | –0.45 (–1.02 to 0.11); p = 0.12 | 0.43 (0.03 to 0.83); p = 0.042 | 0.17 (–0.30 to 0.64); p = 0.47 | 0.22 (–0.22 to 0.66); p = 0.33 |
| 48 months | |||||
| MST | 3.39 | 7.62 | 12.31 | 6.09 | 9.15 |
| MAU | 3.21 | 8.70 | 12.99 | 6.46 | 9.73 |
| Difference (95% CI); p-value | 0.04 (–0.17 to 0.24); p = 0.74 | –1.08 (–1.68 to –0.49); p = 0.00082 | 0.18 (–0.50 to 0.87); p = 0.6 | 0.29 (–0.47 to 1.04); p = 0.46 | –0.08 (–0.86 to 0.70); p = 0.84 |
| Variable | Scale/score | ||
|---|---|---|---|
| Couple Conflict Tactics Scale | Conners ADHD T score | Conners Learning and Language T score | |
| 24 months | |||
| MST | 5.16 | 66.87 | 62.19 |
| MAU | 4.56 | 67.08 | 63.47 |
| Difference (95% CI); p-value | –0.12 (–1.44 to 1.20); p = 0.86 | –0.59 (–3.54 to 2.36); p = 0.7 | –1.49 (–3.85 to 0.88); p = 0.22 |
| 36 months | |||
| MST | 5.31 | 64.77 | 61.62 |
| MAU | 4.61 | 65.23 | 62.58 |
| Difference (95% CI); p-value | 0.28 (–0.85 to 1.41); p = 0.63 | –0.30 (–3.58 to 2.99); p = 0.86 | –2.55 (–5.08 to –0.02); p = 0.053 |
| 48 months | |||
| MST | 6.80 | 62.16 | 59.73 |
| MAU | 3.88 | 63.46 | 62.78 |
| Difference (95% CI); p-value | 1.78 (–0.45 to 4.00); p = 0.13 | –1.36 (–5.63 to 2.92); p = 0.54 | –3.04 (–6.23 to 0.16); p = 0.069 |
| Variable | ABCL end point | |||||
|---|---|---|---|---|---|---|
| Friends | Spouse/partner | Personal strengths | Anxious/depressed | Withdrawn | Somatic complaints | |
| 24 months | ||||||
| MST | 1.53 | 1.31 | 46.27 | 58.65 | 59.00 | 54.89 |
| MAU | 1.70 | 1.43 | 44.58 | 59.84 | 60.61 | 54.85 |
| Difference (95% CI); p-value | –0.16 (–0.87 to 0.55); p = 0.65 | –0.12 (–0.80 to 0.57); p = 0.74 | –1.32 (–7.72 to 5.08); p = 0.69 | 1.65 (–2.64 to 5.94); p = 0.46 | –0.20 (–3.48 to 3.08); p = 0.9 | –0.04 (–2.02 to 1.93); p = 0.97 |
| 36 months | ||||||
| MST | 3.01 | 2.32 | 42.37 | 56.65 | 61.80 | 54.78 |
| MAU | 3.23 | 2.43 | 43.17 | 57.95 | 60.91 | 54.27 |
| Difference (95% CI); p-value | –0.21 (–0.92 to 0.50); p = 0.57 | –0.10 (–0.79 to 0.59); p = 0.78 | –0.69 (–3.97 to 2.58); p = 0.68 | 0.60 (–2.80 to 4.00); p = 0.73 | 0.56 (–1.61 to 2.74); p = 0.62 | 0.47 (–1.39 to 2.33); p = 0.63 |
| 48 months | ||||||
| MST | 3.37 | 4.27 | 41.03 | 59.51 | 60.34 | 54.04 |
| MAU | 4.02 | 4.66 | 41.45 | 56.51 | 61.12 | 54.08 |
| Difference (95% CI); p-value | –0.64 (–1.35 to 0.07); p = 0.078 | –0.38 (–1.07 to 0.30); p = 0.28 | 0.46 (–2.41 to 3.32); p = 0.76 | 2.26 (–0.96 to 5.49); p = 0.17 | 0.37 (–1.27 to 2.02); p = 0.66 | 0.38 (–1.00 to 1.76); p = 0.59 |
| Variable | ABCL end point | |||||
|---|---|---|---|---|---|---|
| Thought problems | Attention problems | Aggressive behaviour | Intrusive | Internalising problems | Thought problems | |
| 24 months | ||||||
| MST | 57.59 | 55.07 | 60.05 | 60.37 | 55.87 | 54.89 |
| MAU | 55.07 | 55.50 | 61.84 | 57.21 | 51.48 | 54.85 |
| Difference (95% CI); p-value | 1.60 (–2.23 to 5.43); p = 0.42 | –0.72 (–4.36 to 2.93); p = 0.7 | –0.43 (–3.17 to 2.31); p = 0.76 | 2.65 (–0.40 to 5.70); p = 0.1 | 0.62 (–5.63 to 6.87); p = 0.85 | –0.04 (–2.02 to 1.93); p = 0.97 |
| 36 months | ||||||
| MST | 55.02 | 56.64 | 61.85 | 59.13 | 51.62 | 54.78 |
| MAU | 54.61 | 55.00 | 63.39 | 59.16 | 52.38 | 54.27 |
| Difference (95% CI); p-value | 0.48 (–1.44 to 2.39); p = 0.63 | 0.18 (–1.91 to 2.27); p = 0.87 | –0.78 (–2.90 to 1.35); p = 0.48 | 0.39 (–1.73 to 2.52); p = 0.72 | –1.19 (–6.55 to 4.16); p = 0.67 | 0.47 (–1.39 to 2.33); p = 0.63 |
| 48 months | ||||||
| MST | 53.98 | 54.18 | 63.74 | 60.28 | 56.33 | 54.04 |
| MAU | 54.51 | 54.03 | 64.03 | 60.79 | 53.38 | 54.08 |
| Difference (95% CI); p-value | –0.71 (–2.66 to 1.24); p = 0.48 | 0.11 (–1.71 to 1.93); p = 0.91 | –0.35 (–2.30 to 1.59); p = 0.72 | 0.36 (–1.94 to 2.66); p = 0.76 | 3.74 (–1.45 to 8.93); p = 0.17 | 0.38 (–1.00 to 1.76); p = 0.59 |
| Variable | ABCL end point | ||||
|---|---|---|---|---|---|
| Externalising problems | Total problems | Critical items | Tobacco times per day | Alcohol days drunk | |
| 24 months | |||||
| MST | 57.03 | 58.66 | 58.92 | 1.48 | 1.25 |
| MAU | 57.33 | 58.40 | 58.53 | 1.53 | 1.40 |
| Difference (95% CI); p-value | –0.11 (–3.60 to 3.37); p = 0.95 | –0.84 (–5.36 to 3.67); p = 0.72 | 1.06 (–2.80 to 4.92); p = 0.6 | –0.05 (–0.58 to 0.48); p = 0.85 | –0.15 (–0.58 to 0.29); p = 0.5 |
| 36 months | |||||
| MST | 57.37 | 58.37 | 58.61 | 2.25 | 1.83 |
| MAU | 58.50 | 58.82 | 58.34 | 2.43 | 1.92 |
| Difference (95% CI); p-value | –0.68 (–3.35 to 2.00); p = 0.62 | –0.26 (–3.15 to 2.63); p = 0.86 | 0.65 (–1.48 to 2.77); p = 0.56 | –0.17 (–0.70 to 0.35); p = 0.52 | –0.09 (–0.53 to 0.34); p = 0.68 |
| 48 months | |||||
| MST | 58.22 | 56.47 | 56.95 | 2.34 | 1.87 |
| MAU | 58.87 | 57.89 | 58.09 | 3.07 | 2.52 |
| Difference (95% CI); p-value | –0.55 (–3.38 to 2.29); p = 0.71 | –0.35 (–2.83 to 2.14); p = 0.79 | 0.01 (–1.75 to 1.77); p = 0.99 | –0.73 (–1.25 to –0.20); p = 0.0068 | –0.65 (–1.08 to –0.22); p = 0.0034 |
| Variable | ABCL end point | ||||
|---|---|---|---|---|---|
| Drugs days used | Mean substance use | Depressive problems | Anxiety problems | Somatic problems | |
| 24 months | |||||
| MST | 1.34 | 1.67 | 56.64 | 53.73 | 54.84 |
| MAU | 1.34 | 1.69 | 59.96 | 52.79 | 54.01 |
| Difference (95% CI); p-value | 0.00 (–0.40 to 0.40); p = 1 | –0.02 (–0.97 to 0.93); p = 0.97 | –1.64 (–6.43 to 3.16); p = 0.51 | 0.54 (–1.46 to 2.53); p = 0.6 | 0.42 (–1.75 to 2.58); p = 0.71 |
| 36 months | |||||
| MST | 1.65 | 3.42 | 60.53 | 54.08 | 54.99 |
| MAU | 1.82 | 3.59 | 60.31 | 53.47 | 53.60 |
| Difference (95% CI); p-value | –0.17 (–0.57 to 0.23); p = 0.41 | –0.16 (–1.12 to 0.79); p = 0.74 | –0.23 (–2.58 to 2.12); p = 0.85 | –0.02 (–1.52 to 1.48); p = 0.98 | 0.89 (–0.83 to 2.61); p = 0.32 |
| 48 months | |||||
| MST | 1.88 | 3.39 | 60.72 | 53.07 | 53.87 |
| MAU | 2.44 | 4.91 | 60.38 | 53.57 | 53.77 |
| Difference (95% CI); p-value | –0.56 (–0.96 to –0.16); p = 0.0062 | –1.52 (–2.47 to –0.57); p = 0.0018 | 0.32 (–1.90 to 2.54); p = 0.78 | –0.04 (–1.62 to 1.54); p = 0.96 | 0.16 (–1.10 to 1.42); p = 0.8 |
| Variable | ABCL end point | ||||
|---|---|---|---|---|---|
| Avoidant personality | ADHD problems | Antisocial personality | Sluggish cognitive tempo | Obsessive–compulsive problems | |
| 24 months | |||||
| MST | 60.34 | 58.24 | 56.97 | 57.32 | 53.38 |
| MAU | 60.61 | 58.81 | 58.01 | 58.29 | 52.89 |
| Difference (95% CI); p-value | 0.56 (–2.31 to 3.44); p = 0.7 | –0.52 (–4.97 to 3.92); p = 0.82 | 0.00 (–3.68 to 3.67); p = 1 | –2.07 (–5.12 to 0.99); p = 0.2 | 0.10 (–2.37 to 2.57); p = 0.94 |
| 36 months | |||||
| MST | 63.83 | 61.50 | 59.77 | 60.07 | 52.58 |
| MAU | 62.40 | 60.28 | 59.13 | 59.18 | 52.21 |
| Difference (95% CI); p-value | 1.09 (–1.22 to 3.39); p = 0.36 | 0.57 (–1.71 to 2.85); p = 0.63 | 0.03 (–1.82 to 1.88); p = 0.98 | 0.54 (–1.73 to 2.80); p = 0.65 | –0.27 (–1.67 to 1.13); p = 0.71 |
| 48 months | |||||
| MST | 63.39 | 59.73 | 59.85 | 57.43 | 51.73 |
| MAU | 63.34 | 61.27 | 60.07 | 59.08 | 51.88 |
| Difference (95% CI); p-value | 0.34 (–1.50 to 2.17); p = 0.72 | –0.34 (–3.18 to 2.51); p = 0.82 | –0.27 (–2.45 to 1.90); p = 0.81 | –0.25 (–2.18 to 1.68); p = 0.8 | 0.14 (–1.35 to 1.62); p = 0.86 |
| Variable | FACES-IV | |||
|---|---|---|---|---|
| Cohesion score | Family communication | Family satisfaction | Flexibility | |
| 24 months | ||||
| MST | 58.51 | 36.73 | 32.17 | 46.22 |
| MAU | 60.73 | 37.59 | 33.02 | 48.48 |
| Difference (95% CI); p-value | 1.57 (–1.54 to 4.69); p = 0.32 | –0.17 (–1.22 to 0.89); p = 0.76 | 0.25 (–1.02 to 1.52); p = 0.7 | –2.22 (–4.37 to –0.06); p = 0.046 |
| 36 months | ||||
| MST | 60.76 | 38.43 | 33.59 | 47.70 |
| MAU | 56.72 | 37.19 | 32.17 | 48.18 |
| Difference (95% CI); p-value | 2.17 (–1.26 to 5.59); p = 0.22 | 0.59 (–0.58 to 1.76); p = 0.32 | 1.32 (0.06 to 2.59); p = 0.042 | –0.46 (–2.42 to 1.50); p = 0.64 |
| 48 months | ||||
| MST | 57.16 | 37.71 | 32.67 | 49.45 |
| MAU | 59.44 | 37.88 | 32.74 | 49.30 |
| Difference (95% CI); p-value | 2.41 (–1.78 to 6.59); p = 0.26 | 1.11 (–0.22 to 2.44); p = 0.11 | 1.13 (–0.58 to 2.85); p = 0.2 | –0.82 (–3.41 to 1.76); p = 0.53 |
| Variable | Questionnaire | ||
|---|---|---|---|
| ICUT | General Health Questionnaire | Loeber Caregiver Questionnaire total | |
| 24 months | |||
| MST | 33.30 | 53.63 | 45.92 |
| MAU | 33.84 | 54.32 | 46.48 |
| Difference (95% CI); p-value | –0.37 (–2.04 to 1.29); p = 0.66 | –1.48 (–3.85 to 0.88); p = 0.22 | –0.26 (–1.22 to 0.70); p = 0.6 |
| 36 months | |||
| MST | 33.45 | 52.96 | 46.53 |
| MAU | 32.77 | 56.42 | 46.96 |
| Difference (95% CI); p-value | –0.84 (–2.85 to 1.17); p = 0.41 | –2.09 (–4.71 to 0.53); p = 0.12 | 0.04 (–1.05 to 1.12); p = 0.95 |
| 48 months | |||
| MST | 32.90 | 55.12 | 46.65 |
| MAU | 31.75 | 56.90 | 46.69 |
| Difference (95% CI); p-value | –0.61 (–2.82 to 1.61); p = 0.59 | –2.86 (–6.11 to 0.39); p = 0.089 | 0.03 (–1.11 to 1.17); p = 0.96 |
| Variable | SDQ end point | |||||
|---|---|---|---|---|---|---|
| Conduct problems | Emotional problems | Hyperactivity | Impact | Prosocial | Total difficulties score | |
| 24 months | ||||||
| MST | 4.08 | 3.43 | 5.11 | 2.76 | 6.11 | 15.67 |
| MAU | 4.38 | 3.29 | 5.33 | 2.74 | 6.26 | 15.79 |
| Difference (95% CI); p-value | –0.19 (–0.60 to 0.21); p = 0.35 | –0.23 (–0.59 to 0.14); p = 0.22 | –0.39 (–0.81 to 0.04); p = 0.079 | –0.15 (–0.60 to 0.29); p = 0.5 | –0.06 (–0.47 to 0.35); p = 0.77 | –0.78 (–1.83 to 0.28); p = 0.15 |
| 36 months | ||||||
| MST | 4.49 | 3.42 | 5.81 | 2.80 | 6.08 | 16.62 |
| MAU | 3.92 | 3.58 | 5.70 | 2.76 | 6.20 | 15.99 |
| Difference (95% CI); p-value | 0.10 (–0.37 to 0.57); p = 0.69 | –0.20 (–0.70 to 0.30); p = 0.44 | 0.06 (–0.36 to 0.49); p = 0.78 | 0.04 (–0.53 to 0.61); p = 0.89 | –0.02 (–0.40 to 0.35); p = 0.9 | –0.05 (–1.20 to 1.11); p = 0.93 |
| 48 months | ||||||
| MST | 3.98 | 3.52 | 5.48 | 2.78 | 6.37 | 15.86 |
| MAU | 3.75 | 3.94 | 5.77 | 2.87 | 6.42 | 16.24 |
| Difference (95% CI); p-value | –0.10 (–0.64 to 0.44); p = 0.71 | –0.20 (–0.85 to 0.45); p = 0.54 | 0.07 (–0.51 to 0.65); p = 0.82 | –0.08 (–0.94 to 0.79); p = 0.86 | 0.06 (–0.50 to 0.62); p = 0.85 | –0.62 (–2.05 to 0.82); p = 0.4 |
Appendix 5 Expanded description of Multisystematic therapy
Multisystemic therapy is an intervention for antisocial behaviour. MST is an intensive family- and home-based intervention specifically developed for young people with serious and persistent antisocial behaviour. It aims to prevent reoffending and out-of-home placements. MST was developed in response to research on the multidetermined nature of serious antisocial behaviour, and adopts a social-ecological approach to intervention. The underlying premise of the social-ecological approach embedded in MST is that serious and persistent antisocial behaviour is multicausal; therefore, effective interventions address the multiple sources of offending behaviour that are found not only in the young person (e.g. values and attitudes, social skills and biological factors) but also in his or her social ecology (i.e. the family, school, peer group and neighbourhood). The key risk factors associated with serious and persistent antisocial behaviour have been identified through decades of longitudinal research and include impulsivity and overactivity on the part of the young person; low levels of parental involvement, and harsh, critical parenting; high levels of family conflict and disruption; and the young person’s associations with other deviant peers. Consequently, in MST, the therapist works primarily with the caregiver to improve his or her parenting skills, enhance family relationships, increase support from social networks, encourage school attendance and achievement for the young person, and reduce the young person’s association with delinquent peers.
Multisystemic therapy aims to have an impact on the entire milieu in which the young person operates by using multiple interventions in combinations indicated by the clinical picture. The treatment approach integrates theoretical concepts and techniques from systemic and structural family therapy, parent training, marital therapy, supportive therapy related to interpersonal problems, social skills components, social perspective training, behavioural methods (e.g. contingency contracting) and cognitive therapy techniques (e.g. self-instructional training). The therapist, normally a graduate mental health worker, is trained in MST as part of a standardised training programme and is supervised consistently at all stages of each active intervention they undertake. MST therapists work as part of a team and receive supervision from a qualified senior supervisor. Each accredited team receives further supervision from a representative of the North American MST organisation, which also monitors adherence to the protocol independently of this supervision process. The therapist has an active role as case manager (with typical caseloads of between four and six families), which includes acting as an advocate with outside agencies.
Multisystemic therapy will typically begin by creating a formulation with the parent and young person that identifies the key drivers of a problematic behaviour such as aggression in the home. This includes the individual, parent, family and peer or school drivers that contribute to this problem. Additional drivers of problematic behaviour could originate from schools, treatment providers or other agencies that have been involved with the family. Once all of the drivers have been identified, the young person and parent(s) will have generated solutions with the therapist. Owing to the nature of antisocial behaviour, these will involve parenting skills and (improving) parent–adolescent interactions, for example the contingency contracting noted above. Agreed solutions are be tracked intensively over time with regular follow-up, sometimes on a daily basis, with adjustments to strategies made as more clinical ‘data’ come in. The intensive involvement lessens as the family becomes more skilled and resourceful, and as indigenous supports such as extended family members are brought in as needed or appropriate. Routine feedback about progress is central and is given through discussions and by tracking change via graphs. The sessions usually end when the major treatment goals identified at the beginning of therapy have been met and when sustainability plans have been agreed to address any slippages in the gains and functioning that have been achieved.
Appendix 6 Outcomes from CYPRESS evaluation conducted during the first phase of the trial (October 2012)
Background
Between November 2011 and April 2012, members of your service took part in the CYPRESS procedure as part of the START randomised controlled trial. The intention here was to develop a measure of service quality that allows assessment of the service delivery aspects of complex interventions for children and young people with conduct and related psychosocial problems, and to characterise MST and MAU in the START trial along these dimensions. The measure is intended to have utility across a range of interventions for young people in general, developed as it has been to capture the service delivery frameworks of both MST and usual services.
CYPRESS was developed by Stephen Butler, Stephen Pilling and Cressida Gaffney on the basis of a review of existing measures in the field, as well as research into the central aspects of service delivery that support complex interventions, as an interview-based measure of the service delivery frameworks supporting complex interventions. The opinion of a further two experienced clinicians was called on in the development of the measure; they reviewed an early draft and their considerations were incorporated into the design of CYPRESS. CYPRESS was piloted with two non-START trial teams, and subsequently administered to 17 teams (9 MST and 8 MAU) taking part in the START trial. The results of these interviews were used to compare the service delivery elements supporting MST and MAU, and to characterise the MAU services in the trial.
The measure
CYPRESS comprises three sections, aimed at capturing key issues pertaining to service delivery level factors that characterise a service. These are as follows: service characteristics (scored out of 30), team operation (scored out of 30) and delivery of interventions (scored out of 40). Below are the item headings and one sample item for each of the three sections.
Service characteristics
Item headings are as follows: ‘shared model of care’, ‘population served’, ‘care pathway’, ‘service capacity’, ‘relationship to other services’ and ‘service/team staffing’.
Sample item: ‘shared model of care’ –
Service has a comprehensive and shared view of the model of care provided which is owned by the service.
Team operation
Item headings are as follows: ‘team meetings’, ‘supervision’, ‘staff training’, ‘team communication’, ‘client outcome monitoring’ and ‘quality assurance’.
Sample item: ‘team communication’ –
Team has clear policies and procedures for communicating information about clients and decisions made by the team, with team colleagues, to clients and with other agencies.
Delivery of interventions
Item headings are as follows: ‘range of interventions consistent with model’, ‘assessment’, ‘individualised care’, ‘family/carer involvement’, ‘assertive engagement’, ‘interventions provided in a range of settings’, ‘risk and child protection’ and ‘case management’.
Sample item: ‘assertive engagement’ –
The team has an assertive approach to the engagement of clients and families/carers (e.g. a ‘no drop out’ policy or a stress on overcoming difficulties in engaging with services).
CYPRESS was designed to be accessible and simple to use. The scale was designed to be scored out of 100, with 20 questions to be scored on a five-point scale, from one to five.
The scale is designed in such a way that the possible scores are given alongside a brief description of the features that characterise that particular score, so raters have the specific features of a given rating available at the time of scoring. Furthermore, the CYPRESS manual was developed to guide raters to where further clarification was needed with regard to the scoring scheme.
The presence of two raters was key, and agreement between them on a final score was considered to be important for reliability. Rating by two people was warranted because of the complexity of the data and to reduce the chance of bias in scoring, thus increasing the robustness of the scores allocated to teams.
Characterisation of management as usual
Characterisation and comparison of the different MAU services in the START trial is an interesting part of this endeavour, offering a perspective on the relatively unexplored usual services, seen here in the context of comparison with MST. Given the restrictions on the reporting of outcome data until the trial is completed, the characterisation of MAU will be the main findings reported here.
The teams constituting MAU represented the following categories:
-
child and adolescent mental health services
-
youth offending team
-
family support charity project
-
specialist local authority child safeguarding service
-
specialist local authority family intervention team.
Some key observations on the nature of the MAU services are summarised below.
Service characteristics
Management as usual services were a combination of NHS, local authority, charity and jointly commissioned services. Those services that operated under joint arrangements highlighted some of the tensions that can arise from this way of organising services, for example as regards child protection policy, team communication and training.
Referral reasons in the highest functioning teams were likely to represent problems of a nature both more serious and more complex, with greater numbers of child protection cases and serious difficulties disrupting the family home. Teams varied in terms of whether their service was preventative, curative or both. Although this distinction was not necessarily addressed explicitly in CYPRESS, it became apparent over the course of the interviews with the teams.
Clarity around questions on maximum caseload numbers, that is both whether such a maximum existed and what it was, differed across teams. In the teams that scored more highly on CYPRESS, there was agreement between supervisors and therapists on both of these questions. These issues could not clearly be linked to, or explained by, the actual caseloads.
The teams that scored more highly on CYPRESS comprehensively articulated the nature of the different roles in the team, the ways in which they interact with one another, the formal hierarchies that govern lines of responsibility and decision-making in the team, and detailed descriptions of when and how particular responsibilities are enacted. There was variation in terms of the requirement for professional qualifications across the teams, but what was apparent in the teams that performed highly on CYPRESS was that, where less highly skilled workers were employed, their roles were clearly delineated and their supervision by professionally qualified staff was considered integral to their role.
Team operation
Team meetings and supervision scores were consistently high. Teams across the sample also scored highly on supervision with little differentiation, yet there were examples of less and more effective supervisory practices that were reflected in respondents’ answers but could not be accurately be reflected in scoring because of the scope of the measure. The key difference, and this was very similar to what was seen in MST teams, was that, although supervision was available to everyone, the provision of supervision that offered the chance for reflection varied widely.
It was apparent in all the teams that training is somewhat more variably offered in MAU than in MST teams, where there are very clear expectations for training at induction and regular booster sessions for all. Although a range of professional backgrounds qualify someone to work as a MST therapist, there is compulsory initial training that must be undertaken before they can commence work as a MST therapist. In none of the MAU services was the same uniformity of training opportunities seen.
Delivery of interventions
Higher performing (as measured by CYPRESS) teams reported comprehensive, structured assessments that routinely used multiple sources of information. Assessment practices in the other teams showed more variability, and were characterised by a less systemic approach.
What distinguished between teams that scored more or less highly on CYPRESS as regards interventions was not simply whether or not there was a range of interventions offered by the team, although this was necessary, but whether or not those interventions were available in a timescale that would be appropriate and therefore useful. Furthermore, there was the issue of which professional a child was allocated to, as not all professionals were able to offer the same service, even when functioning in a generic professional role. This is distinct from those instances where children receive different professional input by design in order to access a particular intervention, for example family therapy sessions. This finding could not necessarily be said to have emerged directly from administering CYPRESS in any given setting, but rather from a synthesis of information gathered over the course of interviewing all the teams with whom the raters met.
Risk management and child protection was the other area, along with meetings and supervision, where all teams scored highly. However, those teams that scored relatively lower noted some challenges arising from its implementation where there are slightly different policies in place across two organisations, and a team is ultimately accountable to both.
The approach to family involvement differed across teams, with different emphases on working with the wider system around a young person.
An assertive approach to engagement was observed in most teams, with only a small minority scoring less highly on this item. By and large, assertive engagement was considered an important part of the work with children or young people and their families by all teams interviewed, with the emphasis being on it increasing with increasing levels of severity and risk. On the basis of this small sample, it seemed that the more generic a service, the less likely assertive engagement was to be reported.
General observations
A particularly striking feature of the teams was the degree to which there was agreement between therapists and supervisors. In the highest-scoring teams (as measured by CYPRESS), there was evident shared knowledge and ways of thinking, whereas in the less high scoring teams there were occasional inconsistencies in factual information, and a shared way of talking about the service, both in practical and philosophical terms, was less apparent.
A model of shared knowledge of the cases in the team, albeit at differing levels of detail, was employed in the higher-scoring teams. None of the teams operated this shared case knowledge model to the same extent as it is used in MST, but it was nonetheless in place in the higher-functioning teams.
The general sense of the lowest-scoring MAU services was of more disparate, less cohesive teams, with a broader, less well-delineated remit or statement of population served. These features did not seem here to be related to the size of the team or, indeed, to the wider organisation.
Observations on the nature of management as usual teams
During the interviewing process, an issue emerged that had not been considered during the measure development phase; a key distinction between different MAU teams was that some were services with which involvement was voluntary for all families, and others were statutory services, that is to say those with which families or young people were compulsorily engaged, as a result of child protection or youth justice legislation, whereas some worked with both voluntary and compulsory cases. Staff spoke of the differences in terms of engagement in the light of whether a young person or family’s involvement was voluntary or otherwise.
The question arose during the research process as to who exactly a team considered to be its client: the young person, the parent/carer(s) or the whole family system. This has implications for how a team scores on the items that look at individualised care and family/carer involvement; some workers might consider their practice to be collaborative with the young person to the exclusion of the parent/carer, or indeed vice versa. In MST, the parent/carer is the primary person with whom the therapists work; there is no compulsion for the young person to be involved in the meetings. This is quite different from the practice in some of the usual services interviewed.
Conclusions
Analysis found that median scores on the CYPRESS measure across the three subsections and total score showed significant differences between MST and MAU teams. The MST teams consistently scored higher on average and demonstrated narrower ranges of scores across the three subsections and total score. However, individual MAU teams in several cases scored higher than MST teams. A case comparison explored a number of ways in which the highest- and lowest-scoring MAU teams were different from one another in terms of the service delivery framework in which they work. It should be noted that the findings outlined above represent both data that emerged directly from the CYPRESS procedure and understandings formed by the raters as a result of interviewing a number of teams and synthesising the information gathered.
We concluded that CYPRESS is a viable means of distinguishing between services that provide complex interventions for children and young people. It offers the chance to characterise services on the basis of the service delivery frameworks that support them rather than by the specific features of interventions, and as such can be used across a range of different services. The potential for bias in development, administration of CYPRESS and analysis of scores is noted, and all findings are considered in view of these, yet overall the CYPRESS procedure indicates that there is potential for further development and use of this means of measuring and characterising services. Further development and testing of CYPRESS is recommended.
Appendix 7 Supplement to qualitative study 1
Interview schedules for parent and young person
Interview schedule multisystemic therapy: parent/carer
Introduction
We’d like to find out about your experiences of MST, both good and bad, in your own words. I am not part of the trial of MST; I am a neutral researcher, so I hope you will feel you can be honest with me and say what you really think about it.
I’ll be asking you to think back about your experience of MST, whether things changed during it, and how things have been since it ended. We’re interested to know what about MST was helpful, and what was less helpful, and also about other things that have affected how things are going for you and your family now.
Current situation
To begin with, I’d like to find out about what’s going on for you right now.
-
How are things at the moment?
-
How are things with [young person]?
-
What’s going well?
-
What’s not going so well?
-
-
Do you feel things are any different now compared to before you started MST?
-
If so, how are they different?
-
General experience of multisystemic therapy
So your MST therapist worked with you from _______to _______. I’d like to spend some time now finding out what that time was like for you.
-
How did you find MST?
-
What was most helpful?
-
Was there anything which wasn’t helpful?
-
Changes during multisystemic therapy
-
Did things change at all during MST?
-
What were things like before MST started?
-
What led up to the MST team working with your family?
-
In what way did things change?
-
-
-
[If there were changes], do you think those changes had anything to do with MST?
-
If so, in what way?
-
What was it about MST that helped things to change?
-
Were there other things that affected the changes, besides MST – for example, things to do with yourself or [young person], with you as a family, or with things outside the family?
-
-
How did you feel about the MST therapist ending her visits?
-
Did you feel ready to finish?
-
-
Did you feel you had learnt anything from MST that was helpful at that time?
-
What was the most helpful thing that MST taught you?
-
What was the biggest problem or difficulty?
-
Changes since ending
Now I’d like you to think about how things have been since ending MST.
-
Have things changed since the end of MST?
-
In what way?
-
-
You said things were [e.g. going well] at the end of MST but that things are [e.g. difficult] at the moment. What has happened in between to change things?
-
How do you make sense of that?
-
Do the changes have anything to do with MST?
-
-
You say that [e.g. you are fighting less]. Did MST contribute to that?
-
In what way?
-
Were there other things that affected the changes, besides MST – for example, things to do with yourself or [young person], with you as a family, or with things outside the family?
-
-
Did you learn anything through MST that has stuck with you?
-
Is there anything you took from MST that you now think you could not do without?
-
-
Do you have other sons or daughters?
-
Have you noticed any changes in the way you parent them?
-
Were those changes to do with skills you learnt in MST?
-
Did anything else affect those changes, besides MST – for example, things to do with yourself or [young person], with you as a family, or with things outside the family?
-
-
Was there anything about MST you found less helpful or less important?
-
Was there anything that made it hard to use what you had learnt in MST?
-
Do you have any ideas about why things went the way they did? [why MST didn’t do what you hoped it could/why things got worse again after they seemed to get better, etc.]?
Positive times
Can you think of an example of a time since MST ended when things have gone particularly well, or when things have been difficult but when you handled something well?
-
Can you tell me more about the situation?
-
What did you do when this happened?
-
Did your experience with MST make any difference to what happened in this situation, or to how you or [young person] responded?
Periods of crisis
Can you think of an example of a time since MST ended when things have gone badly, or when you didn’t feel you handled things well?
-
Can you tell me more about the situation?
-
What did you do when this happened?
-
Did your experience with MST make any difference to what happened in this situation, or to how you or [young person] responded?
Future
-
Thinking about the future, are there any things from MST that you think you’ll use or will stick with you?
-
Are there any things about MST that you think won’t be helpful in the future?
-
Other than MST, what do you think will help to keep things going well or help to change things in the future?
-
What might get in the way or make it difficult?
Concluding questions
-
What do you think things would be like now if you hadn’t had MST?
-
Imagine you are giving feedback to the people who developed MST. What would you like to tell them?
-
If your friend was having similar problems within their family, would you recommend MST to them as something that could help? Can you tell me your reasons?
-
I understand that MST is 5 months of really hard work. Do you think it was worth it?
-
I told you at the start that I wanted to understand what’s changed, and how. Have I asked the right questions? Is there anything else we haven’t talked about, anything I’ve missed?
Interview schedule multisystemic therapy: young person
Introduction
I’m here to talk to you about how you found MST. I am not part of the trial of MST; I am part of a team of researchers, so I hope you will feel you can tell me what you really think about it, both any good things and any bad things.
What I’d really like to know is whether things have changed since MST – and if so, how they’ve changed. I’m trying to understand how MST might have helped with any changes. I’m interested to know what about MST was helpful and what wasn’t, and also about other things that have helped you and your family deal with the things you wanted help with.
Current situation
-
So, first of all, how are things going for you at the moment?
-
What’s going well?
-
What’s not going so well?
-
General experiences of multisystemic therapy
-
What led up to the MST team working with your family?
-
Can you tell me a bit about how you were involved in MST?
-
Who [else] was involved in the MST?
-
What were some of the reasons for that?
-
What was that like?
-
How did you feel about that?
-
-
What did you think of MST?
-
What did you like or not like about MST?
-
What was most helpful about MST?
-
Was there anything you didn’t like or thought wasn’t helpful?
-
-
Did you learn anything from MST?
-
Do you think [your mum] learnt anything?
-
What was the most helpful thing that MST taught you?
-
What was the biggest problem or difficulty?
-
Changes
-
Are things now any different to before you started MST?
-
What were things like before MST?
-
[If there are differences now], what’s changed?
-
Is anything different now with [your mum/dad]?
-
Are you doing anything differently?
-
-
-
Do you think those changes had anything to do with MST?
-
If so, in what way?
-
What was it about MST that helped things to change?
-
Were there other things that helped, besides MST – for example, things to do with yourself, with your family, or with things outside the family?
-
-
How have things been since the end of MST?
-
Have things changed since the end of MST?
-
In what way?
-
Have changes that started during MST continued since it finished?
-
Why do you think that is? Tell me some of the reasons.
-
Does this have anything to do with MST?
-
In what way?
-
Were there other things that affected how things have gone, besides MST – for example, things to do with yourself or [your mum/dad], with you as a family, or with things outside the family?
-
-
Did you learn anything through MST that has stuck with you since MST ended?
-
Is there anything you’ve stopped using?
-
Tell me more about that.
-
-
Was there anything that made it hard to use the things you’d learnt?
-
Do you have any ideas about why things went the way they did? [why MST didn’t do what you hoped it could/why things got worse again after they seemed to get better, etc.]?
Future
-
Are there any things from MST that you think will stick with you in the future? Is there anything you’ll continue to use?
-
What might get in the way or make it difficult?
-
Do you think things will change in the future?
-
What do you think will help [keep things on track/help things get better] in the future?
Concluding questions
-
What do you think things would be like now if you hadn’t had MST?
-
Imagine you are talking to the people who developed MST. What would you like to tell them?
-
If your friend was having the same sort of problems as you, would you recommend MST to them as something that could help?
-
Can you tell me why?
-
-
I understand that MST is 5 months of really hard work. Do you think it was worth it?
-
I told you at the start that I wanted to understand what’s changed, and how. Have I asked the right questions? Is there anything else we haven’t talked about, anything I’ve missed?
Analysis stage 2: developing the coding frame
Extract from a transcript (P2)
Suggested themes noted in the margin as part of the development of the coding frame
| Name of code | Code | |
|---|---|---|
| 1. |
How things were before What life was like before and reasons for MST getting involved |
|
|
How things were before for the parent For example stress, isolation |
1.1 | |
|
How things were before for the young person For example at school, with friends, any police involvement or risk to young person |
1.2 | |
|
How things were before in parent–child relationship For example arguments, shouting |
1.3 | |
|
How things were before in the family For example difficulties with other children in family or with wider family |
1.4 | |
|
How things were before: other Anything else in wider environment |
1.5 | |
| 2. |
Experience of MST Descriptions of how participant found the experience of MST and how they got on with the therapist. Include thoughts about MST beforehand |
|
|
Therapeutic relationship For example getting along with; having someone to talk to; trust; confidential; therapist going above and beyond. Include concerns or exceptions |
2.1 | |
|
Experience of MST generally Positive and negative aspects of the MST not included in the therapeutic relationship For example intensity of the time commitment Include whether or not would recommend, any comments for developers |
2.2 | |
| 3. |
What changed or did not change/how are things now? Descriptions of what changed, or what is different now Include exceptions, i.e. what did not change or got worse |
|
|
Changes in the parent For example being calmer now or managing feelings better; not being reactive; thinking things through; understanding difficulties better Include exceptions, e.g. parent still feels isolated |
3.1 | |
|
Changes in the young person For example managing anger better; taking time to cool off; keeping self safe; making different choices; developing maturity, more positive view of their future, involvement in education/employment Include exceptions: lack of change; things that are still same |
3.2 | |
|
Changes in the relationship between child and parent For example talking more; feeling closer; fewer arguments; less escalation; understanding each other better; appreciating the impact of their behaviour on the other |
3.3 | |
|
Changes in the family For example changes in relationships with wider family or in parenting other children |
3.4 | |
|
Changes outside the family For example changes at school; new friends |
3.5 | |
| 4. |
Attributions of change or lack of change: MST Descriptions of what about MST made the difference, i.e. include here where participants are specifically attributing change to MST Include any exceptions in each specific category |
|
|
Specific things for parents For example reward charts, rewards and consequences, rules and contracts Include also: gaining confidence in ideas already using, testing out new ideas, generalising the ideas to other areas, having new ways to respond, for example, ‘thinking things through’, ‘having new options’, etc. Include also ideas that did not work |
4.1 | |
|
4.2 | |
|
4.3 | |
|
The process of MST/general attributions Include comments about how the process of MST was important in the changes that were made – e.g. therapist facilitating discussions; intensity and momentum; having someone to talk to |
4.4 | |
| 5. | Attributions of change or lack of change: non MST | |
|
Descriptions of changes that are not related to MST input For example changes at school/college; moving house; different friends; money pressures; health difficulties; medication; computer games (community and achievement); challenging life events; young person maturing anyway Include exceptions, i.e. things that went wrong |
5.1 | |
|
Other sources of support Descriptions of other sources of support Include exceptions, for example, losing previous support, or other support that was unhelpful |
5.2 | |
| 6. |
Trajectories and timing of changes When change happened and how. For example, was it a gradual process, an epiphany, did it start during MST and continue afterwards? |
|
|
Changes during MST Include descriptions of how things changed during MST, for example, ‘things were looking up’ when MST ended; include feelings towards ending – as this highlights at what stage things were when MST came to an end Include exceptions, that is, stayed the same or got worse during MST |
6.1 | |
|
Changes since MST: changes have continued: Things have continued in the same way since MST |
6.2 | |
|
Changes since MST: things have got better since ending: Things have improved since MST, e.g. ideas have become easier to implement, everybody has got more used to it, confidence increased now doing it alone, etc. e.g. ‘It started the ball rolling’ |
6.3 | |
|
Changes since MST: things have been up and down Descriptions that things are not consistent – sometimes things go well but there are times when things get worse again. e.g. ‘up and down the ladder’; ‘things work for a while’; ‘we’ve hit a rocky patch’ |
6.4 | |
|
6.5 | |
|
‘If it wasn’t for MST’ What things would be like now without MST, e.g. we would not be living together/have a relationship; I would have ‘cracked up’/’strangled him’ NB: this heading is under ‘trajectories’, as it gives a sense of where things were headed before MST – i.e. if they were deteriorating or staying the same |
6.6 | |
| 7. | Future | |
|
Hopes and concerns for the future General comments about the future – i.e. not related to MST Include any descriptions highlighting that participants think more about the future now in general, e.g. ‘She has ambition now’ |
7.1 | |
|
Thoughts about MST in the future Comments about whether MST will continue to influence into the future, e.g. do participants think they will still be using what they learnt? |
7.2 | |
| 8. | Interview process | |
| Use this code where participants comment on the process of the interview itself. For example, comments about it being hard to remember, any confusion expressed about the research and trial vs. therapy itself, what it is like looking back/being asked about it | 8.1 |
|
Extract from initial summary table Three codes (4.1, 6.1 and 6.3) for a single participant (P2) |
||
|---|---|---|
| 4.1 Attributions of change: MST – parent | 6.1 Changes during MST | 6.3 Changes since MST: things have got better since ending |
| ‘Made such a difference’ knowing therapist was coming and would advise. [also 2.1] Having someone to talk to. ‘It works’ to follow new approach and ‘so that’s what I do’Changed the way I deal with things completely. New approach is ‘taking a step back’ and thinking through best way to deal with something, rather than shouting and ‘jumping in with both feet’. (Hard at first to control temper but in control of it now.) Helpful ‘seeing what the problems were as well’‘[MST therapist] gave me the confidence to know what I was doing.’ [Most important thing learnt:] ‘every problem has a solution and you need to think it through’. Revelation to realise you could take time to think rather than dealing then and there. You can only demonstrate what works for yourself. (i.e. others telling you doesn’t help) When young person not taking tablets ‘nothing works’ but still don’t lose temper. [cf. 4.3 and 5.1] [Idea of stepping back and thinking, rather than any particular strategy.] Keeping calm rather than escalating [example of handling difficult situation] Still doing it – keeping calm and thinking through, including when young person stressed [managing difficulties/setbacks?]Using it in other areas of life too. Skills have been put to the test because of very challenging circumstances [cf. 5.1] | Things changed ‘a bit’, during MST but ‘not a huge amount as far as our relationship goes’‘It started the ball rolling for me’Didn’t want to end but it was ok when it came to it. Had given knowledge and confidenceClearer in mind where needed to goAt the time of ending felt had learned things but ‘not so much as I do now’ [cf. 3.1–3.3] | ‘I think it changed gradually ‘cause it takes a long time to get used to doing things in a different way.’ ‘Looking back on it now and the way things are now, it changed the way I deal with things completely.’ ‘It’s evolved really. I think that’s why it’s different now to how it was when we first . . . because I suppose different things work for different families, but yeah, thinking things through and thinking up a strategy that would work and the right incentives for [young person], that’s how it’s worked. So that’s constantly changing I suppose, really’Using what learned in other contexts – it’s useful in ‘every situation’. Might not always solve it but always helpfulRelationship improved. More time to talk (related to [specific circumstances]). Young person moved out for a bit which helped (due to move out again) [cf. 5.1] |
| Participant summary: P2 |
|---|
|
Before/after MST: significant changes in the way parent manages things at home and with young person, specifically taking time to think about how to respond, and generally being calmer, not escalating. She reported fewer changes in the young person, who she feels is depressed, and for whom the biggest difference is whether or not she is taking her medication. Understands young person more now. Talk more Experience of MST: valued the support from the therapist, as she had felt ‘alone’. Getting advice. Having someone to talk to. Everyone should have MST Timing of changes/trajectory: parent described that things changed during MST but not so much as they have now. MST ‘set a ball rolling’. Gradual changes MST attributions: having someone to talk to. A new way of responding – thinking things through. Seeing what problems were. Talking more (especially since MST). Seeing for yourself that it is better when you do not shout. Keeps going because it works (have not really needed paperwork). Getting used to it – ‘evolving’. Useful in other situations too, even when it does not solve it Other factors: parent also reported that there were significant other factors that had affected changes, especially the young person’s depression and difficult recent experience for the young person and family. Having time to talk [because of circumstances] helped, and young person moving out for a while also helped. (Plan for young person to move out again soon seen as positive.) If it was not for MST: would have fallen out beyond repair Future: continuing with being ‘the person I’ve become’ |
| Interview/coding notes |
|
Very rich interview, parent spoke honestly (I thought) and thoughtfully, without much need for prompting. Interesting that parent was very clear about improvement since MST, and that she felt the interview had prompted her to look back and made her realise that what she thought had been important at the time is different to how she sees it now A lot in this interview about links between changes in parent and changes in relationship (even without much change in the young person). Also on trajectories of change and thinking about why things have gone the way they have |
| Example from initial indexing across the entire data set for three codes (4.1, 6.1 and 6.3) | |||
|---|---|---|---|
| Name of code | Examples from initial indexing | Code | |
| 4. | Attributions of change or lack of change: MST | ||
| Specific things for parents |
Specific ideas: fit circles, rewards and consequences, contracts, scales (e.g. anger thermometer) Developing confidence in ideas – including those that had already been tried Testing things out for self – seeing if they work Generalising to other areas – other children, other relationships. Evolving Responding differently: taking a step back; thinking things through; having new options – and knowing that there is a choice in how you respond Following through New understanding (including being able to see previous patterns, cf. 1.3) Exceptions: Ideas parent did not agree with, e.g. ‘too old’ for sticker charts Things moving too quickly – e.g. planned interventions quickly became out of date as young person was presented with new difficulties Other things made it hard to implement ideas, e.g. money implications of rewards made it hard to be consistent, young person not motivated by rewards. Things only working for a while |
4.1 | |
| 6. | Trajectories and timing of changes | ||
| Changes during MST |
Achieved goals and ready to end: no more for therapist to do Hard to trust that enough had been done – changes only just beginning or not yet seen; concerned about ending: felt needed more Changes seen but concern about continuing alone Could not wait to end: ‘I had to get better so she’d go!’ (young person) Nothing had changed Things were worse than before – e.g. MST caused more escalation |
6.1 | |
| Changes since MST: things have got better since ending |
Ideas have become second nature, so it’s not such hard work now (parent) Everybody has got used to it and knows what to expect Experience of handling things alone has built confidence Generalising ideas to other situations and relationships – expanding influence |
6.3 | |
Analysis stage 4: chart development
Chart development: extract from chart for one participant (P2)
Codes from initial indexing are combined and divided into new categories
| Describing trajectory | Attributions of trajectory |
|---|---|
|
Changes during MST: It did change a bit during MST, but not so much as now. It set a ‘ball rolling’ Confidence and knowledge Less change in relationship during MST |
During MST: Having someone to talk to, getting advice New approach – thinking things through and planning what to do – changed the way I deal with things completely Understanding problems Seeing that what doing is working |
|
Changes since MST: Further changes since MST Relationship improved Evolving and gradual Things are up and down, but still using what learned |
Since MST: Looking back – changed way I deal with things Do not need to look back at paperwork because new way works, so that is what parent uses. Every problem that you come across you can apply the things that you have learned Getting used to the way deals with things Understanding young person better Still deal with things in a better way – sticking to what I say; sometimes it doesn’t work but I do not get so angry. Skills have been put to the test since ending Attributions other than MST: young person’s ‘nature’. Two different people depending on whether takes tablets; having time to talk to young person [because of circumstances] – made parent realise that talking helps – [MST helped pave the way for this change] Main thing is whether young person is taking her tablets So much else has happened |
Analysis stage 5: mapping and interpretation
Developing themes: initial thoughts on thematic structure
| Trajectories of change during MST | Attributions of change during MST |
|---|---|
| Descriptions of the trajectory of changes seen or not seen during MST. i.e. not about content but direction of change. Participants sometimes described different levels of changes – for example improvements in one domain but not others. In addition, single changes could be described in a mixture of ways |
Descriptions of what it was about MST that influenced the changes NB these attributions do not have one-to-one correspondence with the trajectories opposite but relate to the type of things participants described as being important in how things went |
|
Got better quickly: goals achieved Some participants said that their goals had been achieved by the end of MST, and once the therapist finished their visits it was felt that there was no more for them to do (e.g. parent 11 and parent 9) |
What helped Descriptions of exceptions: things about MST that were not helpful, or reasons why MST did not help For example things changed too quickly and ideas could not be followed though (e.g. P6) Young person not engaging with therapist or not trying to make changes; parent not following their side of behavioural contract (YP6) Feeling that therapist was biased towards parent (YP5) Some suggestions parent did not agree with (e.g. too old for sticker charts) Descriptions of other things which influenced change Other factors to do with parent, young person or environment |
|
Changes began during MST Some participants said that while they had noticed some ‘signs’ (P10) of change by the end of MST, they still felt there were further changes to be made and that when MST finished it was still a work in progress Sometimes this was a matter of trusting that subsequent changes would be seen (e.g. P4) (NB this is slightly different to those who felt that things got better after MST, although the two categories sometimes went together) |
|
|
Small changes during MST Some participants described that there were some changes during MST, but that these were limited in range/scope. (This was different to the previous category in that participants were describing completed changes rather than works in progress.) For example YP6, who felt that she had taken on board advice about personal safety but nothing else |
|
|
Changes during MST were up and down Descriptions of things improving in fits and starts |
|
|
No change during MST Nothing changing (e.g. YP5) |
|
|
Things got worse during MST For example young person who felt that MST had caused them to have to leave home Other families where deterioration would have happened anyway |
|
| Trajectories of change since MST | Attributions of change since MST |
|
Descriptions of the trajectory of changes seen or not seen in the year following MST. i.e. not about content but direction of change. Participants sometimes described different levels of changes – for example improvements in one domain but not others In addition, single changes could be described in a mixture of ways |
Descriptions of what it was about MST that influenced the changes. NB these attributions do not have one-to-one correspondence with the trajectories opposite but relate to the type of things participants described as important in how things went Also: non-MST influences – idiosyncratic but including other sources of support, and sometimes interaction between MST and other sources of support [either MST helps other support to have influence (P9) or MST sets up other support (P7)] |
|
Things have got better since MST For some families, especially when looking back as part of the interview (e.g. P2), they saw that things had continued to improve since MST, for example ‘It did change during MST, but not so much as now’ |
|
| Keeping going: changes maintained |
Keep using the strategies (active) Things just keep going |
|
Things up and down since ending [NB this is usually in combination with another description (e.g. things generally getting better but there being ups and downs within this)] Good days and bad days but bad days now ‘never as bad as a good day back then’ (P9) |
Sometimes it does not work (for example young person does not always respond to rewards/consequences) (One parent commented that even when it does not work, still does not get angry any more – P2) (link also to other influences – for example when young person meets up with delinquent friend – P1) [?This pattern could just be a description of the way change happens generally – that often things are up and down in life – so not all participants explained attributions for this – sometimes it was more an attribution in itself?] |
|
Changes could not be sustained; things are worse again/back to how they were Sometimes this was a trajectory for one change in particular, while other changes followed a different pattern (e.g. relationship with the school has deteriorated – P3) |
Changes were not embedded enough For example MST not long enough to retrain parent who has long habit of doing things in the old way (P9) Influence of other factors – e.g. a relationship with someone outside the family [ex-partner (P9) or school (P3)] has changed |
| Things continue the same or worse, where MST made no difference | [?Often this pattern reported by young person who had gone into care/moved out (5, 6, 8)] |
Appendix 8 Supplement to qualitative study 2
Interview schedule
Thanks for agreeing to meet with me and talk a bit about how things are going for you now and about your experiences in receiving help. As I mentioned on the telephone, I would like to speak with you about how things are going with your friends, your relationships with your parents, how you feel about the future, things like that. I really want to hear what you think, including good things and bad things, so there are no wrong or right answers to the questions that I will ask. It’s however you see it really.
-
I would like to start by asking you how things have been going over the last month or so? (Prompt: any major activities, things of particular interest, usual routines?)
-
Please could you tell me about your friends? (Prompt: people you hang out with; what are they like, what do you do together?)
-
What do you think makes a good friend?
-
Have you experienced a good friend doing something wrong? (Prompt: if so, how did you feel?)
-
How would you describe your relationship with your parents? (Prompt: what is good about it/not so good about it?)
-
Can you tell me about a good time with your parents?
-
Now tell me about a bad time.
-
How do you feel about your life at present? (Prompt: good things/not so good things?)
-
What do you think it means to become an adult? (Prompt: what is the main difference between being a child and being an adult?)
-
How much control or influence do you think you have over how that future will unfold? (Prompt: up to you to make the most of it vs. see what happens; any abilities you can draw on?)
-
Have you been getting support from any professionals over the last couple of years? (Prompt: if so, who from and what has that help been like?)
-
Do you remember the MST person who saw you about 4 years ago? What do you remember about that? (Prompt: good things/less good things?) (**Only asked of MST group.)
-
Do you think there is help available as you go through the process of becoming an adult? (Prompts: parents, peers, professionals, others?)
-
Looking ahead, how do you feel about your future? (Prompts: exciting vs. worrying, job prospects?)
We would like you to code a selection of short extracts from participants who are young females aged 17–21 years talking about their lives. The extracts we want you to code show their responses to the different domains of their lives (family, relationships, development, work). In coding each extract aim to ask yourself the question ‘On the basis of this extract, would I describe this person’s state as, on balance, “mature” or “stuck”?’ We expect you to be able to code some of the extracts quickly, but others may take more time. Please note that some individuals will not have extracts for each life domain.
We have given illustrations below to help you see how the categories work. Note that these extracts are prototypical illustrations of the material that you will be looking at.
Mature: Individual appears mature or orientated towards maturity. Tone of communication tends to be positive/optimistic. Sense of control/agency over life. Positive current self compared with previous self may be present.
Illustration: ‘I’m now working as a carer, and I have realised how fulfilling it is to be able to make someone else happy’.
Stuck: Individual is stuck and unable to move beyond unfavourable life circumstances. May have loose plans for a better life but nothing more concrete. Tone of communication tends to be dispirited/apathetic. Sense of lack of control/agency over life. Unlikely to be reflection of how current self differs to previous self.
Illustration: ‘I still have trouble with kids at school who won’t stop bullying me’.
List of abbreviations
- ABCL
- Adult Behaviour Checklist
- CAMHS
- child and adolescent mental health services
- CA-SUS
- Child and Adolescent Service Use Schedule
- CD
- conduct disorder
- CI
- confidence interval
- CYPRESS
- Children and Young People – Resources, Evaluation and Systems Schedule
- EQ-5D-3L
- EuroQol-5 Dimensions, three-level version
- GP
- general practitioner
- HR
- hazard ratio
- ICER
- incremental cost-effectiveness ratio
- ICUT
- Inventory of Callous-Unemotional Traits
- IQ
- intelligence quotient
- MAU
- management as usual
- MST
- multisystemic therapy
- NICE
- National Institute for Health and Care Excellence
- OR
- odds ratio
- PNC
- Police National Computer
- QALY
- quality-adjusted life-year
- SD
- standard deviation
- START
- Systemic Therapy for At Risk Teens
- TAM-R
- Therapist Adherence Measure – Revised
