Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 15/70/73. The contractual start date was in November 2016. The final report began editorial review in April 2019 and was accepted for publication in November 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of the authors
Karen Newbigging was a trustee of the Healthy Minds Board from 2012 to 2017 and a National Institute for Health Research (NIHR) Health Services and Delivery Research (HSDR) associate board member from 2016 to 2019. Doreen Joseph reports receiving personal fees during her time as a HSDR Researcher-Led Panel member (2018–20) during the conduct of the study. Benjamin Costello is a director and trustee of Bromsgrove and Redditch Network (BARN), a local council for voluntary services, which is also a volunteer centre; he is also a director and trustee of Redditch Nightstop.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Newbigging et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction and context
This chapter establishes the context for our study, which deployed a range of methods to provide a comprehensive and detailed description of the contribution of the voluntary sector (VS) in supporting people in a mental health (MH) crisis. The experience of a MH crisis can have a profound impact on the individual concerned, as well as on their family, friends and wider social network. If not managed well, a MH crisis can have adverse consequences and may influence a person’s willingness to seek help in the future. Consequently, the provision of effective MH crisis support across England is a cause for concern. However, many people in crisis are unable to access the help they need when they need it, and are dissatisfied with the help if they receive it. 1–4 The VS, which comprises not-for-profit organisations and informal groups, and is also known as the third sector, provides a range of services to support people experiencing a MH crisis. However, although this contribution is not well understood and has not been widely researched, the value of the VS is increasingly recognised and promoted within MH policy, possibly more so than in other areas of service development and delivery.
Defining a mental health crisis
Defining a MH crisis is by no means easy and, as Rapoport5 observed over half a century ago, ‘the term “crisis” is generally used in a rather loose and indeterminate way, covering a variety of meanings and a wide range of experiences’. Common themes in the way the term is used are as follows: (1) a crisis is a time of heightened vulnerability, (2) a crisis is commonly conceptualised as an event, which poses a threat and leads to a sense of disequilibrium, (3) a crisis can be a negative or positive experience, such that a crisis is viewed as a ‘turning point’,6 with both risks and a constructive potential for change and personal transformation, and (4) the resources available to an individual, both their personal coping strategies and the availability and effectiveness of support, will influence their response to a crisis.
Two aspects of a crisis that are commonly identified are the temporal dimension (i.e. an intense, and sometimes sudden, experience with the urgency of the situation emphasised) and the severity of the crisis. For example, Boscarato et al. 7 state that:
Crises can occur when a person encounters an overwhelmingly stressful situation that might exceed their capacity to cope, resulting in feelings of helplessness and tension. Disorganization and confusion might be subsequently experienced, leading to a ‘breaking point’, characterized by psychological decompensation and disturbed or destructive behaviour.
Boscarato et al. 7
Paton et al. 8 distinguish the current definitions of a crisis in a MH context. These are a pragmatic service-oriented approach (i.e. a person coming to the attention of crisis services because of a relapse of an existing MH condition), self-definitions of crisis (i.e. the person defines their own experience and recovery), a risk-focused definition (i.e. the person is at risk of harming themselves or others) and negotiated definitions (i.e. negotiated collaboratively between service users, carers and staff). 8 Traditional descriptions of a crisis emphasise the behavioural and symptomatic elements of a crisis, reflecting a biomedical framing based on clinical assessments of health and risk. 9,10 These are widely contested for neglecting or negating the experiential aspects of a MH crisis11 and they potentially dismiss the agency of the individual and their family or carers in crisis management. This study, therefore, explores crisis experiences and their conceptualisation, as these will have influenced policy, system development and consequently the role of the VS. We began with an inclusive and relatively neutral conception of a crisis as a ‘turning point’, such that a MH crisis is personally disruptive but can provide opportunities to strengthen personal and social resources, and to anticipate and manage MH problems. This definition was subsequently critiqued by the Study Reference Group (SRG) as overly positive, as discussed in Chapter 4.
The policy and practice context for mental health crisis care
Mental health policy
The provision of effective support for people experiencing a MH crisis has been a focus for policy and service development for over 25 years (see Report Supplementary Material 1). The recurrent theme has been ensuring that people experiencing a MH crisis have rapid access to effective support. The policy focus until recently was largely restricted to NHS services. The National Service Framework for Mental Health12 specified the form and function of crisis resolution home treatment teams (CRHTs) for people with a diagnosis of ‘severe mental illness’. The exclusion criteria13 included people with a diagnosis of personality disorder. In 2009, the Department of Health and Social Care14 drew attention to the role of the VS in providing alternatives to inpatient admission and to short-term sanctuary and support.
The inadequacy of a restricted policy focus for MH crisis care has attracted much attention over the last decade. The fragmentation of the crisis care system was identified by the National Audit Office,15 which recommended that specialist crisis provision by CRHTs should be integrated with other MH services, including acute inpatient care. A 2015 report by the Care Quality Commission (CQC)4 on crisis care and a 2016 report published by the Commission on Acute Adult Psychiatric Care16 similarly highlighted the fragmented nature of the MH system, underlining the inconsistency and inadequacy of MH crisis care provision. The CQC found that only 14% of the people surveyed felt that they had been provided with the right response. Those who had contact with different crisis services evaluated VS services much more positively for their warmth, compassion and capacity to listen and for taking people seriously than NHS services, particularly accident and emergency (A&E), CRHTs and community mental health teams (CMHTs). 4 This reinforced the findings from Mind’s1 survey of service users’ experiences of acute crisis, which emphasised the need for humanity, compassion, a less medically dominated response and greater choice and control,17 highlighting the value of user-led crisis services.
The NHS Mandate for 2014–1518 established specific objectives for the NHS to improve MH crisis care and introduced the Crisis Care Concordat (CCC),3 which identified four key stages of the crisis care pathway:
-
access to support before a crisis through the provision of information, preventative activities and supporting self-directed care
-
urgent and emergency access to crisis care
-
the quality of care during a crisis, including alternatives to inpatient admission
-
recovery and relapse prevention, enabling people to stay well.
This was supported by a series of statements, developed in consultation with service users and carers, describing what people could expect when they experienced a crisis across these different domains (as set out in Box 1). We adopted this description of the crisis care pathway as a reference point for understanding individual experience and system organisation.
When I need urgent help to avert a crisis, I, and people close to me, know who to contact at any time, 24 hours a day, 7 days a week.
People take me seriously and trust my judgement when I say I am close to crisis, and I get fast access to people who help me get better.
2. Urgent and emergency access to crisis careIf I need emergency help for my MH, this is treated with as much urgency and respect as if it were a physical health emergency.
If the problems cannot be resolved where I am, I am supported to travel safely, in suitable transport, to where the right help is available.
I am seen by a MH professional quickly. If I have to wait, it is in a place where I feel safe. I then get the right service for my needs, quickly and easily.
Every effort is made to understand and communicate with me.
Staff check any relevant information that services have about me and, as far as possible, they follow my wishes and any plan that I have voluntarily agreed to.
I feel safe and am treated kindly, with respect and in accordance with my legal rights.
If I have to be held physically (restrained), this is done safely, supportively and lawfully, by people who understand I am ill and know what they are doing.
Those closest to me are informed about my whereabouts and the people who need to know are told that I am ill. I am able to see or talk to friends, family or other people who are important to me if I so wish.
I am confident that timely arrangements are made to look after any people or animals that depend on me.
3. Quality of treatment and care when in crisisI am treated with respect and care at all times.
I get support and treatment from people who have the right skills and who focus on my recovery, in a setting that suits me and my needs.
I see the same staff members as far as possible and, if I need another service, this is arranged without unnecessary assessments. If I need longer-term support, this is arranged.
I have support to speak for myself and make decisions about my treatment and care. My rights are clearly explained to me and I am able to have an advocate or support from family and friends if I so wish.
If I do not have the capacity to make decisions about my treatment and care, any wishes or preferences I express will be respected and any advance statements or decisions that I have made are checked and respected.
4. Recovery and staying well/preventing future crisesI am given information about, and referrals to, services that will support my process of recovery and help me to stay well.
I, and people close to me, have an opportunity to reflect on the crisis and to find better ways to manage my MH in the future.
I am supported to develop a plan for how I wish to be treated if I experience a crisis in the future and there is an agreed strategy for how this will be carried out.
I am offered an opportunity to feed back to services my views on my crisis experience.
Reproduced from the Department of Health and Social Care. 3 Contains public sector information licensed under the terms of the Open Government Licence v3.0. See: www.nationalarchives.gov.uk/doc/open-government-licence/.
Through its focus on securing local agreements to improve the crisis care pathway, the CCC stimulated the development of a range of VS initiatives, including places of safety, crisis houses that can provide an alternative to inpatient care and crisis cafes or safe spaces that have the potential to divert people from A&E. This has been facilitated by additional resources being made available by NHS England, the Department of Health and Social Care19,20 and local commissioners. The evaluation of the CCC confirms that the VS is playing an important role in the local delivery of crisis services. 21
The Five Year Forward View for Mental Health2 emphasised that people with a mental illness have the right to the same high quality of care as people with physical health problems. This means that ‘people facing a crisis should have access to MH care 7 days a week and 24 hours a day in the same way that they are able to get access to urgent physical health care’2 (p. 12, emphasis added; contains public sector information licensed under the Open Government Licence v3.0). In outlining the required transformation of MH services, the Five Year Forward View for Mental Health2 asserted that the VS plays an invaluable role and that new models must be developed in partnership with experts by experience, community organisations and VS organisations (VSOs).
Proposals to improve the provision of MH crisis care were announced in NHS England’s Long Term Plan (LTP). 22 The LTP commits to ring-fencing and increasing investment in MH to accelerate the growth of community and crisis services for children, as well as for young people and adults. It proposes that community crisis services be expanded, so that they can be accessed via NHS 111, with additional resourcing to be supplied to provide a 24/7 community-based MH crisis response offering intensive home treatment as an alternative to acute inpatient admission. 22 The LTP also outlines an ‘improved NHS offer of urgent community response and recovery support’22 (p. 14; contains public sector information licensed under the Open Government Licence v3.0), with waiting time targets for a MH crisis response to be introduced in 2020. The LTP expresses a commitment to increasing (1) alternative forms of provision, referring to safe havens and crisis cafes as more suitable than A&E, and (2) the role of crisis houses as preventing admission. Both of these commitments necessarily require the NHS to work in partnership with the VS in order to better meet people’s needs. These policy developments formally recognise that VSOs, and their particular ways of working, offer a specialist ‘niche’ within a wider ecosystem of MH crisis support.
The wider context for MH crisis care includes (1) increasing rates of use of the 1983 Mental Health Act (MHA), which are now at a record high;23 (2) the disproportionately high rates of detention of people from black, Asian and minority ethnic (BAME) communities, which continue unabated;23,24 (3) inequalities in access for other BAME groups; and (4) emerging evidence that an inadequate response or rejection can lead to increasingly desperate behaviour resulting in increased need for the use of section 136 under the MHA. 25 The MHA review identified the positive contribution of the VS in crisis care. 26 In recommending the provision of alternatives to detention and interventions to prevent crisis or the escalation of crisis, the report comments ‘[T]here should be a varied offer and funding of this provision, which will require a considerable change in culture and what services receive funding’24 (p. 86; contains public sector information licensed under the Open Government Licence v3.0). The government has also set an ambition for zero suicides,27 and the contribution of the VS to prevention and access to appropriate support is included in relevant guidance from the National Institute for Health and Care Excellence (NICE). 28 Finally, austerity and the wider welfare benefit reform have been implicated in the increased risk of a MH crisis29 and, together with perceived isolation, are associated with an increased risk of suicide. 29 This association between inequalities and poor MH is recognised by Public Health England’s initiative entitled the ‘Prevention Concordat for Better Mental Health’, which identifies the VS and community sector as contributors to its implementation. 30 All of this raises fundamental questions about the VS’s role in the provision of effective crisis care.
Although an analysis of wider health and social care policy is outside the scope of this study, it is worth noting that the policy context is conducive to the development of the VS. There are a number of specific policy themes that support the role of the VS: (1) an emphasis on prevention and tackling the social determinants of health, (2) a reframing of integrating health and social care by focusing on place-based approaches, which necessarily recognise the role of voluntary and community organisations,31 and (3) the promotion of asset-based community development approaches. The LTP suggests that integrated care systems be created across England by 2021 to organise commissioners and providers and motivate them to prioritise and make decisions about local provision to meet the needs of their population. These integrated care systems will be overseen by a performance and accountability framework, which will include an indicator of how well local systems are working together. The reforms also propose the introduction of integrated care trusts that will bring together primary and community services. Although the VS is identified as a player in this ambitious reform agenda, how this will play out in practice and the impact on the VS are, as yet, unclear.
The voluntary sector
The VS has been conceptualised as a third ‘terrain’ of organisations between the state and market, comprising charities and community groups, underpinned by a sector ethos that typically values accessibility, self-organisation, service-user-defined outcomes, informality and relational-based approaches. 32,33 The VS makes a wide-ranging contribution to MH, including user-led organisations (ULOs), national specialist MH VSOs, VSOs concerned with a specific social issue (e.g. domestic violence or homelessness) or with a client group (e.g. ex-service personnel), and small community organisations, which are ‘under the radar’ by virtue of their size or informality. 34 Across this diverse range of organisations, there is a wide range of approaches and activity, from intensive support, including supported housing and support in a hospital setting, to advocacy, support groups and peer-led networks (e.g. the Hearing Voices Network), peer support, social and leisure activities, and befriending.
In exploring the roles of non-profit organisations in MH, Karlsson and Markström35 identified two broad (and overlapping) groups. One group is organisations providing services, seen as complementary to or alternatives to public sector services. They seek collaboration, are often dependent on state grants and become more like public or private sector organisations through the process of collaboration, but typically retain strong priorities of self-help and peer support. The second group is characterised as voice-giving rather than service-orientated. This group values experiential knowledge and work to bring about change through services and campaigning.
The VS is described as having a ‘comparative advantage’ and Dayson and Wells36 suggest that this comparative advantage derives from three elements, namely how VSOs do their work, who they do it with and the role they play in their community. 36 In particular, VSOs have a distinctive approach to governance, which is characterised by ‘stakeholder ambiguity’. 37 Stakeholder ambiguity occurs because stakeholders are likely to have hybrid and overlapping roles (e.g. managers may be the same as, or relatively equal to, those in ‘volunteer’ and ‘service user’ roles within the organisation). Such relatively ‘flat’ hierarchies are often associated with an ethos of non-judgementalism, encouraging nurture/care and a high degree of ‘relational skill’. 32
These characteristics mean that the VS may be particularly well placed to provide MH crisis support, offering alternative approaches to public sector provision for populations that are ‘seldom heard’ or find themselves excluded by various mechanisms,38 for example women who have offended or are at risk of offending,39 homeless people40 or older people experiencing anxiety and depression. 41 Thus, the VS plays a particular role in advancing equality by facilitating access to support for people from disadvantaged groups who may be reluctant to access public sector services.
Voluntary and public sector relationships
Since 1997, there has been a significant rise in the involvement of the third sector and civil society in delivering public services. 42 VSOs are now firmly embedded in the delivery of public services including health and MH services. This process has happened in an evolving political context including periods of significant government investment under New Labour, as well as periods characterised by austerity and short-lived agendas, such as the ‘Big Society’ agenda, under the coalition government from 2010 and subsequent Conservative governments from 2015. 32 Alongside this, the increasing marketisation of public services has opened up new opportunities for VSOs by way of competition for health contracts, both between VSOs and with public and private sector organisations. 43 Widespread concerns about this involvement in delivering public services have been expressed, potentially compromising some of the VS’s cherished attributes, especially its perceived trustworthiness, political independence and ability to act as an alternative or challenge to the state. 43 For many commentators, the VS’s enhanced role in the delivery of public sector services has come at the price of a drive towards ‘professionalisation’ and more competitive, even unethical, behaviour. 44 Regardless of the rights and wrongs – and there is no clear consensus across what is a very diverse VS – there is a trade-off between (1) aligning more closely with the values and approach of the public (or private) sector while remaining a challenge and providing an ‘alternative’ to them and (2) particularly in the case of MH, genuinely involving service users. This is often expressed in terms of threats to VSOs’ ‘independence’ from the state and market. 45
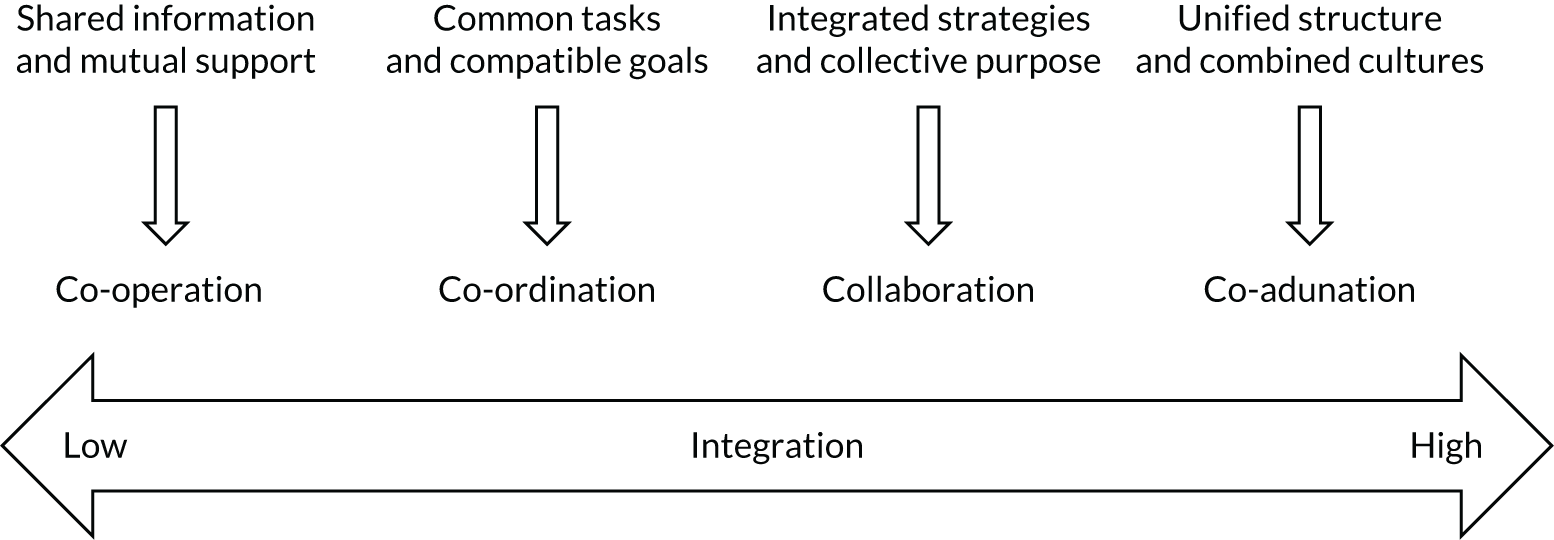
When VSOs work most closely in ‘partnership’ with the public sector, the relationship has been theorised as a collaborative or mutually dependent one arising from the inherent limitations of the two sectors in providing collective services – or, more formally, a system of services45 – suggesting there is some scope for synergy rather than a zero-sum game. This resonates with the CCC’s articulation of the crisis care pathway3 and Crisp et al. ’s16 reiteration of the importance of viewing the MH system as a whole, with synergy between the various elements necessary to provide a timely and effective response. Collaboration and synergistic relationships can have different meanings for the various stakeholders. We draw on the conceptualisation of collaboration by Gray46 as ‘a mechanism by which a new negotiated order emerges among a set of stakeholders’. Therefore, one hypothesis is that a more effective and efficient response to people experiencing a MH crisis will be achieved through effective collaboration between VSOs and public (and in some cases private) sector services. Our understanding of collaboration also draws on the work of Morrissey et al. 47 on MH service system change in a US context, which differentiates between collaboration at the service system level and at the individual client level. This underpins our research design in seeking to understand how different elements of the crisis service system are working together both as a system and for individual service users.
Commissioning the voluntary sector
An increasingly important factor in shaping the relationship between the VS and the public sector has been the rise of commissioning as the foremost mechanism for ‘purchasing’ services from the VS. Public sector commissioners [e.g. within local authorities and Clinical Commissioning Groups (CCGs)] are now required to shape and provide stewardship of local provider ‘markets’. 43 Commissioning was intended to enable a needs-based whole-cycle approach to purchasing services, thereby alleviating issues around fragmentation and allowing VSOs to have a greater influence on defining public services. However, commissioning remains ‘fragmented in policy and practice, between different localities and scales of government’. 48 Commissioning arrangements between the public sector and VSOs sit on a spectrum ranging from narrowly constituted ‘commissioning on price’, which resembles traditional procurement and tendering processes, to ‘intelligent/collaborative’ at the other end. 48 The integrity of commissioning – and the role and standing of commissioners – has also arguably been undermined by austerity and the widespread perception that it is one mechanism for enforcing ‘cuts’ to public services. Miller and Rees49 examined whether or not commissioning has created opportunities to improve the whole system of MH provision, finding that in reality commissioners felt they were ‘subjects’ rather than ‘masters’ of change. Apart from a few promising examples of individual service change, new commissioning arrangements were thought to be unable to bring about systemic change in MH services. This was attributed to a lack of personal expertise and knowledge of local services, limited influence on the whole system, poor communication, fragmented or inconsistent relationships between local authorities, VSOs and NHS services, and competitive tendering processes and contracts, which many VSOs felt limited their creativity or compromised the goals of their service provision. Some commentators have called for much more radical change to commissioning arrangements, including wholesale reform. 50,51 Therefore, linked to an examination of collaboration, understanding the extent to which current commissioning arrangements recognise and support the sustainability and contribution of VSOs to MH crisis care was also an important focus of this study.
This report
This report provides the context, aims, methodology and detailed findings of our study. This chapter has outlined the background for our study, covering the policy and practice context for the VS’s role in MH crisis care. Chapter 2 provides a literature review of relevant research to enable us to map the key concepts and develop the research tools. Chapter 3 describes the aims and methodology for undertaking our study, which involved four work packages (WPs), from outlining the landscape for the VS in MH crisis care to investigating the role at a system and individual level in four (anonymised) case study sites (sites A, B, C and D).
To address the research objectives, we have chosen to present the findings thematically, with each chapter synthesising the data from the different WPs. The Consolidated Criteria for Reporting Qualitative Studies (COREQ)52,53 and the Guidance for Reporting Involvement of Patients and the Public (GRIPP2)54 checklists have been used as guides to ensure comprehensiveness and rigour in reporting our findings. We start with individual experience and foregrounding needs in a MH crisis (see Chapter 4) to establish the reference point for crisis care provision. Chapter 5 describes the different types of VSOs and how they are relevant to meeting these needs. We present a typology of the different types of VSOs and the role they play in MH crisis care. Illustrative descriptions of these different types of organisations are available in the Report Supplementary Material 2. We then present the findings on how people have accessed support from the VS, the nature of the support provided, its quality and adequacy and the difference it has made to people’s lives, both service users and their families/carers (see Chapter 6). We use individual case studies to illustrate people’s experience of accessing help and the VS response. We then examine the relationship between the VS and public sector services, mainly those provided by the NHS, and how well these two sectors are working as elements of a system of MH crisis support to ensure an effective pathway for people needing support in a MH crisis (see Chapter 7).
Finally, we present the findings on the role of commissioning in shaping the contribution of the VS to MH crisis care (see Chapter 8). This includes the sources of funding for VS activity and the relationship with commissioning, including the contracting arrangements, monitoring and the quality of these relationships. We identify the implications for the sustainability of the VS in this area and the recommendations that participants made to strengthen the commissioning of the VS. Chapter 9 provides a synthesis of our findings on the contribution of the VS to MH crisis, the limitations our research and our contribution to addressing the identified knowledge gap. Chapter 10 summarises the implications for policy, practice and further research in this area.
Quotations and illustrative crisis journeys
We have selected quotations to illustrate specific themes, and codes are used to refer to individuals and to maintain anonymity. The codes, which are used in combination, are provided in Table 1. Assigned numbers are sequential for each type of respondent. For example, the first service user to be interviewed in study site A is referred to as ASU1 and a participant in a carers’ focus group in study site B is referred to as BCaFG.
| Code | Participant reference |
|---|---|
| A, B, C and D | Study site |
| Ca | Carer |
| CCG | Clinical Commissioning Group |
| FG | Focus group |
| G | Group |
| LA | Local authority |
| MHP | Mental health professional |
| Po | Police |
| RS1 and RS2 | Regional stakeholders (in regions 1 or 2) |
| S | National stakeholder |
| SU | Service user |
| ULO | User-led organisation |
| VS | Voluntary sector |
We have drawn on data from repeat interviews with service users to illustrate individual crisis journeys (see Figures 5, 6, 9, 10, 12 and 13). These illustrative crisis journeys show how the VS contributes to a patchwork of different types of support at different points in people’s individual journeys. They exemplify how the various types of VSOs reported in Chapter 5 contribute to supporting people with different aspects of their crisis, as well as using public sector services.
Language and choice of terms
Some of the language used in this report will be contested, as it was during our study. We use the term ‘mental health problems’ to describe the wide range of emotional difficulties that people experience, and we have used the term ‘mental illness’ and diagnostic labels as they were used by participants. The term ‘service user’ is used to refer to people who are using or have accessed MH support; we are aware that, because the experience of engagement with MH services is often distressing, disempowering and unwanted, some people prefer the term ‘survivor’. We have used the term ‘black, Asian and minority ethnic’ to refer to people from a wide range of communities serving black or Asian, or people from other racialised, minorities. Finally, we have used the term ‘voluntary sector organisations’ to refer to charities, voluntary organisations and community groups.
Chapter 2 Previous research on the role of the voluntary sector in mental health crisis care
In developing the proposal for this research, it rapidly became clear that the evidence for the contribution of the VS to MH crisis care was scant. We therefore undertook a rapid literature review to identify the knowledge base for the contribution of VSOs to MH crisis care, to map the key concepts and to inform the development of the research tools. Although a systematic review was beyond the scope of this study, our literature review was as comprehensive as possible and followed systematic review principles (see Appendix 1 for details on the method). This chapter provides a summary of the main themes.
Overview of the literature
Thirty papers relevant to the current study were identified (see Appendix 2 for a summary). These included papers from the UK, Canada, the USA, Norway and Australia. The papers fell into five main groups: experiences of a MH crisis and preferences for support (n = 9); evaluation and description of service models, including helplines and peer support (n = 9); alternatives to public sector provision, including comparisons of outcomes and cost-effectiveness, with the majority relating to alternatives to inpatient admission (n = 8); evaluation of new service models, including the VS (i.e. vanguards; n = 2); and the relationship between MH VS providers and MH public sector services (n = 2). The review identified significant gaps in the literature. The majority of the studies were qualitative studies, with five studies considering outcomes using rating scales55–59 and other studies analysing routinely collected data. 20,55,60–64
Conceptualising a mental health crisis
Many papers use the term ‘crisis’, often relying on traditional notions of a crisis. Several papers, however, identify different types of crises or describe important characteristics. The temporal dimensions of a crisis emerge as central, with a crisis as a process or condition and an emergency identified. 9,65 Bonynge et al. ,9 for example, distinguish between moderate (non-acute) crises, in which people are in need of urgent care, and severe crises, which are considered a MH emergency. The latter type of crisis was characterised by observing three or more of the following characteristics: (1) danger to self, (2) danger to others, (3) significant confusion, (4) significant depression and (5) significant functional decline. Sells et al. 66 explored the contexts and conditions for crisis and identified a recursive dynamic between a crisis and its consequences. For example, a chronic illness can lead to a loss of income, role disruption, and challenges to identity and routine, thus contributing to further crises. This suggests that a crisis is not necessarily sudden but can also be triggered by circumstances or life events. 1 Similarly, Gudde et al. 67 and Albert and Simpson68 describe the crisis experience as a process of ‘problem escalation’, with the lack of effective support creating an ‘emergency’, resulting in police intervention, or a cyclical process of short periods of hospitalisation then discharge until another crisis occurs.
Ball et al. 65 argue that there are significant differences between how crises should be understood for people who are living with a serious MH issue. 65 They propose that conceptualising crises in terms of ‘underlying vulnerability’ – traumatic life experiences, troublesome symptoms and ongoing circumstances – instead of a precipitating event leads to a better understanding of how broader conditions for crises are created. Reflecting the situated nature of a MH crisis, Thomas and Longden11 argue for a moral, emotional and contextual approach to understanding crises.
Exploring these dimensions of crises may enable an understanding to be gained of the function and nature of VSO interventions and support, in terms of which point of the crisis process these organisations intervene and what they are aiming to address (preventing readmission or breaking the cycle). It also raises the question of whether or not different services, organisations and individuals have a shared understanding of the crisis process.
Subjective experiences of crisis
Subjective accounts reveal the multifaceted nature of a MH crisis, situated in the context of people’s lives. Despite the inherently personal nature of crises, some common themes are evident: the feeling of ‘emotional darkness’, loneliness and a desire for togetherness, feeling scared and a sense of loss of control. 1,65,69 Hopelessness and seeing no end to the situation may lead to a suicide attempt. A service-user-led study of the experience of CRHTs frames a MH crisis as a journey. 70 Similarly, Gullslett et al. 69 describe MH crises as a ‘continuity of struggles in complex situations’. They identify two dimensions – existential/personal and contextual/social – and, depending on the individual and the situation, one of these might be more dominant. These themes were also identified by the Mind inquiry1 and Ball’s65 situation-specific theory. Other themes included the intervention of others, loss of identity and purpose, alienation, not coping or functioning, hopelessness, despair, self-blame and guilt. These themes were inter-related in complex ways and sometimes conflicting feelings were evident, for instance an awareness of the need for help and a desire to reach out to others, but limited emotional resources or capacity to do so.
Using a phenomenological approach in a study focused on carers’ experiences, Albert and Simpson68 identified that a MH crisis can also be a stressful time for carers. They suggest that they can experience a ‘double deprivation’, often unsupported by staff owing to different understandings of what constitutes a crisis, and not accessing support from their social network, preferring to limit the impact of the MH crisis. This highlights the wider impacts of a crisis and the importance of recognising carers’ knowledge and understanding.
These different experiences and understandings of a crisis indicated that it was important for our research to consider how the crisis experience is conceptualised.
Preferences and crisis responses
Given the intensely personal nature of a MH crisis and the conceptualisation of a MH crisis as a ‘turning point’,6 there is an opportunity for learning and building resilience if effectively supported. 71 Mind’s inquiry into crisis care1 identified four main themes for what people wanted from a crisis support service:
-
to feel cared for, not abandoned
-
choice and control, not coercion
-
a personal caring response rather than a medical one and
-
appreciating that one model does not fit all.
They recommended that there should be a greater range of options to meet different needs, including self-referral options, crisis houses, host families and services provided by peers. Similarly, a consultation exercise by Healthwatch Norfolk72 identified that the help and support provided by community organisations and VSOs, including telephone helplines, drop-ins, cafes, support groups, counselling and therapies, were highly valued and it recommended that their contribution to MH crisis care not be overlooked.
The personal response to a crisis varies from actively seeking help, to managing alone, to others stepping in to seek help. 65 Gudde et al. 67 explored the experiences of people with major mental disorders in a Norwegian context and identified a high threshold for contacting services as a result of previous negative experiences or inappropriate provision. Similar to other studies,1,67 service users wanted easy access to services to enable early intervention and to break a cycle of repeated hospitalisation. 67 Boscarato et al. 7 found that service users did not want a police intervention, with the majority preferring a more informal response. Hutchinson et al. 58 identified that men using a VS MH service were significantly more likely to be unemployed, have forensic histories, have less contact with other health services and have more unmet needs than those attending a service at a MH hospital in the same catchment area. Those attending the VS service cited wanting to escape ‘the system’, with the levels of dissatisfaction with public sector MH services particularly high among African Caribbean groups. These findings suggest that VSOs play an important role in enabling access for people from marginalised groups.
McGrath and Reavy73 underline the different needs of people in a crisis, to counter simplistic assumptions. They identified that people experiencing a MH crisis use space differently to maintain their sense of agency. Those experiencing a psychotic episode preferred outside space, as it ‘appears to open up new zones of fluid possibility, which potentially enables service users to de-centre, stretch out, and disperse some of the burgeoning intensity of experience’. 73 Other people preferred the privacy and the sense of safety afforded by being in an indoor safe space, which helped them restore feelings of agency and strength.
A key question, therefore, is the extent to which service users’ preferences and choices are heard, and the extent of their involvement in planning and defining their own support and recovery. Gudde et al. 67 concluded that service users identified active involvement, with dialogue-based care that placed equal value on their own coping mechanisms (acknowledging that these were not always ‘optimal’), as helpful. This included being understood as a ‘normal’ person, dealing with crises in an everyday context, and respectful, caring relationships.
Voluntary sector mental health crisis services
Crisis houses
One of the most frequently mentioned contributions that VSOs make to the provision of MH crisis support was the provision of alternatives to acute inpatient admission. 74 These are typically crisis houses to be used for up to a few days, or during the day-time or for slightly longer short-term stays of up to 2 weeks. Johnson et al. ’s74 study identified 131 alternatives to hospital admission across England and, although crisis houses are not uniquely provided by the VS, a significant proportion were VSO led.
Some of the perceived advantages of crisis houses over hospital wards, from the perspectives of service users and staff, are that (1) they are more homely (often located in converted residential buildings), less stigmatising and less clinical owing to the fact that they are led by nurses, counsellors, peer supporters and volunteers as opposed to clinicians (e.g. psychiatrists); and (2) pathways to admission can be less fraught, with less coercion and loss of liberty. 59,75 Morant et al. 76 identified the specific benefits of non-clinical crisis houses as providing a more holistic style of care; offering greater autonomy, choice and responsibility to clients; developing strong therapeutic and peer relationships; and enabling people to maintain their connections to ‘normal life’ and the community. This is echoed by Sweeney et al. 59 who found that service user satisfaction and therapeutic alliances were stronger and more positive in crisis houses than in inpatient wards. They attributed this to the homely environment, informal peer support and fewer negative experiences with staff in crisis houses. Thomas and Longden11 commend the Soteria77 and the Sanctuary78 models for their moral imagination, placing empathy at the core of caring.
As well as providing an alternative to admission, crisis houses or other interventions may aim to prevent readmission and promote recovery. 79 Griffiths et al. 80 described a transition intervention service after a stay in a VS crisis house, in response to evidence that 20% of people discharged from inpatient care were being readmitted within 90 days. 81 The intervention was designed to help with living skills, resilience and self-management, and the evaluation found significant improvements in social networks and self-management, although less improvement in the area of work. This highlights the role that VSOs can play in supporting recovery, a highly individualised process to realise people’s strengths and personal aspirations/goals.
Other papers focus on evaluating the value of crisis houses in terms of clinical and/or service outcomes. The evaluation by Larsen and Griffiths55 of the impact of a stay in a non-clinical VS crisis house showed significant increases in all recovery star domains (i.e. managing MH, identity and self-esteem, trust and hope, and self-care) and significant increases in personal goal-scoring data. The service was gate kept by the local MH team as an alternative to acute inpatient hospital admission or providing an intermediate step before returning to the community. Larsen and Griffiths55 highlight the open-door policy, which helped residents maintain independence and connections with the community, and staff training on reflective, compassionate practice, operating on the principle that the recovery process starts as soon as people enter the crisis house. The evaluation by Butt et al. 56 looked at a partnership between a VS crisis house in London and the local home treatment team as an alternative to admission and reported positive improvements in MH and safety, as assessed by service users and clinicians. Croft and İsfan61 also found that short periods of stay in peer respite care reduced inpatient and emergency admissions by up to 9–10 days for each day of stay in peer respite.
A number of factors facilitating the best use of non-clinical crisis houses were identified, including being locally valued, with public sector teams having knowledge of available services and a willingness to promote them, and being designed in collaboration with local MH services in response to local needs so that roles are clearly defined. 55,76 However, public sector staff sometimes found it a challenge to refer to crisis houses appropriately as a result of their small size and limited organisational capacity. 76
There is conflicting evidence on who accesses VS crisis houses, which may reflect the different organisational arrangements, including referral routes and relationships with MH services. Many of the studies tend to position crisis houses as a ‘softer’ alternative that are less appropriate for people with more serious MH issues (i.e. for people who do not require intensive supervision or have specific clinical needs) and, therefore, as less appropriate for compulsorily detained or highly disturbed patients. Crisis houses also seem to offer less comprehensive treatment packages, especially concerning physical health issues. 74,76 There is, therefore, the general suggestion that VSO-led non-clinical crisis houses may be of particular relevance for people who have not yet had contact with secondary MH services. However, Sweeney et al. 59 found that those attending a crisis house were more likely to be known to services and may, therefore, be more likely to seek help. Greenfield et al. ,57 in a randomised controlled trial (RCT) comparing a consumer-managed crisis residential programme (CRP) with four beds to a locked inpatient ward with 80 beds, found a greater severity of ‘illness’ and lower functioning scores for people in the CRP. Although life enrichment and functioning improvements were not significantly greater, self-esteem, social networking and satisfaction all improved for those in the CRP.
Service user involvement and peer support
Peer support is not limited to the VS, but peer support and championing service user involvement have been identified as particular strengths of the VS. Peers act as positive role models of hope and recovery,79 sharing their experiences and learning, and reducing the feeling of stigma and inequality. Gillard et al. 82 identified change mechanisms from peer support for people with MH issues provided by the VS and public sector as building trusting relationships based on shared experience, role modelling living well and recovery, and engaging service users with services and community. Peer support is also a potential benefit for the supporter as well as for the service user, providing a sense of value, a new role and a purpose. 66
User-led organisations are a unique feature of the VS, ranging from those representing a minority ethnic group, to those offering specific services (e.g. art or research), to those operating in particular geographical contexts (e.g. rural or metropolitan). 83 The review identified two evaluations of a survivor-led crisis house for individuals who repeatedly self-harm, Dial House in Leeds,60,84 which found that service users valued their informality, kindness, non-intrusive approach and peer support, and identified benefits in terms of both outcomes and cost-effectiveness.
Cost-effectiveness
A small number of studies have identified that VS provision is cost-effective or have argued that the reduction in the use of statutory MH services has led to potential savings. 64,85 For example, Croft and İsvan’s evaluation of a peer respite programme led to a reduction in the use of inpatient or emergency services, although these decreases were predicted to be time-limited. 61 Fenton et al. 62 identified that a residential crisis programme provided similar outcomes as inpatient care for a significantly reduced cost. Bagley60 identified a £5.17 benefit per £1 invested in Dial House (a ULO) and estimated the total added social value generated over 1 year as £1,757,843.73. Overall, the evidence for the cost-effectiveness of VS provision is scant and this is clearly an area for further inquiry, given the findings that service users prefer residential alternatives to hospital, including those provided by the NHS. 75
Systems, partnerships and processes
The importance of a whole-system approach to effective delivery of crisis care raises questions about how VSOs and the public sector, including the NHS, local authorities and the police, can best work together to ensure an effective and co-ordinated response. Bonynge et al. ,9 for example, scoped out the range of services offered by a US non-profit provider of a MH crisis care system in a rural setting, identifying a mixture of system components: urgent appointments, a crisis hotline, professional on-call services and five crisis beds (with a maximum stay of 72 hours). In examining how the system worked as a whole, they identified that distance was a challenge for mobile crisis services in rural settings, but that the combination of crisis services offered together reduced inpatient admissions by 11% and that many clients achieved stabilisation in the short period of time they used the crisis service. However, although people may use different services, the pathways to help are not always clear, with Healthwatch Norfolk72 identifying that approximately 50% of its respondents did not know who to contact if they needed help urgently.
A number of studies have considered the relationship between the VS and public sector services. The study by Johnson et al. 74 of alternatives to standard inpatient care found high levels of collaboration with NHS staff for non-clinical community-based alternatives, predominantly provided by the VS. Belling et al. 86 investigated the factors influencing the continuity of care by CMHTs through 113 semistructured interviews with MH staff, general practitioners (GPs), social workers and two VSOs. Alongside democratic and empowering leadership styles and decision-making, face-to-face communication facilitated cross-boundary working, including with the VS. Some poor communication between public sector and VS staff was noted, and was attributed to the high mobility of some people with MH issues resulting in highly complex networks of care and multiple interfaces at which communication breakdowns can happen. Information technology (IT) systems and information sharing between organisations was also cited as a significant problem.
Conclusion
The majority of papers identified in this literature review were concerned either with crisis houses or with the emotional or practical experiences of a MH crisis. Although the grey literature identified the particular role of the VS in MH in terms of longer-term, more holistic support, there are few academic studies that explore this. The dominant narrative in academic studies is focused on the VS and crisis houses and reducing admission to inpatient beds. Consequently, there is a gap in understanding the ‘whole system’ of crisis support, across the crisis journey described in the CCC. This includes sparse evidence on (1) a wide range of outcomes, (2) the collaboration between the VS and the public sector at the system and individual levels and (3) cost-effectiveness.
Chapter 3 Research design and methods
This chapter outlines the aims of our research, the research design and the methods adopted to address these aims. Additional details, including interview topic guides and questionnaires, are available in Appendices 3–15.
Aims and objectives
The primary aim of this research was to identify the contribution of the VS to MH crisis care and to identify the implications for policy and practice to strengthen the crisis care response. The specific objectives were to:
-
identify the different types of VS support being commissioned and/or provided to respond to the needs of people experiencing a MH crisis
-
develop a taxonomy of the different organisational types and forms of VS support available, service models (including characterising their relationships with public sector provision) and populations served
-
explore the configuration and the experience of a MH crisis system, including the factors and processes that facilitate the successful contribution of the VS to effective crisis care pathways
-
understand the crisis journey for individuals and their families and individual service user needs in a crisis, and how VSOs contribute to meeting their needs.
The scope of the study was MH crisis care in England. Assessments of clinical outcomes or cost-effectiveness, as well as comparisons with different types of service provision, were beyond the scope of this study.
Research design and methods
The design involved the use of multiple methods, both quantitative and qualitative, to provide a comprehensive and detailed analysis of the contribution of the VS to MH crisis care. The quantitative and qualitative methods complemented one another, with the quantitative methods providing an ‘extensive’ approach,87 to describe the landscape of VS provision, whereas the qualitative methods enabled an ‘intensive’87 investigation of meaning, experiences, relationships and processes. The study design ensured that the qualitative work was capable of being related to the wider picture through locating the qualitative data in a typology of VSOs derived from the quantitative data. To address the research objectives, the study was organised around four distinct but interconnecting WPs (Table 2).
| Objective (WP) | Research question(s) | Subquestions | Research method | Data collection and analysis | Outputs |
|---|---|---|---|---|---|
| (1) To identify the different types of VS MH crisis support (WP1 and WP2) | What is the contribution of the VS to MH crisis support? |
|
National scoping |
|
|
| (2) To develop a taxonomy of the different forms of VSO support available (WP1 and WP2) |
|
|
Mapping of VS support in two contrasting regions of England |
|
|
| (3) To explore the configuration and the experience of a MH crisis system (WP3) | How does the VS fit within the crisis system? |
|
Comparative case study of crisis systems in four CCC areas |
|
|
| (4) To understand the crisis journey for individuals and their families (WP4) | How does the VS support people experiencing a MH crisis? |
|
Comparative case study of crisis systems in four CCC areas |
|
|
The heart of the study was the comparative case study, at the system level (WP3) and at the level of individual service users and their families (WP4). The decision to use a case study design was threefold: (1) case study designs are particularly useful for enabling a real-time exploration of phenomena that are complex and dynamic;88 (2) it enabled an intensive examination of the VS contribution, contextualising both individual experience; and the VSOs within a system, to explore the relationships between VSOs and different system elements, and (3) the intensive examination had the potential to generate theoretical insights that could be applied in other contexts and provide the basis for subsequent evaluative work in relation to outcomes. The following section describes the four WPs, followed by data analysis and synthesis, methods adopted to ensure rigour, the research team composition, patient and public involvement (PPI) and ethics approval.
Work package 1: national scoping exercise
The focus for this WP was to identify the range of support that VSOs are providing to people experiencing a MH crisis. It involved reviewing the evidence and building a national picture of the contribution of the range of VS providers of MH crisis care in England. It comprised four elements: (1) a literature review (see Chapter 2), (2) assembling a database of candidate VSOs providing MH crisis care in England, (3) a national survey of VSOs to identify the type of crisis support being commissioned/provided and to whom, the type of organisation providing the support and the main methods of working, and (4) a purposive sample of interviews with national stakeholders (e.g. policy-makers, professional organisations and service user organisations) and national VSOs to provide further details on the different forms of VSOs, the type of crisis support they provide and how this contributes to the MH crisis care pathway.
Developing the database of candidate voluntary sector organisations
To develop the database for the survey, we identified the relatively small numbers of organisations that are active in the field of MH provision from a number of large databases. Appendix 3 describes the sources used, the process for selecting the candidate organisations for the survey and the decisions we made. We used the International Classification of Nonprofit Organizations (ICNPO) to help identify organisations of interest to this study. The result was a core list of 1982 charities, distributed across subsets of the ICNPO as follows:
-
MH and crisis intervention (n = 682)
-
other health (n = 215)
-
hospitals and rehabilitation (n = 51)
-
housing (n = 337)
-
civic and advocacy organisations (n = 85)
-
social services (n = 612).
We corroborated this against national surveys of third sector organisations in England,89,90 which have found that approximately 1% of charities and social enterprises (about 1800 organisations out of a total of 180,000) consider MH to be one of their three main areas of activity. This suggests that our number of charities (1982) is of the right order of magnitude and this list of VSOs was used as the basis for our survey.
National survey of providers
The purpose of the survey was to identify the range and types of services provided by VSOs to support people experiencing a MH crisis. A structured survey instrument was developed to capture information about the VSO and its scope (local, regional or national), income, and organisation and activity in relation to MH crisis care. This was piloted via relevant networks of the Study Steering Group members (SSG) (see Report Supplementary Material 3) and their comments were used to prepare the final version. The survey combined tick boxes and opportunities to provide free-text responses for the domains summarised in Box 2 (see also Appendix 4). The resulting Bristol Online Survey was sent to the 1982 VSOs identified and was promoted on the research web page and via social media.
-
Organisational form.
-
Whether or not organisations consider that they are involved in the provision of crisis support, and the form it takes.
-
How crisis services are organised and delivered.
-
Target populations and reach.
-
Aims and intended outcomes of provision.
-
Operational model and details.
-
Challenges and key determinants of success in providing MH crisis care.
-
Potential examples of positive practice.
Response rates were monitored and the survey was kept open for the duration of the data collection period from May 2017 to August 2018 to maximise responses. Two e-mail reminders were sent and a small number of telephone calls were made to non-respondents in those regions in which the response rate was lower (approximately 30 selected on a random basis) to encourage responses. Follow-up calls with a small number of VSOs generated illustrative examples of the different types of VS contribution (see Report Supplementary Material 1).
Survey respondents
Of the 1982 candidate charities, we established that:
-
a number declined to participate (n = 22)
-
a number of organisations had ceased to exist (n = 39) and
-
in some cases, the e-mail could not be delivered and/or it was impossible to locate accurate details (n = 105).
A further examination of the charitable objects identified that 204 of the remaining non-respondents were not providing direct services (i.e. grant-giving bodies, national offices or cases in which MH was very peripheral to the main aim of the charity). This left 1612 organisations. We received 220 responses, of which 171 were usable responses, making an overall response rate of 13.7% and a usable response rate of 10.6%. As the main function of the survey was to understand the breadth of VS provision, the responses were considered sufficient to develop an idea of classifications, which were then built on through the interviews at the national and regional levels, which in turn provided more detailed accounts of what some of those different types of VSOs were offering. The survey data were supplemented by interrogating information from the CCC, information from the positive practice website,91 information provided by participants and internet searching, to provide a list of crisis-specific VSOs across England. This information was inputted into a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheet and then imported into geographic information software (GIS)92 to provide a map of the location of these VSOs (see Figure 10).
National stakeholder interviews
Interviews were undertaken with a purposive sample of national stakeholders representing policy-makers (e.g. the Department of Health and Social Care), professional bodies (e.g. the Royal College of Psychiatrists, the Royal College of Nursing and the College of Social Work), regulators (e.g. the CQC), national VS providers (e.g. Mind, Turning Point and Rethink) and national service user and carer organisations [e.g. the National Survivor User Network (NSUN)]. Twenty-seven participants were recruited, mainly via these representative organisations, with a small number recruited through snowball sampling (Table 3).
| Participant type | Number of completed interviews |
|---|---|
| Policy and arms-length body representatives | 4 |
| Service user organisations | 3 |
| Professional organisations | 3 |
| VS | 12 |
| Research | 3 |
| Other | 2 |
| Total | 27 |
| Declined | 10: no response or the invitee considered that they were not sufficiently knowledgeable about the VS |
The interviews covered the following aspects (see also Appendix 5):
-
the nature of the contribution that VSOs can make to MH crisis care
-
effective ways of integrating the VS contribution with that of with public sector services
-
challenges and key determinants of VS success in providing MH crisis care
-
potential examples of positive practice and
-
the future for MH crisis care.
Work package 2: regional mapping
Identifying regions and Clinical Commissioning Group areas
This WP contributed to identifying the different types of VSOs and developing the typology by gathering further detail at the regional level. We identified the region and CCG in which our identified VSOs were located by linking the postcode to digital boundary data using GIS. 92 This enabled us to identify areas with relatively high or low levels of VS presence. We identified regions using the definition of the regions on the ADASS website93 on the basis of contrasting expenditure (high and low) on MH services using data on per-capita CCG spending on MH (fifths or quintiles) for 2015/16. 94 The per-capita spend alongside the mean number of VSOs in each region (quintiles) were combined to give an overall indication of investment in the VS (as detailed in Appendix 6). From this, two regions were identified, the highest (RN1) and the lowest (RN2) on this combined measure. This measure does not definitively indicate the level of public investment in VSOs but did provide a basis for comparison. The number of VSOs does say something about the kind of VS activity in the region because these are based on postcodes and, therefore, the higher numbers of VSOs are actually registered in those regions and so are potentially locally rooted and active. The regions identified covered a large enough area to enable variations in the distribution and access to VS crisis support to be investigated. Because of the differences in the number of CCGs in the two regions (11 vs. 33), we took the pragmatic decision to focus on a subregion of RN2.
Within these regions there were two data collection methods: (1) targeted interviews with commissioners, VSOs and MH providers (n = 14) to identify additional activity that had not been picked up through the national scoping exercise and to explore the regional context for MH crisis care, the interface between VSOs and public sector services, and what factors facilitate effective crisis care pathways (see Appendix 7), and (2) further promoting the survey (used in WP1) to organisations identified from the interviews. Participants were identified through initial contacts with the relevant CCC and/or CCG leads, as well as additional snowball sampling. The main focus for the analysis was to identify variation within and between the two regions, the factors that have shaped this and the potential impact on MH crisis care delivery at the local level. This included variations in provision, capacity and crisis support. The analysis supported the development of the initial taxonomy developed in WP1, and the qualitative data were imported into NVivo (QSR International, Warrington, UK) and analysed alongside the data from the national stakeholder interviews undertaken in WP1, the stakeholder interviews in WP3 and the narrative interviews in WP4.
Work packages 3 and 4: comparative case studies of the voluntary sector contribution
The heart of the study was the comparative case studies, which enabled a detailed investigation of the VSOs’ contribution to MH crisis care. It focused on investigating how the VS elements of the MH crisis care system work together with public sector provision, and identified the challenges and determinants of success from the perspective of commissioners, VS and public sector providers, volunteers, service users and carers. We investigated the contribution of VSOs to the MH crisis care system (WP3) and at an individual level for service users, their families and carers (WP4). Each site had an academic lead and three co-researchers, with all team members being involved in data collection in at least two sites.
Selection of the case study sites
In selecting our case study sites, we adopted a realist approach to sampling,69 recognising that case study research moves back and forth between ‘ideas’ and ‘evidence’. Our original proposal was to identify case studies on the basis of sustainability and transformation partnerships (STPs), but variation, in terms of prioritising MH crisis care and the relationship with the VS, became evident in WP2. In adopting a realist approach, we necessarily surfaced our theoretical proposition that underpinned our sampling strategy (i.e. people experiencing a MH crisis have a wide range of needs and the VS forms one element of a wider MH crisis system able to respond). As the purpose of the CCCs was to bring together system partners, the CCC areas were, therefore, judged to be more fruitful than STPs in providing a context and connections for our research aims. We sought to identify sites that were information-rich (i.e. where there was VS provision of MH crisis support) but we made a deliberate choice not to restrict our sample to CCC areas that were being promoted as positive practice. Therefore, the selection criteria for selecting specific sites were refined as data emerged to enable us to select contrasting sites. The sampling criteria for CCC areas were:
-
Geography: case study sites were selected to include VS provision in rural, urban and coastal settings, and to ensure a geographic spread across England.
-
Population: sites were selected to (1) reflect variations in population density, which we anticipated would have an impact on access, and (2) include significant populations from BAME communities, specifically South Asian communities and African and Caribbean communities, because of the over-representation of African and Caribbean people detained under the MHA and the known barriers to accessing services for these populations.
-
Types of VS provision: cases were selected to provide contrast in terms of the types of type 1 VS provision identified from the earlier phases of work (e.g. a site with a crisis house and one without).
The four sites selected were located in East England, London, North-East England and the West Midlands. Table 4 provides a summary of the key features of the sites. Each site had a range of the different types of VSOs (see Chapter 6, Table 13). For formal crisis VSOs, two sites had crisis beds, provided by a housing association (site B) or a national MH VSO (site D), and two sites had a face-to-face appointment system, which was accessed either through self-referral (site C) or via the NHS (site A). All sites had a helpline provided by a national organisation, and two sites also had local helplines (sites A and C) and a range of other elements of VS provision including user-led services (sites A and C).
| Site | Description | Population (% BAME) | Population density (per km2, 2018) | Socioeconomic deprivation score (Index of Multiple Deprivation rank out of 326, 2015) | Public sector homeless per 1000 (2017–18) | Hospital admissions for MH per 100,000 (2017–2018 for CCG data) | Detentions under the MHA per 100,000 (2017–18) | Suicide rate (all persons) per 100,000 (2016–18) |
|---|---|---|---|---|---|---|---|---|
| A | Large rural areas, with two main centres of population: a university and a town with a relatively large migrant population | 852,523 (10% BAME) | 252 | 4.5% in the most deprived areas and 15% in the least deprived areas nationally | 1.1 | 234 | 21 | 10.45 |
| B | Satellite town, high BAME population, largest migrant group is South Asian. Many economically deprived wards | 327,378 (50% BAME; 20% of total population are South Asian) | 3725 | 20% of LSOAs in the most deprived areas and 55% in the bottom 20% nationally | 0.5 | 335 | 67 | 8.9 |
| C | Inner city, high BAME population, highly mobile population | 314,200 (48% BAME; 27% of total population identifies as black) | 11,000 | 35% of LSOAs in the most deprived areas nationally | 2.7 | 299 | 46 | 6.8 |
| D | Mix of urban, rural and coastal areas with ex-industrial towns. Some very deprived areas, mainly white population | 471,992 (6.5% BAME; largest group is South Asian) | 1361 | 25% of LSOAs in the most deprived areas nationally | Not available | 253 | CCG1: 31 CCG2: 85 | 11.9 |
Work package 3: the voluntary sector contribution within the crisis care system
To understand how the MH crisis care system was operating in each site, data were gathered to identify how different organisations providing MH crisis care worked together, the contribution of the VS to the MH crisis system, and what factors facilitated effective collaboration so that service users and their carers/families could access appropriate support. In each site, two data collection methods were used, as outlined in the following sections.
Semistructured interviews with key stakeholders
The key stakeholders interviewed included service user and carer organisations; local authority and NHS commissioners of MH crisis services and services for specific groups (i.e. learning disability and substance abuse services); NHS staff from a variety of crisis-related services (i.e. CRHTs, psychiatric liaison in A&E and first response services) and professional roles including team managers, GPs, psychiatrists, MH nurses, psychologists and community development workers; the police; councils for voluntary services; and Healthwatch. Participants were identified from initial interviews and web-based searches of the particular site. There were 13–27 stakeholders interviewed in each site (Table 5). The variation in the sample size for each site reflects the geography, organisational arrangements and availability of VSOs.
| Site | Participant type (n) | |||||
|---|---|---|---|---|---|---|
| Commissioners | NHS staff | VSOs | Service user/carer groups | Other | Total | |
| A | 5 (3 CCGs, 2 local authorities) | 6 | 14 | 2 | 0 | 27 |
| B | 1 CCG | 4 | 6 | 1 | 1 | 13 |
| C | 3 (1 CCG, 2 local authorities) | 6 | 11 | 0 | 1 | 21 |
| D | 2 CCGs | 4 | 11 | 0 | 0 | 17 |
| Total | 11 (7 CCGs, 4 local authorities) | 20 | 42 | 3 | 2 | 78 |
The lines of inquiry for these interviews covered the following areas (see Appendix 8):
-
the crisis needs being met by different elements of the crisis care system
-
how well the system responds to the diversity of the needs of the whole population
-
how these different elements work together to provide an integrated MH crisis care pathway
-
the quality of current arrangements
-
the key challenges faced and how these are being addressed and
-
the current and likely future pressures on services.
Two members of the research team (usually a pairing of an academic researcher and a co-researcher) undertook the interviews, and how the interview would be conducted was agreed beforehand.
Two focus groups
Two focus groups, one for service users and one for carers, were held. These aimed to understand their experiences of VS provision and how this fits within the MH crisis care system. They provided an opportunity for a ‘collective conversation’96 and provided an important reference point for how their needs were met by the response of VSOs and the wider system. Focus group participants were recruited via the VSOs, service user and carer organisations, local authorities and NHS MH trusts in each case study site. Steps were taken to ensure diversity in the sample in terms of demographic characteristics, a range of MH problems and a range of crisis experiences. The criteria for inclusion were:
-
having experience of using VS MH crisis care in the past 2 years
-
being aged ≥ 16 years
-
having the capacity to consent to be involved in a research interview.
The focus groups were attended by 30 service users and 22 carers (Table 6), with it proving easier to recruit in some of the case study sites than others. Recruitment was particularly challenging in site A, in part reflecting the large rural nature of this site.
| Case study site | Service user focus group | Carer focus group |
|---|---|---|
| A | 3 (2 women, 1 man) | 2 (1 woman, 1 man) |
| B | 9 (6 women, 3 men) | 7 (5 women, 2 men) |
| C | 12 (8 women, 4 men) | 6 (4 women, 2 men) |
| D | 6 (3 women, 3 men) | 7 (5 women, 2 men) |
| Total | 30 (19 women, 11 men) | 22 (15 women, 7 men) |
Most participants were successfully recruited via VSOs and, consequently, limited demographic details were available. The focus groups in site B were predominantly made up of people of African Caribbean heritage. There were nearly twice as many women as men in both types of focus groups, and many participants had experience of using public sector services as well as VSOs.
All participants spoke English, although there was the option to use interpreters where necessary. The focus groups were co-facilitated by a co-researcher with relevant experience. The purpose of the focus groups was to understand the MH crisis system and, therefore, the topic guide covered experiences and needs in a MH crisis, experiences of the services used, how participants chose which services to access, how the different services they had used compared with each other and the pathway between these services, and recommendations for improving MH crisis support (see Appendix 9).
Work package 4: the voluntary sector contribution at an individual level
This element of the case studies aimed to develop a granular picture of individual crisis journeys to illuminate the VS contribution for individuals experiencing a MH crisis and to understand the operalisation of the interface between the VSO and different services.
Service user recruitment for narrative interviews
Different recruitment methods to identify service users were used across the sites, reflecting different arrangements for MH crisis care provision (Table 7). As VSOs did not always keep sufficient information on people using their services to enable recruitment, NHS organisations also facilitated recruitment. Potential participants were provided with information about the study (i.e. the participant information sheet) and could either complete a slip or send an e-mail indicating they were willing to take part and provide their contact details or give permission for the VSO or NHS to pass on details. The criteria for inclusion were:
-
having experience of using VSOs and an episode of NHS care within the last 6–12 months for support with crisis management
-
being aged ≥ 16 years
-
having the capacity to consent to be involved in a research interview.
| Site | Recruitment methods | Number of potential participants recruited | Actual number of service user participants | Number of family/carer participants interviewed | Number of potential service user participants recruited for repeat interviews | Actual number of service user participants re-interviewed |
|---|---|---|---|---|---|---|
| A | Majority recruited via the NHS, with two recruited via a VSO | 20 (1 person lacked capacity, 3 were unavailable for interview) | 16 | 3 | 8 | 6 |
| B | Recruited by a mix of VSOs and the NHS | 10 (1 person admitted to hospital) | 9 | 4 | 5 | 4 |
| C | Majority recruited by VSOs | 14 (1 unavailable for interview) | 13 | 4 | 9 | 6 |
| D | Recruited by a mix of VSOs and the NHS | 12 (3 unavailable for interview) | 9 | 0 | 4 | 4 |
| Total | 56 | 47 | 11 | 26 | 20 | |
Sample
Forty-seven participants met the inclusion criteria and agreed to take part in a narrative interview. Subject to their consent, a carer or family member was also approached to be interviewed. However, this proved difficult, as a substantial number of service users either were unable to identify anybody or declined to give permission. In total, 11 carers were interviewed, in addition to the 22 carers who had participated in the focus groups.
On completion of the initial interview, each service user participant was invited to complete a brief questionnaire to capture demographic data (Table 8; see also Appendix 10). Ninety-one per cent of the sample agreed (n = 43), although not all of the sample completed every question.
| Group | Gender identity (F : M : NG : T : O)a | Age (years) | Ethnicity (%) | Sexual orientation (%) | Disability (%) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Range | Mean | Median | White | White other | Asian/mixed | Black/African/Caribbean/Black British | Heterosexual | Gay | Lesbian | Bisexual | Prefer not to say | Other | None | Physical | Mental | Learning disability | ||
| Site Ab | 5 : 3 : 0 : 0 : 0 | 17–55 | 35 | 35 | 69 | 13 | 6 | 13 | 69 | 0 | 0 | 19 | 13 | 0 | 31 | 25 | 44 | 0 |
| Site Bc | 5 : 3 : 0 : 0 : 0 | 25–63 | 47 | 50 | 50 | 0 | 13 | 13 | 75 | 0 | 0 | 0 | 25 | 0 | 25 | 38 | 50 | 0 |
| Site Cc | 6 : 5 : 0 : 0 : 0 | 25–60 | 44 | 49 | 67 | 9 | 0 | 24 | 73 | 0 | 0 | 18 | 0 | 9 | 73 | 18 | 9 | 9 |
| Site Dd | 5 : 3 : 0 : 0 : 0 | 24–57 | 43 | 43 | 75 | 0 | 13 | 13 | 100 | 0 | 0 | 0 | 0 | 0 | 50 | 13 | 25 | 0 |
| Total sample | 3 : 2 : 0 : 0 : 0 | 17–63 | 41 | 38 | 65 | 7 | 12 | 16 | 77 | 0 | 0 | 12 | 9 | 2 | 44 | 23 | 33 | 2 |
The responses indicate that were more women than men, and no one identified as non-binary or transgender. There was no upper age limit and a woman of 82 years was recruited but lacked the capacity to consent. Thirty-seven per cent of the sample was from BAME communities. Despite certain sites being included to ensure a diverse population, particularly in terms of the BAME population, we were surprised that this group was less represented in our sample than expected. A young Asian service user commented that ‘mental health issues are often swept under the carpet in Islamic/Asian culture and there is fear of stigma’. In the context of the over-representation of black men under the MHA and more limited treatment options, we selected site C because of its high BAME population, but only a few BAME service users responded, possibly reflecting the limited VS offer for BAME service users, despite their disproportionate representation as inpatients in the local NHS Trust.
Narrative interviews
For each person, information on their experience of a MH crisis and their crisis care trajectory was gathered through separate narrative interviews71 with the person (and their carer, if appropriate). Narrative interviews were adopted to enable a rich description of the unfolding of events and actions from the participants’ perspectives and to gain insights into their MH crisis experience. 97 Narrative interviews differ in format from a structured or semistructured qualitative interview and potentially reduce the likelihood of a participant rehearsing their experience as they might for a clinical interview. The narrative interviews explored similar themes to the focus groups, but from an individual perspective: the extent of a MH crisis, what made it a crisis, the context and factors for the most recent and previous crises, the support and service(s) used, the quality and adequacy of the support and service(s), and a comparison with other services. Prompts were provided as necessary (see Appendices 11–13 for topic guides). Interviews generally lasted about an hour and took place either at the person’s home or in an agreed convenient location, usually the VSO, with a couple of interviews taking place on NHS premises. If the person became upset, the offer of taking a break or concluding the interview was made. Care was taken to check how the person felt at the end of the interview and arrangements were made to facilitate access to additional support, as necessary.
An amendment to the original protocol was made to undertake repeat interviews on the recommendation of the SRG. This was reinforced by the literature review, which conceptualised a MH crisis as building over time34,40 as opposed to a singular episode. Fifty-five per cent of the service user sample (n = 26) were invited to take part in a repeat interview and these participants were selected on the basis of the quality of information provided in the first interview. Forty-three per cent of the original sample were subsequently re-interviewed (n = 20); as regards the remainder, either they did not respond to the invitation or their MH had clearly deteriorated, including a person who took their own life. The repeat interviews were undertaken 4–6 months later to gather further information on the MH crisis trajectory and to analyse shifts in perceptions of the MH crisis experience (see Appendices 12 and 13). During the repeat interview, participants were encouraged to describe their experience after the previous interview using a timeline to map the process and to identify the resources that they had used.
Data saturation
Our sample size and sampling method were designed to enable us to explore variation, complexity and detail to provide a rich picture of the VS contribution to MH crisis care. 98 As it was evident fairly early on that similar themes from the service user and carer focus groups and interviews were emerging – particularly in relation to the crisis experience, views of public sector services and views of the helpful aspects of the VS – we actively sought data to disconfirm this and extend our understanding. However, saturation is a contested concept99 and, with more time and resources, it is possible that we could have sampled more widely to include people with a broader range of protected characteristics and smaller VSOs that go ‘under the radar’.
Data analysis
The findings from each stage of the study were integrated with the findings from each of the WPs, which informed subsequent WPs. WP1 informed the focus for the regional mapping and provided the basis for the development of a typology, refined as a result of WP2, which was used as a sampling frame for the case study site selection.
Database and survey analysis
Identifying the candidate organisations and the analysis of the survey responses was an important first step in identifying the different types of MH VSOs and what they offered to people experiencing a MH crisis. Quantitative data from the survey questionnaires were imported into Stata® (StataCorp LP, College Station, TX, USA) for analysis and were used to generate descriptive statistics to identify the characteristics of the organisations providing services, definitions of crisis, their activities including access arrangements, resources, challenges they encountered, and partnership working with other VSOs and with public sector services. The resulting analysis was used to develop a typology of the different types of VS contributions in MH care, as described in Chapter 5. This was used as a sampling frame for the selection of the case study sites and to locate the field of activity. Qualitative free-text responses were imported into NVivo 12 for analysis and categorising into emergent themes.
This analysis was supplemented by desk-based research to enable us to map the location of formal MH crisis care provision by inputting the postcodes for the location of different types of VSOs (24-hour vs. non-24-hour) into GIS. This enabled us to map their location and explore variations in access.
Qualitative data analysis
With permission, the focus groups and interviews were recorded and transcribed verbatim by a professional transcribing service. Field notes were also taken during and after the interview or focus group. To maintain anonymity and confidentiality, unique identifiers for participants were used throughout the analysis. The transcripts were not returned to participants for comment or correction, although, if they requested it, they were sent the cited extracts for their consent to be included in this report. All data were imported into NVivo 12 to assist in data management and analysis. The qualitative data were explored in different ways using NVivo, to compare data across different participants, different types of VSOs, and within and across case study sites.
The analytic strategies reflected the research objectives to understand the contribution of VSOs in responding to people experiencing MH crises. The interview and focus group data from national, regional and local interviews were analysed thematically, both deductively to reflect the research methods and literature and inductively to capture the richness of participants’ accounts. This combined approach enabled us to address the specific research objectives but also allowed us to explore participants’ experience and discover how they assigned meaning to their experience. 100 Further narrative analysis on the individual service user data are being undertaken for publication.
A 2-day coding workshop was held for the research team. This began with considering our individual experience and viewpoints and how these might influence our interpretation of the data. Subsequently, a sample of transcripts were read and discussed, to identify the initial themes and group the codes into categories to develop an initial coding frame. A workshop was also held with the SRG to ascertain the SRG members’ perspectives on a sample of transcripts and ensure good engagement with the data. An initial set of transcripts were subsequently coded and the coding frame refined in the light of this (see Appendix 14). Transcripts were, subsequently, coded by two main coders (KN and BC) with additional coding by six other members of the team (RI, JR, MA, DJ, CD and BN). This was an inherently interpretive task and the inclusion of co-researchers, in particular, enabled us to benefit from diverse perspectives on the data. In the analysis, we explored patterns and similarities between different data sources and accounts, for example comparing the perceptions of a MH crisis between people with lived experience and VS staff, commissioners and MH staff. Because of the wealth of data, an adapted version of the framework method100 was used and this involved the research team exploring selected codes to identify differences and discrepancies between participant types and case study sites (e.g. conceptualisations of a MH crisis and service users’ experience of VS crisis support). Our analysis of cross-case comparisons was shared and explored at a workshop involving the SRG and SSG, and graphic facilitation was used to maximise engagement with our overall analysis. The main themes from the cross-case comparisons provide a focus for this report. The findings from the within-case analysis are being fed back to each of the study sites.
The data from the repeat interviews were analysed alongside other interview data. However, the drawings and narratives were used to map individual journeys, capturing individual experience and how individuals had used different services. This report provides six individual crisis journeys to illustrate access, impacts or the interface between VSOs and public sector services.
Data synthesis
The purpose of the data synthesis was twofold. First, the synthesis data provided by WP1 and WP2 were used to guide additional sampling and data collection. Second, the data from the case studies were used to clarify and elaborate on the data collected in the earlier stages of the study. We were able to locate the qualitative data on experiences and outcomes of VS MH crisis support within the typology derived from the quantitative data. Within each site, a combination of the analysis from the different methods enabled us to develop a holistic profile of that site and to triangulate our data. The integration of data across the sites enabled cross-case comparisons to be made. This was an iterative process focused on the research objectives and exploring the relationships and tensions between the following variables:
-
the type of crisis needs
-
the type of VS provision and activities
-
individual respondent characteristics
-
the interface between the VS and public sector services and
-
organisational form and commissioning arrangements.
This report presents the major themes from our analysis and describes the range of experiences of the VS, including divergent and minor themes.
Rigour
The strategies employed to ensure the rigour of the study were:
-
the adoption of a multimethod approach to provide a detailed examination of the contribution of the VS to MH crisis care
-
comparing the candidate database with comparable databases
-
the use of COREQ52,53 for reporting findings from the focus groups and interviews and the GRIPP254 checklist for reporting on PPI
-
service user and carer involvement to strengthen the credibility and validity of the study
-
development of the coding frame by the whole research team, and validation with the SRG
-
double coding 10% of transcripts to identify discrepancies and interpretative differences
-
an audit trail, through the use of NVivo.
Research team
The research team comprised 11 people: five academics (two female and three male), five co-researchers (four female and one male, all with a wide range of experience) and one advisor (a male carer). Further detail on the support arrangements for the co-researchers is provided in the sections below. The team met face to face, approximately every 6 weeks, depending on the WP. Training was provided for the whole research team and covered:
-
collecting data through interviews and focus groups
-
ethics considerations and good practice in research, recognising the vulnerability of the target population
-
analysing data and the use of NVivo
-
reporting findings and dissemination.
Nine members of the team (MA, SB, BC, CD, DJ, RI, BN, KN and JR) were involved in data collection. For every study site, there were four researchers (an academic and three co-researchers) and each person was allocated two sites. The focus groups were always undertaken by two researchers, namely an academic and a co-researcher, and this was also the case for the majority of the interviews. Following the focus groups and interviews, there was an opportunity to debrief and to reflect on participants’ accounts and on the interview process.
Service user, carer and public involvement
Conceptualisation and purpose
In this study, those involved in PPI were predominantly, but not exclusively, defined as people with lived experience of a MH crisis (i.e. service users, family members and carers). The purpose of this was to draw on a range of direct experiences of MH crisis support and different interpretive frameworks. The conceptualisation of involvement in this study has its theoretical foundations in a critical analysis of the power asymmetries in knowledge production. Experiential knowledge provides a different perspective because it is closer to lived experience than traditional forms of academic knowledge. 101–103 Involvement was designed so that service users and carers were able to shape, change and challenge the research process and knowledge development.
Involvement methods
In the early stages of developing the proposal, there was involvement via Suresearch,104 a network of over 100 MH service users, survivors and their allies involved in research and education. Service user and carer involvement was, subsequently, built into all stages of the study and took the following forms:
-
Co-researchers: five people with lived experience of a MH health crisis were recruited and involved at all stages of the research, including data collection, analysis and dissemination. The research team also included a carer. Recruitment, training and involvement of co-researchers, including payment and reimbursement of expenses, was advised by Suresearch and consistent with INVOLVE good-practice guidance. 105–110 Each co-researcher was teamed up with an academic for ongoing support and supervision.
-
Members of the SRG: eight people were recruited (with representation from MH service users and carers) to act as a critical friend, inform the development of the research tools and lines of inquiry, and comment on emergent findings.
-
Representation in the SSG: members of the SRG were represented in the SSG, which, as well as providing expert advice, provided overall governance of the project and ensured that the key milestones were met. Both the chair of the SSG and the chair of the SRG brought lived experience of MH crisis and there were three other service users in the SSG (see Report Supplementary Material 3).
The two main methods for public involvement were the development of a website providing updates and blogs on the project, and an open event that was held as part of the Economic and Social Research Council Festival of Social Science. 111
Impact
Service users and carers were active participants in the research process and were able to shape, change and challenge the language used, the research methods and the process as it progressed. This led to significant changes in the study, including:
-
reflecting on the use of language, for example the use of the term ‘service user’ and recasting ‘demand’ as ‘need’
-
defining the scope of VSOs that contribute to supporting people with experience of a MH crisis
-
reflecting on the nuanced understanding of personal experiences of a MH crisis, leading to the definition of a MH crisis as a process rather than a unique event, and contesting the conception of a crisis as a ‘turning point’
-
highlighting the social and economic factors implicated in people’s experience and their negative and potentially long-lasting impact
-
understanding the importance of undertaking repeat interviews with service user participants to reflect the changing nature of the MH crisis experience, which led to a protocol amendment and securing additional funding to undertake repeat interviews
-
inequalities in access for BAME groups informing the case study site selection
-
contributing specialist knowledge and contacts/networks to enable access to specific communities
-
emphasising the importance of hearing from carers and family members.
Evaluation
The quality and impact of the public involvement was reflected on by the SRG and evaluated by With-You consultancy, a service-user-led organisation with membership of the NSUN Research Network (see Report Supplementary Material 4 for the evaluation report). 112 The evaluation drew on good practice and the National Involvement Partnership’s National Involvement Standards113 (known as the 4PI), which set out standards relating to the principles, purpose, presence, process and impact of involvement. Qualitative methods were used, notably interviews with the research team and with SSG and SRG members, and a focus group for SRG members. The interviews and the focus group were audio-recorded and transcribed. Thematic analysis was undertaken by all members of the evaluation team and a draft report was circulated to participants for accuracy.
The independent evaluation suggested that, on the whole, involvement in the study was characterised by a substantial number of successes. Evaluation participants spoke positively about the consistency of service user/carer involvement throughout the project, the equal opportunities for involvement, the meaningful nature of involvement in all aspects of the research process and the avoidance of tokenism, the recognition of the value of experiential knowledge of distress/MH service use, and the flexibility of involvement. Evaluation participants also highlighted the inclusivity and diversity of the project, acknowledging the constraints with regard to the ‘representativeness’ of involvement. Even though evaluation participants indicated that they would value more clarity with regard to job descriptions and procedures, this need for further clarity appeared to be counterbalanced by the genuine nature of involvement and the increased opportunities for learning that the project afforded. Finally, evaluation participants were very clear about the positive impact of service user/carer involvement in the crisis care research project, that is, the impact on the research project itself and on the individual people involved.
Approval by research ethics committees
Standards of good practice for research were followed114 and the project was undertaken in compliance with the Data Protection Act115 and University of Birmingham policies relating to the conduct of research. The University of Birmingham Humanities and Social Sciences Ethical Review Committee (RG16-153) granted ethics approval for WP1 and WP2. Ethical approval for WP3 was granted by West of Scotland Research Ethics Committee 4 (18/WS/0022) and approved by the Health Research Authority (IRAS 211953). Once these approvals were obtained, the research governance bodies for the relevant NHS trusts reviewed the application to confirm participation. Care was taken at the beginning of each interview to ensure that individuals had the capacity to consent to participate. As the study involved people with experience of a MH crisis, who were potentially vulnerable, we kept the well-being of participants under active review and made adjustments as necessary. During the early interviews in WP4, we identified several participants whose needs were not being met, and we subsequently contacted a health or social care professional, usually their GP, regarding our concerns. One participant took their own life during the course of the study. The question of whether or not the research had contributed was considered and there was no suggestion that it had. Appropriate action was taken, as advised by the SSG chair and clinical advisor, the sponsor, the Research Ethics Committee and the National Institute for Health Research (NIHR). This included an urgent amendment to the interview protocol and the participant information sheet to ensure the routine collection of a clinicians details, if we had concerns about a participant’s welfare.
Chapter 4 Experiences of a mental health crisis
This chapter starts with participants’ experiences of a recent MH crisis and considers the relevant context and factors they identified, what they felt their needs were and the impact of the crisis on their lives. The different conceptions of a MH crisis by the various participants are compared. Although this chapter primarily draws on data from WP4, these findings are presented first as a reference point for reporting our subsequent findings.
Experiencing a mental health crisis
More than half of the service user participants reported a previous experience of having a MH crisis (n = 34), although a number of people were unsure whether this was their first crisis or not (Figure 1). There was a higher percentage of people in site C (36%) reporting it as their first crisis, reflecting recruitment mainly via the VS, than in the other sites, where participants were also recruited via the NHS. More than half of the sample (58%) had been accessing VS support for less than a year (Table 9). By contrast, two-thirds (67%) had been using MH services for more than 3 years, although this was particularly the case in sites B and D.
FIGURE 1.
Crisis experience of participants in the study sites.
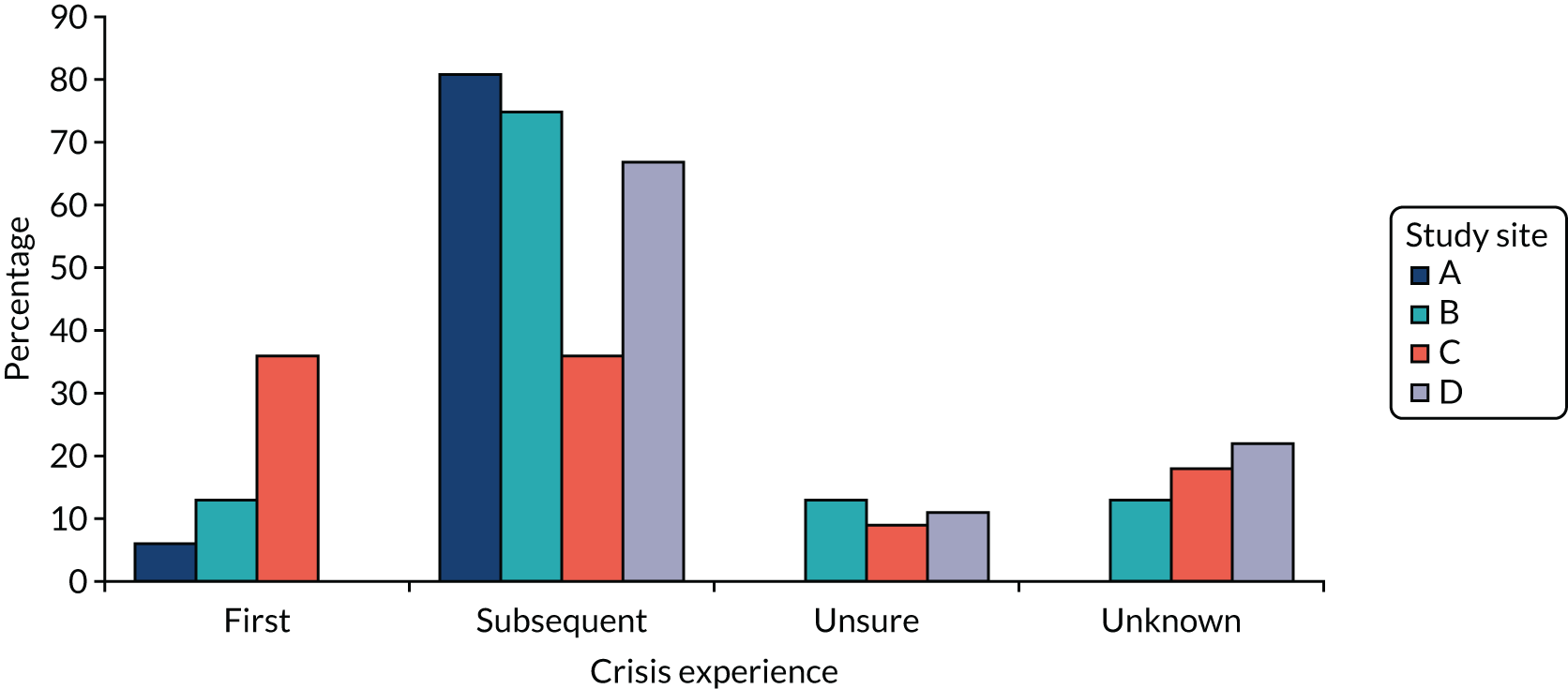
| Study site | Length of contact with VSOs (%) | Length of contact with MH services (%) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| < 3 months | 3–6 months | 6–12 months | 1–3 years | 3–5 years | > 5 years | Undisclosed | < 3 months | 3–6 months | 6–12 months | 1–3 years | 3–5 years | > 5 years | Undisclosed | |
| A | 19 | 13 | 25 | 13 | 19 | 5.5 | 5.5 | 0 | 12.5 | 6.5 | 6.5 | 12.5 | 56 | 6 |
| B | 12.5 | 0 | 37.5 | 0 | 25 | 12.5 | 12.5 | 0 | 0 | 0 | 25 | 0 | 75 | 0 |
| C | 9.1 | 18.2 | 27.3 | 18.2 | 18.2 | 9.1 | 0 | 9.1 | 18.2 | 0 | 18.2 | 36.4 | 18.2 | 0 |
| D | 25 | 12.5 | 38 | 12.5 | 0 | 12.5 | 0 | 0 | 12.5 | 12.5 | 12.5 | 12.5 | 50 | 0 |
| Total | 16.2 | 11.6 | 30.2 | 11.6 | 16.3 | 9.3 | 4.6 | 2 | 12 | 5 | 14 | 16 | 49 | 2 |
Service user participants described a wide variety of crisis experiences across the sites. A distinction can be drawn between (1) ‘a situational crisis’, with service user participants describing their experience of crisis as a ‘one-off’ event or a response to a specific situation (e.g. severe work stress or relationship break-up), (2) ‘a traumatising crisis’, when the crisis was associated with previous trauma (e.g. abuse, assault or loss) and was triggered by a specific situation resonant of this (e.g. an abusive relationship), and (3) a crisis as an element of ongoing MH issues (e.g. depression and bipolar conditions were commonly mentioned). For some people, it was a combination of events or situations coupled with pre-existing trauma or MH issues. Some participants also said that they could not identify a particular trigger. The following sections outline aspects of the experience that were identified.
‘Falling into a million pieces’
For the majority of service user participants, the crisis experience was described as ‘overwhelming’, as bringing a sense of ‘falling apart’ and as a ‘dark place’ to be:
I just couldn’t focus, face anything. I just literally shut down, became very scared, the voices telling me that I’m better off dead, and it was a horrendous 3 years. And then she left, which was even worse because I had nothing then.
ASU2
This experience of being overwhelmed, losing control and uncertainty about life was likened to ‘falling into a million pieces’ and ‘a car crash’, conveying a sense of interruption and disruption. The range of experiences described included extreme anxiety, profound sadness, ‘paranoid beliefs’ and suspicions about other people, hearing voices, self-harm, suicidal feelings and isolation:
It’s like a very, very dark place to be and . . . your nervous system will collapse and [this] means you become more anxious, you become like a jelly and . . . it’s a hard time.
BSU8
Sometimes, the experience was accompanied by intense feelings of anger or exhaustion:
It’s like where it can go from 0 to 100 in a split second . . . where all the coping mechanisms that I’ve had and the help and support just suddenly seem to disappear. I end up on this track that is destructive and . . . then I feel trapped and that’s when it all goes to an enormous crisis.
CSUG
For some, exhaustion reflected the effort that was needed to appear to be coping:
My teachers thought I was fine because during school I would just get on with my work. After school I used to just be really depressed. I couldn’t cope with the anxiety . . . I was panicking so I was crying, struggling breathing because I wasn’t breathing properly. I felt overwhelmed.
ASU4
Rarely, the crisis experience was accompanied by feelings of elation and happiness, as was the case for one person who felt they had special powers and could fly.
Suicidal feelings and self-harm
Suicidal feelings and self-harm were commonly described and were often cited as the reason for contacting a service (both the VS and the public sector). Self-harm was usually repeated and, for some participants, was a way of coping and, therefore, was not seen as a crisis:
I wouldn’t call Crisis or I wouldn’t call a hotline to say I really want to self-harm, can you help me stop. I wouldn’t really be that bothered, to be honest. I wouldn’t consider that a crisis.
ASU5
Suicidal feelings often persisted or emerged at different times; they were rarely an isolated experience:
I got into severe depression and had severe suicidal thoughts constantly.
DSU9
A number of people described having made a suicide attempt previously:
You have thoughts in your head saying suicide or you’re going to do something to yourself or hurt yourself; mine was kind of like a suicide but I snapped out of it, I was seeing things like people coming in the room and things . . . and it’s an experience you’ve got to think about because people don’t understand us.
BSU3
For some participants, there was a recognition that mentioning suicidal feelings would mean they were able to access support quicker:
I can understand it, but it’s unfortunate because . . . I think you learn that very quickly that you’re based on what you’ve got to say in order for somebody to see you.
CSU10
However, there were also instances in which self-ham and suicidal feelings were dismissed, notably by public sector services.
Isolation
There was an association between the crisis experience and isolation, with a number of factors affecting this. The first of these was feeling unworthy:
I hear voices sometimes telling me that no one gives a shit and like no one loves me and all this stuff, and I don’t believe them but sometimes it’s hard not to, you know?
ASU13
The second was a feeling of being unsafe, and so withdrawal and avoiding people or customary activities created a sense of security:
I’ve learned . . . that I can separate myself from people, especially my siblings and my parents, to cut myself off and give them that space so that they haven’t got a power over me to hurt me or impact me in a way.
CSU9
Third, and associated with a sense of shame, was the awareness of MH-related stigma and a perception that they would be judged unfavourably by family, employers and community members:
You know if you suffer from mental health in the Asian community, there’s a stigma attached and they think that ‘she’s gone, she doesn’t know what she’s doing and everything’.
BSUFG
Finally, isolation was identified as a consequence of the crisis experience, with a complex interaction between escalating poor MH, social impact, reduced capacity to perform tasks and usual roles, and poor access to services.
Factors implicated in the experience of a mental health crisis
A wide and complex range of factors were identified as influencing MH and resulting in a crisis, as summarised in Table 10. The three most commonly mentioned factors were family factors (breakdown, conflict or loss), issues related to MH, and housing.
| Factor | Examples |
|---|---|
| Abuse in adulthood | Domestic abuse, rape, racism, cuckooing, financial abuse, exploitation |
| Adverse childhood experiences | Childhood sexual abuse, bereavement and loss, not loved as a child, parental MH problems |
| Alcohol and substance abuse | Alcohol or illegal drug use |
| Family factors | Divorce or relationship breakdown with partner, access and custody issues regarding children, caring responsibilities, conflict over money, parental expectations |
| Financial factors | Debt, welfare benefit cuts, appeals |
| Housing issues | Homelessness, insecure housing, poor state of accommodation |
| Issues related to MH | History of MH problems (diagnoses of schizophrenia, personality disorder and postnatal depression were referred to), relapse in MH, labelling as a self-fulfilling prophecy, medication, difficulty accessing services or support, relapse in MH |
| Adverse events and stress | Serious accidents, bereavement, immigration-related issues, imprisonment |
| Physical health | Complex physical health problems, pain, arthritis, mobility problems |
| Work and education | School or employment-related stress or anxiety, redundancy |
Several participants dated their first experience of a crisis back to childhood, including parental loss and experiences of neglect and/or abuse, with subsequent events retriggering or resonating with this earlier experience. Racism and alienation was also identified as an explanation of the crisis presentation of black African and black Caribbean men and their disproportionate detention under MH legislation:
Racism is a factor, and it is not always blatant or overt. It comes subtly through your surroundings, through the media and so forth. When you’re struggling with feeling marginalised, low self-esteem, meeting racism everywhere you go, it impacts on you subconsciously, or consciously.
CVS7
The precarity of individual circumstances was also identified as having a bearing on MH. For example, an asylum seeker was experiencing a MH crisis because of the fear of deportation as a result of their immigration papers having not been sorted by the Home Office, and was subsequently sectioned. Similarly, housing was identified as a critical factor, particularly in site C, which had the highest rate of homelessness. The practice of ‘cuckooing’, where vulnerable people with MH problems are targeted by drug dealers who then take over their homes, was mentioned:
It starts off like friendship and they think oh god this is nice but then they start doing things to keep them under control like demeaning them; I’ve seen . . . where they’ve made them cut their toenails and stuff, to demean them and degrade them and to keep them in it.
CVS8
It was evident that, alongside complex social situations, several participants experienced complex difficulties, including experiences of MH problems co-occurring with substance use, a diagnosis of autism spectrum disorder and/or a diagnosis of personality disorder:
I’ve got multiple diagnoses; one of them is psychotic tendencies. I don’t realise when I am in a psychotic episode and I need help. The other thing is I have borderline personality disorder, with that I don’t know when it’s escalating but I do know when I am at the top and really stressed.
DCaFG
This could also serve to fuel negative stereotypes, intersecting with other forms of stigma (e.g. related to addiction or learning disabilities) and detract from people having their needs met.
Impact of the crisis
The impact of the crisis was often profound and, for some, the experience had shaped their lives:
The impact of recovering really from a crisis in a space of a few days has a knock on effect on people’s lives and for me it’s really stolen a lot of my life, you know; I’m 40 now and I’ve just got my mental health on track.
ACa3 (friend and service user)
From participants’ responses, it was possible to identify different types of impact, which interacted:
-
emotional impacts, undermining self-belief and self-worth
-
impacts on social networks and directly on family members and carers (as discussed later in this chapter)
-
changes in personal circumstances as a consequence of the MH crisis (e.g. relationship breakdown, unemployment and isolation)
-
changes arising from the service response (e.g. the sense of not being understood, being arrested by the police, being detained under the MHA in hospital, medication changes or access to different forms of treatment or therapy) and
-
changes in behaviour or perspectives.
These impacts could be negative but could also be positive, particularly when the experience led to an individual reappraising their circumstances or approach to life, on their own or with the support of informal networks or services. This was evident for those service users we re-interviewed who had reflected on the crisis experience and made changes as a consequence. These were sometimes attributed to the VSO response, as discussed in Chapter 6, but also reflected individual agency.
Service user needs in a mental health crisis
Reflecting the intensity of the experience and the sense of threat, the most commonly cited need was to feel safe – ‘to be in the safety zone’ or ‘a calm place where you could talk to people’:
You just want to be wrapped up. Safe-guarded if you like; know you’re in a safe place because perhaps you feel threatened.
ASUFG
It was evident that safety is relational – ‘building trust and confidence’, ‘being heard’, ‘reassured’, ‘accepted’ and ‘not being judged’:
I was really fed up because it was like a really vicious cycle I couldn’t escape and it was doing my head in, it was dragging me down, and I just wanted to talk to someone who would like help me reason it out and bring me thinking positively again to get me out of that deep, dark place.
CSUFG
‘Kindness’, ‘being listened to and not being dismissed’, ‘time and space to make sense of the experience’, ‘being treated with care’, ‘compassion’, ‘understanding’ and ‘humanity’ are how participants described what they needed:
When I’m in crisis or going into crisis I need people to be kind rather than kind of tough love approach, it doesn’t work with me.
BSU4
Listening and being able to share openly were important, but some participants also sought guidance – ‘a guru, someone to show me, guide me’:
Sometimes, it’s just being reminded of what I need to do and I know that sounds really silly because I know it and I should be able to do it myself, but when I can’t think because there’s too much going round in my head and I feel like I need to self-harm to be calm enough to be able to then distract myself so it’s safe to stop it going any further, but I feel like – and sometimes that phone call stops the self-harm, does that make any sense?
ASU13
It was evident that some people had ongoing, and sometimes highly complex, needs. For example, one man described having had difficulties since childhood following his mother’s death and an abusive relationship with his father. He identified as having learning difficulties and had been a regular user of crack cocaine. Living in a homeless hostel, he had been in three different prisons in the preceding 9 months, the most recent because he hit someone for spitting on him when he was homeless.
Family members’ and carers’ experiences
The definition of a carer is a family member, relative or friend who provides care for someone close to them who has physical and/or mental difficulties. Some participants were also caring for an elderly relative or had child-care responsibilities. Those that cared for someone with a MH problem did not necessarily consider themselves a carer, highlighting the reciprocal nature of caring and other roles as more important:
There’s certain connotations to it [identity as a carer] that I probably don’t really want to identify myself with. Because it’s not like that all the time; that isn’t how I would describe our relationship or what’s going on. Also I’m not infallible and I also have ups and downs or whatever, so sometimes she has to look after me. So it feels a bit kind of one-sided to call me a carer.
CCa1 (partner)
It was clear from the carers we interviewed that, in general, they were under strain, with some also experiencing their own MH difficulties. One carer had made a suicide attempt because ‘something tipped them over’, whereas another had self-harmed:
We . . . often get carers not only caring for somebody with a mental health problem, but they have their own mental health problem . . . I think stats say 80% of carers have some impact on their own mental health.
DVS4
Many of the carers had been providing support for many years. This included people who had been young carers (children or young adults) of parents or siblings who were suffering from mental distress. A participant’s father commented, ‘he’s witnessed the things from day 1, from 19, ‘cause it affected him. He had a breakdown himself . . . he was crying, when he saw me in bed’. Another participant had been a young carer for her mother and three of her siblings who were diagnosed with bipolar affective disorder, and one with paranoid schizophrenia:
Life has been strung out on managing, supporting to manage crises, but what the issue was that I didn’t really understand mental health, I didn’t understand what a crisis was, the language used in the field, to help me understand what was taking place with my siblings.
S2
There were also parents supporting their adult children who worried about the future in the event of their own death and were not confident that the services would care for them. In one situation, grandparents, with two teenage children, were supporting their daughter and were looking after her 4-year-old child while she was an inpatient. Multiple caring roles were not uncommon:
I’m happy to identify myself as a carer, which means as well as having a mum who’s very physically frail and has memory loss, most directly we’ve got three sons in their 20s and the middle one has Aspergers and the youngest, who’s 23, now has quite severe anxiety and depression.
ACFG1
All carers expressed a strong sense of responsibility, often associated with continual anxiety about the person they cared for:
Well, fear of her hurting herself, her killing herself, you know, that kind of thing. Fear of dangerous consequences or loss and that’s an understandable fear isn’t it, to have?
ACa2 (husband)
In several instances, they or another close friend or family member had intervened to prevent the person from harming or killing themselves:
It would be very frightening . . . ‘OK what do I do with this situation bar trying to wrestle him to the ground and restrain him’, because he would reach a point where sometimes you walk in and he’d be head butting the wall or he’d have taken a Stanley knife to himself and carved all over his stomach.
ASU2 (son)
The interventions to prevent a suicide generally involved calling services, usually the police. In other situations, a family member or carer had been contacted because of concern that the person was about to kill themselves. For example, the police contacted a man because they were worried that his father might be about to take his own life by jumping off a bridge. One carer (a mother) had been a victim of assault by her son:
I have another son – I had to get us out. So as soon as I could extricate myself, we ran out of the door and as I shut the door I heard a bang and he’s thrown the knife after us and it was embedded in the front door. Another time he was pushing the knife in here, oh he’s held various implements at me. He’s broken some teeth, my teeth, he got me in a headlock once.
ACaFG
Clearly, these experiences had an impact on their relationship with the person for whom they care and, indeed, on wider family members, including children. This was in a context of austerity and the reductions to public services and welfare benefits, which served to increase the stress for some carers or family members:
We’ve seen significant rise in our caseloads of carers from all walks of life having problems with housing and their mental health suffering as a result – attempted suicide, things like that. And people who are agoraphobic, who won’t go out . . . they can’t access the benefits, ‘cause they can’t get down to the job centre.
RN2
Conceptions of a mental health crisis
Stakeholders commented on the difficulty of defining a MH crisis. Nonetheless, there was a broad consensus that a crisis is marked by acute distress, an increasing inability to cope and the need for an immediate response:
This is quite hard to articulate. I would say if someone’s thoughts, feelings, compulsions, are having an immediate effect on their ability to carry on normal life – so at one extreme that could be very suicidal tendencies, at the other one it could be this sort of crippling fear of leaving the house. And somebody needs some help straight away, and it’s not always immediately obvious what the help is that they need and that’s part of the struggle.
ACa2 (husband)
For service users and carers, the urgency involved in needing an immediate response should be considered in the social and personal context of their lives, as they often described the crisis experience as a process that unfolds over time.
Crisis as a disruptive process
So it’s really hard to define crisis when it’s over a long term. I think for me it’s whether crisis is just when it’s perceived by the outside world to be a crisis because she’s nearly killed herself. That for me is quite a different definition from what I saw as somebody close to her, who was somebody ebbing towards it and away from it, towards it and away from it.
ACa3 (and service user)
Service users typically contextualised the crisis experience in what was happening in their life; relationship problems, historical and current abuse or trauma, racism, debt, and alcohol or substance use were common:
It was a series of minor crises all along the way really, and then coming more and more frequently. So it’s like about how many you’re getting, and how close together they’re all getting really. How many times a week I feel like I feel suicidal, or feel like I need to call the Samaritans. And when there’s no space between those experiences, I guess that’s a crisis.
CSU5
For some participants, crisis was described as an everyday occurrence, often reflecting fundamental existential doubts about the value of living, overwhelming impulses to self-harm, recurrent symptoms of voices or a persistent feeling of not being able to cope:
I have them every day. Well I’m a dramatic person, but I have them a lot of the time . . . where I feel sort [whispers] of suicidal or I feel like I hear voices and I just want it to stop. Like yesterday, I wanted it to stop and I was like well if I just kill myself, it didn’t matter.
ASU10
This negotiation with the self was common, with the person balancing various factors, including locating it in a spiritual context:
Well in the Quran it says . . . that if something is that severe that it is affecting your health or it’s going to put your health at risk, because we see suicidal as not halal. It’s a bad sin if you commit suicide. But if you feel like you have no other way out, you feel trapped and you feel forced, the only way you can end what’s going on is by ending your life.
DSU4
The factors that were considered in such self-negotiations reflected the resources available (including support and experience of previous responses), the potential for life changes, access to the means to kill themselves, and the meaning of suicide, including the anticipated impact of the act. This process of self-negotiation is portrayed in Figures 2 and 3 (produced by a member of our SRG), with how people think about self-harm (Figure 2) contrasted with the lived experience of self-harm (Figure 3).
FIGURE 2.
How people think self-harm works. Reproduced with permission from Rachel Rowan Olive (https://rachelrowanolive.co.uk), February 2019, personal communication.

FIGURE 3.
The experience of self-harm. Reproduced with permission from Rachel Rowan Olive (https://rachelrowanolive.co.uk), February 2019, personal communication.

The distinction between the first experience and subsequent experiences of a MH crisis was identified by both the service user participants and SRG members. This was viewed as shaping sense-making, the capacity to identify triggers and, thus, self-management. By contrast, some service user participants reported that they were relatively unaware of what was happening and observed that it was those close to them who recognised the signs. This included instances in which a family member or friend, recognising the severity of the situation, had intervened to prevent the person from taking their own life.
Voluntary sector organisations’ conceptions of a crisis
A wide range of definitions of a crisis existed between VSOs, reflecting the breadth of their activity. Suicidal ideation and self-harm were most commonly mentioned by survey respondents, as illustrated in Table 11.
| Rank | Definition | Frequency (%) |
|---|---|---|
| 1 | Suicidal thoughts/plans or risk of harm to self or others | 24 |
| 2 | Loss of control/reality/emotional instability/not coping | 15 |
| 3 | Intense distress | 12 |
| 3 | Mental health presentation or deterioration | 12 |
| 4 | An emergency requiring immediate help | 8 |
| 5 | Self-definition | 6 |
| 5 | Need for support or inability to access services | 6 |
| 5 | Social circumstances (e.g. carer no longer coping, homelessness, benefits withdrawal) | 6 |
| 6 | Requiring clinical services or admission to acute psychiatric care | 5 |
| 7 | Impact on well-being | 2 |
| 8 | Defined in their wellness recovery action plan | 1 |
This focus was evident in the interviews with VSOs, and provided a richer and multifaceted conception of a crisis to emerge. Those VSOs that identified as providing a specific crisis service (see Chapter 5) emphasised the importance of self-definition of the crisis experience (i.e. taking what the person defined as a crisis as the starting point):
In our experience, a crisis means different things to different people. So we have some people that call because they’re suicidal and then we’ve got the other end where somebody’s not able to contain their anxiety.
CVS2
This went hand-in-hand with the importance of acceptance and validating experience. A crisis as a disruptive process was often linked to a lack of personal resources to be able to cope, resonating with the service user experience of being overwhelmed, and linked to the idea of social threat and limited psychological strategies or social resources to be able to respond to circumstances. One crisis-specific VSO, for example, assessed how well-supported people were feeling alongside the intensity of distress and the suicidal thoughts reported:
What we find is that, generally speaking, people may come in with extremely high levels of distress as well as extremely high levels of how suicidal they’re feeling and generally quite low levels of how supported they’re feeling.
CVS3
A crisis was also described by VSOs in terms of being unwell or a relapse in a person’s MH. As with service user accounts, this was often situated in an individual personal and social context, particularly by those VSOs providing support to people who had experienced a life crisis, for example homeless charities or those supporting survivors of rape or domestic violence, such that the life event as a crisis and the MH crisis were inextricably linked:
Other people that have . . . been through a very traumatic incident, like they’ve been raped, and they need support today to help them through that. They might be worried about being pregnant, about a sexual health issue or they might have HIV, so those people could also be deemed to be in crisis.
DVS5
Public sector conceptions of a mental health crisis
Policy-makers, managers and staff also identified the importance of a MH crisis being subjectively defined:
I think one of the absolute crucial things is that you accept the crisis as the patient or the service user defines it. So a crisis is what bothers the service user and/or their relatives to prompt them to actually seek help.
CMHP1
The importance of listening to people in a crisis and validating their experience was recognised:
The . . . worst thing you can do when someone feels that they’re in a crisis is to tell them that they’re not, they don’t meet criteria for a crisis service. It just seems like the least validating thing that you could do. We wanted to be really strong on that message, that if someone says they’re in crisis, they need immediate help, and there’s a wide range of what that help might be, but they need something.
S5
Although many of the strategic stakeholders (i.e. commissioners and MH staff) expressed the view that a subjective definition was important, those with operational roles commonly interpreted a crisis in terms of a diagnosable illness. They also suggested that adopting a wider definition had implications for the service:
We were looking for a diagnosable mental health problem; you know, mental disorders. That is not what we see come through the door now, you know, and of course a crisis service has to respond to what people believe a crisis is and, you know, what we see come through the door are very much people that need help with social prescribing, with housing, with benefits.
DMHP5
Some participants identify situational crises as distinct from people with mental illness and the implications for support – signposting for practical support or needing active support for mental illness. Some VSOs did understand a MH crisis in terms of deteriorating MH, and this was more likely to be those VSOs that considered that they lacked expertise in this area and would, therefore, refer people to more specialist support.
The shifting conception of a MH crisis was sometimes situated in the historical context of a service-focused definition of a crisis as a consequence of the National Service Framework for Mental Health. The evolution of the crisis definition was framed as moving from having ‘two versions of the truth’ (i.e. the official definition and the lived experience of a crisis) to a single version. However, it also reflected that there are different types of MH crises and a wide range of needs:
A quite narrow definition of crisis as a sort of situation in which people are at higher risk of a hospital admission if they’re not provided with some sort of fairly intensive support . . . It’s crucial to also bear in mind that there’s a broader set of crises where people are really distressed and there’s a strong sense that something must be done straight away . . . what we’ve described it, although I think there’d be less clumsy ways of describing it as a sort of subacute crisis.
S22
Conceptions of risk were also linked to definitions of crisis, and covered the risk of harm to self and others, the support available and MH history:
Some . . . people when they become more unwell become very risky, either in terms of self-harm or in terms of irritability and risk of hitting out at other people, or in terms of suicidal thoughts. So when people are referred to us, we’re always assessing their risk and whether it’s safe for them to remain at home, either with or without our support.
AMHP3
Risk was mentioned by VSOs and was implicit in the conception of a crisis by service users when they described the intensity of suicidal feelings and self-harm. Risk was also used, particularly by carers, to refer to risk-taking and risky behaviour as a form of self-harm, as in ‘drinking to oblivion, drug taking, and risky sex’.
The critical difference between public sector conceptions of a crisis (particularly of NHS managers and staff) and those of service users and VSOs was the conception of crisis as an event requiring an urgent response as opposed to a process:
To me, it’s somebody who is not coping with their feelings, their day-to-day life, and that’s a broad spectrum, that can be from people who are sad and that sadness escalates to despair like that [snaps fingers], to somebody that you can’t sit and reason with them.
AMHP5
This conception has shaped service development, including the relationship with VSOs, bringing with it the challenge of establishing when and how public sector services should respond:
So that was a big tension when we started and the debate is not everything that is a crisis needs a mental health input necessarily and so I think that means that mental health organisations get anxious that they’re going to be somehow responsible for making a response to things, which can be like a social crisis, can be all kinds of different things that happen to people . . . In addition I think generally not wanting to over-medicalise distress or social crisis.
AMHP2
The conception of a crisis was reflected in how services are configured, for example crisis support as emergency or out-of-hours provision: ‘to interchange it with out-of-hours support almost so, like, on an evening or a weekend, because traditional services are probably seen as nine to five’ (DVS7). The extent to which VSOs shared the conception of a MH crisis as an event requiring an urgent response reflected their objectives and/or the proximity of their relationship to the NHS and what they were being commissioned to provide. However, service users and carers also defined a MH crisis in terms of the need for an urgent response, often linking this to the intensity of suicidal feelings or self-harm.
Crisis as a turning point
The conception of a MH crisis as a turning point was contested by the SRG for overshadowing the negative aspects and impacts of the crisis experience. In the repeat interviews, some service user participants, however, identified that the experience had made them realise that they had to make a life change to maintain their MH. A crisis as a window of opportunity was identified by carers and by MH staff:
I also see crisis as sometimes a good thing because it’s a chance for things to change when problems are very stuck; sometimes a crisis is a helpful way of actually changing things for the better.
BCaFG
Changing things for the better included the person leaving a relationship or a job that was causing too much stress. Service users and carers also identified the crisis experience as ‘a ticket’ to getting access to much needed support from services through enabling services to understand the gravity of their situation:
There are so many gaps in mental health services that people say ‘well it seems necessary to have a crisis to get care’; in other words, if you don’t have a crisis nowadays from a carer’s point of view, it sometimes feels very, very difficult to just have your needs taken seriously.
ACaFG
Crisis as a missed opportunity was also implicit in the disappointment people felt in the crisis response and the subsequent support failing to enable a person to address their difficulties, develop preventative strategies and address the underlying reasons for the crisis, as explored in Chapter 6.
Summary
The intensity of distress was described by service user participants, and the overwhelming nature of these feelings was associated with needing to be understood and to be treated with compassion and humanity. The narratives identified the experience of a MH crisis as a biographical disruption: an intense and extreme experience that disrupts everyday life and potentially has far-reaching consequences. A corollary of this is that the experience, and the response, cannot be disconnected from the personal and social context of living. This conception contrasts with a narrow definition of a MH crisis as an episode requiring an urgent response, which means that the underlying difficulties may not be addressed. We identified nuanced and important differences in the conceptions of a MH crisis that are enacted through the policy discourse, service configuration and professional behaviour, all of which may influence the contribution of VSOs and their relationship with public sector services. We explore this in more detail in subsequent chapters.
Chapter 5 The contribution of the voluntary sector to mental health crisis support
This chapter synthesises the findings from the different WPs to provide an overview of the contribution of the VS to MH crisis support. It is evident that there is a wide range of VSOs providing support to people experiencing a MH crisis. From the database analysis, survey findings and regional mapping, we developed a typology of the different VSOs and the role they play. Illustrative profiles of these different types of organisations are available as Report Supplementary Material 2 and further examples are available on the Positive Practice website. 91
Organisational arrangements: charities, social enterprises or community groups?
Table 12 summarises the characteristics of the organisations that we surveyed and compares them with our sampling frame and with a wider population of organisations (covering six subsets of the ICNPO) from which the sampling frame was drawn.
| Characteristic | All organisations in the relevant ICNPO categories | Sampling frame | Survey respondents |
|---|---|---|---|
| Proportion that are companies | 0.31% | 0.65% | 0.62% |
| Income | |||
| < £25,000 | 54.0% | 22.5% | 17.1% |
| £25,000–100,000 | 19.3% | 20.6% | 24.4% |
| £100,000–500,000 | 17.0% | 26.9% | 31.7% |
| £500,000–1M | 4.2% | 8.7% | 13.4% |
| £1–10M | 4.7% | 15.5% | 11.0% |
| > £10M | 0.7% | 5.9% | 2.4% |
| Mean income | £495,889 | £3,283,029 | £2,255,004 |
| ICNPO category | |||
| Civic and advocacy organisations | 7.6% | 4.2% | 5.4% |
| Hospitals and rehabilitation | 10.0% | 2.5% | 3.0% |
| Housing | 15.4% | 17.8% | 7.3% |
| Mental health and crisis intervention | 1.7% | 32.6% | 53.3% |
| Other health services | 4.2% | 10.6% | 13.3% |
| Social services | 61.0% | 32.2% | 15.1% |
The salient points of this are as follows:
-
Compared with the main ICNPO categories of interest, those that we identified for our sampling frame are likely to be larger (mean income of £3.28M) and are more likely to be charitable companies (the proportion that are companies is nearly twice as high in the sampling frame as in the ICNPO categories).
-
This is also true of the charities that responded to our survey. Although their mean income is lower than that of the organisations that formed the sampling frame, this is probably because our sampling frame included some very large organisations and survey response rates from such organisations are low. The median incomes of these two groups are almost identical (£152,771 and £154,020, respectively).
-
These results suggest that there are broad similarities between the survey respondents and the subset of charities that are of interest to our study.
We have not compared these results with the wider charity population – there seems little to be gained from comparisons with large numbers of Scout groups, village halls, Women’s Institutes, etc. – but, for charities as a whole, the median expenditure is approximately £16,000 and the proportion that are also companies is 27%. The majority of survey respondents were local in their focus (70%), with 12% describing themselves as regional and 18% as national, meaning that 30% of the organisations are larger than a typical (i.e. local) charity. Therefore, the VSOs in our sample are typically larger and more formalised than the charity population as a whole.
All of the VSOs in the sample were registered charities, but there were variations in organisations’ perceptions of themselves. First, some VSOs were keen to be seen as ‘more than’ a charity – emphasising their business-like approach. Other VSOs emphasised their grassroots origins, volunteer workforce, altruistic values and foundational ethos of user involvement. Some VSOs rejected the paternalistic connotations of ‘charity’:
We don’t want to be a charity; people feel it inhibits what people can do. I think there are arguments for and against that, but we are regulated as a company and of course you know that the financial regulations as a company is more tough than the regulation as a charity.
S24
Second, the degree of closeness to the public sector is far from simple (as discussed in Chapter 7). It can involve VSOs either opting to work closely ‘in partnership’ with the public sector (regardless of their exact sources of funding or ‘resource base’) or seeking direct funding for their work through grants or contracts from the public sector (typically in commissioning processes).
Often, VSOs are adept at blending a complex mixture of funding sources and ‘hiding the wiring’, but this can play out in many different ways in terms of the degree to which they seek to integrate themselves with statutory services, or indeed maintain a high degree of independence or autonomy. We will explore this further in Chapters 7 and 8.
Types of voluntary sector organisations providing mental health crisis care support
From the survey, VSOs that could be formally described as a ‘crisis service’ were in the minority. Just under one-third of respondents said that they actively promoted crisis support services and 13.5% of the total number of respondents characterised themselves as crisis services. A further 19% said that they provided some services to people in crisis. This suggests that we need to distinguish between ‘formal’ crisis VSOs and ‘informal’ crisis VSOs (i.e. those services explicitly established for crisis support vs. those VSOs set up for other purposes – such as dealing with a specific population or with general MH – that also provide crisis support). From the survey data, we identified five different types of VSOs that are contributing to MH crisis support. The different types of VSOs may overlap, but this distinction, as illustrated in Figure 4, was useful for mapping the different VSOs and their contribution to MH crisis care. They were:
-
Type 1: VSOs explicitly set up to provide crisis support and that promote access to support in a crisis for people experiencing mental distress. There are three broad forms of type 1 VSOs: those providing accommodation (crisis houses); those providing a safe space, listening and social activities; and those providing telephone helplines for people who are feeling suicidal or in a MH crisis.
-
Type 2: VSOs active in general MH that provide a wide range of services for people experiencing MH problems, including support in a crisis (officially and unofficially, for example branches of larger MH VSOs and ULOs).
-
Type 3: VSOs set up to support a specific population that may be vulnerable to MH crisis [e.g. women, members of the lesbian, gay, bisexual, transgender and queer (LGBTQ) community, those who are deaf, BAME communities, refugees and ex-military personnel]. These organisations are particularly knowledgeable about the issues facing a particular group of people and, although they do not have a specific focus on MH, they often cover a wide range of health and welfare issues.
-
Type 4: VSOs providing a response to a psychosocial or contextual crisis (e.g. bereavement, pregnancy, rape, domestic violence or homelessness), which means they are likely to encounter people experiencing a MH crisis.
-
Type 5: community and social organisations used by the whole population or particular groups (e.g. churches and faith organisations, welfare and social support).
FIGURE 4.
Voluntary sector organisations providing support in a MH crisis.

Type 1 VSOs were most commonly identified by statutory services as contributing to crisis care.
Table 13 provides a description of the prime functions of the different types of VSOs illustrated in Figure 4.
| Type of VSO | Function | Characteristics | Form | Examples |
|---|---|---|---|---|
| Type 1: MH crisis specific |
|
|
|
|
| Type 2: general MH VSOs providing a wide range of services for people experiencing a MH crisis | To promote the well-being and recovery of people experiencing a MH problem |
|
|
|
| Type 3: VSOs set up to support a specific population that may be vulnerable to MH crisis | To promote the rights and well-being of a specific population |
|
|
|
| Type 4: VSOs set up to respond to specific social issues or life events | To enable people to respond well to a specific social crisis and/or life event |
|
|
|
| Type 5: community and social organisations open to the whole population | To provide social care and welfare support, often as part of a wider mission |
|
Social clubs, activity groups and faith-based organisations |
|
Approach
Across the different types of VSOs, the following characteristics were identified as defining their approach:
-
having staff and volunteers with lived experience
-
blurring the boundary between being a service user and a peer or volunteer
-
being responsive to community needs
-
being flexible
-
having a strengths-based approach
-
involving service users and/or carers/families in the organisation and governance.
Many of these features reflected the VSO’s relationship with communities, whether this was a specific population or a geographical area, combined with a ‘can-do’ attitude:
We’ve got that absolute direct finger on the pulse out there working within community groups, picking up networking with other relevant VSOs, feeling the groundswell and thinking there’s a real need here; right we’ve got to do something about it.
S18
In some instances, this resulted in the initiative being taken to develop MH crisis-specific services, which had the following features in common:
-
a positive stance on MH underpinned by a social model paying attention to the social context of people’s lives
-
providing space and time for the individual to speak about their distress
-
providing a safe, calm and welcoming environment and relational safety
-
informality and providing a light touch in terms of assessment and notekeeping.
Frequently mentioned values underpinning the approach of VSOs included putting the person first, kindness, compassion, humanity and hope. The approach of VSOs was often contrasted with that of statutory services and the NHS, in particular in terms of their flexibility and their capacity to be more focused on an individual’s needs:
So for us not being tied rigidly to six sessions, not being tied rigidly to the entry criteria and not being tied rigidly to geographical criteria are extremely important.
CVS3
One participant attributed the more favourable assessment of VSOs to the fact that the expectations of these services are different from those of statutory service provision:
When something’s voluntary, I think people have . . . a different relation to it because when something is a state provision and you pay taxes . . . we have a right to it . . . You don’t really have that in the same way about a voluntary organisation, you don’t have that expectation, it’s something that is kind of benevolent and it’s there for you despite the fact that you haven’t done anything to sort of warrant that.
CCa1
More commonly, the key axis for comparison was the biomedical (often referred to as a clinical) approach of NHS services versus the social approach of the VS:
You know the biggest issue we have with people is loneliness and isolation. We know that. But loneliness and isolation I think could be dealt with in different ways. Third sector are far better at it than we are. We’re trained clinicians. We will diagnose a dead stick.
CMHP6
A clinical approach was characterised by diagnoses, formality, social distance, demand (as opposed to need) and bureaucracy, including thresholds for determining access. In contrast, a social approach was described in terms of the contextualisation of the crisis, ‘person-centredness’ and need, reduced social distance, open access and responsiveness:
Informal I’d say, because when you come in you’re not frightened of the procedures, the bureaucracy aspect is taken away and like there’s nobody bugging you, . . . you just come in.
ASU4
An important aspect of the VS approach was ‘normalising’ people’s MH crisis experience, which reflected the blurred boundaries between service users and staff, meaning that people could identify with and connect to each other more readily than the us/them approach experienced in encounters with NHS services:
Often they try to normalise the person’s recovery, . . . they support self-management . . . they’re very much part of their recovery in that way. And also when you’re working with other agencies, they aren’t medicalising the problem. You’re getting far more of a person-centred sort of social oriented view of the person, which I think is more normalising for people.
AMHP6
Participants also identified that the VS was better positioned to take a more holistic view of the crisis experience and, thus, was more responsive to the complexity of people’s lives:
I think the voluntary sector’s far more open to the . . . notion of complexity. [It] isn’t really an issue because they just appreciate that people come with all sorts and their very existence is based on seeing people and doing that work . . . They seem to exist a bit closer to the community they serve . . . and so I think they’re a bit more – it sounds terrible to say – person centric as opposed to diagnosis centric.
BCaFG
The social approach was consistently identified by service users as supportive and a helpful first step in enabling them to ‘recalibrate’ (i.e. to become calmer, recover their sense of self and to start to address their difficulties, as discussed in Chapter 6). This approach provides the foundation for a different kind of relationship, namely an accepting and non-judgemental relationship, which extended to the response to suicide and self-harm:
I get the feeling that a lot of people who work in the voluntary sector have gone through problems themselves and they understand more where you’re coming from. I’d quite often experience with the NHS, maybe because I wasn’t dealing with the problem very positively, but the NHS people would get annoyed with me and frustrated.
ASU6
Having more time was also identified as a distinctive aspect of the approach of VSOs in contrast with the NHS, as one peer support worker observed:
GPs only have 7 minutes, so no time to explore. It’s like they have a split personality; ask ‘what’s your symptoms, ‘cause it’s really awful you feel that way’, but they won’t say ‘we’re going to help you through that experience so you get stronger’.
CVS7
The VS is rich and diverse and there will obviously be differences in the extent to which these approaches and values are operationalised in responding to people in a crisis.
Service provision
The VSOs described in Table 13 offer a wide range of services, as illustrated in Table 14. The following sections describe, in more detail, these interventions.
| Type of support | Income (n) | |||||
|---|---|---|---|---|---|---|
| < £25,000 | £25–100,000 | £100–500,000 | £500,000–1M | £1–10M | > £10M | |
| Information/signposting | 22 | 35 | 47 | 19 | 17 | 4 |
| Peer support | 12 | 12 | 21 | 12 | 10 | 2 |
| Advocacy | 2 | 2 | 11 | 23 | 9 | 6 |
| Mentoring | 2 | 5 | 3 | 6 | 6 | 1 |
| Listening | 16 | 24 | 30 | 15 | 6 | 2 |
| Attending groups | 7 | 16 | 21 | 10 | 8 | 1 |
| Therapy sessions | 5 | 13 | 19 | 7 | 7 | 2 |
| Review meetings | 0 | 9 | 16 | 8 | 8 | 1 |
| Recreation | 4 | 7 | 11 | 5 | 6 | 1 |
| Using computers | 6 | 12 | 7 | 9 | 8 | 1 |
| Total number of responses | 70 | 123 | 175 | 83 | 66 | 15 |
| Number of organisationsa | 24 | 37 | 49 | 21 | 17 | 4 |
Signposting and information
Nearly all VSO survey respondents identified signposting as a core activity and, based on the interviews, this was typically to another VSO that could provide more tailored support or services that that VSO did not provide, such as advocacy or specialist counselling for survivors of trauma and abuse. For example:
We try and resolve our crises between us, so we’ll do informal support, offering a bit of peer support, a lot of signposting, and if necessary we can then intervene and get crisis involved, but we also signpost to [a local VSO] which is a telephone service . . . they have a link to proper services in the area, but will also obviously give information out around the Samaritans, crisis cafes.
Peer support VSO
Peer support
Peer support (i.e. support for people in or around a crisis, from people with lived experience of mental distress or a crisis) featured frequently as an intervention provided by paid peer support workers and/or volunteers:
It’s a mental health crisis line and it’s peer led, so it’s delivered by carers and people that have used services themselves. And it’s informal, emotional support where people feel listened to by somebody that’s been there.
CVS2 (paid peer support workers)
This included peer support provided by service-user-led VSOs and formalised peer support programmes:
We’ve got a peer support programme, so we’ve got a team of volunteers, people who have different types of lived experience of mental distress . . . We aim to match people based on that lived experience, so you’re talking to someone and receiving support from someone, like emotional support mainly, from someone who really kind of gets it and who kind of understands.
CVS1 (voluntary peer support workers)
Peer support was provided in various ways including face to face (both one-to-one and in groups), on the telephone, through text services and via e-mail, as well as in various settings including in the community, in group meeting places or in formal service settings such as sanctuaries, crisis houses or hospital wards. Peer support might also include the use of social media, as in the case of a recently established organisation to address (often unaddressed) MH needs in the African community:
So we started this Facebook group, [name], where we deliver Facebook Live and we’ve noticed that a lot more people engaged on Facebook Live rather than face to face and, you know, you see people coming to inbox as well [for culturally sensitive advice].
DVS6
Peer support was also offered through less formal methods, for example by supporting service user and self-help groups.
Listening
The value of listening and creating a space for people to express their distress is a core activity of type 1 crisis services. The importance of listening carefully and attending to what the person wants – ‘[s]omebody that does listen, you know that they do listen, which she does’ (BSU2) – cannot be underestimated:
There’s not many places I think where somebody would get a solid hour and a half of unrushed, listening space or being with space and that is something that we as the voluntary sector can provide, that nobody else can provide. So meeting that need for people who need that, who need exactly that: time and space.
AVS3
Non-judgemental listening, validating personal experience and conveying hope were identified as important factors, and distinct from counselling and formal therapies:
I just felt listened to. I felt understood, and I’m very aware that most of them are volunteers and not trained. I think, in some respects, that was actually a good thing in that I was talking to a human being, not a professional who, you know, makes their own decisions and it just gave you that space to go ‘life is shit’, but having someone there to reassure me that it’s going to get better. And it just helped me look at things slightly differently in a more positive light, you know.
CSU7
Similarly, being able to be present, to be alongside someone, was emphasised by both the VSOs and service users:
I remember one of the team leaders, who was a member of staff that I’d worked with for a long time, her gift was being able to sit in silence with somebody for hours without being drawn into filling a space and filling their minds with all the things that she had to say. That was always very powerful, just being able to be present.
AVS7
This included the value of opening up the space to discuss suicidal feelings without judgement or intervention.
Psychological therapy and counselling
Some VSOs provide psychological therapies or counselling and have been specifically established for this purpose (e.g. a service that was providing counselling for children and young people). In other instances, the VSO providing the crisis service (type 1) would be part of a wider VSO MH service (type 2) and would, therefore, refer someone to this service for a specific course or activity. This included counselling and psychological therapies, provided on an individual or group basis. Some VSOs (types 3 or 4) provided specialist counselling (e.g. for survivors of rape and for carers) and would receive referrals from other VSOs for this purpose. We also heard of community-based therapy and counselling, including one run by a church and one at a community centre.
Support and/or activity groups and recreation
The provision and/or facilitation of various groups emerged as a very strong element of VS activity across all case study areas, particularly in type 2 and 3 VSOs, and the nature and focus of these groups varied considerably. They included groups focused on dealing with elements of people’s MH (e.g. hearing voices, anxiety groups and personality disorder groups), activity groups such as art, dance and exercise, groups for specific people (e.g. women’s groups, carers’ groups and groups for people from particular ethnicities or for victims of domestic abuse) and groups aimed at fostering social connections and mutual support, based on social activities:
We run various different groups – resilience groups, creative groups; we run a hearing voices group that’s connected to the Hearing Voices Network. We have a social club that runs two evenings a week; on the Friday a meal is cooked by one of the members. We have an art group . . . resilience group, and friendship group; groups that are running throughout the week.
AVS13
The MH-focused groups were often more formalised, underpinned by a programme of activities and resources to improve self-management and build resilience. The social groups were more likely to have activities that were determined by the group and were supported, rather than led, by a paid worker or volunteer.
Supporting people in their interactions with public services
Formal and informal support is provided by VSOs to service users in their relationship with public services and this includes peer support, statutory advocacy, peer advocacy and informal support. As noted above, many VSOs have peer support as a central strand of their delivery and this includes supporting people at meetings with statutory services: ‘it was really good because the peer support worker (a volunteer) she actually went to the doctors, helped get B out the house’ (ASULO). This also includes support for the carers of those who have experienced a MH crisis and enabling them to influence MH service provision:
There’s a lot of work going on with [the NHS MH trust] and ourselves and other carer organisations across the patch really about how carers can get involved, issues around confidentiality, information sharing, all of that stuff is being looked at director level . . . the trust self-assessment, how carer-friendly they are, how we involve carers, how you involve patients and carers . . . We work really closely with [the trust] to make sure to try and support carers who are coming into contact with mental health services.
DVS4
Advocacy
The VSOs concerned with advocacy are type 2 VSOs: they do not provide a specific crisis service but they provide a specific form of expertise (as well as broader support in some cases). This includes statutory advocacy for people detained under the MHA (independent mental health advocacy), which is often considered a time of crisis:
The advocate brings expertise and supports the client to ensure they understand the legislation that attaches to a section under the Mental Health Act. The advocate’s role is to support the individual to (a) access services; (b) probably access legal advice and legal representation and when they’re not able to access services or legal advice representation or decisions are made about them staying in the unit for longer, to help them understand those decisions.
BVS6
Similarly, a ULO in site D, which is based in the hospital and provides free office space close to the crisis assessment suite, offers support to service users whatever their situation:
The type of referral that we take – because people can self-refer and staff can refer – the type of referral varies enormously. It can be somebody who really needs support and access or just making sure they get their voice across in whatever service they’re going to. It might be to see a psychiatrist, it might be even if somebody’s an inpatient and they have a particular meeting that they need something with them.
DCaFG
Informal support
This is distinct from a formal advocacy role, and often broader – in terms of liaising with statutory services or chasing a response, signposting people to the appropriate statutory services, providing a space and context for people to engage with statutory services or being present or ‘alongside’ someone (either service users or carers) as they navigate the system: ‘[w]e would sit on the phone with someone while they contacted the crisis team and if possible wait with them until they got there’ (peer support VSO).
One example was a drop-in service for homeless people, the majority of whom have long-standing MH problems. They regularly liaise with statutory sectors to enable their service users to access the support they need, such as NHS Improving Access to Psychological Therapies (IAPT) services. Their attempts are often frustrated, such that someone’s MH deteriorates and they face detention under the MHA. Nonetheless, they continue to look out for the interests of the individual:
If the mental health team require to section [someone] and they have the relevant documentation, we do allow them to use a room. We hope and what we want to have happen is that person’s dignity is preserved. And if the decision is their mental health is such that they really need to be placed in a ward, then it’s a question of how that is handled. We want that person’s privacy, dignity to be protected and you know, it can be dreadful.
CVS11 (type 4)
Practical support and developing life skills
A range of practical support and activities to promote life skills are provided by type 2, 3 and 4 VSOs, including time management, budgeting, self-care, domestic skills, IT literacy skills and support with job applications:
So they [the VSO] created a chore list, sat down with me and my wife and was like ‘right, on this day you do this, [BCa3] will do this, you do this, [BSU4] does this, you do this, [BSU4] does this and stick to it’ and like checklists and it has worked. I mean, I still do 75% of stuff but we’re doing good progress towards actually having a fair share of what each other does.
BCa3 (husband) (type 1 crisis house)
Mentoring
Scant mention was made of mentoring in relation to MH crisis for type 1 VSOs, but mentoring was offered in relation to broader life issues and traumas:
People say ‘I’m not happy, I feel I can’t develop my life’, so we’ve gone through mentoring the refugees and asylum seekers and help them to develop their own life and bring them to activities, involve them in the volunteering, trying to divert their mind from where they are focusing at the moment.
AVS11
Mentoring is distinct from peer support, although these were sometimes blurred, with mentoring focused on identifying and realising opportunities for personal development.
Support for carers and family members
There were instances when the VSO was supporting both the carer and the service user (see, for example, the quotation of BCa3 above). However, the experience of carers and their role was often not recognised by VS or public sector services, with the exception of carers’ organisations, whose prime objective was to support carers and family members. These VSOs offered a range of support, including social support, carers’ assessments under the Care Act (including an assessment of the impact of the caring role on their health and well-being) and, if they were having financial difficulties, a benefit check. They could also receive support from a carer’s support worker to take them out for a couple of hours a week, to provide respite and emotional support. Some family members and carers attended a carers’ support group and this support is valued:
It makes people feel less isolated, as though they’re not the only ones coping with whatever’s going on. And carers often feel they’re helpless . . . one lady . . . whose son’s had psychosis, she just feels so helpless that she can’t cure . . . her son and stop this hurt that he’s having, and make him like he was a few weeks ago.
AVS10
This was viewed as important preventative work for both the carer and the person they care for.
Who is providing the services?
Over three-quarters (77%) of usable responses reported the presence of employees. This is a very high proportion relative to the third sector as a whole. National survey data show that around 35% of English charities had paid employees in 2008 and 2010. 34 This figure is even higher than that derived from Charity Commission records for organisations with incomes greater than £500,000. 116 The number of volunteers appears to increase with the number of employees until the VSO reaches more than 50 employees (Table 15).
| Number of employees | Number of volunteers | ||||
|---|---|---|---|---|---|
| None | < 10 | 10–50 | > 50 | Total | |
| None | 0 | 12 | 15 | 10 | 37 |
| < 10 | 1 | 23 | 42 | 5 | 71 |
| 10–50 | 1 | 7 | 18 | 11 | 37 |
| > 50 | 0 | 4 | 4 | 10 | 18 |
| Total | 2 | 46 | 79 | 36 | 163 |
The capacity of VSOs was repeatedly highlighted as problematic and the short-term nature of funding contracts in many cases makes the retention of skilled paid staff problematic, as discussed in Chapter 8. Pressures were identified in being able to respond to increasing needs and this is challenging in terms of providing accommodation for the service and providing an appropriate response while maintaining volunteer recruitment, training and support.
The skills of the workforce were raised and there was sometimes a sense from public sector participants that the VS needed to be upskilled in some areas, particularly in dealing with people perceived as presenting a higher degree of risk:
I’m frankly happy with the voluntary sector provision, they’ve done a fantastic job, they’ve got [the crisis house], they’ve got the [well-being centre]. I would like some retreats that they can go to from host families maybe and some crisis cafes where they can drop in and then maybe a little bit more qualified staff to run them because most of it is done in the voluntary sector; they sometimes need a bit of training in dealing with seriously mentally unwell people.
BMHP1
Furthermore, the view of the VS being less equipped to deal with people viewed as severely ill was also expressed by VSO participants, who acknowledged the clear delineation of roles between the VS and the public sector:
So for us it is more a lower risk client group because we aren’t clinically trained. We are housing and support workers. And that is what we do . . . So if it was here, it’s about keeping that client safe and finding out what makes a happy life for that person . . . And for us it’s about the risks that come with that from the client themselves. You know, so we don’t have an exclusion criteria per se but if somebody does present with a significant risk to themselves, staff or others, then this wouldn’t be the appropriate placement for them.
DVS1
The VS staff have a wide range of backgrounds, including social work, nursing, forensic psychology, and the prison service as well as working for other VSOs. Development, training and supervision were provided, and this was emphasised by the type 1 VSOs. For example, a type 1 VSO (safe space) had ensured that all staff went on Applied Suicide Intervention Skills Training (ASIST). However, the demanding nature of providing a response was recognised and clearly some VSOs felt less equipped than others:
Just in terms of we’re not counsellors, we’ve done mental health first aid but, it’s quite a demanding situation to be in if someone calls in a crisis. I had [a person in crisis] yesterday, they’re still obviously in quite a bad state.
CVS4
Arrangements to build the capacity of volunteers to respond to people in a crisis through training, support and supervision were also described:
We provide the training (3 days and an evening) and then they work on the line with an experienced volunteer and very closely supervised . . . and then we have group supervision as well. So all the volunteers talk about how well supported they are on the line.
AVS13
Many of the VS participants described their commitment to their clients and to the organisation’s aims of providing a responsive service to make a difference to people’s lives. This often reflected their personal experience:
From a volunteering point of view, people are incredibly generous with their time because everybody knows somebody who’s been affected by [suicide] and I think, quite honestly, a lot of people have thought about suicide, even if only to distance themselves from the idea. I think that means that there’s a lot of love and empathy for people that are feeling suicidal and it’s fantastic to be able to, on some level, bring that community together and have people who are feeling suicidal experience that caring that a lot of people do have towards people who are feeling at their lowest point.
CVS3
This contributed to the sense that, in some instances, VSOs went ‘above and beyond’ to respond to service users’ needs. Support and supervision mechanisms were identified as critical to protecting the welfare of VSO staff and volunteers. These included debriefing, peer support and the ready availability of a more senior staff member.
Voluntary sector support across the crisis journey
In this and the following two chapters, we have provided examples of the contact that different participants made with services across their journeys. These were developed from the narrative interviews and in the repeat interviews; we invited participants to sketch out their crisis journey. We subsequently developed a schematic representation that also draws on their explanation of their journey. The importance of illustrating individual journeys is to demonstrate the ways in which the various different VSO types contributed to supporting people with different aspects of their crisis, using some of the different kinds of interventions identified. To ensure anonymity we have used non-binary description, unless gender was an important aspect of the narrative. Although all service user participants had some contact with public sector services, only some received support from a type 1 VSO across their whole journey, whereas others received support from a type 1 VSO in combination with the other types of VSOs. Some service users received no support from a type 1 VSO at all, but received valuable support from type 2 and 3 VSOs in combination with public sector services. Some of these variations are related to the availability and awareness of services between local areas (see Chapter 6 for more details) and some relate to differing personal contexts, needs, referral routes and relationships between services. However, what they all indicate is the complex nature of individual journeys and how active people often are in managing this for themselves. Figures 5 and 6 show the contacts that different participants made with services across their journeys. Statutory sector services are coloured light blue and VSOs are coloured orange. It should be noted that not all participants gave specific time scales for when services were contacted or for how long, but where possible an indication is given.
Figure 5 illustrates how one woman (DSU4) drew on different types of VSOs to address the trauma of domestic abuse, which was associated with depression and suicidal feelings. DSU4 had accessed a course run by a community organisation (type 5), support from a specialist sexual violence charity (type 4), cognitive–behavioural therapy from a type 2 VSO and counselling from a type 4 VSO. DSU4 accessed the same type 5 service on two occasions. The first course/programme that was offered by this service was not completed by DSU4, but accessing this type 5 service had a profound impact on her well-being and prevented potential loss of life; it enabled her to have a better understanding of their position (the course helped DSU4 to understand that the abuse ‘wasn’t my fault at all; in fact it was probably the opposite’) and gave her the confidence to leave their abusive relationship, which, they thought, saved their life. DSU4 revisited the same type 5 service, a type 4 service for domestic violence survivors and public sector services the following year. This was at a time when DSU4 had suicidal feelings and had hit ‘rock bottom’. Completing the type 5 course (which she had not completed the year before) helped to alleviate suicidal feelings and, she thought, had again saved their life: ‘I don’t think I’d be here if I hadn’t done this course’. DSU4 continued to receive support from this type 4 service and continued to have regular GP check-ups throughout 2018 and 2019. A growing pressure from family members to reconcile with DSU4’s abusive partner led DSU4 to seek cognitive–behavioural therapy from a type 2 VSO and counselling from a type 4 VSO; by accessing these services, DSU4 became more self-reliant, drawing on her personal resources and using self-help measures in preference to VS and public sector services.
FIGURE 5.
An illustration of the contribution of the VS across the crisis journey (site D).
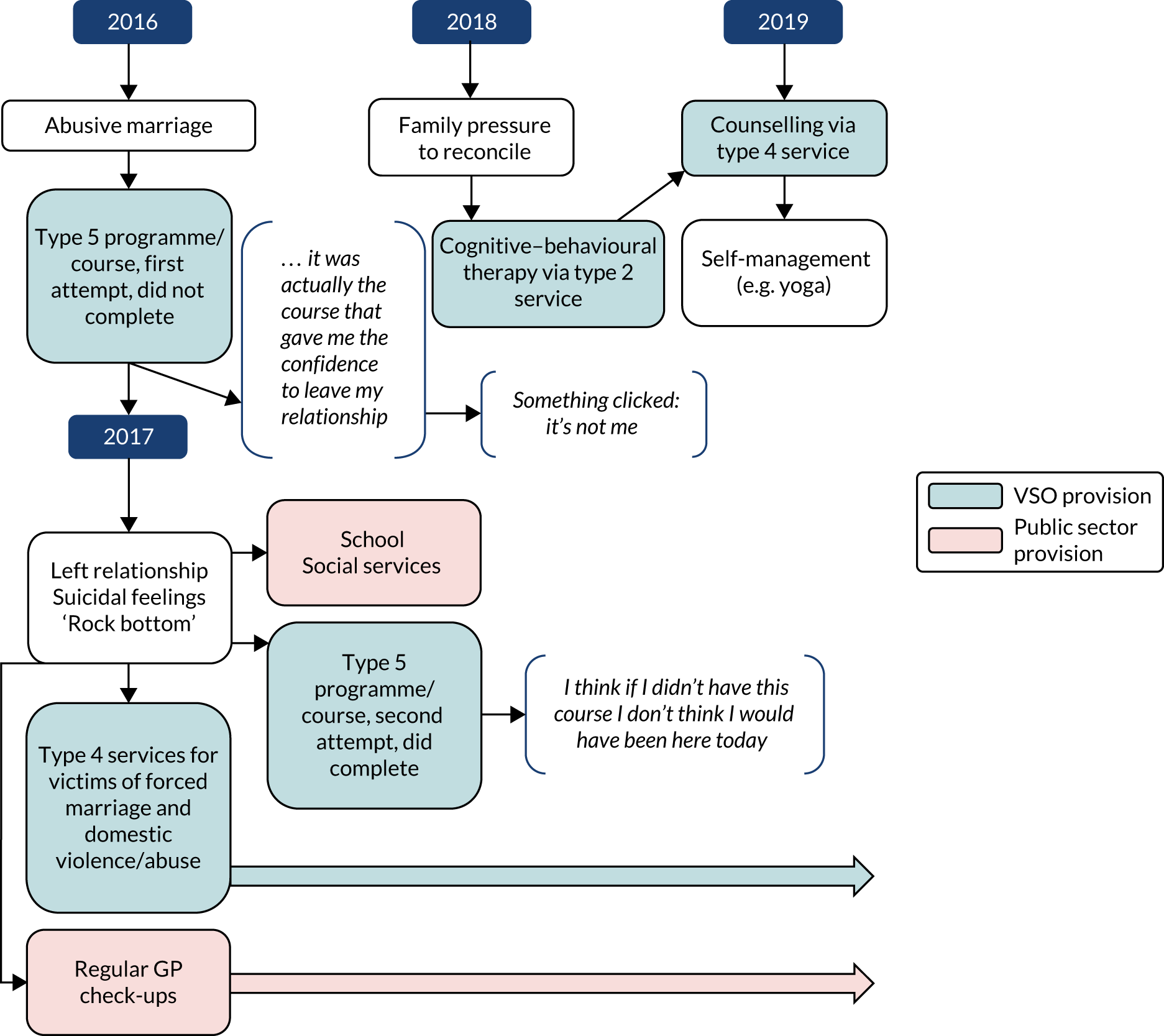
Figure 6 illustrates the complexity of another participant’s (BSU7) situation and how they drew on various VSOs, as well as on the NHS, for support. The context of BSU7’s MH crisis is multifaceted and relates to adverse life events, religion and spirituality, and cultural identity. Following a breakdown related to childhood abuse and an abusive relationship in adulthood, BSU7 was told by fellow church-goers that they were ‘possessed by the devil’. BSU7 believed this and the ensuing spiritual angst and pressure from the church contributed to a heightened and ongoing crisis. The nature of the support that BSU7 relied on from the church as a type 5 service contributed to their subsequent crisis. This led BSU7 to seek support from other local groups and they found support from various type 2, 3 and 4 services. BSU7 did utilise – and in some cases was signposted to – NHS services, but BSU7 did not have a good experience with these public services and often returned to seeking help from VSOs. BSU7’s crisis was exacerbated by repeated questioning of their religion as a consequence of consulting different type 5 religious organisations, which espoused conflicting religious ideas and the nature of BSU7’s crisis. It was as a result of support from a type 3 organisation that BSU7 was able to reflect on how their experiences and religious questions were affecting their cultural identity; this enabled BSU7 to ‘feel new emotions’. However, although this helped BSU7 to see how the uncertainty of their religious views and changing cultural identity had contributed to their crisis, these new emotions ultimately led to an episodic crisis during which BSU7 turned to a national helpline for support.
FIGURE 6.
An illustration of the contribution of the VS across the crisis journey (site B).
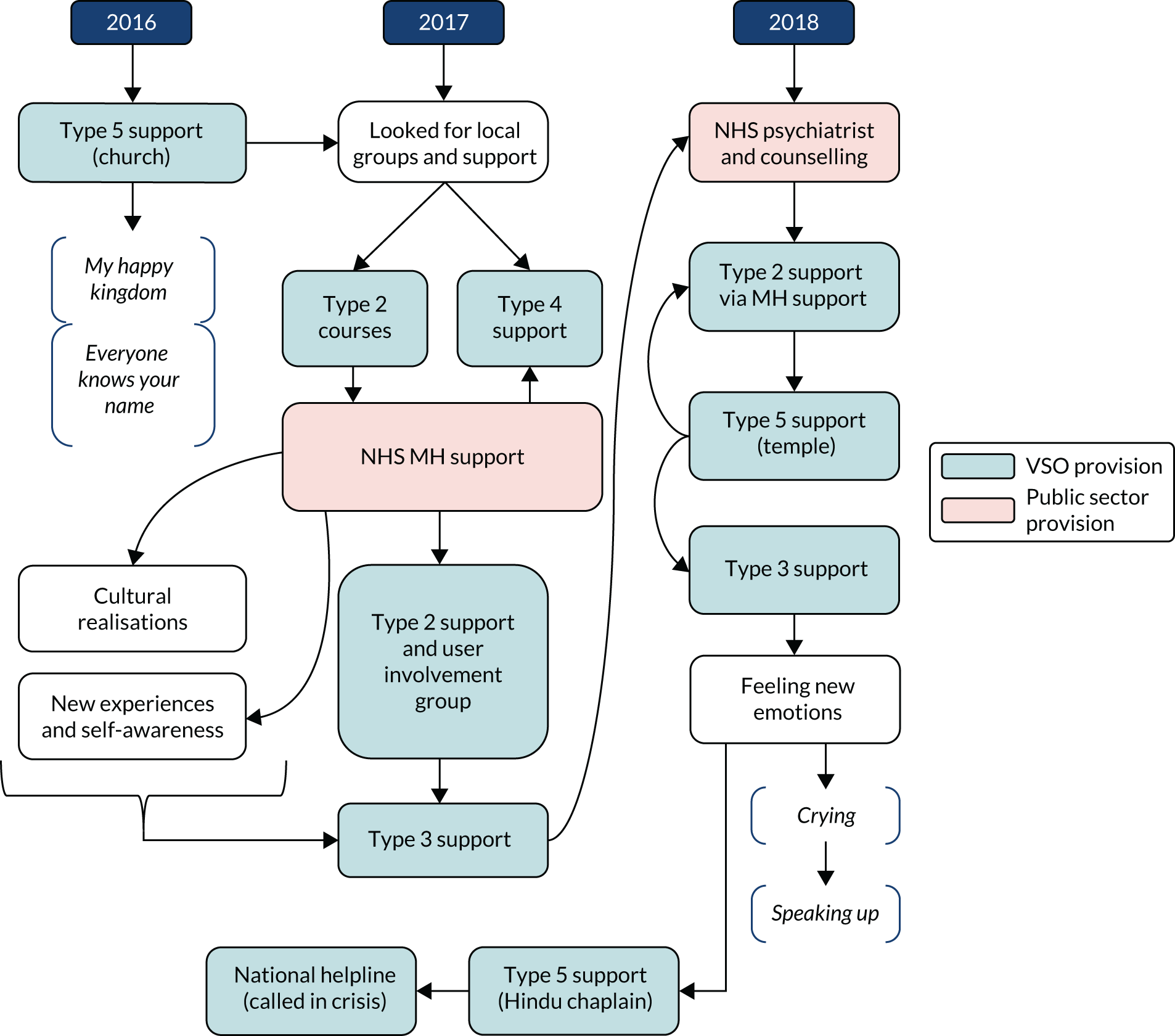
These journeys illustrate the complex and multifaceted support mechanisms that are offered by VSOs. Services, both VS and public sector, are often used in tandem. Service users seek support from VSOs for a wide range of needs and the support they receive is often specific to their situation or circumstance, and often different types of VSOs offer different types of support that complement each other. It is also plain to see that VSOs are not a ‘one-stop-shop’, nor is a service user’s engagement with them transitory; service users can and do revisit VSOs, and their pathway through VSOs is often winding and non-linear.
Summary
Through the use of multiple methods, we have identified the breadth and range of the VS contribution to MH crisis care. Type 1 VSOs are most commonly identified as having a role to play in MH crisis care because they are (1) one of the elements providing an urgent response to someone in crisis and (2) formally commissioned by the public sector to do so and/or access to their crisis support is via the NHS. As well as an immediate response to a MH crisis provided by type 1 VSOs, type 2 VSOs offer preventative activities, support recovery and quality of life for people. Type 3 and 4 VSOs offer specific skills and knowledge in engaging with and responding to people who may not access statutory MH services or are experiencing a specific life event. Our findings, therefore, suggest that the nature of the VS is distinctive and, in comparison with public sector services, the VS is responsive to a wide range of MH needs.
Chapter 6 The right help at the right time: accessibility, adequacy and quality of voluntary sector mental health crisis support
Given the wide range of needs of people experiencing a MH crisis, getting the right help at the right time depends on the availability and adequacy of the MH service context and the MH crisis system. This chapter reports on how people access support from the VS, including the availability of services and the barriers to access; the nature of the support provided; its quality and adequacy; and the difference it made to people’s lives (including both service users and their families or carers). The context of the wider MH crisis system as regards the VS contribution will be discussed in the following chapter.
The contribution of voluntary sector organisations in the case study sites
The typology described in Chapter 5 guided the selection of the case study sites used to investigate different types of contribution, particularly in relation to type 1 crisis services and their relationships with NHS services. Table 16 provides an overview of the VSOs in each site, identified by participants. All of the sites had a helpline with a local branch of a national VSO and two of the sites had user-led helplines, through which callers could access peer support (sites A and C). Two of the sites had a crisis house (sites B and D), both of which provided beds for people in a crisis, and the other two sites offered a safe space out of hours (sites A and C). In three of the sites, access to crisis-specific VSOs, notably the crisis houses in sites B and D and the safe space in site A, was determined by the NHS, whereas all of the helplines were open access. In each of the sites, there was a wide range of the other types of VSOs, reflecting the local political and organisational context for how the VS had evolved to respond to local needs.
| Case study site | Type of VS provision | ||||
|---|---|---|---|---|---|
| Type 1: crisis specific | Type 2: general MH | Type 3: population focused | Type 4: life issues focused | Type 5: examples of VSOs providing wider social support | |
| A |
|
|
|
|
|
| B |
|
|
|
|
|
| C |
|
|
|
|
|
| D |
|
|
|
|
|
Access to voluntary sector crisis support
Access to crisis support is predicated on identifying the need for support, by the person themselves; by a close relative, friend or carer; by a member of the public; or by public services, such as the police. Although many participants referred to several factors, the most commonly cited factor was the intensity of the experience, particularly the level of distress and the perceived risk of harm or to life. Most commonly, service users commented that they had accessed support from type 1 VSOs because they thought that their situation would escalate and possibly lead to self-harm or suicide. People may have made contact with the other types of VSOs (i.e. not type 1 services) when they were experiencing a crisis and two factors influenced this: first, the existence of an established relationship with the VSO or community organisation, thus providing an obvious point of contact, albeit limited by its availability out of hours, and, second, whether or not the crisis was intimately linked to the person’s social context or a specific life issue (e.g. sexual and/or domestic violence, homelessness or insecurity about leave to remain associated with seeking asylum).
The factors identified as influencing access in a crisis can be broadly split into system- and individual-level factors, as illustrated in Figure 7 and described below.
FIGURE 7.
Factors influencing the decision to contact crisis services.
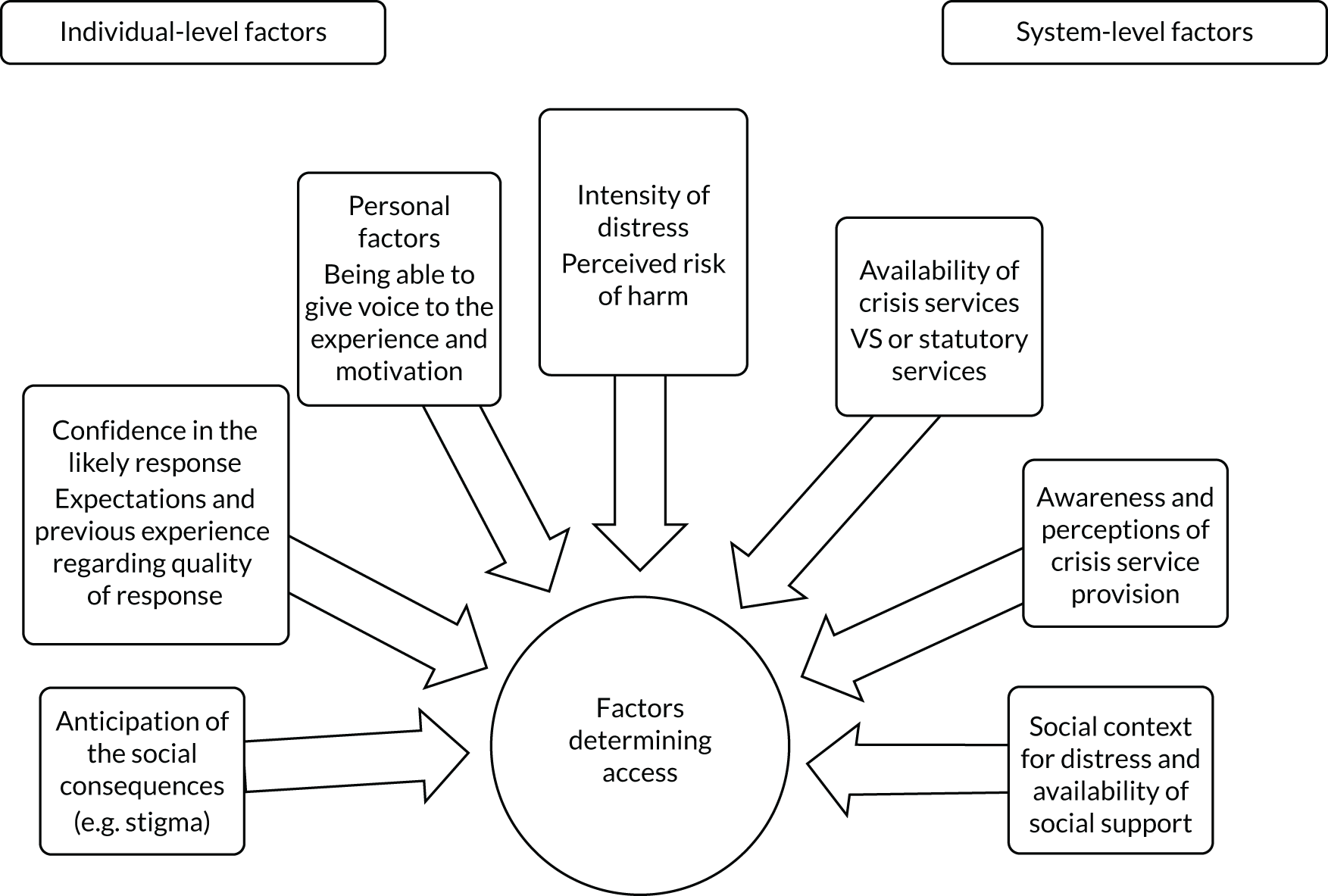
System-level factors determining access
Location and availability of voluntary sector crisis services
Access to VS support in a crisis is dependent on the configuration of the crisis system and the range and availability of VS services. Figure 8 illustrates the distribution of type 1 VSO provision across England and distinguishes between availability in terms of 24-hour provision (e.g. crisis houses) and non-24-hour provision (e.g. safe spaces, crisis cafes and sanctuaries), including both VSO and hybrid models (i.e. NHS and VSO joint provision). This map does not provide a comprehensive picture, as new services are rapidly emerging, reflecting the current policy focus and investment in MH crisis care. 19 In addition to these VS services, there are a wide range of helplines, including both national [the most well-known of which are the Samaritans117 and the Campaign Against Living Miserably (CALM)]118 and local helplines that provide listening services and access to further support. These include those that are user led, providing a peer service; those targeted at specific groups, for example CALM focused on men; those that cover a specific area, for example Nightlink for Cornwall residents,119 and some that are both population and locality specific (e.g. Womankind in Bristol). 120
FIGURE 8.
Map of type 1 VSOs in England. © OpenStreetMap contributors. Data available under Open Database License.
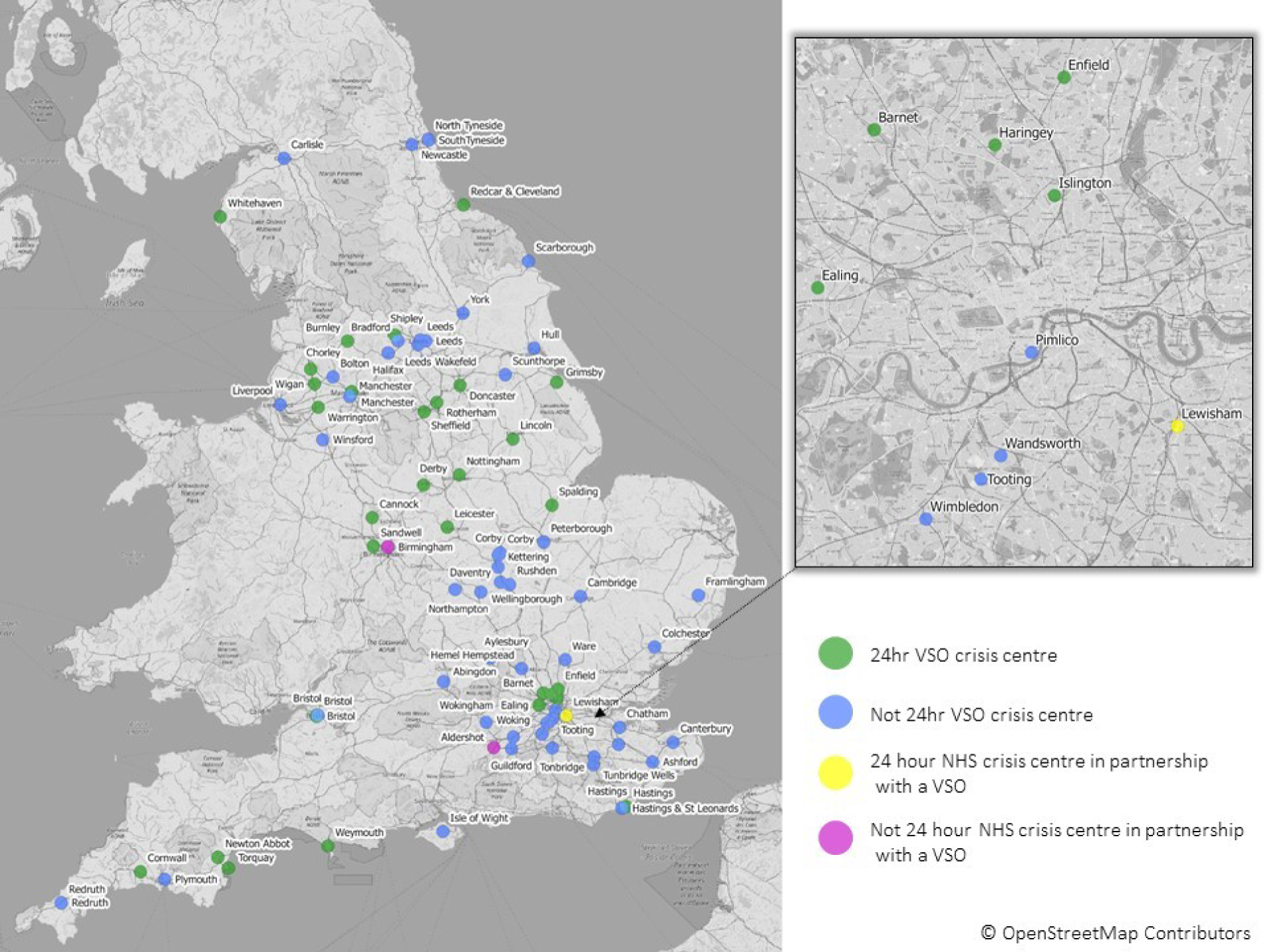
Figure 8 highlights significant variation in the availability of VS provision and demonstrates that people living in more rural areas are underserved. VSOs are typically located in the main centres of populations and thus access is problematic for people in rural areas with limited public transport links and a limited income. One type 1 VSO would arrange taxis for people living in rural areas, but this arrangement did not appear to have been sustained and some people were unwilling to travel far. From the regional mapping in WP2, it was clear that even within the same region there were variations in provision that did not align with population density or deprivation (see Appendix 15). London-based services were reported as having something of an advantage because people were often able to access VSOs in other boroughs or VSO provision had developed to meet specific needs, reflecting greater population density. Access to VSOs was clearly challenging for participants who had moved from an area with provision to an area without provision, and we did not find evidence that there had been collaboration between VSOs in different areas to address this.
Of the national survey respondents, half identified that their services were open only on weekdays, with a further sixth open at weekends and one-third open in the evenings or at ‘other’ times (presumably outside usual day-time working hours). The out-of-hours provision was more likely to be type 1 services and had been introduced to address this identified gap in support. From the mapping, we identified that some type 1 services were available only one or two evenings a week, typically at the weekends, and this was more likely in rural areas. Some VSOs had experimented with both the location and the timing of their services to increase access.
The threats to the sustainability of the VSO and the contraction of public services also have an impact on service availability. One psychiatrist observed, for example, that the closure of a community drop-in service for people in crisis had adversely affected rapid access to support for African and Caribbean men. This appeared somewhat short-sighted given the disproportionate rates of detention for this population.
Eligibility criteria
The eligibility criteria for access also meant that certain groups were commonly excluded by VSOs and by public sector services. For VSOs, the exclusion criteria referred to by survey respondents were:
-
people who use substances, particularly those under the influence of alcohol or drugs
-
people under certain age limits, particularly under 16 or 18 years of age
-
people with violent behaviour or with convictions for sexual offences, arson or violent behaviour
-
people who could not engage with the service or who abused the service (e.g. abusive calls to a helpline)
-
more rarely, people with a diagnosis of psychosis under the care of specialist MH services.
Other VSOs had criteria that reflected their objectives and, therefore, were targeted at a specific population, (e.g. women’s centres) or restricted access to a specific geographical patch. These criteria were by no means universal and it was evident that some VSOs were flexible in their interpretation, for example recognising that, for some people, substance use provided symptom relief.
Awareness and perceptions of voluntary sector crisis service provision
Overall, there was a lack of awareness of what the VS provided among MH staff and service users. Indeed, we found it difficult to find information about VS crisis services when we were developing Figure 8. Although this was largely because some of these services are new or yet to be established, a general lack of information about how to access support in a crisis and what the VS provides was evident:
I think more work needs to be done to promote mental well-being and awareness of crisis services, because even I had to go and look at a leaflet like this to find out what is being offered. How readily available is this to people with poor mental health . . ., so promotion and education can create an awareness about provision of these services, so that everybody knows what to do when they’re going through a mental health crisis.
BMHP1
Generally, people knew of the large VSOs, but were less likely to know about smaller organisations or were unaware that types 3 and 4 make an important contribution to crisis care through offering specialist tailored services. This is further compounded by the instability of funding for the VS, which leads to changes in the landscape of provision:
Finding out that information is quite hard and patchy and, in the meantime, if you then are going out to see somebody who you want to signpost, you don’t want to do them the disservice of signposting them to something that doesn’t exist.
AMHP3
Often, ULOs had established networks, and information about them was communicated by word of mouth. People were often given leaflets or signposted to other VSOs but, in some instances, they may not have had much understanding of what they were being signposted to or how these organisations could help. Knowing what was available was even more challenging for carers and family members. The one exception to this was the Samaritans:
I rang the Samaritans. When it gets really bad you end up thinking that everyone will be better off without you and I remember locking myself in a bathroom because it got really that bad that I was going to slit my wrists. I remember getting to the bathroom but I had my phone and I rang the Samaritans and I was crying down the phone to the Samaritans and they talked to me and calmed me down and things were getting okay.
ASU3
People who had used NHS services in a crisis were more likely to be knowledgeable about VS provision. This was often not the case for people experiencing a MH crisis for the first time: ‘I was thinking what’s the [safe space], what am I doing, where am I . . . is it a hospital, is it a group, is it a . . . what? Because they hadn’t explained to me what it was!’ (ASU5, repeat interview).
Once people had used a specific VSO, they found access easier and, in some instances, although the type 1 service was technically gatekept by the NHS service, some participants mentioned that they had rung the VS directly or known what to say to facilitate access:
But you can ask to go there, say things to make them kind of trigger something to make them suggest the [safe space], you can just say ‘can I go to the [safe space]’ and they’ll say ‘yeah’ or whatever. But no one’s mentioned [it], it’s almost like it’s a secret. You’ve got to be in this little club, like it’s some little secret place that no one’s meant to know about.
ASU5
The reasons given for the NHS gatekeeping direct access to type 1 VSOs included ensuring that people were directed to the right place and that people were not acutely unwell and, thus, did not require specialist NHS services (e.g. the CRHT). The effectiveness of the gatekeeping arrangement was contingent on a well-developed and accurate understanding of the VS offer, as well as on positive collaboration between the sector and the NHS service, as will be discussed in Chapter 7. It was clear that this gatekeeping role could serve as a barrier to access, with service users expressing a preference for open access. However, in site A, the introduction of an NHS crisis helpline was evidently serving to facilitate access, as illustrated by a woman with an experience of postnatal depression, who on the repeat interview described how much her situation had changed. As illustrated in Figure 9, ASU6’s journey began with postnatal depression, followed by an eating disorder. This led to hospital admission under the MHA and a year of treatment from an NHS community personality disorder service. ASU6 subsequently attended the local Recovery College, which contrasted positively with her experience of other NHS services. Following discharge from NHS community services, ASU6 was repeatedly overdosing, calling 999 and ending up in A&E. When an NHS helpline was introduced, linked to NHS 111 and promoted via crisis cards, ASU6 began calling this service and accessing the safe space as an alternative to overdose. The VS staff enabled access to counselling, which ASU6 identified as a major influence on subsequent recovery from both long-term difficulties and repeated crisis experiences.
FIGURE 9.
Access to VS crisis support (site A).
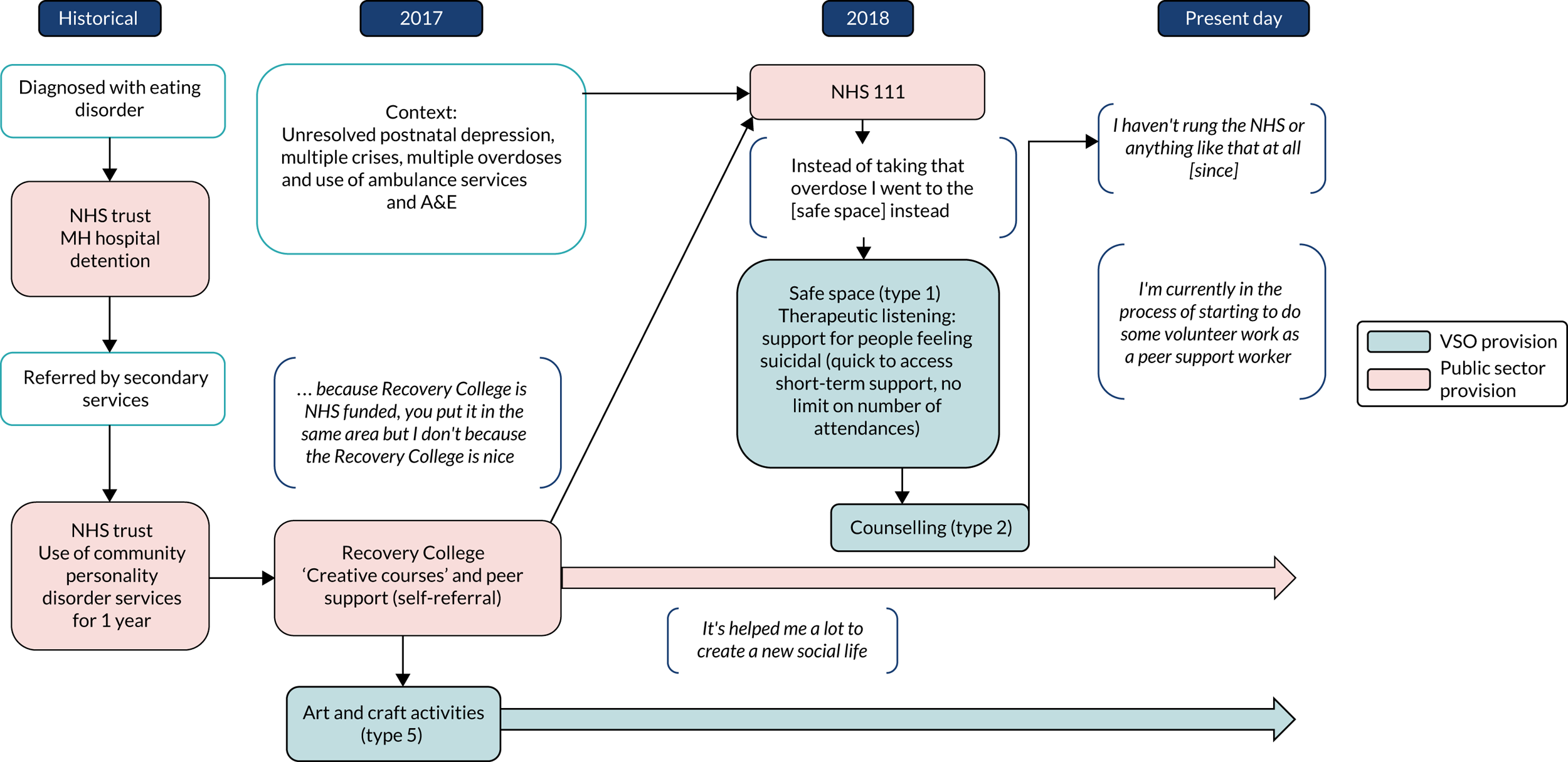
Social context for distress and availability of social support
As noted in Chapter 4, the social context and ready availability of support is intimately linked to the conception of a MH crisis. There was a reasonable range of VSOs providing support to people experiencing specific life events and VSOs that engaged with specific populations. These organisations would receive referrals from other VSOs that recognised their specific expertise and contribution. This was less reported by MH staff, with the exception of a specific VSO direct-access hostel for homeless people. Families and carers provide an important element of crisis care support, but, as noted earlier, many participants were estranged or living at a distance from their families. For those who had a supportive relationship, VSO crisis services (with the exception of carers’ organisations), like the public sector, were generally not engaging well with these support networks.
The role of community and the social context was explicitly mentioned by three VSOs, which were developing and running initiatives that recognised the importance of community and had initiatives targeted at building community capacity by, for example, creating spaces for social groups, such as a knitting group, to meet. The community was also identified as a barrier to access, as noted by a MH VSO focusing on the black community:
Within the black community as well I think mental health problems is a big kind of disgrace, kind of shame . . . It’s actually getting individuals to say ‘I have a mental health problem’.
BVS4
This stigma operates at an individual level and is not restricted to BAME communities, as discussed in the following section.
Individual-level factors determining access
Being able to give voice to the experience and motivation
Language is obviously a barrier to accessing support, although it was not widely identified by the VSOs in our study. Some VSOs do provide specific services to address this; for example, the Sahak Asian Mental Health Helpline for Gujarati, Hindi, Punjabi, Urdu and English speakers living in Kent and Crawley. 121 Despite being fluent in English, it can be important to express your feelings in your first language in a MH crisis, as there is not necessarily conceptual equivalence with English, as was observed by a Brazilian participant.
It was common for people to feel unable to express their needs because of the intensity and complexity of their crisis experience, associated with a sense of powerlessness. In some instances, this reflected a long-standing lack of confidence associated with low self-esteem:
I find it really hard to find a voice really and I think also it’s just when I think, it’s also like dealing with how when things go wrong . . . I always struggle with that as well. Again it all comes back to the self-esteem really and how pretty much everybody has higher than me.
DSU9
Racism and powerful stereotypes could also serve to silence people and engender a sense that they would not be listened to and that their experiences would be misinterpreted. Keeping quiet could also be a deliberate avoidance of the experience or could be the result of feeling that to share your experience would be to ‘burden people’:
I’ve learned who I need to talk to when I think things are becoming a bit overwhelming and even just to the extent of friends and family members who have always been there but you don’t always want to burden people with your problems.
CSU8
Framing distress as a ‘burden’ was often linked with suicidal feelings – no longer wanting to be a ‘burden to the world’ or to family – or with experiences of public sector services and ‘being made to feel a burden’. Similarly, some participants referred to shame, anxiety about not being understood and a nihilistic attitude that it would make no difference:
Mine was the voices, commands . . . It’s frightening, really, really frightening because you don’t know if you’re going to damage yourself or damage somebody but with mine I kept to myself. I wouldn’t talk, I wouldn’t go near nobody and it kept me going for a while but I gave up, I said to him I needed help and it’s a big thing for me . . . because if it wasn’t for [him] I wouldn’t be here.
BSU3
Loss of motivation was also identified and was associated with poor MH and with medication and substance use, particularly by VSOs and carers/families. This was notable for type 3 and 4 VSOs that were engaging with people who were either overlooked by, or who had little faith in, public sector services:
They’re quite clearly in crisis because their teeth are falling out, they’re inappropriately dressed for the weather and they’re not eating properly and all these [are] clear signs that things are going horribly wrong and yet, there’s no kind of desire really on their part to want to engage.
CVS6
The understanding of the difficulty people might experience in taking the step to access support was, however, recognised by VSOs that responded promptly or supported people in engaging with other services:
She was the one who said shall I put my details forward and honestly if I hadn’t said yes and if she hadn’t done it herself, I probably wouldn’t have . . . I was just not in the right place to just cope again with more questions [and] referring myself . . . I think it’s important, somebody else having the volition to put your details to somebody else.
CSU2
In addition, VSOs play an invaluable role in enabling people to have a voice, through advocacy, or facilitating access to crisis support, particularly for those who may be unaware of their needs for support.
Expectations and confidence in the likely response
Overall, service user participants indicated that they would contact a named VSO in the future, should the need arise. A minority of service user participants said that they would prefer to access public sector services, usually their GP, or would not seek any support. It was suggested that ethnic heritage was a factor in this. For example, despite a high suicide rate among Eastern European communities in one of the study sites, it was reported that people from these communities would avoid seeking help and, if they did, it would tend to be via A&E.
Participants also described accessing VS services either when their experience of NHS services had been poor or when they felt that NHS services had not met their needs:
At the beginning I actually spent 7 weeks in hospital and even out of there when the nurses were unavailable I always ended up calling them [a peer-run helpline] from my hospital room because I needed to talk to someone.
CSUFG
Alternatively, they were not being listened to:
I’ve been like pushed from pillar to post in three hostels and I was going to be homeless and everything. It’s times like that when you’re really down and you just think ‘oh, what do I do now?’ and then I was in one hostel, and I phoned the police and said I was going to jump out of the window onto the main road and with me saying that there was police everywhere. The policeman was really nice, he sat and spoke to me and then took me to the VSO crisis service.
ASU12
Consequently, people who had previous experience of a crisis, exercised their judgement in which service they would access, and compassion and humanity were important criteria. Two participants in one of the study sites chose to access a VSO service over 60 miles away because of the positive response that they had when they phoned a service that also offered short-term counselling. The identity of the service was also relevant in determining whether that service would understand the person’s specific cultural or social context and, thus, provide a helpful response.
Anticipation of the social consequences
Concerns about the potential social response, including from public sector services, were identified as a potential barrier to access, with reference to MH-related stigma:
People don’t really – not everybody – don’t really understand when you’re at that suicidal point because a lot of people think that when you take your life you’re being selfish. So there’s that stigma there as opposed to actually I’m in a really, really rotten place and that’s just the tip of the iceberg to explain.
CSUFG
This was apparent even when services were available:
It’s a case of ‘oh, who is going to be there, oh, who is going to see me, will they know me, oh and they know that I’ve got a problem’. That’s the fear . . . to be labelled. So people don’t seek the help because they’re afraid of who else is there.
DSU5
The social and community context, therefore, plays a role in determining if the person and/or their family seeks help:
This particular family had quite collective cultural traits in that their identity was all about the contribution they made to their family and to the community group, so . . . if success is shared by the family, shame is shared, anything that goes wrong is shared and it’s a stigma for other people as well. I think they were just really concerned that it would be shame . . . for the family the priority wasn’t only [getting help], it was parallel to make sure it doesn’t get out.
ACCG5
Conversely, commitments to other people (i.e. children and work) and to pets motivated some participants to acknowledge difficulties and seek help.
Signposting and referral routes
There are several potential routes through which people might access services and most VSOs had more than one. As Table 17 shows, there is a relatively high degree of self-referral, which does not vary by organisational size.
| Income | Self-referred | Family | Drop-in | Community MH services | Other VSO | Crisis/psychiatric | Primary care | Other |
|---|---|---|---|---|---|---|---|---|
| < £25,000 | 0.61 | 0.18 | 0.32 | 0.25 | 0.11 | 0.14 | 0.21 | 0.36 |
| £25,000–100,000 | 0.8 | 0.35 | 0.13 | 0.33 | 0.3 | 0.13 | 0.23 | 0.45 |
| £100,000–500,000 | 0.71 | 0.31 | 0.23 | 0.33 | 0.37 | 0.17 | 0.31 | 0.48 |
| £500,000–1M | 0.91 | 0.55 | 0.23 | 0.41 | 0.55 | 0.27 | 0.41 | 0.64 |
| £1–10M | 0.72 | 0.17 | 0.11 | 0.39 | 0.06 | 0.22 | 0.39 | 0.22 |
| > £10M | 0.25 | 0.25 | 0 | 0.25 | 0 | 0 | 0 | 0.25 |
| Total | 0.73 | 0.31 | 0.2 | 0.33 | 0.29 | 0.17 | 0.29 | 0.44 |
Both stakeholders and service user participants identified easy methods for self-referral as facilitating access:
We operate an online referral system or you pick the phone up to us and we get you in, you don’t have to fill out a complex form . . . We know from doing the online referrals that we’re getting more self-referrals because people are browsing the internet late at night, they can make a referral there and then and we’ll pick it up and follow that up with them.
DVS5
However, access to VS services that are crisis specific (type 1) and the other types of VS support differed in our study sites (see Table 18). Access to two crisis houses and one safe space was being gatekept by the NHS in three of the sites, although one was considering moving to open referral. By contrast, a wider range of VSOs provide open access, as was also the case for crisis-specific helplines and user-led services. This was highly valued by people in crisis needing support. After self-referral, the most common routes are via primary care and community MH services (see Table 17). GPs, MH staff and the police, however, were more likely to signpost than to refer to VSOs. This may have reflected their limited awareness of the VS, but governance concerns were also raised, meaning that some staff were more comfortable leaving it to the individual service user to pursue VSOs rather than make a direct referral:
If you’re referring someone on to a public sector service you tend to refer them, to voluntary services you tend to signpost, though some of them you would refer to, like a large established VSO but I think there is a danger that you might be signposting people to things that are inappropriate or possibly have changed their remit.
AMHP3
The perspective that the VSO was plugging the gap for people who were either unable to access public sector services or on a waiting list is supported by our data. Waiting lists for psychological therapies and specialist services (e.g. people identifying with a personality disorder or experience of abuse) were commonly referred to. It was not uncommon for people to self-refer to a VSO while on a waiting list, or to be signposted to a VSO by the public sector. For example, one participant had been simultaneously referred to IAPT and a VSO by her GP, who anticipated a waiting list for the NHS service. Participants also identified other gaps, as summarised in Table 18.
| Area | Description | Access | Gaps identified |
|---|---|---|---|
| Site A | Two VS safe spaces available from 18.00 to 01.00 by appointment | Access triaged by the NHS, single point of access |
|
| Volunteer-run helpline 7 days a week from 07.00 to 23.00 provided by a ULO | Self-/open referral | ||
| Samaritans helpline and drop-in | Self-/open referral | ||
| Site B | Crisis house managed by a housing organisation | Access gatekept by the NHS CRHT |
|
| Samaritans helpline and drop-in in neighbouring borough | Open referral | ||
| Site C | Peer-run helpline 7 days a week (Monday–Friday, 18.00–00.00; Saturday and Sunday 12.00–00.00) provided by a MH organisation | Self-/open referral |
|
| Three face-to-face peer appointments with people presenting at A&E | Referral by GPs/NHS MH services | ||
| Safe space in neighbouring borough | Self-referral | ||
| Samaritans helpline and drop-in | Self-referral | ||
| Helpline for specific BAME group | Self-referral | ||
| Site D | Crisis house managed by a national MH VSO | Access gatekept by the NHS CRHT |
|
| Samaritans helpline and drop-in | Open referral | ||
| Nationally | Crisis house for people feeling suicidal | All self-referral | |
| Face-to-face support for people feeling suicidal, by appointment | London based, so may not be accessed by those living at a distance | ||
| Samaritans helpline | |||
| CALM helpline for men | |||
| SANEline |
Quality of voluntary sector support
The quality of the VS response was widely praised, in particular the way in which people’s concerns were taken seriously with kindness, sensitivity and responsiveness – ‘a place where time did not matter, you’re number one’ (ASU3):
The staff here are absolutely amazing, you know. They’ve got such a way of explaining things, without hurting anyone’s feelings, without, with just . . . getting their point across, without offending anyone. And it might not be about a situation, it might just be an example you know.
DSU4
Although being able to see the same person was identified by some participants as important, for many it was the consistency of the approach and relational safety that was critical:
It’s somewhere where somebody is just one-to-one with a person; it’s confidential, very confidential, because I had problems with the confidentiality because my workplace was a place that they couldn’t keep anything safe and, you know, I lost trust in people. Here, I felt safe.
CSU11
Many of the participants indicated that they would use a named VSO in the event of a future crisis, with a sense of having a safety net:
The fact that I feel I can go back to them if there was something that was ever wrong, the fact that I know how to get help now and if you ask my husband I don’t think he would know how to get any help for me. They’ve been really, really helpful; if they weren’t there, I don’t think I would be sitting here right now, that’s how crucial they’ve been.
ASU3
The provision of the service by peers with similar experiences made a difference:
That initial conversation at the [safe space] made a huge difference because I . . . felt like for the first time there was an option where if you have a mental health crisis you can sort of learn to deal with it with somebody, not just yourself, because it makes it 10 times less stressful when you do it with somebody who knows exactly what you’re going through . . . It made a difference, it made me feel better and I did feel better.
ASU4
There was also a sense that having peer supporters involved reciprocity and the organisation being a collective effort. One participant had, however, been put off by the VS staff not being qualified MH professionals, although the manner and approach of the volunteer had helped her establish a trusting relationship. There was clearly a high degree of trust and the quality of relationships created a sense of safety, where it was possible to ‘talk about anything’. This included discussing suicidal feelings without a fear of being judged, which was often contrasted negatively with experiences of the NHS:
There’s something about the [type 1 safe space] . . . Everyone I . . . encountered there, and they are all volunteers, they were tremendously friendly and supportive in a way that I think is not necessarily characteristic of accessing the health-care facility. I felt like people really kind of cared about me [and] you can’t kind of underestimate how important that is to people in that situation.
CSU10
Increasing the size of VSOs and the formalisation of the service model through commissioner-led crisis models was identified as potentially posing a threat to this ethos and approach: ‘[T]he bigger VSOs become, the more restricted they become, the harder it is to engage people on a compassionate level’ (CVS7).
It was suggested by one VSO participant that there may be lessons from the formalisation of advocacy services through the introduction of public sector advocacy (i.e. independent MH advocacy): ‘a pushback to return to the “grassroots” of advocacy where they had more time for people; take more grassroots inspiration and action’ (BVS6).
Most of the dissatisfaction with the VSOs usually focused on access and lengthy waiting times for follow-on sessions for one-to-one support or therapeutic programmes. A small number of people found the informality and lack of privacy challenging:
The fact that it wasn’t like a GP’s office, it wasn’t a medical professional, is also kind of off-putting . . . I felt very awkward about meeting an entirely new person that I’d never seen before in my life and then just pouring everything out to them. And while there’s also a lot of other people just walking through this house and sometimes in the room you’re in potentially they’re just hearing snippets of the conversation.
ASU15 (repeat interview)
Nevertheless, this young man who described social anxiety had used the VSO on several occasions. Rarely, negative staff attitudes were mentioned and the highly positive evaluation was in stark contrast with that of NHS provision, as presented in the next chapter. The general theme, however, was that being listened to and being taken seriously is of great importance, whatever the service: ‘[M]an I did feel a lot worse after getting off that phone call [VS helpline], so much worse. They just make you feel like you’re just not important’ (DSUFG).
This raises questions about how to maintain a respectful and positive approach to people experiencing a MH crisis. Negative comments about VS and public sector staff suggest that responding well to people experiencing a crisis can challenge the emotional and psychological resources of staff. Similarly, maintaining an informal and friendly approach (as opposed to a technical and didactic approach) to courses offered by the VS was highlighted, alongside the individual skill of the course leaders in engaging course participants and maintaining an individualised approach.
Adequacy of voluntary sector provision
Variation in availability of voluntary sector organisation services
As discussed earlier, there is significant variation in VSO provision, particularly between urban and rural areas (see Figure 8) and the availability of VSO crisis provision out of hours (see Table 16). Appendix 15 provides information on two regional case studies (referred to as regions 1 and 2) in WP2 to illustrate this in detail. It is, therefore, evident that the current alternatives to public sector provision are a matter of geography – ‘the postcode lottery is a big issue’ – and will affect people’s experience and the availability of alternatives to admission.
The other factors that were identified, by regional case studies 1 and 2, as shaping VSO provision were as follows: (1) the initiatives of the VSOs in responding to identified local needs, such as suicide hotspots, which means that some needs may go unmet (e.g. there was no specific provision for farmers or agricultural workers in region 1 or the increasing population of asylum seekers and refugees in region 2); (2) the outreach by large national VSOs into these areas to provide crisis support and address an identified gap; and (3) the investment in VSO crisis provision, which was facilitated by the CCC, and additional investment, albeit short-lived in region 1. In region 2, this was in progress, with a crisis service redesign under way, involving service users and carers.
Demographic inequalities
Inequalities for particular groups were highlighted across the study sites, notably people from specific BAME communities, asylum seekers and refugees, children and young people, members of the LGBTQ community, people with learning disabilities, homeless people, people who use substances and older people. There are major gaps in whose needs are being met and how, by the way in which a MH crisis is understood and how the crisis system is organised:
The methods that people use to engage them, the pamphlets, they’re not going to be reading any of that. The way that those certain communities communicate [can] be very different from the Caucasian way of communicating. It’s neither good or bad, it’s just different. So until people have an understanding of how to reach certain groups, and also there’s a lot of issues around trust and mistrust and more young black men being sectioned and dying in custody and in care, than average, so trust is definitely broken.
CCCG1
The lack of attention to the demographic diversity was often evident in the way the VSO was commissioned and in the service model:
I think one of the things that we’re concerned about is the way things are currently commissioned, is the fact that we are commissioning specific services. What we need is to commission accessible services. Now none of our services would exclude anybody but they probably, by design, would not necessarily appear accessible to certain groups of people . . . If the need is being met, it is being met by default.
BCCG1
It was, therefore, evident that mainstream VSOs may not be well geared to meet the needs of a diverse population:
If you’re a Muslim woman would you be happy to go to the crisis centres? . . . I’m just thinking, how do they manage different language? People from different countries might have had a completely different experience of mental health services. They might have been forced to have treatment. They might be very, very fearful of speaking to people about that kind of thing.
ALA1
This was underlined by the experience of system reform in site A. The VSO model had first been introduced into a relatively affluent area with a relatively small BAME population (11%). After its initial success, the decision was made to replicate the model in a more socioeconomically deprived area with a higher BAME population (23%). This floundered and it became evident that a more thoughtful approach was needed, leading to consultation with local communities to redesign and promote the service. The often rapid demand by CCGs to introduce VS crisis provision could countermand this.
Evidence of an equalities perspective driving system design, either for the VS or the public sector, was, however, in short supply. One London-based open-access crisis service that was being accessed by people living outside London reported receiving few referrals from BAME communities. The ethnic identity and profile of the VSO can influence help-seeking preferences, reflecting the need for trust and safety. Some VSOs had evolved to tackle inequalities and promote the interests of particular groups (type 3), and social and community organisations, such as some churches for black communities (type 5), were providing a wide range of support to both service users and carers. These initiatives were somewhat separate from MH VSOs (type 2) unless they were specifically providing MH support and were promoted as such. For example, one VSO was supporting people with both MH and learning disabilities, including autistic spectrum disorders. Other type 2 MH VSOs were addressing inequalities through peer support, recovery initiatives and adopting a holistic approach, which encouraged personal development and inroads into work and other opportunities.
As noted previously, with the exception of carer-focused VSOs, the approach to working with carers and families appeared to be underdeveloped. One husband described the anxiety he felt because his wife, who had repeatedly made serious suicide attempts on railway lines, was allowed to leave a VS crisis service at 1 a.m., without alerting him. There was also scant evidence of crisis planning by VSOs and, in some instances, the VSO kept few service user details, reflecting an ethos and commitment to informality.
It proved difficult to determine the adequacy of the VS contribution without understanding the context of the crisis system. For example, housing was identified as major gap in site C, with an increasing homeless population and ‘a massively high threshold’ for supported accommodation. The wider crisis system is considered in Chapter 7.
Impacts of voluntary sector support
As well as being highly valued, service users identified the difference that VS support had made to them, in terms of both the immediacy of the crisis experience and the longer-term impacts on their well-being. These impacts were consistent with meeting the needs that they had identified, as presented in Chapter 4.
For individuals, carers and their families
‘Rebooting my mind’
The support from the VS was identified as enabling people to better manage their MH. In the immediacy of the crisis, time and space away from the context of the crisis, provided by crisis houses and safe spaces, allowed the person to ‘take stock’:
Well [the crisis house] helped me out a lot ‘cause when I got there, that give me a good break for 3 weeks away from everything. It took a lot of stress off me, give me chance to reboot my mind and get me going again, and then work from there.
BSU5 (repeat interview)
Although the impact of immediate support on calming the situation was positively evaluated, the limitations, particularly of helplines, were acknowledged: ‘just calm you down a bit but they’re not going to fix you’ (BSU4, repeat interview).
Giving voice to experience and being listened to
Being able to give voice to the experience cannot be underestimated and many participants referred to the freedom offered by the VSO to ‘be me’, reflecting the sense of relational safety discussed previously. Being listened to, the support in ‘talking you down’ and ‘taking the pressure off my head’, and helping people to feel calmer led to the crisis being deescalated:
Personally, I think it’s been excellent. I was made to feel very, very welcome and it filled a need; I was under no pressure and it was having somebody who actually sit and listens to you, and doesn’t judge you anything and doesn’t put you under pressure to speak. She was always there so was always there for me to speak to, to speak questions. But she never put any pressure on me . . . and I found her voice very reassuring. She helped me a lot.
DSU5
Although listening is identified as one of the core activities of the VS response, it was evident, as implied above, that this was an active, not a passive, process:
It wasn’t just listening and being compassionate. It was sometimes suggesting where things maybe weren’t serving me very well, thought patterns. Or just useful images or strategies to deal with things. But it wasn’t formalised like that, it was just things that came from his life experience . . . My experience was that, as well as listening and keeping track of where I was, he would also try hard not to tell me what to do ever, but make suggestions sometimes.
CSU10
Participants also described how this process of active listening had conveyed hope and enabled them to feel that they could deal with the situation: ‘somebody was there listening to me and also saying you can do it, you can go through, you know’ (CSU11):
Finding that relationship where I felt I could open up to someone and I thought I could actually let someone in, which I’d never been able to do before, was a big eye opener for me; it gives you that sense of, well, actually, I can do this. She hasn’t come at it as the textbook, she’s coming at it as a human being . . . Someone that can actually relate to you that’s been through that type of trouble and crap and can actually say, well, you know, I get bad days too, it’s normal, you’re not getting someone going ‘oh my god, you have a hyper day or you’ve gone manic, let’s get you on the next medication’.
DSU2 (repeat interview)
The provision of support by peers facilitated a sense of solidarity and of being understood, and this was highlighted in relation to BAME VSOs:
I’ve learned a lot since I’ve been here [type 2 VSO] and the staff are like a family to us, you know; they treat us with respect . . . They’ll help you in any way but if you don’t help yourself you’re not going to get anywhere . . . So I need a place I come there for, so, I fancy, black communities it’s like we don’t get much help.
BSU3
Developing strategies for addressing challenges and future crises
Reflecting on the crisis experience and VSO support, several participants described how they learnt something about themselves and changed their perspective:
I kind of just accept it as ‘that’s my life’ really and I don’t really spiral on the negative things that happened anymore. When I think about bad things that happened in the past I stop myself and start thinking about positive things that have happened in the past, and try and relive those memories.
ASU3
For some, this was identifying specific triggers and, for others, it was a sense of what was missing in their life that they needed to address. The benefits of courses offered by the VS and specific VS therapeutic support were identified as enabling participants to develop a better understanding of themselves and to develop practical strategies to manage their MH:
My anxiety levels are just getting to the point now where they’re non-existent and it’s the same with the mental health; it’s just, like, the [VS] course has helped me that much; I would say it helps you control your overthinking, learns you how to deal with unresolved grief, definitely; helps you to like yourself more, as a person, and the ability to learn that everybody’s human and they make mistakes. It’s not hanging onto that, it’s like hanging onto the past and going round in a groundhog day, whereas I’ve learned to let go of it with the [VS] course . . . now I feel different about myself altogether.
DSU3 (repeat interview)
This course, run at a community centre, aimed to enable people to make sense of their experience, offered practical strategies and increased self-awareness and the potential for self-management. For this man, who had made a suicide attempt, the course proved more effective than counselling, which he had previously accessed via his GP, and he attributed this to meeting people encountering similar issues. While aiming to increase an individual’s repertoire for dealing with symptoms, such as panic attacks or suicidal thoughts, such courses also build a sense of solidarity. Furthermore, the value of signposting to other services, including programmes or therapeutic support provided by other VSOs or providing information and support in relation to wider issues, notably housing or welfare benefits, was highlighted: ‘[I]t makes a lot of difference and [she] gets the ball rolling quick, and more people getting help and seen to calms people down because somebody’s coming to listen to you’ (BCaFG).
Carers also highlighted the value of information and VS courses that had helped them develop a better understanding of MH and improved their strategies for coping with their situation:
I’ve attended quite a lot of different courses myself and had I not, I wouldn’t be where I am today because at least I have the understanding, i.e. when a crisis is approaching or what to do in a crisis . . . Well I can say it’s definitely helped me and it’s also helped me to cope well in my caring role.
CCaFG
Preventing suicide and self-harm
Several participants reported the difference that the VSO had made in terms of preventing suicide and self-harm:
As a gay you are not welcome . . . and then . . . every Wednesday I was, going there [type 1 safe space]. My life was without direction and it was so difficult for me. I’m telling you, without all this help I would have not survived.
CSU12
Figure 10 illustrates the crisis journey for this man, who sought asylum in the UK because of persecution in his home country owing to his sexuality. The VS featured in his journey through a range of services in combination, including, but not limited to, specific MH crisis support. He received support from a type 1 VSO via a referral from his hospital consultant, who also referred him for psychological therapy at the same time. Although he viewed the NHS psychological therapy very positively, he had to wait months for access. During this time, he was able to access the type 1 VSO within a week of being referred. Alongside this crisis-specific support, he also received support from multiple type 3 VSOs, which addressed specific issues in his personal context, relating to his sexuality, his status as a refugee at the time of the crisis and his distressing dealings with the Home Office (which had detained and questioned him about his reasons for seeking asylum). The legal support he received from a national asylum seeker VSO (type 3) assisted him in gaining asylum seeker status and being released from detention, which was a significant factor in his MH crisis. The ongoing support of a local refugee and asylum seeker VSO (type 3) helped meet some of his basic needs. In addition, he developed social connections and gained acceptance through attending a LGBTQ network (type 3).
FIGURE 10.
The impact of the VSO on a crisis journey (site C).
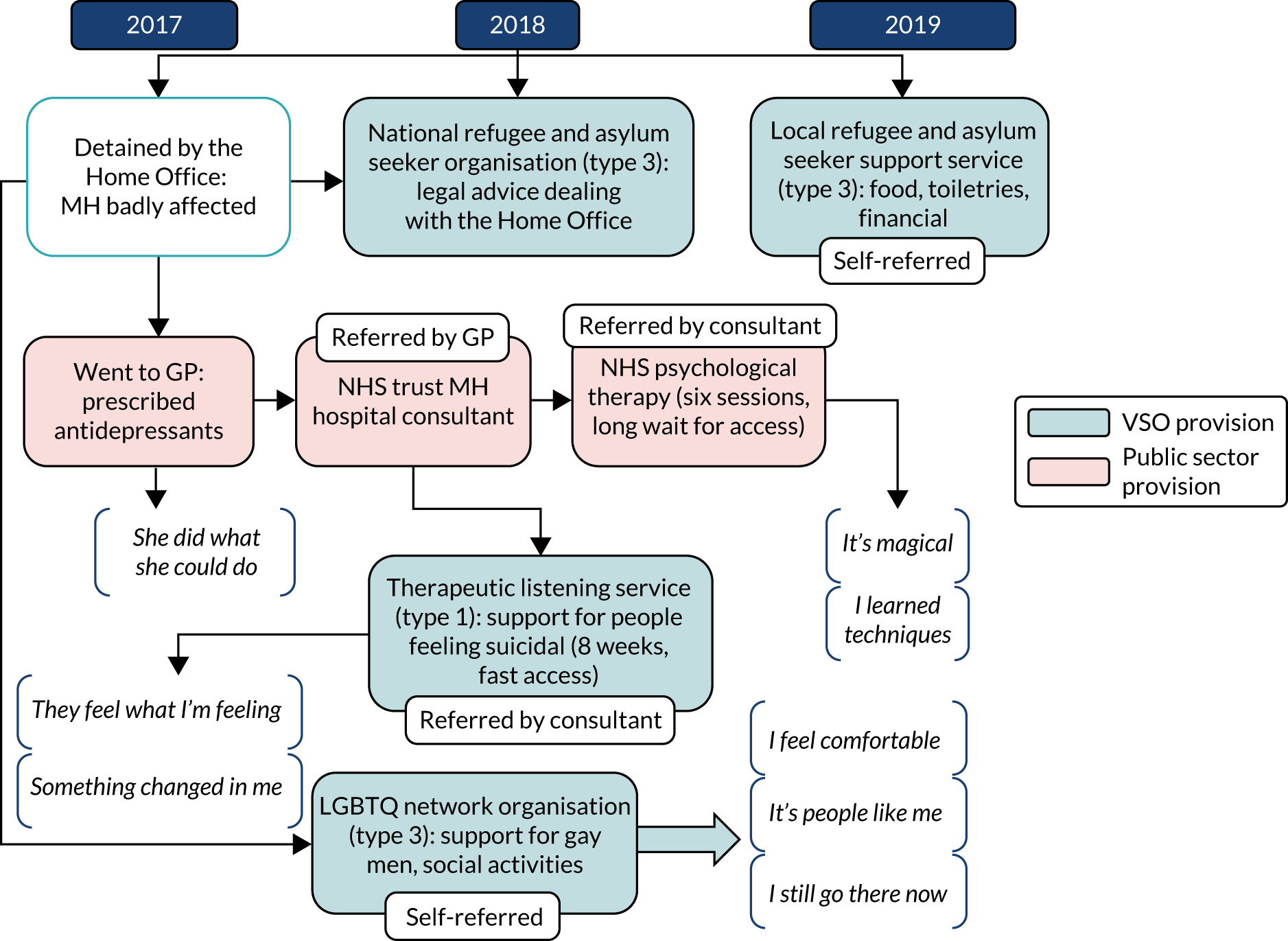
The participant who took their own life during the study had used two type 1 VSOs on several occasions, as well as NHS MH services, including inpatient admissions. They were on a waiting list for a programme offered by a type 2 VSO but possibly enabling them to address their complex difficulties would have required specialist psychotherapeutic support, which they did not appear to have been offered.
Increasing social connection and support
The input from VSOs had enabled some participants to evaluate their social support and to develop new connections through VSO activities and through peer support. The value of the opportunity to become a volunteer or peer supporter was identified by several participants and, for some, gave meaning to the difficult nature of the crisis experience. Several VSOs offered training to become a peer supporter, whereas others provided other volunteering roles or opportunities, which also provided structure and social connection.
Volunteering and employment
For some, volunteering could provide a path to employment:
My whole experience prior to that had been not functioning, not sleeping, just not really there to be honest. It was volunteering in [type 2 retail shop] that has just enabled me to have more of a life. It was when I was put behind the till in the shop that my mind started to work again.
DSU9
In addition, a small number of participants had used VSO support while still in work or off work because of MH difficulties, and this had enabled them to retain their job or change direction. Others had used their skills or developed new skills through the various activities offered (usually by type 2 and 3 VSOs). For example, one participant had developed their passion for art and now runs a local gallery.
Impact on public sector services
Influencing the attitudes and behaviours of mental health staff
When there is a well-developed working relationship between the VS and the public sector, the VS ethos was identified as having a positive impact on staff behaviour and attitudes:
It’s been brilliant because they have a good impact on our team culture, you know, so we play to each other’s strengths . . . it makes [MH staff] think twice about how they’re speaking about patients . . . it challenges them as well, doesn’t it, makes them think, well, actually – so I think it’s just powerful, they’ll ask questions which we need to hear.
AMHP2
This participant suggests that VSO involvement opens the professional–user dynamic up to scrutiny and models a different approach, and this was particularly evident for VSOs providing advocacy.
Reducing the use of public sector services
Investment in the VSO was identified as having an impact on the public sector resources and mode of operation to transform the crisis system:
If you invested a small amount into the voluntary sector you can do that outside of all of that discussion and vested interest. That can immediately have an impact on demand and on A&E flows and everything, and then you have sort of already started to disrupt the system. So it is a bit of a disrupter of the system.
S2
Several participants reported not using public sector services because they received support from a VSO, and these benefits were also identified by commissioners:
They [safe space] are really important in keeping a certain cohort out of hospital, out of crisis, and is really well utilised . . . These are people who are living in supported accommodation, who will come with a minder maybe or they’ll come on their own. They know they’re going to have [a meal] – there’s a routine to it, and there’s a community to it, and also it’s different every time . . . there’s also support with benefits, there’s support with information on navigating if you want help with anything. They will make an effort to find people, the right people to come, so that they can signpost and help.
CCCG1
Access to crisis beds (sites B and D), which provide respite and an alternative to hospital admission, was viewed positively and prevented the crisis from escalating. In particular, the benefits of avoiding the potentially negative consequences of hospital admission were identified:
What those crisis beds do is that they can remove people from the social chaos and enable them just to take a stock and . . . be safe with that 24/7 support that isn’t nursing care; . . . so they’re not being medicated or not being sort of rapidly tranquilised, they’re not being restrained, they’re not being observed continually . . . But were that service not there, the likelihood is they would end up in hospital; we know, to some extent, that people going into hospital doesn’t always mean that they will immediately [be] better off. It triggers off a whole other set of consequential outcomes, so some of which are usually quite poor.
BCCG1
Access to the safe space in site A was also having a positive impact on A&E attendances and inpatient admissions, although whether this was due to system reform or the availability of the VS safe space is unclear.
Evaluating the impact of voluntary sector organisations
Specific VSOs have been evaluated, as identified by the literature review (see Chapter 2). In the study sites, however, there was limited evaluation of the VSO impact. This was explained in terms of respecting that people were in crisis and, as well as being methodologically difficult, a concern that an evaluation focus might detract from responding well. There was a genuine interest in knowing how to approach this, rather than defensiveness on the part of the VSOs. The following methods were being used:
-
commissioning independent research, including from service user organisations
-
capturing narratives about individual experience
-
using red and green tokens for people leaving the service to indicate satisfaction or dissatisfaction
-
interviews with service users on their experience by a service user group [one group was using a values framework (working together, personalisation, inclusion, empathy and honesty] to assess experience
-
the recovery star, most frequently mentioned by type 2 VSOs.
However, the extent to which demographic data were captured and used to inform service development was limited. Commissioners were, however, using data on service use in some areas to identify the impact of commissioning the VSO on service use, particularly on A&E.
Summary
Whether or not people experiencing a MH crisis are able to access the right support in a timely manner provides an indication of the capacity of the wider MH system and reflects the specific context for the evolution of the VSO. The access to type 1 VSOs tends to be restricted by NHS services. Although this may mean that people with higher needs or people presenting with greater risks are assessed by MH staff, self-referral, a rapid response and face-to-face support are clearly valued by service users. It is notable that some people preferred to use VSOs rather than the public sector. The VS services in our study were widely appreciated, evaluated positively and trusted by people in crisis. They offer specific expertise and peer support, and their distinctive contribution is their ethos and approach, which is highly relational and socially oriented. They play an important role in both prevention and recovery by enabling people to manage their MH better, facilitating access to a wider range of support and services, and by enabling people to develop their social networks.
There is work to do in ensuring that VSOs are engaging and providing services to diverse communities, and those that have skills and knowledge of specific life events are factored into the crisis response at a local level. Although this is primarily a descriptive study, we were able to identify a range of positive impacts through VS support, including enabling people to re-evaluate their lives, develop strategies for coping with distress and develop better support networks. The mechanisms by which the VS achieves these positive impacts were often interlinked and, in some instances, were delivered alongside public sector provision. There is a risk that this contribution may be overlooked by the public sector and/or that VSOs work in isolation from each other. This poses questions about how the different organisations can effectively collaborate, while recognising their individual contributions.
Chapter 7 The relationship between the voluntary sector and public sector
The focus for this chapter is the relationship between the VS and public sector services, mainly those provided by the NHS. We examine the findings on how well the range of services in these two different sectors are working as elements of a system of crisis support to ensure an effective pathway for people needing support in a crisis. We draw on data from the repeat interviews to illustrate this.
The wider crisis system in the study sites
Alongside families, communities and the VS, the crisis system includes a wide range of public sector services: NHS 111, GPs, ambulance services, A&E, psychiatric liaison, CRHTs, local authority services, the police and, where it exists, street triage, and social housing (provided by VSOs, housing association or local authorities). For people to be able to access timely support, policy-makers and commissioners proposed that these different elements needed to work as a system, maximising their different contributions through the crisis journey:
So if you have proper signposting information, advice, access for all the different age groups, you know, web tools, counselling services, so people can access easily, you’ll be able to support people earlier to access the right support at an earlier time. So if you have individuals that end up in a mental health crisis or any other crisis, you have the services that are able to respond in an efficient and timely manner . . . We’re talking about crisis resolution home treatment teams. Now we’re talking about an NHS crisis helpline, so we have that service able to meet people’s needs at the time of crisis. The [next] element is good quality care and treatment . . . and a good standard of care is at a similar level across the whole country. But what actually happens after crisis? How do all the systems work together to make sure that it’s effective and efficient so that individual doesn’t have to go back into crisis again, regardless of the time frame?
ACCG1
There was a highly varied notion of a ‘system’ across the sites. However, all of the study sites had a CRHT, locality community MH teams and psychiatric liaison services. It was clear that the CCC, together with additional investment, had created an opportunity for system development in identifying and bringing together different organisations. In site A, there has been an ambitious system redesign taking place over the last 3 years, with the remodelling of the crisis system in tandem with the introduction of an NHS helpline that provided a single point of access to MH crisis support and a redesign of primary care support and the VS support for recovery. Additional resources had been made available to support this and this included investment in a VS safe space, which would receive referrals via the NHS helpline team, which triaged callers based on need and the assessment of risk. The helpline and safe space worked in close collaboration, including joint meetings and supervision. There was also an out-of-hours VSO helpline run by a ULO, as well as a national suicide helpline. The feedback was generally positive:
I think we’ve got a lot more crisis care, I think it’s a lot better than it was . . . We are working much better together as different organisations; we have regular meetings, so that’s working well. So I think actually the crisis support that is available locally is quite good.
AULO1
Sites B and D had specific crisis pathways designed with the VS, but not an overall system:
I think we could do with more of an integrated crisis [system], definitely. At the moment all we’ve got are very overstretched staff trying to deal with people in crisis. Referrals to the crisis team who are also overstretched and if the beds at [the crisis house] are taken people are ending up in [hospital]; it is just trying to keep people safe.
BMHP3
Site B had a 24-hour crisis team and a well-established street triage service operating a ride-along model with a MH nurse and police officer. There was also psychiatric liaison at the local general hospital’s A&E department, from which the crisis team could refer people to the commissioned four-bed VS crisis house where they could stay for up to 3 weeks as an alternative to hospital admission. Service users had been heavily involved in co-producing the CCC and subsequently developed a specification for community safe spaces for people in crisis, and were awaiting the decision from the commissioners. In site D, the CCC had also facilitated the development of the system of crisis care. Funding had been made available through the CCC for an NHS crisis assessment suite and the CCC was attributed with leading to much-improved relationships between the MH trust and the police. There was an NHS walk-in face-to-face crisis service in one of the main urban centres and four CRHTs for different patches, with one gatekeeping access to the VS crisis house (two beds alongside supported housing) on behalf of the other CRHTs. There was also a street triage system operating across the area, a crisis assessment suite for those subject to a section 136 and an out-of-hours VS helpline. These developments were set within a broader context of an NHS and local authority ‘movement to involve the voluntary sector’, although it was unclear how these developments related to each other.
The CCC in site C related to a NHS trust, which covered three other CCC areas. The NHS trust in this site had a 24-hour MH crisis line with options for professionals and service users/carers. Callers to the NHS crisis line were referred to the local VS peer-led crisis line, and vice versa, depending on which service they would be better supported by. There was also a crisis assessment team that linked the police, ambulance service and MH teams, so that first responders encountering someone with a MH need could access advice from a MH specialist by telephone or in person if necessary. This was linked to a section 136 suite in the local acute MH hospital, and there was a psychiatric liaison suite available at the nearby general hospital A&E. Consultants and nurses in the psychiatric liaison suite, community teams and crisis assessment teams, and GPs all regularly referred people to the local VS appointment-based listening service, although it was not a commissioned service.
The overall context of underfunding was identified as impeding the effectiveness of the MH system. In particular, the austerity measures taken by local authorities and the NHS were specifically noted as adversely affecting thresholds for access to services and eligibility criteria for social care, the investment in the VS and the provision of wider support playing an important role in supporting a person’s recovery. In site C, for example, cuts were being made by the local authority to care packages and supported housing placements.
Adequacy of the crisis system
Fragmented systems and unmet needs
As discussed in Chapter 4, a conception of a MH crisis as an episode requiring urgent and emergency response is driving the design of the crisis system. Unsurprisingly, therefore, we identified a range of system gaps, with needs going unmet or not being met well. This was evident across service user and carer participants, and was heightened for people from BAME communities. For example, the importance of early intervention to prevent crises leading to the over-representation of African and Caribbean men who are detained under MH legislation was reinforced as a systemic gap. There were also specific gaps for people who used substances or who had a learning disability, reflecting the separate commissioning arrangements for these two groups. People living in rural areas, people leaving prison, homeless people and people moving between areas also struggled to access crisis support from public sector services and the VS. Similar gaps were noted for children and older people, including those with dementia. Local commissioners and providers were often aware of these gaps and their impact on access and service use, but there was often a sense that these were yet to be addressed:
[People] particularly from South East Asia, [including] second- and third-generation individuals who are living within our community and they all have different needs and have a different context. I think we’ve still got work to do in those areas as well to make sure that we understand the kind of cultural stigma and make sure that we’re supporting those individuals to access our services . . . That’s particularly an issue in terms of our . . . care services as much as our urgent care services, because what we’re seeing in some cases is over-representation of that group within our urgent care services and then under-representation within some of our more generic community mental health teams. So we’re doing work to try and understand that.
DMHP1
A lack of resources was cited as a factor, despite additional resourcing. A fragmented system made consistency and follow-up challenging, and these problems were identified in discharge from A&E, in discharge from acute inpatient care, between primary care and specialist MH services, and between CRHTs and the rest of the MH system. In addition, service users who were parents also highlighted the difficulties in getting support for their children who were autistic or also experiencing MH difficulties.
Service thresholds and ‘responsibility tennis’
The system’s fragmentation was often attributed to the defined criteria and restricted thresholds for accessing different NHS and local authority services, most notably CRHTs, CMHTs and IAPT:
In terms of the statutory services, they have to be in dire need before they are taken on. You know what they see as a crisis and what we see as a crisis are two different things. We’ve got people threatening to commit suicide and even attempted it and they’re still not urgent enough for them, you know. What’s urgent, more than that?
RS1
In site C, there was a waiting list for MHA assessments and this was attributed to police shortages. Although MH staff suggested that the thresholds for CRHTs had relaxed, this did not seem to be matched by the experience of service users and their families, and this was a source of frustration for them and for MH staff. Furthermore, there was concern that the threshold for access would become even tighter:
Not meeting the criteria, that is the major sticking point. And everyone’s budgets are being squeezed, so I think in the future, unfortunately, the criteria’s going to get smaller; well, it’ll be a smaller amount of criteria but the higher end.
AMHP4
Alongside thresholds for accessing specific specialist services, there were waiting lists for psychological therapies, notably IAPT, and several participants had been waiting for more than a year, necessitating us to write to their GP to raise concern:
So there’s the time – there’s the sense of being passed around, that, and also the time that that takes as well, and then obviously your circumstances can change in that time.
DSU2
There was a definite lack of specialist services for people identifying as having a personality disorder and, across the sites, evidence that the needs of those who self-harm or experience suicidal thoughts and present to services repeatedly are not being well met. Therefore, people could find themselves ‘batted’ from one service to another:
I feel like I’m seen as a difficult patient so it’s hard . . . because I’ve got eating problems mixed in with depression and suicidal ideation, so I’ll be passed from the eating disorders team back into the affective team, eating disorders back into affective and essentially none of them really know what to do. So when I’m with the eating disorders team, they don’t want to do any therapy and don’t want to do any treatment, ‘cause they’re like ‘ah, but then you’re more likely to take an overdose and that’s too risky’ and then when you’re with the affective team they’re like ‘your weight’s too low, we can’t work with you unless you’re at a higher weight, therefore we can’t do anything’. So then you’re, like, stuck in this in between, so they’ve just never really done anything.
DSU6
Indeed, MH staff referred to disagreements occurring between them in relation to risk and the most suitable service, indicating a lack of clarity about roles in crisis care. One participant eloquently described this dynamic as ‘responsibility tennis’:
It’s about trying to call up anybody that will listen to try and get some support but it ends up being tennis; you call up this person, they don’t care . . . I’ve had to call up the crisis assessment [team] and they’ve said to me ‘they’re on our books under the community team, you’ll have to speak to them’, so you call up the community mental health team and they say ‘oh we can’t deal with that, if they’re in danger call the police’ and you just end up bouncing round, ‘oh speak to the GP’, and everybody doesn’t want to take on the risk, no one wants to deal with the problem.
CVS8
This included passing the responsibility for action back to the individual experiencing the crisis. Several participants commented on the reluctance of a CRHT to accept a referral, including self-referral, emphasising self-reliance.
Gaps in prevention and recovery
One consequence of a MH crisis being conceptualised as an episode requiring an urgent response is that the follow-up after a crisis episode could be somewhat haphazard: ‘a cliff edge’. Although type 2 VSOs, along with Recovery Colleges, were offering courses and programmes to enable people to address their difficulties and develop strategies for coping, these had not been offered to or factored into crisis planning for many of our participants:
I think there’s a gap, it’s maybe called a pre-crisis, because they intervene when there is a crisis, but there’s always a build up and why does a crisis always, in 9 out of 10 cases, end up in hospital. There could be an intervention before hospital . . . because speaking to people who’ve been sectioned and . . . they say ‘well, why am I here?’ and then they can realise that something is not right with them and they want support before . . . they have to wait until something drastic happens.
CCaFG
In site A, people in a crisis were referred by the NHS and were able to be seen the same day at a safe space. Some participants observed that, since the introduction of this new service, the crisis system had much improved. However, it was evident that, although getting immediate access was possible, there was a major shortfall in the support and psychotherapeutic options for people to address their underlying difficulties. Approximately one-third of people were repeat callers to the NHS helpline and were also using the safe space on a regular basis. It was clear that more than an immediate response was needed for this group of people, who were described in terms of ‘having a personality disorder’:
It’s nice that she’s not in the position other people are where they find themselves completely unable to leave the house and they cannot hold down a job and cannot hold down personal relationships and all of those things. The provision, she feels, is geared very much towards them and it kind of leaves her out. She’s in that squeezed middle part where she’s unwell but she’s not unwell enough to get treatment.
ACa3 (husband)
There were several instances in which participants had been referred for a course, provided usually by a type 2 VSO, and, although there was some delay, it was common for contact to be maintained:
I think the voluntary sector is really valuable. What I like about them is despite that you’re on a waiting list, they will contact you and tell you this is where you’re at. They don’t just leave you in the dark. Whereas with the NHS it’s just there – how long is a piece of string? You’ve been waiting there, you’re not going to get any contact or anything like that.
ASU3 (repeat interview)
This situation was challenging for carers, when support (through either the VS or the public sector) was not evident:
It could actually be lethal because you could be suicidal again, then obviously it’s deeply troubling, frustrating and upsetting and all of that. So that made it harder for her to deal with it. A lot of the conversations that we would be having . . . would be about helping her to cope with that feeling and sort of being in that system, which was quite difficult to negotiate; didn’t know whether you were being looked after, didn’t know what was happening next.
CCa1
Relationship with public sector services
Appreciation of and views of the voluntary sector contribution to crisis care
As noted earlier, awareness of VS provision was generally patchy and best for VSOs that were commissioned to provide crisis services. MH staff and commissioners sometimes struggled to name services or were unaware that the service no longer existed. This does not necessarily mean that they were not appreciative of their role in providing an alternative to public sector services:
There’s a big group of people that go to emergency departments that do not need admission, do not need a bed but do need some sort of psychological therapeutic intervention ‘cause they’re obviously in distress. It’s about working through that distress with people, and there’s something about being able to divert people to a place that’s set up to deal with people’s sort of mental distress as opposed to sitting in an A&E department . . . There’s stuff that they need to talk, they need to work through that’s not about needing an inpatient admission.
CMHP6
The existence of short-term contracts and retendering exercises affecting the landscape of VSO provision was identified as making it difficult for MH staff to have current knowledge of VSO provision. One study site had a service directory developed by a VSO, which was highlighted as a useful resource, although the VSO had not been able to secure resources to keep it up to date.
The value of the VS contribution to crisis care in providing a distinctive and potentially complementary offer was promoted by strategic stakeholders, at national and local levels:
What they offer that’s distinctive or unique is that they bring lived experience to what the person is coming to them with. So they’re bringing, not technical knowledge, they’re bringing experiential personal knowledge and so there’s an element of identification or support that’s different.
S6
The key difference between the two sectors was consistently identified as reflecting the origin of VSOs from grassroots activity, the relational style of working and the involvement of people with lived experience as peers and volunteers (see also Chapter 5):
We call it ‘the additionality’ because quite a lot of things are happening within organisations that aren’t being commissioned. It’s good practice how they’re developed, working alongside people for many years and actually shaping their organisation, listening to the people who are being supported. And that’s a really big untapped resource, is staff who worked alongside people for a long time and actually have done an awful lot of learning and that’s how the sector has developed.
S9
The perspectives of MH staff on the value and skill set of the VS varied and, when there were close working relationships, the VS contribution was welcomed. For some, however, there was a sense that VS provision is inferior to public sector provision, namely a ‘poor relation’, and that VS staff are not skilled: ‘a kind of happy clappy people that aren’t staff or aren’t clinically experienced enough to manage, you know, high risk services’ (AVS7). This is clearly a source of frustration to VSOs, which, in some instances, have professionally qualified staff, but in any event have other relevant skills and experience and offer a different approach:
Third sector offer is a different skill, which is somehow in that moment, in that dynamic, . . . is not kind of saying ‘I’m making you better, it is my job to make you better’. There is something about ‘we’re in it together, you and I’.
AVS7
This was associated with a sense that public sector services did not always appreciate the complexity and range of needs of people being supported by VSOs. On the other hand, other participants flagged concerns about whether the VS capacity was adequate:
The training is maybe a 1-day mental health first aid or Deprivation of Liberty Safeguard (DOLS) or whatever, then they’re left holding the most chaotic people and feeling like ‘I’m holding this baby here and they tell me they’re going to kill themselves, they tell me seeing dead people, they’re becoming aggressive, they need to be sectioned or they need to be taken to a place of safety’.
RS2
By contrast, other participants stressed the importance of the VS in ‘plugging a gap’ created by service closures, notably local authority day centres and acute day hospitals, and the increasing thresholds for accessing NHS and local authority services:
So maybe the voluntary sector, traditionally its role has been it sort of picks people up without, with less criteria and can act then as a sort of wraparound or preventive way or pick people up who have fallen through the net.
ALA2
A lack of appreciation of the role of the VS could impede effective pathways or result in inappropriate referrals or signposting. This was identified by the crisis house in site D, where the VSO crisis beds were reporting underoccupancy and, thus, were not being used to good effect. This was explained by the VSOs in terms of their lack of involvement in referral decisions:
If they’re presented at A&E they’ll be seen by triage or something like that, assessed and gone ‘well, crisis bed suitable’. Then we’ll get a phone call . . . It’s never a phone call like ‘[O]h we’ve got so and so here, we’re considering them for the crisis bed. What do you think?’. We don’t get that phone call.
DVS1
This lack of understanding of the VS could also serve as a barrier to accessing public sector services:
Self-referral to the NHS response team should be OK, but I came across a voluntary sector worker [who] had been dealing with a case where they’d tried and tried and tried following their own interventions to get an assessment through from the NHS response team and had failed to do so and finally managed to get a GP to be heard, but even the GP struggled to get a response.
ALA1
A similar experience recounted by carers hinted at a fractious relationship between primary care and specialist MH services.
Collaboration between voluntary and public sector services at a system level
The quality of relationships is predicated on an awareness and mutual understanding of each other’s contribution. The close working relationship in site A was positively evaluated by a wide range of stakeholders, and there were regular meetings between the safe space manager and the relevant NHS staff: ‘we’ve come on leaps and bounds actually in the last few years’ (AVS3). There was some scepticism from a service user perspective as to the extent to which ‘warm words’ were being translated into practice. A risk that the type 1 VSO had become ‘part of the gang’ was identified and, thus, the contribution of other types of VSOs was potentially being overlooked. Positive relationships between the relevant NHS services (i.e. CRHTs) and the crisis houses were also described in sites B and D, although the formalisation of this relationship was restricted to referral arrangements. In site C, the landscape of crisis provision was dominated by the MH trust but the well-being hub run by a VSO was viewed as having increased access and reduced the number of people using social care services.
A range of ways of developing better relationships and mutual understanding were described:
We have twice yearly training days, the advance nurse practitioner sets those up and wrote out to all the voluntary sector and we have stalls, a marketplace that if there’s anything new in their area they can come and let us know about it, so that worked really well.
DMHP3
These clearly took time, and commitment, to mature to ensure that the VS was viewed as an equal partner:
They can be quite bolshy and when they become equal partners with us they start saying ‘well, what about if we did and what about if we did that?’. So I’ve never felt that we were dominant, we’re the commissioners so we could be quite dominant and bully, but in actual fact a lot of the time [it has] been really refreshing because they’ve reminded us of things that we ought to be doing . . . it’s a reminder of practices we’ve got into.
S17
In addition, VSOs were also working with primary care services; for example, a type 3 VSO in site A described working with a local GP surgery to support people who were recently discharged from hospital and at risk of isolation.
By contrast, some VSOs emphasised the importance of independence from public sector services, recognising that some people choose to use a VSO in preference to the NHS. Unease with the degree of closeness of the NHS was also expressed, with one participant describing one VSO with a close working relationship as ‘a tentacle of the NHS’ and another suggesting that ‘the VS now needed a VS!’. At the heart of this is concern that the values and ethos of the VS may be compromised. Some VSOs, reflecting their engagement with communities and their staffing by people with lived experience, also advocate, in the widest sense, for MH service users and/or carers. This includes offering a radical critique of public sector services, which may not be well received by the public sector and may challenge the development of collaborative relationships, inadvertently fuelling unhelpful stereotypes. For example, one VSO raised concerns about the failure to address negative attitudes and the apathy of NHS MH services to challenge the status quo in relation to their response to people from BAME communities:
[Racism is] like there being an elephant in the room, and it takes a dump, and everyone’s trying to talk about other [superficial] things, whilst trying to pretend they can’t smell it.
CVS7
In this instance, the VSO was trying to address this by being ‘proactive in making sure that we don’t allow ourselves to become part of the [apathetic] culture’ (CVS8) and actively supporting people from BAME communities.
The importance of maintaining this independent stance was emphasised by different types of VSOs, while recognising the need to keep the communication channels open: ‘we’re highly critical of them but we’ve got good relationships’ (BVS1). The extent of the closeness to the NHS, therefore, emerged as an important dimension to consider. Figure 11 depicts the degree of integration between the different VSOs and the NHS that we identified.
FIGURE 11.
The relationship between the VS and the public sector.
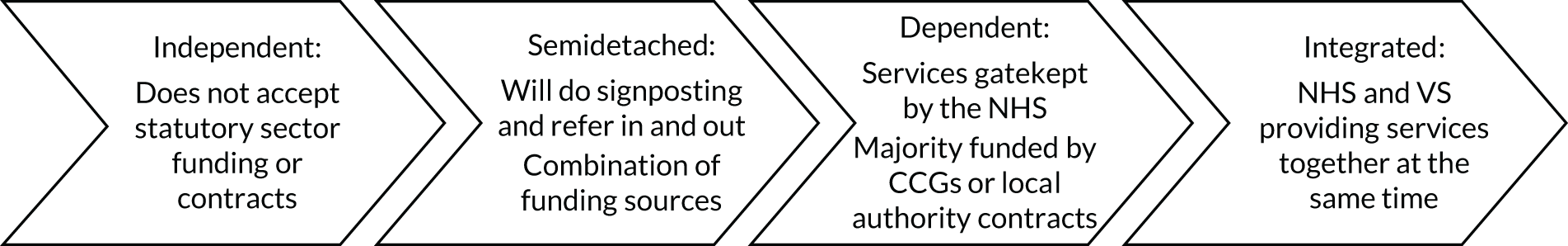
As well as funding arrangements, which are discussed in Chapter 8, the three main indicators of integration between the public sector and the VS at a system level were access arrangements (see also Chapter 6), the extent of information sharing and how risks were managed for individuals.
Access arrangements
In sites A, B and D, MH staff decided on appropriate referrals based, in part, on a risk assessment and gatekept access to type 1 VSOs:
If we’re going to refer people to them, we do the assessing bit, because we think that that’s the bit that we do, that we’re good at, but then they’re really good at being there with people, spending that time doing the de-escalation and then also talking about what next.
AMHP2
When the system was less developed, participants voiced their frustration with repeated assessments, which often failed to materialise into support, as discussed later.
Information sharing
In site A, decisions were judiciously made about the amount of information shared ‘because we don’t want the [safe space] to become a medical place’ (AMH1). Greater information sharing was identified as being useful for people who had complex situations and were using a wide range of services, when contact with services was construed as symptomatic of their difficulties:
I know that there are people that are touching lots of different services, but we don’t know what they’re touching unless they tell us. And it’s how can we make it more effective. I’m just thinking of a couple of ladies who are touching everything but they’re clearly not getting what they need to be able to move forward [reference to NHS trust services, VSO type 2 services, social care and occasional police and ambulance intervention], so getting a bit of what [they] need from everyone, but how can we join that up?
AMHP1
Thus, information sharing to agree ‘a treatment plan’ was seen as facilitating a more considered approach, and was referred to in sites A and C. Similarly, in site B, there was joint working between the NHS and the VSO for people in the crisis house, with joint planning and joint reviews. Furthermore, the importance of shared learning following serious incidents relied on both trust and sharing information. The introduction of the General Data Protection Regulation was identified as affecting information sharing arrangements, although this was yet to be worked through.
Risk management
At a strategic level, VSOs were involved in suicide prevention: ‘[I]t’s an area where people are trying to work together to look for solutions in areas that have caused problems before and just been kind of never addressed in a cross-group sort of way’ (AVS13).
The VSOs had various systems and policies in place to manage risk, including risk registers and lone worker policies, which involved liaison with public sector services:
On an individual level when we’re working with clients, we have really robust systems, so things like risk assessments are conducted as a matter of course. If we visit them in the home, for example, we have really clear processes around making sure the environments are risk assessed and in the mental health units as well, we’re linking with staff to check that the person’s safe to meet with. Often if you’re under a Section you could be a risk to yourself and others.
BVS6
In site A, as MH professionals decided on referrals to the type 1 VSO, the NHS MH service continued ‘to hold the risk’. Risks associated with suicide and self-harm could lead to referral to public sector services, and this was often the case if the VSOs felt that they did not have the relevant skills or expertise:
So if we have clients that would need 15-minute observations, that would be a high risk for us, because we can’t keep that person safe. They would either go to hospital or the crisis team would find an alternative placement for them, dependent on their needs. So for us it is more a lower risk client group because we aren’t clinically trained. We are housing and support workers.
BVS5
Other VSOs explicitly engaged with risk:
Running crisis houses, you are going to inevitably have more people that at least try to take their own lives even if they don’t actually manage to and so we had to sort of educate trustees to say this will happen. It’s a high risk . . . or we can be in it because we believe that we can provide a better experience and we have to try and manage the risk.
S10
Risk management was also framed as ‘a dynamic process’ and one VSO in site D was developing a harm minimisation approach: ‘embedding the recovery approach within our services, which has a focus upon harm minimisation and being far more informed than we were previously’ (DMH1). VSOs had a more comprehensive conception of risk than public sector services and referred to risks to individual welfare, of homelessness, of domestic violence, of substance abuse and of deteriorating MH that VSOs were often managing. This included assertively following individuals up if there was evidence of self-neglect or if they did not turn up as expected, and liaising with NHS services to access appropriate support:
We have been working with [a young woman] and her mood has been progressively worsening. She’s been really struggling and her protective factors have been reduced over the last few weeks, so we started to raise concerns last week with the GP. Today her mum took her to A&E after ringing the NHS helpline, but they had just suggested they should wait until the evening when they might be able to see her. Her mum took her to A&E, A&E tried to send her back to the NHS. I had to liaise with A&E and say ‘look, we’re really concerned about this girl because she’s extremely vulnerable if she’s there and she’s presenting in this distress after isolating herself for the last couple of weeks and not eating, not drinking, she is a serious risk and should be assessed’. So I had to have a long conversation with the psychiatric liaison team just so that they would do an assessment and they’ve finally conceded to do that today.
AVS6
This illustrates the ‘responsibility tennis’ between NHS organisations that we referred to earlier. Indeed, we identified a number of people who were under specialist MH services and situations in which the risks were known but not being managed. This included one woman with psychotic symptoms who had not turned up to a safeguarding meeting and, as far as we could gather, there had been no follow-up. Generally, however, communication about risks was shared when type 1 services were being gatekept:
If there’s something about risk we want to share, we’d pick up the phone as well, we’d send the referral form or we’ll pick up the phone and let them know if there’s something that doesn’t come across on paper really or that is of high enough risk that we’re concerned about it.
DVS3
There was also the view that the VS may not be equipped to assess the level of risk to the individual and others in the crisis house unless MH practitioners were part of the team.
Collaboration between voluntary and public sector services at an individual level
Policy-makers and commissioners often referred to crisis care pathways but we found little evidence of effective pathways across the crisis experience, outlined in the CCC (see Chapter 1). In site A, despite a clear pathway between the NHS helpline and the type 1 crisis service, the complexity of the crisis journey was evident:
Working out all those pathways, different systems you know, different services, trying to work together is difficult for staff – how difficult it must be for actual service users, trying to go through that pathway.
ACCG1
The pathways across the sites were compromised by the difficulties in accessing NHS services that have been discussed. A number of themes emerged for collaboration at an individual level. First, the extent to which needs were being appropriately met in the absence of an articulation of a coherent system and the restricted conception of a crisis as an episode. Service user participants described going round in circles and being repeatedly assessed by NHS services, and to a lesser extent VS services, without this seeming to lead anywhere:
The NHS side of things was just like repeated assessments and she felt like she was continually going back and saying the same stuff and then she just wouldn’t hear anything for ages; she didn’t know whether she was on a waiting list or not . . . it’s harder to cope with stuff like that when you’re depressed and it’s easier to accept stuff like that when you’re not depressed, so she did feel quite abandoned by the NHS.
CCa1
Figure 12 illustrates the journey of a participant, ASU14, who used both NHS and VSO services extensively and had contact with two VSOs out of their area. ASU14 repeatedly self-harmed and their journey dramatically illustrates the lack of resolution of their difficulties, despite the contribution of the various VSOs being appreciated for their supportive and empathic approach.
FIGURE 12.
An illustration of a crisis journey using both NHS and VS support (site A).
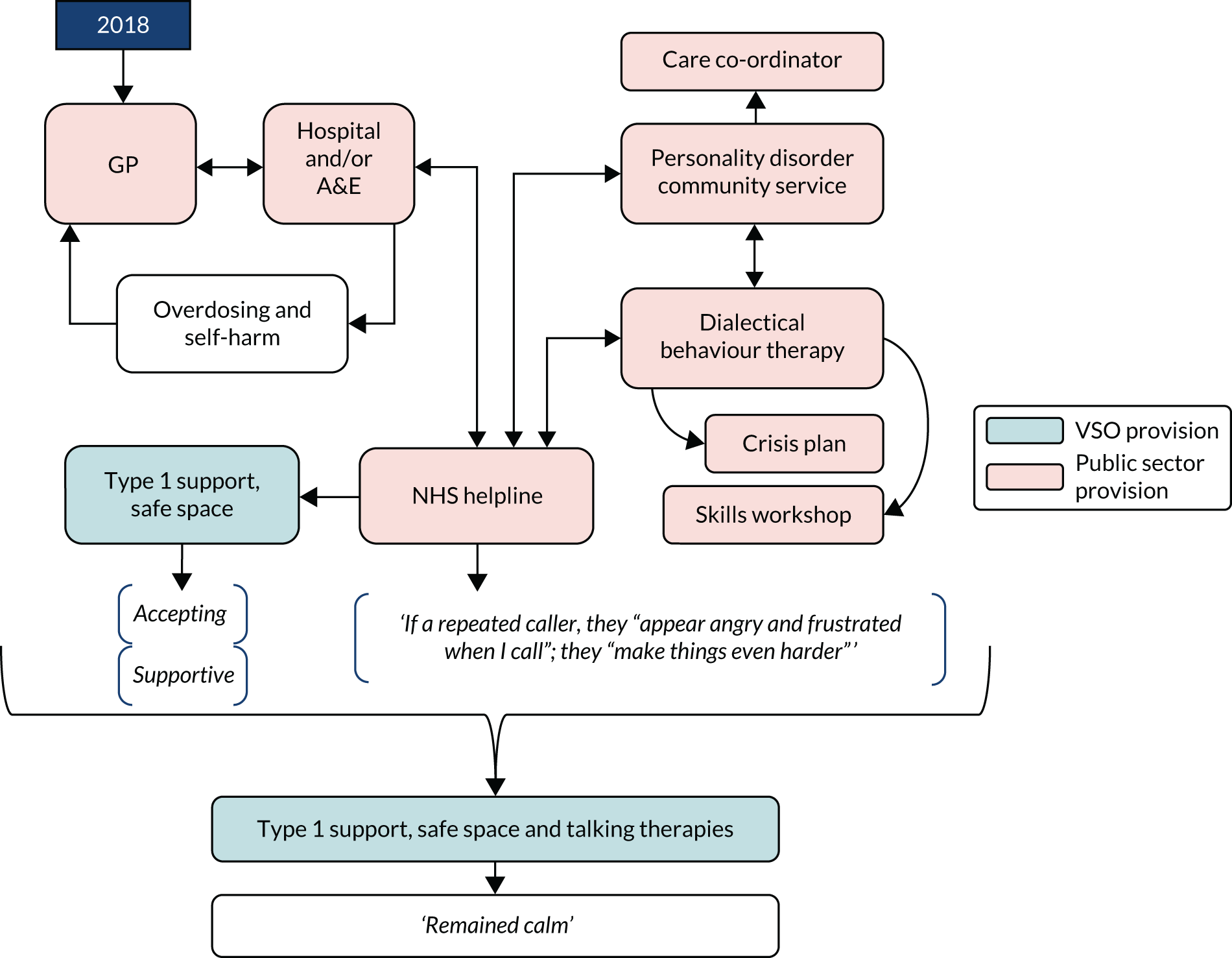
The second theme was the agency of service users in accessing support and ‘project managing’ their crisis. The degree to which this was understood and formalised into a crisis plan was unclear, as few participants referred to a crisis plan.
Third, when the NHS was gatekeeping access to type 1 VSOs, access had improved, but this provision was short term and the VS often had limited capacity for ongoing support. There were clear exceptions to this, for example a VSO for homeless people and a CRHT working together to address the complex array of presenting difficulties for their mutual clients.
The general picture, however, is that the VS is contributing to a patchwork of different types of support, at different points in people’s individual journeys through services, in combination with other VSOs, as well as in combination with public sector services. Figure 13 illustrates this for a participant, BSU4, who had repeated MH crises and had made extensive use of the VSO crisis house, to which they could self-refer. BSU4 also frequently presented at A&E and accessed the CRHT. Despite collaboration between the CRHT, the crisis house and acute admission wards, this pattern was repeated. At the repeat interview, aside from getting a dog, BSU4 described their situation as having changed dramatically because of a change of psychiatrist who reviewed their diagnosis, reduced their medication and referred them for specialist psychotherapy. For BSU4, their involvement with type 1 VSOs was interspersed between frequent public sector service provision/support. This journey reflects how the VS and public sector services can complement each other; for BSU4, type 1 services went hand-in-hand with various public sector services to support their individual crisis needs, but their use of these VSOs was limited by the time limits operating for these services.
FIGURE 13.
An illustration of a crisis journey using both NHS and VS support (site B).
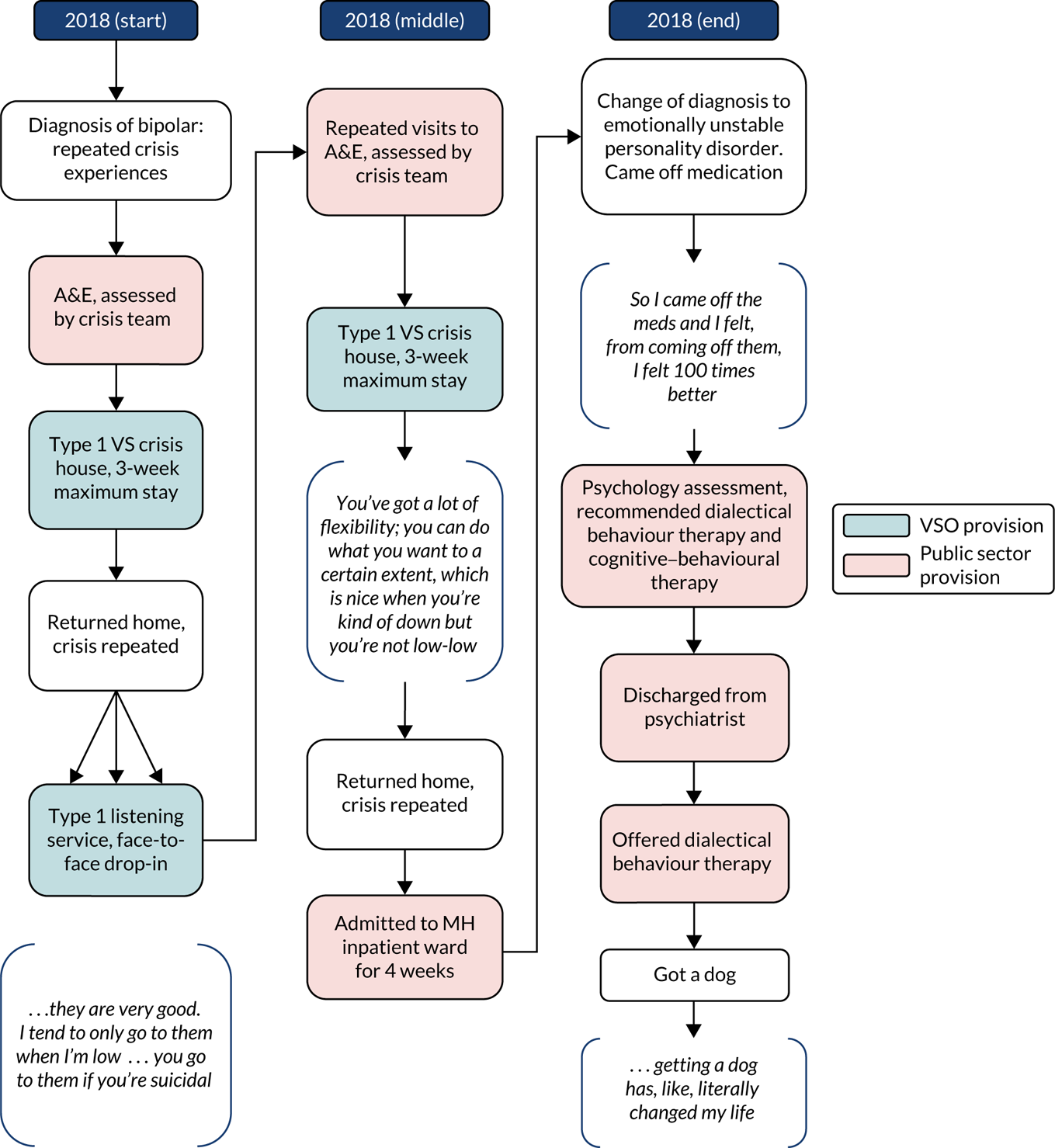
Recommendations for improving the crisis system
As well as commissioning, discussed in the next chapter, participants were able to identify what was needed to improve the crisis system and to better realise the contribution of the VS within this. Some of these have been picked up elsewhere and cover many of the gaps summarised in Table 18. Overall, participants wanted to see a broader range of services, not only those providing an accessible and flexible response to the immediate MH crisis, but also those that enabled people to anticipate and prevent a crisis and to address the underlying issues; abuse, previous trauma, substance use and housing were specifically identified. The crisis event should, therefore, lead to something better:
I think it’s about providing more support, preventative and post-support treatments and exploring more opportunities and giving more flexibility to the types of solutions available; don’t always use the same things. Listen to people, listen to the clients that are actually impacted . . . and more emphasis on supporting people with mental health issues with those two or three key areas of life, empowerment, housing and employment.
BVS6
The importance of this support being needs-led face-to-face support was stressed and participants wanted responsive flexible services: ‘to have an agency just simply called “Help”’. This included readily available peer support:
To have a group where even people who feel like they’ve come out of it or people are still in it or just people could exchange their feelings about it and make everybody feel there’s no shame there, there’s no . . . you know, so many people go through things and so many people are still going through things that, you know, there’s got to be a much more open approach to it.
CSU8 (repeat interview)
The value of the VS was clearly recognised and many participants recommended a better appreciation of this contribution, which would entail upskilling staff, effective collaboration between the VS and the public sector and greater investment in the VS:
The VCS I think should be a key part. I always think when you’re planning MH services this is where we get it wrong. When we plan mental health services we say ‘we’re going to give another 2 billion to the NHS’ and actually I think that’s wrong. What we should say is ‘we’re going to give 1 billion to the NHS and 500,000 to the local authority and 500,000 to the VCS, and we’re going to make them all work together’ and plan the services around the service user.
S17
The potential cost benefits of investment in the VS were also noted:
I have been sectioned three times in the 1 year. My first admission was a bereavement, well, a potential bereavement of my mother. The key thing is to avoid admission, isn’t it? The cost of admission when they cost it out is horrendous. All the money could be saved elsewhere if you didn’t have to go through all this bureaucracy. There’s a lot of money to be saved that could be used for the crisis.
ASUG
Overall, these recommendations were envisaging a crisis system with effective collaboration between all of the different elements, including between VSOs. There was the suggestion that there should be clear standards for crisis support, so that people knew what support they could expect. These would necessarily be underpinned by a commitment to equality: ‘[I]f someone’s going through a crisis, they’re treated equally, doesn’t matter what their cultural background is, don’t matter about their status in society, they’re all treated equally and with the best practice that’s available’ (CCaFG).
This principle of equality was referring not only to people with protected characteristics but also to people with different kinds of MH difficulties, and participants wanted a better response to people who self-harm, people who use alcohol and/or drugs, people who are diagnosed with a ‘personality disorder’ and people who do not easily engage with a standard model of provision.
Summary
The crisis system in the different sites was generally underdeveloped, although the CCC had stimulated some redesign. This was most advanced in site A, where an NHS helpline had been introduced with a first response service attached and a route through to a safe space. Nonetheless, across the sites, there was evidence of a wide range of unmet needs, including for people from BAME communities, young people and people with complex needs related to substance use, learning disabilities or homelessness. The closeness of the relationship with public sector services varies, from VSOs that are committed to maintaining their independence to VSOs that are closely aligned with NHS crisis services and that determine who will access the VSO. Some VSOs provide a radical critique of public sector provision, and maintaining this in a context of competitive tendering may prove challenging.
The relationship between type 1 VSOs and NHS services was most developed and where there was evidence of a mutual understanding of each other’s roles. The awareness and appreciation of other types of VSOs was less developed and there was a general lack of up to date information about what was available. GPs and MH staff would, therefore, signpost rather than refer to these services because of concerns over governance.
Effective collaboration at the level of the individual service user is focused around providing an urgent and immediate response and there was little evidence of a coherent pathway, although VSOs and NHS services would refer to each other. Both the absence of a preventative approach and a lack of continuity to enable people to address the relevant contextual factors were evident. Thus, some people go from crisis to crisis, without adequate support or resolution. The understanding that a crisis represents a window of opportunity for longer-term change appears to be being missed across the crisis system, although is being addressed to some extent by the VS.
Despite this, the VS contribution was widely appreciated and this was evident even for those participants whose difficulties had not been resolved. Participants were often critical of their experience of NHS services and identified the lack of responsiveness of CRHTs, thresholds to accessing services and waiting lists as compromising their access to crisis support. They were also critical of dismissive and insensitive attitudes, and referred to a mistaken view of agency as shifting responsibility back to the person experiencing a crisis. Participants agreed about the need to develop the crisis care system, which would better recognise the contribution of the VS.
Chapter 8 Moving forward: the development and sustainability of the voluntary sector
The breadth and diversity of the VS present a challenge to local commissioners. In this chapter, we consider the findings on the role of commissioning in shaping the VS contribution to crisis care. This includes the sources of funding for VS activity, the relationship with commissioning, the contracting arrangements, monitoring and the quality of these relationships. We draw out the implications for the sustainability of the VS in this area and the recommendations that participants made for strengthening the commissioning of the VS.
The important role of commissioning of the voluntary sector
Market stewardship
Commissioners are expected to perform a market stewardship role,122 attempting to shape the elements of the crisis care ‘system’ that they have a degree of control over. Nevertheless, the data strongly suggest that commissioning is something of a blunt tool for shaping outcomes in terms of system design. The exception to this was site A, where commissioners have led an ambitious programme of service redesign, with consequences for VSOs. In other sites, by contrast, there appears to be a lot of ‘noise’ in the system. For instance:
The challenges of the commissioner I think is to get conventional organisations to work unconventionally. So the way you might want to change something from how it is to how you want it to be might be the way you contract it; so, at the moment, we might have sort of quite prescriptive service specifications . . .
BCCG1
Unfortunately, there does not appear to be a great deal of trust between commissioners and providers, particularly for smaller organisations that have lost their funding. This is perhaps exacerbated by the overall funding context, which is clearly deteriorating, meaning that commissioners are closely associated with ‘cuts’. Nevertheless, there is widespread recognition – by both VS respondents and commissioners – that commissioning needs to be used to attempt to shape the system in more creative and collaborative ways, particularly prior to the delivery phase, to move towards an ‘integrated care system so you’re not necessarily looking at contracting it as one whole thing, you’re trying to get a system to work together more effectively’.
In site B this was being operationalised through joint working of staff, joint training, etc., and the success of this multiagency approach was put down to strong leadership. It is also important to say that there are clearly indications of good relationships between commissioners, VS providers and other stakeholders in the system. For instance, the CCC and its associated engagement and networking arrangements has led to good engagement between different components of ‘the system’:
I was pleased that both carers and service users were able to describe to commissioners what we thought a better voluntary sector offer would look like and we said it needs to be less fragmented, not just if you’re lucky enough a few weeks of this and then a gap and then a few weeks of something else.
ACaFG
Another key task for commissioners is to engage provider organisations throughout the full cycle of commissioning, and indeed there was evidence of VS and community engagement in the commissioning cycle, in order to inform the development and delivery of improved services and outcomes. For instance, in site D, one organisation runs a ‘community mental health ambassador’s programme’:
Basically the CCG realised they weren’t engaging with the local public very well in terms of how they commission and plan local health services, so we’ve been running that project for about 3 years now and it’s just a community engagement project . . . we take [patients] to the governing body every 2 months. And a lot of them are kind of project workers or volunteers themselves with different groups so we’re linked into like asylum seekers and refugees, the LGBT community, people with epilepsy . . . people with learning difficulties, the blind community, the deaf community, so it’s like a total mix.
DVS7
Clinical Commissioning Group respondents equally reflected on the particular value of the involvement of the VS throughout the commissioning cycle:
[A]ctually I think that’s where we learn, that’s where we get our best learning from, why it happened and why did they do it and then we’ll learn from the voluntary sector from their experience.
BCCG1
A complex world: commissioning and the lack of system coherence
Despite the mixed picture described above, there’s no doubting that commissioning is viewed as problematic by a range of stakeholders, but particularly by VSOs that have a negative experience of commissioning, while generally accepting that it is a necessary feature of the public service landscape. This was reflected in comments bemoaning ‘upheaval’ or uncertainty in commissioning arrangements:
So the commissioning changes quite frequently . . . which causes difficulties. The thing that could be better in terms of commissioning is working together a lot better. Commissioning is a constant challenge, especially round here, because CCGs are really strapped financially, so they’re constantly reviewing services.
DVS2
A major theme in the data concerns the complexity of commissioning and associated arrangements and the lack of ‘join-up’ in the system. This is not always necessarily solely about the commissioning process, but is also about the wider complexity of the system:
I think the need to go through panels and things, they can be quite good, but actually there can be meetings on meetings and huge amounts of paperwork and just so that you’re allowed to then refer them to a project . . . In our borough you’ve got the mental health panel [that] deals with the mental health housing and then there’s another panel, which I sit on, which deals with complex needs . . .
CVS6
Indeed, there is a strong sense that separate commissioning arrangements sitting within different ‘pots’ or different public service areas have ‘on the ground’ consequences and make it very difficult, if not impossible, to join up services to meet the needs of groups or individual service users:
They sit outside of the trust, even if we do manage to build up relationships, so all of those things that make care better, I think their funding . . . they have to tender every 3 years and it’s different in every area. For me, we got asked that question at CCG and the commissioning arrangements very much make it difficult and I don’t think the NHS should have a monopoly on crisis care, but if we try to refer in to one of the organisations and they say no, we’re very stuck.
DMHP3
Funding sources, relationships with other ‘fields’ and sectors
Funding sources
From the development of the study database, we noted that charities operating in the field of MH are likely to be considerably more reliant on public funding than the charity population as a whole. The sources of income, identified through the survey, are summarised in Table 19. Contract income is clearly very important, with at least 70% of all charities in the survey receiving incomes greater than £100,000 from local authorities; the proportion is lower for the NHS and CCGs and rises as organisational size increases. Over 80% of organisations with incomes greater than £500,000 receive income in the form of contracts. Variations by size are less noticeable for charitable sources of income such as legacies and fundraising, but there is a clear gradient in the likelihood of drawing on earned sources of income for larger organisations and for social enterprise activities. Interestingly, notwithstanding a widespread perception that grant income from the public sector has declined in significance, there is a suggestion that a significant minority of organisations receive grants from local authorities and the NHS. There are also indications that the likelihood of obtaining grants goes up with size, probably reflecting greater organisational capacity. It is also the case that, for some VSOs, independence from public sector services defines their ethos and, therefore, they do not seek or accept public sector funding.
| Income (banded) | CCG | Local authority | NHS | Other | Any |
|---|---|---|---|---|---|
| < £25,000 | 0.14 | 0.04 | 0.07 | 0 | 0.14 |
| £25,000–100,000 | 0.17 | 0.15 | 0.03 | 0.13 | 0.35 |
| £100,000–500,000 | 0.33 | 0.48 | 0.19 | 0.1 | 0.71 |
| £500,000–1M | 0.5 | 0.73 | 0.27 | 0.14 | 0.81 |
| £1–10M | 0.44 | 0.89 | 0.44 | 0.28 | 0.94 |
| > £10M | 0.75 | 0.75 | 0.75 | 0 | 0.75 |
| Total | 0.3 | 0.41 | 0.18 | 0.11 | |
| Legacies | Fundraising | Earned | Social enterprise | Other | |
| < £25,000 | 0.79 | 0.71 | 0.14 | 0.04 | 0.07 |
| £25,000–100,000 | 0.7 | 0.68 | 0.1 | 0.03 | 0.07 |
| £100,000–500,000 | 0.73 | 0.67 | 0.5 | 0.1 | 0.04 |
| £500,000–1M | 0.64 | 0.68 | 0.36 | 0.18 | 0.05 |
| £1–10M | 0.72 | 0.67 | 0.56 | 0.28 | 0.17 |
| > £10M | 0.75 | 0.5 | 0.25 | 0.25 | 0 |
| Total | 0.72 | 0.68 | 0.32 | 0.1 | 0.07 |
| Big Lottery | Comic Relief | Other charitable organisations | Local authority | NHS | |
| < £25,000 | 0.11 | 0.04 | 0.36 | 0.29 | 0.07 |
| £25,000–100,000 | 0.35 | 0.15 | 0.45 | 0.2 | 0.5 |
| £100,000–500,000 | 0.23 | 0.08 | 0.65 | 0.48 | 0.21 |
| £500,000–1M | 0.41 | 0.09 | 0.59 | 0.55 | 0.18 |
| £1–10M | 0.56 | 0.28 | 0.61 | 0.33 | 0.28 |
| > £10M | 0.5 | 0 | 0.25 | 0.5 | 0.25 |
| Total | 0.3 | 0.11 | 0.53 | 0.37 | 0.16 |
The funding context: from ‘feast to famine’ – declining funding and increasing demand
This section first examines the wider funding context in which commissioning arrangements sit, before moving on to consider specific criticisms of commissioning and its influence on crisis services. It was very clear from interviews at all levels – from national stakeholders to regional commentators and case study respondents – that a major overarching feature affecting MH services (and indeed all related policy fields) has been declining resources, while at the same time needs and demand are perceived to have been increasing:
In the 16 and a half years that I’ve been a consultant, I’ve been here for that time just in this borough, we had a huge provision back in the day of feast and the years of famine have led to a constriction of third sector provision because it’s been decommissioned.
CMHP1
There is also a sense that resources are being spread very thin and that often the VS is seen as an afterthought or receives only the ‘crumbs’; for instance:
[H]ere, as happens in lots of other places, there’s been less funding for mental health in the last few years and, as you’d expect, it’s split between the acute trust and the mental health trust
ACaFG
A strong narrative emerged that funding has declined as a result of public sector austerity, and respondents were clear that, where once public funders and commissioners were almost ‘throwing’ money at providers, including those from the VS, now the landscape is completely transformed:
Well we’ve had a tremendous amount of money taken out the system, you know, both in local authority and in health . . . and we don’t have parity. I think this council spends about 15% of its budget on mental health and I don’t think the CCG spends more than that. Well that’s not good enough, you know, when the demand’s increasing.
CVS5
A number of respondents from different vantage points echoed the idea of falling funding in tandem with the identification of greater need in the ‘system’:
Increased demand for the services and I think the services are geared to be able to meet the demand, that’s a huge, huge issue that’s likely to stretch the services further. At the moment, every service in the country is now running into financial trouble; we’re having staffing cuts, we’re having increasing demand for the services . . . I don’t see any positive new developments happening, everything seems to be shrinking.
BMHP1
This potentially compromised the effectiveness of commissioning to deal with variability in access and quality across the areas, as noted in Chapter 6:
I don’t think the mental health commissioning in Middletown was very effective. I didn’t get a chance to look at that because they all needed to make savings. Middletown’s been even worse hit than Centreville, mainly because they’re so small so the economies of scale aren’t there.
ALA1
Furthermore, it was argued that this systemic austerity was affecting the ability of services to experiment and innovate:
Things have changed so much, that actually people are being so cautious. And it means that you can’t, whenever you’re trying to kind of think of ways of evidence in what we want to do, we’d have to do it in such small ways that it wouldn’t be a good example of what our idea would be.
CMHP2
This, it would appear, is affecting all public sector services, and thus having an impact on relationships across sectors, whether or not they are directly implicated in crisis services or wider MH, including other public services such as the police: ‘[B]ecause to say everything is stretched is a real understatement. It’s at breaking point. It’s at breaking point’ (BPo1).
By contrast, some participants pointed out that the increased emphasis on MH policy, and ministerial statements, have meant that some now perceive that more money is going into MH and this has caused some problems:
What’s a bit of a challenge is balancing people’s perceptions, because of the media, everybody thinks that money’s just been thrown at mental health now and we’re actually finding it harder now than ever to get money because even the grant givers, like the Lottery and people like that, it’s harder to get them because more people are competing. They don’t open the grant giving as much as they used to, so it is harder.
DVS2
Alternatively, more money is being made available but is not reaching VSOs or front-line services:
I think as well recently there has been some political statements about extra money going into mental health for example. So say if x money did go into mental health, where’s it going, is it going towards the trust or is it going towards the actual providers that are delivering face to face?
DVS5
This broader picture, which was consistent across the national, regional and case study data, sets the tone for participants’ understanding of the commissioning landscape. However, it does at times make it difficult for people to disentangle the effects that ‘cuts/austerity’ are having on available resources and relationships between public sector services and VS services, and between VSOs themselves. For instance, it is not surprising that VSOs themselves report an increase in the sense that they are in competition with each other and that they are less likely to share information through a spirit of collaboration, but it is not always clear that commissioning and individual commissioners are necessarily to blame for this.
Impact on voluntary sector organisations: contracting arrangements and the quality of relationships
In addition to the broader resource picture outlined earlier, respondents often described problems with funding arrangements related to public sector funding that were of a longer-term nature. These were reported to create considerable uncertainty and, at times, upheaval for VSOs and indeed for the wider ecosystem of provision and service users. For instance, as regards the loss of funding for a project training service users to tell their stories of MH crisis to public sector services providers, one respondent stated that ‘[I]t was a shame because that gave people some ownership and a bit of pride as well’ (BVS4). Indeed, more widely across site B, it was found that numerous organisations stated that services had stopped as a result of short-term piecemeal funding, and they were searching for ways to keep these – often very specialist or niche – services going, including through voluntary action if necessary. Interestingly, however, VSOs in site B were less critical of the commissioning process than in other sites, and they felt relatively valued by the public sector. In most areas, there was, however, a palpable sense of uncertainty and insecurity, for staff, volunteers and service users:
They’ve said we’ll . . . be given 3 months’ notice if they do finish the service, but the issue is how do you keep staff and train them up and then how do you keep the staff if you can’t, you don’t know from one day to the next whether your service is going to continue. And that’s the same with all the voluntary sector services, there’s no continuity.
AVS2
Clients are anxious . . . ‘am I going to see the same worker, you said to me, you know, will you still be here’, you know, ‘we hope so’. There’s no guarantees. That’s the biggest issue at the moment, trying to provide a continuous service for people who are very unwell in lots of areas, including mental health.
AMHP4
Furthermore, it is clear that service user organisations could be very aware of the impact of funding uncertainty on services they valued and relied on:
A lot of the people working in the [VSO safe space] were really worrying about their money because the funding was only approved every 6 months, so how do you plan service ahead in years to come with Five Year Forward View or whatever you want to call it, if you’ve only got funding every 6 months and you don’t know whether you’re going to get it.
AULO
Again, this was widely reported across the study sites:
There’s the issues in terms of commissioning with third sector agencies as well, so not just the amount of money but also the contracting processes where organisations are living on 12 month/24 month up to a year contracts if they’re lucky, and how that can then impact within the system in terms of relationship building.
DMHP1
Nevertheless, there was an air of realism for many VSOs when they are discussing recent changes in the funding landscape. Typically, this is characterised as the scaling up of contracts (so that they are easier for commissioners to manage), while reducing the overall budget. They recognise that there is not much they can do to influence this (and, indeed, neither can public sector funders); there is an element of fatalism:
There is now one contract, which has seen all, bar three, of the organisations lose all of their funding and one of those organisations had closed. So we are one of the lucky three. But what the local authority said is ‘we don’t want nine, we want one because it’s easier and while we’re doing that, we’ll knock a third of the total budget off the top in order to make some savings’. So where we used to have £1.2 million for this, we’ve now got £900,000 or whatever.
AVS1
In other cases, crucially, respondents make a distinction between the impact of the financial stringencies (and changes) in the wider funding landscape and their disquiet with specific contracting arrangements. One VS respondent, for example, described how the contracts they are being offered are very limiting and bureaucratic in terms of financial reporting:
I feel that the new contract that they proposed was so bureaucratic and so intrusive of people and such a barrier to their rights that it was an important stance for us, as the local charity that’s done it for all these years, to stand back and say ‘hey we’re not doing this. It’s completely wrong’.
CVS8
In effect, the charge is that commissioners, seen as distant from the reality of front-line delivery, are inappropriately interfering in and inhibiting effective delivery:
For me, it’s breaking down the funding to such a point that they’re going to stop making quality decisions about whether the person deserves the advocacy or not. What does a broker have to do with advocacy? Nothing. They have prioritised the financial management . . . They’ve made us report monthly, they’ve made us allocate everything to postcodes, like the amount of work needed just to report back to them where your 120 hours was spent, they want to know what activity you were doing, they want to know everything you could imagine: ‘how long did you spend reading the documents?’.
CVS8
Similarly, the issues described are often less of a systemic nature and seemingly more down to local instances of what could be considered to be poor practice, or the sense that quite simply poor – and ultimately counterproductive – decisions are being made: ‘cutting their nose off to spite their face because of contracts based on price, for which they have then got a worse service than they would have done for not much extra money’. As has been noted in previous research on commissioning,123 these issues are often of a longer-term nature, for instance when grants pre-date the advent of more contemporary commissioning processes:
I’m not so sure whether sometimes there’s been value for money in the way that some of the money is being spent. I think now they’re paying the price and, unfortunately, it’s the likes of us and other organisations who’ve got contracts with them that are now being reviewed because they’ve got to somehow make the savings, which is very frustrating.
DVS2
It is important to note that additional funding for the development of crisis support has been made available and, as a result, there has been rapid growth in the VS in respect of crisis support. In mapping VS provision across England, we have identified a whole raft of new services being developed, particularly safe spaces. It was not uncommon for these to be funded for a short period (e.g. 6 months) to establish the need, before they were then commissioned for a longer period.
Navigating complexity: failure to divert funding towards prevention and to co-ordinate services across different service fields
Both public sector and VSO respondents expressed considerable frustration about the seeming inability of public sector commissioners to ‘bend’ resources towards preventative services, which is argued to be an area in which VSOs excel in providing services and in which it is understood that there would be system-wide benefits resulting from an expansion in services:
Continuing to build on that conversation between the trust and NHS and voluntary and community sector . . . and working with the likes of the CCG to get them to put some money where their mouth is because everyone says prevention is massively important but, when push comes to shove in a financially constrained world, the money for the prevention gets used up by the delivery of the actual crisis service.
AVS1
Next, there seem to be very specific issues that affect specialist services, which, in many cases, overlap with or have an impact on crisis services and thus the quality of crisis pathways. For instance, in site D, we considered specialist sexual and domestic violence services. After describing the complex funding arrangements that the VSO had in place, including a mix of central and local public sector contracts, Lottery funding and long-running grants, the respondents felt strongly that the nature of the service was not always well understood by commissioners:
For me, I think it’s a massive issue, the fact that the CCG, apart from the IAPT service, don’t seem to recognise the value and the impact that [type 4 VSO] has on the survivors of sexual violence. So [type 4 VSO] having to go searching for funding everywhere that you can find it, when really I think there should be a CCG commitment to support the specialist sexual violence services.
DVS5
Furthermore, like in other areas, the argument here is that ‘generic’ IAPT services, on the ground, are not specialist enough to understand the particular needs of victims of sexual violence – some of whom experience a MH crisis – who therefore risk not having their needs met. There is a strong sense that CCGs do not adequately recognise the role of specialist VSOs – whether through financial stringency or lack of knowledge – and that includes the range of local VS domestic violence organisations. So neither the specialist issue(s) nor the role of the VS in addressing or tackling it is recognised:
I don’t think necessarily the commissioners have a good idea of the needs of sexual abuse within that bigger broader picture of domestic abuse. I think they’re probably getting the outcomes and the outputs, but they’re not distinguishing well what were the needs, so how many of those clients did you counsel for domestic abuse, or how many were childhood. I don’t think they’re getting that level of detail. I think, to them, as long as they’ve got that service in place, they’ve got somewhere they can signpost people.
DVS5
A further factor in site D is that IAPT services were being recommissioned as a single service across a wider geographical area, so there was uncertainty about what future services will look like. The point was echoed by national stakeholders, with one participant reporting that their domestic violence/rape services received no CCG funding and relied on multiple funding sources to survive, in a context of increasing waiting lists. However, it is important to note that this issue of whether or not commissioning agencies sufficiently recognise and value ‘specialisms’ varies between sites. For instance, in site B, where there appears to be a recognition of some but not all specialist services, respondents spoke highly of commissioned drug and alcohol services. They also supported the BAME-specific services provided, which even extended to BAME-specific domestic violence services, but conversely services for the LGBTQ community were said to be ‘non-existent’ and public sector services had nowhere to signpost or refer people to who were experiencing a crisis related to their sexuality/gender identity.
Commissioner–voluntary sector organisation relationships: towards better integrated and ‘collaborative’ commissioning
A deeper issue underlying the themes outlined earlier is the sense that commissioners and VSOs can view each other with a mixture of incomprehension and a lack of trust – the relationship is quite fraught – and this clearly bodes ill in terms of improving the quality of commissioned services, service outcomes and integration between public sector and VSO-provided services. A central issue is a fundamental mismatch between the understandings of the sector held by commissioners and VSOs:
Integration I think between the [place of safety] and, you know, it’s the same old chestnut, between the [place of safety] and [the NHS helpline], which is provided by our mental health trust, it’s just an ongoing battle for people to work together and for public sector service not to see third sector as inferior and a little bit vice versa. [The] third sector sort of think ‘oh well they don’t care about us’.
ACCG2
These issues are clearly interlinked: VSOs often feel that commissioners do not understand the complexity of the issues in the front-line day-to-day service arena, but more problematic is the fact that they also do not understand the distinctive and potentially unique offer of local VSOs. In addition, the behaviour and decisions of individual commissioners or teams cannot be entirely disentangled from more structural constraints on commissioning, particularly the trend discussed earlier towards competitive tendering and upscaling of contracts:
I think that what’s happened in the system is that the VS’s contribution isn’t necessarily appreciated . . . Commissioners tend to focus their energies on the big contracts and when you’re talking about the voluntary sector, you’re talking about small amounts of money; they don’t actually invest in them to the degree that they should invest in them, considering that they’ve got the potential to take up quite a lot of slack at quite a lot less cost than these big institutions have.
S2
What VSOs are often calling for from commissioners is a recognition that VSOs can be professional, when required, but also operate in ways that are different from public sector organisations, and that includes combining mission, ethos and the very varied approaches described in Chapter 5. VSOs require commissioners to recognise this distinctive offer while commissioning in ways that are appropriate and proportional, that do not ‘kill the golden goose’, and that allow the VS to operate in ways that are complementary to, rather than competing with, the public sector. There was some sympathy for the constraints that commissioners face:
I think it’s such an awful place to be at the moment, commissioning. I mean, I’ve had very extreme experiences of commissioning. I’ve had really supportive commissioners that are so apologetic for what they’re putting you through because the process is awful.
S18
Key recommendations to improve commissioning included more resources on a longer-term basis; more integrated commissioning and, consequently, joined up services; greater recognition of what the VS offers and how it’s role in commissioned services can be sustained (rather than gradually run down); and, finally, greater involvement of potential beneficiaries (i.e. service users and carers), the VS and communities (including specialist health disorder and protected characteristic communities) in the commissioning cycle.
Summary
As this chapter has shown, it is widely recognised that commissioners are operating in a particularly difficult contemporary context – and some sympathy with them was expressed – given continued public sector austerity and the constraints that the commissioning process places on individual commissioners. Participants recognised the centrality of commissioning in regulating and delivering funding and the sense was that it must be improved, with genuine co-commissioning with people with relevant experience. However, a bigger challenge comes from some of the participants who suggested that the commissioning approach is fundamentally flawed, in particular that commissioning is actively inhibiting or damaging the quality of services delivered in the VS, by adopting a business model.
Chapter 9 Discussion
In this chapter, we synthesise and explore the findings presented in the previous chapters to distil the contribution of the VS to MH crisis care. We start by considering the experience of a MH crisis and the meaning it has for people with direct lived experience, both service users and carers. This establishes a reference point for considering the contribution of the VS and the wider crisis system that represent particular meanings of crisis. Finally, we discuss the limitations and contribution of our research.
A mental health crisis as biographical disruption
From the accounts of people who have experienced a MH crisis, it is clear that this is rarely experienced as a one-off event. The theoretical origins of crisis started with Lindeman and the Coconut Grove Fire. 124 This approach relates to an identifiable catastrophic event in people’s lives (e.g. floods, fires, redundancy and loss), but is not necessarily appropriate for people experiencing MH problems, when an individual’s context sets the stage for the MH crisis. 65 Our findings indicate that a MH crisis has meaning in the context of an individual’s life and is a process, often unfolding over time. Indeed, some service users viewed their lives as an ongoing crisis, often accompanied by profound existential doubts, reflecting the findings of Gudde et al. 67 and Gullslett et al. 69
This conception of a MH crisis as a process resonates with the concept of biographical disruption that has emerged from sociological approaches to illness. 125 Drawing on Giddens’ description of a ‘critical situation’ as ‘a disruption of taken-for-granted assumptions and behaviours’,126 Bury125 locates the experience of a chronic illness in an individual’s biography. This is not to imply that a MH crisis heralds long-standing difficulties; instead, the elements identified by Bury as characterising a ‘biographical disruption’ are relevant here: a recognition of pain and suffering and a possible awareness of death; disruption to everyday life and the forms of knowledge that underpin them; and affecting social relationships, potentially disrupting reciprocity and mutual support. 125 We identified four important elements of the crisis experience: the intensity of the distress, including suicidal feelings and self-harm; the meaning of that experience; the availability and use of support, both social and service support; and the personal and social context of the experience. Locating these elements in a biographical frame strongly supports the contention that a MH crisis is a uniquely personal experience1 and that self-definition is critical, as promoted by many of our participants. It potentially goes further, as argued by Williams (p. 62),127 in providing a bridge between the ‘personal troubles of illness and broader public issues of social structure’,125,127,128 which in the case of MH include stigma and discrimination.
Recasting a MH crisis as a ‘biographical disruption’ crisis contrasts with a narrow biomedical discourse, which has driven policy and practice developments until more recently. Such a discourse has far-reaching implications and risks not only decontextualising experience, but also rendering it unknowable. The struggle by participants to define a MH crisis hints at an ambivalence and, in some instances, rejection of such a narrow understanding of the crisis experience. Nonetheless, a MH crisis as an episode requiring an urgent and emergency response currently underpins the development of the MH crisis system. Our data, therefore, support advocacy of a crisis response that takes a broad view of MH and distress, is person centred, and is responsive to individual needs and wishes (see, for example, the CCC3 and MHA review recommendations26).
The distinctive value of the voluntary sector
Many of the participants in our study had complex difficulties across the MH spectrum, from psychotic symptoms to depression, anxiety and substance use, with several identifying as having a personality disorder. Many reported strong suicidal feelings and a smaller number self-harmed on a regular basis, with one person killing themselves during the course of the study. Although there was no formal assessment of need or diagnosis, our sense was that the participants had significant levels of need that were not being addressed by MH services, which had, in some instances, led them to seek support from a VSO.
It is clear that the VSO offer is distinctive and potentially unique. It is characterised by its relational qualities and attributes, including kindness, the capacity to listen and compassion. This is combined with the blurring of the boundary between service users, peers and staff to facilitate responsiveness to need and community engagement. This emphasis on relationships is typical of a socially oriented approach that contextualises the MH crisis. It is distinct from the approach found in the public sector, which individualises MH problems and pays scant attention to the factors that have contributed to the crisis or to strengthening social networks. Being accepted ‘for the person I am’ and creating the space and time to work through the issues and challenges raised by a MH crisis means that the VS contribution is widely valued. The capacity to engage, particularly with people who have lost faith in public sector provision, is important, particularly in the context of the use of the MHA and the suicide rates for people who missed their last appointment with MH services. 29 Both the commissioning and the organisation of the specific VS contribution were identified as important influences on the ethos and approach, with the suggestion that the value of this could be compromised by greater alignment with a more commercial model.
Framing a MH crisis as a biographical disruption provides a theoretical basis for explaining why the VS contribution is valued; it locates the crisis experience in a social and biographical context, creating the conditions for people to hold uncertainty and explore the meaning of the experience. Indeed, Bury125 argues that a fundamental feature of a biographical disruption is that it entails a fundamental rethinking of the person’s biography and self-concept, as well as decisions about seeking help and mobilising resources. Williams, building on Bury’s theoretical contribution, identifies ‘narrative’ reconstruction128 as a core task in making sense of the illness experience, in this case a MH crisis, and the changing relationship between the self and the social world. This resonates with theoretical constructions of a MH crisis as ‘a turning point’ with opportunities for narrative reconstruction, which may or may not be facilitated by engagement with MH support.
Indeed, the people we spoke to were not passive bystanders in their experience, but were actively searching for meaning and support in an intense and potentially overwhelming experience. We have illustrated how people will actively seek out different sources of support, through the VS and the NHS, if they feel they are not getting the support they need. Appreciating the agency of people in a MH crisis is a clear feature of the VS. This includes agency in relation to suicide, which was valued by participants and contrasted with their perceptions of the risk-averse nature of public sector MH services. The conception of agency was, however, nuanced, with a recognition that, for some people, agency is constrained and that extra efforts are needed to engage with and support them. Another dimension of the VS contribution, consistent with Bury’s exposition of a biographical disruption,125 is that it provides opportunities for social connection and leads to the possibility for mutuality, reciprocity and solidarity through the provision of peer support and/or user-led services.
The contribution of the voluntary sector to crisis care
Given the nature of the crisis experience, the service response is critical. We found that VS support was generally highly valued, regardless of the outcome. This is consistent with other studies that have identified respectful, flexible and consistent support with people in crisis at the centre of decision-making is highly valued. 129 Our findings illustrate the breadth and depth of the VS contribution to supporting people in a MH crisis. There is a wide range of activity, from ULOs to large charities, such as St Andrews Healthcare, which employs 4500 staff and provides services in a similar manner to the NHS.
The VS offers not only a distinctive approach but also a wide range of support across the five types of VSOs that we have distinguished. They appear better equipped than public sector services to support particular groups of people and we identified three groups for whom this may be the case: (1) people, predominantly women, who identified as having a personality disorder or complex post-traumatic stress disorder (Dial House in Leeds130 is recognised for its expertise in working with trauma, which is generally lacking in public sector services);131 (2) groups that are reluctant or fearful of engagement with public sector services, notably people from BAME communities and specifically from African Caribbean communities (the African Caribbean Community Initiative provides an example of culturally appropriate support, underpinned by an African ethic of care);132 and (3) people from specific communities or who have experienced a life event for whom a wide range of skills, knowledge and expertise are required to provide support, for example victims of domestic abuse (e.g. the support provided by Women’s Aid133) and asylum seekers and refugees (e.g. Freedom from Torture134). The unifying themes across these different types of organisations is the importance of peer support and the relatively flat hierarchies, with role boundaries blurred. Indeed, some of the VSOs avoided the term ‘service user’, preferring visitor, volunteer or peer, conveying a sense of communal effort.
Despite this, the contribution of VSOs is often narrowly understood in policy and by the public sector, and in relation to crisis care it is limited to those VSOs that we have characterised as type 1 (crisis specific) or type 2 VSOs (general MH), which make an important contribution to other aspects of the crisis journey, namely prevention and recovery. Types 3 (population specific) and 4 (life event focused) provide specialist support, peer support and engagement with communities that are, often inaccurately, described as ‘hard to reach’ and this type of support is generally not available in the NHS. The skills and capacity evident in these types of VSOs challenge stereotyped assumptions of the VS as ‘a poor relation’. Furthermore, constraining the public sector focus to types 1 and 2 VSOs in crisis support risks increasing inequalities by skewing the funding towards these VSOs at the expense of VSOs serving marginalised and/or racialised communities.
The ability of the VSOs to respond to needs will reflect the legacy of specific VS activity, current capacity and specialist skills. Indeed, we have identified variation in the availability of VS support, not only on the urban–rural axis, but also in terms of particular groups, whose needs are not being well met by the public sector and may also be missing out on VS provision. This demands that greater attention be paid to population diversity, the experience, manifestation and interpretation of distress, and help-seeking preferences. Although, it is argued that the VS has a comparative advantage37 in engaging and responding to the needs of otherwise marginalised groups, there is some evidence from our study that the development of mainstream VS provision crisis care may not be particularly accessible or attractive for particular groups. This requires further investigation and needs to consider ‘under the radar’ organisations34 that are not being commissioned, as well as other forms of VSOs: social enterprises and community interest companies, for instance. Indeed, the quality of commissioning was identified as having a significant impact on the VS provision of crisis support. A better understanding of how population diversity can drive the commissioning of crisis support (both VS and public sector) and wider MH services is needed.
The sustainability of the VS has long been an issue and the rapid expansion of the VS provision of MH crisis care needs to be underpinned by realistic expectations and to support sustainability, as well as potentially innovation and growth. A factor that is relevant to sustainability that emerged partly from the data but also from our experience of undertaking the research was the ‘emotional labour’ of supporting people in a crisis. Recently popularised, the concept of ‘emotional labour’ was originally described by James135 as ‘the labour involved in dealing with other peoples’ feelings, a core component of which is the regulation of emotions’. The intensity of the experiences that participants described to us was troubling. Maintaining the VS’s collaborative advantage (i.e. the capacity to provide a consistent, kind and non-judgemental flexible response) demands that the well-being of staff and volunteers is a priority. This means ensuring that adequate arrangements for support and supervision are in place, which need to be factored into bids and properly recognised by commissioners. The negative evaluations of NHS services, in particular the behaviour and dismissive attitudes of some staff, suggest that this needs to be a priority for these services too.
The voluntary sector as a key element of a crisis care system
Although it focused on the VS contribution, our study has identified that this is contingent on the organisation of the rest of the crisis system. The framing of a MH crisis as an episode emerged as problematic because it compromises ongoing support and the opportunity to develop strategies for preventing crises in the future by addressing the underlying issues, such as trauma, and strengthening social resources. A limited reliance on an urgent and emergency response means that re-presentation, particularly through A&E and section 136 of the MHA, is probably inevitable, costly and an indicator of an ineffective system. 136 Our findings reinforce the systemic problems previously identified by the Audit Commission,15 Mind,1 the CQC4 and Crisp et al. 16 among others. They are a source of frustration for people in crisis, their families/carers and the relevant staff, and are not a good use of resources, personal or public. Indeed, comparing our data with the domains from the CCC (see Box 1), it is clear that there are unmet needs and substantial gaps in support to address underlying difficulties, early intervention and recovery to stay well. Although the VS does contribute here – ‘plugging the gap’ – it was also evident that there was ‘a cliff edge’ for some participants, notably those people with persistent suicidal feelings or self-harm. This was exacerbated by thresholds for access to support for CRHTs, suggesting that the emphasis on fidelity to the model137 should be examined further in the context of a systemic crisis response. Lengthy waiting lists for therapy and a restricted number of sessions also raise questions about the capacity of both the VS and the NHS to respond. The framing of a crisis as an episode underpinning system design also meant that people were often signposted or referred from one service to another without a sense of a journey or a thoughtful pathway for them, and we have provided illustrations of this.
The wider context for these systemic difficulties, including austerity, welfare benefit reform, racism, violence and abuse, were identified by participants. The relationship between inequalities, socioeconomic deprivation and poor MH is inescapable,138–140 with an association between social adversity and suicide. Indeed, our SRG observed that there needs to be a fundamental shift in thinking from seeing services as ‘a safety net’ – albeit one that has an increasing number of holes leading to increased need – to creating firm and stable ‘building blocks’ (e.g. employment and housing). This resonated with the location of a MH crisis in the life course and supports the argument for a robust preventative approach, as others have called for. 138,141,142
The system redesign in one of our sites showed promise, particularly because this redesign went hand in hand with investment in primary care MH and investment in the VS to provide recovery and social support, as well as a type 1 VSO. Nonetheless, there were still issues to address for people who were presenting in crisis. The rationale for gatekeeping access to type 1 VSOs is that people with a diagnosable mental illness and higher levels of risk will be triaged and referred to a CRHT or an equivalent. However, the definitions of need and risk require some examination, as a significant proportion of people who kill themselves have been thought to need less intensive service support after the acute episode has subsided, although many of their risk factors may be unchanged. 143 This raises questions about access to VSOs and the extent to which they should be gatekept via the NHS. Service users value open access and self-referral, and it is likely that some people will be disadvantaged in the moves to make access to crisis support easier if a single point of access is introduced.
Addressing inequalities is a focus for some VSOs and they make a contribution to supporting people in a crisis that needs to be better recognised. Those VSOs that are crisis specific have generally not been designed with equalities in mind. We have, therefore, identified clear inequalities in access along a number of dimensions: (1) the urban–rural axis, (2) ethnicity, (3) substance use, (4) age (both younger and older people) and (5) people with a learning disability and/or diagnosis of autistic spectrum disorder, as well as a lack of support for carers. The proposed transformation of community and crisis services, and the MHA review’s promotion of alternatives to detention and interventions to prevent crisis or the escalation of crisis provides the opportunity to address these inequalities, through investment and collaboration with VSOs that are designed to respond to the needs of these groups.
The shifting shape of the voluntary–public sector relationship
The extent to which the VS works closely and collaboratively with public sector services varies considerably and reflects a complex set of factors including specific organisations’ strategic objectives, ethos and mission, and, crucially, their funding mix. For instance, an organisation that receives little or no public funding has a strong emphasis in its mission on campaigning and/or advocacy, or has governance features such as service-user leadership, and may have good reasons for holding the public sector at ‘arm’s length’. At the other end of the spectrum, some receive a high proportion of their income from the public sector and see it as important to deliver crisis services in partnership with the public sector and to contribute to system integration, innovation and improvement. Nevertheless, our data indicate that it is important to recognise the diversity of views on offer. For some, in advocating for a more coherent and ‘seamless’ crisis system that involves a diversity of providers, there is a risk that the pluralistic nature of the VS will be diluted in a move towards more ‘providers’ under the control of public funders. Allied with this is the fear that a move towards integration risks the creeping control of the more bureaucratic and risk-averse NHS extending into the ‘independent’ VS, reflecting long-standing fears in the academic VS literature. 43,48 Indeed, we identified that, through commissioning, the public sector was influencing the VS methods of operation, potentially compromising VSOs’ values and ethos. An example of this was VSOs shifting from open access to thresholds or waiting times for access or limiting the time that people in crisis were allocated.
Gadja’s144 continuum of integration provides a framework for both understanding this diversity of perspectives within the VS and assessing the strength of partnerships, and is potentially useful in exploring the shifts in the VS–public sector relationship. As illustrated in Figure 14, the degree of integration ranges from co-operation to co-adunation (i.e. a single structure combining the VS and the public sector). Building on this, Figure 15 provides a heuristic to illustrate the VS contribution along the elements of a crisis response, identified by the CCC, and the extent of integration between the different types of the VS and the public sector. In mapping the different VSOs, we noted the emergence of hybrid models of crisis services (usually safe spaces) being introduced by NHS trusts in partnership with a VSO, which are close to the definition of collaboration in Gadja’s model. It was also evident that NHS trusts can develop successful alternatives to inpatient admission, as has been the case with the Drayton Park Crisis House for women in Islington. 145
FIGURE 15.
Typology for the relationship with public sector services.

The growing evidence base for alternatives to inpatient admission emphasise the importance of collaboration between crisis house staff and other MH services. 146 In our examination of the VS’s role, we note in particular that such successful examples rest on a recognition of the distinctive contribution of the VS to the collaboration, and a determination that these contributions are not stifled. In particular, as Chapter 8 makes clear, commissioners need to be adept at understanding the VS and recognising and actively supporting the VS contribution (most obviously financially, but also in terms of requirements and appropriate monitoring). From other research, in cases in which this has worked particularly well there is a ‘mutual dependence’ between the public sector and the VS in the delivery of a service (or set of services), and their associated outcomes. 49 Concern was voiced that the radical critique that some VSOs offer in advocating for their client group would also be compromised, thus representing a loss to the crisis system as a whole, was reflected in the observation that ‘the VS now needs a VS’. Thus, there are tensions that need to be recognised and worked through by the VS and the public sector in a way that is respectful of and safeguards the distinctive and diverse contributions of the VS. Potential issues that need to be addressed include developing satisfactory governance arrangements, good commissioning models, such as alliance contracting, and arrangements for information sharing and risk management.
Limitations/reflexive account
Sampling and recruitment
Providing a profile of the field for people experiencing MH crises may be a flawed endeavour, and we ran the risk of aggregating together the experience of a heterogeneous range of VSOs. Furthermore, identifying charities that operate in a specialist field of activity is challenging, which we sought to overcome by using a range of methods, including database analysis, stakeholder interviews and a national survey. The survey response rate was low and, in part, this reflected our approach, which was to be as inclusive as possible and encompass the widest possible range of MH charities that might be involved in crisis care. However, a disadvantage of this approach was that it was likely that we included organisations that considered themselves outside the scope and, therefore, did not respond. Nonetheless, the response rate is broadly comparable with other studies of the VS, which tends to have limited capacity to respond. 147 Alternative methods, such as telephone interviewing, might have increased the response rate, but would have been resource intensive. As an exhaustive national mapping exercise was beyond the scope of this project, the response rate was judged to be ‘good enough’ to build on in the later data collection exercise, through regional mapping and local case studies, to identify the broad range of services that are available.
One of the difficulties in undertaking this study was the informality of some VSOs, which is precisely what makes them distinctive and attractive to services users. It did mean, however, that in some of the study sites, the VSOs did not keep contact details for service users and it initially proved difficult to recruit participants meeting our inclusion criteria through this route. Thus, service user participants for the narrative interviews were also recruited by the NHS (requiring an amendment to the protocol). Recruitment via the NHS may have had an impact on the study in two ways. First, the level of acuity of these participants may have been higher than a sample recruited via VSOs. Second, participants, both service users and carers, sometimes did not distinguish the service provider (i.e. a public sector service or a VSO), particularly if they had limited experience of services. On the other hand, some participants had been triaged by MH staff and thus may represent a sample of people who do not have a conventional diagnosis of mental illness, but did include a significant number of people with suicidal ideation and impulses.
Carer recruitment for interviews was particularly difficult and many service users were unable to identify a relevant family member or did not want them to be approached. In a small number of instances, an invitation was sent to the carer but no response was received (n = 3). We were more successful in recruiting unrelated carers to focus groups. The difficulties in carer recruitment in MH services have been noted elsewhere and, as Ridley and Hunter148 observed, these are likely to reflect the complex and sensitive nature of the relationships involved and the hidden role of carers.
The accounts of the NHS response were highly critical and those of the VS were generally positive. Despite purposive sampling, participants may have been motivated to take part because of a particularly negative or positive experience, including NHS care failing to meet their needs. However, our findings in his regard are consistent with those of the CQC4 and Crisp et al. 16 on acute inpatient care. The limited focus on the relationship between the VS and primary care, which was identified as an important element of the crisis system, was relatively unexplored in our study.
Study methods
We had proposed to compare the four case study sites through capturing local views on the adequacy and quality of the service through a key informant questionnaire that differentiated different elements of the local crisis system (see Appendix 16). The response to this was poor, despite being promoted via the Clinical Research Networks in the sites. We suspect that this reflected a lack of a well-designed crisis system and the only site where we had a reasonable response was site A, in which efforts have been made to redesign the system. We have therefore not included these findings, as they were too patchy to be useful. Nonetheless, the questionnaire, which we adapted from Morrissey et al.,47 may have some utility in facilitating systems thinking, as it outlines elements of a MH crisis system and could be used to ascertain the adequacy and quality of local provision (as summarised in Appendix 16). 149
Critical perspective on patient and public involvement
As noted earlier, the independent evaluation of service user and carer involvement in the study (see Supplementary Material 4) commended the approach and breadth of involvement. Nonetheless, a number of areas were identified in which this could be strengthened. These included:
-
an explicit discussion about the principles of involvement as a useful starting point in team building
-
greater clarity about the roles and expectations, balanced against the requirement for flexibility and adaptation to emerging findings and learning during the research process
-
greater recognition of the administration role in supporting people with lived experience with the practical aspects of involvement.
Importantly, the evaluation commented on the emotional labour involved given the focus of the study. Guidance for academic researchers in supporting co-researchers and clarity about arrangements for people to take time off from the project were recommended. The evaluation also raised interesting questions about the nature of leadership, which was understood as an inverted model of leadership, with the chief investigator role providing sufficient resources, communication and boundaries to enable others to take on the work. Finally, the scope to strengthen this to enable greater co-production with the ultimate aim of work led by service users and carers was highlighted.
Contribution
Our study gathered rich data on the crisis experience and response. It documents, and provides evidence for, perspectives and perceptions of the VS in MH services that, although well established, have not been documented and evidenced fully. A key contribution of this study is to address this knowledge gap to address the questions of what is being provided by the VS to those experiencing a MH crisis, where it is being provided and to whom. We have developed a number of resources that will provide the basis for further research and practice development, namely (1) a database of organisations that potentially provide support to people in a MH crisis, (2) a typology for identifying the diversity of VSOs supporting people in a MH crisis, (3) a map of the current provision of formal crisis services and (4) our original mapping of individual service user journeys, which illustrates not only how the VS complements and addresses gaps in provision but also the exercise of service user agency. Finally, we have made a theoretical contribution to the conceptualisation of a MH crisis, finding evidence for a shift from a narrow biomedical framing of a crisis as an urgent event to a more contextual understanding that locates the crisis experience in a personal and social context, as a ‘biographical disruption’.
Chapter 10 Conclusion and implications
Summary
Our study has explored the value of VSOs in supporting people in a crisis and has identified the wide range of activities that not only provide an immediate response but also contribute to prevention and recovery. It has shown the VS to be attractive and acceptable to people in a crisis, that the VS has social value and that the VS can potentially address the complex interactions between MH, inequality and socioeconomic conditions. There is also evidence that the VS can provide a cost-effective alternative to public sector provision, particularly inpatient care. However, the understanding and awareness of the VS contribution is not fully realised and the VS can be viewed as ‘a bit player’ in the provision of crisis care.
Although our study focused on the contribution of the VS to MH crisis care, it has thrown the adequacy and quality of crisis care into sharp relief. In doing so, it has identified significant gaps, with crisis provision often a patchwork of services rather than a pathway or coherent system. The need to address this is recognised by the NHS LTP, which proposes the expansion of community crisis services to be accessed via NHS 111 and additional resourcing to enable a 24/7 community-based MH crisis response offering intensive home treatment and alternatives to acute inpatient admission. Recognition of the VS contribution and the routine involvement of the VS in NHS care pathways could help to translate this aspiration into reality. Indeed, the NHS LTP could potentially use the VS as a fulcrum for localised community support, as opposed to complementing or providing an alternative to public sector provision. At a strategic level, this suggests that increasing investment for community and crisis services, identified in the LTP, could be effectively deployed to increase investment and expand VS provision in MH crisis care.
To conclude, our study was a descriptive study and, thus, it provides a platform for further research to contribute to addressing the identified gaps in MH crisis research. 8 The VS provision for children and young people, older adults and specific communities, particularly BAME communities, as well as people who use substances, requires further investigation. The expansion of VSOs in MH crisis care provides a good opportunity to evaluate the different models of VSO provision, including the degree of integration with the public sector, and their outcomes – short- and long-term – including the cost-effectiveness and impact on advancing equalities. Finally, ethnographic studies would enhance our understanding of people’s crisis journeys and the role of VS and public sector service support in promoting the capacity of individuals, families and their social networks to respond to the range of MH crises.
Implications
From our findings, we identified the following implications, taking account of the CCC’s commitment to an inclusive definition of a MH crisis and the NHS LTP commitment to increasing alternative forms of provision for those in a crisis: Department of Health and Social Care, NHS England, Public Health England, Sustainability and Transformation Partnerships/Integrated Care systems/commissioners, local NHS mental health and local authority providers, and their partners.
Effective commissioning
-
NHS England should ensure that the transformation in MH crisis services includes the expertise of the VS and that transformation resources are directed at both statutory and VS services. This would be helped by developing a needs-led understanding of a MH crisis, which should specify how the NHS and local authorities can collaborate effectively with the breadth of VSOs.
-
Public Health England should offer local authorities support to ensure that there is a rigorous and robust understanding of the local demography and the diversity of the population to underpin the development of crisis support. This must pay specific attention to the gaps in support and to the needs of those people who are experiencing a crisis because appropriate services are not available (i.e. for BAME communities, people who also use substances and homeless people). This will be evidenced by local commissioning plans. Public Health England could support this by benchmarking, sharing information and relevant research, including good practice in addressing inequalities.
-
The Department of Health and Social Care and NHS England must ensure that all public sector organisations, not just those that are clearly identified as providing support in a crisis, have a better recognition of what the VS offers. The typology from our study should be formally adopted by the Department of Health and Social Care when the CCC action plan is updated and aligned with the NHS LTP.
-
CCG and local authority commissioners should ensure people, service users, and carers and families with personal experiences of a MH crisis across the protected characteristics are engaged and supported in being involved in commissioning and co-producing the crisis care system. This includes information and training on how commissioning works to enable participation on an equal basis.
-
CCG and local authority commissioners should ensure that the VS and communities are involved in the commissioning cycle in a safe and fair manner. This needs to go hand-in-hand with simplifying the commissioning process to encourage local groups that are disadvantaged by the current arrangements.
-
NHS England should ensure that there is sustainable funding in VS crisis care provision, including in ULOs. This includes organisations and grassroots organisations with local knowledge and engagement with people in, or at risk of, a crisis, who may not be using mainstream VS or public sector provision (e.g. BAME or LGBTQ organisations). The funding allocation should include funding to support staff, as well as volunteer training and supervision.
Improving access to voluntary sector crisis support
-
NHS England should develop and promote an interactive map of VS crisis provision to be made available nationally 24/7 to anyone who needs it. The map should be linked to information about the support available locally and nationally. It must be kept up to date, via commissioning contracts, and be linked to the NHS website. It will provide information on what these VSOs provide, how they could help if you are experiencing a crisis, how you can access them and when they are available.
-
Local systems should ensure that access arrangements are co-ordinated that include a single point of access to appropriately trained staff via NHS 111, and that recognise that some people will choose alternatives to NHS provision.
-
NHS England should ensure that every locality in England provides 24/7 access to non-clinical alternatives to mainstream inpatient provision, which is appropriate to meet the diverse needs of the local population. This includes crisis houses, peer support, safe spaces and walk-in services, including those provided by ULOs and community organisations.
-
Information needs to be readily available to service users, carers and their families so they know that they can ask for an advocate, peer support or someone they trust if they feel unable to explain their situation and make their wishes known.
-
NHS, local authority and VS providers need to make information available so that service users (and carers and their families if appropriate) know that they should be involved in co-producing a crisis plan that sets out what support is available in the event of a further crisis, and how they can access support to enable them to address the contributory factors.
Improving the collaboration between voluntary sector organisations and public sector services
-
Local systems should have arrangements in place across the range of support to avoid crisis and help people stay well. This should involve developing protocols to provide individuals with a follow-up session after a crisis episode, and an appropriate service response by public sector services and VSOs for people who experience crises repeatedly to support long-term management and engagement with the VS.
-
Commissioners and NHS providers need to review the thresholds for different services, hand-offs and the barriers to accessing support in a smooth way between different services (including in the NHS and VSOs) and to reduce the waiting times for support to address the contributory factors for the crisis episode.
-
The arrangements for information-sharing between VSOs and public sector services needs to be clarified, taking account of relevant guidance150 and recognising that, for some VSOs, this will not be appropriate.
-
Local authorities and NHS England should review and develop housing provision to support people with ongoing MH difficulties to access housing and avoid evictions. Action on housing should be included in the updated CCC.
-
Local authorities should ensure access to advocacy or peer support for people experiencing a crisis who find it difficult to express their views on support and treatment preferences, as proposed by the MHA review.
-
NHS providers should ensure that every person has a co-produced crisis plan, which includes the action(s) to take in the event of a future crisis, and includes the role of the VS, as appropriate.
Voluntary sector providers
-
Voluntary sector providers should actively contribute, promote and update information on the services relevant to crisis prevention and crisis support provided by the organisation.
-
Voluntary sector providers should review if their services are helpful and relevant for the local population, and work with commissioners to develop equal access for marginalised groups. This is likely to include investment in upskilling and working in close partnership with specific groups, as well as direct service provision.
-
Voluntary sector providers should review the ethnic diversity of the workforce to ensure that it properly reflects the demographic diversity.
-
Voluntary sector providers should ensure that every person has a co-produced crisis plan, which includes the action(s) to take in the event of a future crisis and risk management.
-
Voluntary sector providers should develop methods for working with carers and family members so that they are well informed and able to support the person in a crisis, as appropriate.
-
Voluntary sector providers should ensure there is good-quality training, supervision and support so that staff well-being is protected, and should recognise the impact of traumatic events and support people experiencing a MH crisis.
Research and academic community
-
Research should be conducted on the organisation and operation of whole systems of crisis care, encompassing both VSO and statutory services.
-
Type 1 (i.e. crisis-specific) VSOs should be investigated to determine how they work, their different organisational arrangements, the populations served, their methods of operation and the outcomes (both MH and social) they are achieving for people in a MH crisis.
-
An evaluation should be undertaken of how the other types of VSOs are responding and contributing to enabling people to avoid a crisis and helping people stay well.
-
The VS and NHS provision should be compared in relation to the provision of crisis houses and safe spaces, including integrated models, and the cost-effectiveness and outcomes from different arrangements.
-
An investigation should be undertaken on how equalities can best be advanced for different population groups, with a focus on models of co-commissioning based on population need and effective models of VSO targeted support.
-
An evaluation should be conducted of different arrangements for PPI in research.
Acknowledgements
The research team is grateful to all those who participated in this study and to the organisations in the case study sites for their support and help with recruiting participants. We would particularly like to thank all those people with direct personal experience of a MH crisis who gave their time freely to share their views and to revisit profoundly challenging periods in their lives. We are indebted to members of the SSG (chaired by Dr Jacqui Dyer, MBE) and the SRG (chaired by Dr Jo Barber) for their insights, encouragement and guidance. We would especially like to thank Rachel Rowan Olive, a MH service user/survivor, illustrator and SRG member for allowing us to include her illustrations (see Figures 2 and 3) about the experience of self-harm in this report. Administrative support was provided by Francesca Tomaselli and we are grateful to her for the day-to-day management of practical aspects of the study. We are also grateful to James Bowles who mapped the distribution of relevant VSOs, Alex Davis who contributed to the study design and to the development of the research tools, and provided expert knowledge on the context for crisis provision. We would also like to acknowledge the invaluable and consistent support from Suresearch.
We commissioned With-You Consultancy to undertake an independent evaluation of PPI and we thank Karen Machin and her team for this. We would like to thank Laura Broderick, graphic and creative facilitator, Think Big Picture, for her illustrations of a final workshop which have been used to illustrate the scientific summary. Finally, we are grateful to NIHR for the funding and would like to thank them and West Midlands Clinical Research Network for their support and helpful advice.
Contributions of authors
Karen Newbigging (https://orcid.org/0000-0001-8764-528X) was the chief investigator for the study and was responsible for co-ordinating the research and providing intellectual oversight. She co-designed the study with Alex Davis, John Mohan and James Rees. Karen was responsible for the ethical conduct of the study and was the lead in the case study element, undertaking fieldwork in three of the four sites. She contributed to coding and synthesis, and led the drafting of the final report.
James Rees (https://orcid.org/0000-0003-0545-782X) contributed to the study design in relation to the VS. He co-ordinated and undertook fieldwork in one of the regional sites in WP2 and in one of the four case study sites. He contributed to coding, synthesis of the findings and the drafting of Chapters 3, 5 and 8 of the report.
Rebecca Ince (https://orcid.org/0000-0002-0725-7912) undertook the literature review and developed the national survey and topic guides for the focus groups and interviews. She analysed the databases and, with Karen Newbigging, developed the typology of VSOs. Rebecca undertook fieldwork in one of the regional sites in WP2 and in two of the four case study sites. She contributed to coding, synthesis of the findings and drafted Chapter 2 of the report.
John Mohan (https://orcid.org/0000-0002-6063-3454) contributed to the study design in relation to literature on the VS. He constructed the database of candidate organisations for the national survey in WP1 and he contributed to relevant sections of the final report.
Doreen Joseph (https://orcid.org/0000-0003-0405-0067) contributed to the development of the research tools and undertook fieldwork in two of the four case study sites. She contributed to coding, synthesis of the findings and drafting of sections for the report.
Michael Ashman (https://orcid.org/0000-0003-4195-0208) contributed to the development of the research tools and undertook fieldwork in three of the four case study sites. He contributed to coding, synthesis of the findings and drafting of sections for the report.
Barbara Norden (https://orcid.org/0000-0002-8455-5702) contributed to the development of the research tools and undertook fieldwork in two of the four case study sites. She contributed to coding, synthesis of the findings and the drafting of the service profiles.
Ceri Dare (https://orcid.org/0000-0002-6762-506X) contributed to the development of the research tools and undertook fieldwork in two of the four case study sites. She contributed to coding and synthesis of the findings.
Suzanne Bourke (https://orcid.org/0000-0002-5581-8622) contributed to the development of the research tools and undertook fieldwork in two of the four case study sites. She contributed to the drafting of the service profiles.
Benjamin Costello (https://orcid.org/0000-0003-4744-5659) undertook fieldwork in one of the case study sites. He contributed to coding, synthesis of the findings and developing the crisis journey diagrams.
Publications
Newbigging K, Mohan J, Rees J, Harlock J, Davis A. Contribution of the voluntary sector to mental health crisis care in England: protocol for a multimethod study. BMJ Open 2017;7:e019238.
Conference presentations
Ince R. Voluntary sector mental health crisis support: a landscape of opportunity, creativity and fragility. Voluntary Sector Studies Network Day Conference, 9 May 2018, York Saint John University, York, UK.
Ince R, Rees J. Towards a typology of third sector engagement and their ‘niche’ in the multi-sectoral ecosystem of mental health crisis support. Social Policy Association Annual Conference, 6 July 2018, University of York, York, UK.
Newbigging K, Ince R. Conceptualising a mental health crisis. Qualitative Research in Mental Health, 20 September 2018, Berlin, Germany.
Newbigging K. The contribution of the voluntary sector to mental health crisis care in England. The European Network for Mental Health Service Evaluation, 6 June 2019, Lisbon, Portugal.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review. However, owing to the sensitivity of the data and the possibility that the location of the participants may be identified, there may be limitations on the data that can be shared.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Mind . Listening to Experience: An Independent Inquiry into Acute and Crisis Mental Healthcare 2011.
- Mental Health Taskforce . Five Year Forward View for Mental Health 2014.
- Department of Health and Social Care (DHSC), Crisis Care Concordat . Mental Health Crisis Care Concordat: Improving Outcomes for People Experiencing Mental Health Crisis 2014.
- Care Quality Commission . Right Here, Right Now: Mental Health Crisis Care Report 2015.
- Rapoport L. The state of crisis: some theoretical considerations. Soc Serv Rev 1962;36:211-17. https://doi.org/10.1086/641243.
- Hobbs M. Crisis intervention in theory and practice: a selective review. Br J Med Psychol 1984;57:23-34. https://doi.org/10.1111/j.2044-8341.1984.tb01577.x.
- Boscarato K, Lee S, Kroschel J, Hollander Y, Brennan A, Warren N. Consumer experience of formal crisis-response services and preferred methods of crisis intervention. Int J Ment Health Nurs 2014;23:287-95. https://doi.org/10.1111/inm.12059.
- Paton F, Wright K, Ayre N, Dare C, Johnson S, Lloyd-Evans B, et al. Improving outcomes for people in mental health crisis: a rapid synthesis of the evidence for available models of care. Health Technol Assess 2016;20. https://doi.org/10.3310/hta20030.
- Bonynge ER, Lee RG, Thurber S. A profile of mental health crisis response in a rural setting. Community Ment Health J 2005;41:675-85. https://doi.org/10.1007/s10597-005-6427-2.
- Bonynge ER, Thurber S. Development of clinical ratings for crisis assessment in community mental health. Brief Treat Crisis Interv 2008;8. https://doi.org/10.1093/brief-treatment/mhn017.
- Thomas P, Longden E. Madness, childhood adversity and narrative psychiatry: caring and the moral imagination. Med Humanit 2013;39:119-25. https://doi.org/10.1136/medhum-2012-010268.
- Department of Health and Social Care . National Service Framework for Mental Health. Modern Standards and Service Models 1999.
- Department of Health and Social Care . The Mental Health Policy Implementation Guide: Crisis Resolution Home Treatment Teams 2001.
- Department of Health and Social Care . New Horizons: Towards a Shared Vision for Mental Health: Consultation 2009.
- National Audit Office . Helping People Through Mental Health Crisis: The Role of Crisis Resolution and Home Treatment Services: Report by the Comptroller and Auditor General 2007.
- Crisp N, Smith G, Nicolson K. Old Problems, New Solutions: Improving Acute Psychiatric Care for Adults in England. London: Royal College of Psychiatrists; 2016.
- Mind . Mental Health Crisis Care: Commissioning Excellence for Black and Minority Ethnic Groups: A Briefing for Clinical Commissioning Groups 2013.
- Department of Health and Social Care . The Mandate – A Mandate from the Government to NHS England: April 2014 to March 2015 2014.
- Department of Health and Social Care . £15 Million Boost for Local Mental Health Crisis Services 2018. www.gov.uk/government/news/15-million-boost-for-local-mental-health-crisis-services (accessed 28 April 2020).
- Home Office . Alternative Places of Safety. The West Sussex Pilot Evaluation 2015 2015.
- Gibson S, Hamilton S, James K. Evaluation of the Crisis Care Concordat Implementation. London: McPin Foundation; 2016.
- NHS England . The NHS Long Term Plan 2019.
- Care Quality Commission . Monitoring the Mental Health Act in 2016 17 2018.
- Department of Health and Social Care (DHSC) . Independent Review of the Mental Health Act 1983: Supporting Documents 2019.
- Bendelow G, Warrington C, Jones A-M. Section 136 in Sussex. Brighton: University of Brighton; 2016.
- Department of Health and Social Care (DHSC) . Modernising the Mental Health Act: Increasing Choice, Reducing Compulsion – Final Report of the Independent Review of the Mental Health Act 1983 2018.
- Department of Health and Social Care (DHSC) . Cross-Government Suicide Prevention Workplan 2019.
- National Institute for Health and Care Excellence . Preventing Suicide in Community and Custodial Settings 2018.
- Appleby L, Kapur N, Shaw J, Hunt I, Ibrahim S, Gianatsi M, et al. The National Confidential Inquiry into Suicide and Homicide by People With Mental Illness. Annual Report: England, Northern Ireland, Scotland and Wales 2017.
- Public Health England . Prevention Concordat Programme for Better Mental Health n.d. www.gov.uk/government/publications/prevention-concordat-for-better-mental-health-consensus-statement/prevention-concordat-for-better-mental-health (accessed 10 March 2020).
- Local Government Association . Stepping up to the Place: The Key to Successful Health and Care Integration 2016.
- Macmillan R. ‘Distinction’ in the third sector. Volunt Sect Rev 2013;4:39-54. https://doi.org/10.1332/204080513X661572.
- Froggett L, Agger A, Damgaard B, Hagedorn Krogh A, Sørensen E. Collaborative Governance and Public Innovation in Northern Europe. Soest: Bentham Science Publishers; 2015.
- Mohan J. Mapping the Big Society: Perspectives from the Third Sector Research Centre 2011.
- Karlsson M, Markström U. Non-profit organizations in mental health: their roles as seen in research. Volunt Int J Volunt Nonprofit Organ 2012;23:287-301. https://doi.org/10.1007/s11266-011-9196-2.
- Dayson C, Wells P. Voluntary and community sector policy under the coalition government. People Place Policy 2013;7:91-9. https://doi.org/10.3351/ppp.0007.0002.0006.
- Billis D, Glennerster H. Human services and the voluntary sector: towards a theory of comparative advantage. J Soc Policy 1998;27:79-98. https://doi.org/10.1017/S0047279497005175.
- Flanagan SM, Hancock B. ‘Reaching the hard to reach’ – lessons learned from the VCS (voluntary and community sector). A qualitative study. BMC Health Serv Res 2010;10. https://doi.org/10.1186/1472-6963-10-92.
- Hatchett V, Pybis J, Tebbet-Duffin U, Rowland N. Provision of mental health interventions in women’s centres: an exploratory study. Couns Psychother Res 2015;15:88-97. https://doi.org/10.1002/capr.12026.
- Taylor HC, Stuttaford MC, Broad B, Vostanis P. Listening to service users: young homeless people’s experiences of a new mental health service. J Child Health Care 2007;11:221-30. https://doi.org/10.1177/1367493507079568.
- Dowrick C, Martin S, Chew-Graham C, Ray MG. Mental Health and Older People: A Guide for Primary Care Practitioners. Basel: Springer; 2016.
- Rees J, Mullins D, Bovaird T. Third Sector Partnerships for Public Service Delivery: An Evidence Review. Birmingham: University of Birmingham, Third Sector Research Centre; 2012.
- Milbourne L, Cushman M. From the third sector to the big society: how changing UK government policies have eroded third sector trust. Int J Volunt Nonprofit Organ 2013;24:485-508. https://doi.org/10.1007/s11266-012-9302-0.
- Benson A. The Devil that has Come Amongst Us. The Impact of Commissioning and Procurement Practices. Brussels: National Coalition for Independent Action; 2014.
- Lipsky M, Smith SR. Nonprofit organizations, government, and the welfare state. Polit Sci 1989;104:625-48. https://doi.org/10.2307/2151102.
- Gray B. Collaborating: Finding Common Ground for Multiparty Problems. San Francisco, CA: Jossey-Bass; 1989.
- Morrissey JP, Calloway M, Bartko WT, Ridgely MS, Goldman HH, Paulson RI. Local mental health authorities and service system change: evidence from the Robert Wood Johnson Foundation Program on Chronic Mental Illness. Milbank Q 1994;72:49-80. https://doi.org/10.2307/3350338.
- Rees J. Public sector commissioning and the third sector: old wine in new bottles?. Public Policy Adm 2014;29:45-63. https://doi.org/10.1177/0952076713510345.
- Miller R, Rees J. Mental health commissioning: master or subject of change?. Ment Health Rev J 2014;19:145-55. https://doi.org/10.1108/MHRJ-04-2014-0013.
- Lowe T. Performance management in the voluntary sector – responding to complexity. Volunt Sect Rev 2017;8:319-31. https://doi.org/10.1332/204080517X15006273841592.
- Lloyds Bank Foundation for England and Wales . Commissioning in Crisis 2016.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349-57. https://doi.org/10.1093/intqhc/mzm042.
- Booth A, Hannes K, Harden A, Noyes J, Harris J, Tong A, et al. Guidelines for Reporting Health Research: A User’s Manual. Hoboken, NJ: Wiley-Blackwell; 2014.
- Staniszewska S, Brett J, Simera I, Seers K, Mockford C, Goodlad S, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. Res Involv Engagem 2017;3. https://doi.org/10.1186/s40900-017-0062-2.
- Larsen J, Griffiths C. Supporting recovery in a third sector alternative to psychiatric hospital admission: evaluation of routinely collected outcome data. J Ment Health Train Educ Pract 2013;8:116-25. https://doi.org/10.1108/JMHTEP-04-2013-0016.
- Butt MF, Walls D, Bhattacharya R. Do patients get better? A review of outcomes from a crisis house and home treatment team partnership. BJPsych Bull 2019;43:106-11. https://doi.org/10.1192/bjb.2018.105.
- Greenfield TK, Stoneking BC, Humphreys K, Sundby E, Bond J. A randomized trial of a mental health consumer-managed alternative to civil commitment for acute psychiatric crisis. Am J Community Psychol 2008;42:135-44. https://doi.org/10.1007/s10464-008-9180-1.
- Hutchinson G, Gilvarry C, Fahy TA. Profile of service users attending a voluntary mental health sector service. Psychiatr Bull 2000;24:251-4. https://doi.org/10.1192/pb.24.7.251.
- Sweeney A, Fahmy S, Nolan F, Morant N, Fox Z, Lloyd-Evans B, et al. The relationship between therapeutic alliance and service user satisfaction in mental health inpatient wards and crisis house alternatives: a cross-sectional study. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0100153.
- Bagley A. Leeds Survivor Led Crisis Service: A Social Return on Investment Analysis – Summary. Leeds: Real-Improvement; 2012.
- Croft B. İsvan N. Impact of the 2nd story peer respite program on use of inpatient and emergency services. Psychiatr Serv 2015;66:632-7. https://doi.org/10.1176/appi.ps.201400266.
- Fenton WS, Hoch JS, Herrell JM, Mosher L, Dixon L. Cost and cost-effectiveness of hospital vs residential crisis care for patients who have serious mental illness. Arch Gen Psychiatry 2002;59:357-64. https://doi.org/10.1001/archpsyc.59.4.357.
- Griffiths A, Gale K. Independent Evaluation of the North East Hampshire and Farnham Vanguard: Aldershot Safe Haven Service. Southampton: Wessex Academic Health Science Network; 2017.
- Gofal Cymru Care Ltd . The Community Crisis House Model: An Evaluation of Wales’ First Crisis House n.d.
- Ball JS, Links PS, Strike C, Boydell KM. ‘It’s overwhelming . . . everything seems to be too much’: a theory of crisis for individuals with severe persistent mental illness. Psychiatr Rehabil J 2005;29:10-7. https://doi.org/10.2975/29.2005.10.17.
- Sells D, Sledge WH, Wieland M, Walden D, Flanagan E, Miller R, et al. Cascading crises, resilience and social support within the onset and development of multiple chronic conditions. Chronic Illn 2009;5:92-102. https://doi.org/10.1177/1742395309104166.
- Gudde CB, Olsø TM, Antonsen DØ, Rø M, Eriksen L, Vatne S. Experiences and preferences of users with major mental disorders regarding helpful care in situations of mental crisis. Scand J Public Health 2013;41:185-90. https://doi.org/10.1177/1403494812472265.
- Albert R, Simpson A. Double deprivation: a phenomenological study into the experience of being a carer during a mental health crisis. J Adv Nurs 2015;71:2753-62. https://doi.org/10.1111/jan.12742.
- Gullslett MK, Kim HS, Andersen AJ, Borg M. ‘Emotional darkness without solutions’: subjective experiences of mental health crisis. Int J Ment Health 2016;45:161-70. https://doi.org/10.1080/00207411.2016.1185875.
- Shaw B, Stapleton V. Reality of Crisis. Nottingham: Becky Shaw; 2010.
- Ashman M, Halliday V, Cunnane JG. Qualitative investigation of the wellness recovery action plan in a UK NHS crisis care setting. Issues Ment Health Nurs 2017;38:570-7. https://doi.org/10.1080/01612840.2017.1300840.
- Healthwatch Norfolk . Using Urgent and Emergency Services at Times of Mental Health Crisis 2017.
- McGrath L, Reavey P. Seeking fluid possibility and solid ground: space and movement in mental health service users’ experiences of ‘crisis’. Soc Sci Med 2015;128:115-25. https://doi.org/10.1016/j.socscimed.2015.01.017.
- Johnson S, Gilburt H, Lloyd-Evans B, Osborn DP, Boardman J, Leese M, et al. In-patient and residential alternatives to standard acute psychiatric wards in England. Br J Psychiatry 2009;194:456-63. https://doi.org/10.1192/bjp.bp.108.051698.
- Howard L, Flach C, Leese M, Byford S, Killaspy H, Cole L, et al. Effectiveness and cost-effectiveness of admissions to women’s crisis houses compared with traditional psychiatric wards: pilot patient-preference randomised controlled trial. Br J Psychiatry Suppl 2010;53:s32-40. https://doi.org/10.1192/bjp.bp.110.081083.
- Morant N, Lloyd-Evans B, Gilburt H, Slade M, Osborn D, Johnson S. Implementing successful residential alternatives to acute in-patient psychiatric services: what can we learn from professional stakeholders’ perspectives?. Psychiatr Prax 2011;38. https://doi.org/10.1055/s-0031-1277831.
- Mosher LR. Soteria and other alternatives to acute psychiatric hospitalization: a personal and professional review. J Nerv Ment Dis 1999;187:142-9. https://doi.org/10.1097/00005053-199903000-00003.
- Esaki N, Benamati J, Yanosy S, Middleton JS, Hopson LM, Hummer VL, et al. The Sanctuary model: theoretical framework. Fam Soc 2013;94:87-95. https://doi.org/10.1606/1044-3894.4287.
- Meddings S, Byrne D, Barnicoat S, Campbell E, Locks L. Co-delivered and co–produced: creating a recovery college in partnership. J Ment Health Train Educ Pract 2014;9:16-25. https://doi.org/10.1108/JMHTEP-04-2013-0011.
- Griffiths CA, Heinkel S, Dock B. Enhancing recovery: transition intervention service for return to the community following exit from an alternative to psychiatric inpatient admission – a residential recovery house. J Ment Health Train Educ Pract 2015;10:39-50. https://doi.org/10.1108/JMHTEP-09-2014-0027.
- Gerson LD, Rose LE. Needs of persons with serious mental illness following discharge from inpatient treatment: patient and family views. Arch Psychiatr Nurs 2012;26:261-71. https://doi.org/10.1016/j.apnu.2012.02.002.
- Gillard S, Gibson SL, Holley J, Lucock M. Developing a change model for peer worker interventions in mental health services: a qualitative research study. Epidemiol Psychiatr Sci 2015;24:435-45. https://doi.org/10.1017/S2045796014000407.
- Rose D, MacDonald D, Wilson A, Crawford M, Barnes M, Omeni E. Service user led organisations in mental health today. J Ment Health 2016;25:254-9. https://doi.org/10.3109/09638237.2016.1139070.
- Beckett J, D’Angelo G, Pattison L, Walker T. Self-harm Evaluation Project: An Evaluation of Services for Individuals Who Repeatedly Self Harm Focusing on A&E and Leeds Survivor Led Crisis Service (Dial House). Leeds: Leeds Survivor Led Crisis Service; 2012.
- Morgan K, Chakkalackal L, Cyhlarova E. Life Lines: Evaluation of Mental Health Helplines. London: Mental Health Foundation; 2012.
- Belling R, Whittock M, McLaren S, Burns T, Catty J, Jones IR, et al. Achieving continuity of care: facilitators and barriers in community mental health teams. Implement Sci 2011;6. https://doi.org/10.1186/1748-5908-6-23.
- Sayer A. Method in Social Science. London: Routledge; 2010.
- Yin RK. Case Study Research and Applications: Design and Methods. London: SAGE Publications Ltd; 2017.
- Social Research Institute . National Survey of Third Sector Organisations, 2008 2010.
- Office for Civil Society . National Survey of Charities and Social Enterprises, 2010 2013.
- Positive Practice . Positive Practice Directory n.d. http://positivepracticemhdirectory.org/ (accessed 20 March 2019).
- Esri . What Is GIS? – Geographic Information System Mapping Technology n.d. www.esri.com/en-us/what-is-gis/overview (accessed 1 April 2019).
- Association of Directors of Adult Social Services . ADASS Regions n.d. www.adass.org.uk/regions2 (accessed 10 June 2020).
- NHS England . CCG Breakdown of QIPP from 2015 16 Plans n.d. www.england.nhs.uk/wp-content/uploads/2015/10/ccg-plans-publication.xlsx (accessed 10 June 2020).
- Ministry of Housing, Communities and Local Government . The English Indices of Deprivation 2019 (IoD2019) 2019.
- Kamberelis G, Dimitriadis G. Focus Groups. New York, NY: Routledge; 2013.
- Rejnö Å, Berg L, Danielson E. The narrative structure as a way to gain insight into peoples’ experiences: one methodological approach. Scand J Caring Sci 2014;28:618-26. https://doi.org/10.1111/scs.12080.
- Morse JM. The significance of saturation. Qual Health Res 1995;5:147-9. https://doi.org/10.1177/104973239500500201.
- Baker SE, Edwards R. National Centre for Research Methods Review Paper: How Many Qualitative Interviews is Enough?. Southampton: National Centre for Research Methods; 2012.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-117.
- Beresford P. Developing the theoretical basis for service user/survivor-led research and equal involvement in research. Epidemiol Psichiatr Soc 2005;14:4-9. https://doi.org/10.1017/S1121189X0000186X.
- Russo J, Beresford P. Between exclusion and colonisation: seeking a place for mad people’s knowledge in academia. Disabil Soc 2015;30:153-7. https://doi.org/10.1080/09687599.2014.957925.
- Beresford P, Boxall K, Staddon P. Mental Health Service Users in Research: Critical Sociological Perspectives. Bristol: Policy Press and Bristol University Press; 2013.
- Davis A, Jeffreys S, Minteh S. Growing a Service User and Carer Research Resource: A Report of a Pilot Project Designed to Develop a Local Network of Service User and Carer Researchers in Mental Health Research 2014.
- Branfield F, Beresford P, Andrews EJ, Chambers P, Staddon P, Wise G, et al. Making User Involvement Work. York: Joseph Rowntree Foundation; 2006.
- Beresford P. From ‘other’ to involved: user involvement in research: an emerging paradigm. Nord Soc Work Res 2013;3:139-48. https://doi.org/10.1080/2156857X.2013.835138.
- Omeni E, Barnes M, MacDonald D, Crawford M, Rose D. Service user involvement: impact and participation: a survey of service user and staff perspectives. BMC Health Serv Res 2014;14. https://doi.org/10.1186/s12913-014-0491-7.
- Pandya-Wood R, Barron DS, Elliott J. A framework for public involvement at the design stage of NHS health and social care research: time to develop ethically conscious standards. Res Involv Engagem 2017;3. https://doi.org/10.1186/s40900-017-0058-y.
- INVOLVE . Public Involvement in Research: Values and Principles Framework. 2015.
- NSUN . The National Involvement Partnership 4PI National Involvement Standards 2013. www.nsun.org.uk/faqs/4pi-national-involvement-standards (accessed 10 March 2020).
- Ince R. Crisis, What Crisis. Birmingham: University of Birmingham; 2018.
- Ormerod E. Survivor Researcher Network: Mental Health Knowledge Built by Service Users and Survivors. London: NSUN; 2018.
- Faulkner A, Yiannoullou S, Kalathil J, Crepaz-Keay D, Singer F, James N, et al. Involvement for Influence. 4PI National Involvement Standards. London: NSUN; 2015.
- Social Research Association . SRA Good Practice Guides. What Is High-Quality Social Research? 2015. https://the-sra.org.uk/SRA/Resources/Good-practice/SRA/Resources/Good-Practice.aspx?hkey=ccb6430d-24a0-4229-8074-637d54e97a5d (accessed 29 June 2020).
- Great Britain . Data Protection Act 2018 2018. www.legislation.gov.uk/ukpga/2018/12/contents/enacted (accessed 1 April 2019).
- Clifford D, Mohan J. The sources of income of English and Welsh charities: an organisation-level perspective. Volunt Int J Volunt Nonprofit Organ 2016;27:487-508. https://doi.org/10.1007/s11266-015-9628-5.
- Samaritans . Help Us Be There for Emily n.d. www.samaritans.org/support-us/emily1/?gclid=Cj0KCQjwnKHlBRDLARIsAMtMHDH_1mix7bRi5w2U2B-xsChF6r5bEFQezu_uu3r6oKFUGnwofg74iGoaAtMfEALw_wcB (accessed 7 April 2019).
- CALM . Campaign Against Living Miserably n.d. www.thecalmzone.net/ (accessed 21 March 2019).
- Re-Gain (Cornwall) . Listening, Supporting, Empowering n.d. www.re-gain.org.uk/index.html (accessed 21 March 2019).
- Womankind Bristol . Women Supporting Women. n.d. www.womankindbristol.org.uk/ (accessed 21 March 2019).
- Rethink Mental Illness . Help in Your Area n.d. www.rethink.org/services-groups/services/service?serviceGroupId=rethink-sahayak-asian-mental-health-helpline (accessed 22 March 2019).
- Institute for Government . What Is Market Stewardship 2015. www.instituteforgovernment.org.uk/publication/what-market-stewardship (accessed 4 April 2019).
- Rees J, Miller R, Buckingham H. Commission incomplete: exploring the new model for purchasing public services from the third sector. J Soc Policy 2017;46:175-94. https://doi.org/10.1017/S0047279416000362.
- Lindemann E. Symptomatology and management of acute grief. Am J Psychiatry 1944;101:141-8. https://doi.org/10.1176/ajp.101.2.141.
- Bury M. Chronic illness as biographical disruption. Sociol Health Illn 1982;4:167-82. https://doi.org/10.1111/1467-9566.ep11339939.
- Giddens A. Central Problems in Social Theory: Action, Structure, and Contradiction in Social Analysis. Berkeley, CA: University of California Press; 1979.
- Williams S. Chronic illness as biographical disruption or biographical disruption as chronic illness? Reflections on a core concept. Sociol Health Illn 2000;22:40-67. https://doi.org/10.1111/1467-9566.00191.
- Williams G. The genesis of chronic illness: narrative re-construction. Sociol Health Illn 1984;6:175-200. https://doi.org/10.1111/1467-9566.ep10778250.
- Farrelly S, Brown G, Rose D, Doherty E, Henderson RC, Birchwood M, et al. What service users with psychotic disorders want in a mental health crisis or relapse: thematic analysis of joint crisis plans. Soc Psychiatry Psychiatr Epidemiol 2014;49:1609-17. https://doi.org/10.1007/s00127-014-0869-1.
- Leeds Survivor Led Crisis Service . Dial House n.d. www.lslcs.org.uk/services/dial-house/ (accessed 5 April 2019).
- High Intensity Network . High Intensity Network n.d. https://highintensitynetwork.org/ (accessed 5 April 2019).
- African Caribbean Community Initiative . About Us n.d. www.acci.org.uk/about-us (accessed 5 April 2019).
- Women’s Aid . What We Do n.d. www.womensaid.org.uk/what-we-do/ (accessed 5 April 2019).
- Freedom from Torture . Freedom from Torture n.d. www.freedomfromtorture.org/homepage (accessed 5 April 2019).
- James N. Emotional labour: skill and work in the social regulation of feelings. Sociol Rev 1989;37:15-42. https://doi.org/10.1111/j.1467-954X.1989.tb00019.x.
- O’Brien A, Sethi F, Smith M, Bartlett A. Public mental health crisis management and Section 136 of the Mental Health Act. J Med Ethics 2018;44:349-53. https://doi.org/10.1136/medethics-2016-103994.
- Lloyd-Evans B, Bond GR, Ruud T, Ivanecka A, Gray R, Osborn D, et al. Development of a measure of model fidelity for mental health Crisis Resolution Teams. BMC Psychiatry 2016;16. https://doi.org/10.1186/s12888-016-1139-4.
- Marmot M. Fair Society, Healthy Lives: The Marmot Review. London: Marmot Review; 2010.
- Knapp M. Mental health in an age of austerity. Evid Based Ment Health 2012;15:54-5. https://doi.org/10.1136/ebmental-2012-100758.
- Wilkinson RG, Pickett KE. Income inequality and social dysfunction. Annu Rev Sociol 2009;35:493-511. https://doi.org/10.1146/annurev-soc-070308-115926.
- Campion J, Coombes C, Bhaduri N. Mental health coverage in needs assessments and associated opportunities. J Public Health Oxf Engl 2016;39:813-20. https://doi.org/10.1093/pubmed/fdw125.
- Burstow P, Newbigging K, Tew J, Costello B. Investing in a Resilient Generation: Keys to a Mentally Prosperous Nation. Birmingham: University of Birmingham; 2018.
- Appleby L. Safer services: conclusions from the report of the National Confidential Inquiry. Adv Psychiatr Treat 2000;6:5-15. https://doi.org/10.1192/apt.6.1.5.
- Gajda R. Utilizing collaboration theory to evaluate strategic alliances. Am J Eval 2004;25:65-77. https://doi.org/10.1177/109821400402500105.
- Howard LM, Rigon E, Cole L, Lawlor C, Johnson S. Admission to women’s crisis houses or to psychiatric wards: women’s pathways to admission. Psychiatr Serv 2008;59:1443-9. https://doi.org/10.1176/ps.2008.59.12.1443.
- Ryan T, Nambiar-Greenwood G, Haigh C, Mills C. A service evaluation of a community-based mental health crisis house in inner city Liverpool. Ment Health Rev 2011;16:56-63. https://doi.org/10.1108/13619321111157990.
- Chapman T, Robinson F. Key Findings from the Northern Rock Foundation Third Sector Trends Study in North East England. Newcastle upon Tyne: Northern Rock Foundation; 2015.
- Ridley J, Hunter S. Subjective experiences of compulsory treatment from a qualitative study of early implementation of the Mental Health (Care & Treatment) (Scotland) Act 2003. Health Soc Care Community 2013;21:509-18. https://doi.org/10.1111/hsc.12041.
- Morrissey JP, Johnsen MC, Calloway MO, Epstein MH, Kutash K, Duchnowski A. Outcomes for Children and Youth with Emotional and Behavioral Disorders and Their Families: Programs and Evaluation Best Practices. Austin, TX: Pro-Ed; 1998.
- NHS England and NHS Improvement . Information Sharing Policy 2018.
- Caplan G. Principles of Preventive Psychiatry. New York, NY, USA: Basic Books; 1964.
- West Dorset CCG. ‘The Safe Haven’ Aldershot: Evaluation Report 2015. www.dorsetccg.nhs.uk/wp-content/uploads/2018/07/Annex-9-Aldershot-safe-haven-evaluation-report.pdf (accessed 10 March 2020).
- Residential alternatives to acute psychiatric hospital admission: systematic review. Br J Psychiatry 2009;195:109-17. https://doi.org/10.1192/bjp.bp.108.058347.
- Marjanovic S, Garrod B, Dubow T, Pitchforth E, Lichten CA, Elston J, et al. Transforming urgent and emergency care and the Vanguard Initiative: learning from evaluation of the Southern Cluster. Rand Health Q 2018;7.
- Charity Data Download . Registered Charities in England and Wales n.d. http://data.charitycommission.gov.uk/ (accessed 21 March 2019).
- Alcock P, Mohan J. Third Sector Research Centre Research Data Collection. Colchester: Economic and Social Research Council; 2013.
- National Council of Voluntary Organisations (NCVO) . UK Civil Society Almanac 2019. What Does the Voluntary Sector Mean n.d. https://data.ncvo.org.uk/profile/voluntary-sector-definition/ (accessed 11 June 2020).
- Salamon LM, Anheier HK. The Emerging Nonprofit Sector: An Overview. Vol. 1. Manchester: Manchester University Press; 1996.
- Morris D. Charities and the big society: a doomed coalition?. Leg Stud 2012;32:132-53. https://doi.org/10.1111/j.1748-121X.2011.00216.x.
Appendix 1 Literature review method
Review question
The review question was ‘how does the VS contribute to MH crisis care?’. This covered evidence relating to service user experience and outcomes, the relationship with public sector services and the cost-effectiveness of VSOs.
Search strategy
A comprehensive search strategy was adopted to identify the breadth of literature in this area, including grey literature and journal articles. The Health Services Management Centre Knowledge and Evidence Service undertook the search. The review was conducted between May and August 2017 and was updated between November 2018 and January 2019.
Sources
The following bibliographic databases were searched: Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane, EMBASE, Health Management Information Consortium (HMIC), MEDLINE, Social Care Online Sociological Abstracts and Web of Science™ (Clarivate Analytics, Philadelphia, PA, USA). Searches were restricted to English-language papers and limited to 2000 onwards, following the focus of the National Service Framework for Mental Health12 on crisis provision. A Google search was undertaken, limited to papers from 2000 onwards using the terms ‘mental health crisis’ and ‘voluntary sector’. Citation tracking was also used – references of or from relevant papers identified through the database searches were followed through to find more recent or other relevant papers. Survey respondents were also invited to send relevant evaluation reports.
Search terms
The search terms used were as follows:
(“mental health” OR “mental illness” OR “psychiat*”) AND (“crisis” OR “emergency” OR “urgen*”) AND (“charit*” OR “voluntary sector” OR “third sector”)
Inclusion and exclusion criteria
Inclusion criteria
-
Participants: adults aged ≥ 16 years.
-
Definition of crisis: related to MH, mental illness or psychiatric emergency.
-
Interventions: interventions or services to MH crisis care, including prevention and recovery, relevant to VS provision.
-
Contexts: international.
-
Literature published from 1 January 2000 and before 1 November 2018.
-
English language.
-
Empirically based papers.
Exclusion criteria
-
Refers only to public sector service provision.
-
Provision for children or young people aged < 16 years.
-
Commentary, policy and book chapters.
-
Not available in English.
-
Published before 1 January 2000 or after 1 November 2018.
Two reviewers (RI and KN) and (BC and KN) independently reviewed the abstracts for inclusion in the review. Zotero (George Mason University, VA, USA) was used to manage the data sources. The findings from the review are presented in Appendix 2.
Quality appraisal
A systematic quality appraisal was not undertaken, as this was a scoping review including diverse types of material. However, observations about the relevance to the current study and factors influencing the robustness of the findings were noted.
Appendix 2 Summary of papers included in the review
| Study details | Publication type | Aim | Method | Findings | Relevance to study |
|---|---|---|---|---|---|
| Albert R, Simpson A. Double deprivation: a phenomenological study into the experience of being a carer during a mental health crisis, 201568 | Journal article | Carers’ experience of crisis and interactions with professional services | Eight qualitative, phenomenological interviews with carers during a MH crisis |
Highly negative experience for carers – ‘double deprivation’ – often unsupported by staff, also protecting their social network rather than receiving support Useful for recognising wider impacts of crisis, highlighting ‘informal’ support/care and the need for recognition of carers’ knowledge and understanding ‘Process’ of crisis – build up, then slow/ineffective response by MH services, then escalating into calling police or hospitalisation Understanding of crisis – difference between carers’ and staff members’ view of what constitutes a crisis |
Very relevant – themes represent personal experiences of carers Small sample of eight carers |
| Bagley A. Leeds Survivor Led Crisis Service: a social return on investment analysis – summary Report, 201260 | Report | SROI analysis prepared for LSLCS | SROI methodology | A £5.17 benefit per £1 invested was found. A sensitivity analysis determined the impact of varying all of the significant assumptions used to calculate this figure. From this, the authors recommended that a range of between £4 and £7 per £1 invested be used to describe the SROI for LSLCS. Using the figure of £5.17, the total added social value generated by LSLCS over 1 year works out as £1,757,843.73 | Used standards to develop the SROI methodology, which is described in great detail |
| Ball JS, Links PS, Strike C, Boydell KM. ‘It’s overwhelming . . . everything seems to be too much’: a theory of crisis for individuals with severe persistent mental illness, 200565 | Journal article | Comparison of the crisis experience for individuals with severe persistent mental illness with the traditional model of crisis | Grounded theory, qualitative study, in-depth interviews, 14 participants (7 men, 7 women) |
Traditional crisis models do not apply to crises among individuals with severe persistent mental illness. Crisis is a poorly understood phenomenon but underlying vulnerability [life experiences, circumstances (e.g. abuse, homelessness, poverty), symptoms (e.g. hearing voices)] sets the stage for crisis Crisis experiences are characterised by feeling overwhelmed, lacking control or feeling scared or lonely. The study identified different types of crisis manifestation ranging from the most common manifestations of agitation, anger and aggression to being low, feeling anxious and euphoria. Immediate responses to crises involve help-seeking behaviour, managing alone or others getting help The difference between this and ‘traditional’ understandings of a crisis (based on Caplan, 1969151) is that, instead of symptoms associated with mental illness being an after effect or legacy of a poorly managed crisis, people are managing ongoing symptoms already, which when exacerbated can precipitate a crisis without an external event or trigger |
Canadian context Helpful for distinguishing between first crisis episode and subsequent episodes Helps outline cyclical nature of crisis |
| Beckett J, D’Angelo G, Pattison L, Walker T. Self-harm evaluation project: an evaluation of services for individuals who repeatedly self harm focusing on A&E and Leeds Survivor Led Crisis Service (Dial House), 201284 | Report | To evaluate services provided to people who repeatedly self-harmed from within the NHS and at LSLCS, also referred to as Dial House | Interviews with 20 people, all of whom had used A&E and 10 of whom had not used Dial House |
Service users valued the non-intrusive approach and the opportunity for peer support at Dial House, but sometimes felt that they could be upset by other visitors. Some A&E participants avoided the service because of links with people connected to Dial House (other visitors, people living nearby, etc.) People liked the non-medical environment of Dial House and being able to have a bath and a meal there People appreciated being treated with respect and kindness |
Small-scale study |
| Belling R, Whitlock M, McLaren S, Burns T, Catty J, Jones IR, Wykes T. Achieving continuity of care: facilitators and barriers in community mental health teams, 201186 | Journal article | Continuity of care between NHS and social services | 113 semistructured interviews with MH staff in trusts, VSOs, GPs, social work, etc. |
Role of VSOs in achieving continuity of care Positive elements: facilitating decision-making and information transfer as a result of prioritising face-to-face high-quality contact with clients Issues: some poor communication between statutory service and VS service staff, high mobility of people with MH issues leads to very complex networks of care, and multiple interfaces where communication breakdowns can happen Issues around blurred roles between social care and medical staff sometimes led to uncertainty and confusion IT systems and information sharing were huge problems |
Satisfactory Calls for better training and more resources, which is a little obvious |
| Bonynge ER, Lee RG, Thurber S. A profile of mental health crisis response in a rural setting, 20059 | Journal article | Case study of the crisis system in a rural setting – US setting | Observed a not-for-profit provider and its patients over a 12-month period |
Distinguishes between moderate and severe crises – severe being MH emergencies (gives criteria) Mixture of system components: urgent appointments, crisis hotline, professional on-call services (13 MHPs, respond within 2 hours) and five crisis beds (72 hours) Distance was a challenge for mobile crisis services in rural settings Combination of crisis services reduced inpatient admission by 11%. Challenges notions of ‘frequent flyers’ (82% used the service once), as many achieved stabilisation in the short period of time they used the crisis service |
Helpful for system overview and components Relevant for the regional comparison or case study sites Biomedical framing |
| Butt MF, Walls D, Bhattacharya R. Do patients get better? A review of outcomes from a crisis house and home treatment team partnership, 201956 | Journal article | Evaluates the outcomes from a partnership between a VS crisis house in Tower Hamlets and the local home treatment team. The crisis house offers a brief residential alternative to psychiatric hospital admission | Collected clinician-reported (HoNOS) and patient-reported (DIALOG) outcome scores from 153 successive admissions between June 2015 and December 2016, to assess the effectiveness of the service model | Found a statistically significant improvement in 9 out of 10 domains of HoNOS and 3 out of 8 domains of DIALOG. Concluded that a partnership between a home treatment team and a crisis house can result in positive outcomes for patients, as determined by both clinicians and patients | Highly relevant but small-scale study |
| Croft B, İsvan N. Impact of the 2nd story peer respite program on use of inpatient and emergency services, 201561 | Journal article | Investigated the relationship between peer respite, provided by a community organisation, and the use of inpatient and emergency services among adults receiving publicly funded behavioural health services | Compared outcomes for matched pairs of 139 users of peer respite and 139 non-users of respite with similar histories of service use and clinical and demographic characteristics. A two-stage regression model first predicted the likelihood of inpatient or emergency service use after the peer respite start date and then predicted hours of inpatient and emergency service use among 89 individuals who used any inpatient or emergency services |
The odds of using any inpatient or emergency services after the programme start date were approximately 70% lower among respite users than among non-respite users, although the odds increased with each additional respite day. Among individuals who used any inpatient or emergency services, a longer stay in respite was associated with fewer hours of inpatient and emergency service use. However, the association was one of diminishing returns, with negligible decreases predicted beyond 14 respite days Concluded that, for some individuals, peer respites may increase meaningful choices for recovery and decrease the behavioural health system’s reliance on costly, coercive and less person-centred modes of service delivery |
Highly relevant, considering peer-support model of respite care |
| Fenton WS, Hoch JS, Herrell JM, Mosher L, Dixon L. Cost and cost-effectiveness of hospital vs residential crisis care for patients who have serious mental illness, 200262 | Journal article | Evaluation of the cost and cost-effectiveness of a residential crisis programme compared with treatment received in a general hospital psychiatric unit for patients who have serious mental illness in need of hospital-level care and who are willing to accept voluntary treatment | Patients in the public MH system (n = 119) willing to accept voluntary acute care were randomised to the psychiatric ward of a general hospital or a residential crisis programme. Unit costs and service utilisation data were used to estimate episode and 6-month treatment costs from the perspective of the government. Episodic symptom reduction and days residing in the community over the 6 months after the episode were chosen to represent effectiveness |
The mean (standard deviation) acute treatment episode costs were 44% lower in the residential crisis programme than in the general hospital. Treatment groups did not differ significantly in symptom improvement or community days achieved. Incremental cost-effectiveness ratios indicate that, in most cases, the residential crisis programme provided near-equivalent effectiveness for significantly less cost The McAuliffe House programme model was based on Soteria and Crossing Place, a residential crisis facility that has operated in Washington, DC, since 1977. This model strives to provide a small home-like environment that emphasises continuity with outpatient treatment providers and community networks. The medical responsibility for each patient is maintained by the patient’s outpatient psychiatrist |
US context One of the few economic evaluations Close relationship with public MH services vis-à-vis clinical responsibility |
| Gillard S, Gibson SL, Holley J, Lucock M. Developing a change model for peer worker interventions in mental health services: a qualitative research study, 201582 | Journal article | How does involvement of peer support affect, influence or produce change | 71 interviews with peer workers, staff and service users in public sector, partnership and VS services | Change mechanisms identified as building trusting relationships based on shared experience, role modelling living well and recovery, and engaging service users with services and community | Relevant for identifying how peer support influences change but scope wider than crisis |
| Gofal Cymru. The community crisis house model: an evaluation of Wales’ first crisis house64 | Report | Evaluation of a crisis house providing short-term (up to 7 days) intensive 24-hour specialist MH support to people who are assessed by the local crisis intervention and home treatment teams as needing additional support to avoid admission to hospital | Draws on data from service use and service user feedback in the first 2 years of operation | Key messages from the first 2 years of service delivery:
|
Descriptive rather than an evaluation |
| Greenfield TK, Stoneking BC, Humphreys K, Sundby E, Bond J. A randomized trial of a mental health consumer-managed alternative to civil commitment for acute psychiatric crisis, 200857 | Journal article | Comparing a consumer-managed CRP with a locked inpatient ward for people who have been sectioned in the USA | RCT comparing outcomes: costs, level of functioning, psychiatric symptoms, self-esteem, life enrichment and service satisfaction |
Four beds, 8-day stay. Addiction counsellor, self-help principles, transition to assertive outreach support (AO) after discharge. Psychiatric unit was 80 beds on locked wards, 6 days, no AO after discharge Greater severity of illness and lower functioning scores for the CRP baseline Lower costs per initial stay for the CRP. More readmissions for the CRP, so total costs for a year were about even. However, better aftercare and more severe symptoms produced more appropriate aftercare and treatment including readmission. Life enrichment and functioning improvements not significantly greater for the CRP, except for social activity functioning. However, symptoms (both self- and interviewer rated) – especially psychoticism, self-esteem and service user satisfaction – were all greater in the CRP |
US context Hierarchy of knowledge is evident – highlights lack of RCTs as the gold standard, this study being the first |
| Griffiths A, Gale K. Independent evaluation of the North East Hampshire and Farnham Vanguard: Aldershot Safe Haven Service, 201763 | Report | Evaluation of the Safe Haven model launched in early 2014 in Aldershot. Builds on a previous evaluation of the use of and feedback on services152 | Analysis of service user feedback and data on use of the Safe Haven and the predicted impact on savings to the NHS, police deployment and the use of section 136 between August 2016 and July 2017 |
Feedback demonstrates how much service users value the service and suggests that the Safe Haven is an established part of the local MH pathway Predicted savings of £72,864 to emergency departments by offering an alternative Prediction: if the service prevented 5% of crisis attendances from resulting in a psychiatric admission (with an average length of stay of 42.2 days), it would save £439,088 |
Relevant, but draws on secondary data to estimate costs Service user information gleaned from service user feedback forms |
| Gudde CB, Olsø TM, Antonsen DØ, Rø M, Eriksen L, Vatne S. Experiences and preferences of users with major mental disorders regarding helpful care in situations of mental crisis, 201367 | Journal article | Experiences of and preferences for helpful care in situations of mental crisis from the perspective of people diagnosed with major mental disorders in Norway | Qualitative individual interviews with 19 users diagnosed with major mental disorders (13 men, 6 women), aged 22–60 years | The preferences of the majority of users were to have a clear understanding of their own problems and ways of handling these, and for early help from providers whom they know well, and who are open to dialogue and reflection. A clear majority had a high threshold for contacting the MH system owing to negative experiences and a lack of user involvement in treatment planning and implementation | Small-scale study but relevant |
| Gullslett MK, Kim HS, Andersen AJ, Borg M. ‘Emotional darkness without solutions’: subjective experiences of mental health crisis, 201669 | Journal article | Subjective experiences | Phenomenological approach: generating theory from experiences |
Summarised a MH crisis as a ‘continuity of struggles in complex situations’ Identified two dimensions of a MH crisis: (1) existential (personal) and (2) social (context). The impact of structures around the person (e.g. demanding social situations or environments) was noted. Depending on the circumstances and the individual, one dimension can be more dominant in the crisis than another Key themes: ‘feeling out of control’, ‘emotional darkness’ and the paradox of ‘loneliness and seeking togetherness’ occurring simultaneously. This translates into a tension between wanting to withdraw and recognising the need to be open to receiving help Hopelessness and seeing no end to the situation: this feeling, in particular, often led to a suicide attempt Can draw on experiences and structures to use them as strategies (warnings and coping) |
Very relevant and makes a theoretical contribution |
| Healthwatch Norfolk, 201772 | Report | To highlight where local services are working well in preventing or reducing escalation of MH care crises and to identify how services can be improved | Multiple methods including:
|
60% of survey respondents were able to plan for times of crisis to some extent, but 40% were not. People were using many different services at times of MH crises. The pathway to help and support is not always clear. Almost half did not know whom to contact in an emergency. Some people who were already receiving MH treatment and care may have had a ‘crisis care plan’ in place (18%) but half (50%) did not have a plan but stated that they wanted one. Knowing which service to contact is difficult. People do not know if they are meant to call NHS 111 or go to A&E |
Relevant Consultation rather than research |
| Home Office20 | Report | Evaluation of the introduction of an alternative place of safety (APoS) run by a third sector organisation, how it would work in practice and identify any lessons learnt for expansion of the scheme |
|
A much lower number of people presented to the APoS than was anticipated. Limited quantitative and qualitative data for the pilot evaluation | Relevant but too limited by the sample size |
| Hutchinson G, Gilvarry C, Fahy TA. Profile of service users attending a voluntary mental health sector service, 200058 | Journal article | Compared male service users at a VS MH service with a statutory service run by a hospital in London |
Interviews with service users attending the VS service over a 6-month period. Social functioning was assessed using the Global Assessment Scales for Symptoms and Disability and the extent to which needs were being met was assessed using the Camberwell Assessment of Need Demographic characteristics were compared between the two groups |
The service users attending the VS service were significantly more vulnerable and disadvantaged (e.g. in unemployment) and were more likely to have lower levels of functioning (Global Assessment of Functioning) and more unmet needs, including numeracy and literacy skills. They were also more likely to have forensic histories. Both patient groups reported problems with intimate relationships and the need for daytime activities Those attending the VS service had less contact with other health services, particularly GPs, and many cited the reasons for this as wanting to escape ‘the system’, which they saw as the police and health service combined Highlights need for culturally sensitive activities in terms of food, leisure and social activities, which were provided by a VSO specifically targeted at Jamaican people Suggests that service users attending VS services are likely to be more socially and materially deprived than those attending public sector services and ‘specific strategies are required to assist these organisations in meeting the many needs of the service users’ |
Acknowledges high levels of dissatisfaction with statutory MH services in African Caribbean groups, as well as high levels of reported MH issues VSOs need support to support these individuals, rather than an assumption being made that they are already good at doing it |
| Johnson S, Gilburt H, Lloyd-Evans B, Osborn DP, Boardman J, Leese M, et al. In-patient and residential alternatives to standard acute psychiatric wards in England, 200974 | Journal article | Describes the range of residential crisis alternatives: VS and NHS based, some private providers | National cross-sectional survey of alternatives to acute psychiatric care in England | Identified 131 alternatives, some of which were managed by the VS. Of the 131, the following were managed by a VSO: two of four therapeutic wards for specific populations (e.g. with a diagnosis of early psychosis or personality disorder), all 11 non-clinical alternatives (fewer clinical staff) and two of five specialist crisis houses (e.g. for women or people with psychosis; more clinical). Most residents had a history of hospital admission for MH, except for those in the non-clinical alternatives |
Outlines residential crisis care Does not assess quality or outcomes |
|
Larsen J, Griffiths C. Supporting recovery in a third sector alternative to psychiatric hospital admission: evaluation of routinely collected outcome data, 201355 Griffiths CA, Heinkel S, Dock B. Enhancing recovery: transition intervention service for return to the community following exit from an alternative to psychiatric inpatient admission – a residential recovery house, 201580 |
Journal article | Evaluation of the impact of a crisis house on MH recovery (the recovery star) and personal goal scoring | Data collected routinely on entry and exit from Rethink Mental Illness Crisis House as part of the support-planning process |
Significant increases in all recovery star domains (managing MH, identity and self-esteem, trust and hope, self-care) and significant increases in personal goal scoring data of 2.5 points. Shows people made significant progress during their stay at the recovery house Crisis house designed in collaboration with local MH team to serve local needs. Gatekept. People come either after a hospital admission as a step down before returning to the community or instead of going to hospital Champions reflective practices (staff putting themselves in service users’ shoes, training on not making judgements) No clinical staff, but clinical teams can visit. Close collaboration with local MH teams is essential to effective delivery. Open-door policy enables links with community and maintains independence. Recovery approach begins when they enter |
Champions being locally bespoke, but this is in conflict with CQC findings that local variation means a lack of service in some places |
| Lloyd-Evans B, Slade M, Jagielska D, Johnson S. Residential alternatives to acute psychiatric hospital admission: systematic review, 2009153 | Journal article | To assess the effectiveness and cost-effectiveness of, and satisfaction with, residential alternatives to standard acute inpatient MH services | A systematic search identified controlled studies comparing residential alternatives with standard inpatient services. Studies were described and assessed for methodological quality | Twenty-seven relevant studies were identified. Nine studies of moderate quality provided no contraindication to identified alternative service models and limited preliminary evidence that community-based alternatives may be cheaper and individuals more satisfied than in standard acute wards | Highly relevant and systematic study |
| McGrath L, Reavey P. Seeking fluid possibility and solid ground: space and movement in mental health service users’ experiences of ‘crisis’, 201573 | Journal article | An analysis of the way in which service users move through and within space, to establish agency and (dis)order while distressed | Two methods were used:
|
Experience of movement and moving between spaces and engaging different people in those spaces as part of the process of crisis. Participants described moving towards fluid, outside spaces, with agency described as being established through seeking and utilising, greater possibilities for action and engaging others. In addition, the opposite pattern of movement was when participants described moving indoors, using the private space of the home to establish order and restore feelings of agency and strength, in contrast with having overwhelming experiences in public spaces. Connections between these patterns of movement and particular forms of distress are discussed. It is argued that community and private spaces are integral to the ways in which selfhood, agency and action are experienced in mental distress, which in turn has implications for policy, treatment and community action | Small-scale study raising an interesting hypothesis |
| Marjanovic S, Garrod B, Dubow T, Pitchforth E, Lichten CA, Elston J, et al. Transforming urgent and emergency care and the Vanguard Initiative: learning from evaluation of the Southern Cluster, 2018154 | Report | Evaluation of three urgent and emergency care Vanguards: Barking and Dagenham, Havering and Redbridge System Resilience Group; Cambridgeshire and Peterborough CCG; and South Devon and Torbay CCG | The evaluation was rooted in a theory-driven framework. It identified the intervention logic and co-produced evaluation indicators. It used a combination of qualitative and quantitative methods, workshops, key informant interviews, surveys, indicator data dashboards, reflection and learning workshops | Identified enablers and challenges:
|
Site specific and not all MH. Findings not particularly helpful, as largely focused on the NHS |
| Mind. Listening to experience, 20111,17 | Report | Service users’ experience of acute and crisis care | An independent panel was established to carry out an inquiry into acute and crisis MH care. A call for evidence was run, hearings were held and a range of services were visited | Four key areas were identified to focus on raising all services to the level of the best:
|
Very relevant from a service user perspective |
| Morant N, Lloyd-Evans B, Gilburt H, Slade M, Osborn D, Johnson S. Implementing successful residential alternatives to acute in-patient psychiatric services: lessons from a multi-centre study of alternatives in England, 201276 | Journal article | Explores successful features and limitations of five residential alternative services in England and factors that facilitate or impede their initial and sustained implementation and success | Qualitative interviews with MH staff | Provided a more holistic style of care. Retained connections to ‘normal life’ and community; offered greater autonomy, choice and responsibility to the clients; and developed strong therapeutic and peer relationships. Seen as less appropriate for sectioned or highly disturbed patients, offering less comprehensive treatments, especially concerning physical health issues, and sometimes a challenge to use appropriately owing to the small size and organisational capacity. Facilitators of the best use of non-clinical alternatives were being locally valued and able to respond to local needs in the MH system, having clear roles as well as adaptability to circumstances, and the local public sector team having knowledge and awareness of the alternative and being willing to promote it | Included two VS alternatives. No service user perspectives, although explored elsewhere. |
| Morgan K, Chakkalackal L, Cyhlarova E. Life lines: evaluation of mental health helplines, 201285 | Report | Descriptive study of the use of and views on MH helplines | Four groups of stakeholders were selected:
|
Most helplines received in excess of 1000 calls per month, and the majority of calls lasted between 5 and 30 minutes Staff generally believed that resources and capacity were the main pressing issues for helplines, as many calls could not be answered straight away, or individual calls needed to be limited to a daily allowance Most of the GPs surveyed (73%) were aware of MH helplines and over half felt that helplines were a useful service and could prevent crises However, concerns were expressed by some GPs about the evidence of the benefits of helplines and helpline staff expertise; a lack of awareness about such services among health professionals was also mentioned. Nevertheless, helplines were seen to have the potential to provide an additional tool for GPs and to deliver a cost-effective means of support out of hours CMHTs viewed helplines’ role as providing support for patients when other MH services are not available, and offering help to someone in a crisis. They viewed helplines as complementary to secondary MH services, as helplines could reduce the burden on those services 60% of callers were currently receiving some support for MH and 78% had a MH diagnosis. The largest proportion of callers had called either once (39%) or over 10 times (20%), suggesting that callers seek either one-off information or otherwise are likely to be regular callers. Almost all callers felt that the helpline had helped them: they felt listened to and they valued the safe space to talk |
Descriptive study of 9 helplines that volunteered to take part. Illustrates the value of helplines in a crisis system, diversity of organisation and provision, and the pressures on helplines |
| Sells D, Sledge WH, Wieland M, Walden D, Flanagan E, Miller R, Davidson L. Cascading crises, resilience and social support within the onset and development of multiple chronic conditions, 200966 | Journal article | Relationship between chronic illness and psychosocial crisis | Phenomenological approach. Qualitative semistructured interviews with 33 adults in primary care in an urban area | Multiple physical and emotional crises often ‘cascading’ from one event (e.g. an accident). Limitations imposed by treatments led to further crises (e.g. mobility, sickness or loss of income). Disruption to roles, identity, routine, etc., contributed to further crisis. Receiving and providing personal/social support helped maintain a sense of personal value and in coping with daily life. Simply the awareness of the presence of others was a comfort, including practical and emotional support from family and friends. Equally important was the role as caregiver – giving a sense of importance and value, a new role and a purpose – which contributed to positive adaptation |
Highlights the role of and preference for support from an informal network. Highlights reciprocal caregiving as therapeutic Contributes to our understanding of crisis as a longitudinal and cumulative process |
| Shaw B, Stapleton, V. Reality of crisis: the experience of having a crisis and of accessing CRHTs, 201070 | Report | Service user experience of a MH crisis and how it affects their perception of CRHTs | Semistructured interviews with 36 people experiencing a MH crisis during a defined 2-week period across Nottinghamshire and Lincolnshire |
People defined a crisis as a journey and emphasised the importance of continuity The experience of access to CRHTs was variable The interpersonal skills of CRHTs were critical in whether or not service users positively evaluated the service response Being able to identify purpose and meaning in their life was important for recovery |
A service-user-led study Focus on service user experience of CRHTs Contribution to the understanding of the recovery process |
| Sweeney A, Fahmy S, Nolan F, Morant N, Fox Z, Lloyd-Evans B, et al. The relationship between therapeutic alliance and service user satisfaction in mental health inpatient wards and crisis house alternatives: a cross-sectional study, 201459 | Journal article | Compares service user satisfaction and therapeutic alliance (i.e. relationship and trust between service users and staff) between inpatient wards and crisis houses |
Mixed methods – quantitative to assess characteristics and satisfaction of service users, and qualitative interviews to assess therapeutic alliance 16 inpatient wards, four crisis houses. Neighbouring London NHS trust areas Service user participants: 247 inpatients, 108 in crisis houses Qualitative: 15 inpatients, 14 in crisis houses |
Service user satisfaction and therapeutic alliance was stronger and more positive in crisis houses than in wards Homely environment, informal peer support and fewer negative experiences with staff contributed to greater satisfaction in crisis houses. There was a perception of less loss of liberty and autonomy in crisis houses than in wards. The crisis houses are linked into the local acute service systems: |
It is possible that these findings are the result of differences in service users (e.g. crisis house users are more likely to be known to services and more likely to seek help themselves). But the general characteristics of clients in the two environments were the same |
| Thomas P, Longden E. Madness, childhood adversity and narrative psychiatry: caring and the moral imagination, 201311 | Journal article | Theory building, feminist perspective challenging ‘technological paradigm’ in caring and encouraging moral, emotional, context-aware approach | Literature and theoretical review | Gives examples of the Soteria and the Sanctuary models as positive examples of moral imagination – greater empathy for those who suffer are put at the core of caring. Cites these as alternatives to ‘technological paradigm’ (i.e. medical model), which focuses on measurements, abnormalities, physical causes, cures, etc. Calls for understanding mental illness as having its roots in a social context, rather than as inherent to the person | Not empirically based but helpful for exploring philosophical views of mental illness and relationships between those who are cared for and carers |
Appendix 3 Development of the database for the survey
Database of candidate voluntary sector organisations
This section outlines the decisions we made to develop the database for the survey.
There are over 200,000 non-profit organisations (registered charities, companies limited by guarantee, community interest companies, industrial and provident societies, etc.) in England and Wales. Although organisations will supply some information about their activities at the point of registration (e.g. with Companies House), this is often in the form of very general categories, such as the Standard Industrial Classification (SIC) and, therefore, is not very informative about specific fields of activity such as MH. We focused in this project on registered charities, which account for by far the majority of third sector organisations, supplemented by other data provided by bodies that represent and support third sector organisations working in particular fields of activity.
Charity Commission register data
We use a combined version of the registers of charities for England and Wales and for Scotland supplied by the Third Sector Research Centre’s research partners the National Council of Voluntary Organisations (NCVO). The NCVO augments the data captured for regulatory purposes with other fields including a classification of organisations and geographical information, both of which are relevant for this study. The regulatory data are open and publicly available. 155
At the time we commenced the project, there were around 190,000 charities on the registers of the various regulators of charities in the UK (the Charity Commission for England and Wales, the Office of the Scottish Charity Regulator and the Charity Commission for Northern Ireland). Our exclusion criteria for the database were as follows:
-
Charities not based in England, using the information supplied in their governing documents or in regulatory returns. There are small numbers of organisations that appear on more than one of these registers, but it is almost unheard of for a social service or health charity to be registered in Scotland or Northern Ireland and to be operating in England. This gave 158,426 organisations.
-
Not currently active [defined as having submitted no non-zero financial returns in the past 5 years (2011–15) prior to the start of the study in 2016]; this left 156,177 organisations. 156
-
Charities that are directly controlled by the NHS (which usually have a fundraising purpose, such as the endowments of teaching hospitals), that provide benefits only to restricted sets of the population (which are known as benevolent organisations, providing support to members of a specific occupational group, e.g. Aged Mineworkers’ Homes) or that are independent schools. This left 152,741 organisations. 157
For the remaining organisations, we searched through their charitable objects – a document, usually created at the time of initial registration with the relevant regulator, which specifies the purposes for which an organisation has been established – for those operating in the area of MH. This involved text searches for key words or phrases including ‘mental’. This reduced the numbers to 9262 charities.
This figure is much larger than estimates from large national surveys that asked third sector organisations to rank the areas of activity that best characterised what they did (see National survey data: what organisations think). 89 The discrepancy arises for two reasons:
-
Some will be false positives – text descriptions of charitable objects will include phrases or words such as ‘regimental’ and ‘environmental’; these satisfy search criteria in that they encompass the text string ‘mental’ but we are unlikely to be interested in them unless other ancillary information suggests that we would. For example, a regimental charity supporting ex-service personnel might well be relevant, given the increased prevalence of mental illness in this group of the population.
-
Some potential candidate organisations were identified because of the way in which charitable objects are constructed. Many charities use, in their objects, standard phrases such as ‘promotion of physical and mental well-being’, ‘develop emotionally, mentally, physically’ and ‘purposes of physical and mental recreation’. Such phrases often occur in the governing documents of generic organisations providing premises and a social focus, such as community centres and village halls, or in those of sports organisations that wish to demonstrate that they have a wider public purpose. However, we judged that it was unlikely that the primary purpose of this provision was support for those experiencing MH crises.
We therefore refined our selections by considering only those entities whose objects included the word ‘mental ‘ or ‘ mentally’, either independently or in combination (e.g. ‘mental health’, ‘mental sickness’, ‘mental well-being’, ‘mental distress’ and ‘mental illness’). However, it was not possible to envisage all of the possible ways in which a reference might be made to mental illness in the objects of charities. The suggested text strings would miss organisations such as the Samaritans, whose objects (which are fairly standard across branches) refer to working to assist ‘persons who are suicidal, despairing or in distress’. Therefore, we included some such organisations on the basis of the team’s prior knowledge of entities that were likely to be delivering crisis support.
We were also able to use the ICNPO, developed by Salamon and Anheier,158 which is now widely accepted as authoritative. This breaks down the fields in which non-profits work into subsectors (e.g. health-related organisations are subclassified as hospitals and rehabilitation centres, nursing homes, MH and crisis intervention centres or medical research or in a residual ‘other’ field). The ICNPO schema has been applied to the population of charities by NCVO, using text data from the Charity Commission to match organisations to this classification. 90 This is a largely automated process with an element of machine learning so that it is refined over time and they have been doing it for over 10 years. Because it is automated, it does mean that its usage needs to be combined with further primary research to avoid the risk of leaving out organisations of substantive interest. The main area in which we were interested was ICNPO 3300, ‘mental health and crisis intervention’. By combining NCVO’s classification with our own searches based on combinations of the foregoing phrases or words, we found around 7000 charities that contained some reference to mental illness in their governing documents. These were distributed quite broadly across the ICNPO, suggesting that many were organisations that had only incidental connections with MH. We therefore excluded organisations in all those ICNPO categories in which the proportion of charitable objects that make reference to MH was under 10%, leaving 3125 charities, with two additional ICNPO categories represented: nursing homes and social services.
We further removed those charities that were not also a charitable company, as, without the protections offered by company status, such organisations cannot legally enter into contracts or employ people, and the trustees can be personally liable for anything that goes wrong. 159 We judged that charities operating in this area would not be willing to take such risks if they wanted to recruit and retain volunteer trustees and, therefore, exclusions on this basis left 1551 charities.
In short, our starting point was as follows:
-
all charities either in the ICNPO class 3300 (‘mental health and crisis intervention’) or that include variants of terms relating directly to MH in their objects: 7371 organisations
-
the above, but restricted to only those subsets of the ICNPO in which at least 10% of charities have such references in their objects: 3125 charities
-
the above, but restricted further, to organisations that were registered as companies: 1551 charities.
However, as this was a largely automated approach, there was a risk that we would be missing potential candidate organisations. Therefore, we supplemented this with further inquiries. These focused on six subsets of the ICNPO, which we believed to be substantively relevant to our work because of concerns with housing, advocacy, other health services, hospitals, social services and MH. Searching through these criteria, our exclusion criteria involved the following:
-
Organisations were removed for which there was anything indicating that they were specifically set up to serve causes that were not being explored by the present project. This covered:
-
specific illnesses or disabilities (e.g. cancer and diabetes)
-
children’s services
-
charities identified as medical or social care facilities (e.g. hospices and nursing homes), friends of medical practices (e.g. Leagues of Friends) or medical equipment funds (e.g. appeals for scanners)
-
sports organisations
-
horticulture (this term often appears connected to ‘mental well-being’ in objects).
-
-
Further clarification was sought by analysis of the information available on the Charity Commission website and/or by using information from the websites of individual organisations. This led us to exclude charities whose sole or principal focus was on leisure and recreation (e.g. maintaining a building, a youth club or specific sports), transport or furniture; charities whose principal purpose was to provide grants as opposed to service provision; and organisations whose primary objectives appeared to be environmental.
We scrutinised the social service category in more depth because of the numbers of organisations in this field – with over 12,000 charities involved – and the likelihood that many of these would at least touch on MH issues in their activities. Within the social services category, a text search of the objects of charities for the string ‘mental’ resulted in 2787 organisations. We filtered out the types that we definitely wanted to exclude under steps (1) and (2) as above. We also searched for other relevant terms such as ‘addiction’, ‘homeless’, ‘abuse’ and ‘substance’ in the objects and checked through these to assign relevance. This left 2383 social care organisations to check through. In this heterogeneous field, it can be difficult to rule organisations out on the basis that they have no connection with MH care, but we removed organisations that had reported no income and entities that appeared to be specifically about child or early-years support (e.g. Home Start). We left in a number of organisations that were recognisable as charities that dealt with vulnerable people, and we also included charities serving elderly people or providing personal care as, after checking a sample, they appeared to provide services to other groups with support needs. For broadly similar reasons, we included organisations that appeared to provide general support and advice to specific groups in which the incidence of mental illness was likely to be higher than in the general population (e.g. the LGBTQ community, people with visual or hearing impairment and ethnic minority groups).
Having approached the challenge of identifying candidate organisations in two slightly different ways, we produced, from the more focused exploration of specific subsets of the Charity Commission data, a core list of 1982 charities. The ICNPO breakdown was as follows:
-
3300: ‘mental health and crisis intervention’ (682 organisations)
-
3400: ‘other health’ (215 organisations)
-
3100: ‘hospitals and rehabilitation’ (51 organisations)
-
6200: ‘housing’ (337 organisations)
-
7100: ‘civic and advocacy organisations’ (85 organisations)
-
4100: ‘social services’ (612 organisations).
National survey data: what organisations think
To corroborate this selection, we drew on national surveys of third sector organisations in England, commissioned by the then Office for the Third Sector, the mechanism through which the Labour government institutionalised its relationships with voluntary organisations and social enterprises. 89,90 Although dated (the surveys were undertaken in 2008 and 2010), the value of these surveys is that they are very large (with over 40,000 respondents) and that charities are actually asked what they do, who they serve and what they consider to be their most important sources of income, as well as asked to provide other information about barriers and constraints. They were given many options in terms of, for example, choice of beneficiary group or type of activity. The data thus provide a different kind of baseline from that available from the Charity Commission data. Third sector organisations were asked what they thought were their three ‘main areas of activity’. From the survey data, we estimate that roughly 1% of charities and social enterprises (about 1800 organisations out of a total of 180,000) thought that MH was one of their three main areas of activity. This suggests that our total of 1982 charities was of the right order of magnitude.
Listings produced by umbrella organisations
What are known as ‘umbrella’ organisations in the third sector provide infrastructural support to voluntary organisations, such as specialist advice; some have a remit to support organisations in a particular geographical area (e.g. a council for voluntary services operating in a particular local authority), whereas others represent the interests of organisations in general (e.g. NCVO), specific types of organisation (e.g. the Social Enterprise Coalition) or organisations operating in a particular field (e.g. the CCC).
We cross-referenced our selected list with a list of organisations associated with the CCC. However, this generated very few organisations that had not been flagged through our search of the Charity Commission data
Financial information: registered charities
For these registered charities, we have a reasonably complete financial history for at least the last 15 years, although we cannot break down income sources for all of them in much detail. This enabled us to provide a profile of the relative size of organisations. Unfortunately, we do not have reliable data on the income sources of our organisations and we do not pursue that issue in this project.
Appendix 4 E-survey tool of voluntary sector organisations in England
Appendix 5 Interview schedule for national stakeholder interviews
Appendix 6 Identification of two regions
Figure 16 compares the regions by per-capita spend, drawing on benchmarking data. 94 The North East was the highest on both normal and weighted spend per capita. The South East was lowest for actual spend and second lowest for weighted spend per capita, with the North West lowest for weighted spend, but third highest for actual spend. If the proposed ‘subregion’ in the South East is considered, the average is £141.98 for actual spend, which would still be the lowest, and the average weighted spend is £159.20, which would still put it second lowest to the North West. According to the quintiles data (Table 20), the chosen ‘subregion’ scores a little higher than the South East overall, but is still lower than all of the other regions.
FIGURE 16.
Regions by per-capita spend. E, East of England; EM, East Midlands; NE, North East; NW, North West; SE, South East; SW, South West; WM, West Midlands; YH, Yorkshire and The Humber. 94
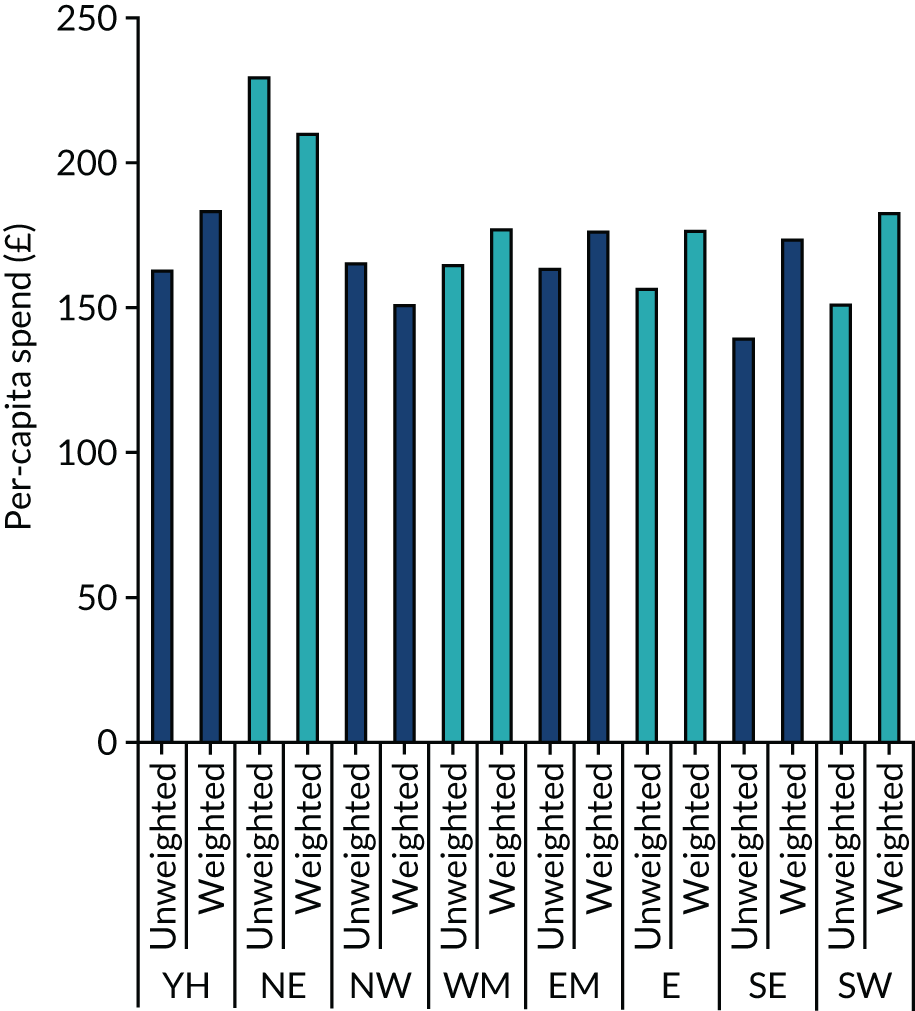
| Region | Abbreviation | Mean MH spend per capita per CCG (quintiles) | Mean number of VSOs per CCG (quintiles) | Combined |
|---|---|---|---|---|
| North East | NE | 4.55 | 1.82 | 6.37 |
| South West | SW | 2.23 | 3.23 | 5.46 |
| Yorkshire and Humber | YH | 3.45 | 1.91 | 5.36 |
| East of England | E | 2.90 | 2.40 | 5.30 |
| West Midlands | WM | 3.14 | 2.00 | 5.14 |
| North West and Cumbria | NW&C | 2.94 | 1.64 | 4.58 |
| East Midlands | EM | 2.79 | 1.68 | 4.47 |
| South East | SE | 2.16 | 1.92 | 4.08 |
| Kent and Sussex | 2.30 | 2.10 | 4.40 |
Appendix 7 Regional interviews: lines of inquiry
-
Role in relation to MH and crisis provision.
-
The range of MH crisis services in the region.
We are particularly interested in VS services:
-
Examples of particularly good practice in the region.
-
Gaps in types of services (e.g. drop-ins, crisis houses).
-
The best places to live for people who might be experiencing a MH crisis and the implications of this for service design.
-
Areas/places where people struggle to access crisis services? What are the reasons for this?
-
(If appropriate) Details on how the organisation fits into the local system and what it offers.
-
Has there been an assessment locally of the needs of people experiencing a MH crisis. If so, the key messages?
-
Commissioning and contracting, and the main funding sources for MH crisis services.
-
Information about the outcomes for people experiencing a MH crisis in this area.
-
The quality of the relationship like between public sector and VS services in this region?
-
Examples of particularly good practice in the region.
-
Anyone who might be good for us to speak to about this?
Appendix 8 Interview schedule for case study stakeholder interviews
Appendix 9 Focus group topic guide
-
The experience of the most recent MH crisis.
-
What events led up to it.
-
What about it meant it was a crisis.
-
-
The experience of a previous MH crisis or crises, if relevant.
-
Differences in use of services?
-
-
Which services were used and for what function?
-
Whether there was a choice and, if so why were these chosen.
-
-
Access to these services and factors influencing this.
-
Eligibility.
-
Urgency.
-
Options?
-
-
Experience of these different services and how they compared with each other.
-
The difference using these services make to individual capacity to deal with the crisis.
-
How did these services support recovery or transition to another service?
-
-
What the person thinks could be improved about crisis support.
-
What are the most prominent characteristics of a MH crisis?
-
What services might help at different points of/types of crisis.
-
What the person would do in the event of a MH crisis in the future.
-
Appendix 10 Service user demographic questionnaire
Appendix 11 Topic guide for the narrative interviews
-
Tell me about your experience of the most recent MH crisis.
-
What events led up to it.
-
What about it meant it was a crisis.
-
-
Experience of previous MH crisis or crises, if relevant.
-
Differences in use of services?
-
-
Which services were used and for what function?
-
Whether there was a choice, if so why were these services chosen.
-
-
Access to these services and factors influencing this.
-
Eligibility.
-
Urgency.
-
Options?
-
-
Experience of these different services and how they compared with each other.
-
The difference using these services made to individual capacity to deal with the crisis.
-
How did these services support recovery or transition to another service?
-
-
What the person thinks could be improved about crisis support.
-
What are the most prominent characteristics of a MH crisis?
-
What services might help at different points of/types of crisis?
-
What would you do in the event of a MH crisis in the future?
-
Appendix 12 Topic guide for carer interviews
-
The experience of the most recent MH crisis and their role and involvement.
-
Experience of a previous MH crisis or crises, if relevant, and their role and involvement.
-
Which services were used, when and what for.
-
Access to these services and factors influencing this.
-
Experience of these different services.
-
The difference using these services made to individual capacity to deal with the crisis.
-
What the person would do in the event of a mental health crisis in the future.
Appendix 13 Script for the repeat service user interviews
Preparation: read previous interview.
The purpose of this interview is to catch up with you, to see whether you have accessed any support since we last met and to get your views on the experience of having a MH crisis and what you have taken from it. As before, we need your consent. Do you have any questions before I ask you to sign the consent form?
Lines of inquiry:
-
What has happened between now and when we last met in [month]?
-
We want to understand your crisis journey and how you have used different services during this time. Can you draw it for us on this piece of paper?
-
What worked well and/or did not work well? Why do you think it worked well?
-
Have your reflections on your experience changed anything?
-
What have you taken from the experience?
-
Prompt: are there particular things that you have discovered about yourself or as a result of your crisis experience?
-
-
What conclusions have you reached on the value of the support that you received from the VS and other support?
-
How well do you think your MH needs are now being met? If they are not being met, how could these be met?
-
Any other thoughts?
Thank you for your support with our research; it is really appreciated. Here is a small token of our appreciation.
There is no need for the participant to complete the questionnaire, as we already have this, unless they did not complete a questionnaire at the first interview.
Appendix 14 Coding frame
| Node | Descriptor |
|---|---|
| Approach of the VS | The approach of the VS |
| Alternative to psychiatry | Providing an alternative to psychiatric care |
| Comparison with the statutory sector | Comparisons between the VS and the statutory sector (i.e. NHS and VS services) |
| Distinctiveness | The distinctive features of the VS |
| Independence | The approach to independence of the VS from the perspective of statutory services |
| Innovation | The types of innovation by the VS |
| Led by people with personal experience of a crisis | A VS crisis service led by people with experience of the VS |
| Organisational aims | The organisational aims of the VSO |
| Organisational culture | A description of the organisational culture |
| Peer- or survivor-led service | A VS crisis service led by people with experience of the VS |
| Range | The different approaches to VS provision |
| Social model | A model emphasising social and structural factors |
| Values | The values of the VSO |
| Carers | The role of carers in a MH crisis |
| Challenges | The challenges experienced by carers |
| Experiences of support | The experience of the support systems used when the person being cared for is in a crisis |
| Multiple roles | More than one role |
| Personal crisis experience | The experience of the carer having a crisis (e.g. being a service user and a carer) |
| Reciprocal caring | The reciprocal nature of support between the carer and service user |
| Relationship with service user | The quality of the carer’s relationship with the service user |
| Commissioning arrangements | How VS MH crisis care is being commissioned |
| Directing the provision | The role of commissioners in directing the crisis care provision by the VS |
| Models of commissioning | How VS crisis services are commissioned (e.g. hub and spoke, spot purchased, contracted) |
| Monitoring | How VS provision is monitored |
| Relationship between VS and commissioners | The quality of the relationship between the VS and commissioners |
| Rules | Rules or regulations regarding commissioning that affect how the VS is commissioned |
| Values | The values of the individuals and/or organisations commissioning VS crisis support |
| Community voice | The voice of community organisations in relation to MH crisis care |
| Conceptions of people in a MH crisis | Conceptions and views of people in a MH crisis |
| Context for the MH crisis | Social, economic and other problems relevant to the MH crisis experience |
| Abuse in adulthood | Abuse experienced during adulthood |
| Adverse childhood experiences | Any adverse experience (e.g. trauma, physical/sexual/emotional abuse) during childhood/adolescence |
| Age | A specific mention of age as a relevant factor |
| Alcohol and substance abuse or misuse | Alcohol and/or substance use/misuse |
| Cultural | Cultural factors relevant to the crisis experience |
| Racism | Discrimination on the basis of race |
| Family factors | Crisis arising owing to family factors (e.g. a breakdown in relationships, familial bereavement, divorce) |
| Financial factors | Crisis arising owing to financial factors (e.g. loss of income, debt) |
| Housing issues | Crisis arising owing to housing issues (e.g. loss of permanent housing, inability to afford rent/mortgage, homelessness) |
| MH diagnosis | Crisis arising owing to MH diagnosis (e.g. personality disorder) |
| Life events | MH crisis related to general life events (not otherwise specified in other nodes) |
| Medication | Medication as a contributory factor for the MH crisis |
| No reason | The service user reports that there is no (apparent) reason for MH crisis |
| Physical illness | Crisis arising owing to physical illness |
| Reason for accessing crisis care | Influences on the person that led them to seek support in a crisis |
| Relapse in MH | MH crisis as a result of a relapse in poor MH |
| Relationship breakdown | Other types of relationship breakdown |
| Resilience | The reasons for strength or assistance in preventing or responding to the MH crisis |
| Service transitions | Transitions (positive or negative) between different services (e.g. child and adolescent MH services and adult services) |
| Social breakdown and isolation | Crisis arising owing to a breakdown in social relationships or feeling isolated (not otherwise related to the person’s family) |
| Trauma and adverse life events in adulthood | Crisis arising owing to trauma or adverse life events in adulthood (not related to abuse in adulthood; e.g. post-traumatic stress disorder) |
| Work and education | Crisis arising owing to work or education |
| Crisis system | The organisation of the crisis system |
| Access to crisis care | Access to care and support in a MH crisis |
| Access prerequisites | The conditions defining access (e.g. eligibility criteria) |
| Availability of services | The availability of crisis services |
| Awareness of how to access | An understanding and awareness of how to access crisis services |
| Barriers | Barriers to access |
| Exclusions | Exclusions from crisis services |
| Inequalities | Inequalities for specific population groups |
| Level of need/demand | The level of need/demand for crisis services (could be over- or underuse) |
| Managing need/demand | The approach to managing need/demand for crisis services |
| Reason for accessing crisis care | Influences on the person that led them to seek support in a crisis |
| Waiting time | How long a person waited before they were able to access crisis care |
| Adequacy | The adequacy of the crisis system |
| Effectiveness | The effectiveness of the crisis system |
| General recommendations | Recommendations for improving the crisis system |
| Non-VS support in a crisis | Support other than from the VS used in a MH crisis |
| Churches and faith groups | Support offered by churches or faith groups |
| Criminal justice system and police | Support offered by the criminal justice system, including police |
| Families and friends | Support from family and friends who are not carers |
| Housing | Housing support |
| Local authority and social care | Support offered by the local authority or social care |
| NHS | Support offered by the NHS |
| Other (e.g. leisure, school, workplace) | Support offered by other support system or service (e.g. leisure, school, workplace) |
| Pathways (e.g. between VS and statutory services) | The pathways between different elements of the crisis system |
| Quality | The quality of the crisis system |
| Workforce | General workforce issues for the crisis system |
| Evidence | The evidence that is used to inform the development of crisis services |
| Experience of VS support | The experience of VS support |
| Consistency | The consistency of the support |
| Continuity | The continuity of the support |
| Environmental | Environmental features |
| Prevention | Preventing crisis or relapse |
| Quality of VSO provision | The quality of VSO provision |
| Good practice | An example of good practice in the VS |
| Standardisation | The standardisation of the quality of MH crisis care by the VS |
| Relational | The quality of the relationship with service users |
| Responsiveness | The responsiveness to service users and local needs |
| Restrictions on service | Any restrictions on service use |
| Funding context | The context for the funding of VS crisis services |
| Austerity | The impact of austerity on funding VS crisis services |
| Awareness of funding opportunities | The awareness of funding opportunities by the VS |
| MH services | Funding for MH services |
| Impact of the crisis response | The impact of the crisis or crisis response on service users |
| Education | The impact of a MH crisis on a service user’s education (e.g. withdrawal from course, not handing in work, change in marks/grades) |
| Employment | The impact of a MH crisis on a service user’s employment (e.g. work absenteeism/presenteeism, resigning, losing job, reducing hours) |
| Family and social relationships | The impact of a MH crisis on a service user’s familial and social relationships |
| Finances | The impact of a MH crisis on a service user’s finances (e.g. loss of income) |
| Future prospects | The impact of a MH crisis on a service user’s future prospects (e.g. prospects of employment, meaningful relationships) |
| Housing | The impact of a MH crisis on a service user’s housing situation (e.g. losing fixed abode) |
| Personal development | The impact of a MH crisis on personal development |
| Self-awareness | The impact of a MH crisis on a service user’s self-awareness of their MH needs |
| Meanings of crisis | What crisis means to participants |
| Temporal dimension | The time dimension of the meaning of crisis (e.g. urgent, imminent) |
| Nature of crisis work | The nature of crisis work (e.g. emotional labour) |
| Personal history and motivation | The personal history and motivation of participants in relation to MH crisis care |
| Aspirations | The aspirations of participants for MH crisis care |
| Commitment | A commitment to improving MH crisis care |
| Drivers | The factors driving the individual in relation to changing MH crisis care |
| Policy and political context | The policy context for the development of MH crisis care |
| Health policy | The health policy context for the development of MH crisis care |
| Mental health policy | The MH policy context for the development of MH crisis care |
| National campaigns | The role/context of national campaigns in/for the development of MH crisis care |
| Political context | The wider political context for the development of MH crisis care |
| Welfare policy | The welfare policy context for the development of MH crisis care |
| Power dynamics | Reference to power dynamics |
| Between NHS and VS | Reference to the power dynamic between the NHS and VS |
| Between services and service users | Reference to the power dynamic between VS services or statutory services and service users |
| Between VSOs | Reference to the power dynamic between different VS services |
| Collaboration | Collaboration between VS services |
| Competition | Competition between VS services |
| Relationship with statutory services | The relationship with statutory services |
| Cultural comparisons | Comparisons of the organisational culture between VS and statutory services that may affect relationships and/or delivery of crisis services |
| Partnership working | Partnership working between VS and statutory services |
| Data sharing | The approach to sharing data about people using their crisis services between VS and statutory services |
| Risk sharing | Risk sharing between VS and statutory services |
| Quality of relationships | The quality of relationships between VS and statutory services |
| Service user experience of a crisis | The service user’s experience of a crisis |
| Feeling safe | Feeling safe in a crisis |
| Intervention of family or friends | Reference to the intervention of family and friends |
| Isolation | Feeling isolated in a MH crisis |
| MH background | Reference to previous experience of MH issues |
| Relationships (e.g. staff and peers) | The service user’s experience of the effect of a MH crisis on their relationships (e.g. strain on or a breakdown in relationships, including social, professional and familial relationships) |
| Risk management | A sense of being at risk or in danger during a MH crisis |
| Self-care | Self-care measures that a service user has taken |
| Self-harm or suicidal feelings | The experience of self-harm or suicidal feelings |
| Service user experience of VS crisis response | The service user’s experience of VS crisis response |
| Being listened to | Being listened to and heard |
| Feeling safe | Feeling safe in a crisis |
| Journey | The crisis journey |
| Relationships (e.g. staff and peers) | The nature of relationships |
| Retraumatising | The experience of a crisis response as retraumatising or triggering |
| Service user needs in crisis | The service user’s needs in a crisis |
| Consistent response | The need for a consistent response |
| Feeling safe | Approaches to ensuring safety during a MH crisis |
| Housing | Accommodation needs during a MH crisis |
| Physical care | The need for physical care |
| Range of needs | A wide range of needs |
| Social | The need for social support |
| Someone to talk to | The need for someone to talk to |
| Stability | The need to feel stable during a MH crisis |
| Unmet needs | Unmet needs |
| Service user voice | How service users have a voice in the design and provision of MH crisis services |
| Advocacy | The use of advocacy to enable service users to have a voice in the design and provision of MH crisis services |
| Challenging stigma | Activities to challenge stigma regarding a service user’s experience of a MH crisis |
| Service user inability to express self | The service user feeling too overwhelmed or inarticulate to express feelings or needs |
| Mechanisms | The mechanisms, other than advocacy, to enable service users to have a voice in the design and provision of MH crisis services |
| Specific features in local context | Relevant factors in the local context |
| Views of the VS | Views of the VS by non-VSOs |
| Additionality | The view that VSOs will add to MH crisis care |
| Cheaper | The assumption that the VS is cheaper than the NHS |
| Misconceptions | Assuming that the VS can do or is doing something that, in fact, it is not |
| Non-stigmatising | The view that the VS is non-stigmatising |
| Plugging the gap | The view that VSOs will plug gaps in the MH crisis care system |
| Unity | Views about a united voice for campaigning, influencing service provision and accountability |
| VS voice | How VSOs have a voice in the design and provision of MH crisis services |
| Campaigning | Specific campaigning activity by VSOs to influence the design and provision of MH crisis services |
| Influencing | Activity by VSOs, other than specific campaigning, to influence the design and provision of MH crisis services |
| VS impact | The impact of VS crisis services |
| Measurement | The measurement of the impact of VS MH crisis services |
| Type | The type of impact of VS crisis services |
| VSO | How the VSO is organised |
| Access | Access to VS support |
| Assessment processes | The assessment processes used |
| Community organisation | A community organisation |
| Delivery challenges | Challenges in the delivery of MH crisis care (e.g. pressures for specialist facilities) |
| Governance | The governance arrangements for VSOs |
| Leadership | Leadership arrangements |
| Location | VSO location |
| Outreach | Provision in different settings |
| Scale | The scale of the VS operation |
| VS capacity | The capacity of the VSO to respond |
| Workforce | Workforce profile |
| VSO service provision | The type of service provision for MH crisis support by VSOs |
| Activity groups | Leisure and recreational activity groups |
| Avoiding inpatient admission | Avoiding admission to inpatient care by providing an alternative service or intervention |
| Bereavement support | Support following bereavement |
| Counselling/psychological therapy | The provision of counselling or psychological therapy |
| Crisis house | A crisis house |
| Drop in | A drop-in facility |
| Employment support | Employment support (paid and voluntary) |
| Helpline | The provision of a helpline |
| Listening | Listening |
| One-to-one support | One-to-one support |
| Peer support | Peer support |
| Practical support | Support with daily living and navigating services |
| Prevention | Activity to prevent a crisis or relapse |
| Recovery | Recovery-focused activities |
| Risk management | The approach to risk management |
| Self-management | The provision of self-management support |
| Training public sector professionals | Training public sector professionals |
| Response to suicide/self-harm | The specific response to suicide or self-harm |
| Safe space | The provision of a safe space |
| Signposting | Signposting to other services |
| Social inclusion | Supporting social inclusion |
| Support groups | Support groups proving emotional support |
| Timing | The timing of the intervention |
| VSO development | The development of VSOs |
| Challenges | Challenges for the development of VSOs |
| Opportunities | Opportunities for the development of VSOs |
| Sustainability | The sustainability of VSOs |
Appendix 15 Regional case studies
Region 1
This region comprised four distinct areas of local government: three largely rural counties and one unitary authority. These were covered by two NHS partnership trusts. The areas were geographically diverse, including coastal areas, small cities and large towns (but no major urban centre), and rural and agricultural areas. Socioeconomically, region 1 is commonly assumed to be wealthy, but interview participants noted specific pockets of deprivation and high need. These were found particularly in coastal and inland towns, each with specific issues such as high rates of substance abuse, a local suicide hotspot or a large proportion of residents from the armed forces. Some of these areas were targeted for pilot studies of VS crisis services, some of which did not extend beyond the pilot phase.
There was significant variation in the availability of VS crisis services both across the region and within the four areas it was made up of. One area housed a number of crisis cafes open out of hours on different days, as well as a VS crisis telephone line. Another area had a residential crisis house that was gatekept by the local CRHT and an out-of-hours safe space (notably, these were both located in the same town, whereas other towns in the area with particular needs had no face-to-face crisis services), while another area had an integrated ‘hardship’ crisis service. There had also previously been a service-user-led pilot of an out-of-hours crisis cafe-style safe space in one of the areas identified as having a high level of need, which did not last beyond the initial 6-month pilot, largely because of underuse. It was noted by a local peer support organisation that the short-term nature of pilot projects such as this one made it difficult to confidently signpost people to crisis services. The fourth area – a largely rural county – had no VS crisis services at all apart from voluntary peer support for people in distress. The sparsest provision was in the most rural areas, in which both VS services such as safe spaces and statutory services such as A&E departments with psychiatric liaison involved long drives or were very difficult to access without a car owing to a lack of reliable public transport infrastructure. There were, however, a number of long-standing VS providers of type 2 services across the region in all areas.
Region 2
This region was made up of 12 local authority areas, including two major urban areas that were considered city regions (both forming combined authorities). The region contained two predominantly rural county council areas and 10 unitary authorities of varying levels of urbanity and scale. In short, there were two large conurbations and two large rural areas, and the region had a significant coastline, which all presented challenges in terms of access and providing services across a very diverse area. The region was covered by two NHS foundation trusts. Overall, the region had a post-industrial character and contained large areas in which communities faced significant deprivation. As can be expected from this brief description, the area was socioeconomically mixed, with deprivation often concentrated in neighbourhoods in urban areas and also somewhat in isolated coastal and rural towns and, owing to distance and relatively fragmented public transport, it could be difficult to travel around the area. The region was noted for high rates of suicide and this was reflected in local MH priorities, including those of some of the VSOs that we spoke to. For instance, some of the smaller VSOs focused on male MH concerns and suicide reduction, including in the rural areas.
One conurbation had a relatively high-profile ‘complex needs’ programme that was led by a VSO and funded by a large national grant maker, reflecting the prevalence of substance abuse and rough sleeping, often closely linked to MH problems. In this area there also appeared to be a relatively active VS role in terms of safe spaces and a Recovery College. In the other conurbation, the local crisis ‘system’ appeared to be closely shaped by statutory organisations (including the provision of various interventions to improve access and response to those in a crisis) and the VS, although the part played by the VS in this was often seen as supplementary and somewhat peripheral: people were ‘signposted’ to VS services as necessary. This latter area also had a VS-delivered crisis house, but this provision was small and not widely known about, and access was gatekept by the area’s crisis teams. Like region 1, region 2 was very diverse and VS provision was much sparser in the rural areas.
Appendix 16 Elements of a crisis care system
| Immediate access to information, signposting and support (e.g. call centres, information hubs-ins) |
| Listening services (e.g. helplines, open-access drop-ins) |
| Well-being and ongoing support services (e.g. peer support, well-being workshops) |
| Safe space/crisis cafe |
| First responders (e.g. street triage, place of safety) |
| A&E liaison |
| CRHTs |
| Crisis accommodation (VS and public sector) |
| Culturally sensitive services (e.g. for specific communities) |
| Psychological therapy and counselling (to address underlying psychological difficulties, e.g. trauma-focused services) |
| Advocacy (to support people to have a voice) |
| Community MH services (to provide ongoing support and recovery) |
| Carers’ support |
| Other |
Glossary
- Crisis house
- Crisis houses offer safe short-term accommodation and support to people experiencing a mental health crisis. They are used when home treatment is not suitable or as a short-term alternative to hospital admission.
- Crisis resolution home treatment team
- Crisis resolution home treatment teams treat people with severe mental health conditions who are currently experiencing an acute and severe psychiatric crisis that, without the involvement of the crisis resolution home treatment team, would require hospitalisation.
- Integrated care system
- The NHS Long Term Plan set out the aim that every part of England will be covered by an integrated care system by 2021, replacing sustainability and transformation partnerships. An integrated care system involves close collaboration between NHS organisations, in partnership with local councils and others, taking collective responsibility for managing resources, delivering NHS standards and improving the health of the population they serve.
- Market stewardship
- Market stewardship takes a broader approach than traditional commissioning and considers how to set the rules of the market so that competition between providers works effectively.
- Personal budget
- A personal budget comprises the financial resources allocated by the local authority to pay for care or support to meet a person’s assessed needs.
- Randomised controlled trial
- A randomised controlled trial follows a research design in which similar people are randomly assigned to two (or more) groups to test a specific treatment or other intervention.
- Safe space
- A safe space is a non-clinical space that, usually out of hours, provides support in a crisis and offers listening and/or peer support. They are also known as sanctuaries, havens or crisis cafes.
- Sustainability and transformation partnership
- Sustainability and transformation partnerships were created to bring local health and care leaders together to plan for the long-term needs of local communities and to improve health and care in the areas they serve.
- Third sector
- The third sector is broadly defined as all organisations operating outside the formal state or public sphere that are not trading commercially for profit. This includes charities and voluntary organisations, community groups, social enterprises, co-operatives and mutuals. Although these organisations are exceptionally diverse, they share a broad common theme of being value driven.
- Voluntary sector organisation
- In this report, we use the term ‘voluntary sector organisations’ to refer to charities, voluntary organisations and/or community groups.
- Wellness recovery action plan
- A wellness recovery action plan is a self-designed prevention and wellness process that anyone can use to get well, stay well and live their life the way they want.
List of abbreviations
- A&E
- accident and emergency
- BAME
- black, Asian and minority ethnic
- CALM
- Campaign Against Living Miserably
- CCC
- Crisis Care Concordat
- CCG
- Clinical Commissioning Group
- CMHT
- community mental health team
- COREQ
- Consolidated Criteria for Reporting Qualitative Studies
- CQC
- Care Quality Commission
- CRHT
- crisis resolution home treatment team
- CRP
- crisis residential programme
- GIS
- geographic information software
- GP
- general practitioner
- GRIPP2
- Guidance for Reporting Involvement of Patients and the Public
- IAPT
- Improving Access to Psychological Therapies
- ICNPO
- International Classification of Nonprofit Organizations
- IT
- information technology
- LGBTQ
- lesbian, gay, bisexual, transgender and queer
- LTP
- Long Term Plan
- MH
- mental health
- MHA
- Mental Health Act
- NCVO
- National Council of Voluntary Organisations
- NIHR
- National Institute for Health Research
- NSUN
- National Survivor User Network
- PPI
- patient and public involvement
- RCT
- randomised controlled trial
- SRG
- Study Reference Group
- SSG
- Study Steering Group
- STP
- Sustainability and Transformation Partnership
- ULO
- user-led organisation
- VS
- voluntary sector
- VSO
- voluntary sector organisation
- WP
- work package
Notes
-
Examples of voluntary sector organisations providing support in a mental health crisis
-
Membership of the Study Steering Group and the Study Reference Group
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/hsdr08290).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.