Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 14/156/23. The contractual start date was in October 2016. The final report began editorial review in October 2019 and was accepted for publication in April 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Gavin D Perkins reports that he is a National Institute for Health Research senior investigator (2015 to present).
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Bion et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Background and context
High-profile failures in health care,1–3 the paradigm for which were the events at the Mid-Staffordshire NHS Foundation Trust,4 demonstrate the important contribution that staff attitudes and behaviours make to the experience of health care and to patient outcomes. They also show how easy it is for good intentions to be subverted, and how entire organisational cultures can become dysfunctional through the actions or inactions of individuals. Despite a near-universally expressed desire to provide the best possible care to their patients, staff may find themselves hampered by ‘inner context’ factors, such as power differentials, inadequate leadership, burdensome bureaucracy and overlapping and competing priorities, or conflicting organisational and personal values and beliefs that are aggravated by ‘outer context’ factors, such as health service pressures or attitudinal changes within wider society. 5,6 These factors may give rise to individual behaviours that at the micro level degrade patient experience of care from ‘excellent’ to ‘good’ or from ‘good’ to ‘poor’, and in the aggregate contribute to failure of whole organisations.
Our hypothesis is that dysfunctional behaviours that are harmful to both patients and staff can be mitigated by promoting insight and empathy through effective reflective learning at the level of the individual and of the organisation. We developed a preliminary logic model that links theories of behaviour change with those of learning to create a reflective learning framework (RLF). The tangible expression of this framework is a toolkit that links meaningful feedback from patients and staff to stimulate effective reflection ‘on-action’ and ‘in-action’ to promote optimal care.
Patient and staff experiences offer important insights into health-care quality
Patient and staff experiences offer important insights into the quality of health care, which complement organisational-level data on processes and outcomes. 7–9 Patient experience is an explicit outcome measure in the UK NHS10,11 and in the regulation of care quality. 12 All NHS trusts are required to collect patient experience data through surveys13,14 and additional insights are available through patient complaints. 15 In the USA, patients are surveyed through the Hospital Consumer Assessment of Healthcare Providers and Systems,16 whereas in Australia health organisations are required to involve consumers in accreditation processes. 17 Staff experience also provides insights into care quality: earlier action on staff concerns could have mitigated failings in care. 4 The NHS staff survey18 has been conducted annually since 2003. Patients and staff appear to share complementary insights into care quality: patient satisfaction is higher in hospitals in which nurses also reported better care quality. 19,20 Patient and staff perceptions appear to offer both overlapping and unique insights into safety in hospital. 21
Patient and staff experience is strongly influenced by staff attitudes and behaviours
The NHS National Inpatient Survey13 asks respondents to rate their overall experience on a scale of 0 (‘very poor’) to 10 (‘very good’). In 2017, 50% of respondents rated their experience as ≥ 9. 13 This indicates that there are substantial opportunities within the health system for ‘learning from excellence’. 22 However, ‘good’ ratings by patients (as opposed to ‘very good’) may also disguise important opportunities for improvement. 23 A survey by Healthwatch England (London, UK) reported that half of those experiencing substandard care do not report it. 24 Patients who respond to surveys with perfect ratings but with negative free text frequently describe lapses in staff behaviours and attitudes,25 such as communication, empathy, courtesy, consideration, compassion and patient focus. A study of patient-reported safety incidents26 found that 22% were related to communication failures alone, whereas a systematic review of patient complaints27 judged that one-third of complaints were related to staff–patient relationships. This may well be an underestimate given that staff behaviours are mentioned in up to two-thirds of all complaints (Queen Elizabeth Hospital Birmingham local data on file). Attitudes and behaviours of other members of staff are also important determinants of staff (dis)satisfaction, as demonstrated by the 487,727 respondents to the NHS staff survey18 in 2018. Taken together, patient and staff experience, both positive and negative, provide an important opportunity for improvement through behaviour modification.
Patient and staff experience data are not used optimally to change behaviours
Despite this investment in data acquisition, health systems have difficulty using patient and staff experience data to improve care, particularly the non-technical skills related to attitudes, behaviours and culture. 28–30 Reflective learning underpins approaches to improving non-technical skills, but the processes by which experiences are translated into reflection, and reflection into behavioural change, are not well understood. Using patient experience to improve care is not a trivial task. 31 Lapses in care are usually multifactorial, the product of interactions between the individual and the ‘system’; however, from the perspective of the patient, quality is largely about trust-based relationships with specific individuals,32 not ‘systems’. Trust boards and quality governance committees must contend with the competing priorities of hundreds of quality indicators each month and may prioritise avoiding falling below a quality threshold rather than achieving higher values of a performance standard once met. A review in 201233 that examined how hospitals had used research from the UK National Inpatient Survey concluded that ‘simply providing hospitals with patient feedback does not automatically have a positive effect on quality standards’. Even trusts with a tradition of collecting and using patient survey data may struggle to convert these data into tangible improvements. 34 In a study of 50 clinical and managerial staff in three English hospitals, Sheard et al. 35 found that ward staff had difficulty using patient feedback, and the collection of patient experience feedback was a ‘self-perpetuating industry’ conducted ‘at the expense of pan-organizational learning or improvements’. 35 They concluded that ‘macro and micro prohibiting factors come together in a perfect storm which [prevents] improvements being made’. 35 In a systematic review, Gleeson et al. 36 reported that ‘patient experience data were most commonly . . . used to identify small areas of incremental change to services that do not require a change to clinician behaviour’. 36 Institutional commitment to using patient feedback may not be reflected at the front line, where single individuals can adversely influence other members of staff. 37 Conversely, front-line staff can struggle to get their voices heard at senior levels; one of the recommendations of the Mid Staffordshire NHS Foundation Trust inquiry4 was to establish ‘Freedom to Speak Up Guardians’ in all NHS trusts to ensure that staff concerns are heard and acted on. 38 These findings indicate that changing behaviours requires a change in underlying attitudes at individual, group and organisational levels. How is this best achieved?
Reflection as behaviour
Behavioural modification is a universal preoccupation, and behavioural sciences now inform government policy. 39 A large number of techniques exist and a proposed behaviour change taxonomy has so far identified 93 different interventions. 40,41 However, evidence supporting the primacy of one technique over another is not strong. 42,43 Many interventions involve personal insight development through reflection, but few behaviour change theories express this explicitly. One which does is the Capability, Opportunity, Motivation – Behaviour (COM-B) framework,44 which assimilates 19 behaviour change theories into a single framework in which the behaviour of interest has three determinants, each with two subtypes: capability (physical and psychological), opportunity (physical and social) and motivation (reflective and automatic). The automatic subtype for motivation relies on heuristics, is engaged in conditions of complexity and stress, and maps to Daniel Kahneman’s ‘System 1’ thinking. 45 The reflective component of motivation is slower, more effortful and analytical (Kahneman’s ‘System 2’ thinking). These two subtypes of motivation map to the ‘peripheral’ and ‘central’ routes described in the elaboration likelihood model of persuasion. 46,47 Factors influencing motivation (particularly the automatic subtype) are summarised by the acronym MINDSPACE (messenger, incentives, norms, defaults, salience, priming, affect, commitment and ego). 48 As the behaviour of interest here is reflection itself, we need to consider both the automatic factors that influence the desire to reflect and the more effortful elements of ‘reflecting on the need for reflection’.
We next consider how theories of reflection as a behaviour link to theories of reflective learning as a tool for personal insight development.
How does reflection stimulate learning?
Kolb and Fry49 presented reflection as a four-stage model: experience, observation, analysis and recalibration. Schön50 described reflection ‘in-action’ and ‘on-action’. Others emphasise the importance of an emotional component to reflective learning,51 including the ‘disorientating dilemma’:52 the realisation that there is a gap between desired and actual behaviours. Sandars53 describes reflection as a metacognitive process that creates a greater understanding of self and situation to inform future actions: looking back to look forward. This involves a transition from tacit to explicit knowledge54 in which socially acquired norms of behaviour55 are modified either through individual reflection or, more powerfully, through group activities. 56 The process shares similarities with Broadwell’s57 four stages of competence: unconscious incompetence (unaware of problem), conscious incompetence (data received, now being processed), conscious competence (using data to improve or disseminate excellence) and unconscious competence (effortless excellence). Effective reflection appears to involve making this transition while recalibrating and reinterpreting experience in-action and on-action.
Reflective learning could be deployed more effectively to improve care quality
First described by Dewey in 1933,58 reflective learning is now a mandatory tool in the education, appraisal and revalidation of health-care professionals. In the UK, the General Medical Council (GMC) and others define reflective practice as:
The process whereby an individual thinks analytically about anything relating to their professional practice with the intention of gaining insight and using the lessons learned to maintain good practice or make improvements where possible.
General Medical Council. 59
They state that:
. . . reflecting on . . . experiences is vital to personal wellbeing and development, and to improving the quality of patient care.
General Medical Council. 59
Reflection is incorporated in all UK health-care postgraduate training programmes and is evidenced in professional portfolios, which, for doctors, must include multisource feedback from patients and colleagues. The Nursing & Midwifery Council require five written reflections over 3 years by nurses for revalidation. 60
However, despite the widespread promotion of reflection as a tool for self-improvement, evidence that it actually improves performance is weak,61–63 as is the evidence that feedback from patient experience surveys promotes effective reflection. 64 We are biased towards favourable events and judgements65,66 and tend to reject adverse patient feedback,67 thereby missing the opportunity to learn from either through critical analysis. Poor performers additionally lack insight into their abilities. 68 It takes emotional strength and resilience to take a critical view of one’s own skills, particularly those relating to attitudes and behaviours given that these touch us personally; undesirable information is processed as a threat with physiological correlates that can actually impede learning. 69 In the UK, doctors are concerned that honest reflections documented in personal portfolios might incriminate them in a court of law. 66 Guidance on reflective practice for doctors70 proposes that solely negative events and errors should be used for reflection, rather than permitting a mix of both negative and positive events. The GMC also mandates reflecting on ‘significant events’, which are defined as ‘any unintended or unexpected event, which could or did lead to harm of one or more patients’59 (Reproduced with permission from the General Medical Council. 59 © 2020 General Medical Council. All rights reserved), in guidance on supporting information for appraisal and revalidation. 71 The emphasis on negative events could be viewed as diminishing the value of learning from positive experiences and role models. 22 The current emphasis on reflection for appraisal has had the effect of diminishing its potential for translation into lifelong reflective practice. 72 If reflective learning is to be effective, it must involve more than just completing a form and ticking boxes.
Could communication skills training substitute for training specifically in reflection? A review of 243 studies73 of teaching communication skills to medical undergraduates identified only 16 interventional studies, and of these only two reported behavioural outcomes, making it difficult to determine whether or not ‘communication skills’ are sufficient or even if such courses are effective at all. At postgraduate level, the effects of communication skills training appear to be weak or evanescent. 74–79 In one randomised controlled trial (RCT) of staff training in end-of-life care,80 communication skills were associated with worse depression among patients in the intervention group.
By contrast, interventions that focus on engaging staff in workplace-based activities, which improve teamworking,81 insight, patient-centred care and empathy, may be more effective and more durable. 82–93 The Cleveland Clinic offers short videos on empathy,94 and similar internet-based resources demonstrate how emotion may be engaged to stimulate reflection and promote mutual understanding. 95,96 For reflective learning to improve patient and staff experience, it probably needs to influence hearts as well as minds. Techniques for reflection need to be based on insights from behavioural sciences and evaluated using relevant process and outcome measures. In summary, the work of reflection must become a social enterprise rooted in a community of learning. This is the ethos of the Patient Experience And Reflective Learning (PEARL) project.
Aims and objectives
The aims of the PEARL project were to develop methods for acquiring patient and staff experiences; to use those experiences to promote effective reflection, insight and empathy; and to develop tools that would help staff apply effective reflection in clinical practice to improve care. In the longer term, our aim is to evaluate the impact of the toolkit through a RCT.
Specific objectives were:
-
establishing surveys for recording patient and staff experience
-
determining attitudes to and uses of patient and staff experience data
-
determining attitudes to, techniques for, barriers to and opportunities for reflective learning
-
developing a RLF – a programme theory or logic model – linking experiential feedback to reflective learning and change
-
mapping factors that influence reflective learning to the COM-B framework of behaviour change
-
developing and piloting methods in the form of a toolkit to incorporate effective reflection in routine practice.
Chapter 2 Methods
Parts of this chapter have been reproduced from the PEARL protocol by Brookes et al. ,97 previously published in BMJ Open. This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/. The text below includes minor additions and formatting changes to the original text.
Workstream 1: introduction and overview of workstreams
The PEARL project was conducted over a 3-year period at the following NHS trusts: University Hospitals Birmingham NHS Foundation Trust (Queen Elizabeth Hospital), Heart of England NHS Foundation Trust (these two have since merged) and Newcastle upon Tyne Hospitals NHS Foundation Trust (Royal Victoria Infirmary and Freeman Hospital). This was a mixed-methods project combining both qualitative and quantitative data with patient and staff co-design techniques. The project consisted of four interlinking workstreams (WSs):
-
Workstream 1 (WS1) included setting up the project and establishing and supporting the local project teams to form the collaboration (see Appendix 1).
-
Workstream 2 (WS2) involved developing, disseminating, collating and reporting the patient and relative survey and the staff survey.
-
Workstream 3 (WS3) involved the ethnographic work, which was conducted in two phases.
-
Workstream 4 (WS4) was the co-design of the RLF and the toolkit.
We describe these in detail below.
Location
The project was located in the acute medical units (AMUs) and intensive care units (ICUs) of the four participating hospitals.
Acute medical units are generally the first point of emergency admission to hospital for patients, usually from the emergency department (ED) or following direct referral by general practitioners in the community. Of those admitted, around 40% of patients may be discharged home from the AMU within 48 hours and 60% transferred to general or specialist wards for continuing care. Specialist acute physicians will generally work 12-hour daytime shifts in the AMU, providing twice-daily ward rounds; weekend cover may be provided by acute physicians or by a general physician on duty. Nurse-to-patient ratios may be in the region of 1 : 6. The clinical team has to cope with large numbers of patients, a rapid turnover and making quick and accurate diagnostic and therapeutic decisions in conditions of uncertainty.
Intensive care units care for the most severely ill patients in the hospital using highly trained staff and complex equipment. Nurse-to-patient ratios are usually 1 : 1 or 1 : 2, providing care to one of the most vulnerable populations in health care, requiring burdensome technical support for multiple failing organ systems and experiencing a mortality rate of around 30%. 98 Intensive care consultants usually conduct two ward rounds per day, 7 days per week, and provide continuous care for periods of several days, or whole weeks, as well as undertaking regular night duties to maximise continuity of care. Providing reliable care in this complex environment requires both high-level technical and non-technical skills. Non-technical skills include effective teamworking, situational awareness and leadership, and the ability to integrate information across locations and over time to co-ordinate communication and actions, and to provide care with compassion.
Participants
Each participating unit established a local project team consisting of clinical, managerial and administrative staff as well as patient and relative representatives with experience of the AMU or ICU. Teams held bimonthly local project team meetings that were chaired by a non-executive director (executive director at one trust).
Staff on the units participated in interviews and observations (carried out as part of WS3) as well as the co-design work to develop interventions to enhance reflection (WS4).
Participants in the experiential data collection workstream (WS2) were patients and relatives who had spent time in the AMU or ICU. Their experiences were collected through the PEARL project patient and relative experience survey. Staff experience data were collected from staff whose primary working area was the AMU or ICU at the participating trusts, using the PEARL project staff experience survey.
Project set-up
Local project leads for each participating unit were appointed. The leads then established a local project team, which consisted of medical, nursing, allied health professional (AHP), administrative and managerial colleagues from their units. The teams were also encouraged to invite patient and relative representatives. Once established, the team agreed local arrangements for project delivery following confirmation of capacity and capability for their site. Existing opportunities for feedback and reflection were identified. With direction from the central project team, local teams held meetings once every 2 months to review project outputs, encourage team reflection (e.g. through existing meetings, team briefs and formal reports) and consider methods for incorporating feedback in routine practice.
In addition, we held four plenary workshops (three of which were co-design activities), nine facilitated local co-design meetings (three in each centre) and one further local co-design meeting without central facilitation. Our ethnographers observed all of these activities and provided feedback on each.
Workstream 2: the PEARL project patient and relative survey and staff survey
General aspects of survey development
The aim of the PEARL project surveys was to acquire experiential data from patients, relatives and staff that could be fed back to the local teams as evidence of the need for reflection, and as a motivating stimulus. We were sensitive to the need to avoid duplicating existing survey work and to minimise the burden on recipients of the surveys and the administrative load for local teams. We describe first the generic considerations for both surveys, followed by the specific development of each survey.
A survey subgroup was established, which consisted of project management committee members (including patient representatives) and the local project leads. A scoping review was undertaken of English-language surveys that had been used in the UK and focused on the experience of care of patients or relatives, or the experience of providing care by health-care staff.
Data acquisition varied between these surveys: some employed questions and others used statements with strength of agreement ratings. The working group, therefore, prioritised a standard approach for the patient and staff surveys, expressing a preference for the use of statements with strength of agreement ratings using a 5-point Likert scale. A limited number of direct questions were also included in the patient and relative survey.
Survey statements were selected or excluded through iterative discussion. The focus of attention was to identify those aspects of health-care behaviours that were within the competence and capability of individuals to address. We aimed as far as possible to preserve the original wording of the source surveys to retain questionnaire validity; where questions had been used, these were edited to statements. For the staff survey, we also conducted a modified Delphi process to prioritise the final set of questions (see Staff experience survey).
For the format of the surveys, we considered at an early stage whether these should be paper based or web based. A study from the Netherlands comparing both formats in colorectal registry cancer patients found a preference for paper surveys among respondents aged > 70 years, which was offset by a trend for web-based responses among those aged < 70 years. 99 A study from Denmark100 found lower response rates, higher completion rates and much lower administrative costs for an e-mailed web-based survey than the postal paper-based format; however, they did not factor in the costs of developing or hosting the web-based survey. Patients may not possess, and medical record departments do not universally record, e-mail addresses or mobile telephone numbers (for social media applications) for sending out invitations to complete the survey, and fewer young people now use e-mail as a primary mode of communication. The local project teams and the patient representatives were of the view that paper-based surveys were preferable at this stage, but recognised that these would in the future be supplanted by web-based approaches.
Participant information sheets accompanied each survey, explaining their purpose and that completion was optional, not mandatory. Questionnaires were anonymous; no person-identifiable information was collected.
The research ethics committee approved implied consent for those respondents who returned the completed questionnaires using the free-post return envelopes.
Analysis was undertaken by the central project team. Each completed survey was reviewed, focusing particularly on the free text to ensure that if serious concerns had been raised the relevant local project lead could be informed for subsequent investigation.
Responses were allocated subject numbers and reported to the Clinical Research Network using the National Institute for Health Research’s (NIHR’s) Central Portfolio Management System for uploading research accruals. Dissemination logs outlining the numbers of surveys disseminated were kept locally, with figures reported to the central team to allow calculation of response rates for each unit.
Surveys were scanned using Formic software (Formic Solutions, Uxbridge, UK) and the data uploaded to a spreadsheet for analysis. Data were presented to the units as standardised reports that showed the proportion of respondents selecting each level of strength of agreement with each statement. The data management team checked a random sample of 10% of the responses to ensure that there were no problems with the scanning. When issues were identified the data management team would undertake further action: either check all data or request a new scan of surveys. Free-text responses were transcribed manually and listed verbatim in the reports. They also underwent thematic analysis using NVivo software (QSR International, Warrington, UK).
Patient and relative experience survey
Questions from the following existing UK-validated questionnaires were reviewed for inclusion by the survey subgroup:
-
NHS National Inpatient Survey13
-
Jenkinson et al. ’s Picker Patient Experience Questionnaire101
-
Sullivan et al. ’s Reduced NHS National Inpatient Survey AMU questionnaire102
-
Family Satisfaction in ICU survey103
-
NHS Friends and Family Test. 14
From these surveys, we extracted those questions that were most relevant to attitudes and behaviours and were applicable to any acute care area in the hospital. We excluded questions that related to logistics (e.g. waiting list delays), related to technical aspects of care (e.g. complications of treatment) or were location specific (e.g. outpatient clinic attendance). This allowed us to use the same survey for the AMUs and the ICUs. We focused on questions relating to non-technical aspects of care (e.g. care delivery and communication), which could be influenced by individual members of staff.
The survey that best met our criteria was the Family Satisfaction in ICU survey,103 which provided the majority of the questions in the final set and obviated the need to undertake a prioritisation exercise for question selection. An additional question was from the Friends and Family Test. 14 Two free-text options were included to ask which aspects of care could be improved and what went well. Limited demographic information was requested. Respondents were given the option of providing their contact details if they wanted a response from the local project lead.
We chose not to offer the survey in languages other than English, partly on grounds of cost–benefit (the process of translation, reverse translation and validation for multiple languages would have added considerable complexity) but mainly because the aim of the survey was to obtain sufficient information to provide material for staff reflection, not to provide a comprehensive assessment of the clinical service, which was the responsibility of the trust.
The final survey that was developed was reviewed and piloted by the whole collaboration prior to implementation.
Eligibility
The PEARL project patient and relative experience survey was offered on alternate days to patients who had been in the AMU for ≥ 24 hours and to patients who had been in the ICU for ≥ 48 hours, to take into account the numbers of patients and the median length of stay for each type of unit. Family members were invited to complete the survey if the patient did not have full capacity to do so. Units liaised with their informatics departments to create automated lists of eligible patients on a weekly basis. A letter accompanied each survey, which contained information on the purpose of the enquiry. If patients had died during their hospital stay, a different letter was sent to the next of kin, expressing condolences and asking if they would mind completing the survey from their perspective. Surveys were accompanied by a pre-paid return addressed envelope.
Dissemination
The PEARL project patient and relative survey was distributed for a continuous 2-year period from June 2017 to May 2019. Participating units were given three different options for disseminating the PEARL project patient and relative experience surveys to eligible participants:
-
option 1 – offer the questionnaire on unit discharge (implied consent from the return of the questionnaire)
-
option 2 – take consent and provide questionnaire on unit discharge
-
option 3 – clinical team post out the questionnaire following hospital discharge (implied consent from the return of the questionnaire).
During piloting, hospital teams used the method most suitable for their unit (unit size and capacity varied widely). The teams found that personally handing out the questionnaires to patients on the unit was very time-consuming and, therefore, all units moved to posting out the questionnaires following discharge from hospital.
Surveys were sent with the appropriate cover letter, participant information sheet and pre-paid return envelope. Completed surveys were sent back to the central project team for processing and analysis.
Surveying bereaved families
Previous studies have shown that satisfaction with care is often higher in bereaved families; therefore, we did not want to exclude these families from the PEARL project. Each local team was encouraged to liaise with the bereavement services in their trust for support with any interactions project staff may have with the families at a sensitive time. An appropriately adapted cover letter for families of the bereaved accompanied the PEARL project questionnaire, clearly providing the contact details of the local project lead at each site for the relatives to make contact with if they felt upset and wanted to speak or meet with someone from the research team. Counselling was available for families, which was provided through the bereavement departments at trusts, if they felt that they would benefit from this.
Processing and analysis
Once the completed questionnaires arrived to the central team they were initially reviewed, and any serious concerns were flagged to the appropriate local project leads for investigation.
Responses were allocated subject numbers and logged as a research accrual with NIHR’s Central Portfolio Management System. Each centre recorded the number of surveys distributed and reported these data to the central team to allow calculation of response rates for each unit.
Surveys were developed and prepared for digital scanning. The responses were digitised, analysed and reported to each local project team on a quarterly basis. Once the surveys were scanned, the data management team would take a random sample of > 10% of the data and check that there were no issues with the scanning. When issues were identified, the data management team would undertake further action: either check all data or request a new scan of surveys.
Data were presented to the units as standardised reports that showed the proportion of respondents selecting each level of strength of agreement with each statement. Performance–importance plots (PIPs) were also provided to illustrate the relationship between the level of satisfaction with each item in the questionnaire and how that particular item influenced overall satisfaction. Free-text responses were transcribed and underwent thematic analysis using NVivo software. Using sentiment analysis, the first node divided free text into positive or negative responses; those containing both were allocated to both categories. Within each of these categories, secondary coding employed emergent themes as these were identified by the researchers reviewing the data.
The reports that were returned to the centres were a graphical representation of the survey data returned in the previous quarter, even if they were from an earlier quarter. Data from the NHS Friends and Family Test for the corresponding time period were obtained for the corresponding hospital sites or trusts and an estimate for the national AMU and ICUs. Not all organisations use the Friends and Family Test in ICUs and each trust has different naming conventions for their ICUs/AMUs, so we may not have captured the results of the Friends and Family Test for all AMUs/ICUs.
In addition to the stacked bar charts and pie charts, a domain score was calculated for experience of communication and experience of care, and PIPs were also generated. The domains are a weighted score of all relevant indicators in which a strong positive statement is given a score of 100, a positive statement a score of 80, a neutral statement a score of 50, a negative statement a score of 20 and a strong negative statement a score of 0.
Performance–importance plots were generated for each unit and for the combined ICU/AMU. The PIPs report the correlation between each question and the overall satisfaction score and how many respondents chose the ‘best’ answer for this question. From the median values for each axis, four quadrants are identified: areas performing well, areas in higher need of improvement, areas potentially overperforming and areas that may need improvement but are a lower priority.
Staff experience survey
Development of the survey: Delphi method for prioritisation and selection of survey items
The aim of the PEARL project staff survey was to gain insights into individual, contextual and organisational influences on staff behaviour that might affect patient experience. This included attitudes towards reflection and to the use of patient experience data.
As with the patient and relative survey, it was felt that there was no single existing survey that met our requirements for the project. Therefore, we assembled material from four existing UK-validated surveys that focused on staff experience and patient safety: the NHS Staff Survey18 from 2016, Hospital Survey on Patient Safety Culture,104 Teamwork and Safety Climate Survey105 and the GMC Trainee Survey. 106 To these we added questions derived from the PEARL project ethnography topic guides. These were based on the COM-B44 framework and the theoretical domains framework. 107 Where the original surveys employed questions, we converted these to statements using a 5-point strength of agreement Likert scale, retaining as much of the original phrasing as possible (as with the patient and relative experience survey).
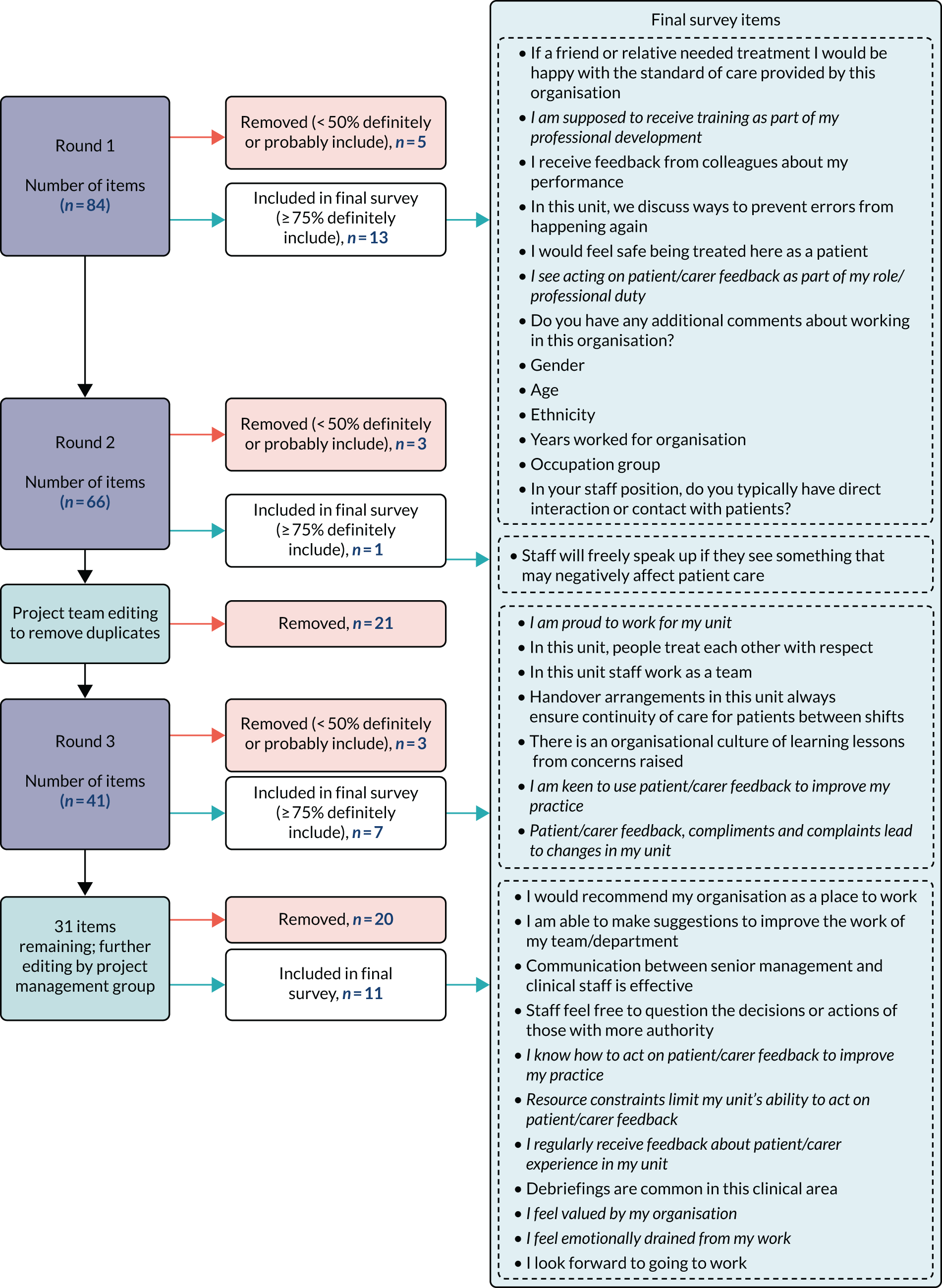
We used a prioritisation method (Delphi) for statement selection because of the diversity and range of options available. The statements were circulated by e-mail to the collaboration and the respondents were asked to rate each statement using a four-point scale: ‘definitely include’, ‘probably include’, ‘probably exclude’ and ‘definitely exclude’. Each e-mail ‘round’ carried forward the outputs from the preceding round.
Responses were categorised as follows:
-
Statements that achieved ≥ 75% agreement to definitely include did not go into the next round, but were extracted and reserved for the final survey.
-
Statements that achieved ≥ 50% agreement to either definitely or probably exclude were removed.
-
Statements that achieved < 100% but ≥ 50% agreement to either definitely or probably include were retained for the next round.
Following three rounds of Delphi prioritisation, a final set of survey questions emerged to form the final PEARL project staff survey. The Delphi process and outputs are presented in Figure 1. Basic demographic questions were included along with one free-text question asking ‘Do you have any additional comments about working in this organisation?’.
FIGURE 1.
The PEARL project staff survey Delphi methodology flow chart. Italic text indicates an item developed from PEARL ethnography topic guides.
Eligibility
The PEARL project staff survey was offered to all clinical, administrative and managerial staff whose primary working area was the AMU or ICU at the participating hospitals. This included doctors (consultants to foundation grade), nurses (bands 5 to 8), administrative and clerical staff (including operational managers), health-care assistants, maintenance and ancillary staff, AHPs and pharmacists. Dissemination logs were maintained locally, with figures reported to the central team to allow calculation of response rates for each unit.
Sampling and consent
The staff survey was distributed twice for a 2-month period during the PEARL project (January to February 2018 and January to February 2019). As with the patient survey, implied consent applied and the surveys were anonymous.
Dissemination
Local units were advised to use the method of dissemination most appropriate for them. Options included via staff pigeon holes, attachment to monthly payslips, at weekly/monthly staff meetings, in staff/locker rooms or posting out. Questionnaires were disseminated with a pre-paid return envelope for completed responses to be sent back to the central project team for processing and analysis.
Processing and analysis
As with the patient and relative survey, once the completed staff surveys were received by the central team a random sample of 10% was reviewed by the data management team and any issues identified were resolved before further processing. All free text was transcribed and classified using NVivo; any serious concerns were flagged to the appropriate local project leads for investigation.
The responses were digitised, analysed and reported to each local project team as standardised reports that showed the proportion of respondents selecting each level of strength of agreement with each statement. In addition to the stacked bar charts and pie charts, an overall domain score was calculated for staff experience. The domain score was calculated using the responses to statements relating to perceptions of care quality and the working environment and excluded those statements relating to personal reflection: a strong positive statement was weighted with a score of 100, a positive statement with a score of 80, a neutral statement with a score of 50, a negative statement with a score of 20 and a strong negative statement with a score of 0. Data from the NHS staff Friends and Family Test for the corresponding time period were obtained for the corresponding hospital sites or trusts. National comparative data for AMUs and ICUs were estimates because different naming conventions for these units between trusts meant that some may have been omitted. For the second survey, comparisons were made with the results of the first survey.
Survey validity and reliability
Before disseminating the first survey, we decided to exclude any question with any of the following response characteristics:
-
a non-response rate of > 10%
-
a lack of discrimination (defined as > 70% of all respondents ‘strongly agreeing’ or ‘strongly disagreeing’ with the statement)
-
redundant (defined as questions with an item-scale Cronbach’s α of < 0.7).
Based on the initial analyses of the first survey, no question met any of the above criteria; therefore, all questions were retained for the second round. Following the second round the analyses were repeated and again no question met any of the above criteria for removal.
Workstream 3: ethnography – phase 1 and phase 2 methods
Workstream 3 took place in two phases.
Phase 1 aimed to investigate current use of patient experience data, to explore options for the feedback of data as part of the reflective learning process and to investigate experiences of, barriers to and opportunities for workplace-based reflective learning.
Phase 2 focused on observations of local co-design meetings and of the implementation and piloting of components of the toolkit in practice. Findings from both phases were used to inform the development of the RLF and toolkit in WS4.
Phase 1
Ethnographic research that was conducted in phase 1 focused on gaining insight into attitudes and practice relating to feedback and reflection on patient experience, through observing day-to-day practice and interviewing a purposive sample of staff across the sites. Topic guides were developed to ensure consistency between ethnographers for phases 1 and 2.
Our key aims for phase 1 were to:
-
systematically describe the approaches used to feedback experiential and quality and performance metrics in ICUs and AMUs
-
obtain staff views about credibility, utility and impact of different approaches to feed back patient experience data
-
explore staff engagement with reflective learning based on patient experience data and identify how individual and group reflection can be promoted in practice
-
identify the factors that affect the extent to which reflection is translated into action at the front line of practice
-
inform the co-design of the RLF and toolkit.
We conducted observations and interviews in eight acute care units (three AMU-type and five ICUs) in the three NHS trusts participating in the PEARL project, between May and December 2017. Characteristics of the sites were as follows:
-
Site P1 had an ICU and a high-dependency unit (HDU), referred to jointly as ‘critical care’, as well as a separate large AMU.
-
Site P2 had an ICU and a separate clinical decisions unit (CDU) (equivalent to an AMU) with an acute medical clinic attached to it.
-
Site P3 was split over two sites: one site had two ICU wards with attached HDUs and an AMU (referred to as the ‘assessment suite’) and the other site had one ICU with an attached HDU.
We conducted > 140 hours of observations in ICUs and AMUs, including 81 informal documented conversations with a wide range of staff. We collected relevant documents, such as newsletters and photos of patient experience displays, in the units. Observations were recorded as written field notes and audio-recorded debriefs. We undertook 45 formal, semistructured interviews with a purposive sample of staff members, including administrative, nursing and medical staff, sampled to include diversity in their role and level of involvement in trust activity around patient experience data. Interviews and observational visits were conducted in two rounds (May to June 2017, prior to the introduction of the PEARL project patient experience questionnaire, and November to December 2017, after data collection had started). We conducted 36 interviews in round 1, which were focused on the collection and use of patient experience data and engagement in reflection, and nine interviews in round 2, which focused in more detail on reflection in practice. Interviews lasted between 10 and 90 minutes (mean 38 minutes). Informed consent was obtained for interviews. Breakdown by site is shown in Table 1.
| Interview characteristic | P1 | P2 | P3 |
|---|---|---|---|
| Approximate observation time (hours) | 43 | 49 | 55 |
| Interviews (n) | |||
| Formal | 15 | 14 | 16 |
| Informal | 17 | 23 | 41 |
| Staff (n) | |||
| Medical | 5 | 6 | 6 |
| Nursing | 6 | 7 | 7 |
| Administrative | 4 | 1 | 3 |
Phase 2
Phase 2 involved observations and interviews. The main aim of phase 2 was to gain insight into staff experiences of using tools to select and design interventions to promote reflection in practice in order to inform the development and implementation of the reflective learning toolkit.
We conducted observations of the local project team meetings in which sites piloted components of the draft toolkit that had been designed to support the selection of reflective practice interventions, and planned for implementation (April to May 2019). We conducted interviews with members of staff at each site who had attended these meetings in order to gain feedback on the approach taken in the meetings and how well the draft toolkit components had worked as well as to capture their experiences of developing and trialling their selected interventions (June 2019). We observed four meetings in total (site P1, two meetings; sites P2 and P3, one meeting each). The first meeting at site P1 lasted approximately 1 hour and the second meeting was approximately 2.5 hours long; the meetings at sites P2 and P3 lasted around 2 hours. Observations were recorded as written field notes and audio-recorded debriefs. We conducted 15 interviews (June to July 2019) with a range of staff (five per site) about their experience of choosing interventions during the meeting and the progress in implementing any chosen interventions on the ICU or AMU wards. Informed consent was obtained for all interviews. Interviews lasted between 26 and 85 minutes (mean 49 minutes). Breakdown by site is outlined in Table 2.
| Interview characteristic | P1 | P2 | P3 |
|---|---|---|---|
| Approximate meeting observation time (hours) | 3.5 | 2 | 2 |
| Number of interviews (n) | 5 | 5 | 5 |
| Staff (n) | |||
| Medical | 1 | 4 | 3 |
| Nursing | 4 | 1 | 2 |
Analysis of phases 1 and 2
Interviews and observation debriefs were recorded and professionally transcribed verbatim; anonymisation took place during transcription. We conducted regular team debriefs during the data collection period to reflect on emerging findings and guide ongoing data collection, and we discussed findings with the wider team. Analysis of data from phases 1 and 2 was conducted separately.
For phase 2 we conducted an analysis to characterise the features of meaningful patient experience feedback and to explore the barriers to and facilitators of effective reflection on patient experience in practice. A thematic analysis approach was taken to analyse the transcripts of the interviews and observational data. 108 A subset of interviews was read in close detail and open-coded to create a code frame and initial thematic categories; these were discussed with the wider study team. The coding frame was then applied to the remaining interviews and observational data transcripts. As new themes arose, there was flexibility to extend the coding frame to capture these. We used case studies, narrative reports and visual data displays as ways of facilitating comparison across sites and synthesising findings. Findings from the analysis of phase 1 data were used throughout the co-design process to inform the development of reflective practice interventions and the toolkit as a whole. Phase 2 data were subject to a separate thematic analysis closely linked to the aims of identifying lessons for development of the toolkit. NVivo 11 software was used to support the management, coding and querying of the data.
Workstream 4: co-design of the reflective learning framework and development and piloting of the toolkit
Introduction
Co-design refers to a set of practices that can be used to allow diverse stakeholders to come together to address a shared issue. The ‘co’ prefix refers to the participatory nature of the activity and ‘design’ refers to both the technical skills and practices of design and the unique approach to problem-solving approach used by designers.
Co-design has previously been used in health care. The most widely published approach is experience-based co-design, which accesses the experiences of patients and relatives and staff from videoed interviews109 or directly in interactive group discussions. The PEARL project co-design approach was supported by the Translating Knowledge into Action (TK2A) theme110 of the NIHR Collaborations for Leadership in Applied Health Research and Care Yorkshire and Humber. The TK2A theme is a multidisciplinary team of health service researchers who have developed over the last 10 years111 methods drawn from design practice, with a focus on the use of creative practice to support the successful sharing and synthesising of knowledge. 112
The reflective learning framework
The RLF is the programme theory or logic model for the PEARL project. It is the health services equivalent of a systems specification in computing or a drug’s mechanism of action. It describes how reflective learning might ‘work’. We developed the RLF iteratively throughout the project, making modifications to the theory as we gained insights from the ethnographic work and from our observations of the co-design process for the toolkit. We based our approach on that recommended by Davidoff et al. 113
We defined reflective learning as an experiential process of personal insight development in which one’s own and others’ experiences are used to produce a change in attitudes and behaviours. We characterised the features of effective reflective learning based on Dewey’s58 three phases of reflection (retrospection, self-evaluation and reorientation), to which we subsequently added Gibbs’ six-step cycle114 and Schön’s50 categorisation of reflection occurring in-action or on-action.
In mapping out the factors affecting engagement in effective reflective learning, we drew on the COM-B framework. 44 With effective reflective learning as the behaviour of interest, the COM-B framework identifies three domains of determinants, each with two subtypes: capability (physical and psychological), opportunity (physical and social) and motivation (reflective and automatic). As the COM-B framework was both parsimonious and evidence based, we decided to incorporate it in our preliminary version of the RLF. An important element of our conceptualisation is that the ‘B’ in COM-B signifies engagement in effective reflective learning: completing the cycle of insight development, attitude change and resulting change in interpersonal behaviour and practice.
This framework incorporates the dynamic in which an input (e.g. experiential information from the surveys) would, depending on the ‘COM’, result in the behaviour of effective reflective learning (primary output). This would generate measurable changes in attitudes and practices, and enhanced care delivery and teamworking (proximal and distal outcomes).
Iterative versions of the RLF were developed by the core project team and presented for critique at the co-design workshops. Participants at the co-design workshops reviewed the RLF for both understandability and scientific credibility and provided feedback that was used in the next iteration. The COM-B framework was used to classify interventions to drive engagement in effective reflective learning as these emerged from the co-design process. We show the evolution of the RLF in Chapter 3.
Toolkit co-design
The co-design meetings
Three facilitated and supported local meetings were held at each of the three sites (nine meetings in total) plus three plenary workshops for all participants. A fourth local meeting was then conducted by each team working without an external facilitator or project team support.
There were three main aims of the co-design meetings:
-
to identify ‘touchpoints’ – key moments in the experience of health care – that provide insights into how we use reflection to understand ourselves and others
-
to understand how different individuals may experience reflection
-
to create or adapt interventions to promote reflective learning in the workplace.
Participants
The co-design meeting participants included a broad range of patients and staff, not just members of the PEARL project team. There were between 10 and 20 attendees, which resulted in manageable and productive meetings. Patients and relatives were equal contributors; they received prior explanation about the purpose of the meetings and the facilitators ensured that they had time and space to develop their own ideas and voice. Mutual understanding emerged from this process. For example, a mother and son gave important insights into communication behaviours, such as staff directing questions and information to the mother when it was quite possible to communicate directly with her son (the patient). Conversely, at the end of one co-design session, an erstwhile patient said that he had not realised how emotional the experience of delivering acute care was for the staff. These and many other insights provided useful examples for linking the COM-B theory to practical reflection tools.
Planning
Each co-design meeting was planned in advance by the PEARL project management committee and facilitator. Recognising that taking time out of the working day is often difficult, local teams were asked to obtain approval from managers and colleagues, and allowances were made for last-minute variations in the number of participants, consequent on the demands of the clinical services. A meeting room was booked, with refreshments and lunch, for a minimum of 4 hours.
Facilitation
Facilitation of the nine co-design local meetings and the three workshops was provided by the Art and Design Research Centre, Sheffield Hallam University (Sheffield, UK). Skilled and sensitive facilitation was essential to promote the flow of conversation, manage emotions, permit periods of silence, allow humour to release tension and ensure that everyone had an opportunity to express their ideas and opinions, regardless of status, seniority or specialty. The facilitation team comprised three members of the TK2A team. The theme lead and clinical researcher are a nurse and physiotherapist, respectively, both having worked on creative co-design projects across a broad range of topic areas for the last 10 years. The third member of the TK2A team is a designer who has worked in health-care contexts and co-design since completing their doctorate. The team were able to function as experts in the co-design process but could claim independence from the team, unit and hospital. A scribe recorded key points, conclusions and actions, and how these were derived. Each meeting was observed by two ethnographers for subsequent distillation and analysis.
The tools and techniques used for co-design were based in part on the NIHR’s Better Services by Design website. 115 The process was underpinned by the ‘double diamond’ approach (‘discover, define, develop, deliver’) in which the first workshop focuses on the key issue, the second expands the discussion to consider the wider context, the third refocuses on developing specific interventions and the final workshop allows participants to report their piloting of the interventions.
Each session started with a brief summary of the purpose of the project and a recap of the preceding activities. The facilitator then invited everyone to introduce themselves, followed by an ‘ice-breaker’ exercise to promote the conditions required for co-design to take place, after which the group undertook the activities described below. Each small working group (between two and four for each meeting, dependent on numbers) was supported by the facilitators and team. Plenary sessions allowed sharing of discussions and outputs. A summary was constructed at the end from all of the participants.
Co-design 1: reflectable moments
The aim of this first workshop was to allow the group to explore the meaning of reflection and how it ‘works’. Participants were invited to describe ‘reflectable moments’: events or activities that stimulated reflection in themselves or others, what feelings were aroused, how these feelings were used to gain insight into oneself or others and how those insights could stimulate generalisable learning. This process aroused emotions that the facilitator channelled into creative energy.
Participants modelled reflectable moments using cut-out figures (Figure 2) to recreate the characters and situations that they had encountered. This allowed the participants to tell their story with both realism and a degree of detachment, recognising the benefits of making the intangible tangible through creative practices. 116
FIGURE 2.
Co-design meeting 1 resources. (a) Cut-out figures; and (b) reflection wheel.

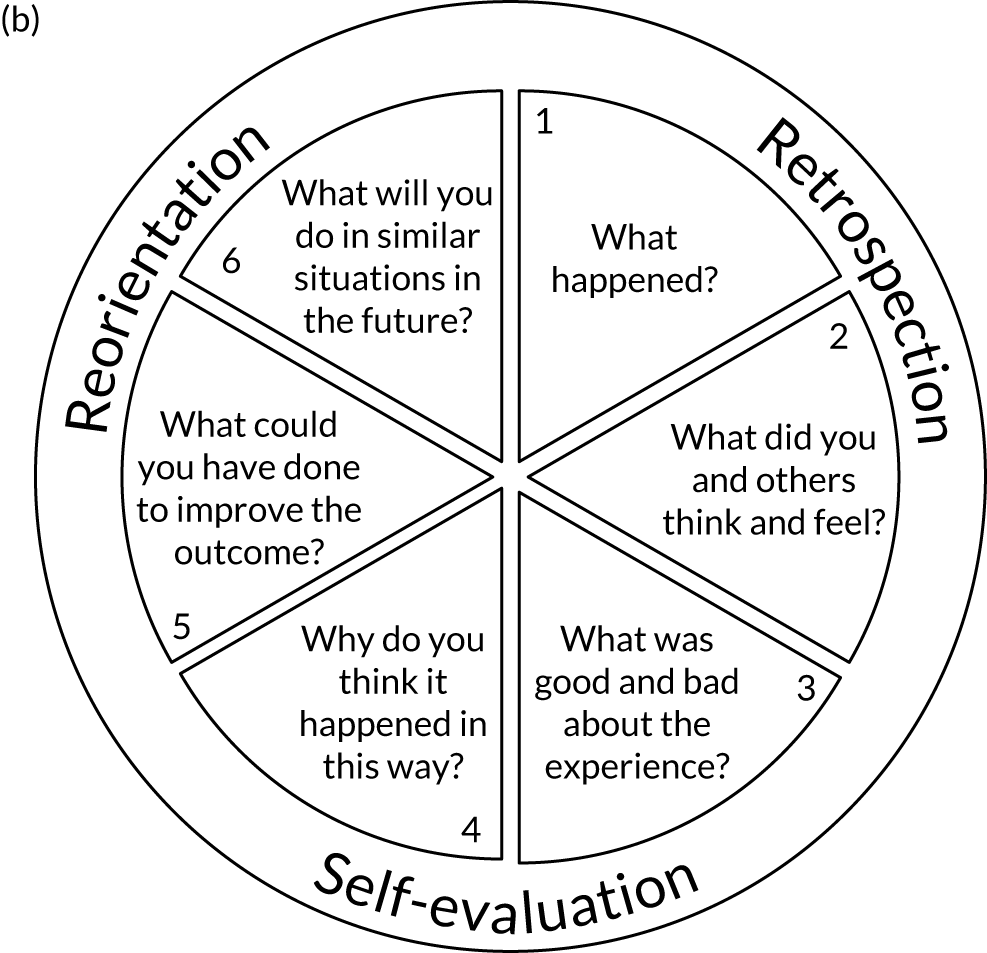
Analysis of the thought processes used by the participants allowed us to combine the three-stage Dewey model58 and six-step Gibbs cycle114 into a single ‘reflection wheel’. It was also clear that individuals varied in their approaches to reflection: in-action, on-action, solitary and group.
Co-design 2: reflection personae
The second workshop gathered participants’ opinions and experiences of reflective behaviours as demonstrated by others, by creating reflective character types or personae. Individuals may accommodate more than one reflection stereotype, but isolating these in caricatures permits participants to focus on specific issues and promotes examination of one’s own attitudes to reflective learning.
The participants were invited to form four groups to consider one each of the following types: the ‘groupie’, the ‘ruminator’, the ‘loner’ and the ‘non-reflector’ (Figure 3).
FIGURE 3.
Co-design meeting 2 resources. (a) Reflection personae; and (b) reflective learning activities table.
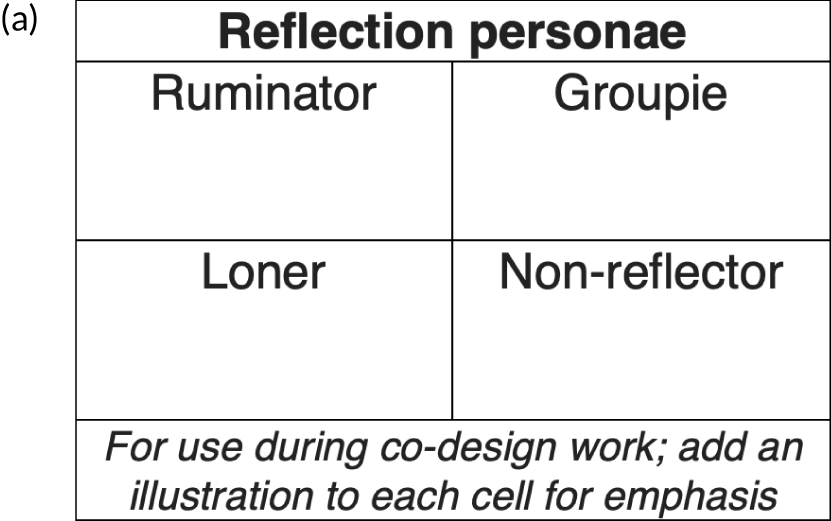
For each of these personae:
-
Small group session 1 – participants created a fictitious but believable character based on that reflection type using the template (20 minutes).
-
Plenary session 1 – participants described that character to the other groups (5 minutes for each group).
-
Small group session 2 – participants discussed how each character would respond to a good feedback scenario and a negative feedback scenario (20 minutes).
-
Plenary session 2 – participants considered what actions or interventions might promote effective use of feedback by each character (5 minutes for each group).
The scribe classified outputs from plenary session 2, which were subsequently transcribed using the 2 × 2 table to categorise actions and interventions according to whether they were predominantly in-action or on-action interventions and for use by groups or individuals.
Co-design 3: designing interventions to incorporate reflection in everyday activities
The third meeting was conducted twice: the first time it was facilitated and supported by the PEARL project management committee and the second time it was conducted independently by the local teams using additional tools. We describe here the second of these two meetings.
Participants were asked to examine the list of prioritised reflection tools and activities (see Table 9).
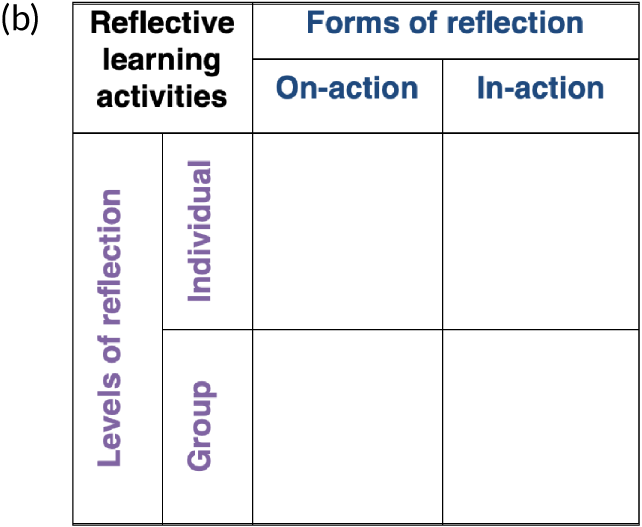
In step 1, participants were given polling cards to give their private views on the extent to which the unit staff had the capability, opportunity and motivation to reflect on patient and staff experience (Figure 4). The anonymous responses were collected, the scores for each element (capability, opportunity and motivation) were summed and the percentage agreement for each proposition was determined by dividing the sum of the scores for each element by the number of respondents and multiplying by 100.
FIGURE 4.
Co-design meeting 3 resources.
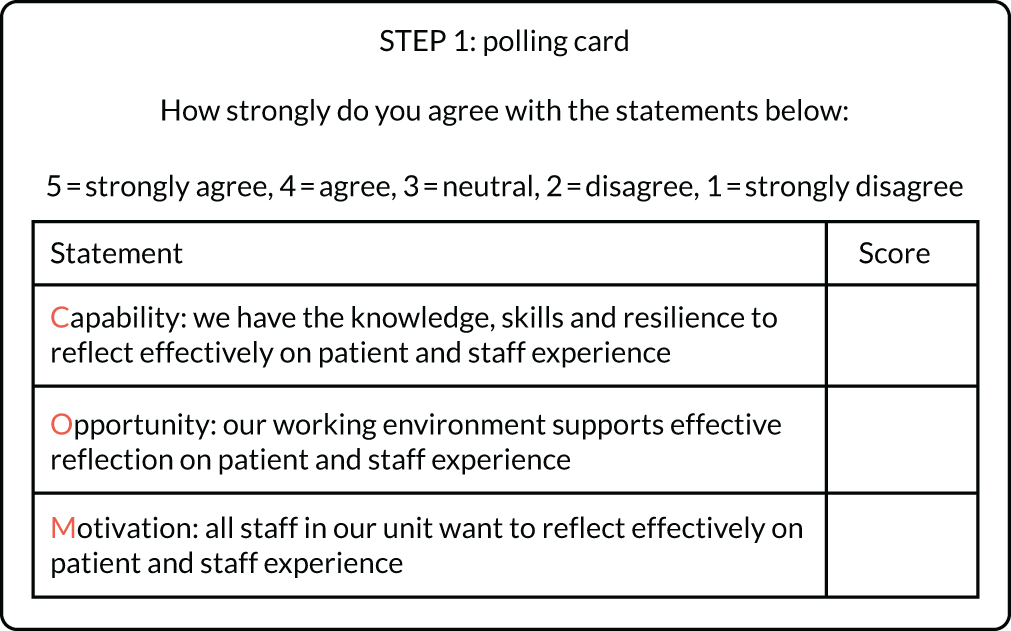
In step 2, the difference between the actual percentage agreement and the maximum percentage agreement (100%) provided an indication of the perceived gap between the current position and the ideal position for each element of the framework. Participants were asked to discuss the possible reasons for each gap, for example by asking ‘What would be needed for you to give this element a top rating of 5?’.
In step 3, based on the gap analysis, from the list of prioritised interventions (see Table 9) and working in small groups the participants developed a maximum of three using the reflection specification template (Table 3). Participants were asked to focus on actions or activities that promote reflection, not on those that ‘fix the problem (identified using the feedback collected)’. For example, when considering how to enhance reflection during handovers or ward rounds, using a checklist is unlikely to promote reflection (although it will be highly beneficial for many other reasons), whereas starting the handover or round with some feedback from one of the surveys, encouraging input on the round from the relatives or ending the round with a quick debrief, could stimulate reflection by giving everyone a voice.
In step 4, in plenary session, participants presented their activity to the whole group. A task management and delivery plan was completed for each activity.
In step 5, teams were asked to pilot the intervention using rapid cycle approaches (test, evaluate, retest and spread) and provide feedback to the final plenary workshop.
| Reflection intervention | |
| Describe briefly here the nature of the intervention (e.g. ward round, handover, debriefing, posters, coffee mornings, induction training) and then complete the right-hand column below: | |
| What will you do? | • |
| Why will this activity help staff be reflective? | • |
| Who can participate in this activity? | • |
| When will it occur? In-action (‘hot’), near action (‘warm’), or on-action (‘cold’)? | • |
| Where will the reflection take place/be located? | • |
| How can the reflection be structured or supported? | • |
| Barriers: what might limit the effectiveness of this reflection? | • |
| Enablers: what factors might make the reflection more effective? | • |
| Outputs: what impact will this particular act of reflection have? | • |
Prioritisation of the reflection activities and tools
We identified potential candidate tools and interventions for inclusion in the toolkit in several ways. During the co-design meetings and workshops, staff identified numerous methods for promoting reflective learning. Some of these activities were already in routine use, others were aspirational and some were unconstrained by practical considerations. The ethnographers also identified and described approaches for reflection in practice from their observations and interviews.
We combined the outputs of these nine workshops with the findings from the observational and interview work undertaken by the ethnographers to assemble a list of tools and activities that had the potential to enhance reflective learning. This list was then circulated to the local project teams as a questionnaire, with the request that each member rated each of the tools or activities for effectiveness and feasibility using a 5-point Likert scale (5 = strongly agree, 4 = agree, 3 = neutral, 2 = disagree and 1 = strongly disagree). Effectiveness was defined as ‘the likely impact of the activity if it were to be introduced to your unit’. Feasibility was defined as ‘the likelihood that it could be introduced and would be acceptable to most staff’.
Responses were aggregated and median ratings were determined. The following cut-off points were used to determine inclusion, exclusion or further consideration:
-
inclusion – effectiveness median of 4 or 5
-
exclusion – effectiveness median of 1 or 2, or effectiveness median of 3 and feasibility median of 1, 2 or 3
-
further consideration – effectiveness median of 3 and feasibility median of 4 or 5.
The outputs from this process are described in Chapter 3.
Patient and public involvement
The PEARL project has put patients and relatives at the centre of the research because they were involved in the inception in the initial design, contributing as full collaborators. There was patient and public involvement (PPI) representation on all of our project teams and committees. The central project team had two PPI representatives, the Project Steering Committee had one PPI representative and the local project teams had eight PPI representatives.
Patient and public involvement representation in the local project teams were as follows: site 1 benefited from two PPI representatives, one of whom was disabled, and sites 2 and 3 each had three PPI representatives. A benefit of the PPI members attending was the opportunity for local leads to consult with them about the running of the project locally (such as raising awareness of the patient and relative experience survey). Patients and relatives also offered their thoughts on the feedback received in the reports from the project surveys, and contributed to actions that were taken as a result of the feedback.
The PEARL project is a developmental project using co-design to develop the RLF. To develop the framework, the PPI representatives in the local project teams were equal partners in the co-design meetings and the facilitated plenary workshops (described above). They have informed decisions about the extent to which PPI representatives can contribute to this type of co-design process. An example of PPI engagement is that they developed the cue cards that were used in group work for stimulating effective reflection.
All PPI representatives who have been involved in the project are full members of the PEARL project collaboration and are acknowledged as co-authors in all publications and project outputs. They will also participate in dissemination activities.
Chapter 3 Results
Given the inter-related nature of the four workstreams, we present the project outputs by theme rather than by workstream.
Overview
There was excellent engagement by the three trusts, with the AMUs and ICUs working together to form a unitary local project team at each centre. This was a comparatively novel collaboration for the staff because acute medicine and intensive care medicine are distinct specialties working in separate locations. Each local project team included patient representatives, with the initial contact being made through existing unit-based patient groups, Patient Advice and Liaison Service (PALS) or personal interaction after a period of clinical care. The fast-paced throughput of the AMUs made it more difficult for the staff to establish longer-term relationships with patients, unless the acute physicians also undertook follow-up clinics. The patient representatives supported the co-design meetings and workshops, with a median of two members from each centre attending each session.
Each local project team was chaired by a non-executive director (two centres) or an executive director (one centre). The choice of the executive director was made by the chief executive of that trust. The chairpersons tended to provide support locally rather than engage in the plenary workshops.
The PEARL project patient and relative experience survey
Respondents and response rates
The PEARL project patient and relative survey was distributed continuously for 2 years from June 2017 to May 2019. A total of 18,616 surveys were disseminated and 4747 responses were received (overall response rate 25.5%). Response rates were higher in ICUs (35.4%) than in AMUs (20.1%) (Table 4).
| Trust | AMU/ICU | Number of eligible patients | Number of questionnaires administered | Number of questionnaires returned | Per cent of eligible patients receiving questionnaire | Response rate (%) |
|---|---|---|---|---|---|---|
| Site 1 | AMU 1 | 8508 | 6131 | 1212 | 72.1 | 19.8 |
| ICU 1 | 5574 | 3177 | 1112 | 57.0 | 35.0 | |
| Site 2 | AMU 2 | 5173 | 3276 | 593 | 63.3 | 18.1 |
| ICU 2 | 784 | 426 | 114 | 54.3 | 26.8 | |
| Site 3 | AMU 3 | 4125 | 2642 | 620 | 64.0 | 23.5 |
| ICU 3 | 1357 | 1051 | 342 | 77.5 | 32.5 | |
| ICU 4 | 1206 | 937 | 380 | 77.7 | 40.6 | |
| ICU 5 | 1413 | 976 | 374 | 69.1 | 38.3 | |
| All AMUs | 17,806 | 12,049 | 2425 | 67.7 | 20.1 | |
| All ICUs | 10,334 | 6567 | 2322 | 63.5 | 35.4 | |
| Overall | 28,140 | 18,616 | 4747 | 66.2 | 25.5 | |
Approximately 60% of surveys were completed by the patient, 20.5% by family members and the remainder by both the patient and the relative. Given the difference in the severity of illness, it was expected that more ICU than AMU responses would have been completed by the relative; however, this was not the case: the distribution of respondents in the categories was similar for both AMUs and ICUs (Table 5).
| Trust | AMU/ICU | Patients, n (%) | Relatives, n (%) | Patients supported by a relative, n (%) | Unknown, n (%) | Total, n |
|---|---|---|---|---|---|---|
| Site 1 | AMU 1 | 705 (58.2) | 275 (22.7) | 220 (18.2) | 12 (1.0) | 1212 |
| ICU 1 | 702 (63.1) | 220 (19.8) | 180 (16.2) | 10 (0.9) | 1112 | |
| Site 2 | AMU 2 | 381 (64.2) | 108 (18.2) | 101 (17.0) | 3 (0.5) | 593 |
| ICU 2 | 46 (40.4) | 37 (32.5) | 30 (26.3) | 1 (0.9) | 114 | |
| Site 3 | AMU 3 | 446 (71.9) | 86 (13.9) | 83 (13.4) | 5 (0.8) | 620 |
| ICU 3 | 167 (48.8) | 117 (34.2) | 56 (16.4) | 2 (0.6) | 342 | |
| ICU 4 | 258 (67.9) | 66 (17.4) | 54 (14.2) | 2 (0.5) | 380 | |
| ICU 5 | 255 (68.2) | 65 (17.4) | 53 (14.2) | 1 (0.3) | 374 | |
| All AMUs | 1532 (63.2) | 469 (19.3) | 404 (16.7) | 20 (0.8) | 2425 | |
| All ICUs | 1428 (61.5) | 505 (21.7) | 373 (16.1) | 16 (0.7) | 2322 | |
| Overall | 2960 (62.4) | 974 (20.5) | 777 (16.4) | 36 (0.8) | 4747 | |
The self-identified ethnicity of the respondents was predominantly white British (88.8%) (Table 6).
| Trust | AMU/ICU | White, n (%) | Non-white, n (%) | Unknown, n (%) | Total |
|---|---|---|---|---|---|
| Site 1 | AMU 1 | 1055 (87.0) | 131 (10.8) | 26 (2.1) | 1212 |
| ICU 1 | 966 (86.9) | 125 (11.2) | 21 (1.9) | 1112 | |
| Site 2 | AMU 2 | 468 (78.9) | 111 (18.7) | 14 (2.4) | 593 |
| ICU 2 | 93 (81.6) | 18 (15.8) | 3 (2.6) | 114 | |
| Site 3 | AMU 3 | 590 (95.2) | 20 (3.2) | 10 (1.6) | 620 |
| ICU 3 | 321 (93.9) | 12 (3.5) | 9 (2.6) | 342 | |
| ICU 4 | 362 (95.3) | 13 (3.4) | 5 (1.3) | 380 | |
| ICU 5 | 361 (96.5) | 7 (1.9) | 6 (1.6) | 374 | |
| All AMUs | 2113 (87.1) | 262 (10.8) | 50 (2.1) | 2425 | |
| All ICUs | 2103 (90.6) | 175 (7.5) | 44 (1.9) | 2322 | |
| Overall | 4216 (88.8) | 437 (9.2) | 94 (2.0) | 4747 | |
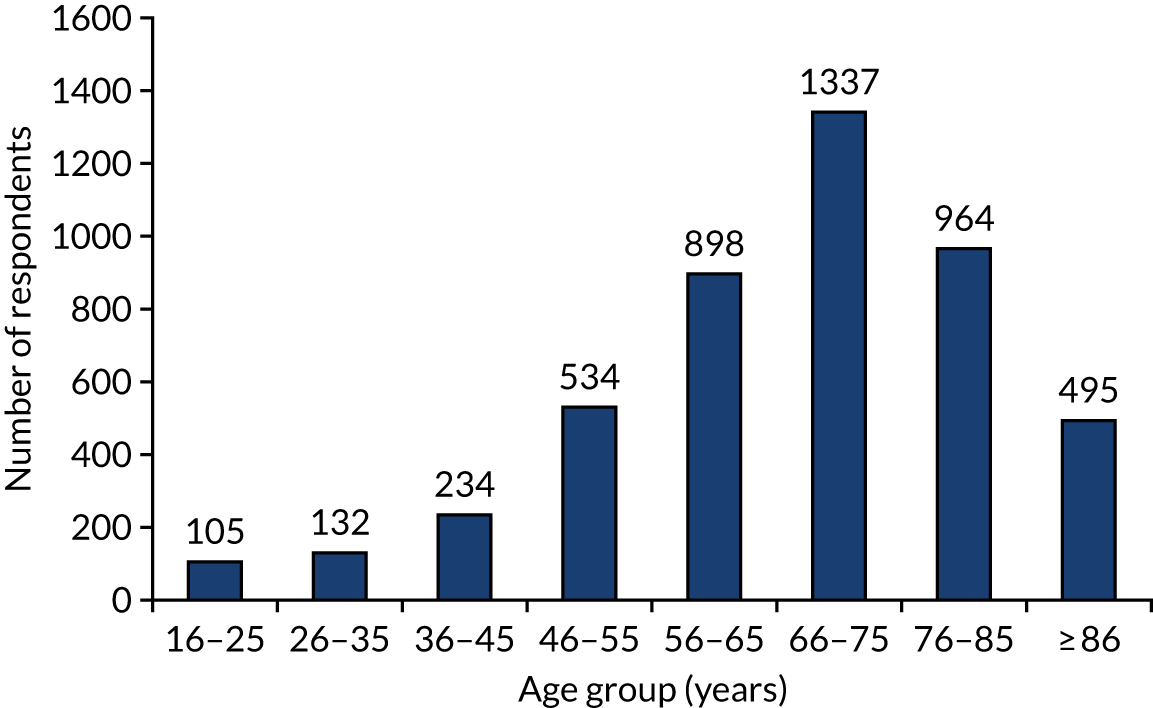
Age characteristics of the respondents are shown in Figure 5. In total, 59.8% (n = 2796) of respondents were aged ≥ 66 years.
FIGURE 5.
The PEARL project patient and relative survey: respondents by age.
Quantitative analysis of survey responses
Respondent ratings from ICU patients and relatives were more positive for all questions than for AMUs. In response to the NHS Friends and Family Test question ‘How likely are you to recommend our unit to friends and family if they needed similar care or treatment?’, 93.5% of ICU patients and relatives selected ‘extremely likely’ or ‘likely’, compared with only 74.3% of AMU respondents (p < 0.0001). This difference was also evident in response to the question ‘How would you rate the overall quality of care you/your relative received in the unit?’: 93.1% of ICU respondents selected ‘excellent’ or ‘good’, compared with 72.0% of AMU respondents (p < 0.0001). There was concordance between patients and relatives in the ICU in their responses: 93.9% of ICU patients selected ‘extremely likely’ or ‘likely’, compared with 92.0% of ICU relatives in response to the Friends and Family Test; 93.4% of patients rated care as ‘excellent’ or ‘good’, compared with 92.3% of relatives. In AMUs, however, patients rated care more positively than relatives: 76.2% of patients compared with 66.7% of relatives selected ‘extremely likely’ or ‘likely’ to the Friends and Family Test question, and 74.4% of patients but only 62.6% of relatives rated AMU care as ‘excellent’ or ‘good’ (p < 0.0001).
All other questions in the PEARL project patient and relative experience survey (excluding question 5, ‘were you ever in pain?’) were phrased as statements with a 5-point Likert scale of agreement for responses (strongly agree to strongly disagree). Notable differences were seen between ICU and AMU respondents, with higher ratings for perceptions of being treated with dignity and respect in ICU respondents (97.0%) than in AMU respondents (88.9%) (p < 0.0001). No other differences were evident between responses from patients and responses from relatives. Confidence in staff was high for both the ICU and the AMU, but again differences were apparent: ICU respondents were more likely to express confidence in doctors (97.7%) and nurses (96.5%) than AMU respondents (88.8% and 88.3%, respectively).
All respondents stated that they were more likely to get answers that they could understand from both doctors (89.2%) and nurses (92.7%) in the ICU than in the AMU [77.6% (p < 0.0001) and 80.2% (p < 0.0001), respectively]. Relatives stated that they were more likely to understand the responses they received from nurses than responses they received from doctors (ICU 93.2% vs. 86.9%, p < 0.0001; AMU 78.6% vs. 72.7%, p < 0.0001).
Significant differences were seen in response to the statement ‘I was able to speak to a doctor when I wanted to do so’: 75.4% of ICU respondents agreed or strongly agreed with this statement, compared with 53.7% of AMU respondents (p < 0.0001). No difference in response was seen between ICU patients and ICU relatives; however, there was a notable difference between AMU patients and AMU relatives: 57.1% of patients agreed or strongly agreed with the statement, compared with 45.8% of relatives (p < 0.0001).
Analysis using performance–importance plots
To illustrate the relationship between the level of satisfaction with each item in the questionnaire and how that particular item influenced overall satisfaction, PIPs were generated. As described in Chapter 2, the PIP compares the percentage of ‘best response’ ratings for each survey item with the correlation coefficient of each item and the overall weighted satisfaction score. Figures 6 and 7 include guidance on interpreting such plots.
FIGURE 6.
Performance–importance plot: aggregated ICU patient survey responses (n = 2322).

FIGURE 7.
Performance–importance plot: aggregated AMU patient survey responses (n = 2425).

The results for ICU respondents are shown in Figure 6 and for AMU respondents in Figure 7. Each survey statement is identified by a number. The survey statement responses relating to communication are coded dark blue and those relating to clinical care are coded light blue. The two questions relating to overall satisfaction are coded orange.
Three conclusions can be drawn from inspection of these plots. The first is that all of the responses relating to communication are clustered in or near the left-upper quadrant, indicating that perceptions of the adequacy of communication strongly determine overall satisfaction. The second is that ICU respondents have a higher median best satisfaction rating (54%) overall than AMU respondents (31%). The third is that, despite this difference between AMUs and ICUs, the pattern is retained: patient and relative experience of communication with staff remains the main driver of (dis)satisfaction.
There are several plausible explanations for these differences between AMUs and ICUs. Compared with ICUs, AMUs have much lower nursing and medical staffing intensities, a higher patient throughput, shorter lengths of stay and, therefore, less time for staff to establish fiduciary relationships with patients and families. It is also likely that, given the high throughput and short length of stay, the AMU data are ‘contaminated’ by patient and relative experiences acquired before AMU admission (e.g. in the ED or a ‘holding area’ awaiting admission) and after transfer out of the AMU to other wards in the hospital with even lower staffing levels.
However, the purpose of the survey is to provide staff with quantitative and qualitative data that can be used as the raw material to promote reflective learning at both the individual and the organisational level. Here, a very clear message emerges: the technical aspects of care are by and large well delivered and it is the non-technical, behavioural aspects of care that affect patient and relative experience.
Analysis of free-text responses
Of the 4747 survey responses received, 3275 (69%) had additional comments relating to how care could be improved and what was done well. Free-text responses from patients and relatives were substantially positive (≈ 60% of comments).
Positive feedback
Most of the positive feedback related to general aspects of the service for both AMUs and ICUs:
First-class service all round.
Keep up the excellent work.
Around one-third of the positive feedback received referred to the high level of care and compassion that was shown to both the patients and their relatives on the units:
The whole family were treated with respect and kept up to date with everything going, the family we were not pushed out and were able to stay with the patient round the clock. All staff showed empathy and respect.
Most positive feedback was generic, referring to all of the staff in the units without singling out professional groups. Sometimes, positive comments referred to named individuals: we reported these separately from the main report to the local project lead. The following descriptors for those individuals were frequently used: caring, friendly, fantastic, excellent, compassionate, polite and kind. The professionalism shown by all staff was also noted. This gave patients and their relatives confidence in the individuals treating them and the care that they received:
My only comment is how excellent all the staff are, and what an extremely frightening time for me and my relatives, they helped put us all at our ease with their confidence, skills and abilities.
Negative feedback
Negative feedback was provided by around one-third of respondents and related predominantly to the following four categories: staffing and resources, communication, the unit environment, and care and compassion.
Staffing and resources
Feedback for this category was more frequently cited by respondents who had spent time in the AMU rather than the ICU. ICU patients often commented on noticeable differences once they were moved from the ICU to general wards:
Excellent care in the intensive care unit, but due to staff shortage not so good on the ward.
Although a number of respondents described staff as being ‘rushed off their feet’, there was a sense of gratitude from patients and their relatives as they appreciated and understood the difficulties that the staff faced while providing care:
I think they did most things well and the nurses were always cheerful even though they never seemed to have enough time.
Comments were also made relating to the lack of continuity of care between shifts. Often a shift would end and new nursing staff were allocated; however, time was not spent getting to know the individual needs of the patient or where in the care pathway the patient was.
Furthermore, patients and relatives on one particular AMU noted how staff were having to manage with the limited resources available to them, highlighting the need for investment in new equipment and improved technology.
Issues relating to communication
As with the feedback relating to staffing and resources, negative comments associated with issues in communication were more frequent from AMU respondents than ICU respondents. There were several different themes that arose relating to poor communication.
A number of comments referred to the use of appropriate language that patients and relatives could understand. Feedback was received from both ends of the scale; some respondents complained that they did not understand and would have appreciated ‘less complex language’, whereas other respondents would have preferred more technical details and medical terminology:
Clinical care cannot be faulted but discussions with family could benefit from review – we were treated like we were stupid, just because we do not wear suits does not reflect intelligence.
A number of respondents mentioned the issue of having to repeat themselves numerous times to the different staff members (in both the AMU and the ICU):
More communication between patient and doctors and relatives. More communication between staff –should not have to keep repeating self to all new staff especially when one is ill and cannot always remember everything.
Even when patients and relatives did repeat themselves, they often felt that they were not listened to, with their concerns being passed from one staff member to another without being addressed:
The doctor on the ward did not listen to my concerns although I believe I expressed them logically and clearly.
A number of negative free-text comments were received from patients and relatives on the AMU regarding issues in communication during the discharge process. Relatives arrived at units to find that patients had been moved to another clinical area or prepared for discharge without the relative being informed.
Finally, a number of complaints were received referring to staff members (specifically nursing staff) having inappropriate conversations in front of patients and relatives:
Staff should have personal conversations during their own time and not on wards while patients are trying to listen to doctors talking to them. Doctors should not have to remind nurses of this.
Issues relating to the unit environment
A frequently cited source of dissatisfaction related to the high levels of noise at night. Patients on ICUs made comments referring to the sounds of equipment, whereas patients on AMUs complained about nurses talking loudly while they were trying to sleep:
Sleeping was a problem. Nurses were quite loud at night they had a good chat about a planned night out, which was annoying while trying to sleep.
A number of patients made comments about difficulties sleeping because of the uncomfortable beds and requested for lights to be dimmed where possible.
Some patients and relatives were not happy with the standard of cleanliness on the units:
My bed sheets were dirty; pillowcase had dried vomit on it!!
Furthermore, on AMUs some patients and relatives raised concerns about the appropriateness of the location of the patient on the ward. These comments were often made by relatives of patients who had died; they would have preferred more privacy at such a difficult time. Comments were also received from those with disabilities:
My son is severely disabled and we would have been better in a cubicle with a hoist.
Issues with care and compassion
Issues relating to lapses in care and compassion were split fairly equally between AMUs and ICUs. A large number of these negative comments were about nursing staff, relating to rudeness in particular:
Staff need more training with compassion, patient needs, respect and to keep patient dignity. Nurses were rude.
Further negative feedback was received regarding staff members making inappropriate and insensitive comments about the care of the patient. These comments were largely received from patients suffering from mental health conditions, who often felt that the staff did not treat them with the respect that they deserved because they were admitted because of their mental illness. Some comments identified issues that were of concern to patients but were not recognised as important by the staff member:
No one asked me if I had had my bowels opened neither did anyone ask me when I was back on the ward. On the day that I was being discharged I did mention to a nurse that I hadn’t done so since the day before my operation. Her comment was ‘Oh yes I’m like that when I am away from home’. This to me was a most inappropriate reply. The problem caused me a great deal of pain and discomfort which took 3 weeks to be resolved with laxatives.
Some comments were made relating to issues with the medical care received. Examples include patients asking numerous times for dressings to be changed but being ignored, and doctors prescribing meal supplement drinks and nurses not administering them. Other comments referred to confusion around tests and investigations:
I was taken for CT [computerised tomography] scan twice by mistake. Once the porter had the wrong patient, and the second time was 4 hours after I’d had CT scan as my name was on the list twice!
A difference in the level of care received during the day and night on AMUs was noted:
Some nurses on night shift didn’t take care of the wounds properly when dressing it (cleaning and cream).
Other less frequent complaints were made in regard to the food, discharge process and waiting times, and pain management.
The PEARL project staff experience survey
Response rates
Two rounds of the PEARL project staff survey were conducted in January and February 2018 and 2019. In 2018, 1694 surveys were distributed to AMU and ICU staff, of which 681 completed questionnaires were returned (response rate 40.2%) (Table 7). In 2019, 1541 surveys were distributed and 870 completed questionnaires returned (response rate 56.46%). Surveys were supplied with a freepost return envelope, allowing respondents to complete the survey anonymously before returning it to the central project team for processing and analysis. Aggregated reports that outlined findings for each unit were provided.
| Year | Trust | AMU/ICU | Number of questionnaires distributed (n) | Number of questionnaires returned (n) | Response rate (%) |
|---|---|---|---|---|---|
| 2018 | Site 1 | AMU 1 | 192 | 74 | 38.5 |
| ICU 1 | 676 | 268 | 39.6 | ||
| Site 2 | AMU 2 | 95 | 40 | 42.1 | |
| ICU 2 | 189 | 91 | 48.2 | ||
| Site 3 | AMU 3 | 121 | 61 | 50.4 | |
| ICU 3 | 150 | 47 | 31.3 | ||
| ICU 4 | 135 | 49 | 36.3 | ||
| ICU 5 | 136 | 51 | 37.5 | ||
| Overall | 1694 | 681 | 40.2 | ||
| 2019 | Site 1 | AMU 1 | 139 | 59 | 42.4 |
| ICU 1 | 563 | 357 | 63.4 | ||
| Site 2 | AMU 2 | 150 | 69 | 46.0 | |
| ICU 2 | 130 | 82 | 63.1 | ||
| Site 3 | AMU 3 | 112 | 26 | 23.2 | |
| ICU 3 | 149 | 73 | 49.0 | ||
| ICU 4 | 133 | 106 | 79.7 | ||
| ICU 5 | 165 | 102 | 61.8 | ||
| Overall | 1541 | 874 | 56.7 | ||
Quantitative analysis of survey responses
Survey performance
There was a high degree of internal consistency between survey statements (Cronbach’s alpha = 0.924). The most highly correlated questions were those of the Friends and Family Test and ‘Staff will freely speak up if they see something that may negatively affect patient care’ (r = 0.6922).
Aggregated responses
There was no significant difference in the overall domain scores between the first and the second surveys for AMUs (63.1 vs. 67.9) and ICUs (68.9 vs. 68.1).
To facilitate interpretation of the results of the survey we have combined ‘strongly agree’ with ‘agree’, and ‘strongly disagree’ with ‘disagree’ and have excluded non-response rates, which were low (mean non-response rate, 1.11%; average number of non-responders, n = 17). Considering all of the responses from both types of unit combined (Table 8), 90.2% of staff had confidence in the standard of treatment provided, 84.4% were proud to work for their unit, around 80% were positive about teamworking and handover arrangements and 86% would feel safe being treated as a patient in their unit. Less positively, more than half of the respondents did not feel valued by their trust, 30% felt that staff were not treated with respect and 36.5% felt unable to make quality improvement suggestions. Almost half of the respondents (47.7%) considered communication between senior management and clinical staff to be ineffective and felt unable to question those with more authority (45.7%).
| Statement | Agree | Neutral | Disagree | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| 1. If a friend or relative needed treatment I would be happy with the standard of care provided by this organisation | 1391 | 90.2 | 58 | 3.8 | 93 | 6.0 |
| 2. I would recommend my organisation as a place to work | 1181 | 76.5 | 124 | 8.0 | 238 | 15.4 |
| 3. I feel valued by my organisation | 739 | 48.0 | 380 | 24.7 | 420 | 27.3 |
| 4. I look forward to going to work | 875 | 56.8 | 209 | 13.6 | 456 | 29.6 |
| 5. I am proud to work for my unit | 1300 | 84.4 | 61 | 4.0 | 179 | 11.6 |
| 6. In this unit, people treat each other with respect | 1074 | 69.8 | 190 | 12.3 | 275 | 17.9 |
| 7. I am able to make suggestions to improve the work of my team/department | 977 | 63.5 | 207 | 13.5 | 355 | 23.1 |
| 8. I am supported to receive training as a part of my professional development | 1136 | 73.5 | 165 | 10.7 | 245 | 15.8 |
| 9. In this unit staff work as a team | 1225 | 79.3 | 114 | 7.4 | 205 | 13.3 |
| 10. Handover arrangements in this unit always ensure continuity of care for patients between shifts | 1234 | 80.6 | 106 | 6.9 | 191 | 12.5 |
| 11. Communication between senior management and clinical staff is effective | 807 | 52.3 | 275 | 17.8 | 460 | 29.8 |
| 12. Staff feel free to question the decisions or actions of those with more authority | 837 | 54.3 | 331 | 21.5 | 373 | 24.2 |
| 13. In this unit, we discuss ways to prevent errors from happening again | 1191 | 77.4 | 113 | 7.3 | 234 | 15.2 |
| 14. I would feel safe being treated here as a patient | 1329 | 86.0 | 58 | 3.8 | 159 | 10.3 |
| 15. Staff will freely speak up if they see something that may negatively affect patient care | 1248 | 80.7 | 88 | 5.7 | 210 | 13.6 |
| 16. There is an organisational culture of learning lessons from concerns raised | 1074 | 70.1 | 119 | 7.8 | 340 | 22.2 |
| 17. I receive feedback from colleagues about my performance | 917 | 59.4 | 278 | 18.0 | 349 | 22.6 |
| 18. I regularly receive feedback about patient/carer experience in my unit | 764 | 49.9 | 317 | 20.7 | 450 | 29.4 |
| 19. I see acting on patient/carer feedback as part of my role/professional duty | 1325 | 86.7 | 32 | 2.1 | 172 | 11.2 |
| 20. I am keen to use patient and carer feedback to improve my practice | 1424 | 92.8 | 7 | 0.5 | 103 | 6.7 |
| 21. I know how to act on patient/carer feedback to improve my practice | 1234 | 80.5 | 53 | 3.5 | 245 | 16.0 |
| 22. Resource constraints limit my unit’s ability to act on patient/carer feedback | 665 | 43.6 | 248 | 16.3 | 613 | 40.2 |
| 23. Patient/carer feedback, compliments and complaints lead to changes in my unit | 811 | 53.0 | 133 | 8.7 | 587 | 38.3 |
| 24. Debriefings are common in this clinical area | 537 | 35.1 | 535 | 34.9 | 460 | 30.0 |
| 25. I feel emotionally drained from my work | 761 | 49.4 | 381 | 24.7 | 398 | 25.8 |
Staff were very positive about feedback and reflection. The great majority of respondents (92.8%) wished to use patient and carer feedback to improve their practice, 86.7% considered it a professional duty to do so and 80.5% felt that they knew how to do this. By contrast, 22.2% of respondents disagreed that there was a culture of learning from the concerns raised, 43.6% said that resource constraints limited their unit’s ability to act on patient feedback and only 53% considered that feedback would lead to changes in the unit. Almost half of respondents felt emotionally drained by their work.
Comparisons between trusts, units and staff
The responses from one of the three trusts were generally less positive than for the other two trusts, with lower ratings for recommending the trust if family members needed treatment, for recommending the trust as a place to work, feeling valued, being proud of their unit and perceptions of teamworking. This trust also had higher rates of feeling emotionally drained. Attitudes to feedback, reflection and practice improvement did not differ between sites.
The AMU staff tended to give less positive ratings of teamworking and collaboration, communication, safety, contextual factors and well-being, but shared the same perspectives as ICU staff in terms of their responsibilities and desire to use feedback to improve practice.
Doctors were more positive than non-doctors for most domains but were less likely to agree that they received patient feedback (42.1% vs. 53.3%) and that they knew how to act on patient/carer feedback to improve practice (71.5% vs. 83.6%). Both groups were equally committed to using feedback to improve practice. Trainee doctors gave similar ratings to consultants in terms of speaking up and raising concerns, but only 29.1% of trainees agreed that they received patient experience feedback (consultants 56.9%).
Emotional exhaustion was common, but with a seniority and professional gradient: junior nurses were most likely to agree that they felt emotionally drained (57.2%), followed by senior nurses (51.8%), junior doctors (39.1%) and consultants (38.2%).
Analysis of free-text responses
Of the 1551 PEARL project staff experience survey respondents, 35% provided additional free text about working at their organisation. The proportion of positive to negative free-text comments was the reverse of that seen with the patient survey: approximately 78% of staff free text contained negative comments. These predominantly related to lack of training and progression opportunities, issues with teamworking, staff feeling unsupported in their roles, communication and the overall impact of working on staff well-being.
Positive comments
Respondents appreciated working in a team-based environment, which allowed them to be creative and to achieve high standards of care. Pride in work was a common theme:
I feel proud to work for this organisation, it’s dynamic, innovative and has high standards. I also feel extremely lucky to work with the team that I have, who are friendly, respectful caring and responsive.
Good organisation. Good team culture, all levels approachable.
Being treated with respect, and being able to raise concerns, were essential:
The work within the team on the floor is exceptional. All members of the multidisciplinary team work well together with respect and dignity.
I would recommend this trust as a good place to work. I do feel comfortable about raising concerns if necessary. Our manager is very approachable and supportive.
Pastoral support evidenced by regular senior–junior staff meetings were considered important:
Good environment to work in. More frequent meetings with senior staff on progress/performance would be beneficial and help me to feel more valued rather than just a number.
In addition, direct experience of local care was influential:
Family members been treated here. Happy with care received.
Negative or critical comments
Issues relating to staffing levels
The pressure of understaffing in both AMUs and ICUs was noted by staff from all occupational groups. Staff expressed clear concerns about the impact of inadequate staffing levels on staff well-being, with increased stress and lack of job satisfaction being reported. A number of comments linked understaffing with adverse consequences for patient safety:
Low staffing levels can make the unit feel unsafe and affect staff satisfaction. Staff are feeling burnt out and drained.
Staff well-being
Both AMU and ICU staff members described the adverse impact on staff well-being of poor staffing levels, feeling unappreciated, lack of respect shown by colleagues and safety concerns. The impact of these factors on retention of staff and high staff turnover was also noted:
I don’t feel appreciated at this unit. I feel this unit can make me so stressed out it effects my life outside of work.
Issues relating to training and progression
Comments regarding issues with personal training were received from nursing staff and junior doctors. A large proportion of these respondents worked in the ICU. Causes of this included a lack of funds to support professional development and high workload from understaffing. The lack of opportunities for nurses to progress to more senior grades was also noted:
Lack of money and high workload stop changes and staff training education from happening. Study days are often cancelled in order to put the attending staff to work on the unit.
Although the opportunities for training were considered to be limited, in one unit the high quality of the training, when it did occur, was noted:
The unit is so busy and dynamic that opportunities to do training are limited. However the quality of on-ward teaching from all staff is high.
Team working and respect
Negative comments in this category were largely received from nursing staff, bands 5 and 6 in particular. Often, a feeling of a lack of respect shown by their senior colleagues was noted:
It is sadly clear that the senior managers/nursing team at times may not respect each other (junior team members and new starters are aware of this). It makes me really sad that some of our most committed staff members may be leaving based on poor culture and this is something that needs to be worked on and addressed.
Comments that were made by AHPs in this category referred to a poor relationship with senior doctors. Physiotherapists in particular felt that their professional advice and knowledge was often disregarded during multidisciplinary team meetings:
Variable respect between the team. Extremely dependent on consultant working and the level of respect with which they treat the rest of the MDT [multidisciplinary team] . . . appears to disregard nursing or AHP opinion in favour of his own. Even in situations where the former team members know an individual patient very well.
Communication issues
As reported by the patients and relatives, issues with communication were expressed by staff of all occupation groups on both the AMU and the ICU. Staff also often referred to a lack of feedback received from their managers, and hearing from them only if there is was problem:
I feel that communication between senior management staff and clinicians could be improved.
I never receive feedback on how I am doing in my role. Only ever hear from managers if there is a problem. No regular contact from team leaders or managers.
Larger organisational issues
Some comments were received that linked to larger organisational issues, lack of appreciation, praise and recognition and wider national NHS issues. A large proportion of this feedback was provided by consultants. The general state of the NHS is a clear concern for consultants, as is the working of their trust and individual unit:
I feel that in general [trust] is a good organisation and is one which I am happy to work for, but recently I feel there are a lot of increasing demands and pressures put on staff. The workload is increasing with sicker patients and more expected of staff. I feel that morale has decreased because staff feel under pressure and under valued. I am aware that these issues are not specific to [trust], but are wide felt in the NHS. I feel that more staff and better training would help relieve some of these pressures.
Unit environment
Comments raising concerns about the unit environment were received from both the AMU and the ICU; however, the issues raised for each unit were different. Negative feedback about the ICU environment referred to a lack of dedicated work/desk space for doctors on the units:
One major issue is the lack of dedicated handover area for doctors. There are also no dedicated areas for doctors to sit and work on the units. This is a major factor affecting quality and safety of our work.
Negative comments about the environment from one AMU specifically referred to the lack of basic working equipment. Some patients and relatives who had spent time on this unit had also noted this issue:
Lack of good, working equipment adds to frustration.
Pride in unit and organisation
Despite raising a large number of concerns about working in the AMU and the ICU, staff still expressed how proud they were of their units. This was displayed by staff of all occupation groups:
I enjoy working for this unit and I enjoy my role enormously.
Proud of a fantastic unit.
Ethnography phase I: approaches to feedback and to reflective learning
Patient experience data
Patient experience data are collected in different forms, which fall into three broad categories. Formal data are collected and collated at the organisational level, such as questionnaires/surveys (including the PEARL project survey) and the Friends and Family Test, and through non-solicited mechanisms, such as complaints, contacts via the PALS or recognition of individual members of staff through local awards. Informal data available to individual front-line staff about patient experience come from items such as ‘thank you’ cards and gifts from patients/relatives and bedside comments. In between these formal and informal sources of feedback are other forms of feedback that front-line staff receive that are generated as part of organisational activities; however, these types of feedback are not collated and used formally for organisational activities. These include patient stories generated when patients are invited to come back and share their experiences, and individual-level feedback that is collected for mandatory revalidation or appraisals. We refer to these three different types of feedback as happening ‘above-the-line’, ‘below-the-line’ and ‘between the lines’, respectively (Figure 8).
FIGURE 8.
Forms of feedback. M&M, morbidity and mortality. a, Facebook, Inc., Menlo Park, CA, USA; URL: www.facebook.com.
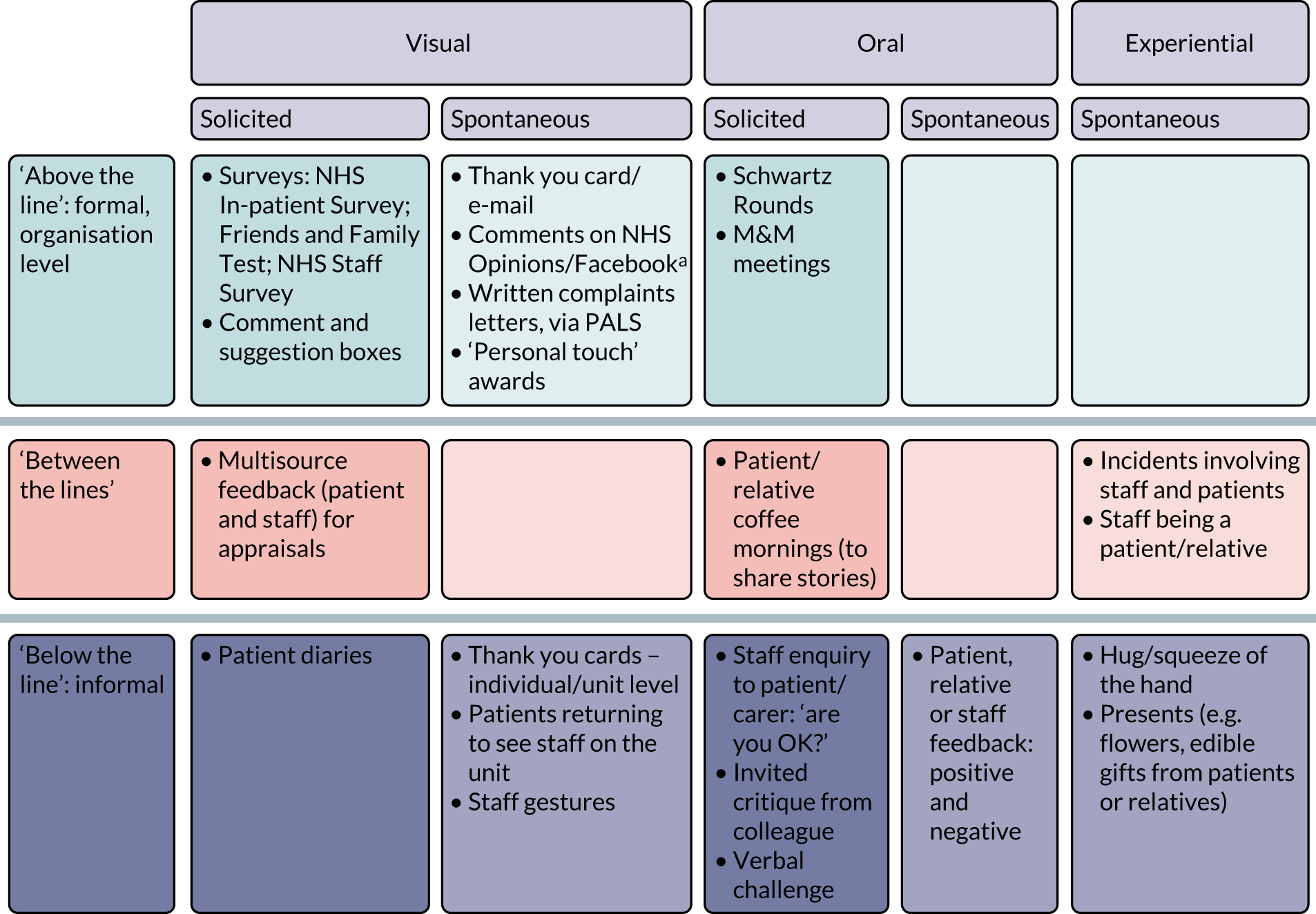
If all types of data are taken into account, there are currently a broad range of sources of patient experience data potentially available as a stimulus for reflection. Sites varied in their approaches to actively gathering formal data on patient experience and in the extent to which staff had access to the different forms of feedback. In terms of formal sources of data, where questionnaires were being used these were usually administered during the patient’s stay, but were often not used systematically, and the approach was widely described as being ‘hit and miss’. The Friends and Family Test was used in some of the AMUs but did not tend to be used in the ICUs at any site. A few ICUs, or sections of ICUs, did try to collect regular patient or relative data through the use of questionnaires/forms. Not every ICU had formal, regular collection of patient experience data; some ICUs collected patient experience data on an annual or 2-yearly basis, whereas others used forms, such as the ‘Take two minutes’ form, or ‘suggestion boxes’ in the relatives’ room to collect relatives’/patients’ experiences. All sites had systems for collating and feeding back complaints.
Doctors who collected patient experience data for the purpose of their own appraisals were able to collect from any ward in the hospital including the AMUs and the ICUs; however, it seemed that the doctors felt that it was difficult to hand out patient surveys in these locations.
In terms of organisational opportunities for staff to hear patient stories, in some participating ICUs (usually those with extended stays) staff had the opportunity to attend follow-up clinics or coffee mornings to hear about patients’ experiences from patients and relatives/carers; however, these sessions were primarily designed to help patients’ reorientation as opposed to a means of generating patient experience feedback. AMUs did not have a similar scheme.
All staff had the opportunity to receive informal patient feedback, for example at the bedside or through receiving thank you letters, but this was more likely to occur on ICUs, where patients had extended stays. In addition, some staff felt that nurses and other ward-based staff were more likely than doctors to receive verbal patient experience feedback because they were more of a consistent presence on the ward.
Barriers to data collection: formal patient experience data
In terms of barriers to collecting patient experience data through formal data collection systems, such as surveys, there were differences between the ICUs and the AMUs. On the whole, the AMUs were described as very busy, with a high turnover of patients and a pressure to free bed spaces, which made collecting formal patient experience data challenging. Some patient groups on these units (e.g. toxicology patients, those with delirium or dementia and those not having English as a first language) were sometimes considered unsuitable to approach to collect data from; occasionally relatives would be approached to ask for feedback, but this was difficult because there had been little time to build up a relationship with the relatives. In the ICUs there were similar groups of patients (e.g. those with delirium or dementia, those who were sedated or those who were critically ill) whom staff considered could not be directly approached; however, relatives would be asked more often for feedback. This was generally considered to be easier on ICUs than on AMUs because the staff had had more time to build up a relationship with the relatives and, therefore, found them easier to approach; the staff across all sites described how they got to know some patients and families very well. However, relatives of those who had passed away did not tend to be asked for feedback on any of the units at any of the sites:
So the last thing they’re bothered about is filling out a form, so response rates are not great. And again the staff are dead busy, so trying to gather patient experience [is difficult], you always find that in acute sector, in emergency sector.
Interview (int) 043, admin
Ways in which patient experience data are fed back and the impact of this
We observed numerous ways in which formal data from surveys and other organisational activities, such as complaints monitoring, were fed back to the staff. Some feedback was provided actively (e.g. feedback at handover) whereas other feedback required the staff to actively seek out data. Across the different sites, there were those who placed a high value on formal patient experience collected through survey methods and those who placed a lower value on it. This was demonstrated in attitudes to and engagement with patient feedback and on how valuable the outputs were perceived to be. Staff wanted to receive data in various ways; for example, many front-line staff preferred to see free-text comments from surveys (as well as or instead of graphs and figures) because these were more impactful and helped them see what they had done well or to identify concrete issues for improvement. Staff responded differently depending on who presented the data and how they were presented. Negative feedback presented in a judgemental way was seen as more likely to be resisted or ignored. Survey data were fed back via many different mechanisms, which included active feedback in which the staff were informed about the data through face-to-face encounters, e-mails or noticeboards.
Patient experience was also discussed at various meetings at the sites where a variety of grades attended, some quite senior, depending on the purpose of the meeting and the hospital site. Efforts were made to cascade this information to more junior staff, but this had varying levels of success:
With the patient feedback forms, we get a lot, a lot of feedback. So every shift, before we start our shift we do our expectations, which are things that have gone well, not so well, things we need to improve on or things we have improved on, and we do get a lot of patient feedback in there.
Int 029, nurse
There were also ‘passive’ mechanisms for feeding back, in which the member of staff would have to go and find the data on, for example, a poster display on a ward, the trust dashboard or the hospital Facebook page (Facebook, Inc., Menlo Park, CA, USA; URL: www.facebook.com). Across the sites different members of staff had responsibility for patient experience data. Each site had staff designated as being involved in patient experience through either patient experience teams or patient services. Some clinical staff at each site had also taken on or been given the role of collecting, analysing and disseminating patient experience data. All sites had mechanisms for feeding back complaints, and it was also common for complimentary e-mails that had been received by the organisation, which named members of staff, to be forwarded on so that the staff member knew that they had been praised.
Feedback obtained through informal means, such as direct feedback from a patient at the bedside, was highly valued. If the verbal feedback at the bedside was negative, it gave the staff a chance to address the issue before anything was escalated further (i.e. became a formal complaint). Informal feedback tended to be reflected on by an individual but was not always integrated into formal structures for collating feedback at a unit or trust level or for prompting learning and reflection at a group level.
Overall, nurses were often more aware of all types of patient feedback than doctors, and there was a common view that nurses received more ‘bedside feedback’. There seemed to be more awareness across staff groups of informal patient feedback, such as thank you cards, and unit-level compliments and complaints than patient feedback obtained through survey methods. Many staff claimed that they received no information about patient experience, despite survey data being made available (e.g. on ward noticeboards or trust dashboards). There was, however, an appetite among staff for wanting to know how they were doing:
We may get feedback from survey results, but certainly I don’t – I’m not aware of where to look for it.
Int 045, nurse
It would be nice to get some patient feedback, positive or negative, because that’s how you improve or . . . change your clinical practice or your . . . practice in general.
Int 025, doctor
Responding to feedback
The type of feedback that front-line staff wanted was around the care that they provided (e.g. ‘were they gentle, kind, caring?’); however, they also wanted ‘actionable’ feedback from which they could make a change or an improvement. Patient experience data that were not within the control of staff to act on were felt to be of little value:
Depending on what the results are, some of the things we can’t change. I know last month there were people complaining about the use of the visitors’ waiting area, it’s not very big, but any area that isn’t a ward in the hospital is like gold dust . . . There’s nothing else we can do, we have no rooms. So some of the things that come back were ‘we need a bigger waiting area’, however, we can’t.
Int 001, admin
There were several barriers to engaging with patient feedback. In terms of survey data, there were issues related to the ‘faith’ that staff had in the data, and whether or not they were valid, reliable and legitimate. There were concerns around bias in terms of which and how many patients were providing data; some very low response rates to surveys were recorded for some units. Within and across sites there were different levels of engagement with patient experience survey data, which was demonstrated by some staff not knowing what data were collected in their unit or how these were was fed back to the staff. Granularity of data were also important; some staff placed lower value on the data fed back if they could not relate to them personally or if they were combined with other data from other units that had different experiences.
Engagement with patient experience data was undermined in some staff groups by the perception that patient feedback was a ‘nurse type’ activity; however, all levels of staff admitted to this not necessarily being their top priority on occasions. Some staff expressed views that sometimes ‘clinical’ results were more meaningful and important than patient ‘experience’ feedback. Other barriers included too much focus on negative feedback and the lack of priority given to patient experience in meetings.
Staff in managerial and improvement roles were more likely than other staff to see survey patient experience data, including numerical data, as valuable for identifying problematic issues and guiding their efforts to improve their service. Quantitative data were seen as valuable for showing trends and having the potential to reflect practice at the unit level. For front-line staff, informal mechanisms, including feedback at the bedside and coffee mornings, tended to provide richer and more engaging feedback and were described as being more likely to prompt reflection. They were most likely to engage emotionally with informal, personal feedback and to be motivated to change their practice based on it. Staff suggested that there would be value in trying to collate and share these types of informal qualitative data at the level of the unit:
And as a manager, when I can’t be here 24/7, so getting the feedback from the patients also gives you that reassurance that actually when you’re not here the care is being delivered to the standard that you would expect . . . And I think as managers you want hard facts and figures, so you want percentages, numbers and that sort of thing.
Int 041, nurse
They’ve just started running regular coffee mornings as support for patients . . . [at] their last meeting . . . there was a lot in there about noise and sleep at night. And then I worked a night shift the next day and everybody’s shouting down the ward at 2 o’clock in the morning, I’m like ‘shut up’!
Int 011, doctor
Reflective practice
Reflective practice activities
All staff were familiar with the term ‘reflective practice’ once it had been described to them. Reflective practice took several forms across the sites and across different staff levels. Staff said that they were taught how to reflect during their medical training, which mainly involved writing reflective pieces. Some staff had portfolios in which they continued to write reflective pieces. Consultants also talked about encouraging the doctors to reflect and teaching them how to do it. Doctors and nurses were required to demonstrate reflective practice for appraisal and revalidation purposes; here, the approach was more formalised and tended to be in writing, plus a discussion with a more senior member of staff. Staff felt that they were more likely to reflect on clinical aspects of practice and could more easily come up with examples of changing their clinical practice, as opposed to their attitudes and behaviours, after reflecting on an event:
I think most of us prefer to concentrate on the clinical aspects and not the sort of non-clinical and reflecting about those topics . . . I guess maybe, there isn’t a structure and there shouldn’t be a structure for the non-clinical reflections they tend to be very superficial because you don’t really know what you are doing. So you just stop, after like a line of reflection . . . we are not taught to reflect particularly well.
Int 014, doctor
Although staff were less likely to initially describe reflection as something that they did in everyday practice, on prompting they were able to describe examples of spontaneous reflection in day-to-day practice:
I asked her if she tends to reflect on things during the day and then she . . . said actually yes she does do that an awful lot . . . She said that a couple of weeks ago she’d had a patient who was really upset, and she said that all that day she spent time thinking about how she could have dealt with the patient better and how she could have made the patient feel more at ease and more comfortable, and so she said actually she reflects on that sort of thing quite often.
Observation
Attitudes towards and engagement with reflection
On the whole, the staff who were interviewed and observed had very positive attitudes towards reflection. Staff were able to articulate reasons for and the impact of reflecting, which included improving their clinical skills and professional development as a clinician, to make the patient’s experience better, to enable staff members to be better able to handle situations, to de-stress and to reassure themselves that they were doing a good job. Staff believed that reflection could make a difference; there was some belief that reflection helped remind staff of how to do their job well and gave a deeper understanding of situations that might arise. Managers used reflection to facilitate learning.
There were, however, some negative views expressed concerning reflection. These were that some staff felt that others reflected inadequately, that there was usually no time to reflect, that even if someone reflected there was little impact from this and that there was some resistance to the mandatory nature of some reflection activities. There was an indication that staff attitudes towards reflection could change over time, with a generally more favourable attitude developing with experience:
I guess maybe I saw reflection, in the early years I reflected on negative incidents, and it had very, reflection had negative connotations. Something I’d done, I’d done wrong . . . Whereas now maybe reflection is a kind of, it’s not necessarily that something wrong has happened, maybe it’s something that I could just learn from . . . I’m much quicker to see the positives in reflection now than I used to be.
Int 053, doctor
Practicalities of reflection
All respondents talked about ‘doing reflection’. What this entailed varied among people but included thought and written reflections, with spoken reflections being either with one other person or in a group setting. Reflections were both formal and informal, with formal reflections tending to be required for revalidation, appraisal and complaints procedures, whereas informal reflections often happened in the coffee room, on the way home or at home. The timing of the reflection varied: sometimes reflection happened as the event was taking place, but more often it took place later and some said that they reflected constantly. On the whole, respondents said that they were encouraged and expected to reflect as part of their practice, and that some opportunities were already in place for this (such as through supervisions). Barriers to reflection included the lack of ability to reflect effectively. Some respondents felt that the ability of some doctors to reflect was really poor, which was because they were not taught how to do it properly. There was also evidence of a lack of understanding of ‘closing the loop’ on reflection through gaining insight and changing practice; for example, some described having a chat with colleagues in a coffee room or simply thinking over things themselves as reflection. Other barriers included little support to facilitate the reflection process, lack of prioritisation of reflection (particularly compared with quality improvement), lack of time or space to reflect (either individually or in group settings) and a low level of motivation to reflect if there was little confidence that it would make a difference:
When I go home I like to vent a little bit, and that’s kind of how I get things off my mind sometimes. And then I’m absolutely fine. Whether you call that reflection or not, I don’t know.
Int 027, nurse
Sometimes I wonder though whether, you know, you’re so ingrained in the way you do something, you can reflect on it all you like and think I’m going to be slightly different and then you find out you’re no different than you were before.
Int 010, admin
Staff said that they valued both negative and positive feedback to reflect on but that negative feedback was the most likely to result in a change in their behaviour or the system. However, staff also described the risk of rumination, in which negative experiences could be thought about without resolution.
There were a variety of ways in which staff were prompted to reflect, which included being involved in a positive or a negative incident (clinical or patient experience). This incident could be their own practice or someone else’s. Patient experience feedback could prompt refection if it was personally meaningful and/or emotionally engaging. Reflection was also prompted in a more intangible way when there was a gradual realisation that a change was required to improve patient experience. Staff also reflected on their personal experiences of health care, such as times when they had been the relative of a patient in intensive care; these experiences could transform their perspectives on how patients experienced acute care:
Speaking from someone that’s experienced that side when my dad happened to be in intensive care and whatever, and in A&E [accident and emergency], it’s very important. And I’ve seen both sides of it.
Int 003, nurse
Co-design meetings and workshops
As described in Chapter 2, we conducted three facilitated co-design meetings at each centre (nine in total) linked to three facilitated plenary workshops for the whole collaboration. Each centre held one further local co-design meeting without external facilitation. The workshops allowed the three centres to share and feed back their experiences, the central project team to provide scientific support and the whole collaboration to participate in developing reflection tools and activities.
Staff from both the AMUs and the ICUs attended all nine facilitated local meetings; patient representatives attended all except one local meeting and participated in all of the plenary workshops. Ethnographers observed all meetings and provided generalised feedback at the plenary workshops. The degree of collaboration and mutual respect was impressive, as was the capacity of team members to provide constructive challenge and self-criticism. Rather than providing a separate forum for the patient representatives, we chose to include them with the clinical staff from the start. In the early stages of the project, the facilitators needed to ensure that the patient representatives were able to express their views, but they became more confident and empowered as the project proceeded.
The co-design meetings
At the start of the first meeting in each centre, following introductions, participants were invited to describe touchpoints or ‘reflectable moments’ that had happened during clinical practice and stimulated reflection and personal insight in themselves or in others. Many of these accounts, from both staff and patients, were emotionally charged and at times transforming, in the sense that there was little need thereafter to explain why effective reflection was important. It also demonstrated that, once emotional engagement had occurred, it needed to be balanced by sufficient distance to permit objective analysis and the transition to ‘conscious competence’. This was achieved in the second half of the meeting by asking participants to create a reflective learning scene or event using pre-prepared cardboard cut-out figurines and ward furniture, which participants could personalise. There was excellent engagement by team members in this activity, but the team members varied in the extent to which the events were used to describe personal learning. The clinical staff in particular tended to focus their attention on producing better care rather than ‘better reflection to produce better care’. Indeed, throughout the project we had to emphasise the need for clinical participants (including core project team members) to focus on reflection as the behaviour, not the secondary outcome of better care.
In the second set of local co-design meetings, participants used stylised characters (‘personae’) to discuss individual differences in reflective learning. Themes that started to emerge from these discussions included the need for organisational support for reflective learning, integrating reflection in continuing professional development activities, training in reflection, senior role models, reflection mentors or ‘buddies’ to provide individual support and prompts for reflection. ‘Loners’ or ‘ruminators’ were perceived as needing 1 : 1 support to encourage participation in group activities. Non-reflectors were perceived as problematic if this was associated with dysfunctional behaviours and a lack of insight, in which case forms of mandated feedback (multisource/360-degree feedback), senior engagement and sanctions and challenges could be deployed if there was organisational support for speaking up. There was a desire for methods of evidencing reflection that would not compromise confidentiality or diminish authenticity, and for demonstrating that reflection had resulted in learning, either individually or at an organisational level.
Teams were invited to the third set of co-design meetings to test a method for developing two reflection interventions. In the first half of the meeting, teams were asked to identify and discuss the various opportunities for reflection that they had experienced, or would have liked to be made available, in their units; 31 opportunities were identified, ranging from solitary reflection on-action at home to formal reflection meetings or reflection in-action. Teams then selected the two opportunities that they considered the most effective, and in the second half of the meeting they developed these ideas using the reflection specification template (see Table 3). This provided a ‘dry run’ for the final team meetings that were held locally without external facilitation (described in detail below and in the second phase of the ethnography observations).
Plenary workshops
The four workshops were held on 14 June 2017, 15 February 2018, 20 December 2018 and 4 June 2019. The workshops were held in the conference park of the University of Birmingham, Birmingham, from 10.30 to 16.00, with a break for lunch. There was variation in attendance, which was driven in large part by the constraints of the clinical service. There was PPI representation at each workshop.
Following the first scene-setting plenary workshop, the second, third and fourth workshops were interdigitated with the local co-design meetings. For each workshop, the morning session enabled teams to report on progress with reflective learning activities and on how they had used the patient and staff survey reports. This allowed teams to share experiences and learn from each other. The central project team members then provided de-identified feedback on ethnographic observations, discussed pedagogic considerations (methods of reflection and learning) and reviewed tools and techniques for behaviour change. In the afternoon sessions, teams undertook practical exercises and the day concluded with a summary from the chairperson of the steering committee.
In the second and third workshops we introduced to the local teams various models of COM-B as a framework linking forms of reflection (on-action and in-action, group and solitary) to determinants of reflection (capability, opportunity and motivation) and their subdomains, and thence to factors influencing those domains. We show this in Figures 9–12. This framework was considered too complicated to be used as a practical tool by the local teams but functioned well conceptually and for diagnostic and developmental applications by the central project team. The high-level elements of capability, opportunity and motivation proved to be useful classifiers of the reflective learning interventions that were prioritised by the local teams following workshop 3. In workshop 4, the participants presented the reflective learning tools that they had selected, developed and piloted. We describe this in detail in the next section.
FIGURE 9.
The PEARL project COM-B reflection framework. CPD, continuing professional development; M&M, morbidity and mortality; MSF, multisource feedback; QI, quality improvement.
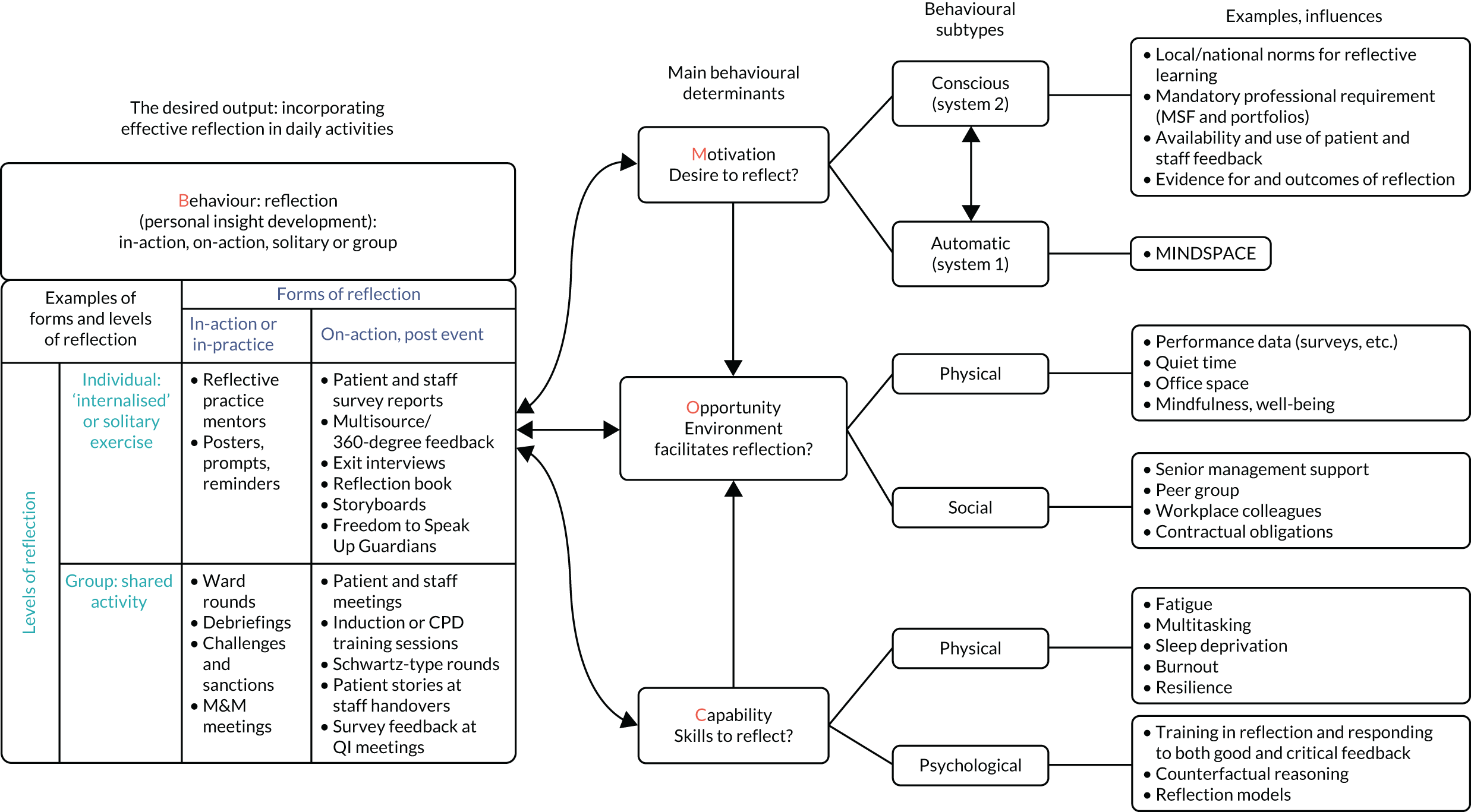
FIGURE 10.
The PEARL project COM-B reflection framework: motivation to reflection (MINDSPACE). MSF, multisource feedback.
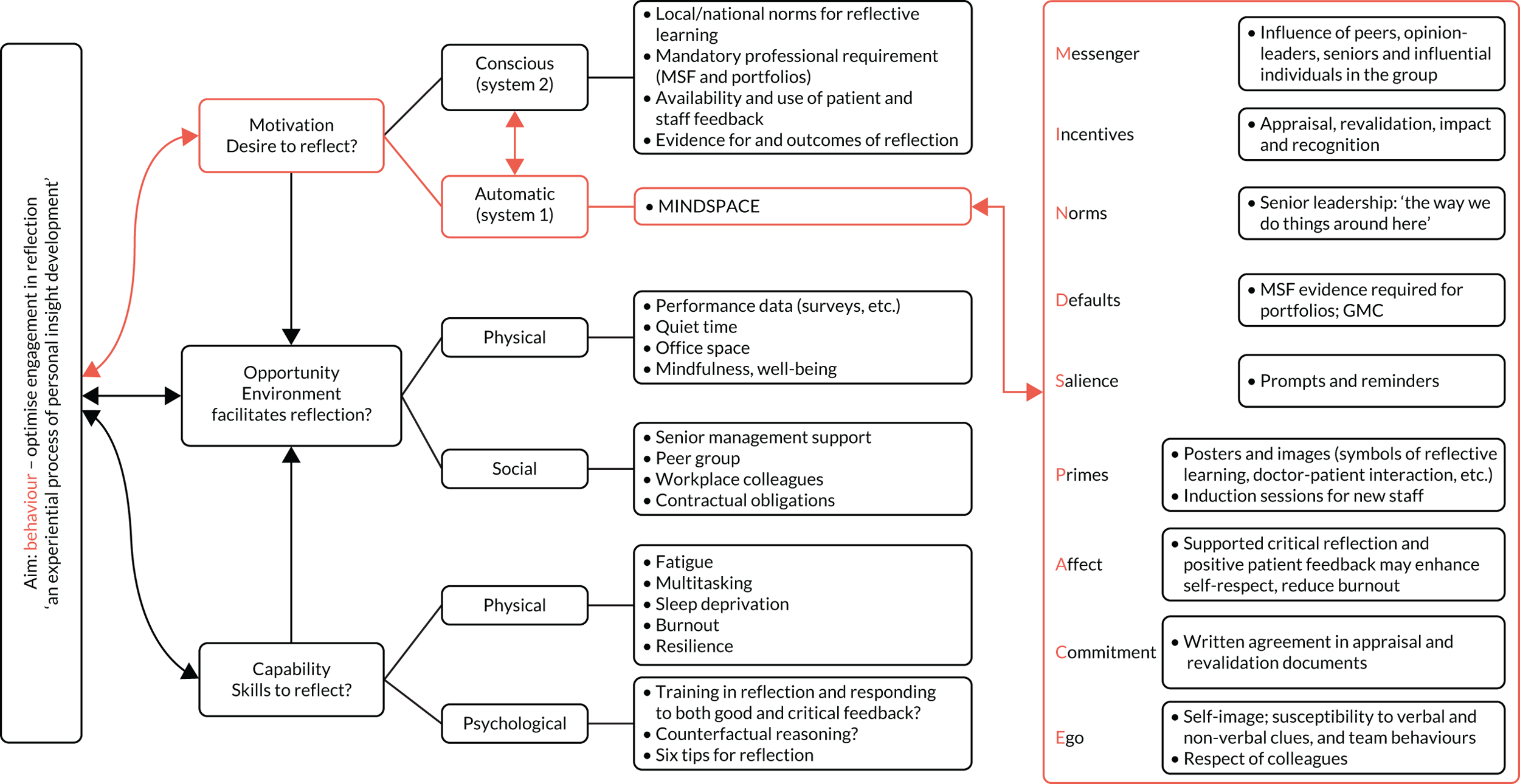
FIGURE 11.
The PEARL project COM-B reflection framework: opportunity to reflect. MSF, multisource feedback.
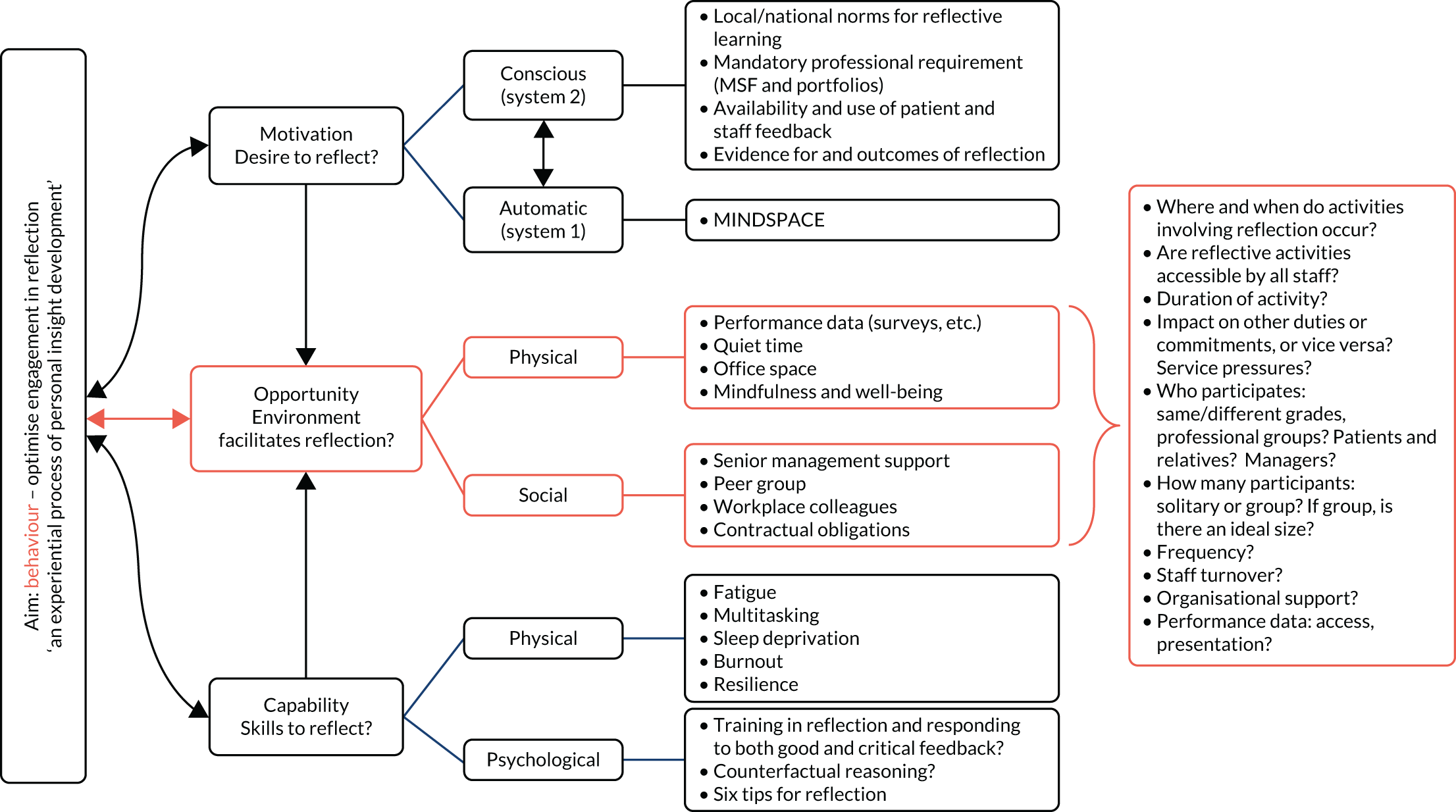
FIGURE 12.
The PEARL project COM-B reflection framework: capability to reflect. MSF, multisource feedback.
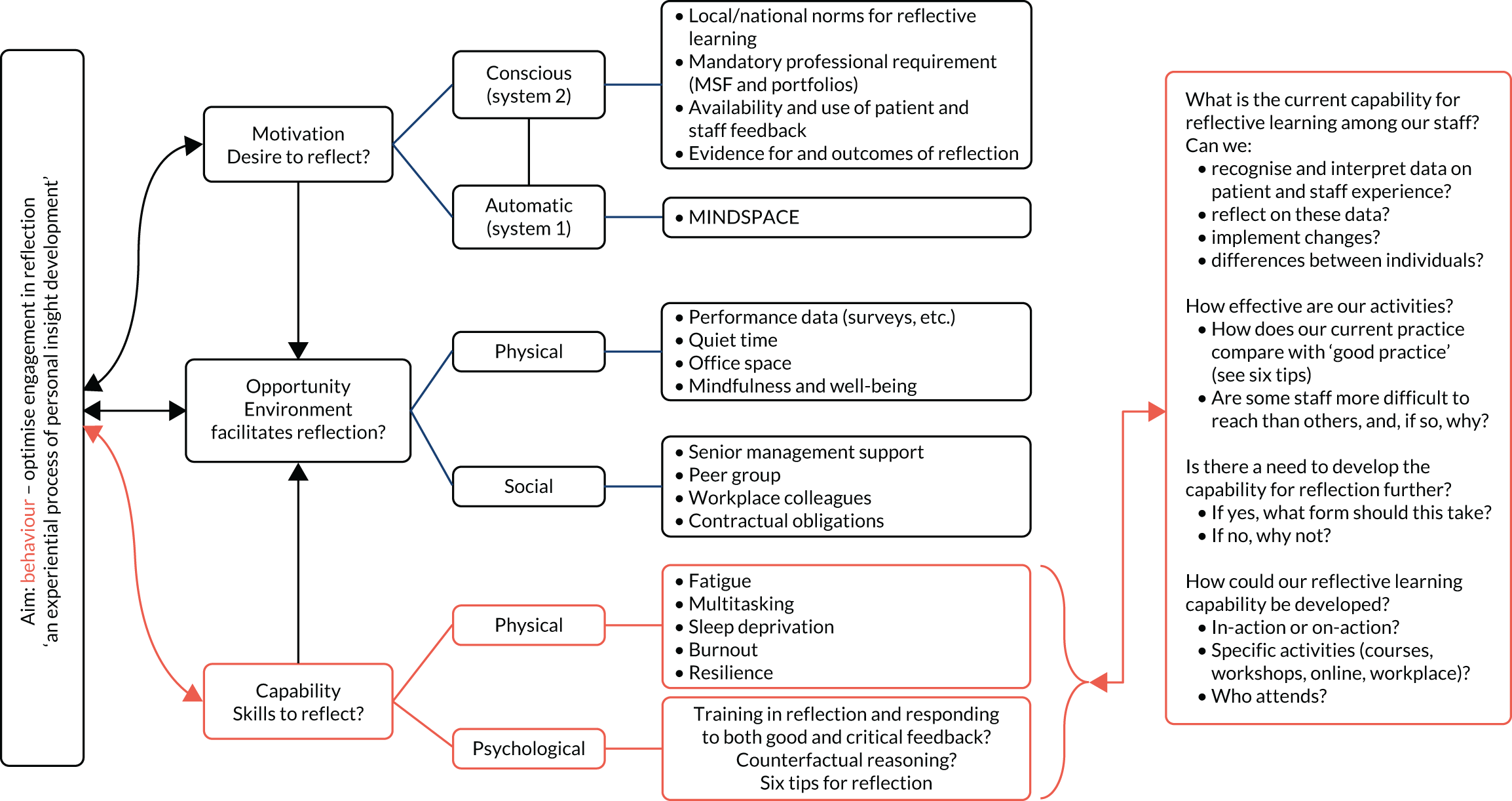
Prioritisation of reflection tools
Participants were invited to rate 49 proposed reflective learning tools and activities (see Chapter 2). Of these, 13 were excluded, three were merged into one activity, 30 met the criteria for inclusion and three were included following review by the project management team. The 33 retained items were discussed further by the project management team, edited, amalgamated where there was substantial similarity in function and classified in accordance with the contribution each would make to addressing capability, opportunity or motivation. The final set consisted of 25 items for incorporation in the toolkit (Table 9).
| Themes | Tool or activity | Capability | Opportunity | Motivation |
|---|---|---|---|---|
| Obtain meaningful feedback | ||||
| Documenting experiences | Patient and staff surveys with free-text comments | ✓ | ✓ | |
| Staff rating of colleagues for excellence in using reflection to enhance patient and staff experience | ✓ | ✓ | ||
| 360-degree/multisource feedback | ✓ | ✓ | ||
| Exit interviews for departing staff to provide feedback on working environment | ✓ | ✓ | ||
| Sharing ‘reflectable moments’ | Reflection book or Post-It NoteTM (3M, Cynthiana, KY, USA) box in the workplace for written comments | ✓ | ||
| Unit storyboards displaying anonymised patient and staff experiences | ✓ | |||
| Extranet collation of anonymised patient and staff experiences [e.g. Health Talk online (www.healthtalk.org; accessed June 2020)] | ✓ | |||
| To reflect effectively | ||||
| Patient involvement | Patient and staff group meetings to hear and reflect on patient stories | ✓ | ✓ | |
| Patient or relative participation in quality improvement meetings | ✓ | ✓ | ||
| Prompts | Posters or screen savers in the workplace | ✓ | ||
| Support systems, critical friends, mentors and role models | Freedom to Speak Up Guardian champions or confidential contacts | ✓ | ✓ | |
| Peer support/staff well-being/social media groups to share reflections | ✓ | ✓ | ||
| Reflective practice mentors/role models/champions trained to provide local support using toolkit and to stimulate reflection in others | ✓ | ✓ | ||
| Reflection skills: how to reflect | Training in reflection skills | ✓ | ||
| Staff induction training to include patient and staff feedback | ✓ | ✓ | ||
| Techniques and models for reflection, reflection diaries, templates, checklists or applications | ✓ | |||
| Time out from clinical work, continuing professional development sessions or study days on reflection including role play, patient and staff stories and feedback | ✓ | ✓ | ✓ | |
| Written reflection in portfolios for appraisal/revalidation | ✓ | ✓ | ||
| Group reflection activities | Group reflection (e.g. Schwartz-type rounds), away days | ✓ | ✓ | ✓ |
| Informal staff room chats, ‘coffee cup conversations’ | ✓ | ✓ | ||
| Patient/staff stories before staff handovers | ✓ | ✓ | ✓ | |
| In clinical practice | ||||
| Reflection during clinical activities | Handovers | ✓ | ✓ | |
| Ward rounds | ✓ | ✓ | ||
| Debriefings | ✓ | ✓ | ||
| Morbidity and mortality or clinical review meetings | ✓ | ✓ | ||
Final co-design meeting and workshop 4
Following workshop 3, each team held a final local co-design meeting without external facilitation to develop a limited number of reflection tools, describing the activity using the reflection specification template and piloting the activity at least once before reporting their experience with this at the final plenary workshop 4. The teams had some difficulty with the exercise in which participants were invited to express their strength of agreement with the statements about unit capability, opportunity and motivation to reflect. One centre provided numeric responses from the ICU and the AMU separately, one provided a combined rating for all units and one was unable to conduct the rating exercise. The difficulty appeared to be with summing participants’ Likert scale responses and expressing this as a group percentage. For those teams that did provide responses, the mean (range) agreement was 76% (75–80%) for capability, 46.6% (25–67%) for opportunity and 71% (68–80%) for motivation, suggesting that the participants viewed lack of opportunity as the predominant barrier to effective reflection.
A total of 11 activities based on nine themes were developed (Table 10), with varying degrees of piloting because the interval between the local co-design meetings and workshop 4 was only 3–4 months. The ethnographic evaluation of this phase is described below.
| Activity | n |
|---|---|
| Schwartz-type rounds | 1 |
| Reflective practice mentors | 1 |
| Reflective practice meetings | 2 |
| ICU patient and staff coffee mornings | 2 |
| Staff induction training to include patient and staff survey feedback | 1 |
| Patient and relative participation in quality improvement meetings | 1 |
| Posters prompting reflection | 1 |
| Patient and relative feedback storyboard | 1 |
| Positive feedback from surveys announced at clinical handovers | 1 |
Ethnography phase 2: toolkit design phase
As well as feeding in the findings from phase 1 to the design of workshops and development of the toolkit, the ethnography team observed and provided formative feedback from local team meetings and project workshops during the toolkit design phase. In addition, the team observed and documented the fourth set of local co-design meetings (see Chapter 2) to capture experiences of piloting the process of selecting and implementing toolkit interventions. The team also interviewed 15 members of staff, five at each participating site, about their experience of piloting the implementation of some of the reflective learning tools.
Meeting logistics
As described in Chapter 2, a meeting was planned by each hospital taking part in the study to select up to three interventions for each unit to aid or promote reflection. The core project team provided guidance on how to run these meetings, with a pre-designed slide set and a pre-meeting telephone call with the project leads. The meetings were observed by an ethnographer. Interviews were conducted with a sample of meeting participants, who were chosen to access the views of people with a variety of roles; interviews were conducted by telephone following the meetings. The focus was on optimising the approach for sites to select and implement interventions: key lessons learned about how to optimise the approach are included in Selecting interventions.
A variety of staff from the ICUs and the AMUs attended these meetings including, among others, consultants, registrars, matrons and nurses; one hospital site also had PPI representatives. There was variation among the participants in terms of seniority within the hospital and familiarity with the PEARL project. For all of the meetings there was a good mix of staff present; however, it was felt that attendance by more senior staff and a wider mix of hospital staff, such as physiotherapists and health-care assistants, would have benefited the discussion and selection of interventions:
Because obviously I’m quite a junior sister to the unit . . . I think from both our point of view, and just seeing who was involved in the other teams at the other trusts, I feel like maybe we weren’t represented enough from more senior staff.
Int 017, nurse
The obvious staff groups that weren’t represented would be allied health professionals, so I’m talking about physiotherapists . . . and pharmacists and people like that. They’re not kind of absolute core members of the team . . . but they are there a lot of the time, and should probably be represented as far as possible.
Int 038, doctor
The meetings took place at different times during the day at the hospital sites, with breakfast meetings and lunchtime meetings being two of the options. There were disadvantages to both time slots, with respondents generally feeling that people were rushing to leave the breakfast meeting and that lunchtime meetings were delayed because morning activities were over-running. Although all the sites had scheduled different lengths of time for the meeting, ranging from 1 to 2.5 hours, all respondents commented that more time was necessary and that the meeting felt rushed at the end:
There’s something about that there should have been more time, definitely and there should have been more time then to go through these activities contributing to reflection because that was not discussed. It was literally they were given the list, quickly choose one, quickly discuss it.
Observation
There were staff attending the meetings who were less familiar with the PEARL project and the methodology; although time was given to provide background information, some respondents felt that this was inadequate. This was particularly the case for one of the exercises that required staff to judge the ‘capability’, ‘opportunity’ and ‘motivation’ for reflection already present, so that a ‘gap’ could be identified. It was felt that this exercise was overly complicated and, although it did create discussion, it was not used by all to select interventions:
I think I added two slides in, and I did make some changes. I think, because at the meeting there were some people who were new to PEARL. Completely, they needed at least one slide that actually explained the capability, opportunity, motivation model. And what sort of things we were looking for.
Int 035, doctor
The meetings were viewed positively on the whole; they were described as being very constructive with lots of enthusiasm from the participants. During the meetings there were occasions when groups were working together; this may have been a unit with different disciplines discussing ideas or it may have been those from a similar discipline but different grades working together. What was observed was that these groupings gave an opportunity for exchanges of ideas and learning from others, be that a different unit, discipline or grade. Further discussions, through e-mail or formally planned meetings, took place after the initial meeting to help develop ideas:
It was actually one of the, I felt, one of the better meetings that I’d been to regarding PEARL. I think it was very well attended, people were very enthusiastic, and seemed keen and interested in it. There was quite a lot of revelation during our meeting, you know, the ITU [intensive therapy unit] nurses discovering that the CDU nurses had no staff room.
Int 036, nurse
Overall, negative comments about the meeting that highlighted areas for improvement included the length of time allowed for the meeting, there not being enough background for new people, the need for a broader spectrum of staff to attend and the complexity of some of the exercises. There were different views expressed about the selection process for the interventions, with the view being that the key criteria should be that the interventions should be practical and feasible, whereas some felt that this potentially restricted their creativity:
I think we were quite constrained to what was said, and it may have been that more ‘out of the box’ suggestions might have come up, but because of the format we did just come up with things that . . . were not particularly ‘out of the box’, were not particularly novel.
Int 038, doctor
Selecting interventions
There were a variety of approaches taken to select the interventions; very few of the groups used the capability, opportunity, motivation exercise, described above, that focused on identifying the gaps to then inform the selection of interventions:
I think from our point of view, because we were already in the process of certainly starting the coffee mornings, they were already running, that one seemed very obvious, because actually we could build upon it and do it within the reflective PEARL framework.
Int 020, nurse
I think we went through them and looked at what was practical and what might not be practical.
Int 057, doctor
I think it almost gave it a bit more of an impetus to sort of go OK, this might have a bigger impact, but a bit trickier, but actually why don’t we go with it.
Int 039, doctor
Approaches taken to select the interventions included:
-
voting on the supplied list of interventions
-
developing an idea that was already ongoing
-
selecting an intervention that was feasible to implement in a short time period
-
choosing interventions that were felt would have a lot of impact.
After the interventions had been selected, the teams had to outline the plans for implementing them. Some found this harder than others, depending on whether the intervention was already in place to some degree or if it was a completely new idea. There were tensions evident in some groups in which the discussion about the potential intervention focused on the potential problems without taking a solution-focused approach.
The respondents expected the interventions that they had selected to have an impact on reflection, but could not always say how much impact or how long this might last. Some commented that they hoped the intervention would last beyond the life of the project. There did appear to be a trade-off between impact and feasibility, with interventions that were seen as easier to do expected to have less impact than other interventions that required more time and resources. One issue that caused problems for groups was finding suitable metrics that would give evidence that reflection had taken place. Concern was raised regarding how impact would be measured and, therefore, how staff would know that the intervention had made a difference:
I think the main issue with us was like that it was . . . about the metrics, wasn’t it? I think that was my main issue . . . we had patient feedback from like coffee mornings, and that was given to staff as well who came along, but we have no official way of measuring [impact].
Int 017, nurse
Will the intervention make a difference to certain individuals? Yes, I’m sure it will. And therefore in that respect, it’s worth doing. Will it make a difference that’s measurable in any way, whether, in terms of staff morale or staff sickness rates or patient experience? I’d love to think it will but I think it will be very difficult to show.
Int 037, doctor
Implementing interventions
Many of the selected interventions had been implemented following the meeting; therefore, it was possible during the interviews for the respondents to comment on the ones that they were involved with. Some interventions had been quite successful and were starting to become embedded in the unit or used beyond the original plan; this was often the case when the intervention was already partly under way and some staff members had taken ownership of the intervention (e.g. patient coffee mornings). Other interventions proved more problematic and either had not been started or had been tried with the realisation that amendments were needed if the implementation was to continue. Reasons for the intervention not working included practical limitations; for example, the discovery that reflecting during handover was ineffective because there was not enough time, or that staff at the end of their shift were exhausted and were, therefore, not engaging well. A common feature of the interventions chosen, however, was that sites had primarily chosen interventions that provided improved access to patient feedback, put prompts in the environment to encourage reflection or provided an opportunity for reflection to take place, such as through time in meetings or interaction with reflection mentors:
As I said, the mandatory training days slot, we’ve almost embedded that actually, it’s almost become a permanent fixture.
Int 059, nurse
A notable omission from the interventions selected was the use of frameworks or models of reflection to ensure that reflection was effective, in particular ensuring that staff ‘closed the loop’ on reflection to ensure that there are changes in attitudes and behaviours. One exception to this was one site that developed and displayed a poster illustrating the steps involved in completing a reflective cycle. This was developed further by the project management team, with the centre involved to create the PEARL project reflective cycle.
Respondents indicated that they would continue to work on the interventions that they had selected, as well as look to implement other ideas. There also seemed to be a ‘knock-on’ effect, with some interventions being used more widely as other members of staff became aware of them and saw other opportunities for their implementation:
The education side, we were just literally launching them [feeding back about patient experience from the coffee mornings] . . . and as a result of the PEARL, [person 5], our matron, has actually asked, after listening the other day to what we were actually doing with the role play and things, she’s actually asked us to present it to band 6 and band 7 meetings and things like that.
Int 017, nurse
Staff suggestions for the final toolkit
Staff were asked about the main challenges to be overcome in promoting the take-up of the toolkit in hospitals. These included the following:
-
Reflection was seen as very important by the respondents but was also acknowledged as easy to avoid when there were intense time pressures.
-
The ability of staff to have the time and opportunity to go and reflect if it meant them leaving their patients.
-
Staff may not feel motivated to reflect, for whatever reason, and, therefore, culture change may be necessary to motivate these staff to reflect – this is challenging.
-
There was concern raised about the legal implications of doing written reflection and how that may impact the staff member and how they choose to reflect.
-
Staff identified that having a means of capturing that reflection had taken place through some kind of metric as an important but challenging element of the toolkit.
-
Staff felt that it would be challenging to introduce the toolkit if there was not enough support from the organisation and buy-in from senior staff.
-
It was seen as important to make sure that the ‘right’ people were involved from the start of introducing the toolkit to promote its use.
-
For the toolkit to be successful it was felt that it needed to be introduced with lots of promotion and maybe a social media campaign, so that all staff were aware that it was taking place.
-
A further challenge was having interventions that were not heavily reliant on one member of staff to make them successful.
-
Tools need to be sustainable beyond the initial PEARL project support.
Staff were asked in interviews to give feedback on what they thought was important to include in the toolkit and implementation plan. One of the main responses was to have examples in the toolkit of how the intervention had worked in other units and enough guidance to be able to replicate the intervention but with the flexibility to adapt it to their specific requirements. Staff wanted prompts that they could use to help direct their reflection and exercises they could do to help facilitate discussion and reflection. There was also a request to have some background information on how the PEARL project developed, details on the ‘science’ behind behaviour change and a glossary (because it was felt that some staff may not be familiar with all the terminology) included in the toolkit:
So I think a little bit of guidance, which is where I see the reflection mentors coming in, so that people are reassured that what they’re doing, that they are sort of doing it in a beneficial way. Because we can all just chat about things, but I think to really actually, if we’re going to use this toolkit to benefit the staff, maybe just a little bit of guidance about the background to why we did PEARL, what we found from PEARL, this is why we’ve come up with this toolkit, and you know, we want it to help you, and this is how we envisage it helping.
Int 035, doctor
Key features that staff wanted to be included in the toolkit and in the plan to support its implementation were:
-
examples of where the tool has worked in other units (this could be built into an electronic repository or hard-copy examples)
-
background on the PEARL project and details on the ‘science’ behind behaviour change and reflection
-
glossary of terms used
-
simple, straightforward tools that could easily be picked up and used
-
access/pointers to other useful resources
-
tools that could be completed in a few minutes
-
ways of measuring the impact so that there is evidence that reflection has happened or that the tool has worked
-
strong branding in the toolkit and maybe some publicity to support its launch
-
guidance/tips on how to use the tool – maybe also a video guide.
What excellent reflection would look like
For most staff, a successful outcome from the PEARL project would be reflection becoming normalised and something that happened naturally on the unit and did not feel like a tick-box exercise. It was felt that staff would feel more valued if they were given time and space to reflect and that this was an activity that was encouraged by more senior staff. Excellence would also be indicated by having measurable changes happening as a result of the interventions:
If you get PEARL embedded into the culture of a unit in the same way, that it’s just something we do, I think that would be the ideal utopian state.
Int 038, doctor
I think excellent would look like . . . that people’s reflection would be both a personal thing and an individual thing, but also a team dynamic and a change. I think personally for it to be excellent we need to demonstrate change. Whether that change is of attitudes, behaviours, changes of practices or changes of the environment.
Int 019, nurse
Chapter 4 Synthesis
Linking the PEARL project findings to the Capability, Opportunity, Motivation – Behaviour model
The PEARL project highlights two paradoxes. The first is that, despite the beneficent intentions of the great majority of health-care staff, our surveys show that a notable proportion of patients and relatives, and of staff themselves, experience staff attitudes and behaviours that are amenable to improvement. The second paradox is that, although all staff endorsed the concept of reflective learning to improve care, and the great majority considered that they reflected frequently or ‘all the time’, they found it difficult to describe how reflection functioned or give examples of how it changed behaviours. ‘Reflection’ appeared to be synonymous with ‘thinking’ (or perhaps with ‘ruminating’), not necessarily with learning or behaviour change.
The behaviours that strongly influence patient satisfaction are those related to communication rather than the more technical aspects of care. Although this may appear unimportant to (or may not even be noticed by) some busy health-care staff, for patients and relatives suboptimal behaviours degrade ‘excellent’ care to merely ‘good’, or ‘good’ to ‘poor’, and for some they transmute grief into grievance, persisting in memory long after the event. For staff, adverse behaviours by colleagues contribute to dissatisfaction and work-related stress, which impede teamworking and speaking up and diminish self-respect and feeling valued. These deficits are accentuated by power gradients, and could affect patient satisfaction and patient safety. By contrast, the excellent behaviours of potential role models are to some extent taken for granted and infrequently subjected to constructive analysis, which means that opportunities for generalisable learning may be missed.
Adverse behaviours may well be stimulated or exacerbated by service pressures but they are not fully explained by them; the ‘Good Samaritan’ experiment showed that individuals respond differently to the needs of others despite being exposed to the same (randomised) conditions of urgency. 117 Moreover, the majority of patient and relative survey responses identified excellent care and high levels of satisfaction despite exposure to the same service pressures. Although we explicitly chose the most acute areas of the hospital to conduct the PEARL project, the overall levels of satisfaction are higher than comparable national data, so acuity alone is not the explanation. However, context matters, as is evident from comparison of the two surveys between ACUs and ICUs, and the views expressed to our ethnographers. The (better staffed) ICUs tend to have higher patient and staff ratings than AMUs for several aspects of clinical practice and organisational support, but there was no difference in the enthusiasm of staff between both types of unit for using feedback to learn and improve care. When the behaviour in question is reflective learning, contextual differences disappear.
Current approaches to reflection, although intended to be formative, tend to be used in a summative manner to determine progression to the next stage of training or for revalidation. Written reflections in portfolios were regarded as lacking impact, perhaps because in creating these reflections it may be easier to focus on technical rather than behavioural aspects of care delivery, because a mandated and standardised approach to documentation diminishes authenticity or because of fears of exposing the writer to criticism or litigation. The PEARL project surveys provided staff with meaningful feedback about patient and staff experience in a manner that was relevant and personal and that was presented in such a way that it was easy to assimilate and difficult to ignore. By presenting survey data in quantitative and qualitative forms, the survey reports engaged both the analytical and the emotive mind, providing the motivation to reflect, to learn and to improve. One of the teams likened the discovery that their care was less than perfect to a group grief reaction118 in which initial denial gradually evolves into acceptance and improvement. The gap between manifest and desired behaviours – the disorientating dilemma – challenges us personally and touches on who we are, on our norms and on our social settings. Effective reflection, therefore, demands personal resilience and the skills to conduct critical self-evaluation: capability is a key element in effective reflection. Organisations can maximise the benefits of reflective learning by ensuring that staff are valued, empowered, supported in developing critical self-evaluation and able to access professional development time to do this in a safe and supportive environment. This is the third element of the COM-B framework: the opportunity to reflect.
The use of the COM-B framework in diagnostic mode appeared to have some merit despite that during the final non-facilitated co-design meeting some of the local teams seemed to have difficulty in converting the outputs of the ranking exercise into a percentage (see Final co-design meeting and workshop 4). For the three groups providing responses, there was agreement that the main barriers to effective reflection were those impeding opportunity to reflect. The exercise would probably have been completed by all teams had we asked them to perform the ranking exercise alone and performed the calculation for them separately.
Therefore, we find that the COM-B framework has potential as a diagnostic tool in considering the various factors that influence reflective learning. We consider next the development of the PEARL project logic model, linking feedback, reflection and learning to better care.
The reflective learning framework
Our initial logic model for reflective learning (Figure 13) polarised behaviours as suboptimal or exemplary, and attempted to describe the resolution of the disorientating dilemma through an interplay between tacit and explicit knowledge and progression through four stages of awareness of competence. Although the PEARL project did not explicitly set out to test theories of learning, we found no evidence to deny the validity of these concepts. However, the design of this model did not lend itself to prospective testing, and nor did it offer a useful foundation on which to build a practical toolkit for use in the clinical environment.
FIGURE 13.
Preliminary logic model for reflective learning. FS-ICU, Family Satisfaction in the Intensive Care Unit.
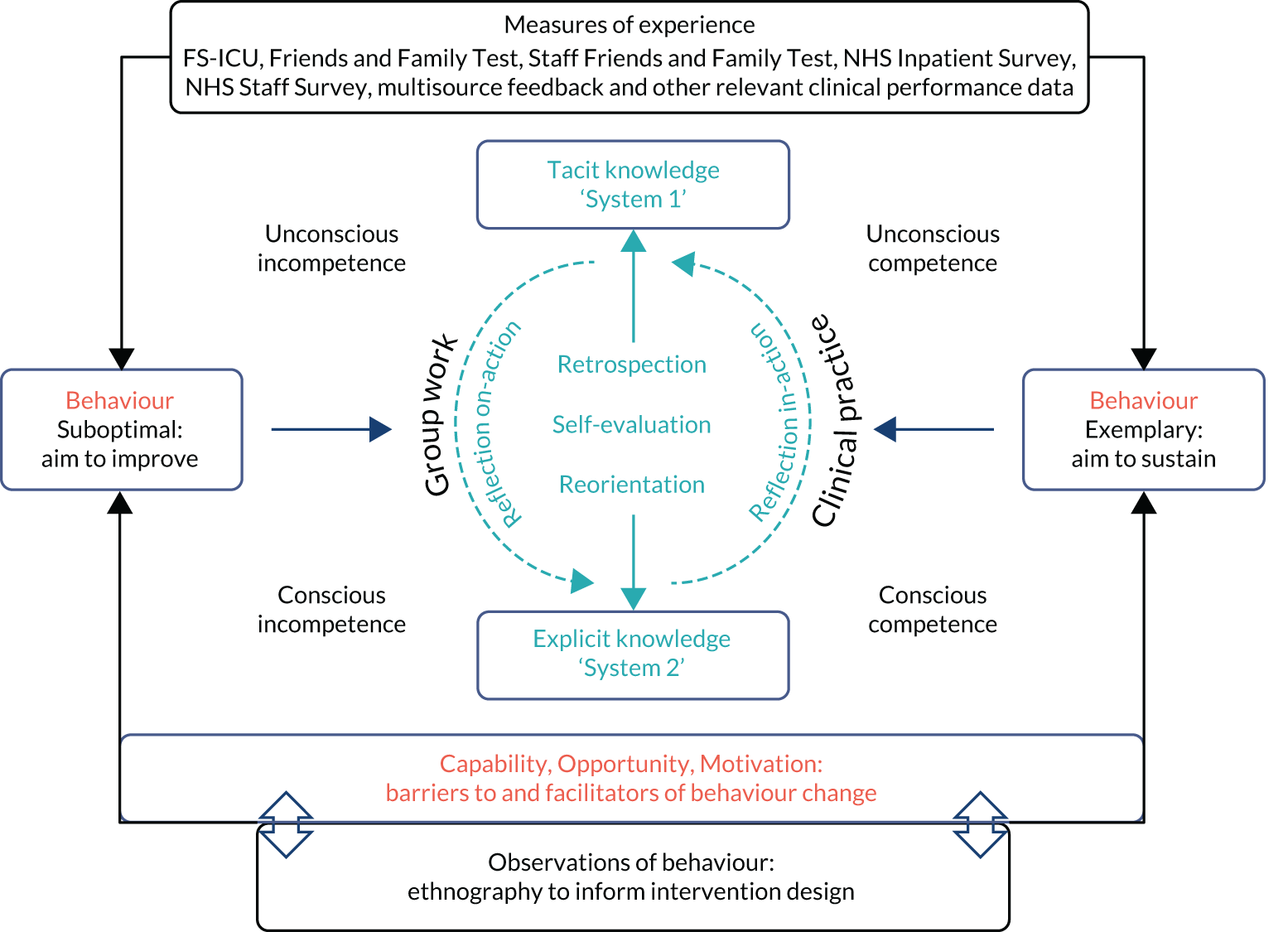
As we acquired experience and information from our collaborators on their approaches to reflective learning, it became clear that a linear model was preferable, linking meaningful feedback to effective reflection (the target behaviour) and thence to proximal and distal outcomes (Figure 14). The proximal outcomes would be improvements in behaviours in the clinical environment and distal outcomes would be patient and staff experiences of care. The model is agnostic to the type of behaviour described in the initial feedback given that both positive and negative experiences can be used to promote learning. We found that this model satisfactorily described the processes by which individuals make use of experiences through reflection. The model could also be used predictively to explain variations in reflection as the target behaviour based on differences in access to experiences, such as meaningful feedback, or differences in capacity, opportunity and motivation to use those experiences effectively.
FIGURE 14.
The PEARL project logic model of reflective learning.
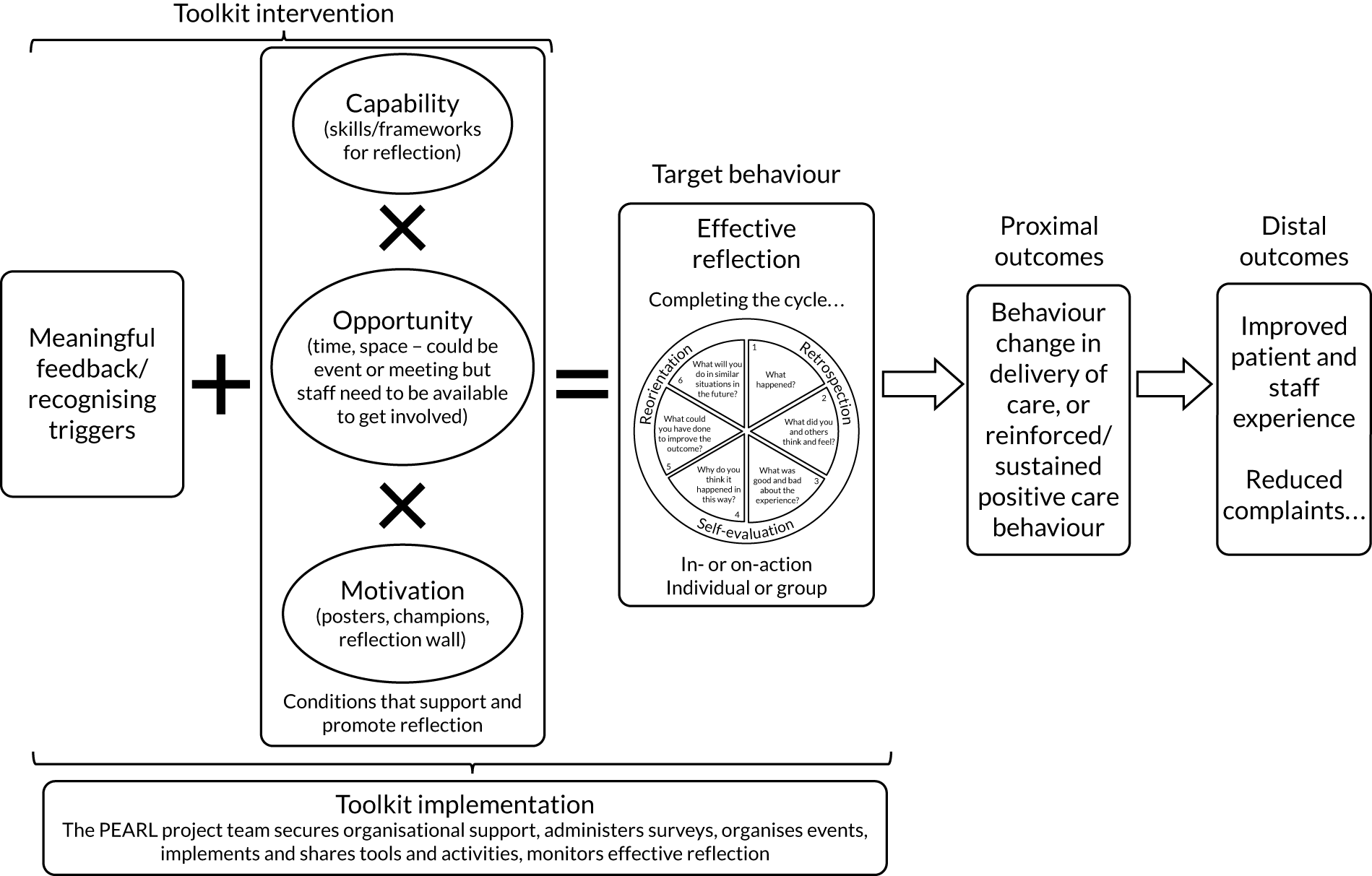
To describe effective reflection we combined Dewey’s58 three-step process of retrospection, self-evaluation and reorientation with Gibbs’ six-stage cycle of reflective learning114 to create the PEARL project ‘reflection wheel’ (Figure 15). This encourages the user to view reflection as a creative exercise in self-improvement, reducing the risk of ruminative recycling.
FIGURE 15.
The PEARL project reflection wheel.
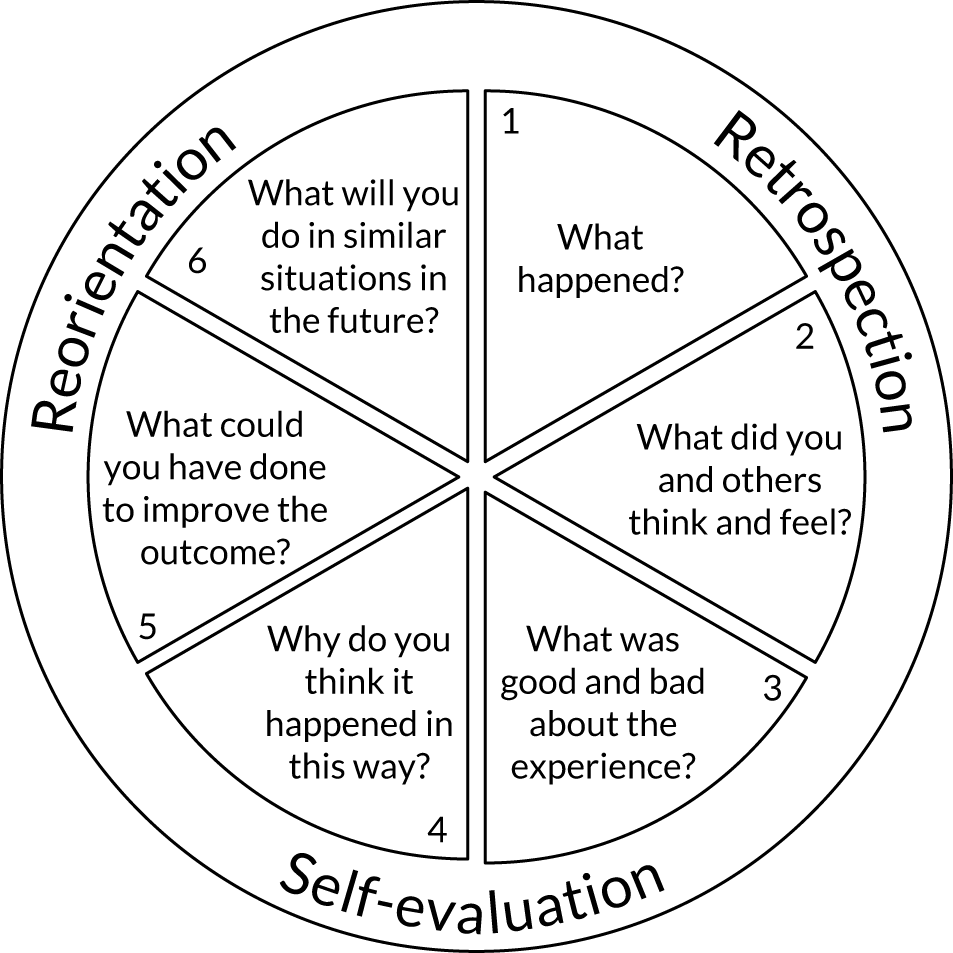
From framework to toolkit
The final stage in the evolution of the RLF was to present the reflective learning interventions (see Table 9) in a form suitable for use in the clinical environment. Working with the Art and Design Research Centre, Sheffield Hallam University, four templates were evaluated by the local project teams, with a clear preference for a boxed and layered design in which an introductory booklet describing the background, theory and outputs of the PEARL project is followed by two sections containing A5-sized mini guides to practical tools for meaningful feedback and effective reflection and one section with A4-sized guides of reflection in clinical practice. Beneath this lies a resources section containing the surveys, sample reports, posters and cue cards. The toolkit box is attractively presented to stimulate a degree of curiosity and a desire to see what lies inside. The inside of the lid contains a storyboard in the form of a cartoon, and interposed between the box lid and the introductory booklet is a (non-glass) mirror inscribed with the PEARL project reflection wheel.
The mini guides were developed by the project management team with feedback from the local teams, incorporating the reflection specifications used by the local teams for the nine reflection activities produced in their final co-design meetings. The focus for each was to convey as synoptically as possible the key elements needed to get the activity under way. A standard format was employed, with sections for describing the activity, resources required and ‘top tips’. Figure 16 is an example for patient and staff group meetings. The ‘COM’ box indicates which of the three components of the COM-B framework this activity addresses.
FIGURE 16.
The PEARL project toolkit example effective reflection mini guide.
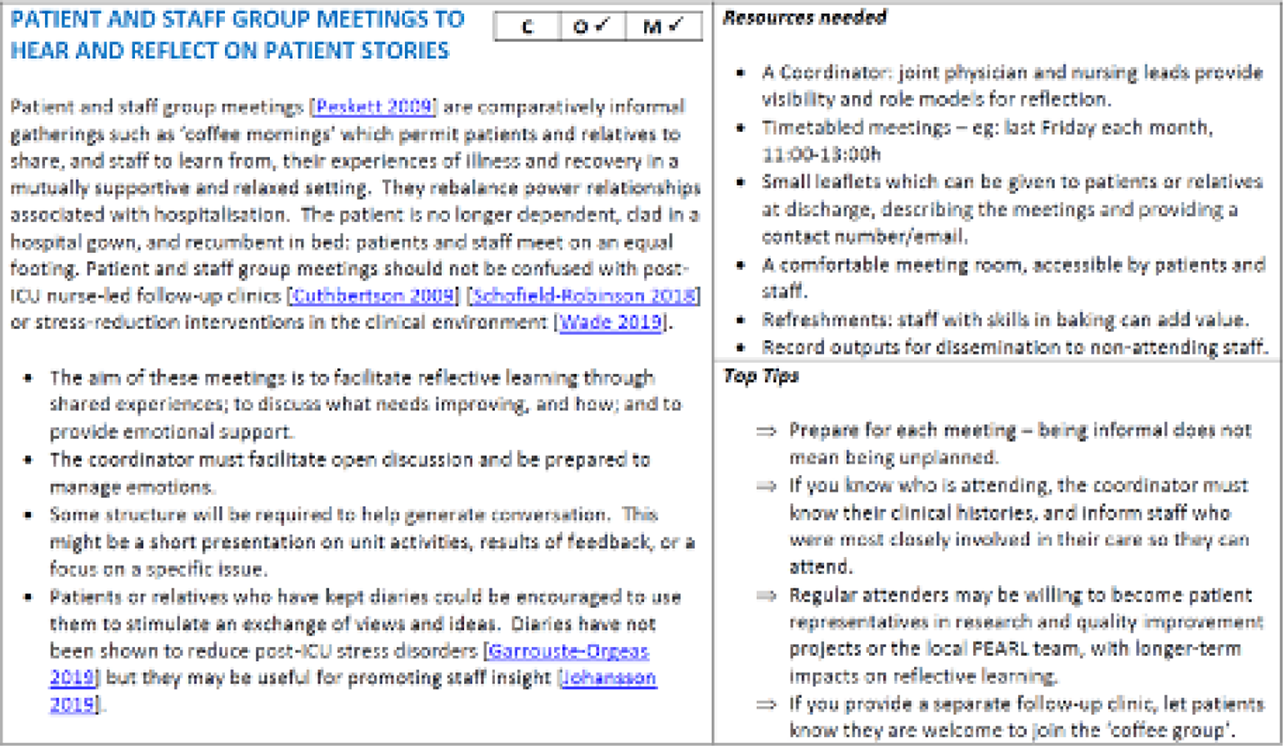
Chapter 5 Discussion
Overview
The PEARL project is a novel mixed-methods exploratory study that aims to improve patient and staff experiences of the health-care system by enhancing staff insight and empathy through reflective learning. Over 3 years we formed a highly effective collaboration of clinicians, patients and researchers; developed two surveys to measure patient, relative and staff experiences of health care; provided regular feedback reports to local teams and explored their use of the data; worked with clinicians and patients to co-design reflective learning interventions; and evolved a behaviour change model of reflective learning. This logic model provided a framework with which we have created a toolkit containing activities that will help health-care staff acquire meaningful feedback, use that feedback for effective reflection and ultimately apply reflective learning in the clinical environment to produce better outcomes for patients and staff.
Local leadership was crucial for successful project delivery. We combined senior managerial support with strong clinical leadership to encourage staff participation and to identify and welcome patients as collaborators in the local project teams. To minimise creating additional work for already very busy staff, we asked teams to integrate project work as far as possible in existing activities. This approach should facilitate sustainability after the end of the project.
The PEARL project surveys were an essential element in providing meaningful feedback combining quantitative and qualitative data in an easily accessible format. The surveys provided an easy justification for team meetings. For the patient surveys, the PIPs provided information (not just ‘data’) showing that patients’ and relatives’ satisfaction with care is determined by their perceptions of how well staff communicate, especially doctors. This finding held true for both ICUs and AMUs, despite the difference in overall satisfaction. Medical staff who make time for patients and relatives, who listen as well as talk and who use accessible language will enhance patient experience and are valuable role models for trainees. Free-text comments brought quantitative data to life and engaged the emotions, which helped to motivate staff to address matters of concern; positive narrative feedback helped teams to recognise excellence and enhance morale. The value of positive feedback was two-fold: to make negative feedback more palatable and, and where detail was provided, to offer benchmarks for excellence.
The staff surveys revealed strong support for reflection as a professional duty and for improving patient care, and they provided a rich source of materials on which to reflect, by exposing concerns about care quality, pressures of work and emotional exhaustion, and evidence of opportunities to flatten hierarchies and promote empowerment, ‘voice’ and teamworking. The contextual differences between AMUs and ICUs in staff experience, combined with the absence of differences in the desire of staff to use patient feedback to improve care, should stimulate organisations to reflect on how best to support staff in hard-pressed clinical areas: effective reflection and staff well-being are complementary.
The key finding from our ethnographic observations is that reflective learning is not a simple task. Despite (or possibly because of) the widespread requirement for written reflections to form part of professional portfolios for appraisal and revalidation, and despite the strong endorsement by staff of the use of patient experience to promote reflective learning, few clinical staff seem to analyse the processes involved in using feedback and apply them creatively for critical self-analysis and reorientation. This was not necessarily from a lack of desire to do so, but probably because their primary desire was to improve care directly, rather than improving insight and empathy as the more proximate target. However, as we know, if we could mandate better care just through providing checklists, there would be no need for reflection and no high-profile organisational failures in health care. Therefore, we had to provide regular reminders to participants that the task in hand was to design interventions to enhance reflection, not to design ‘better ward rounds’ or other clinical activities, despite these being the ultimate desired outcomes. Closing the loop on reflection is central to making reflection creative: using experiences to learn, to improve and to design a better health-care system. The creative element stops reflection from being rumination. Our reflective learning model and the PEARL project wheel are designed to promote this approach.
The PEARL project logic model has the potential to be used both diagnostically to evaluate the reflective learning environment and predictively to test behavioural interventions. Our data are highly preliminary and require large-scale prospective testing; however, among front-line staff we find strong support for the use of patient and staff feedback for reflection and a wide range of ideas about how to make feedback accessible and meaningful and how to use it to best effect. Staff perceive the main obstacle to effective reflection to be the lack of opportunities to reflect in the workplace. This is probably symptomatic of the workload pressures of the health service, as reflected in the high rates of work-related stress reported in the staff survey and observed by patients and relatives in their free-text responses to the patient survey.
Not all members of staff will be as highly motivated as the local PEARL project teams, who will need to make reflection ‘part of what we do’ every day and create an ethos of reflective learning as the norm, not the exception, and diffuse this throughout their units and trusts. Real-world stories make a profound difference by engaging emotions and making experiences relevant. Seeing the world through others’ eyes takes imagination, time and effort, and these can be constrained by the demands of a busy clinical environment. Many of the PEARL project tools, therefore, take these factors into account.
We identified many sources of feedback regarding patient experiences, both formal and informal; however, staff often missed opportunities to use these experiences, perhaps because some were highly personal or regarded as less legitimate because they were informal. All experiences are legitimate for reflection. In addition, sometimes the most transient experiences are the most affecting: a raised eyebrow or a shrug of the shoulders, or an affectionate embrace or squeeze of the hand, may ‘speak volumes’ and are well worth subjecting to analysis. Guidance on recognising triggers for reflection and finding ways of using and sharing these experiences is also included in the toolkit. Our patient representatives developed ‘cue cards’, which can be used not only as a resource in group discussions but also to allow staff to record events occurring during clinical work for later exploration and analysis.
An important but possibly undervalued element in professional development activities is enjoyment. The local teams not only maintained momentum for 3 years but grew in terms of interest, participation and ownership during that time, with excellent engagement by unit staff in promoting the surveys, completing the staff survey and using the survey reports to promote reflection. The co-design meetings and plenary workshops included time for socialising, with refreshments and lunch included. The meetings were expertly facilitated, and the sense of creating something new seemed to engage all of the participants and foster innovative thinking. The PEARL project was a worked example of how reflection in practice can contribute to staff well-being,119–123 which could also be a relevant outcome metric in evaluating the PEARL project. This approach was carried through to the design of the toolkit itself. We chose a mix of contents, from short accessible guides for use in the clinical environment to more discursive accounts of the science of reflective learning, and presented them in a format that should appeal to a wide range of staff. The tools ranged from a poster, which could be displayed behind lavatory doors (without removal by hospital estates management), to short guides on setting up Schwartz-type rounds124 or PEARL surveys, to full reports of the patient and staff surveys. Effective reflection is challenging; however, it can also be creative and ultimately fulfilling.
The PEARL project toolkit is not the end of the PEARL project: it is the beginning. Our intention is to build on this work by evaluating the toolkit as a complex intervention125 in a prospective randomised step-wedge trial.
Robustness of the study and limitations
The PEARL project is a novel approach to developing reflective learning. We have empowered staff and patients from AMUs and ICUs to collaborate with content experts to create a range of tools to gather meaningful feedback, to use that feedback for effective reflection and to reflect in clinical practice with the intention of improving patient and staff experience. As far as we can tell, the project outputs – the RLF and toolkit – are unique in this context.
The surveys were a central element of the PEARL project. Setting them up required the AMU and ICU staff to work together in their local project teams to develop the best method for dissemination and to use the feedback to promote reflection and compare results between units. Regular reports helped to maintain interest and focus. However, the analysis of the questionnaires and preparation of these reports was onerous, despite using machine-readable forms, and took the combined resources of the project manager, a data clerk and our statistician. We do not regard this as sustainable outside the environment of a funded research project. Web-enabled electronic surveys will be required for future work.
Similarly, the extraction, transcription and analysis of the free-text contributions from both surveys was time-consuming. We are undertaking an exploratory study of machine-learning analysis of free text, with the intention of developing methods for automated thematic analysis that could be applied prospectively to web-based surveys.
A strength of the PEARL project was the broad range of participants, particularly our patient and relative contributors. We recognise that the PEARL project collaborators represent those who are committed to reflection and quality care, and may, therefore, be more invested in the project outputs than those who come to it de novo. However, we did not find resistance when we piloted the toolkit in the three centres. We do not regard them as atypical: the respondents to the staff surveys were similarly committed to reflection as a means of improving care quality. It is nevertheless very likely that a large-scale study with more centres will reveal differences in local contexts and cultures, which may act as barriers to adoption of the toolkit. A potential weakness of the surveys is under-representation of certain ethnic groups. For example, white respondents represented 70% of the total respondents for the two trusts situated in Birmingham; however, at the last reported population census in 2011, 57.9% of the local urban population were in this category. 126 We do not know if this represents reduced engagement by non-white populations or language barriers. It was not possible logistically or financially to translate the patient survey into non-English languages. We will conduct subanalyses to explore possible ethnic differences in the experience of health care, but this was not the main purpose of the patient survey, which was to provide feedback that could be used by staff for promoting reflection, and in this respect it served that purpose well.
Chapter 6 Conclusions
Implications for practice
In the PEARL project, we have shown that staff in AMUs and ICUs have a strong desire to improve practice through reflective learning and that this desire seems to be independent of variation in contextual factors that affect staff experience, such as workload and staffing pressures, or the experience of being valued and heard. Indeed, staff view reflective learning as an instrument for addressing some of these workplace-based challenges and stressors. However, the ability of the individual to actually perform reflection effectively is not independent of organisational context. To convert desire into action, positive staff attitudes towards reflection need organisational support, paralleled by evidence that the organisation itself is capable of reflective learning. The first implication for practice is that trusts should understand that effective reflection needs to be led, practised and demonstrated by senior executive leadership, senior clinical staff and middle management.
Because the desire to use reflection effectively is context independent, we would assert that the PEARL project can apply to all fiduciary relationships, not just to those in health care. The second practice implication of our work, therefore, is that the PEARL project should be generalisable.
The current approaches to reflective learning are perceived as suffering from deficiencies, such as a lack of authenticity, a focus on short-term or summative outcomes or a failure to effect genuine change. We have also shown that staff prioritise certain aspects of reflection over others. They tend to reflect on their own clinical practice rather than specifically on their patients’ experiences; to select the more technical aspects of health-care delivery rather than attitudes and behaviours as examples of reflection; and to focus on interventions or activities that enhance access to feedback and opportunities for reflection instead of dissecting the (effortful) mental processes required for performing effective reflection. The third implication, therefore, is that for reflection to become effective it needs to be ‘unpackaged’, to become explicit and deliberate in the initial stages: the phases of conscious incompetence and conscious competence in reflective learning. Get this right and effective reflection will become a virtuous habit (unconscious competence).
By using co-design techniques with front-line staff and patients and relatives, together we have developed reflective learning tools that can be integrated with existing professional development activities and can be locally owned and adaptable, so that individual units can participate in this creative process and share their work between units or between trusts. The toolkit is not intended to be a static entity: it is a beginning, not an end. Our fourth implication is that staff must make the PEARL project their own creative enterprise and participate in a networked community of practice. This approach is considered to have contributed to the success of the Future Hospital Programme. 127
We have found the COM-B framework to be a valuable approach for describing reflection in terms of capability, opportunity and motivation. By combining the COM-B framework with pedagogic theories of learning we have created a composite model that has diagnostic potential, for example by identifying that staff tend to focus on opportunities for reflection more than on capability or motivation. Another example is provided by the unit that had better than expected staff ratings of their capability to reflect, and then realised that they had two members of staff who were employed as mental health nurses who discharged this responsibility primarily by providing staff support through workplace-based mentorship in reflection, thus an impact on capability. Our fifth implication for practice, therefore, is that the PEARL logic model could be employed in a predictive manner to evaluate different approaches for enhancing reflection to improve patient and staff experience and to explore how variations in context influence reflection. This links to our recommendations for further research.
Further research recommendations
Although the toolkit has considerable face validity, it cannot be assumed that all that is required for successful implementation is to deliver the box to the units and trusts who wish to use it. There is a substantial gap between developing a promising intervention and applying it effectively in a new context. 128–130 Moreover, we regard the toolkit not only as a preliminary offering requiring further development but as a platform for local staff to adopt, adapt, revise and recreate the tools in their own units. If it is received as an immutable and perfectly formed set of commandments for reflection, it will suffer the same fate as many other well-intentioned best practice recommendations.
The toolkit should be evaluated as a complex intervention125 in a mixed-methods, prospective, randomised, stepped-wedge cluster trial. This method allows all units to be in both control and intervention arms and gives the trial team time to undertake the cluster inductions. It also provides the best approach to evaluate the impact of context on fidelity of adoption and application of the PEARL project. Study metrics would include process measures (adoption, development and use of the toolkit), proximate outcomes (staff survey responses) and distal outcomes (patient survey responses, staff absenteeism and complaints).
A prospective cluster RCT would provide a firm foundation for evaluating other research questions.
How do local cultures influence reflective learning?
A collaborative local culture with quality-focused inclusive leadership is essential for the success of quality improvement interventions,131 and we would propose to characterise trusts and units in terms of organisational subcultures6 before and towards the end of the intervention. We would propose to evaluate two hypotheses among others. The first is that compliance-orientated organisations may be less susceptible to behavioural modification than collaboration-orientated organisations. The second is that, within whole organisations, multiple subcultures (cliques/clans, hierarchies, developmental and rational) can be identified, which are driven largely by the impact of single individuals.
How do social media create communities of learning?
We would wish to establish web-enabled surveys and to create moderated social media support groups in parallel with the roll-out of the toolkit. Disseminating outputs and sharing experiences in a concise and targeted manner is essential for reaching busy staff members, who may respond differently depending on the way information is presented (‘narrative for nurses’ and ‘data for doctors’ would be one such meme).
Are the results of locally driven experiential surveys more potent influencers than standardised national surveys?
We know that survey results are more influential the closer they are to the subjects themselves. Data and narrative are also complementary. We would, therefore, propose to compare the PEARL project surveys with the results from national surveys (NHS Inpatient Survey, NHS Staff Survey and the GMC Trainee Survey) in terms of how these various sources are used to influence practice and learning, and the extent to which their results influence staff.
Acknowledgements
The PEARL project team are grateful to the Study Steering Committee for their invaluable support: Professor Rebecca Lawton, Mr Harry Turner, Professor James Neuberger and Professor Stephen Brett. Dr Remi Bec and Mrs Cheryl Grindell were instrumental in the planning and delivery of the co-design workshops. We also thank Mrs Sue Pargeter (Health Services and Delivery Research programme manager) and Mrs Claire Price for their support.
Collaborators
Janet Willars, Caroline Higenbottam, Fiona Wyton, Emma Fellows, Katie Moss, Lauren Cooper, Luke Flavell, Jackie Flavell, James Raeside, Mary Hawkesford, Hannah Laugher, Tim Jones, Susan Nevitt, Kelly Naylor, Julie Sampson, Joanna Mann, Sarah Ballinger, Teresa Melody, Grainne Buggy, Lucie Linhartova, Jessica Thompson, Sikander Majid, Panchani Diviyesh, Patricia Thorpe, Alina Shaha, Rebecca Carvell, Anita Joshi, Karen Kneller, Helen Halliday, Collette Iles, Ingrid O’Neil, Gill Yeoman, Claire Randell, Helena Korovesis, Carmen Scott, Helen Doherty, Kay Protheroe, Leigh Dunn, Kath McCourt, Stephen Perks, Trishna Chakravorty, Cheryl Grindell, Remi Bec, Leah Duffy, Elaine Tracey, Caite Nee, Sarah Vince, Isabelle Barrow, Neil Alderson, Christine Straughan, Kirstie Cullen, Ian Spencer, Marie Thomas, Andrew Cox, Ralph Arnold, Shane Butlin, Victoria Smith, Jianxia Sun and Louise Swan.
Contributions of authors
Julian Bion (https://orcid.org/0000-0003-0344-5403) (Chief Investigator) was responsible for the overall design, management and conduct of the study, with extensive experience in health services research, pedagogic development and intensive care medicine.
Olivia Brookes (https://orcid.org/0000-0002-7944-4231) (Project Manager and Collaborator) managed the day-to-day running of the project under the chief investigator, managed governance and study set-up and the processing, analysis and presentation of study findings.
Celia Brown (https://orcid.org/0000-0002-7526-0793) (University of Warwick) has a strong academic background in pedagogic research and is the lead for medical education and reflection in the PEARL project WS4. She contributed to our understanding of how reflection is used to achieve learning.
Carolyn Tarrant (https://orcid.org/0000-0001-7356-5342) [Associate Professor in Health Psychology and Joint Group Lead of the Social Science Applied to Healthcare Improvement Research (SAPPHIRE) group, University of Leicester] was the lead for the ethnographic workstream (WS3), directing a group of ethnographers making original observations of practice.
Julian Archer (https://orcid.org/0000-0001-9983-9655) (Professor in Medical Education Research, University of Plymouth) was our expert on multisource feedback, advising on how to convert feedback into effective reflection.
Duncan Buckley (https://orcid.org/0000-0001-7432-4188) (Patient and Public Representative) provided extensive experience of the totality of the emergency care pathway. He also provided insights into patient–staff interactions.
Lisa-Marie Buckley (https://orcid.org/0000-0002-4755-8904) (Patient and Public Representative) provided extensive experience of the totality of the emergency care pathway. She also provided insights into patient–staff interactions.
Ian Clement (https://orcid.org/0000-0001-9854-6674) (Intensive Care Consultant, Newcastle upon Tyne Hospitals NHS Foundation Trust) advised on practical aspects of reflective learning and helped co-design the reflection toolkit.
Felicity Evison (https://orcid.org/0000-0002-9378-7548) (Project Statistician) oversaw the quantitative analysis from the patient and staff survey instruments.
Fang Gao Smith (https://orcid.org/0000-0002-8095-0609) (Local Lead for the Intensive Care Unit, Birmingham Heartlands Hospital) advised on practical aspects of reflective learning and helped co-design the reflection toolkit.
Chris Gibbins (https://orcid.org/0000-0001-8322-8139) (Consultant in Acute Medicine, Newcastle upon Tyne Hospitals NHS Foundation Trust) advised on practical aspects of reflective learning and helped co-design the reflection toolkit.
Emma-Jo Hayton (https://orcid.org/0000-0002-8672-2957) (Acute Medicine Lead, Birmingham Heartlands Hospital) advised on practical aspects of reflective learning and helped co-design the reflection toolkit.
Jennifer Jones (https://orcid.org/0000-0001-6936-6092) (Ethnography Research Fellow) organised and collated information from interviews and near-patient observations and was responsible for the analysis of qualitative data.
Richard Lilford (https://orcid.org/0000-0002-0634-984X) (PEARL Methodologist) advised on study design.
Randeep Mullhi (https://orcid.org/0000-0002-2387-7126) (Local Lead for the Intensive Care Unit, Queen Elizabeth Hospital) advised on practical aspects of reflective learning and helped co-design the reflection toolkit.
Greg Packer (https://orcid.org/0000-0002-7353-6581) (Trainee Representative, Intensive Care Local Team at Queen Elizabeth Hospital) was responsible for analysis of data from the GMC survey.
Gavin D Perkins (https://orcid.org/0000-0003-3027-7548) (Professor of Intensive Care Medicine, University of Warwick) was the lead for debriefing and feedback in the PEARL project.
Jonathan Shelton (https://orcid.org/0000-0002-7940-6796) (Intensive Care Consultant, Newcastle upon Tyne Hospitals NHS Foundation Trust) advised on practical aspects of reflective learning and helped co-design the reflection toolkit.
Catherine Snelson (https://orcid.org/0000-0002-1790-0780) (Acute Medicine Lead, Queen Elizabeth Hospital) advised on practical aspects of reflective learning and helped co-design the reflection toolkit.
Paul Sullivan (https://orcid.org/0000-0003-4672-658X) (Society of Acute Medicine) represented the Society of Acute Medicine in the PEARL project and provided expertise in quality improvement in acute medicine.
Ivo Vlaev (https://orcid.org/0000-0002-3218-0144) (Professor of Behavioural Sciences, University of Warwick) advised the PEARL project on behaviour change theory and techniques and lead this aspect of the toolkit development.
Daniel Wolstenholme (https://orcid.org/0000-0003-1507-6043) (NIHR CLAHRC Yorkshire and the Humber) was the co-design facilitator leading the co-design workshops and helped with the design of the toolkits.
Stephen Wright (https://orcid.org/0000-0002-7011-0606) (Senior Intensive Care Consultant, Newcastle upon Tyne Hospitals NHS Foundation Trust) advised on practical aspects of reflective learning and helped co-design the reflection toolkit. He also advised the project on the family satisfaction survey.
Data-sharing statement
Requests for access to data should be addressed to the corresponding author. The qualitative study data generated are not suitable for sharing beyond those contained within the report. Further information can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Kirkup B. The Report of the Morecambe Bay Investigation 2015. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/408480/47487_MBI_Accessible_v0.1.pdf (accessed September 2019).
- Kirkup B. Report of the Liverpool Community Health Independent Review 2018. www.england.nhs.uk/publication/report-of-the-liverpool-community-health-independent-review/ (accessed September 2019).
- Gosport Independent Panel . Gosport War Memorial Hospital: The Report of the Gosport Independent Panel 2018. www.gosportpanel.independent.gov.uk/media/documents/070618_CCS207_CCS03183220761_Gosport_Inquiry_Whole_Document.pdf (accessed September 2019).
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry 2013. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/279124/0947.pdf (accessed September 2019).
- Dixon-Woods M, Baker R, Charles K, Dawson J, Jerzembek G, Martin G, et al. Culture and behaviour in the English National Health Service: overview of lessons from a large multimethod study. BMJ Qual Saf 2014;23:106-15. https://doi.org/10.1136/bmjqs-2013-001947.
- Mannion R, Davies H. Understanding organisational culture for healthcare quality improvement. BMJ 2018;363. https://doi.org/10.1136/bmj.k4907.
- World Health Organization (WHO) . The World Health Report 2000. Health Systems: Improving Performance 2000.
- Institute of Medicine Committee on Quality of Health Care in America . Crossing the Quality Chasm: A New Health System for the 21st Century 2001.
- Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2012-001570.
- Department of Health and Social Care (DHSC) . High Quality Care For All. NHS Next Stage Review Final Report 2008.
- NHS Digital . About the NHS Outcomes Framework n.d. https://digital.nhs.uk/data-and-information/publications/ci-hub/nhs-outcomes-framework (accessed February 2019).
- Care Quality Commission . NHS Patient Experience Survey Programme: Outline Programme 2017 18 n.d. www.cqc.org.uk/file/151928 (accessed February 2019).
- Care Quality Commission . Adult Inpatient Survey 2017 n.d. www.england.nhs.uk/statistics/2018/06/13/overall-patient-experience-scores-2017-adult-inpatient-survey-update/ (accessed February 2019).
- NHS . Friends and Family Test n.d. www.england.nhs.uk/fft/ (accessed February 2019).
- NHS Digital . Data on Written Complaints in the NHS n.d. https://digital.nhs.uk/data-and-information/publications/statistical/data-on-written-complaints-in-the-nhs (accessed February 2019).
- Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) . Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) n.d. www.hcahpsonline.org/ (accessed February 2019).
- Australian Commission on Safety and Quality in Health Care (ACSQHC) . The National Safety and Quality Health Service Standards 2012.
- NHS Survey Coordination Centre . NHS Staff Survey 2019 n.d. www.nhsstaffsurveys.com/Page/1056/Home/NHS-Staff-Survey-2018/ (accessed February 2019).
- Aiken LH, Sermeus W, Van den Heede K, Sloane DM, Busse R, McKee M, et al. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ 2012;344. https://doi.org/10.1136/bmj.e1717.
- Flott K, Darzi A, Mayer E. Care pathway and organisational features driving patient experience: statistical analysis of large NHS datasets. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-020411.
- Lawton R, O’Hara JK, Sheard L, Reynolds C, Cocks K, Armitage G, et al. Can staff and patient perspectives on hospital safety predict harm-free care? An analysis of staff and patient survey data and routinely collected outcomes. BMJ Qual Saf 2015;24:369-76. https://doi.org/10.1136/bmjqs-2014-003691.
- Learning from Excellence . Learning from Excellence: A Call to Learn from What Goes Well in Healthcare n.d. https://learningfromexcellence.com/ (accessed February 2019).
- Burt J, Newbould J, Abel G, Elliott MN, Beckwith J, Llanwarne N, et al. Investigating the meaning of ‘good’ or ‘very good’ patient evaluations of care in English general practice: a mixed methods study. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-014718.
- Healthwatch . Suffering in Silence: Listening to Consumer Experiences of the Health and Social Care Complaints System 2014.
- Gallan AS, Girju M, Girju R. Perfect ratings with negative comments: learning from contradictory patient survey responses. Patient Experience J 2017;4:15-28. https://doi.org/10.35680/2372-0247.1234.
- O’Hara JK, Reynolds C, Moore S, Armitage G, Sheard L, Marsh C, et al. What can patients tell us about the quality and safety of hospital care? Findings from a UK multicentre survey study. BMJ Qual Saf 2018;27:673-82. https://doi.org/10.1136/bmjqs-2017-006974.
- Reader TW, Gillespie A, Roberts J. Patient complaints in healthcare systems: a systematic review and coding taxonomy. BMJ Qual Saf 2014;23:678-89. https://doi.org/10.1136/bmjqs-2013-002437.
- Sheard L, Marsh C, O’Hara J, Armitage G, Wright J, Lawton R. The patient feedback response framework – understanding why UK hospital staff find it difficult to make improvements based on patient feedback: a qualitative study. Soc Sci Med 2017;178:19-27. https://doi.org/10.1016/j.socscimed.2017.02.005.
- Martin GP, Aveling EL, Campbell A, Tarrant C, Pronovost PJ, Mitchell I, et al. Making soft intelligence hard: a multi-site qualitative study of challenges relating to voice about safety concerns. BMJ Qual Saf 2018;27:710-17. https://doi.org/10.1136/bmjqs-2017-007579.
- Armstrong N, Brewster L, Tarrant C, Dixon R, Willars J, Power M, et al. Taking the heat or taking the temperature? A qualitative study of a large-scale exercise in seeking to measure for improvement, not blame. Soc Sci Med 2018;198:157-64. https://doi.org/10.1016/j.socscimed.2017.12.033.
- Flott KM, Graham C, Darzi A, Mayer E. Can we use patient-reported feedback to drive change? The challenges of using patient-reported feedback and how they might be addressed. BMJ Qual Saf 2017;26:502-7. https://doi.org/10.1136/bmjqs-2016-005223.
- Scott DAH, Grant SM. A meta-ethnography of the facilitators and barriers to successful implementation of patient complaints processes in health-care settings. Health Expect 2018;21:508-17. https://doi.org/10.1111/hex.12645.
- DeCourcy A, West E, Barron D. The National Adult Inpatient Survey conducted in the English National Health Service from 2002 to 2009: how have the data been used and what do we know as a result?. BMC Health Serv Res 2012;12. https://doi.org/10.1186/1472-6963-12-71.
- Lee R, Baeza JI, Fulop NJ. The use of patient feedback by hospital boards of directors: a qualitative study of two NHS hospitals in England. BMJ Qual Saf 2018;27:103-9. https://doi.org/10.1136/bmjqs-2016-006312.
- Sheard L, Peacock R, Marsh C, Lawton R. What’s the problem with patient experience feedback? A macro and micro understanding, based on findings from a three-site UK qualitative study. Health Expect 2019;22:46-53. https://doi.org/10.1111/hex.12829.
- Gleeson H, Calderon A, Swami V, Deighton J, Wolpert M, Edbrooke-Childs J. Systematic review of approaches to using patient experience data for quality improvement in healthcare settings. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-011907.
- Sheard L, Marsh C, O’Hara J, Armitage G, Wright J, Lawton R. Exploring how ward staff engage with the implementation of a patient safety intervention: a UK-based qualitative process evaluation. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-014558.
- Care Quality Commission . Freedom to Speak Up Guardians n.d. www.cqc.org.uk/national-guardians-office/content/national-guardians-office (accessed February 2019).
- Behavioural Insights Team . The Behavioural Insights Team n.d. www.behaviouralinsights.co.uk/ (accessed February 2019).
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81-95. https://doi.org/10.1007/s12160-013-9486-6.
- Michie S, West R, Sheals K, Godinho CA. Evaluating the effectiveness of behavior change techniques in health-related behavior: a scoping review of methods used. Transl Behav Med 2018;8:212-24. https://doi.org/10.1093/tbm/ibx019.
- Johnson MJ, May CR. Promoting professional behaviour change in healthcare: what interventions work, and why? A theory-led overview of systematic reviews. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-008592.
- Chauhan BF, Jeyaraman MM, Mann AS, Lys J, Skidmore B, Sibley KM, et al. Behavior change interventions and policies influencing primary healthcare professionals’ practice-an overview of reviews. Implement Sci 2017;12. https://doi.org/10.1186/s13012-016-0538-8.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6. https://doi.org/10.1186/1748-5908-6-42.
- Kahneman D. Thinking, Fast and Slow. London: Penguin Random House; 2012.
- Petty RE, Cacioppo JT. The effects of involvement on responses to argument quantity and quality: central and peripheral routes to persuasion. J Pers Soc Psychol 1984;46:69-81. https://doi.org/10.1037/0022-3514.46.1.69.
- O’Keefe D, Dillard JP, Shen L. The SAGE Handbook of Persuasion: Developments in Theory and Practice. Thousand Oaks, CA: SAGE Publications Ltd; 2012.
- Dolan P, Hallsworth M, Halpern D, King D, Metcalfe R, Vlaev I. Influencing behaviour: the mindspace way. J Econ Psychol 2012;33:264-77. https://doi.org/10.1016/j.joep.2011.10.009.
- Kolb DA, Fry RE, Cooper C. Theories of Group Process. New York, NY: John Wiley & Sons; 1975.
- Schön DA. The Reflective Practitioner: How Professionals Think in Action. New York, NY: Basic Books; 1983.
- Pedler M, Burgoyne J, Boydell T. The Learning Company: A Strategy for Sustainable Development. Maidenhead: McGraw–Hill Publishing Company; 1996.
- Mezirow J. A critical theory of adult learning and education. Adult Educ 1981;32:3-24. https://doi.org/10.1177/074171368103200101.
- Sandars J. The use of reflection in medical education: AMEE Guide No. 44. Med Teach 2009;31:685-95. https://doi.org/10.1080/01421590903050374.
- Nonaka I, von Krogh G. Tacit knowledge and knowledge conversion: controversy and advancement in organizational knowledge creation theory. Organization Science 2009;20:635-52. https://doi.org/10.1287/orsc.1080.0412.
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977;84:191-215. https://doi.org/10.1037//0033-295x.84.2.191.
- Aronson L. Twelve tips for teaching reflection at all levels of medical education. Med Teach 2011;33:200-5. https://doi.org/10.3109/0142159X.2010.507714.
- Broadwell MM. Teaching for learning (XVI). The Gospel Guardian 1969;20:1-3a. www.wordsfitlyspoken.org/gospel_guardian/v20/v20n41p1-3a.html (accessed June 2020).
- Dewey J. How We Think: A Restatement of the Relation of Reflective Thinking to the Educative Process. Lexington, MA: D.C. Heath and Company; 1933.
- General Medical Council . The Reflective Practitioner – Guidance for Doctors and Medical Students n.d. www.gmc-uk.org/education/standards-guidance-and-curricula/guidance/reflective-practice/the-reflective-practitioner---guidance-for-doctors-and-medical-students (accessed June 2020).
- Royal College of Nursing . Revalidation Requirements: Reflection and Reflective Discussion n.d. www.rcn.org.uk/professional-development/revalidation/reflection-and-reflective-discussion (accessed September 2019).
- Roessger KM. The effect of reflective activities on instrumental learning in adult work-related education: a critical review of the empirical research. Educational Research Review 2014;13:17-34. https://doi.org/10.1016/j.edurev.2014.06.002.
- Winkel AF, Yingling S, Jones AA, Nicholson J. Reflection as a learning tool in graduate medical education: a systematic review. J Grad Med Educ 2017;9:430-9. https://doi.org/10.4300/JGME-D-16-00500.1.
- Ferguson J, Wakeling J, Bowie P. Factors influencing the effectiveness of multisource feedback in improving the professional practice of medical doctors: a systematic review. BMC Med Educ 2014;14. https://doi.org/10.1186/1472-6920-14-76.
- Boiko O, Campbell JL, Elmore N, Davey AF, Roland M, Burt J. The role of patient experience surveys in quality assurance and improvement: a focus group study in English general practice. Health Expect 2015;18:1982-94. https://doi.org/10.1111/hex.12298.
- Kappes A, Faber NS, Kahane G, Savulescu J, Crockett MJ. Concern for others leads to vicarious optimism. Psychol Sci 2018;29:379-89. https://doi.org/10.1177/0956797617737129.
- McKee M, Stuckler D. Reflective practice: how the world bank explored its own biases?. Int J Health Policy Manag 2016;5:79-82. https://doi.org/10.15171/ijhpm.2015.216.
- Farrington C, Burt J, Boiko O, Campbell J, Roland M. Doctors’ engagements with patient experience surveys in primary and secondary care: a qualitative study. Health Expect 2017;20:385-94. https://doi.org/10.1111/hex.12465.
- Ehrlinger J, Johnson K, Banner M, Dunning D, Kruger J. Why the unskilled are unaware: further explorations of (absent) self-insight among the incompetent. Organ Behav Hum Decis Process 2008;105:98-121. https://doi.org/10.1016/j.obhdp.2007.05.002.
- Garrett N, González-Garzón AM, Foulkes L, Levita L, Sharot T. Updating beliefs under perceived threat. J Neurosci 2018;38:7901-11. https://doi.org/10.1523/JNEUROSCI.0716-18.2018.
- Academy of Medical Royal Colleges . Academy and COPMeD Reflective Practice Toolkit n.d. www.aomrc.org.uk/wp-content/uploads/2018/08/Reflective_Practice_Toolkit_AoMRC_CoPMED_0818.pdf (accessed September 2019).
- General Medical Council . Meeting Our Revalidation Requirements: Overarching Principles n.d. www.gmc-uk.org/registration-and-licensing/managing-your-registration/revalidation/guidance-on-supporting-information-for-appraisal-and-revalidation/meeting-our-revalidation-requirements---overarching-principles (accessed July 2020).
- The UK Medical Revalidation coLLAboration (UMbRELLA) . Evaluating the Regulatory Impact of Medical Revalidation 2018. www.gmc-uk.org/-/media/documents/umbrella-report-final_pdf-74454378.pdf (accessed September 2019).
- Sanson-Fisher R, Hobden B, Waller A, Dodd N, Boyd L. Methodological quality of teaching communication skills to undergraduate medical students: a mapping review. BMC Med Educ 2018;18. https://doi.org/10.1186/s12909-018-1265-4.
- Papageorgiou A, Loke YK, Fromage M. Communication skills training for mental health professionals working with people with severe mental illness. Cochrane Database Syst Rev 2017;6. https://doi.org/10.1002/14651858.CD010006.pub2.
- Ditton-Phare P, Loughland C, Duvivier R, Kelly B. Communication skills in the training of psychiatrists: a systematic review of current approaches. Aust N Z J Psychiatry 2017;51:675-92. https://doi.org/10.1177/0004867417707820.
- Moore PM, Rivera Mercado S, Grez Artigues M, Lawrie TA. Communication skills training for healthcare professionals working with people who have cancer. Cochrane Database Syst Rev 2013;3. https://doi.org/10.1002/14651858.CD003751.pub3.
- Brighton LJ, Koffman J, Hawkins A, McDonald C, O’Brien S, Robinson V, et al. A systematic review of end-of-life care communication skills training for generalist palliative care providers: research quality and reporting guidance. J Pain Symptom Manage 2017;54:417-25. https://doi.org/10.1016/j.jpainsymman.2017.04.008.
- Oladeru OA, Hamadu M, Cleary PD, Hittelman AB, Bulsara KR, Laurans MS, et al. House staff communication training and patient experience scores. J Patient Exp 2017;4:28-36. https://doi.org/10.1177/2374373517694533.
- Chung HO, Oczkowski SJ, Hanvey L, Mbuagbaw J, You JJ. Educational interventions to train healthcare professionals in end-of-life communication: a systematic review and meta-analysis. BMC Med Educ 2016;16. https://doi.org/10.1186/s12909-016-0653-x.
- Curtis JR, Back AL, Ford DW, Downey L, Shannon SE, Doorenbos AZ, et al. Effect of communication skills training for residents and nurse practitioners on quality of communication with patients with serious illness: a randomized trial. JAMA 2013;310:2271-81. https://doi.org/10.1001/jama.2013.282081.
- Haynes AB, Edmondson L, Lipsitz SR, Molina G, Neville BA, Singer SJ, et al. Mortality trends after a voluntary checklist-based surgical safety collaborative. Ann Surg 2017;266:923-9. https://doi.org/10.1097/SLA.0000000000002249.
- Derksen F, Bensing J, Lagro-Janssen A. Effectiveness of empathy in general practice: a systematic review. Br J Gen Pract 2013;63:e76-84. https://doi.org/10.3399/bjgp13X660814.
- Kelm Z, Womer J, Walter JK, Feudtner C. Interventions to cultivate physician empathy: a systematic review. BMC Med Educ 2014;14. https://doi.org/10.1186/1472-6920-14-219.
- Dwamena F, Holmes-Rovner M, Gaulden CM, Jorgenson S, Sadigh G, Sikorskii A, et al. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev 2012;12. https://doi.org/10.1002/14651858.CD003267.pub2.
- Mazzi MA, Rimondini M, Deveugele M, Zimmermann C, Moretti F, van Vliet L, et al. What do people appreciate in physicians’ communication? An international study with focus groups using videotaped medical consultations. Health Expect 2015;18:1215-26. https://doi.org/10.1111/hex.12097.
- Agledahl KM, Gulbrandsen P, Forde R, Wifstad A. Courteous but not curious: how doctors’ politeness masks their existential neglect – a qualitative study of video-recorded patient consultations. J Med Ethics 2011;37:650-4. https://doi.org/10.1136/jme.2010.041988.
- Beach MC, Sugarman J, Johnson RL, Arbelaez JJ, Duggan PS, Cooper LA. Do patients treated with dignity report higher satisfaction, adherence, and receipt of preventive care?. Ann Fam Med 2005;3:331-8. https://doi.org/10.1370/afm.328.
- Laganá L, Gavrilova L, Carter DB, Ainsworth AT. A Randomized controlled study on the effects of a documentary on students’ empathy and attitudes towards older adults. Psychol Cogn Sci 2017;3:79-88. https://doi.org/10.17140/PCSOJ-3-127.
- Nelson SW, Germann CA, MacVane CZ, Bloch RB, Fallon TS, Strout TD. Intern as patient: a patient experience simulation to cultivate empathy in emergency medicine residents. West J Emerg Med 2018;19:41-8. https://doi.org/10.5811/westjem.2017.11.35198.
- Pollak KI, Alexander SC, Tulsky JA, Lyna P, Coffman CJ, Dolor RJ, et al. Physician empathy and listening: associations with patient satisfaction and autonomy. J Am Board Fam Med 2011;24:665-72. https://doi.org/10.3122/jabfm.2011.06.110025.
- Buckman R, Tulsky JA, Rodin G. Empathic responses in clinical practice: intuition or tuition?. CMAJ 2011;183:569-71. https://doi.org/10.1503/cmaj.090113.
- Amutio-Kareaga A, García-Campayo J, Delgado LC, Hermosilla D, Martínez-Taboada C. Improving Communication between physicians and their patients through mindfulness and compassion-based strategies: a narrative review. J Clin Med 2017;6. https://doi.org/10.3390/jcm6030033.
- Kiosses VN, Karathanos VT, Tatsioni A. Empathy promoting interventions for health professionals: a systematic review of RCTs. J Compassionate Health Care 2016;3. https://doi.org/10.1186/s40639-016-0024-9.
- Cleveland Clinic . Empathy: The Human Connection to Patient Care 2013. www.youtube.com/watch?v=cDDWvj_q-o8 (accessed February 2019).
- TEDx Talks . TEDxMaastricht - Fred Lee - ‘Patient Satisfaction or Patient Experience?’ 2011. https://www.youtube.com/watch?v=tylvc9dY400 (accessed February 2019).
- EIRMC . Say This, Not That: Patient Experience Video. Eastern Idaho Regional Medical Center 2013. www.youtube.com/watch?v=r842Ylpa-nQ (accessed February 2019).
- Brookes O, Brown C, Tarrant C, Archer J, Buckley D, Buckley LM, et al. Patient experience and reflective learning (PEARL): a mixed methods protocol for staff insight development in acute and intensive care medicine in the UK. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2019-030679.
- Hutchings A, Durand MA, Grieve R, Harrison D, Rowan K, Green J, et al. Evaluation of modernisation of adult critical care services in England: time series and cost effectiveness analysis. BMJ 2009;339. https://doi.org/10.1136/bmj.b4353.
- Horevoorts NJ, Vissers PA, Mols F, Thong MS, van de Poll-Franse LV. Response rates for patient-reported outcomes using web-based versus paper questionnaires: comparison of two invitational methods in older colorectal cancer patients. J Med Internet Res 2015;17. https://doi.org/10.2196/jmir.3741.
- Ebert JF, Huibers L, Christensen B, Christensen MB. Paper- or web-based questionnaire invitations as a method for data collection: cross-sectional comparative study of differences in response rate, completeness of data, and financial cost. J Med Internet Res 2018;20. https://doi.org/10.2196/jmir.8353.
- Jenkinson C, Coulter A, Bruster S. The Picker Patient Experience Questionnaire: development and validation using data from in-patient surveys in five countries. Int J Qual Health Care 2002;14:353-8. https://doi.org/10.1093/intqhc/14.5.353.
- Sullivan P, Harris ML, Bell D. The quality of patient experience of short-stay acute medical admissions: findings of the Adult Inpatient Survey in England. Clin Med 2013;13:553-6. https://doi.org/10.7861/clinmedicine.13-6-553.
- Wall RJ, Engelberg RA, Downey L, Heyland DK, Curtis JR. Refinement, scoring, and validation of the Family Satisfaction in the Intensive Care Unit (FS-ICU) survey. Crit Care Med 2007;35:271-9. https://doi.org/10.1097/01.CCM.0000251122.15053.50.
- Surveys on Patient Safety Culture . SOPS™ Hospital Survey: Version 1.0 – Hospital Survey on Patient Safety n.d. www.ahrq.gov/sites/default/files/wysiwyg/professionals/quality-patient-safety/patientsafetyculture/hospital/resources/hospscanform.pdf (accessed September 2019).
- Hutchinson A, Cooper KL, Dean JE, McIntosh A, Patterson M, Stride CB, et al. Use of a safety climate questionnaire in UK health care: factor structure, reliability and usability. Qual Saf Health Care 2006;15:347-53. https://doi.org/10.1136/qshc.2005.016584.
- General Medical Council . National Training Surveys n.d. www.gmc-uk.org/education/how-we-quality-assure/national-training-surveys (accessed September 2019).
- Atkins L, Francis J, Islam R, O’Connor D, Patey A, Ivers N, et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implement Sci 2017;12. https://doi.org/10.1186/s13012-017-0605-9.
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analyzing Qualitative Data. London: Routledge; 1994.
- Locock L, Robert G, Boaz A, Vougioukalou S, Shuldham C, Fielden J, et al. Testing accelerated experience-based co-design: a qualitative study of using a national archive of patient experience narrative interviews to promote rapid patient-centred service improvement. Health Serv Deliv Res 2014;2. https://doi.org/10.3310/hsdr02040.
- National Institute for Health Research . Translating Knowledge Into Action n.d. http://clahrc-yh.nihr.ac.uk/our-themes/translating-knowledge-into-action (accessed June 2020).
- Chamberlain P, Wolstenholme D, Dexter M, Seals E. The State of the Art of Design in Health An Expert-Led Review of the Extent of the Art of Design Theory and Practice in Health and Social Care. Sheffield: Sheffield Hallam University; 2015.
- Langley J, Wolstenholme D, Cooke J. ‘Collective making’ as knowledge mobilisation: the contribution of participatory design in the co-creation of knowledge in healthcare. BMC Health Serv Res 2018;18. https://doi.org/10.1186/s12913-018-3397-y.
- Davidoff F, Dixon-Woods M, Leviton L, Michie S. Demystifying theory and its use in improvement. BMJ Qual Saf 2015;24:228-38. https://doi.org/10.1136/bmjqs-2014-003627.
- Gibbs G. Learning by Doing: A Guide to Teaching and Learning Methods. Oxford: Further Education Unit; 1988.
- Better Services by Design . Better Services by Design 2015. https://bsbd.org.uk/bsbd/ (accessed September 2019).
- Cooke J, Langley J, Wolstenholme D, Hampshaw S. ‘Seeing’ the difference: the importance of visibility and action as a mark of ‘authenticity’ in co-production. Comment on ‘Collaboration and Co-production of Knowledge in Healthcare: Opportunities and Challenges’. Int J Health Policy Manag 2017;6:345-8. https://doi.org/10.15171/ijhpm.2016.136.
- Darley JM, Bateson CD. ‘From Jerusalem to Jericho’: a study of situational and dispositional variables in helping behaviour. J Pers Soc Psychol 1973;27:100-8. https://doi.org/10.1037/h0034449.
- Kübler–Ross E. On Death and Dying. New York, NY: Macmillan Publishers Ltd; 1969.
- Maben J, Taylor C, Dawson J, Leamy M, McCarthy I, Reynolds E, et al. A realist informed mixed-methods evaluation of Schwartz Center Rounds® in England. Health Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06370.
- The Health Foundation . Improving the Health and Wellbeing of 1.6m NHS Employees 2019. www.health.org.uk/news-and-comment/newsletter-features/improving-the-health-and-wellbeing-of-1.5m-nhs-employees (accessed September 2019).
- NHS Employers . Evidence Base Health and Wellbeing: Evidence Base n.d. www.nhsemployers.org/retention-and-staff-experience/health-and-wellbeing/developing-your-health-and-wellbeing-strategy/evidence-base (accessed September 2019).
- The King’s Fund . Encouraging Staff Wellbeing in Health and Care 2016. www.kingsfund.org.uk/events/encouraging-staff-wellbeing-health-and-care (accessed September 2019).
- Chartered Institute of Personnel and Development . Health and Well-Being at Work 2019. www.cipd.co.uk/knowledge/culture/well-being/health-well-being-work (accessed September 2019).
- The Point of Care Foundation . Schwartz Rounds n.d. www.pointofcarefoundation.org.uk/our-work/schwartz-rounds/ (accessed February 2019).
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and Evaluating Complex Interventions. Medical Research Council; 2019.
- Birmingham City Council . 2011 Birmingham Population &Amp; Migration Topic Report 2011. www.birmingham.gov.uk/downloads/file/9742/2011_birmingham_population_and_migration_topic_report (accessed September 2019).
- Frith L, Hepworth L, Lowers V, Joseph F, Davies E, Gabbay M. Role of public involvement in the Royal College of Physicians’ Future Hospitals healthcare improvement programme: an evaluation. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-027680.
- Tarrant C, O’Donnell B, Martin G, Bion J, Hunter A, Rooney KD. A complex endeavour: an ethnographic study of the implementation of the Sepsis Six clinical care bundle. Implement Sci 2016;11. https://doi.org/10.1186/s13012-016-0518-z.
- Dixon-Woods M, Leslie M, Tarrant C, Bion J. Explaining Matching Michigan: an ethnographic study of a patient safety program. Implement Sci 2013;8. https://doi.org/10.1186/1748-5908-8-70.
- Dixon-Woods M, McNicol S, Martin G. Ten challenges in improving quality in healthcare: lessons from the Health Foundation’s programme evaluations and relevant literature. BMJ Qual Saf 2012;21:876-84. https://doi.org/10.1136/bmjqs-2011-000760.
- Fulop NJ, Ramsay AIG. How organisations contribute to improving the quality of healthcare. BMJ 2019;365. https://doi.org/10.1136/bmj.l1773.
Appendix 1 The PEARL collaboration
Writing Committee
Julian Bion, chief investigator and corresponding author. Professor of Intensive Care Medicine, University of Birmingham, Birmingham, UK.
Olivia Brookes, PEARL Project Manager Research, Development & Innovation, University Hospitals Birmingham NHS Foundation Trust, Birmingham, UK.
Celia Brown, Population Evidence and Technologies, University of Warwick, Coventry, UK.
Carolyn Tarrant, SAPPHIRE group, University of Leicester, Leicester, UK.
Duncan Buckley, PPI Representative, Birmingham, UK.
Lisa Marie Buckley, PPI Representative, Birmingham, UK.
Felicity Evison, Informatics Department, University Hospitals Birmingham NHS Foundation Trust, Birmingham, UK.
Jennifer Jones, SAPPHIRE group, University of Leicester, Leicester, UK.
Ivo Vlaev Behavioural Science, University of Warwick, Coventry, UK.
Daniel Wolstenholme, NIHR CLAHRC Yorkshire and Humber, Sheffield, UK.
Co-applicants
Julian Archer, Royal Australasian College of Surgeons, Melbourne, VIC, Australia.
Ian Clement, Critical Care, Newcastle upon Tyne Hospitals NHS Foundation Trust, Newcastle upon Tyne, UK.
Fang Gao, Smith Institute of Inflammation & Ageing, University of Birmingham, Birmingham, UK.
Chris Gibbins, Acute Medicine, Newcastle upon Tyne Hospitals NHS Foundation Trust, Newcastle upon Tyne, UK.
Emma Hayton, Acute Medicine, University Hospitals Birmingham NHS Foundation Trust, Birmingham, UK.
Richard Lilford, Applied Health Research & Delivery, University of Warwick, Coventry, UK.
Randeep Mullhi, Critical Care, University Hospitals Birmingham NHS Foundation Trust, Birmingham, UK.
Greg Packer, Critical Care, University Hospitals Birmingham NHS Foundation Trust, Birmingham, UK.
Gavin Perkins, Critical Care Medicine, University of Warwick, Coventry, UK.
Jonathan Shelton, Critical Care, Newcastle upon Tyne Hospitals NHS Foundation Trust, Newcastle upon Tyne, UK.
Catherine Snelson, Critical Care and Acute Medicine, University Hospitals Birmingham NHS Foundation Trust, Birmingham, UK.
Paul Sullivan, Acute Medicine, Chelsea and Westminster NHS Trust, London, UK.
Stephen Wright, Critical Care, Newcastle upon Tyne Hospitals NHS Foundation Trust, Newcastle upon Tyne, UK.
Collaborators
Janet Willars.
Caroline Higenbottam.
Fiona Wyton.
Emma Fellows.
Katie Moss.
Lauren Cooper.
Luke Flavell.
Jackie Flavell.
James Raeside.
Mary Hawkesford.
Hannah Laugher.
Tim Jones.
Susan Nevitt.
Kelly Naylor.
Julie Sampson.
Joanna Mann.
Sarah Ballinger.
Teresa Melody.
Grainne Buggy.
Lucie Linhartova.
Jessica Thompson.
Sikander Majid.
Panchani Diviyesh.
Patricia Thorpe.
Alina Shaha.
Rebecca Carvell.
Anita Joshi.
Karen Kneller.
Helen Halliday.
Collette Iles.
Ingrid O’Neil.
Gill Yeoman.
Claire Randell.
Helena Korovesis.
Carmen Scott.
Helen Doherty.
Kay Protheroe.
Leigh Dunn.
Kath McCourt.
Stephen Perks.
Trishna Chakravorty.
Cheryl Grindell.
Remi Bec.
Leah Duffy.
Elaine Tracey.
Caite Nee.
Sarah Vince.
Isabelle Barrow.
Neil Alderson.
Christine Straughan.
Kirstie Cullen.
Ian Spencer.
Marie Thomas.
Andrew Cox.
Ralph Arnold.
Shane Butlin.
Victoria Smith.
Jianxia Sun.
Louise Swan.
Project Steering Committee
Rebecca Lawton, chairperson.
Stephen Brett.
James Neuberger.
Harry Turner.
List of abbreviations
- AHP
- allied health professional
- AMU
- acute medical unit
- CDU
- clinical decisions unit
- COM–B
- Capability, Opportunity, Motivation – Behaviour
- ED
- emergency department
- GMC
- General Medical Council
- HDU
- high-dependency unit
- ICU
- intensive care unit
- MINDSPACE
- messenger, incentives, norms, default, salience, priming, affect, commitment, ego
- NIHR
- National Institute for Health Research
- PALS
- Patient Advice and Liaison Service
- PEARL
- Patient Experience And Reflective Learning
- PIP
- performance–importance plot
- PPI
- patient and public involvement
- RCT
- randomised controlled trial
- RLF
- reflective learning framework
- SAPPHIRE
- Social Science Applied to Healthcare Improvement Research
- TK2A
- Translating Knowledge into Action
- WS
- workstream
