Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 14/04/16. The contractual start date was in March 2016. The final report began editorial review in December 2018 and was accepted for publication in June 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Fiona Lobban and Vanessa Pinfold were the originators of the Relatives’ Education And Coping Toolkit (REACT) and, therefore, are not independent researchers. Jo Rycroft-Malone is Programme Director of the National Institute for Health Research (NIHR) Health Services and Delivery Research (HSDR) programme, which funded this research, and is chairperson of the funding committe, and, at the time that the project was funded, was the deputy chairperson of the commissioned workstream of the NIHR HSDR programme.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Lobban et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Background and rationale
In this chapter, we outline the potential benefits of digital health interventions (DHIs) to support self-management of long-term health conditions and describe the implementation challenges in reducing the gap between the potential that DHIs can deliver and what is currently available to service users and carers. We then consider the specific example of long-term mental health problems, and make the case for the need to better support relatives who care for people with psychosis or bipolar disorder. Finally, we describe the design and development of the Relatives’ Education And Coping Toolkit (REACT) and its use in this study to explore the factors affecting its implementation within early intervention for psychosis (EIP) teams in NHS trusts across England.
Digital health interventions in the NHS
Recent decades have seen a significant increase in the development and use of DHIs to support health-care delivery. DHIs can be defined as programmes that provide support and treatment for physical and/or mental health problems via a digital platform or device, for example a website or an app (an application, typically downloaded by a user to a mobile device). The support provided can be emotional, decisional and/or behavioural. 1,2 Many are available directly to users through the internet or app stores, whereas others are designed to be offered as part of broader health-care packages.
In this study, we were interested specifically in the use of DHIs in supporting patients and relatives to self-manage long-term mental health conditions, although much of the rationale and learning are potentially generalisable to long-term physical health conditions. The prevalence of long-term health problems has increased as the population ages, and costs to public health services are substantial. 3 By supporting people to understand their condition better, identify factors influencing the severity of symptoms, spot early signs of relapse, adopt strategies to manage these early signs and learn when and where to seek help most effectively, it is argued that we can improve the quality of life of individuals and their families, and save public money. 4
The attraction of DHIs to support long-term conditions is easy to see. They offer the potential for widespread dissemination of high-quality, standardised care, accessible at the user’s convenience. Hence, they are particularly suited to rural areas and developing countries, where face-to-face service delivery can be very challenging but access to mobile technology is developing at pace. 5
Self-management interventions are designed to empower users, and digital delivery offers the added potential of uniting people online to share their experiences and harness the power of peer support. Although DHI development costs can be substantial, ongoing delivery is likely to be more cost-effective than face-to-face support.
Research evidence to support the feasibility, acceptability and effectiveness of DHIs in mental health is mounting. Data exist to support the short-term benefits of web-based psychological treatments for depression and anxiety disorders, compared with waiting list controls. 6,7 Online interventions are being rapidly developed for psychosis and bipolar disorder, where data support their feasibility and acceptability. 8–11 For these reasons, there has been a strong policy push to develop the UK’s digital health provision. 12
The implementation challenge
The successful implementation of DHIs in routine health-care services is far more limited than in research. Despite substantial investment in development, many DHIs are not adopted by their intended users, are abandoned, fail to scale up locally or spread to other settings, or are not sustained over time. The challenges can be systemic (i.e. difficulties in embedding an intervention in existing health services) or at the individual level, with low uptake levels among service users, although the two issues can be connected, for example if users feel that the intervention is not well supported by their health-care professionals.
Attempts to offer an online cognitive–behavioural therapy programme, Beating the Blues, at scale in UK mental health services13 and as part of routine care in the USA14 highlighted great difficulties in getting patients to use the programme or staff to integrate it into practice. In many ways, this is unsurprising; this is a relatively new field of enquiry and the process of change will inevitably take time. However, given the substantial implementation gap that still exists for non-digital health interventions,15 it is crucial that we do not assume that the transition from evidence to impact is inevitable. We urgently need to understand the main factors inhibiting the implementation of DHIs and use this understanding to better inform their design, evaluation, commissioning and delivery, and maximise their potential benefits.
This understanding should also mitigate the potential harm of inadequately tested DHIs, such as the increased risk of serious of breaches of confidentiality for personal and sensitive data;16 expensive information technology (IT) failures;17–19 potential increases in health inequalities;20 and lack of evidence-based commissioning, resulting in ineffective or harmful interventions being offered in clinical practice.
Psychosis and bipolar disorder
Psychosis is an umbrella term that covers many conditions, the common feature of which is a loss of touch with reality. The lifetime prevalence of a psychotic episode ranges from 5% to 7%, with the majority having only one episode. 21 Approximately 0.48% of the population develop more enduring mental health problems such as schizophrenia,22 which is estimated to cost the economy of England over £5B annually. 23
The most common manifestations of psychosis are believing things that are generally accepted to be untrue by other people (delusions); being unable to think clearly and so sounding muddled and confused (thought disorder); and experiencing things that are not really happening, for example hearing or seeing things that other people cannot (hallucinations).
Bipolar disorder is the third most common mental health cause of disability globally,24 affecting 1–4.5% of adults25 and costing the English economy £5.2B annually, largely due to inadequate treatment. 23 Bipolar disorder is characterised by episodes of extreme low mood (depression) and extreme high or irritable mood (mania or hypomania in its milder form). Self-harm and suicidal behaviour, excessive spending, sexual disinhibition and heightened irritability can all escalate during mood episodes, and psychotic symptoms are also more likely to occur. Between episodes, functioning may return to normal levels, but many people will continue to report problematic subsyndrome levels of depression that affect their functioning and relationships. 26
The need to support relatives
Relatives of people with severe mental health problems (primarily psychosis and bipolar disorder) provide the vast majority of care. This saves the NHS an estimated £1.24B per year in the UK,27 but is associated with high levels of distress in relatives;28,29 significant practical, financial and emotional burdens;30 stigma; worry; shame and guilt;31 trauma;32 and loss. 33,34
Factors that increase the negative impact of psychosis on carers include being a female carer;35 living with the person with psychosis; young patient age and awareness of the patient’s suicidal ideation;36 reduced social support and family resources;36,37 use of emotion-focused coping strategies;38,39 and the beliefs that relatives hold about psychosis, particularly about its cause and control. 40–42
The frequency of suicide attempts within the bipolar disorder population is higher than for many other populations affected by mental health issues, and this is a distressing situation for carers to manage. 43 During periods of mania, extravagant spending, irritability and inappropriate and disproportionate behaviour become more frequent and extreme. 44–46 The challenge of learning to cope with manic and depressive episodes can not only negatively affect the service user but also diminish the carer’s and their family’s quality of life, with carers expressing feelings of helplessness, anger and anxiety. 47,48
It is important to note that some relatives also report positive aspects of caring for someone with a severe mental health problem, including identifying personal strengths, feeling a sense of love, caring and compassion, developing new insights about their lives and living, and greater intimacy with others as a result of their journey of coping with mental illness. 49,50
Relatives of people with psychosis or bipolar disorder face many common needs. These include how best to support someone in their recovery journey; how to deal with a mental health crisis; how to manage difficult situations; how to manage stress; and how to understand and navigate mental health services and the treatments they offer.
Furthermore, mental health services are often structured such that people with a psychosis or bipolar disorder diagnosis are managed within the same teams (e.g. community mental health teams or EIP teams). Therefore, interventions to support relatives that work across these conditions make practical sense.
The Relatives’ Education And Coping Toolkit intervention
To examine in depth the major factors affecting the implementation of an online self-management toolkit for relatives of people with psychosis or bipolar disorder in UK mental health services, this study employed a multiple case study design and used the understanding gained to develop an implementation plan to support uptake and use. Through strategic use of theory to guide our data collection, analysis and interpretation, we aimed to ensure that the key factors identified, and the strategies needed to maximise successful implementation, would be generalisable to other DHIs offered within clinical teams.
The programme that formed the basis for this study was REACT, a supported self-management toolkit offered by EIP teams, providing easily accessible evidence-based information and support for relatives of people with psychosis or bipolar disorder as recommended by the National Institute for Health and Care Excellence (NICE) guidelines. 51,52 It has been shown to be effective in reducing distress and improving perceived support and ability to cope in relatives of people with psychosis in EIP services. 53
A comprehensive recovery-focused toolkit, REACT was originally offered in paper form to relatives of people with psychosis, with telephone and e-mail support from ‘REACT supporters’ from the clinical team. It was subsequently made available online, and broadened to cover relatives of people with bipolar disorder,54 with online support from members of the clinical team via confidential direct messaging, and from other relatives through a restricted-access forum moderated by the REACT supporters.
REACT was designed to be offered by a non-professional support worker (or equivalent) currently working in an EIP team, as it does not require highly trained health professionals, but does require experience in supporting psychosocial interventions, availability and flexibility. Importantly, support workers are relatively inexpensive, reducing cost barriers to further implementation.
In the REACT trial, one NHS trust employed and trained relatives with lived experience of supporting someone with psychosis or bipolar disorder as REACT supporters for relatives across the UK. However, for this study, serving EIP staff within each individual trust were given this role, identifying the most appropriate supporters (professional or non-professional), based on available staff resources and structure.
REACT supporters were trained for the role using standardised training materials provided online by the research team as part of our initial implementation plan. REACT contained 12 key modules, each consisting of high-quality standardised written information, videos of clinical experts or experts by experience sharing their knowledge and experiences to illustrate key points, and self-reflection tasks to ensure that content was personalised to the user. All videos of relatives telling their own stories were retold by actors to preserve anonymity. The modules included What is Psychosis?, What is Bipolar Disorder?, Managing Positive Symptoms, Managing Negative Symptoms, Managing Mood Swings, Dealing With Difficult Situations, Managing Stress (Doing Things Differently), Managing Stress (Thinking Differently), Understanding Mental Health Services, Treatment Options, Dealing With Crises and The Future.
Figure 1 is a screenshot of the home page, which outlines the modules. A full description of each is given elsewhere. 55 REACT also includes a resource directory that signposts users to a wide range of relevant national and local resources. A ‘meet the team’ page ensures that relatives are fully informed about who is delivering the content of the website. Logos for the relevant NHS trust, Lancaster University, Lancashire Care NHS Trust, University College London (UCL), Liverpool Clinical Trials Research Centre (CTRC) and the McPin Foundation are prominently displayed on the log-in page. ‘Mytoolbox’ offers users a confidential space to save links to any information sources they may want to access easily in future, including specific content within the toolkit, their self-reflection tasks and external web links. A blog page offers a flexible space for additional communication with website users, which can be edited by REACT supporters. Each of the participating trusts could edit some elements of the toolkit to allow limited tailoring to their location or to a particular organisation (Table 1).
FIGURE 1.
Screenshot of the REACT toolkit homepage, showing modules and features. Reproduced with permission from Lobban et al. 56 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original.

| Editable function | Description |
|---|---|
| Logo | |
| Meet the team | Introduces the trust staff including the IMPART lead and REACT supporters |
| Emergency contact information | REACT is not a crisis intervention and so directs relatives to appropriate crisis support |
| Availability and contact e-mail addresses for REACT supporters | Hours available and how often the forum and direct messages are checked to manage expectation |
| Resources directory | Staff can edit the content to ensure that local knowledge is captured and shared |
| Forum welcome message, rules of use and suggested topic areas for discussion | This is an opportunity to introduce the forums and mention any particular rules, monitoring times or anything else appropriate |
Context: early intervention for psychosis teams
This study investigated the implementation of REACT within EIP teams in NHS mental health trusts: REACT was offered online and supported by a member of the EIP team.
Early intervention for psychosis teams are part of public sector clinical services in England, providing localised early intervention (EI) support to people with early signs of psychosis and/or other severe mental health problems (including bipolar disorder). Depending on the size of the NHS trust, there may be also be further embedded units, delivering care to distinct geographically defined areas.
Early intervention for psychosis teams were established to deliver care in line with NICE guidelines51 to people during the ‘critical period’ of the first 3 years following the onset of psychosis, and to reduce the duration of untreated psychosis, which has been shown to predict long-term outcomes. 57 Most teams work with people who have developed symptoms of psychotic illness for the first time for up to 3 years following their first contact with services (specific criteria vary between services). In the UK, EIP teams generally consist of a mix of psychiatrists, psychologists, care co-ordinators (social workers, community psychiatric nurses, occupational therapists) and support workers.
Although EIP services have not been immune to the funding challenges faced by all mental health services in the UK,58 they have received additional funding to facilitate the implementation of NICE guidelines and to meet the access and waiting time (AWT) standards for mental health services59,60 published in 2015 and mandated from April 2016. These standards required EIP teams to deliver eight standards, two of which were:
Where patients are in contact with their families, family members to be offered family intervention (FI).
Carers to receive focused education and support.
However, a national audit of EIP teams in England in 2016 showed poor implementation. 61 Of most relevance to this study, only 50% of relatives received a carer-focused education and support programme, and only 31% were offered structured family intervention, with only 12% receiving it. 61 Offering REACT was expected to help services to be compliant with the NICE Quality Standards for both psychosis (NICE Quality Standard 8062) and bipolar disorder (NICE Quality Standard 9563) by offering carers access to an education and support programme. Specifically, the guidelines recommend that carers are given written and verbal information in an accessible format about the diagnosis and management of psychosis and schizophrenia, positive outcomes and recovery, types of support for carers, role of teams and services, and getting help in a crisis.
When providing information, carers should be offered support if necessary. Importantly, REACT was not designed to replace structured face-to-face family interventions.
Relevant previous and parallel research
REACT was itself developed as part of a National Institute for Health Research (NIHR) Research for Patient Benefit-funded study to design and test the feasibility and acceptability of a self-management toolkit to support relatives of people with psychosis. 64 This involved a systematic review of the literature to identify the key components of interventions that were effective in improving outcomes for carers;65 focus groups with relatives to understand their experiences and what they want from a support intervention;66,67 and a feasibility trial to determine the acceptability of the intervention, preference for type of support, rates of recruitment and retention, and an estimate of the likely effect size on a range of outcomes for relatives. 53
Initially, REACT was offered as a series of paper booklets, supported by a support worker in an EIP team by e-mail or telephone. To increase accessibility, it was developed into an online intervention, and a clinical and cost-effectiveness trial was funded by NIHR under its Health Technology Assessment efficient design call for randomised controlled trials (RCTs) that tested efficient trial designs that could help address the problem of growing costs of large-scale definitive trials. 68
This funding offered the opportunity to test the online REACT intervention in an entirely online trial. REACT was offered nationally online, with REACT supporters drawn from trained relatives with lived experience of supporting someone with psychosis or bipolar disorder. The aim was to test the clinical effectiveness and cost-effectiveness of REACT. Funding was awarded for 36 months with a start date of October 2015. The results of the trial have not yet been published.
In parallel, we secured funding for this study through the NIHR Health Services and Delivery Research funding stream. 69 The aim was to identify the factors affecting the successful delivery of an online intervention within EIP services. In this study, REACT was offered online within a series of NHS trusts, supported by staff in the trusts’ EIP teams. Although the IMPlementation of A Relatives’ Toolkit (IMPART) study included baseline and follow-up measures of outcomes for relatives, it was not designed to test clinical effectiveness, as there was no control group that was not receiving the intervention. The focus of this study was on understanding the process of implementation. This study was funded for 30 months from March 2016.
The two studies were complementary and used the same measures and follow-up period, giving the potential to compare both the reach and the outcomes achieved by providing REACT in these very different ways. This allows us to answer questions about which is likely to be the most effective service provision model, and to compare the effectiveness of peer- and clinician-supported approaches.
Research team
Our team included UK-based relatives, clinicians [clinical psychologists, psychiatrists, general practitioners (GPs)], academics, statisticians and health economists, with a common interest in developing and evaluating new ways to support people with mental health problems and their relatives. The team in its entirety came together specifically for this project. Although team members varied in background, training, epistemological and ontological stance, some important factors underpinned their successful collaboration:
-
a commitment to improving the lives of people with mental health problems and their relatives in non-stigmatising, empowering and recovery-focused ways
-
a recognition of the invaluable role that relatives play in supporting people with mental health problems, and the current lack of adequate support available to them
-
an interest in ensuring that evidence-based health care is delivered to service users and carers appropriately and in a timely fashion
-
an interest in the challenges of implementation of complex interventions into complex organisational systems
-
a commitment to identify efficient ways to carry out publicly funded research to provide value for money to the UK taxpayer.
The research was made possible by the involvement of our six participating NHS trusts. To ensure openness and transparency during data collection, we agreed to keep data confidential and to anonymise the trusts and individual participants. The six trusts were therefore allocated common bird habitats as pseudonyms, and the teams within them were named after birds likely to live within this habitat (thank you to Professor William Sellwood for this ornithological expertise).
Liverpool CTRC was extremely helpful in supporting this study. Although not funded directly, the centre supported the consent and data collection processes. It had built an online data collection infrastructure as part of the Health Technology Assessment-funded REACT trial, and adapted this for the purpose of this study.
Study management and oversight
Project Management Group
The initial Project Management Group (PMG) consisted of the grant holders who were responsible for developing the study ideas and delivering the project. This group included a relative who had spend many years supporting a family member with a diagnosis of schizophrenia (SF); two clinical academic psychologists (FL and SHJ) based in Lancaster; a clinical academic psychiatrist with a lead role nationally in EIP services (SJ) and a clinical academic GP who is director of an eHealth centre at UCL (EM); a trial statistician (CJS); a consultant clinical psychologist with a lead role in development and roll-out of EIP services (JS); the director of the McPin Foundation, which promotes service user involvement in research (VP); an internationally acclaimed expert in implementation theory and practice (JR-M); and a clinical lead for EIP teams in a local NHS trust (RS). The group met monthly via teleconference.
Additional members of the operational team based mainly in Lancaster evolved to include a lecturer in mental health with a special interest in implementation (and who joined the PMG) (NRF); two carer researchers; an IT developer (AW); five research associates over the lifetime of the project (VA, BG, EL, CM and PO); an individual who provided administrative support (BM); and two trainee clinical academics in psychiatry (GA-A) and clinical psychology (JB). They all met weekly in relation to specific tasks throughout the project and attended the PMG as required. Research associates based at the London site joined this operational meeting via teleconference.
Study Steering Group
A Study Steering Group (SSG) was appointed to oversee the project on behalf of the project sponsor (Lancaster University) and project funder (NIHR) and to ensure that the project was conducted to the rigorous standards set out in the Department of Health and Social Care’s Research Governance Framework for Health and Social Care70 and the Guidelines for Good Clinical Practice.
The group was chaired by a clinical academic and expert in the delivery of mental health interventions in the NHS (Professor David Kingdon) and included a service user or relative (this role was occupied by three people throughout the course of the study), a senior clinical academic with relevant methodological expertise in health service research, a senior NHS manager in EIP services and a representative of Lancaster University as sponsoring organisation. The SSG met before the start of the study, at the end of the pilot phase and then annually until the end of the study. All meetings took place via teleconference.
Patient and public involvement strategy
The project was designed to involve relatives at every stage and level of decision-making. The funding bid was developed with a carer who had been involved in the original REACT toolkit evaluation and who was a co-applicant on this grant. Roles were designed and costed on the independent SSG for two patient and public involvement (PPI) experts. A co-ordinating agency (the McPin Foundation) was appointed to lead on the PPI programme, drawing on experience from other studies and their involvement in the development of the original REACT toolkit. We anticipated that involving relatives would improve the delivery of the project and the experience of relatives in the research process, and ensure that findings were more effectively disseminated. PPI involvement and a reflection of the challenges around PPI are given in Appendix 1.
Chapter 2 Aims, design and theoretical frameworks
This chapter sets out the overarching aims and objectives of the study. It describes the overall design and theoretical frameworks on which the study builds. The study is set out in three phases, the detailed methods and results of which are outlined in Chapters 3–7.
A full protocol56 for the study was published early in the study process following the guidance provided by the Standards for Reporting Implementation Studies (StaRI) statement. 71
Overall study aims and objectives
The overall aims of the study were to identify critical factors affecting the implementation of an online-supported self-management intervention for relatives of people with recent-onset psychosis or bipolar disorder into routine clinical care, and to use this information to inform an implementation plan to facilitate widespread use and inform wider implementation of DHIs.
The objectives were to:
-
measure the uptake and use of REACT by NHS EIP teams and relatives
-
identify critical factors affecting implementation of REACT
-
identify resources required (and cost implications) for successful implementation of REACT in EIP teams
-
investigate the impact of REACT delivered by EIP teams on relatives’ self-reported outcomes
-
develop a user-friendly REACT implementation plan and related resources to facilitate widespread use and dissemination
-
use the findings from this study to further develop theories of implementation of digital interventions in real-world practice.
Study design
This study used a theory-driven multiple case study design,72 taking a mixed-methods approach that integrated quantitative assessments of outcome (delivery, use and impact of REACT) and qualitative assessments of the mechanisms of implementation through observation, document analysis and in-depth interviews. The study was theoretically informed by normalisation process theory (NPT)73 and the non-adoption, abandonment, scale-up, spread and sustainability (NASSS) framework. 74
Our cases were six NHS trusts in England. Case studies can be particularly useful when trying to understand the implementation of a complex intervention in a real-world setting in which the process or context cannot be controlled. REACT was a ‘complex intervention’75 because it depended on the actions of individuals across different contexts and individuals adapting their behaviour over time. The intervention also produced multiple outcomes that needed to be understood. Implementation was made more complex by the dynamic context in which the intervention was situated, with competing demands on the system. A mixed-methods approach bringing together quantitative and qualitative assessments was therefore required to understand this complexity.
We also designed the study to have extensive input from stakeholder groups at each trust to ensure that the implementation plans were collaboratively designed and refined.
Theoretical frameworks
The IMPART study was theory driven while remaining strongly embedded in practice. Theory helped to guide our data collection and to frame our analysis, ensuring that we were drawing on previous learning about what was likely to be important, but also contributing our findings to a body of knowledge that could inform other studies.
However, we were careful to use theory only where appropriate, and actively seek data that did not fit our theoretical frameworks. There were many models, frameworks and theories that we could have used to guide our work and ensure that our findings could be interpreted within a theoretical framework that supported their potential to be generalised. 76 Our aim was to choose those frameworks that were most appropriate for each of our aims and the context in which this work took place.
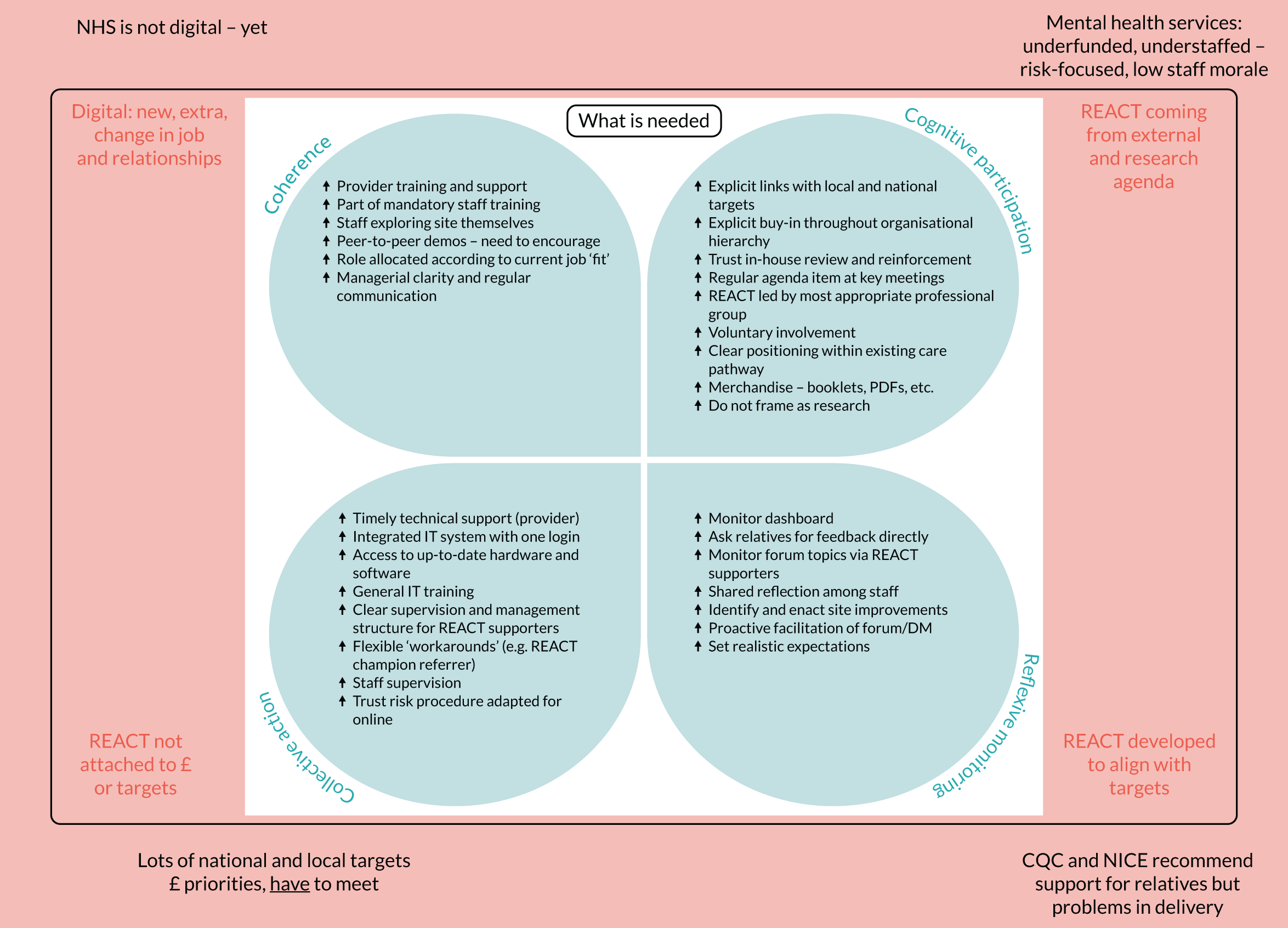
Normalisation process theory is a theory of action that focuses on a person’s actions rather than individual attitudes and beliefs (www.normalizationprocess.org; accessed 6 December 2019). NPT began as a model (normalisation process model) of the factors that promote or inhibit the routine work of embedding a new health technology into practice. The key constructs identified were interactional workability, relational integration, skill-set workability and contextual integration. The model has since been developed into a theory that includes the normalisation process model as constituting ‘collective action’ and adds concepts of ‘coherence’ (how actors make sense of a set of practices), ‘cognitive participation’ (the means by which they participate in them) and ‘reflexive monitoring’ (how these practices are then appraised). 77 Each construct represents a generative mechanism of social action. That is, each construct represents the different kinds of work that people do as they work around a set of practices, whether these are a new technology or the trial of a complex intervention (Figure 2).
FIGURE 2.
Model of the components of NPT. Reproduced from May C, Finch T. Implementing, embedding, and integrating practices: an outline of normalisation process theory. Sociology 43(3), pp. 535–54. 73 Copyright © 2009 by BSA Publications Ltd. Reprinted by permission of SAGE Publications, Ltd.
Normalisation process theory is concerned with three core problems:
-
Implementation – the social organisation of bringing a practice or practices into action. This is defined as a pattern of organised, dynamic and contingent interactions in which individuals and groups work with a complex intervention, within a specific context or health system, over time.
-
Embedding – the processes through which a practice or practices become (or do not become) the routine everyday work of individuals and groups.
-
Integration – the processes by which a practice or practices are re-enacted and sustained among the social matrices of an organisation.
Normalisation process theory was chosen for use in the IMPART study for several reasons. First, NPT focuses specifically on the work carried out by staff to understand the process by which a complex health-care intervention is implemented, embedded and integrated (or not), and as we anticipated that more of our data would come from talking to staff, this matched our focus of concern. Second, NPT is a formal theory and, as such, facilitated the development of testable hypotheses in phase 1 of the study to help focus the collection and analysis of data in phase 2. Third, NPT has clear implementation constructs and a website with clear guidelines on understanding and guiding the implementation process. This allowed all members of the multidisciplinary team to learn about the theory independently (as well as within the group) and ensured a clear reference point for those working with the data and the coding framework. Finally, NPT has also been extensively applied in eHealth settings,78–80 allowing us to more easily compare our findings with previous studies.
Normalisation process theory proved a very useful model for guiding our collection and analysis of data from staff working in EIP teams. However, it was not easily adapted to help understand the experiences being offered by REACT or the wider context in which staff were operating. Both of these were essential to building an explanation of the implementation of REACT. To integrate our findings across all elements of the study, we therefore drew on the NASSS framework,74 which aims to help predict and evaluate the success of a technology-supported health or social care programme.
The NASSS framework was developed from an extensive systematic review of previous technology implementation frameworks, and a series of six empirical case studies, each testing a different type of technology-supported programme (e.g. video consultations, pendant alarm systems, care organising software) in different health-care settings. The framework outlines seven key domains that are important to consider in determining the success of implementation: the condition or illness, the technology, the value proposition, the adopter system (staff and patients/relatives), the organisation, the wider social context and the evolution (interaction and mutual adaptation) of these domains over time.
The NASSS framework was published after the study protocol was funded and, therefore, did not inform the study at the outset. However, while conducting data analysis and interpretation, we found that it provided a useful framework for explaining the findings as a whole. Therefore, the domains from the NASSS framework were used to structure and present our findings in Chapter 8. A diagram of the framework is presented in Chapter 8 (see Figure 19).
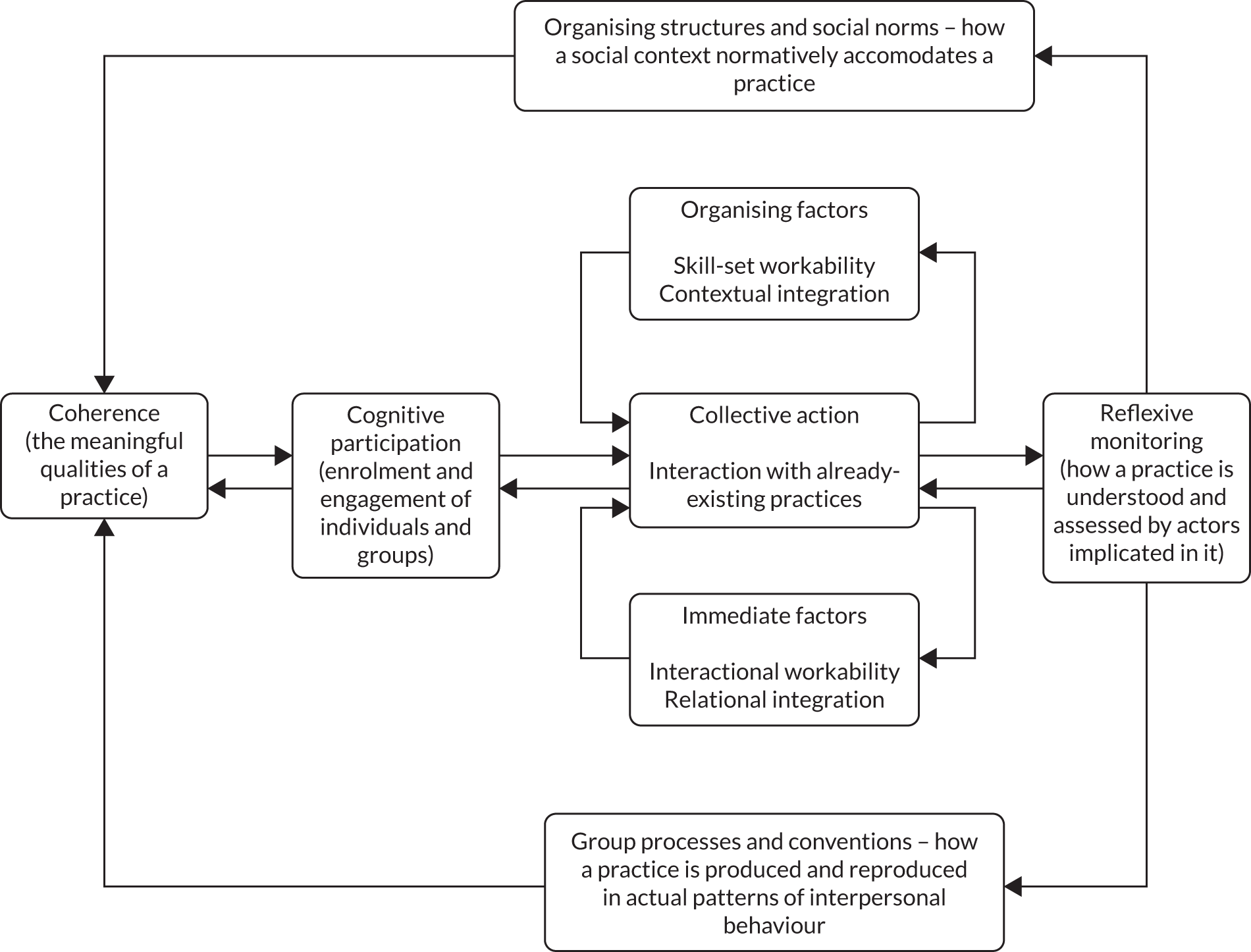
Three phases of the IMPART study
We used our iterative case study design flexibly, adapting our approach in response to activity on the ground. While maintaining a focus on specific trusts at each time point, we maintained good links with all trusts and listened to what was happening at each. The study was divided into three phases. The design is shown in Figure 3.
FIGURE 3.
Flow chart showing the design of the IMPART study. IPv, implementation plan version; SRG, stakeholder reference group. Reproduced with permission from Lobban et al. 56 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original.
Phase 1: hypothesis generation
In phase 1, we outlined an implementation theory identifying the factors that we hypothesised would influence successful implementation of REACT and how they would lead to successful outcomes. Our study theory was informed by NPT, with specific hypotheses further informed by:
-
a systematic review of relevant implementation studies of DHIs for people with psychosis or bipolar disorder and/or their relatives to identify factors affecting implementation81
-
qualitative analysis of data relevant to implementation from the REACT feasibility trial,53 including interviews with EIP staff who have worked as REACT supporters and relatives who used REACT
-
stakeholder workshops including staff and relatives at each participating trust
-
synthesis of these data informed by our clinical and theoretical expertise in this area.
Phase 2: hypothesis testing
In phase 2, we used a case study design to test our hypotheses about which factors would influence the implementation of REACT. We developed an implementation plan to address these factors, and made it available in successively more developed forms across three waves.
Phase 2 was conducted across two geographical regions (North of England and South of England), with three NHS trusts participating in each. All six trusts were given the REACT toolkit and initial implementation plan [implementation plan version (IPv) 1] at the start of phase 2. The implementation plan included an online manual of detailed instructions outlining roles and responsibilities for key staff implementing REACT and face-to-face training sessions within each trust. Guidance for relatives on using REACT is embedded within the toolkit.
We collected detailed case study data in two of our participating trusts (one in each region) as wave 1. Key factors affecting implementation were identified and then discussed with stakeholders in the two trusts in wave 2. The research team worked collaboratively with these stakeholders to design IPv2 in these trusts. Further data were collected to test the impact of this and to identify additional factors affecting implementation. A third iteration (IPv3) was then developed with staff in the final two wave 3 trusts. Data from this wave, combined with ongoing longitudinal data from the four trusts in waves 1 and 2, informed the final version (IPv4).
Phase 2 required a mixed-methods approach, in which we collected quantitative data to describe the levels of implementation and outcomes within each trust, and qualitative data to identify the key factors that could explain these patterns of implementation. Consistent with the case series design, our data were first analysed within each trust before we attempted to analyse and explain similarities and differences between trusts.
The methods are described in detail in Chapter 4, and the design and objectives are summarised in Table 2.
| Objective | Data collected |
|---|---|
| Measure uptake and use of REACT by NHS EIP teams and relatives |
Number of clinician accounts created (quantitative) Number of relatives invited to use REACT (quantitative) Number of relative accounts active (quantitative) Levels of use of REACT by relatives (quantitative) |
| Identify resources required (and cost implications) for successful implementation of REACT in EIP teams | Online resources survey completed by staff at end of phase 2 (quantitative) |
| Investigate the impact of REACT delivered by EIP teams on relatives’ self-reported outcomes | Questionnaires assessing distress, well-being, quality of life and eHealth literacy, completed by relatives online at first use of REACT and at 12 and 24 weeks’ follow-up (quantitative) |
| Identify critical factors affecting implementation of REACT |
Stakeholder reference groups (qualitative) Interviews with key stakeholders including staff and relatives (qualitative) Document analysis (qualitative) Meeting observations (qualitative) |
Developing the implementation plans
In this study, we have used the term ‘implementation plan’ (or sometimes ‘implementation strategy’ or ‘implementation intervention’) according to the definition by Proctor et al. 82 to refer to a wide range of ‘methods or techniques used to enhance the adoption, implementation, and sustainability’ of an intervention (in this case, REACT). Implementation strategies have been widely reported in the literature across a wide range of contexts, interventions, and user groups, but identifying what is likely to work for whom, in what context and in relation to a specific intervention remains a challenge. Attempts have begun to meet this challenge, with the development of taxonomies to define and classify the array of strategies to facilitate further testing (e.g. Powell et al. 83 and Leeman et al. 84). Although offering helpful suggestions, this work did not yet help us to identify the best strategies to implement REACT. Therefore, we relied on a pragmatic analysis of our data from phase 2, and the NPT framework, to guide our successive versions of the implementation plan.
To develop successive implementation plan iterations in a time frame to suit the project and the needs of trusts, we needed the agility to make sense of the ‘bigger picture’ and then develop, implement and evaluate each new iteration. As far as possible, this was linked to specific data sources (interviews, workshops, documents and meeting observations) but did not rely on a full thematic analysis or coding of transcribed data, which would have been unfeasible in the time available. Regular multidisciplinary research team meetings and stakeholder reference group (SRG) meetings within the trusts ensured that this analysis remained grounded in the data. This was referred to as ‘level 1 analysis’, and is distinguished from level 2 analysis, which was much more detailed and involved coding of interview, document and meeting data using a framework analysis85 informed by NPT and our study hypotheses generated in phase 1.
We did not use NPT to guide our data collection or analysis with relatives, although we did consider this. Although the NPT framework could be usefully adapted to accommodate the very important role of the service user in delivering complex health-care interventions, we felt that this was beyond the scope of the study. We therefore approached our data more inductively and used an open thematic analysis to identify emerging themes.
Consistent with the accelerated creation-to-sustainment (ACTS) model described by Mohr et al. ,86 our approach to developing the implementation plans recognised that the success and sustainability of any DHI depended on understanding people’s experiences and the health service setting in which the DHI was intended to be used. Asking health professionals to engage with something new when resources (e.g. time and staffing) are scarce requires us to develop flexible and low-effort ways to facilitate this. New practices, particularly digital ones such as REACT, are often introduced with the promise of time and cost saving or enabling services to meet targets that are not currently being met. However, in the short term (and before these benefits materialise), staff are asked to invest time to learn new skills, become familiar enough with a new technology to be able to use or recommend it, and often to interact with service users in a different way.
The implementation of a DHI may also be one of a range of research activities that a trust or service is currently involved in. Therefore, our implementation plans were developed using collaborative iterative cycles developed through face-to-face workshops, and drawing on appreciative inquiry approaches,87 to recognise and enhance aspects that were working well while providing a safe context to identify what needed to be changed.
Phase 3: finalising the implementation plan
The aim of phase 3 was to synthesise all of the data across all six trusts to identify the key factors affecting implementation and develop a national implementation plan for REACT IPv4 (objective 4), but also to draw out the generalisable learning for the delivery of DHIs into NHS services (objective 5). We used local ‘data analysis days’ to engage staff in the analysis of trust-level data; key staff involved in REACT roles across all trusts in integration of findings across trusts; and the whole project team including carer relatives in a final 2-day ‘explanatory synthesis event’ in which we produced the final explanatory synthesis outlined in Chapter 8. We also presented the iterative development of the implementation plans and drew on all of the study data to agree a final version of IPv4.
Ethics
Ethics approval for the IMPART study was granted by the Health Research Authority and the East of England – Cambridge South Research Ethics Committee (reference 16/EE/0022). All EIP staff in each of the participating trusts were made aware of the study, and organisational research and development (R&D) approval was given for the research team to monitor the use of REACT and be present in the trust. All participants (staff and relatives) who provided additional individualised data (interviews, workshops, relatives’ questionnaires) provided informed written consent prior to participating in the study.
Chapter 3 Phase 1: hypothesis generation
The aim of phase 1 was to develop a study-specific logic model identifying the factors that we hypothesised would influence successful implementation of REACT. This model was informed by implementation theory and later served as a guide to data collection and analysis, making explicit our underlying assumptions and ensuring that analytic generalisations based on our findings could inform the growing field of implementation science. 72
We operationalised our model as a series of propositions in the form of:
X will happen, if Y.
For this study, this became:
The implementation of REACT is more likely to be successful, if . . . [list of key factors].
Most implementation theories are ‘mid-range theories’, defined as useful frameworks to guide practitioners in a general sense. 88 They may tell us the kind of factors likely to be important, but do not identify specific factors in any one context. For this, we need to generate a programme-specific logic model that integrates mid-range formal theories with informal theories (i.e. ideas and learning based on the previous evidence and experience of key stakeholders).
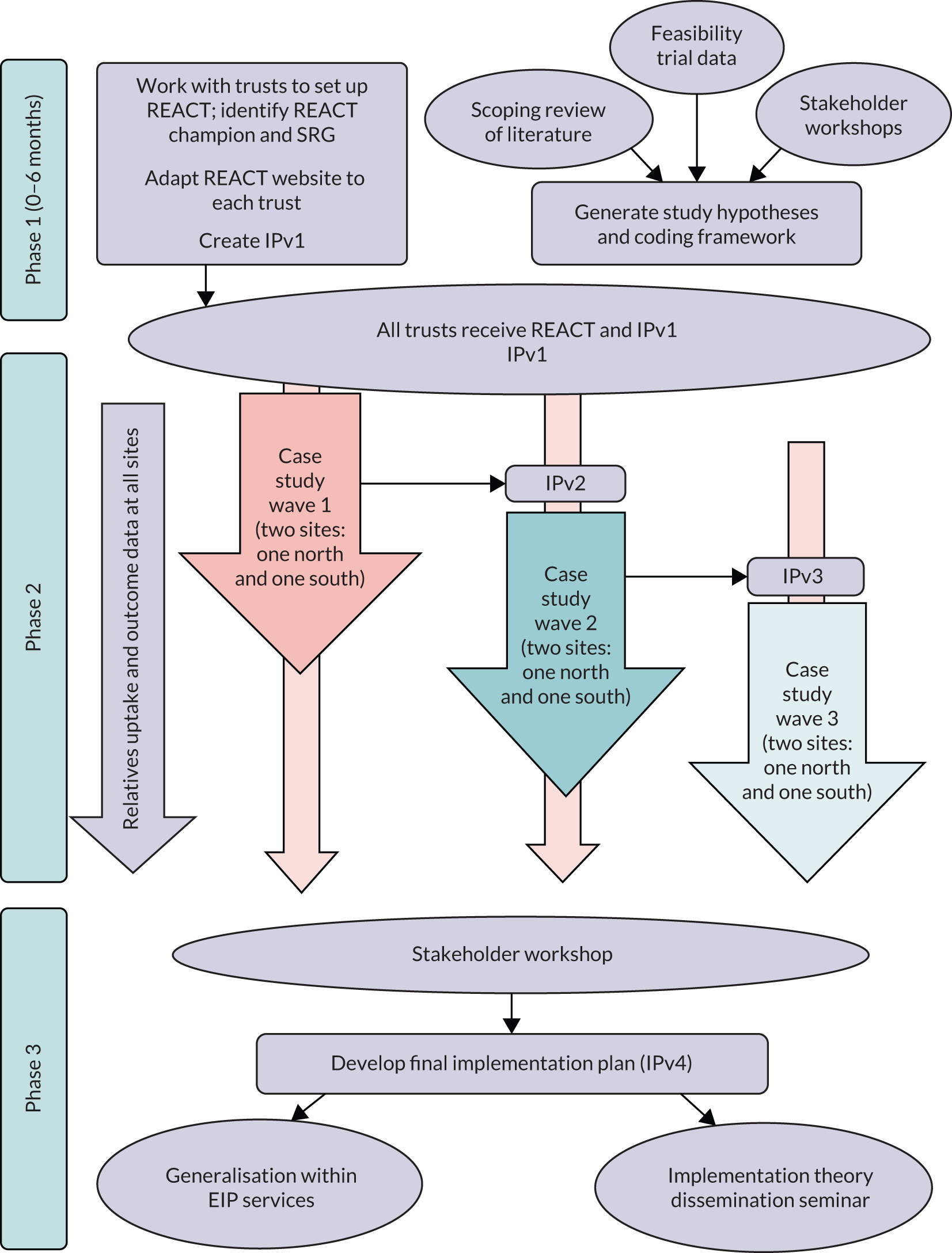
Developing the IMPART study logic model
Our logic model was informed by four key elements:
-
NPT73
-
a systematic review of relevant implementation studies of DHIs for people with psychosis or bipolar disorder and/or their relatives81
-
qualitative analysis of data from the REACT feasibility trial,53 including interviews with EIP staff and relatives
-
SRGs, including staff and relatives at each participating trust.
Synthesis of the findings from each element was informed by the clinical and theoretical expertise of our research team. The process is shown in Figure 4.
FIGURE 4.
Generation of study-specific hypotheses and study logic model.
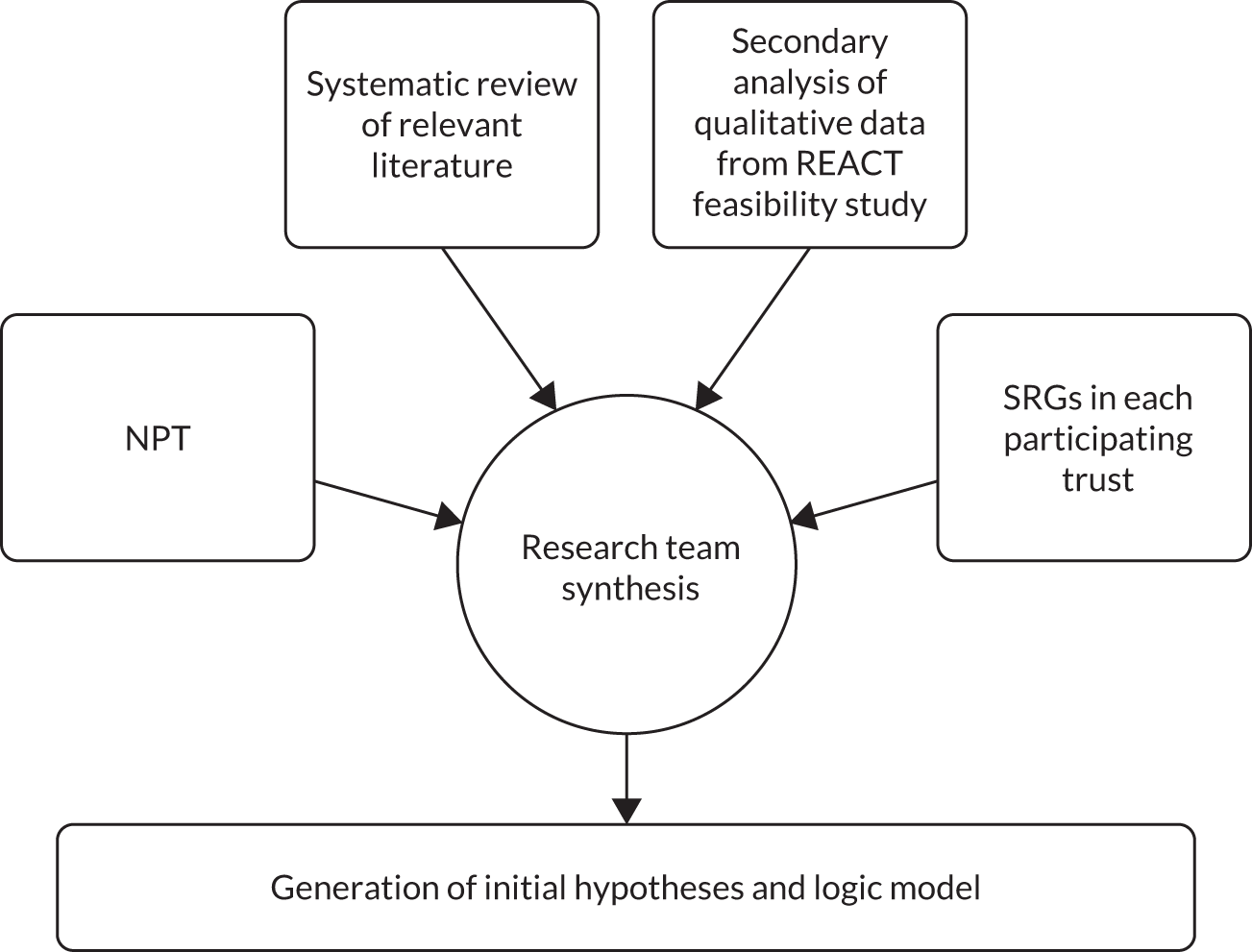
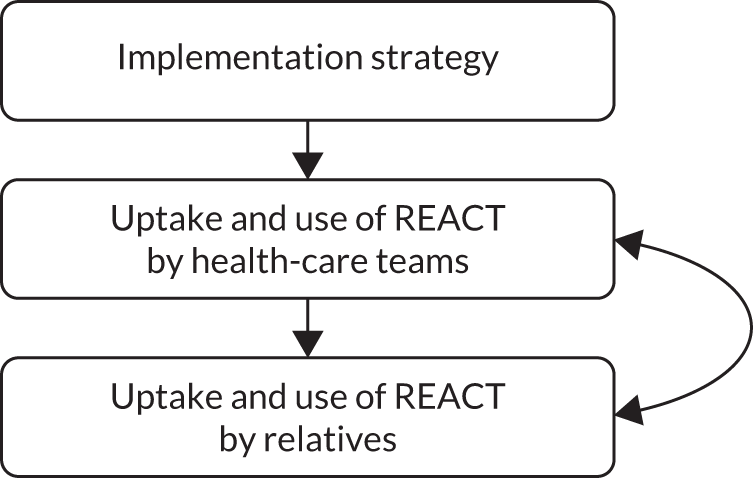
Our preliminary work, prior to the grant, had led us to hypothesise that uptake and use of REACT by relatives would be best encouraged by embedding REACT into routine health care, thus ensuring that relatives were introduced to the intervention by a trusted professional, who would subsequently promote its ongoing use. NPT suggested that this embedding into routine health care would be itself facilitated by positive feedback from relatives (reflexive monitoring, Figure 5). Thus, although our primary outcomes related to uptake and use by health-care professionals, we were also interested in uptake and use by relatives.
FIGURE 5.
Preliminary logic model at the time when the grant was submitted.
Developing the IMPART study-specific hypotheses
The methods and findings for each of the four pieces of work in phase 1 that informed the study-specific hypotheses are published in full elsewhere (NPT73 and the literature review81) or as appendices to this report (see Appendix 2 for the secondary analysis and Appendix 3 for the SRG report). In this chapter, we focus on the key findings from each and explain how these were synthesised to form the IMPART study-specific hypotheses. Appendix 4 shows how the key findings from each element in phase 1 informed the final study-specific hypotheses and evaluates these hypotheses in the light of the study’s findings.
Normalisation process theory
Normalisation process theory was used to inform the structure of the framework into which our hypotheses were organised, and which then guided our data collection and analysis. The framework was used flexibly and, in phase 2, evolved to include additional constructs. However, in phase 1, we used the 16 core components, organised within the four core constructs of NPT as outlined on the NPT toolkit:89
-
coherence – the sense-making work people do individually and collectively when faced with operationalising a set of practices
-
cognitive participation – the relational work that people do to build and sustain a community of practice around a new technology or intervention
-
collective action – the operational work people do to enact a set of practices
-
reflexive monitoring – the appraisal work people do to assess and understand how the new intervention affects them and others.
We used the online toolkit to train the whole team to ensure that everyone had a good understanding of the theory. Although our team included internationally recognised experts in the field of implementation science (notably JR-M and EM), it was important that all team members, including carer researchers, and other methodological and clinical experts also had a thorough working knowledge of the theory so that everyone could contribute to the data analysis.
We then used this shared understanding to map the findings from our literature review, secondary analysis of REACT feasibility study data and SRG meetings into the framework. This helped to develop the generic mid-range NPT components into study-specific hypotheses for the IMPART study. The process for this is presented in Appendix 4, Tables 27–31.
As an example, the NPT component ‘relational integration’ in the construct ‘collective action’ hypothesises that an intervention is more likely to succeed if staff maintain their trust in each other’s work and expertise throughout the intervention. Data from all three studies in phase 1 contributed to making this a study-specific hypothesis in REACT:
REACT is more likely to be successfully implemented (more relatives are invited to use it) if REACT is offered as part of an integrated package of care for relatives, and not a stand-alone intervention; access is restricted to relatives already supported within the team; staff can see and are confident that the forum is well managed; staff can see and are confident that direct messages are being responded to; REACT supporters and IMPART leads are clear and confident about managing risk identified in REACT.
Systematic literature review
We conducted a systematic review of studies published between January 1995 and October 2017 that identified factors affecting implementation of DHIs for people with psychosis or bipolar disorder, or their relatives. 81 In this chapter, we focus on the key factors relevant to understanding the work undertaken by staff to implement DHIs, and the uptake and use by service users or relatives. The review identified 26 eligible papers describing DHIs for service users, but none aimed at supporting relatives. This further highlighted the need for the IMPART study.
The majority of factors for effective implementation of DHIs were focused on the characteristics of staff supporting the DHIs, or the design of the intervention. The first key finding was that users were more likely to engage with a DHI if it was facilitated by a staff member or peer supporter, and had been proposed by a staff member who could understand and clearly articulate its benefits. Enthusiastic staff can serve as champions for DHIs, reinforcing engagement among service users and providing practical guidance. They can also mitigate the experience of DHIs as generic and impersonal. The importance of human support in successful implementation was a strong theme across several studies, and is consistent with the findings of other systematic reviews. 90
Engagement among service users was facilitated by the DHIs’ accessibility (independently, in their own time and in their own home) and the ability to share information with friends and family. Some felt that the DHIs made communication with staff members easier on issues such as drug and alcohol use, which they would have found difficult to broach face to face, or relieved the boredom of time spent in inpatient facilities.
Key barriers to engagement for both staff and service users were concerns about cybersecurity, complexity and poor interoperability. Concerns about data privacy or security were associated with disengagement. DHIs that were difficult to use or time-consuming did not succeed, and DHIs that did not integrate with existing IT systems were found to be frustrating, either because they required additional logins or because important information was not being shared between platforms. DHIs that were considered either too complex for users or too simplistic were also less likely to be sustained by staff or service users.
Some service users expressed concerns about the potentially negative impact of a DHI on their mental health, with reports of increases in paranoia or other exacerbations of symptoms. Symptom severity, particularly episodes of acute ill health, and negative symptoms of schizophrenia were barriers to engagement. These factors highlighted the importance of user-centred design in all aspects, and including all users.
Finally, cost was a consistent factor in the review. Although digital interventions are promoted as offering potential long-term savings, insufficient funding in the short term was linked to inadequate staff time, training, space and necessary equipment, all of which negatively affected implementation.
These factors were mapped onto the relevant NPT framework constructs.
Secondary analysis of REACT feasibility study data
The aim of this secondary analysis was to identify factors affecting implementation of REACT (in its paper version) during the REACT feasibility trial (2008–12). 53 This was a stratified RCT in which 103 relatives were allocated to receive either treatment as usual (TAU) or TAU plus the paper-based REACT toolkit intervention, in a ratio of 1 : 1. Compared with TAU only, those receiving the intervention showed reduced distress and perceived increased support and ability to cope at 6-month follow-up.
Participants were relatives, partners or close friends of people experiencing psychosis who were supported by EIP services in three participating trusts. Each participant was offered an initial face-to-face session introducing the toolkit and agreeing arrangements for support, which was offered by e-mail or telephone (relatives’ preference) for up to 1 hour per week over 6 months, with a minimum of monthly contact.
Six REACT supporters working across the EIP teams were trained and offered monthly group supervision for the duration of the project. The first 14 relatives to complete the 6-month follow-up were invited to take part in a qualitative interview about their experiences of REACT. Twelve consented but one data file was corrupted and could not be analysed. Interviews were also conducted with the four supporters still involved in the study at the end.
Our secondary analysis of these data sought to identify specific factors affecting implementation of REACT. Despite the toolkit being mainly offered in paper form during the trial [an online Portable Document Format (PDF) was also available], we still felt that the data had important insights to offer into the process of implementing this self-management toolkit for relatives as part of an existing care pathway. See Appendix 2 for a detailed description of the methods, participants and findings. Appendix 2, Table 25, provides a summary of the main findings.
The key themes to emerge from our analysis were the importance of timing (when REACT is offered); the perceived benefits for the relative; that structure and delivery of the support; and the balancing of the REACT supporter role with other job demands.
Timing
Both relatives and supporters identified the need for REACT to be offered to relatives as early as possible to ensure that it was available as they were making sense of the challenges they faced and developing ways of coping. It should therefore be clearly identified as an early step in the care pathway. However, an early offer should be regularly followed up with prompts to explore the use of REACT and highlight its potential value to relatives:
Everybody I met loved it, there was not criticism for the toolkit, except for ‘I’ve already figured this information out for myself, but had this been [there] a year ago . . . [it] would have been a godsend’.
REACT supporter
[My supporter] used to ring me and I would say, oh, something trivial was bothering me; he said, well why don’t you look at section this, section that, and I shouldn’t have to be prompted but, he would and then I would start reading it again then you know, . . . I was really yes, into it then.
Relative
Perceived benefits for relatives
REACT supporters were motivated to offer the intervention to relatives when they saw it as being directly relevant to the diverse range of relatives they worked with, easily accessible, engaging and up to date. Their work was driven by wanting to see specific benefits for relatives, including feeling valued in their role and developing greater knowledge about mental health and services, which would lead to greater confidence to engage with services and indirectly improve their relationship with service users:
It does really benefit if people understand what they are dealing with – I think that’s half the battle . . . [otherwise] they are just fighting against the unknown really all the time.
REACT supporter
Relatives highlighted the use of case studies as particularly engaging as they realised that they were not alone in the problems they faced. Even those who felt that they would have benefited from earlier access to REACT valued the reassurance of information that was consistent with the understanding they had already developed:
It confirmed what you had worked out for yourself, that you were actually on the right line.
Relative
Structure and delivery of support
Relatives and REACT supporters were in agreement that REACT would not work as a stand-alone intervention, and that support was crucial. REACT supporters saw their key role as listening to relatives and directing them back to relevant parts of the toolkit at an appropriate pace. Relatives valued support for giving prompts to visit particular modules, elaborating on topics in REACT with additional resources, talking through ways to manage specific scenarios and offering reassurance when appropriate. Although e-mail and other online written communication offered convenience and an opportunity to compose the content, both parties felt that face-to-face (ideally) and/or telephone support was necessary for engagement:
You need at least an initial contact face to face so then you know who you are talking to.
Relative
And it did help to – much more so than I think you could do on the phone – it did help to build that rapport and therapeutic relationship with the participant.
REACT supporter
REACT supporter role
REACT supporters found adding this role to their existing work a challenge, particularly finding the time to carry out the associated tasks and attending supervision. Some also felt that keeping boundaries between the role and other aspects of their job was not always easy. One supporter struggled with how best to manage negative feedback from a relative about another member of the clinical team. This highlights the importance of allocating REACT supporter roles to staff who have time and appropriate skills, and to ensure that they receive regular support and supervision.
These factors were mapped onto the relevant NPT framework constructs.
Stakeholder reference groups
Stakeholder reference groups met in each participating trust during phase 1 of the IMPART study. The aims were to:
-
establish good working relationships with key stakeholders in each trust
-
finalise delivery of REACT and IPv1
-
explore the views of EIP staff, service users and relatives on factors they thought likely to affect the implementation of REACT in their trust.
Each trust identified an IMPART lead to provide ‘on the ground’ insights into the workings of a particular site and to help researchers to access key data sources. Leads were asked to identify potential SRG members – ideally senior trust board members or EIP service leads, EIP team managers or clinicians, two EIP support workers, two EIP relatives and two EIP service users – and to help set up and co-chair the SRG meeting, held on NHS premises.
All SRG meetings were attended by at least two members of the IMPART research team: a research associate and the North of England or South of England site lead or PPI lead. See Appendix 3 for a detailed report of the methods and results forms including key themes arising from these meetings (see also Appendix 3, Figure 20).
The SRGs were well attended and provided invaluable predictions about factors that would be likely to affect implementation within each trust. However, staff were generally at a clinical and managerial level, with no involvement of senior trust representatives. In some trusts, the IMPART lead chose to hold separate staff and service user/relative meetings owing to fears that meetings would be used to air dissatisfaction with services.
There was a high level of consistency between trusts in terms of the factors considered likely to affect implementation of REACT. These factors included the promotion of its potential to meet the needs of relatives, saving staff time, helping trusts to meet their clinical targets, the flexibility of trusts to adapt REACT to their specific needs, staff confidence in the content and in their role in offering REACT, and the commitment of resources at an organisational level:
We need to make some decisions about the level of support we can give to it and whether or not we can afford to support the instant messaging and the forum, so I guess [we need] to have a clearer idea of what you think the time resource will be.
Staff member
Stakeholders felt that a key strength of REACT was its availability to relatives without requiring service user consent, as this targeted a currently unmet need.
Initial engagement from staff was anticipated to depend on engendering a sense of ownership of REACT within each team, which would be facilitated by ensuring that staff had easy access to the website and training, and by allocating key people to REACT roles. Ongoing use of the intervention by staff would be facilitated by the ability to monitor relatives’ levels of use, and to change and update the content in response to their feedback:
Will you be using any of the things that get spoken about in the forum to kind of tailor the toolkit? So if there are lots of discussions about sleep or diet will you then use that maybe to add to the toolkit for the future?
Staff member
Important barriers that stakeholders felt would need to be addressed before staff and relatives would engage were primarily linked to the REACT group (the online forum) and included confidentiality, security and privacy of data (mainly a concern of relatives); the challenge of managing disclosed risk of harm; and the website being used to air negative feedback (mainly a concern of staff).
The latter was particularly evident in one trust and was clearly linked to experience of an earlier online intervention in which some members of staff had been ‘trolled’. Most stakeholders felt that such risks could be managed by restricting access to the forum to invited relatives, and by having clear ground rules and regular moderation by a REACT supporter.
Despite the credibility of the intervention being clearly enhanced by multidisciplinary input to its development, including from service users/carers and health-care professionals, some concerns were expressed about lack of fit between the content of the toolkit and the ethos of the service. In one trust in particular, REACT was perceived as too medicalising by defining diagnostic terms such as schizophrenia. Staff in this trust wanted more content that focused on well-being and recovery than they felt was currently included:
It just seems to me that a lot of the discussion’s been around lifestyle stuff and families wanting to have more information about well-being in general – I just wonder if this is a very medical model and it’s coming from a very kind of, you know, medical perspective, and actually it needs to open up a little bit more to those kind of life.
Staff member
Challenges were also identified in using REACT to meet the diversity of relatives in terms of language, age, confidence with IT and reading skills. Generally, stakeholders felt that REACT was not suitable for those whose first language was not English, who were older, who were less IT confident or who had a lower reading ability:
[In] my family I’m the only one who speaks English for example, and how would they access this?
Service user
Relatives and staff in all trusts were clear that although they would value the information and peer support offered by REACT, particularly if offered early in their journey, it should be offered as part of an integrated package of care and should not replace face-to-face support:
It’s going to tick the ‘information for relatives and carers’ box, but I don’t want it to be instead of actually getting face-to-face contact and support with care co-ordinators and things like that.
Staff member
Key factors identified by the SRGs as likely to affect implementation of REACT were mapped onto the relevant NPT framework constructs.
Synthesis and generation of study-specific hypotheses
Guided by the online toolkit (www.normalizationprocess.org; accessed 6 December 2019), we began by developing our team-wide understanding of NPT’s four core constructs, then its 16 construct components, and then took the related questions from the interactive toolkit to generate a list of propositions relating to the general processes that NPT predicts are likely to lead to successful implementation of an intervention.
Once the analyses of the systematic review, REACT feasibility trial and SRG data were complete, we used another ‘data day’ to map the key findings from each of these data sets onto the NPT construct components. By using the structure of the NPT toolkit questions, we were then able to synthesise these data sources to generate our propositions specific to the IMPART study (see Appendix 4, Tables 27–30, column 5).
The propositions that resulted from this process under each of the four core NPT constructs are described in the following sections.
Coherence
REACT is more likely to be successfully implemented (i.e. more relatives will be invited to use it) if:
-
all staff have easy and independent access to the toolkit in their own time, with clear guidance on what it is, who it is for and what it offers
-
staff are given an opportunity to discuss whether or not, and how, to use REACT within their service; decisions from this are visibly endorsed at senior management level
-
staff can access training that clearly outlines their roles and responsibilities in delivering REACT
-
staff are able to view the content of the REACT toolkit and can see clear benefits for staff and/or relatives, such as –
-
accessibility
-
relevance
-
credibility
-
reassuring
-
non-stigmatising
-
fits with EIP service ethos
-
clear user involvement
-
inclusive
-
safe to use.
-
Cognitive participation
REACT is more likely to be successfully implemented (i.e. more relatives will be invited to use it) if:
-
there is a clear lead (‘champion’) who drives REACT forward within the trust
-
staff make explicit links between REACT and existing key trust targets and priorities
-
key roles are appropriately allocated
-
training is provided for tasks that may require new skills (e.g. forum moderation)
-
staff have a sense of ownership and take responsibility for promoting REACT within the service and offering REACT to relatives (and do not see this as the role of the researchers)
-
delivery of REACT is included as a regular agenda item at relevant operational meetings within clinical teams.
Collective action
REACT is more likely to be successfully implemented (i.e. more relatives will be invited to use it) if:
-
staff carry out their roles and responsibilities as outlined in the ‘how-to’ manual and have the resources to allow them to do this. Key tasks include –
-
IMPART lead creating REACT supporter and clinician accounts
-
all staff inviting relatives (requires access to computer and relatives’ details)
-
REACT supporters regularly moderating the forum (requires regular access to the online forum)
-
REACT supporters providing timely responses to direct messages
-
regularly updating blogs and local resources
-
-
REACT is offered as part of an integrated package of care for relatives, and not a stand-alone intervention
-
access is restricted to relatives already being supported within the team
-
staff can see and are confident that the forum is being well managed
-
staff can see and are confident that direct messages are being responded to
-
REACT supporters and IMPART leads are clear and confident about managing risk identified on REACT
-
IMPART lead and REACT supporter roles are allocated to people with the time, skills, organisational role and support to carry them out
-
REACT is clearly visible within the relevant clinical care pathway trust policy documents
-
REACT is customised with accurate trust details
-
staff are allocated time for training, supervision and carrying out their tasks specifically related to REACT
-
staff have easy access to computers or tablets and IT support to enable their online tasks related to REACT
-
staff can work easily between REACT and existing electronic health-care record/IT systems.
Reflexive monitoring
REACT is more likely to be successfully implemented (i.e. more relatives will be invited to use it) if:
-
staff can access regular data that show that relatives are using REACT
-
feedback from relatives is reviewed and shared as part of an operational meeting and can inform ongoing work
-
staff are able to gather direct feedback from relatives they have invited to use the website (if positive, this facilitates implementation)
-
staff are able to request or enact improvements to REACT as they see fit.
Discussion
The aim of this chapter was to explain the development of our study-specific model for the IMPART study. We created a list of hypotheses in the form of propositions about factors likely to affect the successful implementation of REACT, drawing on a mid-range theory (NPT), relevant data from a review of existing literature, our previous feasibility study and SRGs in each participating trust.
The process of developing these propositions helped our team to better understand NPT as a theory, and specifically its relevance to the IMPART study, and to operationalise each of the NPT constructs. They have guided our data collection by telling us the kind of data we are likely to need to test each one, and have informed the development of topic guides for staff interviews.
Integrating the three data sets into a NPT framework was not without challenges. NPT’s focus is the work undertaken by staff to deliver the intervention rather than the work undertaken by the user to then engage, although it does indirectly acknowledge the importance of user engagement in the reflexive monitoring of staff. In contrast, a substantial number of our data focused on the engagement of the end user with the DHIs, and so highlighted factors associated with characteristics of the DHIs or of the user. Although it would be possible to adapt NPT to explore the work undertaken by the relatives to engage with REACT, this was beyond the scope of this project. Therefore, data relevant to this engagement is not included in the NPT framework, but is used in Chapter 8 to help interpret the data collected from relatives set out in Chapter 7.
The hypotheses derived from phase 1 are revisited in Chapter 8, and tested in the light of the data collected in phase 2 (see also Appendix 4).
Chapter 4 Phase 2: methods
This chapter details the methods used for phase 2 of the IMPART study. The primary aims of phase 2 were to:
-
test our hypotheses about which key factors would influence the implementation of REACT across our six participating NHS trusts
-
develop an implementation plan.
An additional aim was to assess the effectiveness of REACT. We follow StaRI71 where appropriate.
Design
As described in Chapter 2, the design was a theory-driven multiple case study design72 using a mixed-methods approach integrating quantitative assessments of outcome (delivery, use and impact of REACT) and qualitative assessments of mechanisms including observation, document analysis and in-depth interviews with staff and relatives.
Context
The study took place across six NHS trusts in England. This context is described in detail in Chapter 1.
Sites
Preserving the anonymity of participating trusts and teams was of particular importance in this study owing to the sensitive nature of the data collected from carers and staff. A multilayered taxonomy of birds and habitats was used to identify trusts and teams within each trust.
Trusts were selected to be geographically and ethnically diverse to maximise the generalisability of findings. A summary is given in Table 3, drawing on the Royal College of Psychiatrists College Centre for Quality Improvement (CCQI) audit in 2014;92 specific figures are not provided so that trusts are not easily identifiable.
| Trust | Location | Wave | Population served | Summary data estimated from CCQI 2014 audit92 |
|---|---|---|---|---|
| Woods | South of England | 1 | Approximately 0.5 million people; large ethnic diversity; approximately half identify as white British; urban setting | Approximately 47% of service users and their families were offered family intervention; half of carers were offered education and support |
| Moor | North of England | 1 | Approximately 0.5 million people; predominantly white British; over half living in a rural setting | Approximately 3% of service users and families were offered family intervention; 6% of carers were offered education and support |
| Ocean | North of England | 2 | Over 2.5 million people in large urban area; vast majority identify as white British | Approximately 32% of service users and families were offered family intervention; 87% of carers were offered education and support |
| Seashore | South of England | 2 | Approximately 0.75 million people in an urban and ethnically diverse setting | Approximately 42% of service users and families were offered family intervention; 71% of carers were offered education and support |
| Lakes | North of England | 3 | Approximately 1.5 million people across a predominantly rural location; majority of the population identify as white British | Approximately 62% of service users and their families were offered family intervention; 30% of carers were offered education and support |
| Marsh | South of England | 3 | Approximately 1.5 million; mostly urban with rural pockets; predominantly white British | Approximately 3% of service users and their families were offered family intervention; 74% of carers were offered education and support |
Participants
Participants were all staff in EIP teams and relatives or close friends of someone with bipolar disorder and/or psychosis, referred by staff to use the REACT toolkit, and who then consented to take part in the study (subsequently referred to as research relatives). Relatives who did not wish to take part in the research were still able to access REACT and their data were used only in summarising levels of clinical activity (subsequently referred to as clinical relatives).
Staff were initially informed about REACT and the IMPART study through the IMPART leads. Staff and relatives were invited to SRGs and to other group workshops by the IMPART leads, with support from the research team. Individual staff were approached directly by the research team and invited to take part in individual interviews. A detailed description of sampling and procedure for individual and group interviews is given in Process evaluation.
Relatives were invited to use REACT via an invitation e-mail from a staff member, with instructions on how to set up an account. Relatives who visited the website were also invited by e-mail to take part in the collection of research data, and had the choice of completing questionnaires, taking part in an interview (see Chapter 7) or both. Relatives could use the REACT intervention without participating in the research, although all REACT users had to agree to terms and conditions that permitted collection and analysis of basic demographic and website use information. Relatives who agreed to participate in the research provided informed consent online before being asked to complete any research measures.
Description of the intervention
The REACT intervention is described in detail in Chapter 1.
A separate instance of the REACT toolkit was set up for each of the six NHS trusts. This allowed each trust to manage its own website, restricting access to invited relatives. Each trust was clinically responsible for its website, including moderating the forum and responding to direct messages.
Description of implementation plan version 1
The first version of the implementation plan, IPv1, was informed by the hypotheses described in Chapter 3, and designed to be deliverable at minimal cost. It had the following components, each promoting NPT core constructs.
Personalisation of the intervention to each trust
This was intended to engender a sense of ownership and legitimisation. Each trust was able to customise some elements of the website content including adding a logo, times that the forum/direct messaging services were actively moderated and by whom, emergency contacts, and photos and biographies of the trust’s REACT supporters and IMPART leads.
Initial familiarisation with the intervention
This was aimed at building coherence and cognitive participation.
Pilot REACT
All six trusts received pilot versions of REACT on 19 September 2016. During this pilot phase, the research team responded to feedback from the trusts.
Training
An online manual of instructions for delivery and use of REACT was provided to all staff in the pilot phase, and was updated throughout the study in response to feedback. Each trust had at least one face-to-face training session, offered as soon as possible after the website went live. Some had more sessions to accommodate separately located EIP teams. The training provided an overview of the importance of carer information and support and NICE guidelines, an outline of key components of the REACT website, aims of the IMPART study and key roles, and how to use REACT.
Establishing local champions
This promoted cognitive participation. An IMPART lead was identified in each trust to work with the research team to assist with the research process, and within the trust to implement REACT.
Each IMPART lead held a senior role in the EIP and had expressed interest in the study, but roles and selection varied between leads. For Moor and Woods Trusts, the IMPART leads were co-applicants of the project and senior clinicians in their trusts. In Ocean, the first IMPART lead had been involved in the development of REACT. In Seashore and Marsh, senior clinicians were recruited; in Lakes, a senior psychiatrist with an interest in research took on the role.
The IMPART leads were encouraged to customise their trust’s REACT website with support from the research IT team. They also helped set up a SRG of staff and service users or relatives in each trust as described in Chapter 3. These groups met periodically throughout the study, initially to support the research process, but quickly evolved to become an important data source. Finally, IMPART leads were often instrumental in allocating REACT supporter roles within the EIP service.
Establishing workflows
This promoted coherence, activation and reflexive monitoring. Staff needed accounts in order to visit the REACT toolkit, invite relatives and monitor whether or not their invitation had been accepted. An account was created by the research team for each IMPART lead who then created REACT supporter accounts for the people moderating the website and clinician accounts for staff who could refer relatives to the website. Clinicians then created accounts for relatives. This ensured that control over access to REACT remained with the trust staff. Table 4 shows each of the key roles related to REACT and the different levels of website access for each role. Figure 6 shows the pathway through the REACT website.
| Role | Description of role | Access |
|---|---|---|
| IMPART lead | Provide a link between the research team and clinical service. Provide access to key data sources. Create accounts for REACT supporters and all staff | Full access to REACT trust website, with information regarding all signed-up clinicians, REACT supporters and relatives. Could not access forums and direct messages |
| REACT supporter | Support the relative to use and get the most out of the toolkit. Moderate the REACT group forum and respond to direct messages from relatives. Update local information on the resource directory | Access to all aspects of REACT toolkit including forum and direct messages, and details of relatives who have been invited |
| Clinician | Invite relative to use REACT, both verbally and by sending them an online invitation | Sign up relatives only; could access toolkit modules |
| Relative | End users of REACT | Access to REACT toolkit, including forum and direct messages |
FIGURE 6.
Pathway through the REACT intervention. CTRC, clinical trials research centre.
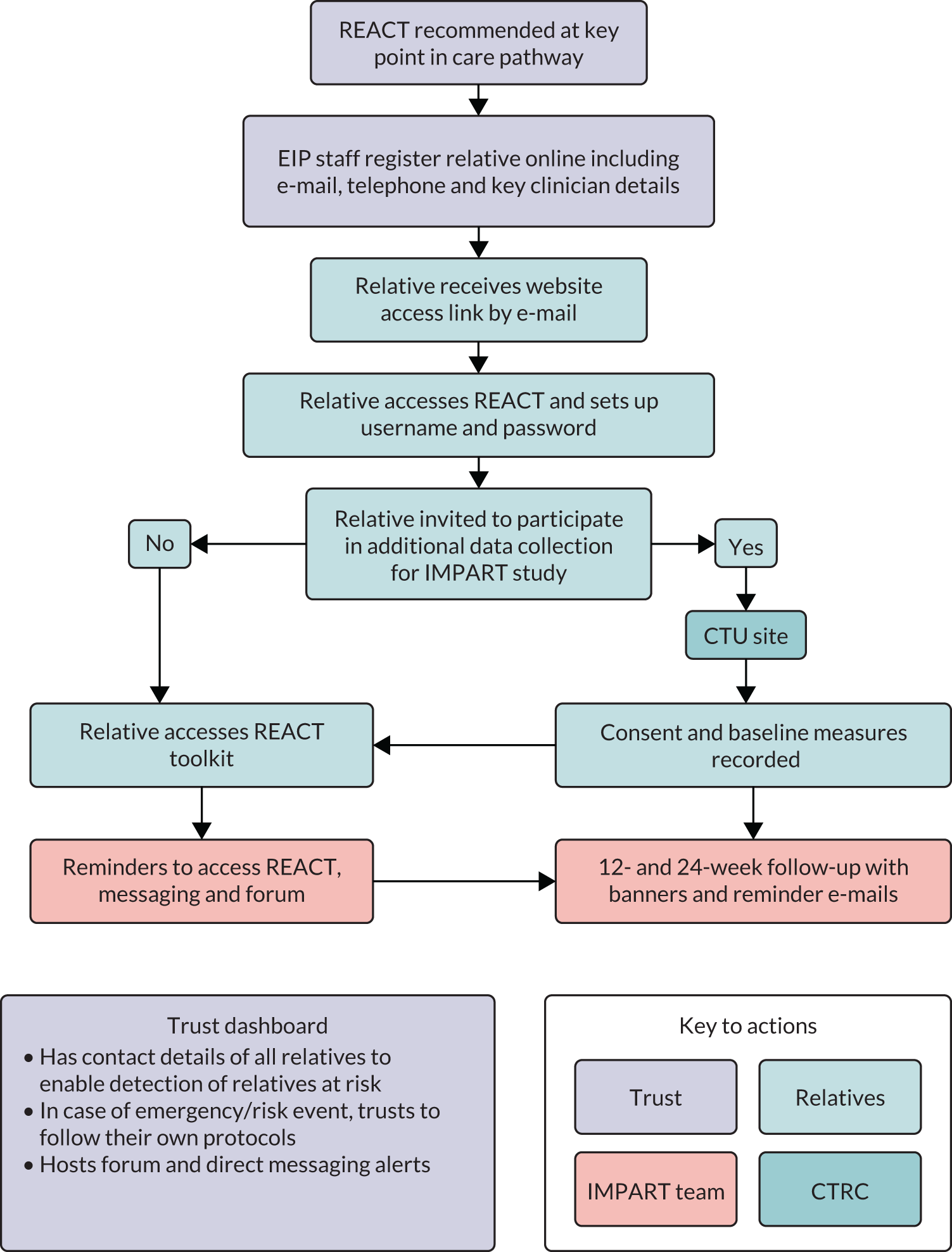
Go live
REACT went live for all six trusts on 21 November 2016. Trusts were informed by an e-mail sent to each IMPART lead explaining that feedback on the pilot had been addressed and REACT was live in their trust. Instructions on how to deliver and use REACT were available via the online manual, and face-to-face training was available via the research team. This was followed up by telephone to arrange training. Figure 6 shows the pathway of how relatives were invited to use REACT.
Developing and delivering the implementation plans
All trusts received IPv1 at the start of wave 1. IPv2 was developed with stakeholders during waves 1 and 2 and delivered to the two trusts in wave 2 (Ocean and Seashore). IPv3 was further developed from additional learning in waves 2 and 3 and delivered to trusts in wave 3 (Lakes and Marsh). The content of these implementation plans is described in detail in Chapter 6.
The final implementation plan (IPv4) was also informed by data from relatives’ interviews (see Chapter 7) and by the development of our explanatory synthesis (see Chapter 8). Figure 7 summarises the iterative ‘You said . . . we did’ action cycles that underpinned this process.
FIGURE 7.
Iterative cycles used to develop REACT implementation plans.
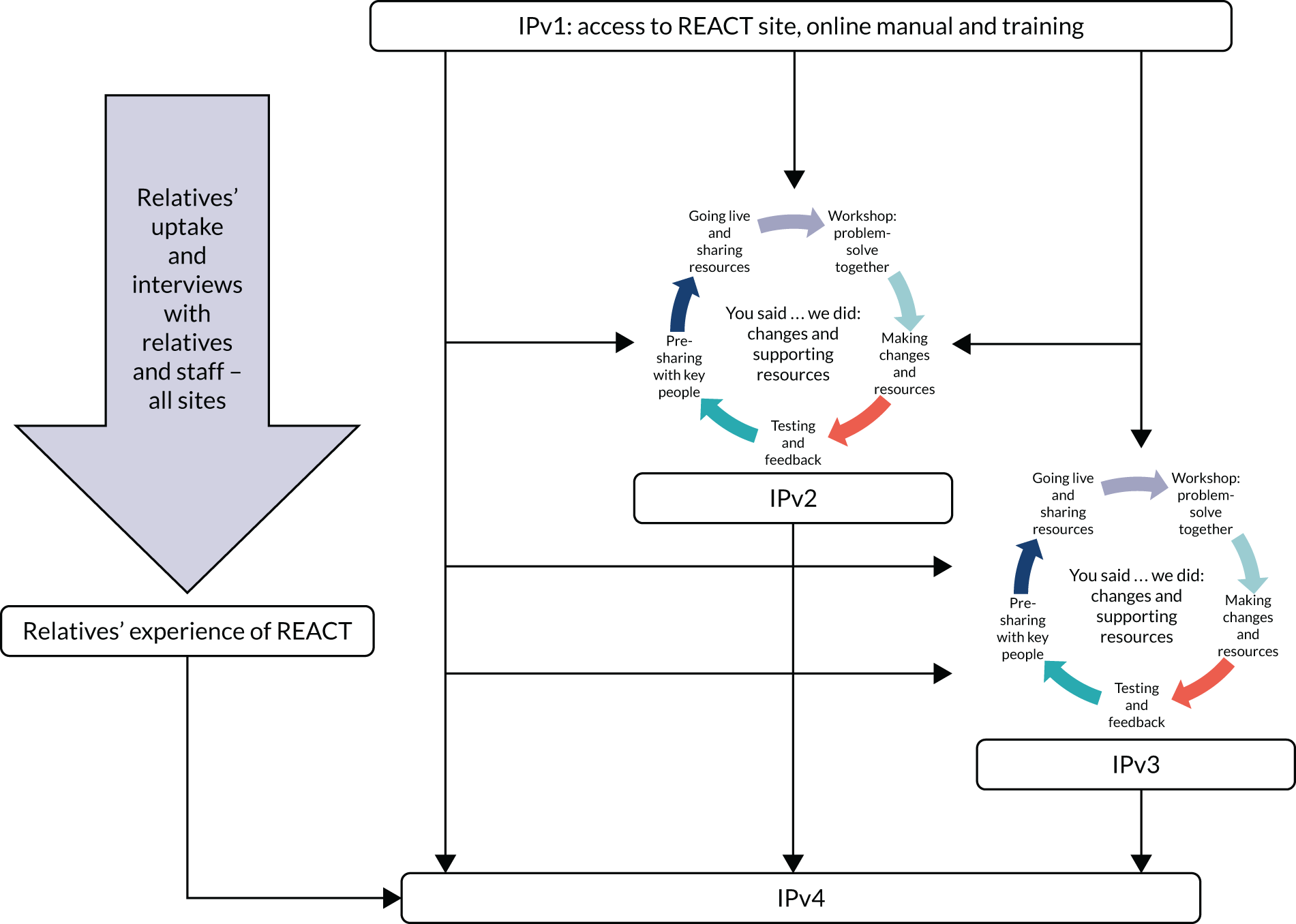
Each action cycle began with a workshop to which EIP staff and relatives were invited to share their experiences of using or not using REACT, and to explore the facilitators of and barriers to use. The workshops were co-facilitated by a member of the research team, the IMPART lead and a carer researcher, and resulted in an agreed list of changes that would better facilitate the implementation of REACT. Staff were encouraged to talk openly about all the challenges they faced, but the workshop facilitators attempted to pull out those challenges that there was some possibility of addressing as part of the implementation plan. Staff were encouraged to expand on issues in individual interviews such as high workloads, lack of IT training and staff turnover, but the workshops aimed to be solution focused to identify practical changes that could be made.
These changes were shared by e-mail and phone with workshop attendees and those unable to join, and further suggestions were invited. Any changes requiring adaptations to the REACT interface were reviewed by the research team with the IT developer to assess feasibility and time scale. Agreed changes to the interface and to the implementation plan were tested and refined with workshop attendees and within the research team before being implemented. Any changes that could not be made were clearly identified alongside reasons why this was not possible. Observations and feedback on each implementation plan were collected to inform subsequent iterations.
This process required fast, agile working, identifying and responding to needs within very short time scales. For this reason, data were analysed at two different levels, described in detail in Analysis.
Evaluation
Implementation outcomes were measured using primarily quantitative measures from clinicians and relatives. Intervention (REACT) outcomes were measured using relatives’ questionnaires covering five areas:
-
distress, using the General Health Questionnaire-28 (GHQ-28)93
-
well-being, using the Carer Well-being and Support Scale (CWS)94
-
quality of life, using the EuroQol-5 Dimensions, five-level version (EQ-5D-5L)95
-
eHealth literacy, using the eHealth Literacy Scale (eHEALS)96
-
relatives’ caring role.
Process evaluation to identify the factors affecting implementation of REACT was understood using primarily staff interviews and workshops, SRGs and some document analysis and meeting observations. We also evaluated the resources required to deliver REACT using an online questionnaire. Study objective and data collection are described in Table 5.
| Objectives | Data | Type of data | Source and time of data collection |
|---|---|---|---|
| Implementation outcomes | |||
| 1. Assess the uptake and use of REACT by NHS EIP teams |
Number of REACT accounts created by clinicians Number of invitations from clinicians to relatives to use REACT |
Service evaluation | All clinicians’ activity during study period |
| 2. Assess the uptake and use of REACT by relatives | The level of use of each module using web analytic statistics; including the number of visits to each website section and total time spent on the website | Service evaluation | All relatives’ activity during 24-week period |
| The number of REACT accounts created by relatives | Service evaluation | All relatives’ activity during study period | |
| Basic demographic information | Service evaluation | Assessed at baseline | |
| Intervention outcomes | |||
| 3. Investigate the impact of REACT on relatives’ self-reported outcomes | Questionnaire data:
|
Research | Self-reported measures completed by research relatives. Data collected at time of registration (baseline) and at 12 and 24 weeks |
| 4. Investigate association patterns between website use and outcomes | Number of visits to each website section and total time spent on the website by relatives | Service evaluation and research | Relatives’ activity during 24-week period |
| Relatives’ self-reported outcome measures as above | Service evaluation and research | Self-reported outcome measures at baseline | |
| Process evaluation | |||
| 5. Understand reasons for observed outcomes | Qualitative data from staff and relative interviews, SRGs, document analysis, meeting observations | Research | Collected throughout phase 2 |
| 6. Iteratively develop an optimal implementation plan | Co-development with staff | Research | Iterative version of implementation plan developed in each wave, finalised during evidence synthesis |
| Resources | |||
| 7. Investigate resources and costs needed for successful implementation of REACT | Questionnaire designed for this study | Service evaluation | Completed by clinicians from each participating NHS trust at the end of the study to enable time to use toolkit in clinical services |
Implementation outcomes
Clinicians’ activity was monitored throughout the study in each trust to assess their engagement with the REACT toolkit, as quantified by the number of accounts they created and the number of invitations they sent to relatives.
We collected basic demographic and web use information from all relatives on the REACT website (research and clinical relatives) to evaluate which users the intervention reached and which modules were most and least visited. The demographic questionnaire [available at www.journalslibrary.nihr.ac.uk/programmes/hsdr/140416/#/documentation (accessed February 2020)] completed at the time of creating an account collected participants’ age, gender, ethnicity, highest education, current employment status and internet access. Website use data were collected during the study period, including the total number of logins to the toolkit, the total number of visits to each module and to the forum, and the total time spent on the website.
Intervention outcomes
Those who agreed to complete the outcome measures (research relatives) provided informed consent online before completing the questionnaires outlined above. These measures were chosen because they have good psychometric properties and were acceptable and sensitive to change in the REACT feasibility trial. 53 Questionnaires were offered at baseline and again after 12 and 24 weeks to ensure that we captured short- and longer-term impacts. Participants received three automated reminder e-mails to complete the questionnaires at each follow-up point. Owing to limited resources, no further efforts were made to follow up non-responders. All data from relatives were collected online, anonymised and downloaded to a database held at the Liverpool CTRC.
Measures
General Health Questionnaire-28
The GHQ-28 assesses the general health of participants during the previous few weeks across 28 items, each assessed on a 4-point Likert scale ranging from ‘not at all’ (0) to ‘much more than usual’ (3). Potential total scores range from 0 to 84, with higher scores indicating worse health outcomes. There are four subscales of seven items each, covering somatic symptoms (items 1–7), anxiety/insomnia (items 8–14), social dysfunction (items 15–21) and severe depression (items 22–28). The tool is also suitable for screening purposes using an alternative binary scoring method (with the two lowest response options scoring 0 and the two highest options scoring 1). Using the latter method, any total score exceeding the threshold value of 4 would classify the respondent as ‘caseness’, indicating that further medical attention was required. 97
Carer Well-being and Support Scale
This tool evaluates relatives’ well-being in the previous 4 weeks and general satisfaction with the support they receive. It has two separate subscales: well-being (32 items) and support (17 items). Well-being is assessed on a 5-point Likert scale from 0 (concerned ‘a lot’) to 4 (‘not at all’ concerned). Support is measured on a 4-point scale from 0 (‘very dissatisfied’ with support) to 3 (‘very satisfied’ with support). The subscales are obtained by adding the item scores, which give a range 0–128 for the well-being subscale and 0–51 for the support subscale. Higher scores indicate better outcomes for carers with regard to their well-being and satisfaction with support. 94
EuroQol-5 Dimensions, five-level version
The EQ-5D-5L is a measure of health-related quality of life and includes a descriptive system and a visual analogue scale (VAS) (EQ-5D-5L VAS). The descriptive system evaluates five dimensions (mobility, self-care, usual activities, pain/discomfort and anxiety/depression) on a 5-point Likert scale from 1 (‘no problems’) to 5 (‘extreme problems’). Participants are asked to indicate their health states on the day of the assessment by selecting the most appropriate statement for each dimension. Answers across the five dimensions can be combined into a five-digit profile number. The UK index score value sets range from –0.594 (where all five dimensions score 5: ‘extreme problems’) to 1 (where all dimensions score 1: ‘no problems’); a higher index score indicates a better outcome for respondents. The EQ-5D-5L VAS asks participants to rate their health on the day of the assessment on a 20-cm vertical VAS, scored from 0 (‘the worst health you can imagine’) to 100 (‘the best health you can imagine’). The selected scores can be used as a continuous measure of health. 95
eHealth Literacy Scale
The eHEALS evaluates participants’ eHealth literacy, including knowledge, comfort and perceived skills in finding, evaluating and applying electronic health information to health problems. The tool operates with eight items scored on a 5-point Likert scale ranging from 1 (‘strongly disagree’) to 5 (‘strongly agree’). Responses are summed for a total score from 8 to 40; higher scores indicate more positive evaluations of the participants’ own health literacy skills. 96
Process evaluation
Factors affecting implementation outcomes were explored through individual staff interviews, SRG workshops, document analysis and meeting observations, and analysed together within the NPT framework, then were used to inform iterative versions of the implementation plan. Interviews with relatives explored their perspective of the implementation of REACT, but were analysed separately using an open thematic coding. Each step is described in the following sections.
Staff interviews
Sampling strategy
A purposive sampling strategy was used to identify key stakeholders, including IMPART leads, REACT supporters, team managers and frontline clinical staff generally referred to as care co-ordinators. We also interviewed people with relevant strategic roles who were likely to play a part in implementing the toolkit in each trust, such as R&D leads and transformation managers.
Quantitative data (e.g. the number of relatives each staff member invited to REACT) and qualitative data from SRGs, workshops and staff interviews were used to identify staff members who were perceived as instrumental to the delivery of REACT, as well as those who were less inclined to promote the toolkit. Opportunity sampling was also used to recruit staff members when delivering training or presentations at trusts.
Development of topic guide for individual staff interviews
The staff interview topic guide [available at www.journalslibrary.nihr.ac.uk/programmes/hsdr/140416/#/documentation (accessed February 2020)] was designed to identify factors affecting implementation of REACT in routine EIP service practice and to test specific mechanisms that were hypothesised to be important. The schedule was broadly structured around NPT’s theoretical framework and the study-specific hypotheses generated in phase 1, but also aimed to elicit important contextual information. The guide was further developed in waves 2 and 3 to test ideas that emerged in interviews and case studies, and to assess the impact of new components in subsequent implementation plans. A separate pro forma was developed for IMPART leads [available at www.journalslibrary.nihr.ac.uk/programmes/hsdr/140416/#/documentation (accessed February 2020)] with contextual information about the EIP and trusts.
Process of staff interviews
We conducted semistructured, audio-recorded interviews with staff members face to face or by telephone at a time and place of their choosing. Although interviews were focused on testing our implementation hypotheses, the topic guide was used flexibly to allow new ideas and contextual information to emerge.
Before the interview, staff members were given a participant information sheet (PIS) [available at www.journalslibrary.nihr.ac.uk/programmes/hsdr/140416/#/documentation (accessed February 2020)] and invited to ask questions before giving written consent [available at www.journalslibrary.nihr.ac.uk/programmes/hsdr/140416/#/documentation (accessed February 2020)]. The PIS made clear that interviews would be recorded and advised that written notes could be taken if preferred. Participants were informed that their data would be anonymised and that anonymised quotations might be used in resulting publications and presentations. Transcripts were cleaned and anonymised prior to analysis. Further data security details are found in Data storage and management.
Meeting observations
The observation pro forma [available at www.journalslibrary.nihr.ac.uk/programmes/hsdr/140416/#/documentation (accessed February 2020)] was derived from Spradley and McCurdey’s98 nine dimensions of descriptive observation and adapted for the IMPART study to test propositions in each context. We aimed to observe naturally occurring meetings suggested by the IMPART lead and SRGs as a potential source of data about the context in which REACT was being implemented. Workshops and presentations were also recorded on observation pro formas.
Document analysis
We aimed to sample EIP, trust and national policy documents that might provide information about how relatives were supported in the trust, and specifically if and how REACT fitted into this strategy. All documents were imported into NVivo version 11 (QSR International, Warrington, UK) and coded as one of two codes: ‘What is the trust offering for relatives?’ and ‘Document’s reference to REACT’. The document analysis supported the interview data by providing contextual information for the implementation of REACT. The documents were also used to identify and compare similarities and differences between trusts.
Reflective diaries
Reflective diaries were kept by the lead researchers throughout the study. They were used to develop the researchers’ interpretation of the data as they were being collected, including contextual non-interview data that were informative to the overall narrative understanding of the process of implementing REACT (e.g. summaries of relevant e-mail correspondence or telephone calls). The diaries also recorded timing of key contextual events to understand how these affected implementation outcomes. Most importantly, these diaries provided a real-time record of the impressions and insights of the researchers on the ground to ensure that this could most effectively inform the final analyses. This was particularly crucial given the change of research staff, meaning that researchers who were closest to the data in wave 1 were no longer working on the project at the time of the final analyses.
Stakeholder reference groups
Stakeholder reference groups took place in all six trusts at key points throughout the study (see Report Supplementary Material 1 for dates). The first groups are described in detail in Chapter 3 and Appendix 3 and were used to inform the development of our study hypotheses. Subsequent SRGs were primarily used to develop iterations of the implementation plan, providing feedback on what was already provided, identifying ongoing challenges and co-developing subsequent versions. The attendees were largely determined by the IMPART leads in collaboration with the research team.
Relatives’ interviews
Sampling
Relatives who consented to complete online questionnaires were also invited to take part in an interview about their experience of being offered REACT. Partway through the study, we applied for an ethics amendment to separate the process of inviting relatives into the research study and inviting them into REACT. This change was in response to feedback from relatives who were confused about whether or not the research questionnaires formed part of the REACT intervention. The baseline research questionnaires were removed from the initial log-in process, and relatives were given the option of completing these later and/or being contacted about taking part in an individual interview or declining to take part in any form of research. The amendment also approved recruitment (via EIP staff) of relatives who had been invited to use REACT but who had not proceeded to access the website and create an account. Our aim was to sample across all six trusts.
Procedure
This part of the study was led by a trainee clinical psychologist (Johanna Barraclough), supervised by Fiona Lobban, and closely supported by the carer researchers and lead researchers at each site, with additional input at the analytic stage from the wider PMG.
Relatives who consented were contacted by a member of the research team by e-mail or telephone, sent a copy of the PIS and consent form [both available at www.journalslibrary.nihr.ac.uk/programmes/hsdr/140416/#/documentation (accessed February 2020)] and offered the opportunity to ask questions. For relatives who agreed to take part, an interview was scheduled at a time and location convenient to them.
Data collection
Interviews took place between May 2017 and May 2018 by telephone or face to face in NHS clinical locations, and lasted 40–70 minutes. Interviews were semistructured in accordance with the interview topic guide [available at www.journalslibrary.nihr.ac.uk/programmes/hsdr/140416/#/documentation (accessed February 2020)], with flexibility to allow issues raised by participants to be fully explored. Topics explored with relatives included their caring role, the process by which they were first introduced to REACT, their initial impressions, their use of REACT, REACT’s pros and cons, any impact that REACT had on them or their family, how REACT compared to other forms of support they had accessed or been offered, and support for REACT from the EIP team. All interviews were audio-recorded and transcribed.
Resources survey
At the end of the study, clinicians were asked to complete an online cost and savings survey to estimate the time and resources used and/or freed up by using REACT in their services. This is available at www.journalslibrary.nihr.ac.uk/programmes/hsdr/140416/#/documentation (accessed February 2020).
Sample size
Our main purpose was to understand the process of evaluation, building a detailed picture in each trust by talking to relevant staff in EIP teams and in the wider organisation. We attempted to sample relatives, including those who had used REACT and those who had not, to interview across all participating trusts. The sample of relatives completing the quantitative measures was determined by the level of implementation.
Analysis
Quantitative data
Descriptive statistics for variables measured on an interval scale were mean, standard deviation (SD), median, range and interquartile range (IQR); for categorical (including ordinal) variables, they were frequency (n) and percentage. Pearson’s correlation coefficient was used to quantify linear associations between interval variables, with Spearman’s rank correlation coefficient being used if the association was potentially non-linear. Independent sample t-tests (using the Satterthwaite approximation for the degrees of freedom where equality of variances could not be assumed) and Pearson’s chi-squared tests were used to explore differences between clinical and research participants. Paired t-tests were used to investigate the mean change from baseline to 12 weeks and to 24 weeks in the research participants’ self-reported scores; effect sizes were estimated by dividing the mean change by the baseline SD. Statistical significance required a two-sided p-value of < 0.05, and 95% confidence intervals (CIs) were presented. All data analyses were performed using IBM SPSS Statistics version 23 (IBM Corporation, Armonk, NY, USA).
Qualitative data: staff
Qualitative data sets collected from trust staff, meeting observations and document analyses were analysed using framework analysis85 and NVivo software. Data were analysed on two levels.
Level 1 analysis
This was a dynamic and agile sense-making process that provided the basis for preliminary explanation building that informed the development of each implementation plan. The analysis drew on themes that were clearly emerging from the data prior to detailed coding into the NPT framework. Themes were identified by the lead researchers at each site, and discussed during fortnightly analysis meetings, and at the monthly PMG meetings. The key factors were then presented and discussed in a workshop setting with key stakeholders from the subsequent wave for further elaboration and testing as part of developing the subsequent implementation plan.
Level 2 analysis
In parallel to the level 1 analysis, all data were uploaded into NVivo and coded line by line. A framework analysis was used to synthesis data from different sources and accommodate multiple researchers’ contributions. The initial framework was developed from NPT and findings from phase 1, then further developed during the study as codes were refined and additional codes were added. Changes to the framework were agreed at fortnightly coding meetings, attended by the lead researchers for the North of England and South of England sites and the chief investigator.
Researchers analysing the data at each site had access to NVivo files, which they used to store and analyse data. At regular intervals, these files were merged, collating the data from the two lead researchers. Previous files were archived and researchers each worked on an individual copy of the most recently merged document. This process was repeated throughout data collection and analysis.
At the end of each wave of phase 2, individuals from the PMG attended one of two ‘data day’ events to analyse the qualitative data from one of the trusts in that wave. Six trust data days were held, one for each trust. To ensure that the analysis had a broad range of perspectives, each was attended by the North of England and South of England lead researchers, the chief investigator, at least one carer researcher and at least one other clinical academic expert. Anonymised summaries of the data were distributed for familiarisation prior to the event. The day then involved the PMG members discussing the themes emerging in each part of the coding framework, the differences between embedded units in the trust and the general narrative emerging from the trust summaries. Areas requiring further exploration were also identified and necessary changes were made to the interview topic guides.
Qualitative data: relatives
Analysis of relatives’ interview data was led by Johanna Barraclough and followed the procedure proposed by Braun and Clarke. 99 This inductive thematic coding method allows themes to emerge from the data rather than relying on a pre-existing framework, but also offers a detailed description of the process that was easy for our carer researchers, who had no formal research training, to become involved in, ensuring multiple perspectives.
The first phase of analysis consisted of thorough immersion in the data by reading the entire data set of interviews several times and recording notes about ideas and meanings in a reflective journal. Ideas about interesting segments of the data were organised into initial codes, which represented areas of meaning. The entire data set of interviews was worked through methodically, with all potential codes marked in the margin of each transcript. A pictorial map of codes was created using sticky notes, enabling visual identification of patterns of meaning while retaining sight of instances of departure. To ensure that the process was valid and rigorous, two members of the research team with experience as carers of a close relative with psychosis or bipolar disorder independently coded six transcripts, each with the results discussed with the lead researcher (Johanna Barraclough). A high level of consistency provided reassurance that the process was appropriate, and discussions about the implications of the codes identified served as a useful foundation for building themes, with the lived experience perspective of the carers providing insight.
The codes were then compiled into a Microsoft Word (Microsoft Corporation, Redmond, WA, USA) document together with supporting quotations from interviews.
The next phase involved taking a broader perspective on the data and grouping the codes into potential themes. The visual sticky note map enabled codes to be grouped into clusters of overarching themes, and a structure of main themes and subthemes emerged, which was then translated into a Microsoft Word document together with supporting quotations. Seven members of the research team, including the two carer researchers and chief investigator, met to review the main researcher’s decisions regarding the potential themes. Discussions centred on whether or not the coded data supported each theme and the scope of each theme, with themes divided or amalgamated as needed. The descriptions given to the themes were discussed for accuracy. Discussions also explored how themes linked together and their illumination of factors affecting implementation of REACT from the participants’ perspective.
Following the meeting, the main researcher reviewed the whole data set once more to verify that the themes were robust, and the diagram was refined to illustrate the story conveyed by the data. This diagram was presented at the explanatory synthesis meeting (described in the following section) and refined further in the light of the process of integrating these data with data from other parts of the IMPART study.
Developing an explanatory synthesis and final implementation plan
Our final explanatory synthesis and IPv4 were informed by our analysis of qualitative and quantitative data from staff and relatives across all trusts, as described previously. Ideally, relatives’ data would have been collected earlier and could have informed early iterations of the implementation plan, but this was not possible.
Trust analysis days
These were held at each trust. IMPART leads invited staff and relatives who had been involved in the IMPART study to attend. The research team presented a preliminary summary of the factors affecting implementation of REACT at that trust, based on the data days analysis described in Level 2 analysis. Participants were encouraged to question, elaborate on and explore these findings, particularly highlighting any areas of misunderstanding or important missing factors. These events were a key step in ensuring that participants felt fully part of the research process, rather than just providers of data.
The IMPART study-wide data day
The IMPART leads and other key staff, including REACT champions and supporters, were invited to a 1-day event to support the interpretation of data gathered across all six trusts. The main aims of the event were to:
-
present the draft final analysis, including overarching themes and key factors affecting implementation developed across the six trusts, and gather attendees’ feedback and reflections
-
present all trusts with each iteration of the implementation plan and gather suggestions for IPv4
-
ensure that attendees had all the information they needed about the immediate future of REACT, including how the findings of the IMPART study would be interpreted alongside those of the parallel REACT trial55
-
maintain a collaborative working relationship and investigate how and if attendees wanted to continue contributing REACT in the year following the end of the IMPART study.
Explanatory synthesis event
All IMPART study team members, including members of the PMG, an IT developer, research associates and carer researchers, were invited to a final 2-day study event. The main aims were to:
-
synthesise the analyses of all of the data collected throughout the study and develop a coherent story, including testing our study-specific hypotheses
-
collaboratively develop an explanatory synthesis to understand the key factors that affected implementation of REACT across all six trusts
-
finalise an implementation plan (version 4) that could be shared with other NHS trusts that were interested in using REACT
-
reflect on the role of NPT in the IMPART study (i.e. successes and challenges) and implications for future development of the theory.
Data storage and management
All participants providing individual or group interview data gave written consent for interviews to be audio-recorded, with the following exceptions. One staff member and one staff group did not wish to be recorded, but consented to handwritten notes recording key points emerging from the discussion. One participant consented to be interviewed but did not consent to any record being made. Her interview informed the reflexive diary of the research associate. All participants were made aware that their data would be anonymised following transcription, and that anonymised quotations might feature in resulting publications and presentations.
Interviews were digitally recorded using encrypted audio-recorders [Philips Pocket Memo (Philips, Guildford, UK) and Olympus DS-2400 (Olympus, Southend-on Sea, UK)], and audio files were uploaded to secure servers at Lancaster University or UCL at the earliest opportunity; original recordings were then deleted from the recorder. Audio-recordings of interviews were sent to the transcriber electronically in a zipped [using 7-zip version 18.01 (Free Software Foundation, Inc., Boston, MA, USA)] password-protected file via a secure file-sharing digital platform [Dropbox (London, UK), Zendto version 4.10 (University of Southampton, Southampton, UK)].
All relatives’ outcome measure data were collected through an online system at Liverpool CTRC and stored on secure servers physically located within access-controlled server rooms and backed up nightly to a separate physical location. All identifiable data were encrypted using a 256-bit encryption algorithm. CTRC servers were subject to penetration testing audits undertaken by University of Liverpool central IT staff.
The IMPART data are stored on a secure server at Lancaster University, which complies with relevant statutory provisions including the Data Protection Act 2018100 and the European Union General Data Protection Regulation. 101 Data held on Lancaster University servers are stored in a resilient storage infrastructure that is dual housed in the university’s data centres (on site). There are multiple levels of redundancy built into these storage arrays – snapshots and backups are automated and created regularly.
University single sign-on credentials are required to access the shared network drive; the principal investigator (PI) controls access to specific folders and ensures that this is monitored regularly.
Chapter 5 Implementation, intervention and resource outcomes: quantitative data
This chapter summarises the quantitative data collected to describe the levels of implementation of REACT within each of the six trusts, the characteristics of the relatives who signed up to REACT, the impact of REACT on relatives’ outcomes measured using online questionnaires, and the resources needed to implement REACT. Chapters 6 and 7 present primarily qualitative data about the process of implementation, which attempt to explain the outcomes presented in this chapter.
Implementation outcomes are presented for each wave. Trusts in each wave received successively more developed implementation plans, which were informed by the qualitative findings of our process evaluation (see Chapter 6). Presenting the data in this way allows us assess whether or not implementation outcomes improved with each iterative version of the implementation plan. Relatives’ characteristics and intervention outcomes are not presented by wave as we did not hypothesise any relationship between implementation plans and relatives’ characteristics or the impact of the intervention. There were also insufficient data to allow any meaningful comparisons to be made between waves.
Implementation outcomes
Staff activity and relatives’ uptake of REACT in each NHS trust
Figures 8–13 and Table 6 present the number of staff accounts created, invitations sent to relatives and accounts created by relatives in each of the six participating NHS trusts. Figure 8 also shows the timing of key research-related activities in each trust.
FIGURE 8.
Timeline of clinicians’ and relatives’ activity in wave 1 trusts: Woods Trust.
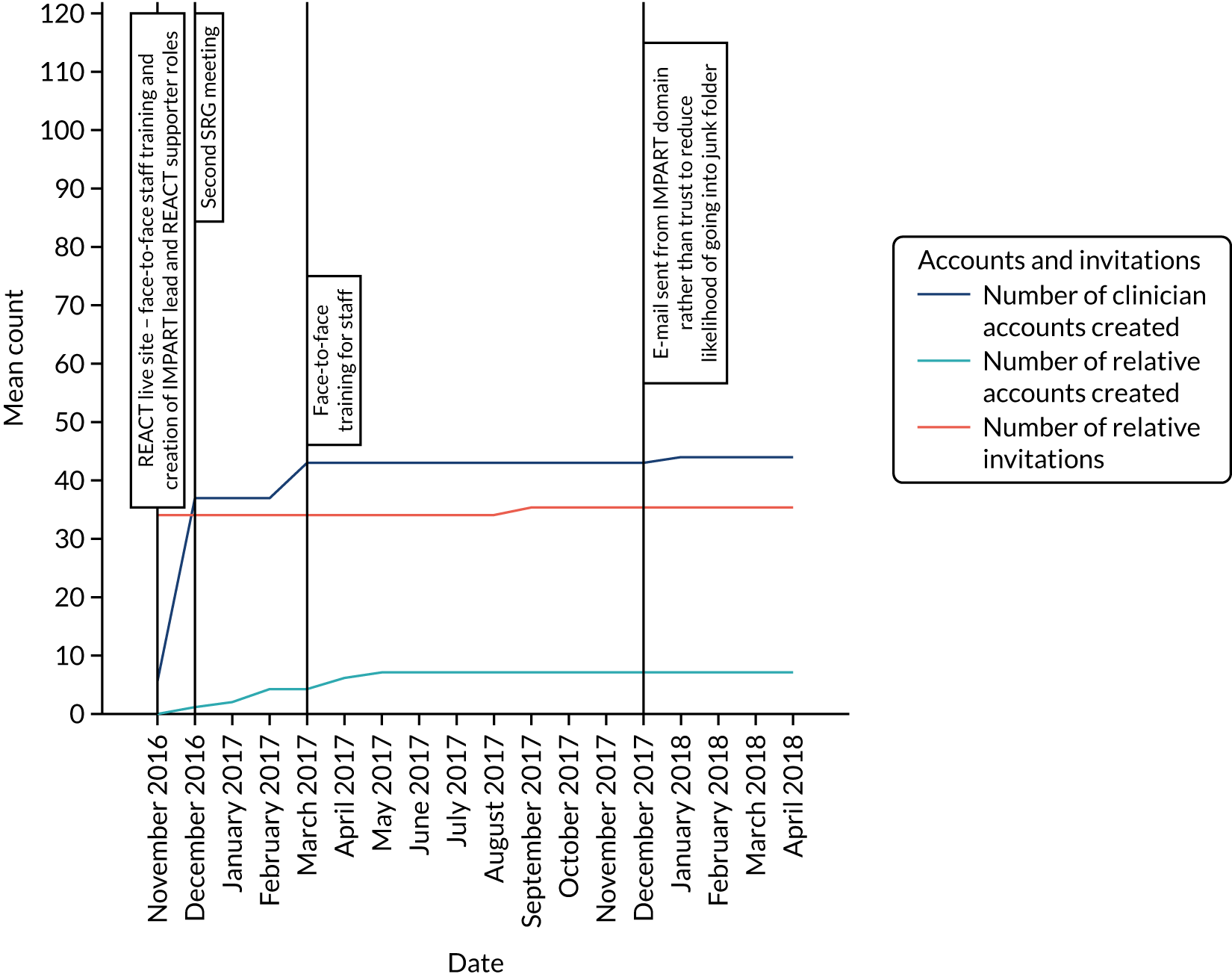
| Summary variable | Wave 1 | Wave 2 | Wave 3 | Mean (SD) | Range | |||
|---|---|---|---|---|---|---|---|---|
| Woods | Moor | Ocean | Seashore | Lakes | Marsh | |||
| Number of clinician accounts created | 44 | 37 | 32 | 63 | 64 | 41 | 46.8 (13.5) | 32–64 |
| Number of clinicians sending invitations (% of clinicians who created accounts) | 8 (18) | 12 (54) | 4 (12) | 18 (29) | 8 (13) | 7 (17) | 9.5 (5.9) | 4–18 |
| Number of invitations sent | 35 | 47 | 40 | 112 | 29 | 92 | 59.1 (34.30) | 29–112 |
| Number of relatives invited (% of caseload) | 29 (6)a | 40 (18)a | 37 (5)a | 93 (24)a | 25 (4)a | 86 (23)a | 51.7 (13.3) | 25–93 |
| Number of relative accounts created (% of caseload) | 7 (1)a | 24 (11)a | 20 (3)a | 38 (9)a | 17 (3)a | 53 (15)a | 26.5 (16.5) | 7–53 |
| CCQI audit: % of relatives offered FI | 47 | 3 | 32 | 42 | 62 | 3 | TNS 31 | |
| CCQI audit: % of carers offered carer-focused education and support | 50 | 6 | 87 | 71 | 30 | 74 | TNS 50 | |
Wave 1 trusts
As seen in Figures 8 and 9, uptake, defined by the numbers of staff accounts created and numbers of relatives invited to use REACT, was relatively low, and similar in both trusts. Although more clinicians set up accounts in Woods than in Moor, subsequent activity was lower in Woods (fewer invitations were sent and fewer relatives signed up to REACT). There were no significant changes over the study period. Research team activity was minimal in wave 1 trusts, which received only IPv1.
FIGURE 9.
Timeline of clinicians’ and relatives’ activity in wave 1 trusts: Moor Trust.

Wave 2 trusts
Wave 2 trusts were given an enhanced implementation plan (IPv2; see Chapter 6). This appears to be associated with additional uptake and use in Seashore, with more relatives invited to register by staff members and more accounts created by relatives, but there was substantially less activity in Ocean throughout the study period, as shown in Figures 10 and 11.
FIGURE 10.
Timeline of clinicians’ and relatives’ activity in wave 2 trusts: Ocean Trust.
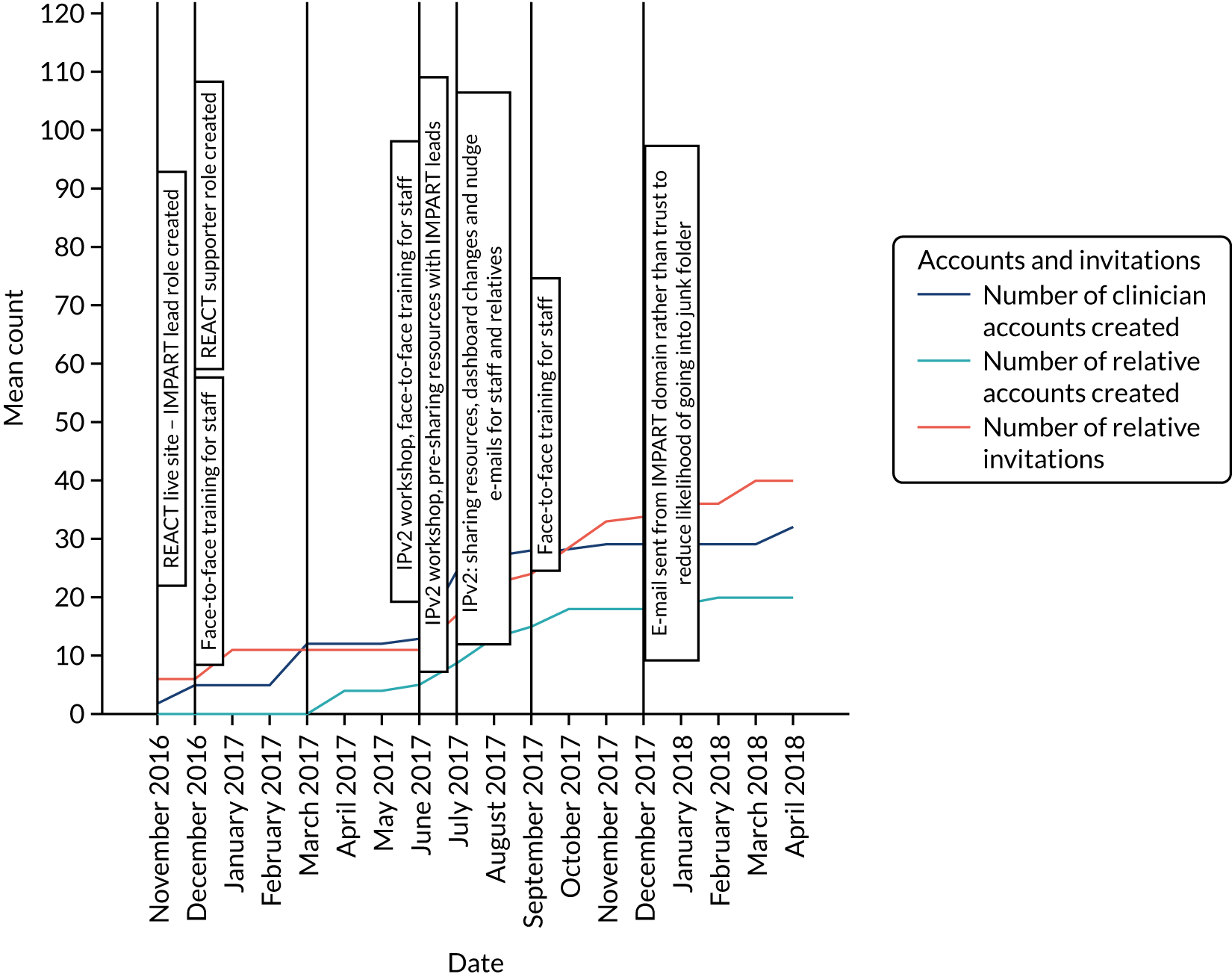
FIGURE 11.
Timeline of clinicians’ and relatives’ activity in wave 2 trusts: Seashore Trust.
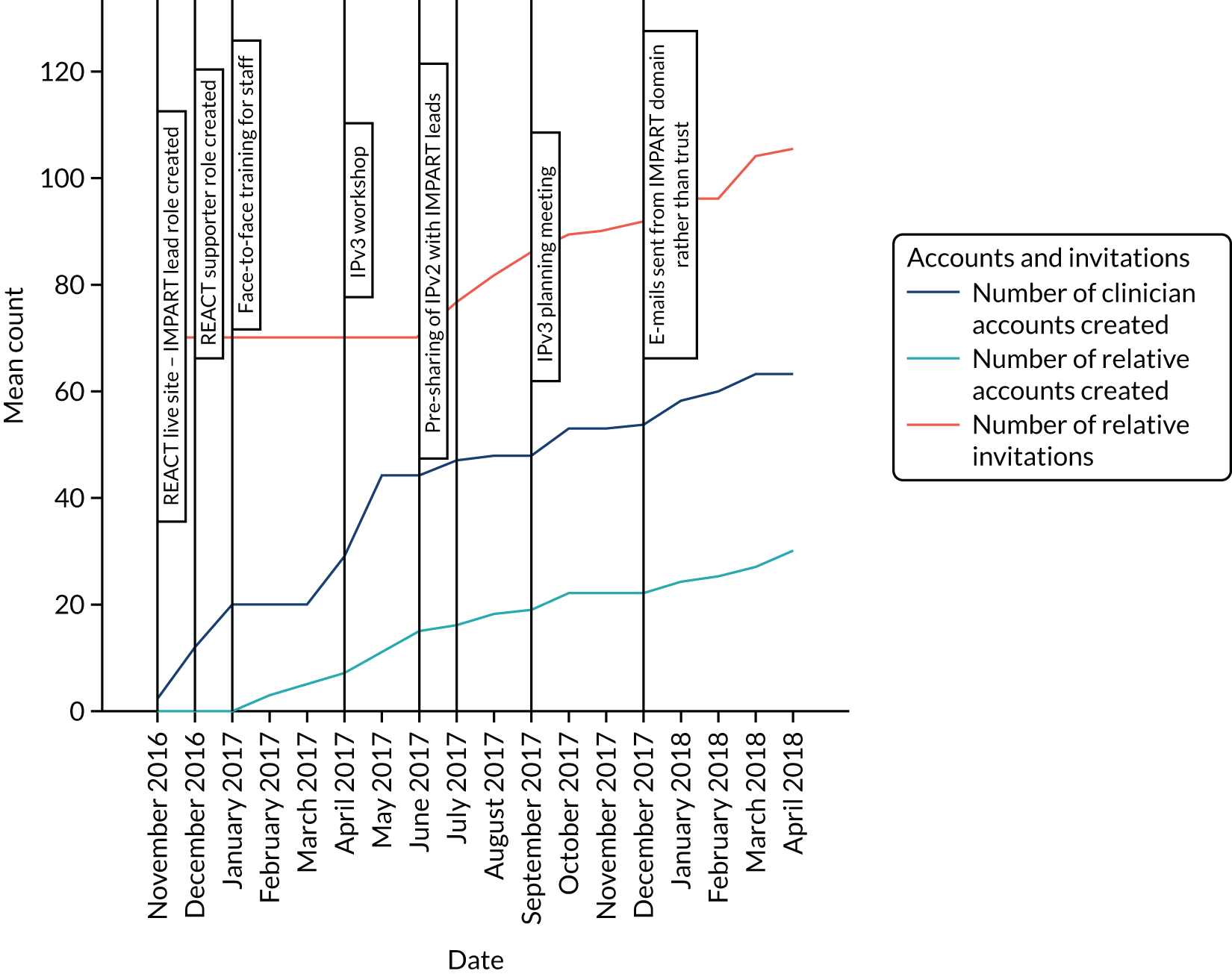
Wave 3 trusts
The two trusts in wave 3 received the most intense implementation plan, the content of which is described in Chapter 6. As in wave 2, the trusts differed in levels of activity, with Marsh Trust showing more activity than Lakes Trust, as seen in Figures 12 and 13. IPv3 appears to be associated with an increase in the number of invitations sent and relatives’ accounts created, but not in the number of clinician accounts created. Marsh Trust was the only trust with more relatives’ than clinicians’ accounts. In contrast, the most clinician accounts were created in Lakes Trust, although the number of relatives’ accounts remained comparatively low.
FIGURE 12.
Timeline of clinicians’ and relatives’ activity in wave 3 trusts: Lakes Trust.
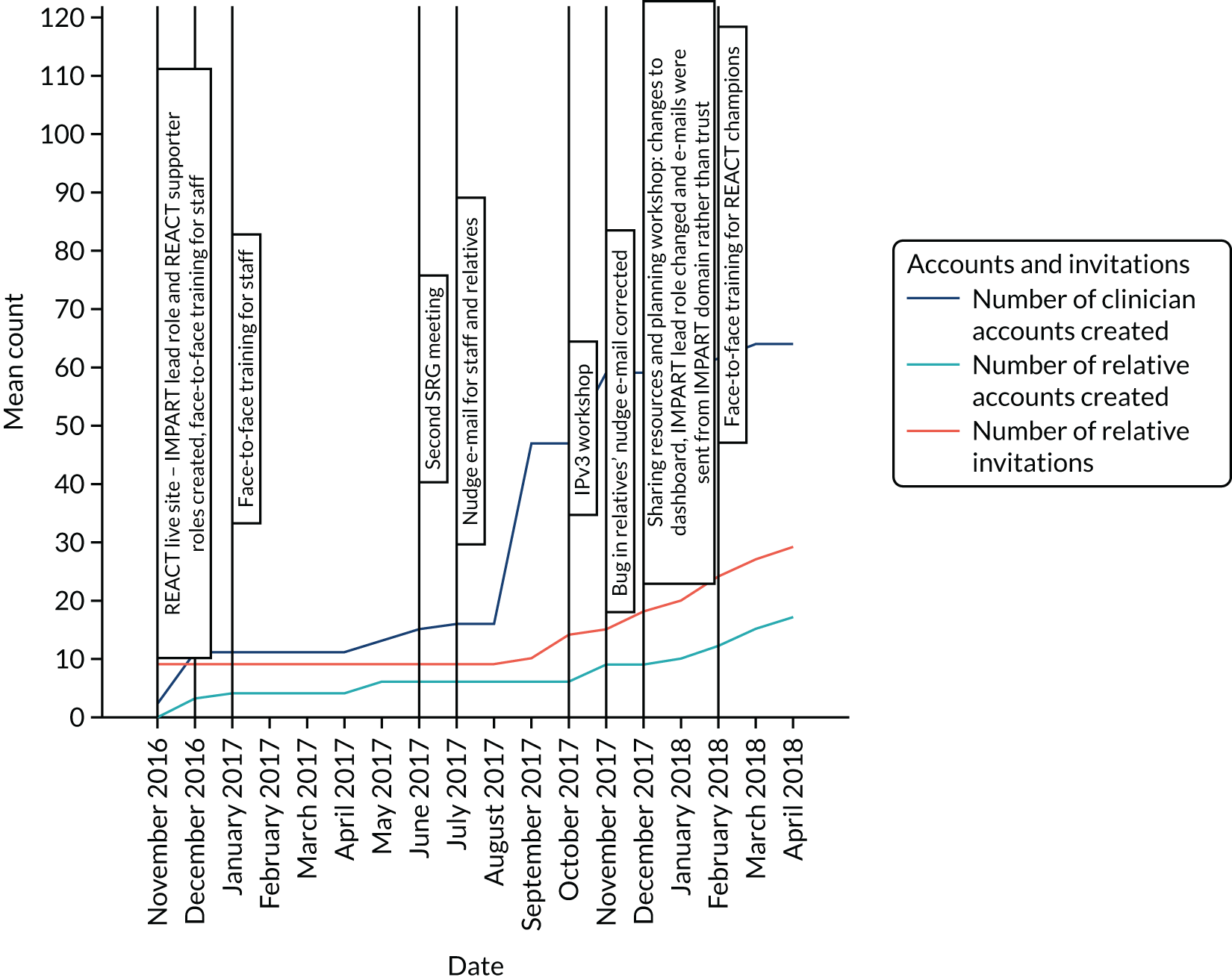
FIGURE 13.
Timeline of clinicians’ and relatives’ activity in wave 3 trusts: Marsh Trust.
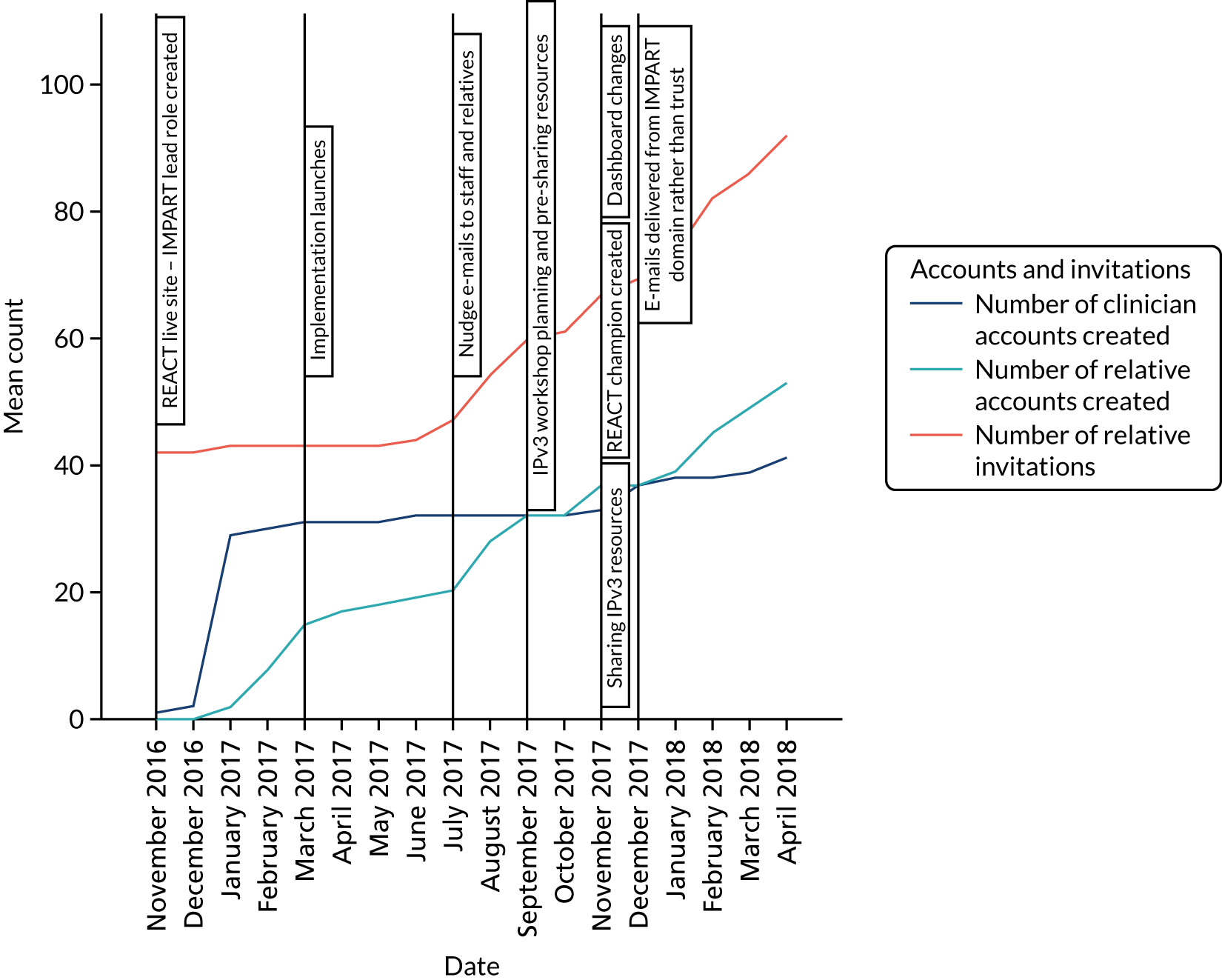
Table 6 provides summary statistics for accounts created by staff, invitations sent in total (including repeat invitations), number of relatives invited and number of relatives’ accounts created. Table 6 also shows summary data for levels of support offered to relatives by each trust prior to using REACT, as reported in the National Audit of Early Intervention Service Providers conducted by the Royal College of Psychiatrists in 2016. 102
The highest number of clinicians signed up at Lakes Trust (n = 64; wave 3) and the lowest number signed up at Ocean Trust (n = 32; wave 2). Seashore Trust (wave 2) sent the most invitations in total (n = 112) and to individual relatives (n = 87), whereas Lakes Trust sent the fewest (despite having the largest number of clinician accounts). A minority of clinicians across all trusts sent invitations, with the fewest being in Ocean (n = 4) and the most in Seashore (n = 18). Marsh Trust had the most relatives’ accounts (n = 53; wave 3), and Woods Trust had the lowest (n = 7; wave 1). High uptake in Seashore may be linked to the lack of other forms of family intervention offered, based on national audit data. According to the audit, Lakes Trust offered family intervention to the highest proportion of relatives (62%), whereas Moor (wave 1) and Marsh offered family intervention to the lowest proportion (3%), much lower than the national sample average of 31%. As for carer-focused education and support, Ocean offered this to the highest proportion of relatives (87%) and Moor to the lowest (3%), again substantially below the sample average of the audit.
Data collection from relatives
Figure 14 illustrates the recruitment and attrition of relative participants. Clinicians across the six trusts sent a total of 355 invitations to relatives; 159 relatives’ accounts were set up across the six participating trusts. Sixty-two participants consented to complete outcome measures, of whom 56 (baseline), 21 (12 weeks) and 20 (24 weeks) completed at least some measures. Sixteen participants completed (at least partially) the measures at all three time points.
FIGURE 14.
Relatives’ demographic and intervention outcome data: recruitment and retention.
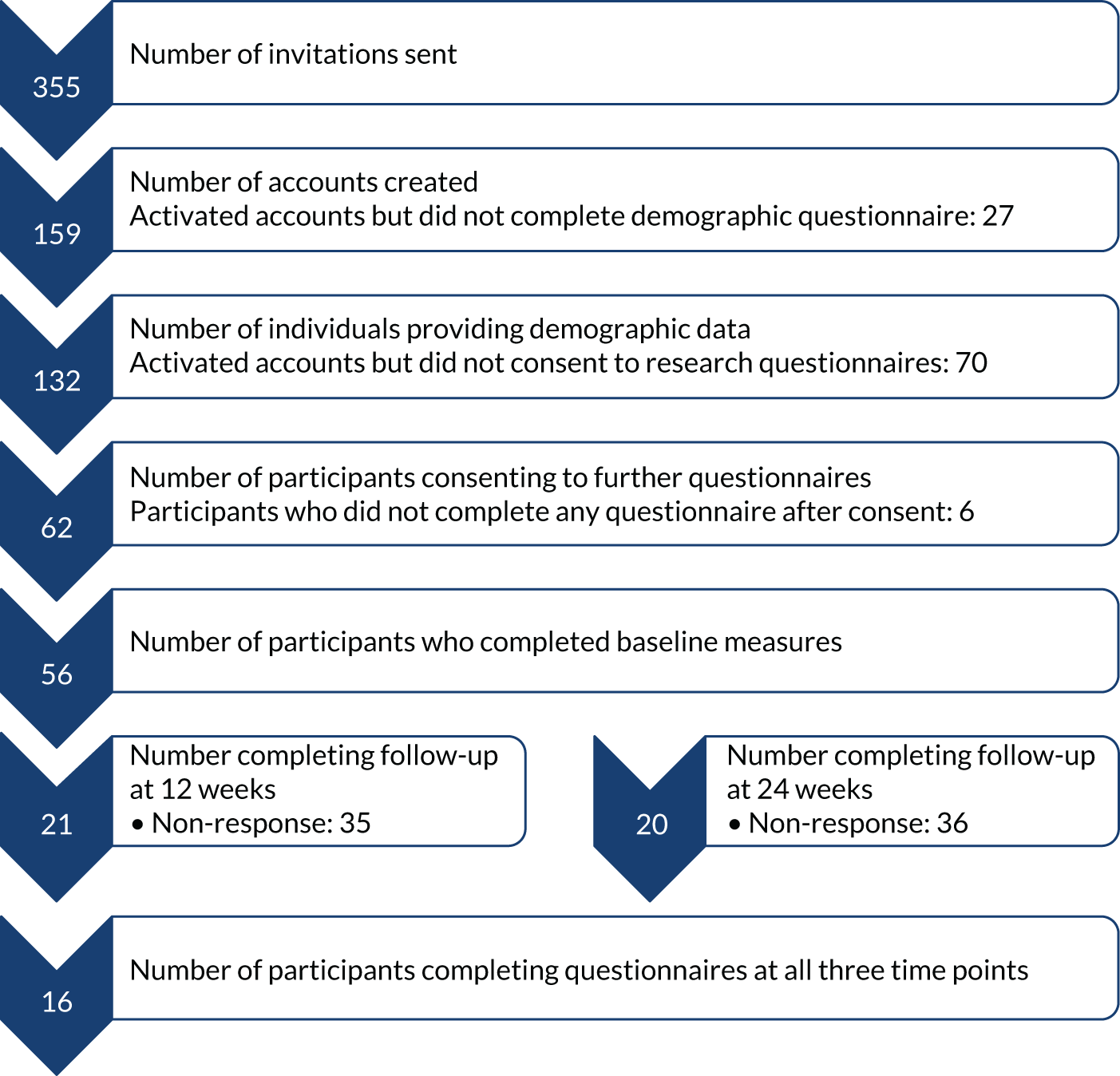
Participants’ characteristics
Table 7 summarises the sociodemographic characteristics of relatives. Comparisons were made between clinical relatives and research relatives, but there were no significant differences in any of the variables. The majority of participants in both groups did not work full time, were aged > 50 years, were female, were from a white ethnic background, used broadband or Wi-Fi to access the internet and were educated to Advanced level (A level) or above.
| Characteristic | Woods (N = 6) | Moor (N = 20) | Ocean (N = 17) | Seashore (N = 28) | Lakes (N = 15) | Marsh (N = 46) | Overall, n (%) |
|---|---|---|---|---|---|---|---|
| Age (years) (n) | |||||||
| 16–25 | 1 | 2 | 1 | 2 | 1 | 1 | 8 (6) |
| 26–35 | – | 4 | – | 2 | 2 | 4 | 12 (9) |
| 36–50 | 1 | 5 | 5 | 10 | 2 | 7 | 30 (23) |
| > 50 | 4 | 8 | 11 | 14 | 10 | 33 | 80 (61) |
| Missing | – | 1 | – | – | – | 1 | 2 (2) |
| Gender (n) | |||||||
| Female | 6 | 16 | 13 | 25 | 10 | 36 | 106 (80) |
| Male | – | 4 | 4 | 3 | 5 | 9 | 26 (19) |
| Missing | – | – | – | – | – | 1 | 1 (1) |
| Ethnicity (n) | |||||||
| Any white background | 3 | 19 | 17 | 15 | 15 | 39 | 108 (82) |
| Any other ethnic background | 3 | 1 | – | 12 | – | 3 | 19 (14) |
| Missing | – | – | – | 1 | – | 4 | 5 (4) |
| Internet access (n) | |||||||
| Broadband or Wi-Fi | 6 | 18 | 17 | 26 | 14 | 44 | 125 (95) |
| Mobile data (3G, 4G) | – | 1 | – | 2 | – | – | 3 (2) |
| No access | – | – | – | – | – | 1 | 1 (1) |
| Intermittent/poor quality | – | – | – | – | 1 | – | 1 (1) |
| Missing | – | 1 | – | – | – | 1 | 2 (2) |
| Education (n) | |||||||
| School leaver | 1 | 3 | 8 | 5 | 5 | 10 | 32 (24) |
| A level or equivalent | 2 | 6 | 3 | 3 | 3 | 10 | 27 (20) |
| Degree | 1 | 4 | 5 | 14 | 6 | 13 | 43 (33) |
| Postgraduate | 2 | 2 | – | 5 | 1 | 9 | 19 (14) |
| Missing | – | 5 | 1 | 1 | – | 4 | 11 (8) |
| Employment (n) | |||||||
| Full time | 2 | 6 | 4 | 6 | 5 | 16 | 39 (30) |
| Part time | 2 | 6 | 8 | 9 | 3 | 10 | 38 (29) |
| Unable because of caring responsibility | 1 | 3 | – | 6 | 1 | 3 | 14 (11) |
| Not in paid employment for other reason | 1 | 3 | 4 | 5 | 5 | 12 | 30 (23) |
| Missing | – | 1 | 1 | 2 | 1 | 5 | 11 (8) |
Table 8 provides information about the caring roles of research participants from the ‘About your caring role’ questionnaire completed at baseline (see Appendix 5 for 12- and 24-week follow-up; this information was not collected from clinical participants). The majority of participants had been in caring roles for > 1 year and had an average of 45 hours of predominantly face-to-face contact with the person they were supporting each week. Most participants reported that caring for their relatives had not affected their employment status or performance, because they either had not been in paid employment prior to their caring role or were still performing the same work. A small number of participants at each assessment point reported either stopping work or reducing their hours owing to their caring role. Participants reported caring for between one and four relatives, with the majority caring for one relative only. Demographic and clinical characteristics of the relatives cared for are also presented in Table 8 (see also Appendix 6). The most common relationships were mother (participant) and child (relative cared for). Individuals who were cared for were primarily aged < 25 years and living at home. The most commonly reported diagnosis was psychosis. However, there were relatively high rates of missing data or instances when participants did not know the diagnosis of their relative.
| Characteristic | Baseline |
|---|---|
| Research participants | N = 53 |
| Duration of caring role, n (%) | |
| < 1 month | 2 (4) |
| < 1 year | 13 (25) |
| > 1 year | 38 (72) |
| Duration of care role (months) | |
| Mean (SD) | 48.4 (68.93) |
| Range (IQR) | 0–284 (9–48) |
| Level of contact (hours/week), mean (SD); range (IQR) | |
| Face-to-face contact | 48.4 (43.56); 2–168 (18–62) |
| Other contact | 9 (15.42); 0–70 (1–10.5) |
| Total contact | 57.4 (46.72); 4–170 (21–82) |
| Impact on work role, n (%) | |
| No: not in paid work before caring role | 15 (28) |
| No: still performing the same work | 26 (49) |
| Yes: reduced working hours | 4 (8) |
| Average reduced working hours, mean (SD), range (IQR) | 12 (2.45); 10–15 (10–14.5) |
| Yes: stopped working | 8 (15) |
| Additional time taken off, n (%) | |
| N/A | 14 (26) |
| No | 18 (34) |
| Yes | 21 (40) |
| Hours taken off in past 12 weeks, mean (SD), range (IQR) | 15.3 (34.22); 0–168 (0–15.5) |
| Number of relatives cared for, n (%) | |
| 1 | 40 (75) |
| 2 | 7 (13) |
| 3 | 3 (6) |
| 4 | 3 (6) |
| Total | 75 |
| Relatives cared for | N = 75 |
| Participant’s relationship to relative(s), n (%) | |
| Mother | 45 (60) |
| Father | 2 (2.67) |
| Grandfather | – |
| Sibling | 3 (4) |
| Wider family | 1 (1) |
| Daughter | 7 (9) |
| Son | – |
| Partner | 5 (7) |
| Friend | – |
| Other | 1 (1) |
| Missing | 11 (15) |
| Age of relative(s) (years), n (%) | |
| < 16–25 | 37 (49) |
| 26–35 | 10 (13) |
| 36–50 | 7 (9) |
| > 50 | 10 (13) |
| Missing | 11 (15) |
| Relative’s diagnosis, n (%) | |
| I don’t know | 5 (7) |
| Bipolar disorder, bipolar affective disorder, manic depression | 6 (8) |
| Schizophrenia | 2 (3) |
| Psychosis | 38 (51) |
| Schizoaffective disorder | 1 (1) |
| Other | 10 (13) |
| Missing | 13 (17) |
| Relative living with participant, n (%) | |
| Yes | 43 (57) |
| No | 19 (25) |
| Missing | 13 (17) |
Web use of relatives
Table 9 summarises the 24-week web use of research and clinical participants, and the results of independent t-tests comparing their web use (see also Appendix 7). The mean number of logins for the group as a whole was 3.78 (SD 4.43), but there was a lot of variation, with a range of 0–31 logins (median 2 logins, IQR 1–8 logins). The mean total time spent on the website was 40.6 minutes (SD 54.54 minutes), with a range of 0–298 minutes (median 20.1 minutes, IQR 4.9–57.5 minutes). In general, the research participants used the website more than the clinical participants, and the difference was significant in the total number of logins, number of visits to modules 1–6 and module 11, number of visits to the forum, total time spent on the website and total number of module visits (composite measure of visits to the 12 different modules).
| Web use variables | Participants, mean (SD) | Independent t-tests | ||||||
|---|---|---|---|---|---|---|---|---|
| Clinical (n = 76) | Research (n = 56) | Overall | t | df | 95% CI | Cohen’s d | p-value | |
| Number of logins | 2.1 (2.56) | 6.1 (5.32) | 3.78 (4.43) | –5.21 | 73.62 | –5.4 to –2.5 | 1.01 | < 0.001 |
| Total number of module visits | 3.2 (6.15) | 7.8 (9.08) | 5.2 (7.84) | –3.26 | 90.88 | –7.4 to –1.8 | 0.61 | 0.002 |
| Number of visits to forum | 0.4 (0.65) | 1.7 (2.47) | 1.0 (1.81) | –4.03 | 60.65 | –2 to –0.7 | 0.81 | < 0.001 |
| Total time spent on website (minutes) | 24.7 (37.84) | 62.1 (65.68) | 40.6 (54.54) | –3.82 | 81.62 | –56.8 to –17.9 | 0.73 | < 0.001 |
Figure 15 displays the average number of visits during the 24-week follow-up period for clinical and research participants to the different sections of the website. Module 1 (‘What is psychosis?’) and the forum were the most frequently visited sections for both clinical and research participants, and module 9 (‘Understanding mental health services’) was the least visited by both groups.
FIGURE 15.
Website use of clinical and research participants.
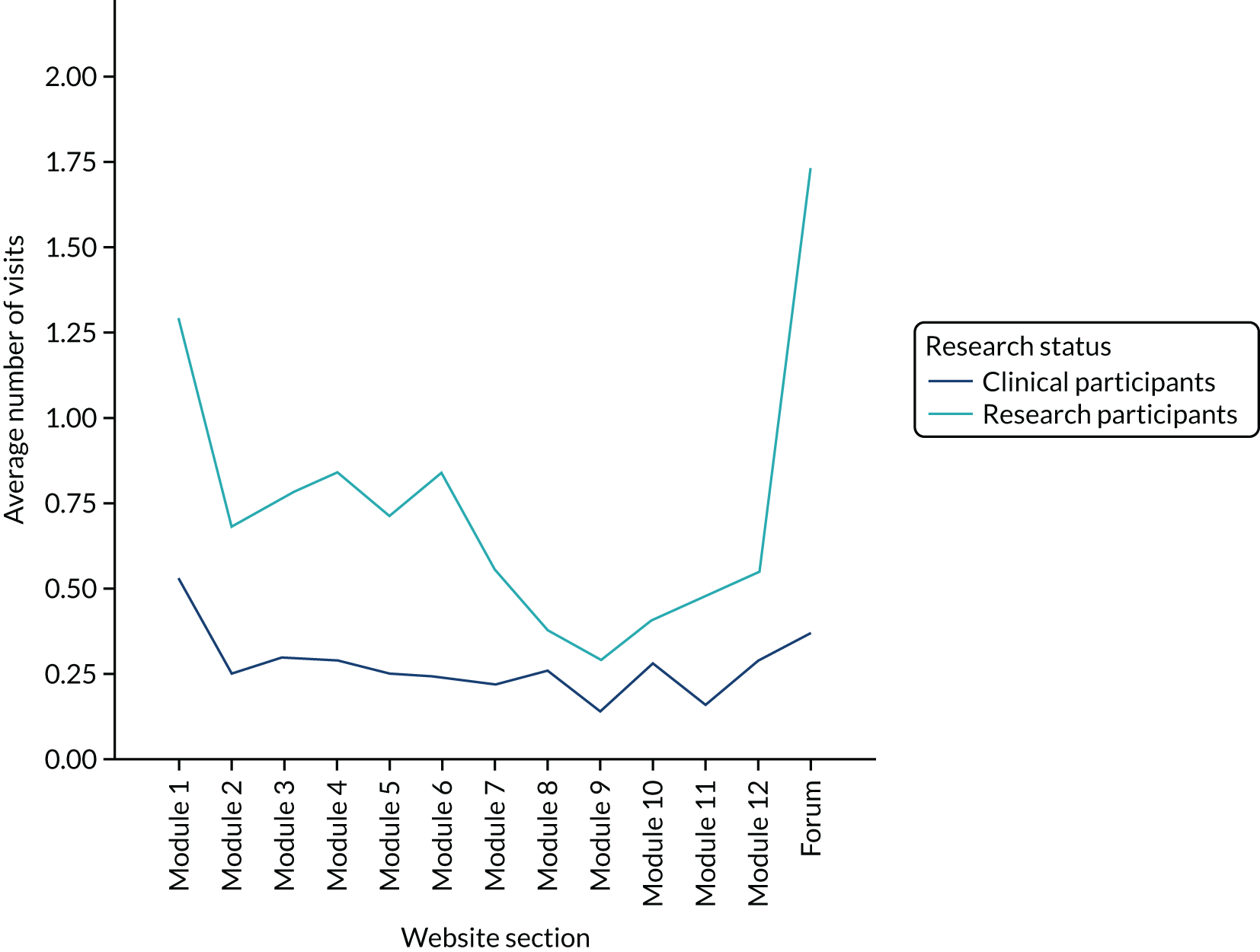
Intervention outcomes
The impact of REACT on relatives self-reported measures
The descriptive statistics of self-reported measures at the three time points are summarised in Table 10. Results regarding the GHQ-28 screening scores (items scored as 0, 0, 1, 1) indicated that 34 participants (60%) scored above the clinical threshold of 4 out of 5 at baseline, compared with 11 (55%) at 12 weeks and 12 (60%) at 24 weeks. The average total GHQ-28 scores (items scored 0–3) were also above the suggested clinical threshold of 23 out of 24 at each follow-up point, confirming high levels of distress in the sample. Mean values of the GHQ-28 total scores, and subscales of social dysfunction, severe depression and anxiety and insomnia, the CWS well-being scale and eHealth literacy all improved with small effect sizes. Paired t-tests with 95% CIs compared baseline scores with those at the 12- and 24-week follow-ups; none of the changes from baseline was statistically significant (see Appendix 8).
| Variable | Baseline | 12-week follow-up | 24-week follow-up | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Mean (SD) | Range (IQR) | n | Mean (SD) | Range (IQR) | n | Mean (SD) | Range (IQR) | |
| GHQ-28 total score | 56 | 31.6 (14.43) | 7–65 (19.8–40) | 20 | 27.3 (9.79) | 13–51 (19.25–30) | 20 | 26.0 (10.28) | 8–45 (20–33) |
| GHQ-28 screening score | 56 | 9.4 (7.48) | 0–27 (3–15) | 20 | 7.6 (6.85) | 0–21 (1.5–11.8) | 20 | 7.1 (6.02) | 0–20 (0.5–11) |
| GHQ-28 somatic symptoms | 56 | 8.2 (4.76) | 1.00–17.00 (4–11.8) | 20 | 7.6 (3.66) | 3–14 (4–10.5) | 20 | 7.2 (3.72) | 0–13 (5.3–10) |
| GHQ-28 anxiety and insomnia | 56 | 10.6 (4.95) | 2–21 (7) | 20 | 8.9 (3.78) | 3–16 (6–12.5) | 20 | 8.5 (4.67) | 1–18 (5.3–13.3) |
| GHQ-28 social dysfunction | 56 | 9.6 (3.26) | 2–20 (7–11.8) | 20 | 8.5 (2.40) | 5–15 (7–10) | 20 | 8.1 (2.34) | 4–13 (7–9) |
| GHQ-28 severe depression | 56 | 3.2 (3.93) | 0–14 (0–6) | 20 | 2.3 (2.11) | 0–7 (0.25–3) | 19 | 2.2 (2.82) | 0–9 (0–4) |
| CWS well-being | 55 | 72.5 (27.66) | 16–127 (47–93) | 19 | 84.2 (24.08) | 12–128 (75–96) | 19 | 87.3 (26.59) | 37–128 (68–107) |
| CWS support | 55 | 33.4 (10.56) | 7–51 (29–41) | 19 | 35.5 (11.46) | 8–51 (32–47) | 19 | 36.3 (12.06) | 9–51 (28–46) |
| eHealth literacy | 54 | 27.6 (5.47) | 16–39 (24–32) | 19 | 29.2 (3.62) | 20–35 (26–32) | 19 | 28.2 (5.89) | 10–36 (25–32) |
| EQ-5D-5L VAS | 54 | 66.3 (25.77) | 0–100 (48.8–82.3) | 19 | 68.2 (27.40) | 0–95 (61–82) | 19 | 66.3 (26.72) | 0–96 (59–80) |
| EQ-5D-5L index | 54 | 0.8 (0.16) | 0.05–1 (0.7–0.9) | 19 | 0.8 (0.08) | 0.68–1 (0.8–0.9) | 19 | 0.8 (0.14) | 0.49–1 (0.7–0.9) |
Resources: costs and savings of implementing REACT
All trusts were given free access to REACT and IPv1 at the start of wave 1. Trusts in waves 2 and 3 received additional resources associated with IPv2 and IPv3 at no cost from the research team. These were estimated to cost approximately £400 per trust, and would be an additional treatment cost if REACT was implemented in routine clinical practice. The plans are described in full in Chapter 6. A summary of estimated item costs is provided in Appendix 9.
Survey responses
Forty-eight staff members completed the costs and savings survey across five trusts (Table 11). Lake Trust had the highest response rate; no staff completed the survey in Woods. The majority of respondents were clinicians who had referred relatives to REACT, followed by REACT supporters. Given the variation in number and role of respondents, it is not valid to make comparisons between trusts or across different waves. However, a general picture across all trusts can be ascertained.
| Role | Number of respondents, by trust | Total (N = 46), n (%) | |||||
|---|---|---|---|---|---|---|---|
| Woods (N = 0) | Moor (N = 6) | Ocean (N = 5) | Lake (N = 17) | Seashore (N = 11) | Marsh (N = 7) | ||
| IMPART lead | – | – | 1 | 1 | 1 | 1 | 4 (9) |
| IMPART lead and REACT supporter | – | 1 | – | 1 | 1 | – | 3 (7) |
| REACT supporter | – | 1 | 2 | – | 4 | 3 | 10 (22) |
| REACT champion | – | – | – | 2 | – | 1 | 3 (7) |
| Clinician | – | 4 | 2 | 11 | 5 | 2 | 24 (52) |
| Support worker | – | – | – | 1 | – | – | 1 (2) |
| Team manager | – | – | – | 1 | – | – | 1 (2) |
Costs
Individual staff time required to implement REACT
Table 12 presents the time spent implementing REACT by staff in each trust. Three types of activity were measured: time spent training and learning about REACT; staff activity within their teams, such as setting up accounts and inviting relatives; and research activity.
| Time | Trust (n) | Total (N = 46), n (%) | ||||
|---|---|---|---|---|---|---|
| Moor (n = 6) | Ocean (n = 5) | Lake (n = 17) | Seashore (n = 11) | Marsh (n = 7) | ||
| Time spent being trained/told about REACT | ||||||
| < 1 hour | 1 | 2 | 2 | 0 | 0 | 5 (11) |
| 1–2 hours | 2 | 1 | 7 | 7 | 4 | 21 (46) |
| 2–5 hours | 3 | 1 | 5 | 2 | 0 | 11 (24) |
| 5–10 hours | – | 1 | 1 | 1 | 1 | 4 (9) |
| > 10 hours | – | – | 2 | 1 | 2 | 5 (11) |
| Total time spent getting familiar with the content and features | ||||||
| None | – | – | 2 | 1 | 1 | 4 (9) |
| < 1 hour | 1 | 2 | 7 | 4 | 2 | 16 (35) |
| 1–2 hours | 3 | 2 | 7 | 4 | 1 | 17 (37) |
| 2–5 hours | 2 | 1 | 1 | 2 | 2 | 8 (17) |
| > 5 hours | – | – | – | – | 1 | 1 (2) |
| Total time spent being trained by the research team | ||||||
| Never trained | 4 | 2 | 4 | 1 | – | 11 (24) |
| < 1 hour | 1 | 1 | 3 | 2 | 1 | 8 (17) |
| 1–2 hours | 1 | – | 9 | 7 | 4 | 21 (46) |
| 2–5 hours | – | 2 | – | 1 | 1 | 4 (9) |
| 5–10 hours | – | – | 1 | – | 1 | 2 (4) |
| Total time spent being shown how to use REACT | ||||||
| Not shown | 2 | 3 | 4 | 5 | 4 | 18 (39) |
| < 1 hour | 2 | 2 | 7 | 4 | 2 | 17 (37) |
| 1–2 hours | 2 | – | 4 | 2 | 1 | 9 (20) |
| 2–5 hours | – | – | 2 | – | – | 2 (4) |
| Total time spent showing REACT to other team members | ||||||
| Did not do | 1 | 2 | 9 | 3 | 4 | 19 (41) |
| < 1 hour | 2 | 2 | 6 | 4 | – | 14 (30) |
| 1–2 hours | 1 | 1 | – | 1 | 1 | 4 (9) |
| 2–5 hours | 2 | – | 1 | 3 | 1 | 7 (15) |
| 5–10 hours | – | – | 1 | – | 1 | 2 (4) |
| Time spent on setting up accounts for other staff members | ||||||
| None | 4 | 2 | 14 | 6 | 5 | 31 (67) |
| < 1 hour | 1 | 2 | 2 | 2 | – | 7 (15) |
| 1–2 hours | 1 | – | – | 2 | 1 | 4 (9) |
| 2–5 hours | – | 1 | – | 1 | 1 | 3 (7) |
| 5–10 hours | – | – | 1 | – | – | 1 (2) |
| Total time spent inviting relatives | ||||||
| None | – | – | 3 | – | 4 | 7 (15) |
| < 1 hour | 1 | 1 | 8 | 5 | – | 15 (33) |
| 1–2 hours | 2 | 1 | 2 | 4 | 2 | 11 (24) |
| 2–5 hours | 2 | 1 | 4 | 2 | 1 | 10 (22) |
| 5–10 hours | – | 2 | – | – | – | 2 (4) |
| 10–15 hours | 1 | – | – | – | – | 1 (2) |
| Time spent receiving supervision (respondents with REACT supporter role)a | ||||||
| n = 2 | n = 2 | n = 1 | n = 5 | n = 3 | n = 13 | |
| None | 1 | 1 | – | – | 2 | 4 (31) |
| < 1 hour | 1 | – | 1 | 4 | 1 | 7 (54) |
| 1–2 hours | – | 1 | – | 1 | – | 2 (15) |
| Time spent supervising REACT supporters (respondents who did not have REACT supporter role)a | ||||||
| n = 5 | n = 3 | n = 17 | n = 7 | n = 4 | n = 36 | |
| None | 4 | 2 | 15 | 3 | 1 | 25 (69) |
| < 1 hour | 1 | – | – | 2 | 1 | 4 (11) |
| 1–2 hours | – | 1 | 1 | 1 | 1 | 4 (11) |
| 2–5 hours | – | – | – | 1 | 1 | 2 (6) |
| 5–10 hours | – | – | 1 | – | – | 1 (3) |
| Total time spent on taking part in research activity | ||||||
| None | – | 1 | 7 | 3 | 1 | 12 (26) |
| < 1 hour | 3 | 1 | 4 | 2 | 2 | 12 (26) |
| 1–2 hours | 1 | 2 | 3 | 1 | 1 | 8 (17) |
| 2–5 hours | – | 1 | 2 | 5 | – | 8 (17) |
| 5–10 hours | 1 | – | – | – | 2 | 3 (7) |
| > 10 hours | 1 | – | 1 | – | 1 | 3 (7) |
Training and learning
Most staff reported having received 1–2 hours of training and that most of this was delivered by the research team. Approximately two-thirds of respondents had spent < 2 hours becoming familiar with the content and features of REACT.
Staff activity in their teams
Approximately 40% of respondents neither showed other team members how to use REACT nor were shown by others in their team. The majority of respondents had never set up an account for other team members. Approximately one-third of the staff had spent < 1 hour inviting relatives, and very few spent > 5 hours. Eighty per cent of REACT supporters had received either no supervision or just under 1 hour of supervision in total during the study period.
Research activity
This is presented separately from clinical activity but is included here, as taking part in the research clearly triggered clinical activity for some staff (see Chapter 6). Most staff members spent < 1 hour on research activities, including taking part in interviews and implementation plan workshops. Approximately 13% of the respondents reported having spent > 5 hours on various research activities.
Organisational activity to implement REACT
The survey also explored time spent discussing REACT in organisational meetings (Table 13). Approximately half of the respondents had seen REACT as a regular agenda item at meetings. These were mostly monthly clinical team meetings, attended by 5–20 people. However, in most instances, REACT was discussed for < 5 minutes and only two respondents reported that REACT was discussed at a regular meeting for > 15 minutes. Other meetings in which REACT had appeared as a standing agenda item included business meetings, EIP steering group meetings, referral meetings and R&D meetings. REACT was an ad hoc agenda item in a clinical improvement group in Seashore, a strategy meeting in Lakes and a mental health care group clinical governance meeting in Moor.
| Discussion of REACT | Trusts (n) | Total (N = 46), n (%) | ||||
|---|---|---|---|---|---|---|
| Moor (n = 6) | Ocean (n = 5) | Lake (n = 17) | Seashore (n = 11) | Marsh (n = 7) | ||
| Have you seen REACT as a regular agenda item at meetings? | ||||||
| Yes | 4 | – | 8 | 6 | 4 | 22 (48) |
| No | 2 | 5 | 9 | 5 | 3 | 24 (52) |
| How often was the meeting?a | ||||||
| n = 4 | – | n = 8 | n = 6 | n = 4 | n = 22 | |
| Monthly | 5 | – | 6 | 6 | 1 | 14 (64) |
| Weekly | 2 | – | – | – | 2 | 4 (18) |
| Other | 1 | – | 2 | – | 2 | 4 (18) |
| Approximately how many people attended the meeting?a | ||||||
| 5–10 | 2 | – | 4 | 3 | – | 9 (41) |
| 11–20 | 1 | – | 3 | 3 | 3 | 10 (45) |
| 21–30 | 1 | – | – | – | 1 | 2 (9) |
| > 30 | – | – | 1 | – | – | 1 (5) |
| How long was REACT discussed at the meeting (minutes)?a | ||||||
| < 5 | – | – | 3 | 6 | 1 | 10 (45) |
| 5–10 | 3 | – | 3 | – | 2 | 8 (36) |
| 10–15 | – | – | 1 | – | 1 | 2 (9) |
| > 15 | 1 | – | 1 | – | – | 2 (9) |
Additional costs
Respondents were asked whether or not any additional resources had been required to deliver REACT. In one trust, it was reported that a computer had been bought; in another, additional software had been bought (although accessing REACT requires only an internet browser).
Savings
The final section of the survey explored whether or not staff members could identify areas where REACT contributed to savings of resources or other benefits to staff or relatives (Table 14). The majority of respondents did not feel that REACT reduced the time they spent supporting relatives. Those who did save time estimated this to be only 1–2 hours across the whole study period. However, > 80% of respondents reported that REACT helped their services to better support relatives by equipping staff members with a resource to share with relatives and helping them to reach both national policy and local service targets to support relatives. Respondents in Ocean also felt that the toolkit improved their confidence and offered a backup for their important conversations with relatives. They highlighted that REACT not saving time was a positive thing as it may indicate staff spending more time communicating with and supporting relatives as a result of having REACT and improved confidence. In Lakes, staff felt that REACT had improved communication with relatives owing to relatives having more understanding of psychosis/bipolar disorder. In Moor, staff reported that REACT was particularly helpful to relatives who do not wish to attend family interventions but were seeking a better understanding of mental health problems. Finally, in Seashore, a member of staff mentioned that REACT fostered thinking of alternative ways to support carers using digital/online resources.
| Discussion of REACT | Trust (n) | Total (N = 46), n (%) | ||||
|---|---|---|---|---|---|---|
| Moor (n = 6) | Ocean (n = 5) | Lake (n = 17) | Seashore (n = 11) | Marsh (n = 7) | ||
| Do you think REACT has saved time you would otherwise have used to support relatives? | ||||||
| Yes | 3 | – | 5 | 3 | 2 | 13 (28) |
| No | 3 | 5 | 12 | 8 | 5 | 33 (72) |
| Total time saved by using REACT (hours)a | ||||||
| n = 3 | n = 0 | n = 5 | n = 3 | n = 2 | n = 13 | |
| < 1 | – | – | 1 | 1 | – | 2 (15) |
| 1–2 | – | – | 4 | 1 | 1 | 6 (46) |
| 2–5 | – | – | – | 1 | – | 1 (2) |
| 5–10 | 1 | – | – | – | 1 | 2 (15) |
| > 10 | 1 | – | – | – | – | 1 (2) |
| Missing | 1 | – | – | – | – | 1 (2) |
| Do you think REACT helped your service/team to support relatives?a | ||||||
| Yes | 6 | 3 | 16 | 7 | 6 | 38 (83) |
| No | – | 2 | 1 | 4 | 1 | 8 (17) |
Summary
Overall, little time was dedicated to REACT in any of the trusts. There was individual variation, but a general pattern seemed to be that staff spent a couple of hours being trained to use REACT, a couple more to familiarise themselves with the content, and then no more than a few hours over the entire study period referring relatives. Very little time was spent in any trust discussing REACT in meetings, and REACT supporters did not receive much supervision in their role. Despite this relatively low level of investment of time, staff still did not generally feel that REACT had saved them time in supporting relatives. It may be (as suggested by one participant) that this was because REACT itself facilitated increased contact with some relatives, as it facilitated communication. However, other benefits were identified, including REACT being seen as a valuable information resource for staff and relatives, and an appropriate way to meet national and local clinical targets.
Relatives who were invited to use REACT were predominantly white British mothers aged > 50 years reporting high levels of clinical distress. On average, they used the website for < 1 hour in total, although there was considerable variation between individuals. All outcome measures showed change in the desired direction over time, but changes were small and none was statistically significant.
There was some evidence to suggest that successively more developed versions of the implementation plan led to greater numbers of relatives being invited to use REACT. However, the relationship was far from straightforward, with wide variation between trusts in the same wave. How the implementation plans were used in each trust and other relevant factors affecting the implementation of REACT are explored in Chapters 6 and 7.
Chapter 6 Implementation outcomes and iterative implementation plans: qualitative data
This chapter presents the final outcome of the analysis of the qualitative data collected across the six participating NHS trusts. Tables 15–22 summarise the factors identified in each trust against the four core constructs of NPT. We describe successive iterations of implementation plans following each wave of data collection, then draw out common findings and important differences relevant to understanding the delivery of REACT. Where appropriate, we draw on quantitative data.
Narrative summaries of the context, key findings against each NPT component, the lead researcher’s reflective summary and feedback from final trust analysis days for each trust are presented in Appendices 10–15 (which include Tables 37–42 describing participants in each trust). Figures illustrating the common barriers and ways to enhance implementation of REACT revealed by these data are in Appendix 16 (see Figures 21 and 22).
Trust summaries and iterative implementation plans
Trust responses to each iteration of the implementation plan are summarised against NPT’s four core constructs:
-
coherence – the sense-making work that people do individually and collectively when faced with operationalising a set of practices
-
cognitive participation – the relational work that people do to build and sustain a community of practice around a new technology or intervention
-
collective action – the operational that work people do to enact a set of practices
-
reflexive monitoring – the appraisal work that people do to assess and understand how the new intervention affects them and others.
Implementation plan version 1
Challenges for this first iteration were to deliver REACT in all six trusts, train staff by providing an online manual followed by face-to-face training, and appoint an IMPART lead as PI in each trust, as described in Chapter 4.
Wave 1 outcomes
Table 15 shows uptake of REACT by staff and relatives in wave 1 trusts. Table 16 shows qualitative outcomes in response to the four NPT core constructs.
| Activity | Trust | |
|---|---|---|
| Woods | Moor | |
| Number of staff accounts | 44 | 37 |
| Number of relatives’ invitations sent | 35 | 47 |
| Number of individual relatives invited (after duplicates removed) | 29 | 40 |
| Number of relatives’ accounts created | 7 | 24 |
| NPT core construct | Trust | |
|---|---|---|
| Woods | Moor | |
| Context |
|
|
| Coherence |
|
|
| Cognitive participation |
|
|
| Collective action |
|
|
| Reflexive monitoring |
|
|
Staff in both trusts in wave 1 could clearly see the potential value of an online toolkit for relatives and for NHS staff:
[Groups] can be very responsive and warm and everything but they’re also yeah you have to get here for 6 o’clock on alternate Tuesdays . . . [A website is] much more kind of accessible and people can read stuff in their own speed.
Woods IMPART lead 04, individual interview
One potential benefit is you can very easily offer I suppose everyone with an internet connection really the same information . . . consistently across the board . . . And hopefully if it’s used then you can get used to working with a family that have a certain knowledge base which I think would be good.
Woods clinician 87, individual interview
Some of our newer staff will really benefit from reading that information and knowing what information is useful to share. Particularly when you’re young, you lack some of the life experience like you know I did.
Woods REACT supporter 03, individual interview
Yeah I think it fits in in terms of reaching the family interventions target and as I said before I think it fits in with the BFT [behavioural family therapy] as well. So it kind of hits a couple of the targets that we’ve got to do I think.
Woods clinician 06, individual interview
However, as Table 16 showed, staff in Woods were under huge pressure with high caseloads and low morale. With REACT seen as a research project and without financial incentives, the team never really signed up. Implementing anything in this team would have been a challenge. Agreement to join the IMPART study was driven by the trust’s R&D agenda:
Trust leadership are very keen on research, although I don’t think that they adequately communicate that enthusiasm to people on the ground . . . I think had you given [managers] the choice they would probably have said well we . . . support research as an important thing but we don’t really feel able to participate at the moment.
Woods IMPART lead 01, individual interview
They’re not necessarily the things that I would clinically say are the most important, but they’ve got money attached to them . . . Sadly they are often the priorities.
Woods clinician 01, individual interview
There was no evidence of REACT being embedded in any care pathways or service structures, or of any team managers directing staff to offer REACT. Staff themselves did not find REACT easy to integrate into their daily practice, or the website easy to use:
People just forget it . . . When you’re doing an assessment, when you’re meeting a family member, you have a thousand and one things on your mind that you’d like to assess and write down and stuff and it’s difficult to remember the spiel.
Woods IMPART lead 04, individual interview
You load up the dashboard, you first get this screen which is kind of sort of meaningless . . . It’s hard to know what does what, it’s kind of trial and error.
Woods IMPART lead 04, SRG meeting
Moor Trust covers a rural area where staff had much smaller caseloads (estimated around 15) but distances to visit service users were great. EIP staff were embedded in general community teams, making formal and peer training challenging. Key individuals were responsible for driving REACT, but beyond these individuals there was low engagement. Trust IT systems ran old web browsers that did not support the encryption algorithm used by REACT (which was configured to require a reasonable strength of encryption and reject known insecure algorithms), and the firewalls blocked videos embedded in the website and hosted on YouTube (YouTube, LLC, San Bruno, CA, USA). Staff did not have access to mobile devices to show relatives REACT in their homes, leading to requests for a paper version.
Concerns were also expressed about the possible impact of REACT on relationships with relatives as a result of more information:
If I was a relative and I went on and I see, ‘Oh we’ve got the right to ask for this and this and this’ – the trust doesn’t provide everything it’s advertising on REACT . . . For example it talks about art therapies . . . As it stands, our service users can’t access that internally. So that’s an issue . . . A lot of the things that are linked to EI we’re still in the very early stages of thinking about how, and that’s not a Moor Trust exclusive issue.
Moor REACT supporter 01, individual interview
As in Woods, REACT was not seen as priority because it was not linked to financial targets, and identification of REACT as being part of the research agenda led staff to look to the research team to engage staff and relatives to use REACT:
You have come today and it has prompted me, reminded me for example about the REACT toolkit.
Moor clinician 03, individual interview
I think you really need to just grab them in the team meeting one day and get them logged on, because I really don’t believe they’ll prioritise logging on.
Moor REACT supporter 03, individual interview
In both trusts, lack of feedback or engagement from relatives very quickly demotivated staff. In Woods, early abandonment was triggered by the REACT supporter leaving and the role not being reallocated:
I think it just feels a bit kind of stagnant.
Woods REACT supporter 01, individual interview
Yeah I’ve given it to a couple of patients, I’ve had a look at it myself, I think it looks really good. But the patients that I’ve given it to they haven’t accessed it . . . I’ve asked them you know a couple of times and it’s, ‘Oh I’ve not got round to it yet’.
Moor clinician 08, individual interview
Implementation plan version 2
Implementation plan version 2 aimed to address some of the issues above. Factors identified in wave 1 fed into workshops in wave 2 trusts where IPv2 was designed and delivered. It attempted to increase staff engagement by making REACT more visible and user friendly. Some elements of IPv2 were further developed in IPv3: these are shown in italic text in Table 17.
| Challenge identified | Implementation plan component in response |
|---|---|
|
1. REACT NHS booklet and insert cards: business card with URL and card for staff to write relatives’ information needed to send the invitation |
|
2. ‘Merchandise’ (described below) |
|
3. Simple, attractive e-mail nudges for relatives and staff |
|
4. A memorable URL, which then directed users to the relevant trust website (URL cannot be published without identifying participating trusts) |
|
5. Planning document issued: Maximising the success of REACT for your EIS |
|
6. User-friendly dashboard with auditing section to show who has been invited to use REACT |
REACT NHS booklets
These booklets, shown in Figure 16, were produced for staff to show to relatives to support their introduction to REACT. Designed to be an attractive description of REACT and its potential benefits for both staff and relatives, the booklets came with a business card with the REACT toolkit Uniform Resource Locator (URL) so that relatives would have the address to hand, and an information card to prompt staff to record the information (name and e-mail address) needed to later send an invitation from the REACT website.
FIGURE 16.
Booklets and merchandise for IPv2. Reproduced from Greenhalgh et al. 74 © Trisha Greenhalgh, Joseph Wherton, Chrysanthi Papoutsi, Jennifer Lynch, Gemma Hughes, Christine A'Court, Susan Hinder, Nick Fahy, Rob Procter, Sara Shaw. Originally published in the Journal of Medical Internet Research (www.jmir.org), 1 November 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on http://www.jmir.org/, as well as this copyright and license information must be included.

The booklet included an invitation to use REACT with or without taking part in the collection of research data (data showed that this was a barrier for relatives – see Chapter 7). It was important that relatives could read a description of REACT without going online. The packs were welcomed, and fitted with how clinicians generally offered services and built relationships with relatives.
In IPv3, minor modifications were made in response to feedback, including using the term ‘friends and family’ on the cover to be more consistent with the terms services used.
Merchandise
Mugs, pens and sticky notes with the REACT URL (see Figure 16) were also suggested by staff at the workshops, to raise awareness within teams and ‘give something back’. However, feedback on the merchandise was mixed. Some reported it serving its purpose: ‘I first became aware of REACT, I think I saw it on a mug and asked somebody about it’, but others were less positive. One person commented ‘I think it’s a waste of funding’. One team offered the merchandise as prizes in a competition for the highest number of relatives invited (Ocean); others handed them out to all staff. Teams were encouraged to use them as they saw fit.
E-mail reminders
E-mails to nudge relatives to visit REACT were already part of the toolkit but were redesigned to be more user friendly, and reminders to staff were introduced. Modifications included significantly reducing the length of the e-mails, making the hyperlink to the toolkit more prominent and increasing visibility of the logo at the head of the e-mail. New subject headers explicitly stated the content or action required.
In IPv3, the source and wording of the e-mails were changed to reduce the likelihood that e-mails went into spam or junk folders.
An easy-to-remember URL
The original URL required users to type in the right trust initials (which for one trust changed during the study). The new URL made it easier for staff and relatives to find the right REACT website and the inclusion of ‘nhs’ within the URL conveyed that REACT was being offered through an NHS service, to differentiate it from the REACT trial website (www.reacttoolkit.co.uk), which was being used in parallel.
Planning document ‘Maximising the success of REACT for your EIS’
This was used to structure a collaborative process with key individuals in the trust to help them to think about what was needed to support REACT in their trust. It could help teams to identify who was best placed to offer REACT, how it fitted with what they already did well, and the existing places where REACT could be promoted to staff and relatives. The final version of the document is available at www.journalslibrary.nihr.ac.uk/programmes/hsdr/140416/#/documentation (accessed February 2020).
In IPv2, this was designed as an internal self-reflection process for staff. In IPv3, it evolved to facilitate a conversation with the identified agents of change, and included a plan for how the conversation would continue to be revisited in the future. Key questions developed as part of the workshops included:
-
Why are we offering REACT? What key targets or aims will it help us meet?
-
How will staff team members be introduced to REACT?
-
Where does REACT fit into the existing care pathway for relatives?
-
Which people in the team/service will carry out each of the key REACT roles?
Dashboard changes
The website front page was upgraded to show clearly how many relatives’ invitations had been sent, and how many had accepted. Quotations from relatives who had found REACT helpful were added and the link to create a relative invitation was given prominence. Names of key functions were changed.
In IPv3, an icon from the main website was introduced so the dashboard was more easily discoverable. An audit function was made available to REACT supporters, REACT champions and IMPART leads so they could easily see which relatives had been invited, and whether or not they had activated an account. Staff were encouraged to follow-up with relatives who had not created an account.
Wave 2 outcomes
Table 18 shows uptake of REACT by staff and relatives in wave 2 trusts. Table 19 shows qualitative outcomes in response to the four NPT core constructs.
| Activity | Trust | |
|---|---|---|
| Ocean | Seashore | |
| Number of staff accounts | 32 | 63 |
| Number of relatives’ invitations sent | 40 | 112 |
| Number of individual relatives invited (after duplicates removed) | 37 | 93 |
| Number of relatives’ accounts created | 20 | 38 |
| NPT core construct | Trust | |
|---|---|---|
| Ocean | Seashore | |
| Context |
|
|
| Coherence |
|
|
| Cognitive participation |
|
|
| Collective action |
|
|
| Reflexive monitoring |
|
|
As in wave 1, most staff who were interviewed understood what REACT consisted of and could easily identify its potential value to relatives and staff:
Much more user friendly, much more sophisticated, much more aesthetically pleasing, and much more modern. There was a carers’ pack that the trust sent out and I was very unimpressed with that pack, just very dry, very sort of legal, not helpful I didn’t think.
Ocean clinician 02, individual interview
There’s BFT [behavioural family therapy] and that’s offered to everybody as well, but I don’t think there’s anything been sort of something you can log on and look at and use at your own time, you know, in your own pace.
Ocean REACT supporter 01, individual interview
In Ocean, there was some concern about the benefits of DHIs to older relatives, and the need to delay the introduction of REACT until the time was right:
A lot of people that come into our service are kind of coming in at their wits’ end and initially all they want is their loved one to get better. So I think usually other than some basic psychoeducation verbally that’s all that they want at that point because it’s just a bit too overwhelming. And usually after a couple of months that’s when you can start kind of drip-feeding it in.
Ocean clinician 04, individual interview
Many staff also felt that DHIs were not inherently as good as face-to-face support, particularly when they were unable to access all of the information that staff were party to:
It does meet a big need but . . . it doesn’t encompass everything. There needs to be that one-on-one, that face-to-face kind of ability for someone to talk to someone about someone you know, especially like professional-wise you know.
Ocean clinician 28, individual interview
Concerns about staff workload, low morale and high rates of staff turnover were also evident in wave 2 trusts. Despite this, there was evidence of engagement: REACT booklets were put in carer welcome packs, and REACT was promoted at friends and family groups.
Interestingly, in both trusts, the IPv2 resources were used to change the way that relatives were signed up to REACT. Rather than all care co-ordinators signing up relatives themselves, care co-ordinators used the booklets to introduce REACT to relatives face to face, and used the cards to get their details, which they then passed to REACT supporters and IMPART leads. This helped care co-ordinators overcome the technical challenges but meant that they were not very familiar with the website content and did not see activity on the dashboard, and so received no feedback about relatives’ use.
Despite generally positive feedback about the IPv2 changes, REACT was still given low priority, either because it was seen as aimed at carers, not service users, or because it was still seen as research:
I have given it to a couple of people when I’ve done first assessments and yeah it probably isn’t seen as a priority with me . . . You go in and start work and developing care plans and things with the clients [and] maybe you don’t always then focus on the carer.
Ocean clinician 05, individual interview
I believe in research, I like the idea of trials and trying to improve, so if I can remember what I’m asked to do I’ll try and get people on board, but we do forget . . . So reminders are good I think.
Ocean REACT supporter 07, individual interview
REACT was also seen as belonging to a particular professional group who sat outside the multidisciplinary team of care co-ordinators:
It shouldn’t be psychology should it, REACT, it’s just an information sharing but because it is held in psychology people are thinking oh it’s another psychology strategy.
Seashore clinician 68, group interview
Staff in Seashore suggested having a ‘REACT champion’ in each team to ensure that REACT remained a regular agenda item and a priority for all staff.
Finally, the demotivating impact of slow uptake by relatives and lack of activity on the forum was evident in both trusts, although there was also evidence that positive feedback inspired staff to use REACT:
I’ve had such nice feedback from people really, relatives really sort of saying I’m so glad you told me about this, ‘cos I’ve been Googling and trying to find stuff out and it’s all just coming back and I don’t understand it, whereas this is kind of it’s easier to access and it’s user friendly I think.
Ocean REACT supporter 02, individual interview
Implementation plan version 3
Implementation plan version 3 was developed during wave 2 and aimed to address some of the key issues identified in wave 1, 2 and 3 trusts. Factors identified in waves 1 and 2 fed into workshops in wave 3 trusts where the implementation plan was designed and delivered.
Implementation plan version 3 primarily addressed concerns over staff not inviting relatives; staff training not being accessed, particularly by new staff members; the need for feedback about sent invitations; and the longevity of someone driving REACT in the trust after the IMPART study ended. All components of IPv2, including those shown in italic text in Table 17, were included in IPv3, which is described in Table 20.
| Key challenges identified | Component of implementation plan |
|---|---|
|
7. ‘Request access’ button for relatives who have not been sent an invitation |
|
8. Staff induction packs for each role |
|
|
|
9. New ‘REACT champion’ role |
|
10. New ‘how-to’ manual with interactive knowledge quiz |
|
11. The newsfeed |
|
12. Printable PDF summary sheets for selected modules |
|
13. Demo version of the REACT website |
‘Request access’ function
Lakes Trust staff felt that a ‘request access’ function would empower relatives who had heard about REACT and allow them to choose when they wanted to be invited. Marsh Trust staff felt that the function was redundant as they already had a working system to generate relatives’ invitations.
Staff induction packs
Staff induction packs were developed as ‘quick start’ guides for the main REACT roles, including IMPART lead, REACT supporter and REACT champion, and were used to train new staff quickly. These were available within the updated online manual described in Updated ‘how-to manual’ and as printed documents. Packs included a table of who does what and posters for staff offices and communal areas and relatives’ waiting areas [available at www.journalslibrary.nihr.ac.uk/programmes/hsdr/140416/#/documentation (accessed February 2020)].
The REACT champion
This new role supporting the IMPART lead was developed to support individual team members to offer REACT, keep REACT on the clinical agenda and ensure that it retained a presence within teams after the completion of the IMPART study. This helped across larger trusts with multiple EIP teams and wider areas to cover. The REACT champion would be the ‘go-to’ person for information on how to use REACT and would work closely with the REACT supporters. The role would ideally be taken by someone already leading on carer support.
Updated ‘how-to manual’
The new manual included mini ‘how-to’ videos for each task and screenshots so that actions could be easily followed. REACT supporter and clinician roles were supported by a quiz to check understanding; completing this resulted in a certificate to use in professional development portfolios.
The newsfeed
The newsfeed was an attempt to increase staff visits to the website and provide feedback about relatives’ activity on the website and other carer-related events. All staff with a REACT login received regular e-mail updates of the most-talked-about topics in their trust forum and any news that REACT supporters wished to share. However, this proved problematic because of the lack of activity on the forums. The forum was the most visited part of the toolkit (see Chapter 5), but this seemed to be largely owing to relatives checking back in the hope that there was activity, rather than responding to a post (see Chapter 7). The newsfeed became in danger of having the opposite effect of decreasing staff engagement by highlighting the lack of uptake, which staff found demoralising.
Printable PDF summaries of REACT toolkit modules
Staff welcomed the printouts of information modules because they helped to overcome the challenge of remembering their log-in details or not having the technology to show relatives the website in home visits. The PDFs gave relatives a clearer idea of toolkit content and increased the number of people responding to the invitation [available at www.journalslibrary.nihr.ac.uk/programmes/hsdr/140416/#/documentation (accessed February 2020)].
Demo version of REACT
This was created for staff in Lakes as requested. The REACT champions used it when they met to become more familiar with the REACT website and practise tasks required to send invitations without ‘breaking’ the live Lakes REACT website or having access to confidential information on the forums to which they were not privy.
Wave 3 outcomes
Table 21 shows uptake of REACT by staff and relatives in wave 3 trusts. Table 22 shows qualitative outcomes in response to the four NPT core constructs.
| Activity | Trust | |
|---|---|---|
| Lakes | Marsh | |
| Number of staff accounts | 64 | 41 |
| Number of relatives’ invitations sent | 29 | 92 |
| Number of individual relatives invited (after duplicates removed) | 25 | 86 |
| Number of relatives’ accounts created | 17 | 53 |
| NPT core construct | Trust | |
|---|---|---|
| Lakes | Marsh | |
| Context |
|
|
| Coherence |
|
|
| Cognitive participation |
|
|
| Collective action |
|
|
| Reflexive monitoring |
|
|
Owing to the study design, wave 3 trusts had the most time to explore and use REACT in a way that suited their existing service. In Marsh, staff had undertaken a lot of work in adapting REACT to fit their service. Specifically, early concerns that the clinical team was unable to support the REACT supporter role meant that this had been adopted by a non-clinical member of the R&D team who also moderated the forum and responded to direct messages.
In contrast, there was little evidence of any activity related to REACT in Lakes before the start of wave 3. This is consistent with the activity graphs shown in Chapter 5 (see Figures 8–13). This seemed to be largely owing to the initial IMPART lead (a senior psychiatrist with strong research links) leaving the post shortly after the start of the study. Although this role was delegated to a colleague (also a psychiatrist), no one in the trust had voluntarily or actively bought into REACT becoming part of the clinical service.
Although the same potential values in offering REACT to relatives were identified in both wave 3 trusts as had been seen in waves 1 and 2, concerns were also raised that impeded the implementation of REACT. The main concern involved the REACT forum: Marsh in particular had previously experimented with online forums with negative consequences, including staff being individually identified and ‘trolled’ online:
My main concerns were I had experience with forums before, and if they are not well maintained, if they are not well administered and moderated, you can have problems . . . It’s not a forum about football or . . . This is a forum about something serious.
Marsh REACT champion 04, individual interview
In Lakes Trust, a lack of trust policies for managing risk online was repeatedly raised by a range of staff. This resulted in staff in the REACT supporter role refusing to moderate the forum for fear of being held responsible for risks they did not know how to manage:
It’s absolutely no chance I’m going to be putting my registration at risk . . . Somebody just says I need help right now, doesn’t get it within 20 minutes, a stereotype saying [?] off the bridge and then well they put a cry for help knowing [that I] was on duty and he didn’t see it.
Lakes REACT champion 03, group interview
Other concerns included a lack of fit between REACT and the ethos of the EIP teams, particularly the general use of DHIs, and use of diagnostic terms. In REACT, common diagnostic terms were defined to help relatives understand what they mean, but EIP teams were keen to avoid these terms as stigmatising and frightening:
I think the first description was one of schizophrenia and I wasn’t impressed with that ‘cos I think that is scary for having that as your first introduction to psychosis . . . We wouldn’t ever give somebody a diagnosis of schizophrenia within the first year probably anyway.
Marsh REACT champion 10, individual interview
Digital health interventions are not commonly used, and require a shift in culture that may be felt to threaten the centrality of the staff role:
I suppose it is a slight break with tradition isn’t it, to use an internet-based source, because I suppose it depends how professionals are; our most valuable tool is ourselves and I don’t know whether there’s something that potentially is a bit daunting about handing that over to something else, i.e. technology.
Marsh clinician 08, implementation workshop
. . . Who’s taking ownership of the information, who’s overseeing the risk and things like that, so I was just sort of reminded about the reticence maybe or the anxiety about health care and health-care professionals sort of losing some of that oversee over what’s happening.
Marsh clinician 08, implementation workshop
The same pressures of workload and prioritisation of financially linked priorities were identified as in the previous waves, resulting in a lack of support for the REACT supporter roles:
If we’ve got our managers saying well . . . there’s £20M to this physical health target . . . it’s quite disheartening for the nurses because all you want to do is serve your patient and in essence you’ve got to come off clinical duty so you can prioritise this target . . . There’s money attached to absolutely everything.
Lakes REACT champion 03, group interview
Also consistent with previous trusts, REACT was strongly identified as a research project. Although in all trusts this actually stimulated clinical activity (see Figures 8–13) because the research interviews and workshops reminded staff about REACT, it was also seen as inherently time limited and as the responsibility of the research team to implement.
In Marsh Trust, this led to the REACT supporter role being taken on by a non-clinical member of the R&D department just to make the project viable. The clinical team did not feel that they had the resources to support REACT but the R&D department was keen to take part in the research and so this collaborative solution was forged. In many ways, this worked well during the lifetime of the IMPART study. The new REACT champion recruited many relatives and gave their contact details to the REACT supporter to sign up, and this generated the highest number of relatives’ accounts of any trust. However a lack of engagement from the rest of the clinical team is likely to lead to REACT being abandoned at the end of the IMPART study.
Staff are used to research projects that are time limited and do not lead to lasting service change. They know that there is no R&D funding after the end of the study. Owing to a lack of infrastructure to sustain interventions developed and tested using research funding, our research team was unable to offer a longer-term solution to this issue, or even promise to make the REACT website available after the end of the study:
We do mention it every week in our team meeting, but it’s under our research headline, and we’re actually involved in about three other research projects, so there is a little bit of fatigue shall I say with research projects, so maybe we need to relocate it under our carers.
Marsh IMPART lead 01, implementation workshop
In Lakes, there was the added complication that REACT was seen as ‘owned’ by psychiatry. The trust already had a comprehensive family therapy service, which would have been the ideal service to support REACT but it was not involved in the intervention. This confused staff:
Yeah I do think there is something a bit odd about a family resource coming from psychiatry not from the family therapists; I do think that is unusual.
Lakes clinician 07, individual interview
Summary
All staff in all six trusts could see clear value in offering REACT to relatives, which was consistent with the findings from the costs and savings survey reported in Chapter 5. However, despite collaborative attempts to develop iterations of the implementation plan that addressed barriers to implementing REACT, other issues remained.
Some of these were linked to limitations in the content and design of the REACT toolkit. Limited time and resources meant that we could tweak some elements of the dashboard or wording of e-mails, but fundamental changes were not possible during the IMPART study. However, we have clear ideas of the required changes to content and design, such as making REACT available as an app that does not require a login at each visit. With additional funding, these can easily be addressed.
Other barriers we are less able to address are described below.
Fears among staff about the growing role of DHIs, their potential to replace staff and their responsibility for risk are understandable and not unreasonable.
The view of research as ‘nice to have’ (or otherwise) but not fundamental to health-care delivery, particularly for staff under such pressure, was not a surprise. Similarly, the lack of infrastructure to continue interventions that have been developed and implemented as research projects was a challenge we were aware of from the outset. However, in both instances, we may have underestimated their direct impact on staff engagement. Change in the NHS takes time, and some trusts were only beginning to really explore the challenges they faced in offering REACT when the end of the study period loomed large and there was no continuation plan:
The thing is with this job . . . there’s change all the time and there’s new systems and new forms to get used to. You know, I think it just takes time for anything new to get embedded.
Marsh clinician 42, individual interview
These wider contextual issues are further elaborated in the explanatory synthesis for the final version of our implementation plan (IPv4) in Chapter 8.
Chapter 7 Relatives’ engagement with REACT: qualitative data
Method
Rationale and design
This section of the IMPART study had a qualitative design to allow relatives’ views and experiences of the implementation of REACT to be captured through a semistructured interview format. The key research question addressed was ‘What are the factors affecting relatives’ engagement with REACT?’.
These data were not analysed in waves, as the iterative nature of the implementation plan design was aimed at changing staff behaviour and getting more invitations sent to relatives, rather than changing the way in which relatives engaged with REACT.
The small number of relatives interviewed from each trust also prevented generalising to the experience of other relatives in that trust. However, we have highlighted instances when the study wave or elements of the implementation plan appear to have relevance, and explore this in the discussion.
The methods are described in detail in Chapter 4. Characteristics of the participants and the key themes are described in the following sections.
Participants
Twenty-three relatives participated in the study, all of whom had internet access at home. Table 23 shows the demography of the sample.
| Participant identifier | Age group (years) | Gender | Ethnic group | Employment | Caring relationship | Time spent on REACT (minutes) |
|---|---|---|---|---|---|---|
| Woods-RE-06 | 51–55 | Female | British | Part time | Mother | 99 |
| Woods-RE-07 | 56–60 | Female | British | Part time | Mother | 78 |
| Woods-RE-08 | 56–60 | Female | White and black Caribbean | Unemployed | Mother | 0 |
| Moor-RE-04 | 16–20 | Female | British | Full time | Sibling | 70 |
| Moor-RE-11 | 46–50 | Male | British | Full time | Father | 0 |
| Moor-RE-09 | 46–50 | Female | British | Part time | Mother | 93 |
| Moor-RE-10 | 51–55 | Female | British | Part time | Mother | 63 |
| Ocean-RE-06 | 51–55 | Female | British | Full time | Mother | 62 |
| Ocean-RE-05 | 46–50 | Female | British | Part time | Mother | 298 |
| Seashore-RE-04 | 56–60 | Female | British | Part time | Mother | 14 |
| Seashore-RE-05 | 41–45 | Female | Other white background | Unable to work because of caring responsibilities | Mother | 22 |
| Seashore-RE-06 | 66–70 | Female | British | Retired | Mother | 63 |
| Seashore-RE-09 | 36–40 | Female | Caribbean | Unable to work because of caring responsibilities | Mother | 114 |
| Seashore-RE-10 | 61–65 | Male | British | Part time | Father | 41 |
| Seashore-RE-11 | 31–35 | Male | Indian | Full time | Sibling | 0 |
| Seashore-RE-12 | 50–56 | Female | Asian or Asian British: Indian | Full time | Mother | 0 |
| Seashore-RE-13 | 66–70 | Female | British | Retired | Mother | 61 |
| Marsh-RE-09 | 51–55 | Female | British | Unemployed | Mother | 35 |
| Marsh-RE-11 | 56–60 | Female | British | Unable to work because of ill-health or disability | Mother | 15 |
| Marsh-RE-03 | 61–65 | Female | British | Retired | Mother | 89 |
| Marsh-RE-10 | 61–65 | Female | British | Full time | Mother | 37 |
| Marsh-RE-12 | 46–50 | Female | British | Full time | Mother | 0 |
| Marsh-RE-08 | 61–65 | Female | British | Retired | Mother | 266 |
Relatives were recruited from five of the six participating trusts. We were unable to recruit any relatives from Lakes, and recruited the most relatives from Seashore. This pattern reflected the number of relatives agreeing to take part in the quantitative measures described in Chapter 5.
There was a high degree of variability in the use of REACT. The mean time spent on REACT was 63 minutes, substantially higher than the mean for all relatives (40 minutes, see Chapter 5). However, this group included relatives who did not use REACT at all, and others who spent nearly 5 hours on REACT. The amount of time spent by each participant on each module and on the forum is detailed in Report Supplementary Material 2.
As described in Chapter 4, emerging themes in the interview transcripts were visually identified by use of sticky notes. The final wall of notes is seen in Figure 17. The final thematic analysis of factors that influenced relatives’ engagement with REACT elicited four overarching themes and associated subthemes, summarised in Box 1.
FIGURE 17.
Sticky notes used to identify emerging themes of relatives’ engagement.
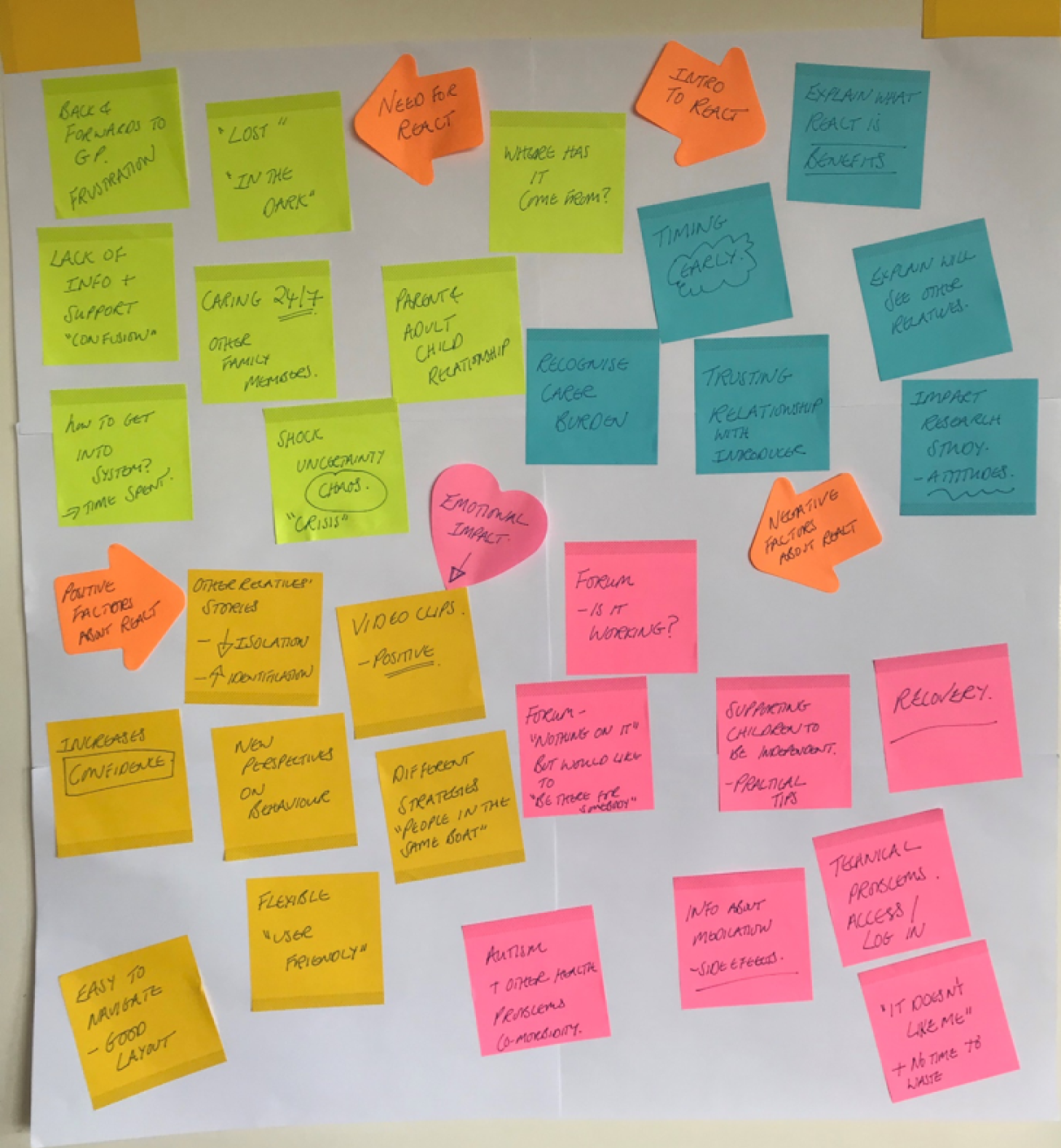
-
Impact of caring role.
-
Family dynamics.
-
Initial contact with health services.
-
Who?
-
When?
-
How?
-
Video clips.
-
Ease of navigation.
-
Empowerment.
-
Technical problems.
-
Inactive forum.
-
Lack of specific information.
The relationship between these themes is presented pictorially by Figure 18. The relatives as participants are represented by the rainwater and their journey is shown by its path as it falls from the clouds to the hills and is captured by various buckets. The first theme, ‘Context’, is represented by the rain cloud, which holds the relatives and the complexity of their individual situations, illustrating the impact of their caring relationships on their emotions and on the practicalities of daily life.
FIGURE 18.
Relationship between key themes in understanding relatives’ experiences with REACT.
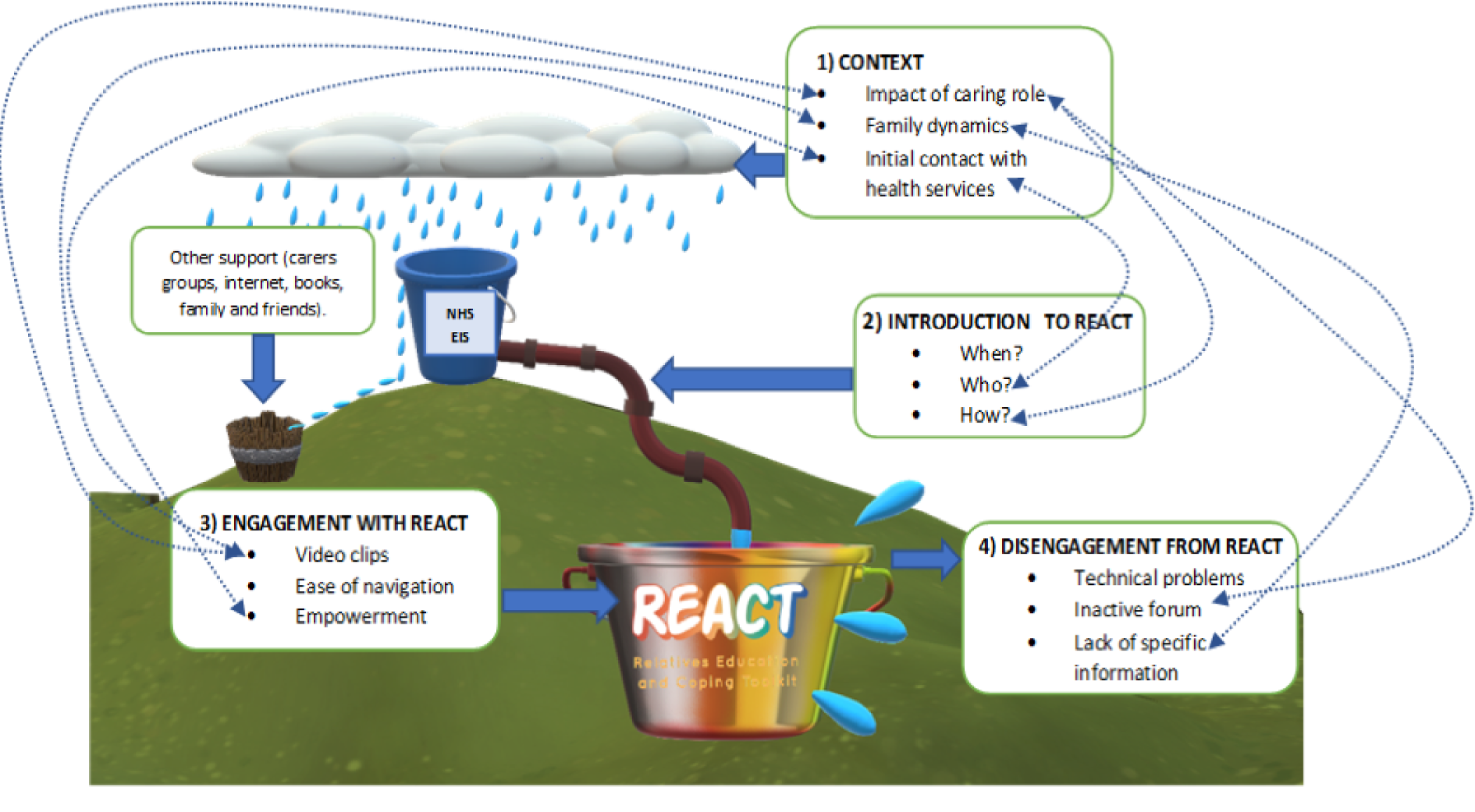
The flow of rainwater from the cloud represents the relatives’ journey to NHS EIP services, shown by the blue bucket. The brown bucket represents other forms of support that relatives may use, either in conjunction with EIP or separately, including support provided by charities and other sources of information.
The second theme, ‘introduction to REACT’, represented by the pipe, describes the way in which the participants are introduced to REACT by EIP staff, with the characteristics of this introduction determining the extent to which they initially engage with the intervention. The bends in the pipe represent the importance of an effective introduction in order to maintain the water flow through to the REACT ‘bucket’.
The third theme, ‘engagement with REACT’, refers to the participants remaining contained within REACT, with the factors that keep them interested grouped into subthemes. Theme 4, ‘disengagement from REACT’, is represented by rainwater escaping from the bucket and shows the aspects of REACT that participants felt could be improved in order to meet their needs.
The diagram shows links between the themes and subthemes as dotted lines. Although each participant’s journey may be linear (a relative of an EIP service user introduced to REACT, and then accessing REACT), the factors that affect their engagement with the intervention link back to their context. This reflects the fact that an in-depth understanding of the situation and experience of being a relative of someone experiencing psychosis or bipolar disorder is fundamental to designing the features of REACT and creating a protocol for the way in which it is introduced to relatives.
Theme 1: context
The first theme captures the essence of the environment into which REACT was introduced, which encompasses family, personal, work, social and practical factors. Understanding context is fundamental to making sense of how relatives engaged with the toolkit. The subthemes combine to illustrate situations experienced by the relatives, which are characterised by chaos, uncertainty, complex family structures and relationships, and difficult interactions with a range of physical and mental health services in the search for clarity and treatment. All of the participants provided rich detail about the experience and effects of caring for a family member.
Impact of the caring role
Participants described their lack of understanding of what was happening to their relative in terms of their illness, and the emotional impact of this uncertainty. One participant conveyed how all of her time and energy were directed towards her relative, which left little space for understanding what was happening to the whole family. This created a feeling of a state of emergency, with no opportunity to gain perspective and analyse the problem. Despite the lack of emotional space to understand the situation, there was a strong desire to make sense of it and understand its origins:
It was very, very difficult to understand what was going on and where it had come from, and you were just so confused . . . you don’t have any space to process it or to understand it.
Mother, aged 56–60 years, Woods 08
The search for meaning and the cause of the difficulties was prevalent in participants’ accounts. In some cases, a sense of guilt emerged as participants questioned whether or not their actions had led to the difficulties being experienced by their relative, with one person questioning whether or not she had done something during pregnancy that had caused the mental health problems besetting her son.
Participants described their reaction to the onset of their relatives’ difficulties as a state of shock, accompanied by fear and uncertainty. This highlighted the trauma associated with the onset of psychosis or bipolar disorder. One participant described how she felt ‘lost’, evoking a sense of isolation and a lack of support and clarity about what was happening. In addition to physical demands of time and energy, the emotionally traumatising impact of shock suggested that the participant’s ability to seek support and process information at this time would be limited, despite this being a real need:
I think initially it was a tremendous shock and very frightening, and we were just lost.
Mother, aged 66–70 years, Seashore 06
The persistent trauma and shock were described as having a negative impact on carers’ own mental health and stress levels. This experience was not characterised by an isolated incident of stress, but continued over an extended period, resulting in high levels of distress. The intensity of the caring relationship was exacerbated by uncertainty about their relative’s behaviour. The need for constant vigilance made the caring role feel all-encompassing:
You just don’t know from you know hour to hour really how they’re going to behave.
Mother, aged 51–55 years, Woods 06
Because it’s so crazy for 2 years, trying to get support for him, and I was thinking . . . I’m going to end up having a mental breakdown.
Brother, aged 31–35 years, Seashore 11
Under these circumstances, the relatives’ own needs became supressed. This highlighted the need for information and support that were easy to access and digest, and could be used flexibly to fit in with the unpredictable nature of the caring role.
Family dynamics
Participants discussed difficulties with balancing the needs of the rest of the family because of the demands of the family member experiencing mental health problems. The challenge of allocating time to roles such as wife or husband, friend, employee or parent to other siblings linked with the previous theme stretched resources. Attending to the needs of other children was difficult, as was maintaining a commitment to work. Three participants felt that they were unable to work because of their caring responsibilities. Others said that they were able to remain in work only because of the flexibility shown by employers. One participant described how valued leisure activities were no longer possible, and acknowledged with resignation that this was part of being a carer. This showed how the needs of carers were often relegated in the face of other demands, sometimes with the carers not even recognising this themselves. Understanding this contextual factor is important in planning for how REACT is introduced and presented, as discussions about identifying and validating the needs of the carer may be required:
Yes, you’re not just the carer really, it’s balancing everybody else’s need in, ‘cos that’s the reality of families isn’t it?
Mother, aged 61–65 years, Marsh 03
I’ve given up work to be there 24/7 for my daughter who basically has had a couple of episodes which initially we thought was brought on by drug-induced psychosis.
Mother, aged 50–56 years, Seashore 12
I ended up being off work with him until April . . . There are big chunks of my life where I’ve had to take time out from what I do to care for [my son].
Mother, aged 46–50 years, Moor 09
Initial contact with health services
This subtheme covers contact between participants and clinical services, both physical and mental health, in the search for clarity at the onset of their relatives’ difficulties. Despite extensive attempts to find someone who could tell them what they should do to support their relative, participants were often very frustrated by the lack of support and information. They described time and effort spent travelling fruitlessly to different clinics. The sense of being excluded from services, and the effort and tenacity required on their part to even identify where help might be found, were palpable:
I’ve gone to one clinic after another and nobody can actually tell me how I get into the system.
Mother, aged 66–70 years, Seashore 13
Some participants contrasted the lack of clarity about what was happening to their relative with physical health, where definite diagnoses and treatment plans are made:
Initially I was very confused as to what was really wrong and I said this many times: if you’re dealing with measles or a broken leg then we’d all know what to do, but where mental health is concerned it’s anybody’s guess it seems.
Mother, aged 66–70 years, Seashore 13
All of this seemed to exacerbate carer distress. Participants spoke about feeling frustrated that their voice was not heard when interacting with services for their relative. In adult services, clinical staff were often reluctant to communicate with them owing to confidentiality. Participants felt that services discounted the value of their knowledge about their child and were excluded from discussions owing to the service user’s status as an adult. This further diminished the role of the participant as the carer. The contrast between how insignificant they felt their role to be considered by clinical staff and the reality of the amount of time and physical and emotional energy put into caring incited strong emotions of anger and sadness, but also reinforced feelings that their own needs as carers were not relevant. This was highlighted when one participant expressed her frustration at not being listened to by clinical staff:
I see him on a day-to-day basis; something’s not right, you know that, your mother instinct comes in.
Mother, aged 50–56 years, Seashore 12
I just think if the professionals actually sat down and interviewed us as well and maybe just not told us all of [son’s] confidential business but just listened to what I had to say.
Mother, aged 56–60 years, Seashore 04
Most frustration was focused on the initial process of trying to access support at the onset of their relatives’ difficulties, and carers primarily described interactions with NHS primary care services such as GPs, rather than the EIP service. Although there was variance in the length of time before appropriate services were accessed, positive experiences did not feature in participants’ descriptions of this initial period. Once participants were able to access EIP services, they described more positive experiences and provision of support.
Theme 2: introduction to REACT
The way in which relatives were introduced to REACT proved to be a key factor in determining their level of engagement. There were three important elements: who they were introduced by, when they were introduced and how they were introduced.
Who?
The personal characteristics and relationship between the participant and EIP staff member as REACT introducer influenced the decision about whether or not to access REACT. A positive relationship with the introducer was characterised by trust and familiarity with the circumstances and needs of the carer, and made relatives more likely to sign up to REACT. The sense that the introducer has the participant’s best interests at heart was fundamental. Participants appreciated the care shown by the introducers and, in particular, that REACT focused on them as carers:
He said it was like . . . a toolkit, you know, you might find it useful, you know just have a look and see what you think, you know it’s being developed, so that’s what I did, I had a look ‘cos I liked him.
Mother, aged 56–60 years, Woods 08
I would go with anything that [care co-ordinator] had said and the person that worked with him previously, you know, they were very good and they just wanted to help.
Mother, aged 56–60 years, Seashore 04
Strong individual relationships emerged when participants felt that they were being listened to, taken seriously and not dismissed:
. . . But it was the Thursday of that week that the people from the EIP team first came, and I have to say they were absolutely brilliant. They spoke to me first, they were very concerned about how I was coping.
Mother, aged 61–65 years, Marsh 08
Early intervention team, amazing, really, really good in [town] – the one thing is that no one pooh-poohs you, they take it seriously.
Mother, aged 61–65 years, Marsh 10
Participants saw REACT as something that worked in conjunction with EIP, rather than being a replacement, with a strong existing relationship with EIP being important for this dynamic, and REACT was viewed as part of a package of care:
The toolkit . . . doesn’t replace the actual contact with the professionals, you know, that [contact] was invaluable, and still is actually. But it is useful in addition.
Mother, aged 46–50 years, Ocean 05
Participants were asked how they would feel about being introduced to REACT by another relative rather than a member of EIP staff, and most saw additional benefits to this. Other carers were viewed as offering potentially greater levels of understanding than clinical staff, which has implications in terms of involving carers to introduce REACT in future:
I think if you’re actually experiencing the problem yourself you really have a better . . . You really understand what’s useful and what’s not useful.
Mother, aged 46–50 years, Ocean 05
When?
Participants wanted REACT to be available to relatives as soon as possible, to address the need for clarity and support during the early phase of their relative’s difficulties. Several participants expressed frustration that REACT had been offered to them too late to be of use. The onset, with its shock and confusion, was the time when information about what was happening would have been much appreciated and could have reduced the trauma of the situation. Participants wanted to better understand what their relative was experiencing in order to provide more meaningful support to them, and felt that REACT could have had a role in providing this if it had been provided at the right time:
I do think the website itself is brilliant but it was probably just too late for us.
Sister, aged 16–20 years, Moor 04
You’re sort of there stumbling around in the dark really, so at that point initially if you’re given information or signposted to things, I think then you can start to then understand, OK, what they’re going through.
Mother, aged 56–60 years, Woods 08
However, some participants acknowledged that too much information early on might have been experienced as overwhelming. Despite this, they still wanted REACT to be available to them early, so that it was there when they felt ready to access it – they could make the decision about when the right time was:
I suppose for me it would have been valuable to give that information when I got a carers’ pack . . . Even if you don’t use it, basically you’ve got it, you know you can look at it.
Mother, aged 61–65 years, Marsh 03
How?
Participants needed to hear the benefits of REACT as part of the introduction. They wanted explicit detail of what was covered and specifically how this could be of value to them. Key to this was a clear message that REACT prioritised the needs of the relative. The opportunity to hear stories from other relatives about their experiences was a significant draw, especially when this was explicitly linked to reducing the sense of isolation that can accompany being a carer.
Although the initial introduction was seen as the most significant interaction in engaging relatives with REACT, gentle reminders from staff were also crucial to ongoing use. The discussions, explanations and ongoing reminders highlighted the importance of REACT being offered as part of an integrated service that included face-to-face contact:
. . . that it was just so important for me to look after myself because I was his primary carer, you know, that role was explained to me as well, and . . . I think it was after the second visit that [care co-ordinator] sent me the contact details or the user details for me to log on to the REACT website.
Mother, aged 61–65 years, Marsh 08
The question of whether or not REACT was introduced in the context of the IMPART research study is significant here, with opinion divided between participants regarding whether or not this motivated them to access REACT.
Some participants felt that engaging in a research project was positive, because it contributed to advancing knowledge that would benefit people in similar circumstances. Others felt that it would put them off using the toolkit as it represented one more demand to add to an already-heavy load:
I was just so grateful for the help that I did get and you know that I did genuinely want to, you know, contribute here in any way that I could . . . for other people.
Mother, aged 61–65 years, Marsh 08
I might have been irritated if somebody said, ‘oh yeah, it’s a research at that point’ ‘cos I was so stressed out . . . ‘Oh, do you think I really want to be worried about research when I’ve got somebody trying to kill themselves?’
Mother, aged 51–55 years, Marsh 09
Theme 3: positive engagement with REACT
If initial engagement with REACT was largely determined by the way it was introduced, ongoing use was more strongly linked to the actual content of REACT. Participants described the features that appealed to them and kept them engaged.
Video clips
Participants were positive about REACT’s use of video clips, which illustrated situations faced by other relatives and how they dealt with them. Watching the clips reduced their feelings of isolation, as they identified with people in similar situations.
They also found the clips useful in suggesting strategies for dealing with difficult periods, and new, helpful ways of communicating with their relative, for example when experiencing scenarios such as hearing voices. (This subtheme links with context and family dynamics.) This enabled participants to change their perspective and improve their understanding of what their relative was going through, which then enabled them to consider different ways of thinking about the situation and change their behaviour:
I found the information on there absolutely brilliant, absolutely brilliant, because some of the people were even talking about the same experiences that I was having.
Mother, aged 61–65 years, Marsh 08
One of the video clips explained it beautifully: she said, ‘even though it may not seem real to us, it actually is a real thing for them, so as convincing as I’m saying to him no that didn’t happen . . . well, you shouldn’t say that to a person because it actually did happen, in their brain it happened’. So yeah . . . there was lots of good videos.
Mother, aged 36–40 years, Seashore 09
REACT usage data for the above participant (Seashore 09) supports her description: she visited the module containing the video clip she referred to three times during her total of eight logins to REACT, suggesting that this was the most engaging module for her.
Empowerment
Having more information about their relatives’ conditions increased relatives’ confidence and made them feel more empowered. When interacting with clinical services, the information they gathered from REACT meant that they felt more equipped to have meaningful conversations and were not so readily dismissed. One participant talked about how REACT reduced her feelings of panic about her relative’s difficulties, and led to a calmer feeling of acceptance:
I felt empowered honestly after having that little session online by myself.
Mother, aged 36–40 years, Seashore 09
We’re not being fobbed off with ‘everything’s going on OK’ [when] really it’s not.
Mother, aged 51–55 years, Moor 10
Once you start listening to other people’s stories or the literature, like I said, it makes you calmer about the situation, that’s what I’m trying to say . . . My attitude now, well not all the time but sometimes, is right we’ll ride the waves and see what happens whereas before I’d be like trying to stop the waves.
Mother, aged 51–55 years, Woods 06
Ease of navigation
Participants found REACT easy to navigate and understand. The modular structure allowed some participants to identify which section of REACT was most relevant to them, and others to work through REACT methodically and sequentially, as preferred. This echoes the earlier theme in which relatives also wanted choice about when they could access REACT:
Well I thought it was bright, and like I say the big boxes to click on to send you further into what you wanting, really easy, and it’s easy to navigate from one to the other, you know you can bounce around it, you don’t have to go step by step anywhere, so you can take bits whenever you want it, so yeah I found it quite user friendly and easy on the eye.
Mother, aged 46–50 years, Moor 09
This participant’s REACT usage data shows that she accessed 10 of REACT’s 12 modules over five separate logins, which supports her description of ease of navigation.
Theme 4: disengagement from REACT
Factors that discouraged participants from using or returning to REACT included technical problems with accessing REACT, a lack of activity on the forum and the omission of important areas of content.
Technical problems
Some participants expressed frustration with problems they had with accessing REACT and with the initial account set-up process. Persistence and additional support from EIP staff were needed in some cases. For some, this meant that REACT was perceived as another task, another problem to overcome, rather than something helpful and supportive. Some participants felt as if they had done something wrong, and REACT added to their feelings of stress and burden rather than helping. One participant referred to REACT as ‘not liking’ them, which evoked an antagonistic relationship and a direct contrast with REACT’s aim of providing support. This emphasised the importance of resolving technical issues quickly, which was not always possible owing to limited resources.
Access issues also occurred because the REACT online trial ran in parallel to the IMPART study. Some IMPART participants used an internet search rather than through the link provided by their trust and accidently reached the REACT online trial website rather than the toolkit hosted by their trust. This problem would not occur in any future implementation of REACT:
I think my husband and I tried and initially there was problems getting onto the website, we were having issues.
Mother, aged 50–56 years, Seashore 12
So I do need to be able to get on it easily ‘cos that’s like another oh god not something else I’ve got to do.
Mother, aged 61–65 years, Marsh 03
Inactive forum
The forum was designed to allow relatives to connect with each other to share experiences, ask questions and exchange information. However, because each trust hosted a separate forum and the number of relatives using REACT in each trust was small, there was very little activity on the forums. This discouraged participants from posting, as they felt that this would make them conspicuous. This also gave the impression that it was not functioning as it should, thereby reducing confidence in the rest of the intervention. Participants wanted a well-populated and fully functioning forum to communicate with other relatives, reduce their sense of isolation and motivate them to revisit REACT to look at new content. Some participants checked the forum several times, and then followed this up by contacting EIP staff about whether or not the forum was active. Their persistence demonstrated the level of interest and need for this feature. REACT usage data support this point, as the forum was the most visited area of REACT, despite the lack of activity. One participant logged into the website eight times to check if anything was posted:
Only thing I was slightly disappointed in was the forum. I mean I don’t know how new the website is but there was just nothing on it, you know, I was hoping to be able to just go in there and read, you know . . . how other people had dealt with them.
Mother, aged 61–65 years, Marsh 08
Well, it didn’t seem to work. I did go on it a few times and initially didn’t get any response and then I mentioned it again to [care co-ordinator], I’m not sure how up and running it is or actually was.
Mother, aged 46–50 years, Ocean 05
Lack of specific information
Participants wanted more information about some topics that were not included in REACT to help in their supporting role. Specific medications and their side effects, comorbid health conditions and recovery were specifically highlighted; for example, participants were concerned about weight gain associated with some medications and wanted more information about this particular side effect, how to address it with their relative and, if necessary, introduce conversations about healthy diet and exercise:
Explain the medication, explain the risk of the medication, you know because . . . there is a lot of side effects, addiction to it. My brother put on about 4 stone in weight within a short period of time because of the medication – nobody told me about that, but how can a family member protect somebody . . . if they don’t know that information?
Brother, aged 31–35 years, Seashore 11
There’s not enough information about clozapine, aripiprazole, the mixtures thereof, getting those right, the side effects of that.
Father, aged 61–65 years, Seashore 10
Some participants said that REACT did not feel relevant to them as it did not provide case studies in which the service user had more than one condition. They had to adapt the information too much for their own situation. Autism, in particular, was a relatively common comorbid issue. Participants need to feel that REACT could be applied to the specifics of their situation and family, that it could be tailored to their needs and that it could account for the differences in families’ situations:
But what we didn’t know at the time, and didn’t know until March of 2017, that [daughter] is autistic as well.
Brother, aged 31–35 years, Seashore 11
Most participants were parents, and some felt that REACT lacked sufficient information about supporting their children to achieve an independent and fulfilling life. They were concerned about what would happen to their son or daughter if they were no longer able to support them, and this led to a desire to help their child to become more independent.
This emphasises the idea that participants feel that the information provided in REACT can be tailored to their individual situation and provide practical strategies for navigating problems. Participants expressed the need to help their relative complete day-to-day tasks independently and support them to build their own skills:
The recovery section was not particularly uplifting . . . and I know it’s a very slow process, even recovery, and just understanding more that how recovery is going to happen. How things move forwards. It just seemed quite a small section.
Mother, aged 46–50 years, Ocean 05
Independence to me means well managing the things you have to do everyday to be able to live independently.
Mother, aged 61–65 years, Marsh 03
Well I need them to be OK, I need them to get on with their lives.
Mother, aged 41–45 years, Seashore 05
Discussion
Relatives described many challenges in their caring role, and valued being offered REACT as a source of information and support. However, they saw REACT as being one tool in a much broader health-care system that they were keen to be more involved with.
Logging on to REACT and taking the time to explore it required time and effort and was often done in response to a recommendation from a key staff member they trusted and whom they felt had their best interests at heart. This staff member was also often called on to help navigate REACT and to overcome technical issues.
Relatives were very keen to learn new information and strategies and listen to other carers who could help them to make sense of and respond to the challenges they faced. Although the modules, particularly the video clips, went some way to meeting this need, there was a lot of disappointment in the lack of activity on the forums. Relatives had excellent ideas about how the content of REACT could be improved and when and how REACT should be offered, and clearly need to be involved in ongoing design and delivery of REACT.
The broader context (see Theme 1: context) and engagement with the specific aspects of REACT (see Theme 3: positive engagement with REACT and Theme 4: disengagement from REACT) are unlikely to be influenced by the iterative versions of the implementation plan described in Chapter 6. However, the process of introducing REACT to relatives (see Theme 2: introduction to REACT) is likely to be influenced by some of the developments made. For example, in wave 2 (IPv2), REACT NHS booklets were provided to staff to use with relatives, and these explicitly highlighted the benefits of REACT for relatives. This may have reminded staff to articulate these benefits when they introduced REACT, which was a key facilitator of relatives engaging with REACT.
Implementation plan version 2 also introduced a planning document to help services to work out how best to integrate REACT into their existing care pathways, which was further developed in wave 3 (IPv3) to structure a strategy meeting to promote ownership with the organisation. Where successful, this would have ensured that REACT was reliably offered early in the relatives’ EIP journey and as part of a coherent package of care, both of which participants described as key facilitators.
The data presented here do not allow us to directly test the impact of each implementation plan, but do support the content as being relevant to enhancing relatives’ engagement as well as staff engagement. However, these data also highlight the importance of nurturing individual relationships between relatives and specific staff members over time, which was not specifically addressed in any of our implementation plans.
Context was clearly very important in determining how relatives engaged with REACT. Consequently, context emerged as a strong theme in the analysis. However, in separating this out, we may have lost the link between key features of the context and how this was affecting relatives’ experiences of being introduced to REACT, factors that enhanced engagement and those that led to disengagement.
Chapter 8 Explanatory synthesis
This chapter integrates the findings from all phases of the study and across all of the data sources, including our observations and insights during the process of the study, to identify the key factors affecting the implementation of REACT.
Our original plan was to develop an explanatory synthesis that best represented these findings, and offer a new framework that could be generalised to other digital technology projects in health service settings. However, there are so many theories and frameworks in the literature, very few of them independently tested, and no guidance as to which is likely to be of most use for a particular purpose. Therefore, rather than develop an additional framework, we examined our findings through the lens of an existing framework: the NASSS framework. 74
Normalisation process theory was the theoretical framework that guided our collection and analysis of qualitative data from staff members within the participating NHS trusts. However, this theory did not readily apply to understanding the experiences of relatives, nor did it capture many of the wider contextual factors that were clearly affecting the implementation of REACT. NASSS was recently developed to help predict and evaluate the success of a technology-supported health or social care programme. It was developed from an extensive systematic review of previous technology implementation frameworks and a series of six empirical case studies, each testing a different type of technology-supported programme (e.g. video consultations, pendant alarm systems and care-organising software) in different health-care settings.
The framework, shown in Figure 19, outlines seven key domains that are important to consider to determine the success of implementation:
-
the condition or illness
-
the technology
-
the value proposition
-
the adopter system (staff and patients/relatives)
-
the organisation
-
the wider social context
-
the evolution (interaction and mutual adaptation) of these domains over time.
FIGURE 19.
The NASSS framework for considering influences on the adoption, non-adoption, abandonment, spread, scale-up and sustainability of patient-facing health and care technologies. Reproduced from Greenhalgh et al. 74 ©Trisha Greenhalgh, Joseph Wherton, Chrysanthi Papoutsi, Jennifer Lynch, Gemma Hughes, Christine A’Court, Susan Hinder, Nick Fahy, Rob Procter, Sara Shaw. Originally published in the Journal of Medical Internet Research (www.jmir.org), 1 November 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on http://www.jmir.org/, as well as this copyright and license information must be included.

The NASSS framework suggests that each of these domains can be characterised by its degree of complexity, and the greater the complexity across the domains, the less successful long-term implementation is likely to be.
The NASSS framework was useful for integrating findings with team learning during the IMPART study. We used it to structure our explanation of key factors affecting the implementation of REACT. As such, we were able to offer an independent evaluation of the applicability of NASSS in a novel setting.
Use of the NASSS framework also enables our findings to be interpreted alongside those of other studies using the same framework. We highlight the issues of complexity in relation to each of the NASSS domains, and identify how this complexity could be better managed. The application of the NASSS framework underpins the presentation of IPv4. Our focus in developing IPv4 was to increase the likelihood of adoption and sustainability of REACT, as the time scale of our study allowed us to capture only this early stage. The content in this chapter is organised around the domains of the NASSS framework.
How successfully was REACT implemented?
We assessed implementation success in terms of how many staff accounts were created, how many relatives were invited and how many relatives’ accounts were activated. However, consistent with the exploratory nature of this study, we had not specified a threshold level for defining implementation as successful. Nevertheless, staff in each trust had implicit ideas about uptake and success of REACT, which affected their behaviour.
Across all six trusts, 355 invitations were sent to relatives, 159 relatives’ accounts were created and 56 relatives completed baseline questionnaires. On average, relatives who created an account visited the website four times and spent 41 minutes on REACT. Given that REACT could potentially have been offered to all relatives supporting someone in the participating teams, these numbers may seem low. On the other hand, many clinicians invited only new relatives who came into the service during the period of the study; these numbers therefore constitute a significant proportion of new relatives.
It is important to note that the aim of our study was not to use researcher activity to maximise recruitment (as we might in a RCT) but to understand what factors affected clinician implementation of REACT. Therefore, we focused on understanding the implementation process of a new DHI in practice and how this differed between trusts.
NASSS domain 1: the nature of the condition
Psychosis and bipolar disorder are both highly complex conditions. The reliability and validity of both terms have been questioned due to the large variation in presentation, outcome and response to treatment in people to whom these labels have been applied. 103 The defining features are extreme and experienced largely internally (such as hallucinations, delusions and extreme mood swings). The risks of social isolation, unemployment, self-harm and suicide are high. 43,46 Consequently, the challenges faced by relatives supporting someone with psychosis or bipolar disorder are significant and fluctuating. Often, these challenges negatively affect the relative’s own social and mental health. 28–34 Of the relatives completing the GHQ-28 in this study, 60% scored about the clinical threshold of 4 out of 5 (items were scored as 0, 0, 1, 1, as recommended for screening) at baseline. Access to support for relatives is highly variable, and despite clinical and government guidelines, many relatives still feel excluded from services. 104
On the whole, staff who engaged in the research were very positive about the concept of an online toolkit to support relatives in EIP services, and felt that this would be an appropriate way to meet their needs for information and support. Relatives could also see value in having an online resource that helped them to make sense of the experiences they were dealing with, particularly if it was available at an early stage in this journey.
However, both staff and relatives emphasised the complexity of the issues faced by relatives, and the need for a DHI to complement rather than replace face-to-face support. Ideally, REACT would be part of a package of care, delivered by a clinical member of staff who also worked with the service user and could involve both family members as partners in the ‘triangle of care’. 105
Unfortunately, pressures on mental health services meant that staff felt unable to prioritise time spent with relatives. Although most of the relatives we spoke to were very positive about the direct support they had received from EIP teams, staff felt that pressure of workload had led them to prioritise service user outcomes above those of carers. Indeed, some suggested that demonstrating a significant impact of REACT on service user outcomes would give it greater value for staff than any impact on carer outcomes. At an organisational level, there was little evidence of relatives being strategically involved in trust activity. It was challenging to include relatives in the SRGs because none of the trusts had existing frameworks through which relatives could be engaged in service development; some trusts actively resisted inclusion for fear of giving relatives an opportunity to complain about the services they were receiving (see Appendix 3, Table 26).
NASSS domain 2: the technology
REACT was developed over a number of years with extensive user involvement. The content was structured around questions that relatives had identified as important; videos and peer forums facilitated the sharing of stories to reduce stigma, increase hope and exchange practical support ideas; and confidential direct messaging was included to address fears around anonymity. The toolkit was branded with NHS and university logos to enhance credibility and engender trust. Versions for each of the six NHS trusts were adapted with trust logos and specific information to make them locally relevant. REACT was piloted in situ, and staff received online and face-to-face training as part of IPv1.
However, there were several limitations of the technology, which caused staff and relatives to fail to adopt or to disengage from the intervention. Insufficient time and resources led to inadequate internal testing within the trusts. Piloting in situ identified early problems that led to a loss of faith in the intervention and subsequent abandonment by staff. Once the website was live, IT issues continued (such as broken links between pages or to external sites) and caused further loss of engagement.
Considerable time was spent with relatives to ensure that the design of REACT was appropriate. For those who accessed it, this seems to have been time well spent. Relatives appreciated many features, particularly the opportunity to hear the stories of others facing similar challenges. However, staff users had not been involved in designing the interface for referring relatives to REACT and many found it to be unappealing and hard to navigate. It looked technical and some staff felt that they were in the ‘back end’ and feared being able to ‘break’ the website. Staff who persevered and explored the changes made in IPv2 and IPv3 found the website simple to use.
Lack of staff involvement in design also led to a technology that integrated poorly with trust IT systems and with general working practices. For example, accessing REACT required a reasonably secure connection to the web server that some outdated browsers on trust computers could not provide. YouTube videos and some textual content (words such as ‘drugs’) were blocked by trust IT firewalls. The need to log in with a username and password was a major obstacle, with REACT (like all externally provided DHIs) not being directly accessible via the trust login. Despite staff being able to set these individually, remembering multiple logins and persevering when these failed were big barriers.
At an even more basic level, REACT required access to a computer and an internet connection. These were not always available to staff in their place of work and, crucially, were rarely available on mobile devices during home visits to allow them to show REACT to relatives. To preserve the privacy of relatives, staff were also unable to access all REACT components (specifically the forum and direct messaging). This led to anxiety about what might be there and, consequently, a reluctance to invite relatives.
Attempts to improve the usability of the website via an online training manual proved largely unsuccessful, as staff reported it being rarely used (web usage data are not useful here as the page is open access and page counts would include visits by the IMPART team). Face-to-face training was more highly valued, but was attended by only a small proportion of staff at each site. More successful were delegating the role of inviting relatives to a small number of individuals (as in Marsh) and appointing a REACT champion to facilitate training and provide peer support (as suggested in Seashore). Ultimately, though, the lack of engagement with staff in the design was a key factor in non-adoption and abandonment of REACT.
Most relatives in EIP services in all trusts were never sent an invitation to REACT. Those who were experienced similar IT frustrations to the staff. Some never received their invitation, which often went into junk folders (solved by changing the originating e-mail addresses and wording of the e-mails). The same challenges of broken links and forgotten log-in credentials existed.
Initially, relatives were invited to take part in the IMPART research study and complete the pre and post questionnaires as part of the log-in process. This took them to a Liverpool CTRC website that, after completing the measures, redirected them to REACT. On some occasions, this redirect did not work, and some relatives mistakenly thought that the questionnaires were the website. As soon as we became aware of this, the system was changed: new users were taken straight to REACT and the research invitations were sent in a separate e-mail.
A frequently cited reason for relatives (and subsequently staff) disengaging from REACT was the lack of activity on the forums. This was the feature that relatives expressed most interest in and tried most often to access. However, despite some relatives experimenting with posts, the lack of activity was disappointing and led to abandonment. Forums require a critical mass of activity (and therefore people) to be successful. They are very hard to get going and require very active moderators to regularly generate topics of interest and reply quickly to posts, until enough people are active and the moderator can take more of a guiding role. Most REACT supporters saw their role as responding to posts rather than proactively generating activity, and given the small number of relatives invited onto REACT in any one trust, these forums were like empty dancefloors that did not encourage participation.
Lack of activity on the forum created a vicious cycle that reduced staff motivation to offer REACT. Staff were very interested to know what was discussed on the forums and so IPv3 included an e-mailed newsfeed that summarised topics of discussion in the hope of engaging staff and motivating them to refer more relatives to REACT. It seemed to have the opposite effect by highlighting the lack of activity, which staff took to indicate lack of interest from relatives. They therefore stopped referring.
NASSS domain 3: the value proposition
Everyone we spoke to in the IMPART study saw value in having an online self-management toolkit to support relatives.
For senior managers, this was facilitated by the 2014 publication of the AWT standards for mental health106,107 and subsequent audits of the ability of each NHS trust to deliver NICE guideline clinical care for people with psychosis, including carer education and support for relatives. REACT was developed specifically to meet this aim and was presented as such during the initial approach to NHS trusts. Some trusts (e.g. Marsh) were also driven by R&D departments that were rewarded for engagement in NIHR portfolio studies. Consequently, recruiting NHS trusts to the study was easy.
Most frontline clinical staff were aware of trust targets and priorities and of national clinical guidelines, although generally less so for those pertaining to carers rather than service users. For them, REACT’s value was as a high-quality, professional resource that educated both relatives and staff. Some staff felt that this improved the quality of the conversations they were able to have because relatives were more informed. REACT was expected to save staff time in the longer term, and allow services to support relatives of service users who did not want their relative to be directly involved in their care.
Benefits identified by relatives included the ability to access support at a time and location that suited them, and support that was directed specifically at their own needs as carers.
However, perceived value was not sufficient to drive activity. The strongest theme in our data was that staff did not have the time to offer REACT. Although many saw that REACT could save time in the long term, their experience was that in the short term engaging with a new way of working would require additional time and resources. Most respondents in the costs and savings survey taken towards the end of the study did not feel that REACT had reduced the time they would otherwise have used to support relatives. Time is fixed, and staff always have the same amount of time.
Given the evident demands on staff time and the pressure services were under, inability to prioritise delivery of REACT was perhaps not surprising. Teams struggled to provide support to service users and manage risk. Staff morale was low, long-term absences were high and frequent staff turnover was the norm, particularly in Woods and Seashore. Staff talked of the very many targets and ‘priorities’ they were supposed to meet, and how they were consequently forced to prioritise within the priorities. As one IMPART lead in Moor Trust put it, ‘REACT is just not the shark nearest the boat’.
Priority was generally given to targets that were service user focused, financially incentivised, nationally endorsed or ‘home-grown’. REACT was carer focused, had no funding attached to its delivery, was not endorsed by NHS England and had been developed and offered by a research team external to the trust.
Relatives also faced time challenges. These were made easier when REACT’s potential value was made explicit and personal to them when it was being introduced. Particularly, relatives were more likely to sign up to REACT if it was introduced by someone in the service with whom they already had a good relationship, whose opinion they trusted and who spent time explaining what was in REACT and why they might benefit from it.
Timing was also crucial. REACT was more highly valued if offered early in the relative’s contact with services, while they were still trying to make sense of what was happening and before they had spent a lot of time and effort finding out information through other means.
REACT was designed to be an adjunctive resource in a comprehensive service. If NHS trusts struggle to deliver other parts of the service for relatives, then its potential value can become a perceived risk. For relatives, the potential risk was that DHIs such as REACT might replace face-to-face support, which was not what they wanted. For staff too, the risk was that relatives might feel ‘fobbed off’ or discover what other services they should have access to. Their frustration would then be directed back at staff and be difficult to manage.
NASSS domain 4: intended adopters
Adoption, non-adoption and abandonment may all be linked to a user’s view of the condition, the technology and the intervention’s perceived value, as outlined above. However, additional aspects of the intended adopters are also important.
In this context, there were two groups of intended adopters: NHS staff and relatives. Both needed to be willing and able to adopt REACT. We therefore identified IMPART leads in each trust, but left the allocation of key roles including the REACT supporters to the discretion of the service. Our hope was that these would be allocated to the staff perceived as most willing and able, and that early adopters would lead the way for other staff to follow. To some extent, this did happened. However, significant obstacles became apparent.
The main obstacle to staff willingness to refer relatives to REACT was a sense of fear and threat. The most fundamental threat was to staff jobs. DHIs are often presented as tools that will enable staff and make their jobs easier, but this is within a context in which many other jobs are being replaced rather than augmented by digital technology,108 and the exact impact of DHIs on NHS jobs cannot be predicted. The fear that REACT could replace face-to-face clinical therapy was present, and had staff questioning whether or not DHIs could ever be as good as face-to-face support (see particularly Woods and Marsh).
Other potential threats came from the potential to be ‘trolled’ on an online forum, or be held responsible for managing risks disclosed online without adequate training or policies being in place. Trolling was a particular fear in Marsh after experiences with an earlier DHI. Fear of being held responsible for risk events was widespread across all trusts and, in one (Lakes), directly led to staff withdrawing support for REACT. None of the trusts seemed able to reassure staff or produce risk policies that had been adapted for online communication.
Finally, for some staff, REACT also threatened to highlight their service’s existing difficulty in meeting relatives’ needs. It was feared that REACT would open up a line of communication with relatives who would be better educated about what services they should be receiving, and consequently request access to services the trust was unable to offer. Staff felt that it would have been difficult to manage these expectations.
Some staff did not adopt REACT because they did not see it as legitimately fitting their role. Either it was perceived as belonging to a different professional group, such as ‘led by psychiatry’ or ‘from psychology’, or it was seen as the role of the research team to deliver REACT. Staff were more familiar with research designs such as RCTs where they would identify potential participants but in which the research team would recruit the participant and deliver the intervention.
Staff had to be able as well as willing, and specific DHI-related skills were important. General confidence in using DHIs was surprisingly low, and fears of ‘breaking the site’ or getting it wrong were not uncommon. Navigating the website and remembering log-in details were challenging, made more difficult by the limitations of the technology design outlined in NASSS domain 2: the technology. Despite 281 staff accounts being created, only 57 staff members ever sent a relative’s invitation.
If relatives who were sent an invitation or made aware of REACT were willing, their ability to navigate the process was also a significant barrier, again mainly owing to the technology design outlined in NASSS domain 2: the technology. Some relatives tried to find REACT through a search engine rather than by following the link in their invitation e-mail. This led them to the REACT trial website, which was running at the same time; when they tried to log in, their details were rejected, causing frustration and abandonment.
NASSS domain 5: the organisation
REACT was designed to help NHS trusts to deliver NICE guideline care by offering carer education and support alongside other recommended interventions, such as structured, face-to-face family interventions; carer support groups; and joint case management. The website could accommodate trust-specific information, such as availability of website moderators, or other aspects of the care and resources directory. Staff feedback in individual interviews and workshops led to improvements to the interface and a planning document to support trusts in thinking through how REACT could best fit their existing service structure and care pathways.
Despite this, there were a number of ways in which REACT did not ‘fit’ with services, impeding implementation. Failure of fit was evident at the level of organisational culture and the specific clinical pathways into which REACT was offered.
Fit with organisational culture
Adopting a DHI into EIP teams required a huge shift in working culture. These teams were historically characterised by people talking to each other and recording activities using pen and paper. Direct human contact was understood to be the main agent of change. An online intervention was not something staff were naturally exposed to or generally seeking. Basic access to IT facilities and staff training was extremely limited, and experience of other digital health systems, including electronic health records, had been generally frustrating.
During our data collection, it was clear neither to us nor to staff who was responsible within trust organisations for the strategic direction of service development and who could facilitate the shift needed for staff to embrace DHIs such as REACT. Many were not sure who needed to give the ‘go ahead’ for staff to use REACT, and the distinction between clinical and operational managers seemed to add to the confusion. Some trusts (e.g. Marsh) had a ‘transformation manager’, but it was not clear how they would support the use of interventions such as REACT.
REACT came into trusts via R&D teams that were very keen to support research in their trust. Although the clinical teams agreed to this happening, often the decision was made by a key senior individual (who often then became the IMPART lead) without much evidence of team consultation. In one trust (Lakes), this person then left the team during the study period.
Several consequences stemmed from this lack of strategic engagement. First was that teams were sometimes being asked to adopt several new approaches in parallel, and change in many directions at once. For example, staff in Seashore were being asked to integrate a new DHI to support service user recovery at the same time as learning about REACT, which caused some confusion. Second, because the intervention had no clear clinical ‘home’ and was not adopted by any specific professional roles, there was no infrastructure or allocated resources to support ongoing sustainability or spread. REACT supporters were not given regular supervision to support their work (> 50% of REACT supporters responding to the costs and savings survey had received < 1 hour of supervision for their REACT role over the entire study period) and, consequently, there were no incentives for them to carry this out. Over time, REACT supporters disengaged from the intervention, leaving the forums often unmoderated. This disengagement exacerbated the fears of clinical staff regarding risk and trolling, which in turn reduced the likelihood of staff to refer relatives to REACT.
In all trusts, there appeared to be a lack of organisational capacity to strategically change practice: to reflect, adapt and reorganise. We noted that teams were constantly fighting to meet immediate service user priorities with low staffing and limited resources. Reported caseloads were higher than the EIP model was designed to accommodate. There was no evidence of any positive impact from the additional EIP funding or the government’s commitment to ‘parity of esteem’ for mental and physical health (although we did not collect comparative data for any physical care services).
Fit with the clinical pathway
In general, EIP teams offered support to relatives in the relative’s own home. Most staff did not have regular access to mobile technology on which they could show REACT to relatives in these face-to-face consultations. REACT was literally out of sight and, therefore, very often out of mind. Even when staff brought REACT to mind, social barriers impeded them from introducing it. Although most relatives had personal computers or tablets, staff did not feel that it was appropriate to ask the relative to log in to their own personal device to be shown the website, particularly as these were often in the bedroom or other private area of the house.
We tried to address this issue by providing (in IPv2) attractively designed REACT NHS booklets that explained what REACT offered and how to access it, and later (IPv3) printable PDF summaries of the REACT modules. These were generally welcomed by staff, and highlighted the complementary benefits of using digital technology alongside other forms of communication.
Staff who did refer relatives to REACT had no subsequent knowledge about whether or not the relative had accepted their invitation and used REACT and, if so, what their impressions of it were. This lack of feedback was demotivating, and led to disengagement among staff. As noted above, our attempt to address this via the newsfeed in IPv3 seemed to have the opposite effect as it highlighted the lack of activity.
Finally, at the time of the study there was no formal way for staff to record REACT-related activity in their electronic note systems, other than as a note in the service user’s electronic record. In all trusts, any staff time spent supporting relatives was recorded in the service user records, as carers do not have an independent record. Consequently, staff caseloads did not accurately reflect the number of people a staff member was working with. As the pressure on systems continues to grow, the cliché that ‘what gets measured gets done’ is likely to become increasingly true.
NASSS domain 6: the wider system
REACT fitted very well into several key government agendas. It had the potential to facilitate a shift towards a paperless NHS by 2020 as set out by NHS Digital;12 it supported the delivery of NICE-recommended care, to increase parity of esteem between mental and physical health;106 and it also had the potential to facilitate meeting the needs of carers as set out in chapter 23 of the Care Act 2014. 109
However, despite this, key factors within the wider system worked against the implementation of REACT.
Despite the commitment of large amounts of money to meet the NHS’s commitment to ‘harness the information revolution’,12,110 our findings suggest that access to up-to-date mobile hardware and software was very limited for frontline NHS staff. Confidence in using digital technology was low and there was no evidence of training or support available within these EIP teams. Anxiety about responsibility for risk was very evident and was situated within a wider context of societal anxiety about data security111 and a blame culture in the NHS. 112
Despite the inclusion of carer targets within the AWT framework, it was difficult for services to prioritise activity to meet these. Our health system reflects our societal system in which health is generally conceptualised within an individualistic framework, in which the focus is on the individual rather than the social structure in which they are situated. 113 Relatives in the UK provide an estimated £1.24B per year of support to the NHS in unpaid caring roles,27 and staff understand the logic of supporting them in terms of longer-term outcomes. However, failure to prioritise carer support seems to reflect the lack of organisational capacity to do much more than short-term risk management. The services taking part in our study were extremely stretched. Although mental health is a government priority, and funding has been targeted towards EIP services more than at other parts of mental health services,106 this is within a context in which annual rates of increase in the overall health budget to meet growing demand have been declining over the past decade. 114
NASSS domain 7: evolution over time
One factor affecting staff non-adoption and abandonment of REACT was that it was perceived as part of their trust’s research agenda rather than as a long-term clinical strategy. However, several staff asked whether or not REACT would continue to be available to them at the end of the project. REACT was wholly funded as NIHR research and, therefore, we were unable to guarantee that REACT would continue to be available and supported. Understandably, this limited the effort and behavioural adaptation that staff were willing to invest in something that might disappear. Some staff questioned whether or not, in this situation, REACT should be offered at all.
There is currently no national infrastructure for tested products funded by public money to be adopted and delivered nationally at the end of the research phase. Survival depends on the developers (who are often clinical academics and not entrepreneurs) finding collaborative partnerships with digital technology partners, private investors or individual commissioners at a trust level, and setting up commercial contracts. REACT was being tested in a large RCT in parallel to this study and, without the data from that research, it was not possible to establish a longer-term delivery model or establish funding for it. We are not alone in facing this challenge. A recent systematic review of meta-analyses of web-based interventions developed and tested in RCTs showed that in only 21.3% of cases (57/268) did a functional website continue beyond the trial. 115
It must be noted, however, that as well as discouraging staff engagement with REACT, the research process also triggered activity. Contact with staff to arrange individual interviews and SRGs was associated with an increase in relatives’ invitations (see Figures 8–13). Similarly, there was some suggestion from the web use data that relatives who signed up to take part in the research study also visited the website more often, although this may just reflect a general tendency to comply with requests.
Conclusion: implementation plan version 4
The NASSS framework hypothesises that the degree of complexity within each of its seven domains will determine whether or not a DHI is successfully implemented. Each domain can be assessed as simple (few components and predictable, e.g. making a sandwich), complicated (lots of components, largely predictable, e.g. building a rocket) or complex (dynamic, multiple interacting elements and unpredictable, e.g. raising a child). 116 However, the domains are interdependent and so it is not possible to identify any one specific factor that underpins implementation success.
In the present study, challenges were identified in all of the seven NASSS domains. The level of complexity in each domain was high. Although this gave clear direction as to what needed to change, it was also somewhat disheartening. Although we might be able to improve the value of REACT and the reliability and interoperability of the technology, build greater capacity to use it in staff and relative adopters, and may even be able to offer support for organisational change at a trust level, we are much less able to reduce the complexity of psychosis (the condition), the wider context of NHS funding or the lack of infrastructure to support long-term funding of DHIs (emergence over time). Despite the apparent culture of in-house development in large technology companies of ‘fail early, fail often’, because of the way in which competitive funding operates in the public health sector, there is no reward for sharing learning about how to overcome barriers, and only DHIs presented as successful are likely to attract further funding.
We have highlighted the main factors that our findings suggested were important in relation to each of these domains, and used them to develop IPv4, set out in Table 24. The strategies map directly onto the factors raised in each of the seven domains. Finally, we have drawn out recommendations that can be used to inform the implementation of other DHIs within similar community health teams.
| NASSS framework | REACT IPv4 |
|---|---|
| 1. Condition |
|
| 2. Technology |
|
| 3. Value proposition |
|
| 4. Intended adopters |
|
| 5. Organisation |
|
| 6. Wider system |
|
| 7. Embedding and adaptation over time |
|
Suggestions for others implementing digital health interventions based on the findings from the IMPART study
The following recommendations are based on the key findings of the IMPART study. They are aimed at people designing and delivering DHIs within the health-care sector and, for this reason, they complement the broader recommendations of Greenhalgh et al. 74
-
All stakeholders, including referrers and end users, should be closely involved in the development, testing and implementation of DHIs at every step of the design process.
-
Allow sufficient time and resources for iterative co-design, internal testing and piloting (and then some more).
-
Identify the potential value of the technology to each stakeholder group within the health-care setting and provide evidence (including data, endorsements and testimonials) that directly targets these values.
-
Understand exactly when, where and how it fits into the care pathway and conduct a risk assessment of all the steps along the pathway to see where implementation could be impeded.
-
Ensure that all stakeholders are actively involved in the service decision to adopt the DHIs, and that they have the opportunity to have their fears and concerns heard and addressed prior to adoption.
-
Understand how change happens within an organisation and ensure that the key agents of change are engaged in the implementation process.
-
Identify champions within the workforce and user groups who will take a lead role in ensuring ongoing sustainability of the intervention.
-
Manage expectations about what can realistically be achieved with the technology.
-
Be transparent about the short-term and long-term costs and savings of delivering the technology. Be careful to include the costs incurred in changing existing practice and training staff in new ways of working.
-
Understand the hardware and software that the organisation is using and design the technology appropriately.
-
Establish a clear communication channel for ongoing stakeholder feedback, and a mechanism to ensure that this can be addressed in a timely manner.
-
Develop a comprehensive training programme for all staff and service users involved in the DHI. This should include a balance of the formal (built into mandatory organisational training programmes) and informal (peer-to-peer support and demonstrations), and should be offered on a rolling basis to ensure that skills are regularly updated and new staff can easily access training.
-
Training should include general IT skills to increase confidence, as well as skills specific to the DHI, and clear guidance on management of risk and responsibility, and should be offered through a range of media (online, face to face, paper) to support different styles of learning.
-
Ensure that the technology is rigorously tested internally and in situ, while managing expectations to ensure that confidence in the technology is not lost during the process.
-
Engage early with the evolving infrastructures and support systems surrounding digital interventions, including the Academic Health Science Networks, NHS Innovation Accelerator, the national accelerator programme, the NHS Technology Adoption Centre117 and others, to establish long-term delivery models as soon as possible.
-
Build in efficient and agile evaluation of the reach and impact of the technology, complying with General Data Protection Regulation101 requirements for the collection of personal data.
-
DHIs are often designed to add value to multicomponent packages of care. It is important to establish that those aspects of care are reliably delivered before assessing the impact of the DHIs.
These recommendations should be considered by those attempting to design or deliver DHIs within a health-care system. However, for DHIs to have significant impact on the UK health-care system, a shift in policy and practice is required at a national level. Our recommendation is that DHIs that are developed with public funding should be made freely available to the NHS. Those that are effective should be adopted and made available via a national and centrally run organisation (such as NHS Digital), rather than commissioned at a local level. Equally rigorous standards should be set to evaluate the effectiveness of commercially developed products, and careful contracting should prevent the risk of price inflation once the health-care system has become reliant on the DHIs.
Chapter 9 Discussion
In this chapter, we revisit the main aims and specific objectives of the study and show how each of these has been met. We outline the strengths and limitations of the study that need to be taken into account when using the study findings. We highlight implications for clinical service delivery, implementation theory and further research. Finally, we reflect on our PPI strategy, which is given in Appendix 1.
Study objectives
The overall aim of the IMPART study was to identify critical factors affecting the implementation of an online supported self-management intervention for relatives of people with recent-onset psychosis or bipolar disorder into routine clinical care, and to use this information to inform an implementation plan to facilitate its widespread use and inform wider implementation of DHIs. Over a funding period of 30 months, we were able to achieve all six objectives listed in Chapter 2.
Measure uptake and use of REACT by NHS early intervention for psychosis teams and relatives
Over the study period of 18 months and across all six trusts, 281 staff accounts were created, 355 relatives’ invitations were sent, 310 relatives were invited and 159 relatives created an account. The most common characteristics of the relatives were that they were white British, a mother and aged > 50 years, and caring for their son/daughter with a diagnosis of psychosis who was living at home.
The mean time spent using the website was 40.6 minutes (SD 54.54 minutes) and the mean number of logins was 3.78 (SD 4.43), although there was considerable individual variation. We do not know how much use of REACT is required for effective change, but these levels of engagement compare relatively favourably with other online interventions, which often show lower than intended engagement118 and in some cases only a minority of participants visited the website more than once. 119
The most common pattern of staff behaviour was 1–2 hours being trained to use REACT (including presentation by the research team), < 2 hours familiarising themselves with the content and < 5 hours referring relatives over the entire study period. REACT appeared as an agenda item for a range of meetings, but was only a regular item at clinical team meetings for approximately half of the staff, and was commonly discussed for < 5 minutes. REACT supporters generally spent longer training and using REACT than other staff did, but received little or no supervision.
Identify critical factors affecting implementation of REACT
Chapter 8 presented a full explanatory synthesis of the critical factors affecting the implementation of REACT. In summary, staff in EIP teams were under great pressure, with high caseloads, several competing priorities and, in some trusts, high levels of staff absence. Staff found it difficult to prioritise time spent supporting carers.
Staff and relatives agreed that REACT could offer an appropriate way to increase access to information and support for carers, but only if it was delivered as part of a comprehensive care package that also included face-to-face support. Staff who used REACT felt that it had facilitated communication with relatives, saw it as a valuable information resource for staff and relatives, and an appropriate way to meet national and local clinical targets, but they did not generally feel that REACT had saved them time in supporting relatives, and may have even increased the amount of contact they had. Staff also reported frustrating practical and technical difficulties.
Relatives were generally very positive about the content of REACT. They valued the comprehensiveness of the modules, and particularly valued hearing about the experiences of other relatives and service users through the videos. However, many reported technical issues and were disappointed by the low level of activity on the forums, making them reluctant to post. This, in turn, made staff less motivated to refer more relatives, creating a vicious cycle working against sustained use.
REACT did not fit with staff members’ current ways of working, which were primarily paper based and community located. This incompatibility was exacerbated by a lack of up-to-date mobile technology. Staff felt that they needed more support and training to use DHIs, and had specific fears about being trolled online and managing risk. Fundamentally, they saw the human relationship as the main agent of change in mental health services, and felt that DHIs somewhat threatened this.
Finally, REACT was offered in the context of the IMPART research study and consequently staff saw the research team, not clinicians, as being responsible for driving it forward. They also recognised that REACT might not be available after the research period and lacked longer-term funding, making them question the value of changing their current working patterns to accommodate REACT.
There was some evidence that the iterative versions of the implementation plans developed during the study (see Chapter 6) led to increasingly more relatives being invited to use REACT. However, the relationship was far from straightforward, with wide variation between trusts.
Some of these factors are consistent with the findings of previous research in this area: specifically, staff concerns about the impact of DHIs on staff–patient (in this case relative) relationships, and the need for appropriate IT equipment, collaborative technology design and training and support have all been identified in other health contexts. 120 The negative impact on staff engagement of poor system design, IT failures and fears that the use of technology will dehumanise care have also been highlighted. 121 Staff fears about managing risk, being trolled online and the negative impact of the research context are unlikely to be particular to REACT, and need further exploration in other contexts.
Identify resources required (and cost implications) for successful implementation of REACT in early intervention for psychosis teams
Here, we outline the main resources required by our final implementation plan (IPv4). We have not allocated specific numerical costs, as these will vary depending on the organisational structure in any one trust (staff costs) and on the number of trusts adopting REACT (cost of delivery per trust).
Implementation plan version 4 (see Chapter 8) was designed to address each of the barriers to implementation and enhance identified facilitators, and hence suggested a fundamental change in the way in which REACT is offered.
Rather than each NHS trust hosting a separate version of REACT, restricted to relatives in their trust only, the intervention could be more easily delivered if it were available nationally from one centrally located and funded source, supported by dedicated trained REACT supporters, and open to all relatives in trusts that adopt the programme. This would overcome the challenges that staff found in dedicating time to the REACT supporter role and in accessing supervision. It would create a much larger population of participating relatives, generating a critical mass to stimulate an active forum. Finally, it would create an effective way to engage relatives as peer workers in the delivery of NHS services as they could be trained as REACT supporters.
Set-up costs
The primary cost for this set-up phase is staff time and a licence fee to adopt REACT. Clinical staff and those with responsibility for organisational strategy, transformational change and IT need to be involved with relatives in a joint review of the pros and cons of using REACT in their service. All identified concerns should be addressed before adoption. Policies (including risk management) should be adapted to accommodate the online nature of REACT. Key roles need to be allocated, and pathways designed, clearly stating who will offer REACT, when, how and with what support. A mechanism should be established to review progress and adapt REACT and the implementation plan at regular intervals.
Ongoing costs
Ongoing costs also primarily involve staff time. IPv4 recommended that a REACT champion should be identified in each team. Their role would be to create and maintain a visible REACT presence for all staff, ensuring that it is a regular agenda item in appropriate meetings. The branded merchandise developed in this study (sticky notes, travel mugs, posters, etc.) could support this. The champions would co-ordinate a rolling programme of staff training (formal and informal) and facilitate communication between the clinical team and REACT hosts.
Staff identified to refer relatives to REACT need time to be trained and to get to know the website. They need REACT booklets that describe the intervention and its benefits, which should also be placed in carer packs. Staff need up-to-date mobile technology that allows them to show the DHIs to relatives in their own homes. No additional software is required.
We estimated the total cost for consumables (merchandise, booklets, posters, etc.) to be approximately £400 per team, based on 20 staff supporting 200 relatives. The cost of licensing REACT per annum would depend on the number of trusts that used it, with more trusts reducing the costs. IT costs would depend on the technology chosen, but is not specific to REACT. Staff costs would vary between trusts.
Savings
REACT is not anticipated to significantly reduce the amount of staff time dedicated to supporting carers. Our data suggest that this time is already less than needed to meet national clinical targets and deliver NICE-recommended care. 51,52 In fact, REACT may increase the time spent communicating with relatives. In the longer term, this should improve carer and service user outcomes (and save money), but would require further testing.
Investigate the impact of REACT delivered by early intervention for psychosis teams on relatives’ self-reported outcomes
Relatives had high GHQ-28 scores at baseline, with approximately 60% scoring above the threshold for clinically significant distress. These levels of distress are consistent with those previously reported for relatives in EIP services. 53,122 Between baseline and the 12- and 24-week follow-ups, there was a general pattern of declining distress, social dysfunction, depression, anxiety and insomnia, and increasing carer well-being and eHealth literacy. However, these changes were small and none was statistically significant.
Develop a user-friendly REACT implementation plan and related resources to facilitate widespread use and dissemination
Implementation plan version 4 is described in full in Chapter 8. In addition to the necessary trust resources outlined against the objective Identify resources required (and cost implications) for successful implementation of REACT in early intervention for psychosis teams (staff time and training, merchandise, licence and IT), other key elements include updating the content and functionality of REACT; identifying a sustainable provider and long-term funding model at the national level; and building a mechanism to ensure that the ongoing audit of the reach, uptake and impact of REACT that is not onerous or perceived as research.
Use the findings from this study to further develop theories of implementation of digital interventions in real-world practice
Normalisation process theory73 was used to understand the work undertaken by staff in participating trusts to implement REACT. The NASSS framework74 was used to synthesise these data with the key factors affecting relatives’ engagement and the wider contextual factors. Rather than developing these theories further, we tested the utility of both in understanding the implementation of REACT.
Normalisation process theory proved very useful in informing data collection and analysis, particularly in relation to the work undertaken by the staff. It also worked well in informing the iterative development of IPv2 and IPv3. This was the majority of our data, and so this theory would have been sufficient to develop an effective implementation plan. However, we were keen to develop this plan further to ensure that it also addressed the complexity of the wider context and the engagement of relatives. We therefore used NASSS to synthesise all of the data from the IMPART study. This led to the development of a final implementation plan (IPv4) that differed significantly from our original implementation plan (IPv1).
The NASSS framework builds on many previous theories, and synthesising our data from staff and relatives in the key domains was relatively straightforward. Working across two different frameworks could have led to theoretical confusion, but in practice it worked very well. The theories proved highly complementary: NPT gave us a detailed focus on staff behaviour, and NASSS allowed us to then integrate the key themes identified by NPT with the data from relatives and the broader contextual factors, to present our explanatory synthesis. In combination, they helped us to meet our study objectives.
Study strengths
Our study was strongly embedded in implementation theory. At a practical level, the use of theory helped focus our data collection and structure our analyses. We were able to test the utility of the NPT and NASSS frameworks in a novel context, and create generalisable knowledge to inform the delivery of DHIs other than REACT, and within contexts other than EIP teams.
Data collection took place across multiple and varied NHS trusts. This increased the external validity and generalisability of the findings, ensuring that our implementation plan, if flexibly used, should facilitate implementation across most NHS trusts in England.
Our research was very timely. The findings are of direct relevance to the government agenda to increase the spread of DHIs12 and to improve mental health services, the delivery of NICE guideline-recommended care106 and specifically support for carers. 109
We examined the perspectives of the end user (relatives) as well as of staff doing the direct work of implementation. This was important because it clearly demonstrated that the way in which REACT is implemented by staff had a direct impact on engagement by relatives, and that relatives’ engagement then fed back to affect the work undertaken by staff.
We designed the study to be collaborative and informed by perspectives of all relevant stakeholders. Relatives formed part of our study team and contributed to its design, data collection and analysis. SRGs were set up at each NHS trust, and attempts were made to include a range of staff roles and relatives and service users in these groups (although this was not always successful in every trust). These groups became the vehicle for co-design of implementation plan iterations.
Study limitations
The main limitations of the study relate to the study design, use of theory and research process.
Study design
The research team had a dual role of delivering REACT while also collecting data to understand the process of implementation. This was confusing for trust clinical staff because it strongly embedded REACT within a research agenda, leading them to assume that REACT would be time limited and driven by the research team. This was a key factor in non-adoption. It also created a tension for the research team. On the one hand, our role was to observe and record, and to intervene only via the strategies outlined in our implementation plans. However, as originators, we also wanted REACT to be viewed positively by staff and, consequently, it was tempting at times to try to facilitate the implementation process. This highlights the need for independent implementation and independent evaluation of DHIs to overcome researcher bias.
Our study design included analysis of data from interviews, observations and document analysis. In the event, the number of data we were able to collect through observation was very limited. We worked with IMPART leads to try to identify meetings in which REACT was likely to be a key agenda item, and asked the meeting chairpersons if we could attend. There were very few meetings in which REACT appeared as a specific agenda item, and, where it was discussed as part of routine clinical practice, the staff did not think it appropriate that we attend the meeting owing to the confidential nature of material being discussed. Therefore, our analysis relied more heavily than we would have liked on interview data and document analysis, with less direct observation being possible.
In the ‘you said . . . we did’ cycles, staff and relatives made suggestions for how the obstacles to using or offering REACT could be overcome. The opportunity to influence the development of REACT was well received and the limits of what could be changed because of time and resources were understood. However, some changes that could not be made, such as offering REACT as a mobile app rather than a website, were repeatedly requested by two trusts (Lakes and Marsh), and this caused frustration for staff as these changes would have overcome the challenge of needing to remember a password.
For relatives, the confusion in our study design came from embedding our research within the clinical delivery of REACT. The invitation to complete questionnaires for the IMPART study initially came as part of the process of setting up a REACT account, leading some relatives to question if this was part (or even the whole) of the intervention. These processes were separated once we became aware of the issue.
Study theory
Normalisation process theory proved a useful theory to guide the collection and analysis of staff data, but was limited (at the time) in helping us to understand relatives’ engagement with REACT or in clearly specifying the wider contextual factors relevant to the implementation of REACT. We added additional codes to our coding framework to accommodate data specifically relevant to understanding the context (within EIP teams, and wider context) and the research process, which was identified as a particularly significant contextual factor. We analysed the relatives’ data using an open thematic approach.
Since the design of the IMPART study, NPT has evolved to more explicitly consider the importance of context. May et al. 123 in particular highlight the interaction between the plasticity of intervention components and the elasticity of contexts in determining success of implementation. Despite this development, we chose to use the NASSS framework to synthesise our findings.
Study process
We were very ambitious in the amount of work we set out to deliver, given the time scale and resources. Our lack of experience in designing and delivering IT projects meant that we underestimated the time and resources needed to deliver this, although this is not uncommon even in large-scale national digital projects. 124 Consequently, some staff were frustrated by IT failures, which, with a part-time IT developer, we could not address immediately. To meet our study objectives, we drew on the additional resources of a Master of Science student (GA-A) who led the systematic review of literature in phase 1, and a Doctorate in Clinical Psychology student (Johanna Barraclough) who led the analysis of interviews with relatives.
We underestimated the speed with which behaviour change can be achieved within the NHS, particularly when the change required is seen as part of a research agenda rather than a clinical agenda. We were unable to interview relatives as early as planned because this depended on REACT first being adopted by staff who could then invite relatives to use REACT. Consequently, these data had less impact on the development of IPv1–3 than planned. This also led to fewer relatives completing the outcome measures within the study period and, therefore, the pre–post analysis of outcome measures was likely to be underpowered to identify any significant changes.
The time frame of the study was limited, including only an 18-month window of observation following the initial deployment of the REACT intervention. Consequently, we were able to observe only the initial stages of adoption/non-adoption and early abandonment. Data collected over a longer time scale would be required to understand scale-up, spread and sustainability. This seems to be a gap in implementation science, with fewer studies funded to understand these stages of implementation. 125 (Note that a request for a funded extension to the IMPART study was rejected.)
Finally, the majority of participants in this study were white British, even in trusts that served populations with high ethnic diversity and, therefore, the generalisability of the findings is restricted to this population. As participants were identified by staff (rather than the research team), this bias may reflect a more general challenge across the services in engaging relatives from minority ethnic groups.
Despite these limitations, our findings have important implications for clinical service delivery, implementation theory and further research, which are outlined in the following sections.
Implications for clinical service delivery
Our findings have clear implications for the development of clinical services in relation to supporting relatives and using digital technology.
Despite extensive government and charity recommendations to involve relatives more actively in supporting people with psychosis or bipolar disorder, and to offer education and support to meet their own needs,51,52,105,109 these remain challenging for staff. Mental health services remain chronically underfunded. 126 Staff interviewed in this study felt unable to meet all of the targets set, and so prioritised within these. They focused primarily on targets that involved working with service users, and those with clear financial incentives attached, at the expense of support for relatives.
One reason for this is likely to be that individual staff caseloads are measured by number of service users. Work to support relatives requires additional time and resources, and historically has not been measured. Reported caseloads in EIP services were much higher than the original target of 15 per full-time-equivalent care co-ordinator. 127 National audits have marked progress in trust delivery of AWT standards. Nationally available averages for 2016 suggest that 16.1% of people with first-episode psychosis in contact with their families took up family intervention, and 37.8% of carers took up carer-focused education and support. 102 Figures for individual trusts and data on how many people were offered and declined family intervention are not currently available. However, there are as yet no financial consequences for failing to hit carer targets. Work that staff undertake with relatives needs to be visible and rewarded, which would require increased funding for mental health services.
If digital health interventions such as REACT were to become part of mental health services, the data suggests that staff and relatives would prefer their funding to augment rather than replace funding for face-to-face support. Staff and relatives were very clear that they did not want DHIs to replace face-to-face interventions, which the evidence supports as the most effective service model. 128
Clinical staff who are asked to implement DHIs need reliable access to up-to-date mobile hardware and secure software. They need to work with integrated systems that require a single login, and training and support to develop their IT skills and confidence. Risk policies need to be adapted for services delivered online, and individual levels of responsibility need to be made clear. DHIs need to be strategically implemented on the basis of service demand, and with longer-term commitment to cycles of review and adaptation, rather than short-term cycles of failure and abandonment. Service demand should be determined through organisational infrastructures that support the meaningful involvement of service users and carers, as well as staff. These elements were not reliably available in any of the participating trusts in this study.
Implications for implementation theory
There are well over 100 implementation theories and frameworks,129 and at least 28 focus specifically on health technologies. 74 With notable recent exceptions,129 there is very little guidance on how to select the theory most likely to be of use to a particular study or project. Rather than develop more theories, existing ones should be tested, and encouraged to evolve over time and contexts, just like the technology-enhanced services they try to understand. Our experience was that NPT and NASSS were useful for different purposes. NPT helped with a detailed analysis of the work undertaken by staff, whereas NASSS was more useful in then situating this work within the wider context, in terms of the health-care setting, the wider political context and the particular point in time. NPT recognises the importance of context, whereas NASSS provided a framework around which to understand factors that are likely to be important, and highlighted the futility of some aspects of the implementation plan in the absence of any control over factors in the wider context.
In particular, adaptations to the functionality of REACT were made to address issues raised by staff around content, usability and feedback; however, without addressing the ways in which DHIs are developed, tested and commissioned within the NHS, staff were unlikely to commit to using REACT as they perceived it as transitory, research driven (rather than clinically driven) and, therefore, of low priority.
The language used to describe concepts within the theories was a challenge. Although members of our team who were more familiar with NPT (EM) found it easy to understand and to use to help make sense of our data, those who were using it for the first time found it more difficult to understand and differentiate the core components. One example was the term ‘cognitive participation’. Those with a background in psychology intuitively interpreted this as being about the beliefs and attitudes held by the staff rather than the relational work that it refers to.
Further work is needed to understand the relative contribution of different theories to help implementation scientists to consider which theory will work best to guide their work in different contexts, and how to work with multiple theories for different levels of explanation.
Implications for future research
Implementation of REACT was so inextricably linked to the behaviour of staff delivering it and the context in which it was situated that we agree with the proposal of Mohr et al. 14 that it is more helpful to consider a DHI such as REACT as a technology-enabled service (TES) rather than a digital product. This has implications for how REACT is developed and tested over time. In this study, the implementation plans have been presented as distinct from the toolkit, but they are actually an integral part of the intervention, and future evaluation should test the effectiveness of the entire TES in the context within which it is being delivered.
Mohr et al. 14 also suggest that a TES cannot be evaluated using traditional efficacy trials. TESs have to be allowed to evolve and adapt in an agile way, otherwise they quickly become redundant. For this reason, trial designs that take several years to deliver, and that prioritise internal validity, may not be fit for this purpose. However, where public money is being used, it is essential that we have robust evidence of effectiveness, and there is an urgent need for new methodologies that allow us to do this.
The parallel RCT evaluating REACT supported by relatives and offered nationally,55 and this implementation study in which REACT was supported by clinicians and offered locally through EIP teams56 both tell us important things. However, integrating the findings will not tell us exactly what works for whom in what context. Future research to evaluate DHIs should consider hybrid designs that allow all aspects of the TES to develop as part of the study, and that test outcomes in situ. Possible designs to consider include realist evaluations130 and the ACTS model. 86 The ACTS model uses an iterative process that includes two basic functions (design and evaluate) across three phases (create, trial and sustain). In the create phase, a minimally viable TES is created, along with an implementation blueprint. In the trial phase, both effectiveness and implementation are evaluated and changes in the TES are made using optimisation and continuous quality improvement strategies. The final phase of sustainment involves the withdrawal of research or donor support, leaving a functioning, continuously improving TES in place.
A key challenge to this design is to balance design flexibility with scientific rigour. There are many aspects to this, but of particular note are the need for transparency to prevent bias (highlighted in this study), especially given the large sums of money at stake, and randomisation to control for the impact of confounding variables (highlighted by the REACT trial131 in which both arms showed substantial improvement over time).
Finally, DHIs are often promoted as interventions that increase accessibility and, for this reason, can reduce unequal access to health care. However, early research shows that differences in access to internet and mobile technology predicted by sociodemographic factors (primarily age and ethnicity) can create a ‘digital divide’ between those with and without access. 132,133 Our findings highlight the additional impact of assumptions that both staff and service users/relatives make about who these interventions are most suitable for, which then determine who is offered them and who uses them. This supports the need to explore many levels of division, including accessibility, skills, engagement and outcomes, in order to ensure that DHIs do not increase rather than reduce existing health inequalities. 134
Acknowledgements
This study is dedicated to Naomi Fisher who very sadly died during the publishing of the final report. She was our warm, funny, generous and incredibly clever colleague and friend who we will remember always. She played an essential role in this study and spent her life trying to improve support for people with mental health difficulties.
The IMPART study was supported by the North West Coast Clinical Research Network, including research support costs. We thank all of the staff and relatives at the six participating NHS trusts and the members of the Study Steering Committee chaired by David Kingdon, Professor of Mental Health Care Delivery within Medicine at the University of Southampton. We also thank Anthony Greenwood, Claire Hilton, Laura Wainwright, Sarah Tambo, Charlotte Rothwell and Samuel Williams for support with data collection or administrative tasks at Lancaster University, and Shashya Wijesinghe and Francesca Bentivegna for similar services at UCL.
We would like to acknowledge the extensive time and effort of all of the staff and relatives who took part in the IMPART study. This work would not have been possible without their generous co-operation. We would like to acknowledge further support for the study from Laura Wainwright and Claire Hilton who conducted the interviews with relatives and REACT supporters (respectively) in the REACT feasibility trial, which was used for the secondary analysis in phase 1. We would like to thank Nic Barnard for helping to pull together the report and make sure it all made sense (hopefully). All errors and confusion are the responsibility of the authors.
We have provided extensive quotations from data collected during this study from all six trusts. These have been carefully edited to ensure that all quotations are anonymous. We have also attempted to hide the identity of individual NHS trusts by allocating bird habitat names. Further data are not openly available because we would not be able to share this without jeopardising anonymity. Data may be available on request.
Contributions of authors
Fiona Lobban (https://orcid.org/0000-0001-6594-4350) (Spectrum Centre for Mental Health Research, Division of Health Research, Faculty of Health and Medicine, Lancaster University) was the chief investigator.
Duncan Appelbe (https://orcid.org/0000-0003-1493-0391) (CTRC, Department of Biostatistics, University of Liverpool) contributed IT design, management and support for the online collection of data from the study participants.
Victoria Appleton (https://orcid.org/0000-0002-7214-0702) (Spectrum Centre for Mental Health Research, Division of Health Research, Faculty of Health and Medicine, Lancaster University) was the lead research associate in the North of England sites in year 1.
Golnar Aref-Adib (https://orcid.org/0000-0003-2220-5317) (Division of Psychiatry, UCL) was author of the systematic review on factors affecting implementation of DHIs for people with psychosis or bipolar disorder and/or their family and friends.
Johanna Barraclough (https://orcid.org/0000-0003-1189-5340) (Spectrum Centre for Mental Health Research, Division of Health Research, Faculty of Health and Medicine, and the Department of Clinical Psychology, Lancaster University) was a trainee clinical psychologist researcher on the study with a focus on relatives’ data collection and analysis.
Julie Billsborough (https://orcid.org/0000-0002-4801-4853) (McPin Foundation) contributed data analysis, co-ran a SRG meeting, gave input into data days, contributed to the report and provided her perspective as a carer.
Naomi R Fisher (https://orcid.org/0000-0002-4851-7207) (Spectrum Centre for Mental Health Research, Division of Health Research, Faculty of Health and Medicine, Lancaster University) led on design of the implementation plans.
Sheena Foster (https://orcid.org/0000-0002-2052-9476) (McPin Foundation) contributed data analysis, co-ran a SRG meeting, gave input into data days, contributed to the report and provided her perspective as a carer.
Bethany Gill (https://orcid.org/0000-0002-8104-3955) (Research Associate, Spectrum Centre for Mental Health Research, Division of Health Research, Faculty of Health and Medicine, Lancaster University) was the North of England site lead research associate in the final year of the project and contributed data collection management and analysis.
David Glentworth was an IMPART lead at a participating trust.
Chris Harrop (https://orcid.org/0000-0002-0644-8127) was an IMPART lead at a participating trust.
Sonia Johnson (https://orcid.org/0000-0002-2219-1384) (Division of Psychiatry, UCL) was the South of England sites lead.
Steven H Jones (https://orcid.org/0000-0002-8801-5113) (Spectrum Centre for Mental Health Research; Division of Health Research; Faculty of Health and Medicine; Lancaster University) was a North of England site lead.
Tibor Z Kovacs (https://orcid.org/0000-0002-1572-4066) was a site PI and IMPART lead at a participating trust.
Elizabeth Lewis (https://orcid.org/0000-0001-8840-4621) (Research Assistant, Spectrum Centre for Mental Health Research, Division of Health Research, Faculty of Health and Medicine, Lancaster University) was the interim North of England sites lead research associate.
Barbara Mezes (https://orcid.org/0000-0002-0799-2423) (Research Associate, Spectrum Centre for Mental Health Research, Division of Health Research, Faculty of Health and Medicine, Lancaster University) wrote the methods and results sections of the quantitative study. She contributed to the conception and design of the quantitative components of the IMPART study and contributed to data collection, checking and analysis, production of graphs and tables and interpretation of results.
Charlotte Morton (https://orcid.org/0000-0003-3848-420X) (Research Assistant, Division of Psychiatry, UCL) was the lead research associate for the South of England sites.
Elizabeth Murray (https://orcid.org/0000-0002-8932-3695) (Research Department of Primary Care and Population Health, UCL) contributed to setting the research questions, designing the research methods and protocol, analysing and interpreting the data and writing the final report.
Puffin O’Hanlon (https://orcid.org/0000-0003-3515-1661) (Research Assistant, Division of Psychiatry, UCL) contributed to study design, protocol writing, data collection and qualitative data analysis.
Vanessa Pinfold (https://orcid.org/0000-0003-3007-8805) (McPin Foundation) was the PPI lead.
Jo Rycroft-Malone (https://orcid.org/0000-0003-3858-5625) (School of Healthcare Sciences, Bangor University) was a co-applicant, advised on the approach to case study data collection and analysis, and commented on drafts of the final report.
Ronald Siddle (https://orcid.org/0000-0002-2303-5148) was a grant holder, REACT lead and REACT supporter at a participating trust.
Jo Smith (https://orcid.org/0000-0002-0277-1680) (School of Allied Health and Community, University of Worcester) was an EIP expert clinical advisor.
Chris J Sutton (https://orcid.org/0000-0002-6406-1318) (Centre for Biostatistics, Division of Population Health, Health Services Research & Primary Care, School of Health Sciences, Faculty of Biology, Medicine and Health, The University of Manchester) gave input to the design and management of the project, support with statistical analysis and reporting of quantitative data, and input to the synthesis and interpretation of study results.
Pietro Viglienghi (https://orcid.org/0000-0002-0699-6596) took part in the pilot and was the IMPART lead at a participating trust.
Andrew Walker (https://orcid.org/0000-0001-6486-6135) (Spectrum Centre for Mental Health Research, Division of Health Research, Faculty of Health and Medicine, Lancaster University) is a digital technologist who was involved in the implementation of the REACT toolkit and the iterative development of the IMPART study. He also contributed data extraction, management and analysis.
Catherine Wintermeyer (https://orcid.org/0000-0002-9164-1334) (Spectrum Centre for Mental Health Research, Division of Health Research, Faculty of Health and Medicine, Lancaster University) was involved in the initial planning of the IMPART project and analysis of the REACT feasibility data.
Publications
Lobban F, Appleton V, Appelbe D, Barraclough J, Bowland J, Fisher NR, et al. IMPlementation of A Relatives’ Toolkit (IMPART study): an iterative case study to identify key factors impacting on the implementation of a web-based supported self-management intervention for relatives of people with psychosis or bipolar experiences in a National Health Service: a study protocol. Implement Sci 2017;12:152.
Aref-Adib G, McCloud T, Ross J, O’Hanlon P, Appleton V, Rowe S, et al. Factors affecting implementation of digital health interventions for people with psychosis or bipolar disorder, and their family and friends: a systematic review. Lancet Psychiatry 2019;6:257–66.
Lobban F, Appelbe D, Appleton V, Billsborough J, Fisher NR, Foster S, et al. IMPlementation of An online Relatives’ Toolkit for psychosis or bipolar (IMPART study): iterative multiple case study to identify key factors impacting on staff uptake and use. BMC Health Serv Res 2020;20:1–3.
Data-sharing statement
The PI and sponsor will ensure that all data are stored in formats that comply with widely accepted standards, in line with the recommendations of the UK Data Service (www.ukdataservice.ac.uk; accessed 6 December 2019) for data sharing, reuse and preservation. Standard protocols will be adopted for naming of files and versioning.
All anonymised new data will be prepared and stored in Lancaster University’s research data repository [via the university’s research information management system, Pure (Elsevier, Amsterdam, the Netherlands)] for a minimum of 10 years beyond the end of the project, under the university’s research data policy.
Ownership of copyright and intellectual property rights for all research conducted for the IMPART study will ultimately be held by Lancaster University, as sponsor. All new research data suitable for reuse will be available with an appropriate Creative Commons Licence (Attribution NonCommercial 4.0 International; CC BY-NC 4.0) that allows reuse by other researchers.
The PI is ultimately responsible for data management and sharing. The Lancaster University research data management team provided guidance on data management and sharing.
Extensive anonymised quotations from data collected during the study have been included in the report. All queries regarding these should be submitted to the corresponding author in the first instance. Access to further available anonymised data may be granted following review and if appropriate agreements are in place.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Aranda-Jan CB, Mohutsiwa-Dibe N, Loukanova S. Systematic review on what works, what does not work and why of implementation of mobile health (mHealth) projects in Africa. BMC Public Health 2014;14. https://doi.org/10.1186/1471-2458-14-188.
- Murray E, Hekler EB, Andersson G, Collins LM, Doherty A, Hollis C, et al. Evaluating digital health interventions: key questions and approaches. Am J Prev Med 2016;51:843-51. https://doi.org/10.1016/j.amepre.2016.06.008.
- House of Commons Health Committee . Managing the Care of People With Long-Term Conditions: Second Report of Session 2014–15 2014.
- Panagioti M, Richardson G, Small N, Murray E, Rogers A, Kennedy A, et al. Self-management support interventions to reduce health care utilisation without compromising outcomes: a systematic review and meta-analysis. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-356.
- Ruzek JI, Yeager CM. Internet and mobile technologies: addressing the mental health of trauma survivors in less resourced communities. Glob Ment Health 2017;4. https://doi.org/10.1017/gmh.2017.11.
- Arnberg FK, Linton SJ, Hultcrantz M, Heintz E, Jonsson U. Internet-delivered psychological treatments for mood and anxiety disorders: a systematic review of their efficacy, safety, and cost-effectiveness. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0098118.
- Drozd F, Vaskinn L, Bergsund HB, Haga SM, Slinning K, Bjørkli CA. The implementation of internet interventions for depression: a scoping review. J Med Internet Res 2016;18. https://doi.org/10.2196/jmir.5670.
- Alvarez-Jimenez M, Alcazar-Corcoles MA, González-Blanch C, Bendall S, McGorry PD, Gleeson JF. Online, social media and mobile technologies for psychosis treatment: a systematic review on novel user-led interventions. Schizophr Res 2014;156:96-106. https://doi.org/10.1016/j.schres.2014.03.021.
- Hidalgo-Mazzei D, Mateu A, Reinares M, Matic A, Vieta E, Colom F. Internet-based psychological interventions for bipolar disorder: Review of the present and insights into the future. J Affect Disord 2015;188:1-13. https://doi.org/10.1016/j.jad.2015.08.005.
- Berry N, Lobban F, Emsley R, Bucci S. Acceptability of interventions delivered online and through mobile phones for people who experience severe mental health problems: a systematic review. J Med Internet Res 2016;18. https://doi.org/10.2196/jmir.5250.
- O’Hanlon P, Aref-Adib G, Fonseca A, Lloyd-Evans B, Osborn D, Johnson S. Tomorrow’s world: current developments in the therapeutic use of technology for psychosis. BJPscyh Adv 2016;22:301-10. https://doi.org/10.1192/apt.bp.115.014654.
- NHS England . Five Year Forward View 2014.
- Gilbody S, Littlewood E, Hewitt C, Brierley G, Tharmanathan P, Araya R, et al. Computerised cognitive behaviour therapy (cCBT) as treatment for depression in primary care (REEACT trial): large scale pragmatic randomised controlled trial. BMJ 2015;351. https://doi.org/10.1136/bmj.h5627.
- Mohr DC, Weingardt KR, Reddy M, Schueller SM. Three problems with current digital mental health research . . . and three things we can do about them. Psychiatr Serv 2017;68:427-9. https://doi.org/10.1176/appi.ps.201600541.
- Haines A, Kuruvilla S, Borchert M. Bridging the implementation gap between knowledge and action for health. Bull World Health Organ 2004;82:724-31.
- Big Brother Watch . NHS-Data-Breaches. A Big Brother Watch Report November 2014 2014. www.bigbrotherwatch.org.uk/wp-content/uploads/2014/11/NHS-Data-Breaches-Report.pdf (accessed 4 August 2017).
- Department of Health and Social Care . Delivering 21st Century IT Support for the NHS: National Strategic Programme 2002.
- National Audit Office . Review of the Final Benefits Statement for Programmes Previously Managed Under the National Programme for IT in the NHS 2013. www.nao.org.uk/wp-content/uploads/2013/06/10171-001_NPfiT_Review.pdf (accessed 15 February 2015).
- Department of Health and Social Care . The Future of the National Programme for IT 2010. http://webarchive.nationalarchives.gov.uk/20120503092804/http://www.dh.gov.uk/en/MediaCentre/Pressreleases/DH_119293 (accessed 15 February 2015).
- Tinder Foundation . Health &Amp; Digital: Reducing Inequalities, Improving Society. An Evaluation of the Widening Digital Participation Programme 2016. http://nhs.tinderfoundation.org/wp-content/uploads/2016/07/Improving_Digital_Health_Skills_Report_2016.pdf (accessed 31 March 2018).
- McGrath JJ, Saha S, Al-Hamzawi A, Alonso J, Bromet EJ, Bruffaerts R, et al. Psychotic experiences in the general population: a cross-national analysis based on 31,261 respondents from 18 countries. JAMA Psychiatry 2015;72:697-705. https://doi.org/10.1001/jamapsychiatry.2015.0575.
- Simeone JC, Ward AJ, Rotella P, Collins J, Windisch R. An evaluation of variation in published estimates of schizophrenia prevalence from 1990–2013: a systematic literature review. BMC Psychiatry 2015;15. https://doi.org/10.1186/s12888-015-0578-7.
- McCrone PR, Dhanasiri S, Patel A, Knapp M, Lawton-Smith S. Paying the Price: The Cost of Mental Health Care in England to 2026. London: The King’s Fund; 2008.
- Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet 2013;382:1575-86. https://doi.org/10.1016/S0140-6736(13)61611-6.
- Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, Petukhova M, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch Gen Psychiatry 2007;64:543-52. https://doi.org/10.1001/archpsyc.64.5.543.
- Paykel ES, Abbott R, Morriss R, Hayhurst H, Scott J. Sub-syndromal and syndromal symptoms in the longitudinal course of bipolar disorder. Br J Psychiatry 2006;189:118-23. https://doi.org/10.1192/bjp.bp.105.013870.
- Andrew A, Knapp M, McCrone P, Parsonage M, Trachtenberg M. Effective Interventions in Schizophrenia – the Economic Case. A Report Prepared for the Schizophrenia Commission 2012.
- Winefield HR, Harvey EJ. Determinants of psychological distress in relatives of people with chronic schizophrenia. Schizophr Bull 1993;19:619-25. https://doi.org/10.1093/schbul/19.3.619.
- Barrowclough C, Tarrier N, Johnston M. Distress, expressed emotion, and attributions in relatives of schizophrenia patients. Schizophr Bull 1996;22:691-702. https://doi.org/10.1093/schbul/22.4.691.
- Lowyck B, De Hert M, Peeters E, Wampers M, Gilis P, Peuskens J. A study of the family burden of 150 family members of schizophrenic patients. Eur Psychiatry 2004;19:395-401. https://doi.org/10.1016/j.eurpsy.2004.04.006.
- Szmukler GI, Burgess P, Herrman H, Benson A, Colusa S, Bloch S. Caring for relatives with serious mental illness: the development of the Experience of Caregiving Inventory. Soc Psychiatry Psychiatr Epidemiol 1996;31:137-48. https://doi.org/10.1007/BF00785760.
- Barton K, Jackson C. Reducing symptoms of trauma among carers of people with psychosis: pilot study examining the impact of writing about caregiving experiences. Aust N Z J Psychiatry 2008;42:693-701. https://doi.org/10.1080/00048670802203434.
- Patterson P, Birchwood M, Cochrane R. Expressed emotion as an adaptation to loss: prospective study in first-episode psychosis. Br J Psychiatry Suppl 2005;48:s59-64. https://doi.org/10.1192/bjp.187.48.s59.
- Jones K. Addressing the needs of carers during early psychosis. Early Interv Psychiatry 2009;3:22-6. https://doi.org/10.1111/j.1751-7893.2009.00127.x.
- Tennakoon L, Fannon D, Doku V, O’Ceallaigh S, Soni W, Santamaria M, et al. Experience of caregiving: relatives of people experiencing a first episode of psychosis. Br J Psychiatry 2000;177:529-33. https://doi.org/10.1192/bjp.177.6.529.
- McDonell MG, Short RA, Berry CM, Dyck DG. Burden in schizophrenia caregivers: impact of family psychoeducation and awareness of patient suicidality. Fam Process 2003;42:91-103. https://doi.org/10.1111/j.1545-5300.2003.00091.x.
- Magliano L, Fadden G, Madianos M, de Almeida JM, Held T, Guarneri M, et al. Burden on the families of patients with schizophrenia: results of the BIOMED I study. Soc Psychiatry Psychiatr Epidemiol 1998;33:405-12. https://doi.org/10.1007/s001270050073.
- Möller-Leimkühler AM. Burden of relatives and predictors of burden. Baseline results from the Munich 5-year-follow-up study on relatives of first hospitalized patients with schizophrenia or depression. Eur Arch Psychiatry Clin Neurosci 2005;255:223-31. https://doi.org/10.1007/s00406-004-0550-x.
- Magliano L, Fadden G, Economou M, Held T, Xavier M, Guarneri M, et al. Family burden and coping strategies in schizophrenia: 1-year follow-up data from the BIOMED I study. Soc Psychiatry Psychiatr Epidemiol 2000;35:109-15. https://doi.org/10.1007/s001270050192.
- Lobban F, Barrowclough C, Jones S. Does expressed emotion need to be understood within a more systemic framework?. Soc Psychiatry Psychiatr Epidemiol 2006;41:50-5. https://doi.org/10.1007/s00127-005-0993-z.
- Onwumere J, Lotey G, Schulz J, James G, Afsharzadegan R, Harvey R, et al. Burnout in early course psychosis caregivers: the role of illness beliefs and coping styles. Early Interv Psychiatry 2017;11:237-43. https://doi.org/10.1111/eip.12227.
- Kuipers E, Watson P, Onwumere J, Bebbington P, Dunn G, Weinman J, et al. Discrepant illness perceptions, affect and expressed emotion in people with psychosis and their carers. Soc Psychiatry Psychiatr Epidemiol 2007;42:277-83. https://doi.org/10.1007/s00127-007-0165-4.
- Chessick CA, Perlick DA, Miklowitz DJ, Kaczynski R, Allen MH, Morris CD, et al. STED-BD Family Experience Collaborative Study Group. Current suicide ideation and prior suicide attempts of bipolar patients as influences on caregiver burden. Suicide Life Threat Behav 2007;37:482-91. https://doi.org/10.1521/suli.2007.37.4.482.
- Fletcher K, Parker GB, Manicavasagar V. Coping profiles in bipolar disorder. Compr Psychiatry 2013;54:1177-84. https://doi.org/10.1016/j.comppsych.2013.05.011.
- Hosang GM, Uher R, Maughan B, McGuffin P, Farmer AE. The role of loss and danger events in symptom exacerbation in bipolar disorder. J Psychiatr Res 2012;46:1584-9. https://doi.org/10.1016/j.jpsychires.2012.07.009.
- Morriss R, Yang M, Chopra A, Bentall R, Paykel E, Scott J. Differential effects of depression and mania symptoms on social adjustment: prospective study in bipolar disorder. Bipolar Disord 2013;15:80-91. https://doi.org/10.1111/bdi.12036.
- Lowenstein JA, Butler DW, Ashcroft K. The efficacy of a cognitively orientated carers group in an early intervention in psychosis service – a pilot study. J Psychiatr Ment Health Nurs 2010;17:628-35. https://doi.org/10.1111/j.1365-2850.2010.01564.x.
- Zendjidjian X, Richieri R, Adida M, Limousin S, Gaubert N, Parola N, et al. Quality of life among caregivers of individuals with affective disorders. J Affect Disord 2012;136:660-5. https://doi.org/10.1016/j.jad.2011.10.011.
- Chen FP, Greenberg JS. A positive aspect of caregiving: the influence of social support on caregiving gains for family members of relatives with schizophrenia. Community Ment Health J 2004;40:423-35. https://doi.org/10.1023/B:COMH.0000040656.89143.82.
- Veltman A, Cameron J, Stewart DE. The experience of providing care to relatives with chronic mental illness. J Nerv Ment Dis 2002;190:108-14. https://doi.org/10.1097/00005053-200202000-00008.
- National Institute for Health and Care Excellence . Psychosis and Schizophrenia in Adults (CG178) No. CG178 2014.
- National Institute for Health and Care Excellence . NICE Clinical Guideline. Bipolar Disorder: The Assessment and Management of Bipolar Disorder in Adults, Children and Young People in Primary and Secondary Care. 2014.
- Lobban F, Glentworth D, Chapman L, Wainwright L, Postlethwaite A, Dunn G, et al. Feasibility of a supported self-management intervention for relatives of people with recent-onset psychosis: REACT study. Br J Psychiatry 2013;203:366-72. https://doi.org/10.1192/bjp.bp.112.113613.
- Honary M, Fisher NR, McNaney R, Lobban F. A web-based intervention for relatives of people experiencing psychosis or bipolar disorder: design study using a user-centered approach. JMIR Ment Health 2018;5. https://doi.org/10.2196/11473.
- Lobban F, Robinson H, Appelbe D, Barraclough J, Bedson E, Collinge L, et al. Protocol for an online randomised controlled trial to evaluate the clinical and cost-effectiveness of a peer-supported self-management intervention for relatives of people with psychosis or bipolar disorder: Relatives Education And Coping Toolkit (REACT). BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-016965.
- Lobban F, Appleton V, Appelbe D, Barraclough J, Bowland J, Fisher NR, et al. IMPlementation of A Relatives’ Toolkit (IMPART study): an iterative case study to identify key factors impacting on the implementation of a web-based supported self-management intervention for relatives of people with psychosis or bipolar experiences in a National Health Service: a study protocol. Implement Sci 2017;12. https://doi.org/10.1186/s13012-017-0687-4.
- Marshall M, Lewis S, Lockwood A, Drake R, Jones P, Croudace T. Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: a systematic review. Arch Gen Psychiatry 2005;62:975-83. https://doi.org/10.1001/archpsyc.62.9.975.
- Rethink Mental Illness . Lost Generation: Why Young People With Psychosis Are Being Left Behind, and What Needs to Change 2014.
- NHS England . Guidance to Support the Introduction of Access and Waiting Time Standards for Mental Health Services 2015.
- Rathod S, Kingdon D, Pinninti N, Turkington D, Phiri P. Cultural Adaptation of CBT for Serious Mental Illness: A Guide for Training and Practice. Hoboken, NJ: John Wiley & Sons; 2015.
- Healthcare Quality Improvement Partnership, Royal College of Psychiatrists . Report of the Early Intervention in Psychosis Audit 2016.
- National Institute for Health and Care Excellence (NICE) . Psychosis, Schizophrenia in Adults; Quality Standard 80 2015. www.nice.org.uk/guidance/qs80 (accessed 6 December 2019).
- National Institute for Health and Care Excellence (NICE) . Bipolar Disorder in Adults. Quality Standard 95 2015. www.nice.org.uk/guidance/qs95 (accessed 6 December 2019).
- Lobban F, Glentworth D, Pinfold V, Minns V, Dunn G, Larkin W, et al. An Evaluation of the Feasibility and Effectiveness of a Supported Self Management Package for Relatives of People With Recent Onset Psychosis. Relatives Education and Coping Toolkit (REACT) Study: NIHR Research for Patient Benefit Final Report. 2012.
- Lobban F, Postlethwaite A, Glentworth D, Pinfold V, Wainwright L, Dunn G, et al. A systematic review of randomised controlled trials of interventions reporting outcomes for relatives of people with psychosis. Clin Psychol Rev 2013;33:372-82. https://doi.org/10.1016/j.cpr.2012.12.004.
- Wainwright LD, Glentworth D, Haddock G, Bentley R, Lobban F. What do relatives experience when supporting someone in early psychosis?. Psychol Psychother 2015;88:105-19. https://doi.org/10.1111/papt.12024.
- Lobban F, Glentworth D, Haddock G, Wainwright L, Clancy A, Bentley R. REACT Team . The views of relatives of young people with psychosis on how to design a Relatives Education And Coping Toolkit (REACT). J Ment Health 2011;20:567-79. https://doi.org/10.3109/09638237.2011.593592.
- Lobban F, Jones S, Johnson S, Minns V, Murray E. An Online Randomised Controlled Trial to Evaluate the Clinical and Cost Effectiveness of the Relatives Education And Coping Toolkit (REACT). NIHR Health Technology Assessment Efficient Designs Call. Southampton: National Institute for Health Research; n.d.
- Lobban F, Jones S, Johnsons S, Minns V, Pinfold V, Rycroft-Malone J, et al. IMPlementation of A Relatives’ Toolkit (IMPART Study): Examining the Critical Success Factors, Barriers and Facilitators to Implementation of an Online Supported Self-management Intervention in the NHS. Southampton: National Institute for Health Research Health Services and Delivery Research; n.d.
- Department of Health and Social Care . Research Governance Framework for Health and Social Care 2005.
- Pinnock H, Barwick M, Carpenter CR, Eldridge S, Grandes G, Griffiths CJ, et al. Standards for Reporting Implementation Studies (StaRI) statement. BMJ 2017;356. https://doi.org/10.1136/bmj.i6795.
- Yin RK. Case Study Research: Design and Methods. Newbury Park, CA: SAGE; 2014.
- May C, Finch T. Implementing, embedding, and integrating practices: an outline of normalisation process theory. Sociology 2009;43:535-54. https://doi.org/10.1177/0038038509103208.
- Greenhalgh T, Wherton J, Papoutsi C, Lynch J, Hughes G, A’Court C, et al. Beyond adoption: a new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. J Med Internet Res 2017;19. https://doi.org/10.2196/jmir.8775.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Medical Research Council Guidance . Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- Nilsen P. Making sense of implementation theories, models and frameworks. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0242-0.
- May CR, Mair F, Finch T, MacFarlane A, Dowrick C, Treweek S, et al. Development of a theory of implementation and integration: normalization process theory. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-29.
- Mair FS, May C, O’Donnell C, Finch T, Sullivan F, Murray E. Factors that promote or inhibit the implementation of e-health systems: an explanatory systematic review. Bull World Health Organ 2012;90:357-64. https://doi.org/10.2471/BLT.11.099424.
- Murray E, Burns J, See TS, Lai R, Nazareth I. Interactive health communication applications for people with chronic disease. Cochrane Database Syst Rev 2005;4. https://doi.org/10.1002/14651858.CD004274.pub4.
- Murray E, Treweek S, Pope C, MacFarlane A, Ballini L, Dowrick C, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med 2010;8. https://doi.org/10.1186/1741-7015-8-63.
- Aref-Adib G, McCloud T, Ross J, O’Hanlon P, Appleton V, Rowe S, et al. Factors affecting implementation of digital health interventions for people with psychosis or bipolar disorder, and their family and friends: a systematic review. Lancet Psychiatry 2019;6:257-66. https://doi.org/10.1016/S2215-0366(18)30302-X.
- Proctor EK, Powell BJ, McMillen JC. Implementation strategies: recommendations for specifying and reporting. Implement Sci 2013;8. https://doi.org/10.1186/1748-5908-8-139.
- Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0209-1.
- Leeman J, Birken SA, Powell BJ, Rohweder C, Shea CM. Beyond ‘implementation strategies’: classifying the full range of strategies used in implementation science and practice. Implement Sci 2017;12. https://doi.org/10.1186/s13012-017-0657-x.
- Ritchie J, Lewis J, Nicholls CM, Ormston R. Qualitative Research Practice: A Guide for Social Science Students and Researchers. Newbury Park, CA: SAGE; 2013.
- Mohr DC, Lyon AR, Lattie EG, Reddy M, Schueller SM. Accelerating digital mental health research from early design and creation to successful implementation and sustainment. J Med Internet Res 2017;19. https://doi.org/10.2196/jmir.7725.
- Cooperrider DL, Srivastva S. Appreciative inquiry in organizational life. Res Organ Change Dev 1987;1:129-69.
- Davidoff F, Dixon-Woods M, Leviton L, Michie S. Demystifying theory and its use in improvement. BMJ Qual Saf 2015;24:228-38. https://doi.org/10.1136/bmjqs-2014-003627.
- May C, Rapley T, Mair FS, Treweek S, Murray E, Ballini L, et al. Normalization Process Theory On-Line Users’ Manual, Toolkit and NoMAD Instrument 2015. www.normalizationprocess.org/npt-toolkit/ (accessed 30 January 2020).
- Granja C, Janssen W, Johansen MA. Factors determining the success and failure of eHealth Interventions: systematic review of the literature. J Med Internet Res 2018;20. https://doi.org/10.2196/10235.
- Lobban F, Appelbe D, Appleton V, Billsborough J, Fisher NR, Foster S, et al. IMPlementation of An online Relatives’ Toolkit for psychosis or bipolar (IMPART study): iterative multiple case study to identify key factors impacting on staff uptake and use. BMC Health Serv Res 2020;20:1-3. https://doi.org/10.1186/s12913-020-5002-4.
- Royal College of Psychiatrists . Report of the Second Round of the National Audit of Schizophrenia (NAS) 2014 2014.
- Goldberg DP, Hillier VF. A scaled version of the General Health Questionnaire. Psychol Med 1979;9:139-45. https://doi.org/10.1017/S0033291700021644.
- Quirk A, Smith S, Hamilton S, Lamping D, Stahl D, Pinfold V, et al. Development and Validation of the Carer Well-Being and Support (CWS) Questionnaire: Report for the National Institute for Health Research Service Delivery and Organisation Programme 2009.
- Herdman M, Gudex C, Lloyd A, Janssen MF, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. https://doi.org/10.1007/s11136-011-9903-x.
- Norman CD, Skinner HA. eHEALS: the eHealth literacy scale. J Med Internet Res 2006;8. https://doi.org/10.2196/jmir.8.4.e27.
- Goldberg D. Manual of the General Health Questionnaire. Windsor: NFER Nelson; 1978.
- Spradley JP, McCurdy DW. Anthropology, the Cultural Perspective. Hoboken, NJ: John Wiley & Sons; 1980.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Great Britain . Data Protection Act 2018 n.d. www.legislation.gov.uk/ukpga/2018/12/contents/enacted (accessed 6 December 2019).
- European Union . EU General Data Protection Regulation n.d. www.gov.uk/government/publications/guide-to-the-general-data-protection-regulation (accessed 6 December 2019).
- Audit of Early Intervention in Psychosis . Report of the Early Intervention in Psychosis Audit 2016.
- Bentall RP. Madness Explained: Psychosis and Human Nature. London: Penguin Books; 2004.
- Vermeulen B, Lauwers H, Spruytte N, Van Audenhove C. P.1.k.038 Experiences of family caregivers for persons with severe mental illness: an international exploration. Eur Neuropsychopharmacol 2015;25. https://doi.org/10.1016/S0924-977X(15)30484-3.
- Worthington A, Rooney P, Hannan R. The Triangle of Care. Carers Included: A Guide to Best Practice in Mental Health Care in England. London: Carers Trust; 2013.
- Department of Health and Social Care . Achieving Better Access to Mental Health Services by 2020 2014.
- NHS England . The Forward View into Action: Planning for 2015 16 2014.
- Levy F. Computers and populism: artificial intelligence, jobs, and politics in the near term. Oxf Rev Econ Policy 2018;34:393-417. https://doi.org/10.1093/oxrep/gry004.
- Department of Health and Social Care . Explanatory Notes: Care Act 2014 – Chapter 23 2014.
- Iacobucci G. NHS plan calls for new models of care and greater emphasis on prevention. BMJ 2014;349. https://doi.org/10.1136/bmj.g6430.
- Department of Health and Social Care . Lessons Learned Review of the WannaCry Ransomware Cyber Attack 2018.
- Wise J. . Survey of UK doctors highlights blame culture within the NHS. BMJ 2018;362. https://doi.org/10.1136/bmj.k4001.
- Triandis HC. Individualism and Collectivism. Abingdon: Routledge; 2018.
- The King’s Fund . The NHS Budget and How It Has Changed 2018. www.kingsfund.org.uk/projects/nhs-in-a-nutshell/nhs-budget (accessed 30 November 2018).
- Rogers MA, Lemmen K, Kramer R, Mann J, Chopra V. Internet-delivered health interventions that work: systematic review of meta-analyses and evaluation of website availability. J Med Internet Res 2017;19. https://doi.org/10.2196/jmir.7111.
- Greenhalgh T. How to improve success of technology projects in health and social care. Public Health Res Pract 2018;28. https://doi.org/10.17061/phrp2831815.
- National Institute for Health and Care Excellence (NICE) . NICE Boosts Support for Innovative Ideas 2013. www.nice.org.uk/news/article/nice-boosts-support-for-innovative-ideas (accessed 30 November 2018).
- Eysenbach G. The law of attrition. J Med Internet Res 2005;7. https://doi.org/10.2196/jmir.7.1.e11.
- Verheijden MW, Jans MP, Hildebrandt VH, Hopman-Rock M. Rates and determinants of repeated participation in a web-based behavior change program for healthy body weight and healthy lifestyle. J Med Internet Res 2007;9. https://doi.org/10.2196/jmir.9.1.e1.
- Brewster L, Mountain G, Wessels B, Kelly C, Hawley M. Factors affecting front line staff acceptance of telehealth technologies: a mixed-method systematic review. J Adv Nurs 2014;70:21-33. https://doi.org/10.1111/jan.12196.
- Huryk LA. Factors influencing nurses’ attitudes towards healthcare information technology. J Nurs Manag 2010;18:606-12. https://doi.org/10.1111/j.1365-2834.2010.01084.x.
- Barrowclough C, Gooding P, Hartley S, Lee G, Lobban F. Factors associated with distress in relatives of a family member experiencing recent-onset psychosis. J Nerv Ment Dis 2014;202:40-6. https://doi.org/10.1097/NMD.0000000000000072.
- May CR, Johnson M, Finch T. Implementation, context and complexity. Implement Sci 2016;11. https://doi.org/10.1186/s13012-016-0506-3.
- Wachter R. Making IT Work: Harnessing the Power of Health Information Technology to Improve Care in England. Executive Summary. London: Department of Health and Social Care; 2016.
- Labrique A, Vasudevan L, Weiss W, Wilson K. Establishing standards to evaluate the impact of integrating digital health into health systems. Glob Health Sci Pract 2018;6:S5-17. https://doi.org/10.9745/GHSP-D-18-00230.
- Lamb N. Discrimination at the Heart of the NHS: Early Intervention in Psychosis: The Failure to Deliver the Same Standards of Access to Evidence-based Treatment for those with Mental Health as those with Physical Health Problems. London: Liberal Democrats; 2018.
- Department of Health and Social Care . The Mental Health Policy Implementation Guide 2001.
- Pharoah F, Mari J, Rathbone J, Wong W. Family intervention for schizophrenia. Cochrane Database Syst Rev 2010;12. https://doi.org/10.1002/14651858.CD000088.pub2.
- Birken SA, Powell BJ, Shea CM, Haines ER, Alexis Kirk M, Leeman J, et al. Criteria for selecting implementation science theories and frameworks: results from an international survey. Implement Sci 2017;12. https://doi.org/10.1186/s13012-017-0656-y.
- Pawson R, Tilley N. Realistic Evaluation. London: SAGE; 1997.
- Lobban F, Akers N, Appelbe D, Iraci Capuccinello R, Chapman L, Collinge L, et al. A web-based, peer-supported self-management intervention to reduce distress in relatives of people with psychosis or bipolar disorder: the REACT RCT. Health Technol Assess 2020;24. https://doi.org/10.3310/hta24320.
- Zillien N, Hargittai E. Digital distinction: status-specific types of internet usage. Soc Sci Q 2009;90:274-91. https://doi.org/10.1111/j.1540-6237.2009.00617.x.
- Kontos E, Blake KD, Chou WY, Prestin A. Predictors of eHealth usage: insights on the digital divide from the Health Information National Trends Survey 2012. J Med Internet Res 2014;16. https://doi.org/10.2196/jmir.3117.
- Scheerder A, van Deursen A, van Dijk J. Determinants of internet skills, uses and outcomes. A systematic review of the second- and third-level digital divide. Telematics Informatics 2017;34:1607-24. https://doi.org/10.1016/j.tele.2017.07.007.
- Wainwright L. Carers’ Needs and Self Management in Bipolar Disorder and Psychosis. n.d.:2009-13.
- Sutton RI, Staw BM. What theory is not. Adm Sci Q 1995;40:371-84. https://doi.org/10.2307/2393788.
Appendix 1 Patient and public involvement strategy
The IMPART project was designed to involve mental health service users and carers at every stage and level of decision-making. The funding bid was developed with a carer who had been involved in the original REACT toolkit evaluation. Roles were designed and costed on the independent SSG for two PPI experts. Advisory groups were planned for each study site, drawing on local carer/service user knowledge and expertise to support the implementation process. A co-ordinating agency, the McPin Foundation, was appointed to lead on the PPI programme, drawing on experience from other studies and its involvement in the development of the original REACT toolkit.
Our successes in the project included ensuring that mental health carers and service users were involved throughout, despite a number of challenges. We created new roles after the study commenced for two peer researchers because we were missing this expertise, particularly when planning data collection workshops and involvement in data analysis. The peer researchers stayed with the study to the end, which worked well. They co-facilitated stakeholder workshops, worked with researchers on the analysis of the relatives’ data, were involved in project management meetings, planned and co-facilitated stakeholder workshops and contributed to report writing as well as to peer review papers.
Carer researchers prioritised which parts of the REACT website to turn into PDF download resources, and helped the team to word e-mails appropriately when inviting carers to take part in the study.
Our challenges included the study carer co-applicant withdrawing from the study near the beginning, the changing role of our local research advisory groups from research advisors to research participants, the length of time it took to gain research passports for our peer researchers and keeping everyone updated on study progress. There were also difficulties with the SSG, appointed by NIHR to oversee our work, ensuring that PPI roles felt meaningful for group members.
Experiences and lessons learnt
In this section, we review the contributions made by different parts of the PPI programme. This section was co-written by Vanessa Pinfold and the carer researchers (Julie Billsborough and Sheena Foster), as well as via e-mail communication with SSG members.
Study Steering Group
The SSG was an independent group, including two people drawing on expertise from experience gained by being a mental health carer or service user.
Throughout the study, meetings were held largely via teleconference, including PMG and SSG meetings. PPI in research often relies on the building of relationships to generate successful partnerships. This was hard to establish using this platform and, when coupled with infrequent meetings, keeping members engaged and up to date on the study was hard. One PPI member of the SSG withdrew because they did not attend several meetings. We recruited another by looking for a service user researcher employed in the sector who could take on the role within their substantive position. However, they were unable to attend any meetings because of several changes in dates and other commitments. By the end, no PPI members were still engaged in the IMPART SSG.
The SSG is a requirement for NIHR-funded studies and is responsible for monitoring progress. One PPI member’s feedback stated that their role felt token and that communication was infrequent. They felt that their contribution was not valued:
I suggest that if we want researchers to include PPI we should be as robust as we are about the arrangements for management of participants/research subjects. Thus, as [a] clear plan, setting out aims and objectives and how researchers will demonstrate they have achieved these; thus, holding a meeting wouldn’t cut the ice on an application review process because the question would be why hold the meeting, what are costs of doing this, what has been done to achieve maximum participation and what changed as a result of the meeting.
PPI member
How can PPI roles be developed in the NIHR monitoring structure to ensure meaningful involvement but remain independent of the research team? A key challenge is that the research team cannot chair the SSG. The group is appointed by NIHR but administered by the research team, leading to blurring of responsibilities. We observe from this experience that greater guidance from NIHR on PPI positions within the SSG would be useful (e.g. role clarity, responsibilities, whistleblowing process), and support and training for people in these roles should be delivered through NIHR so that individuals can remain independent.
Project Management Group
The PMG was chaired by the chief investigator and met via teleconference, first via video link but more successfully using telephone calls. At the start of the project, McPin Foundation staff joined the calls, and helped to plan the set-up of the SRGs and local data collection.
After the carer co-applicant left the team, we looked for other ways to ensure that service user and carer expertise were included in the PMG. This led to the recruitment of two peer researchers, who were invited to PMG meetings. These sessions helped with planning, active communication of project progress and team building. To ensure that everyone contributed and felt involved, the chairperson always asked for individual comments. These meetings were well received by the peer researchers, who found the monthly telephone calls an important mechanism for staying engaged with study progress and assessing how they could add most value to the study, such as offering to interview carers.
Peer researchers
We employed two peer researchers, both with research expertise and experience as mental health carers, to work on IMPART. The roles were developed by the PPI lead and study PI. Careful consideration was given to practical support required to sustain the roles, what specific tasks might be given to the roles, and resourcing. We decided to locate one role with the main team in Lancaster, providing easy access to the study team, including training in NVivo, with key responsibilities for data analysis. The second role was focused on co-facilitating the workshops and making changes to REACT through waves 1 and 2, requiring travel across the six study sites.
Both of these were small roles, not substantive posts, and this limited opportunities for involvement. For example, the peer researchers would have liked to have been involved in collecting interview data. However, there was some confusion about whether or not PPI members of the team required research passports, and once it was established that they did, there were further delays in organising the required documents. This was frustrating for those involved, and is one of the lessons from this study. Feedback from the peer researchers reflected their experiences:
I felt that the PPI involvement has been a bit sporadic and some of the researchers didn’t fully understand the benefits of involving carers or how to involve us.
Peer researcher 1
Generally felt involved with the project but not clear that there was a complete understanding of how they could use carers as peer researchers and the clear benefits from doing so.
Peer researcher 2
In the final 6 months of the study, research passports were gained and involvement increased, leading to greater satisfaction for the peer researchers. Both contributed to the explanatory synthesis days in July 2018 and worked with a Lancaster-based researcher on analysing relatives’ interview data:
Getting involved in analysing the relatives’ data made me feel a lot more involved in the study. It was great to see the interview transcripts and to get a better feel for how relatives viewed REACT.
Peer researcher 1
I think involvement is a learning curve for everyone. I appreciate that it may be difficult to know how best to use someone’s skills, particularly if you haven’t worked with them before.
Peer researcher 2
Recommendations for other studies
When recruiting to PPI roles in research studies, there is a need to recognise carers’ skills above and beyond their caring role. Some carers will have research skills and will have worked as researchers, whereas others will not have this experience. Consider what sort of input you want carers to provide, and when, throughout the study. What caring experiences may people need to have in order to provide the input your study requires? This may sound easy, but it is complicated and can require research teams to be willing to do things differently, including shared decision-making, more detailed planning and training for the wider team in why PPI is important. It also requires PPI contributors to understand the limits of their role and seek clarity early when anything is unclear or feels token. Open two-way dialogue is important to prevent misaligned expectations.
Ensuring that the whole team is on board with PPI in the study is important. Co-applicants may design PPI strategies and support them, but changeover of research staff during projects can lead to less involvement for PPI roles. Plans for training and support are required so that people in PPI roles learn and develop, and feel supported to be fully involved in the research study. This guards against tokenism.
Carers can find it difficult to say – even when working in mental health research – that they do not feel able to take on challenging work at the time. It is important to spend time building relationships with PPI members of the team and ensure that people are able to be honest about the work a study team is offering.
Effort is required to keep PPI members on board throughout a study. This includes good communication and clarity about roles, payment and support on offer. It is more difficult to give input to a research project ad hoc. This needs to be recognised and a strategy put in place to ensure that involvement is meaningful at all points of contact.
Involving carers in research may have its challenges for researchers too. It might be useful to note down which aspects of PPI went well and what could have been improved.
Clarity is needed over who appoints, trains and supports the SSG. If it is to be independent of the research team, it would be helpful if NIHR managed this process, including recruiting members, training, offering support and providing someone within the group to undertake administration. It is difficult for the research team to establish and support an independent group to oversee its own work.
Finally, we reflect that better clarity is required over PPI leadership in studies and the roles and responsibilities of different contributors. Within IMPART, the PPI lead role was split between two people, neither working in the two lead universities, Lancaster University and UCL, but employed and managed by the McPin Foundation. In practice, a lot of the direction of PPI input came from the operational study team, including the chief investigator and study research assistants. Sorting out early how responsibilities are to be allocated, decisions are to be communicated and budgets are to be managed is essential.
Appendix 2 Secondary analysis of REACT feasibility trial data
Introduction
This report looks at two sets of interviews conducted with people taking part in a RCT testing the feasibility and effectiveness of REACT. 53
The main aim of this study was to identify the key factors affecting the implementation of REACT in the feasibility study, and consider how these might inform the development of hypotheses for the IMPART study.
Background
The feasibility trial was a stratified randomised controlled feasibility trial in which 103 participants were allocated with a ratio of 1 : 1 to receive either TAU or TAU plus the REACT intervention. REACT was a paper-based toolkit (also available in online PDFs) supported by members of the participating clinical teams.
Following baseline assessments, independent randomisation was done by a UK clinical trials unit. Participants were relatives, partners or close friends of people experiencing psychosis who were currently being supported by the EIP services within a participating NHS trust. These teams support young people experiencing psychotic symptoms between the ages of 14 and 35 years for a period of up to 3 years. 53 Only relatives in direct contact with EIP services were invited to take part. Only one relative per family (the self-identified main carer) took part in the study, but they were encouraged to share the intervention with other close family members. Additional inclusion criteria included that the first contact with EIP services be within the past 24 months and that participants be aged > 18 years with sufficient understanding of written and spoken English (translations and interpreters were not routinely available). All participants gave written informed consent. The main finding was that, compared with TAU only, those receiving the additional REACT intervention showed reduced distress and increased perceived support and perceived ability to cope at the 6-month follow-up.
For the purposes of the feasibility trial, REACT was a supported self-management package consisting of 13 sections that were modular and could be used flexibly. These modules contained information pertaining to psychosis in general but also had information designed to provide relatives of people with psychosis with specific information for the family, as well as case studies and signposting to other resources. Modules included What is Psychosis?, Managing Positive Symptoms, Managing Negative Symptoms, Dealing with Crises, Dealing with Difficult Behaviour, Managing Stress – Thinking Differently, Managing Stress – Doing Things Differently, Understanding Mental Health Services, Treatment Options, The Future, Resource Directory and Jargon Terms. Participants were given a printed version of the toolkit as well as being offered an online version. Each participant was supported to use the toolkit by somebody working in EIP services in the NHS; these people were called REACT supporters.
Support was targeted at helping relatives to identify the key difficulties they faced and guiding them to find the most relevant information and strategies in the toolkit. Discussion then focused on making these general principles as directly relevant as possible to each individual participant, and on helping relatives to try out new strategies and reflect on the outcomes of this. All relatives were offered an initial face-to-face session in which they were introduced to the toolkit and arrangements for support were agreed. Support was offered by e-mail or telephone (relative’s preference) for a maximum of 1 hour per week over 6 months. To ensure that communication was maintained, supporters were asked to contact relatives monthly as a minimum if the relatives did not respond to appointments or initiate contact.
REACT supporters attended 4 days of training spaced over 3 months, followed by monthly group supervision for the duration of the project.
Forty-seven relatives (92%) had a face-to-face introductory session lasting between 35 and 90 minutes, with a median length of 60 minutes. The number of subsequent support sessions (defined as contacts lasting ≥ 5 minutes) ranged from 0 to 17, with a median number of 3 sessions (IQR 2–6 sessions). The length of support sessions ranged from 5 to 90 minutes, with a median of 25 minutes (IQR 15–40 minutes). Total minutes of REACT supporter contact with relatives over the 6-month intervention period ranged between 0 and 855 minutes, with a median of 125.5 minutes (IQR 75–204 minutes).
Thirty-one participants (61%) received support via telephone only, six (12%) by e-mail only and seven (14%) had a combination of both. Three participants (6%) did not receive any additional support after the introductory session. Only one participant requested access to the online version of the toolkit.
The aim of this study was to identify factors influencing implementation of REACT during the feasibility trial from feedback given by supporters and relatives.
These data were used alongside a scoping review of the implementation literature, and an analysis of the views of relatives and key staff in participating NHS trusts (ascertained in focus groups), to generate hypotheses about what factors may affect the implementation of an online version of REACT in six NHS trusts as part of the IMPART study. The data from all sources were interpreted within the framework of NPT to guide the development of an analysis framework for the IMPART study.
Methods
Ethics approval for collection of interview data in the REACT feasibility trial was given by East of England – Cambridge South Research Ethics Committee (reference 08/H1001/147).
REACT supporters
Six NHS supporters were initially trained to support REACT. All had an interest in mental health. One had been a service user and one was a parent of someone with mental health difficulties. Although feedback about the training was generally positive, one dropped out during training because he had left his post in the service, another dropped out following training because of changes in his role within the EIP team and one was unable to continue owing to ill health. Supporters who remained with the study worked flexibly to cover work across teams, and additional input was required from one of the research team, a trained nurse therapist (REACT supporter 1), to support three participants. Interviews were conducted with the four active supporters at the end of the study: two men and two women, with a mean age of 42 years. Three participants were working or had worked as support time and recovery workers in EIP; the other participant was a nurse, cognitive–behaviour therapist and a family intervention worker. As part of the original study, all participants consented to be interviewed, and for the data to be analysed to understand their experience of their role as REACT supporters.
Materials
A comprehensive topic guide was used to explore the REACT supporters’ experience of providing support in the REACT study. Areas covered included their general impressions of the REACT project and the toolkit, their experiences working with the relatives and whether or not they felt that the support was valuable, and practical issues in delivering REACT as designed.
REACT participants
Participants
Relatives were recruited from NHS EIP services in the north-west of England who had taken part in the REACT trial. 53 The first 14 participants who were contactable by telephone were given information and asked if they would like to take part in an interview. Twelve agreed but two declined, stating that they were too busy. It was felt that 12 participants would provide a manageable data set and as this number was just under one-quarter of those who had received the intervention it was also felt that this was likely to encapsulate the participants’ experiences well. For this analysis, 1 of the 12 interview transcript Microsoft Word documents would not open as the electronic file had become corrupted, so only 11 of the 12 interviews were coded for this report. All relatives had used the printed version of the toolkit.
Ten mothers, one father and one father-in-law, all aged 46–60 years, took part, with all their relatives experiencing an episode of psychosis. They were all white British and the majority (n = 10) were living with their relative. Six were employed full time, five were unemployed or retired and one was in part-time work. Seven were aware of a diagnosis: psychosis (n = 5), depression (n = 1) and bipolar disorder (n = 1). The relatives’ perception of time since diagnosis had a mean of 10.63 months (range 1–28 months).
Relatives were provided with written information and invited to discuss the study with the researcher; if they agreed to take part, they were asked to give written consent.
Procedure
All participants were offered to be interviewed in their own home, at NHS trust premises, at a university or in a public space. Interviews were digitally recorded. The initial part of each interview explored the participant’s experience of supporting their relative with psychosis and their experience of coping, and was analysed and published as part of a Doctor of Philosophy thesis. 135 The second part, which has been used for this report, followed a topic guide exploring four areas: their general experience of using REACT, how they used the REACT toolkit, their view of the REACT support and whether or not anything changed for them as a result of having used REACT. The interviewer made it clear that both positive and negative feedback would be beneficial.
Analysis
For this report, 11 interview transcripts from the REACT relatives and four REACT supporters were read in detail by the researcher (CW). Catherine Wintermeyer had not conducted the interviews and was conducting a secondary analysis of these data, so spent considerable time immersing herself in the data to familiarise herself with the interviews. Each interview was then coded line by line, and codes were discussed in supervision and grouped into subthemes that summarised the key factors identified. Further discussion focused on grouping subthemes and further developing key themes that were relevant to the research question: what are the factors affecting implementation of REACT? Indicative quotations were used to illustrate the themes, and ensure clear links between the data and the findings.
The identified themes were then further refined at a ‘data day’ in which all members of the IMPART PMG worked with these data to finalise the key themes and draw out the implications of the hypotheses generated as part of the IMPART study, bearing in mind the changes to the way REACT was delivered in this study.
Coding the identification of subthemes was done separately for supporters and relatives. However, in identifying the final themes and implications for IMPART hypothesis generation, we attempted to integrate the findings and to present the perspectives of both relatives and supporters in relation to each of the key factors.
Given the distance between the interviews and the analysis in terms of time and location of personnel, no attempt was made to carry out an in-depth interpretative analysis as we did not feel that this would be of value or appropriate to meet the aims of the analysis.
Results
The key factors identified as affecting the implementation of REACT are best described within the following themes:
-
design and content of the toolkit
-
timing of the REACT intervention
-
structure and delivery of support
-
perceived benefits of the toolkit for relatives
-
balancing the REACT supporter role with a general support worker role.
Each theme is outlined in detail in the following sections. Table 25 summarises the key factors affecting the implementation of REACT.
| Factor | REACT supporters | REACT relatives |
|---|---|---|
| Design and content of the toolkit |
|
|
| Timing of the REACT intervention |
|
|
| Structure and delivery of support |
|
|
| Perceived benefits for relatives |
|
|
| Balancing REACT supporter role with general support worker role |
|
Design and content of the toolkit
REACT supporters felt that the content of the toolkit was easy to follow and self-explanatory, as well as being bright, colourful, engaging and written in a friendly way. It was also described as being flexible and matching what families needed at that time, making it acceptable to a broad range of people. The REACT supporters reported that the case studies were helpful for participants too, as they were accessible, funny and they felt that relatives could identify with the specific challenges that the characters were facing, including duration of illness and stigma:
The toolkit is written so simplistically it’s so easy for them to follow.
REACT supporter 2
Toolkit’s very self-explanatory.
REACT supporter 3
It’s flexible so you can titrate the support according to need . . . looks official but it’s kind of informal and cool enough to not to put people off. It looks inviting, it’s easy to read. Erm, the content of the material, er, I think is good . . . is accessible, yes.
REACT supporter 1
Despite this, supporters recognised several limitations to REACT. They felt that REACT was helpful for people who were well organised, literate and used to reading or studying, whereas many of the people they visited had more chaotic lifestyles, were not as literate and did not use printed media, and so were likely to find REACT more overwhelming. The provision of static information that was difficult to update was also noted, implying that an online resource would be more appropriate in this context:
Erm, I think it probably needs fine tuning, as soon as you write something down it’s out of date, and I think that is one of the problems with um with printed material, with a printed resource like that is that, um, people are becoming increasingly used to getting information from a variety of sources, not just printed material. So, so I think in the [pause] it has this limitation in that respect.
REACT supporter 1
One supporter highlighted the fact that REACT was unlikely to meet the needs of all relatives, pointing out that:
We’ve got one size toolkit, but people come in different sizes. So it didn’t meet everybody’s needs.
REACT supporter 1
Relatives were also generally positive about what REACT offered:
Erm . . . at that time I was so desperate that I was just delighted to get anything, I had been all over the internet but you know yourself if you have ever done that it’s mostly either for professionals or for illness-specific type things and what have you. When I got REACT manual, I felt better because it showed me, it first of all it related to what was going on in my house.
Relative 024
Positive comments were made about the structure and layout of the toolkit, with relatives describing it as bright and colourful, which made it appealing to read. Relatives described it as ‘well laid out’, ‘very clear’ and ‘well presented’ with ‘nice colours’. Most relatives liked the modular aspect as they felt that they could access the parts they wanted by just looking at that particular section and they liked being able to take out one particular book instead of holding the whole toolkit:
It’s very nice to look at. I thought it was clear, very colourful. I loved the drawing. I liked the humour in it. Erm I like the fact you can take the books out, so you haven’t got to have all of it in your hand. You can find your way round it on your own.
Relative 046
Key aspects of the toolkit that relatives identified positively included creating a list of helpful telephone numbers for use in a crisis; contact with other services, which made them feel less isolated; self-reflection tasks; and case studies:
Examples in the books are good. The examples of the, you know, the case study things. Because they seemed real. And, er, yeah, I just did find it really useful.
Relative 046
One relative liked the real-life examples but felt that some of the solutions needed ‘a saint to react like that’; nevertheless, they found the different point of view interesting, even if they took only part of it away:
But I like the stories that they did. But having said that you know sometimes, the solutions what they used must be a saint that would think like that you know . . . Erm . . . but like one of them was saying it’s trying to ask you how you would react to it, and erm . . . I don’t think I will ever react like that erm . . . but it was interesting. I mean, they were like saints they way they were reacting to it, but it’s nice to somebody else’s point of view and if you just take a part of it away, I think that’s good.
Relative 040
Another suggestion was for more examples from more complex family situations, including managing the responses of other people involved in the family system:
Like a scenario where there is a family of five and there is a step-dad involved, who is not the natural father and he is having to, the poor wife is having to cope with him, as well as him and them, do you know what I mean, there is, there is . . . I have got to be, I have got to be in the middle of them all, got to keep them all happy.
Relative 032
Overall, the content of the toolkit seemed to cater for many of the needs of the relatives in terms of information they were seeking. However, individual relatives did make suggestions of things they would have liked even more information about, including occupational therapy with suggestions of activities, medication, and family therapy and working together as a family.
Timing of the REACT intervention
Although REACT was offered to relatives in EIP teams in the feasibility study, many of these relatives had been supporting someone with psychosis for many years. Both supporters and relatives felt that the toolkit came too late for these relatives, who have already had to try to find information on the internet to answer their questions (which supporters described as ‘pretty scary’) and figure out a way of dealing with things themselves.
One REACT supporter summarised the issue as:
Everybody I met loved it, there was not criticism for the toolkit, except for ‘I’ve already figured this information out for myself, but had this been a year ago . . . would have been a godsend’.
REACT supporter 3
They suggested that to overcome this problem, REACT needed to be included as an early step in the trust care pathway:
So I think what a good idea would have been is, which I know isn’t always practical in terms of the study, but if this was going to be rolled out as standard in the NHS, was as soon as the person is accepted by the EIP team, their next-of-kin carer was identified and approached and asked ‘Would you like one of these support kits to help you?’.
REACT supporter 3
The REACT supporters reported a lot of variation in how often and when they were called on to give support. In general, relatives who were in crisis or facing a lot of difficulties were more likely to use the support offered. A common pattern for those not in crisis was for the supporter to initially see the relative face to face then speak a week later; contact would then drop to fortnightly, then monthly:
With some of them, they didn’t use it initially. And it’s like with anything else, if you know it’s there, some people just didn’t need to use it . . . but if there was a crisis came up or there was someone who had a particularly, um, one of their children were in the services and they were having a particularly turbulent time with them, I’d hear more from them.
REACT supporter 4
Consistent with the views of the REACT supporters, the REACT relatives felt that the toolkit would have been more useful earlier on and might have changed the way they responded. They also felt that they would have been more likely to read it more in the early stages:
If I had had it there, then I wouldn’t have aged 10 years . . . would have been so much easier for all of us . . . taken the abject fear out of it . . . would have made a very big difference.
Relative 024
Difficult times were often a trigger for turning to the toolkit:
If she has been particularly bad sometimes I have looked just looked through it at whatever I have thought at that moment.
Relative 006
However, this was not universal. Some relatives read the toolkit when they received it, and would only occasionally go back to sections if they were prompted to do so by the supporter:
I didn’t need to keep going to it, because like I say once I have read it . . . seemed to stick with me but sometimes, I would talk to [supporter] as he used to ring me and I would say oh, something trivial was bothering me, he said well why don’t you look at section this, section that, and I shouldn’t have to be prompted but, he would and then I would start reading it again then you know . . . I was really yes, into it then.
Relative 032
Structure and delivery of support
Face-to-face meeting
The first face-to-face meeting was described by REACT supporters as being very useful and likely to increase use by the relatives, as it gave an opportunity to build rapport and establish a relationship with each relative. It also allowed the supporter to know more about who they were talking to before they rang them:
So I, that interview I think was, from my perspective it appeared like a therapeutic one, a useful one for the relative. And it did help to, much more so than I think you could do on the phone, it did help to build that rapport and therapeutic relationship with the participant.
REACT supporter 1
One supporter felt that they could gauge from this meeting the likely level of engagement the relative would have with the toolkit, based on what else was going on in the household and the level of other distractions. Another supporter felt that the initial face-to-face meeting was helpful, but suggested the need for a second one at a later date, to help refocus and give the support sessions a bit more structure.
However, supporters did also identify big challenges in setting up the face-to-face meeting and finding a time to suit both proved difficult, leading to several missed appointments:
I just had one person that I couldn’t get hold of and I think she went through right to about a month before her set period before she actually got the REACT tool . . . just not been in and I’d been chasing her and chasing her and, ah, she cared for her mum and she cared for her daughter and worked full time. So in the end I just arranged and left it under a car in the driveway, so she got the toolkit.
REACT supporter 4
Although there was individual variation, the majority of the REACT relatives felt that the face-to-face meeting was an important element. It helped relatives to build a rapport with the supporter, but also made the whole experience feel more personal:
She did come once just so you know, so we knew each other really because obviously you wouldn’t want to just phone somebody up if you didn’t, you need at least an initial contact face to face so then you know who you are talking to. I am not so sure I would have liked it if they just said well here is a number just ring.
Relative 054
Support provided via e-mail or phone
Support could be provided via the telephone or e-mail. REACT supporters had personal preferences but tried to offer choice to the relatives where possible. Supporters who preferred e-mails highlighted the benefit of being at their desk at a time convenient for them and so felt able to compose a better-quality reply. Telephone calls had to be scheduled, or potentially interrupted other activities:
You know so, e-mails are better because you are actually in one place with nothing else going on. So you can kind of like calm yourself down and there is no kind of like noise . . . more time consuming composing an e-mail, but I think the quality of the information in the e-mail is better. It’s not as rushed, you can think about things . . . For me, e-mail was definitely the choice.
REACT supporter 2
However, another supporter preferred to offer telephone support as she felt that this gave her a truer picture of how things were going for the relative:
Even though you can’t see someone to see their reactions to you face to face or to see what they’ve done in the toolkit, you can, you know the long pauses, you know if the tone of their voice changes and things like that. So you can still pick up on that. On e-mail, we all write e-mails, we all go back and think ‘Oh, I won’t quite say it like that and I’ll put it some other way’ and things like that. So I am not sure that the e-mail really represented how they maybe would have felt.
REACT supporter 3
For the REACT relatives, the key advantage of e-mail support was also in the speed and convenience of doing this at a time to suit them. Some also found that e-mail allowed them to express themselves more openly:
For me being me, the advantages are, I could be more open. I am not a very, you might think because I am sat here talking to you, telling you all my stuff but that is because it’s for research. But I wouldn’t be able to open my heart up normally to people, I am very not like that, erm . . . so the fact that it’s by e-mail you are not face to face and you are not asking you know directly.
Relative 024
Technical failures were a concern. As one relative pointed out:
Well I liked it [e-mail] because it was quick, erm but then like all technology when it’s down, it’s down.
Relative 046
Yes our’s keeps going down our e-mail here, it’s a bit touch and go and it’s no good doing e-mail at work, so I don’t tend to give my e-mail address here because it’s quite bad that wireless free, I don’t know what, the wireless internet since we have had that it’s been dodgy.
Relative 006
Overall, their preference was to have a range of options and a flexibility to their timing and use. For some, the support was evidently the most valued part of the intervention:
And I must admit when I got to the end I think I was really sad that there wouldn’t be that kind of support. Because, I suppose I do think about things quite a lot and I suppose it was the next best thing to counselling really, somebody being in your world with you, erm, and that was the kind of thing that I needed to, somebody to look at how I was coping and make suggestions how I might do it better.
Relative 046
Others felt glad that it was there as an option, but were happy to use the toolkit on their own:
I understood why it was there, how to use it and everything so . . . And then there was only one occasion that I actually felt I needed to ring her . . . but I know that I could have rung more if I had needed to it’s just that I didn’t need to.
Relative 054
Strategies used by supporters to engage relatives
REACT supporters identified several important strategies that they felt they had learnt to facilitate engagement of relatives with REACT. Possibly the most strongly emphasised by all supporters was the need to be flexible with how and when support sessions were scheduled. Some had tried to book these in advance, or at regular times each week, but all felt that they needed to change sessions to suit the relatives’ commitments in order to be able to make contact. This was quite a challenge, particularly when the supporter worked office hours and was not able to offer evening or weekend appointments:
Um, it’s one of the problems I had is that is that I had to decide, the difficulty was that I would set aside say an afternoon every week or every 2 weeks just to do the REACT support but in practice people want you to or need you to be much more flexible . . . So if I set aside Friday afternoon there might be a couple of people who I would reach, but others maybe only had a day, morning off on a Tuesday or whatever, and I think that was the difficulty I found, was being that flexible. And if they weren’t in or they couldn’t answer my call, it’s then finding another time later in the week.
REACT supporter 1
The way in which the support interacted directly with the content of the toolkit was also identified as important but challenging. Supporters tried to balance broader discussion with the relative, listening to their experiences, and following their agenda, with directing them to use relevant parts of the toolkit, and to engage with the self-reflection exercises:
Um, I think you probably need to think more about the interface between the toolkit and the support . . . Um, it feels sort of you know, some of them you’re asking them to disclose their thoughts and feelings and things and that is not that easy to then go and discuss on the phone. Um, so, but however I would think at least with some people to maintain, to establish a connection between them actively you know doing the work on self-management and the support might be a good thing.
REACT supporter 1
Reminders to go back and consult relevant sections of the toolkit were also identified as useful by the REACT relatives, who found it helpful when the REACT supporter was able to elaborate on the content of the toolkit, recommending additional reading or resources to address a particular issue:
If I was worried ‘bout something . . . then he would say have a look in your managing you know things or whatever it was at the time, and have a look in section 4 and it will explain it all to you and you will feel better afterwards and things like that, yes he did, yes he did help me.
Relative 032
You know somebody that knows it or is in, working in that environment, and probably seen it all before or whatever I don’t know it was good to have somebody in the know ring you. And he is quite a funny guy actually, we had a laugh. But yes it was good . . . but with the toolkit when I was reading it you know, I would always start with talking about this, and erm . . . he would always ask me how it related to what I was doing and, you know and . . . or I would ask him questions, regarding the drugs or something like that. And he would always refer to the toolkit, and you know be pointing it out and which is good, great.
Relative 040
Relatives’ engagement was further facilitated by the chance to talk through specific scenarios and gain reassurance and feedback that they were using appropriate strategies to manage the situations they faced, or alternative suggestions of how they could manage the situation:
But I think the feedback from your support is really important. And I found it, I found it reassuring as well. You need to know that you’re doing the right things.
Relative 046
Because, I suppose I do think about things quite a lot and I suppose it was the next best thing to counselling really, somebody being in your world with you erm and that was the kind of thing that I needed to, somebody to look at how I was coping and make suggestions how I might do it better.
Relative 046
Perceived benefits of the toolkit for relatives
Both REACT supporters and relatives were able to identify tangible benefits for the relatives of using REACT.
All of the REACT supporters recognised the advantages of offering information and support to relatives specifically designed for them, focus on their needs, and that empower them to navigate the system they are operating within:
. . . think relatives, and I’ve always said this, they need their own person that they can turn to. Not the care co-ordinator ‘cos you have conflicting, you know, the care co-ordinator’s there for the service user’s best interest. There is no one there and in fact I’ve seen a few times where parents or relatives just get cut out of things. And I just think at the end of the day they’re going to go, they are the main providers of the care, they’ve got to be involved.
REACT supporter 4
Knowing that this support was there, even for those who did not access it regularly, was seen as important:
But I think for a lot of parents, knowing that it was there and that they could ring ‘cos I’d always leave it open.
REACT supporter 4
The main tangible benefit was having access to update to date and accurate information that can be hard to access elsewhere:
It does really benefit if people understand what they are dealing with, it think that’s half the battle rather than if people just don’t understand anything about things, I think they are just fighting against the unknown really all the time.
REACT supporter 2
This was thought to lead to having the confidence to find out more and get more involved with services directly. For example, REACT includes a module outlining confidentiality and how to respond when as a relative you feel you cannot get the information they feel they need, or want to share information you feel staff need to know:
. . . realised that ‘yeah, OK, you can’t tell me the ins and outs because of confidentially but actually I have a voice too, and you probably would learn a lot if you listened to me for 10 minutes’.
REACT supporter 3
. . . saying to them ‘you can ask’ you know and just giving them the confidence through the support to do that.
REACT supporter 3
The indirect benefits of this are hard to determine in these data but there is some suggestion that REACT supporters perceived that engagement with the REACT toolkit might be affecting significant relationships within the family home:
I am not entirely sure if it was the REACT toolkit that changed his perspective, but he was much more . . . I don’t know if it was the support or the toolkit, but it became much more relaxed, much more relaxed as things went on. Uh, I think a little bit more confident that if she were becoming unwell that both she and him would be able to detect, so meaningful changes.
REACT supporter 1
REACT relatives felt that having support specifically aimed at them made them feel more valued, and knowing that there was someone to contact if they did have a problem made them feel more secure:
I need my space to, erm, I suppose to be valued as to what I am doing, do you know what I mean, being his main carer, I think that is all right to be valued as that, do you know what I mean, so I think he gave me that as well. Like, it’s tough this, you know you are doing alright.
Relative 065
Sometimes if nothing had have happened you just feel as if you are just chatting for chatting sake whereas knowing that you could just ring if something did happen was a lot better.
Relative 054
Relatives reported finding REACT reassuring, in that they would recognise strategies that they were already using and this made them feel that they were doing things right:
You can work out things as to what is what, but then it told you, so it confirmed what you had worked out for yourself, that you were actually on the right line.
Relative 008
It also highlighted to them that the challenges they faced were also faced by many other people who were also seeking the same kind of help:
. . . did make me realise that there are other people in the same boat as me, you know, the fact that there is a book actually there, been printed for people who have relatives.
Relative 006
Having contact details for various organisations was described as being helpful, as was having everything held together in one toolkit:
All the information is there in one lump.
Relative 008
Balancing REACT supporter role with general support worker role
The final theme relevant to implementation was discussed by only REACT supporters, and focused on the challenges of integrating their role as REACT supporter with their broader clinical role within the mental health team. REACT relatives talked about the general challenge of finding time to use REACT, but beyond this, did not go into detail that helped identify specific factors that could inform the development of implementation hypotheses for the IMPART study.
In general, supporting REACT seemed to fit well within the role that staff already held within their teams. Delivering the support was not seen as a problem, although attending regular supervision meetings that took place as part of the research project was more problematic, especially as these were held centrally, requiring supporters to travel for up to 1 hour each way.
One of the REACT supporters was also a trained cognitive–behavioural therapist and offered structured family intervention to some families within the trust. For him, the main challenge lay in trying to keep the focus on supporting relatives to use the toolkit, as opposed to offering a more active therapy:
It’s a bit more difficult from my perspective because I was providing sort of general support, rather than therapeutic support, which is what my job is, to be a therapist.
REACT supporter 1
There were also concerns about where the boundaries of the REACT supporter role lay, and when they were doing things to support the relative that might fall outside this, but would fall within a more generic support worker role. For example, one supporter, through talking to the relative, became aware that the person the relative was supporting was not receiving the level of care they should have been from the team. They reported this back to the team meeting, but this was later concerned not to be part of the role:
She’s not blaming me it’s just like, ‘My daughter’s CPN [community psychiatric nurse] hasn’t been here for weeks, um, what can I do about that?’ Or ‘Is that right? Should they be visiting more often?’ or ‘How can I get hold of them?’ or ‘maybe the other person has gone off sick and there’s not a new person here?’. So I think it might not have been in that particular case but in another case I ended up ringing the team involved and saying this is a concern that the relative has passed on, has there been a change of care co-ordinator? What’s happened to them? . . . So, you know, if they wanted a more practical active intervention. Or that might have been more appropriate to the difficulties that they were experiencing at the time.
REACT supporter 1
Finally, supporters expressed some discomfort when put in the position of listening to relatives giving negative feedback about the service, or about specific members of staff. There was uncertainty as to how best to manage this situation, recognising the need for relatives to have a chance to ‘sound off’ but having to choose what to feed back:
I still think that you need somebody that can back it up, so somebody there for the relatives. And I don’t think that that can be like a care co-ordinator, you know it can’t be the same because that’s conflicting. If it was somebody separate that they could just sound off to, you know and say ‘Well, actually I’m not happy about this and I’m not happy about that’ ‘cos I had a lot of that as well . . . I think they forget that I worked for the EIP service, but I was also delivering REACT? You know so I’d get ‘You know so-and-so’s no good and bla-di-blah’. Um, I had to manage that and be very careful.
REACT supporter 4
Discussion
Summary of findings
Interviews with four REACT supporters and 11 REACT relatives who took part in the REACT feasibility trial53 were analysed to identify the key factors affecting their use of the REACT toolkit. Important factors included the design and content of the toolkit, in particular how relevant the content was to meeting the relatives’ needs, and how accessible and engaging the information and presentation were; the timing of when the toolkit was offered, and the flexibility and availability of the support to match when this was most needed by the relatives; the structure and delivery of the support, including the importance of an initial face-to-face introductory meeting followed by a choice of follow-up support by e-mail or telephone, depending on the relative’s preferences, to prompt relatives to use relevant parts of the toolkit, suggest additional resources where relevant, offer reassurance for appropriate coping strategies, and talk through strategies to manage difficult situations; perceived benefits for relatives, including the reassurance of knowing that they are not alone in facing these problems, that the information and support is available and easily accessible in one place, and the knowledge and confidence this provided to help them manage their situation and engage with mental health services; and the ability of the supporters to define the supporter role and differentiate this from other clinical roles they may have within the team, while also integrating the support with the wider clinical service offered to relatives.
Implications for IMPART study hypotheses
The aim of this analysis was to inform the generation of hypotheses for the IMPART study. First, it is important to understand differences in the design of the REACT intervention that is being used in the IMPART study. These changes have come about in response to extensive feedback from relatives in a series of focus groups54 and through the relatives’ advisory group that has helped to develop REACT.
The REACT toolkit used in the feasibility trial was a modular printed self-management toolkit consisting of 12 booklets, and was supported by a member of the EIP service clinical team. Support included an initial face-to-face session followed by telephone or e-mail contact.
Key changes to the REACT toolkit used in the IMPART study include:
-
REACT is offered solely online, with no paper version.
-
The content has been adapted so that it is suitable for relatives and close friends of people with psychosis and bipolar disorder.
-
The content has been extended to include additional modules relevant to bipolar experiences, and more extensive video case studies of clinicians and actors retelling relatives’ stories.
-
REACT is now supported within NHS EIP teams by clinical staff who are able to edit key aspects of the toolkit, including the resource directory where they can add additional resources they feel are relevant. REACT supporters support relatives online using asynchronous direct messages.
-
REACT includes a peer support forum on which relatives can talk with each other. This is moderated by the REACT supporters.
Bearing in mind these modifications, we have considered the implications of these findings for the IMPART study hypotheses, and these are reported in Chapter 3.
Appendix 3 Stakeholder reference group key themes
Introduction
The IMPART study aimed to understand factors influencing the implementation of an online supported self-management intervention for relatives of people with recent-onset psychosis to identify the resources needed to integrate it into routine clinical care, and to use this information to develop a national implementation plan. The study was conducted across EIP services across six NHS trusts, and used a theory-driven case study design to understand the process of implementation of REACT.
The study comprised three phases. The aim in phase 1 was to develop a programme theory of the implementation of REACT in order to guide our case study data collection and analysis. The programme theory comprised a set of theoretical propositions. Theoretical propositions have been described as ‘a [hypothetical] story about why acts, events, structure, and thoughts occur’ (Sutton and Straw;136 Yin72). The IMPART study propositions were based on the propositions of NPT, and refined by findings from three data sources analysed in phase 1: a systematic review of the literature, qualitative data from the REACT feasibility study and qualitative data from SRG focus groups. We used a two-step process to generate the IMPART study propositions:
-
We generated a list of propositions relating to the general processes that NPT predicts are likely to lead to successful implementation, using NPT.
-
We mapped our findings from phase 1 onto NPT constructs to explore whether or not there were any potential impacting factors identified in phase 1 that were inadequately captured by NPT constructs.
This report details the qualitative analysis of the SRGs that were held in each trust during phase 1 of the IMPART study.
The aims of the SRGs as stated in the IMPART study protocol were to:
-
Develop good working relationships with key stakeholders at each trust, including commissioners, service managers, clinical staff, service users and relatives.
-
Generate hypotheses about what the stakeholders believe will be the key facilitators and barriers to the implementation of REACT.
-
Finalise an initial plan (version 1) to facilitate the implementation of REACT, including the rationale and process of integrating REACT into the existing service, and the resources needed to do this.
-
Help to determine the most relevant sources of data relevant to hypothesised implementation factors.
Aims
The aim of the phase 1 SRG focus groups was to explore EIP staff, service user and relatives’ views regarding key impacting factors on the implementation of the REACT toolkit in EIP services.
Methods
Setting: stakeholder reference group focus groups
The phase 1 SRG focus groups were held during phase 1 of the study, between March 2016 and June 2016. At the time of the focus groups, NHS ethics and R&D approvals for the IMPART study had been given, and the research team had given a presentation on the study and the REACT toolkit to participating staff teams. These presentations included the rationale behind the IMPART study, an outline of the IMPART study design, a description of the toolkit, screenshots of key content and an outline of staff roles in delivering it. However, the REACT toolkit was in the process of being adapted for use in each site, and trusts did not have access to the website itself. PIs had been confirmed at each site. Each participating EIP service had been advised to allocate two roles (IMPART lead and REACT supporter) to members of their team in order to facilitate the research and implementation. The role of IMPART lead, as specified to teams, were to (1) provide an insight into the workings of a particular site, facilitate researcher access to key data sources, and meet regularly with the case study researcher, and (2) identify potential members of, assist with setting up, and co-chair the SRG. It was recommended that the REACT supporter role included (1) promoting REACT to other staff and to relatives, (2) moderating the REACT online peer support forum REACT group (check users are adhering to ground rules, stimulate discussion) and (3) providing information and signposting through the REACT direct messaging service.
The IMPART leads in each of the six IMPART study sites were approached and asked to set up a SRG meeting. Meetings were held on NHS premises at each of the six sites. IMPART leads were advised that the group should comprise individuals in their trust who were likely to be involved in the implementation of the REACT toolkit, and would ideally include senior trust board members or EIP service leads, EIP team managers/clinicians, two EIP support workers, two EIP relatives and two EIP service users. In some trusts, SRGs were set up almost independently by the IMPART lead. In others, researchers and the McPin Foundation offered varying levels of support.
The meetings followed a similar format across trusts, and comprised a presentation from the research team followed by a group discussion using a semistructured topic guide. The presentation comprised an introduction to the IMPART study [background, need for improved relatives’ support, the evidence–practice gap for online mental health interventions, study aims, design including timeline, quantitative and qualitative data collection, and expected study output (dissemination of findings and an implementation plan)], an introduction to the REACT toolkit (including descriptions and screenshots of key components), the role of the SRG and the aims for the first SRG meeting.
Participants
Participants in each SRG are shown in Table 26. SRGs in four trusts included both EIP staff and relatives and/or service users. In two trusts, relatives and service users were not invited to the initial SRG meeting, as staff felt that it was important to have an initial discussion with staff before consulting with relatives. In these trusts, a second SRG was held to include relative and service user SRG members. Senior management was noticeably absent from meetings. In most trusts, IMPART leads felt that it was unlikely that senior management staff would see their attendance as necessary. In others, senior management staff were approached but did not respond, or expressed an interest in attending but were unable to attend owing to other commitments.
| Trust | Researchers and staff | Relatives and service users | Researcher notes |
|---|---|---|---|
| Ocean | 9 staff (IMPART lead, 2 clinical psychologists, 6 care co-ordinators); 2 researchers [1 IMPART North site research associate (VA); 1 IMPART North site lead (SJ)] | 1 relative, 1 service user | Organised by the IMPART lead and good turnout. Owing to a variety of staff and a service user and relative’s discussion was focused on ways to implement REACT that suited the relatives, service users and different staff members. It was a very informative meeting and everyone seemed enthusiastic |
| Moor (SRG part 1) | 5 staff (PI, 1 clinical psychologist, 1 clinical team leader, 1 STR worker, R&D director); 2 researchers [1 IMPART North site research associate (VA), 1 IMPART North site lead (SJ)] | None | Organised by the IMPART lead. This SRG was meant to consist of both staff and relatives but it transpired that only staff had been invited to attend this meeting and it was claimed by the IMPART lead that he did not see the point in inviting relatives as we had already developed the toolkit and we would probably not be able to make the changes that they wanted. I was quite shocked by these comments as the toolkit was still being developed and the purpose of the SRG is to ensure stakeholder involvement in the IMPART study. I felt that there was a staff unwillingness to meet with relatives as they believed this would turn into a meeting where the relatives just complained to staff. It was decided that a second SRG would need to be developed to ensure that the relatives were consulted |
| Moor (SRG part 2) | 2 staff (PI, 1 clinical psychologist); 2 researchers [1 IMPART North site research associate (VA); 1 IMPART North site lead (SJ)] | 9 relatives | Organised by VA with help from a relative and then the relative recruited other relatives through a city carers support group. Very well attended by relatives, due to some of these relatives being in service for so long it was very interesting to hear their points of view has they had an extensive knowledge base. They could also discuss points with a ‘less-emotional head’ and with ‘hindsight’, which was valuable information. There were three relatives who were new to EIP and they were understandably more emotional but they could not input the same has they had no comparison and did not yet know ‘how things worked’. Although there was one person who was very negative and did appear to want to complain, this was well managed by keeping on track with the questions and relatives being able to see the questions we wanted answering, also the person who wanted to complain was known to the relatives and staff so they appeared to know how to communicate with him. Overall, this SRG was very insightful and good for building relationships and promoting REACT/IMPART as these relatives were highly involved in the Moor relative’s community |
| Lakes | 2 staff (1 clinical psychologist, 1 IMPART lead); 2 researchers [1 IMPART North site research associate (VA); 1 IMPART North site lead (SJ)] | 2 relatives | Organised by the IMPART lead and actually poor turnout among staff. Only one staff member attended and the IMPART lead. The two relatives that attended were informative and gave their perspective, although it became more of a ‘support’ meeting due to the 2 relatives and just 2 staff members. Lack of staff may be due to IMPART Lead’s reduced working hours/role now that he is retiring and maybe not as influential among the team |
| Marsh (SRG part 1) | 5 staff [1 consultant psychiatrist (PI), 2 team managers, 1 care liaison worker, 1 R&D clinical research co-ordinator]; 1 IMPART South site research assistant (PO) | None | Organised by IMPART lead and all staff considered relevant attended. Relatives not invited due to staff concerns re feasibility and time frame of implementation; senior management (R&D director) unable to attend due to other commitments |
| Marsh (SRG part 2) | 2 staff (2 carer liaison workers); 1 IMPART South site research assistant (PO); 1 PPI co-ordinator | 3 relatives, 1 service user | Organised by carer liaison worker, who also invited relatives and service users to attend – no issues reported with this |
| Woods | 7 staff [1 consultant psychiatrist (PI); 1 team manager, 1 clinical psychologist; 2 care co-ordinators (IMPART leads), 2 assistant practitioners (REACT supporters)]; 1 researcher (PO); 1 PPI co-ordinator | 2 service users, 4 relatives | Organised by PI and researcher. All staff invited to attend but little expressed interest in attendance from care co-ordinators. All staff asked by PI and IMPART leads to invite relatives, several reminders from research staff. All but 1 service user recruited by IMPART leads and REACT supporters. Senior management invited by PI but no response to e-mails |
| Seashore | 11 staff [1 consultant psychologist (PI), 1 service manager, 2 team leads, 3 psychologists, 1 CPN, 1 social worker, 2 assistant psychologists]; 2 researchers [1 IMPART South site research assistant (PO), 1 IMPART South site lead (SIJ)]; 1 PPI co-ordinator | 3 service users, 1 relative | Organised by Seashore PI and IMPART lead, who also invited and encouraged all staff members to attend. No reported difficulties with attendance. All teams asked to identify relatives and service users. Reported difficulties with identifying interested relatives – reasons unclear |
Data collection
A semistructured topic guide was used to ensure that key topics were discussed in each SRG while remaining open enough to allow exploration of related views and experiences. Discussion was led jointly by the IMPART lead and researchers.
The topic guide was designed by the research team to elicit views on:
-
current service provision for carers
-
the REACT toolkit
-
factors that might influence whether or not staff promote the REACT toolkit
-
who will deliver the REACT toolkit
-
factors that might influence whether or not relatives use the REACT toolkit
-
what additional resources might be needed for successful implementation.
Stakeholder reference group members’ names and roles/job titles were also recorded.
Analysis
The SRG meetings were audio-recorded and transcribed verbatim. The transcripts were imported into NVivo 11 for Windows. Data were initially analysed thematically, following an inductive, data-driven process. Initial coding of transcripts was completed separately on one North of England and one South of England transcript by researchers Puffin O’Hanlon, Fiona Lobban, Sonia Johnson, Victoria Appleton, Vanessa Pinfold and MR1, and the remaining transcripts were coded by Puffin O’Hanlon. Initial codes were sorted into themes; emergent themes were discussed among Puffin O’Hanlon, Victoria Appleton, Sonia Johnson and Fiona Lobban throughout analysis. The resulting coding frame (Figure 20) was presented to the IMPART PMG for further group discussion and development at a data clinic. Data clinics are 1-day events scheduled throughout the project that allow the entire project team to come together face to face to facilitate more in-depth data analysis and to offer a reliability check on the analysis process.
FIGURE 20.
Stakeholder reference group thematic structure.
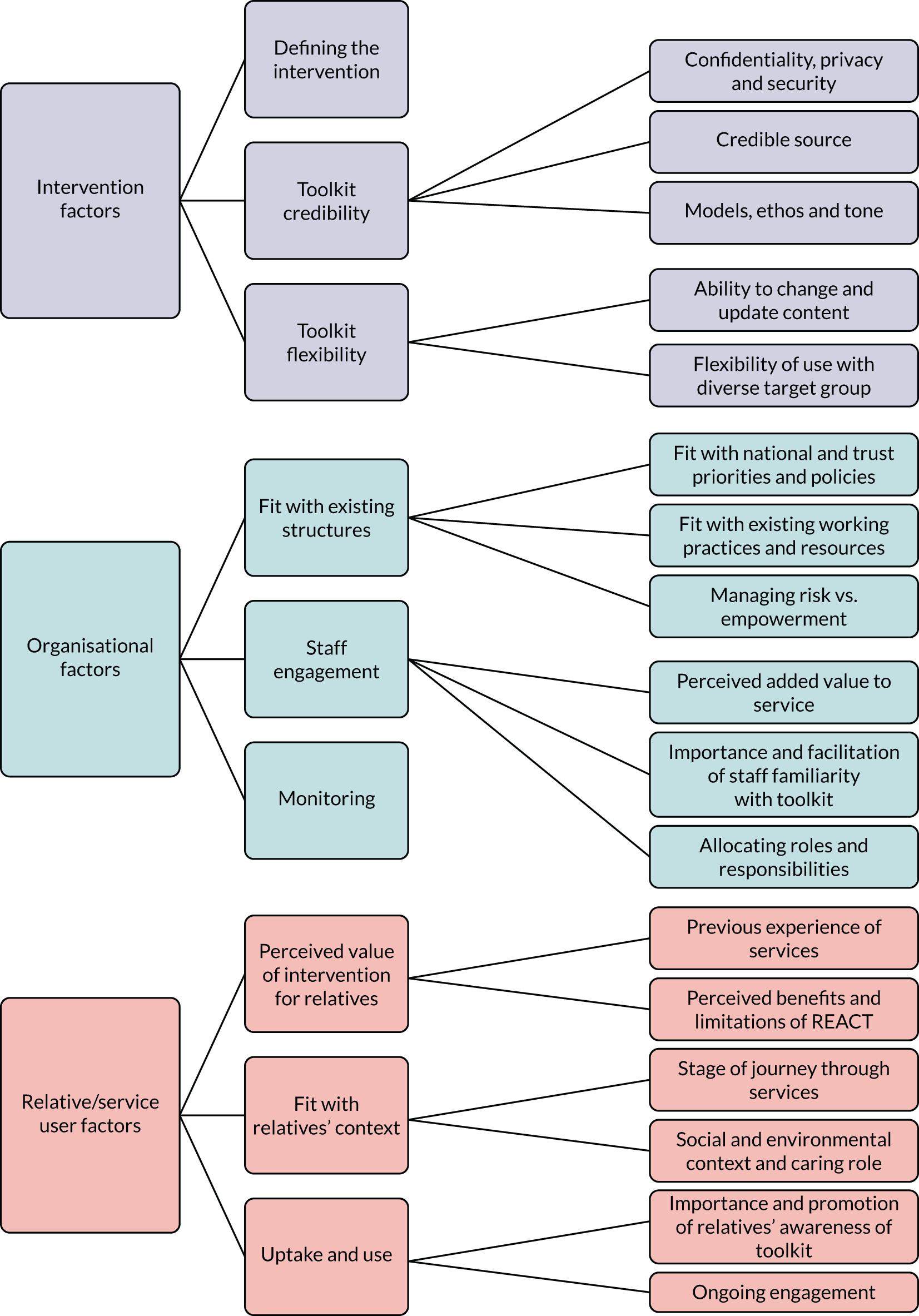
Intervention factors
Defining the intervention
Participants were generally very positive about the principles of REACT (online), and their questions focused around what kind of information was available in REACT (online) and how extensively REACT (online) could be offered within the trust. Clarifying who, how and when people would be able to access REACT (online) was a priority. Specifically, they were keen to know if the toolkit would be suitable for young siblings, service users, relatives of people who were currently in assessment or defined as having an ‘at-risk mental state’, and relatives of people discharged from EIP services, all of whom they felt could benefit. Many relatives expressed the view that the toolkit should be available at the very beginning of their contact with services (e.g. from a GP, at A&E), before contact with EIP services:
It’s difficult to say really without having a closer look at it but if it’s something for carers to keep in touch with each other and feel like there’s other people around, you know experiencing similar things, that’s got to be a good thing you know, I would say.
Relative, Seashore
Toolkit credibility
Confidentiality, privacy and security
Concerns around confidentiality, privacy and security were identified as potential barriers to use. One Seashore service user stated that her parents would not provide any personally identifiable information on the internet (e.g. name or address), and would not use the website if they had to provide this information to access it; another relative from Woods stated that concerns that their use of the website may not be confidential and private may lead to people not using the forum. However, the discussion in this group highlighted the complexity around data privacy by stressing the importance of anonymity to peers on the forum, but being generally accepting of trusted persons (e.g. EIP staff) to link their activity on the website to their personal details for legitimate reasons (e.g. risk management). That the website was accessible to only relatives within the trust was linked to sense of safety, although one relative (Lakes) expressed concern about unauthorised individuals gaining access (e.g. if relatives shared their log-in details). All relatives agreed with the need for clear information on the website about who could access the website and to whom their activity on the website was identifiable to enable them to make an informed choice about what information to share (Ocean and Marsh relatives):
I think, this is just me as a person, I think something like that forum, I want to know who can see it, so I think, you know ‘cos then I can make that informed choice. So if I know this is only accessible to carers and family members who’ve been given the URL and to staff within Ocean, I can make an informed choice about actually what I want to put on there.
Relative, Ocean
[Being identifiable to trust staff] wouldn’t bother me, I mean they’ve got all our details anyway so I think you have to use your common sense really on it, you know I think something inappropriate might be somebody for instance trying to give advice that is not, like say a medical thing you know, but it wouldn’t bother me if my ID was linked at all I think because I don’t know I’d be just using it for the right reasons.
Relative, Marsh
Credible source
Both relatives and staff linked their views of the toolkit to the credibility of contributors to its content. The fact that REACT (online) was developed by a multidisciplinary team of professionals, service users and relatives was seen very positively, as was the peer support from the REACT supporters and other relatives using the forum. Staff stated that this would make the toolkit compare favourably with existing resources, such as the NHS Choices website (Seashore), and would promote learning (Woods, Ocean). Others expressed a general view that the toolkit was a more reliable and credible source of information than other online resources (Lakes, Moor):
The website has been developed along with service users and carers . . . someone who’s actually experienced psychosis . . . and so just to make sure that it differs from the dry NHS Choices website or just a bit more prescriptive rather than directive.
Service user, Seashore
As with anything with service users always, my first thing is if I’m sort of advocating the use of something is what information is there about the evidence base that this is safe, effective, so that families, you know if I’m going to put my time into this that yes this is worth doing.
Staff member, Ocean
I would have used this because trying to get information off the internet there’s that many things on the internet you’ve a lot of it’s not straightforward information, where this it’s coming from the psychiatrists, doctors, people in the profession, so it’s up to date information and at least this is going to give you a better insight to how to cope with the condition.
Relative, Lakes
Models, ethos and tone
The extent to which REACT (online) was fitted with existing frameworks around mental health was important for staff and relatives. Relatives expressed a desire for information and advice that fitted with their understanding of mental health problems and recovery, for example diet and exercise or self-care. Some relatives said that they would be more likely to find the toolkit helpful if content was positive and hopeful, for example posts of positive quotations on the forum or of recovery stories (Marsh). Staff in some trusts (Seashore, Woods, Ocean) stated that clinical staff may resist promoting or using the toolkit if they perceived the content to be diagnostically driven or reliant on a medical model, and thus not in keeping with EIP values:
It just seems to me that a lot of the discussion’s been around lifestyle stuff and families wanting to have more information about well-being in general, I just wonder if this is a very medical model and it’s coming from a very kind of you know medical perspective and actually it needs to open up a little bit more to those kind of life, is it I don’t know what’s on there.
Staff member, Woods
I think as long as it’s perceived as good quality information and in keeping with early intervention sort of values and so on, I think one thing I said there was a big list of diagnosis and I think you answered the question saying it doesn’t sort of sell diagnosis as the be all and end all and I think that would have hit a lot of resistance in EI services if there was a strong emphasis on that.
Staff member, Ocean
Toolkit flexibility
Ability to change and update content
Staff in Seashore, Marsh, Woods and Moor placed importance on the ability to update and change content in order to 1) fit individual trusts through consistency with national and trust guidelines (Moor), service changes (Moor), and service ethos (Seashore), and 2) tailor the toolkit to the needs of users through keeping the local resources directory up to date (Marsh, Moor) and making changes to content based on user feedback (Woods, Moor).
Will you be using any of the things that get spoken about in the forum to kind of tailor the toolkit? So if there are lots of discussions about sleep or diet will you then use that maybe to add to the toolkit for the future?
Staff member, Woods
The new targets . . . mean that the 14 to 35 age range that we’ve all grown and loved is no longer er applicable, it’s 14 to um 65 now . . . so that might change the profile of what we were going to put in there, what is psychosis . . . things that are more relevant to the more mature people.
Staff member, Moor
Flexibility of use with diverse target group
Stakeholders expressed concerns around the ability of the toolkit to meet the needs of their diverse target population. This was compounded by staff uncertainty following recent changes in eligibility criteria for EIP services, and particularly the extension of the age range that EIP serves and the likely increase in young carers and spouses. Views about the suitability of the toolkit for young carers varied, with some viewing this group as more likely to use an online resource (Marsh), while others expressed concern that the content may not be suitable (Marsh, Moor). Whether or not content was appropriate across different diagnoses was also discussed (Lakes, Seashore).
In all trusts, staff and relatives viewed the target population as diverse in terms of age, level of English language proficiency, lifestyle and mental health diagnosis, and questioned to what extent the REACT (online) toolkit would be accessible for different potential users. Staff and service users in all trusts highlighted the fact that the toolkit is available in only the English language, and that a significant proportion of relatives in their trusts would not have sufficient English language proficiency to understand the website content. Options for increasing flexibility, including printing out and translating key content, or using Google Translate (Google Inc., Mountain View, CA, USA), were discussed, but it was generally agreed that Google Translate would not capture key meanings and may even produce misinformation.
Access to and confidence with computers and the internet was also highlighted as an issue. Stakeholders linked computer and internet access and confidence to age (Seashore, Marsh, Ocean, Lakes), with younger generations viewed as more confident with digital technology but less likely to own a computer and more likely to live chaotic lifestyles, and older generations as both less confident and less likely to own a computer. Unreliable 3G access in rural areas was seen as a potential barrier (Moor). Barriers of access were seen as surmountable to varying degrees, depending on (1) whether or not the toolkit could be used on different devices, including smartphones (stakeholders viewed smartphone ownership as higher than laptops or computers, especially among younger carers – Ocean, Moor, Woods, Marsh), (2) ease of use (Woods, Lakes), (3) provision of human support (Marsh) and (4) accessibility at community centres or libraries (Moor, Marsh).
Portability of the intervention, either through printouts or access on smartphones, was seen as important in terms of its ability to meet individual needs:
[In] my family I’m the only one who speaks English for example, and how would they access this.
Service user, Seashore
‘Cos they’re gonna ask different things and they’re also gonna talk about different things, it might have been quite nice to have had a separate forum for the younger ones.
Staff member, Marsh
I mean I’m old so I can be ageist, maybe more people older don’t really use it, don’t feel so comfortable, for some of the younger ones, I think of the over 35s ‘cos we’re talking about services for them too, but maybe some of the younger ones who’d be able to know what to do, they don’t have access to funds or they’re not living in the same place, they’re moving around, or their lives are chaotic and they can’t actually make use of the, maybe some of the carers are in a similar situation.
Staff member, Seashore
I do know quite a few of our established carers who would struggle on a computer, but I mean if it’s something that we can sit in on and just go through with them, but it is if you’re brought up with computers it’s completely different and I mean even work colleagues struggle sometimes with the systems.
Staff member, Marsh
Organisational structures
Fit with existing structures
Fit with national and trust priorities and policies
There was considerable variation within and across trusts regarding the extent to which the toolkit was seen to be a help or a hindrance in meeting national and local priorities and policies. The impact of the new AWT guidance was discussed in all trusts except Woods. Service managers in Seashore and Moor promoted the view that carers’ support should be a priority area for improvement because it is an area of current underperformance. Both highlighted that offering the REACT (online) toolkit would not fully meet AWT requirements for family interventions but spoke of ways they could incorporate it into the care pathway. These included offering the toolkit as one of a broader range of services (Moor, Seashore) or the REACT champion taking a lead on other aspects of family work.
In Marsh, team leads stated that the at-risk mental state pathway was a current priority and source of concern, bringing with it uncertainty over referral rates and workload, and that there would not be adequate staff time available to deliver REACT (online) at present. Staff in Marsh expressed concern that there may be a perceived lack of fit between the toolkit, designed to be used by individual carers, and the ‘whole-family’ approach of the EIP service, where the whole family is involved in care, promoted by the trust:
I think the carer support feature of our current drive to bring all our services up to gold standard is one area that we haven’t quite cracked, I think we’ve quite a lot of carer support but it’s inconsistent and I think this is a good way . . . but there are other areas of carer support we need to be giving in teams that we’re not . . . I wonder if it needs to be seen in that context as to how we’re going to develop carer support generally in all three teams.
Staff member, Seashore
It’s going to tick the information for relatives and carers box, but I don’t want it to be instead of actually getting face-to-face contact and support with care co-ordinators and things like that.
Staff member, Lakes
The importance of having trust policies to guide delivery of an online intervention was discussed in Moor and Ocean, with Ocean staff expressing confidence in managing risk issues with existing policies and procedures, and in Moor there was a perceived lack of policy to guide staff, and a lack of clarity regarding whose responsibility it should be to develop guidance on managing online risk at the senior management level. Moor and Marsh expressed a lack of trust in senior-level support, at the level of buy-in (Moor) or front-line delivery (provision of additional funding for REACT supporter time), even where senior-level support for technological innovation was evident (Marsh):
I think, ‘cos we’ve moved implementation date to July 2017, I think that overcomes a lot of barriers. So we were going with the initial sort of plan I think we’d struggle as well because of where we’re at with implementing the new standards and everything else that’s involved and hopefully by July we’ll be in a much better place.
Staff member, Marsh
I do think that from a director level, from an innovation level, actually there’s probably more focus on implementation of tech now than there’s ever been.
Staff member, Marsh
Fit with existing working practices and resources
Discussion under this theme centred around the fit of the toolkit with existing provision of carer support, and around the extent to which the toolkit would require changes to existing roles or additional resources.
The peer support forum was seen as fulfilling a similar function to a carer support group, although it was seen as potentially more accessible than carer support groups, but lacking face-to-face support (Marsh). The psychoeducation content was seen as fulfilling a similar function to current information given to relatives (e.g. leaflets), while having the added value of being more specific to psychosis and bipolar disorder and, therefore, more relevant than more general information that is currently given:
[The carer’s group is] really valuable the fact that it’s face to face and I think that in itself is valuable and that’s the one thing it has over the IMPART, but it’s also the exclusion of a lot of people because of the geography, the time, we always run it in an evening to try and create more of a space for the carers but it’s the geography of it, so the take up isn’t huge, you know when we think we’ve got 350 open cases and on average we’re getting what eight carers, 8 or 10.
Staff member, Marsh
Each trust was advised by the research team that the amount of staff time required to support the messaging and forum function would be likely to depend on the number of relatives accessing the website, and that it was difficult to give a more accurate estimate before the website was launched. The perceived ease with which moderating the forum and providing the messaging service could be supported within existing structures varied according to the amount of resources they felt it would require and the amount of resources they felt able to access. In Woods, the role had been allocated prior to the SRG to two new dedicated carer workers who had recently been appointed, and apart from clarifying that the role would fit into a 9-to-5 working day, no issues with the task were raised. In Marsh, where there are also two dedicated (but part-time) carer workers, team leads stated that resources for supporting carers were limited and already stretched, and that the toolkit could not be supported without additional staff time. The Marsh carer workers stated that they would feel able to support relatives with using the toolkit as part of the support they already provide, but not able to moderate the forum. In Seashore, staff expressed a general attitude that teams would be able to support the toolkit, which they did not feel would require a significant amount of staff time:
It does need to be moderated, and that it shouldn’t be onerous, it shouldn’t be too much work, someone flicking over it maybe once a week or every now and then I’d guess.
Staff member, Seashore
Marsh and Moor discussed the challenge of delivering the toolkit in terms of a lack of fit between the perceived consistent dedicated block of time required to support the forum and messaging service and the reactive nature of EIP work. The division and co-ordination of the REACT supporter role across teams within one trust was also seen as a challenge in some trusts where the forum is trust wide, but the teams operate relatively independently for all other services (Moor, Ocean).
Staff discussed the ability to draw on existing IT resources, including trust-provided devices such as iPads (Apple Inc., Cupertino, CA, USA) (Woods) or smartphones (Moor), R&D staff time (Marsh, Moor) and IT support (Marsh), as facilitating factors in implementation, but still felt that there was a lot of work to be done to support staff to work with online interventions:
The processes to support staff in working in this sort of way don’t exist in our trust at the moment and probably would need some reflection on how things are actually done and what sort of clinical processes were put in place by the organisation to support it . . . in terms of clinical responsibility if you’re moderating or if you’re providing a response who what level of responsibility, which clinician should be doing it, how are they supervised to do it, all of those sort of things as with any sort of clinical practice would need to be thought through I would have thought.
Staff member, Moor
Managing risk versus empowerment
Perceived risk was almost exclusively associated with the delivery of the peer support forum. The main source of concern was inappropriate content ranging from inappropriate but well-meant advice, to disclosure of possible harm, extreme views and bullying. Staff in Marsh expressed concerns about relatives posting overly negatively about the service or staff (including the risk of threats to staff) and a perceived need for strict moderation procedures that allowed immediate removal of any user threatening staff and linking user identifiers to individuals. This concern seemed to be informed by the team’s previous experience of hosting an open online forum for people experiencing mental health problems.
Staff in Seashore and Ocean also discussed the potential risk of the toolkit leading to misinformation (e.g. regarding diagnosis), although staff in the same SRGs highlighted that such information is accessible to relatives from other sources:
We know full well even from carers’ groups or anything like that we still get people who come in to stir things up, you know, that’s the nature of it, people will never be 100% happy with our service no matter how well we deliver it.
Staff member, Marsh
Strategies to manage risk varied across individuals and across trusts. Staff in Marsh, Moor and Lakes perceived limiting access to EIP relatives from their trust as an effective mechanism for reducing the risk of inappropriate use of the forum. Relatives viewed limited access as providing a sense of safety, but did want relatives who had been able to access the forum to be able to continue to do so after discharge (Marsh). Staff in other trusts discussed the balance between the role of the moderator and ‘self-governance’ by users, through providing clear ground rules, clarity about appropriate use of the forum, directing people to crisis lines, encouraging relatives to report inappropriate posts, enabling individual choice with regard to reading/following potentially distressing or unhelpful posts and trusting users to ‘have a conversation’ (Woods). Staff in Seashore suggested a role for relatives in moderating the forum:
But I think also if we’re able to keep a database and say yes your posts are anonymised but we will maintain contact with who has what PIN number that should reign it in a bit, so we contain it by being a closed forum anyway, but we can contain it more actually just knowing that we do have that, we do know what number is what person it’s just going to work the same way every other forum on the internet works.
Staff member, Marsh
People are going to log on, they’re either going to talk to each other and it will get out of control and then it will stop, or they’re going to talk to each other, it will be fine, or people just won’t use it.
Service user, Marsh
But I think we must be into empowering, I think the idea not just to show responsibility, I think the idea is that a group of carers who were able to commit themselves to this who have a lot to give for obvious reasons, even involved in moderating it.
Staff member, Seashore
Staff engagement
Perceived added value to service
Marsh staff expressed a general view of self-help as a ‘good thing’ and saw REACT (online) as a way for the service to engage groups they have historically struggled to engage (e.g. geographically distant or young carers). Participants in three trusts (Seashore, Moor, Lakes) discussed the extent to which delivery of the REACT (online) toolkit could help their service meet AWT targets with relatively low levels of effort. Participants from the same three trusts (Seashore, Moor, Lakes) highlighted the potential for the toolkit to free up staff time, while at the same time expressing concerns that staff may see the toolkit as adding to their already increased workload at a time of extensive service changes. They stressed the importance of ‘selling’ the time-saving potential of the toolkit when promoting it to staff. The ability to offer the toolkit without service user consent was also highlighted as valuable (Ocean, Seashore); uncertainty around how to work with carers of service users who refuse consent was seen as a continuing problem, and the toolkit as a potential solution. Participants stressed the importance of ensuring that staff are aware of this potential value:
I really want families and carers to have more information, the only thing in the back of my mind is kind of going what are we going to have to do, what care co-ordinators can do in terms of actually . . .
Staff member, Ocean
I think there is still some of that concern amongst staff about confidentiality and I think it’s about us making sure that staff are really aware of what carer’s rights are to information, my sort of stance would be that this information and access to this toolkit, that families would have a right to access this because it’s not like you say identifiable personal information, it’s general information about that is relevant to their family member, so and it’s a very clear statement in all the guidance that that is stuff that carers and families are entitled to, they’re not entitled to any sort of personal information that somebody’s asked to be kept confidential but the sort of general, what is psychosis.
Staff member, Ocean
Importance and facilitation of staff familiarity with the toolkit
Staff familiarity with the toolkit was seen as an essential step towards promoting its use in services. Without this, staff would be unable to appreciate the potential value to the service (Ocean) and the safety and efficacy of the toolkit for relatives (Ocean). In Seashore, familiarity was highlighted as key to engendering a sense of ownership of the website among the staff.
In most trusts, different levels of familiarity were seen as appropriate for different staff groups: care co-ordinators would need to have adequate knowledge of and enthusiasm for the toolkit to introduce it to relatives (Seashore, Moor, Ocean), or be provided with the right information to give out (e.g. in a leaflet, Marsh), but could not be expected to have detailed knowledge given other demands (Moor). Some trusts identified a need for a ‘champion’, a member of staff acting as a ‘resident expert’ (Lakes), who could promote the toolkit to staff and answer questions (Seashore, Moor, Lakes).
Various mechanisms for promoting staff familiarity with the toolkit were suggested, from staff simply having access to the website to look at in their own time (Seashore), to discussing the toolkit at routine meetings, to dedicated training in the toolkit (Moor). The Moor SRG was the only one to discuss staff training. Perceived challenges included competing demands on staff time and attention, although the possibility of combining it with routine training (e.g. IT) was seen as potentially mitigating this. Staff suggested that training needed to compete for staff attention amid other demands, for example by being visual, avoiding big documents or typed instructions, and being delivered by relatives. A role for researchers in promoting staff engagement with the website was also identified in some trusts, from working with the IMPART lead to think through how to promote the website (Seashore), to delivering training (Moor, Marsh):
It would be nice to have the dummy package so we can like go through it as a team and have a look at it, because once again it’s hard to promote something if you don’t really know what you’re promoting. So I think you have to get the team owning it and signing up to like the principles of it and the having it on their agenda, talking about it in meetings, and thinking about is there anything we can do differently to try and promote it in a different way or, so that tends to be how we work really . . . We need a champion.
Staff member, Seashore
It feels to me as though the main focus is staff training, we need staff to know what this is, how to use it, and that from there they then will signpost people into the service.
Staff member, Moor
Allocating roles and responsibilities
Key tasks were generally divided into three broad areas: promoting the toolkit to staff, promoting the toolkit to relatives and supporting the intervention itself through moderating the forum and providing the messaging service. Stakeholders in several trusts expressed the view that promoting the toolkit to staff was a legitimate part of the researcher’s role, including an expectation that researchers would provide training to staff in how to use the toolkit. In Moor, Ocean, Marsh and Seashore, all stakeholders agreed that the task of promoting the toolkit to relatives most naturally fell under the care co-ordinator’s role. In Woods and Marsh, dedicated carers’ workers perceived promoting the toolkit as work that fitted with their role.
Clarity regarding what supporting the forum and messaging service would involve and whose role it would be varied, from a staff member (as yet unidentified) checking the website every now and then (Seashore), to a dedicated staff member dedicating an hour to the task every morning (Marsh). In Moor and Marsh, the REACT supporter role was perceived as requiring dedicated, consistent staff time, and staff from both trusts expressed concern that they would not be able to roll out the toolkit without extra resourcing for staff time. In Woods, where REACT supporter roles had been assigned before the meeting, and both supporters were present, there was little discussion of roles and responsibilities. In some trusts, an additional task of keeping the local resources up to date was also highlighted:
What we’re looking at is daily monitoring on a Monday-to-Friday basis, so rather than going half-heartedly and going, oh we’ll just do it 2 days, we’d rather have someone do it every morning for, well, what’s generated, it could be half an hour it could be an hour, so initially we’re looking at half an hour every morning. So I spoke to [the R&D lead] about him looking at helping us with this.
Staff member, Marsh
We need to make some decisions about the level of support we can give to it and whether or not we can afford to support the instant messaging and the forum, so I guess to have a clearer idea of what you think the time resource will be, we’ve got three teams, I guess we can devise some way of sharing it out between, unless one person says yeah I really want to do that.
Staff member, Ocean
We’ve got two people from the early intervention service, and both of them have got you know a day job but the anticipation is that they’ll do a few hours a week by logging on each day and just seeing what’s going on.
Staff member, Moor
A lot of families want to locate everything with the care co-ordinator and want – so again it comes back to training that care co-ordinator, ‘cos they want everything to come out of that one person and that one person is being asked to do so much more now anyway, so we really need to train them to sell this really well.
Staff member, Moor
Monitoring
Staff in Ocean and Moor stressed the importance of monitoring the extent to which the toolkit was being used and by whom. Researchers advised Ocean and Moor that registration and usage data would be collected by the research team and fed back to trusts. Both Moor and Ocean discussed supplementing these data with further levels of monitoring, including the possibility of conducting an audit of how many relatives on the caseload had been offered the toolkit (Moor), and collating relatives’ feedback via care co-ordinators. Staff in Seashore discussed monitoring the use of the toolkit as an important factor in staff feeling ownership of the toolkit, and as something that should be discussed and addressed in team meetings.
One relative in Seashore wanted the option to give anonymous feedback on the website, and staff in Marsh and Woods stressed the importance of responding to user feedback on the content of the toolkit:
I think we need to find a way of making sure that we’re capturing how much of an issue [internet access] is and where it’s more of an issue and then can develop a plan to make sure we’re not excluding anybody.
Staff member, Moor
I think you have to get the team owning it and signing up to like the principles of it and the having it on their agenda, talking about it in meetings, and thinking about is there anything we can do differently to try and promote it in a different way or, so that tends to be how we work really.
Staff member, Seashore
Interpreting stakeholder reference group data for IMPART study hypotheses
The SRGs were well attended and provided invaluable predictions about factors that would be likely to affect implementation within each trust. However, staff were generally at a clinical and managerial level, with no involvement of senior trust representatives. In some trusts, the IMPART lead chose to hold separate staff and relative groups, as it was felt that this would be more productive owing to fears that the meetings might be hijacked to air dissatisfaction with services.
There was a high level of consistency between trusts in terms of the key factors identified as likely to affect implementation of REACT (online): in particular, promotion of its potential benefits in terms of meeting needs of the relatives, saving staff time, and helping trusts meet their clinical targets; flexible delivery to allow REACT (online) to be adapted to trust-specific needs; staff confidence in the content and their role in offering REACT (online); and commitment of resources at an organisational level. Some important differences, such as the risk of the website being used to air negative feedback, were clearly linked to specific previous experiences of online interventions.
The thematic analysis of the data was inductive, but the research team was simultaneously being trained in NPT and so it is possible that this growing awareness of the theory influenced the kinds of factors being identified and may have led to some important factors being missed.
Appendix 4 Synthesis, generation and outcome of study-specific hypotheses
This appendix sets out how the IMPART research team, guided by NPT, synthesised its analyses in phase 1 of the study into a series of hypotheses of the conditions likely to lead to successful implementation of the REACT intervention.
Tables 27–30 show the generation of hypotheses for each of NPT’s four core constructs:
-
coherence – the sense-making work that people do individually and collectively when faced with operationalising a set of practices
-
cognitive participation – the relational work that people do to build and sustain a community of practice around a new technology or intervention
-
collective action – the operational work that people do to enact a set of practices
-
reflexive monitoring – the appraisal work that people do to assess and understand how the new intervention affects them and others around them.
| NPT core construct components and toolkit questions | Systematic literature review | REACT feasibility study data | SRG data | Study-specific propositions: implementation of REACT more likely to succeed if: |
|---|---|---|---|---|
|
Differentiation: how a set of practices and their objects differ from each other Q: participants distinguish the intervention from current ways of working |
Ability to access intervention easily, independently and in own time will facilitate use | Staff and relatives need easy access to the toolkit with clear guidance on what it is, who it is for and what it offers (defining the intervention) | All staff have easy and independent access to the toolkit in their own time, with clear guidance on what it is, who it is for and what it offers | |
|
Communal specification: working together to build shared understanding of the aims, objectives and expected benefits of a set of practices Q: participants collectively agree about the purpose of the intervention |
Staff need to be involved in planning if, and how, REACT will be implemented within their service | Staff given the opportunity to discuss whether or not and how to use REACT in their service; decisions from this are visibly endorsed at senior management level | ||
|
Individual specification: things people do to help them understand their specific tasks and responsibilities around a set of practices Q: participants individually understand what the intervention requires of them |
Staff need adequate training in how to use REACT and what their specific role is | Clinical staff need to understand exactly who, when and how they will introduce relatives to REACT (timing of REACT intervention) | Staff access training that clearly outlines their roles and responsibilities in delivering REACT | |
|
Internalisation: work to understand the value, benefits and importance of a set of practices Q: participants construct potential value of the intervention for their work |
Staff who enjoy using REACT and can clearly identify potential benefits show greater levels of use Evidence of long-term cost saving (including staff time and travel) will promote greater use Staff identify REACT as being appropriate for the demographic (age, gender, ethnicity) and clinical features (diagnosis, level of distress) of the relatives they are supporting Staff fears about privacy and anonymity need to be aired and addressed |
Clinical staff will invite relatives to REACT if they see the content as directly relevant to the diverse range of relatives they work with, easily accessible, engaging and up to date (design and content of toolkit); and can see specific benefits to relatives (e.g. normalisation, feeling valued, reassurance they are doing what they can, greater confidence to engage with services, positive impact on relationship with service users) (perceived benefits for relatives) |
Clinical staff will invite relatives to REACT if they see it as coming from a credible source, having genuine user involvement and fitting with the broader model, ethos and tone of the team (i.e. psychosocial rather than overly biological model) (toolkit credibility and fit with existing structures) Frontline clinical staff will invite relatives to REACT if they see it as appropriate and able to meet the needs of the diverse range of users across age, language, diagnosis, lifestyle, computer accessibility and confidence (toolkit flexibility) Clinical staff will invite relatives if they see it as a way to better engage relatives who cannot access face-to-face groups, or where service users will not consent to their involvement, while also freeing up staff time (staff engagement) Information about what data are stored, how, and who has access to it needs to be very clear and may determine staff and relatives’ use of the website. Fears around confidentiality and data protection are common (toolkit credibility) |
Staff can view the content of the toolkit and see clear benefits for staff and/or relatives, such as:
|
| NPT core construct components and toolkit questions | Systematic literature review | REACT feasibility study data | SRG data | Study-specific propositions: implementation of REACT more likely to succeed if: |
|---|---|---|---|---|
|
Initiation: the work of key individuals to drive forward new practices Q: key individuals drive the intervention forward |
Enthusiastic staff can serve as champions, reinforcing engagement and providing guidance | Role of a ‘REACT champion’ would support implementation – resident expert who could promote REACT and answer questions (staff engagement) | There is a clear lead (‘champion’) who drives REACT forward within the trust | |
|
Enrolment: work staff do to reorganise themselves and others to collectively contribute to the new practices Q: participants buy in to the intervention |
IMPART lead, REACT supporter and clinical staff roles need to be clearly allocated, and clearly understood by all staff to ensure shared understanding (structure and delivery of support) |
Trusts are more likely to invest resources into delivering REACT if it is clearly seen as being able to deliver on key trust priorities (e.g. meeting AWT initiative). Where there is doubt about this, or competing trust priorities, implementation is likely to be less successful (fit with existing structures) Training that allows staff to look around the website and emphasises the key benefits and addresses safety concerns will lead to greater staff buy-in (staff engagement) |
Staff make explicit links between existing key targets and priorities within the trust and REACT | |
|
Legitimation: work done to ensure that other participants believe that it is right for them to be involved, and that they can make a valid contribution to it Q: participants agree that the intervention should be part of their work |
Staff need training to reduce any disparities between IT skills required for REACT and those possessed by the staff |
Education and support are likely to be seen as legitimate parts of clinical staff roles, but managing a forum may require additional training/support structures (fit with existing structures) Although clinical staff see it as their role to promote REACT to relatives, they see the promotion and training of staff as the role of the research team (staff engagement) |
Key roles are appropriately allocated Training is provided for tasks that may require new skills (e.g. moderating a forum) Staff have a sense of ownership and take responsibility for promoting REACT within the service, and offering REACT to relatives (and do not see this as the role of the researchers) |
|
|
Activation: once under way, participants need to collectively define the actions and procedures needed to sustain a practice and to stay involved Q: participants continue to support the intervention |
Staff need to develop a sense of ownership over REACT by having a regular forum in which decisions can be made about how to deliver REACT within the trust (staff engagement) | Delivery of REACT is included as a regular agenda item on relevant operational meetings within the clinical teams |
| NPT core construct components and toolkit questions | Systematic literature review | REACT feasibility study data | SRG data | Study-specific propositions: implementation of REACT more likely to succeed if: |
|---|---|---|---|---|
|
Interactional workability: interactional work that people do with each other, intervention artefacts, and other elements of a the intervention when they operationalise them in everyday settings Q: participants perform the tasks required by the intervention |
REACT supporters (and IMPART leads and clinical staff) need to ensure that they carry out the key roles on a regular basis as outlined in the how-to manual, for the system to work (balancing REACT supporter role) |
Being able to access the toolkit offline, on a range of devices (phone, tablet, computer) and being able to print out key sections were all seen as likely to increase use of REACT by staff and relatives (toolkit flexibility) Training needs to be targeted to the specific individual roles as different levels of understanding may be required (staff engagement) |
Staff carry out their roles and responsibilities as outlined in the ‘how-to manual’ and have the resources to allow them to do this. Key tasks include:
|
|
|
Relational integration: knowledge work that people do to build accountability and maintain confidence in the intervention and in each other using it Q: participants maintain their trust in each other’s work and expertise through the intervention |
REACT needs to be supported by people so feels personal and part of a package of care for relatives REACT aids communication and relationships between patients (relatives) and the clinical team |
The way in which REACT is introduced to relatives and the support around this is crucial to whether or not it will be used. Flexibility in communication (including online) is welcome, but face-to-face contact and telephone contact is crucial to support any online support (structure and delivery of support) |
Clinical staff need to be aware of trust risk management policies and be confident that risks identified through the REACT website (particularly shared posts on the forum) can be safely managed within existing policy (fit with existing structures) Limiting access to the toolkit to relatives of people currently receiving support from the IT service will reduce anxiety about the forum being used inappropriately, and staff will feel more able to manage it (fit with existing structures) |
REACT is offered as part of an integrated package of care for relatives, and not a stand-alone intervention Access is restricted to relatives already being supported within the team Staff can see and are confident that the forum is being well managed Staff can see and are confident that direct messages are being responded to REACT supporters and IMPART leads are clear and confident about managing risk identified on REACT |
|
Skill-set workability: allocation work that underpins the division of labour set up around a set of practices as they are operationalised in the real world Q: the work of the intervention is appropriately allocated to participants |
REACT supporter role (and IMPART lead) is a key role and needs to be allocated to a member of staff who has the appropriate skills, interest, time and support to carry out this role (balancing REACT supporter role . . .) | Managing the forum, responding to direct messages and updating local resources are seen as additional tasks, not falling under any specific existing job description, that require additional resource and support (staff engagement) | IMPART lead and REACT supporter roles are allocated to people with the time, skills, organisational role and support to carry these out | |
|
Contextual integration: how intervention is managed through allocation of resources, execution of protocols, policies and procedures Q: the intervention is adequately supported by its host organisation |
REACT needs to be integrated into existing electronic health record/IT systems Staff need adequate time, space and equipment to deliver REACT |
Trust care pathways and other relevant policy documents must clearly direct clinical staff as to when and how REACT should be introduced to relatives (timing of REACT) Relatives will engage with REACT only if it is offered as part of a comprehensive intervention integrated with additional support including further information, reassurance and talking through specific scenarios (structure and delivery of support) IMPART leads and REACT supporters must be allocated the appropriate time and support to carry out their roles in REACT (balancing REACT supporter role) |
Trust staff need to customise the REACT toolkit to fit with existing services and local needs of users in that trust including local resource directory, availability of forum, etc. (toolkit flexibility, fit with existing structures) Where roles are not seen as being part of current practice (e.g. managing a forum), staff will require additional time, training and support to deliver this (fit with existing structures) Existing trust IT resources (availability of tablets, computers, and IT support) are likely to have an impact on implementation success (fit with existing structures) Training in REACT needs to be integrated with existing training framework but be attractive (visual) and involve relatives (staff engagement) |
REACT is clearly visible within the relevant clinical care pathways trust policy documents REACT is customised with accurate trust details Staff are given allocated time for training, supervision and carrying out their tasks specifically related to REACT Staff have easy access to computers/tablets and IT support to enable their online tasks related to REACT Staff can work easily between REACT and existing electronic health-care records/IT systems |
| NPT core construct components and toolkit questions | Systematic literature review | REACT feasibility study data | SRG data | Study-specific propositions: implementation of REACT more likely to succeed if: |
|---|---|---|---|---|
|
Systematisation: work of collecting information to determine how effective and useful it is for them and others Q: participants access information about the effects of the intervention |
Trusts very keen for formal structured feedback (audit) on accessibility, percentage take up and levels of use, and relatives’ feedback (monitoring) | Staff access regular data that show that relatives are using REACT | ||
|
Communal appraisal: formal and informal work to evaluate a set of practices – can use many different means to draw on experiential and systematised information Q: participants collectively assess the intervention as worthwhile |
Feedback from relatives is reviewed and shared as part of an operational meeting and can inform ongoing work | |||
|
Individual appraisal: experiential work people do as individuals to appraise the effects on them and the context they are in Q: participants individually assess the intervention as worthwhile |
Staff involvement will be linked to level of patient (relative) involvement | Staff are able to gather direct feedback from relatives they have invited to use the website (if positive then facilitates implementation) | ||
|
Reconfiguration: work to refine procedures, practices or even the intervention itself Q: participants modify their work in response to their appraisal of the intervention |
Clinical staff need to be able to modify the intervention based on user feedback (toolkit flexibility and monitoring) | Staff are able to request or enact improvements to REACT as they see fit |
Guided by the online NPT toolkit (www.normalizationprocess.org; accessed 6 December 2019), we began by developing our team-wide understanding of the four core constructs, then the 16 construct components (four in each core construct), and took the related questions from the interactive toolkit to generate a list of propositions relating to the general processes that NPT predicts are likely to lead to successful implementation of an intervention. The components and their accompanying questions are in column 1 of Tables 27–30. We then used a ‘data day’ to map the key findings of the systematic review, REACT feasibility trial and SRG data analyses onto the components (columns 2–4 of Tables 27–30).
Using the structure of the NPT questions, we were then able to synthesise across these data sources to generate our study-specific propositions (column 5 of Tables 27–30).
Unless otherwise specified, ‘staff’ refers to the whole range of staff working across roles with in the NHS trust; in practice, we acknowledged the need to identify which staff in particular were crucial to each proposition in our data collection.
Finally, Table 31 takes these hypotheses – again set out according to NPT’s core constructs and their components – and evaluates the outcomes at the end of the trial, based on qualitative and quantitative data gathered during the study.
| NPT construct | Implementation of REACT is more likely to be successful if: | Overall trust summary |
|---|---|---|
| Coherence | ||
| Differentiation | All staff have easy and independent access to the toolkit in their own time, with clear guidance on what it is, who it’s for and what it offers | All staff with an account created by their IL could access the toolkit and online ‘how-to’ manual, but limited access to IT, out-of-date browsers and trust firewalls limited access. Staff found it hard to find time to learn about REACT as it did not fit any existing training infrastructure |
| Communal specification | Staff have an opportunity to discuss whether or not and how to use REACT in their service, and decisions from this are visibly endorsed at senior management level | The decision to take part in REACT often came from the trust R&D department or senior staff who took on the IMPART role. Most staff were not part of the decision, and were often unclear as to who had made this decision and who was driving forward this change |
| Individual specification | Staff access training that clearly outlines their roles and responsibilities in delivering REACT | Lack of understanding about roles and responsibilities was evident. Attempts were made to address this with written documents and videos in successive implementation plans but most staff (TMs in particular) were keen for more face-to-face training from the research team. This was delivered early on but was not available to absent or new staff. Peer-to-peer training was valued but delivered ad hoc |
| Internalisation | Staff can view the toolkit and see clear benefits for staff and/or relatives, such as:
|
Staff identified many benefits to REACT for both staff (e.g. time-saving, improved quality of interactions with relatives) and relatives (e.g. high-quality, easily accessible information) Extensive user involvement was identified as a positive aspect of the toolkit. However, the use of diagnostic terms in one of the modules, and limited focus on recovery (1 module out of 12) meant that some questioned its fit with the EIP ethos The biggest barrier to staff engagement was the concern about managing risk on the forum and direct messages |
| Cognitive participation | ||
| Initiation | There is a clear lead (‘champion’) who drives REACT forward within the trust | Each trust began with an IMPART lead, but the need for a peer ‘champion’, whose role was to keep REACT in people’s minds and on meeting agendas, and support staff, became apparent. This was introduced with IPv3, too late for its impact to be evaluated |
| Enrolment | Staff make explicit links between the trust’s existing targets and priorities and REACT | Most staff were very aware of their service’s targets and priorities, and the national drivers for these (e.g. NICE, AWT). However, these were mostly service user related, not carer related. Targets that either were service user focused or had financial incentives were given priority |
| Legitimation |
Key roles are appropriately allocated Training is provided for tasks that may require new skills (e.g. moderating a forum) Staff feel ownership and take responsibility for promoting REACT within the service, and offering it to relatives (and do not see this as the role of the researchers) |
Staff in all trusts saw REACT as a research project, which limited engagement. Staff training was seen as the responsibility of the research team Some staff also felt that the research team should be ‘recruiting relatives’ Lack of experience, training and clear risk management protocols were barriers to RS engagement, and led to RSs in one trust refusing to accept this role |
| Activation | Delivery of REACT is a regular agenda item at relevant operational meetings of clinical teams | There was little evidence that REACT was a regular item for any clinical meetings. If it was, it was a research item. This gave the impression that REACT was not supported by the clinical service and over time led to abandonment |
| Collective action | ||
| Interactional workability | Staff carry out roles as outlined in the manual and have the resources to do this. Key tasks include:
|
ILs in all trusts did create accounts for staff and roles were allocated to RSs. However, lack of allocated time or supervision led to lack of proactive engagement among RSs, and concern among staff about how activity on the website was being managed. This made staff reluctant to refer relatives to REACT |
| Relational integration |
REACT is offered as part of an integrated package for relatives, not a standalone intervention Access is restricted to relatives who are already supported Staff are confident that the forum is well managed Staff are confident that direct messages are responded to RSs and ILs are clear and confident about managing risk identified on REACT |
REACT was restricted to relatives within the EIP teams, and this helped trusts to feel that activity on the website would be manageable However, because staff were unable to see the forum or direct messages, they had concerns about what might be posted and how this would be managed These concerns were exacerbated when the RS was either outside the clinical team (in one trust this was a member of the R&D department) or did not engage proactively with the website, owing to their own concerns about managing the forum |
| Skill-set workability | IL and RS roles are allocated to people with the time, skills, organisational role and support to carry these out | RS and RC roles worked much better when allocated to staff who already had a specialist role supporting carers. ILs were more effective when closely embedded within the clinical team, and not clinical academics, which reinforced the perception of REACT as a research not clinical endeavour |
| Contextual integration |
REACT is clearly visible in the relevant clinical care pathway trust policies REACT is customised with accurate trust details Staff are allocated time for REACT training, supervision and tasks Staff have easy access to IT equipment and support to enable their online tasks Staff can move easily between REACT and existing electronic health-care records and IT systems |
REACT was seen to fit easily within trusts’ care pathways and was included explicitly in service checklists and carer welcome packs. The toolkit was appropriately customised with trust-relevant details However, lack of interoperability between REACT and the trust electronic pathways was a consistently identified barrier Similarly, it did not fit with EIP teams’ usual ways of working in relatives’ homes and without mobile devices |
| Reflexive monitoring | ||
| Systematisation | Staff access regular data that show that relatives are using REACT | Lack of feedback about relatives’ use in early waves and low levels of engagement in later waves were clearly demotivating for staff and led them to stop inviting relatives to REACT |
| Communal appraisal | Relatives’ feedback is shared in operational meeting and informs ongoing work | None of the trusts had a formal feedback structure for relatives or a communal process to discuss this. Some staff shared informal feedback in team meetings |
| Individual appraisal | Staff can gather direct feedback from relatives whom they have invited to use the website (positive feedback facilitates implementation) | In IPv1, staff could not see if relatives had responded to their invitation. This was rectified in IPv2 and IPv3 but still did not provide detailed qualitative feedback. Some staff actively solicited feedback from relatives, but where this was negative, it led to discontinued use by the staff. However, positive feedback also inspired use |
| Reconfiguration | Staff can request or enact improvements to REACT as they see fit | Staff took part in a series of collaborative workshops to identify ways to facilitate REACT. However, time and limited resources meant that many suggestions could not be implemented during the project. Some, such as removing the need for staff and relatives to log in, are being explored for a future redesign of REACT |
Appendix 5 The caring role of participants
Table 32 provides information about the caring roles of research participants and how this varied over time, using data from the ‘About your caring role’ questionnaire completed at baseline and at the 12-week and 24-week follow-ups. This information was not collected from clinical participants.
| Caring role | Time point | ||
|---|---|---|---|
| Baseline (N = 53) | Follow-up 1 (12 weeks) (N = 18) | Follow-up 2 (24 weeks) (N = 18) | |
| Duration of caring role, n (%) | |||
| < 1 month | 2 (4) | – | – |
| < 1 year | 13 (25) | 3 (17) | 3 (17) |
| > 1 year | 38 (72) | 15 (83) | 15 (83) |
| Duration of caring role (months) | |||
| Mean (SD) | 48.4 (68.93) | 57.3 (97.41) | 35.2 (41.61) |
| Range (IQR) | 0–284 (9–48) | 3–415 (12.8–45.8) | 6–186 (15–43.8) |
| Level of contact (hours/week), mean (SD); range (IQR) | |||
| Face-to-face contact | 48.4 (43.56); 2–168 (18–62) | 36.1 (39.36); 0–168 (8.5–52.5) | 50.7 (45.75); 2–168 (14.3–70) |
| Other contact | 9 (15.42); 0–70 (1–10.5) | 9.1 (17.09); 0–70 (0–10.5) | 3 (3.07); 0–10 (1–4.3) |
| Total contact | 57.4 (46.72); 4–170 (21–82) | 45.2 (44.68); 0–168 (18.5–54.8) | 53.7 (45.35); 5–169 (16.3–71.8) |
| Impact on work role, n (%) | |||
| No: not in paid work before caring role | 15 (28) | 7 (39) | 5 (28) |
| No: still performing the same work | 26 (49) | 9 (50) | 7 (39) |
| Yes: reduced working hours | 4 (8) | 1 (6) | 3 (17) |
| Average reduced working hours, mean (SD); range (IQR) | 12 (2.45); 10–15 (10–14.5) | 20; N/A | 16 (6.93); 8–20 (N/A) |
| Yes: stopped working | 8 (15) | 1 (6) | 3 (17) |
| Additional time taken off, n (%) | |||
| N/A | 14 (26) | 9 (50) | 8 (44) |
| No | 18 (34) | 8 (44) | 7 (39) |
| Yes | 21 (40) | 1 (6) | 3 (17) |
| Hours taken off in past 12 weeks, mean (SD); range (IQR) | 15.3 (34.22); 0–168 (0–15.5) | 4; N/A | 9.3 (9.45); 2–20 (N/A) |
| Number of relatives cared for, n (%) | |||
| 1 | 40 (75) | 13 (72) | 11 (61) |
| 2 | 7 (13) | 5 (28) | 3 (17) |
| 3 | 3 (6) | – | 3 (17) |
| 4 | 3 (6) | – | 1 (6) |
| Total number of relatives cared for | 75 | 23 | 30 |
The majority of participants had been in caring roles for > 1 year and had an average of 45 hours’ predominantly face-to-face contact with the person they were supporting each week. Most participants reported that caring for their relatives had not affected their employment status or performance, either because they had not been in paid employment prior to their caring role or because they were still performing the same work. A small number of participants at each assessment point reported either stopping work or reducing their hours because of their caring role.
Appendix 6 Demographic characteristics of relatives
Demographic and clinical characteristics of the relatives cared for by participants at baseline and at the 12-week and 24-week follow-ups are presented in Table 33. The most common relationship was mother (participant) and child (relative cared for). Individuals cared for were primarily aged < 25 years and living at home. The most commonly reported diagnosis was psychosis. However, there were relatively high rates of missing data or instances when participants did not know the diagnosis of their relative.
| Relative characteristic | Time point, n (%) | ||
|---|---|---|---|
| Baseline (N = 75) | Follow-up 1 (12 weeks) (N = 23) | Follow-up 2 (24 weeks) (N = 30) | |
| Participant’s relationship to relative(s) | |||
| Mother | 45 (60) | 14 (61) | 13 (43) |
| Father | 2 (2.67) | 1 (4) | 2 (7) |
| Grandfather | – | – | 1 (3) |
| Sibling | 3 (4) | 1 (4) | – |
| Wider family | 1 (1) | 1 (4) | 1 (3) |
| Daughter | 7 (9) | – | 4 (13) |
| Son | – | – | 1 (3) |
| Partner | 5 (7) | 1 (4) | – |
| Friend | – | 1 (4) | – |
| Other | 1 (1) | – | – |
| Missing | 11 (15) | 4 (17) | 8 (27) |
| Age of relative(s) (years) | |||
| < 16–25 | 37 (49) | 10 (43) | 10 (33) |
| 26–35 | 10 (13) | 4 (17) | 5 (17) |
| 36–50 | 7 (9) | 4 (17) | 1 (3) |
| > 50 | 10 (13) | 1 (4) | 6 (20) |
| Missing | 11 (15) | 4 (17) | 8 (27) |
| Relative’s diagnosis | |||
| I don’t know | 5 (7) | – | – |
| Bipolar disorder, bipolar affective disorder, manic depression | 6 (8) | – | 1 (3) |
| Schizophrenia | 2 (3) | 2 (9) | 4 (13) |
| Psychosis | 38 (51) | 10 (43) | 9 (30) |
| Schizoaffective disorder | 1 (1) | 1 (4) | – |
| Other | 10 (13) | 4 (17) | 6 (20) |
| Missing | 13 (17) | 6 (26) | 10 (33) |
| Relative living with participant | |||
| Yes | 43 (57) | 12 (52) | 10 (33) |
| No | 19 (25) | 5 (22) | 10 (33) |
| Missing | 13 (17) | 6 (26) | 10 (33) |
Appendix 7 Website use of clinical and research participants
Table 34 summarises the 24-week website use of research and clinical participants, and the results of independent t-tests comparing their website use. The mean number of logins for the group as a whole was 3.78 (SD 4.43), but there was a lot of variation, with a range of 0–31 logins (median 2 logins, IQR 1–8 logins). The mean total time spent on the website was 40.6 minutes (SD 54.54 minutes), with a range of 0–298 minutes (median 20.1 minutes, IQR 4.9–57.5 minutes). In general, research participants used the website more than clinical participants, and the difference was significant in total number of logins, number of visits to modules 1–6 and module 11, number of visits to the forum, total time spent on the website and the total number of module visits (composite measure of visits to the 12 different modules).
| Website use variables | Mean (SD) | Median/range (IQR) | Independent t-tests | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| CP (n = 76) | RP (n = 56) | Overall | CP (n = 76) | RP (n = 56) | Overall | t | df | 95% CI | Cohen’s d | p-value | |
| Number of logins | 2.1 (2.56) | 6.1 (5.32) | 3.78 (4.43) | 1/0–17 (1–2) | 4.5/1–31 (2.3–8) | 2/0–31 (1–8) | –5.21 | 73.62 | –5.4 to –2.5 | 1.01 | < 0.001 |
| Number of visits | |||||||||||
| Module 1 | 0.5 (1) | 1.3 (1.22) | 0.9 (1.16) | 0/0–5 (0–1) | 1/0–5 (0–2) | 0/0–5 (0–1) | –3.82 | 104.38 | –1.2 to –0.4 | 0.69 | < 0.001 |
| Module 2 | 0.3 (0.57) | 0.7 (0.77) | 0.4 (0.69) | 0/0–3 (0–0) | 1/0–3 (0–1) | 0/0–3 (0–1) | –3.53 | 97.07 | –0.7 to –0.2 | 0.65 | 0.001 |
| Module 3 | 0.3 (0.69) | 0.8 (1.01) | 0.5 (0.87) | 0/0–3 (0–0) | 0/0–4 (0–1) | 0/0–4 (0–1) | –2.97 | 91.78 | –0.8 to –0.2 | 0.56 | 0.004 |
| Module 4 | 0.3 (0.63) | 0.8 (1.14) | 0.5 (0.92) | 0/0–3 (0–0) | 0.5/0–5 (0–1) | 0/0–5 (0–1) | –3.26 | 79.45 | –0.9 to –0.2 | 0.62 | 0.002 |
| Module 5 | 0.3 (0.57) | 0.7 (1.36) | 0.5 (1) | 0/0–3 (0–0) | 0/0–9 (0–1) | 0/0–9 (0–1) | –2.41 | 69.28 | –0.9 to –0.1 | 0.47 | 0.019 |
| Module 6 | 0.2 (0.54) | 0.8 (1.47) | 0.5 (1.08) | 0/0–2 (0–0) | 0/0–8 (0–1) | 0/0–8 (0–1) | –2.92 | 65.87 | –1 to –0.2 | 0.58 | 0.005 |
| Module 7 | 0.2 (0.62) | 0.6 (1.17) | 0.4 (0.91) | 0/0–4 (0–0) | 0/0–7 (0–1) | 0/0–7 (0–0) | –1.91 | 77.78 | –0.7 to 0.00 | 0.37 | 0.06 |
| Module 8 | 0.3 (0.79) | 0.4 (0.65) | 0.3 (0.73) | 0/0–5 (0–0) | 0/0–2 (0–1) | 0/0–5 (0–0) | –0.87 | 130.00 | –0.4 to 0.1 | 0.16 | 0.39 |
| Module 9 | 0.1 (0.39) | 0.3 (0.62) | 0.2 (0.51) | 0/0–2 (0–0) | 0/0–2 (0–0) | 0/0–2 (0–0) | –1.49 | 85.98 | –0.3 to 0.1 | 0.30 | 0.14 |
| Module 10 | 0.3 (0.74) | 0.4 (0.78) | 0.3 (0.76) | 0/0–5 (0–0) | 0/0–4 (0–1) | 0/0–5 (0–0) | –1.01 | 130.00 | –0.4 to 0.1 | 0.17 | 0.32 |
| Module 11 | 0.2 (0.63) | 0.5 (0.93) | 0.3 (0.79) | 0/0–5 (0–0) | 0/0–4 (0–1) | 0/0–5 (0–0) | –2.46 | 90.95 | –0.6 to 0.00 | 0.41 | 0.027 |
| Module 12 | 0.3 (0.88) | 0.6 (0.93) | 0.4 (0.91) | 0/0–6 (0–0) | 0/0–3 (0–1) | 0/0–6 (0–0) | –1.65 | 115.30 | –0.6 to 0.1 | 0.29 | 0.10 |
| Total number of module visits | 3.2 (6.15) | 7.8 (9.08) | 5.2 (7.84) | 1/0–27 (0–3) | 6/0–50 (1–11.5) | 2/0–50 (0–7) | –3.26 | 90.88 | –7.4 to –1.8 | 0.61 | 0.002 |
| Number of visits to the forum | 0.4 (0.65) | 1.7 (2.47) | 1.0 (1.81) | 0/0–3 (0–1) | 1/0–12 (0–2.8) | 0/0–12 (0–1) | –4.03 | 60.65 | –2 to –0.7 | 0.81 | < 0.001 |
| Total time spent on website (minutes) | 24.7 (37.84) | 62.1 (65.68) | 40.6 (54.54) | 9.7/0–156.5 (1.7–25.7) | 39.45/0–298 (16.3–78.6) | 20.1/0–298 (4.9–57.5) | –3.82 | 81.62 | –56.8 to –17.9 | 0.73 | < 0.001 |
Appendix 8 Paired t-test results
Table 35 shows the results of the paired t-tests comparing baseline scores with those at the 12- and 24-week follow-ups. None of the comparisons was statistically significant. Mean values of the GHQ-28 total scores and subscales of social dysfunction, severe depression and anxiety and insomnia decreased and increased for the CWS well-being subscale and eHealth literacy, all with small effect sizes.
| Variable | Baseline and follow-up 1 (12 weeks) | Baseline and follow-up 2 (24 weeks) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of paired outcomes | Mean change: baseline to follow-up 1 (SD) | t | 95% CI | Cohen’s d | p-value | Number of paired outcomes | Mean change: baseline to follow-up 2 (SD) | t | 95% CI | Cohen’s d | p-value | |
| GHQ-T | 20 | –0.6 (12.6) | 0.21 | –5.3 to 6.5 | 0.05 | 0.83 | 20 | –1.35 (9.9) | 0.61 | –3.3 to 6.0 | 0.12 | 0.55 |
| GHQ-S | 20 | 0.6 (3.9) | 0.69 | –2.4 to 1.2 | 0.16 | 0.50 | 20 | 0.7 (4.3) | 0.73 | –2.7 to 1.3 | 0.23 | 0.48 |
| GHQ-AI | 20 | –0.55 (4.8) | 0.51 | –1.7 to 2.8 | 0.13 | 0.61 | 20 | –1.15 (4.0) | 1.30 | –0.7 to 3.0 | 0.26 | 0.21 |
| GHQ-SDF | 20 | –0.2 (3.4) | 0.26 | –1.4 to 1.8 | 0.08 | 0.80 | 20 | –0.7 (2.7) | 1.16 | –0.6 to 2.0 | 0.28 | 0.26 |
| GHQ-SD | 20 | –0.45 (2.8) | 0.72 | –0.8 to 1.8 | 0.14 | 0.48 | 20 | –0.2 (2.4) | 0.37 | –0.9 to 1.3 | 0.05 | 0.72 |
| CWS-W | 19 | 2.42 (17.5) | 0.60 | –10.9 to 6 | 0.09 | 0.55 | 18 | 3.28 (21.9) | 0.64 | –14.2 to 7.6 | 0.14 | 0.53 |
| CWS-S | 19 | –0.53 (8.5) | 0.03 | –3.4 to 4.6 | 0.08 | 0.79 | 18 | 0.78 (9.4) | 0.35 | –5.4 to 3.9 | 0.08 | 0.73 |
| eHEALS-T | 19 | 1.00 (4.9) | 0.90 | –3.3 to 1.3 | 0.18 | 0.38 | 18 | 0.5 (4.7) | 0.45 | –2.8 to 1.8 | 0.10 | 0.66 |
| EQ-5D-5L VAS | 19 | –2.26 (22.9) | 0.43 | –8.8 to 13.3 | 0.10 | 0.67 | 18 | –4.94 (21.4) | 0.98 | –5.7 to 15.6 | 0.22 | 0.34 |
| EQ-5D-5L index | 19 | 0.01 (0.1) | 0.61 | –0.1 to 0.0 | 0.12 | 0.55 | 18 | –0.01 (0.01) | 0.40 | –0.04 to 0.06 | 0.10 | 0.70 |
Appendix 9 Estimated costs of resource packs
All trusts were given free access to REACT and IPv1 at the start of wave 1. Trusts in waves 2 and 3 received additional resources associated with IPv2 and IPv3 at no cost from the research team. These were estimated to cost approximately £400 per trust, and would be an additional treatment cost if REACT was implemented in routine clinical practice. A summary of estimated item costs is shown in Table 36.
| Item | Quantity | Cost (£) | |
|---|---|---|---|
| Overall | Per unit | ||
| Pens | 40 | 21.4 | 0.53 |
| Sticky notes | 30 | 27.9 | 0.93 |
| Travel mug | 20 | 37.6 | 1.88 |
| Ceramic mug | 20 | 56.12 | 2.8 |
| Booklets with business and insert cards, plastic wallets | 200 | 216.74 | 1.08 |
| Staff induction packs for each IMPART role | 5 | 9.14 | 1.83 |
| Maximising success pack | 1 | 0.3 | |
| Laminated poster | 2 | 0.5 | |
| Postage per team | 2 | 25.96 | 12.98 |
| Implementation pack total per trust | 395.66 | ||
Appendix 10 Lakes Trust case summary
Participants
Please note that trust, team and participant names have been anonymised in quotations in Appendices 10–15.
| Participant identifier | NHS role | REACT role | Number of relative invitations sent | Research activities participated in |
|---|---|---|---|---|
| GO-IL-CP-01 | Psychiatrist | IMPART lead | 0 | Individual interview, SRG |
| Lakes-CL-CP&HRICE-01 | Clinical psychologist and head of research innovation and clinical effectiveness | Clinician | 0 | SRG |
| GR-RS-CC-06 | Care co-ordinator | REACT supporter | 5 | Group interview |
| DU-RC-CC-01 | Community psychiatric nurse | REACT champion | 2 | SRG, individual interview, implementation workshop |
| Lakes-CL-MHN-03 | Community psychiatric nurse | Clinician | 0 | SRG |
| Lakes-IL-CP-02 | Psychiatrist | IMPART lead | 19 | SRG, implementation workshop, individual interview, group interview |
| DU-ST-04 | Lead for CRN | N/A | 0 | Group interview |
| DI-RC-CC-02 | Care co-ordinator | REACT champion | 0 | Implementation workshop |
| DI-RC-CC-03 | Care co-ordinator | REACT champion | 0 | Group interview, implementation workshop |
| DU-CL-Cpsyc-07 | Clinical psychologist | Clinician | 0 | Individual interview |
| GR&CO-CL-TL-08 | Team lead | Clinician | 0 | Individual interview |
| DU&SW-CL-TL-09 | Team lead | Clinician | 0 | Individual interview |
| DU-CL-CC-10 | Care co-ordinator | Clinician | 0 | Individual interview |
| GR-CL-CBT-11 | CBT therapist | Clinician | 0 | Individual interview |
| GR-CL-SW-12 | Support worker | Clinician | 0 | Individual interview |
| GR-CL-CP-13 | Psychiatrist | Clinician | 0 | Individual interview |
| GR-CL-CP-14 | Care co-ordinator | Clinician | 0 | Individual interview |
| GR-CL-SW-15 | Support worker | Clinician | 0 | Individual interview |
| GR-CL-Cpsyc-16 | Psychologist | Clinician | 0 | Individual interview |
| SW-RC-CC-04 | Care co-ordinator | REACT champion | 0 | Individual interview |
Context
Lakes Trust serves a population of 1.5 million, predominantly rural and of white British ethnicity. The trust employs approximately 6000 staff. EI services offer care to 569 people delivered by 46 clinical staff. Seventy-five per cent of patients are in contact with a relative. Compared with other trusts, Lakes Trust offered the largest number of family interventions, with 63% of service users and their families being offered family intervention. In contrast, Lakes Trust’s performance of the NICE standard for carer education was relatively poor, with only 30% of carers being offered carer-focused education and support.
Lakes Trust EIS consists of six teams: Duck, Swan, Grebe, Coot, Diver and Goose. The caseload and population served vary among the teams, for instance Grebe mainly serves a rural population, whereas Duck serves a mainly urban population. The teams operate independently but are managed in pairs: Duck and Swan Team are managed together, as are Grebe and Coot, and Diver and Goose. The original IMPART lead (GO-IL-CP-01) for Lakes was a senior clinician and was a key facilitator in gaining trust support for the IMPART study. The IMPART lead (GO-IL-CP-01) left Lakes Trust in early 2017 and a new IMPART lead took over. The second IMPART lead (Lakes-IL-CP-02) then took over the role, but there was a period of limited activity until December 2018, when REACT started to gain momentum with the second IMPART lead and the trust generally. This trust allocated REACT supporters and REACT champions but their involvement with REACT fluctuated over the study period.
Although some teams appear more committed to carer support than others, the trust as a whole appears to recognise the importance of carer involvement. There are several documents and flyers on the trust website relevant to carers and service users. In addition, as part of initial introductions of relatives into the service, staff members complete a ‘Getting to Know You’ document. This document is integrated as part of their ‘Rio’ system and is advertised on the trust website. However, the teams do not conduct carer’s assessments; any carers identified who need an assessment are referred to local external bodies, such as carers’ groups, where they will complete the assessment.
Lakes Trust received IPv3.
Key findings against normalisation process theory components
Coherence
Differentiation
The majority of staff across Lakes Trust had some awareness of REACT, which has been influenced mainly by the presence of the research team, the IMPART lead and REACT champions. Presentations delivered by the research team are discussed most often as confirming and expanding staff’s initial vague understanding of REACT. However, even where staff have been present at discussions led by the IMPART lead, they have not been fully aware of what REACT is and what input from staff is required. The process of dissemination has not been equal across teams in the trust, which has led to some being more informed than others:
It’s moved forward a little bit further with Grebe than it has in Coot, you know they didn’t seem to have that much knowledge about REACT and I mean [staff member], I shouldn’t really mention names, but you know [staff member] said . . . [staff member] kind of said, she kind of whispered to us I’ve never seen this, you know, I know nothing about this, and I said but we’ve discussed it. You know I’ve talked about it, Lakes-IL-CP-02’s the lead and you know the Goose Diver team and Coot should have more familiarity with REACT than any other service, but actually this team doesn’t seem to be as aware.
GR&CO-CL-TL-08, 7 February 2018, individual interview – Lakes
Brilliant, so could you tell me about when you first became aware of REACT?
The first time I became aware of REACT when you came up to the team, was it about a month ago I think?
Yeah.
Yeah and that was the first time I’d really been aware. I was aware a little bit before that ‘cos we received a box of goodies and things, so I had a little flick through the leaflet but I hadn’t really done much with that. So yeah that was the first time I kind of properly got information about REACT was when you came up that time for our meeting.
SW-RC-CC-04, 30 April 2018, individual interview – Lakes
Lakes Trust has a very positive attitude towards working with families and relatives, evidenced by its existing resources including information booklets, family therapists and behavioural family therapy (BFT)-trained care co-ordinators. For individual staff members who have an understanding of what REACT is and what it involves, comparisons are made between what the staff offer face to face and what REACT offers online. REACT is also compared with other research projects the trust is involved with and external resources, with staff suggesting that REACT has to compete for staff attention:
I mean we’ve got family therapy and family care and family helpers, we’ve got qualified family therapists so obviously families are very very important and carers. We have a number of family therapists in our team now you know there’s two or three that have recently just qualified, trained in behavioural family therapy and a systemic models and stuff like that and I myself have done it as well, I think you have as well DI-RC-CC-03, with a family thing, so we already go out and see families and we educate them about mental health problems, we kind of do what the REACT programme does online but we go out and meet them face to face.
DU-RC-CC-01, 25 April 2018, group interview – Lakes
In some respects yeah, we’re fighting a losing battle because although we’ve got REACT and the iPads, the trust does some really good kind of self-help leaflets and in print but that’s there’s more amount of stuff on social media and the internet and you can take anything you like.
GR-CL-CBT-11, 24 April 2018, group interview – Lakes
Individual specification
Although REACT supporters have had e-mail correspondence with the research team and the IMPART lead and attended presentations and meetings focusing on REACT, REACT supporters are unclear about what the role involves and the commitment required to fulfil the role. REACT supporters’ limited understanding of what the role requires has also influenced the extent to which they have felt able to attempt to integrate the role with their professional role. This is different from the REACT champions who, through discussions and meetings, have been able to understand their role and the tasks they need to undertake to promote REACT:
I think it’s me at the minute, I think we were going to do it between, there’s a week later on that I’m not able to get to but we’re discussing that process, who does what when and how you kind of fit that into other work and how that’s changed, back to the earlier question I think I got an e-mail from Lancaster, I was kind of copied into that e-mail about what REACT was, what IMPART was and what I’d be committing to and at that time it was kind of no longer than an hour a week, but it just feels so much bigger than an hour . . .
Do you say it feels like they’re given an hour as well, how much time a week do you think you would have to give?
I don’t know, I’m kind of the designated, well there’s two of us now in the team, designated to kind of oversee this thing and I still don’t know myself yet what it actually involves.
GR-RS-CC-06, 24 April 2018, group interview – Lakes
Where there has been a limited understanding of what staff are required to deliver REACT, staff members have tended to distance themselves from the intervention rather than seek out opportunities to learn more about it. Staff understanding of what is required to deliver REACT and what they would need to do to use the resource with families largely seems to have come from researcher presence. Awareness of the resource seems to have come from the research team and IMPART leads, but actually knowing what is required has been primarily influenced by the research team:
Was there anything particularly helpful about the introduction that I gave?
I think it was just about having the opportunity to ask questions, but also about kind of seeing it on the screen and looking at it and actually being able to see what it looked like and how it actually worked, because in a leaflet form it just sounds brilliant but it also sounds like a lot of work, when it’s actually not. So I think initially when I saw the leaflet and I read about it I was like right OK I think I’ll be able to think about that soon, but also like it was too much for me to think about, it’s too much work, it’s another thing to do, but by being able to sit down with yourselves and explaining what it was and what it looked like, it wasn’t actually as much as I thought it was going to be, so it was a bit more of a actually I can consider this or I can do this with the next person who I visit. So I think it’s appropriate for, so it didn’t feel as overwhelming.
DU-CL-CC-10, 6 April 2018, individual interview – Lakes
Communal specification
Among staff, particularly managers and REACT supporters, there seemed to be some confusion around what the roles of the staff in the team were. The REACT supporters attended sessions with the IMPART lead and researchers to try to understand their role more. Some confusion appears to be rooted in the language used, specifically ‘supporter’ and ‘champion’, owing to the overlap with ‘carers’ champion’, and how support is offered to this role:
And you said he was going to do another session next week, he was going to, we knew the session was on, I knew it was this week, this afternoon, and he was going to go through things again, ‘cos I think that the supporters are quite anxious about what’s happening and what their role is and what they’re likely to encounter, and I think that’s still very unsure about how it’ll all work.
GR&CO-CL-TL-08, 7 February 2018, individual interview – Lakes
The REACT champion’s meeting started with a discussion about roles as there was some confusion around the REACT supporter and REACT champion with GR-RS-CC-06 and [Grebe REACT supporter]. They thought that GR-RS-CC-06 as the champion and [Grebe REACT supporter] was a supporter because GR-RS-CC-06 would be the main REACT member in the team and [Grebe REACT supporter] would support him (This was decided as [Grebe REACT supporter] is the Carers’ champion and it was suggested by the team lead that GR-RS-CC-06 could support [Grebe REACT supporter] in this role, and in return [Grebe REACT supporter] would support GR-RS-CC-06 in his REACT role. I distributed print outs of the tables of roles, and we all looked at these.) [Grebe REACT supporter] said she though one had to be the champion and one had to be the supporter. After they had read the table of roles, they asked if they could both be supporters and said that actually everything on the REACT champion column of roles was what GR&CO-CL-TL-08 (Grebe and Coot Team Lead) was already doing. They said she has been promoting REACT and keeping it on the agenda. They said that the role sheet had been helpful for outlining their roles.
Observations from REACT champions’ meeting, 7 February 2018
Titled REACT staff and general staff suggested that what REACT aims to do resonates with what the family therapists do already. This appears to have created some confusion and concern among the staff about why the family therapists are not involved with the project. One family therapist discussed that they had not felt able to get involved with REACT because they did not know what their role would involve:
Yeah I do think there is something a bit odd about a family resource coming from psychiatry not from the family therapists, I do think that is unusual.
DU-CL-Cpsyc-07, 3 January 2018, individual interview – Lakes
Just saying about you giving the leaflets out, is anyone else in Diver doing anything with REACT or is it just you?
There’s a couple of us, we get a similar question about why the family therapists are not here?
DI-RC-CC-03, 25 April 2018, group interview – Lakes
Internalisation
Staff were able to identify possible benefits of REACT for relatives and for themselves. Access to information and an interactive platform as well as the possibility of relatives being able to use REACT to help themselves support their relatives were identified as benefits. This was also seen as a positive for staff as if relatives were able to access information independently of them it would help them to manage their working capacity when they are already overwhelmed with caseloads:
I mean relatives would like to look at it so they can support their own child or son, daughter or whoever you know, their husband, wife, they might need those services and they can take a lead role it in.
Yeah exactly yeah, definitely.
A lot of the time it’s just straight if there’s a problem I’ll ring the care co-ordinator and see if we can solve it, whereas if the information’s there they might be able to go and do it themselves.
Yeah exactly.
This would be an incentive for care co-ordinators as well because if you.
Reduce our workload.
DI-RC-CC-03, DU-RC-CC-01, DI-RC-CC-02, 12 December 2017, and Lakes-IL-CP-02, 12 December 2017, group interview – Lakes
The majority of staff members had a general positive attitude towards REACT. However, whether or not staff members felt that REACT has benefit for their work is dependent on their knowledge of the content of the website. Although some staff accepted that the premise of REACT would meet relatives’ needs, it may not offer any benefit if it presents conflicting information. Some staff felt that they could not personally invest in REACT until they have had the opportunity to understand what it contains and make a judgement on whether or not it is suitable. Staff members who believe that REACT aligns with what they discuss in their roles see it as a complementary resource to the existing resources that the trust offer that could help achieve desired outcomes among family, such as shared understanding:
I think families and possibly care co-ordinators they are crying out for information and certainty and what’s going on, what should I do, so in some ways they would find I think it would there’s a real demand for this kind of thing. And obviously online so yeah I think it’s the way forward in lots of ways, my only as I said my only hesitation is it’s what information is being given, who’s that from, what perspective is it and how does it fit with where the family’s at and where the client’s at? So blindly giving information you know there is a difficulty with that particularly in psychosis which is all about how we make sense of the world and what’s real and what’s not, so I’m very very supportive but I am also just have that slight you know who decided what information is being given and how might that fit with what an individual, where that’s at with the work that we’re doing with an individual family. That’s my kind of just confirms I guess, yep.
DU-CL-Cpsyc-07, 3 January 2018, individual interview – Lakes
Another concern raised by staff about REACT was focused more generally on it being something additional to their core work that they would have to undertake. A lot of staff discussed how busy they were and how their role had changed over recent years and that they sometimes struggled to find the time to offer support outside what was mandatory or target driven:
There are so many different issues that we never did 5, 10 years ago that we’re doing now. So we’re not the role of the nurse has diversified into such huge areas, this REACT potentially could be looked on, and I’m not saying it’s looked on now, but by other people it could be looked on as another thing which is just another piece of work that I have to do on top.
DU-RC-CC-01, 12 December 2017, group interview – Lakes
Cognitive participation
Initiation
Both of the IMPART leads, NTIL01 and NTIL02, have been responsible for driving the intervention forward, although this has happened consecutively rather than in parallel. The first IMPART lead, NTIL01, was involved in initiating the set up of REACT in Lakes Trust and took action independent of the research team to drive the intervention forward. NTIL02 has been a predominant factor in the initiation of REACT in Lakes Trust and has undertaken a range of actions, including organising ‘REACT champions’ meetings’ and discussing REACT in team meetings, to revive REACT and drive it forward. This has raised concerns among some staff members, but many have said that they have too many competing priorities to assist him:
So is it NTIL02 that mentions it in the strategy meetings or is it?
Yeah, GO-IL-CP-01 used to, I mean you know GO-IL-CP-01 when we first agreed to be a part of the study it was because we agreed it in a strategy meeting that we thought it would be helpful and then he took the lead from there as well, so it was talked about a lot and then there was a transition where Lakes-IL-CP-02, yeah GO-IL-CP-01 left and Lakes-IL-CP-02 started, and so it kind of it’s come back up again certainly over the last 6 month, it’s become a little bit more proactive and so yeah.
GR&CO-CL-TL-08, 7 December 2018, individual interview – Lakes
The extent to which team managers and senior staff have been involved in driving REACT forward has varied within Lakes Trust. Where a key member or senior member of staff have not been involved in assisting with the promotion of REACT, REACT champions have felt limited in the extent to which they can drive it forward. In other teams, the team manager has been actively involved in promoting REACT and has taken action to implement the resource in the two teams they manage by creating staffing structures that fit with existing roles. One team manager discussed that they felt uncomfortable about asking staff to undertake tasks associated with REACT owing to the volume of mandatory and target-driven tasks they were already giving them:
With Lakes-IL-CP-02 it must be great to have a consultant that you can turn around and look to a consultant and say you know any discussions around that, you know . . . not in there that often and the manager’s just new to be fair, it’s not her fault, we have got a new manager in, she’s now being kind of told from higher up that this is what your job is, she’s focused on targets, ‘cos we have got to achieve targets and goals, we have had another new manager kind of come in to the team who’s taken Coot away from Duck.
There’s loads of dynamics.
There is isn’t there, but that’s the bottom line, the bottom line is there’s a bit of dynamics situation going on where managers are trying to achieve targets, I’m not making excuses, but I’d say since DU&SW-CL-TL-09’s come up the manager, things have been very difficult to try and move forward. Yes I can hand out sheets when I see a patient and stuff but that’s as much as it’s going at the minute you know for me.
DU-RC-CC-01 and DI-RC-CC-03, 25 April 2018, group interview – Lakes
What I’ve done in Grebe is I have a carers’ champion, and then I have GR-RS-CC-06 who’s the REACT supporter, and I’ve actually paired them up so that they support each other, because there’s a lot of work to be done through the carers’ champion that could be useful to REACT, so it was easier to do that, so they’re both doing a dual role, so I think that might be something that I’ll do in the team, but again we’re both small teams and it can be a lot of work you know.
GR&CO-CL-TL-08, 7 December 2018, individual interview – Lakes
Enrolment
In Lakes Trust, staff were hesitant to volunteer to undertake the REACT supporter role. The lack of enthusiasm centres around concerns about the perceived time commitment that the role requires, risk management of the website and the fit with their professional role. Owing to the lack of voluntary undertaking, individuals have been assigned the REACT supporter roles by the original IMPART lead and team managers. The REACT champion role that was available in Lakes Trust was much more appealing to staff:
. . . but people aren’t keen to become representatives or leads in something because again our time’s just so limited.
Yeah, is that what’s stopping people do you think, the time or is there anything else that is possibly putting people off becoming leads or representatives?
I think it’s the time and the level of commitment that it would need, definitely, I don’t think anything else would be like preventing people from doing it, especially personally, I think it’s great so I wouldn’t, it’s just the caseload and time and being able to fit things in, definitely.
DU-CL-CC-10, 6 April 2018, individual interview – Lakes
The involvement of senior staff including team leads, psychiatrists and psychologists was limited to supporting and encouraging others to become involved in delivering REACT. Senior staff did not take on a titled REACT role, despite requests from the IMPART lead mainly owing to the volume of their existing workload. Other members of senior staff discussed that as they usually work on only a one-to-one basis with service users they did not think that REACT would fit with their working pattern:
When Lakes-IL-CP-02 first told you about it, did he ask you like specifically to do anything with it or?
Well he was asking me to sort of be a supporter and I just said absolutely not at this moment in time, I’m working a 60-hour week as it is, I’ll just leave it alone.
Is that what it was like for you at the time, a 60-hour week?
It’s still not far off now.
DU&SW-CL-TL-09, 22 March 2018, individual interview – Lakes
None of the psychologists are involved in our site, have you got psychologists?
No, [psychologist] been asked by Lakes-IL-CP-02 a couple of times but I don’t think.
He was just backed away.
It’s not that vital to their job.
DU-RC-CC-01 and DI-RC-CC-03, 25 April 2018, group interview – Lakes
Legitimation
Staff have conflicting opinions about the extent to which REACT is suitable for Lakes Trust EIS and individual staff roles. Some staff see REACT as a resource that complements NICE guidelines and existing staff roles, in particular the carers’ champion role. There are concerns among other staff about whether or not REACT provides the right level of information for relatives, whether or not it fits with the clinically led service model and whether or not diagnosis topics and the module titles are appropriate for EIS, as this is not usually discussed until individuals are leaving services. Individuals who are concerned about levels of information still deliver REACT, unlike staff who are concerned about the conflicting REACT and therapeutic content:
I think it more comes under the fact that I’m the carers’ champion, I think it’s been involved in that kind of thing.
OK brilliant, and how does the REACT champion role fit with your carers’ champion role?
Quite well yeah, kind of it fits with the caring really well.
SW-RC-CC-04, 30 April 2018, individual interview – Lakes
Yeah, so basically this project fits very well in the NICE guidelines and it’s just how to make team managers aware and how to demonstrate that this is concordant with the guidelines and with audit tool that they’re using.
Lakes-IL-CP-02, 26 October 2018, individual interview – Lakes
Despite the majority of staff attitudes towards REACT being positive, REACT remained low in staff’s priority rankings. Staff admitted that competing pressures presented by their work influenced their ability to deliver REACT and dedicate resources to it. Despite being a trust that has a focus on relatives and carers, REACT as well as work with carers can drop in the priority scale to targets associated with service users and monetary incentives:
So if we are going to scale priorities, where would REACT fit do you think?
Pretty low.
Yeah.
No offence.
DU&SW-CL-TL-09, 22 March 2018, individual interview – Lakes
We’re not going to be allowed to, or we are going to be allowed, it’s important to drive this but then if we’ve got our managers saying well there’s DI-RC-CC-03 and DU-RC-CC-01 there’s 20 million pound to this physical health target if you’ve got to, and that’s OK it’s quite disheartening for the nurses because all you want to do is serve your patient and in essence you’ve got to come off clinical duty so you can prioritise this target, you’ve got to do all the physical health, that’s just an example of there’s money attached to absolutely everything, if with the greatest respect if REACT isn’t got 20 million pounds to it, we’re going to be kneecapped by the managers to say we’ve got to prioritise on the stuff that’s going to keep ourselves going, even though this would keep ourselves going because if you give that education and that support to people who comes.
DI-RC-CC-03, 25 April 2018, group interview – Lakes
Activation
Team efforts to keep REACT on the agenda and sustain its delivery are not equal within Lakes Trust. Diver and Goose’s team meeting agenda had REACT as a regular agenda point but it was forced to compete with other demands. A barrier to sustaining REACT is the other commitments and pressures that the teams also discuss and how decisions are made to prioritise. In Grebe and Coot, REACT is included in the team meetings but at present it does not seem to be something where sustainment and initiation are actively considered, but the enthusiasm of the team manager to sustain the intervention suggests an attempt to facilitate the intervention. In Duck and Swan, there does not appear to have been as much commitment to sustaining REACT as in the other four teams, causing it to become ‘lost’ among staff. There was little evidence of plans to change this:
Whether they do or not I guess we’re all it comes up in my team’s meeting, the Diver some of the team’s meeting it’s always on the agenda, again like everything though it’s which of the 40 plates are you going to drop that are spinning. And that sounds very bad and again probably negative in a way to say because if you were coming at us with and we had five patients each and we had a bit of time we’d just turn around to them during the day and have half an hour time or a lunch then I think it would be far far easier but.
DI-RC-CC-03, 25 April 2018, group interview – Lakes
Yeah and do you think REACT has become a bit has become lost?
I’ve lost sight of it, I don’t think I can speak to the rest of the team, I don’t know how many referrals you’ve had, yeah I don’t know because I haven’t like I said I just haven’t managed to, I’ve lost sight of it and I yeah.
DU-CL-Cpsyc-07, 3 January 2018, individual interview – Lakes
At a more informal level, there was little evidence that REACT is discussed among colleagues unless initiated by an agenda point or a focused REACT meeting. Where it was discussed, it was among individuals who are more invested but was still not considered to be a ‘hot topic’:
Brilliant, do you discuss REACT with anyone at all?
Do I? No.
DU&SW-CL-TL-09, 22 March 2018, individual interview – Lakes
Is REACT discussed amongst your colleagues at all?
Some. I know that of the people who attended the REACT meeting are quite fans of it so I guess the people who are more involved with carers maybe talk about it a little bit more, but I wouldn’t say it was a hot topic.
DU-CL-CC-10, 6 April 2018, individual interview – Lakes
Collective action
Interactional workability
REACT champions and care co-ordinators are able to deliver the intervention to relatives as part of their existing approach, and are able to modify their approach depending on the skill set of the relative. However, a structured mechanism or plan has not been produced for an informed and systematic way for the team to introduce REACT and sign relatives up to the website. This, along with limited knowledge of the website and the process of signing up relatives, has resulted in very few relatives having accounts:
Yeah sure, she was I kind of brought the leaflet with me and initially she didn’t really want anything to do with it because I think the internet’s just quite scary and online kind of stuff was quite intimidating for her, but when we were kind of looking at the site, we kind of I try, like she’s got like a tablet and on the internet but I took my laptop, so there was a few times it wasn’t great because it was like Wi-Fi connection with my laptop and things, but ultimately when she kind of looked at it I think she felt like it was quite like it wasn’t as intimidating as she thought it was going to be, and when we looked at if she never really thought through I’ve got to admit but I’m still in the process of continuously kind of discussing it with her because I think she’s one of these people who will just kind of forget to use it when I’m not maybe there, but once she gets the hang of it and she’s not kind of scared of it I think she would use it on her own.
DU-CL-CC-10, 6 April 2018, individual interview – Lakes
So people were much more enthused about doing it ‘cos I do think that there was some, we haven’t signed anybody up in Grebe and I was really quite surprised at that, I mean I had checked with GR-RS-CC-06 and I was quite surprised because people had taken the cards out, I knew people had taken the cards out but I think that people had said I don’t really know what I’m telling them, the information leaflet is clear, it’s concise and all the rest of it, but it doesn’t actually tell you, you can’t see the site and you can’t see what’s there.
GR&CO-CL-TL-08, 7 February 2018, individual interview – Lakes
Skill-set workability
Staff discuss the need for both clinical and technical competencies in REACT supporters. There is a concern among current REACT supporters around their ability to appropriately complete the technical side of the REACT supporter role. As there is currently minimal activity on the website, this is not an issue at present, but there is a concern that as activity increases the role may be more suitable for someone with more technical knowledge. Managers appear to be aware of the REACT supporter role requiring a balance of technical and clinical skills and have concerns that they have not appropriately allocated the role to individuals that have both of these skill sets:
Although we’ve had REACT for a while there’s not a lot of activity on the site, I think that’ll change in time but I’m probably not best placed to be in a position, being I am computer savvy to an extent but there’s this kind of whole level about that in terms of kind of managing a site and kind of dealing with queries like that, I think these are the difficult questions that come up from other supporters within the locality, lots of what do we do ifs. And I think that stems from this same issue, this target-driven thing, this kind of you need to get certain things done or you’re then accountable to the targets rather than the people you’re sitting in front of.
GR-RS-CC-06, 24 April 2018, group interview – Lakes
It’s also thinking about and I mean that’s more for line managers is thinking about who is going to be able to do it because it is a little bit technical as well and as you could hear from me yesterday, I can manage computers but I’m not great with computers, and actually when I’m thinking about it, one of the people I’ve got identified is really quite and by their own admission would say that they’re quite well with kind of tools on the computer, you know Rio and how to do things and I think hmm, in Grebe we don’t have, we’re all of a similar kind of age bar [staff member] and you know she certainly talks about things in a very different way from how we do and I think you know we need to think about that. You want your experienced staff to be the people that answer the questions but actually you need people that are tech savvy and I’m not convinced that I’ve been that clever with people being tech savvy so.
GR&CO-CL-TL-08, 7 January 2018, individual interview – Lakes
Several staff members at Lakes Trust family therapists are repeatedly identified as an important staff collective to try to engage with the REACT intervention and promote it to. Staff suggest that their experience, skills and working practices would make them suitable for delivering the REACT intervention. However, family therapists have not engaged with the intervention:
And what I suggested I think in the last meeting was that maybe the family therapists or family workers should be pushing REACT because I think from an educational point of view, they’re the ones that are sitting like we are now in a family environment saying you know your son or your daughter’s going through this, it must be terrible, can I suggest REACT? . . . they need to be tuning it to this because I think they need to be playing a part, because I think family therapists, I’m not saying we’ve got more work on than a family therapist has, but they’re the ones that see the families that’s what they do, that’s what their bread and butter is. So if they’re working with families, they need to be selling it as much as we do.
DU-RC-CC-01, 25 April 2018, group interview – Lakes
Relational integration
Staff liability and accountability with regard to the forum and direct messaging service that the REACT intervention offers have been a constant source of concern to REACT champions, REACT supporters and staff generally. Staff have not felt confident that they can safely make use of the intervention and that it could be used as a crisis service, or relatives may see it as an alternative to contacting the team rather than an extension of what the team already provides. This concern has caused individuals to change their REACT roles from supporters to champions so that they did not have to be associated with or responsible for the forum and direct messaging service:
My forever concern was that just the forum on that one, it’s probably well documented you know, not being negative or certainly not to embrace the website, it’s absolutely no chance I’m going to be putting my registration at risk to look over something that’s, but for the confidence, the security, the even if everybody somebody just says I need help right now doesn’t get it within 20 minutes, a stereotype saying [?] off the bridge and then well they put a cry for help knowing DI-RC-CC-03 was on duty and he didn’t see it.
DI-RC-CC-03, 25 April 2018, group interview – Lakes
Staff who are aware of the content and features of the REACT website believe that it will meet the needs of relatives and it complements the messages the teams are delivering. There is a concern that as each team has different internal and external resources that the REACT supporters monitoring the website may not have enough knowledge of what it can offer relatives and as a result may provide inaccurate information to relatives. As the direct messaging service is not filtered by teams within the trust, some planning of how supporters will respond needs to take place:
So when you say that do you think when you say the REACT supporter, do you think for is this like for the messaging service or something like that?
I think it depends on what comes up. For basic support around accessing the site, then it could be any supporter, but I think if it’s something specifically about you know I’ve got this difficulty or my son requires blah blah, it would be more specific if it was the locality worker that was able to respond to that and I suppose that’s some of the work that you’re doing with NTIL02 and the supporters this afternoon, is looking at if it is something quite specific do they then just you know say it was me that was on on a Thursday, I would just say look I’m going to contact the local supporter and do it that way, you know it’s how do we make sure people get the right information, some of it will be generic but some of it has to be a little bit more specific.
GR&CO-CL-TL-08, 7 February 2018, individual interview – Lakes
Contextual integration
There is an effort by a few invested staff members including the IMPART lead, one team lead and the REACT champions to integrate REACT into regular team meetings. However, this effort is influenced by the ability to remember REACT and whether or not REACT can compete with other demands raised in meetings. It was also the same titled REACT staff who raised REACT in meetings and as such the discussion was dependent on their presence in the meetings:
Absolutely. That is one thing that we do 100%, so we had 100% CPA rate, everybody had one, and if this could be a part of CPA [Care Programme Approach] meeting, but I personally try to make it part and even I forget, with all my involvement in REACT I still keep forgetting it.
Do you know if any of the other teams have made it part of their meetings so far?
No I don’t think so.
Lakes-IL-CP-02, 10 October 2017, group interview – Lakes
. . . Whether they do or not I guess we’re all it comes up in my team’s meeting, the Diver some of the team’s meeting it’s always on the agenda, again like everything though it’s which of the 40 plates are you going to drop that are spinning. And that sounds very bad and again probably negative in a way to say because if you were coming at us with and we had five patients each and we had a bit of time we’d just turn around to them during the day and have half an hour time or a lunch then I think it would be far far easier but.
DI-RC-CC-03, 25 April 2018, group interview – Lakes
There was some frustration from titled REACT staff and staff generally that individuals in a position to allocate resources to support the delivery of REACT did not make this available to staff. This meant that staff were having to complete REACT tasks alongside their existing workload, which was not always possible:
. . . or if we had a bit more time, if the managers would say us two or for the IMPART or the REACT leads, have half a day or just have 2 hours, absolutely protected time for it, game on I think that would be much more better, you know, if you wangle a bit of extra funding.
DI-RC-CC-03, 25 April 2018, group interview – Lakes
Are you being given any, is there any like support to free up any time to talk about REACT being given to you or is it just something you’re having to try and fit in yourself with everything else?
Yeah it’s something that we have to try and fit in to our caseload as care co-ordinators yeah.
DU-CL-CC-10, 6 April 2018, individual interview – Lakes
Reflexive monitoring
Systemisation
There was no evidence of formal monitoring of the uptake of REACT within Lakes Trust. Where there was informal monitoring of staff and relative uptake of REACT, staff seemed quite demotivated by the limited uptake of REACT but remained hopeful that activity of both staff and relatives would increase with time. However, this hope of increased activity is met with concerns around ability to continue with the REACT supporter role:
I think as Lakes-IL-CP-02 says I think we’ve got to initially try and get this stage one off the ground and get all the care co-ordinators on board, let everybody know what it’s about, everyone’s got one of them things in their [tray?] but I think probably 50% have read it and I think probably 50% haven’t, and of that 50% I would say how many have actually logged into it and seen what it’s like? Probably none.
DU-RC-CC-01, 12 December 2017, group interview – Lakes
Although we’ve had REACT for a while there’s not a lot of activity on the site, I think that’ll change in time but I’m probably not best placed to be in a position, being I am computer savvy to an extent but there’s this kind of whole level about that in terms of kind of managing a site and kind of dealing with queries.
GR-RS-CC-06, 24 April 2018, group interview – Lakes
Individual appraisal
The EIP team leads are supportive of their staff undertaking REACT roles; however, they voiced concerns around the amount of time staff have to dedicate to the role with regard to fulfilling the tasks and travelling to meetings. The concern seems to resonate with other comments managers have made about the amount of demand and tasks they are having to put on their team owing to internal and external targets:
Like this afternoon, they’re going down to [hospital name] it’s going to take an hour for our staff to go down, an hour there and then probably an hour, hour and a half to come back, so again it takes up a lot of time and we’re asking staff to do that and they do see it as important but we’re asking staff to do that and it’s going to take much longer you know or a lot of time out of their day to do it, so it can be quite tough.
GR&CO-CL-TL-08, 7 February 2018, individual interview – Lakes
Very few staff have received feedback from relatives about REACT, and for those who have, the comments have been mixed. Where relatives have been reluctant to engage with REACT, reasons are similar to those given by staff including availability of time:
I know the one that I introduced to the REACT she wasn’t that bothered because she said she had enough problems finding the time to go on this to look at things, to go onto a forum as well, but then again it’s just things have changed with her family lately and I think if she put a few comments in saying I’m going through this has anybody been through it, possibly I don’t know . . .
DU-RC-CC-01, 12 December 2017, group interview – Lakes
So what do you think of the REACT toolkit so far?
I think it’s very good, yes. I’ve introduced a few people to it and every carer, family member liked it and gave positive verbal feedback.
Lakes-IL-CP-02, 10 October 2017, group interview – Lakes
Communal appraisal
There was very limited evidence of communal appraisal in Lakes Trust. Where there was evidence of communal discussion of REACT, it was often discussed hypothetically and as an idea rather than in relation to reviewing the resource. This was evident for discussions among both staff and relatives:
I think the carers that we had in I think they did have an interest in the forums didn’t they, we had people who were there was only a couple of carers here but one or two of them did say they liked the idea of the forum.
DU-RC-CC-01, 12 December 2017, group interview – Lakes
l’ll keep trying for definite, but before in other ways and other times we’ve met and I know the other people who were involved on another level were sincerely quite impressed and I think they generally could go forward, it’s just we’re so busy.
DI-RC-CC-03, 25 April 2018, group interview – Lakes
Reconfiguration
As part of IPv3, Lakes Trust was able to request resources to aid the delivery of REACT. The two main additional resources the staff requested were having PDF versions of the information on the toolkit and a staff-only version of the REACT website, which REACT supporters could practise using the features of. Staff also requested a change to the instructions above the forum to coincide more closely with their attitudes towards online risk and concern around relatives using the website inappropriately:
No that’s fine. Have you suggested it to any relatives yet [SW-RC-CC-04]?
I have. They were kind of just a little bit overwhelmed by the computer, so I’ve given out some of the handouts, which were useful and I think have been quite a talking point for people and it has made it easier for people that speak with the service users kind of about their experience ‘cos they can refer to the page a bit more, like the language to use and things, I think REACT’s been quite useful, but I’ve not had anybody use the online toolkit.
SW-RC-CC-04, 30 April 2018, individual interview – Lakes
And is that more reassuring for you now as a care co-ordinator with those instructions?
Yeah ‘cos I guess as well you know it would be something that when I’m sitting with a patient I would be able to say [missing] so it wouldn’t feel like it was coming from me because there’s an actual like description on there to say like you know so it wouldn’t be like me kind of speaking, I guess it would be it might be challenging to say that to somebody like a carer and say actually this is what you can’t do, but because it’s there on the screen it’s almost being able to say well this is what it says, so it feels a little bit less intimidating maybe with the carer.
DU-CL-CC-10, 6 April 2018, individual interview – Lakes
Researcher’s reflexive summary
Knowledge of REACT spread slowly through this trust but this was possibly owing to the large geographical spread of the teams and only having one IMPART lead at a time. Once REACT supporters and champions began discussing REACT internally, such as during team meetings, this seemed to increase staff awareness. Staff were generally positive about REACT and could see potential benefits for themselves and relatives, but buy-in was limited by time pressures and competition with mandatory and target-driven work requirements. One of the key barriers to implementation of REACT in Lakes Trust was the concern around risk management and responsibility and liability of the direct message and forum functions on the REACT website. This concern was continuously articulated by REACT champions, REACT supporters, team managers and general staff members throughout interviews and presentations with the research team. This concern was so prominent it had a paralysing effect, with REACT supporters not taking on any roles related to these aspects for fear of their actions leading to something that may affect their professional role, such as an adverse event. There was also confusion and frustration from the EIP staff around the non-involvement and non-action of the family therapists, which became a barrier to implementing REACT in Lakes Trust.
Feedback from final trust analysis days
The final SRG at Lakes Trust was attended by the current IMPART lead (Lakes-IL-CP-02), one REACT supporter and one REACT champion (DI-RC-CC-03). The IMPART lead invited, and asked staff members to invite, relatives to attend the SRG but it was only attended by the three staff members. Despite this, trusts verbalised efforts to work with relatives, but there still remains a lack of integration between staff members and relatives in collaborative working. Apologies were sent from other REACT champions and supporters for their absence, as they had other duties; this further emphasises where research and relatives feature in staff members’ priorities. The staff agreed that the NHS is not digitally orientated, which does create challenges for implementing digital interventions, particularly outdated phones and ‘clumsy’ systems. When discussing coherence findings, the REACT champion explained that they provide psychoeducation to relatives ‘by default’, covering the content of REACT without the label. The IMPART lead suggested that staff do not connect what they provide with what REACT can offer relatives, which they need to do as providing relatives with just a website would not be enough to encourage relatives to visit REACT. For cognitive participation, the REACT supporter explained that their team is currently involved in four research projects and, therefore, external researchers often do not leave lasting impressions. REACT is still seen as another external research project, as opposed to a resource that the trust offers to relatives. For collective action, the IMPART lead explained that checking activity on the forum had fallen off their personal agenda owing to lack of activity, emphasising how reactive this role is and not pro-active. The effects of this lack of activity were discussed further when considering reflexive monitoring, when the IMPART lead discussed feeling demotivated by the lack of uptake of REACT from the relatives they had invited. The REACT supporter suggested that if REACT could be made into an app, this would make it more accessible for staff and relatives. Concluding statements from the staff members included that in principle REACT was a good idea, but is difficult to deliver in practice.
Appendix 11 Marsh Trust case summary
Participants
| Participant identifier | NHS role | REACT role | Number of relative invitations sent | Research activities participated in |
|---|---|---|---|---|
| HE-IL-CP-01 | Consultant psychiatrist | IMPART lead | 0 | SRG, individual interview, IPv3 planning, pre-sharing focus group |
| MOO-CL-CLN-03 | Clinical lead nurse (was interim service lead) | Clinician | 0 | SRG, IPv3 planning, |
| MOO-RC-CPA-04 | Carer practice advisor | REACT champion | 62 | SRG, IPv3 planning, pre-sharing focus group |
| MOO-CL-CT-08 | CBT therapist | Clinician | 0 | Training, IPv3 planning |
| HE-RC-OT-CC-10 | Senior occupational therapist, lead for family intervention and family and friends’ group | REACT champion | 24 | Training, IPv3 planning, pre-sharing, individual interview |
| MOO-CL-TM-20 | Team manager | Clinician | 0 | IPv3 planning |
| RD-RS-ACRC-26 | Assistant clinical research co-ordinator | REACT supporter | 0 | IPv3 planning, individual interview |
| RD-CL-TraM-29 | Transformation manager | Clinician | 0 | Pre-launch, individual interview |
| HE-CL-MS-30 | Medical student | Clinician | 0 | Pre-launch |
| HE-CL-CPN-CC-41 | CPN | Clinician | 11 | Individual interview |
| MOO-CL-OT-CC-42 | Occupational therapist | Clinician | 3 | Individual interview |
| MOO-CL-CPN-CC-49 | CPN | Clinician | 6 | Training and feedback session |
| RD-RS-ACRC-50 | Assistant clinical research co-ordinator | REACT supporter | 1 | Training, phone interview |
| MOO-CL-CPN-CC-51 | Community mental health nurse | Clinician | 1 | Training and feedback session |
Context
Marsh Trust covers a population of 1.3 million, which is mostly urban with pockets of rural regions and predominantly white British. The trust employs approximately 2300 staff, and approximately 400 service users access EI services, which comprise approximately 40 clinical staff. According to the 2016 CCQI audit,102 this trust offered family interventions to approximately 2% of service users and their families, and around 74% of carers were offered carer-focused education and support.
Marsh Trust consists of two EIP teams, Moorhen and Heron, which accept referrals for 14- to 65-year-olds. Moorhen team has a substantially larger caseload than Heron team, with 235 and 133 service users, respectively, and the staffing levels in each team reflect this. This trust initially experienced considerable difficulty in supporting the IMPART study owing to a perceived lack of resources to allocate the REACT supporter role to a clinician. Therefore, the trust’s R&D team played an instrumental role in enabling the implementation of REACT by agreeing to allocate the REACT supporter role to a R&D staff member. There was one IMPART lead and one REACT supporter across both teams, although there were three REACT supporters during the course of the study owing to periods of sick leave.
The two teams varied in terms of their existing sources of information and support for carers. Heron runs a monthly family and friends’ group, which consists of psychoeducation and informal peer support; however, Moorhen team withdrew their carers’ group owing to historical poor attendance. Both teams deliver BFT and have access to a carer practice advisor, whose primary duty is to conduct carers’ assessments. In addition, this trust has received recognition for its commitment to the Triangle of Care105 and working collaboratively with carers.
This trust received IPv3.
Key findings against normalisation process theory components
Coherence
Differentiation
The majority of staff were aware of REACT and understood the rationale for the intervention. Although staff described several resources available for carers in their services, most distinguished REACT from their existing ways of working with relatives and felt that REACT could complement other forms of support:
I mean one of the things that has kind of come up with our care co-ordinators who also do the family intervention is that there is quite a lot of crossover of the information on the REACT tool and some of the work that they do with the FI [. . .] it was still sort of recognised that family intervention is different in that it’s delivered sort of face to face and there are obviously other components involved, but the kind of psychoeducation side of things, I guess it’s felt this is supportive of that if anything, it’s not that it’s sort of taking away.
HE-IL-CP-01, 21 March 2017, individual interview
Staff also drew comparisons between REACT and other research projects; hence, there appeared to be a general perception of REACT as an external research study, rather than an integrated part of the clinical service. The concept of engaging with an online self-management tool was novel to most staff and there were limited comparisons to other technologies hosted by the trust:
. . . do they know this is sort of new in a sense, do they know it’s, is it classed as a pilot or is it how’s it explained to people?
When I tell carers I say it’s a pilot, it’s a study, you know.
And people are invited to participate in the actual study if they want to but they can continue using the website even if they decline.
OK so it’s marketed as a study to them, OK.
15 November 2017, pre-sharing meeting/group interview
Individual specification
Despite widespread awareness of REACT, relatively few staff had a clear understanding of the toolkit content and their own tasks in relation to the intervention. A small minority had logged onto the website independently and felt confident in inviting relatives to the website. Staff understanding of how to use the website was facilitated by researcher-led presentations, independent exploration of the website, conversations with colleagues and use of the online manual. However, few staff were aware of the online manual and many reported that it was difficult to visualise and remember REACT from presentations delivered during team meetings with full agendas:
The session, and it was in a big, the whole team were in a big room and it was great having the slides and that but I think I’d prefer to be doing it as I someone was telling me about it because that’s how, I’m quite visual.
MOO-CL-CPN-CC-51, 21 March 2018, group training and feedback session
Staff with assigned IMPART roles, including the REACT champions, IMPART lead and REACT supporters, had a more detailed understanding of toolkit material and their individual responsibilities. This seemed to be influenced by contact with researchers, including opportunities to collectively discuss and define their roles, and greater provision of training and practical support.
Communal specification
The majority of staff were able to identify the REACT champions in their respective teams, but seemed less aware of the IMPART lead. This was probably influenced by the IMPART lead’s lack of presence in Moorhen and her own understanding of the role as primarily facilitating research rather than clinical delivery of REACT. Most staff had a vague understanding of the responsibilities of the REACT supporter and lacked awareness of who occupied this role in their trust. The supporter’s limited contact with clinical teams seemed to be a barrier to communal understanding of the role, whereas participation in researcher-facilitated meetings increased staff awareness of the supporter’s responsibilities:
Do they [the REACT supporter] just keep an eye on what’s going on, and if there’s anything a bit untoward or they’re worried about they’d contact the care co-ordinator.
MOO-CL-CPN-CC-49, 21 March 2018, group training and feedback session
Although some staff acknowledged their role in offering REACT to relatives, many viewed the tasks of promoting REACT and inviting carers to the website as the champions’ responsibility and, therefore, lacked inclination to learn how to use the website:
. . . obviously I then presumed MOO-RC-CPA-04 our carer support worker would take the lead in putting our relatives, our carers or whatever on, and I found out he only covers the [location] part and most of my clients are [location]. So then I came away and I didn’t know what to do, so I hadn’t used it.
MOO-CL-CPN-CC-51, 21 March 2018, group training and feedback session
In Moorhen, staff’s collective understanding of the champion’s responsibilities was reached by mutual agreement after explicit discussion in a team meeting. However, staff in Heron team appeared reluctant to develop a shared understanding of their individual tasks and, therefore, their understanding of the champion role seemed to develop implicitly:
Yeah we as a team, as I said we found a way of working together, yes OK maybe, I know it’s not the same in the [Heron], it’s slightly different I think, but I’m happy and they’re happy that I deal with carers, that I would get involved in this.
MOO-RC-CPA-04, 16 March 2018, individual interview
. . . it feels a bit like it hasn’t permeated the team and I don’t know quite why, but I do and I am I facilitate the family and friends group, so therefore I’m sort of thinking about that more than maybe other people in the team [. . .] And I don’t know quite why, I mean we have taken that back to the team meeting and I’m repeating it.
HE-RC-OT-CC-10, 18 September 2018, implementation workshop
Internalisation
Staff recognised the potential benefits of REACT for both carers and themselves, such as increasing access to reliable information and complementing face-to-face support, and many found comfort in knowing they had another resource to offer relatives in the context of limited capacity:
I think it’s a good thing, REACT is a good thing because it’s there 24/7 they can go on it when they like [. . .] and I just think it’s a good complement to what we do.
HE-CL-CPN-CC-41, 5 March 2018, individual interview
Yeah I think it’s really good, it’s brilliant, especially as with all the will in the world you’ve only got a certain amount of time when you can do stuff with carers and you’ve got everything else, in that way it’s a really educational tool that anyone can use you know, it’s really good.
MOO-CL-OT-CC-42, 16 February 2018
Despite this, many expressed reservations about the website, particularly in relation to risk management on the peer-support forum, which appeared to stem from a previous negative experience of hosting a local trust forum. Hence, the REACT supporter tasks were perceived as intensive and incompatible with the trust’s resource availability. Some also communicated uncertainties about the value of peer support for relatives, noting that exposure to others’ negative experiences of caring can adversely affect one’s own well-being:
My main concern were I had experience with forums before, and if they are not well maintained, if they are not well administered and moderated, you can have problems, and we can all have problems in this kind of work if you see what I mean, it’s not a forum about football or this is a forum about something serious. So I had my reservation about a forum.
MOO-RC-CPA-04, 16 March 2018, individual interview
I think if it’s like the carers’ group which is as I say been running for a long long time, it’s really great, but when my young person’s parents went, they found it quite negative ’cos sometimes people have been there, you know relatives have been ill for years, and maybe services didn’t provide what they expected and what they wanted, so dad didn’t come away thinking that it was particularly a good group [. . .] So if my person’s on a forum and someone else said oh don’t bother ’cos they’re rubbish or my son’s been like that for 15 years, that would sort of be the negative.
MOO-CL-CPN-CC-51, 21 March 2018, group training and feedback session
Other perceived shortcomings highlighted by staff included the non-intuitive design of the staff interface and the use of diagnostic language that is discordant with language commonly used in their services. Staff’s personal views about the value of digital health technologies was also an important factor affecting their opinions of REACT:
I think the first description was one of schizophrenia and I wasn’t impressed with that ‘cos I think that is scary for having that as your first introduction to psychosis [. . .] I didn’t think that was at all helpful, so that put me off to start with [. . .] We wouldn’t ever give somebody a diagnosis of schizophrenia within the first year probably anyway, even if they you know we would really wait.
HE-RC-OT-CC-10, 12 March 2018, individual interview
I suppose it is a slight break with tradition isn’t it, to use an internet based source, because I suppose it depends how professionals are, our most valuable tool is ourselves and I don’t know whether there’s something that potentially is a bit daunting about handing that over to something else, i.e. technology [. . .] who’s taking ownership of the information, who’s overseeing the risk and things like that, so I was just sort of reminded about the reticence maybe or the anxiety about health care and health-care professionals sort of losing some of that oversee over what’s happening [. . .] I don’t know whether it’s a conscious thing that we’re thinking, we’re probably not thinking oh gosh REACT no we’re going to avoid that, but it’s just not a natural thing.
MOO-CL-CT-08, 18 September 2017, implementation workshop
Cognitive participation
Initiation
A key enabling factor in this trust was the selection of enthusiastic REACT champions, who were perceived by their colleagues as the main drivers of the intervention. The champions worked to drive the intervention forward by raising awareness of REACT among relatives and staff, and most staff relied on the champions to invite relatives to the website. Their motivation appeared to be facilitated by perceived good fit between the intervention and their existing priorities, given that they deliver alternative sources of support for relatives, including carers’ assessments, BFT and a family and friends’ group:
So I think the limitations, well this is just an observation that everybody that’s signed up to REACT apart from one person are people that I work with, so it feels a bit like it hasn’t permeated the team and I don’t know quite why, but I do and I am I facilitate the family and friends group, so therefore I’m sort of thinking about that more than maybe other people in the team. And people I mean it’s true that most of the people in the family and friends’ group tend to be people that I work with, not entirely but people that I’ve had some involvement with.
HE-RC-OT-CC-10, 18 September 2017, implementation workshop
The IMPART lead felt that her role in driving REACT forward reduced over the course of the study, which she attributed to lack of time to perform required tasks and a perception of greater shared responsibility for delivering REACT. The REACT supporters were rarely mentioned by staff, which may be indicative of their limited ability to drive the intervention forward owing to a lack of presence in the teams:
And to be honest now, really, in terms of the website, all that I do is if there’s a new care co-ordinator I get them put onto it, because now the care co-ordinators and particularly in the [Heron] team, our senior OT [occupational therapist], has kind of taken on you know inviting carers and I feel more comfortable.
HE-IL-CP-01, 20 April 2018, individual interview
Enrolment
Staff concerns around the forum and resources were initially major barriers to enrolment. Therefore, the allocation of the REACT supporter role to a member of R&D staff was a key factor in securing staff buy-in, because this provided a solution to the perceived lack of resources in clinical teams and was interpreted by staff as an indicator of managerial support. The SRG and other planning meetings between staff and researchers also played an instrumental role in facilitating enrolment by providing a forum for defining and allocating key tasks and roles.
The REACT champions’ buy-in appeared to be aided by their enthusiasm for supporting carers and perceived fit with existing priorities in their work. However, the IMPART lead later reflected that the demands of the role were higher than anticipated and incompatible with her existing workload:
To be honest I mean it is a struggle, particularly as I say at the beginning of the study, there was more input needed. And I think you know well with all the restraints that we all find ourselves under, you know [. . .] I think if I were asked today to go back and to take on that kind of role, I would be much more reluctant to do so.
HE-IL-CP-01, 20 April 2018, individual interview
Despite a widespread understanding that there were positive reasons for introducing the intervention, building a shared commitment to the delivery of REACT proved to be difficult. Staff buy-in appeared to be limited by perceived lack of time to offer REACT, perceived lack of computer literacy to engage with a digital intervention and a general perception of REACT as a low-priority research activity. Among the few individuals who engaged with REACT, factors that facilitated buy-in included familiarity with the website, frequent contact with carers and perceived good fit with their existing workload and skill set:
Yeah I’m just thinking ‘cos we do mention it every week in our team meeting, but it’s under our research headline, and we’re actually involved in about three other research projects, so there is a little bit of fatigue shall I say with research projects, so maybe we need to relocate it under our carers.
HE-IL-CP-01, 18 September 2017, implementation workshop
There are a few people in our team who are complete, worse than me in terms of being technophobes so that can be a bit of challenge [. . .] I think it’s just the individual’s comfort with technology, so it does tend to be our younger care co-ordinators who are much more comfortable in just doing it, yeah.
HE-IL-CP-01, 20 April 2018, individual interview
Legitimation
Although staff recognised the importance of providing carer support and felt that REACT fitted with their working model, carer education and support was perceived by most as peripheral to their main duty of providing care to service users. Some appreciated the value of REACT in complying with NICE guidelines; however, many attached greater importance to targets for family intervention and carer assessments:
I think we offer, you know it’s part of our job to offer carers, we have to include carers, so I think it would be easy to just use it like every person we offer carers’ assessment, carers’ group [. . .] And part of the EIP NICE care plan, it’s got carers, so that again have you offered the assessment.
MOO-CL-CPN-CC-51, 21 March 2018, group training and feedback session
Even better would be having a service user whose mum had used it and felt better, you know somebody else having that perspective on their mum using it would be brilliant, ‘cos I think our hearts in the team are with the service user, carers and family are definitely definitely there but they are slightly secondary, and so if you could do it from actually as a service user I see my mum feel less anxious about me [. . .]
HE-RC-OT-CC-10, 15 November 2017, pre-sharing meeting
The REACT champions viewed themselves as the right people for the champion role and perceived the work involved in the new practice as a legitimate part of their job. This seemed to be influenced by their personal interest in supporting relatives and perceived fit with their existing role in providing face-to-face support to carers. Other staff members demonstrated limited ownership over the new practice and tended to view REACT as the champions’ responsibility. Contextual factors, including staffing shortages and high workload, and the perception of REACT as a research project also seemed to negatively affect the extent to which REACT was seen as a priority. Furthermore, limited managerial involvement in the implementation effort may have affected the degree to which staff prioritised REACT:
Yeah I’m sort of feeling like it’s good for me because it means that I’ve, you know all of my role is around family so it definitely means that I’m more focused on that . . .
HE-RC-OT-CC-10, 12 March 2018, individual interview
Activation
There was some evidence of continued support for REACT and collective efforts to keep the new practice going, such as the inclusion of REACT as a standing agenda item in Heron’s weekly team meetings. In addition, staff collectively defined actions needed to sustain the delivery of REACT during researcher-facilitated meetings, such as integrating REACT training into the staff induction process and embedding REACT in job descriptions. However, there was little evidence of commitment to putting proposed mechanisms into practice. Furthermore, the provision of REACT supporter time from the R&D department was identified as a barrier to sustaining the delivery of REACT over the longer term as a result of the perceived lack of resource to support this role beyond the study:
I mean we so yeah we do have it on the agenda, I mean certainly whenever we start, when we have a new assessment, we start seeing someone new, and if they’re obviously as a carer, we do mention about REACT or at least the majority of care co-ordinators will remember to mention it.
HE-IL-CP-01, 20 April 2018, phone interview
And also you know past the study, I’m certainly not going to be able to be the one kind of logging everyone on. And I think this goes back to also we’re not going to have a REACT supporter and a research and development team, so it goes back to it is a resource issue, we do need someone to take ownership of that and who’s that going to be? That’s going to be more and more difficult.
HE-IL-CP-01, 15 November 2017, pre-sharing meeting
Collective action
Interactional workability
Although some care co-ordinators promoted REACT to relatives, the majority found it difficult to fit the work involved in the new practice into their daily routines. Perceived time and effort to perform tasks required by REACT and lack of confidence in carrying out key tasks were important barriers:
MOO-RC-CPA-04 does a lot of it because people are so busy with all the other things, chances are they might forget amongst everything else [. . .] Yeah he registers people and it’s like he’ll invite them to REACT if you can’t do it, or if you’re busy or whatever, so that’s really good.
MOO-CL-OT-CC-42, 16 February 2018
So yeah I think I’d use it, now I know how to, and it was just I knew it was going to be simple, it’s just not on my radar.
MOO-CL-CPN-CC-51, 21 March 2018, group training and feedback session
Despite this, the delivery of REACT became part of routine practice for the REACT champions, who integrated the toolkit into their usual ways of working with relatives. For example, the champions offered REACT in conjunction with carers’ assessments and family intervention sessions and promoted the toolkit material at the family and friends’ group:
. . . so we were talking about managing stress anyway, so I’d already planned to do managing stress and then we I’d taken along the thinking differently PDF, and actually what happened was the first half of the group was talking about people’s own experiences of what’s happened in the last month and it was all about exactly this module, it was incredible. So it was and so it just confirmed and sort of helped with the discussion, it was really strange, so we were talking about these common thinking traps and how people had been sort of jumping to conclusions and we were and then it just sort of consolidated it all so it was really really helpful.
HE-RC-OT-CC-10, 12 March 2018, individual interview
Skill-set workability
Staff confidence in contributing to the delivery of REACT appeared to be influenced by individuals’ comfort with technology. However, most reported that using the website was less difficult than they had anticipated:
. . . I think it was the techy elements that I had a few kind of worries about, I’m not hugely technologically minded but [. . .] I think I was worried initially that I would have to be inputting information onto it but in the end, you know it was all well explained and navigating the website was ended up not being too difficult.
HE-IL-CP-01, 20 April 2018, individual interview
Staff also expressed concerns about how risk would be managed on the forum and questioned accountability for adverse events. The trust’s previous negative experience of hosting a forum and lack of clarity around how trust risk protocols can be applied to online contexts seemed to reinforce staff anxieties:
I think that’s probably still a grey area because so far I think what our trust is good at is managing sort of clinical risk [. . .] Online is a different thing, I think we’re not exposed to it enough and therefore we haven’t outlined how that would work, so I think you know managing a forum, as far as I’m aware there’s no formal training for that in the trust, so that’s quite bespoke.
RD-CL-TraM-29, 11 January 2018
Nevertheless, the REACT champion role was perceived to be a good fit with the carer practitioner role owing to frequent contact with relatives and alignment with existing priorities. The REACT supporters generally felt that this role was appropriately allocated to them, although they acknowledged that the tasks of moderating a forum and writing blog posts may require additional training because these are not typical responsibilities for NHS staff.
Relational integration
On the whole, staff were positive about REACT and maintained trust in the toolkit content, suggesting that the information provided on the website is consistent with the message they convey to relatives in their clinical work:
And also from a confidence point of view and it’s easy to read and they’re easy to understand and I you know so for example on Monday you gave me those links to the PDFs, I printed them off, I didn’t look at them beforehand [. . .], I could confidently just print it off, take it to the group, know that it would be relevant for some of the people, you know.
HE-RC-OT-CC-10, 12 March 2018, individual interview
Reservations voiced by staff were mostly in relation to the forum, with prominent concerns about risk and the potential negative impact of exposure to other carers’ negative experiences. Although staff were aware that interactive components of the website were being monitored, most had a limited understanding of how risk was being managed by the REACT supporter:
And are you aware of how the forum is kind of monitored and things in your trust?
Not really, I think MOO-RC-CPA-04’s mentioned it but I can’t really remember how it all works. He’s mentioned it but apart from that I don’t know, I don’t know that much about it to be honest.
16 February 2018, individual interview
Contextual integration
Integration of REACT into existing structures and channels of support for carers was achieved to some degree. The REACT champions described how they included the intervention in their daily work practices and the REACT booklet was included in both services’ welcome packs. REACT was discussed as a regular agenda item in Heron’s weekly team meetings, as prompted by the IMPART lead, and on an ad hoc basis in Moorhen’s monthly business meetings, as prompted by Moorhen’s champion. Hence, the presence of key individuals seemed to facilitate contextual integration through their ability to raise awareness and keep REACT on the agenda:
It’s all on our, you know we’re all very aware of it and you know I think only when it’s sort of mentioned when MOO-RC-CPA-04’s kind of there and puts it up on the agenda but I think it’s not really mentioned specifically I don’t think.
MOO-CL-OT-CC-42, 16 February 2018
Contextual factors also had an important impact on implementation. Staffing shortages, multiple tasks demanding attention and introduction of new systems that require time and inclination to learn were some of the key factors limiting staff engagement with the new practice. The temporary provision of REACT supporter time from the R&D department was also perceived as a barrier to implementation over the longer term because this was intended as a short-term solution for the purpose of the study. Therefore, there was a sense that staff felt that the long-term delivery of REACT would demand important changes to the organisational environment or their routine ways of working:
The thing is with this job I think there’s things all the time and there’s change all the time and there’s new systems and new forms to get used to. You know I think it just takes time for anything new to get embedded [. . .] do you know what I mean, just constantly kind of you know changing so I think it’s just any change takes time really . . .
MOO-CL-OT-CC-42, 16 February 2018
Reflexive monitoring
Systemisation
Staff used a number of ways to monitor and reflect on their implementation efforts. Some accessed information on the dashboard to gauge whether or not relatives had created an account. However, others were unaware of how to access this information and felt that the dashboard was difficult to navigate and understand. There was a consensus that it was important to be able to monitor the uptake of the intervention for audit purposes, although there was no evidence of formal monitoring of REACT:
I know which pending invites I’ve got and I think I have to click users to see how many people are actually signed up . . . also I can only see, again it’s not like a nosey kind of thing, but it’s for that, but I can only see for example I cannot see everybody that’s been invited from our team, I can only see the people I invite. So to audit, it makes it difficult to audit the whole thing if you see what I mean.
MOO-RC-CPA-04, 18 September 2018, Implementation workshop
‘Cos I suppose it is an intervention isn’t it, that we’re offering, and we can’t audit, I mean we’ve obviously got our targets and one of the main ones is everyone should be offered family intervention, and obviously in an ideal world we would but we can’t do that, so this is sort of like the next best thing if you like, and we’re not knowing yeah we can’t audit that and see how many people have taken it up and been active on the website.
MOO-CL-TM-20, 18 September 2017, implementation workshop
Some recalled occasions when they received positive feedback from carers about REACT; however, requests for feedback were not implemented consistently and staff reported that their degree of contact with relatives affected their ability to obtain feedback. Research focus groups attended by carers also provided a forum for staff to hear about carers’ experiences of using the intervention.
Individual appraisal
Although staff maintained their view of REACT as a valuable resource, they seemed disappointed by the perceived low uptake by relatives and limited activity on the forum. Several staff felt that more detailed information about relatives’ use of the website, including number of visits to the website and which pages they accessed, would improve their ability to appraise the intervention:
Sometimes some websites, especially forums, there’s so much talking about the forum, I’m talking about the site as a whole you know, it tells you how many people are online say, how many were online yesterday or you know it’s not.
Which pages are they accessing regularly.
Well I do not know whether you can go into details and that, it’s just to see whether it’s used.
15 November 2017, pre-sharing meeting
Nevertheless, staff highlighted some personal benefits of REACT for their work, such as having a reliable resource to signpost to and saving time, indicating that they saw value in their efforts to promote the toolkit:
The benefits are that I’ve got somewhere that I can go to that I know that the information’s accurate and up to date and that it’s beneficial from the time point of view.
HE-RC-OT-CC-10, 12 March 2018, individual interview
Communal appraisal
There was limited evidence of formal monitoring or collective efforts to appraise the toolkit. However, the majority of staff were aware that there had been limited forum activity and that a substantial proportion of relatives had not registered for an account. This shared understanding appeared to be facilitated by collective discussions at researcher-facilitated meetings and occasional feedback from the champions in team meetings:
So we did discuss it a while ago and I remember people were saying that they weren’t sure whether the people were actually using it or not, you know whether we can see that or not, which would be good to know, if people are using it.
MOO-CL-OT-CC-42, 16 February 2018, individual interview
Reconfiguration
There was some evidence of reconfiguration in the early stages of the study, whereby staff adapted the delivery of REACT in response to perceived lack of resources in clinical teams. Specifically, the REACT supporter role was allocated to a member of staff outside the EIP service and the supporter’s responsibilities were modified to fit with this model. For example, the supporter was not expected to promote the toolkit to carers owing to a lack of contact with relatives. In addition, one IMPART lead role was allocated across both teams and implementation of REACT was delayed until the trust decided how they could adequately support its delivery.
Researcher’s reflexive summary
There appeared to be a widespread awareness of REACT among Marsh Trust staff and a shared understanding of the rationale and anticipated benefits of the intervention. However, staff with assigned IMPART roles tended to have a clearer understanding of their individual responsibilities for facilitating implementation. Despite a good level of awareness, there was a sense of reluctance among care co-ordinators to invest time in contributing to the work involved in implementing REACT. Staff with allocated roles, particularly the REACT champions, demonstrated greater commitment to delivering the intervention, which seemed to be facilitated by perceived fit with their existing priorities and frequent contact with carers. Hence, the integration of REACT into existing practices was largely dependent on the efforts of the REACT champions. The involvement of R&D staff in the delivery effort appeared to be both a help and a hindrance, because this reinforced the view of REACT as a short-term research project and limited longer-term thinking about how implementation could be sustained beyond the study. However, owing to Marsh Trust previously experiencing ‘trolling’ of staff on trust forums, the reluctance of clinical staff to undertake the REACT role meant that the R&D team taking on the REACT supporter role was the only option.
Feedback from final trust analysis days
All staff apart from new staff and students were aware of REACT, but few staff had used the website. Trust staff across both teams agreed that the results were a valid interpretation of what had happened with REACT within their trust and there was consensus that the key themes discussed were accurate. The REACT booklet is in the carers’ packs for both teams, but this did not appear to be common knowledge among the staff. There remained some negative attitudes around the forum: one staff member reported that she had received a panicky e-mail from the REACT supporter asking her to get in touch with the carer because of a post on the forum; however, the staff member said that she could not see the forum and that it would have been helpful to see what had been posted. Another staff member suggested that the online forum could be ‘tricky’ and made comparisons to the family and friends’ group, which they occasionally co-facilitated. They suggested that some carers might find the forum upsetting or that the forum could be dominated by certain individuals, such as those who are typically more vocal in the carers’ group. The REACT champion for Moorhen was the main individual discussing REACT with relatives and creating relative invitations, and he was happy to do this on behalf of other staff members.
Appendix 12 Moor Trust case summary
Participants
| Participant identifier | NHS role | REACT role | Number of relative invitations sent | Research activities participated in |
|---|---|---|---|---|
| Moor/GRO-IL-Cpsyc-01 | Clinical psychologist | IMPART lead | 3 | Individual interview, SRG |
| LA-RS-TL-01 | Clinical team leader | REACT supporter | 1 | SRG |
| Moor-CL-CPsyc-01 | Clinical psychologist | Clinician | 0 | SRG |
| Moor-CL-RDL-02 | R&D lead | Clinician | 0 | SRG |
| PI-RS-STR-02 | STR worker | REACT supporter | 10 | Individual interview, SRG |
| HA-CL-CC-03 | Care co-ordinator | Clinician | 3 | Individual interview |
| PI-CL-CC-04 | Care co-ordinator | Clinician | 6 | Individual interview |
| PI-CL-CC-05 | Care co-ordinator | Clinician | 0 | Individual interview |
| PI-CL-CC-06 | Care co-ordinator | Clinician | 6 | Individual interview |
| PI-CL-CC-07 | Care co-ordinator | Clinician | 6 | Individual interview |
| PI-RS-CBT-03 | Cognitive therapist | Clinician | 1 | Individual interview |
| CH-CL-OT-08 | Occupational therapist | Clinician | 2 | Individual interview |
| CH-CL-MHN-09 | Mental health nurse | Clinician | 0 | Individual interview |
| CH-CL-CC-10 | Care co-ordinator | Clinician | 5 | Individual interview |
| LA-CL-MHP-11 | Mental health practitioner | Clinician | 0 | Individual interview |
Context
Moor Trust serves a population of approximately half a million people who are predominantly white British, with over half living in a rural setting. The trust offers mental health and community care through approximately 4000 staff. The EI service delivers care to 216 service users through 24 staff. In this trust, 95% of EI patients report being in contact with a relative.
Moor Trust has one EIP team operating through a hub and spoke model, which accepts individuals aged 14–65 years. Staff members are not located centrally as a team, but are integrated with the community mental health team. The average caseload for full-time care co-ordinators is 13.5 service users, which is small comparative to other trusts; however, owing to the rural nature of Moor Trust, staff have considerably lengthier journeys between service users. Moor Trust had one IMPART lead who’s base is Grouse: one of six locations the EIP team operated from. The IMPART lead was a clinical psychologist and a senior member of staff within the EIP team. In addition to participating in IMPART, Moor Trust also participated in an initial pilot trial that created awareness of REACT among some staff prior to the introduction of IMPART.
Moor Trust received IPv1.
Key findings against normalisation process theory components
Coherence
Differentiation
The majority of staff had an understanding of what REACT is and were able to explain the content and features of REACT. Staff were aware of the information available on REACT and discussed its suitability for both staff and relatives, and were also able to describe the interactive features of REACT, including the forum and messaging features:
OK so my understanding now it that it’s a self-help toolkit for relatives, so they can work through various modules and just get the information, or they can actually do the reflection sheets and stuff and have it almost like a work book, and they can access peer support from other relatives, and some feedback from us via the supporters, and hopefully make the whole experience a bit less distressing.
LA-RS-TL-01, 20 January 2017, individual interview
Staff were able to distinguish REACT from current ways of working, including paper-based leaflets and BFT. There was some confusion as to the background of REACT; one staff member did not understand the research element of REACT, which led to some confusion when offering REACT to a relative:
I’ve had two feedback from two carers. The first one she said she wasn’t very happy, she said she didn’t realise it was a research, and she wasn’t happy about taking part in that research ‘cos I didn’t give her that information. And I didn’t because I didn’t know it was a research.
PI-CL-CC-07, 5 June 2017, individual interview
Individual specification
Although staff had a general awareness of REACT and its content, they were often less clear on how to explain and offer REACT to relatives. Only a few staff members attended the training session organised by the research team so other staff were investigating the REACT website themselves. With staff having only limited availability to look at the website themselves, many felt that they still did not fully understand the resource and their role in offering it to relatives:
I deliver it to all my patients’ families. But I’m not really sure how to deliver it still.
OK, in terms of?
What it is, you know what do we call it, what is it, is it information kind of site, or I don’t really know how to deliver it.
And do you think it’s because there’s a few different things involved in the toolkit or is it because you haven’t had the training?
Possibly, yeah I haven’t had the training and no one’s really told me what it exactly is.
PI-CL-CC-07, 5 June 2017, individual interview
. . . just wondered if you could tell me if you know anything about REACT? And if so what do you know?
Yeah, I know a little bit about it. I’ve tried to get some of my patients’ families on there, but I’m still in the process of kind of figuring it out myself a little bit. So I am trying to go on it when I have even just a spare few minutes, just to kind of get a bit of a feel of it but from what I’ve been on it so far it’s been really really good I think.
PI-CL-CC-06, 5 June 2017, individual interview
Communal specification
The team lead for Moor’s EIP, who is also a REACT supporter, considered what would be needed from other senior members of the team in order to support the delivery of REACT. The extent to which there is a communal understanding of the roles of other members of the team remains less clear:
It would be good to log on and look around it, only because we’re going to have the locality leads there, so the team leads who are managing the EI staff, and I need them to take on board that they need to be, as well as me, they need to be checking in their supervision and they need to be checking with their staff.
LA-RS-TL-01, 20 January 2017, individual interview
There is some concern among staff that certain members of the team, including nurses and newer members of staff, are not familiar with providing resources for relatives to help themselves. This suggests that the role of offering REACT may have been inhibited by existing working patterns and attitudes towards help:
I think what they haven’t what they’re not yet at ease with, and I get it, is the idea of giving people the responsibility to go away on their own, so I think I think nurses are the worst for that although this may be really [missing word] but that risk thing of don’t worry I’ll tell you it all, here’s the advice and here’s what to do in this scenario, and resisting that a little bit and kind of going how do you think you could manage it, how do you like to manage it, I don’t think they’re quite there yet with that, and so the idea, whilst they’re whilst there’s no doubt it will save them heaps and heaps of time.
PI-RS-CBT-03, 5 June 2017, individual interview
Internalisation
The potential benefits of REACT identified by staff were mainly focused on themselves and service users. For staff, REACT was viewed as a resource that can help improve their own knowledge and reduce their workload, which eases pressures and helps them to meet targets. Specifically, staff believe that offering REACT will help them meet targets around family intervention but that BFT meets them more comprehensively. There was less evidence that staff had considered the benefit of REACT for relatives apart from that it offered information independent of the service:
So I think actually I think some of our newer staff will really benefit from reading that information and knowing what information is useful to share. Particularly when you’re young, you lack some of the life experience like you know I did.
PI-RS-CBT-03, 5 June 2017, individual interview
Yeah I think it fits in in terms of reaching the family interventions target and as I said before I think it fits in with the BFT as well. So it kind of hits a couple of the targets that we’ve got to do I think.
PI-CL-CC-06, 5 June 2017
Cognitive participation
Initiation
The IMPART lead, clinical leads and REACT supporters were responsible for driving REACT forward through signing up staff, inviting relatives and monitoring and commenting on the forum. However, there was some confusion about what was required from staff, which may have inhibited REACT being driven forward:
. . . And has Moor/GRO-IL-Cpsyc-01 signed up all the practitioners then? Or who’s signing up the staff to REACT so that they can sign up the relatives?
I’m presuming that Moor/GRO-IL-Cpsyc-01 and PI-RS-STR-02, because the people who are on there at the moment, there’s one from West, so I’m presuming that PI-RS-STR-02’s, and there’s one from South, and I’m presuming that Moor/GRO-IL-Cpsyc-01, but I’m seeing Moor/GRO-IL-Cpsyc-01 on Thursday, it’s those little bits that I’m no 100% sure about just yet. I’m pretty sure, ‘cos he sent kind of direction around and sometimes you just need to send direction repeatedly because staff are getting overwhelmed with.
LA-RS-TL-01, 20 January 2017, individual interview
In addition to certain staff members, the research team assisted with driving the intervention forward. The presence of the research team in meetings and individual interviews often prompted action from staff members. In addition, when asking about meetings that staff could use as platforms to promote REACT, this often resulted in the team asking the research team to present. The researchers were invited to attend meetings to talk about REACT as staff members believed that they would discuss REACT more comprehensively:
I think that presence like yes, obviously you have come today and it has prompted me, reminded me for example about the REACT toolkit.
HA-CL-CC-03, 3 May 2017, individual interview
Enrolment
Barriers to staff engagement and commitment include an increase in caseload for care co-ordinators and the demands of targets. The IMPART lead expressed concern that staff could not deliver the same level of care or engage in activities outside what is mandatory and target driven:
I’m sure that my organisation would probably say we’re still delivering fantastic care, but I can’t really imagine that the same number of care co-ordinators could deliver as good a care with more people than they used to with fewer people. So I think it’s a general, it’s probably a general reduction in their willingness to do extra things ‘cos the access target is what the managers are focusing on and when the managers focus on something that’s what probably gets done almost to the exclusion of other stuff.
Moor/GRO-IL-Cpsyc-01, 14 August 2017, individual interview
Legitimation
There were concerns among some staff who were more involved with REACT, such as the REACT supporters, that other members of staff would not log on to REACT and explore the website independently and that it would be up to the research team to facilitate this:
. . . I think you’re right, that is the selling point by a really long shot and I think I wouldn’t like we I wasn’t there but I said to PI-RS-STR-02 I think you really need to just grab them in the team meeting one day and get them logged on, because I really don’t believe they’ll prioritise logging on.
PI-RS-CBT-03, 5 June 2017, individual interview
Activation
The IMPART lead for Moor felt well placed in his role to help sustain REACT but was concerned about how staff would continue to use the resource. There was concern that staff would offer REACT once to relatives and then not use it in the future or not revisit modules. There is some effort to maintain discussion of REACT on team and individual levels during meetings and supervision:
I think as far as our staff are concerned, they are probably getting to the point where there’s a family issue comes up in supervision, then they are delivering it and it’s a sort of like fire once missile, they probably are doing it, and then as far as they’re concerned I think the staff’s mentality is I put them in touch with a source of information and support and it probably occasion of us saying are you getting on alright with it? But I don’t think that they would believe that they’re doing a lot with that, I think they would believe that they’ve just introduced them to somewhere where they can get some additional support or whatever. I mean that’s not exactly the case here, occasionally things come up and they might in the original REACT we used to talk people through it and say right you need to go to chapter 6, this is about this and we need to go there, I don’t think that our workers are actually doing that with people, I think they are leaving them to get on with it to some extent.
Moor/GRO-IL-Cpsyc-01, 14 August 2017, individual interview
Yeah it’s discussed in the EIP forum which is held monthly, it’s not discussed monthly, it’s not discussed at each one but it does get discussed occasionally in there, and then I suppose just in our supervision. If I’ve got a family member maybe that’s using it or someone new to the service, it might get discussed in my supervision as to whether that’s appropriate to offer it.
LA-CL-MHP-11, 30 November 2017, individual interview
Collective action
Interactional workability
Staff members were able to offer REACT to relatives and saw it as an additional resource that relatives could be signposted to. However, technical issues with the trust were often discussed as a factor that might prevent this. Staff often struggled to perform the tasks required to deliver REACT because of issues with Moor Trust hosting an out-of-date browser:
I would also with each patient I’ve asked if they would like the REACT website sharing with them. So things like that, I would class REACT as a resource that’s available to them.
LA-CL-MHP-11, 30 November 2017, individual interview
. . . there was one bit I couldn’t get on because of the browsers that we use, but that’s an issue.
And what was the bit? Was it videos or?
It was I think it was the resources bit, I’d have to get on and show you, but that’s an issue internally . . . It’s unsupported, I need a better browser. I get that with anything external and I have got Chrome, so I don’t know whether that would.
LA-RS-TL-01, 20 January 2017, individual interview
Staff who had high caseloads of older relatives did not have a high success rate with signing up relatives, despite attempts to encourage them to use the resource:
What it was, was it wasn’t simple to the demographic in our area, ‘cos it is, it is acceptable in our area, what it is in my caseload I don’t have a lot of the younger people on my caseload, I have the older end, in that you know some of them are in their late 50s coming up to some of them even just going up to 60 age bracket, so even though I try to take my information leaflet along with me and say what REACT is about, and a very, they seem to have accepted that it’s a useful resource, very you know sort of very kind of me to offer it, but because they’re not clued up with computers, that computer age and literacy, they decline, they say thank you but no thank you, we don’t want to bother with it.
CH-CL-MHN-09, 14 June 2017, individual interview
Skill-set workability
There was evidence that the REACT supporter who monitored the forum did not feel equipped to respond to clinical questions as he regarded the role as supportive not clinical. The REACT supporter was able to direct questions to staff more suitably qualified to answer these questions. The REACT supporter was more confident in his role of inviting relatives on behalf of clinicians than answering clinical questions:
I have had one or two questions from relatives that aren’t relative to what my role is with the website like clinical questions, which I have forwarded on to the CPNs [community psychiatric nurses] and also like responded to like clarifying my role as a supporter and not like a clinical role [word missing] and they should be directing those questions to the CPN.
So you are actually saying that on the forum they are asking questions that you think . . .
No I got a question from somebody like in a personal message . . . Who was asking about well basically like about a clinical question about their relative’s psychosis.
PI-RS-STR-02, April 2017, individual interview
Relational integration
The clinical lead for Moor Trust EIS was concerned about the discordance between the content of what therapeutic interventions are available generally and what Moor’s EIS service is actually capable of offering. There appeared to be concern that REACT may prompt relatives to ask questions of the service that they might not have answers to:
Funnily enough that’s who I was going to talk to just before you arrived, ‘cos I’m very conscious in looking through if I was a relative and I went on and I see oh we’ve got the right to ask for this and this and this, the trust doesn’t provide everything it’s advertising on REACT, so that’s something that we need to think about . . . for example it talks about art therapies. We have very limited access and that was who I was speaking to just before you came, the art therapist, and I just happened to see her. As it stands, our service users can’t access that internally. So that’s an issue. Obviously all the health and well-being and the education, so a lot of the things that are linked to EI we’re still in the very early stages of thinking about how, and that’s not a Moor Trust exclusive issue, that’s you know.
LA-RS-TL-01, 20 January 2017, individual interview
There is evidence that staff view REACT as a way of complementing current work with relatives, which reinforces the expertise of staff and gives them a chance to follow up psychoeducation with relatives at a later date:
And I think the REACT it gives us a chance to work with them on that website as well as we just kind of give the leaflets out and it might have just got a bit forgotten about, whereas the REACT gives us a chance to follow things up I think.
PI-CL-CC-06, 5 June 2017, individual interview
Contextual integration
There was good evidence of reorganisation in order to deliver REACT effectively, through incorporation of it in a process checklist for families. REACT was presented as a ‘must do’ by the clinical lead; however, some staff did struggle initially with incorporating REACT into their existing workload. REACT was also introduced to new staff as part of their induction to working in the trust EIS:
Yeah so they have a process, checklist process about working with families as a whole, and within that they’re expected to so everybody should be offered access to this, once they’ve been accepted into the three year pathway, they should be offered access to this, they should be offered an assessment, a BFT assessment, and we should be offering them kind of external things like a carer’s assessment and stuff like that. So it’s been presented as a must do really, because that’s it’s that important.
LA-RS-TL-01, 20 January 2017, individual interview
OK and who told you about it in October?
My supervisor, so within our training when I was first inducted into the service.
OK, can you tell me a bit about your REACT training when you were first inducted?
That’s going back quite a bit, we were just basically shown the service and told how we can make a referral for family members of patients to get registered on it.
LA-CL-MHP-11, 30 November 2017, individual Interview
Reflexive monitoring
Systemisation
Staff have sought feedback from relatives but have found that they have not used the website. The main source of feedback has been relayed to staff through the research team members who spoke to relatives independently about REACT. Staff seemed to place high importance and value on relative feedback as it can be infrequent:
I actually got a really nice e-mail from one of the relatives, so I could actually if you wanted me to just say a snippet of, ‘cos the relatives said it’s just so good to know that we’re being listened to and I got positive praise for the trust.
Oh they’d love that. Anything like that, because it feels like it’s so far and few between that sort of feedback.
LA-RS-TL-01, 20 January 2017, individual interview
Yeah I’ve given it to a couple of patients, I’ve had a look at it myself, I think it looks really good. But the patients that I’ve given it to they haven’t accessed it, and when – I don’t know why that is, I don’t know if it’s a time thing, I’ve asked them you know a couple of times and it’s oh I’ve not got round to it yet, so but I’ve looked at it, I think it’s a good site, I think it’s very usable and really helpful, but for whatever reason.
CH-CL-OT-08, 14 June 2017, individual interview
Individual appraisal
The REACT supporter’s appraisal of the content of REACT and its usefulness for relatives was more positive than their appraisal of the forum. As the forum was not as active as first hoped, it was suggested that hosting it over a larger platform may be more appropriate:
I think for anybody coming into the service from the outside like you know somebody’s relative whose only knowledge of it is what they have seen like in the presentation of their relative then it is going to help a lot. But it is how the practitioner sells it to start with, and the uptake on the site. If it was a national thing, and there were thousands of people signed up to it then I think it would be really good on the forums and on the sort of, with people linking up with each other side of it.
PI-RS-STR-02, April 2017, individual interview
Communal appraisal
Although there was limited evidence of communal appraisal of REACT at the time of the interview, there were plans in place from the clinical lead to discuss REACT at trust-wide EIS meetings:
How is the delivery of REACT going in your team then, in the service?
I mean I guess I’m waiting for feedback because that will I mean the process and stuff only went out last week, so we have our forums monthly, so I’ll be kind of reviewing that every month and hopefully if I see more and more practitioners going on there that shows me that they’ve yeah.
LA-RS-TL-01, 20 January 2017
Reconfiguration
There is evidence that staff at Moor Trust modified the intervention through printing off aspects of the toolkit as it is not always appropriate to, or possible to, view REACT online when visiting people’s homes. Owing to limited staff resources, staff have also used their own personal devices to show relatives REACT in their own homes. These modifications to the toolkit further demonstrate the digital and technical difficulties that staff at Moor Trust face:
Yes and so you print it off as well so you don’t really show them online it is more of a print-off erm . . .
Sessions yes we don’t really have the, unless erm . . . they have got internet in their homes, we wouldn’t really have internet. I mean, to be honest I have to use my own iPhone to get somebody on REACT the other day [laughs] in their house . . . Yes so we wouldn’t tend to, I wouldn’t tend to use the internet. I mean I did offer with the older people to do that with them, but they declined.
PI-CL-CC-04, 23 May 2017, individual interview
Do you think that if you had used the REACT toolkit you would have printed off stuff from that as well to use that?
Probably yes, especially if they found something particularly useful.
PI-CL-CC-05, 5 June 2017, individual interview
Researcher’s reflexive summary
Generally, staff members had a good awareness of REACT and who it was for, but it was less clear how aware they were of the content of the modules and how much independent exploration of the website had taken place. The main benefits staff perceived of REACT were for the staff themselves; only a few members talked about the potential benefits for relatives. The IMPART lead and clinical lead appeared to be the key forces for driving REACT forward among staff but it was the REACT supporter who was the key individual responsible for sending out relative invitations on behalf of other staff members. Having the REACT supporter available to invite relatives was helpful for staff as there seemed to be several technical barriers to them being able to do this themselves.
Feedback from final trust analysis days
The final SRG was attended by the IMPART lead, two REACT supporters and another member of staff. One REACT supporter discussed that he had spent a lot of time sending relative invitations on behalf of care co-ordinators but did not spend time going out to carers and promoting REACT himself because he had not been asked to. The member of staff said that they asked the REACT supporter to invite relatives for them as they find it difficult to remember how to get on to the website because it is not something she has to use every day and is not something they can do when working away from the office. Staff discussed that there has been a limited amount of activity on the website with regard to both the forum and direct messages. Where there have been direct messages, these have often been around clinical matters rather than about the website, and the REACT supporter has required the assistance of the IMPART lead to answer these. Staff discussed the difficulty of getting activity going when they only get around five new cases a year each, and not all of them will have a family member who is interested in or will use REACT.
Staff agreed that the trust-specific technology often created difficulties for them trying to use REACT. Issues raised were ‘dreadful’ trust smartphones, the trust not having Google Chrome (Google Inc., Mountain View, CA, USA) as the automatic search engine, laptops taking up to 30 minutes to load and not wanting to use relatives’ broadband when trying to demonstrate REACT in people’s homes. The IMPART lead and REACT supporter were currently monitoring the uptake of REACT but they did not know how successful this was as it is easy for staff to just write ‘offered REACT’ but no one is perusing it beyond this and only a few will revisit it with relatives. The staff said that REACT had been put on the checklist but the extent to which the checklist is followed varies; despite it being mandatory, some people still do not use it.
Appendix 13 Ocean Trust case summary
Participants
| Participant identifier | NHS role | REACT role | Number of relative invitations sent | Research activities participated in |
|---|---|---|---|---|
| SH-IL-LPFPI-01 | Lead practitioner for psychological interventions | IMPART lead | 20 | Individual interview, implementation workshop, SRG |
| SH-RS-STR-01 | STR worker | REACT supporter | 4 | Individual interview, implementation workshop |
| GA-RS-CC-02 | Social worker | REACT supporter | 0 | Individual interview, implementation workshop |
| PE-RS-10 | Unknown | REACT supporter | 0 | Training |
| GA-IL-Cpsyc-02 | Clinical psychologist | IMPART lead | 12 | Training, individual interview |
| PE-RS-Cpsyc-04 | Clinical psychologist | IMPART lead/react supporter | 0 | Individual interview, implementation workshop, SRG |
| PE-RS-05 | Unknown | REACT supporter | 0 | Training |
| SH-CL-CC-01 | Care co-ordinator | Clinician | 0 | Training, individual interview |
| SH-CL-CC-02 | Care co-ordinator | Clinician | 0 | Training, individual interview |
| GA-CL-CC-03 | Care co-ordinator | Clinician | 0 | Training, individual interview |
| SH-RS-STR-06 | STR worker | REACT supporter | 11 | Individual interview; implementation workshop |
| SH-CL-CC-04 | Care co-ordinator, mental health nurse | Clinician | 0 | Individual interview |
| SH-CL-CC-05 | Care co-ordinator | Clinician | 0 | Individual interview |
| SH-CL-CC-06 | Care co-ordinator | Clinician | 0 | Individual interview |
| PE-CL-PT-07 | Psychological therapist | Clinician | 0 | Individual interview |
| PE-CL-CC-08 | Care co-ordinator | Clinician | 0 | Individual interview |
| PE-CL-CC-09 | Care co-ordinator | Clinician | 0 | Individual interview |
| PE-CL-CC-10 | Care co-ordinator | Clinician | 0 | Individual interview |
| PE-RS-CC-07 | Care co-ordinator | Clinician | 0 | Individual interview |
| PE-CL-CC-11 | Care co-ordinator | Clinician | 0 | Individual interview |
| PE-CL-CC-12 | Care co-ordinator | Clinician | 0 | Individual interview |
| PE-CL-CC-13 | Agency care co-ordinator | Clinician | 0 | Individual interview |
| GA-CL-CC-14 | Care co-ordinator | Clinician | 0 | Individual interview |
| PE-CL-CC-15 | Care co-ordinator | Clinician | 0 | Individual interview |
| PE-CL-CC-16 | Care co-ordinator | Clinician | 0 | Individual interview |
| PE-CL-STR-17 | STR worker and carers champion | Clinician | 0 | Individual interview |
| PE-CL-CC-08 | Care co-ordinator | Clinician | 0 | Individual interview |
| PE-CL-Cpsyc-19 | Clinical psychologist | Clinician | 0 | Individual interview |
| PE-CL-CC-20 | Care co-ordinator | Clinician | 0 | Individual interview |
| GA-CL-Cpsyc-21 | Clinical psychologist | Clinician | 0 | Individual interview |
| GA-CL-CC-22 | CPN/care co-ordinator | Clinician | 0 | Individual interview |
| GA-CL-SWS-23 | Social work student | Na | 0 | Individual interview |
| GA-CL-CC-24 | Care co-ordinator | Clinician | 0 | Individual interview |
| GA-CL-CC-25 | Care co-ordinator/independent placement support worker | Clinician | 0 | Individual interview |
| GA-CL-SW-26 | Locum (assessment team, social work background) | Na | 0 | Individual interview |
| GA-CL-CC-27 | Care co-ordinator | Clinician | 0 | Individual interview |
| SH-CL-CC-28 | Care co-ordinator | Clinician | 0 | Individual interview |
| SH-CL-CC-29 | Care co-ordinator (CPN) | Clinician | 0 | Individual interview |
| SH-CL-CC-30 | Care co-ordinator (social worker) | Clinician | 0 | Individual interview |
| SH-CL-TL-31 | Team lead | Clinician | 0 | Individual interview |
| SH-CL-CC-32 | Care co-ordinator | Clinician | 0 | Individual interview |
| PE-CL-TL-33 | Team lead | Clinician | 0 | Individual interview |
Context
Ocean serves an urban area of 2.7 million people, with a majority white British population. The trust employs just under 5000 staff. EI services have 28 clinical staff delivering care to 740 service users across three teams. Forty per cent of EI patients were in contact with a relative.
Ocean Trust EIS is commissioned to serve individuals aged 14–65 years and is divided into three teams: Petrel, Shearwater and Gannet. Petrel and Shearwater are the largest teams with caseloads of 273 and 257, respectively. Gannet team is smaller, with a caseload of 155, and the staffing in these teams is reflective of this. Staffing in Petrel has been a particular issue for the trust owing to high turnover of staff and agency staff as well as staff having long-term absence due to sickness. Shearwater and Gannet have had more stable staffing, but across the trust care co-ordinators have caseloads often in the high 20s as opposed to the recommended 12–15.
Resources for, and relationships with, relatives are varied across the teams within the trust. Staff at Petrel are trained to deliver family therapy and are aware that it should be offered, but are unable to do so owing to a lack of time and difficult caseloads. Where support to relatives and carers is offered, this is a referral to an individual external to EIP. In Shearwater and Gannet, regular family and friends groups were run by the teams and they sent a carers’ pack to families of individuals who join the service. Shearwater is also responsible for completing carers’ assessments, whereas Gannet and Petrel refer on to the local authority.
Each of the three teams had an IMPART lead and a REACT supporter; however, the leads and supporters in Shearwater and Gannet were more involved than those in Petrel.
Ocean Trust received IPv2.
Key findings against normalisation process theory components
Coherence
Differentiation
Knowledge of REACT and its content varied across teams in Ocean Trust, with staff at Shearwater having the most intricate knowledge of the website and staff at Petrel having a very limited understanding. Most staff cite attendance at meetings led by their IMPART leads and/or the research team as the source of their understanding of REACT:
Well it’s an online tool for carers and relatives and friends and family. The aim being for everyone to access a clear, a clear resource that gives them clear information and be able to direct them to whatever they want to look at. Obviously offers the psychoeducation bit but then it offers the ongoing support via the forum and the mediator and stuff, and obviously the ability then to speak to other carers as well, which I think’s a key thing.
SH-CL-CC-28, 18 December 2017, individual interview – Ocean
. . . So can you tell me briefly what your understanding of REACT is?
It’s an online toolkit for relatives, I don’t know much more. I know did somebody come in and have a talk about it recently? I don’t know. I don’t know much about it is the honest answer.
PE-CL-STR-17, 21 November 2017, individual interview – Ocean
Where staff have an understanding of what REACT offers, comparisons are made to other sources of support for relatives internal and external to Ocean Trust, including family therapy, carers’ assessments and carers’ packs. REACT was often viewed as positively different owing to it being dynamic and online:
OK yeah. So how does REACT compare to alternative sources of support for relatives in your trust?
Much more user friendly, much more sophisticated, much more aesthetically pleasing, and much more modern. There was a carers’ pack that the trust sent out and I was very unimpressed with that pack, just very dry, very sort of legal, not helpful I didn’t think.
SH-CL-CC-02, 18 December 2017, individual interview – Ocean
. . . I mean like I said there’s BFT and that’s offered to everybody as well, but I don’t think there’s anything been sort of something you can log on and look at and use at your own time you know in your own pace.
SH-RS-STR-01, 3 July 2017, individual interview – Ocean
I think it’s more accessible and direct, ‘cos most people do access the internet now and don’t particularly want to go to groups if they’re busy or doing other things. So it makes it more accessible that way.
GA-CL-CC-24, 29 November 2017, individual interview – Ocean
Individual specification
Care co-ordinators were instructed by IMPART leads to utilise the booklet insert cards developed for IPv2 to introduce relatives to REACT and return their details to the IMPART lead or REACT supporter to generate the REACT invitation. The majority of care co-ordinators understood this routine and what they needed to do as individuals for relatives to be invited to REACT. Care co-ordinators did not view their actions as a role or requirement, but just a task they had been asked to do:
So when you were first told about it were you asked to do, were you asked to take any role or to do anything with REACT?
Me personally no, I can’t recall that no. Other than obviously encourage people to use it and that if and to take obviously names back to SH-IL-LPFPI-01 it might have been SH-RS-STR-01 as well, but SH-IL-LPFPI-01 as the one, takes names of families who were interested back to SH-IL-LPFPI-01 and he could arrange for you know if they’re interested for them to be signed onto it.
SH-CL-CC-28, 18 December 2017, individual interview – Ocean
There were differences in understanding among REACT supporters around what their role involved. Where REACT supporters worked closely with their IMPART lead and had attended researcher-led training sessions, there was a clearer understanding of what their role required from them. For other REACT supporters, the absence of training and support left them unsure how to deliver REACT:
Yeah I mean generally I don’t think it’s that big of an ask to ask us to be involved in trying to approach people to sign up. The actual website side of things, I didn’t realise how much editing, I thought I was just going to be authorised to sign people up, I didn’t realise that I’d have full editing capabilities for the website and I’m still not entirely sure what I’m expected to do, am I expected to log in every so often and check for inappropriate comments or I don’t know what I’m actually expected to do on that front.
PE-RS-CC-07, 14 September 2017, individual interview – Ocean
Communal specification
Shared understanding of the roles of staff within the team have been gained through attendance at team meetings and training, delivered independently by staff and also with the assistance of the research team. Staff understand what is required to deliver REACT as a team, and the distinction between the roles of care co-ordinators and REACT supporters:
OK, so when have you been given the information?
We’ve been given the information through the team meetings, and we have two nominated workers who’ve done the training and they can access putting people on the website, so we will go out, offer the intervention to families that we work with, gain their contact details and e-mail and then they’ll get set up on the system by the two nominated workers, who have access to the system. And then the carers, parents, can access the information then.
GA-CL-CC-24, 29 November 2017, individual interview – Ocean
Staff who have not attended training, or do not have a specified individual role, have a limited understanding of who and what is involved in delivering REACT to relatives. For instance, the team leads are aware of REACT and who is responsible for leading it within the team, but do not know what the roles within the team are and what is needed to deliver the intervention:
OK, what’s he been doing with REACT do you know?
I don’t fully know, I know he’s like the allocated person and he has all the materials and stuff but yeah beside from that I don’t know in depth what he’s been doing.
PE-CL-TL-33, 2 February 2018, individual interview – Ocean
Internalisation
Staff evaluate the potential benefits of modality and the content of REACT separately. Staff identify that REACT meets a need for information, which has perceived benefits for both staff and relatives and, as such, the response towards the content of REACT is largely positive. However, staff opinions of REACT being an online resource are often more varied, even for individual staff members:
. . . there may be a benefit of some kind of online use of doing that, one person particularly, but that I can think of, but again her internet skills, she’s a retired woman, you know who’s not particularly computer savvy, and her internet skills aren’t particularly great, so you know I think there’s some probably some really useful things that REACT can do but it might not necessarily reach the people who most need it because of their limitations in their online skills but also not everyone has a laptop, not everyone has a smartphone, so in some senses that sort of online approach already excludes those people.
GA-CL-CC-14, 21 November 2017, individual interview – Ocean
The majority of staff members believed that the forum had the possibility to be positive for relatives in reducing social isolation, offering peer support and offering an alternative accessible resource to what the trust offers, such as the friends and family group. REACT supporters who monitor the forum discussed how the flexibility of the role allowed it to fit with their existing workload, meaning that dedicated time was not required. Where potential risk of the forum is discussed, it did not appear to overly concern staff as they were confident that REACT was being monitored:
I think it’s just ‘cos as a supporter and as an STR worker we have duty days, so that can be part of our duty day, would be to look at the forums and answer questions, ‘cos sometimes we’re waiting for duty work to come in, so I think it is viable, it is yeah.
SH-RS-STR-01, 3 July 2017, individual interview – Ocean
What about are there any risks that you think it presents?
I suppose unhelpful stuff could go on in the forum, potentially, if someone was unhappy with the service or kind of sharing information that perhaps wasn’t too accurate maybe on them forums. But that’s a risk that could happen outside of REACT, it’s not something that’s particular to REACT itself is it, and it will be monitored on there so I suppose yeah I can’t think of any immediate risk.
SH-CL-CC-30, 18 December 2017, individual interview – Ocean
Cognitive participation
Initiation
Each team within Ocean had an IMPART lead, and in Shearwater and Gannet team the IMPART leads are repeatedly identified by staff members as the leads for REACT. Shearwater’s IMPART lead was the first to undertake the role and has been very active in promoting and sustaining REACT within the team, which he has done alongside the REACT supporters within the team, who are also mentioned by staff as individuals who promote and run REACT. In Gannet, the IMPART lead is identified as the key individual too, but their promotion of REACT is not as clearly remembered by staff and has been discussed on a less frequent basis:
So who showed it to you?
It was SH-IL-LPFPI-01, SH-IL-LPFPI-01‘s like the lead, he’s the lead family therapy, so he’s been involved in leading the trial.
SH-CL-CC-28, 18 December 2017, individual interview – Ocean
I do remember now but it’s not something that’s cropped up loads, I have to say, it’s been mentioned a few times in meetings and GA-IL-Cpsyc-02s tried to promote it.
GA-CL-CC-25, 7 December 2017, individual interview – Ocean
In Petrel, the IMPART lead did not display the same level of ownership of REACT as the other leads, and requested support from the research team to drive REACT forward. The activity of the clinical studies officer including delivering REACT resources was also discussed as an action that engaged staff:
You could tell people refocus I suppose, you know kind of come once in a while to that, or pop down, that kind of like but I think the important thing is to just actually get cracking in terms of signing people up.
PE-RS-Cpsyc-04, 21 June 2017, individual interview – Ocean
Enrolment
The REACT supporter role was not enforced or made mandatory, but discussed with staff in team meetings and individually with staff identified as potentially suitable to be supporters by the IMPART leads. The decision to become a REACT supporter was influenced by what the role would involve and a personal interest in REACT:
IMPART lead thank you yeah, so he’s IMPART lead and I think it was him that first asked would I be interested and asked me go come along to a focus group initially at [town name] a steering group or whatever.
There’s a lot of different ones.
Yeah and I went along there and really sort of you know spat me interest really to become involved in it and then when he was asking for supporters I said yes I’d do that, so that’s how I got involved in it.
SH-RS-STR-01, 3 July 2017, individual interview – Ocean
The IMPART leads were very conscious of the high workload and burden Ocean staff were experiencing as part of their professional role and, as such, planned to implement a model of delivering REACT that would involve minimal effort from staff. The IMPART leads allocated staff the task of gathering relatives’ details and returning them to the leads or supporters, hoping that the contribution from staff would be minimal enough for them to engage with REACT and not ‘overwhelm’ staff. Plans were also made to include information booklets about REACT in initial assessment packs to accommodate REACT within existing staff tasks:
. . . just kind of the burden factor is something that scares people off, really quickly, so kind of even having care co-ordinators and supporters and all that kind of stuff like, people could potentially run the risk of switching off, whereas using care co-ordinators or selling the benefits to them like oh just giving them one small task to do, the most important one which is just mention this to your relative will you, give them this, and then give me whatever or get them to sign this and put their details. Essentially is it just their phone number, their e-mail and their name?
PE-RS-Cpsyc-04, 21 June 2017, individual interview – Ocean
Where relationships with relatives can already be under strain, staff are particularly cautious about directing staff away from the service to external resources including REACT. Staff do not want relatives to feel as though as they are offering REACT so as not to provide services themselves:
. . . Yeah do you think there’s anything particularly easy or difficult about implementing something like REACT in services, apart from as you say it’s a lot to remember?
I think that’s all it is really is that there is so much to remember like it all comes down to the care co-ordinators to offer it to people and we’re trying to remember all of the support services that are available, all the other like resources that we’ve got for the person, ‘cos it’s very rare that someone needs one thing, we’ve got all these research studies and it’s quite a lot of overlap in there and it’s just trying to remember everything without sounding like you’re just reaming off a list, well would you like therapy via this research and would you like this research and we can refer you here. It can start to feel like you’re just you don’t want the person to feel like you’re fobbing them off when you’re saying I could do this but I’d rather you accessed that there. So it’s trying to do it sensitively, it’s not always a good time, then it can get put off, we’ve just got so much to remember, and you want it to stay personal, it’s just the sheer amount of things we’ve got to remember.
PE-RS-CC-07, 14 September 2017, individual interview – Ocean
Legitimation
The majority of care co-ordinators perceive working with carers, and by extension REACT, to be a legitimate part of their role and a resource they should be offering. Staff believe that REACT has the potential to fit with their priorities around carers, but not their targets. Despite the perceived fit with their roles and duties, offering REACT to relatives is often considered a low priority among staff, with the service user and target-driven work being considered as higher priorities:
It’s probably you know I have given it to a couple of people when I’ve done first assessments and yeah it probably isn’t seen as a priority with me, it should be, that you go in and start work and developing care plans and things with the clients that maybe you don’t always then focus on the carer because you have you’re aware that they’ve received the pack and they access support separately from you so.
SH-CL-CC-05, 25 August 2017, individual interview – Ocean
The team leads in Ocean Trust did not engage with REACT to the same extent as other staff members, but this appeared to be due with them not perceiving REACT to fit with their roles. The team leads do not engage in clinical work and have a largely managerial role so perceive having an overview of REACT to be sufficient for them. As one lead grouped REACT with ‘research stuff’, it suggests that REACT has not been integrated at the senior staff level and is seen as external research rather than an internal resource:
That’s fine. What are your views on the REACT toolkit?
I don’t really know it very well to be honest and to be honest, because we do have a lot of different research stuff going on, I just know the basics of it and it’s the care co-ordinators who sort of deal with it more, so I’m not really sure of the . . .
SH-CL-TL-31, 18 December 2017, individual interview – Ocean
I suppose one of the tricky things is my role that I’m quite often all over the place at different meetings and that’s why I’m not getting involved in some of those discussions and meetings where REACT has been mentioned. So I’m not sure really but I think I don’t know it’s tricky really because for me I feel obviously I need to have an awareness that it’s going on, and that it could be something that people need to look at, but I suppose I wouldn’t be directly referring people in, so I’m not sure kind of to what level I need to know about it if that makes sense.
PE-CL-TL-33, 2 February 2018, individual interview – Ocean
Activation
There is some evidence that Ocean Trust is considering the actions that need to be completed to maintain awareness, and sustain the delivery of REACT, but these have mainly been discussed by the IMPART leads and REACT supporters. Actions suggested included discussing REACT in business meetings and team meetings and organising regular meetings with IMPART leads and REACT supporters across the trust. There was evidence that discussions involving REACT had evolved from a standing agenda point to introduce REACT by a key individual to something that is discussed on a case-by-case basis by staff generally. Barriers to staff involvement in planning include the perception of REACT as external research and concern that staff would not act on the instruction of others:
Yeah so we meet every week, we’ll go through any sort of new referrals, feedback from assessments and then just any ongoing cases that we want to bring to the team for a discussion. And if there is a bit of an issue with you know a carer or something, you know we might say have you considered REACT as a solution really, problem-solving, that might be something we want to consider just to kind of prompt each other, so that’s generally how it’s sort of brought up, unless it’s sort of in a business meeting, it might be something GA-IL-Cpsyc-02 specifically wants to share about it, like an update or something, then it would be yeah.
GA-CL-CC-22, 28 November 2017, individual interview – Ocean
We do forget, we are asked to do quite a lot of different, and I believe in research, I like the idea of trials and trying to improve, so if I can remember what I’m asked to do I’ll try and get people on board, but we do forget and things are changing all the time, so reminders are good I think . . . so I think someone coming in, you don’t have to come in every week, you don’t have to come in every month, but if numbers are looking like they’re dropping off a bit it might be quite useful for someone to come in and remind us of the benefits, ‘cos I could do it but they wouldn’t listen to me.
PE-RS-CC-07, 14 September 2017, individual interview – Ocean
Collective action
Interactional workability
In Ocean Trust, the majority of staff members are involved in delivering REACT; however, tasks completed by staff differ according to whether they are a titled REACT member (IMPART lead or REACT supporter) or a care co-ordinator. In Ocean Trust, care co-ordinators do not have logins to REACT, and so use the resources developed for IPv2 to gather relatives’ details and return them to IMPART leads or REACT supporters, who then complete the invitation process. This model works well for care co-ordinators, as they do not have the resources to complete the sign-up process when visiting relatives. However, in Petrel team, delivery of REACT is limited to the REACT supporter:
Just mainly just kind of if you give me your e-mail address or you put it on this card and you can either send it to SH-IL-LPFPI-01 in the office or I can take it back but I haven’t kind of gone on a visit and sort of logged on and kind of gone oh look at this, you need to see it, ‘cos we don’t have laptops or owt like that and it just seems a bit cheeky to sort of get somebody to not cheeky but don’t normally kind of get people to access their computers during a visit.
SH-CL-CC-02, 18 December 2017, individual interview – Ocean
Staff are able to incorporate offering REACT into their day-to-day working practices to complement existing trust resources and therapies, such as BFT. However, there are differences among individual staff members in when they would offer REACT to relatives, with some staff members being concerned about overwhelming relatives and so delaying giving information until a time they feel it would be most helpful for the relative:
Yeah, for instance I’m working with a family that’s a bit there’s quite a lot of conflict and it’s a bit split up at the moment, so my client’s a male client, he was living at home, his mental health brought then such a degree that it was impacting on his marriage and his relationship with his children, so he had a bit of respite over with his mum, so I kind of offered them BFT family intervention with the children and the wife and the grandma, and also offered them access to the REACT website for them to access more information around psychosis and their understanding of the difficulties that the son and husband were going through, to kind of get an understanding about some of the complexities and difficulties and about treatment.
GA-CL-CC-24, 29 November 2017, individual interview – Ocean
Again it’s swings and roundabouts, it depends a lot of people that come into our service are kind of coming in at their wits end and initially all they want is their loved one to get better. So I think usually other than some basic psychoeducation verbally that’s all that they want at that point because it’s just a bit too overwhelming. And usually after a couple of months that’s when you can start kind of drip feeding it in, and it might be after like I’m thinking about the couple of people I’ve referred to REACT, it’s over 6 months after they’ve been in the service for that then to seem something that they could do, ‘cos otherwise they’ve just said that they’ve been a bit overwhelmed, it’s a bit too much, they haven’t got time yeah.
SH-CL-CC-04, 25 August 2017, individual interview – Ocean
Skill-set workability
The tasks allocated to care co-ordinators to deliver REACT seem to fit well with existing staff practices, which could be owing to consideration of the IMPART leads to try to prevent overburdening care co-ordinators. The REACT supporters at Shearwater and Gannet are positive about the fit between their role as a REACT supporter, their professional NHS role and their technological abilities. Having computer literacy has allowed the REACT supporters to navigate the process of inviting relatives and monitoring the forum with ease. However, lack of technology confidence has created concern and fear in Petrel’s REACT supporter who has reacted by not completing supporter duties:
Perfect right, I think you’re really computer literate as well so do you think that helps?
That helps yeah, I mean I would be happy to, and I am happy to go through and because it is so easy, like you say I do know a little bit about computers and stuff like that, but when you’re using it it’s just point and click, point and click, you know so it’s really easy and I think that’s been great.
SH-RS-STR-01, 3 July 2017, individual interview – Ocean
I only went onto it as a supporter about 2 weeks before I went on leave and then I was on leave for 2 weeks, so I did have a quick look on it before I went off to try and familiarise myself with it for what I was asking people to use it, and for me I’m not very technological, because it gave me like for editing powers, so I could actually edit the site, it scared me a bit, and I didn’t want to go into it too much in case I did something I shouldn’t.
PE-RS-CC-07, 14 September 2017, individual interview – Ocean
Relational integration
There was a largely positive consensus among staff that REACT can provide relatives with the information and support they need to an extent. Staff often discussed the importance of face-to-face contact with relatives with regard to regular contact, and in therapeutic capacities such as BFT, and that it is still needed and cannot be replaced by REACT:
Well I think it meets the need massively but then not fully you know, it’ll never meet unless there’s a person talking to you and a person who knows a relative so you know, so it does meet a big need but it wouldn’t be the whole, it doesn’t encompass everything. There needs to be that one on one, that face-to-face kind of ability for someone to talk to someone about someone you know, especially like professional wise you know.
SH-CL-CC-28, 18 December 2017, individual interview – Ocean
Among staff, there was some pessimism that both staff and relatives would perform the actions required for REACT to be successful, including completing the sign-up process. In particular, there was concern among staff about whether or not the forum would be moderated sufficiently by staff and used appropriately by relatives:
There’s hardly any activity on the forums, people are not asking questions. And it’s difficult to get to that kind of critical mass of people on there to start generating stuff. The activity that we have had is one or two relatives just asking specific questions, usually unrelated to the material in the toolkit.
SH-IL-LPFPI-01, 11 September 2017, group interview – Ocean and Seashore
Contextual integration
Staff in Ocean are able to integrate the resources developed to support the delivery of REACT into existing resources such as carers’ packs to make information about REACT available to every carer known to the service. However, this action led to some staff members not discussing REACT with relatives because they knew that they would have received information in the pack. The REACT supporters at Shearwater are also displaying the REACT resources in the office to promote REACT to staff:
Yeah we’ve got a parenting carers’ pack, carers’ pack basically, and it’s got the information about the services we provide for parents, the parents’ group and carers’ group, we have we do the BFT family group therapy, it’s got Gannet carers’ contact details in there and information about them, and local information that they can access. And I think the REACT, you know the REACT online service, that information’s in there as well.
GA-CL-CC-24, 29 November 2017, individual interview – Ocean
I noticed there’s some merchandise brought over and I wondered if that helped with prompting people to remember REACT or to think about signing people up, so having a pen or?
These are all on our main desk in the office, so anybody can pick them up, anyone can look at them, so we’ve deliberately kept them out so they are there every day and people walk past that desk every day so they can’t help but not look at them so.
SH-RS-STR-06, 14 August 2017, individual interview
However, the extent to which REACT has been integrated at an organisational level was not as apparent. REACT was not integrated into pathways, plans or staff introductions. Staff who joined the trust after the presentations by the IMPART leads and the research team were introduced to REACT by the trust’s clinical studies officers, suggesting that REACT is still encompassed with research as opposed to integrated with the service:
Yeah. And I know you’re new, but did you have any induction training where REACT was mentioned or anything like that?
No, we had a brief induction to the sort of general some of the general research that the trust is doing as a whole, and CSO CRN [clinical studies officer, clinical research network] briefly sort of told me what his role is and some of the research that is happening at the minute in the trust but that was it and I’m not even sure if that was discussed specifically.
PE-CL-CC-15, 21 November 2017, individual interview – Ocean
Reflexive monitoring
Systemisation
There was limited evidence that staff were formally monitoring use of the REACT website and uptake of invitations among relatives themselves. Staff do not appear to be having conversations with relatives about REACT after they have offered it to them. Where staff have investigated uptake of REACT, this has been through approaching the IMPART leads to ask. Staff have not been able to check for themselves owing to the mechanism employed in Ocean Trust where only the IMPART leads and REACT supporters send out relative invitations:
Do you know if those relatives are using REACT?
I think one is, I do not know about the other one, I think it was only two but I think one is, I’m not sure about the other one though, so I’ve not really to be honest I’ve not asked her about it.
SH-CL-CC-28, 18 December 2017, individual interview – Ocean
Good and you said it’s good now that you’ve seen some of your relatives using it. How do you know that your relatives are using it?
Because SH-IL-LPFPI-01 tells me that they’ve gone on and signed in, they’ve used his link.
So it SH-IL-LPFPI-01 monitoring it or are you asking SH-IL-LPFPI-01 if people are?
Oh I ask SH-IL-LPFPI-01, did so and so’s wife, ‘cos so I get their details don’t I, like their e-mail address and I give it to SH-IL-LPFPI-01. SH-IL-LPFPI-01 sends them a link and then apparently if they activate it it comes up on the thing on the side, so yeah.
SH-CL-CC-01, 18 December 2017, individual interview – Ocean
Individual appraisal
There was limited individual appraisal of REACT within Ocean Trust, which was perhaps due to several of the team admitting that REACT still felt new to them at the time of the interview. Staff have received some informal feedback from relatives about REACT, which appeared to have come through individual discussions. Positive feedback from relatives appears to have reaffirmed staff’s initial positive impressions of REACT. Positive feedback from relatives appears to be an important factor in the way staff appraise REACT as it has the ability to change staff’s opinion of the resource:
But just saying that it has been really useful, and that’s really nice because I initially thought this could be something that people will find really easy to access, it’s going to have relevant information, relevant support, and then I don’t see too much of the difficulty in getting that out there, and that’s the feedback that I’ve had, and that is how it’s been. So I don’t think that’s really changed, if anything it’s been even better because I’ve had such nice feedback from people really, relatives really sort of saying I’m so glad you told me about this, ‘cos I’ve been Googling and trying to find stuff out and it’s all just coming back and I don’t understand it, whereas this is kind of it’s easier to access and it’s user friendly I think.
GA-RS-CC-02, 13 September 2017, individual interview – Ocean
Communal appraisal
There was no evidence of communal appraisal of REACT within Ocean Trust. Staff did not discuss using formal data about REACT to evaluate the resource or discuss impact.
Reconfiguration
Staff discussed that they did not have compatible or suitable NHS equipment to demonstrate REACT to relatives when they met relatives. In response to this, staff often used the booklets developed for IPv2 to introduce relatives to REACT and would use the insert cards to take the relative’s details back to the IMPART lead or REACT supporter. Staff have also used their own personal equipment to demonstrate REACT:
And then we can go out then, I use my own personal phone ‘cos obviously my work phone doesn’t let me go on the internet, or I’ll ask them to get their iPad out and I’ll show them that way. And then it’s there on their memory then isn’t it, so yeah, I do like it though, it’s just about us remembering to go out there and sell it to them as well.
SH-CL-CC-01, 18 December 2017, individual interview – Ocean
There have been suggestions from staff about how REACT could be delivered in the future, with suggestions of training relatives directly and offering REACT as a paper-based document rather than an online resource. One suggestion repeated by Ocean staff is that they would have preferred to have their own login to REACT so they could explore the website themselves. Under the current model Ocean Trust uses, it is only the REACT supporters and IMPART leads who can log in to the website, so other members of staff have only been able to view what has been presented to them:
I don’t know really, I think that it I think that if care co-ordinators individually would be able to log on and do it, I think they would. I don’t think it, I don’t know, I mean maybe it hinders it a bit if you’re sort of having to wait for me or GA-IL-Cpsyc-02 to be around to kind of pass on the card or the information or whatever to say can you log this person on, can you log this person onto the system. I think it’s good to have a couple of dedicated people who know about it, who go to the meetings and feedback to the team, in terms of inviting people to use it, I don’t know, I think that could potentially be put out to other people as well.
GA-RS-CC-02, 13 September 2017, individual interview – Ocean
. . . I’ve not actually, I’ve got to be open, I haven’t actually been on and seen the site myself, it’s only the information what we’ve been given. I think that would be useful for us to have been able to access the site.
GA-CL-CC-24, 29 November 2017, individual interview – Ocean
Researcher’s reflexive summary
The majority of staff were aware of REACT and were able to discuss who it was for and the content and features of the toolkit. Very few staff had explored the website independently, and knowledge of REACT was developed through attendance at presentations and training sessions. Lack of independent exploration of the website was in part owing to only a limited number of staff, the IMPART leads and REACT champions, having logins to REACT. This decision to limit logins was made by the IMPART leads in an attempt to limit additional work for care co-ordinators; however, some staff still felt that it was difficult to deliver REACT because of the volume of other mandatory, target-driven work they had. Some staff members discussed that they would have liked the opportunity to log on to REACT themselves so they could explore the content of REACT independently. REACT supporters felt well suited to discussing REACT with relatives and sending invitations, but were often concerned about their clinical and technology skills for monitoring the website and forum.
Feedback from final trust analysis days
The final SRG was attended by the IMPART leads from Shearwater and Petrel and four other members of staff from Shearwater. Shearwater’s IMPART lead discussed that IPv2 booklets were being placed in the carers’ packs by the administration team but the uptake from relatives remained low. Petrel’s IMPART lead discussed the benefit of the resource but that difficulties facing the team had meant that only limited effort was invested.
Staff discussed the length of the process for inviting relatives to use REACT as a difficulty, especially when relatives would sometimes lose information that they would pass on, and suggested that an automatic invitation process would be helpful. Staff agreed that the NHS is not yet equipped for digital, and the lack of resources creates difficulties in delivering REACT: in particular, the log-in process and sending relatives’ invitations through e-mail, as often this is not recorded correctly in notes. Staff agreed that REACT is a useful resource but with limited time and headspace it is often difficult to think about REACT and anything else that is not a mandatory requirement. There was some difference in opinions about who should be supporting the IMPART leads, with staff suggesting carer champions but the carer champion explaining that with this role and a caseload of 30 they could not possibly take on an additional role. Petrel’s IMPART lead discussed the lack of support from senior management and said that this support would be needed as well as REACT being incorporated into targets to be delivered effectively. Staff said that they had received limited feedback from relatives but attributed this to the forum being quiet. Staff remained concerned about the unknown issues that REACT might raise. There is also concern that as the forum grows it might be used to post negative comments about staff and the service.
Staff disagreed that relatives should be given information about REACT as early as possible as they are often already overwhelmed with information and there are often things such as carers assessments that happen after a couple of weeks and it can be used to support this plan, which staff see as a better fit. Staff were also concerned that offering REACT could be seen by relatives as ‘fobbing off’ when they want face-to-face support and information, so they are cautious about how they introduce REACT to relatives and believed that it needed to be delivered in conjunction with face-to-face support.
Appendix 14 Seashore Trust case summary
Participants
| Participant identifier | NHS role | REACT role | Number of relative invitations sent | Research activities participated in |
|---|---|---|---|---|
| PL-IL-CPsy-01 | Principal clinical psychologist/clinical research domain lead | IMPART lead | 1 | SRG, individual interview, implementation workshop |
| GU-IL-CPsy-02 | Clinical psychologist | IMPART lead | 6 | SRG, implementation workshop |
| SA-IL-CPsy-03 | Clinical psychologist | IMPART lead | 2 | Implementation workshop, group interview |
| PL-RS-APsy-02 | Assistant psychologist | REACT supporter | 26 | Implementation workshop, |
| GU-RS-APsy-03 | Assistant psychologist/vocational worker | REACT supporter | 10 | Implementation workshop, individual interview |
| SA-RS-APsy-04 | Assistant psychologist | REACT supporter | 17 | SRG, implementation workshop, individual interview |
| PL-CL-MHN-CC-01 | Community mental health nurse | Clinician | 0 | SRG |
| GU-CL-TM-02 | Team leader (senior nurse practitioner) | Clinician | 7 | SRG, individual interview |
| SE-CL-HPsy-09 | Head of psychology and lead for psychosis pathway | Clinician | 0 | Individual interview |
| GU-CL-HAP-16 | Honorary assistant psychologist | Clinician | 0 | Implementation workshop |
| GU-CL-HAP-17 | Honorary assistant psychologist | Clinician | 23 | Implementation workshop, individual interview |
| GU-CL-SW-19 | Social worker/senior practitioner, carer champion | Clinician | 3 | Individual interview |
| SA-CL-CPN-CC-24 | CPN, care co-ordinator | Clinician | 1 | Implementation workshop |
| SA-CL-ST-25 | EIS student | Clinician | 0 | Implementation workshop |
| SA-CL-STW-34 | Star worker | Clinician | 0 | Individual interview, implementation launch |
| PL-CL-CPsy-39 | Locum clinical psychologist | Clinician | 0 | Individual interview |
| GU-CL-CPN-41 | CPN, treatment and recovery team – non-EIP staff | Clinician | 1 | Individual interview |
| GU-CL-HAP-43 | Honorary assistant psychologist | Clinician | 4 | Individual interview |
| SA-CL-CPN-CC-51 | CPN | Clinician | 2 | Individual interview |
| SA-CL-SW-CC-52 | Social worker | Clinician | 0 | Individual interview |
| SA-IL-CPsy-53 | Clinical psychologist | IMPART lead | 12 | Group interview |
| SA-CL-HAP-57 | Honorary assistant psychologist | Clinician | 15 | Group interview |
| SA-CL-CPsy-68 | Clinical psychologist | Clinician | 0 | Group interview |
Context
Seashore Trust serves an urban and ethnically diverse population of approximately 750,000 people. The trust employs more than 3500 staff and around 412 individuals receive care from EI services delivered by 35 clinical staff. The 2016 national CCQI audit102 indicates that this trust offered family interventions to approximately 43% of service users and their families, and around 71% of carers were offered education and support programmes.
Seashore Trust is comprised of three EI services, which serve an age range of 18–35 years. Sandpiper has the largest caseload (172), followed by Plover (129) then Gull (111). This trust experienced high staff turnover during the study, particularly in Plover where all care co-ordinators and the team manager left the service within a couple of months. There was an IMPART lead and REACT supporter in each team, although Sandpiper and Plover experienced a period with no REACT supporter owing to staff turnover, and the IMPART lead also changed in Sandpiper.
In terms of existing provisions for carers, all three teams deliver family interventions and run their own family and friends’ groups, although Plover’s group stopped temporarily owing to staffing shortages. Carers’ assessments are occasionally conducted in house, although the bulk of assessments are conducted by an external carer worker. Gull team is able to refer service users and their families to a local systemic therapy clinic and is the only team that has a service welcome pack, which includes information for carers. All teams have links to local recovery colleges with courses specifically for carers.
This trust received IPv2.
Key findings against normalisation process theory components
Coherence
Differentiation
There was good awareness of REACT across the three teams, with the exception of decreased awareness in Plover following a period of high staff turnover. Although many felt that the availability of carer-specific resources was limited, REACT was most frequently compared to BFT and a family and friends’ group, and it was commonly described as a valuable adjunct to existing care:
I think my vision of it is a way to kind of interact with other carers I think, access more support in the future, but it’s just kind of almost like a quick collection of things. I see it more of like a really handy useful thing rather than a streams and volumes and dates and organisations and stuff, I think it’s kind of REACT is a first point of call, rather than going to a group and organising carers’ assessments and groups and have a little bit of a touch with REACT and then see and then expand from there.
GU-CL-CPN-41, 20 October 2017, individual interview
Staff also drew comparisons between REACT and a new NHS Digital initiative aimed at service users, which was rolled out in parallel with REACT, and there was some evidence of confusion between the two initiatives:
One of our best care co-ordinators who’s very experienced, I asked him all about his experience of using it [REACT] and it quickly became apparent he didn’t know what it was. And this is a guy who’s been to so many presentations and I’ve talked to him one to one, he was getting it confused with the other initiative that was going on at the same time which is in this trust . . .
PL-IL-CPsy-01, 25 October 2017, individual interview
Individual specification
Coherence was strong among a few key individuals who had allocated roles for facilitating implementation, namely the REACT supporters and IMPART leads. These individuals were clear about their responsibilities for delivering the intervention and assisting colleagues with REACT, which appeared to be aided by collective discussions about their roles and use of the online manual. However, aside from these individuals, relatively few staff members had detailed knowledge of REACT or had spent any significant amount of time on the website, and most were unclear about their own roles in the implementation effort. Some attributed their lack of clarity to insufficient training and lack of exposure to the website, whereas others lacked motivation to learn about the toolkit:
Well I haven’t really, I haven’t used it, I just know that it’s a resource of information for people who are experiencing difficulties.
And where have you learnt about it mainly?
Mainly at the presentations in the morning, when people like yourself have come along and said look this is what we’ve got, we’ve got a toolkit here and off you go.
SA-CL-SW-CC-52, 23 November 2017, individual interview
Communal specification
Most staff were aware of key individuals championing REACT in their teams and had a basic understanding of what their roles entailed. However, there was a poor communal understanding among staff of what the new practice required of them individually. There appeared to be a shared expectation for one or two individuals, namely the REACT supporters, IMPART leads and honorary placement students, to carry out the work involved in delivering the intervention. This seemed to be influenced by the profession that these individuals were associated with and the lack of a forum for building a collective understanding of tasks and roles beyond researcher-facilitated meetings. High staff turnover, particularly in Plover, was an additional obstacle to maintaining awareness of REACT and associated roles:
. . . I think it was just kind of assumed that it was myself and SA-IL-CPsy-03 who would just kind of take the lead ‘cos we had the titles of kind of REACT lead and supporter, and I think whenever the management have been approached they’ve kind of been like well that’s SA-RS-APsy-04 and SA-IL-CPsy-03’s thing to do, so it kind of gets knocked back a bit to us, so it kind of it’s the same kind of vibe with kind of family interventions again in general, it’s like it seems to become a psychology thing unfortunately rather than being a whole-team thing.
SA-RS-APsy-04, 25 July 2017, individual interview
. . . I can’t recall anyone going through the modules clearly with us, I think it was like your team signed you up like so GU-IL-CPsy-02 as the lead just sent everyone logins and said off you go, have a look at it yeah, hence why I was thinking some team time to look at it together, so we all feel confident, we can ask questions.
GU-CL-TM-02, 21 November 2017, individual interview
Internalisation
Most staff appreciated the value of the REACT intervention for their work, such as having a reliable source of information for carers, and there was a sense that some felt empowered to support carers because of the availability of a resource specifically designed to address their needs:
I find it tremendously kind of, there’s comforting, but tremendously pleasing to be able to say that there is a good resource, we have it, here it is, this is something that I can recommend, having not had that for so many years, and giving out quite dodgy information on a sheet to people, to actually say here is a really good website, that’s great.
PL-IL-CPsy-01, 11 September 2017, group interview
. . . it’s nice to know oh right this is something I have that’s up my sleeve and it kind of gives me a sense of like a purpose [. . .] now I feel like yeah I’m a specialist in carers’ needs and I have a specialist tool for you and I think it’s really useful.
GU-CL-CPN-41, 20 October 2017, individual interview
Staff also discussed limitations of REACT, including the appearance, content and usability of the website, and negative first impressions affected initial engagement with the intervention. Perceived costs were highlighted, in terms of time required to deliver REACT, and some care co-ordinators felt that the costs outweighed the benefits in the context of their existing workload. In addition, negative views about technology limited staff’s ability to construct the value of REACT for their work:
Yeah my initial sense was that it looked very serious, sorry, it felt a bit dry somehow [. . .] it didn’t feel particularly easy to navigate or eye catching, I don’t know what it was. Kind of put me off a little bit, but then once I started going on to the information and stuff you know I think it was all there.
GU-CL-SW-19, 23 November 2017, individual interview
Well the first thing for me is I suppose because of my age as well is that it’s not the kind of website that I would automatically approach [. . .] so I would never sign up for something like this, because I would see it as another hassle to do, it’s something else, it’s another password I’m going to forget, I may well get unsolicited and unwanted spam and e-mails that I have to go in and adjust my account settings in order to reduce . . .
SA-CL-SW-CC-52, 23 November 2017, individual interview
Cognitive participation
Initiation
The REACT supporters and IMPART leads were central to the implementation effort. The supporters assisted their colleagues in using REACT and, in most cases, offered to invite interested relatives to the website on behalf of their colleagues. The IMPART leads worked to drive the intervention forward by assigning the supporter roles and offering ongoing support, as well as raising staff awareness of REACT and considering ways to embed REACT within existing structures:
I think I probably I’ve been taking the main role in the team in terms of talking to people about it, and trying again like signing the care co-ordinators up and showing them and things like that, so yeah I think myself and SA-IL-CPsy-03 probably keep it in people’s heads yeah.
SA-RS-APsy-04, 25 July 2017, individual interview
Nonetheless, the leads and supporters suggested that several factors affected their ability to drive the intervention forward, including their professional orientation, the degree of managerial support and their physical presence in the team. Specifically, the association of REACT with psychology staff encouraged a shared perception of REACT as a psychological intervention and acted as a barrier to initiation by care co-ordinators, particularly in Sandpiper. Difficulty in securing managerial support in Sandpiper and Plover was also identified as a barrier by the IMPART leads, who acknowledged that team managers have a stronger influence over care co-ordinators’ workloads and the extent to which tasks are prioritised. In addition, staff in all teams perceived researchers as key drivers of REACT through frequent contact and provision of promotional merchandise, which helped to maintain awareness and prompt activity:
You guys are good ‘cos I think without regular prompting from the IMPART team we probably wouldn’t do half as much as we do, I certainly as an IMPART lead need that regular reminding . . .
PL-IL-CPsy-01, 11 September 2017, group interview
Enrolment
Although staff understood the purpose of REACT and recognised the need for their service to support carers, such understanding did not appear to translate into a willingness to contribute to the work involved in implementing the intervention. A key barrier to securing staff buy-in was the perceived time and effort required to deliver REACT in the context of existing high workload. A common perception of REACT as a psychological tool and a research project, and lack of managerial backing were also important factors limiting engagement:
I think the biggest issue we’ve had is convincing care co-ordinators that it’s less work rather than more [. . .] we’re fighting this uphill battle as it were, looking for reasons not to do it, because they assumed it was more work. Yeah. So I think that’s the biggest hurdle to overcome, is the more work thing, trying to convince people it’s less work and in their interests.
PL-IL-CPsy-01, 25 October 2017, individual interview
. . . I think if REACT had been introduced as not research but just something we’re going to do from now, that by the way we might evaluate, possibly it might have been seen as more of an infrastructural thing, this is what we will do, but yeah. The kiss of death is kind of true, but people switch off as soon as you go this is a person from X university and they’re going to talk about this project. You can see half the team sort of go oh god and fold their arms and how many more minutes have we got to put up with this, no matter what the project is . . .
PL-IL-CPsy-01, 25 October 2017, individual interview
Nevertheless, there appeared to be some variation in enrolment between teams. There was greater evidence of personal investment in the delivery of REACT among Gull staff, which seemed to be facilitated by a shared commitment to working with carers and managerial support for REACT. It is also noteworthy that the initial training session was held at Gull’s team base and predominantly attended by Gull staff:
We’ve had a really good buy-in from care co-ordinators, and it hasn’t been extra work ‘cos it’s just been, so they talk to carers and they ask for e-mail addresses and then they just send them to GU-CL-HAP-17 and I, and we put them on the REACT tool so [. . .] we’re all quite family and friends orientated I don’t know, carer orientated as a team, and it comes up in meetings every week, you know it’s in the big meeting about carers we’re talking to and if you’re in CPA [Care Programme Approach] you’ll talk to the carers there, why not just offer the tool?
GU-RS-APsy-03, 7 April 2017, group interview
Legitimation
Many staff acknowledged that carer support is a ‘core intervention’ under the EIP model, and thus indicated that REACT is a legitimate part of their role and the support their service provides. In addition, several recognised the role of REACT in helping their service to meet audit targets around carer education and support:
. . . I think for me it is one of the priorities ‘cos it’s one of the ways that we can offer support to carers and that’s part of the core part of our job, it’s one of the core interventions.
GU-CL-SW-19, 23 November 2017, individual interview
Despite this, there was a strong sense that targets for family and carer support are viewed as secondary to targets concerning the service user, and consequently supporting relatives was seen as a legitimate but relatively low-priority task:
[REACT] would make it so much easier for us to provide that carers’ support and information which is kind of one of the targets, but I guess because within the targets there’s the kind of family and psychological support isn’t necessarily the first priority, then probably REACT would become part of that kind of let’s think about that later on, yeah.
SA-RS-APsy-04, 25 July 2017, individual interview
Prioritising, yeah – which does feel uncomfortable, because my original point about carer support as an afterthought – this is a very good example of how that happens. It’s that when we can’t deliver the essentials for our clients, in the first instance, carers go to the back of the queue.
GU-IL-CPsy-02, 4 April 2017, group interview
Although IMPART leads and REACT supporters viewed the delivery of REACT as a legitimate part of their jobs, they felt that the allocation of these roles to psychologists negatively affected the extent to which non-psychology staff members felt that it was right for them to be involved. IMPART leads proposed that greater management involvement would offer a stronger lever for driving implementation forward in their teams:
It shouldn’t be psychology should it REACT, it’s just an information sharing but because it is held in psychology people are thinking oh it’s another psychology strategy rather than actually it’s just MDT, it’s just information.
SA-CL-CPsy-68, 10 April 2018, group interview
I think senior momentum is quite important in our teams [. . .] if the team manager makes it apparent this is just a part of the job, so REACT isn’t just a kind of something you do like a form you fill out every 3 months and that’s it, REACT is actually part of the structure of what you do [. . .] having a manager that will alongside asking about the reds and the ambers and who’s still in hospital and who’s back in the country and in trouble, so alongside the other more important criteria of risk management which can easily take over everything, prioritising REACT, have you asked them, have you given them the website, that’s important.
PL-IL-CPsy-01, 11 September 2017, group interview
Activation
There was limited evidence of staff willingness to collectively define actions needed to sustain the delivery of REACT. Although discussions during researcher-facilitated meetings generated some suggestions for overcoming existing challenges, there was a lack of commitment to putting such mechanisms into action. Staff reported that REACT is a regular agenda item in Gull’s team meetings; however, there was a consensus across the three teams that an allocated ‘champion’ is needed to maintain awareness and prompt staff activity:
I think it is having the person who’s the champion, to keep the impetus going of someone each week, you know that’s their job each week to hound care co-ordinators and keep it on the agenda really, ‘cos I think it could slip off the agenda if it’s not.
GU-IL-CPsy-02, 10 October 2017, individual interview
Cognitive participation
Interactional workability
The delivery of REACT became normalised for the REACT supporters, who promoted the toolkit in their interactions with relatives and supported colleagues in offering REACT. However, there was a sense that the implementation effort was predominantly a solo activity rather than a collective effort by all staff members. Indeed, this is illustrated by the fact that the delivery of REACT came to a halt in Sandpiper and Plover when the REACT supporters left the services and did not resume until new supporters were assigned. Hence, this highlights the paradoxical impact of having few key individuals dedicated to driving implementation forward:
. . . the assistant psychologist who was being our champion locally, PL-RS-APsy-02, he left, end of July, so there was no one that particularly could be there running it on a day-to-day basis, ringing carers and inviting them, and he was also given the carers’ group I think so that’s also and without his input in this team it really hasn’t thrived I don’t think.
PL-IL-CPsy-01, 25 October 2017, individual interview
Skill-set workability
Staff confidence in performing tasks required by the intervention appeared to be mixed and largely dependent on individuals’ IT skills and familiarity with the REACT website. Furthermore, perceived and actual difficulties in accessing the website negatively affected staff’s confidence to contribute to the delivery of REACT. REACT supporters expressed some concerns about their suitability for the role but generally felt adequately equipped; however, they found it difficult to evaluate their ability to carry out required tasks due to lack of activity on the website. IMPART leads felt that the role was appropriately allocated to them, although some acknowledged that senior management have greater authority to implement new practices:
I think everyone would be able to use it, would have the kind of capability to use it, it would just be getting that initial like getting on it and having I think the logins and things like that were a little bit difficult because everyone’s got so many logins for different things, and people forget their passwords and that makes it a little bit more difficult.
SA-CL-STW-34, 10 January 2018, individual interview
Relational integration
Although most staff appreciated the potential benefits of REACT, some appeared to lose trust in the intervention. Several staff emphasised that relatives prefer face-to-face support and questioned whether or not REACT could meet their needs, particularly in the light of perceived low uptake and limited forum activity. Scepticism concerning digital health technologies and perceived and real barriers to accessing the website also negatively affected staff’s confidence in the intervention:
I think it’s age but also I think it’s the fact that it’s so formal and the fact that you know you have to sign into it, you have to have a password, you have to have a login, do you know it’s you have to you’ve got to commit time to it, it’s not just readily available to you, and all those little barriers would be sufficient for me to say no, I can’t be arsed . . .
SA-CL-SW-CC-52, 23 November 2017, individual interview
Some staff expressed concerns that carers may come to a different understanding of their relative’s illness to that of the team owing to dissonance between diagnostic language used on the REACT website and language used by clinical staff. Nonetheless, several indicated that the online toolkit had a positive impact on their interactions with carers:
Well you’re sort of hit with the bipolar and so like diagnosing people and I think that’s the interesting thing ‘cos we don’t diagnose people with unspecified non-organic psychosis [. . .] so it’s like you know instantly the carers will be looking at it going whoa what’s this you know like we’re already giving a diagnosis and what do I look at, what’s relevant yeah. So I don’t know I suppose having the information given in a format that we actually use, yeah.
GU-CL-TM-02, 21 November 2017
Contextual integration
There was some evidence of integration of REACT into existing practices, such as the incorporation of REACT booklets within Gull’s service welcome packs and promotion of REACT at family and friends’ groups across the three teams. Furthermore, REACT was occasionally mentioned in team meetings, although this was largely dependent on prompting by a few key individuals or researcher presence.
Reflecting staff’s views on role legitimacy, psychology staff members with assigned roles made an effort to embed REACT within their existing structures, such as audits of psychological interventions; however, permeating the rest of the team proved to be more difficult:
I think there is something to be said that throughout the entire time that REACT has been here it’s always been held by psychology, to hold it in mind, so it’s us who will hold it in mind to try and keep it on the agenda and have regular points like this, where we will try to think OK well what’s working, what’s not working, and to try and systematise our processes like embedding it within the carers’ group or within the supervisory structures and so on, etc. It’s just the rest of the system is harder to keep it held in mind because of the staff turnover and other health care professionals as has been noted, but we will definitely always keep it in mind ‘cos it’s an excellent resource to be able to use, but it’s just keeping it going.
SA-IL-CPsy-03, 10 April 2018, group interview
It was clear that contextual difficulties were a major barrier to implementation, including high caseloads, staff turnover and multiple tasks competing for attention. Staff lacked the headspace for REACT and did not view it as a priority, despite recognising its potential value for carers and the service. Although there was a strong narrative that managerial support offers a stronger lever for implementation, it was evident that, even in Gull team where managerial support was strong, it was difficult to prioritise REACT above tasks that were perceived as more pressing:
The manager in my team is very supportive of it, but I think it’s care co-ordinators being overworked by other demands you know. We’ve got someone leaving now and we’re not allowed to have a locum in place of them, they’ve got more caseload, they’ve got to do the CPAs, they’ve got to do the safeguarding, they’ve got to do the. Well those are subjects, that feels more a priority than signing people up . . .
GU-IL-CPsy-02, 15 June 2017, implementation workshop
Reflexive monitoring
Systemisation
Monitoring and reflecting on relatives’ uptake of REACT was an important factor affecting staff’s appraisal of the intervention and their implementation efforts. Some staff used their pending invitations and congratulatory e-mails as an indicator of relatives’ engagement with REACT, and few sought feedback from relatives they invited to the website. There was also some evidence of formal monitoring, such as logging relative invitations on an existing carers’ database in Gull and including REACT in an audit of psychology interventions in Sandpiper. Most were disheartened by the uptake of the intervention and felt demotivated to continue inviting relatives to the website:
. . . I mean I’ve signed up a lot a of people to REACT, well I’ve told a lot of carers about it, entered their e-mails, and then I think out of about probably about six or seven that I’ve done so far they’ve all I think about two have then gone and registered [. . .] that then demotivates you as a staff member ‘cos you kind of think well if they’re not bothering with it you know why am I, I’ve got so many things to think about you know and so that’s I think it’s just one of those things where it’s there’s the issue on both sides, who keeps you motivated and engaged with it?
GU-CL-TM-02, 21 November 2017, individual interview
. . . so what we are doing in [Sandpiper] is that we’re developing a kind of audit, it means we’re kind of auditing the target that care co-ordinators will use at CPAs to have a look at all of the interventions and REACT will be part of that so a lot of them are getting used to just offering and understanding that it’s something we have to do as part of the early intervention plan.
SA-RS-APsy-04, 7 April 2017, group interview
Individual appraisal
Perceived low uptake of REACT negatively affected staff’s appraisals of their implementation efforts as worthwhile and many reported that they found it difficult to comment on the usefulness of the intervention owing to limited feedback from relatives. Some suggested that more detailed usage information would facilitate their ability to evaluate the toolkit. Nevertheless, perceived positive effects of the intervention on staff’s interactions with carers appeared to facilitate positive appraisals:
I think when it first came I think everyone was really excited, but I don’t know if it’s made a difference to how people deal with carers [. . .] it’s a really brilliant tool, so people handing out asking for e-mail addresses and myself and GU-CL-HAP-17 were getting lots of e-mail addresses from parents, but because parents weren’t taking it up, people didn’t notice, people haven’t noticed it, so I think people are less, putting it out there a lot less.
GU-RS-APsy-03, 20 October 2017, individual interview
. . . I think it’s a way of giving them some form of independence and empowerment to go out there, do some research, gain some knowledge, and when they have conversations with me later on, they feel they’re able to have a conversation on a higher level because there’s some understanding now because they have gained some knowledge, so they know the basics now, so they don’t feel I’m asking a silly question . . .
SA-CL-CPN-CC-51, 4 December 2017, individual interview
Communal appraisal
There was some evidence of communal appraisal, such as conversations about uptake and forum activity during team meetings; however, collective discussions using formal data were a rare occurrence and were often prompted by researcher presence:
. . . I remember SA-RS-APsy-04 fed back and saying that people weren’t really using it and just kind of hearing about you know from people about how many people have been using it [. . .] It was mentioned in the team meeting, she discussed it and then we talked about it when the mugs and things like that were given out, so we knew that obviously it had been quite difficult to encourage people to sign up but we wanted to bring it to people’s attention.
SA-CL-STW-34, 10 January 2018, individual interview
Reconfiguration
There was limited evidence of reconfiguration, other than an apparent decline in staff’s willingness to invite carers to REACT owing to perceived lack of engagement with the intervention. In addition, Gull staff reported that they included REACT booklets in their welcome packs because of feedback from carers that it would have been helpful to receive the toolkit at an earlier point in their contact with services:
There have been maybe a few people that I’ve spoken to on the phone that have said it’s really helpful. But also kind of mixed so kind of yeah it’s really helpful but this would have been better at the beginning [. . .] which has been good because it’s kind of made us think OK let’s put these in all our welcome packs and that’s kind of like something we’ve learnt from people’s opinion on it.
GU-CL-HAP-17, 19 July 2017, individual interview
Researcher’s reflexive summary
Staff in Seashore Trust showed a good understanding of the purpose of REACT and were generally able to construct the value of the intervention for their work. However, such understanding and appreciation of the potential benefits of the toolkit were not necessarily sufficient to motivate staff to play an active role in implementing the intervention. The extent to which staff engaged with the new practice was largely a result of contextual factors, including workload, staff turnover and degree of managerial support, as well as human factors such as computer literacy. Although staff with assigned roles were highly motivated and facilitated integration of REACT within existing structures, most faced resistance in building a collective commitment to the intervention in their respective teams. In addition, staff were quickly demotivated by perceived poor uptake of the intervention; hence, it seems important for staff to see value in their implementation efforts and to manage expectations in order to maintain engagement.
Feedback from final trust analysis days
Staff agreed that the log-in process is a barrier for both staff and relative engagement with REACT, but would want to keep the log-in process so that staff could monitor relatives’ use of the website. Staff suggested that there is annoyance and frustration among staff about being asked to do anything new and that our findings could be about any new initiative, not just REACT. Staff were not sure why some are more aware of NICE guidelines and AWT targets than others. The IMPART lead said that on the EI drop-down portal (linked to Rio) there is a tick box for offering carer education and support; some staff members did not appear to be aware of this. Staff suggested that there is an increasing drive in the trust towards collecting data and staff are aware that they are being monitored for audits and targets.
Appendix 15 Woods Trust case summary
Participants
| Participant identifier | NHS role | REACT role | Number of relative invitations sent | Research activities participated in |
|---|---|---|---|---|
| WA-RS-AP-03 | Assistant practitioner | REACT supporter | 2 | Individual interview |
| WA-CL-OT-CC-72 | Occupational therapist, care co-ordinator | Clinician | 0 | Individual interview |
| WA-CL-SW-CC-89 | Locum social worker, care co-ordinator | Clinician | 0 | Individual interview |
| WA-CL-OT-CC-12 | Occupational therapist, care co-ordinator | Clinician | 0 | Individual interview |
| WA-CL-TM-06 | Team manager | Clinician | 0 | Individual interview |
| TH-CL-MHN-CC-27 | Mental health nurse, care co-ordinator | Clinician | 0 | Individual interview |
| TH-CL-AP-87 | Assistant practitioner | Clinician | 5 | Individual interview |
| TH-IL-MHN-CC-04 | Mental health nurse, care co-ordinator | IMPART lead | 4 | SRG, individual interview |
| TH-CL-TM-05 | Team manager (job share) | Clinician | 0 | SRGs |
| WO-CL-PsyR-02 | Psychology lead for the recovery and rehabilitation division | Clinician | 0 | Individual interview |
| TH-CL-TM-01 | Team manager (job share), interim service manager | Clinician | 0 | Individual interview |
| TH-IL-SW-CC-02 | Social worker, AMPH | IMPART lead | 0 | SRG, individual interview |
| WA-IL-SW-CC-03 | Social worker, AMPH, care co-ordinator | IMPART lead | 0 | SRGs, individual interview |
| TH-RS-CW-01 | Assistant practitioner, carer worker | REACT supporter | 12 | SRGs, individual interview |
| WA-IL-CP-01 | Consultant psychiatrist | IMPART lead | 5 | Individual interview, SRG |
Context
Woods Trust serves an urban population of around half a million people, of whom almost half identify as white British. The trust employs approximately 2000 staff, and around 500 service users access care from EI services delivered by 36 staff. Fewer than half of service users have an identified relative and, according to the 2016 national CCQI audit,102 approximately 48% of service users and their families were offered family interventions and 50% of carers were offered education and support.
Woods Trust consists of two EI teams, Thrush and Warbler, which accept referrals for individuals aged 18–65 years, and both teams have a caseload of 256 service users in total. This trust experienced high staff turnover and long-term sickness, particularly in Warbler, where half of the team left within the first 6 months of the case study. Warbler had two IMPART leads and one REACT supporter, and Thrush had one IMPART lead and one REACT supporter; however, there were some role changes due to periods of sick leave and perceived incompatibility with workload.
In terms of existing provisions for carers, both services have an assistant practitioner who leads on carer support and provides in-house carers’ assessments and a fortnightly family and friends’ group across both teams. The teams also offer BFT and paper-based information, and staff are able to refer relatives to a trust-wide carers’ group, a local service for carers and a recovery college.
This trust received IPv1.
Key findings against normalisation process theory components
Coherence
Differentiation
Most staff described REACT as an online resource for carers and differentiated the toolkit from carers’ assessments, BFT and a family and friends’ group. The majority of staff recalled learning about the toolkit from researchers and it was clear that REACT was viewed as a research project as opposed to an integrated part of the EI service:
I think at the moment it probably still feels that it’s research, that it’s still fairly new and that we’re still getting to grips with it I guess, I don’t – personally yeah I don’t see it yet as being part of the whole package . . .
WA-CL-TM-06, 24 October 2018, individual interview
Individual specification
REACT supporters, IMPART leads and team managers were generally clear on their individual tasks in relation to the toolkit, which appeared to be aided by researcher-led training and other meetings and practical support from researchers. Most care co-ordinators were only vaguely aware of their role in promoting REACT to relatives and had a limited understanding of how to use the website. However, those who had independently explored the website tended to have a more detailed understanding of the toolkit and how to perform required tasks:
I think it was hard to get a viewpoint ‘cos I couldn’t really picture what it was too well and I understood it was a relatives’ toolkit but because I wasn’t able to see the website and wasn’t able to actually see the toolkit, I don’t think I really got it until the point where I was able to kind of click and look into it and see what was actually there [. . .] I think that’s the first time I was like ‘oh this is actually really cool’, whereas before I was kind of like ‘I don’t really know what it is’.
TH-RS-CW-01, 8 May 2017, individual interview
Communal specification
Managers tended to have good understanding of REACT supporter, IMPART lead and care co-ordinator roles, but awareness at different levels was variable. For the most part, care co-ordinators were not fully aware of who occupied REACT supporter and IMPART lead roles and what those roles entailed. Forums for discussing tasks and roles appeared to be limited to REACT supporter supervision and researcher-facilitated meetings:
The first thing is to make sure that we’re getting a vote of confidence to know what it is, at the moment I think it’s been kept within this meeting really, there’s probably a few people on each team who know about it, but I think it needs general a bit more education for the team as a whole about it.
TH-CL-TM-05, 15 December 2016, SRG
I’m not sure if TH-IL-MHN-CC-04 does anything for this study or if it’s the other study, it might be the totally wrong study [. . .] I know there was some people meant to be leading, be a reference point for it, but I’m not really sure, might be the wrong study.
TH-CL-AP-87, 14 March 2017, individual interview
Internalisation
Staff appreciated potential benefits of REACT for carers, such as greater accessibility to reliable information and empowering carers to do their own research. Some also identified potential benefits for themselves in their professional roles, such as offering a standardised approach for all care co-ordinators and providing a useful go-to source of information for promoting a shared understanding between clinicians and carers:
It’s much easier to access and much more available than for example a group [. . .] [groups] can be very responsive and warm and everything but they’re also yeah you have to get here for 6 o’clock on alternate Tuesdays, versus just go to the website, so it’s much more kind of accessible and people can read stuff in their own speed.
TH-IL-MHN-CC-04, 8 May 2017, individual interview
I think one potential benefit is you can very easily offer I suppose everyone with an internet connection really the same information and kind of yeah level of information consistently across the board which is quite useful, ‘cos with sort of any approach it varies from care co-ordinator to care co-ordinator to relationship with the person, so I think having that is quite useful, like a standardised approach, yeah I think that can be useful. And hopefully if it’s used then you can get used to working with a family that have a certain knowledge base which I think would be good.
TH-CL-AP-87, 14 March 2017
Nevertheless, staff often balanced potential benefits with perceived shortcomings of REACT, including the non-user-friendly design of the staff interface, overemphasis on diagnosis and lack of face-to-face engagement. Many emphasised that REACT should be an additional resource rather than a substitute for face-to-face professional or peer support. Those who had not seen the website found it difficult to form an opinion and many felt that they needed relatives’ feedback to construct the value of the intervention. Some were sceptical about the value of digital interventions and online forums in general and, therefore, sceptical of REACT:
. . . I guess ambivalent in a sense, because as I said before it’s good to have something which can be accessible at any time during the – you know because they, obviously, it can be difficult to kind of get out and meet other people. I’m, you know, a little bit sceptical of online forums in terms of actually properly kind of feeling you’re engaging with other people. You know and I think that’s something that I’m, you know I’m a little bit kind of unsure about.
TH-IL-SW-CC-02, 16 November 2016, individual interview
Cognitive participation
Initiation
The primary WA-IL-CP-01 played a key role in introducing REACT to the trust and was perceived by staff as the main driver of the intervention. WA-IL-CP-01 facilitated management buy-in to the intervention by discussing REACT regularly at senior managers’ meetings; however, WA-IL-CP-01’s ability to drive REACT forward was limited by a lack of physical presence in the teams and a strong association with research. REACT was also strongly associated with the IMPART research assistant, who drove the intervention forward through presentations and regular contact with key individuals. Consequently, this encouraged a shared perception of REACT as an external research project rather than EIS core business:
. . . mainly my role has been just saying please could you make use of it. But possibly that’s been a little bit counterproductive because I’m the person who says you know can you possibly recruit somebody for this research study or whatever, I’m very much identified with research in the team, so in retrospect I probably would have tried hard not to have any kind of to sort of steer clear of its implementation in the team really . . .
WA-IL-CP-01, 26 July 2017, individual interview
. . . I only associate it when yourself or others come in and talk about this research study, and I forget that it’s a tool that you know I could use it.
WA-CL-OT-CC-72, 6 June 2017, individual interview
Team managers seemed keen to be involved, although they were hesitant in allocating IMPART roles owing to concerns about burdening staff who were already stretched. Once allocated, the IMPART leads and REACT supporters’ willingness to drive the intervention forward was variable, with some showing enthusiasm and others expressing ambivalence about the project. Perceived fit with existing role and workload and individuals’ IT confidence appeared to be important factors affecting their willingness to drive REACT forward:
I mean like TH-IL-MHN-CC-04 is on it isn’t he, he gets how to do it online, he’ll definitely push it, knows how to make it straightforward. I think the major is, I mean I imagine at whatever time there’s always going to be people who say I’m too busy to do it . . .
WA-IL-SW-CC-03, 3 January 2017
Enrolment
The process of defining and allocating key roles was challenging, given that managers were concerned about burdening staff with additional tasks. Although managers were keen for the delivery of REACT to be a shared responsibility to minimise additional workload, there was little evidence of attempts to secure wider staff buy-in. Nevertheless, a key facilitator of enrolment was senior management support for the allocation of the REACT supporter role as a mandatory part of carer workers’ role and it was felt that their supervisors would be best placed as IMPART leads:
Yeah, so TH-RS-CW-01, basically she’s a new member of staff and certain roles were identified for her, so she didn’t volunteer, she was basically assigned, you’re going to do this. And when I heard that I was going to be supervising her, and I heard that she’d took on this work and that there was a need for an IMPART lead I at the time thought, well actually if I’m supervising maybe that makes sense that I take that on. Not actually realising that – yeah I mean it’s not so much work, but it is kind of – the issue with it was actually it, I just really couldn’t get myself to think about it because I had so much other stuff to think about.
TH-IL-SW-CC-02, 16 November 2016, individual interview
Stakeholder reference group meetings and other meetings with researchers appeared to be important for building staff buy-in by offering opportunities to discuss tasks and roles, and practical training sessions increased staff’s confidence in using the website. Despite this, many reported that they lacked headspace for anything new, and high staff turnover, particularly in Warbler, presented an additional challenge to maintaining a communal understanding of individual responsibilities for delivering REACT:
Initially, well I mean to be honest I was a little bit reluctant ‘cos I felt that it would be something complex I have to learn about, do you know like I needed to know how to sell idea, I thought we would have like a solid target to meet and that side of things. So that was me being a little bit anxious, how do I accommodate this in my like daily schedule?
WA-RS-AP-03, 6 June 2017, individual interview
. . . I think just having a headspace for anything new that takes work and you’re not doing on autopilot is quite hard.
TH-CL-TM-01, 19 December 2016, individual interview
Legitimation
Staff were clear that REACT fits with the EI model of supporting carers and senior staff understood that the toolkit could meet a perceived need and help the trust to achieve the audit target for carer education and support. Nevertheless, staff placed greater weight on targets concerning service users and targets that are financially incentivised, whereas REACT tended to be viewed as a good-practice, optional extra:
It’s easier when it actually meets a target because we’re so short of staff for the targets that anything that’s not directly linked to the targets gets really second priority now [. . .] And so this one [REACT] is the easiest one of any innovation recently because it so clearly meets a gap that we’ve got.
WO-CL-PsyR-02, 20 December 2016, individual interview
. . . generally things that have money attached to them that will keep, you know from my point of view they’re not necessarily the things that I would clinically say are the most important, but they’ve got money attached to them [. . .] And so we’re slightly at the mercy of those, so they are the, sadly they are often the priorities.
TH-CL-TM-01, 19 December 2016, individual interview
There was a sense that research is valued in the team, although many felt that research activities could not be prioritised during challenging times. Therefore, the common perception of REACT as a research project was a significant barrier to legitimation. There was a strong narrative that contextual factors, including high caseloads, staff turnover and increasing audit requirements, were a barrier to performing any tasks that were not mandatory or were perceived as non-priority:
. . . I think [the managers’] view probably would have been that we just shouldn’t do any research while things have been as difficult as they have in the past couple of years [. . .] trust leadership are very keen on research, although I don’t think that they adequately communicate that enthusiasm to people on the ground [. . .] I think had you given people like TH-CL-TM-01 and TH-CL-TM-05 the choice they would probably have said well we [. . .] support research as an important thing but we don’t really feel able to participate at the moment.
WA-IL-CP-01, 26 July 2017, individual interview
I think there’s an awful lot of new stuff happening right now, which makes it quite difficult for people to know what they should be focusing on [. . .] you know one week we’re saying this is the absolute priority, and then the next week we’re saying, actually that’s no longer absolute priority, you know. I think that given how high caseloads are and how stretched people are, and how low, you know morale is low in one of the teams because of staffing changes.
TH-CL-TM-01, 19 December 2016, individual interview
Activation
There was some evidence of willingness to sustain the delivery of REACT, such as the inclusion of REACT as a standing agenda item in REACT supporters’ supervision and integration of REACT in the 8-week assessment checklist. However, staff reported that REACT rarely came up in team meetings or clinical discussions, and there was a sense that staff held researchers responsible for keeping the new practice going. Staff suggested a number of ways to embed REACT within existing structures during researcher-led meetings and interviews, yet there was little evidence of a collective effort to improve delivery in practice:
[From researchers] I think it’s only the way in which we hear about it, so I think maybe if it was like a top-down approach from you know the managers instilling in us you know that this is stuff we can be using, if we need help come to them, they should be on top of it . . .
WA-CL-OT-CC-72, 6 June 2017, individual interview
Collective action
Interactional workability
REACT supporters appeared to integrate REACT into their daily routines, such as offering the toolkit as part of carers’ assessments and family and friends’ groups, and occasionally encouraging care co-ordinators to promote REACT to relatives. However, the delivery of REACT was primarily dependent on the activity of these few key individuals, with limited evidence of a shared commitment to implementing the intervention:
[REACT supporters] do offer it to relatives they see. And to people in the relatives’ group and then sign people up [. . .] I think other people very intermittently offer it to relatives as well with encouragement from the REACT supporters and from me, but I think that’s very spasmodic [. . .] My impression is not that it’s very widely put forward otherwise by staff [. . .] I think the managers feel that the carers’ support workers are providing encouragement for it to be used, which I think they are, but it’s not been owned as a sort of whole-team responsibility . . .
WA-IL-CP-01, 26 July 2017, individual interview
Care co-ordinators indicated that REACT did not fit easily into their routine work practices and identified a number of barriers, including multiple tasks demanding time and attention, limited face-to-face contact with relatives and perceived and actual difficulties in using the website:
. . . people just forget it, you have a lot of things on your mind, when you’re doing an assessment, when you’re meeting a family member, you have a thousand and one things on your mind that you’d like to assess and write down and stuff and it’s difficult to remember the spiel of oh by the way we have this website full of lots of information and yeah just getting everyone to remember to do that is quite difficult actually.
TH-IL-MHN-CC-04, 8 May 2017, individual interview
. . . you load up the dashboard, you first get this screen which is kind of sort of meaningless, and it’s hard, there’s all the things you need to do on the left but it’s hard to know what does what, it’s kind of trial and error . . .
TH-IL-MHN-CC-04, 15 December 2016, SRG
Skill-set workability
Most staff reported feeling sufficiently confident in their IT skills to use the website and some were already using iPads in their work; however, managers suggested that staff lacked the capacity or inclination to learn new systems in the context of high workload and other changes to their usual ways of working:
. . . even people in the team who you know probably are reasonably technologically savvy outside work, don’t necessarily have the capacity or time or inclination I suppose to look into all the different ways of doing things in a new way, because things are constantly being done and changed.
TH-CL-TM-05, 12 June 2017, individual interview
Delivering REACT was perceived to be a good fit with the carer workers’ role due to frequent contact with carers and alignment with their existing priorities, although they expressed uncertainty about their ability to moderate a forum. IMPART lead roles were seemingly taken on with an expectation that required tasks would be minimal, and the allocation of these roles was later seen as a poor choice by managers because of incompatibility with their high workload:
It fits in quite well ‘cos I work with carers so it’s one of the resources I give for support most of the time, and so I guess my role is probably the one that REACT fits into the best, ‘cos I work with carers all the time.
TH-RS-CW-01, 8 May 2017, individual interview
Relational integration
Although staff generally reported that digital interventions have a place in EIS work, many appeared to lack confidence in the ability of REACT to meet carers’ needs and expressed doubt about whether or not relatives would use the website appropriately. Staff were clear that face-to-face support is superior to online support and some raised concerns that relationships between carers and clinicians could be challenged if carers came to a different understanding of service users’ problems to that held by the team through using the website:
. . . there’s this feeling I think both among the managers and the staff, they don’t quite seem to see a digital intervention as something that’s sort of real and high quality, I think they kind of feel that they’re offering relatives something that’s a little bit sort of weird and tricksy and not quite the real stuff that they as mental health professionals are supposed to be offering and I think that’s quite sort of wide spread, almost just like embarrassment in offering this.
WA-IL-CP-01, 26 July 2017, individual interview
. . . if something’s told to them from a professional or a doctor and is slightly different to what’s on [REACT] [. . .] they might I suppose want to challenge or undermine, I’m not sure it’s a massive risk but you can explain your reasons why, it’s just the situation that happens, I’m not sure it’s massively risky but yeah it could cause a bit of disgruntlement I suppose.
TH-CL-AP-87, 14 March 2017, individual interview
Perceived and actual technical difficulties seemed to lead to a loss of trust in the REACT website, and perceived low uptake and lack of forum activity negatively affected staff’s trust in carers to effectively make use of the intervention:
I also think the sort of sign-up interface for staff is quite clanky and hard to find your way into [. . .] not that I’ve logged onto it regularly but it’s always a bit sort of irritating really.
WA-IL-CP-01, 26 July 2017, individual interview
Contextual integration
Integration of REACT into existing work practices was largely dependent on the work of the REACT supporters, such as through family and friends’ groups and carers’ assessments. Staff reported that REACT occasionally came up organically in clinical discussions and team managers sometimes prompted staff in team meetings, although collective discussions were most often initiated by researcher presence. Perceptions of REACT as a research activity and a sense of lack of ownership over the project seemed to limit efforts to integrate REACT into existing service structures:
People do mention it you know, I’ve heard it kind of organically in conversations in the office, we were talking about a client’s carer or relative or something, about their needs, and someone said send them to REACT [. . .] there’s an increasing awareness of it.
TH-IL-MHN-CC-04, 8 May 2017, individual interview
. . . I think at least for me it does feel more like a research that carers can benefit from [. . .] rather than something that we should be implementing as part of EIS [. . .] I mean I imagine if it was part of policy, people would just remember it more, it just feels more important and something that needs to be done, instead of one of these extra things that need to be remembered, yeah.
TH-RS-CW-01, 8 May 2017, individual interview
There was a strong narrative from all staff that the recent period had been a particularly challenging time for the teams and that contextual difficulties were a major barrier to implementing REACT, with high staff turnover, high caseloads and low morale and team cohesion leaving little headspace for anything new. Despite appreciating the potential value of REACT, staff did not feel able to deliver this additional resource within the current climate:
So like the average caseload now in [Warbler] is around 30, and in [Thrush] around 26 I think [. . .] which obviously, compared to the ideal for an EI team of 15 is double [. . .] So what’s that meant is that the care co-ordinators now don’t have any time to do the EI model that they used to do when they had a lower caseload [. . .] So we’ve actually not been able to get anywhere near the staffing that we calculate that we need to meet the second part of the standard, which is the thing about the interventions.
WO-CL-PsyR-02, 20 December 2016, individual interview
There was also some suggestion that the trust was not equipped technologically to host a digital intervention because IT systems were perceived as unreliable and most staff were unable to access the internet on their work phones. Although the teams had access to iPads through another study, a large proportion of staff rarely used iPads in their work, which seemed to reflect a lack of confidence and training:
I think also all the IT systems at work are pretty awful really, we’ve got terribly slow internet and frequent problems logging in to the most basic things, and I think there’s something about the sort of rubbish nature of the IT systems and you’ve seen the phones the staff get given that don’t really do the internet, and I think there’s something about all that that sort of I think it just creates a mindset where you know people may be sort of inhabitants of the digital world outside work but somehow at work it doesn’t really seem like we are in that age . . .
WA-IL-CP-01, 26 July 2017, individual interview
Reflexive monitoring
Systemisation
There was some evidence of efforts to monitor relatives’ use of the website, although staff seemed to view the evaluation of REACT as the research team’s responsibility. The SRG offered a forum for staff to hear about carers’ experiences of using the toolkit; however, most had not sought feedback in their own interactions with relatives. Some accessed information on the dashboard, including pending invitations and active users, as an indicator of relatives’ uptake of the intervention and tended to find this disheartening. Limited access to information about the effects of REACT and their implementation efforts seemed to leave staff feeling unsure about where they might be going wrong and at a loss for what more they could do:
I think it’s just not seeing any kind of outcomes coming from registering people and it looks like there’s no activity on the site, I guess I mean people might be logging on, the few that have actually registered, but I guess there’s no way of monitoring it, no way of knowing that people are actually finding it helpful or useful.
TH-RS-CW-01, 8 May 2017, individual interview
Individual appraisal
Staff generally maintained their belief that the toolkit was a good resource, although they found it difficult to assess whether or not the intervention was useful without feedback from carers. Staff reported feeling demotivated by the low uptake of REACT by relatives and lack of forum activity, and this seemed to leave staff questioning whether or not their efforts to promote the toolkit were worthwhile:
I think it just feels a bit kind of stagnant and a bit just like it just feels like you’re kind of registering people but there’s no outcome and you’re just not getting any, it’s kind of you’re just registering but it just goes into a void and you’re not getting any feedback from it. And I guess it probably reduces the motivation to do it, and it kind of puts REACT in terms of like putting it in the front of your memory and remembering it every time you see a carer, you probably don’t do it as often because it’s not really producing much from you registering yeah. It’s tough.
TH-RS-CW-01, 8 May 2017, individual interview
Communal appraisal
There was little evidence of formal monitoring or collective efforts to appraise the intervention beyond the occasional mention in team meetings and some discussions between IMPART leads and REACT supporters:
Just in sort of the team meetings when we’ve talked about individuals and we’ve talked about carers’ needs and we’ve talked about people that might need referring for you know carers’ support, that’s been one of the things that’s been fed back and they’ve used it. So it hasn’t been formalised, I don’t know whether you do have formal feedback form that you want us to use now or in the future, so I wouldn’t be able to tell you that.
WA-CL-TM-06, 24 April 2017, individual interview
Reconfiguration
There was very little evidence of reconfiguration, other than some indication that staff modified their efforts to promote the intervention in response to perceived low uptake by relatives.
Researcher’s reflexive summary
Staff in Woods Trust demonstrated a reasonable understanding of REACT and most were able to appreciate the potential value of the intervention. Despite this, high staff turnover was an obstacle to maintaining widespread awareness of the toolkit and a communal understanding of individual responsibilities in the delivery effort. Although the REACT supporters integrated the toolkit into their routine work practices, the delivery of REACT was predominantly a solo activity rather than a collective effort. Contextual difficulties, including staff turnover and high workload, appeared to be an important factor limiting staff’s willingness to play an active role in implementing the intervention and there was a sense that staff would have struggled to implement anything new during this challenging time. However, the implementation effort seemed to be further hindered by the common perception of REACT as a low-priority research activity, which limited staff buy-in and ownership over the intervention.
Feedback from final trust analysis days
Several staff members had an awareness of REACT but only one staff member in attendance reported using REACT once and that it happened a long time ago. The team lead explained that staff originally involved with REACT had now left the EIS team. The present staff did not know how to use REACT and stated that more training is needed if they were to offer it again. There was some tension regarding who’s responsibility it was to sustain and collect feedback from relatives about REACT. Staff felt that these tasks were the researcher’s responsibility, highlighting that REACT was still perceived as a research project as opposed to part of the service. The team lead stressed the distinction that REACT is currently a research project and that other mandatory and legal requirements, such as carer’s assessments, have to be prioritised. Staff agreed that usability of REACT was an issue, with the log-on process making accessibility difficult. Staff agreed that there was a need for REACT, but being hosted via a digital platform created issues for their EIS population, with many not having access to devices or the internet. Overall, few members of staff were vocal in providing feedback, which was probably influenced by staff’s general lack of knowledge about the IMPART study and REACT and their consequent inability to comment on what had happened to REACT in their trust.
Appendix 16 Common barriers to and promoters of implementation of REACT
Figures 21 and 22 summarise the common barriers to implementation of REACT and the ways that implementation can be enhanced, based on the data explored in Chapter 6.
FIGURE 21.
The main factors affecting the implementation of REACT. CQC, Care Quality Commission.
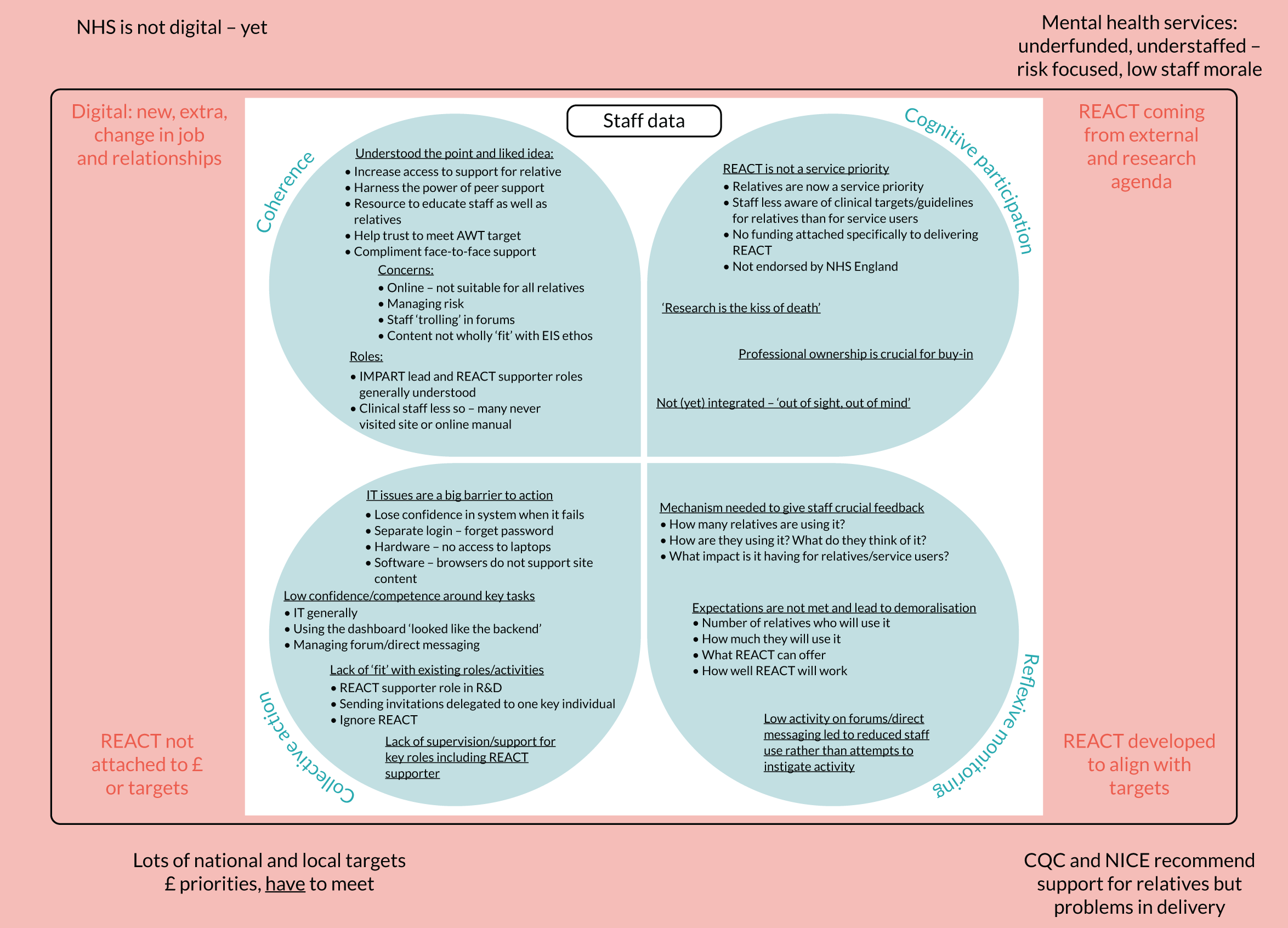
FIGURE 22.
Ways to enhance the implementation of REACT. CQC, Care Quality Commission; DM, direct messaging.
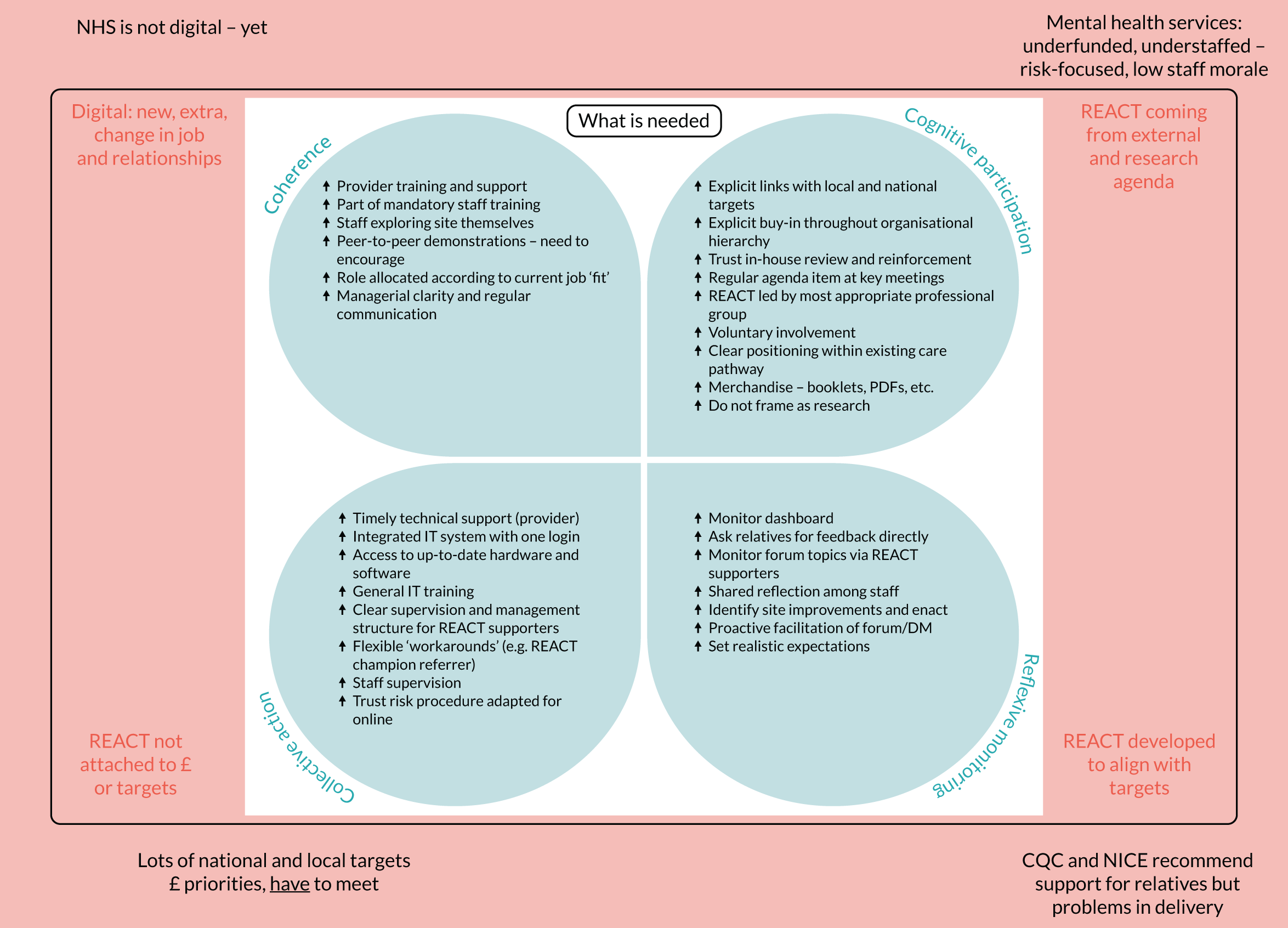
Glossary
- Bipolar disorder
- A mood disorder characterised by periods of low mood (depression) and periods of elevated mood (hypomania or mania).
- Digital health intervention
- An intervention delivered via digital technologies, such as smartphones, websites and text messaging.
- Early intervention in psychosis team
- Part of public sector clinical services in England that provide early intervention support to people with early signs of psychosis and/or other severe mental health problems (including bipolar disorder) in a particular geographical locality in England.
- eHealth
- An alternative term for a digital health intervention.
- EuroQol-5 Dimensions, five-level version
- A measure of health-related quality of life developed by the EuroQol Group. The latest version assesses five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Ratings can be given for each across five levels of severity.
- NHS trust
- A health-care delivery organisation that covers a defined geographical area of England.
- Non-adoption, abandonment, scale-up, spread and sustainability framework
- Developed to help predict and evaluate the success of a technology-supported health or social care programme.
- Normalisation process theory
- This theory was developed to describe the process by which a new health-care intervention becomes (or does not become) part of normal everyday practice.
- Psychosis
- A state in which people perceive or interpret the world around them very differently than do others. Psychosis most frequently manifests as having beliefs that are not shared by others and do not have a basis that is understandable to others (often called delusions); not being able to think clearly and so sounding muddled and hard to follow (often called thought disorder); and experiencing, for example hearing or seeing, things that other people cannot (often called hallucinations).
- Relatives’ Education And Coping Toolkit
- An online supported self-management toolkit for relatives or friends of people with psychosis or bipolar disorder.
- Technology-enabled service
- Health service in which technology plays a role alongside many other face-to-face components.
List of abbreviations
- ACTS
- accelerated creation to sustainment
- AWT
- access and waiting time
- BFT
- behavioural family therapy
- CCQI
- College Centre for Quality Improvement
- CI
- confidence interval
- CPN
- community psychiatric nurse
- CTRC
- Clinical Trials Research Centre
- CWS
- Carer Well-being and Support Scale
- DHI
- digital health intervention
- eHEALS
- eHealth Literacy Scale
- EI
- early intervention
- EIP
- early intervention for psychosis
- EIS
- Early Intervention Service
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- GHQ-28
- General Health Questionnaire-28
- GP
- general practitioner
- IMPART
- IMPlementation of A Relatives’ Toolkit
- IPv
- implementation plan version
- IQR
- interquartile range
- IT
- information technology
- NASSS
- non-adoption, abandonment, scale-up, spread and sustainability
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NPT
- normalisation process theory
- Portable Document Format
- PI
- principal investigator
- PIS
- participant information sheet
- PMG
- Project Management Group
- PPI
- patient and public involvement
- R&D
- research and development
- RCT
- randomised controlled trial
- REACT
- Relatives’ Education And Coping Toolkit
- RS
- REACT supporter
- SD
- standard deviation
- SRG
- stakeholder reference group
- SSG
- Study Steering Group
- StaRI
- Standards for Reporting Implementation Studies
- TAU
- treatment as usual
- TES
- technology-enabled service
- UCL
- University College London
- URL
- Uniform Resource Locator
- VAS
- visual analogue scale
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/hsdr08370).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.