Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 14/04/40. The contractual start date was in January 2016. The final report began editorial review in August 2019 and was accepted for publication in March 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Diane Sellers reports grants and personal fees from Nutricia Advanced Medical Nutrition (Trowbridge, UK) and personal fees from Nutricia Global (Danone, Hoofddorp, the Netherlands) outside the submitted work.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Craig et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Context
Evidence reviews recommend that health and social care professionals attend to non-clinical factors and ensure that there is consistent and structured support for children with neurodisability and their caregivers in care pathways when a gastrostomy feeding tube (GFT) is recommended, ensuring that decision-making is informed. 1,2 The provision of psychosocial support (PSS) is an under-researched area and this study aimed to explore how these recommendations have been implemented in practice to identify exemplar models. In short, the study aimed to identify what PSS exists for parents of children with neurodisability with complex feeding needs and for children, how PSS is accomplished in different service models and local configurations of health and social care. It also aimed to identify any gaps in provision, with a view to delivering minimum standards of PSS and making recommendations for change.
Neurodevelopmental conditions, such as cerebral palsy, are the most common cause of disability, estimated to affect 3–4% of children in the UK. 3 This population of children are also the most frequent users of health services. 4 Research suggests that parents of disabled children (70% of mothers and 40% of fathers of severely disabled children) are vulnerable to stress as a result of the demands of care, which can, in turn, negatively affect children’s well-being and family functioning. 5 Indeed, there is research to suggest that chronic stress, associated with caring for children with multiple and complex needs, can negatively affect caregivers’ quality of sleep, physical health and immune function. 6,7
Children with cerebral palsy are at particular risk of oromotor problems affecting their ability to obtain an adequate nutritional intake by mouth, including difficulties chewing, swallowing and feeding, with implications for their nutrition, growth and overall health. 8 Dysphagia, although often under-recognised in this population of children, is common,9 with a reported prevalence ranging from about one-fifth of children with cerebral palsy of any degree10 to 99% in children with severe cerebral palsy and intellectual disability. 11 Pulmonary aspiration is also common (where food or fluid enters the airway), resulting in poor respiratory health, and is considered a significant cause of premature death in this group of children. 12 Caregivers report that mealtimes are prolonged and stressful. 13,14 A GFT, surgically placed in the child’s stomach, is usually recommended where a child’s swallow is considered unsafe and/or growth is compromised, and commercially prepared feeds obtained on prescription are administered through the GFT. Following gastrostomy, insertion stress may also increase in the short term for some families as a result of complications of the procedure, aftercare, the need to learn new nursing techniques and the grief associated with coming to terms with a medicalised way of feeding and other psychosocial sequelae. 15–18
Moreover, the recommendation of gastrostomy can generate parental opposition to the procedure,19 creating conflicts about the feeding management of children and the decision to have a GFT. A systematic review of 11 qualitative research studies conducted in the UK, Canada and Australia1 highlighted the decisional conflicts that parents experience when considering a GFT and the role of services in shaping parental experiences of care and ameliorating stress. Eight out of the 11 studies reported that health-care professionals (HCPs) did not provide enough support to families. Four studies reported that families felt pressured to accept a GFT and six studies reported that professionals failed to appreciate the difficulty of the decision-making process for parents and the impact of GFT feeding on child and family life. Lack of information, conflicting information and lack of opportunity to meet with other families, in addition to concerns about the operative procedure, were also reported.
Conflicts may also arise in schools and other institutional settings between parents and surrogate feeders. Parents may support oral feeding while surrogate feeders have concerns about the safety of feeding children orally owing to the risk of aspiration. 20 It is unclear how disagreements about children’s feeding and growth are managed by professionals, and the attitudes of professionals towards the use of safeguarding legislation where conflicts arise are unexplored. This is compounded by the lack of strong evidence on the effectiveness of a GFT,21 although the intervention is associated with improvements in children’s health, weight gain and maternal mental health. 22,23 We aimed to explore professionals’ experiences of managing conflict.
There is a growing parent-led movement in the use of blended diets (BDs) (i.e. blended food prepared at home and inserted into the GFT). It is estimated that 500 children start BDs each year;24 the continuing number is unknown. However, not all professionals support the practice because of concerns about the risk of gastrointestinal infection, undernutrition and GFT blockages (because many GFTS are not designed for BDs), although there is little robust evidence to support these concerns. 25 The British Dietetic Association (BDA) has developed a policy statement about the use of BDs to create a permissive culture of open discussion between parents and dietitians and offers recommendations in the absence of national guidance;26 where dietitians believe it is in the interests of the child, they can suggest a BD, providing that this is in keeping with their employer’s policy. This raises another potential area for conflict around children’s feeding management, and we aim to examine local practice in relation to BDs in our case study, although this will be discussed in depth in future publications.
This research builds on the doctoral study27 and subsequent work of the chief investigator, who was involved in conducting a prospective controlled trial on the benefits23 and costs28 of GFT interventions and an interview study on parental support needs. 29 This work suggested that clinicians prioritised children’s growth and nutrition and less attention was afforded to parental, particularly mothers’, anxieties about GFT feeding in everyday contexts. Mothers’ narratives were often underpinned by a sense of blame for having failed to establish, or maintain, oral feeding and, hence, children’s growth. The recommendation of a GFT challenged culturally available narratives on ‘good mothering’ and normative child development mediated through oral feeding and mealtimes invoked as sites of intimacy, pleasure, child participation, socialisation and inclusion. 30,31 The emotional side of the decision-making process was often neglected in clinical decision-making despite being a clearly emotive issue for both parents and clinicians. It is through this, and other bodies of work that have also investigated the social meanings that parents attach to GFT interventions, that a range of PSS needs have emerged. 14,18,32–34
In this study we aim to focus on how services provide PSS. As we progressed through the study, this term evolved to place greater emphasis on the emotional aspects; hence, the term psychosocial and emotional support (PSE) is a recommendation. We drew on a broad definition of PSS that includes the practical issues of having to learn new feeding regimes and nursing procedures in caring for a child with a GFT (which also have psychosocial effects, as our study illustrates), including replacing GFTs and what are, arguably, additional stressors when things go wrong [e.g. infection of the gastrostomy site (stoma), GFTs getting blocked], in addition to the actual decision-making process. In this study we aimed to use the term PSS as a means of emphasising the non-clinical aspects of decision-making and support. However, this was often difficult for professionals to disentangle and, therefore, presented a tension throughout the study because professionals understood support, including PSS, through the lens of their professional background, risk and clinical practice. This is discussed further in Chapter 6 and in relation to the analytical construct of ‘hidden work’, a finding of the research.
Aims and objectives
The overall aim of the study was to explore how different neurodisability services meet the PSS needs of children/young people with complex feeding needs and their families when making a decision to have a GFT and issues that arise following surgery.
We aimed to (1) identify different service support models nationally, (2) compare the implementation and operation of support and key resource differences and (3) provide an estimate of their costs.
Research objectives
-
Establish a national (UK) picture of models and practice via an online survey.
-
Compare the implementation and operation of four contrasting service models and practice using a collective case study research methodology.
-
Analyse how support is accomplished in different organisational structures, including health and social care sectors, and the role of schools in supporting children and families.
-
Provide rich description of contrasting supportive practices and the interface between services and other key agencies.
-
Identify different features of service configurations and supportive practices and analyse their costs, specifically to (1) assess the resources required for each of the models considered and how these costs impinge on health and social care services and (2) estimate the costs of providing psychosocial care.
-
Identify whether or not any models of support utilise service user involvement or third-sector organisations (i.e. families with experience of GFT feeding or voluntary organisations) and analyse how service users/family support organisations interface with the formal health and social care sectors and how they are resourced.
-
Analyse professionals’ understanding of support issues and how services provide support, the support needs of young people and their families and how these were met.
-
Derive best practice guidance on support issues from an explication of the service models identified in the study and service specifications and make recommendations for change to inform commissioning decisions and set standards of support for children and families.
-
Make recommendations for embedding support for a wider constituency of children with complex health needs and their families, including recommendations for training and skilling the wider children’s workforce, by deriving general principles of how services can provide support and where in the care pathways this should happen.
Structure of report
The report is formed of six chapters. Chapter 2 details the methodological approach and methods for the three-phase mixed-methods study, including the national survey, the collective case study, the study of resource utilisation and costs, and willingness to pay (WTP) for PSS. We outline our theoretical model used throughout the report and our public and patient involvement (PPI) work in the same chapter. There is also a discussion of data integrity. Chapter 3 presents the findings of the web-based survey (WBS). Chapter 4 describes each of the four cases in our case study in detail. Chapter 5 details the findings of the resource use, costings and WTP studies. Chapter 6 summarises the findings of the study in relation to our synthesis model.
Chapter 2 Research methodology
Research design
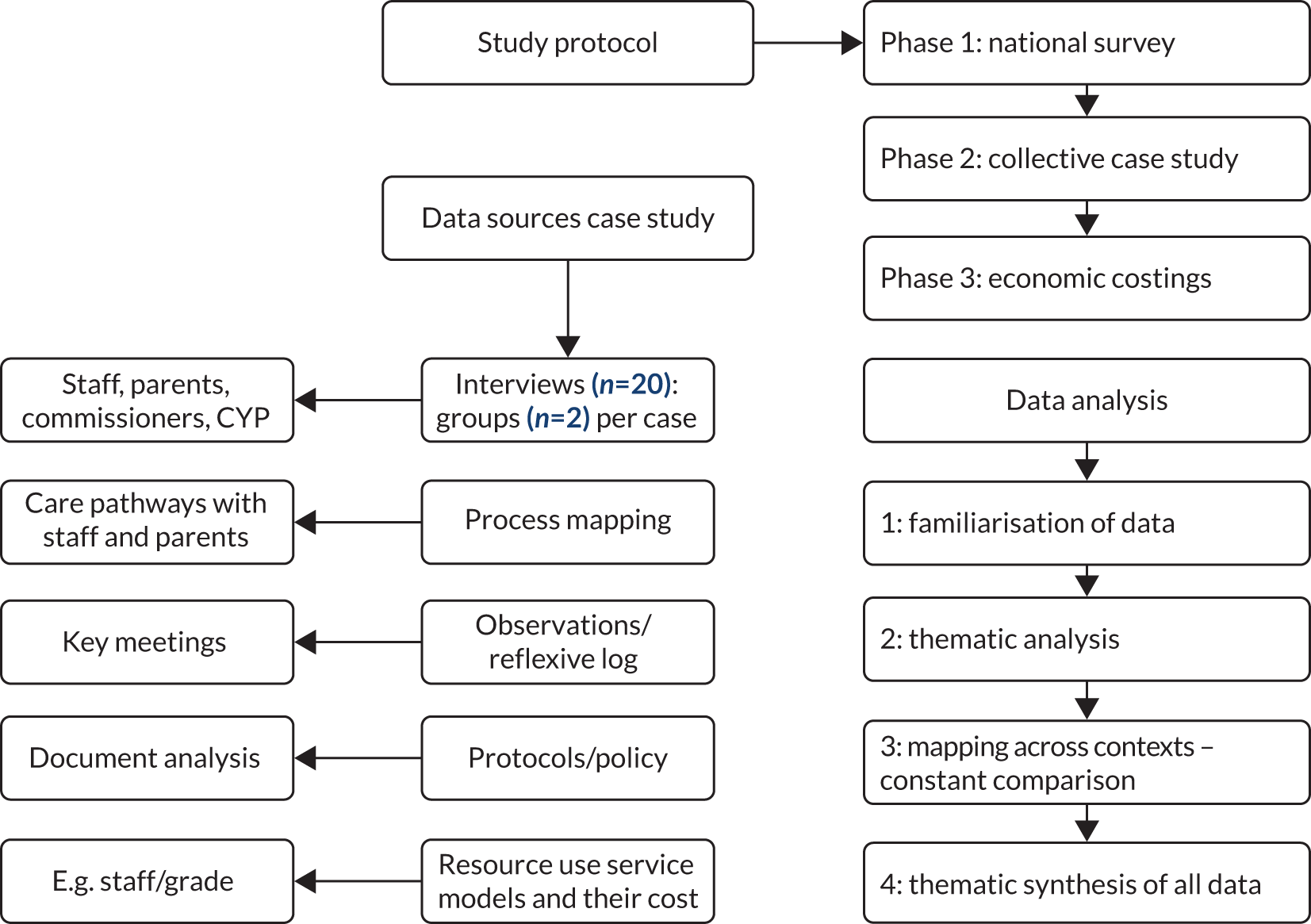
The research design was an explanatory, sequential mixed-methods approach with a qualitative, collective case study as the dominant or priority method. 35 The study entailed three phases: an exploration of service delivery support through a WBS to explore and scope best practice and identify case study sites for phase 2 (phase 1), a case study of four exemplar services (phase 2) and an estimate of the resources and costs of PSS (phase 3). The results of the WBS were used to inform the case study and data from phase 2 were used to inform the WTP study in phase 3. Data were kept ‘analytically distinct’35 across the three phases and are synthesised in a final chapter, although the findings of each phase fed into the next. Figure 1 illustrates the work scheme.
FIGURE 1.
Work scheme. CYP, children and young people.
Phase 1: web-based provider survey mapping practice
Phase 1 of the project addressed objective 1 and involved a web-based national survey of policy and practice distributed to all disability feeding teams in the UK using a professional database (round 1) hosted by the British Academy of Childhood Disability (BACD). The BACD is a multidisciplinary organisation and subgroup of the Royal College of Paediatrics and Child Health. The database was established for the purposes of research and to improve child health and service development initiatives. On our behalf, the BACD e-mailed all leads of disability services registered nationally with a link to our WBS.
The survey (see Appendix 1) aimed to provide a picture of established practice in relation to PSS. In addition, we aimed to identify further case study sites from the findings of the survey.
Fifty-four questions, including open-ended questions, were intended to gather data on the following themes: type of organisation, care pathways, how PSS was delivered and by whom, access, perceptions of best practice support (open-ended), areas for improvement and associated barriers (open-ended), parental peer involvement, and information about resolving conflict (including the use of safeguarding). Respondents were also asked if they would be willing to participate in phase 2, an in-depth qualitative case study of practice. The WBS was sent out to our PPI group for comment and was piloted informally, in-house, with members of the Project Advisory Group (PAG) and selected clinicians and academics.
Owing to an initial poor response rate (see Appendix 2 for the dissemination log), and on the advice of the BACD to expand our methods of dissemination, we e-mailed our survey link to research managers of the research and development (R&D) departments of all trusts using the National Directory of NHS Research Offices to cascade our survey link to the relevant staff/clinicians at child development centres (CDCs)/disability services (including their equivalent in Scotland) and feeding teams. This required permission for a non-substantial amendment from the Health Research Authority (HRA)/Camden and King’s Cross Research Ethics Committee (REC). In addition, we disseminated the link through various professional networks identified through the project co-investigators, including gastroenterology, speech and language therapy, and dietetics. In Scotland, we distributed the WBS through the National Managed Clinical Network for Children with Exceptional Healthcare Needs (NMCN CEN), NHS National Services Scotland. As R&D departments had to assess for capacity and capability, the deadline was extended.
Data were collected between July 2016 and May 2017; this period included a pause to obtain permission to disseminate the survey link through the R&Ds. The survey was designed, and data analysed, using Qualtrics XM (Provo, UT, USA) and exported into Microsoft Excel® 2016 (Microsoft Corporation, Redmond, WA, USA) for analysis. Open-ended questions were analysed thematically, drawing on approaches described by Braun and Clarke. 36 Text was organised into meaningful categories, compared across all responses and labelled using principles borrowed from constant comparative analysis. 37 Codes were stored in an Excel spreadsheet with illustrative quotations.
Phase 2: collective case study
We drew on Stake’s description of a ‘collective case study’38 for phase 2, that is, an instrumental case study that ‘provides insight into a phenomenon of interest’39 to gain an understanding of how support for children and parents was accomplished across complex care landscapes in four sites. ‘Collective case study’ describes a methodological approach whereby a number of individual cases are purposefully sampled because of their variety, range, contradictions or complexity. 40 Each case is investigated in depth but a common set of questions are asked of each to make comparisons. Robson describes a case study as ‘a strategy for doing research which involves an empirical investigation of a particular contemporary phenomenon within its real-life context using multiple sources of evidence’. 41 This is important when analysing complex health-care organisations and systems of care because it allows for both depth and breadth of analysis through multiple data sources and the differing perspectives of key players. 42,43
The cases are intended to provide exemplars of different service configurations and four cases were chosen to balance the need for a small sample to facilitate in-depth data collection and sufficient scope to explore variations in support in different local systems. In this study, a ‘case’ covers the local health and social care system rather than a single service so that these issues and linkages can be explored. Because these local configurations were sometimes complex, crossing health, education and social care boundaries, the cases often emerged through a mapping of the care landscape and was an iterative process. 44 Segar et al. 44 noted that, rather than having clear boundaries, ‘fuzziness and emergence are inherent to the case’.
Selection criteria case study sites: integration and support
Previous research on organisational case studies has selected sites according to best practice or performance criteria; for example, the Birthplace study45 selected sites according to the findings of the 2007 Health Commission Services Review. However, there were no policy recommendations to inform the selection of neurodisability services. Given the lack of guidance on models of service delivery, and how services should provide support, we identified cases in terms of the integration of PSS as a proxy for the structured support recommended in evidence reviews and also aimed to look at variation. We developed a four-step approach to the selection of cases (Figure 2).
FIGURE 2.
Development of a case study site selection framework. CSO2, case study site 2; CS03A, case study subsite 3A; PI, principal investigator.
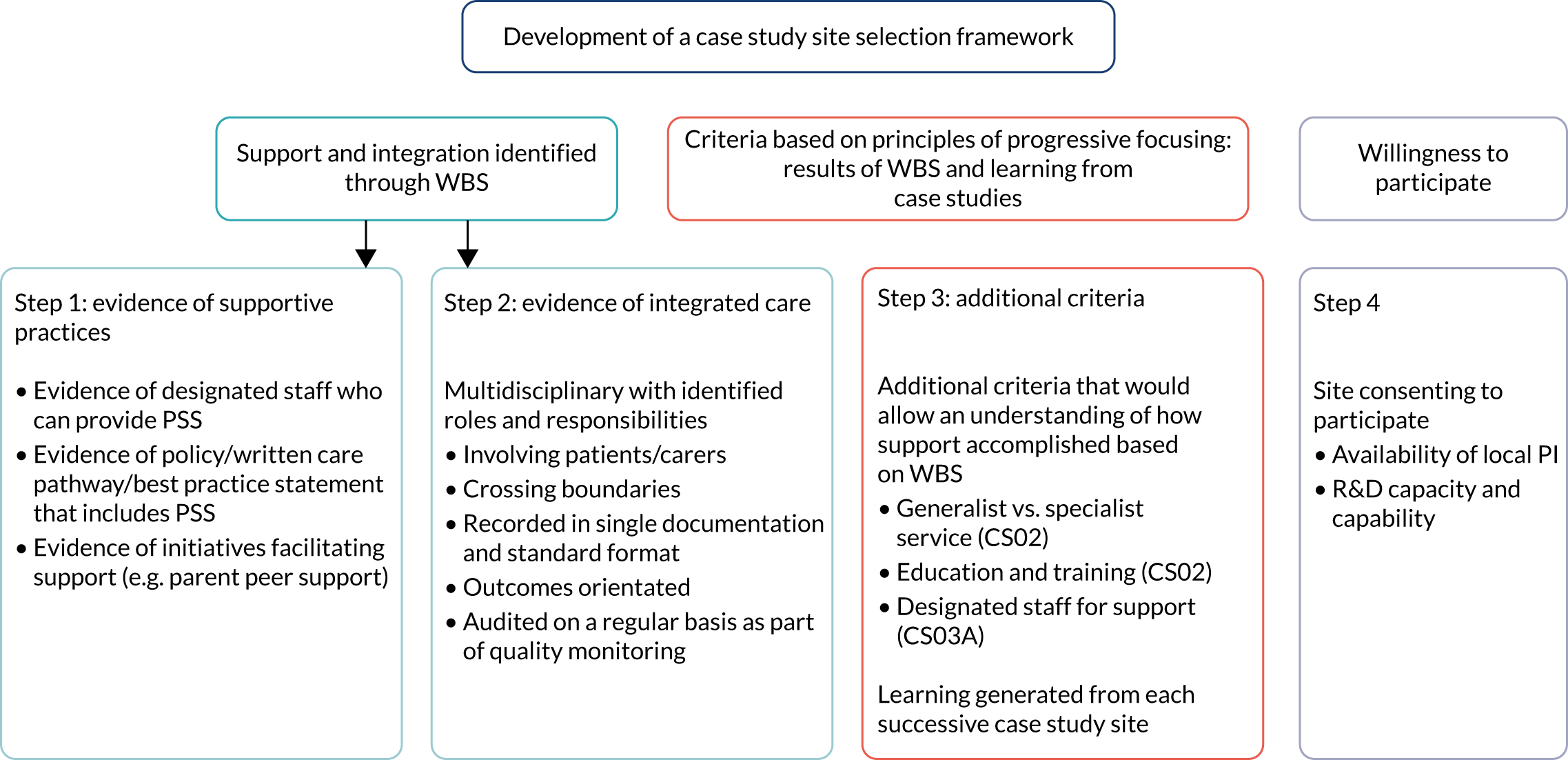
Steps 1 and 2
We initially aimed to identify services from the WBS using the criteria of support (step 1) and integrated care pathways (step 2) (Figure 3). We operationalised ‘higher’ levels of support as involving designated staff offering PSS and written care pathways that included PSS. Our operational definition of integrated care, as a care pathway approach, was ‘structured multidisciplinary care plans which detail essential steps in the care of patients with a specific clinical problem’. 46 The standards of integrated care pathways are provided in step 2. We asked respondents in our WBS to indicate which of the criteria outlined in steps 1 and 2 applied to their service to guide our case study selection. 47
FIGURE 3.
Preliminary selection criteria integration vs. support.

Step 3
Step 3 involved using the learning garnered from our first case study and WBS and applying these findings to the selection of subsequent cases, drawing on ideas from Stake’s progressive focusing methodology,48 which allowed additional criteria to emerge in relation to our study aims. For example, as it became clear that some services had examples of best practice but no formal care pathway, and on the advice of members of the PAG, we adopted a more flexible approach to the selection of our cases using theoretical criteria. 48
Step 4
Willingness to participate was also an important criterion as an indication of staff or organisations’ willingness to learn or show case examples of best practice. Interest and ‘opportunity to learn’ were therefore privileged over ‘typicality’ of service. 39
It should be noted that, although the initial criteria of integration and support (see Figure 3) informed the selection of case study 1, the results of our WBS, and our PAG, suggested that not all services would have written care pathways and that support was often provided generically as part of the multidisciplinary team (MDT). Assumptions that care involving designated staff equated to a higher level of support was problematised through our findings. Indeed, the concepts of ‘high’ and ‘low’ integration and support are themselves discursive constructions and highly contested in the absence of evidence and guidance. Therefore, we chose additional sites according to theoretical sampling and what those services could tell us about PSS initiatives using theoretical sampling based on the learning and experience garnered from the field work.
Selection of case study sites
All case study site services, apart from the service at case study site 2 (CS02), which was described as a generic service, were specialist services in which MDTs delivered care to children with complex feeding needs. All sites referred to specialised tertiary centres for the placement of a GFT. Three of our cases were based in England and one in Scotland (we do not provide exact regional locations to preserve anonymity). Two of our case study sites were in the 20% most deprived authorities in England, with approximately one-fifth of children living in low-income families; one of our case study sites was in one of the least deprived authorities, with approximately 7% of children living in low-income families. 49 The cases and rationale for their selection were as follows:
-
Case study site 1 (CS01) was selected because it met our initial criteria of integration and support. We initially designated this site as high in integration, between health and education via a co-located special school, and support (defined as availability of designated staff). In addition, there was a strong parental network organised around the school.
-
Case study site 2 (CS02) was chosen because it was an example of a generalist, rather than a neurodisability, service, where children were cared for by a MDT and staff had generic responsibility for all children but specialised in caring for children with complex feeding needs. Staff were supported by the NMCN CEN, which serves as a forum for disseminating best practice across Scotland. The WBS identified that the NMCN CEN had developed a training module for staff specifically on the importance of providing emotional support to parents when making decisions about GFT feeding. This was also underpinned by policy, that is, a best practice statement and guideline based on research findings. 50 Education and training were identified as aspects of best practice in our WBS and as gaps by some staff in our first case study.
-
The services of a psychologist were available at case study subsite 3A (CS03A) but were not available at case study subsite 3B (CS03B), reflecting an inequality in access to resources, although both services were homed in the same NHS trust. Both sites referred children who needed a GFT to the same tertiary centre [case study tertiary site 3C (CS03C)], which had recently implemented a nurse assessment model. We selected CS03A to specifically examine (1) the experiences of parents of younger children and (2) the role and function of designated staff to offer support (e.g. a psychologist), a theme raised in the WBS. The comparison was felt to be useful in understanding commissioning, staffing arrangements and resources: themes identified in our WBS as barriers and levers in the provision of PSS.
-
Our final site, case study site 4 (CS04), could be described as a hospital-based, district service. There was no written care pathway. This site was a mini case study because the recruitment of parents was particularly difficult. Moreover, the tertiary referral centre did not have capacity to participate.
Data collection
Interviews with key stakeholders
We conducted semistructured interviews and focused group discussions in each case with a theoretical sample of service managers, staff (health care, social care, education) and parents and children (the children were included whenever possible). In addition to face-to face interviews we offered participants telephone or Skype™ (Microsoft Corporation, Redmond, WA, USA) interviews. We used visual mapping of service configurations as an interview aid with professionals, where possible, to better understand referral pathways in local systems of care. 51 Interview schedules were semistructured and required a degree of flexibility depending on where families were in their feeding journey (see Report Supplementary Material 2 and 3). Flexible interviews were necessary for children to accommodate their communication preferences.
Observations and document review
This was not an ethnographic study so the role of observation and review of documents operated as follows: prior to the interviews we obtained key documents relevant to the case study (e.g. service documents, care plans, care pathways, mission statements, protocols on eating and drinking) to sensitise us to the context of service delivery and identify aspects that could be corroborated in interviews. We conducted observation of selected aspects of services at key junctures, including appointments and meetings with family groups. Non-participant observations aimed to provide a baseline understanding of the context of care and sensitise us to the influences of this on care delivery. Both observation and document review helped to highlight issues of relevance that could be explored in interviews and assist with triangulation of data.
Data management
Interviews were audio-recorded, transcribed, de-identified and stored in NVivo version 11 (QSR International, Warrington, UK). Key documents and notes of observation were added to the NVivo database alongside interviews.
Analysis of data
The lack of research on how services provide support to children and families, coupled with diversity of provision due to a lack of guidance on how services should be organised, and the complex nature of family journeys (which often traversed multiple health-care organisations, education and social care), provided the rationale for a largely descriptive approach to the case study to provide sufficient contextual detail. 52 Our approach to analysis involved four levels:
-
description of services to highlight how support was accomplished across each service configuration and their contexts, building on the findings of the WBS
-
visual service mapping highlighting linkages in and between services to illustrate pathways and complexity derived from interviews and checked in feedback sessions
-
themes highlighted in the WBS
-
theoretical model of decisional conflict.
The original plan was to analyse the qualitative interviews using a framework analysis53 combined with a narrative approach to provide rich illustrations and storied accounts. However, the case study generated to some extent heterogeneous data in line with our progressive focusing methodology, which allowed us to focus on different strengths of services in each of our cases to illustrate how support was accomplished across a diverse array of organisations we have loosely termed ‘local service configurations’. Therefore, our cases cut across health care, social care and educational provision and across different sectors of provider. This provided a rationale for a prioritised focus on a thematic analysis,54 which we felt was more sensitive to the different perspectives and the dynamic nature of the project.
An analytical framework was developed in relation to the research questions, findings from the WBS and model of decisional conflict. 1,55 Care was taken to attend to similarities and differences in the data in and across case study sites using principles derived from constant comparative analysis where possible. 37 Data were organised in relation to our theoretical framework and are presented in a synthesis model in Chapter 6. It should be noted that not all key themes are presented in every case study site to the same degree of analysis; in some cases there were no data relating to that theme or there was less evidence of a particular phenomenon in that setting.
Theoretical model and data synthesis
We drew on Manhant et al.’s1,55 model of decisional conflict as a way of organising and categorising data specifically on decisions about feeding. Based on a systematic review of qualitative interview studies, the model outlined three sources of decisional conflict between HCPs and families arising from the recommendation of a GFT, including the values that parents attach to the meaning of feeding and GFTs; the child and family context, including unique family circumstances; and processes of care, which includes characteristics of organisations or care configurations, how these and HCPs interact with families to make decisions and the role of support and information. This theoretical framework informed the interview schedules as well as the analysis and synthesis of data.
Data synthesis
We collected and analysed the WBS (phase 1) and the case study data in two consecutive phases, with the qualitative case study being the primary component. Themes identified in the WBS were explored in greater depth in interviews in the case study and used to identify case study sites for phase 2. The phase 2 case study data were used to inform the scenarios in the WTP study in phase 3; otherwise, analysis in each phase remained distinct. We present findings in terms of a synthesis model that takes into account structures and outcomes in addition to processes of care and populate this model with our descriptive themes in Chapter 6. 56
Recruitment of staff and families
All staff and families were approached by the appointed principal investigator or research nurse at each case study site. The research team did not have direct contact with families initially. The research nurses contacted families by phone to advise them an information pack would be sent out, with their permission, inviting them to participate in the study. Packs were then sent out and followed up with a telephone reminder by the local staff 2 weeks later. Health-care staff received e-mail invitations advising them about the research, followed by the information packs and e-mail reminders. The local principal investigators and research nurses also sent out packs to school-based staff where the clinical teams delivered clinics. Consent forms were returned to the research team. Parents consented for their children to participate. Inclusion criteria are described in Appendix 3.
Phase 3: resource utilisation and cost implications of psychosocial support
We adopted a two-step approach to the study of costs of support, comprising an estimate of the resources involved (study 1) and WTP for support (study 2). Resource questionnaires were developed and disseminated to parents and staff across all case study sites via the local principal investigators or research nurses (study 1) and a survey was disseminated more widely through social media (study 2).
Study 1: estimation of resource use
Questionnaires on resource use concerning health service appointments were sent out to 103 parents and carers of children who had had a GFT or in whom placement of a GFT was being considered (see Report Supplementary Material 4). Information requested included demographic data concerning the child; details of HCP appointments related to the GFT in the previous 12 months; the length of each appointment, who was present and what issues were discussed; and whether or not emotional PSS was given and, if so, for how much time. Further questions asked if their problem was resolved and if they would have liked specific appointments to discuss emotional psychosocial issues. Questions were also asked about their satisfaction with each appointment and if they were offered the opportunity to talk to other parents or families and, if not, if they would have liked the opportunity to do so. The questionnaire also asked how satisfied parents were overall with their care on a scale from 1 to 5, and provided free-text comments on their child’s feeding and the PSS that they received or would like to have received. Questionnaires were also sent to HCP staff (see Report Supplementary Material 5). In Chapter 4, we report mainly on data from the parental questionnaire as well as reporting on the training and confidence in supporting families from the professional questionnaire.
Study 2: willingness to pay
Parents and HCPs were asked to value two different services: a hypothetical model of care that reflected usual practice across all four case study sites (service A) and service B, which reflected an enhanced care package of support based on data gleaned from the interviews and organised around the principles of structured and consistent support. 1 They varied slightly in terms of professional support and the frequency and type of psychological support offered. The aim of such questioning was to determine what value parents would put on each service relative to the other and, therefore, which model of care (service A or B) they would prioritise and thereby express a strength of preference for, using a hypothetical ‘purchasing price’ as a measure of such value (see Report Supplementary Material 6 for descriptions of the two hypothetical service scenarios).
The questionnaire and scenarios were piloted with our PPI parent group for ease of completion and among members of the PAG. Owing to the amount of time it would have taken to gain permission to disseminate the questionnaire through our case study sites, we decided to seek ethics approval through the University of Hertfordshire and distribute our questionnaire through professional and parental networks and social media, including Facebook (Facebook, Inc., Menlo Park, CA, USA; www.facebook.com) and Twitter (Twitter, Inc., San Francisco, CA, USA; www.twitter.com). The questionnaire was distributed via Qualtrics from 3 April 2019 to 28 May 2019.
Patient and public involvement
Involving parents and young people in the process of research
A PPI reference group was formed comprising three parents and three young people and organised by Triangle (Brighton, UK) (co-applicant), an independent organisation that provides consultancy and advocacy services that enable children and young people to communicate about important matters. Triangle conducted the PPI on our behalf. The research team provided Triangle with a brief, or instrument, and asked for comment. Triangle liaised with parents and children on our behalf. In relation to children’s participation, a member of the research team usually observed the consultation. Our lay chairperson was involved in all aspects of the research study.
Input into data collection tools and project information sheets
Parents provided feedback on project information sheets. Parents also provided feedback on the form and content of the WBS; this task was not accessible to young people. We asked for feedback from parents on the scenarios used in the WTP questionnaire in terms of wording and ease of understanding.
The young people’s PPI group gave feedback on the content of the children’s interview schedule, which included social stories about children eating. The comments the young people made included concerns about the social stories that involved a child choking (used to illustrate that oral feeding was unsafe), which they felt could raise anxiety. This was removed. Their comments ‘we are all different’ and ‘only people who have been trained by my SLT [speech and language therapist] should help me with eating and drinking’ were, with their permission, used on the project website. Parents provided feedback on the interview schedule for professionals and parents by commenting on the wording of questions and the content of the interview schedule and made suggestions to simplify questions and ask additional questions.
Input into the website
The young people’s PPI group and parents’ group provided feedback on the project website hosted by the University of Hertfordshire. The feedback addressed the visual appeal, potential audience and content. One parent felt that the images of children implied that all children with gastrostomies were wheelchair users and advised us to change this, which we did. There was a comment that the characters portrayed needed to be more ethnically diverse. We made these changes. Use of the term PPI was also questioned: one parent felt that it had medical and insurance connotations. We changed the wording to ‘community engagement’.
It also became apparent that the website was not accessible to children through the university system: it took substantial time to locate the website using its augmentative and alternative communication (AAC) systems because of the length of the URL and the number of clicks involved. This was partly a result of the ways in which universities manage website pages, which researchers have little control over. Therefore, we purchased an independent URL to make the website more directly accessible. We also provided feedback to the PPI group on what changes we had made in response to its involvement, in line with best practice guidance. 57
Outputs
We fed back our results to parents and asked them to read our lay summary for ease of understanding. Parents and children commented on the minimum standards of support, which are included as supplementary information.
Ethics approval
Ethics approval was obtained from the HRA National Research Ethics Service Committee Camden and King’s Cross (REC reference 16/LO/0214).
The WTP study was reviewed by the University of Hertfordshire’s Health, Science, Engineering & Technology Ethics Committee with Delegated Authority (reference UH03705) and received ethics approval.
Written consent from parents and staff to participate in interviews was obtained.
Box 1 indicates changes to the original protocol.
The survey was disseminated through R&D departments of trusts using the National Directory of NHS Research Offices and a range of professional networks, in addition to the BACD database. This required a non-substantial ethics committee amendment.
Phase 2: case studyWe amended the protocol to offer telephone or Skype interviews to staff and parents to maximise opportunities for participation.
We had initially planned to use framework analysis as an approach to the analysis of qualitative data supplemented by a storied approach to participants’ narratives. We adopted a thematic analysis to the qualitative data. We had planned to use Greenhalgh et al. ’s42 organisational theory of factors influencing diffusion of innovation and barriers to implementation in relation to our data. However, the data did not lend themselves to this approach, although we have described the barriers to implementation of PSS. We use Mahant et al. ’s1 model of decisional conflict as described in the protocol.
Phase 3: resource utilisation and costsIt was not possible to assess costs from children’s clinical records because it became apparent that PSS is generally not recorded in the clinical notes as a distinct activity. Rather, support was integrated into the clinical appointments and children and families were rarely referred to a psychologist or specialist where this would be recorded.
We changed the timing of the dissemination of the resources questionnaire to coincide with the initial invitation to participate, rather than later, owing to concerns about sample attrition and low response rates.
Owing to the small number of questionnaires returned by parents, the cost analysis draws on data across all four cases in the case study rather than four separate models. Similarly, in the WTP study, we aggregated data across parents and professionals, given that professionals were the largest participant grouping.
TimescaleThe project was paused for 12 months, from 2017 to 2018, owing to a change of sponsor while the project moved to the University of Hertfordshire.
Integrity of data
Generalisability
We aimed to use the case study to bring into relief approaches to embedding PSS in a variety of settings through interviews with a range of stakeholders, observations of care processes and a review of service documents. We concur with Sharpe et al. ,40 who argue that the different views of a range of participants across diverse contexts allows for some degree of generalisability, particularly when supported by additional data from other sources, in our case from phases 1 and 3 and the case study with data from across the four cases.
Interviews were coded by an independent researcher (JL) and checked by another researcher (EB). The chief investigator (GC) also reviewed 10% of transcripts for coding.
The case study has also been reported with regard to Rodgers et al. ’s58 consensus standard for the reporting of case studies in organisations (see Report Supplementary Material 1).
Member checking
Feedback sessions were conducted at two case study sites (CS01 and CS04), which involved face-to-face meetings with HCPs, and descriptive information about the case studies was sent to two sites (CS02 and CS03) for comment to validate the findings. The mapping of services was either sent to the principal investigators at each site for comment or discussed in feedback sessions.
Triangulation
Cohen et al. ’s59 definition of triangulation as an approach that maps out and explains the richness and complexity of a phenomenon by studying it from more than one standpoint reflects the way in which triangulation was handled in this study. To this end, a range of professionals and services were identified using theoretical sampling and we employed different methods to provide data (interviews, document review and observation). These different data sources provided a more balanced and holistic picture of services, which can often look, feel and be experienced as different from varying perspectives and across case study sites. Theoretical triangulation and synthesis was used by applying Mahant et al. ’s1 model of decisional conflict, and themes were compared across case study sites.
Chapter 3 Results of the web-based survey scoping best practice
The WBS was disseminated through two distinct routes. The first route was via the BACD database during July and October 2016. The WBS was opened 71 times; 30 respondents provided no information beyond the initial consent, leaving 41 respondents. After the removal of duplicates (n = 2) and the responses of a respondent who had indicated that there was no feeding team, this left 38 respondents. The second route was via the R&D departments of individual NHS trusts, which resulted in a time delay reflecting the need for additional permissions. Between December 2016 and May 2017, the WBS was opened 47 times; 21 respondents provided no information beyond consent, leaving 26 respondents. There were 64 WBSs returned with different degrees of completion, which explains variations in the denominator. We disseminated the WBS through professional networks during both periods. Owing to the multiple routes we used to disseminate the WBS, we do not have a denominator, and hence response rate, for the WBS.
Respondents
Table 1 illustrates the number of responses to the survey questions. Most respondents were based in services in England (83%). There were no responses from Northern Ireland, which may be the result of a different mechanism of dissemination (see Appendix 2). The WBS was completed by a range of professionals, although those with a dietetic background, and paediatric consultants, represented the highest number of respondents. We report on the main themes that we aimed to explore in phase 2 and that would help identify additional case study sites; namely the delivery of PSS, perceptions of good practice, areas for improvement and associated barriers and levers. Table 2 provides a thematised account of responses from the open-ended questions. In addition, we report on parental involvement and decisional conflict.
| Responses | n (% of completed responses) |
|---|---|
| In which nation is your service based? (N = 63) | |
| England | 52 (83) |
| Wales | 5 (8) |
| Scotland | 6 (9) |
| Northern Ireland | 0 (0) |
| Professional background of person completing survey (N = 49) | |
| Consultant paediatrician | 10 (20) |
| Dietetics | 14 (29) |
| Children’s community nursing | 7 (14) |
| Nurse specialist | 4 (8) |
| Other | 7 (14) |
| School nurse | 1 (2) |
| SLT | 3 (6) |
| Staff nurse | 2 (4) |
| Consultant gastroenterology | 1 (2) |
| About care pathways | |
| Does your service have any of the following?a (N = 35) | |
| Written care pathway | 13 (37) |
| Best practice statement guidance | 7 (20) |
| Multidisciplinary guidance | 9 (26) |
| Written dysphagia policy | 9 (26) |
| Other | 13 (37) |
| About the PSS offered | |
| Is PSS offered to the following groups? (N = 45) | |
| Children | 24 (53) |
| Young people | 22 (49) |
| Parent/carer | 31 (69) |
| No PSS offered | 20 (44) |
| Is PSS documented or formalised? (N = 43) | |
| Yes | 15 (35) |
| No | 28 (65) |
| Do you have a process/tool in place to measure outcome of PSS? (N = 38) | |
| Yes | 7 (18) |
| No | 31 (82) |
| Do children/families have to meet a threshold to receive PSS? (N = 25) | |
| Yes | 7 (28) |
| No | 18 (72) |
| How well do you feel your service supports children/families? (N = 44) | |
| Very well | 8 (18) |
| Room for improvement | 29 (66) |
| Not very well | 6 (14) |
| No support | 1 (2) |
| Is there something you would like to do differently to improve the PSS offered? (N = 43) | |
| Yes | 38 (88) |
| No | 5 (12) |
| Parental peer support | |
| Does your team offer referrals to other parents who have experience of gastrostomy? (N = 38) | |
| Yes | 23 (60.5) |
| No | 15 (39.5) |
| If yes, is the referral formalised in any way? (N = 23) | |
| Yes | 19 (82) |
| No | 4 (18) |
| Are there any established parent or voluntary groups that you work with as part of your service? (N = 35) | |
| Yes | 6 (17) |
| No | 29 (83) |
| Decisional conflict (N = 39) | |
| Does the service have written guidance or approaches to managing conflict when the parents/child disagree? | |
| Yes | 8 (21) |
| No | 31 (79) |
| In the last 12 months | |
| Has children’s weight/growth raised concern about safeguarding?b (N = 34) | |
| Yes | 30 (88) |
| No | 4 (12) |
| Have you or your team used safeguarding legislation in relation to children’s feeding/weight/growth? (N = 34) | |
| Yes | 16 (47) |
| No | 18 (53) |
| Do clinicians/therapists receive clinical supervision/guidance/support when working with children and families who disagree? (N = 41) | |
| Yes | 31 (76) |
| No | 10 (24) |
| Question | Themes |
|---|---|
| Please identify three key aspects of your service that you feel are examples of good practice in delivering PSS to children and families? |
|
|
|
| What changes would you like to make? |
|
| What would help you to make those changes? |
|
| What barriers, if any, would you need to overcome to make those changes? |
|
Psychosocial support
A total of 44% of respondents reported not offering PSS according to the definition provided, and approximately half of respondents reported offering some form of PSS to children and young people. Possibly owing to the severity of children’s disability or young age, PSS was mainly offered to parents. In approximately two-thirds of cases, PSS was not documented or formalised and most respondents had no method of measuring the outcome of a PSS intervention. In a small number of cases, children/families had to reach a threshold, or meet criteria, to receive support. For example, one service indicated that ‘a child must be less than 4 years of age and attending a local CDC to be eligible for clinical psychology input’ and that ‘this resource is not readily available to other branches of the feeding team’.
Perceptions of good practice
Respondents were asked to identify three key aspects of good practice in their service. Staffing arrangement such as dedicated feeding clinics, MDT working and specialist staff were mentioned:
The service is just dedicated to enterally fed patients, so the clinical expertise is very specific, and the advice provided is current and from experienced clinicians.
Very good multidisciplinary teamworking and communication between whole team across all sites.
Of interest was the support provided from a clinical psychologist to the rest of a team:
Opportunity for individual sessions with a clinical psychologist. [Their] presence increases all the team members’ awareness of issues, which we discuss at team workshops.
This specialist support contrasted with services where PSS was integrated within the appointment:
We address nutritional, physical and emotional aspects of feeding problems simultaneously.
Practice approaches included values-based, family-centred and holistic care that recognises that approaches other than traditional biomedical ones are important. Having access to up-to-date knowledge was also mentioned and the importance of high-quality clinical care. Linking families together was perceived as an aspect of good practice.
Areas of change needed in the provision of psychosocial support and perceived levers and barriers
Two-thirds of respondents felt that they could improve on how they delivered PSS, which might be an indication of practitioners who were more reflexive about service improvements. It may also be easier to respond in this way rather than endorse a more negative response. The majority (88%) of respondents felt that they would like to do things differently.
Perceived barriers to implementing changes were identified, including commissioning, workforce issues and the need for better communication across teams:
Different services being commissioned by different trusts. For example, in [name of area] speech therapy and community paediatrician is provided by [name of trust] while dietetics and children community nurse by [name of different trust].
Workforce issues were also raised, suggesting the need for support for staff in addition to parents:
High levels of stress experienced in looking after children with complex neurodisability and their families.
The need for improved communication between services and the tertiary centre, and within the service, were also mentioned so that HCPs had advanced notice of those children due to have surgery:
If medical staff bringing children in to insert a tube, more communication with wider team so they can give support.
Peer–parent support
A number of services indicated that they linked families considering a GFT for their child with those families who had experience, sometimes through signposting to national parent organisations, although this did not appear to be a formalised arrangement. There was an acknowledgement that families had opportunities to meet parents through schools:
Actually no [i.e. not formalised], but I wanted to say that it is by means of PINNT [Patients on Intravenous and Naso-gastric Nutrition Treatment (Christchurch, UK); a support and advocacy group for people receiving home artificial nutrition]. In addition, many of the families already know other families with a child with a gastrostomy from their shared special needs school. So, when they come to my nurse-led clinic, most have already seen a gastrostomy. This may increase or decrease their anxiety.
We have used Contact A Family [London, UK] in the past but do not routinely signpost families in this way.
Similarly, several services reported that they had relationships with established parent or voluntary groups, although this was not specifically feeding related:
[Name of city] parent-carers – mutual participation in meetings. Not specific to feeding.
[Name of national organisation], part of our NHS organisation, involving parents and young people in service design. Not specifically for feeding issues.
When asked in what way parents or groups were involved in supporting families considering a GFT, responses included ‘additional and independent support’. Resourcing parental involvement was also raised as an issue:
We did have a support group, we did run for families who tube feed but we haven’t had a meeting for a long while as it’s very time-consuming to arrange and we struggle with time in work to arrange but it is something that we are hoping to restart soon.
One service mentioned that a food and nutrition group involved two parent members in addition to school and HCPs.
Decisional conflict
Few services had written guidance or approaches to managing conflict when parents disagreed with the recommendation of a GFT and 88% reported that children’s feeding, weight or growth had raised safeguarding concerns. Just under half reported using safeguarding frameworks because of concerns, although it is possible that this was due to additional concerns. The majority of respondents reported that they had access to clinical supervision when dealing with disagreements.
Summary of survey findings
Evidence reviews have suggested that services should offer consistent and structured support in care pathways to ensure high-quality decision-making when families consider a GFT for children. The results of our WBS suggested that a range of practitioners delivered support. The majority of services did not appear to have a formalised way of documenting PSS or of measuring the outcomes of PSS initiatives, which we aimed to explore further in our case study because this has implications for services’ ability to monitor and evaluate PSS provision through audit and research, which may prove useful in justifying resources, given that lack of resources was mentioned as a barrier to developing PSS. Indeed, one barrier to the implementation of PSS initiatives mentioned was the lack of evidence of effectiveness.
Although difficult to determine different typologies of service from survey responses, reflecting a limitation of the method, respondents made the distinction between specialist (e.g. specialist enteral clinics) and generalist services. The availability of designated staff (e.g. a psychologist) to offer PSS was mentioned as an aspect of best practice and perceived as an opportunity to improve care. This contrasted with approaches in which PSS appeared to be integrated within clinical appointments. We aimed to explore these different staffing arrangements of specialist and generalist services, and designated PSS compared with integrated PSS offered by a MDT, in our case study. There was some evidence of children having to meet thresholds to receive PSS, perhaps from designated staff, and access to a psychologist was available in some branches of one service but not others. Inequality in the provision of PSS is a theme we therefore aimed to investigate further.
Not all services offered PSS to children, which may reflect a lack of expertise in communicating with children who, as often the case in this population, are non-verbal (between 42% and 60% of these children are estimated to have a communication impairment). 10,60 Although some services appeared to have involved local parent groups in general service developments, this was not feeding specific, but indicates the potential availability of resources in the locale for developing peer support initiatives. Professionals also signposted families to national organisations, but we do not know if this was followed through. Generally, peer-to-peer parent support was arranged informally and on an ad hoc basis. Concerns about time and resourcing to do this well were raised. There was some ambivalence about whether peer-to-peer parent support was beneficial or could raise anxiety. An example of how the parent voice could be embedded in practice was provided by parents sitting alongside HCPs and teachers on a food and nutrition group in one service. Parental peer support was explored in phase 2.
Children’s weight and growth raised safeguarding concerns for the majority of respondents, with little evidence of guidance to support staff. How clinicians manage conflict, risk and safeguarding was explored in our case study.
Perceived barriers to change were identified, including staffing arrangement, facilities, resources and commissioning. Resourcing and competing needs were dominant themes, reflecting an awareness of financial constraints as a barrier to providing PSS. These themes were explored in phase 2.
Limitations
It proved very difficult to disseminate a WBS nationally, despite extensive efforts, following a poor response rate using a professional database. Appendix 2 illustrates an extract from our dissemination log using the BACD database. This suggests that only 43 out of 225 recipients initially opened the e-mail containing the survey link sent to CDCs (our target audience) by the BACD on our behalf, with 11 out of 43 opening the survey link. Low response rates to surveys involving doctors are commonly reported, including rates of 29% in Canada61 and 30% in the UK. 62 Moreover, the research team had to rely on gatekeepers to disseminate the survey. Future efforts could second a member of the BACD to help with telephone reminders to improve response rates, and there is evidence that incentives increase participation;63 however, these approaches would have implications for resourcing.
Information request overload may have had some bearing. Anecdotal evidence from our networks suggest that clinicians receive many requests for information, including for research, commissioner requests and national professional body surveys. The length of the WBS may have been a factor affecting the differences in responses to questions, although evidence that length affects response fatigue is not conclusive;64 rather, WBS content, interest and motivation in the context of time pressures may be factors. However, responses to questions later in the survey did appear to wane. Given the lack of formalised and documented approaches to recording PSS, it is possible that respondents may have had to find the answers to the survey from different data sources and hence left the survey but then did not return to complete it.
As a result of the above, we are unable to claim that the results are representative, although we did identify topics worthy of further exploration in our case study. Methodologically, surveys are a crude tool for capturing data about complex services crossing boundaries. For example, there was some evidence to suggest that responses reflected PSS across services rather than individual services. Similarly, it proved difficult to classify services and models of psychosocial support from the responses provided in the WBS. There was a tendency of staff to respond with stock responses such a ‘MDT working’ as an aspect of best practice, which provided little insight into how teams functioned. This is a limitation of the method. There are also methodological issues regarding individual responses that ‘speak’ on behalf of whole teams and services, hence the need for a mixed-methods study that allowed us to explore the themes raised in this WBS.
Chapter 4 Findings of the collective case study
Structure of the results chapters of the case study
This chapter details each of the four case study sites. Each case begins with an overall description based on documents and interviews, and this is followed by an outline of how support is delivered in relation to our themes developed from an analysis of interviews, observations and review of service documents. Each case is accompanied by a service map detailing the relationship between key nodes in the service and ‘referral pathways’ where possible, although pathways were often informal and crossed different sectors of provision, including education. These maps were produced iteratively, with the aim of highlighting complexity, and served as a focus for reflection in feedback sessions with teams where possible.
Interview participants
Table 3 illustrates the number of participants interviewed (including joint interviews or group discussions). These were children (n = 3), parents (n = 26) and staff (n = 58) across the four case study sites. The small number of children interviewed reflected their young age, severity of cognitive impairment and parental gatekeeping (access and consent issues). However, there was a group of children involved in the PPI group; these children’s involvement is detailed in Chapter 2, Patient and public involvement. There were 40 hours of observation of care processes.
| Participant | CS01 | CS02 | CS03 | CS04 |
|---|---|---|---|---|
| Parent | 11 | 9 | 5 | 1 |
| Child | 2 | 0 | 0 | 1 |
| Staff | 20 | 15 | 15 | 8 |
To maintain confidentiality, professional and biographical information is presented in aggregate in Report Supplementary Material 7 rather than per case study.
Case study site 1
Overall description of the case
Case study site 1 is described as a specialist clinical service and a co-located, charitable-funded special school and associated services. The clinic saw children attending the co-located special school and children in the local catchment who may have attended other schools in the area. Figure 4 shows the configuration of care at CS01. There had been a recent move in this setting to pool budgets for health and education, and clinical services received payment from education and NHS Clinical Commissioning Groups (CCGs), with agreed levels of funding for each child. However, for older children (aged 19–25 years), funding for health was described as ‘piecemeal’ (in an orientation interview) and dependent on NHS Continuing Healthcare assessment funding, reflecting inequities in service provision for young people.
FIGURE 4.
Configuration of care: CS01. CCN, children’s community nurse; GP, general practitioner.
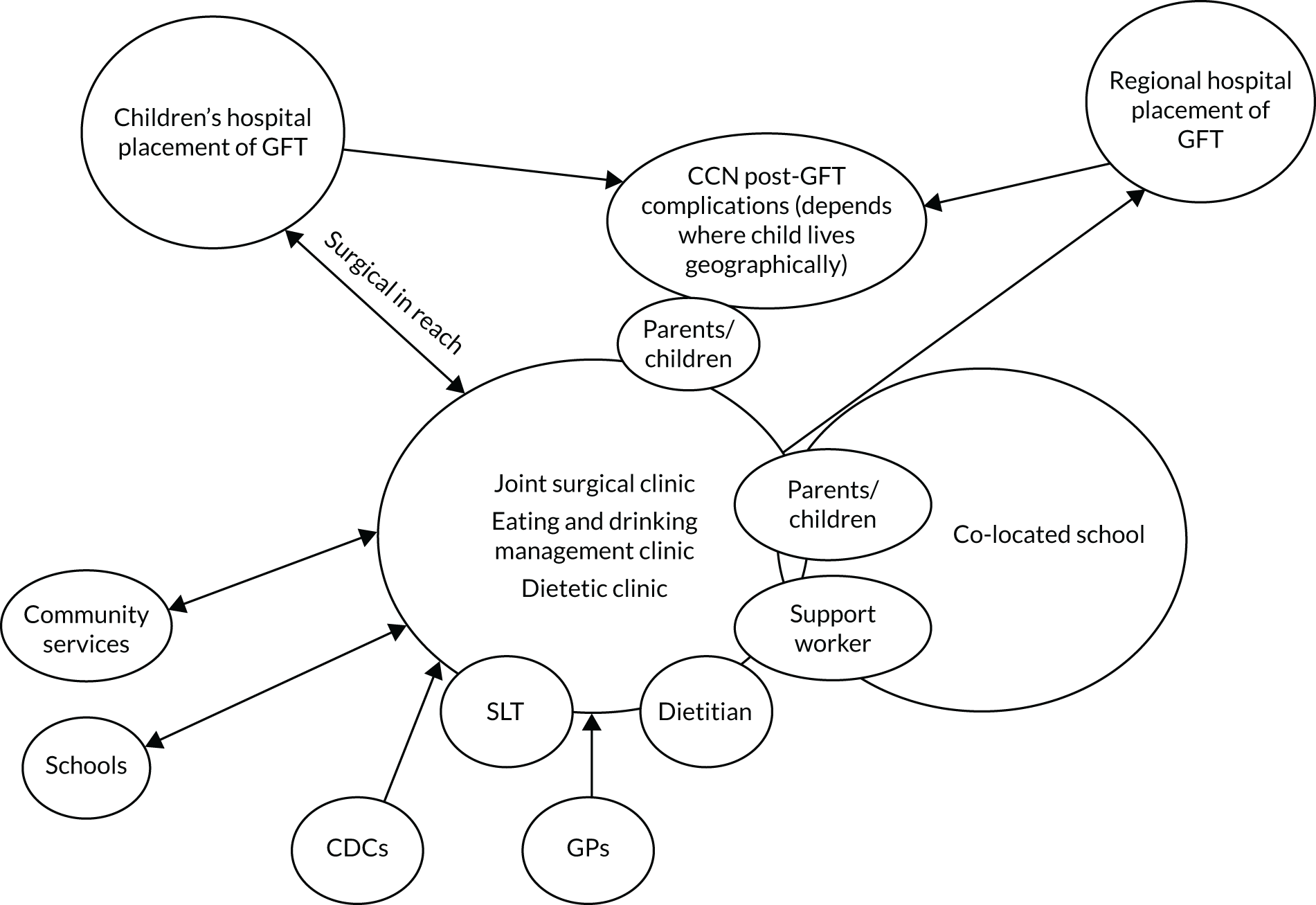
The CS01 clinical service provided a range of specialist health-care services for children and young people with neurodisability and complex feeding needs/GFT. Referrals to outpatient services could be made through any NHS HCP and were accepted without prior approval, provided that they could be accommodated by the outpatient clinic allowance set out in the contract financial schedule. The allowance for outpatient clinics was therefore used to provide outpatient access to non-pupils (as described in the service specification document for the CS01 clinical service; details omitted to preserve anonymity). Pupils attending the co-located special school had an assigned paediatrician who visited the school and was linked with the school therapists, nurses and teachers. This helped to simplify referrals to the clinical services and the joint assessment of children.
Staffing arrangement
The nutrition team, which was part of the nutrition service that provides clinical care to children and young people with complex neurodisability, included a paediatrician, dietitian, nutrition nurse specialist and SLT and offered a dietetic clinic. Team meetings, which were attended by clinical staff, parents and school representatives, aimed to address any issues around feeding. A paediatrician was linked to the nutrition clinic and therefore came in direct contact with pupils at the CS01 school. There were three main clinics where children and families could be seen: a dietetic clinic, a drinking and management clinic and a joint surgical clinic (discussed later as an aspect of integrating community and tertiary services).
The dietetic clinic was run by a senior paediatric dietitian, lead clinician and nutrition nurse specialist. The clinic was for children and young adults for whom there are dietary or nutritional concerns, and all individuals fed by a GFT or nasogastric (NG) feeding tube were reviewed in this clinic once per year to ensure that their intake was nutritionally adequate (sources: Dietetic Clinics leaflet developed by the CS01 clinical service; CS01 dietetic clinic observation notes).
The eating and drinking management clinic was run by the specialist SLT, who was the clinical lead for eating and drinking difficulties. The service was for children and young adults who have complex eating and drinking needs and who did not attend the co-located school. Referrals could be made to this service by the SLT, general practitioner (GP) or paediatrician. The clinics were held monthly throughout the year. Funding was covered through a service-level agreement or individually commissioned service (source: Eating and Drinking Management Clinic leaflet developed by the CS01 clinical service).
Integrating support
A named paediatrician co-ordinated the MDT for nutrition and took responsibility for ensuring that PSS was provided. A key worker scheme operated through the school to cater for social care needs and represent children at health meetings. In general, however, the health team viewed the paediatrician as the ‘key worker’, although this term was not used. The joint surgical clinic included a consultant paediatrician in neurodisability, visiting paediatric surgeon from the local children’s hospital (tertiary centre), paediatric dietitian, paediatric SLT and nutrition nurse. This clinic was for children aged < 19 years with feeding issues that required a surgical opinion about the need for a GFT. Investigations were organised from the clinic. Referrals could be made to this service by either a paediatrician or a GP. Clinics were held six times per year (source: Joint Surgical Clinic leaflet developed by the CS01 clinical service). Surgery for the insertion of a GFT was performed at the tertiary hospital, with the surgeon leading the process and community nurses supporting the parents before and after surgery (CS01, S10, FG).
Integrating support: health and education
This case study site provided a highly specialised and resource-intensive service characterised by a high level of integrated care between NHS therapy and health services and education, which enabled support around the decision-making phase of a GFT for school-aged children, post-gastrostomy care and feeding choices before and after surgery. Integrated care was enabled through a three-way partnership between the clinical services, co-located school and children/families. Integration was manifested in the way that health care was personalised to the needs of individual children, embedded in the school curriculum and co-produced by teachers and therapists working together (therapists were involved in teaching and teachers were involved in health care).
Parents interviewed at CS01 identified their main support as coming from the co-located school, where multidisciplinary working takes place, facilitated by the partnership between the school, parents and clinical services. They often compared their experiences with previous experiences of their child in other locations:
They’re very sensitive to the needs of the children here [in the school] and they group them accordingly . . . I can honestly say that [name of child], and all the children here, they’re in a very good place. And I think in order [to achieve] . . . what constitutes a good environment for children with needs, is having the clinical services, the experienced staff all the time and the school together.
CS01, parent (P)2, focus group (FG)
The benefits of integrated health care in minimising health-care burden (e.g. attending appointments, time out of school to attend appointments) were valued by parents:
All schools around the country for children with physical disabilities should be like [CS01 school]. When you come to [CS01] you can say that and I always say ‘give a child and a parent 6 months and you’ll see the difference in both of them’, because the child has the team behind them, and the parent gets their life back.
CS01, P1, joint interview (JI)
The views of parents were supported by members of the school and clinical staff, but for them the emphasis was less on the co-location aspect of the school and more on the place where the MDT came together. As one of the teachers said:
In terms of the way the school is joined up with clinical services, we are a multidisciplinary team, or that’s one way to describe it. We join up with the therapists, as well as the nursing and doctor team. We have a bleep system where we can call nurses . . . We had a doctor in the classroom yesterday and three nurses.
CS01, staff member (S6), individual interview (II)
It is important to bear in mind that the clinical services at CS01 were not only for those children in the special school. Other children could access the clinical service as an outpatient but could not access all services owing to the unique funding arrangements at CS01. However, we were not able to conduct interviews with families attending other schools.
Psychosocial support
Policy and guidelines
Children’s rights to psychosocial, emotional support (although not specifically about feeding) were enshrined in a charter that underpinned the work of the school and the clinical services. It was co-produced by children and young people in conjunction with care staff, allied HCPs and nursing and teaching staff. The charter stated that to be as healthy as possible, children can ‘[r]ely on an adult to have up-to-date information about their health needs and impairments, including psychosocial and emotional needs, as well as their health and medical needs’ (source: charter outlining children’s rights while in the care of services developed jointly between the clinical services, school and children and young people). The charter then stated that ‘these rights must be actively supported and embedded in practice at [CS01]’. The values and rights are reinforced through staff induction, ongoing training and integrated teamworking, and feature in job descriptions (local principal investigator, CS01, 2019, personal communication).
Staffing arrangement: psychosocial support
At CS01, support for feeding issues could be provided by any member of the MDT and was usually provided as part of the appointment. There was a psychologist, clinical psychologist and psychiatrist within the clinical services; the psychologist worked with children with behavioural difficulties in the school. Psychologists did not routinely participate in appointments with families but could be drawn on as the need arises and can support the team. A clinician reflected on how this works:
So, you need to go up a tier, and when I say up a tier, involve someone else if it’s not working well. So, here, for example, we have a behavioural therapist who works within this team; it isn’t part of our clinics, but if there was a concern, then I would involve them because they’re more rehearsed and have more skills. And then again, it’s that integrated working, working together to try and do it better.
CS01, S10, FG
Feeding practices: risks, values and emotions
Clinicians generally had a good appreciation of the values that parents attached to feeding a disabled child and the difficulty that some families experienced accepting a recommendation to have a GFT and, in some cases, to stop feeding children orally:
I think it’s a very mechanical way of feeding a child and I think if you’re a mum, sort of loving, nurturing and caring is really closely wrapped up in feeding, so I think if you’re having to do something that’s so clinical in terms of nurturing your child, you’re removing some of the closeness and bonding and relationship factors within that relationship. So, I think that’s really important that that’s managed carefully.
CS01, S3, II
The risks associated with oral feeding and association with poor respiratory health were seen as a particular stumbling block for parents:
And I think in some cases where there has been a real danger, a real worry about aspiration and [children] becoming repetitively unwell with chest infections . . . it’s sometimes quite hard for parents to believe it’s to do with their eating and drinking. . . . I think parents have had a lot of resistance to that idea, because I think probably, it’s almost parents feeling that it’s their own fault that their child has been ill.
CS01, S4, II
The emotional aspect of the consultation and parental need for support was acknowledged:
We do give emotional support because we explain to them exactly what we’re going to do, and what the benefits and the disadvantages are. We also listen to the parents and sometimes they say, ‘No, no way, I don’t want this’. [Murmurs of agreement.] Well, we don’t want to force them to have it, we understand that, but we do try to convince them it’s really in the interests of the child, and we will try to convince them, so it’s actually very emotional work you do, you can’t change that.
CS01, S1, JI
However, another professional in the same group felt that the support they provided to families was not always enough. The professional commented that the practice of documenting that the risks and benefits of the procedure had been explained to parents in the clinical notes might address the medicolegal aspects of a surgical intervention, but did not always guarantee that the emotional aspects of the procedure had been addressed to the satisfaction of parents. The consequences of not having adequately prepared families for the procedure were evident in an example recounted by the clinician, although it was stressed that this was not a typical case:
They [the family] didn’t feel supported . . . so, they just felt it just all happened so quickly, and they didn’t really know what was happening.
CS01, S2, II
In one observation of the joint surgical clinic involving the MDT [surgeon, consultant paediatrician, dietitian and SLT] prior to the clinic, a child’s case was discussed, including the medical history, current feeding issues and potential solutions, and recommendations were identified jointly. The parent (father) was then brought in. He engaged in conversation with the SLT and dietitian, who recommended that he made a one-to-one appointment within the next few weeks to make sure that fluid intake was under control. The observer noticed that, although care was taken in the meeting to check the father’s wishes, emotional issues were not raised or discussed (CS01 clinic observation notes).
Another member of staff felt that having additional appointments separate to routine clinical appointments would improve how the team communicated and delivered support. There was a feeling that a lot of communication was happening in e-mails that was not the optimal way to provide support:
I would like to identify set points where a conversation is had with the child outside of a clinic appointment, because I don’t think that that . . . I think it’s a bit ad hoc at the moment, and I’m sure that some people are getting missed in terms of that.
CS01, S8, JI
The nurses were perceived to have a key role in providing support to families because they were the ones working closely with children and were better able to address parental concerns about the lived experience of having a GFT, for example what it means to have a GFT, how parents would manage the GFT and how parents would feed their child. Dietitians were also seen as playing a key role.
The dilemmatic65 and emotional nature of feeding practices, particularly where a child is not able to communicate her own preference, is nicely summed up in a joint interview involving two mothers in which one mother is reflecting on feeding her child by mouth even though her child has a GFT. The second mother clearly recognises the importance of oral feeding to her friend’s maternal identity. This psychosocial aspect of feeding contrasts with the very factual approach to explaining the risks of the procedure and does, perhaps, speak to the complexities involved in supporting parents. Information about risk appeals to reason but not to the emotional investments in feeding a child food by mouth:
It’s like I said, feeding, it’s an issue, but is it my issue? How much of it is my issue and how much of it is [name of child]’s issue? I know what [name of child]’s issues are. She physically finds it [eating] hard work.
But how does it impact on [name of mother] as her mother?
But psychologically, I know it [child not eating] upsets me but does it upset [name of child]? Is [name of child] thinking, ‘thank god I haven’t got to eat anymore’? I’m thinking, ‘I want my child to eat’, and [name of child] is probably thinking, ‘thank god I haven’t got to go through that every mealtime’. Do you know what I mean? I don’t know.
CS01, JI
Post-gastrostomy support
Many parents felt that post surgery was when care could break down, with parents being insufficiently prepared before discharge. Parents had to learn new nursing procedures post gastrostomy, such as replacing the gastrostomy button. There was a recognition that in learning these new skills they avoided trips to hospitals and saved the services money. There was a perception that some clinical staff in hospitals could not perform these tasks, attesting to the skills and experience parents developed:
I’ve found that not enough nurses or even doctors know about inserting the [name of gastrostomy device]. We’ve taken [name of child] to [name of hospital] on a number of occasions before I became used to inserting the [name of gastrostomy device] myself, but not many know how to insert the [name of gastrostomy device] button. On the last occasion that we had to go to [name of hospital] to do it, I had to do it myself and I think more training needs to be given to all of the nursing staff and to some junior doctors.
CS01, P2, FG
One parent described how she had accidentally perforated her son’s bowel trying to replace a gastrostomy button and how she needed to build skills to perform the task. In conversations about practical support, parents in the FG talked about care after surgery being very much a case of the ‘luck of the draw’, for example being discharged from the ward after surgery with or without a care plan for feeding, getting good support from the home enteral feeding company from which the nurses could be helpful or unhelpful, and good or poor access to community nurses.
Procurement and equipment
Obtaining the right equipment and spare parts were viewed as a ‘lottery’ reflecting local procurement policies. Parents reported having to negotiate or ‘battle’ to obtain equipment:
It is luck of the draw in everything though [murmurs of agreement] because we’ve just been swapped our community nurses, so we’re now in a different area. I don’t know if I should be naming areas or names, but the previous one, difficult to get equipment, difficult to get even two extra syringes a month!
Oh, yeah!
You e-mail, phone, plead your case.
Mmn.
CS01, P2, P7, FG
The practical difficulties and frustrations involved in obtaining equipment reflected an ongoing need for support across the life course, although these needs were met to some extent through parental peer support. By way of example, in the FG parents began to advise each other about how to resolve some of the issues raised in the above extract.
When asked who the ‘go to’ person for help was when difficulties arose, the parents clearly indicated that this would depend on the issue at hand. Different people based in different locations had various roles in providing advice and support, delivering supplies and managing equipment. Some parents demonstrated that they were sophisticated service navigators in finding the services, people and solutions (including equipment) that they required to solve the problems they experienced. Others, however, may be less adept.
Parent peer support
Case study site 1 was characterised by a strong parental network facilitated by the unique and integrated relationship between the school and clinical services, an active group of parents, a support worker available to facilitate communication between the school and clinical services, a space for parents to meet, an on-site café and a site-specific social media site. Those parents who drove their children to school (car parking facilities are available) were often able to meet with each other. Both HCPs in the clinical services and staff members in the school commonly expressed the view that parental peer support was highly beneficial because it enabled parents to discuss issues openly, including the benefits of GFT feeding, without feeling undue pressure from professionals, and offered advice on post-gastrostomy care. This was confirmed by the parents themselves:
And that’s a lot of how you get information with kids like ours; it’s not because the professionals are telling you but because you hear it from other people, other parents.
CS01, P1, JI
I think often parents have more useful information than professionals . . . and they are easier to get hold of than, for example, consultants.
CS01, P2, FG
Seeking online medical advice and support from other parents about a GFT (pre and post GFT insertion) seemed to be a common practice:
Facebook is a great tool for parents to chat and share experiences and information. There’s a lot of groups now on Facebook, feeding groups and blended diet groups, reflux groups, so I got a lot of information from groups.
CS01, P2, FG
This was confirmed by a teaching assistant:
[The group] only started a couple of years ago; it’s a Facebook group and they also meet; they have regular social events. They have clinical information meetings as well, whereby whether you’re a parent that’s over in [name of place] or whether you’re a parent that’s 2 miles down the road, and you’ve got a query about your child but you don’t know whether to take it to a clinician, you can just pile it in and other parents are quite often very helpful at saying, ‘Oh, have you thought of this support or that support?’, or somebody says, ‘Oh, the gastrostomy is looking a bit sore; have you tried any tapes underneath it that will work?’.
CS01, S5, II
Parent coffee mornings were a feature of the partnership with the co-located school and information sharing at CS01. These sessions ran every half-term and were led by the support worker, an individual whose role was to link the school and clinical services but who also had a key role in supporting families around funding issues. The sessions also offered parents the opportunity to Skype, which was useful for parents who did not live within a reasonable commuting distance. An observation of the parent coffee morning session that aimed to address a specific issue (BDs) revealed that, in addition to parents/carers, they were attended by various professionals at both clinical services and the school, including a SLT, nurse, consultant paediatrician, dietitian and support worker as well as school staff members. Parents were able to share their concerns and experiences; staff members listened attentively and offered solutions.
The success of the parent support network was evidenced by the fact that parents at other schools (where parental networks were absent or less well developed) also made use of the network at CS01, which served as a hub of support. However, it was reported that not all parents accessed parental support events or group meetings at CS01 or on Facebook (CS01, P1, parents FG). This could raise the issue of equity of access to support for those parents who would have liked peer involvement.
Decision-making
Parents at CS01 were asked about the process of decision-making for a GFT. The emotional side of the decision was mentioned extensively by all parents, who referred to the decision as ‘horrific’, ‘unnatural’ and ‘the hardest decision as parents’ they ever had to make. There was a suggestion that having a GFT was not ‘what normal able-bodied people would do’ (CS01, P5, IPI). The importance of food and feeding was mentioned and a sense of failure when unable to feed a child. As one mother said:
I felt like I’d failed because the only thing you want to do for your child really is feed them, isn’t it? So, it’s the most important thing you can do for your child, it’s the first thing you do for your child and you continue to do it until they learn to do it for themselves, don’t you? . . . They were asking us to make a decision which, for me, was a very scary decision; again, it feels so abnormal.
CS01, P5, IPI
There were also concerns about how parents would manage feeding with a GFT in the context of family mealtimes, and how others beyond the family would react or cope:
I was worried about other kids feeling alienated by it, not understanding, and I didn’t want people to have any more reason than they already had to be disconnected from [name of child] really, to kind of judge him as different . . . I worried about the extended family; you know, so much revolves around eating together, going out and eating; I just couldn’t imagine it really.
CS01, P5, II
Despite the concerns and the emotions regarding the decision, there was a recognition that in many cases there was no option: the parent(s) had ‘run out of options’, were exhausted with the efforts of trying to feed the child and understood that the child’s health was deteriorating. Parents felt that presenting the GFT as a temporary, rather than a permanent, intervention was something that would have helped, giving them hope that the child might eat by mouth at some point in the future.
Thus, the key concepts for parents included fear of the unknown, feelings of guilt and maternal failure, learning to accept a different (‘abnormal’) way of feeding, the potential for stigma or perceived difference, the conflict engendered when weighing up the options or indeed of not having an option, and having to manage new nursing procedures and medicalised ways of feeding post surgery. The management of equipment and supplies was particularly burdensome owing to local procurement policies.
Decisional conflict
Staff at CS01 were cognisant of the emotional aspects of the decision for parents and families. When asked how staff supported the decision-making process, a dietitian explained that it was often an individualised decision depending on a family’s acceptance of the situation and child and family circumstances:
It really depends on the family; I think you have to make a decision, a pre-emptive decision on how you may feel the parents will take it, depending on the amount of time you’ve worked with them, their personality, the experiences they’ve had. Also, the experience of the child and the young person and what they’ve been through, if they’ve had a tube in the past, if other people have said it to them, if even they’ve thought about it as an option. So, I would certainly want to tell the family that we need to give everyone the benefit of the doubt at first, and we’re not at all pointing the finger or giving any blame to anybody, because I think the first initial thought is of guilt from the parents that they’re not providing the right nutrition for their child.
CS01, S8, JI
There were instances where the decision was not straightforward and it was generally agreed that multidisciplinary working, where decisions were shared and made collectively, was necessary before going down the safeguarding route. In comparison, staff in the community were perceived to be more isolated:
My feeling is, talking to some other therapists in the community, that they’re much more isolated in that decision-making process with families, and that’s quite scary. Whereas here, I think it’s much more of a collective responsibility.
CS01, S8, JI
There was a perception that therapists working alone in the community were much more likely to prescribe a nil-by-mouth feeding regime following video-fluoroscopy. This had resulted in a protocol at CS02 to ensure that video-fluoroscopy was repeated as part of a MDT approach.
When asked about potential conflicts, staff suggested that they usually agreed among themselves on the decision, but where there was a difference of opinion it was necessary to be consistent in the presentation of information to parents:
So, we need to be consistent, not necessarily to say we disagree, but if we disagree, we need to have that discussion without the parents there, not to confuse them. Not on the decision they make, but on the information we deliver.
CS01, S2, II
However, because of the value parents attached to feeding children orally, and the assumed quality of life associated with oral feeding, HCPs tried to go the extra mile to support families to manage the risk. For example, building in physical exercise to improve muscle tone and swallow function prior to eating a meal was one strategy personalised to the needs of a child.
The HCPs also spoke about the emotional impact on them of managing conflict and issues about safeguarding:
I can think of another instance where the parents were very much into healthy eating and the child was not thriving . . . and you can see a very chaotic child in front of you and I was not being able to . . . I wasn’t getting anywhere in my conversations, so it can be intensely frustrating at that point. [Murmurs of agreement.] And also, in the back of your mind, there is always the question, is this a safeguarding issue? [Murmurs of agreement.]
CS01, S9, FG
Guidance on eating and avoiding choking and aspiration was available for parents/carers and school staff (source: eating and drinking guidance at CS01). This drew on a system of traffic light codes that identified the level of experience needed by the person assisting the child. According to the document the assigned assistance code is reviewed every term by the speech and language therapy team.
A member of staff who was the lead for safeguarding recalled only one instance of involvement with a child who needed to be fed in a particular way because of safety considerations. Another member of staff described the conflict she felt between her safeguarding role and her role providing support for parents:
Obviously if there are significant safeguarding concerns, they need to be addressed, but I think with my role it’s very much about building up trust and relationships with families, and I’m very keen for that to be done.
CS01, S4, II
School staff and clinicians at CS01 therefore aimed to support families with decision-making, establish a relationship of trust, provide consistency of information and involve parents in decision-making. Staff members were mindful of safeguarding issues and formal proceedings were rare.
Blended diets
Blended diets, in which blended food that is prepared at home (as opposed to formula only) and administered through a GFT, were highly topical at CS01, with a parent coffee morning devoted to the use of BDs. Although not officially recommended, at CS01 there appeared to be a permissive approach towards BD use, with some staff members offering more proactive support. However, it was suggested that conflicts arose – not just between HCPs and parents but also between HCPs themselves – when the child was considered ‘very malnourished’ (CS01, Pr FG). Although school policies allowed food prepared at home to be administered in school, they did not permit the blending of school meals, suggesting a form of risk management whereby parents rather than the institution owned the risk. 20
Staff training
In relation to the training of carers, parents at CS01 took on a major role as ‘feeding experts’ and provided guidance and training to school staff on how to feed their children orally, whether that be in the school or in the community. In the FG, one of the parents (CS01, P2, FG) described their role as follows, with others in the FG signalling agreement:
I come in to do training, I’m training someone up, a different person, and I’m quite surprised to see how many children are eating orally; it’s nice to see it. But on the other hand, I do understand with some parents, there’s no choice and it is too unsafe. [Murmurs of agreement.] They’re very good at listening and we’ve trained very good carers here I think.
CS01, P2, FG
Thus, the important aspects about the training of staff from the viewpoint of parents was that they considered it their responsibility to ensure that staff knew how to feed their children and that they were best placed to give this guidance because of their often considerable experience of looking after one or more children with feeding problems.
School staff members attend induction training that includes training on supporting communication and eating and drinking for children and young people with complex neurodisability. Training on GFT use is provided by the nursing team. When asked about any training or preparation they may have had to offer emotional support to parents and families, clinical and teaching staff members highlighted a gap. One professional shared a concern about the lack of formal training in psychology and how approaches should be tailored to the needs of individual children:
I think [I] find it very difficult because we’ve had no training in psychology, and I think [name of professional] is typically on the forefront of it and I do feel quite vulnerable, because I don’t know the exact strategy to give them. I haven’t been trained in cognitive behavioural therapy or behavioural change or anything, and I find it sometimes a struggle to work out how I can motivate a family without having learnt psychology knowledge.
CS01, S8, JI
Teaching staff interviewed at CS01 were also parents of children with gastrostomies. Thus, they had experiences and backgrounds that influenced their knowledge of caring for children with complex feeding needs. One described her training and rationale:
I am gastrostomy trained and jejunostomy trained, and I am able to do everything that needs to be done in class. I also support parents, and the reason I trained to do gastrostomies and jejunostomies was not only because my [child] had it, but also because I like to know what I’m expecting my staff to do, and I also like to be able to converse with parents about what their children need.
CS01, S6, II
This teacher described that through caring for her own child her knowledge was gained through experience rather than formal training. Since becoming a teacher, she had received formal training, with observation by nurses and SLTs until competent. This was made possible by having the clinical services on site.
There were ‘strict’ controls in place whereby staff were not allowed to feed children until the training had been undertaken successfully. However, none of the teaching staff members referred to training to cope with the emotional aspects of GFT feeding.
Summary
In conclusion, while staff at the forefront of feeding, especially those in the school, were well trained for the physical procedures involved in feeding, it appeared that specialist training on how to provide emotional support to parents/carers or children was lacking. Informal sources of training through shared learning among members of the MDT, including psychologists where needed, were mentioned. Psychologists did not form part of the core team, although they could be drawn on as and when required to support staff. Some parents held the view that although emotional support was important there were potential barriers to how this could be provided. In a feedback session with parents, for example, concerns about referrals to professionals outside the team (e.g. a psychologist) were raised as these may be construed as the team ‘passing the buck’ and adding to the burden of appointments. Concerns were raised about the amount of time it would take to get an appointment with a specialist for PSS. Some parents also felt that, because the children often had complex needs, emotional support should be available for a broader spectrum of issues across the life course, not just related to feeding.
Case study site 2
Overall description of the case
Case study site 2 was a generalist service with a highly specialised MDT for children with complex feeding needs. The team was employed by a Scottish Health Board within NHS Scotland. Children and families were seen at home, a clinic, a school or in other community locations. Referrals came into the service via paediatrician, paediatric dietitian, SLT or GP. The service served an area with a large rural catchment.
Staffing arrangement
Each child with complex feeding needs had input from a consultant paediatrician, dietitian, SLT and children’s community nurse (CCN) who cared for children until either GFT feeding was no longer required or they transition into adult services. The MDT aimed to see children with complex feeding needs as close to their homes as possible in line with the Health and Social Care Delivery Plan. 66
There were established links with specialists at the tertiary hospital (included a paediatric gastroenterologist and paediatric nutrition nurse specialist), although this was 45 miles away. Further assessment of children took place at the gastroenterology clinic at the tertiary centre before appointments with surgeons for the placement of a GFT. Post-gastrostomy care was the responsibility of the local MDT. The CCN team provided the immediate care regarding the gastrostomy site (stoma). The paediatric dietitian organised the initial delivery of the GFT feeds and equipment to the child and family home, after which the CCN team arranged the delivery of the feeds. Figure 5 shows the configuration of care at CS02.
FIGURE 5.
Configuration of care: CS02. HV, health visitor; OT, occupational therapist; SCBU, special care baby unit.
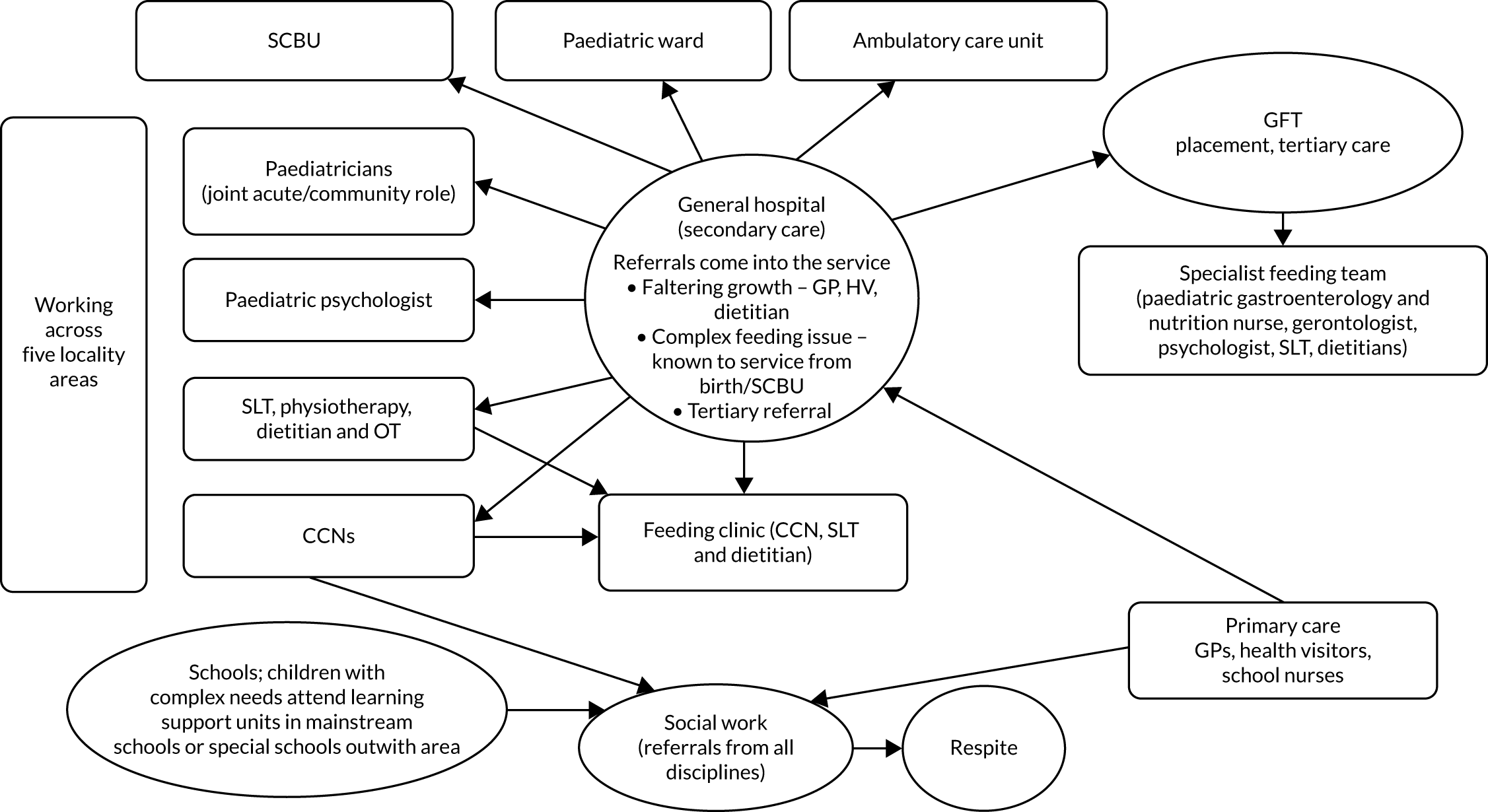
Integrating support
There were two mechanisms for integrating support: meeting around the child (MAC) and home enteral feeding clinic for children (HEFCC).
Meeting around the child
A MAC involved the CCN, paediatrician, SLT, dietitians and consultant paediatricians. Also in attendance were parents/carers, school staff members, health visitors and children’s social workers. Health visitors would be involved with younger children but did not have a role in caring for the child’s GFT. A MAC was part of the child’s planning process following the principles of getting it right for every child (GIRFEC). 67 Getting it right for every child is the policy directive in Scotland that aims to support families by making sure that children and young people can receive help, at the right time, from the right people. A MAC took place in the setting that was convenient for the child and family, and the frequency depended on the child’s and family’s needs and the availability of staff. Once needs were identified, support for the child was provided from the team around the child (TAC) through a Child’s Plan and co-ordinated by a lead professional. In addition, children with complex feeding needs would have a named dietitian, CCN, SLT and paediatrician.
Home enteral feeding clinic for children
Children and young people with complex feeding needs were usually seen every 6 months in the HEFCC as part of a MDT review. There were regular, monthly HEFCC meetings with MDT members including the CCNs, SLT and dietitians. These team members also provided outreach visits, based on the individual child’s needs, across a large geographical patch. Paediatric dietitians provided a specialist dietetic service to infants and children who require home enteral (GFT) feeding. They also provided shared dietetic care for those children requiring specialist services at tertiary centres. The paediatricians had a joint hospital and community role. A HEFCC could be delivered in schools.
Psychosocial support
Policy and guidance
The need for emotional support was enshrined in a best practice statement68 and clinical guidelines that recommended psychosocial assessment, including of the psychosocial impact of commencing GFT feeding for the child and family, and referral to a paediatric psychologist. The NMCN CEN aims to strengthen specialist services for children with complex and exceptional health-care needs in Scotland. The NMCN CEN is one of a range of specialist networks within the National Network Management Service (NNMS) that aims to drive improvement and has co-ordinated several initiatives to facilitate PSS, including a best practice statement and additional resources. These include:
-
An information leaflet for parents/carers whose children need help with feeding. It recognises that the impact of GFT feeding is different for everyone and supports discussions around the feelings that parents may experience.
-
A digital versatile disc (DVD) called How Does It Feel: The Emotional Impact of Tube Feeding that discusses the emotional impact of GFT feeding.
-
An e-learning toolkit developed in partnership with the University of Stirling. One of the modules, ‘The emotional impact of tube feeding’, aims to develop knowledge and experience around the potential emotional impact for families when changing from oral to GFT feeding. It emphasises the need for continuing support.
Staffing arrangement: psychosocial support
The multidisciplinary model at CS02, involving professionals from the CCN team, in consultation with their colleagues, was reported as a key aspect of support in relation to GFT feeding. Parents at CS02 were typically referred to either community nurses or individuals such as the dietitian and the SLT as sources of support:
I think the community nurses have always been good at listening. There were times when I really relied on them a lot just to talk about different aspects of [my child’s] health; I’m sure feeding would have come into it.
CS02, P2, II
The community nurse, that’s who I usually go to about any worries. I can just quickly message her and say, ‘What do you think? Could you come out and have a look?’.
CS02, P3, II
We were being given home visits at the beginning, which was key. It started when the speech therapist paid a home visit and we had the conversation about my child having made a choice basically that he doesn’t want anything orally. And she then suggested a home visit with a dietitian. And the dietitian was able to give us much more information on the medical aspects of what was involved with having the operation and then the feeding after the operation.
CS02, P8, II
The [paediatrician] was a massive influence on us for the first few years when we were here, and she was really supportive.
CS02, P5, II
An important feature was the continuity of relationship with these HCPs:
In terms of the medical team in the hospital and the services, apart from the nurse those who most helped with the decision were our paediatrician and our neurologist; they were both very involved and they’re still our doctors . . . It’s important to us that our neurologist and our paediatrician have always stayed the same.
CS02, P5, II
One of the important things is having people who know us and know our child . . . She’s been our community nurse for 8 and a half years, so we’ve got a really good relationship.
CS02, P6, II
By contrast, another parent identified a lack of support from the GP in the decision-making process and subsequently:
I feel like our GPs, and it doesn’t matter whether we’re in [that place] or [another place], don’t know my child at all and they make very little effort to get to know [my child]. And therefore, they’re not supporting me, they’re not supporting the rest of our family.
CS02, P5, II
At CS02, any member of the MDT could refer parents for specialist PSS. However, despite policy and guidance recommendations, there was no established process for the MDT to record psychosocial assessment or monitor that it had taken place. Those parents who were interviewed did not comment on any such referrals, although none would have been at the stage of having had a recent gastrostomy or change of feeding system. Interviews with staff members suggested that such referrals were rare and used on an ‘as required’ basis rather than a routine requirement for all children who are GFT fed. It would seem that paediatric psychologists, although embedded in other chronic-disease MDTs, such as diabetes MDTs, would see children with complex feeding needs and their parents less routinely:
Because with other services in the hospital, we’re kind of proactively a member of the multidisciplinary team and we hear about kids, like in the diabetes service, I’m quite involved in their team. Whereas with the feeding, they’ve obviously got their network of people that are involved and then I think they’d have to reach a . . .
Point.
Point, and then think, oh, maybe we’ll ask the psychologist, because it hasn’t really come to us that much, and maybe that’s a wee bit of something that needs to be looked at.
CS02, S3, II
Involvement of a psychologist tended to occur after the feeding intervention to work on oral feeding rather than during the decision-making phase:
I could talk more in terms of having seen families where they’ve maybe had NG [nasogastric] tubes or had PEG [percutaneous endoscopic gastrostomy] feeding, but this is now later, where they’re trying to re-establish more oral feeding. And I think there can be quite a lot of difficult issues at this point. I felt the cases I’ve seen, and I know my colleague has had a couple of cases too, there’s often been quite heightened maternal anxiety: the children are not getting enough nutrition or they’re not eating a wide variety of foods or textures.
CS02, S3, II
The need for emotional support
A children’s social worker saw his role as a listening ear and acknowledged the emotional nature of the assessment process – ‘taking the parent back through the cycle of grief’ (CS02, S2, II) – but this support was of a more general nature and time limited; support was seen as the role of the health services.
Staff members in a learning support unit based in a school made the point that the emotional needs of parents, families and children can vary depending on the individual. They provided two contrasting examples:
For one family, because [the child] is so competent, we don’t feel the need to support the family in that at all. But then we have another [child] who is in [name of school], who the dietitian and paediatrician actually are quite keen to put on PEG feeding, but the parents are very much against it for a number of reasons. There are huge issues around [the child’s] eating and [the child’s] mum is very anxious about [the child] not gaining weight, and that then creates a bit of a tension between school and home sometimes because she’s not always convinced that we’re doing our best, which is coming out in her anxiety.
CS02, S9, JI
A nurse manager also commented that, although many parents become very knowledgeable about the technical aspects of care involved with GFT feeding their child, they were parents first and foremost and needed to be supported as parents and their emotional needs catered for.
Parents expressed different needs for emotional support. One mother reflected on the decision and, with hindsight, felt that she did not cope well and could have benefited from support:
And I definitely think there were parts within my life, looking back now, where I don’t think I did cope very well, and I think I probably was suffering depression and things like that. And it’s only now I’ve come through it all that I can look back and think, ‘God, how did I even get up in the morning!?’. I think when I look back, it could have been an easier experience had I had more support emotionally, rather than me just putting on a brave face, saying, ‘that’s fine’.
CS02, P5, II
Another parent (CS02, P6, II) felt that the situation had changed from one where emotional support was not offered to the current position where specialist nurses were identified with whom a bond could be made. When asked about the provision of emotional support, another parent referred to support from a SLT, though made the point that it was also necessary to come to terms with the situation herself:
The speech therapist was the person that had left the door open and said, ‘Any questions, any worries, phone me or I’ll come and pay a home visit’. But I think I’d had so much information, there was only so much you could take in and it was just, for me personally, coming to terms with the fact that he was going to be fed this way. So really it was for me to do that, it wasn’t anybody out there that was ever going to help me with that; I had to personally get around to that myself.
CS02, P8, II
Similarly, other parents were equivocal about the need for emotional support and presented a stoical front of having to ‘get on with it’, which may be an artefact of the timing of the research in relation to parental decision-making, given the passage of time. Moreover, different issues trigger different anxieties and support needs. The practical support needed around managing the GFT may be a more pressing issue than managing the emotional labour involved. Historical accounts of decision-making and support needs may also be constructed differently from more recent accounts in which parents are in the heart of the decision. Notwithstanding these limitations, parental accounts were often still very vivid, and they used emotive terminology to describe their experiences: oral feeding was ‘terrifying’ because of the risk of aspiration and chest infections; the reaction to the recommendation of a GFT was either ‘scary’ or parents felt ‘relieved’.
The role of schools
There was no special school provision at CS02, and most children either attended a learning support unit in a mainstream school or had a shared placement between the learning support unit and the mainstream school. Some children would attend special school in other areas of Scotland or England. Nonetheless, in interviews, parents did identify schools as a source of support:
Yeah, [the school] is fantastic. Really, really open door. On the phone all the time. If they have a problem or they’re not sure of anything going on with [my child], they’re straight on the phone and I’ll come down, because I’m lucky, I just live [distance] away, so I can come down. And any training, they’re straight on it with the additional needs assistants, and pretty much all the ANAs [additional needs assistants] are trained up to deal with [my child].
CS02, P8, II
Another parent explained that school staff support did vary according to the issue that needed to be resolved and that the CCN was the main point of call for more complex issues:
There is a school nurse as I said but I think [my child’s] needs are so complex and so specialised that the community nurses tend to come into the school if there’s a [serious] issue or problem, rather than the school nurse, because CCNs are trained to deal with complex needs on a much more regular basis than the school nurses.
CS02, P8, II
Attempts to integrate therapy and education, as at CS01, were also evident in the learning support unit, for example in the introduction of problem-solving activities involving food and feeding practices into the curriculum for all children. This was felt to enable non-verbal children to express food preferences (CS02, S9, JI).
Parent peer support
There was no formal parental peer support group at CS02, although individuals were generally encouraged to engage with other parents and carers. The parents varied in the extent to which they felt that they needed or wished to relate to other parents. Reasons for not seeking out peer support included other work and family commitments, good existing personal and/or professional support networks, distance from the hospital and the feeling that there were unlikely to be other parents with similar issues.
Some parents had made informal contact with other parents (e.g. CS02, P8, II, and CS02, P6, II). One mother discussed informal meet-ups over coffee but stated that a more formal group event would not be something that appealed:
There are a couple of mums I meet up with occasionally and have a coffee with and just air everything out with them, and yeah, so I’ll have that but I’m not one for groups and things like that. That’s not my thing at all! I’d rather go out and have a nice cup of coffee and everything. Although that’s different though from having coffee with friends, because those mums have children with complex needs or disabilities, so they completely know where you’re coming from and they understand you.
CS02, P6, II
Clinical and teaching staff members at CS02 confirmed that they would suggest contact with other families if they considered that it would be helpful to the parents, though two did sound a note of caution that it would be important not to breach confidentiality. A paediatrician additionally raised several barriers to parents meeting up, including distance, geographical spread and lack of transport:
Part of the problem I think with this area is that you’re very aware that it’s quite difficult to put similar children together with other children, so you may be dealing with quite different conditions in their needs for gastrostomy feeding. And the parents are very spread out, finances and transport aren’t easy.
CS02, S1, JI
A social worker confirmed that they had experience of linking up families in the past that had resulted in unintended, positive consequences by families sharing the same carers, but issues of confidentiality were also raised:
We did run a support group for a short period of time, looking at linking families with other services and, as a result, they were then able to link up and to share: share difficulties, share positives, share advice of how to get things that they had previously got in the past. However, we can’t go around saying, ‘Oh, by the way, your neighbour up the street also has a child who is gastrostomy fed’. But by doing that support group, it linked them, and they were then able to link with each other and realise where in the locality [the other families] actually were. And as a result, quite a lot of them now use the same carers for their packages of care.
CS02, S2, II
Other clinical staff did not feel the need for a formal support group or for them to suggest linking with other families because there was a perception that families were doing this themselves using social media.
Decision-making
Parents at CS02 did refer to the process they went through when deciding to have GFT feeding, although these accounts were historical rather than recent. The decision to GFT feed was often a result of problems such as recurrent chest infections, compromised growth and an unsafe swallow:
. . . he needed more and at the time with the nasogastric tube, he was getting overnight feeds plus what they call bolus feeds. I think the decision was that it wasn’t quite enough and that fitting the PEG would make it a lot easier for him to cope with, and maybe less anxious about the whole business. And that kind of proved to be right, and we managed to get larger quantities into him that way.
CS02, P3, II
Not all parents felt negative about the decision if they felt that it was in the child’s best interest (e.g. CS02, P5, II) and that a GFT would benefit their child and help them to thrive. One parent (CS02, P6, II) admitted that she did not like the decision because it was ‘another step away from normality and into [a] medical [way of feeding]’ but accepted the decision when it was felt that there was no viable, safe alternative. The emotional and stressful nature of mealtimes also influenced the decision to elect for GFT feeding:
[The child] was about [age] when we got to the point where it was just becoming dangerous. [The child] was dangerously underweight, wasn’t eating, it was really, really stressful; every single mealtime, everybody was in tears. So, the nurse sat me down and said, ‘I think we need to be a bit more serious about this’. And it was the best decision ever!
CS02, P5, II
Various strategies for managing conflict were proposed by HCPs (e.g. CS02, S6, FG, and CS02, S4, II). These included explaining the advantages of GFT feeding for the child, engaging the parents in the decision, and referring the parents on to other professionals who may be better placed to advise or who could offer more weight or gravitas.
Decisional conflict
Professionals also stressed the importance of a team approach and relationships with families in arriving at jointly agreed decisions so that disagreements were uncommon:
I think we’re quite lucky that we know our families really well and because we’re such a small team, it’s not like the families are seeing loads of different people. I think we’ve always come to a joint decision with families.
CS02, S6, FG
Strategies also involved emphasising quality of life and challenging ideas that GFT feeding was regressive. Advice that oral feeding could become less pressurised and more enjoyable was another strategy adopted, although this was not safe for all children. There was a recognition that parents had different views about a GFT and simple questions asking where they were in their thinking helped staff to assess families’ preparedness to accept a GFT rather than any formal assessment:
I think we recognise that, well, for no two people is it the same, but for some they just cannot function . . . so functioning with a gastrostomy is the way they want to go and for others it’s the exact opposite, that a gastrostomy is a heart-rending medical intervention taking away their ability to orally feed their child. So we’re upfront and we ask them [what they think about it], because essentially we will take them through the fact that actually in the vast majority of cases, oral feeding becomes a much more pleasurable, enjoyable, less pressurised and social activity where actually your feed can be supplemented by gastric feeding.
CS02, S5, JI
Professionals were also aware of the possible tensions in managing disagreements, including the need to respect parental choice while ‘balancing up duty of care and medical needs’ (CS02, S3, II) and acting as ‘advocates for all of the children that we work with’ (CS02, S9, JI).
At the tertiary centre, which received patients for surgery from a wider catchment area, HCPs could not recall a case where safeguarding had been used around the decision-making phase for gastrostomy.
At the school, one staff member raised the issue of feeding and safeguarding. They had had concerns about parents orally feeding a child who aspirated and felt that, because schools were a front-line service responsible for the health and well-being of children, they were duty bound to act (CS02, S9, JI).
Blended diets
There was little evidence of parents using BDs at CS02, although at the tertiary centre, which covered a wider catchment area, staff reported an increase in the use of BDs more generally. It is of interest, perhaps, that professionals felt that there were more issues around safeguarding in relation to parental adherence post gastrostomy, particularly in relation to BDs, than at the decision-making phase:
Sometimes the more tricky bit comes where the family is managing the feed after the tube is in.
OK.
So you’re possibly going to run into situations there more than the actual getting the tube.
The compliance associated with it.
Yeah, because some families choose to do their own thing, and it’s not always the best thing, but they think they’re doing right. And then there’s the blenderised diet, it’s a big thing that’s coming out and it’s not the wrong thing to do, but it’s whether they’re doing it right. So that’s more your area where you might raise child protection for us as opposed to the getting of the tube.
CS02, Pr1, Pr2, JI
These risks and tensions (a pattern repeated across all sites) are discussed in more detail in Chapter 6.
Staff training
Training resources with a focus on the emotional aspects of GFT feeding were available. This included the NMCN CEN DVD How Does It Feel: The Emotional Impact of Tube Feeding, which was developed based on consultation with parents and carers, a young person who was previously GFT fed and professionals. There was evidence of formal educational provision: the NMCN CEN e-learning toolkit that had been developed in partnership with the University of Stirling as an online module. This toolkit explores best practice in caring for and supporting children, young people and their families and those who support them. It develops knowledge and experience around the potential emotional impact for families when changing from oral to GFT feeding and emphasises the need for continuing support. However, it is not mandatory to complete the module and it does not include a formal assessment tool for assessing the need for PSS.
When asked about training, school staff suggested that they had received ‘informal’ training to learn how to use the GFT, although the nurses who provided the training would have considered this to be formal. They also referred to care plans and guidance that, although not formal training, gave the ‘necessary information’ to assist parents and families in the care and utilisation of the equipment. They also mentioned that a commercial company was sometimes involved in informing staff and/or parents.
A health visitor and school nurse expressed in an interview that they felt that, because they rarely dealt with children and young people with feeding difficulties, there was a danger of them becoming deskilled. School nurses were not routinely involved in decisions about gastrostomy, or any care, in relation to GFT feeding; rather, their role focused on supporting the parents and other family members. They also commented that, although the ANAs in schools received training on the technical aspects of care, there was a perception that this placed a lot of responsibility on them. The CCN team would be responsible for offering one-to-one support for school staff and regular training updates (e.g. actions to take if a child’s GFT falls out and giving medication via the GFT):
For the ANAs, the outreach nurses tend to come from the hospital and train them, but because they don’t train them about absolutely every aspect that they’re going to come across, it’s really difficult, and they can get quite anxious.
CS02, S8, JI
The CCNs also received annual updates on managing gastrostomies run by the enteral feeding companies that offered hands-on sessions. The issue of resources and competing needs for training was also raised by staff in schools:
Training obviously would be good, but where do you stop, because there’s so many conditions that would be useful for us to know a bit more about in the community. [Murmurs of agreement.] And whether our managers would say, ‘Yes, it’s important for you to go and learn about that, as opposed to going to do something else it’s difficult to judge’.
CS02, S8, JI
These differences contrast with staff in the special school at CS01, although in the case of CS01 there were more children who were GFT fed in the special school. Maintaining skills is more difficult when the number of GFT-fed children is small.
Inequity in provision
Access to short-term breaks and respite care could be challenging as not all services were able to provide the level of support required for GFT or NG feeding tube feeding (CS02, S6, FG, and CS02, S2, II). In addition, it was felt that inequities might arise for families in remote settings whose GPs or local nurses lacked appropriate training. Children schooled outside the service catchment area were also felt to be disadvantaged because support from HCPs, specifically physiotherapists and SLTs, would not be available because they would be unable to cross over into the area where the family lived.
Health-care professionals also queried whether or not psychological services had the expertise to offer interventions for non-verbal children with complex needs compared with other children with long-term conditions:
I don’t know whether or not psychology could support children with a learning disability to get around behaviours about eating because of the learning disability. We deal with some children who are incredibly complex: autistic, non-verbal, a completely different set of motivations and barriers and boundaries. I don’t know that psychology would be able to have a significant impact and maybe that’s why it’s a gap.
CS02, S6, FG
Need for integrated working
A paediatrician (CS02, S1, JI) indicated the need for more integrated working in that children and families tended to have to go to different settings and people for their service:
And we do multidisciplinary working around them, but it’s not in one setting, a one-stop shop. So, we’d have a speech therapist, they might see a dietitian, I might see them, we might get a psychologist involved, but we don’t have a way of doing all that together, which I think would be much better and more timely, and probably then offset some of the problems.
CS02, S1, JI
This fragmentation also affected the management of the GFT site:
I’m not sure we have a co-ordinated approach to [the management of gastrostomies]. We tend to go, ‘Oh, we’ll try this’, and somebody will say, ‘Try that’, and you speak to somebody else and they say, ‘Have you tried this?’. And you know, that I think seems to me to be a bit fragmented and I don’t know whether that’s because of a lack of expertise in one individual. We have lots of different people; even within community children’s nursing, we have four or five individuals who are all looking after children across a geographical spread. We have seven consultants looking after a range of children across a geographical spread. So, we may lack some real expertise. This can cause a lot of discomfort for children and distress for families and seem to take a while to sort out.
CS02, S1, JI
The issues of parents having to go to multiple localities, the turnover of staff and the requirement to repeat information to different people were raised by a health visitor and a school nurse; both felt that a more co-ordinated service could be achieved:
There’s a problem here that seems to be with the speech and language therapists: they only get short-term contracts. So, somebody might develop a relationship with one, and then they ring up and discover she’s gone! And parents do not like repeating themselves over and over to different professionals, to a whole bunch of people. I think there’s various things been attempted in the past, like specialised notes – passport-type things – to try and cut down that. But it’s difficult because again the rurality we’re in, these children are mainly in mainstream schools, and because our capacity and workload is really stretched.
CS02, S8, JI
Summary
Guidance at CS02 recommended that parents be assessed for their PSS needs and referred to a paediatric psychologist, yet pathways for referral were not always clear and there was no mention of assessment tools by staff. Referrals to the paediatric psychologist were not routine but made on an ‘as and when required’ basis, although there was a feeling expressed by staff that the children may fall through a gap because they were mainly non-verbal communicators. Parents appeared to value relationship continuity. Parental groups were less in evidence than at CS01, with some parents preferring to receive support from professionals. Barriers to parental peer support were professional and parental perception of need and usefulness, and the geographical spread of parents, which may leave some parents at a disadvantage in remote areas where services are less developed. Child care and transport were also mentioned, and professionals had some concerns about confidentiality issues in putting parents in contact with each other.
Case study site 3
Overall description of the case
Case study site 3 is described as two contrasting services that refer to the same tertiary referral service. Therefore, we present CS03 as two subsites (CS03A and CS03B) and one tertiary centre (CS03C) (Figure 6).
FIGURE 6.
Configuration of care: CS03.
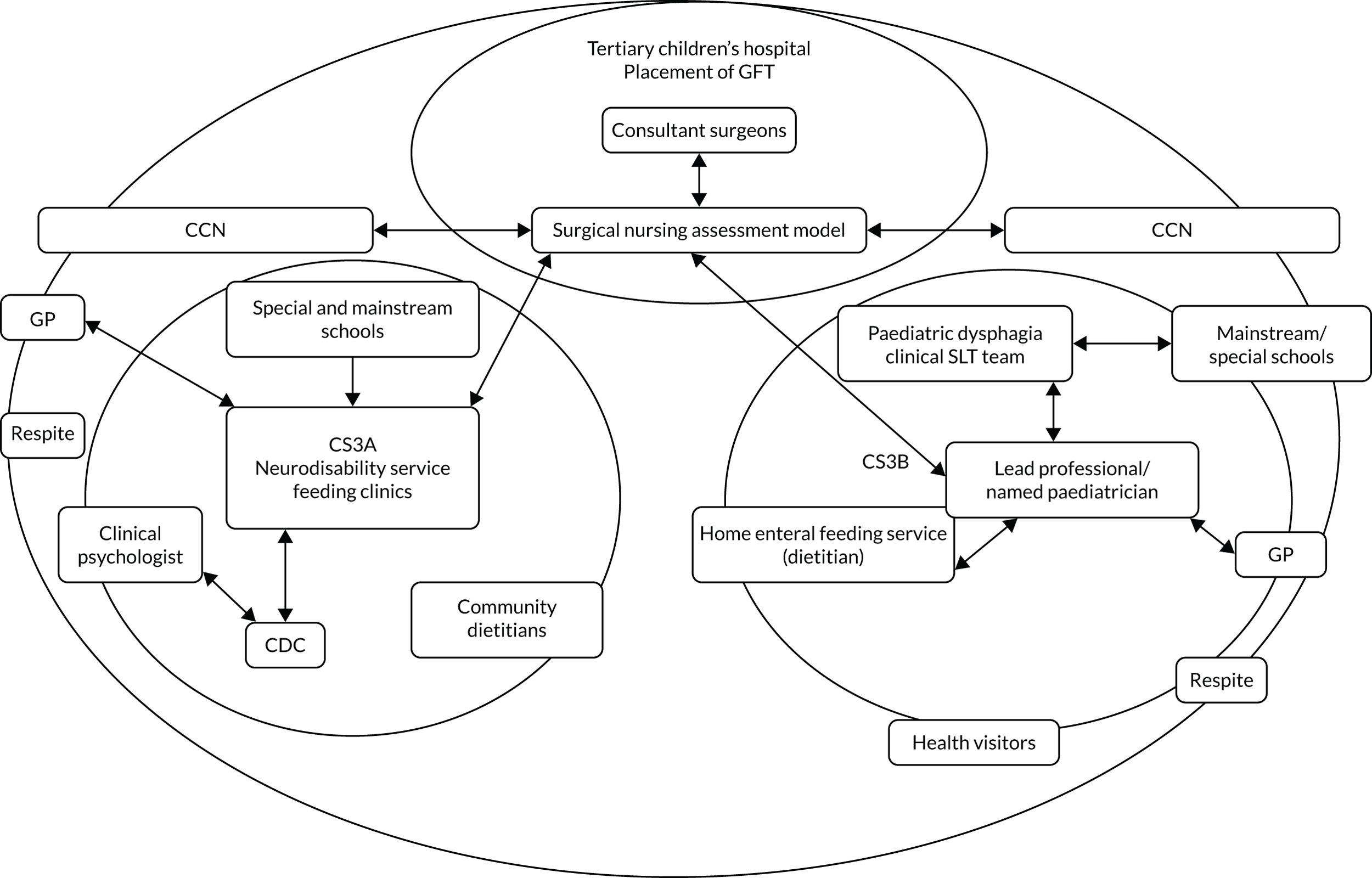
Both subsites can be described as district secondary care neurodisability services and were chosen to highlight comparative differences in resourcing, organisation and ways of working, although both services were employed by the same trust. CS03B did not have a fully integrated feeding clinic or access to a psychologist for support (a feature, until recently, of CS03A) and, therefore, relied on the lead professional to co-ordinate care involving a ‘virtual’ team. Of interest was a recently implemented surgical nurse assessment model at the tertiary centre that aimed to integrate, or link, community and tertiary health services and support families through the decision-making process. Differences between CS03A and CS03B were attributed to historical factors and leadership.
Staffing arrangement
At CS03A there was a dedicated feeding team and clinics. Feeding team meetings took place at schools or in the community and consisted of a paediatrician, dietitian, SLT, OT and, sometimes, school staff. If the feeding clinic was conducted in school(s), the teacher, teaching assistant and CCN attended. There were different feeding clinics:
-
the CDC clinic (only for children who are seen by the MDT and aged 0–3 years; most children are aged 0–2 years)
-
three school clinics for children attending special schools
-
two additional outreach clinics, one in the city and one in a rural area.
Referrals came from SLTs and paediatricians. Criteria for referrals to the feeding clinic were in place.
At the core of the CDC was a therapy group where preschool children are assessed. With regards to feeding, children were seen together with the SLT, dietitian and paediatrician, who were always present in the clinic, and OT or clinical psychologist for certain groups of children and parents. Between feeding clinic appointments, individual members of the MDT may have seen the child on their own and communicated with the rest of the team by e-mail.
Conversely, CS03B did not have a fully integrated feeding clinic and access to a psychologist was not usual practice. The community paediatrician, SLT, OT, dietitian and CCN saw the parent/child in a range of locations including clinics, at home, at school or nursery. CS03B offered clinics, school visits or home visits of usually a single profession, although there were some joint visits with therapists. In the past there had been joint visits involving a SLT and a dietitian, but, because the dietitian was hospital-based and employed by another trust at the time of conducting the research, joint visits were rare. Referrals to the service came through the GP, health visitor, school nurses or other primary care providers. Children seen were between the ages of 0 and 19 years.
Integrating support
Lead professional
Both subsites (CS03A and CS03B) relied on the lead professional, usually a paediatrician, to co-ordinate care. However, the organisational structure of teamworking was more informal at CS03B:
We don’t have very much of a formal service [to support feeding issues], so it maybe that I invite the speech therapist, for example, into my clinic to see them jointly. I would see them and then ask the speech therapist and probably the dietitian to see and they may end up seeing them jointly with the specialist health visitor or it may be that they have individual assessments. If they’re in the special school the community nurse, the specialist school nurse would also be involved.
CS03B, S2, IPI
The mode of working was described as ‘partially multidisciplinary’ owing to the lack of a formal specialist feeding clinic involving all members of the MDT. Instead, a ‘virtual multidisciplinary team’ (CS03, BS8, IPI) operated where staff members communicated with each other about children and families via e-mail and telephone. Although a multidisciplinary feeding clinic had been advocated for a long time, the service did not have the backing or funding for this.
The tertiary nurse assessment model: integrating community and tertiary health services
At the tertiary centre, children aged up to 16 years were eligible for a referral for assessment and placement of a GFT. There was no lower age limit; rather, the criterion for eligibility for GFT insertion was weight (≥ 4.5 kg). The hospital was the referral centre for up to 12 other hospitals. The service, therefore, covered a large geographical patch and provided outreach for a regional clinic. Recent changes meant that all referrals for the placement of a GFT were assessed by the surgical nursing team, in a nurse-led clinic, prior to families seeing the surgeons. Before this, children were referred directly to the surgical outpatients clinic. This change was implemented to reduce the amount of time it took for children to be accepted onto the waiting list for surgery. Nurses were given enhanced training to be able to perform this role. The nurses conducted pre-surgical assessments, trained the CCNs in the management of the GFT and, occasionally, trained school nurses and other staff. In terms of post-gastrostomy support, they contacted parents 6 weeks after the gastrostomy to check whether or not there were any complications associated with the procedure. This model is discussed in Integrating community and tertiary services: the surgical nurse assessment model.
Psychosocial support
Policy and guidelines
The document review identified two documents that specifically referred to the provision of support. The first (which covered both CS03A and CS03B) outlined the clinical objectives of the NHS feeding team. The second documented the feeding team’s clinical pathway, stipulating a MDT approach (defined as numerous professionals working together within a single agency) to provide support to parents. A core team is described in this document as ‘a paediatrician, dietitian and SLT’ (service document CS03). Other professionals may also include occupational therapists (OTs), physiotherapists, school or community nurses, clinical psychologists and preschool and school staff including early support key workers. The roles of this core feeding team were elaborated. Referral criteria to the feeding team included children known to at least two of the services involved. This document also suggested that the team would offer ‘support around decision making processes regarding non-oral feeding’ and ‘support for parents to manage increasing risk of aspiration in changing or progressive conditions’.
As part of the feeding assessment, the clinical pathway suggested providing opportunities to assess parental concerns, including the amount of time spent feeding and emotions around feeding. Emotional support appeared on a list of potential concerns rather than as a theme in its own right. Both CS03A and CS03B were expected to provide generalised support around feeding through goal-based outcomes jointly agreed with parents. Packages of care offered included ‘[s]upport around decision making processes regarding non-oral feeding’.
Staffing arrangement: psychosocial support
The parents interviewed at CS03A identified several members of the MDT who were involved in their children’s care. The number of individuals involved reflects the complexity of children’s care needs:
So, we’ve got a dysphagia speech and language therapist. We’ve got a dietitian locally. [The child is] also involved in a trial on [place name 1], which is a way to do the [name of diet] without having to do the [name of diet]. So, we’ve also got a dietitian based up at [place name 2] as well, our community paediatrician, and we’ve got a brilliant school nurse because [our child] is in a special school, and we’ve got a community nurse.
CS03A, P1, IPI
We’ve got the social worker. Then [the people we relate to have] got to link to each other and mainly we do the school pre-medical meeting once on every 3 months or 2 months, so that you’ve got the community nurse, you’ve got the health care, community health, and you’ve got the dietitian, you’ve got the school people, you know, you’ve got the [name] social worker and you’ve got everything, the paediatrician, paediatrician doctor, the consultant because she is heading the meeting, and then we’ve got the speech and language therapist.
CS03A, P2, II
In a FG of professionals, staff confirmed their roles in relation to what appeared to be a complex terrain of care influenced by geography and commissioning arrangements. The paediatrician described working across a specific geographical patch but also seeing children with complex feeding needs from the wider area. One of the community-based OTs reported seeing some preschool children in group therapy. The SLT described her role as providing community-based support to children with complex needs and feeding difficulties aged 0–19 years, from hospital discharge and for as long as needed. The paediatric dietitian worked only in the community, in schools, and provided a service to the feeding clinic in one of the schools. Her role was to ‘support nutritional assessments and children who are either orally fed or require enteral support’ (CSO3A, S1):
We work quite closely with three specialist health visitors, so with some of our most complex children we’ve been able to get to know them a bit and they get to know their families and feeding issues so that’s been quite helpful, again for longer-term support. And they visit in the home and they typically visit once a month.
CS03A, S1, FG
At the tertiary centre, specialist gastroenterology nurses would see parents and the child and assess and advise on the need for a GFT, including before a referral was made, reflecting a unique aspect of the model:
We book them into our nurse-led clinic and we run through why the gastrostomy’s been indicated, we talk about how the procedure would be undertaken, we discuss what will happen when the child’s in hospital, what will happen when they go home, what educational needs that they will need while they’re in. We discuss any concerns or queries that parents have got, and we would then put them on the waiting list. Also, prior to a referral even happening, we can meet with a family, discuss the pros and cons of a gastrostomy tube versus a nasogastric tube and whether it’s going to be beneficial for this child as part of, really, their counselling, I suppose, of having a feeding tube.
CS03C, S1, FG
Support was also provided by the CNN team, which was described as playing an important role in offering support, particularly after GFT placement, or when changes in feeding practice were needed, although the service was under pressure. Although documented as part of the core team, when professionals were asked about the early years support workers, these posts were reported to have been scaled back. There was a perception that these workers had administrative roles in organising meetings with teams around the child rather than roles supporting families around feeding.
Variations in the provision of support
When staff FG participants at CS03 were asked whether or not there were any variations in the support provided, the shared view was that services aimed to provide the same level of service to every child and that, if there were variations, this was based on individual need. However, variations in support from a clinical psychologist were apparent and not all children had access to psychological support. Although the psychologist reported that support was structured and embedded in care pathways (CS03A, S5, IPI) it was clear that involvement of a psychologist was inconsistent within different clinics in the same trust:
There is no psychology provision in any of the other feeding clinics, so the other members of the team provide some of the support, but there’s no clinical psychology provision. I think it is very important to have access to psychological support, emotional support, and it’s very important to have a multidisciplinary team that works with a child, looking specifically at feeding.
CS03A, S5, IPI
Staff in the FG also acknowledged the limited support available from a psychologist across the patch. They were aware of groups of children who would not be seen by therapists post gastrostomy. For example, children with autism who restrict their own diet for sensory reasons did not receive support because the service was commissioned for children with severe development delay only. However, it was not clear that children always fell into structured diagnostic categories; this raises questions about commissioning along diagnostic categories, which results in resources for some children and not others. 69
Staff were aware of the emotional issues for parents around GFT feeding and felt that adequate support was not always available.:
The needs are huge.
Yeah.
I think we all recognise that feeding is a very emotive issue for parents, it’s kind of one of the most basic things that a parent feels like they should be able to do for their child and if they can’t, then I think a lot of parents take that very personally and feel quite disempowered as a parent if they’re not feeding their child, by whatever method. The amount of support available is probably not as great as we would like, I think we all try, but there definitely is room for more. In one of our feeding clinics, at our child development centre clinic, we have funding for a clinical psychologist, although that’s a very small group of children, and there’s only one person and obviously they don’t all have a relationship with her, so I think the reality of it is that most of the psychosocial support comes from all of us, because we’re the ones that have the long-term relationship.
CS03A, S6, S9, FG
Staff suggested that they spent a considerable amount of their time providing PSS. For example:
The amount of time that I spend on psychosocial stuff is huge, the majority of what I do really is that, so if I’m in a home visit it might take me on average an hour, and the assessment of feeding will probably take me 15, 20 minutes, and the rest of that appointment is discussion and psychosocial support, and reassurance, so quite a huge proportion of what I do is psychosocial stuff, not just around gastrostomy, obviously around the whole complexities of having a child with complex needs.
CS03A, S1, FG
When talking about the need for emotional support, staff provided a rationale for its importance but also indicated that formal input from a psychologist was not always the answer given the individual needs of families when living with, and caring for, a disabled child. This is one of several quotations that illustrates this point:
And in terms of specifically in psychosocial support, I don’t think there’s much need for most families to have an actual formal psychology input. What there is a need for is that long-term relationship with a member of the health care team who can journey with them and support them on establishing the child’s feeding by whatever method, but I don’t know how you fund that because it’s not the same person for each family.
CS03A, S1, FG
The team also acknowledged that any psychologist would need to be integrated into the team because parents did not always want to take up the offer of an appointment with a psychologist. However, it was recognised that integrating a psychologist into the team, given the frequency of clinics (every 4–6 months), would affect relationship building and continuity, and that it might be better to introduce the psychologist in the weekly therapy groups where structured goal-based therapy took place. However, the burden to families of attending weekly clinics was acknowledged.
At CS03B, clinic staff confirmed that there was no formally commissioned psychological service to provide PSS. Most staff considered the provision of emotional support as part of their role, and as part of the role of the team, including the paediatricians, dietitian and nurses. Specialist health visitors were also involved but only in one geographical part of CS03B, reflecting variations in resources within the patch.
A consultant paediatrician summarised the situation:
We have limited options, we don’t have any direct access to any mental health [or] psychology support, so the options that I would tend to use would be things like specialist nurse support and information, so that’s it’s specifically if we’re looking down the gastrostomy pathway, information and support through the community children’s nursing team, the school nursing team, and then consideration of contact with other families who have been through the same process, so some of it is about providing information, so that everything becomes less scary; the more informed you are, maybe then the better decision-making you can make, supporting with others that have gone through the pathway but we haven’t got, in our team we haven’t got a specific psychology support available.
CS03B, S8, IPI
There appeared to be a lack of appropriate materials to reinforce the information provided in clinics other than that produced by a commercial feed company in conjunction with a parents’ organisation (Carers UK, London, UK). A community dietitian described the resources as useful tools for those parents who wanted to read around the topic. However, it was unclear whether or not these resources were made available to parents, and there may be ethics concerns about providing information produced by the commercial feeds sector. A parent suggested the need for explanatory materials for children and families:
I really think a great little booklet to come home with that answers questions that you can show your family that you can read through [would be good]. Also, I think, social stories that children can have, we’re going to go to hospital and there’s a picture of the hospital, and then I’m going to have this put in my tummy and I’m going to have a magic sleep and all those things that children have through social stories would have been really helpful because then I could use those for his siblings as well.
CS03B, P6, IPI
This parent also described the need for support for the whole family and not just mothers. As she became responsible for passing on information to the wider family, she felt that this was to the detriment of her own support needs:
In the end I felt that my time at home was also looking after my family who were worried about it, so I wasn’t necessarily able to just concentrate on my emotional care involved in our decision to have [the child] tube fed because I was asking and answering a lot of questions from my family. And when you have a big family, and everyone’s got his well-being and concerns at heart, I was finding I was looking after everybody else, so I don’t necessarily think that the parents’ emotional support is at the forefront, no I don’t.
CS03B, P6, IPI
Conversely, another parent (CS03B, P4, II) felt more need for practical information rather than emotional support. This was linked to the fact there was little choice about their child having a GFT:
I didn’t feel that we needed the emotional support, it was more the physical support you need, telling you what to do and what you’re doing wrong. Emotionally we didn’t have much choice, so we’d just got to get on with it; with everything that’s happened to [the child], you’ve just got to have your head down, there’s no point in sitting around mulling it over.
CS03B, P4, II
When asked about the need for PSS, another parent preferred to talk about his concerns around housing and welfare benefits, for example the difficulties involved in lifting and moving a disabled child and negotiating stairs.
Feeding practices: risks, values and emotions
One parent (CS03A, P1, IPI) identified the need for improvements in the ‘psychosocial and the emotional’ support offered. This parent distinguished between professionals who went by ‘the textbook’ and advised a nil-by-mouth feeding regime owing to concerns about an unsafe swallow and those who adopted a ‘real-life’, pragmatic approach to oral feeding. This parent spoke of the difficulty of denying a child food in the context of family mealtimes and recommended the need for an individualised approach to support.
Technically ice cream and chocolate are not purees but, and so technically he shouldn’t have them, but it’s remembering the importance of quality of life and living in a family and, you know, he’s got a younger sister, how can I say well she can have chocolate and he can’t?
CS03A, P1, II
The quotation reflects the values this parent attaches to food and feeding in family contexts. Here, the theoretical risk associated with eating certain foods is minimised in favour of the child’s assumed quality of life and ensuring that all children are treated equally.
Parent peer support
There was no formalised parent support group at CS03. One parent mentioned a small support group that she ran every 3 weeks on a drop-in basis at CS03B, but it was unclear if this was widely known about. Staff across all sites acknowledged the importance of peer support and reported that they put individual parents in contact with others. Staff also talked about how parents who were linked with each other to provide support, especially through the school system, although they recognised that peer support would not suit all families:
I have to say special schools are brilliant at that as well, because obviously they’ve got the child every day and they are feeding them, so they’re very good at working with parents and identifying other parents that also provide peer support, which we have found hugely powerful actually . . . But whilst they’ve been really helpful, for some families, it doesn’t work for everyone. Some families are quite private.
CS03A, S1, FG
Maintaining confidentiality was at the forefront of the minds of the team and participants stressed the importance of asking permission from families before putting parents in contact with each other. This put the onus on the new family to proactively seek out those parents willing to talk about their experiences. In an observation of a clinical session, the paediatrician suggested that the mother (CS03A, P9, II) could ask the school nurse if she could facilitate contact with another parent to see what a GFT looked like on another child. The mother said she would like that. Caution about how relationships were managed was advised, in particular matching parents and the accuracy of information passed on and shared:
You’ve got to be really careful that we’re not opening a can of worms [when introducing parents to each other]. We need to make sure that those parents are well matched and their children, because I’ve had parents who’ve said, ‘My friend’s little boy, he used to eat and then he got his gastrostomy, and then his speech therapist said he couldn’t have any tasters any more, and now he’s lost his swallow and now he will never eat again’. And I’m thinking, ‘Well actually that’s not quite true’. So, some parents can pick up what they want to hear, so you’ve just got to make sure you know exactly, have all your ducks in a row.
CS03B, S7, IPI
Although there was no formal parent support group at the tertiary centre, staff reported that they used Facebook, having created a professional group, and could invite parents to join the group and put them in contact with others. Again, they emphasised the role of special schools as the place where parents were likely to meet and know each other:
So what about the role of parental peer support, it’s not a common practice?
I always ask, not in a formal way, but I do always ask, ‘Do you know any other?’, because they tend to run in circles, these families.
They all go to special needs schools together, and they’ll say, ‘Oh, I’ve seen someone at my son’s school that’s got one and I’ve spoken to their mum about it’. I would always ask that, but we don’t have a formal way of saying, ‘Make sure you go and see someone with a gastrostomy’.
We do also have a Facebook, we as a team are on Facebook as a professional group as such and we have, lots of our parents who have gastrostomies, or children have gastrostomies, are on there as a group, so if there is a parent that wants to, and doesn’t have access, we can signpost them to that group and add them to that group so they could ask questions of those families. It doesn’t tend to happen very often because most of our parents, as I’ve said, their kids, if they’ve got complex needs, are in a special needs school and have got, they talk to other parents about how things work and all this sort of thing.
CS03C, S1, S2, FG1
Peer contact may not be consistently offered, however. Whereas one mother at CS03B stated that she would have liked the opportunity to talk to other parents before the GFT had been placed, another parent did not:
The other parents, what type of support do you get from them because they are in the same situation as I am, so how can you expect from someone if they are in the same situation as you are? . . . And I’m a type of person, I don’t want to put my pressure onto somebody else.
CS03A, P2, II
The research suggests that schools can play an important role in facilitating parental networking and, hence, support.
Decision-making
Staff were asked about strategies for facilitating the decision-making process when recommending a GFT. A community dietitian referred to having a conversation with the parents, providing as much information as possible (face to face and by reference to written information), showing pictures of the procedure and identifying the advantages of the procedure and the positive impact it can have on the child’s life. The importance of having good relationships with families was stressed, alongside an experienced team that allowed them to proactively identify those children who might need a GFT:
One of the things that we’ve got, one of the bonuses we’ve got is we’ve got good relationships with these families and we’ve got lots of experience between us so we can almost predict and pre-empt which children are going to almost certainly need one.
CS03A, S1, FG
Other staff also talked about persuasion rather than coercion, which they felt was neither possible nor desirable, and the importance of setting goals around nutrition, which facilitated decision-making for parents:
So we cannot force parents, of course, to accept the solution, so we will, we will work on the feeding as, but it will not be myself working on the feeding, it will be the paediatrician and the other professionals, and they will make home visits and try to help the parents implement feeding plans. And we set very specific goals for nutrition and safety of swallow and we monitor the child’s progress, and the question of gastrostomy is mentioned, discussed with them throughout, and when the goals are not met for natural feeding, then usually the parents get closer to that decision. We also try to bring them in contact with other parents who have had, who have gone through the same and went for a gastrostomy.
CS03A, S5, IPI
And some parents find the idea of having a gastrostomy and their child having to undergo surgery so abhorrent that it’s quite traumatic for them, so we just have to have repeated gentle conversations really and reassurance that what they need to focus on is what is in the best interests of their child.
CS03B, S2, IPI
Others felt that parents often came to their own conclusions on the need for a GFT. One parent (CS03A, P1, IPI) suggested that the decision had been very challenging because she was unable to admit to anybody how difficult it was ‘getting fluids into’ the child. The decision was helped by talking with other mothers whose children had the same condition and being ‘open and honest’ about how hard she was finding it in a feeding clinic appointment a few weeks later. When the team suggested a GFT, the mother felt relief because she had wanted the team to suggest it rather than her ask for it, which may have been interpreted as an admission of an inability to cope.
Another parent discussed the inevitability of the decision (drawing on military metaphors, e.g. ‘losing the battle’ and ‘biting the bullet’), and reluctance to accept the decision that they nevertheless later suggested, which proved very worthwhile:
So we started getting things in place, such as talking with the doctor about the feed and the gastrostomy, and we had the dietitian and all, lots of people involved, and the speech and language [therapist] because of the tongue movements trying to move the food round the tongue, all these people were involved. But we started losing the battle really, because we couldn’t get the volume of food we needed into her and she was losing, she was looking dreadful. So, we bit the bullet. I’m glad we did but at the time you think ‘What am I doing to her, poor thing?’. But at the time, you think ‘Yeah, I don’t want to do this’, but it was worth it, looking back it was worth it.
CS03B, P4, II
Integrating community and tertiary services: the surgical nurse assessment model
This case highlights a recently implemented nursing assessment model that served to integrate the tertiary and community health services and provide support for parents before and after gastrostomy. Therefore, the surgical nurses were actively involved in assessing children for a GFT and supporting families through the decision-making process and contacted parents 6 weeks post surgery to check if any complications had arisen. They also offered training to community nurses. A member of the surgical team discussed the rationale for the implementation of the model, which was to reduce the waiting period for children to have surgery for a GFT:
So, previously we had a pathway where the children were seen in one of our outpatient clinics by one of the surgeons directly, and we tried to involve the nurses at that point in time, and it became evident that quite a lot of children were having to wait quite a long time to get into one of our outpatient clinics. And so, we identified that our surgical nurse specialists could be trained and educated to deliver a lot of the information that we were giving the families, because it’s, typically, very similar from one case to the next. We thought they could provide a more holistic service, particularly because they have, perhaps, a greater time with the family themselves than the surgeons will have been able to have within the constraints of a busy outpatient clinic.
CS03C, S21, II
The nurses talked about the provision of emotional support as integral to their role. The support needs of parents were related to the apparent ‘elective’ nature (i.e. associated with parental choice rather than heath-care professional decision) of gastrostomy (which meant that the onus of responsibility for the decision was perceived to lie with parents), concerns about the procedure ‘going wrong’, whether or not the GFT would be permanent and whether or not the child would still be able to feed orally:
So what are the common concerns of parents?
I think the main concern . . . is they won’t be able to feed orally, so they think that, I guess whether they don’t know the technicalities of it or whether they think that professionals will just automatically want to use the gastrostomy over feeding orally. A lot of our families, of course, spend a long time feeding these children purees, and, actually, that’s what they’re happy to do, but I think that’s probably the main concern and, is it permanent, is this going to be forever?
And I think a lot of them, especially the kids with complex needs, they’ve, yes, they’ve, any other operation the child’s ever had, they’ve had because somebody said they need to have it, whereupon a gastrostomy is never a, ‘Your child needs to have it’, it’s a, ‘It could be a benefit’, so it always falls down to being the parent’s decision, and I think they really struggle with the, ‘This is their fault’, if they make that decision and it doesn’t go right, it’s their fault, they’ve put their child through that. So, it’s the first, probably, just really big decision they’ve made about an operation where someone’s not said, ‘Your child has to have this’, it’s a choice rather than a decision that’s made for them in some ways.
CS03C, S1, S2, FG1
The nurses reported different pathways for children depending on whether the referral came from the community or internally. The number of appointments and length of appointments (ranging from 20 to 50 minutes with a nurse or 15 minutes with a surgeon) were reported to vary according to families’ needs, the professional involved and the timetabling of the clinic. In straightforward cases, where a family was generally positive about a GFT, the child would be seen, assessed and be placed on a waiting list and then seen again on the day of surgery. However, more appointments were often necessary; for example, where parents were not happy to proceed with surgery or if there was a conflict of opinion between the parents and the community medical team about the child’s need for a GFT:
So we’ve got one specific child I can think of at the moment that we have seen about four or five times in clinic because each time [the GFT]’s to go in and we discuss again, and the parents go away and go, ‘No, we don’t want it’, and then they get pushed back into the clinic because the medical professionals say ‘No, no, they need a gastrostomy’, they come and see us again and we talk about it, parents say ‘No’ and walk away again. So, we do sometimes see them a few times to go through and discuss it.
CS03C, S2, FG1
It is of interest, perhaps, that the surgical team viewed gastrostomy as an elective procedure and privilege parental choice. However, the local referring team may have viewed this differently. This issue has been discussed in the literature in relation to the management and ownership of risk and how these positions – that is, who owns or manages the risk of a child having/not having a GFT – shifts between parents and different professionals throughout the referral process. 20
A member of the surgical team (CS03C, S21, II) felt that they offered some element of PSS in explaining the pros and cons of the procedure and associated risks and offering reassurance about the need for a GFT. Where there was not complete parental ‘buy-in’, parents would be invited back to another appointment having had time to consider all the information. However, they felt that parents had usually made the decision to have a GFT by the time they had their surgical consultation, and at that stage their emotional concerns often related to the waiting list rather than the decision to have a GFT. Variations in waiting times (4–6 months where families accessed the nurse-led clinic for the first time or 3–4 months where the families had decided to proceed) were a result of both parent and provider delay. The team were interested in streamlining the referral process by ensuring that all families were referred to the nurse specialists in the first instance.
When asked about the need for a psychologist, one team member (CS03C, S21, II) suggested that such a resource would be better placed in the community. However, as other members of the team (e.g. CS03C, S1, FG) pointed out, they had no resources or funding for psychology support. The community nurses were seen as the families’ first point of call for support, with back-up from the nurses at tertiary level as required. Moreover, the nurses were not aware of any psychological resource in any of the geographical areas they covered. The idea that specific diagnoses provided a passport to resources was again reinforced and gaps identified for children with neurodisability and their families:
For us, we have no resources at all, so as a surgical team we have no funding for psychology or support. So, if, when it comes to the neurodisabilities, it’s very difficult because there isn’t anything acutely in the hospital . . . So, if they’re cystic fibrosis, renal, intestinal failure, each of those teams have got psychology support included in their package, so our renal team, our cardiac team, our gastro team, they’ve all got psychologists attached to them.
CS03C, S1, FG1
The surgical team also followed families up post surgery to check on any issues, although aftercare was generally the preserve of the CCN team. The PSN generally served as a linking role between families and the CCN, ensuring that families were in contact with the CCN pre gastrostomy, and ensuring appropriate linkages with the CCN and dietitians post gastrostomy. However, the team recognised that contact between the CCN and families pre gastrostomy was more likely when a child had a GFT and would therefore be known to the CCN team. There was recognition of a lack of resources in the CCN team, and there were variations in the timing and number of visits made by CCNs to families. There was an acknowledgement that parents had to become proficient at managing the GFT because less support was available beyond the immediate post-operative period (two points of contact as a minimum are recommended by the tertiary team: at day 10 and week 4):
In the ideal world, and this world is not ideal, the referral would go pre-operatively, the community team would meet the family before the surgery, they would go through how they’re going to do their education and even, potentially, do some of the teaching beforehand, but the staff in the community, they don’t have enough staff to do that, so it’s very much we get the referral in and they meet them afterwards.
I think they are good at the follow-up, though.
They are very good at the follow-up most of the time. I think, eventually, [the amount of contact has] gone down; when the child’s had a gastrostomy for a long time, the support gets less and less and less because the parents are supposed to know what they’re doing.
CS03C, S1, S2, FG1
There was also an acknowledgement that there was more contact between the CCN team and families because the former was tasked with delivering the equipment needed for GFT feeding, which also provided opportunities for interactions; these opportunities had decreased, however, since home delivery companies performed the function. Because different areas had different contracts with feeding and equipment companies, it was not clear what provision was available and whether or not this depended on the contract and procurement.
Decisional conflict
When making decisions about whether or not their child should have a GFT, parents typically described how it was often quite a lengthy process. Reasons given for the need for a GFT included the child not putting on weight or becoming ‘dangerously underweight’, not being able to take enough food orally or having problems with choking. Where disagreements arose, staff suggested that it was a matter of weighing up the risk to the child of not going ahead with the procedure. In terms of concerns about feeding, other professionals would be involved and, in extreme cases, the team would be prepared to refer the family to other agencies, such as social care (CS03B, S7, IPI).
A paediatrician summarised the process whereby parents would be encouraged to make a decision for their child to have a GFT. Again, a multidisciplinary approach appeared to be key in managing situations where there were safeguarding concerns:
We look first of all at do we have any safeguarding concerns and then look at whether we need to support the family down that route, but usually it’s taking a multidisciplinary approach involving the specialist from the hospital who would, if we’ve got to the point where the child is referred but then they don’t want to go ahead with it, and to see then what, how we can support the decision-making. If it hasn’t got to that, is usually, depending on urgency we try a softly approach, so that parents have time to get used to the decision, to be able to make it in a supported way.
CS03B, S8, IPI
Staff were asked if there were ever disagreements in the team about a child’s need for a GFT, and all suggested that it was rare for other staff involved with the family not to agree with the decision, although there was some recognition that differences in opinion could arise between staff in the community and acute sectors:
We in the community are good at looking at that bigger picture and saying, do you know what, don’t worry about that for the moment, or let’s just focus on this, or what is needed here, whereas the acute teams just see one problem and fix that one problem.
CS03A, S1, FG
A paediatrician (CS03B, S2, IPI) felt that conflict was more likely in families who were resistant to the child having a GFT placed. These conflicts can impose additional burdens on mothers, who are usually the ones to attend clinical appointments, in terms of managing information, emotions and relationships with the wider family, and may suggest a need for greater support.
Interviews with staff at the tertiary centre suggested that it was rare for safeguarding issues to affect the decision-making process and that the concerns and conflicts that did arise were similar to those reported at other case study sites. Strategies employed were to guide families by outlining the pros and cons of GFT feeding and not putting undue pressure on them. The nursing team were aware, however, of a few cases where issues of safeguarding had arisen, and they worked closely with the surgeons and the community paediatrician in these examples. In general, when safeguarding was raised, feeding was usually part of a bigger issue. In the community services there were procedures in place for safeguarding where the team could refer to the safeguarding nursing team, but, given that the teams had developed relationships with families, they felt that they were more likely to resolve the issue without recourse to a referral to another team. Procedures were also being formalised.
Blended diets
As at other sites, BDs occupied a grey area of practice. A service document outlined the tension: ‘although current policy does not recommend blenderised tube feeding due to lack of scientifically supporting evidence, providing balanced information that is currently available from a health professional is essential and good practice’ (source: service document, CS03). Staff adopted a pragmatic approach, given that parents were already adopting the practice, but would offer support only following a risk assessment in line with trust guidance (CS3A, S16), as was common across all case study sites. Resourcing support was a major concern. Staff made the distinction between ‘supporting’ and ‘recommending’ BDs (CS03A, S6).
Post-gastrostomy support
Post-gastrostomy support was provided by the surgeon, the paediatric surgical nurse specialists and the community nurses post discharge, although it was suggested that when, very occasionally, things did not go according to plan or parents were worried, families would tend to contact the surgical nursing team rather than the community nurses at this point. The surgeon also described the support post surgery that was received by the child and their family, including the link with the community:
After a gastrostomy is placed, the surgeon is primarily involved in the post-operative care of the child, making sure they’re recovered from the operation completely, but the child spends, typically, a day or two on the surgical ward whilst we ensure that they’re able to tolerate the feed. We make sure the parents have got adequate teaching and training for what they are going to need to do at home, we make sure that the dietitian’s plan is in place, so that they know exactly what feeding regime they’re going to have, and the surgical nurse specialist will always make sure that they’ve got that adequate information before they go home . . . For all children, we touch base with their community nurses to make sure the community nurses know what’s going on and that they’re aware what the plan is and the specific need for that individual child.
CS03C, S21, II
However, one parent, whose child had experienced post-discharge complications that resulted in readmission, felt that they had not been adequately prepared prior to the GFT placement. Staffing shortages meant that they were not shown how to manage the equipment beforehand and there was little hands-on practice following surgery:
But at the same time, I do feel like me and [husband] probably could have done with a bit of more support in the way of maybe counselling or something but, you know, someone to chat through maybe a bit more about. Because I think when we came home and in the early hours of the morning when all this stomach fluid was coming out, it was quite traumatic.
CS03B, P3, II
The stressors experienced in the example provided by this parent included a lack of tutoring and preparedness in managing the equipment and feeds caused by a feeling of their child having been discharged too soon, with little opportunity for familiarisation prior to surgery, owing to ‘staffing issues’, the side effects of the procedure (which were experienced as ‘scary’) and the child’s eventual readmission to hospital This resulted in a lack of sleep over several nights and associated worries about the child’s health. This example illustrates the psychosocial sequela post surgery and the need for support not only during the decision-making phase.
Staff training
Apart from the psychologist at CS03A, none of the staff members identified any specific training to support the emotional and psychosocial aspects of families’ decision-making, though most drew on their initial professional training and some had backgrounds in learning disability or autism. Training mentioned by one or more participants included a counselling module, generic team training around how to have difficult conversations, statutory and mandatory training, continuing professional development (CPD) courses and a paediatric module provided by the BDA (not feeding specific). Informal learning from senior and experienced colleagues and through observations in feeding clinics was also mentioned. Similarly, although the paediatric surgical nurses were all paediatric trained, extensive formal training for complex feeding as part of nurse training had not been undertaken, only the occasional study day. Nevertheless, the nurses discussed ways in which they gained their knowledge, the main being ‘on the job’ or through ‘hands-on training’. However, training in PSS was not part of this training.
A view that offering support was ‘common sense’ was also suggested, but this perhaps underestimates the skills involved in supporting parents making difficult decisions. For example, one parent recounted that a clinician had offered to put her in touch with the school to ‘teach her’ how to feed her child. Although the suggestion was made with good intent, it was perceived by the parent as undermining her parenting skills.
Summary
Historically, CS03A has had input into the feeding team from a psychologist, but only a limited number of children were able to access this support through the CDC. Moreover, it was noted that these children and families may not be those most in need of support, illustrating ways in which a resource can create inequities within the service. Support was generally provided by the MDT and there were mixed views about the need for a psychologist for all families and how a psychologist could be best embedded in the MDT in ways that did not add to the appointment burden of parents. Relationship continuity provided by professionals known to families was mentioned as an important factor by staff and parents, as was the supportive role of schools. A recently implemented nursing assessment model at the tertiary centre responsible for placing gastrostomies, initially designed to reduce waiting times, ensured that the first point of contact was the nursing team, rather than surgeon, which may have allowed a space to provide support to families. The team also provided support to the local community nursing team and, indeed, when there were shortages of CCNs they were sometimes able to provide support, particularly at follow-up, which was formalised. Some surgical staff adopted strategies to persuade families to accept a GFT that would suggest a more utilitarian approach to food – that is, a child can or cannot eat and that technically a GFT offers a different way of delivering nutrition – which contrasts with the social meaning of food and feeding that many parents valued and community staff were aware of at the other case study sites. These different understandings may also reflect professional roles and location (that is, the type of advice offered by the surgical team in the acute sector versus that offered by professionals based in the community).
Case study site 4
Overall description of the case
Case study site 4 provides a district disability, hospital-based service, in line with the BACD’s Quality Principles for Paediatric Disability Services. 70 It was described as a consultant-led team with expertise in paediatric disability. Although not a CDC, the service model drew on some aspects of a CDC but saw children aged 0–18 years. Professional expertise in the trust and in the community was drawn on as and when required. This site was selected because the composition of teams could vary and members were bought together in a flexible way depending on need and the expertise required. Housed under one roof, it offered a one-stop shop, particularly as, until recently, gastrostomies were placed on-site. Figure 7 illustrates the configuration of care.
FIGURE 7.
Configuration of care: CS04. BF, breastfeeding; VFSS, video-fluoroscopic swallow study.
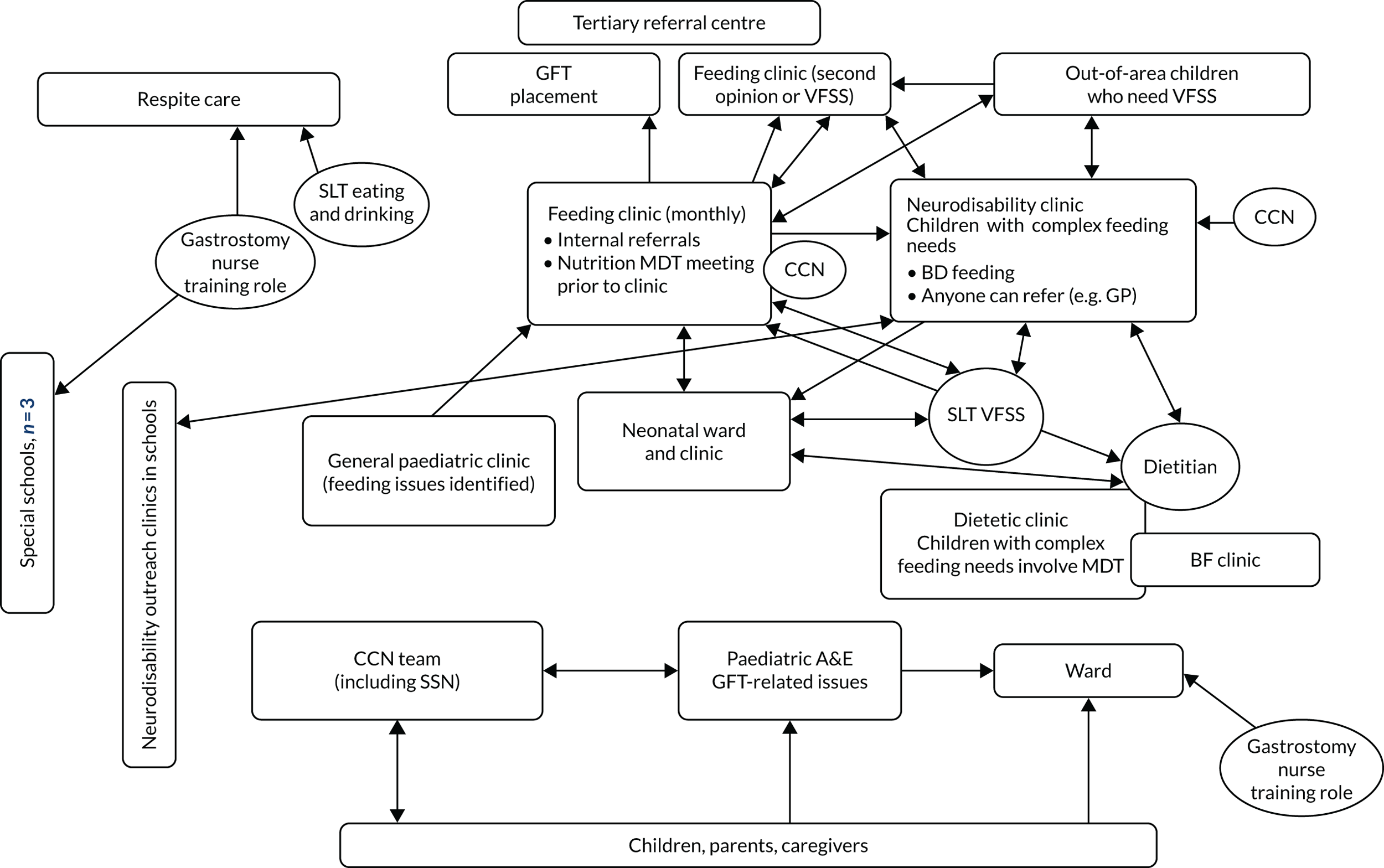
Staffing arrangement
There was a three-tiered feeding pathway for children with complex feeding needs who could be seen in the neonatal clinic, neurodisability clinic or feeding clinic. There was no formal feeding care pathway. Any professional could refer to the paediatric disability service, although most referrals came from within the hospital because most children were already under the care of a consultant with a special interest in the field of practice. In addition, referrals could be received from primary care practitioners (e.g. health visitors, GPs) and special educational needs co-ordinators. Historically, gastrostomies were placed in-house by a consultant with gastroenterology expertise. Gastrostomies are now done in a regional paediatric surgical centre, although post-surgery support is devolved back to the local CCN team and the dietitian.
A feeding clinic was held monthly in the children and young person’s service based in the hospital, which usually involved a range of HCPs, including a paediatrician with gastroenterology expertise, a CCN, a dietitian and a SLT with expertise in dysphagia. Appointments were either unidisciplinary or multidisciplinary, with any of the above professionals participating. There were monthly operational meetings that included the paediatric disability team, specialist support team, disabled children’s social work team, CCNs and allied HCPs to facilitate communication and problem-solving. There was also a local specialist support team for children and young people with physical and medical needs in mainstream schools, comprising a senior specialist teacher, specialist paediatric OT and nurses. The paediatricians also ran clinics at several special schools that had specialist school nurses employed by the trust. Community nurses supported children post surgery and there was input from a dietitian. Gastroenterology nurses also provided support prior to gastrostomy. Community nurses played a key role in decision-making.
Clinical psychology formed part of children and young people’s services [Child and Adolescent Mental Health Service (CAMHS)]. In theory, support could be accessed through referral as required, including specialist clinical psychology support where children and young people were identified as having a learning disability. There was no psychologist in the paediatric disability service.
All of the above professionals provided support for families, either individually or together. This was on an ‘as and when required’ basis, tailored to the needs of the individual child, young person and family/carers. Some families were offered more frequent outpatient clinic appointments where the need was greater. Children with complex disability also often had an emergency health-care plan that highlighted what to do in an emergency and when to seek help and advice from professionals at that time. Telephone support was offered to families and they could contact any of the team members should they need further advice.
A local group run by a physiotherapist, OT and SLT supported children and their families/carers with complex needs from an early age, although this is not feeding specific. Referrals were made by consultants. The group, which ran for 10–12 weeks, provided an opportunity to assess children and families and identify additional needs. The group ran in term time and was limited to six places because space constraints limited numbers. In a feedback session it was felt that this group could provide a space to further embed emotional support for families considering a GFT for their child.
Generally, if a family came under the catchment area of the service, they were likely to receive care from the service from a very early age until the child transitioned into adult services at the age of 18 years. This would be a different model from a CDC, which would see children only at a very early age. Professionals therefore commented that they knew their families very well and all knew each other as professionals. There was a sense of relationship continuity and care provided by this service model. However, inequity in care provision was identified for referrals originating from outside the region. These families could not access the community nursing team or the SLT because these services were the responsibility of the local providers. This affected a small group of families annually and the reasons for referrals out of patch tended to be parental choice and changes in local teams.
All appointments with families were underpinned by the use of a traffic light tool71 that aimed to facilitate communication in the consultation. Families indicated the issues that they would like to focus on by ticking a pre-formed list of issues, including feeding, or by noting any concerns in a free-text box. The tool was also designed to celebrate positive aspects of children’s development. The tool, developed with the input of disabled young people, parents and other experts, was widely available to all neurodisability services. Although PSS was not included, it could be adapted to include this, thus enabling parents to assert their right to PSS. There was also a podcast explaining the use of the tool available on YouTube (YouTube, LLC, San Bruno, CA, USA; www.youtube.com). 72
Speech and language therapists (SLTs) played a key role in assessing children. Referrals to the SLT team were triaged through a referral form in addition to letters that clearly stated that the referral was for an assessment around ‘eating, drinking or swallowing’. The SLT interviewed stated that the SLT team tended to see children only where there were specific concerns about choking or swallowing. Children with behavioural/sensory feeding issues (e.g. children with autism) would be referred to the autism team. SLTs would also see children from the neonatal ward if there were concerns about swallow safety and there was need for support around oral feeding.
One parent reflected on the support offered from various professionals in relation to feeding:
We were in touch with the dietitian and the consultant sees her every 6 months. If I need the community nurse, I’ve got them, you know, on my phone, I’d just ring up for advice . . . When we first introduced food it was a battle, and I used to get myself really, really upset about it, and the speech therapist used to come out and she would say, ‘Don’t make mealtimes a battle, put it out, if she wants it she’ll eat it, if she doesn’t, just take it away and try at the next sitting down’, which is what we did, and as I say it’s just gradually built up from that.
CS04, P1, II
Observations of a multidisciplinary nutrition meeting prior to the feeding clinic, and of the feeding clinic itself, evidenced multidisciplinary working. This involved a senior specialist dietitian and a paediatric consultant along with the parents. At one meeting, the dietitian offered to send the mother some information on playful eating and provided a few tips on how to introduce new food and textures into the child’s diet. She advised the parent that the child needed to explore different textures by touching and playing with the food, which was viewed to be as important as eating, and parents were advised not to worry about mess.
Post-gastrostomy care
Post-surgery care was provided by a specialist gastroenterology nurse:
We talk about general care after the surgery. After the fitting of the tube we visit them regularly and gradually reduce the visits when families become more confident with it, if they need us more, we continue with regular visits. You need to know your families and we provide individualised care to each child. There is a big impact on the family if the child can’t feed. The dietitian also sees them, and the multidisciplinary team discusses the family’s anxieties and feeding issues.
CS04, S1, II
As in other cases, both CCNs and specialist school nurses were involved in supporting children who had GFTs and their families. Referrals came from the hospital into the CCN team. One member of staff (CS4, S7, IPI) felt that a direct referral to the school nursing team would avoid duplication of effort. However, as CCNs were responsible for providing care out of term time and during other periods when the school nurses were not working, overlap may be inevitable when ensuring continuity of care. In special schools, staff were trained by the school nurses to manage feeding, and in mainstream schools the teaching assistants were trained to manage feeding.
Integrating support
Lead professional
Care was co-ordinated by the lead consultant, who drew together relevant HCPs depending on the needs of the child; hence, the model involved a bespoke way of working. This contrasted with the lead professional described at CS03B, at which there was no dedicated feeding team and staff were not housed under one roof or in the same trust.
Psychosocial support
Although in theory there was access to psychological support through CAMHS (as at all case study sites), this was not routine practice and for many children they would be too young to access this service. There was no psychologist at the paediatric disability service because this was not commissioned by the CCG. This contrasts with the availability of support for children with other long-term conditions and disability (e.g. chronic fatigue and diabetes) – a familiar pattern across all case study sites. Families and caregivers had to approach their GP for parental mental health issues. The following extract illustrates, to some extent, the complexity of pathways into mental health services and how children with neurodisability, and their families, fall through the gaps:
So when a parent is in distress about issues relating to feeding, what referrals are available to you? Is there a psychologist available, or any other professional?
Not really, I mean that’s, there isn’t, I mean we have CAMHS, children and young peoples’ psychological service, but you really have to be accessing, you have to, well, I mean a lot of our children don’t even meet the criteria for accepting referrals. So, we can make referrals, but they often get rejected, and it’s normally just about the team trying to support that family. Health visitors can be, some of the health visitors can be really helpful in supporting the little ones with feeding, and sometimes community nurses again, because they’re going in a bit more regularly. They can be very good in supporting with feeding. And then, so we do have some children’s nurses who go out to those who’ve got very specific medical needs, and sometimes we use them as well with feeding. So, we just, there isn’t, well there is something that we can refer onto, but often the children don’t meet its criteria unfortunately, so there’s a gap there.
CS04, S11, IPI
Professionals had different views on the added value of having a psychologist in the team. Concerns about including a psychologist included cost, recruitment difficulties, level of expertise and how they would be integrated into the wider team. There was also a feeling that other members of the workforce had those skills:
So, now I don’t, so yes, it would be wonderful to have a psychologist in the team and to be involved with every family. Having worked in teams where psychologists have been there it’s been very valuable and very useful; however, psychologists are extremely expensive resources and, you know, we have general recruitment difficulties across mental health teams as well as paediatric teams in our area. I don’t think our families lose out because they haven’t got a psychologist in the team, I’m sure that, you know, value could be added for some cases particularly the ones where there’s that tricky conversation, but they are very few and far between, I would say only one every, maybe one in 4 or 5 years, so you couldn’t justify a psychologist based on that.
CS4, S2, IPI
However, views on the benefits of including a psychologist in the team were influenced by the difficulties they had experienced in resourcing other posts. For example, one consultant reflected on a failed attempt to persuade commissioners to provide additional support for CCNs. Although CCNs were valued highly by parents (and other staff), their role, it was suggested, was poorly understood and undervalued by commissioners. They also had concerns that, to pay for a psychologist, cuts would have to be made elsewhere because trusts were not looking for ‘new business’ and there was ‘no money to pay for more staff’; instead, the resource would have to be paid from efficiency savings such as ‘more joined-up working’, ‘effective use of the feeding clinic’ and ‘reducing the number of appointments with different professionals’.
It was highlighted that, as support is not always available in the community, particularly at weekends, families may need to go to accident and emergency (A&E):
I think we need a few more community nurses as well. So, if a child has a tube and they have a problem at the weekend they need to go into A&E, so looking at kind of the weekend support around tube feeding. I think sometimes some families can just go straight up, like phone ahead and go up to one of the paediatric wards but that depends on if the ward’s full or not, I would have thought, you know, it’s a trip to A&E at the weekend for families if the tube’s come out for example. And our community nurses, they’ve got less time now as well, so I think they’re fairly stretched.
CS04, S9, IPI
The pressure on the CCN team, and the possible under-resourcing of the team, was emphasised at CS03 and contrasts, perhaps, with CS02, where resource constraints were not foregrounded in staff narratives. The CCN team at CS02 was provided by a Health Board rather than the CCGs typical of the English system, although we cannot say if these perceived differences were due to differences of commissioning arrangements, caseload or factors relating to the locality of each case.
The need for PSS early in the feeding journey was identified by a nurse:
Yeah, ah-ha. I suppose it would be helpful mainly for parents who are thinking about going down the road for gastrostomy; it’s quite hard, thinking of coming to terms with, that your child is probably, is not going to eat. You know, so I think support that way. I mean at the moment we do have a child who has an NG tube in, and she doesn’t have anything orally, but parents don’t want to have a gastrostomy fitted, because they believe she’s going to eat in the future, and I think it’s just, you know, it’s going to take a lot of time for them to realise that their child is never, probably is going to eat, or they’re never going to eat an efficient diet and in the meantime, you know, the child has an NG tube in, and pulling it out regular and, you know, all the things that come with having an NG tube. So, I think if there was more support around that, then maybe that may, that may help.
CS4, S7, IPI
The importance of early intervention was stressed by another member of the team (CS04, S9, II) who felt that a drop-in feeding group for young children with swallowing difficulties being weaned on to solids, a model adopted in a London children’s hospital, would be helpful. However, barriers to establishing such a group at CS04 were the problem of travelling with children on public transport and a recognition that funding for transport for families had been cut.
Similarly, a consultant felt that, with more time, the service could proactively identify problems:
I suppose maybe having a bit more time to do a bit more with the families would be good, if we had, you know . . . we could do more support, possibly, if we had more time to dedicate to them. That might be useful, we could do more frequent reviews then and pick up on problems maybe early or possibly if there were some. Because, as I say, at the minute we rely sometimes on the families contacting us if they’re concerned.
CS04, S6, II
Peer parental support
Professionals relied on informal contact and support between parents rather than having formalised referrals. Moreover, it was felt that parent-to-parent contact was happening organically around the clinic. One consultant reflected on the growth of social media, which, they thought, had, perhaps, taken over the role of clinicians in facilitating parental networking:
When I first started working in community 20-odd years ago there was no social media whereas now they all know each other because of Facebook and Twitter and things like that and they meet at the outpatients appointment, they swap, they’ll friend each other and before you know it you’ve got a little support group going on social media. I think some families definitely do that because social media [has] taken over from us a little bit now.
CS04, S3, IPI
However, one parent (CS04, P1, II) identified the need for a support group to share experiences and to discuss coping strategies with other parents, which challenged staff assumptions that peer support had developed organically. A staff member (CS04, S6, IPI) mentioned that in MDT meetings there was often discussion about ways of stimulating more contact between parents and families, and they thought that nurses could do more to suggest this. Another member of staff noted the benefits of peer parental contact:
As a team we’ll maybe identify that our parent might benefit from speaking to another parent about, if they were going to try a blended diet for example or around a PEG but I think that’s done fairly carefully in that the community nurse might identify a family and ask if they would be OK, you would be checking permission with both sides before introducing. More commonly, it’s actually parents just get in touch with other parents through various networks, be it social media, Facebook groups or Portage [www.portage.org.uk/about/what-portage; accessed August 2020].
CS04, S9, IPI
Transitions into adult services were identified as a potential area for improvement, although this was contested by another member of staff who felt that there was joint working and a slow transfer to help facilitate the move:
A disability liaison nurse and social worker look at the transition care at 16 years old; at 18 years old they leave the special school. They also leave the paediatric neuro team and transition the adult team, so the paediatric team do home visits up to the age of 18.
CS04, S3, II
Are there particular issues for older children and transitions in terms of referral pathways and support?
There is room for improvement in referral pathways into adulthood. District community nurses don’t take them on after they transition into adult care, so there is less in the adult arena. Homeward take over and disability nurses could get involved and [their] patients tend to go into hospital for any issues that may arise.
CS04, S1, II
The need for parent information about GFT feeding was identified, suggesting that there may not be collective knowledge about the resources available developed by commercial companies, or concerns about their use.
Decision-making
Feeding problems were monitored and, when it became clear that an alternative form of feeding was going to be needed, the community nurses played a role in supporting families. There were monthly meetings with the MDT and community nurses. As at other sites, staff reflected on the emotional impact of the suggestion of a GFT, which parents viewed as artificial, and the impact on family mealtimes, and feelings of guilt at not being able to feed a child:
They may resent or resist suggestions of what are often seen as artificial methods of feeding and I think a lot of what we try to do is keep that territory as neutral as we can from as an earlier stage as possible so that families don’t feel they’re failing by having to resort to those things but those are things that are there to try and help them make the next step in terms of supporting their child’s development and feeding, where that’s possible.
CS04, S5, II
Most HCPs interviewed agreed that families and carers needed to be actively involved in decision-making about a GFT. There was a feeling that parents received a lot of information before the procedure, including about the use of toys with a button or PEG to see what a GFT looked like.
The decision-making process was also described as quite complex owing to the involvement of multiple family members (parents are often accompanied by other family members, such as grandparents) who may or may not be involved in children’s care. Therefore, HCPs had to understand how the family as a whole made a decision, as portrayed in the following quotation:
Generally the demographic of the local population is that people don’t really move away so they have quite complex family networks, and grandparents, other relatives, often come to appointments with the family, and decision-making’s interesting in that you obviously can provide all the information to families but sometimes, not always, a lot of families will want you to try and guide them as to the right decision and they don’t always like it if you just say these are the options, these are the pros and cons, what do you want to do?
CS04, S4, IPI
With the expectation that families should take a lead role in decision-making, the observation that some families tried to hand back responsibility for the decision to the consultant was considered undesirable as professionals wanted families to make an informed choice and become well versed in the pros and cons of gastrostomy and GFT feeding:
There’s this temptation for a lot of families to sort of hand over the decision to you to make as the professional, which isn’t really how you would normally do a consultation, you know, you’d really want the family to be paramount in terms of having information and then being able to make that decision.
CS04, S4, IPI
Decisional conflict
Disagreements between professionals regarding GFT placement were not reported by staff because of a culture of ‘open discussion’. Disagreements with families were usually managed by going at the families, own pace:
It’s usually, that’s usually where there’s a safety issue, where the swallow clearly isn’t safe on the video, fluoroscopy and so the family want to continue to feed the child. Those are the only situations where we’ve run into difficulties, but we’ve managed to work those through with families and it’s not been a matter of interprofessional disagreement, it’s more been a matter of being able to help the family to see what the safety issues are.
CS04, S2, II
Although the tertiary centre had a role in influencing parental decisions by offering a surgical opinion, it was generally felt that the bulk of the work of supporting families came from the local referring team. In exceptional cases, children with very complex needs requiring additional support could be referred to the feeding/neurodisability clinic at the tertiary centre.
Blended diets
Another potential area for conflict surrounded the use of BDs. As at other sites, staff at CS04 highlighted the tensions between a lack of official support for BDs and increasing use by families: ‘We have certainly got a few on the caseload, yes, and managed without any national guidelines for it, and it’s not actively encouraged from a professional point of view’ (CS04, S3, IPI). This will be discussed in the final chapter.
Staff training
Staff were trained in their clinical areas and were competent to provide clinical care but training very much focused on these aspects:
So, they [the feeding clinic team members] have all had training, so all our nurses have postgraduate degrees, they’ve got their clinical skills course that they’ve completed, they’re prescribers as well. The speech and language therapists that are involved in children with feeding issues are dysphagia competent in line with their respective colleges and they’ve had relevant training in communication skills, et cetera. So, we’re very, we’re lucky that we’ve got a team that is, you know, been well trained and is practising regularly.
CS04, S2, II
Staff were also involved in training each other on the clinical and technical aspects of feeding (e.g. in the case of premature or other newborns, SLTs provide extra support to NICU staff to establish whether or not oral feeding is appropriate, and CCNs are also involved in training school staff in the management of gastrostomies). Specialist school nurses also reported in-house training on nutrition and feeding pumps/GFT management by gastrostomy specialist nurses (CS04, S7, IPI). SLTs reported training health visitors to enable them to provide more general feeding support and advice (e.g. weening process), to avoid unnecessary referrals and to enable the SLTs to better focus on children with an increased risk of poor growth (CS04, S9, IPI), but there was little formal training in the psychosocial aspects of feeding and support, although generic CPD courses may have relevance and transferable learning. Nurses may have had some generic training in mental health, but some felt that additional training in counselling skills could be useful (CS04, S1, II).
Summary
Case study site 4 provided an example of a three-tiered feeding pathway housed under one roof where the composition of teams was flexible. Input of team members was dictated by children’s needs and, therefore, similar to teamworking at CS03B. Care was co-ordinated by the lead professional. However, there was no written care pathway. The general view was that additional support from a psychologist may be beneficial but not for all parents and that a range of staff, with the right training, could provide PSS. Cost considerations were considered a barrier. Staff felt that they would like to offer more proactive support in detecting feeding difficulties sooner and develop parental peer support further. The role of the CCN appeared key in supporting families, although there was a feeling that the team needed strengthening, as at CS03.
It was difficult to recruit parents into this study; hence, the views of families were not well represented. Therefore, we were not able to triangulate views expressed by staff with those expressed by parents, although observations were used. The issue of recruitment is discussed in Chapter 6.
Chapter 5 Results of the resource use and willingness to pay for support
Resource use
In this chapter we report the results from the parental resource use questionnaire, including the number of appointments and the support received in minutes from each health-care, social services or educational professional. From the HCP questionnaire we report on training to provide support and perceived confidence in providing support.
A total of 21 out of 103 questionnaires were received from parents or carers (response rate 20%; see Appendix 1). The average age of children was 2 years 3 months and 16 out of 21 had a GFT. The mean number of appointments over the previous 12 months was 2.25, none of which had been arranged to discuss PSS. When asked if they would have liked such an appointment, nine caregivers said no, seven said yes and three did not know.
Eight out of 21 respondents completed the question on appointments and support, with five reporting receipt of PSS over eight appointments. A summary is set out in Table 4.
| Parent or carer (n = 8) | Appointment number | Emotional support offered in appointments in previous 12 months (minutes) | HCP(s) providing support | Cost (£)a |
|---|---|---|---|---|
| 1 | 1 | 15 | Surgeon | 317.37 |
| 2 | 30 | Dietitian, paediatrician, community nurse, surgeon, health visitor | ||
| 3 | 60 | Community nurse, surgeon | ||
| 4 | 20 | Paediatrician | ||
| 2 | 0 | 0 | 0 | |
| 3 | 1 | 30 | Dietitian, community nurse | 17.00 |
| 4 | 0 | 0 | 0 | |
| 5 | 1 | 0 | 0 | |
| 2 | 15 | Dietitian, surgeon | 19.25 | |
| 6 | 1 | 60 | Paediatrician, dietitian, OT, surgeon | 227.00 |
| 7 | 1 | 5 | Nurse | 4.00 |
| 8 | 0 | 0 | 0 | |
| All (average) | 1.5 | 32.5 | 76.42 |
Parents reported between zero and four appointments where they discussed psychosocial issues, with time spent on emotional support lasting up to 60 minutes, averaging at 32.5 minutes. In terms of the unit cost of the HCPs’ time, the time spent on PSS ranged in cost from £0.00 to £317.37 per child per year, with an average of £76.42 per family for the year at 2017 prices. 73
Respondents were asked who they went to for PSS the last time they had a worry or anxiety about their child’s feeding. The replies were school nurse or dietitian (n = 5), community clinic (n = 3), doctor or community nurse (n = 2), online support (n = 1), SLT (n = 1) and a social group (n = 1). Three respondents reported that the issue they sought support for was resolved, 17 reported that it was partially resolved and one reported that it was not at all resolved. Only one respondent reported that a HCP had offered the opportunity to speak to another parent but that they did not take it up because they were already in contact with a parent. Twelve out of 21 (57%) reported that they would have liked such an opportunity, eight (38%) reported that they would not and one (5%) did not know.
Satisfaction with care
When asked about their satisfaction with the support received the last time they had a worry or anxiety about their child’s feeding, 16 reported being fairly or very satisfied, three reported being partially satisfied, one reported being not very satisfied and one reported being not at all satisfied. When asked about their overall satisfaction with the care related to their child’s GFT or feeding problems, eight reported being fairly or very satisfied, six reported being partly satisfied, four reported being not very satisfied and one reported being not at all satisfied.
Health-care professionals’ confidence and training in providing psychosocial support
A total of 31 out of 109 questionnaires were received from HCPs (response rate 28%), who were asked about how confident they were in providing PSS to families using a five-point Likert scale as well as about what training, if any, they had received to do this. Responses (including type of professional) are provided in Tables 5 and 6.
| Profession | Respondents, n (N = 31) |
|---|---|
| Paediatrician | 8 |
| SLT | 5 |
| Dietitian | 4 |
| Paediatric surgeon | 4 |
| Surgical nurse | 3 |
| Psychologist | 2 |
| School nurse | 2 |
| CCN | 2 |
| Paediatric gastrostomy nurse | 1 |
| Total | 31 |
| Level of confidence | n | Received training | Type of training |
|---|---|---|---|
| Very | 4 | 4 | 2 medical, 1 psychological, 1 NMCN CEN (online and DVD) |
| Fairly | 10 | 2 | 1 medical, 1 psychological |
| Somewhat | 10 | 0 | |
| Not very | 6 | 1 | 1 medical |
| Not at all | 1 | 0 | |
| Total | 31 | 7 |
Few of the HCP respondents (7/31) had received specialist training for PSS. Among these, specialist training for PSS was usually part of medical or formal professional training. Only one nurse (the only one to report being very or fairly confident) had received training and this was provided by the NMCN CEN (online and DVD training). There was a tendency for those with more confidence in providing PSS to have received relevant training. These results support the interview data from phase 2, during which a lack of specific training was identified.
Willingness to pay
A total of 168 respondents started the survey. Among these, 148 consented to their data being used for the purpose of research. A total of 103 completed the rating of service A (usual care) and 96 completed the rating of service B (enhanced support involving some provision for access to a psychologist and a more formalised approach to peer parental support) (see Chapter 3). Respondents were asked how much they would value a package representing the current provision and one representing the enhanced provision. Because parents would not be asked to pay for this PSS, and we did not wish to imply that they would, we used the preferred term ‘value’. Table 7 illustrates the types of respondent – professional or parent – who completed the survey. The majority of respondents were HCPs (72%).
| Relationship | n (%) |
|---|---|
| Parent/carer of a child with neurodisability and complex feeding needs | 18 (19) |
| Parent/carer of a disabled child without complex feeding needs | 5 (5) |
| HCP | 68 (72) |
| Decision-maker/commissioner/manager of a service | 3 (3) |
| Other | 1 (1) |
Table 8 provides information about respondents’ household composition. Report Supplementary Material 7 provides additional demographic detail including sex, age, education level, employment status, annual household income, country of residence and ethnicity.
| Household composition | n (%) |
|---|---|
| With partner | 65 (70) |
| With other adult(s) | 10 (11) |
| Alone as a single householder | 12 (13) |
| Other | 6 (6) |
| Total | 93 |
Respondents were predominantly female (96%), aged between 25 and 54 years (85%), residing in England (80%), living with a partner (70%) and in paid employment (81%); 86% had a degree at either bachelor’s or master’s level and the majority were from the higher-income brackets. This reflects that the survey was completed mainly by HCPs.
Table 9 sets out the frequency of values, expressed in Great British pounds, attached to service A, which represents usual care for PSS, and service B, which represents the enhanced package.
| Service | Value (£), n (%) | Total | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 50 | 100 | 150 | 200 | 250 | 300 | 350 | 400 | 450 | 500 | ||
| A | 4 (4) | 11 (11) | 9 (8) | 7 (7) | 13 (13) | 16 (15) | 6 (6) | 3 (3) | 10 (10) | 2 (2) | 22 (21) | 103 |
| B | 1 (1) | 7 (7) | 2 (2) | 2 (2) | 7 (7) | 3 (3) | 8 (8) | 6 (6) | 12 (13) | 7 (7) | 41 (43) | 96 |
Figure 8 represents the change scores in the values respondents assigned to services A and B and demonstrates that most people’s scores changed between 0 and 300 when valuing the two different services in favour of service B.
FIGURE 8.
Change scores assigned to services A and B.
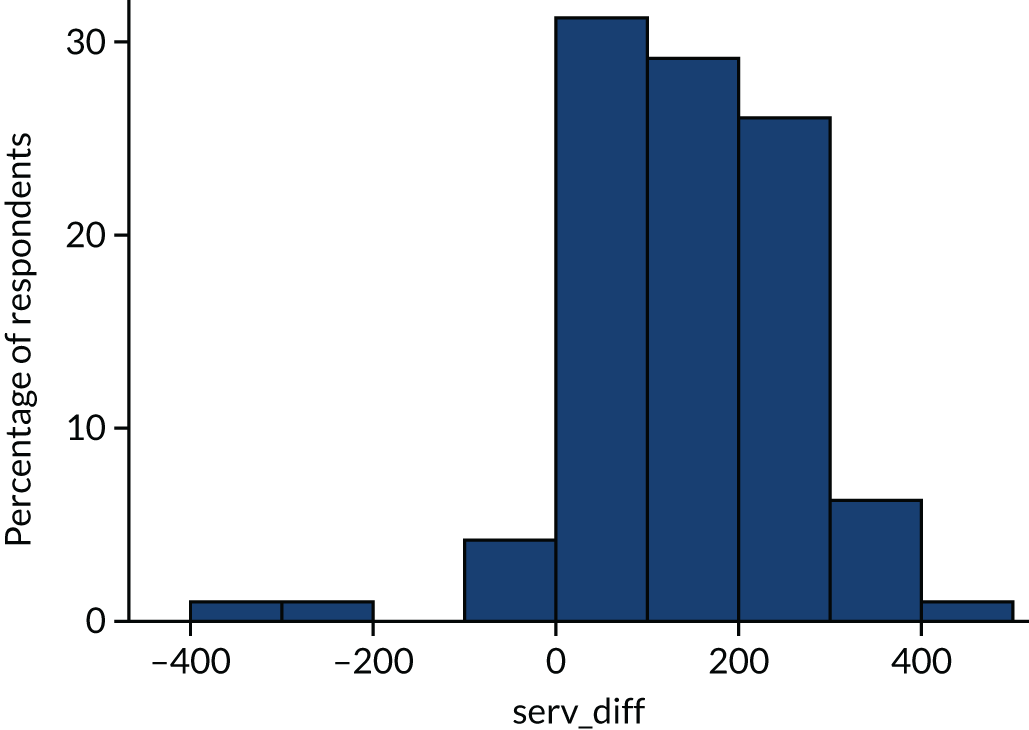
Table 10 sets out the means, standard deviation (SD) and 95% confidence intervals (CIs) of values assigned to services A and B. Because a preliminary analysis indicated that the data were skewed, a non-parametric Wilcoxon signed-rank test was used to measure the difference in values between the two services. The median ranks for service B were significantly higher than those for service A, demonstrating a preference for enhanced support with involvement of a psychologist and parental peers, which was statistically significant (n = 96; p < 0.001).
| Service | n | Mean value, £ (SD; 95% CI) |
|---|---|---|
| A | 96 | 259.90 (158.72; 227.73 to 292.05) |
| B | 96 | 374.48 (149.74; 344.14 to 404.82) |
A two-sample t-test (unequal variances assumed) was used to assess whether or not there was a significant difference in WTP between parents and HCPs. Mean WTP for service A (carers, £252.17; HCPs, £262.33; p = 0.8090) and WTP for service B (carers, £306.52; professionals, £395.89; p = 0.0519) showed no significant difference in WTP between them. There was also no significant difference in WTP by household income group for service A (p = 0.5550) and B (p = 0.6852) using a one-way analysis of variance.
Conclusion on use of resources for psychosocial care
The number of parents or carers responding and reporting discussion on psychosocial issues during routine appointments was small and, as a result, the evidence on service costs to the NHS, social services and educational services is not strong. This reflects the challenge of researching a relatively small population. Those who responded may have been motivated to respond if they had experienced more discussion around PSS and so may have had higher than the average contact. The average estimate of costs is £76.42 per child per year at 2017 prices,73 with the highest single estimate being £317 for one child for 1 year. These figures suggest that the implementation of PSS into regular appointments would possibly add a percentage point to overall costs. In a previous study,28 we reported the overall net costs of GFT placement compared with pre-gastrostomy costs to be £147.96 per week per child at 2002 prices. 28 This is equivalent to £10,500 per year at 2017 prices. 73
We were not able to estimate value in terms of quality of life (to estimate opportunity cost to services) but instead provided WTP estimates, which were intended to assess the societal value of the services. When the cost estimates were compared with the estimates of WTP, which were £259.00 (95% CI £227.73 to £292.05) for scenario A (n = 96) and £374.00 (95% CI £344.14 to £404.82) for scenario B, it becomes clear that these values far exceed the costs estimated from our sample. However, a limitation of these values is that they can be biased by the respondents’ ability to pay. This was analysed in the analysis of variance, which showed no significant difference in WTP by household income.
Psychosocial support during appointments was provided by a range of HCPs, including doctors, nurses, teachers, dietitians, OTs, SLTs and health visitors. Appointments took place in hospitals, at GP practices, at community health centres and at schools. The professionals involved received salaries from different budget sources, there being no central budget for this care. Costs of support were therefore spread between a number of budgets. Parental peer support was valued but not offered consistently. Apart from our previous study on costs of gastrostomy,28 there is very little information on resource use and none for PSS for this cohort of children and families. Future studies may be required.
Chapter 6 Discussion
Evidence reviews recommend that professionals attend to the non-clinical aspects of decision-making involving a GFT (including the values that parents attach to feeding children), to ensure consistent and structured support in care pathways, although structured support is not clearly defined. 1,2 This study aimed to identify exemplar models of PSS to examine how these recommendations are implemented in practice. Given that PSS was integrated into children’s clinical appointments, PSS as a discourse and practice was difficult for professionals to disentangle from their routine clinical care. This was reflected in interviews with professionals, who mainly discussed PSS provision through the lens of their professional and clinical practice and in relation to risk management. Therefore, PSS as an embodied practice was relatively muted and also had ‘leaky’ boundaries where clinical ‘care’ and PSS were often used interchangeably; this semantic shift represented a tension throughout the study and is discussed later in this chapter in relation to the analytical construct of ‘hidden work’.
For the purpose of this study we initially interpreted structured PSS as support that was integrated through a care pathway. However, given the complexity of families’ journeys, which cross service boundaries, and the general absence of written pathways, we identified mechanisms that enabled the integration of children’s care at critical junctures and that served as foci for the integration and provision of PSS, even in the absence of explicit pathways. Haggerty et al. 74 question whether or not formal care pathways lead to improvements in care and suggest that a more useful approach is to look at whether or not care is experienced as ‘connected and coherent’. Others suggest that care co-ordination can involve a range of strategies that fall along a continuum, including co-located services, services characterised by collaboration, and integrated services. 75 We elaborate further in relation to our reflections on different service configurations and mechanisms for the integration of care and PSS.
Parents also differed in their need for PSS, which problematises, perhaps, the concept of structured support when a ‘one-size-fits-all’ approach is adopted. Such approaches are considered harmful when they undermine people’s own coping strategies and fail to build on resilience and contrast with the concept of personalised care, as expressed, for example, in terms such as MAC and TAC, used at some case study sites. 76 We were also concerned that structured support could be defined by commissioners in terms of a set number of appointments, or quantity of time, which could limit the amount of support available; hence, we prefer to use the term ‘enabling structures’ for structures that support the provision of personalised psychosocial interventions.
Integration and theorisation of data
Our initial model for the analysis of data was based on that of Mahant et al. 1,55 This model identified three overarching areas in which decisional conflict could arise when families make a decision to have a GFT for their child: the values parents attach to oral and GFT feeding; the context of child and family decision-making; and processes of care that describe the characteristics and capacity of services to support high-quality decision-making. The results of our provider survey highlighted a number of themes that referred to the wider structural capacity of services in supporting families; therefore, we used the Donabedian56 framework as a rationale for the synthesis and presentation of findings (Figure 9). This framework views service quality as determined by structures, processes and outcomes. We populated the framework with descriptive themes that emerged from phase 1 and were investigated in depth in our case study (phase 2). We also recognise that structures, processes and outcomes are interrelated rather than discrete entities. In addition, we identified three analytical constructs from our case study in relation to PSS and processes of care. Whereas our descriptive themes presented in the case study remained close to the data, our analysis brought an interpretative element that generated three new constructs:77
-
hidden work
-
expressing emotional vulnerability
-
negotiations around risk and values.
FIGURE 9.
Synthesis model of findings. IT, information technology.
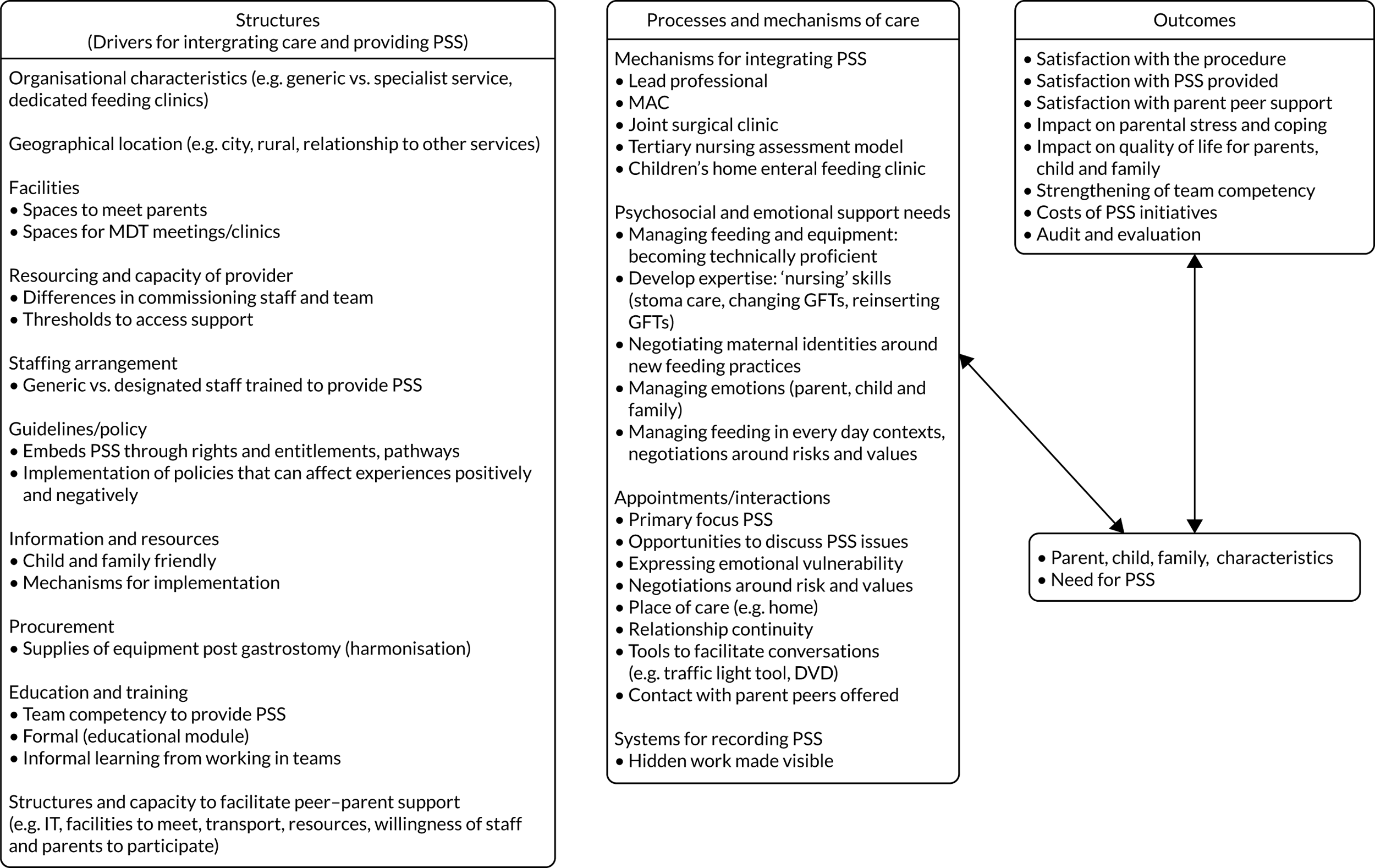
Support needs of parents
Support needs of parents can be summarised under five main headings:
-
managing emotions and relationships (parents’, children’s and other family members’) around the decision to have a GFT and thereafter
-
negotiating maternal identities around new feeding practices
-
managing feeding and equipment and becoming technically proficient
-
developing expertise in ‘nursing’ skills (e.g. stoma care, changing GFTs)
-
managing feeding in everyday contexts, including negotiations around risks and values.
Reflections on different service configurations in our case study
Our research design does not allow us to say if there is one right way of delivering care. However, we have attempted to draw out enabling features that might move us towards an ‘ideal’ service configuration in terms of how PSS can be embedded at different stages of the child and family journey. These are detailed in our synthesis of findings in Figure 9. Table 11 provides a comparative overview of the different services on key characteristics identified in our synthesis model. We offer reflections on the strengths of different service configurations with reference to a range of mechanisms that served to integrate care and PSS. These included the following:
-
having a lead professional (e.g. CS01, CS03, CS04)
-
the integration of health and education (CS01)
-
MACs (CS02)
-
innovative approaches that integrated care between the community and tertiary services [e.g. a joint surgical clinic (CS01) and a tertiary nurse assessment model (CS03)]
-
a HEFCC (CS02).
| Descriptor | Site | ||||
|---|---|---|---|---|---|
| CS01 | CS02 | CS03A | CS03B | CS04 | |
| Structures | |||||
| Organisational characteristics | |||||
| Generic service for children with exceptional health-care needs | ✗ | ✓ | ✗ | ✗ | ✗ |
| Specialist neuro/disability service | ✓ | ✗ | ✓ | ✓ | ✓ |
| Multidisciplinary feeding clinic | ✓ | ✗ | ✓ | ✗ | ✓ |
| Multidisciplinary HEFCC (non-paediatrician led) | ✗ | ✓ | ✗ | ✗ | ✗ |
| Formalised mechanism linking community and tertiary health services | ✓ | ✗ | ✓ | ✓ | ✗ |
| Integrated health and education with co-located school through pooled budgets | ✓ | ✗ | ✗ | ✗ | ✗ |
| Clinics held in special schools through service level agreements/service specifications | ✓ | ✓ | ✓ | ✓ | ✓ |
| Guidelines/policy | |||||
| Written care pathway (PSS not explicitly mentioned) | ✗ | ✗ | ✓ | ✓ | ✗ |
| Best practice statement (emotional support mentioned) | ✗ | ✓ | ✗ | ✗ | ✗ |
| PSS for children embedded through rights charter (not feeding specific) | ✓ | ✗ | ✗ | ✗ | ✗ |
| Trust guidance on BDs | ✓ | ✗ | ✓ | ✓ | ✓ |
| Formalised, ongoing parental representation in services with opportunities to input into policy and practice | ✓ | ✗ | ✗ | ✗ | ✗ |
| Staffing arrangement | |||||
| PSS provided by MDT members | ✓ | ✓ | ✓ | ✓ | ✓ |
| Some access for families to designated, trained staff for PSS, although not usual practice | ✓ | ✗ | ✗ | ✗ | ✗ |
| Education and training | |||||
| Formal training available in understanding PSS needs of parents making the decision for a child to have a GFT | ✗ | ✓ | ✗ | ✗ | ✗ |
| Processes and mechanisms of care | |||||
| Mechanisms for integrating PSS | |||||
| Lead professional (paediatrician) | ✓ | ✗ | ✓ | ✓ | ✓ |
| Joint surgical clinic linking community and tertiary health care pre and post gastrostomy | ✓ | ✗ | ✗ | ✗ | ✗ |
| Tertiary nursing assessment model linking community and tertiary health care services pre and post gastrostomy | ✗ | ✗ | ✓ | ✓ | ✗ |
| HEFCC (non-paediatrician led) | ✗ | ✓ | ✗ | ✗ | ✗ |
| MACs (usual practice) | ✗ | ✓ | ✗ | ✗ | ✗ |
| Appointments/interactions | |||||
| PSS integrated within appointment, although not the primary focus | ✓ | ✓ | ✓ | ✓ | ✓ |
| Tools to facilitate conversations (e.g. DVD, traffic light tool) | ✗ | ✓ | ✗ | ✗ | ✓ |
| Formal system for recording provision of PSS | ✗ | ✗ | ✗ | ✗ | ✗ |
| Peer-to-peer parent support consistently offered to families considering a GFT as part of care plan | ✗ | ✗ | ✗ | ✗ | ✗ |
Case study site 1
Case study site 1 was a specialist neurodisability service with dedicated feeding clinics and a large number of enabling features, including a high level of integration and a relatively high level of PSS achieved through integration with a co-located school, and task-sharing between health and educational staff. Care was co-ordinated by a lead paediatrician. In addition, there was a high level of parental involvement, including representation on feeding committees and parent-led use of social media (e.g. Facebook). This level of integration had been achieved through strong leadership, policy underpinning the partnership and the funding model, which included pooled budgets (recently implemented). In addition, a joint surgical clinic held in the community health services, involving a surgeon from the tertiary centre at which gastrostomies are placed, served to integrate care in line with research recommendations. 29 This example of shared care contrasted with models in which tertiary service involvement was largely limited to a consultation with families for the placement of a GFT (e.g. CS04).
Although parental access to psychologists for support was not usual practice, members of the MDT had access to psychologists and psychiatrists for additional support as required. Although there was no written care pathway, the right to emotional support for children more generally was leveraged through the shared clinical services and school’s children’s charter, informed by a rights-based discourse and developed with children and families. Competency in providing PSS was strengthened through shared learning among team members. Although the model was highly specialised, and not necessarily replicable, it showcased elements of best practice that could be explored for adoption in other services subject to the availability of funding.
Case study site 2
Case study site 2 is an example of a generalist service for children with exceptional health-care needs tailored to a rural context and staffed by a MDT. The provision of PSS was enabled through a best practice statement that specifically mentioned the need to provide emotional support based on research evidence. Resources to support children and families could be leveraged through MACs. The model offered a different approach for achieving high levels of support for a small number of children, with assistance from a national managed network (NMCN CEN). The network disseminated best practice, including a DVD for families considering a GFT, produced with parental involvement. There was an educational module on the provision of PSS available through e-learning and developed in conjunction with a local university and the NMCN CEN. However, this training was not mandatory and was available only to individual members of the NMCN CEN, raising access and implementation issues.
Despite the challenges of care provision in rural areas, care appeared to be person- and relationship-centred and, hence, PSS was achieved in a relatively informal way. Relationship continuity across the life course was particularly strong with the CCN team. Problems following surgery were likely to be identified by the CCNs or in the 6-monthly reviews of children in the therapist/nurse-led, home enteral feeding clinic. This was a strong feature of the model given that research suggests that dedicated enteral feeding teams can reduce hospital re-admissions for GFT-related complications from 23% to 2% post surgery. 78 The enteral feeding clinic also specialised in supporting oral feeding following GFT insertion, which parents, more generally, valued.
Case study site 3
Case study site 3 was a specialist neurodisability service and our case highlighted uneven provision both within and between services, with risk of gaps in community settings. Whereas CS03A had a feeding clinic, CS03B did not. Teams were co-ordinated by a named paediatrician; however, the model of teamworking at CS03B was described as serial, rather than multidisciplinary, with some members of the MDT employed by different trusts, attesting to the fragmentation of health services delivery. Staff saw families individually and the team communicated by telephone, e-mail or face to face at MDT liaison meetings. It was unclear if or how this affected families. Although there is no research to suggest which models of care work best in terms of child health outcomes, parents may have preferred the ‘one-stop shop’ approach afforded by the feeding clinic model. National Institute for Health and Care Excellence (NICE) guidance on the care of children with cerebral palsy (not feeding specific) recommends that children should be cared for by a core multidisciplinary team. 79 The model of service delivery at CS03B appeared to rely more heavily on the lead paediatrician to co-ordinate and integrate care involving professionals across different trusts. There was a written care pathway but PSS was not explicitly stated. Of interest was the availability of the services of a psychologist at CS03A, although only particular groups of children were able to access the services through the CDC, based on the criterion of age, reflecting inequity in access within and across services. No similar resource existed at CS03B. Moreover, additional restrictions to accessing the services of the psychologist at CS03A were implemented during our study.
A recently implemented surgical nurse assessment model at the tertiary centre at which gastrostomies were placed provided an alternative model of integrating the community and tertiary services and supported families to make a decision about the need for a GFT. The surgical nursing team based at the tertiary centre at CS03 conducted an initial assessment of children’s need for a GFT and provided support to families before and after surgery, a model, as at CS01, that could be considered an example of best practice given that our provider survey (phase 1) identified gaps in communication between community and tertiary centres. Follow-up post surgery, at specified time points, allowed any problems arising from the placement of a GFT to be identified and actioned. The tertiary centre’s use of social media (e.g. Facebook) provided an opportunity for the provision of information to families.
Case study site 4
Case study site 4 was a district, hospital-based service where teams were co-located. The composition of teams varied according to need and, hence, there was a fluidity to how teams functioned. As at CS03B, the co-ordination of care was reliant on the lead professional. However, co-location is not a proxy for integration or a ‘unitary construct’ but a ‘complex set of relationships, organisational structures, and other features meant to help practices deliver care’. 75 The difficulty in capturing this complexity was reflected in the service map at CS04, which has a three-tier feeding pathway (although unwritten), a further indication of the high level of specialisation. This level of specialisation was reflected in the fact that, until recently, gastrostomies were also placed within the service. This function then transferred to the tertiary centre, which had minimal involvement in supporting the majority of children referred, which contrasted with the model of care at CS03. There were strong links with the CCN team, which was viewed as the ‘eyes of the service in the community’, although reported to be under pressure. An important aspect of care was the traffic light tool (a communication aid developed with the input of parents) widely adopted by clinicians, which aimed to empower parents in clinical consultations. The tool could be adapted to help guide conversations around PSS issues related to children’s feeding and GFT placement.
Overall impressions
Medical models of working, which may be more dominant where the lead professional is medically or surgically trained, may support the integration of teams and services but be less effective in involving parents and ensuring that PSS is integrated routinely in care. Parental roles were stronger at CS01, typified by strong leadership and the integration of health and education through pooled budgets, although there was evidence of a strong partnership prior to this funding model. Nurse-led models can be very effective for ensuring PSS is integrated and provided, as at CS03 and in the CCN teams described at CS02 as well as at other case study sites, but they require sufficient staffing resources to be effective. Different models are likely to work for more rural settings, as at CS02, which was a generalist service staffed by a MDT responsible for children with exceptional health-care needs. There may be a role for psychologists in advising and supporting generic staff to integrate PSS, which may be a more feasible and effective use of resources than aiming to refer all parents routinely to psychologists.
Commissioning and procurement
A key point to note in our study is the variation in resources across a relatively small set of case study sites in addition to variations within services. This was particularly marked at CS03A and CS03B. However, CS03, and to some extent CS04 (where paediatricians and services were hospital based), is probably more representative of models of services in England. These variations, often historical in nature, may reflect adaptations to local contexts and local commissioning in England, but funding issues may require a national response to ensure parity and efficiency of provision.
Different procurement policies by hospital trusts potentially affected the lived experience of caring for children fed by a GFT. This was very clear at CS01 when parents were asked who the ‘go to’ person was when an issue arose. The ensuing conversation focused on the complexity of obtaining supplies and equipment owing to procurement policies that, at times, appeared unfathomable to parents. There was talk of a ‘post code lottery’, reflecting the wide catchment area that children came from and an inequality in provision. Parents demonstrated their expertise as skilled navigators of services in trying to obtain the equipment they needed. Previous research has described the stress parents experience over obtaining feeds and equipment and, hence, this is an area where support can be provided. 80
Who provides psychosocial support: team members and designated roles?
Across all case study sites the provision of PSS was deemed the responsibility of the MDT, rarely a designated specialist, and provided in the context of children’s clinical appointments. However, few professionals had received training in PSS initiatives (7/31 in our costing study) other than during their formal professional training which, arguably, would not be sufficient to produce clinical expertise. 81 This was confirmed by the professional questionnaire in phase 3, in response to which few respondents (4/31) reported feeling very confident in providing PSS. Professionals who participated in the phase 3 costings questionnaire appeared more confident if they had received specific training.
Generally, PSS was enacted by various members of the team at different points in the child and family feeding journey but was rarely formalised or documented in tangible ways, which also made costs of care difficult to estimate. Although professionals reported spending a considerable amount of time and effort supporting families in general, PSS as a discourse and practice appeared to be secondary to the more technical aspects of clinical care and was relatively hidden. Moreover, it was unclear whether or not the support offered by teams was what families wanted, and emotional support, where needed, was a gap highlighted by both providers and parents.
Although staff believed that families had access to psychologists through CAMHS, in reality many children did not reach the threshold (e.g. through the presence of harm to themselves or others) for this support and it was often unclear if parents had to be re-referred for support through their GP, highlighting a tension, perhaps, around ‘adults’ as ‘patients’ or ‘carers’ in children’s services. Moreover, where access was available, pathways were often unclear. Different views were expressed on the need for psychologists by both professionals and parents. Discussion of the inclusion or exclusion of psychologists in the context of funding was particularly prevalent at CS03 and CS04, and costs were a perceived barrier to including specialised staff offering PSS in teams unless savings were made elsewhere. The view that commissioners expected ‘more for less’ and issues of affordability informed responses rather than what staff felt was needed. Conversely, in feedback sessions, parents mentioned they would like the choice of seeing a psychologist, but were concerned about the burden of additional appointments if psychologists were not integrated into teams, and that a referral might suggest that parents were not coping. The provision of enhanced PSS involving a psychologist was valued by both HCPs and parents in the WTP study (phase 3). Although not statistically significant, parents attached a lower value to the enhanced service than did professionals. This may be because professionals were valuing their own time and input, whereas most of the parents had not experienced the support described in the enhanced scenario.
There was a view that the CCN team was best placed to offer support, although these services were described as ‘under pressure’ in some areas, including at CS03 and CS04. Nursing teams can play an important role in caring for children post gastrostomy, including during stoma-related complications and replacing devices,82 which may prevent hospital admissions.
There was little mention of the role of key workers in interviews in our study. This may, in part, be due to differences in terminology and understandings of the role, which can make comparisons across service models difficult. 83 HCPs did not view them as part of the multidisciplinary feeding team. Although the literature emphasises the roles of key workers in co-ordinating care5 and providing emotional support,84 not all families have key workers85 (reports suggest that approximately one-third of children have access in the UK) and there have been problems implementing these schemes. 86 Hence, in our study it was usual practice for the lead professional to co-ordinate care, including PSS. However, if the leads are doctors, they may see families with less frequency than other professionals. In Scotland the term ‘key contact’ was used and the type of professional would depend on the child’s age (e.g. a head teacher for school-aged children or a health visitor for children aged < 5 years), although this did not specifically relate to feeding. The confusion over terminology was confirmed by our parents in our PPI reference group. One parent stated that the term ‘key worker’ was ‘overused’ and hence it was difficult to identify who the key worker was and, in their view, key workers did not provide emotional support. Moreover, staff members at CS03 confirmed that early-support key workers, although they used to be available, were now scaled back and did not attend clinical appointments or offer support around feeding.
Although MACs provided a mechanism of support for children with complex needs at CS02, these were not used at other sites for feeding-related support. In some areas, particularly at CS03, MACs were perceived to be associated with safeguarding owing to resource constraints. A recent report from the National Audit Office, Pressures on Children’s Social Care,87 seems to confirm the impact of austerity on services: ‘Local Authorities have responded to financial pressures by prioritising child protection work and reducing spending on non-statutory children’s services’ (reproduced with permission from The National Audit Office87). In some areas, ‘Multidisciplinary Reviews’ or ‘Child in Need Reviews’ are used and may serve as a means of assessing and meeting some families’ need for support.
Information and resources
There was a general lack of child- and parent-friendly materials except at CS02, which had access to a DVD produced for parents by the NMCN CEN. Information provision was often technical, and some leaflets included drawings of older adults rather than children. Moreover, it was unclear how parents accessed the information. Some recent materials (appropriate for children) were identified in feedback sessions with staff, produced by a home enteral feeding company in conjunction with Carers UK, but not all professionals were aware of these resources and there may be ethics barriers to promoting materials by companies that produce infant formula in addition to commercial feeds. Parents were also using social media to obtain information. For example, at CS01 parents solicited advice from others through Facebook.
Structures to facilitate peer-to-peer parent support
No site had a formal approach to involving parents as peer supporters, although there was some evidence of clinicians putting families in contact with each other or directing parents to people or agencies who could facilitate this. However, this was not consistent. Professionals generally valued the idea of parent peer contact but expressed concerns about confidentiality and ensuring that parents were well matched. There was a concern that peer contact could have negative consequences if not appropriately managed. This was identified as a potential barrier. Some groups of parents valued the opportunity to meet other parents and receive information about their experience of having to make a decision about their child being fed via a GFT; others, particularly at CS02, tended to value the expertise of professionals. The way parental support is presented may also be an issue. Coffee mornings or social events featured in most cases, which appealed to parents, whereas the term and concept of a ‘parent support group’ did not always resonate. Parents’ involvement was more active at CS01, which again may attest to the uniqueness of the partnership between school and health-care services. Facilities for parents to meet certainly helped, and parents were actively involved in joint committees between health care and education. However, the parent group was not professionally led and appeared to form organically around the school, supported by a staffing resource. The school was able to serve as a focus for galvanising parental involvement through well-established networks and more casual contacts, although not all parents were involved. There was also evidence of some parents setting up their own group in other areas (CS03B).
We were not able to investigate the role of nurseries in offering support for preschool children, but there are similar networks of parents in early-years provision that would be worthy of further study. The success of parental networks at some sites (e.g. CS01) was such that there was a ripple effect to schools outside the case study site. However, not all parents accessed parental networks, which may raise issues of equity in terms of accessing support. Not all parents felt that they needed to access parental support, and for some, owing to geography and distance, attendance at parental events was not possible. Staff often perceived that parents were accessing support through social media, but little is known about these interactions. Nurses at one tertiary centre used social media (e.g. Facebook) to introduce parents to each other.
Processes and mechanisms of care
Processes of care include the interactions of staff with parents as opposed to the clinical tasks that are performed. We identified three analytical constructs governing processes of care: hidden work, expressing emotional vulnerability and negotiations around risk.
Hidden work
This construct describes the hidden work that both parents and professionals enact. Although most professionals had a good understanding of the values that parents attached to oral feeding and the conflicts that can arise when making the decision to gastrostomy feed a child, they struggled to articulate how they specifically delivered PSS. Theoretical approaches to support were rarely mentioned. Indeed, staff may not have a theoretical understanding of what they do when they support families. The more embodied the work the more difficult it may be to articulate practices that are taken for granted, and, methodologically, interviews are not the best tool to analyse practice. The inability to describe work unless doing it and the tendency of hidden work to be undervalued or not recognised have been noted in other studies. 39 Allen,88 for example, in a study of nurses’ organisational practices, suggests that the hidden nature of work becomes normalised through everyday practice, including the effort involved in the organisation and co-ordination of patient care. Allen88 suggests that the culture of ‘measure and manage’ in contemporary health care renders particular types of work invisible and tends to privilege task-focused work over relationally focused care. The invisibility of the skill involved in supporting families was evident in one professional’s claim that a ‘common sense’ approach to support was needed, which underestimates the skill both acquired and needed. Indeed, our research suggests that the provision of effective emotional support requires a lot of skill.
The lack of recognition and value of the work involved in providing PSS may be a reason why it is not recorded in children’s records, which in turn conspires to ensure that the work remains hidden. Moreover, it may not be deemed appropriate to note the care of parents in medical records for children who are the primary patient. This invisibility of PSS in health records rendered the economic costings of care all the more difficult in phase 3; yet, as Bowlby89 notes, ‘[t]he performance of informal caring involves a person using resources – people, ideas, material objects, as well as time and space to care – accessed through particular places and spaces at particular times’.
There was a parallel in the hidden work enacted by professionals and that of parents managing their own emotions and the emotions of other family members when making a decision to feed their child via a GFT as well as in the support that they offered other families as peers. Managing a myriad of relationships with professionals and navigating complex care systems was another aspect of this hidden work; for this reason, perhaps, many parents preferred to receive PSS from a known individual to minimise relationship burden.
Following surgery, parents became highly proficient at dealing with the practical and technical aspects of gastrostomy feeding and learnt what were arguably new nursing tasks. This journey from novice to expert, however, became an imperative, rather than a choice, where support from services appeared to wane over time. Moreover, the consequences of not managing the GFT could result in long journeys and admission to hospital, which many parents wished to avoid. The development of expertise may also provide an opportunity to take back control of children’s care and feeding as witnessed by the amount of time some parents spent training school staff before allowing them to feed their children (as evidenced at CS01) and the adoption of BDs, which inevitably placed parents as risk managers – another aspect of hidden caring work.
The research also highlighted the impact on professionals of having to manage decisional conflict and to support families through difficult decisions about children’s feeding, which they too experienced as emotionally demanding. This indicates a need for emotional support for professionals too, through clinical supervision. Support from a psychologist might prove useful in these contexts.
Expressing emotional vulnerability
Not all families viewed a GFT negatively; hence, families’ need for PSS varied and may reflect difference in values and family contexts,90 suggesting that a personalised, approach, tailored to individual children and families, rather than a pre-structured approach, is warranted. It may also have reflected the timing of the research in relation to the gastrostomy; for example, many parents provided a historical account, whereas the need for support may be more readily expressed when parents are at the centre of making the decision. Although some parents minimised their need for PSS, their narratives about their experiences were vivid and drew on emotive terminology (e.g. ‘terrified’, ‘scared’) even when considerable time had lapsed.
Some presented a stoical front, minimising their need for support, reflecting, perhaps, cultural differences in expectations about health-care services. There was a sense of needing to get on. Some parents’ narratives reinforced a division between the need for emotional or practical support and generally emphasised the latter. However, families may not be able to assert their needs for PSS for a variety of reasons, not least because they felt that asking for support, or counselling, may signify emotional vulnerability and inability to cope, something that many parents would be keen to avoid. Some parents reported that there was not enough time to raise the issue of emotional support in a busy clinic (it can be difficult for parents to intervene in the flow of clinical tasks), reflecting a temporal dimension to the meanings parents attach to spaces as places of care. 89 Bowlby89 argues that, because spaces are socially defined, professionals should attend to ‘how people feel about the timing and placing of the caring relationship in which they are involved’. More neutral spaces may help parents to discuss their concerns. Asking for help with the technical and practical aspects of GFT care may be an easier and more immediate demand in the face of having to learn new nursing procedures. Parents did expect to be tutored in the care of the GFT, although some reported more support in this area was needed before discharge from tertiary centres at which the GFT was placed. The side effects of the procedure in the immediate aftermath of surgery and beyond were certainly experienced as traumatic by some parents, suggesting an important touch point where additional support may be needed.
At a feedback session in one service, clinicians felt that, given the need for support was unique to families, they should take the lead in communicating their needs. There was some frustration expressed about parents who wanted to ‘push the decision back onto the clinicians’. No doubt this was underpinned by an attempt to democratise and share decision-making and hence minimise decisional conflict. 91 However, it can position families into ‘unwilling collaborators’ in decisions about their child’s feeding even though they may feel they lack expertise. 27
Negotiations around risk and values: decisional conflict
Our analysis was informed by Mahant’s model of decisional conflict. 1 Both professionals and parents were involved in negotiations around risk, including on the safety of oral feeding, that is the risk of oral aspiration, the use of blended feeding, which was generally not recommended by services, and the decision to have a GFT. Previous research identified tensions between professional and parental values, with professional practice focused on the biomedical aspects of care (e.g. nutrient intake and weight gain) and parents focused on the lived experience of feeding a disabled child. However, this distinction is perhaps too binary, because many professionals in our case study demonstrated an appreciation of the values parents attach to food, feeding and mealtimes and indeed shared these values. This is a positive finding, suggesting that professionals were aware of the issues highlighted by studies conducted > 15 years ago. 27 Major conflicts around feeding between professionals and families were rarely reported in interviews. Rather, professionals reported that they respected parental wishes and were prepared to go at the families’ own pace in making feeding decisions. The consensus was that you could not force a medical intervention on parents who did not want it. However, some professionals expressed concerns about how to respect parental wishes and while also ensuring the best interests of the child. This would seem to support the findings in the provider survey, which suggested a generalised concern about feeding and safeguarding, although this was rarely actioned. This may reflect a team decision, despite individual concerns, and the availability of support through clinical supervision. Alternatively, it may be the case that concerns about feeding are rarely the sole reason for safeguarding.
The assumed risks associated with oral feeding, and an unsafe swallow, were often minimised by professionals in favour of the child’s quality of life, which, in line with parents’ views, was assumed to be better if feeding was normalised in family contexts. However, the extent to which professionals were willing to accept parents’ desire to feed their child by mouth was also dependent on the way that teams operated and whether or not there was multidisciplinary teamworking with an ethos of collective responsibility for risk management. There appeared to be an ethos of ‘risk feeding’ – that is, measures were put in place to minimise the risks associated with oral aspiration – rather than recommending a strict nil-by-mouth feeding regime, to respect caregivers’ wishes. Some professionals felt that a GFT could help normalise feeding by mouth because the pressure on children and families is reduced if most of the nutrients are delivered by GFT.
The use of BDS appeared to be a particularly contentious area given the lack of evidence and professional consensus to recommend the practice. 92 Resourcing issues were also raised as a barrier by staff to their use, including an anticipated increase in the size of professionals’ caseloads. The use of BDs post gastrostomy attests to the values parents attach to food and feeding practices,93,94 although BDs were mainly supported for medical, rather than social, reasons in clinical arenas. Professionals had to balance the wishes of parents against professional and institutional guidance and ‘supported’ rather than ‘recommended’ BDs and, therefore, located their practice in the grey area of risk management in feeding. 20 Inevitably, institutions adopted a position of compromise on the use of BDs, which was sometimes experienced as contradictory. For example, in one school, only food prepared at home could be blended and put in the GFT, whereas school meals could not; one hospital would permit only a mix of formula and BD if a child was admitted. Therefore, parents would have to adapt food preparations in line with different institutional policies, or agree to these adaptations, and, hence, engage in negotiations around the management and ownership of risk20 – another aspect of hidden work and source of stress.
Outcomes
Although this was not a systematic study of outcomes following gastrostomy, parents generally viewed gastrostomy favourably, as documented in the research literature,95 although many recalled problems in the immediate aftermath of surgery and being faced with having to learn new feeding practices and nursing skills. Side effects of the procedure resulted in families having to seek health care, involving travel and sometimes admission to hospital, or required parents to develop expertise in managing the nursing care of their children themselves, particularly as support from services waned over time. Research has documented the benefits of gastrostomy feeding, including reductions in psychological distress over time (e.g. at 12 and 18 months post surgery). 96,97 However, problems that children and families experience when using home enteral nutrition overnight include sleep disturbance, dislodgement and blocking of GFTs, and problems with the pumps delivering feeds are also reported. 80 Models of care that support families in the immediate aftermath of surgery, such as the CCN team and the home enteral clinic at CS02, and the tertiary nursing assessment model at CS03, have the potential to improve care post surgery by minimising the side effects of treatment and preventing readmissions to hospital. 78,98 Models of care that better prepare families for surgery, as at CS03, where children were assessed by nurses at the tertiary centre where the GFT was placed prior to appointments with surgeons, may also provide important spaces for families to discuss issues of concern. In this example, the surgical nurses additionally provided an important link between families and the CCNs, who also provided support, although there was a perception that these services were under-resourced. Schools also play an important role, and there was evidence of significant task-sharing between health-care and educational staff at CS01, a service characterised by high levels of integration between health-care and education. At other case study sites (e.g. CS02), school staff would not necessarily engage in nursing activities, which would be the role of the CCN team.
Research on health outcomes for paediatric neurodisability has demonstrated that parents value emotional well-being as an aspect of health. 99 In our study, little was recorded in the children’s notes that could be utilised to evaluate this aspect. Recording of satisfaction with the procedure, or the PSS provided, was generally absent, as were any quality-of-life measures for children and families. Data on the impact of parental peer support, given that this was an informal arrangement, were not captured, nor was the effect of training on team performance. A systematic review of core outcomes reported that ‘life impact and resource use’ were under-represented in research studies. 100 The authors of the review suggest that these outcomes are either undervalued or not measured owing to a lack of standardised tools. This also presented difficulties with phase 3 of this research on costing PSS. A recent study analysing children’s medical records in Sweden101 demonstrated that clinicians emphasised biological and nutritional outcomes post gastrostomy, whereas information on psychosocial aspects was only sparsely documented. The authors concluded that information relating to medical intervention goals dominated and was prioritised over psychological aspects, despite the involvement of psychologists and social workers in setting these goals – findings that were supported in this study.
The lack of documented outcomes is not surprising given the hidden nature of PSS work. Professionals reported that they spent considerable time supporting families. If such investment of time is to be valued then this work needs to be rendered visible through appropriate documentation and evaluation to show the potential to improve the quality and experience of decisions about children’s feeding, parental enablement and the PSS provided, including the overall impact across the life course. It may also help to obtain resources.
Equally, there were no mechanisms in place to record or evaluate the impact of specialist training on the team. If training was focused specifically on assessing and meeting the PSS needs of parents, or staff with specialist skills were involved in supporting parents or teams, this could prove an effective use of resources. This is important given that austerity has led not only to services being cut but also to professionals having less time with children. 102 Team training, which strengthens the ‘collective competence’ of the team, could ensure that PSS is consistently embedded103,104 rather than left to individual interest, and could also draw on the expertise of parents as trainers. 105
Implications for practice and services
Integrating psychosocial support
In interviews, HCPs report spending significant time supporting children and families, but because PSS is integrated into appointments it is undocumented and therefore not recognised or valued, and provision may therefore be inconsistent.
The challenge for services is how to better integrate PSS into clinical ways of working by creating spaces dedicated to PSS initiatives that can also be documented, audited and evaluated. The different mechanisms for integrating care identified in this study could serve as foci for strengthening PSS initiatives in these enabling structures.
Because there were differences in parental need for PSS, a personalised approach using appropriate assessments by a named staff member, with training and with continuity of the professional involved, could also ensure effective use of resources. Given that parents and children may not be able to assert their need for PSS in time-limited appointments dominated by clinical aspects, appointments where the primary focus is PSS or longer appointments with dedicated time may enable parents to discuss their concerns. Flexibility will be important because parents’ need for PSS may not coincide with appointments and parents may find it difficult to talk about their feelings in the presence of their children. PSS could be formalised as part of standard care, which would help to normalise emotional vulnerability, and standards of support could be developed and shared with children and families (see Report Supplementary Material 8). Because professionals had different ideas about parents’ PSS needs, ranging from a discussion about the risks involved in placing a GFT to an understanding of the emotional impact of the decision (e.g. a grief journey), we recommend the term ‘psychosocial emotional support’ to ensure that appointments focus on values and emotions in addition to clinical risks and tasks. Service providers could offer home visits, which have been shown to be valued, although this would incur costs for travel and additional time.
Parents also expressed a preference for receiving support from someone they knew, which suggests the importance of relationship continuity, which may be an important factor when considering how to integrate support from a designated member of staff (e.g. psychologist or equivalent), where available. School staff also have an important role to play in wrapping support around the child and family and could be more proactively involved in supporting families through team training. Lead professionals have a role in co-ordinating this support, which also needs to be recognised.
Where access to a psychologist or equivalent professional with specialist training is available, it would be helpful to parents and staff to know how to obtain this access, should they choose, and what to expect through clear pathways. Careful attention to the use of language (terminology), as well as how the issue of PSS and the opportunity to see a specialist is raised, will be needed to avoid the suggestion that parents cannot cope and, hence, reinforce the sense of failure that many parents may already feel.
The provision of child- and family-friendly information using social stories106 could also be better integrated into care as a standard and entitlement to ensure equity of access. There was evidence of a DVD for parents at CS02, which could be shared, and online resources made available through professional and parental networks.
Mechanisms for recording and auditing PSS may help to make the case for additional resources and could provide useful costings information. National guidance on how to code and capture data will be necessary107 to minimise discrepancies in coding to compare service data. Coded and structured data could then be exploited for secondary purposes. 108
Training and education
Staff may benefit from specialised training that brings a psychological approach to the way teams work specifically tailored to the PSS needs of this group of children and families and could form part of induction or appraisal as a means of embedding training. This is important given the assertion that, although services can make a difference to the health-care needs of children, they are less able to meet the social and emotional needs of families. 109 Team training, including staff from education and social care, would be particularly beneficial to strengthen collective competency. This would ensure a systems-based approach to embedding and providing psychological support, rather than an approach based on the initiative, skills or interests of individual practitioners. There is evidence for the benefits of interprofessional education110,111 and, in the context of quality improvement initiatives, it can improve practice. 112 There was evidence of an online training resource at CS02 and this could be made more widely available for educational purposes. Parents can also play an important role in delivering professional education. Training for professionals could focus on how to enable decision-making through guided and structured conversations with families, drawing on research evidence. 90 Communication tools, such as the traffic light tool at CS04, where parents could identify their priorities for the appointment, could be adapted to ensure that PSS was the primary focus.
Parent peer support
Establishing a formal register of parents willing to talk to others may overcome concerns about confidentiality using models adopted by many charities [e.g. the peer-moderated group run by Together for Short Lives (Bristol, UK)]. Services could encourage the development of parental networks through coffee mornings. Social media can play an important role for those parents living in rural areas, geographically dispersed or preferring support at arm’s length to face-to-face support, or where there are space restrictions. There was evidence of parent-led Facebook groups where parents solicited advice from each other, and professional groupings used Facebook to connect parents in our study.
The suggestions we have made here are of relevance to the wider children’s services and workforce, particularly the training of staff to incorporate a psychological dimension in their practice and the potential role of social media.
Strengths and limitations of the study
Methodological limitations
We conducted a qualitative case study with a focus on four service configurations chosen, in part, from the findings of a WBS that produced a low yield of responses. Therefore, we cannot claim that these services are representative of all services. However, we chose sites based on what they could tell us about how PSS was provided and integrated into children’s care and the factors that enabled services to provide the support they offered based on the findings of the WBS and additional theoretical criteria. A study on the organisation of midwifery units51 similarly chose four sites, and generalisation in that study was seen to work on a ‘conceptual and theoretical level’. We believe that our analytical constructs (hidden work, expressing emotional vulnerability and negotiations around risk) are theoretically generalisable and reflect processes of care for families regardless of the different characteristics of the services we chose to study. We also recognise that the mechanisms for the integration of care that we have presented may not be exhaustive, and that our findings are provisional, given that services are often in a state of change. Indeed, we witnessed changes in the organisation of care at two sites over the course of our study – a finding reported elsewhere. 113 It is of interest that a survey of 100 parents conducted in New South Wales, Australia, reported overlapping concerns with those reported by some families in this study: families expressed dissatisfaction with their care and the support they received both before (42%) and after (36%) surgery – themes that resonate with some parents’ experiences in our study (although not all), albeit in a different context. 114
It proved extremely difficult to disseminate a national survey (phase 1) outside a professional database of leads of child development teams. Dissemination through the R&D networks of different trusts required a considerable amount of administrative work given that each R&D department must assess their capacity and capability to participate in research studies. We had little control over the dissemination of the questionnaire. The survey was disseminated during a transition period for the HRA in England and Wales, which led to considerable delays and inconsistency in the process of obtaining permissions. This undoubtedly led to a poorer response rate than anticipated, and we have discussed further methodological limitations of surveys as tools to capture organisational practice in the context of complex service configurations in Chapter 1. There were also differences between responses reported in the WBS and actual practice. For example, 15 out of 35 respondents stated that PSS was formalised, and 19 out of 23 respondents stated that referrals to other parents were formalised, yet our field work (phase 2) suggested this was not the case. These differences may be due, in part, to sampling or an artefact of the methods used. We were better able to probe and tease out these differences in interviews.
Interviews can also have their limitations when used to identify everyday practices that remain hidden. 39 Ethnographic observations of care, and reflective interviews with teams and parents, following clinical consultations may prove a more effective approach to understanding the delivery of PSS in real time. This may prove challenging to organise where facilities and time are limited.
The system of permissions
The permissions process for the case study research was also administratively onerous given the fragmentation of services (community services coming under one trust and tertiary services another) and where members of the MDT were employed by different trusts. Each case required at least two sets of permissions. In one case an additional set of permissions would have been required to interview one member of the MDT employed by a different trust. Because this was not an efficient use of research time, some members of the MDT were not interviewed. Assessments of capacity and capability often took several months, particularly in the second half of the study, owing to concerns about the General Data Protection Regulation (GDPR). 115 One R&D department made an application to the Caldicott Guardian because our research involved children, demonstrating an additional level of governance not required elsewhere. Therefore, the model of research governance proved challenging for a project requiring a more iterative and flexible approach – an important characteristic of progressive focusing. Regional and cross-sector approvals would to help minimise the administrative burden for studies of this type and complexity.
Parent and child participation
It proved difficult in some cases to engage parents and children in the research. The research team did not have direct access to parents and relied on research nurses to disseminate information about the project. Before sending information by post, the services contacted parents by telephone to seek their permission to participate and send out the information. However, the research team, concerned that this might affect response rates, felt that the first contact messaging should be nuanced in a way that encouraged participation and consent on receipt of the information. We also asked services to advertise the project through their social media and via posters in clinics (which needed additional approvals). In addition, our lay chairperson contacted local parent groups informally, where these existed, to inform them about our study. It is also possible that families were dealing with more pressing issues that took priority in the face of cuts to local services,102 and some of our case study sites were drawn from areas characterised by higher than average levels of deprivation, which may have affected participation rates. One service cautioned that, historically, parents did not participate in qualitative studies, suggesting a culture that is biomedical research dominated. Poor parental recruitment in palliative care research as a result of professional gatekeeping has been reported. 116
It can also take time to access children because of the need to work with gatekeepers, including parents, who provide consent to interview children. 117,118 An audit of consent forms across two case study sites revealed that just over half of parents did not consent to their child participating in research. Most parents when asked to consent left the box blank, or actively refused, or put ‘not applicable’. Reasons for refusal included that the child was ‘non-verbal’ and that the child had global developmental delay and could not speak. One parent agreed providing they were present to assist with communication. There are particular challenges to interviewing children in this population (approximately 42–60% are estimated to have communication impairments)10,60 due to the different modalities that they use to communicate and how these interactions are interpreted. 119 For this reason we planned to video-record interviews. However, one service would not allow us to video the interviews of children on their premises, although the research had received ethics approval. Moreover, the service was not able to provide rooms for interviews owing to space limitations. For those parents who did provide consent, it proved logistically difficult to arrange interviews owing to children’s schooling and the need for permission to video-record on school premises, as well as illness that prevented participation. Because some parents lived a considerable distance away from health centres, with little public transport, travel to families’ homes made it difficult for researchers conducting field work at a distance and Skype interviews would not be suitable.
It also took time to establish a relationship of trust with children and learn their preferred way of communicating, which would have required repeated visits, with the potential to affect children’s schooling and family life. Gaining children’s assent to participate could take up to 30 minutes, and in the case of one child 20 minutes was their maximum attention span. One interview had to be conducted through the child’s teaching assistant, but researchers have questioned the validity of children’s views expressed through intermediaries. 120 Therefore, we have not presented data from children in this report in any substantive way. However, our PPI work involving children provides a particularly powerful example of children’s views on the right to support.
Timescapes and experiences
Parents’ accounts of their experiences were often historical and reflected diverse timescapes. Hence, issues took on different significance depending on where parents were in their child’s feeding journey. For example, in some cases decisions about gastrostomy were made, and the surgery undertaken, many years ago, and the children were now in their teens, whereas other experiences were much more recent. In some instances, decisions had yet to be made. Thus, parents’ narratives were located in the past and present. However, the accounts of staff almost invariably described their experiences as a provider of care in a service at the case study site under investigation and in relation to current practice, which often served to support the views expressed by families. Moreover, parents of older children provided data on the experiences of GFT feeding across the life course, not previously reported, which adds to our understanding of support issues beyond the decision-making phase.
Moreover, owing to the complexity of children’s needs and the severity of their neurodisability, children often received care from multiple health providers in different locations. Parents sometimes discussed their experiences in relation to services within and outside the boundaries of the case study sites. Parental narratives therefore traversed these complex timescapes and landscapes of care.
Resource use, costings and willingness to pay
Response rates for the costings questionnaire from both parents (20%) and professionals (28%), although comparable to that reported in a study costing key worker schemes (30%),121 warrant further discussion. An audit of consent forms at two case study sites revealed that just under one-quarter of parents did not consent to participate in one, or both, of the phase 3 studies. It is of interest that 30% of staff did not consent to participate either, although at this stage the costings questionnaire had not been included in the information packs. We later changed the stage at which the questionnaire was disseminated so that it was included with the consent forms for fear of sample attrition. For example, owing to a change of sponsor, the project was paused for 1 year at the time that the questionnaires were sent to CS01 for dissemination; however, owing to indemnity issues, they were not sent out until after the pause. This inevitably led to a loss of momentum and continuity. There was much discussion in the PAG about whether or not sending the questionnaires with the consent forms contributed to information overload. We asked the local research nurses to advise parents that they did not need to complete the costings questionnaire at the same time as the consent forms and that they could receive assistance to complete the forms from the research team to maximise consent.
Higher response rates (e.g. 71%) were reported in a study on the cost-effectiveness of gastrostomy,28 but that study took place at a tertiary centre with a higher volume of children than the community services in our study. Parents were recruited directly in clinics by an onsite researcher who had formed a relationship with the families because the research design, involving multiple data collection points, necessitated frequent contact with the families, before and after the placement of a GFT. The researcher was therefore known to the families. The researcher was able to assist families with the completion of forms at the hospital or by telephone. Gatekeeping was also minimised. However, in our study researchers were very much ‘outsiders’ to the services and not allowed to approach families directly. Future costing studies may therefore need to be conducted at the regional or tertiary centres to capitalise on the volume of patients, although much of the support will have taken place in the community, sometimes over many months or years.
Low response rates are not surprising given that we were looking for a particular cohort of children. Moreover, parents may be wary of participating in research if they feel that this could result in the withdrawal of services that are already perceived to be under threat. 87,102 Indeed, this was confirmed by a professional at one case study in conversation with a parent. Professionals may have similar misgivings about costings research in a climate of cuts and limited resources, particularly where services may be under review, as was the case at one of our sites. One clinician, for example, did not agree to the WTP aspect of the study and refused to advertise the study to parents because it might be misconstrued as requiring payment for health care.
Our estimates of cost were based on the responses of eight parents, five of whom reported that they had received PSS in the previous 12-month period; therefore, the results have to be interpreted with caution, as should the estimates of time provided, given that self-reporting of time spent in activities may be over- or underestimated. 13 Other parents either indicated that they had not attended appointments in the previous 12-month period or left this section blank. There was a perception in our case study that parents had to learn to manage what could arguably be described as nursing tasks post gastrostomy. They may have resolved their issues themselves or through other means, for example by telephone, and not received appointments per se. Again, this reflects the problem of researching small populations with health disparities122 where data are lacking or simply not recorded because PSS is not recognised or valued as a distinct activity by services and commissioners. However, this is an important finding.
Notwithstanding the limitations, a key strength of this study lay in the use of a mixed-methods approach, gathering data from a range of perspectives where possible. This meant that professional reports of if and how PSS was provided, for example, could be balanced by the views and reported experiences of parents and carers, and a range of professional experiences were captured. In addition, the use of observation, although only limited data are reported directly here, provided a third ‘observer’ perspective that added to our capacity to triangulate the findings. The case study has also showcased several initiatives in providing PSS that will help services to further develop and embed resources. The case study has also highlighted gaps in service delivery and the training needs of staff.
Implications for future research
Potential areas for future research include:
-
A study to develop, pilot and validate an instrument to assess PSS co-produced with families.
A scoping study of existing tools to assess PSS and their relative strengths and limitations. This would identify gaps and the need for the development of a brief tool, co-produced with parents. The tool should be easy to implement in busy clinics and should document outcomes that are in line with agreed service goals and that are important to parents.
-
The development and evaluation of parent peer support initiatives for families considering a GFT for their child.
Parents expressed different views about peer-to-peer parent support, with some strongly in favour. Although the evidence for peer support schemes is not conclusive,123 there is evidence of benefit in mental health services. Schemes have produced modest cost savings,124 although they are resource intensive to establish. In our study, professionals emphasised the importance of matching parents, and this was also raised in Shilling’s study,123 along with a number of methodological considerations when planning studies, including time frames, comparators and measurement of health outcomes. A feasibility study would provide important contextual information influencing outcomes125 and could inform a future trial involving formal quality-of-life outcome measures.
-
An exploration of professional and parental attitudes towards costing studies and barriers to participation.
In a systematic review of peer support123 no studies of cost were identified. Similarly, an absence of studies on costings, attributed to a lack of suitable outcome measures or an undervaluing of studies involving costs, has also been reported in neurodisability research. 100 A qualitative study exploring professional and parental attitudes and barriers to participation in costings studies, and the acceptability of tools to collect data and outcome measures, may help to inform the design of future studies.
-
A study to develop and evaluate the role of parent trainers in training packages for health and social care professionals.
Our study identified the need for appropriate training packages for teams and that parent trainers could play a role in meeting this gap126 given their expertise. Standards of delivery and jointly agreed competencies would be needed. Training packages co-produced with parents and professionals would ensure appropriate content.
Acknowledgements
The authors thank all the professionals, parents and children who participated in research interviews or FGs or completed research questionnaires, the children and parents who formed our PPI reference group and others who provided feedback informally and all the staff from the voluntary agencies and professional bodies who helped disseminate our WTP questionnaire through their professional and parental networks.
The authors thank the anonymised principal investigators at two case study sites.
The authors thank Ms Helen Cockerill, Ms Jane Shaw, Dr Brindha Dhandapani, Dr Susan Protheroe, Dr Karen Horridge, Dr Mark Whiting, Dr Eilis Kennedy and Mr Habib Aziz as members of the G-PATH (gastrostomy feeding and psychosocial support pathways) Project Advisory Group.
The authors thank Dr Megan Smith (Research Fellow, University of Hertfordshire), who assisted with the design, collection and preliminary analysis of the data for the WTP study (phase 3), and Mr Nigel Smeeton (Statistician) for statistical advice and the analysis of the WTP study.
The authors thank Dr Judith Lathlean (Independent Consultant), who assisted with the analysis of the qualitative data.
Contributions of authors
Gillian M Craig (https://orcid.org/0000-0001-5132-7378) (Reader, Public Health, Social Science) contributed to writing the protocol, undertook the analysis of the qualitative case study data and associated write-up, analysed the national survey data, wrote the first draft of the report, critically reviewed the manuscript and agreed the final version.
Eva Brown Hajdukova (https://orcid.org/0000-0001-6127-7001) (Research Fellow) undertook the analysis of the qualitative case study data and associated write-up, critically reviewed the manuscript and agreed the final version.
Celia Harding (https://orcid.org/0000-0002-5192-2027) (Senior Lecturer, Speech and Language Therapy) contributed to writing the protocol and other sections of the report, commented on revised drafts, critically reviewed the manuscript and agreed the final version.
Chris Flood (https://orcid.org/0000-0001-5170-7792) (Senior Lecturer, mental health and health economics) contributed to writing the protocol, the costings and resource use analysis and write-up, critically reviewed the manuscript and agreed the final version.
Christine McCourt (https://orcid.org/0000-0003-4765-5795) (Professor, Maternal and Child Health, Case Study Research) contributed to writing the protocol and other sections of the report, commented on revised drafts, critically reviewed the manuscript and agreed the final version.
Diane Sellers (https://orcid.org/0000-0002-3090-2107) (Speech and Language Therapy) contributed to the writing of sections of the report, commented on revised drafts, critically reviewed the manuscript and agreed the final version.
Joy Townsend (https://orcid.org/0000-0002-7912-9856) (Emeritus Professor, Health Economics) contributed to writing the protocol and the costings and resource use analysis and write-up, critically reviewed the manuscript and agreed the final version.
Dawn Moss (https://orcid.org/0000-0001-7013-0925) (Consultant Nurse Specialist) contributed to the writing of sections of the report, commented on revised drafts, critically reviewed the manuscript and agreed the final version.
Catherine Tuffrey (https://orcid.org/0000-0002-6308-1173) (Consultant Paediatrician) contributed to the writing of sections of the report, commented on revised drafts, critically reviewed the manuscript and agreed the final version.
Bryony Donaldson (https://orcid.org/0000-0001-6256-028X) (Dietitian) contributed to the writing of sections of the report, commented on revised drafts, critically reviewed the manuscript and agreed the final version.
Maxime Cole (https://orcid.org/0000-0002-8633-9149) (Co-director, Triangle; PPI) undertook PPI with parents and young people, contributed to the writing of sections of the report, commented on revised drafts, critically reviewed the manuscript and agreed the final version.
Anna Gill (Lay Chairperson of PAG; PPI) contributed to the writing of sections of the report, commented on revised drafts, critically reviewed the manuscript and agreed the final version.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Mahant S, Jovcevska V, Cohen E. Decision-making around gastrostomy-feeding in children with neurologic disabilities. Pediatrics 2011;127:e1471-81. https://doi.org/10.1542/peds.2010-3007.
- Ferluga ED, Sathe NA, Krishnaswami S, Mcpheeters ML. Surgical intervention for feeding and nutrition difficulties in cerebral palsy: a systematic review. Dev Med Child Neurol 2014;56:31-43. https://doi.org/10.1111/dmcn.12170.
- Emerson E. Deprivation, ethnicity and the prevalence of intellectual and developmental disabilities. J Epidemiol Community Health 2012;66:218-24. https://doi.org/10.1136/jech.2010.111773.
- Allard A, Fellowes A, Shilling V, Janssens A, Beresford B, Morris C. Key health outcomes for children and young people with neurodisability: qualitative research with young people and parents. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2013-004611.
- Sloper P. Models of service support for parents of disabled children. What do we know? What do we need to know?. Child Care Health Dev 1999;25:85-99. https://doi.org/10.1046/j.1365-2214.1999.25220120.x.
- Gallagher S, Phillips AC, Carroll D. Parental stress is associated with poor sleep quality in parents caring for children with developmental disabilities. J Pediatr Psychol 2010;35:728-37. https://doi.org/10.1093/jpepsy/jsp093.
- Gallagher S, Phillips AC, Drayson MT, Carroll D. Parental caregivers of children with developmental disabilities mount a poor antibody response to pneumococcal vaccination. Brain Behav Immun 2009;23:338-46. https://doi.org/10.1016/j.bbi.2008.05.006.
- Reilly S, Skuse D, Poblete X. Prevalence of feeding problems and oral motor dysfunction in children with cerebral palsy: a community survey. J Pediatr 1996;129:877-82. https://doi.org/10.1016/S0022-3476(96)70032-X.
- Reilly S, Wisbeach A, Carr L, Southall A, Martin C. Feeding Problems In Children: A Practical Guide. Abingdon: Radcliffe Medical Press; 2000.
- Parkes J, Hill N, Platt MJ, Donnelly C. Oromotor dysfunction and communication impairments in children with cerebral palsy: a register study. Dev Med Child Neurol 2010;52:1113-19. https://doi.org/10.1111/j.1469-8749.2010.03765.x.
- Calis EA, Veugelers R, Sheppard JJ, Tibboel D, Evenhuis HM, Penning C. Dysphagia in children with severe generalized cerebral palsy and intellectual disability. Dev Med Child Neurol 2008;50:625-30. https://doi.org/10.1111/j.1469-8749.2008.03047.x.
- Emerson E, Hatton C, Robertson J, Roberts H, Baines S, Evison F, et al. People with Learning Disabilities in England 2011. Durham: Improving Health and Lives – Learning Disabilities Observatory; 2012.
- Sullivan PB, Lambert B, Rose M, Ford-Adams M, Johnson A, Griffiths P. Prevalence and severity of feeding and nutritional problems in children with neurological impairment: Oxford Feeding Study. Dev Med Child Neurol 2000;42:674-80. https://doi.org/10.1017/s0012162200001249.
- Spalding K, McKeever P. Mothers’ experiences caring for children with disabilities who require a gastrostomy tube. J Pediatr Nurs 1998;13:234-43. https://doi.org/10.1016/S0882-5963(98)80050-X.
- Calderón C, Gómez-López L, Martínez-Costa C, Borraz S, Moreno-Villares JM, Pedrón-Giner C. Feeling of burden, psychological distress, and anxiety among primary caregivers of children with home enteral nutrition. J Pediatr Psychol 2011;36:188-95. https://doi.org/10.1093/jpepsy/jsq069.
- Enrione EB, Thomlison B, Rubin A. Medical and psychosocial experiences of family caregivers with children fed enterally at home. JPEN J Parenter Enteral Nutr 2005;29:413-19. https://doi.org/10.1177/0148607105029006413.
- Pedersen SD, Parsons HG, Dewey D. Stress levels experienced by the parents of enterally fed children. Child Care Health Dev 2004;30:507-13. https://doi.org/10.1111/j.1365-2214.2004.00437.x.
- Thorne SE, Radford MJ, McCormick J. The multiple meanings of long-term gastrostomy in children with severe disability. J Pediatr Nurs 1997;12:89-9. https://doi.org/10.1016/S0882-5963(97)80029-2.
- Sleigh G, Brocklehurst P. Gastrostomy feeding in cerebral palsy: a systematic review. Arch Dis Child 2004;89:534-9.
- Craig GM, Higgs P. Risk owners and risk managers: dealing with the complexity of feeding children with neurodevelopmental disability – negotiating and communicating health risk. Health Risk Soc 2012;14:627-37. https://doi.org/10.1080/13698575.2012.717610.
- Gantasala S, Sullivan PB, Thomas AG. Gastrostomy feeding versus oral feeding alone for children with cerebral palsy. Cochrane Database Syst Rev 2013;7. https://doi.org/10.1002/14651858.CD003943.pub3.
- Pemberton J, Frankfurter C, Bailey K, Jones L, Walton JM. Gastrostomy matters – the impact of pediatric surgery on caregiver quality of life. J Pediatr Surg 2013;48:963-70. https://doi.org/10.1016/j.jpedsurg.2013.02.012.
- Craig GM, Carr LJ, Cass H, Hastings RP, Lawson M, Reilly S, et al. Medical, surgical, and health outcomes of gastrostomy feeding. Dev Med Child Neurol 2006;48:353-60. https://doi.org/10.1017/S0012162206000776.
- Smith T, Micklewright A, Hirst A, Gowan H, Baxter J. Annual BANS Report 2010. A Report by the British Artificial Nutrition Survey (BANS), a Committee of BAPEN 2010.
- Coad J, Toft A, Lapwood S, Manning J, Hunter M, Jenkins H, et al. Blended foods for tube-fed children: a safe and realistic option? A rapid review of the evidence. Arch Dis Child 2017;102:274-8. https://doi.org/10.1136/archdischild-2016-311030.
- British Dietetic Association (BDA) . Policy Statement: The Use of Blended Diet With Enteral Feeding Tubes 2019. www.bda.uk.com/uploads/assets/2ae537f0-6dab-483f-be7b2abd5f6b20cf/191111-Blended-Diets-Policy-Statement-FINAL-COUNCIL-APPROVED.pdf (accessed 14 March 2020).
- Craig G. Mother Knows Best: Gastrostomy Feeding and Disabled Children – Professional and Parental Discourses. London: University College London; 2004.
- Townsend JL, Craig G, Lawson M, Reilly S, Spitz L. Cost-effectiveness of gastrostomy placement for children with neurodevelopmental disability. Arch Dis Child 2008;93:873-7. https://doi.org/10.1136/adc.2007.133454.
- Craig GM, Scambler G, Spitz L. Why parents of children with neurodevelopmental disabilities requiring gastrostomy feeding need more support. Dev Med Child Neurol 2003;45:183-8. https://doi.org/10.1017/s0012162203000355.
- Craig GM, Scambler G. Negotiating mothering against the odds: gastrostomy tube feeding, stigma, governmentality and disabled children. Soc Sci Med 2006;62:1115-25. https://doi.org/10.1016/j.socscimed.2005.07.007.
- Craig GM. Horror and disgust: gastrostomy feeding and identity transformation. Radical Psychol 2010;8.
- Craig GM. Psychosocial aspects of feeding children with neurodisability. Eur J Clin Nutr 2013;67:17-20. https://doi.org/10.1038/ejcn.2013.226.
- Brotherton AM, Abbott J, Aggett PJ. The impact of percutaneous endoscopic gastrostomy feeding in children; the parental perspective. Child Care Health Dev 2007;33:539-46. https://doi.org/10.1111/j.1365-2214.2007.00748.x.
- Brotherton A, Abbott J. Mothers’ process of decision making for gastrostomy placement. Qual Health Res 2012;22:587-94. https://doi.org/10.1177/1049732311423841.
- Tariq S, Woodman J. Using mixed methods in health research. JRSM Short Rep 2013;4. https://doi.org/10.1177/2042533313479197.
- Braun V, Clarke V, Cooper H, Camic PM, Long DL, Panter AT, et al. APA Handbook of Research Methods in Psychology, Volume 2: Research Designs – Quantitative, Qualitative, Neuropsychological, and Biological. Washington, DC: American Psychological Association; 2012.
- Fram SM. The constant comparative analysis method outside of grounded theory. Qual Rep 2013;18:1-25.
- Stake RE. The Art of Case Study Research. Thousand Oaks, CA: SAGE Publications Ltd; 1995.
- Swinglehurst D, Greenhalgh T, Russell J, Myall M. Receptionist input to quality and safety in repeat prescribing in UK general practice: ethnographic case study. BMJ 2011;343. https://doi.org/10.1136/bmj.d6788.
- Sharpe R, Benfield G, Lessner E, DeCicco E. Scoping Study for the Pedagogy Strand of the JISC E-Learning Programme 2005. https://d1wqtxts1xzle7.cloudfront.net/34884524/scoping_study_final_report_v4.1_.pdf?1411721391=&response-content-disposition=inline%3B+filename%3DScoping_Study_for_the_Pedagogy_strand_of.pdf&Expires=1600707248&Signature=TWNLDBWkPI6YWGPYqygFNFcIwL0teMU16g7BkFgcQA-WEO~jJbz4S90MGf~DFLhnwbiZVOe7oANDd-ToYVPEZaWfSkU3E6M9UbWwMA99eDZHhCdWexv-k3-mkHO79LAcyjdE-8GKMbUiKjYvgh7koJKHT8bRPlEh7be0IO6vsX5O9LFT6cNr4XBXmA-GowoOXU67PckAxJ4~qgg1kSpQtgM2Z6pH6R09c2fn~YNd43PzvNqD5EZM02D-4LAQV6-MNNk1sIXVWI1zNdlv6wS8XD8-GfuluZwz8fTW7n1PZbR7B09s3nBh0g9cDhind6CnWihmWYoRmQzHLsalP1sWrQ__&Key-Pair-Id=APKAJLOHF5GGSLRBV4ZA (accessed 18 September 2020).
- Robson C. Real World Research: A Resource for Social Scientists and Practitioner Researchers. Oxford: Wiley-Blackwell; 1993.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581-629. https://doi.org/10.1111/j.0887-378X.2004.00325.x.
- Yin RK. Case Study Research: Design and Methods. Thousand Oaks, CA: SAGE Publications Ltd; 2003.
- Segar J, Checkland K, Coleman A, McDermott I, Russell J, Greenhalgh T, et al. Case Study Evaluation: Past, Present and Future Challenges. Bingley: Emerald Group Publishing Limited; 2015.
- Hollowell J, Puddicombe D, Rowe R, Linsell L, Hardy P, Stewart M, et al. Perinatal and maternal outcomes by planned place of birth for healthy women with low risk pregnancies: the Birthplace in England national prospective cohort study. BMJ 2011;343. https://doi.org/10.1136/bmj.d7400.
- Campbell H, Hotchkiss R, Bradshaw N, Porteous M. Integrated care pathways. BMJ 1998;316:133-7. https://doi.org/10.1136/bmj.316.7125.133.
- Cook JV, Dickinson HO, Eccles MP. Response rates in postal surveys of healthcare professionals between 1996 and 2005: an observational study. BMC Health Serv Res 2009;9. https://doi.org/10.1186/1472-6963-9-160.
- Stake RE, Denzin NK, Lincoln YS. The Sage Handbook of Qualitative Research. Thousand Oaks, CA: SAGE Publications Ltd; 2005.
- Public Health England (PHE) . Public Health Profiles 2019. https://fingertips.phe.org.uk (accessed 14 January 2020).
- NHS Quality Improvement Scotland . Caring for Children and Young People in the Community Receiving Enteral Tube Feeding: Best Practice Statement 2007. www.healthcareimprovementscotland.org/previous_resources/best_practice_statement/caring_for_children_and_young_.aspx (accessed 14 March 2020).
- McCourt C, Rayment J, Rance S, Sandall J. An ethnographic organisational study of alongside midwifery units: a follow-on study from the Birthplace in England programme. Health Serv Deliv Res 2014;2. https://doi.org/10.3310/hsdr02070.
- Dopson S. The potential of the case study method for organisational analysis. Policy Politics 2003;31:217-26. https://doi.org/10.1332/030557303765371708.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-117.
- Braun V, Clarke V, Hayfield N, Terry G. Thematic Analysis: Handbook of Research Methods in Health Social Sciences. Singapore: Springer Nature Singapore Pte Ltd; 2018.
- Mahant S, Cohen E, Nelson KE, Rosenbaum P. Decision-making around gastrostomy tube feeding in children with neurologic impairment: Engaging effectively with families. Paediatr Child Health 2018;23:209-13. https://doi.org/10.1093/pch/pxx193.
- Donabedian A. The quality of care. How can it be assessed?. JAMA 1988;260:1743-8. https://doi.org/10.1001/jama.260.12.1743.
- Mathie E, Wythe H, Munday D, Millac P, Rhodes G, Roberts N, et al. Reciprocal relationships and the importance of feedback in patient and public involvement: a mixed methods study. Health Expect 2018;21:899-908. https://doi.org/10.1111/hex.12684.
- Rodgers M, Thomas S, Harden M, Parker G, Street A, Eastwood A. Developing a methodological framework for organisational case studies: a rapid review and consensus development process. Health Serv Deliv Res 2016;4. https://doi.org/10.3310/hsdr04010.
- Cohen L, Manion L, Morrison K. Research Methods in Education. London: Routledge; 2002.
- Yin Foo R, Guppy M, Johnston LM. Intelligence assessments for children with cerebral palsy: a systematic review. Dev Med Child Neurol 2013;55:911-18. https://doi.org/10.1111/dmcn.12157.
- Cunningham CT, Quan H, Hemmelgarn B, Noseworthy T, Beck CA, Dixon E, et al. Exploring physician specialist response rates to web-based surveys. BMC Med Res Methodol 2015;15. https://doi.org/10.1186/s12874-015-0016-z.
- Royal College of Physicians (RCOP) . SAS Physicians Survey 2018 2018. www.rcplondon.ac.uk/projects/outputs/sas-physicians-survey-2018 (accessed 14 March 2020).
- Asch DA, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol 1997;50:1129-36. https://doi.org/10.1016/S0895-4356(97)00126-1.
- Rolstad S, Adler J, Rydén A. Response burden and questionnaire length: is shorter better? A review and meta-analysis. Value Health 2011;14:1101-8. https://doi.org/10.1016/j.jval.2011.06.003.
- Billig M, Condor S, Edwards D, Gane M, Middleton D, Radley A. Ideological Dilemmas: A Social Psychology of Everyday Thinking. Thousand Oaks, CA: SAGE Publications Ltd; 1988.
- Scottish Government . Health and Social Care Delivery Plan 2016. www.gov.scot/publications/health-social-care-delivery-plan (accessed 14 March 2020).
- Coles E, Cheyne H, Rankin J, Daniel B. Getting It Right for Every Child: A National Policy Framework to Promote children’s Well-Being in Scotland, United Kingdom 2016;94:334-65. https://doi.org/10.1111/1468-0009.12195.
- NHS Quality Improvement Scotland . Gastrostomy Tube Insertion and Aftercare: (for Adults Being Cared for in Hospital or in the Community) – Best Practice Statement 2007. www.evidence.nhs.uk/search?om=[%7B%22srn%22:[%22Healthcare%20Improvement%20Scotland%22]%7D]%26q=peg+feeding+guidelines%26sp=on (accessed 14 March 2020).
- Avdi E, Griffin C, Brough S. Parents’ constructions of professional knowledge, expertise and authority during assessment and diagnosis of their child for an autistic spectrum disorder. Br J Med Psychol 2000;73:327-38. https://doi.org/10.1348/000711200160543.
- British Academy of Childhood Disability (BACD) . Quality Principles For Paediatric Disability Services 2016. https://hubble-live-assets.s3.amazonaws.com/bacd/redactor2_assets/files/83/QualityPrinciples.pdf (accessed 5 August 2020).
- Ireland P, Horridge KA. The Health, Functioning and Wellbeing Summary Traffic Light Communication Tool: a survey of families’ views. Dev Med Child Neurol 2017;59:661-4. https://doi.org/10.1111/dmcn.13370.
- YouTube . Health, Functioning and Wellbeing Summary Traffic Light Communication Tool n.d. www.youtube.com/watch?v=Zx4idZRPcy4 (accessed August 2020).
- Department of Health and Social Care (DHSC) . NHS Reference Costs 2017 2018.
- Haggerty JL, Reid RJ, Freeman GK, Starfield BH, Adair CE, McKendry R. Continuity of care: a multidisciplinary review. BMJ 2003;327:1219-21. https://doi.org/10.1136/bmj.327.7425.1219.
- Ginsburg S. Colocating Health Services: A Way to Improve Coordination of Children’s Health Care?. New York, NY: Commonwealth Fund New York; 2008.
- Pupavac V. Therapeutic governance: psycho-social intervention and trauma risk management. Disasters 2001;25:358-72. https://doi.org/10.1111/1467-7717.00184.
- Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008;8. https://doi.org/10.1186/1471-2288-8-45.
- Kurien M, White S, Simpson G, Grant J, Sanders DS, McAlindon ME. Managing patients with gastrostomy tubes in the community: can a dedicated enteral feed dietetic service reduce hospital readmissions?. Eur J Clin Nutr 2012;66:757-60. https://doi.org/10.1038/ejcn.2012.19.
- National Institute for Health and Care Excellence . Cerebral Palsy in Under 25s: Assessment and Management 2017. www.nice.org.uk/guidance/ng62 (accessed 13 August 2020).
- Evans S, Holden C, MacDonald A. Home enteral feeding audit 1 year post-initiation. J Hum Nutr Diet 2006;19:27-9. https://doi.org/10.1111/j.1365-277X.2006.00662.x.
- Benner PE, Tanner CA, Chesla CA. Expertise in Nursing Practice: Caring, Clinical Judgment, and Ethics. New York, NY: Springer Publishing Company; 2009.
- Cunningham S, Best C. Guidelines for routine gastrostomy tube replacement in children. Nurs Child Young People 2013;25:22-5. https://doi.org/10.7748/ncyp2013.12.25.10.22.e331.
- Hillis R, Brenner M, Larkin PJ, Cawley D, Connolly M. The role of care coordinator for children with complex care needs: a systematic review. Int J Integr Care 2016;16. https://doi.org/10.5334/ijic.2250.
- Carter B, Thomas M. Key working for families with young disabled children. Nurs Res Pract 2011;2011. https://doi.org/10.1155/2011/397258.
- Greco V, Sloper P. Care co-ordination and key worker schemes for disabled children: results of a UK-wide survey. Child Care Health Dev 2004;30:13-20. https://doi.org/10.1111/j.1365-2214.2004.00381.x.
- Liabo K, Newman T, Stephens J, Lowe K. A Review of Key Worker Systems for Children with Disabilities and Development of Information Guides for Parents, Children and Professionals. Cardiff: Wales Office for Research and Development; 2001.
- National Audit Office . Pressures on Children’s Social Care 2019. www.nao.org.uk/wp-content/uploads/2019/01/Pressures-on-Childrens-Social-Care.pdf (accessed 14 March 2020).
- Allen D. The Invisible Work of Nurses: Hospitals, Organisation and Healthcare. London: Routledge; 2014.
- Bowlby S. Recognising the time—space dimensions of care: caringscapes and carescapes. Environ Plan A 2012;44:2101-18. https://doi.org/10.1068/a44492.
- Nelson KE, Lacombe-Duncan A, Cohen E, Nicholas DB, Rosella LC, Guttmann A, et al. Family experiences with feeding tubes in neurologic impairment: a systematic review. Pediatrics 2015;136:e140-51. https://doi.org/10.1542/peds.2014-4162.
- Wyatt KD, List B, Brinkman WB, Prutsky Lopez G, Asi N, Erwin P, et al. Shared Decision Making in pediatrics: a systematic review and meta-analysis. Acad Pediatr 2015;15:573-83. https://doi.org/10.1016/j.acap.2015.03.011.
- British Dietetic Association (BDA) . The Use of Blended Diet With Enteral Feeding Tubes 2019. www.bda.uk.com/resource/the-use-of-blended-diet-with-enteral-feeding-tubes.html (accessed 14 March 2020).
- Breaks A, Smith C, Bloch S, Morgan S. Blended diets for gastrostomy fed children and young people: a scoping review. J Hum Nutr Diet 2018;31:634-46. https://doi.org/10.1111/jhn.12563.
- Breaks A. What factors affect the decision of parents to select blended tube feeding for their gastrostomy fed child?. Clin Nutr ESPEN 2017;22:121-2. https://doi.org/10.1016/j.clnesp.2017.07.018.
- Downs J, Wong K, Ravikumara M, Ellaway C, Elliott EJ, Christodoulou J, et al. Experience of gastrostomy using a quality care framework: the example of rett syndrome. Medicine 2014;93. https://doi.org/10.1097/MD.0000000000000328.
- Åvitsland TL, Birketvedt K, Bjørnland K, Emblem R. Parent-reported effects of gastrostomy tube placement. Nutr Clin Pract 2013;28:493-8. https://doi.org/10.1177/0884533613486484.
- Sullivan PB, Juszczak E, Bachlet AM, Thomas AG, Lambert B, Vernon-Roberts A, et al. Impact of gastrostomy tube feeding on the quality of life of carers of children with cerebral palsy. Dev Med Child Neurol 2004;46:796-800. https://doi.org/10.1017/s0012162204001392.
- Klek S, Szybinski P, Sierzega M, Szczepanek K, Sumlet M, Kupiec M, et al. Commercial enteral formulas and nutrition support teams improve the outcome of home enteral tube feeding. JPEN J Parenter Enteral Nutr 2011;35:380-5. https://doi.org/10.1177/0148607110378860.
- Morris C, Janssens A, Shilling V, Allard A, Fellowes A, Tomlinson R, et al. Meaningful health outcomes for paediatric neurodisability: stakeholder prioritisation and appropriateness of patient reported outcome measures. Health Qual Life Outcomes 2015;13. https://doi.org/10.1186/s12955-015-0284-7.
- Kapadia MZ, Joachim KC, Balasingham C, Cohen E, Mahant S, Nelson K, et al. A core outcome set for children with feeding tubes and neurologic impairment: a systematic review. Pediatrics 2016;138. https://doi.org/10.1542/peds.2015-3967.
- Backman E, Granlund M, Karlsson AK. Documentation of everyday life and health care following gastrostomy tube placement in children: a content analysis of medical records [published online ahead of print February 14 2019]. Disabil Rehabil 2019. https://doi.org/10.1080/09638288.2019.1573383.
- Horridge KA, Dew R, Chatelin A, Seal A, Macias LM, Cioni G, et al. Austerity and families with disabled children: a European survey. Dev Med Child Neurol 2019;61:329-36. https://doi.org/10.1111/dmcn.13978.
- Shinners J, Franqueiro T. Individual and collective competence. J Cont Edu Nurs 2017;48:148-50. https://doi.org/10.3928/00220124-20160321-02.
- Franqueiro T, King M, Brown D. Transforming the workforce from individual to collective competence. J Contin Educ Nurs 2017;48:440-1. https://doi.org/10.3928/00220124-20170918-02.
- Limbrick P, Limbrick P. Family-centred Support for Children with Disabilities and Special Needs: A Collection of Essays. Clifford: Interconnections; 2007.
- Gray C, White AL, McAndrew S. My Social Stories Book. London: Jessica Kingsley Publishers; 2002.
- Spencer A, Horridge K, Downs D. Empowering clinical data collection at the point of care. Arch Dis Child 2015;100:815-17. https://doi.org/10.1136/archdischild-2014-307972.
- Robertson AR, Fernando B, Morrison Z, Kalra D, Sheikh A. Structuring and coding in health care records: a qualitative analysis using diabetes as a case study. J Innov Health Inform 2015;22:275-83. https://doi.org/10.14236/jhi.v22i2.90.
- Abbott D, Watson D, Townsley R. The proof of the pudding: what difference does multi-agency working make to families with disabled children with complex health care needs?. Child Fam Soc Work 2005;10:229-38. https://doi.org/10.1111/j.1365-2206.2005.00362.x.
- DiMaria-Ghalili RA, Mirtallo JM, Tobin BW, Hark L, Van Horn L, Palmer CA. Challenges and opportunities for nutrition education and training in the health care professions: intraprofessional and interprofessional call to action. Am J Clin Nutr 2014;99:1184-93. https://doi.org/10.3945/ajcn.113.073536.
- Reeves S, Perrier L, Goldman J, Freeth D, Zwarenstein M. Interprofessional education: effects on professional practice and healthcare outcomes (update). Cochrane Database Syst Rev 2013;3. https://doi.org/10.1002/14651858.CD002213.pub3.
- Hammick M, Freeth D, Koppel I, Reeves S, Barr H. A best evidence systematic review of interprofessional education: BEME Guide no. 9. Med Teach 2007;29:735-51. https://doi.org/10.1080/01421590701682576.
- Greenhalgh T, Humphrey C, Hughes J, Macfarlane F, Butler C, Pawson R. How do you modernize a health service? A realist evaluation of whole-scale transformation in London. Milbank Q 2009;87:391-416. https://doi.org/10.1111/j.1468-0009.2009.00562.x.
- ACI Gastroenterology and Nutrition Networks GENCA . A Clinician’s Guide: Caring for People With Gastrostomy Tubes and Devices 2014. https://aci.health.nsw.gov.au/about-aci/e-news?a=220992 (accessed August 2020).
- GOV.UK . Guide to the General Data Protection Regulation n.d. www.gov.uk/government/publications/guide-to-the-general-data-protection-regulation (accessed August 2020).
- Steele R, Cadell S, Siden H, Andrews G, Smit Quosai T, Feichtinger L. Impact of research participation on parents of seriously ill children. J Palliat Med 2014;17:788-96. https://doi.org/10.1089/jpm.2013.0529.
- Powell MA, Smith AB. Children’s participation rights in research. Childhood 2009;16:124-42. https://doi.org/10.1177/0907568208101694.
- Shaw C, Brady L-M, Davey C. Guidelines for Research with Children and Young People. London: National Children’s Bureau Research Centre; 2011.
- Sargent J, Clarke M, Price K, Griffiths T, Swettenham J. Use of eye-pointing by children with cerebral palsy: what are we looking at?. Int J Land Comm Disord 2013;48:477-85. https://doi.org/10.1111/1460-6984.12026.
- Lewis A, Porter J. Interviewing children and young people with learning disabilities: guidelines for researchers and multi-professional practice. Br J Learn Disab 2004;32:191-7. https://doi.org/10.1111/j.1468-3156.2004.00313.x.
- Beecham J, Sloper P, Greco V, Webb R. The costs of key worker support for disabled children and their families. Child Care Health Dev 2007;33:611-18. https://doi.org/10.1111/j.1365-2214.2007.00740.x.
- Korngiebel DM, Taualii M, Forquera R, Harris R, Buchwald D. Addressing the challenges of research with small populations. Am J Public Health 2015;105:1744-7. https://doi.org/10.2105/AJPH.2015.302783.
- Shilling V, Morris C, Thompson-Coon J, Ukoumunne O, Rogers M, Logan S. Peer support for parents of children with chronic disabling conditions: a systematic review of quantitative and qualitative studies. Dev Med Child Neurol 2013;55:602-9. https://doi.org/10.1111/dmcn.12091.
- Simpson A, Flood C, Rowe J, Quigley J, Henry S, Hall C, et al. Results of a pilot randomised controlled trial to measure the clinical and cost effectiveness of peer support in increasing hope and quality of life in mental health patients discharged from hospital in the UK. BMC Psychiatry 2014;14. https://doi.org/10.1186/1471-244X-14-30.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Medical Research Council Guidance . Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- Neef NA. Pyramidal parent training by peers. J App Behav Anal 1995;28:333-7. https://doi.org/10.1901/jaba.1995.28-333.
Appendix 1 Web-based survey
Appendix 2 Dissemination log of web-based survey
Dissemination through BACD.
Invitation sent 14 July 2016:
-
225 recipients (CDC list).
-
43 opened the e-mail.
-
11 clicked on the link.
Sent 22 July 2016 (BACD members):
-
348 recipients.
-
134 opened the e-mail.
-
5 clicked on the link.
Sent 9 August (CDC list) – reminder:
-
225 recipients.
-
44 opened the e-mail.
-
6 clicked on the link.
Northern Ireland Cerebral Palsy Register: sent 14 July 2016 and reminder 8 September 2016.
Royal College of Speech and Language Therapists (RCSLT) newsletter 18 July 2016 and 8 September 2016 (Facebook and Twitter).
British Association for Community Child Health: 19 July 2016 and 8 September 2016.
Paediatric Gastroenterology, Hepatology and Nutrition: 19 July 2016.
Dietitians interested in special children (DISC): 13 July 2016 and 8 September 2018.
Parenteral and enteral nutrition group of the British Dietetic Association (PENG): 1 August 2016 and 8 September 2016.
National Nutrition Nurses Group: 21 September 2016.
British Association of Parenteral and Enteral Nutrition (BAPEN): 21 September 2016.
Appendix 3 Inclusion and exclusion criteria
Children and young people
Inclusion criteria:
-
neurodisabling conditions and complex feeding needs, such as cerebral palsy, attention deficit hyperactivity disorder, autism spectrum disorder, Down syndrome
-
GFT or GFT recommended in the past/future
-
age 5–25 years
-
reasonable level of communication, including use of AAC
-
ability to express needs and preferences.
Exclusion criteria:
-
lack of ability to express needs and preferences
-
age < 5 years
-
absence of neurodisabling condition (e.g. GFT owing to cystic fibrosis or severe skin disorder).
Parents/family members/caregivers
Inclusion criteria:
-
parent(s)/family member(s)/caregiver(s) of a child/young person with a neurodisabling condition and complex feeding needs who may also receive nutrition via a GFT or a GFT has been recommended
-
parent(s)/family member(s)/caregiver(s) of a child/young person aged 0–25 years.
Professionals
Inclusion criteria:
-
work with families of children with a neurodisabling condition and complex feeding needs or manage services or commission services
-
work for services that have indicated a willingness to participate in the research and have capacity to participate.
All
Exclusion criteria:
-
already involved in research studies that would suggest that participation in this research would be too onerous.
Glossary
- Blended diet
- A diet that includes blended food that is prepared at home (as opposed to formula only) and administered through a gastrostomy feeding tube.
- Children and young people
- People aged 0–25 years.
- Gastrostomy feeding tube
- A tube surgically inserted into the stomach through the abdomen to supply nutrition.
- Multidisciplinary team
- A group of professionals with different professional backgrounds (e.g. doctors, nurses, speech and language therapists, dietitians). Composition may vary across services, as may the involvement of other professionals in health and social care.
- Neurodisability
- ‘Neurodisability describes a group of congenital or acquired long-term conditions that are attributed to impairment of the brain and/or neuromuscular system and create functional limitations. A specific diagnosis may not be identified’ (Morris C, Janssens A, Tomlinson R, Williams J, Logan S. Towards a definition of neurodisability: a Delphi survey. Dev Med Child Neurol 2013;55:1103–8).
- Psychosocial support
- Includes the following:processes to facilitate shared decision-making, including mechanisms for resolving conflict or maintaining a therapeutic relationship when parents/children disagree with the recommendation of a gastrostomy feeding tube or the safety of oral feedingprovision of child-centred and age-appropriate information and the equivalent for families on all aspects of tube feeding, including medical and social aspects and any risks and benefitsprovision of emotional or psychological support for coming to terms with a different way of feeding that offers parents, young people and children the opportunity to explore their concerns about feeding and the values they attach to food, eating, feeding by mouth and feeding by gastrostomy feeding tube in the context of the child and family and their everyday livespractical support in managing gastrostomy feeding tubes and feeds, including new nursing proceduresfinancial advice in terms of out-of-pocket expenses incurred as a result of gastrostomy feeds, where applicableopportunities to reinstate oral feeding following gastrostomy, where appropriate.
- Stoma
- A surgically created opening in the stomach or intestine to insert a gastrostomy feeding tube.
- Structured support
- Support that is consistently provided as part of a care plan or care package. This may be during the decision-making phase, the period immediately after surgery and/or in the longer term. It may be offered by a designated professional, member of a multidisciplinary team or layperson/parent.
List of abbreviations
- AAC
- augmentative and alternative communication
- A&E
- accident and emergency
- ANA
- additional needs assistant
- BACD
- British Academy of Childhood Disability
- BD
- blended diet
- BDA
- British Dietetic Association
- CAMHS
- Child and Adolescent Mental Health Service
- CCG
- Clinical Commissioning Group
- CCN
- children’s community nurse
- CDC
- child development centre
- CPD
- continuing professional development
- CS01
- case study site 1
- CS02
- case study site 2
- CS03
- case study site 3
- CS03A
- case study subsite 3A
- CS03B
- case study subsite 3B
- CS03C
- case study tertiary site 3C
- CS04
- case study site 4
- DVD
- digital versatile disc
- FG
- focus group
- GFT
- gastrostomy feeding tube
- GP
- general practitioner
- G-PATH
- gastrostomy feeding and psychosocial support pathways
- HCP
- health-care professional
- HEFCC
- home enteral feeding clinic for children
- HRA
- Health Research Authority
- MAC
- meeting around the child
- MDT
- multidisciplinary team
- NG
- nasogastric
- NMCN CEN
- National Managed Clinical Network for Children with Exceptional Healthcare Needs
- OT
- occupational therapist
- PAG
- Project Advisory Group
- PEG
- percutaneous endoscopic gastrostomy
- PPI
- public and patient involvement
- PSE
- psychosocial and emotional support
- PSS
- psychosocial support
- R&D
- research and development
- REC
- Research Ethics Committee
- SLT
- speech and language therapist
- TAC
- team around the child
- WBS
- web-based survey
- WTP
- willingness to pay
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/hsdr08380).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
