Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 17/06/06. The contractual start date was in May 2018. The final report began editorial review in September 2019 and was accepted for publication in April 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Cotterill et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Parts of this chapter have been reproduced from our review protocol. 1,2 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Health workers routinely carry out behaviours that affect patient diagnoses, care, treatment and recovery. Many of these behaviours have clear guidelines for best practice. Examples include appropriate ordering of diagnostic tests,3,4 appropriate prescription of antibiotics,5,6 regular recall of patients with long-term conditions,7 hand-washing8 and choice of wound dressings. 9 Health workers face many challenges when following evidence-based professional practice, such as lack of time, competing demands and requests from patients. The issue of implementing best practice findings from clinical research to practice is termed the second translational gap,10 and can have significant impacts on patient and population health. Although there are no reliable published estimates, to our knowledge, of how well health professionals follow best clinical practices overall, we can draw on a couple of illustrative examples. In England, the USA and Canada it is estimated that 37%, 27% and 66% of patients with high blood pressure have their condition controlled, respectively, and health professionals can support improvement through prescribing medication, regular review of patients and lifestyle advice. 11 In England alone, 700 quality-adjusted life-years could be saved annually through just a 15% increase in this figure. 11 One out of 20 hospital admissions are caused by adverse drug events,12 and approximately half of these globally are believed to be preventable, owing to lapses in best practice in terms of prescribing or monitoring behaviours by clinicians. 13 There is evidence that social influences are important in clinical practice. 14,15
Social norms interventions
One proposed solution has been to implement behaviour change interventions based on social or peer norms. 16 Social norms are the implicit or explicit rules that a group uses to determine values, beliefs, attitudes and behaviours. A social norms intervention seeks to change the clinical behaviour of a target health worker by exposing them to the values, beliefs, attitudes or behaviours of a reference group or person. These social norms interventions can form part of an audit and feedback (A&F) initiative,17–19 or may be developed as another behaviour change intervention. 20 These are often interventions with reach: they can be implemented across multiple health workers and settings at low cost, so there is the potential for large absolute gain. We use the term target to refer to a health worker at whom a social norms intervention is aimed, with a view to changing their clinical behaviour. We use the term reference group or reference person to mean a person or group of people whose values, beliefs or behaviours are exposed to the target.
The ability of social norms to affect behaviour has been considered within several behaviour change theories and theoretical frameworks. For example, ‘subjective norm’ is a construct within the theory of planned behaviour,21 which describes subjective norm as an individual’s perceptions of whether valued others think one should perform a behaviour, combined with a motivation to comply with others’ beliefs. The theory of normative social behaviour22 proposes that behaviour can be changed through normative mechanisms, and has made distinctions between descriptive norms (beliefs concerning the prevalence of a behaviour) and injunctive norms (beliefs concerning what one feels they ought to do based on others’ expectations, linked to social approval). A descriptive norms message provides the target with information about the behaviour of others in the reference group. Examples of descriptive norms interventions include giving the target information about the behaviour of a reference person or group, or comparison of the target’s behaviour with the behaviours of a reference person or group. An injunctive norms message provides the target with information about the values, beliefs or attitudes of the reference group, conveying social approval or disapproval. Examples of injunctive norms interventions include providing the target with information about whether or not the behaviour has the approval/disapproval of the reference group or person; exposure (actual or promised) of the target’s behaviour to a reference group; and praise, commendation, applause or thanks (actual or promised) from a reference group or person.
The theoretical domains framework23 (which has drawn its domains and their content from multiple theories of behaviour change) includes a ‘social influences’ domain, which includes several normative constructs: social norms, social comparisons, group norms, descriptive norms and injunctive norms. The social influences domain goes beyond social norms to include a broader range of social concepts, such as emotional and practical support, demonstrating a behaviour and changing the social environment. The idea of using social norms as a behavioural intervention is present across disciplines (politics, economics, psychology and health) and there is variation between disciplines in how social norms are described.
Behaviour change techniques
The behaviour change technique (BCT) taxonomy v1 (the current version) is a list of 93 distinct BCTs that are used in behaviour change interventions. 24 A BCT is ‘a technique . . . proposed to be an active ingredient’24 of a behavioural intervention that contributes to behaviour change. We have chosen to identify and classify social norms intervention components in terms of the BCT taxonomy v1 because, based on international consensus, the taxonomy defines and labels all active ingredients of interventions. It incorporates previous behaviour change taxonomies and has involved significant effort from leaders in the field, and considerable investment from the Medical Research Council and the National Institute for Health Research (NIHR) in developing the taxonomy. We believe that this is the most reliable tool currently available that can define BCTs. The names of BCTs that are included in the taxonomy have been italicised whenever they are used in this report.
The BCT taxonomy groups BCTs into categories, and none of the categories directly relate to social norms. This is perhaps surprising, given that the concept of social norms occurs in so many theories of behaviour change, including the Theoretical Domain Framework, but extensive work by a panel of experts resulted in the hierarchy of the taxonomy, and clearly it needs to meet the needs of a large and diverse community of researchers. An earlier version of the taxonomy had a ‘social influence’ category,23 which does not appear in the current version. 24 The BCT taxonomy v124 includes five BCTs that we believe involve social norms: social comparison (6.2), information about others’ approval (6.3), credible source (9.1), social reward (10.4) and social incentive (10.5). 24 The numbers in brackets follow the labelling of the BCTs in the BCT taxonomy v1. We have discussed this selection of social norms BCTs carefully, both within the research team and with our independent Study Steering Committee (SSC) of international experts.
Social comparison
‘Draw attention to others’ performance to allow comparison with the person’s own performance. Note: being in a group setting does not necessarily mean that social comparison is actually taking place.’24
‘Example: Show the doctor the proportion of patients who were prescribed antibiotics for a common cold by other doctors and compare with their own data.’24
Information about others’ approval
‘Provide information about what other people think about the behaviour. The information clarifies whether others will like, approve or disapprove of what the person is doing or will do.’24
‘Example: Tell the staff at the hospital ward that staff at all other wards approve of washing their hands according to the guidelines.’24
Credible source
‘Present verbal or visual communication from a credible source in favour of or against the behaviour. Note: code this BCT if source generally agreed on as credible e.g. health professionals, celebrities or words used to indicate expertise or leader in field and if the communication has the aim of persuading.’24
‘Example: Present a speech given by a high status professional to emphasise the importance of not exposing patients to unnecessary radiation by ordering x-rays for back pain.’24
The following two social norm BCTs have been amended slightly to ensure that the definition is sufficiently tight to allow us to identify and delineate interventions. Further details of the reasons for change are available in the protocol. 2
Social reward
The original definition of social reward was ‘Arrange verbal or non-verbal reward if and only if there has been effort and/or progress in performing the behaviour (includes ‘Positive reinforcement’). Examples: Congratulate the person for each day they eat a reduced fat diet’. 24
Our new tighter definition is as follows: arrange praise, commendation, applause or thanks if and only if there has been effort and/or progress in performing the behaviour (includes ‘positive reinforcement’). Example: arrange for a family doctor to be sent a thank you note for each week that they reduce their level of antibiotic prescribing.
Social incentive
The original definition for social incentive was ‘Inform that a verbal or non-verbal reward will be delivered if and only if there has been effort and/or progress in performing the behaviour (includes ‘positive reinforcement’). Examples: Inform that they will be congratulated for each day that they eat a reduced fat diet.’24
Our new tighter definition is as follows: inform that praise, commendation, applause or thanks will be delivered if and only if there has been effort and/or progress in performing the behaviour (includes ‘positive reinforcement’). Example: promise a family doctor in advance that they will be sent a thank you note for each week that they reduce their level of antibiotic prescribing.
Why it is important to undertake this research
There are health service contexts in which modification of the behaviour of health workers may have a beneficial effect on patient diagnosis, care and treatment, and on the costs of health care. These contexts include situations in which health workers are expected to follow evidence-based professional practice, such as prescribing, ordering tests, choosing treatments and adhering to guidelines. There are challenges in implementing recommended practice findings from clinical research into practice, referred to as the second translational gap. 10 Providing social norms interventions to health workers may help overcome these barriers to implementing recommended practice through a number of ways, including persuading them that they should change their individual behaviour, working collaboratively with their peers to develop action plans and change the organisation of care, observing good practice from other organisations and gaining support from senior managers. 16 This systematic review will summarise evidence on the use of social norms interventions to influence clinicians to implement recommended clinical behaviours. In advance of starting this review, our pilot work indicated that there were > 90 trials investigating the use of social norms interventions. A systematic review of the evidence was required to establish whether or not these interventions are effective, and what factors influence their effectiveness.
Health workers frequently receive A&F, which involves ‘providing a recipient with a summary of their performance over a specified period of time’. 17 Social norms interventions are sometimes included as one component of A&F, such as when the health worker is shown information about their own performance and also a comparison with their peers. 18,19 A&F has already been shown to be effective in changing health worker behaviour, but with large variation in outcomes depending on the context and the intervention design. 25 There is a need to understand the components for successful A&F. 17,26 The effects or mechanisms of the ‘social influence’ constituents of A&F have been identified in a systematic review as topics for further research. 17 As noted earlier, interventions based on social influence include social norms interventions; however, social influence is a broader concept that covers emotional and practical social support, changes to the social environment and modelling of behaviour. 23 Our review may contribute to this important research agenda by systematically examining the evidence for using social norms interventions with health workers.
Prior to starting the review and during its implementation we spoke to members of the public about this proposal and asked which aspects of the research were important and relevant to them. They told us that the research might contribute to cost savings to the NHS by reducing waste (e.g. waste of prescriptions or tests) without reducing patients’ quality of care, and provide opportunities for standardisation (e.g. use of social norms interventions to encourage nurses to use standard wound dressings when appropriate rather than ordering multiple types), which would affect costs. They identified the potential for social norms methods to be used in the curriculum for training health professionals. Patient safety is very important: patients suffer if antibiotics are wrongly prescribed and there is broader concern about antibiotic resistance. Social norms approaches could be applied to other health worker behaviours and could lead to changes in ways of thinking. Changes in health worker behaviour may lead to changes in patient behaviour too, for example patients may copy the health worker’s example of hand-washing. Patients told us that it would be interesting to extend this research in the future to how patients perceive staff behaviour and how health workers are influenced by social norms of patients, for example asking for/not wanting antidepressants or making comments about hand-washing. ‘Maybe the review will lead to broader research including patients in the social comparison equation. That seems important to me’ (PPI group member). Patients felt that they could have a role in social norms interventions, for example by reminding health workers to wash their hands or telling the general practitioner (GP) that they do not expect to be prescribed antibiotics for a cold; however, they were cynical about whether or not doctors would listen to patients when they present best practice (example was given of a relative who had better care in Australia, but the doctor in the UK did not want to hear about it). In response to this observation, we made sure to record any studies in the review that considered the role of patients in social norms interventions.
Scoping review
Prior to starting the systematic review, we conducted a scoping review. The purpose of the scoping review was to test out the search and screening procedures for the planned systematic review and provide information to help estimate the number of eligible studies and the amount of work involved. A systematic literature search on social influences (carried out on 9 November 2016) revealed a total of 3644 potentially eligible abstracts for our systematic review, after removing duplicates. Screening of these titles/abstracts generated 264 titles that met our initial screening criteria regarding study type, population and intervention. Reading the full text of 100 out of the 264 screened abstracts resulted in 42 being excluded, 51 being included and seven requiring further information. Among the 51 included papers, there were 35 unique trials. From this we estimated that there would be at least 135 articles and 93 unique trials in our review.
Before the scoping review we discussed our plans widely, including with the members of the SSC. This led us to revise the search strategy from the earlier work, aligning the search and coding framework more closely to social norms BCTs in the BCT taxonomy v1. 24 We also made a decision very early in the project to use the term ‘social norms interventions’ rather than ‘social influences’. This was because ‘social norm’ is a more specific term for the interventions we are interested in, whereas ‘social influence’ is used elsewhere in the literature as a broader term encompassing a wide array of behaviour change strategies, such as emotional or practical social support from others, restructuring the social environment and modelling or demonstrating behaviour. 23,27
Aim and research questions
The overall aim was to conduct a systematic review to assess, among health workers, the impact of social norms BCTs compared with controls (alternative interventions, no intervention or comparison of one social norms BCT with one or more other social norms BCTs) with compliance to evidence-based professional practice. The review addressed two research questions:
-
What is the effect of social norms interventions on the clinical behaviour of health workers, and resulting patient outcomes?
-
Which contexts, modes of delivery and behaviour change techniques are associated with the effectiveness of social norms interventions on health worker clinical behaviour change?
These questions were explored using forest plots and metaregression; network meta-analysis was undertaken to rank the effectiveness of the social norms interventions.
Chapter 2 Methods
Parts of this chapter have been reproduced from our review protocol. 1,2 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Changes to the protocol
The published protocol differs from the funding proposal in the ways listed below, and these changes were approved by NIHR during the early months of the project:
-
Change in terminology – ‘social norms’ replaces ‘social influence’. The justification for this was twofold. First, the term ‘social influence’ is a domain within the Theoretical Domains Framework23 and encompasses a broad range of social concepts, such as emotional and practical support, demonstrating a behaviour and changing the social environment, as well as social norms; it is not specific enough for the purpose of this review. Second, ‘social norms’ better captures the core mechanism by which we expected the interventions to have an effect.
-
We added to our inclusion criteria a requirement that included studies must state a behaviour that is being targeted for change. This was not a fundamental change from the earlier version, but was stated more clearly than previously.
-
Change from ‘health professional’ to ‘health worker’. This is a clarification rather than a change to the original inclusion criteria. It was always our intention to include all staff providing health care, and this change of terminology makes clear that not all health workers have professional qualifications.
Inclusion criteria
The inclusion criteria for the review were based on the population, types of intervention and study designs, as follows.
Population
The population of interest was health workers (including managers) responsible for patient care in a health-care setting. Health workers in training were included, but only if they were in a health-care setting (i.e. not in campus or laboratory environments). Any health-care setting was eligible, including primary care, secondary care, care homes, nursing homes and patients’ own homes. Interventions taking place in simulated environments were not eligible for inclusion.
Interventions
A social norms intervention seeks to change the clinical behaviour of a target health worker by exposing them to the values, beliefs, attitudes or behaviours of a reference person or group. We looked for the five BCTs that we considered to have a social norms element to them: 6.2. social comparison, 6.3. information about others’ approval, 9.1. credible source, 10.4. social reward and 10.5. social incentive. However, we were open to including studies that met all other inclusion criteria and had a social norms element, even if they did not include any of these five BCTs.
Included studies must have stated a clinical behaviour of health workers that was targeted for change through the use of social norms. If the behaviour was not specified, it was not possible to determine which aspects of an intervention were relevant to the anticipated behaviour change. Indeed, the BCT taxonomy v1 coding guidance states that the target behaviour needs to be specified and BCTs must target that behaviour for BCTs to be coded. 28 Clinical behaviour here is defined as any behaviour that is performed within a (non-simulated) environment that affects patient diagnosis, care, treatment or recovery. We have reported the number of studies identified by our search that met all other inclusion criteria but did not mention a target behaviour.
Comparators
All comparators were eligible for inclusion, including alternative interventions, no intervention or comparison of one social norms BCT with one or more other social norms BCTs.
Study designs
Only randomised controlled trials (RCTs) were included in the review. All designs of RCTs (cluster, factorial, parallel, cross over and stepped wedge) were eligible for inclusion. The justification for restricting the review to RCTs was that the review is concerned with the effectiveness of social norms, and RCTs are the best method for assessing the effectiveness of an intervention.
We included both published and unpublished research. Studies had to be reported in English because the research team had no resource for translation from other languages.
Search strategy
The search strategy was developed using an extensive iterative scoping process, involving the whole team including an information specialist (Jane Roberts). Lists of possible search terms were suggested by team members; these were developed into search strategies by Jane Roberts, who then ran preliminary searches. A sample of the titles and abstracts were reviewed closely by Sarah Cotterill and Mei Yee Tang and discussed by the wider team. This review involved consideration of whether searches were too inclusive or too restrictive, and examination of resulting abstracts to look for potential additional search terms.
The searches were based on three groups of terms: population, interventions and study design.
Population
A list of population terms was developed by looking at Cochrane reviews25,29 that included a similar population of health workers, augmented by job roles included in the UK national workforce data set produced by NHS Digital. 30
Interventions
Social norms interventions are not described consistently in the literature, and different terms are used in various academic disciplines. This presented us with the challenge of finding appropriate search terms to make sure that we would discover the full range of literature on this topic. We were aware that many studies involving A&F contain a social comparison element;25 therefore, we looked at the search terms that were used in a previous systematic review of A&F. 25 We omitted anything relating solely to ‘audit’, as this was not relevant for this review.
During the scoping phase, various feedback terms were tried out. The use of ‘feedback’ alone produced many irrelevant papers, such as those relating to educational feedback and electronic feedback. The final search, following extensive trial and error in the piloting phase, included ‘feedback’ when used alongside other relevant terms (audit, monitoring, peer, performance, data, individualised, web, personalised, comparative, team, practitioner, practice and clinical or social). We also included ‘benchmark’. We included some overall terms that are used in the literature on social norms: ‘norm’ used close to ‘social’, ‘descriptive’, ‘peer’ or ‘subjective’; ‘social influence’; ‘benchmarking’; ‘social or peer comparison’; and ‘social competition’. Terms that appeared in behavioural economics literature were included: ‘social proof’, ‘image motivation’ and ‘warm glow’.
Additional search terms were developed for each of the five social norms BCTs by looking at the text used to describe them in the BCT taxonomy v1,24,31 extensive discussion in the team and examining relevant articles. Additional terms for information about others’ approval and credible source included ‘positive reinforcement’, ‘congratulate’, ‘praise’ and ‘commendation’. Terms for social reward and social incentive included ‘social’, ‘verbal’ and ‘non-verbal’ alongside ‘incentive’ or ‘reward’. Finally, the search included terms to describe theories that are used to explain interventions based on social norms: the Theory of Planned Behaviour,32 the Theory of Reasoned Action,33 the Theoretical Domains Framework,34 Social Cognitive Theory,35 and the Theory of Normative Social Behaviour. 22
Study design
The search for RCTs was taken directly from the Cochrane RCT search described in the Cochrane Handbook for Systematic Reviews of Interventions. 36 This was translated into other relevant databases.
The search was developed in MEDLINE and then adapted for other databases. Terms relating to the same concept (e.g. different types of health workers) were combined using the Boolean operator ‘OR’ and different concepts (e.g. health workers and social norms) were combined using ‘AND’. The search strategy was tailored for the different electronic databases using medical subject headings (MeSH) where appropriate, wildcard symbols and truncations (see Appendix 1). Backward- and forward-citation searching was not conducted owing to time and resource constraints.
Published literature was systematically searched on 24 July 2018 in electronic databases relevant to health and social care: Ovid MEDLINE, Ovid EMBASE, Healthcare Databases Advanced Search (HDAS) – Cumulative Index to Nursing and Allied Health Literature (CINAHL), HDAS British Nursing Index (BNI), Cochrane Central Register of Controlled Trials (CENTRAL), Ovid PsycINFO and Web of Science (see Appendix 1 for search strategies and Appendix 1, Table 15, for the results).
Data collection
Study selection
The process for identifying studies for review followed the stages of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. 37
All references generated from the search were managed in Covidence (Melbourne, VIC, Australia): an online screening and data extraction tool for systematic reviews. All reviewers were provided with instructions for both the title and the abstract, and full-text screening stages (see Appendix 2). At the title and abstract screening stage there was an initial learning phase (305 studies), during which the coders worked steadily through the task, applying the inclusion criteria to the papers and stopping after small batches to discuss any discrepancies as they went along. Disagreements and uncertainties were discussed with the wider research team. This process enabled the main coder to build up a high level of consistency. For the remaining studies, one reviewer (MYT) independently screened all of the titles and abstracts against the inclusion criteria, and another researcher (SC, SR or JW) screened a sample of 20% of the records. These were randomly selected using a random integer generator (www.random.org; accessed 1 September 2020). By the time that 20% of the records (493 studies) had been screened, there was very little difference between the decisions of the two coders, and we were confident that the main coder could make the exclusion decisions with reliability. Inter-rater reliability on these 493 studies was good38 (kappa = 0.68). Where there was any hesitation on her part about whether to include or exclude, she erred on the side of inclusion and continued to discuss any uncertainties with the wider team.
All of the studies at the full-text stage were independently screened by two researchers from the screening team (MYT, SC or SR). The two reviewers screened the papers concurrently using Covidence, and were not aware of the other person’s recommendation until after they had entered their own. The screening involved reading the full-text paper and deciding whether or not the paper met the eligibility criteria (a population of health workers in a health-care setting, a social norms intervention targeted at clinical behaviour change and a RCT). If the study was excluded, the reviewer entered a reason for exclusion. Any disagreements over the recommendation to exclude or the reason for exclusion were flagged up by Covidence and the two reviewers met to discuss. If they were unable to come to a consensus, there was moderation by a third researcher or discussion at a team meeting.
Data extraction and management
For efficiency, data extraction was conducted in three stages: stage 1 involved extraction of all data apart from the details of the intervention, stage 2 was the BCT coding (carried out by a different team concurrently with stage 1) and stage 3 was carried out later, because it relied on data collected during the BCT coding (e.g. we needed to identify which aspects of the intervention were based on social norms to assess the frequency or format of the social norms intervention). Data from included studies were extracted using data extraction forms derived from the Cochrane Effective Practice and Organisation of Care data collection form. 39
Stage 1 data extraction
See extraction form in Appendix 3, Tables 16 and 17.
Data were independently extracted by two researchers from the data extraction team (MYT, LH, SR and SC). Any disagreements were referred to a third researcher for consideration or discussed at a research team meeting.
Data extracted were:
-
setting of the trial (e.g. primary)
-
country in which trial was conducted
-
design of trial
-
aim of the trial
-
unit of allocation
-
primary outcome
-
secondary outcomes
-
time points
-
statistical analysis
-
inclusion/exclusion criteria (and whether or not the inclusion criteria targeted participants based on low target performance)
-
methods of recruitment
-
number of randomised clusters, if randomised RCT
-
subgroups measured (both health workers and patients)
-
target behaviour
-
total number of patients and health workers randomised
-
type of health worker targeted by the intervention
-
withdrawals and exclusions (after randomisation)
-
number of participants (both patients and health workers) randomised to group
-
number of clusters randomised to group, if cluster RCT
-
type of control
-
outcomes
-
quality assessment (risk of bias).
Stage 2 data extraction: coding of behaviour change techniques
See the BCT extraction form in Appendix 5, Table 19.
Specific BCTs were independently double coded using the BCT taxonomy v124 by at least two researchers. A BCT extraction form was produced to guide the process. Each study’s intervention descriptions from all of the relevant papers (e.g. protocol, process evaluation and main findings) were collated by Mei Yee Tang and transposed to the BCT extraction form so that the second coder (RP, SC or JR) could have the information required for BCT coding available in the one document for each study. All coders had access to the full papers on Covidence, so that they were able to find further relevant information that could help them with the coding task. Following coding, for each study Mei Yee Tang transferred the BCT codes and information extracted by both coders onto a single final BCT extraction form. As part of this process, any discrepancies were highlighted by Mei Yee Tang and the disagreements were resolved through discussion or by the moderation of another coder.
For each study, BCTs were separately coded for all arms (i.e. the control arm and all intervention arms). Mei Yee Tang coded BCTs for all studies, which were then independently double coded by another trained coder within the research team (SC, RP or JR). BCT coders also recorded the target population, target behaviour, whether or not guidelines were provided as part of the intervention and the direction of change in the behaviour that was desired.
Training
All coders completed online training on the coding of BCTs (www.bct-taxonomy.com/; accessed 1 September 2020) and attended a workshop facilitated by co-applicant Rachael Powell and study steering committee member Marie Johnson prior to starting the coding process. To ensure that all coders were familiar with the BCT coding process and coded consistently, a random sample (using www.random.org; accessed 1 September 2020) of three studies was selected for coding by all coders (MYT, RP, SC and JR). All coders coded the three intervention descriptions independently before meeting to discuss any issues that arose. This practice exercise with all BCT coders was repeated again on another four randomly selected studies. The two practice sessions helped to refine the coding process and revise the BCT extraction form (see Appendix 5, Table 19). A decision log was kept throughout the BCT coding process to record any decisions that were made to ensure the consistency of coding. Details are provided in Appendix 6.
Behaviour change techniques inter-rater reliability
Inter-rater reliability for each of the BCTs that were present at least once across all intervention arms was assessed using the prevalence-adjusted and bias-adjusted kappa (PABAK) statistic (see Appendix 7, Table 20), which adjusts for both the prevalence and the occurrence of BCTs. 40 In circumstances in which prevalence is low, the widely used chance-corrected kappa statistic is likely to underestimate reliability as it is highly dependent on prevalence. 41 To calculate the PABAK, the kappaetc module in Stata® I/C 14.0 (StataCorp LP, College Station, TX, USA) was used to produce the Brennan–Prediger statistic. 42,43
Stage 3 data extraction: trial and intervention characteristics
See the stage 3 data extraction form in Appendix 4, Table 18.
Information relating to trial and intervention characteristics [focused on the social norms element(s) only] was extracted during stage three of data extraction using Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) by Sarah Cotterill and Mei Yee Tang:
-
Did the inclusion criteria target participants based on low target performance?
-
Frequency and intensity of intervention.
-
Format of intervention.
-
Source of the intervention (i.e. the person delivering the intervention).
-
Was this person delivering the intervention internal or external to the target person’s organisation?
-
Reference group/person used as the comparison/source of approval.
-
Type of comparison.
The processes of the third stage of data extraction, along with the accompanied instructions, were refined through piloting (see Appendix 4 for the final version). Six studies were independently extracted by Sarah Cotterill and Mei Yee Tang. The instructions were refined during this pilot phase and some categories were added to ensure that extraction was as consistent as possible. The piloting process was repeated until a high level of agreement was reached between the two coders.
In the protocol, we had envisaged that we would contact authors for additional information if the data needed to calculate effect sizes were not adequately reported in the paper. We were not able to do this owing to time constraints, but we made efforts to search for additional papers, including process evaluations and protocols. Once all of the data were extracted, they were transferred to Stata for analysis.
Assessment of risk of bias
As part of the first stage of data extraction, risk of bias for each included study was independently assessed by the data extractors (LH, MYT, SC and SR) using The Cochrane Collaboration tool for assessing risk of bias36 across a range of criteria: selection bias, performance bias, detection bias, attrition bias, reporting bias, selective outcome reporting and other biases. Included studies were classified as having a high, low or unclear risk of bias for each criterion. All risk-of-bias criteria were added as part of the data extraction form in Covidence. Where disagreements occurred, a discussion between the two extractors took place to resolve the disagreement or a third data extractor would be brought in when an agreement could not be reached. Percentages of high/low/unclear judgements for each risk-of-bias criterion across included studies were calculated and reported as a bar chart to provide a summary of the risk of bias across criteria domains (see Figure 2). Text summaries across each criteria of bias were produced in line with The Cochrane Collaboration’s guidance for large reviews. 36 Judgements for each risk-of-bias criterion for all included studies were reported (see Appendix 15, Figure 20).
Data analysis
Outcomes and prioritisation
The primary outcome for the review was compliance of the health worker with the desired behaviour at the time point closest to 6 months post intervention. We expected studies to report different behaviours (e.g. prescribing, hand-washing and test ordering) and we expected studies to measure those behaviours in different ways. We converted any observed measure of health worker behaviour into a standardised mean difference (SMD) between groups in terms of compliance with the desired behaviour. Common examples included the mean number of times a behaviour was performed per health worker or the mean rate of behaviour (e.g. percentage of the population for whom antibiotic items were dispensed). At times, compliance was reported as a binary outcome, such as compliance versus non-compliance on a single occasion, and was expressed either in a binary format or using an odds ratio.
We used the methods of Chinn44 to convert binary outcomes to a SMD with associated standard errors (see Appendix 8 for the formula).
If several measures of compliance were reported in sufficient detail to enable the analysis of a trial, we used the following criteria to select the outcome for the primary analysis, in decreasing order of importance: (1) observed measure rather than self-report, (2) appropriate adjustment for clustering, (3) continuous measure, (4) final score rather than percentage change or change from baseline, (5) described as the primary outcome, (6) used to calculate the sample size and (7) reported first.
The secondary outcome for the review was patient health-related outcomes that were likely to result from targeting the health worker behaviour. These were converted to a SMD using a similar approach.
Some trials incorporated baseline measurements into their analyses. This was carried out either by adjusting for baseline values of the outcome measure or of other prognostic variables in an analysis of covariance (ANCOVA), or by reporting outcomes as changes from baseline. We have prioritised ANCOVA-adjusted estimates of the treatment effect where relevant or those from logistic regression, given that these are generally more precise. Change scores cannot be pooled through conversion to SMDs.
Missing data
Our preferred approach to dealing with missing data was to take steps to try to obtain them. We searched for companion papers by author searching and citation searching. Contacting trial authors was not possible owing to limited resources and the large number of studies. We imputed estimates of standard deviations where necessary by using any available information, such as p-values, confidence intervals (CIs), ranges or standard errors of baseline data, by pooling standard deviations from other similar studies that use the same type of outcome or by searching for trials that used the same outcome. Where necessary, for cluster randomised trials we imputed a value of the intraclass correlation coefficient (ICC) by pooling across similar studies.
Unit of analysis issues
Where any of the studies in the review were cluster randomised trials, we extracted both raw summary measures (e.g. means and numbers having had the event) and adjusted standard errors from appropriately analysed trials. Where it was not possible to obtain the adjusted SMD and its standard error directly, the methods that were used to calculate the SMD and standard error are shown in Appendix 9, Table 21.
Several studies had more than two relevant arms (e.g. two different social norms interventions and a control group). In each case, we extracted data on any comparison that was relevant to our primary research question, while avoiding double counting where possible. Where relevant, we combined study arms that contained identical BCTs. In cases with two different social norms interventions and a single control arm, where possible we divided the number of health-care workers in the control arm approximately evenly between the comparisons to avoid double counting, while retaining the correct intervention effect. In studies with more than one candidate control arm, we chose the comparison that provided the more pure test of social norms (e.g. social norms intervention + X vs. X is a more pure test of social norms than social norms intervention + X vs. usual care).
Where a study was a factorial trial analysed appropriately using linear or logistic regression, we extracted the covariate and standard error that best assessed the effect of social norms BCTs, for example a covariate comparing all arms containing a social norms BCT with all arms without.
Analysis of skewed data
If the primary outcome data were heavily skewed, meta-analyses based on SMDs of the untransformed data would be expected to produce biased estimates. In some cases, compliance was reported as ‘mean per cent compliance’ or similar, and there is a likelihood that this outcome is skewed when close to 0% or 100% owing to it being bounded. We removed data likely to be skewed (where mean compliance was close to 0% or 100%) in a sensitivity analysis.
Utilising the behaviour change technique coding in the analysis
The approach we took to utilising the BCTs in the meta-analysis was to create an Excel file of all the trials, listing the intervention and control BCTs on separate rows. We subtracted the control arm BCTs from the intervention arm BCTs to identify the BCTs that would be expected to be responsible for the differences between the two arms.
Using the five types of comparison (extracted during the BCT coding process), listed in Box 1, allowed us to separate out three different tests of social norms:
-
‘Pure’ test of social norms intervention alone (comparisons 1 and 2, see Box 1).
This involved trials with social norms BCT(s) in the intervention arm and no BCTs in the control arm (comparison 1). These trials were the purest test of social norms interventions: the BCTs being tested were those found in the intervention arm. For trials in which an intervention arm including a social norms BCT combined with other BCTs was tested against a control arm containing the same other BCTs (comparison type 2), the control arm BCTs were subtracted from the intervention arm to reveal the BCTs that would be expected to account for differences in outcome. For example, if the study tested social comparison and instructions on how to perform the behaviour (intervention arm) against instructions on how to perform the behaviour (control arm), the comparison type would be ‘social comparison’.
-
‘Complex’ test of a social norms intervention alongside one or more other BCTs (comparison 3, see Box 1)
This involved trials in which an intervention arm including a social norms BCT combined with other BCTs was tested against a control arm containing none of the same BCTs (comparison 3). The control arm was deducted from the intervention arm to reveal the test involved in the comparison. For example, if the study tested a complex intervention such as credible source, feedback on behaviour, social support unspecified and behavioural practice/rehearsal (intervention arm) against social support unspecified and behavioural practice/rehearsal (control group), the comparison would be ‘credible source’ and ‘feedback on behaviour’ versus control.
-
Social norms intervention occurring in both arms (comparisons 4 and 5; see Box 1)
In some studies, two different social norms interventions were compared (comparison 4) or the same social norms intervention appeared in both arms (comparison 5). Where social norms interventions occurred in both arms of a trial, the study did not provide useful information for the meta-analysis, because these trials do not test the effect of social norms interventions, but they were potentially useful to the review as follows:
-
Any study that directly compared one social norms BCT against another (e.g. social comparison vs. credible source) could potentially be included in the network meta-analysis.
-
Any study that compared the same social norms BCT in both arms, with the addition of other BCTs (e.g. with the addition of social support in one of the arms) or comparing differing modes of delivery (e.g. social comparison delivered in person or by e-mail) could potentially be included in the metaregression.
-
Any study where social norms BCT(s) were delivered in both arms as a control intervention, for the purpose of testing a separate intervention, in which the social norm was a minor part were not included in any analysis.
-
Comparison 1: social norms BCT vs. any control.
Comparison 2: social norms BCT + X vs. X.
Comparison 3: social norms BCT + X vs. any control.
Comparison 4: social norms BCT type A vs. social norms BCT type B.
Comparison 5: social norms BCT + X vs. social norms BCT + Y.
In summary, the information extracted for the analysis describes the BCTs that were tested in the study rather than all of the BCTs that make up the intervention. In some cases (comparison 1) the content of the comparison is the same as the content of the intervention arm, but in most cases (comparison 2 and 3) the content of the comparison is what is left of the intervention when the control arm is taken away. We regard this as the part of the intervention that was actively tested in the trial. A limitation of this approach is that we may have missed some interaction effects.
Feedback on behaviour
Early on in our coding, we observed that the BCT ‘feedback on behaviour’ was often found to be presented alongside a social norms BCT. The implementation of three social norms BCTs (social comparison, social incentive and social reward) would seem to be greatly facilitated by combination with ‘feedback on behaviour’. Social comparison, defined as ‘draw attention to others’ performance to allow comparison with the person’s own performance’,24 does not by definition require feedback on the target’s own behaviour to be provided, but providing such feedback (e.g. performance data) would be expected to facilitate comparison. Social reward, ‘arrange verbal or non-verbal reward if and only if there has been effort and/or progress in performing the behaviour’,24 and social incentive, ‘inform that a verbal or non-verbal reward will be delivered if and only if there has been effort and/or progress in performing the behaviour’,24 similarly do not require feedback on the target’s behaviour to be provided (e.g. the behaviour could be monitored by others without feedback to make the reward/incentive process clear to a target), but feedback on the behaviour fits very well with these social norms BCTs and might be expected to facilitate the action of these BCTs.
Because of the high prevalence of feedback on behaviour (present in 88/100 comparisons), we combined ‘feedback on behaviour’ with the social norms BCT with which it appeared for the purpose of primary analyses: in the forest plots we have listed each social norm with or without feedback. However, it was important to unpick the separate effects of feedback on behaviour: this was examined as part of the metaregression. As a sensitivity analysis, we examined the overall effects of social norms interventions with and without feedback on behaviour.
Data synthesis
Criteria for study data to be meta-analysed
We included in a meta-analysis those studies that report a primary outcome measure (clinical behaviour of a health worker) or secondary outcome (patient outcome) that can be converted into a SMD.
Planned approach for meta-analysis
Research question (RQ) 1: what is the effect of social norms interventions on the clinical behaviour of health workers, and the resulting patient outcomes?
The comparisons used in the analysis to answer RQ1 are shown in Appendix 10, Table 22. We stratified the studies in the forest plot according to the type of comparison (see Utilising the behaviour change technique coding in the analysis) and the type of target behaviour, and pooled estimates across strata. The aim of this was to provide some initial insight into whether or not, and how, treatment effects vary systematically in trials using different social norms techniques, while remaining aware of the likely confounding by other trial characteristics. We considered I2 and tau when interpreting heterogeneity, but did not use it as the basis for analytic decisions. We preferred a fixed-effects approach rather than a random-effects approach to meta-analysis, which we consider to yield a summary of the evidence in these trials (i.e. the average effect), rather than an estimate of a common underlying treatment effect. However, we also reported a random-effects analysis.
Research question 2: which contexts, modes of delivery and BCTs are associated with health worker clinical behaviour change? To address this research question, we followed steps 1 to 3.
Step 1 – we explored sources of variation using forest plots and narrative description. In addition to those comparisons used in RQ1, we included the following types of comparison in a narrative description: (1) social norms intervention A versus social norms intervention B and (2) social norms intervention + X versus social norms intervention + Y, where X and Y are any BCT or combination of BCTs, and A and B are either two different types of social norms BCT or the same social norms BCT delivered by two different methods.
Step 2 – we undertook an exploratory analysis using multivariable metaregression to investigate sources of heterogeneity and explain variation in the results. Metaregression is an appropriate regression method in which weights are assigned to studies/subgroups based on the standard error of the treatment effect. Appendix 11, Table 23, shows the predictor variables together with anticipated parameterisations that we included in the metaregression analyses. Although controlling for multiple predictors at once is desirable, in practice this was governed by the number of trials and the observed distributions of the variables. We allowed for trials from the different comparisons to enter into a single metaregression given that we anticipated we would be able to control for comparators and co-interventions in the regression. We had intended to categorise the control conditions, but were unable to do this robustly.
Step 3 – we used network meta-analysis to explore which social norms BCT, combination of social norms BCTs or combination of social norms BCT with other BCTs, if any, appears most effective. We considered two broad approaches for network meta-analysis, and made the decision to employ type (a) after consultation with our SSC.
-
Network meta-analysis
We examined data from all trials to look at the most commonly occurring combinations of social norms BCTs, either alone or alongside other BCTs. We built and examined a network diagram including social norms BCTs and commonly occurring combinations of social norms BCTs with other BCTs, plus control. Decisions about whether or not to ‘lump together’ BCTs or combinations of BCTs into categories were made after careful discussion by the project team. The justifications were recorded. The geometry of the network diagram was evaluated and no revisions were required to achieve a connected network. Fixed-effects and random-effects network meta-analyses were fitted in Stata.
-
Multi-components-based network meta-analysis. 45
Each intervention in the review would have been considered as a combination of BCT components. We would include all social norms BCTs along with other commonly found BCTs in a components-based network plot. This type of analysis ideally requires all available trials that test the BCT components of interest; our search strategy was not appropriate for this as we were focusing on the social norms components only. We therefore decided not to pursue this approach.
The results from direct and indirect evidence were compared to check for consistency. Trials grouped by comparison were examined to assess transitivity. Metaregression did not identify any clear potential effect modifiers; therefore, although we planned in the protocol to include these in the model, this did not happen.
Additional analyses
We carried out the following sensitivity analyses for the primary outcome:
-
include only studies with a low risk of bias (for the key domains of allocation concealment, sequence generation, attrition, selective outcome reporting and other sources of bias)
-
exclude continuous outcomes reported as ‘mean percentage’ that were < 20% or > 80%, as these are unlikely to come from a normal distribution
-
include only studies in which the standard deviation was not imputed
-
using alternative values of imputed ICC
-
studies with and without feedback on behaviour.
Publication bias
We aimed to minimise the impact of reporting biases by performing a comprehensive search for eligible studies. We investigated the impact of publication bias in the reported studies using a funnel plot.
Patient and public involvement
We recruited members of the public from two sources: (1) PRIMER (Primary Care Research in Manchester Engagement Resource: https://sites.manchester.ac.uk/primer/about-primer/; accessed 1 September 2020), a public involvement group in the Centre for Primary Care, University of Manchester, and (2) an advertisement on Citizen Scientist, which is based at Salford Royal NHS Foundation Trust and promotes research and patient and public involvement (PPI) opportunities for members of the public. We advertised for anyone aged > 18 years who had used any type of NHS service: we were not looking for people with any particular condition or experiences.
Mr Manoj Mistry has been involved in the review from the start. He has a wealth of past experience of involvement in research and was an invaluable part of the review. He had input into the proposal before we submitted the funding bid and he was a member of the SSC, bringing a patient and carer perspective to the meetings. He attended all three SSCs and played a full and active role in the committee’s discussions.
Two PPI events were planned for this study. The first event took place in August 2018 at the University of Manchester. The aim of the first event was to discuss how the review would be relevant to members of the public, and to get feedback on the overall design of the review. Six members of the public (two female, four male), including Mr Manoj Mistry, participated in the workshop, and they discussed with us the relevance of the review for patients and carers. They felt that patients can have a role in changing health worker behaviour, for example by reminding health workers to wash their hands or telling the GP that they do not expect to be prescribed antibiotics for a cold, although they were cynical about whether or not doctors would listen to patients when they present potential best practice (example given of a relative who had better care in Australia, but the doctor in the UK did not want to hear about it). In response to this observation, we made sure to record whether or not any studies in the review considered patients’ role in social norms interventions (e.g. use of the information about others’ approval BCT, where the approval came from patients) (see Appendix 12, Table 24, for a short report of the meeting).
We had feedback from four public contributors on the Plain English summary, and Mr Manoj Mistry has reviewed this description and account of our PPI activity.
A second PPI workshop took place in October 2019 at the University of Manchester to discuss how best to disseminate the findings to a wider audience. Four of the original group members (including Mr Manoj Mistry) attended. We presented the preliminary findings from the SOCIAL study and asked the group what they considered to be the most important messages from a public perspective. We also asked the group to suggest suitable language for presenting the findings to a lay audience. They suggested that the main messages should be that the study provides evidence that social norms interventions can encourage the medical community to change behaviour, leading to better outcomes for patients.
One or two things make social norms interventions even more effective:
-
right message (i.e. the use of different social norms BCTs)
-
right place (i.e. context)
-
right method (i.e. mode of delivery).
Authority of the message sender is crucial.
Messages from all sources are important, including those from patients.
We plan to follow this approach when we write summary materials for a lay audience. There was concern (from some) about the term ‘behaviour change’. Alternatives were ‘influence’ or ‘improve’, but they did not all agree. The group wanted us to avoid being preachy or patronising or using a telling-off approach to health workers: they talked about health workers being ‘encouraged’ by social norms interventions, rather than ‘directed’. The group felt that social norms messages would also be useful with people who teach and mentor students and young professionals. The lack of effect for face-to-face delivery of social norms interventions was viewed as surprising.
Chapter 3 Results
Identification of included studies
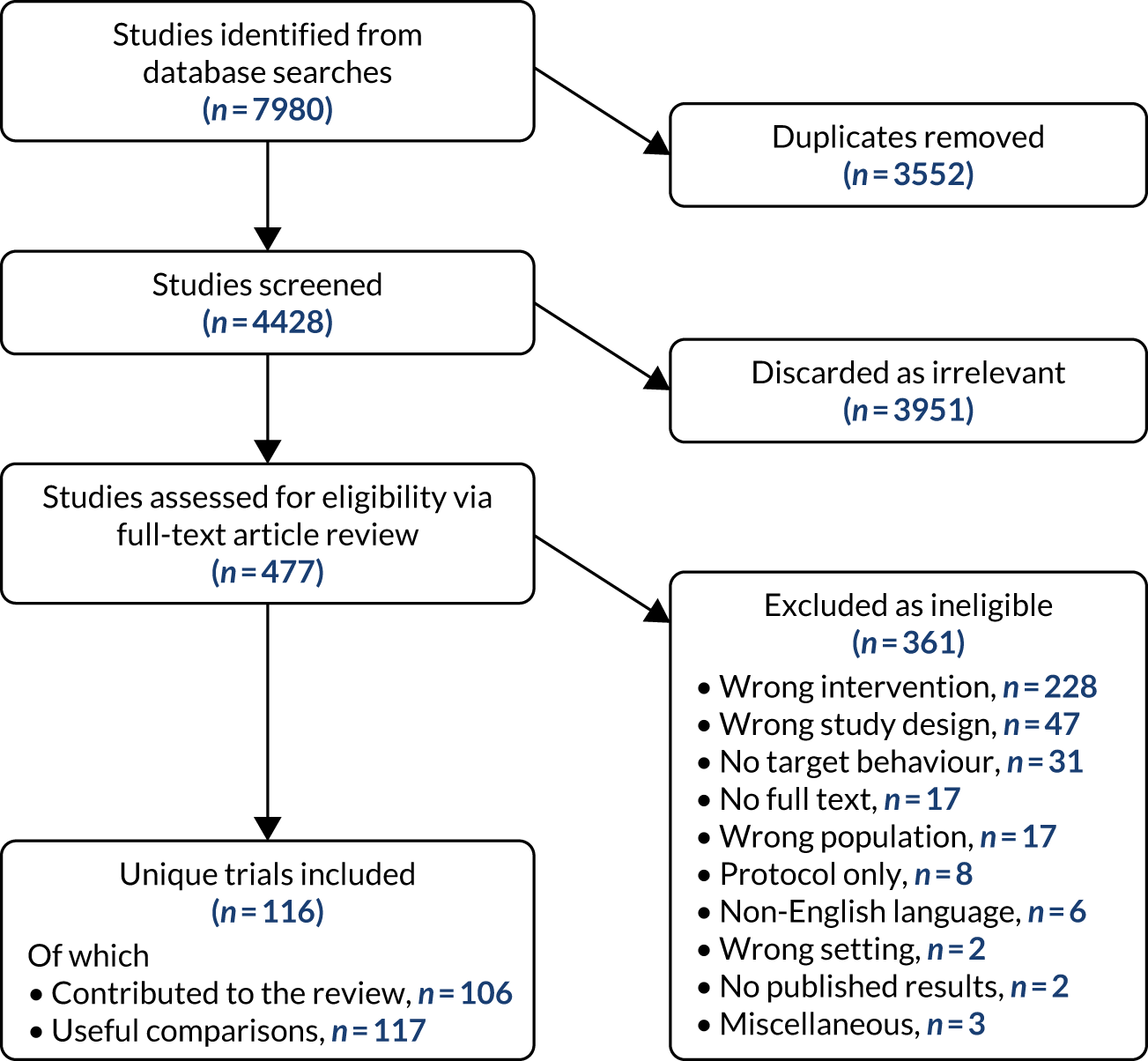
Of the 7980 studies identified using database searches, 3552 were identified as duplicates leaving 4428 separate studies to be screened. Of these, 3951 were discarded as irrelevant to the research questions under consideration, leaving 477 to be assessed for eligibility by full-text review of publications. Of these, 361 were excluded as ineligible for various reasons, as described in Figure 1. There were 116 studies that met the inclusion criteria, and 106 of these contributed findings to the review. Some of the 106 studies had more than one trial arm, and there were a total of 117 comparisons that tested the effect of social norms on the clinical behaviour of health workers. The remaining 10 studies met all of the inclusion criteria but did not provide usable outcome data: two reported the overall effect but did not compare the results between groups,46,47 six reported results unclearly or incompletely,48–53 one trial was discontinued before completion54 and one did not report results on our primary or secondary outcomes. 55 Searches for companion papers were unsuccessful and authors were not contacted owing to limited time. A brief description of the studies is provided in Appendix 13, Table 25.
FIGURE 1.
The PRISMA flow chart of the SOCIAL review.
Characteristics of included studies
Study characteristics
A detailed summary of study characteristics is shown in Table 1. Over half of the included trials were conducted in North America (Canada: n = 15, 14.2%; USA: n = 45, 42.5%) and the most common settings were primary care (n = 57, 53.8%) and hospitals (including both inpatient and outpatient: n = 31, 29.3%). GPs were the most frequently targeted type of health worker (n = 45, 42.5%), with many studies also targeting a mixture of health workers (n = 35, 33.0%). In terms of target behaviour, 40 studies (37.7%) aimed to change prescribing behaviours (including vaccinations), with 25 (23.6%) concerned with the overall management of conditions/communications (e.g. being friendly during consultations) and 21 (19.8%) focusing on arranging, conducting or administering tests/assessments (e.g. performing HbA1c testing). Of the 106 trials that contributed findings to the review, the majority (n = 70, 66%) were cluster RCTs, with 31 RCTs (29.2%), four stepped-wedge designs (3.8%) and one two-arm matched-cluster RCT. The majority of trials (n = 103, 97.2%) did not explicitly target participants with a low target performance. This is surprising, because the literature on social norms strongly suggests that social comparison is more likely to be successful if it is addressed to low performers: telling a high performer that they are already doing more than their peers does not motivate them to improve. 56,57 It is possible that some of the trials took place in contexts where the performance of all the health professionals was generally low at baseline, so they did not need to specifically seek out low performers to target, but no information was provided to support such an assumption. A complete list of all trials and their characteristics is included in Appendix 14, Table 26.
| Study characteristic (n = 106) | Frequency | % |
|---|---|---|
| Country | ||
| Australia | 8 | 7.5 |
| Canada | 15 | 14.2 |
| Denmark | 4 | 3.8 |
| UK | 13 | 12.3 |
| Netherlands | 6 | 5.7 |
| USA | 45 | 42.5 |
| Other/multiple | 15 | 14.2 |
| Setting | ||
| Primary (GP/general practice nurses) | 57 | 53.8 |
| Hospital (inpatient and outpatient) | 31 | 29.3 |
| Community | 4 | 3.8 |
| Care/nursing home | 4 | 3.8 |
| Mixed | 7 | 6.6 |
| Other | 3 | 2.8 |
| Type of health worker | ||
| Doctor (primary care) | 45 | 42.5 |
| Doctor (secondary care) | 19 | 17.9 |
| Other (nurse/dentist/AHP/pharmacist) | 7 | 6.6 |
| Mixture/whole team | 35 | 33.0 |
| Target behaviour | ||
| Prescribing (including vaccinations) | 40 | 37.7 |
| Hand-washing/hygiene | 4 | 3.8 |
| Tests/assessments | 21 | 19.8 |
| Referrals | 3 | 2.8 |
| Management communications | 25 | 23.6 |
| Other | 2 | 1.9 |
| Multiple behaviours | 11 | 10.4 |
| Type of trial | ||
| Cluster RCT | 69 | 65.1 |
| Factorial | 4 | 3.8 |
| RCT | 28 | 26.4 |
| Stepped wedge | 4 | 3.8 |
| Matched pairs, cluster RCT | 1 | 0.9 |
| Targeted at low baseline performance?a | ||
| No | 103 | 97.2 |
| Yes | 2 | 1.9 |
| Unclear | 1 | 0.9 |
| Intervention characteristic (n = 117) | Frequency | % |
| Source | ||
| Peer | 6 | 5.1 |
| Investigators | 83 | 70.9 |
| Supervisor/senior colleague | 2 | 1.7 |
| Patient | 1 | 0.9 |
| Respected source | 15 | 12.8 |
| Other | 1 | 0.9 |
| Not reported | 9 | 7.7 |
| Internal/external deliveryb | ||
| Internal | 17 | 14.5 |
| External | 81 | 69.2 |
| Unclear/not reported | 19 | 16.2 |
| Reference group | ||
| Peer | 97 | 82.9 |
| Professional body | 1 | 0.9 |
| Senior person | 9 | 7.7 |
| Patient(s) | 1 | 0.9 |
| Multiple | 4 | 3.4 |
| Unclear/not reported | 5 | 4.3 |
| Direction of change | ||
| Increase | 85 | 72.6 |
| Decrease | 30 | 25.6 |
| Maintenance | 0 | 0.0 |
| Unclear | 2 | 1.7 |
| Format | ||
| Face-to-face meeting | 16 | 13.7 |
| 10 | 8.5 | |
| Written (paper) | 29 | 24.8 |
| Separate computerised | 10 | 8.5 |
| Mixed | 18 | 15.4 |
| Unclear/not reported | 34 | 29.1 |
| Frequency | ||
| Only once | 35 | 29.9 |
| Twice | 10 | 8.5 |
| More than twice | 45 | 38.5 |
| Unclear/not reported | 27 | 23.1 |
Intervention characteristics
Details of intervention characteristics are shown in Table 1. Of the 117 comparisons, many were delivered using a written (paper) format (n = 29, 24.8%) or utilised a mixed format (e.g. face to face and written) (n = 18, 15.4%). Participants in 45 (38.5%) interventions received the intervention more than twice, whereas 10 comparisons delivered the intervention twice (8.5%) and 35 (29.9%) delivered the intervention only once. In the majority of comparisons, the investigators were the source of the intervention (k = 83, 70.9%) and the intervention was delivered by someone external to the target health worker’s organisation (k = 81, 69.2%). In 97 (82.9%) of the comparisons, the reference group/person was the target health worker’s peer. In terms of the desired direction of change, 85 (72.6%) studies aimed to increase the behaviour. There was a lack of clarity in reporting across many intervention characteristics within the included studies. For example, in 34 (29.1%) interventions, the format was unclear or not reported and the frequency of the intervention was unclear or not reported in 27 (23.1%) comparisons.
Description of the behaviour change techniques
The frequency of specific social norms BCTs occurring within the 100 comparisons that tested social norms interventions against a control are shown in Table 2. We found tests of social comparison (n = 79), credible source (n = 7) and social reward (n = 2) against control. Some studies tested more than one social norms BCT together: social comparison and credible source (n = 6), social comparison and social reward (n = 2) and multiple social norms BCTs (more than two) together (n = 4). The social norms interventions often occurred alongside other BCTs, and 22 different techniques were identified (see Table 2).
| Behaviour change technique | n |
|---|---|
| Social norms BCTs | |
| 6.2 Social comparison | 90 |
| 9.1 Credible source | 18 |
| 10.4 Social reward | 5 |
| 6.3 Information about others’ approval | 4 |
| 10.5 Social incentive | 1 |
| Other BCTs | |
| 2.2 Feedback on behaviour | 88 |
| 3.1 Social support (unspecified) | 25 |
| 4.1 Instruction on how to perform the behaviour | 20 |
| 7.1 Prompts/cues | 19 |
| 5.1 Information about health consequences | 18 |
| 1.2 Problem-solving | 12 |
| 1.1 Goal-setting (behaviour) | 9 |
| 8.1 Behavioural practice/rehearsal | 5 |
| 1.4 Action planning | 4 |
| 6.1 Demonstration of the behaviour | 4 |
| 1.3 Goal-setting (outcome) | 3 |
| 2.3 Self-monitoring of behaviour | 2 |
| 2.7 Feedback on outcome(s) of behaviour | 2 |
| 12.5 Adding objects to the environment | 2 |
| 1.7 Review outcome goals | 1 |
| 2.1 Monitoring of behaviour by others without feedback | 1 |
| 5.3 Information about social and environmental consequences | 1 |
| 8.2 Behaviour substitution | 1 |
| 9.2 Pros and cons, final | 1 |
| 10.3 Non-specific reward, final | 1 |
| 12.1 Restructuring the physical environment | 1 |
| 10.1 Material incentive (behaviour) | 1 |
The 117 comparisons belonged to the three comparison categories as follows (Table 3):
-
Pure comparisons. There were 36 comparisons that offered a ‘pure’ test of social norms interventions. Most of these tested social comparison (33 comparisons). There were far fewer comparisons testing credible source (n = 3), social reward (n = 1), social comparison and credible source together (n = 2), or social comparison and social reward together (n = 2).
-
Comparisons involving other BCTs. Social comparison was combined with social support (unspecified) (n = 7), prompts and cues (n = 5), information about health consequences (n = 4) and instruction on how to perform the behaviour and prompts/cues (combined) (n = 5). Combined interventions involving social comparison with more than two other BCTs or where the combination occurred only once in the study were combined into one group: social comparison and other BCTs (n = 25). Credible source did not occur more than once with any one particular BCT, so there is one category of credible source with other BCTs (n = 4) and another of social comparison and credible source with other BCTs (n = 4). There was one example of social reward with other BCTs (n = 1). Where more than two social norms BCTs occurred together, they were combined in a category (n = 4).
-
Social norms BCTs in both arms. There were 17 comparisons in which both arms involved social norms interventions (Table 4).
| Social norms interventions comparison types | n (%) |
|---|---|
| Pure comparisons | |
| Social comparison | 33 (28) |
| Credible source | 3 (3) |
| Social reward | 1 (1) |
| Social comparison and credible source | 2 (2) |
| Social comparison and social reward | 2 (2) |
| Comparisons involving other BCTs | |
| Social comparison and social support (unspecified) | 7 (6) |
| Social comparison and prompts/cues | 5 (4) |
| Social comparison and information about on health consequences | 4 (3) |
| Social comparison and instruction on how to perform the behaviour & prompts/cues | 5 (4) |
| Social comparison and other BCTs | 23 (21) |
| Credible source and other BCTs | 4 (3) |
| Social comparison and credible source and other BCTs | 6 (3) |
| Social reward and other BCTs | 1 (1) |
| Multiple social norms BCTs and other BCTs | 4 (3) |
| Social norms BCTs in both arms | |
| Social norms BCTs both arms | 17 (15) |
| Total (n) | 117 |
| Comparison type | Frequency |
|---|---|
| Same social norms intervention in both arms, testing some other intervention (n = 11) | |
| Credible source and feedback on behaviour vs. credible source and feedback on behaviour with other BCTs | 1 |
| Social comparison vs. social comparison and goal-setting | 1 |
| Social comparison and feedback vs. social comparison and feedback plus information about others’ approval and other BCTs | 1 |
| Social comparison and feedback vs. social comparison and feedback with other BCTs | 7 |
| Social comparison and feedback vs. social comparison and feedback with a patient-level intervention | 1 |
| Comparison of two social norms interventions (n = 2) | |
| Credible source and social comparison and feedback on behaviour and other BCTs vs. social comparison and feedback on behaviour | 1 |
| Social comparison and credible source and feedback on behaviour vs. credible source | 1 |
| Testing different variants of the same social norms intervention (n = 4) | |
| Social comparison vs. social comparison, no other BCTs | 2 |
| Credible source vs. credible source | 1 |
| Social comparison and feedback and social support (unspecified) vs. social comparison and Feedback plus social support (unspecified) | 1 |
| Total | 17 |
Variation in trial characteristics by type of social norms intervention
Table 5 shows the key trial characteristics by the type of comparison. In total, 33 different comparisons were a pure test of ‘social comparison’ and these were quite varied in terms of type of target behaviour, type of health-care worker and type of setting; similarly, those trials that tested social comparison alongside other BCTs were also quite varied. There were 13 comparisons that tested ‘credible source’ alone or with other BCTs and four that included social reward, and again these were spread over a range of behaviours, contexts and settings. Reassuringly, there is no clear pattern to suggest that the use of BCTs was restricted to particular behaviours, contexts or settings, and this is consistent with the regression results, which suggested that the results were consistent after adjustment.
| Trial characteristic | Social norm comparison category, n (%) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Social comparison | Credible source | Social reward | Social comparison and credible source | Social comparison and social reward | Social comparison and social support (unspecified) | Social comparison and prompts and cues | Social comparison and information on health consequences | Social comparison and instructions and prompts/cues | Social comparison and others BCTs | Credible source and other BCTs | Social comparison and credible source and other BCTs | Social reward and other BCTs | Multiple social norms and other BCTs | |
| Comparisons with primary outcome data (n) | 33 | 3 | 1 | 2 | 2 | 7 | 5 | 4 | 5 | 25 | 4 | 4 | 1 | 4 |
| Target behaviour | ||||||||||||||
| Prescribing | 15 (45) | 1 (100) | 1 (50) | 2 (100) | 2 (29) | 1 (20) | 3 (75) | 1 (20) | 11 (44) | 1 (25) | 1 (25) | 1 (25) | ||
| Hand/hygiene | 1 (25) | 1 (100) | 1 (25) | |||||||||||
| Tests | 7 (21) | 1 (14) | 3 (60) | 1 (25) | 3 (60) | 4 (16) | 1 (25) | 1 (25) | ||||||
| Referrals | 2 (8) | 1 (25) | ||||||||||||
| Manage conditions | 5 (15) | 3 (100) | 1 (50) | 2 (29) | 1 (20) | 5 (20) | 2 (50) | 2 (50) | ||||||
| Other | 12 (14) | 1 (4) | ||||||||||||
| Multiple | 6 (18) | 1 (14) | 1 (20) | 2 (8) | ||||||||||
| Type of HCP | ||||||||||||||
| Doctor: GP | 16 (48) | 1 (50) | 2 (100) | 4 (57) | 2 (40) | 1 (25) | 4 (80) | 11 (44) | 2 (50) | 1 (25) | 1 (25) | |||
| Doctor: secondary | 4 (12) | 3 (100) | 1 (14) | 1 (20) | 1 (20) | 2 (12) | 1 (25) | 1 (25) | 1 (25) | |||||
| Other HCP | 4 (12) | 1 (100) | 1 (4) | 0 (0) | 1 (25) | |||||||||
| Mixed/team | 9 (27) | 1 (50) | 2 (29) | 2 (40) | 2 (40) | 1 (20) | 10 (40) | 2 (50) | 2 (50) | 1 (100) | 1 (25) | |||
| Setting | ||||||||||||||
| Primary | 18 (55) | 1 (50) | 2 (100) | 4 (57) | 4 (80) | 1 (25) | 5 (100) | 17 (68) | 2 (50) | 1 (25) | 1 (25) | |||
| Hospital | 6 (18) | 3 (100) | 2 (29) | 1 (20) | 2 (50) | 6 (24) | 2 (50) | 2 (50) | 1 (100) | 2 (50) | ||||
| Community | 1 (3) | 1 (100) | 1 (50) | 1 (25) | ||||||||||
| Care/nursing | 0 (0) | 1 (14) | 1 (25) | 1 (4) | 1 (25) | |||||||||
| Mixed | 7 (21) | |||||||||||||
| Other | 1 (3) | |||||||||||||
Outcome measures
Using the criteria described in Chapter 2, Outcomes and prioritisation, we selected a single primary outcome measure of compliance with desired behaviour for each relevant comparison. Of the 117 comparisons used in the review, 32 (27%) provided an odds ratio, 42 (35%) provided raw binary data and 43 (37%) provided mean with standard deviation (standard deviations were imputed where necessary).
Risk of bias
A summary of each risk-of-bias item across the included studies (n = 106) is shown in Figure 2. Individual risk-of-bias assessments for all of the included studies can be found in Appendix 15, Figure 20.
FIGURE 2.
Review authors’ judgements about each risk-of-bias item presented as percentages across all included studies (n = 106).
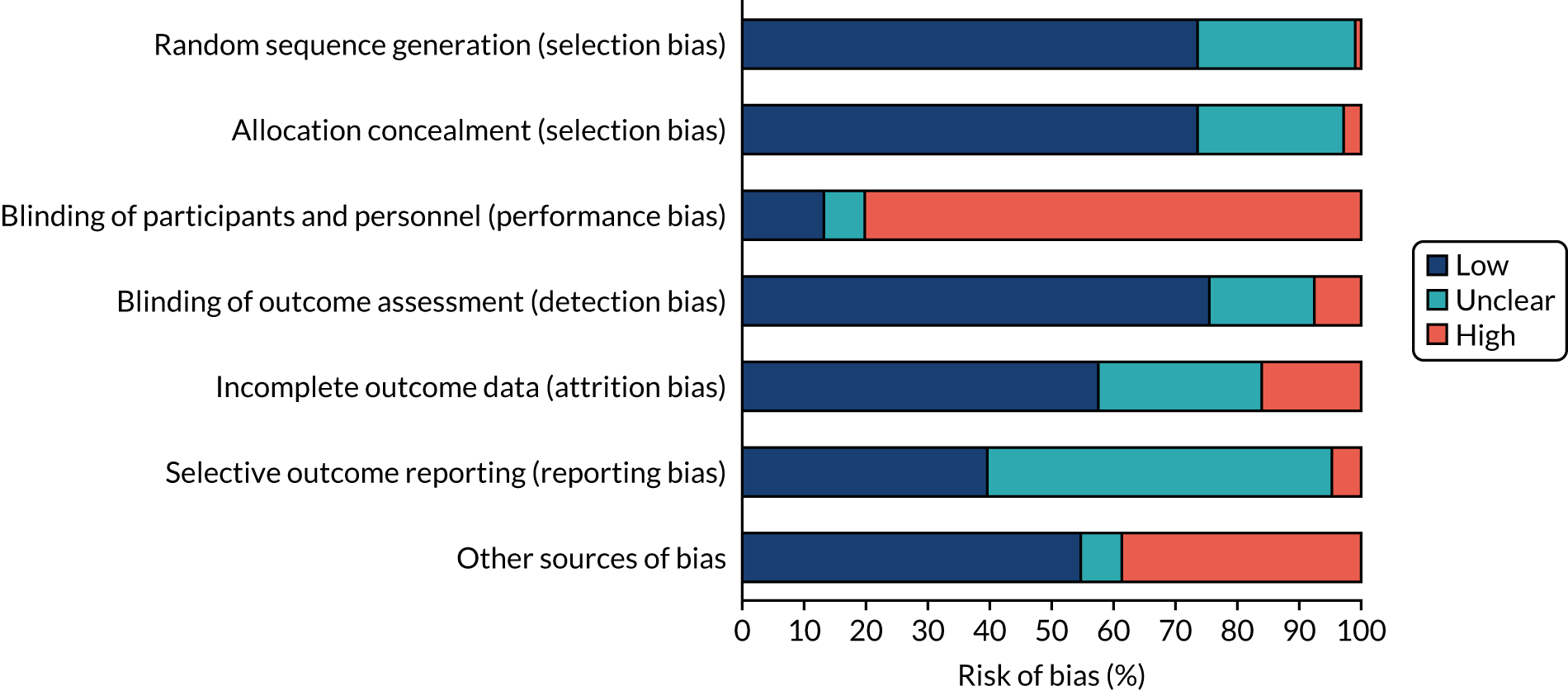
Allocation
In terms of random sequence generation, methods were deemed sufficient to produce comparable groups for the majority of studies (n = 78, 73.6%) and were, therefore, considered to be at low risk of bias. Only one study was rated to be at high risk of bias, and this was because of the original randomisation being rejected because of a perceived lack of balance between groups. All other studies (n = 27) were rated as unclear because of insufficient information to permit a judgement. The majority of studies were also rated to be at low risk of bias for allocation concealment (n = 78, 73.6%), primarily because of recruitment and consent being conducted before randomisation took place. Three studies were rated to be at high risk of bias because randomisation took place before recruitment and/or obtaining consent. The remaining studies (n = 25) were considered unclear because there was insufficient information available, or because recruitment/consent had occurred post randomisation and it was unclear whether or not participants were aware of their allocation at the time of enrolment/consent.
Blinding
Many of the studies were cluster trials, randomised at the hospital or clinic level, making the blinding of participants and personnel impractical. Owing to this clustering, most studies were rated to be at high risk of bias (n = 85). Fourteen studies were considered to be at low risk of bias owing to participants/personnel being unaware of the study aims and hypothesis, intervention content and existence of other groups/interventions, or being unaware that they were taking part in a trial. Studies rated as unclear (n = 7) lacked clarity in reporting the blinding of participants and whether or not participants were aware of the intervention or study aims and outcomes. For blinding of outcome assessment, most studies (n = 80) obtained data from electronic health records, online reports or databases or routinely collected data, in which the outcome assessors were blind to group allocations and were, therefore, rated to be at low risk of bias. Eight studies were judged to be at high risk of bias where participants selected consecutive patient records to contribute to the outcome assessment (so could have selected groups based on good practice), where participants selected the patients and collected the data or where outcome measures were recorded by participants. The remaining studies (n = 18) were judged to be unclear because of a lack of information or lack of clarity in terms of whether or not outcome assessors were blinded to allocation.
Incomplete outcome data
Over half of the included studies (n = 61) were considered to be at low risk of bias for incomplete outcome data for the following reasons: no drop-outs/low attrition, attrition evenly distributed across groups, drop-out reasons unlikely to be connected to interventions, analysis conducted on intention-to-treat basis and different patients before and after. Seventeen studies were rated to be at high risk of bias as they had large numbers of drop-outs, a lack of discussion of drop-out reasons, unequal (or unreported) attrition across groups or reasons for drop-outs being related to the intervention. The remaining studies (n = 28) were judged to be unclear as a result of insufficient or unclear reporting of attrition.
Selective reporting
Where outcomes appeared to have been reported as stated in the protocol (or where there was only one outcome and this was adequately reported), studies were judged to be at low risk of bias for selective outcome reporting (n = 42). Five studies had made changes from the planned outcomes in the protocol, or had ambiguously reported the primary outcome at registration (enabling multiple interpretations), and were, therefore, considered to be at high risk of bias. Studies that had no available protocol and had multiple outcomes, or several ways of reporting outcomes, were categorised as being unclear (n = 59).
Other potential sources of bias
No potential other sources of bias were identified for over half of the included studies (n = 58). A small number of studies (n = 7) were rated as unclear for reasons including a lack of clarity in whether or not adjustments were made for clustering in the analysis, an unclear unit of analysis for some statistical tests and only summary trial methods and data reported. The remaining studies (n = 41) were judged to be at high risk of bias for the following reasons: no adjustment for clustering in analyses; poor reporting (particularly of outcome data, therefore making interpretation difficult); potential problems with the study design (e.g. stepped-wedge, step-wise regression); concerns over analysis processes (e.g. extreme values replaced or excluded); important baseline differences between groups or large differences in participant numbers across arms; and analysis within rather than between groups.
Effects of interventions: health worker behaviour (primary outcome)
Overall effect
There were 100 comparisons suitable for meta-analysis. Figure 3 shows the SMD summarised by type of BCT comparison in a fixed-effects meta-analysis. From this plot we can see that, as expected, there is a large amount of heterogeneity with an overall I2-value of 85.4%. Overall, combined data suggest that, on average, interventions that include social norms components were associated with a modest improvement of 0.08 SMD (95% CI 0.07 to 0.10). Forest plots showing each individual study in the review, by the social norm BCT used in the study, are in Appendix 17, Figures 22–26.
FIGURE 3.
Fixed-effects forest plot summarised by type of comparison. CS, credible source; SC, social comparison; SR, social reward. Note that SR (one comparison) and SR and other BCTs (one comparison) have been combined in this graph to improve presentation.
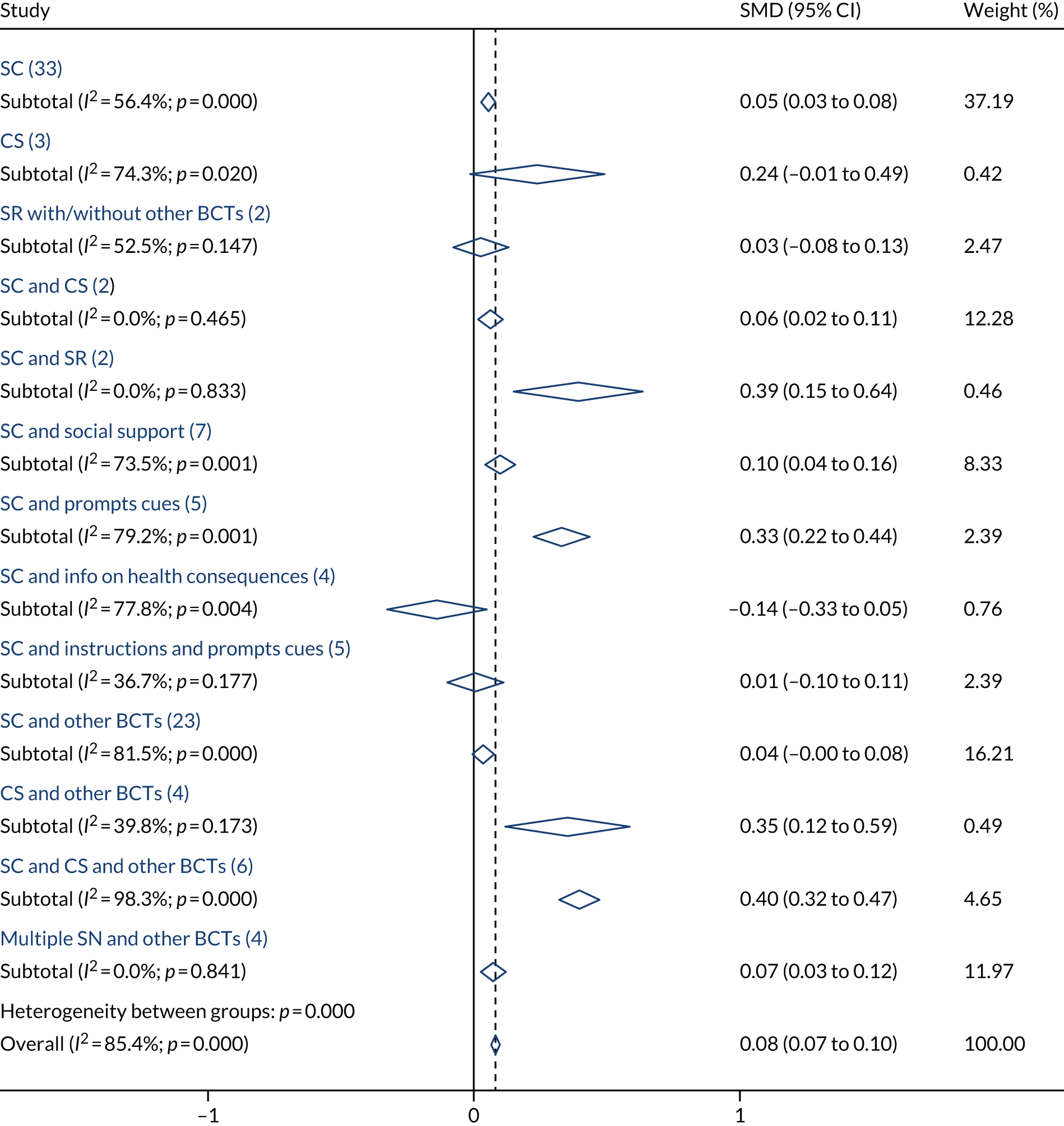
The I2 is interpreted as a measure of the proportion of variability owing to heterogeneity between studies. This can be calculated only when two or more studies are included in the same subgroup/meta-analysis, as can the p-value alongside I2 that tests the null hypothesis that I2 = 0. Note that I2 is related to precision and rapidly approaches 100% when the number of studies is large. 58 τ2 is an alternative measure of heterogeneity, calculated only during a random-effects meta-analysis, and can be interpreted as the between-study variance.
Note that most trials in this review were randomised at a cluster level and the unit of analysis may be patient, health-care worker or a larger unit, such as clinic or hospital. With that in mind, it is impossible to report ‘N’ for each trial in any consistent way. In the meta-analysis, the weights were calculated based on the standard error of the SMD extracted from the individual trials, which has been adjusted for clustering where necessary. The number of comparisons is reported for each subgroup in brackets on all forest plots. Forest plots showing the effect in every individual study, summarised by social norms intervention, are included in Appendix 1 (see Figures 22–26).
Figure 4 shows the SMD, summarised by the type of BCT comparison in a random-effects meta-analysis. Similar conclusions can be drawn when looking at the random-effects result compared with the fixed-effects result; however, using weights from a random-effects meta-analysis suggests a larger overall SMD (0.16, 95% CI 0.11 to 0.21, I2 = 85.4%, τ2 = 0.043) and a wider CI, because the random-effects meta-analysis attributes more weight to smaller trials.
FIGURE 4.
Random-effects forest plot summarised by type of comparison. CS, credible source; SC, social comparison; SR, social reward.
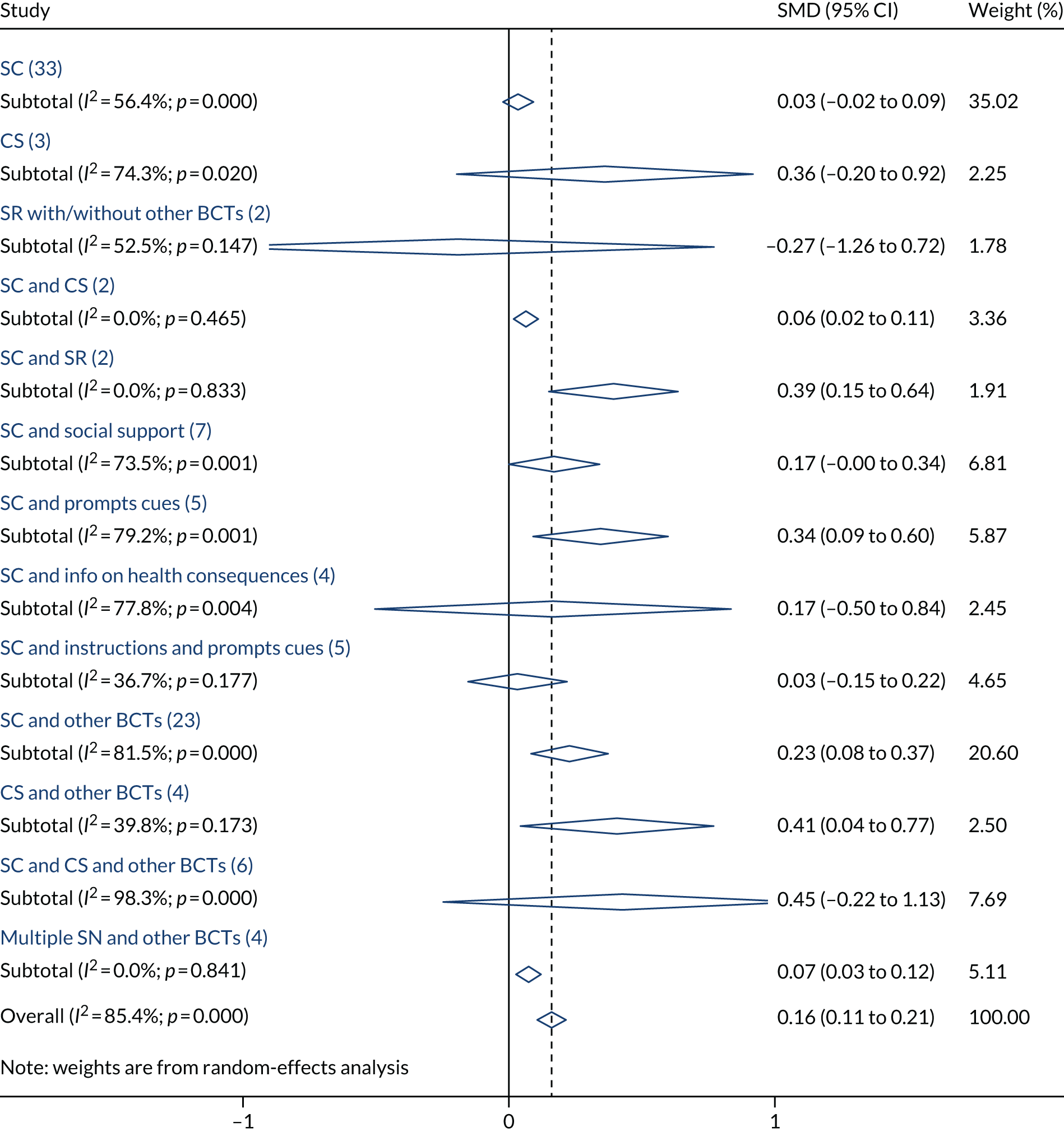
Illustration of standardised mean differences
For this review, we converted all measures of the effectiveness of health worker behaviour into a common scale: the SMD (standardised effect size). SMDs can be difficult to interpret. To illustrate how the observed average standardised effect sizes translate into real health-care scenarios, we have converted the SMD into a risk difference (difference in percentage points) for a range of typical baseline compliance rates (Table 6). This was carried out in two steps: (1) transforming the SMD into an odds ratio using a method suggested in the Cochrane handbook36 section 12.6.3, and (2) transforming the odds ratio into a risk difference, using a method proposed by Grant. 59
| Typical baseline compliance | Expected improvement (percentage points) | Illustration | |
|---|---|---|---|
| Social norms interventions on average O.08 SMD | Credible source interventions on average 0.3 SMD | ||
| 20% | 2 | 10 | In a population in which the appropriate tests are ordered 20% of the time, we would expect a social norms intervention, on average, to increase the rate of compliance by 2 percentage points to 22% |
| 40% | 4 | 13 | In a population in which prescribing guidelines are being adhered to 40% of the time, we would expect a credible source intervention, on average, to increase the rate of compliance by 13 percentage points to 53% |
| 60% | 3 | 12 | In a population in which recommended referrals are being made 60% of the time, we would expect a social norms intervention, on average, to increase the rate of referral by 3 percentage points to 63% |
| 80% | 2 | 10 | In a population in which the rate of antibiotic prescribing is 80%, we would expect a credible source intervention, on average, to reduce the rate of prescribing by 10 percentage points to 70% |
Investigation of social norms behaviour change techniques
Note that owing to the high prevalence of the BCT feedback on behaviour (present in 88/100 comparisons), in the forest plots we have combined feedback on behaviour with the social norms BCT with which it appeared; that is we have listed each social norms BCT with or without feedback. Later we examine the separate effect of feedback on behaviour as part of the metaregression and as a sensitivity analysis.
We summarised the SMDs by the type of social norms comparison (see Figure 3). There is little consistency in SMDs when looking at the different types of social norms interventions being tested, with subgroup CIs that do not overlap each other and that are inconsistent with the overall effect. Interventions including credible source appear to have larger effect sizes on average than other social norms interventions, and this is true for both credible source on its own (n = 3) (SMD 0.24, 95% CI –0.01 to 0.49) and credible source combined with other BCTs (n = 4) (SMD 0.35, 95% CI 0.12 to 0.59), although the CIs are wide. Credible source combined with social comparison (n = 2) had an average effect of 0.06 SMD (95% CI 0.02 to 0.11), and credible source combined with social comparison and various other BCTs (n = 6) appeared to be the most effective of all, with a SMD of 0.40 (95% CI 0.32 to 0.47). Comparisons that were a ‘pure’ test of social comparison (with or without feedback, n = 33) appeared to have a small effect (SMD 0.05, 95% CI 0.03 to 0.08), and the size of the effect is similar when social comparison is combined with various other BCTs (n = 23) (SMD 0.04, 95% CI –0.00 to 0.08). Social comparison appeared to be very effective when combined with prompts/cues (n = 5) (SMD 0.33, 95% CI 0.22 to 0.44), but ineffective when combined with both prompts/cues and instruction on how to perform the behaviour (n = 5) (SMD 0.01, 95% CI –0.10 to 0.11). Social reward appeared to be very effective when combined with social comparison (n = 2) (SMD 0.39, 95% CI 0.15 to 0.64), but only one study looked at social reward on its own and found a negative effect. We need to interpret these observations cautiously owing to the large amount of heterogeneity and the differences in contexts and settings.
In an attempt to ease interpretation, Figure 5 shows a re-categorisation of Figure 3. In this plot, all comparisons that test each of the social norms BCTs (social comparison, credible source and social reward), whether alone or alongside other BCTs, have been combined. Trials that combine two or more social norms BCTs have been put together in one group. As before, comparisons that test credible source (n = 7), either alone or in combination with other BCTs, appear to be the most effective on average (SMD 0.30, 95% CI 0.13 to 0.47). The effect of social comparison (n = 77) appears to be very small (SMD 0.06, 95% CI 0.04 to 0.8). There is little evidence to suggest that social reward is effective (SMD 0.03, 95% CI –0.08 to 0.13), but this is based on only two trials. Trials involving a mixture of more than one social norms BCT (n = 14) have a larger than average effect (SMD 0.13, 95% CI 0.10 to 0.16).
FIGURE 5.
Fixed-effects forest plot summarised by alternative categorisation of BCTs.
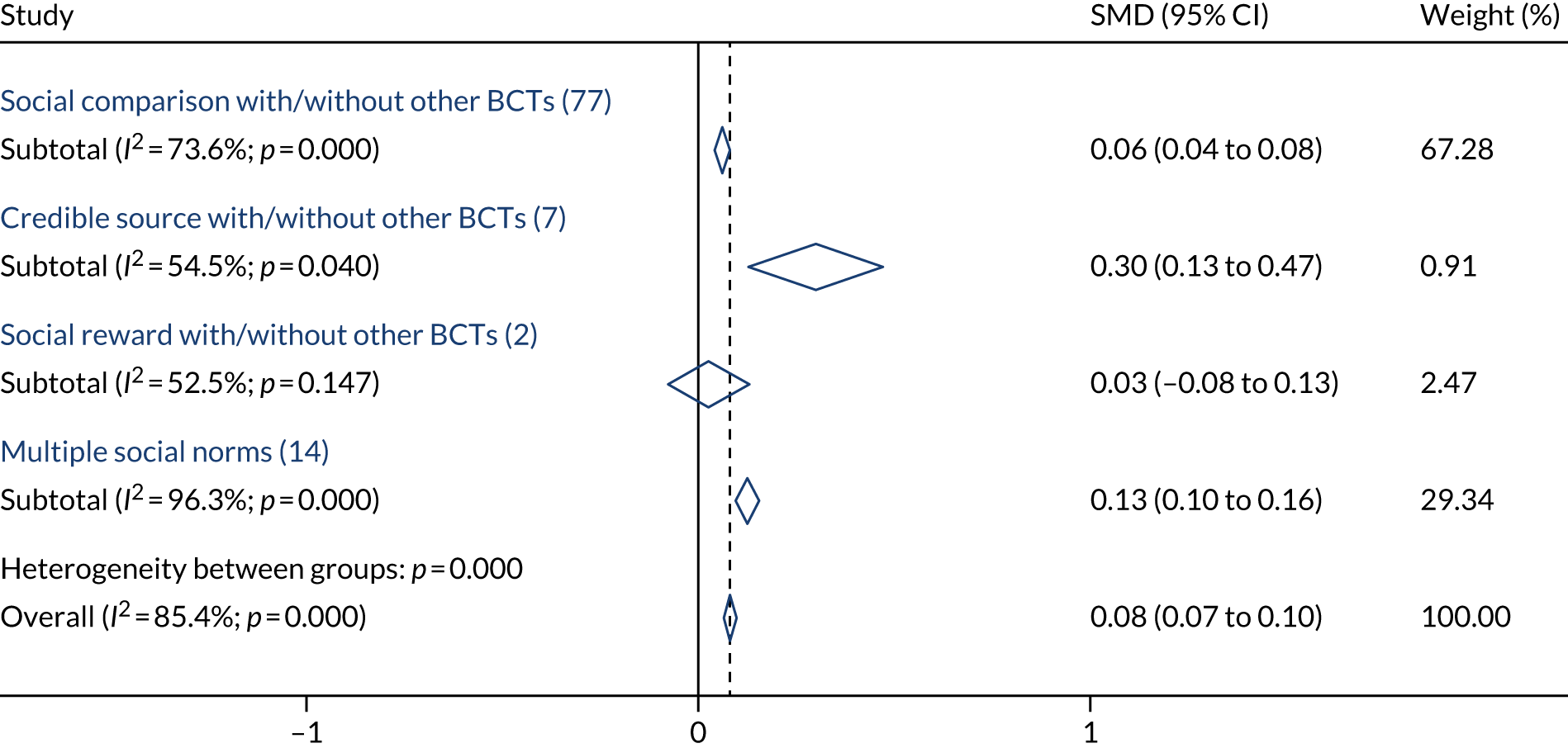
Illustrative case studies
The purpose of this review is to offer a structured summary across all of the 106 studies, but we have included some illustrative case studies (Table 7) to provide a concrete example of each of the three intervention types that were found to be the most effective (credible source and social comparison, social comparison with prompts/cues, social comparison and social reward).
| Details of study | Outcome measure, SMD (95% CI) | Control arm | Intervention description (BCTs coded) |
|---|---|---|---|
| Credible source and social comparison | |||
|
Hallsworth et al. (2016)60 RCT Doctor (primary care) Aim: to reduce the number of unnecessary prescriptions of antibiotics by GPs in England |
The rate of antibiotic items dispensed per 1000 population 0.13 (0.03 to 0.29) |
Delayed intervention (after the end of the trial) No BCTs were coded |
A letter was sent to GPs from the Chief Medical Officer. The letter stated that the practice was prescribing antibiotics at a rate higher than 80% of practices in its NHS local area team, and used three concepts from the behavioural sciences. The first was social norms information about how the recipient’s practice’s prescribing rate compared with other practices in the local area. Second, the letter was addressed from a high-profile figure, with the assumption that this would increase the credibility of its content. Finally, the letter presented three specific, feasible actions that the recipient could do to reduce unnecessary prescriptions of antibiotics: giving patients advice on self-care, offering a delayed prescription and talking about the issue with other prescribers in his or her practice. The letter was accompanied by a copy of the patient-focused ‘Treating your infection’ leaflet, which acted to reinforce the message of the letter by supporting delayed or reduced prescribing (9.1 credible source, 6.2 social comparison, 2.2 feedback on behaviour, 4.1 instruction on how to perform the behaviour) |
| Social comparison and prompts/cues | |||
|
Vellinga et al. (2016)61 Arm A Cluster RCT Doctor (GP) Aim: to increase the number of first-line antimicrobial prescriptions for suspected UTIs in adult patients |
Adherence to guidelines for antimicrobial prescribing in primary care 0.55 (0.32 to 0.77) |
Phase 1: a coding workshop – routine coding for UTIs using standardised codes were demonstrated. The purpose of this was to facilitate the generation of electronic A&F reports (not available to control until after the trial). Control practices then provided ‘usual care’ for the remainder of the intervention No BCTs were coded |
Arm A: phase 1 – a coding workshop (same as control). Phase 2: interactive workshops were designed to promote changes in antimicrobial prescribing for the treatment of UTIs by presenting an overview of prescribing and antimicrobial resistance, discussing the role of the GP in the spread of AMR. A computer prompt was developed for use within the selected general practice management software system. This prompt summarised the recommendations for first-line antimicrobial treatment and appeared on the computer screen when the GP entered the International Classification of Primary Care code (U71) for ‘cystitis, urinary infection, other’. This prompt also reminded the GP to collect patients’ mobile telephone numbers. Electronic A&F reports were available to download by GPs. These reports provided the practice with information on antimicrobial prescribing for UTIs in comparison with the aggregated information from the other practices participating in the intervention (7.1 prompts/cues, 2.2 feedback on behaviour, 6.2 social comparison) |
| Social comparison and social reward | |||
|
Persell et al. (2016)62 2 × 2 × 2 factorial Doctor (GP) Aim: to reduce inappropriate antibiotic prescribing for ARIs |
Physician rate of oral antibiotic prescribing for non-antibiotic-appropriate ARIs, acute sinusitis/pharyngitis and all other diagnoses of respiratory infection 0.44 (–0.06 to 0.94) |
Intervention 1 (accountable justifications): clinicians received electronic health record alerts summarising the treatment guidelines corresponding to the ARI diagnosis for which the antibiotic was being written, prompted the clinician to enter a free-text justification for prescribing an antibiotic, and informed the clinician that the free-text justification provided would be included in the patient’s medical record in which it would be visible to other clinicians. Clinicians were also informed that if no free-text justification was entered, a default statement ‘No justification for prescribing antibiotics was given’ would appear in the record. If the antibiotic order was cancelled, no justification was required, and no default text appeared. Alerts were suppressed for patients with comorbid chronic conditions that exempted these patients from clinical guidelines (4.1 instruction on how to perform the behaviour, 7.1 prompts/cues). Intervention 2 (suggested alternatives): when entering an ARI diagnosis for a patient, clinicians received a computerised alert containing multiple non-antibiotic prescription and non-prescription medication choices as well as educational materials that could be printed and given to the patient (7.1 prompts/cues) |
Intervention 3 (peer comparison): clinicians received e-mailed monthly performance feedback reports that included the clinician’s individual antibiotic prescribing rates for non-antibiotic-appropriate ARIs and, as a benchmark, the antibiotic prescribing rate for clinicians who were in the 10th percentile within the clinic (i.e. the lowest rates of inappropriate antibiotic prescribing). If clinicians were among the 10% of their peers with the lowest prescribing rates, the e-mailed reports told clinicians ‘You are a top performer.’ If clinicians were not among the 10% best, the e-mailed report told clinicians ‘You are not a top performer. You are prescribing too many unnecessary antibiotics.’ The proportion of ‘Top Performers’ could be > 10% of clinicians if > 10% of clinicians had an inappropriate antibiotic prescribing rate of zero (2.2 feedback on behaviour, 6.2 social comparison, 10.4 social reward) |
Variation in context and mode of delivery
We have summarised the SMD in various contexts and modes of delivery to examine where, how and with whom social norms interventions are most likely to be effective.
Type of health-care worker
Figure 6 shows the SMD summarised by the type of health-care worker in a fixed-effects meta-analysis. The effect of social norms interventions appears to be quite consistent when comparing GPs with doctors in secondary care as the type of health-care worker targeted (not shown), with an overall effect with doctors (n = 68) of 0.08 SMD (95% CI 0.07 to 0.10). We found no evidence that social norms interventions were effective with nurses or allied health professionals (AHPs) (SMD –0.01, 95% CI –0.12 to 0.11), although the number of comparisons was small (n = 5). The effect with other health workers, many of which were mixed groups such as doctors/nurses or nurses/AHPs (n = 27), was 0.08 SMD (95% CI 0.07 to 0.10).
FIGURE 6.
Fixed-effects forest plot summarised by type of health-care worker.

Target behaviour
Figure 7 shows the SMD summarised by the type of target behaviour in a fixed-effects meta-analysis. Interventions targeting prescribing behaviour (n = 40) appeared to be the most effective, on average (SMD 0.11, 95% CI 0.09 to 0.13). The effect of social norms interventions appeared to be reasonably consistent across other types of target behaviour, including test ordering (n = 21) and management of/communication about conditions (n = 23). Social norms interventions appear to be less effective with hand-washing (n = 3, SMD 0.04, 95% CI –0.05 to 0.13) and referrals (n = 3, SMD –0.08, 95% CI –0.23 to 0.07), but the number of studies is small.
FIGURE 7.
Fixed-effects forest plot summarised by target behaviour.
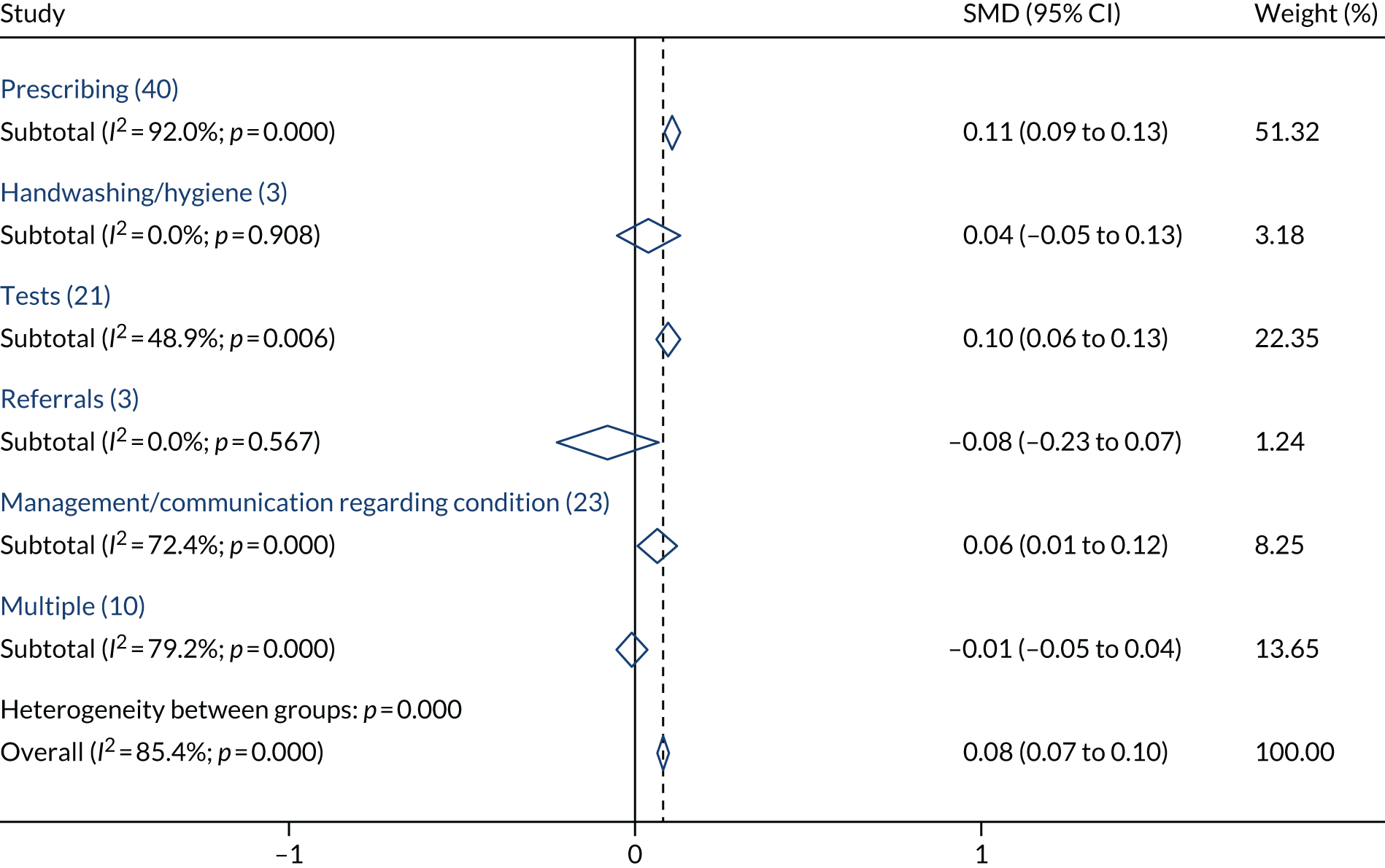
We have not presented a forest plot summarising the SMD by whether or not the participants were targeted based on low baseline performance, because there were only two trials that did this.
Health-care setting
Figure 8 shows the SMD summarised by health-care setting in a fixed-effects meta-analysis. The effect of social norms interventions appeared to be slightly lower in primary care settings (SMD 0.07, 95% CI 0.05 to 0.09) (n = 56) than in hospital settings (SMD 0.12, 95% CI 0.07 to 0.18) (n = 27), but both are consistent with the overall effect. Trials taking place in community settings (n = 4) and care/nursing home settings (n = 4) appear to be less effective on average; however, both CIs do overlap with the overall effect. Trials conducted in mixed settings (n = 9) appear to be more effective on average (SMD 0.35, 95% CI 0.27 to 0.42).
FIGURE 8.
Fixed-effects forest plot summarised by health-care setting.
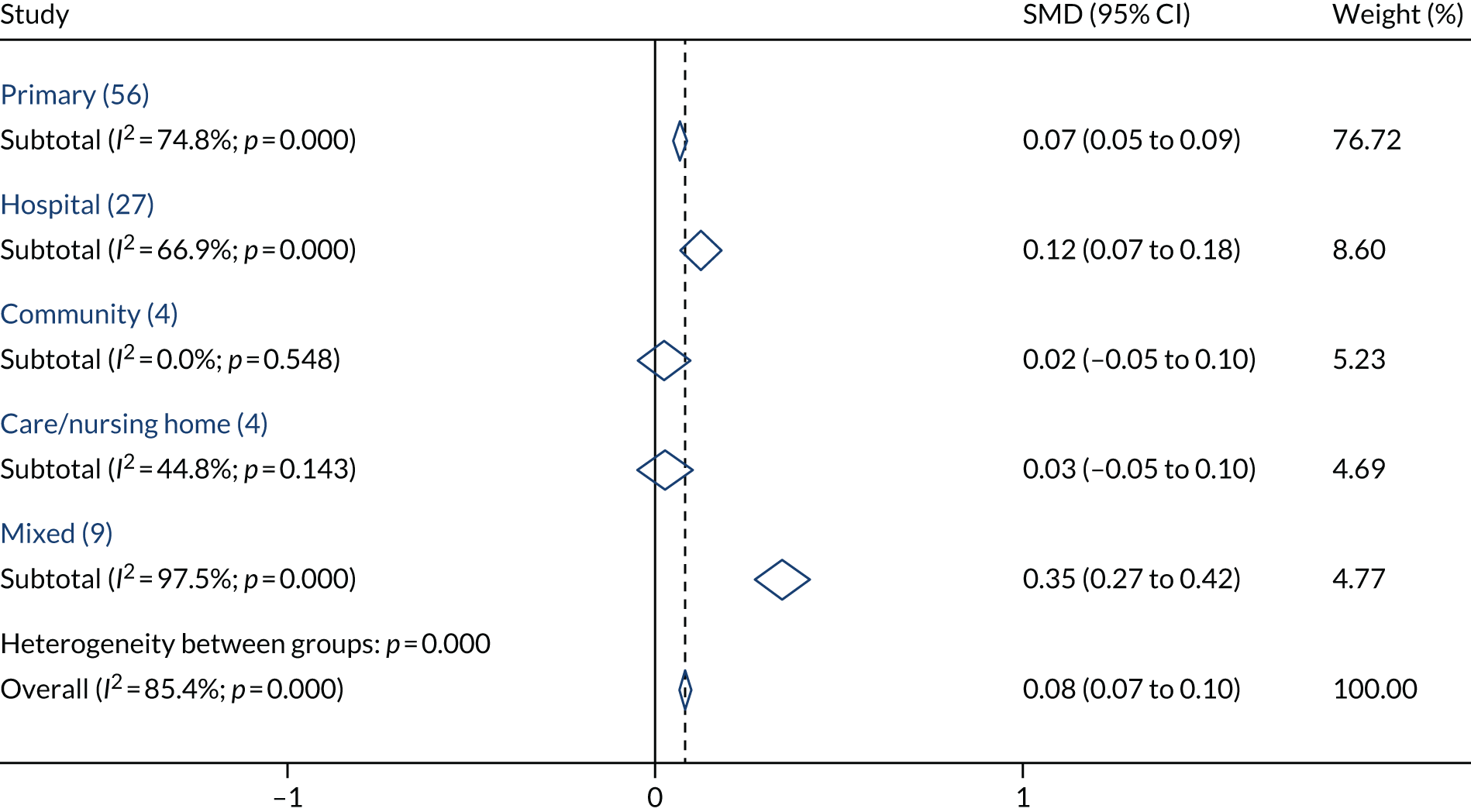
Reference group
The reference group is the person or persons that the target is compared with or receives approval from. Figure 9 shows the SMD summarised by the type of reference group within the trials. The effect of social norms interventions appeared to be reasonably consistent across different types of reference group, with most CIs overlapping, and there was general consistency of each group with the overall effect. Most trials (n = 84, 82.9%) had peers as the reference group (SMD 0.08, 95% CI 0.06 to 0.10). Only one trial had patients as the reference group; the effect was consistent with other studies (SMD 0.10, 95% CI –0.17 to 0.37) but the CI was wide because of the low weight in the review.
FIGURE 9.
Fixed-effects forest plot summarised by reference group.

Benchmarks
When social comparison interventions are delivered, they sometimes include a benchmark: this may be a peer-related benchmark, such as the top 10% or 20% of performers among their peer group, or it may be an external benchmark, such as a performance target set by a royal college. If no benchmark is set, the social comparison usually reports the average performance among peers. The downside of the average approach is that the above-average performers will receive feedback suggesting that they are already performing better than their peers, which may lead them to reduce their effort. 56 Figure 10 shows the SMD summarised by the type of benchmark that was used. Only trials involving social comparison have been included, because benchmarking is not relevant to the other social norms interventions. The effect of social norms interventions appeared to be reasonably consistent, regardless of whether a peer benchmark (13 studies: SMD 0.06, 95% CI 0.02 to.011) or the average performance (67 studies: SMD 0.11, 95% CI 0.09 to 0.13) was included: the CIs overlap and there is general consistency of each group with the overall effect.
FIGURE 10.
Fixed-effects forest plot summarised by benchmark.

Source of the intervention
Figure 11 shows the SMD summarised by the source of the intervention (i.e. the person delivering the intervention) in a fixed-effects meta-analysis. The effect of social norms interventions appeared to be consistent across the different sources, with the exception of supervisor/senior colleague (n = 2), which appeared to be, on average, less effective (SMD –0.28, 95% CI –0.56 to 0.01). In most trials, the source of the intervention was the investigator (n = 72) (SMD 0.08, 95% CI 0.06 to 0.10) or a respected source (n = 11) (SMD 0.09, 95% CI 0.03 to 0.16). The credible sources that were found in the literature included:
-
nurses in management positions who encouraged change in various behaviours to improve hospital stroke care63
-
a ‘highly respected senior clinician’ who persuaded doctors of the harms and limited diagnostic benefit of X-ray for lower back pain64
-
maternal–fetal medicine specialists, perinatologists or obstetricians who were influential with colleagues, who championed the use of corticosteroids to colleagues in antenatal care65
-
nurse facilitators with master’s degrees and specialist training who promoted changes in preventative care in general practices66
-
opinion leaders nominated by a peer for their expertise in obstetric care67 or breast cancer surgery68
-
a clinical co-ordinator regarded as a ‘credible role model’ in managing patients with congestive heart failure69
-
a letter to poorly performing GPs from the Chief Medical Officer about their rates of antibiotic prescribing. 60
The other categories occurred infrequently and we should interpret these results with caution owing to some wide CIs.
FIGURE 11.
Fixed-effects forest plot summarised by source of intervention.
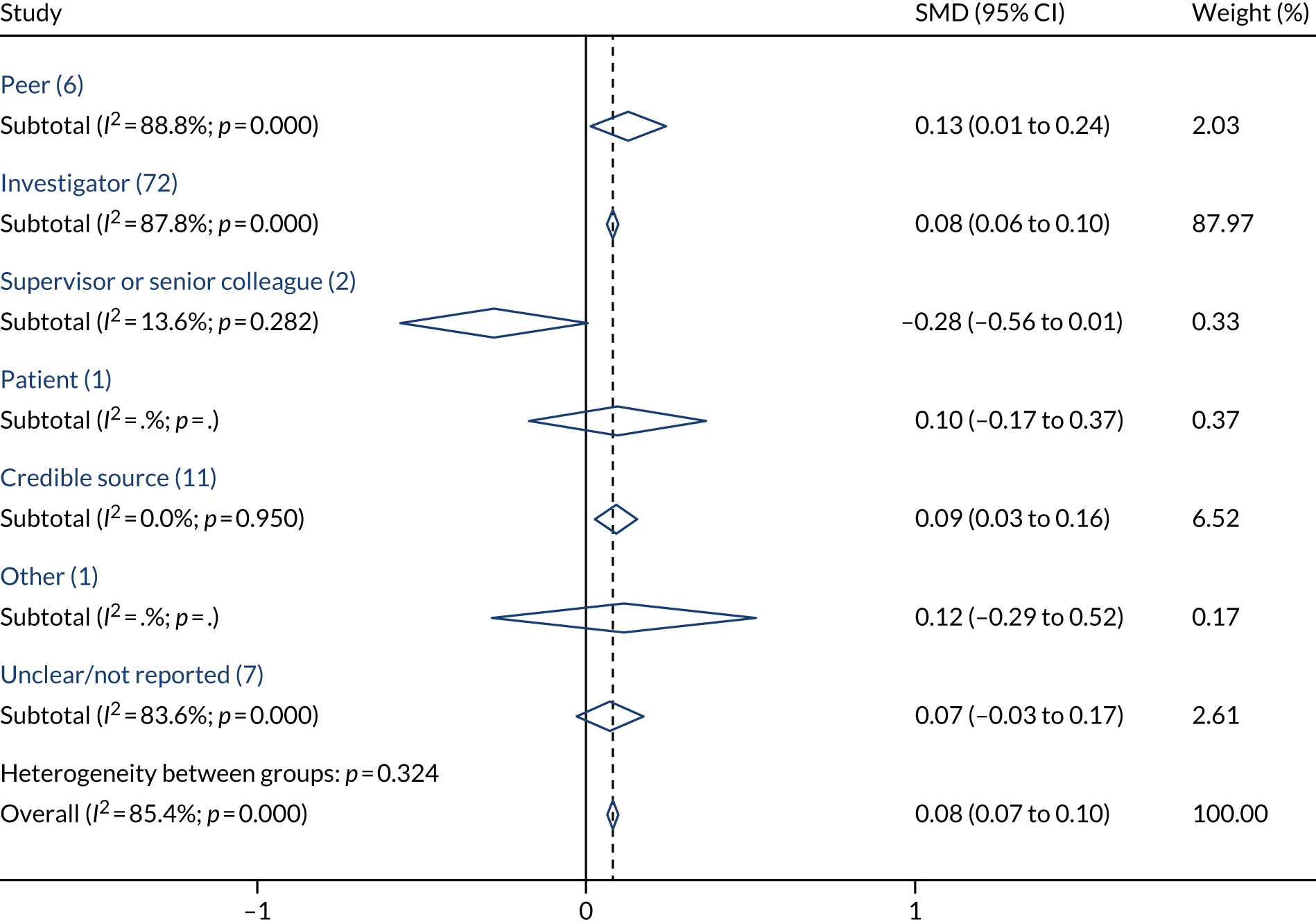
Direction of change targeted
Figure 12 shows the SMD summarised by the intended direction of change in the behaviour in a fixed-effects meta-analysis. The social norms intervention appeared to be, on average, slightly less effective when the intervention was aimed at increasing a behaviour (n = 70) (e.g. more hand-washing) (SMD 0.06, 95% CI 0.04 to 0.09) than when it was aimed at decreasing a behaviour (n = 28) (e.g. prescription of antibiotics) (SMD 0.10, 95% CI 0.08 to 0.12), but both CIs are consistent with the overall effect.
FIGURE 12.
Fixed-effects forest plot summarised by the direction of change targeted.
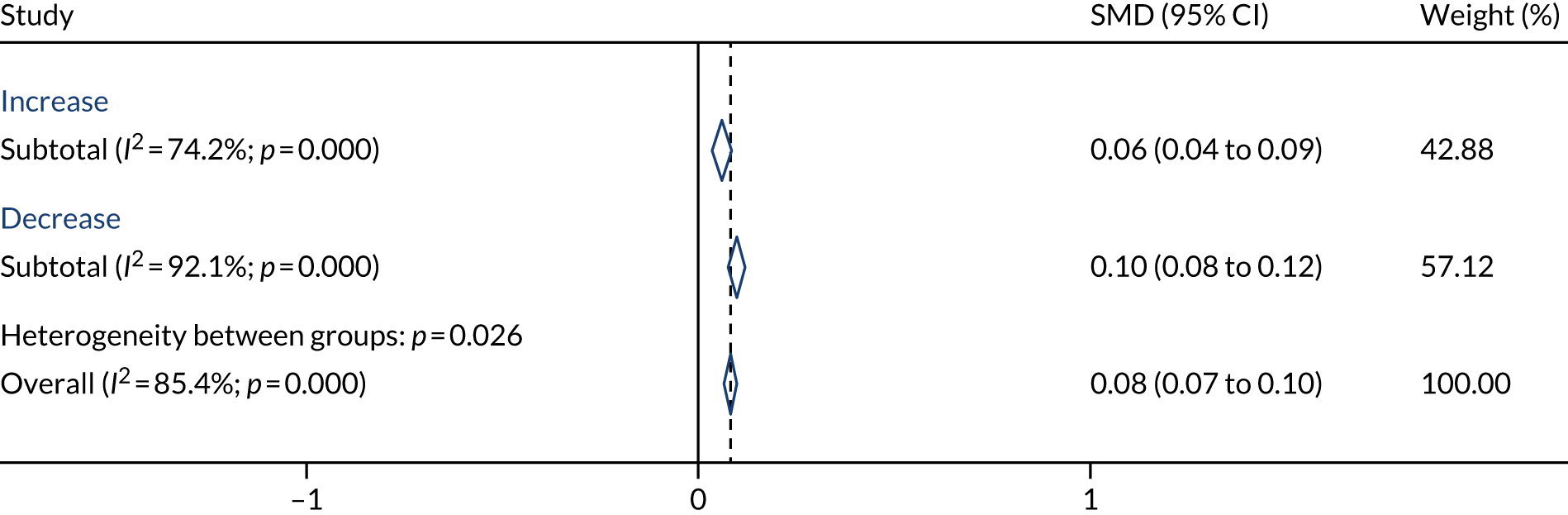
Frequency of the intervention
Figure 13 shows the SMD summarised by the frequency/intensity of the interventions in a fixed-effects meta-analysis. The effect of the social norms interventions appeared to be, on average, most effective when the intervention was delivered only once (n = 28) (SMD 0.25, 95% CI 0.21 to 0.30). It appeared to be less effective, on average, when delivered more frequently (n = 47) (SMD 0.06, 95% CI 0.04 to 0.08).
FIGURE 13.
Fixed-effects forest plot summarised by frequency of the intervention.

Format of the intervention
Figure 14 shows the SMD summarised by the format of the intervention. Trials delivered via computerised methods whereby the intervention was posted on a website or other computerised format that was not integrated into the health-care worker’s workflow (n = 8) appeared to be more effective than average (SMD 0.23, 95% CI 0.15 to 0.31). By contrast, interventions delivered face to face (n = 14) appeared to be ineffective, on average, with a SMD of –0.01 (95% CI –0.06 to 0.03). Trials with an e-mailed (n = 9), written (n = 25) or a mixed format (n = 14) appeared to be reasonably consistent with each other and with the overall effect.
FIGURE 14.
Fixed-effects forest plot summarised by format of intervention.
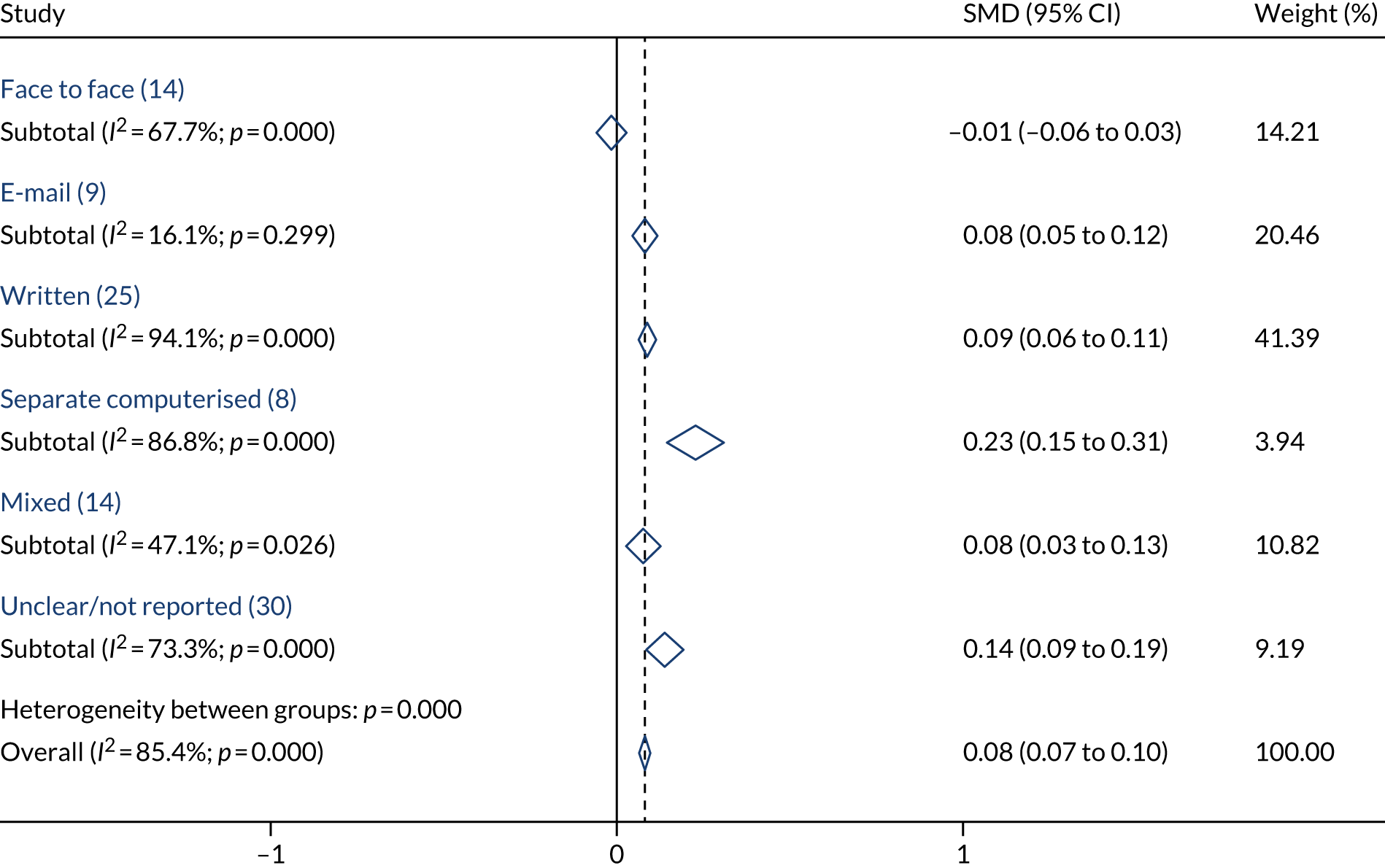
Person delivering the intervention
Figure 15 shows the SMD summarised by whether the person who delivered the intervention was internal or external to the target’s organisation in a fixed-effects meta-analysis. Most (n = 68) interventions were delivered by an external person, often the investigator. The effect of social norms interventions, on average, seemed to be consistent across internal sources (n = 17) (SMD 0.11, 95% CI 0.05 to 0.17) and external sources (n = 68) (SMD 0.08, 95% CI 0.06 to 0.10). However, this should be interpreted cautiously given the wide CIs for internal sources.
FIGURE 15.
Fixed-effects forest plot summarised by person delivering the intervention.

Studies with social norms behaviour change techniques in both arms
There were 17 comparisons in which both arms involved social norms interventions. These are summarised in Appendix 16, Figure 21. Most of these involved social comparison in both arms, with feedback on behaviour20,70–77 or without feedback18 (n = 10), and typically they were studies that tested some other combination of BCTs in the intervention arm, but had A&F offered as part of usual care in both arms. One study tested a combination of BCTs in the intervention arm, but had credible source in both arms as part of usual care. 78 None of these studies offered any interesting insights for the review because they were designed to test the effect of other interventions.
Only two studies had a different social norms BCT in each arm, which offered a head-to-head comparison. One study tested the effect of credible source, social comparison and feedback on behaviour and other BCTs against social comparison and feedback, with an estimated SMD of 1.30 (95% CI 0.50 to 2.10),79 suggesting that credible source with other BCTs has a high effect compared with social comparison and feedback. Another study found no evidence of a difference between social comparison, credible source and feedback, and credible source alone, with an estimated SMD of 0.29 (95% CI –0.39 to 0.98). 80
There were four studies that examined the effect of different variants of social comparison (n = 3) or credible source (n = 1). Wright et al. 81 offered formal educational sessions led by a highly regarded surgeon (credible source) to both arms of the trial, and offered one-to-one ‘academic detailing’ by the highly regarded surgeon to a local opinion leader. The addition of academic detailing was effective compared with the educational sessions alone (SMD 0.32, 95% CI 0.08 to 0.56). Kiefe et al. 82 found that providing social comparison where the average performance for the top 10% of the physicians was reported was more effective than social comparison reporting the mean performance of other physicians (SMD 0.25, 95%CI 0.13 to 1.37). Schneider et al. 83 similarly tested benchmarked social comparison (best 10% of GPs) with the median performance, and found no evidence of an effect (SMD 0.03, 95% CI –0.05 to 0.56). There was no evidence of a difference in outcome when a similar social comparison intervention was provided to each arm, where the intervention arm was given the information in a work book and the control arm received a graphical computer slide show (SMD –0.04, 95% CI –0.52 to 0.44). 84
Investigation of behaviour change techniques, settings and contexts, using metaregression
Metaregression: social norms behaviour change techniques and other behaviour change techniques (with feedback on behaviour behaviour change techniques)
For metaregression, we used all of the 100 comparisons that tested the effect of social norms BCTs with two additional comparisons79,80 that had different social norms BCTs in each arm. Metaregression allows us to examine the effect of all social norms BCTs plus other common BCTs simultaneously in the same analysis, by using binary covariates for the presence/absence of each BCT in the intervention being tested. When all of the social norms BCTs and other commonly used BCTs are included together in a metaregression (Table 8), only credible source stands out as being clearly effective, which suggests that using credible source in an intervention improves compliance with the desired behaviour by an average SMD of 0.29 (95% CI 0.08 to 0.50). Note that there is a large amount of heterogeneity, and that after taking into account the effect of BCTs the residual variation owing to heterogeneity is 85.4%.
| Covariate (BCT code) | Effect, SMD (95% CI) | p-value |
|---|---|---|
| Social norm BCTs | ||
| Social comparison (6.2) | 0.01 (–0.25 to 0.26) | 0.96 |
| Credible source (9.1) | 0.29 (0.08 to 0.51) | 0.01 |
| Social reward (10.4) | 0.06 (–0.38 to 0.51) | 0.77 |
| Information about others’ approval (6.3) | –0.07 (–0.65 to 0.50) | 0.80 |
| Social incentive (10.5) | –0.27 (–1.28 to 0.73) | 0.59 |
| Other BCTs | ||
| Feedback on behaviour (2.2) | 0.14 (–0.15 to 0.42) | 0.35 |
| Information about health consequences (5.1) | –0.10 (–0.35 to 0.15) | 0.42 |
| Prompts/cues (7.1) | 0.05 (–0.17 to 0.27) | 0.67 |
| Social support (unspecified) (3.1) | 0.07 (–0.14 to 0.28) | 0.52 |
| Instruction on how to perform the behaviour (4.1) | –0.05 (–0.27 to 0.17) | 0.65 |
Metaregression: social norms and other behaviour change techniques (without feedback on behaviour behaviour change techniques)
Social comparison and feedback on behaviour commonly appear together in the same intervention; therefore, including both of these in the same metaregression would probably cause multicollinearity problems. Repeating the regression reported in Table 8 but excluding feedback on behaviour gives similar results (Table 9), but suggests that social comparison may also have an effect, improving compliance with desired behaviour by an average SMD of 0.12 (95% CI 0.00 to 0.23). The effect of credible source remains fairly consistent (SMD 0.31, 95% CI 0.10 to 0.52). This result is similar to that seen in the forest plots. There is no evidence from this metaregression to suggest that adding other BCTs alongside social comparison or credible source offers any additional improvement once the effect of the social norms BCTs has been taken into account; however, these BCTs were seen only in a small number of trials and the heterogeneity is substantial (residual I2 = 85%; τ2= 0.10), so we must interpret this observation cautiously.
| Covariate (BCT code) | Effect, SMD (95% CI) | p-value |
|---|---|---|
| Social norm BCTs | ||
| Social comparison (6.2) | 0.12 (0.00 to 0.23) | 0.06 |
| Credible source (9.1) | 0.31 (0.10 to 0.52) | 0.01 |
| Social reward (10.4) | 0.15 (–0.26 to 0.55) | 0.48 |
| Information about others’ approval (6.3) | –0.17 (–0.71 to 0.37) | 0.54 |
| Social incentive (10.5) | –0.06 (–0.95 to 0.83) | 0.90 |
| Other BCTs | ||
| Information about health consequences (5.1) | –0.10 (–0.35 to 0.15) | 0.43 |
| Prompts/cues (7.1) | 0.07 (–0.14 to 0.28) | 0.50 |
| Social support (unspecified) (3.1) | 0.10 (–0.10 to 0.30) | 0.34 |
| Instruction on how to perform the behaviour (4.1) | –0.05 (–0.27 to 0.18) | 0.69 |
Metaregression: contexts and settings
When including the chosen regression coefficients for factors connected to context and settings, either independently or simultaneously with a constant term, there is no clear evidence that any of these factors are related to treatment effect (Table 10). Very little variability has been explained by the inclusion of these covariates (residual I2 = 85.6%; τ2 = 0.11). The metaregression conducted was a random-effects metaregression, whereas earlier exploratory forest plots were fixed effect; fixed-effect metaregression is not recommended as a valid method85 because it assumes that all heterogeneity can be explained by the regression covariates, and it leads to a high risk of type 1 errors. The difference between random-effect and fixed-effect analyses explains, in part, why subgroups that appeared quite separate on forest plots do not lead to statistically significant covariates in the metaregression. Metaregression is also subject to low power and overfitting, and although we have 102 comparisons included, this may not be sufficient to lead to stable covariate estimates.
| Setting/context | Single variable regression, SMD (95% CI) | Multivariable regression, SMD (95% CI) |
|---|---|---|
| Health-care worker | ||
| Doctor vs. other | –0.02 (–0.21 to 0.16) | –0.04 (–0.24 to 0.16) |
| Behaviour | ||
| Prescribing vs. tests | 0.10 (–0.12 to 0.33) | 0.12 (–0.12 to 0.36) |
| Management/communication vs. tests | 0.08 (–0.18 to 0.34) | 0.08 (–0.21 to 0.38) |
| Other vs. tests | –0.10 (–0.36 to 0.17) | –0.11 (–0.42 to 0.20) |
| Setting | ||
| Secondary care vs. primary care | 0.03 (–0.17 to 0.23) | 0.02 (–0.20 to 0.25) |
| Other vs. primary care | –0.01 (–0.24 to 0.22) | –0.05 (–0.30 to 0.20) |
| Direction of change required | ||
| Increase vs. decrease | –0.01 (–0.19 to 0.18) | 0.00 (–0.23 to 0.23) |
| Format | ||
| Face to face vs. written | 0.04 (–0.23 to 0.32) | 0.07 (–0.24 to 0.37) |
| Computer (including e-mails) vs. written | 0.07 (–0.19 to 0.33) | 0.07 (–0.21 to 0.34) |
| Mixed/unclear vs. written | 0.09 (–0.12 to 0.30) | 0.10 (–0.13 to 0.34) |
Investigation of behaviour change techniques, settings and contexts, using network meta-analysis
Network meta-analysis is a suitable method to rank the social norm BCTs from most effective to least effective. For the network meta-analysis, we used all of the 100 comparisons that tested the effect of social norm BCTs with two additional comparisons79,80 that had different social norm BCTs in each arm. Some regrouping was carried out to the social norm categories to reduce the number of categories and avoid small groups: all comparisons testing social reward with or without other BCTs were combined, all comparisons testing credible source with or without other BCTs were combined and all comparisons testing social comparison and credible source with or without other BCTs were combined. The number of comparisons available for each of the social norm BCTs is shown in Table 11, and the diagram of how they are networked in shown in Figure 16.
| Intervention group | Type of control group | Total | |
|---|---|---|---|
| 0. Control | 1. Social comparison | ||
| 1. Social comparison | 33 | N/A | 33 |
| 2. Credible source | 7 | 0 | 7 |
| 3. Social reward | 2 | 0 | 2 |
| 4. Social comparison and credible source | 8 | 2 | 10 |
| 5. Social comparison and social reward | 2 | 0 | 2 |
| 6. Social comparison and social support (unspecified) | 7 | 0 | 7 |
| 7. Social comparison and prompts/cues | 5 | 0 | 5 |
| 8. Social comparison and information about health consequences | 4 | 0 | 4 |
| 9. Social comparison and instruction on how to perform the behaviour and prompts/cues | 5 | 0 | 5 |
| 10. Social comparison and other BCTs | 23 | 0 | 23 |
| 11. Other multiple social norm BCTs | 4 | 0 | 4 |
| Total | 100 | 2 | 102 |
FIGURE 16.
Network diagram to showing the available comparisons. 0, any control; 1, social comparison; 2 credible source; 3, social reward; 4, social comparison and credible source; 5, social comparison and social reward; 6, social comparison and social support (unspecified); 7, social comparison and prompts/cues; 8, social comparison and information about health consequences; 9, social comparison and instruction on how to perform the behaviour and prompts/cues; 10, social comparison and other BCTs; 11, other multiple social norm BCTs.
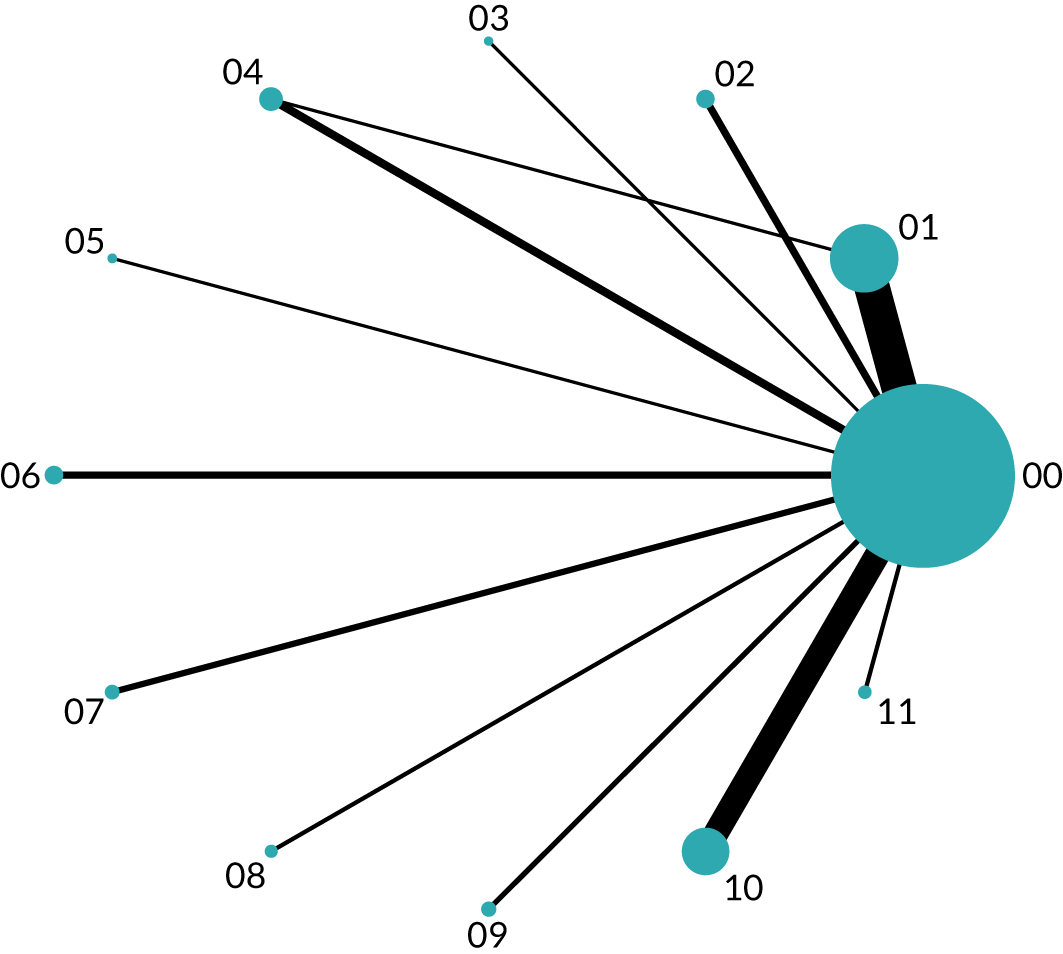
Network meta-analysis gives similar effect sizes and CIs to those seen in the meta-analysis (see Figure 3), but also allows us to rank the social norms interventions from best to worst (Table 12). The evidence from 102 tests of social norm BCTs suggests that the most effective interventions contain social comparison and social reward (SMD 0.39, 95% CI 0.15 to 0.64), social comparison and prompts/cues (SMD 0.33, 95% CI 0.22 to 0.44) or credible source (SMD 0.30, 95% CI 0.13 to 0.47). Social comparison on its own (SMD 0.05, 95% CI 0.03 to 0.08) or combined with social support (unspecified) (SMD 0.10, 95% CI 0.04 to 0.16) or other BCTs (SMD 0.04, 95% CI 0.00 to 0.08) all appear to be more effective than control, on average, in improving compliance with the desired behaviour; however, they were associated with a very modest effect size. The use of credible source and social comparison together (SMD 0.16, 95% CI 0.12 to 0.20), and other combinations of two or more social norm BCTs together (SMD 0.07 95% CI 0.03 to 0.12), similarly have a modest effect on behavioural outcomes. There is no evidence to suggest that social reward (SMD 0.03, 95% CI –0.08 to 0.13), social comparison, instruction on how to perform the behaviour and prompts/cues (SMD 0.01, 95% CI –0.10 to 0.11), or social comparison and information about health consequences (SMD –0.14, 95% CI –0.33 to 0.05) offer benefit above control; however, in all cases the CIs were wide and we cannot rule out a modest effect.
| Effect | Effect, SMD (95% CI) | Probability of being the best intervention (%) |
|---|---|---|
| Social comparison and social reward vs. control | 0.39 (0.15 to 0.64) | 59.2 |
| Social comparison and prompts/cues vs. control | 0.33 (0.22 to 0.44) | 22.2 |
| Credible source vs. control | 0.30 (0.13 to 0.47) | 18.6 |
| Social comparison and credible source vs. control | 0.16 (0.12 to 0.20) | 0.0 |
| Social comparison and social support (unspecified) vs. control | 0.10 (0.04 to 0.16) | 0.0 |
| Other multiple social norm BCTs vs. control | 0.07 (0.03 to 0.12) | 0.0 |
| Social comparison vs. control | 0.05 (0.03 to 0.08) | 0.0 |
| Social comparison and other BCTs vs. control | 0.04 (0.00 to 0.08) | 0.0 |
| Social reward vs. control | 0.03 (–0.08 to 0.13) | 0.0 |
| Social comparison, instructiona and prompts/cues vs. control | 0.01 (–0.10 to 0.11) | 0.0 |
| Social comparison and information on health consequences vs. control | –0.14 (–0.33 to 0.05) | 0.0 |
Sensitivity analyses
Tables 13 and 14 show that our main conclusion is robust: there is little change in our average SMD when we impute alternative values for the ICC when required, exclude trials in which the standard deviation was imputed, remove trials reporting mean per cent compliance in which the mean compliance was close to 0% or 100%, or include trials at only low risk of bias on each domain. Note that we decided before analysis not do a sensitivity analysis on ‘risk of bias due to blinding’, as we believe blinding to be difficult/impossible in social norm interventions and, as expected, it was rarely seen; however, we must bear in mind that our review is at risk of bias owing to this lack of blinding.
| Analysis | Effect, SMD (95% CI) | Number of comparisons |
|---|---|---|
| Full data set | 0.08 (0.07 to 0.10) | 100 |
| Using imputed ICC = 0.2 instead of 0.1 | 0.08 (0.06 to 0.10) | 100 |
| Using imputed ICC = 0.05 instead of 0.1 | 0.09 (0.07 to 0.10) | 100 |
| Removing trials with imputed SDs | 0.09 (0.07 to 0.10) | 94 |
| Removing trials reporting mean per cent compliance close to 0% or 100%a | 0.07 (0.05 to 0.08) | 77 |
| Keeping only trials at low risk of bias owing to allocation concealment | 0.11 (0.09 to 0.13) | 72 |
| Keeping only trials at low risk of bias owing to sequence generation | 0.08 (0.06 to 0.10) | 74 |
| Keeping only trials at low risk of bias owing to selective outcome reporting | 0.09 (0.07 to 0.11) | 41 |
| Keeping only trials at low risk of bias owing to attrition | 0.10 (0.08 to 0.12) | 57 |
| Keeping only trials at low risk of bias owing to other biases | 0.09 (0.07 to 0.11) | 59 |
| Removing trials in which ‘feedback on desired behaviour’ was not part of the tested intervention | 0.08 (0.07 to 0.10) | 88 |
| Analysis | Effect, SMD (95% CI) | Number of comparisons |
|---|---|---|
| Full data set | 0.16 (0.11 to 0.22) | 100 |
| Using imputed ICC = 0.2 instead of 0.1 | 0.16 (0.10 to 0.21) | 100 |
| Using imputed ICC = 0.05 instead of 0.1 | 0.16 (0.11 to 0.21) | 100 |
| Removing trials with imputed SDs | 0.18 (0.12 to 0.23) | 94 |
| Removing trials reporting mean per cent compliance close to 0% or 100%a | 0.12 (0.07 to 0.16) | 77 |
| Keeping only trials at low risk of bias owing to allocation concealment | 0.18 (0.12 to 0.25) | 72 |
| Keeping only trials at low risk of bias owing to sequence generation | 0.17 (0.10 to 0.23) | 74 |
| Keeping only trials at low risk of bias owing to selective outcome reporting | 0.22 (0.13 to 0.31) | 41 |
| Keeping only trials at low risk of bias owing to attrition | 0.18 (0.13 to 0.24) | 57 |
| Keeping only trials at low risk of bias owing to other biases | 0.13 (0.09 to 0.18) | 59 |
| Removing trials in which ‘feedback on desired behaviour’ was not part of the tested intervention | 0.17 (0.12 to 0.23) | 88 |
In an additional unplanned sensitivity analysis, we excluded comparisons that did not include feedback on behaviour alongside the social norm BCT being tested. Conclusions would be similar whether or not comparisons that included feedback on behaviour were included.
Publication bias
There is some evidence of funnel plot asymmetry, with several SMDs lying on the right-hand side outside the predicted funnels (Figure 17). This means that the review may be missing some unpublished negative trials, or may include more positive trials than justified owing to selective outcome reporting. We should review the results cautiously in the light of the risk of outcome reporting bias, especially when we look at the magnitude of the extreme positive trials in relation to the overall treatment effect.
FIGURE 17.
Funnel plot: the intervention effect estimates from individual studies against the standard error.
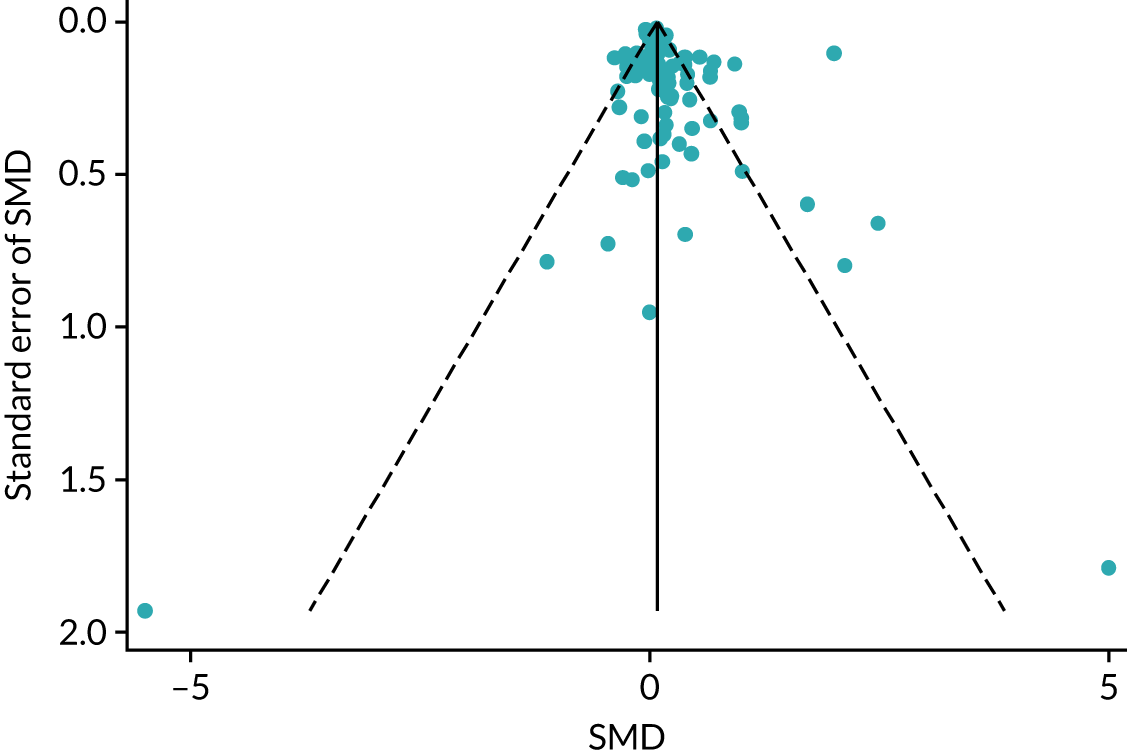
Effects of interventions: patient health outcomes (secondary)
Figure 18 shows the SMD among patient outcomes (14 comparisons), grouped by type of BCT comparison, in a fixed-effects meta-analysis. Only a subset of comparison types is represented compared with the results for primary (health worker behaviour) outcomes, given that not all studies reported a patient outcome. As for health worker behaviour outcomes, heterogeneity is high with an overall I2 = 91.5%. Combined data from these 14 comparisons suggest that interventions with a social norm component were associated with an improvement in patient outcomes of 0.17 SMD (95% CI 0.14 to 0.20), on average. However, this is strongly influenced by those studies testing social comparison, in particular Bentz et al. 87 (weight 46%) with an estimated SMD of 0.36 (95% CI 0.32 to 0.40) and Beck et al. 86 (weight 31%) with an estimated SMD of 0.00 (95% CI –0.05 to 0.05). Estimates consistent with a null effect were found for all studies testing social comparison combined with social support (unspecified), prompts/cues, instruction on the behaviour plus prompts/cues or other BCTs. A larger positive effect of 0.86 SMD (95% CI 0.29 to 1.44) is found for the test of a credible source intervention, but this is from one small study (weight 0.3%). 67 These results for patient outcomes should be interpreted cautiously owing to a large amount of heterogeneity among studies, and to the small number of studies in some groups.
FIGURE 18.
Patient outcomes: fixed effects summarised by type of comparison (15 comparisons). CS, credible source; SC, social comparison; SR, social reward.
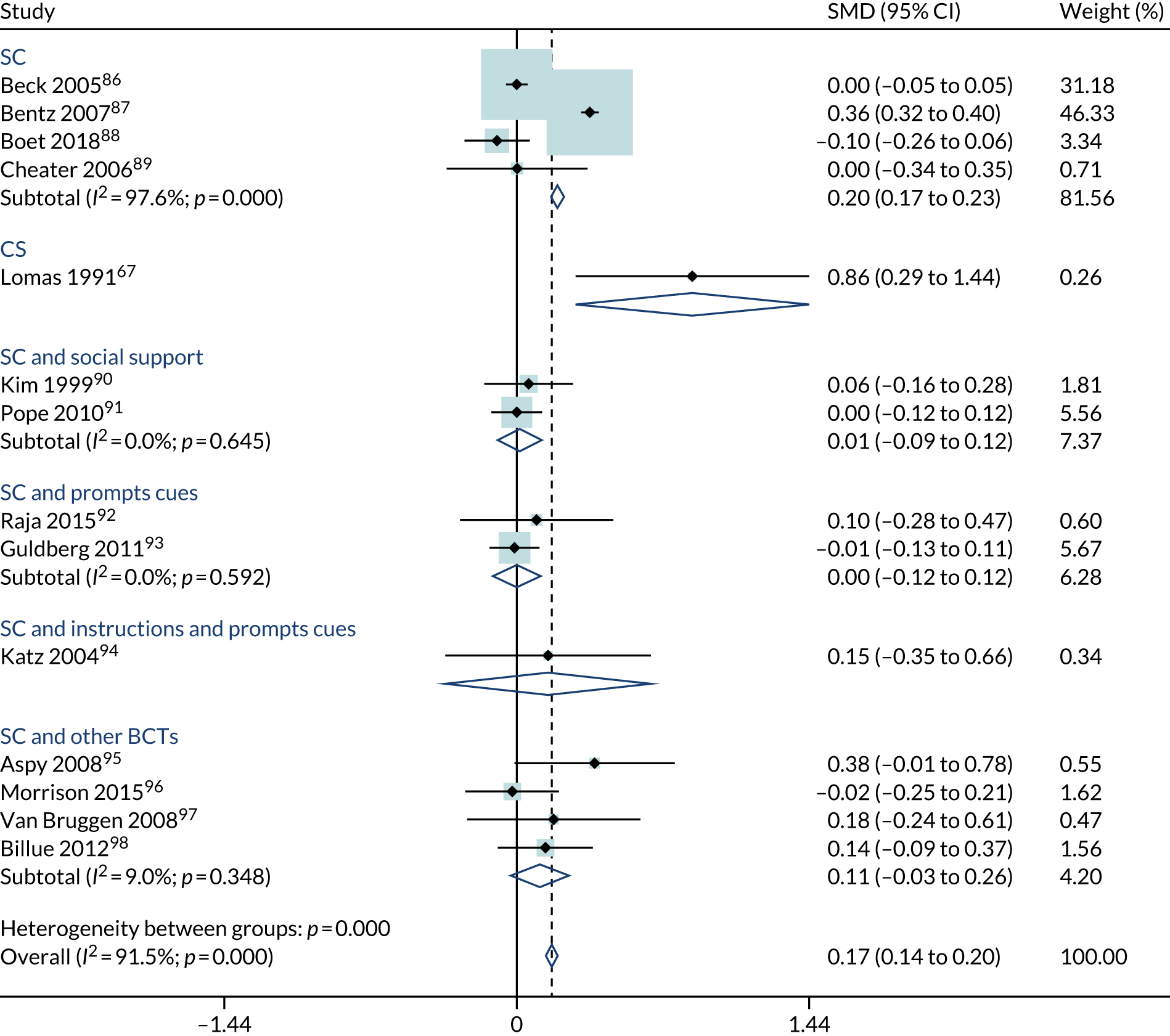
Both the patient outcomes and the target behaviours varied across the studies. To illustrate the findings, we offer some examples of studies included in the review. Ivers et al. 18 targeted GP behaviour in arranging testing and prescribing for people with diabetes, and the patient outcome was mean systolic blood pressure. Aspy et al. 95 targeted primary care physicians, encouraging them to offer a mammogram to appropriate women patients, and the patient outcome was the proportion of eligible patients who had a mammogram. Lomas et al. 67 targeted secondary care doctors, encouraging them to reduce the offer of caesareans to women who had previously had caesareans, and the patient outcome was the proportion of vaginal births. Billue et al. 98 targeted GP behaviour in intensifying medication for a range of health conditions, and the patient outcome was the proportion of patients with controlled diabetes. In studies in which there was more than one health outcome, we chose the study’s primary outcome, and if that was not clear, we chose the first outcome that was reported.
Figure 19 shows the SMD among patient outcomes (14 comparisons), grouped by type of BCT comparison, using a random-effects meta-analysis. As for the fixed-effects analysis, only a subset of comparison types is represented compared with the results for primary outcomes, given that not all studies reported a patient outcome.
FIGURE 19.
Patient outcomes: random effects grouped by type of comparison (14 comparisons). CS, credible source; SC, social comparison; instructions, instruction on how to perform the behaviour; social support, social support (unspecified).

The overall estimate of effect is less precise and slightly attenuated compared with the corresponding fixed-effects analysis, with an overall estimated SMD of 0.11 (95% CI –0.02 to 0.24). The results for 12 out of the 14 comparisons are consistent with no effect, exceptions were Lomas et al. ’s67 (weight 3.5%) test of a credible source intervention, with an estimated SMD of 0.86 (95% CI 0.29 to 1.44) and Bentz et al. ’s87 (weight 10%) test of a pure social comparison intervention, with an estimated SMD of 0.36 (95% CI 0.32 to 0.40). However, the overall estimated group SMD for pure social comparison interventions is 0.08 (95% CI –0.18 to 0.34), consistent with no effect. As for the corresponding fixed-effects analysis, the results should be interpreted cautiously owing to a high amount of heterogeneity and relatively few comparisons in each group.
Chapter 4 Discussion
Summary of findings
Social norms interventions can be an effective approach to changing the clinical behaviour of health workers. Interventions that include a social norms component were associated with an improvement in health worker behaviour outcomes of 0.08 SMD (95% CI 0.07 to 0.10) (n = 100 comparison). To illustrate the size of this effect, if, among GPs, the baseline rate of conducting annual reviews and blood tests for people with diabetes was 40%, a SMD of 0.08 would be equivalent to a 4% increase, from 40% to 44%, in the conduct of the annual reviews. Social norms interventions were associated with an improvement in patient outcomes of 0.17 SMD (95% CI 0.14 to 0.20) (n = 14 comparisons), on average. There was a large amount of heterogeneity, with some studies reporting substantially higher or lower effects for social norm interventions. This heterogeneity was investigated by examining the effect of variation in BCT, context and mode of delivery, by using forest plots, metaregression and network meta-analysis.
Social norm behaviour change techniques
There were three types of social norms intervention that were the most effective, on average, in changing health worker behaviour: social comparison together with social reward (SMD 0.39, 95% CI 0.15 to 0.64), social comparison together with prompts/cues (SMD 0.33, 95% CI 0.22 to 0.44), and credible source, either alone or in combination with other BCTs (SMD 0.30, 95%CI 0.13 to 0.47).
Other interventions had a more modest effect, but still appeared to be better than control: social comparison when delivered on its own (SMD 0.05, 95% CI 0.03 to 0.08), with social support (unspecified) (SMD 0.10, 95% CI 0.04 to 0.16) or with other BCTs (SMD 0.04, 95% CI 0.00 to 0.08). Combining credible source with social comparison (SMD 0.16, 95% CI 0.12 to 0.20), and other combinations of two or more social norm BCTs (SMD 0.07 95% CI 0.03 to 0.12) also had a modest average effect.
Interventions involving social reward or information about others’ approval appeared to be ineffective, but this is based on a very small numbers of trials. There was only one trial of social incentive, which showed no evidence of an effect.
These findings were consistent across forest plots, regression and network meta-analysis.
Concomitant behaviour change techniques
We examined whether or not the addition of other BCTs with the social norm BCTs was associated with any improvement in effect. The most frequently occurring BCT was feedback on behaviour (found in 88/100 comparisons); more often than not, health workers were provided with feedback on their own behaviour at the same time as they received interventions telling them about the behaviour of others or the approval of others. It was not possible in this study for us to completely untangle the effect of social comparison and feedback, but the sensitivity analysis suggests that the effect is similar whether or not feedback on behaviour is delivered alongside social comparison.
Interventions that tested social comparison with the addition of social reward (n = 2) or prompts/cues (n = 5) were more effective than social comparison alone, but when social comparison was delivered alongside prompts/cues plus information about health consequences (n = 4) or instructions on how to perform the behaviour and prompts/cues (n = 5) the intervention was ineffective. It may be that prompts and cues enhance social comparison when the behaviour is well understood by the recipient, but the prompts were ineffective when there was a need for instructions or education. Social comparison with social support (unspecified) (n = 7) was effective in changing health worker behaviour and had a similar size of effect to social comparison alone. However, these additional BCTs occurred in a relatively small number of trials, too small to show any additive effect in the metaregression.
Contexts
We explored the contexts in which social norms interventions were delivered. We found that social norms interventions were effective with different types of health workers. However, they may be less effective with nurses and AHPs than with doctors, although the number of studies with nurses and AHPs was low. Social norms interventions have been successful in targeting a wide range of clinical behaviours, including prescribing, tests, and management and communication around health conditions, but may be ineffective with hand-washing and referrals. They were equally effective in primary and secondary care, but may be less effective in community and care home settings, although the number of studies in those settings was low. The effect of social norms interventions appears to be reasonably consistent across different types of reference group (peers, senior persons, patients and mixed populations). Social norms interventions appear to be, on average, slightly more effective at reducing behaviours (e.g. reducing antibiotic prescriptions) than increasing them (e.g. increasing hand-washing).
Modes of delivery
Interventions appear equally effective regardless of who delivers them; there is some indication that interventions delivered by supervisors were less effective, but the number of such studies was small. The effect is similar regardless of whether the intervention comes from an internal or external source, although the number of interventions from internal sources was low. Delivering the intervention once is sufficient: there was no evidence of an increased effect from more frequent delivery. All methods of delivery of social norms interventions were effective apart from face to face; delivery by website appeared to be the most effective method.
In summary, the review provides robust evidence that social norms interventions were effective in changing the clinical behaviour of health workers: credible source, social comparison and social reward were all found to be more effective than control. Credible source was found to be very effective. Social comparison is very effective when combined with social reward or prompts/cues, but there is still an effect when social comparison is delivered on its own or with social support (unspecified), credible source or other BCTs. Social norms interventions have been implemented in a variety of contexts and we did not find strong evidence that the effectiveness varies by context. In terms of modes of delivery, delivering the intervention once was sufficient and sending the intervention by website or other computerised format was the most effective.
Quality of the evidence
Across some domains (e.g. random sequence generation, allocation concealment and blinding of outcome assessment), the majority of trials (> 70%) were judged to be at low risk of bias. The risk of bias was high for the blinding of participants and personnel, with 80% high risk, owing to the nature of the interventions used and preponderance of cluster trials in the review. When we looked at only the trials at low risk of bias for each key domain in a sensitivity analyses, our overall treatment effect changed very little, suggesting that the results were robust and not strongly influenced by the trials at high/unclear risk of bias; we cannot rule out the possibility of response bias owing to lack of blinding.
Strengths and limitations
The review was carefully designed and executed to minimise bias. The selection of studies, data extraction and BCT coding were all undertaken by two independent coders, and any discrepancies were resolved by discussion or involvement of a third coder: this reduces the risk of errors or inconsistencies in the review. All coders received appropriate training. A strength of the review is that the review team thought long and hard about the choice of data to extract: we wanted to avoid the danger of extracting so much data that we would risk spurious findings. We concentrated on those features that were considered relevant in earlier reviews, and those that seemed to have particular relevance to the topic. 16,17,25 Despite this, it is possible that we failed to extract some important design features. Another strength is that we did not exclude any studies on the basis of their choice of outcomes, and we converted any available outcome into a SMD: this meant that we were able to use all of the available evidence and summarise it all together in one analysis.
Trials were excluded from the review where the intervention did not target a specific behaviour, for example we would exclude a trial if the intervention was aimed at a health worker with the intention of reducing patient blood pressure, but did not make explicit to the health worker what behaviour(s) were expected of them to achieve the reduction. These exclusions occur because the focus of this review is the behaviour change of health workers. If a behaviour is not specified, it is not possible to determine whether or not an intervention actually targeted that behaviour, and change in that behaviour (our primary outcome) cannot be assessed. This approach is consistent with that of the BCT taxonomy v1;24 to identify an intervention component as a BCT using the BCT taxonomy, a crucial requirement is that the intervention component in question targets the behaviour that the intervention aims to address. There is a potential risk that we have excluded some studies that may have added to the review where there was a target behaviour and an intervention that did target that behaviour, but we were unable to determine this because of poor reporting. In the future we plan to undertake a separate review of those studies that did not include a target behaviour.
The large number of studies retrieved prevented us from requesting additional information from authors. There were 10 studies without suitable outcome measures that we could not include in the meta-analysis. The size of the review makes it unlikely that the missing 10 studies would have had an effect on the review outcome, particularly as many of them were small studies. There were studies for which we imputed missing information relating to the outcomes, such as ICCs and standard deviations. Sensitivity analyses suggest that the missing information has not had a significant impact on the review.
The primary approach to meta-analysis was based on a fixed-effects approach. 99 The fixed-effects analysis summarises the evidence in these trials, rather than estimating a common underlying treatment effect. 100 We are aware that this topic is highly contested, and we have also presented random effects for the most important analyses, as planned. In every one of our analyses, both the fixed-effects and the random-effects approaches produced a result in the same direction, with the fixed-effects approach resulting in a lower effect for the intervention (SMD 0.08 vs. 0.16): this is because of the random-effects approach giving greater weight to smaller studies. We believe that we would have come to similar conclusions, regardless, whether we had chosen fixed effects or random effects as our primary analysis.
In this review, we combined different types of outcomes in the same analysis in an attempt to provide an overall summary of all of the available evidence on social norms interventions in a single review. The trials used came from a variety of different contexts and settings, and utilised different trial designs and units of analysis. This has led to a very heterogeneous review, and we acknowledge the limitations of this approach. The magnitude of effects for the most promising behaviour change interventions were approximately 0.3 SMDs, which, relative to the between-study variability (τ2 = 0.2), does seem to indicate an important effect.
All of the meta-analysis was undertaken on the basis of comparisons: we subtracted the BCTs in the control arm from those in the intervention arm to obtain a list of BCTs that were actively tested in each study. The active ingredient that we were testing was what was left of the intervention when the control arm was taken away. We consider this the most suitable approach to examine the effect of the various social norm BCTs; however, a limitation of this approach is that we may have missed some interaction effects. A few of the studies were complex in the sense that both arms contained multiple BCTs. In these cases, we simplified them to the core comparison of interest for the review. One example is a study by Boet et al. 88 that tested social comparison (with feedback on outcome of the behaviour and instruction on how to perform the behaviour) against a control group that received the same components (feedback on outcome of the behaviour and instruction on how to perform the behaviour) but without social comparison. This was coded as social comparison versus control. Another example is a study by Bentz et al. 94 that tested social comparison [with social support (unspecified), feedback on behaviour, instruction on how to perform the behaviour and prompts/cues] against a control group that received all the same techniques, but without the social comparison and feedback on behaviour. This was coded as social comparison vs. control. These complex interventions and controls represent a minority of the trials: most studies were much simpler. An issue with overly complex interventions and controls is that it makes it very difficult to isolate which ingredients, among many, are contributing to the overall effect.
We used the BCT taxonomy v124 to code all of the BCTs that were included within the intervention or control arms of the trials. The BCT taxonomy is based on a significant body of research, but it is unlikely to be fully comprehensive; the authors acknowledge and anticipate that extension or modification could be appropriate in the future. It is, therefore, possible that on occasion BCTs that do not yet feature in the BCT taxonomy could have been presented alongside social norm BCTs and were missed during the BCT coding exercise.
The asymmetry of the funnel plot suggests that the review may have missed some unpublished negative trials. Unpublished studies were eligible for the review, but our search strategy was not successful in finding them. We did not have the resources to contact authors of included studies to ask them if they knew of other relevant but unpublished material. It is possible that there are unpublished documents that we did not include. We only considered studies written in English, which may have also excluded some relevant studies from the review. We selected a single behaviour outcome from every trial using published trial reports; it is possible that this put the review at risk of selective outcome reporting, although we tried to minimise this by using a prespecified selection hierarchy. A sensitivity analysis including only those trials with either a relevant prespecified primary outcome or a single relevant behavioural outcome suggested that the results were robust to selective outcome reporting.
Discussion of findings in relation to the literature
A Cochrane systematic review25 summarised 140 studies and examined the effect of A&F on health worker behaviour and patient health outcomes. The authors found that A&F led to a small improvement on average (weighted median adjusted per cent change relative to control was 1.3%, interquartile range 1.3% to 28.9% in continuous outcomes), but there is a wide variation in effect. The review authors and others have recommended future research to explore this variation and, in particular, to identify factors relating to the intervention design, context and the recipient. 17 The results of our review make a contribution to this agenda by suggesting aspects of the design of A&F interventions that are associated with positive outcomes: (1) making it clear that a credible source approves of the desired behaviour; (2) feedback on an individual’s behaviour is likely to be more effective if it is accompanied by drawing attention to the behaviour of their peers; (3) complex interventions involving multiple social norms seem to be effective; and (4) social comparison seems to be enhanced by the use of prompts and cues, such as providing lists of patients with suboptimal management101 or sending guideline-based recommendations with test results102 to support decision making, or computerised pop-ups when particular codes are entered into an electronic system,61 but the benefit of prompts and cues may hold only when the health worker understands how to do the behaviour. The effect of social norms interventions seemed to be reasonably consistent across the contexts we explored: social norms interventions worked across a range of health professionals, behaviours and settings. By contrast to an earlier review of A&F,25 delivering the intervention once appeared to be sufficient and sending the intervention by website or other computerised format was most effective. Our results align with findings from a recent synthesis of qualitative literature on A&F,16 which found that letting health professionals know how their performance relates to that of their peers (social comparison) and providing opportunities for peer discussion [social support (unspecified)] were valuable in changing behaviour.
A recent overview of systematic reviews on promoting professional behaviour change in health care summarised 67 reviews and found that the most effective interventions were educational outreach using academic detailing, A&F feedback and reminders. 103 Using normalisation process theory as a theoretical lens, the authors concluded that interventions that seek to ‘restructure and reinforce new practice norms’ (opinion leaders, educational meetings and materials/guidelines) and those that ‘associate practice norms with peer and reference group behaviours’ (academic detailing, A&F) are most likely to be successful in changing clinical behaviour, and that combining the two approaches together may be particularly effective by creating clear rules of conduct and encouraging individuals to follow their peers. 103 Interventions that seek to change attitudes were found to be less likely to be successful. The importance given to peer and reference group behaviours in this previous study certainly justifies our efforts to identify which social norms interventions are associated with success. We found a lack of clarity around terms that are commonly used in the literature about health worker behaviour change. An example is academic detailing, where a target health worker receives individual support or advice from someone else with expertise in that area. We found that academic detailing appeared frequently as a technique but its precise content was usually not specified. We agreed to treat academic detailing like other ‘packages’ in the BCT taxonomy v1 that are not well-defined (e.g. cognitive–behavioural therapy or counselling) and code it as social support (unspecified). This is based on the idea that the health worker is getting some unspecified support, but we cannot precisely pin it down. If the paper included a detailed description of the content of the academic detailing, we added other BCT codes, if indicated, such as credible source if the person delivering the intervention was a credible source who provided approval of the behaviour. Similarly, opinion leaders occurred fairly frequently, sometimes without clarity of what was involved, and were coded only as credible source when we felt that it clearly met the definition in the BCT taxonomy v1.
The BCT taxonomy v124 was used in this review to classify the BCTs in the intervention and control arms of the included studies: we categorised both the social norm techniques and the accompanying techniques. Four coders (two experienced health psychologists, one health services researcher and one librarian) were provided with a half-day of training by experts and an online course (www.bct-taxonomy.com/), and managed to achieve fairly high levels of inter-rater consistency, which adds to the evidence40 that the taxonomy is a consistent and reliable tool for classifying BCTs. Social norms are not explicitly considered as a category of BCTs in the BCT taxonomy. Instead, social norms appear across three categories: comparison of behaviour, comparison of outcomes and reward or threat. This might seem surprising given how often social norms appear in various behaviour change theories,21–23 but the structure of the BCT taxonomy was determined through a careful process involving 18 experts grouping BCTs according to their ‘similar active ingredients’,24 with an aim of creating a structure that facilitates use rather than one that is theory based. We defined a social norms intervention as one seeking to change the clinical behaviour of a target health worker by exposing them to the values, beliefs, attitudes or behaviours of a reference group or person, and we then selected BCTs from the taxonomy that met this definition, involving one of the BCT taxonomy developers in that discussion. This classification worked well for our purposes, but the use of this group of social norm BCTs by other research teams would strengthen the evidence for its utility.
Implications for policy and practice
Our research provides strong evidence from many studies to suggest the following implications for policy and practice:
-
Social norms interventions targeting health workers are effective in both changing the clinical behaviour of health workers and improving outcomes for patients, and should continue to be implemented (102 studies).
-
Social comparison, where a target health worker is provided with information about the clinical behaviour of their peers, allowing them to make a comparison with their own behaviour, is, on average, effective and should continue to be implemented. It is effective both on its own and as part of a complex intervention, and is more effective than simply providing feedback on the target’s behaviour (81 studies).
-
Credible source (where the target health worker understands that a clinical behaviour has the approval of someone they regard as a credible source) is, on average, effective and should continue to be implemented. It is effective both on its own and as part of a complex intervention (15 studies).
-
Social comparison can be enhanced by the use of prompts/cues, such as providing lists of patients to support decision-making (such as those who have test results that warrant investigation), or computerised pop-ups when particular codes are entered into an electronic system. The benefit of prompts and cues may not apply when the behaviour is not well understood by the health worker or they need to learn new skills to undertake it (10 studies).
-
Social norms interventions can be used to good effect across a wide range of health contexts:
-
They are effective in changing the behaviour of doctors (68 studies) and other health workers (12 studies).
-
They can be used successfully to change a variety of behaviours, such as prescribing (40 studies), ordering and conducting tests (21 studies), managing long-term conditions and improving communication with patients (23 studies).
-
They are suitable for use in both increasing behaviour (e.g. more frequent contact with patients or increase in blood testing for a particular condition) (70 studies) or reducing behaviour (e.g. fewer prescriptions for antibiotics or reduction in the number of unwarranted blood tests) (28 studies).
-
They can be used successfully in both primary (56 studies) and hospital care (27 studies).
-
-
Mode of delivery:
-
The source of the intervention can be internal or external.
-
Formats including e-mail (9 studies), written (25 studies), web based (8 studies) and mixed (14 studies) have all been used successfully.
-
Our review provides weaker evidence to suggest the following implications for policy and practice:
-
By contrast to earlier research, our study found that delivering the intervention once (28 studies) appeared to be more effective than delivering the intervention multiple times (47 studies). However, this finding could also be explained by other differences between studies. For example, it is plausible that multiple-time delivery would be used when the desired behaviour is difficult or associated with intractable problems.
-
Sending the intervention by website or other computerised format may be more effective (8 studies) than more costly written (25 studies) or face-to-face methods (14 studies).
Recommendations for further research
-
Credible source has been identified as an effective intervention component, but was included in only 18% of the comparisons identified in this review. For this reason, it seems not to be commonly used for changing clinical behaviours and people responsible for behaviour change policy in this setting may not be familiar with it. Additional work is needed to develop credible source interventions for use in the NHS. As a first step, a narrative synthesis of the trials using credible source in this review, together with the qualitative papers, process evaluations and protocols associated with those trials, would provide a more detailed picture of the credible source interventions that are associated with more successful outcomes.
-
Social comparison is currently used more frequently in the NHS than credible source. We identified a high level of heterogeneity in the effectiveness of social comparison. We have started to unravel this heterogeneity and this research suggests that social comparison can successfully be enhanced by the addition of social reward, prompts/cues or social support (unspecified), but further research would provide more depth to these findings.
-
Qualitative work with health workers, managers and policy-makers is needed to understand the acceptability and feasibility of credible source, social comparison and social reward interventions and to understand who the most credible ‘credible sources’ are.
-
The authors of the BCT taxonomy v1 anticipate that it will be subject to future revision. On the basis of this study we would welcome the creation of a new category ‘social norms’, bringing together the five BCTs used in this study. However, we recognise that the taxonomy is used for many purposes and across disciplines, so other perspectives will need to be considered.
-
The methodological quality of trials was mixed. The review included some large factorial trials that tested several behaviour change interventions simultaneously; this design can be an efficient way of exploring different components of behaviour change interventions and their interactions. Some trials used novel methods to minimise bias such as ‘attention’ controls in which participants were given the identical behaviour change intervention for an alternative target behaviour: this type of design is to be encouraged.
-
The quality of trial reporting was mixed and in many cases it was difficult to extract the necessary information required in this review. Poor trial reporting needs to be addressed in future trials of social norms interventions with health professionals. When assessing the risk of bias, we identified 45 (42.5%) studies with incomplete outcome data and, although a few studies had explicitly changed outcomes since the protocol (n = 5, 4.7%), many more reported multiple outcomes and did not have a published protocol (n = 59, 55.7%), making it impossible to assess whether or not there had been selective outcome reporting. Use of guidelines, such as SPIRIT104 and CONSORT,105 would lead to improvement. In addition, the reporting of the details of interventions was poor. In 34 (29.1%) studies, the format of the intervention was unclear or not reported, and the frequency of the intervention was unclear or not reported in 27 (23.1%) interventions. This poor reporting of interventions in behavioural public policy research has been reported elsewhere,106 and could be addressed by consistent use of the Template for Intervention Description and Replication (TIDieR) framework107,108 and the BCT Taxonomy. 24
-
Trials were excluded from the review where the intervention did not target a specific behaviour. We plan to undertake a separate review of those studies that did not include a target behaviour, to assess whether or not the effects of those interventions vary from the effects found in the current review.
Chapter 5 Conclusions
Social norms interventions are an effective method of changing the clinical behaviour of health workers and have a positive effect on patient outcomes. Although the overall result is modest and very variable, there is the potential for social norms interventions to be applied at a large scale. The most effective social norms interventions are providing communication in favour of the desired behaviour from a credible source, and social comparison combined with prompts/cues. These interventions can be effective in a variety of NHS contexts.
Acknowledgements
We thank the independent members of the Study Steering Committee: Robbie Foy (chairperson), Professor of Primary Care, University of Leeds; Marie Johnston, Professor of Health Psychology, University of Aberdeen; Sofia Dias, Professor in Health Technology Assessment, University of York; and Manoj Mistry, lay member. They were very generous with their time and provided encouragement and wise counsel throughout the project. Marie Johnston came from Aberdeen to run a training workshop on BCT coding. We are grateful to Jack Wilkinson who was employed as a researcher in the early stages of the review until he was successful in winning a University of Manchester presidential fellowship.
Contributions of authors
Sarah Cotterill (https://orcid.org/0000-0001-5136-390X) (Senior Lecturer, Health Services Research and Statistics) conceived of the idea for the review and managed the project. She led the writing of the funding proposal and the study protocol, and was involved in screening, data extraction and BCT coding. She attended research group meetings that directed the research. She helped to prepare the data for analysis and undertook descriptive analysis. She led the drafting of the final report and the response to reviewer comments.
Mei Yee Tang (https://orcid.org/0000-0002-3116-6025) (Research Associate, Psychology) was employed as a researcher throughout the project. She contributed to the protocol and was involved in screening, data extraction and BCT coding. She attended research group meetings that directed the research. She was involved in drafting the final report and responding to reviewer comments and approved the final version.
Rachael Powell (https://orcid.org/0000-0002-8023-8873) (Senior Lecturer, Health Psychology) was the lead for health psychology. She was a co-applicant on the funding proposal, contributed to the protocol and was involved in screening and BCT coding. She attended research group meetings that directed the research. She was involved in drafting the final report and responding to reviewer comments and approved the final version.
Elizabeth Howarth (https://orcid.org/0000-0003-3462-3946) (Research Associate, Statistics) was involved in data extraction and conducted the meta-analysis of patient health outcomes. She was involved in drafting the final report and approved the final version.
Laura McGowan (https://orcid.org/0000-0002-4054-9300) (PhD student, Psychology) helped to prepare the data for analysis and undertook descriptive analysis. She was involved in drafting the final report and responding to reviewer comments and approved the final version.
Jane Roberts (https://orcid.org/0000-0003-3878-0404) (Librarian, Information Retrieval) wrote the search strategies and ran the searches. She was involved in BCT coding. She was involved in drafting the final report and approved the final version.
Benjamin Brown (https://orcid.org/0000-0001-9975-4782) (Senior Academic GP and Honorary Consultant, Primary Care) was the clinical lead. He was a co-applicant on the funding proposal and contributed to the protocol. He attended research group meetings that directed the research. He was involved in drafting the final report and responding to reviewer comments and approved the final version.
Sarah Rhodes (https://orcid.org/0000-0002-5837-801X) (Research Fellow, Statistics) was the lead statistician. She was a co-applicant on the funding proposal, contributed to the protocol and was involved in screening and data extraction. She attended research group meetings that directed the research. She converted all the outcome measures to SMDs, conducted the meta-analysis, metaregression and network meta-analysis of the health worker behaviour outcomes and prepared the results for publication. She was involved in drafting the final report and responding to reviewer comments and approved the final version.
Publications
Cotterill S, Powell R, Rhodes S, Roberts J, Tang MY, Wilkinson J. The Impact of Social Norms Interventions on Clinical Behaviour Change among Health Workers: Protocol for a Systematic Review. PROSPERO 2016:CRD42016042718. URL: www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42016042718 (accessed 3 September 2020).
Cotterill S, Powell R, Rhodes S, Brown B, Roberts J, Tang MY, Wilkinson J. The impact of social norms interventions on clinical behaviour change among health workers: protocol for a systematic review and meta-analysis. Syst Rev 2019;8:176.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Cotterill S, Powell R, Rhodes S, Roberts J, Tang MY, Wilkinson J. The Impact of Social Norms Interventions on Clinical Behaviour Change Among Health Workers: Protocol for a Systematic Review n.d. www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42016042718 (accessed 3 September 2020).
- Cotterill S, Powell R, Rhodes S, Brown B, Roberts J, Tang MY, et al. The impact of social norms interventions on clinical behaviour change among health workers: protocol for a systematic review and meta-analysis. Syst Rev 2019;8. https://doi.org/10.1186/s13643-019-1077-6.
- Hamilton W, Watson J, Round A. Investigating fatigue in primary care. BMJ 2010;341. https://doi.org/10.1136/bmj.c4259.
- National Institute for Health and Care Excellence (NICE) . Cardiovascular Disease: Risk Assessment and Reduction, Including Lipid Modification 2014.
- Davies SC, Fowler T, Watson J, Livermore DM, Walker D. Annual report of the Chief Medical Officer: infection and the rise of antimicrobial resistance. Lancet 2013;381:1606-9. https://doi.org/10.1016/S0140-6736(13)60604–2.
- Hawker JI, Smith S, Smith GE, Morbey R, Johnson AP, Fleming DM, et al. Trends in antibiotic prescribing in primary care for clinical syndromes subject to national recommendations to reduce antibiotic resistance, UK 1995–2011: analysis of a large database of primary care consultations. J Antimicrob Chemother 2014;69:3423-30. https://doi.org/10.1093/jac/dku291.
- National Institute for Health and Care Excellence (NICE) . Type 2 Diabetes in Adults: Management 2015.
- Loveday HP, Wilson JA, Pratt RJ, Golsorkhi M, Tingle A, Bak A, et al. epic3: National evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect 2014;86:S1-70.
- National Institute for Health and Care Excellence (NICE) . Chronic Wounds: Advanced Wound Dressings and Antimicrobial Dressings 2016.
- Cooksey D. A Review of UK Health Research Funding. London: Her Majesty’s Stationery Office; 2006.
- Public Health England . Tackling High Blood Pressure: From Evidence into Action 2014.
- Pirmohamed M, James S, Meakin S, Green C, Scott AK, Walley TJ, et al. Adverse drug reactions as cause of admission to hospital: prospective analysis of 18 820 patients. BMJ 2004;329:15-9. https://doi.org/10.1136/bmj.329.7456.15.
- Howard RL, Avery AJ, Slavenburg S, Royal S, Pipe G, Lucassen P, et al. Which drugs cause preventable admissions to hospital? A systematic review. Br J Clin Pharmacol 2007;63:136-47. https://doi.org/10.1111/j.1365-2125.2006.02698.x.
- Whiting P, Toerien M, de Salis I, Sterne JA, Dieppe P, Egger M, et al. A review identifies and classifies reasons for ordering diagnostic tests. J Clin Epidemiol 2007;60:981-9. https://doi.org/10.1016/j.jclinepi.2007.01.012.
- van der Weijden T, van Bokhoven MA, Dinant GJ, van Hasselt CM, Grol RP. Understanding laboratory testing in diagnostic uncertainty: a qualitative study in general practice. Br J Gen Pract 2002;52:974-80.
- Brown B, Gude WT, Blakeman T, van der Veer SN, Ivers N, Francis JJ, et al. Clinical Performance Feedback Intervention Theory (CP-FIT): a new theory for designing, implementing, and evaluating feedback in health care based on a systematic review and meta-synthesis of qualitative research. Implement Sci 2019;14. https://doi.org/10.1186/s13012-019-0883-5.
- Ivers NM, Sales A, Colquhoun H, Michie S, Foy R, Francis JJ, et al. No more ‘business as usual’ with audit and feedback interventions: towards an agenda for a reinvigorated intervention. Implement Sci 2014;9. https://doi.org/10.1186/1748-5908-9-14.
- Ivers NM, Tu K, Young J, Francis JJ, Barnsley J, Shah BR, et al. Feedback GAP: pragmatic, cluster-randomized trial of goal setting and action plans to increase the effectiveness of audit and feedback interventions in primary care. Implement Sci 2013;8. https://doi.org/10.1186/1748-5908-8-142.
- Carney PA, Abraham L, Cook A, Feig SA, Sickles EA, Miglioretti DL, et al. Impact of an educational intervention designed to reduce unnecessary recall during screening mammography. Acad Radiol 2012;19:1114-20. https://doi.org/10.1016/j.acra.2012.05.003.
- Huis A, Schoonhoven L, Grol R, Donders R, Hulscher M, van Achterberg T. Impact of a team and leaders-directed strategy to improve nurses’ adherence to hand hygiene guidelines: a cluster randomised trial. Int J Nurs Stud 2013;50:464-74. https://doi.org/10.1016/j.ijnurstu.2012.08.004.
- Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process 1991;50:179-211. https://doi.org/https://doi.org/10.1016/0749-5978(91)90020-T.
- Rimal RN, Real K. How behaviors are influenced by perceived norms: a test of the theory of normative social behavior. Communic Res 2005;32:389-414. https://doi.org/10.1177/0093650205275385.
- Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci 2012;7. https://doi.org/10.1186/1748-5908-7-37.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81-95. https://doi.org/10.1007/s12160-013-9486-6.
- Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard-Jensen J, French SD, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev 2012;6. https://doi.org/10.1002/14651858.CD000259.pub3.
- Gardner B, Whittington C, McAteer J, Eccles MP, Michie S. Using theory to synthesise evidence from behaviour change interventions: the example of audit and feedback. Soc Sci Med 2010;70:1618-25. https://doi.org/10.1016/j.socscimed.2010.01.039.
- Ivers NM. Optimizing Audit and Feedback Interventions to Improve Quality in Primary Care 2014.
- Michie S, Johnston M, Abraham C, Francis J, Hardeman W, Eccles M. BCT Taxonomy Starter Pack for Trainees 2014. www.bct-taxonomy.com/pdf/StarterPack.pdf (accessed 3 September 2020).
- Merriel A, van der Nelson HA, Lenguerrand E, Chung Y, Soar J, Ficquet J, et al. Emergency training for in-hospital-based healthcare providers: effects on clinical practice and patient outcomes. Cochrane Database Syst Rev 2016;5. https://doi.org/10.1002/14651858.CD012177.
- NHS Digital . A Guide to the Staff Group, Job Role and Area of Work Classifications Used in ESR 2019. https://digital.nhs.uk/data-and-information/areas-of-interest/workforce/national-workforce-data-set-nwd-guidance-documents (accessed 3 September 2020).
- Michie S, Wood CE, Johnston M, Abraham C, Francis JJ, Hardeman W. Behaviour change techniques: the development and evaluation of a taxonomic method for reporting and describing behaviour change interventions (a suite of five studies involving consensus methods, randomised controlled trials and analysis of qualitative data). Health Technol Assess 2015;19. https://doi.org/10.3310/hta19990.
- Ajzen I. The theory of planned behavior. Organ Behav Hum Decision Proc 1991;50:179-211. https://doi.org/10.1016/0749-5978(91)90020-T.
- Fishbein M, Ajzen I. Belief, Attitude, Intention, and Behavior: An Introduction to Theory and Research. Reading, MA: Addison-Wesley; 1975.
- Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A. Making psychological theory useful for implementing evidence based practice: a consensus approach. BMJ Qual Saf 2005;14:26-33. https://doi.org/10.1136/qshc.2004.011155.
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986.
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. London: The Cochrane Collaboration; 2011.
- Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med 2009;6. https://doi.org/10.1371/journal.pmed.1000097.
- Altman DG. Practical Statistics for Medical Research. London: Chapman & Hall; 1991.
- Effective Practice and Organisation of Care (EPOC) . Data Collection Form: EPOC Resources for Review Authors 2013.
- Abraham C, Wood CE, Johnston M, Francis J, Hardeman W, Richardson M, et al. Reliability of identification of behavior change techniques in intervention descriptions. Ann Behav Med 2015;49:885-900. https://doi.org/10.1007/s12160-015-9727-y.
- Chen G, Faris P, Hemmelgarn B, Walker RL, Quan H. Measuring agreement of administrative data with chart data using prevalence unadjusted and adjusted kappa. BMC Med Res Methodol 2009;9. https://doi.org/10.1186/1471-2288-9-5.
- Gwet KL. Handbook of Inter-Rater Reliability: The Definitive Guide to Measuring the Extent of Agreement Among Raters Advanced Analytics. Gaithersburg, MD: Advanced Analytics, LLC; 2014.
- Klein D. Implementing a general framework for assessing interrater agreement in Stata. Stata J 2018;4:871-90. https://doi.org/10.1177/1536867X1801800408.
- Chinn S. A simple method for converting an odds ratio to effect size for use in meta-analysis. Stat Med 2000;19:3127-31. https://doi.org/10.1002/1097-0258(20001130)19:22<3127::AID-SIM784>3.0.CO;2-M.
- Caldwell DM, Welton NJ. Approaches for synthesising complex mental health interventions in meta-analysis. Evid Based Ment Health 2016;19:16-21. https://doi.org/10.1136/eb-2015-102275.
- Bar-Zeev Y, Bonevski B, Bovill M, Gruppetta M, Oldmeadow C, Palazzi K, et al. The Indigenous Counselling and Nicotine (ICAN) QUIT in Pregnancy Pilot Study protocol: a feasibility step–wedge cluster randomised trial to improve health providers’ management of smoking during pregnancy. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-016095.
- Michael SS, Babu KM, Androski C, Reznek MA. Effect of a data-driven intervention on opioid prescribing intensity among emergency department providers: a randomized controlled trial. Acad Emerg Med 2018;25:482-93. https://doi.org/10.1111/acem.13400.
- Brunette MF, Dzebisashvili N, Xie H, Akerman S, Ferron JC, Bartels S. Expanding cessation pharmacotherapy via videoconference educational outreach to prescribers. Nicotine Tob Res 2015;17:960-7. https://doi.org/10.1093/ntr/ntv006.
- Colon-Emeric CS, McConnell E, Pinheiro SO, Corazzini K, Porter K, Earp KM, et al. CONNECT for better fall prevention in nursing homes: results from a pilot intervention study. J Am Geriatr Soc 2013;61:2150-9. https://doi.org/10.1111/jgs.12550.
- Forrest CB, Fiks AG, Bailey LC, Localio R, Grundmeier RW, Richards T, et al. Improving adherence to otitis media guidelines with clinical decision support and physician feedback. Pediatrics 2013;131:e1071-81. https://doi.org/10.1542/peds.2012-1988.
- Hampshire A, Blair M, Crown N, Avery A, Williams I. Action research: a useful method of promoting change in primary care?. Fam Pract 1999;16:305-11. https://doi.org/10.1093/fampra/16.3.305.
- Wadland WC, Holtrop JS, Weismantel D, Pathak PK, Fadel H, Powell J. Practice-based referrals to a tobacco cessation quit line: assessing the impact of comparative feedback vs. general reminders. Ann Fam Med 2007;5:135-42. https://doi.org/10.1370/afm.650.
- Wattal C, Goel N, Khanna S, Byotra SP, Laxminarayan R, Easton A. Impact of informational feedback to clinicians on antibiotic-prescribing rates in a tertiary care hospital in Delhi. Indian J Med Microbiol 2015;33:255-9. https://doi.org/10.4103/0255-0857.153582.
- Paul CL, Piterman L, Shaw JE, Kirby C, Forshaw KL, Robinson J, et al. Poor uptake of an online intervention in a cluster randomised controlled trial of online diabetes education for rural general practitioners. Trials 2017;18. https://doi.org/10.1186/s13063-017-1869-8.
- Szczepura A, Wilmot J, Davies C, Fletcher J. Effectiveness and cost of different strategies for information feedback in general practice. Br J Gen Pract 1994;44:19-24.
- Schultz PW, Nolan JM, Cialdini RB, Goldstein NJ, Griskevicius V. The constructive, destructive, and reconstructive power of social norms. Psychol Sci 2007;18:429-34. https://doi.org/10.1111/j.1467-9280.2007.01917.x.
- Nomura H, John PC, Cotterill S. The use of feedback to enhance environmental outcomes: a randomised controlled trial of a food waste scheme. Local Environment 2011;16:637-53. https://doi.org/10.1080/13549839.2011.586026.
- Rücker G, Schwarzer G, Carpenter JR, Schumacher M. Undue reliance on I(2) in assessing heterogeneity may mislead. BMC Med Res Methodol 2008;8. https://doi.org/10.1186/1471-2288-8-79.
- Grant RL. Converting an odds ratio to a range of plausible relative risks for better communication of research findings. BMJ 2014;348. https://doi.org/10.1136/bmj.f7450.
- Hallsworth M, Chadborn T, Sallis A, Sanders M, Berry D, Greaves F, et al. Provision of social norm feedback to high prescribers of antibiotics in general practice: a pragmatic national randomised controlled trial. Lancet 2016;387:1743-52. https://doi.org/10.1016/S0140-6736(16)00215–4.
- Vellinga A, Galvin S, Duane S, Callan A, Bennett K, Cormican M, et al. Intervention to improve the quality of antimicrobial prescribing for urinary tract infection: a cluster randomized trial. Can Med Assoc J 2016;188:108-15. https://doi.org/10.1503/cmaj.150601.
- Persell SD, Doctor JN, Friedberg MW, Meeker D, Friesema E, Cooper A, et al. Behavioral interventions to reduce inappropriate antibiotic prescribing: a randomized pilot trial. BMC Infect Dis 2016;16. https://doi.org/10.1186/s12879-016-1715-8.
- Lakshminarayan K, Borbas C, McLaughlin B, Morris NE, Vazquez G, Luepker RV, et al. A cluster-randomized trial to improve stroke care in hospitals. Neurology 2010;74:1634-42. https://doi.org/10.1212/WNL.0b013e3181df096b.
- French SD, McKenzie JE, O’Connor DA, Grimshaw JM, Mortimer D, Francis JJ, et al. Evaluation of a theory-informed implementation intervention for the management of acute low back pain in general medical practice: the IMPLEMENT cluster randomised trial. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0065471.
- Leviton LC, Goldenberg RL, Baker CS, Schwartz RM, Freda MC, Fish LJ, et al. Methods to encourage the use of antenatal corticosteroid therapy for fetal maturation: a randomized controlled trial. JAMA 1999;281:46-52. https://doi.org/10.1001/jama.281.1.46.
- Baskerville NB, Hogg W, Lemelin J. Process evaluation of a tailored multifaceted approach to changing family physician practice patterns improving preventive care. J Fam Pract 2001;50:W242-9.
- Lomas J, Enkin M, Anderson GM, Hannah WJ, Vayda E, Singer J. Opinion leaders vs audit and feedback to implement practice guidelines. Delivery after previous cesarean section. JAMA 1991;265:2202-7. https://doi.org/10.1001/jama.1991.03460170056033.
- Guadagnoli E, Soumerai SB, Gurwitz JH, Borbas C, Shapiro CL, Weeks JC, et al. Improving discussion of surgical treatment options for patients with breast cancer: local medical opinion leaders versus audit and performance feedback. Breast Cancer Res Treat 2000;61:171-5. https://doi.org/10.1023/a:1006475012861.
- Hayes RP, Baker DW, Luthi JC, Baggett RL, McClellan W, Fitzgerald D, et al. The effect of external feedback on the management of medicare inpatients with congestive heart failure. Am J Med Qual 2002;17:225-35. https://doi.org/10.1177/106286060201700605.
- Mold JW, Aspy CA, Nagykaldi Z. Oklahoma Physicians Resource/Research Network . Implementation of evidence-based preventive services delivery processes in primary care: an Oklahoma Physicians Resource/Research Network (OKPRN) study. J Am Board Fam Med 2008;21:334-44. https://doi.org/10.3122/jabfm.2008.04.080006.
- Koff MD, Brown JR, Marshall EJ, O’Malley AJ, Jensen JT, Heard SO, et al. Frequency of hand decontamination of intraoperative providers and reduction of postoperative healthcare-associated infections: a randomized clinical trial of a novel hand hygiene system. Infect Control Hosp Epidemiol 2016;37:888-95. https://doi.org/10.1017/ice.2016.106.
- Quinley JC, Shih A. Improving physician coverage of pneumococcal vaccine: a randomized trial of a telephone intervention. J Community Health 2004;29:103-15. https://doi.org/10.1023/b:johe.0000016715.91811.4b.
- Baker R, Farooqi A, Tait C, Walsh S. Randomised controlled trial of reminders to enhance the impact of audit in general practice on management of patients who use benzodiazepines. Qual Health Care 1997;6:14-8. https://doi.org/10.1136/qshc.6.1.14.
- Mourad SM, Hermens RP, Liefers J, Akkermans RP, Zielhuis GA, Adang E, et al. A multi-faceted strategy to improve the use of national fertility guidelines; a cluster-randomized controlled trial. Hum Reprod 2011;26:817-26. https://doi.org/10.1093/humrep/deq299.
- Hysong SJ, Simpson K, Pietz K, SoRelle R, Broussard Smitham K, Petersen LA. Financial incentives and physician commitment to guideline-recommended hypertension management. Am J Manag Care 2012;18:e378-91.
- Weitzman S, Greenfield S, Billimek J, Hava T, Schvartzman P, Yehiel E, et al. Improving combined diabetes outcomes by adding a simple patient intervention to physician feedback: a cluster randomized trial. Isr Med Assoc J 2009;11:719-24.
- Desveaux L, Gomes T, Tadrous M, Jeffs L, Taljaard M, Rogers J, et al. Appropriate prescribing in nursing homes demonstration project (APDP) study protocol: pragmatic, cluster-randomized trial and mixed methods process evaluation of an Ontario policy-maker initiative to improve appropriate prescribing of antipsychotics. Implement Sci 2016;11. https://doi.org/10.1186/s13012-016-0410-x.
- Rask KJ, Kohler SA, Wells KJ, Williams JA, Diamond CC. Performance improvement interventions to improve delivery of screening services in diabetes care. J Clin Outcomes Manag 2001;8:23-9.
- Soumerai SB, McLaughlin TJ, Gurwitz JH, Guadagnoli E, Hauptman PJ, Borbas C, et al. Effect of local medical opinion leaders on quality of care for acute myocardial infarction: a randomized controlled trial. JAMA 1998;279:1358-63. https://doi.org/10.1001/jama.279.17.1358.
- Sauaia A, Ralston D, Schluter WW, Marciniak TA, Havranek EP, Dunn TR. Influencing care in acute myocardial infarction: a randomized trial comparing 2 types of intervention. Am J Med Qual 2000;15:197-206. https://doi.org/10.1177/106286060001500503.
- Wright FC, Law CH, Last LD, Klar N, Ryan DP, Smith AJ. A blended knowledge translation initiative to improve colorectal cancer staging [ISRCTN56824239.]. BMC Health Serv Res 2006;6. https://doi.org/10.1186/1472-6963-6-4.
- Kiefe C, Allison J, Williams O, Person S, Weaver M, Weissman N. Improving quality improvement using achievable benchmarks for physician feedback: a randomized controlled trial. JAMA 2001;285:2871-9. https://doi.org/10.1001/jama.285.22.2871.
- Schneider A, Wensing M, Biessecker K, Quinzler R, Kaufmann-Kolle P, Szecsenyi J. Impact of quality circles for improvement of asthma care: results of a randomized controlled trial. J Eval Clin Pract 2008;14:185-90. https://doi.org/10.1111/j.1365-2753.2007.00827.x.
- Braybrook S, Walker R. Influencing prescribing in primary care: a comparison of two different prescribing feedback methods. J Clin Pharm Ther 1996;21:247-54. https://doi.org/10.1111/j.1365-2710.1996.tb01146.x.
- Higgins JP, Thompson SG. Controlling the risk of spurious findings from meta-regression. Stat Med 2004;23:1663-82. https://doi.org/10.1002/sim.1752.
- Beck CA, Richard H, Tu JV, Pilote L. Administrative Data Feedback for Effective Cardiac Treatment: AFFECT, a cluster randomized trial. JAMA 2005;294:309-17. https://doi.org/10.1001/jama.294.3.309.
- Bentz CJ, Bayley KB, Bonin KE, Fleming L, Hollis JF, Hunt JS, et al. Provider feedback to improve 5A’s tobacco cessation in primary care: a cluster randomized clinical trial. Nicotine Tob Res 2007;9:341-9. https://doi.org/10.1080/14622200701188828.
- Boet S, Bryson GL, Taljaard M, Pigford AA, McIsaac DI, Brehaut J, et al. Effect of audit and feedback on physicians’ intraoperative temperature management and patient outcomes: a three-arm cluster randomized-controlled trial comparing benchmarked and ranked feedback. Can J Anaesth 2018;65:1196-209. https://doi.org/10.1007/s12630-018-1205-0.
- Cheater FM, Baker R, Reddish S, Spiers N, Wailoo A, Gillies C, et al. Cluster randomised controlled trial of the effectiveness of audit and feedback and educational outreach on improving nursing practice and patient outcomes. Medical Care 2006;44:542-51. https://doi.org/10.1097/01.mlr.0000215919.89893.8a.
- Kim CS, Kristopaitis RJ, Stone E, Pelter M, Sandhu M, Weingarten SR. Physician education and report cards: do they make the grade? Results from a randomized controlled trial. Am J Med 1999;107:556-60. https://doi.org/10.1016/S0002-9343(99)00293-4.
- Pope JE, Thorne JC, Cividino AA, Lucas K. A randomized controlled trial of rheumatologist education impacting on systematic measurements and treatment decisions in rheumatoid arthritis (RA): results of the Metrix study. Arthritis Rheum 2010;10.
- Raja AS, Ip IK, Dunne RM, Schuur JD, Mills AM, Khorasani R. Effects of performance feedback reports on adherence to evidence-based guidelines in use of CT for evaluation of pulmonary embolism in the emergency department: a randomized trial. Am J Roentgenol 2015;205:936-40. https://doi.org/10.2214/AJR.15.14677.
- Guldberg T, Vedsted P, Kristensen J, Lauritzen T. Improved quality of Type 2 diabetes care following electronic feedback of treatment status to general practitioners: a cluster randomized controlled trial. Diabetic Medicine 2011;28:325-32. https://doi.org/10.1111/j.1464-5491.2010.03178.x.
- Katz DA, Muehlenbruch DR, Brown RL, Fiore MC, Baker TB. Effectiveness of implementing the Agency for Healthcare Research and Quality Smoking Cessation Clinical Practice Guideline: a randomized, controlled trial. J Natl Cancer Inst 2004;96:594-603. https://doi.org/10.1093/jnci/djh103.
- Aspy CB, Enright M, Halstead L, Mould JW. Oklahoma Physicians Resource/Research Network . Improving mammography screening using best practices and practice enhancement assistants: an Oklahoma Physicians Resource/Research Network (OKPRN) study. J Am Board Fam Med 2008;21:326-33. https://doi.org/10.3122/jabfm.2008.04.070060.
- Morrison LJ, Brooks SC, Dainty KN, Dorian P, Needham DM, Ferguson ND, et al. Improving use of targeted temperature management after out-of-hospital cardiac arrest: a stepped wedge cluster randomized controlled trial. Crit Care Med 2015;43:954-64. https://doi.org/10.1097/CCM.0000000000000864.
- van Bruggen R, Gorter KJ, Stolk RP, Verhoeven RP, Rutten G. Implementation of locally adapted guidelines on type 2 diabetes. Family Practice 2008;25:430-7. https://doi.org/10.1093/fampra/cmn045.
- Billue KL, Safford MM, Salanitro AH, Houston TK, Curry W, Kim Y, et al. Medication intensification in diabetes in rural primary care: a cluster-randomised effectiveness trial. BMJ Open 2012;2. https://doi.org/10.1136/bmjopen-2012–00095-.
- Poole C, Greenland S. Random-effects meta-analyses are not always conservative. Am J Epidemiol 1999;150:469-75. https://doi.org/10.1093/oxfordjournals.aje.a010035.
- Higgins JPT, López-López JA, Becker BJ, Davies SR, Dawson S, Grimshaw JM, et al. Synthesising quantitative evidence in systematic reviews of complex health interventions. BMJ Global Health 2019;4. https://doi.org/10.1136/bmjgh-2018-000858.
- Peiris D, Usherwood T, Panaretto K, Harris M, Hunt J, Redfern J, et al. Effect of a computer-guided, quality improvement program for cardiovascular disease risk management in primary health care: the treatment of cardiovascular risk using electronic decision support cluster-randomized trial. Circ Cardiovasc Qual Outcomes 2015;8:87-95. https://doi.org/10.1161/CIRCOUTCOMES.114.001235.
- MacLean CD, Gagnon M, Callas P, Littenberg B. The Vermont diabetes information system: a cluster randomized trial of a population based decision support system. J Gen Intern Med 2009;24:1303-10. https://doi.org/10.1007/s11606-009-1147-x.
- Johnson MJ, May CR. Promoting professional behaviour change in healthcare: what interventions work, and why? A theory-led overview of systematic reviews. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-008592.
- Chan AW, Tetzlaff JM, Altman DG, Laupacis A, Gøtzsche PC, Krleža-Jerić K, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med 2013;158:200-7. https://doi.org/10.7326/0003-4819-158-3-201302050-00583.
- Schulz KF, Altman DG, Moher D. CONSORT Group . CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med 2010;152:726-32. https://doi.org/10.7326/0003-4819-152-11-201006010-00232.
- Cotterill S, John P, Johnston M. How better reporting standards could advance behavioural public policy: useful tools for reporting interventions and evaluations. Policy and Politics n.d.
- Campbell M, Katikireddi SV, Hoffmann T, Armstrong R, Waters E, Craig P. TIDieR-PHP: a reporting guideline for population health and policy interventions. BMJ 2018;361. https://doi.org/10.1136/bmj.k1079.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Gould GS, Bovill M, Pollock L, Bonevski B, Gruppetta M, Atkins L, et al. Feasibility and acceptability of Indigenous Counselling and Nicotine (ICAN) QUIT in Pregnancy multicomponent implementation intervention and study design for Australian Indigenous pregnant women: a pilot cluster randomised step-wedge trial. Addict Behav 2019;90:176-90. https://doi.org/10.1016/j.addbeh.2018.10.036.
- Awad AI, Eltayeb IB, Baraka OZ. Changing antibiotics prescribing practices in health centres of Khartoum State, Sudan. Eur J Clin Pharmacol 2006;62:135-42. https://doi.org/10.1007/s00228–005–0089–4.
- Barnett KN, Bennie M, Treweek S, Robertson C, Petrie DJ, Ritchie LD, et al. Effective Feedback to Improve Primary Care Prescribing Safety (EFIPPS) a pragmatic three-arm cluster randomised trial: designing the intervention. Implement Sci 2014;9. https://doi.org/10.1186/s13012-014-0133-9.
- Beidas RS, Becker-Haimes EM, Adams DR, Skriner L, Stewart RE, Wolk CB, et al. Feasibility and acceptability of two incentive-based implementation strategies for mental health therapists implementing cognitive-behavioural therapy: a pilot study to inform a randomized controlled trial. Implement Sci 2017;12. https://doi.org/10.1186/s13012-017-0684-7.
- Bhatia RS, Ivers NM, Yin XC, Myers D, Nesbitt GC, Edwards J, et al. Improving the appropriate use of transthoracic echocardiography: the Echo WISELY trial. J Am Coll Cardiol 2017;70:1135-44. https://doi.org/10.1016/j.jacc.2017.06.065.
- Bhattacharyya O, Harris S, Zwarenstein M, Barnsley J. Controlled trial of an intervention to improve cholesterol management in diabetes patients in remote Aboriginal communities. Int J Circumpolar Health 2010;69:333-43. https://doi.org/10.3402/ijch.v69i4.17629.
- Brinkman WB, Geraghty SR, Lanphear BP, Khoury JC, del Rey JAG, DeWitt TG, et al. Effect of multisource feedback on resident communication skills and professionalism – a randomized controlled trial. Arch Pediatr Adolesc Med 2007;161:44-9. https://doi.org/10.1001/archpedi.161.1.44.
- Brown B, Young J, Smith DP, Kneebone AB, Brooks AJ, Egger S, et al. A multidisciplinary team-oriented intervention to increase guideline recommended care for high-risk prostate cancer: a stepped-wedge cluster randomised implementation trial. Implement Sci 2018;13. https://doi.org/10.1186/s13012-018-0733-x.
- Buntinx F, Knottnerus JA, Crebolder H, Seegers T, Essed GGM, Schouten H. Does feedback improve the quality of cervical smears? A randomized controlled trial. Br J Gen Pract 1993;43:194-8.
- Butler CC, Simpson SA, Dunstan F, Rollnick S, Cohen D, Gillespie D, et al. Effectiveness of multifaceted educational programme to reduce antibiotic dispensing in primary care: practice based randomised controlled trial. BMJ 2012;344. https://doi.org/10.1136/bmj.d8173.
- Cánovas JJ, Hernández PJS, Botella JJA. Effectiveness of internal quality assurance programmes in improving clinical practice and reducing costs. J Eval Clin Pract 2009;15:813-19. https://doi.org/10.1111/j.1365-2753.2008.01100.x.
- Colon-Emeric CS, Lyles KW, House P, Levine DA, Schenck AP, Allison J, et al. Randomised trial to improve fracture prevention in nursing home residents. Am J Med 2007;120:886-92. https://doi.org/10.1016/j.amjmed.2007.04.020.
- Curtis JR, Olivieri J, Allison J, Gaffo A, Juarez L, Kovac S, et al. A group randomized trial to improve safe use of nonsteroidal anti-inflammatory drugs. Am J Manag Care 2005;11:537-43.
- Curtis JR, Westfall AO, Allison J, Becker A, Melton ME, Freeman A, et al. Challenges in improving the quality of osteoporosis care for long-term glucocorticoid users: a prospective randomized trial. Arch Intern Med 2007;167:591-6. https://doi.org/10.1001/archinte.167.6.591.
- Eccles M, Steen N, Grimshaw J, Thomas L, McNamee P, Soutter J, et al. Effect of audit and feedback, and reminder messages on primary-care radiology referrals: a randomised trial. Lancet 2001;357:1406-9. https://doi.org/10.1016/S0140-6736(00)04564-5.
- Elouafkaoui P, Young L, Newlands R, Duncan EM, Elders A, Clarkson JE, et al. An audit and feedback intervention for reducing antibiotic prescribing in general dental practice: the RAPiD cluster randomised controlled trial. PLOS Med 2016;13. https://doi.org/10.1371/journal.pmed.1002115.
- Eltayeb IB, Awad AI, Mohamed-Salih MS, Daffa-Alla MA, Ahmed MB, Ogail MA, et al. Changing the prescribing patterns of sexually transmitted infections in the White Nile Region of Sudan. Sex Transm Infect 2005;81:426-7. https://doi.org/10.1136/sti.2004.014001.
- Ferguson TB, Peterson ED, Coombs LP, Eiken MC, Carey ML, Grover FL, et al. Use of continuous quality improvement to increase use of process measures in patients undergoing coronary artery bypass graft surgery: a randomised controlled trial. JAMA 2003;290:49-56. https://doi.org/10.1001/jama.290.1.49.
- Fiks AG, Mayne SL, Michel JJ, Miller J, Abraham M, Suh A, et al. Distance-learning, ADHD quality improvement in primary care: a cluster-randomized trial. J Dev Behav Pediatr 2017;38:573-83. https://doi.org/10.1097/DBP.0000000000000490.
- Foster JM, Hoskins G, Smith B, Lee AJ, Price D, Pinnock H. Practice development plans to improve the primary care management of acute asthma: randomised controlled trial. BMC Fam Pract 2007;8. https://doi.org/10.1186/1471-2296-8-23.
- Foy R, Penney GC, Grimshaw JM, Ramsay CR, Walker AE, MacLennan G, et al. A randomised controlled trial of a tailored multifaceted strategy to promote implementation of a clinical guideline on induced abortion care. BJOG 2004;111:726-33. https://doi.org/10.1111/j.1471-0528.2004.00168.x.
- Fuller C, Michie S, Savage J, McAteer J, Besser S, Charlett A, et al. The Feedback Intervention Trial (FIT) – improving hand-hygiene compliance in UK healthcare workers: a stepped wedge cluster randomised controlled trial. PLOS ONE 2012;7. https://doi.org/10.1371/journal.pone.0041617.
- Gerber JS, Prasad PA, Fiks AG, Localio AR, Grundmeier RW, Bell LM, et al. Effect of an outpatient antimicrobial stewardship intervention on broad-spectrum antibiotic prescribing by primary care pediatricians a randomized trial. JAMA 2013;309:2345-52. https://doi.org/10.1001/jama.2013.6287.
- Gjelstad S, Fetveit A, Straand J, Dalen I, Rognstad S, Lindbaek M. Can antibiotic prescriptions in respiratory tract infections be improved? A cluster-randomized educational intervention in general practice–the Prescription Peer Academic Detailing (Rx-PAD) Study. BMC Health Serv Res 2006;6. https://doi.org/10.1186/1472-6963-6-75.
- Goff DC, Gu L, Cantley LK, Parker DG, Cohen SJ. Enhancing the quality of care for patients with coronary heart disease: the design and baseline results of the Hastening the Effective Application of Research Through Technology (HEART) trial. Am J Manag Care 2002;8:1069-78.
- Hayashino Y, Suzuki H, Yamazaki K, Goto A, Izumi K, Noda M. A cluster randomized trial on the effect of a multifaceted intervention improved the technical quality of diabetes care by primary care physicians: the Japan Diabetes Outcome Intervention Trial-2 (J-DOIT2). Diabet Med 2016;33:599-608. https://doi.org/10.1111/dme.12949.
- Heller RF, D’Este C, Lim LLY, O’Connell RL, Powell H. Randomised controlled trial to change the hospital management of unstable angina. Med J Aust 2001;174:217-21. https://doi.org/10.5694/j.1326-5377.2001.tb143238.x.
- Hemkens LG, Saccilotto R, Leon Reyes S, Glinz D, Zumbrunn T, Grolimund O, et al. Personalized prescription feedback using routinely collected data to reduce antibiotic use in primary care: a randomized clinical trial. JAMA Int Med 2017;177:176-83. https://doi.org/10.1001/jamainternmed.2016.8040.
- Herbert CP, Wright JM, Maclure M, Wakefield J, Dormuth C, Brett-MacLean P, et al. Better prescribing project: a randomized controlled trial of the impact of case-based educational modules and personal prescribing feedback on prescribing for hypertension in primary care. Fam Pract 2004;21:575-81. https://doi.org/10.1093/fampra/cmh515.
- Horbar JD, Carpenter JH, Buzas J, Soll RF, Suresh G, Bracken MB, et al. Collaborative quality improvement to promote evidence based surfactant for preterm infants: a cluster randomised trial. BMJ 2004;329. https://doi.org/10.1136/bmj.329.7473.1004.
- Houston TK, Sadasivam RS, Allison JJ, Ash AS, Ray MN, English TM, et al. Evaluating the QUIT-PRIMO clinical practice ePortal to increase smoker engagement with online cessation interventions: a national hybrid type 2 implementation study. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0336-8.
- Howe A. Detecting psychological distress: can general practitioners improve their own performance?. Br J Gen Pract 1996;46:407-10.
- Kaufman RM, Stanworth S, Taljaard M, Yazer MH, Reeves C, Delaney M, et al. Trial of feedback on blood use. Transfusion 2016;56.
- Kennedy CC, Ioannidis G, Thabane L, Adachi JD, Marr S, Giangregorio LM, et al. Successful knowledge translation intervention in long-term care: final results from the vitamin D and osteoporosis study (ViDOS) pilot cluster randomized controlled trial. Trials 2015;16. https://doi.org/10.1186/s13063-015-0720-3.
- Reynolds E, Shea J. Kogan . Effectiveness of report cards based on chart audits of residents adherence to practice guidelines on practice performance: a randomized controlled trial. Teach Learn Med 2003;15. https://doi.org/10.1207/S15328015TLM1501_06.
- Liddy C, Hogg W, Russell G, Wells G, Armstrong CD, Akbari A, et al. Improved delivery of cardiovascular care (IDOCC) through outreach facilitation: study protocol and implementation details of a cluster randomized controlled trial in primary care. Implement Sci 2011;6. https://doi.org/10.1186/1748-5908-6-110.
- Lim WY, Hss AS, Ng LM, John Jasudass SR, Sararaks S, Vengadasalam P, et al. The impact of a prescription review and prescriber feedback system on prescribing practices in primary care clinics: a cluster randomised trial. BMC Fam Pract 2018;19. https://doi.org/10.1186/s12875-018-0808-4.
- Mayne SL, duRivage NE, Feemster KA, Localio A, Grundmeier RW, Fiks AG. Effect of decision support on missed opportunities for human papillomavirus vaccination. Am J Prev Med 2014;47:734-44. https://doi.org/10.1016/j.amepre.2014.08.010.
- McClellan WM, Millman L, Presley R, Couzins J, Flanders WD. Improved diabetes care by primary care physicians: results of a group-randomised evaluation of the Medicare Health Care Quality Improvement Program (HCQIP). J Clin Epidemiol 2003;56:1210-7. https://doi.org/10.1016/S0895-4356(03)00198-7.
- McCluskey A, Ada L, Kelly PJ, Middleton S, Goodall S, Grimshaw JM, et al. A behavior change program to increase outings delivered during therapy to stroke survivors by community rehabilitation teams: The Out-and-About trial. Int J Stroke 2016;11:425-37. https://doi.org/10.1177/1747493016632246.
- McPhee SJ, Bird JA, Jenkins CN, Fordham D. Promoting cancer screening. A randomized, controlled trial of three interventions. Arch Internl Med 1989;149:1866-72. https://doi.org/10.1001/archinte.1989.00390080116025.
- Meeker D, Linder JA, Fox CR, Friedberg MW, Persell SD, Goldstein NJ, et al. Effect of behavioral interventions on inappropriate antibiotic prescribing among primary care practices a randomized clinical trial. JAMA 2016;315:562-70. https://doi.org/10.1001/jama.2016.0275.
- Metlay JP, Camargo CA, MacKenzie T, McCulloch C, Maselli J, Levin SK, et al. Cluster-randomized trial to improve antibiotic use for adults with acute respiratory infections treated in emergency departments. Ann Emerg Med 2007;50:221-30. https://doi.org/10.1016/j.annemergmed.2007.03.022.
- Mold JW, Fox C, Wisniewski A, Lipman PD, Krauss MR, Harris DR, et al. Implementing asthma guidelines using practice facilitation and local learning collaboratives: a randomized controlled trial. Ann Fam Med 2014;12:233-40. https://doi.org/10.1370/afm.1624.
- O’Connell DL, Henry D, Tomlins R. Randomised controlled trial of effect of feedback on general practitioners’ prescribing in Australia. BMJ 1999;318:7182-11. https://doi.org/10.1136/bmj.318.7182.507.
- O’Connor PJ, Sperl-Hillen J, Johnson PE, Rush WA, Crain AL. Customized feedback to patients and providers failed to improve safety or quality of diabetes care: a randomized trial. Diabetes Care 2009;32:1158-63. https://doi.org/10.2337/dc08-2247.
- Patel M, Kurtzman GW, Kannan S, Small D, Morris A, Honeywell S, et al. Effect of an automated patient dashboard using active choice and peer comparison performance feedback to physicians on statin prescribing: the pre-scribe randomized clinical trial. J Gen Intern Med 2018;33:174-5. https://doi.org/10.1001/jamanetworkopen.2018.0818.
- Pimlott NJ, Hux JE, Wilson LM, Kahan M, Li C, Rosser WW. Educating physicians to reduce benzodiazepine use by elderly patients: a randomized controlled trial. CMAJ 2003;168:835-9.
- Raasch BA, Hays R, Buettner PG. An educational intervention to improve diagnosis and management of suspicious skin lesions. J Contin Educ Health Prof 2000;20:39-51. https://doi.org/10.1002/chp.1340200108.
- Sandbaek A, Kragstrup J. Randomized controlled trial of the effect of medical audit on AIDS prevention in general practice. Fam Pract 1999;16:510-4. https://doi.org/10.1093/fampra/16.5.510.
- Soleymani F, Rashidian A, Dinarvand R, Kebriaeezade A, Hosseini M, Abdollahi M. Assessing the effectiveness and cost-effectiveness of audit and feedback on physician’s prescribing indicators. Value Health 2014;17. https://doi.org/10.1016/j.jval.2014.08.473.
- Søndergaard J, Andersen M, Vach K, Kragstrup J, Maclure M, Gram LF. Detailed postal feedback about prescribing to asthma patients combined with a guideline statement showed no impact: a randomised controlled trial. Eur J Clin Pharmacol 2002;58:127-32. https://doi.org/10.1007/s00228-002-0454-5.
- Søndergaard J, Andersen M, Støvring H, Kragstrup J. Mailed prescriber feedback in addition to a clinical guideline has no impact: a randomised, controlled trial. Scand J Prim Health Care 2003;21:47-51. https://doi.org/10.1080/02813430310000564.
- Stewardson AJ, Sax H, Gayet-Ageron A, Touveneau S, Longtin Y, Zingg W, et al. Enhanced performance feedback and patient participation to improve hand hygiene compliance of health-care workers in the setting of established multimodal promotion: a single-centre, cluster randomised controlled trial. Lancet Infect Dis 2016;16:1345-55. https://doi.org/10.1016/S1473-3099(16)30256-0.
- Thomas RE, Bernard Lewis C, Ramsay C, Eccles M, Grimshaw J. Effect of enhanced feedback and brief educational reminder messages on laboratory test requesting in primary care: a cluster randomised trial. Lancet 2006;367:1990-6. https://doi.org/10.1016/S0140-6736(06)68888-0.
- Tjia J, Field T, Mazor K, Lemay CA, Kanaan AO, Donovan JL, et al. Dissemination of evidence-based antipsychotic prescribing guidelines to nursing homes: a cluster randomized trial. J Am Geriatr Soc 2015;63:1289-98. https://doi.org/10.1111/jgs.13488.
- Trietsch J, van Steenkiste B, Grol R, Winkens B, Ulenkate H, Metsemakers J, et al. Effect of audit and feedback with peer review on general practitioners’ prescribing and test ordering performance: a cluster-randomised controlled trial. BMC Fam Pract 2017;18. https://doi.org/10.1186/s12875-017-0605-5.
- Verstappen W, van der Weijden T, Sijbrandij J, Smeele I, Hermsen J, Grimshaw J, et al. Effect of a practice-based strategy on test ordering performance of primary care physicians – a randomized trial. JAMA 2003;289:2407-12. https://doi.org/10.1001/jama.289.18.2407.
- Voorn V, Marang-van dMP, Hout A, Hofstede S, So-Osman C, Akker-van MM, et al. The effectiveness of a de-implementation strategy to reduce low-value blood management techniques in primary hip and knee arthroplasty: a pragmatic cluster-randomized controlled trial. Implement Sci 2017;12. https://doi.org/10.1186/s13012-017-0601-0.
- Wang Y, Li Z, Zhao X, Wang C, Wang X, Wang D, et al. Effect of a multifaceted quality improvement intervention on hospital personnel adherence to performance measures in patients with acute ischaemic stroke in China: a randomized clinical trial. JAMA 2018;320:245-54. https://doi.org/10.1001/jama.2018.8802.
- Watkins RS, Moran WP. Competency-based learning: the impact of targeted resident education and feedback on pap smear adequacy rates. J General Intern Med 2004;19:545-8. https://doi.org/10.1111/j.1525-1497.2004.30150.x.
- Winickoff RN, Coltin KL, Morgan MM, Buxbaum RC, Barnett GO. Improving physician performance through peer comparison feedback. Medical Care 1984;22:527-34. https://doi.org/10.1097/00005650-198406000-00003.
- Winslade N, Eguale T, Tamblyn R. Optimising the changing role of the community pharmacist: a randomised trial of the impact of audit and feedback. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010865.
- Young JM, D’Este C, Ward JE. Improving family physicians’ use of evidence-based smoking cessation strategies: a cluster randomization trial. Prev Med 2002;35:572-83. https://doi.org/10.1006/pmed.2002.1111.
Appendix 1 Search strategies
| Database | Number of results | Date of search |
|---|---|---|
| Ovid MEDLINE | 1486 | 23 July 2018 |
| Ovid EMBASE | 2134 | 24 July 2018 |
| HDAS CINAHL | 943 | 24 July 2018 |
| HDAS BNI | 286 | 24 July 2018 |
| Cochrane CENTRAL | 584 trials (1999 total) | 24 July 2018 |
| Ovid PsycINFO | 470 | 24 July 2018 |
| Web of Science | 2112, 2120 | 19 July 2018 and 30 July 2018 |
Database: Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations
Date range searched: 1946 to week 2 July 2018.
Date searched: 23 July 2018.
Search strategy
-
(anaesthetist* or anesthetist* or audiologist* or cardiologist* or chiropodist* or clinician* or consultant* or cadet* or counsellor* or dentist* or dermatologist* or dietician* or Doctor* or GP or GPs or gynaecologist* or gynecologist* or matron* or midwife or midwives or neurologist* or nurse* or nutritionist* or obstetrician* or oncologist* or optometrist* or orthodontist* or orthoptist* or orthotist* or osteopath* or paediatrician* or pediatrician* or paramedic* or pathologist* or pharmacist* or phlebotomist* or physician* or physiologist* or physiotherapist* or podiatrist* or practice manager* or practice staff or practitioner* or prosthetist* or psychiatrist* or psychologist* or psychotherapist* or radiographer* or radiologist* or registrar* or rheumatologist* or surgeon* or therapist* or urologist* or anesthesiologist* or prescriber* or sonographer*).ab,ti. (1,380,041)
-
exp Health Personnel/ (462,248)
-
exp CONSULTANTS/ (6476)
-
((ambulance or associate or audiology or cardiology or chiropody or clinical or dental or dermatology or family or gynaecology or gynecology or health or healthcare or “health care” or hospital or house or medical or midwifery or neurology or nursing or nutrition or obstetrics or oncology or optometry or orthodontic or paediatric* or pediatric* or pathology or pharmacy or physiology or physiotherapy or podiatry or psychiatry or psychology or “public health” or radiolog* or rheumatology or surgical or therapy or trainee or urology or respiratory or magnetic resonance imaging) adj2 (assistant* or cadet* or director* or manager* or officer* or personnel or practice or practitioner* or professional* or provider or receptionist* or resident* or scientist* or secretar* or specialist* or staff or technician* or technologist or visitor* or worker*)).ab,ti. (499,319)
-
1 or 2 or 3 or 4 (1,895,700)
-
benchmark*.ab,ti. (30,808)
-
((audit or monitoring or peer or performance or data or individualised or individualized or web or personalised or personalized or compar* or team or practitioner or practice or clinical or social) adj2 feedback).ab,ti. (6421)
-
FEEDBACK, PSYCHOLOGICAL/ (3122)
-
((social or descriptive or peer or subjective) adj2 (norm or norms)).ab,ti. (5654)
-
social influence.ab,ti. (1497)
-
Social Norms/ (747)
-
BENCHMARKING/ (12,165)
-
((social or peer*) adj2 comparison*).ab,ti. (1649)
-
social competition.ab,ti. (109)
-
social proof.ab,ti. (17)
-
image motivation.ab,ti. (8)
-
warm glow.ab,ti. (27)
-
((social or verbal or non-verbal or nonverbal or non verbal) adj2 (incentive or incentives or reward or rewards)).ab,ti. (637)
-
positive reinforcement.ab,ti. (1439)
-
“congratul*”.ab,ti. (505)
-
praise.ab,ti. (1720)
-
commendation.ab,ti. (68)
-
Reinforcement, Social/ (1036)
-
credible source.ab,ti. (100)
-
Peer Influence/ (273)
-
theory of planned behavio?r.ab,ti. (2518)
-
theory of reasoned action.ab,ti. (453)
-
theoretical domains framework.ab,ti. (249)
-
social cognitive theory.ab,ti. (1344)
-
“theory of normative social behavio?r*”.ab,ti. (21)
-
6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 (64,961)
-
randomized controlled trial.pt. (463,949)
-
controlled clinical trial.pt. (92,495)
-
“randomiz*”.ab,ti. (447,770)
-
“randomis*”.ab,ti. (89,649)
-
placebo.ab. (187,269)
-
Clinical Trials as Topic/ (184,102)
-
randomly.ab,ti. (288,777)
-
trial.ti. (180,410)
-
RCT.ab,ti. (15,807)
-
32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 (1,188,749)
-
exp Animals/ (21,630,632)
-
Humans/ (17,157,286)
-
42 not (42 and 43) (4,473,346)
-
41 not 44 (1,094,500)
-
5 and 31 and 45 (1486)
Database: Ovid EMBASE
Date range searched: 1974 to 3 July 2018.
Date searched: 24 July 2018.
Search strategy
-
(anaesthetist* or anesthetist* or audiologist* or cardiologist* or chiropodist* or clinician* or consultant* or cadet* or counsellor* or dentist* or dermatologist* or dietician* or Doctor* or GP or GPs or gynaecologist* or gynecologist* or matron* or midwife or midwives or neurologist* or nurse* or nutritionist* or obstetrician* or oncologist* or optometrist* or orthodontist* or orthoptist* or orthotist* or osteopath* or paediatrician* or pediatrician* or paramedic* or pathologist* or pharmacist* or phlebotomist* or physician* or physiologist* or physiotherapist* or podiatrist* or practice manager* or practice staff or practitioner* or prosthetist* or psychiatrist* or psychologist* or psychotherapist* or radiographer* or radiologist* or registrar* or rheumatologist* or surgeon* or therapist* or urologist* or anesthesiologist* or prescriber* or sonographer*).ab,ti. (1,960,089)
-
exp health care personnel/ (1,342,608)
-
((ambulance or associate or audiology or cardiology or chiropody or clinical or dental or dermatology or family or gynaecology or gynecology or health or healthcare or “health care” or hospital or house or medical or midwifery or neurology or nursing or nutrition or obstetrics or oncology or optometry or orthodontic or paediatric* or pediatric* or pathology or pharmacy or physiology or physiotherapy or podiatry or psychiatry or psychology or “public health” or radiolog* or rheumatology or surgical or therapy or trainee or urology or respiratory or magnetic resonance imaging) adj2 (assistant* or cadet* or director* or manager* or officer* or personnel or practice or practitioner* or professional* or provider or receptionist* or resident* or scientist* or secretar* or specialist* or staff or technician* or technologist or visitor* or worker*)).ab,ti. (679,603)
-
1 or 2 or 3 (2,881,143)
-
“benchmark*”.ab,ti. (36,669)
-
((audit or monitoring or peer or performance or data or individualised or individualized or web or personalised or personalized or compar* or team or practitioner or practice or clinical or social) adj2 feedback).ab,ti. (8968)
-
psychological feedback/ (148)
-
((social or descriptive or peer or subjective) adj2 (norm or norms)).ab,ti. (6586)
-
social influence.ab,ti. (1678)
-
social norm/ (1918)
-
benchmarking/ (2281)
-
((social or peer*) adj2 comparison*).ab,ti. (1938)
-
social competition.ab,ti. (114)
-
social proof.ab,ti. (18)
-
image motivation.ab,ti. (8)
-
warm glow.ab,ti. (36)
-
17 ((social or verbal or non-verbal or nonverbal or non verbal) adj2 (incentive or incentives or reward or rewards)).ab,ti. (786)
-
positive reinforcement.ab,ti. (1856)
-
“congratul* ”.ab,ti. (592)
-
praise.ab,ti. (1997)
-
commendation.ab,ti. (82)
-
credible source.ab,ti. (110)
-
peer pressure/ (1879)
-
theory of planned behavio?r.ab,ti. (2951)
-
theory of reasoned action.ab,ti. (485)
-
theoretical domains framework.ab,ti. (343)
-
social cognitive theory.ab,ti. (1564)
-
“theory of normative social behavio?r* ”.ab,ti. (19)
-
5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 (67,494)
-
randomized controlled trial/ (511,149)
-
“randomized controlled trial (topic)”/ (149,003)
-
controlled clinical trial/ (460,071)
-
“randomiz*”.ab,ti. (651,632)
-
“randomis*”.ab,ti. (134,394)
-
placebo.ab. (267,600)
-
“clinical trial (topic) ”/ (94,526)
-
randomly.ab,ti. (385,072)
-
trial.ti. (253,539)
-
RCT.ab,ti. (29,215)
-
30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 (1,652,219)
-
exp animal/ (24,606,612)
-
human/ (19,708,224)
-
41 not (41 and 42) (4,898,388)
-
40 not 43 (1,521,835)
-
4 and 29 and 44 (2134)
Database: Cumulative Index to Nursing and Allied Health Literature (searched via Healthcare Databases Advanced Search)
Date range searched: 1937 to July 2018.
Date searched: 24 July 2018.
Search strategy
-
(anaesthetist* OR anesthetist* OR audiologist* OR cardiologist* OR chiropodist* OR clinician* OR consultant* OR cadet* OR counsellor* OR dentist* OR dermatologist* OR dietician* OR Doctor* OR GP OR GPs OR gynaecologist* OR gynecologist* OR matron* OR midwife OR midwives OR neurologist* OR nurse* OR nutritionist* OR obstetrician* OR oncologist* OR optometrist* OR orthodontist* OR orthoptist* OR orthotist* OR osteopath* OR paediatrician* OR pediatrician* OR paramedic* OR pathologist* OR pharmacist* OR phlebotomist* OR physician* OR physiologist* OR physiotherapist* OR podiatrist* OR practice manager* OR practice staff OR practitioner* OR prosthetist* OR psychiatrist* OR psychologist* OR psychotherapist* OR radiographer* OR radiologist* OR registrar* OR rheumatologist* OR surgeon* OR therapist* OR urologist* OR anesthesiologist* OR prescriber* OR sonographer*).ti,ab (685,003)
-
exp “HEALTH PERSONNEL”/ (460,134)
-
exp CONSULTANTS/ (6768)
-
exp COUNSELORS/ (2836)
-
((ambulance OR associate OR audiology OR cardiology OR chiropody OR clinical OR dental OR dermatology OR family OR gynaecology OR gynecology OR health OR healthcare OR “health care” OR hospital OR house OR medical OR midwifery OR neurology OR nursing OR nutrition OR obstetrics OR oncology OR optometry OR orthodontic OR paediatric* OR pediatric* OR pathology OR pharmacy OR physiology OR physiotherapy OR podiatry OR psychiatry OR psychology OR “public health” OR radiolog* OR rheumatology OR surgical OR therapy OR trainee OR urology OR respiratory OR magnetic resonance imaging) ADJ2 (assistant* OR cadet* OR director* OR manager* OR officer* OR personnel OR practice OR practitioner* OR professional* OR provider OR receptionist* OR resident* OR scientist* OR secretar* OR specialist* OR staff OR technician* OR technologist OR visitor* OR worker*)).ti,ab (306,659)
-
(1 OR 2 OR 3 OR 4 OR 5) (1,102,321)
-
(benchmark*).ti,ab (7103)
-
((audit OR monitoring OR peer OR performance OR data OR individualised OR individualized OR web OR personalised OR personalized OR compar* OR team OR practitioner OR practice OR clinical OR social) ADJ2 feedback).ti,ab (4258)
-
((social OR descriptive OR peer OR subjective) ADJ2 (norm OR norms)).ti,ab (3664)
-
(“social influence”).ti,ab (647)
-
“SOCIAL NORMS”/ (777)
-
BENCHMARKING/ (6186)
-
((social OR peer*) ADJ2 comparison*).ti,ab (1032)
-
(“social competition”).ti,ab (6)
-
(“social proof”).ti,ab (14)
-
(“image motivation”).ti,ab (2)
-
(“warm glow”).ti,ab (8)
-
((social OR verbal OR non-verbal OR nonverbal OR non verbal) ADJ2 (incentive OR incentives OR reward OR rewards)).ti,ab (214)
-
(“positive reinforcement”).ti,ab (364)
-
(congratul*).ti,ab (754)
-
(praise).ti,ab (1230)
-
(commendation).ti,ab (78)
-
exp “REINFORCEMENT (PSYCHOLOGY)”/ (7087)
-
(“credible source”).ti,ab (35)
-
“PEER PRESSURE”/ (774)
-
(“theory of planned behavio?r”).ti,ab (746)
-
(“theory of reasoned action”).ti,ab (377)
-
(“theoretical domains framework”).ti,ab (186)
-
(“social cognitive theory”).ti,ab (1035)
-
(“theory of normative social behavio?r*”).ti,ab (0)
-
(“randomized controlled trial”).pt (83,342)
-
(“clinical trial”).pt (86,031)
-
(randomiz*).ti,ab (145,263)
-
(randomis*).ti,ab (36,299)
-
(placebo).ab (40,900)
-
exp “CLINICAL TRIALS”/ (241,787)
-
(randomly).ti,ab (64,596)
-
(trial).ti (80,310)
-
(RCT).ti,ab (13,964)
-
(33 OR 34 OR 35 OR 36 OR 37 OR 38 OR 39 OR 40 OR 41) (373,368)
-
exp ANIMALS/ (79,723)
-
HUMAN/ (1,706,502)
-
43 NOT (43 AND 44) (72,224)
-
42 NOT 45 (369,810)
-
(7 OR 8 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18 OR 19 OR 20 OR 21 OR 22 OR 23 OR 24 OR 25 OR 26 OR 27 OR 28 OR 29 OR 30 OR 31) (32,595)
-
(6 AND 46 AND 47) (943)
Database: British Nursing Index (searched via HDAS)
Date range searched: 2008 to July 2018.
Date searched: 24 July 2018.
Search strategy
-
(anaesthetist* OR anesthetist* OR audiologist* OR cardiologist* OR chiropodist* OR clinician* OR consultant* OR cadet* OR counsellor* OR dentist* OR dermatologist* OR dietician* OR Doctor* OR GP OR GPs OR gynaecologist* OR gynecologist* OR matron* OR midwife OR midwives OR neurologist* OR nurse* OR nutritionist* OR obstetrician* OR oncologist* OR optometrist* OR orthodontist* OR orthoptist* OR orthotist* OR osteopath* OR paediatrician* OR pediatrician* OR paramedic* OR pathologist* OR pharmacist* OR phlebotomist* OR physician* OR physiologist* OR physiotherapist* OR podiatrist* OR practice manager* OR practice staff OR practitioner* OR prosthetist* OR psychiatrist* OR psychologist* OR psychotherapist* OR radiographer* OR radiologist* OR registrar* OR rheumatologist* OR surgeon* OR therapist* OR urologist* OR anesthesiologist* OR prescriber* OR sonographer*).ti,ab (249,905)
-
“MEDICAL PERSONNEL”/ OR DENTISTS/ OR “NURSE PRACTITIONERS”/ OR NURSES/ OR “NURSING ASSISTANTS”/ OR PARAMEDICS/ OR PHARMACISTS/ OR “PHYSICIAN ASSISTANTS”/ OR PHYSICIANS/ OR “VISITING NURSES”/ OR “SCHOOL NURSES”/ OR “FAMILY PHYSICIANS”/ OR HOSPITALISTS/ OR SURGEONS/ OR “SURGEONS GENERAL”/ (90,414)
-
((ambulance OR associate OR audiology OR cardiology OR chiropody OR clinical OR dental OR dermatology OR family OR gynaecology OR gynecology OR health OR healthcare OR “health care” OR hospital OR house OR medical OR midwifery OR neurology OR nursing OR nutrition OR obstetrics OR oncology OR optometry OR orthodontic OR paediatric* OR pediatric* OR pathology OR pharmacy OR physiology OR physiotherapy OR podiatry OR psychiatry OR psychology OR “public health” OR radiolog* OR rheumatology OR surgical OR therapy OR trainee OR urology OR respiratory OR ‘magnetic resonance imaging’) ADJ2 (assistant* OR cadet* OR director* OR manager* OR officer* OR personnel OR practice OR practitioner* OR professional* OR provider OR receptionist* OR resident* OR scientist* OR secretar* OR specialist* OR staff OR technician* OR technologist OR visitor* OR worker*)).ti,ab (104,652)
-
(1 OR 2 OR 3) (315,078)
-
(benchmark*).ti,ab (1473)
-
((audit OR monitoring OR peer OR performance OR data OR individualised OR individualized OR web OR personalised OR personalized OR compar* OR team OR practitioner OR practice OR clinical OR social) ADJ2 feedback).ti,ab (788)
-
((social OR descriptive OR peer OR subjective) ADJ2 (norm OR norms)).ti,ab (554)
-
(“social influence”).ti,ab (80)
-
BENCHMARKS/ (124)
-
((social OR peer*) ADJ2 comparison*).ti,ab (120)
-
(“social competition”).ti,ab (0)
-
(“social proof”).ti,ab (5)
-
(“image motivation”).ti,ab (0)
-
(“warm glow”).ti,ab (1)
-
((social OR verbal OR non-verbal OR nonverbal OR ‘non verbal’) ADJ2 (incentive OR incentives OR reward OR rewards)).ti,ab (24)
-
(“positive reinforcement”).ti,ab (50)
-
(congratul*).ti,ab (146)
-
(praise).ti,ab (367)
-
(commendation).ti,ab (16)
-
(” credible source”).ti,ab (14)
-
“PEER RELATIONSHIPS”/ (111)
-
(“theory of planned behavio?r”).ti,ab (194)
-
(“theory of reasoned action”).ti,ab (63)
-
(“theoretical domains framework”).ti,ab (26)
-
(“social cognitive theory”).ti,ab (238)
-
(“theory of normative social behavio?r*”).ti,ab (0)
-
(“controlled clinical trial”).pt (103)
-
(“clinical trial”).pt (1993)
-
(randomiz*).ti,ab (10,533)
-
(randomis*).ti,ab (13,753)
-
(placebo).ab (4521)
-
“CLINICAL TRIALS”/ (11,795)
-
(randomly).ti,ab (7058)
-
(trial).ti (10,477)
-
(RCT).ti,ab (854)
-
(30 OR 31 OR 32 OR 33 OR 34 OR 35 OR 36 OR 37 OR 38) (36,001)
-
(5 OR 6 OR 8 OR 9 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18 OR 19 OR 20 OR 21 OR 22 OR 23 OR 24 OR 25 OR 26 OR 27 OR 28) (4166)
-
(4 AND 39 AND 40) (0) (Will not run on the hdas interface. Error occurs.)
-
(39 AND 40) (286) (As a compromise have run the ‘BCT’ terms and the RCT filter instead)
Database: Cochrane Central Register of Controlled Trials
Date range searched: up to July 2018.
Date searched: 24 July 2018.
Search strategy
-
#1. (anaesthetist* or anesthetist* or audiologist* or cardiologist* or chiropodist* or clinician* or consultant* or cadet* or counsellor* or dentist* or dermatologist* or dietician* or Doctor* or GP or GPs or gynaecologist* or gynecologist* or matron* or midwife or midwives or neurologist* or nurse* or nutritionist* or obstetrician* or oncologist* or optometrist* or orthodontist* or orthoptist* or orthotist* or osteopath* or paediatrician* or pediatrician* or paramedic* or pathologist* or pharmacist* or phlebotomist* or physician* or physiologist* or physiotherapist* or podiatrist* or practice manager* or practice staff or practitioner* or prosthetist* or psychiatrist* or psychologist* or psychotherapist* or radiographer* or radiologist* or registrar* or rheumatologist* or surgeon* or therapist* or urologist* or anesthesiologist* or prescriber* or sonographer*) (151,905)
-
#2. MeSH descriptor: [Health Personnel] explode all trees (8572)
-
#3. MeSH descriptor: [Consultants] explode all trees (38)
-
#4. ((ambulance or associate or audiology or cardiology or chiropody or clinical or dental or dermatology or family or gynaecology or gynecology or health or healthcare or “health care” or hospital or house or medical or midwifery or neurology or nursing or nutrition or obstetrics or oncology or optometry or orthodontic or paediatric* or pediatric* or pathology or pharmacy or physiology or physiotherapy or podiatry or psychiatry or psychology or “public health” or radiolog* or rheumatology or surgical or therapy or trainee or urology or respiratory or “magnetic resonance imaging”) adj2 (assistant* or cadet* or director* or manager* or officer* or personnel or practice or practitioner* or professional* or provider or receptionist* or resident* or scientist* or secretar* or specialist* or staff or technician* or technologist or visitor* or worker*)) (1579)
-
#5. #1 or #2 or #3 or #4 (154,716)
-
#6. benchmark* (1170)
-
#7. ((audit or monitoring or peer or performance or data or individualised or individualized or web or personalised or personalized or compar* or team or practitioner or practice or clinical or social) adj2 feedback) (466)
-
#8. MeSH descriptor: [Feedback, Psychological] this term only (471)
-
#9. ((social or descriptive or peer or subjective) adj2 (norm or norms)) (89)
-
#10. “social influence” (219)
-
#11. MeSH descriptor: [Social Norms] this term only (53)
-
#12. MeSH descriptor: [Benchmarking] this term only (122)
-
#13. ((social or peer*) adj2 comparison*) (866)
-
#14. “social competition” (3)
-
#15. “social proof” (3)
-
#16. “image motivation” (1)
-
#17. “warm glow” (1)
-
#18. ((social or verbal or non-verbal or nonverbal or “non verbal”) adj2 (incentive or incentives or reward or rewards)) (167)
-
#19. “positive reinforcement” (214)
-
#20. congratul* (39)
-
#21. praise (189)
-
#22. commendation (2)
-
#23. MeSH descriptor: [Reinforcement, Social] this term only (71)
-
#24. “credible source” (10)
-
#25. MeSH descriptor: [Peer Influence] this term only (18)
-
#26. “theory of planned behavio?r” (196)
-
#27. “theory of reasoned action” (70)
-
#28. “theoretical domains framework” (33)
-
#29. “social cognitive theory” (673)
-
#30. “theory of normative social behavio?r*” (0)
-
#31. #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 (4154)
-
#32. #5 and #31 (1999)
Database: Ovid PsycINFO
Date range searched: 1806 to week 3 July 2018.
Date searched: 24 July 2018.
Search strategy
-
(anaesthetist* or anesthetist* or audiologist* or cardiologist* or chiropodist* or clinician* or consultant* or cadet* or counsellor* or dentist* or dermatologist* or dietician* or Doctor* or GP or GPs or gynaecologist* or gynecologist* or matron* or midwife or midwives or neurologist* or nurse* or nutritionist* or obstetrician* or oncologist* or optometrist* or orthodontist* or orthoptist* or orthotist* or osteopath* or paediatrician* or pediatrician* or paramedic* or pathologist* or pharmacist* or phlebotomist* or physician* or physiologist* or physiotherapist* or podiatrist* or practice manager* or practice staff or practitioner* or prosthetist* or psychiatrist* or psychologist* or psychotherapist* or radiographer* or radiologist* or registrar* or rheumatologist* or surgeon* or therapist* or urologist* or anesthesiologist* or prescriber* or sonographer*).ab,ti. (475,811)
-
exp Health Personnel/ (125,953)
-
exp CLINICIANS/ (9108)
-
exp psychologists/ (30,765)
-
exp therapists/ (30,979)
-
exp counselors/ (12,843)
-
((ambulance or associate or audiology or cardiology or chiropody or clinical or dental or dermatology or family or gynaecology or gynecology or health or healthcare or “health care” or hospital or house or medical or midwifery or neurology or nursing or nutrition or obstetrics or oncology or optometry or orthodontic or paediatric* or pediatric* or pathology or pharmacy or physiology or physiotherapy or podiatry or psychiatry or psychology or “public health” or radiolog* or rheumatology or surgical or therapy or trainee or urology or respiratory or magnetic resonance imaging) adj2 (assistant* or cadet* or director* or manager* or officer* or personnel or practice or practitioner* or professional* or provider or receptionist* or resident* or scientist* or secretar* or specialist* or staff or technician* or technologist or visitor* or worker*)).ab,ti. (158,838)
-
1 or 2 or 3 or 4 or 5 or 6 or 7 (599,269)
-
“benchmark*”.ab,ti. (7399)
-
((audit or monitoring or peer or performance or data or individualised or individualized or web or personalised or personalized or compar* or team or practitioner or practice or clinical or social) adj2 feedback).ab,ti. (6239)
-
((social or descriptive or peer or subjective) adj2 (norm or norms)).ab,ti. (10,209)
-
social influence.ab,ti. (4465)
-
Social Norms/ (7479)
-
((social or peer*) adj2 comparison*).ab,ti. (4744)
-
social competition.ab,ti. (198)
-
social proof.ab,ti. (57)
-
image motivation.ab,ti. (10)
-
warm glow.ab,ti. (74)
-
((social or verbal or non-verbal or nonverbal or non verbal) adj2 (incentive or incentives or reward or rewards)).ab,ti. (1033)
-
positive reinforcement.ab,ti. (2681)
-
“congratul* ”.ab,ti. (1056)
-
praise.ab,ti. (3944)
-
commendation.ab,ti. (134)
-
Social Reinforcement/ (1531)
-
credible source.ab,ti. (96)
-
Peer Pressure/ (713)
-
theory of planned behavio?r.ab,ti. (4094)
-
theory of reasoned action.ab,ti. (1226)
-
theoretical domains framework.ab,ti. (48)
-
social cognitive theory.ab,ti. (2727)
-
“theory of normative social behavio?r* ”.ab,ti. (31)
-
9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 (53,015)
-
clinical trial.md. (21,174)
-
“randomiz* ”.ab,ti. (65,985)
-
“randomis* ”.ab,ti. (8914)
-
placebo.ab. (36,895)
-
Clinical Trials/ (10,978)
-
randomly.ab,ti. (66,420)
-
trial.ti. (26,281)
-
RCT.ab,ti. (3557)
-
33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 (167,864)
-
8 and 32 and 41 (470)
Database: Web of Science
Searching the following indexes:
-
Science Citation Index Expanded (1900 – present).
-
Social Sciences Citation Index (1900 – present).
-
Arts & Humanities Citation Index (1975 – present).
-
Conference Proceedings Citation Index- Science (1990 – present).
-
Conference Proceedings Citation Index- Social Science & Humanities (1990 – present).
-
Book Citation Index– Science (2005 – present).
-
Book Citation Index– Social Sciences & Humanities (2005 – present).
-
Emerging Sources Citation Index (2015 – present).
Date searched: 19 July and 30 July 2018.
Search strategy
| # | Results | Search terms |
|---|---|---|
| # 34 | 2112 |
#33 AND #26 AND #3 Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 33 | 1,359,758 |
#32 OR #31 OR #30 OR #29 OR #28 OR #27 Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 32 | 17,590 |
TS = RCT Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 31 | 353,646 |
TI = trial Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 30 | 338,102 |
TS = randomly Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 29 | 236,066 |
TS = placebo Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 28 | 92,236 |
TS = randomis* Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 27 | 746,089 |
TS = randomiz* Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 26 | 237,058 |
#25 OR #24 OR #23 OR #22 OR #21 OR #20 OR #19 OR #18 OR #17 OR #16 OR #15 OR #14 OR #13 OR #12 OR #11 OR #10 OR #9 OR #8 OR #7 OR #6 OR #5 OR #4 Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 25 | 1 |
TS = “theory of normative social behavio?r*” Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 24 | 3388 |
TS = “social cognitive theory” Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 23 | 329 |
TS = “theoretical domains framework” Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 22 | 1215 |
TS = “theory of reasoned action” Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 21 | 2173 |
TS = “theory of planned behavio?r” Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 20 | 1895 |
TS = “Peer influence” Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 19 | 139 |
TS = “credible source” Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 18 | 534 |
TS = “social reinforcement” Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 17 | 260 |
TS = commendation Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 16 | 9477 |
TS = “praise” Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 15 | 1232 |
TS = congratul* Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 14 | 1795 |
TS = “positive reinforcement” Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 13 | 1917 |
TS = ((social or verbal or non-verbal or nonverbal or “non verbal”) NEAR/2 (incentive or incentives or reward or rewards)) Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 12 | 460 |
TS = “warm glow” Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 11 | 26 |
TS = “image motivation” Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 10 | 66 |
TS = “social proof” Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 9 | 381 |
TS = “social competition” Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 8 | 5791 |
TS = ((social or peer*) NEAR/2 comparison*) Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 7 | 6870 |
TS = “social influence’ Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 6 | 15,835 |
TS = ((social or descriptive or peer or subjective) NEAR/2 (norm or norms)) Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 5 | 19,569 |
TS = ((audit or monitoring or peer or performance or data or individualised or individualized or web or personalised or personalized or compar* or team or practitioner or practice or clinical or social) NEAR/2 feedback) Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 4 | 167,874 |
TS = benchmark* Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 3 | 1,755,025 |
#2 OR #1 Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 2 | 583,153 |
TS = ((ambulance or associate or audiology or cardiology or chiropody or clinical or dental or dermatology or family or gynaecology or gynecology or health or healthcare or “health care” or hospital or house or medical or midwifery or neurology or nursing or nutrition or obstetrics or oncology or optometry or orthodontic or paediatric* or pediatric* or pathology or pharmacy or physiology or physiotherapy or podiatry or psychiatry or psychology or “public health” or radiolog* or rheumatology or surgical or therapy or trainee or urology or respiratory or “magnetic resonance imaging”) NEAR/2 (assistant* or cadet* or director* or manager* or officer* or personnel or practice or practitioner* or professional* or provider or receptionist* or resident* or scientist* or secretar* or specialist* or staff or technician* or technologist or visitor* or worker*)) Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
| # 1 | 1,399,895 |
TS = (anaesthetist* or anesthetist* or audiologist* or cardiologist* or chiropodist* or clinician* or consultant* or cadet* or counsellor* or dentist* or dermatologist* or dietician* or Doctor* or GP or GPs or gynaecologist* or gynecologist* or matron* or midwife or midwives or neurologist* or nurse* or nutritionist* or obstetrician* or oncologist* or optometrist* or orthodontist* or orthoptist* or orthotist* or osteopath* or paediatrician* or pediatrician* or paramedic* or pathologist* or pharmacist* or phlebotomist* or physician* or physiologist* or physiotherapist* or podiatrist* or practice manager* or practice staff or practitioner* or prosthetist* or psychiatrist* or psychologist* or psychotherapist* or radiographer* or radiologist* or registrar* or rheumatologist* or surgeon* or therapist* or urologist* or anesthesiologist* or prescriber* or sonographer*) Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI Timespan = All years |
Appendix 2 The SOCIAL systematic review: screening instructions
Title and abstracts
-
1a. All studies will be ordered by title. To be included, a paper has to meet all of the inclusion criteria outlined below. If in any doubt, include the paper into the next stage of full-stage screening for a more detailed examination.
-
Study type: the review includes RCTs, including a range of designs (cluster, factorial, parallel, crossover and stepped wedge).
-
If the title/abstract says ‘randomised’ and no further information – include.
-
If the title/abstract states e.g. ‘allocated’ or ‘assigned to groups’ – include.
-
If in any doubt about whether or not it is a RCT – include.
-
-
Population:
-
health workers responsible for patient care in a health-care setting
-
health workers in training will be included (but only if they are in a health-care setting, not in a campus environment).
-
-
Intervention:
-
Aims to change clinical behaviour of health workers. Clinical behaviour here is defined as any behaviour that is carried out within a (non-simulated) clinical environment/setting.
-
A social norms intervention:
-
A social norms intervention seeks to change the clinical behaviour of a target health worker by exposing them to the values, beliefs, attitudes or behaviours of a reference group or person. The intervention could be either descriptive norms or injunctive norms based.
-
A descriptive norms message provides the target with information about the behaviour of the reference person/others in the reference group. Examples inlcude:
-
giving the target information about the behaviour of a reference person or group
-
comparison of the target’s behaviour with the behaviours of a reference person or group.
-
-
An injunctive norms message provides the target with information about the values, beliefs or attitudes of the reference person/group, conveying social approval or disapproval.
-
Providing the target with information about whether or not the behaviour has the approval/disapproval of the reference group or person.
-
Exposure of the target’s behaviour to a reference group.
-
Offer to expose the target’s behaviour to a reference group.
-
Praise, commendation, applause or thanks from a reference group or person.
-
Promise of praise, commendation, applause or thanks from a reference group or person.
-
-
-
-
-
1b. Any papers (e.g. protocols and process evaluations) linked to trials that are not the main trial paper but fulfil the criteria outlined above will also be included and kept in a separate folder on Covidence (see 2 below), to flag that the main trials for these papers need to be located and further examined at full-text screening.
Any relevant systematic reviews identified at the title and abstract stage will also be kept in a folder on Covidence to identify any other relevant studies that may be eligible for inclusion into the present review.
-
2. The review will be set up in Covidence (www.covidence.org): an online screening and data extraction tool for systematic reviews.
-
All of the references generated from the database searches will have any duplicates removed and be imported into Covidence. All of these references will be displayed in ‘Screen references’ under ‘Title and abstract screening’.
-
As per the protocol, one reviewer (MYT) will independently screen all of the titles and abstracts. Under ‘Review settings’, the number of ‘Reviewers required for screen’ will be ‘1’.
-
In the first instance, SC/JW/SR will also double screen ‘X number/proportion’ of studies. These will be randomly selected using a random integer generator (www.random.org; accessed 1 September 2020).
-
A second reviewer (JW) will screen a sample of 20% of the records. These will be randomly selected using a random integer generator (www.random.org; accessed 1 September 2020).
-
All of the inclusion criteria outlined in (1) will be added to Covidence, so will be shown at the top of the page as reminders of the criteria that need to be fulfilled to be included to the next stage of full-text stage screening.
-
A decision will be made for each paper by selecting ‘No’, ‘Maybe’ or ‘Yes’ on Covidence next to the paper.
-
Full-text screening
-
All studies should be ordered by title on Covidence. To be included, a paper has to meet all of the inclusion criteria outlined below:
-
Study type: RCT (cluster, factorial, parallel, crossover and stepped wedge).
-
Population:
-
Health workers responsible for patient care in a health-care setting.
-
Health workers in training will be included (but only if they are in a health-care setting, not in a simulated or campus environment).
-
-
Intervention:
-
Aims to change clinical behaviour of health workers. Clinical behaviour here is defined as any behaviour that is carried out within a (non-simulated) clinical environment/setting.
-
A social norms intervention:
-
A social norms intervention seeks to change the clinical behaviour of a target health worker by exposing them to the values, beliefs, attitudes or behaviours of a reference group or person. The intervention could be either descriptive norms or injunctive norms based.
-
A descriptive norms message provides the target with information about the behaviour of the reference person/others in the reference group. Examples include:
-
giving the target information about the behaviour of a reference person or group
-
comparison of the target’s behaviour with the behaviours of a reference person or group.
-
-
An injunctive norms message provides the target with information about the values, beliefs or attitudes of the reference person/group, conveying social approval or disapproval.
-
providing the target with information about whether or not the behaviour has the approval/disapproval of the reference group or person
-
exposure of the target’s behaviour to a reference group
-
offer to expose the target’s behaviour to a reference group
-
praise, commendation, applause or thanks from a reference group or person.
-
promise of praise, commendation, applause or thanks from a reference group or person.
-
-
We anticipate that the reference person or group could include:
-
people with the same profession or occupation as the target
-
people employed by the same organisation (unit of employment) as the target
-
people who deliver, administer, manage, commission or make policy on health services
-
professional bodies such as royal colleges, trade unions.
-
-
-
-
Appendix 3 Stage one data extraction guidance
| Section | Field | Notes | Codes |
|---|---|---|---|
| Identification | Setting | 1 Primary (GP and general practice nurses) | |
| 2 Hospital: inpatient | |||
| 3 Hospital: outpatient | |||
| 4 Mental health | |||
| 5 Community (district nursing, pharmacy, opticians, podiatry) | |||
| 6 Care/nursing home | |||
| 7 Other | |||
| If other add free text | |||
| Country | Free text | ||
| Methods | Design | For stepped wedge choose ‘other’ and enter ‘stepped wedge’ | |
| Most trials in this review can be considered cluster randomised – and the most important bit of information is the unit of allocation that is captured elsewhere; however, we need to be consistent. For a trial in which the unit of allocation is the health worker and data are collected at a patient level, we should class the trial as ‘cluster randomised’ | |||
| Unit of allocation | |||
| Primary outcome | Describe selected behaviour compliance outcome | ||
| Secondary outcomes | Describe selected patient outcome | ||
| Time points | List all reported, including baseline, in months since randomisation (for compliance with target behaviour) | ||
| Statistical analysis | Brief description of statistical analysis, including any adjustment for clustering. Note any problems/errors | ||
| Population | Target behaviour (short summary) | 1 Prescribing | |
| 2 Hand-washing | |||
| 3 Test ordering | |||
| 4 Referrals | |||
| 5 Other | |||
| 6 Unclear | |||
| If other add free text after the number | |||
| Target behaviour (full) | Add free-text description, as described in the paper, e.g. ‘Prescribing of antibiotics’ | ||
| Total number randomised | Report the number of patients and number of health workers | ||
| Type of health worker | The profession of the person who was the target of the intervention | 1 Nurse | |
| 2 Doctor: GP | |||
| 3 Doctor: secondary care | |||
| 4 Pharmacist | |||
| 5 AHP | |||
| 6 Other | |||
| If other add free text after the number | |||
| Interventions | Number of participants randomised to group | Both patients and health professionals where relevant | |
| Number of clusters randomised to group | Only cluster RCTs | ||
| Description |
Copy and paste ALL details given by the authors about the intervention. Please include details from any of the study papers Flag or paste link(s) to supplementary material(s), where appropriate |
||
| Type of control | 6 Variation of SN | ||
| 7 Usual practice | |||
| 8 Attention control | |||
| 9 Concomitant intervention | |||
| 10 Unsure | |||
| 11 Other (add details) | |||
| Outcomes | See note below on extracting outcomes | ||
| Use ‘add note’ to add extra information e.g. ICC, adjusted values | |||
| Choose time point closest to 6 months | |||
| Quality Assessment | See Cochrane Handbook, chapter 836 | Please use ‘other sources of bias’ to make a judgement on methods of analysis in the case of cluster RCTs | |
| Rate risk of bias (note 2 below) in relation to compliance with target behaviour | |||
| See also section 16.3.2 of the Cochrane Handbook ‘Assessing risk of bias in cluster-randomised trials’36 |
Aim: standardised mean difference and standard error (adjusted for clustering if necessary).
| Scenario | What to extract | Aim |
|---|---|---|
| Scenario 1: individually randomised, numerical outcome | Extract mean and standard deviation by group | Calculate SMD and standard error in Stata |
| Scenario 2: individually randomised, binary outcome | Extract number having event and totals by group | SMD=3πlnORStandard error SMD = √3/π × standard error log OR |
| Scenario 3: cluster randomised, numerical outcome | Extract mean and standard deviation by group. Extract detail required to calculate ‘design effect’ – e.g. ICC, adjusted and unadjusted standard errors |
Calculate SMD and standard error in Stata Multiply standard error by the variance inflation factor |
| Scenario 4: cluster randomised, binary outcome | Extract number having event and totals by group. Extract detail required to calculate ‘design effect’ – e.g. ICC, adjusted and unadjusted standard errors |
Calculate SMD and standard error as above Multiply standard error by the variance inflation factor |
where M is average cluster size.
Where ICC is not given, either (a) use ICC from a similar study or (b) use ratio of adjusted/unadjusted standard errors to estimate the variance inflation factor.
(See section 16.3.6 of Cochrane Handbook.)36
Appendix 4 Stage three data extraction form (with guidance provided to the data extractors)
Use –1 throughout for not applicable and –2 for not reported
Only code arms that have social norms as part of the intervention: code any arms without social norms as –1 throughout.
| Section | Field | Notes | Codes |
|---|---|---|---|
| Trial information | 1. Does inclusion criteria target participants based on low target performance? | 0. No | |
| 1. Yes | |||
| 9. Unclear | |||
| Intervention information | 2. Frequency and intensity of intervention | Mixed total of all the times that any social norm element of the intervention was delivered | 1. Once only |
| 2. Twice | |||
| 3. More than twice | |||
| 9. Unclear/not reported | |||
| 3. Format | Focus on the social norm elements |
|
|
| 4. Source of the intervention (i.e. the person delivering the intervention) | Focus on the social norm elements. If the source is unclear, err on the side of interpreting this as the investigator |
|
|
| 5. Is the person delivering the intervention internal or external to the target person’s organisation? | Focus on the social norm elements. If the source is the investigator, assume this is external unless says otherwise | 1. Internal | |
| 2. External | |||
| 9. Unclear/not reported | |||
| 6. Reference group/person |
Group/person used as (a) the comparison (social comparison) or (b) source of approval (other BCTs) If the intervention includes more than one type of social norm and the reference groups are different, code as ‘multiple’ If researchers intervene with one person and then that person intervenes with HCPs, code as that person |
1. Peer | |
| 2. Professional body | |||
| 3. Senior person (e.g. manager, policy-maker, commissioner) | |||
| 4. Patient(s) | |||
| 5. Other | |||
| 6. Multiple | |||
| 9. Unclear/not reported | |||
| If other add free text | |||
| Does the author explicitly describe this as SN? | 0. No | ||
| 1. Yes | |||
| Direction of change in behaviour that is desired |
|
Appendix 5 Behaviour change techniques coding template form
| Target population: | |||
|---|---|---|---|
| Target behaviour: | |||
| Arm | MYT BCTs | Initials BCTs | Final agreed BCTs |
|
Control (Name) |
|||
| If guidelines present |
Guideline unspecified (delete as appropriate): Yes/No (list BCTs below) Guideline BCTs (list): |
Guideline unspecified (delete as appropriate): Yes/No (list BCTs below) | Guideline unspecified (delete as appropriate): Yes/No (list BCTs below) |
|
Intervention 1 (Name) |
|||
| If guidelines present |
Guideline unspecified (delete as appropriate): Yes/No (list BCTs below) Guideline BCTs (list): |
Guideline unspecified (delete as appropriate): Yes/No (list BCTs below) | Guideline unspecified (delete as appropriate): Yes/No (list BCTs below) |
| Section | Field | Notes | Codes (delete as appropriate) |
| Methods | Type of comparison |
Type 1 SN vs. any control This could be social norm vs. current practice, social norm vs. nothing, social norm vs. a non-social norm BCT Type 2 SN + X vs. X This is any trial where it is the social norms element that is being tested E.g. social comparison with audit vs. audit alone E.g. credible source with education vs. education alone Type 3 SN + X vs. any control This is any trial where the social norms element packaged with other BCTs is being tested E.g. social norms with education and audit vs. usual practice E.g. multifaceted intervention with social norms element v nothing Type 4 Either two different social norm interventions or the same social norm interventions packaged in different ways E.g. social comparison vs. social reward Social comparison via e-mail vs. social comparison face to face Type 5 The social comparison element is identical in each arm, but the other interventions differ E.g. social comparison with reminders vs. social comparison without reminders E.g. credible source with education vs. credible source without education |
|
| Interventions | Does the author explicitly describe this as SN? | 0 No | |
| 1 Yes | |||
| Is SN a substantial part (type 3 above)? | 0 No | ||
| 1 Yes | |||
| 2 Unsure | |||
| Concomitant intervention (type 2, 3 or 5 above) | 0 No | ||
| 1 Yes | |||
| Direction of change in behaviour that is desired |
|
||
Appendix 6 Behaviour change technique coding decision log
It was agreed that all coders would do the following.
Code academic detailing as 3.1. social support (unspecified). We found that ‘academic detailing’ appeared quite frequently, and often its precise content was not specified. We agreed to treat academic detailing like other ‘packages’ in the BCT taxonomy v1 that are not well defined (e.g. cognitive–behavioural therapy or counselling) and code it as ‘social support (unspecified)’. This is based on the idea that the health professional is getting some unspecified support, but we cannot precisely pin it down. If the paper included a detailed description of the content of the academic detailing we added other BCT codes, if indicated. We discussed this with Marie Johnson, member of our steering committee, and author of the BCT taxonomy v1.
Guidelines were coded for BCTs, as with other text describing interventions. If BCTs could not be identified within guidelines, these were coded as ‘Guidelines (unspecified)’.
Where health workers were provided with a list of patients for the purpose of prompting them to a clinical behaviour (e.g. a list of patients with high blood pressure and not on recommended medication), these were coded as 7.1. prompts/cues.
Forced choices (such as when a GP gets a pop-up box when trying to prescribe antibiotics and has to choose between specified options) were coded as 7.1. prompts/cues.
Continuing medical educational credits were not coded as 10.3. non-specific reward unless there was evidence that the credits are contingent on progress towards performing the behaviour (e.g. rather than completion of educational modules).
Appendix 7 Inter-rater agreement for behaviour change technique coding (PABAK)
| BCT label (ordered according to frequency) | N in which BCT was present across the included unique armsa | PABAK | 95% CI |
|---|---|---|---|
| Social norm BCTs | |||
| 6.2. Social comparison | 117 | 0.92 | 0.87 to 0.97 |
| 9.1. Credible source | 24 | 0.83 | 0.76 to 0.91 |
| 6.3. Information about others’ approval | 10 | 0.96 | 0.92 to 1.00 |
| 10.4. Social reward | 5 | 0.97 | 0.93 to 1.00 |
| 10.5. Social incentive | 1 | 0.99 | 0.97 to 1.00 |
| All other identified BCTs (present at least once) | |||
| 2.2. Feedback on behaviour | 130 | 0.79 | 0.71 to 0.87 |
| 4.1. Instruction on how to perform the behaviour | 48 | 0.65 | 0.55 to 0.75 |
| 3.1. Social support (unspecified) | 41 | 0.83 | 0.75 to 0.90 |
| 7.1. Prompts/cues | 29 | 0.79 | 0.71 to 0.87 |
| 5.1. Information about health consequences | 26 | 0.80 | 0.72 to 0.88 |
| 1.2. Problem-solving | 17 | 0.86 | 0.79 to 0.93 |
| 12.5. Adding objects to the environment | 14 | 0.88 | 0.82 to 0.94 |
| 1.1 Goal-setting (behaviour) | 10 | 0.91 | 0.85 to 0.97 |
| 2.7. Feedback on outcome(s) of behaviour | 10 | 0.87 | 0.80 to 0.93 |
| 6.1. Demonstration of the behaviour | 6 | 0.97 | 0.93 to 1.00 |
| 8.1. Behavioural practice/rehearsal | 5 | 0.98 | 0.96 to 1.00 |
| 1.3. Goal-setting (outcome) | 4 | 0.95 | 0.91 to 0.99 |
| 1.4. Action planning | 4 | 0.91 | 0.86 to 0.97 |
| 2.3. Self-monitoring of behaviour | 4 | 0.93 | 0.88 to 0.98 |
| 12.1. Restructuring the social environment | 3 | 0.98 | 0.96 to 1.00 |
| 12.2. Restructuring the social environment | 3 | 0.97 | 0.93 to 1.00 |
| 5.3. Information about social and environmental consequences | 3 | 0.98 | 0.96 to 1.00 |
| 1.7. Review outcome goal(s) | 2 | 0.97 | 0.93 to 1.00 |
| 10.1. Material incentive (behaviour) | 2 | 0.98 | 0.96 to 1.00 |
| 2.1. Monitoring of behaviour by others without feedback | 2 | 0.96 | 0.92 to 0.99 |
| 9.2. Pros and cons | 2 | 0.97 | 0.94 to 1.00 |
| 1.9. Commitment | 1 | 0.99 | 0.97 to 1.00 |
| 10.3. Non-specific reward | 1 | 0.98 | 0.96 to 1.00 |
| 2.5. Monitoring of behaviour without feedback | 1 | Ratings do not vary | |
| 3.2. Social support (practical) | 1 | 0.97 | 0.93 to 1.00 |
| 8.2. Behaviour substitution | 1 | 0.99 | 0.97 to 1.00 |
Appendix 8 Formula for converting binary outcomes to standardised mean differences
Appendix 9 Methods used to calculate standardised mean difference and standard error, where appropriate
| Scenario | What was extracted | Method |
|---|---|---|
| Scenario 1: cluster randomised, numerical outcome |
Mean and standard deviation by group Detail required to calculate ‘design effect’ – e.g. ICC |
Calculate SMD and standard error Multiply standard error by the variance inflation factor to account for clustering |
| Scenario 2: cluster randomised, binary outcome |
Number having event and totals by group Detail required to calculate ‘design effect’ – e.g. ICC |
SMD=3πln ORStandard error SMD = √3/π × standard error log OR Multiply standard error by the variance inflation factor to account for clustering |
where M is average cluster size.
Variance inflation factor = square root of design effect.
(See section 16.3.6 of Cochrane Handbook.)36
Appendix 10 Comparisons used in the analysis for research question 1
| Scenario | Interventions | Controls | |
|---|---|---|---|
| 1 | Social norm intervention | vs. | Any control |
| 2 | Social norm intervention + X | vs. | X |
| 3 | Social norm intervention + X | vs. | Any control |
Appendix 11 Predictor variables to be included in the metaregression
| Covariate | Parameterisation |
|---|---|
| Social intervention techniques | |
| Social comparison | Binary (0 = No, 1 = Yes) |
| Information about others’ approval | Binary (0 = No, 1 = Yes) |
| Credible source | Binary (0 = No, 1 = Yes) |
| Social incentive | Binary (0 = No, 1 = Yes) |
| Social reward | Binary (0 = No, 1 = Yes) |
| Timing of outcome measurement | Continuous (months) |
| Who delivers the intervention? | |
| Internal | Categorical variable (it may be necessary to combine categories depending on frequencies of each in the data set) |
| External | |
| Unclear | |
| Frequency of intervention | |
| Once | Categorical variable |
| More than once | |
| Format of the intervention | |
| Active (e.g. face to face, telephone) | Categorical variable |
| Inactive (e.g. e-mail, letter) | |
| Mixed | |
| Not clear | |
| Type of health worker | Categorical variable |
| Type of behaviour | |
| Prescribing | Categorical |
| Hand-washing | |
| Test ordering | |
| Referrals | |
| Other/mixed | |
| Baseline performance | Continuous (proportion meeting standard) |
| Concomitant interventions | |
| None | Categorical |
| Other BCT | |
| Other active | |
| Direction of change required | |
| Increase | Categorical |
| Decrease | |
| Maintenance | |
| Unclear | |
| Control group | |
| None/usual care | Categorical |
| Attentional control | |
| Active control | |
| Other BCT | |
| Risk of bias | |
| Low risk | Categorical |
| Unclear risk | |
| Reference group | |
| Health-care worker | Categorical |
| Other | |
| Who is intervention directed at: | |
| Individual | Categorical |
| Team | |
| Unclear | |
Appendix 12 Summary of the first patient and public involvement workshop, August 2018
| Summary of PPI discussion | How suggestions were addressed |
|---|---|
| Doctors may be influenced by feedback from their peers on best practice, but they often they will not listen to patients when they present potential best practice (example given of a relative who had better care in Australia, but the doctor in the UK did not want to hear about it). Patients can have a role, e.g. by reminding health workers to wash their hands or by telling the GP that they do not expect to be prescribed antibiotics for a cold | If studies included patients as a reference group, we recorded that and considered whether it was effective |
| Social norms feedback could come from within the same organisation, within the region or from a wider national source. If health workers get feedback from only their own organisation, it may mean that they are not being exposed to current best practice and innovation from elsewhere | We recorded the source of the feedback, and considered which sources are the most effective |
| In medical school, future doctors are exposed to the most up-to-date ideas, but after that they may learn only about the practices that are adopted locally | |
| We may expect to see differences in the results of the feedback if it is given by a peer at the same level or one from a higher level/more experienced | |
| When providing social norms feedback it is important that there is benchmarking against good practice: do not want to change behaviour unless it will lead to patient benefit. There is no use in telling health workers about the behaviour of their peers unless either (a) there is already evidence that the behaviour is known to lead to positive outcomes for patients or (b) the outcome for patients will be measured |
We recorded whether or not the social norms intervention is accompanied by provision of information (but were unable to assess whether or not the information is evidence based) We reported what proportion of studies reported on patient outcomes and assessed whether or not social norms interventions are effective on patient outcomes |
| Any change in behaviour will be most effective if it is long term, not just short term | We have not been able to consider long-term effects |
| Will the review include studies involving volunteers, as well as paid health-care workers? | We included volunteers if they were involved in providing health care in a health-care setting |
Appendix 13 Studies that have no suitable outcome data
| Study (first author and year) | Description of study | Issue with the outcome data |
|---|---|---|
| Bar-Zeev 201746 | Stepped-wedge cluster trial examining the effect of a complex intervention involving social comparison compared with usual care on health providers’ management of smoking during pregnancy |
We located the main trial results paper,109 a stepped-wedge trial that did not report the control and intervention phases separately, so the trial outcomes were not a controlled test of the intervention |
| Brunette 201548 | Cluster RCT examining whether face-to-face or video delivery of a combined educational outreach and social comparison is more effective in increasing prescriptions for smoking cessation among prescribers | The mean difference at 6 months can be read from a graph, but neither the n nor the SD were clearly reported, so not usable |
| Colon-Emeric 201349 | Cluster RCT examining whether or not social comparison with social support (unspecified) is more effective than usual care in promoting falls-prevention behaviour among nursing home workers | The outcome was not reported in sufficient detail; the only information is that baseline scores improved for all groups combined, with no significant difference between intervention and control facilities |
| Forrest 201350 | Factorial cluster RCT comparing the effect of social comparison and ‘clinical decision support’ on adherence to treatment guidelines by physicians | This was a factorial study that was not reported appropriately. We were unable to extract reliable outcome data: there may be a mistake in the headings in table 3. Percentage difference between groups is reported. There are unit of analysis issues |
| Hampshire 199951 | Cluster RCT comparing the effect of social comparison with or without problem-solving on the provision of child health surveillance in primary care | No useful numerical results reported |
| Wadland 200752 | Cluster RCT comparing the effect of social comparison with prompts and cues on referral to a smoking cessation quit line by primary care physicians | No useful numerical results reported |
| Michael 201847 | RCT examining the effect of social comparison compared with usual care on prescription of opioids by emergency medicine physicians | Results not presented by intervention and control group |
| Paul 201754 | Cluster RCT examining the effect of social comparison with social support (unspecified) compared with usual care on management of diabetes by GPs | The trial was discontinued because of a lack of response from GPs |
| Szczepura 199455 | Cluster RCT testing the effect of different ways of presenting feedback (including social comparison) on immunisation and prevention behaviours in general practice | No numerical results reported on health worker behaviour or patient outcomes |
| Wattal 201553 | Cluster RCT testing the effect of social comparison on prescribing of antibiotics by hospital doctors | Table 1 is the average dose at all measurement periods (pre and post) so it does not show the effect of the intervention. Table 2 does show the effect, but it is divided into subgroups. We considered combining the subgroups and taking the mean immediately prior to intervention and mean 6 months later, but there was also no SD |
Appendix 14 Study and intervention characteristics of each included comparison
| Study (first author and year) | Study characteristics | Intervention characteristics | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Country | Setting | Type of health worker | Target behaviour | Type of trial | Low target performance? | Format | Frequency | Source | Internal/external delivery | Reference group | BCTs | Direction of change | |
| Aspy 200895 | USA | Primary | Doctor: GP | Tests | Cluster RCT | No | Mixed | More than twice | Investigator | External | Peer | SC and other BCTs | Increase |
| Awad 2006110 Arm A | Other/multiple | Primary | Mixed or team | Prescribing | RCT | No | Unclear/not reported | Only once | Unclear/not reported | Unclear/not reported | Peer | SC | Increase |
| Awad 2006110 Arm B | Other/multiple | Primary | Mixed or team | Prescribing | RCT | No | Unclear/not reported | Only once | Unclear/not reported | Unclear/not reported | Peer | SC and other BCTs | Increase |
| Baker 199773 | UK | Primary | Doctor: GP | Management/communication regarding condition | Cluster RCT | No | Unclear/not reported | Only once | Unclear/not reported | Unclear/not reported | Peer | SN in both arms | Increase |
| Barnett 2014111 Arm A | UK | Primary | Doctor: GP | Prescribing | Cluster RCT | No | More than twice | Investigator | Unclear/not reported | Multiple | SC and CS | Increase | |
| Barnett 2014111 Arm B | UK | Primary | Doctor: GP | Prescribing | Cluster RCT | No | More than twice | Investigator | Unclear/not reported | Multiple | Multiple SNs and other BCTs | Increase | |
| Baskerville 200166 | Canada | Primary | Doctor: GP | Management/communication regarding condition | RCT | No | Mixed | Unclear/not reported | Unclear/not reported | Unclear/not reported | Unclear/not reported | CS and other BCTs | Increase |
| Beck 200586 | Canada | Hospital | Other HCP | Prescribing | Cluster RCT | No | Written | Only once | Investigator | Unclear/not reported | Unclear/not reported | SC | Increase |
| Beidas 2017112 | USA | Community | Other HCP | Prescribing | RCT | No | Only once | Supervisor or senior colleague | Internal | Senior person | SR | Increase | |
| Bentz 200787 | USA | Primary | Mixed or team | Management/communication regarding condition | Cluster RCT | No | Written | More than twice | Investigator | Internal | Peer | SC | Increase |
| Bhatia 2017113 | Other/multiple | Mixed | Mixed or team | Tests | Cluster RCT | No | Mixed | More than twice | Investigator | External | Peer | SC | Decrease |
| Bhattacharyya 2010114 | Canada | Mixed | Mixed or team | Prescribing | Cluster RCT | No | Unclear/not reported | Unclear/not reported | Investigator | Internal | Peer | SC | Increase |
| Billue 201298 | USA | Primary | Doctor: GP | Prescribing | Cluster RCT | No | Separate computerised | Twice | Investigator | External | Peer | SC and other BCTs | Increase |
| Boet 201888 | Canada | Hospital | Doctor: secondary care | Management/communication regarding condition | Cluster RCT | No | More than twice | Investigator | External | Peer | SC | Increase | |
| Braybrook 199684 | UK | Primary | Doctor: GP | Prescribing | RCT | No | Mixed | Only once | Investigator | External | Professional body | SN in both arms | Decrease |
| Brinkman 2007115 | USA | Hospital | Doctor: secondary care | Management/communication regarding condition | RCT | No | Unclear/not reported | Unclear/not reported | Investigator | External | Multiple | Multiple SN and other BCTs | Increase |
| Brown 2018116 | Australia | Hospital | Doctor: secondary care | Referrals | Stepped wedge | No | Mixed | Only once | Credible source | Internal | Senior person | SC and CS and other BCTs | Increase |
| Buntinx 1993117 | Other/multiple | Mixed | Mixed or team | Tests | RCT | No | Unclear/not reported | Only once | Investigator | External | Peer | SC | Increase |
| Butler 2012118 | UK | Primary | Mixed or team | Prescribing | Cluster RCT | No | Face to face | Only once | Investigator | External | Peer | SC and other BCTs | Decrease |
| Cánovas 2009119 | Other/multiple | Primary | Doctor: GP | Multiple | RCT | No | Unclear/not reported | Unclear/not reported | Investigator | External | Peer | SC | Increase |
| Carney 201219 | USA | Hospital | Other HCP | Tests | RCT | No | Separate computerised | Unclear/not reported | Investigator | External | Peer | SC and other BCTs | Decrease |
| Cheater 200689 Arm A | UK | Primary | Other HCP | Multiple | Cluster RCT | No | Written | Unclear/not reported | Investigator | External | Peer | SC | Increase |
| Cheater 200689 Arm B | UK | Primary | Other HCP | Multiple | Cluster RCT | No | Written | Unclear/not reported | Investigator | External | Peer | SC | Increase |
| Colon-Emeric 2007120 | USA | Care/nursing home | Mixed or team | Prescribing | Cluster RCT | No | Written | More than twice | Investigator | Unclear/not reported | Peer | SC and social support | Increase |
| Curtis 2005121 | USA | Other | Doctor: GP | Prescribing | RCT | No | Written | Twice | Investigator | External | Peer | SC | Increase |
| Curtis 2007122 | USA | Mixed | Mixed or team | Multiple | Cluster RCT | No | Separate computerised | Unclear/not reported | Investigator | External | Peer | SC | Increase |
| Desveaux 201677 | Canada | Care/nursing home | Mixed or team | Prescribing | Cluster RCT | No | Separate computerised | More than twice | Investigator | External | Peer | SN in both arms | Decrease |
| Eccles 2001123 Arm A | UK | Mixed | Doctor: GP | Tests | Factorial | No | Unclear/not reported | Twice | Investigator | External | Peer | SC | Decrease |
| Eccles 2001123 Arm B | UK | Mixed | Doctor: GP | Tests | Factorial | No | Unclear/not reported | Twice | Investigator | External | Peer | SC | Decrease |
| Elouafkaoui 2016124 | UK | Community | Other HCP | Prescribing | Cluster RCT | No | Unclear/not reported | More than twice | Investigator | External | Peer | SC | Decrease |
| Eltayeb 2005125 | Other/multiple | Primary | Mixed or team | Prescribing | RCT | No | Unclear/not reported | More than twice | Investigator | External | Peer | SC | Decrease |
| Ferguson 2003126 | USA | Hospital | Doctor: secondary care | Prescribing | Cluster RCT | No | Unclear/not reported | Unclear/not reported | Investigator | External | Peer | SC | Increase |
| Fiks 2017127 | USA | Primary | Doctor: GP | Management/communication regarding condition | Cluster RCT | No | Mixed | Twice | Investigator | External | Peer | SC and social support | Increase |
| Foster 2007128 | UK | Primary | Doctor: GP | Management/communication regarding condition | RCT | No | Written | Only once | Investigator | External | Peer | SC and other BCTs | Increase |
| Foy 2004129 | UK | Hospital | Doctor: secondary care | Referrals | Matched pairs cluster RCT | No | Unclear/not reported | Unclear/not reported | Investigator | External | Peer | SC and other BCTs | Increase |
| French 201364 | Australia | Primary | Doctor: GP | Tests | Cluster RCT | No | Mixed | Unclear/not reported | Credible source | Internal | Peer | CS and other BCTs | Decrease |
| Fuller 2012130 | UK | Hospital | Mixed or team | Hand-washing/hygiene | Stepped wedge | Unclear | Mixed | More than twice | Investigator | External | Unclear/not reported | SR and other BCTs | Increase |
| Gerber 2013131 | USA | Primary | Doctor: GP | Prescribing | Cluster RCT | No | Mixed | More than twice | Investigator | External | Peer | SC and other BCTs | Decrease |
| Gjelstad 2006132 | Other/multiple | Primary | Doctor: GP | Prescribing | Cluster RCT | No | Written | Unclear/not reported | Investigator | Internal | Peer | SC and social support | Decrease |
| Goff 2002133 | USA | Primary | Doctor: GP | Prescribing | Cluster RCT | No | Unclear/not reported | More than twice | Unclear/not reported | Unclear/not reported | Peer | SC and instructions and prompts/cues | Increase |
| Guadagnoli 200068 | USA | Hospital | Doctor: secondary care | Management/communication regarding condition | Cluster RCT | No | Face to face | Unclear/not reported | Credible source | Internal | Peer | CS | Increase |
| Guldberg 201193 | Denmark | Primary | Doctor: GP | Multiple | Cluster RCT | No | Separate computerised | More than twice | Investigator | External | Peer | SC and prompts/cues | Increase |
| Hallsworth 201660 | UK | Primary | Doctor: GP | Prescribing | RCT | Yes | Written | Only once | Credible source | External | Peer | SC and other BCTs | Decrease |
| Hayashino 2016134 | Other/multiple | Primary | Doctor: GP | Multiple | Cluster RCT | No | Written | More than twice | Investigator | External | Peer | SC | Increase |
| Hayes 200269 | USA | Hospital | Doctor: secondary care | Management/communication regarding condition | Cluster RCT | No | Face to face | Unclear/not reported | Credible source | Unclear/not reported | Unclear/not reported | CS | Increase |
| Heller 2001135 | Australia | Hospital | Mixed or team | Multiple | Cluster RCT | No | Mixed | Unclear/not reported | Credible source | Unclear/not reported | Multiple | SC | Unclear |
| Hemkens 2017136 | Other/multiple | Primary | Doctor: GP | Prescribing | RCT | No | Mixed | More than twice | Investigator | External | Peer | SC | Decrease |
| Herbert 2004137 | Canada | Primary | Doctor: GP | Prescribing | Cluster RCT | No | Written | Unclear/not reported | Investigator | External | Peer | SC | Increase |
| Horbar 2004138 | USA | Hospital | Mixed or team | Prescribing | Cluster RCT | No | Unclear/not reported | Unclear/not reported | Investigator | External | Peer | SC and other BCTs | Increase |
| Houston 2015139 | USA | Primary | Mixed or team | Referrals | Cluster RCT | No | Separate computerised | Unclear/not reported | Investigator | External | Peer | SC and other BCTs | Increase |
| Howe 1996140 | UK | Primary | Doctor: GP | Management/communication regarding condition | RCT | No | Unclear/not reported | Only once | Investigator | External | Peer | SC and other BCTs | Increase |
| Huis 201320 | Netherlands | Hospital | Other HCP | Hand-washing/hygiene | Cluster RCT | No | Unclear/not reported | Twice | Investigator | External | Peer | SN in both arms | Increase |
| Hysong 201275 | USA | Primary | Mixed or team | Management/communication regarding condition | Factorial | No | Separate computerised | More than twice | Investigator | External | Peer | SN in both arms | Increase |
| Ivers 200318 | Canada | Primary | Doctor: GP | Multiple | Cluster RCT | No | Written | More than twice | Investigator | External | Peer | SN in both arms | Increase |
| Katz 200494 | USA | Primary | Mixed or team | Management/communication regarding condition | Cluster RCT | No | Unclear/not reported | Only once | Investigator | External | Peer | SC and instructions and prompts/cues | Increase |
| Kaufman 2016141 | USA | Hospital | Doctor: secondary care | Prescribing | Cluster RCT | No | More than twice | Investigator | Unclear/not reported | Peer | SC | Decrease | |
| Kennedy 2015142 | Canada | Care/nursing home | Mixed or team | Prescribing | Cluster RCT | No | Unclear/not reported | Unclear/not reported | Investigator | External | Peer | SC and CS and other BCTs | Increase |
| Kiefe 200182 | USA | Other | Mixed or team | Prescribing | RCT | No | Written | Unclear/not reported | Investigator | External | Peer | SN in both arms | Increase |
| Kim 199990 | USA | Primary | Doctor: GP | Multiple | Cluster RCT | No | Written | Only once | Other | Unclear/not reported | Peer | SC and social support | Increase |
| Koff 201671 | USA | Hospital | Mixed or team | Hand-washing/hygiene | RCT | No | More than twice | Investigator | Unclear/not reported | Peer | SN in both arms | Increase | |
| Kogan 2003143 | USA | Mixed | Mixed or team | Management/communication regarding condition | Cluster RCT | No | Written | Only once | Supervisor or senior colleague | Internal | Peer | SC | Increase |
| Lakshminarayan 201063 | USA | Hospital | Mixed or team | Management/communication regarding condition | Cluster RCT | No | Unclear/not reported | Unclear/not reported | Credible source | Internal | Senior person | CS and other BCTs | Increase |
| Leviton 199965 | USA | Hospital | Doctor: secondary care | Prescribing | Cluster RCT | No | Face to face | Only once | Credible source | External | Senior person | CS and other BCTs | Increase |
| Liddy 2011144 | Canada | Primary | Doctor: GP | Multiple | Stepped wedge | No | Face to face | Unclear/not reported | Investigator | External | Peer | SC and other BCTs | Increase |
| Lim 2018145 | Other/multiple | Primary | Doctor: GP | Prescribing | Cluster RCT | No | Written | More than twice | Investigator | External | Peer | SC | Decrease |
| Lomas 199167 | Canada | Hospital | Doctor: secondary care | Management/communication regarding condition | Cluster RCT | No | Mixed | More than twice | Peer | Internal | Unclear/not reported | CS | Unclear |
| MacLean 2009102 | USA | Primary | Mixed or team | Tests | Cluster RCT | No | Written | More than twice | Investigator | Internal | Peer | SC and prompts/cues | Increase |
| Mayne 2014146 Arm A | USA | Primary | Mixed or team | Prescribing | Cluster RCT | No | Unclear/not reported | More than twice | Investigator | External | Peer | SC and other BCTs | Increase |
| Mayne 2014146 Arm B | USA | Primary | Mixed or team | Prescribing | Cluster RCT | No | Unclear/not reported | More than twice | Investigator | External | Peer | SC & other BCTs | Increase |
| McClellan 2003147 | Australia | Community | Mixed or team | Management/communication regarding condition | Cluster RCT | No | Mixed | Unclear/not reported | Credible source | External | Peer | SC and CS | Increase |
| McCluskey 2016148 | USA | Primary | Doctor: GP | Tests | Cluster RCT | No | Face to face | Only once | Investigator | External | Peer | SC and instructions and prompts/cues | Increase |
| McPhee 1989149 | USA | Hospital | Doctor: secondary care | Tests | RCT | No | Face to face | More than twice | Investigator | External | Peer | SC and information on health consequences | Increase |
| Meeker 2016150 | USA | Primary | Doctor: GP | Prescribing | Cluster RCT | No | More than twice | Investigator | External | Peer | SC and SR | Decrease | |
| Metlay 2007151 | USA | Hospital | Doctor: secondary care | Prescribing | Cluster RCT | No | Unclear/not reported | Only once | Investigator | External | Peer | SC and information on health consequences | Decrease |
| Mold 200870 | USA | Primary | Mixed or team | Management/communication regarding condition | RCT | No | Unclear/not reported | Only once | Investigator | External | Peer | SN in both arms | Increase |
| Mold 2014152 Arm A | USA | Primary | Doctor: GP | Management/communication regarding condition | Cluster RCT | No | Face to face | More than twice | Peer | Internal | Peer | SC | Increase |
| Mold 2014152 Arm B | USA | Primary | Doctor: GP | Management/communication regarding condition | Cluster RCT | No | Face to face | More than twice | Peer | Internal | Peer | SC | Increase |
| Morrison 201596 | Canada | Hospital | Mixed or team | Management/communication regarding condition | Stepped wedge | No | Unclear/not reported | More than twice | Unclear/not reported | Unclear/not reported | Peer | SC and other BCTs | Increase |
| Mourad 201174 | Netherlands | Other | Mixed or team | Multiple | Cluster RCT | No | Mixed | Twice | Investigator | External | Peer | SN in both arms | Increase |
| O’Connell 1999153 | Australia | Primary | Doctor: GP | Prescribing | Cluster RCT | No | Written | Twice | Investigator | External | Peer | SC | Decrease |
| O’Connor 2009154 Arm A | USA | Primary | Doctor: GP | Tests | RCT | No | Unclear/not reported | More than twice | Investigator | External | Peer | SC and instruction on how to perform the behaviour and prompts/cues | Increase |
| O’Connor 2009154 Arm B | USA | Primary | Doctor: GP | Tests | RCT | No | Unclear/not reported | More than twice | Investigator | External | Peer | SC and instructions and prompts/cues | Increase |
| Patel 2018155 | USA | Primary | Doctor: GP | Prescribing | Cluster RCT | No | Unclear/not reported | Unclear/not reported | Investigator | External | Peer | SC | Increase |
| Peiris 2015101 | Australia | Primary | Mixed or team | Tests | Cluster RCT | No | Unclear/not reported | Unclear/not reported | Investigator | External | Peer | SC and prompts/cues | Increase |
| Persell 201662 | USA | Primary | Doctor: GP | Prescribing | Factorial | No | More than twice | Investigator | External | Peer | SC and SR | Decrease | |
| Pimlott 2003156 | Canada | Primary | Doctor: GP | Prescribing | RCT | No | Written | More than twice | Investigator | External | Peer | SC and information on health consequences | Decrease |
| Pope 201091 | Canada | Hospital | Doctor: secondary care | Other | RCT | No | Face to face | Only once | Investigator | External | Peer | SC and social support (unspecified) | Increase |
| Quinley 200472 | USA | Primary | Doctor: GP | Prescribing | Cluster RCT | Yes | Written | Only once | Investigator | External | Peer | SN in both arms | Increase |
| Raasch 2000157 | Australia | Primary | Doctor: GP | Tests | RCT | No | Mixed | Only once | Peer | External | Peer | SC and social support (unspecified) | Increase |
| Raja 201592 | USA | Hospital | Doctor: secondary care | Tests | RCT | No | More than twice | Unclear/not reported | Internal | Peer | SC and prompts/cues | Increase | |
| Rask 200178 | USA | Primary | Mixed or team | Tests | Cluster RCT | No | Written | Only once | Credible source | External | Senior person | SN in both arms | Increase |
| Sandbaek 1999158 | Denmark | Primary | Doctor: GP | Management/communication regarding condition | RCT | No | Written | Unclear/not reported | Investigator | External | Peer | SC and other BCTs | Increase |
| Sauaia 200080 | USA | Hospital | Mixed or team | Management/communication regarding condition | Cluster RCT | No | Mixed | Twice | Credible source | Unclear/not reported | Peer | SN in both arms | Increase |
| Schneider 200883 | Other/multiple | Primary | Doctor: GP | Management/communication regarding condition | Cluster RCT | No | Unclear/not reported | Unclear/not reported | Unclear/not reported | Unclear/not reported | Peer | SN in both arms | Increase |
| Soleymani 2014159 | Other/multiple | Mixed | Mixed or team | Prescribing | RCT | No | Written | Only once | Investigator | External | Peer | SC and other BCTs | Decrease |
| Søndergaard 2002160 Arm B | Denmark | Primary | Doctor: GP | Prescribing | Cluster RCT | No | Written | More than twice | Investigator | External | Peer | SC | Increase |
| Søndergaard 2003161 | Denmark | Primary | Doctor: GP | Prescribing | Cluster RCT | No | Written | Only once | Investigator | External | Peer | SC | Decrease |
| Soumerai 199879 | USA | Hospital | Doctor: secondary care | Prescribing | Cluster RCT | No | Face to face | Only once | Credible source | External | Senior person | SN in both arms | Increase |
| Stewardson 2016162 Arm A | Other/multiple | Hospital | Mixed or team | Hand-washing/hygiene | Cluster RCT | No | Face to face | More than twice | Credible source | Internal | Senior person | SC and CS and other BCTs | Increase |
| Stewardson 2016162 Arm B | Other/multiple | Hospital | Mixed or team | Hand-washing/hygiene | Cluster RCT | No | Face to face | More than twice | Patient | External | Patient(s) | Multiple SN and other BCTs | Increase |
| Thomas 2006163 | UK | Primary | Doctor: GP | Tests | Factorial | No | Written | More than twice | Investigator | External | Peer | SC | Decrease |
| Tjia 2015164 Arm B | USA | Care/nursing home | Mixed or team | Prescribing | Cluster RCT | No | Unclear/not reported | Only once | Investigator | External | Peer | SC and other BCTs | Decrease |
| Tjia 2015164 Arm A | USA | Care/nursing home | Mixed or team | Prescribing | Cluster RCT | No | Unclear/not reported | Only once | Investigator | External | Peer | SC and information on health consequences | Decrease |
| Trietsch 2017165 | Netherlands | Primary | Doctor: GP | Multiple | Cluster RCT | No | Face to face | More than twice | Investigator | External | Peer | SC and other BCTs | Decrease |
| van Bruggen 200897 | Netherlands | Primary | Mixed or team | Tests | Cluster RCT | No | Unclear/not reported | Only once | Unclear/not reported | Unclear/not reported | Peer | SC and other BCTs | Increase |
| Vellinga 201661 Arm A | Other/multiple | Primary | Doctor: GP | Prescribing | Cluster RCT | No | Separate computerised | Only once | Investigator | External | Peer | SC and prompts/cues | Increase |
| Vellinga 201661 Arm B | Other/multiple | Primary | Doctor: GP | Prescribing | Cluster RCT | No | Separate computerised | Only once | Investigator | External | Peer | SC and other BCTs | Increase |
| Verstappen 2003166 Arm A | Netherlands | Primary | Doctor: GP | Tests | RCT | No | Mixed | More than twice | Credible source | External | Senior person | SC and CS and other BCTs | Decrease |
| Verstappen 2003166 Arm B | Netherlands | Primary | Doctor: GP | Tests | RCT | No | Written | More than twice | Investigator | External | Peer | SC | Decrease |
| Voorn 2017167 | Netherlands | Hospital | Doctor: secondary care | Other | Cluster RCT | No | Twice | Investigator | External | Peer | SC and other BCTs | Decrease | |
| Wang 2018168 | Other/multiple | Hospital | Mixed or team | Management/communication regarding condition | Cluster RCT | No | Separate computerised | More than twice | Peer | Internal | Peer | SC and social support | Increase |
| Watkins 2004169 | USA | Hospital | Doctor: secondary care | Tests | RCT | No | Unclear/not reported | Only once | Investigator | External | Peer | SC and other BCTs | Increase |
| Weitzman 200976 | Other/multiple | Primary | Doctor: GP | Tests | Cluster RCT | No | Face to face | Only once | Investigator | External | Peer | SN in both arms | Increase |
| Winickoff 1984170 | USA | Hospital | Doctor: secondary care | Tests | Cluster RCT | No | Written | More than twice | Investigator | Internal | Peer | SC | Increase |
| Winslade 2016171 | Canada | Community | Other HCP | Management/communication regarding condition | RCT | No | Written | Only once | Investigator | External | Peer | Multiple SN and other BCTs | Increase |
| Wright 200681 | Canada | Hospital | Doctor: secondary care | Tests | Cluster RCT | No | Mixed | More than twice | Credible source | External | Senior person | SN in both arms | Increase |
| Young 2002172 | Australia | Primary | Doctor: GP | Management/communication regarding condition | Cluster RCT | No | Face to face | Only once | Peer | Unclear/not reported | Peer | SC and other BCTs | Increase |
Appendix 15 Risk-of-bias judgements across each domains for each included study
FIGURE 20.
Risk-of-bias judgements across each domains for each included study.
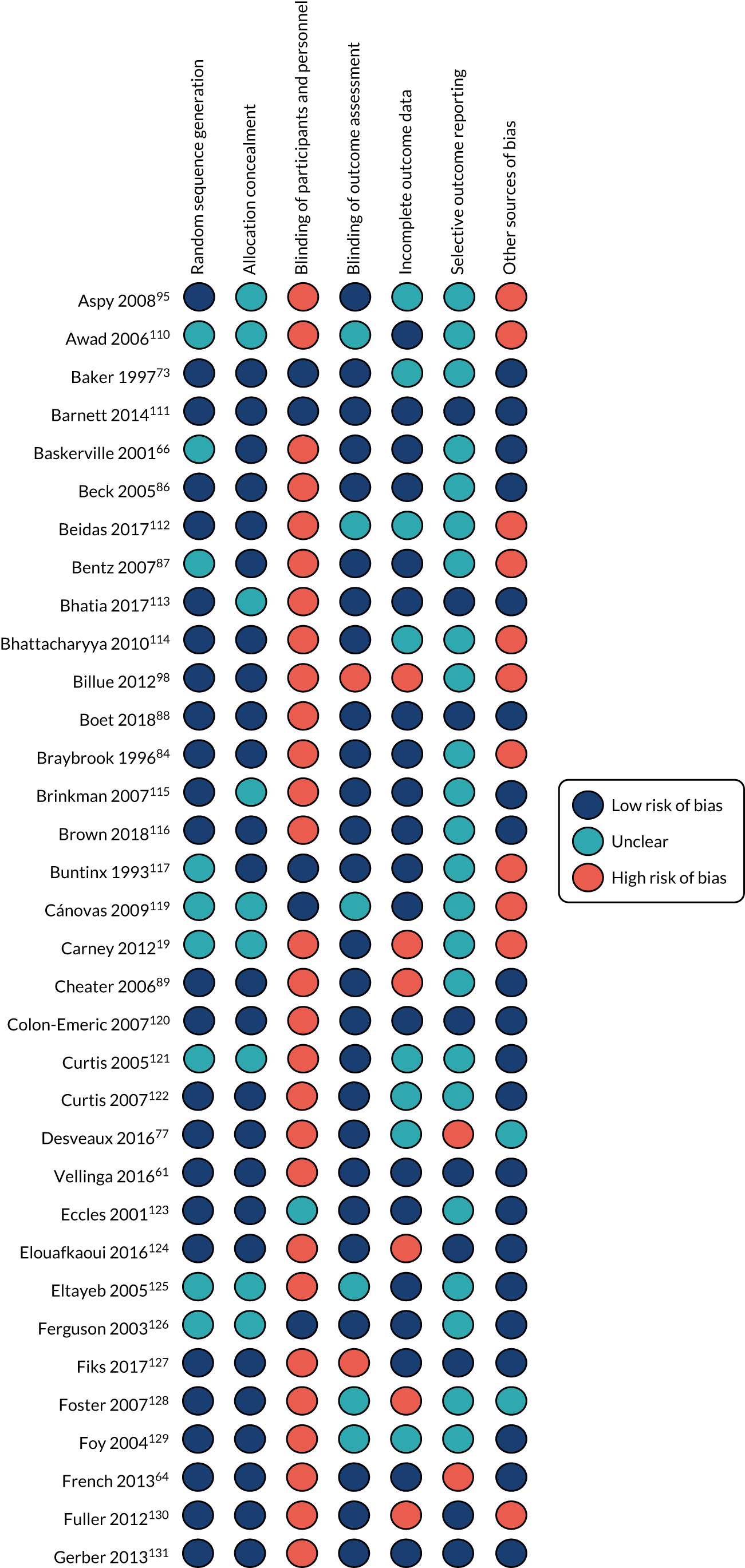
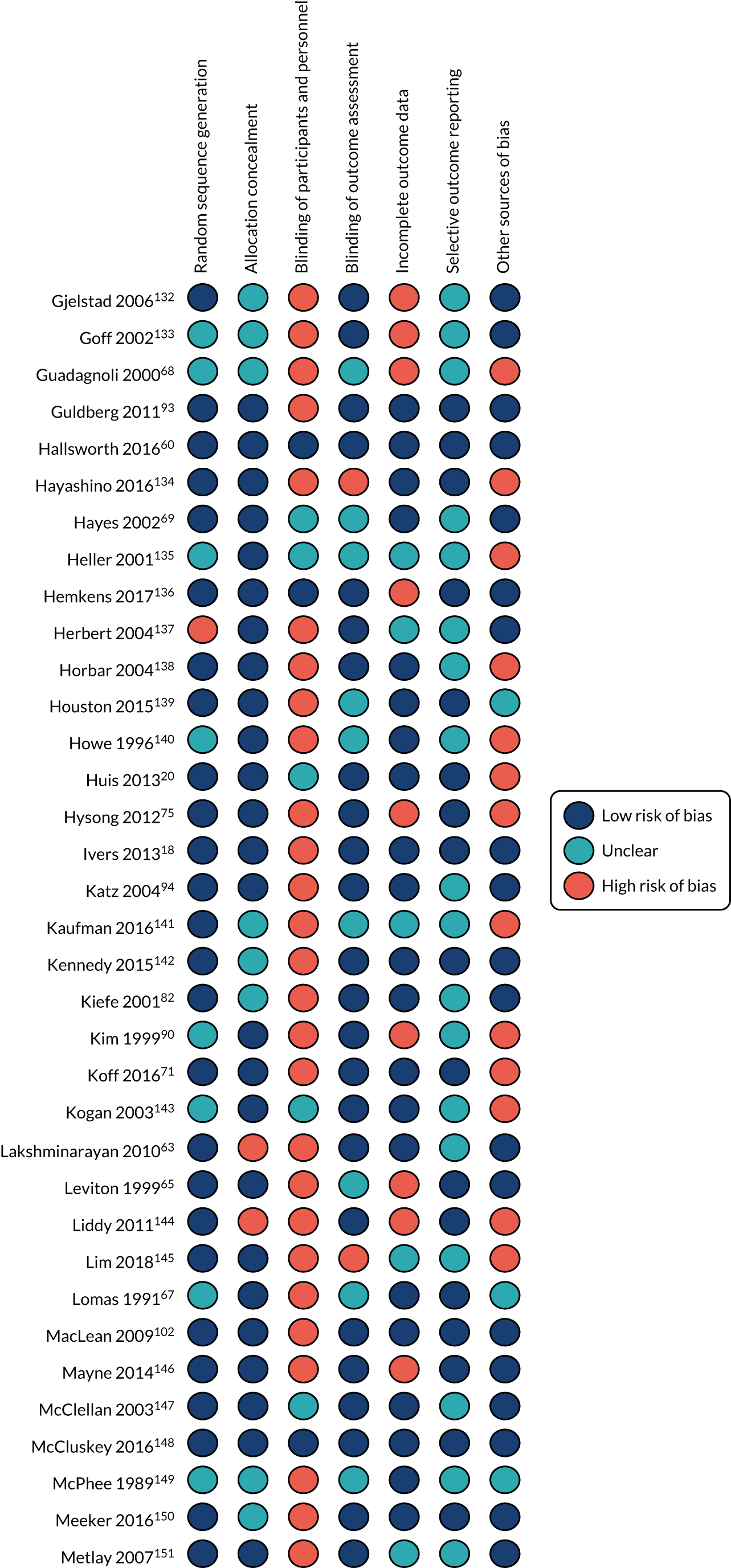
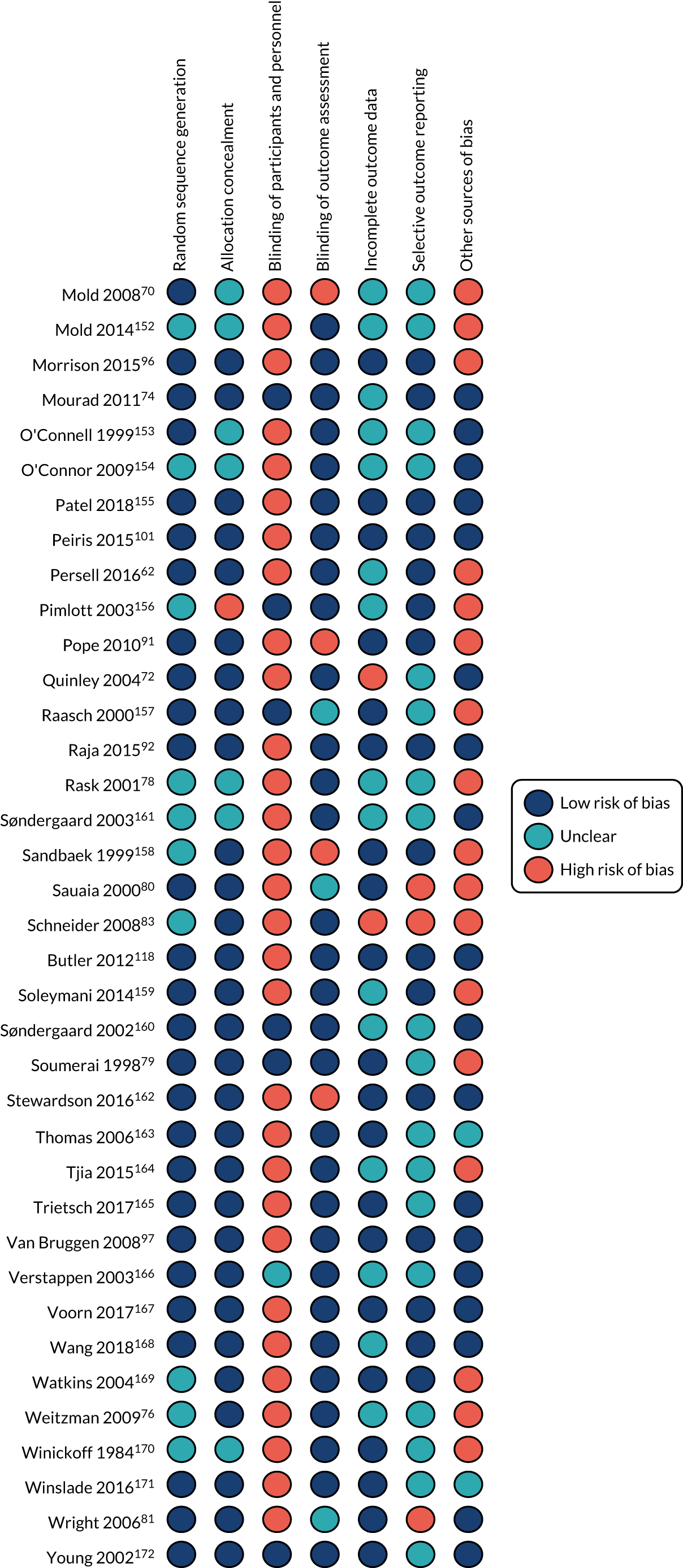
Appendix 16 Studies with social norm interventions in both arms: forest plot
FIGURE 21.
Fixed-effects forest plot showing studies with social norm interventions in both arms.
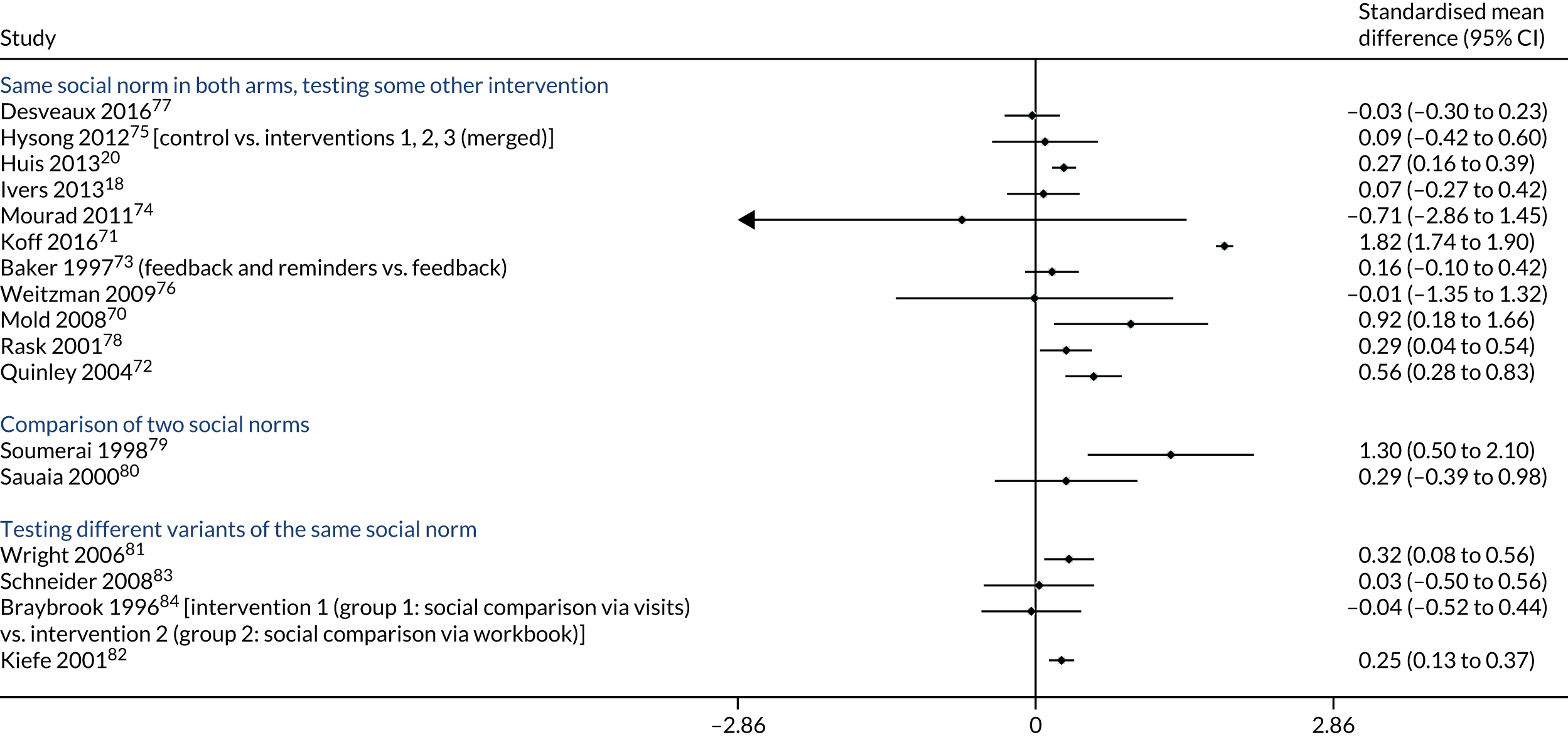
Appendix 17 Forest plots showing individual studies, by social norms behaviour change techniques
FIGURE 22.
Fixed-effects meta-analysis of trials testing social comparison with or without feedback on behaviour.

FIGURE 23.
Fixed-effects meta-analysis of trials testing social comparison with other BCTs.
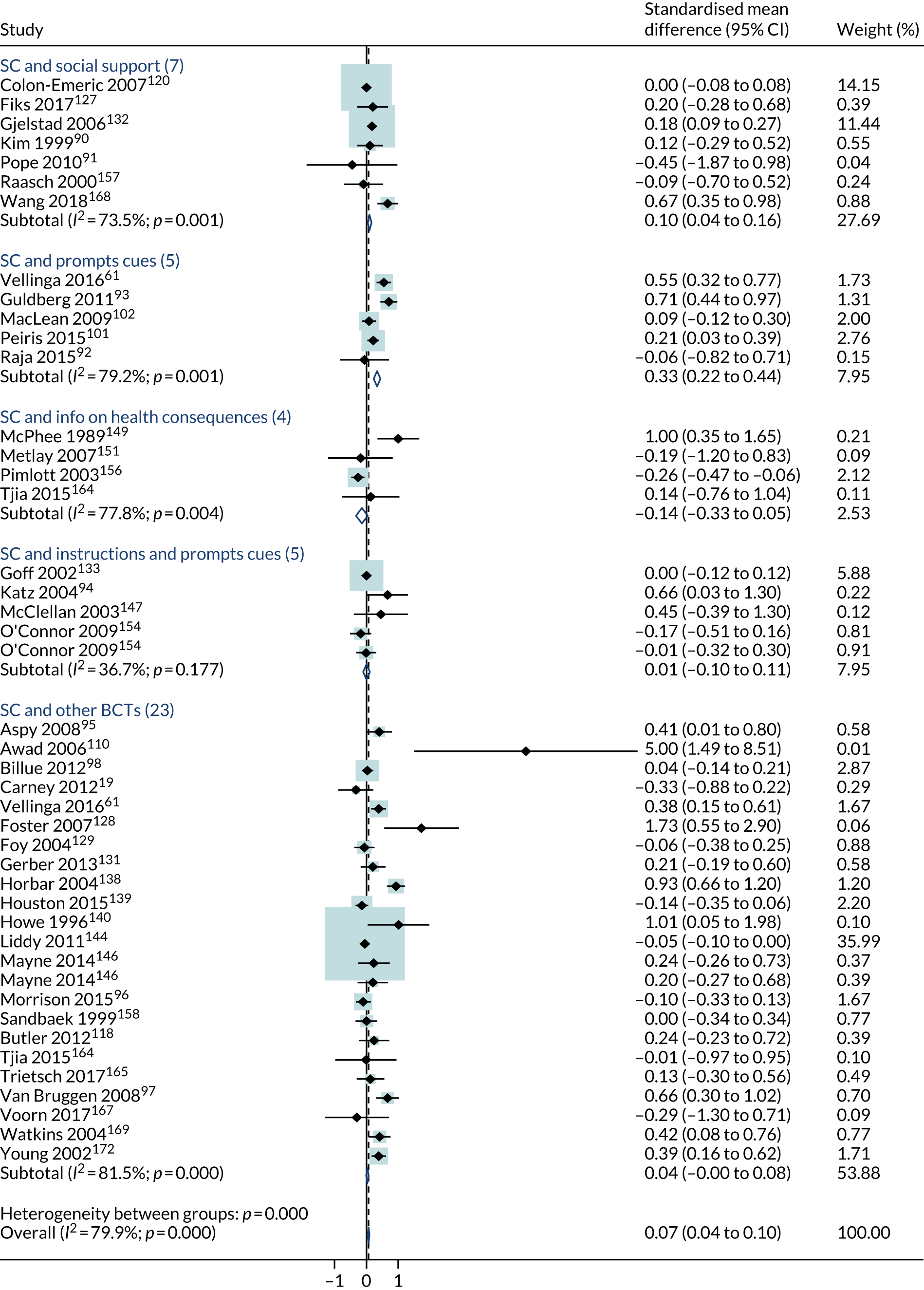
FIGURE 24.
Fixed-effects meta-analysis of trials testing credible source.
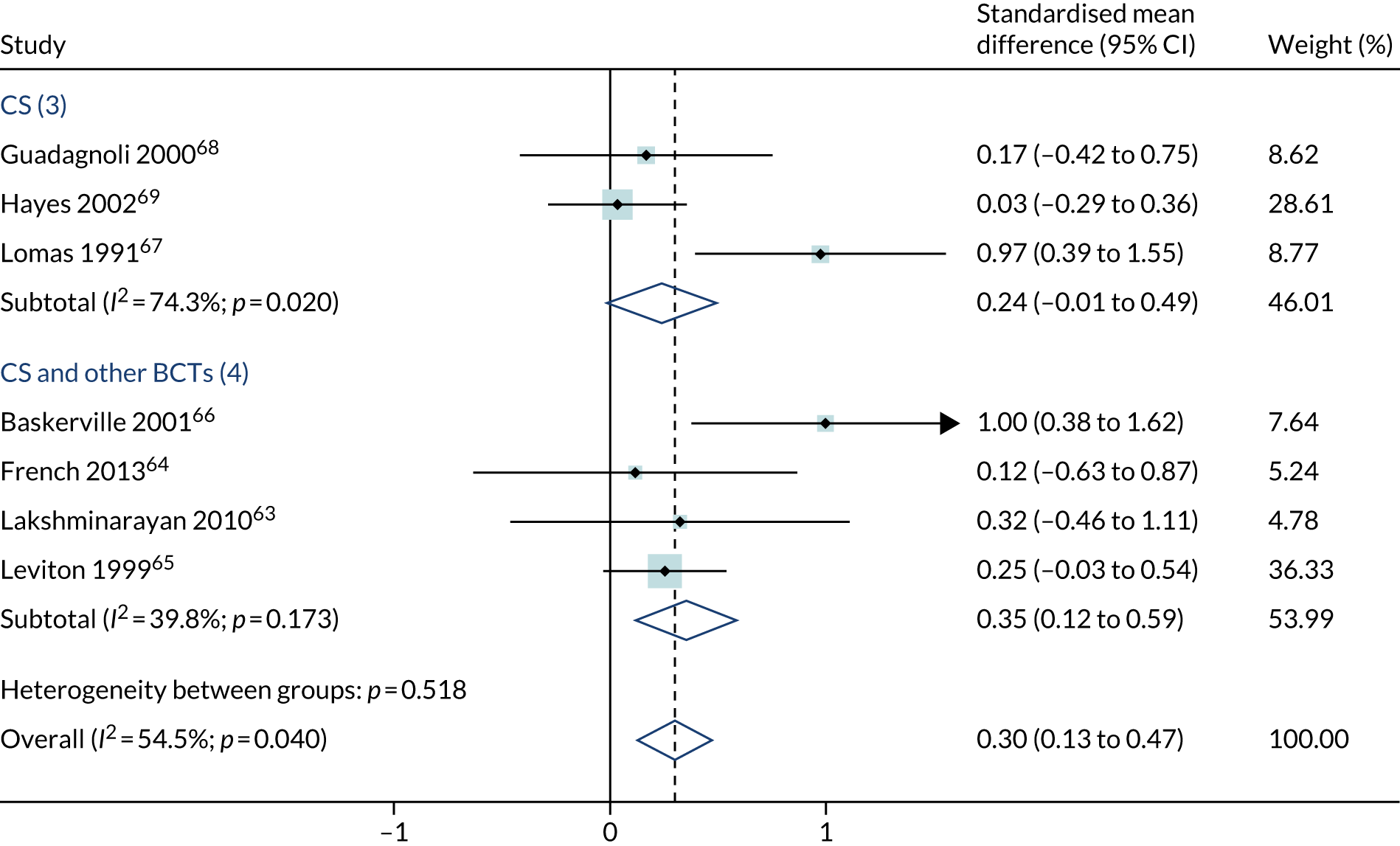
FIGURE 25.
Fixed-effects meta-analysis of trials testing social reward.

FIGURE 26.
Fixed-effects meta-analysis of trials testing multiple social norm BCTs.
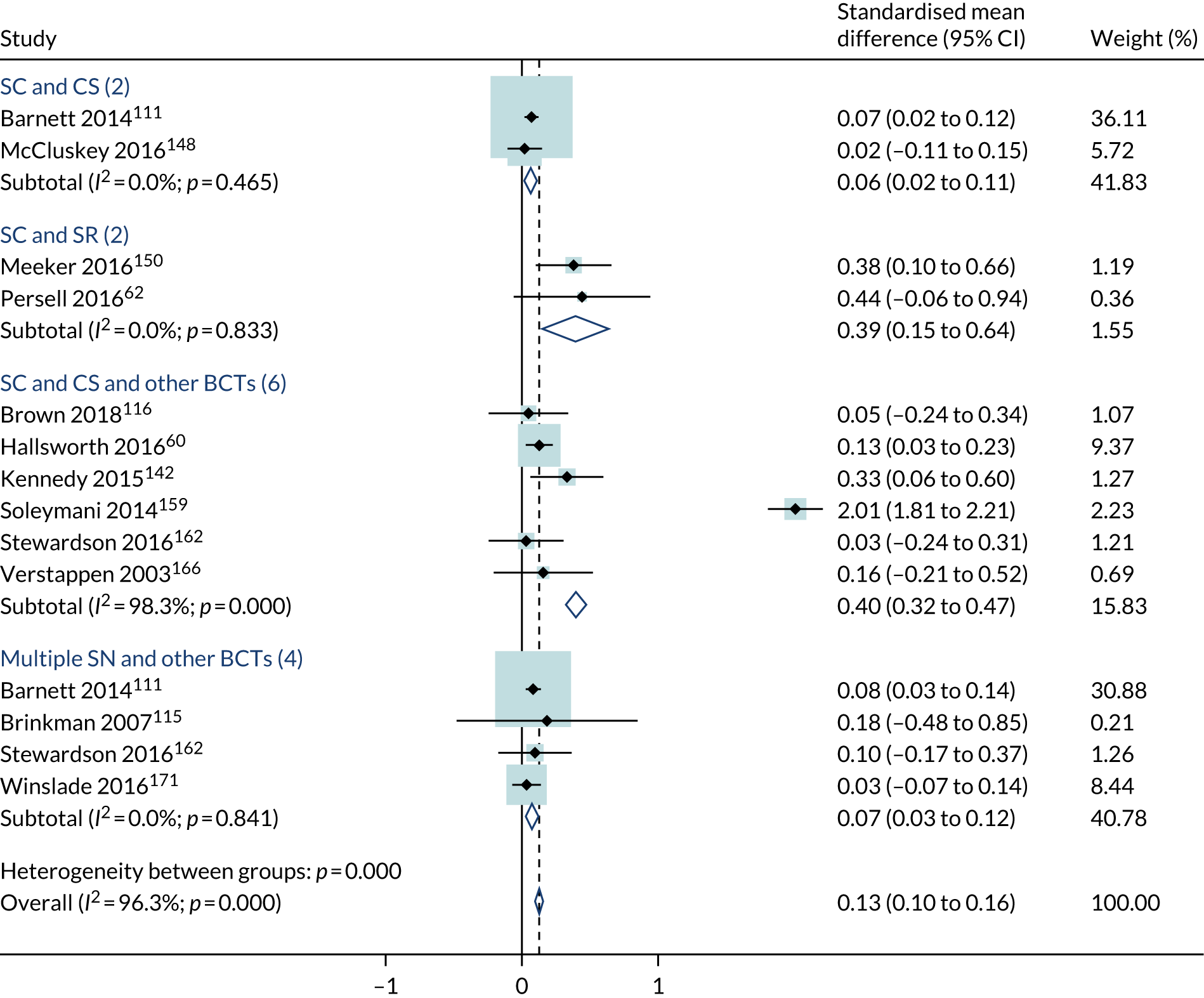
List of abbreviations
- A&F
- audit and feedback
- AHP
- allied health professional
- ANCOVA
- analysis of covariance
- BCT
- behaviour change technique
- BNI
- British Nursing Index
- CENTRAL
- Cochrane Central Register of Controlled Trials
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- GP
- general practitioner
- HDAS
- Healthcare Databases Advanced Search
- ICC
- intraclass correlation coefficient
- MeSH
- medical subject heading
- NIHR
- National Institute for Health Research
- PABAK
- prevalence-adjusted and bias-adjusted kappa
- PPI
- patient and public involvement
- PRISMA
- Preferred Reporting items for Systematic Reviews and Meta-Analyses
- RCT
- randomised controlled trial
- RQ
- research question
- SMD
- standardised mean difference
- SSC
- Study Steering Committee
- TIDieR
- Template for Intervention Description and Replication
