Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 13/54/25. The contractual start date was in April 2015. The final report began editorial review in December 2019 and was accepted for publication in June 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Renedo et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Context
Transitions from paediatric to adult health services cause problems worldwide, particularly among young people living with a long-term condition affecting their health and future life. 1,2 Improvement of young people’s health and their health-care experiences during the period of transition to adult services has become an important priority area both in the UK3–5 and internationally. 6 Health transition is a gradual process that spans the period from early adolescence to adulthood and continues until the person adjusts and is fully established as an adult patient in adult care services. 7 It constitutes a significant developmental phase7,8 when multiple difficulties arise from the interaction between young people’s health condition and physical, psychological and social developmental changes,9,10 including transitions occurring in other areas of life. Transition to adult care is crucial for those with long-term conditions. This is a time of increased medical vulnerability. 11 Multiple demands emerge from the diverse social contexts of the young person beyond health care, including demands for increased competency and autonomy in self-management10 of their own condition and societal expectations about how the young person should develop into a responsible adult, including achieving particular educational and career goals. All these demands and parallel transitions in other aspects of a young person’s life occur against the background of changes in their health care as the young person is transferred to adult services. For young people, pursuing aspirations to live a ‘normal’ life while simultaneously self-managing their condition during transition can prove very taxing. 9
Young people’s experiences of care across the health-care system during the process of transition to adult care, including the clinical care they receive and any support they are given to prepare them for adult services (i.e. transitional care), can have a major impact on their health and future life. 1,2 Poor experiences of care during the transition period are likely to disengage young people from services, lead to poor health outcomes and shape their future adult patterns of engagement with services. 12
One long-term condition for which the period of transition to adult health-care services is a particularly challenging period13–16 and for which there is a need for better health care17,18 is sickle cell disorder (SCD). SCD is an inherited blood disorder characterised by an abnormal haemoglobin that results in sickle-shaped red blood cells that tend to fragment, leading to anaemia, jaundice, fatigue and extreme tiredness. During physical stresses the sickled red cells block small blood vessels, causing excruciating, severe painful episodes, splenic hypofunction with consequent increased susceptibility to severe infection, and chronic organ damage resulting in significant disability and reduction in life expectancy. 19 Episodic acute painful episodes are a constant threat for people with SCD and can become more frequent with age. 20 They are unpredictable, can be excruciating and sometimes emerge together with acute chest syndrome, stroke and infections. 21 They require timely medical treatment. Both acute painful episodes and chronic pain affect everyday life and can have important long-term health implications. Almost one-third of people with SCD report having pain nearly every day, and over half report pain for more than half of the time. 22 There is a high prevalence of other comorbidities among young people with SCD, including asthma, cardiac dysfunction, chronic lung disease, avascular necrosis of the long bones and organ damage. 15,23
Sickle cell disorder poses an important global public health challenge. 24 In the UK, between 12,500 and 15,000 people live with SCD,21 with London accounting for the majority of the national SCD cases and SCD-related hospital admissions. 25 The vast majority of patients live in London or larger urban conurbations in the UK. 26 Approximately 250 new cases are identified every year via newborn screening in England. 27 SCD is the most common genetically inherited significant health-threatening condition among newborns in England. It predominantly affects people of black African and African-Caribbean origin. 28
Sickle cell disorder provides an excellent case study for examining transition to adult health-care services. It is a complex condition that is rapidly becoming more common in the UK,29 and SCD patients aged 16–20 years report poorer experiences of care than those in other age groups, particularly during emergency attendances. 18 People with SCD who are aged 20–29 years are hospitalised more often than those in other age groups and have the highest rates of short-duration emergency admissions for SCD painful episodes. 25 This suggests that care needs to improve during transition into adult services so that young people are better equipped to avoid these emergency hospitalisations when they reach adulthood. Similar outcomes have been found among patients in the USA, where acute care utilisation and rehospitalisation rates among 18- to 30-year-old patients are higher than in any other age group,30 suggesting that young people reaching adulthood need extra support to avoid hospitalisations and poor health outcomes. 15 McLaughin and Ballas31 also showed that mortality among US children with SCD on chronic transfusions is very high if these children are not adequately followed up in adult clinic following transfer from paediatric services.
In the USA, overall childhood mortality rates have decreased significantly, but mortality has increased among young adults at the age corresponding to transition between paediatric and adult care. 13 In the USA, many young people move to adult services with poor preparation and support. 14
Despite evidence indicating that there are gaps in transitional care for young people with SCD in many different settings, we lack knowledge about what works to improve care during transition,32 about the type of support SCD patients need during this period and about the ways in which their social contexts mediate their experiences of transition and problems during this period. Poorly managed and poorly supported transitions can have major negative sequelae, not just for young people but also for their families and health services, including poor treatment compliance, health deterioration, disengagement with services and increased rates of emergency hospitalisations,5,32,33 sometimes with life-threatening consequences.
Transition is a period of vulnerability for young people with any long-term condition. 34 However, the unpredictability of SCD and the threat of painful episodes bring additional challenges. 35,36 There is also stigma associated with SCD because of poor understanding of the condition both socially and among health-care staff, which increases the burden on young people with the condition. 36–38 Patients can be stereotyped as drug-seekers39 (i.e. abusing pain relief and being addicted to opioid painkillers). 40
Sickle cell disorder can be ‘racialized’. 41–44 In England, black African and African-Caribbean communities are most affected by SCD,28 as well as by the negative health and social impacts of societal inequalities. 28,45,46 Health services for SCD are limited compared with those for patients living with ‘disorders such as cystic fibrosis, which primarily affects people of Northern European descent’. 43 Complicating this further is the stigma associated with the SCD diagnosis in some communities. 47
Quality transitional care to prepare young people to adjust to adult services is increasingly considered a central element of any youth-friendly health-care service. 48,49 Improvements in transitional care need to be grounded in comprehensive understanding of the holistic needs and experiences of patients during transition,4 including across the health-care system (i.e. beyond specialised care), and consider their wider social contexts (such as relationships, education, work and other life transitions). Limited research from the USA50–52 has explored the role of health-care service components in achieving successful transition for patients with SCD. We lack understanding, however, about how transitions between child and adult health-care services interact with wider social contexts. For other long-term conditions, although there is a considerable body of research on how transition is supported in specialist care, there is little research examining how experiences of clinical care across the health-care system (i.e. beyond specialised care) affect the transition process. 53 SCD transitional care needs to include consideration of developmental issues beyond health and should take into account the young person’s perspective on their own transition to adulthood and adult services. 15 However, young people’s voices are not usually included in health-care transition research to the extent needed54 and their experiences of transitions in care outside specialist services across the health-care system remains largely unexamined. Top-down approaches to health-care service planning55 that do not involve patients dominate current provision. 56 Self-management of SCD is demanding and requires close self-monitoring [e.g. keeping hydrated (drinking water), keeping warm, resting, avoiding arduous physical activity, and being attentive and responsive to signs of a possible painful episode]. 57,58 These self-management practices are inculcated in young people with SCD as a form of ‘self-regulatory governance’. 58
Listening to children’s and young people’s voices – and acting on what they say – is crucial to help develop better, more youth-friendly services7 and adolescent-responsive health systems59 and enabling educational and work contexts6 to help young people to stay healthy. Survey data and superficial accounts of young people’s experiences, which often treat young people as passive subjects, need to be supplemented with in-depth understandings of wider factors influencing health. 60 Understanding young people’s experiences across the health-care system and in their wider social context during the process of transition is crucial.
Our qualitative research study explored the experiences of young people with SCD as they transitioned from paediatric to adult NHS services, with a focus on how their clinical experiences were integrated into their whole lives. We examined the world beyond the clinical realm and investigated wider aspects of young people’s lives that affect their SCD transitions, such as education, relationships and work. 61 We adopted a ‘slow co-production’ approach56 and involved patients as research participants and also as team collaborators (see Chapter 3) in an in-depth qualitative exploration that aimed to produce ‘patient-centred knowledge’. 56,61 By engaging in this way, that is with young people’s own experiences and voiced needs, we aimed to inform service provision that meets the NHS goal of providing ‘patient-centred’ transitional care5,62 and to help inform global efforts to improve adolescent health.
Chapter 2 Research objectives
The objective of this study was to inform transitional care and support for young people. We used a sociological, person-centred approach, looking beyond the clinical context to other areas also affected during transitions to adulthood. Our specific aims are listed below:
-
to examine experiences of health-care transition from the patient perspective, taking into account social aspects of young people’s lives outside health-care services
-
to examine how young people with SCD move from using paediatric to adult health-care services
-
to examine how social context affects transition
-
to investigate young people’s experiences of living with SCD during transition to adulthood
-
to examine how health-care transition affects young people’s health-care-related behaviour and quality of life
-
-
to understand how current health care meets the holistic needs of young people with SCD during transition
-
to explore how young people experience care relationships and interactions with health-care providers during transition
-
to understand young people’s concerns during health-care transition
-
to explore how these relate to health-care professionals’ views
-
-
to understand the type of support young people with SCD require to improve their transition experiences and develop recommendations to improve NHS transitional care for this population
-
to use the findings to inform the development of resources to support the successful move of young people with SCD into adulthood and adult care successfully
-
to reflect on how lessons from SCD can be applied to health-care transitions more generally.
Chapter 3 Patient and public involvement
We worked closely with non-clinical, non-academic SCD experts (i.e. patient and carer representatives) throughout. Patient and carer experts Cherelle Augustine, Nordia Willis and Patrick Ojeer [hereafter referred to as CA, NW and PO and collectively as patient and public involvement (PPI) experts] were involved in the project from its inception, working on developing the research questions and funding proposal, advising on the project throughout data collection and being involved in parts of the substantive analytical work, as well as playing an important part in dissemination activities. 46 Their work has been vital to ensure that patient perspectives have been central during study design, data analysis and knowledge translation. 46,56
In our role as academic researchers we adopted a responsive approach to working with PPI experts in the project, as well as with other patients, carers and patient groups. Our previous experience suggested that this would help ensure that patients were involved in a meaningful and sustainable way. For instance, we soon discovered that large stakeholder and steering group meetings would be inappropriate and difficult to achieve. Instead, we worked with our PPI experts to ensure that we were holding smaller, more appropriate meetings (sometimes one to one). These smaller meetings meant that we were able to adapt to the needs and other commitments of those involved, as well as to reschedule meetings to accommodate other commitments or illness.
During the project, as well as regular meetings with PPI experts, we held discussions with SCD patient charities and with patient group representatives from the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care Northwest London (CLAHRC NWL) SCD Early Years Steering Group. This group developed and validated a patient-reported experience measure for SCD. 18 The NIHR CLAHRC NWL was a programme funded by NIHR to facilitate collaborations between researchers, clinicians and patients to help ensure that research evidence was translated into health-care practice. 63 The NIHR CLAHRC NWL SCD Early Years Steering Group included clinicians and paediatricians (including one specialising in SCD) as well as others who work in different conditions affecting children and young people. Through these different fora we discussed the development of study materials, findings, the practical implications of the findings and how to move forward, including how best to translate our findings into outputs that would benefit patients.
Involvement during inception and initial stages of the project
The idea for the project originated from our interactions with patients and patient charities during our investigation into patient involvement in SCD health-care improvement in the NIHR CLAHRC NWL. 64–66 NW and CA [two young people with SCD and founders of Broken Silence (London, UK), a charity organisation for young people with SCD] and PO (father of a SCD patient) were involved from the start. We worked with them to identify research questions and to understand their transition experiences and obtain their views on the project’s aims and methods, all of which we incorporated into the final study.
PO emphasised that the aims should be to assess how transitional care enables patients to be treated in accordance with the NHS ethos ‘no decision about me without me’. 67 Our objectives were formulated accordingly.
Broken Silence highlighted the need to create tangible resources that would benefit patients, particularly to empower them. This influenced CM’s and AR’s original idea of using research findings to co-produce support resources with young adults with SCD to help patients achieve better self-care and be better able to navigate the health-care system. As we explain later, we used our findings to inform a programme for young people that supports this aim (see Chapter 9).
We consulted CA and other young people at various stages of the development and design of study materials (i.e. information sheet, consent form and topic guides). They advised us not to use the term ‘disease’ in our project title and tag line (i.e. ‘This Sickle Cell Life: voices and experiences of young people with sickle cell’) and gave input when we liaised with the graphic designer over the look and feel of the project materials.
Patient and public involvement experts have extensive networks,65 and for this project CA, NW and PO helped us broaden our reach to different stakeholders. We drew on their networks to launch the project and elicit comments and suggestions during later stages (e.g. during analysis and during the process of reflecting on how the findings might be translated into practice).
With the help of our PPI contacts and via their networks we arranged a launch event that was attended by many people with SCD, with some travelling considerable distances to do so. Participants also included service providers, researchers and postgraduate students. They were enthusiastic about the project. We presented study aims, answered questions about the project and invited comments and suggestions. Participants gave us insights and suggestions for data collection and analysis. We arranged the event so that participants would have time to network with one another over tea and biscuits. Participants reported finding the event enjoyable, meeting new people and following up with people they had met at our event (e.g. being able to invite new contacts to a SCD workshop for patients and carers).
Involvement during data collection
CA helped us recruit interviewees from outside health-care services, which was one of our planned ways to include those who might engage with services less often. After discussions with CA, and noting her deep knowledge and excellent ideas for the project, we arranged a contract and an amendment of ethics approval for her to conduct some of the interviews for the project. We provided training to prepare her to conduct interviews (on qualitative research interviewing and ethics). CA found patient recruitment outside services difficult (as did we; see Chapter 5) and was unable to recruit any further interviewees. We continued working with her on other aspects of the project, including data analysis, write-up and dissemination.
Involvement during analysis and knowledge translation
The PPI experts informed the analysis and interpretation of the data and helped us think about how to translate findings into useful resources to support transitions. They facilitated relationships with charities working with people with SCD and also assisted with work to help get the findings into practice. During our meetings, we also answered questions about the project and invited comments and suggestions for further analysis and interpretation. The PPI experts contributed with ideas for further analysis, helping put the data into context.
Patient and public involvement experts collaborated on analysing and disseminating findings. Their additional role as authors46 emerged from our discussions of the findings and analysis for which they provided substantive insights. We (academics) worked with the PPI experts to develop ways of writing together that were not unduly burdensome for them while also ensuring that they had appropriate authorial voice. We wished to balance the types of tasks that it was reasonable for non-academic authors to do while avoiding unethical ‘gift’ authorship. One article has been published at time of writing. 46 There has been considerable interest from others in our process of writing together and we hope to explore this further together, reflecting on what worked well and what worked less well during the co-authorship process. We hope to write about our reflections so that others can try out similar experiments and/or comment on the process.
The Sickle Cell Society (London, UK), a national patient charity representing the sickle cell community, NIHR CLAHRC NWL and CA were all involved in translating our findings into practice. We presented our analysis and discussed it with them in a reflective session on knowledge translation and implications for practice. They helped us decide how best to translate findings into useful resources to support transitions. This collaboration resulted in our findings feeding into the development of a programme delivered by the Sickle Cell Society to support transitions for young people with sickle cell and their families [see Chapter 2, objective (d)]. The programme’s second phase is greatly informed by our findings as well as issues prioritised by the Sickle Cell Society and its network of individuals and families affected by SCD. The work includes a public awareness campaign that aims to address the wider social context of transitions identified in our study (e.g. lack of awareness and knowledge about sickle cell in school contexts, among peers and at work). We include more information about the programme in Chapter 9.
During knowledge translation, CA arranged and joined us in a meeting with the patient charity Sickle Cell & Young Stroke Survivors (www.scyss.org). We discussed our findings and ways to put them into practice via useful resources to improve transitions for young people with SCD. The meeting helped us put the data into context as well as providing useful discussions about the development of resources.
Our discussions with PPI experts in the project, sickle cell disease specialists, SCD charities, PPI/co-production experts and health-care quality improvement professionals resulted in our changing our original plan, which was to co-produce project output resources via collaborative workshops. We originally proposed four workshops with young patients with SCD to discuss the findings and reflect on ways in which they could be translated into useful resources, including a digital story/film. As our study progressed, emerging findings and our engagement meetings with various stakeholders helped us realise the importance of:
-
Addressing the wider social context of young people (e.g. developing resources targeted not at young people with SCD themselves but at others who also have an impact on their life and health care). This also dovetails with our findings that highlight the importance of removing responsibility for improvement from young people with SCD to avoid perpetuating the idea that the locus of control for the condition rests solely in the young person.
-
Working with patient charities who were already working with young people with SCD and representing their voices (as detailed above) to translate the findings into resources. We were also alerted to the existence of SCD digital stories, including one about transition.
We changed our plan to accommodate our new knowledge of the situation and the preferences of the people we were working with. Instead of creating workshops and a film we worked with the engagement team &Us at the Royal College of Paediatrics and Child Health (RCPCH) to deliver a participatory event to collaboratively reflect on the findings, their implications and next steps (e.g. co-produce ideas for improving transition). &Us involved young people in the planning of the event, and we also engaged stakeholders via the NIHR CLAHRC NWL Early Years Steering Group, from whom numerous ideas emerged to shape and guide the event. We worked with the &Us project team to take advantage of their expertise in events run by, and for, young people. Young people with SCD and other long-term conditions participated in the event and the discussions it generated about outputs for the project.
The participatory event also involved other key stakeholders, including carers of people with SCD, representatives from NHS England and school staff. We were careful to ensure that we included accident and emergency (A&E) doctors and non-specialist health-care providers, both because our findings had indicated that they were particularly important stakeholders when it comes to improving transitions and also because they were identified by the PPI experts as key stakeholders (see Chapter 9). NW co-delivered part of the event and PO participated in it. We used participatory approaches throughout the plan for the event.
The event has generated meetings with various stakeholders and facilitated further discussions about the implications of our findings for practice and further issues identified by participants (including young people) at the event (see Chapter 9).
Reflections on patient and public involvement challenges and facilitators
It takes time and resources to build meaningful and sustainable PPI relationships. We had already developed relationships with PPI experts prior to grant development and funding application. Had we not had this relationship we would not have developed the project in the first place (i.e. the PPI experts had sensitised us to the importance of the issues and they were crucial in shaping the study with us).
Advantages of taking a co-productive, dialogical approach included a flexible and responsive approach to involvement that considered how non-academic partners wanted to participate and how they were able to participate, long-term engagement of PPI experts in the project (i.e. from inception to dissemination), PPI input iteratively shaping the research process and knowledge produced throughout, and the chance for PPI experts to see how their input was shaping different aspects of the project. Challenges included structural constraints to do with the grant writing and funding process, lack of time to support joint writing and lack of academic structures to support writing with non-academic partners.
We were subjected to funding deadlines that were not flexible enough to incorporate PPI at the late stages of the funding application. The turnaround time to respond to reviewer comments was far too short for us to ensure that PPI experts had an input. We had approximately 1 week between receiving comments and the deadline for our response.
We requested an extension; however, this was refused because the funding panel meeting date was fixed and the turnaround time limited accordingly. Not only were we unable to include the external PPI experts in the response to reviewers, but a key member of the academic team was also unavailable during that week. In the context of a chronic condition where individuals may need to rest this is particularly problematic because participants should not be expected to put their health at risk to respond to unexpected and tight deadlines. The tight turnaround time, without prior notice of the deadlines involved, would also disproportionately disadvantage those with caring responsibilities who may need to plan time to meet short deadlines. We fed these reflections back to NIHR at the time and so the specific procedures may now have changed. We note that NIHR has been highly supportive of our PPI involvement efforts throughout and has taken limitations of its processes seriously. In addition, NIHR supported us when we wished to implement better PPI strategies that deviated from our original plan.
Meaningful and sustainable PPI throughout the project has been assisted by having dedicated resources to ensure that PPI experts are paid for their time, commitment from all partners to collaborative working to meet the goal of improving the lives of young people with SCD and flexibility. 56
A flexible approach to respond to PPI expert needs and preferences was crucial. 65 We tried to ensure that the meeting formats encouraged dialogue and that times and locations were convenient. Our aim was to make the project’s ‘participatory spaces’65 as inclusive and collaborative as possible. For instance, our smaller meetings were often informal and included coffee shop meetings, workshops and ad hoc one-to-one teleconferences to discuss specific issues. These different formats enabled us to share ideas and critical reflections with one another in ways that encouraged dialogue.
The work was time-consuming for PPI experts. Having resources to pay them for their time on the project was important. As researchers we were paid for our time working on the project and we wanted the time and expertise of PPI experts to be recognised too. NIHR also recognised the importance of these payments and agreed to fund them.
We present quotations from PPI experts reflecting on their involvement in the project, with their permission:
Working with the LSHTM [London School of Hygiene & Tropical Medicine] team on the This Sickle Cell Life transition project has been an absolute pleasure. Not only has my point of view and experience as a person living with sickle cell disease been utilised and considered as professional expertise. I have been empowered and trained to partake in the project in a more hands-on role and been invited at every stage of the project to contribute and co-produce content based on the research outcomes.
Quotation 1, CA reflecting on her participation
What stood out about working in the project was that I was listened to fully and that it was truthful; researchers were not trying to steer me in a particular direction. You get involved in research projects and they often have a predicted hypothesis. Our presence [PPI experts] was always at the forefront, I was involved at every stage. This is true working together, what I define as working together as a team.
Quotation 2, NW reflecting on her participation
What I have appreciated is working in a co-productive way; the team’s receptiveness to suggestions and their open-minded attitudes. We have all worked on equal footing. I have felt acknowledged as an equal partner. I have always been recognized at the decision-making process and have been able to see my contribution. This was reflected at the participatory event with RCPCH where it really felt that it was our work, the work of the whole team. In other PPI projects there is not such feeling.
Quotation 3, PO reflecting on his participation
Chapter 4 Literature review
Health care for sickle cell disorder
In adult health services long-term clinical care for SCD is predominantly provided by haematologists, who are mostly based in large teaching hospitals that may not be close to patients’ homes. In paediatric services, care is often led by paediatric haematologists in collaboration with paediatricians with an interest in haemoglobinopathies at local centres. The differences in service delivery structure and access to expertise may affect young people’s experiences of care when they are transitioning from child to adult services. Acute painful episodes requiring medical attention are usually managed outside the specialist services in the nearest hospital, in A&E departments or on general (non-specialist) paediatric/medical wards. The disadvantage for people with SCD is that expertise in managing the condition may be severely limited or completely absent in non-specialist health services. 68 In recent years increased attention has been paid to meeting the need for better SCD care in the UK. 18 This has led to the creation of dedicated pain management day centres for SCD in many hospitals, tailored transition care clinics for young people moving between specialist paediatric and adult services, the establishment of an NHS Specialist Commissioning Group for SCD and thalassaemia, and development of National Institute for Health and Care Excellence guidance21 and Sickle Cell Society standards for care. 68
Hospital admissions rates among people with SCD as primary diagnosis in England rose between 2001/2 and 2009/10, from 21.2 per 100,000 population to 33.5 per 100,000 population. 25 Most of the admissions lasted < 24 hours, but hospital readmissions and in-hospital mortality among SCD patients were highest among those with comorbidities and from the most socioeconomically deprived areas. 25,69 Painful episodes are the most common reason both for attending emergency services and for hospitalisations among people with SCD. 70 They can be excruciatingly painful and require timely treatment not only to alleviate pain but also because they can be accompanied by other acute complications [e.g. stroke, liver or splenic sequestration, acute chest syndrome (a life-threatening complication of SCD) and infections]. 21 Treatment of painful episodes often requires strong analgesics and the reassessment of response to pain relief every 30 minutes until pain is improving and for at least 4 hours afterwards. 21 Careful monitoring for complications during treatment of painful episodes is also essential. Poor monitoring of respiration after administration of opioids can lead to death. 71
One US study showed that patients with SCD waited significantly longer for pain relief on acute presentation to the A&E department than patients presenting with pain from renal colic (chosen as a comparable condition). 72 The patient-reported experience measure developed and validated for children and young people in the UK by Chakravorty et al. 18 has substantiated this finding. There is a widespread problem of poor knowledge about SCD among non-specialist health-care providers and the general public, as well as an overall poorer experience of care in the emergency setting than in planned specialist care. Lack of timely provision of pain relief is of particular concern. 18 Failure to manage acute painful episodes adequately can lead to morbidity. 73 Management of painful episodes is an excellent example of an aspect of care for which it is not only desirable but essential that SCD patients and clinicians work together to achieve optimum health outcomes. Engaging with patients’ pain reports with an attitude of ‘empathy and acceptance’20 is crucial for developing trusting care relationships and should be part of physical/clinical management. 20,74 In the UK, national guidelines21 emphasise that health-care providers should treat patients who are experiencing a painful episode as experts in their own condition, and must take patients’ own views and preferences into account. However, patients with SCD experiencing painful episodes can be seen as ‘problem patients’. 75 Lack of legitimacy of SCD patient voices extends far beyond the clinic. Our paper on patient experiences of pain management18 was rejected from one journal based on a reviewer’s and editor’s claim that patient perspectives cannot be considered as a source of evidence on their own without further supportive evidence/data.
Living with sickle cell disorder
Sickle cell disorder research has been dominated by a biomedical model that ignores the social dimensions of the disease. 76–79 However, we know that people’s social context plays a key role in supporting or undermining how they cope with SCD. 78,79 The attitudes of others to the condition and their ‘disabling responses’, including lack of sensitivity to young people’s concerns, can make young people with SCD feel excluded and misunderstood. 79 Experiences of living with SCD while trying to live a ‘normal’ life are complex for young people. 79 The unpredictability of the condition makes the SCD experience uncertain, with periods of acute pain threatening the person’s sense of autonomy24 as well as affecting school attendance79,80 and employment. 81 Coping experiences need to be understood not only in relation to personal resources and capabilities but also in the broader context of how others respond to the condition and the life changes experienced during transitions to adulthood. 79 With some exceptions (see, for example, Dyson et al. 24,58,80 and Atkin and Ahmad79) there is little research on the experiences of young people living with SCD80 and, in particular, on how the social context in which they live shapes these experiences. We know, for example, that young people’s negative experiences of how others react to their condition and self-management practices (e.g. being denied drinking water or toilet breaks) at school mediate their experience of SCD, making their illness experiences worse80 and limiting their ability to cope. 79 Support at school is poor. 24 The stress created by teachers’ and peers’ responses can contribute to triggering painful episodes. 24 School policies (e.g. attendance and active participation in physical activities) and routines have also been found to be disabling of young people’s attempts to maintain health. These may completely contradict clinic recommendations for self-care. 58 Experiences of racism can also be part of the life of individuals with SCD and intensify the experiences of marginalisation that they already encounter because of their condition. 24,79 The invisibility of SCD symptoms contributes to others failing to appreciate the seriousness of the condition, including SCD pain experiences. This in turn affects how others react to young people’s SCD,58,79 often with insensitivity. 79
Pain is central to the experience of living with SCD and has a significant impact on quality of life. Communicating pain to others, including health-care providers, can be a challenge for individuals with SCD, who see their pain experiences as ineffable. 82,83 Research shows that people with SCD find that their pain reports are not always taken seriously and can be treated with scepticism. 79,82 Some children and young people with SCD may minimise the expression of pain to avoid worrying their parents or peers79,83 and can develop pain coping strategies (e.g. watching television, listening to music, socialising)82,84–86 that may not make their pain visible to observers. 82 These coping strategies may mean that others disbelieve pain reports. 83 The fact that the condition manifests in very different ways in different people can also contribute to others’ disbelief of young people’s reports of their illness experiences and self-management needs. 24
People living with SCD engage in ‘bracketing SCD’24 in their life, distancing themselves from the condition and not making it a central aspect of their identity. 79,87 Attending to social aspects of young people’s illness experiences and the role of others on the development of coping strategies and self-identity is crucial,78 particularly during transition to adulthood. Identities include ideas we form about ourselves and our bodies, as well as understandings of how we should behave, that can affect how we act in relation to health,88–90 and this in turn can affect our health. Our in-depth sociological approach and conceptual framework,61 which we present below, contributes to such understanding by locating health-care transitions in the broader social context of young people’s lives and their transitions to adulthood. In doing so, we respond to calls for social science approaches to SCD and move away from research that has located the problem within internal (physical or psychological) characteristics of the person. 24
Conceptual framework: transition and the importance of identity development
Health literature around transition between paediatric and adult health-care services often implies that transition to adulthood is a linear process at the end of which young people are independent,91 adopt healthy adult lifestyles and are economically productive. 6 Adolescence is framed as a vulnerable and problematic phase that needs to be addressed through transitional care support. 91 In this view, young people are potentially ‘at risk’92 (e.g. not adhering to treatment or disengaging from services)3 and in need of improvement. During transition, they must become autonomous, compliant and responsible adults who take control of their condition. 91 In line with this implied view, transitional care recommendations and guidelines in the UK and elsewhere focus on encouraging young people to develop into ‘patient experts’, with the necessary health literacy and skills to take individual responsibility for self-management of their condition. 3,6,93,94 There is also an implication that developing adult-like rationality will result in healthy behaviours. 91
However, there are multiple interconnecting factors beyond individual capabilities that influence young people’s understandings and responses to health issues. For this reason, it is essential to move beyond the linear conceptualisation of transition to take account of more complex features of the phenomenon. Here, we draw on sociological and anthropological literature that views transitions as messy and non-linear processes that involve identity development. 95–97
We conceptualise health-care transition as a lengthy, complex and dynamic process98,99 that continues after the transfer into adult services4,100 and interacts with other aspects of transitions to adulthood (e.g. starting sexual relationships or moving from education to work). Borrowing from biosocial and ecological approaches to transition,17 we take young people’s wider social contexts into account, including the micro-system (e.g. home, health services, school, friends) and the macro level of sociocultural norms and attitudes circulating in young people’s social groups (e.g. connected with adolescence, health and illness) and the interactions between these. This approach helps us move beyond the clinical realm and examine how health-care transition intersects with transitions to adulthood within the wider social context, including within education, work and social life. We contribute to this model by focusing on the role of identity development during transition. 61
Life-long health-related habits develop during transitions to adulthood. 101 Young people are urged to improve their self-management skills and health-related knowledge during this transition period. 5,6 However, transitions, including health transition, require not only skills development but also the development of new identities (i.e. a sense of who one is and how one should behave as an adult, for instance as an adult rather than a child patient). 61,102 Identity formation and the tensions around identity development are crucial during transitions and any effort to support young people during this period should take these developmental issues into account. 10 Identities shape individuals’ approach to health90,103 and health-related practices. 90,104 Understanding how identities develop during transitions can help in understanding why young people move into healthy adult life successfully or not, especially in relation to how they adapt to their health conditions. 105
We lack understanding of how health transition shapes young people’s identities or how these identities contribute to how they develop into adult patients.
Transitions can be conceptualised as complex and non-linear, involving intense identity work. 95,96 Identities function as ‘recipes for living’ or ‘interpretative frameworks’ through which health behaviours and health experiences are mediated. 88 Transitions involve multiple changes in young people’s lives that produce ‘ruptures’ in their existing habits, knowledge and self-definitions. 106 Ruptures during transitions require young people to redefine their identities and understandings so that new ways of acting can emerge. During this process, young people must reconstruct understandings of what constitutes an ‘adult’ and an ‘adult patient’ for themselves, as well as negotiate related values and ideas about these concepts circulating in their sociocultural environments. 107 These concepts and related social ideas are functional for the young person. They work as frames of reference for them to make sense of their new experiences and to develop identities that regulate their behaviours in new contexts and relationships. 107 The identities they develop during transition are the outcome of young people’s efforts to address changes in their lives and to respond to normative ideas and demands about how one should behave as an adult that circulate in their social contexts,107,108 including, for example, ideas around healthy lifestyles, self-management and demands from educational and health-care systems.
How identities develop during transition can help us understand whether or not young people develop images of themselves that help them adapt to their condition, engage in protective health practices and function effectively through the different life changes they experience. A focus on identity also offers a way to take into consideration the role of the social context in organising young people’s transition experiences and shaping their sense of self. Particularly important during transition is the process of working through the ambivalence and tension between different self-images and establishing an integrated adult identity to navigate the demands of adult life. 109 We hypothesised that living with a long-term condition may prolong this identity development process and make it more challenging. 61
Chapter 5 Methodology
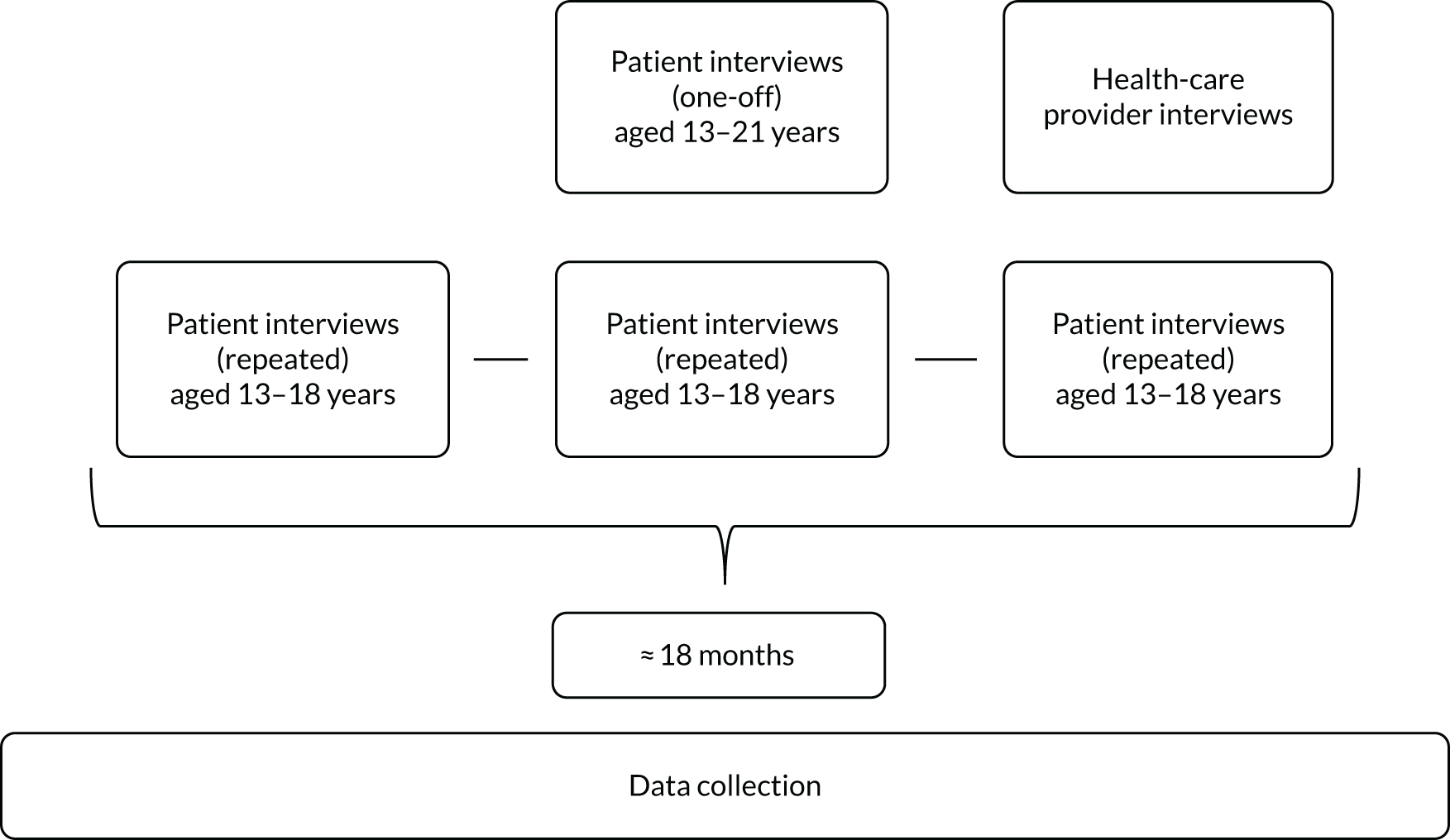
We explored the lived experiences of participants and their views on transition. We used a longitudinal, qualitative design (Figure 1).
FIGURE 1.
Data collection.
We recruited participants from as wide a range of locations as possible in two cities (i.e. London and another large English city).
London is the UK city with most cases of SCD,25 and we added another UK city to provide a point of comparison. We do not name this city because outside London there are comparatively few people with SCD and we do not wish to compromise confidentiality.
Data collection comprised 80 interviews with 48 young people with SCD (30 women and 18 men aged 13–21 years). This included 27 one-off interviews (17 interviews with 19- to 21-year-olds and 10 interviews with 13- to 18-year-olds) and 53 repeated interviews with 21 13- to 18-year-olds, interviewing them two or three times over a period of approximately 18 months.
The longitudinal element of the study included repeated interviews with younger participants to capture their experiences during the process of transitioning, as well as any changes happening over time during this period. This approach was useful to capture the evolving experience of the unpredictable nature of SCD110 and developmental processes. 111
We conducted single interviews with older participants who had already been transferred to adult care. We included this wide range of ages because transition is a dynamic process and we wanted to cover ages when the concept of transition is introduced in health-care services through to the post-transfer period in adult services. It was also important to include younger participants (aged 13–15 years) because the concept of transition is generally first introduced at this age, making their concerns and experiences particularly relevant. Interviewing older participants who had already been transferred to adult services allowed us to capture both their retrospective accounts and their current experiences of adult services, which we approached as part of the ongoing transition process.
Interviews
Patient interviews
We recruited participants via sickle cell disease specialist health-care services and from communities via our network of contacts with patient advocates. For recruitment via health-care services, clinical staff from those services first approached potential participants and told them about the study, giving them the opportunity to be contacted by us if they were interested in participating. Among those potential participants, 16 whom we approached did not go on to participate (in most cases because they did not return our calls or were busy). We originally proposed to conduct approximately 105 interviews across different age groups. During the analysis we conducted alongside data collection we reached thematic saturation112 (i.e. when the key themes about transition and the experience of living with SCD were being addressed and new interviews added little extra information). At that point we closed recruitment to the project. In addition, recruitment was very challenging. Partly for this reason, we enlisted the help of PPI expert CA (who has SCD; see Chapter 3); however, CA was also unable to recruit any further participants and we judged that the difficulties of recruiting new participants and the resources that would have been required would most likely not be offset by extra information gained from new interviews.
Patient interview topic guides were shaped by discussions with PPI experts in the project56 and fully reflected our research questions to explore young people’s experiences of navigating health transitions beyond clinical settings to consider the wider context of young people’s lives. We explored their experiences of receiving health care as well as experiences of growing up and moving into adulthood, including changes they were experiencing in their life more generally, such as in education, relationships and life at home and work, and how these inter-related with their health experiences. Topic guides for follow-up interviews were informed by specific topics that emerged in first interviews on which we wanted to follow up. In repeated interviews we also captured their lived experiences and changes since the previous interview. Eliciting good-quality accounts from the youngest participants proved difficult using traditional interview techniques. Participants told us that SCD and life with SCD was not something that they were used to talking about. For example, they found it hard to articulate their pain experiences verbally. They said that others’ lack of experience of this type of pain made articulating it harder because others would not be able to understand their experiences. To help participants describe their experiences we gave them a pen and paper and asked them to draw their experiences of living with SCD (e.g. pain experiences and managing SCD in other spaces of their life outside hospital) and to talk while they drew to tell us about the representations they were producing (see Appendix 2). Once they finished the drawing we also asked them to explain the representation they had produced and used the conversation to introduce follow-up questions. The drawings helped them use imagery and metaphors to represent what they described as ineffable experiences. One participant told us that drawing provided an alternative mode of expression. The dynamics of the interview suggested that the act of drawing and doodling while talking also created a more relaxed space, where the focus was moved from the young person to the drawing and what the drawing represented.
AR conducted the interviews. As we explain in Chapter 3, we had hoped for CA (a PPI expert) to conduct some interviews through recruitment outside health-care services, but unfortunately she was unable to recruit and conduct interviews. AR is a white university researcher without SCD and her position may have influenced what participants did or did not want to report (see Chapter 7, Limitations of the study). AR was not an employee at any of the health service or recruitment sites.
Health-care provider interviews
AR conducted 10 interviews with health-care providers from specialist SCD teams.
The health-care provider interviews explored experiences of providing care for patients with SCD undergoing health-care transition (either preparing for transfer or having undergone transfer to adult services), as well as their views on best approaches to transitional care.
We adopted a flexible approach to conducting interviews to respond to participants’ needs and preferences. Participants chose interview locations and times. Interviews with young people were mostly conducted in homes, with some in hospitals. Provider interviews were conducted in the health-care settings where they work.
Interviews with patient participants lasted between 60 and 90 minutes and those with providers were 45–60 minutes long. All interviews were audio-recorded and transcribed verbatim by a transcription agency, with checks for accuracy by the research team. We took fieldnotes after interviews to record our experiences of conducting the interview, key topics discussed by participants, characteristics of interview locations and other reflections about how different aspects of the interview might have influenced the interview dynamics, including what young people told us.
Analysis
We used NVivo version 11 server software (QSR International, Warrington, UK) to organise the data. For the analysis of interviews we adopted an inductive, iterative approach following some of the steps of grounded theory,112 a particularly useful approach to studying lived experiences of chronic illness, and thematic analysis. 113 We developed the coding frame inductively from the interview data set. We started with open line-by-line coding to stay close to the data and moved in later stages to more focused coding to synthesise, categorise and compare the text data. 112 The coding frame was also in part based on our original interest in understanding young people’s experiences of transition in different arenas of their life, including their experiences of interacting with health-care services during this period. The coding frame and the emerging analytical themes were refined alongside repeated rounds of coding and ‘memo-writing’112 (about codes, about emerging analytical themes and about each case/participant) and via regular reflective dialogues with patient and carer PPI experts. The analysis focused not only on what participants were saying (i.e. the ‘whats’ of their experiences) but also on how their experiences and views were recounted in the interview situation. 114
We also attended to the types of social positions participants adopted at different points of the interview, which helped us identify the type of identities they were constructing through their narratives. 61,64,104 In the analysis we took into consideration the interactional and socially constructed nature of interview narratives,114 reflecting on the ways in which we as white academic researchers without SCD might have participated in the co-production of data (i.e. what participants reported) and how participants positioned themselves in the interview. We reflected on contextual issues, such as how the physical location of the interview (i.e. health-care services vs. home), might have shaped the relationship between interviewee and interviewer, rapport between them and the data generated. The interviewer, AR, introduced herself as a researcher who was independent of participants’ health-care services, with no connection with any type of service provision. We wanted to minimise possible participant concerns about being judged by us (e.g. about whether or not they were taking responsibility for their condition). The study information leaflets were designed to be youth friendly (we worked on these resources with young people; see Chapter 3) and clearly communicated researcher independence. In an attempt to be more approachable we also did not include our academic work titles (e.g. Dr) in study materials. Trying to conduct interviews on participants’ ‘home turf’ was also a deliberate attempt to facilitate rapport with participants.
Changes to the original protocol
We originally planned to collect diary data from 15 patient interviewees to supplement their interview accounts of their experiences during transition. We invited interview participants to volunteer to complete diaries in which we asked them to tell us about their everyday life with SCD. We gave them an open brief and an opportunity to talk (via audio-recorder) or write about or take photographs that related to their thoughts, feelings and experiences of living with SCD. Completion rate was low and diaries were very short (in most cases they contained one or two brief diary entries). We received only six diaries from the 24 participants who had volunteered to complete them. We had offered this activity to many participants because we had anticipated low levels of completion. We also adopted a flexible and open approach to the task, offering young people a choice of audio, photographic or written formats. We received one photographic diary (consisting of just one photograph accompanied by a sentence explaining why this had been chosen to explain the participant’s experiences), two written diaries and three audio-recorded diaries that were transcribed verbatim. We analysed the diaries using a thematic approach. These did not yield different/additional data, although they sometimes added detail or nuance as well as reiterated issues explored in the interviews. We had chosen diaries as a complementary data collection technique because they are thought to be non-intrusive ways of collecting longitudinal data about health-care and social experiences during transition. 115 Our participants, however, fed back to us that the diaries interfered with their daily responsibilities (e.g. homework) and with their desire not to think about their condition.
We originally planned 15 interviews with specialist health-care providers to compare young people’s concerns about and views on transition with those of specialist SCD health-care staff. Our emerging findings, however, indicated that the problems they experienced were not within specialist services and so we reduced the total number of interviews. The 10 interviews gave us a sense of the context of specialist care and helped contextualise patient accounts of specialist services.
We originally planned to analyse contemporaneous medical case notes for diary participants, with their consent, to compare the clinical records of their health status and treatment alongside their subjective diary and interview accounts of transition experiences (e.g. having many pain crises might have an important effect on transition experiences). We did not engage in this task because we had so few diaries and also because the interviews gave us detailed accounts of timings and experiences of painful episodes, acute hospitalisations or SCD-related complications.
In response to our findings, engagement with various stakeholders and discussions with PPI experts, we changed our original plan to conduct four workshops with young people with SCD to co-produce output resources. Instead, we conducted a participatory event (reported in Chapter 9). We explain the reasons behind these changes in Chapter 3.
Ethics approval
We received a favourable ethics opinion for the study from the London School of Hygiene & Tropical Medicine (LSHTM) (reference 10107) and approval from the NHS Research Ethics Committee (reference 15/LO/1135). Participants aged 16–21 years and parents/carers of 13- to 15-year-olds gave informed consent to participate. The 13- to 15-year-olds additionally provided their own informed assent. At the end of each interview we gave participants referral information about external agencies they could contact for support on issues raised. We gave patient participants gift vouchers to compensate them for their time. To protect anonymity we identify only participant age range in our reporting, not exact age.
Chapter 6 Results
During transitions, young people find it challenging to develop and practise patient expertise, including involvement in decisions about their own care [see Chapter 2, objectives (a) and (b)]. We report some of our findings elsewhere,46,61,83,116 and some of the interview quotations used in the other publications are reproduced in this report (in some cases the quotes have undergone minor edits for readability).
In the quotations presented in this report, we have used ‘[ . . . ]’ to indicate where we have cut text from the interview transcript. Short pauses are indicated with ‘( . )’, and ‘. . .’ indicates that the interviewee did not finish the sentence.
Young people struggle with health-care transitions. There are tensions between the expectations of them as adult patients (e.g. being independent and engaging in good self-care) and the realities of the disabling environments they have to navigate [see Chapter 2, objectives (a) and (b)]. On the one hand, adults in the health-care context (e.g. health-care providers) and parents/carers demand that the young person must learn more about their condition and body and act responsibly to stay healthy. On the other hand, when young people attempt to practise these new behaviours and use their patient expertise, for instance by making requests about the care they receive, they are often disregarded. This disregard typically manifests in non-specialist health-care settings during unplanned visits (e.g. in A&E and on general hospital wards if they are admitted as inpatients for unplanned care). 46,116 Disregard for their voice is also manifested in their social context via their schools and peers.
These findings form four key themes: (1) the push for young people to engage in self-care, (2) obstacles to achieving self-care, (3) young people’s mistrust of hospital care and (4) the problems young people encountered in their schools and social contexts. We present these in detail below and end the section by describing how young people navigate the obstacles they encounter.
The push for young people to engage in responsible self-management and develop patient expertise
Transition involves young people trying to discipline themselves in response to the push for responsible self-management and patient expertise that they experience from health-care services and carers while also often working hard in other areas of their life (e.g. education and work) to become the type of adult they are expected to be (e.g. self-actualising and productive) [see Chapter 2, objective (a)]. 61
Young people growing up with SCD develop personalised knowledge about how SCD affects them. 46,61 Participants presented themselves at the interview as being – and working on becoming – disciplined patients who take responsibility for self-monitoring and managing their condition, with expertise in their own body and knowledge of SCD. They described themselves as knowledgeable about their bodily limits, their pain experience and the therapeutic practices and medications that work for their individual bodies. Their personalised knowledge includes differentiating the types of pain episodes and their consequences. They talked about increasingly learning about the timing of pain events and how different types of pain involve different lengths of recovery. They spoke about knowing which pain relief medication to take (depending on the stage of their painful episode) and talked about regulating how much pain relief medication they take. They said that this is important to ensure that stronger pain relief would be effective when needed. They often talked about being aware of risks to their health and of practices that are good or bad for their condition, including which pain relief and medication would be ineffective or inappropriate for them. They asserted their patient expertise, explaining that they know their body and how it is affected by SCD better than anyone else, yet they still recognise that the transition between paediatric and adult services is a process that involves commitment to learning about themselves and how the condition affects them. Participants talked about always carrying water and pain relief medication with them. They articulated extensive awareness and monitoring of their own body. They talked about listening to their own body, monitoring it (e.g. temperature, types and levels of pain), drinking water, avoiding cold weather and regulating their social life to stay healthy:
I always have water and my medicine in my room [ . . . ] I don’t go out as often, I’ve realised that, um, I like to study more [ . . . ] I know how to keep myself warm with clothing and stuff before anything else [ . . . ] I arrange my sleeping patterns in a way, like I’m getting enough sleep and stuff. So right now I’m trying to prevent feeling really tired and having fatigue [ . . . ] since I was younger they’ve always told me like water is the main thing [ . . . ] So I’m keeping hydrated and stuff [ . . . ] I just try and do it [read up on SCD] as much as possible so I’m learning about it each time [ . . . ] so I understand.
Quotation 4, A6, 16- to 18-year-old woman.
For participants, transition to adulthood involves learning to regulate everyday life and behaviours temporally and spatially to avoid and manage pain episodes. For instance, participants choose to manage a pain episode at home when possible, because for them this facilitates rest and a quick recovery. They have learned about the importance of responding promptly to the first signs of a potential crisis to avoid the pain episode escalating and having to be admitted to hospital. Participants also talked about regulating their behaviour spatially to self-manage their condition:
I have to be aware, just in case I do get sick. ’Cause sometimes in the day it could also just hit me [ . . . ] So I have to be just, like, aware, to make sure that I don’t overdo myself, or I don’t walk too much [ . . . ] especially in, like, really hot weathers or really cold weathers, so I have to make sure to, like, not go out for too ( . ) for a really long period of time. And also to always drink water [ . . . ] to keep myself hydrated [ . . . ] I try to make sure that I’m not going out too ( . ) too often, or if I do go out with my friends I’d make sure to go around [the neighbourhood] and not too far away, and make sure that my mum knows exactly where I am in case I do fall ill, then she’d be able to pick me up.
Quotation 5, Z1, 16- to 18-year-old woman.
For instance, participants typically talked about staying at home and avoiding socialising to manage SCD-related fatigue. When planning social activities or choosing where (or whether or not) to go to university, participants expressed a desire to stay close to home and hospitals (see Quotation 5). They talked about planning carefully ahead of social outings. This includes thinking about travel arrangements and about where activities take place to ensure access to their hospital in the case of an emergency or access to a lift to avoid fatigue. Participants said that they had developed their own techniques to self-manage a pain crisis and know how to ration pain relief to ensure its effectiveness. They regulate their social and everyday life around their self-management needs.
When speaking during interview, participants (more typically younger ones) produced accounts in which they addressed themselves in their talk and asked themselves to improve their self-management behaviour and become more responsible patients (see Quotation 7). For instance, they referred to the need to listen to their own body and monitor their body temperature and energy levels to avoid pain episodes (see Quotations 9 and 10). Calls for self-improvement to become a disciplined patient (who cares for themself) were more common among younger participants and echoed the discourses about individual responsibility that were conveyed by doctors/nurses and family/carers. Older participants presented themselves as already having moved into this type of responsible patienthood. For instance, they reported on their competent self-management practices. Participant Z1 (aged 16–18 years) (see Quotations 5 and 8) presented herself as expert in her own body and actively addressing its needs. She positioned herself as knowledgeable about pain and about how to manage it and talked about how socialising is an aspect of her life that she needs to carefully regulate to ensure that she maintains health. Although more common among older participants, younger ones also positioned themselves as having autonomy in self-care and being knowledgeable about their condition:
I know what I have to do to keep myself well [ . . . ] everything they [doctors, nurses] tell me to do, like get sleep or do this, I just do them, because I know it’s crucial for me.
Quotation 6, U10, 13- to 15-year-old boy
You have to be on top of all your appointments, you have to be on top of your prescriptions for instance, you can’t run out of them, things like that. You just have to be aware of yourself and look after yourself [ . . . ] just have to ( . ) be more aware of my sickle cell and not get caught up in everything. I don’t really know how to explain that but ( . ) if I am doing my [university degree] here, I just have to remember if I’m in the library all night, to eat well, to drink well, to keep warm, not do anything that’s unnecessary like go out in the rain, if I don’t need to. I just think you have to be more aware of it and it’ll be fine.
Quotation 7, I7, 19- to 21-year-old woman
I can cope on my own [ . . . ] I know when to take my tablets, I know when I have to like take a like break [ . . . ]. I know that like if I do, like, overexert myself then I will get ill and I’d know, like, I just know when I need to stop.
Quotation 8, Z3, 19- to 21-year-old man
Participants talked about transitioning into healthy adulthood in individualising terms (as an issue dependent on their own actions and self-improvement into disciplined patienthood). When asked about what type of support and resources would help them in their transition, their responses framed transition as a matter of personal change (i.e. an issue to be managed by the individual). They did not generally refer to how others could help them, but instead located control of health and of moving into healthy adult life within a purposeful and independent self who takes responsibility for their own health. Participants framed successful health-care transition as an individual change: a process of developing health-related knowledge and learning how to actively monitor their own body while regulating behaviour and their own life to maintain their own health. For instance, when talking about how to achieve a healthy future, participant E4 (see Quotation 10) talked in individual terms, focusing on better self-management and healthy lifestyle choices:
I have to try and be, yeah, you have to try and like relax more and [ . . . ] like not use a lot of my energy and like keep drinking water and stay away from like heaters [ . . . ]
Quotation 9, I5, 13- to 15-year-old girl (emphasis added by authors).
The reasons like I’m ill [ . . . ] is ’cause I wasn’t really paying attention to the way I was feeling. [ . . . ] I could have prevented it [pain crisis] if I’d paid attention [ . . . ] I should pay attention to this. ’Cause, yeah, attentiveness, that’s the thing I need to work on [ . . . ] I think I’m slowly getting there [ . . . ] like trying to change it [ . . . ] I am paying more attention in everything, really.
Quotation 10, E4, 19- to 21-year-old woman (emphasis added by authors).
Transition as a process of becoming a self-disciplined patient is learned through relationships with health-care professionals and echoed in relationships with parents and carers (see Quotations 11, 15 and 16). Participants talked about older adults’ constant reminders to take responsibility for their health (e.g. to stay hydrated and wear warm clothes) and about the risks of not doing so (see Quotations 15 and 16). Although this could be annoying for the young person, these exhortations could act as a reminder ‘to help me to stay healthy’ (E4, 19- to 21-year-old woman). Participants’ interview accounts illustrate how reminders to take responsibility are internalised and work to encourage them to be disciplined patients. At interview they addressed themselves in talk, drawing on someone else’s voice (presumably adult carer or health-care professional) to remind themselves about the type of adult patient they ought to be and about the consequences of not taking individual responsibility (see Quotation 11). Here, they were echoing the self-management and involvement in own care discourses they heard from health-care professionals and carers. Participants E4 and I5 (see Quotations 9 and 10) asked themselves to improve self-management practices and learn how to listen to their own bodies to avoid pain crises. Participant O7 (see Quotation 11) draws on what we interpret as the nurse’s voice to remind himself about the risks of not taking responsibility:
I didn’t care that much, um, but then [ . . . ] as you get older you know that you really need to start doing it [taking medication, attending appointments] [ . . . ] sometimes you get tired and you like you don’t want to take any medication, and you don’t want to go into hospital, um but then when they [doctors/nurses] tell you what the consequences will be, you get to understand more [ . . . ] she [nurse] told me what will happen if I don’t take it and how [ . . . ] there’s a possibility I could die, and then she said I won’t be able to [practise favourite sport] and so when I heard that [ . . . ] I thought, OK, I have to start taking it then [ . . . ] I’ve just mostly learned about how to keep my ferritin levels down [ . . . ] they check it at hospital so they’ll know if I’ve had medication or not. And so it makes you think, oh they’re going to find out [that I am not taking medication] anyway, so [ . . . ] oh I should just grow up and do it [ . . . ] and just take my medication and just go to the hospital, because it’s only helping you.
Quotation 11, O7, 13- to 15-year-old boy (emphasis added by authors).
They’d [doctors and nurses] always be like, yeah, you should be taking antibiotics. We know more about your condition than you do, we’ve done all this research, this is this, is this, you know? [ . . . ] just kind of felt like every time I went there, they would tell me all the possibilities of my condition and all the bad things that could happen because I had sickle cell. And all the things that I had to be doing and how I had to be like, I had to be on medication for the rest of my life.
Quotation 12, I9, 19- to 21-year-old woman
It [going to routine clinic appointments with a specialist team] teaches me just to look after myself. [Interviewer: How?] It just, you just, you realise like you’ve gotta look after yourself.
Quotation 13, Y4, 19- to 21-year-old man
Although participants talked about parents’ reminders to engage in self-management practices as if they were annoying (see Quotation 16), the parent gaze nevertheless works as a reminder to take responsibility. One participant told us how, after a long hospital stay, she had made the decision to start taking responsibility to engage in desired self-management practices. Her parents’ comments about an unhealthy lifestyle might have helped foster a sense of individual responsibility for the consequences of her choices:
My [mum/dad] was just telling me, you probably didn’t drink water, you probably didn’t do your exercise. ’Cause I probably wasn’t drinking water ’cause, um, the only thing I would drink is like fizzy drinks [ . . . ] I tend to drink a lot of water now [ . . . ] that’s the key.
Quotation 14, I8, 13- to 15-year-old girl.
They [parents]’re kind of, you know, lecturing me, or just reminding me every hour to drink water and to keep warm and things.
Quotation 15, A5, 16- to 18-year-old woman
My mum, they either just come one like in the middle of the day and say, I know you haven’t been drinking enough. And the thing is, I probably have. I’m not going to show you every time I’m drinking water, oh look I’m drinking water. I feel like I’m old enough to be thinking that by myself. Maybe when I was a lot younger, but that has been something that’s constantly annoyed me for a while, is people telling me what they think that I should be doing, even though I’m probably doing it anyways.
Quotation 16, I7, 19- to 21-year-old woman
Obstacles to enacting patient expertise: being disregarded and feeling invisible
As we have shown above, young people growing up with SCD developed an in-depth sense of individual responsibility for their own condition and personalised knowledge about their body and how it is affected by SCD. However, participants talked about having their expertise questioned or disregarded both during health-care encounters in non-specialised unplanned hospital settings and in interactions with others in their social contexts [see Chapter 2, objectives (a) and (b)] [see Health-care context (non-specialist hospital unplanned care) and Social context].
Health-care context (non-specialist hospital unplanned care)
Participants did not report having any problems with their transition from specialist SCD paediatric services to specialist SCD adult services. However, they did encounter barriers when they sought non-specialist unplanned hospital care, including hospital wards and A&E departments for painful episodes. Here we present participants’ experiences of health care during transition, focusing on their experiences of non-specialist unplanned clinical care outside the organised ‘transitional care’ they receive to prepare them to move into adult services [see Chapter 2, objectives (b) and (c)].
Participants encountered barriers to negotiating quality care and to being involved in decisions about their own care. 46,116 They told us that their voices are not always heard or acted on. Participants talked about not being listened to in those settings when using their expertise in their own body and condition and when trying to discuss with non-specialist staff how to manage their own care. 46,116 They described having their expertise questioned or disregarded by, for example, staff giving them a particular medication despite their protests that the medication would be ineffective or by staff inserting cannulas in areas of their bodies where participants had already explained that it would not work or would cause pain (see Quotations 18 and 19). Staff not listening to participants also translated into being discharged too early or not being admitted to hospital when they should have been (see Quotation 26). For instance, one participant talked about telling hospital staff he was still feeling unwell and needed to stay longer in hospital. He said that he was not taken seriously, was released and had to be readmitted the next day. Another participant found it difficult to convince staff that she had to stay in hospital because she felt unwell and the next day she was diagnosed with a chest infection. Older participants articulated more explicitly than younger ones their realisation that they are not always perceived as knowledgeable about their bodies and condition, that non-specialist staff lack knowledge about SCD and the frustration that comes from these experiences:
They [staff]’re always patronising. And they think I don’t know what’s best for me [ . . . ] they can’t just do whatever, they have to know how I feel, about what I’m feeling.
Quotation 17, U3, 16- to 18-year-old man.
The doctors that I’ve experienced [in A&E] do not help. Because I had ( . ) it wasn’t a crisis, but I had a weird pain here, and so when we went they gave me naproxen, which is just a different form of ibuprofen. And even though I said ibuprofen doesn’t work, that’s what they gave me, and they told us to go home.
Quotation 18, A6, 16- to 18-year-old woman.
If they [ward staff] were looking for a vein but they couldn’t find one and I was telling them where the veins were and they weren’t really listening [ . . . ] My veins collapse a bit and like when they look for one they can’t find one but like I know where they all are, so then I’ll be trying to tell them where it is and they weren’t really listening and they’ll just be, like, moving my arm around a lot and it would hurt.
Quotation 19, A1, 13- to 15-year-old girl.
Occasions when participants’ requests for pain relief were ignored exemplify the barriers they face in utilising their patient expertise. They talked about the frustration and stress of knowing how important it is to act quickly to respond to painful episodes but not having their request for pain relief treated as urgent (see Quotation 22). Participants reported delays in receiving pain relief and not being given the right pain relief or an adequate dose. They reported that non-specialist hospital staff ignore them when they say that they are in pain or question them about the degree of pain they are experiencing. They said that staff refuse to discuss with them how their pain should be managed. Participants told us of staff asking them to wait and giving them excuses regarding why delays were necessary (e.g. staff being busy). Participants told us of times when they had tried to explain to staff what method or amount of pain relief worked best for them but had been ignored. They were not able to be involved in deciding how their pain should be managed and their reports were questioned or disregarded. They said they know when they need medication and how frequently it should be administered, but they felt ‘ignored’ and judged when asking for it:
She’s supposed to be giving me pain relief every 2 hours, she’s ignoring me for half the day. I keep on asking her, you know, can I have my tablets now? She’s like OK, I’m getting them, and then an hour later I still can’t find her.
Quotation 20, I6, 19- to 21-year-old man.
The nurses are different on each ward. So it depends on the nurse itself, they’re gonna be mean or kind. So you just don’t know what you’re going to get when you’re on [ . . . ] Sometimes you’re just calling out in pain and you know you need your medication but no one’s coming. And it’s like your pulse is going up and no one’s here [ . . . ] Sometimes they’re, they’ll take their time coming [ward nurses] to get to you. [ . . . ] I feel sad ’cause sometimes it upsets me, like I feel like I’m neglected.
Quotation 21, O3, 19- to 21-year-old woman.
You might have ringed [sic] the bell maybe about, I don’t know, five, six times and, er, while you’re rolling around, they [ward nurses]’re really busy, moving around helping other people and stuff. So you might have to hold on a bit, er, longer than you’d normally hold on. So you might still be in pain and then, er, they’d only come to you, you know, maybe 2, 3 hours even after. And then of course they’d tend to you and by then it might, it, the pain might have risen so much that, you know, it’s, it’s, the painkillers won’t work so then you might have to use stronger painkillers [ . . . ] if you hold the pain for too long, um, it gets worse than it was before.
Quotation 22, O4, 19- to 21-year-old man.
Participants’ history of pain and of treatment fed into their personal expertise and they used this to assess and respond to their care needs. However, this experience-based expertise appeared to be disregarded and their reports about pain questioned or undermined, making participants feel judged and misunderstood. Participant I10 (see Quotation 23) talked about feeling that his patient expertise was not being recognised by staff. Participants were knowledgeable about their care needs and how pain relief works on their body. Participant I10 could self-assess whether or not a pain episode would continue into the following day. He drew on this knowledge to explain to staff his need to stay in hospital; however, he was not listened to. Having to wait for long periods before receiving medication makes participants feel ‘abandoned’, with delays also worsening their pain (see Quotation 22). They told us that the stress caused by waiting for pain relief makes the pain worse and makes it less likely that the subsequent dose will work:
They [staff] just kept on coming in and telling me that er erm erm that it’s OK for me to go home ’cause, ’cause when they asked me what’s the scale of like 1 to 10 of your pain, I told them at the moment it’s not, it’s not bad, it’s about er 3 or 2, so it’s not bad at all, but I told them that erm if I go home erm like at that, at that moment if I went home, I would pretty much be back tomorrow morning ’cause the erm medicines that they gave me would wear off. But I don’t think they were listening to me [ . . . ] they must have thought that maybe I didn’t know what I was talking about.
Quotation 23, I10, 16- to 18-year-old man.
Some participants understood delays in terms of staff overwork. However, others perceived delays in pain relief as being rooted in staff scepticism about their pain experience. Some participants told us about feeling that they are seen as liars or ‘drug addicts’ (see Quotations 24 and 25). One participant overheard ward nurses discussing his pain in sceptical terms:
They [ward nurses] say it [that you are a drug addict] amongst themselves and then you can hear it. So they’ll be like saying it, you’ll be laying in there and they’ll be out here talking, and be like oh, he just wants, you can hear them whispering to each other, you know, maybe his pain’s not that bad he just wants some morphine. You know, and you kind of like overhear it.
Quotation 24, I6, 19- to 21-year-old man
It was a bad experience really [being in the ward] [ . . . ] The doctors just didn’t really believe, not believe but they thought I was like faking or like doing it to get medication [analgesia] as if I like was addicted to medication. [ . . . ] But I can be laughing but still in pain and that’s what people need to understand, like nurses and doctors and even people in general, that I can be in pain, anyone can be in pain and like still be laughing because we know how to, people, like kids or, you know, kids know how to deal with the pain and we just try to distract ourselves.
Quotation 25, O1, 13- to 15-year-old girl.
When I was in, admitted [ . . . ] they would like sometimes say, uh there’s nothing wrong with her, uh she’s lying about her illness [ . . . ] It was difficult especially ’cause I was in pain, like I dunno ( . ) Why I would lie about something about coming to hospital? It doesn’t even make sense.
Quotation 26, Z1, 16- to 18-year-old woman.
Participants know where on their bodies cannulas are best inserted and where insertion attempts will not work. Nevertheless, they told us of times when they had tried to explain to health-care staff the best place to insert a cannula and staff would ignore them. Many disliked needles and how staff inserted intravenous cannulas in their bodies, often in places where they knew from past experience would not be successful. Participants also talked about staff inserting cannulas too abruptly. The consequences of staff not listening to them about how to manage their body and being too ‘rough’ were scars, heavy bleeds and pain (see Quotations 29 and 30). One participant talked about feeling dismissed by a doctor and characterised his attempts to give her an injection as being ‘stabbed’ when he knew she did not like injections (I9, 19- to 21-year-old woman) (see Quotation 28):
At the [children’s ward] they put the needle erm here, then the vein collapsed and then they started going here. Erm at [adult ward] they went back to here [the one that collapsed] and the first few times I told them that it’s not gonna work and it was like they weren’t listening to me [ . . . ] they would still try and do it. [ . . . ] And erm then it would fail, so it felt like they were putting a needle in for no reason.
Quotation 27, U5, 19- to 21-year-old man.
The same doctor who was talking down to me and made me feel very small. He, um, he, basically he tried to get an injection like four time[s], he knew I don’t like injections. He tried it four times, didn’t get it [ . . . ] He tried four times, didn’t get it. Then he got this, like, demon injection [laughs] and just like stabbed my artery. And for days my hand was like this.
Quotation 28, I9, 19- to 21-year-old woman
[I had] this arterial line but it was in my groin and they attached it with stitches, but then a doctor ripped it out without cutting the stitches off and it was bleeding, it was terrible [ . . . ] He was trying to take the arterial line out and the nurse said, you need to take the stitches out. But because I was so, so disorientated I was so out of it because I was in pain, and I was sick, I didn’t know what was going on [ . . . ] it was crazy.
Quotation 29 E1, 19- to 21-year-old woman.
[Hospital staff] left a bit of it [midline in A5’s arm], like, hanging out for, um, it was because I was having a PCA [patient-controlled analgesia] and fluids at the same time. And he left it hanging out so it was easier for the nurses. [ . . . ] They [hospital staff] pushed it all the way in, to the point where it was uncomfortable and hurt a bit. Um, but when I told them, they wouldn’t really do anything about it.
Quotation 30, A5, 16- to 18-year-old woman.
Not having a voice in interactions with staff and not being attended to in a timely way was also typical in situations where participants asked for assistance they required because they were immobile. For instance, participant Z1 told us she had asked staff to take her to the toilet and was told ‘I don’t have time, you have to ask another nurse’ (see Quotation 31). 116 Another two participants who were not able to walk properly were allocated beds far away from the toilet. They told us that their requests for help to go to the toilet or for a commode were not treated with urgency and they were made to feel a nuisance for requesting basic help. For instance, participant U2 told us about a time when she asked for a commode because she was on a drip and her legs were hurting. She could overhear the nurse talking to the other nurse saying ‘All the time this one needs a commode, commode’. She told us this made her feel ‘really upset’:
You’d press it, and like she wouldn’t come, and like you’d always keep pressing it. You could hear it ringing in the nurses’ station, but no nurse would, you know, come to, to me to see like if there’s anything wrong or anything. So you know, you’d be just waiting and waiting. And at that time, I think I needed the toilet or something, because I couldn’t walk, so I needed someone to take me there. But no one would come, so I had to wait for like half an hour or so to just, until they decided to come.
Quotation 31, Z1, 16- to 18-year-old woman.
Participant A5 (see Quotation 32) told us about staff not responding to her requests for help despite explicit manifestations of her lack of bodily autonomy (i.e. she had her wheelchair and crutches with her and had explained to staff she was unable to walk to the bathroom). She explained how, instead of responding to her requests for help, nurses ‘went ahead and did things how they usually do it and did it their way’. She ended up being taken to the bathroom by her parents during their daily visits:
The doctors and nurses, they, they encouraged me, they didn’t really force me, they, they just kind of kept nagging at me to try and walk to the, um, the bathroom, instead of having to use a commode. Um, and I kept telling them that I couldn’t do it ’cause it was too painful and I, I had to use a wheelchair. But, um, they didn’t really listen at all.
Quotation 32, A5, 16- to 18-year-old woman
Participant E5 (see Quotation 33) talked about the frustration of not having her voice heard when explaining to hospital staff that she should be put in the children’s ward (when admitted for painful episode) because she had not been transferred to adult services yet. She said she knew the protocol for ward admission, but her voice was not heard and staff often moved her from ward to ward because ‘they can’t, they don’t know where to, where I should be’. She described how ‘tiring’ it was having to move because she would have to walk and get out of bed. Others also told us about being moved between different wards while they were in pain during a single hospital stay:
It’s just sometimes, like, if I’m admitted, [ . . . ] it’s, like, a bit of a, it’s like, really weird, because they’re like, you should [be] on the [adult ward] because you’re [16- to 18-years-old], [ . . . ] they [doctors]’re always getting confused [ . . . ] It’s just, it’s kind of tiring. Especially if [ . . . I] have to walk around, or if I had, like, if I’ll be in a bed and I have to go somewhere different. [ . . . ] So [ . . . ] I’ve been moved from a ward to another, and back again, then back to A&E, and then back to another ward. [ . . . ] They don’t know where to – where I should be. So, it’s kind of like, here we go again [ . . . ] And obviously I’ll be . . . there’s no one going to be there to fight my corner, because mum’s not going to be there. And so it’ll be like explaining to them, like – no, this is what it is, this is what it is [ . . . ] So I want to try and, I want to try and stay, like, as healthy as I can. That way I don’t have to put myself in that, like, position.
Quotation 33, E5, 16- to 18-year-old woman.
When talking to us about how her transition experience could be improved, participant E5 (see Quotation 33) said that hospital staff ‘need to listen’ because ‘I am the patient so I know what’s kind of best for me’. Participants told us about the frustration of trying to repeat to staff what care practices are suitable or unsuitable for their SCD and how SCD affects them personally. From experiences such as those described above, participants became aware of the difficulties of using their patient voice to communicate their SCD expertise and knowledge of their own body when they were being treated by non-specialist health-care staff.
Participants reported that they find it hard to make themselves heard when trying to be involved in their own care for two main reasons: (1) the invisibility of SCD symptoms (particularly of pain-related suffering) and (2) the lack of knowledge of SCD among non-specialist staff. Health-care transitioning involved becoming aware of how non-specialist staff may have limited or no knowledge of SCD. Participant U9 told us that nurses do not seem to know that SCD is an inherited condition (see Quotation 35). Another participant (U5, 19- to 21-year-old man) told us about a time when a paramedic gave him too high a dose of morphine, an analgesic the participant had never had before. Participant U5 said the paramedic ‘didn’t know anything’ about SCD. Participants often said that non-specialist staff should learn about SCD as well as take seriously their request for pain relief:
I want them [nurses] to like, um, understand my condition, and if I, uh, if I’m in pain I should get some medicines.
Quotation 34, U2, 16- to 18-year-old woman
Nurses asked me, she said, oh you have sickle cell, I said yeah, she said how long have you had it? And I was just like, I was born with it [laughter] kind of thing. So I just thought they don’t understand really [ . . . ] the last thing I wanna do when I’m sick is start explaining stuff all the time to each person that comes.
Quotation 35, U9, 19- to 21-year-old man.
I would like to be, so, so, so they under, understand it more. So, whenever I go to like A&E, then I have to explain to some of the doctors sometimes like what it is, like what pain I’m in ’cause they don’t really like, they don’t really understand.
Quotation 36, O2, 16- to 18-year-old woman
Some participants said that, instead of listening to their reports of pain and how to treat it, staff judge their need for pain relief based on their poor knowledge of SCD and their limited experience of treating a few SCD patients, or their knowledge of other conditions that cause pain. Participants explained to us that SCD pain is different from other types of pain and talked about the difficulties of translating their pain experience in ways that are accessible to others. 83 They explained that each person with SCD is affected differently and emphasised the idiosyncratic nature of the condition. 83 One participant, for instance, mentioned that staff would sometimes compare her with other SCD patients, or with patients with other conditions (see Quotation 39). Participants talked about how people who have not experienced SCD pain cannot understand it. Their accounts indicated that they considered their pain to be ineffable:83
They [staff in the ward where she reported being ignored]’d only had one other sickle cell patient before me. I’m not sure how they handled her, but they didn’t handle that well with me, it was very bad [ . . . ] that’s what they kept referring to when they were partially ignoring me, they’d just tell me: ‘we’ve had someone else with sickle cell before’, and that was sort of the end of the discussion. Because they, whatever they did, they figured it worked with this other person, but it didn’t work with me. [ . . . ] It [sickle cell] varies from one person to the next.
Quotation 37, Z2, 19- to 21-year-old woman.
They [staff] haven’t . . . sometimes they’ve read my notes or not read my notes and there’s like a lot of notes. [ . . . ] It’s like ( . ) mm, like that they wouldn’t like really understand what’s, like even though I have sickle cell they wouldn’t really understand how it affects me, I’d have to like explain it every time.
Quotation 38, U4, 13- to 15-year-old boy
They [nurses]’ll assume that let’s say my pain score is at a 5 or a 4, when really it could be at an extreme 10 and still be there laughing and being happy [ . . . ] sometimes they [doctors]’re not trained or the, their speciality of, maybe they might be more into cancer research or to people with different, different, different cases than sickle cell. Sometimes they’ll think that, they’ll try and compare, I feel sometimes they try to compare the two, like two different cases with one another and sometimes they get it twisted because it might not be the same case. Maybe that person might be feeling pain, but they need to understand that my pain might be 10 times worse and that I could be, other people have a different pain tolerance. Some people can be crawling, or crawling around because they’re in pain or scream, sometimes people are even cursing, but with me I’m usually with pain I’ll try to be calm and breathe in and breathe out, so that it’s more calming and try and get control of the pain.
Quotation 39, O1, 13- to 15-year-old girl.
Participant I6 was knowledgeable about the difference between SCD pain and other forms of pain, and about the difficulties of articulating the degree of the pain:
[At the A&E of a particular hospital they are] slower with giving the medication, the pain relief, [ . . . ] they just like think you’re a drug addict or something, [laughs] he just wants to feel ( . ) some morphine. [ . . . ] Because they’re always like, [ . . . ] how hard – like, on a scale of 1 to 10 how tough’s the pain? And if you say anything below like 5, then they’ll say: ‘we’re not going to give you no morphine [laughs] because you don’t need it’. But really you do, even when it’s at, even when the pain’s at like a 5 level, you need the [morphine].
Quotation 40, I6, 19- to 21-year-old man.
Participants had learned how to control pain and were used to being in pain. 83 They knew how to engage in breathing exercises to stay calm. They had also learned to try to conceal signs of their pain from others, so that they could carry on with life and avoid focusing on their pain. 83 They talked about keeping pain to themselves in their everyday lives to avoid others becoming alarmed, particularly family and peers, and because they were embarrassed to express pain in front of strangers. They said that this meant that they often did not show the types of signs of pain that others might expect and use to assess their need for pain relief. They were aware that the degree of their pain is often invisible to others (see Quotation 42). 83 Participants explained that health-care staff would assess their pain based on how they looked (see Quotation 41) as opposed to listening to their reports of being in pain and of needing pain relief. Participant Z2 (see Quotation 46) told us that staff would listen to her requests for pain relief only when they saw very obvious visual expressions of acute pain (e.g. when she was crying or shouting). She tried to question staff about why they were not listening to her. As the situation did not improve she went home to self-manage her pain there. She explained that she ‘couldn’t get better in their care’:
People think that I can, if I’m laughing and I’m fine, if my [family] come to see me then I’m fine, then they’ll just think, ah you’re fine, and they won’t give me my medication on time [ . . . ] Like the nurses, the nurses all think because I’m laughing they’ll think that my pain score is like 5 or 3.
Quotation 41, O1, 13- to 15-year-old girl.
As much as I was saying that it’s really hurting it’s like they couldn’t really see it in my face. And I don’t really know why they didn’t think to do the blood test earlier but when they did it, it was like my haemoglobin was so low and then like they called me back.
Quotation 42, U9, 19- to 21-year-old man.
Of course now [pain] it’s not visible at all ’cause I could just hold it in for as long as I can. But I think maybe a few years ago I, it is visible. [ . . . ] If you can’t see that that person’s in pain and they are then, er, it’s gonna make it difficult to get them treated because, you know, he looks fine. [ . . . ] It’s like in, in A&E when I was in the emergency, if you look fine or you look like you’re not in pain then they’re gonna take a very long time to, you know, get in contact with you and get you sorted out. So I think it’s, it was much easier when I was a bit younger to get seen because you’d be screaming, you’d be in a lot of pain and they could see it. And, ’cause they can see it, they can react to it. But yeah, now, now, now it’s just, er, it’s not as easy to, to get across that you’re in a lot of pain ’cause they can’t see it. So yeah, it is a bit more difficult, visibility.
Quotation 43, O4, 19- to 21-year-old man.
When I was transitioning and loads of people had no idea what it was and I was so confused, I thought, I thought, I thought, you know, this is a hospital, they should know exactly what it is. But, er, it turns out a lot of people don’t know what it is. [ . . . ] Nurses had no clue what it is. They know what every, everything else is but sickle cell, they don’t really know what it is. So they find it more difficult to look after a patient with sickle cell. So I was a bit, you know, confused.
Quotation 44, O4, 19- to 21-year-old man
When I’m in hospital at times I don’t look as much in pain, ’cause I’m really, since I’ve been having like crisis from so young I’m really good at coping with pain and stuff so I might not look as sick as other people and I think sometimes that works against me. [ . . . ] Sometimes, they [health-care staff at ward] don’t really listen to how you feel at times, they kind of just look at you and think, oh you look OK, we’ll let you go sort of thing. And even sometimes like I’ve had pains in my legs and I’ve been to [hospital] and erm, they, they, they’ve like just, erm, not admitted me when maybe they should have.
Quotation 45, U9, 19- to 21-year-old man.
I sort of got ignored [in the ward] when I was calm and everything was fine, and I needed my tablets to be a constant, like every 4 hours [ . . . ] I’d be left for about 8 hours, and then suddenly I’d get like a really bad sickle attack [ . . . ] And I was even more stressed out because no one was listening, and I’d go for all these hours without like any tablets [pain relief]. And then the doctor would react after or during, whilst I was having a really bad sickle attack, or I’d be like crying, or in the bed like hunched over. And that was the only time that she would listen, but when I was calm and OK, or just sat there and go OK, I need my tablets, right, I need it now, I’ve been tracking the times, and they’d be like OK, and then not come back. [ . . . ] She’d only see when I was in pain, and then she’d react, and then it was too late. [ . . . ] It went on for about 5 days [ . . . ] the second I say I’m not fine, for doctors they don’t seem to always react.
Quotation 46, Z2, 19- to 21-year-old woman.
Participant I9 (see Quotation 47) talked about staff at A&E undermining her personal account of being ill by conducting multiple tests to find biomedical evidence of her accounts of her own symptoms and failing to find them:
You don’t want to feel like they’re judging you [A&E staff] and you’re kind of like over-reacting and you’re just being silly and you’re wasting their time. [ . . . ] [They] check your heart, they check your blood, they check like stuff [ . . . ] and your haemoglobin may not be low at that point, [ . . . ] they check things that don’t really affect your situation. So if I’m feeling pain and my haemoglobin isn’t low [ . . . ] oh you’re fine, and send you home [ . . . ] it would be nicer if they, like, asked you, how are you? You know, how are you feeling? What do you think could be the cause, what’s going on with you? As opposed to, yeah, your haemoglobin’s fine, your heart rate’s fine, your oxygen’s fine, get out. You know? ’Cause then you kind of feel like you don’t even know how to take care of your, yourself. You kind of go, like, you’re not looking at the right signs, feel like you’re wasting their time.
Quotation 47, I9, 19- to 21-year-old woman.
Some participants talked about the stigma around pain relief and of being aware of stereotypes about drug-seeking. These participants saw this as a further barrier to staff listening to their pain reports. They talked about staff distrusting their complaints:
There was one time where I needed [oral morphine liquid] and you know the whole situation where there are some, some patients who get addicted to it. [ . . . ] So they, they might think that I was gonna get addicted to morphine or they [doctors/nurses in the hospital ward] might think that I was giving them the wrong, wrong instructions, that I’m not supposed to have morphine. So then it makes it a bit, a bit more difficult to communicate. [ . . . ] I remember asking for morphine and they just, they didn’t want to give it to me. They, they thought I wasn’t in the right place to ask for it or something like that. [ . . . ] They were just like, um, you know, we’re gonna have to ask the doctor.
Quotation 48, O4, 19- to 21-year-old man.
Being in pain and unable to speak under the effects of strong analgesics and being unaccompanied by relatives pose additional challenges for young people with SCD. In these situations, it is difficult for young people to advocate for themselves. Participants said that having relatives present to advocate for them and to relay information to staff is important to ensure good care. 46 For instance, they talked about how their parents or other family members will tell staff about medication reactions, allergies and remind them that they need to administer additional doses of pain relief medication. Some participants explained how their specialist consultants, who knew their SCD history and personal care needs, had played a role advocating for good care for them when admitted to non-specialist wards. One participant told us about a time when her consultant had insisted she was moved to another ward to receive better care. A couple of participants told us about the advantage of having a familiar face on the ward. One of them told us about a time when there was a ward nurse who knew a member of her family. A second participant told us about being cared for by a nurse who had treated her in the past. Both liked the nurses checking up on them and being asked how they felt or if they needed anything.
Sickle cell disease specialist health-care professionals’ views: gap in transitional care
Participants did not report having any particular problems with the SCD care they received in specialist services. Sickle cell disease specialist providers talked about how poor patient experiences in non-specialist adult contexts (e.g. abrupt transition from child to adult wards) can be an additional challenge for young people during health transition. They talked about the importance of the transitional care support young people receive in sickle cell disease specialist services, that is the support sickle cell disease specialist services give to young people so that they can adjust to adult services, develop a voice and patient expertise [see Chapter 2, objectives (b) and (c)]:
Commonly the biggest hurdle for transitioning patients is not as much the transitioning of their, the transfer of their clinical care but the transfer between paediatric department to adult hospital ward [ . . . ]. [Addressing this problem] needs to be a government initiative that, that alters that in terms of how teenagers are transitioned [ . . . ] because we have [in specialist services] a transitioning culture that has been continuous. But we don’t have a continuous transitioning culture in the hospital. They go from the children’s ward straight to the adult’s ward, and that’s not transitioning. [ . . . ] The biggest challenge, you know, in a sense it becomes a victim of our own success with the patients because we’re so good at, at, transitioning them [within specialist services], you know. We make it so much easier, so much more talked about, it, it sort of flows nicely and then they end up in somewhere where they completely hate [adult ward in non-specialist care].
Quotation 49, Z7
Participant Z7 went on to discuss the need to address discontinuity in transitional care in specialist compared with non-specialist services to improve the transition experience. She highlighted the need for non-specialist ward and A&E services to work closely with specialist teams. Specialist providers highlighted the abrupt nature of transitions from child to adult wards. Transitional care support in specialist services is gradual and starts several years before the actual transfer, whereas the transition from children to adult wards outside those specialist services is abrupt. The first time on an adult ward can be a very difficult experience for young people. This issue could be resolved with ‘standalone’ sickle wards or young people’s wards.
Specialist SCD care works to support transitions by trying to develop the young person, giving them the confidence and resources to be involved in their own care and to take ownership of their condition. Participant Z8 talked about the importance of developing this expertise so that young patients can have a voice and be actively involved in their care when attending non-specialist services:
So we start discussing this and trying to get them independent but at that time they are still under the nests of their mum or their parents. [We give them information about and] underline, erm, what their illness or their condition is. So [that] they understand why they’re taking it [treatment. e.g. penicillin V, folic acid] [and about] their normal HB [haemoglobin] levels so they know what it is. When they present to A&E, erm, they can actually ask, what’s my HB today? You know, just make them more independent in their care, managing their care as well. It also goes into what triggers will cause them to have, to come into hospital to have a painful crisis, erm, what to avoid, what not to avoid. You know, just being aware of them and their condition as an individual [ . . . ] is really a brilliant bridge in terms of getting to know them better, erm, in terms of getting them to understand where they are in their condition and what they’re looking forward to in terms of when they leave paediatrics and go into adult. [ . . . ] if they’re going to uni [university] being able to meet a GP [general practitioner] there, being able to tell the GP, well this is who I am, this is what I have, this is my normal HB, this is what happens when I become unwell.
Quotation 50, Z8 (emphasis added by authors)
Helping young patients learn to be heard and be involved in their own care in non-specialist health-care services means helping them develop knowledge about SCD and how it affects them personally. Specialist providers talked about the importance of young people developing expertise in their own body and condition. Participant Z8 (see Quotation 50) explained that this learning is crucial for young people to ‘transfer’ information about themselves to non-specialist staff caring for them.
We want them to learn about their condition [ . . . ] They ask us the information as well erm, you know, what’s my haemoglobin level? We tell them. Erm how much blood have I had today? So it’s, it’s little stepping stones in to becoming independent for their own bodies and treatment, so that’s what I would say the difference would be. Just getting that independence.
Quotation 51, Y1
So if their HB [haemoglobin]’s normally 80 or 90 grams, erm, and they, you know, they can say to the doctors, what is my HB today? And the doctor say it’s 60, you can say well my HB’s normally 80 and that’s probably why I’m feeling this unwell and I’ve been feeling this way, you know, having a good record of what’s been happen, last week this happened and I was feeling light headed or this happened. You know, being able to give a really good, erm, report of what’s happening with them is, I think, is what is important as well, in terms of what you’re referring to. So we can develop that now.
Quotation 52, Z8 (emphasis added by authors)
Developing knowledge of their own body and condition is not enough for active involvement in self-care. Specialist health-care provider Z6 (see Quotation 53) argued that young people also need to develop a voice to demand good care and question the type of care they are given. Developing a voice is important because non-specialist staff do not always have experience of treating SCD. It is also important to be able to articulate feelings of pain and discomfort when clinical tests are not always a good indicator (see Quotation 54):
You might have to ask for your drugs rather than the nurses, where on a paediatric ward you’ve got a nursing ratio of one to three, you know, or one to four [ . . . ] and you have, have to actively say, OK I’m due this now can I have my [pain relief medication], and that’s, you know, that’s quite a big thing for a 16-year-old. [ . . . ] once you’re on top of it is much easier to keep control. Erm, whereas once you start chasing it it’s much harder to break [ . . . ] if you [ . . . ] hit it hard and you get on top of it and you break the cycle you’re much more likely to win more quickly and get, and get it [pain] under control and recovering more quickly.
Quotation 53, Z6
The numbers [haemoglobin levels] that you’re seeing don’t necessarily reflect the way that they’re feeling because it’s not just the haemoglobin protein going to, that’s, that’s, that’s affecting fatigue, is it? It’s lots of different things that play into that, that symptom.
Quotation 54, Z10
Participant Z6 talked about the role that specialist services play in supporting young people to become actively involved in their own care and exercise their voice so that they can move to adult services feeling equipped to negotiate quality care:
I always say [to patients], erm, don’t ever let anybody do anything to you if you don’t understand why and you don’t know. And you should always ask us. If we ever ask you to do something and you don’t know why we’re doing it to you and you don’t understand then it, then it’s your job to ask us and it’s our job to tell you in a way that you can understand [ . . . ]
Quotation 55, Z6 (emphasis added by authors)
One main concern for specialist providers was disengagement with specialist services (e.g. regular clinic attendance). Accordingly, working on the relationship with the young person was seen as an important element of good transitional care. Specialist staff often talked about the importance of building trust and engaging the young person. They said that, to achieve this, it is important to adopt a non-didactic approach. Accompanying the young person along the transition journey and developing a dialogue with them to address individual needs, preferences and concerns, including beyond health, was seen as an ideal approach. Adopting this flexible and more holistic approach is crucial to avoid making the services experiences ‘too painful’ for young patients (Z6), as this is a period when specialist staff risk losing young patients’ engagement with services and treatment (see Quotation 56). This flexible approach might include, for instance, avoiding clinical examinations if the young person finds this particularly embarrassing and offering alternatives in terms of treatment options and how they want to engage with services:
We’re also really aware that this is the point that we can lose them to services and we can lose their engagement in their treatment. Um so it’s not just about making sure that they like the service, it’s about making sure that they trust us and they will talk to us [ . . . ] but I think it is crucial that we don’t make ourselves something else that you can rebel against. You know, I’m not here to tell you what to do, I’m here to give you the information so that you know what the best thing is for yourself, but if there’s any things that we can do to help you work out what the best thing is for yourself, then speak to us. [ . . . ] So we try to make it that we’re approachable and we’re not telling them off [ . . . ] [the major transition challenge is] particularly, uh I guess it’s building trust, um getting them used to us.
Quotation 56, Y3 (emphasis added by authors)
I think that’s, that’s one of the really challenging and rewarding things is to have somebody walking through to the room and, and be just kind of not engaged with this at all, this is just not, not where I want to be right now and to really understand that and bring them along and tr, and try and work in a kind of, well how do we make this work for you? [ . . . ] OK well how about if we don’t examine you, you know, today, would that make you feel any better? [ . . . ] So would you prefer it if actually next time we did a Skype™ [Microsoft Corporation, Redmond, WA, USA]? Or we FaceTimed [Apple Inc., Cupertino, CA, USA]? Or we had a chat? [ . . . ] and kind of trying to hold on to that relationship [ . . . ] is about having shared priorities, you know, and, and as a medic you make, we make judgements on the balance of risk all the time and so the balance of risk fa, for not doing something right, nor ( . ) versus keeping someone engaged with the system.
Quotation 57, Z6 (emphasis added by authors)
Building trust involves taking account of how clinical care fits into the context of the young person’s life and recognising parallel transitions (e.g. going out to parties). Specialist providers talked about how they try to work with young people during transition, taking into account their needs and preferences, by involving them in dialogue about wider issues happening in their life, including their life priorities and aspirations (see Quotation 58). This non-didactic approach includes involving the young person in conversation and critically reflecting on barriers from their social life that might compromise their self-care:
Uh, try to get the young person to identify that they’re not taking the medicines as prescribed so that they’re owning it as an issue and then work out if they really want to be on the medicine, try to agree a strategy but very much with them being allowed to be honest about what they’re doing and not doing. [ . . . ] part of my role will be to try to anticipate what happens next and also to give them routes back in when they’ve opted out [from taking medication]. [ . . . ] We’ve just got to try to go with them on that one and try to sort of work out, well this is the downside, that’s the bad point about stopping the tablets, this would be the benefits, meh, check an understanding of the long term as well as short term issues and try to encourage them to review it for themselves.
Quotation 58, Y2 (emphasis added by authors)
Distrust, trying to stay out of hospital and resorting to oneself (pushing oneself into self-reliance)
Young people often have limited patient voice when they attend non-specialist services. 46,116 They navigate this gap in transitional care by learning how to rely on themselves and opting to manage pain episodes at home in an attempt to avoid bad hospital experiences. 116 Transitioning into adult care can mean no longer trusting non-specialist hospital care and learning that SCD is often misunderstood. Young people learn that staff may not respond to their needs and may not allow them to be involved in decisions about their care. Participants pushed themselves to manage painful episodes at home despite knowing this could pose a health risk. Going to hospital for unplanned care was viewed as a last resort [see Chapter 2, objectives (a), (b) and (c)]:
If I’m seriously ill, I’d come into hospital but if I’m ill and I feel like I can stay at home, I’ll stay at home [ . . . ] If I need [ . . . ] more pain management I’ll come here [hospital], if not then stay at home. [ . . . ] You just know in yourself really, like [when to go to hospital]. When I was younger I think I used to, er, be in hospital a lot more [ . . . ] but now I’m older I can bear with it [pain]. [ . . . ] I felt like I’d rather stay at the other one [children’s ward] [clears throat]. ’Cause you don’t know ‘em. When, when you’re with like older people you don’t know, that person like could probably just die.
Quotation 59, Y4, 19- to 21-year-old man.
Over time, repeated experiences of not being heard and experiences of delays in pain relief and of not having basic care needs met contributed to participants’ distrust of services (see Quotation 60). 116 Participant Z2 explained how one particular experience of being ‘ignored’ when she asked for pain relief, which caused her ‘stress’ and more pain, had a major impact on her trust in non-specialist hospital care:
Once that had happened I sort of changed how I behaved in hospitals. Like I tried to make sure that I was heard, because I didn’t want to fall back into that time. [ . . . ] Even now when I go back I still don’t fully trust them, even in different hospitals, it, it doesn’t really matter to me. I try to avoid the hospital as much as I can, not specifically because of that experience, but that has had a very big impact on my trust with like doctors and nurses, in understanding sickle cell.
Quotation 60, Z2, 19- to 21-year-old woman.
Participants have come to anticipate negative experiences, including having their voice and expertise disregarded or questioned. In the case of participant I9 (see Quotation 62), the experience of being disregarded by A&E doctors had shaped her decision to self-manage at home. It had also made her realise the drawbacks of an invisible condition/symptoms. She feels that she has to ‘look iller’ than she is to be taken seriously by A&E doctors. She had started questioning whether or not she really needs to access health-care services:
One of the main things is the kind of, the attitude that some of the staff have and, erm, I feel like I’m not listened to [ . . . ] And they just ignore me. And I’m not sure if it’s like, if it’s actually like that or if I’m kind of just imagining it but, erm, but it does affect my mood still.
Quotation 61, A5, 16- to 18-year-old woman.
I always felt like it [treatment from A&E doctors] was kind of condescending and it was kind of like, yeah, you don’t really have this. You don’t fit the textbook definition, so you shouldn’t be here. As opposed to why are you feeling like this? How are you feeling? What could possibly be wrong? Let’s try and solve it.
Quotation 62, I9, 19- to 21-year-old woman.
Trying to avoid hospital care during a painful episode involves participants utilising their bodily expertise and knowledge of their condition. They know how to assess what pain relief they need based on the different types of pain they experience. They also said that they know how to ration pain relief medication so that subsequent doses will continue to work. They have also learnt their own pain soothing remedies (e.g. self-massage using ointments or breathing techniques). Participants draw on this expertise to self-manage at home and go to hospital only when they need stronger pain relief:
Only a few years ago, that’s when I was able to kind of cope better, and I had a better understanding of the kind of medicine I need, and if I need like the strongest out of the painkillers or just like a little bit. So I kind of developed and kind of grew on to how to take care of it myself. Until I reached this point, where I feel like I don’t need to go hospital sometimes, or sometimes I do, then. And as you grow older you’re going to be able to know the different types of pain also, like if it’s going to be a mild crisis, or if it’s going to be a really severe crisis.
Quotation 63, Z1, 16- to 18-year-old woman.
Participants reported that they distrust non-specialist staff:
I try my best to hold it [pain] at home, even though I know it, it’s, it’s the worst option, I shouldn’t be doing this, I should go straight in. [ . . . ] There might not be any chairs in A&E, you might not even get like a, a bed to be on until they call you out [ . . . ] The whole emergency area, was a massive deal ’cause that, that could also, um, make me decide if I want to go into hospital or not. And, um, yeah, and the wards of course. The wards might not be as helpful, as nice, so you might be a bit scared to go [ . . . ] Sometimes you’re not too sure if the nurse who’s looking after you – you’re not too sure if they understand you enough. So they might give you some medications that you can’t have or they might give you medications that – um, you know, the wrong dose.
Quotation 64, O4, 19- to 21-year-old man.
Some said that when they cannot avoid a hospital admission they are more prone to double-checking care practices to avoid mistakes they have experienced in the past, such as being given the wrong medication or overdoses. One participant reported having started watching nurses’ care practices to check whether or not they are doing things ‘right’ (e.g. when being given medication). Another participant told us about a time when she had to phone her mother because nurses were about to give her medications she had never heard of. She explained to us that she wanted to check with her mother whether or not she could take them.
Participants also reported a desire to make any hospital stay as short as possible. For instance, while recovering from an acute painful episode at ward one participant drew on her expertise about how different types of analgesia interacted with her body to ask for the analgesic she calculated would enable her to leave hospital as quickly as possible. She explained that she did not want to be given codeine because this would make her fall asleep, which meant a longer hospital stay.
Social context
Young people with SCD also encounter barriers to enacting their patient expertise when interacting with others in their social context (e.g. with friends, peers and adults at school/work) (see Quotation 67) [see Chapter 2, objectives (a) and (c)]. Participants talked about others questioning or undermining their reports of acute pain. They also told us of the opposite. Sometimes others would be overprotective and over-react to their signs of pain, ignoring participants’ explanations that the situation was not an emergency. Participants presented themselves as aware of what their body allows them to do and of what self-management practices to engage in, but explained that it can be difficult to enact this patient expertise because of others’ lack of knowledge. They talked about how they feel that they are not listened to. Even when they explain SCD and their self-management needs to others they find that others forget what they have told them and subsequently ask why they are engaging in certain self-management practices or why they cannot participate in certain activities, either in an attempt to prevent painful episodes or because of fatigue (e.g. taking a break to rest when playing football). Participants told us about friends forgetting about their SCD and how it affects them and having to repeat their explanation (see Quotation 66). They talked about the frustration of having to constantly remind others what SCD is and explain their self-care behaviour. They find this constant repeating and trying to explain to others ‘tiring’ (I4), ‘annoying’ (U4) and ‘irritating’ (A7). Some participants explicitly said that they do not like being asked too many questions about SCD. They expect that others will not understand or in the future will ask again and question their behaviour. There was a shared sense of hopelessness, that others will never understand the condition (see Quotation 65) and a feeling that there is ‘no point’ in trying to explain it:
When it happens in public when I’m around friends or if I’m in uni [university] or something, that’s when it gets really irritating ’cause I, [ . . . ] I can explain it but I know that you won’t understand it so there’s no point in me in explaining it. [ . . . ] And the ones that don’t understand it, I just [ . . . ] I just make jokes about it, say ‘oh I’m just half a man’, like ‘you’re better than me’. Most times I just make jokes about it. It doesn’t affect me. [ . . . ] I know that they won’t understand it so sometimes if I’m, if I’ve got enough energy to explain it, I’ll explain it and [ . . . ] I’ll just make jokes about it saying, ‘oh I’m, I’m tired, I’m, I’m lazy’, just blame it on that.
Quotation 65, U5, 19- to 21-year-old man (emphasis added by authors)
Sometimes I feel like I have to explain why I can’t do certain things or why I have to, um, drink so much water [ . . . ] sometimes I feel like there’s no point in telling someone because they, they’ll forget or they won’t remember or that they, they won’t believe it or think it’s rubbish or something.
Quotation 66, A5, 16- to 18-year-old woman
I feel like you get different kinds of sickle pain, so it might, you might have sickle pain but you might be able to deal with it yourself. And if you say that they’ll [friends] say, oh you can’t deal with it yourself, go to hospital or something. And that’s not really necessary. I feel like ( . ) you have to really listen to the person who has the sickle cell to understand what they want and understand how they’re coping ( . ) because you think that you might know but you probably, probably don’t.
Quotation 67, I7, 19- to 21-year-old woman
School
Participants talked about teachers not understanding their condition and needs and not listening to their expert voices. Participant I7 told us that teachers disregard her expertise in her own body and condition (see Quotation 68). She told us of a time when a teacher went to hospital with her. She tried to explain to hospital staff that it was difficult to cannulate her to get bloods and that her teacher had said ‘oh, no, the doctor knows what they’re doing’. After talking about this at the interview she emphasised her expertise in her own body and condition and the need for others to take it seriously (see Quotation 68). She also told us about school staff being overprotective at times and not believing her reports of feeling fine and of having recovered fully from painful episodes. Instead, they insisted on monitoring her and asked her to visit the medical centre:
But, I know what I’m doing as well but they [school staff] wouldn’t really understand that I’ve done it so many times that ( . ) they need to listen to me as well.
Quotation 68, I7, 19- to 21-year-old woman
Participants said that teachers would question their explanations about how they felt and undermine the severity of their pain (see Quotation 69). Participant A5, for instance, told us that teachers ‘refused to believe’ that her SCD is severe and how much it affects her. She told us about a time when a teacher asked her to go outside with the other peers. She explained that the wheelchair could not go on the grass. There was no wheelchair exit. The teacher disregarded her explanation and the severity of her SCD (‘she really didn’t think it was that bad’) and ‘forced’ her to go out on her crutches, despite the fact that she had explained she ‘was in too much pain to walk’:
They don’t feel what I feel. Like when I get pains and stuff so if I have a tummy pain they’ll say drink water, which is OK but if it gets to the point where my tummy pain is above excruciating I’ll have to go to the nurse and I’ll have to stay out of lessons, not stay out of lessons but not go to lessons and probably go home, ’cause the pain is so much.
Quotation 69, O1, 13- to 15-year-old girl
Participants told us about teachers, who, despite being aware of their diagnosis, complained about low attendance or late arrival. Participant U1 talked about explaining to teachers that she cannot do certain things because of her SCD, but said that telling them about it did not really ‘work that much’ and they would ‘forget it’ so she had to remind them. Some participants said that teachers questioned or denied their requests to go to the toilet or to drink water in class even when they had an agreement with the school that allowed them to do this. On some occasions, participants reminded teachers about their SCD and of how these practices were part of their self-management, but most frequently participants said that they did not mention SCD as an explanation for their behaviour or needs. Participant I5 told us teachers thought her requests to go to the toilet for her SCD were ‘an excuse’ to get out of lesson. Participant O7 (see Quotation 70) said that he was asked to push his limits during physical education and the teacher gave him a detention when he stopped running because he was fatigued. Participant A1 (see Quotation 71) told us that teachers thought she was making excuses when she told them that she had not done homework because she was ill or when she was late to class because she had struggled to walk from one classroom to another:
We had to run round like a room like as many times as we could, and he kept getting me to go and so when I knew I’d got, I’ve reached my limit, he, he said, oh keep going, keep going now, keep going, keep going faster and faster, and I just stopped, so I don’t really care if they say something because I know me better than they know me [ . . . ] I stopped, and then he said I had a detention, but I didn’t go, I didn’t go really because I explained to him after, if I can’t do something then I stop, because I like to try and get as well as I can and I try to do as well as I can possibly do, but when I reach my limit that’s me done [ . . . ] I told him [I have SCD], I don’t know if he remembers.
Quotation 70, O7, 13- to 15-year-old boy
I don’t think they [teachers] were really that concerned. [ . . . ] Like if you would try to explain to them like the situation they wouldn’t really wanna hear it, they would just think it will just be like an excuse. [ . . . ] If you were behind on work or like you couldn’t do a piece of work or you missed a few lessons, sometimes if you tried to explain it to them they wouldn’t understand like how, yeah, how serious it was and they would just think it was just an excuse or like if you were late to lesson you said it was ’cause like you can’t walk that fast, that, like that far in that space of time, they would think you were just like, yeah, you were just using it as an excuse.
Quotation 71, A1, 13- to 15-year-old girl
They just have to understand that I’m going to be out of school maybe a lot [ . . . ] that was a problem in my other school, I used to get, um ( . ) told a lot that I was just always like bunking off school, that I was faking it and stuff like that. [ . . . ] So it did get irritating when people used to say that I used to lie about being sick and stuff like that [ . . . ] There was a teacher that thought I was lying.
Quotation 72, Y5, 16- to 18-year-old woman
There were a couple of them who every time I, I was absent because I was in a lot of pain they erm, they’d ask me why and they thought I was just being truant. And erm, when I was in hospital I remember one of the teachers coming up to me and saying that, erm, that I was kind of, erm, exaggerating how bad the pain was.
Quotation 73, A5, 16- to 18-year-old woman (emphasis added by authors)
Work
Experiences of others not understanding the seriousness of SCD and undermining their reports of pain or requests for help also took place at work. Participant Z3 (see Quotation 74) told us that his work colleagues and his manager do not really understand his needs. Participants often mentioned the invisibility of symptoms and lack of awareness about SCD as the main factors in not being understood and not being heard. For instance, participant U9 (see Quotation 76) talked about others’ reactions when he told them about not being able to do certain things and about his pain, ‘[it] just goes over their heads’. Colleagues would judge the severity of the pain based on how he looked:
So they know that like obviously I’m, I can get ill and whatever but I don’t think they know like the extent of what it is. Yeah, like they don’t know what exactly happens [ . . . ] they don’t really understand. Do you know what I mean? [ . . . ] If I’m standing up like ’cause some days it’s just, it’s not busy so they’re like, oh you have to get off the till and whatever. So sometimes I’m like, I just, I’ll be standing up and I’ll be like, like I need to sit down, like my legs are killing or whatever. So they’ll be like, but they, they’ll be like OK but they wouldn’t be like, oh OK like it’s, like I dunno, they don’t, they don’t understand like why, you know what I mean?
Quotation 74, Z3, 19- to 21-year-old man
There’s certain people that just don’t understand it at all. . . . I work at erm a [shop] in town and erm my boss, I have so many different managers [ . . . ] my boss, my manager, er my first manager I ever had, she didn’t know [ . . . ] I told them [about my SCD] but then they just didn’t [ . . . ] They didn’t know what sickle cell was, but like though you know when someone’s not really bothered, they don’t really want to listen or anything like that, so that was the first two [managers] [ . . . ] I told them I had sickle cell and everything and they just saw it as erm, oh erm if you want to take five minutes [to rest for self-management] that’s fine, just do, like that. They didn’t really, they just brushed it off like, they weren’t really paying attention.
Quotation 75, U5, 19- to 21-year-old man
If I tell you that I’m not feeling very good then you should just accept it rather than, rather than think, thinking about how I look with your eyes.
Quotation 76, U9, 19- to 21-year-old man
One of the main issues that makes it difficult for young people to convey their patient expertise to others in their social environments, including both work and school contexts, is the general lack of public understanding and awareness about SCD. Participants expected that people would not know about SCD or understand the condition and its implications. Participants often compared SCD with other conditions and positioned it as having less status than other better-known illnesses (e.g. cancer or diabetes). They told us about others not having heard of the condition and described the difficulties of trying to explain to someone who has never heard of SCD what it is and how it affects them (see Quotation 77). Even when peers have heard of it, they generally know only basic biomedical information provided in school science lessons (e.g. that it is a genetic inherited condition related to blood). When we asked them about how their transition experiences could be better supported, participants talked about the need for others in their environment, and society in general, to learn about SCD. They talked about the need for others to be ‘educated’ about SCD to avoid having to ‘explain it every time’ (U3), with some also saying that lack of understanding about the condition can lead to young people being stereotyped. For instance, participant U3 talked about the need for teachers to learn about the condition the same way they know about other conditions because without this knowledge they ‘don’t know how to help’ and cannot enable young people’s self-management at school (see Quotation 72):
I want people to know, I want people to understand [ . . . ] make, be aware and let people know that we are suffering in, like silence I suppose. ’Cause it’s like we’re just forgotten about [ . . . ] we have to keep telling people what it is and how it affects us. It’s like what, when is someone gonna finally understand what it, what it’s go . . . what it’s about and how it affects us in a bad way [ . . . ] knowing what, what we go through.
Quotation 77, O3, 19- to 21-year-old woman
I feel like some people don’t even know about the condition. They don’t, they’ve never heard of it. [ . . . ] I still have to explain it often. It kind of gets irritating [ . . . ] I usually would explain it, just a quicker version [ . . . ] I get pains quite often, and that’s just a, it’s just a quick way of saying it.
Quotation 78, A7, 16- to 18-year-old man (emphasis added by authors)
When participants talked about others ‘knowing’ they had SCD, in general, this would refer to knowing about the diagnosis but not necessarily understanding the condition and how it affects their life:
And even my friends who know about it, they don’t really know about it, they’ve not researched it, they don’t know the smaller side of things. Like if I get extremely tired, to just let me take a break, or the, even the extreme side of things, if I’m in a lot of pain, what to do. I’ve given them like step by step examples, because I just worry if something were to actually happen that I’m not around the right people to deal with it. Because I’m not really able to do much in a high-pressure situation with the sickle attack.
Quotation 79, Z2, 19- to 21-year-old woman
Transitional tactic: social silencing
Participants said that, as a result of their social experiences, they prefer to avoid talking about SCD (see Quotations 80 and 81). This social silencing involves not wanting to disclose the condition to others because of the expectation that those others will not listen or will not understand either the condition or their illness experience. Not wanting to disclose or disclosing to only a few close friends was common. Those who did disclose explained that they kept SCD to themselves and did not really talk about it. Participants reported that they avoid talking about their needs and how SCD affects them. Social silencing also involves not asking for support and not using SCD as an explanation (e.g. for being fatigued or arriving at school late). Social silencing helps protect participants from having to constantly explain SCD to others. In addition, it helps those younger participants who struggle to explain SCD to others who they expect will not know about it. It also helps participants to avoid being treated differently and to maintain a sense of ‘being normal’:
There are times where they [friends] don’t really get it because, when I get tired doing, well playing basketball, for example, they just think I’m really lazy but sometimes it’s not that, it’s just I have sickle cell [ . . . ] I often think, it’s just they don’t understand, erm, like sometimes I can’t be bothered to explain the whole thing. Yeah, I’ve been doing a lot of explaining a lot during high school as well about my illness, and then sometimes I can’t be bothered so I just don’t tell them, I just let them think that I’m lazy.
Quotation 80, I3, 16- to 18-year-old man (emphasis added by authors)
I was off school I think for about a week and a half and everyone would just be like . . . I came back to school and found out everyone was saying, ‘ah she’s always faking this and that’, but then I was just like, ‘I don’t really care if you think I’m faking it, continue thinking I’m faking it, it doesn’t really bother me any more’. [ . . . ] I just left them, I’d be just like, ‘that’s your own opinion, if you think I’m faking it, OK, well done, [snigger] well done, I was legit at home being sick, so . . .’
Quotation 81, Y5, 16- to 18-year-old woman
Participant Y5 also told us about not telling teachers she had SCD and not using SCD to explain her behaviour (e.g. looking fatigued in class, having to rest while doing sport and having to stop walking while out socialising). She said it would be good for teachers to know she had SCD so that they could understand her behaviour. She told us that she sometimes was ‘not really engaged in class’ and ‘can fall asleep in class, so it would be helpful for them to know’ so that they do not think she’s ‘just being a disruptive child in class’. She explained that teachers had told her before that she was ‘not focused’ and that she ‘should go to bed earlier’. Similarly, participant I3 told us that he does not use SCD to explain his behaviour to teachers when he is unable to concentrate at college or struggling to stay awake. Participant U9 (see Quotation 82) said that he knows his limits and will tell friends when he cannot do something, but does not explain that this is because he has SCD:
Sometimes I might just say I can’t do X, Y, Z because I’m sick or blah, blah, blah, but I don’t really get into like really deep details, I usually just say like I’m sick or whatever, [sniffing] or like I’m having a crisis and they might not really know what that means but I just say it anyway. And like I think they, they understand to an extent, and they don’t bother me about it, if that makes sense? [ . . . ] You don’t have to go into too deep detail but if they just know that when you’re sick it means like just leave it alone then that’s it. [ . . . ] Just say I’m not well, I never say what it is.
Quotation 82, U9, 19- to 21-year-old man
Interaction with others has taught participants to expect that others do not understand SCD. These expectations contribute to social silencing. Participant I3 (see Quotation 80) explained that he has decided to stop trying to explain SCD to others. He has learned how to protect himself by either not talking about it or by keeping the explanation short, even when this involves others potentially seeing him as lazy rather than experiencing SCD-related fatigue or pain. Similarly, participant O7 has developed a sense of hopelessness about trying to explain his health needs to teachers and told us that there is ‘no point’ telling teachers all over again. Teachers not remembering about his SCD was a sign of ‘how much they’ll actually care’. Participant U5’s narrative indicated that he has lost hope that others will understand his condition. He expects that others ‘won’t understand’ and has decided to silence his condition and explain it only when he has ‘the energy’. On most occasions, he said, he prefers not to use SCD as an excuse, instead attributing his behaviour (e.g. lack of stamina) to being ‘tired’ or ‘lazy’. He told us about occasions when he explained it was because of SCD, but that others did not understand. He said he had learned to deal with these situations by keeping his explanation short and making ‘jokes’ by saying he was ‘half a man’ (see Quotation 65):
I just prefer to say [to school/college peers] I was just ill or if they ask me why I [have access to school/college elevator] I just say, oh ’cause I need it ’cause like I have like really bad knees. So sometimes I prefer not to say like the reason [ . . . ] ’cause after they ask me more questions and it’s like the questions they get almost every time you tell someone what, what sickle cell is. So sometimes like the work, the questions get boring [ . . . ] You have to answer them over and over again [ . . . ] I’ve heard a lot of, oh she doesn’t look like she’s got like a disability, I don’t have, but then I, I sometimes I say, I don’t have to look different or be like in a wheelchair [ . . . ] I don’t have to look different or be in a wheelchair to be a disabled, I can be standing up, talking fine but still have a problem that’s inside me and really affect[s] me.
Quotation 83, O1, 13- to 15-year-old girl
It gets kind of tiring. I mean trying to get them to understand. I mean after a while if they don’t understand I’ll just tell them to, oh just Google [Google Inc., Mountain View, CA, USA] it and it will, it will tell you more [giggles].
Quotation 84, I4, 16- to 18-year-old woman
Another typical form of social silencing is to keep the explanation short. This is a strategy that participants have developed to deal with the constant questioning. Participant A7 (see Quotation 78) referred to this as giving ‘a quicker version’ of SCD and how it affects him. Some participants provide the short version (see Quotations 82 and 85). Short versions typically refer to biomedical aspects (e.g. shape of red cells, lack of oxygen) and give a brief reference to pain but lack details about how SCD affects the individual and about the experience of living with it. Participant O3, for instance, told us about disclosing to friends but not telling ‘the full story about sickle cell’. Another participant, Y4, said that he would not go into any explanation about what SCD is and how it affects him with his peers because they learn about it in school science lessons and they can also find information via internet searches:
They’ll ask me, what is sickle cell? And I’m just like, oh you, it’s like you get pains in your joints and you just get really bad pain, that’s what I, I say to them. But it’s not exactly that, there’s more to it, and like [ . . . ] when some people ask me, I’m just like, it’s to do, something to do with your bones and your joints, and pain, and that’s it.
Quotation 85, U2, 16- to 18-year-old woman
I drew it [a sickle-shaped cell] on the piece of paper like a diagram and then he [friend] figured it out and then I told him to research it because I didn’t really want to explain it because I never know how I’m going to explain it and it’s just long to explain. So he searched it and then he just researched it.
Quotation 86, U4, 13- to 15-year-old boy
Silencing becomes important when the person believes that others will not know about SCD. Silencing protects participants from having to constantly repeat to others what SCD is and how it affects them. Although participants often said that others do not need to know about their SCD, they also said that it would be useful if people knew about the condition. They recognise the importance of others being aware of their condition and knowing how to look after them if they need help during a severe pain episode. Participants emphasised that others need to learn about SCD and take their voices seriously because in a crisis there might be no time for explanations or the person may not be able to speak. For instance, participant I3 (see Quotation 87) talked about moving to higher education and the importance of having friends know about SCD:
Say I can’t walk to the kitchen to get the medicine I would have to ask my mum to get it for me, um, if the pain’s unbearable then they would have to like call 911, I mean 999. So hopefully my friends, if I have to trust, the friends I trust they would be responsible and sensible of the situation and help me through it, [ . . . ] sometimes, um, if you get someone who is irresponsible he wouldn’t take it, take the situation serious, so that, that wouldn’t be nice if like I’m in pain and they would be like, oh, it’s nothing serious, and like that.
Quotation 87, I3, 16- to 18-year-old man
It would be a lot helpful, so that they know that, oh it’s ’cause of this, that’s why I’m feeling sick, but if I’m just looking weak they might just think it’s like a little cold or something like that, like I say, it be better to know that I’ve got sickle cell, so that they can help me [ . . . ] it will help them to know that I have got it, so that they will know what to do.
Quotation 88, Y5, 16- to 18-year-old woman
Participant E2 (see Quotation 89) told us that he had begun to disclose to teachers and friends that he has SCD, but still does not talk proactively or in detail about it. He believes that disclosing might nevertheless prevent others from misperceiving his behaviour. Participant E5 (see Quotation 90) has also started telling work colleagues about her SCD. She has started being assertive about needing a rest when she feels tired; however, when she is tired, rather than resting, she engages in less energy-consuming activities because she worries about being seen as lazy. She also explained that she takes annual leave for routine clinic appointments. Participant U6 was an exception. She had started to bring leaflets to teachers to help them understand SCD:
Then [once I told them I had SCD] knew that, oh OK, this is why you miss so much of school, de, de, de, you’re not lazy whereas they thought I was just missing school on purpose because I didn’t really want to tell people about my condition ( . ) because I didn’t feel comfortable about telling them.
Quotation 89, E2, 19- to 21-year-old man
If they [work colleagues] don’t really know what’s going on. They can be like, ‘oh you’re always lazy’ or ‘you’re always tired’ and so that’s a big thing, especially when I’m working because I want to be up on my feet looking at [people she looks after]. So I have to say, guys I’m feeling a bit more tired than usual and they are, always: ‘communicate on how we’re feeling because then everything can run smoothly’ [ . . . ] I just decided to tell everyone. That way everybody knows, it’s out there so instead of thinking I’m not doing it for the sake of not doing it, I’m not doing it because I genuinely do feel tired or I genuinely do feel slower than usual.
Quotation 90, E5, 16- to 18-year-old woman
Difficulties developing and consolidating new adult identities: the adult patient versus the adult outside health-care contexts
Managing interdependent and contradictory demands on the self: being a disciplined patient versus a self-actualising student/professional
Young people with SCD encounter difficulties when trying to develop adult identities that help them to achieve life goals while simultaneously staying healthy [see Chapter 2, objectives (a) and (c)]. We have discussed this in detail elsewhere. 61 Participants’ narratives illustrate tensions between demands for self-preservation (i.e. the push to develop responsible self-management practices and patient expertise) (see The push for young people to engage in responsible self-management and develop patient expertise) and demands for self-actualisation to become competent students and professionals. 61 Health-care discourses exhorting young people to take responsibility for themselves and their own health clash with wider disciplinary discourses governing adolescence and transitions to adulthood. The plural demands on the young person with SCD play out in the identities they are trying to develop as they move into adulthood, and these demands create tensions that are difficult to resolve. For example, schools demand that young people excel academically, but excelling at school is difficult for young people who have to spend time in hospital, who are in pain or who have to rest regularly to avoid painful episodes. At the same time, health-care staff and parents demand that young people take individual responsibility and become competent at self-management. For participants, trying to respond to these competing self-disciplining demands translates into conflicting identities: on the one hand, their disciplined patient self and, on the other hand, their self-actualising self who wanted to meet education and career goals.
To be responsible patients, participants have to engage in relentless self-disciplining to stay healthy while trying to meet other responsibilities and life goals. 61 This involves, for instance, carefully regulating their everyday life to avoid painful episodes and minimise the impact of these on their education. Participants draw on their expertise of their own body and manage pain by themselves so that they can resume educational and work responsibilities as soon as possible. For instance, to recover quickly, participants avoid hospital as much as possible so that they can stay at home to rest more comfortably. They explained that a hospital stay means a longer recovery time and more time missed from school or work. They talked about responding quickly to the first signs of a severe pain episode to avoid it escalating and about resting to prevent a pain crisis. These practices are important to avoid hospital admission, which participants felt would negatively affect their educational performance or disappoint work colleagues. Participant U10 told us about listening to his own body and resting and responding to his body’s needs by doing what the doctors and nurses tell him to do to reduce the impact of SCD on his education:
[ . . . ] if I’m sick I won’t have any school at all. So it’s better off missing 1 day than missing all the lessons [ . . . ]
Quotation 91, U10, 13- to 15-year-old boy.
Like, say that I had like a deadline in and maybe, I feel like, oh I’ve gotta start earlier because just in case something happens and I’m not able to do it or something. [ . . . ] when it comes to my work I plan in advance. So obviously I make sure that I like have enough time to get the work done and completed just in case like I do have a crisis and I’m not able to do it for like a week or two, that I just, I know that I’ve still got some time to have, to do it, like to be able to do it and still get like a good grade from, from it.
Quotation 92, Z3, 19- to 21-year-old man
I feel. Erm, yeah, I don’t know. Nervous. [ . . . ] That I won’t get the highest marks that I can get. [ . . . ] I just want the highest. [ . . . ] The highest mark possible which is an A*. [ . . . ] I’d want at least one A* but if I got like a C or a D I’d feel like a failure.
Quotation 93, E6, 13- to 15-year-old girl
Participants talked about self-disciplining in areas of their life outside health, such as education and work. They often talked about trying their best (see Quotation 93), staying ‘focused’ and working on self-improvement. Trying to control pain and tiredness is a typical strategy to try to achieve this. They presented themselves at interview as working on self-improvement, and echoed messages on personal achievement and self-efficacy typically promoted in educational environments. They also talked about trying to do their best at education and work. Participants talked about being active and productive. For example, participant A6 (see Quotation 4) presented herself at interview as responsible in terms of SCD self-management and knowledge, and in terms of being responsible in her studies. She talked about regulating her social life and going out less to study more ‘because I feel sometimes I haven’t learnt it’. She positioned herself as taking individual responsibility for self-management of SCD and actively seeking to improve her health and prevent painful episodes. In a subsequent interview she told us about her concerns about going to university. She wanted to make sure she was going to be ‘safe’ and ‘focusing on my learning, and making sure that I’m trying my hardest’. Similarly, participant Z3 (see Quotation 92) positioned himself in his narrative as a disciplined patient and as trying hard to achieve a good education. In the interview he said that he had achieved the grades he needed to get into his chosen degree course despite having missed a great deal of college because of his SCD. However, he framed his achievement somewhat negatively, saying it ‘wasn’t the best [he] could have done’ and that ‘[he] wanted to do better for [himself]’, perhaps reflecting a consciousness of adults’ wishing to shape young people into responsible and high-achieving adults. Later in the interview he told us about ‘always get[ting] drilled in, like, we need to have good GCSEs [General Certificates of Secondary Education], need to have good grades’ [reproduced with permission from Renedo et al. 61 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text].
Participants talked about disciplining themselves in terms of time management (see Quotation 92) and regulating social interactions (e.g. avoid friends’ distractions during class) to help them stay focused and meet deadlines. For instance, participant Z4 (see Quotation 94) told us about working hard to achieve career goals and positioning himself at interview as more responsible than his university peers:
I have a, er, a big inspiration, which is to be successful in the future [ . . . ] just keep on working hard [to achieve this] [ . . . ] keep studying [ . . . ] I like to focus and work a lot, but sometimes [students during lectures] will, like, lose concentration and do silly stuff [ . . . ]
Quotation 94, Z4, 19- to 21-year-old man.
I stay at home more than I go out and I, before I go out I make sure I’ve done all my work, school work [ . . . ] I don’t let it [SCD] stop me from doing anything. [ . . . ] I just think OK, I’m going to set myself a goal, and then say if I’m [doing exercise], I’ll say, I’m gonna at least get to this point, and then if I think I can do better, I’ll do better. I think, ah don’t stop, don’t stop, don’t stop now.
Quotation 95, O7, 13- to 15-year-old boy
Some participants meet deadlines by factoring in the possibility of a painful episode and doing extra work during the times they are well. This sometimes involves pushing their bodies by working late at night or not taking time off work. It also means missing out on socialising (e.g. avoiding distractions during class). Participant U9 told us that missing school ‘forced me to work faster and harder all the time’ (see Quotation 96). The self-actualising student/professional might have to ignore signs of pain or tiredness and push their body to the limit in pursuit of academic and work achievement:
[ . . . ] usually, like I, I work really hard like, and I work really fast because a lot of the time in school I would be out for so long that I have to catch up. [ . . . ] If I like missed a few days I don’t want it to look like, like I’m not as useful to the team [at work]. [ . . . ] I didn’t want to feel like I was like taking, taking the piss or anything but it, I think again, it’s like the laziness thing, it’s like in my head maybe [ . . . ] sometimes I’ll be reluctant to take time off [from work] or I’ll try, or I’ll just take painkillers and go rather than, erm, not going.
Quotation 96, U9, 19- to 21-year-old man.
When I’m in hospital and I wanna work, and I try or I get too tired and I can’t, it’s just a bit frustrating [ . . . ] I take my books with me but if I’m getting too tired then I have to stop and not doing as much as I want to, and that’s why it upsets me.
Quotation 97, I7, 19- to 21-year-old woman.
I take my work very seriously, and even if I’m ill I like to still keep in contact [with peers from the same working team at university]. It tends to be that other people don’t like to keep in contact with me, because they think I can’t handle it.
Quotation 98, Z2, 19- to 21-year-old woman
Like I don’t want it to slow me down or like my progress and that just because I have sickle cell, it don’t mean like it can stop me from doing what I wanna do [ . . . ] During the day, maybe [ . . . ] I don’t do as much work as I should at the last lesson ’cause I’m tired [ . . . ] I just do the work at home, like when I have my nap [ . . . ] I don’t really have time to like do anything to stop me getting tired, ’cause I have to like do my best [at General Certificates of Secondary Education] even though I am tired. [ . . . ] Then [if I get ill] like all that time’s wasted because I try, I actually try my best and then something, this is stopping me from doing what I wanna do.
Quotation 99, O6, 13- to 15-year-old girl (emphasis added by authors)
Developing an aspirational adult self requires young people to push themselves. Participants were aware of the punishing consequences of not listening to their bodies and managing health needs. Participant I7 (see Quotation 97) tried to work while unwell in hospital. Her quotation illustrates the self-regulation for achievement and self-actualisation that we found in the young participants’ narratives. Participant Z2 (see Quotation 98) told us about trying to produce university work while off sick. Participant U2 (see Quotation 100) told us about trying to avoid hospital as much as possible and instead manage pain at home because she had revision to do and because she did not want this to affect her attendance, which was already below the acceptable level. She said that all of these factors would affect her educational progress. In a subsequent interview, participant U2 spoke about making sure she has breaks during college to rest, drink liquids (both recommended SCD self-management practices) and regain energy to avoid falling asleep. This is important so that she can continue to focus for the rest of the day:
If I go hospital then I’m going to have to stay there for like I don’t know how many days and then I’m going to miss a lot of time off of college and then my attendance is going to be low. [ . . . ] So I don’t, I don’t want to go in hospital because of that reason. [ . . . ] I may not be able to progress into my other course that I want to do.
Quotation 100, U2, 16- to 18-year-old woman
Cultivating the aspirational adult is in tension with the patient self, who is conscious of the impact on health that pushing body limits can cause. Participant I3 (see Quotation 101) said he should do more sports and talked about trying to control his low stamina when doing sports (e.g. ‘I push myself’), which in the past had led to acute pain episodes. In the final interview he talked about transitioning towards a healthy and more active lifestyle. He talked about being more in control of his health and making healthy choices. He also talked about disciplining himself by working hard to achieve success in life: ‘I want to try and do my best so I work twice as hard [ . . . ] I’ll push myself and make it a competition to try and get ahead of everyone else or be a good person’. In previous interviews he had positioned himself as trying to work harder to be ‘successful in the future’ and about not letting SCD ‘hold me back’ from his life goals:
I’m trying to work on my cardiovascular so I can . . . my heart can pump like oxygen round more. That will benefit me [ . . . ] I’m more active this time, yeah. [ . . . ] I’ve been researching a lot. [ . . . ] I’ve been around going online, and stuff like, what type of fruit I could eat, that’s really beneficial like, [ . . . ] and like iron as well, iron deficiency, um, trying er, you know, make a, improve my health like health style, lifestyle, so I’m trying to become more fitter [ . . . ] the only way I could make improvement or continue going over crisis is by improving my body that’s why I’m taking care of it. [ . . . ] I do try to push myself um, to do work [at college when feeling tired] but if I can’t, I probably just relax, talk to some friends, stuff like that. Um, yeah, and then when break time comes I eat something, relax a bit and then sometimes I do have the energy to do some work, try and push myself and then later on I rest and then complete the work or try and finish all of it.
Quotation 101, I3, 16- to 18-year-old man.
Participants reported that they want to become fitter, but that cultivating a sporty self is difficult. They talked about trying to exercise and the frustration of getting tired. Although this was more typical of the boys and men, women also talked about needing to work on themselves to develop stamina and improve body performance:
I want to improve my health, but it’s hard at the same time because you know, one part of you needs to improve my health and the other part of me can’t let that happen, otherwise I’d be in pain. [ . . . ] I would push myself [at the gym] um, to the limit I know that, you know, as soon as I get to this part I have to stop. And then I would use a steam room or a sauna, and I will sit there um, for a long time, so if there was any chance of having a crisis that I could treat my body at the same time, instead of, you know, walking out into the cold, and then putting myself at risk more. So I, I knew that if I wanted to improve my health in that way I had to like balance it with keeping myself warm and keeping myself hydrated, and making sure that I was OK before I, you know, before I did the exercise and after.
Quotation 102, A6, 16- to 18-year-old woman
The threat of developing stigmatising identities: the ‘lazy’ self
As we have seen above, cultivating the aspirational adult who wants to work hard to develop and perform well exists in tension with being a responsible patient who rests or stays at home to stay healthy. The difficulties in trying to develop self-actualising adult identities while trying to be a disciplined adult patient were sometimes played out in stigmatising identities (i.e. one’s own or others’ characterisations of the young person with SCD as ‘lazy’). 61 Participants frequently talked about being ‘lazy’ or about their concerns that others perceived them as lazy (see Quotations 103–105). They talked about SCD-related fatigue and self-management practices (resting) as something unproductive and lazy, despite also recognising them as important aspects of self-care:
Sometimes it’s tiring ’cause then I can’t be bothered to do it and I just feel lazy. I’m lazy most of the time, like I can’t be bothered to get up, or like my bones just feel weak so I just sit in my bed all day. [ . . . ] I don’t know, it’s just, just don’t really bother to do stuff, so I’m just sitting in one place for like more than 5 hours. [ . . . ] Some people call me lazy.
Quotation 103, O6, 13- to 15-year-old girl
Only my laziness [can stop me from getting a degree] most of the time, yeah. I prefer to just sit down all the time, not do anything, I feel lazy so . . .
Quotation 104, E6, 13- to 15-year-old girl
If, if I can’t do something people will say, oh, you’re being lazy [ . . . ] because of my sickle cell I do have to let people know what I have because if I get tired they’ll wonder why I’m just so tired all the time and I don’t want people to think I’m being lazy by sitting down.
Quotation 105, A2, 19- to 21-year-old woman
I’ll get a crisis today as in at night time. ( . ) That’s when it will affect me so I would have to call my manager and let them know ( . ) I’m sick, de, de, de, de whereas they might think I’m lying and I just don’t want to go.
Quotation 106, E2, 19- to 21-year-old man
Interviews were permeated with examples of having to rest to manage SCD fatigue. However, at points in the interview participants distanced themselves from images of someone just staying at home and not doing much, shifting to positions that constructed their identity as more active, working on self-improvement and cultivating a transformative self. For instance, they would talk about being productive and distanced themselves from others whom they saw as letting their condition ‘hold [them] back’ by ‘sit[ting] at home’. Participant Z4 told us about a time when he was admitted to hospital and stayed in bed watching television. He characterised his preferences for doing this rather than engaging in other hospital activities (e.g. ward school) as a ‘lazy’ choice. This was in contrast to other self-positions he adopted at interview (see Quotation 94), when he talked about staying focused and working hard to succeed in life and achieve career goals:
I’m always feeling tired. So like when I’m feeling tired I, I don’t like, I don’t like doing nothing, so sort of I’m like lying in bed or go sleep. But, being, being in bed all day like it’s not, it’s like, it’s just not, not, not good really, it’s just like, being tired all the time, lying in bed like, you’re not doing nothing, are ya? It’s like, I wanna like try my best and not, like, not get into bed.
Quotation 107, O2, 16- to 18-year-old woman.
There’s been days where I don’t do anything and then I’ll get used to not doing anything, so I’ll get into the habit of being lazy.
Quotation 108, O1, 13-15-year-old girl.
That’s the only thing I’m worrying about at the moment. So yeah, studies and work, just being able to keep a steady attendance, not missing stuff. Um, and of course, when you miss days and stuff, they might think you’re not as motivated and they might think you’re just missing days for the sake of it.
Quotation 109, O4, 19- to 21-year-old man
Participants were concerned about others seeing them as lazy, and some said that they were called ‘lazy’ by others. Note how participant O2 (see Quotation 107) might be either addressing herself in talk (e.g. ‘You’re not doing nothing, are ya?’) or imagining herself being addressed by someone else who might be perceiving her as lazy. Resting seemed not to be an appropriate practice for her and she talked herself into becoming more active. Similarly, participant O1 (see Quotation 108) also self-identified as ‘lazy’ for wanting to stay in bed when tired and unwell. However, she ‘force[s]’ herself to go to school or help her parents with household chores. Pushing herself is important to try to cultivate an aspirational adult identity and avoid developing what she sees as inappropriate habits. This type of narrative performance of real-life strategy might help her increase her distance from a ‘lazy’ self.
Participant I3 spoke about how his fatigue impedes exercise. His friends know about his SCD, but they sometimes still forget about it. At different points in the interview (see Quotation 101) he aligned himself with more active forms of being (e.g. doing sports and working on improving stamina, working hard to achieve educational goals), constructing a social identity that distances him from a ‘lazy’ self:
There are times where they [friends] don’t really get it because, when I get tired doing, well playing basketball, for example, they just think I’m really lazy.
Quotation 110, I3, 16- to 18-year-old man
Some older participants have disclosed their condition to avoid being seen as lazy (see Quotation 111). Participant E5 disclosed her condition at work because of a past experience of a teacher who did not know she had SCD and who perceived her fatigue as a sign of laziness. This experience might have encouraged her to be more open about it:
So they [work colleagues] know like I get tired or, and I can like go out [have a break] I let them know so that I feel like I’m not like, I don’t want to seem like I’m slacking or anything. [ . . . ] because I guess sometimes I’m just lying down like not doing anything, ’cause sometimes I get tired and then they, I feel like they’re looking at me like she’s not doing anything, why? But, and yeah, and then so I told them, they’re like OK, it’s fine.
Quotation 111, E5, 16- to 18-year-old woman
Participant E5 still makes herself stay active and asks colleagues to give her things to do, perhaps because she is concerned that they will see her as being lazy. She has asked them to ‘try and keep’ her ‘moving’. She does not want to ‘sit around’ and wants to keep her ‘energy up’ because if she stops she will be ‘more sluggish’. In a subsequent interview she explained that ‘many, many, many people think I’m just lazy or I’m just always tired’. She had started warning her work colleagues when she is feeling ‘a bit more tired than usual’.
Learning how to protect others: relationality of sickle cell disorder and pain experience
Sickle cell disorder and pain experiences have crucial relational dimensions,83 and participants placed great importance on the impact of their condition on significant others [see Chapter 2, objective (a)]. Participants’ accounts of their SCD experiences were told through and against significant others – mainly parents, but also other family members and friends. When asked about their individual experiences, participants often introduced significant others’ experience to tell us about how their SCD affects those others. In doing this, they seemed to emphasise that their SCD (including SCD pain) affects others more than themselves. This was typical when they spoke about pain experiences, as we have detailed elsewhere. 83 The gaze of the other as observer of their pain or as affected by their pain was explicit in their narratives. Participant Y5 (see Quotation 112), rather than talking about herself not being able to bear the ongoing pain episodes, introduced her mother’s experience and emphasised it over her own. Similarly, participant I3 (see Quotation 113) spoke about how his mother is affected by his pain, prioritising this over a personal account of his own pain-related suffering. Participant I3 conceals his pain not only to protect his mother but also to protect himself from seeing his mother suffer at the sight of him in pain:
I used to have literally a [pain] crisis nearly every day, so there was some times my mum couldn’t bear it, every week I’d be in hospital for about a weekend or something like that.
Quotation 112, Y5, 16- to 18-year-old woman.
When I get a crisis I think I said, mentioned in the other interview, like a crisis my mum, like, worries about me and then I worry, like, that kind of breaks my heart [ . . . ] Sometimes I don’t show it but I do actually worry about my mum. It breaks my heart when I see my mum like upset when I’m, when I’m in pain and stuff like that because I don’t want her to worry about me like that.
Quotation 113, I3, 16- to 18-year-old man.
Part of participants’ concern for parents’ experiences of their own painful episodes and their condition was wanting to avoid worrying or being a burden to their parents. Their narratives were of a young person wanting to protect others from their SCD and who learn over time how to keep their SCD private (by disguising pain and trying to manage painful episodes alone as much as possible). Participants talked about not wanting to disturb family dynamics and not wanting to be a burden to their family. For instance, participant I8 wondered how life without SCD would be because ‘it’s stressing my mum out, it’s stressing my dad out, it’s stressing me out’:
It’s normally not just, um, it, obviously it’s not just the person who’s having the pain, it’s the people around them that have to do other things for them, so then they have the sort of stress, as well. [ . . . ] sometimes it feels like you’re annoying other people just like by having pain and like stopping what they [parents]’re doing for, for yourself, um, so then it just like, you don’t want them to feel that they have to stop everything and that they can, um, do things for themselves.
Quotation 114, U8, 13- to 15-year-old girl.
I feel a bit like a burden to my parents ’cause I have pain all, all the time and they have to deal with it all the time. And, um, part of me feels like I’m doing them a favour by staying in my room so that they can just get on with whatever they have to do and not worry about me.
Quotation 115, A5, 16- to 18-year-old woman.
Sometimes I feel like I’m annoying them for like my sickle cell. [ . . . ] My mum has to like wake up early for like work and stuff, and like it, like it comes, when it comes in like the evening and taking me to the hospital, they stay there for like a lot of hours and then we get back on like 4 a.m. and like she still has to wake up to go to work. And, um, I just feel like, like I’m annoying them.
Quotation 116, I5, 13- to 15-year-old girl
When telling us about a pain episode for which he had to be admitted to hospital, participant I6 told us about feeling ‘upset’ because of how this had affected his partner. He introduced the experience of his partner into his narrative to explain that she had to ‘get out of bed’ to call the ambulance and go to hospital with him. Concerns about being a ‘burden’ to others (e.g. partner, family) were common. Participant O1 also gave more prominence to her mum’s experience of one of the worst experiences in hospital when she was not given pain relief in time. The nurses were ‘rude’:
And it’s like, of course mum already has trouble with me ’cause she’s always in hospital with me, she doesn’t, she’s already stressed out and it just gets her even more stressed out [with nurses being rude].
Quotation 117, O1, 13- to 15-year-old girl
In a subsequent interview, when telling us about how she might depict her pain in a drawing, participant O1 told us she would also draw her family to represent pain, saying ‘It’s not a nice thing for them to come and see me in pain’. She also told us about a time when she was under the effects of strong pain relief and half asleep, and heard her family members crying. She added:
I feel like – sometimes I feel like it’s my fault that they have to be here or have to like see me in this, like, circumstances.
Quotation 118, O1, 13- to 15-year-old girl
Participants also introduced others into the narratives in other ways. For instance, they talked about being observed and subject to others’ judgements and reactions during pain episodes. For instance, participant A5 talked about her pain experience as being ‘on stage’ (see Quotation 120). Participants were concerned about shocking or worrying others. They talked about the stress of seeing others worrying about them or looking ‘scared’ and the frustration of not being able to talk. When we asked participant I10 about his experience of attending A&E, he talked about being embarrassed at being seen in pain ‘in front of everyone who’s watching’. Another participant (A1) told us that she liked the fact that hospital nurses were not affected by her pain because they did not know her personally. She said this contrasted with her mother, who became stressed, which in turn made her stressed and ‘feel worse’. They also worried about being judged as over-reacting. When telling us about attending hospital for a painful episode, participant I3 told us about being ‘left in pain for hours’ and staff not giving him pain relief and how this affected his mother (see Quotation 119):
They didn’t do anything to try and get my pain down and my mum was really upset, and I was pretty upset as well ’cause I was in so much pain and they took like hours to try and, erm, try and give me pain relief as, as well. That was another thing that I, my mum didn’t really like about [hospital].
Quotation 119, I3, 16- to 18-year-old man
I wouldn’t, I wouldn’t draw myself alone [A5 on how she might make a drawing to depict her pain], um, I, I think I might actually like draw myself on stage in pain and, um, ’cause, ’cause, when I do have a crisis, my, my parents, you know, they like tell the whole family what’s happening and, um, so there are a lot of people involved.
Quotation 120, A5, 16- to 18-year-old woman.
I literally fell over [during a painful episode] [ . . . ] I couldn’t speak, and I could just see her [family member], she was just in my eyesight, and she was like freaking out and stressing out [ . . . ] and just because I’m seeing them panic and I can’t say anything, like calm down, it’s OK, it’s not, it’s, well it’s bad but it’s not too bad. And because I can’t communicate that and all I’m seeing is them panicking, it makes me panic that they’re panicking, or it makes me stress out because they’re panicking.
Quotation 121, Z2, 19- to 21-year-old woman
Participants talked about having learned how to suppress pain expression to conceal it from others as part of self-managing their painful episodes. 83 For instance, they talked about keeping SCD to themselves, to ‘firm it’, ‘to mask’ pain and ‘control[ling] [pain] in other people’s eyes’ (Z2). 83 Participant Z1 told us that she had learnt to ‘put a brave face on’. She also explained that she did not want her parents to experience her pain. Participant U2 told us about having moved to adult specialist services and preferring not to have her parents in the consulting room to protect them from when she talked about pain with the doctor. She said that the parent did not like ‘when I’m, when I talk about that how I’m in pain’, explaining that it is ‘uncomfortable’ and makes him ‘sad’. She had learnt that her parent did not like seeing her in pain through his past reactions to her painful episodes when she had seen him looking ‘sad’. Now she opted to keep pain away from him. At the final interview, participant O1 (see Quotation 118) told us that she was trying to prevent her mother from realising she was in pain because she did not want her to worry or not sleep because she had to get up early for work and ‘it’s not nice to have, only having what, 3 hours of sleep left?’.
Chapter 7 Discussion
The sociological, in-depth qualitative approach allowed us to examine experiences of health-care transition from the perspective of young people with SCD, taking into account aspects of their life outside services, including education, work and social relationships. By focusing on the development of young people’s adult identities we have illustrated how aspects of their social life interact with their health transitions and their movement into adult patienthood with SCD [see Chapter 2, objective (a)]. We have shown that young people with SCD can struggle to develop a coherent sense of adult self as they are caught between conflicting demands on the self that emerge from their health-care and social contexts (i.e. to perform as both disciplined responsible patients and self-actualising student/professionals). 61 Identity development during transitions involves relentless self-disciplining in different aspects of life, and young people seeing themselves as in constant need of improvement to reconcile these plural demands on the self. 61 Transitioning to adult health-care services also involves developing tactics to respond to the obstacles that young people encounter when trying to enact their patient expertise, both in non-specialist hospital care settings and in their wider social context [see Chapter 2, objectives (a) and (b)]. These obstacles, and the tactics young people develop in response, can create a ‘risk space’ for young people. This is a space that hampers the development and practice of ‘expert patient’ identities and the consolidation of adult identities, while promoting social relationships that can hinder young people’s ability to maintain health, self-manage their condition, pursue aspirations in life and have a good quality of life as they move into adulthood. Below we discuss these key findings in relation to the study objectives and research questions.
Young people’s experiences of care during health-care transition
A key challenge in successful transition for young people with SCD relates to failing to be recognised as experts in their own condition. They can experience poor care in the health care that they receive outside specialist care, including experiencing barriers to having a say in their treatment based on their knowledge of their condition and being prevented from using their patient expertise. Our participants were able to draw on their extensive experienced-based knowledge of their body and their condition, grounded in diligent health self-monitoring. As we have shown, however, their status as ‘patient experts’ – knowledgeable about their condition and their bodies – was too often disregarded. It was disregarded first inside non-specialist hospital settings, such as when they attended A&E for painful episodes or when they were admitted to non-specialist hospital wards,46,116 and, second, outside health-care services, in their relationships with peers, teachers and work colleagues.
On the one hand, young people with SCD experience a push from adults for responsible self-management and development of patient expertise (transition demands typically come from the health-care context and are also conveyed through carer/parent relationships). On the other hand, their attempts to enact these are hampered in relationships with non-specialist health-care providers, leading to young people having difficulties in being involved in own care and using their patient expert knowledge to negotiate better-quality care. They are also hampered in their social contexts. Lack of knowledge about SCD among health-care staff and poor engagement with young people’s voices are key disabling features inside and outside hospitals that can hamper young people’s attempts to enact expert patienthood as they move into adulthood. Young people in our study were trying to respond to transition demands for active involvement in their own care, health literacy, responsibility for self-management and expertise of their own body. However, their relationships with others limited the practice of these behaviours and posed an obstacle to them having their voices heard.
Young people did not tell us about any concerns with their transition from specialist paediatric to specialist adult services, but they encountered barriers to enacting their patient expertise and receiving high-quality care in unscheduled non-specialist hospital settings. 46,116 The main areas of concern were poor pain relief management, poor management of basic care and body needs, non-specialist staff not knowing enough about SCD and barriers to involvement in decisions about their care.
Participants’ pain relief needs were not always managed in a timely way, and sometimes they did not receive adequate pain relief. Participants said that their basic bodily needs were not met, such as when they needed a visit to the toilet or during cannula insertion. They said that staff responded in ways that suggested that they were not listening to, or open to acting on, what the young person said. Non-specialist staff communicated their scepticism directly when they questioned the young person’s assertions about their needs or preferences, or expressed their scepticism indirectly when they delayed treatment.
Problems with response times for pain relief from emergency health-care staff,18 poor knowledge of SCD among providers in unscheduled care settings18,39 and patients not being involved in treatment decisions39,117 constitute barriers for all SCD patients. However, these are likely to be more acute during transition to adult care. Unaccompanied young patients may not yet have developed skills to advocate for themselves and demand high-quality care. The young person in pain might also find it difficult to speak to communicate their knowledge, needs and concerns. 118 These problems of poor care are also likely to be more pronounced when sickle cell disease specialists are not available as advocates, such as in hospitals without specialist clinics.
For young people with SCD, transitioning between paediatric and adult health-care services involves a process of understanding that unplanned non-specialist hospital care can be poor and recognising that they may not be seen as having a legitimate voice in these health-care contexts. 46,116 Young people learn about different aspects of poor care, particularly that their condition is often not understood by non-specialist staff who will not always listen to their requests, be responsive to their needs or allow them to have a say in decisions about their own care. Young people with SCD developed mistrust in, and disengagement from, non-specialist hospital care and developed tactics to stay out of hospital as much as possible. Owing to their experiences of poor care, transition involved young people pushing themselves into self-reliance and into learning how to call on their expertise in their own body and condition to confine care to their home environment. Providers do not always listen to young people’s pain reports. 119 Our study shows how these types of care experiences shape young people’s health-care transition into a process through which they learn how to rely on their own resources as much as possible to avoid unplanned hospital care.
Young people are recommended to take increased responsibility in managing their health, and this is at the heart of transitional care policies and guidance5,59,120 and the ‘self-regulatory governance’ for responsible self-management that the clinic encourages. 58 Although taking responsibility for self-management of painful episodes is important, resorting to self-reliance is taxing. It pushes young people to self-manage pain at home as much as possible to avoid or delay non-specialist hospital care, with the awareness that this can be risky. Pain becomes more difficult to treat if it is not promptly managed,118 and delaying hospital care can lead to complications. 121 Participants seemed to be resorting to adult-like skills of self-management and self-efficacy as a tactic to address their concerns about poor-quality care, rather than as a positive transition skill that they were learning as part of their move into adulthood.
Delaying possible hospital attendance for as long as possible means that pain is likely to be very intense on arrival and as a consequence people might find it especially difficult to communicate with staff about their pain and treatment needs. 118 The inability to speak and uncertainty regarding whether or not care needs will be met and whether or not one’s voice will be taken seriously create additional stress. In this situation, staff willingness to hear and act on patient voice and expertise is crucial for quality care. Because SCD affects people in very different ways, generalisations about different cases and a one-size-fits-all approach to care are not appropriate. Young people have expertise grounded in a history of living with SCD and receiving care, which can help non-specialist staff tailor their care to patients’ needs more effectively, improving experiences and outcomes. This is particularly important in the case of emergency care, when staff might not be able to access medical records and patients and carers can play a crucial role in brokering knowledge about treatment and the condition. 122
We examined how health-care transitions shape young people’s health-related behaviour and quality of life [see Chapter 2, objective (a)]. Avoiding care and resorting to self-reliance may be established and taken into adult life, as patterns of health behaviour are often developed during adolescence and young adulthood. 93,120 This may help explain why the highest rates of emergency admissions are among those aged 20–29 years:25 this is the time when parents’ and carers’ involvement and influence lessens and when disengaging from hospital may be more possible for young people with bad experiences of unplanned care. Care experiences during the period of transition to adult health-care services, which include lacking a voice and uncertainty about quality of care, can exacerbate what is already a very uncertain illness experience. 36 Although resorting to self-management of painful episodes may help young people exert some control in an otherwise unstable landscape, it can also pose a risk to their health. Cumulative experiences of struggling to be heard may deter a young person from trying to act as a ‘knowledge broker’122 with respect to their own condition and body to try to improve the care they receive.
Ensuring that children and young people are involved in their own care and that they can participate in health-care service improvement is crucial for youth-centred services. 2,123 There is an increasing mandate for health-care professionals to listen to and take into account children and young people’s views, involving them as experts in their own care. 2 Our research illustrates that, despite good intentions, in the case of SCD transitions there is still work to be done. Developing voice as a patient and being encouraged to act with agency in health-care encounters are fundamental if young people are to move into adult services feeling confident that they are involved in their own care. This is particularly important in the case of SCD care, which has historically been racialised in the UK. 43 In addition to the general problem of lack of voice experienced by young people in health-care services,124,125 in the case of SCD patients there may also be a dimension of racism in their voices being dismissed. 41,43,126
Sickle cell disorder is a condition that is ignored or ‘rendered invisible’. 24,82 Biomedical indicators appear to have more weight in clinical encounters than patient expert voices and symptom reports. 82 We found that the invisibility of pain and patients’ ability to control its expression seemed to contribute to staff scepticism and delays in receiving pain relief. There are other issues that compound the situation further (e.g. stereotyping SCD patients as drug-seekers117,127 and the fact that not all service providers are familiar with SCD or its treatment). 39
There is a clear contradiction between referring to young patients as experts and requesting that they behave as such and what happens in practice in micro-encounters of therapeutic treatment when their expertise is questioned. As our study illustrates, for children and young people to raise their voices to ensure that they are listened to and acted on, it is not enough to have policies mandating participation/involvement, nor is it enough to educate young people themselves. A wider enabling environment is essential to facilitate young people’s voices and expertise. Without this, we risk alienating young people not only from involvement in their own care but also from participating in wider aspects of health care, such as service improvement, research and service commissioning and governance.
Social-psychological aspects of young people’s lives that interact with health-care transition
Social silencing: protecting self and others
There are obstacles in young people’s social contexts that make it difficult for them to talk about their illness experiences and use their patient expertise to explain self-management needs and other health-related practices. Other people’s lack of knowledge about what SCD is and understanding of how the condition affects young people’s lives, coupled with past experiences of being disregarded or not taken seriously, contributed to young people resorting to social silencing. The young people we interviewed have learned to expect that others will not understand their condition and will question their patient expert voice and/or not listen to it. The consequent sense of hopelessness has made our participants opt to keep their illness experience to themselves. Social silencing involves not wanting to disclose, or disclosing only to a few people, and keeping the explanation short. Even when disclosing to others, young people still individualise their illness experience, not asking for support nor using SCD to explain their behaviour. They do not share details with others about how the condition actually affects them or what it means to live with it.
Young people use social silencing as a strategy to protect themselves in relationships with others who do not know about SCD and who will undermine its seriousness or who fail to listen to young people’s patient expert voice. Social silencing works by protecting young people at the social-psychological level. It creates a ‘safe’ space for young people, preventing feelings of frustration at not being heard, not being taken seriously or being misunderstood, while helping them maintain a sense of normality (i.e. not being identified with a chronic health condition). However, social silencing can have negative consequences, because it contributes to making SCD less visible. Lack of public awareness and understanding of the condition in young people’s social context can be perpetuated through social silencing and prove risky for the young person. It can potentially hamper young people’s attempts to stay healthy and reduce their quality of life as they move into adulthood. Social silencing can make it more difficult for young people to get help when they need it, for example in the case of a painful episode. It can contribute to the creation of a ‘risk’ space where young people might not be able to talk about their needs and be understood, but are instead further stigmatised by others. Lack of talk about SCD and general public awareness can contribute to particular images of young people as lazy rather than suffering from SCD-related fatigue, something our participants were particularly concerned about. Young people with SCD struggle to be heard by adults in educational and health-care contexts. 79 Our study adds understanding to this issue by shedding light on how struggling to have a voice as an expert patient and to use this expertise in interactions with others affects young people’s behaviour, sense of self and relationships with others during transition to adulthood.
Another form of social silencing is developed as one starts protecting significant others from the impacts of SCD. In the interviews, young people seemed to prioritise how their SCD affects significant others (e.g. parent suffering by seeing them in pain) over how it affects themselves. Young people’s perceptions of the impact of SCD on significant others and the feeling of being a burden to them contribute to the larger illness experience, adding stress to what is already a very painful and uncertain condition. Our findings illustrate the relational dimensions of the SCD experience [i.e. how the condition is lived and accounted through and against others, particularly significant others (family) and one’s own perception of their experiences of the young person’s SCD]. 83 As one moves into adulthood, keeping SCD private by trying to self-manage alone and disguising pain becomes a way of protecting others and oneself from extra suffering. This form of individualising their illness experiences becomes part of young people’s repertoire of self-management tactics as they move into adulthood.
Difficulties developing adult identities
Health-care transitions shape young people’s identities and help ‘make’ particular kinds of adult patients. 61 This focus on identity formation can help us understand the difficulties young people experience as they try to consolidate new self-understandings to guide their health-related behaviour as they move to adulthood. Young people with SCD can struggle to develop a coherent sense of adult self as they are caught between conflicting demands for self-preservation and self-actualisation. 61 The way in which identities develop during transitions involves young people seeing themselves as in need of improvement to reconcile the demands on the self to perform as both disciplined responsible patients and self-actualising student/professionals. Our study has found that the development of adult identities poses an additional challenge during transition for young people with SCD. All young people experience the complexities of ‘making’ a coherent and consistent adult identity;96,106 however, these are rendered even more difficult for young people with SCD.
Developing new identities during transition for young people with SCD can be exhausting. It involves young people seeing themselves as in need of improvement in different areas of their life to respond to competing demands from different intersecting life transitions. This translates into relentless self-disciplining and self-monitoring to try to do both at the same time; that is, to produce bodily efficacy and stay healthy while working hard to respond to competing demands for self-actualisation to become competent and successful adults, while simultaneously managing the threat of stigmatising identities linked to SCD-related symptoms (such as someone being ‘lazy’). Messages about individual responsibility, self-management and active involvement in own care that circulate in health-care contexts today – and are conveyed by parents – intersect with competing demands for achievement from schools that are often not compatible. For instance, schools demand that young people excel and become entrepreneurial, competent individuals,128,129 but excelling at school is far more difficult for young people who spend time in hospital or who have to rest regularly to avoid having a pain crisis. School demands that can conflict with young people’s efforts to protect their health (including self-care practices such as staying hydrated) include emphasis on regular attendance, engagement in physical activities and non-interruption of lessons for toilet or water breaks. 58 Young people with SCD are ‘dys-positioned’ between these conflicting adults’ demands emerging from health-care services and school contexts. 58 Young people with SCD can struggle to develop a coherent, unified sense of self as they are caught between these interdependent self-disciplining identities that are difficult to reconcile. 61
These difficulties in developing adult identities can pose a risk to young people’s health and quality of life. Young people can engage in exhausting and continuous attempts to consolidate their self-disciplining identities to try to conform to normative ways of being an adult while trying to maintain health. Our findings illustrate how ‘pushing oneself’ might develop into a resourceful yet risky tactic to try to meet education and work responsibilities while helping respond to social expectations about academic achievement. Patient participants emphasised individual responsibility and the young person as a purposeful agent, and they did not generally refer to the role others could perform in supporting their journey. This individualisation of illness makes the journey more onerous for young people, who might not seek help from others. Difficulties in enacting the self-actualising and competent student/professional identity can be played out in a ‘lazy’ identity that is disempowering and stigmatising. 61 This risk to the sense of self of young people with SCD can be compounded by teachers’ and peers’ misperception of SCD-related fatigue as a property of someone being lazy. 76,80 Young people with SCD are aware of these misrepresentations and try to distance themselves from ‘lazy’-stigmatising identities by pushing their body limits when unwell and/or disguising their fatigue. 61
Implications for the health-care transition of other long-term conditions
Findings from this study can be applied to the understanding of health-care transitions in other long-term conditions, such as diabetes, asthma, epilepsy, inflammatory bowel disease or arthritis [see Chapter 2, objective (e)]. Our insights into identity development during transition offer a way to understand young people’s experience of growing up with a long-term condition. The conflict between multiple adult identities (patient and non-patient), difficulties in trying to reconcile them to formulate a coherent sense of self and the self-disciplining and self-regulation for self-improvement that our participants deployed61 may well be shared by other young people. The conflicting demands on time and effort for health preservation versus academic achievement and the inevitable self-imposed pressure to be ‘successful’, both as a patient and as a student, is applicable to all young people with a long-term condition. Understanding how young people living with a long-term health condition work to craft new identities as they move to adulthood should also be the focus of attempts to improve health-care transition and the support young people receive as they move to adulthood. Many long-term conditions share the requirement that young people develop both health-care autonomy and autonomy as an adult more generally, which may add additional difficulties to the general experience of moving to adulthood. 130 Young people with diabetes, for instance, experience similar moral demands to exert control over themselves that can translate into young people engaging in multiple and competing self-disciplining practices. 131 In looking at identity formation, our study adds an understanding of how these competing demands can become the source of young people’s struggles to formulate identities that help them stay healthy but still allow them to meet other life goals. Tensions in reconciling conflicting adult identities might shed light on the difficulties young people with other long-term conditions encounter during transition to adulthood when trying to develop images of themselves as adult patients to guide their health-related actions.
Some of our other findings are likely to apply to transition in other long-term conditions, particularly our analyses of how becoming an expert patient is experienced and developed in encounters in health-care and social settings, and the implications for disengagement with services and for social silencing of the condition. Adults’ push for responsible self-management and emphasis on self-advocacy that is at odds with the barriers young people with SCD encounter when trying to practise their expertise in their own body and condition should be explored further in other health conditions. The lack of status as patient experts and lack of voice that young people with SCD experience in encounters with acute non-specialist health-care staff during transition to adult services, and the obstacles to accessing adequate and timely medical care and having basic bodily care needs met, may well be experienced by young patients with other long-term conditions, particularly when these are less known or affect already marginalised groups. Similar barriers to high-quality unplanned hospital care might exist for young people with more common conditions during their transition to adult services. Despite being one of the most common conditions for children and young people, asthma, for example, is generally poorly understood and managed in non-specialist health-care settings, in some cases leading to fatal outcomes. 132 Barriers to recognition of patient expertise could extend well into adulthood. For example, adults with diabetes have found similar obstacles to having their knowledge of their own body and condition recognised in health-care encounters, with non-specialist health-care professionals mistrusting their patient expertise. 133 There needs to be a shift in emphasis from ‘self-care/advocacy’ to acknowledging the need to recognise young people’s voices. This may well also apply to other conditions. Our study underscores the importance of ensuring that young people’s voices are listened to and acted on to deliver youth-friendly7 and adolescent-responsive services59 across the health-care system and, particularly, although not exclusively, during the transition period. Without this, we risk young people learning how to delay hospital care and resort to self-management at home because of their negative experiences of care. Involvement in decisions about care, staff attitudes, including respect, and active listening to patients’ concerns and pain management are all issues related to the key domains of youth-friendly and patient-centred care that young people with long-term conditions report as integral to the quality of their health-care experiences. 134,135
Social silencing might also be shared with other young people living with long-term conditions that are less common, less represented in society or have an element of stigma associated to them. For instance, we know that children and young people with human immunodeficiency virus often deal with their condition in silence, confining talk to clinical spaces where they become used to accessing only medicalised framings of their condition and not its social aspects, such as how it affects their life and how it will shape the future. 136,137 Silencing and narrow medicalised framings of a long-term condition may limit young people’s ability to integrate their condition into their everyday life as they transition to adulthood, and articulate a fuller version of what it means to be an adult with SCD. It may also bring health risks. Young people living with long-term conditions may prefer not to disclose their condition, but they nevertheless recognise that it is useful for others to understand their condition, for instance for support during medical emergencies. 138 For example, school-based interventions educating peers have improved quality of life for children with asthma. 139
The transitional tactic of learning how to make one’s illness experience private to protect significant others from suffering and avoid being a burden is something other young people living with long-term conditions might also practise increasingly as they move into adulthood. For instance, as children with cystic fibrosis grow, their parents’ role as emotional protectors of their children (from knowing the severity of their condition) tends to reduce while children’s desire to protect their parents from distressing information about their health grows. 140 Children who are terminally ill learn from adults how to avoid conversations about their diagnosis and death, and engage in these silencing practices as a way of protecting their parents. 141 Our analysis of the relationality of SCD and the processes by which the illness experience is lived through and against significant others, with young people making efforts to avoid others’ suffering, highlights this additional burden for young people transitioning to adulthood. This should be examined further in other long-term conditions.
Limitations of the study
Our findings are derived from interviews with a group of young people with SCD in London and one other city in England. We do not claim that our sample of young people represents all experiences of young people with SCD. However, our findings provide insights into how social-psychological aspects of young people’s lives and health care shape their experiences and inform their behaviour during transition to adulthood. These findings are likely to be relevant to other young people with SCD and young people with other long-term conditions. We have discussed our findings with young people with SCD and stakeholders, including patient charities, carers and specialist clinicians, throughout the analysis and dissemination process (see Chapter 3), and our findings resonated with their experiences. Our analysis was also refined and informed through these participatory processes (see Chapter 3). In addition, themes relating to quality of unplanned hospital care were also prominent in a separate study of patient-reported experience measures in SCD,18 suggesting that they do apply more widely.
Our findings are based on what participants chose to tell us, which may have been influenced by how they perceived the research and interviewer AR whose background and identity (i.e. a white adult academic researcher without SCD) differed from their own. We considered how our identities influenced the interview dynamic and analysis. The type of identities participants present through interview narratives and their narratives are contingent on the interview situation and relationship with the interviewer. We are mindful that the interview situation might have invited young people to present themselves through socially desired ‘modes of subjectification’. 142 This might explain why they produced identities that portrayed themselves as responsible and working on developing disciplined forms of being an adult patient. As researchers, we made efforts to avoid being perceived as adult experts similar to the adults they encountered in health-care and education settings, who were relaying disciplinary demands about responsibility in health and achievement in education and work. As we explain in Chapter 5, we presented ourselves as researchers independent of their health-care services and outsiders to the health-care services context. Our research leaflets were youth friendly, and we tried to conduct most interviews in participants’ ‘home turf’ (see Chapter 5). Even when conducting interviews at hospital settings, young people seemed comfortable talking and asserting their patient expertise and drew on their expert voices to speak about different issues during the interview, including about the type of care they wanted and the need for others to listen to their voices. Despite these efforts, the position of the interviewer as white university researcher without SCD may have influenced what participants did and did not report. For example, this could be why participants did not talk explicitly about racism in relation to their discussions of their voices and patient expertise being disregarded. 41,43,126 We did not ask them directly whether or not they thought their care was racialised, but they also did not bring it up in the interviews when accounting for how others responded to them.
Chapter 8 Conclusions
Empowering young people and providing youth-friendly, person-centred care
Our findings have implications for improving care across the health-care system (beyond specialist care) during transitions [see Chapter 2, objective (c)] to make services youth friendly,134 developmentally appropriate and adolescent responsive. 59,143 The transitional care efforts of planned/specialist-led services to empower young people to take responsibility for their own health, to self-advocate for their own needs and navigate health-care services may not be enough to achieve successful transitions. Our findings suggest that young people must be supported and their skills developed and enabled across the health-care system, including during interactions with non-specialist staff. Transitional support work delivered within specialist services often emphasises developing individual patient skills, such as confidence to move into adult services, self-management and health literacy. 5 There is evidence that some transitional care approaches of specialist-led service features, such as joint paediatric/adult clinics and specific age-banded clinics, work to support young people adjust to adult services. 1,144 Our research suggests that transitional care should also look beyond specialist-led clinics and be accompanied by additional efforts across the health-care system to help make acute general care a safer place for young people to practise their patient expertise during transitions.
Focusing only on ‘improving’ young people’s behaviours and skills so that they can confidently move into adult services without addressing the barriers they face when they access unplanned care in general services can have important negative consequences (e.g. disempowering and disengaging young people and reinforcing the barriers to treatment that transitional care seeks to address). Even when the young person has transition-‘readiness’ skills (e.g. health literacy, self-management knowledge, communication and advocacy skills), if their patient expertise is disregarded or undermined in a service, preventing them from using those skills, or if they are not involved in decisions about their treatment, they may develop mistrust in that service and perhaps in health-care services more widely. 116
An emphasis on self-management for successful transition should not be interpreted as an issue for individual patients, leaving them to handle problems on their own. Developing self-management skills should include guidance and support from health-care teams, including from non-specialist health-care professionals, to promote positive youth skills development. 7 Health-care professionals could play a role in supporting young people to advocate for themselves and communicate with staff. It is important for young people to develop ‘diplomacy’ skills46 and learn how to present themselves in health-care encounters to ensure that they are heard by health-care staff, although it could be argued that this should not be necessary. Developing assertiveness and these diplomacy skills involves encouraging young people to communicate with staff in a way that they would be perceived as co-operative rather than adversarial. 46 Although developing self-advocacy skills is recognised as important in SCD transitions,17 learning these diplomatic skills46 is not something that is emphasised in guidelines on transition. However, these skills may be crucial for young people with SCD, even if they should expect to be heard and respected regardless. These diplomacy skills are important to protect health and navigate health-care systems as they move into adulthood to (1) convey the seriousness of SCD pain and receive timely care, (2) build relationships with ward staff to prime them to recognise when the young person’s health deteriorates rapidly and (3) develop rapport with specialist consultants and specialist nurses who can then advocate for them at non-specialist wards and have power to encourage improvements in SCD care in these settings. It should not be necessary for young people to accommodate ways of communicating with staff that are seen as more ‘correct’ or appropriate, particularly when they are in severe pain or distress. Nor should it be necessary for young people to perform as ‘sick’82 to make their suffering visible in a certain way simply to convince staff to take it seriously. Developing understanding of the value of listening to young patients, particularly their reports about pain, should be a priority within health-care systems and in training of health-care staff.
Preparing young people to move into adult services through skills building is important for transition. 3 However, it is also crucial to make structural and organisational changes to tailor services to young people and create enabling spaces for them to practise their transition-readiness skills and patient expertise while having a voice in care encounters throughout the whole health system, not just in specialist services. 116 We need to move beyond simply focusing on ‘support[ing] young people in fitting in with the health-care system’ and instead work on engaging with their experiences to consider how health services can meet their needs. 91 This is an important step towards creating an enabling health-care context for young people to enact transition readiness.
Health-care services that are youth friendly and adolescent responsive to support young people through transition to adult care should include inpatient adolescent wards145 and developmentally appropriate care. 7,146 Our work suggests a particular need to work closely with hospital staff to train them in transitional care147,148 (SCD care in particular119), compassionate care149,150 and in communication skills, such as how to engage with young people and listen to their voices, to ensure that young people can influence their health care. 145,150 Barriers to good transitions may be partly due to lack of focus in medical training on young people as a distinct patient group with specific health needs. 151 To address these barriers, staff should be trained in issues around adolescent health so that care is youth centred and focused on young people’s needs. 123 We also suggest working on improving staff attitudes towards young people,119 to help them both to recognise their status as experts in their own body and condition and to recognise that their voice is legitimate. Staff respect and openness to listening to patients’ voices and involvement in their own care are issues young people identify as central to positive experiences of care. 134,135 Improving staff attitudes may be achieved through an experiential learning component148 that includes the participation of young people145 and perhaps using clinical simulation techniques. 152 For young people to be taken seriously it is also important that staff learn about pain to empathise, instead of stereotyping the young person in severe pain as a ‘difficult patient’. 84 If young people are to be involved in their own care, and more widely in health-care services improvement, their patient expertise needs to be recognised ‘on the ground’ in the micro-encounters with health-care professionals who care for them.
Creating these enabling environments to support young people’s involvement will also include organisational strategies, such as increasing visibility of systems for young people to make suggestions for improvement and complaints,2,125 as well as increasing awareness among staff about patients’ rights to have their voices heard. 125 Initiatives such as the implementation of patient-held health and well-being passports153 with personal information about a patient’s care, and acting on this information, may help ensure that care is responsive to young people’s needs. This may be particularly useful when the young person is unable to communicate because of poor health. In the UK, guidance is now available on ways to improve young people’s health care, which could help address some of the problems we have found in our study with regard to poor quality of care in unplanned non-specialist settings. 145,150
Working with young people’s wider context
Sickle cell disorder illness experience and pain is an individual experience that may involve significant suffering. Our study has indicated the importance of the relational dimension of SCD and how young people’s illness experience cannot be abstracted from the social relationships in which they engage in their everyday life [see Chapter 2, objectives (a) and (c)]. These relationships can constitute an additional source of stress and burden for young people and can limit their ability to self-manage and practise their patient expertise.
Working on young people’s wider social contexts, including educational contexts (e.g. schools80,154 and universities), is essential to create enabling spaces for young people to use their patient expertise and have it recognised to protect their health while still consolidating self-actualising adult identities that help them achieve their life goals. Substantial work is needed in this wider social context to raise awareness about the condition, educate the public and address stigma and stereotyping associated with SCD-related fatigue and use of opioids for pain relief. In schools, this could involve increasing awareness about the condition among teachers and peers through different subjects of the curriculum going beyond biomedical aspects to promote knowledge about SCD lived experiences. 76 Whole school-based educational approaches have succeeded in increasing peer understanding of other long-term conditions, such as asthma. 139 McCann et al. 139 found that improved knowledge of asthma among non-asthmatic school peers was associated with a significant positive impact on children with asthma, such as improvements in their self-esteem and quality of life. School support should be in place regardless of whether or not the young person wants to openly speak about the condition and whether or not staff can remember the specifics of SCD as a medical condition. 24,87 School support should focus on holistic responses targeting the whole school rather than simply the individual knowledge and practices of teachers (e.g. changing school uniform so that long trousers that protect from the cold are allowed). 24 The aim is to create a culture in the school that ‘en-ables’24 young people to achieve their goals and their academic and social potential. Dyson155 has produced a comprehensive school guideline to support young people with SCD at school, which is published online as an open education source.
Young people with SCD may wish to prevent their family members worrying about them and so under-report pain or ill health. One way to address this may be working with families and carers to help them understand these internal conflicts and facilitate open conversations at home about the additional stress young people experience in trying to protect them from the suffering and impact of the condition. Allowing open conversations about the condition and its impact on individuals may help reduce stigma associated with SCD in the community.
Reconciling and consolidating adult identities as an indicator of successful transitions
Although mainstream health-care transition work often emphasises improving young people’s individual skills, such as their health-related knowledge and confidence to move into adult life,5 young people must also be supported to navigate the complexities that we have discussed in this report [see Chapter 2, objective (c)]. Health-care transition support programmes could help young people negotiate the complexities of their competing patient and non-patient adult identities. Helping them reconcile these identity conflicts may help them move into adulthood in a healthy way.
The problems around developing adult identities could be addressed in health-care transition support work. For sickle cell disease specialist providers, key indicators of whether or not a transition has been successful include completing key developmental milestones, achieving educational and employment goals and having children. 16 The consolidation of multiple adult identities could also be added as a success indicator.
Health-care staff should be wary of how the practices and discourses permeating relationships with young people in health-care contexts, including clinical care relationships and any type of transitional support they receive, relay disciplinary demands on the young person participating in defining what they can and should become. Transition support programmes should work with young people in collaborative ways, encouraging their participation and critical reflective dialogue156 so that they can develop awareness of, and critique, the social conditions that shape their adult identities. This participatory reflective work could help young people move away from individualising views of health and transition that focus the locus of control of success on improvements at the personal/individual level. Instead of dictating to young people who they should become and pushing them to conform to normative forms of adulthood, we should work with them in dialogue. A participatory approach is essential if we are to encourage young people’s agency to cultivate self-specified and fulfilling identities. 61
Recommendations for research
Future studies could examine perceptions among A&E staff and general medical health-care professionals of SCD (beyond the biomedical and clinical care aspects), including examining their attitudes towards young people with SCD and the impact of these perceptions in practice (e.g. via observations of care practices). This could provide insights about the specific issues to be addressed in training and in collaborative or advocacy work with sickle cell disease specialist providers. It would be useful to examine how young people’s voices and agency manifest in hospital settings where they receive unplanned acute care, and what can be done to improve those interactions with health-care staff to enable young people to raise their voices and use their patient expertise in these interactions.
Another important area of future inquiry would be to examine dynamics between family members and carers and young people, and how relationships influence health-care transitions. Such research could examine parent–carer interactions at home and hospital settings. It could investigate how the nature of this relationship affects the young person’s ability to develop adult identities and an adult voice to help exert control over their life and engagement with health-care services.
Future research might also include developing, implementing and evaluating a whole-school intervention to increase understanding of SCD among teachers and peers,139 including a participatory component to enable critical reflections156–158 on how SCD and transition affect young people’s lives. This research could examine the impact of such interventions on the quality of life of young people with SCD and their agency to raise their voices about their condition and needs, as well as identity development, as they transition to adulthood.
Chapter 9 Impact
This section of the report details how our project has sought to generate a range of different activities across the diverse contexts that affect the lives and well-being of children and young people with SCD.
This Sickle Cell Life participatory stakeholder event: reflecting on the implications of findings for practice
We held a participatory event for This Sickle Cell Life on 2 April 2019. The aim of the event was to help move our research findings into practice to improve experiences of young people with SCD. We engaged directly with key stakeholders (i.e. young people, including those with SCD and other long-term and/or chronic conditions, parents and carers, policy-makers, clinicians and researchers). We worked with the RCPCH &Us involvement team at the RCPCH to plan and facilitate the day-long workshop because of their expertise in children and young people’s engagement. We centred young people at each stage of the planning to ensure that the event was relevant and was designed by and for young people. We hired a professional photographer and an illustrator for the event to ensure that we had visual outputs to share that would help to keep attendees engaged throughout the workshop and help spread the message on social media. In advance of the event, the RCPCH &Us team contacted UK grime rapper and musician A-Star, who had recorded a music video about his life experience with SCD159 and he responded with a video message to play at the event.
At the event, we presented research findings and asked attendees to reflect on them, drawing on their different backgrounds and experiences. We also asked them to work together to co-produce innovative ideas for resources to health-care transitions for young people with SCD. We worked with participants to co-produce ideas about the implications of the research while listening to young people’s experiences of both SCD and wider representation and involvement initiatives to think about the context, issues and potential solutions.
The participatory workshop offered more than a unidirectional process of disseminating findings. It fostered dialogue between young people, carers and others who we had identified in the research as particularly important outside specialist services (e.g. educational staff, A&E doctors and non-specialist health-care providers). We aimed to make the day as interactive and fun as possible to ensure that everyone felt that they could have a say in their responses to our research findings and to ensure that they felt heard. We also wanted to ensure that they felt that the day had been worth their time and energy to attend.
Fifty people attended the event. Attendees included:
-
young people aged 13–18 years (both with and without SCD/sickle cell trait and other long-term health conditions)
-
youth health advocates affiliated to RCPCH &Us
-
SCD patient experts
-
parents and carers of children and young people with SCD
-
academic researchers
-
representatives of the following organisations that have a role in the care of young people and/or in influencing the support they receive in their everyday life
-
NHS England
-
multiple NHS hospital trusts, including non-specialist doctors who did not have extensive prior knowledge of SCD, as well as non-specialist nurses and hospital managers
-
paediatric nurses and others from the Roald Dahl’s Marvellous Children’s Charity (Amersham, UK), a charity that provides expert care and support for children with serious health conditions across the UK
-
social services
-
council staff
-
NIHR CLAHRC NWL
-
staff from the Sickle Cell Society, including the society’s director.
-
After hearing about This Sickle Cell Life research findings and what young people said would help their SCD patient experience, stakeholders – especially young stakeholders – asked the researchers a series of questions in a game show style as a way of continuing the dialogue between researchers, young people and SCD advocates. Twenty-three questions were developed to ask the research team, patient representatives and voluntary sector group in quick-fire rounds, with extra questions answered by the panel after the event. These additional answers were shared with attendees through the event report. After this question-and-answer session we screened the SCD awareness music video created by A-Star. 159 After screening the video, participants worked in groups to collaboratively reflect on the implications of our findings for practice and draw on their own experiences and expertise to co-produce ideas to improve transitions for young people with SCD at different levels, from health services to other social contexts of young people’s lives.
Young people, parents and carers, activists and clinicians worked together to devise co-produced recommendations for health-care providers and the government (see Appendix 1). These recommendations were the culmination of the event and input was gathered from across the group. Ideas emerged from a discussion–solution–action framework, including topics from increasing non-specialist clinical knowledge of SCD care to supporting identity development through transition. For example, participants explored the idea of a ‘universal sickle plan’ to address a problem they identified through their discussions. In the scenario of a universal sickle plan:
-
the problem is lack of shared information between departments/professionals on SCD care
-
the solution is a universal sickle plan available in paper and as an application that includes a standard operating protocol (e.g. first-line treatment, medications, fluids, allergies, a SCD/thalassaemia checklist)
-
the action should be exploration with NHS England, King’s Health Partners (London, UK) and the Sickle Cell Society.
During the event the photographer took photos to document the day. The illustrator captured many of the conversations that happened over the course of the day and represented the research and its lived impact on young people with long-term health conditions.
The event was positively received by attendees. Feedback from young people attending the event was very positive. When asked to sum up the day in three words in (confidential) feedback forms, responses included ‘motivating, inspiring, toolkit’, ‘insightful, fun, sociable’, ‘great, fulfilling’, ‘clever, thoughtful, eventful’ and ‘educative, fun, brainstorming’. Evaluation feedback from non-specialist NHS clinicians was also positive.
We asked attendees to make pledges about what actions they would take after having attended the workshop to support the future of This Sickle Cell Life (i.e. our research project). Many made specific pledges. For instance, one respondent pledged to improve hospital emergency department training and another wrote of their intention to amplify the voices of young people at their emergency centre when designing care approaches. Another pledged to encourage people from black and minority ethnic communities to donate blood to help people with SCD or thalassaemia. Another pledged to discuss their condition more openly with others, writing: ‘If I can help one person, then that’s one person whose life I have added to. I’m the voice of the Silent Sickler!’. One of the attendees, a secondary school teacher, pledged to share the A-Star video in their school as part of a ‘turbo teaching’ session. Others said that they would share the video more widely among their social networks.
We also had the opportunity to communicate with wider SCD, thalassaemia and chronic conditions communities:
-
The professional photographer and the illustrator we had hired for the event produced a range of media content for dissemination. Many attendees tweeted and shared online their own photographs of the illustrations throughout the day to their own networks, including youth and school networks, as well as charities, policy groups and NHS health trusts.
-
Musician A-Star also retweeted photos taken by attendees of our event on the day (see www.twitter.com/AstarMusicUK) to his 5300 Twitter (URL: www.twitter.com, Twitter, Inc., San Francisco, CA, USA) followers.
Over the summer, the RCPCH &Us team compiled a delegate event report as an outcome of the This Sickle Cell Life event and distributed it to event attendees.
After the event, RCPCH &Us committed to organising additional meetings with key stakeholders. These included:
-
Meetings with staff at the Sickle Cell Society who were introduced at our participatory stakeholder event.
-
Meetings (being arranged) with strategic partners to review the potential for including a universal SCD plan in the development of NHS England digital health solutions (including mobile phone applications).
-
A ‘mop-up’ session with youth delegates and young volunteers supporting the next steps, including analysing outreach data and a document summarising recommendations for change based on our research findings and the participatory workshop being distributed to key stakeholders.
-
An outreach tour to enhance stakeholder engagement at two secondary schools in Milton Keynes, UK, and Lincoln, UK. In July 2019, 130 young people participated in discussions about their awareness of SCD and how to improve this in school settings. The school sessions echoed comments in the research and the event in April, with general knowledge around SCD being minimal and a clear steer from students to increase knowledge, skills and understanding about the condition through lessons, events and having the opportunity to hear from SCD role models.
Students said:
It could be explained so it helps other students showing what it is, how you get it and how to help people with it.
We need to know: What it is? What does it do to you? What are the effects?
Explain it in a simple way in science or in a (not boring) assembly.
One of the health-care managers who attended our participatory event invited RCPCH &Us to run a subsequent engagement event with NHS emergency care staff in Manchester, UK, in autumn 2019. In addition, RCPCH &Us plans to speak with non-specialist health workers from paediatrics, general medicine and emergency medicine about the co-designed recommendations and how to improve patient experiences for young people with SCD.
The Roald Dahl’s Marvellous Children’s Charity has been in touch with RCPCH &Us about more joint work on SCD and to share the learning. The charity arranged for a young person with SCD and their parent, who both attended our April event, to present their experiences of SCD care at the conference on health-care transition in May 2019.
Some of the young people and parents who participated in the event have subsequently become more involved in other health projects to share their experiences and increase awareness of others. This involvement includes (1) joining a national research project into improving quality improvement measures for general practitioners, acute settings and for those with long-term conditions (April 2019) and (2) being more involved in the work of RCPCH, including joining the Infants, Children and Young People’s Engagement Committee (July 2019) and participating in wider discussions, such as about indoor air pollution, skills for paediatricians and Doctor of Philosophy (PhD) research on individual decision-making, and also helping to set RCPCH engagement priorities for the coming year.
Blog by the Royal College of Paediatrics and Child Health &Us team
As well as contributing our own thoughts on our research findings from This Sickle Cell Life to our Dialogue, Evidence, Participation and Translation for Health (DEPTH) research blog [URL: https://blogs.lshtm.ac.uk/depth/ (accessed 18 August 2020)], we wanted to hear from some of the people we had engaged with at our dissemination event and amplify their viewpoints to the wider community. We are looking into hosting blogs from attendees at the event that will feature their reflections on the research. The RCPCH &Us team are also planning to write a blog from their perspective of having involved young people in both the planning and delivery of the event. We will be publishing this blog on our DEPTH website [URL: www.lshtm.ac.uk/research/centres-projects-groups/depth#updates (accessed 18 August 2020)].
Sickle Cell Society Self Over Sickle programme
Our findings have helped to shape a programme, the Self Over Sickle (SOS) programme, devised by the Sickle Cell Society to support transitions for young people with SCD and their families [see Chapter 2, objective (d)]. The programme promotes improved physical, psychological, social and emotional well-being for young people aged 16–25 years, with resources available online, through social media, podcasts and live in-person conversation events that are also livestreamed to listeners remotely. The programme aims to combine issues identified in our research that we discussed with SOS project staff through various reflective sessions on knowledge translation in 2018 and 2019 (including the participatory event described above) with those identified as important by the Sickle Cell Society. The programme’s focus on transition is not limited to health care as it also addresses other aspects of transitions to adulthood, such as dating, relationships and education.
The SOS programme seeks to empower individuals and influence the wider social environment. Our research findings shaped SOS programming as follows.
Social silencing
The SOS programme focuses on peer-led conversation between young people who tackle the social silencing of SCD [influenced by our findings (see Chapter 6, Transitional tactic: social silencing) and a paper on the limitations and social complexities of seemingly straightforward pain scales used in clinical care83] and building confidence in vocalising the SCD experience to the uninitiated (reflecting our findings and papers46,116). As part of the SOS programme, the Sickle Cell Society is devising an advertising campaign designed to address our findings about the link between social silencing and lack of public awareness about SCD (see Visibility).
Self-actualisation and self-preservation
These are themes that emerged in our findings about identity development during transition61 (see Chapter 6, Difficulties developing and consolidating new adult identities: the adult patient versus the adult outside health-care contexts). The SOS programme attendees agreed that the issues they experience are not always clinical but are often internal battles of self-actualisation. 61 Young people often know the facts and figures about their condition but find personal concerns harder to articulate (see Chapter 7, Social silencing: protecting self and others). For example, the SOS programme kickstarted, both during and after the sessions, personal conversations between young people with SCD, who expressed surprise and excitement at being able to discuss their conditions with other people ‘just like’ them. Topics included late period onset, how SCD affects dating, when and how to ask for pain medication46,116 and the NHS pain scale. 83 The SOS programme engaged with our finding that young people with SCD default to referring to their condition using biomedical, rather than social, definitions to their peers based on secondary school science lessons. The SOS programme highlights holistic approaches to articulating the condition.
Visibility
The SOS programme is working to make SCD more visible with a billboard advertising campaign. This initiative was influenced by findings of social silencing and by discussions at our participatory event, in which Nordia Willis, one of the key PPI experts in This Sickle Cell Life, spoke about how young people with SCD do not see the condition represented in wider society. The billboard campaign aims to raise awareness about SCD and its effects.
Participatory work
The SOS programme was conceived as an expert delivery approach. However, SOS programme staff discussed involvement and co-production approaches with Cherelle Augustine, a PPI expert in This Sickle Cell Life, and with SOS regional representatives who also live with SCD, and concluded that advice about SCD is best received from others with the condition. As a result of these discussions, the SOS programme adopted a peer-led approach.
Concrete end product
Cherelle Augustine advised that participatory approaches should always generate an end product that is useful to participants involved in the project. The SOS programme podcast,160 upcoming ad campaign and YouTube series (URL: www.youtube.com, YouTube, LLC, San Bruno, CA, USA),161 built with input from young people with SCD via social media162 and in-person SOS programme advocacy events, are tangible evidence of participant involvement. The products condense themes previously discussed with young people with SCD into short, accessible and shareable video clips and tips, emphasising the theme of transition based on feedback from user groups and the This Sickle Cell Life participatory stakeholder event. This initiative led to the SOS programme ‘40-day challenge’ for service users, advocates and carers to celebrate 40 years of the Sickle Cell Society, with 40 challenges uploaded to social media channels using the hashtag #40FOR40. The challenge aims to encourage conversations about SCD and is partly informed by our research findings on social silencing and the need to address SCD stigma.
Images of Innovation
We were selected by the LSHTM to showcase This Sickle Cell Life in the Images of Innovation exhibition in September 2019. The exhibition was set up to celebrate 120 years of health innovation at the institution and invited researchers to contribute a visual representation of research at the institution. The brief was to ‘creatively capture an innovative project you or your team have been undertaking in a single image, accompanied by a short description’ to illustrate how research has an impact. We entered an image made by the artist who illustrated our participatory event and were selected to represent the project in the exhibition, enabling us to start conversations with a wider group of people who were interested in improving health care for people with long-term conditions, working with children and young people and participatory approaches to research.
Social media
We wished to communicate with a wide range of stakeholders, including patients and carers, charities, activists, clinicians, policy-makers and the general public. We created a Twitter account (URL: https://twitter.com/ThisSCLife) (Figure 2) in June 2015 and from 2017 onwards we have posted an update from the project, a news story or interacted with sickle cell charities, health groups, activists and clinicians every weekday. Our Twitter account connects with > 1100 activists, patients and clinicians and totals nearly 500 followers. In addition, we have communicated with a strikingly wide range of different Twitter users, including not just academic and clinical researchers but SCD campaign groups, awareness days campaigners and Black History Month campaigners. One of our most successful campaigns has been sickle cell research ‘threads’ that unpack our published academic articles across 10–15 linked tweets for a bite-sized precis of our research findings.
FIGURE 2.
Screenshot of our project Twitter account.
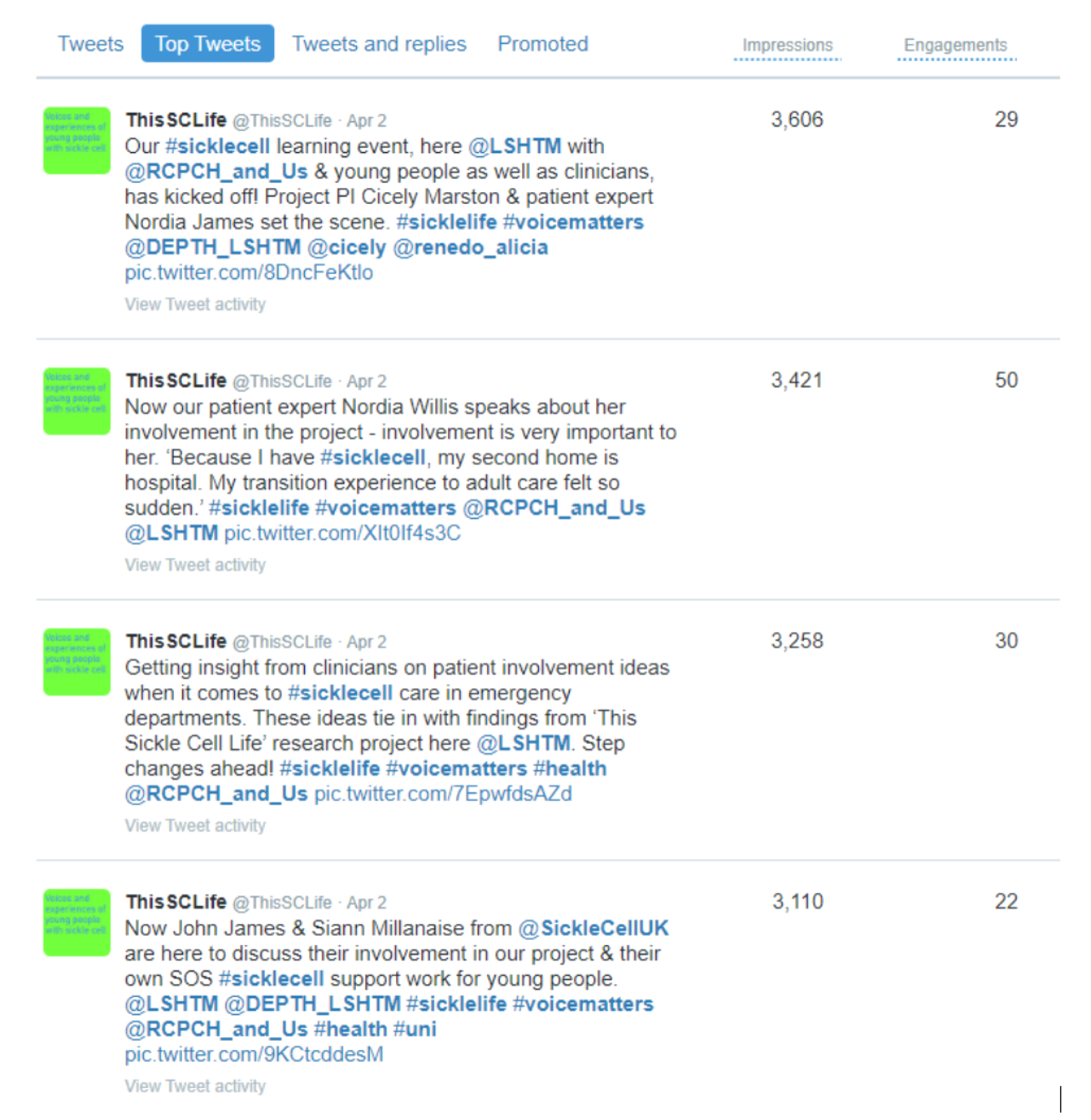
At our participatory event in April 2019 (i.e. the This Sickle Cell Life participatory stakeholder event described above) we ran two hashtags for our Twitter account (see Figure 2): #SickleLife and #VoiceMatters. Event organisers as well as attendees live tweeted using these hashtags throughout the day, building our engagement for those who could not attend in person, including for health reasons. The RCPCH &Us team, NIHR CLAHRC NWL and LSHTM spokespeople also tweeted throughout the day, which generated further interest in our participatory work as well as our research findings. For example, the NIHR CLAHRC NWL, which has 2700 online followers, engaged with many followers who work on improving quality of health-care services in the NHS and globally. Meanwhile, RCPCH &Us had > 2500 impressions on their This Sickle Cell Life event tweets. Our Twitter analytics reports showed that our most viewed (impressions) and retweeted (engagements) outputs on social media in 2019 were from our SCD event (Figure 3), with a significant boost in new followers, new interactions – nearly 2500 on the day of the event (see Figure 3) – and new ‘reads’ of our research, across both blog hits and academic article downloads.
FIGURE 3.
Twitter analytics snapshots of interactions with our DEPTH research group Twitter account.

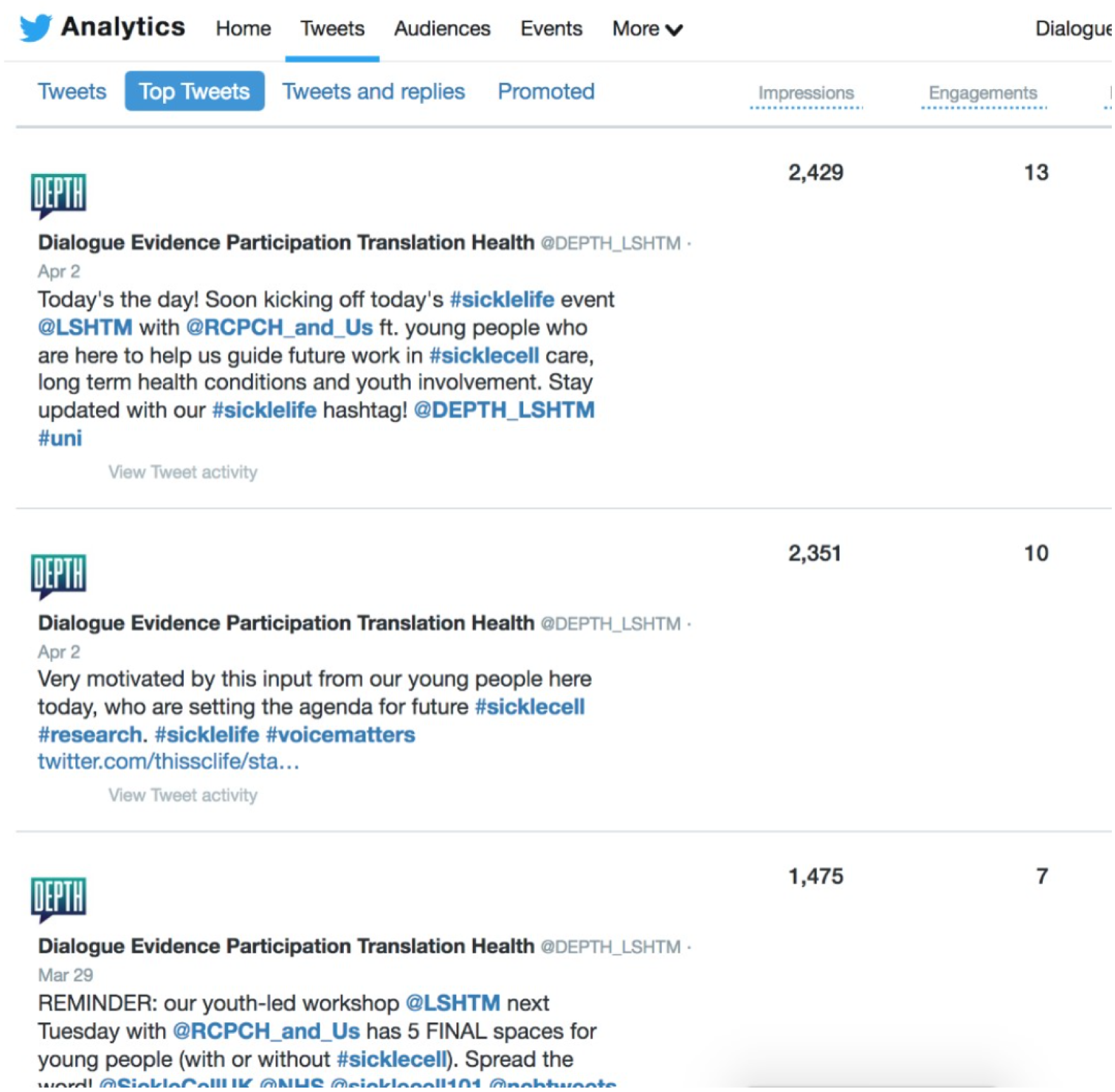
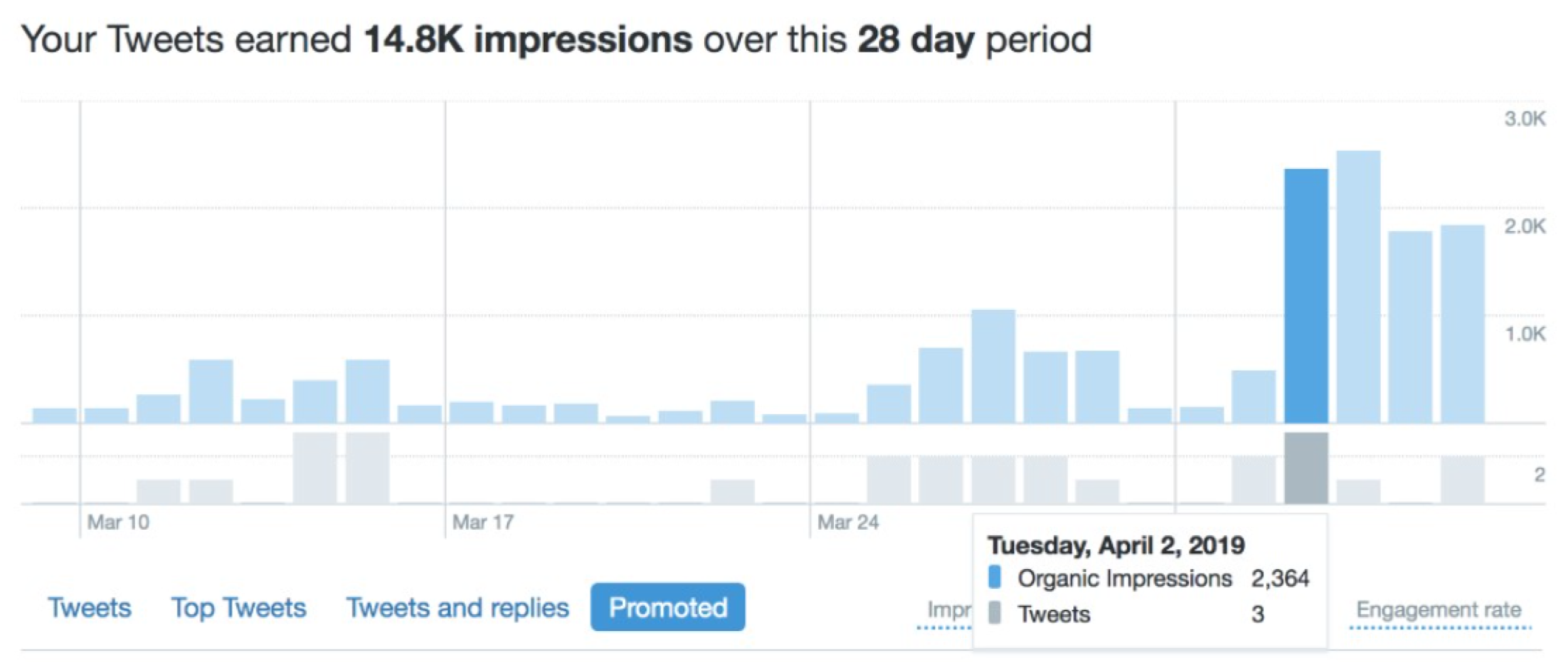
We also created a LSHTM-hosted This Sickle Cell Life webpage [URL: www.lshtm.ac.uk/research/centres-projects-groups/this-sickle-cell-life (accessed 18 August 2020)]. We have used this platform to disseminate our latest research findings and update readers on project progress. We are committed to making our research as accessible as possible to non-specialists and particularly to people with SCD, including, most importantly, the young people who were involved as interviewees, advisors and event participants. With this in mind, we have included lay summaries of our peer-reviewed journal articles on our website, all written in plain English, as a supplementary resource to the usual academic abstracts. We have also written blogs about our SCD research, participation and co-production for our DEPTH research WordPress site (www.wordpress.com, WordPress Foundation, San Francisco, CA, USA) [URL: https://blogs.lshtm.ac.uk/depth/ (accessed 18 August 2020)]. Our blog, started early in 2019, has 1300 hits already, with a traffic spike following our participatory stakeholder event in April 2019.
Academic conference engagement
Lead researcher AR presented a paper reporting on young people’s difficulties developing and consolidating new adult identities61 at the British Sociological Association Medical Sociology Group Annual Conference in Glasgow in September 2018. She discussed early research findings with other sociologists in the academic community.
Invited presentation at the UK Forum on Haemoglobin Disorders national meeting
We presented evidence at the UK Forum on Haemoglobin Disorders educational and training meeting in November 2018. The forum is a national organisation that formulates national policy for screening and management of SCD, thalassaemia and related conditions. At this meeting we presented findings and received helpful questions and feedback on the implications of our work for practice. One health-care professional, for instance, told us they would use our findings to advocate for health-care service improvements for young people with SCD.
Invited panel discussion at the NIHR CLAHRC NWL panel discussion ‘powerful partnerships’
Principal investigator CM and lead researcher AR were invited to discuss our co-produced This Sickle Cell Life project at a panel during the event ‘Making a Difference – A Journey with Collaborations for Leadership in Applied Health Research Northwest London’ on 6 June 2019. Among the other panellists who were reflecting on the topic of partnership in health care with us were the musician A-Star, a representative of the SOS transition programme and a representative of the Sickle Cell Society. At the panel we discussed our collaboration with different stakeholders throughout the project, including with PPI experts, specialist clinicians and Sickle Cell Society members. We also responded to questions from the audience.
Serendipitous and additional impacts
One positive outcome of This Sickle Cell Life has been the extent to which the findings have been taken up and disseminated without explicit involvement or funding from the research project grant. There may well be further activities unknown to us. Independent activities we are aware of include one of our PPI experts Nordia Willis presenting the findings at a nursing training session as part of general nursing education, with an estimated audience of > 100 trainees. Another of our PPI experts, Patrick Ojeer, sent information about This Sickle Cell Life to a large USA-based network of haemotology specialists [URL: www.haematology.org (accessed 18 August 2020)] that he was part of and This Sickle Cell Life was featured in a follow-up all-subscriber e-mail newsletter to US clinicians. Our research also received a special mention at the Treating Haemoglobinopathies 2020 National Conference in central London in January 2020.
Acknowledgements
We thank all the participants who gave their time to the project, and Cherelle Augustine, Nordia Willis, Patrick Ojeer and Dr Paul Telfer for their expert input.
We are grateful for the input of the NIHR Clinical Research Network and the NIHR CLAHRC NWL.
Contributions of authors
Alicia Renedo (https://orcid.org/0000-0001-7159-1723) (Assistant Professor, Social Science) was lead researcher, conceived and designed the study, participated in co-production processes, collected and analysed the data and led the writing.
Sam Miles (https://orcid.org/0000-0003-0836-1209) (Research Fellow, Social Science) participated in co-production processes, analysed the data and wrote the report.
Subarna Chakravorty (https://orcid.org/0000-0003-3862-3230) (Specialist Paediatric Consultant, Haematology) contributed to the design of the study, advised during the project and provided input into the report.
Andrea Leigh (https://orcid.org/0000-0002-9238-7382) (Specialist Paediatric Consultant, Haematology) contributed to the design of the study, advised during the project and provided input into the report.
John O Warner (https://orcid.org/0000-0001-7123-6369) (Emeritus Professor, Asthma) contributed to the conception of the study, advised during the project and provided input into the report.
Cicely Marston (https://orcid.org/0000-0002-5529-4646) (Professor of Public Health, Director of DEPTH Research Group) was principal investigator, conceived, designed and led the project, participated in co-production processes, analysed the data and wrote the report.
All authors approved the final version of the manuscript.
Publications
Miles S, Renedo A, Marston C. Slow co-production’ for deeper patient involvement in health care. J Health Des 2018;3:57–62.
Miles S, Renedo A, Augustine C, Ojeer P, Willis N, Marston C. Obstacles to use of patient expertise to improve care: a co-produced longitudinal study of the experiences of young people with sickle cell disease in non-specialist hospital settings. Crit Public Health 2019:1–11.
Renedo A, Miles S, Chakravorty S, Leigh A, Telfer P, Warner JO, et al. Not being heard: barriers to successful transition into adult care for children and young people with chronic conditions – evidence from ‘this sickle cell Life’ research. BMC Health Serv Res 2019;19:876.
Renedo A, Miles S, Marston C. Transitions to adulthood: self-governance and disciplining in the making of patient citizens. Sociol Health Illn 2019;42:481–95. https://doi.org/10.1111/1467-9566.13019.
Collins P, Renedo A, Marston C. Communicating and understanding: pain limitations of pain scales for patients with sickle cell disease and other painful conditions [published online ahead of print August 1 2020]. J Health Psychol 2020.
Data-sharing statement
The data sets generated and analysed for this study contain sensitive personal data that were collected from children and young people. These data will not be made freely available by depositing them in a publicly available repository. However, we will accept legitimate requests to access the data. Requests should be made to the corresponding author. All requests will be considered on a case-by-case basis.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Crowley R, Wolfe I, Lock K, McKee M. Improving the transition between paediatric and adult healthcare: a systematic review. Arch Dis Child 2011;96:548-53. https://doi.org/10.1136/adc.2010.202473.
- Department of Health and Social Care (DHSC) . You’re Welcome – Quality Criteria for Young People Friendly Health Services 2011.
- Department of Health and Social Care (DHSC) and Department for Education and Skills . Transition: Getting It Right for Young People 2006.
- Department of Health and Social Care (DHSC) . Transition: Moving on Well 2008.
- National Institute for Health and Care Excellence (NICE) . Transition From Children’s to Adults’ Services. Quality Standard 2016.
- World Health Organization (WHO) . Global Accelerated Action for the Health of Adolescents (AA-HA!): Guidance to Support Country Implementation 2017.
- Farre A, McDonagh JE. Helping health services to meet the needs of young people with chronic conditions: towards a developmental model for transition. Healthcare 2017;5. https://doi.org/10.3390/healthcare5040077.
- Scal P. Improving health care transition services: just grow up, will you please. JAMA Pediatr 2016;170:197-9. https://doi.org/10.1001/jamapediatrics.2015.3268.
- Waldboth V, Patch C, Mahrer-Imhof R, Metcalfe A. Living a normal life in an extraordinary way: a systematic review investigating experiences of families of young people’s transition into adulthood when affected by a genetic and chronic childhood condition. Int J Nurs Stud 2016;62:44-59. https://doi.org/10.1016/j.ijnurstu.2016.07.007.
- Christie D, Viner R. Adolescent development. BMJ 2005;330:301-4. https://doi.org/10.1136/bmj.330.7486.301.
- Wijlaars LPMM, Hardelid P, Guttmann A, Gilbert R. Emergency admissions and long-term conditions during transition from paediatric to adult care: a cross-sectional study using Hospital Episode Statistics data. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-021015.
- Hargreaves DS, Greaves F, Levay C, Mitchell I, Koch U, Esch T, et al. Comparison of health care experience and access between young and older adults in 11 high-income countries. J Adolesc Health 2015;57:413-20. https://doi.org/10.1016/j.jadohealth.2015.05.015.
- Hamideh D, Alvarez O. Sickle cell disease related mortality in the United States (1999–2009). Pediatr Blood Cancer 2013;60:1482-6. https://doi.org/10.1002/pbc.24557.
- McPherson M, Thaniel L, Minniti CP. Transition of patients with sickle cell disease from pediatric to adult care: assessing patient readiness. Pediatr Blood Cancer 2009;52:838-41. https://doi.org/10.1002/pbc.21974.
- DeBaun MR, Telfair J. Transition and sickle cell disease. Pediatrics 2012;130:926-35. https://doi.org/10.1542/peds.2011-3049.
- Stollon NB, Paine CW, Lucas MS, Brumley LD, Poole ES, Peyton T, et al. Transitioning adolescents and young adults with sickle cell disease from pediatric to adult health care: provider perspectives. J Pediatr Hematol Oncol 2015;37:577-83. https://doi.org/10.1097/MPH.0000000000000427.
- Treadwell M, Telfair J, Gibson RW, Johnson S, Osunkwo I. Transition from pediatric to adult care in sickle cell disease: establishing evidence-based practice and directions for research. Am J Hematol 2011;86:116-20. https://doi.org/10.1002/ajh.21880.
- Chakravorty S, Tallett A, Witwicki C, Hay H, Mkandawire C, Ogundipe A, et al. Patient-reported experience measure in sickle cell disease. Arch Dis Child 2018;103:1104-9. https://doi.org/10.1136/archdischild-2018-314955.
- Piel FB, Steinberg MH, Rees DC. Sickle cell disease. N Engl J Med 2017;376:1561-73. https://doi.org/10.1056/NEJMra1510865.
- Redding-Lallinger R, Knoll C. Sickle cell disease – pathophysiology and treatment. Curr Probl Pediatr Adolesc Health Care 2006;36:346-76. https://doi.org/10.1016/j.cppeds.2006.07.002.
- National Institute for Health and Care Excellence (NICE) . Sickle Cell Acute Painful Episode: Management of an Acute Painful Sickle Cell Episode in Hospital 2012.
- Smith WR, Penberthy LT, Bovbjerg VE, McClish DK, Roberts JD, Dahman B, et al. Daily assessment of pain in adults with sickle cell disease. Ann Intern Med 2008;148:94-101. https://doi.org/10.7326/0003-4819-148-2-200801150-00004.
- Powars DR, Chan LS, Hiti A, Ramicone E, Johnson C. Outcome of sickle cell anemia: a 4-decade observational study of 1056 patients. Medicine 2005;84:363-76. https://doi.org/10.1097/01.md.0000189089.45003.52.
- Dyson SM. Sickle Cell and the Social Sciences: Health, Racism and Disablement. Oxford: Routledge; 2019.
- Aljuburi G, Laverty AA, Green SA, Phekoo KJ, Banarsee R, Okoye NV, et al. Trends in hospital admissions for sickle cell disease in England, 2001/02–2009/10. J Public Health 2012;34:570-6. https://doi.org/10.1093/pubmed/fds035.
- National Haemoglobinopathy Register . NHR Information Service Patient Number by Centre and Diagnosis: National Haemoglobinpathy Register 2016. www.nhr.nhs.uk/wp-content/uploads/2016/05/NumberPatientsByCentre.pdf (accessed 10 June 2019).
- Public Health England . NHS Sickle Cell and Thalassaemia Screening Programme Data Report 2017 to 2018 2020. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/870090/Sickle_cell_and_thalassaemia_screening_annual_data_report_1_April_2017_to_31_March_2018.pdf (accessed 6 November 2020).
- Hickman M, Modell B, Greengross P, Chapman C, Layton M, Falconer S, et al. Mapping the prevalence of sickle cell and beta thalassaemia in England: estimating and validating ethnic-specific rates. Br J Haematol 1999;104:860-7. https://doi.org/10.1046/j.1365-2141.1999.01275.x.
- Streetly A, Clarke M, Downing M, Farrar L, Foo Y, Hall K, et al. Implementation of the newborn screening programme for sickle cell disease in England: results for 2003–2005. J Med Screen 2008;15:9-13. https://doi.org/10.1258/jms.2008.007063.
- Brousseau DC, Owens PL, Mosso AL, Panepinto JA, Steiner CA. Acute care utilization and rehospitalizations for sickle cell disease. JAMA 2010;303:1288-94. https://doi.org/10.1001/jama.2010.378.
- McLaughlin JF, Ballas SK. High mortality among children with sickle cell anemia and overt stroke who discontinue blood transfusion after transition to an adult program. Transfusion 2016;56:1014-21. https://doi.org/10.1111/trf.13418.
- Campbell F, Biggs K, Aldiss SK, O’Neill PM, Clowes M, McDonagh J, et al. Transition of care for adolescents from paediatric services to adult health services. Cochrane Database Syst Rev 2016;4. https://doi.org/10.1002/14651858.CD009794.pub2.
- Nakhla M, Daneman D, To T, Paradis G, Guttmann A. Transition to adult care for youths with diabetes mellitus: findings from a universal health care system. Pediatrics 2009;124:e1134-41. https://doi.org/10.1542/peds.2009-0041.
- Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC. The age of adolescence. Lancet Child Adolesc Health 2018;2:223-8. https://doi.org/10.1016/S2352-4642(18)30022-1.
- Lebensburger JD, Bemrich-Stolz CJ, Howard TH. Barriers in transition from pediatrics to adult medicine in sickle cell anemia. J Blood Med 2012;3:105-12. https://doi.org/10.2147/JBM.S32588.
- Blake A, Asnani V, Leger RR, Harris J, Odesina V, Hemmings DL, et al. Stigma and illness uncertainty: adding to the burden of sickle cell disease. Hematology 2018;23:122-30. https://doi.org/10.1080/10245332.2017.1359898.
- Jenerette CM, Brewer CA, Edwards LJ, Mishel MH, Gil KM. An intervention to decrease stigma in young adults with sickle cell disease. West J Nurs Res 2014;36:599-61. https://doi.org/10.1177/0193945913512724.
- Jenerette CM, Brewer C. Health-related stigma in young adults with sickle cell disease. J Natl Med Assoc 2010;102:1050-5. https://doi.org/10.1016/S0027-9684(15)30732-X.
- Maxwell K, Streetly A, Bevan D. Experiences of hospital care and treatment-seeking behavior for pain from sickle cell disease: qualitative study. West J Med 1999;171:306-13.
- McCaffery M, Grimm MA, Pasero C, Ferrell B, Uman GC. On the meaning of ‘drug seeking’. Pain Manag Nurs 2005;6:122-36. https://doi.org/10.1016/j.pmn.2005.08.002.
- Bediako SM, Moffitt KR. Race and social attitudes about sickle cell disease. Ethn Health 2011;16:423-9. https://doi.org/10.1080/13557858.2011.552712.
- Tapper M. In the Blood: Sickle Cell Anemia and the Politics of Race. Philadelphia, PA: University of Pennsylvania Press; 1999.
- Dyson SM. ‘Race’, ethnicity and haemoglobin disorders. Soc Sci Med 1998;47:121-31. https://doi.org/10.1016/S0277-9536(98)00023-9.
- Pletcher MJ, Kertesz SG, Kohn MA, Gonzales R. Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. JAMA 2008;299:70-8. https://doi.org/10.1001/jama.2007.64.
- All-Party Parliamentary Group on Sickle Cell and Thalassaemia . Sickle Cell Disease and Thalassaemia: A Health Check July 2009. England 2009.
- Miles S, Renedo A, Augustine C, Ojeer P, Willis N, Marston C. Obstacles to use of patient expertise to improve care: a co-produced longitudinal study of the experiences of young people with sickle cell disease in non-specialist hospital settings. Crit Public Health 2019:1-11. https://doi.org/10.1080/09581596.2019.1650893.
- Adeyemo TA, Ojewunmi OO, Diaku-Akinwumi IN, Ayinde OC, Akanmu AS. Health related quality of life and perception of stigmatisation in adolescents living with sickle cell disease in Nigeria: a cross sectional study. Pediatr Blood Cancer 2015;62:1245-51. https://doi.org/10.1002/pbc.25503.
- Viner RM. Transition of care from paediatric to adult services: one part of improved health services for adolescents. Arch Dis Child 2008;93:160-3. https://doi.org/10.1136/adc.2006.103721.
- Department of Health and Social Care (DHSC) . You’re Welcome Quality Criteria: Making Health Services Young People Friendly 2007.
- Telfair J, Myers J, Drezner S. Transfer as a component of the transition of adolescents with sickle cell disease to adult care: adolescent, adult, and parent perspectives. J Adolesc Health 1994;15:558-65. https://doi.org/10.1016/1054-139X(94)90139-T.
- Telfair J, Ehiri JE, Loosier PS, Baskin ML. Transition to adult care for adolescents with sickle cell disease: results of a national survey. Int J Adolesc Med Health 2004;16:47-64. https://doi.org/10.1515/ijamh.2004.16.1.47.
- Sobota A, Neufeld EJ, Sprinz P, Heeney MM. Transition from pediatric to adult care for sickle cell disease: results of a survey of pediatric providers. Am J Hematol 2011;86:512-15. https://doi.org/10.1002/ajh.22016.
- Bhawra J, Toulany A, Cohen E, Moore Hepburn C, Guttmann A. Primary care interventions to improve transition of youth with chronic health conditions from paediatric to adult healthcare: a systematic review. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-011871.
- Betz CL, Lobo ML, Nehring WM, Bui K. Voices not heard: a systematic review of adolescents’ and emerging adults’ perspectives of health care transition. Nurs Outlook 2013;61:311-36. https://doi.org/10.1016/j.outlook.2013.01.008.
- Withers AL, Green R. Transition for adolescents and young adults with asthma. Front Pediatr 2019;7. https://doi.org/10.3389/fped.2019.00301.
- Miles S, Renedo A, Marston C. Slow co-production’ for deeper patient involvement in health care. J Health Des 2018;3:57-62. https://doi.org/10.21853/JHD.2018.39.
- Oni L, Dick M, Smalling B, Walters J. Care and Management of Your Child with Sickle Cell Disease: A Parent’s Guide. London: NHS Sickle Cell and Thalassaemia Screening Programme; 2006.
- Dyson SM, Atkin K, Culley LA, Dyson SE, Evans H. Sickle cell, habitual dys-positions and fragile dispositions: young people with sickle cell at school. Sociol Health Illn 2011;33:465-83. https://doi.org/10.1111/j.1467-9566.2010.01301.x.
- McDonagh JE, Farre A, Gleeson H, Rapley T, Dovey-Pearce G, Reape D, et al. Making healthcare work for young people. Arch Dis Child 2018;103. https://doi.org/10.1136/archdischild-2017-314573.
- Robert G, Cornwell J, Locock L, Purushotham A, Sturmey G, Gager M. Patients and staff as codesigners of healthcare services. BMJ 2015;350. https://doi.org/10.1136/bmj.g7714.
- Renedo A, Miles S, Marston C. Transitions to adulthood: self-governance and disciplining in the making of patient citizens. Sociol Health Illn 2019;42:481-95. https://doi.org/10.1111/1467-9566.13019.
- Department of Health and Social Care (DHSC) . Getting It Right for Children, Young People and Families: Maximising the Contribution of the School Nursing Team: Vision and Call to Action 2012.
- Caldwell SE, Mays N. Studying policy implementation using a macro, meso and micro frame analysis: the case of the Collaboration for Leadership in Applied Health Research & Care (CLAHRC) programme nationally and in North West London. Health Res Policy Syst 2012;10. https://doi.org/10.1186/1478-4505-10-32.
- Renedo A, Marston C. Healthcare professionals’ representations of ‘patient and public involvement’ and creation of ‘public participant’ identities: implications for the development of inclusive and bottom-up community participation initiatives. J Community Appl Soc 2011;21:268-80. https://doi.org/10.1002/casp.1092.
- Renedo A, Marston C. Spaces for citizen involvement in healthcare: an ethnographic study. Sociology 2015;49:488-504. https://doi.org/10.1177/0038038514544208.
- Renedo A, Marston CA, Spyridonidis D, Barlow J. Patient and public involvement in healthcare quality improvement: how organizations can help patients and professionals to collaborate. Public Manage Rev 2015;17:17-34. https://doi.org/10.1080/14719037.2014.881535.
- Department of Health and Social Care (DHSC) . Equity and Excellence: Liberating the NHS 2010. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/213823/dh_117794.pdf (accessed 22 September 2020).
- Sickle Cell Society . Standards for the Clinical Care of Adults With Sickle Cell Disease in the UK 2018. www.sicklecellsociety.org/sicklecellstandards/ (accessed 11 June 2019).
- Aljuburi G, Laverty AA, Green SA, Phekoo KJ, Bell D, Majeed A. Socio-economic deprivation and risk of emergency readmission and inpatient mortality in people with sickle cell disease in England: observational study. J Public Health 2013;35:510-17. https://doi.org/10.1093/pubmed/fdt100.
- Yusuf HR, Atrash HK, Grosse SD, Parker CS, Grant AM. Emergency department visits made by patients with sickle cell disease: a descriptive study, 1999–2007. Am J Prev Med 2010;38:536-41. https://doi.org/10.1016/j.amepre.2010.01.001.
- Lucas SB, Mason DG, Mason M, Weyman D. A Sickle Crisis? A Report of the National Confidential Enquiry into Patient Outcome and Death 2008 2008.
- Lazio MP, Costello HH, Courtney DM, Martinovich Z, Myers R, Zosel A, et al. A comparison of analgesic management for emergency department patients with sickle cell disease and renal colic. Clin J Pain 2010;26:199-205. https://doi.org/10.1097/AJP.0b013e3181bed10c.
- Wilson BH, Nelson J. Sickle cell disease pain management in adolescents: a literature review. Pain Manag Nurs 2015;16:146-51. https://doi.org/10.1016/j.pmn.2014.05.015.
- Inoue S, Khan I, Mushtaq R, Sanikommu SR, Mbeumo C, LaChance J, et al. Pain management trend of vaso-occulsive crisis (VOC) at a community hospital emergency department (ED) for patients with sickle cell disease. Ann Hematol 2016;95:221-5. https://doi.org/10.1007/s00277-015-2558-x.
- Anie KA, Steptoe A, Bevan DH. Sickle cell disease: pain, coping and quality of life in a study of adults in the UK. Br J Health Psychol 2002;7:331-44. https://doi.org/10.1348/135910702760213715.
- Dyson SM, Atkin K, Culley LA, Dyson SE. The educational experiences of young people with sickle cell disorder: a commentary on the existing literature. Disabil Soc 2007;22:581-94. https://doi.org/10.1080/09687590701560196.
- Swanson ME, Grosse SD, Kulkarni R. Disability among individuals with sickle cell disease: literature review from a public health perspective. Am J Prev Med 2011;41:390-7. https://doi.org/10.1016/j.amepre.2011.09.006.
- Dyson SM. First conference of the worldwide initiative on social studies of haemoglobinopathies: sickle cell over the next 100 years. Am J Prev Med 2011;41:413-16. https://doi.org/10.1016/j.amepre.2011.09.009.
- Atkin K, Ahmad WI. Living a ‘normal’ life: young people coping with thalassaemia major or sickle cell disorder. Soc Sci Med 2001;53:615-26. https://doi.org/10.1016/S0277-9536(00)00364-6.
- Dyson SM, Abuateya H, Atkin K, Culley L, Dyson SE, Rowley D, et al. Reported school experiences of young people living with sickle cell disorder in England. Br Educ Res J 2010;36:125-42. https://doi.org/10.1080/01411920902878941.
- Bediako SM. Predictors of employment status among African Americans with sickle cell disease. J Health Care Poor Underserved 2010;21:1124-37. https://doi.org/10.1353/hpu.2010.0945.
- Ciribassi RM, Patil CL. ‘We don’t wear it on our sleeve’: sickle cell disease and the (in) visible body in parts. Soc Sci Med 2016;148:131-8. https://doi.org/10.1016/j.socscimed.2015.11.033.
- Collins P, Renedo A, Marston C. Communicating and understanding pain: limitations of pain scales for patients with sickle cell disease and other painful conditions [published online ahead of print August 1 2020]. J Health Psychol 2020. https://doi.org/10.1177/1359105320944987.
- Bergman EJ, Diamond NJ. Sickle cell disease and the ‘difficult patient’ conundrum. Am J Bioeth 2013;13:3-10. https://doi.org/10.1080/15265161.2013.767954.
- Marlowe KF, Chicella MF. Treatment of sickle cell pain. Pharmacotherapy 2002;22:484-91. https://doi.org/10.1592/phco.22.7.484.33675.
- Pack-Mabien A, Labbe E, Herbert D, Haynes J. Nurses’ attitudes and practices in sickle cell pain management. Appl Nurs Res 2001;14:187-92. https://doi.org/10.1053/apnr.2001.26783.
- Dyson SM, Atkin K, Culley LA, Dyson SE, Evans H, Rowley DT. Disclosure and sickle cell disorder: a mixed methods study of the young person with sickle cell at school. Soc Sci Med 2010;70:2036-44. https://doi.org/10.1016/j.socscimed.2010.03.010.
- Campbell C. Migrancy, masculine identities and AIDS: the psychosocial context of HIV transmission on the South African gold mines. Soc Sci Med 1997;45:273-81. https://doi.org/10.1016/S0277-9536(96)00343-7.
- Gervais MC, Jovchelovitch S. Health and identity: the case of the Chinese community in England. Soc Sci Inform 1998;37:709-29. https://doi.org/10.1177/053901898037004008.
- Jovchelovitch S, Gervais MC. Social representations of health and illness: the case of the Chinese community in England. J Community Appl Soc Psychol 1999;9:247-60. https://doi.org/10.1002/(SICI)1099-1298(199907/08)9:4%3C247::AID-CASP500%3E3.0.CO;2-E.
- Allen D, Gregory J. The transition from children’s to adult diabetes services: understanding the ‘problem’. Diabet Med 2009;26:162-6. https://doi.org/10.1111/j.1464-5491.2008.02647.x.
- Kelly P. Youth at risk: processes of individualisation and responsibilisation in the risk society. Discourse Stud 2001;22:23-3. https://doi.org/10.1080/01596300120039731.
- Sawyer SM, Afifi RA, Bearinger LH, Blakemore SJ, Dick B, Ezeh AC, et al. Adolescence: a foundation for future health. Lancet 2012;379:1630-40. https://doi.org/10.1016/S0140-6736(12)60072-5.
- Kane M, Bibby J. Listening to Our Future: Early Findings from the Young People’s Future Health Inquiry 2018. www.health.org.uk/sites/default/files/Listening%20to%20our%20future.pdf (accessed 10 June 2019).
- Arnett J. Emerging Adulthood: The Winding Road from the Late Teens Through the Twenties. New York, NY: Oxford University Press; 2004.
- Renold E, Ringrose J. Schizoid subjectivities? Re-theorizing teen girls’ sexual cultures in an era of ‘sexualization’. J Sociol 2011;47:389-40. https://doi.org/10.1177/1440783311420792.
- Durham D, Durham D, Solway J. Elusive Adulthoods. Bloomington, IN: Indiana University Press; 2017.
- Lugasi T, Achille M, Stevenson M. Patients’ perspective on factors that facilitate transition from child-centered to adult-centered health care: a theory integrated metasummary of quantitative and qualitative studies. J Adolesc Health 2011;48:429-40. https://doi.org/10.1016/j.jadohealth.2010.10.016.
- Blum RW, Garell D, Hodgman CH, Jorissen TW, Okinow NA, Orr DP, et al. Transition from child-centered to adult health-care systems for adolescents with chronic conditions. A position paper of the Society for Adolescent Medicine. J Adolesc Health 1993;14:570-6. https://doi.org/10.1016/1054-139X(93)90143-D.
- Colver A, Pearse R, Watson RM, Fay M, Rapley T, Mann KD, et al. How well do services for young people with long term conditions deliver features proposed to improve transition?. BMC Health Serv Res 2018;18. https://doi.org/10.1186/s12913-018-3168-9.
- Hagell A, Shah R, Coleman J. Key Data on Young People 2017. London: Association for Young People’s Health; 2017.
- Viner R. Transition from paediatric to adult care. Bridging the gaps or passing the buck?. Arch Dis Child 1999;81:271-5. https://doi.org/10.1136/adc.81.3.271.
- Tarrant M, Hagger MS, Farrow CV, Jetten J, Haslam C, Haslam A. The Social Cure Identity, Health and Well-Being. East Sussex: Psychology Press; 2012.
- Marston C, Renedo A, Nyaaba GN. Fertility regulation as identity maintenance: understanding the social aspects of birth control. J Health Psychol 2018;23:240-51. https://doi.org/10.1177/1359105317726367.
- Côté JE. The enduring usefulness of Erikson’s concept of the identity crisis in the 21st century: an analysis of student mental health concerns. Identity 2018;18:251-63. https://doi.org/10.1080/15283488.2018.1524328.
- Zittoun T. Transitions: Development Through Symbolic Resources. Greenwich: InfoAge; 2006.
- Duveen G, Lloyd B, Duveen G, Moscovici S, Jovchelovitch S, Wagoner B. Development as a Social Process: Contributions of Gerard Duveen. Oxford: Routledge; 2013.
- Hermans HJM. The dialogical self: toward a theory of personal and cultural positioning. Cult Psychol 2001;7:243-81. https://doi.org/10.1177/1354067X0173001.
- Erikson EH. Identity: Youth and Crisis. New York, NY: Norton; 1968.
- Fuggle P, Shand PA, Gill LJ, Davies SC. Pain, quality of life, and coping in sickle cell disease. Arch Dis Child 1996;75:199-203. https://doi.org/10.1136/adc.75.3.199.
- Calman L, Brunton L, Molassiotis A. Developing longitudinal qualitative designs: lessons learned and recommendations for health services research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-14.
- Charmaz K. Constructing Grounded Theory. London: SAGE Publications Ltd; 2006.
- Attride-Stirling J. Thematic networks: an analytic tool for qualitative research. Qual Res 2001;1:385-40. https://doi.org/10.1177/146879410100100307.
- Hosltein JA, Gubrium JF, Denzin NK, Lincoln YS. The Sage Handbook of Qualitative Research. Thousand Oaks, CA: SAGE Publications Ltd; 2011.
- Alaszewski A. Using Diaries for Social Research. Thousand Oaks, CA: SAGE Publications Ltd; 2006.
- Renedo A, Miles S, Chakravorty S, Leigh A, Telfer P, Warner JO, et al. Not being heard: barriers to successful transition into adult care for children and young people with chronic conditions – evidence from ‘this sickle cell Life’ research. BMC Health Serv Res 2019;19. https://doi.org/10.1186/s12913-019-4726-5.
- Haywood C, Beach MC, Lanzkron S, Strouse JJ, Wilson R, Park H, et al. A systematic review of barriers and interventions to improve appropriate use of therapies for sickle cell disease. J Natl Med Assoc 2009;101:1022-33. https://doi.org/10.1016/S0027-9684(15)31069-5.
- Jenerette CM, Brewer CA, Ataga KI. Care seeking for pain in young adults with sickle cell disease. Pain Manag Nurs 2014;15:324-30. https://doi.org/10.1016/j.pmn.2012.10.007.
- Mulchan SS, Valenzuela JM, Crosby LE, Diaz Pow Sang C. Applicability of the SMART model of transition readiness for sickle-cell disease. J Pediatr Psychol 2016;41:543-54. https://doi.org/10.1093/jpepsy/jsv120.
- Sawyer SM, Drew S, Yeo MS, Britto MT. Adolescents with a chronic condition: challenges living, challenges treating. Lancet 2007;369:1481-9. https://doi.org/10.1016/S0140-6736(07)60370-5.
- Ballas SK. Pain management of sickle cell disease. Hematol Oncol Clin North Am 2005;19. https://doi.org/10.1016/j.hoc.2005.07.008.
- O’Hara JK, Aase K, Waring J. Scaffolding our systems? Patients and families ‘reaching in’ as a source of healthcare resilience. BMJ Qual Saf 2019;28:3-6. https://doi.org/10.1136/bmjqs-2018-008216.
- Kennedy I. Getting it Right for Children and Young People: Overcoming Cultural Barriers in the NHS So As to Meet Their Needs. London: Department of Health and Social Care; 2010.
- Curtis K, Liabo K, Roberts H, Barker M. Consulted but not heard: a qualitative study of young people’s views of their local health service. Health Expect 2004;7:149-56. https://doi.org/10.1111/j.1369-7625.2004.00265.x.
- Association for Young People’s Health (AYPH) . Young People’s Views on Involvement and Feedback in Healthcare: Report of a Brief On-Line Survey of Young People 2014.
- Rouse CM. Uncertain Suffering: Racial Health Care Disparities and Sickle Cell Disease. Oakland, CA: University of California Press; 2009.
- Shapiro BS, Benjamin LJ, Payne R, Heidrich G. Sickle cell-related pain: perceptions of medical practitioners. J Pain Symptom Manage 1997;14:168-74. https://doi.org/10.1016/S0885-3924(97)00019-5.
- Fendler L, Hultqvist K, Dahlberg G. Governing the Child in the New Millennium. New York, NY: Routledge; 2001.
- Jeffrey C. Geographies of children and youth I: eroding maps of life. Prog Hum Geogr 2010;34:496-505. https://doi.org/10.1177/0309132509348533.
- Heaton J, Räisänen U, Salinas M. ‘Rule your condition, don’t let it rule you’: young adults’ sense of mastery in their accounts of growing up with a chronic illness. Sociol Health Ill 2016;38:3-20. https://doi.org/10.1111/1467-9566.12298.
- Balfe M. Diets and discipline: the narratives of practice of university students with type 1 diabetes. Sociol Health Illn 2007;29:136-53. https://doi.org/10.1111/j.1467-9566.2007.00476.x.
- Levy ML, Fleming L, Warner JO, Bush A. Paediatric asthma care in the UK: fragmented and fatally fallible. Br J Gen Pract 2019;69:405-6. https://doi.org/10.3399/bjgp19X704933.
- Snow R, Humphrey C, Sandall J. What happens when patients know more than their doctors? Experiences of health interactions after diabetes patient education: a qualitative patient-led study. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-003583.
- Ambresin AE, Bennett K, Patton GC, Sanci LA, Sawyer SM. Assessment of youth-friendly health care: a systematic review of indicators drawn from young people’s perspectives. J Adolesc Health 2013;52:670-81. https://doi.org/10.1016/j.jadohealth.2012.12.014.
- Britto MT, DeVellis RF, Hornung RW, DeFriese GH, Atherton HD, Slap GB. Health care preferences and priorities of adolescents with chronic illnesses. Pediatrics 2004;114:1272-80. https://doi.org/10.1542/peds.2003-1134-L.
- Bernays S, Paparini S, Seeley J, Rhodes T. ‘Not taking it will just be like a sin’: young people living with HIV and the stigmatization of less-than-perfect adherence to antiretroviral therapy. Med Anthropol 2017;36:485-99. https://doi.org/10.1080/01459740.2017.1306856.
- Bernays S, Seeley J, Rhodes T, Mupambireyi Z. What am I ‘living’ with? Growing up with HIV in Uganda and Zimbabwe. Sociol Health Illn 2015;37:270-83. https://doi.org/10.1111/1467-9566.12189.
- Kaushansky D, Cox J, Dodson C, McNeeley M, Kumar S, Iverson E. Living a secret: disclosure among adolescents and young adults with chronic illnesses. Chronic Illn 2017;13:49-61. https://doi.org/10.1177/1742395316655855.
- McCann DC, McWhirter J, Coleman H, Calvert M, Warner JO. A controlled trial of a school-based intervention to improve asthma management. Eur Respir J 2006;27:921-8. https://doi.org/10.1183/09031936.06.0035604.
- Iles N, Lowton K. What is the perceived nature of parental care and support for young people with cystic fibrosis as they enter adult health services?. Health Soc Care Community 2010;18:21-9. https://doi.org/10.1111/j.1365-2524.2009.00871.x.
- Bluebond-Langner M. The Private Worlds of Dying Children. Princeton, NJ: Princeton University Press; 1978.
- Rabinow P, Rose N. Biopower today. Biosocieties 2016;1:195-217. https://doi.org/10.1017/S1745855206040014.
- World Health Organization . Steering the Transition from Adolescent-Friendly Projects to Adolescent-Responsive Health Systems n.d. http://apps.who.int/adolescent/second-decade/section6/page8/sdolescent-responsiveness.html (accessed 20 August 2019).
- Colver A, McConachie H, Le Couteur A, Dovey-Pearce G, Mann KD, McDonagh JE, et al. A longitudinal, observational study of the features of transitional healthcare associated with better outcomes for young people with long-term conditions. BMC Med 2018;16. https://doi.org/10.1186/s12916-018-1102-y.
- Goddard A, Wolfson L, Wolfson E. On the Margins of Medical Care. Why Young Adults and Adolescents Need Better Healthcare: A Report to the Future Hospital Programme of the Royal College of Physicians 2015.
- Farre A, Wood V, Rapley T, Parr JR, Reape D, McDonagh JE. Developmentally appropriate healthcare for young people: a scoping study. Arch Dis Child 2015;100:144-51. https://doi.org/10.1136/archdischild-2014-306749.
- McDonagh JE, Viner RM. Lost in transition? Between paediatric and adult services. BMJ 2006;332:435-6. https://doi.org/10.1136/bmj.332.7539.435.
- Wright RJ, Howard EJ, Newbery N, Gleeson H. ‘Training gap’ – the present state of higher specialty training in adolescent and young adult health in medical specialties in the UK. Future Healthc J 2017;4:80-95. https://doi.org/10.7861/futurehosp.4-2-80.
- Reddin CD, Cerrentano E, Tanabe P. Sickle cell disease management in the emergency department: what every emergency nurse should know. J Emerg Nurs 2011;37:341-5. https://doi.org/10.1016/j.jen.2010.04.014.
- Royal College of Physicians . Acute Care Toolkit 13. Acure Care for Adolescents and Young Adults 2015.
- Gleeson H, Turner G. Transition to adult services. Arch Dis Child Educ Pract Ed 2012;97:86-92. https://doi.org/10.1136/archdischild-2011-300261.
- Cantrell MA. The importance of debriefing in clinical simulations. Clin Simul Nurs 2008;4:e19-e23. https://doi.org/10.1016/j.ecns.2008.06.006.
- Wood D, Wood D, Williams A, Koyle MA, Baird AD. Transitioning Medical Care Through Adolescence to Adulthood. Berlin: Springer; 2019.
- Dyson S, Atkin K, Culley L, Dyson S. Critical realism, agency and sickle cell: case studies of young people with sickle cell disorder at school. Ethnic Racial Stud 2014;37:2379-98. https://doi.org/10.1080/01419870.2013.809130.
- Dyson SM. Sickle Cell and Thalassaemia: A Guide to School Policy (Second Edition) 2016. www.dora.dmu.ac.uk/handle/2086/12182 (accessed 8 July 2019).
- Freire P. Pedagogy of the Oppressed. Harmondsworth: Penguin; 1990.
- Freire P. Education for Critical Consciousness. London: Continuum; 2005.
- Guareschi PA, Jovchelovitch S. Participation, health and the development of community resources in Southern Brazil. J Health Psychol 2004;9:311-22. https://doi.org/10.1177/1359105304040896.
- A Star – Hidden Pain Ft. Leke 2019. https://www.youtube.com/watch?v=gPaX0kXj_jQ.
- Sickle Cell Society . Self Over Sickle n.d. www.sicklecellsociety.org/selfoversickle/ (accessed 13 October 2020).
- Sickle Cell Society . 001 THE SELF OVER SICKLE PODCAST n.d. www.youtube.com/watch?v=8g89Igd5xKY (accessed 13 October 2020).
- Self Over Sickle . Self Over Sickle n.d. www.instagram.com/selfoversickle/ (accessed 13 October 2020).
Appendix 1 Co-produced recommendations from the This Sickle Cell participatory dissemination event
Discussion: improving understanding of emergency department staff to support sickle cell disease/thalassaemia care from the first professional contact to discharge
Solution
Improve materials, networking, information sharing, emergency department pathway, patient involvement in experience of care tracking, training, etc.
Action
Identify current best practice by specialist nurses and share through royal colleges (e.g. the Royal College of Emergency Medicine and the Royal College of Nursing).
Discussion: increase knowledge and awareness of sickle cell disease/thalassaemia across professionals and the public
Solution
Create bite-size training that can be delivered through online short video links, e-mails and patient-led micro-teach sessions.
Action
Review existing materials through the Sickle Cell Society and Roald Dahl’s Marvellous Children’s Charity specialist nurses and feedback from the summer roadshow.
Discussion: creating a project that supports identity development through transition through mentoring and advocacy
Solution
Identify mentoring/advocate programmes where training can be delivered on SCD/thalassaemia, identify funding for specific SCD/thalassaemia advocates and develop a dashboard and quality improvement link to audit and policy.
Action
Review existing provision and funding with key partners.
Discussion: lack of shared information between departments/professionals on sickle cell disorder care
Solution
Create a universal sickle plan available in hardcopy and as an application that includes a standard operating protocol (e.g. first-line treatment, medications, fluids, allergies, a SCD/thalassaemia checklist).
Action
Exploration with NHS England, King’s Health Partners and the Sickle Cell Society.
Appendix 2 Example of drawing used during interview to help interviewee discuss their experience of living with sickle cell disorder
List of abbreviations
- A&E
- accident and emergency
- CLAHRC NWL
- Collaboration for Leadership in Applied Health Research and Care Northwest London
- DEPTH
- Dialogue, Evidence, Participation and Translation for Health
- LSHTM
- London School of Hygiene & Tropical Medicine
- NIHR
- National Institute for Health Research
- PPI
- patient and public involvement
- RCPCH
- Royal College of Paediatrics and Child Health
- SCD
- sickle cell disorder
- SOS
- Self Over Sickle
