Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 14/04/02. The contractual start date was in April 2016. The final report began editorial review in March 2019 and was accepted for publication in August 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Maxwell et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction, background and aims
Introduction
Pelvic organ prolapse (POP) affects women of reproductive age and beyond; it is a condition seen in up to 50% of parous women and up to 75% of women attending outpatient gynaecology clinics. 1,2 Treatment options for prolapse include surgery and conservative management [with pessaries or pelvic floor muscle training (PFMT)]. A high proportion of women go on to have surgical intervention, which is often prone to failure, with the same prolapse recurring or another prolapse occurring in another location, which can lead to repeated operations. 3 Mesh-related complications are frequently reported, and have a removal rate of up to 35%. 4 In Scotland, in 2014, the use of synthetic mesh implants in the treatment of POP was suspended; this suspension was subsequently introduced in NHS England in 2018.
These highly publicised suspensions of synthetic mesh implants make the need for non-surgical options to treat this condition even more pressing. 5 Clear evidence of the clinical effectiveness and potential cost-effectiveness of PFMT in the management of prolapse is now available. This evidence concludes that PFMT should be recommended as a first-line treatment for POP. 6 The Pelvic Organ Prolapse PhysiotherapY (POPPY) trial was a multicentre randomised controlled trial of the clinical effectiveness and cost-effectiveness of individualised PFMT compared with a lifestyle-advice leaflet in women with newly diagnosed symptomatic stage I, II or III prolapse. 6 The POPPY trial constitutes the largest, most rigorous, pragmatic trial of PFMT for prolapse and, as such, provides the necessary evidence to inform future practice. Individualised PFMT provided by specialist women’s health physiotherapists (WHPs) was found to be effective in reducing women’s symptoms of prolapse and in improving prolapse-related quality of life. It also showed potential to be a cost-effective treatment. However, knowledge of efficacy and effectiveness is not enough to ensure implementation.
Background
In the UK, there is currently limited availability, and variation in the availability, of specialist WHPs to deliver PFMT to the large numbers of women who may benefit from it. 7,8 In the UK, there are approximately 800 specialist physiotherapists working in women’s health, as registered with the Pelvic, Obstetric and Gynaecological Physiotherapy (POGP) group. The number of women aged > 40 years in the UK (based on the 2011 census9) is approximately 15.9 million; taking a symptomatic estimate of 10% into account means that there are approximately 2600 symptomatic women for each specialist physiotherapist in the UK. It is unlikely that PFMT will be available to meet the demand unless it can be delivered in other formats, for example by other types of health-care professionals (HCPs).
Implementation science is an emerging field involving complex and multilevel processes. 10 It aims to advance knowledge of implementation by providing generalisable knowledge that will be useful for other settings and contexts. It can help to identify barriers to implementation, but should also extend this to how and why implementation processes are effective. 11 To do this, we need to study implementation strategies and the contexts and processes in which implementation strategies are delivered. Such research is a necessary step in the Medical Research Council’s evaluation of complex interventions framework. 12
Research to improve the implementation of evidence-based PFMT was required. Delivery methods that can enhance service capacity and increase the availability and choice for women are required, but these need to be tested to ensure that the outcomes achieved under trial conditions are maintained. We needed to know whether or not the NHS could deliver PFMT using different staff skill mixes and/or different numbers of sessions and still maintain the benefits observed under trial conditions. We also needed to know how PFMT is implemented in everyday practice and understand the barriers to and facilitators of successful uptake and delivery. It was anticipated that this knowledge would enhance the likelihood of PFMT being rolled out more widely if service models could be successfully tailored to suit different local circumstances and resources, thereby increasing the availability of such services for the many women who would benefit from this treatment.
In addition, trial follow-up rarely extends to more than 1 or 2 years post trial. An observed reduction in ‘further treatment’ following PFMT was initially established in the POPPY trial. A record linkage-based study of longer-term follow-up of the original POPPY trial participants would show whether surgery is prevented or delayed by the use of PFMT. These data would help inform NHS managers as to what long-term benefits they might expect if they implemented PFMT.
Aims
Overall aims
-
To maximise the delivery of effective PFMT for women with prolapse through the study of its implementation in three diverse settings. This would involve developing different service delivery models, such as using different staff skill mixes, with the format of delivery being determined locally.
-
To assess the impact of PFMT on longer-term treatment outcomes using linked health-care data for the majority of the original POPPY trial participants (i.e. those based in Scotland).
Specific aims
-
To understand the barriers to and facilitators of implementing PFMT across varying NHS locations from managerial, delivery staff and women’s perspectives and experiences, and to develop different models of delivery in response to these.
-
To explore the potential for different groups of staff skill mix to deliver PFMT without compromising the achievement of clinical outcomes.
-
To explore fidelity or variation to the PFMT protocol (e.g. number of sessions) and the impact of any variations.
-
To establish the levels of support required by non-specialist physiotherapists to deliver PFMT.
-
To explore the acceptability and outcomes for women of different delivery models.
-
To establish the costs and benefits associated with each model of delivery.
-
To contribute to knowledge of how and why implementation processes are successful (or not) through exploring what works, for whom and in what circumstances.
-
To establish whether or not the benefits observed among the POPPY trial participants are maintained at longer-term follow-up and across different NHS settings.
Chapter 2 Overview of methodology, study design, intervention description and patient and public involvement
Methodology
Theoretical frameworks
The study was informed by two theoretical frameworks from implementation science theory: the realist evaluation framework13 and the reach, effectiveness, adoption, implementation and maintenance (RE-AIM) framework. 14 The realist evaluation approach was used to understand how the intervention was implemented in different study sites, what contextual factors influenced its implementation and what ‘mechanisms of action’ lead to successful (or unsuccessful) delivery and outcomes. The RE-AIM framework was used to determine the overall public health effect of the intervention, using specific and standard ways of measuring the key indicators of potential impact and the widespread adoption and sustainability. The combination of both of these frameworks enabled us not only to evaluate the intervention’s internal and external validity, but also to take account of the context in which the intervention was delivered and identify the mechanisms that made it work (or not) to produce the observed outcomes. Realist evaluation is explained in more detail in Chapter 4, alongside its methods, and the realist evaluation findings are presented in Chapter 5.
The RE-AIM framework
The RE-AIM framework, developed by Glasgow et al. ,14 is designed to enhance the quality, speed and health impact of efforts to translate research into practice, and is based on five dimensions: reach, efficacy/effectiveness, adoption, implementation and maintenance. Its purpose is to expand the assessment of interventions beyond efficacy to multiple criteria that may better identify the translational quality and public health impact of health interventions, balancing the emphasis on internal and external validity. The RE-AIM framework helped to focus on important outcomes for implementation research at both the individual (recipient/use) and the organisation/system level (agents of delivery). The specific aspects of the RE-AIM framework are explained in the following paragraphs, along with the types of data gathered in this study for each of these aspects, which are presented across the findings chapters (see Chapters 4–6 and 9).
Reach
Reach refers to the absolute number, proportion and representativeness of the target population that is touched by the intervention. In this study, reach was assessed by exploring whether or not the increased service capacity resulted in or could lead to changes in the target population (e.g. reaching those with mild to moderate POP, the number of referrals from various sources and increased accessibility of PFMT in local areas). Reach was assessed using both qualitative and quantitative data.
Effectiveness
Effectiveness refers to the impact of an intervention on important outcomes. In the context of this study, effectiveness was explored both quantitatively (i.e. whether or not the different models of PFMT service delivery remained effective when compared with the outcomes from the original POPPY trial) and qualitatively (i.e. the experience of improvement reported by women and staff delivering PFMT and the experience of quality of care reported by women).
Adoption
Adoption refers to the willingness by the target settings, institutions and staff to implement, support and embed the intervention into their routine practice. In this study, adoption was assessed by the extent of uptake of PFMT by staff, the continued participation (or dropout) in the delivery of PFMT and the level of support provided by services and staff for the adoption of PFMT delivery.
Implementation
Implementation refers to the fidelity and consistency of intervention delivery as intended, and the cost of the intervention. In this study, implementation was monitored using the qualitative data on how the intervention was delivered locally and the extent to which it was implemented by the services as intended, as well as the quantitative data on the service delivery costs for different models of delivery.
Maintenance
Maintenance refers to the extent to which an intervention becomes institutionalised or part of the organisational practices/policies. At individual level, it refers to long-term outcomes of the intervention. In this study, the maintenance of intervention effects in individuals and settings over time was monitored via the outcomes data and the record linkage-based follow-up of the original POPPY trial participants, who were based in Scotland. It was also assessed through qualitative data on the future plans of study sites to continue the intervention and to train more staff in PFMT delivery.
Design
This study included the following components.
Realist evaluation
A realist evaluation was carried out that used case studies of implementation of PFMT delivery in three varying NHS settings (see Chapters 4 and 5). The realist evaluation allowed for substantial local stakeholder engagement and for local sites to make decisions on how to deliver PFMT [e.g. using different skill mixes such as specialist physiotherapists, women’s health nurses and junior (band 5) physiotherapists, as well as different numbers of sessions] (Figure 1). The realist evaluation would elicit local folk theories around how implementation was supposed to work [context–mechanism–outcome (CMO) configurations], track how implementation was working (including fidelity to the PFMT protocol) and lead to an understanding of what influenced outcomes.
FIGURE 1.
The PROPEL intervention flow chart. EQ-5D-5L, EuroQol-5 Dimensions, five-level version; ICIQ-UI SF, International Consultation on Incontinence Questionnaire – Urinary Incontinence Short Form; POP-Q, Pelvic Organ Prolapse Quantification; POP-SS, Pelvic Organ Prolapse Symptom Score; PROM, patient-reported outcome measure; PROPEL, PROlapse and Pelvic floor muscle training: implementing Evidence Locally. Reproduced from Maxwell et al. 15 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated. This figure includes minor additions and formatting changes to the original figure.
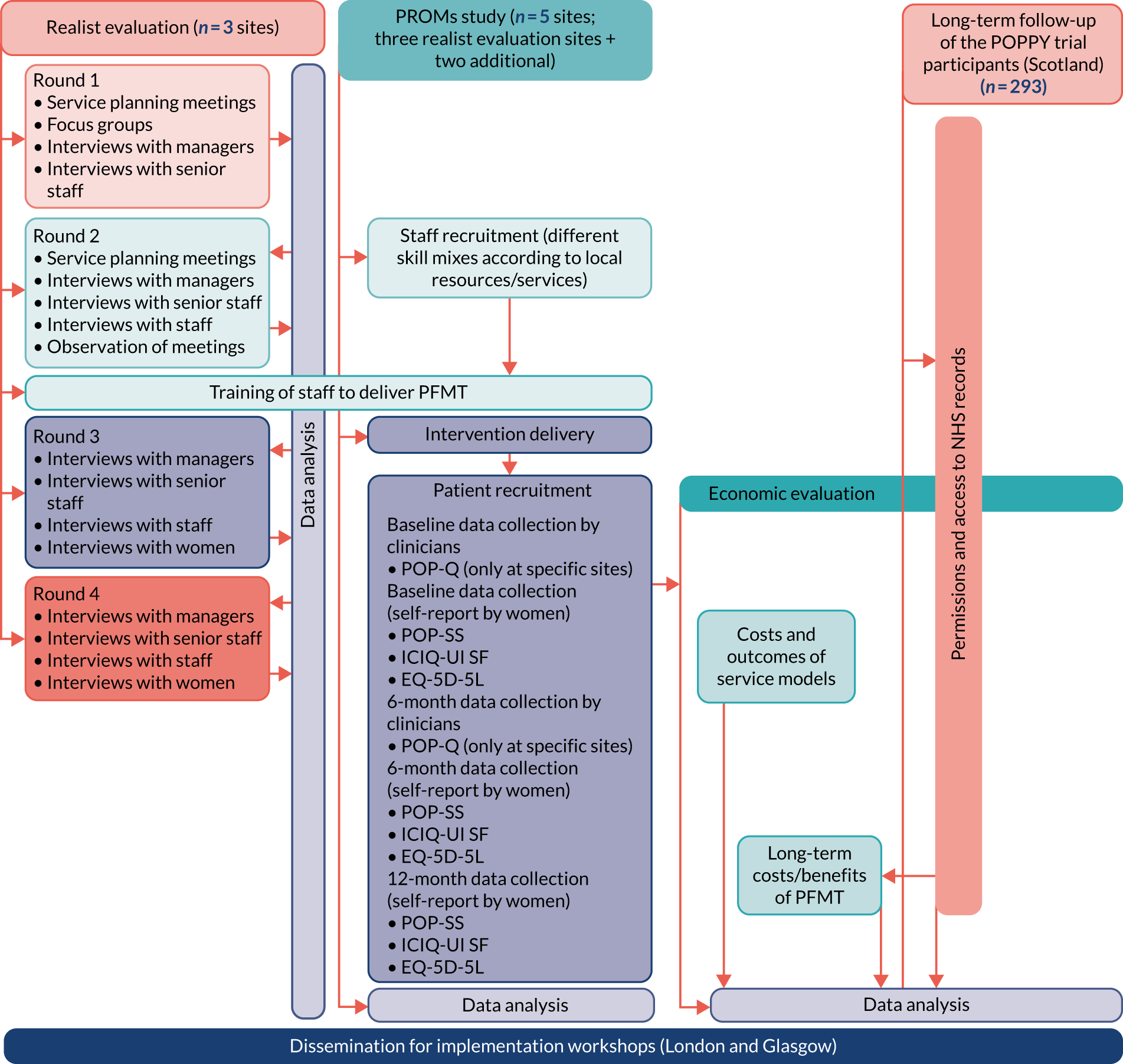
Patient-reported outcome measures study
A robust patient-reported outcome measures (PROMs) study, which used the same outcome measures as the original POPPY trial, was conducted in five NHS sites (three case study sites plus two additional sites, see Figure 1) to observe the outcomes for women receiving the different models of care (see Chapter 6). It was intended that, in the skill mix of staff across sites, there would be a mix of specialist physiotherapists, other physiotherapists and different types of nursing roles. It was also intended that the skill mix of staff would allow for a comparison of the specialist-delivered outcomes with the non-specialist-delivered outcomes. This would also allow comparison of the delivery of PFMT by specialist physiotherapists in the everyday world of the NHS with those observed in trial conditions.
Longer-term follow-up
Longer-term follow-up of up to 6 years of the original POPPY trial participants was carried out using record linkage of hospital and outpatient data [provided by Information Services Division Scotland via the NHS electronic Data Research and Innovation Service (eDRIS) (see Chapter 7).
Economic evaluation
An economic evaluation was carried out, which was concerned with the associated costs and outcomes of different service delivery models for delivering PFMT. In addition, an economic assessment of the long-term costs associated with accessing further pelvic prolapse treatment over time was conducted for the original POPPY trial participants, who were resident in Scotland (Chapter 8).
The applicability of study findings and outcomes
Finally, ‘dissemination and implementation workshops’ (in England and Scotland) were run to discuss the applicability of study findings and outcomes with service managers/women’s HCPs/general practitioner (GP)/patient and public representatives from across the country, with discussion of implications for planning of local services and identification of any further key barriers to or facilitators of change (see Chapter 9).
Intervention description
The PROlapse and Pelvic floor muscle training: implementing Evidence Locally (PROPEL) intervention that was being evaluated in this study is fully described using the Template for Intervention Description and Replication (TIDieR) checklist (see Appendix 1). 16 Participants attended an initial assessment and treatment visit with a PROPEL intervention clinician to determine their personalised PFMT protocol, and the patient was provided with any additional lifestyle information deemed necessary to assist with their treatment. Further appointments were scheduled at the patient’s and clinician’s discretion; the sessions progressed using the PFMT protocol until the clinician or patient decided that no further appointments were required, at which point the patient was discharged from the service. Alternatively, if it became apparent that the patient’s condition was more complex than initially thought, the clinician had the choice to refer the patient to specialist physiotherapy. During each appointment, clinicians completed a clinician assessment form to record all information.
Training to deliver pelvic floor muscle training
Staff who were identified in round 2 of the realist evaluation as potential staff to deliver the PROPEL intervention were approached by either specialist physiotherapists or a consultant within their trust. The staff who were to deliver the PROPEL intervention attended a 1-day training session held within their site. The training session was developed specifically for the PROPEL intervention and in conjunction with the POGP. It was delivered by two POGP-registered specialist physiotherapist trainers to a maximum of five new staff per site. In addition, a member of the research team was present at all training sessions to ensure that all questions regarding study specifics could be answered. Training manuals were produced and provided to the participants. Further details on the training are provided in Appendix 2.
Patient and public involvement
The Bladder and Bowel Foundation (BBF) (Kettering, UK) was an initial partner in this research and a co-applicant that contributed to the study design and provided expertise concerning the involvement in this study of women with prolapse. The BBF specifically provided input to the discussions on the delivery options women may receive, on the issues of recruitment of women and on the feasibility of patient data collection processes. They also provided members’ views of their experiences of health care and how they would value opportunities for PFMT, and the likelihood of its acceptability to women with POP.
However, the intention that the BBF would continue to be represented throughout the conduct of this study as a full partner and member of the project management team was not realised, because the BBF ceased to exist just at the point of the PROPEL intervention commencing. We then worked to identify another organisation that could step in to fulfil the role of the BBF. On the advice of our Study Steering Committee (SSC) we approached PromoCon (Worsley, UK), which later became Bladder and Bowel UK, as an organisation that represented people with bowel and bladder problems, and PromoCon agreed to become a part of the PROPEL intervention team. However, the process of understanding the organisational commitment and who would be able to take on the lead role within the PROPEL intervention from within PromoCon was confounded by the organisation’s own impending changes and its move to forming Bladder and Bowel UK. Therefore, it took some time within the PROPEL intervention to secure the support of another patient and public involvement (PPI) organisation; this had an impact on our ability to recruit individual women with experience of POP to sit on our project management group (PMG) and our SSC.
With the help of Bladder and Bowel UK, we finally recruited two PPI representatives: one became part of the PMG and the other joined the SSC. We continued to try and recruit further PPI representatives well into the 2 years after the study initially began, but without any further success. However, the two women recruited to the PMG and the SSC remained with the study to the end and contributed greatly to our meetings and how we communicated with both women and HCPs.
Although our PPI representatives were not actively involved in data collection or analysis tasks, they did provide input to project management, commenting on project documentation and reports to the funder, but, specifically, they were extremely valuable in discussing local site problems. There were difficulties in getting sites up and running and there were issues concerning staff attrition rates (mainly as a result of illness or retirement), which all affected the ability of sites to recruit sufficient numbers of women. Our PPI representatives were sympathetic to these issues, but also offered insight and sometimes solutions, such as contacting other local women’s groups to raise awareness of the study.
Our PPI representatives had always been intended to support dissemination of these findings to lay audiences and were included as key participants in our proposed dissemination and implementation workshops, which were intended, for example, for NHS managers, service leads, urogynaecologists, and physiotherapists with a remit for POP. One of our PPI partners attended two workshop events (London and Glasgow) and was a powerful voice not only in the telling of her own experiences, but also in encouraging managers and HCPs to take the PROPEL intervention findings on board and act on them. The feedback from the dissemination events overwhelmingly rated the contribution of the PPI representative as ‘excellent’.
We will continue to work with our PPI representatives in producing further outputs for lay audiences and will also disseminate these via Bladder and Bowel UK.
The experiences of our PPI representatives of working with the PROPEL intervention are described as follows:
I welcomed the opportunity, my first, to be involved as PPI representative in this project.
In my view anything that reduces the number of women having to undergo surgery can only be good for patients. Having increased numbers of skilled staff and reducing the costs involved in surgery would also be of benefit for NHS trusts.
I did find it difficult to offer any specific input to the project, particularly latterly when I was less able to attend meetings. I found the experience interesting and would certainly participate as PPI in the future.
PPI representative 1 (PMG)
I feel very privileged to have been a PPI on this study as the subject matter is very relevant to my patient experience within the NHS. I work within the NHS (in an unrelated field) so have (a little) understanding of the difficulties faced on a daily basis with staffing and funding issues. But more importantly I have years of patient experience and know how difficult I personally found it to access women’s health physiotherapy in my area. Hence, I appreciated being involved in a study that could not only improve patient outcome, but look at the implementation aspect of providing an NHS service.
Having never been involved in a research project before, I found the team supportive, friendly and above all willing to listen. It is sometimes difficult partake in discussions when you are not experienced or qualified in the field, but I felt that the patient voice was heard. I feel my experience with administrating an online support group for women with pelvic pain and prolapse helped with my ability to voice the patient point of view.
My highlight was speaking about my patient experience at the dissemination meetings. It was well received and I felt it emphasised why the research was undertaken and what a difference it could make to patient outcomes. It was fantastic to hear of the success of the project and that physiotherapy works in terms of patient improvement and cost savings. I look forward to being involved in the next study. Thanks to the PROPEL team for all their hard work.
PPI representative 2 (SSC)
Chapter 3 Description of case study sites and implementation of training
Introduction
The PROPEL intervention initially aimed to include three diverse sites across the UK in which to develop new models of PFMT service delivery. These three sites, A, B and C, had been identified during the funding application process and were keen to be involved in the study from this stage. It became apparent during the recruitment of women to the PROMs study and from the delays in sites to implement the new models that we would find it difficult to reach our recruitment target through these three original sites. Through one of our co-applicants who had previously been on the executive committee of the POGP, we sent out an invitation to around 20 women’s health services throughout Scotland and England. We had a number of positive responses, which resulted in the recruitment of two further ‘light-touch’ sites to the study. By this stage in the study, round 1 of data collection for the realist evaluation had been completed in sites A, B and C and the decision was made, with the agreement of the PMG, not to include these two new sites in the full realist evaluation, but to gain some reflection on their experiences of setting up and delivering PFMT in their regions. This decision was made to avoid further delays in recruiting women to the PROMs study and to maximise follow-up of women, while at the same time adding to our knowledge of ‘what works’ for implementation.
Overview of sites
Site A
This site had two components for delivering PFMT to women with prolapse in a secondary care setting:
-
community continence service
-
two hospital-based women’s physiotherapy services.
In both settings, the teams delivering PFMT were composed of band 7 [Agenda for Change (AfC)] and band 6 (AfC) specialist WHPs. Service planning meetings (SPMs) were held with the community and hospital teams separately, as they functioned under different management. Clinicians from these three teams had previously taken part in the POPPY trial.
Community
Initially, the community lead indicated that there was a need for an increase in capacity and was keen for continence nurses to be involved and be trained to deliver the PROPEL intervention. In addition, the community lead had indicated that they wanted to use group sessions for women with prolapse to educate them about PFMT before they were referred on for one-to-one treatment. After discussion with the team, it emerged that there was strong resistance to clinical groups other than physiotherapists being trained to deliver PFMT. In addition, not all of the physiotherapists in the team felt that they had the capacity to take part in the PROPEL intervention. Ultimately, two physiotherapists from the community agreed to participate.
Hospital
At the first SPM, the lead of the hospital service indicated that their preference was to not change their model of PFMT service delivery, citing staff shortages. After discussion among the core research team, the decision was made that we would use this as an opportunity. A total of nine specialist WHPs were recruited from the two hospital-based teams to deliver the PROPEL PFMT intervention to women with prolapse. This meant that they could continue with their normal service while the research team were able to collect data on the outcomes of PFMT, as delivered by specialist WHPs in a real NHS setting outside the constraints of a trial setting. It was agreed that they would continue to deliver the same specialist service to women recruited to the PROPEL intervention, including any adjunct therapies that they would prescribe normally. Nine specialist WHPs took part in the study, initially to recruit women to the focus groups in round 1 of the realist evaluation with a view to deliver PFMT through the PROPEL intervention in the two hospital teams. Six months into the project, the service lead approached the research team with fears that, because of further staff shortages, they were unsure if they would be able to continue to be involved in the PROPEL intervention. A number of meetings followed during which the research team provided the site with options that would enable them to continue their involvement in the PROPEL intervention, in a decreased capacity if necessary. This resulted in the loss of one of the hospital-based teams’ participation and a reduction in members of the team taking part in the remaining team.
At the end of the service planning process at this site, it was confirmed that five specialist WHPs from the hospital team and two from the community team would take part in the PROPEL intervention. The benefit of using this model of service delivery were twofold. First, we would be able to see if the outcomes obtained by specialist physiotherapists in the PROPEL intervention were comparable with those seen in the POPPY trial. Second, this specialist model provided us with a comparison group, similar to that in the POPPY trial, to use as a benchmark for the outcomes achieved by other clinician groups recruited and trained across the other four study sites.
Site B
Site B was a rural site with a large geographical area and an existing model of PFMT service delivery by a small number of specialist WHPs in hospital settings. Owing to the large area that this service was required to cover, they had concerns around the capacity of the existing service and the accessibility of this service to women. It was these issues that had led them to become involved in the PROPEL intervention at the outset.
From the outset, the central research team and the local principal investigator (PI) had difficulties engaging key managerial stakeholders in the service planning process. This was, in part, attributed to major changes taking place in the urogynaecology service locally in both a physical and organisational capacity. SPMs took the form of a more bottom-up approach to planning the new model of service delivery, with one specialist WHP leading the development process for the model that would be used in the PROPEL intervention. The local PI was very motivated and had previously been involved in providing additional training in this area with clinicians who had a special interest in this area of service delivery. Like site A, the service planning took longer than anticipated; consequently, there were delays in recruiting women to the realist evaluation and the PROMs study. There was significant discussion about which clinicians would be trained to deliver the PROPEL intervention. During discussion with the SSC about the groups of clinicians who were being trained to deliver the PROPEL intervention, we were advised that sites A–E set up a triage step within their referral process for potential PROPEL intervention participants. In site B, this meant that all women referred with POP received an initial assessment, which was carried out by a specialist WHP who identified if the woman met the inclusion criteria for the study. Only at that point were women approached about participating in the study.
This site had the most diverse clinical mix taking part in the study: district nurses, continence lead nurse specialists, musculoskeletal and general physiotherapists and urogynaecology nurses. The mix in the staff who were trained meant that the point of delivery of the new model of service was also a lot more diverse and was much more accessible for the women receiving this intervention. The large number of clinicians trained at this site and their diverse roles resulted in the point of delivery of PFMT services moving from a hospital to a community-based setting in many cases. It also meant that women who consented to take part in the PROPEL intervention could receive their treatment closer to home, as the clinicians trained for the PROPEL intervention were located across a variety of places in this site. Eight clinicians were trained to deliver the PROPEL intervention.
Site C
This urban site previously delivered limited PFMT services through a small number of specialist WHPs in a hospital setting. Similar to site B, this site was interested in moving these services to a community-based setting so that they were more accessible. At the initial SPM, which was the best-attended meeting at this site, it was highlighted that a community-based urinary continence team, which included physiotherapists and band 6 and 7 (AfC) nurses, was the preferred model of PROPEL PFMT intervention service delivery. The lead of this team indicated at this meeting that they would have to take this proposal to their management before this could be taken forward; however, they were keen to see this happen. One week following this meeting, the research team were informed by the site’s research and development department that the proposed community continence team were currently involved in another research project and would not have the capacity to take part in the PROPEL intervention alongside this existing project. It was agreed that further possible models of service delivery would be discussed at the next scheduled SPM.
The next SPM was poorly attended; despite this, further possible models of service delivery were discussed, which still focused on having a community-based element to the PROPEL PFMT intervention service delivery. SPM attendees identified community-based physiotherapists, who were not part of the continence team, as possible participants. They also discussed the possibility of training a number of urogynaecology nurses who were based in the hospital, to supplement the community physiotherapists. Following this meeting, the research team received interest directly from a number of these physiotherapists. Unfortunately, these physiotherapists did not have the support of their managers and were therefore unable to take this model of service delivery forward.
At this stage in the planning process, the research team flagged up the issues around the slow progress in setting up a new model of PFMT delivery to the independent SSC in this site. It was decided that this site would need to be given a deadline to have identified the clinicians who would be taking part in the PROPEL intervention, so that this site could be taken forward without causing catastrophic delays to the study. Finally, the decision was made locally that, despite wanting to set up a community service, this would not be possible at that time; instead, it was decided to follow up with a model using urogynaecology nurses based in the hospital to deliver the new service delivery model. Three nurses agreed to be trained to take part in the PROPEL intervention.
Sites D and E
Each of these were urban sites with a wide socioeconomic spread. As discussed previously, these sites were recruited as ‘light-touch’ sites to be involved in the women’s PROMs study only and not in the realist evaluation. The result of not having to go through the data collection process around the service planning for new models of service delivery was that these sites were set up more quickly and started recruiting only shortly after the original three sites. Site D implemented a model of service delivery that was made up of four band 6 and 7 (AfC) musculoskeletal physiotherapists. Site E implemented a model of service delivery that was made up of two band 5 (AfC) nurses and two physiotherapists: one band 5 and one band 6 (AfC).
Womens’ input into service planning for the PROPEL intervention
The women’s focus group data that were collected in round 1 of data collection for the realist evaluation were summarised and fed back at a SPM at each of the sites. The focus group study was designed so that each site had data on the issues that were important to women currently using these services; this included topics around awareness of women in the existing service, referral pathways and treatment received. These data were collected and fed back to sites so that the views of women could be considered in the process of designing a new model of delivering PFMT to women in the PROPEL intervention.
Overall, 26 clinicians were initially trained to deliver the PROPEL intervention (Table 1). In total, six of these withdrew from the study prior to treating any women using the PROPEL intervention protocol. They cited a number of reasons for this, including injury, lack of confidence, lack of capacity, organisational issues and moving away from their current post.
| Site | Service context | Service model adopted | Skill mix trained |
|---|---|---|---|
| A | Urban, POPPY site | No change. Existing primary and secondary care provision of specialist physiotherapy. Referrals triaged | Specialist physiotherapists (existing team):
|
| B | Rural | The PROPEL intervention PFMT training was provided to a variety of clinicians over a large geographical area. This included clinicians with special interest, district nurses, continence nurses and physiotherapists. The PROPEL intervention women were triaged by specialist physiotherapists prior to referral to the PROPEL intervention service. Community based and secondary care based |
Musculoskeletal physiotherapists, band 6 (n = 2) General physiotherapist, band 6 (n = 1) District nurses (n = 2) Lead nurse specialist in continence, band 6 (n = 1) Urogynaecology (n = 2) |
| C | Urban | New provision of PFMT delivery developed for the PROPEL intervention based in secondary care. Consultant triaged and referred to the PROPEL intervention service provided by urogynacology nurses | Urogynaecology nurses:
|
| D | Urban | Community health-care setting. Current PFMT service delivered by small number of specialist physiotherapists. Four clinicians to deliver the PROPEL intervention service in a community health-care setting | Musculoskeletal physiotherapist, 1 × band 5, 2 × band 6 and 1 × band 7 |
| E | Urban | Current PFMT service delivered by small number of specialist physiotherapists. Four trained clinicians to deliver the PROPEL intervention service in a community health-care setting |
Urogynaecology nurse (n = 2) Physiotherapists (band 5, n = 1 and band 6, n = 1) |
Training
Pelvic floor muscle training
Clinicians at sites B–E received the same standardised training as outlined in Appendix 2; assessors at these sessions completed a checklist to verify the completion of aspects of the training, using the checklist in Appendix 3. As the staff identified in site A were already fully trained specialist WHPs, they were not required to undertake this training. Instead, these clinicians undertook a training session with members of the PROPEL intervention research team, which focused on the paperwork that they would be required to complete during the treatment of women recruited locally to the study. These staff were also given copies of the self-report questionnaires that the women would be receiving, so that they were familiar with what women in the study would be asked to complete.
Pelvic Organ Prolapse Quantification System training
Although the Pelvic Organ Prolapse Quantification System (POP-Q) is a validated research tool for objectively measuring the stage of prolapse in women, it is not a measure that is commonly used in the clinical setting (see Appendix 4). 18,19 As seen in Chapter 2, Design, and Figure 1, it was planned to carry out the POP-Q assessment at baseline and at the 6-month follow-up for each woman recruited to the PROMs study. It quickly became apparent from meetings with the staff who would be delivering PFMT locally that the POP-Q assessment was not a commonly used clinical measure, even among the specialist WHPs.
In site A, the POP-Q training was delivered to the staff delivering the PROPEL intervention by a consultant urogynacologist who was working in this site. Each clinician taking part in the PROPEL intervention was given the option of completing a simplified POP-Q staging assessment or a full POP-Q assessment on women at baseline when they attended their first appointment, and again 6 months after a woman began her treatment (see Appendix 5).
The specialist WHPs in site B who were involved in triaging women for the PROPEL intervention were provided with similar training from a urogynaecologist working in another specialist women’s health centre. After this training had been completed, all POP-Q assessments at this site were carried out by a band 7 (AfC) specialist WHP at the time of a woman’s triage appointment. On completion of their PFMT treatment by the newly trained clinicians, women then attended an extra appointment with the band 7 specialist WHP, who completed their follow-up POP-Q assessment. Owing to the geographical area and the constraints that this imposed on the specialist physiotherapists, only a proportion of the women recruited to the PROPEL intervention at this site received these baseline and follow-up POP-Q assessments.
Similarly in site C, it was the consultant gynaecologist who undertook the baseline and follow-up POP-Q assessments with women, rather than the newly trained urogynaecology nurses. They were, therefore, well placed to complete the POP-Q baseline assessment at the triage stage. For their follow-up POP-Q assessment, women were invited to come back in for an additional appointment with the consultant after completion of their PFMT treatment.
The POP-Q was a secondary outcome measure. Owing to the difficulties and time delays the research team encountered in organising the POP-Q training for clinicians, in both sites A and B, the decision was made by the PMG [and ratified by the National Institute for Health Research (NIHR)] that we would not carry out the POP-Q assessments on the women recruited in the two light-touch sites. The delays between clinicians receiving the PFMT intervention training and the recruitment of women were 4, 2.5 and 4 months in sites A, B and C, respectively. These delays were incurred as a result of these three sites requiring training to carry out the POP-Q assessments.
Chapter 4 Realist evaluation methods
Parts of this chapter are adapted with permission from Abhyankar et al. 17 This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data. The text below includes minor additions and formatting changes to the original text.
Realist evaluation approach
Realist evaluation belongs to the family of theory-based evaluation approaches. Theory-based evaluations aim to clarify the ‘intervention theory’, that is clarify how intervention activities are understood to cause or contribute to outcomes and impacts. Realist evaluation was used in this study to understand how the intervention was implemented in different study sites, what contextual factors influenced its implementation and what ‘mechanisms of action’ led to successful (or unsuccessful) delivery and outcomes.
Realist evaluation has emerged in response to the need for knowledge that extends beyond that obtained by the traditional outcome-focused evaluation approaches that ask the question – is the intervention effective? Realist evaluation is founded on the premise that interventions are complex and are introduced into social systems that are also complex. It maintains that no interventions are universally effective, but that some things work for some people in some contexts. Realist evaluation therefore asks what is it about the intervention that works, for whom, in what contexts and why. 20
Realist evaluation contends that it is not interventions that work; rather, it is the people involved in interventions who make them work. Interventions introduce opportunities, resources or ideas for change, but whether or not these actually lead to the intended outcomes depends on how people react to, interpret and act on these resources. It is people’s reasoning and capacity in response to the intervention elements that represent the real ‘mechanisms of action’ in any intervention. These mechanisms of action are, however, contingent on the social context in which people work. Certain contexts enable people to act, whereas others place limits on people’s behaviour. 21 Realist evaluation thus seeks to explain the complex relationship between the mechanisms activated by the intervention, the context that influences their workings and the intended and unintended outcomes they produce. The explanatory proposition of realist evaluation is that interventions work (have successful outcomes – O) only in so far as they introduce appropriate ideas and opportunities (mechanisms – M) to groups in the appropriate social and cultural conditions (contexts – C). The task of an evaluation is to identify the linked patterns of contexts, mechanisms and outcomes (CMO configurations) to explain how particular outcomes were brought about by certain mechanisms being triggered in certain contexts. 20
This study aimed to implement a complex intervention, the delivery of PFMT using different staff skill mixes, in complex NHS systems consisting of a number of actors, varying resources, diverse geographical locations and service configurations. The implementation also involved actions and decisions from people in multiple roles at different levels, for example from service managers and finance directors at organisational level to front-line staff delivering and supporting the PFMT intervention, as well as women receiving PFMT. Given the interplay of multiple factors operating in different personal or organisational contexts with different priorities and goals, realist evaluation provided an appropriate framework and methodology to explore and explain the implementation of PFMT.
Realist evaluation typically involves three broad phases. Phase 1 seeks to identify the ‘folk’ theories about how and why the intervention will bring about change. This involves eliciting ideas about how the intervention is expected to be implemented and work, what intended and unintended outcomes are likely, what may be their mechanisms of action and what contextual factors may enable or constrain these mechanisms. Data are gathered from those involved in the implementation of the intervention and its key stakeholders. These data are used to build hypotheses about the causal relationships between specific contexts, mechanisms and outcomes; these are known as the CMO configurations. Phase 2 involves testing these theories by gathering data on the actual implementation process; this unfolds the mechanisms and outcomes and impacting contexts. In the third and final phase, the intervention theories are refined through iterative data analyses and interpretation to provide middle-range theory statements about why and how the intervention worked, for whom and in what contexts.
Phases and methods of realist evaluation
The realist evaluation was conducted in three broad phases, using a longitudinal, multiple case study design. The five study sites described in Chapter 3 were considered as ‘cases’, although the full realist evaluation was conducted in three sites only. Cases were defined at the level of the NHS trust in England and NHS Health Board in Scotland, as these represent the units through which health services are organised, governed and delivered in local areas. Defining the ‘cases’ at the level of these broad units helped to ensure that the influence of contextual conditions at various levels (i.e. from financial, organisational and managerial level to clinician, practice and patient level) was encompassed in the evaluation.
Data collection
The three phases of the realist evaluation aimed to identify, test and refine a theory explaining how and why the PROPEL intervention worked (or not). It involved data collection at four time points over an 18-month implementation period. The methods used in each phase are outlined in the following sections. Table 2 presents the number and type of data sources collected in rounds 1 to 4.
| Round | SPMs | Managers/service leads | Senior clinicians | Staff delivering PFMT | Women |
|---|---|---|---|---|---|
| 1 | Total, n = 12
|
Total, n = 5
|
Total, n = 2
|
No interviews in this round |
Total, n = 21 Focus groups, n = 17Interviews, n = 4 (all in site C) |
| 2 | Total, n = 26
|
Total = 6
|
Total = 3
|
Total = 11
|
No interviews in this round |
| 3 | N/A | Total, n = 10
|
Total, n = 4
|
Total, n = 10
|
Total, n = 18
|
| 4 | N/A | Total, n = 5
|
Total, n = 2
|
Total, n = 18
|
Total, n = 15
|
Phase 1: identifying folk theories of change
Phase 1 took place during the planning stages of the intervention through two rounds of data collection and aimed (1) to track local decisions on what to implement and how, rationales for service delivery decision-making and ideas about how implementation is supposed to work and (2) to elicit folk theories of change from the implementers and key stakeholders of the intervention about how the intervention was intended to be implemented and work in their areas, for example the likely outcomes of the intervention, possible mechanisms of action and potential contextual influences.
Rounds 1 and 2: development and operationalisation of the service delivery models
Focus groups with women who were receiving care for prolapse in each study site were conducted in round 1, to provide service user input to the local SPMs, where the models for PFMT service delivery were discussed and decided on. The focus groups explored women’s experiences of prolapse and treatments, their experiences of local services and care, their preferences for service delivery models, acceptability of PFMT and their visions for a responsive and woman-centred service. Women aged ≥ 18 years who were seeking and receiving care for prolapse through the local gynaecology/women’s health service in each site were eligible to take part. Women were identified and recruited by either the specialist pelvic floor dysfunction physiotherapists/WHPs or the consultant gynaecologists/urogynaecologists in local sites. The initial plan was to hold four focus groups across the three sites (one site would host two focus groups because of the large geographical size of the service area), with a minimum of four and a maximum of 10 participants per focus group. However, participant availability prevented a focus group being held in one location (site C), because of the geographical location and the inability of participants to travel. Instead, four individual telephone interviews were conducted with consenting participants in that area, using the same topic guide as for the three focus groups. The combined use of focus groups and individual interviews for pragmatic reasons may have lowered the homogeneity in the data collection process, with a potential threat to the trustworthiness of findings. 22 However, the absence of any observed differences in the type of data collected by each method and the convergence of key themes across the two methods suggests enhanced trustworthiness of findings. 23
Focus groups were conducted in private rooms at local hospitals and were facilitated by two researchers. The focus groups each lasted approximately 1 hour and involved four, five and nine participants. The telephone interviews lasted approximately 20–30 minutes. Focus groups and interviews were recorded digitally, transcribed verbatim and summarised by the research team. The summaries were presented at the SPMs to enable inclusion of service user voice into the decisions about service design.
The liaison specialist physiotherapist in each site identified and invited local service managers, clinical leads, consultants and other relevant staff groups to attend a series of SPMs. The first SPM was convened in round 1, and aimed to familiarise the attendees with the evidence base for PFMT and discuss its potential benefit for local management of POP. Members of the research team attended this meeting to explain and reinforce study aims. The planning team then discussed the current service provision and the local capacity issues, as well as how these might be addressed with the available or an extended staff pool. Initial options for service delivery models were discussed with ‘actions’ for any fact-finding, involvement of others or other actions necessary to help finalise decisions about service models.
A second SPM was convened in round 2 by study sites to finalise the service delivery model to be implemented, plan the operationalisation of the new model within current service structures and identify staff groups for training in PFMT delivery. The meeting involved the same attendees as the first meeting, plus any new members as deemed appropriate by the local service. Members of the research team attended this meeting to ensure that study aims and objectives were met and to observe the decision and planning process. Both meetings were audio-recorded to track the decisions being made as well as the folk theories around how implementation is supposed to work, what may be the likely outcomes and what contextual factors may impede or facilitate the implementation. The decisions were finalised over two planning meetings in sites A and B and three meetings in site C.
Two rounds of individual semistructured interviews were conducted with a number of stakeholders in each site to identify local theories of change. Service leads or managers and senior practitioners (urogynaecology consultants/senior nurses or allied health-care professionals/GPs) who were likely to be key decision-makers were identified from the SPM attendees and invited to take part in round 1 and 2 interviews. Further interviewees were identified using a snowballing technique. The interviews were conducted by a member of the research team, either face to face or via telephone, and were facilitated by topic guides developed specifically for the purpose of the interview round. Round 1 interviews explored the contextual detail about the site (e.g. how care is currently organised, gaps in the service and need for change, and proposals for changes in service delivery), anticipated barriers to and facilitators of implementation (e.g. resources, capacity issues, training, funding and buy-in from stakeholders), potential mechanisms (e.g. attitudes towards PFMT delivery by non-specialists and the challenges to implementation of different proposals) and anticipated outcomes. Round 2 interviews explored staff views about the operationalisation of the decisions about service delivery models, attitudes and reactions of various staff towards the new service model, how this will be translated to the staff groups identified for PFMT training and service delivery, the potential barriers to and facilitators of implementation of the new model, the involvement of and potential impact on other staff groups or services, and intended and unintended outcomes. The exception to this was site A, where the staff groups were interviewed only once, in round 2, as this site was not implementing any changes to its existing service models. The interviews in this site focused more on understanding how the current service was organised and working, what worked well and why and what areas needed improvement.
In round 2, additional interviews were also conducted, with the staff being asked about delivering PFMT under the new service model to explore their views on the new service model, their involvement in PFMT delivery, their expectations of training and the new role, their concerns and anticipated problems and how these might be overcome, and the anticipated impact on their professional role. In site A, which was not implementing any changes, these interviews focused on understanding how the service was delivered and working, what worked well and why, what needed improvement and what it was about their service and care that led to positive outcomes for women. Interviewees were identified from staff lists provided by local service leads. Interviews were conducted by members of the research team, either face to face or by telephone, and were facilitated by topic guides that were relevant to those staff groups.
Phase 2: testing the folk theories
The initial folk theories of change were tested by collecting data on contexts, mechanisms and outcomes at the operational level in each study site, to explore how the intervention was implemented and worked in different areas. This was carried out through two further rounds of data collection. Round 3 took place ‘during’ the implementation stages once staff had begun to deliver PFMT to women under the new service model, and focused on exploring how the new service model was operating and any problems that had arisen during implementation. Round 4 took place after the intervention period had ended, as dictated by the achievement of site-specific recruitment and treatment target, and focused on exploring whether or not the implementation was perceived to be successful, whether or not/how the intervention worked, what lessons were learnt from implementation and the plans for continuation of PFMT delivery locally. In this phase, data were also collected from staff in the light-touch sites D and E, to explore the implementation process, barriers, facilitators and outcomes in those areas.
Rounds 3 and 4: delivering and reviewing the models
Round 3 interviews with service leads/managers explored the process of referrals to newly trained staff, any anxieties or concerns around training and support, service delivery, local resources required for delivery and any perceived effect on women, staff and services. Round 4 interviews explored service leads’/managers’ perceptions of success of the models, the models’ sustainability, modifications that may be necessary, key drivers for success, areas and extent of perceived impact, and future plans for further expansion of services.
Round 3 interviews with consultants/senior nurses/allied HCPs/GPs explored their views on implementation and the perceived impact on other service areas. Round 4 interviews explored their views of the overall implementation and impact, key drivers for success and views on continuation or expansion of services.
Round 3 interviews with staff delivering PFMT explored their experiences and views of implementation, concerns regarding their role in its delivery, problems experienced in service delivery and perceived impact on factors such as women’s outcomes and their workload. Round 4 interviews explored their overall experience of delivering PFMT and the impact they felt that their role had for women and services, and key drivers of success.
Round 3 interviews with women receiving PFMT from the newly trained staff explored their expectations and experiences of PFMT treatment, experience of care, and perceived impact on symptoms and quality of life. Round 4 interviews explored their experience of the intervention, adherence to therapy appointments and the prescribed PFMT programme; perceptions of treatment, outcome and care; and intentions to continue with PFMT.
Interviews were conducted via telephone by a member of the research team and were guided by topic guides that were specific to the participant groups being interviewed.
Data analysis
Round 1 and 2 data analysis
Data from round 1 and 2 interviews and SPMs were transcribed verbatim and analysed using the thematic framework approach adapted for use in realist evaluations. 24,25 Data analysis proceeded in parallel with data collection. A coding frame was developed in round 1 using data from two transcripts (one from a service lead/manager and one from a senior practitioner), the summaries of the first SPM from sites B and C and the three core concepts from realist evaluation: CMO. Two members of the research team (PA and JW) read and reread the transcripts to familiarise themselves with the data. Data from the transcripts were sectioned into ‘meaningful units of analysis’, which were essentially segments of data containing discrete bits of information. Each unit was assigned a code that reflected the meaning of the data segment in relation to the main topics covered in the interviews, for example problems in service, current and potential enablers and barriers, and interim and long-term outcomes. The codes were initially assigned by two researchers independently, but were subsequently compared and refined until they accurately described the meaning contained.
Codes from the four transcripts and meeting summaries were then considered together to look for similarities, which were either merged into one or grouped together under higher-order themes. The codes were also classified as describing a context, a mechanism or an outcome. Codes describing any pre-existing factors outside the control of intervention designers, such as social or service structures, enabling or disabling conditions, resources, relationships, cultures, staff/service capacities and motivations, were categorised as contexts. Codes that suggested a change in people’s minds and actions (e.g. reasoning, feelings, behaviours, judgements, decisions and attitudes at individual, interpersonal, social and organisational levels) in response to the changes introduced by the implementation, as well as those described as interim outcomes of the intervention, were considered as mechanisms. Finally, codes that described the intended and unintended consequences of the intervention at the level of women, staff or services were classified as outcomes.
Following these classifications, an initial coding framework was developed that was then systematically applied by another researcher with experience in qualitative research to all of the transcripts from rounds 1 and 2. New codes were added as they emerged from subsequent data. Once all of the data had been coded, the content of the coding framework was revisited and refined. The coding framework was used to summarise the data for each study site to capture the site-specific processes of implementation and theories of change. Specifically, the coded data were used to identify linked patterns of CMOs and generate initial CMO configurations (i.e. hypotheses about what mechanisms would be triggered in each site, under what condition/contexts, to achieve what outcomes). Once the theories of change were identified for each site, these were compared across the sites to note similarities and differences. Although the sites differed in terms of macro-level contextual factors (e.g. geographic location, organisation of care and existing service models), a number of micro-level contextual factors were similar across the sites (e.g. staffing issues, support and buy-in from management and availability of resources). This meant that it was possible to look for patterns of CMOs that cut across the site boundaries. Cross-case comparisons were used to then identify an overall folk theory of how the intervention will work through different mechanisms being trigged in different contexts to generate diverse outcomes.
Round 3 and 4 data analysis
Data from rounds 3 and 4 were analysed using the thematic framework approach, similar to that described in phase 1. Briefly, a coding frame was developed using data from four round 3 transcripts (one from each participant group: service manager, senior practitioner, delivering staff and women, from across the three sites). Two researchers (PA and another researcher with experience in qualitative research) independently read and reread the transcripts and coded smaller segments of data. The codes were compared, discussed and refined until the meaning and content of each was agreed. The codes were then grouped into higher-order themes according to the similarities and relationships among them. They were also classified according to the concepts of CMOs, to explore how the different contexts influenced the implementation of the intervention, what mechanisms of actions were triggered and what outcomes were produced. Codes were classified as context if they described something that existed prior to the implementation or something that had developed/emerged/changed during the intervention, but was unrelated/not attributed to the intervention itself. Codes were classified as mechanisms if they described activities or actions taken by those implementing the intervention/touched by the intervention, including their thought processes, feelings, decisions and reactions. Codes were classified as outcomes if they described something that happened as a result of the intervention, whether intended or unintended and whether higher-level outcomes or indicators of higher-level outcomes. The initial coding frame was applied systematically to all data from rounds 3 and 4 (by TA), adding further codes or categories as they emerged from the data.
Once all of the data had been coded, the next step was to identify CMO patterns in the data. Initially, this process was carried out at the level of individual study sites to provide a ‘story of implementation’ by understanding the outcomes of implementation in each site, their underlying mechanisms of action and the contextual factors triggering those mechanisms. Data from each transcript were summarised and tabulated using a framework consisting of rows that indicated a data source and columns that indicated the CMOs. The data summaries were compared across the participants to develop overall CMO configurations for the site in the next phase of analysis.
The next phase of analysis focused on ‘testing’ the initial theories of change identified in phase 1 for their adequacy in explaining the observed CMO patterns. This involved explicitly comparing the observed CMO patterns (how and why the intervention actually worked or not) with the hypothesised CMO patterns (how and why it was expected to work). The analytical process was outcome led; that is, we began with the groups of outcomes that were anticipated in phase 1 folk theories to result from the intervention (e.g. women’s health outcomes, reach of intervention) and looked for evidence in the phase 2 data on how much or how well those outcomes were achieved in each site. An attempt was also made to map these outcomes to the elements of the RE-AIM framework to begin an assessment of the impact, adoption and sustainability of the intervention. We then sought to explain the observed outcomes in each site, by looking for the possible linked mechanisms and contextual factors that appeared to trigger those mechanisms. These constituted the site-specific CMO configurations.
Theory refinement
Phase 3: refining intervention theories
Once the site-specific CMOs were developed that explained when, why and for whom certain outcomes were achieved (or not), cross-case comparisons were performed to refine the CMOs and develop middle-range theories about the intervention. For each outcome, we compared and contrasted the CMO models emerging from all three sites, as well as the two light-touch sites. The analysis was carried out a higher level of abstraction, transcending the individual sites. The CMOs were refined by identifying the facilitating or impeding contextual factors that were common across the sites, and re-examining the linked mechanisms in relation to each outcome. This meant that a particular CMO was now able to explain the workings of the intervention in more than one site where the specific contextual factors were present.
Chapter 5 Findings of the realist evaluation
Parts of this chapter are adapted with permission from Abhyankar et al. 17 This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data. The text below includes minor additions and formatting changes to the original text.
Phase 1: folk theories of change – how was the intervention expected to work?
In rounds 1 and 2, participants in each site described the wider context in which their service operated in, the current configuration of the service for prolapse care, the perceived gaps in service and the key drivers for change. This description was followed by an account of proposed service models and implementation plans, anticipated and unanticipated outcomes, explanations of how the intervention was expected to work and the existing and potential barriers and facilitators likely to affect implementation.
The PROPEL intervention introduced an opportunity to deliver PFMT using different staff skill mixes to a wider population of women with prolapse than that currently reached by specialist physiotherapy services. The PROPEL intervention provided an opportunity for sites to reconfigure local service and referral pathways, and supported provision of training in PFMT delivery to new staff skill mixes. The PROPEL intervention also provided some limited resources to support the new models of service delivery, such as specialist physiotherapist time to support those newly trained while they engaged in recruiting and delivering PFMT to the study population. Across the three sites, the intervention was expected to affect three key sets of outcomes: (1) have an impact on public health by way of widening the reach and accessibility of PFMT to the target group in local areas, (2) have an impact on women’s health by way of improvements in prolapse symptoms and quality of life and/or reduction in surgeries and (3) have an impact on services by way of shortened waiting lists for PFMT and a reduction in specialist workload, so that their resources can be focused on more complex cases.
The context and organisation of prolapse care varied significantly across the three sites. Several contextual factors were identified in round 1 and 2 data that seemed likely to influence the implementation of the intervention, which, in turn, would affect the achievement of anticipated outcomes. In the following section, we describe the context in each site before articulating the initial CMOs that emerged from data explaining how the intervention was likely to work and what factors were expected to facilitate or impede the implementation.
Context of care in study sites
Site A
Site A was a large urban area with primary and secondary provision of specialist physiotherapy services for women with prolapse. It was a previous participant in the POPPY trial, and several POPPY trial physiotherapists were providing input into prolapse care. The service had been well established for over a decade and offered PFMT to women with prolapse through specialist physiotherapists working in the acute and community settings. The staff expressed pride in the service, describing it as providing gold-standard care. The reasons for this were cited as:
-
all specialist physiotherapists being highly trained in PFMT for prolapse
-
having good working relationships and flow of communication with nurses, consultants, pain clinics and incontinence services
-
having a team approach to practice and respect for each other among different professionals
-
having adequate levels of staffing and resources to deliver the service.
Improvements were seen to be needed in raising awareness among GPs about prolapse and PFMT to enable direct referrals, in improving waiting times and referral pathways and in improving follow-up care. The team’s motivation for taking part in the study was to showcase their gold-standard service, rather than implement any changes.
Site B
Site B, in contrast to site A, had a large geographic spread in remote and rural areas with limited availability of specialist physiotherapy services. The incontinence service worked closely with the physiotherapy service, but was seen mainly as a ‘pad provision’ service that needed to become more holistic and proactive in assessing and treating urinary incontinence. Both services suffered from shortages of staff; specialist physiotherapists were few in number and the continence service lacked a clinical lead at the time of the study. The geographic spread of the area meant that the patients and staff had to travel long distances for care, which was compounded by shortages of staff. Despite the challenges, there were high levels of motivation among the staff; many had a special interest in women’s health and the service had a history of training musculoskeletal physiotherapists in delivering PFMT on a needs basis. Nurses and physiotherapists were enthusiastic about being trained in PFMT delivery and were supported and encouraged by their managers.
Site C
Site C was an urban area with limited specialist physiotherapy provision available for prolapse, where women were triaged by the urogynaecology consultants. There was said to be a lack of co-ordination between primary care and secondary care services with regards to incontinence and prolapse. There was enthusiasm about the PROPEL intervention among acute and community nurses, management and some consultants, and there was a perceived need for service redesign.
Theories about how the intervention would work, for whom and in what contexts
Four sets of CMO configurations were identified from the data, which contained folk theories around how each of the intended outcomes would be brought about and what may facilitate or impede these processes (Figure 2). The data also revealed an unintended outcome that was expected to affect implementation. Each CMO is described briefly and illustrated via a diagram.
FIGURE 2.
The CMO configurations 1–4. C, context; M, mechanism; O, outcome. Reproduced with permission from Abhyankar et al. 17 This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data. The figure includes minor additions and formatting changes to the original figure.
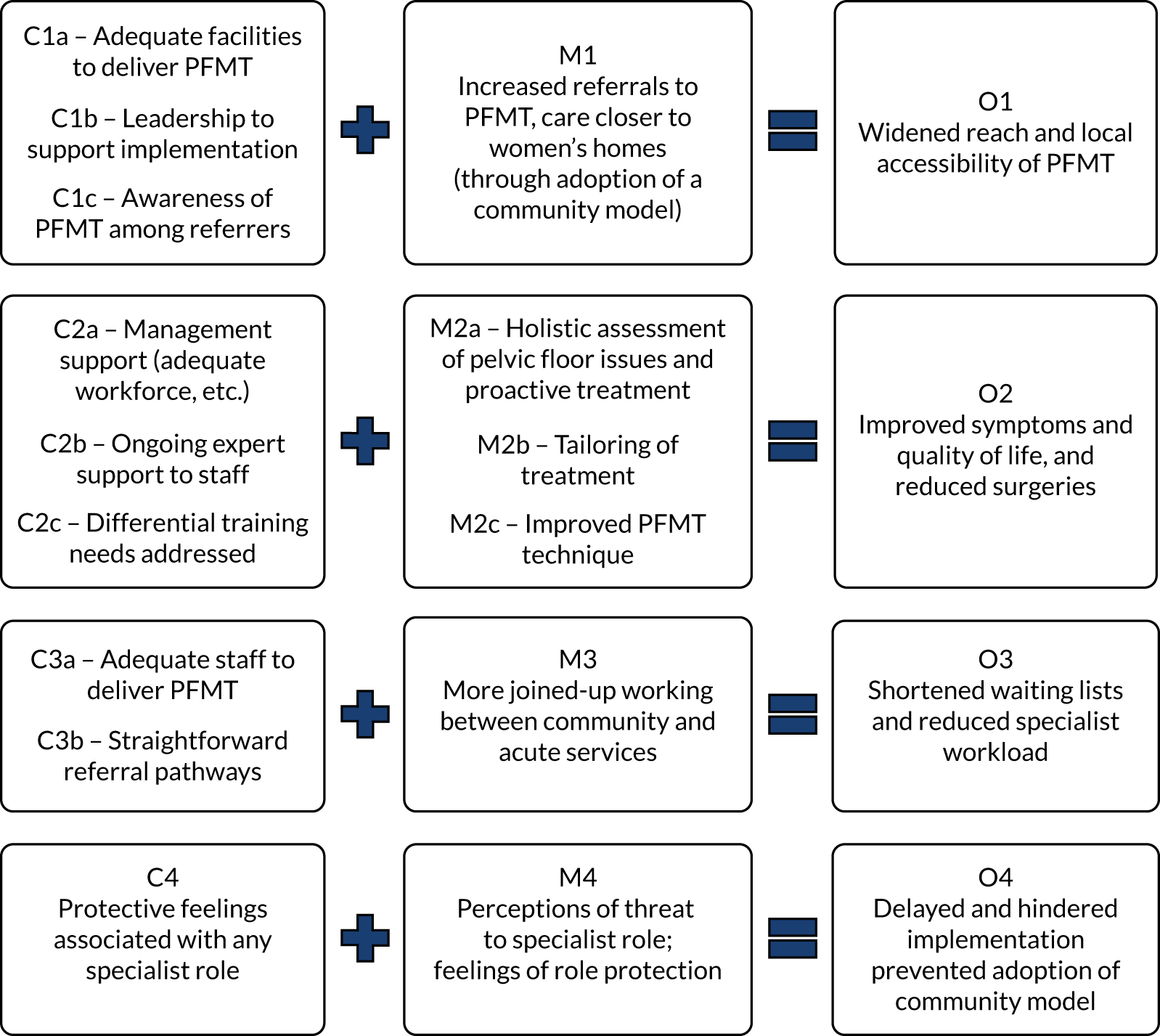
Context–mechanism–outcome configuration 1: widening the reach of pelvic floor muscle training through increased local provision of care
It was anticipated that using different staff skill mixes to deliver PFMT would widen the reach and accessibility of PFMT in local areas because it would increase the number of referrals to PFMT and increase the provision of PFMT in the community, closer to women’s homes, through adoption of a community model of service delivery. This mechanism was dependent on whether or not adequate facilities (e.g. private rooms in clinics) were available to carry out internal assessments and deliver PFMT, whether or not there was strong leadership in services to support the work and whether or not GPs and other potential referrers were aware of PFMT and new referral options. In sites B and C, there were concerns that a lack of appropriate facilities may be a challenge to successful implementation.
Context–mechanism–outcome configuration 2: improving women’s health outcomes through holistic and proactive care
The intervention was also expected to improve women’s symptoms, improve quality of life and reduce the need for surgeries. This would be achieved by enabling the newly trained staff to perform more holistic assessments of urinary incontinence and pelvic health issues, and provide proactive treatment in the form of PFMT by enabling them to tailor the treatment and advice based on accurate internal assessments and by informing women of the correct PFMT technique. Whether or not these mechanisms would materialise depended on whether or not there was adequate support from the service leads and/or management in terms of ensuring that there was dedicated time for staff to deliver PFMT; whether or not there was a sufficient workforce to deliver existing and new services, and whether or not they had manageable workloads; whether or not ongoing support by specialist physiotherapy staff was available to newly trained staff; and whether or not the differential training needs of different skill mixes (e.g. nurses vs. physiotherapists) were acknowledged and addressed. In sites B and C, the staff shortages and existing staff roles and workload were expected to act as barriers to successful implementation. Worries were also expressed about the impact on the workload of the newly trained staff if the demand for the number of referrals increased as a result of greater awareness of PFMT among GPs and women.
Context–mechanism–outcome configuration 3: improving service organisation through joined-up working
The intervention was expected to improve service delivery by reducing specialist workload and shortening waiting lists. This was expected to result from more joined-up working between physiotherapy teams and nursing teams in the community and acute settings. This was possible only if there were an adequate number of staff trained to deliver PFMT and if the referral pathways were straightforward. There were some concerns that the pressure to reduce the waiting lists may actually lead to inappropriate referrals to newly trained staff, which, in turn, would increase rather than decrease the waiting times and the specialist workload.
Context–mechanism–outcome configuration 4: implementation difficulties due to role protection issues
In addition to the intended mechanisms and outcomes, the interviewees anticipated a fourth, rather unintended, mechanism that had already started to unfold and affect the implementation processes during the initial stages, leading to some undesirable outcomes. With the intervention bringing the prospect of training other skills mixes, particularly staff in the lower banding/grade, this triggered perceptions of threat to the role of practitioners specialising in pelvic health or PFMT and activated feelings of role protection among these staff. A reluctance was sensed among the specialist staff, particularly in sites A and C, to train nurses of a lower band to perform the higher-skilled tasks (e.g. deliver PFMT, which has been a specialist job), as it was felt to be causing a disservice to the specialist profession. This reluctance was also observed in the form of some ‘hostility’ at the SPMs. The feelings of role protection were said to be always present, but these were observed to resurface and intensify as a result of the PROPEL intervention. This mechanism of ‘role protection’ hindered and delayed the process of implementation in sites A and C, and prevented the adoption of a community model of PFMT delivery involving band 5 community nurses. Site A continued their service through hospital- and community-based specialist physiotherapists without making any changes to the service model, whereas site C had to abandon the plans for training nurses or physiotherapists in the community and adopted a hospital-based model involving hospital-based urogynaecology nurses.
Phase 2: testing the folk theories
The way in which the PROPEL intervention was implemented and worked in each site is presented in Tables 3–5 in the form of site-specific CMOs. These CMOs report the outcomes of the implementation that were observed in each site and attempt to explain how and why these outcomes were achieved, for whom and in what contextual conditions. The outcomes include those that were expected in the initial theories of change, as well as those unintended and unanticipated.
| Context | Actor | Mechanism | Outcome |
|---|---|---|---|
| Site A | |||
|
|
|
|
|
|
|
|
| Site B | |||
|
|
|
|
|
ANP and community nurse for continence |
|
|
|
|
|
|
|
|
|
|
| Site C | |||
|
|
|
|
|
|
|
|
|
|
|
|
| Site D (light-touch site) | |||
|
|
|
|
|
Newly trained musculoskeletal physiotherapists |
|
|
| Site E (light-touch site) | |||
|
|
|
|
| Context | Actor | Mechanism | Outcome |
|---|---|---|---|
| Site A | |||
|
|
|
|
| Specialist physiotherapists have autonomy over appointment system (can make their own appointments) |
|
|
|
| Site B | |||
|
|
|
|
|
Newly trained musculoskeletal physiotherapists and CLN |
|
|
|
|
|
|
| Site C | |||
|
|
|
|
|
|
|
|
|
|
|
|
| Site D (light-touch site) | |||
|
|
|
|
| Site E (light-touch site) | |||
|
|
|
|
| Context | Actor | Mechanism | Outcome |
|---|---|---|---|
| Site A | |||
|
|
|
|
| Site B | |||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Site C | |||
|
|
|
|
|
|
|
|
|
|
|
|
| Site D (light-touch site) | |||
|
|
|
|
| Site E (light-touch site) | |||
There was good implementation support from managers:
|
|
|
|
Phase 3: refined intervention theory – how did the PROPEL intervention work, for whom and in what contexts?
The site-specific CMOs were compared and contrasted in a cross-case analysis to develop refined theories about the intervention. At this stage, the outcomes were also mapped explicitly to the indicators of impact that were suggested by the RE-AIM framework. During this process, we classified the specific outcomes of the PROPEL intervention as being related to one of the RE-AIM framework indicator areas, and sought to explain the patterns of outcomes observed in the theory-testing phase by comparing and contrasting their linked patterns of mechanisms and of triggering contexts in different sites. We first looked for the common patterns of mechanism and outcome links and then identified the contexts in which they were contingent. In the following sections, we present the refined CMOs that represent a middle-range theory about the impact that the PROPEL intervention had, what mechanisms of action brought about that impact, for whom and in what contexts.
Reach: impact on access to pelvic floor muscle training
In the PROPEL intervention, ‘reach’ referred to the extent to which the PROPEL intervention, the delivery of PFMT by different HCPs, reached the target population that it was intended to reach. It was hypothesised that the intervention would widen the access to PFMT by increasing the awareness of and referrals to PFMT and increasing the availability of trained staff who were delivering care close to women’s homes in the community. The extent to which this was achieved following implementation of the intervention varied across the study sites, depending on the presence or absence of two key contextual factors: (1) the receptiveness of the clinical setting and (2) the level of awareness of PFMT among potential referrers. The CMOs were refined based on this knowledge and are described in the following paragraphs and illustrated in Figures 3 and 4.
FIGURE 3.
Refined CMOs explaining the impact of the PROPEL intervention on access to PFMT: role of receptiveness of service. C, context; M, mechanism; O, outcome. Reproduced with permission from Abhyankar et al. 17 This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data. The figure includes minor additions and formatting changes to the original figure.
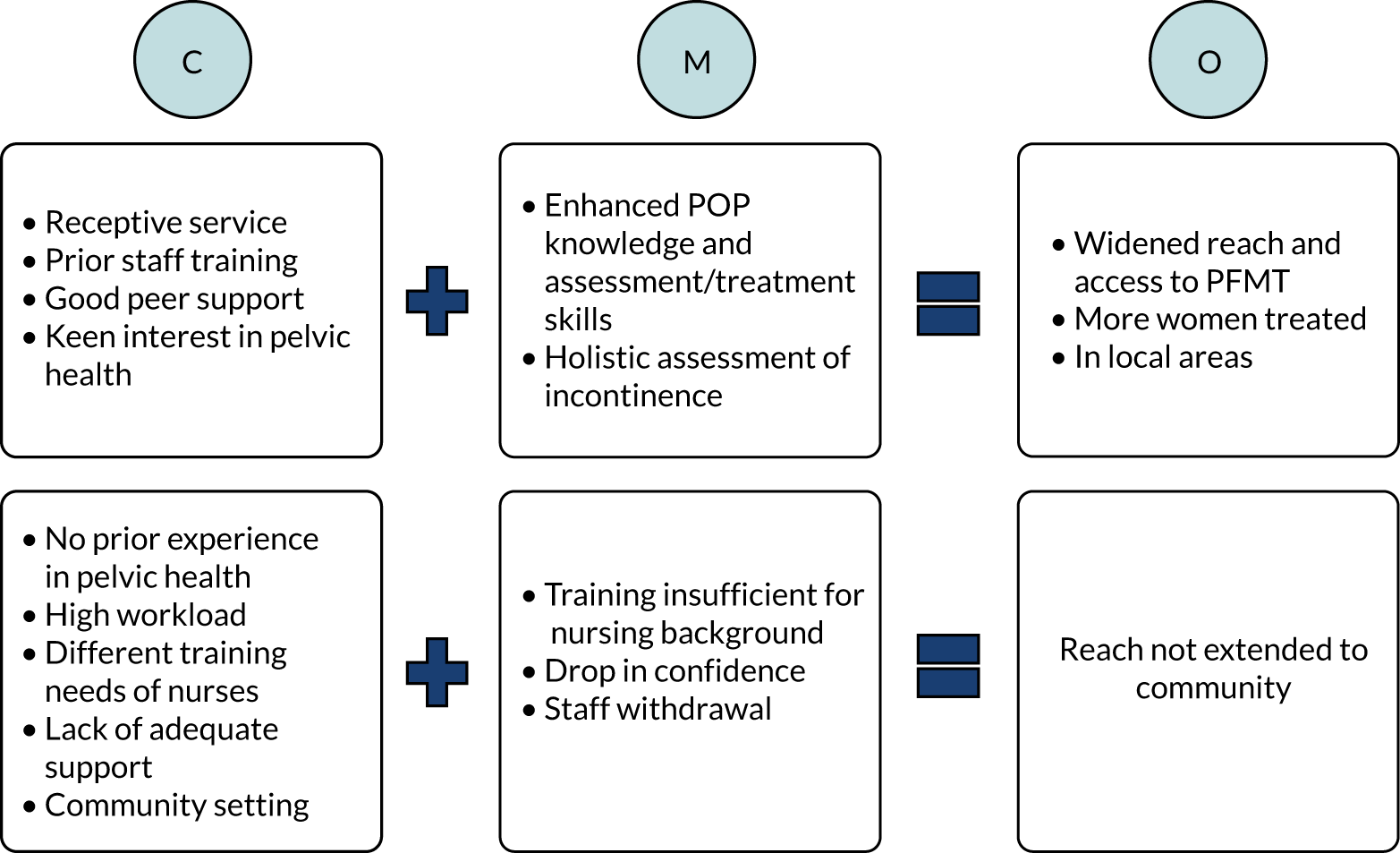
FIGURE 4.
Refined CMOs explaining the impact of the PROPEL intervention on access to PFMT: role of team’s awareness of PFMT services. C, context; M, mechanism; O, outcome. Reproduced with permission from Abhyankar et al. 17 This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data. The figure includes minor additions and formatting changes to the original figure.
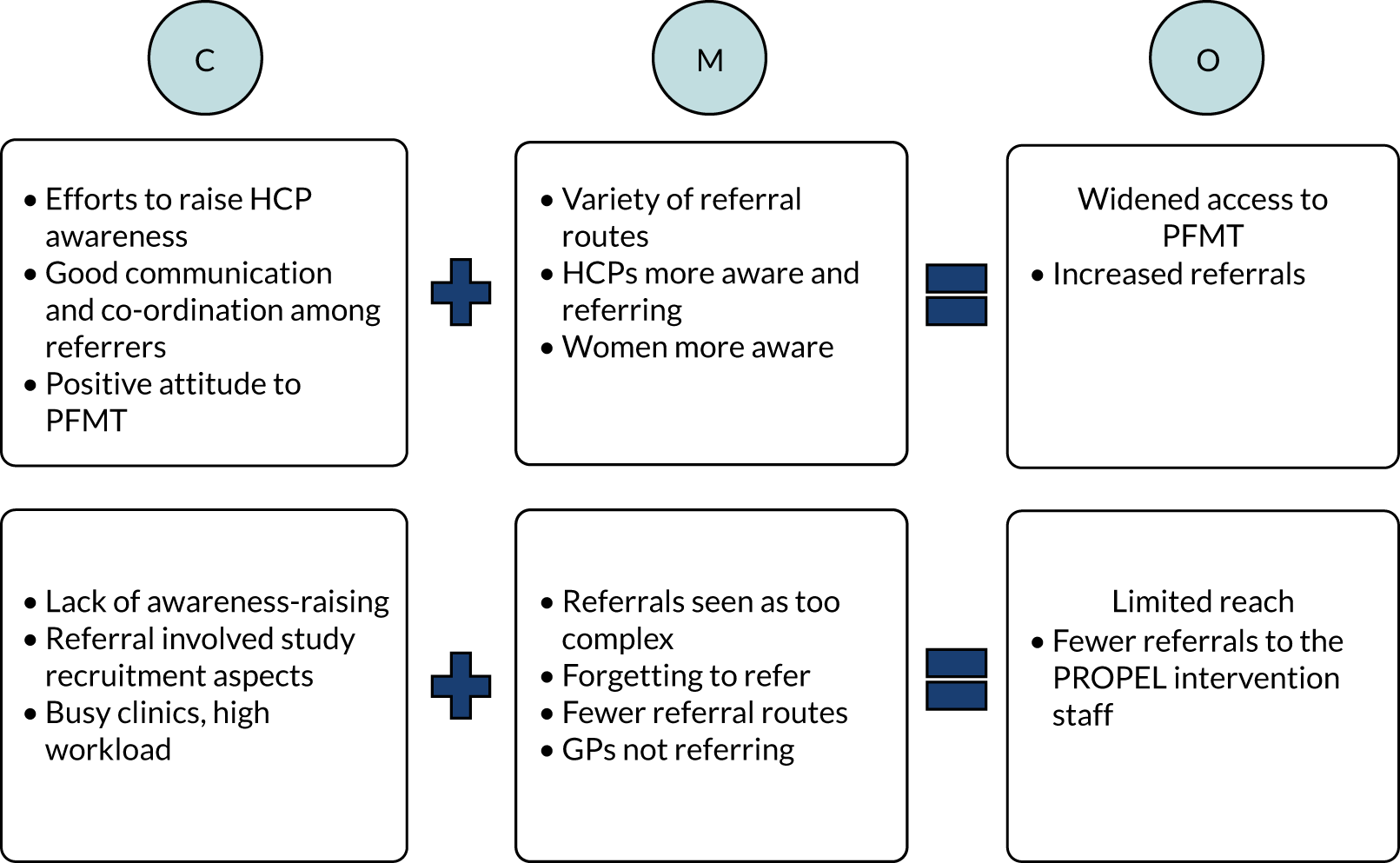
The access to PFMT widened in areas where the service was receptive to the PROPEL intervention (Figure 3). This included the staff and management having a keen interest in pelvic health issues and women’s health, the service already having started providing additional training to other staff to increase their capacity and having good peer support networks in place. This was mainly observed in the case of musculoskeletal and general physiotherapists, and some nurses. In these contexts, the PROPEL intervention training enhanced staff’s knowledge of prolapse and their skills and confidence in its assessment and treatment. The transition to doing internal assessments and PFMT was easier and faster for these skill mixes as a result of their basic physiotherapy training or continued professional development training in pelvic health assessment and management. Nursing staff who dealt with urinary incontinence extended their knowledge and skills beyond prolapse and applied this to women with incontinence and other pelvic health issues. Their enhanced knowledge led them to become more holistic in the assessment of pelvic issues and proactive in providing treatment.
However, different sets of mechanisms and outcomes were observed in the case of nurses working in the community who had no prior experience or training in pelvic health. A key underlying mechanism was low levels of adoption by community nursing staff, which was reflected in their withdrawal from the study. For the district nurse, the training was felt to be inadequate to address their knowledge and skill gap, as they did not have the level of understanding of physiology that physiotherapy training provided. This lowered their confidence and led to withdrawal from the study. For the advanced nurse practitioner for incontinence, their existing workload and a mismatch of expectations from their role led to withdrawal. The community setting was considered inappropriate for prolapse assessment and PFMT delivery; internal assessments were not feasible in people’s homes or care homes and PFMT was deemed unsuitable for older people and those with dementia, both of whom comprised the main aspect of the community nursing role. As a result, contrary to original intentions, PFMT failed to be extended to community settings.
Another reason for the difference in the reach of PFMT was the level of awareness of PFMT services among professionals who could refer women to PFMT (Figure 4). In contexts where the teams made an effort to raise other HCPs’ awareness of PFMT, there was good communication and co-ordination among referrers and there were favourable attitudes to PFMT, access to care was widened. This was because there were a variety of direct referral routes available: GPs and consultants were referring patients to these services, as well as women who were more aware of PFMT spreading the word in community. In contrast, the referrals were restricted in areas where not much effort had been made to raise awareness among potential referrers, which meant that their referral patterns remained unchanged. Referrals were also restricted because the consultants remained distant and disengaged in the PROPEL intervention, and other possible referral routes were not exploited (e.g. through urogynaecology nurses). Referral involved study recruitment, which was difficult to do in busy, short-staffed clinics. The process of referral to the PROPEL intervention was seen as being more complex than routine referrals hence it was often forgotten.
Effectiveness: impact on symptoms, quality of life and care experience
Effectiveness in the context of the PROPEL intervention was concerned with the impact of PFMT delivery by different staff skill mixes on women’s symptoms, quality of life and experience of care. It was anticipated that the PROPEL intervention would improve women’s symptoms and quality of life, and reduce the need for surgery by improving their PFMT technique, providing better tailoring of treatment and improving holistic assessment of urinary incontinence and related issues. The outcome study revealed that there was a significant improvement in outcomes after the intervention compared with before, but there were no significant differences in outcomes across the five sites and across different delivering staff and across different service models. This suggested that the outcomes were comparable regardless of which study site PFMT was delivered in, by whom and through which model. However, the staff’s and women’s perceptions of their outcomes were found to differ from the actual clinical evidence of improvement and across different sites, owing to differences in implementation processes. The refined CMOs below explain these differences in perceived outcomes (Figure 5).
FIGURE 5.
Refined CMOs explaining the impact of the PROPEL intervention on women’s health. C, context; M, mechanism; O, outcome; UI, urinary incontinence. Reproduced with permission from Abhyankar et al. 17 This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data. The figure includes minor additions and formatting changes to the original figure.

Many women and staff reported improvements in their prolapse symptoms (e.g. muscle control and strength) and incontinence problems. In some cases, the experience of improvement was greater than the clinical evidence. When improvements in symptoms were reported, the underlying mechanisms appeared to include women receiving better explanations of prolapse and the role of PFMT from the delivering staff, receiving feedback on their performance from internal assessments, provision of a tailored and structured PFMT routine, receiving advice on the correct PFMT technique and receiving techniques for exercising regularly, all of which improved women’s adherence to exercises. The reported improvements in quality of life resulted from staff enabling women’s self-management of their symptoms by offering tips and advice on lifestyle, which helped to improve women’s bladder control and increase their confidence to resume previous activities. There was an overall person-centred approach, as staff were seen as approachable and motivational, to dedicate enough time, to reduce women’s embarrassment and to make women comfortable during their visits. This resulted in a positive and satisfactory experience of care. All of the above mechanisms were triggered in contexts where the staff were adequately trained and confident, where the staff had expert support available throughout and when the referrals were appropriate for the level of care they provided.
In contrast, certain contextual factors failed to trigger the mechanisms that led to perceptions of improvement in symptoms, quality of life and care. This was particularly the case when the staff delivering PFMT were located in an acute ward setting. Both the delivering staff and the women reported less improvement in symptoms, despite the clinical improvement that was observed in the PROMs study indicating otherwise. A number of factors present in these contexts seemed to trigger certain mechanisms that led to a lesser experience of improvement. First, there was a time gap between training and PFMT delivery that led to an initial loss of confidence among delivering staff. Second, the specialist physiotherapy team was located separately and there was a lack of clarity and communication on both sides about the delivering staff’s support needs. This triggered another mechanism, whereby the staff resorted to supporting each other by doing joint clinics, which helped with care and their confidence.
Adoption: impact on service delivery
Adoption refers to the willingness of institutions and staff to implement an intervention and to support the intervention’s adoption into routine practice. In this study, one of the indicators of adoption, the uptake and continued participation (or drop out) by staff, was already reflected in the mechanism, leading to wider (or restricted) reach of PFMT to target populations. Another indicator of the extent to which the intervention was adopted into practice is the effect of the PROPEL intervention on the services in which PFMT was delivered by other skill mixes. Favourable impact on service outcomes would indicate higher levels of adoption, whereas unfavourable impact would indicate lower levels of adoption. It was hypothesised that the intervention would reduce waiting times and specialist workloads by creating more joined-up working between acute services and community services. Although there was little evidence for this mechanism in the theory-testing phase, a number of other outcomes and their underlying mechanisms ensued, for instance, to impact workloads and pressures on delivering staff, as well as their professional colleagues, the organisation and functioning of the services and the perceived support from wider team (Figure 6).
FIGURE 6.
Refined CMOs explaining the impact of the PROPEL intervention on service delivery. C, context; M, mechanism; O, outcome. Reproduced with permission from Abhyankar et al. 17 This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data. The figure includes minor additions and formatting changes to the original figure.
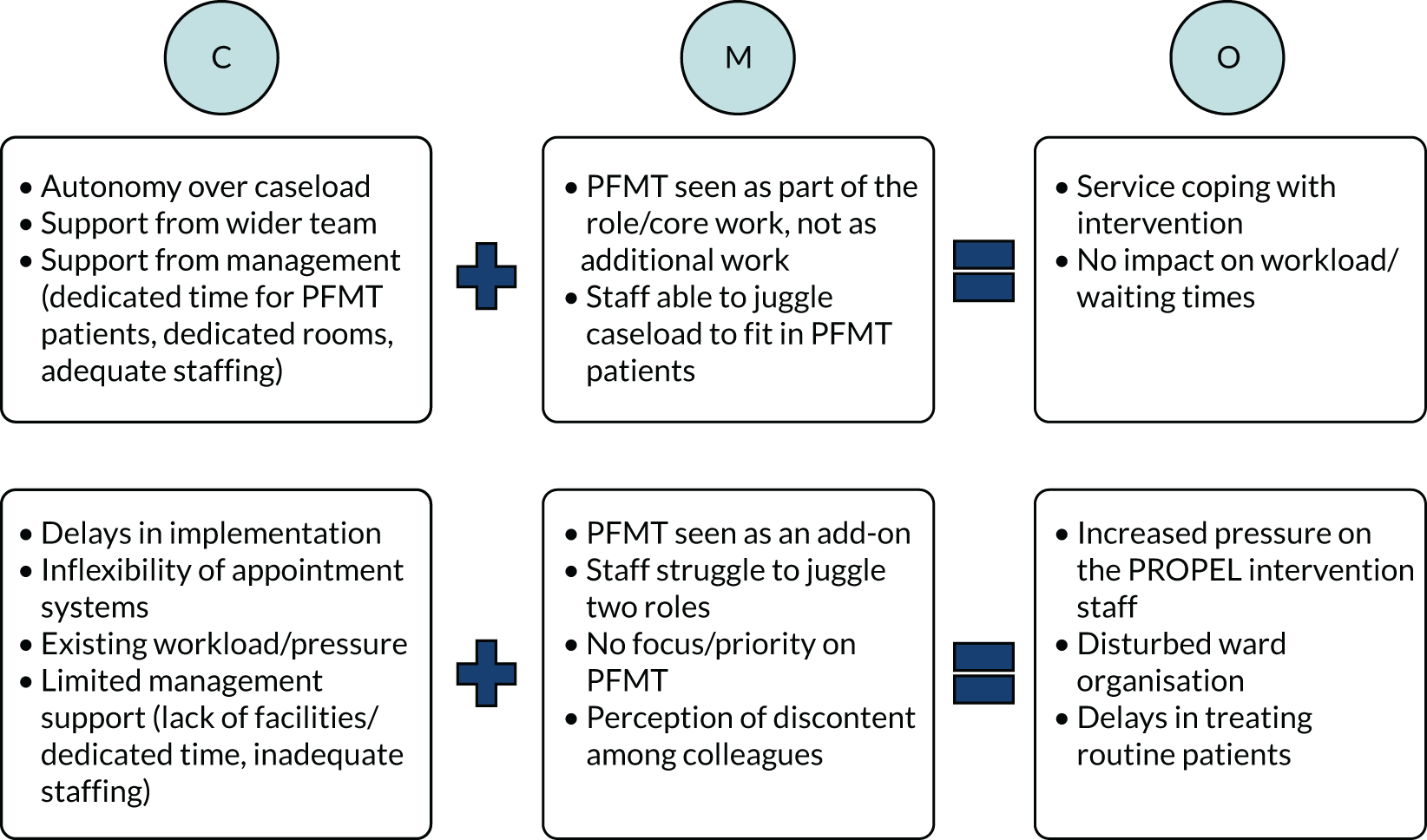
The intervention was better integrated and adopted into the routine service in some areas than in others, and had little disruptive impact on workload, service organisation or waiting times in such areas. This was observed particularly in contexts where practitioners, mainly physiotherapists and, in some settings, nurses, had some degree of autonomy over managing their bookings and caseloads and the wider team supported their involvement in PFMT delivery. Their service management also provided support by allowing dedicated time for PFMT delivery, making rooms available for assessment and treatment, and providing adequate staffing resources. This triggered the mechanism wherein PFMT was seen as part of their core role, rather than as an add-on. It also enabled the staff to juggle their own caseload to allow for the prolapse patients.
Contrary to this, service disruption was reported in some areas in the form of disturbed ward organisation, delays in treating routine patients, and increased pressure on delivering staff, particularly in the cases of nurses in the acute ward setting and the community setting. This was because PFMT delivery in these settings was seen as an add-on and not given a priority or due recognition. Staff had to juggle two roles and required additional administrative support. Team colleagues were perceived to be discontent with staff’s involvement in PFMT, as they often had to provide cover for the PROPEL intervention staff in their day jobs. This resulted in doubts about the extent to which such an intervention may be supported by the wider team. Several unfavourable factors in the context played a role in triggering these mechanisms. First, delays in implementation and inflexibility of the patient booking systems meant that slots for the PROPEL intervention patients remained unfilled during early phases and led to delays in the treatment of routine patients, as slots could not be allocated to them. Second, existing workload pressures in the service areas, as well as a lack of dedicated time for PFMT, a lack of appropriate facilities and inadequate staffing resources, put additional pressure on delivering staff.
Implementation: impact on implementation plans
Implementation refers to the extent to which the PROPEL intervention was delivered/implemented as intended by the services. During the implementation phase, the services in sites A, B and C considered and debated various models of service delivery and potential staff skill mixes, with the overall intention of widening access to PFMT in local communities. Whether or not this intention was accomplished was determined by the strength of the tendency of staff groups to protect professional roles and boundaries (which could prevent change), which was triggered in certain contextual conditions (Figure 7).
FIGURE 7.
Refined CMOs explaining the impact of the PROPEL intervention on implementation plans. C, context; M, mechanism; O, outcome. Reproduced with permission from Abhyankar et al. 17 This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data. The figure includes minor additions and formatting changes to the original figure.
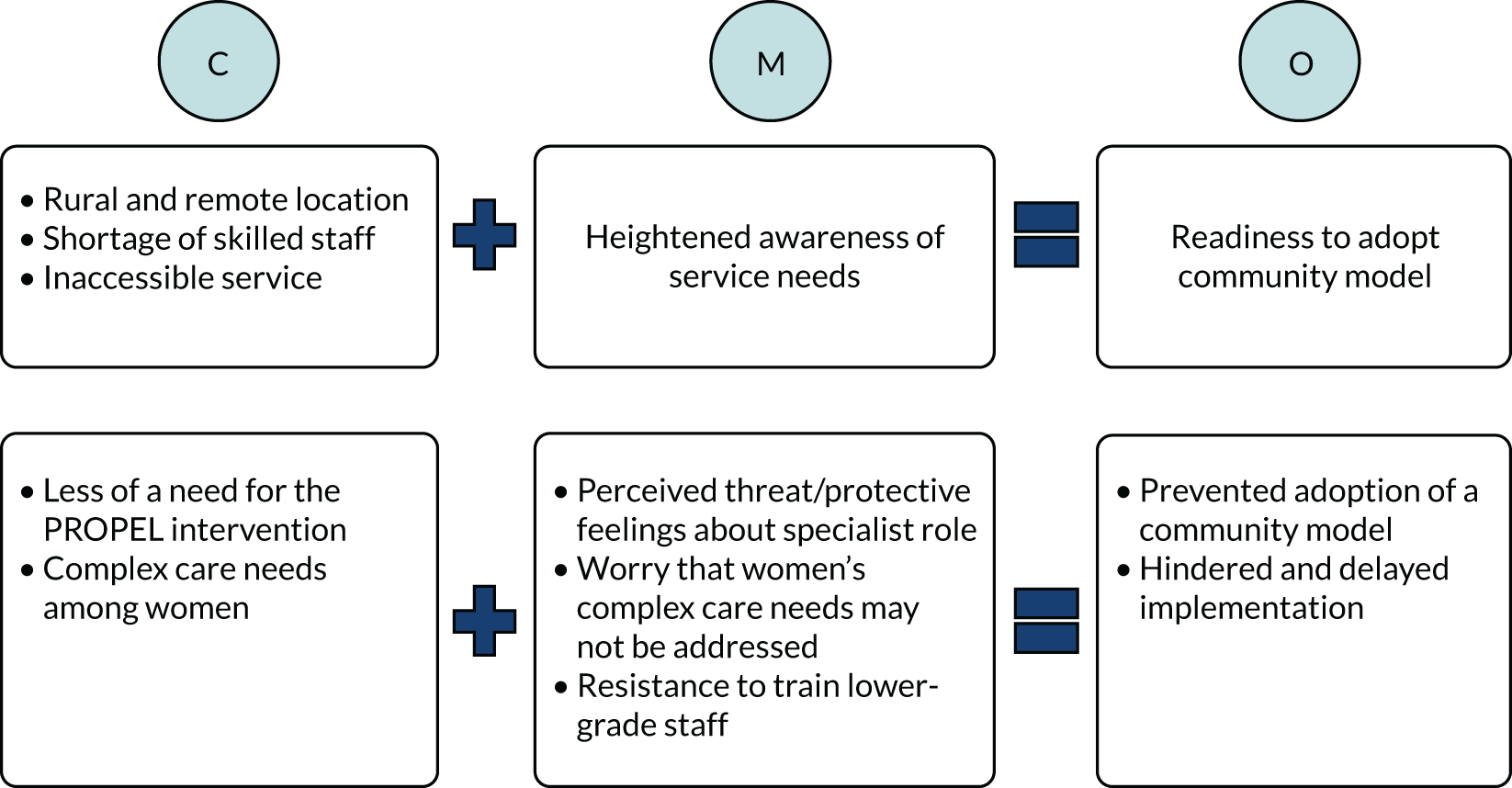
In remote and rural contexts, where there were significant staff shortages and service was inaccessible in many areas, there was heightened awareness of the service needs among the implementers, at least at the implementation stage, which led to an increased readiness to adopt a community model and train nursing staff in the community. However, in other contexts with adequate specialist capacity where there was less of a need for such an intervention, the implementers were less convinced of the requirement for the PROPEL intervention. This triggered feelings of threat to their role and protective feelings about their role among the specialist or higher-grade staff. These staff were also concerned that training lower-grade staff may not address women’s complex care needs adequately and would have a negative effect on standard of care. These feelings resulted in preventing the adoption of a community model, resistance to train lower-grade nurses and significant delays in implementation.
Summary of findings from the realist evaluation
In summary, an outcome evaluation of the PROPEL intervention, showed that women’s outcomes improved regardless of the service model and skill mix through which PFMT was delivered. The realist evaluation provided more insights into the extent to which, how and why the intervention worked (or not) in diverse contexts that differed in their geographical locations, service organisation, type of service model used, skill mix trained and availability of support structures and resources. Findings from the realist evaluation suggest that implementation of PFMT that is delivered by different clinicians in the context of the UK NHS would probably be successful if:
-
the training of PFMT delivery is adequately tailored to the needs of the different skill mix
-
there is awareness about prolapse and PFMT among women, GPs and other HCPs
-
the referral systems are open, flexible and well co-ordinated
-
there is sufficient buy-in at organisational levels and strong managerial support in terms of resources, training, time, autonomy and staffing
-
the wider team supports the delivery of PFMT through different staff skill mixes
-
the tendencies to protect professional roles and boundaries (and thereby prevent change) are acknowledged, addressed and managed effectively and balanced with the population needs.
Chapter 6 The patient-reported outcome measures study
This chapter describes the methods and results of the quantitative analysis of self-reported outcome data collected from the PROPEL intervention participants. This section of the report addresses original research questions 2 and 3.
Primary research questions
-
Does the intervention, as implemented, improve POP symptoms in women at the 6-month follow-up? (research question 2).
-
Does the effect of the intervention on POP symptoms at the 6-month follow-up differ when the intervention is delivered by specialist physiotherapists compared with when it is delivered by other HCPs? (research question 3).
Secondary research aims
-
Applying the primary research questions to POP symptoms at the 12-month follow-up (research question 2).
-
Applying the primary research questions to secondary outcomes, including other pelvic floor-related outcomes (severity of prolapse and incontinence) and service-related outcomes (number of health service contacts) (research question 2).
Study design
The study was an observational prospective cohort study that compared PROMs pre and post intervention. The PROMs study was concerned with answering the specific aims to explore the differences in clinical outcomes with the different skill mixes and to understand the variations of PFMT protocol. Furthermore, data from the PROMs study were used to establish the costs and benefits of each model.
Recruitment of patients
Women with stages I–III POP who were referred to a local service were recruited to the study. All participants were required to have an internal exam by a specialist clinician (i.e. physiotherapist, GP or consultant) to determine their eligibility for the study. Women were determined to be eligible if they met the following criteria.
Inclusion criteria
The inclusion criteria were women who:
-
were aged ≥ 18 years
-
presented with symptomatic stage I, II or III prolapse of any type and who were suitable to be referred for PFMT
-
were willing to take part in the research and comply with necessary data collection.
Exclusion criteria
The exclusion criteria were women who:
-
were pregnant or < 1 year postnatal
-
had prolapse greater than stage III
-
had pelvic cancer, cognitive impairment or neurological disease (as indicated by referral source or patient/carer reported at assessment consultation).
Outcome measures
The primary outcome measure was the Pelvic Organ Prolapse Symptom Score (POP-SS), which consists of seven items that relate to the frequency of different prolapse symptoms, each with a five-point Likert scale response set (0–4). The total is the sum of the seven questions and the possible scores range from 0 to 28, with higher scores indicating greater symptom severity. The POP-SS was treated as a continuous variable.
Secondary outcome measures consisted of two pelvic floor-related outcomes. These were (1) objective prolapse severity stage (measured using the POP-Q) (which was treated as an ordinal scale) and (2) urinary symptoms [measured using the International Consultation on Incontinence Questionnaire – Urinary Incontinence – Short Form (ICIQ–UI SF)]. 26 The ICIQ-UI SF score was calculated as the sum of the first three items (relating to frequency, volume of leakage and interference with everyday life). The ICIQ-UI SF score was treated as a continuous scale with a possible range from 0 to 21, with higher scores indicating worse symptoms.
Service-related outcomes were also included as secondary outcome measures, specifically the need for further treatment, defined as the number of NHS contacts during the follow-up period. These outcome measures were treated as count data.
Sample size
We assumed that the minimum clinically important difference in the POP-SS was 2 points and that the standard deviation (SD) of the differences in POP-SS between baseline and follow-up was 5.5 points (close to what has been observed in the POPPY trial). A sample size of 120 paired observations (with two-sided alpha = 0.05) would, therefore, provide 80% power to detect important differences in POP-SS.
Analysis methods
In research question 2, paired t-tests were conducted to compare POP-SSs at baseline with those at 6-month follow-up.
In research question 3, independent-samples t-tests were used to compare the mean change in POP-SS from baseline to 6-month follow-up in women who were seen by specialist physiotherapists with the mean change in women who were seen by other HCPs.
In addition, for research question 2, a linear mixed model was used to estimate the change in POP-SS between baseline and 6 months, adjusted for covariates. This model had ‘POP-SS’ as a dependent variable, ‘measurement time point’ as an independent variable, and ethnicity, parity, age and body mass index (BMI) change during follow-up fitted as fixed effects in the multilevel model, as well as a random effect for participant. 27
In addition, for research question 3, a linear mixed model was used to estimate the difference in change in POP-SS (from baseline to 6 months) between women treated by specialist physiotherapists and those who were treated by other HCPs, adjusted for covariates. This model had ‘change in POP-SS between baseline and follow-up’ as a dependent variable, and a factor variable for ‘professional delivering the intervention’ as an independent variable. Other covariates, for example baseline POP-SS, ethnicity, parity, age and BMI, were fitted as fixed effects in the multilevel model, along with a random effect for site. 27
The same methods were repeated for the secondary outcomes when sufficient data were available. Further tests for the presence of a dose–response relationship between the intervention and the outcomes were performed by testing for a relationship between outcomes and level of adherence. Adherence was measured as the time spent doing pelvic floor exercises during the previous month. A sensitivity analysis was also carried out to test the effect of excluding participants who had surgery during follow-up.
Participant flow
A total of 102 women were recruited to the study. Baseline questionnaires were available from 91 women, and 71 women completed the 6-month follow-up questionnaire, for whom 68 questionnaires were matched to baseline questionnaires. Seventy-two participants with baseline or 6-month follow-up questionnaires also had a clinical assessment form. Eight participants had a clinical assessment form only, and 59 participants had baseline and 6-month follow-up questionnaires plus a clinical assessment form. Participant flow is summarised in Figure 8.
FIGURE 8.
The PROMs study participant flow.
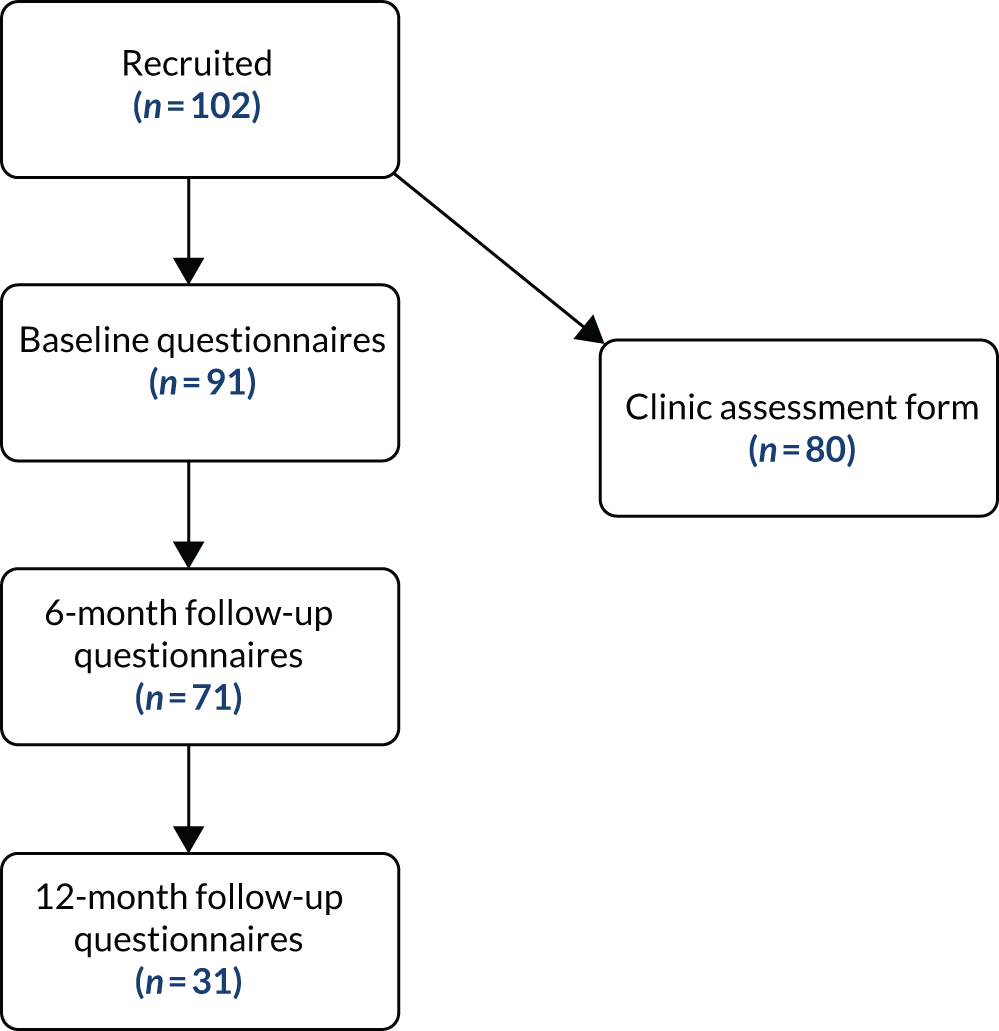
Baseline characteristics
The baseline characteristics of the sample are summarised in Tables 6 (continuous measures) and 7 (categorical measures). The ‘6 months’ and ‘12 months’ columns show the effect of missing data on the distribution of these characteristics at each follow-up point, by summarising the baseline data for those who responded only at 6 months and 12 months, respectively. Overall, the distribution of participant characteristics is stable from baseline to the 6-month follow-up.
| Variable | Baseline | 6 months | 12 months |
|---|---|---|---|
| Age (years) | |||
| Mean (SD) | 57.5 (11.5) | 59.1 (11.2) | 58.6 (12.4) |
| Range | 32.1–78.6 | 32.5–79.2 | 33.0–79.5 |
| Total (n) | 87 | 70 | 30 |
| BMI (baseline report) (kg/m2) | |||
| Mean (SD) | 27.1 (4.6) | 27.0 (4.5) | 26.6 (4.4) |
| Range | 17.9–42.6 | 17.9–42.6 | 17.9–35.6 |
| Total (n) | 76 | 58 | 24 |
| Number of months aware of having prolapse (baseline report) | |||
| Mean (SD) | 46.3 (94.6) | 43.6 (87.0) | 30.3 (47.9) |
| Range | 1–504 | 1–480 | 2–240 |
| Total (n) | 85 | 63 | 27 |
| Number of months of bothersome symptoms of prolapse (baseline report) | |||
| Mean (SD) | 23.77 (43.31) | 25.24 (49.31) | 19.62 (25.06) |
| Range | 1–324 | 1–324 | 2–120 |
| Total (n) | 82 | 62 | 29 |
| Do your prolapse symptoms interfere with physical activity? (e.g. walking, housework or exercise) 0 points (not at all) to 10 points (a great deal) (baseline report) | |||
| Mean (SD) | 4.34 (3.35) | 4.06 (3.31) | 3.52 (3.05) |
| Range | 0–10 | 0–10 | 0–10 |
| Total (n) | 90 | 67 | 31 |
| Do your prolapse symptoms interfere with social activity? (e.g. going out of the house, shopping or work) 0 points (not at all) to 10 points (a great deal) (baseline report) | |||
| Mean (SD) | 3.39 (3.33) | 3.30 (3.33) | 2.87 (3.07) |
| Range | 0–10 | 0–10 | 0–10 |
| Total (n) | 90 | 67 | 31 |
| Does your prolapse give you problems with personal hygiene? 0 points (not at all) to 10 points (a great deal) (baseline report) | |||
| Mean (SD) | 2.81 (3.16) | 2.51 (2.89) | 2.32 (2.86) |
| Range | 0–10 | 0–10 | 0–10 |
| Total (n) | 90 | 67 | 31 |
| Overall, how much do your prolapse symptoms interfere with your everyday life? 0 points (not at all) to 10 points (a great deal) (baseline report) | |||
| Mean (SD) | 4.42 (3.05) | 4.13 (3.01) | 3.52 (2.74) |
| Range | 0–10 | 0–10 | 0–10 |
| Total (n) | 90 | 67 | 31 |
| Overall, how much do your prolapse symptoms interfere with your sex life? 0 points (not at all) to 10 points (a great deal) (baseline report) | |||
| Mean (SD) | 4.21 (3.44) | 4.15 (3.27) | 4.24 (3.22) |
| Range | 0–10 | 0–10 | 0–10 |
| Total (n) | 68 | 46 | 21 |
| Variable | Baseline, n (valid %) | 6 months, n (%) | 12 months, n (%) |
|---|---|---|---|
| Ethnicity | |||
| White | 78 (97.5) | 59 (100) | 25 (100) |
| Asian | 2 (2.5) | 0 (0.0) | 0 (0.0) |
| Missing | 22 | 43 | 77 |
| Site | |||
| A | 30 (29.4) | 22 (32.4) | 6 (19.4) |
| B | 27 (26.5) | 20 (29.4) | 15 (48.4) |
| C | 8 (7.8) | 5 (7.4) | 1 (3.2) |
| D | 20 (19.6) | 10 (14.7) | 7 (22.6) |
| E | 17 (16.7) | 11 (16.2) | 2 (6.5) |
| Missing | 0 | 34 | 71 |
| Education | |||
| University or college degree | 24 (29.6) | 19 (32.2) | 8 (25.8) |
| University or college less than degree level | 21 (25.9) | 13 (22.0) | 3 (9.7) |
| Upper secondary school qualification | 8 (9.9) | 6 (10.2) | 6 (19.4) |
| Lower secondary school qualification | 15 (18.5) | 11 (18.6) | 4 (12.9) |
| None of the above | 13 (16.0) | 10 (16.9) | 4 (12.9) |
| Missing | 21 | 43 | 71 |
| Ring or pessary (baseline report) | |||
| Yes | 3 (3.3) | 2 (2.94) | 0 (0.0) |
| No | 88 (96.7) | 66 (97.1) | 31 (100) |
| Missing | 11 | 34 | 71 |
| Constipation (baseline report) | |||
| Yes | 31 (37.8) | 23 (38.3) | 10 (37.0) |
| No | 51 (62.2) | 37 (61.7) | 17 (45.9) |
| Missing | 20 | 42 | 75 |
| Chest/respiratory symptoms (baseline report) | |||
| Yes | 13 (16.0) | 8 (13.3) | 4 (14.8) |
| No | 68 (84.0) | 52 (86.7) | 23 (85.2) |
| Missing | 21 | 62 | 75 |
| Smoker (baseline report) | |||
| Yes | 7 (8.6) | 6 (10.2) | 3 (11.5) |
| No | 74 (91.4) | 53 (89.8) | 23 (88.5) |
| Missing | 21 | 43 | 76 |
| Parity | |||
| 0 | 1 (1.3) | 1 (1.8) | 0 (0.0) |
| 1 | 13 (16.5) | 11 (19.6) | 2 (8.0) |
| 2 | 38 (48.1) | 27 (48.2) | 13 (52.0) |
| 3 | 17 (21.5) | 11 (19.6) | 6 (24.0) |
| 4 | 7 (8.9) | 5 (8.9) | 4 (16.0) |
| ≥ 5 | 3 (3.8) | 1 (1.8) | 0 (0.0) |
| Missing | 23 | 46 | 77 |
Results
Primary outcome results (Pelvic Organ Prolapse Symptom Score)
The distribution of scores on the primary outcome (POP-SS) was explored visually in a histogram (Figure 9). Before intervention, that is, at baseline, there were 88 POP-SSs available. The distribution of these scores is shown in Figure 9. Similarly, the POP-SSs available at the 6-month follow-up were examined to evaluate the distribution of the scores. At 6 months post intervention, 68 POP-SSs were available. The distribution of these scores is shown in Figure 10.
FIGURE 9.
Histogram of the primary outcome, POP-SS: all baseline questionnaires.
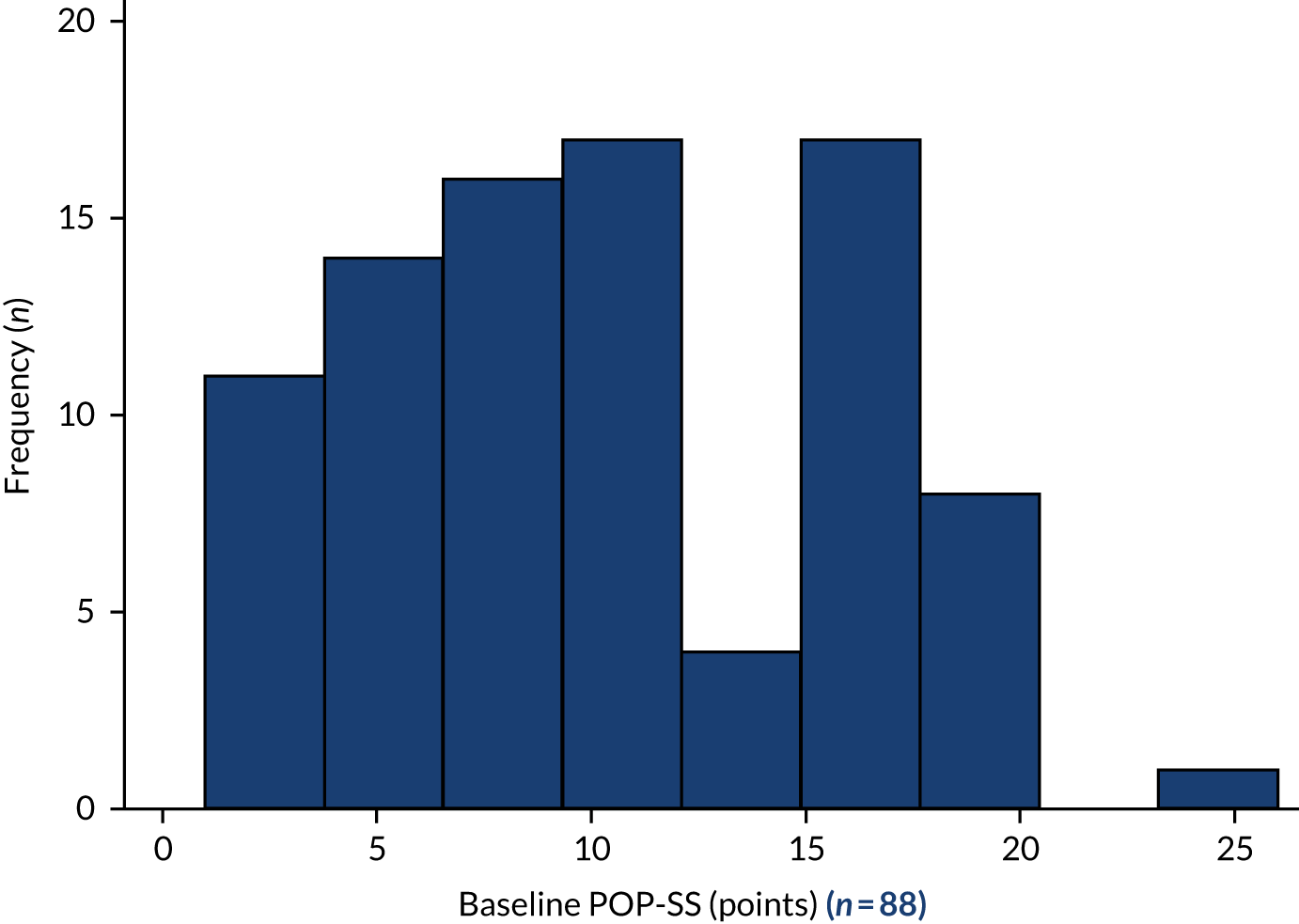
FIGURE 10.
Histogram of the primary outcome, POP-SS: full sample.

Results for women who had paired data available at baseline and 6-month follow-up
The primary comparison is between the scores at baseline and the scores at 6-month follow-up among the women for whom both sets of observations are available. There were 65 women with both baseline and 6-month POP-SSs. Initially, we examined the distribution of the scores at baseline and 6-month follow-up visually in frequency histograms (Figures 11 and 12, respectively).
FIGURE 11.
Histogram of the primary outcome, POP-SS paired data: baseline.
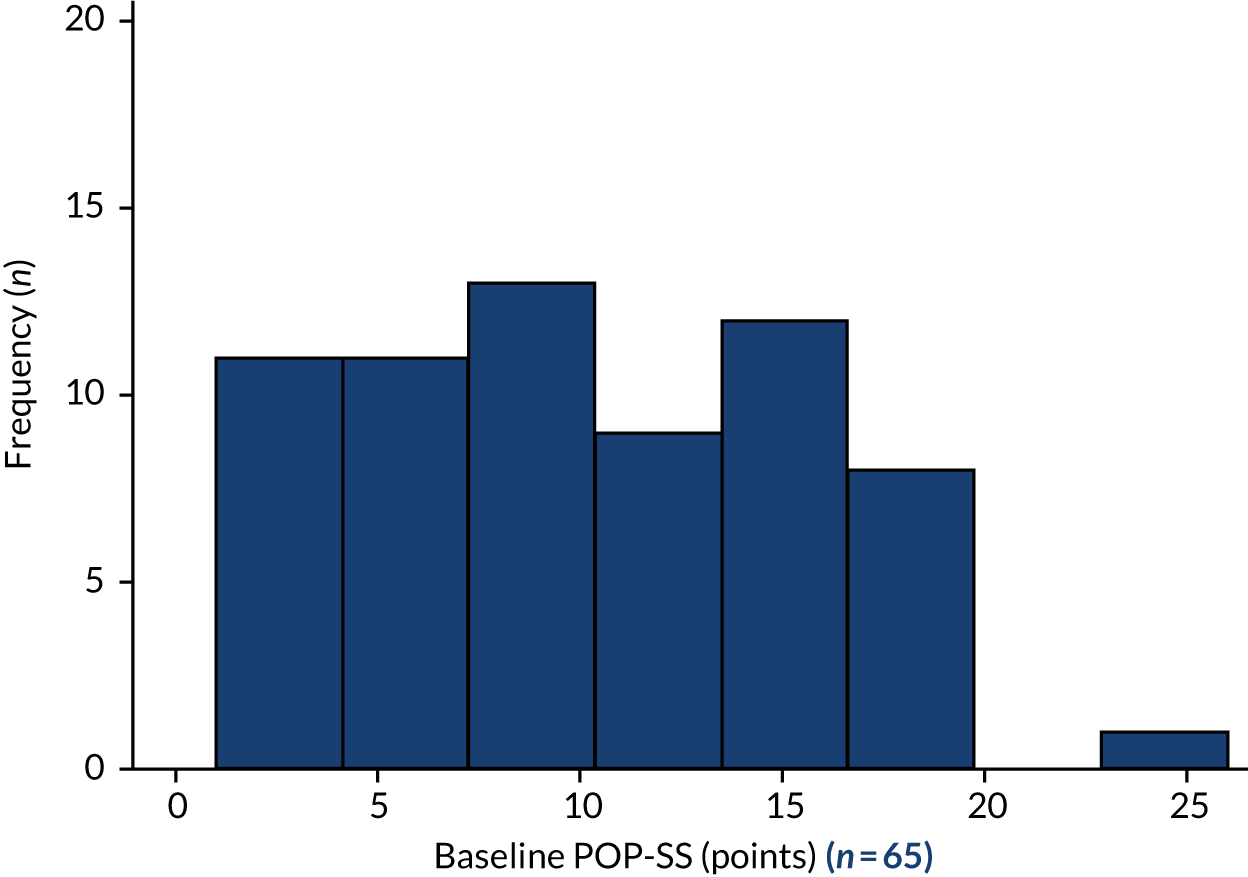
FIGURE 12.
Histogram of the primary outcome, POP-SS paired data: 6 months.
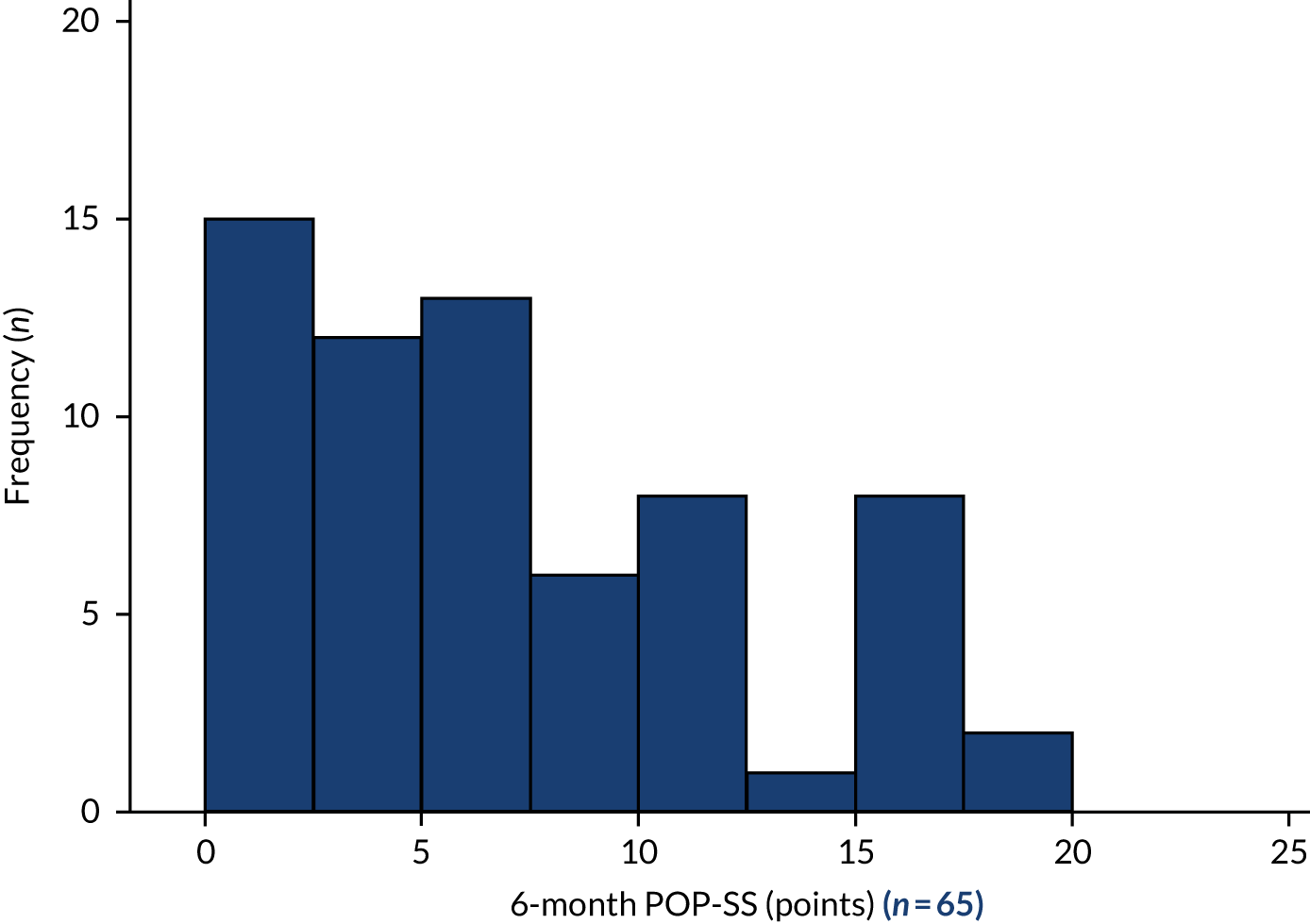
The primary quantitative research question regarding whether or not there was a significant change in the POP-SSs between baseline and 6-month follow-up (research question 2) was evaluated with a paired t-test (Table 8). A Wilcoxon matched-pairs signed-rank test was also significant (p < 0.001). Prolapse symptom severity was significantly lower at the 6-month follow-up than at baseline. The estimated difference in POP-SS between baseline and 6-month follow-up is 3.20 points [95% confidence interval (CI) 2.00 to 4.40 points].
| Variable | n | Mean | Standard error | SD | 95% CI | Paired means t-test |
|---|---|---|---|---|---|---|
| POP-SS (points) at baseline | 65 | 10.18 | 0.70 | 5.63 | 8.79 to 11.58 | t = 5.3142, df = 64; p < 0.001 |
| POP-SS (points) at 6 months | 65 | 6.98 | 0.65 | 5.23 | 5.69 to 8.28 | |
| Difference (points) | 65 | 3.20 | 0.60 | 4.85 | 2.00 to 4.40 |
Estimating the effects of the intervention from the mixed-effects model
The effect of the intervention was also evaluated with linear mixed models (Table 9). Linear mixed models allow computation of appropriate standard errors for correlated, repeated-measures data and estimate subject-specific conditional effects with adjustment for covariates. 27 The first model had POP-SS as a dependent variable and time as an independent variable (baseline vs. 6-month follow-up). That is, the coefficient for ‘time (baseline vs. 6 months)’ in the model estimates the conditional difference in means on the POP-SS between baseline and 6-month follow-up. A random effect of participant was included in the model to control for repeated measures. The second model also included parity and age, as assessed at baseline, and BMI, as measured at baseline and 6-month follow-up. The third model included ethnic group. A second random effect of site was also tested in the models; however, the effect was not significant and so was dropped and is not included in the results presented. We recognise that the degrees of freedom (df) in the described models are very low. The models are presented for illustration only, as they were part of the planned analysis. The estimated effect is very similar to the paired t-test, which estimated the treatment effect as a 3.20-point improvement in POP-SS, and here the fully adjusted model estimates the effect as a 3.48-point improvement.
| Variable | Coefficient (95% CI) | ||
|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |
| Time (effect of the intervention) | –3.34 (–4.46 to –2.22) | –3.50 (–4.96 to –2.06) | –3.48 (–4.93 to –2.04) |
| Parity (baseline) | 1.03 (–0.04 to 2.10) | 0.88 (–0.23 to 2.00) | |
| BMI (change from baseline) | 0.11 (–0.15 to 0.38) | 0.11 (–0.15 to –0.38) | |
| Age (baseline) | –0.01 (–0.10 to 0.12) | 0.01 (–0.10 to 0.13) | |
| Ethnic group: white | 0 | ||
| Ethnic group: Asian | 6.80 (–3.86 to 17.45) | ||
| Ethnic group: missing | 1.21 (–2.47 to 4.88) | ||
| Random effect of participant estimate | 16.34 (10.60 to 25.18) | 14.42 (8.07 to 25.76) | 13.79 (7.68 to 24.76) |
| Total (n) | 91 | 56 | 56 |
Next, we began to explore the second research question by examining how the baseline POP-SSs varied by site (Table 10). The mean POP-SSs ranged from 9.57 points (SD 5.52 points) in site E to 15.71 points (SD 3.25 points) in site C.
| Site | Total patients (n) | Baseline POP-SS, mean (SD) | 6-month follow-up POP-SS, mean (SD) | Mean difference (95% CI) |
|---|---|---|---|---|
| A | 22 | 10.50 (5.95) | 6.55 (4.34) | –3.95 (–6.11 to –1.80) |
| B | 19 | 9.16 (5.00) | 6.53 (5.54) | –2.63 (–5.28 to 0.02) |
| C | 5 | 16.00 (2.74) | 12.2 (3.63) | –3.80 (–6.49 to –1.11) |
| D | 10 | 9.90 (5.63) | 6.40 (4.93) | –3.50 (–7.67 to 0.67) |
| E | 9 | 8.67 (6.22) | 6.78 (6.92) | –1.89 (–4.67 to 0.89) |
Table 10 indicates that the effect of the intervention is significant when considering either site A or site C alone only. This analysis, however, does not allow us to compare effects across sites. The comparison by site was conducted in a general linear model. POP-SS at 6 months was the dependent variable. The effect was estimated by an interaction term between ‘site’ and ‘baseline POP-SS’. The interaction term and the main effect of ‘site’ were not statistically significant. That is, we cannot reject the null hypothesis of no difference in effect of the intervention between sites. This result was expected, given that the study was not powered to detect between-site differences.
Comparison of intervention delivery by specialist physiotherapists versus delivery by other health-care professionals
The second quantitative research question (research question 3) concerned whether or not the effect of the intervention varied according to whether it was delivered by specialist physiotherapists or other HCPs. The sample was divided into two groups: women who were seen by specialist physiotherapists and women seen by another HCP. The difference in the change in POP-SS between baseline and 6-month follow-up was compared between the two groups; the results are shown in Table 11.
| Group | Total (n) | Mean change in POP-SS (points) from 0 to 6 months | Standard error | SD | 95% CI |
|---|---|---|---|---|---|
| Seen by specialist physiotherapist | 22 | –3.95 | 1.03 | 4.86 | –6.11 to –1.79 |
| Seen by other HCP | 43 | –2.81 | 0.74 | 4.86 | –4.31 to –1.32 |
| Combined | 65 | –3.20 | 0.60 | 4.85 | –4.40 to –2.00 |
| Difference | 1.14 | 1.27 | –1.41 to 3.69 |
There is no evidence to reject the null hypothesis of there being no difference between the intervention delivered by specialist physiotherapists and the intervention delivered by other HCPs. In the mixed-effect model, the effect of ‘being seen by a specialist’ was not significant before and after adjustment of covariates and random effect of centre.
Secondary research questions
The Pelvic Organ Prolapse Symptom Score at 12 months
The difference in the mean POP-SS between baseline and 12-month follow-up was assessed using a paired-samples t-test (Table 12). At the 12-month follow-up, POP-SSs were available for 30 women only. The scores at 12-month follow-up were, on average, significantly lower than those at baseline, with a difference over time of 2.73 points (95% CI 0.99 to 4.48 points; p = 0.003).
| Variable | Total (n) | Mean | Standard error | SD | 95% CI |
|---|---|---|---|---|---|
| Baseline POP-SS (points) | 30 | 9.70 | 1.00 | 5.48 | 7.65 to 11.75 |
| 12-month follow-up POP-SS (points) | 30 | 6.97 | 0.92 | 5.05 | 5.08 to 8.85 |
| Difference (points) | 30 | 2.73 | 0.85 | 4.68 | 0.99 to 4.48 |
International Consultation on Incontinence Questionnaire – Urinary Incontinence Short Form at 6 months
Table 13 summarises the change in the ICIQ-UI SF score from baseline to 6-month follow-up. Paired data were available for ICIQ-UI SF scores for 39 women at baseline and 6-month follow-up. The change in ICIQ-UI SF score is also significant between baseline and 6-month follow-up (p = 0.0028).
| Variable | Total (n) | Mean | Standard error | 95% CI | Paired means t-test |
|---|---|---|---|---|---|
| Baseline ICIQ-UI SF score | 39 | 7.77 | 0.53 | 6.69 to 8.84 | t = –3.1947, df = 38; p = 0.0028 |
| 6-month follow-up ICIQ-UI SF score | 39 | 6.23 | 0.51 | 5.20 to 7.26 |
Stage of prolapse (Pelvic Organ Prolapse Quantification System) at 6-month follow-up
There were 34 POP-Q scores available at baseline and 27 POP-Q scores available at the 6-month follow-up. From these scores, most women were deemed to be at stage II of prolapse. At baseline, eight women (23.5%) were at stage I, 25 women (73.5%) were at stage II and one woman (2.9%) was at stage III of prolapse. At the 6-month follow-up, 12 women (44.4%) were at stage I, 14 women (51.9%) were at stage II and one woman (3.7%) was at stage III of prolapse.
There were 26 women with a POP-Q score at both baseline and 6-month follow-up. A Wilcoxon matched-pairs signed-rank test was used to test the equality of the distributions at baseline and at 6-month follow-up; there was no significant difference between the distributions (p = 0.0956).
Number of visits to a health-care professional
Figure 13 shows the distribution of health-care visits in the 6 months before baseline; there was a mean of 1.76 visits (SD 1.40 visits, range 0–10 visits, n = 85 participants).
FIGURE 13.
Graph of the distribution of health-care visits 6 months before baseline.
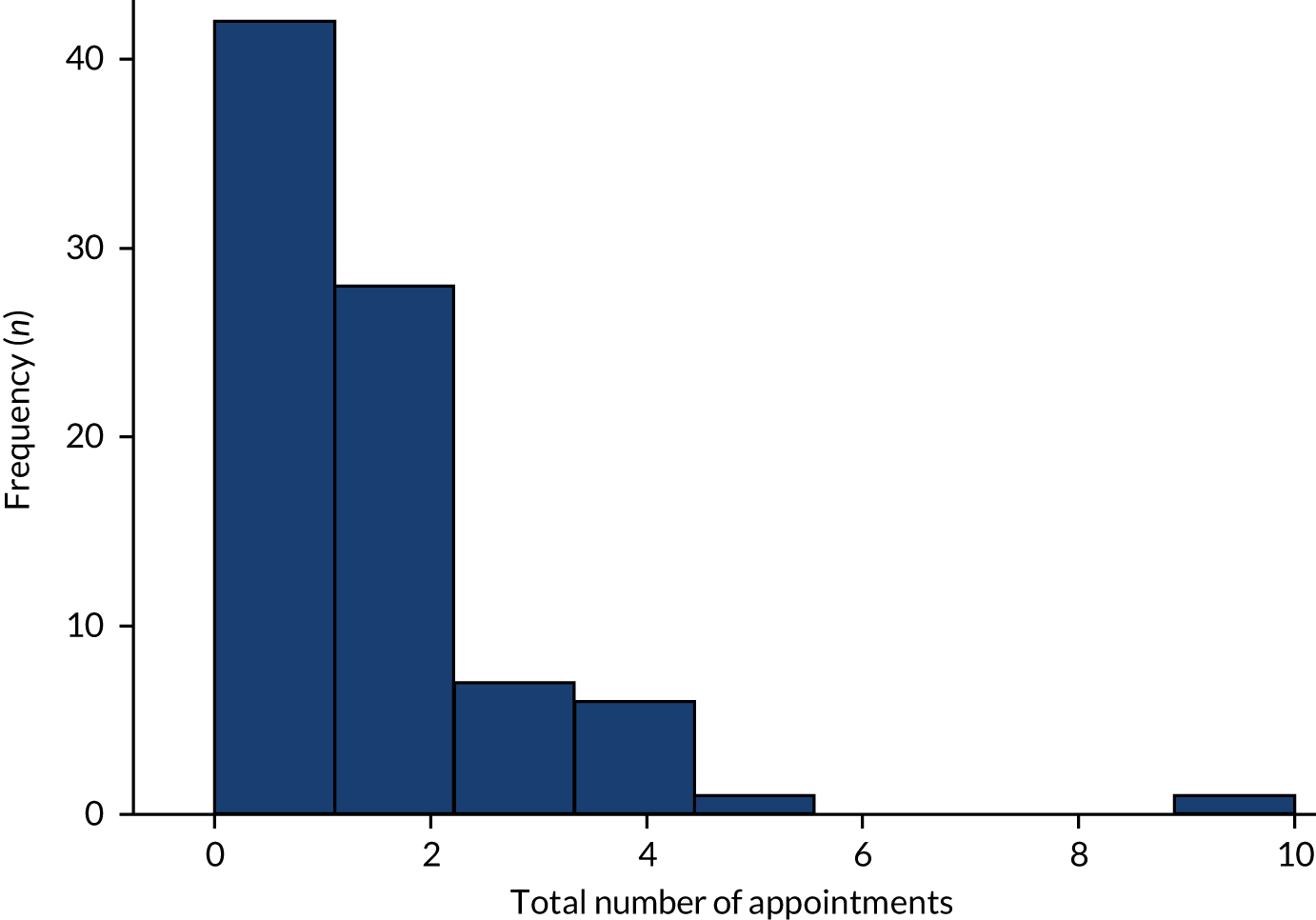
The mean number of health-care visits in the 6 months between baseline and 6-month follow-up was 0.92 visits (SD 1.33 visits, range 0–4 visits, n = 65 participants) (Figure 14). The distribution of the count of health-care visits is not normally distributed; therefore, a non-parametric matched-samples test was employed to test the difference in distributions between baseline and the 6-month follow-up.
FIGURE 14.
Number of GP and nurse appointments between baseline and the 6-month follow-up questionnaire.
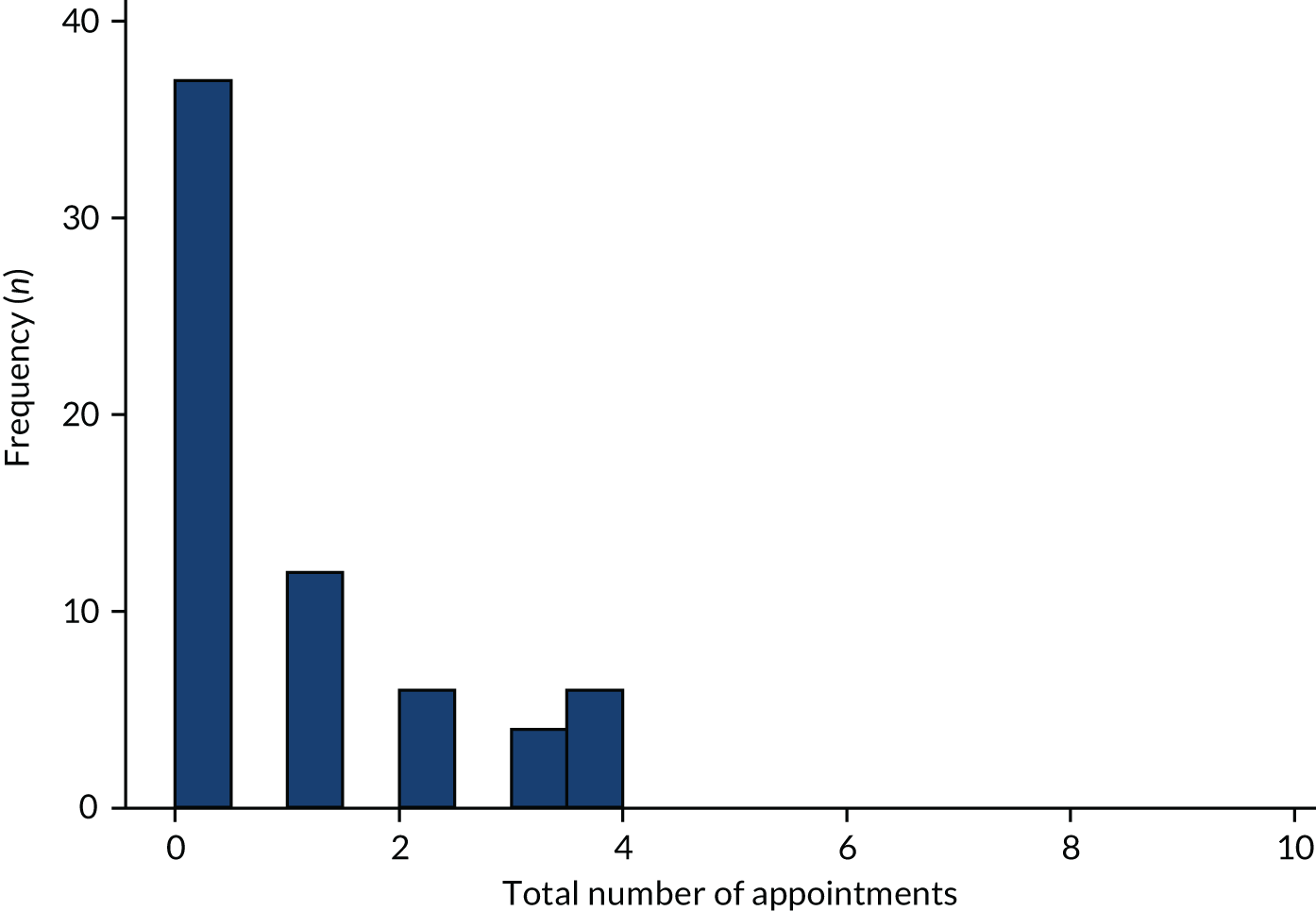
Table 14 summarises the number of appointments for women with paired data before and after the intervention (n = 59). There was a significant reduction in the number of health-care visits after the start of the intervention (Wilcoxon signed-rank test z = 3.663; p < 0.001).
| Appointments by period | Total (n) | Mean (SD) | Median (IQR) | Range |
|---|---|---|---|---|
| Total appointments in the 6 months prior to baseline | 59 | 1.73 (1.51) | 2 (1–2) | 0–10 |
| Total appointments between baseline and 6-month follow-up | 59 | 0.96 (1.36) | 0 (0–2) | 0–4 |
Association between adherence and prolapse symptoms
Adherence was assessed as the self-reported frequency of performing pelvic floor exercises. At the 6-month follow-up, one woman (1.45%) reported that she did not do pelvic floor exercises, two women (2.90%) reported that they did them a few times per month, one woman (1.45%) did them a few times per week, six women (8.70%) did them once per week, 10 women (14.49%) did them once per day and 49 women (71.01%) reported that they did pelvic floor exercises a few times per day.
Most women reported performing pelvic floor exercises a few times per day. We compared the change in the POP-SS from baseline to 6-month follow-up between women who performed pelvic floor exercises a few times per day and women who performed pelvic floor exercises less frequently (i.e. once per day or less); we found no evidence of a difference between these groups. The mean change in the POP-SS for those performing exercises a few times per day (n = 49) was a reduction of 3.75 points, and the mean change in those performing pelvic floor exercise less frequently (n = 19) was a reduction of 2.05 points. This was not a statistically significant difference, as determined by an independent-samples t-test (t = 1.2642, df = 61; p = 0.2110). The non-parametric correlation between the pelvic floor exercise frequency and the change in POP-SS between baseline and 6-month follow-up is also not significant (Spearman’s rho = –0.135; p = 0.2912).
Sensitivity analyses
In total, four women reported having surgery between baseline and the 6-month follow-up, and three women had a pessary. The primary outcome analysis was repeated with these cases excluded as a sensitivity analysis. Table 15 shows the result of a paired t-test comparing before scores with after scores on the POP-SS, with the women who had treatment (i.e. surgery or pessary) in the 6 months after baseline excluded. The result remains statistically significant.
| Variable | Total (n) | Mean | Standard error | SD | 95% CI |
|---|---|---|---|---|---|
| Baseline POP-SS (points) | 58 | 10.17 | 0.76 | 5.77 | 8.66 to 11.69 |
| 6-month follow-up POP-SS (points) | 58 | 7.03 | 0.71 | 5.37 | 5.62 to 8.45 |
| Difference (points) | 58 | 3.14 | 0.67 | 5.09 | 1.80 to 4.48 |
Chapter 7 The POPPY trial participant data linkage study
This chapter describes the long-term follow-up of participants in the POPPY trial by linking participants’ trial data with hospital admissions data.
Methodology
Brief description of the POPPY trial/sample
The multicentre randomised POPPY trial showed PFMT to be an effective treatment for POP. The current analysis examines the follow-up data on secondary care usage for trial participants in Scotland (n = 293 women).
Primary research question (research question 5)
Are women who were randomised to the POPPY trial intervention in Scotland less likely to receive further secondary care treatment related to their prolapse during the follow-up period than women who were randomised to the control group?
Trial design
The trial was a parallel-group, multicentre, randomised controlled trial with data linkage follow-up.
Linkage approval process
An application was made to the Public Benefit and Privacy Panel for Health and Social Care in 2017. Following a Tier 1 review (April 2017), the application was initially referred for a Tier 2 (out-of-meeting review) review but was subsequently referred to a Tier 2 panel (November 2017) that required the PI to attend this meeting to respond to questions. Approval was obtained from the Tier 2 Public Benefit and Privacy Panel (PBPP Application 1617-0049/Semple: Using linked data to follow up longer-term outcomes of POPPY trial participants) in January 2018. NHS National Services Scotland’s eDRIS then carried out the linkage of the POPPY trial data with the SMR0028 and SMR0129 data sets (Scottish Morbidity Records for outpatients and inpatients, respectively). Anonymised linked data files were made available for analysis via the National Safe Haven.
Linked data set
The data set contained International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10)30 diagnosis codes, Office of Population Censuses and Surveys Classification of Interventions and Procedures (OPCS)31 procedure codes and the time since randomisation for any outpatient attendances, day cases or inpatient episodes with at least one of the following diagnosis or procedure codes relating to pelvic floor disorders:
-
pelvic organ prolapse diagnosis (N81 Female genital prolapse or N99.3 Prolapse of vaginal vault)
-
urinary incontinence diagnosis (N39.3 Stress UI, N39.4 Overflow/Reflex/Urge UI or R32 Unspecified UI including enuresis)
-
faecal incontinence diagnosis (K62.2 Anal prolapse, K62.3 Rectal prolapse or R15 Faecal incontinence)
-
pelvic organ prolapse procedure [P18 Other obliteration of vagina including colpocleisis, P22-P24 Vaginal prolapse and vault repairs, P26 Introduction of supporting pessary into vagina, Q07-Q08 Excision of uterus or Q54 Operations on other ligament of uterus (including uterine suspension)]
-
urinary incontinence procedure (M51-M58 Operations to support outlet of female bladder)
-
faecal incontinence procedure (A70 Neurostimulation of peripheral nerve or H57 Other operations on the anal sphincter to control continence).
Primary outcome
The primary outcome measure was the occurrence of any related secondary care treatment for pelvic floor disorders during follow-up, using routinely collected individually linked hospital episode data (defined as OPCS4 procedure code P18, P22-P24, P26, Q07-Q08, Q54, M51-M58, A70 or H57 as main operation or other operation or ICD-10 diagnosis code N81, N99.3, N39.3, N39.4, R32, K62.2, K62.3 or R15 as main or other condition). The primary outcome measure was expressed as a binary variable.
Secondary outcomes
Secondary outcome measures included the participant receiving a related operation, the participant receiving treatment specifically for prolapse, the participant experiencing urinary incontinence and faecal incontinence, the participant receiving a pessary or neurostimulation, and the time to first treatment. All outcomes were treated as binary variables, with the exception of the time-to-event outcome.
Timing of the study outcome assessments
The follow-up period was from initial randomisation to the original POPPY trial on 26 September 2007 to the date of data linkage (May 2018), that is approximately 11 years. Randomisation date was recorded with reduced precision in the linked data set to prevent re-identification of participants.
Statistical analysis
Baseline patient characteristics were reported. Categorical data were presented using counts and percentages and continuous data were presented using the number of patients, mean, median, SD, minimum, maximum and interquartile range, as appropriate. The variables included:
-
age – categorised as 25–44 years, 45–64 years, or 65–79 years
-
parity – number of births at baseline
-
BMI – at baseline
-
prolapse symptom severity (POP-SS) at baseline
-
stage of prolapse (POP-Q), categorised as stage I, II or III
-
motivation for prolapse surgery, levels 1 and 2
-
intervention status at baseline for the POPPY trial – physiotherapy (PFMT) or control (lifestyle advice leaflet).
Mixed-effects logistic regression was conducted to estimate treatment effects [odds ratios (ORs) and 95% CIs], with the binary outcome measure as the dependent variable and the intervention group status as the binary independent variable. Analyses were adjusted for the same variables as used in the original POPPY trial analysis [baseline symptom severity (POP-SS), prolapse stage (POP-Q) and motivation for prolapse surgery]. In addition, treatment centre was included as a random effect and age group was included as an additional covariate, because over an 11-year follow-up period the effect of age may increase. Cox regression was used to analyse time-to-event data. A sensitivity analysis of the primary outcome was conducted to examine the effect of missing data.
Results
The baseline characteristics of participants included in the analysis are summarised in Tables 16 and 17. The distribution of characteristics is similar to that of the full POPPY trial sample.
| Variable | Intervention (physiotherapy), n (%) | Control (lifestyle advice leaflet), n (%) | Total, n (%) |
|---|---|---|---|
| Status of surgery | |||
| 1 | 18 (12.1) | 15 (10.4) | 33 (11.3) |
| 2 | 131 (87.9) | 128 (89.6) | 259 (88.7) |
| Stage of prolapse | |||
| I | 18 (12.1) | 17 (11.8) | 35 (12.0) |
| II | 107 (71.8) | 108 (75.0) | 215 (73.4) |
| III | 24 (16.1) | 19 (13.2) | 43 (14.7) |
| Age group (years) | |||
| 25–44 | 20 (13.4) | 23 (16.0) | 43 (14.7) |
| 45–64 | 92 (61.7) | 91 (63.2) | 183 (62.5) |
| 65–79 | 37 (24.8) | 30 (20.8) | 67 (22.9) |
| Parity | |||
| 0 or 1 | 19 (12.8) | 15 (10.4) | 34 (11.6) |
| 2 | 70 (47.0) | 59 (41.0) | 129 (44.0) |
| 3 | 41 (27.5) | 49 (34.0) | 90 (30.7) |
| 4 | 17 (11.4) | 17 (11.8) | 34 (11.6) |
| Missing | 2 (0.7) | 4 (2.8) | 6 (2.1) |
| Total | 149 (50.9) | 144 (49.1) | 293 (100) |
| Variable | Intervention (physiotherapy) | Control (lifestyle advice leaflet) | Total (n) |
|---|---|---|---|
| BMI | |||
| Total (n) | 144 | 135 | 279 |
| Mean | 27.3 | 27.2 | |
| SD | 4.9 | 4.4 | |
| Range | 17.4–46.1 | 20.2–41.0 | |
| Months of bother | |||
| Total (n) | 131 | 128 | 259 |
| Mean | 22.4 | 22.0 | |
| SD | 33.4 | 35.9 | |
| Range | 0–192 | 1–240 | |
| Prolapse symptom severity (POP-SS) | |||
| Total (n) | 142 | 135 | 277 |
| Mean | 10.5 | 10.1 | |
| SD | 6.0 | 5.8 | |
| Range | 0–28 | 0–27 | |
During the follow-up period, 15 participants (5%) died (Table 18). The mortality rate was 5% in both groups.
| Variable | Intervention (physiotherapy), n (%) | Control (lifestyle advice leaflet), n (%) | Total, n (%) |
|---|---|---|---|
| Alive | 141 (94.6) | 137 (95.1) | 278 (94.9) |
| Died | 8 (5.4) | 7 (4.9) | 15 (5.1) |
| Total | 149 (100) | 144 (100) | 293 (100) |
Women receiving treatment during follow-up
The overall proportion of women receiving any treatment was 48.1% (141/293): 43.6% (65/149) in the intervention group and 52.8% (76/144) in the control group (Table 19). This corresponds to a number needed to treat of 11; that is, 11 women would need to receive the physiotherapy intervention in order to prevent one further treatment during follow-up.
| Variable | POP-SS imputed at median (n = 293), OR (95% CI) | Complete case (n = 277), OR (95% CI) | p-value for imputed |
|---|---|---|---|
| Intervention | 0.61 (0.37 to 0.99) | 0.59 (0.36 to 0.98) | 0.047 |
| Prolapse symptom severity | 1.05 (1.00 to 1.09) | 1.05 (1.00 to 1.10) | 0.037 |
| Status of surgery | 0.53 (0.24 to 1.19) | 0.53 (0.23 to 1.21) | 0.126 |
| Stage of prolapse: II (reference category stage I) | 2.03 (0.90 to 4.66) | 1.89 (0.82 to 4.35) | 0.091 |
| Stage of prolapse: III (reference category stage I) | 3.00 (1.07 to 8.41) | 2.84 (1.00 to 8.07) | 0.036 |
| Age band 45–64 years (reference category < 45 years) | 1.82 (0.86 to 3.86) | 1.95 (0.90 to 4.22) | 0.116 |
| Age band 65–79 years (reference category < 45 years) | 4.62 (1.90 to 11.36) | 4.99 (1.97 to 12.62) | 0.001 |
The mixed-effects logistic regression on ‘any treatment during follow-up’ (primary outcome measure) with adjustment for baseline prolapse symptom severity, motivation for prolapse surgery, age group and prolapse stage, with a random effect of centre and missing prolapse symptom severity imputed at median, estimates a significant treatment effect (OR 0.61, 95% CI 0.37 to 0.99; p = 0.047). The estimated parameters from the model are shown in Table 19.
The likelihood ratio test for the mixed-effects logistic regression model compared with a model with fixed effects only (likelihood ratio test χ2 = 2.74; p = 0.0489) indicated that the random effect of centre is required. The 95% CI for the coefficient for the effect of the intervention does not include zero; therefore, the effect of the intervention is statistically significant and is associated with a reduction in the log-odds of any treatment during follow-up. The adjusted OR of 0.61 corresponds to a relative risk reduction of 0.80, indicating that the probability of the need for further treatment is 20% lower in the group receiving the physiotherapy intervention than in the control group after adjustment for covariates.
The sample is relatively small; therefore, missing POP-SS values were imputed at the median. The complete-case analysis is shown for comparison in Table 19.
Women receiving conservative treatment during follow-up
The rates for conservative treatment (defined as receiving either a pessary or a neurostimulation in either an outpatient or an inpatient setting) were 12.8% in the intervention group and 16.7% in the control group. There was no difference between groups (χ2 = 0.896; p = 0.344) and the linear mixed model (Table 20) corroborates this finding, by estimating an OR of 0.66 (95% CI 0.33 to 1.33; p = 0.244). There is no evidence that the intervention reduced the need for conservative treatment during follow-up.
| Variable | OR (95% CI) | p-value |
|---|---|---|
| Intervention | 0.66 (0.33 to 1.33) | 0.244 |
| Prolapse symptom severity score at baseline (missing imputed at median) | 0.94 (0.88 to 1.01) | 0.086 |
| Preference for surgery | 2.34 (0.46 to 11.84) | 0.303 |
| Stage of prolapse II (reference category stage I) | 0.75 (0.24 to 2.33) | 0.619 |
| Stage of prolapse III (reference category stage I) | 0.92 (0.24 to 1.31) | 0.906 |
| Age band 45–64 years (reference category < 45 years) | 2.87 (0.65 to 40.14) | 0.122 |
| Age band 65–79 years (reference category < 45 years) | 13.09 (1.59 to 107.75) | 0.017 |
The rates for receiving any related operation (OPCS4 code P18, P22–P24, P26, q07–Q08, Q54, M51–M58, A70 or H57) were 32.9% (49/149) in the intervention group and 36.1% (52/144) in the control group. The rates are lower for this outcome than for the primary outcome measure, as this outcome counts the procedures specified above only, rather than any treatment for or diagnosis of pelvic floor disorders. The linear model to compare groups is summarised in Table 21 (OR 0.78, 95% CI 0.47 to 1.32; p = 0.356). When the outcome measure is limited to any prolapse procedure, the results are very similar. The proportion of participants having any prolapse surgery is 32.8% (49/149) in the intervention group and 34.0% (49/144) in the control group, which is very similar to the proportions quoted above because nearly all of the women who had a procedure had treatment that included a prolapse procedure. Frequencies for the outcome of any urinary incontinence surgery (M51–M58) and the outcome of any faecal incontinence surgery (H56–57) cannot be reported because of low numbers. In summary, there is no evidence that the intervention reduced the need for these types of treatment during follow-up.
| Variable | OR (95% CI) | p-value |
|---|---|---|
| Intervention | 0.78 (0.47 to 1.32) | 0.356 |
| Prolapse symptom severity score at baseline (missing imputed at median) | 1.08 (1.03 to 1.13) | 0.001 |
| Preference for surgery | 0.46 (0.20 to 1.05) | 0.066 |
| Stage of prolapse II (reference category stage I) | 2.24 (1.16 to 5.79) | 0.097 |
| Stage of prolapse III (reference category stage I) | 3.54 (1.15 to 10.92) | 0.028 |
| Age band 45–64 years (reference category < 45 years) | 1.72 (1.32 to 3.91) | 0.197 |
| Age band 65–79 years (reference category < 45 years) | 2.79 (1.09 to 7.14) | 0.032 |
Analysis of time to first treatment
We examined whether or not there was any difference between the intervention group and the control group in the time until treatment during follow-up. That is, we investigated whether or not the intervention was effective in delaying any further prolapse treatment. First, we examined whether or not the overall follow-up periods were similar between the intervention group and the control group. The time in follow-up (i.e. the time at risk and under observation) was found to be comparable between the groups. The mean time in follow-up in the intervention group was 9.36 years (SD 262.5 days) and the mean in the control group was 9.32 years (SD 267.9 days).
The survival function for the intervention group and the control group is shown in Figure 15. The survival function shows how the proportion of women in the two groups who had not received any further treatment declined over time.
FIGURE 15.
Kaplan–Meier survival estimates by intervention status.

A Cox regression was used to test whether or not women in the control group were likely to receive treatment sooner than women in the intervention group. The Cox regression model (Table 22), which was stratified by preference for surgery and included 264 subjects and 125 failures, estimated that there was a significant hazard ratio in favour of the intervention group of 0.65 (95% CI 0.46 to 0.94; p = 0.020). This indicates that the intervention did delay the need for further treatment and that, during follow-up, women in the treatment group had a 35% lower hazard for treatment.
| Variable | HR (95% CI) | p-value |
|---|---|---|
| Intervention | 0.65 (0.46 to 0.94) | 0.020 |
| Prolapse symptom severity score at baseline (missing imputed at median) | 1.06 (1.02 to 1.09) | 0.001 |
| Stage of prolapse II (reference category stage I) | 1.48 (0.77 to 2.85) | 0.245 |
| Stage of prolapse III (reference category stage I) | 2.40 (1.13 to 5.13) | 0.023 |
| Age band 45–64 years (reference category < 45 years) | 1.66 (0.88 to 3.10) | 0.115 |
| Age band 65–79 years (reference category < 45 years) | 2.58 (1.29 to 5.17) | 0.008 |
| BMI | 0.95 (0.91 to 0.99) | 0.014 |
When the outcome was restricted to time to surgery (Table 23), the number of failures was 91 and the hazard ratio was 0.71 (95% CI 0.47 to 1.08; p = 0.112).
| Variable | HR (95% CI) | p-value |
|---|---|---|
| Intervention | 0.71 (0.47 to 1.08) | 0.112 |
| Prolapse symptom severity score at baseline (missing imputed at median) | 1.08 (1.04 to 1.12) | < 0.001 |
| Stage of prolapse II (reference category stage I) | 1.47 (0.67 to 3.22) | 0.335 |
| Stage of prolapse III (reference category stage I) | 2.65 (1.09 to 6.44) | 0.031 |
| Age band 45–64 years (reference category < 45 years) | 1.56 (0.78 to 3.15) | 0.211 |
| Age band 65–79 years (reference category < 45 years) | 2.22 (1.00 to 4.91) | 0.049 |
| BMI | 0.95 (0.91 to 1.00) | 0.036 |
Missing data
The results of the sensitivity analysis of the primary outcome (any treatment) to examine the potential effect of missing data are summarised in Table 24. This analysis used a mixed-effects model similar to the main analysis, but with multiple imputation by chained equations. Two variables only were missing data (BMI and POP-SS). The data were checked for missing completely at random by logistic regression of missingness in these variables against the values of covariates included in the above analyses. Missingness in POP-SS was predicted by centre and missingness in BMI was predicted by age group, with missing data most likely in the youngest age group. Data were assumed to be missing at random. 26 Missing data were imputed through chained equations, with BMI imputed through regression and POP-SS imputed as truncated regression. The variables in the imputation models included all of those in the analysis models. No auxiliary variables were included. There were 100 imputed data sets created with a burn-in of 10. Trace plots were inspected to confirm the stability of the chain at the specified burn-in. The result is similar to the main analysis, but with a slightly lower OR of 0.60 in favour of PFMT (95% CI 0.37 to 0.99; p = 0.046).
| Variable | OR (95% CI) | p-value |
|---|---|---|
| Intervention | 0.60 (0.37 to 0.99) | 0.046 |
| Prolapse symptom severity score at baseline | 1.05 (1.00 to 1.10) | 0.034 |
| Preference for surgery | 0.53 (0.24 to 1.19) | 0.126 |
| Stage of prolapse II (reference category stage I) | 2.03 (0.89 to 4.64) | 0.093 |
| Stage of prolapse III (reference category stage I) | 3.00 (1.07 to 8.641) | 0.037 |
| Age band 45–64 years (reference category < 45 years) | 1.84 (0.87 to 3.89) | 0.112 |
| Age band 65–79 years (reference category < 45 years) | 4.70 (1.92 to 11.48) | 0.001 |
Summary of findings
The data linkage study provides evidence that PFMT reduces the overall long-term risk of requiring hospital treatment for pelvic floor disorders, over a post-intervention period of > 10 years. There is also evidence that PFMT extends the time for which hospital treatment is not required.
Chapter 8 Economic evaluation of pelvic floor muscle training
Introduction
The economic evaluation for the PROPEL intervention was concerned with the associated costs and outcomes of different service delivery models for delivering PFMT. In addition, an economic assessment of the long-term costs that were associated with accessing further pelvic prolapse treatment over time was conducted for the original POPPY trial participants, who were resident in Scotland. The multicentre randomised POPPY trial had found that individualised PFMT was effective in reducing the symptoms of prolapse, provided improvements in quality of life and showed potential to be cost-effective in women. 6
Objectives of the research
The research objectives were to:
-
provide estimates of the costs of each service delivery model involved in the PROPEL intervention
-
determine the patient outcomes following PFMT using the EuroQol-5 Dimensions, five-level version (EQ-5D-5L), for each delivery model
-
estimate the long-term costs associated with accessing further pelvic prolapse treatment over time to inform estimates of the potential cost-effectiveness of PFMT.
Methods
Models of provision
The comparator site for the purpose of the economic evaluation was site A, which operated with the same PFMT delivery model before and after the PROPEL intervention.
Resource use and costs
Perspective
The perspective of the primary economic analysis was the UK NHS. In all cases, resource use and costs relate to consultations in primary and secondary care for prolapse or prolapse-related symptoms only.
Resource use data
The PROPEL intervention service delivery models for pelvic floor muscle training
Associated resource use data for the delivery of PFMT per site were obtained from the clinical centres. Cost categories included were staff costs (AfC band and specialism) and activity data (e.g. the number of treatment sessions and duration of appointments) for the delivery of PFMT. Resource use data for community-based care and patient resources for further pelvic prolapse treatment were collected using participant-completed questionnaires. Associated resource implications for the delivery of PFMT were assessed per site.
The POPPY trial longitudinal follow-up
Follow-up data on secondary care resource use and costs for POP treatment in secondary care (inpatient and outpatient data) for the POPPY trial participants in Scotland were accessed to estimate the longitudinal costs. The time period was 11 years (2007–18).
Health service costs
Costs to the UK NHS were calculated using the national average unit costs for primary care resource use [Personal Social Services Research Unit (PSSRU)]32 and for secondary care resource use (Scottish Health Service Costs33 and NHS Reference Costs 2017/1834). The PROPEL intervention costs were incurred within a 12-month period, so a discount rate was not applied. The costs were reported in 2017/18 Great British pounds (GBP) (Table 25). The original POPPY trial costs base year was 2009. Longitudinal follow-up data were adjusted using UK gross domestic product deflators (2017 base year). 35
| Resource item | Unit | Unit cost (£) | Source |
|---|---|---|---|
| NHS health-care resource use | |||
| Consultant referral to physiotherapy | Visit | 158 | NHS Reference Costs 2017/18,34 WF01B consultant-led, non-admitted, face-to-face attendance, first |
| Triage appointment | PWH | 55 | Assumes cost of band 7 specialist physiotherapist |
| Allocated cost per attendance (physiotherapy) | Per attendance | 17 | Scottish Health Service Costs33 (R046) |
| Staff involved in delivery of PFMTa | |||
| Band 7 specialist physiotherapist | PWH | 55 | PSSRU Unit Costs of Health and Social Care 2018,32 table 12. Hospital-based scientific and professional staff |
| Band 6 physiotherapist specialist | PWH | 46 | PSSRU Unit Costs of Health and Social Care 2018,32 table 12. Hospital-based scientific and professional staff |
| Band 7 physiotherapist | PWH | 55 | PSSRU Unit Costs of Health and Social Care 2018,32 table 12. Hospital-based scientific and professional staff |
| Band 6 physiotherapist | PWH | 46 | PSSRU Unit Costs of Health and Social Care 2018,32 table 12. Hospital-based scientific and professional staff |
| Band 5 physiotherapist | PWH | 35 | PSSRU Unit Costs of Health and Social Care 2018,32 table 12. Hospital-based scientific and professional staff |
| Band 6 district nurse | PWH | 45 | PSSRU Unit Costs of Health and Social Care 2018,32 table 13. Hospital-based nurses |
| Band 5 staff nurse | PWH | 37 | PSSRU Unit Costs of Health and Social Care 2018,32 table 13. Hospital-based nurses |
| Community health-care resource use | |||
| GP | Per surgery consultation | 28 | PSSRU Unit Costs of Health and Social Care 2018,32 table 10. 3b General Practitioner – unit costs |
| Practice nurse | PWH | 36 | PSSRU Unit Costs of Health and Social Care 2018,32 table 10. 2 Nurse (GP practice) |
Health-related quality-of-life data
The EQ-5D-5L data were collected at baseline and at the 6- and 12-month follow-ups. The EQ-5D-5L provides a single utility-index score for use in analysis. 36 Average scores were calculated at each time point for the whole participant sample and by site using the index calculator tool from EuroQol. 37 Changes in scores between baseline and 6 months were calculated and tested using the parametric paired t-test for statistically significant differences in health-related quality-of-life (HRQoL) scores, before and after PFMT. This time scale was in line with the primary outcome analysis.
Statistical analyses were performed using IBM SPSS Statistics version 24.0 (IBM Corporation, Armonk, NY, USA) and Microsoft Excel® 2010 (Microsoft Corporation, Redmond, WA, USA). Conventional levels of significance (5%) were used.
Results
Costs of each delivery model
To calculate the costs for one cycle of PFMT treatment, data about the band and specialism of staff members delivering the treatment were used. The average cost for the delivery pathway at each site was calculated, as shown in Table 26, using available data for 70 participants. The total cost comprised the average staff costs for referral, triage and treatment, and a proportional allocation of overheads to reflect that all services within a hospital share facilities. An allocated cost of £17.00 per attendance for physiotherapy (table R046)33 was used for overheads. The estimated mean cost per patient for an episode of PFMT (2017–18 GBP) was £438.91 in site A; it was £464.43 in site D, £434.97 in site B, £353.53 in site C and £339.36 in site E. The costs per site assume that each patient attends all of their PFMT treatment sessions. Excluding overheads, the mean costs were £353.91 in site A, £349.97 in site B, £268.53 in site C, £362.43 in site D and £288.36 in site E.
| Activity | Site A (N = 24) | Site B (N = 16) | Site C (N = 7) | Site D (N = 14) | Site E (N = 9) |
|---|---|---|---|---|---|
| Referral cost (£): consultant | 157.53 | 157.53 | 157.53 | 157.53 | 157.53 |
| Triage cost (£): band 7 specialist physiotherapist | 55.00 | 55.00 | 0.00a | 55.00 | 55.00 |
| PFMT treatment cycle | |||||
| Initial appointment time (minutes) | 60 | 60 | 60 | 40 | 45 |
| Number of treatment sessions | 4 | 4 | 4 | 5 | 2 |
| Duration of treatment sessions (minutes) | 30 | 30 | 30 | 30 | 30 |
| Total average clinic time per woman (minutes)b | 180 | 180 | 180 | 190 | 105 |
| PFMT delivery by staff | |||||
| Band 7 specialist physiotherapist (n) | 3 | ||||
| Band 6 physiotherapist specialist (n) | 21 | ||||
| Band 7 physiotherapist (n) | 2 | 1 | |||
| Band 6 physiotherapist (n) | 13 | 12 | 5 | ||
| Band 5 physiotherapist (n) | 3 | ||||
| Band 6 nurse (district nurse) (n) | 3 | ||||
| Band 5 nurse (staff nurse), (n) | 7 | ||||
| Average cost per patient (£)c | 141.38 | 137.44 | 111.00 | 149.90 | 75.83 |
| Total cost per patient excluding overheads allocation (£) | 353.91 | 349.97 | 268.53 | 362.43 | 288.36 |
| Overheads allocated cost (by number of attendances) | 85.00 | 85.00 | 85.00 | 102.00 | 51.00 |
| Total cost per patient including overheads (£) | 438.91 | 434.97 | 353.53 | 464.43 | 339.36 |
There was no difference between sites in terms of resource use for referral to physiotherapy triage. Site C was the only site that operated direct referral to initial appointment without triage, and had the lowest average cost to deliver PFMT as part of the PROPEL intervention. The total clinical time to deliver PFMT per patient was 180 minutes for sites A, B and C, 190 minutes for site D and 105 minutes for site E. It should be noted that site C increased its treatment follow-up sessions from three (usual care) to four sessions (the PROPEL intervention) per patient. This increased the time per treatment cycle from 150 minutes (usual care) to 180 minutes (the PROPEL intervention), which increased the average staff cost for a treatment cycle from £92.50 to £111.00 during the research study, and increased the total cost from £335.03 to £353.53. The average staff cost per patient during the PROPEL intervention was £141.38 in site A, £137.44 in site B, £111.00 in site C, £149.90 in site D and £75.83 in site E.
For a small number of participants at each site, the information about which clinical specialist had provided treatment was unavailable (two participants in site A, three in site B, one in site D and three in site E); a sensitivity analysis to test the impact of this on the average costs was conducted. To generate a range of the average cost, it was first calculated presuming that all ‘unknown’ were treated by the lowest-cost clinical staff member, and was next recalculated presuming that the highest-cost clinical staff member delivered the treatment. The average cost per patient ranges were £141.00–144.00 in site A, £136.50–137.65 in site B, £149.24–152.81 in site D and £70.00–84.00 in site E.
Health service costs
Participants reported their use of health-service resources for further pelvic prolapse treatment. Between baseline and 6 months, 71 participants provided this information (Table 27). Between baseline and 6 months, participants sought further treatment for POP from a GP a total of 44 times and from a practice nurse a total of 17 times. All of the visits were accounted for by 29 (41%) participants. The combined number of visits per participant ranged from 1 to 4. By site, the number of GP appointments for POP was 17 (median 0) in site A, 11 (median 0) in site B, 6 (median 1) in site C, 5 (median 0.5) in site D and 5 (median 0) in site E. By site, the number of practice nurse appointments for POP was 2 (median 0) in site A, 7 (median 0) in site B, 1 (median 0) in site C, 2 (median 0) in site D and 5 (median 0) in site E. In total, 37 (52%) participants did not visit a GP or practice nurse for POP. Very small differences were seen between delivery sites; these were very unlikely to be statistically or clinically significant.
| Category | Unit cost (£) | Unit (n) | Cost (£) |
|---|---|---|---|
| Prolapse treatment | |||
| Pessarya | 204.97 | 3 | 615 |
| Physiotherapyb | – | 55 | – |
| POP consultation with GP | 28 | 44 | 1408 |
| POP consultation with practice nurse | 36 | 17c | 153 |
| Urinary incontinence | |||
| Physiotherapyb | – | 17 | – |
| Drug treatmentd | – | 5 | Unknown |
| Surgery | |||
| Vaginal repaire | 1630 | 2 | 3260 |
| Abdominal hysterectomyf | 2649 | 1 | 2649 |
| Vaginal hysterectomyf | 2649 | 1 | 2649 |
| Total | 10,733 | ||
Participants reported if they had attended physiotherapy appointments. However, as it was not clear if these were related to their PROPEL intervention appointments, these were not included in the cost calculations, to prevent double-counting. Other costs incurred by the PROPEL intervention participants were reported, which included consultations for non-POP-related matters with their GP (80 appointments) or practice nurse (39 appointments). Seven participants reported that they had taken days off work: two participants as a result of POP (1 day and 35 days) and five for non-POP issues (1 day, 1 day, 4 days, 5 days and 30 days). Although these are relevant to the analysis from a societal perspective, they are not part of the current analysis.
Health-related quality-of-life outcomes
The EQ-5D-5L data were available for 84 participants at baseline, 68 participants at 6 months and 30 participants at 12 months. Around half of all participants indicated that they had slight or moderate problems on the EQ-5D-5L domains of pain, anxiety/depression and usual activities. Mean utility increased over time: baseline, mean 0.791 (SD 0.179); 6 months, mean 0.827 (SD 0.160); and 12 months, mean 0.866 (SD 0.117). The EuroQol visual analogue scale (EQ-VAS) demonstrated the same trend: baseline, mean 77.4 (SD 18.3); 6 months, mean 79.6 (SD 18.2); and 12 months, mean 82.9 (SD 11.5).
Table 28 shows the mean utilities by time point for all participants and by site. A paired-samples t-test was conducted to compare utility at baseline with utility at 6 months, and to compare utility at baseline with utility at 12 months, for all of the PROPEL intervention participants. Differences were not statistically significant between baseline and 6 months [paired t(df = 60) = 1.163; p = 0.25, two-tailed] or between baseline and 12 months [paired t(df = 25) = 0.113; p = 0.911, two-tailed]. With the exception of site C, a large proportion of participants at each site reported a maximum health-state utility value (1.000) at baseline. This may account for the inability of mean utility scores to significantly improve over time. Paired-sample t-tests of longitudinal differences between baseline and 6 months for participants within each research site were not statistically significant: site A t(df = 19) = 1.418 (p = 0.172), two-tailed; site B t(df = 18) = 0.655 (p = 0.521), two-tailed; site C t(df = 4) = 0.875 (p = 0.431), two-tailed; site D t(df = 6) = 0.121 (p = 0.907), two-tailed; and site E t(df = 9) = 0.959 (p = 0.363), two-tailed.
| Site | Maximum utility reported at baseline, % (n) | Mean EQ-5D-5L score (n participants) | ||
|---|---|---|---|---|
| Baseline | 6 months | 12 months | ||
| Total PROPEL intervention participants | 25 (21) | 0.791 (84) | 0.827 (68) | 0.866 (30) |
| A | 32 (8) | 0.830 (25) | 0.825 (23) | 0.883 (6) |
| B | 29 (7) | 0.836 (24) | 0.857 (21) | 0.846 (15) |
| C | 0 (0) | 0.753 (6) | 0.805 (5) | 1.000 (1) |
| D | 27 (4) | 0.702 (15) | 0.721 (7) | 0.888 (6) |
| E | 14 (2) | 0.758 (14) | 0.852 (12) | 0.827 (2) |
For change over time, 61 participants completed the EQ-5D-5L at baseline and at 6 months [mean utility gain n(61) = 0.019 (95% CI –0.006 to 0.043)]. Comparing participants receiving specialist physiotherapist care (n = 20) with participants receiving care from other clinical staff (n = 41), the mean utility gain for the participants receiving specialist physiotherapist care was higher [n(20) = 0.035 (95% CI –0.011 to 0.082)] than for others [n(41) = 0.012 (95% CI –0.019 to 0.041)]. The differences were not statistically significant [t(df = 59) = 0.817; p = 0.417, two-tailed].
A total of 25 participants completed the EQ-5D-5L at baseline, 6 months and 12 months. Utility scores for those who had received specialist physiotherapist treatment (n = 5) were compared with those who received treatment from other clinical staff (n = 20). An independent-samples t-test indicated that there was no statistically significant difference in improvement in HRQoL from baseline to 12 months between the groups [t(df = 23) = –0.602; p = 0.553, two-tailed].
The POPPY trial longitudinal outcomes
Long-term costs that were associated with accessing further pelvic prolapse treatment were estimated using follow-up data for 293 women involved in the POPPY trial. NHS Scotland Scottish Morbidity Record (SMR) data for F2 Gynaecology and CB Urology health-care utilisation was accessed for the period 2007–18. For the SMR-00 data set, no F2 and CB episodes had a main condition recorded; therefore, it was not possible to filter in or out only POP-relevant episodes on that basis. The main operation codes were used and were predefined as P18, P22–P24, P26, Q07–Q08, Q54, M51–M58, A70 and H57. It should be noted that operation code is a non-mandatory code field for SMR-00. No relevant operation code for POP was recorded in CB episode data for either SMR-00 or SMR-01. No further analysis was carried out for CB specialty. Resource use costs for each episode’s main operation were valued in prices using the UK NHS Reference Costs 2017/18. 34
Table 29 presents the resource use costs for available data regarding F2 gynaecology outpatient and inpatient episodes of care. Owing to issues of confidentiality, SMR-01 data cannot be broken down further. Information is presented in aggregate to meet the data protection requirements of the NHS National Services Scotland’s Statistical Disclosure Control Protocol Version 3.0. 39 Resource use costs were estimated for 111 F2 outpatient episodes of care, using the main operation code of interest. Resource use costs were estimated for 109 F2 inpatient episodes, using the main operation code of interest recorded. Inpatient costs (2017–18 prices), excluding excess bed-days, were higher for the control group (£172,458.70; 53%) than for the intervention group (£154,544.02; 47%). Including excess bed-days, the difference in costs between the groups was £21,480.26, retaining a 53% and 47% split. Longitudinal follow-up data about health-care resource use for prolapse treatment by the POPPY trial participants indicated that the overall total costs for the control group were higher than for the intervention group (53% and 47%, respectively). The difference is potentially an artefact of the adjustment of 2017–18 prices, using the UK deflator series. 35
| SMR record type | Physiotherapist (treatment) costs (£) | Leaflet (control) costs (£) |
|---|---|---|
| SMR-00: outpatienta | 9112.08 | 10,200.04 |
| SMR-01: inpatient | 154,544.02 | 172,458.70 |
| SMR-01: inpatient – excess bed-daysb | 8723.24 | 12,288.82 |
| Total | 172,379.36 | 194,947.56 |
Outpatient (SMR-00)
In total, 5004 episodes of outpatient care was recorded for all participants. A total of 1419 F2 episodes were recorded between 2007 and 2018. No main condition code was recorded. A total of 84% of records had no main operation or other operation code recorded. Of 226 F2 records with a main operation code, 129 F2 records had an operation code of interest recorded as a main or other operation. Excluding ‘did not attend’ episodes, resource use costs were estimated for 111 episodes of care that had a procedure of interest recorded as main operation.
Figure 16 compares all episodes of care between POPPY trial groups, and compares identifiable POP-relevant episodes of care between groups (2007 to 2010 are supressed because of low numbers). The numbers of episodes of health-care treatment shown in Figure 16 indicate a broadly similar pattern of resource use by both groups.
FIGURE 16.
Comparison of the health-care resource utilisation between the POPPY trial control and treatment group participants, gynaecology specialty: all episodes of care vs. POP-relevant coded episodes of care. Note that lines start at different points owing to small numbers within years.
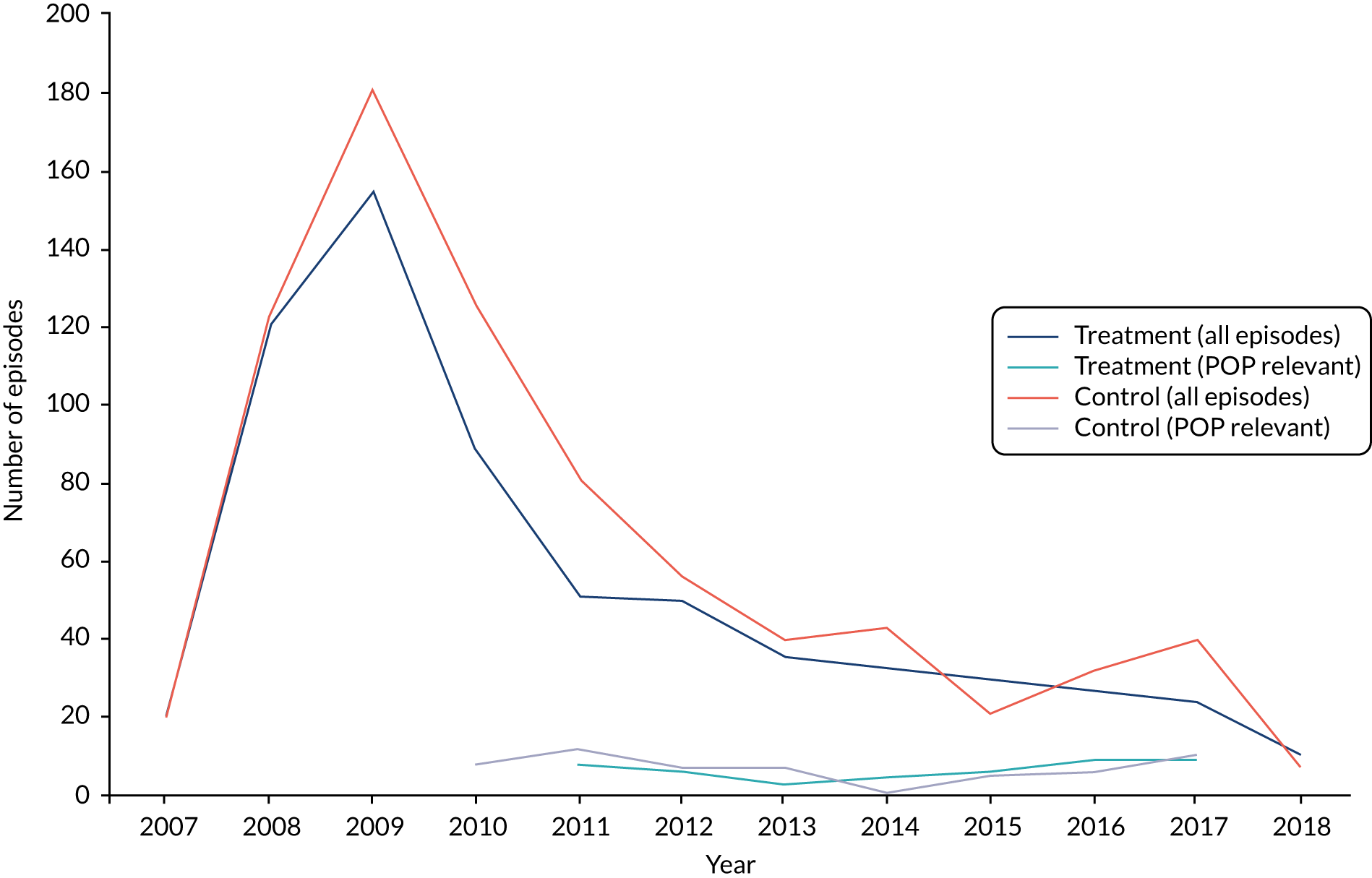
New appointments accounted for 41% of the intervention group and 30% of the control group episodes of care. Table 30 summarises the POP-relevant outpatient resource use costs.
| POPPY trial group | SMR-00 | Units (n) | Unit cost (£) | Total (£)a |
|---|---|---|---|---|
| Intervention | P26 procedure (MA23Z, outpatient) | 52 | 183.52 | 9112.08 |
| Control | P26 procedure (MA23Z, outpatient) | 59 | 183.52 | 10,200.04 |
The total estimated outpatient resource use costs were lower for the intervention group than for the control group: £9112.08 and £10,200.04, respectively (2017–18 GBP prices). Given that it was not possible to use a condition code to filter records in or out, and that 84% of records did not have any procedure codes recorded, it was not possible to determine how many data were missing. It is not possible to conclude whether or not there is a difference in the absolute number or timing of use of outpatient health-care resources between groups since the POPPY trial.
Surgery (SMR-01)
In total, 1153 episodes of inpatient care had been recorded for all participants, including 166 F2 episodes. Of 166 episodes, 137 episodes recorded a main condition code and 126 a main operation code. A total of 109 F2 episodes recorded at least one procedure code of interest. Table 31 indicates that, overall, the control group received more procedures of interest than the intervention group.
| Procedures of interest | Number of proceduresa | |
|---|---|---|
| Intervention group | Control group | |
| Colporrhaphy/repair (P22, P23, P24, Q54) | 52 | 67 |
| Hysterectomy (Q07, Q08) | 5 | 5 |
| Incontinence (M53) | < 5 | 8 |
Comparison between groups indicates that patterns of admission were broadly similar during the period 2007–18, with a total of 50 health-care episodes for the intervention group and 59 for the control group. The total number of excess bed-days (based on the average stay of the POPPY trial participants by main operation code) was 20 for the intervention group and 28 for the control group. The timing of more expensive procedures, cost-adjusted to 2017–18 prices using the UK deflator series,35 drives some of the difference in total cost. For the physiotherapy group, 35% of the main operation codes were for expensive operations (> £4000), most of which had occurred in earlier years and, therefore, were deflated for cost-adjustment. In contrast, 21% of the main operation codes for the control group were for expensive operations carried out in later years and, therefore, costs were subject to less adjustment.
Discussion
The economic analysis assessed the costs of each clinical site’s delivery model of PFMT. The total cost of the specialist physiotherapist delivery model was calculated at £434.13 per woman attending for PFMT during the PROPEL intervention (2017/18 GBP). This includes the cost of consultant referral, specialist physiotherapist triage, the initial assessment appointment and treatment sessions delivered by specialist physiotherapists (AfC band 7 or band 6), and proportional overheads. At the other PROPEL intervention sites, delivery varied in terms of referral pathway, the amount of clinical contact time to deliver PFMT that women could access and the mix of clinical staff delivering PFMT. Services that were delivered using higher-band physiotherapists only were more costly than services delivered by other staff mixes.
The headline costs indicated that, generally, services that were delivered using higher-band physiotherapists only were more costly. In common with other clinical studies, the introduction of the PROPEL intervention was accompanied in some clinical sites by an increase in staff for the duration of the project. Changes in resources may provide the opportunity to reduce waiting lists, as was the case for site D during the PROPEL intervention, or to enable access to treatment for more patients. Future research into sustainable changes to resources is advised.
Changes in utility, measured using the EQ-5D-5L (secondary outcome), indicated that the PROPEL intervention participants had a high self-reported level of HRQoL, with 31% of participants reporting maximum utility at 6 months (37% at 12 months). This was also reflected in the participants’ responses to the EQ-VAS. Utility improved by 0.019, on average, over 6 months: 0.035 for specialist physiotherapists and 0.012 for other clinicians (with no significant difference between these groups). The primary outcome indicated that statistically significant differences in POP-SSs were found in sites A and C, comparing baseline with 6 months. Comparison between sites was not possible. The economic outcomes indicated that no statistically significant difference was found between baseline and 6 months within any site. There was a greater magnitude of improvement in EQ-5D-5L scores for women who received PFMT treatment from specialist physiotherapists than for women who received the treatment from other HCPs, but this was not a statistically significant difference.
During the POPPY trial, the mean cost of PFMT was £306.86 (95% CI £250.74 to £368.29) for one woman taking part (2009 prices) [mean cost £349.45 (95% CI £285.54 to £419.41) for 2018 prices]. 6 Longer-term benefits were not considered as part of the study. Longitudinal follow-up data of the POPPY trial participants did not indicate a difference in the use of health-care resources between the groups. Interpretation of outpatient health-care resource use between the groups is limited by the absence of coding reference information. On the basis of the available follow-up data obtained from the administrative data sets, there is no observed difference in resource use between the groups at 11 years post PFMT.
Limitations
The intention had been to use site A as a comparator site to compare the costs and benefits of the different mixes of staff (band and specialism) delivering PFMT. Changes to the number of clinical sites involved, to recruitment and to the follow-up period for participants precluded this analysis comparing sites.
The allocation of overheads was carried out by a simple multiplication of the number of attendances by the NHS Reference Costs34 for overheads. This may not be accurate for all clinical sites, particularly where clinical space may not be immediately accessible and identification of a facility may incur additional costs. Adjustment to reflect local service delivery conditions should take this into account.
Chapter 9 Dissemination for impact
Introduction and methods
The PROPEL intervention aimed to deliver an evidence base for alternative models of care to increase the capacity within services for delivering the evidence-based PFMT intervention for POP (as supported by the POPPY trial). To support further dissemination of this evidence (from the POPPY trial and the PROPEL intervention), we included dissemination activities that would also extend opportunities for further data collection on potential barriers and facilitators beyond the PROPEL intervention sites to a wide range of interested stakeholders across the UK.
Two ‘dissemination for implementation’ workshops were held: one in London and one in Glasgow, with 72 participants and 48 participants, respectively. The participants constituted specialist physiotherapists, physiotherapists, consultant urogynaecologists, women’s health fitness instructors and nurses. The majority of participants rated the workshop as meeting their objectives extremely well/very well, with a small minority (n = 6 across two events) rating the workshop as average in meeting their objectives. Most of the participants had attended the workshop to ‘identify how services may be changed to reach more women’ and to ‘find out about the results of PROPEL’. Following the workshop, the majority thought that their service could initiate some change and could identify actions to take forward.
Workshops consisted of sharing the preliminary findings of the PROPEL intervention but also included an ‘action-planning’ component for service managers and those responsible for the delivery of non-surgical interventions for prolapse, which allowed them to start planning a local service redesign that could deliver PFMT to larger numbers of women. These events also acted as ‘data gathering’ opportunities: gathering further data on the potential opposition and barriers to implementation, and how services can make sense of the study findings and apply them to their own services. We encouraged all participants to leave with an action plan.
The dissemination and implementation workshops were delivered according to a theoretically driven structure that detailed problems, solutions (mechanisms for action) and actions. We have used this theory-driven workshop structure previously.
Individual and group perceived barriers to and facilitators of delivering PFMT and delivery using non-specialist roles were mainly recorded using sticky notes posted on group boards, alongside group feedback of key points at several intervals during the day-long workshops. The sticky notes were gathered and collated at the event by the research team and were collectively reported back to the event audience to reflect the broad consensus on the barriers to and facilitators of delivering PFMT. These sticky notes were retained and their key themes were confirmed in a secondary coding exercise by ED, KB and MM, with specific attention given to understanding the levels of opposition and action, the discussion of barriers and whether or not the study findings influenced the development of solutions to these barriers, what other study findings are likely to influence adoption and implementation (e.g. financial data) and which models of delivery seem more favourable for wider adoption and implementation.
It is not surprising that most of the barriers, often representing the absence of something, were also noted as facilitators when the same thing was present or available. The same themes were evident across both workshops; therefore, the data from both events were combined. The main themes are presented and their content is briefly described in the following sections.
Workshop findings
Awareness-raising in primary care
Awareness-raising in primary care was one of the prominent themes from the workshops and was seen as an essential starting point in making changes to women’s care pathways. It was suggested that GPs lacked knowledge of PFMT and the default action was to refer patients to urogynaecology, where the outcome was more likely to be less conservative options. The GP-to-consultant treatment route bypassed the most conservative treatment options, such as PFMT and pessaries.
Several participants thought that they could use the PROPEL study findings to talk to GPs in their local area, and some participants proposed this as a first step in an action plan. There were suggestions of training GPs in pelvic health and using the evidence base for PFMT to raise their awareness that something can be implemented to improve the lives of women and that a prolapse is not something to ‘put up with’.
Awareness-raising among women
Raising awareness among women was referred to as a barrier, in the sense that women would not know that they could opt for more conservative treatment options and, therefore, they would not be able to discuss alternative preferences with their GP. The discussions on raising awareness among women were mostly concerned with ideas as to how this could be carried out. It was recognised that there were many health-care encounters for women where the issue of pelvic health could be raised (e.g. when undergoing a smear test, especially for raising awareness among young women, or antenatal and postnatal appointments). This could be as both general advice (do you know about PFMT? Do you understand why PFMT is important? Do you know how to do PFMT?) and possible identification of prolapse or pelvic problems.
The promotion of continence products (e.g. television advertising) was seen as something that needed to be counteracted, as it ‘normalised’ bladder problems and prevented women from considering alternative solutions. Campaigns that promote pelvic health are needed in order to educate and inform women and raise awareness of prolapse and alternative treatment options. It was also suggested that women should be able to self-refer and that this might increase the uptake of PFMT for prolapse as a first-line treatment.
Staffing resources and staff time
As with the findings of the PROPEL intervention, the availability of staff and staff time was seen by workshop participants as the main barrier to initiating service change, such as that carried out within the PROPEL intervention. Each potential staff group was noted as already having a full workload/caseload and their time available for new patient groups and interventions was seen to be limited. However, it was also recognised that there were larger numbers of nurses and musculoskeletal physiotherapists; therefore, if services for PFMT were to increase, then these staff groups did seem more likely to have availability to account for this. There were also examples of current services being unable to recruit specialist physiotherapists and posts being left unfilled.
Resources: funding and space
In addition to staffing resources, other resources, such as clinic space, were also mentioned. There were general comments around funding, which could be for posts, other resources needed to run a PFMT clinic or resources for enabling training. The PROPEL intervention had reported that some staff had difficulty in sourcing rooms to see women, and that workshop participants similarly told of a lack of availability of rooms to deliver their current services. If these problems were limiting current services, any further service provision was, therefore, even more limited. There was some discussion of seeking to deliver more services in the community where space may be available.
Training
The PROPEL intervention had informed workshop participants about the PFMT training and how this was delivered. However, this was an area of concern for specialist physiotherapists, who raised concerns about the availability of specialists to provide support to staff and provide any further education needed post training. There were also concerns that other staff groups (non-specialists) would not be able to manage complex cases or the multitude of issues that prolapse patients can present with. Many thought that 1 day of training was not enough and that this should be accompanied by clinical supervision or ‘shadowing’ in clinics to increase experience. There were also some suggestions that additional virtual training and update sessions could be provided. (This was also raised by participants on the training course, and additional support was accessed at most sites, even if this was peer support from other newly trained colleagues.)
Educating other professionals (e.g. GPs and consultants) to understand other HCP roles was also seen as enabling referrals to other types of services.
Funding for training and training opportunities was seen as being limited within the NHS at present.
Champions/enthusiasts
It was acknowledged that, even with the PROPEL intervention, the successful implementation of the different models had often relied on a local enthusiast or a champion who had led the way to make it happen. This included identifying who could be trained and convincing them and others (their managers) that this would be a good thing, and liaising with the research team to help organise the training locally. They were also involved in helping to triage women locally, to help the new referral system work. Although the workshops enabled participants to consider even small initial steps that they could take to move towards change, participants saw a person with some degree of seniority or access to decision-makers as being a strong facilitator to change happening at a strategic and service level.
Multidisciplinary team working and clinical pathways
Some of the reasons for limited referrals to some roles within the PROPEL intervention were disjointed teamworking and a lack of clarity on referral pathways, or overly complicated referral pathways. To overcome these problems, there needs to be more multidisciplinary teamworking and everyone in the team needs to be on the same page with regard to the appropriate clinical pathways. This also includes the primary care team having a better understanding of all of the possible clinical pathways and roles of others.
Management support
For substantial change to happen, there always has to be management support. Without this, training could be wasted, as staff time may not subsequently become available to enable working with women with prolapse, and resources such as treatment rooms may not be made available. Although many workshop participants were ready to consider change and to take some immediate action, this could get them only so far without the additional support and actions from others. There was also recognition that, although one manager may agree with the need to change, what needs to change and how change could be achieved, managers work in sectors that do not necessarily communicate to each other (e.g. hospital and community). Options to develop new services could be seen as one sector trying to offload burden to another sector. The transfer of potential savings from one sector to another never happens and, therefore, even robust financial evidence will do little to convince sectors to carry out things differently.
Conclusion
These workshops have added to the knowledge that was generated in the PROPEL intervention, confirming and identifying additional barriers to and facilitators of introducing new models of delivery for PFMT for increasing the capacity and availability of PFMT for women with prolapse. The following activities could follow on from this study to begin to address some of the concerns and raise the potential for change on a wider scale across the NHS:
-
Develop awareness-raising training for GPs and information for urogynaecologists about the benefits of PFMT as a first-line treatment.
-
Develop new guidelines for practice nurses, midwives and continence services to capitalise on existing opportunities for early identification and intervention, for example by advising women about PFMT during routine smear tests and perinatal appointments.
-
Develop public health campaigns for women of all ages (including teenagers), including, for example, a digital versatile disc (DVD) or animation to encourage understanding of pelvic health and exercises.
-
Engage with gynaecological service leads to reconfigure care pathways that include PFMT as a first-line treatment option.
-
Undertake work to improve care pathways for women with prolapse, including self-referral pathways for PFMT.
Chapter 10 Discussion, conclusions and implications
The overall aims of the PROPEL intervention were to study the implementation and outcomes (including costs) of different models of delivery of PFMT for women with POP, in order to increase the service provision of PFMT across contrasting NHS sites. This was conducted using a realist evaluation, alongside the collection of robust outcomes similar to those utilised in the original POPPY trial of PFMT for prolapse. The economic evaluation for the PROPEL intervention was concerned with the associated costs and outcomes of different service delivery models for delivering PFMT. In addition, an economic assessment of the long-term costs associated with accessing further pelvic prolapse treatment over time was conducted for the original POPPY trial participants resident in Scotland.
Implementation and outcome studies
The models of delivery included a specialist WHP-delivered service, which was used as a gold-standard comparison for other models. It was also seen as important to understand the delivery of such specialist-delivered services outside the trial conditions, in the real world of the NHS. All other services across four other sites implemented various models, with musculoskeletal physiotherapists, other physiotherapists and nurses delivering PFMT. All services except one operated a model whereby women were triaged by a specialist or consultant and referred, as appropriate, for PFMT delivery by the newly trained staff groups.
A realist evaluation was conducted alongside a robust PROMs study to understand ‘what works’, taking into account the impact that the local context has in influencing what works. The realist evaluation was based on multiple case studies of the implementation and outcomes of PFMT delivery in three contrasting NHS settings, sites A, B and C (see Chapter 4) (with the PROMs study involving five sites: sites A–E). The realist evaluation methods allowed for engagement of local stakeholders from the outset, which permitted a detailed exploration of how local sites made decisions on how to deliver PFMT (e.g. using different skills mixes) and how these were implemented. This enabled an understanding of what helped or hindered service delivery, of how the services integrated or affected other services or HCPs and of any potential influences on outcomes for women. The focus of ‘what works and for whom’ included the views of service managers, consultants/referral agents and those delivering PFMT, as well as the views of the women in receipt of PFMT services. However, given the overall positive outcomes for women (all models were effective for women), the presentation of findings focused more on the different models and HCPs delivering PFMT and what worked for ‘implementation’.
When there is a perceived need for services (as a result of a lack of an existing service), this is a driver for change. The service with the most established model of specialist physiotherapist-delivered PFMT was the service that was the most resistant to trying alternative models, regardless of need (e.g. staff absences and increasing waiting times for women were reported during this study). The lack of available services in rural areas was a driver for training many different staff types and initiating ‘workarounds’ to enable triage and referrals to the new services.
Staff who were newly trained within the PROPEL intervention and who had some level of prior knowledge of women’s health issues and of the physiology of the pelvic region were more comfortable with this new role and were more likely to feel confident following the 1-day training.
The following are required to successfully implement PFMT for prolapse:
-
The provision of adequate training that is tailored to needs of different staff skill mixes.
-
An increased awareness of PFMT among GPs and other HCPs.
-
Well-co-ordinated and flexible referral systems.
-
Wider (multidisciplinary) team support and/or buy-in.
-
Organisational and managerial support with effective leadership.
-
A receptive setting (some community nursing and acute wards may not be appropriate).
For the PROMs study, five NHS sites were recruited to deliver PFMT using a range of delivery models. Site A constituted an exclusively WHP-specialist service model that then acted as a comparator for models involving delivery by ‘other’ staff groups (i.e. nurses, physiotherapists), as developed by sites B–E.
A total of 102 women were recruited to the PROMs study from across the five sites and a total of 65 women provided both baseline and 6-month POP-SSs (the primary outcome measure). The mean POP-SS at 6-month follow-up was significantly lower than that at baseline, indicating that prolapse symptom severity had reduced. The mean difference between baseline and 6 months represented a clinically meaningful difference. A significant improvement was still observed when comparing baseline with 12-month POP-SSs (although numbers were low).
There was no statistically significant difference in the improvement of symptoms obtained from PFMT delivery by specialist physiotherapists (mean change in POP-SS = –3.95) compared with PFMT delivery by other HCPs (mean change in POP-SS –2.81 points) (mean difference 1.14 points, t = 0.89, df = 63; p = 0.37).
Additional (secondary) outcomes showed that there was a significant reduction in the number of health-care visits after the start of the intervention (mean of 1.73 appointments in the 6 months prior to baseline compared with 0.96 appointments between baseline and 6-month follow-up, Wilcoxon signed-rank test z = 3.663; p < 0.001).
The economic evaluation found that the key difference between models in determining costs was the staff grade (NHS band) and the overall length of time practitioners spent with the women (hours). The baseline HRQoL score was already high in this population, which may have affected our ability to improve this. There were no significant differences in HRQoL between women seen by specialist physiotherapists and women seen by other practitioners. The average EQ-5D-5L scores did not indicate a deterioration in HRQoL for any model of delivery. The limited participant numbers precluded assessment of cost-effectiveness for the models of delivery.
The headline costs indicated that, generally, services delivered using higher-band physiotherapists only were more costly. In common with other clinical studies, the introduction of the PROPEL intervention was accompanied in some clinical sites by an increase in staff for the duration of the project. Changes in resources may provide the opportunity to reduce waiting lists, as was the case for site D during the PROPEL intervention, or to enable access to treatment for more patients. Future research into sustainable changes to resources is advised.
In an analysis of the long-term follow-up data of 293 of the original POPPY trial participants (both intervention and control participants), the main outcome measure was any related secondary care treatment during follow-up using routinely collected individually linked hospital episode data. This showed (using a mixed-effects logistic regression on any treatment during follow-up with random effect of centre) that the effect of the intervention (PFMT) is statistically significant and is associated with a reduction in the log odds of any treatment during follow-up. People in the intervention group had a lower hazard for any treatment.
Longitudinal follow-up data of the POPPY trial participants did not indicate a difference in the use of health-care resources between the groups. Interpretation of outpatient health-care resource use between groups is limited by the absence of coding reference information. On the basis of the available follow-up data obtained from the administrative data sets, there is no observed difference in resource use between the groups at 11 years post PFMT.
The dissemination and implementation workshops were attended by 120 participants (72 in London and 48 in Glasgow) and identified key barriers (and facilitators) in line with those observed in the realist evaluation. The presentation of the PROPEL intervention findings allowed for the discussion of the possibility of different ways to deliver PFMT. This ‘evidence base’ helped the majority of participants to shift into thinking that ‘change’ was possible and to begin developing action plans to discuss with their local services.
Limitations of the study
This study allowed for local services in three areas (one in England and two in Scotland) to determine how they would implement/deliver PFMT. It was originally anticipated that all sites might implement PFMT delivered by a mix of specialists and other HCPs, and that there would be more higher-level co-ordination of referral pathways to fit seamlessly with referrals (from primary care), triage and treatment with PFMT. The reluctance of one site to train non-specialist physiotherapists meant that we had to find other sites that were, or were willing to start, delivering alternative models. However, this did then provide a strong specialist service against which to evaluate the outcomes compared with other staff delivery.
The negotiation of implementation of different models in other sites and the availability of staff for training incurred delays in implementation, which inevitably affected the recruitment of participants to the outcome study and, therefore, long-term follow-up of women beyond 6 months. The ‘failure’ to pursue some proposed models meant that we needed to re-think how PFMT could be delivered in the face of these barriers; this, in turn, has contributed to our understanding of such barriers. This study has also been conducted in the everyday world of the NHS, where staff absences and shortages are common. The fact that staff could be identified and trained, and that PFMT was implemented with successful outcomes, bodes well for other services being able to attempt similar changes.
The number of women recruited to the PROMs study was lower than anticipated (target: 120 women) and the recruitment rates varied across sites, which hampered cross-site comparisons. The slow rate of recruitment also affected our ability to continue with 12-month follow-up for a large proportion of the women. However, there were sufficient women recruited to enable the key research questions to be answered in relation to the effectiveness of PFMT in improving prolapse symptoms and in determining whether or not the use of non-specialist physiotherapists would result in significantly reduced beneficial outcomes for women.
Logistically, it was not possible to make widespread use of the POP-Q in this study. The use of this measure requires a high level of skill in conducting a physical examination and may also require additional visits by women in studies using the POP-Q. The use of non-specialist physiotherapists working in different settings and geographical locations meant that POP-Q assessments required the additional availability of someone trained in its use to travel to different locations, often to assess one woman. This provision was not possible for most sites.
We have endeavoured to follow up women in the longer term using routinely available and linked health data. Whereas inpatient records are robust indicators of treatment outcomes, outpatient records are more variable in their availability and their accuracy of recording of treatments and procedures. The majority of the POPPY trial participants were resident in Scotland, which made accessing and linking hospital-based activity possible, but did not make accessing and linking primary care data possible. However, the number of original POPPY trial participants (n = 293) available for long-term follow-up was sufficient to enable a robust analysis.
Implications for policy
An NHS review has revealed that there are currently hundreds of women now undergoing surgery to have mesh implants removed. Although a repair using mesh is not the only surgical procedure for prolapse, it has constituted a common procedure in favour of more traditional procedures. Most mesh devices were launched without clinical trials to support their effectiveness, meaning that complication rates were never established prospectively. The National Institute for Health and Care Excellence banned the use of vaginal mesh to treat prolapse in December 2017. Recognising the potential scale of the problem, and in response to lobbying, the UK government announced a review into how the NHS addresses concerns about medical treatments, including vaginal mesh devices. This review is led by Baroness Cumberlege. 40 Following presentation of the PROPEL intervention findings at our dissemination and implementation workshops, the Chartered Society of Physiotherapists approached the PROPEL intervention team to input its findings to this review. These were submitted in February 2019. The PROPEL study was discussed at an oral hearing. 41 Informed by the PROPEL study, the Chartered Society of Physiotherapists made the following recommendations to the review:
-
Women who have had a prolapse or stress urinary incontinence should be referred for PFMT as a first line of treatment.
-
Increase the specialist physiotherapy workforce and train non-specialists to provide PFMT.
Similarly, the Scottish government has initiated its own response to the mesh concerns. A Scottish independent review42 of the use, safety and efficacy of transvaginal mesh implants in the treatment of stress urinary incontinence and POP in women was initiated in response to growing public concern about the number of women experiencing serious complications. At this time, the Cabinet Secretary for Health and Wellbeing asked NHS Scotland to consider suspension of transvaginal mesh procedures pending the outcome of this review. 42 Concluding this review in 2017, its chairperson expressed the hope that their report would go some way to ensuring that the voices of patients continue to be valued, and that they could be assured that future NHS prolapse interventions would be evidence based and audited in order to deliver the best possible outcome with minimum adverse effect. 42
The PROPEL intervention began by listening to women in our three case study sites and gave this information to the local teams to consider in their development and delivery of services. We have ensured that the implementation of PFMT using different models of delivery was subject to a robust outcomes evaluation (using the same primary and secondary outcomes as the original POPPY trial). This has provided a strong evidence base, on which other NHS sites can build, to deliver an evidence-based intervention for women with prolapse that does indeed minimise the potential for adverse effects.
The independent review (Scotland)42 found that current research studies on safety and effectiveness have not provided sufficient evidence on the long-term impact of mesh surgery. They recommended that the lack of long-term follow-up and related outcome data, including information on quality of life and activities of daily living, should be addressed.
The POPPY trial and the PROPEL intervention have both focused on robust outcomes data and the primary outcome has been based on a measure that captures women’s views of their prolapse symptoms and quality of life. This study has also conducted more long-term follow-up of the original POPPY trial participants. We believe that this adds to the strength of evidence for PFMT.
Following an invitation to the Chief Medical Officer for Scotland to our dissemination and implementation workshop in Glasgow, the Scottish government responded with an invitation to present our findings at a meeting that took place in February 2019. These findings were shared with the Consultant in Public Health Medicine, the Government’s Oversight Group and the Senior Medical Officer. The level of interest in our findings at national policy level indicates the relevance of our work for both policy and practice.
Conclusions
It is possible to train different staff types/skill mixes to effectively deliver PFMT to women. Women’s self-reported outcomes significantly improved across all service models delivering PFMT. The PROPEL intervention has demonstrated how different models and service contexts can affect implementation, but, if these are addressed in advance, then there will be a greater likelihood of successful integration with existing health-care pathways and greater opportunities for ensuring that (non-specialist) staff delivering PFMT are supported to deliver PFMT with appropriately triaged patients and appropriate clinical supervision. Services delivered by higher-band physiotherapists only were more costly than services delivered by other staff mixes. No statistically significant difference in the improvement of HRQoL between baseline and 6 months within any site, or from baseline to 12 months between participants treated by specialist physiotherapists and participants treated by other clinical staff, was found. Small participant numbers prevented an assessment of cost-effectiveness.
The realist evaluation combined with the robust outcomes data confirms that PFMT can be successfully delivered using a range of staff/skill mixes and in different NHS settings, and that outcomes are not compromised by different delivery models. This study provides examples of delivery of PFMT (beyond delivery by specialist physiotherapists) by clinicians (i.e. nurses, other physiotherapists) who have an interest in women’s health.
Implications for practice
The evidence supports training a broader range of HCPs with an interest in women’s health and/or with a knowledge of physiology/body muscles to deliver PFMT to women.
Delivery of PFMT by other clinicians was supported by specialist physiotherapists undertaking triage of women to determine their suitability for PFMT. The role of the specialist physiotherapist could then be enhanced, to provide education and support to other HCPs to enable them to safely deliver PFMT to women while managing more complex cases of POP themselves.
Increasing the use of and referral to PFMT as a first-line treatment was facilitated by improved multidisciplinary team working across urogynaecology services and improved communication with primary care. A review of existing pathways to PFMT could identify areas for improvement.
Primary care referrals to PFMT as a first-line treatment for POP would probably increase with more awareness-raising (of POP and PFMT) and education for GPs and other primary HCPs.
The following activities could follow on from this study to begin to address some of the concerns above and raise the potential for change on a wider scale across the NHS:
-
Develop awareness-raising training for GPs and information for urologists and urogynaecologists about the benefits of PFMT as a first-line treatment.
-
Develop new information for practice nurses, midwives and continence services to capitalise on existing opportunities for early identification and intervention, for example by advising women about PFMT during routine smear tests and perinatal appointments.
-
Develop public health campaigns for women of all ages (including teenagers), including, for example, a DVD or animation, to encourage understanding of pelvic health and exercises.
-
Engage with gynaecological service leads to reconfigure care pathways that include PFMT as a first-line option.
-
Undertake work to improve care pathways for women with prolapse, including self-referral pathways for PFMT.
Research recommendations
This evaluation provides a toolkit of outcomes that could be used in routine service delivery, especially the POP-SS outcome measure, which is a relatively easy-to-use, self-complete measure that has now been widely evaluated. Routine evaluation of outcomes could provide more widespread evidence for PFMT delivery by HCPs.
Logistically, it was not possible to make widespread use of the POP-Q in this study. A study comparing the ability of the self-complete POP-SS tool to correlate with the (physical) changes in POP severity (as measured by a clinical assessment using the POP-Q) could help further studies to determine whether the POP-SS is sufficient or we need to input further resources in pelvic health research to ensure that there is more robust completion of the POP-Q examination.
The follow-up study included inpatient and outpatient attendances for a large proportion of original POPPY trial participants. Further studies might explore the information available in primary care and whether or not this has a bearing on assessing the impact of PFMT in the longer term.
The ‘activities’ outlined in Implications for practice would benefit from being grounded in ‘intervention development’ research, which includes input from HCPs (across sectors) and women with POP to ensure that the content of interventions and the formats of delivery are optimised for maximum impact and reach. This would include ‘implementation’ research associated with intervention delivery.
Acknowledgements
We would like to acknowledge the three NHS sites that took part in the whole of the PROPEL intervention: NHS Highlands, NHS Greater Glasgow and Clyde and University Hospitals of Leicester NHS Trust. The time and efforts that were given have been incredible. We are also indebted to the two sites that took part in our PROMs study, Medway NHS Foundation Trust and Southend University Hospital NHS Foundation Trust; without the participation of these sites we could not have completed the PROPEL intervention on time with the robust data that we achieved. We also thank the women who took part in the PROPEL intervention when they did not have to, but gave their time to complete our questionnaires and interviews.
We would also like to thank our PPI and health-care representatives who contributed to the development and conduct of the study, and especially for their contribution to our dissemination workshops.
The authors would like to acknowledge the support of the eDRIS Team (National Services Scotland) for its involvement in obtaining approvals, provisioning and linking data and the use of the secure analytical platform within the National Safe Haven.
The authors would like to thank Bladder and Bowel UK for its involvement and support during the PROPEL intervention, in particular Karen Irwin, service manager and clinical nurse specialist.
Thanks also go to our:
-
PMG (additional to authors) – Mary Macfarlane.
-
SSC – Professor Jo Jackson, University of Essex; Dr Fiona Harris; Suzanne Kent; Julie Ellis; and Janice Faulkner.
-
Regional research support services for their help in recruitment and data collection tasks within the study sites.
Finally, we would like to thank NIHR for supporting this work.
Contributions of authors
Margaret Maxwell (https://orcid.org/0000-0003-3318-9500) (Professor of Health Services and Mental Health Research, Director of the Nursing, Midwifery and Allied Health Professions Research Unit) is lead author of the report and, as such, contributed substantially to writing the report (specifically all abstracts and summaries, and Chapters 1, 8 and 9), as well as editing contributions to all other chapters. She was PI of the study.
Karen Berry (https://orcid.org/0000-0001-6795-4149) (Project Manager and Research Fellow) was the lead researcher who led all of the data collection activity and contributed to its writing (specifically Chapters 2 and 3, and all of the appendices) and was editorial lead for the entire report.
Sarah Wane (https://orcid.org/0000-0002-1766-882X) (Research Associate and Lead Research Fellow during maternity cover for KB) contributed to all data collection activity and, specifically, the qualitative data collection and analysis. She contributed to editing the final report, specifically Chapters 2 and 3.
Suzanne Hagen (https://orcid.org/0000-0002-9741-9160) (Professor of Health Services Research, Deputy Director of the Nursing, Midwifery and Allied Health Professions Research Unit) was the PI of the original POPPY trial and contributed substantially to the PROMs study methods and the long-term follow-up study using data linkage to routine NHS data. She edited the final report, with specific attention to the Scientific summary and Chapters 8 and 9 and the intervention description in Appendix 1.
Doreen McClurg (https://orcid.org/0000-0002-2872-1702) (Professor of Pelvic Floor Physiotherapy) led the adaptation and implementation of training in PFMT for non-specialists. She contributed to editing the final report with specific contributions to Chapters 8 and 9 and sections related to PFMT training and its delivery.
Edward Duncan (https://orcid.org/0000-0002-3400-905X) (Associate Professor of Applied Health Research) contributed expertise to the realist evaluation and the planning, running and data collection and analysis of the dissemination and implementation workshops. He contributed to editing the final report and, specifically, Chapters 8 and 9.
Purva Abhyankar (https://orcid.org/0000-0002-0779-6588) (Lecturer, Faculty of Health and Sports Science) led the realist evaluation and conducted the data analysis for its evaluation. She wrote Chapters 4 and 5 and edited other sections of the final report, with specific attention to reporting of the realist evaluation in the Abstract, Scientific summary, and the Discussion and Conclusions in Chapter 9.
Andrew Elders (https://orcid.org/0000-0003-4172-4702) (Statistician, Nursing, Midwifery and Allied Health Professions Research Unit) was the lead statistician on the PROPEL intervention and contributed to the PROMs study and the POPPY data linkage follow-up study in all aspects, from inception and design to data management, analysis and write-up. He co-wrote Chapters 5 and 6, and edited other sections of the final report, with specific attention to reporting of the outcomes and data linkage studies in the Abstract, Scientific summary, and the Discussion and Conclusions in Chapter 9.
Catherine Best (https://orcid.org/0000-0002-3652-2498) (Lecturer/Statistician, Nursing, Midwifery and Allied Health Professions Research Unit) was a statistician in the PROPEL intervention who contributed to data management and analysis for the PROMs study and the POPPY data linkage follow-up study. She co-wrote Chapters 5 and 6, and edited other sections of the final report, with specific attention to reporting of the outcomes and data linkage studies in the Abstract, Scientific summary, and the Discussion and Conclusions in Chapter 9.
Joyce Wilkinson (https://orcid.org/0000-0002-1008-1882) (Lecturer, Faculty of Health and Sports Science) contributed expertise to the realist evaluation and conducted data analysis for the realist evaluation alongside PA and SW. She contributed to Chapters 4 and 5 and edited other sections of the final report, with specific attention to reporting of the realist evaluation in the Abstract, Scientific summary, and the Discussion and Conclusions in Chapter 9.
Helen Mason (https://orcid.org/0000-0002-9303-2794) (Professor of Health Economics and Deputy Director Yunus Centre for Social Business and Health at Glasgow Caledonian University) led the economic evaluations within the PROPEL intervention in relation to the PROMs study and the POPPY data linkage follow-up study. She co-wrote Chapter 7 and edited other sections of the final report, with specific attention to reporting of the economic evaluations in the Abstract, Scientific summary, and the Discussion and Conclusions in Chapter 9.
Linda Fenocchi (https://orcid.org/0000-0003-2536-8234) (Researcher in Heath Economics at Glasgow Caledonian University) conducted the analysis for the economic evaluation of the models of service delivery and their outcomes and for the economic evaluation of the longer-term follow-up of the POPPY trial participants. She co-wrote Chapter 7 and edited other sections of the final report, with specific attention to reporting of the economic evaluations in the Abstract, Scientific summary, and the Discussion and Conclusions in Chapter 9.
Eileen Calveley (https://orcid.org/0000-0001-8731-2338) (Research Fellow) contributed to the inception of the PROPEL intervention and the overall design and planning of the study and its early set-up stages. She contributed ongoing expertise to data collection and was specifically involved in the planning, organisation and analysis of the dissemination and implementation workshops. She contributed to editing the final report.
Karen Guerrero (https://orcid.org/0000-0001-9591-059X) (Lead Consultant in Urogynaecology, Queen Elizabeth University Hospital) was the lead clinician (Scotland) and contributed to the inception of the PROPEL intervention and the overall design and planning of the study and its implementation in one of the realist evaluation sites. She contributed to editing the final report, specifically its conclusions and recommendations.
Douglas Tincello (https://orcid.org/0000-0002-6385-851X) (Professor of Female Pelvic Medicine and Reconstructive Surgery, University Hospitals of Leicester NHS Trust) was the lead clinician (England) and contributed to the overall planning of the study and its implementation in one of the realist evaluation sites. He specifically contributed to the dissemination and implementation workshops, facilitating data collection at these events and contributing to analysis. He contributed to editing the final report, specifically its conclusions and recommendations.
Publication
Abhyankar P, Wilkinson J, Berry K, Wane S, Uny I, Aitchison P, et al. Implementing pelvic floor muscle training for women with pelvic organ prolapse: a realist evaluation of different delivery models. BMC Health Serv Res 2020;20:910.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Beck RP, McCormick S, Nordstrom L. A 25-year experience with 519 anterior colporrhaphy procedures. Obstet Gynecol 1991;78:1011-18.
- Swift S, Woodman P, O’Boyle A, Kahn M, Valley M, Bland D, et al. Pelvic Organ Support Study (POSST): the distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am J Obstet Gynecol 2005;192:795-806. https://doi.org/10.1016/j.ajog.2004.10.602.
- Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 1997;89:501-6. https://doi.org/10.1016/S0029-7844(97)00058-6.
- Iglesia CB, Fenner DE, Brubaker L. The use of mesh in gynecologic surgery. Int Urogynecol J Pelvic Floor Dysfunct 1997;8:105-15. https://doi.org/10.1007/BF02764826.
- Hagen S, Stark D, Maher C, Adams E. Conservative management of pelvic organ prolapse in women. Cochrane Database Syst Rev 2004;2. https://doi.org/10.1002/14651858.CD003882.pub2.
- Hagen S, Stark D, Glazener C, Dickson S, Barry S, Elders A, et al. Individualised pelvic floor muscle training in women with pelvic organ prolapse (POPPY): a multicentre randomised controlled trial. Lancet 2014;383:796-80. https://doi.org/10.1016/S0140-6736(13)61977-7.
- Hagen S, Stark D, Cattermole D. A United Kingdom-wide survey of physiotherapy practice in the treatment of pelvic organ prolapse. Physiotherapy 2004;90:19-26. https://doi.org/10.1016/S0031-9406(03)00003-8.
- Hagen S, Stark D, Dougall I. A survey of prolapse practice in UK women’s health physiotherapists: what has changed in the last decade?. Int Urogynecol J 2016;27:579-85. https://doi.org/10.1007/s00192-015-2864-9.
- Office for National Statistics . Population Estimates for UK, England and Wales, Scotland and Northern Ireland, Mid–2011 and Mid–2012. 2013. https://webarchive.nationalarchives.gov.uk/20160105225204/www.ons.gov.uk/ons/rel/pop-estimate/population-estimates-for-uk--england-and-wales--scotland-and-northern-ireland/mid-2011-and-mid-2012/index.html (accessed 27 January 2020).
- The Health Foundation . Evidence Scan: Improvement Science 2011.
- Proctor EK, Powell BJ, Baumann AA, Hamilton AM, Santens RL. Writing implementation research grant proposals: ten key ingredients. Implement Sci 2012;7. https://doi.org/10.1186/1748-5908-7-96.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. https://doi.org/10.1136/bmj.h1258.
- Pawson R, Tilley N. Realistic Evaluation. Newbury Park, CA: SAGE Publications Ltd; 1997.
- Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health 1999;89:1322-7. https://doi.org/10.2105/AJPH.89.9.1322.
- Maxwell M, Semple K, Wane S, Elders A, Duncan E, Abhyankar P, et al. PROPEL: implementation of an evidence based pelvic floor muscle training intervention for women with pelvic organ prolapse: a realist evaluation and outcomes study protocol. BMC Health Serv Res 2017;17. https://doi.org/10.1186/s12913-017-2795-x.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Abhyankar P, Wilkinson J, Berry K, Wane S, Uny I, Aitchison P, et al. Implementing pelvic floor muscle training for women with pelvic organ prolapse: a realist evaluation of different delivery models. BMC Health Serv Res 2020;20. https://doi.org/10.1186/s12913-020-05748-8.
- Persu C, Chapple CR, Cauni V, Gutue S, Geavlete P. Pelvic Organ Prolapse Quantification System (POP-Q) – a new era in pelvic prolapse staging. J Med Life 2011;4:75-81.
- Stark D, Dall P, Abdel-Fattah M, Hagen S. Feasibility, inter- and intra-rater reliability of physiotherapists measuring prolapse using the pelvic organ prolapse quantification system. Int Urogynecol J 2010;21:651-6. https://doi.org/10.1007/s00192-009-1089-1.
- Pawson R. Evidence-based policy: in search of a method. Evaluation 2002;8:157-81. https://doi.org/10.1177/1358902002008002512.
- Pawson R, Manzano-Santaella A. A realist diagnostic workshop. Evaluation 2012;18:176-91. https://doi.org/10.1177/1356389012440912.
- Morse JM. A review committee’s guide for evaluating qualitative proposals. Qual Health Res 2003;13:833-51. https://doi.org/10.1177/1049732303013006005.
- Lambert SD, Loiselle CG. Combining individual interviews and focus groups to enhance data richness. J Adv Nurs 2008;62:228-37. https://doi.org/10.1111/j.1365-2648.2007.04559.x.
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analyzing Qualitative Data. Abingdon: Routledge; 1994.
- Abhyankar P, Cheyne H, Maxwell M, Harris F, McCourt C. A realist evaluation of a normal birth programme. Evid Based Midwifery 2013;11:112-19.
- Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn 2004;23:322-30. https://doi.org/10.1002/nau.20041.
- Snijders TAB, Bosker RJ. Multilevel Analysis: an Introduction to Basic and Advanced Multilevel Modeling. Newbury Park, CA: SAGE Publications; 2011.
- Information Services Division Scotland . Outpatient Appointments and Attendances – Scottish Morbidity Record (SMR00) 2016. www.ndc.scot.nhs.uk/National-Datasets/data.asp?ID=1&SubID=4 (accessed 27 January 2020).
- Information Services Division Scotland . General Acute Inpatient and Day Case – Scottish Morbidity Record (SMR01) 2016. www.ndc.scot.nhs.uk/National-Datasets/data.asp?ID=1&SubID=5 (accessed 27 January 2020).
- World Health Organization . International Statistical Classification of Diseases and Related Health Problems 10th Revision 2016. https://icd.who.int/browse10/2016/en (accessed 27 January 2020).
- NHS . OPCS Classification of Interventions and Procedures n.d. www.datadictionary.nhs.uk/web_site_content/supporting_information/clinical_coding/opcs_classification_of_interventions_and_procedures.asp (accessed 27 January 2020).
- Curtis L, Burns A. Unit Costs of Health and Social Care 2018. Canterbury: PSSRU, University of Kent; 2018.
- NHS . Scottish Health Service Costs 2018. www.isdscotland.org/Health-Topics/Finance/Publications/2018-11-20/2018-11-20-Costs-Report.pdf (accessed 27 January 2020).
- Department of Health and Social Care (DHSC) . NHS Reference Costs 2017 18 2018.
- HM Treasury . GDP Deflators at Market Prices, and Money GDP September 2018 (Quarterly National Accounts) n.d. www.gov.uk/government/statistics/gdp-deflators-at-market-prices-and-money-gdp-september-2018-quarterly-national-accounts (accessed 24 January 2019).
- EuroQol . EQ-5D-5L Health Questionnaire. English Version for the UK. 2009. https://euroqol.org/wp-content/uploads/2019/10/Sample_UK__English__EQ-5D-5L_Paper_Self_complete.pdf (accessed 27 January 2020).
- EuroQol Research Foundation . EQ-5D User Guides n.d. https://euroqol.org/publications/user-guides/ (accessed 27 January 2020).
- Information Services Division Scotland . Scottish Drug Tariff Part 3 APPLIANCES 2019. www.isdscotland.org/health-topics/prescribing-and-medicines/scottish-drug-tariff/Docs/May-2019/2019-05-SDT-PART3V2.pdf (accessed 29 January 2020).
- NHS . National Services Scotland Statistical Disclosure Control Protocol Version 3.0. n.d. www.isdscotland.org/About-ISD/Confidentiality/disclosure_protocol_v3.pdf. 2015 (accessed 4 March 2019).
- The Independent Medicines & Medical Devices Safety Review . News n.d. www.immdsreview.org.uk/news.html (accessed 27 January 2020).
- The Independent Medicines & Medical Devices Safety Review . Written Evidence. Evidence Submitted to the Review Following Its Oral Hearings n.d. www.immdsreview.org.uk/downloads/Evidence/FOR%20PUBLICATION%20-%20Evidence%20Submitted%20Following%20Oral%20Hearings.pdf (accessed 27 January 2020).
- Scottish Government . Transvaginal Mesh Implants Independent Review: Final Report n.d. www.gov.scot/publications/scottish-independent-review-use-safety-efficacy-transvaginal-mesh-implants-treatment-9781786528711/ (accessed 27 January 2020).
- Laycock J, Jerwood D. Pelvic floor muscle assessment: the PERFECT scheme. Physiotherapy 2001;87:631-42. https://doi.org/10.1016/S0031-9406(05)61108-X.
- Female Genital Mutilation Act 2003. London: The Stationery Office; 2003.
- Scottish Parliament . Prohibition of Female Genital Mutilation (Scotland) Act 2005 2005.
Appendix 1 The PROPEL TIDieR checklist
Pelvic floor muscle training
Intervention
The intervention was PFMT. The aim of this implementation study was to assess whether or not PFMT delivered by different skill mixes of clinicians would elicit the same outcomes in women with stages I–III prolapse as those seen in the POPPY trial.
Materials
A 1-day training course for intervention providers.
Procedures
The anatomy/function of pelvic floor muscles were explained. Training was given in ‘the knack’ – correctly contracting pelvic floor muscles and precontracting against increases in abdominal pressure. An internal assessment of pelvic floor muscles was carried out to correct exercise technique and assess muscles [using the Pressure, Endurance, Repetitions, Fast contractions, Every Contraction Timed (PERFECT) scheme43]. Tailored lifestyle advice was given when appropriate.
Provision
Provided by POGP registered trainers. Training outlined in Appendix 2.
Delivery
Face-to-face, one-to-one delivery. Home-based practice and outpatient clinics.
Regimen
Home pelvic floor muscle exercises plus 3–6 appointments with clinician delivering PFMT. Duration of physiotherapy appointments unclear.
Tailoring
Yes, home exercise programme modified at each appointment on basis of examination findings and diary recordings. Clinicians decided how many appointments each participant needed.
Modification
No modifications were made.
Adherence
Clinic appointments monitored by clinicians delivering the intervention.
Control
There was no control as this was an implementation study.
Appendix 2 The PROPEL intervention training outline
The training for the PROPEL intervention clinicians was carried out by experienced pelvic health physiotherapists and tutors on the Pelvic, Obstetric and Gynaecological Physiotherapy Professional Network workshops of the Chartered Society of Physiotherapy. There was a mixture of professions and grades participating in the workshops.
The content of this 1-day programme was a modification of the 3-day ‘POGP Pelvic Health Physiotherapy female urinary dysfunction’ entry-level course and the 1-day ‘POGP Pelvic Health Physiotherapy POP, advancing your practice, better understanding of POP’ course. These workshops are designed to be carried out sequentially, as the first provides general background plus practical training in vaginal examination, and the second develops further knowledge in the specialty. Mentoring post workshop is recommended.
Pre-course reading was recommended. See below.
Vaginal assessment practicals included tutor demonstration, participant assessment on a tutor and, when applicable, peer-to-peer examinations. Consent was documented.
A skills checklist for the PROPEL intervention training pelvic floor and vaginal assessment practical session was also completed for each participant. See below.
Programme
| Time | Topic | Tutor |
|---|---|---|
| 09.00–10.00 | Introductions, background and research protocol | |
| 10.00–10.30 | Professional issues | |
| 10.30–11.00 | POP: background | |
| 11.00–11.15 | Coffee | |
| 11.15–12.30 | Subjective assessment | |
| 12.30–1.00 | Lunch | |
| 13.00–13.30 | Objective assessment | |
| 13.30–15.30 | Practical | |
| 15.30–16.15 | Treatment planning, advice and exercises | |
| 16.15–16.45 | Questions |
Recommended pre-attendance learning
Professional issues learning tasks:
-
Familiarise yourself with the consent policy used within your organisation.
Ensure that you are aware of the key components of valid consent, including capacity, the requirements relating to information-sharing, as well as the documentation requirements of your organisation.
Reflect on the process you use when seeking consent for a vaginal examination and consider whether or not this fulfils your statutory and professional obligations.
-
Familiarise yourself with your organisation’s chaperone policy.
Consider the process used by you/your organisation in order to establish whether or not a chaperone is required for vaginal examination and reflect on whether or not this fulfils your professional/organisational obligations.
-
Familiarise yourself with the confidentiality requirements of your organisation, including those relating to recently enacted legislation such as the Female Genital Mutilation Act (2003)44 or the Prohibition of Female Genital Mutilation (Scotland) Act (2005). 45
Ensure that you know how to disclose or escalate any concerns you have relating to patient confidentiality issues.
-
Familiarise yourself with the relevant sections of your organisation’s infection prevention/control policy.
Ensure that you know how to apply the infection prevention/control policy to ensure safe and effective practice in relation to patients attending as part of the PROPEL intervention.
Additional background learning/knowledge update
The tutor team also recommends that you review the anatomy of the pelvic floor prior to attending the study day. The following YouTube (YouTube, LLC, San Bruno, CA, USA) link is a useful 10-minute tutorial showing the three-dimensional arrangement of the pelvic floor complex: www.youtube.com/watch?v=P3BBAMWm2Eo (accessed 30 January 2020).
Other useful resources relating to POP include:
-
www.nhs.uk/conditions/prolapse-of-the-uterus/Pages/Introduction.aspx (accessed 30 January 2020).
-
www.rcog.org.uk/en/patients/menopause/pelvic-organ-prolapse/ (accessed 30 January 2020).
Relevant pages of the Royal College of Obstetricians and Gynaecologists, with good links to other sites and surgical options:
-
http://pogp.csp.org.uk/publications/pelvic-organ-prolapse-physiotherapy-guide-women (accessed 30 January 2020).
The POP patient information leaflet of the POGP, which will be given to all women in the PROPEL intervention:
-
www.yourpelvicfloor.org/conditions/pelvic-organ-prolapse/ (accessed 30 January 2020) – The pelvic organ prolapse patient information leaflet of the International Urogynaecology Association (IUGA), providing a concise overview of the condition.
-
www.csp.org.uk/videos/customized-pelvic-organ-prolapse-quantification-exercise-quick-score-entry (accessed 30 January 2020).
Demonstration of a POP-Q measurement; note: this is for information only.
Important information about the practical session on vaginal examination:
This training day includes a practical session on vaginal examination. The aim of the session is for you (as a participant) to practise the examination that you will perform on patients as part of the PROPEL intervention assessment.
Format of the teaching session: one tutor will demonstrate the vaginal examination, using the other tutor as a model. Following this you will be able to practise the examination by peer or tutor examination in small groups. There will be no more than four participants per group.
Tutor examination will involve a tutor acting as the model. Peer examination involves one or more participants acting as the model. Each participant makes their own decision whether or not they act as a model. If you choose to act as a model, you will decide whether this is for one or more examinations and you have the right to opt in or out of the practical sessions at any time.
It is recognised that peer examination can be advantageous. Participants on similar courses who have acted as a model often recommend it as a valuable learning experience, but it is not a requirement. The advantages of acting as a model include you developing a personal insight into the patient experience, including comfort and/or dignity issues. This may allow better communication with your patients as to what they may experience when you examine them in clinical practice. The disadvantages are likely to vary on an individual basis. There may be no disadvantages to you personally; however, such disadvantages may include feelings of discomfort, embarrassment or lack of modesty, as well as relationship boundary issues with fellow learners and/or an exacerbation of legacy of prior sexual abuse and/or trauma. There should be no perception of coercion to participate as a model and you will not be asked to justify your decision.
If you choose to act as a model, you have the right to decline to be examined by any specific course participants owing to embarrassment or other factors. In the case of a participant declining to complete at least one vaginal examination on a model, it will not be possible to complete the skills checklist and the participant will not be able to complete the programme.
You will be provided with a consent form, which must be printed and brought with you to the PROPEL intervention training day. Further information will be given at the training day and you will have the opportunity to observe a demonstration of the examination before you decide on the extent of your involvement in the practical session. Once you have a better understanding of what is required and have had the opportunity to ask any questions you may have about the session, you will be asked to complete the form.
If you would like the opportunity to talk to one of the tutors prior to the training, regarding any aspect of the practical session (including any health issues), then please contact the PROPEL intervention team who will put you in touch with one of the tutors.
Appendix 3 The PROPEL intervention training skills checklist
Appendix 4 The PROPEL intervention Pelvic Organ Prolapse Quantification System assessment form

Appendix 5 Project timeline
| Study tasks | Year and month | |||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2016 | 2017 | 2018 | 2019 | |||||||||||||||||||||||||
| November | December | January | February | March | April | May | June | July | August | September | October | November | December | January | February | March | April | May | June | July | August | September | October | November | December | January | February | |
| Round 1 | ||||||||||||||||||||||||||||
| Round 2 | ||||||||||||||||||||||||||||
| Round 3 | ||||||||||||||||||||||||||||
| Round 4 | ||||||||||||||||||||||||||||
| Clinical recruit/training | ||||||||||||||||||||||||||||
| Patient recruitment (realist evaluation) | ||||||||||||||||||||||||||||
| Patient recruitment (outcomes) | ||||||||||||||||||||||||||||
| Baseline | ||||||||||||||||||||||||||||
| 6 months | ||||||||||||||||||||||||||||
| 12 months | ||||||||||||||||||||||||||||
| Data linkage | ||||||||||||||||||||||||||||
| Analysis (realist evaluation) | ||||||||||||||||||||||||||||
| Analysis (outcomes) | ||||||||||||||||||||||||||||
| SSC meetings | ||||||||||||||||||||||||||||
| PMG meetings | ||||||||||||||||||||||||||||
| Dissemination | ||||||||||||||||||||||||||||
List of abbreviations
- AfC
- Agenda for Change
- BBF
- Bladder and Bowel Foundation
- BMI
- body mass index
- CI
- confidence interval
- CMO
- context–mechanism–outcome
- df
- degrees of freedom
- DVD
- digital versatile disc
- eDRIS
- electronic Data Research and Innovation Service
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- EQ-VAS
- EuroQol Visual Analogue Scale
- GBP
- Great British pounds
- GP
- general practitioner
- ICIQ-UI SF
- International Consultation on Incontinence Questionnaire – Urinary Incontinence Short Form
- HCP
- health-care professional
- HRQoL
- health-related quality of life
- ICD-10
- International Statistical Classification of Diseases and Related Health Problems, Tenth Revision
- NIHR
- National Institute for Health Research
- OPCS
- Office of Population Censuses and Surveys Classification of Interventions and Procedures
- OR
- odds ratio
- PFMT
- pelvic floor muscle training
- PI
- principal investigator
- PMG
- project management group
- POGP
- pelvic, obstetric and gynaecological physiotherapists group
- POP
- pelvic organ prolapse
- POPPY
- Pelvic Organ Prolapse PhysiotherapY
- POP-Q
- Pelvic Organ Prolapse Quantification System
- POP-SS
- Pelvic Organ Prolapse Symptom Score
- PPI
- patient and public involvement
- PROM
- patient-reported outcome measure
- PROPEL
- PROlapse and Pelvic floor muscle training: implementing Evidence Locally
- PSSRU
- Personal Social Services Research Unit
- RE-AIM
- reach, effectiveness, adoption, implementation and maintenance
- SD
- standard deviation
- SMR
- Scottish Morbidity Record
- SPM
- service planning meeting
- SSC
- Study Steering Committee
- TIDieR
- Template for Intervention Description and Replication
- WHP
- women’s health physiotherapist
