Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 13/10/86. The contractual start date was in September 2014. The final report began editorial review in April 2019 and was accepted for publication in March 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Beresford et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Background and study overview
About autism
Autism is a spectrum of developmental conditions that change the way people communicate and experience the world around them. 1 Diagnostic characteristics are pervasive difficulties since early childhood, including reciprocal social communication and restricted, repetitive interests and behaviours. 2 Around half of autistic adults have learning disabilities (LDs). Earlier diagnostic classifications imposed diagnostic labels according to the presence of learning disabilities or functional ability (e.g. Asperger syndrome, high-functioning autism). Although no longer used as diagnostic labels, some autistic people choose to continue to use them for themselves. Improved recognition and awareness of autism over the years has seen a substantial rise in the estimated prevalence from 4 out of 10,000 people in the mid-1960s to the current estimate of ≈ 1% of the adult population,3 with around half diagnosed as autistic without LDs.
The health and well-being of autistic adults
There is now a robust evidence base on the health and other outcomes of autistic adults. Autistic adults without LDs experience poorer outcomes than the general population in many areas of their lives,4,5 including mental health, particularly anxiety and depression;6–11 social isolation;12–15 employment;16–19 and achieving independent living. 20 More recent evidence also points to poorer physical health outcomes and increased risk of suicide. 21,22 Co-occurring mental health problems may be the primary source of impairment23 and in themselves may directly impact other outcomes, such as managing everyday life, work and independent living. Other studies have highlighted potential impacts on family members, particularly parents, with reports of unmet information and support needs, and negative impacts on health outcomes. 24
Despite this evidence, a number of studies conducted in different countries report difficulties accessing diagnostic services and wide-ranging unmet needs. 25,26 A lack of specialist autism adult services, particularly for autistic adults without LDs, is a key reason for this. 27 Indeed, it has been estimated that not providing long-term, low-intensity, holistic support for this population is likely to result in higher costs to individuals and society. 28
The notion of a Specialist Autism Team
In England, widespread concern about the health, social and economic outcomes of inadequately supporting autistic adults culminated in the cross-government Autism Act (2009)29 and Autism Strategy (2010). 30 These placed responsibility on the NHS and local authorities (LAs) to improve support and services for autistic adults. Both the Autism Act29 and the Autism Strategy30 stipulated the need for autism-specific provision, including specialist community-based, multidisciplinary teams to develop, co-ordinate and deliver services. National Institute for Health and Care Excellence (NICE) guidance published shortly after31 also recommended that each locality had such a team, referring to them as Specialist Autism Teams (SATs), and further specified their multidisciplinary nature and roles (Box 1).
In each area a specialist community-based multidisciplinary team for adults with autism (the specialist autism team) should be established. The membership should include:
-
clinical psychologists
-
nurses
-
occupational therapists
-
psychiatrists
-
social workers
-
speech and language therapists
-
support staff (e.g. staff supporting access to housing, educational and employment services, financial advice, and personal and community safety skills).
The specialist autism team should have a key role in the delivery and co-ordination of:
-
specialist diagnostic and assessment services
-
specialist care and interventions
-
advice and training to other health and social care professionals on the diagnosis, assessment, care and interventions for adults with autism (as not all may be in the care of a specialist team)
-
support in accessing, and maintaining contact with, housing, educational and employment services
-
support to families, partners and carers where appropriate
-
care and interventions for adults with autism living in specialist residential accommodation
-
training, support and consultation for staff who care for adults with autism in residential and community settings.
NICE, 201231
Reproduced with permission from NICE. 31 © NICE [2012] Autism spectrum disorder in adults: diagnosis and management. Available from www.nice.org.uk/guidance/cg142 All rights reserved. Subject to Notice of rights. NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this product/publication.
The term used by NICE to describe this type of provision in its more recently published Guidance Implementation Resources (GIRs),32 and by the government in its updated strategy for autism (Think Autism. Fulfilling and Rewarding Lives, the Strategy for Adults with Autism in England: An Update),33 is ‘multi-agency local autism team’. Overall, the proposed functions or roles of these teams were generally unchanged. However, compared with the NICE 2012 guideline,31 the 2014 GIRs32 appear to place additional emphasis on particular roles or functions, namely, ‘up-skilling’ professionals in other services and the provision of autism-specific, preventative social inclusion and well-being interventions. These are interesting developments that reflect a wider re-emphasis on supporting self-management and prevention. The 2014 GIRs32 also appear to signal a recognition that, for a condition emerging as more prevalent than previously thought, exclusively ‘specialist’ provision is not a sustainable model and an important part of the role of a specialist service should be upskilling other professionals and services.
The lack of evidence underpinning policy and practice
The Guideline Development Group (GDG) that was responsible for the NICE guideline31 on management of adults with autism5 made the following comment:
. . . while there is no doubt that guidance on the development and organisation of care for people with autism is needed, it is nonetheless very challenging to develop. In significant part this relates to the very limited evidence base . . .
National Collaborating Centre for Mental Health. 5
Indeed, the group noted that the evidence base was even more limited with respect to autistic adults without LDs than that for autistic adults with LDs and autistic children.
Thus, in terms of its recommendation for the development of SATs, the GDG drew on the Common Mental Health Disorders Guideline34 and studies that explored the views and experiences of autistic adults, carers, partners and other family members. 5 As a result, although advocating the broad principles and role of SATs, the GDG could not advocate a particular structure or model of service delivery.
The dearth of evidence faced by the NICE GDG in 2012 remains a significant issue and barrier to evidence-informed care, management, service development and policy development. 27,32,35,36 A number of reports identify the relative underinvestment of health and care services research concerning the care and support of autistic adults compared with other lifelong conditions. 36,37 Other reports make the point that, historically, within autism research, the attention and investment has been on neurobiology and cognitive research, which has had little or no impact on the lives of autistic people. 38
The call to develop an evidence base on Specialist Autism Teams
The Autism Act29 and NICE guidance’s31 recommendation that localities have a ‘Specialist Autism Team’ has tasked commissioners and practitioners with developing a new type of provision in the absence of any robust evidence about what it should look like in terms of its organisation, service structure, delivery and practice characteristics. The NICE GDG recognised this, and one of its key research recommendations was that as SAT provision emerged and developed this should be evaluated, with particular attention paid to identifying service characteristics associated with positive outcomes (Box 2). This study was developed specifically in response to this call for evidence. To our knowledge, this remains the only study of this sort of provision for autistic adults without LDs. 32
The Department of Health’s autism strategy (2010) proposes the introduction of a range of specialist services for people with autism; these will usually be built around specialist autism teams. However, there is little evidence to guide the establishment and development of these teams.
There is uncertainty about the precise nature of the population to be served (all people with autism or only those who have an IQ of 70 or above), the composition of the team, the extent of the team’s role (for example, diagnosis and assessment only, a primarily advisory role or a substantial care co-ordination role), the interventions provided by the team, and the team’s role and relationship with regard to non-statutory care providers. Therefore it is likely that in the near future a number of different models will be developed, which are likely to have varying degrees of success in meeting the needs of people with autism. Given the significant expansion of services, this presents an opportunity for a large-scale observational study, which should provide important information on the characteristics of teams associated with positive outcomes for people with autism in terms of access to services and effective co-ordination of care.
NICE, 2012 p. 4231
Reproduced with permission from NICE. 31 © NICE [2012] Autism spectrum disorder in adults: diagnosis and management. Available from www.nice.org.uk/guidance/cg142 All rights reserved. Subject to Notice of rights. NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this product/publication.
Study aims
This was the first study of ‘Specialist Autism Team’-type provision. The overall aim was to generate an evidence base on this novel model of care and support service for autistic adults that would be pertinent and valuable to commissioners, practitioners and the autism community and could support evidence-informed implementation of national policy, and service and practice development. Although specific to the English context, the dearth of provision for autistic adults means that the findings may be a useful resource more widely, as other countries seek to improve services and support for autistic adults. 27
The key research questions the study sought to address were:
-
What models of providing SATs currently exist?
-
Is there a particular service model(s) that performs better in terms of achieving positive outcomes for its users?
-
What characteristics of SATs are associated with positive outcomes?
-
What is the ‘added value’ to individuals of the support and care functions of a SAT beyond the diagnostic assessment process?
-
What is the service user experience and does it differ between SATs?
-
What are the costs of the different models of SATs, how are they being funded and how do they compare in terms of costs and cost-effectiveness?
Study design and structure
To address these questions, a two-stage study was conducted.
Stage 1 (the mapping study) identified services in England that fulfilled the NICE criteria of a SAT, described the service characteristics and investigated whether or not it was possible to create a typology of different SAT service models.
Stage 2 (the evaluation study) was a mixed-methods investigation of SATs that sought to:
-
describe the implementation and delivery of SATs
-
describe the outcomes of using SATs at 12 months after entry into the service and, where possible, at 18 and 24 months after entry into the service
-
identify and explore features of service organisation, delivery and practice, and individual characteristics, that are associated with user outcomes
-
estimate the costs of different models of SATs and investigate cost-effectiveness
-
describe the experiences of using a SAT
-
conduct an initial comparison of outcomes for individuals diagnosed and then supported by a SAT with a cohort of individuals who received a diagnostic assessment only.
Figure 1 illustrates the overall design and flow of the study.
FIGURE 1.
Overview of the study.

Stage 1: the mapping study
Multiple data sources [survey of Autism Leads across England, searches of Clinical Commissioning Groups (CCGs) and local authority (LA) websites and published reports] were used to identify services in England that, potentially, fulfilled the NICE guideline31 description of a SAT in terms of functions and staffing. All identified services were subject to a two-stage screening process, with additional data collected directly from the services potentially fulfilling the NICE criteria after the first stage of screening. Data on services identified as SATs were subject to structured content analytical techniques to describe them, to identify service characteristics that distinguished them and to test whether or not they could be organised into a typology of SAT service models. Purposive sampling techniques were used to identify SATs to act as research sites for stage 2. Stage 1 took place in late 2014 and 2015.
Stage 2: the evaluation of Specialist Autism Teams
Stage 2 comprised a mixed-methods observational study of two cohorts [the SAT cohort and the Diagnosis-Only (DO) cohort] and a nested qualitative study of the views and experiences of senior members of SATs.
The SAT cohort comprised users of SATs, who were recruited at the time of their first full assessment appointment. Individuals in this cohort included those referred to the SAT who were already diagnosed with autism [the ‘Support-Only’ (SO) group] and those referred for diagnostic assessment and ongoing support [the ‘Diagnosis and Support’ (D&S) group].
Three of the research sites also provided a regional or national diagnostic assessment service for individuals living outside its CCG/LA boundaries via block contracts with neighbouring CCGs or on a case-by-case basis. The DO cohort comprised individuals who accessed the diagnostic assessment service at these sites via this pathway. Thus, these individuals did not receive any post-diagnosis support from the SAT.
The SAT and DO cohorts were followed up for 12 months from the point of the first full assessment appointment (T0). Outcomes and resource use data were collected at 3 (T1), 6 (T2) and 12 months (T3) for the whole cohort. T3 was our primary outcome time point. For those recruited early to the study, it was decided that outcome data would also be collected at 18 (T4) and 24 (T5) months, as this would provide initial data on longer-term outcomes.
A purposively selected subsample of service users from both cohorts was recruited to take part in a semistructured, in-depth interview about their experiences as service users, perceived outcomes and views on factors (service-level and individual-level characteristics) that affected outcomes. Where the interviewee gave permission, a family member (e.g. a parent or partner) nominated by the interviewee was also invited to take part in an interview.
The nested qualitative study of senior SAT practitioners used individual interviews and focus group discussions to collect data on their views and experiences of setting up, managing and delivering a SAT; factors affecting outcomes; and ensuring sustainable developments and improvements in the care and support for autistic adults without LDs.
Finally, for the economic evaluation element, SAT service leads were asked to provide relevant financial information.
Study delivery
Stage 2 recruitment and data collection took place between February 2016 and November 2018, with all study participants followed up to at least the 12-month follow-up time point.
We encountered two obstacles in delivering the study. First, recruitment of research sites to the study, which was originally scheduled to take 4 months, took over 1 year. Reasons for this included (1) needing to bring additional sites on board to replace a large research site that withdrew well into study set up because of capacity and commissioning issues; (2) two sites having to pause study set up because of recommissioning processes; and (3) in some sites, limitations to the local research and development support available and/or a lack of autism expertise among clinical studies officers. Second, resource limitations meant that the majority of sites could not collect or provide data on service-level outcomes (e.g. intervention take up and retention) for stage 2 of the study.
On a separate note, a proposed element of stage 2 (i.e. seeking views on support, training and advice from services/staff who refer to the service and/or care for adults with autism in residential and community settings) was not pursued. This was for a number of reasons. SATs were providing services only to autistic adults without LDs, almost all of whom lived independently. The two research sites that provided the most extensive consultancy and supervision of other services/professionals withdrew from the study prematurely owing to capacity (and a third site also operating in this way failed to open); therefore, accessing referrers/services with the experience of using the SAT for more than one case was significantly affected. In addition, the majority of referrals were via the diagnostic pathway or self-referral.
Ethics considerations
Stage 1 (the mapping study) was defined as a service audit by the Health Research Authority and did not require ethics approval. The Health Research Authority’s North West – Greater Manchester West Research Ethics Committee reviewed and approved stage 2 (Research Ethics Committee reference 15/NW/0708) and all substantial amendments.
Public and service user involvement
When developing the funding application, we surveyed members of the National Autistic Society (London, UK) to ascertain their interest and support for the project, and their views on the key questions that the research should address. Strong support for the study was expressed; this appeared to be driven by experiences of high levels of unmet need and the lack of specialist autism services.
A project advisory group (PAG), comprising autistic adults without LDs, was appointed. PAG members were recruited through an advertisement that was placed on the National Autistic Society’s website that provided details of the application process, including hyperlinks to an information sheet (explaining the project, its objectives and what being on the PAG would involve) and a short application form. The application form collected information that allowed us to ensure that a range of experiences and characteristics were represented on the PAG (e.g. age, age at diagnosis, experience of using any autism-specific services and geographical location). Over 70 individuals applied. Applications were reviewed by the research team and 14 individuals were invited to an afternoon ‘project advisory group recruitment event’ that was held at the head office of the National Autistic Society. The purpose of this event was for applicants to meet the research team and experience some of the tasks and activities that they might be expected to do as a member of the PAG (e.g. reviewing information sheets, small group tasks and discussions). It also provided the research team with the opportunity to observe the group working together. Eleven individuals attended the event and, at the end of the event, all indicated they were willing be on the PAG.
We used face-to-face meetings to consult with the PAG. These were held in a central London venue that was routinely used by the National Autistic Society and was previously checked as being suitable for use by autistic adults. Those unable to attend meetings had the opportunity to share comments and views via a telephone call with a member of the research team or via e-mail. In between meetings, we consulted with the group via a closed Facebook group (Facebook, Inc., Menlo Park, CA, USA; URL: www.facebook.com). This was something that the majority of individuals asked to be created in preference to using e-mail for communication. We also provided project updates via Facebook.
All elements of the project were discussed with the group, with particular attention paid to those elements in which autistic adults without LDs were directly involved as research participants. Examples of the sorts of issues that we brought to the group included:
-
content and layout of all stage 2 recruitment materials
-
the wording of questions for the demographic and the resource use questionnaires used for the outcomes evaluation
-
formatting and layout of the outcomes evaluation questionnaire
-
the reminder process when questionnaires were not returned
-
content and ordering of the topic guide for the user interviews (process evaluation)
-
tools to use to facilitate interviews
-
issues to consider when recruiting to and setting up interviews for the process evaluation (reported in Appendix 6)
-
adjustments required to interview technique
-
minimising anxiety associated with anticipating and during interviews.
In addition, individual members of the PAG met with the member of the research team who conducted the service user interviews. These meetings were used both to review draft topic guides and as a training experience for the researcher with respect to interacting with and interviewing autistic adults without LDs. We cannot emphasise enough the contribution the PAG made to this project.
Chapter 2 Stage 1: identifying and describing ‘Specialist Autism Team’ services
Introduction
Stage 1 was a necessary preliminary to the evaluation stage of the project. It identified and described services across England that fulfilled the NICE’s31 definition of a SAT (see Box 1), thus allowing us to identify our research sites. It also generated important standalone evidence regarding the way and extent to which localities are implementing SAT provision.
The key objectives were to:
-
identify SATs currently operating in England
-
describe their characteristics (structure, delivery and ways of working) and examine the differences and similarities between them
-
test whether or not service characteristics cluster together in such a way that a typology of SAT service models can be recognised.
Methods
Identification of services potentially fulfilling Specialist Autism Team criteria
An overview of the process by which SATs were identified is shown in Figure 2. Data collection instruments are available in Report Supplementary Material 1.
FIGURE 2.
The process of identifying SATs.
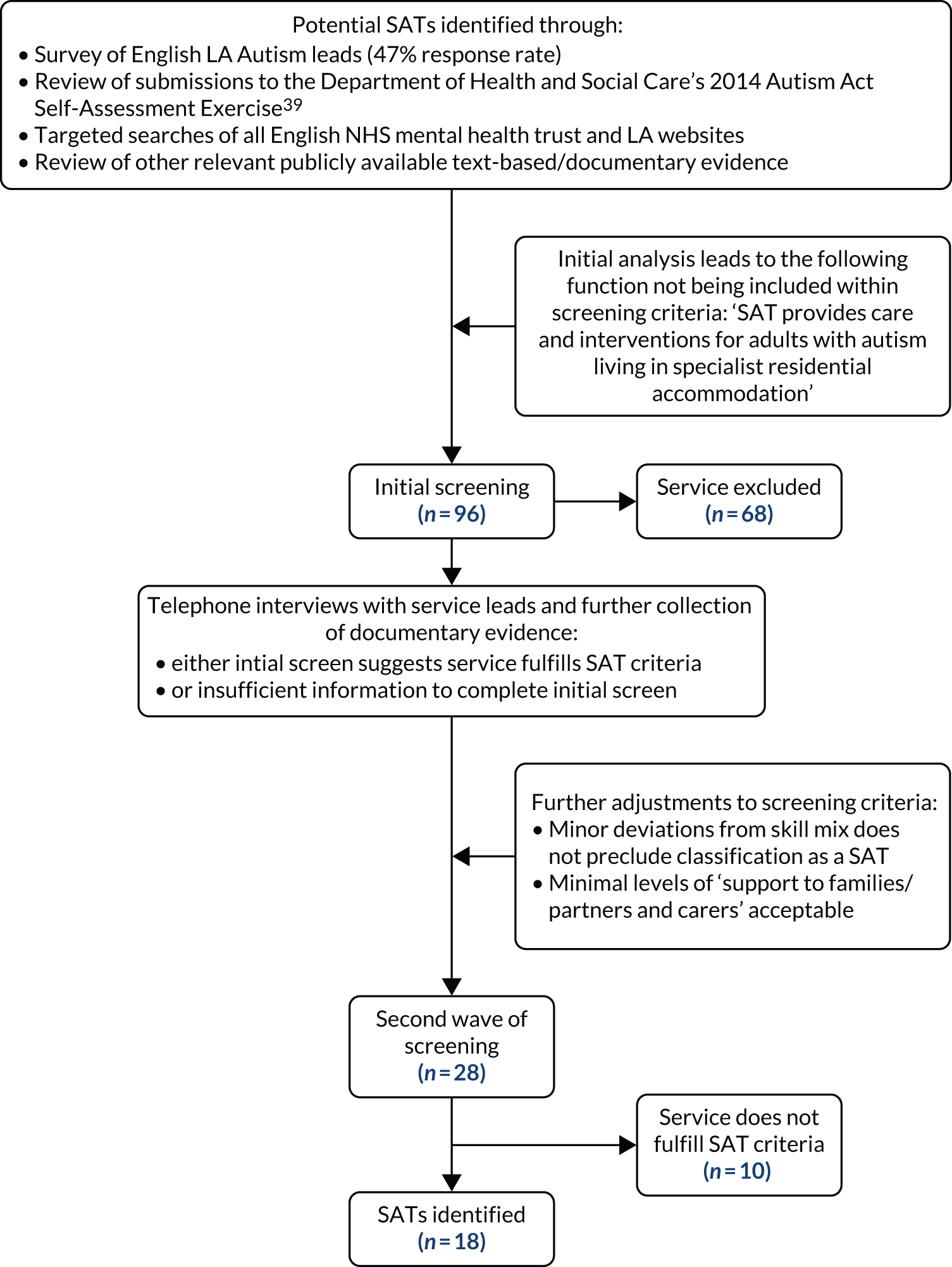
A survey of Autism leads across England, web searches and reviews of documentary evidence identified services that, potentially, fulfilled the NICE description of a SAT in terms of functions and staffing. Information gathered on identified services (n = 96) was independently scrutinised by at least two members of the research team. It soon became apparent that the predominant population served by potential SATs were autistic adults without LDs. In response, one of the functions of SATs set out in the NICE guidance31 – ‘care and interventions for adults with autism living in specialist residential accommodation’ – was not used as an inclusion criterion (NICE 2012 Autism spectrum disorder in adults: diagnosis and management. Available from www.nice.org.uk/guidance/cg142 All rights reserved. Subject to Notice of rights. NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this product/publication). Where insufficient information had been identified to allow a screening decision, services were taken forward to next stage of data collection. Twenty-eight services were taken through to this stage. The main reasons why services were lost at this screening stage were that they provided (1) diagnostic assessment service only or (2) social care provision with no integrated pathway to/from a diagnostic assessment service.
Structured telephone interviews with service leads of ‘potential SATs’ (n = 28) gathered further data. These interviews were conducted from late 2014 to mid-2015. Interviews, lasting 50–75 minutes, were audio-recorded and a detailed summary was subsequently generated. The topics covered included:
-
commissioning and funding arrangements
-
the population served and eligibility criteria
-
the structure of the service
-
the service/team composition
-
the diagnostic assessment process
-
the approach to meeting health, social care and other needs (e.g. deliver interventions, refer on and/or ‘up-skill’ other services)
-
the wider service context (local availability of other specialist autism provision, including third sector).
The interviewees were asked to supply any relevant publicly available documentary evidence (e.g. annual reports/audits, service commissioning briefs and invitations to tender for services) that was not already collected. Where interviews were not achieved (n = 6/28), further extensive efforts were made to gather publicly available documentary evidence.
Using the data gathered, a detailed ‘service description’ of each potential SAT was created and organised under the following high-level headings:
-
service history and overview
-
staffing, skill mix and location
-
structure of the service and commissioning and funding arrangements
-
eligibility criteria and referral
-
services/interventions offered
-
ways of working
-
the care pathway
-
discharge and caseload.
Before the final screen and informed by an initial analysis of the data, further adjustments to the inclusion criteria were made. First, minor deviations in skill mix from the NICE guidance31 were not used as exclusion criteria. Second, any degree of intensity of ‘support to families/partners and carers’ was acceptable.
‘Service descriptions’ were independently scrutinised by at least two members of the research team. Where necessary, follow-up telephone calls/e-mails with services were carried out to gather additional information. Final decisions regarding whether or not a service (or configuration of services) was classified as a SAT were made in the context of a review of evidence and discussion involving two or more members of the research team.
Data analysis
We had proposed to use cluster analysis to analyse the data and support the generation of a typology of models of service delivery. However, a first look at the data made it apparent that this was neither feasible nor appropriate. First, there were just 18 SATs in our sample. Second, it was clear that these were complex and highly idiosyncratic services and there were no patterns in the co-occurrence of certain features or characteristics. Third, and related to the previous point, no relevant existing evidence was available that could inform selecting certain service characteristics/organisational features to prioritise in the development of a typology.
Service descriptions were, therefore, subject to structured content analysis. 40 Qualitative data were interrogated for descriptive evidence on service characteristics and explanations given for service characteristics or ways of working, etc. Data were also extracted into Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheets to facilitate comparison between SATs and the identification of any consistent clustering of service characteristics or features. Analytical writing, with iterations shared and commented on by all members of the research team, supported data analysis and conclusion drawing. We also carried out a brief descriptive analysis of all relevant quantitative and qualitative data that were collected to generate high-level information about specialist autism provision in localities without a SAT.
Results
Services identified as SATs varied in a number of service characteristics. There were no consistent patterns in the way certain characteristics co-occurred and, as a result, it was not possible to develop a typology of SAT service model into which services could be allocated.
The number of Specialist Autism Teams identified and their broad characteristics
Eighteen localities in England were identified as having a SAT (based on the revised inclusion criteria reported in Methods).
A number of factors influenced both the original ‘design’ of services and the changes to service features/characteristics over time. External influencers were the funding available, the service specifications set out in commissioning briefs and the nature and extent of multiagency working. These were, to some extent, interdependent. Internal influences were personal clinical opinion and cumulative clinical experience acquired through running a SAT.
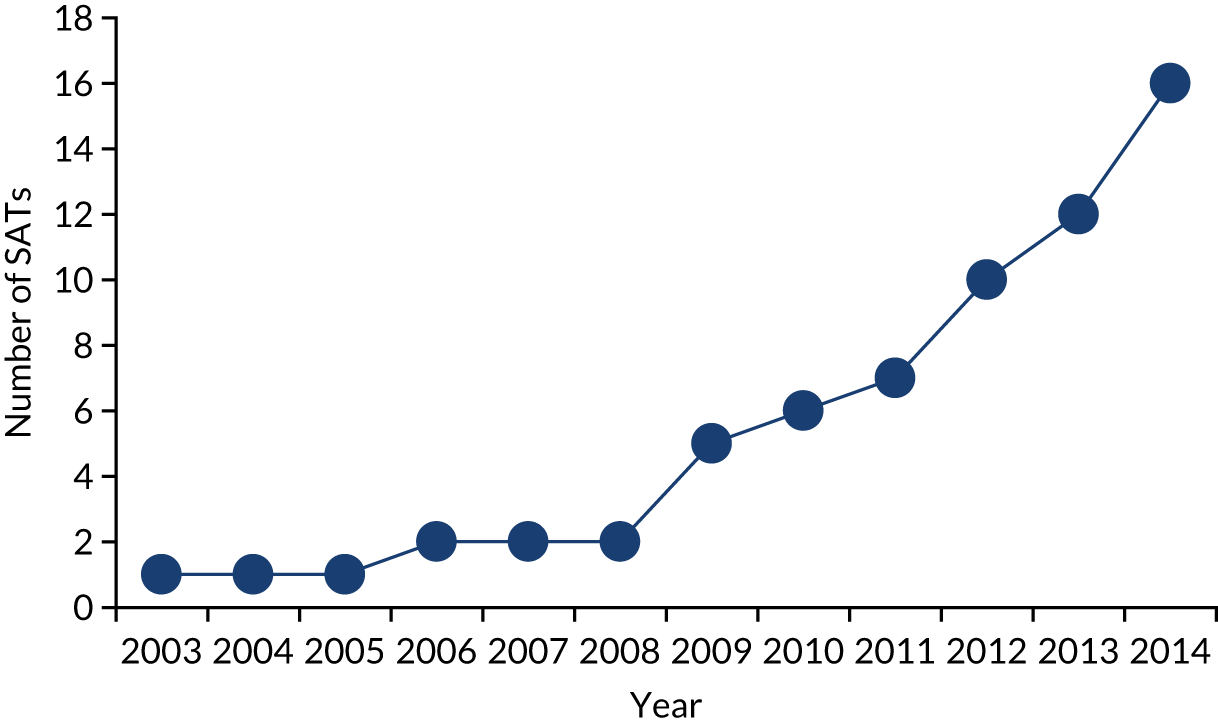
The majority of SATs came into existence from 2009, with only two existing prior to that date (Figure 3). For those more recently established, the Autism Act,29 Autism Strategy30 and 2012 NICE guidance31 were identified as providing the impetus or justification for the development of the SAT.
FIGURE 3.
The number of SATs in existence by year (missing data, n = 2).
The loss of Specialist Autism Teams
A very small number of services were identified that, previously, would have been regarded as fulfilling the criteria for a SAT. Owing to a reduction in NHS funding and/or a loss of LA involvement, services had constricted to being a diagnostic service.
Population served
Entry into the service was commonly via a diagnostic assessment. The majority of SATs (n = 16/18) also accepted referrals of adults without LDs who were already diagnosed with autism. The proportion of ‘already diagnosed’ referrals within these services varied from < 10% to around half. Only one-quarter of SATs accepted self-referrals. All SATs operated an eligibility criterion of an IQ of > 70. The explanation for this selective approach was a perceived gap in support for autistic adults without LDs, and a belief that there were significant differences in the types of provision and expertise needed for autistic adults with LDs compared with those without LDs.
Organisational features
Autism-specific versus neurodisability service
The majority of SATs were autism-specific services (n = 15), but three were based within a wider neurodisability service.
Organisational structure and funding arrangements
A number of different organisational structures and funding arrangements were identified. Within each, different commissioning and funding arrangements were observed.
The majority of SATs were a single service (n = 12), typically based in the local community mental health trust. A number of different commissioning and funding models were reported:
-
CCG sole commissioner with a SAT fully funded from the health budget.
-
CCG sole commissioner with a LA-seconded social worker post.
-
CCG lead commissioner in joint health/social care commissioning arrangement; SAT mainly funded by CCG, and LAs contributing a relatively small proportion of funding for a social work post.
-
LA-led commissioner (as per role of autism lead for locality) in joint health/social care commissioning arrangement; approximately equal financial contributions from health and LA.
Where the CCG had geographical boundaries that covered more than one LA, financial contributions and involvement by LAs varied.
Three SATs comprised two services jointly delivering SAT provision to a locality. Diagnostic assessment was provided by an NHS service, and support for social/everyday living support needs was provided by the LA (adult social care teams) and, in one locality, in partnership with a third-sector provider. Two types of commissioning arrangement were observed. First, the SAT was jointly commissioned (LA as the lead commissioner) with approximately equal financial contributions coming from CCG and LA. Second, the two services were separately commissioned by the CCG and LA, but had established joint-working practices.
Finally, a ‘hub and spoke model’ was observed. Here, three localities had commissioned a neighbouring, well-established (single-service) SAT to deliver diagnostic assessment, mental health intervention and advice services. Different commissioning arrangements (CCG as the sole commissioner vs. CCG as the lead commissioner with LA involvement) meant that there were differences between localities in terms of LA social work/social care involvement. In two localities these staff were seconded into the service, in the other a joint-working arrangement was in place.
Staffing and skill mix
The size of the team (in terms of whole-time equivalents) did not necessarily reflect the size of a locality’s population. Constraints in funding were reported. The NICE guidance31 recommended a multidisciplinary team, with a range of professions represented. All SATs were multidisciplinary, but considerable variation in approaches to staffing were observed.
Clinical psychology was the only profession represented in all SATs, with diagnostic assessment the dominant aspect of that role. Within each SAT, the proportion of staffing resource assigned to clinical psychology ranged from < 15% to 50%. Differences in the time requirements of diagnostic assessment protocols and whether or not the SAT delivered specific mental health interventions, rather than referring to another service, appeared to determine this. Typically, if psychiatry featured in the staff team it represented a small proportion of staffing resource. The exception was one service in which the diagnostic assessment was led by psychiatry and not clinical psychology.
Around two-thirds of SATs had a (mental health or social care) social work post. Many SATs also had generic posts in which a set of competencies and autism expertise, rather than a particular professional qualification, were required. Speech and language therapists (SLTs), social workers, mental health nurses and/or occupational therapists occupied these posts. The whole-time equivalent of total staffing resource allocated to generic posts ranged between 25% and 35%. Specific SLT and occupational therapist posts were unusual, although in some SATs had relatively high whole-time equivalents.
Around two-thirds of SATs also employed staff who did not hold a professional qualification. These were typically assistant psychology posts, but other ‘support’ posts were also used. The roles that they assumed included initial/screening assessments, supporting diagnostic assessments and co-facilitating group-delivered interventions. Support workers were more likely to be involved in meeting social/social care needs, such as being involved in running ‘drop-in’ sessions/support groups and providing individuals with community-based ‘low intensity’ support. A few SATs also employed ‘employment support workers’. The proportion of staff resource assigned to ‘support worker’ posts ranged between 20% and 50%.
The diagnostic assessment
Specialist Autism Teams differed in their diagnostic assessment protocols and each was unique. Protocols varied in terms of the:
-
use of published diagnostic tools and/or clinical interview protocols [e.g. Diagnostic Interview for Social and Communication Disorders (DISCO)]41
-
approaches involving informants for the developmental history
-
number of sessions (from one to around four)
-
number of professionals involved (between one and three)
-
decision-making process
-
process by which the outcome of the assessment was shared with the client.
There was wide variation in reported rates of diagnosis between SATs, ranging from < 50% to > 80%. SAT professionals believed that this variation could be attributed to a number of factors, including referrals to longer-established services potentially being ‘harder’ to diagnose (i.e. present more subtly), between-clinician differences and differences in diagnostic assessment protocols.
Psychoeducational support regarding diagnosis
All SATs offered a psychoeducation intervention after diagnosis. As an approach, such interventions integrate psychotherapeutic and educational elements. Their objective is to develop understanding and acceptance of autism, address information needs and support the development of adaptive strategies to manage everyday life. The content of psychoeducation interventions was broadly similar across SATs. Some SATs used a multisession, group-delivered intervention, others used two or more individually delivered sessions and a few offered flexibility regarding mode of delivery, which was based on the individual’s needs.
Needs assessment and ‘care planning’
All SATs conducted a comprehensive needs assessment (covering mental health, social care, employment, housing and sensory needs). This took place either within the diagnostic assessment process or when ‘already diagnosed’ referrals entered the service. This resulted in a ‘care plan’ that incorporated the ‘offer’ from the SAT in terms of interventions and support, and any planned onward referrals or signposting. Services varied in the extent to which the care plan was co-produced with the service user.
Types of care provided by Specialist Autism Teams
The interventions being delivered by SATs could be organised as two ‘levels’ of care, both of which were included in the care plan:
-
supporting self-management – interventions that increase knowledge and understanding of autism, improve or develop coping/problem-solving skills and self-efficacy, and develop informal support networks
-
managing or addressing specific mental health and/or social needs in which the specialist nature or severity of needs and/or the individual’s capacity to self-manage mean that professional support/intervention is required.
Most SATs did not manage forensic cases or individuals with significant or ‘high-risk’ mental illnesses. If involved, they typically assumed an advisory/consultancy role.
Supporting self-management
A range of interventions to support self-management were reported (Table 1). Information provision and psychoeducation were provided by all SATs, and almost all offered informal support groups. Provision of other self-management interventions was idiosyncratic.
| Intervention | Notes/further information | Prevalencea |
|---|---|---|
| Supporting knowledge and understanding of autism | ||
| Psychoeducation intervention | Typically manualised, group-delivered interventions | Universal |
| Written information | One service also provided DVDs (digital versatile disks) | Universal |
| One-off seminars/workshops | Programme of topic areas covered | Unusual |
| Facilitating connections with peers and wider autism (or other) community | ||
| Signpost to third-sector/user-led autism groups | Verbal recommendations and provision of written information. Includes local community-based, virtual and national groups | Universal |
| Informal support group | Regular, informal gatherings, often held in a public venue (e.g. local café). ‘Hosted’ by SAT staff. (One SAT occasionally introduced social outings and another organised a walking group) | Common |
| ‘Drop-in’ serviceb | Regular (weekly, bimonthly or monthly) service comprising advice/information provision, and an opportunity for informal contact with staff and other autistic people. May offer one-to-one appointments. Social activities (e.g. social/interest groups) may also take place | Less common |
| Support peer-led social/interest groups | SAT supports initial set up (e.g. introducing potential members) and/or maintenance (e.g. venue and administration support) of a peer-led interest/activity group (e.g. badminton, music or theatre) | Unusual |
| Signpost to local mental health recovery group | Achieved through information provision and advice nearing discharge | Unusual |
| Developing coping/problem-solving skills | ||
| Psychoeducation intervention | Typically manualised, group-delivered interventions | Universal |
| Training in problem-solving/coping skills | Often delivered as manualised group intervention. One SAT also offered mindfulness classes | Universal |
| Information and advice about services/sources of support | ||
| Written information | For example, contact details and information leaflets about other services and benefit entitlements | |
| Informal support group | See earlier notes in table | Common |
| ‘Drop-in’ serviceb | See earlier notes in table | Less common |
| Telephone advice serviceb | If available staff cannot provide information, referred as ‘duty query’ to team meeting for discussion | Less common |
| Facilitating inclusion/access to mainstream/community activities | ||
| Support inclusion in ‘mainstream’ group/club | Staff actively support ‘introduction’ into existing mainstream/community-based groups/clubs (e.g. local arts project or sports club) | Unusual |
Specialist Autism Teams differed according to the priority given to offering interventions that supported self-management. Commissioning arrangements, clinical opinion and/or availability of autism-specific voluntary sector groups/services in their locality accounted for this. A small number of SATs were distinctive in the relative high priority and investment that was given to this aspect of their service. Others reported that they had plans to expand this aspect of their work. Although psychoeducation was delivered soon after diagnosis, other self-management interventions were not confined to a specific time point in the care pathway. Practitioner judgement (particularly in terms of clients’ readiness) and, in the case of rolling programmes of group-delivered interventions, the availability of an intervention influenced when an individual might access such interventions. In some SATs, self-management interventions were explicitly used as a way of ‘stepping down’ care.
Management of specific mental health and/or social needs
Where identified mental health, social care, employment, housing and sensory needs were sufficiently severe to require direct therapeutic intervention from a suitability qualified professional, there were substantial differences in the ways that this was approached:
-
One-to-one work – as well as direct work with the individual, this could also include contact with other agencies/organisations (e.g. employer, landlord or LA housing department) in an advocacy role.
-
Manualised, group-delivered interventions.
-
‘Supported referral’ to another service. By ‘supported referral’, we mean that SAT staff support the engagement of an individual with the service (e.g. attending assessments, supporting an individual to complete application for benefits, co-working with the service during assessment and care planning). Services/agencies that SATs referred to included:
-
community mental health services for psychological well-being interventions
-
LAs for assessment of eligibility for statutory social care provision
-
secondary adult mental health services (more severe mental health difficulties)
-
specialist employment support services (statutory and third sector)
-
welfare/benefits services.
-
Specialist Autism Teams differed in the types of need that were managed within the team and those that were routinely managed through a ‘supported referral’. This variously depended on commissioning arrangements, the perceived suitability of mainstream services, an individual’s ability to engage or cope with a mainstream intervention, the skills/competencies of the team and, in terms of accessing statutory assessment of social care need, the nature of the involvement of the LA in the SAT.
In some SATs, management of employment, welfare and/or housing needs occurred only when significant mental health needs were also present. Where this was not the case, signposting (e.g. providing information about sources of support and contact details for agencies) was used.
For mental health needs, a small minority of SATs reported that it was highly unusual for them to undertake direct work. More common was a time-limited intervention (e.g. cognitive–behaviour therapy for anxiety). Sometimes this preceded a referral to a mainstream psychological well-being service. In one SAT, mental health interventions were spot purchased, as the CCG commissioned the diagnostic assessment only. In terms of social needs (i.e. social care, employment, housing and welfare needs), commissioning arrangements and the skill mix of the team determined whether a SAT was directly involved or used a supported referral to address a need. Finally, SATs varied considerably in the extent of resources directed to specialist sensory processing interventions; this reflected differences in clinical opinion regarding their effectiveness.
Management and oversight of the care plan
There were two broad approaches to overseeing implementation of the care plan: managed care and episodic involvement.
In the majority of sites (n = 14), a named member of the team held responsibility for co-ordinating and overseeing implementation of the care plan; we refer to this as ‘managed care’. In some SATs, this individual was also presented to the service user as their ‘named contact’ while they were in the service. In 12 SATs, there was no predefined duration for an individual to be in the service, but there was an aspiration to achieve discharge (or for the client to use drop-in type provision only) for the majority of clients within at least 1 year. However, in two SATs all referrals were eligible to receive up to a maximum number of sessions (11 or 12 sessions). In one of these SATs, there was no time limit by which these sessions had to be delivered. Both of these SATs used ‘named contacts’, and one-to-one work was a core feature of both.
A second approach was ‘episodic involvement’. Here, the individual is placed on waiting list(s) for each intervention identified in the care plan, receiving each intervention when it becomes available, should they choose to. Two SATs adopted this model. There is no review prior to discharge, rather the individual is regarded as no longer ‘in the service’ once the last intervention has been delivered/offered.
Type of discharge
The majority of SATs operated closed discharge. Two SATs used an open discharge system in which individuals could re-refer themselves to the service within the first 12 months post discharge. A further two SATs used stepped discharge, offering monthly contact from the service for the first 6 months post discharge.
Changes in delivery models and practice
Many, and, particularly, the longer established, SATs reported ways in which their service had changed or evolved. These were driven by one of more of the following factors:
-
unprecedented levels of demand for the service caused by unanticipated numbers of referrals and/or high levels of unmet need
-
changes in commissioning arrangements
-
reductions in funding
-
observing existing practices (e.g. open-ended involvement) were creating a dependency on the service
-
cumulative clinical experience of working with adults with autism.
Changes implemented included introducing triaging of referrals in terms of level of need, shifting from individual to group-delivered interventions, the introduction of, or increased investment in, preventative and low-intensity support in terms of social inclusion and self-management.
Advice and training to mainstream services and professionals
One of the functions of SATs stipulated in government strategy and clinical guidance is to upskill other professionals and services in their locality. All SATs were delivering on this, although the resource and priority allocated to this varied according to whether or not such activities were included in service specification and the staff views on the suitability of mainstream services/interventions for autistic adults.
Some delivery models were fundamentally based on upskilling and co-working with other services to deliver care and support to autistic adults. Here, clinical leads believed that this was the only sustainable way to meet demand for specialist autism provision. Aside from this, SATs reported upskilling a wide range of professionals/services, including mental health learning disability (LD) teams, adult social care mental health and LD teams, general practitioners (GPs), police, prison service, employers and local industry. Box 3 summarises the types of upskilling work that SATs undertook.
Design and/or delivering of training to staff working in services that interact with/support adults with autism.
Routinely provide other agencies/professionals opportunities for consultation with a team member/whole team regarding management of a particular case or more strategic supervision/advice. Most SATs provided this in a responsive way; one SAT offered bookable, 30-minute consultation slots with the whole team (two available each week).
Supporting mainstream services to deliver interventions (e.g. statutory social care assessments, employment support, mental health therapies), or co-delivering intervention with mainstream staff.
Co-creation of autism-suitable interventions/adaptation of generic interventions delivered by mainstream services (e.g. well-being interventions delivered by primary care/community mental health teams).
Access to the Specialist Autism Team by the wider community of autistic adults
To make themselves available for low-level support and advice to the wider population of autistic adults without LDs living in their locality, a small number of SATs offered an open drop-in service. However, service leads reported that it was highly unusual for someone not previously known to them to attend or, indeed, this had never occurred. One SAT ran a programme of open workshops/seminar on various topics related to autism.
Support to family members and supporters of autistic adults
Supporting family members is the final identified function of SATs. This aspect of provision was not prioritised and SATs undertook limited or no direct work in this area. Where it was provided, the types of support offered included:
-
provision of written information
-
responding to simple requests for advice (raised at drop-in or via telephone calls to the service)
-
leading informal ‘family member’ support group meetings
-
enabling and hosting a peer-led support group
-
extending an existing drop-in services for use by family members
-
organising and hosting occasional social events for autistic adults and their families
-
at diagnosis, offering the opportunity to attend an individually delivered post-diagnosis psychoeducational intervention with the individual being diagnosed.
Many SATs regarded local third-sector groups and peer-led networks as an important source of support for family members. Where this was the case, SATs signposted and promoted them. There were instances of joint work with these organisations (e.g. support groups and social events). Some SATs, however, reported such partnerships were not available in their locality.
Specialist autism provision for adults with autism/no learning disabilities in localities without Specialist Autism Teams
In localities that did not have a SAT service, one or both of the following types of provision were observed.
Diagnostic services
Autism diagnostic assessments were reported as being provided by one of the following arrangements:
-
non-specialist autism local NHS service
-
service-level agreement with specialist autism diagnostic assessment service in the region
-
spot purchasing of specialist autism diagnostic assessments.
Some of the specialist autism diagnostic services for which we collected data during stage 1 reported a frustration at the limitations placed on them, and the services and support they could provide, by funding/commissioning arrangements.
Services solely commissioned/provided by local authorities
As expected, we identified a large number of specialist services for autistic adults solely commissioned/provided by LAs. Sometimes these services were delivered in-house, or specialist autism third-sector providers had been commissioned. These included organisations specific to a locality and national organisations (e.g. National Autistic Society). They included both ‘autism without LDs’ and ‘whole spectrum’ services. None of these services, on their own, fulfilled the criteria for a SAT. If an specialist autism diagnostic/mental health service existed in their locality (which was unusual), there were no joint-working arrangements.
Summary
This mapping study has revealed whether or not, and how, localities in England have implemented the Autism Act29 and NICE’s recommendation for a SAT. We did not identify a single instance of the NICE ‘Specialist Autism Team’ model being fully implemented with respect to all autistic adults. Rather, it has stimulated the development of new provision specifically for autistic adults without LDs. Indeed, many services reported that the decision to focus on this population arose from the recognition of a (total) lack of specialist autism services for this group and significant concerns about their outcomes/well-being. Their situation was contrasted to autistic adults with LDs who were perceived to be (relatively) well served by NHS and LA LD services.
Given the specific focus of SATs on autistic adults without LDs, it is not surprising to find that the SATs identified did not wholly align with the NICE guidance31 on SATs. First, although always multidisciplinary and delivering multiple functions, they are not typically multiagency. However, all SATs reported systems or pathways that connected them to other agencies, particularly LA social care and housing departments, and specialist autism third-sector organisations. Second, except for individuals with complex mental health problems, their emphasis was on delivery of care and support, referring onto and supporting access to other services, rather than assuming a care co-ordination role. Finally, their work with carers/supporters was typically minimal. This might simply reflect prioritisation of work within the context of constrained resources and/or may indicate lower levels of need among family members of autistic adults without LDs than family members of autistic adults with LDs. Alternatively, it may reflect a lack of understanding or recognition of the support needs of this group.
An objective of stage 1 was to discover if SATs could be classified according to a typology of service models based on their structural and organisational characteristics and ways of working. Our work has revealed the complexity of SATs. This partly arises from the fact that the functions and roles of SATs are so wide ranging. Thus, there is potential for differences between SATs both in the emphasis given to the different roles/functions and, within each role/function, differences in practices and ways of working. Furthermore, staffing of a service is often one of the dimensions used to define service model typologies. 42 However, we found that, for some posts, generic competencies and an expertise in autism were more important than specific professional qualifications. Layered on top of these issues, but not necessarily influencing them, are the more ‘straightforward’ organisational dimensions (such as commissioning arrangements and the organisational location of the service).
A consequence of this complexity, and the relatively small number of SATs currently operating, meant that a distinct typology that was meaningful across the entire set of roles/functions of a SAT was not identified. It is, however, very clear that there are a number of service-level characteristics (as well as some higher-level structural/organisational characteristics) on which SATs differ.
In our study protocol, based on work carried out to support development of the funding application, the following service characteristics were identified as potentially distinguishing between SATs. These were:
-
caseload – autism without LDs versus all autism
-
‘virtual’ versus co-located teams
-
professional composition
-
extent of diagnostic assessment
-
to deliver interventions versus consultation/support to other services
-
the wider service context (local availability of other specialist autism provision, including third sector)
-
the level and nature of partnership between health and social care.
Findings from this mapping work indicate that many of these characteristics did indeed serve to distinguish between SATs. The exceptions are that SAT provision is for autistic adults without LDs only and diagnostic assessment is consistently a core and substantive aspect of provision and, in a minority of SATs, the only pathways into the service.
The implications of these findings for stage 2 of this project were that, in the absence of a typology of service models, the focus shifted from a comparison of service models to exploring the impact of service-level (and some individual) characteristics on outcomes, costs and cost-effectiveness. Indeed, this had always been a key research objective as set out in the protocol.
Chapter 3 The research sites
Introduction
This chapter describes the services that acted as research sites for the evaluation study. We focus on reporting whether or not research sites represented service characteristics that were identified by the mapping study (see Chapter 2) and distinguished between services.
Characteristics of the sites
Sociodemographic and population characteristics
Sites varied in the size of the population they served and their geographical size. Most were localities representing a single CCG and LA. They represented a range of deprivation and urban/rural characteristics (see Appendix 1, Table 24).
Organisational characteristics
Four sites were neurodevelopmental services and the remainder were autism-specific services (Table 2). Two (sites D and H) were multiteam services, with separate teams delivering the diagnostic assessment and ongoing support functions; these teams were not co-located. One multiservice SAT (site D) was commissioned entirely by the local CCG. In the other (site H), the diagnostic assessment service was commissioned by the CCG and the ongoing support service by the LA. Close joint-working arrangements ensured continuity of care between the services.
| Site ID | Year established | Autism or ND service | Commissioner | LA funding/resource contribution | Single vs. multiteam | Hold and co-ordinate complex cases? |
|---|---|---|---|---|---|---|
| A | 2003 | Autism only | CCG | Part-fund social inclusion hub (via carers grant)a | Single | No |
| B | 2014 | Autism only | CCG | None | Single | No |
| CAb | 2009 | ND | CCG | None | Single | No |
| Dc | 2009 | Diagnostic assessment service is ND | CCG | None | Multi | Yes |
| E | 2011 | ND | CCG | None | Single | Yes |
| F | 2012 | Autism | CCG | In some districts, part-time social work post seconded to serviced | Single | No |
| H (Ha and Hb)e | 2013 | Diagnostic assessment service is ND | Ha: CCG Hb: LA | Funds Hb | Multi | No |
| IAb | 2014 | ND | CCG lead | LA social work posts seconded to service | Single | No |
| J | 2014 | Autism | Joint, LA lead | Joint funded by LA and CCG | Single | No |
The different patterns of commissioning and funding identified in the mapping study (see Chapter 2) were represented in the research sites. Among the single-service SATs, three out of the seven had no LA involvement. In another (site A), the LA contributed to the funding of the drop-in service. One (site J), however, was jointly commissioned (with relatively equivalent levels of funding) by the LA and NHS. In two other sites (sites F and IA), the CCG was lead commissioner, with the LA seconding social work posts. However, in site F, which had three LAs within its boundaries, LAs varied in whether or not they invested in the service.
Thus, the range of organisational characteristics observed across all SATs identified in the mapping study (see Chapter 2) were represented in the sites recruiting to the study.
Service lead and skill mix
Seven research sites were clinical psychology led and the remaining two sites were nurse led (site CA) and psychiatry led (site J) (see Appendix 1, Table 25). The only profession represented across all sites was clinical psychology. In the majority of services (n = 7), the staff team included four or more professional disciplines (e.g. psychiatry, clinical psychology, mental health nursing, speech and language therapy, and occupational therapy) or roles (e.g. autism clinical specialist and specialist autism support worker). The remaining two services both had clinical psychologists and autism clinical specialists/support workers, with the latter working across a range of needs. Sites varied in the relative resource allocated to staff with the same professional qualification. However, as reported in Chapter 2 (and also discussed in Chapter 5), care should be taken when interpreting this given that services reported, on occasion, prioritising autism expertise and a generic skill set over discipline-specific expertise. Overall, research sites represented the different patterns of staffing and skill mix observed in the mapping study (see Chapter 2).
Eligibility and referral pathways
The research sites represented both open and closed referral processes observed in the mapping study (see Chapter 2). Four out of the nine sites operated an open referral process, including self-referrals (Table 3). The majority (n = 6) accepted referrals of those already diagnosed. A further two accepted such referrals, but only for those on their complex care pathway. This represented a very small minority of their caseload. Only one service triaged referrals at the intake assessment stage, prioritising referrals in terms of severity of mental health symptoms or social need.
| Site ID | Does the service accept self-referrals? | Which services are able to refer? | Does the service accept those already diagnosed? | Does the service triage referrals? |
|---|---|---|---|---|
| A | Yes | Open | Yes | No |
| B | Yes | Open | Yes | No |
| CAa | No | Any statutory health/social care | Yes | Exceptionally |
| Db | No | Any statutory health/social care | No, except complex care pathway | No |
| E | No | Any statutory health/social care | No, except complex care pathway | No |
| F | No | GP | Yes | Yes |
| H (Ha and Hb)c | Yes | Open | Yes | No |
| IAa | No | Any statutory health care | Yes | No |
| J | Yes | Open | No | No |
Diagnostic assessment processes
The majority of research sites were using a standardised diagnostic assessment tool (Table 4). The number of sessions used to complete the diagnostic assessment process ranged from one to four or more. Rates of diagnosis ranged from 36% to 90%. Where the assessment was completed in a single session, this tended to be a half-day appointment. Practice varied in terms of the number of staff involved and when service users learnt the outcome of the assessment. The majority of services conducted a single feedback appointment, after which service users were offered a psychoeducational intervention. In one site (site D), the mental health and social needs assessments were split between the two teams delivering the service. This range in approach to diagnostic assessment in the research sites was expected given that findings from the mapping study indicated services were idiosyncratic in their approach and practice. Work soon to be completed by Newcastle University45 on diagnostic assessment practices in England provides further analysis of this issue.
| Site ID | Typical number of sessions | Standardised assessment tool? | Staff involved | Were referrals told diagnosis at assessment appointment? | How report of diagnostic (and needs) assessment (and care plan) shared with individual | Timing of feedback appointment(s) | Typical number of feedback appointments | Proportion diagnosed |
|---|---|---|---|---|---|---|---|---|
| A | One | DISCO | One clinician (clinical psychologist, specialist autism nurse or autism clinical specialist), then consult team | No | Posted to service user before feedback appointment | Not specified | One | 60% |
| B | One | ADOS-2, ADI-R | One clinician (clinical psychologist or specialist autism nurse), then consult team | No | Posted to service user before feedback appointment | Not specified | One | 90% |
| CA | One | ADOS-2, ADI-R | Two members of the team (clinical psychologist, nurse consultant, SLT) | Yes. Unless need to consult with team | At feedback appointment | Specify 4 weeks | ‘User-determined’ | 53% |
| D | Approximately four | See site E | Threea | 61% | ||||
| E | Approximately four | ADOS-2 | Two members of team (including clinical psychologist). If necessary, consult team | No | At feedback appointment | Not specified | Two/three | 47% |
| F | Three | No | One clinician (clinical psychologist). Then consult team | No | Draft report sent to service user | Not specified | One | 85% |
| H | Approximately four |
ADOS-2 DISCO (if complex) |
One clinician (clinical psychologist) | No | At feedback appointment | Specify up to 4 weeks | One | 47% |
| IA | One | No | One clinician (clinical psychologist), SLT may also be involved | Yes. Unless need to consult with team | Posted to service user before feedback appointment | Within weeks | One | 50% |
| J | One | No. Plan to introduce ADOS-2 | Two members of team, led by psychiatrist. Then consult team | No | Posted to service user before feedback appointment | Within weeks | One | 36% |
Delivery of the care plan: key features
A range of delivery and practice characteristics were represented in the research sites (Table 5). The three approaches to the management and oversight of the care plan identified in the mapping study (see Chapter 2) and approaches to addressing specific presenting needs (direct work vs. supported referral) were represented. The range of intensity of involvement with supported referrals that was reported by the mapping study was not fully represented by the research sites. Unfortunately, the service that had invested the most in supporting non-specialist services to deliver care and interventions had to withdraw from being a research site.
| Site ID | Management and oversight of care plan | Dominant mode of delivering psychoeducation | Routinely do one-to-one work regarding mental health problems | Management of presenting social care needs (daily living skills, community care assessment) | Communication/social skills interventions (one to one and/or group) | Approach to employment support | Type of discharge | Drop-in-type provision while in service? | Drop-in-type provision after discharge? |
|---|---|---|---|---|---|---|---|---|---|
| A | Managed, no named contact | Group | Yes | Supported referral | No | Supported referral | Stepped | Yes | No |
| B | Managed, no named contact | Group | Yes | Supported referral | No | Supported referral | Stepped | No | No |
| CA | Managed and named contact | One to one | Yes | Supported referral | Yes, SLT led | Supported referral | Open | No | No |
| Da | Managed and named contact | One to one | Yes | In house | Yes, not led by SLT | Direct work | Open | Yes | No |
| E | Episodic | One to one | No | Supported referral | Yes, not led by SLT | Supported referral | Closed | No | No |
| F | Episodic | Group | Yes | Supported referral | No | Direct work | Closed | No | No |
| H (Ha and Hb)b | Managed and named contact | Group | No | In house | Yes, not led by SLT | Direct work | Open | Yes | Yes |
| IA | Managed, no named contact | Group | Yes | In house | Yes, SLT led | Supported referral | Closed | No | No |
| J | Managed and named contact | One to one | Yes | In house | Yes, SLT led | Direct work | Closed | Yes | No |
In terms of group-delivered interventions, each service had developed its own; none was a published, manualised intervention. With respect to communication/social skills interventions, in some services this was led by a SLT, in others this was not the case.
The research sites also represented the three types of discharge observed in the mapping study (see Chapter 2), and the use or non-use, of drop-in provision. Unfortunately, the service in which drop-in provision was (perhaps) the most developed had to withdraw from acting as a research site.
Provision for carers
The research sites varied in provision for carers (see Appendix 1, Table 26). This ranged from signposting to receiving care and support alongside the family member, where appropriate (site CA). Three services (sites D, E and H) described their provision as being limited to a psychoeducational intervention post diagnosis. Another service (site IA) provided limited access to a more general support group-type provision. A couple of services noted that take-up of carers support was higher among parents than other family members. All but one service (site J) reported that there were active local autism carers groups to which they were routinely signposted. This sort of provision was not available in site J’s locality. This range of provision for carers and, overall, its limited nature is representative of the wider findings from the mapping study (see Chapter 2).
Training and consultancy
Training and consultancy was a core element of the range of services provided by the SATs acting as research sites. All but one site were commissioned to routinely deliver autism awareness training and/or more specialist training in their trust and, often, to other statutory services (see Appendix 1, Table 27). Less common, reported by only three sites, were autism awareness activities in the local community among the public. All sites reported providing advice to services/professionals in their locality on a case-by-case basis, although one site reported that this was unusual. Such input was not restricted to NHS or LA services. One site (site F) also offered an ‘advisory clinic’ (two appointments available per week) whereby individual professionals or whole teams could consult with the SAT. Again, this was used by a range of statutory agencies. In addition to these services and activities, one site (site C) had developed e-learning packages for its trust and LA.
Summary
This chapter reports the characteristics of the research sites. Overall, it demonstrates that the range of service characteristics identified as serving to distinguish between SATs in England (see Chapter 2) were represented in our research sites. However, some elements of service delivery and practice were not fully represented, including the full range of drop-in provision and the more intensive approaches to ‘upskilling’ professionals working in mainstream services [e.g. GPs, community mental health teams (CMHTs) and improving access to psychological therapies (IAPT)]. This was principally because of the withdrawal of a research site during study set-up.
Chapter 4 Leading and delivering a Specialist Autism Team
Introduction
This chapter concerns senior practitioners’ views and experiences of leading and delivering a SAT. The material reported in this chapter was collected during interviews with service leads during stage 1 and a workshop for senior practitioners (see Appendix 2 for the methodological report). A unique identifier system is used in this and the following chapter to ensure anonymity of services while allowing scrutiny of representativeness of quotations. We divide the chapter into three main sections:
-
the challenges facing SATs
-
aspects of services working well
-
sustainability.
The challenges facing Specialist Autism Teams
Increasing numbers of referrals
A very significant concern for all services was the number of referrals. All services reported a year-on-year increase. In addition, all reported an increase in the proportion of referrals who had complex needs. Critically, none had received an equivalent increase in funding. Indeed, a minority had experienced a constriction in available resources (e.g. loss of funding for posts, post being frozen, withdrawal or reduction of LA involvement):
We’ve constantly historically doubled over [the 4 years existed] . . . And pretty much the same amount of money.
SAT1
. . . the number of referrals are constantly increasing. We thought 7 years ago that we’d have a mass input and then it would slow down. Unfortunately it hasn’t, and we’ve got no more staff than we had to start with.
SAT2
As well as the increasing rates of autism diagnoses in children, services believed that there were three main reasons for this situation. First, mainstream/generic services could be unwilling to work with this population, even with supervision from a SAT. Second, other services were referring to the service as means of managing their own caseload. Third, the absence of any other non-LD, specialist autism provision in the locality.
Issues with service throughput
Services operating a more open-ended care pathway were, unsurprisingly, more likely to identify issues with service throughput. More generally, a reluctance of mainstream services (e.g. CMHT and IAPT) to accept referrals and the absence or loss of low-level community support services, such as third-sector services, peer-led groups/networks and LA provision, were identified as adversely affecting throughput:
. . . the [third-sector organisation] withdrew everything . . . virtually all their volunteering services and all that sorta stuff, which was a big loss . . . and unfortunately the cutbacks in terms of the voluntary sector and local authority and all of those sorts of thing (means) virtually all support has gone.
SAT2
Services acting as care co-ordinators for those with complex needs reported the additional difficulty of being unable to discharge these service users because of the complexity of their needs or the absence of another specialist autism service on which to refer. This further compounded the issue of long waiting lists:
We’re only supposed to care co-ordinate eight people. We’ve got 11 people at the moment and a lot waiting . . . massive pressure of people coming through who are very, very complex, that do need specialist care co-ordination but we can’t do it. And it’s a real area of stress for us trying to find out where those people can go. It’s very difficult to ‘review and move on’ the people that we have got because their needs remain constant and they don’t get better . . . so it’s really difficult, that.
SAT4
Increasingly constrained resources
Increasing numbers of referrals and growing caseloads within the context of unchanged levels of resource meant that all services reported an increase in wait times, both at referral to the service and in the delivery of the interventions set out in the care plan. Inadequate financial resources were attributed to both commissioners’ demands and within-trust cost-improvement programmes:
They [commissioners] are putting a lot of pressure on us to change our practice and looking at really limiting what interventions we’re going to be able to do.
SAT3
All services had changed their service offer or aspects of practice to manage these pressures. Staff described the strain and sense of conflict experienced when they felt that the quality of care and service users’ outcomes were being compromised:
. . . we’re just getting bigger and bigger waiting lists . . . and how do you deal with that? Do you sacrifice to some extent the quality of your assessment and try and just do it as best, you know, when your commissioners are just saying, ‘well the NICE guidelines are only guidelines, the quality standards are just guidelines’.
SAT5
Cos that’s what we’re talking about, trying to change our referral process, our assessment process and still maintain quality, because people aren’t giving us any more money.
SAT4
Concerns about the negative impacts of changes in practice/provision on the quality of provision and user outcomes particularly centred on the diagnosis and assessment process (e.g. in the clinic rather than at home and conducting the assessment in a single session), wait times for interventions once diagnosed and the intensity of support that could be provided. Examples given here include increasing the use of group-delivered interventions, which may not suit all service users, and reducing the intensity or duration of one-to-one work:
There are some cases [undergoing diagnostic assessment] that we talk about an awful lot and deliberate about a lot. And people are different at home and different when they come to the office, different in, you know, different environments.
People do need time to process their diagnosis . . . but they shouldn’t be waiting months inbetween getting the diagnosis and getting the intervention.
We [now only] offer eight (one-to-one) sessions. That’s only very recently – we did have a much more ongoing approach but, cos obviously, the amount of referrals [mean] we’ve got to limit that . . .
SAT6
We’re doing more groups now to try and free up some of our time to do more of the one-to-one stuff. Having clinics as opposed to going out and doing that kind of more bespoke stuff, even though it’s not preferable, that’s kind of helped us, managed to keep our heads above water.
SAT5
Resource constraints also meant that some services found that their community-based provision was delivered in less-than-adequate venues, which was particularly an issue for those with sensory sensitivities:
. . . the financial squeeze means we’ve got no money to pay for anything, so you’re trying scrambling about trying to find some free rooms somewhere, and usually they’ll end up in some horrible old NHS community building which isn’t great. It’s that kind of practical thing . . . And you know if you don’t get it right then it won’t work.
SAT2
At the same time, services noted that constrained resources had specifically driven, or were driving, what was regarded as positive service innovation. Examples included introducing a weekly drop-in service for individuals on waiting lists for interventions and setting up a ‘supervision and consultation’ service to support mental health locality teams. We return to the issue of managing demand and ensuring sustainability in a later section of this chapter (see Ensuring sustainable improvements).
The impact of wider resource constraints across statutory services
Services also noted the impact of the wider issue of (increasingly) constrained resources across statutory services. They partly attributed the perceived reluctance of other services to accept referrals as part of a wider strategy by these services to manage their demand:
Everyone is under massive amounts of pressure with the resources they have. We see a pattern . . . We try and refer to adult social care, they come back to us because they don’t have a learning disability, or we try and signpost them to the community mental health team [and we get the response] . . . ‘no, they’ve autism, they’re not eligible’. So we just keep finding these barriers for this client group.
Our clients do go to the commissioner for mental health to request funding [for specialist psychological interventions]. It’s very hit and miss as to whether they get it unfortunately.
SAT6
Alternatively, when referrals were accepted, long waiting times were a strong possibility:
. . . we do have a referral pathway for Community Care Assessments . . . if you’ve got 2 years to wait to get one. So it’s not, that’s not great.
SAT5
The impact of the commissioning cycle
A minority of services described the impact of an annual or bi-annual commissioning cycle. It was regarded as affecting recruitment and as a significant barrier to strategic planning. Delays in commissioning decisions had led to one service being commissioned on a month-to-month basis for a period of time:
. . . 'cause of the commissioning recruitment’s been a massive problem, because we can’t offer people 3- to 4-week posts . . . no one has a job like that; and also, forward planning.
SAT8
Aspects of services working well
The previous section has described the challenges faced by SATs and the (potential) threats to quality of care and service users’ experiences. Despite this, all senior practitioners readily identified features of their service that (they believed) were working well.
Core service features
Those with very holistic multidisciplinary teams consistently identified this as a very positive aspect of their service, including the contribution of all disciplines to the diagnostic and needs assessment process. Depth of autism expertise was another feature that services highlighted as key to accurate diagnoses and needs assessments. Many services spoke very positively about specific group-delivered psychoeducational and skills development interventions.
Specific features
Further specific examples of service provision regarded as working well, as identified by senior practitioners, included:
-
involving ex-service users in developing information resources, acting as peer mentors in psychoeducational interventions, volunteering at drop-in services and running autism awareness/training programmes
-
commissioning a third-sector provider of specialist employment support to deliver work/employment interventions
-
offering a drop-in service for those waiting to receive one-to-one sessions
-
implementing stepped discharge arrangements; here, examples included after formal discharge, service users being able to telephone into the service for a 6-month period and providing access to a ‘drop-in’ type service
-
in localities with strong user- or carer-led groups, collaborative working with these groups to support access to some form of ongoing support and autism-specific network.
Motivated and committed staff team
Finally, a number of senior practitioners noted that, despite the challenges, staff were highly motivated and committed to the service. One service lead gave evidence of this in the way staff were prepared to assume additional roles to enable the service to function.
Sustainability
From the outset of our interactions with SAT practitioners, there was a recurring theme of evolving delivery models and practice driven by both the wider (limited) resource context and the cumulative clinical experience. Many services reported a degree of naivety when setting up their service in terms of how they would work and the level of demand for their service:
When we first started we were really naive. We thought we’ll be an all singing all dancing do everything for everybody service, and we’ve learnt very quickly that you can’t.
SAT2
When asked about future redevelopments in the functions and balance of work carried out by SATs that were required to ensure sustainable improvements in support for autistic adults without LDs, four features of service design, delivery and practice by SATs were identified:
-
greater emphasis on the ‘consultation and supervision’ function
-
continued and greater resource and attention to supporting self-management and minimising dependency
-
working, where possible, with local peer-led networks
-
introducing/increased resourcing of drop-in services and other low-level support.
Services differed in terms of the extent to which they addressed, or had changed their ways of working to reflect, these features. However, and importantly, for each of these features, at least three services had extensive experience with each of these aspects of service delivery, design and practice. The following sections report senior practitioners’ views about and experiences of these features, including potential barriers to implementation.
Greater emphasis on ‘consultation and supervision’ function
Service leads believed that a change of emphasis or attention to acting as autism consultants and offering supervision to mainstream services was one of the key solutions to ensuring that adults with autism (without LDs) accessed services in a timely way. This might involve specific joint working or supervision of a specific case, supporting services with adjustments to their services and interventions (e.g. IAPT and Community Care Assessments), and more general autism awareness and education across the workforce.
Although recognising that integrating a consultative function within their delivery model was key, a note of caution was sounded in terms of the potential risks it posed for inappropriate and potentially harmful care and misdiagnosis:
. . . and you get people coming on a day’s training thinking they’re expert. That’s a danger, especially with diagnosis sometimes.
SAT9
For SATs to achieve a greater emphasis on consultative support to mainstream services, senior practitioners stressed that shifts in understanding and attitude were required within SATs, among professionals in other services and at the trust level.
Changes required to shift to a ‘consultation and supervision’ approach
For SATs, senior practitioners noted that staff have to be prepared to work in this way, with the consequence of having less direct contact with service users. There also had to be an acceptance that working in this way may not rapidly result in efficiencies; it required significant ‘upstream’ investment of time:
. . . [it is] necessary to conceptualise [it] as long-term goal. It’s gonna take 5 years, and then take another 5 years; it’s an ongoing piece of work, isn’t it?
SAT9
However, current pressures on SATs meant that it was very challenging to work with this longer-term view. This was identified as a significant barrier to putting more resources into taking this approach:
And I just don’t have the time, nor does everybody else. . . . It takes as long to do consultations as it does to see people really. It’s time-consuming to do it properly.
SAT5
For mainstream services, it was noted that there had to be an understanding and acceptance of this new way of working. All services reported this to be very challenging and a number of reasons for this were identified. First, the ‘consultation and supervision’ model is relatively unusual in mental health services and, thus, as a way of working, it is poorly understood:
I think the default mode is, if you’re a specialist service you will take more responsibility.
SAT9
In addition, it was service leads’ experience that some professional groups (GPs and adult psychiatry were mentioned here) were very difficult to engage. This was attributed to a lack of understanding of autism (e.g. regarded as a childhood condition) and a lack of interest and/or time:
Some are interested but, to be quite frank, the vast majority are not and they don’t have time to be interested.
SAT2
They’re not really, not enough people coming to, for supervision, or to training days . . . but we just keep plugging away. You’ve just got to keep doing it.
SAT9
Furthermore, it was noted that the process of ‘educating’ other services about using SATs for consultation and supervision, rather than as a service to refer on to, needed to be continual because of staff turnover. The example was given of IAPT services that use assistant psychologists who do not typically stay long in a post:
There’s new staff and . . . then new service managers. So it’s just reiteration.
SAT9
Finally, senior practitioners noted that resistance to a ‘consultation and supervision’ model may be stronger in situations in which a well-established SAT was trying to shift towards this approach:
I think you’re in a better position if you’ve said that from the start than if you suddenly try and change along the way.
SAT5
To address this, one service reported that it was developing a ‘consultation contract’ which set out the roles of the SAT and mainstream services.
For trusts, senior practitioners stressed the need for recognition of the resource implications to mainstream services of taking on greater responsibility for the care of autistic adults, and to ensure that staff training needs are properly met:
Trusts need to see the value. So we need the trust to want the people to be able to do that and to give them the time to do that in the context of everything else they’ve got to do, like you said, otherwise you’re just fighting a losing battle . . .
Ensuring the correct balance between consultative approaches and direct work
Despite support for an increased emphasis from SATs on providing consultation and supervision to mainstream services, there was also strong agreement that such an approach does not obviate the need for SATs to do any direct work or deliver interventions to autistic adults without LDs. This was because mainstream services are, by their nature, generalists and staff cannot be expected to have specialist autism skills nor to deliver autism-specific interventions:
It’s about reasonable adjustments, I suppose, isn’t it? Just like you would your workplace. You can’t expect [mainstream] providers to do the things we may want them to do. But you could expect them to make some tweaks, to make it more accessible.
SAT9
. . . there’s not a lot of services out there to do a lot of the work we want done. If it’s anxiety and depression, great, IAPT. If it’s primary care, go to your GP. But what about psychosexual work, what about the whole range of things that people with autism struggle with?
SAT9
Supporting self-management and minimising dependency
Service leads agreed that the overall approach of SATs should be to minimise service users’ dependency on the service and develop their self-management abilities. This was an aspect of provision that had often already seen significant changes in some services.
A post-diagnosis psychoeducation intervention, covering information about autism and living with autism, was regarded as the critical starting point to supporting self-management:
. . . enable people to get to this point where they’re very aware of their condition, they’re very aware of what’s going to be difficult, and what then to do about it. And also people need to take that responsibility too, about making those choices about [for example] who you’re going to disclose to . . .
All services also offered other interventions, typically group delivered, that related to acquiring skills and understanding which enabled or supported self-management (e.g. social skills, coping skills and anxiety management).
Group delivery was, typically, regarded as a positive decision rather than being regarded as a solution to very limited resources. Indeed, a lack of adequate, protected time for practitioners to prepare for, deliver and review group-delivered interventions affected the quality of the intervention and the outcomes achieved. Identified benefits included the opportunity to hear and learn from others’ experiences, and using ex-service users as co-facilitators or speakers. In addition, the opportunity for self-development associated with simply going along to a group was stressed. A potential additional benefit was that groups (or some members) sometimes chose to continue to meet informally after the intervention was completed:
. . . we’ve got some self-sustaining groups that go on from there [group-delivered intervention].
SAT7
However, although advocating group-delivered interventions, practitioners made it clear that this required investing time in preparing and supporting individuals to attend:
Lots of people with autism would say, ‘I can’t do a group’, but actually they can, it’s just they’re very anxious and it’s something that’s really scary to them. So, a lot of preparation work with them helps them go into that group . . . And making sure facilitators in that group are people who can hold that group, which is a skill in itself when you’ve got lots of different people . . .
SAT7
In addition to specific interventions, senior practitioners described more general ways of working with service users that supported self-management and minimised the risk of individuals becoming dependent on the service. Often these had been developed in response to observing undue dependency and/or a realisation that previous approaches to care were unsustainable:
[we give the message from the start that] . . . we cannot scoop you up and fix you, that’s the message, because everybody comes and families come thinking you’re going to scoop them up nicely, fix them, and then give them back, and we’re not able to do that . . . Because it’s not fixable.
SAT2
Yes, I’m an information giver, I’m somebody who can enable, but they don’t look to me to solve anything they want.
We made a decision several years ago now about things that we wouldn’t do . . . and it might sound really simple, but it’s things like not filling in forms with people. So we spend probably as much time not filling in forms as we would if we actually filled it in for them. So it’s about that emotional resilience to show them that they, they can do it. So it’s kind of short-term pain for long-term gain really.
SAT2
Working with local peer-led networks
Services with strong local peer-led groups (including those for carers) consistently identified them as a core element to a sustainable framework of long-term support for autistic adults without LDs and their families. Connecting individuals to these groups was seen by some service leads as a key function of their service and a whole-team awareness of potential support groups/networks was important:
It’s just about using what’s out there and being really knowledgeable as a team about what is out there.
It was noted that information provision may not be sufficient and that more proactive support may be required to enable service users to engage with such provision:
I think it’s about signposting to whatever services there are out there, to get them to be engaged with those services . . . Linking them into local groups, getting them into them. Getting the carers into anything you can get them into so that the carer feels they’ve got somewhere to go to as well.
We’ve got to use what we’ve got and it’s a matter of getting people into them. Making them, helping them to feel that they’ve got something outside of your service.
Practitioners suggested that the geographical characteristics of a locality (i.e. rural vs. urban) may affect the number and range of peer-led networks and other third-sector organisations with which SATs can partner.
Drop-in services and other low-level support
A number of services used drop-in services or telephone contact as a means of providing ongoing, low-level support. For some, access to such support was time limited and was the way in which stepped discharged was managed:
So we have this step-down service now where they can still link in with the service for 6 months after, perhaps have a telephone clinic each month; and then they tend to kind of just go off and obviously if they need to come back they can come back, but that seems to have worked really well.
SAT5
Others, however, offered service users the open facility to telephone the service for one-off contact and four services provided a weekly drop-in that was open to ex-service users. All those providing this sort of low-level, ongoing support were strong believers in its value. Specifically, it was identified as serving to pre-empt problems or crises, nurture independence and self-management skills and reduce the sense of isolation:
I’ve got somebody who rings me twice per year who’s been discharged for 4 years but they still they still ring twice per year. But that’s what keeps them going, they don’t go into crisis and end, end up, using loads and loads of services. And it’s generally only a quick phone call about probably nothing but it’s just a, a check in that we’re still there and they’re still there and it’s a 5-minute call and they’re gone; and, and I think that, you can’t replace that really, that’s, that’s really invaluable.
SAT5
. . . it’s the ‘there when you’re needed’ level of support. It might be a 5-minute conversation it might take half an hour. But just holding their hand through some difficulties until they learn to do it themselves. I think it’s really valuable and I have increasingly less contact with people as they learn to manage these situations themselves. They generalise a lot better from that than from didactic teaching. People can turn up for half an hour and then we won’t see them again for 6 months, and then they’ll come again. But they know it’s there.
SAT6
With (our drop-in service), the idea of that is to help people network and then move on to back into mainstream.
SAT5
Light touch, access when you need it. Drop-in services are great . . . a little bit can, can go a long way, can’t it?
SAT9
There was a high level of interest among those not currently offering such services. However, some spoke of the difficulties of persuading commissioners that provisions such as this should be included in their service specification.
Summary
This chapter has reported senior practitioners’ experiences of leading and delivering a SAT. Unanticipated rates of referral and difficulties with securing onward referrals or discharging service users were presented as putting SATs under considerable strain. This was compounded by a lack of a commensurate increase in resources. All services had restricted their service offer or changed their models of service delivery to manage this situation. Unsurprisingly, this was felt to affect the quality of care that they were able to provide. Despite this, all believed in the value of their service and identified elements that were working particularly well. Autism expertise, multidisciplinary teams, and psychoeducational and self-development interventions were highlighted. Specific innovative practices or models of service delivery were described.
There was clear evidence that service design, delivery and practice had evolved and was evolving. This was driven partly by resource constraints and the pressures on services. Alongside this was the fact that SATs were a new model of service provision, set up in the relative absence of a body of clinical experience and knowledge to draw on, and no evidence base on service design, delivery and intervention effectiveness.
In reflecting on this learning, senior practitioners identified four features of SAT delivery models and practice that, they believed, would help ensure sustainable improvements in support for autistic adults without LDs. These were (1) placing greater emphasis on and investment in upskilling and supporting mainstream services to deliver care and support; (2) working in ways and delivering interventions that nurtured self-management skills and did not foster a dependency on the SAT; (3) where possible, collaborating with peer-led networks; and (4) providing drop-in services and other forms of low-intensity, ongoing support. However, senior practitioners noted the challenges associated with seeking to invest in and implement such developments within a context of immediate and pressing demands on their own services. Furthermore, the more general context of resource constraints meant services may be unwilling or not have the capacity to change how they work with and use SATs.
Chapter 5 Factors affecting outcomes: practitioners’ views
Introduction
This chapter reports the second element of the findings from the nested qualitative study of SAT practitioners. Here, we report on two main themes. First, understanding and assessing the outcomes of SATs. Second, individual- and service-related factors that may affect outcomes. These findings, and those presented in the subsequent two chapters reporting service users’ views, provide important and useful contextual evidence before we turn, in Chapter 8, to report findings from the quantitative evaluation of SATs. A description of the methods can be found in Appendix 2.
Understanding and assessing outcomes
Practitioners emphasised the diversity of the population who are referred to their services in terms of functioning, complexity and need. They believed that these factors significantly affected both the support individuals wanted or needed from the SAT, and the outcomes which could be achieved.
Some people don’t want anything, they’ll go ‘Thanks a lot, that’s my diagnosis, I’m fine with that, cheers!’. Other people will be like, you know, living in terrible circumstance and socially isolated.
Related to this point was the extent that any change associated with using a SAT, particularly in the lives of individuals with more complex needs, may or may not be observable or amenable to measurement:
There is improved outcomes, but there may not be a lot of change. So there might be more scaffolding around their lives and more access to support, which does improve the outcomes for them and will mean there are differences in their day-to-day life, but they might not massively change their routines or their social isolation particularly, but they’ll be more supported. It’s still an improved outcome, but it’s not a lot of change.
Practitioners also spoke about potential conflicts between outcomes and individual differences in the priority given to different outcome domains:
People that have really severe anxiety . . . you can encourage them and enable people to become more socially aware and involved, but that increases their anxiety so that it will be negative for them. But it’s about what’s the biggest gain, isn’t it, really? It’s whether it’s worth it for your anxiety to go up.
Finally, a lack of understanding of autism and resultant unrealistic expectations of the service could result in disappointment and frustration among service users:
. . . they’re expecting everything to be cured by the diagnosis or the intervention.
Person-centred factors associated with outcomes
Functioning and complexity of need
As already noted, practitioners reported a great range in functioning and complexity of need among those referred to their services. These were felt to affect the type of impact that a SAT could expect to achieve. For some, maintaining existing health and functioning or preventing further decline are appropriate outcomes. For others, positive change, sometimes quite specific to a particular aspect of their lives, can be hoped for or expected:
Some of it’s about current functioning. So, like for our complex clients, it’s still improved outcomes, but it’s not a lot of change. And then we’ve got people who are, have jobs, they have families and that kind of thing. They have more of an idea about what they want to do [achieve from using the service].
Ownership of the referral
Practitioners identified three types of referrals: those highly engaged and positively wanting an autism diagnosis, those with mixed feelings and anxiety about the process and passive participants. The last group typically comprised those in which parents have driven the referral:
There’s a massive range, isn’t there? There’s some people that are incredibly motivated and really want a diagnosis, and some people that are a bit ambivalent, and some people that other people are saying: ‘Oh, I think this is an issue for you’.
Reaction to the diagnosis
A strong and consistent theme within practitioners’ discussions was the way that service users’ reactions to their diagnosis affected longer-term outcomes. For some, this reaction was closely related to ownership, or not, of the referral. Thus, in some cases, the diagnosis fulfils a (potentially long term) desire to make sense of their lives. Here, seeking a referral or self-referral may not be precipitated by a particular difficulty or crisis, but a readiness or desire to make sense of themselves and their lives:
There are individuals where the diagnosis can give them sort of a clarity. It can give them an understanding of what it, why they’ve had these difficulties. Those people that are kind of, almost on a sort of quest of understanding why . . . It’s a positive thing in a way cos it kind of makes sense.
It’s about acceptance of the diagnosis when you’ve always felt different and lost and, you know, having an explanation of how that can help you understand yourself and move with things.
Importantly, psychoeducation was regarded as playing a critical role in supporting positive outcomes from being diagnosed.
Engagement with the interventions offered by the service
Practitioners believed that engagement with the service following diagnosis was affected by ownership of the referral and reaction to the diagnosis (as described above). Crucially, they may affect engagement with psychoeducation interventions, which was the first intervention typically offered. Lack of engagement with this was regarded as having the potential to stymie ongoing engagement with the service and/or the potential for positive impact of subsequent interventions:
Outcomes would be improved for people who either will or can engage in [psychoeducation interventions]. But it’s whether they have that ability, or whether they have severe anxiety, to be able to do that.
Mental health difficulties, such as anxiety and depression, were also implicated. In general, practitioners referred to service users having different levels of motivation in terms of wanting or feeling able to make changes in their lives:
. . . its’ about the level of motivation to want to do something and change something.
Family support
Senior practitioners agreed that family members’ responses to the diagnosis can differ widely. For example, a diagnosis of autism may improve one couple’s relationship, as it provides an explanation for why a partner behaves in the way that they do. For another couple, however, an individual may find the realisation that certain things about their partner cannot be changed is a catalyst for ending their relationship. Therefore, overall, families were regarded as having the potential to facilitate or hinder positive outcomes. This was attributed partly to existing family relationships and dynamics, but also to family members’ ability and willingness to understand the additional challenges faced by autistic people, and what they can do to accommodate specific needs:
It can be a really, really positive thing if they have a supportive family . . . then having that diagnosis will possibly enable some more empathy or understanding around the difficulties and can improve things like family dynamics at home.
Across these discussions, the value of family members receiving psychoeducation related to the diagnosis of autism was highlighted.
The intersection of individual need and service characteristics
Another key factor that was thought to affect user outcomes was the ‘fit’ between the support and the interventions provided by a SAT and individuals’ needs. This was not necessarily about severity or complexity of need. In some instances, for example, it concerned whether or not services were able to offer low-level support on an ad hoc basis for those individuals who, for the majority of the time, managed their everyday lives independent of formal support:
[There are some] who don’t need very much support but need to be able to access informal support, so a telephone call or a ‘cuppa tea’ kind of chat as and when they need it as opposed to something formal, eight sessions kind of thing. And if that can be made available to them, they seem to have very, very good outcomes.
However, practitioners also noted that the types of needs presented by service users, and their ability to identify specific and realistic aspects of their lives that they wanted to change, could affect whether or not substantive changes in outcomes were observed. They explained that some needs or difficulties are more amenable to change or address, or that it is reasonably straightforward to equip individuals with self-management skills:
People who have sensory issues, so where you can actually [help them with] coping strategies for dealing with those things, you know, practical things that can help on a day-to-day basis.
The people that are goal-driven but also have realistic expectations. They’ve gone into the service with a clear idea of what their chosen outcome is and then work with someone towards it.
Service characteristics associated with outcomes
One of the sessions at the senior practitioner workshop explored views about aspects of service design and practice perceived to affect service user outcomes. We used a small group-work activity in which participants ranked 13 service characteristics in order of their relative impact on service user outcomes. Rankings were then used to stimulate a whole-group discussion on this issue.
The quality of the diagnostic assessment process
There was strong consensus that the quality of the diagnostic and needs assessment process was important in terms of supporting positive outcomes. All participants believed that their service provided this, and this service characteristic was stressed as distinguishing SATs from other diagnostic pathways.
Skill mix with autism expertise
Skill mix of the team, specifically its multidisciplinary nature, was consistently regarded as one of the most important service characteristics in terms of supporting positive outcomes. Practitioners noted that some key skills are shared across different professions and it may be the case that it is the skill set, rather than the professional qualification, that is the key issue. Integral to this was autism expertise. Indeed, some noted that, on occasion, when considering the skill mix in a team, this expertise was prioritised over a particular professional being represented on the team. Practitioners from one service described the value of having someone with direct experience of autism within the team:
The skill mix of the team is vitally important.
We all bring different things to the team from our professional backgrounds so it’s useful to have a mix of professions with experience . . . [of supporting autistic people without LDs].
We need skill mix, but it isn’t so much your profession, it’s about your skills and knowledge of autism.
Alternative modes of intervention delivery
Another service characteristic seen to have the potential to impact outcomes was services’ ability to be flexible in the way that they provided care and support to accommodate service users' needs and preferences. Two components were identified: the overall delivery model (time-/session-limited vs. open-ended contact) and the mode of delivery (i.e. individual vs. group). The first quotation below comes from a senior practitioner working across two SATs, one mainly using group-delivered interventions and the other using individual work alongside groups:
You can see the difference being able to offer groups and individual work alongside, or just individual work. It makes quite a big difference.
There’s so many positives of both approaches [time/session-limited vs. open-ended].
There are so many people that identify as our services as ‘I’ve been using you for years, and I don’t use you very often but I’ve got that if I need it’. Whereas other people respond so much better to ‘I’ve have these sessions and I go and then I’m never going to see you again’. I just think they’re both equally as important.
Services should be able to be flexible around the individual’s needs.
Having a ‘named contact’
Service users having a ‘named contact’ in the service was regarded as, potentially, impacting outcomes. It was also noted that it was very relevant to service user experience:
A key worker is really important for people. Like a contact, somebody that you can form a relationship with and contact.
We have a named contact primarily because of feedback from the service users. They [said they] don’t like being passed from pillar to post [because] they might move through different professionals in the team. So one person holds responsibility for that service user while they’re moving through. Then, if they need to ring, they leave a message specifically for that person.
Not all services had a formal ‘named contact arrangement’. However, it was reported that this could happen informally on an ad hoc basis:
. . . they will tend to ‘take’ to one of the members of staff and call them.
Local authority involvement
Some practitioners regarded LA involvement in the SAT as one of the more important factors potentially affecting service user outcomes. Specifically, it was seen as supporting a holistic approach and direct access to community care assessments:
. . . in terms of local authority involvement, we all felt it was really important and crucial to a holistic autism service with social work involvement.
Features of service organisation and delivery with less influence on outcomes
Service characteristics identified as being less likely to affect individual outcomes were if a service was autism-only or a neurodevelopmental service, and whether the service was delivered by a single team or two/three teams, each delivering specific functions.
Engagement with Specialist Autism Teams by other services involved
Finally, the extent to which other services that were also involved with a service user (e.g. owing to co-existing mental or physical health conditions) sought advice and input from the SAT was felt to have the potential to determine the extent to which SATs could support improvements or maintain the status quo in people’s lives. Practitioners commented that there was still room for significant improvement in the understanding of autism within mainstream provision:
If you’ve got somebody that is already getting regular support from the physical or mental health service, it would help [these] professionals to actually understand the difficulty, where they [service user] might be coming from, and what the difficulties might be.
Summary
This chapter reported senior SAT practitioners’ views about the outcomes that SATs can expect to achieve, and the impact individual and service user characteristics may have on outcomes.
The great diversity among service users in terms of complexity of need and what they hope to achieve from a referral to a SAT was emphasised. A number of individual characteristics were identified as having the potential to affect outcomes. These included functioning and complexity of need, ‘ownership of the referral’, reaction to the diagnosis, engagement with interventions offered by the SAT and the quality and nature of family support. The fit between service users’ needs and the support and interventions provided by a SAT was also identified as key in determining the extent to which positive outcomes were achieved.
Service characteristics that were regarded as having the potential for greatest impact on user outcomes included richness of skill mix/the multidisciplinary nature of the team, being able to offer alternative ways to receive an intervention (e.g. group vs. one-to-one sessions), service users having a ‘named contact’ and LA involvement. Whether the SAT service was autism-only or a neurodevelopmental service was regarded as relatively unimportant, as was the organisational structure (single vs. multiteam).
Finally, the extent to which other services also caring for or supporting the service user implemented autism-specific adjustments to their own practice or delivery was regarded as having the potential to affect the outcomes achieved by a SAT.
Chapter 6 Impacts of using a Specialist Autism Team or diagnostic assessment service
Introduction
This is the first of three chapters reporting the views and experiences of service users. Here, we present qualitative data generated from a question included in the study questionnaire at the 12-month follow-up (T3). The question sought to capture, at a high level, study participants’ descriptions of the impacts on their lives of using a SAT (SAT cohort) or, for our comparator cohort, a diagnostic assessment service (DO cohort).
Method
Data were collected at T3 (i.e. 12 months after participants attended their first full assessment appointment) through two questions that were included in the T3 outcomes questionnaire. The first, a fixed-response question, asked ‘Overall, how would you describe the impact (or difference) that the [name of service] has had on your life?’. Response options were ‘positive impact’, ‘little or no impact’ or ‘negative impact’. Respondents were then invited to explain their chosen response with the instruction ‘If you wish, please tell us in what ways the [name of service] has impacted on your life, or why it has not had much impact.’. A blank text box (equivalent to A5 size in hard-copy version) was provided.
These questions were originally included to inform the development of the topic guide used for the qualitative interviews with service users (reported in Chapter 7) and for the sampling framework for this component of the study (as we wanted the range of the perceived impact to be represented). However, given that over half of participants chose to provide a brief account of their experiences, it was decided that this data set should be subject to analysis using qualitative content analysis techniques. Appendix 3 provides an account of the analytical process.
The sample
Over half the T3 sample (138/260) completed both questions, as follows:
-
SAT cohort, n = 106/164 (64.60%)
-
D&S group, n = 74/133 (55.65%)
-
SO group, n = 32/75 (42.70%)
-
-
DO cohort, n = 32/52 (61.50%).
Appendix 4, Table 30, provides an overview of the sample characteristics.
Findings
Overall impression of the service
In total, 60.4% of respondents reported that the service had a positive impact on their lives, 33.8% reported little or no impact and 5.8% reported a negative impact. However, examination of the qualitative data suggests that a positive impact rating does not necessarily indicate a singularly positive experience and outcome. Rather, a more mixed experience was possible, with some describing the support that they had received as insufficient (Table 6). This table also displays the difference between cohorts. Thus, although 60.0% of SAT D&S group respondents and 56.3% of DO respondents reported a positive impact, this figure was much lower (28.1%) for SAT SO group respondents.
| Impact rating | DO cohort | SAT cohort | Whole sample | |||||
|---|---|---|---|---|---|---|---|---|
| D&S group | SO group | |||||||
| n (%) | Rank | n (%) | Rank | n (%) | Rank | n (%) | Rank | |
| Positive | 18 (56.3) | 1 | 45 (60) | 1 | 9 (28.1) | 2 | 72 (51.8) | 1 |
| Positive but insufficient | 6 (18.7) | 3 | 5 (6.7) | 3 | 1 (3.1) | 4 | 12 (8.6) | 3 |
| Little/no | 7 (21.9) | 2 | 22 (29.3) | 2 | 18 (56.3) | 1 | 47 (33.8) | 2 |
| Negative | 1 (3.1) | 4 | 3 (4.0) | 4 | 4 (12.5) | 3 | 8 (5.3) | 4 |
| Total | 32 | 75 | 32 | 139 | ||||
In explaining the reason for a non-positive rating, a range of unmet needs (e.g. mental health difficulties, family understanding of autism and access to social care) and/or inadequacy of support were described. DO cohort respondents typically wrote more generically about insufficiencies, often stating simply that they needed more follow-up support after diagnosis than had been offered, both for themselves and for their family. The following sections report further findings from the content analysis that shed light on why respondents from different cohorts may have had different experiences.
The accounts of positive impact
Appendix 5, Table 31, summarises results of the content analysis of respondents’ accounts of the positive impact(s) that the SAT had on their lives. It shows that positive impacts were wide ranging in nature, with 18 different types of impact identified. These were grouped into seven broad categories:
-
understanding and acceptance of diagnosis and self
-
improved mental health and coping
-
help with employment and education
-
access to other services
-
improved social skills, relationships and networks
-
contact with supportive practitioners
-
reduced sense of isolation.
The number and range of positive impacts experienced varied between cohorts (see Appendix 5, Table 31). All types of positive impact were reported by at least one D&S group respondent. However, the range of positive impacts experienced by SO group and DO cohort respondents was more limited (10/18 and 7/18, respectively). It is notable that ‘contact with supportive practitioners’ was reported only by SAT cohort respondents. This impact category includes a number of different aspects of supportive practice, including being made to feel valued, feeling understood, being treated with respect and staff being experts in autism, easy to contact and responsive to individual need. The follow extract illustrates the significance of such an experience:
Being understood and being treated with such respect and compassion was a hugely beneficial experience after not having been very understanding or compassionate with myself.
SU37, SAT cohort: SO group
The most frequently reported type of positive impact, which was observed across the three cohorts, was ‘greater understanding of self’. Examination of the qualitative data linked to this code provides some explanation as to what this concept means and why it was valued. First, it referred both to their current lives and to their past experiences. Second, ‘greater understanding of self’ had allowed respondents to be more accepting and forgiving of themselves. They described both specific effects or changes (e.g. worrying less about why they behaved as they did, ceasing to label themselves as ‘weird’, changing job/career to one more suited to them) and more global positive impacts, such as increased confidence and self-esteem and improved well-being and/or mental health:
I no longer worry or analyse my thoughts and actions like I used to. I feel much more at ease and finally feel that I understand myself as a person. Although I still struggle with anxiety, I am grateful that I have been given answers. The fact that I am now aware I have Asperger’s is great, it makes sense and provided me with what I have needed all my life – answers and closure.
SU39, SAT cohort: D&S group
I can now learn to live with who I am and what I am capable of/and what I am not. I don’t feel I have to push myself as much to fit in (which caused me the most stress). I still have other problems with moods and sensory issues. I am learning more about this condition all the time.
SU40, SAT cohort: D&S group
It is worth noting here that although respondents across all cohorts reported ‘increased understanding of self’, only respondents in the D&S and SO groups reported that they had benefited from ‘help with accepting and/or seeing the strengths of their diagnosis’. Comments such as the following were made:
It’s given clarity in my life. I know the reason why I’m the way I am. And thanks to [name of service] I look at my condition in a positive manner.
SU41, SAT cohort: D&S group
Given the connection respondents made between greater understanding and acceptance of self, it perhaps is not surprising that improved mental health (including self-esteem) was also one of the most frequently reported positive impacts. Indeed, scrutiny of responses related to improved self-esteem or mental health revealed that such changes were most frequently linked to improved self-understanding. However, for a minority, improved mental health was attributed to other interventions provided by the service (e.g. sessions with a psychologist, joining hobby groups and receiving additional support at university):
I feel strongly that if I had not been sent to the [name of service] team when I had I would not be in such a positive place as I am today. I will always have difficulties with mental health but I now have coping mechanisms and a support system in place which I would never have had without this team. Thank you.
SU42, SAT cohort: D&S group
The accounts of little or no impact
Table 7 provides an overview of respondents’ reasons for why the services that they used had little or no impact on their life. This group represented 22 out of 75 D&S respondents, 18 out of 32 SO group respondents and 7 out of 32 DO group respondents. Across all groups, the most frequent reason for little or no impact (27/47) was that no support had been received.
| Reason | DO cohort (n = 7) | SAT cohort | ||||
|---|---|---|---|---|---|---|
| D&S group (n = 22) | SO group (n = 18) | |||||
| Frequency | Rank | Frequency | Rank | Frequency | Rank | |
| Not received any support | 7 | 1 | 12 | 1 | 8 | 1 |
| Support provided was insufficient | 0 | – | 4 | 3 | 3 | 3 |
| Support provided was unsuitable | 0 | – | 5 | 2 | 5 | 2 |
| Decided did not want help | 0 | – | 1 | 4 | 2 | 4 |
As would be expected, among DO cohort respondents, little or no impact was solely attributed to not receiving any input or support from the service after the diagnostic assessment process was complete. Notions of isolation were evident and this could offset any positive impacts of being diagnosed. For example:
They diagnosed and left me. The diagnosis was positive as it helped me claim PIP [Personal Independence Payment]. Being left alone and questioning my entire life due to my diagnosis was a negative, left entirely to my own devices.
SU43, DO cohort
These respondents also described the types of issues that they continued to struggle with or the types of support that they wanted. These included coming to terms with the diagnosis, managing mental health problems, helping with relationship difficulties, finding out about/connecting with support groups/services for autistic people and managing difficulties with employment/workplace.
Among the SAT cohort, not receiving input or support from a service was attributed to either the service not being in touch since the diagnostic or needs assessment, or the respondent still being on a waiting list for a group intervention(s). A sense of frustration was observed in many responses:
After my first two appointments in which I was assessed and then told the result, I have not had any further contact with [name of service] other than when I inquired when I would receive the report of my assessment, which I did not get until almost 12 months after my diagnosis. Since my diagnosis I have not been given any information about help/support that is available.
SU44, SAT cohort: D&S group
They have totally failed to put on group sessions. I’ve not heard from them in months.
SU45, SAT cohort: D&S group
The second most frequently reported reason among the SAT cohort for a service having no impact was that the support received did not (fully) address the individual’s needs. This was either because the desired support had been unavailable or not offered (e.g. employment support, explaining the diagnosis to relatives, etc.) or because a respondent was discharged from a service before they felt ready:
It’s a bit like having the carpet pulled from under your feet. It would only have an ongoing positive impact if the support was ongoing. It’s a bit like trying to help a homeless person by giving him exactly six nights of accommodation and then nothing.
SU46, SAT cohort: D&S group
A third reason that SAT cohort respondents rated the service they used as having little or no impact was that the support/interventions offered or provided were regarded as unsuitable. Where further detail was provided, it typically concerned being offered group-delivered (as opposed to a one-to-one) intervention(s). Finally, a small proportion of SAT cohort respondents reported declining any/further input because of other demands on their time or because they felt too old to change how they lived their lives.
The accounts of negative impact
Just 8 out of 139 respondents rated the service that they had used as having a negative impact on their life. In the majority of cases (6/8) this was because the respondent had not been offered any post-diagnosis support.
Summary
This chapter has reported findings from our analysis of responses to two questions used in the T3 (12-month follow-up) questionnaire to explore study participants’ views on the impact(s) on their lives of using a SAT or a diagnostic assessment service. Over half of the T3 sample completed both questions. These data provide a useful, first, and high-level, insight into service users’ views and experiences. This complements data from our in-depth, semistructured interviews with a smaller subsample of study participants and is reported in Chapters 7 and 9.
The majority of respondents reported that the service they used had a positive impact on their lives; for some (and across all cohorts), negative impacts or insufficient support rendered this positive impact partial. The types of reported impact reveal the potential for SATs to have a positive impact across many life domains. However, the full range of impacts was represented only in the accounts of respondents from the D&S group. SO respondents were less likely to report a positive impact. It is not clear from these data why this may be the case.
Where respondents reported little/no impact or a negative impact, this was typically because they had not received any support/interventions in addition to the diagnostic/needs assessment. Other reasons included that respondents were still waiting to receive an intervention (in all instances, this was for a group-delivered intervention) and that the interventions/support offered were regarded as unsuitable. Group, as opposed to one-to-one, delivery was the most common reason to refuse or drop out of an intervention. Other reasons for little or no impact included insufficient intensity or duration of support, or that the service did not address their priorities. A small minority of respondents reported choosing not to engage with the service owing to pressures of time or because they felt that they were too old to change well-established coping strategies.
Chapter 7 Experiences of using a Specialist Autism Team
Introduction
This chapter turns to the experiences of individuals who used a SAT and forms part of the study’s qualitative evaluation. Appendix 6 provides an account of the methods. Briefly, 29 individuals, representing all research sites, were recruited approximately 12 months after their first full assessment appointment. A purposive sampling frame ensured representation of age and gender, and reported impact of the service. Semistructured, in-depth interviews explored pathways into the service, expectations, outcomes, views on factors affecting outcomes and service user experiences. The chapter is organised into the following sections:
-
pathways into the service
-
hopes and expectations at the outset
-
views about the specialist nature of the services
-
experiences of the diagnostic assessment process
-
the extent to which individuals’ needs were met
-
the impact of characteristics of service delivery and practice on outcomes
-
practical barriers affecting access to SATs.
Pathways into the service
Of the 29 individuals recruited, 21 had not previously been diagnosed with autism (D&S group). The majority had initiated their referral to a SAT. For some, this had been triggered by their own research into autism or their experiences of difficulties at work, social difficulties or problems with their mental health. Others had made or sought a referral at the suggestion of others. For a minority, a parent or health professional (e.g. GP or psychiatrist) had decided and organised the referral. A further eight interviewees were already diagnosed with autism (SO group). For the majority, their referral had been instigated either by a professional already working with them or by a family member. A minority had self-referred, and reported being helped or encouraged to do so by a parent. One individual had used the SAT previously.
Hopes and expectations at the outset
Among those who were not previously diagnosed with autism, the diagnostic assessment was regarded as having the potential to offer an explanation for the various struggles they had experienced over their lives. A number spoke of how they hoped having a diagnosis would give them ‘peace of mind’, ‘closure’ or ‘validation’:
I was just looking for validation, and to have a word to explain my difficulties so I didn’t just need to put them down to me being a bit ‘weird’.
SU14, 18 years
I said [to GP] that I’ve got like 20 years left and I just want some sort of peace, because I beat myself up about how I feel and I’m, I feel I’m inadequate.
SU21, 62 years
Some were not seeking or felt the need for, any further assistance from the SAT. Others, however, wanted help with one or more, sometimes quite substantial, difficulties in their lives (e.g. mental health, social isolation/social skills, independent living and accessing adjustments at work or college). A few also hoped that having a diagnosis would help others (e.g. family and work colleagues) to understand them better.
Those already diagnosed were typically much more specific about the help or support that they wanted, perhaps reflecting a greater understanding of autism, its potential impacts and intervention options. Needs were wide-ranging and included mental health difficulties, social isolation, managing day-to-day life, sleep difficulties, sensory issues and work/employment issues.
Regardless of diagnostic history, many interviewees reporting mental health needs indicated that they had previous, not necessarily successful, experiences of generic/mainstream mental health provision.
Views about the specialist nature of the services
When speaking of their experiences of using a SAT, interviewees often described or referred to ‘autism-friendly’ practices. These, in themselves, were regarded as evidence of the specialist nature of the service. A number of interviewees specifically described ‘feeling understood’ or referred to the fact that the SAT was staffed by professionals with an expertise in autism. Feeling that they were using a service that understood them was an emotional support in itself. Together, these engendered confidence and engagement with the service:
By offering support for it and stuff like that, and they work with people that have it. So that, that put my mind at ease, that I’m definitely not alone and, that there is people that understand it and that offer support for it.
SU9, 18 years
They are understanding, kind, caring and all that type of stuff. They don’t judge you, they’re amazing at what they do. If you come in with a problem they’ll listen to you and that type of stuff, so yes, I would recommend someone who’s got autism to go and see them.
SU25, 21 years
Experiences of the diagnostic assessment process
All SATs had a unique diagnostic assessment protocol (see Chapter 3). There were, however, no noticeable differences in interviewees’ overall level of satisfaction with the way that the assessment process was managed, which was either positive or neutral. There were no spontaneous complaints, for example, about the number of sessions involved or the duration of the process.
That was not to say, however, that some found it a difficult process that caused them anxiety and unease. Being the centre of attention, having to describe private matters or admit to struggling with, what others might regard as, straightforward, everyday tasks caused embarrassment. The use of open-ended questions and having more than one assessor involved were sources of anxiety. Finally, a few interviewees were unhappy that their parents had to be involved and some reported finding some of the assessment tasks (e.g. story-telling and shape completion) childish and patronising.
Some interviewees found the requirement to recall childhood experiences particularly difficult. Undergoing this brought back difficult memories and had caused some interviewees to become upset during the assessment. One interviewee described this as ‘re-traumatising’ (SU47).
The predominant emotional response to being diagnosed with autism was a sense of relief: at having suspicions confirmed or having an explanation for and validation of struggles throughout their life. However, for many, this was followed by a more mixed set of emotions. [We explore this in more depth in a later chapter (see Chapter 9), which focuses particularly on experiences of the diagnostic assessment process from the perspective of SAT users and those accessing only a diagnostic assessment.]
In terms of other short-term outcomes, some described the way an autism diagnosis per se enabled or opened access to a particular form of support, such as welfare benefits (e.g. Employment and Support Allowance) or adjustments at work or college. Indeed, for some, this had been the primary motivation for their referral to the SAT, with some subsequently self-initiating access to these. The great majority of our interview sample, however, had additional needs that required further input and support from the SAT.
Extent to which individuals’ needs were met
Within interviewees’ accounts, four broad areas of need, varying between individuals, were identified:
-
understanding and coming to terms with/accepting their autism diagnosis
-
strategies and skills to support successfully managing everyday life and situations
-
mental health or social needs (social needs = social care, employment, housing and welfare needs) presented at referral or identified/emerging during the time with the service
-
emotional support to overcome or endure a period of difficulty.
Based on the evidence gathered in their interviews, we allocated interviewees to one of three groups in terms of the levels of unmet needs at discharge from the SAT (or, if still with the service, ≈ 12 months after the first full assessment appointment):
-
Needs predominantly met. This group can be further distinguished:
-
lower levels of need at referral
-
higher levels of need at referral.
-
-
Met and unmet needs. This group can be further distinguished in terms of why some needs remained unmet:
-
service did not address the full range of presenting needs
-
some needs only partially met by discharge
-
needs predominantly unmet.
-
Organising the sample in this way allowed us to investigate systematically whether or not, and how, features or characteristics of service delivery and practice affected service users’ accounts of the ways a SAT did or did not help them. This was one of the primary objectives of this element of the overall project, and we report our findings in Service characteristics: impacts on outcomes. First, however, we offer a broad description of these three groups and their experiences.
Needs predominantly met
Eight of our interviewees, across six SATs, reported their needs to be fully or predominantly met by the service. This included individuals not previously diagnosed and individuals already diagnosed with autism. Some individuals had very substantial and wide-ranging difficulties at the point of referral (e.g. homelessness, redundancy, depression and suicidal ideation) and described the considerable impacts that receiving support from a SAT had on their lives:
When I was diagnosed I was not far off being incapable of work and now I’m 6 months into a new job and coping incredibly well, despite massive upheaval and significant change. And I’m doing that at the same time as trying to move house and coping with the rug being pulled out from under my identity in terms of my diagnosis. There is no universe in which I would be coping half as well if it wasn’t for the support I’ve received.
SU35, 33 years
I felt they went above and beyond, and I am truly grateful. I wanted to complete this interview to express that, as I can’t thank them enough.
SU22, 37 years
Others had sought referral to the SAT for a diagnostic assessment and did not identify themselves as having any additional support needs. In these instances, the diagnosis often enabled individuals to self-initiate any changes or resolve problems in their lives, and they had not required support from the SAT to achieve this:
The main thing I really wanted was the diagnosis for work. I had support that I needed from ex-wife and friends so I wasn’t really looking for any sort of ongoing support from the service.
SU18, 62 years
Met and unmet needs
Thirteen interviewees, across seven SATs, were allocated to the ‘mixed experience’ group, with some of their needs remaining unmet or only partially addressed. Although half regarded themselves as still ‘in the service’, no interviewees were actively engaged when we interviewed them. Unmet or partially met needs were attributed to ‘ineffective’ interventions and limitations of the SAT in terms of format, duration, intensity, scope and flexibility of the support available: we return to these issues in detail in Service characteristics: impacts on outcomes. Reports of refusing, not using or dropping out of the interventions/support offered were much more common in this group than in the ‘needs met’ group. The cause of limitations to the support received was most frequently attributed to funding constraints within the NHS and participants expressing sympathy for SAT practitioners. Nevertheless, a number of people expressed disappointment at the help they received.
Needs predominantly unmet
Seven interviewees, across four SATs, were allocated to the unmet needs group. All reported that, aside from the diagnostic assessment, the support they had received had not helped. All had been discharged or had disengaged from the service. The unmet needs that were reported were wide ranging and, in some cases, quite significant or dehabilitating. They were consistently attributed to limitations in the support offered by the SAT and/or the support/interventions being delivered in a way that they could not access (e.g. group-delivered interventions). We return to these issues in detail in Service characteristics: impacts on outcomes.
Some presented the experience of being discharged and/or being offered intervention/support as inadequate or inaccessible, with language that indicated a sense of rejection and a perceived lack of compassion on the part of the service; for example, ‘thrown out’ (SU8) and ‘ticked off [waiting list]’ (SU17), as well as:
The service is like, is almost like detached, it’s like doesn’t even wanna try and help. . . . I feel like I’m not getting across, like I can’t get across how bad it is kinda thing.
SU47, 20 years
Another common theme in this group’s accounts was a frustration that needs had been articulated or identified during assessment, but not then addressed:
It felt like there was a disconnect between the person doing the diagnostics and the follow-up. Identifying an issue is isn’t the same as providing solutions or help with the issue.
SU12, 28 years
A noteworthy difference in experience between the ‘unmet needs’ group and the ‘needs met’ and ‘mixed experience’ groups was that the ‘unmet needs’ group were more likely to describe waiting times for the diagnostic assessment as being problematic, with some having waited > 2 years. It is possible that these waiting times increased the severity of personal difficulties or the hope vested in how the SAT would impact their lives, which, in turn, heightened or coloured their emotional response to their experiences of using a SAT. Despite this sense of frustration and disappointment, as with the ‘mixed experience’ group, interviewees also referred to the high level of demand for services and lack of funding as an explanation as to why they had received so little support.
Service characteristics: impacts on outcomes
This section reports characteristics of service delivery and practice that, based on our analysis of interviewees’ accounts, appear to be associated with outcomes (that is, the extent to which needs were met). They are as follows:
-
scope of and access to psychoeducation about autism
-
the service’s overall model of care delivery
-
availability of an alternative to group-delivered interventions
-
timeliness of group-delivered interventions
-
approach to managing referrals to other services.
Scope of and access to psychoeducation about autism
A range of emotional reactions and responses to an autism diagnosis were described. Positive (e.g. relief) and negative (e.g. anger, distress or grief) emotional responses were reported, with some individuals experiencing both, simultaneously and/or over time. All SATs offered an extended psychoeducation intervention (i.e. an intervention seeking to increase understanding of autism, self-understanding and self-management skills) via either group or one-to-one sessions. However, not all SATs offered one-to-one work for those unable to attend a group (see Availability of alternatives to group-delivered interventions).
Individuals in the ‘needs met’ and ‘mixed experience’ groups typically spoke very highly of the psychoeducation that they had received:
It ended a lifetime’s worth of feeling inadequate and feeling worthless.
SU36, 21 years
Aspects of psychoeducation identified as being particularly helpful included content that gave insight into how autism may affect them, including the positive aspects of the condition; sharing experiences, including speakers with positive stories of living with autism (group delivery only); and learning coping techniques for dealing with difficulties commonly experienced by autistic people (e.g. sensory overload and anxiety). A dominant theme in these individuals’ accounts was the impact on the way that they viewed themselves: feeling more accepting or forgiving of themselves. Some also spoke of feeling less need to mask autistic behaviours and/or seeing the positive side of the condition:
It [the diagnosis] could have been life-changing in a way that left me stranded and in fact it has been life-changing in a way that’s given me enormous support and enormous hope, and a new capacity for thinking about myself and the world around me.
SU35, 33 years
By contrast, those in the unmet needs group had either not accessed this intervention (owing to long waiting lists or feeling unable to attend a group) or dropped out early because they found it unhelpful. Being unable to access (good) psychoeducation appeared to be a key influence in whether or not individuals had been able to resolve any negative emotional reactions to the diagnosis.
The service’s overall model of care delivery
All of the individuals in the ‘met needs’ group with support needs extending beyond the diagnostic assessment had attended SATs that provided individualised managed care that was overseen and co-ordinated by a single member of the SAT, who also acted as the ‘named contact’ for the service user. For individuals experiencing a mental health crisis, being able to contact their ‘named contact’ outside appointment times was consistently regarded as extremely valuable. As well as responding to needs that the individual was aware of on referral or were identified in the assessment process, this model of care was also able to respond to needs emerging during the time that the individual was in the service. Furthermore, in adopting this model of care, these services typically had the skills and expertise within the team to respond directly to a wide range of support needs. Where required, they supported referrals to other services/agencies:
It has been individualised to me, I’ve felt seen and heard and respected during the entire thing, but the breadth, but also that the breadth of professionals involved has meant that I’ve had several different appropriate touch points, each of which has had a measurable significant impact like, and it, it’s been, yeah, it’s been fantastic. Considering, considering what a shitty, complicated weird situation it has been it has been, the, the service has been brilliant.
SU35, 33 years
She does things that I wouldn’t have ever known about, having the one to ones . . . I think they’ve exceeded what I expected with it, they’ve explained it [the diagnosis] to me so I understand it, and try to put coping methods in place. That’s exceeded what I expected.
SU15, 47 years
There was some evidence that limiting the duration of individualised managed care (e.g. the SAT being able to offer only a fixed number of sessions) could mean that some needs remained unmet at discharge. This was observed among individuals in the ‘mixed experiences’ group attending such services, especially those with complex and long-standing difficulties. However, even in SATs not working to a fixed number of sessions, a few individuals in the ‘mixed experience’ group believed that they were discharged before they were ready to leave:
I was hoping to stay a client. But they thought that I had all the support I needed, that’s why, but I don’t feel that, because they thought I was finished but I wasn’t, and I didn’t get a chance to explain that to them.
SU9, 18 years
By contrast, interviewees whose SATs did not work within an individualised model of care, offering instead a limited range of interventions and referring elsewhere to address other needs, consistently typically reported (at least some) unmet needs. A later section, Approach to managing referrals to other services, further explores practices around referring to other agencies or sources of support, and how this may be implicated in needs remaining unmet.
Availability of alternatives to group-delivered interventions
Many SATs used groups to deliver one or more interventions. Typically, this was a positive choice, with group delivery perceived as the best approach to achieve the specific objectives of that intervention (see Chapter 4). However, not all SATs offered one-to-one sessions if an individual felt unable to attend a group-delivered intervention. The lack of an alternative to group delivery of an intervention was a frequently cited reason for a need remaining unmet. In these cases, the individual had either refused or dropped out of the intervention early on. In both situations, no alternative (i.e. one-to-one session) was offered.
The most common reason for refusing or dropping out of a group-delivered intervention centred on social anxiety and/or a lack of confidence about being in a group. For some, past experiences of finding groups emotionally draining or distressing contributed to this decision. Other reasons, less frequently described, included an unwillingness to spend time with and/or be seen with other autistic people, particularly if they were perceived to be more severely affected; fears that hearing others’ experiences may be upsetting; and not believing that sharing experiences would be of use or value. An experience of a poorly facilitated group (e.g. not keeping to time/agenda and feeling that distressed participants were not well supported) was another reason for drop out.
Two interviewees spoke positively about the support that was given to attend a group-delivered intervention. Valued practices included pre-meetings with the group facilitator to hear more about what would happen; having the chance to view or be reassured about the suitability of the venue in terms of lighting, etc.; and allowing and supporting participation in group discussions via written, as opposed to verbal, contributions. Similar or complementary practices were suggested by interviewees who had not taken up a group-delivered intervention, but felt that, with support, it might have been possible. These interviewees also suggested offering a mentor or buddy to accompany individuals.
Timeliness of group-delivered interventions
Some of the interviewees who attended SATs using group-delivered interventions spoke of long gaps between the offer of support being made and the relevant group starting. This increased the risk of needs remaining unmet in a number of ways: individuals’ willingness to attend the group diminished or the intervention was regarded as no longer relevant or seen as coming too late to be useful. Some interviewees described how the presenting need increased in severity during the waiting period, which made attending the group more problematic. Finally, and in addition, a lack of communication from the SAT while waiting for a group to start (this could be several months) was, for some, a source of further anxiety with concerns that the SAT had forgotten about them.
Approach to managing referrals to other services
The ways in which individuals were referred to other agencies or sources of support to address needs that could not be met by the SAT also appeared to influence whether or not needs were met. We use the term ‘supported referrals’ to describe instances where SATs assisted with completing application forms (e.g. benefits); arranged and/or accompanied individuals to appointments with other agencies or organisations (e.g. employers, housing officers and social services); and/or acted as an advocate in meetings with other agencies. These sorts of practices were consistently reported by individuals in the ‘needs met’ and many of those in the ‘mixed experience’ group:
She’s very like to the point, very like, this is what she needs, this is what she’s like entitled to type of thing. I do think they like fight your corner for you, not that you should have to fight your corner, but like I do think it’s quite like a driven service.
SU7, 27 years
Experiences such as these contrasted with those who had been ‘signposted’ (i.e. provided with information and contact details for other agencies or other potential sources of support) with regard to an identified need. There was very little evidence that signposting was actively used or successful; as a result, needs remained unmet. For example, two interviewees spoke of being given the contact details for social or housing services. One had made no attempt to contact the service, the other had attempted to visit the service, but it had been closed and he had not returned.
Practical barriers affecting access to Specialist Autism Teams
A few interviewees reported practical barriers to accessing services or interventions that were offered by their SAT, which resulted in needs remaining unmet. This included, for those in employment, running groups during working hours only. Others had not attended group sessions or used a drop-in service because it would have involved them using public transport and/or journey times were considered too long. Finally, some reported forgetting and, therefore, missing appointments.
Summary
This chapter reported the findings from interviews with users of SATs that explored experiences of using SATs, outcomes experienced, and the perceived impact of service characteristics and ways of working on outcomes. A key analytical tool used was to split the sample into three groups according to whether, at 12 months after entry into the service, interviewees reported needs were, as follows: predominantly met, a mix of met and unmet, or predominantly unmet. We then investigated whether or not and how service characteristics and ways of working played a role in these experiences and outcomes.
Interviewees described a number of pathways into the service and a diversity in the level and type of presenting needs. Many were hoping the diagnostic assessment process might yield answers or confirm suspicions. Despite experiencing very different diagnostic assessment protocols and processes, overall, interviewees were quite satisfied with the way that the assessment process was managed, although many found it an uneasy and anxiety-provoking experience. For a few, the diagnosis enabled them to independently address specific difficulties or support needs. Many, however, had a number of needs for ongoing support from the SAT. These included understanding, coming to terms with and accepting the diagnosis; needing support to develop strategies to better manage everyday life and situations; specific mental health and social needs; and emotional support needs.
Five characteristics of service delivery and practice were identified as affecting the extent to which SATs had addressed service users’ needs. They were as follows: (1) the scope of and access to psychoeducation about autism; (2) the service’s overall model of care delivery; (3) the availability of an alternative to group-delivered interventions; (4) the timeliness of group-delivered interventions; and (5) the approach taken to managing referrals to other services. Finally, a few interviewees reported some practical barriers to accessing support and interventions offered by the SAT.
Chapter 8 The quantitative evaluation and factors affecting outcomes
Introduction
This chapter reports the quantitative elements of our observational study. After a description of the study design and methods, findings are reported with respect to the three main objectives.
Objectives
The objectives of this aspect of the study were as follows:
-
to describe changes in outcomes between entry into a SAT and 12 months later (T3), and to offer an initial description of longer-term outcomes
-
to explore whether or not individual and service characteristics are associated with T3 outcomes
-
to explore whether or not outcomes differ between individuals diagnosed and then supported by a SAT, and a cohort of individuals who received a diagnostic assessment only.
Study design
The study was an observational study of two cohorts: the main SAT cohort and a smaller DO cohort.
The Specialist Autism Team cohort
This cohort comprised users of SATs who were recruited at the time of their first full assessment appointment. Individuals in this cohort included those referred to the SAT but already diagnosed with autism (the SO group), and those referred for diagnostic assessment and ongoing support (the D&S group).
The Diagnosis-Only cohort
Three of the SATs that acted as research sites also provided a regional or national diagnostic assessment service for individuals living outside its CCG/LA boundaries via block contracts with neighbouring CCGs or on a case-by-case basis. The DO cohort comprised individuals who accessed one of these regional diagnostic assessment services; thus, these individuals did not receive any post-diagnosis support from the SAT.
Methods
Setting
Nine SATs (referred to as ‘research sites’) that were broadly representative of the range of service characteristics and ways of working observed in current SAT provision in England (see Chapter 3).
Study participants
The SAT cohort inclusion criteria for participants were that they were:
-
diagnosed with autism by the SAT or already had a confirmed diagnosis when referred
-
able to give informed consent, as judged by SAT practitioner in the research sites.
The DO cohort inclusion criteria for participants were that they were:
-
living outside the geographical commissioning boundaries of the SAT to which the individual has been referred
-
referred to a SATs regional/national diagnostic assessment service
-
able to give informed consent, as judged by SAT practitioner in the research sites.
Variables: standardised outcome measures
Outcomes were captured immediately prior to, at or immediately after the first full (diagnostic/needs) assessment appointment (T0), and at the following follow-up time points: 3 months (T1), 6 months (T2) and 12 months (T3) after T0. For those recruited earlier in the study, 18- (T4) and 24-month (T5) follow-ups were also possible. The following suite of standardised outcome measures and categorical outcome indicators was used (further details are provided in Appendix 7).
Primary outcome
-
World Health Organization Quality of Life Assessment, Abbreviated Version (WHOQOL-BREF)46 psychological domain (higher scores = better outcome).
Secondary outcomes: standardised measures
-
General Health Questionnaire (12-item version) (GHQ-12)47 (higher scores = worse outcome).
-
EuroQol-5 Dimensions, five-level version (EQ-5D-5L)48,49 (higher scores = better outcome).
-
Interpersonal Support Evaluation List – Short Form (ISEL-SF): belonging support subscale50 (higher scores = worse outcome).
-
WHOQOL-BREF social domain (higher scores = better outcome).
-
WHOQOL-BREF physical domain (higher scores = better outcome).
-
WHOQOL-BREF environment domain (higher scores = better outcome).
Secondary outcomes: categorical indicators – daytime occupation/usual activities
-
Difficulty with managing usual activities of daily living: EQ-5D-5L item ‘Usual activities (e.g. work, study, housework, family or leisure activities)’. Response options: no, slight moderate or severe problems.
-
Availability of information needed for daily living: question 13, WHOQOL-BREF – ‘How available to you is the information that you need in your day-to-day life?’. Response options: not at all, a little, moderately, mostly or completely.
-
Employment status: working versus seeking work versus not working because of sickness/disability.
-
Satisfaction with capacity for work: question 18, WHOQOL-BREF – ‘How satisfied are you with your capacity for work?’. Response options: very dissatisfied, dissatisfied, neither satisfied nor dissatisfied, satisfied or very satisfied.
-
Satisfaction with leisure time: standalone question – ‘I am satisfied with how I spend my free time’. Response options: definitely true, probably true, probably false or definitely false.
Secondary outcomes: access to autism-specific networks and support
The following items, from the study’s Client Service Receipt Inventory (CSRI), were used as indicators of connections with and use of autism-specific networks:
-
membership of an autism-specific regional or national third-sector organisation
-
membership of an autism-specific online-only group, community or forum
-
in the past 4 weeks, number of contacts with/use of either of the above.
Other service evaluation data
At T3, respondents were asked to rate the impact of the SAT on their life as positive impact, little or no impact, or negative impact. This was followed by a space in which respondents were invited to describe the ways that the SAT had affected their life or why it did not have much impact (see Chapter 6). At T3, respondents reported their status with the SAT (still using or discharged) and used a checklist to indicate the concerns on which the SAT had worked with them.
Study recruitment and retention
Recruitment and T0 (baseline) data collection took place within the following time window: from no longer than 3 weeks prior to the start of the full assessment (that is, diagnostic and needs assessment or, for those already diagnosed, needs assessment) to no later than 7 days after (see Appendix 8 for an account of the recruitment and data collection process). Figure 4 summarises recruitment and retention to the study. The recruitment rate was 57.20% (424/741). Over one-quarter (n = 114; 26.88%) of participants became ineligible for the study after the diagnostic assessment did not diagnose them with autism (n = 103) or the individual withdrew from the diagnostic assessment process (n = 11). Retention to the study at T3 (primary follow-up time point) was as follows: SAT D&S group, 133 out of 164 participants (81.1%); SAT SO group, 75 out of 88 participants (85.2%); and DO cohort, 52 out of 56 participants (92.8%).
FIGURE 4.
Flow chart: recruitment and retention to the study (not all participants complete each wave).
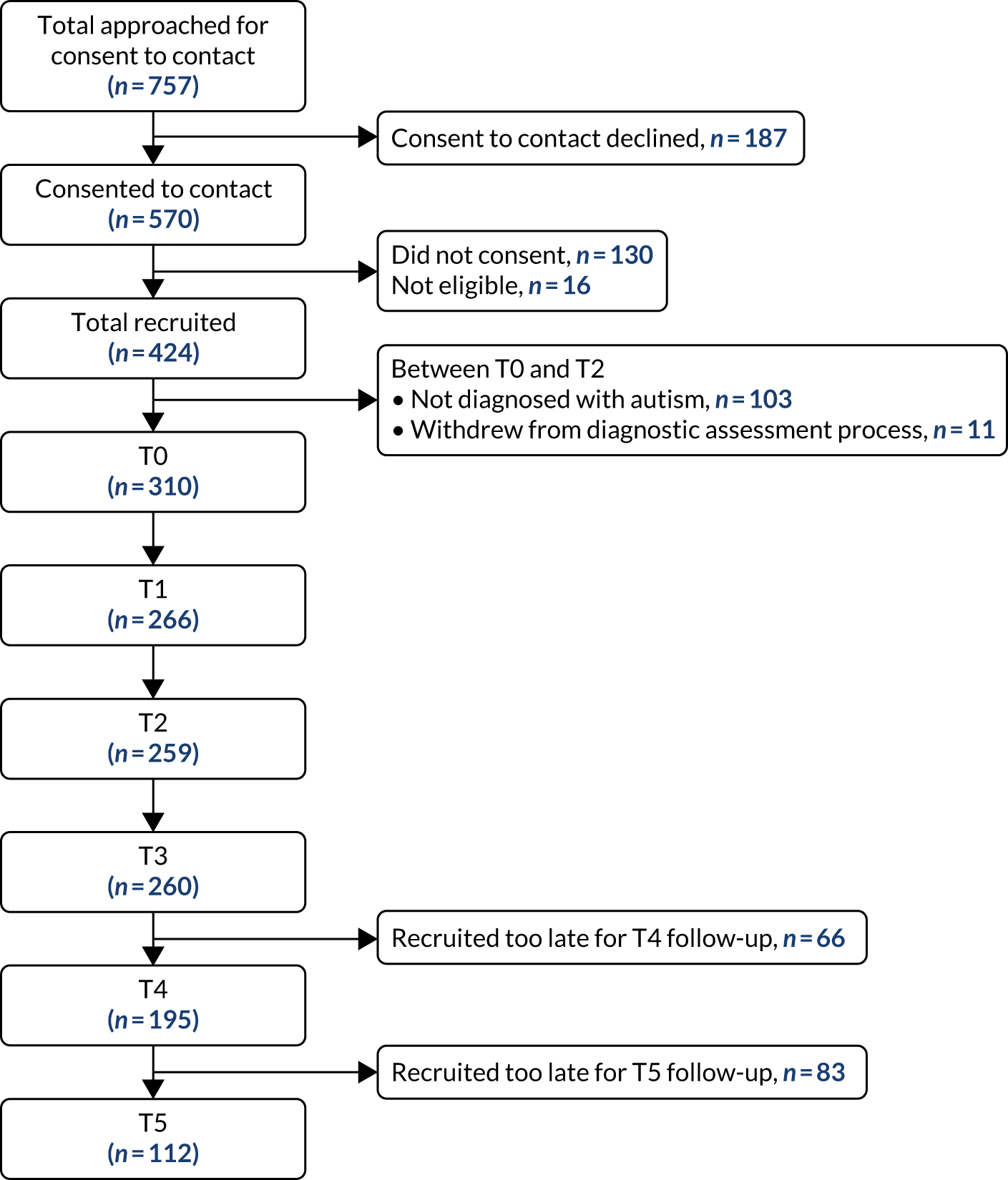
Analytical plan
The statistical software Stata® 14.2 (StataCorp, College Station, TX, USA) was used.
Sample characteristics
Descriptive statistics were used to describe the sociodemographic characteristics of the SAT and DO cohorts. For continuous variables, the means, standard deviations, median, maximum and minimum values were calculated. Categorical data were calculated as counts and percentages.
Outcomes
Standardised outcome measure scores and outcome indicator data were summarised descriptively at each time point. Mean score, standard deviations, median and range were used to describe scores on standardised measures. Categorical data were explored using frequency counts and percentages.
Within the SAT cohort, the D&S and SO groups were treated separately for the descriptive analyses. The reason for this was twofold. First, the nature and range of support and interventions available to the two groups differed, particularly in terms of psychoeducation. Second, their demographic and outcome characteristics differed. Findings from the process evaluation that suggested that the two groups differed in their motivations and objectives for seeking support from a SAT (see Chapter 7) support this approach. t-tests compared mean scores on standardised outcome measures at T0 and T3, and the effect size was calculated. Categorical outcome indicators were analysed using contingency tables, McNemar’s chi-square and chi-square tests of symmetry, in which necessary response options were collapsed. Similar tests were used to conduct exploratory descriptive analyses of outcomes at the 18- (T4) and 24-month (T5) follow-ups.
Service and individual characteristics affecting Specialist Autism Team cohort outcomes
To investigate the association between individual and service characteristics on T3 outcomes, generalised linear regression modelling techniques were used. Characteristics were added one at a time to the model, with only those significant (p < 0.05) retained for the final model. All analyses were controlled for age, gender and outcome score at baseline, and were accounted for clustering by site.
Comparing the Diagnosis-Only cohort and the Diagnosis and Support group
For the comparison of T3 outcomes of the D&S group and DO cohort, the same approach to an initial analysis of baseline and outcomes data was used. We then conducted two sets of analysis of covariance (ANCOVA):
-
using only WHOQOL-BREF psychological domain scores at 12 months
-
including the following: baseline WHOQOL-BREF psychological domain, age and gender.
Analyses were repeated for GHQ-12 (Likert scoring). It was not possible to repeat for EQ-5D-5L because distribution of scores was asymmetric.
Results: sample characteristics
Appendix 9, Table 32, presents the characteristics of study participants.
Sociodemographic characteristics
Diagnosis and Support group
The mean age was 31.1 years (range 18–69 years). Over half (57.1%) of the participants were male and the majority (80.4%) were single. Most (60.0%) participants had received further or higher education. Over half (57.1%) were no longer living with parents. In terms of employment status, the largest group (39.9%) were those unable to work because of illness or disability. Less than one-third (30%) were in paid work, a further 8.6% were looking for work and 15.3% were students.
Support-Only group
The mean age was 26.5 years (range 17–55 years). The majority of the participants were male (62.5%) and were single (90.1%). Most (58.6%) participants had received further or higher education. Over two-thirds (70.5%) were still living with their parents. One-third (33.3%) were students, only 13.8% were in paid work and a similar proportion (12.6%) were looking for work. Just under one-third of participants were unable to work because of illness or disability.
Within the SAT cohort, there were statistically significant differences between the D&S group and the SO group in terms of relationship status [χ2 = 4.740, degrees of freedom (df) = 1; p = 0.0295], whether or not they were living in the parental home (χ2 = 17.346, df = 1; p = 0.000) and the proportion of the sample who were students (χ2 = 10.669, df = 1; p = 0.001). There was also a statistically significant difference in age (mean difference 4.64 years; p = 0.0026), with the D&S group, on average, being older.
Diagnosis-Only cohort
The mean age was 35.23 years (range 18–64 years). The majority (64.3%) of participants were male and over two-thirds (67.9%) were single. Most (71.4%) participants had received further or higher education. Most (62.5%) had left the family home and almost half (45.5%) were in paid employment.
Differences between the D&S group and the DO cohort were non-significant, except for employment status and age. Here, a higher proportion of the DO cohort were working (χ2 = 4.59, df = 1; p = 0.0322) (as opposed to job-seeking/unable to work) than in the D&S group. There was also a statistically significant difference in age (mean difference 4.11 years; p = 0.0033), with the DO cohort, on average, being older.
Outcomes at baseline
Scores on standardised outcome measures at baseline are presented in Appendix 10, Tables 33 and 34. The SO group WHOQOL-BREF psychological domain mean score was significantly higher than that of the D&S group and DO cohort. No other differences between groups in baseline outcome scores were observed.
Discharge status at T3
At T3 (12-month follow-up), the SAT cohort study participants were asked to report if they had been discharged (and date of discharge) or were still in the service (Figure 5). The quality of data was poor; 13.5% of responses were coded as missing data (highly unusual in this study and perhaps indicating uncertainty) and a further 20.1% were coded as ‘study participant uncertain’ (based on information provided under the ‘other’ response option). Just under 40% reported that they were still using the service and over one-quarter (26.9%) had been discharged. From the data we have, it would appear that the D&S group were more likely to have been discharged at T3.
FIGURE 5.
Status at T3 (12-month follow-up) in (a) the D&S group and (b) the SO group [n (%)].
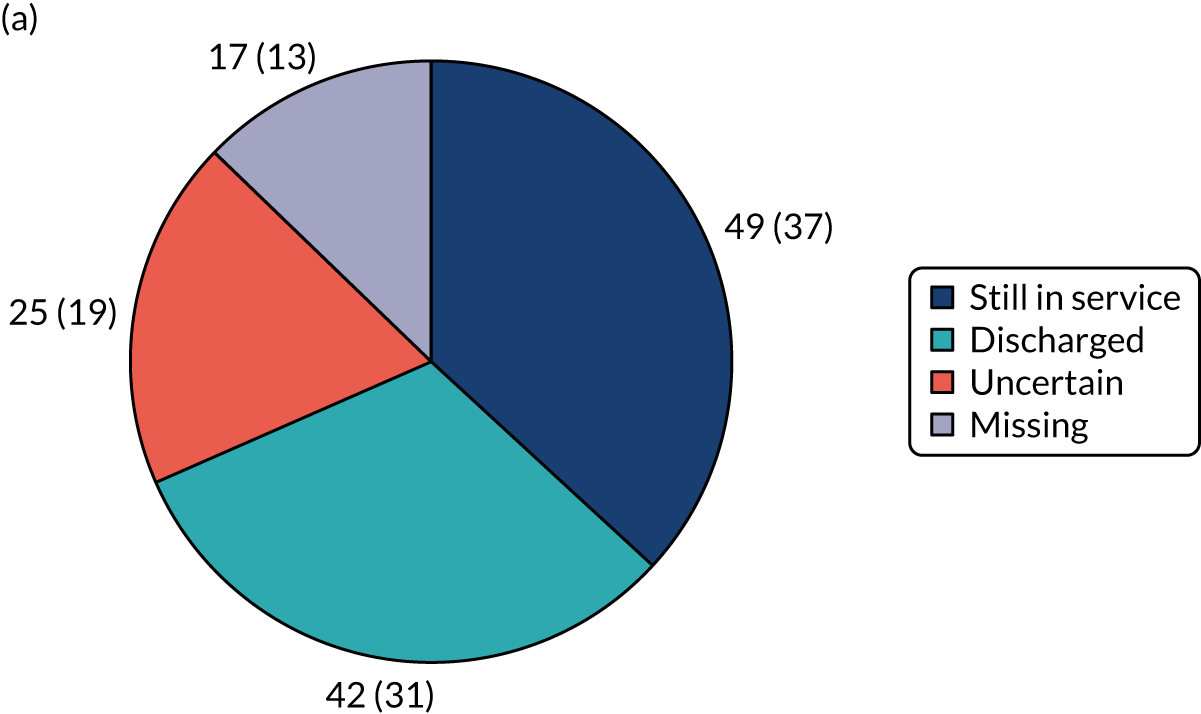
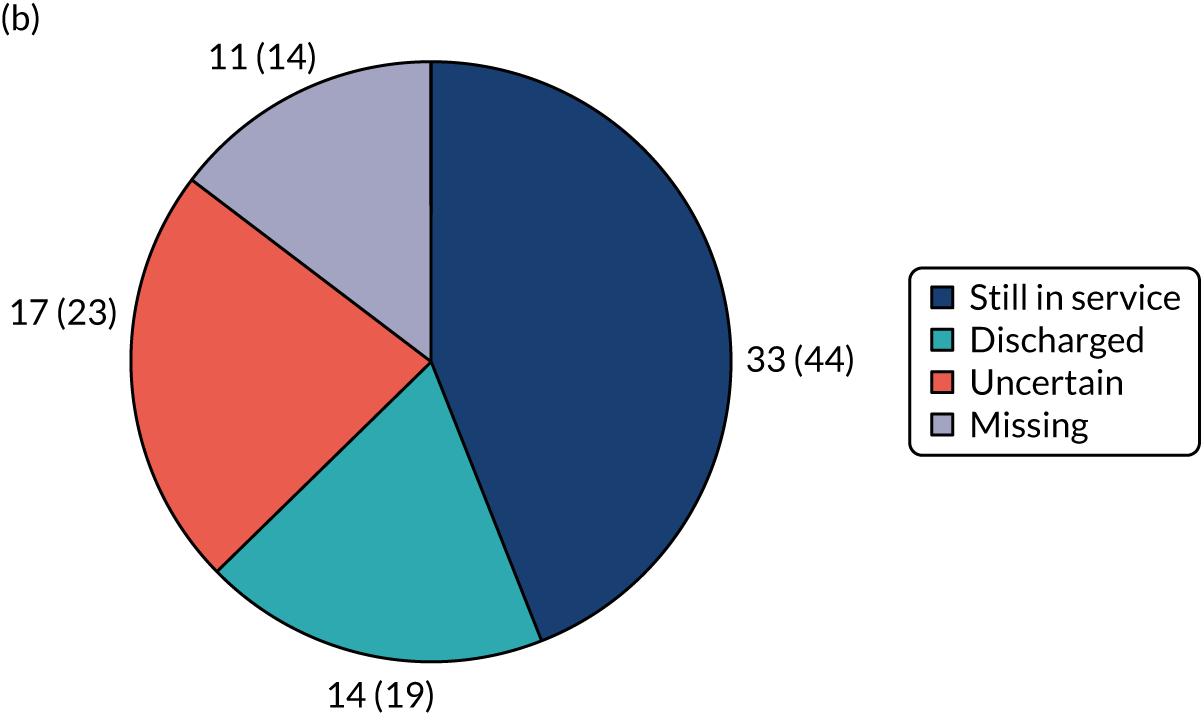
When the study was designed, and in consultation with service leads, we had expected the majority of study participants to be discharged by T3.
Concerns worked on: Specialist Autism Team cohort
At the 12-month follow-up (T3), we used a checklist to ask about the concerns that participants had worked on with the SAT (Figures 6 and 7). There was no difference between the D&S and the SO groups in the total number of concerns worked on. However, there were some differences in the type of concern. For example, a smaller proportion of the SO group reported working on understanding of autism, living with autism and family members’ understanding of autism. By contrast, compared with the D&S group, a greater proportion of the SO group had worked on employment, financial and social network/relationship issues. Across both, around one-third reported that they had worked on managing anxiety and/or other emotional difficulties.
FIGURE 6.
Concerns worked on with the SAT: D&S vs. SO groups.
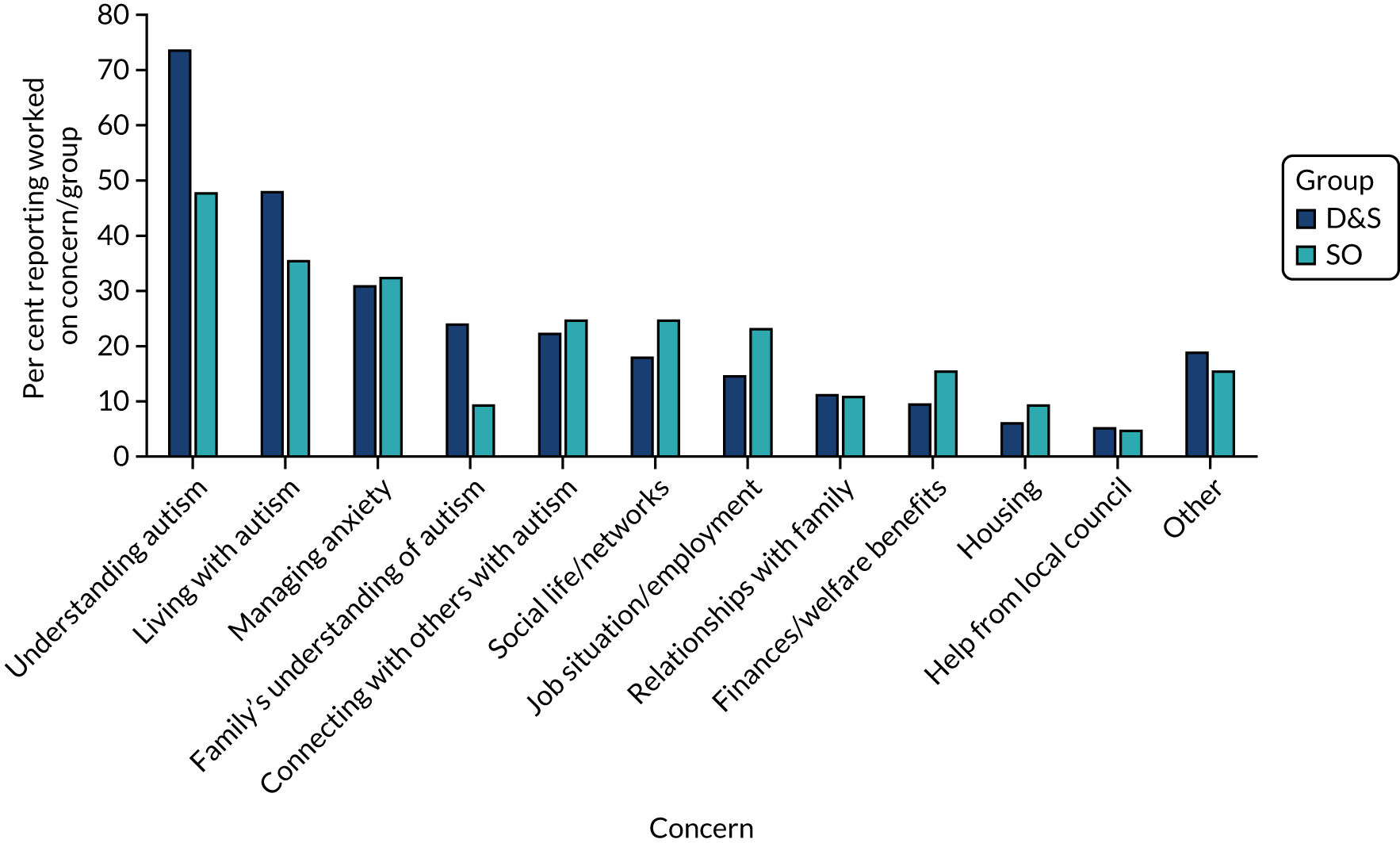
FIGURE 7.
Distribution of D&S vs. SO groups in terms of number of concerns worked on.
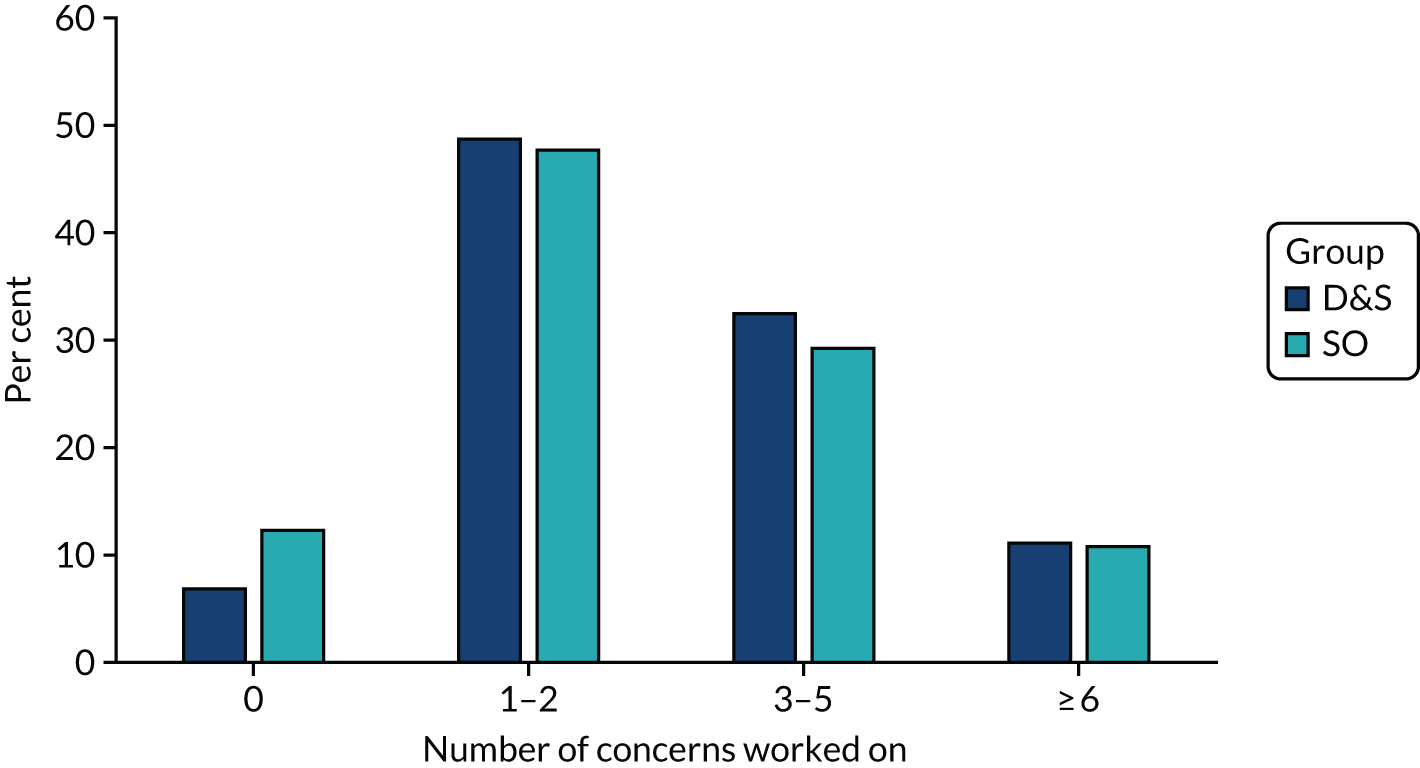
Results: Specialist Autism Team cohort outcomes
Tables presenting descriptive analyses of outcomes (standardised measures and categorical indicators) at each time point are presented in Appendix 11, Tables 35–40. This section focuses on presenting the results on changes in outcomes between T0 and T3. At the outset, we note that there were no significant differences in the baseline (T0) scores on any outcome measures between those retained at T3 and those not retained. There were also no significant differences in sociodemographic characteristics, except that men were more likely to drop out of the study than women. Overall, retention to the study was > 80%.
Mental health
Table 8 describes changes in mental health outcomes for the D&S and SO groups between T0 and T3. For both of the groups, differences in WHOQOL-BREF psychological domain and GHQ-12 mean scores between T3 and T0 were not significant. For the D&S group, the proportion of the sample scoring below the GHQ-12 clinical threshold (i.e. sample mean score at T0) increased between T0 and T3, with this increase being statistically significant (p < 0.01). This was not the case for the SO group.
| Outcome | Sample size | Time point, mean score | Difference in mean score (95% CI) | p-value | Effect sizea | |
|---|---|---|---|---|---|---|
| T0 | T3 | |||||
| D&S group | ||||||
| WHOQOL-BREF psychological domain | 132 | 38.43 | 40.09 | 1.65 (–4.11 to 0.80) | 0.19 | 0.12 |
| GHQ-12 | 133 | 18.24 | 17.14 | 1.11 (0.05 to 2.26) | 0.06 | 0.16 |
| GHQ-12 caseness: movement around cut-off pointb | ||||||
| T3 (n) | ||||||
| Above cut-off point | Below cut-off point | Total (n) | ||||
| T0 (n) | Above cut-off point | 32 | 28 | 60 | ||
| Below cut-off point | 10 | 63 | 73 | |||
| Total | 42 | 91 | 133 | |||
| McNemar’s χ2 = 8.53 (df = 1); exact p = 0.0051 | ||||||
| SO group | ||||||
| WHOQOL-BREF psychological domain | 75 | 43.31 | 42.60 | 0.71 (–2.43 to 3.85) | 0.65 | 0.05 |
| GHQ-12 | 74 | 17.41 | 17.16 | 0.25 (–1.62 to 2.13) | 0.79 | 0.03 |
| GHQ-12 caseness: movement around cut-off pointb | ||||||
| T3 (n) | ||||||
| Above cut-off point | Below cut-off point | Total (n) | ||||
| T0 (n) | Above cut-off point | 16 | 17 | 33 | ||
| Below cut-off point | 18 | 24 | 42 | |||
| Total | 34 | 41 | 75 | |||
| McNemar’s χ2 = 0.8658 (df = 1); exact p = 1.0 | ||||||
Quality of life
For the D&S group, no statistically significant changes in scores from T0 to T3 were observed in measures of health-related quality of life (EQ-5D-5L) and the other WHOQOL-BREF domains (social, physical and environmental) (Table 9). This was also the case for the SO group, except for WHOQOL-BREF social domain scores, for which a statistically significant deterioration was observed (p < 0.05), representing a small effect.
| Outcome | Sample size | Time point, mean score | Difference in mean score (95% CI) | p-value | Effect sizea | |
|---|---|---|---|---|---|---|
| T0 | T3 | |||||
| D&S group | ||||||
| Quality-of-life domains | ||||||
| Health-related quality of life (EQ-5D-5L) | 130 | 0.70 | 0.68 | 0.03 (–0.01 to 0.06) | 0.13 | 0.13 |
| WHOQOL-BREF social | 133 | 44.64 | 45.39 | 0.75 (–4.80 to 3.29) | 0.71 | 0.03 |
| WHOQOL-BREF physical health | 131 | 52.52 | 52.91 | 0.40 (–3.00 to 2.21) | 0.76 | 0.03 |
| WHOQOL-BREF environment | 133 | 56.98 | 55.43 | 1.55 (–0.89 to 3.99) | 0.21 | 0.11 |
| Perception of social networks | ||||||
| ISEL-SF belonging subscale | 132 | 6.84 | 6.79 | 0.05 (–0.42 to 0.53) | 0.83 | 0.02 |
| SO group | ||||||
| Quality-of-life domains | ||||||
| Health-related quality of life (EQ-5D-5L) | 74 | 0.73 | 0.72 | 0.01 (–0.04 to 0.06) | 0.74 | 0.04 |
| WHOQOL-BREF social | 75 | 47.22 | 41.67 | 5.56 (0.63 to 10.49) | 0.03 | 0.23 |
| WHOQOL-BREF physical health | 74 | 55.28 | 54.98 | 0.30 (–3.08 to 3.68) | 0.86 | 0.20 |
| WHOQOL-BREF environment | 75 | 57.09 | 55.54 | 1.55 (–1.77 to 4.87) | 0.36 | 0.11 |
| Perception of social networks | ||||||
| ISEL-SF belonging subscale | 75 | 6.41 | 6.31 | 0.12 (–0.53 to 0.75) | 0.74 | 0.04 |
Perception of social networks
In terms of perceptions of social networks (measured using the ‘belonging’ subscale of the ISEL-SF), changes in score between T0 and T3 were not significant for either the D&S group or the SO group (see Table 9).
Daily living: occupations and activities
Five categorical indicators of daily living were used in the study:
-
perceived ability to manage the usual activities of daily living, captured using the relevant item of ED-5D-5L
-
perceived sufficiency of information needed for daily living, assessed using the relevant item of WHOQOL-BREF
-
change in employment status of those in paid work, job-seeking or unable to work because of illness or disability at T0
-
satisfaction with capacity for work, assessed using the relevant item of WHOQOL-BREF
-
satisfaction with how they spent free time, captured using an item designed for this study.
Managing usual activities of daily living
In the D&S group at T0, 57 study participants reported that they were unable to manage, or had severe or moderate problems managing, the usual activities of daily living (Table 10). At T3, 26 (45.6%) of these individuals reported no or slight problems in this domain of their life; this change was statistically significant (p < 0.05). In the SO group at T0, 24 out of 75 study participants reported not being able, or having moderate to severe problems, to manage the usual activities of daily living. At T3, 12 of these individuals reported no or slight problems. This change was not statistically significant.
| Outcome | Number of participants | ||||
|---|---|---|---|---|---|
| Managing usual activities of daily living (EQ-5D-5L usual activities domain)a | |||||
| D&S group | |||||
| T3 | |||||
| Unable/severe problems | Moderate problems | No/slight problems | Total | ||
| T0 | Unable/severe problems | 6 | 3 | 5 | 14 |
| Moderate problems | 8 | 14 | 21 | 43 | |
| No/slight problems | 2 | 9 | 64 | 75 | |
| Total | 16 | 26 | 90 | 132 | |
| Symmetry test: χ2 = 8.36 (df = 3); p = 0.0392 | |||||
| SO group | |||||
| T3 | |||||
| Unable/severe problems | Moderate problems | No/slight problems | Total | ||
| T0 | Unable/severe problems | 4 | 2 | 4 | 10 |
| Moderate problems | 3 | 3 | 8 | 14 | |
| No/slight problems | 3 | 11 | 37 | 51 | |
| Total | 10 | 16 | 49 | 75 | |
| Symmetry test: χ2 = 0.82 (df = 3); p = 0.846 | |||||
| Availability of information needed for daily living (WHOQOL-BREF q13)a | |||||
| D&S group | |||||
| T3 | |||||
| Not at all/a little/moderately | Mostly/completely | Total | |||
| T0 | Not at all/a little/moderately | 44 | 23 | 67 | |
| Mostly/completely | 19 | 47 | 66 | ||
| Total | 63 | 70 | 133 | ||
| Mcnemar’s χ2 = 0.38 (df = 1); p = 0.537 | |||||
| SO group | |||||
| T3 | |||||
| Not at all/a little/moderately | Mostly/completely | Total | |||
| T0 | Not at all/a little/moderately | 26 | 8 | 34 | |
| Mostly/completely | 14 | 27 | 41 | ||
| Total | 40 | 35 | 75 | ||
| Mcnemar’s χ2 = 1.64 (df = 1); p = 0.2000 | |||||
Availability of information needed for daily living
The change in the proportion of the sample reporting having sufficient information for daily living between T0 and T3 was not significant for either the D&S or the SO group (see Table 10).
Employment status
Among study participants at T0 in paid work, job-seeking or unable to work because of illness or disability, the proportion of whom reporting a change in employment status (i.e. not working to working), or remaining in work, at T3 was non-significant for the D&S and the SO group (Table 11).
| Outcome | Number of participants | ||||
|---|---|---|---|---|---|
| Employment statusa | |||||
| D&S group | |||||
| T3 | |||||
| Paid work | Unable to work owing to illness/disability or job-seeking | Total | |||
| T0 | Paid work | 28 | 7 | 35 | |
| Unable to work owing to illness/disability or job-seeking | 9 | 44 | 53 | ||
| Total | 37 | 51 | 88 | ||
| Mcnemar’s χ2 = 0.25 (df = 1); p = 0.617 | |||||
| SO group | |||||
| T3 | |||||
| Paid work | Unable to work owing to illness/disability or job-seeking | Total | |||
| T0 | Paid work | 8 | 0 | 8 | |
| Unable to work owing to illness/disability or job-seeking | 1 | 26 | 27 | ||
| Total | 9 | 26 | 35 | ||
| Satisfaction with capacity for work (WHOQOL-BREF Q13)b | |||||
| D&S group | |||||
| T3 | |||||
| Very dissatisfied/ dissatisfied | Neither | Very satisfied/satisfied | Total | ||
| T0 | Very dissatisfied/dissatisfied | 44 | 19 | 9 | 72 |
| Neither | 8 | 11 | 8 | 27 | |
| Very satisfied/satisfied | 58 | 8 | 17 | 31 | |
| Total | 44 | 38 | 34 | 130 | |
| Symmetry test: χ2 = 5.08 (df = 3); p = 0.1659 | |||||
| SO group | |||||
| T3 | |||||
| Very dissatisfied/ dissatisfied | Neither | Very satisfied/satisfied | Total | ||
| T0 | Very dissatisfied/dissatisfied | 25 | 11 | 1 | 37 |
| Neither | 5 | 3 | 4 | 12 | |
| Very satisfied/satisfied | 3 | 8 | 14 | 25 | |
| Total | 33 | 22 | 19 | 74 | |
| Symmetry test: χ2 = 4.58 (df = 3); p = 0.205 | |||||
Satisfaction with capacity for work
The proportion of the sample reporting changes in their satisfaction with their capacity for work at T3 compared with T0 was non-significant for both the D&S and the SO groups (see Table 11).
Satisfaction with how they spent their free time
The proportion of the sample reporting changes in their satisfaction with how they spend their free time at T3 compared with T0 was non-significant for both the D&S and the DO groups (Table 12).
| Outcome | Number of participants | |||
|---|---|---|---|---|
| I am satisfied with how I spend my free timea | ||||
| D&S group | ||||
| T3 | ||||
| Definitely/probably true | Probably/definitely false | Total | ||
| T0 | Definitely/probably true | 42 | 21 | 63 |
| Probably/definitely false | 21 | 48 | 69 | |
| Total | 63 | 69 | 129 | |
| Mcnemar’s χ2 = 0.00 (df = 1); p = 1.000 | ||||
| SO group | ||||
| T3 | ||||
| Definitely/probably true | Probably/definitely false | Total | ||
| T0 | Definitely/probably true | 29 | 11 | 40 |
| Probably/definitely false | 13 | 22 | 35 | |
| Total | 42 | 33 | 75 | |
| Mcnemar’s χ2 = 0.17 (df = 1); p = 0.683 | ||||
Access to autism-specific networks and support
Membership
No significant change in the membership of local/regional/national autism-specific voluntary sector organisations and/or online forums/communities was observed in the D&S group or the SO group. In both groups, at T3, the great majority were not members of any such group or organisation [D&S: 109/132 (82.6%); SO: 62/74 (83.8%)] (Table 13).
| Outcome | Number of participants | ||||
|---|---|---|---|---|---|
| Membership of autism-specific voluntary organisations/online community | |||||
| D&S group | |||||
| T3 | |||||
| Member of organisation and/or community | No memberships | Total | |||
| T0 | Member of organisation and/or community | 2 | 6 | 8 | |
| No memberships | 21 | 103 | 124 | ||
| Total | 23 | 109 | 132 | ||
| Mcnemar’s χ2 = 2.00 (df = 1); p = 0.1573 | |||||
| SO group | |||||
| T3 | |||||
| Member of organisation and/or community | No memberships | Total | |||
| T0 | Member of organisation and/community | 5 | 7 | 13 | |
| No memberships | 8 | 54 | 61 | ||
| Total | 12 | 62 | 74 | ||
| Mcnemar’s χ2 = 0.07 (df = 1); p = 0.7963 | |||||
| Any contact with autism-specific voluntary organisations/communities? | |||||
| D&S group | |||||
| T3 | |||||
| One or more contacts | No contact | Total | |||
| T0 | One or more contacts | 11 | 9 | 20 | |
| No contact | 26 | 87 | 113 | ||
| Total | 37 | 98 | 133 | ||
| Mcnemar’s χ2 = 8.53 (df = 1); p = 0.0051 | |||||
| SO group | |||||
| T3 | |||||
| One or more contacts | No contact | Total | |||
| T0 | One or more contacts | 8 | 10 | 18 | |
| No contact | 7 | 49 | 56 | ||
| Total | 15 | 59 | 74 | ||
| Mcnemar’s χ2 = 0.4669 (df = 1); p = 0.6291 | |||||
Contacts
In terms of contacts with any autism-specific third-sector organisations, at T0, 113 out of 133 (84.9%) participants in the D&S group had had no contact with any such organisation in the previous 4 weeks (see Table 13). By T3, 26 (23.0%) of the T0 ‘no-contact’ group had had some sort of contact with an autism-specific organisation in the previous 4 weeks. This change was statistically significant (p < 0.01). This overall positive change in contacts with autism-specific third-sector organisations was not observed in the SO group. However, at T0, a greater proportion of individuals had been in contact with such an organisation than those in the D&S group [D&S group: 20/133 (15.1%); SO: 18/74 (24.4%)].
Longer-term outcomes
For individuals recruited early to the study, the opportunity was taken to collect longer-term follow-up data at 18 (T4) and 25 (T5) months (D&S group: T4, n = 94/133, T5, n = 62/133; SO group: T4, n = 56/88, T5, n = 42/88). Tables reporting our descriptive analyses are presented in Appendix 12. We offer a brief overview of findings here.
Mental health
For the D&S group, at T4, no statistically significant changes in mental health outcomes were observed (see Appendix 12, Tables 41 and 42). At T5, and not observed at T3, statistically significant improvements in scores on the WHOQOL-BREF psychological domain (p < 0.01, small effect size) and GHQ-12 (p < 0.05, small effect size) were observed (see Appendix 12, Tables 41 and 42). However, unlike at T3, movement of the sample from above to below the clinical threshold (using the sample mean as the threshold) was non-significant.
For the SO group, a statistically significant deterioration in the WHOQOL-BREF psychological domain score between T0 and T4 was observed (p < 0.001, medium effect size) (see Appendix 12, Tables 43 and 44). However, by T5, this deterioration, although still observed, was non-significant (see Appendix 12, Tables 43 and 44). In terms of other mental health outcomes, no statistically significant changes were observed between T0 and T4 or T0 and T5. This pattern of results replicates findings for T0 to T3.
Quality of life
For the D&S group, no statistically significant changes in scores of quality-of-life measures (EQ-5D-5L, WHOQOL-BREF social, physical health and environment domains) were observed between T0 and T4 and T0 and T5 (see Appendix 12, Tables 45 and 46). These findings align with those observed for T0 to T3.
For the SO group, there were no statistically significant differences in scores of these measures between T0 and T4 or T0 and T5 (see Appendix 12, Tables 47 and 48). This aligns with findings for T0 to T3; however, for that time period a significant deterioration in WHOQOL-BREF social domain score was observed.
Perception of social networks
For the D&S group, no statistically significant changes were observed in study participants’ perceptions of the quality of their social networks between T0 and T4 or T0 and T5 (see Appendix 12, Tables 45 and 46) (ISEL-SF belonging subscale). For the SO group, the findings were the same (see Appendix 12, Tables 47 and 48). All of these findings align with those observed for T0 to T3.
Daily living: occupations and activities
For the D&S group, just under half (48.8%) of those reporting that they were unable to manage or had severe/moderate problems in managing usual daily activities at T0 reported no or slight problems at T4 (see Appendix 12, Table 49). This aligns with findings for T0 and T3 (statistically significant). This proportion increases when comparing T0 with T5 (59.3%), with this increase being significant (p < 0.05) (see Appendix 12, Table 50). No other statistically significant changes in our indicators of daily living (i.e. perceived availability of information needed for daily living, employment status, satisfaction with capacity for work and how spend free time) between T0 and T4 or T0 and T5 were observed. This aligns with findings from T0 and T3.
For the SO group, half (10/20) of those participants reporting being unable to manage, or having severe or moderate problems managing, activities of daily living at T0 reported no or slight problems at T4 (see Appendix 12, Tables 50 and 51). A similar proportion (9/18) was also observed at the T5 time point (see Appendix 12, Table 52). These proportions are similar to those observed at T3 and for the T0 to T3 analysis. The change in the proportion of the T4 and T5 participants reporting a positive change in availability of information to manage daily life and satisfaction with their leisure time compared with T0 was non-significant. The overall patterns of results appear to be similar to the findings for T0 and T3.
Membership of autism-specific organisations/communities
In the D&S group, at T4, the proportion of individuals who had become members of an autism-specific organisation since T0 (13.7%) was similar to that observed at T3 (see Appendix 12, Table 53). By T5, however, the proportion of T0 non-members who reported having become a member of an autism-specific organisation had increased to 20.6% (see Appendix 12, Table 53). In terms of contact with such organisations in the previous 4 weeks, at T4, 15.3% of those at T0 reporting ‘no contact’ had had at least one contact with such an organisation in the previous 4 weeks. At T5, this proportion rose to 24.5%: a figure similar to that observed at T3 (which was statistically significant). At both time points, cell counts preclude testing for clinical significance.
For the SO group, as at T3, very few individuals who were not members of autism-specific organisations at T0 had become members at either T4 or T5 (see Appendix 12, Table 54). Finally, in terms of contacts with autism-specific organisations in the previous 4 weeks, as at T3, only a small minority had had any contact with such groups in the 4 weeks prior to T4 and T5.
Results: service and individual characteristics associated with Specialist Autism Team cohort outcomes
A key objective of the quantitative evaluation was to investigate whether a particular service or individual characteristics are associated with outcomes. For these analyses, we focused on mental health outcomes only.
The selection of characteristics to explore in the quantitative evaluation was strongly informed by findings from the mapping study (see Chapter 2) and our qualitative research with SAT practitioners (see Chapters 4 and 5) and service users (see Chapters 7 and 9). Individual characteristics are set out in Table 14 and they include sociodemographic characteristics; diagnostic status at referral; health and functioning at referral; informal resources and support at the 12-month follow-up (T3); input from the SAT on self-management; and status in the service at T3. Service characteristics (Table 15) focused on high-level organisational, structural and delivery features.
| Characteristic | Variable |
|---|---|
| Sociodemographic | |
| Age | Age in years |
| Gendera | Male or female |
| Diagnostic status at referral | |
| Reason for referral | D&S vs. SO |
| Health and functioning at T0 | |
| Mental health at referral (T0) | T0 GHQ-12 score (Likert scoring) |
| Functioning at referral (T0) | T0 EQ-5D-5L ‘usual activities’ domain scoreb |
| Informal resources and support at T3 | |
| Social networks at T3 | T3 ISEL-SF belonging subscale score |
| Perceived availability of information to manage day-to-day life at T3 | T3 WHOQOL-BREF Q13c (availability of information needed in day-to-day life) |
| Contact with autism-specific groups/communities at T3 | Contact vs. no contact with autism-specific organisation/online community in previous 4 weeks |
| Status in service | |
| Still under SAT at T3 | In service vs. discharged |
| Service characteristic | Variable value (or label) | Allocation of research sites to characteristic |
|---|---|---|
| Organisational/structural characteristics | ||
| LA involvement (indicator of social care expertise and easier access to LA support) | CCG | A, B, C, D, E, F |
| Joint CCG/LA | Ha, Hb, IA, J | |
| Single vs. multiservice team (D&S group only) | Single service | A, B, CA, E, F, IA, J |
| Multiservice | D, Ha | |
| Diagnostic assessment process (D&S group only) | ||
| Autism only vs. ND service | Autism only | A, B, F, J |
| ND | CA, D, E, Ha, IA | |
| Dominant mode of delivering psychoeducation post diagnosis | Group | A, B, F, Ha, IA |
| One to one | CA, D, E, J | |
| Delivery | ||
| Skill mix (in addition to clinical psychology, number of professional disciplines represented on team) (indicator of degree to which SAT takes an holistic approach) | 2 or 3 disciplines | A, B, Ca, D, Ha, Hb |
| ≥ 4 disciplines | E, F, IA, J | |
| Routinely do one-to-one work regarding mental health problems | Yes | A, B, CA, D, F, IA, J |
| No | E, Ha, Hb | |
| Delivery of care plan | Managed | A, B, Ca, D, Ha, Hb, IA, J |
| Episodic | E, F | |
| Drop in provision and/or named contact while in service | Yes | A, Ca, D, Ha, Hb, J |
| No | B, E, F, IA | |
| Discharge practice (separate analysis: outcomes at T4 and T5) | ||
| Type of discharge | Closed | E, F, IA, J |
| Stepped | A, B | |
| Open | Ca, D, Hb | |
Generalised linear regression modelling techniques were used. Characteristics were added one at a time to the model, with only those significant (p < 0.05) retained for the final model. All analyses controlled for age, gender and outcome score at baseline, and accounted for clustering by site.
Modelling statistics [statistical significance, regression coefficients and 95% confidence intervals (CIs)] were used to allocate characteristics to one of four categories:
-
strong evidence found of an association between the characteristic and the outcome measure
-
some evidence found of an association between the characteristic and the outcome measure
-
weak evidence found of an association between the characteristic and the outcome measure
-
no evidence found of an association between the characteristic and the outcome measure.
Characteristics with no evidence of association with T3 mental health outcomes
Regression analysis explored, one at a time, the association between individual and service characteristics and mental health outcomes (WHOQOL-BREF psychological domain, GHQ-12). Individual characteristics for which no evidence was found of an association between the characteristic and the T3 mental health outcomes were:
-
diagnostic status at referral (i.e. D&S group vs. SO group)
-
functioning at referral (EQ-5D-5L usual activities domain)
-
contact with autism-specific groups/communities at T3.
The status in service (i.e. discharged vs. still in service) was significantly associated with T3 mental health outcomes. However, it was not taken forward to modelling owing to the large numbers of missing data (42/180, 23%).
Service characteristics for which we found no evidence of an association between the characteristic and the T3 mental health outcomes were:
-
LA involvement in commissioning/funding the service (taken to indicate social care expertise and easier access to LA services)
-
single versus multiteam service structure
-
autism versus neurodevelopmental service
-
mode of delivering psychoeducation post diagnosis
-
whether or not they routinely do one-to-one work for (non-complex) mental health problems.
Characteristics with evidence of association with T3 mental health outcomes
Tables 16 and 17 present outputs from the multiple regression modelling for T3 for the WHOQOL-BREF psychological domain and GHQ-12, respectively. Varying degrees of strength for evidence of an association (almost always in the same direction) were observed for all individual and service characteristics with one or both of the mental health outcomes.
| Coefficient | p-value | 95% CI | |
|---|---|---|---|
| T0 WHOQOL-BREF psychological domain score | 0.55 | 0.000 | 0.39 to 0.72 |
| Individual characteristics | |||
| Age (years) | 0.09 | 0.007 | 0.02 to 0.15 |
| Gender (reference: male) | 1.00 | ||
| Female | –2.37 | 0.077 | –5.01 to 0.26 |
| T0: GHQ-12 score | –0.49 | 0.023 | –0.92 to –0.07 |
| T3: ISEL-SF belonging subscale score | –1.34 | 0.002 | –2.18 to –0.50 |
| T3: availability of information (reference: not/little/moderately) | 1.00 | ||
| Mostly/completely | 5.52 | 0.032 | 0.47 to 10.56 |
| Service characteristics | |||
| Skill mix (reference: zero to two disciplines) | 1.00 | ||
| Four or more disciplines | 7.39 | 0.001 | 3.18 to 11.61 |
| Delivery of care plan (reference: episodic) | 1.00 | ||
| Managed | 4.59 | 0.082 | –0.58 to 9.75 |
| Drop in provision and/or named contact while in service (reference: yes) | 1.00 | ||
| No | 0.34 | 0.684 | –1.29 to 1.97 |
| Constant | 26.15 | 0.000 | 11.68 to 40.61 |
| Coefficient | p-value | 95% CI | |
|---|---|---|---|
| T0 GHQ-12 score | 0.37 | 0.000 | 0.25 to 0.49 |
| Individual characteristics | |||
| Age (years) | 0.03 | 0.531 | –0.07 to 0.13 |
| Gender (reference: male) | 1.00 | ||
| Female | 1.44 | 0.033 | 0.12 to 2.76 |
| T3: ISEL-SF belonging subscale score | 0.60 | 0.000 | 0.30 to 0.91 |
| T3: availability of information (reference: not/little/moderately) | 1.00 | ||
| Mostly/completely | –2.86 | 0.009 | –5.02 to –0.70 |
| Service characteristics | |||
| Skill mix (reference: zero to two disciplines) | 1.00 | ||
| Four or more disciplines | –2.14 | 0.000 | –3.33 to –0.96 |
| Delivery of care plan (reference: episodic) | 1.00 | ||
| Managed | –1.00 | 0.064 | –2.05 to 0.06 |
| Drop in provision and/or named contact while in service (reference: yes) | 1.00 | ||
| No | –1.58 | 0.005 | –2.70 to –0.47 |
| Constant | 8.51 | 0.000 | 4.03 to 12.99 |
Individual characteristics
-
Age: there was moderate evidence of an association between age and WHOQOL-BREF psychological domain score at T3, but no evidence of association was found between age and GHQ-12 scores.
-
Gender: there was moderate evidence of an association between gender (women faring worse) and GHQ-12 score at T3, and a weak association between gender (women faring worse) and WHOQOL-BREF psychological domain score at T3.
-
Mental health at entry to the service: there was moderate evidence of an association between T0 GHQ-12 scores and WHOQOL-BREF psychological domain scores at T3.
-
Informal social networks: there was strong evidence of an association between T3 ISEL-SF belonging subscale scores (perceived availability of social network) and WHOQOL-BREF psychological domain and GHQ-12 (Likert) scores at T3.
-
Availability of information (WHOQOL-BREF, q. 1346): there was strong evidence of an association between perceived availability of information to manage everyday life and WHOQOL-BREF psychological domain and GHQ-12 scores at T3, with greater sufficiency of information associated with better mental health outcomes.
Service characteristics
-
Skill mix: there was strong evidence of an association between skill mix and both mental health outcomes, with greater skill mix (i.e. four or more professional disciplines working in the service) associated with better outcomes.
-
Delivery of care plan: there was weak evidence of an association between WHOQOL-BREF psychological domain and GHQ-12 scores at T3, and delivery of the care plan, with managed (as opposed to episodic) care associated with better outcomes.
-
Drop-in provision and/or named contact: no evidence of an association was found between this characteristic and WHOQOL-BREF psychological domain outcome scores at T3. For GHQ-12 score at T3, there was moderate evidence that a lack of drop-in/named contact was associated with better T3 scores.
Results: comparison of the Diagnosis and Support group and the Diagnosis-Only cohort
The final component of our quantitative evaluation of SATs was to compare outcomes of individuals not previously diagnosed with autism in terms of their care pathway. That is, either they had accessed a SAT (D&S group of the SAT cohort) or they had accessed a regional/national diagnostic assessment service (DO cohort). We report findings from the qualitative interviews with service users relevant to this element of the study in Chapter 9.
The opportunity to incorporate a DO cohort into the study emerged part way through the study and was carried out with the full support of the Study Steering Committee and funder. At the time that this element of the study was conceived, there were very few existing studies from which to base power calculations. This affected the accuracy of our original power calculations and, as revealed by post hoc power calculations, resulted in an underestimation of sample size requirements. Thus, findings should be treated as preliminary.
Changes in mental health around the point of diagnosis
A descriptive analysis of mean GHQ-12 scores at T0, T2 (post-diagnosis time point) and T3 (12-month follow-up) was carried out, and results for the D&S group and DO cohort were compared (Figure 8).
FIGURE 8.
Mean GHQ-12 scores at baseline, post diagnosis and the 12-month follow-up in (a) DO cohort and (b) D&S group.
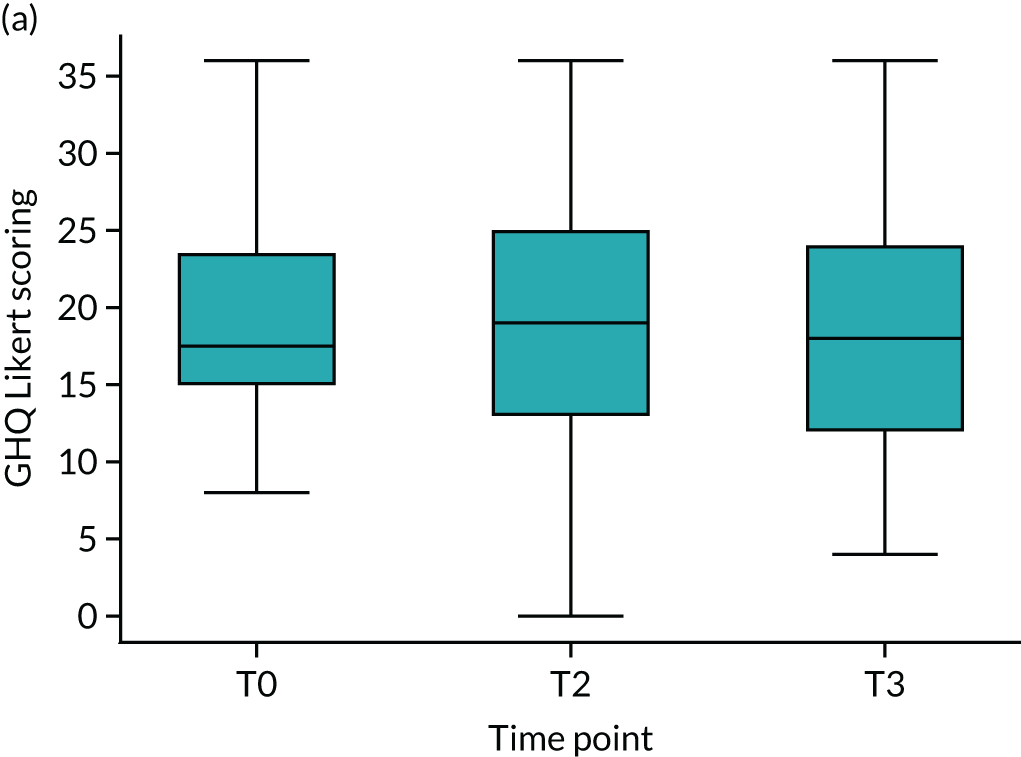
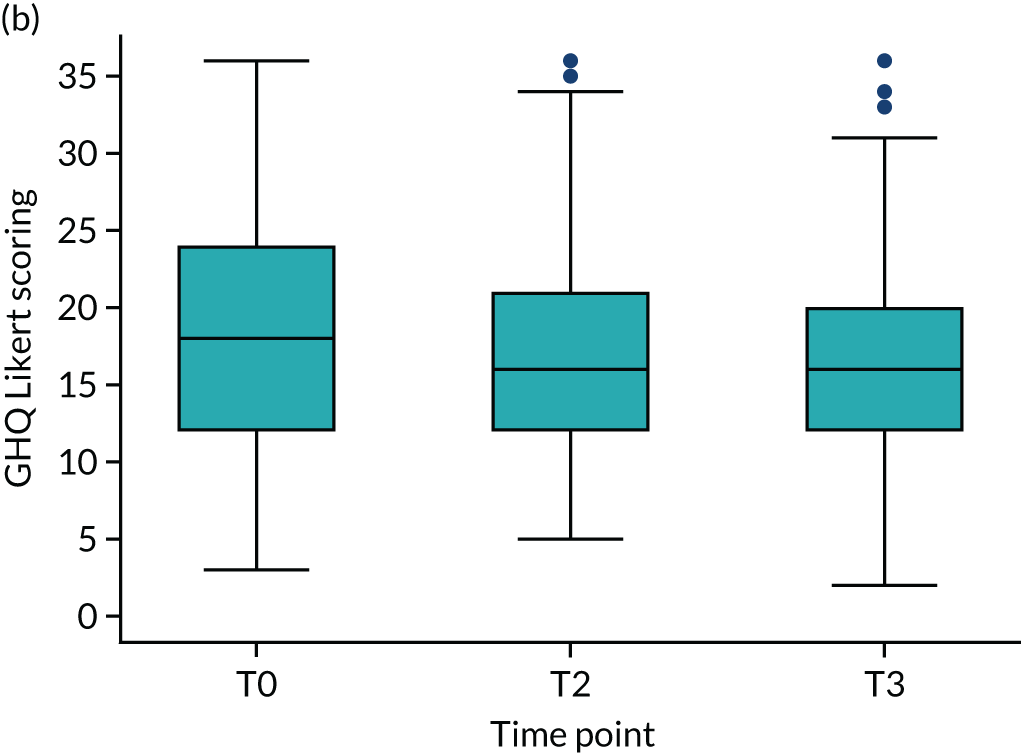
The overall trajectory of the mean GHQ-12 score for the D&S group was in a positive direction. This was not the case for the DO cohort, with evidence of a deterioration between T0 and T2.
Outcomes at the 12-month follow-up
There were no statistically significant changes in the DO cohort mental health outcomes at T3 compared with T0 (Table 18).
| Outcome | Sample size | Time point, mean score | Difference in mean score (95% CI) | p-value | Effect sizea | |
|---|---|---|---|---|---|---|
| T0 | T3 | |||||
| WHOQOL-BREF psychological domain | 52 | 34.47 | 38.54 | 4.071 (–9.25 to 1.11) | 0.12 | 0.22 |
| GHQ-12 | 52 | 19.60 | 18.40 | 1.192 (–1.39 to 3.78) | 0.36 | 0.13 |
| GHQ-12 caseness: movement around cut-off pointb | ||||||
| T3 (n) | ||||||
| Above cut-off point | Below cut-off point | Total | ||||
| T0 (n) | Above cut-off point | 12 | 9 | 21 | ||
| Below cut-off point | 10 | 21 | 31 | |||
| Total | 22 | 30 | 52 | |||
| McNemar’s χ2 = 0.05 (df = 1); p = 1.00 | ||||||
Similarly, no statistically significant changes in outcomes were observed in terms of quality of life (EQ-5D-5L, WHOQOL-BREF social, physical and environment domains) and perceptions of social networks (ISEL-SF belonging subscale) (see Appendix 13, Table 55). Likewise, no changes were observed on indicators of daily living or regarding access to autism-specific networks (see Appendix 13, Tables 56 and 57).
Comparing T3 mental health outcomes for the Diagnosis-Only cohort and Diagnosis and Support group
We then used ANCOVA to compare the T3 mental health outcomes of the DO cohort with those of the D&S group. This was repeated, restricting the D&S group to those individuals who used SATs that also provided a regional diagnostic service and recruited to the DO cohort. Outputs are presented in Appendix 14 (Table 58: WHOQOL-BREF psychological domain; Table 59: GHQ-12). No significant differences in mental health between the two groups were observed at T3.
Summary
This chapter has reported findings from the quantitative elements of our observational study. First, we presented a descriptive account of outcomes and changes in outcomes of users of SATs, separated into two groups according to the reason for their referral to the SAT (D&S vs. SO). Second, we reported our investigation into the association between certain service and individual characteristics and outcomes. Finally, we presented findings from an initial exploration of differences in outcomes between individuals diagnosed and then supported by a SAT (D&S group) and individuals who used a diagnostic assessment-only service (DO cohort).
A statistically significant, positive change in the proportion of study participants scoring below the GHQ-12 clinical threshold (sample mean) was observed in the D&S group, but not in the SO group. No other significant changes in mental health outcomes were observed. No statistically significant changes in perceived social support and other quality-of-life domains were observed in the D&S group. In the SO group, a deterioration in social quality of life was observed.
With respect to daytime occupation/usual activities, in the D&S group, a statistically significant proportion of study participants reported no longer having severe or moderate problems managing the usual activities of daily living at T3. This was not observed in the SO group. No statistically significant changes in other indicators of daytime occupation/activities (i.e. perceived availability of information required for daily living, employment, satisfaction with capacity for work and satisfaction with leisure time) were observed in either group.
In terms of access to autism-specific networks and support, for the D&S group, although the proportion with membership of an autism-specific organisation/community did not change, a statistically significant proportion who reported no contacts with such organisations at T0 reported at least one contact in the 4 weeks prior to T3 data collection. This was not observed in the SO group.
Our second set of analyses investigated the association between individual and service characteristics on mental health outcomes. We found no evidence of an association between T3 mental health outcomes and diagnostic status at referral (i.e. D&S vs. SO), functioning at referral or contact with autism-specific communities. We also found no evidence of an association between the T3 mental health outcomes and the following service characteristics: LA involvement, service structure (single vs. multiteam), autism versus Neurodevelopmental service, predominant mode of delivering psychoeducation (group vs. one to one) and whether or not the service routinely offers one-to-one work for (non-complex) mental health problems.
Multiple regression modelling work found moderate evidence of an association between at least one mental health outcome and age and gender. There was also strong evidence of an association (in a positive direction) between mental health outcomes and social support, and greater sufficiency of information to manage everyday life at T3. Furthermore, there was strong evidence that richer skill mix was associated with better mental health outcomes. In addition, weak evidence was found of an association between how the care plan was delivered (managed vs. episodic) and mental health outcomes (favouring managed care). For the final service characteristic taken forward to the modelling work, the evidence regarding the association between access to drop-in provision and/or a named contact was equivocal.
Finally, we reported findings from an initial exploration of outcomes of individuals who used a regional diagnosis assessment service (DO cohort), comparing them with individuals diagnosed by a SAT (D&S group). First, we looked at the trajectory of mental health outcomes. This exploratory analysis indicates a potential differential impact of receiving a diagnosis of autism between the DO cohort and the D&S group. Second, we compared DO cohort outcomes at baseline (T0) with outcomes at the 12-month follow-up time point (T3); no statistically significant changes were observed. Finally, we compared T3 mental health outcomes of the DO cohort with our D&S group. No significant differences were observed. We would note that these analyses were underpowered and, therefore, no conclusions can be drawn. However, the lack of improvement in outcomes of the DO cohort at the 12-month follow-up, and deteriorations in mental health outcomes in the immediate post-diagnosis time period, do indicate areas of potential concern that require further research. The following chapter reports findings from a second, qualitative component of this work in which we describe and compare the experiences of individuals from the D&S group and DO cohort.
Chapter 9 Experiences of an autism diagnosis with and without post-diagnosis support
Introduction
This chapter reports the experiences and impacts of receiving an autism diagnosis, comparing the accounts of those who received extended psychoeducation and access to other support (D&S group of SAT cohort) with those who received only a diagnostic assessment (DO cohort). This chapter, thus, presents our second set of evidence on this topic, with the previous chapter reporting findings from an initial comparative exploration of outcomes.
Methods
Given that we report our qualitative research with service users over two non-consecutive chapters, we have chosen to report the methods in an appendix (see Appendix 6). To summarise, 37 autistic adults and 10 family members were interviewed. The sample comprised 22 individuals from the SAT cohort’s D&S group (representing all research sites) and nine individuals from the DO cohort (representing the main research site that recruited to the DO cohort plus one of the other two). In terms of family members, three were relatives (all parents) of individuals in the DO cohort and eight were relatives of individuals in the SAT D&S group.
Findings are organised around four topics:
-
hopes and expectations on referral for diagnostic assessment
-
emotional responses to the diagnosis
-
experiences of follow-up session(s) and psychoeducation
-
several months on – the perceived impact of the diagnosis.
We note that there is, on occasion, a small overlap between the findings reported in this chapter and the findings reported in Chapter 7. This has been necessary to provide sufficient context to some of the findings.
Hopes and expectations on referral
Many interviewees had suspected that they were autistic for some time, often years, prior to the diagnostic assessment. A minority, however, did not think that this was the case and agreed to the assessment only to satisfy the referring practitioner. Some interviewees reported that, at the time of referral, they were having one or more, sometimes quite substantial, difficulties in their lives for which they were seeking help and support (e.g. mental health problems, independent living, social isolation and adjustments at work or college). A few also recalled hoping that a diagnosis would help others (e.g. family and work colleagues) to understand them better.
Emotional responses to the diagnosis
Although interviewees had typically been seeking a diagnosis, reactions were multifaceted and often shifted over time. Most interviewees said that, at least initially, they had reacted positively to the diagnosis, referring primarily to feelings of ‘relief’. This relief centred on having an explanation for and validation of the struggles that they had experienced in their life. For some, this put an end to years of not being believed or, in their experience, being perceived as ‘mad’, ‘crazy’ or ‘a pain’:
Me and my mum sat and cried with relief, because my mum thought she was going barmy, and it was just more of a relief that somebody like professional actually had acknowledged what we’d said and finally agreed with us . . . So it was just a lot of relief that somebody had actually listened and believed what I was saying.
SU28
Some further articulated a sense of hope that they would (finally) get the help that they needed and be able to make changes to their life:
I’m not mad, this is the way I’m made. Yay, I can get help.
SU30
However, it was common for initial feelings of relief to be combined with or superseded by feelings of shock, anxiety and confusion. The following extract is the same interviewee as the penultimate quotation above:
I think I found it quite difficult initially. I’d got the clarity and it was nice to have it recognised, but then at the same time it was like, well got this label now, right, what do I do with it? And then trying to come to terms with it and accepting it was difficult.
SU28
In addition, another interviewee said:
In the first couple of days it was quite a relief to understand that these problems that I was having, or I am having, should I say . . . it made me think, ‘Right, I can deal with that now’. So that was helpful. But then sort of from that, the next few weeks, months, it just kind of ate away at me every single day. I just kind of thought, ‘Oh my god, I’ve got this condition, I don’t know what it means, I don’t know how to deal with it, I don’t know how to live a normal life now.’.
SU32
For a small minority of participants, the immediate reaction was entirely negative. They attributed this to not wanting to have ‘something wrong’ with them, particularly something that was not ‘curable’:
After she’d given me the diagnosis, I was like ‘Right, so what can I do about it?’. And she said ‘You don’t sound very happy.’ [And I said] ‘No, well obviously I’m not very happy because someone’s just told me I can’t do certain things. Just by saying to me you’re autistic, that’s telling me you can’t do anything about it.’ I’m a doer, I spend my life finding ways to deal with things, even if I can’t solve it I need to be able to do something. So I felt quite at a loss.
SU33
Whether or not interviewees described their initial reaction as positive or negative, feelings of frustration and loss featured in many interviewees’ accounts of their reaction to diagnosis. Interviewees of all ages had reflected on how life might have been different if they had been diagnosed earlier in life:
Initially the Asperger’s diagnosis upset me more than other mental health diagnoses I’d had in the past and I couldn’t explain why. I was diagnosed at age 58 and I’d loved to have known much earlier than that because then I could have tried to moderate or control it and my life could have been different, relationships might have worked.
SU1
I was grieving the fact that if I had been diagnosed when I was 9 I might not have been suicidal . . . and I might never have been homeless and I might have received the support that I clearly so desperately needed.
SU35
As the following quotation demonstrates, for at least some people, grief and loss remained an experience a year after receiving the diagnosis:
I’m grieving 20 lost years of my life. And I think perhaps there’s something there about adult diagnosis that is not necessarily taken seriously enough. Most of us have gone through hell and back. From speaking to others, a lot of us have gone through awful things as much because we were misdiagnosed or undiagnosed, as because of our autism itself.
SU35
Interviewees also described finding it difficult to understand how they could have struggled with life for so many years, coming into contact with a wide range and/or number of practitioners over that period, without their autism being recognised. Some described feelings of frustration and anger towards practitioners and/or family members. Again, for some, this sense of frustration was still being experienced when we interviewed them several months after receiving the diagnosis:
I was also a bit frustrating thinking, ‘I’m in my late 40s and nobody has noticed this. How can it have gone on for so long with all the problems at school and with other things and nobody noticed?’. I feel a bit annoyed with my parents they didn’t pick up on it. At school they knew I was having massive problems and stuff. That side of it frustrates me, because they’ve been living with it as well, and have difficulties with this and that.
SU15
Family members’ accounts
Family members’ accounts of their partner’s or son’s/daughter’s reaction to learning their diagnosis fell quite evenly into one of three types. Some believed it had been a relief to their family member. One parent recalled being surprised at the level of their son’s relief. This had made them realise that they had been unaware of how much the diagnosis meant to their child:
He was thrilled to know why he’d been feeling the way he had for so long, and we didn’t know he was suffering like that.
F3
Others described their relative’s reaction as neutral or ambivalent. Interestingly, these observations did not always tally with their partner’s or child’s account where, as well as providing a new understanding of themselves, feelings of shock, depression and anxiety were described.
A further group reported a very negative reaction, with one describing high levels of distress:
The diagnosis completely floored her. She was beside herself and because she suffers with other mental health issues she literally says, ‘Well that’s it, my life’s over, I may as well not even be here’.
F9
Another spoke of how, although she felt very positive about her son getting a diagnosis because it ‘opened doors all over the place’ (F4), her son’s response had been very different. She further explained that he still (approximately 12 months after diagnosis) got ‘depressed’ if he thought about it.
Experiences of follow-up session(s) and psychoeducation
For the DO cohort, the diagnostic assessment package purchased by the referring agencies included the offer of a single follow-up meeting. Some also offered a single post-diagnosis/psychoeducational group session.
By contrast, those using a SAT were offered at least one follow-up session, plus a psychoeducation intervention delivered via either a group session and/or a series of one-to-one sessions (see Chapter 3). The objective of psychoeducation is to increase the understanding of autism, self-understanding and self-management skills (see Chapters 2 and 4).
It was at this point, therefore, that the experiences of care and support diverged significantly for DO and SAT (D&S group) cohorts. Furthermore, although many DO cohort interviewees said that those providing the assessment had made it clear that there would be no longer-term support after the diagnostic assessment, there was some evidence that at least some may not have fully appreciated the limits to what the service could offer.
Diagnosis-Only cohort interviewees
Diagnosis-Only cohort interviewees consistently described the follow-up session as including a discussion of the written report of the diagnostic assessment; being provided with information leaflets about autism; being encouraged to seek further information from the internet; and being signposted to relevant services.
Two elements of this session were regarded as valuable and helpful: explanations as to which aspects of their difficulties were linked to autism (and which were not) and advice on living with autism (e.g. encouragement to develop daily routines and techniques for avoiding ‘meltdowns’).
However, shortcomings and concerns with regard to other aspects of the feedback session were described. First, some reported that information leaflets were age inappropriate (e.g. targeted at young people) or included negative suggestions about what autism meant for people. Second, some who had followed the advice to use the internet as a source of information described coming across information and statistics that were highly negative about the implications of being autistic. This rendered interviewees feeling worried for their future.
Finally, signposting to other services (e.g. social services and employment advisors) was typically regarded as ineffectual and even demoralising. All of those advised to contact other services had not done so, pointing out that the very fact that they were autistic made this difficult, even if they were ‘high-functioning’:
They [service] say your diagnosis opens doors. What doors? I find that quite difficult, because somebody, for me, has to open the door else I can’t get through it.
SU33
Thus, a clear and strong theme in the DO cohort interviewees’ accounts was the insufficiency of the input that they had received post diagnosis. Indeed, for some, there was a sense of an experience of abandonment in their accounts:
What I got was I got a diagnosis and then they gave me a few leaflets and said ‘There you go, good luck, you won’t be seeing us again, take care, bye.’. And that was really frustrating.
SU27
You shouldn’t be diagnosed and then left to your own devices. There was disappointingly little . . . I got something from them [the diagnosis]. I suppose I should be grateful for that. Some people get nothing at all.
SU10
Among those interviewees who described being shocked or confused by their diagnosis, the limited nature of follow-up support seemed to be particularly problematic, exacerbating negative emotional responses. For example, one participant, who had not expected to be diagnosed, said that discharge left her feeling like she had been in a ‘hit and run accident’ (SU30). Another participant said diagnosis because it ‘opened doors all over the place’, her son’s response had been very different that if it had not been for the support offered by people outside the service he would have felt like he had been ‘hung out to dry’ (SU27).
Family members’ accounts
Where the service user’s reaction was neutral or relieved, and/or it felt like there was little need for support, parents were satisfied with the input received. By contrast to this, a parent whose daughter became very upset by the diagnosis described contacting the service for advice, and was dismayed that nothing could be offered other than a follow-up session scheduled a number of weeks later, once reports had been completed.
Specialist Autism Team cohort interviewees
The SAT cohort interviewees who attended the psychoeducation intervention offered were, overall, very positive about this intervention:
It ended a lifetimes worth of feeling inadequate and feeling worthless.
SU36
It was valuable beyond words. It [the diagnosis] could have been life-changing in a way that left me stranded and in fact it has been life-changing in a way that’s given me enormous support and enormous hope, and a new capacity for thinking about myself and the world around me.
SU35
Aspects of the intervention that were identified as particularly helpful included:
-
content that gave insight into how autism may affect them, including the positive aspects of the condition
-
content on dealing with disclosure of diagnosis
-
learning coping techniques for dealing with difficulties commonly experienced by autistic adults (e.g. sensory overload, anxiety and dealing with social situations)
-
being directed to other reliable sources of information
-
listening to and/or sharing experiences (group-delivery only)
-
speakers with positive stories of living with autism (group-delivery only).
A dominant theme in these individuals’ accounts was the impact on how they viewed themselves. They spoke about feeling more accepting or forgiving of themselves. Some also described feeling less need to mask their autistic behaviours and/or the positive aspects of being autistic:
It helped me gain a deeper understanding of my own struggles and why I have them, but it also emphasised that having autism has given me a lot of strengths which is not something I had considered before.
SU36
However, a small proportion of individuals had not accessed any psychoeducation input. For the majority, this was because the SAT that they used offered only a group-delivered intervention that they were unable or unwilling to attend. In addition, one interviewee had waited 1 year to receive psychoeducational input. He described enduring months of sleep difficulties, regularly staying up into the early hours to reread the lengthy assessment report (over 150 pages) in an attempt to understand the diagnosis and its potential impact over the course of his life.
Family members’ accounts
Family members typically described the psychoeducation that their partner/child had received as highly beneficial. However, in one instance, there had been a very substantial delay in the follow-up sessions being offered, of which the parent was highly critical.
Perceived impacts of diagnosis
Positive impacts
All participants said that being diagnosed with autism had some positive impacts, although the nature and extent of this varied considerably.
The most commonly reported positive impact was an increased understanding of self, including why they found certain environments or situations difficult. Some believed that this understanding had reduced their anxiety and/or led to improvements in self-esteem. Others reported that it had enabled them to develop strategies to help them cope better with life (e.g. developing a better morning routine and making greater use of calendars and lists) and taking more care of themselves (e.g. allowing themselves more ‘downtime’, avoiding ‘meltdown’ triggers and ending difficult relationships). Having the diagnosis was also said to have helped family and friends to better understand their behaviour and the things that they found difficult or challenging. In some cases, this resulted in improved relationships.
A second way that being diagnosed with autism had achieved positive impacts in interviewees’ lives was that it had reduced interviewees’ sense of isolation. Comfort was drawn from simply knowing that there were other people who had similar life experiences to their own. Very occasionally, interviewees reported joining a local autism group or had friends disclose that they were also autistic.
A third mechanism by which being diagnosed had a positive impact was the way it enabled access to practical assistance, such as welfare benefits (Personal Independence Payments, Employment Support Allowance, Disabled Students Allowance), university/college/workplace assessments, adjustments and support.
Fourth, being diagnosed caused improvements in the quality of care and support received from other services, with practitioners using diagnostic assessment reports to help direct care or respond more appropriately to an individual’s needs. Finally, and occasionally, it had triggered other family members to undergo an autism diagnostic assessment.
Negative impacts
Set against these positive experiences, some interviewees reported long-standing or unresolved difficulties related to the diagnosis. The characteristics of this group are consistent. It comprised all interviewees from the DO cohort and those from the SAT cohort (3/20) who had received very limited or no psychoeducational input because either they had chosen not to or they had been unable to access the psychoeducational intervention offered.
Among those in our sample from the DO cohort, more than half said that they were still struggling to come to terms with and understand their diagnosis and the implications it may have for their lives:
. . . still quite overwhelming at times . . . the diagnosis in what it actually means. It’s very much a positive thing. However there isn’t a day that goes by that the A word doesn’t flit through my thoughts. It’s everywhere, life-changing.
SU29
I just don’t understand it and I don’t get the condition, I don’t, and as much as I try and read about it, it just doesn’t make any sense to me.
SU32
I want to understand what happens now. So it’s kind of like I’ve been given a diagnosis and a pile of paperwork and it’s like, well, what does this actually mean? Is this gonna hold me back at work, is it gonna hold me back in university, do I need to compensate for the way that I act socially? I don’t really know, I don’t really know what it means.
SU27
The vast majority of DO cohort interviewees said that they wanted further help to understand and come to terms with their diagnosis. Some described how they were still actively searching for information and sources of support. Even those who were initially relieved to be diagnosed and continued to view the diagnosis positively spoke of struggling or feeling overwhelmed by it at times. As a result, they were keen to point out the importance of high-quality psychoeducation and wider post-diagnostic support:
It’s a dedicated assessment centre so I believe it does well what it does. However . . . diagnosis is a traumatic experience, life-changing. Some will handle it better than others. I guess I’m one of the lucky ones who is quite positive about the diagnosis and life in general and have found ways to self-manage quite well . . . others are not.
SU29
A few of the DO cohort interviewees believed that receiving the diagnosis had caused a significant detrimental effect on their mental health:
I spent a year thinking I needed to die because of what someone had told me, because there’s nothing for you if you’re autistic, because you can’t change the way you are.
SU33
Even a year down the line I’m still seeing it as kind of a death sentence like, right, that’s it, my life’s over, I don’t know how to deal with this condition and everything, and you end up looking at everything differently, and it triggers loads of stuff off that you might not necessarily have thought of before, and I think that can then get you quite stressed and quite anxious.
SU32
In all of these cases, interviewees attributed the severity of their mental health difficulties to the fact that psychoeducation and other post-diagnostic support had not been available to them. Two interviewees explained that they had eventually sought help from a ‘therapist’ (unclear if this was an NHS referral or private practitioner) when their feelings of anxiety and depression and suicidal thoughts spiralled to an unmanageable level.
Family members’ accounts: impacts on the individual
Family members of individuals from both cohorts described positive impacts of their family member receiving a diagnosis. These included their relative seeming more ‘comfortable’ with themselves, and that it had enabled access to practical support related to participating in everyday life and supporting achievement of things they had hoped for (e.g. travelling overseas).
Family members of SAT cohort interviewees also typically regarded the diagnosis as opening access to additional care and support (including that directly provided by or accessed through the SAT). This had brought a range of, sometimes very significant, benefits. These included improvements in mental health, greater independence, an improved ability to manage everyday life and assistance with disclosure of their diagnosis to work colleagues:
Since he’s had the assessment he’s not talked of killing himself . . . he’s not actually said, since then, that, I might as well hang myself or I wish I could just cut my head off. He hasn’t said anything horrible like that, since this has been going on with these, you know, weekly meetings, etc. So they must be doing something, mustn’t they?
F4
By contrast, some family members of DO cohort interviewees saw no positives coming from the diagnosis, per se. Furthermore, when the diagnosis did not then lead to additional support (and potentially positive impacts for the individual), this could be a source of frustration:
It was time consuming to do and where did it get us? Although they’ve said you now have an official diagnosis, it’s like so what? Because it doesn’t help, it doesn’t do anything for her, she can’t access any services.
F7
One parent (DO cohort) firmly believed that the diagnosis had had a negative impact on her child’s life:
She’ll say . . . ‘I can’t help it. I’ve got Asperger’s. I’m on the autistic spectrum. There’s nothing I can do about it.’ It’s not changed her behaviour as such because she’s always had meltdowns, but it’s as if she thinks it is her lot now and how life has to be.
F9
Family members’ accounts: impacts on themselves
Parents who were closely involved in their child’s life also reported impacts on their own lives. For the couple of other family members we interviewed, impacts were minor or much less significant.
Across both cohorts, parents reported that the diagnosis, in itself, had been sufficient to have a positive impact on family relationships. This was for two reasons. First, having some understanding of the condition meant that situations that might trigger upset or arguments could be avoided. Second, it prevented family members misinterpreting behaviour as deliberately difficult.
However, where individuals had reacted negatively to the diagnosis, support from the service appeared to play a major role in determining whether or not and how this affected parents:
She constantly tells us ‘you’re rubbish, you’re a bad parent, you don’t do this, you don’t support me, you’re not getting me any help, you’re not getting me this, you’re not getting me that’. You do feel . . . well yeah, I am a rubbish person.
F9
This contrasts sharply with another family’s experience in which the individual received a one-to-one psychoeducation intervention. This parent reported a marked improvement in her son’s mental health, which, in turn, led to significant improvements in their own levels of stress.
Finally, few family members said that they wanted help for themselves. Instead, they explained that by helping the individual, services would also be helping the family. A minority, however, did express a desire for support. Suggestions included, for emotional support, having access to a parent/carer support group and information about other possible sources of support.
Summary
This chapter has reported the experiences and impacts of receiving an autism diagnosis. We compared the accounts of those who, post diagnosis, received extended psychoeducation and access to other support (sampled from the SAT cohort, D&S group) with those of individuals who had been diagnosed by a regional/national autism diagnosis service in which no psychoeducation was available (sampled from our DO cohort). A small number of family members were also interviewed.
Many, but not all, interviewees said that they had expected to be diagnosed with autism. Some described quite significant issues or difficulties that they hoped an autism diagnosis would (help to) resolve. The initial response to the diagnosis was typically one of relief and a sense of explanation. For a minority of our sample, however, the reaction was one of wanting to reject the diagnosis, and the loss of hope and control that they believed it brought. Among those whose initial reaction was positive, emotions typically became more mixed. Notions of frustration that they were not diagnosed earlier and grief over ‘lost years’ were common themes. For some, these feelings were still present at the time we interviewed them, several months after the diagnosis. Family members’ observations of their relative’s reaction are reasonably aligned, but also revealed evidence of emotional experiences hidden from them.
The DO and SAT cohort interviewees reported differences in the quality, duration and intensity of psychoeducational support accessed post diagnosis. This led to very different experiences and impacts. Almost all SAT cohort interviewees had accessed and spoke very highly of the psychoeducational support that they had received in terms of its content and the influence and impact it had on them. Those who attended group-delivered psychoeducation noted the value of hearing positive stories from peers and the opportunity to be exposed to shared experiences. A small number, however, had not accessed the psychoeducation intervention offered by their SAT. This was usually because it was a group-delivered intervention and they had felt unable to attend (some SATS did not offer one-to-one sessions as an alternative). A couple had experienced significant delays in the intervention being provided.
The DO cohort interviewees, although valuing the opportunity for the explanations and advice that a follow-up session offered, also described the insufficiency of input. For some, this, in itself, had been a very difficult experience, with notions of abandonment emerging from their accounts. In addition, there was a consensus among these interviewees that provision of written information was of limited value and advice to use the internet to locate further information carried risks. Finally, none had pursued services to which they had been signposted.
We carried out our interviews around 12 months after the start of the diagnostic assessment process, with diagnosis typically having taken place around 6–9 months previously. By this stage, all participants could identify a positive impact of being diagnosed with autism. However, the nature and extent of this varied considerably.
An increased understanding of self was frequently described, and some believed that this had directly led to improvements in their well-being. It also enabled them to develop more effective coping strategies. A reduced sense of isolation, which was brought about by simply knowing that others had the same experience, and improvements in relationships with family and friends were also reported. In addition, among those using other (mainstream) services, diagnostic assessment reports had been used by these practitioners to improve care provided.
However, some DO cohort interviewees reported long-standing or unresolved difficulties that were associated with the diagnosis. Some described difficulties with acceptance and/or understanding of autism. Almost all DO cohort interviewees, including those who had been relieved to receive the diagnosis, said that they wanted further help understanding and coming to terms with the diagnosis. A few believed that receiving the diagnosis had caused a deterioration in their mental health. In all instances, they attributed this to the lack of psychoeducation and other post-diagnostic support.
Family members’ accounts broadly align with those of their relatives. Again, among those drawn from the DO cohort, there was a frustration with the lack of support. We also asked family members about the impact on themselves of their relative being diagnosed. Positive impacts on family relationships were often described. However, they also noted the impact that deteriorations in the well-being of their relative had on them, with increased levels of stress and hopelessness described. The majority of family members did not want support for themselves, rather they pointed to the benefits to them of their relative receiving the care and support they needed.
Chapter 10 The economic analysis
Introduction
The economic analysis comprised a number of components and concerned only the SAT cohort. SATs were costed based on financial information provided by each service or its managing organisation. Service utilisation patterns were costed and compared between the SO group and the D&S group. Interindividual variations in service utilisation were examined by reference to differences in participant and SAT characteristics. Links between the service utilisation costs in the 12-month period after baseline and the primary outcome score at the 12-month follow-up point were explored, again adjusting for differences in individual and SAT characteristics. We looked at how costs differed by service characteristics. We examined the cost-effectiveness of different service arrangements by bringing together the cost findings and both the primary outcome (WHOQOL-BREF psychological domain) and the quality-adjusted life-year (QALY) gain. We used regression analyses of variations in both costs up to the 12-month point and these two outcomes at 12 months to generate parameters that allowed examination of cost-effectiveness of different service characteristics. As with almost any study, there are limitations to the data available and, for some analyses, sample sizes are low.
Methods
Setting
The setting was the same as that for the outcomes evaluation (see Chapter 8).
Study participants
Inclusion criteria for the SAT cohort and characteristics of sample members are described in Chapter 8.
Costs of Specialist Autism Teams
The SAT costs (measured in Great British pounds) were calculated using financial information (overall annual budget for 2017–18) obtained by the research team from each SAT or its managing organisation, combined with data on the total number of clients supported in each site (also obtained from SATs themselves), to give an overall average cost per study participant for each SAT. It was not possible to carry out microcosting of activities within the SATs because of the considerable time that any such exercise would have taken, nor did those services hold information in a way that would allow separate costing of their various diagnostic and post-diagnostic activities. The advantage of top-down costing is that it is easier to operationalise than microcosting, considerably less time-consuming for the researcher and considerably less intrusive for services. An exploration of cost variations partially compensated for this disadvantage by including regressors that reflect key service and individual components in the analyses.
Some, but not all, SATs provided us with high-level budgetary information. Where financial information was missing, costs were imputed, taking into account differences between SATs in the proportion of D&S and SO service users on caseloads, as this potentially has an effect on average per-person costs. This was estimated from the proportions in our study sample. When we later analysed cost variations and cost-outcome links, we used both SAT costs and (other) service costs.
Service utilisation and associated costs
Service utilisation patterns (health, social care and other statutory sectors) for individuals were collected with an adapted version of the CSRI that was created specifically for this study. It was completed at each time point, covering a retrospective period of 4 weeks.
Services provided within the SAT were assumed to be covered by the SAT budget. However, contacts with professionals and services reported in the CSRI are likely to represent some double-counting, as we know generally that study participants can find it hard to attribute professionals to specific roles and/or services. We, therefore, conducted additional analyses to test how sensitive key findings were to the possibility of some degree of double-counting. We did this, for example, in the cost variations analyses by setting each of the largest cost components to zero (to represent no contact with that particular service outside the SAT) and examining whether or not it affected comparisons between different types of SATs/SAT characteristics.
The CSRI also collected information on employment status (allowing calculation of productivity costs associated with days off because of sickness absence) and privately borne costs. It was not possible to collect data from family members or others on the amount or nature of unpaid care and support. If a participant was categorised as being in full-time paid employment, the number of days taken off work in the last 3 months was multiplied by the number of hours worked per day (assumed to be 7) multiplied by the minimum wage (£7.83 for adults). If an individual worked part time, the number of hours worked per week was divided by 5 working days to obtain the number of hours per day. This was multiplied by the minimum hourly rate at that time of £7.83. If someone was self-employed, the costs for lost productivity were treated in the same way as for a full-time worker. For other work status responses, such as trainee, voluntary worker, job-seeking, not working owing to sickness/disability, student, maternity/paternity leave, carer and retired, we did not attach monetary values to them and cost was assumed to be zero.
The focus of the economic evaluation, as set out in the prespecified analysis plan, was costs between baseline and 12 months that were computed from data collected for 4-week retrospective periods at 3 months (T1), 6 months (T2) and 12 months (T3), and interpolated between time points to get a full 52-week costing. Sample sizes at 18 and 24 months were insufficient to conduct robust analyses, and analysis beyond 12 months was not part of the original design for the study. Unit costs utilised in our analyses are given in Table 19.
| Category | Unit costs | Source |
|---|---|---|
| GP consultation | £31 per 9.22 minutes, including direct care | Unit Costs of Health and Social Care 2018 51 |
| Psychologist | £43 per hour, £0.72 per minute | Unit Costs of Health and Social Care 2018 51 |
| Occupational therapist | £43 per hour, community occupational therapist | Unit Costs of Health and Social Care 2018 51 |
| Nurse | £59 per face-to-face consultation | Unit Costs of Health and Social Care 2018 51 |
| SLT | £34 per hour | Unit Costs of Health and Social Care 2018 51 |
| Social worker | £44 per hour | Unit Costs of Health and Social Care 2018 51 |
| Support worker | £23 per hour | Unit Costs of Health and Social Care 2018 51 |
| Police officer | £48 per hour | Unit Costs of Health and Social Care 2018 51 |
| Private cost | £74 for other therapist, adults, one to one | 2017/18 Reference Costs and Guidance 52 |
| Fixed group | £16 for delivery by a non-specialist | Unit Costs of Health and Social Care 2018 51 |
| Support group | £16 for delivery by a non-specialist | Unit Costs of Health and Social Care 2018 51 |
| Social group | £16 for delivery by a non-specialist | Unit Costs of Health and Social Care 2018 51 |
| Outpatient | £140 per visit | 2017/18 Reference Costs and Guidance 52 |
| Accident and emergency | £160 per visit | 2017/18 Reference Costs and Guidance 52 |
| Walk-in centre | £160 per visit | 2017/18 Reference Costs and Guidance 52 |
| Day case | £742 for day case | 2017/18 Reference Costs and Guidance 52 |
| Inpatient care | £6161 for non-elective short stay | 2017/18 Reference Costs and Guidance 52 |
| Minimum hourly rate | £7.83 minimum wage rate per hour for adults (≥ 25 years) | UK government website (2019)53 |
Statistical tests
Independent t-tests compared means for the annual health and social care costs and societal costs by different cost components. Bootstrapping was used (bias corrected) owing to skewed costs.
Cost variations
In analyses of variations in cost, the dependent variable was cost over the 12-month period between T0 and T3, calculated as above. Multivariate statistical analyses were conducted to explore to what extent the observed variations in some cost measures between individuals in the sample were associated with characteristics of those individuals and of the SATs that provided their support and/or diagnosis. Given the absence of previous research on SATs to guide the selection of variables, the analyses examined associations with potentially all individual characteristics measured at baseline (using measures described in Chapter 8), in particular the effects of different SAT characteristics (again, described earlier; see Table 15), although we were parsimonious in inclusion of independent variables given the sample size.
Generalised linear modelling was used for these analyses to allow flexibility to address probable skewness in the dependent variables. We tested for the best-fitting distributional form. Site-specific variance clustering was considered in the regression equations with robust standard errors. All baseline variables for the individual and SAT service characteristics were tested for statistical significance using a p-value of 0.05 and were explored for potential inclusion in the model. They were added one at a time to the cost model given statistical significance and theoretical importance. Variables considered for potential inclusion were the following:
-
individual characteristics at baseline
-
age
-
gender
-
ethnicity
-
marital status
-
highest educational qualification
-
living arrangements (living alone, living with others)
-
accommodation type (rented, student halls, own/mortgaged)
-
work situation
-
time off employment/education
-
EQ-5D-5L five domains individually (mobility, self-care, usual activities, pain/discomfort and anxiety/depression)
-
membership to an autism-specific organisation or online
-
met with voluntary support worker
-
attended local group meeting
-
contacted a helpline
-
have e-mail contacts with autism organisation
-
WHOQOL-BREF physical, psychological, social and environmental domains
-
GHQ-12 scores
-
-
service characteristics
-
LA involvement
-
multiservice team versus single-service team
-
neurodevelopmental versus autism only
-
dominant mode of delivering psychoeducation post diagnosis
-
skill mix
-
routinely do one-to-one work regarding mental health problems
-
delivery of care plan
-
drop-in provision and/or named contact while in service.
-
We did not include discharge practice (closed, stepped, open) as this information was not available at T3.
Cost–outcome links
The analysis of cost–outcome links focused on the primary outcome, WHOQOL-BREF psychological domain, as the dependent variable, measured at 12 months, which was regressed on study participant characteristics at T0, SAT characteristics, and costs both at T0 and over the 12-month period that followed. Again, generalised linear modelling was used for these analyses, adjusting for clustering by site, and again both D&S and SO groups were identified and included in the same multiple regressions. Individual cost components for each service cost were included separately in the cost–outcome link regression to explore whether or not differences in costs may be driving differences in outcome.
The 17 cost components included were GP, psychologist, occupational therapist, nurse, SLT, social worker, support worker, group activities lasting a fixed number of sessions, support group, social group, outpatient care, accident and emergency, walk-in centre, day case, inpatient care, police officer and private appointment with other therapists.
These were included in the regressions along with age, gender, WHOQOL-BREF psychological domain at T0, diagnostic status at referral (SO vs. D&S) and baseline health and social care costs.
Cost-effectiveness analysis
We examined cost-effectiveness in this observational design by estimating a number of regression equations: one with cost measured over 12 months as a dependent variable (first for health and social care costs and then for societal costs); one with the primary outcome at 12 months (WHOQOL-BREF psychological domain score) as a dependent variable (again, separately from health and social care and societal perspectives, given that we needed to adjust for baseline costs); and one with QALYs measured over the period from baseline to 12 months as a dependent variable (from health and social care and societal perspectives, in turn). QALYs were calculated from EQ-5D-5L scores and UK societal weights, using ‘area-under-the-curve’ calculations. Generalised linear modelling was used, adjusting for clustering by site.
We examined estimated coefficients on each of the service characteristics (LA involvement, multiservice team vs. single service, etc.) in each equation to see whether or not these characteristics were significantly associated with cost or outcome variations. In principle, we could interpret these coefficients as measures of incremental changes in cost and effectiveness, and then compute incremental cost-effectiveness ratios between two variants of a particular service characteristic. We have generally not carried this out below, as this adds little to our narrative summary of the results.
Statistics package
The statistical software Stata® 14.2 and SPSS version 24 (Statistical Product and Service Solutions, SPSS Inc., Chicago, IL, USA) were used.
Results
Specialist Autism Team costs
Cost information was obtained from four of the nine SATs. One SAT (multiservice delivery model) provided partial information. Of the remainder, two declined to provide cost information, whereas the other two agreed to provide cost information but did not deliver it, despite reminders. For the SATs with cost information, average costs per client were estimated based on the method described in Costs of Specialist Autism Teams. This costing did not take account of other functions/services included in commissioning arrangements (e.g. training/support to staff in mainstream services, public awareness raising and provision of low-level support post discharge). The average cost per client for the four SATs from which we could obtain budget data and information on the total number of service users per year were £360, £768, £781 and £2951. Differences between SATs may be linked to operational scale (for example, the lowest-cost SAT supported more than four times as many autistic people than the highest-cost SAT), location (influencing some input prices), characteristics of people being supported and the range of services delivered (e.g. some SATs did not accept referrals from those already diagnosed and the extent of direct work). We can examine the last two potential sources of variation with data collected in this study. For SATs that did not provide financial information, we imputed from these observed cost data (see Costs of Specialist Autism Teams).
Comprehensive support costs
Service utilisation data and costs for services provided by SATs (captured by SAT budgets) were summed to give a subtotal for the health and social care costs. In addition, costs were calculated for employment-related and other ‘formal’ sectors (police officer contacts) (see Appendix 15, Tables 60 and 61).
Significant differences in costs between D&S and SO groups over the 12-month period were found in relation to accessing three professions/interventions: psychologist (p = 0.05), nurse (p = 0.05) and fixed-session, group-delivered interventions (p = 0.05) (see Appendix 15, Table 62). These are key features of SAT provision. Sensitivity analyses to address the possibility that there was double-counting between the SAT budgets and the service utilisation reported by study participants were, therefore, conducted.
Aggregating costs across the different service components revealed that the D&S group had service-related costs totalling £2546 over the 12-month period, compared with £1699 for the SO group. Societal costs (again excluding SAT costs for the moment) summed to £2733 for the D&S group and £1931 for the SO group (see Appendix 15, Table 60).
Aggregated costs for each 4-week period of data collection by time point and group (D&S vs. SO) are shown in Table 20. At baseline, the total health and social costs were £125 for the D&S group (n = 164) and £151 for the SO group (n = 88). Costs increased over time, probably as a result of SAT involvement, although comparisons between time points should be made cautiously because of sample attrition: individuals for whom costs were available are not identical between time points. There were no significant differences in costs between the D&S and SO groups at any individual time point.
| Time point | Cost measure | D&S group | SO group | Test of difference in mean costs | |||||
|---|---|---|---|---|---|---|---|---|---|
| n | Mean (£) | SD (£) | n | Mean (£) | SD (£) | t | p-value | ||
| T0 | Health and social care | 164 | 125.07 | 213.83 | 88 | 151.26 | 238.57 | –0.89 | 0.37 |
| Societal | 164 | 210.52 | 493.13 | 88 | 179.22 | 321.65 | 0.54 | 0.59 | |
| T1 | Health and social care | 99 | 170.58 | 601.93 | 58 | 225.95 | 359.18 | –0.64 | 0.53 |
| Societal | 138 | 194.41 | 354.93 | 77 | 200.86 | 345.90 | –0.13 | 0.90 | |
| T2 | Health and social care | 87 | 168.92 | 202.84 | 44 | 183.91 | 216.58 | –0.39 | 0.70 |
| Societal | 137 | 149.26 | 268.42 | 70 | 166.03 | 264.61 | –0.43 | 0.67 | |
| T3 | Health and social care | 90 | 272.27 | 594.05 | 45 | 192.33 | 255.91 | 0.86 | 0.39 |
| Societal | 133 | 240.09 | 603.19 | 75 | 141.05 | 242.69 | 1.36 | 0.18 | |
Cost variations
As noted earlier, analyses of cost variations took each measure of cost over the 12-month period between T0 and T3 as a dependent variable, which was regressed on individual characteristics at baseline and SAT characteristics, adjusting for clustering by site. Generalised linear modelling with gamma distribution and identity link was used for these analyses as the best-fitting model with the lowest Akaike information criterion (AIC) values among other generalised linear modelling model specifications. As noted above, two series of regression analyses were conducted: health and social care costs, and societal costs.
Health and social care costs
Some individual characteristics at baseline were significantly associated with health and social care costs over the 12-month period to T3 (Table 21):
-
The SO group had lower costs than the D&S group (difference of £1107).
-
Women had higher costs than men, the average difference being £534.
-
People living with parents, foster carers or guardians at the start of the study tended to have lower costs than those who were not (difference of £770).
-
A 1-point higher WHOQOL-BREF psychological domain score at baseline was associated with a £17 lower cost.
-
People who had higher baseline costs were more likely to have higher 12-month costs.
Other individual characteristics were not associated with health and social care cost differences.
| Characteristic | Coefficient | Robust standard error | z | p > z | 95% CI |
|---|---|---|---|---|---|
| Diagnostic status on referral [1 = already diagnosed (SO), 0 = not yet diagnosed (D&S)] | –1107.21 | 116.30 | –9.520 | 0.000 | –1335.14 to –879.27 |
| Baseline health and social care cost (£) | 4.65 | 1.11 | 4.190 | 0.000 | 2.48 to 6.83 |
| Age (years) | –7.35 | 17.60 | –0.420 | 0.676 | –41.84 to 27.15 |
| Gender (1 = female, 0 = male) | 533.58 | 145.72 | 3.660 | 0.000 | 247.97 to 819.18 |
| Living with parents at T0 (1 = yes, 0 = no) | –770.23 | 328.53 | –2.340 | 0.019 | –1414.14 to –126.31 |
| Time off work/education because of illness (1 = yes, 0 = no) | 594.23 | 388.99 | 1.530 | 0.127 | –168.19 to 1356.64 |
| WHOQOL-BREF psychological domain score at T0 | –17.33 | 3.51 | –4.940 | 0.000 | –24.20 to –10.45 |
| LA involvementa | –1251.46 | 991.27 | –1.260 | 0.207 | –3194.31 to 691.38 |
| Team structureb | –197.13 | 434.78 | –0.450 | 0.650 | –1049.29 to 655.03 |
| Autism vs. ND servicec | –348.57 | 87.57 | –3.980 | 0.000 | –520.20 to –176.95 |
| Psychoeducationd | 404.49 | 267.16 | 1.510 | 0.130 | –119.12 to 928.11 |
| Skill mixe | 2481.10 | 551.29 | 4.500 | 0.000 | 1400.59 to 3561.60 |
| One-to-one workf | –114.57 | 389.18 | –0.290 | 0.768 | –877.37 to 648.20 |
| Delivery of care plang | 3107.13 | 644.48 | 4.820 | 0.000 | 1843.96 to 4370.30 |
| Constant term | –30.69 | 744.21 | –0.040 | 0.967 | –1489.31 to 1427.94 |
Looking at the service characteristics (see Table 21), those significantly associated with T3 health and social care costs were:
-
Autism versus neurodevelopmental services – individuals in SATs with a neurodevelopmental service had lower costs than individuals in SATs with an autism-only service (difference of £349).
-
Skill mix – individuals in SATs that involved four or more professional disciplines had higher costs than individuals in SATs that involved only two or three disciplines (difference of £2481).
-
Delivery of care plan – individuals in SATs with a managed approach to care plan delivery had higher costs than individuals in SATs that used an episodic approach (difference of £3107).
The service characteristic of drop-in provision and/or a named contact while in the service (1 = no; 0 = yes) does not appear in the regression results because of multicollinearity.
We noted earlier the possibility of double counting of some costs if sample members reported contacts with professionals whose costs were, in fact, already accounted for in our estimates of SAT delivery costs. Professions/services for which double counting was judged most likely to have occurred were as follows: consultations with nurses, psychologists or support workers. Analysis of these profession/service costs found that they differed according to service characteristic (see Appendix 15, Table 63). We conducted sensitivity analyses by re-running the health and social care cost regression after removing costs for the two largest cost components (nurses and psychologists) both singly and in combination. The significance of some service characteristics was sensitive to the measurement of costs: when psychologist costs were set to zero, psychoeducation became statistically significant; when nurse costs were set to zero, and when both nurse and psychologist costs were set to zero, both psychoeducation and one-to-one working became statistically significant. (Full details available on request.)
Societal costs
A second series of analyses focused on societal cost variations. Total societal costs included costs for police officers, private out-of-pocket payments for private appointments with other therapists and costs associated with productivity losses owing to sickness absence, in addition to the total annual health and social care costs analysed above. The same set of individual and service characteristics was explored for their associations with costs as for the health and social care costs analyses, with variables retained or excluded depending on statistical significance, taking into account correlations with other variables. Analyses were adjusted for clustering.
A number of individual characteristics at baseline were significantly associated with societal costs over the 12-month period to T3 (Table 22). The SO group had lower costs than the D&S group (difference of £1020).
-
Women had higher costs than men, with the average difference being £599.
-
A 1-point higher WHOQOL-BREF psychological domain score at baseline was associated with a £20 lower cost.
-
People who had higher baseline costs were more likely to have higher 12-month costs.
Other individual characteristics were not associated with health and social care cost differences.
| Characteristic | Coefficient | Robust standard error | z | p > z | 95% CI |
|---|---|---|---|---|---|
| Diagnostic status at referral (1 = SO, 0 = D&S) | –1020.21 | 113.14 | –9.020 | 0.000 | –1241.96 to –798.47 |
| Baseline societal cost (£) | 3.59 | 1.47 | 2.450 | 0.014 | 0.71 to 6.46 |
| Age (years) | 17.78 | 10.40 | 1.710 | 0.087 | –2.60 to 38.16 |
| Gender (1 = female, 0 = male) | 599.12 | 192.93 | 3.110 | 0.002 | 220.99 to 977.26 |
| Time off work/education owing to illness (1 = yes, 0 = no) | 829.07 | 501.41 | 1.650 | 0.098 | –153.68 to 1811.83 |
| WHOQOL-BREF psychological domain score at T0 | –20.07 | 4.26 | –4.720 | 0.000 | –28.42 to –11.73 |
| LA involvementa | –388.92 | 683.62 | –0.570 | 0.569 | –1728.80 to 950.95 |
| Team structureb | –679.16 | 200.38 | –3.390 | 0.001 | –1071.90 to –286.43 |
| Autism vs. NDc | –113.17 | 154.94 | –0.730 | 0.465 | –416.84 to 190.50 |
| Psychoeducationd | 827.23 | 91.82 | 9.010 | 0.000 | 647.27 to 1007.18 |
| Skill mixe | 2495.06 | 411.13 | 6.070 | 0.000 | 1689.25 to 3300.86 |
| One-to-one workf | –873.47 | 229.93 | –3.800 | 0.000 | –1324.13 to –422.81 |
| Delivery of care plang | 2976.92 | 556.50 | 5.350 | 0.000 | 1886.20 to 4067.65 |
| Constant term | –30.69 | 744.21 | –0.040 | 0.967 | –1489.31 to 1427.94 |
Looking at the service characteristics, five were significantly associated with T3 societal cost variations:
-
Team structure – individuals in SATs with multiservice teams had costs that were on average £679 lower than those for individuals in SATs with a single team structure.
-
Psychoeducation – individuals in SATs for which the dominant mode of delivering psychoeducation post diagnosis was one to one had £827 higher costs than individuals in SATs that used group delivery.
-
Skill mix – individuals in SATs that involved four or more professional disciplines had higher costs than individuals in SATs that involved only two or three disciplines (difference of £2495).
-
One-to-one work – individuals in SATs that routinely providing one-to-one work regarding (non-complex) mental health problems had lower costs than individuals in SATs without such an approach (difference of £873).
-
Delivery of care plan – individuals in SATs with a managed approach to care plan delivery had higher costs than individuals in SATs that used an episodic approach (difference of £2977).
We conducted equivalent sensitivity analyses for societal cost variations, as reported above, for health and social care cost variations. In this instance, the analyses showed that the pattern of the service characteristics was not sensitive to the measurement of psychologist or nurse costs. (Again, details are available on request.)
Cost–outcome links
Examination of the cost–outcome links focused on the primary outcome: WHOQOL-BREF psychological domain. Seventeen cost components (over the 12-month period to T3) were included (GP, psychologist, occupational therapist, nurse, SLT, social worker, support worker, group activities lasting a fixed number of sessions, support group, social group, outpatient care, accident and emergency, walk-in centre, day case, inpatient care, police officer and private appointment with other therapists), along with referral group, age, gender, WHOQOL-BREF psychological domain at T0 and baseline societal costs.
The regression equation is presented in Appendix 15, Table 64. Some individual and SAT characteristics were found to be associated with inter-individual differences in outcome (broadly consistent with the analyses reported in Chapter 8), but there was no significant association between the WHOQOL-BREF psychological domain at 12 months and the total annual societal costs. Significant predictors were baseline WHOQOL-BREF psychological domain scores and GP costs. In other words, differences in GP costs and WHOQOL-BREF psychological domain scores at baseline were driving some differences in the WHOQOL-BREF psychological domain scores at T3.
Cost-effectiveness analysis
The cost-effectiveness of different service characteristics was examined by looking at the estimated coefficients on service characteristic indicators in the cost and outcome regressions. The cost regressions (one for health and social care costs and one for societal costs) have been reported in Cost variations. In this section we report the outcome regressions, first for WHOQOL-BREF psychological domain and then for QALYs. Again, we used generalised linear modelling and found that a Gaussian family distribution and identity link had the best fit (lowest AIC values).
In the first regression (WHOQOL-BREF psychological domain, health and social care perspective) (see Appendix 15, Table 65), three of the service characteristics indicators were significantly associated with T3 outcome variations:
-
Team structure – individuals in SATs with multiservice teams had, on average, a 5-point higher score on the WHOQOL-BREF psychological domain than individuals in SATs with a single team structure, taking into account other covariates.
-
Autism versus neurodevelopmental service – individuals in SATs with a neurodevelopmental service had, on average, a 10-point lower score on the WHOQOL-BREF psychological domain than individuals in SATs with an autism-only service.
-
One-to-one work – individuals in SATs that routinely provided one-to-one work regarding (non-complex) mental health problems had, on average, a 17-point higher score on the WHOQOL-BREF psychological domain than individuals in SATs with a single team structure.
In the second regression (WHOQOL-BREF psychological domain), this time from a societal perspective (see Appendix 15, Table 66), four of the service characteristics indicators were significantly associated with T3 outcome variations:
-
Local authority involvement – individuals in SATs with joint LA and CCG arrangements had, on average, a 9-point lower score on the WHOQOL-BREF psychological domain than individuals in SATs with just CCG arrangements, taking into account other covariates.
-
Team structure – individuals in SATs with multiservice teams had, on average, a 4-point higher score on the WHOQOL-BREF psychological domain than individuals in SATs with a single team structure.
-
Autism versus neurodevelopmental – individuals in SATs with a neurodevelopmental service had, on average, a 10-point lower score on the WHOQOL-BREF psychological domain than individuals in SATs with an autism-only service.
-
One-to-one work – individuals in SATs that routinely provided one-to-one work regarding (non-complex) mental health problems had, on average, a 20-point higher score on the WHOQOL-BREF psychological domain indicator than individuals in SATs in which this was not routinely offered.
The third and fourth regressions took QALYs over the 12-month period as a dependent variable and analysed variations from, first, a health and social care perspective and, second, a societal perspective (in the adjustment for baseline cost). We also adjusted for baseline utility score (computed from EQ-5D); outputs are presented in Appendix 15, Tables 67 and 68.
In the first regression, three service characteristics were significantly associated with QALY variations:
-
Local authority involvement – individuals in SATs with joint LA and CCG arrangements had, on average, a 0.683 higher QALY score than individuals in SATs with CCG arrangement only, taking into account other covariates.
-
Autism versus neurodevelopmental service – individuals in SATs with a neurodevelopmental service had, on average, a 0.182 lower QALY score than individuals in SATs with an autism-only service.
-
One-to-one work – individuals in SATs that routinely provided one-to-one work regarding (non-complex) mental health problems had, on average, a 0.395 lower QALY score than individuals in SATs with a single team structure.
From a societal perspective, the same three service characteristics were significantly associated with QALY variations over the 12-month period:
-
Local authority involvement – individuals in SATs with joint LA and CCG arrangements had, on average, a 0.585 higher QALY score than individuals in SATs with just CCG arrangements, taking into account other covariates.
-
Autism versus neurodevelopmental service – individuals in SATs with a neurodevelopmental service had, on average, a 0.194 lower QALY score than individuals in SATs with an autism-only service.
-
One-to-one work – individuals in SATs that routinely provided one-to-one work regarding (non-complex) mental health problems had, on average, a 0.381 lower QALY score than individuals in SATs with a single team structure.
Bringing these analyses together, the findings in relation to the effects of service characteristics on costs, self-reported psychological quality of life and QALYs can be summarised as follows (Table 23):
-
Local authority involvement – from a health and social care perspective, there are no cost or psychological quality-of-life differences between SATs with joint LA/CCG arrangements or SATs that are only CCG-led. From a societal perspective, there is no cost difference for joint LA/CCG SATs, but psychological quality of life is slightly worse (9 points on a scale that runs from 0 to 100 points). However, LA involvement was associated with higher QALY scores over the 12-month period. Overall, the cost-effectiveness of joint LA/CCG arrangements rests on the credibility of the QALY results.
-
Team structure – psychological quality-of-life outcomes are slightly better for SATs with multiservice teams than for single team structures; however, the difference is only 4 or 5 points on the 100-point scale. Health and social care costs do not vary with this service arrangement, but societal costs are slightly lower for multiservice SATs. QALYs do not vary with team structure. Overall, these findings do not suggest major differences from a cost-effectiveness standpoint between team structures.
-
Autism versus neurodevelopmental service – psychological quality-of-life outcomes are 10 points lower for individuals in SATs with a neurodevelopmental service rather than an autism service, which is marked on a scale running from 0 to 100 points. QALYs were also lower. Health and social care costs are slightly lower for neurodevelopmental service SATs and there is no difference in societal costs. Overall, these findings point to a cost-effectiveness advantage for autism-only services.
-
Psychoeducation – there was only one significant difference between SATs whose dominant mode of delivery of psychoeducation post diagnosis was one-to-one delivery compared with SATs in which there was group delivery: societal costs were slightly higher for the former. Sensitivity analyses suggest that one-to-one delivery of psychoeducation might be slightly less costly (health and social care costs only) if our measurement of psychologist costs included some double-counting. Overall, however, there is no strong cost-effectiveness case for either one-to-one or group delivery.
-
Skill mix – in the case of skill mix, there are no observable differences in psychological quality of life according to the richness of skill mix in the SAT being used, nor any differences in QALYs; however, individuals supported by SATs that had four or more professional disciplines had substantially higher costs than individuals in SATs that had only two or three disciplines. On cost-effectiveness grounds, and in terms of psychological quality-of-life and QALY outcomes, arrangements in which fewer professions are included appear to be preferred.
-
One-to-one work – individuals using SATs that routinely provide one-to-one work for people with (non-complex) mental health problems have substantially better psychological quality-of-life outcomes than individuals using SATs not using one-to-one approaches either at no higher cost (health and social care perspective) or at reduced costs (societal perspective). On the other hand, QALYs were lower with one-to-one work. Sensitivity analyses suggest that one-to-one work might be slightly more costly (health and social care costs only) if both the psychologist and the nurse had been double-counted, although the difference was not great. Overall, given that psychological quality of life was the primary outcome and that the validity of QALYs generated from the EQ-5D has not been established for autistic people, we conclude that one-to-one work by SATs is a cost-effective way to deliver support for people experiencing mental health problems, as indicated by changes in self-reported psychological quality of life.
-
Delivery of care plan – individuals in SATs with a managed approach to delivering care plans had significantly higher costs, yet psychological quality-of-life outcomes and QALYs were unaffected. Overall, we would conclude that an episodic approach appears to be more cost-effective than a managed approach with respect to this particular outcome.
| Service characteristic | Health and social care perspective | Societal perspective | ||
|---|---|---|---|---|
| Cost | Outcome | Cost | Outcome | |
| LA involvement | No difference | No difference in WHOQOL-BREF PD; QALYs higher | No difference | WHOQOL-BREF 9 points lower; QALYs higher |
| SAT structure | No difference | WHOQOL-BREF PD 5 points higher | £679 lower | WHOQOL-BREF 4 points higher |
| Autism vs. ND services | £349 lower | WHOQOL-BREF PD 10 points lower; QALYs lower | No difference | WHOQOL-BREF 10 points lower; QALYs lower |
| Mode of delivering psychoeducation | No difference | No difference | £827 higher | No difference |
| Skill mix | £2481 higher | No difference | £2495 higher | No difference |
| One-to-one work for presenting mental health problems | No difference | WHOQOL-BREF PD 17 points higher; QALYs lower | £873 lower | WHOQOL-BREF 20 points higher; QALYs lower |
| Approach to delivering care plan | £3107 higher | No difference | £2977 higher | No difference |
Summary
Our economic evaluation had a number of elements. We calculated the cost of each SAT from locally provided data. We calculated other service-related costs, but also noted that double-counting of some components is possible, although our exploration via sensitivity analyses suggests that this would have had little impact on our overall findings. We observed cost variations across the sample, and explored these in a series of multiple regression analyses. We similarly explored variations in the primary outcome measure (WHOQOL-BREF psychological domain) and QALYs measured over a 12-month period to explore the relative cost-effectiveness of different service arrangements.
Mean service-related costs of supporting this sample of autistic adults in contact with SATs were £2240 (health and social care) and £2453 (societal). Numerous individual and service characteristics appeared to be linked to cost variations. Annual health and social care costs were lower for:
-
people already diagnosed with autism (SO group) than those not previously diagnosed (D&S group)
-
men
-
people living with parents, foster carers or guardians
-
people with higher WHOQOL-BREF psychological domain scores at baseline
-
people with lower baseline costs.
Annual societal costs were lower for exactly the same groups of people, except there was no societal cost difference associated with living arrangement (with parents, etc.).
In addition, we found that both cost measures were associated with some of the service characteristics identified as distinguishing between SATs. For health and social care costs, significant associations were found with autism versus neurodevelopmental services, skill mix (number of professional disciplines involved) and delivery of care plan (managed vs. episodic). For societal costs, significant associations were found with team structure (multiservice vs. single team), psychoeducation (one-to-one vs. group delivery), skill mix, one-to-one work for people with mental health problems and delivery of care plan.
When we looked at cost-effectiveness, and in terms of psychological quality-of-life outcomes, the strongest evidence that was found suggested that autism-only services were more cost-effective than neurodevelopmental services; arrangements involving a smaller number of professionals appear more cost-effective; one-to-one work with people experiencing with mental health problems was cost-effective; and an episodic approach is more cost-effective than a managed approach to delivering care plans. When we measured effectiveness with QALYs, the pattern of cost-effectiveness was slightly different. However, it has not been established if the EQ-5D-5L is a suitable instrument for generating QALYs for autistic adults, and we would suggest caution in interpreting these particular findings.
Chapter 11 Discussion
Introduction
In this chapter, we consider the strengths and limitations of this study, before moving on to discuss and synthesise the study findings, placing them, where possible, within the context of existing evidence.
Strengths and limitations
Strengths
To the best of our knowledge, this is the first study to investigate SAT provision in England – a model of care consistently set out in government strategy since 2011 and recommended by NICE. The study has identified and described the approaches taken by localities to set up such provision, and explored practitioners’ experiences of implementing and delivering SATs. In the main study phase, and using a mixed-methods approach, we evaluated such provision, seeking to investigate and understand SATs from the perspective of practitioners, service users and family members, as well as tracking service users’ outcomes and their use of a wide range of specialist and generic services. A key objective of this chapter is to synthesise and integrate findings from these various elements of the study. Hopefully we have achieved this and, in doing so, have demonstrated the benefits afforded by the mixed-methods design.
Overall, the services recruited to the study as research sites represented well the range of approaches taken to SAT provision. Retention to the study and data completeness were excellent. All outcome measures performed well, including those not previously used with this population. We believe that this indicates that the outcomes evaluated and standardised measures chosen, in consultation with our PAG, were appropriate and meaningful. In addition, we worked with the PAG on the design and layout of the study questionnaire booklet. Thus, the hard copy was printed on pale-yellow paper with a dark-blue print, the layout was uncluttered and, where required, shading was used to distinguish between rows/items. Furthermore, at the 12-month follow-up, our primary time point and where highest retention was observed (> 85%), we included a question about the specific impact of the SAT on participants’ lives, with the option of using a free-text response format to describe experiences. Over half of the study participants took the opportunity to briefly share their experiences (reported in Chapter 6). As well as generating data, we believe that this also supported retention. Levels of retention also lend support to other strategies used. These included hard and online versions of questionnaires, the use of personalised/non-automated text message and e-mail alerts immediately prior to a data collection time point, and a three-stage reminder process using both electronic (e-mail, text message) formats and letters. At the same time, it is vital to acknowledge the commitment of study participants to this research.
In England, the care and support of autistic people remains a policy priority and there is a long-term commitment to improve provision. 33,54 Thus, the findings from this study (that commenced in 2014) remain highly relevant. Furthermore, although its focus has been on a model of care and service delivery in England – given the limitations in provision and service development in other countries, and a desire on their part to address this issue – the findings have a wider use and application. 27
The study was designed and carried out in the absence of a broader evidence base on autistic adults without LDs. There was, for example, a very limited literature to draw on to inform the selection of outcome measures when the study was being designed in 2013. Since then, however, there has been a burgeoning awareness of the need for a robust evidence base to inform the care and support of autistic adults without LDs. 27,37,55 Although the last couple of years have seen the publication of studies on outcome measurement or service design and delivery,27,37,55 the evidence base remains very limited. Thus, this study comprises a significant contribution not only with respect to models of providing care and support to autistic adults without LDs, but also methodically; for example, learning about recruitment and retention, data collection and outcomes measurement. With respect to outcomes measurement, members of the research team (EM and BB) have conducted an evaluation of the psychometric properties of the GHQ-12 using Rasch analysis (available from the authors).
Limitations
There are a number of limitations that are important to detail given their implications for the extent to which conclusions can be drawn.
Stage 1 sought to identify services that fulfilled NICE’s description of multidisciplinary, community-based provision for autistic adults: referred to by NICE as ‘Specialist Autism Teams’. We did not identify any service that fully aligned with NICE’s descriptive criteria of SAT provision. The key deviation was that all of the services identified worked exclusively with autistic adults without LDs, although some provided consultancy to other services with regard to all autistic adults. For this reason, this is not a study limitation but rather a ‘limitation’ of implementation of the SAT provision model. However, it does mean that the findings and conclusions drawn cannot inform service development for autistic adults with LDs.
Other variations in the integrity of NICE’s vision for SATs were also observed between SATs. For example, differences in the provision for carers, engagement in upskilling practitioners in mainstream services, extent of multidisciplinarity (and, by implication, holistic approach to care and support) and the provision or not of longer-term, low-intensity support. We have explored why services differed in the extent to which they have or could fully implement SAT provision, and this has generated useful and important evidence.
Evaluating the impact of different structural arrangements and approaches to care and service delivery on service user outcomes and resource use was a core study objective. A key finding from stage 1 was that each SAT was idiosyncratic. This meant that we could not cluster SATs into different ‘types’ or service models and then go on to evaluate and compare the different models using one or two exemplar services per model. Thus, as specified in the study protocol, we moved on to investigate how service characteristics (e.g. structural features, delivery approaches and ways of working) may affect user outcomes and resource use.
It is important here to note that in the quantitative component of this investigation, for each characteristic, the research sites clustered together differently. This was exacerbated by needing to have nine research sites to fulfil the sample size requirements within the study timeline. (The study had more research sites than originally planned owing to withdrawal of a large SAT early in study set-up, slower than expected throughput and, hence, recruitment in some sites, and significant delays in recruitment opening in two sites because of delays in the recommissioning processes.) These issues can, to some extent, be managed in the analytical process. However, it remains that we need to be careful in the interpretation of some findings and the weight given to them.
Finally, for the economic evaluation, data regarding SAT funding, budgets and caseloads were secured from fewer than half of the research sites. Perceived vulnerabilities with respect to funding and commissioning arrangements may have inhibited sharing of budgetary and costs information with the research team. Imputation was used to derive estimated costs for each site; however, the wide variation between sites mean that findings should be treated with caution. Taking a top-down approach to understanding service costs meant that a breakdown of staff costs/resource by the different SAT functions (e.g. diagnostic assessment, mental health interventions, drop-in provision and work with other groups, such as training and consultancy) was not possible. The very different approaches taken by SATs to, for example, the diagnostic assessment process (as reported in Chapter 3, Diagnostic assessment processes) illustrate the limitations of the top-down approach. They also serve to demonstrate the need for caution when interpreting findings. Certainly, to carry out microcostings would have required a substantial additional research resource. However, on reflection and in hindsight, given the novelty of the delivery model and the lack of existing research, this may have been a worthwhile investment.
In terms of the qualitative elements, one site was under-represented in the sample of service users interviewed for the study. This was because, unexpectedly, it closed recruitment quite early in the study timeline and there were, therefore, limited numbers of study participants eligible for interview (i.e. had used a service ≈12 months) when these took place towards the end of the study. However, this site was well represented in the sample who provided written accounts of their experiences within the T3 study questionnaire (reported in Chapter 6). In addition, although we used a sampling frame to ensure representation of a range of characteristics and experiences, the sample recruited to interview was self-selecting, although we note that > 70% of those invited were interviewed.
Furthermore, we did not recruit as many family members to the qualitative evaluation as had been planned. Given the topic of the interview, it was essential that the autistic adults chose whether or not a family member was also invited to take part in the study. Fourteen (out of 38) agreed to this and, of these, nine family members were recruited. This means that the conclusions we can draw regarding family members’ views of the impacts that using a SAT had on their relative (e.g. child, partner) are limited. In addition, our understanding of family members’ needs, and the actual or potential role SATs played in meeting those needs, is partial. It is important to note here that many of the interviews we did conduct with family members revealed significant concerns and difficulties, both for themselves and the autistic person. This accords with findings from existing research that has looked at family members of autistic adults. 24,56
Once the study was under way, a small additional element was introduced that offered an exploratory comparison of the outcomes and experiences of those on a diagnostic pathway provided by a SAT (D&S group of the SAT cohort) with those diagnosed by a regional/national diagnostic assessment service (DO cohort) in which no post-diagnosis support was available. It is important to highlight the initial nature of these findings. The quantitative evaluation was underpowered and the number recruited to our qualitative study was limited. Furthermore, we do not know if and how the quality of the diagnostic assessment process from which the DO cohort was recruited compares with other diagnostic services in England. The particular challenges associated with discriminating autism from co-occurring mental health problems is well documented,57 and indicates the need for a high level of expertise. Senior practitioners in our research sites believed that they offered high-quality diagnostic assessments (including at least one feedback session). However, they noted that this was not necessarily the case for other diagnostic assessment pathways operating across the country. Thus, these findings cannot be generalised and more research is certainly required in this area.
Finally, all sites reported higher than expected levels of demand on their service that had not been matched by an increase in resources. In addition, in two of our sites, there were extended periods during which a key post (e.g. specialist practitioner, clinical psychology) was unfilled. The consequence for all services was longer wait times between intake and full assessment and, potentially, longer wait times for interventions set out in the care plan. Findings from our qualitative data collected from service users (see Chapters 6 and 7) indicate that this may affect both the service user experience and the impact.
The implementation of Specialist Autism Team provision in England
Stage 1 of the study (see Chapter 2) sought to identify localities in England that had a SAT. The key findings from stage 1 of this study are:
-
SAT provision in England has been developed specifically for autistic adults without LD.
-
In 2015, (just) 18 localities in England were identified as having a SAT.
-
SATs differ according to a number of service characteristics.
The rationale for specifically developing provision for autistic adults without LDs was consistent across SATs; namely, the lack of any specialist services for this group, concerns about unmet need and evidence about increased risk of poor outcomes: a deficit identified by national audits of autism provision. 58 None of the SATs was fully ‘compliant’ with the NICE guidance on roles, function and skill mix. Resource and/or commissioners’ service specifications constrained the scope of services. For example, direct provision of care and support for carers and autistic adults in the community who were not currently ‘in the service’ was often very limited.
Our findings suggest that the Autism Act 200929 and the NICE guidance31 stimulated the development of SATs across England, with two-thirds of SATs established from 2010 onwards. However, access to such provision remains very limited, with just 18 SATs identified. Representing this statistic in terms of numbers of LAs indicates that individuals living in less than one-sixth (25/152, 16%) of LAs in England have access to a SAT. Differences in the data collected mean that we cannot directly compare our findings with the fourth (2016) national review of progress in implementing the Autism Act. 58 However, they do describe that just 16% of LAs report access to specialist autism post-diagnostic needs assessments (e.g. mental health) for autistic people without learning disabilities, which, given this is a clear SAT function, indicates that our mapping work is likely to have identified all, if not the great majority, of SATs in England.
Clearly, the extent to which SATs have been implemented has, to date, been very limited. On the other hand, this mapping study has generated strong evidence that it is possible to implement such provision, and there are different ways of setting up such a service (e.g. the single vs. multiteam model, models of LA involvement).
The NICE guidance31 made clear statements about the functions of a SAT and the need for a multidisciplinary approach. However, no evidence-informed guidance could be offered on service characteristics, such as models of organisation and delivery and ways of working. As a result, differences in the implementation and operationalisation of this guidance were anticipated. Our findings confirm that this is the case, with SATs varying in a number of characteristics. These included organisational features; staffing and skill mix; diagnostic assessment protocols; interventions used to address presenting needs; priority given to supporting self-management; the extent to which they engaged with supporting family members and upskilling professionals in mainstream services; and the approaches taken to delivering such support. The specific interventions being provided also varied; for example, many provided group sessions on living with autism, but each was unique. The funding available, the extent of statutory social care involvement (i.e. LAs) and clinical opinion strongly influenced the specific characteristics and practices of services.
The absence of an evidence base had the potential to affect a number of different decision-making processes related to the establishment of SATs. This included the content of service specifications developed by commissioners and the funding allocated. Furthermore, although the resources available impacted decisions made by professionals involved in designing and delivering SATs, their own clinical opinions and cumulative clinical experience sometimes strongly influenced service characteristics. This is also the case for the specific interventions provided for which, again, evidence on effectiveness and user experience is extremely limited. 35,59–61
Such observations are, by no means, unexpected. Statutory provision is unavoidably influenced and constrained by available resources, and clinical experience is an inevitable but valuable contributor to clinical decision-making and, more recently, service design. 62,63 However, as with other studies, these findings highlight the need for investment in developing an evidence base that can support and inform issues of the design and delivery of services for autistic adults. 36,38
Implementing and delivering a Specialist Autism Team
A nested qualitative study of the experiences of senior practitioners within SATs provided another layer of understanding of SATs and built on the findings from the mapping study. As reported in Chapter 4, this piece of work revealed the range of challenges that senior staff encounter as they lead and deliver SATs. In addition, throughout the chapter, the learning accrued through cumulative clinical experience is a strong theme. This is not surprising. We should remember that the majority of services that we evaluated were relatively ‘young’. All had been developed in the absence of any research evidence to guide service design and delivery, and there were very few SATs already in existence on which to model service design. (Indeed, prior to acting as research sites for this study, none of our research sites was aware of the existence of many of the other research sites.)
Interviews and focus groups with senior practitioners revealed a process of them learning about effective ways of working with autistic adults without LDs, and a growing understanding of models of working and service delivery that are feasible and sustainable. To some extent, the external and internal pressures of constrained resources, experienced relatively more acutely in mental health and LAs,54,64 meant that services had (rapidly) become critically reflective and solution-focused.
All services were extremely concerned about the number of referrals. Both well-established services (for which a decline in demand, at least via the diagnostic assessment pathway, might be expected) and those more recently opened reported a year-on-year increase. The number, and its increasing nature, had not been anticipated. Importantly, none had received additional commensurate funding and a few had seen a reduction in funding. Furthermore, none believed that the level of demand would fall. Certainly, it is likely that increased awareness of autism among professionals and the public has contributed to increased demand for diagnostic assessment in adulthood. 65 SAT practitioners also believed that the lack of any other non-LD autism-specific provisions in the locality and mainstream services’ reluctance to work with autistic adults (with their own resource constraints increasing that resistance) were the key drivers to growing numbers of referrals into the SAT. Furthermore, these factors also made for difficulties for SATs trying to refer to other services (e.g. IAPT and CMHT) and, for some service users, discharging them from the service.
In response to these pressures, all of the services in our study had revised their service offer or ways of working. It was felt that these changes had, in some way, compromised the quality of care, including the wait time (both for assessment and for interventions), the intensity of support provided or a lack of flexibility in how care was provided; for example, offering only group-delivered interventions. However, there were also examples of innovations that had been implemented in response to these constraints that senior practitioners felt had been particularly successful.
Supporting sustainability
An important component of this nested study concerned distilling learning and opinions about whether or not and how SAT provision should further develop. All services were convinced of the importance and value of SATs having a core role in the care and support of autistic adults without LDs, both those needing/newly diagnosed and those diagnosed as children or earlier in adulthood. However, to ensure that there are sustainable improvements in support for autistic adults without LDs, senior practitioners believed that some shifts in the role of SATs, and the emphasis and priority given to certain functions by such services, was required. They were as follows:
-
while maintaining the availability to provide specialist autism interventions and support, placing greater emphasis and resource on consultation and supervision of practitioners working in mainstream/generic services
-
ensuring practice and interventions offered supported self-management rather than fostered dependency
-
developing and investing in the low-intensity support available post discharge; ideally, but not only, this would incorporate collaborative working with local peer-led networks.
Such suggestions are not to say that senior practitioners believed that the vision of SATs set out by NICE needed modification. The guideline31 clearly specifies SATs as being responsible for providing and/or co-ordinating care and support (our emphases), and the Autism Strategy30 identified autistic adults without LDs as being likely to particularly benefit from preventative support. Rather, they believed that service specifications may need revising. Based on their experiences to date, senior practitioners emphasised that such changes require ‘buy-in’ and commitment from commissioners. They noted, however, that it had proved very challenging, or indeed impossible, to secure funding for, for example, drop-in services or other preventative-type provision. The absence of an evidence base on the impacts and effectiveness of low-intensity support was a barrier to making a case for incorporating such provision in the SAT offer.
With respect to increasing the emphasis given to the consultative role, it is important to note that senior practitioners were very clear that it would not remove the need and demand for specialist autism interventions provided by practitioners with extensive expertise in autism, and for those with complex needs. They also noted the potential risks associated with under-trained professionals assuming a level of autism-expertise or competence.
Furthermore, adopting a consultative/supervision model was dependent on mainstream services being willing and allowed to work in this way. Although ‘consultative’ models of health-care delivery have been implemented in other fields of health care, it is not a familiar approach in community adult mental health. The recently published NHS Long Term Plan,54 however, points in that direction, noting the requirement for health-care providers to ‘make reasonable adjustments’ so that autistic people can access and use their services.
Supporting self-management, making available long-term low-intensity support from SATs (e.g. telephone ‘clinics’ and drop-in services) and supporting autistic adults to connect with peer-led groups and communities all point to building resilience and preventing future difficulties, even crises. We noted earlier the challenge of making the case for investing in such provision, although some modelling work published by the National Audit Office demonstrated that such provision for autistic adults without LDs may be cost-saving, or at least cost neutral. 28 Wider evidence indicates a potential benefit of supporting self-management and for its integration within the care of people with long-term conditions. 66,67 However, robust evidence of their impact and effectiveness for autistic adults without LDs is required. 36,68
However, and particularly with respect to the notion of promoting community-led and peer-led support, it is important to also draw attention to findings from stage 2 concerning the membership and contact with autism-specific third-sector organisations and peer-led groups and communities (see Chapter 8). We found that less than one-quarter of study participants were members of an autism-specific voluntary organisation, with a similar proportion having had any contact with such an organisation in the 4 weeks prior to each data collection time point. Although an increase in contacts with such organisations was observed at the 12-month follow-up, and appeared to be sustained into the longer term, it is important to remember that, for the majority, no change was observed. This finding highlights that some people may be unable, even with support, to use peer support. Equally, and as we report in Chapter 8, others may be disinterested or unwilling to do so.
The evaluation of the Specialist Autism Teams
Domains of impact
Chapter 6 reported findings from our analysis of free-text data collected at T3 on the ways that SATs had affected study participants’ lives (or not). Over half of the T3 respondents responded to this question. The impacts described were wide ranging and serve to illustrate the range of needs that an autistic adult without LDs may have. We organised them into seven broad categories: understanding of autism, acceptance of self, improved mental health, reduced sense of isolation, improved relationships and social networks, help with employment and education, and supporting access to other services. In addition, the positive impact of contact with supportive and autism-expert practitioners was reported. Together, these provide evidence that some degree of holistic care was being achieved by the SATs we evaluated. Our data on service users’ reports of the number and range of concerns that they had worked on with their SAT (see Chapter 8) corroborate this, as do findings from our in-depth semistructured interviews with service users (see Chapter 7).
Thus, in these interviews, a similarly wide range of needs was described. In addition, it was clear that interviewees varied considerably in the severity and complexity of their needs. For example, some of those referred via the diagnostic assessment pathway (and including post-diagnostic psychoeducation) identified no further needs for which they required the support of the SAT. Others, however, had multiple and/or long-standing needs and difficulties. In terms of perceived outcomes of using a SAT, we heard a range of experiences. Some described their needs as being fully or predominantly met and this included those who, on referral to the service, had significant difficulties. Others had a more mixed experience, with some needs being met and others remaining unmet. The accounts of a third group indicated that their needs remained predominantly unmet. In a subsequent section (see Factors affecting outcomes of using a Specialist Autism Team) we report our findings as to why there were these different experiences.
Outcomes
Overall, and in line with other studies,24,69 on all domains of the WHOQOL-BREF mean scores were lower for the sample members than for UK norms. 70,71 With respect to the GHQ-12, compared with other studies that have used this measure, a greater proportion of our sample were scoring above the population mean clinical threshold (> 80% vs. 40%). 72,73 Using EQ-5D to generate utility scores, the sample had markedly worse generic health-related quality of life than that for population norms (e.g. 0.696 for those aged 23–34 years compared with an England norm of 0.919). 74
A number of changes in outcomes were observed between baseline and 12-month follow-up (T3) (see Chapter 8). For the D&S group, a statistically significant improvement in the proportion of study participants scoring below the GHQ-12 clinical threshold was observed. Although the WHOQOL-BREF psychological domain mean score also improved, this was not a statistically significant change. The picture for the SO group is different, with no statistically significant improvements in mental health observed.
With respect to our secondary outcome measures (EQ-5D-5L, WHOQOL-BREF social, physical and environmental domains, ISEL-SF belonging subscale), for the D&S group, changes in the mean score between T0 and T3 were slight and non-significant. The same pattern of findings was observed for the SO group, except for the WHOQOL-BREF social domain, for which a statistically significant (p < 0.05) deterioration was observed at T3.
We also investigated changes in outcomes using a set of categorical indicators that assessed two broad domains: daytime occupation/usual activities and access to autism networks and support. For the D&S group, a statistically significant increase (p < 0.05) in the proportion of participants reporting no/slight problems with managing daily living was observed. However, there was no evidence of a positive change in terms of perceived availability of information needed for everyday living, employment status, satisfaction with capacity for work and satisfaction with leisure time. For the SO group any changes were non-significant.
In terms of access to autism networks and support, for the D&S group there was no significant change in the levels of membership of autism-specific local/regional/national groups and/or online-only communities. Indeed, at T3, less than one-fifth were members of such an organisation/community. However, there was a significant increase (p < 0.01) in the proportion of the sample who reported some contact with such an organisation/community in the 4 weeks prior to T3. That said, it is important to note that the majority (73.9%) had no contact. For the SO group, membership levels also remained low at T3 (16.1%). Unlike the D&S group, no significant change in levels of contact was observed.
To summarise, for the D&S group, there was some evidence of improvement in mental health, ability to manage everyday living and use of autism-specific third-sector/peer-led organisations at T3. Findings for the SO group differed, with the statistically significant change observed only being a deterioration in social quality of life (as measured by WHOQOL-BREF’s Social domain). We would note that the size of the SO group is relatively small and, therefore, detecting changes in outcomes may be compromised.
There are a number of possible explanations for the differences observed between the D&S and the SO groups. Thus, the groups differed in their sociodemographic characteristics. Overall, the SO group was younger and, therefore, more likely to have been diagnosed in childhood. This also meant that they were more likely to be students and to be living with their parents. Thus, the potential support networks of the two groups may differ and this may have affected outcomes. In addition, at baseline, the SO group reported a better mental health quality of life. This may indicate, for at least some, that needs were less severe or less pervasive in their impact.
An alternative or additional explanation is that some participants in the SO group may have unresolved difficulties regarding their autism diagnosis that meant that they were unable to (fully) benefit from the interventions provided by the SAT. SATs do not routinely offer a psychoeducational intervention to those referred to their service who are already diagnosed (i.e. the SO group). However, recent studies report that young adults diagnosed as children may hold incorrect beliefs about autism. 75,76 Furthermore, evidence is starting to emerge on the potential role of psychoeducation in preventing poor mental health outcomes because it seeks to support understanding, personal acceptance and a positive view of autism. 77,78
It may also be the case that the expectations and needs of the D&S group and the SO group differed. In our interviews with service users, those sampled from the SO group interviewees reported a wide range of, sometimes quite specific, needs associated with managing everyday life and social relationships. By contrast, and aligning with other research,79,80 the expectations of the D&S group were strongly centred on the diagnostic assessment, particularly as a means to offering sense or validation of their lives. That is not to say, however, that some also had quite significant mental health and/or social needs. However, these needs tended to be expressed in more global terms. Therefore, it is possible that the ‘lack of fit’ between the users’ needs (and expectations) and the care and support SATs offered was greater for the SO group than for the D&S group. Other findings lend some support to this argument. First, there was a difference between groups in the proportion reporting that the SAT did not work on any of their concerns (12.3% vs. 6.8%) (see Chapter 8). In addition, the SO group was more likely to report little, no or a negative impact of using a SAT, with the lack of positive impact attributed to no, or unsuitable or insufficient, support being offered (see Chapter 6). Finally, and not possible for us to investigate, we do not know whether there are routine differences in the quality or intensity of support offered by SATs to these two groups.
Factors affecting outcomes of using a Specialist Autism Team
A key objective of the study was to generate evidence on what a SAT should ‘look like’ in terms of its characteristics and ways of working. Our quantitative and qualitative data both contributed to addressing this objective.
Service characteristics
We found no evidence of an association between outcomes and any organisational or structural features investigated, namely LA involvement in commissioning/funding, the structure of the SAT (single vs. multiteam) and whether the service was an autism-specific service or a wider neurodevelopmental service. Findings from the economic evaluation align with this apart from the autism-specific versus neurodevelopmental service characteristic, for which (after adjusting for other baseline covariates) an advantage in favour of autism-specific SATs was observed. These indicate, in a very preliminary way, that different approaches to the broad organisational set-up of SATs may be acceptable. However, we would stress that these are initial findings and evidence of no association should not be interpreted as an absence of association. We have no evidence from our qualitative data that contradicts these findings with respect to single versus multiteam structure and autism-specific versus neurodevelopmental service provision.
However, our finding of no evidence that LA involvement is associated with user outcomes does require further discussion. Services that we classified as having LA involvement varied in how this was operationalised (e.g. the LA seconded the social work post vs. the LA part-funded specialist autism support workers or drop-in provision), although for all services, it supported access to community care assessments. Cell counts meant that these different models of LA involvement had to be collapsed into a single characteristic, which does mean that we have to be careful in how we interpret this finding. In our analysis of service user interviews, active support with accessing other services was identified as being associated with needs being met (see Chapter 7). Senior practitioners believed that LA involvement could be an important and valuable feature of SATs (see Chapter 5), offering the ability to carry out or smooth access to social care assessments and promoting collaborative working between the SAT and the adult social care teams more widely. However, they also noted very long waiting lists for LA social care assessments, which may offer further explanation for our findings. Finally, the proportion of SAT users who needed and were eligible for LA social care was likely to be relatively small (see Appendix 16, Table 69). This means that any impacts on outcomes may not have been discernible given the size and nature of the sample recruited to this study.
We did, however, find strong evidence of an association between skill mix and outcomes, with greater skill mix associated with better mental health outcomes. These findings align with wider evidence on the positive impact of richer skill mix in mental health services. 81 Our qualitative evidence consistently supports and offers explanations for this. The ‘fit’ between service users’ needs and what a SAT was able to provide, which was at least partly determined by skill mix, was identified by service users and SAT practitioners as key to the impacts SATs could achieve (see Chapters 5–7). Richness of skill mix can be taken as an indicator of the extent to which a truly holistic approach can be achieved. This emerged as one of the core explanations for differences in service users’ experiences and the degree to which they felt their needs were met by the SAT (see Chapter 7). This perspective also provides an explanation for seemingly contradictory findings from the economic evaluation that did not find richer skill mix to be more cost-effective in terms of psychological quality of life. We also note the tentative nature of conclusions drawn from the economic evaluation.
With respect to the overall model of care delivery, we applied the broad classification of managed versus episodic care. Managed care was defined as the active, ongoing review and monitoring of the care plan and its impacts. SATs allocated to ‘managed care’ included those in which the service user was actively involved in review and forward planning. ‘Episodic care’ describes a model in which there is minimal review and oversight of progress through a set of interventions determined at needs assessment. Episodic care should not, however, be regarded as less holistic in the range of care and support offered. We found weak evidence that managed care was associated with better mental health outcomes at the 12-month follow-up. Again, findings from our qualitative research accord with this. It appeared that it facilitated a responsive approach, meaning that the needs emerging during the time in the service could be responded to, which was something that was highly valued. It also supports goal-focused approaches to care and support. However, episodic care is associated with lower costs and so may be seen as more cost-effective.
In some SATs, the managed care model included service users having a ‘named contact’ within the service whom they could get in touch with between appointments or group sessions. Many of these SATs also offered some form of informal drop-in service (see Chapter 3). Another, although not offering a named contact, did provide a ‘drop-in’ service, but not necessarily at the outset of joining the service. Findings from our qualitative research with senior SAT practitioners and service users (see Chapters 5 and 6) indicated that having a named contact was an important feature of service delivery in terms of the potential to affect outcomes (and service user experience). We also knew from our interviews with service users that, for some, the opportunity for low-intensity, reactive contact with the service, such as that afforded by a drop-in service, was valued. We, therefore, decided to group these two features into a single service characteristic (drop in provision and/or named contact) and tested for an association with outcomes at the 12-month follow-up. Findings were mixed. There was no evidence of an association between this characteristic and psychological quality of life (WHOQOL-BREF psychological domain). However, there was moderate evidence of an association between not offering drop in provision and/or a named contact and more positive mental health outcomes. This is unexpected and, as already described, runs firmly counter to the shared view of service users and practitioners.
In terms of features of service delivery, there was no evidence that the mode by which SATs typically delivered psychoeducation (group vs. individual) was associated with outcomes. Findings from the economic evaluation similarly conclude that, in terms of cost-effectiveness, there is no strong case for either mode of delivery. Our interviews with service users revealed the different benefits of both modes of delivery (see Chapter 7). For those who found attending groups very difficult, this could act as a significant barrier to take up, an issue perhaps more acute in, but not unique to, autistic adults. 82 At the same time, certain aspects of group delivery were identified by service users as extremely helpful. These included the opportunity to hear others’ experiences (including positive ‘peer role models’) and a reduced sense of isolation. Indeed, these benefits were the rationale given by senior practitioners to use group delivery, but they also noted the importance of having resources available to support, where required, attendance of a group. Finally, we note here that all senior SAT practitioners believed that their psychoeducation was of high quality, a position re-iterated by our qualitative data (see Chapters 6, 7 and 9). It is important to stress, therefore, that this finding should not be generalised to other models of diagnostic provision.
We also found no evidence that routinely offering one-to-one work for (non-complex) mental health problems (as opposed to group-delivered interventions or supported referrals) was associated with mental health outcomes. However, in terms of psychological quality of life, findings from our economic evaluation provide preliminary evidence of the value of SATs providing one-to-one work for non-complex mental health problems. A number of factors may be at play here. First, all SATs sought to refer on to mainstream community mental health services (e.g. IAPT), and one-to-one work with non-complex cases was typically limited in its duration and intensity. Second, all SATs routinely offered at least one (typically) group intervention to improve managing anxiety and psychological resilience. The lack of evidence on their effectiveness, and the effectiveness of generic IAPT interventions for autistic adults without LDs, make it difficult to further specify possible explanations for this finding. Another factor pertinent here may be the positive emotional impact of simply feeling understood (because of the service’s autism expertise) that service users described (see Chapter 7).
Individual characteristics
We found no evidence that referral pathway (D&S vs. SO) was associated with mental health outcomes. In terms of associations between individual characteristics and mental health outcomes at T3, we found moderate evidence of an association between age and mental health quality of life (WHOQOL-BREF psychological domain) at T3, but this was not the case for GHQ-12 scores at T3. In terms of gender, there was moderate evidence that gender (favouring men) was associated with mental health quality of life at T3, with a similar pattern of findings (weak) for GHQ-12 scores. There was also moderate evidence that mental health at T0 (GHQ-12 score) was associated with mental health outcomes at T3.
Three further person-centred factors (all assessed using a categorical indicator) were investigated as predictors of T3 mental health outcomes:
-
contact with autism-specific communities
-
having the information needed to manage everyday life
-
social networks/support.
These factors are all, we would argue, amenable to intervention.
No evidence was found of an association between contact with autism-specific communities (in the previous 4 weeks) and mental health outcomes. We note that this is a very crude indicator of the extent to which individuals were using autism-specific communities as a source of support; small cell counts meant that we could not look at the intensity or nature of those contacts and we asked only about the previous 4 weeks. These limitations may offer some explanation for our finding. At the same time, it is important to refer to observed levels of membership and contacts with an autism-specific group/community (see Chapter 8). At T3, fewer than one in five individuals were members of an autism-specific group/community, and less than one-quarter reported any contact with such an organisation in the previous 4 weeks. Furthermore, our evidence on longer-term outcomes (18- and 24-month follow-up) does not indicate that such support is taken up post discharge (see Chapter 8 and Appendix 12, Tables 53 and 54). At the same time, it is important to note that SAT staff regarded such groups/communities as an important contributor to providing long-term, low-intensity support to autistic adults without LDs (see Chapter 4). This accords with other research,79,83–85 and the NICE guideline recommends SATs work in partnership with such organisations. To our knowledge, however, there have been no studies of their effectiveness, neither could we find any literature on reach and take-up of such provision. 35,68
We found strong evidence of an association (in a positive direction) between perceived availability of information to manage everyday life and T3 mental health outcomes. A recent qualitative review of autistic adults’ experiences of self-determination and quality of life describes the role that information plays in supporting self-determination, and the literature on self-management of long-term conditions also points to its importance. 86,87 However, we do note that this finding should be regarded as a ‘first look’ at this issue. We used a single question from the WHOQOL-BREF as our indicator of satisfaction with availability of information to manage everyday life. This reveals nothing about the type of information and the purposes for which it may be used. However, our descriptive analysis suggests that around half of the study participants reported inadequacies in the availability of information they needed for daily life (see Chapter 8).
Finally, we found strong evidence of an association between perceived availability of social support and mental health outcomes at T3. This is not unexpected; the association between social support/social isolation and depression is well established, although evidence regarding its association with anxiety is more preliminary. 88 Our measure of perceived social support (belonging subscale of ISEL-SF) captured both support from the family and friendship groups. We have already discussed the role of SATs in supporting autistic adults without LDs to make connections with peers. A further role is supporting family understanding of autism and, indeed, one-quarter of our sample reported that the SAT had worked on this concern (see Chapter 8). Our qualitative research with service users revealed that addressing family members’ understanding of autism was a valued element of SAT service provision (see Chapter 6). It was, however, sometimes reported as an unmet need. Findings from our mapping study revealed that care and support of family members was one aspect of provision set out in the NICE guideline that services did not prioritise, often because of resource constraints (see Chapters 3 and 4). However, we know from other research that family members may struggle to accept the diagnosis, with this having a significant negative impact on autistic adults themselves. 80
Comparing outcomes and experiences of the Diagnosis-Only cohort and Diagnosis and Support group
Finally, we compared experiences and outcomes of individuals diagnosed and receiving post-diagnosis support from a SAT (D&S group) with those diagnosed via a national/regional diagnostic assessment service (the DO cohort). We collected two sets of evidence. First, we collected the same outcome data from the DO cohort as for the SAT cohort (see Chapter 8). Second, we interviewed a subsample of the DO cohort and, for some of these, a member of their family (see Chapter 9). We remind the reader here that the DO cohort sample was small, thus findings are initial and exploratory.
We found evidence of a potential difference between the DO cohort and the D&S group in the trajectory of mental health outcomes from baseline to 12-month follow-up. Evidence of a potential deterioration in mental health (GHQ-12 score) in the immediate post-diagnosis period, as observed in the DO cohort, was not seen in the D&S group. No statistically significant change on any of the study’s outcome measures and indicators was observed in the DO cohort between T0 and T3. This contrasts with observed improvements in mental health, ability to manage everyday life and contacts with autism-specific groups/communities found for the D&S group. Our analyses comparing T3 mental health outcomes of the DO cohort with those from the D&S group were underpowered.
The interviews with individuals representing the DO cohort and D&S group revealed, to start, a commonality of experience of the diagnostic assessment process. The majority expected to be diagnosed and experiences of the actual process were typically positive. However, learning the diagnosis triggered a range of emotions. Relief was the typical first response; however, a minority despaired the lifelong nature of the condition. Among those whose initial response had been positive, this soon shifted to a more mixed set of emotions. There was talk of frustration about not being diagnosed earlier and grief for the ‘lost years’. For some, these feelings were still being experienced when our interviews took place (around 6–9 months post diagnosis). Family members’ accounts suggest that such negative emotional experiences, and the investment individuals may place in the diagnostic assessment process, may be hidden from them.
The accounts of the D&S group and the DO cohort interviewees diverged substantially when experiences of post-diagnosis support were discussed. This was clearly located in the significant differences in the quality, duration and intensity of psychoeducational support that they could access post diagnosis. D&S group interviewees spoke highly of post-assessment feedback session(s) and psychoeducation interventions (typically group delivered), and described the impact that these had on them in terms of understanding, (self-) acceptance and a sense of being supported. By contrast, DO cohort interviewees – who within the diagnostic assessment package had a single feedback session and, sometimes, a single group psychoeducation session – described such support as insufficient. The experience of inadequate support was itself a negative experience, with notions of abandonment an evident theme in their accounts.
At the time of our interviews around 6–9 months post diagnosis, all interviewees said that being diagnosed had brought some positive impacts, particularly in terms of self-understanding (something we observed more widely among study participants; see Chapter 6). However, some DO cohort interviewees reported long-standing or unresolved difficulties associated with the diagnosis, and almost all expressed the need for further support with understanding and coming to terms with the diagnosis. A few believed that receiving the diagnosis had subsequently caused a deterioration in their mental health. In all instances, this was attributed to the lack of psychoeducation and other post-diagnostic support.
Previous qualitative and quantitative studies of adults’ experiences of being diagnosed with autism also report relief as a predominant emotional response, and that the diagnosis offered an explanation for their experiences of life. 84,89–92 They too describe the potential range of emotions, both positive and negative, which may be experienced. 79,91,93,94 Similarly, they also report how the diagnosis may facilitate improvements in family relationships and the support received from other services or educational establishments/the workplace. 79,91 Studies that specifically explored immediate post-diagnosis support describe experiences of inadequate support that resulted in unanswered questions and a sense of isolation and dismay. 80,89,90
We believe that our findings make an important, new contribution to the existing, small evidence base. First, by interviewing individuals around 6–9 months post diagnosis, it has been possible to explore medium-term impacts and experiences. Second, we have compared the impact of different post-diagnosis provision on individuals’ and family members’ experiences. This has revealed the negative impacts, which are potentially longstanding, that may occur as a result of inadequate psychoeducation support after diagnosis. It also offers evidence of the wider impacts and benefits associated with being diagnosed within the context of a SAT, which has the potential to address, at least in the short to medium term, (some of) the needs of autistic adults without LDs.
Chapter 12 Conclusions
Summary of findings and implications
Eighteen services in England that fulfilled NICE’s description of a SAT were identified. All had been developed specifically for autistic adults without LDs. Although some had existed before the Autism Act 200929 and subsequent NICE guideline,31 most had been established in response to these. All had been commissioned because of concerns about the lack of access of specialist diagnostic assessments for adults, concerns about the well-being and outcomes of autistic adults without LDs and the absence of any specialist provision for this group. It would appear, however, that the majority of localities in England do not offer this type of provision. That said, the findings from this study suggest that it is possible to develop and provide a service that aligns with the NICE guideline31 and government’s Autism Strategy30 for a multidisciplinary, community-based service for autistic adults (without LDs) and their families, and that also supports other services involved in the care and support of this group. The services identified varied in accordance with a number of service characteristics, and these did not cluster sufficiently for it to be possible to develop a service typology.
Senior practitioners working in SATs strongly believed in the value and unique contribution of their services. The multidisciplinary nature of the service, staffed by practitioners who are specialist in autism, was seen as a critical feature. However, sustaining high-quality care was challenging owing to unanticipated levels of demand (not matched by increased funding), and the lack of other services being willing and available to share the care and support of autistic adults without LDs. Given that SATs are a new type of provision, and with very little evidence and relatively limited clinical experience to draw on, it was, perhaps, unsurprising to find that many services had developed and evolved their provision and ways of working.
Looking forward, and to ensure sustainable care and support for autistic adults without LDs, senior practitioners believed that it would be necessary for their ‘consultative and supervision’ role in mainstream services to be expanded, although this was dependent on the collaboration of mainstream services and with the support of commissioners. In addition, investment was required to allow them to provide specialist, low-intensity, ongoing support (e.g. drop-in services), thus offering long-term continuity of care. There was strong agreement in the value and importance of involving and collaborating with the local autistic community to achieve such provision. Finally, and connected to the notion of low-intensity and long-term support, senior practitioners wanted to be able to invest more in interventions and ways of working that nurtured self-management and self-resilience.
The study collected quantitative and qualitative evaluation data. Findings from the quantitative evaluation demonstrate the wide range of need, health and functioning among those referred to SATs, and this was also observed in the qualitative data. Some people are referred with quite specific needs that are amenable to relatively straightforward interventions. Others are more complex. Evidence from our qualitative study indicates that both can benefit from a SAT, and our quantitative data demonstrates the range of needs and concerns that SATs may address. Findings from our quantitative evaluation indicate that using a SAT may be associated with improved mental health (as indicated by movement from above to below clinical threshold), perceived ability to manage everyday life and, for a minority, increased use of autism-specific groups/communities for support and advice. There was some evidence that these benefits may be sustained into the longer term. However, significant improvements were not observed in our global and health-related quality-of-life measures, and these potential benefits were observed only in those accessing the SAT through the diagnostic assessment pathway (although we note small sample sizes for the SO pathway). Overall, deteriorations in scores on standardised measures were not observed; this may indicate that, for some at least, use of a SAT prevented deteriorations in health and well-being.
The accounts of service users recruited to our qualitative study revealed a range of experiences in terms of the needs that they had when entering the service. For some, the diagnostic assessment and subsequent psychoeducation was sufficient, whereas others had substantial and wide-ranging difficulties. Included in our sample were individuals who believed that using a SAT had resulted in very considerable improvements in their lives. For those whose needs remained unmet or undermet, this was attributed to deficiencies in the duration, intensity, scope and flexibility of the support that the SAT was able to offer. The ability of services to offer, where required, one-to-one work rather than group-delivered interventions, longer-term involvement and less holistic provision were key barriers to meeting need. Taken together, these findings indicate that, as model of care, SATs have the potential to deliver expert, holistic care and support. However, insufficiencies in resource and lack of collaborative working with other services, sometimes reluctant to share involvement in the care of autistic adults without LDs, hinders what can be achieved.
An initial exploration of our quantitative data on the effects of individual and service characteristics on outcomes found strong evidence that richer skill mix was associated with better mental health outcomes and, although evidence is weaker, managed care approaches were more favourable than episodic involvement in delivering care plans. These findings accord with evidence from our interviews with service users, who also stressed the importance of a named contact within the service: something that often co-occurs with managed care. Findings from our economic evaluation show that some of these outcome improvements are achieved at only higher costs, which may prove a challenge to wider implementation; the economic evaluation also suggested that one-to-one work with SAT users with mental health problems could be cost-effective. There was also strong or moderate evidence that different structural models are acceptable for SATs; for example, single or multiple teams involved in service delivery, and locating the provision in autism-specific or neurodevelopmental services. Such evidence is useful to those seeking to develop or re-design such provision.
We found strong evidence of an association between mental health outcomes and quality of social networks and perceived availability of information to manage everyday life. These are both domains in which SATs have the potential to intervene and, to some extent, point to providing social inclusion interventions and drop-in type provision, something for which many SATs had little designated resource. Two further findings from the study are relevant here. First is the relatively minimal engagement of the study sample, even post discharge, with autism-specific third-sector or peer-led groups or organisations, including online communities and forums. Second, among those who took part in our interview study, no one had successfully pursued and used services (including autism-specific groups/communities) that had been ‘signposted’ to them. Indeed, for the majority, no attempts had been made. It is clear that simply providing information, with the expectation that the service user will act on it, is ineffective or insufficient for many individuals. It may be the case that, compared with non-autistic people, autistic people without LDs face additional challenges in pursuing signposts. The presence of mental health difficulties may be a further barrier. Overall, however, very little is understood about what is often a core feature of service provision.
The final element of our evaluation was a small-scale comparison of individuals living outside commissioning boundaries of a SAT, but referred to the SAT for diagnostic assessment only (the DO cohort), with those who had accessed SATs via the diagnostic assessment pathway (the D&S group of our SAT cohort). The very different post-diagnosis experiences and perceived outcomes reported by the two groups point to the fundamental importance of high-quality and extended psychoeducation following diagnosis. It appeared to be the linchpin in the trajectories of the two groups, and serves to illustrate the significance and implications of diagnosing someone with autism.
Implications
The notion of a SAT was developed by the GDG convened by NICE to develop guidance on the diagnosis and management of autism in adults. This was a novel service model and the GDG acknowledged that the research evidence available to support and inform the way that this recommendation was operationalised and implemented was very limited. It called for research that would help to define those aspects of service organisation and delivery that best support positive outcomes. This was the primary objective of this study.
This study has shown that it is possible to set up such a service. However, very few localities have been able to achieve this. Findings support the notion of SATs and have demonstrated the benefits and positive impacts they can achieve; however, they need to be sufficiently resourced. Importantly, our findings suggest that different organisational structures are possible, including different approaches to integrating health and social care into a single provision (e.g. jointly commissioned vs. separate teams with joint-working arrangements).
The National Institute for Health and Care Excellence called for evidence on what a SAT should look like in terms of staffing and the interventions that it should provide. Autism-specific expertise, interventions and adjustments to service provision were identified as critical to the achievement of positive changes in people’s lives. With respect to staffing, overall, our findings support a diversity of professions (or rich skill mix) within the service and a holistic, individualised approach to care and support. In terms of interventions, we believe that the findings make a strong case for extended post-diagnosis psychoeducation, and interventions and practice that nurture self-management with respect to mental health, managing day-to-day life and strengthening social networks. This should include the provision of low-intensity, drop-in-type advice and support after discharge. There is some limited evidence indicating that it may be cost-effective for SATs to deliver one-to-one mental health interventions in service, rather than supporting referrals to, for example, IAPT.
The great majority of those referred to SATs have mental health needs and addressing these is fundamental to achieving positive changes in other life domains. Some SATs operated on a model whereby non-complex mental health problems (or those not directly arising from autism diagnosis) were managed by referring on to generic community mental health services. However, such referrals (i.e. handover, assessment and intervention) need to be supported by the SAT, with that support being available to both the individual and the receiving service. To make this work, commissioning arrangements need to include sufficient resource for SATs to be able to do this and for mainstream services to be required (and sufficiently resourced) to accept such referrals. The same argument applies to other statutory services.
Findings from this study do not support the use of signposting (i.e. simply providing information about another statutory or third-sector service, or community support group/network). Given that autistic adults may encounter additional barriers to initiating an approach to a new organisation, any service working with autistic people should consider reviewing its use of signposting. In addition, services should not assume that peer-led/autism-community organisations and networks, or support groups/networks run by autism charities, are widely used or replace specialist autism services providing or being available for advice and support on a longer-term basis to autistic adults living in their locality.
Finally, and aligning with existing evidence, findings from this study raise significant concerns about the insufficiency or lack of post-diagnosis psychoeducation provided by services that offer only diagnostic assessment.
Research recommendations
Research concerning the lives, care and support of autistic adults without LDs is newly emerging but burgeoning. As has been noted elsewhere,95 investment at this early stage in the development of a core outcome set, in partnership with autistic adults without LDs, would help to ensure the best return on that investment. This may require the development of new measures or adaptation of existing ones. 96
Based on the findings of this study, and to further develop the evidence-base required by commissioners and professionals with responsibility for the care and support of autistic adults, we make the following recommendations for future research:
-
Informed by and drawing on the findings of this study, a large-scale, mixed-methods observational study comparing the effectiveness and cost-effectiveness of SAT provision with diagnostic assessment-only provision, and including family members’ outcomes. This would generate further, and more definitive, evaluation evidence and allow further, more complex, exploration into service design/delivery characteristics associated with outcomes.
-
Identification and evaluation of approaches to SATs providing a ‘consultation and supervision’ function to mainstream services involved in the care and support of autistic adults without LDs.
-
Identification, description and evaluation of approaches to provide low-intensity, long-term specialist autism support to autistic adults without LDs.
-
Studies that develop the evidence base on existing ‘manualised’ interventions being delivered by SATs, such as psychoeducational and self-management interventions should be designed to answer the questions: what works for whom and under what circumstances?
-
Work to identify and describe the information needs that enable autistic adults without LDs to manage everyday life and how these needs can be best met.
-
Research that furthers our understanding of how autistic people without LDs respond to and use signposting and ways to improve the impact of signposting.
Acknowledgements
Dr Tom Berney was a co-applicant and provided clinical supervision to the research team. We are grateful for his input and insights.
The National Autistic Society was a co-applicant and supported the patient and public involvement work, development and execution of the dissemination and impact strategy. In particular, we acknowledge the support and contributions of Carol Povey, Tom Madders and Tim Nicholls.
The research would like to thank the PAG for their support and commitment to this project. Their insights and contributions were invaluable.
We also thank the Study Steering Committee, chaired by Professor Richard Hastings, for their advice, input and support.
We also thank Teresa Frank for the administrative support she provided across the course of the project, and for the administrative support provided by Emily Dunn and Karen Overend.
We also acknowledge the work and contribution of Dr Wendy Mitchell to stage 1 of the project and establishing the PAG.
Contributions of authors
Bryony Beresford (https://orcid.org/0000-0003-0716-2902) (Professor, Health and Social Care Services Research) was the lead applicant and principal investigator. She oversaw delivery of the project, led all aspects of the work (except the economic evaluation), and supervised the research team, except the health economist team.
Suzanne Mukherjee (https://orcid.org/0000-0002-9012-0369) (Research Fellow) contributed to stage 1 data collection and analysis, recruitment of stage 2 research sites and study set-up, and qualitative research with SAT practitioners. She also led the second iteration of qualitative data analysis and write-up of all qualitative elements, and supported work with the PAG.
Emese Mayhew (https://orcid.org/0000-0002-6024-8273) (Research Fellow) was responsible for research administration databases and support to study administrators, oversaw data management and conducted quantitative analyses.
Emily Heavey (https://orcid.org/0000-0003-0920-7705) (Research Fellow) carried out all qualitative data collection (service users, family members), developed analytical framework, coded all data and contributed to write-up of qualitative data.
A-La Park (https://orcid.org/0000-0002-4704-4874) (Assistant Professorial Research Fellow) worked on data collection and analysis for economic evaluation.
Lucy Stuttard (https://orcid.org/0000-0001-7205-7151) (Research Fellow) contributed to stage 1 data collection and analysis, recruitment of stage 2 research sites and study set-up, oversaw early stages of outcomes data collection and data management processes, and supported work with the PAG.
Victoria Allgar (https://orcid.org/0000-0002-5228-2623) (Senior Research Fellow, Statistics) was a co-applicant. She oversaw the statistical analysis of outcomes evaluation and supervised researchers working on quantitative analyses.
Martin Knapp (https://orcid.org/0000-0003-1427-0215) (Professor, Health and Social Care Policy) was a co-applicant. He led all aspects of the economic evaluation and supervised the researchers working on the economic evaluation.
Publication
Mayhew E, Stuttard L, Beresford B. Assessment of the psychometric properties of the GHQ-12 in an English population of autistic adults without learning difficulties [published online ahead of print 11 July 2020]. J Autism Dev Disord 2020.
Data-sharing statement
Available data have been included in the appendices. Any queries or data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Autistica . What Is Autism 2019. www.autistica.org.uk (accessed 24 February 2020).
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders (DSM-5) 2013. www.psychiatry.org/psychiatrists/practice/dsm (accessed 24 February 2020).
- Brugha TS, McManus S, Bankart J, Scott F, Purdon S, Smith J, et al. Epidemiology of autism spectrum disorders in adults in the community in England. Arch Gen Psychiatry 2011;68:459-65. https://doi.org/10.1001/archgenpsychiatry.2011.38.
- National Autistic Society . Review of Implementation of the Autism Strategy 2013.
- National Collaborating Centre for Mental Health . Autism: Recognition, Referral, Diagnosis, and Management of Adults on the Autism Spectrum. National Clinical Guideline Number 142 2012. www.ncbi.nlm.nih.gov/books/NBK299070/ (accessed 24 February 2020).
- Buck TR, Viskochil J, Farley M, Coon H, McMahon WM, Morgan J, et al. Psychiatric comorbidity and medication use in adults with autism spectrum disorder. J Autism Dev Disord 2014;44:3063-71. https://doi.org/10.1007/s10803-014-2170-2.
- Croen LA, Zerbo O, Qian Y, Massolo ML, Rich S, Sidney S, et al. The health status of adults on the autism spectrum. Autism 2015;19:814-23. https://doi.org/10.1177/1362361315577517.
- Gillberg IC, Helles A, Billstedt E, Gillberg C. Boys with Asperger syndrome grow up: psychiatric and neurodevelopmental disorders 20 years after initial diagnosis. J Autism Dev Disord 2016;46:74-82. https://doi.org/10.1007/s10803-015-2544-0.
- Hofvander B, Delorme R, Chaste P, Nydén A, Wentz E, Ståhlberg O, et al. Psychiatric and psychosocial problems in adults with normal-intelligence autism spectrum disorders. BMC Psychiatry 2009;9. https://doi.org/10.1186/1471-244X-9-35.
- Joshi G, Wozniak J, Petty C, Martelon MK, Fried R, Bolfek A, et al. Psychiatric comorbidity and functioning in a clinically referred population of adults with autism spectrum disorders: a comparative study. J Autism Dev Disord 2013;43:1314-25. https://doi.org/10.1007/s10803-012-1679-5.
- Lugnegård T, Hallerbäck MU, Gillberg C. Psychiatric comorbidity in young adults with a clinical diagnosis of Asperger syndrome. Res Dev Disabil 2011;32:1910-17. https://doi.org/10.1016/j.ridd.2011.03.025.
- Huang AX, Wheeler JJ. High-functional autism: an overview of characteristics and related issues. Int J Spec Educ 2006;21.
- NHS Digital . Autism Spectrum Disorders in Adults Living in Households Throughout England 2009.
- Howlin P, Mawhood L, Rutter M. Autism and developmental receptive language disorder – a follow-up comparison in early adult life. II: social, behavioural, and psychiatric outcomes. J Child Psychol Psychiatry 2000;41:561-78. https://doi.org/10.1111/1469-7610.00643.
- Howlin P, Alcock J, Burkin C. An 8 year follow-up of a specialist supported employment service for high-ability adults with autism or Asperger syndrome. Autism 2005;9:533-49. https://doi.org/10.1177/1362361305057871.
- Barnard J, Harvey V, David P, Prior A. Ignored or Ineligible? The Reality for Adults with Autism Spectrum Disorders. London: National Autistic Society; 2001.
- Hurlbutt K, Chalmers L. Adults with autism speak out: perceptions of their life experiences. Focus Autism Other Dev Disabil 2016;17:103-11. https://doi.org/10.1177/10883576020170020501.
- Jennes-Coussens M, Magill-Evans J, Koning C. The quality of life of young men with Asperger syndrome: a brief report. Autism 2006;10:403-14. https://doi.org/10.1177/1362361306064432.
- Howlin P, Goode S, Hutton J, Rutter M. Adult outcome for children with autism. J Child Psychol Psychiatry 2004;45:212-29. https://doi.org/10.1111/j.1469-7610.2004.00215.x.
- Knapp M, Romeo R, Beecham J. The Economic Consequences of Autism in the UK. London: Mental Health Foundation; 2007.
- Kirby AV, Bakian AV, Zhang Y, Bilder DA, Keeshin BR, Coon H. A 20-year study of suicide death in a statewide autism population. Autism Res 2019;12:658-66. https://doi.org/10.1002/aur.2076.
- Richa S, Fahed M, Khoury E, Mishara B. Suicide in autism spectrum disorders. Arch Suicide Res 2014;18:327-39. https://doi.org/10.1080/13811118.2013.824834.
- Maddox BB, Gaus VL. Community mental health services for autistic adults: good news and bad news. Autism Adulthood 2019;1:15-9. https://doi.org/10.1089/aut.2018.0006.
- Grootscholten IAC, van Wijngaarden B, Kan CC. High functioning autism spectrum disorders in adults: consequences for primary caregivers compared to schizophrenia and depression. J Autism Dev Disord 2018;48:1920-31. https://doi.org/10.1007/s10803-017-3445-1.
- Camm-Crosbie L, Bradley L, Shaw R, Baron-Cohen S, Cassidy S. ‘People like me don’t get support’: autistic adults’ experiences of support and treatment for mental health difficulties, self-injury and suicidality. Autism 2018;23:1431-41. https://doi.org/10.1177/1362361318816053.
- Crane L, Adams F, Harper G, Welch J, Pellicano E. ‘Something needs to change’: Mental health experiences of young autistic adults in England. Autism 2019;23:477-93. https://doi.org/10.1177/1362361318757048.
- Murphy CM, Wilson CE, Robertson DM, Ecker C, Daly EM, Hammond N, et al. Autism spectrum disorder in adults: diagnosis, management, and health services development. Neuropsychiatr Dis Treat 2016;12:1669-86. https://doi.org/10.2147/NDT.S65455.
- Clark F, Scharasschkin A, Xu D. Supporting People with Autism Through Adulthood. Model to Assess the Financial Impacts of Providing Multi-disciplinary Support Services for Adults with High-functioning Autism/Asperger Syndrome. London: National Audit Office; 2009.
- Great Britain . Autism Act 2009 2009. www.legislation.gov.uk/ukpga/2009/15/contents (accessed 14 October 2020).
- Department of Health and Social Care (DHSC) . Fulfilling and Rewarding Lives: The Strategy for Adults With Autism in England 2010. https://webarchive.nationalarchives.gov.uk/20130104203954/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_113369 (accessed 14 October 2020).
- National Institute for Health and Care Excellence (NICE) . Autism Spectrum Disorder in Adults: Diagnosis and Management. Clinical Guideline 142 2012. www.nice.org.uk/guidance/cg142 (accessed 24 February 2020).
- National Institute for Health and Care Excellence (NICE) . Autism in Adults. Evidence Update May 2014. A Summary of Selected New Evidence Relevant to NICE Clinical Guideline 142 ‘Autism: Recognition, Referral, Diagnosis and Management of Adults on the Autism Spectrum’ (2012) 2014. https://arms.evidence.nhs.uk/resources/hub/1035112/attachment (accessed 24 February 2020).
- Department of Health and Social Care (DHSC) . Think Autism. Fulfilling and Rewarding Lives, the Strategy for Adults With Autism in England: An Update 2014. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/299866/Autism_Strategy.pdf (accessed 24 February 2020).
- National Institute for Health and Care Excellence (NICE) . Common Mental Health Problems: Identification and Pathways to Care. Clinical Guideline CG123 2011.
- Lorenc T, Rodgers M, Rees R, Wright K, Melton H, Sowden A. Preventative Co-Ordinated Low-Level Support for Adults With High-Functioning Autism. Systematic Review and Service Mapping 2016. https://eppi.ioe.ac.uk/CMS/Portals/0/PDF%20reviews%20and%20summaries/Autism%20support%202016%20Lorenc%20report.pdf (accessed 24 February 2020).
- National Autistic Taskforce . National Autism Project – The Autism Dividend – Reaping the Rewards of Better Investment 2017. http://nationalautismproject.org.uk/wp-content/uploads/2017/01/autism-dividend-report.pdf (accessed 24 February 2020).
- Autistica . A Review of the Autism Research Funding Landscape in the United Kingdom 2018. www.autistica.org.uk/downloads/files/Autistica-Scoping-Report.pdf (accessed 24 February 2020).
- Pellicano E, Dinsmore A, Charman T. What should autism research focus upon? Community views and priorities from the United Kingdom. Autism 2014;18:756-70. https://doi.org/10.1177/1362361314529627.
- Public Health England (PHE) . Autism Self-Assessment Framework 2014 – Results 2014. http://webarchive.nationalarchives.gov.uk/20160704150527/http://www.improvinghealthandlives.org.uk/projects/autsaf2014results (accessed 14 October 2020).
- Assarroudi A, Heshmati Nabavi F, Armat MR, Ebadi A, Vaismoradi M. Directed qualitative content analysis: the description and elaboration of its underpinning methods and data analysis process. J Res Nurs 2018;23:42-55. https://doi.org/10.1177/1744987117741667.
- Leekman SR, Libby SJ, Wing L, Gould J, Taylor C. The Diagnostic Interview for Social and Communication Disorders: algorithms for ICD-10 childhood autism and Wing and Gould autistic spectrum disorder. J Child Psychol Psychiatry 2002;43:327-42. https://doi.org/10.1111/1469-7610.00024.
- Parker G, Spiers G, Cusworth L, Birks Y, Gridley K, Mukherjee S. Care closer to home for children and young people who are ill: developing and testing a model of service delivery and organization. J Adv Nurs 2012;68:2034-46. https://doi.org/10.1111/j.1365-2648.2011.05893.x.
- Lord C, Rutter M, le Couteur A. Autism Diagnostic Interview-Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J Autism Dev Disord 1994;24:659-85. https://doi.org/10.1007/BF02172145.
- Lord C, Risi S, Lambrecht L, Cook EH, Leventhal BL, DiLavore PC, et al. The Autism Diagnostic Observation Schedule–Generic: a standard measure of social and communication deficits associated with the spectrum of autism. J Autism Dev Disord 2000;30:205-23. https://doi.org/10.1023/A:1005592401947.
- Wigham SIB, LeCouteur A, Berney T, Wilson C, Petrou A, Ensum I, et al. Manuscript in preparation. Newcastle University; 2019.
- World Health Organization (WHO) . The World Health Organization Quality of Life (WHOQOL)- BREF 2004.
- Goldberg DP. General Health Questionnaire. London: GL Assessment Ltd; 1992.
- EuroQol Group . EuroQol - a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208. https://doi.org/https://doi.org/10.1016/0168-8510(90)90421-9.
- Janssen MF, Pickard AS, Golicki D, Gudex C, Niewada M, Scalone L, et al. Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: a multi-country study. Qual Life Res 2013;22:1717-27. https://doi.org/10.1007/s11136-012-0322-4.
- Cohen S, Hoberman HM. Positive events and social supports as buffers of life change stress. J App Soc Psychol 1983;13:99-125. https://doi.org/10.1111/j.1559-1816.1983.tb02325.x.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2018. Canterbury: Personal Social Services Research Unit, University of Kent; 2018.
- NHS Improvement . 2017/18/Reference/Costs/and/Guidance 2018. https://improvement.nhs.uk/resources/reference-costs/ (accessed October 2020).
- GOV.UK . National Minimum Wage and National Living Wage Rates n.d. www.gov.uk/national-minimum-wage-rates (accessed 14 October 2020).
- NHS . Online Version of the The NHS Long Term Plan 2019. www.longtermplan.nhs.uk/online-version/ (accessed 24 February 2020).
- Howlin P, Taylor JL. Addressing the need for high quality research on autism in adulthood. Autism 2015;19:771-3. https://doi.org/10.1177/1362361315595582.
- Herrema R, Garland D, Osborne M, Freeston M, Honey E, Rodgers J. Mental wellbeing of family members of autistic adults. J Autism Dev Disord 2017;47:3589-99. https://doi.org/10.1007/s10803-017-3269-z.
- Wigham S, Rodgers J, Berney T, Le Couteur A, Ingham B, Parr JR. Psychometric properties of questionnaires and diagnostic measures for autism spectrum disorders in adults: a systematic review. Autism 2019;23:287-305. https://doi.org/10.1177/1362361317748245.
- Public Health England . Autism Self-Assessment Exercise 2016. Detailed Report and Thematic Analyses 2017. https://dera.ioe.ac.uk/29444/1/Autism_self_assessment_framework_2016_report.pdf (accessed 24 February 2020).
- Rodgers J, Ofield A. Understanding, recognising and treating co-occurring anxiety in autism. Curr Dev Disord Rep 2018;5:58-64. https://doi.org/10.1007/s40474-018-0132-7.
- Pallathra AA, Cordero L, Wong K, Brodkin ES. Psychosocial interventions targeting social functioning in adults on the autism spectrum: a literature review. Curr Psychiatry Rep 2019;21. https://doi.org/10.1007/s11920-019-0989-0.
- Spain D, Blainey SH. Group social skills interventions for adults with high-functioning autism spectrum disorders: a systematic review. Autism 2015;19:874-86. https://doi.org/10.1177/1362361315587659.
- Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. BMJ 1996;312:71-2. https://doi.org/10.1136/bmj.312.7023.71.
- Carr VL, Sangiorgi D, Büscher M, Junginger S, Cooper R. Integrating evidence-based design and experience-based approaches in healthcare service design. HERD 2011;4:12-33. https://doi.org/10.1177/193758671100400403.
- Iacobucci G. Budget cuts force local councils into ‘narrow’ focus on social care, warns watchdog. BMJ 2018;360. https://doi.org/10.1136/bmj.k1113.
- Russ V, Kovshoff H, Brown T, Abbott P, Hadwin JA. Exploring the role of empathy in understanding the social-cognitive profile for individuals referred for autism spectrum disorders assessment in adulthood [published online ahead of print July 26 2018]. J Autism Dev Disord 2018. https://doi.org/10.1007/s10803-018-3693-8.
- The Health Foundation . Helping People Help Themselves. A Review of the Evidence Considering Whether It Is Worthwhile to Support Self-Management 2011. www.health.org.uk/sites/default/files/HelpingPeopleHelpThemselves.pdf (accessed 24 February 2020).
- Taylor SJC, Pinnock H, Epiphaniou E. A rapid synthesis of the evidence on interventions supporting self-management for people with long-term conditions. Health Serv Deliv Res 2014;2. https://doi.org/10.3310/hsdr02530 (accessed 24 February 2020).
- Lorenc T, Rodgers M, Marshall D, Melton H, Rees R, Wright K, et al. Support for adults with autism spectrum disorder without intellectual impairment: systematic review. Autism 2018;22:654-68. https://doi.org/10.1177/1362361317698939.
- Khanna R, Jariwala-Parikh K, West-Strum D, Mahabaleshwarkar R. Health-related quality of life and its determinants among adults with autism. Res Autism Spectr Disord 2014;8:157-67. https://doi.org/10.1016/j.rasd.2013.11.003.
- Skevington SM, McCrate FM. Expecting a good quality of life in health: assessing people with diverse diseases and conditions using the WHOQOL-BREF. Health Expect 2012;15:49-62. https://doi.org/10.1111/j.1369-7625.2010.00650.x.
- Mason D, McConachie H, Garland D, Petrou A, Rodgers J, Parr JR. Predictors of quality of life for autistic adults. Autism Res 2018;11:1138-47. https://doi.org/10.1002/aur.1965.
- Moss P, Howlin P, Savage S, Bolton P, Rutter M. Self and informant reports of mental health difficulties among adults with autism findings from a long-term follow-up study. Autism 2015;19:832-41. https://doi.org/10.1177/1362361315585916.
- Picardi A, Fagnani C, Medda E, Toccaceli V, Brambilla P, Stazi MA. Genetic and environmental influences underlying the relationship between autistic traits and temperament and character dimensions in adulthood. Compr Psychiatry 2015;58:178-88. https://doi.org/10.1016/j.comppsych.2014.12.018.
- Janssen MF, Szende A, Cabases J, Ramos-Goñi JM, Vilagut G, König HH. Population norms for the EQ-5D-3L: a cross-country analysis of population surveys for 20 countries. Eur J Health Econ 2019;20:205-16. https://doi.org/10.1007/s10198-018-0955-5.
- Coleman-Fountain E, Beresford B, Thomas W, Hujala A, Laulainen S, McMurray R. The Management of Wicked Problems in Health and Social Care: An International Text. Abingdon: Routledge; 2018.
- Cage E, Di Monaco J, Newell V. Experiences of autism acceptance and mental health in autistic adults. J Autism Dev Disord 2018;48:473-84. https://doi.org/10.1007/s10803-017-3342-7.
- Kapp SK, Gillespie-Lynch K, Sherman LE, Hutman T. Deficit, difference, or both? Autism and neurodiversity. Dev Psychol 2013;49:59-71. https://doi.org/10.1037/a0028353.
- Cooper K, Smith LGE, Russell A. Social identity, self-esteem, and mental health in autism. Eur J Soc Psychol 2017;47:844-54. https://doi.org/10.1002/ejsp.2297.
- Hickey A, Crabtree J, Stott J. ‘Suddenly the first fifty years of my life made sense’: experiences of older people with autism. Autism 2018;22:357-67. https://doi.org/10.1177/1362361316680914.
- Crane L, Batty R, Adeyinka H, Goddard L, Henry LA, Hill EL. Autism diagnosis in the United Kingdom: perspectives of autistic adults, parents and professionals. J Autism Dev Disord 2018;48:3761-72. https://doi.org/10.1007/s10803-018-3639-1.
- Lawes A, Marcus E, Pilling S. What Staffing Structures of Mental Health Services are Associated with Improved Patient Outcomes? A Rapid Review. London: National Collaborating Centre for Mental Health; 2017.
- Dombrowski SU, O’Carroll RE, Williams B. Form of delivery as a key ‘active ingredient’ in behaviour change interventions. Br J Health Psychol 2016;21:733-40. https://doi.org/10.1111/bjhp.12203.
- Southby K, Robinson O. Information, advocacy and signposting as a low-level support for adults with high-functioning autism spectrum disorder: an example from the UK. J Autism Dev Disord 2018;48:511-19. https://doi.org/10.1007/s10803-017-3331-x.
- Lewis LF. Realizing a diagnosis of autism spectrum disorder as an adult. Int J Ment Health Nurs 2016;25:346-54. https://doi.org/10.1111/inm.12200.
- Müller E, Schuler A, Yates GB. Social challenges and supports from the perspective of individuals with Asperger syndrome and other autism spectrum disabilities. Autism 2008;12:173-90. https://doi.org/10.1177/1362361307086664.
- Kim SY. The experiences of adults with autism spectrum disorder: self-determination and quality of life. Res Autism Spectr Disord 2019;60:1-15. https://doi.org/10.1016/j.rasd.2018.12.002.
- Panagioti M, Richardson G, Small N, Murray E, Rogers A, Kennedy A, et al. Self-management support interventions to reduce health care utilisation without compromising outcomes: a systematic review and meta-analysis. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-356.
- Wang J, Mann F, Lloyd-Evans B, Ma R, Johnson S. Associations between loneliness and perceived social support and outcomes of mental health problems: a systematic review. BMC Psychiatry 2018;18. https://doi.org/10.1186/s12888-018-1736-5.
- Lewis LF. Exploring the experience of self-diagnosis of autism spectrum disorder in adults. Arch Psychiatr Nurs 2016;30:575-80. https://doi.org/10.1016/j.apnu.2016.03.009.
- Jones L, Goddard L, Hill EL, Henry LA, Crane L. Experiences of receiving a diagnosis of autism spectrum disorder: a survey of adults in the United kingdom. J Autism Dev Disord 2014;44:3033-44. https://doi.org/10.1007/s10803-014-2161-3.
- Powell T, Acker L. Adults’ experience of an Asperger syndrome diagnosis: analysis of its emotional meaning and effect on participants’ lives. Focus Autism Other Dev Disabil 2015;31:72-80. https://doi.org/10.1177/1088357615588516.
- Huws JC, Jones RS. Diagnosis, disclosure, and having autism: an interpretative phenomenological analysis of the perceptions of young people with autism. J Intellect Dev Disabil 2008;33:99-107. https://doi.org/10.1080/13668250802010394.
- Jones RSP, Quigney C, Huws JC. First-hand accounts of sensory perceptual experiences in autism: a qualitative analysis. J Intellect Dev Disabil 2009;28:112-21. https://doi.org/10.1080/1366825031000147058.
- Punshon C, Skirrow P, Murphy G. The ‘not guilty verdict’: psychological reactions to a diagnosis of Asperger syndrome in adulthood. Autism 2009;13:265-83. https://doi.org/10.1177/1362361309103795.
- Brugha TS, Doos L, Tempier A, Einfeld S, Howlin P. Outcome measures in intervention trials for adults with autism spectrum disorders; a systematic review of assessments of core autism features and associated emotional and behavioural problems. Int J Methods Psychiatr Res 2015;24:99-115. https://doi.org/10.1002/mpr.1466.
- McConachie H, Mason D, Parr JR, Garland D, Wilson C, Rodgers J. Enhancing the validity of a quality of life measure for autistic people. J Autism Dev Disord 2018;48:1596-611. https://doi.org/10.1007/s10803-017-3402-z.
- Bibby P, Brindley P. 2011 Rural–urban Classification of Local Authority Districts and Similar Geographic Units in England: A User Guide (Revised January 2017). London: Office for National Statistics; 2017.
- Ministry of Housing, Communities and Local Government . English Indices of Deprivation 2015 2015.
- Miles MB, Huerman AM, Saldana J. Qualitative Data Analysis: A Methods Sourcebook. Thousand Oaks, CA: SAGE Publications Ltd; 2013.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-117.
- Boeije H. A purposeful approach to the constant comparative method in the analysis of qualitative interviews. Qual Quant 2002;36:391-409. https://doi.org/10.1023/a: 1020909529486.
- Kamio Y, Inada N, Koyama T. A nationwide survey on quality of life and associated factors of adults with high-functioning autism spectrum disorders. Autism 2013;17:15-26. https://doi.org/10.1177/1362361312436848.
- Payne TJ, Andrew M, Butler KR, Wyatt SB, Dubbert PM, Mosley TH. Psychometric evaluation of the interpersonal support evaluation list–short form in the aric study cohort. SAGE 2012;2. https://doi.org/10.1177/2158244012461923.
Appendix 1 Chapter 3 tables
| Site ID | Sociodemographic and population characteristics | Size of area (mile2) | |||
|---|---|---|---|---|---|
| Approximate adult population in locality served by SAT | Number of LAs co-terminus with CCG | Relative deprivationa | Rural–urban classification97 | ||
| A | 377,500 | 1 | 4/152 | Urban with major conurbation | 44 |
| B | 219,500 | 1 | 60/152 | Urban with major conurbation | 59 |
| CA | 243,000 | 1 | 8/152 | Urban with minor conurbation | 29 |
| D | 212, 000 | 1 | 40/152 | Urban with major conurbation | 54 |
| E | 175,000 | 1 | 120/152 | Urban with major conurbation | 41 |
| F | 605,000 | 3 | 78/152 | Includes mainly rural with hub towns, urban with significant rural and urban with city and towns | 832 |
| 121/152 | |||||
| 128/152 | |||||
| H | 126,500 | 1 | 144/152 | Urban with major conurbation | 15 |
| IA | 439,500 | 1 | 48/152 | Urban with minor conurbation | 142 |
| J | 199,000 | 1 | 9/152 | Urban with major conurbation | 8 |
| Site ID | Clinical lead | Clinical psychologist | Psychiatrist | Social worker | Occupational therapist | Speech and Language Therapist | Nurse consultant | Mental health nurse | Autism support workera | Autism clinical specialistb | Assistant psychologist |
|---|---|---|---|---|---|---|---|---|---|---|---|
| A | Clinical psychologist | 8 | 0 | 0 | 0 | 0 | 0 | 20 | 26 | 10 | 0 |
| B | Clinical psychologist | 2 | 0 | 0 | 0 | 0 | 0 | 10 | 0 | 0 | 10 |
| CA | Autism nurse consultant | 16 | 2 | 0 | 0 | 12 | 10 | 2 | 6 | 0 | 10 |
| D | Clinical psychologist | 4 | 2 | 0 | 10 | 0 | 0 | 0 | 10 | 0 | 6 |
| E | Clinical psychologist | Yesc | Yesc | 0 | 0 | Yesc | 0 | Yesc | Yesc | 0 | Yesc |
| F | Clinical psychologist | 19 | 0.25 | 5d | 5e | 0 | 0 | 4d | 0 | 0 | 12 |
| Haf | Clinical psychologist | Yesc | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Hbf | Autism clinical specialist | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 15 | 0 |
| IA | Clinical psychologist | Yesc | Yesc | 10 | 4 | 8 | 0 | 4 | 0 | 0 | 0 |
| J | Psychiatrist | 4 | 7 | 5 | 10 | 3 | 0 | 0 | As requiredg | 0 | 0 |
| Site ID | Description of provision for carers | Partnerships with third-sector organisations |
|---|---|---|
| A | Signpost to carers’ organisations | Able to signpost to active local autism carers group(s) |
| B | Signpost to carers’ organisations | Able to signpost to active local autism carers group(s) |
| CA | Described as ‘integral to the service’; may attend one-to-one sessions with service user (joint interventions) | Able to signpost to active local and regional autism carers group(s) |
| D | Two psychoeducation sessions post diagnosis | Able to signpost to active local and regional autism carers groups |
| E | Two psychoeducation sessions post diagnosis | Able to signpost to active local and regional autism carers groups |
| F | Able to contact service for requests with signposting and advice, if appropriate, contacts are discussed by the team | Able to signpost to active local autism carers group(s) |
| Ha | Offer three psychoeducational sessions for families/carers post diagnosis | Able to signpost to active local autism carers group(s) |
| Hb | Do not formally offer support but will provide informal support/advice if appropriate and service user agrees | |
| IAa | Offer a support group led by psychologist for a fixed number of sessions. Predominantly attended by parents | Able to signpost to active local autism carers group(s) |
| J | Six weekly carers events. Have speakers plus time to chat/raise issues. Predominantly attended by parents | No active local autism carers group(s) |
| Site ID | Training for specific services | Joint working | Routine advisory service | Public awareness activities |
|---|---|---|---|---|
| A | Monthly awareness training sessions across trust | Advise services/professionals on a case-by-case basis regarding autism-specific adjustments | No | Not reported |
| B | Monthly awareness training sessions across trust | Advise services/professionals on a case-by-case basis regarding autism-specific adjustments | No | Not reported |
| CA | One-off and rolling training programmes to statutory agencies (NHS, LA, police and prison service) and private sector organisations | Advise services/professionals on a case-by-case basis regarding autism-specific adjustments | No | Contribute to community awareness raising activities |
| D | Runs training for CMHT | Not routinely provided | No | Not reported |
| E | One-off and rolling training programmes to statutory agencies (e.g. NHS, LA, police and prison service) | Advise services/professionals on a case-by-case basis regarding autism-specific adjustments | No | Not reported |
| F | Deliver training to psychiatrists on diagnosing autism | Advise services/professionals on a case-by-case basis regarding autism-specific adjustments | Each week, two 30-minute consultation appointments available for booking by teams/professionals in statutory services | Not reported |
| H(a and b) | Run training workshops on request. Wide range of agencies (e.g. police, adult education, CMHT and social care) | Advise services/professionals on case-by-case basis regarding autism-specific adjustments | No | Not reported |
| IAa | Rolling programme of 1 day’s introduction to autism training open to all LA and trust staff. Provide bespoke training to statutory and private organisations | Advise to services/professionals on a case-by-case basis regarding autism-specific adjustments | No | Monthly public seminar for autistic people and family members |
| J | One-off and rolling training programmes to statutory agencies (NHS, LA, police and prison service) and other organisations (e.g. businesses) | Advise services/professionals on a case-by-case basis regarding autism-specific adjustments | No | Run awareness-raising events |
Appendix 2 The nested qualitative study with senior practitioners
Study objectives
The objectives of the nested qualitative study of senior practitioners’ views and experiences were as follows to:
-
understand and describe the implementation and delivery of SAT-type provision
-
identify and describe the external and within-service factors that support or hinder the operation of the service and the quality of care and support provided
-
explore and report senior practitioners’ cumulative experiences of providing care and support to autistic adults without LDs
-
secure senior practitioners’ views on the factors that affect the impact of their services on individuals’ lives
-
explore views regarding aspects of service organisation and delivery (within SATs and across the wider service context) that support the development of sustainable long-term care for autistic adults without LDs, and experiences of implementing such approaches.
Findings from this nested study are reported in Chapters 3–5.
Methods
Data were collecting using:
-
Individual telephone interviews with one practitioner (or a joint interview with up to three senior practitioners) in each research site. This was followed up, where required, with e-mail conversation to address missing information or points of clarification.
-
An overnight workshop to which all sites were invited. The workshop schedule is presented in Table 28 and participant details in Table 29.
Interviews and workshop discussions were audio-recorded and verbatim transcripts were created. Qualitative content analysis and thematic analysis were used to analyse the data. Thematic frameworks are set out in Box 4, with data coded using this framework. Analytical writing and mind mapping were used to map and explore the interconnections between the themes and the structure of the presentation of the data.
| 8.45 | Taxis from hotel |
| 9.00 | Arrive: tea/coffee available |
| 9.15 | Introductions, housekeeping and plan for the day |
| 9.25 |
Overview of the SHAPE project: objectives, impact and current progress (Presentation by research team) |
| 9.45 |
Overview of findings from national mapping exercise (Presentation by research team) |
| 10.05 |
Introducing each service: the speed-dating way (Each service gives a 4-minute presentation about its service) |
| 10.45 |
Reflection on current approaches to delivering ‘Specialist Autism Team’ provision (Whole-group discussion) |
| 11.00 | Coffee and cakes |
| 11.30 |
Experiences of delivering a ‘Specialist Autism Team’ service: what helps and hinders you meeting your objectives? (Small group work and feedback) |
| 12.15 |
What works and for whom? (Small-group work and whole-group discussion) |
| 1.00 | Lunch |
| 1.45 |
Dos and do nots: learnings about autism-specific practice (Individual tasks and whole-group discussion) |
| 2.30 |
Involving adults with autism in research: learnings from the SHAPE project (Presentation by research team) |
| 3.00 | Comfort break |
| 3.15 |
The issue of sustainability: what service features/ways of working need to be present, both within the Specialist Autism Team and the wider service context? (Small-group work and feedback) |
| 4.00 |
Aspirations for the future (Service representatives work together followed by feedback) |
| 4.15 | ‘Take aways’ |
| 4.25 | Closing comments |
| 4.30 | Depart |
| Site ID | Role (profession) | |
|---|---|---|
| Attended | Registered to attend, gave late apologies | |
| A | Service leadb (clinical psychology) | |
| B |
Acting service lead (clinical psychology) Senior team member (clinical psychology) |
Senior team member (autism nurse consultant) |
| C | Service lead (autism nurse consultant) | Senior team member (SLT) |
| D | Service lead (occupational therapy) | |
| E | Service lead (autism nurse consultant) | |
| F | Declined invitation to attend workshop owing to capacity issues | |
| H |
Service leadc (senior autism practitioner) Support worker |
Service leadd (clinical psychology) |
| I |
Service lead (speech and language therapy) Senior team member (clinical psychology) |
|
| J | Senior practitioner (occupational therapy) | |
Commissioning issues:
-
commissioning cycle
-
instability
-
planning
-
-
resource/resource constraints
-
changes
-
impacts on provision/quality
-
private providers
-
-
wider context of cost improvement
Volume:
-
number of referrals
-
changes
-
waiting lists
-
-
sources of referrals
-
child and adolescent mental health services
-
lack of other autism-specific services
-
support needs trajectory
-
-
caseload
-
complexity
-
barriers to discharge
-
support needs trajectory
-
-
commissioner/resource response.
Response to increased demand:
-
impact on provision
-
impact on mode of delivery
-
group vs. one to one
-
home vs. clinic
-
limiting offer
-
-
concerns
-
managing expectations.
Maintaining quality:
-
managing/supporting group delivery
-
information and communication to service users.
Consultation/supervision role:
-
potential impacts/benefits
-
concerns
-
barriers
-
SAT time/resource
-
short-termism
-
changing old habits
-
lack of engagement
-
understanding
-
interest
-
pressure on mainstream service
-
stability/churn of staff
-
-
-
trust responsibilities
-
innovative practice.
Self-management vs. dependency:
-
rationale for prioritisation
-
practices and interventions to support self-management/reduce dependency
-
managing discharge
-
barriers to resourcing/delivering.
Low-level ongoing support:
-
models of practice
-
experiences of providing
-
factors supporting/hindering approach.
Wider context – local autism and carer communities:
-
models of joint working
-
involvement in service design/development
-
service user evaluation.
Factors affecting outcomes:
-
individual – positive
-
‘theory of impact’
-
-
individual – negative
-
‘theory of impact’
-
-
family-level factors
-
‘theory of impact’
-
-
service characteristics
-
‘theory of impact’
-
other.
-
Appendix 3 Analysis of free-text responses
Qualitative content analysis is a technique used to describe and interpret textual data using a systematic process of coding to identify categories, themes and patterns within the data. 40 The analytical process was as follows:
-
Participants’ responses to the T3 open question on ways in which the service had impacted (or not) on their life were entered into a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheet by researcher A, alongside their rating of the impact (positive, little/no, negative). Guided by the results emerging from other elements of the research as to the factors that affected experiences, data on the type of service received (‘diagnostic assessment only’, ‘diagnostic assessment and support’ or SO) were also entered into the spreadsheet.
-
Researcher A then reviewed the whole data set to (1) remove any respondents whose response did not relate to the open question (e.g. commenting on the usefulness of the research study rather than the service) and (2) check whether or not there was concordance between the impact rating and the qualitative data. This revealed that some of those who reported rating the impact as positive reported that, although the impact was positive, the support provided was not sufficient to deal with their needs. It was, therefore, decided to create a fourth impact (‘positive impact but insufficient support’) to capture these nuances within the data.
-
Next, the qualitative data were re-read, this time with a focus on ways in which the service had positively impacted participants’ lives, as well as reasons given for the service having little/no or a negative impact. Based on this review, an initial list of codes was created.
-
The initial list of codes was added to the Microsoft Excel spreadsheet so that the final table included the qualitative response alongside the list of potential codes. All qualitative responses were then read again, and a note was made on the spreadsheet of any codes that appeared within the qualitative response. Where data did not correspond to an existing code, an additional code was created and added to the spreadsheet. The focus was on creating a comprehensive list of codes so that no data were left uncoded.
-
Next, a count of the number of times a code was endorsed by participants was carried out and a short summary report compiled. The results of this initial content analysis were shared with researcher B to allow for discussion of whether or not the codes made conceptual sense, and whether any codes should be removed or collapsed. This resulted in a final coding framework that included 18 ways in which services have a ‘positive impact’, four reasons for services having ‘little or no impact’ and two reasons for services having a ‘negative impact’.
-
After updating the database in line with the final list of agreed codes, the frequency count of the number of times that codes appeared in the data was carried out, with comparisons made between participants in the different study groups [i.e. DO cohort, SAT cohort (D&S and SO groups)].
-
Finally, researcher A examined the qualitative data linked to each code to develop a deeper understanding of the meaning and significance of each code, and to check for any links between codes.
Appendix 4 The T3 impact question: respondent characteristics
| Characteristic | Cohort, baseline measure | ||
|---|---|---|---|
| DO | SAT | ||
| D&S group | SO group | ||
| Age (years) | |||
| Mean (SD) | 38.3 (13.2) | 34.5 (13.1) | 28.7 (11.9) |
| Median (range) | 40.5 (18–64) | 31.0 (18–69) | 23.0 (17–55) |
| Gender, n (%) | |||
| Male | 18 (56.3) | 37 (50.0) | 14 (43.8) |
| Female | 14 (43.8) | 35 (47.3) | 17 (53.1) |
| Neither | 0 (0) | 2 (2.7) | 1 (3.1) |
| Total | 32 (100) | 74 (100) | 32 (100) |
| Relationship status, n (%) | |||
| Single | 20 (62.5) | 60 (81.1) | 28 (87.5) |
| Long-term partnership | 12 (37.5) | 14 (18.9) | 4 (12.5) |
| Total | 32 (100) | 74 (100) | 32 (100) |
| Educational qualifications, n (%) | |||
| No qualifications | 2 (6.3) | 5 (6.8) | 1 (3.1) |
| GCSE/O levels | 5 (15.6) | 20 (27.0) | 10 (31.3) |
| Further education | 8 (25.0) | 19 (25.7) | 12 (37.5) |
| Higher education | 17 (53.1) | 30 (40.5) | 9 (28.1) |
| Total | 32 (100) | 74 (100) | 32 (100) |
| Independent living, n (%) | |||
| Lives with parents | 12 (37.5) | 26 (35.1) | 20 (62.5) |
| Independent | 20 (62.5) | 48 (64.9) | 12 (37.5) |
| Total | 32 (100) | 74 (100) | 32 (100) |
| Employment status, n (%) | |||
| Paid work | 16 (50) | 27 (36.5) | 3 (9.4) |
| Student | 3 (9.4) | 6 (8.1) | 12 (37.5) |
| Job-seeking | 0 (0) | 6 (8.1) | 1 (3.1) |
| Disabled | 7 (21.9) | 28 (37.87) | 12 (37.5) |
| Other | 6 (18.8) | 7 (9.5) | 4 (12.5) |
| Total | 32 (100) | 74 (100) | 32 (100) |
Appendix 5 Types of positive impact
| Type of impact | DO cohort (n = 24) | SAT cohort | ||||
|---|---|---|---|---|---|---|
| D&S group (n = 50) | SO group (n = 10) | |||||
| Frequency | Rank | Frequency | Rank | Frequency | Rank | |
| Understanding and acceptance of diagnosis and self | ||||||
| Increased understanding and acceptance of self | 15 | 1 | 26 | 1 | 4 | 1 |
| Help with coming to terms with diagnosis/seeing strengths of autism | 0 | – | 6 | 5 | 1 | 4 |
| Increasing others understanding of diagnosis (e.g. family, friends, colleagues) | 3 | 4 | 5 | 6 | 0 | – |
| Improved mental health and coping | ||||||
| Improved mental health/self-esteem | 4 | 3 | 12 | 2 | 1 | 4 |
| Development of coping strategies | 2 | 5 | 4 | 7 | 2 | 3 |
| Adjustments to medication | 0 | – | 3 | 8 | 0 | – |
| Help with employment and education | ||||||
| Access to adjustments/support at work/college/university | 5 | 2 | 3 | 8 | 0 | – |
| Access to/improved support from other services | ||||||
| Support from other services (e.g. housing, employment, social care) | 1 | 6 | 4 | 7 | 3 | 2 |
| Signposting to other services | 0 | – | 4 | 7 | 0 | – |
| Provided other practitioners with information on needs | 0 | – | 1 | 10 | 0 | – |
| Improved social skills, relationships and networks | ||||||
| Improved social skills and/or relationships | 1 | 6 | 3 | 8 | 0 | – |
| Meeting others similar to myself | 0 | – | 7 | 4 | 2 | 3 |
| Attendance of social/hobby groups | 0 | – | 1 | 2 | 3 | |
| Contact with supportive practitioners | ||||||
| Staff were understanding/respectful/supportive | 0 | – | 9 | 3 | 2 | 3 |
| Access to staff with expertise in autism | 0 | – | 2 | 9 | 1 | 4 |
| Practitioners easy to contact/responsive to needs | 0 | – | 3 | 8 | 2 | 3 |
| Reduced sense of isolation | ||||||
| Reassurance of knowing there is a service that can help if needed | 0 | – | 3 | 8 | 0 | – |
| Feeling less alone knowing others have the same condition | 0 | – | 1 | 10 | 0 | – |
Appendix 6 Qualitative study of service users and family interviews: design and methods
Objectives
The qualitative component of the study addressed or contributed to addressing the following of the study’s overall objectives:
-
identify and explore features of service organisation, delivery and practice, and individual characteristics that are associated in user outcomes
-
describe the experiences of using a SAT
-
conduct an initial comparison of outcomes for individuals diagnosed and then supported by a SAT with a cohort of individuals who received a diagnostic assessment only.
Design
Single, in-depth, semistructured interviews with a subsample of study participants and, with their permission, a member of their family were carried out. Interviews took place at around the 12-month follow-up time point. In the original design (based on anticipating the identification of distinct types of service model and evaluating one or two exemplar services per model), it was proposed that we would interview 40 study participants and 20 family members. These remained our target sample sizes.
We purposively sampled to represent the following characteristics:
-
research site
-
the different groups – D&S and SO groups within the SAT cohort, and the DO cohort
-
within each group
-
perceived impact of service at the 12-month follow-up (using impact rating question in T3 questionnaire with the following response options: positive impact; little or no impact or negative impact)
-
age
-
gender.
-
Recruitment took place over a 4-month period and the profile of the recruited sample was reviewed on an ongoing basis against the sampling framework. Service users were offered a range of ways to participate in an interview: face to face, telephone and instant messenger. Telephone interviews were used with family members. Interviews took place between March and August 2018.
Methods
Our PAG developed a ‘checklist of practice’ for the research team to support autism-friendly practices throughout process involved in taking part in an interview (Box 5). Members of the PAG provided orientation and training on living with autism and adjusting communication/interview techniques and facilitation strategies. We consulted with the PAG about the content of the topic guide, with drafts iteratively piloted with three members of the PAG.
-
Duration should generally not last more than an hour, but be prepared for flexibility.
-
Remember that some people will be quite talkative, others will be more reticent.
-
Interviewers will need to be softly spoken and able to speak clearly. Avoid strong accents.
-
Consider using visual tools/cues within the interview as something to look at/work on – reducing need for eye-to-eye contact.
-
Consider where would be good places to do interviews. Do you need to offer choice over place of interview?
-
Consider using a visual/physical cue that the interviewee can use to signal when they do not want to answer a question, or wants interview to close (e.g. red and yellow cards).
-
Consider offering choice of gender of interviewer.
-
Do not try to recruit too far in advance.
-
Be clear when interviews need to be completed by.
-
Explain the purpose of the interview and provide information about timings, structure, etc. It is better to overestimate how long the interview will take when providing information about how long the interview will be.
-
Highlight value and importance of people’s own views and experiences.
-
Explain to people that they can bring someone along to support them and/or a calming object.
-
Consider if it is appropriate to check if the interviewee has any sensory impairments or dyslexia, and to ask if there are any modifications to the way that the interview happens that would help?
-
Provide information about the questions/sorts of topics to be covered in advance of the interview. Leave a space between each question or topic in case the person wants to write a few notes. If the interview may not necessarily follow a particular order, explain this.
-
Make it clear that they can choose not to answer some questions.
-
Remind interviewees that they can have someone with them for support and/or a calming object.
-
Provide a photograph of the researcher.
-
Provide contact information, including mobile/text.
-
If aware that the interviewee has a support worker, explain that it is fine to let them know about the interview or offer to do so.
-
Call the day before to remind/confirm arrangements and remind re contact details. Let the person know if there are times when you will not be contactable (e.g. no telephone signal).
-
Do not wear perfume or use strongly scented products that day.
-
Be punctual. Consider calling to say, ‘I’m on time, I’ll be there in 5 minutes’.
-
If delayed on the way to the interview, get in touch and, if possible, give a new arrival time. This should be precise rather than vague.
-
Let the interviewee instigate hand-shaking (or not).
-
Check the interviewee’s name – how would they like to be called?
-
Ask how they are and how they feel about having the interview that day. Check that they are happy to continue. If the interviewee is feeling anxious, etc., check if there’s anything you can do. Remind the person about having someone with them and/or a calming object.
-
Remind the interviewee about the structure of the interview at the beginning and keep doing this throughout, noting when moving on to a new topic. Within this, remind them that they do not have to answer questions and can close the interview at any time.
-
Offer the chance for a break(s), and re-offer this during interview if it feels appropriate/needed.
-
Offer thanks during the interview when ending one topic and moving on to another topic. Reassure people that they are providing important and valuable information.
-
Keep to the timings described (e.g. how long the interview will last), and make sure that the interviewee knows you are taking responsibility for how long the interview will last, and that all the questions are covered. If would like to extend duration, check rather than just press on.
-
If appropriate, tailor questions specifically to the individual’s experiences and reduce demand for accurate recall (e.g. . . . our research record says you started using the Asperger team in June 2017 . . .).
-
Avoid using questions that demand them to recall information if we have the information already.
-
Ask one question at a time. Avoid multiple questions within a single utterance.
-
Use short, clear questions (e.g. instead of saying ‘I would like you to think back . . . ’, just say ‘think back . . . ’).
-
Ask about specific things, rather than asking vague, general questions.
-
Try to make sure that the questions are relevant and the individual will feel able to answer them.
-
Silence is OK – remember the 8-second rule!
-
Do not automatically rephrase questions; give the person time to think about their answer.
-
Consider offering the alternative of writing answers down.
-
Make a clear statement that the interview is finished and that the recorder is switched off.
-
Check if they have any questions/concerns about the interview.
-
Reassure them of the value of their contribution. Repeat thanks for contribution.
-
Be clear about what happens after the interview, for example how the researcher will use the information gathered during the interview.
-
Provide a mechanism for people to get in touch if they want to clarify something they said, or want to add further comments.
-
If the interview does not take place in the person’s home, check if they would like some quiet time before leaving the place in which the interview happened.
Recruitment: service users
Queries were run on the study data set to identify participants who were eligible for interview (in terms of their time point in the study) and generate relevant sampling information.
An invitation letter, information sheet and response form were posted to 53 study participants. Individuals notified their interest in taking part in an interview either via returning the response form (indicating that they were interested or not interested) or via e-mail or text message. Thirty-nine individuals responded and agreed to take part in an interview, with 38 interviews completed. After two failed arrangements to conduct an instant messenger interview with the final interviewee, we did not pursue further. Of those who did not take part (n = 14), six responded indicating that they were not interested in taking part and eight did not return a response form.
The sample comprised 19 men, 17 women and two people choosing to identify as neither male nor female. The majority (30/38) described themselves as white British, three as white other, two as mixed ethnicity and the remainder described themselves as either Asian/Asian British or ‘other’. Most (33/38) were single/separated or divorced. They ranged in age from 17 to 62 years. Nine were from the DO cohort, 22 from the D&S group of the SAT cohort and eight from the SO group.
Recruitment: family members
At the end of the interviews with service users, they were asked if there was someone in their family who might have a perspective on their (i.e. service user) outcomes and experiences. If this was the case, we sought agreement to approach them about taking part in the study. However, we did not pose this request where it was clear from the interview that no family members had been involved with or observed their use of the service, or where asking this question might cause discomfort (e.g. where evidence of no current contact with family or significant discord). Fourteen service user interviewees provided contact details of a family member whom they were happy for us to approach about taking part in an interview.
These individuals were contacted via the method suggested by the participant (e-mail, post or telephone), with nine agreeing to be interviewed. All individuals except one were parents. Of these, the majority were parents of young adults (< 25 years). All study groups [SAT cohort (D&S and SO groups) and DO cohort] were represented.
Following the interview, all individuals taking part in an interview were sent a multistore shopping voucher (high street and online) with the thank you letter.
Data collection
For the service user interviews, all modes of data collection were used. Those choosing face to face also chose where the interview took place. Type and location of interviews were as follows:
-
telephone interview – 19/38
-
face to face – 15/38
-
chose interview at home – 6/15
-
chose interview in ‘public place’ – 9/15
-
café – 8
-
library – 9
-
-
-
instant messenger – 3/38.
In addition, one study participant requested an e-mail interview. Here, a simplified version of the topic guide was devised and reviewed by a member of the PAG. The interview was administered as a number of blocks of questions, with each block being sent after receipt of the previous. Where clarification was required, specific additional questions were added to the subsequent block of questions.
All verbal interviews were audio-recorded. On a couple of occasions in which interviewees had requested interviews in a ‘public place’, the researcher had concerns about the quality of the recording because of ambient noise levels and/or the interviewee being very softly spoken, so notes were also taken during the interview.
Family member interviews were conducted over the telephone.
The interviews with service users covered the following topics:
-
services/interventions received from the service
-
history of/reasons for referral
-
expectations
-
experiences of the assessment process and perceived outputs and outcomes
-
experiences of services/interventions received and perceived outputs and outcomes
-
impacts of service on life domains
-
extent to which needs met
-
factors supporting or hindering outcomes, impacts and needs met
-
experiences of discharge
-
suggested improvements to provision.
The interviews with family members covered the following topics:
-
nature of involvement with the service
-
expectations of the service for the service user
-
views on the service user’s experience and perceived impacts
-
family member’s own experience of the service
-
suggested improvements to provision.
The topic guides are available in Report Supplementary Material 2.
Data analysis
Two members of the research team (EH and SM) led the analysis of the qualitative data, with the analysis supported by NVivo 12.1 (QSR International, Warrington, UK). Verbatim transcripts were created. The broad approach was thematic99,100 and the constant comparative method101 was used to support the analytical process. Following data immersion by one member of the research team and discussions within the team, an initial thematic framework organised around key themes/topics covered in the topic guide was developed. High-level themes are set out in Box 6. Transcripts were indexed in NVivo using this framework. Emily Heavey carried out all data extraction. This was independently checked by Suzanne Mukherjee. Alongside this work, short summaries of interviews were prepared to support the analytical process. Iterations of analytical writing were used to build and test descriptive and explanatory analyses. Emily Heavey led on the analytical and writing phase, with ongoing discussions and reviews of writing by the two other members of the research team (SM and BB).
Expectations and overall opinions:
-
expectations and reasons for going
-
recommendations
-
overall impression.
Services used, offered and declined:
-
diagnostic assessment
-
reaction to diagnosis
-
assessment of needs
-
drop-in centre
-
information
-
group work
-
social or hobby group
-
one-to-one sessions
-
named contact
-
referrals to other services
-
other.
Areas worked on or not worked on with the service:
-
understanding autism
-
living with autism
-
managing anxiety and other emotional difficulties
-
social life/social networks
-
connecting with others with autism
-
job situation/employment
-
finance issues/welfare benefits
-
help from local council
-
housing
-
family relationships
-
family understanding of autism.
How the service is run:
-
waiting times and pre-discharge follow-up
-
environment and set-up
-
staff
-
discharge and post-discharge follow-up.
Appendix 7 Description of outcome measures
World Health Organization Quality-of-Life Instrument, abbreviated version (WHOQOL-BREF)46
The WHOQOL-BREF is made up of 26 items comprising two global questions and 24 items capturing the following domains: physical health (seven items), psychological health (six items), social relationships (three items) and environment (eight items). Respondents complete the measure with respect to the previous 2 weeks. The response format is a five-point scale. Raw scores are transformed into standardised scores. A higher score indicates better subjective quality of life. The WHOQOL-BREF psychological health domain was our primary outcome. The other domains were secondary outcomes. It has been used to explore quality of life among populations of adults with autism18,102 and a recent UK psychometric evaluation of the measure reports good psychometric properties. 96
General Health Questionnaire (12-item version)47
The 12-item version of the General Health Questionnaire (GHQ-12) was used to measure mental health. It focuses on two major areas: the inability to carry out normal functions and the appearance of new and distressing experiences. It comprises 12 items, with each item rated on a four-point scale: less than usual, no more than usual, rather more than usual and much more than usual. The Likert scoring method (0, 1, 2 and 3) was used alongside a categorisation of ‘caseness’, or clinical threshold defined as scoring above the mean for the study sample. 72,73
EuroQol-5 Dimensions, five-level version48,49
This standardised measure of health status provides a descriptive profile of health-related quality of life with respect to five domains (mobility, self-care, usual activities, pain/discomfort and anxiety/depression) and a single index value of health status. It is a self-report measure comprising five items. Respondents report difficulty with each domain in terms of one of five levels: no problems, some problems, moderate problems, severe problems and extreme problems (coded 1 to 5, respectively). The five-digit figure that is generated is then converted into a single-weighted index score.
Interpersonal Support Evaluation List – Short Form: belonging support subscale50
The Interpersonal Support Evaluation List – Short Form is a measure of perceived social support. A more recent large-scale psychometric evaluation has confirmed the four-factor structure of the measure. 103 It comprises four, 4-item subscales, one of which is the belonging support subscale that captures the perceived availability of others to interact socially. Respondents indicate on a four-point scale (definitely true, probably true, probably false and definitely false) the extent to which each statement (or item) is true for them. It is scored 0 to 3, and positive are reversed scored; thus, a lower score indicates greater perceived availability of others to interact with socially. This measure replaced the one originally proposed in our funding application (The Inventory of Socially Supportive Behaviours – Short Form) following feedback from our User Advisory Panel.
Appendix 8 Quantitative evaluation: recruitment procedure and data collection processes
Recruitment materials and processes were developed in consultation with our User Advisory Group and practitioners working in SATs. Core features and stages of the recruitment process were:
-
introduction to the study by the SAT – either via a letter, at intake or at the first full assessment appointment
-
individual consents to contact by clinical studies officer (CSO) in a face-to-face meeting in the clinic, a home visit or by post
-
according to the preferred mode of contact, the CSO establishes contact, shares the PIS and consents to the study
-
respondent consents and completes the T0 questionnaire.
Local modifications of the process were devised to align with individual service’s usual processes and practices and, therefore, minimise disruption and resource demand on the services. In terms of subsequent data collection time points, study participants indicated their preference at T0: postal, online/electronic survey (using Qualtrics software: www.qualtrics.com, accessed 15 October 2020) or home visit by a local CSO to assist with completion. The research team administered data collection from T1 onwards, directly managing administration of postal and electronic surveys, and liaising with local CSOs when a home visit was required.
To support retention, for postal and electronic survey administration, the following process was used at each follow-up data collection time point:
-
Text message alerting the study participant to expect to receive study questionnaire booklet (via post or e-mail).
-
Study questionnaires sent to participant.
-
If the questionnaire was not returned after 9 days from initial administration, a text message reminder was sent.
-
If the questionnaire was not returned after 16 days from initial administration, the questionnaire booklet was re-sent in the preferred format.
-
If the questionnaire was not returned after 25 days from initial administration, a final text message reminder was sent.
In addition, at each data collection time point, study participants were sent a £20 shopping voucher (multiple stores, high street and online) on receipt of a completed study questionnaire booklet.
Appendix 9 Characteristics of study participants
| Characteristic | SAT cohort (N = 252) | SAT cohort: D&S group (N = 164a) | SAT cohort: SO group (N = 88) | DO cohort (N = 56) |
|---|---|---|---|---|
| Age (years) | ||||
| Mean (SD) | 29.51 (11.7) | 31.1 (12.03) | 26.5 (10.45) | 35.23 (13.28) |
| Median (range) | 25 (17–69) | 27 (18–69) | 21 (17–55) | 31.5 (18–64) |
| Gender, n (%) | ||||
| Male | 148 (60.1) | 93 (57.1) | 55 (62.5) | 36 (64.3) |
| Female | 94 (37.4) | 64 (39.3) | 30 (34.1) | 20 (35.7) |
| Neither | 9 (3.5) | 6 (3.7) | 3 (3.4) | 0 (0.0) |
| Relationship status, n (%) | ||||
| Single | 211 (84.1) | 131 (80.4) | 80 (90.9) | 38 (67.9) |
| Long-term partnership | 40 (15.9) | 32 (19.6) | 8 (9.1) | 18 (32.1) |
| Educational qualifications | ||||
| None | 24 (9.6) | 15 (9.2) | 9 (10.3) | 7 (12.5) |
| GCSE/O levels | 70 (27.9) | 43 (26.4) | 27 (31.0) | 9 (16.1) |
| Further education | 92 (37.0) | 56 (34.4) | 36 (41.4) | 19 (33.9) |
| Higher education | 64 (25.5) | 49 (30.1) | 15 (17.2) | 21 (37.5) |
| Independent living, n (%) | ||||
| With parents | 132 (52.6) | 70 (42.9) | 62 (70.5) | 21 (37.5) |
| Left family home | 119 (47.4) | 93 (57.1) | 26 (29.5) | 35 (62.5) |
| Employment status, n (%) | ||||
| Paid workb | 61 (24.5) | 49 (30.1) | 12 (13.8) | 25 (45.5) |
| Student | 54 (21.6) | 25 (15.3) | 29 (33.3) | 4 (7.3) |
| Job-seeking | 25 (10.5) | 14 (8.6) | 11 (12.6) | 3 (5.5) |
| Unable to work owing to illness/disability | 92 (37.0) | 65 (39.9) | 27 (31.0) | 16 (29.1) |
| Other | 16 (6.4) | 10 (6.1) | 8 (9.2) | 7 (12.7) |
Appendix 10 Specialist Autism Team and Diagnostic-Only cohorts: baseline scores – standardised outcome measures
| Cohort/group | Sample size | Mean (SD) | Median (range) | t-test | ||
|---|---|---|---|---|---|---|
| WHOQOL-BREF psychological domain | Difference in mean score (95% CI) | p-value | ||||
| SAT cohort: SO group | 88 | 44.2 (18.8) | 45.83 (0–87.5) | SO vs. D&S | –5.39 (–10.42 to –0.36) | 0.04 |
| SAT cohort: D&S group | 164 | 38.81 (19.61) | 33.33 (0–95.83) | |||
| DO cohort | 56 | 34.61 (19.93) | 33.33 (0–80) | D&S vs. DO | 4.20 (–1.81 to 10.20) | 0.17 |
| GHQ-12 | Difference in mean score (95% CI) | p-value | ||||
| SAT cohort: SO group | 88 | 17.17 (7.31) | 16 (0–36) | SO vs. D&S | 1.16 (–0.74 to 3.05) | 0.23 |
| SAT cohort: D&S group | 164 | 18.33 (7.27) | 18 (3–36) | |||
| DO cohort | 56 | 19.54 (7.61) | 17.5 (8–36) | D&S vs. DO | –1.21 (–3.45 to 1.04) | 0.29 |
| GHQ-12 caseness: under vs. at or above whole sample mean score at baseline | χ2 test | p-value | ||||
| Under mean score, n (%) | At or above mean score, n (%) | Pearson’s χ2 (df) | ||||
| SAT cohort: SO group | 88 | 55 (62.5) | 33 (37.5) | 0.991 (2) | 0.61 | |
| SAT cohort: D&S group | 164 | 92 (56.1) | 72 (43.9) | |||
| DO cohort | 56 | 32 (57.1) | 24 (42.9) | |||
| Cohort/group | Sample size | Mean (SD) | Median (range) | t-test | ||
|---|---|---|---|---|---|---|
| Health-related quality of life (EQ-5D-5L) (2017 tariff) | Difference in mean score (95% CI) | p-value | ||||
| SAT cohort: SO group | 87 | 0.72 (0.21) | 0.78 (0.09–1) | SO vs. D&S | –0.03 (–0.09 to 0.02) | 0.25 |
| SAT cohort: D&S group | 163 | 0.69 (0.22) | 0.73 (–0.12–1) | |||
| DO cohort | 53 | 0.67 (0.22) | 0.70 (0.05–1) | D&S vs. DO | 0.02 (–0.05 to 0.09) | 0.50 |
| ISEL-SF belonging subscale | ||||||
| SAT cohort: SO group | 88 | 6.35 (2.82) | 6 (0–12) | SO vs. D&S | 0.54 (–0.21 to1.30) | 0.16 |
| SAT cohort: D&S group | 164 | 6.89 (2.92) | 7 (0–12) | |||
| DO cohort | 56 | 7.30 (2.84) | 7 (0–12) | D&S vs. DO | –0.41 (–1.30 to 0.47) | 0.36 |
| WHOQOL-BREF social relationships domain | ||||||
| SAT cohort: SO group | 88 | 47.96 (24.9) | 50.00 (0–100) | SO vs. D&S | –4.18 (–10.61 to 2.25) | 0.20 |
| SAT cohort: D&S group | 163 | 43.79 (24.56) | 41.67 (0–100) | |||
| DO cohort | 55 | 39.24 (18.19) | 41.67 (0–91.67) | D&S vs. DO | 4.55 (–2.57 to 11.66) | 0.21 |
| WHOQOL-BREF physical health domain | ||||||
| SAT cohort: SO group | 87 | 55.43 (19.41) | 57.14 (3.57–92.86) | SO vs. D&S | –3.83 (–8.99 to 1.34) | 0.15 |
| SAT cohort: D&S group | 163 | 51.61 (19.91) | 50 (3.57–100) | |||
| DO cohort | 56 | 53.64 (21.36) | 53.57 (14.29–92.86) | D&S vs. DO | –2.03 (–8.22 to 4.16) | 0.52 |
| WHOQOL-BREF environment domain | ||||||
| SAT cohort: SO group | 87 | 56.86 (16.27) | 59.38 (15.63–93.75) | SO vs. D&S | –0.85 (–5.23 to 3.53) | 0.70 |
| SAT cohort: D&S group | 164 | 56.01 (17.13) | 56.25 (3.13–96.88) | |||
| DO cohort | 56 | 56.10 (19.74) | 56.25 (15.63–96.88) | D&S vs. DO | –0.09 (–5.56 to 5.38) | 0.97 |
Appendix 11 Specialist Autism Team cohort: outcomes at each time point
| Cohort/group | T0 | T1 | T2 | T3 | T4 | T5 |
|---|---|---|---|---|---|---|
| D&S group | ||||||
| WHOQOL-BREF psychological domain | ||||||
| Sample size | 164 | 138 | 137 | 132 | 95 | 61 |
| Mean (SD) | 38.81 (19.61) | 39.52 (20.05) | 39.96 (19.49) | 40.09 (20.62) | 38.77 (19.21) | 42.21 (19.96) |
| Median (range) | 33.33 (0–95.83) | 37.5 (4.17–100) | 37.5 (0–100) | 41.67 (0–95.83) | 37.5 (0–83.33) | 41.67 (0–91.67) |
| GHQ-12 | ||||||
| Sample size | 164 | 138 | 137 | 133 | 95 | 62 |
| Mean (SD) | 18.33 (7.27) | 17.13 (6.97) | 17.12 (7.18) | 17.14 (7.56) | 17.53 (7.78) | 17.05 (6.68) |
| Median (range) | 18 (3–36) | 16 (0–33) | 16 (5–36) | 16 (2–36) | 16 (4–36) | 16.5 (4–36) |
| GHQ-12 caseness: under vs. at or above sample mean score at T0 | ||||||
| Under, n (%) | 92 (56.1) | 84 (60.9) | 88 (64.2) | 91 (68.4) | 60 (63.2) | 38 (61.3) |
| At/above, n (%) | 72 (43.9) | 54 (39.1) | 49 (35.8) | 42 (31.6) | 35 (36.8) | 24 (38.7) |
| Sample size | 164 | 138 | 137 | 133 | 95 | 62 |
| SO group | ||||||
| WHOQOL-BREF psychological domain | ||||||
| Sample size | 88 | 76 | 68 | 75 | 56 | 42 |
| Mean (SD) | 44.2 (18.8) | 45.23 (19.66) | 41.74 (19.29) | 42.6 (19.63) | 36.89 (18.4) | 39.88 (18.15) |
| Median (range) | 45.83 (0–87.5) | 45.83 (8.33–87.5) | 45.83 (4.17–87.5) | 45.83 (0–95.83) | 37.5 (4.17–83.33) | 39.58 (8.33–75) |
| GHQ-12 | ||||||
| Sample size | 88 | 77 | 70 | 75 | 56 | 42 |
| Mean (SD) | 17.17 (7.31) | 14.91 (6.27) | 17.34 (7.61) | 17.16 (6.9) | 19.39 (6.82) | 17.12 (7.54) |
| Median (range) | 16 (0–36) | 14 (3–32) | 16.5 (0–36) | 16 (5–34) | 19 (7–33) | 16 (4–36) |
| GHQ-12 caseness: under vs. at or above sample mean score at T0 | ||||||
| Under, n (%) | 50 (56.8) | 56 (72.7) | 39 (55.7) | 41 (54.7) | 25 (44.6) | 25 (59.5) |
| At or above, n (%) | 38 (43.2) | 21 (27.3) | 31 (44.3) | 34 (45.3) | 31 (55.4) | 17 (40.5) |
| Sample size | 88 | 77 | 70 | 75 | 56 | 42 |
| Cohort/group | T0 | T1 | T2 | T3 | T4 | T5 |
|---|---|---|---|---|---|---|
| D&S group | ||||||
| Health-related quality of life (EQ-5D-5L) (2017 tariff) | ||||||
| Sample size | 163 | 138 | 137 | 131 | 95 | 62 |
| Mean (SD) | 0.6 (0.22) | 0.6 (0.23) | 0.6 (0.25) | 0.67 (0.27) | 0.69 (0.24) | 0.65 (0.25) |
| Median (range) | 0.73 (–0.12–1) | 0.73 (–0.15–1) | 0.73 (–0.18–1) | 0.76 (–0.17–1) | 0.76 (–0.17–1) | 0.71 (–0.25–1) |
| WHOQOL-BREF social relationships domain | ||||||
| Sample size | 163 | 137 | 137 | 133 | 95 | 61 |
| Mean (SD) | 43.79 (24.56) | 43.8 (23.67) | 45.1 (23.42) | 45.39 (23.5) | 45.18 (21.76) | 40.85 (24.14) |
| Median (range) | 41.67 (0–100) | 41.67 (0–100) | 50 (0–100) | 50 (0–100) | 41.67 (0–91.67) | 41.67 (0–83.33) |
| WHOQOL-BREF physical health domain | ||||||
| Sample size | 163 | 138 | 137 | 132 | 95 | 61 |
| Mean (SD) | 51.61 (19.91) | 52.23 (19.87) | 52.61 (20.4) | 52.73 (20.77) | 51.95 (22.13) | 53.34 (21.59) |
| Median (range) | 50.00 (3.57–100) | 53.57 (0–100) | 53.57 (3.57–100) | 57.14 (3.57–100) | 53.57 (0–100) | 57.14 (3.57–96.43) |
| WHOQOL-BREF environment domain | ||||||
| Sample size | 164 | 138 | 137 | 133 | 95 | 61 |
| Mean (SD) | 56.01 (17.13) | 55.1 (17.33) | 54.72 (19.12) | 55.43 (17.71) | 54.57 (18.28) | 56.51 (17.27) |
| Median (range) | 56.25 (3.13–96.88) | 56.25 (12.5–100) | 53.13 (3.13–100) | 56.25 (3.13–100) | 56.25 (0–100) | 56.25 (3.13–90.63) |
| SO group | ||||||
| Health-related quality of life (EQ-5D-5L) (2017 tariff) | ||||||
| Sample size | 88 | 77 | 70 | 75 | 56 | 42 |
| Mean (SD) | 17.17 (7.31) | 14.91 (6.27) | 17.34 (7.61) | 17.16 (6.9) | 19.39 (6.82) | 17.12 (7.54) |
| Median (range) | 16 (0–36) | 14 (3–32) | 16.5 (0–36) | 16 (5–34) | 19 (7–33) | 16 (4–36) |
| WHOQOL-BREF social relationships domain | ||||||
| Sample size | 88 | 76 | 68 | 75 | 56 | 42 |
| Mean (SD) | 47.96 (24.9) | 49.67 (22.17) | 42.4 (22.71) | 41.67 (22.42) | 41.44 (24.44) | 43.25 (24.71) |
| Median (range) | 50 (0–100) | 50 (8.33–100) | 45.83 (0–91.67) | 41.67 (0–83.33) | 41.67 (0–91.67) | 50 (0–91.67) |
| WHOQOL-BREF physical health domain | ||||||
| Sample size | 87 | 77 | 67 | 75 | 56 | 42 |
| Mean (SD) | 55.43 (19.41) | 58.53 (19.08) | 54.69 (19.8) | 55.1 (19.35) | 51.02 (19.89) | 53.23 (19.08) |
| Median (range) | 57.14 (3.57–92.86) | 58.33 (12.5–96.43) | 57.14 (7.14–92.86) | 57.14 (14.29–89.29) | 53.57 (10.71–92.86) | 53.57 (10.71–96.43) |
| WHOQOL-BREF environment domain | ||||||
| Sample size | 88 | 77 | 69 | 75 | 56 | 42 |
| Mean (SD) | 56.86 (16.27) | 58.33 (18.47) | 55.39 (17.48) | 55.54 (17.08) | 54.58 (17.29) | 54.09 (17.67) |
| Median (range) | 59.38 (15.63–93.75) | 59.38 (3.13–93.75) | 59.38 (18.75–87.5) | 56.25 (15.63–93.75) | 54.69 (15.63–90.63) | 51.56 (6.25–93.75) |
| Cohort/group | T0 | T1 | T2 | T3 | T4 | T5 |
|---|---|---|---|---|---|---|
| D&S group | ||||||
| ISEL-SF belonging subscale | ||||||
| Sample size | 164 | 138 | 137 | 132 | 95 | 62 |
| Mean (SD) | 6.89 (2.92) | 7.07 (2.96) | 6.82 (2.92) | 6.79 (2.82) | 6.71 (3.02) | 6.77 (3.25) |
| Median (range) | 7 (0–12) | 7 (0–12) | 7 (0–12) | 7 (0–12) | 7 (0–12) | 7 (0–12) |
| SO group | ||||||
| ISEL-SF belonging subscale | ||||||
| Sample size | 88 | 76 | 70 | 75 | 56 | 42 |
| Mean (SD) | 6.35 (2.82) | 5.46 (2.83) | 6.46 (2.75) | 6.31 (2.91) | 6.41 (2.82) | 6.5 (3.04) |
| Median (range) | 6 (0–12) | 5 (0–12) | 7 (0–12) | 6 (0–12) | 6 (1–12) | 7 (0–12) |
| Cohort/group | T0 | T1 | T2 | T3 | T4 | T5 |
|---|---|---|---|---|---|---|
| D&S group, n (%) | ||||||
| Managing usual activities of daily living (EQ-5D-5L usual activities domain) | ||||||
| Unable | 4 (2.4) | 1 (0.7) | 1 (0.7) | 5 (3.8) | 3 (3.2) | 2 (3.2) |
| Severe problems | 15 (9.1) | 9 (6.5) | 11 (8.0) | 11 (8.3) | 7 (7.4) | 3 (4.8) |
| Moderate problems | 55 (33.5) | 44 (31.9) | 34 (24.8) | 26 (19.7) | 22 (23.2) | 13 (21.0) |
| Slight problems | 36 (22.0) | 39 (28.3) | 42 (30.7) | 45 (34.1) | 26 (27.4) | 22 (35.5) |
| No problems | 54 (32.9) | 45 (32.6) | 49 (35.8) | 45 (34.1) | 37 (38.9) | 22 (35.5) |
| Sample size (n) | 164 | 138 | 137 | 132 | 95 | 62 |
| Availability of information needed for daily living (WHOQOL-BREF q13) | ||||||
| Not at all | 8 (4.9) | 8 (5.8) | 9 (6.6) | 8 (6) | 8 (8.4) | 2 (3.3) |
| A little | 25 (15.2) | 21 (15.2) | 21 (15.4) | 23 (17.3) | 18 (18.9) | 9 (14.8) |
| Moderately | 49 (29.9) | 39 (28.3) | 41 (30.1) | 32 (24.1) | 22 (23.2) | 19 (31.1) |
| Mostly | 56 (34.1) | 53 (38.4) | 46 (33.8) | 54 (40.6) | 34 (35.8) | 25 (41) |
| Completely | 26 (15.9) | 17 (12.3) | 19 (14.0) | 16 (12) | 13 (13.7) | 6 (9.8) |
| Sample size (n) | 164 | 138 | 136 | 133 | 95 | 61 |
| SO group, n (%) | ||||||
| Managing usual activities of daily living (EQ-5D-5L usual activities domain) | ||||||
| Unable | 1 (1.1) | 1 (1.3) | 0 (0.0) | 3 (4.0) | 1 (1.8) | 1 (2.4) |
| Severe problems | 10 (11.4) | 5 (6.6) | 7 (10.0) | 7 (9.3) | 10 (18.2) | 4 (9.8) |
| Moderate problems | 17 (19.3) | 13 (17.1) | 20 (28.6) | 16 (21.3) | 10 (18.2) | 11 (26.8) |
| Slight problems | 24 (27.3) | 31 (40.8) | 18 (25.7) | 20 (26.7) | 17 (30.9) | 11 (26.8) |
| No problems | 36 (40.9) | 26 (34.2) | 25 (35.7) | 29 (38.7) | 17 (30.9) | 14 (34.1) |
| Sample size (n) | 88 | 76 | 70 | 75 | 55 | 41 |
| Availability of information needed for daily living (WHOQOL-BREF q13) | ||||||
| Not at all | 4 (4.5) | 3 (3.9) | 2 (2.9) | 4 (5.3) | 1 (1.8) | 1 (2.4) |
| A little | 15 (17.0) | 14 (18.2) | 16 (23.2) | 13 (17.3) | 12 (21.4) | 9 (21.4) |
| Moderately | 23 (26.1) | 20 (26) | 21 (30.4) | 23 (30.7) | 17 (30.4) | 13 (31) |
| Mostly | 34 (38.6) | 29 (37.7) | 23 (33.3) | 22 (29.3) | 17 (30.4) | 17 (40.5) |
| Completely | 12 (13.6) | 11 (14.3) | 7 (10.1) | 13 (17.3) | 9 (16.1) | 2 (4.8) |
| Sample size (n) | 88 | 77 | 69 | 75 | 56 | 42 |
| Cohort/group | T0 | T1 | T2 | T3 | T4 | T5 |
|---|---|---|---|---|---|---|
| D&S group, n (%) | ||||||
| Employment status | ||||||
| Paid work | 49 (30.1) | 44 (31.9) | 39 (28.9) | 41 (31.3) | 32 (33.7) | 24 (38.7) |
| Student | 25 (15.3) | 17 (12.3) | 15 (11.1) | 13 (9.9) | 10 (10.5) | 5 (8.1) |
| Job-seeking | 14 (8.6) | 6 (4.3) | 10 (7.4) | 10 (7.6) | 5 (5.3) | 3 (4.8) |
| Unable owing to illness/disability | 65 (39.9) | 51 (37) | 54 (40.0) | 47 (35.9) | 31 (32.6) | 25 (40.3) |
| Other | 10 (6.1) | 20 (14.5) | 17 (12.6) | 20 (15.3) | 17 (17.9) | 5 (8.1) |
| Sample size (n) | 164 | 138 | 135 | 131 | 95 | 62 |
| Satisfaction with capacity for work (WHOQOL-BREF q18) | ||||||
| Very dissatisfied | 36 (22.3) | 23 (16.7) | 29 (21.2) | 24 (18.2) | 18 (18.8) | 13 (21.3) |
| Dissatisfied | 53 (32.7) | 53 (38.4) | 49 (35.8) | 35 (26.5) | 24 (25.3) | 18 (29.5) |
| Neither satisfied/dissatisfied | 36 (22.2) | 32 (23.2) | 30 (21.9) | 38 (28.7) | 25 (26.3) | 10 (16.4) |
| Satisfied | 30 (18.5) | 26 (18.8) | 18 (13.1) | 27 (20.5) | 23 (24.2) | 19 (31.2) |
| Very satisfied | 7 (4.3) | 4 (2.9) | 11 (8.0) | 8 (6.1) | 5 (5.3) | 1 (1.6) |
| Sample size (n) | 162 | 138 | 137 | 132 | 95 | 61 |
| Satisfaction with leisure time (standalone item: ‘I am satisfied with how I spend my free time’) | ||||||
| Definitely true | 24 (14.7) | 19 (13.8) | 18 (13.1) | 22 (16.7) | 14 (14.7) | 9 (14.8) |
| Probably true | 53 (32.5) | 43 (31.2) | 37 (27.1) | 41 (31.0) | 36 (37.9) | 21 (34.4) |
| Probably false | 52 (31.9) | 53 (38.3) | 61 (44.5) | 36 (27.3) | 25 (26.3) | 19 (31.1) |
| Definitely false | 34 (20.9) | 23 (16.7) | 21 (15.3) | 33 (25.0) | 20 (21.1) | 12 (19.7) |
| Sample size (n) | 163 | 138 | 137 | 132 | 95 | 61 |
| SO group, n (%) | ||||||
| Employment status | ||||||
| Paid work | 12 (13.8) | 11 (14.7) | 9 (12.9) | 11 (14.9) | 10 (17.9) | 11 (26.2) |
| Student | 29 (33.3) | 19 (25.3) | 21 (30.0) | 21 (28.4) | 18 (32.1) | 9 (21.4) |
| Job-seeking | 11 (12.6) | 9 (12) | 4 (5.7) | 11 (14.9) | 8 (14.3) | 5 (11.9) |
| Unable owing to illness/disability | 27 (31.0) | 23 (30.7) | 25 (35.7) | 26 (35.1) | 16 (28.6) | 13 (31) |
| Other | 8 (9.2) | 13 (17.3) | 11 (15.7) | 5 (6.8) | 4 (7.1) | 4 (9.5) |
| Sample size (n) | 87 | 75 | 70 | 74 | 56 | 42 |
| Satisfaction with capacity for work (WHOQOL-BREF q18) | ||||||
| Very dissatisfied | 16 (18.4) | 10 (13.5) | 11 (16.4) | 12 (16.0) | 13 (23.2) | 7 (16.7) |
| Dissatisfied | 25 (28.7) | 20 (27.0) | 22 (32.8) | 21 (28.0) | 19 (33.9) | 15 (35.7) |
| Neither satisfied/dissatisfied | 19 (21.8) | 21 (28.4) | 19 (28.4) | 23 (30.7) | 12 (21.4) | 10 (23.8) |
| Satisfied | 24 (27.6) | 17 (23) | 13 (19.4) | 17 (22.7) | 12 (21.4) | 7 (16.7) |
| Very satisfied | 3 (3.4) | 6 (8.1) | 2 (3.0) | 2 (2.7) | 0 (0.0) | 3 (7.1) |
| Sample size (n) | 87 | 74 | 67 | 75 | 56 | 42 |
| Satisfaction with leisure time (standalone item: ‘I am satisfied with how I spend my free time’) | ||||||
| Definitely true | 16 (18.2) | 12 (15.8) | 8 (11.4) | 9 (12.0) | 5 (8.9) | 3 (7.1) |
| Probably true | 30 (34.1) | 26 (34.2) | 22 (31.4) | 33 (44.0) | 18 (32.1) | 14 (33.3) |
| Probably false | 24 (27.3) | 28 (36.8) | 23 (32.9) | 19 (25.3) | 17 (30.4) | 15 (35.7) |
| Definitely false | 18 (20.5) | 10 (13.2) | 17 (24.3) | 14 (18.7) | 16 (28.6) | 10 (23.8) |
| Sample size (n) | 88 | 76 | 70 | 75 | 56 | 42 |
| Cohort/group | T0 | T1 | T2 | T3 | T4 | T5 |
|---|---|---|---|---|---|---|
| D&S group, n (%) | ||||||
| Are you a member of any autism-specific voluntary organisations or charities? | ||||||
| None | 155 (94.5) | 119 (86.2) | 111 (81.0) | 109 (82.6) | 79 (84.0) | 47 (77.0) |
| Only ‘local/regional group or national organisation’ | 2 (1.2) | 7 (5.1) | 10 (7.3) | 11 (8.3) | 8 (8.5) | 9 (14.8) |
| Only ‘online-only group/forum’ | 7 (4.3) | 9 (6.5) | 11 (8.0) | 8 (6.1) | 5 (5.3) | 5 (8.2) |
| Both | 0 (0.0) | 3 (2.2) | 5 (3.6) | 4 (3.0) | 2 (2.1) | 0 (0.0) |
| Sample size (n) | 164 | 138 | 137 | 132 | 95 | 62 |
| Number of contacts with any autism-specific voluntary organisation or charity in past 4 weeks? | ||||||
| 0 | 140 (85.4) | 102 (73.9) | 94 (68.6) | 96 (72.2) | 76 (80) | 47 (75.8) |
| 1 | 19 (11.6) | 23 (16.7) | 34 (24.8) | 22 (16.5) | 15 (15.8) | 12 (19.4) |
| 2 | 3 (1.8) | 13 (9.4) | 8 (5.8) | 11 (8.3) | 4 (4.2) | 2 (3.2) |
| 3 | 1 (0.6) | 0 (0.0) | 1 (0.7) | 4 (3.0) | 0 (0.0) | 1 (1.6) |
| 4 | 1 (0.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Sample size (n) | 164 | 138 | 137 | 133 | 95 | 62 |
| SO group, n (%) | ||||||
| Are you a member of any autism-specific voluntary organisations or charities? | ||||||
| None | 74 (85.1) | 61 (79.2) | 56 (82.4) | 61 (81.3) | 42 (77.8) | 37 (88.1) |
| Only ‘local/regional group or national organisation’ | 9 (10.3) | 13 (16.9) | 9 (13.2) | 11 (14.7) | 8 (14.8) | 2 (4.8) |
| Only ‘online-only group/forum’ | 3 (3.4) | 2 (2.6) | 2 (2.9) | 2 (2.7) | 3 (5.6) | 2 (4.8) |
| Both | 1 (1.1) | 1 (1.3) | 1 (1.5) | 1 (1.3) | 1 (1.9) | 1 (2.4) |
| Sample size (n) | 87 | 77 | 68 | 75 | 54 | 42 |
| Number of contacts with any autism-specific voluntary organisation or charity in past 4 weeks? | ||||||
| 0 | 67 (77.0) | 63 (81.8) | 54 (78.3) | 60 (80) | 42 (77.8) | 33 (78.6) |
| 1 | 16 (18.4) | 11 (14.3) | 11 (15.9) | 12 (16) | 11 (20.4) | 7 (16.7) |
| 2 | 4 (4.6) | 2 (2.6) | 2 (2.9) | 2 (2.7) | 1 (1.9) | 2 (4.8) |
| 3 | 0 (0.0) | 1 (1.3) | 2 (2.9) | 1 (1.3) | 0 (0.0) | 0 (0.0) |
| 4 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Sample size (n) | 87 | 77 | 69 | 75 | 54 | 42 |
Appendix 12 Specialist Autism Team cohort: longer-term outcomes
| Outcome | Sample size (n) | Time point, mean score | Difference in mean score (95% CI) | p-value | Effect sizea | |
|---|---|---|---|---|---|---|
| T0 | T4 | |||||
| WHOQOL-BREF psychological domain | 95 | 38.27 | 38.77 | 0.50 (–3.53 to 2.53) | 0.74 | 0.03 |
| GHQ-12 | 95 | 18.64 | 17.53 | 1.12 (–0.40 to 2.63) | 0.15 | 0.15 |
| GHQ-12 caseness: movement around cut-off pointb | ||||||
| T4 (n) | ||||||
| Above cut-off point | Below cut-off point | Total (n) | ||||
| T0 (n) | Above cut-off point | 25 | 18 | 43 | ||
| Below cut-off point | 10 | 42 | 52 | |||
| Total | 35 | 60 | 95 | |||
| Mcnemar’s χ2 = 2.29; (df = 1); p = 0.185 | ||||||
| Outcome | Sample size (n) | Time point, mean score | Difference in mean score (95% CI) | p-value | Effect sizea | |
|---|---|---|---|---|---|---|
| T0 | T5 | |||||
| WHOQOL-BREF psychological domain | 61 | 37.13 | 42.21 | 5.08 (–8.93 to –1.23) | 0.01 | 0.34 |
| GHQ-12 | 62 | 19.29 | 17.05 | 2.24 (0.51 to 3.98) | 0.01 | 0.33 |
| GHQ-12 caseness: movement around cut-off pointb | ||||||
| T5 (n) | ||||||
| Above cut-off point | Below cut-off point | Total (n) | ||||
| T0 (n) | Above cut-off point | 18 | 15 | 33 | ||
| Below cut-off point | 6 | 23 | 29 | |||
| Total | 24 | 38 | 62 | |||
| Mcnemar’s χ2 = 3.86 (df = 1); p = 0.078 | ||||||
| Outcome | Sample size (n) | Time point, mean score | Difference in mean score (95% CI) | p-value | Effect sizea | |
|---|---|---|---|---|---|---|
| T0 | T4 | |||||
| WHOQOL-BREF psychological domain | 56 | 42.80 | 36.89 | 6.01 (2.58 to 9.45) | 0.00 | 0.47 |
| GHQ-12 | 56 | 18.16 | 19.39 | –1.23 (–3.15 to 0.69) | 0.20 | 0.17 |
| GHQ-12 caseness: movement around cut-off pointb | ||||||
| T4 (n) | ||||||
| Above cut-off point | Below cut-off point | Total (n) | ||||
| T0 (n) | Above cut-off point | 21 | 7 | 28 | ||
| Below cut-off point | 10 | 18 | 28 | |||
| Total | 31 | 25 | 56 | |||
| Mcnemar’s χ2 = 0.53 (df = 1); p = 0.629 | ||||||
| Outcome | Sample size (n) | Time point, mean score | Difference in mean score (95% CI) | p-value | Effect sizea | |
|---|---|---|---|---|---|---|
| T0 | T5 | |||||
| WHOQOL-BREF psychological domain | 42 | 41.27 | 39.88 | 1.39 (–3.28 to 6.05) | 0.55 | 0.09 |
| GHQ-12 | 42 | 18.31 | 17.12 | 1.19 (–1.55 to 3.93) | 0.39 | 0.14 |
| GHQ-12 caseness: movement around cut-off pointb | ||||||
| T5 (n) | ||||||
| Above cut-off point | Below cut-off point | Total (n) | ||||
| T0 (n) | Above cut-off point | 9 | 13 | 22 | ||
| Below cut-off point | 8 | 12 | 20 | |||
| Total | 17 | 25 | 42 | |||
| Mcnemar’s χ2 = 1.19 (df = 1); p = 0.383 | ||||||
| Outcome | Sample size (n) | Time point, mean score | Difference in mean score (95% CI) | p-value | Effect sizea | |
|---|---|---|---|---|---|---|
| T0 | T4 | |||||
| EQ-5D-5L | 94 | 0.68 | 0.69 | 0.004 (–0.04 to 0.03) | 0.81 | 0.03 |
| WHOQOL-BREF social domain | 95 | 42.37 | 45.17 | –2.81 (–7.21 to 1.59) | 0.21 | 0.13 |
| WHOQOL-BREF physical domain | 95 | 52.20 | 51.95 | 0.24 (–2.96 to 3.46) | 0.88 | 0.02 |
| WHOQOL-BREF environment domain | 95 | 56.64 | 54.57 | 2.08 (–0.74 to 4.90) | 0.15 | 0.15 |
| ISEL-SF belonging subscale | 95 | 7.21 | 6.71 | 0.51 (–0.11 to 1.12) | 0.10 | 0.17 |
| Outcome | Sample size (n) | Time point, mean score | Difference in mean score (95% CI) | p-value | Effect sizea | |
|---|---|---|---|---|---|---|
| T0 | T5 | |||||
| T5 (24-month follow-up) | ||||||
| EQ-5D-5L | 62 | 0.67 | 0.65 | 0.02 (–0.01 to 0.10) | 0.04 | 0.11 |
| WHOQOL-BREF social domain | 61 | 41.67 | 40.85 | 0.82 (–5.28 to 6.92) | 0.79 | 0.03 |
| WHOQOL-BREF physical domain | 61 | 52.20 | 53.34 | 1.14 (–5.08 to 2.79) | 0.56 | 0.07 |
| WHOQOL-BREF environment domain | 61 | 56.78 | 56.51 | 0.28 (–3.41 to 3.97) | 0.88 | 0.02 |
| ISEL-SF belonging subscale | 62 | 7.19 | 6.77 | 0.42 (–0.37 to 1.21) | 0.29 | 0.14 |
| Outcome | Sample size (n) | Time point, mean score | Difference in mean score (95% CI) | p-value | Effect sizea | |
|---|---|---|---|---|---|---|
| T0 | T4 | |||||
| EQ-5D-5L | 54 | 0.717 | 0.66 | 0.06 (–0.01 to 0.12) | 0.078 | 0.244 |
| WHOQOL-BREF social domain | 56 | 47.25 | 41.44 | 5.80 (–0.35 to 11.95) | 0.06 | 0.25 |
| WHOQOL-BREF physical domain | 55 | 56.64 | 50.91 | 3.73 (–0.28 to 7.75) | 0.07 | 0.25 |
| WHOQOL-BREF environment domain | 56 | 55.60 | 54.58 | 1.03 (–2.46 to 4.52) | 0.56 | 0.08 |
| ISEL-SF belonging subscale | 56 | 6.46 | 6.41 | 0.05 (–0.67 to 0.77) | 0.88 | 0.02 |
| Outcome | Sample size (n) | Time point, mean score | Difference in mean score (95% CI) | p-value | Effect sizea | |
|---|---|---|---|---|---|---|
| T0 | T5 | |||||
| EQ-5D-5L | 40 | 0.68 | 0.69 | 0.01 (0.08–0.06) | 0.84 | 0.03 |
| WHOQOL-BREF social domain | 42 | 49.11 | 43.25 | 5.85 (–1.37 to 13.07) | 0.11 | 0.25 |
| WHOQOL-BREF physical domain | 42 | 52.93 | 53.23 | –0.30 (–4.88 to 4.28) | 0.89 | 0.02 |
| WHOQOL-BREF environment domain | 42 | 56.47 | 54.09 | 2.38 (–2.53 to 7.29) | 0.33 | 0.15 |
| ISEL-SF belonging subscale | 42 | 6.64 | 6.50 | 0.14 (–0.78 to 1.07) | 0.75 | 0.05 |
| Measure | Number of participants (n) | ||||
|---|---|---|---|---|---|
| Managing usual activities of daily living (EQ-5D-5L usual activities domain)a | |||||
| T4 | |||||
| Unable/severe problems | Moderate problems | No/slight problems | Total | ||
| T0 | Unable/severe problems | 5 | 3 | 4 | 12 |
| Moderate problems | 3 | 12 | 18 | 33 | |
| No/slight problems | 2 | 7 | 41 | 50 | |
| Total | 10 | 22 | 63 | 95 | |
| Symmetry test, χ2 = 5.51; p = 0.138 | |||||
| Availability of information needed for daily living (WHOQOL-BREF q13)a | |||||
| T4 | |||||
| Not at all/a little/moderately | Mostly/completely | Total | |||
| T0 | Not at all/a little/moderately | 34 | 14 | 48 | |
| Mostly/completely | 14 | 33 | 47 | ||
| Total | 48 | 47 | 95 | ||
| McNemar’s χ2 = 0.00 (df = 1); p = 1.0 | |||||
| Employment statusb | |||||
| T4 | |||||
| Paid work | Unable to work owing to illness/disability or job-seeking | Total | |||
| T0 | Paid work | 23 | 5 | 28 | |
| Unable to work owing to illness/disability or job-seeking | 8 | 25 | 33 | ||
| Total | 31 | 30 | 61 | ||
| McNemar’s χ2 = 0.69 (df = 1); p = 0.405 | |||||
| Satisfaction with capacity for work (WHOQOL-BREF q18)a | |||||
| T4 | |||||
| Very dissatisfied/dissatisfied | Neither | Very satisfied/satisfied | Total | ||
| T0 | Very dissatisfied/dissatisfied | 32 | 10 | 10 | 52 |
| Neither | 6 | 10 | 5 | 21 | |
| Very satisfied/satisfied | 4 | 5 | 12 | 21 | |
| Total | 42 | 25 | 27 | 94 | |
| Symmetry test, χ2 = 3.57 (df = 3); p = 0.312 | |||||
| Satisfaction with leisure timec | |||||
| T4 | |||||
| Definitely/probably true | Probably/definitely false | Total | |||
| T0 | Definitely/probably true | 35 | 10 | 45 | |
| Probably/definitely false | 14 | 35 | 49 | ||
| Total | 49 | 45 | 94 | ||
| McNemar’s χ2 = 0.67 (df = 1); p = 0.414 | |||||
| Measure | Number of participants (n) | ||||
|---|---|---|---|---|---|
| Managing usual activities of daily living (EQ-5D-5L usual activities domain)a | |||||
| T5 | |||||
| Unable/severe problems | Moderate problems | No/slight problems | Total | ||
| T0 | Unable/severe problems | 4 | 2 | 3 | 9 |
| Moderate problems | 0 | 7 | 16 | 23 | |
| No/slight problems | 1 | 4 | 25 | 30 | |
| Total | 5 | 13 | 44 | 62 | |
| Symmetry test: χ2 = 10.2 (df = 3); p = 0.017 | |||||
| Availability of information needed for daily living (WHOQOL-BREF q13)a | |||||
| T5 | |||||
| Not at all/a little/moderately | Mostly/completely | Total | |||
| T0 | Not at all/a little/moderately | 24 | 8 | 32 | |
| Mostly/completely | 6 | 23 | 29 | ||
| Total | 30 | 31 | 61 | ||
| McNemar’s χ2 = 0.29, (df = 1); p = 0.593 | |||||
| Employment statusb | |||||
| T5 | |||||
| Paid work | Unable to work owing to illness/disability or job-seeking | Total | |||
| T0 | Paid work | 18 | 3 | 21 | |
| Unable to work owing to illness/disability or job-seeking | 5 | 20 | 25 | ||
| Total | 23 | 23 | 46 | ||
| McNemar’s χ2 = 0.50 (df = 1); p = 0.480 | |||||
| Satisfaction with capacity for work (WHOQOL-BREF q18)a | |||||
| T5 | |||||
| Very dissatisfied/dissatisfied | Neither | Very satisfied/satisfied | Total | ||
| T0 | Very dissatisfied/dissatisfied | 25 | 4 | 7 | 36 |
| Neither | 3 | 5 | 2 | 10 | |
| Very satisfied/satisfied | 2 | 1 | 11 | 14 | |
| Total | 30 | 10 | 20 | 60 | |
| Symmetry test: χ2 = 3.25 (df = 3); p = 0.354 | |||||
| Satisfaction with leisure timec | |||||
| T5 | |||||
| Definitely/probably true | Probably/definitely false | Total | |||
| T0 | Definitely/probably true | 19 | 7 | 26 | |
| Probably/definitely false | 10 | 24 | 34 | ||
| Total | 29 | 31 | 60 | ||
| McNemar’s χ2 = 0.53 (df = 1); p = 0.467 | |||||
| Measure | Number of participants (n) | ||||
|---|---|---|---|---|---|
| Managing usual activities of daily living (EQ-5D-5L usual activities domain)a | |||||
| T4 | |||||
| Unable/severe problems | Moderate problems | No/slight problems | Total | ||
| T0 | Unable/severe problems | 2 | 2 | 2 | 6 |
| Moderate problems | 2 | 4 | 8 | 14 | |
| No/slight problems | 7 | 4 | 24 | 35 | |
| Total | 11 | 10 | 34 | 55 | |
| Symmetry test: χ2 = 4.11 (df = 3); p = 0.250 | |||||
| Availability of information needed for daily living (WHOQOL-BREF q13)a | |||||
| T4 | |||||
| Not at all/a little/moderately | Mostly/completely | Total | |||
| T0 | Not at all/a little/moderately | 22 | 9 | 31 | |
| Mostly/completely | 8 | 17 | 25 | ||
| Total | 30 | 26 | 56 | ||
| McNemar’s χ2 = 0.06 (df = 1); p = 0.81 | |||||
| Employment statusb | |||||
| T4 | |||||
| Paid work | Unable to work owing to illness/disability or job-seeking | Total | |||
| T0 | Paid work | 8 | 0 | 8 | |
| Unable to work owing to illness/disability or job-seeking | 0 | 17 | 17 | ||
| Total | 8 | 17 | 25 | ||
| McNemar’s χ2 = 0.00; p = 1 | |||||
| Satisfaction with capacity for work (WHOQOL-BREF q18)a | |||||
| T4 | |||||
| Very dissatisfied/dissatisfied | Neither | Very satisfied/satisfied | Total | ||
| T0 | Very dissatisfied/dissatisfied | 24 | 2 | 1 | 27 |
| Neither | 5 | 2 | 3 | 10 | |
| Very satisfied/ satisfied | 3 | 7 | 8 | 18 | |
| Total | 32 | 11 | 12 | 55 | |
| Symmetry test: χ2 = 3.89 (df = 3); p = 0.274 | |||||
| Satisfaction with leisure timec | |||||
| T4 | |||||
| Definitely/probably true | Probably/definitely false | Total | |||
| T0 | Definitely/probably true | 17 | 11 | 28 | |
| Probably/definitely false | 6 | 22 | 28 | ||
| Total | 23 | 33 | 56 | ||
| McNemar’s χ2 = 1.47 (df = 1); p = 0.225 | |||||
| Measure | Number of participants (n) | ||||
|---|---|---|---|---|---|
| Managing usual activities of daily living (EQ-5D-5L usual activities domain)a | |||||
| T5 | |||||
| Unable/severe problems | Moderate problems | No/slight problems | Total | ||
| T0 | Unable/severe problems | 2 | 3 | 1 | 6 |
| Moderate problems | 1 | 3 | 8 | 12 | |
| No/slight problems | 2 | 5 | 16 | 23 | |
| Total | 5 | 11 | 25 | 41 | |
| Symmetry test: χ2 = 2.03 (df = 3); p = 0.567 | |||||
| Availability of information needed for daily living (WHOQOL-BREF q13)a | |||||
| T5 | |||||
| Not at all/a little/moderately | Mostly/completely | Total | |||
| T0 | Not at all/a little/moderately | 13 | 8 | 21 | |
| Mostly/completely | 10 | 11 | 21 | ||
| Total | 23 | 19 | 42 | ||
| McNemar’s χ2 = 0.22 (df = 1); p = 0.637 | |||||
| Employment statusb | |||||
| T5 | |||||
| Paid work | Unable to work owing to illness/disability or job-seeking | Total | |||
| T0 | Paid work | 5 | 0 | 5 | |
| Unable to work owing to illness/disability or job-seeking | 0 | 15 | 15 | ||
| Total | 5 | 15 | 20 | ||
| McNemar’s χ2 = 0.00; p = 1.00 | |||||
| Satisfaction with capacity for work (WHOQOL-BREF q18)a | |||||
| T5 | |||||
| Very dissatisfied/dissatisfied | Neither | Very satisfied/satisfied | Total | ||
| T0 | Very dissatisfied/dissatisfied | 14 | 4 | 1 | 19 |
| Neither | 6 | 4 | 1 | 11 | |
| Very satisfied/satisfied | 2 | 2 | 7 | 11 | |
| Total | 22 | 10 | 9 | 41 | |
| Symmetry test: χ2 = 1.07 (df = 3); p = 0.785 | |||||
| Satisfaction with leisure timec | |||||
| T5 | |||||
| Definitely/probably true | Probably/definitely false | Total | |||
| T0 | Definitely/probably true | 11 | 7 | 18 | |
| Probably/definitely false | 6 | 18 | 24 | ||
| Total | 17 | 25 | 42 | ||
| McNemar’s χ2 = 0.08 (df = 1); p = 0.782 | |||||
| Measure | Number of participants | |||
|---|---|---|---|---|
| T4 (18-month follow-up) | ||||
| Membership of autism-specific voluntary organisations and/or online community? | ||||
| T4 | ||||
| Member of organisation and/or community | No memberships | Total | ||
| T0 | Member of organisation and/or community | 3 | 4 | 7 |
| No memberships | 12 | 75 | 87 | |
| Total | 15 | 79 | 94 | |
| McNemar’s χ2 = 4.00 (df = 1); p = 0.077 | ||||
| Any contact with autism-specific voluntary organisations/communities? | ||||
| T4 | ||||
| One or more contacts | No contact | Total | ||
| T0 | One or more contacts | 7 | 10 | 17 |
| No contact | 12 | 66 | 78 | |
| Total | 19 | 76 | 95 | |
| McNemar’s χ2 = 0.18 (df = 1); p = 0.670 | ||||
| T5 (24-month follow-up) | ||||
| Membership of autism-specific voluntary organisations and/or online community? | ||||
| T5 | ||||
| Member of organisation and/or community | No memberships | Total | ||
| T0 | Member of organisation and/or community | 2 | 1 | 3 |
| No memberships | 12 | 46 | 58 | |
| Total | 14 | 47 | 61 | |
| McNemar’s χ2 = 9.31 (df = 1); p = 0.003 | ||||
| Any contact with autism-specific voluntary organisations/communities? | ||||
| T5 | ||||
| One or more contacts | No contact | Total | ||
| T0 | One or more contacts | 2 | 7 | 9 |
| No contact | 13 | 40 | 53 | |
| Total | 15 | 47 | 62 | |
| McNemar’s χ2 = 1.80 (df = 1); p = 0.26 | ||||
| Measure | Number of participants | |||
|---|---|---|---|---|
| T4 (18-month follow-up) | ||||
| Membership of autism-specific voluntary organisations and/or online community? | ||||
| T4 | ||||
| Member of organisations and/or community | No memberships | Total | ||
| T0 | Member of organisation and/or community | 4 | 3 | 7 |
| No memberships | 7 | 39 | 46 | |
| Total | 11 | 42 | 53 | |
| McNemar’s χ2 = 1.60 (df = 1); p = 0.344 | ||||
| Any contact with autism-specific voluntary organisations/communities? | ||||
| T4 | ||||
| One or more contacts | No contact | Total | ||
| T0 | One or more contacts | 6 | 5 | 11 |
| No contact | 6 | 36 | 42 | |
| Total | 12 | 41 | 53 | |
| McNemar’s χ2 = 0.09 (df = 1); p = 0.763 | ||||
| T5 (24-month follow-up) | ||||
| Membership of autism-specific voluntary organisations and/or online community? | ||||
| T5 | ||||
| Member of organisation and/or community | No memberships | Total | ||
| T0 | Member of organisation and/or community | 3 | 2 | 5 |
| No memberships | 2 | 35 | 37 | |
| Total | 5 | 37 | 42 | |
| McNemar’s χ2 = 0.00; p = 1.00 | ||||
| Any contact with autism-specific voluntary organisations/communities? | ||||
| T5 | ||||
| One or more contacts | No contact | Total | ||
| T0 | One or more contacts | 4 | 4 | 8 |
| No contact | 5 | 29 | 34 | |
| Total | 9 | 33 | 42 | |
| McNemar’s χ2 = 0.11; p = 1 | ||||
Appendix 13 Diagnosis-Only cohort: changes in non-mental health outcomes – T0–T3
| Measure | Outcome |
|---|---|
| Health-related quality of Life (EQ-5D-5L) (2017 Tariff) (n = 48) | |
| Mean score | T0 = 0.670; T3 = 0.680 |
| Difference in mean score | 0.0105 |
| 95% CI | –0.070 to 0.489 |
| p-value | p = 0.724 |
| Effect sizea | 0.051 |
| ISEL-SF belonging subscale (n = 52) | |
| Mean score | T0 = 7.35; T3 = 6.96 |
| Difference in mean score | 0.385 |
| 95% CI | –0.36 to 1.13 |
| p-value | p = 0.307 |
| Effect sizea | 0.143 |
| WHOQOL-BREF social domain (n = 51) | |
| Mean score | T0 = 38.89; T3 = 42.48 |
| Difference in mean score | 3.595 |
| 95% CI | –9.44 to 2.25 |
| p-value | p = 0.222 |
| Effect sizea | 0.173 |
| WHOQOL-BREF physical domain (n = 52) | |
| Mean score | T0 = 53.43; T3 = 51.85 |
| Difference in mean score | 1.580 |
| 95% CI | –2.85 to 6.01 |
| p-value | p = 0.477 |
| Effect sizea | 0.099 |
| WHOQOL-BREF environment domain (n = 51) | |
| Mean score | T0 = 56.39; T3 = 55.23 |
| Difference in mean score | 1.155 |
| 95% CI | –2.55 to 4.86 |
| p-value | p = 0.534 |
| Effect sizea | 0.088 |
| Measure | Number of participants | ||||
|---|---|---|---|---|---|
| Managing usual activities of daily living (EQ-5D-5L usual activities domain)a | |||||
| T3 | |||||
| Unable/severe problems | Moderate problems | No/slight problems | Total | ||
| T0 | Unable/severe problems | 6 | 2 | 0 | 8 |
| Moderate problems | 2 | 5 | 9 | 16 | |
| No/slight problems | 1 | 4 | 22 | 27 | |
| Total | 9 | 11 | 31 | 51 | |
| χ2 = 2.92 (df = 3); p = 0.404 | |||||
| Availability of information needed for daily living (WHOQOL-BREF q13)a | |||||
| T3 | |||||
| Not at all/a little/moderately | Mostly/completely | Total | |||
| T0 | Not at all/a little/moderately | 15 | 8 | 23 | |
| Mostly/completely | 13 | 16 | 29 | ||
| Total | 28 | 24 | 52 | ||
| χ2 = 1.19 (df = 1); p = 0.275 | |||||
| Employment statusb | |||||
| T3 | |||||
| Paid work | Unable to work owing to illness/disability or job-seeking | Total | |||
| T0 | Paid work | 15 | 4 | 19 | |
| Unable to work owing to illness/disability or job-seeking | 3 | 12 | 15 | ||
| Total | 18 | 16 | 34 | ||
| χ2 = 0.14 (df = 1); p = 0.706 | |||||
| Satisfaction with capacity for work (WHOQOL-BREF q18)a | |||||
| T3 | |||||
| Very dissatisfied/dissatisfied | Neither | Very satisfied/ satisfied | Total | ||
| T0 | Very dissatisfied/dissatisfied | 20 | 6 | 4 | 30 |
| Neither | 4 | 0 | 2 | 6 | |
| Very satisfied/ satisfied | 5 | 1 | 10 | 16 | |
| Total | 29 | 7 | 16 | 52 | |
| Cell counts too low for analysis | |||||
| Satisfaction with leisure timea,c | |||||
| T3 | |||||
| Definitely/probably true | Probably/definitely false | Total | |||
| T0 | Definitely/probably true | 19 | 9 | 28 | |
| Probably/definitely false | 9 | 15 | 24 | ||
| Total | 28 | 24 | 52 | ||
| χ2 = 0.00 (df = 1); p = 1.00 | |||||
| Indicator of access to autism-specific organisations | ||||
|---|---|---|---|---|
| Membership of autism-specific voluntary organisations and/or online community? | ||||
| T3 | ||||
| Member of organisation and/or community | No memberships | Total | ||
| T0 | Member of organisation and/or community | 6 | 1 | 7 |
| No memberships | 7 | 38 | 45 | |
| Total | 13 | 39 | 52 | |
| McNemar’s χ2 = 4.50 (df = 1); p = 0.034 (note: small cell counts) | ||||
| Any contact with autism-specific voluntary organisations/communities? | ||||
| T3 | ||||
| One or more contacts | No contact | Total | ||
| T0 | One or more contacts | 7 | 3 | 10 |
| No contact | 5 | 37 | 42 | |
| Total | 12 | 40 | 52 | |
| McNemar’s χ2 = 0.50 (df = 1); p = 0.480 | ||||
Appendix 14 The T3 mental health outcomes: Diagnosis-Only cohort versus diagnostic and support group
| ANCOVA | Adjusted means | 95% CI | F-statistic | p-value |
|---|---|---|---|---|
| Using total D&S group | ||||
| Model 1 (n = 182) | 91.34 | < 0.001 | ||
| Comparing T3 WHOQOL-BREF psychological domain scores | ||||
| DO cohort | 40.93 | 36.87 to 44.99 | ||
| D&S group | 39.25 | 36.69 to 41.81 | ||
| Difference in means | –1.680 | –6.48 to 3.12 | 0.48 | 0.491 |
| Controlling for | ||||
| T0 WHOQOL-BREF (psychological) | 182.41 | < 0.001 | ||
| Model 2 (n = 181) | 40.47 | < 0.001 | ||
| Comparing T3 WHOQOL-BREF psychological domain scores | ||||
| DO cohort | 41.91 | 37.58 to 46.24 | ||
| D&S group | 40.82 | 37.57 to 44.07 | ||
| Difference in means | –1.087 | –5.85 to 3.68 | 0.20 | 0.653 |
| Controlling for | ||||
| T0 WHOQOL-BREF (psychological) | 64.77 | < 0.001 | ||
| GHQ-12 score at T0 | 7.22 | 0.008 | ||
| Age | 1.20 | 0.276 | ||
| Gender | 2.62 | 0.107 | ||
| Using D&S subsample (identical diagnostic assessment protocol to DO cohort) | ||||
| Model 1 (n = 94) | 41.79 | < 0.001 | ||
| Comparing T3 WHOQOL-BREF psychological domain scores | ||||
| DO cohort | 40.21 | 36.03 to 44.39 | ||
| D&S group | 36.52 | 31.89 to 41.15 | ||
| Difference in means | –3.69 | –9.93 to 2.54 | 1.38 | 0.242 |
| Controlling for | ||||
| T0 WHOQOL-BREF (psychological) | 83.34 | < 0.001 | ||
| Model 2 (n = 93) | 16.60 | < 0.001 | ||
| Comparing T3 WHOQOL-BREF psychological domain scores | ||||
| DO cohort | 41.50 | 36.54 to 46.47 | ||
| D&S group | 38.08 | 32.80 to 43.36 | ||
| Difference in means | –3.42 | –9.84 to 2.99 | 1.12 | 0.292 |
| Controlling for | ||||
| T0 WHOQOL-BREF (Psychological) | 41.91 | < 0.001 | ||
| T0 GHQ-12 | 0.00 | 0.946 | ||
| Age | 0.44 | 0.511 | ||
| Gender | 2.13 | 0.148 | ||
| ANCOVA | Adjusted means | 95% CI | F-statistic | p-value |
|---|---|---|---|---|
| Using total D&S group | ||||
| Model 1 (n = 183) | 30.43 | < 0.001 | ||
| Comparing T3 GHQ-12 | ||||
| DO cohort | 17.88 | 16.04 to 19.72 | ||
| D&S group | 17.46 | 16.30 to 18.61 | ||
| Difference in means | –0.424 | –2.60 to 1.75 | 0.15 | 0.701 |
| Controlling for | ||||
| T0 GHQ-12 | 59.79 | < 0.001 | ||
| Model 2 (n = 182) | 12.67 | < 0.001 | ||
| Comparing T3 GHQ-12 | ||||
| DO cohort | 17.36 | 15.34 to 19.38 | ||
| D&S group | 16.78 | 15.28 to 18.29 | ||
| Difference in means | –0.574 | –2.80 to 1.65 | 0.26 | 0.611 |
| Controlling for | ||||
| T0 GHQ-12 | 22.48 | < 0.001 | ||
| T0 WHOQOL-BREF (Psychological) | 0.93 | 0.336 | ||
| Age | 0.04 | 0.844 | ||
| Gender | 1.92 | 0.168 | ||
| Using D&S subsample (identical diagnostic assessment protocol to DO cohort) | ||||
| Model 1 (n = 94) | 8.67 | < 0.001 | ||
| Comparing T3 GHQ-12 | ||||
| DO cohort | 18.40 | 16.31 to 20.49 | ||
| D&S group | 19.36 | 17.04 to 21.69 | ||
| Difference in means | 0.966 | –2.16 to 4.09 | 0.38 | 0.541 |
| Controlling for | ||||
| T0 GHQ-12 | 16.81 | < 0.001 | ||
| Model 2 (n = 93) | 4.23 | 0.002 | ||
| Comparing T3 GHQ-12 | ||||
| DO cohort | 17.31 | 14.83 to 19.79 | ||
| D&S group | 18.75 | 16.11 to 21.39 | ||
| Difference in means | 1.439 | –1.77 to 4.65 | 0.79 | 0.375 |
| Controlling for | ||||
| T0 GHQ-12 | 4.12 | 0.046 | ||
| T0 WHOQOL-BREF (Psychological) | 1.98 | 0.163 | ||
| Age | 0.55 | 0.461 | ||
| Gender | 1.70 | 0.196 | ||
Appendix 15 Economic evaluation outputs
| Group | Statistic | Bias | SE | Bootstrapped 95% CI | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| GP | ||||||
| D&S (n = 148) | Mean | 209.63 | 0.61 | 20.61 | 168.90 | 256.57 |
| SD | 248.97 | –1.10 | 21.87 | 205.77 | 288.23 | |
| SE mean | 20.47 | |||||
| SO (n = 79) | Mean | 207.24 | 0.46 | 26.63 | 158.47 | 261.38 |
| SD | 229.94 | –2.51 | 18.02 | 196.26 | 259.17 | |
| SE mean | 25.87 | |||||
| Psychologist | ||||||
| D&S (n = 148) | Mean | 267.10 | –0.92 | 48.18 | 183.98 | 366.95 |
| SD | 597.50 | –25.34 | 161.47 | 334.31 | 856.97 | |
| SE mean | 49.11 | |||||
| SO (n = 79) | Mean | 154.38 | 1.55 | 32.62 | 92.80 | 222.72 |
| SD | 294.04 | –3.10 | 39.68 | 205.83 | 364.85 | |
| SE mean | 33.08 | |||||
| Occupational therapist | ||||||
| D&S (n = 148) | Mean | 124.08 | 0.84 | 79.44 | 33.17 | 283.44 |
| SD | 951.80 | –168.51 | 539.22 | 118.26 | 1619.58 | |
| SE mean | 78.24 | |||||
| SO (n = 79) | Mean | 24.84 | –0.26 | 10.79 | 7.90 | 45.14 |
| SD | 97.22 | –5.81 | 28.41 | 40.11 | 132.01 | |
| SE mean | 10.94 | |||||
| Nurse | ||||||
| D&S (n = 148) | Mean | 323.60 | –0.13 | 110.13 | 161.44 | 536.10 |
| SD | 1349.28 | –116.76 | 546.17 | 395.29 | 2112.17 | |
| SE mean | 110.91 | |||||
| SO (n = 79) | Mean | 97.39 | –0.10 | 27.71 | 48.09 | 153.27 |
| SD | 236.32 | –5.96 | 43.34 | 151.31 | 297.83 | |
| SE mean | 26.59 | |||||
| SLT | ||||||
| D&S (n = 148) | Mean | 11.23 | –0.02 | 4.50 | 3.54 | 19.49 |
| SD | 54.45 | –1.71 | 12.21 | 28.66 | 72.37 | |
| SE mean | 4.48 | |||||
| SO (n = 79) | Mean | 4.21 | –0.03 | 3.16 | 0.00 | 10.21 |
| SD | 27.74 | –3.93 | 13.65 | 0.00 | 42.87 | |
| SE mean | 3.12 | |||||
| Social worker | ||||||
| D&S (n = 148) | Mean | 26.17 | 0.28 | 12.55 | 5.45 | 52.08 |
| SD | 150.62 | –7.40 | 46.88 | 54.25 | 217.06 | |
| SE mean | 12.38 | |||||
| SO (n = 79) | Mean | 16.34 | –0.51 | 8.79 | 3.42 | 32.43 |
| SD | 79.52 | –7.26 | 28.05 | 31.29 | 113.42 | |
| SE mean | 8.95 | |||||
| Support worker | ||||||
| D&S (n = 148) | Mean | 130.71 | 1.10 | 39.71 | 67.88 | 215.32 |
| SD | 474.23 | –18.25 | 139.49 | 194.94 | 693.33 | |
| SE mean | 38.98 | |||||
| SO (n = 79) | Mean | 181.28 | –5.18 | 67.94 | 72.65 | 307.31 |
| SD | 615.10 | –64.17 | 224.87 | 151.41 | 896.28 | |
| SE mean | 69.20 | |||||
| Group activities lasting a fixed number of sessions | ||||||
| D&S (n = 148) | Mean | 40.18 | 0.38 | 7.74 | 26.08 | 56.04 |
| SD | 95.83 | –0.39 | 10.73 | 72.64 | 114.95 | |
| SE mean | 7.88 | |||||
| SO (n = 79) | Mean | 18.49 | –0.25 | 7.95 | 6.43 | 32.84 |
| SD | 70.89 | –4.07 | 20.27 | 35.97 | 97.56 | |
| SE mean | 7.98 | |||||
| Support group | ||||||
| D&S (n = 148) | Mean | 45.46 | 0.18 | 8.81 | 29.86 | 62.39 |
| SD | 106.65 | –0.96 | 14.51 | 79.43 | 130.41 | |
| SE mean | 8.77 | |||||
| SO (n = 79) | Mean | 34.99 | 0.19 | 16.20 | 10.60 | 67.31 |
| SD | 141.92 | –9.55 | 49.50 | 50.91 | 212.49 | |
| SE mean | 15.97 | |||||
| Social group | ||||||
| D&S (n = 148) | Mean | 34.89 | –0.14 | 11.95 | 17.15 | 57.77 |
| SD | 144.54 | –6.97 | 38.99 | 78.05 | 197.25 | |
| SE mean | 11.88 | |||||
| SO (n = 79) | Mean | 60.08 | 0.79 | 17.07 | 31.03 | 96.60 |
| SD | 155.83 | –2.17 | 25.98 | 106.08 | 200.68 | |
| SE mean | 17.53 | |||||
| Outpatient care | ||||||
| D&S (n = 148) | Mean | 289.88 | –0.93 | 60.56 | 181.28 | 409.95 |
| SD | 732.16 | –12.12 | 127.27 | 483.39 | 952.01 | |
| SE mean | 60.18 | |||||
| SO (n = 79) | Mean | 329.30 | –1.98 | 81.93 | 181.50 | 499.18 |
| SD | 715.82 | –25.96 | 141.70 | 483.87 | 914.64 | |
| SE mean | 80.54 | |||||
| Accident and emergency | ||||||
| D&S (n = 148) | Mean | 77.54 | 0.26 | 23.17 | 39.30 | 122.95 |
| SD | 281.22 | –4.01 | 46.78 | 194.67 | 358.81 | |
| SE mean | 23.12 | |||||
| SO (n = 79) | Mean | 59.42 | –1.40 | 28.94 | 12.89 | 112.22 |
| SD | 263.96 | –15.03 | 74.53 | 119.14 | 358.68 | |
| SE mean | 29.70 | |||||
| Walk-in centre | ||||||
| D&S (n = 148) | Mean | 91.63 | 1.34 | 24.30 | 50.51 | 143.16 |
| SD | 289.98 | –1.98 | 43.82 | 205.13 | 366.41 | |
| SE mean | 23.84 | |||||
| SO (n = 79) | Mean | 105.64 | 1.45 | 43.33 | 33.48 | 195.60 |
| SD | 367.69 | –10.23 | 88.01 | 189.00 | 510.29 | |
| SE mean | 41.37 | |||||
| Day case | ||||||
| D&S (n = 148) | Mean | 32.69 | 0.21 | 23.24 | 0.00 | 79.05 |
| SD | 280.24 | –28.00 | 122.01 | 0.00 | 427.43 | |
| SE mean | 23.04 | |||||
| SO (n = 79) | Mean | 91.86 | –1.24 | 55.24 | 0.00 | 196.58 |
| SD | 465.30 | –34.87 | 159.32 | 0.00 | 658.63 | |
| SE mean | 52.35 | |||||
| Inpatient care | ||||||
| D&S (n = 148) | Mean | 162.82 | –0.49 | 61.54 | 57.97 | 286.88 |
| SD | 759.50 | –19.11 | 150.29 | 464.62 | 991.53 | |
| SE mean | 62.43 | |||||
| SO (n = 79) | Mean | 101.68 | –4.74 | 67.76 | 0.00 | 217.10 |
| SD | 634.93 | –82.80 | 274.60 | 0.00 | 897.16 | |
| SE mean | 71.44 | |||||
| Police officer | ||||||
| D&S (n = 148) | Mean | 12.69 | –0.13 | 4.77 | 4.42 | 22.18 |
| SD | 56.30 | –1.71 | 11.78 | 31.53 | 74.30 | |
| SE mean | 4.63 | |||||
| SO (n = 79) | Mean | 25.75 | –0.30 | 13.80 | 3.92 | 50.81 |
| SD | 121.29 | –7.70 | 37.80 | 25.72 | 168.88 | |
| SE mean | 13.65 | |||||
| Private appointments with other therapists | ||||||
| D&S (n = 148) | Mean | 37.49 | –0.83 | 18.65 | 10.94 | 71.72 |
| SD | 228.10 | –23.76 | 87.90 | 83.56 | 341.86 | |
| SE mean | 18.75 | |||||
| SO (n = 79) | Mean | 216.81 | –0.26 | 94.10 | 77.98 | 400.40 |
| SD | 832.63 | –54.50 | 277.11 | 317.33 | 1216.59 | |
| SE mean | 93.68 | |||||
| Days taken off owing to sickness | ||||||
| D&S (n = 148) | Mean | 155.29 | –0.73 | 49.54 | 68.26 | 248.48 |
| SD | 622.82 | –25.01 | 159.14 | 289.45 | 863.90 | |
| SE mean | 51.20 | |||||
| SO (n = 79) | Mean | 48.88 | –1.27 | 25.64 | 11.10 | 93.72 |
| SD | 233.64 | –21.46 | 83.51 | 60.19 | 329.97 | |
| SE mean | 26.29 | |||||
| Health and social care costs | ||||||
| D&S (n = 164) | Mean | 2546.21 | –2.82 | 277.94 | 2122.26 | 3079.15 |
| SD | 3496.49 | –198.124 | 1079.46 | 1763.57 | 5131.56 | |
| SE mean | 273.03 | |||||
| SO (n = 88) | Mean | 1669.44 | 2.9 | 219.34 | 1267.34 | 2108.41 |
| SD | 2003.87 | –26.483 | 280.589 | 1423.11 | 2453.65 | |
| SE mean | 213.613 | |||||
| Societal costs | ||||||
| D&S (n = 164) | Mean | 2733.54 | –3.97 | 293.92 | 2271.11 | 3308.36 |
| SD | 3714.10 | –175.88 | 1040.63 | 2046.85 | 5262.59 | |
| SE mean | 290.02 | |||||
| SO (n = 88) | Mean | 1931.08 | 5.40 | 259.29 | 1449.79 | 2493.76 |
| SD | 2347.04 | –30.33 | 317.00 | 1713.76 | 2880.36 | |
| SE mean | 250.20 | |||||
| Cost (£) | Mean difference | Bootstrapa bias | Standard error | Significance (two-tailed) | BCaa 95% CI | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Health and social care costsb | 876.77 | –5.73 | 352.25 | 0.024 | 199.29 | 1620.76 |
| Societal costsb | 802.46 | –9.37 | 387.99 | 0.046 | 78.07 | 1575.64 |
| Cost component | Levene’s test for equality of variances | t-test for equality of means | Significance (two-tailed) | Mean difference | Standard error difference | 95% CI | |||
|---|---|---|---|---|---|---|---|---|---|
| F-statistic | Significance | t-test | df | Lower | Upper | ||||
| GP | 0.35 | 0.56 | 0.34 | 229.00 | 0.73 | 11.65 | 33.96 | –55.26 | 78.56 |
| Psychologist | 4.18 | 0.04 | 2.00 | 226.24 | 0.05 | 116.58 | 58.38 | 1.53 | 231.63 |
| Occupational therapist | 2.83 | 0.09 | 0.95 | 231.00 | 0.34 | 98.78 | 104.17 | –106.47 | 304.03 |
| Nurse | 5.04 | 0.03 | 2.01 | 164.94 | 0.05 | 225.46 | 112.44 | 3.45 | 447.47 |
| SLT | 5.16 | 0.02 | 1.33 | 229.11 | 0.19 | 7.08 | 5.32 | –3.41 | 17.57 |
| Social worker | 1.39 | 0.24 | 0.57 | 230.00 | 0.57 | 10.08 | 17.72 | –24.84 | 45.00 |
| Support worker | 0.39 | 0.53 | –0.50 | 231.00 | 0.62 | –35.58 | 71.62 | –176.69 | 105.53 |
| Fixed group | 11.58 | 0.00 | 1.99 | 214.38 | 0.05 | 21.68 | 10.92 | 0.16 | 43.20 |
| Support group | 0.57 | 0.45 | 0.61 | 230.00 | 0.54 | 9.97 | 16.29 | –22.13 | 42.06 |
| Social group | 3.53 | 0.06 | –1.13 | 231.00 | 0.26 | –22.76 | 20.09 | –62.34 | 16.82 |
| Outpatient | 0.21 | 0.65 | –0.39 | 231.00 | 0.70 | –38.42 | 98.43 | –232.36 | 155.53 |
| Accident and emergency | 0.14 | 0.71 | –0.13 | 230.00 | 0.90 | –5.60 | 44.75 | –93.78 | 82.58 |
| Walk-in centre | 0.39 | 0.53 | –0.24 | 231.00 | 0.81 | –10.14 | 43.13 | –95.13 | 74.85 |
| Day case | 5.33 | 0.02 | –1.01 | 116.85 | 0.32 | –55.18 | 54.80 | –163.70 | 53.34 |
| Inpatient | 0.08 | 0.78 | 0.15 | 231.00 | 0.88 | 15.49 | 103.21 | –187.88 | 218.85 |
| Police officer | 3.22 | 0.07 | –0.84 | 231.00 | 0.40 | –9.90 | 11.76 | –33.07 | 13.26 |
| Private costs | 18.61 | 0.00 | –1.86 | 89.10 | 0.07 | –169.37 | 91.18 | –350.54 | 11.80 |
| Days taken off | 6.88 | 0.01 | 1.89 | 208.33 | 0.06 | 106.70 | 56.40 | –4.48 | 217.87 |
| Service characteristic | Costs over 12-month period to T3 (£) | |||||
|---|---|---|---|---|---|---|
| Nurse | Psychologist | Support worker | ||||
| Mean | SE | Mean | SE | Mean | SE | |
| LA involvement | ||||||
| Joint LA/CCG | 101.06 | 29.17 | 246.52 | 47.94 | 241.46 | 92.27 |
| CCG | 237.13 | 75.64 | 186.27 | 33.83 | 98.16 | 26.61 |
| Team structure | ||||||
| Multiservice | 53.43 | 18.15 | 272.35 | 78.58 | 114.55 | 39.01 |
| Single service | 247.29 | 78.91 | 192.25 | 34.37 | 97.72 | 27.59 |
| Autism vs. ND | ||||||
| ND | 309.88 | 168.42 | 253.58 | 45.79 | 111.64 | 24.52 |
| Autism only | 166.45 | 43.84 | 175.23 | 41.99 | 93.61 | 35.47 |
| Psychoeducation | ||||||
| Dominant mode is one-to-one sessions | 333.55 | 191.49 | 198.74 | 45.99 | 91.11 | 23.54 |
| Group delivered | 164.70 | 41.34 | 206.05 | 41.14 | 104.44 | 33.89 |
| Skill mix | ||||||
| Number of professional disciplines is four or more | 155.45 | 38.93 | 165.14 | 30.25 | 123.25 | 59.17 |
| Number of professional disciplines is two or three disciplines | 227.06 | 80.15 | 210.96 | 37.26 | 130.31 | 32.94 |
| One-to-one work | ||||||
| Routinely do one-to-one work for mental health problems | 91.86 | 25.99 | 218.77 | 43.14 | 222.7 | 81.56 |
| Not routinely carried out | 245.21 | 78.45 | 192.66 | 35.03 | 98.68 | 27.58 |
| Delivery of care plan | ||||||
| Managed | 216.82 | 74.84 | 218.27 | 35.42 | 129.94 | 30.93 |
| Episodic | 175.76 | 45.94 | 125.68 | 25.26 | 122.81 | 73.16 |
| Drop-in provision and/or named contact while in the service | ||||||
| No drop-in provision | 171.63 | 43.24 | 168.22 | 32.12 | 136.12 | 66.31 |
| Drop-in provision available | 219.43 | 77.19 | 208.29 | 36.02 | 126.13 | 31.74 |
| Coefficient | Standard error | z | p > z | 95% CI | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Diagnostic status at referral (1 = SO; 0 = D&S) | –1.489 | 2.061 | –0.720 | 0.470 | –5.529 | 2.552 |
| Age (years) | 0.106 | 0.084 | 1.270 | 0.205 | –0.058 | 0.270 |
| Gender (1 = female; 0 = male) | –0.050 | 1.865 | –0.030 | 0.978 | –3.705 | 3.605 |
| WHOQOL-BREF psychological domain score at T0 | 0.760 | 0.050 | 15.120 | 0.000 | 0.662 | 0.859 |
| Costs (£) | ||||||
| Societal at T0 | 0.002 | 0.002 | 0.900 | 0.366 | –0.002 | 0.006 |
| GP | –0.011 | 0.004 | –2.640 | 0.008 | –0.020 | –0.003 |
| Psychologist | –0.002 | 0.002 | –0.810 | 0.420 | –0.007 | 0.003 |
| Occupational therapist | 0.002 | 0.003 | 0.810 | 0.418 | –0.003 | 0.008 |
| Nurse | –0.002 | 0.002 | –1.000 | 0.318 | –0.007 | 0.002 |
| SLT | –0.018 | 0.020 | –0.910 | 0.363 | –0.058 | 0.021 |
| Social worker | –0.001 | 0.010 | –0.130 | 0.900 | –0.021 | 0.019 |
| Support worker | 0.001 | 0.003 | 0.350 | 0.725 | –0.004 | 0.006 |
| Fixed group | –0.001 | 0.012 | –0.070 | 0.941 | –0.025 | 0.024 |
| Support group | 0.009 | 0.009 | 1.080 | 0.280 | –0.008 | 0.026 |
| Social group | 0.001 | 0.006 | 0.100 | 0.917 | –0.012 | 0.013 |
| Outpatient | 0.001 | 0.002 | 0.940 | 0.350 | –0.002 | 0.004 |
| Accident and emergency | 0.008 | 0.005 | 1.710 | 0.088 | –0.001 | 0.017 |
| Walk-in centre | 0.004 | 0.003 | 1.160 | 0.247 | –0.003 | 0.010 |
| Day care | 0.000 | 0.003 | 0.060 | 0.952 | –0.005 | 0.006 |
| Inpatient care | –0.003 | 0.002 | –1.690 | 0.091 | –0.006 | 0.000 |
| Police officer | 0.013 | 0.011 | 1.190 | 0.234 | –0.008 | 0.034 |
| Private appointments with other therapist | –0.003 | 0.002 | –1.420 | 0.154 | –0.006 | 0.001 |
| Constant term | 9.460 | 3.942 | 2.400 | 0.016 | 1.735 | 17.185 |
| Coefficient | Robust standard error | z | p > z | 95% CI | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Diagnostic status at referral (1 = SO; 0 = D&S) | 1.011 | 1.249 | 0.810 | 0.418 | –1.437 | 3.459 |
| Baseline health and social care costs (£) | 0.001 | 0.003 | 0.330 | 0.740 | –0.005 | 0.007 |
| Age (years) | 0.038 | 0.070 | 0.550 | 0.584 | –0.098 | 0.175 |
| Gender (1 = female; 0 = male) | –1.023 | 2.779 | –0.370 | 0.713 | –6.470 | 4.423 |
| Living with parents at T0 (1 = yes; 0 = no) | 1.950 | 2.105 | 0.930 | 0.354 | –2.176 | 6.075 |
| Time off work/education owing to illness (1 = yes; 0 = no) | –3.089 | 2.722 | –1.130 | 0.256 | –8.424 | 2.246 |
| WHOQOL-BREF psychological domain score at T0 | 0.724 | 0.079 | 9.110 | 0.000 | 0.568 | 0.880 |
| LA involvementa | –6.075 | 4.726 | –1.290 | 0.199 | –15.338 | 3.188 |
| Team structureb | 4.874 | 1.928 | 2.530 | 0.011 | 1.095 | 8.653 |
| Autism vs. NDc | –9.986 | 0.943 | –10.590 | 0.000 | –11.835 | –8.138 |
| Psychoeducationd | 2.631 | 2.138 | 1.230 | 0.219 | –1.560 | 6.822 |
| Skill mixe | –5.872 | 4.000 | –1.470 | 0.142 | –13.712 | 1.967 |
| One-to-one workf | 17.097 | 1.152 | 14.840 | 0.000 | 14.839 | 19.355 |
| Delivery of care plang | –6.762 | 5.247 | –1.290 | 0.197 | –17.046 | 3.522 |
| Constant term | 19.905 | 6.063 | 3.280 | 0.001 | 8.022 | 31.787 |
| Coefficient | Robust standard error | z | p > z | 95% CI | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Diagnostic status at referral (1 = SO; 0 = D&S) | 1.696 | 1.344 | 1.260 | 0.207 | –0.939 | 4.330 |
| Baseline societal cost (£) | 0.004 | 0.002 | 2.260 | 0.024 | 0.001 | 0.007 |
| Age (years) | –0.022 | 0.063 | –0.350 | 0.728 | –0.145 | 0.101 |
| Gender (1 = female; 0 = male) | –2.780 | 1.938 | –1.430 | 0.151 | –6.578 | 1.019 |
| Time off work/education owing to illness (1 = yes; 0 = no) | –4.399 | 2.342 | –1.880 | 0.060 | –8.988 | 0.190 |
| WHOQOL-BREF psychological domain score at T0 | 0.714 | 0.074 | 9.630 | 0.000 | 0.568 | 0.859 |
| LA involvementa | –8.574 | 3.364 | –2.550 | 0.011 | –15.168 | –1.980 |
| Team structureb | 4.002 | 1.771 | 2.260 | 0.024 | 0.531 | 7.472 |
| Autism vs. NDc | –9.966 | 0.797 | –12.500 | 0.000 | –11.528 | –8.404 |
| Psychoeducationd | 1.077 | 1.074 | 1.000 | 0.316 | –1.028 | 3.181 |
| Skill mixe | –4.977 | 3.031 | –1.640 | 0.101 | –10.917 | 0.962 |
| One-to-one workf | 19.510 | 1.536 | 12.700 | 0.000 | 16.499 | 22.520 |
| Delivery of care plang | –5.490 | 3.576 | –1.540 | 0.125 | –12.499 | 1.519 |
| Constant term | –30.69 | 744.21 | –0.040 | 0.967 | –1489.31 | 1427.94 |
| Coefficient | Robust standard error | z | p > z | 95% CI | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Referral (1 = SO; 0 = D&S) | –0.059 | 0.058 | –1.020 | 0.309 | –0.173 | 0.055 |
| Age (years) | 0.001 | 0.002 | 0.310 | 0.758 | –0.004 | 0.005 |
| Gender (1 = female; 0 = male) | 0.039 | 0.039 | 0.990 | 0.320 | –0.038 | 0.115 |
| Living with parents at T0 (1 = yes; 0 = no) | –0.004 | 0.059 | –0.070 | 0.941 | –0.121 | 0.112 |
| Time off work/education owing to illness (1 = yes; 0 = no) | –0.105 | 0.045 | –2.350 | 0.019 | –0.194 | –0.017 |
| Baseline utility score | 0.681 | 0.124 | 5.470 | 0.000 | 0.437 | 0.925 |
| Baseline health and social care cost (£) | 0.000 | 0.000 | 0.260 | 0.791 | 0.000 | 0.000 |
| LA involvementa | 0.638 | 0.234 | 2.730 | 0.006 | 0.179 | 1.096 |
| Team structureb | 0.007 | 0.093 | 0.080 | 0.937 | –0.175 | 0.190 |
| Autism vs. NDc | –0.182 | 0.086 | –2.110 | 0.034 | –0.351 | –0.013 |
| Psychoeducationd | 0.161 | 0.094 | 1.710 | 0.087 | –0.023 | 0.345 |
| Skill mixe | –0.283 | 0.196 | –1.440 | 0.149 | –0.667 | 0.102 |
| One-to-one workf | –0.395 | 0.121 | –3.270 | 0.001 | –0.632 | –0.159 |
| Delivery of care plang | –0.274 | 0.216 | –1.270 | 0.204 | –0.698 | 0.149 |
| Constant term | 0.459 | 0.239 | 1.920 | 0.055 | –0.009 | 0.927 |
| Coefficient | Robust standard error | z | p > z | 95% CI | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Referral (1 = SO; 0 = D&S) | –0.062 | 0.055 | –1.120 | 0.263 | –0.171 | 0.046 |
| Baseline societal cost (£) | 0.000 | 0.000 | –1.290 | 0.197 | 0.000 | 0.000 |
| Age (years) | 0.001 | 0.002 | 0.580 | 0.564 | –0.003 | 0.005 |
| Gender (1 = female; 0 = male) | 0.051 | 0.039 | 1.310 | 0.191 | –0.026 | 0.128 |
| Time off work/education owing to illness (1 = yes; 0 = no) | –0.085 | 0.046 | –1.860 | 0.062 | –0.175 | 0.004 |
| Baseline utility score | 0.634 | 0.126 | 5.010 | 0.000 | 0.386 | 0.882 |
| LA involvementa | 0.585 | 0.218 | 2.680 | 0.007 | 0.157 | 1.013 |
| Team structureb | 0.042 | 0.093 | 0.450 | 0.652 | –0.141 | 0.225 |
| Autism vs. NDc | –0.194 | 0.085 | –2.280 | 0.023 | –0.361 | –0.027 |
| Psychoeducationd | 0.163 | 0.088 | 1.860 | 0.063 | –0.009 | 0.335 |
| Skill mixe | –0.247 | 0.192 | –1.290 | 0.197 | –0.623 | 0.129 |
| One-to-one workf | –0.381 | 0.113 | –3.360 | 0.001 | –0.603 | –0.159 |
| Delivery of care plang | –0.235 | 0.208 | –1.130 | 0.258 | –0.642 | 0.173 |
| Constant term | 0.442 | 0.234 | 1.890 | 0.059 | –0.016 | 0.901 |
Appendix 16 Assessment by local authority for care or support needs: Specialist Autism Team cohort
| Response options | T0 (n = 201), n (%) | T3 (n = 204), n (%) |
|---|---|---|
| No | 176 (87.56) | 170 (83.33) |
| Waiting | 8 (3.98) | 5 (2.45) |
| Currently being assessed | 5 (2.49) | 7 (3.43) |
| Yes, not eligible | 4 (1.99) | 8 (3.92) |
| Yes, have care plan and receive direct payments | 7 (3.48) | 11 (5.39) |
| Yes, have care plan and council manage my individual budget | 1 (0.5) | 3 (1.47) |
| Total | 201 (100) | 204 (100) |
List of abbreviations
- AIC
- Akaike information criterion
- ANCOVA
- analysis of covariance
- CCG
- Clinical Commissioning Group
- CI
- confidence interval
- CMHT
- community mental health team
- CSO
- clinical studies officer
- CSRI
- Client Service Receipt Inventory
- D&S
- Diagnosis and Support
- df
- degrees of freedom
- DISCO
- Diagnostic Interview for Social and Communication Disorders
- DO
- Diagnosis Only
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- GDG
- Guideline Development Group
- GHQ-12
- General Health Questionnaire – 12
- GIR
- Guidance Implementation Resource
- GP
- general practitioner
- IAPT
- improving access to psychological therapies
- ISEL-SF
- Interpersonal Support Evaluation List – Short Form
- LA
- local authority
- LD
- learning disability
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- PAG
- project advisory group
- QALY
- quality-adjusted life-year
- SAT
- Specialist Autism Team
- SHAPE
- Supporting adults with High-functioning Autism and asPerger syndromE
- SLT
- speech and language therapist
- SO
- Support Only
- T0
- baseline assessment
- T1
- 3-month assessment
- T2
- 6-month assessment
- T3
- 12-month assessment
- T4
- 18-month assessment
- T5
- 24-month assessment
- WHOQOL-BREF
- World Health Organization Quality Of Life assessment, abbreviated version
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/hsdr08480).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
