Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 16/115/18. The contractual start date was in December 2017. The draft report began editorial review in September 2019 and was accepted for publication in May 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2021. This work was produced by Burton et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2021 Queen’s Printer and Controller of HMSO
Chapter 1 Background
At both national and local levels, there is a general consensus that the NHS could get better at ensuring that the least effective interventions are not routinely performed, or only performed in more clearly defined circumstances.
Ellul et al. 1
The challenge
Across the globe, health and care systems are under pressure to demonstrate that actions to ensure efficient use of resources are prioritised, but do not compromise the quality of the care provided to patients and the public. Alongside this growing emphasis on more efficient use of resources for health and care services2 is the stark reality of overspending across health services. In the UK, for example, just 5% of NHS providers overspent their annual budgets in 2010/11. However, two-thirds of NHS trusts were in deficit by 2015/16. 3 In the USA, it has been estimated that 30% of medical spending is unnecessary. 4 The problem is further compounded when non-evidence-based decisions are known to have poor outcomes, can cause harm and/or are of low value, but nonetheless continue to be made.
Government policy in high-income economies highlights the importance of the delivery of health and care that is efficient, is prudent and makes best use of resources when these may be limited. In the UK, Realistic Medicine5 promotes treatment that is focused on the probability of benefit rather than the possibility of benefit. In her second report, the Chief Medical Officer for Scotland outlines how the intention of Realistic Medicine5 is to place the patient at the centre of decision-making, utilising a personalised approach to their care while concurrently reducing harm and waste. The challenges to these ambitions are certainly not underestimated, in particular when the desire to provide safe, personalised care at an individual level may be in tension with broader aims of Realistic Medicine, notably when ‘tackling unwarranted variation in care, managing clinical risk, and innovating to improve, are essential to a well-functioning and sustainable NHS’. 5
In Wales, the principles of prudent health care6 have been launched, primarily to discourage the tendency to intervene when a lesser intervention might suffice. The policy driver for prudent health is a ‘healthier’ Wales, the Welsh Government’s long-term plan for health and care, which informs much of today’s health agenda across Wales. Prudent health-care principles are applied by the Bevan Exemplars (i.e. health professionals who test out innovation at the heart of care provision) and Bevan Advocates (i.e. public representatives who work to support the principles by sharing experiences and developing person-centred approaches to support prudent health care). 7,8 What is apparent through scrutiny of these and other examples of similar policy drivers across the globe is the emphasis on the importance of using only clinical and other practices that are effective, valuable and reflect a high quality of care for patients. A foundation for both the Scottish and Welsh initiatives, together with the What Works Network in England, is the robustness of an evidence base on which to verify decisions. 9
Current policy drivers include the Choosing Wisely10 campaign in Canada and the USA. The Choosing Wisely mission is a proactive campaign to encourage conversations between clinicians and patients, thereby helping people to choose care that is safe, is evidence based and does not duplicate interventions the person may have already received. Additionally, the use of low-value practices is an area of growing interest for the patient and public agenda, which is too often faced with reports of poor practice, wastage and duplication of services. Although there is potential for the patient and the public agenda, as a significant channel, to drive improvements in this area (e.g. challenging expectations around antibiotic prescribing), the success of these approaches are often not captured by meaningful data.
There is often insufficient consideration about how best to stop or withdraw existing practices and services that have been identified as low value, non-evidence based or unsafe. This is the knowledge gap that has led to this review being undertaken. To provide managers, commissioners and service leaders with practical information on how to successfully change/replace practices, meaningful evidence is required to understand the challenges and complexities involved, and provide solutions to ultimately improve service efficiency and quality. Despite reflecting a renewed dedication to evidence-based health care,11 researchers have previously highlighted that stopping interventions, policies and practices lacks guidance for practitioners and managers. 12
De-implementation at practice level
Although still in its infancy, interest is developing across health and care in de-implementation. 11,13,14 De-implementation is often described, at practice level, as a process of disinvesting or abandoning practices or interventions that may be harmful or ineffective,11 or no longer necessary. 15 Although the term is associated with ‘stopping practices that are not evidence based’,4 or the discontinuation of interventions that should be stopped,15 to date, a comprehensive definition of de-implementation at practice and service level is largely absent. This review aims to address this gap.
Furthermore, although there may be an assumption that de-implementation is the reverse process of implementation, with some transferability of the mainstay implementation theory and frameworks between the two, McKay et al. 15 suggest that de-implementation should be considered separately from recognised stages of implementation, including adoption and sustainability. Although many similarities may be apparent in the literature,15 which cross-reference the work of others,4,16 the factors that shape the processes of implementation and de-implementation are likely to be different and, if similar, work in different ways. 11 In one example, Hahn et al. 14 found that the usual strategies for implementation success, such as improving awareness and knowledge, were unlikely to be effective for de-implementation.
Prasad and Ionnidis11 refer to de-implementation as the abandonment of practices (i.e. a process that is contingent on a multitude of factors, not only research evidence, but also financial and professional conflicts, and cultural and societal values). 17,18 The process of de-implementation as the abandonment of existing practice is also supported by Voorn et al.,19 who argue that theory and evidence about agents, barriers, facilitators and interventions is limited. There are reports from individual studies that have specifically paid attention to de-implementation. For example, van Bodegom-Vos et al. 4 explored the literature and analysed data about implementation and de-implementation from two studies among Dutch orthopaedic surgeons. The authors4 conclude that further research is required to understand the required leadership and champion characteristics that can accelerate the process of de-implementation. The authors4 also call for more research to establish the factors that influence the success (or not) of de-implementation and to provide better understanding of the range of de-implementation strategies.
De-implementation at system level
According to Robert et al. ,20 system-level approaches focus on ‘policies to remove interventions from across wider geographical areas and/or patient populations, and strategic reconfiguration of services leading to organisational downgrading or closure’. Therefore, closing acute and community services, stopping the particular use of a medical technology and removing drugs from a formulary would fall under this remit. 20 They found a stark contrast between expert and practice opinion about what should determine related decisions, underpinned by technical and political processes. For Robinson et al. ,21 priority-setting and rationing was seen as one of resource scarcity when referring to withdrawing or cutting services. Williams et al. 22 describe the replacement and removal of interventions and services as they become obsolete or are superseded by others.
A recognised priority for international health-care financing23 is de-implementation under the guise of disinvestment. This is an underdeveloped area, especially regarding the lack of overt disinvestment frameworks in use. 24 According to Harris et al. ,25 there is little evidence to guide health-care staff and systems to take a systematic approach towards disinvestment. Paprica et al. 26 agree that there is a lack of guidance and point to political and social factors that can hinder evidence-informed disinvestment strategies. This approach is not always related to a whole service, as there can be partial or selective disinvestment approaches. 26 Elshaug et al. 23 suggest an ever-present economic dimension in their definition of disinvestment, as ‘healthcare practices, procedures, technologies, or pharmaceuticals that are deemed to deliver little or no health gain for their cost, and thus do not represent efficient health resource allocation’. It is unclear whether or not disinvestment always includes the shifting of resources to other health services and technologies that have greater clinical effectiveness or cost-effectiveness, although this is assumed by Polisena et al. 27 and Rooshenas et al. 12 in their definitions. There appears to be better clarity about the concept of rationing, mainly that it is focused on the one core idea of limiting or denying a potentially beneficial treatment because of its scarcity. 28 Dickinson et al. 29 conceptualise rationing as ‘the withholding of resources to the cost of individual patients’, compared with priority setting, which applies to populations.
Previous reviews
The study of de-implementation has gained impetus in recent years. Norton et al. 30 sought evidence of de-implementation research grants funded in the UK and the USA. The authors included only 20 grant proposals focused on de-implementing across a range of health services and practices. We sought the evidence from previous reviews about de-implementation and found that Niven et al. ,13 which, to date and to our knowledge, is the sole evidence review of de-implementation. Niven et al. 13 set out to systematically review the literature on de-adoption and used scoping review methodology for the task. The authors found a large number of different terms relating to the process of de-adoption with no established taxonomy. Niven et al. 13 suggest that lack of clarity is having a negative impact on communication and ‘branding’. When terms such as knowledge translation and implementation science are well established, Niven et al. 13 suggest that de-adoption and de-implementation as ‘natural antonyms of adoption and implementation, ought to be used as terms that brand the process of reducing or removing low-value clinical practices’. 13 The review authors propose a model that providers and decision-makers can use to guide efforts to de-adopt ineffective and harmful practices. The complexity of de-adoption is highlighted in their review, as is the potential of employing an active change intervention for successful de-adoption. 13 Crucially, the review identifies a number of questions for further research ‘to determine an ideal strategy for identifying low-value practices, and facilitating and sustaining de-adoption’. 13
We conclude from this review and current discourse about de-implementation and de-adoption that further understanding of the dimensions of both is required to inform health and care stakeholders how best to move forward. For managers and clinicians this included the need to disentangle the practices that may be ineffective for one population group but effective for another, and better understand the factors that determine why practices should be de-implemented or de-adopted. There exists a clear gap in the evidence to enable managers and service leaders to understand how best to de-implement using different approaches when they may be operating in different circumstances. In Chapter 2 we explain the rationale for choosing a realist approach for the review in conjunction with the review aims and objectives articulated below.
Review questions
The main aim of this review was to produce useful programme theory and practical guidance for policy-makers, managers and clinicians to help them with de-implementation processes and procedures.
The objectives of the review were to:
-
generate a concept analysis of de-implementation
-
identify and map the range of different de-implementation approaches and/or strategies currently being utilised across health and care, paying attention to ways in which they are assumed to work
-
produce a typology of de-implementation types, processes and contexts
-
examine and understand the range of anticipated and unanticipated impacts of these approaches and/or strategies across different settings and stakeholders, paying attention to contextual conditions that influence these impacts
-
generate an evidence-based realist programme theory that explains the successful processes and impacts of de-implementation
-
explore, through stakeholder engagement in the review methods, decision-making processes associated with de-implementation
-
produce recommendations about ways in which different approaches and/or strategies can help managers and service leaders plan and prioritise de-implementation in a systematic and efficient manner
-
stimulate a wider debate about avoiding and stopping services that are considered wasteful, of low value and non-efficient for future provision.
Summary
In this first chapter we have sought to provide the important context for this subject across health and care today. What has emerged in this chapter is the lack of clarity about the concept of de-implementation and the levels at which de-implementation operates. These knowledge gaps, together with the suggestion that future research is focused on ‘similarities and differences between the study of de-implementation of health practices and programs and related areas of inquiry, such as health-care delivery, implementation science, improvement science, and others’,30 have led to this review. In the next chapter we report on the methods employed for the review.
Chapter 2 Review methods
Introduction
As articulated in Chapter 1, this review drew on realist principles to address the review aims and objectives, as well as significant research team experience. 31–33 In this chapter we present the review methods and follow published publication standards (i.e. points 5–13 from the list of items to be included when reporting a realist synthesis). 34 Further details of the review methods are presented in the published review protocol. 35
Changes in the review process
No changes were made to the published protocol.
Rationale for using realist synthesis
Realist synthesis was considered to be the most appropriate method to use for this review. In Chapter 1, reference to the fact that there is likely to be a complex array of approaches to de-implementation operating in a variety of contexts means that realist synthesis is a natural fit for this review. Realist synthesis is theory driven,36 whereby the focus is on understanding underlying elements or mechanisms of a programme that interact within contexts to result in success or failure. Using this approach is a recognition that programmes are implemented in different contexts and, hence, operate through different mechanisms to produce different patterns of outcomes. 37 Therefore, a realist synthesis can facilitate an evidence-based explanation of how complex programmes operate within different conditions.
A realist review begins with the construction of an initial programme theory, developed through the collection of evidence from the literature and relevant stakeholders (Phase 1). This initial theory is refined to create a final programme theory that provides plausible explanations of why certain interventions work (or do not work) in certain circumstances. This is an iterative rather than linear process, as the theory is repeatedly tested and refined with accumulating knowledge (Phases 2 and 3). The realist methodology is a theory driven, interpretive approach to uncover underlying mechanisms that account for why people change because of the intervention resource. The interpretive approach is driven by various forms of reasoning (e.g. deductive methods and inductive reasoning), but fundamental to the realist method of inquiry is abductive or retroductive reasoning. 38 Retroduction is a mode of inference in which events are explained by postulating (and identifying) mechanisms that are capable of producing outcomes. According to Wynn and Williams,39 retroduction is characterised by the use of causal mechanisms as the basis for explanation.
In realist synthesis, programme theory ‘describes how an intervention may work to change people’s behaviours’. 40 The intervention is not the theory but a ‘resource’ people choose to use to help behaviour change. 41 To construct programme theories, different sources of evidence are sought through a systematic process that includes stakeholder engagement, an overview of relevant extant theory40 and scrutiny of primary research of the topic under the lens. 42 In this case, the focus was on de-implementation of programmes or interventions.
In realist synthesis, programme theory is expressed as conjectured and then final context–mechanism–outcome (CMO) configurations. Mechanisms describe ‘the pathway from resource to reasoning and response’,40 and resources can be described as those that are ‘material, cognitive, social or emotional’. 31 The reasoning and response may stem from the perspectives of the receivers, the organisers and/or those involved in the delivery of programmes/interventions.
Review strategy
Programme theory development and refinement involves a number of interconnected steps. As is usual, in this realist synthesis, stages were conducted in an iterative rather than linear fashion, in contrast to a traditional systematic review approach. 43 As agreed in our funded protocol, the realist synthesis was undertaken over four phases (see Appendix 1):
-
concept analysis and initial programme theory development
-
retrieval, review and synthesis of evidence
-
refining programme theory
-
programme theory evaluation.
The review process iterated between theory development, interrogation of evidence and theory refinement based on the team’s previous experiences. 32,33
Scoping the literature
The review was preceded by a scope of the evidence34 to outline the possible theoretical underpinnings of de-implementation and to clarify understanding. We determined a list of key words from our initial team conceptualisation of de-implementation and undertook a preliminary scope of evidence using a related published search strategy. 13 For this initial scoping search, we undertook a title-only search in Cumulative Index to Nursing and Allied Health Literature (CINAHL) and MEDLINE, limited to human and English language, using TI (disinvest* OR dis-invest* OR ‘decrease use’ OR discontinu* OR dis-continu* OR abandon* OR reassess* OR re-assess* OR obsole* OR ‘medical reversal’ OR contradict* OR withdraw* OR ‘health technology reassessment’ OR deimplement* OR de-implement*) N3 (healthcare or technolog* or device* or intervention* or health practi?e* or medical or medical practi?e* or procedur* or drug or drugs or biotechnology*) and found 100 results in CINAHL and 1123 results in MEDLINE. A percentage of these were screened for titles of interest to the review. We also carried out a search to identify relevant reviews and guidelines. We found 55 titles that appeared initially of interest to this element of the review.
Theoretical platform
The theoretical platform guided the literature scoping and consultation work with stakeholders. To initiate the process, we undertook a desktop exercise to consider the range of different theories and approaches that underpin the implementation research evidence base. Elements of these theories provided the platform for Phase 1 work and the following:
-
innovation and unlearning, for example the role of context and systems in challenging and renewing organisational memory (e.g. Cegarra-Navarro et al. 44)
-
organisational psychology (i.e. stages of renewal and decline) (e.g. Lester et al. 45)
-
habit formation and breaking habits, including how habits are formed (e.g. Lally et al. 46) and the role of habit in implementing research on clinical behaviour change (e.g. Nilsen et al. 47)
-
ecology and life cycle assessment (e.g. Atkins et al. 48)
-
health-care rationing (e.g. Rooshenas et al. 12) and the ethics of rationing (e.g. Scheunemann and White28)
-
technology adoption and the diffusion of innovations (e.g. Rogers49 and Greenhalgh et al. 50)
-
implementation and knowledge mobilisation (e.g. Rycroft-Malone et al. 51 and Ferlie et al. 52)
-
decision-making theories and strategic decision-making (i.e. rational and non-rational) (Oliveira53)
-
organisational management, complexity thinking, resource-based view (e.g. Plesk and Wilson,54 and Burton and Rycroft-Malone55)
-
leadership and theories of leadership (e.g. The King’s Fund,56–58 Tomlinson,59 West et al. 60 and Wong and Cummings61)
-
efficiency/prudent systems and processes (e.g. Aylward et al. 62 and The King’s Fund63)
-
nudge and behaviour change (Sunstein and Thaler,64 Marteau et al. ,65 Evans and Stanovich66 and Parkinson et al. 67)
-
human factors/cognitive task analysis (e.g. Catchpole68 and the Agency for Healthcare Research and Quality69)
-
persuasion theories used as a stage in the diffusion process (e.g. Rogers70) and attitude change (e.g. Wood71)
-
organisational sociology, with focus on culture and power as contextual factors and receptive contexts (Pettigrew and Whipp72).
Phase 1: concept analysis
In Phase 1, a concept analysis of ‘de-implementation’ was undertaken. The rationale for undertaking this work at this stage was twofold:
-
There is an identified conceptual confusion surrounding the term ‘de-implementation’ and the desire for better clarity.
-
There is a requirement for better understanding to inform the development of the initial programme theory.
Background
‘De-implementation’ was the overarching concept for this review. However, as articulated in Chapter 1, the term is used inconsistently and interchangeably within the extant literature. 73 For example, de-implementation may describe explicit and directional functions (i.e. withdrawal or stopping interventions) or abandoning medical practices when evidence of efficacy is weak or absent, or when harm is demonstrated. 11 However, for this review, we consider that de-implementation may also be more implicit and, at best, inferred within theories that inform the implementation research evidence base.
Concept analysis
A concept analysis is defined as a formal, linguistic procedure used to determine the essential attributes of a concept. It focuses on the use of words to explain phenomena. 62 Concept analysis is a technique that requires critical approaches to uncover subtle elements of meaning embedded in concepts, where a concept is thought of ‘. . . as mental constructions; they are our attempts to order our environmental stimuli . . . that contain defined attributes’. 74
Process
Drawing on the results of the scoping search, we identified clustered attributes (i.e. antecedents, process and outcome) and specified model, related and contrary cases that place the concept in context. We aimed to identify empirical referents that could be used to evaluate the occurrence of the concept in practice, policy or research. Walker and Avant’s74 concept analysis procedure was followed. The procedure describes an iterative eight-step process:
-
Select a concept.
-
Determine the aims and purposes of analysis.
-
Identify all uses of the concept that are discovered.
-
Determine the defining attributes.
-
Identify a model case.
-
Identify borderline, related, contrary, invented and illegitimate cases.
-
Identify antecedents and consequences.
-
Define empirical referents.
Search strategy for the concept analysis
The search strategy for the concept analysis entailed a restricted scoping review of the literature,75 instigated by the 43 terms identified by Niven et al. 13 We undertook a title-only search in CINAHL and MEDLINE, limited to human and English language, using TI (disinvest* OR dis-invest* OR ‘decrease use’ OR discontinu* OR dis-continu* OR abandon* OR reassess* OR re-assess* OR obsole* OR ‘medical reversal’ OR contradict* OR withdraw* OR ‘health technology reassessment’ OR deimplement* OR de-implement*) N3 (healthcare or technolog* or device* or intervention* or health practi?e* or medical or medical practi?e* or procedur* or drug or drugs or biotechnology*). We also used snowballing techniques to identify clusters of relevant papers and checked references lists of relevant published reviews.
Results
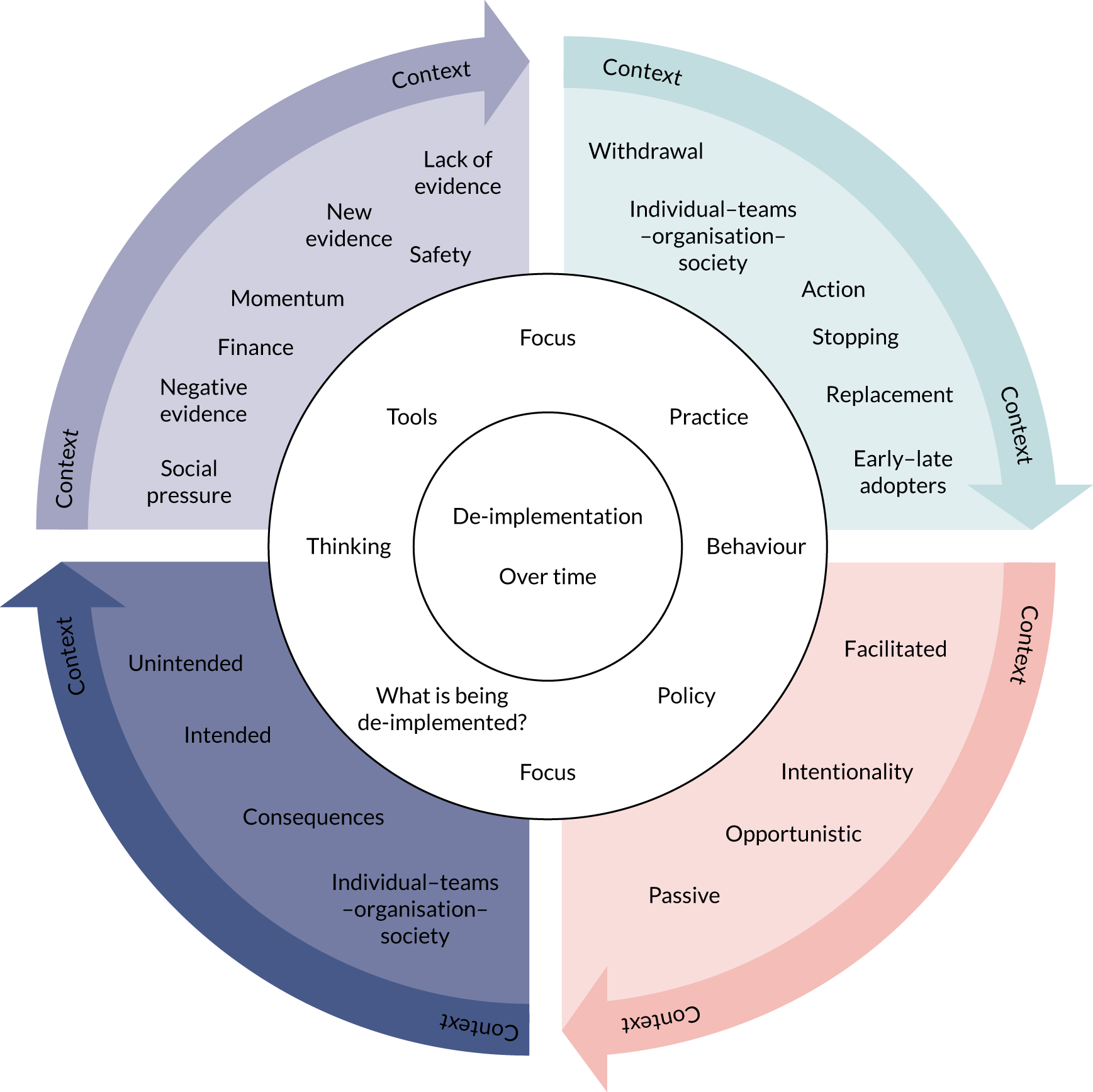
In total, the search returned 214 papers, representing 26 terms that referred to de-implementation (Table 1). PJ, CRB, LW, BH and JRM undertook desktop work to develop and agree an extraction template. We extracted data from a total of 38 papers selected on the basis of their descriptive depth across the range of terms identified in the papers or suggested by stakeholders. These were used to develop an initial framework of de-implementation attributes represented in Figure 1.
| Terms | Number of papers |
|---|---|
| Abandonment | 2 |
| Contradicted | 1 |
| De-adoption | 11 |
| De-commissioning | 5 |
| Decreased use | 2 |
| De-implementation | 31 |
| De-innovate | 1 |
| De-prescribing | 33 |
| Discontinuation | 7 |
| Disinvestment | 52 |
| Elimination | 1 |
| Evidence reversal | 1 |
| Exnovation | 3 |
| Health technology reassessment | 7 |
| Low value | 13 |
| Medical reversal | 12 |
| Mis-implementation | 2 |
| Obsolete/obsolescence | 3 |
| Overuse/overdiagnosis/overtreatment | 7 |
| Rationing | 7 |
| Reduce inappropriate testing | 2 |
| Substitution | 2 |
| Withdraw | 8 |
| De-escalation | 0 |
| Desist | 0 |
| Disincentivise | 0 |
| Retract | 0 |
FIGURE 1.
Concept analysis defining attributes and antecedents.
Uses of the concept
Van Bodegom-Vos et al. 4 differentiated between terms such as de-adoption and discontinuation as clinician initiated, whereas terms such as disinvestment and de-implementation required a strategy to be in place for abandonment to occur. According to van Bodegom-Vos et al. ,4 de-implementation is the preferred term to apply to the reduction of procedures with little evidence base, as it can incorporate a wider range of approaches than just the removal of financial incentives. Wang et al. 76 described four types of change related to de-implementation:
-
partial reduction
-
complete reversal
-
substitution with related replacement
-
substitution with unrelated replacement of existing practice.
Critical attributes
We identified five critical attributes for de-implementation. The attributes identified are described in Table 2.
| Critical attribute | Description |
|---|---|
| What is being de-implemented | This is the focus of change and relates to one or more context areas, such as clinician behaviour change or organisational policy |
| Push or driving force | Factors motivating the de-implementation process (e.g. lack of evidence of effectiveness, financial constraints or safety issues) |
| Nature of action | What is the continuum of the de-implementation process from complete termination to replacement with another innovation? |
| Degree of intentionality | To what extent is the de-implementation process intentional and planned or passive and opportunistic? |
| Consequences | Intended or unintended and at what level, in what context and over what time? |
What is being de-implemented?
This attribute is the focus for change, directed either at behaviours (e.g. clinicians or managers) or more broadly at policy level, with both contexts often being targeted simultaneously. 19
Push or driving force
There are several reasons why the de-implementation of a process or procedure becomes prominent at certain times. New evidence can emerge that shows a better way of proceeding, there may be concern about the safety of a procedure or there can be the removal of incentives.
Goal of the action
This attribute describes the goal of the de-implementation strategy. For procedures with safety issues, the objective may be to withdraw the drug or procedure entirely. However, in other contexts, the procedure may be of value to a particular defined group, but not for the majority, and so the de-implementation approach is to reduce the number of people who do not derive benefit. In many cases, the low-value procedure could be replaced by a more effective alternative (i.e. a case of medical reversal that can in certain contexts be an effective stratagem). 77
Degree of intentionality
This attribute highlights the purposefulness of the de-implementation process. The strategy adopted for the abandonment of a procedure may be passive as clinicians increasingly adopt a newer intervention, but this process is not actively initiated or led, leading to the eventual stopping of the procedure. Other strategies may be planned and facilitated, such as the closure of a facility.
Consequences
The results of the de-implementation process may not have been as intended (e.g. the strategy may have had the objective of stopping the procedure, but the strategy achieved only a diminution in practice).
Case studies
Walker and Avant’s74 concept analysis process proceeds through the development of several cases that represent all the attributes of the concept (i.e. a model case, a borderline case that has some attribute and a contrary case that clearly does not contain attributes of the concept). Walker and Avant74 stipulate that the cases can be taken from real-life examples, literature or cases constructed by authors. For all three case examples in our concept analysis, we have drawn on evidence from the literature on de-implementation, rather than construct our own cases. We found that having examples drawn from evidence is a useful starting point for further refinement of the concept.
Model case
A model case is an example that articulates the attributes within the concept. Walker and Avant74 recommend that the model case should be a ‘pure case’. A study by Schondelmeyer et al. 78 serves as a model exemplar.
What is being de-implemented
Clinician behaviour was the target of the intervention and stopping or reducing the use of continuous pulse oximetry (CPO) in children with wheezing, specifically preventing the overuse of CPO for children who were on room air with decreased need for bronchodilator medication. 78
Driving force
The need for the de-implementation of CPO related to safety issues for the patient (i.e. alarm fatigue) and evidence from national organisations, such as Choosing Wisely (Philadelphia, PA, USA), for the lack of evidence in its widespread use. 78
Nature of action
The objective of the de-implementation process was the reduction of CPO use, not its withdrawal, as in certain patient groups CPO is recommended. There was also an element of substitution, with intermittent pulse oximetry replacing CPO. 78
Degree of intentionality
De-implementation was planned using the Plan, Do, Study, Act quality improvement cycle. A period of staff engagement preceded the implementation of the project and included a consensus-based agreement that blood oxygen saturation of ≥ 90% on room air for 2 hours or the reduction of salbutamol treatment to over 2-hourly periods constituted withdrawal of CPO monitoring. The de-implementation intervention consisted of a local guideline that emphasised waste reduction and patient safety related to alarm fatigue. This information was distributed to all nurses and doctors during staff meetings and educational conferences. In addition, at nurse handovers, reminders of the guidelines were given with a three-question assessment tool that determined the need for CPO continuation. 78
Consequences
The primary outcome measure was the median time per week that children were on CPO. The pre de-implementation time was 10.7 hours and post intervention it was 3.1 hours. There were no significant differences in intensive care readmissions when compared with a control unit. 78
Borderline case
Borderline cases are examples where most, but not all, attributes are referenced. A study by Kost et al. 79 is outlined below.
What is being de-implemented
Again, it was clinician behaviour that was targeted in reducing low-value procedures identified by the Choosing Wisely campaign. Procedures were low-back pain X-rays, antibiotics for sinusitis, Papanicolaou tests for women aged < 21 years or women who have had a non-cancerous hysterectomy, annual electrocardiography screening for low-risk patients, and scanning of women with no risk factors who are aged < 65 years and men with no risk factors who are aged < 70 years for osteoporosis. 79
Driving force
As identified by Choosing Wisely, in the case of each of these procedures there is a lack of evidence as to their value without further risk indicators. There are financial incentives in de-implementing these five practices. 79
Nature of action
The aim was to stop, or at least substantially reduce the number of, these procedures in the identified populations. There was no indication of substitution with other procedures. 79
Intentionality
The de-implementation initiative was on the passive continuum, with a 1-hour in-person seminar or webinar reviewing the five Choosing Wisely recommendations. 79
Consequences
A chart review (of 1089 patients) was employed 6 months pre de-implementation and 6 months following de-implementation. Results showed some intended and unintended consequences, including reduction in sinusitis antibiotic prescribing (statistically significant) and osteoporosis scanning; however, there was no change in use of low-back pain imaging, Papanicolaou tests or annual electrocardiography procedures. The absence of de-implementation in these three procedures may be due to high rates of adherence to the guidelines before the de-implementation intervention was initiated. 79
This borderline case79 has most of the attributes, but critically lacks an adequate de-implementation strategy as in the model case. In addition, this study79 highlights the increasing difficulty of de-implementing low-value procedures that already have a high disinvestment outcome.
Contrary cases
Contrary cases show minimal attributes that signify the concept, and we denote this through a paper by Chamberlain et al. 80 The paper80 tracks National Institute for Health and Care Excellence (NICE) guidelines for the overuse of caesarean sections in women with hepatitis, endometrial biopsies to investigate infertility and varicocele operations to treat infertility in men.
What is being de-implemented
Clinician decision-making and behaviour are the targets of the NICE guideline recommendations for the three procedures. 80
Driving force
NICE recommendations indicated that there is a lack of evidence to support continuation of the procedures. The NICE reminder prompts had not been previously evaluated and the Chamberlain et al. 80 study assessed the impact of four reminders for each procedure over a 12-year period.
Nature of action
NICE recommended that these procedures are discontinued without substitution. 80
Degree of intentionality
The NICE guidelines’ recommendations are a passive method of communicating discontinuation of the procedures, and the study drew on opportunistic data collected through the national Hospital Episode Statistics 6 years before guidance and 6 years post guidance. 80
Consequences
The outcomes were unintended, in that the three procedures did not decrease in line with the NICE disinvestment advice. Indeed, there was an increase in procedural use of endometrial biopsies and caesarean sections in women with hepatitis. 80
Empirical referents of de-implementation
According to Walker and Avant74, empirical referents are ‘categories of actual phenomena that demonstrates the occurrence of the concept itself’. The focus of most de-implementation strategies is clinician decision-making behaviours, usually to reduce habitual practices. However, other areas for de-implementation would rest at the organisational and policy levels. The driving force of de-implementation is an essential attribute, as it initiates and provides a rationale for de-implementation. The drivers may be on a continuum from strong to weak, as the force of negative evidence or patient safety would push disinvestment quicker than weaker evidence. The action attribute is again on a referent continuum from stopping to a reduction in the procedure. Substitution with a more effective procedure may result in greater de-implementation of the low-value procedure and different strategies maybe required for early and late adopters. As described in the model case, if the de-implementation strategy is planned and facilitated, then there is a greater chance of a reduction in the process or procedure.
Summary
The process of concept analysis enabled the extraction of the defining attributes of de-implementation within health and social care. Five critical attributes were noted as essential to understanding de-implementation. These were (1) the focus of change, (2) the reasons or push to pursue de-implementation, (3) the extent of de-implementation that is achievable, (4) the degree of planning involved and (5) the intended or unintended consequences. The five critical attributes provided a basis for initial theory development. Case studies were helpful to explicate how de-implementation functions in different contexts.
Initial programme theory development
The concept analysis was part of the Phase 1 work to help the development of the initial programme theory; the construction of a practical framework to represent the ideal about de-implementation, what works, how and under which conditions; and seek evidence about de-implementation of programmes and interventions. This work drew on the initial searches completed to develop the concept analysis, and theory and evidence that we considered relevant, as articulated already in the scoping and theoretical platform sections.
Stakeholder engagement (Phase 1)
Phase 1 work to develop the initial programme theory additionally included consultation with stakeholders. Stakeholder engagement is essential to the success of a realist synthesis. For this review, stakeholder engagement was designed to help elaborate on the review context, refine the review questions, contribute to initial programme theory development, interpret the evidence and assist with dissemination. Here, we report on the stakeholder engagement programme of work to contribute to initial programme theory development.
Stakeholders were purposively sampled to ensure representation from relevant constituencies (i.e. health and care services managers, organisational leaders, patients and the public representation). We identified stakeholders from across different areas of the NHS in the UK. Included were service and clinical managers, senior clinicians, service commissioners and representatives from patient and public involvement groups.
Discussions with stakeholders throughout the study took place in individual telephone interviews (see Appendix 2) or in a workshop format (see Appendix 3). Discussions were designed to be more open ended in the early stages of the review to develop an understanding of the complexities of the contexts in which de-implementation efforts are situated. In total, 10 stakeholders consented to take part, comprising four patient representatives and six clinicians and/or service managers. Discussions became more focused on particular parts of the initial programme theory as the review progressed. Integration of data was guided through the principles of framework analysis. 81
Initial programme theory
The culmination of the work undertaken in Phase 1 was the development of a framework (see Figure 1) that provides an initial explanation of the complexity of de-implementation, and the contextual conditions that underpin the process. This was subsequently used to bound theoretical development. The conceptual components of de-implementation in health care are:
-
De-implementation = f (what is being de-implemented; push or driving force; nature of action; degree of intentionality), which results in intentional and unintentional consequences, over time, for different stakeholders.
Our initial perspective was that de-implementation is associated with five main variables that operate in time and context. The first variable is what is being de-implemented. This is the focus of change and can relate to one or more context areas, such as clinician behaviour change or organisational policy. The second variable is the driving force for de-implementation (e.g. lack of evidence of clinical effectiveness or cost-effectiveness, financial constraints or safety issues). The third variable of nature of the action is the continuum of the de-implementation process from complete termination to replacement with another innovation. The fourth variable is intentionality, that is, to what extent the de-implementation process is intentional and planned or passive and opportunistic. Finally, the outcomes of de-implementation can be both intentional and unintended. Through an iterative process of discussion among the project team and referencing back to the initial proposal literature, we developed elements of the initial programme theory. These were in the form of ‘if–then’ statements that linked different components of the initial programme theory. The development and prioritisation of these statements were regularly discussed with key stakeholders throughout Phase 1 via face-to-face meetings and telephone calls. The statements were then used to guide the search and synthesis of evidence from the literature.
Phase 2: searching processes
Primary search of databases
The major health, social and welfare databases were searched using keywords identified through search development and database-specific ‘keywords’ associated with the initial programme theory, adapted for each information source. Key terms around the main concept were identified from key literature reviewed during the scoping phase and also taken from Niven et al. 13 It was noted that a single shared terminology, for example a medical subject heading term for de-implementation, is lacking. There were no date limits or material type restrictions on the search. Methodological filters were not used to avoid excluding any potentially relevant papers. Systematic searches were conducted in 11 databases subscribed to by Bangor University, Bangor, UK: MEDLINE and CINAHL via EBSCOhost, Applied Social Sciences Index and Abstracts, Social Services Abstracts, International Bibliography of the Social Sciences, Social Science Database, Sociological Abstracts and the Sociology Database via ProQuest, the National Institute for Health Research (NIHR) Journals library, the Cochrane Library and The Campbell Collaboration. See Appendix 4 for an example search strategy. Our search was not limited to health and social care and we sought evidence to capture the emergence of the ‘what matters is what works’ philosophy,82 and international policy campaigns to improve efficiency in health and social care services (e.g. the American Board of Internal Medicine Foundation). 83
Selection and appraisal of documents
The searches took place in April and May 2018. References were stored in Mendeley database software (Mendeley Desktop; Elsevier, London, UK). The systematic databases search yielded 7964 references. After removing duplicates, 5262 hits remained for title screening. Hits for each database are shown in Appendix 5. An abstract shift was completed on the 5262 remaining papers and this left 239 references that were deemed relevant to the research question.
Within the primary search of 5262 papers, a large proportion of articles were on the specific topic of de-prescribing. De-prescribing is a specific type of process for reducing low-value interventions, but represented the largest element within the literature on de-implementation. These papers were reviewed in a separate sift of the evidence. A total of 136 de-prescribing articles were chosen for full-text review. A key feature of a realist review is theory formulation, and literature is examined that best supports the development of the programme theory.
The original scoping review conducted for proposal submission included 212 references. After duplicates were removed, the remaining 154 papers along with the 239 papers identified in the database search provided a total of 393 papers for full-text review. Other members of the project team then subjected these 393 papers to an independent assessment, and this reduced the number of papers for extraction to 92. Exclusion of a large number of papers at this stage was because of the evidence base being largely descriptive.
Alerts were set up for the database searches and were scanned up to December 2018. Three additional papers were added through snowballing, from database alerts and from project group and stakeholders (see Appendix 5). Internet-based searches for grey literature were conducted for workforce development project reports, national inspection and regulation quality reports, and evaluative information about these initiatives (see Appendix 5 for a list of the organisations searched). Although none of this grey literature evidence was included in the final data analysis, it was useful to inform/contextualise the findings. The final number of papers for inclusion to support the programme theory was 42.
Data extraction
Screening for relevance to the initial programme theory involved a systematic approach, using a system developed in a previous funded realist study. 84 Evidence was excluded unless it related to one or more of the programme theory areas. In realist synthesis, the programme theories being ‘tested’ are made visible through bespoke data extraction forms. 31 In this review, a bespoke extraction template was developed around the initial programme theory (see Appendix 6). Evidence was included if we considered it to be ‘good and relevant enough’. 42 PJ, LW, CRB, JRM and BH undertook member checking in the reviewing and extracting processes, and any discrepancy in opinions about the relevance of evidence was resolved through discussion. PJ, CRB and LW undertook data extraction from the identified 92 papers. Following the data extraction process, 42 papers were deemed to be relevant for inclusion and analysis. These were primarily intervention studies. Thirty-seven papers related to de-prescribing across acute and community settings, seven papers reported on interventions, including reducing imaging for low-back pain, and diagnostic test ordering. One paper reported on a realist evaluation of an included intervention for reducing benzodiazepine use in older adults. The 42 papers (see Appendix 7 for list of final included papers) were then subjected to a realist critique to help identify mechanisms that underpinned the interventions, and the contextual conditions that were necessary to trigger them.
Analysis and synthesis processes
The realist synthesis is theory driven and uses abduction to understand CMO configurations. Synthesis is a process of triangulation, so that different sources of evidence are considered in a process of theory development, testing and refining. To provide structure, we organised the extracted information into data tables that represent the different bodies of evidence that inform the programme theory areas. We then undertook an abductive and retroductive approach85 to understand the best explanation of the cause in the evidence about de-implementation and look for recurring patterns in the data. We then linked the patterns to form a refined programme theory, consisting of CMOs (i.e. explanatory statements reflecting the complexity of de-implementation strategies and processes). This process was facilitated by the further development of a set of plausible hypotheses – again in the form of ‘if–then’ statements about what might work, for whom, how, why and in what circumstances – about de-implementation (see Appendix 8).
Phase 3
To test and refine the programme theory, in Phase 3 we provided a check of validity of the evidence in relation to ‘what works’, how and under which conditions in the current approaches to de-implementation of health and care practice and interventions. We conducted a further 21 telephone interviews using the sampling strategy identified in Phase 1, and analysed the data to test the synthesis findings and refine the programme theory. A semistructured interview schedule (see Appendix 9) ensured that the interviews were focused on ‘sense-checking’ from the participants’ perspectives (see Appendix 10 for an overview of participants’ roles). The interviews were conducted by telephone and lasted no longer than 30 minutes. All interviews were audio-recorded and transcribed.
Phase 4
The purpose of Phase 4 was to develop actionable recommendations for interventions that help the de-implementation of low-value treatments and services. This is discussed fully in Chapter 4.
Ethics process for the review
The study fell outside the scope of NHS and social care requirements for ethics review; however, we sought ethics approval from Bangor University’s Health and Medical Sciences Research Ethics Committee to conduct the interviews. Approvals were granted on 22 May 2018 (research proposal number 2017-16242).
As we were enrolling participants for telephone interviews and workshops who were NHS staff, we did require research governance approval from the NHS. Approvals were granted on 24 August 2018 (reference 18/HCRW/0001).
Chapter 3 Findings
The theory development, refinement and testing process, as described in Chapter 2, led to the elaboration of six CMO configurations. The total number of papers used in the analysis was 42, and these are described in Appendix 5. The nature of the interventions used in the included studies is discussed in Chapter 4. We now present each of the six CMOs. We suggest that the CMOs should not be seen as mutually exclusive, as how the different elements of each interact is important.
Context–mechanism–outcome 1: nudging professional practice
De-implementation interventions that attempt to change clinician behaviour in the context of fast or habitual decision-making (context) may be effective when they include aspects of precommitment, accountable justification and benchmarking performance against peers. Changes in practice may be prompted by slowing decision-making through increasing attention to the low-value practice behaviour (mechanism 1), ensuring that practice is consistent with an individual patient’s expectations (mechanism 2) and prompting professionals’ concerns about professional reputation (mechanism 3). Effectiveness was mixed across changes to professional behaviour, with impacts visible on communication with patients (outcome 1) and in some aspects of prescribing practice (outcome 2) (Figure 2).
FIGURE 2.
Context–mechanism–outcome 1.
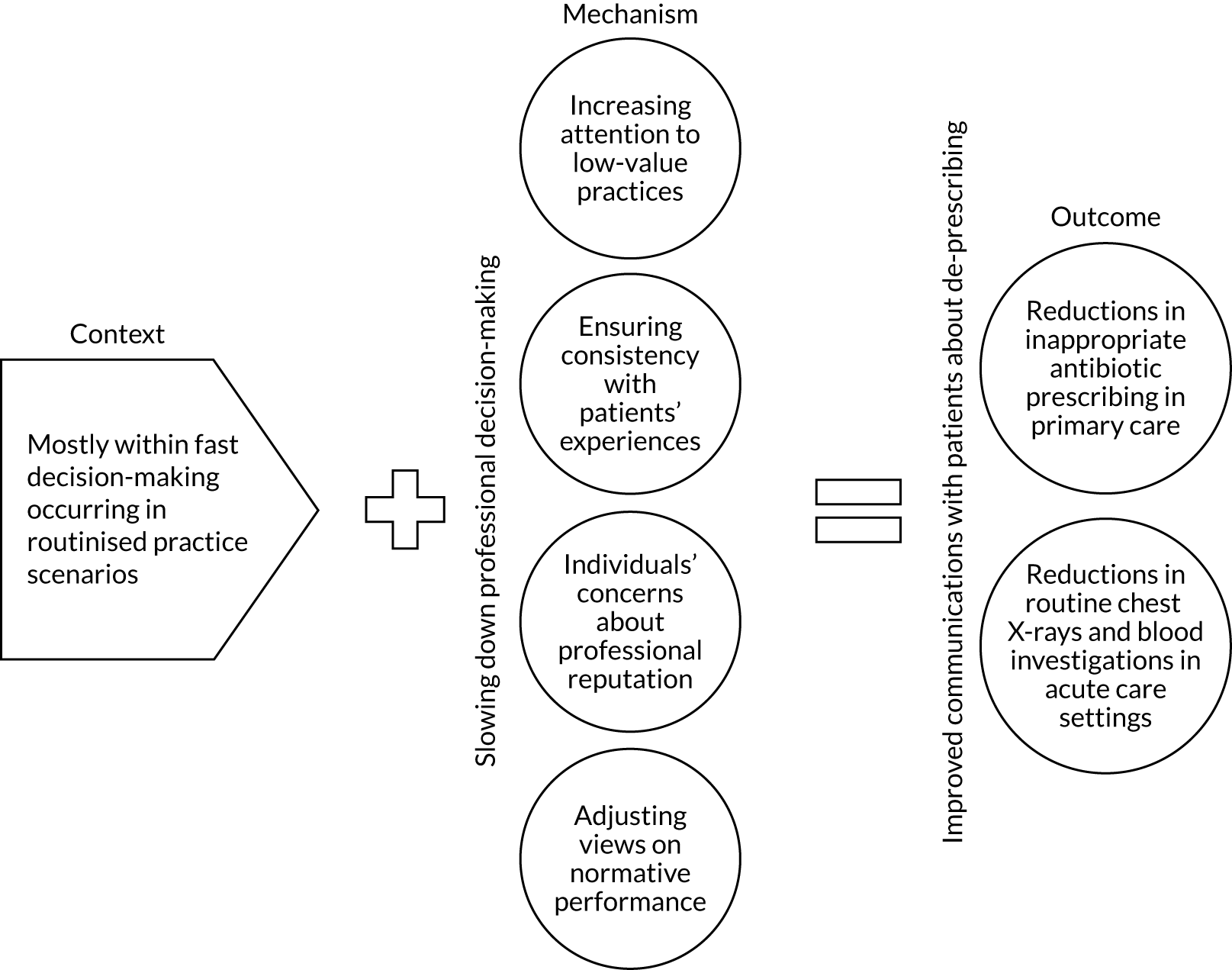
Context
The included evidence indicates that interventions that were designed to disrupt the contexts in which clinicians’ decision-making processes were operating, and to make these processes more conscious and deliberate, show promise for de-implementation. A reliance on intuitive or ‘fast’ thinking86 to reduce cognitive load within the everyday demands of professional practice can interfere with the thinking necessary for the more deliberative and scientific approaches required to limit low-value care.
Within the studies included in this analysis, many of the service contexts are routine primary care clinical decision-making by physicians.
The Meeker et al. 87 study intervention explicitly included information to physicians that their prescribing rates would be monitored. To some degree, the very positive results from this simple public declaration of precommitment to de-implementation may be due to an awareness of practice surveillance.
The Kullgren et al. 88 and the Trumbo et al. 89 studies were aligned with the Choosing Wisely campaign, which may have influenced, in some way, clinicians’ decisions to precommit to de-implementation. However, the influence of a national campaign warrants further attention, as neither of these studies88,89 demonstrated significant instrumental changes to practice.
Increasing attention to low-value practice
Precommitment is a professional’s statement of intent in which they make visible to others that they will behave in certain ways. Precommitment was generated and communicated in different ways, including the use of invitations to professionals to precommit to de-implementation,87,88 point-of-care reminders for those who did precommit88 and/or general declarations of professional intention (e.g. a poster with a signed photograph of the professional made visible to the patient). 87
A simple public declaration of physicians’ intention to de-implement was tested within outpatient primary care clinics in the USA. It focused on the inappropriate use of antibiotics for acute respiratory infections. 87 These declarations comprised a poster with a signed photograph of the physician made visible to all patients, and committed the physician to the reduction in inappropriate antibiotic prescribing. The intention to de-implement was elicited after a presentation on the study in a standard clinic meeting. If physicians participated in the study, they were informed that this would involve randomisation to display a poster of precommitment within their own patient examination rooms and that, regardless of randomisation, all their antibiotic prescribing data would be monitored. The study intervention ran over a 12-week period, commencing mid-February to accommodate one flu cycle. Baseline data summarising 10 months’ antibiotic prescribing practice were extracted from the electronic health record.
The study was small. A total of 14 physicians completed the study, with data available for 954 patient care episodes. The adjusted baseline rate of inappropriate antibiotic prescribing was similar for the intervention and control practices, at 43.5% and 42.8%, respectively. Nevertheless, at the end of the 12-week trial, the inappropriate prescribing pattern decreased to 33.7% for the intervention clinicians and increased to 52.7% for the controls. The data did not demonstrate any ‘workaround’ by physicians by selecting antibiotic-appropriate diagnosis codes. There was an increase in the reduction of inappropriate prescribing rates for each additional month that the poster was displayed, although this failed to reach statistical significance.
Kullgren et al. 88 incorporated precommitment into a more comprehensive professional behavioural de-implementation intervention that was evaluated in a 12-month stepped-wedge cluster randomised controlled trial (RCT) of 45 primary care physicians in six practices in the USA. The intervention was designed to reduce the incidence of orders of low-value interventions, and was designed to nudge decision-making away from the low-value practice by raising professionals’ awareness of evidence-based recommendations to de-implement very close to the decision point. The precommitment was in the form of an invitation to comply with recommendations for the management of three clinical problems: imaging in uncomplicated low back pain and headaches, and the prescription of antibiotics for acute sinusitis. Precommitment was obtained after a presentation about the de-implementation study. If clinicians did precommit, this was in the form of a signed statement after the initial study presentation. Medical administrative staff were provided with training to identify potential patients who fell into one of the three clinical problems and then applied a Post-it® note (3M Cynthiana, KY, USA) on the patient’s documentation that was immediately visible to the physician during consultation. Training was in the form of a brief (10-minute) individual session, reinforced with a one-page summary of their role. These staff-applied point-of-care prompts were introduced to physicians, reminding them of their signed precommitment statement. Paper-based prompts were used as these were thought to minimise the risk of computer fatigue and to increase visibility. Prompts were attached to a patient education handout to support physicians’ attempts to reduce low-value interventions. Weekly e-mails with links to resources to improve communication with patients about low-value services were also sent to participating physicians.
Electronic health record data were used to measure the primary effect of the intervention (i.e. any reduction in physicians’ ordering of targeted low-value clinical interventions). Any potential for physicians to order different interventions rather than simply to cease ordering was also evaluated. The collection of electronic ordering data was supplemented by a physician survey that included attitudinal items about intervention components. A sample of physicians was also invited to participate in a telephone interview that explored how their practice was influenced (or not) through their precommitment and associated reminders.
Primary outcome analysis demonstrated no reduction in the incidence of low-value orders other than a small but statistically significant reduction in back pain imaging orders [–1.2%, 95% confidence interval (CI) –2.0% to –0.5%; p = 0.001]. A sensitivity analysis that reviewed clinical encounters with relevant clinical codes, rather than those encounters solely identified by the trained medical administrative staff, showed reductions in inappropriate orders for all three clinical problems during the intervention period. However, these effects were not sustained over a 3-month follow-up period. Reductions in the ordering of imaging for uncomplicated low back pain were mirrored by an increase in the percentage of visits with a potential alternative order of minimal value (1.9%, 95% CI 0.5% to 3.3%; p = 0.007).
Survey data demonstrated that most physicians (63.6%) found patient education handouts helpful, and precommitment itself was thought to be helpful by nearly half (47.7%) of those physicians who completed the survey. Fewer physicians felt that the precommitment reminders (31.8%) and other resources to support communication (20.4%) were helpful. Interview data suggested that the patient education handouts were most helpful in facilitating communication during the clinical encounter, even for ‘the more difficult patients where I would have been tempted not to follow guidelines’. 88
Although the qualitative data indicate that the intervention materials helped in the communication process with patients, the overall results of this study of precommitment as a means of de-implementing low-value interventions were disappointing. The authors conclude that the limited effect of precommitting to reducing the use of low-value treatments without alternative management strategies may be due to the feeling physicians have ‘. . . to do something’. 88
Other strategies identified in the synthesis to increase professionals’ awareness of low-value practices include both the use of suggested alternatives and accountable justification. Both strategies, along with feedback on performance relative to peers, were evaluated in the context of inappropriate antibiotic prescribing in 47 US primary care practices. 90 The ‘suggested alternatives’ intervention comprised an alert on the electronic health record that highlighted to physicians that a prescription of antibiotics would not be generally indicated for the particular diagnosis, and an alternative course of action was suggested. In addition to increasing attention to a low-value practice, the assumption was that ‘prescribers may infer that a suggested alternative ought to be considered, thus reducing the likelihood that an antibiotic would be prescribed’. 90 Although the accountable justification intervention similarly drew attention to the low-value practice, physicians were required to complete an additional activity through the electronic health record to make an inappropriate prescription for antibiotics. This activity was completion of a free-text justification of the treatment decision. Physicians were also informed that this justification would be visible with the patient’s notes as an ‘antibiotic justification note’. A 2 × 2 × 2 factorial design was used to test different combinations of no intervention with these two interventions and a peer comparison intervention across the 47 primary care practices. Findings showed no statistically significant reduction in prescribing rates for the ‘suggested alternatives’ intervention. However, the absolute difference for accountable justification was –18.1% (difference in differences –7.0%, 95% CI –9.1% to –2.9%). Increasing the sense of professional accountability was anticipated to trigger reputational concerns and a desire to act in line with recommendations within clinical guidelines.
Individuals’ concerns about professional reputation
In the Meeker et al. 90 study, independent, statistically significant reductions in inappropriate antibiotic prescribing were seen for both ‘accountable justification’ and ‘peer comparison’ interventions. As above, the requirement to provide a justification for sustaining a low-value, unrecommended intervention may have worked through triggering professionals’ concerns about their reputations in different ways (i.e. reminding clinicians of the low-value nature of the prescribed intervention, forcing an additional level of critical scrutiny of the decision itself and raising concerns about professional reputation through the documentation of an unadvised course of action).
However, ‘peer comparison’ was also shown to be effective. This monthly e-mail-based intervention provided participating physicians with a ranking (i.e. highest to lowest inappropriate prescribing rate). Those in the lowest decile of prescribers were informed that they were ‘top performers’, whereas others were informed that they were ‘not a top performer’. The absolute difference for peer comparison was –16.3% (difference in differences –5.2%, 95% CI –6.9% to –1.6%), with the authors90 pointing to the positive reinforcement provided to those who managed to successfully reduce inappropriate prescribing. Three studies89,91,92 of performance feedback that included an element of social comparison were identified, although in only one study91 the feedback alone was the focus of investigation. Social comparison feedback is a technique that ‘. . . provides participants with information on their own performance compared to their peers to correct misperceptions about norms that may drive overuse of some tests’. 91 Trumbo et al. 89 included comparative performance feedback alongside education and other supportive interventions. However, in a study by Sacarny et al. ,92 feedback to physicians included the statement that performance was being placed under official administrative scrutiny. Although the previous two studies88,90 focused on physicians’ ordering of investigations within inpatient settings, this study focused on ‘off-label’ prescribing of antipsychotic medication for older and disabled adults. All of these studies were conducted in the USA.
The de-implementation intervention investigated by Sacarny et al. 92 attempted to manipulate concerns about professionals’ reputations. The investigation was conducted across a study population of 5055 primary care physicians who were the highest prescribers of an off-label antipsychotic medication enrolled in the Medicare programme. The evaluation design was a placebo-controlled parallel-group investigation of comparative performance in the form of three peer comparison letters to each of 2528 physicians randomised to the experimental intervention. These letters indicated that individuals’ prescribing of antipsychotic drugs was high relative to their peers and was under review by Medicare. The letters were clearly worded to draw attention to inappropriate levels of prescribing and were sent several months apart over the 9-month intervention period. The control group of physicians (n = 2527) received ‘placebo’ letters about medicine regulations. A baseline cohort of patients were identified from those receiving the study medication from any study provider up to 1 year prior to the study, and these patients were classified as being either ‘guideline concordant’ or as having ‘low-value prescribing’ against prespecified clinical criteria.
The intervention demonstrated a decrease of 11.1% (95% CI 9.2% to 13.1%; p < 0.001) in existing and new prescribing practices compared with the control group who received ‘placebo’ letters. The intervention also produced a decrease of 27.1% in the volume of new antipsychotic drug prescriptions over 9 months (95% CI 23.1% to 31.1%; p < 0.001), which persisted over a 2-year period. The authors conclude that letters providing comparative performance data and indication of external surveillance to the ‘highest prescribing physicians in the Medicare programme led to statistically significant, persistent decreases’ in antipsychotic prescribing. 92 The use of both the ‘carrot’ and ‘stick’ approach to providing performance feedback was also attested to in our stakeholder engagement, as in the quotation below from a clinical director of cardiology during a telephone interview:
. . . so I met with the individual [consultants] first and then with their teams, them and their teams and the individual meetings were basically ‘look here’s your data, you’re losing the organisation £1,000,000 a year, you’re keeping people in too long, and more people are dying than they should’. My approach was ‘how can I help you to improve this’ and you know what I also said was ‘obviously if these things can’t improve I’m going to have to look at whether you should be supervising other junior doctors, I’m going to have to look at what you can and can’t do’.
Academic_M5
Adjusting views on normative performance
Ryskina et al. 91 used a single-blinded RCT to evaluate a simple social comparison performance feedback intervention. Social comparison feedback is a technique that ‘. . . provides participants with information on their own performance compared to their peers to correct misperceptions about norms that may drive overuse of some tests’. 91 The clinical focus of the study was in-hospital laboratory routine test ordering, which is long considered to be an overused practice in the USA. In Ryskina et al. ’s91 study, 114 physicians were randomly allocated to one of two groups: a control group that received no feedback or an experimental group that received a personalised e-mail of their routine laboratory ordering (including blood count, metabolic panel, liver function and common coagulation tests) compared with the average of all clinicians from the previous week’s test ordering. These individuals also had access to a continuously updated and personalised dashboard that provided the context to these data, including patient-level details. No statistically significant reduction in the experimental group physicians, in terms of the count of routine laboratory orders placed by each physician per patient-day, was identified, regardless of individual physicians’ pre-intervention ordering rates relative to their peers. However, there was a general reduction in laboratory testing. Ryskina et al. 91 surmised that there may have been ‘cross-contamination’ between the groups, but also that the intervention group did not access their review e-mails and personalised dashboards regularly. This lack of engagement may be because of the clinicians having to physically access the e-mails themselves, presenting an added barrier. However, if the information was automatically accessible without needing to access the data then the difficulty for the physician would be reduced.
In addition to comparative performance feedback, Trumbo et al. 89 provided additional support to enable staff to reduce unnecessary ordering of chest X-ray investigations within two critical care settings [i.e. cardiovascular intensive care units (CVICUs) and medical intensive care units (MICUs)] in one US hospital over a 9-month period. The intervention provided information about Choosing Wisely’s evidence of the consequences of daily routine chest X-rays through a face-to-face session with staff members at each unit, giving feedback on current chest X-ray ordering rates and providing a rationale for reducing routine ordering. ‘Peer champions’ were recruited from each unit following this session. Two advanced nurse practitioners from the CVICU and three physicians (residents) from the MICU volunteered as peer champions. Their role was to co-ordinate data responses and encourage colleagues to adhere to the recommendations, as well as providing weekly feedback on X-ray ordering. Improvement science methods, including Plan, Do, Study, Act cycles, were used to facilitate de-implementation. There were no control settings on the evaluation design. The two critical care units were compared against their pre-intervention X-ray ordering data. The CVICU achieved a small but statistically significant fall in X-ray ordering from a pre-intervention rate of 1.16 (interquartile range 1.06–1.28) chest X-rays per patient per day to a post-intervention rate of 1.07 (interquartile range 0.94–1.21; p < 0.001) chest X-rays per patient per day. The MICU, which had a pre-intervention rate lower than the CVICU, showed no change over a 33-week period. Quantitative data were augmented by observation and semistructured interviews with stakeholders. Reasons for differences between the intensive care units were related to the turnover of staff and reduced quality improvement initiatives in the MICU that showed no significant decrease in X-ray ordering. Trumbo et al. 89 reported ‘messaging about reducing unnecessary tests went well when framed at the unit level but may be counterproductive if used to question individual ordering decisions’. 89 Although it is unclear from the presented data why this conclusion was drawn, two clinical incidents (unrelated to chest X-rays) that occurred during the study time frame may have posed additional de-implementation challenges.
The provision of comparative performance feedback has been linked to both prompt reputational concerns about being a professional outlier and correct views on normative performance. This mechanism is extended in studies that focused on more supportive forms of peer and collegial mentoring. Here, there was an explicit focus on using peer support as a means for de-implementation,93 albeit as part of a complex array of education, training, printed information and ongoing external facilitation. This comprehensive strategy was evaluated in a cluster randomised trial93 covering 765 patients from 72 units in 32 Norwegian nursing homes. The purpose of the trial93 was to limit the use of inappropriate prescribing of antihypertensive medication. The primary outcome was the number of antihypertensive medications prescribed (with description defined as fewer drugs at month 4 than at baseline), together with patients’ systolic blood pressure and pulse measurements.
Findings showed that the medications were significantly reduced in the intervention group (n = 43, 32%) compared with control (n = 11, 10%). Blood pressure increased for the intervention patients from 128 ± 19.5 mmHg to 143 ± 25.5 mmHg at 4 months, but at 9 months this fell back to the pre-intervention average of 134 mmHg, with no effect on pulse. Gulla et al. 93 concluded that in long-term hospital care the introduction of planned medication reviews with collegial mentoring can reduce antihypertensive drug prescribing and potential side effects without increasing patient blood pressure in the longer term. However, following the termination of the study, the difference between the intervention and control units became negligible, with the authors emphasising that continued collegial support and education are essential for achieving sustained de-implementation.
Outcomes
Three groups of de-implementation interventions, drawing on ideas from behavioural economics on behaviour change, were identified across the evidence: (1) seeking professionals’ precommitment to de-implement, (2) seeking accountable justification for sustaining low-value practices and (3) benchmarking professionals’ performance against peers. As complex interventions with multiple components, and depending on contextual conditions, each study intervention had the potential to trigger any or all of the four submechanisms that we have identified. Consequently, we are not able to identify outcomes associated with each of these submechanisms. Our summary indicates the observed outcomes of interventions that, broadly speaking, were designed to slow decision-making, and make this more thoughtful and deliberate. 88
There is mixed evidence on the impact of obtaining precommitment in delivering prescribing behaviour change away from low-value clinical interventions. Interventions that solely raise awareness of low-value practices appear to have little impact on de-implementation, even when these are delivered close to clinical decision points, although this has been tested in few clinical scenarios. Disrupting routine fast decisions through the use of precommitment that also raises patients’ expectations around de-implementation87 may be more effective. In addition, professionals’ concerns around delivering treatment that is consistent appear to be more effective in reducing inappropriate prescriptions of antibiotics. Precommitment appears to work in terms of changing dialogue with service users, but this may be dependent on the precommitment being made explicit to patients. As a result, the precommitment may be more associated with a desire to be congruent with expectations, rather than with the clinical issue per se.
The findings from Meeker et al. ’s87 study are encouraging. The study intervention was of minimal cost and was more effective than a more comprehensive approach to precommitment. 88 Although not translating into instrumental changes to prescribing practices, materials such as reminders, patient education materials and online resources to support communication with patients were found to be appreciated by physicians in this study.
Collegial or peer support approaches to reducing low-value treatments and tests appear to have some effect, but in a much wider package of de-implementation activity, or through invoking professional rivalry90 and concerns about individual performance with respect to peers. However, providing an additional threat associated with sustaining the low-value practice was also seen to be effective. 92 Peer evaluation of practice, in the context of pharmacist review of physician practice, did not appear to be effective in delivering change in prescribing of practice.
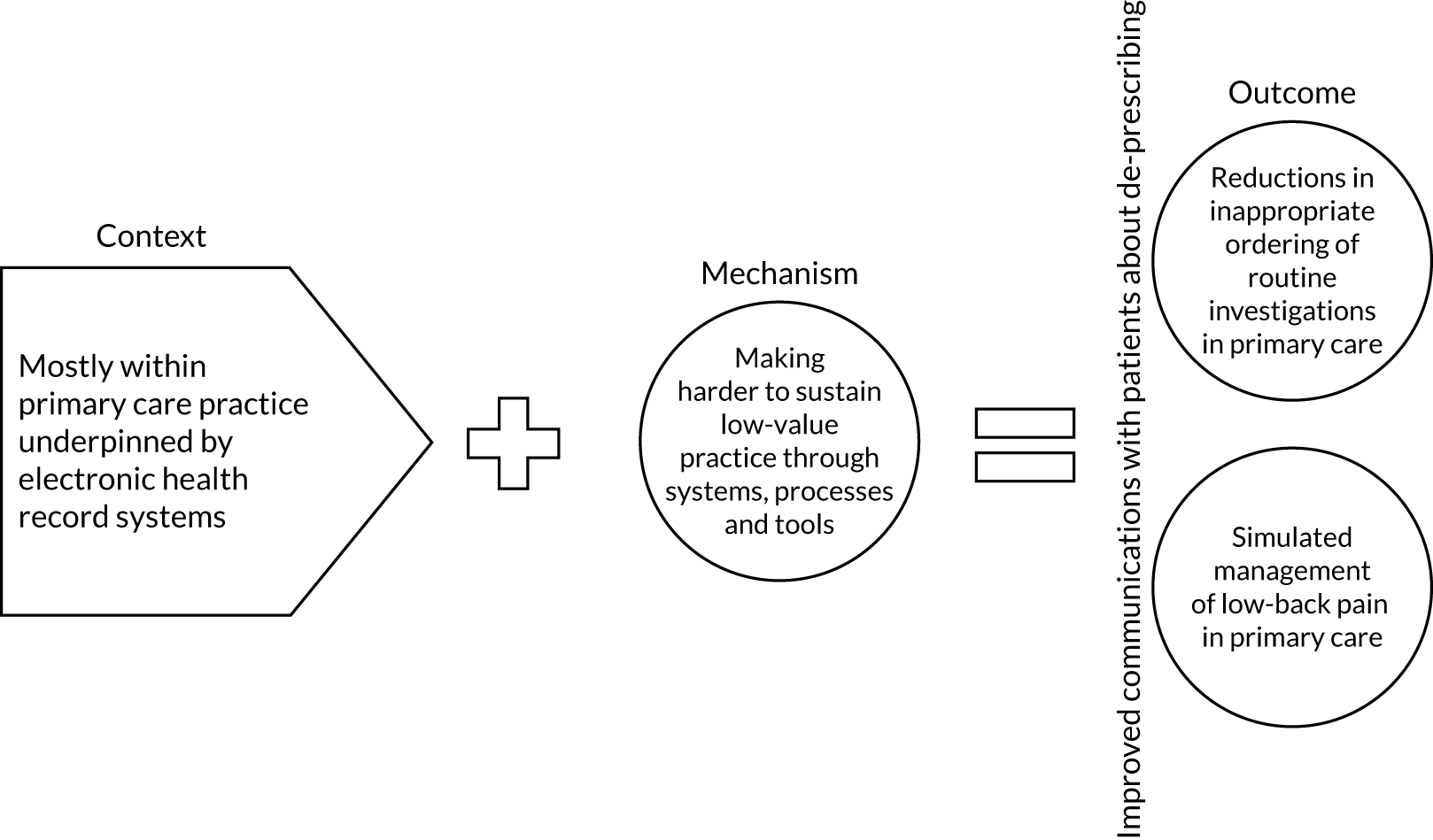
Context–mechanism–outcome 2: designing de-implementation through technology
In the context of clinical practice underpinned by electronic health records, de-implementation interventions that amend the design of these systems (context) may be successful when their design makes sustaining low-value practice harder (mechanism). Things may be made harder by changing information displays/choice options. Impacts were demonstrated in the reduction of orders for unnecessary diagnostic tests (outcome) (Figure 3).
FIGURE 3.
Context–mechanism–outcome 2.
Context
The context of this aspect of de-implementation programme theory is the propensity for institutional systems to influence clinical decision-making in ways that make implementation easier or de-implementation harder. The studies94,95 here focus essentially on making changes to electronic health records, such as setting the default decision option to the preferred setting. Preference in this sense is the selection of a high- rather than a low-value treatment decision. As with the first CMO, the practice scenario in which much of this evidence is located is in primary care, and the selection of diagnostic tests or treatment options by physicians. The use of computer systems is now universal and increasing, and so designing systems with de-implementation as an objective may be an expedient way to reduce low-level treatments.
A number of studies included in this synthesis made the evidence surrounding treatment options more visible in a variety of ways, including colour coding. 94 Here, a colour-coding system of dots was integrated into menu options for the ordering of routine diagnostic tests within primary care settings. The dots represented the strength of evidence and recommendations for the use of each diagnostic test, as specified by the United States Preventive Services Task Force (USPSTF). 96 A reference group of primary physicians were involved in agreeing the changes to the menu options, and physicians were still able to select additional tests, if desired, by searching for the test name. Diagnostic tests coded with green dots had been recommended by USPSTF, the tests coded red had not been recommended and those diagnostic tests with a yellow dot had been recommended in only some circumstances. The analysis of this trial did not specifically examine the effects of colour coding the strength of evidence. The synthesis did not pursue this line of analysis any further, as the evidence associated with making evidence of effectiveness explicit, for example through clinical guidelines, was not within our remit.
Making it harder to sustain low-value treatment options
Since 2011, primary care physicians in Portugal have had to use an electronic health records system for ordering diagnostic and laboratory tests in primary care. Routine practice required clinicians to order tests either by searching for a specific test or by selecting from a shorter short-cut menu organised around major clinical domains (e.g. basic, cardiovascular, rheumatology, respiratory). Rather than select individual tests from the short-cut menu, physicians were also able to order the full complement of tests by selecting an ‘all’ function for that menu. Concerns that tests were variably over-requested with preventative intentions or to meet patients’ expectations prompted Martins et al. 94 to evaluate the impacts of amending the presentation of choice options within the health record system. In addition to colour coding the strength of recommendations as above, two additional amendments were evaluated:
-
the removal of some diagnostic tests from short-cut menus (including uric acid, serum protein electrophoresis, sedimentation rate, electrocardiogram and chest X-ray)
-
the addition of some diagnostic tests to short-cut menus (including high-density lipoprotein cholesterol).
The electronic health record software modifications were implemented in May 2012, and evaluated in a parallel randomised trial design over 8 months across the equivalent of nine primary health-care centres. We assessed the impact on ordering of (1) tests removed from the electronic health record, (2) tests added to the electronic health record, (3) tests coded with green dots (i.e. those recommended by USPSTF) and (4) tests coded with red dots (i.e. those not recommended by USPSTF). The most significant impact detected in the trial was for the ordering of tests other than electrocardiography, which had been removed from short-cut menus. When ‘low-value’ tests were removed from choice options, although the prescription rates of low-value diagnostic and laboratory tests in the control group were consistent, a reduction from 31.3 prescriptions before software modification to 13.9 prescriptions afterwards was observed. As the authors comment, the ‘results demonstrate the importance of testing and evaluating various aspects of medical informatics programs to improve efficiency and contribute to improved clinical practice and clinical outcomes’. 94
More subtle changes to information displays were evaluated by Soon et al.,95 albeit within a hypothesised practice scenario around the management of low-back pain in primary care. Soon et al. 95 showed that the withdrawal of options from clinicians’ choice menus can positively influence behaviour change and make sustaining low-value practice harder. However, amending the layout of options can, in theory, effect similar changes. The layout changes evaluated in this study included a partition display of treatment options related to the practice scenario. The partition display drew on the assumption that ‘people are less likely to select items listed horizontally than those listed vertically’. 95 In practical terms, all treatment options were open to clinicians, but those options that were considered low value were presented horizontally rather than vertically on a computer screen. These partition display changes were evaluated against a control, where all treatment options were listed horizontally, alongside a default option and a combination of default and partition display. The default option listed only recommended treatment options, together with a selection prompt for clinicians to use to see additional low-value treatment options.
These combinations of displays were evaluated in a 2 × 2 factorial randomised trial among primary care physicians (n = 120) in Australia. Participants were asked to complete four clinical vignettes of patients with low-back pain. Two vignettes linked the scenario with six imaging options, and the other two vignettes linked the scenario with six medication options. Within each scenario, participants were asked to select a minimum of one and maximum of three treatment options. Participants were randomised to the same condition (i.e. control, partition display, default display or partition display plus default) for all four vignettes. The primary outcome was the proportion of scenarios for which study participants opted for a minimum of one low-value option.
Although the partition display group showed no effect in reducing the selection of low-value treatments, the default display group that listed the high-value options reduced the odds of choosing a low-value option by 44% (odds ratio 0.56, 95% CI 0.37 to 0.85; p = 0.006). The partial display group failed to demonstrate a significant impact on low-value option selection independently or on combination with the default display group. This RCT showed the benefits of using electronic systems that make it harder for clinicians to access low-value options and easier to retrieve high-value tests, but in quite transactional ways. Put simply, presenting more effective treatment options and ‘hiding’ low-value options within information displays and treatment options appears to work. Importantly, Soon et al. 95 included an examination of participants’ propensity for critical reflection within decision-making and, on that basis, were able to suggest that ‘these findings suggest that [this approach] may be most effective in situations where thinking “slow” is difficult or discouraged’. 95
Outcomes
For CMO 2, we found that deliberate efforts to make it harder to sustain low-value practices resulted in short-term outcomes not dissimilar to those identified for CMO 1. When technological adaptations were reported to be successful, they had an impact on test ordering habits. 94,95 We concluded that longer-term outcomes are likely to follow with better use of time and workload for staff, and improved health outcomes for patients.
Context–mechanism–outcome 3: enhancing capability to de-implement through improving professionals’ practice
The potential to increase professionals’ capability to de-implement when there is concern or uncertainty about, or variation in, a specific practice issue or problem (context) and increasing knowledge of, and skills related to, the evidence to drive de-implementation (mechanism) can lead to reductions in the rates of inappropriate ordering of routine investigations and in inappropriate prescribing (outcome) (Figure 4).
FIGURE 4.
Context–mechanism–outcome 3.
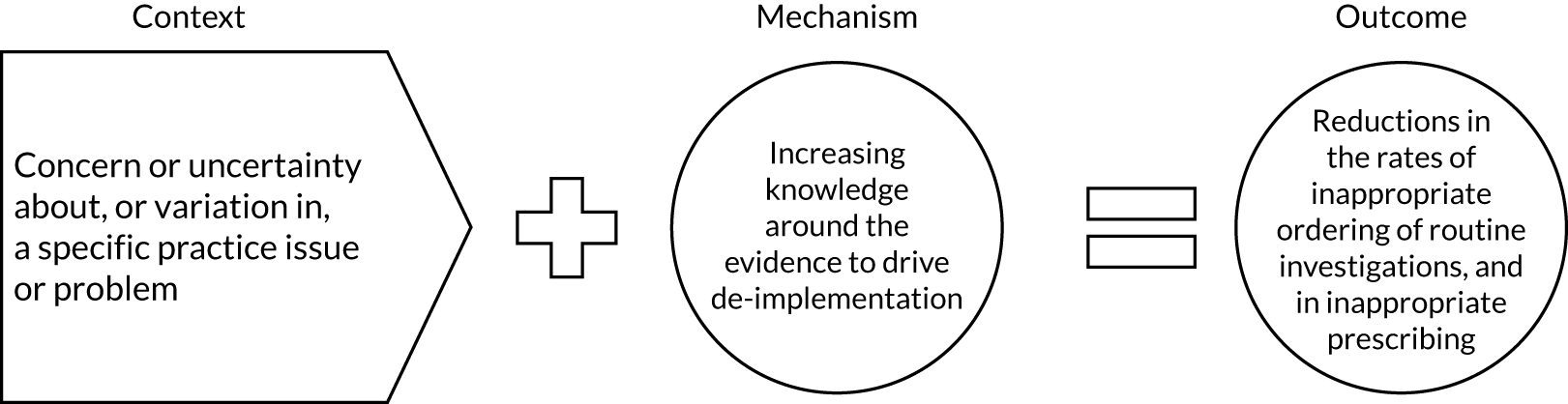
Context
The context for this CMO is uncertainty, variation in practices, identification of a problem in clinical care, or a desire to reduce harm. Evidence to support this CMO drew from papers93,97–100 focused on the following:
-
reducing inappropriate nuclear myocardial perfusion image testing in a US care facility in a pretest–post-test study using a brief multimodal educational intervention97
-
reducing polypharmacy in older patients in community settings98
-
reducing the use of indwelling urinary catheters99
-
training nursing home nurses about medication use100
-
limiting the use of inappropriate prescribing of antihypertensive medications. 93
The evidence of de-implementation interventions that featured in this CMO was educational in nature. The interventions consisted of multimodal approaches, with various combinations of information giving, feedback on individual performance, collegiate peer support, education plus regular evaluation, and/or being implemented ‘close’ to practice. In one study,97 the intervention consisted of a 1-hour interactive lecture tailored to resonate with the specific specialties under question, for example the cardiology department focusing on heart failure assessment, primary care practitioners looking at heart disease screening and hospital physicians focusing on chest pain evaluation. The authors describe how they employed a ‘collaborative tone focused on improving patient care and used a peer to deliver a multimodality approach’. 97
Bregnhoj et al. 98 described a RCT in which a combined or single educational intervention with a control group of general practitioners (GPs) was introduced. The combined educational intervention consisted of an interactive meeting around polypharmacy and prescribing for older people, together with feedback from a senior clinical pharmacologist on GP prescribing habits in patients who the GPs had identified for the study. The second group of GPs received polypharmacy education without pharmacological feedback on identified patients. The control group received neither option. In a parallel-group RCT reported by Fenton et al. 101 the participants consisted of 31 physicians (control, n = 30) and the intervention involved standardised patient instructors delivering two 20-minute visits to the physicians. Additionally, personalised feedback was provided for the physicians involved.
Juola et al. 100 carried out a secondary analysis of a cluster RCT, investigating whether or not training nursing home staff about medication use would lead to a reduction in falls among residents with cognitive impairment. Twenty wards were randomised in this Finnish study. Nurses working in the intervention wards received two 4-hour interactive training sessions based on constructive learning theory, which involved problem-based learning and learner-centred approaches around harmful medications related to their patient group. Additionally, ‘nurses were encouraged to present and discuss actual resident cases from their own wards’. 100 Nurses in the control group received the intervention post analysis.
Menegueti et al. 99 describe a quasi-experimental study conducted in a nine-bedded intensive care unit of a tertiary care hospital in Brazil. The study was carried out over 12 years. Phase 1 of the implementation involved reminders to staff of prevention measures. In Phase 2, biannual training for all clinical staff was based on Centers for Disease Control and Prevention guidance for prevention of catheter-associated urinary tract infection. The topics included:
. . . criteria for indication of use of indwelling urinary catheter which consisted of patients who: have urinary retention, bladder obstruction or coagulation problems that prevent them from having an intermittent catheter, undergone an urological procedure or had urethra trauma.
Menegueti et al. 99
Training was supplemented in a third phase by a denominated checklist ‘to evaluate the indication and/or maintenance of any indwelling urinary catheter’. 99 In a further phase, the training was exchanged for mandatory training for new staff plus a daily checklist.
Finally, in a cluster RCT of 765 patients from 72 units in 32 Norwegian care homes, Gulla et al. 93 used a complex intervention strategy called COSMOS (i.e. COmmunication, Systematic assessment and treatment of pain, Medication review, Occupational therapy Safety). The context for this paper was uncertainty regarding the benefits of treating care home patients with multimorbidities with antihypertensive drugs. The strategy comprised an educational programme to implement the COSMOS intervention, medication review, family engagement and facilitation, including collegial mentoring from peers and clinical targets around blood pressure related to nursing home patients. The educational programme was multidisciplinary and ‘covered research-based knowledge about communication with relatives and patients through advance care planning, pain assessment and treatment, the rationale for multidisciplinary medication review, and organisation of activities for all included patients. The education program also included role-playing and patient-centred discussions’. 93
Increasing knowledge and skills around the evidence to drive de-implementation
In the Winchester et al. 97 study, an increase in knowledge or skills emerged through the process of persuading physicians and advanced practice providers to reduce inappropriate testing. Increasing knowledge through education was viewed as a low-cost approach, which ‘if applied properly, could help curtail the unnecessary use of medical test and procedures’. 97 Increasing knowledge was considered to change the behaviour of the service providers in this case, as the underlying issue was an identified lack of knowledge as opposed to fixed habits or false beliefs.
In the paper by Menegueti et al. ,99 increasing knowledge and skills via the training was enhanced by the introduction of a daily checklist to support decision-making:
Three days per week, the physician and nurse of the Infection Control Service reviewed the decisions with the clinical staff, and discussed any cases that did not conform to the indication criteria . . . In this phase, the addition of the checklist intended to facilitate the decision-making by the clinical team.
Menegueti et al. 99
In the other evidence included in this CMO, studies focused on de-implementation issues related to medication (i.e. polypharmacy and reduction in inappropriate or harmful medication). In the Gulla et al. 93 study, an increase in knowledge or skills relating to a decrease in the use of antihypertensive drugs in care home patients was assumed through the process of implementing a complex multimodal intervention. However, the authors reported that the effects were not long-lasting, highlighting the importance of sustainability:
. . . we expected that the effect of collegial mentoring, multidisciplinary collaboration between physicians and nursing staff, and education would last beyond the four-month period. However, our results demonstrated that the main effects [of collegial mentoring, collaboration between physicians and nursing staff, and education] were concentrated between baseline and month four, and that significant differences between the intervention and control units diminished over time. Sustained collaboration, education and learning are crucial prerequisites for person-centred care.
Gulla et al. 93
In the Juola et al. 100 study, although nurses’ knowledge about medications was not assessed prior to the intervention, the authors hypothesise that the comprehensiveness of the nurses’ prior education could have been a contributory factor towards intervention success:
Registered and practical nurses in Finland receive a comprehensive education (3.5 and 2.5 years’ duration, respectively). This education includes teaching about medications. This is different to the situation in some other countries where aged care wards are often staffed by aged car workers with lower levels of formal education.
Juola et al. 100
Therefore, attention should be drawn to increased knowledge and the potential of this to improve the capability of staff to de-implement.
Collegiate and peer support
We noted that in some of the evidence presented in CMO 3, the presence of collegiate peer support associated with the educational nature of the intervention. In the Winchester et al. 97 study, for example, materials (i.e. lecture delivery and poster displays distributed throughout the care facility) were designed so as to maximise collaborative peer support without practitioner shaming:
. . . the tone of the lectures and poster was purposefully one of collaboration. None of the materials focused on shaming or punishing providers for ordering rarely appropriate tests. We informed providers that the goal of the initiative was to work together to achieve the best for our patients.
Winchester et al. 97
In the Gulla et al. 93 paper, collegial mentoring forms part of the medication review component of the intervention:
The physician was in charge of all medical decision in the meeting; the nurse provided updated knowledge about the patients’ situation, and the researcher gave provided decision support by initiating discussions, giving support in difficult decisions and supplementing with relevant research on the field (collegial mentoring).
Gulla et al. 93
Being implemented ‘close’ to professionals’ practice
We additionally noted in this CMO that a pattern emerged with interventions designed to include an element of closeness to the practitioners’ own work or workplace. This was often in relation to the professionals’ subject areas, but also included other efforts to fit with the work area. In the Menegueti et al. 99 study, for example, during the training ‘the clinical team was presented with the rates of utilisation of indwelling urinary catheters and the number and rates of CAUTI [catheter-associated urinary tract infection] occurring in the past 6 months’. 99
An interactive educational intervention with actual prescriber patients was described in the Juola et al. 100 paper:
The sessions involved interactive discussion about the list of harmful medication and suitable alternatives. To demonstrate the relevance, nurses were encouraged to present and discuss actual resident cases from their own wards.
Juola et al. 100
Patient-centred discussion formed part of the educational programme in the COSMOS intervention described in the Gulla et al. 93 paper. In the Winchester et al. 97 study, the detail of the printed posters used suggests forethought to fit closely with the professionals’ work:
. . . size was chosen because the primary care clinics have official notice boards which accommodate this poster size. Posters were distributed, two for each clinical site, with the request that they be posted in the providers’ work areas for easy reference.
Winchester et al. 97
The authors conclude that tailoring the intervention to the targeted professionals in this way changed behaviours, as ‘prior data showed that the patterns of rarely appropriate testing differed by specialty. Using education tailored to the audience may have enhanced the effect’. 97
The notion of making education fit closely with the professional’s work in de-implementation activities, as supported by data, also resonated through the telephone interviews undertaken in Phase 3 of the synthesis:
I think a lot of people go back to personal experience and I think what is quite powerful is actually patient stories. I think patient stories when we take it down to the individual can actually be far more powerful than some of the very academic written evidence about some of this stuff.
Nurse and allied health professions clinical director B9
Feedback on individual performance
We noted in this CMO an attempt to test feedback on individual practitioner performance and its potential for enhancing de-implementation efforts. Bregnhøj et al. 98 included feedback on patient medication as one of the combined intervention constituents. GPs in the combined intervention group, following attending the educational meeting, received ‘written recommendation targeting medication problems identified while rating the Medication Appropriateness Index (MAI). Afterwards, the GPs were contacted by telephone by a senior clinical pharmacologist (JS) to discuss any uncertainties concerning the recommendations given’. 98 However, the authors point out that this approach can be more expensive and time-consuming than an educational approach alone.
Outcomes
In this CMO, the data pointed to outcomes in the form of reductions in the rates of inappropriate ordering of routine investigations, reductions in harmful/inappropriate medications or clinical practices. We found that engaging practitioners through co-produced and interactive education methods can highlight a lack of knowledge around the de-implementation of, for example, routine tests and medications. However, although often valued by the professional, the evidence demonstrated little impact on subsequent instrumental outcomes.
In CMO 3 we found that when enhancing knowledge or skills about de-implementation emerged, the design and delivery of the different multimodal activities, including education, also delivered outcomes that are considered significant. For example, positive effects on de-implementing inappropriate patient testing were noted in the Winchester et al. 97 study. In this case, the proportion of appropriate myocardial perfusion image testing increased from 80.5% to 95.2% and remained at 92.7% at 4 months post intervention. The percentage of inappropriate testing initially decreased from 4.9% to 1.3% and then remained at 1.4% (p < 0.001). This paper97 highlights (in the context of professionals’ lack of knowledge of test effectiveness) that educational interventions that incorporate elements of fit with professionals’ work or workplace can have positive effects to reduce inappropriate patient testing.
Combining education and feedback can lead to improved medication appropriateness in older people. 98 Inappropriate prescribing was measured through the MAI and showed that prescribing behaviour improved in the combined intervention group, but not in the single education group or control group. The regression analysis showed that the estimated difference in the combined intervention group was a 5-point improvement (95% CI –7.3 to –2.6) in MAI score, and change in number of medications in the combined intervention group consisted of a significant decrease of –1.03 (95% CI –1.7 to –0.30). In this case, the combined intervention group, which included efforts to fit with the professionals’ work through integrating group discussions on patient cases within the educational meeting, coupled with specific feedback from clinical pharmacists on actual patients being treated by the GP, led the authors to conclude that ‘a combined intervention consisting of an interactive educational meeting for GPs and feedback to GPs on participating patients’ medication by clinical pharmacologists and a clinical pharmacist can improve medication appropriateness in elderly patients exposed to polypharmacy’. 98
Combining education plus a checklist led to huge reductions in the incidence of catheter-associated urinary tract infection among patients in an intensive care unit in the Menegueti et al. 99 study:
The number of CAUTI [catheter-associated urinary tract infection] decreased substantially over the 4 phases (60 in 24 months during baseline, 64 in 48 months in the biannual training phase, 23 in 48 months in the checklist and biannual training phase, and 3 in 24 months in the checklist and initial training phase).
Menegueti et al. 99
Particular styles used for educational activities (i.e. engaging style and real patient examples) can lead to instrumental outcomes (e.g. reduced incidence of falls). 100 In the Juola et al. 100 paper, outcomes were assessed at baseline and at 6- and 12-month follow-up and showed a reduction in harmful medication use in the intervention group (–11.7%, 95% CI –20.5% to –2.9%; p = 0.009), but remained constant in the control group (3.4%, 95% CI –3.7% to 10.6%; p = 0.34). Patients in the intervention wards with a Mini Mental State Examination score of > 10 had significantly fewer falls than patients in the control wards. There were 171 falls in the intervention wards, compared with 259 falls in the control group, with an incidence rate ratio of 0.72 (95% CI 0.59 to 0.88; p < 0.001). Juola et al. 100 hypothesised that the engaging learning style employed (i.e. incorporating the nurses’ own medication management practices) contributed to the success of the intervention.
Gulla et al. 93 concluded that in long-term hospital care the introduction of planned medication reviews with collegial mentoring can reduce antihypertensive drug prescribing. Findings showed that the medications were significantly reduced in the intervention group (n = 43, 32%) compared with the control group (n = 11, 10%). Blood pressure increased among the intervention patients from 128 ± 19.5 mmHg to 143 ± 25.5 mmHg at 4 months, but at 9 months this fell back to the pre-intervention average of 134 mmHg, with no effect on pulse.
Context–mechanism–outcome 4: ‘watchful waiting’ as an active intervention
Clinicians may face difficulties in managing situations where they are uncertain about diagnoses or where patients themselves request interventions that have demonstrable low value (context). In these contexts, interventions that seek to enhance professionals’ communication skills, utilise ‘watchful waiting’ as an alternative active intervention strategy or that engage directly with patients, can enhance patients’ sense of validation of their concerns without resorting to sustaining the low-value practice (mechanism). When this occurs, it is possible to see an increase in patients’ sense of autonomy and motivation to disengage from the low-value practice, an improvement in the quality of the patient–professional relationship and reductions in low-value practices, such as inappropriate routine investigations and prescribing (outcome) (Figure 5).
FIGURE 5.
Context–mechanism–outcome 4.

Context
This CMO configuration highlights the importance of patient preferences being incorporated into de-implementation strategies. Citing the range of media that the public are exposed to, and both the direct and the indirect personal experiences of health care, Keijzers et al. 102 suggest that ‘patients tend to believe that investigations and treatment are always beneficial’. Evidence from research is only one source of knowledge available to both patients and professionals in informing decision-making within health care. Therefore, there is the potential for too optimistic a view of effectiveness for an intervention and an underestimation of the harms associated with that intervention. 103
Validating patients’ health concerns
Diagnostic worries on the part of patients was cited by Fenton et al. 101 and May et al. 104 as one factor associated with overuse of low-value tests in US primary care. Specifically, the use of magnetic resonance imaging for recent-onset uncomplicated low back pain, dual-energy X-ray absorptiometry screening for women aged < 65 years without osteoporosis risk factors and neuroimaging for recent-onset headache. The hypothesis that improving the patient-centredness of professionals’ communication with patients would reduce the need for ordering these investigations was tested by Fenton et al. 101 Although an evaluation failed to demonstrate any overall significant impact of this hypothesis, an observational analysis of this study completed by May et al. 104 provided evidence of communication styles associated with de-implementation.
Fenton et al. 101 designed a brief 20-minute intervention to improve patient-centredness, comprising two visits by standardised patient instructors to US primary care physicians, during which a six-step patient-centred communication strategy was utilised: (1) developing understanding of a patient’s concerns, (2) validating these concerns through empathy and normalisation, (3) providing reassurance when possible, (4) explaining that risks outweigh the benefits of tests, (5) flexibly negotiating alternatives and (6) exploring for residual concerns. Instructors used different techniques to support implementation of this communication strategy, including performing the role of patients requesting two of these low-value tests and feedback on physicians’ performance. The impact of this strategy was evaluated against a control intervention that comprised visits by instructors and the provision by e-mail of guidelines on these clinical topics. No attention appears to have been paid to broader aspects of patient-centredness within the primary care experience.
The patient-centred communication strategy was evaluated in a RCT of 61 physicians. The primary outcome was whether or not physicians ordered any of the three low-value tests in follow-up visits from other standardised patients trained to request the tests. Providing instruction on communication drawing on two of the three low-value tests provided an opportunity to investigate any intervention carry-over to the third test (i.e. neuroimaging for recent-onset headache). Up to three follow-up visits from standardised patients per physician participant over a 3- to 12-month period were planned. Seventy-eight visits for control physicians were completed; of the 77 completed visits for trained physicians, and in addition to a standardised measure of patient-centred communication, the fidelity of the patient-centred communication behaviours was assessed in audio-recordings in all but one of these visits. All participating physicians were asked 2–4 weeks after each visit whether or not they suspected that they had seen a standardised patient. Visits were suspected at similar rates by both groups of physicians. Physicians in the intervention group were also asked to rate the quality and relevance of the training. In summary, and despite a positive qualitative evaluation of the training itself, it was not associated with any difference in the odds of subsequent test ordering from standardised patients (adjusted odds ratio 1.07, 95% CI 0.49 to 2.32).
A post hoc observational analysis of this trial completed by May et al. 104 assessed the association between whether or not low-value tests were ordered during the visits by standardised patients, and five specific communication behaviours related to the strategy outlined above: (1) normalisation, (2) reassurance around specific features of the case, (3) explaining that the risks of testing outweigh the benefits, (4) suggesting that tests will be ordered if symptoms persist, and (5) suggesting evidence-based alternatives for residual concerns. The relationships between these behaviours and whether or not physicians subsequently ordered the requested low-value test were evaluated in a series of regression analyses.
Of these behaviours, the provision of reassurance and alternative evidence-based strategies were used most commonly (95.5% and 97.4%, respectively) and normalisation the least (6.5%), all irrespective of whether or not a low-value test was ordered. Only for risks outweighing benefits (57.1%) and watchful waiting (67.5%) were statistically significant differences observed. Low-value tests were ordered less often when watchful waiting (88% vs. 12%; p < 0.001) and risks outweighing benefits (65% vs. 37%; p = 0.002) were utilised by physicians. Subsequent adjusted analyses demonstrated the overwhelming contribution of watchful waiting communication techniques (marginal effect –38%, 95% CI –44.3% to –31.7%). Although this was a secondary analysis relying on the post hoc coding of patient–physician–consultant communication, the authors104 conclude that watchful waiting, in which patient worries are acknowledged and a future route towards testing is available if problems persist, is a simple and effective communication technique for reducing low-value testing in primary care. The authors104 suggest that this strategy is ‘supported by theories of patient autonomy and control’, and that reassurance alone might be seen by some patients as a passive rejection of their concerns.
However, the use of watchful waiting as a prospective intervention in its own right was a strong theme within the evidence of this synthesis. For example, Keijzers et al. 102 make a compelling case for deliberate clinical inertia, or ‘the art of doing nothing’, as a positive response to situations when there is uncertainty whether or not the benefits of intervention may be outweighed by harm. Keijzers et al. 102 argue that the appropriate context for deliberate clinical inertia is shared decision-making, reinforcing that even doing nothing is an active strategy requiring discussion, knowledge sharing and agreement between patients and professionals. Although patients may have some unrealistic expectations about the value of modern health care, professionals may similarly fear the risk of litigation associated, for example, with missing rare diagnoses. Therefore, knowledge of the strength of evidence, clinical experience and confidence, alongside transparent communication and a fundamental focus on patients’ best interests are all required. 102 Sun et al. 105 highlight that there can be variable requirements of the evidence for watchful waiting. Using the inappropriate use of antibiotics for acute otitis media in children as an exemplar case study, Sun et al. 105 highlighted in an observational analysis of 250 children that, where patients met guideline criteria for prescription of antibiotics for acute otitis media, then there was 100% compliance with a recommendation to prescribe. However, when guidelines indicated that watchful waiting was the recommendation, ‘current practice in this emergency department instituted watchful waiting only 4.9% of the time’. 105
The following framework for the implementation of clinical inertia is presented to reframe ‘doing nothing’ as ‘doing something’:105
-
empathy and acknowledgement
-
symptom management
-
clinical observation
-
education about the natural course of the condition
-
managing expectations (in the context of patient values and concerns)
-
shared decision-making.
This framework for watchful waiting has been developed and evaluated in a number of studies included in the evidence base for this synthesis, largely within the context of reducing low-value or ineffective prescribing practice. For example, Little et al. 106 undertook a randomised trial that involved 315 children aged between 6 months and 10 years who presented with otitis media. The trial was based around general practices in the south-west of England. The watchful waiting intervention was the delay in providing antibiotics until 72 hours post consultation. Importantly, parents could collect the antibiotics if they felt that their child was not improving. The control group received immediate antibiotic medication, and both groups also received written advice sheets appropriate to their group allocation. Results showed that symptoms generally resolved after 3 days, with the children who were prescribed with immediate antibiotics having shorter illness (–1.1 days, 95% CI –0.54 to –1.48 days), fewer nights disturbed (–0.72 days, 95% CI –0.30 to –1.13 days) and slightly less paracetamol consumption (–0.52 spoons/day, 95% CI –0.26 to –0.79 spoons/day). Parents of 36 of the 150 children in the watchful waiting group used the delayed antibiotic prescriptions, with 77% of the parents being very satisfied with the process. Fewer children in the delayed group had diarrhoea, and fewer parents believed in the effectiveness of antibiotics and in the need to see the doctor for future episodes of infection.
The approach to watchful waiting evaluated by Little et al. 106 did contain a safety net for both clinician and parents, in that the antibiotics could be collected at a later date if the child’s condition did not improve. This risk reduction approach to watchful waiting was also alluded to in the stakeholder telephone interviews:
. . . but many years ago I used to work elsewhere in general paediatric practice and I found if you take the 5 minutes to explain to the patient who’s expecting you to give antibiotics for the viral illness, why they don’t need antibiotics, most of them will get it, not all, but most . . . I think also how much you watch and wait will depend on the urgency of the situation but also the competency . . . do you know what I mean? I think, again there were parents that I would see with a child in an emergency room and I would think actually I trust these parents and I’m pretty sure this is a viral and we’ll do whatever we need to do to confirm that and we can give them a safety net and they can go home. You might meet a different set of parents where you think, do you know what I’m not sure they’ll be able to come with this, and maybe we need to help them in a different way. I think it’s a big ask isn’t it, certainly for GP colleagues who are at the front line, I just think and understand that their time is so limited.
Clinical medical director B6
In a US study, MacGeorge et al. 107 recruited, through a participant panel, 134 parents who had children aged ≤ 5 years and who had been advised to undertake a watchful waiting approach to treating their child’s otitis media. An online survey asked the parents to recall the interaction with the health professional, then coded for five aspects of content. The findings showed that up to 27% of the participants did not comply with the watchful waiting advice and immediately obtained the antibiotics for their child. The parents who adhered to the watchful waiting approach had been given greater explanation of the symptoms of otitis media, received instruction on how to monitor and respond to the child’s pain, and provided with a follow-up opportunity. The authors concluded that clinicians can improve patient adherence with a watchful waiting strategy through better education around antibiotic side effects, and reinforce the importance of a ‘safety net’ through advice on monitoring the condition with the option of follow-up contact, which validates patients’ concerns and provides reassurance.
In other clinical contexts, the use of watchful waiting as an effective strategy has been explored using a pragmatic randomised trial design, comparing observation of patients with acute, uncomplicated diverticulitis with the existing practice of administering intravenous antibiotics four times daily for 48 hours. 108 In total, 528 patients were included, with a median time to recovery of 14 days in the observational group and a median time to recovery of 12 days in the standard treatment group (p = 0.15; hazard ratio for functional recovery = 0.91; lower limit of one-sided 95% CI 0.78). Hospital stay was shorter for the watchful waiting group (2 days vs. 3 days; p = 0.006), but findings are limited to confirmed mild forms of diverticulitis. Pradhan et al. ,109 in an overview of systematic reviews and RCTs describing watchful waiting and brief education in the management of low back pain, highlighted the importance of patient communication and education through activity modification and reassurance. Their review, however, showed that for chronic low-back pain, watchful waiting may not be an effective strategy to employ because exacerbation of symptoms increases the likelihood of patient anxiety and depression. To examine the cost savings of a watchful waiting approach to acute otitis media, Sun et al. ’s105 cost–utility analysis of a retrospective sample of 250 children with acute otitis media attending emergency departments in the USA highlighted the potential additional costs of watchful waiting to patients and families. In this case, these costs could include parents’ time away from work, the costs of additional analgesia, and the logistics of future consultations and visits, if required, as part of the watchful waiting strategy.
The importance of health-care provider education about watchful waiting as an active clinical intervention with patients was attested to in a secondary analysis of a scenario-based intervention involving a woman with depression. Meredith et al. 110 examined factors that could increase primary care clinicians’ inclination to favour watchful waiting as a strategy to manage depression. Findings showed that the tendency to use watchful waiting as an approach among the clinicians was low, with only 34 (20%) reporting a high tendency to use watchful waiting. Clinicians were significantly more likely to choose such a strategy if they had greater psychological knowledge or thought that the need to treat the physical or medical condition was more important than treating the depression. Watchful waiting was less likely to be utilised if there was limited access to other mental health professionals. In our telephone interviews, we found that senior clinicians also employed the use of watchful waiting as a technique, but they acknowledged that it was a difficult decision to make:
Oh very very much so, I do see that [watchful waiting], I often and I see colleagues on ward rounds sometimes and the sensible thing to do is nothing . . . doctors, nurses you know all of us in the medical profession, the hardest thing we find is to do nothing.
Clinical medical director M7
The same clinician also commented that a substitution strategy, such as sending to another health-care practitioner, was not useful unless it was seen as effective:
. . . if we’re doing it [substitution] just because we want to give them something, what I mean is if I’m sending to physiotherapy, they don’t need rather than antibiotics they don’t need then I’m just wasting a different resource if you know what I mean. But I think yes there are probably other resources that we can take better advantage of, then you think some of it is probably communication amongst ourselves and patients and families as well.
Clinical medical director M7
Increasing patient involvement in their treatment through shared decision-making and incorporating patient preferences was highlighted by several stakeholders during telephone interviews:
. . . I believe the only way to support patients is to have clearly shared understanding and shared ownership of that risk to a greater extent as you can so that means being fully involved with the patient and shared decision-making, which means making sure that they’ve had the relevant information presented back to them in such a way that they can understand it and weigh it up. And we think we do that very well but very often we don’t for a variety of reasons, time being one of them, but I think if patients understand your process of clinical reasoning and are happy to go along with that thread then it’s much easier to jointly manage that clinical risk and you can reassure them that they don’t need the test or investigation.
Commissioner B10
The context of this CMO configuration recognises the important influence that patients’ expectations can have on the outcome of consultations, particularly in relation to low-value diagnostic testing and drug regimes in primary care. Across the evidence base for watchful waiting, there is consistent recognition of the importance of shared decision-making as the context for de-implementation in this way. However, some de-implementation interventions have focused primarily on a patient perspective. Tannenbaum et al. 111 undertook to reduce the use of benzodiazepines by older adults in Canada by direct patient education. Reflecting evidence of the positive impact of direct-to-consumer marketing by the pharmaceutical industry, their hypothesis was that direct-to-patient education could reduce the inappropriate consumption of benzodiazepines.
The hypothesis was tested in a cluster RCT in which community-dwelling adults in Canada, aged ≥ 65 years and currently receiving benzodiazepine therapy, were allocated to the educational intervention or to usual care. Clustering by the 30 community pharmacies involved was used to evaluate the potential for contamination between service users in the same pharmacy. The intervention itself was underpinned by a programme theory of patient empowerment, in which greater knowledge on the part of service users was expected to drive ‘shared decision-making to deprescribe’ (Tannenbaum et al. ). 111 The educational intervention included a self-assessment about the risks of benzodiazepine use; presentation of the evidence of harm; statements designed to create dissonance about safety; peer champion stories to raise perceptions of self-efficacy; suggestions about alternative strategies for dealing with insomnia/anxiety; and stepwise recommendations for tapering drug use. Complete cessation of benzodiazepine at 6 months post intervention was achieved in 27% of those receiving the educational intervention compared with 5% of those who did not (prevalence difference 23%, 95% CI 14% to 32%). Moreover, nearly two-thirds of all those in receipt of the educational intervention went on to initiate conversations with either their physician or pharmacist, and over half attempted discontinuation in some form.
The programme theory for this intervention was further evaluated in a realist evaluation of the trial data. 112 This provided an opportunity, through a mix of qualitative and quantitative analyses, to disentangle the contribution of potential mechanisms that reduced consumption: (1) increased motivation through greater knowledge and understanding, (2) building capacity to taper through increased self-efficacy or (3) the provision of opportunities to discuss consumption with a health-care provider. The analysis demonstrated that, within the context of reducing benzodiazepine use in older adults, de-implementation mechanisms that ‘target patient motivation and capacity . . . yield successful outcomes where healthcare providers are supportive, and patients do not have competing internal competing desires to remain on drug therapy’. 112
Outcomes
This evidence suggests that providing training, albeit brief, to health professionals to help them navigate de-implementation in the face of patients’ requests for low-value tests is appreciated. 101 This may not easily translate into improvements in overall or specific patient-centred communication styles, or subsequent changes in professionals, ordering behaviours. Tannenbaum et al. 111 demonstrated that an, albeit complex, educational intervention delivered to patients had the potential to initiate discussions with health-care professionals about de-implementation. Over one-quarter of those who received the intervention (although one where there was evidence of potential for harm) went on to discontinue consumption. However, a strategy of watchful waiting appears to be productive in helping patients and professionals, alike, navigate the complexities of de-implementation. Through a co-produced approach to decision-making, reciprocity can be achieved for patient and health-care provider, in that the patient feels that their needs are taken into account and the health-care practitioner is reassured that they are still providing the best care for the patient. Through a process of watchful waiting, both parties can contribute to a reduction of inappropriate and low-value treatments. Many patients can be reassured that this strategy is acceptable if it is appropriately presented as a way of monitoring the patient’s condition without undermining their concerns.
Context–mechanism–outcome 5: supporting staff to de-implement
De-implementation strategies may be less effective when there are strong interpersonal relationships that can develop between clinicians and patients (context). Better communication and engagement with stakeholders, including patients, and professionals’ confidence building can validate concerns around potential risks of de-implementation, the quality of patient care and service ethos (mechanism), leading to a mitigation of professionals’ emotional burden (outcome) (Figure 6).
FIGURE 6.
Context–mechanism–outcome 5.
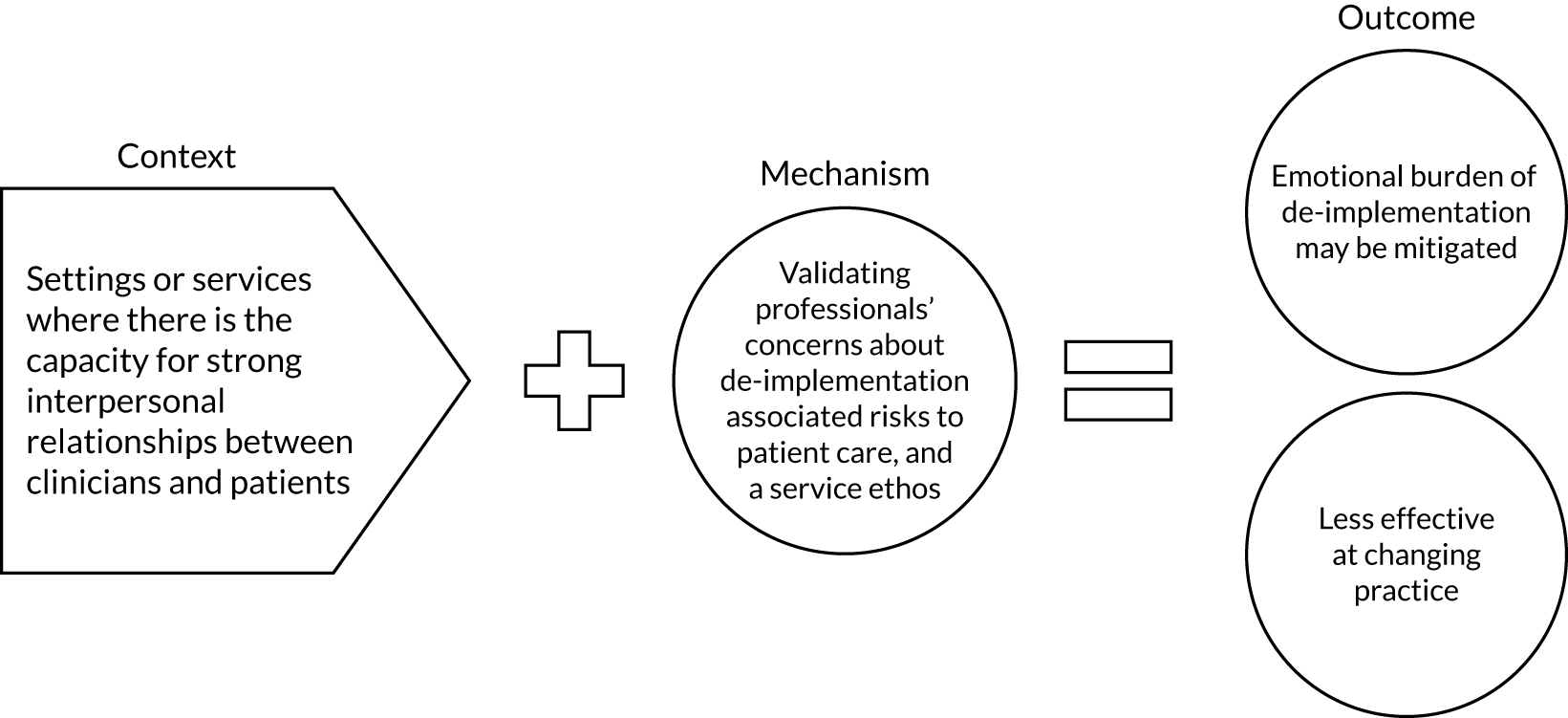
Context
The context for this CMO is the relationship between practitioners and patients. Practitioners are in direct contact with patients and their families, and care provision can extend over a prolonged period of time. These relationships influence the delivery of service provision, as they are not just a technical exercise but in large part built on patients’ trust in the health professional. Indeed, models of clinical decision-making emphasise the rational and cognitive components of the process and underplay the emotionality that also influences the choices made. 113 De-implementation (or disinvestment) has negative connotations with health professionals and the public, in that withdrawal of services is equated with saving money rather than improving care. 114 If treatments are de-implemented, even if there is evidence for their lack of efficacy, there will also be an attendant emotional component for practitioners and patients. The approach taken to de-implementing a service or treatment needs to address the emotional effects on professionals.
Letting go
Mitchel et al. 115 investigated the reaction of health service staff to the de-implementation of a patient-oriented service, that is the removal of weekend allied health staff, such as dietitians and physiotherapists, on several acute hospital wards. The original de-implementation trial was a two-stepped-wedge cluster RCT conducted between 2014 and 2015 among patients in two hospitals in Australia. The primary outcomes were length of patient stay, unplanned readmission and adverse patient events. Haines et al. 116 concluded that ‘. . . having no weekend allied health service on these wards was no worse than having the newly developed service that was brought back in, and indeed was superior for some outcomes’. 116 The Mitchel et al. 115 study used observation and focus groups with a total of 156 hospital staff before the commencement of trial 1 (i.e. the de-implementation phase). The resultant transcripts were thematically analysed and generated five broad themes: (1) immediate negative reaction with patient and staff consequences, (2) an excuse to save money, (3) incompatibility with health service values, (4) bending rules to circumvent the trial protocol and (5) disinvestment as opportunity. Mitchel et al. 115 used Kubler-Ross’s117 responses to the grief model to explain the reactions of staff to the forthcoming de-implementation, beginning with shock and denial, leading to anger and ending with acceptance. The authors point out that de-implementation directly threatens professional identity that impedes clinicians from questioning their own service provision. This qualitative research showed that the potential negative impact on patients of de-implementing a service, as perceived by health-care providers, needs to be explained to the staff involved. In addition, the research showed that the quality of the service to patients can be maintained and improved through the de-implementation of a service. As Mitchel et al. 115 conclude:
Staff saw the project as a threat to patient safety and quality of care and to meeting patient flow targets, resulting in conflict between the healthcare workers’ professional and organisational identities.
Mitchel et al. 115
Likewise, one consultant physician/dentist commented:
. . . I remember that being quite difficult a scenario to do so because it meant letting go of something which we’ve always done like this and either we haven’t had any major complications, problems or side effects or downfalls to it, but never the less other people did and so there was a difficult process.
Consultant physician/dentist M9
Meaningful engagement
In a narrative review, Day et al. ,2 in examining challenges facing the Choosing Wisely campaign in Australia, note that there is little evidence to show how disinvestment should be conducted. However, the authors2 conclude that if disinvestment is to work then transparent engagement with the clinical community around quality of care and patient safety is essential for success. In relation to the emotional challenges facing clinicians, our interviews show the pressure of maintaining a de-implementation strategy:
. . . if one has had a bad experience [of de-implementation] this is going to scar one quite significantly and the challenges of future cases are going to be potentially if one has had a bad experience.
Consultant physician/dentist M10
Within the context of health technology reassessment, in its broadest meaning, Soril et al. 118 conducted an evidence review of systematic reviews, followed by an expert stakeholder consultation. Their aim was to illustrate concepts that optimise the health technology reassessment process. The review stage synthesised systematic reviews that described or evaluated frameworks or experiences with health technology reassessment. Identified reviews were then appraised to identify primary articles for the analysis. Synthesis of the evidence identified the significant factors involved in health technology reassessment, and a diagram representing these factors was created. This schematic of ‘conceptual groupings’ was then presented to stakeholders, who were made up of clinicians, academics and health managers (sample size not stipulated). Over a 1-month period, stakeholders debated the schematic developed from the literature, through online and face-to-face discussion with the authors, until consensus was reached. The final schematic that emerged outlined the de-implementation process and consisted of six key questions that planners should ask when considering reassessing or de-implementing a health technology.
-
What is the value of the technology?
-
What is the current utilisation gap?
-
What are the available tools and resources?
-
What are the levers for change?
-
What is the desired outcome(s)?
-
Who are the foundational actors?
The central question that underpins health technology reassessment was the identification and engagement of the people involved in the process, and the necessity to have ‘meaningful engagement’, with transparency and authenticity of process delivery with all stakeholders. This was also reflected in our telephone interviews:
. . . if I reflect on the ones we’ve done [de-implementation] in a positive way, it’s always about being honest from the outset and being clear with people and not being ambiguous because once you’re ambiguous and maybe not being truthful from the outset you lose the stakeholders that you need to progress things.
Nurse and allied health professions clinical director B7
Fear
As for engagement with public stakeholders, Daniels et al. 119 looked at how health-care leaders view public involvement in disinvestment decision-making, employing a Q study method and interviews. Fifty-five NHS managers, comprising medical (n = 16), allied health professional (n = 10), nursing leads (n = 8) and administrators (n = 21), agreed to participate in stage 1. Q methodology is a procedure in which statements are rank ordered for significance by individuals and are then sorted through factor analysis. Once this procedure was completed with the 55 NHS managers, 20 participants agreed to telephone interviews based on the Q-sort analysis. The Q-sort produced three broad factors: (1) those health managers who advocated public involvement in de-implementation, (2) managers who were cautious supporters and (3) managers designated the ‘freedom of choice group’, who supported public involvement but believed that the public should be free to participate or not. Through the follow-up interviews, it was apparent that all the groups were more cautious about public involvement in the disinvestment process. Daniels et al. 119 state that ‘. . . in part, respondent fears that public input might take an adversarial form’. The authors highlight the importance of recognising the emotional elements facing clinical managers who make de-implementation decisions when there is a pushback by the public to these decisions:
Participation is required that allows for the expression of discord and emotion alongside consensus-building and rational argument.
Daniels et al. 119
Likewise, one commissioner commented:
And the context of course, so it depends on the level of risk . . . it depends what the stakes are, so if the stakes are low, it’s easier to take the risk isn’t it, if the stakes are high . . . they are unlikely to tolerate that risk for obvious reasons.
Commissioner B10
Information-giving/engagement
In an Australian study, Hodgetts et al. 120 used a co-design approach and deliberative engagement with all stakeholders involved in assisted reproductive technology (ART) treatment. A systematic review showed that ART effectiveness decreases with advancing maternal age, particularly after the age of 42 years, and therefore becomes a low-value treatment. With the findings from the review, stakeholder engagement sessions were instigated, consisting of three groups: (1) a consumer group, comprising patients and partners who had experienced ART; (2) a community forum group who represented the south Australian population more generally; and (3) a group of clinicians with experience in ART. The forums included ‘. . . the provision of accessible information by content experts, facilitation by an independent professional, small and larger group deliberation and the generation of policy guidance’. 120 Each stakeholder group attended two sessions several weeks apart. In the first session, each group considered the results of the review and from these discussions proposed a policy for ART funding in Australia. In the second session, each group received the outputs from the other groups, resulting in further deliberation. Each group’s discussions were transcribed and analysed through a thematic approach. Surprisingly, the consumer groups’ discussions did not show the self-interest of funding of ART that would have been expected. Instead, they recognised the limits on health spending. Similarly, the community group and clinicians also recognised that health provision should meet the needs of all patients, not just one sector, and ART should not be considered any different from other medical conditions. The findings indicate that a strategy of full engagement, including building the communication skills of all stakeholders, can be a way of reducing professionals’ concerns. The importance of engaging the wider stakeholders was also referred to by a health service commissioner whose quote supports the conclusions of Hodgetts et al. :120
They [clinicians] are influenced very much influenced by patient and family experience and patient voice that does help and I think hard facts behind it and showing improvement with regards to things that really speaks home . . .
Consultant physician/dentist M3
Relationships and leadership
In an opinion piece, Gupta and Moriates121 discuss the importance of leadership in creating a culture in which low-value practices are discouraged. The authors121 outline four steps these leaders need to take:
-
engage front-line providers, particularly through patient-centred rationale
-
create infrastructure to support improvements
-
use value-based incentives
-
be visible and show commitment.
In addition, Gupta and Moriates121 state that leaders should also build up an infrastructure that enables staff to communicate and feel confident in making their concerns known through the visibility of shared goals. These leadership qualities were also evident in a three-round Delphi study conducted by Robert et al. 20 Thirty international experts who had extensive experience and responsibility in decommissioning either through research or in practice contexts were recruited. Participants came from Australia (n = 6), Canada (n = 3), the UK (n = 20) and Ireland (n = 1). Their expertise included removal of treatments or prescribed drugs from practice, relocation and reconfiguration of services, and closure of services and departments. The Delphi method is used to ascertain a range of opinions on a particular topic, with the intent of producing a consensus around the topic in question. 122 The method uses a group of participants known as ‘panellists’ who are specially selected for their particular expertise on a topic. There is then a series of two or more sequential questionnaires known as ‘rounds’. Following each round, the researcher collates opinions, and redistributes potential consensus statements to the panellists until there is agreement or consensus around the issue. In the Robert et al. 20 study, three rounds were undertaken. In round 1, participants identified factors that they thought were involved in decommissioning. These responses were analysed through content analysis and formed into an 88-statement Likert scale for round 2. The Likert statements were computed for consensus and those statements receiving low scores were redistributed to participants in round 3, together with the overall results from round 2, with open-ended comments. Opinions from the final round of consensus meetings were grouped into three interlinked categories: (1) change management and implementation, (2) evidence and information and (3) relationships and political dimensions. The consensus from the expert panel showed how ‘messy’ the process of de-implementation is in reality,20 with political and financial decisions eclipsing professional concerns. The unsystematic approach to de-implementation can cause tensions for professionals, and conclusions drawn by Robert et al. 20 from the Delphi study included ‘. . . a strong leadership team, engaging clinical leaders from an early stage, and establishing a clear rationale for change’. 20 The importance of leadership and relationships was also endorsed by the following quotes from clinical directors:
But for bringing around change, you need skilled leaders that’s for sure, I guess that’s what this quality improvement work is like, certainly in our health trust and it’s a national thing but people who are trained to bring about quality improvement through staff engagement and de- . . . whatever it’s called . . . de-implementation is a quality improvement initiative isn’t it.
Clinical medical director B1
. . . you need the basis of good relationships, so before you can even get into being a mature team, because that’s cohesive, you’ve got to spend time on just having those relationships.
Nurse and allied health professions clinical director B7
Outcomes
For CMO 5, the evidence suggests that de-implementation is a process that can generate unease and concerns among health-care professionals. Mitchel et al. 115 outlined how staff react emotionally to the removal of a service that they believed helped their patients, even when there was little supporting research evidence of its efficacy. De-implementation can heighten health professionals’ emotional involvement if they perceive that the removal of a service harms their patients. To counter the emotional burden of de-implementation, health-care professionals need to have organisational structures, such as building long-term relationships with stakeholders that would enhance confidence and skills to communicate concerns, which can then mitigate emotional burden. 119
Context–mechanism–outcome 6: aligning multiple perspectives
In the context of embedded low-value practices (context), when there are no financial disincentives, a whole-system approach to de-implementation would appear to be more effective. When a whole-system approach to de-implementation includes combinations of a multicomponent de-implementation intervention, engagement of the multiprofessional team and advocacy or service user involvement, the perception of a more aligned approach fosters trust (mechanism), which then can bolster success in generating behaviour change predominantly within de-prescribing (outcome) (Figure 7).
FIGURE 7.
Context–mechanism–outcome 6.
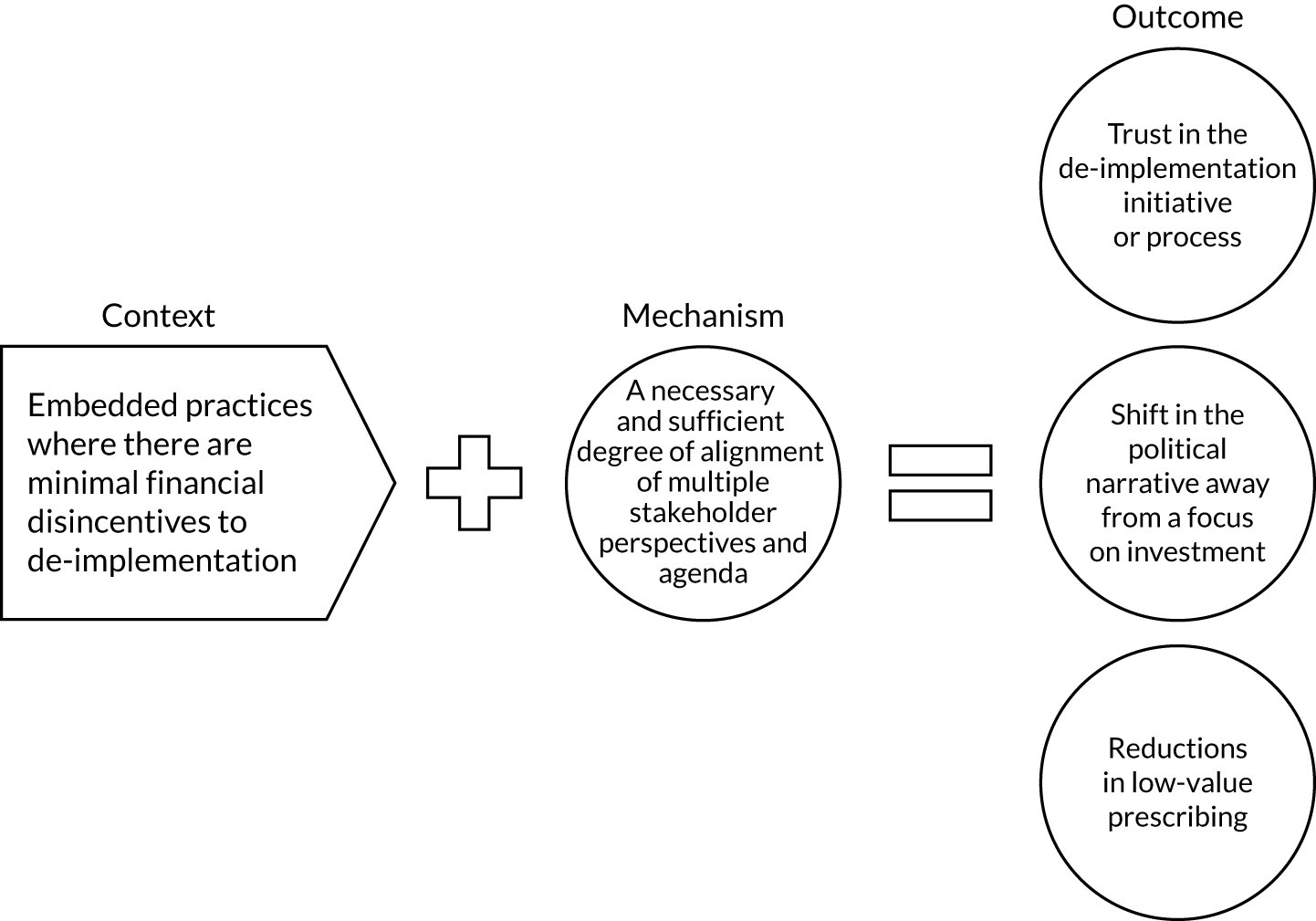
Context
The evidence included in this synthesis reflects a recognition of the challenges of de-implementing low-value practices when these are deeply embedded within health-care systems. As Montini and Graham17 highlight:
. . . practice patterns are located within a social structural context so that even the strongest evidence’s influence is mitigated by the conditions of the context in which health care is practiced.
Montini and Graham17
The influence of context is well established within the implementation literature, although the theoretical, methodological and practical consequences are debated. The same issues apply within de-implementation. Based on a historical analysis of radical mastectomy for breast cancer, the authors17 provide a compelling account of ‘historical entrenchment’ of this intervention, and the different factors that influenced de-implementation towards a less aggressive modified procedure. This case highlights the potential influence of de-implementation from clinical paradigms, or the major worldviews and theories that explain health problems and their resolution (e.g. a theory of cancer as a local disease); payment systems that reward more, rather than less, intervention; professional vested interests in the co-ordination and leadership of disease management pathways; consumer awareness of alternatives to the status quo and degrees of public pressure for change; and the availability of alternative procedures that have potential to add value to health outcomes or experiences.
A necessary and sufficient degree of alignment of multiple stakeholder perspectives
The de-implementation of radical mastectomy was associated with some degree of alignment of different factors, as it occurred ‘at a time when there was convergence in clinicians’ and patients’ awareness of the scientific evidence, patients expressing their preferences for an alternative, and when there were other viable treatments to offer instead of radical mastectomy. 17 Successful de-implementation appears to be dependent on the development of a sufficient degree of alignment between different perspectives, specifically those of relevant stakeholders. The evidence demonstrates a number of ways in which this alignment can be achieved.
The use of a multidisciplinary approach to de-prescribing in primary care settings was investigated in five primary care general practices in England, focusing on shared medicines management for older patients between the GPs and community pharmacists. 123 The Randomised Evaluation of Shared Prescribing for Elderly people in the Community over Time trial implemented an interrupted time series design ‘to estimate the effect of pharmaceutical care on the appropriateness of prescribing; patients’ knowledge, adherence, and quality of life; and the incidence of adverse events. 123 Pharmaceutical care was recommended as an alternative method for reviewing medication prescribed for older people to both improve health and reduce unnecessary hospital admissions, specifically by ‘improving communication between the pharmacist . . . the patient, and the GP’ (e11). Training consisted of theory and practice of pharmaceutical care, and practical exercises in collaboration with the GP. The study failed to demonstrate any statistically significant impact of the complex intervention, which the authors attributed to difficulties the pharmacists had in accessing full patient data and arranging meetings with the GPs:
Pharmacists were also typically unable to gather full and detailed clinical histories, which led to frustration on the part of some GPs when their prescribing was questioned.
e15
Richmond et al. 123 explain the non-significant result to the lack of a relationship between GP and pharmacist, suggesting that without this rapport it was difficult for the pharmacist to influence GP prescribing. However, Spinewine et al. 124 found that adding pharmaceutical care to the usual prescribing management programme in an inpatient hospital setting reduced the overuse, misuse and underuse of medicines for older patients. In a RCT of 203 Belgian patient participants aged ≥ 70 years, pharmaceutical care was provided from admission to discharge and delivered by a specialist clinical pharmacist who had direct contact with the medical team and patients. The appropriateness of prescribing on admission, at discharge and 3 months after discharge was measured, and patients in the intervention group were significantly more likely than control patients to have an improvement in underuse criteria from admission to discharge. This comprehensive intervention resulted in better medication management for the intervention group, as indicated by scores on the MAI, and in the Assessing Care of Vulnerable Elders underuse criteria from admission to discharge (odds ratio 9.1, 95% CI 4.2 to 21.6, and odds ratio 6.1, 95% CI 2.2 to 17.0, respectively).
We also found evidence data to show success of a multiprofessional approach to engagement within long-term care settings. 125 Here, a multidisciplinary approach in the form of the Multidisciplinary Multistep Medication Review (3MR) in nursing home settings was evaluated in a pragmatic clustered randomised trial. The experimental intervention consisted of an assessment of the resident’s perspective, medical history, medications review, and a meeting between the physician and the pharmacist, and implementation of medication changes. This Dutch study had 59 nursing home wards and allocated 16 care of the elderly physicians and 26 wards to the control group, and 16 care of the elderly physicians and 33 wards to the intervention. The 3MR intervention is a four-step process, in which the elderly care physician and pharmacist began by assessing each patient’s situation through a patient-completed questionnaire (with assistance if required) and completing a review of medical charts, including blood results. In step 2, the pharmacist reviewed the prescribed medication using the Screening Tool to Alert to Right Treatment/Screening Tool of Older Persons' Prescriptions (START/STOPP) and Beers Criteria. Step 3 was a multidisciplinary meeting, in which patient data were reviewed and decisions taken to withdrawing inappropriate medications, leading to the final step of implementation. Findings showed that, in comparison with usual care, the multicomponent intervention de-prescribed at least one drug for 39.1% of patients compared with 29.5% in the control group (adjusted relative risk 1.37, 95% CI 1.02 to 1.75). Commenting on their findings, Wouters et al. 125 indicated that the 3MR system needs to be repeated to coincide with changes in the patient’s condition, from prevention to palliative and comforting care. Additionally, the authors125 suggested that further research needs to be done to find better ways of incorporating patient preferences in the de-prescribing process.
The main reasons for the success of this intervention appear to be the structured approach employed and the direct contact between the multidisciplinary team. A structured approach was realised through a therapeutic plan, involving the patient, pharmacist and other professionals. In addition, high levels of pharmacist visibility were reported through the presence of the pharmacist on the unit 4 days per week (e.g. taking part in ward rounds), with access to medical records, and having direct contact with patients and their family carers. The pharmacist conducted a medication assessment on admission and provided a patient record and care plan. The intervention was also noted to contain a degree of opportunity-seeking, whereby the pharmacist discussed the opportunity to improve/optimise prescribing with the prescriber, who could accept or reject the intervention. Furthermore, the pharmacist answered all questions that health-care professionals asked about medications. At discharge, the pharmacist provided written and oral information on treatment changes to the patient or caregiver, as well as written information to the GP.
Other examples of the potential success of structured approaches using multidisciplinary teams across both hospital and community care were reported by Crotty et al. 126 Crotty et al. 126 suggested that multidisciplinary case conferences can increase appropriate prescribing and reduce the use of inappropriate medications in residential care. This clustered randomised trial evaluated the impact of multidisciplinary case conferences on the appropriateness of medications and on patient behaviours in Australian care settings for older people, with 154 participants having medication problems and/or challenging behaviours. The two case conferences were chaired by the GP, held at the residential home and consisted of a geriatrician, a pharmacist, residential care staff and a representative of the Alzheimer’s Association. The case conferences developed a multifaceted approach to the management of the patients, with the patient’s GP augmenting the discussion through the medical records, the Alzheimer’s Association representative contributing with advice on non-pharmaceutical interventions and the care home staff expanding on issues recorded in the patient case notes. Outcomes were measured with the MAI and patient behaviour assessed with the Nursing Home Behavior Problem Scale. Findings showed that medication appropriateness improved in the intervention group (MAI mean change 4.1, 95% CI 2.1 to 6.1) compared with the control group (MAI mean change 0.4, 95% CI –0.4 to 1.2; p < 0.001), with a significant reduction in the MAI score for use of benzodiazepines (mean change control –0.38, 95% CI –1.02 to 0.27, vs. mean change intervention 0.73, 95% CI 0.16 to 1.30; p = 0.017). However, there was no improvement in resident behaviour because of low levels of behavioural problems at baseline. Surprisingly, improvements in medication management were seen only in residents who were discussed in the case conferences; there was no carry-over to other residents in the nursing homes, demonstrating the importance of a co-ordinated approach where all members of the team are aware of the strategies for appropriate medication management.
This section discusses evidence from studies that look at more centralised multiservice health systems, rather than localised interventions. Spinewine et al. 124 suggested that the positive findings of their study were due to the whole-system approach, which involved the multidisciplinary team having high visibility of the pharmacist, who would have built up a relationship with the medical team. The importance of an effective multidisciplinary team for the management of the de-implementation process was reiterated by many participants in our telephone interviews, as this example testifies:
We are quite fortunate in a way that we work in a very close knit team and we all have . . . we come from different backgrounds and we have a very big collaborative in terms of also debating things quite intensely and yes we’re debating it and we’re looking at it but it requires a certain openness and trust of people to actually be able to do it.
Consultant physician/dentist M9
In a cross-sectional survey of eight community services in northern England, Gray et al. 127 assessed the variation in treatment and management of complex wounds. Data from 3179 patients with a total of 5632 complex wounds were evaluated. The data showed a substantial variation in the use of antimicrobial dressings, ranging from 18% to 69%. The authors’ recommend that a systematic approach should be instigated, bringing together clinicians, managers and policy-makers to identify de-implementation priorities. Similarly, Montini and Graham17 conclude their historical analysis of a de-implementation challenge with the view that to ‘. . . facilitate de-implementation . . . intervening in the broader context in which clinicians work – the social, political, and economic realms – rather than focusing on healthcare professionals’ behaviour, may indeed be a fruitful approach to effect change’. 17 Peiro,128 in a narrative review, discusses the complexity of de-implementation across different country contexts. The starting point for this review is the international challenge of disinvestment in low-value practices, with the reluctance of some national contexts to address the controversies associated with that disinvestment. There may be disagreements across different stakeholders as to the evidence for many low-value treatments, together with underlying psychological and sociological barriers that can undermine de-implementation at a much broader level. A plea to build ‘internally sustainable [health] systems’ requires a whole-system approach that is transparent. 128 The paper128 argues for an organisational approach to de-implementation through building trust between stakeholders, and highlights that there may be a small proportion of patients who require treatments that are considered ineffective for the majority.
An exemplar organisational framework to guide de-implementation is described by Parchman et al. 129 Parchman et al. 129 argue for behavioural, organisational and cultural change as requirements to overcoming the challenges of de-implementing low-value care. The framework, which is primarily focused on the challenges of overuse, describes four necessary conditions for de-implementation:
. . . addressing low-value care; build a culture of trust, innovation and improvement; establish shared language and purpose; and commit resources to measurements.
Parchman et al. 129
Pivotal to their framework is the use of ‘sense-making conversations’ where different stakeholders, in this case professionals, teams and groups across health-care services and organisations, can achieve alignment between the potential for harm associated with overuse of low-value interventions and understandings of the scale of the overuse challenge in stakeholders’ daily practice. Alignment in this sense is associated with ‘shared norms of behaviour, shared language, and a shared vision for co-ordinated action around reducing use’. 129 Although essentially a narrative text located at the interface of patient and professional dialogue around decision-making, Parchman et al. 129 appear to reject the concept of ‘value’ in favour of ‘harm’ as the focus for alignment around a common language. The authors129 argue that harm, rather than value, may have more resonance with patients and professionals alike, and that harm can be used to describe de-implementation challenges at a population level. For example, the consequence of overuse of services is reduced access for those patients who may, indeed, benefit from them.
The transferability of economic approaches to the allocation of health resources to de-implementation challenges, such as disinvesting in services, specifically the programme budgeting and marginal analysis method, has been considered. 130 As with other approaches to de-implementation, although there may be a shared goal across stakeholders, such as improving population health, differences in organisational objectives may still minimise the success of specific methods, such as programme budgeting and marginal analysis. Success in these terms related principally from moving to agreement that ‘something needs to be done’, to instrumental changes to service configurations and availability. Mortimer130 argues for greater specification in economic dimensions of de-implementation as a key requirement, including being specific about required budgetary contexts of de-implementation [such as any financial constraints to be delivered, the scope of budgets relevant to the de-implementation initiative and the (lack of) potential for financial recovery], and greater attention to the constituency and ‘democratic’ accountability of stakeholder representation. Budgets should have specific investment proposals linked to de-implementation proposals and an orientation towards ‘shift-lists’, rather than ‘wish-lists’, when the business case is made for de-implementation. Project strategy groups should include stakeholder representatives, but also have advisors who have experience of, and are supportive of, de-implementation. There is a concern that stakeholder engagement in de-implementation is often weighted against disinvestment and towards the status quo, hampered by stakeholders’ specific interests and lack of access to specific knowledge required for success (e.g. of the evidence base).
The use of financial resources in de-implementation, as highlighted by Mortimer,130 was also raised in data collected through telephone interviews, especially linked to patient or service improvements directly relevant to the health-care team:
I would say financial incentives to consultants aren’t necessarily the most viable, I think actually if you say that you can have something back for your services, it’s probably more attractive to a lot of consultants. Some are going to be kind of guided by financial rewards themselves but actually a lot of them will say, ‘if you can have something extra for your service or an extra member of staff or that kind of thing it would actually change practice because actually that would be a win for most of us’.
Consultant physician/dentist B5
The importance of a whole-system approach to directing de-implementation in a health service is also recommended by Hollingworth et al. 131 Hollingworth et al. 131 adopted a multimethod approach that included a rapid systematic review; use of Hospital Episode Statistics; non-participant observation of two primary care trusts; Clinical Commissioning Group meetings, including document analysis; and a case study of de-implementation of carpal tunnel release surgery. The authors131 found a large geographical variation for many procedures, with Clinical Commissioning Group meetings dominated by investment strategies, rather than de-implementation. The authors131 recommend an increased role for central NHS support to encourage commissioners to think about de-implementation by providing relevant evidence to facilitate decision-making. However, Montini and Graham17 argue that historical, economic, professional and social factors can hinder de-implementation efforts. Therefore, if a programme or practice has been in place for a long time and is well integrated into public health systems, it may be highly resistant to de-implementation and may include financial and professional interests that are dependent on the service. It may be difficult to de-implement and replace some low-value programmes without a change in the social milieu surrounding them.
Outcomes
Embedded practices are often reinforced through a variety of professional, public, policy and system-level factors. Engaging stakeholders appears to be effective in developing some form of shared space in which de-implementation can occur. The empirical evidence for this CMO is primarily located within interventions that have brought clinical colleagues together to work on de-implementation challenges. There is evidence that, for inappropriate drug prescribing, a whole-system approach that employs multidisciplinary groups, including patients and families, and which is aligned to a clear objective, is effective (for example124–126). Evidence of the effectiveness for strategies for de-implementation of broader scope, such as decommissioning and disinvesting in services, relies more on the reports of those with experience of the process. De-implementation efforts within a whole-system approach are likely to be more effective if such systems can foster trust between appropriate stakeholders. Trusting relationships encourage stakeholders to proceed with the de-implementation process in the knowledge that all involved are working in the best interests of the patients. More broadly, financial incentives can be useful in the de-implementation process if, again, there is an open strategy that clearly indicates how the service will benefit.
Chapter 4 Discussion and conclusions
Introduction
In this final chapter, we revisit the aims and objectives of the synthesis and provide a summary of the main challenges associated with this review. We provide a recap of the main findings from Chapter 3 and a commentary on the nature of interventions that informed the review findings. We additionally comment on our understanding of contextual conditions and characteristics that underpin the evidence base for the review. In the light of the initial programme theory and the conceptualisation of de-implementation, we consider the implications of the review findings for health and care services going into the future. Discourse around the wider significance of our findings for stakeholders are included. Finally, we offer a suite of practical solutions for managers and practitioners based on new understanding of what works, and the particular de-implementation strategies that can support efforts to minimise low-value care for patients and improve efficiencies across health and care settings.
Revisiting the aims of the evidence synthesis
Our aim at the start of this review was to provide explanatory evidence to inform managers and practitioners of how de-implementation strategies best work to reduce low-value care and improve efficiency across health and care. On commencing the review, we used de-implementation as an umbrella term to represent how to stop interventions/programmes that are embedded in practice but (1) for which supporting evidence is lacking or weak and (2) have minimal gain for patients or, at worst, are considered harmful. We additionally aimed to provide clarity about the concept of de-implementation. From the work undertaken in Phase 1, we developed an initial programme theory that suggests that what works (i.e. successful de-implementation) is dependent on:
-
the focus (i.e. the nature of what is being de-implementation)
-
momentum (i.e. factors that drive de-implementation)
-
the actions (i.e. the actions that characterise de-implementation)
-
the degree of intentionality of de-implementation
-
the intentional and unintentional consequences for different stakeholders in context, and over time.
The initial programme theory was informed through the findings from the concept analysis and is denoted in the following:
De-implementation = f (what is being de-implemented; push or driving force; nature of action; degree of intentionality), which results in intentional and unintentional consequences, over time, for different stakeholders.
Challenges of the review
At this point in this chapter, we consider it opportune to report on some of the challenges and the subsequent learning we have encountered during the course of this review. The first challenge was related to the scope of the synthesis and the nature of evidence required to inform the initial programme theory development. The scope of the synthesis was compounded by the mass of different terms to describe de-implementation, as reported in Chapter 2. To ensure direction regarding the nature of the evidence, we used the concept analysis to guide our decision-making process in weighing up the utility of data to inform and explain our theory development and refining process.
We acknowledge that we encountered logistical challenges in getting stakeholders together for theory development and refinement. On reflection, this is not surprising, as we had specifically targeted busy front-line managers and clinicians for stakeholder engagement. The challenges related to meetings planned to produce initial theoretical threads based on experience and expertise. We overcame this challenge by being flexible, meeting individuals at suitable times to fit with their schedules and making best use of telephone interview methods to collect data.
Weighing up the nature of evidence that underpins our theory development and refinement, it is apparent that there is dominance of some areas of practice (e.g. de-prescribing). However, by threading the elements of the initial programme theory through the systematic search process, we stayed true to the realist approach by focusing on finding the best evidence to inform and refine programme theory development. This reflects the ethos within realist approaches, as opposed to prioritising the quality and nature of the data/evidence within.
The final challenge we encountered was in ensuring that we stayed true to the underpinnings of realist methodology when reviewing and analysing evidence. We attempted to overcome this particular challenge by paying more attention to realist critique within the selected papers, placing greater emphasis on understanding the nature of the interventions, and always seeking the inter-relationships between contexts and mechanisms, and how this leads to particular outcomes, as reported in Chapter 3.
Summary of review findings
The final review findings are collectively described as CMO configurations. Together, they represent a final programme theory, an explanatory account of what works, how and under which circumstances or conditions. In a nutshell, this theory represents how de-implementation in health and care services has the potential to be successful.
Context–mechanism–outcome 1
De-implementation interventions that attempt to change clinician behaviour in the context of fast or habitual decision-making (context) may be effective where they include aspects of precommitment, accountable justification and benchmarking performance against peers. Changes in practice may be prompted by slowing decision-making through increasing attention to the low-value practice behaviour (mechanism 1), ensuring that practice is consistent with an individual patient’s expectations (mechanism 2) and prompting professionals’ concerns about professional reputation (mechanism 3). Effectiveness was mixed across changes to professional behaviour, with impacts visible on communication with patients (outcome 1) and in some aspects of prescribing practice (outcome 2).
Context–mechanism–outcome 2
In the context of clinical practice underpinned by electronic health records, de-implementation interventions that amend the design of these systems (context) may be successful when their design makes sustaining low-value practice harder (mechanism). Things may be made harder by changing information displays/choice options. Effectiveness was demonstrated in the reduction in orders for unnecessary diagnostic tests (outcome).
Context–mechanism–outcome 3
The potential to increase professionals’ capability to de-implement when there is concern or uncertainty about, or variation in, a specific practice issue or problem (context) and increasing knowledge of, and skills related to, the evidence to drive de-implementation (mechanism) can lead to reductions in the rates of inappropriate ordering of routine investigations and in inappropriate prescribing (outcome).
Context–mechanism–outcome 4
Clinicians may face difficulties in managing situations where they are uncertain about diagnoses or where patients themselves request interventions that have demonstrable low value (context). In these contexts, interventions that seek to enhance professionals’ communication skills, utilise watchful waiting as an alternative active intervention strategy or that engage directly with patients, can enhance patients’ sense of validation of their concerns without resorting to sustaining the low-value practice (mechanism). When this occurs, it is possible to see an increase in patients’ sense of autonomy and motivation to disengage from the low-value practice, an improvement in the quality of the patient–professional relationship and reductions in low-value practices, such as inappropriate routine investigations and prescribing (outcome).
Context–mechanism–outcome 5
De-implementation strategies may be less effective when there are strong interpersonal relationships that can develop between clinicians and patients (context). Better communication and engagement with stakeholders, including patients, and professionals’ confidence building can validate concerns around potential risks of de-implementation, the quality of patient care and service ethos (mechanism), leading to a mitigation of professionals’ emotional burden (outcome).
Context–mechanism–outcome 6
In the context of embedded low-value practices (context), when there are no financial disincentives, a whole-system approach to de-implementation would appear to be more effective. When a whole-system approach to de-implementation includes combinations of a multicomponent de-implementation intervention, engagement of the multiprofessional team and advocacy or service user involvement the perception of a more aligned approach fosters trust (mechanism), which then can bolster success in generating behaviour change predominantly within de-prescribing (outcome).
Summary of the interventions
One of the initial review aims was to identify and map the range of different de-implementation approaches and/or strategies currently being utilised across health and care services. From the data, we identified a range of interventions that provide the foundations for our analysis of contexts, mechanisms and outcomes. We found that the nature of interventions identified in the included studies review were located in the following domains:
-
a nudge (e.g. precommitment, accountable justification and peer comparison)
-
a decision-support system design [e.g. active promotion of evidence-based choices, removing or changing information displays/choice options, additional information to be inputted by clinicians (in low-value practice situation)]
-
workforce development, education and training
-
patient-mediated interventions
-
system re-design.
Across these domains, we identified a range of specific intervention components (Table 3) that may provide insight for the development of future de-implementation strategies for further testing.
| Intervention component | Source |
|---|---|
| Interventions that include element(s) from electronic systems (e.g. medical records system, software modifications, computerised decision-making support, campaign with tag line, visual display/checklist) | Meeker et al.,90 Soon et al.95 and Rysinka et al.91 |
| Interventions that include elements of face-to-face approaches (e.g. onsite education, interactive lecture, training session feedback) | Gulla et al.,93 Meeker et al.,90 Trumbo et al.,89 Bregnhøj et al.,98 Fenton et al.,101 Juola et al.,100 Winchester et al.,97 Crotty et al.,126 Keijzers et al.,102 Menegueti et al.,99 Richmond et al.,123 Spinewine et al.124 and Sun et al.105 |
| Interventions that include written elements (e.g. a booklet, vignettes, poster displays, letters, peer comparison letters) | Kullgren et al.,88 Meeker et al.,87 Meeker et al.,90 Sacarny et al.,92 Little et al.,106 Martin and Tannenbaum,112 Tannenbaum et al.,111 Trumbo et al.89 and Winchester et al.97 |
| Interventions revolving around an individual (e.g. a peer champion/de-implementation leaders) | Gulla et al.,93 Trumbo et al.,89 Hodgetts et al.,120 Keijzers et al.,102 Menegueti et al.,99 Meredith et al.132 and Parchman et al.129 |
| Improvement programme | Gulla et al.93 |
| Interventions that are focused on standards or programmes [e.g. improvement programme (prescribing), protocol/systematic approach to patient assessment] | Martins et al.,94 Haines et al.,116 Daniels et al.,108 Gupta and Moriates,121 Hodgetts et al.,120 Hollingworth et al.,131 MacGeorge et al.,107 Martin and Tannenbaum,112 Mitchel et al.,115 Montini and Graham,17 Mortimer,130 Peiro,128 Robert et al.,20 Pradhan et al.,109 Soril et al.,118 Spinewine et al.124 and Wouters et al.125 |
Through a clearer understanding of the profile of different interventions located within the specific domains, Table 3 provides a basis for assessment when different de-implementation strategies are planned across health and care services. Additionally, there is clearer justification for choosing particular strategies that match with the problem/requirement.
Context
Before moving to appraise the theory drawn from the review findings, a consideration of the contexts within which the evidence for this review were drawn is required. Although the mechanisms we have uncovered provide understanding for how the intervention is assumed to work, in the realist sense, mechanisms are always contingent on certain contexts/conditions. In assessing the nature of the evidence, we have previously noted that much of it is located within specific literature (e.g. de-prescribing). There were characteristics that denote the contexts or conditions in this review. The particular contexts were associated with ‘fast’ decision-making86 and routine decisions. We note that evidence was more likely to be derived from primary care or campaigns situated in secondary care, involving approaches such as surveillance, or related to diagnostics and low-value care.
Theory areas
In this section we provide a precis of the theoretical learning we extracted through the development of the final programme theory. The final programme theory is represented in Table 4.
| CMO heading | Mechanism | De-implementation intervention | Context | Outcome |
|---|---|---|---|---|
| Nudge | Slowing down professional decision-making by:
|
Precommitment Accountable justification Feedback on performance relative to peers |
Mostly within fast decision-making occurring in routinised practice scenarios |
Improved communications with patients about de-prescribing Reductions in the rates of: |
| Design | Re-designing systems to make it harder to sustain low-value practice | Embedding decision support within electronic health records | Mostly within primary care practice, underpinned by electronic health record systems |
Improved communications with patients about de-prescribing Reductions in the rates of inappropriate ordering of routine investigations in primary care The simulated management of low-back pain in primary care |
| Capability | Increasing individual professionals’ capability | Multimodal educational interventions, with various combinations of information giving, feedback on individual performance, collegiate and peer support, and implemented ‘close’ to practice | Concern or uncertainty about, or variation in, a specific practice issue or problem | Reductions in the rates of inappropriate ordering of routine investigations, and in inappropriate prescribing |
| Watchful waiting | Sense of validation of patients’ health concerns |
Interventions directed towards clinicians’ use of communication strategies Watchful waiting as an active intervention strategy Patient-mediated interventions |
Diagnostic uncertainty or requests from patients for low-value treatments or diagnostic tests |
Reciprocity in the patient–professional relationship Increases in patients’ sense of autonomy and motivation to de-implement Reductions in the rates of inappropriate ordering of routine investigations, and in inappropriate prescribing |
| Emotion | Validating professionals’ concerns about de-implementation-associated risks to patient care, and a service ethos | Staff communication skills and confidence building | Settings or services where there is the capacity for strong interpersonal relationships between clinicians and patients |
Emotional burden of de-implementation may be mitigated Less effective at changing practice |
| Alignment | A necessary and sufficient degree of alignment of multiple stakeholder perspectives |
A multiprofessional approach Whole-system approaches |
A multiprofessional approach Whole-system approaches |
Trust in the de-implementation initiative or process Shift in the political narrative away from a focus on investment Reductions in low-value prescribing |
Nudge
Nudge theory, developed by Sunstein and Thaler,64 suggests that small changes in the context or choice architecture surrounding certain behaviours can persuade people to adopt desired behaviours. Therefore, in the case of de-implementation, this can support the relinquishing of processes that show little evidence of efficacy. The idea of nudge is not to force health-care providers to take a certain course of action, but to present a context in which the favoured behaviour is brought to the fore. Nudge is a process that operates within the context of decisions taken that are routine or habitual, as occurs in everyday decision-making, including clinical care. We had previously identified how nudge and behaviour change might feature in the review. From our initial theoretical territory through to review data, behavioural insights resonated and informed programme theory development and refining. In the theoretical platform reported in Chapter 2, and through the work of Sunstein and Thaler,64 we had anticipated that the introduction of ‘choice architecture’ to nudge people in a given direction would trigger mechanisms related to decisions notwithstanding the freedom to choose, a key ethos of nudge-type interventions. Other evidence we included in the theoretical territory mapping (see Chapter 1) included the work of Martreau et al. 65–67
In CMO 1, we additionally found that nudge theory is supported by intervention processes that are more deliberate and conscious. Precommitment strategies for professionals work best when they are kept simple and are consistent with patient expectations.
Design
Previous evidence, such as that presented by The Health Foundation, has shown the potential of default systems to influence behaviours across health and care:
Default options have been shown to have considerable influence on behaviours and are present across health care, in order sets, bundles and care protocols, technological prompts and communication strategies, as well as patterns of practice that are effectively ‘hidden’ defaults.
Perry et al. 133
The impact of using, or re-designing defaults may be associated with significant changes in professional behaviour. Consequently, careful design, implementation and evaluation will be key.
Our review findings have additionally uncovered the potential benefits of employing deliberate ways (which are transactional in nature) of hiding or removing low-value options in electronic health records systems. This approach makes it more difficult to continue practising/using low-value interventions or medicines management.
Capability
The significance of educating for professional capability highlights the ‘extent to which individuals can adapt to change, generate new knowledge, and continue to improve their performance’. 133 The theory in CMO 3 suggests that, when there is uncertainty or variation in practices or in addressing a clinical problem, the provision of education that increases professional capability can lead to a reduction in the rates of inappropriate actions (e.g. prescribing or investigation/test ordering).
Narrative
In a reflective narrative, Keijzers et al. 102 recognise the complexity for clinicians of ‘deliberate clinical inertia’ to reduce the risks for patients of overzealous management. Medical clinicians are biased to intervene, partly through the expectations of patients who believe that most tests and treatments are generally beneficial. An important driver for clinicians is perceived risk for them if the patient’s condition deteriorates because a test or treatment has not been prescribed, causing harm by omission rather than commission. Clinicians are not reprimanded for sanctioning a treatment, but can be scrutinised for not doing so if this is the ‘standard’ expectation. One key area that can persuade more clinicians to think about ‘doing nothing’ is to re-frame the idea as ‘watchful waiting’ or ‘active surveillance’. Watchful waiting is the key theory represented in CMO 4, in which the patient’s concerns are acknowledged and opportunities for follow-up are available if there are any changes. Watchful waiting also provides the clinician with a stratagem that can limit the use of low-value treatments without losing patient trust when there are uncertainties about diagnosis or patients request low-value interventions.
Emotion
A systematic review by Kozlowski et al. 113 on the role of emotion in clinical decision-making found ‘. . . sufficient evidence to conclude that clinicians’ experienced emotions and their perceptions and understanding of others’ emotions can and do influence their decisions’. 113 Emotional bias is an aspect that limits de-implementation, particularly if there is a strong interpersonal relationship between clinician and patient. Within CMO 5, we found that de-implementation strategies may be less effective when there are strong interpersonal relationships between clinicians and patients. Clinical decision-making has been viewed through the prism of rationality, but there is increasing evidence that decisions are influenced by emotions arising from choices made by the clinician.
System
Context–mechanism–outcome 6 extends the context to the organisation and system delivery that is an essential scaffold to strengthen the likelihood of de-implementing low-value practices. Essentially, the organisation needs to have procedures in place that do not just focus on implementing changes within the system, but also take account of what low-value practices need to be removed.
Collectively, the summary of theory represents the areas within the final programme theory.
Review objectives
At the start, the review was driven by a particular set of objectives. Below, we consider how we have met each objective:
-
Identifying and mapping the range of different de-implementation approaches and/or strategies currently being utilised across health and care, paying attention to ways in which they are assumed to work.
To achieve this objective, we captured evidence and have provided a clearer identification of a range of interventions that have the potential to underpin successful de-implementation strategies across health and care.
-
Producing a typology of de-implementation types, processes and contexts.
We achieved this objective through the production of the concept analysis in Phase 1 of the review.
-
Examining and understanding the range of anticipated and unanticipated impacts of these approaches and/or strategies across different settings and stakeholders, paying attention to contextual conditions that influence these impacts.
This objective was achieved through capture of data that reflect a closer understanding of the outcomes within the programme theory.
-
Generating an evidence-based realist programme theory that explains the successful processes and impacts of de-implementation.
This objective was achieved through production of a final programme theory.
Actionable recommendations
The review findings lead to actionable recommendations for de-implementation, which we describe as a practical 11-point plan, designed for the attention of practitioners and managers across health and care settings:
-
to provide alternative interventions, including watchful waiting, when there is no high-value alternative, ensuring that there is a time frame for review
-
to remove low-value options from decision-making, systems, processes and tools
-
to engage service users in de-implementation by amending expectations around low-value care and treatment options
-
to consider opportunities for surveillance of low-value practices
-
to avoid reliance on enhancing communication skills alone to deliver de-implementation strategies
-
to assess the degree of alignment between public, professional and patient narratives around de-implementation at different levels (i.e. local and national)
-
to carefully consider the consequences of de-implementation for patient and professional relationships
-
to carefully manipulate concerns about professionals’ reputation by seeking additional justification for low-value treatment options and benchmarking professional practice
-
to embed uncertainty about negative evidence and decision-making in pre-registration education
-
to consider the nature of decision-making around low-value practice, including how it is supported by systems, processes and tools
-
to raise awareness of low-value practice through education and training, as part of a broader approach and across pre and post registration education curricula.
Conclusions
The review has stimulated a wider debate about avoiding and stopping services that are considered wasteful, of low value and non-efficient. In conclusion, the findings from this realist synthesis provide clear evidence of what to pay attention to to successfully de-implement low-value or non-efficient practices across health and care settings. Our review has highlighted the implications of de-implementation for health and care, and for patients and the public, and we offer an 11-point plan for action. This review provides a more coherent understanding of the concept of de-implementation and a theory-driven explanatory account of how to proceed.
The synthesis findings were presented in interim form to the NICE Implementation Strategy Group in August 2019. Following publication of the final report, and associated scientific and professional journal papers, we will recommend a series of strategies that will help managers and clinicians de-implement low-value processes, and disseminate these recommendations through the following channels: a range of blog posts to engage different audiences with the study and the findings; presence and presentation at relevant national and international conferences focused on the strategies to improve efficiency and value in health and care; creative animation easily accessible on YouTube (www.youtube.com, YouTube, LLC, San Bruno, CA, USA).
Recommendations for research
The review offers the following recommendations for research:
-
Further investigation of decision-making processes outside type 1 decisions is required to identify opportunities for successful de-implementation.
-
Further investigation is required to identify opportunities for new interventions that draw on non-traditional theories (e.g. design, aesthetics) and organisational theories to gain new insights.
-
Research should aim to further the theoretical basis for de-implementation, taking into account the discourse relating to practice (e.g. decommissioning services).
-
Research should consider how de-implementation can be investigated in the context of randomised controlled trials.
-
Research should aim to further enhance the description of, and therefore gain clearer clarity around, programme theory and de-implementation interventions.
-
Research should consider de-implementation and implementation as polar entities on a continuum of knowledge-informed change and learn about different issues that are more or less evident along the continuum.
-
Research should consider further conceptual development of de-implementation.
Acknowledgements
We would like to acknowledge the contribution and support of stakeholders and participants who engaged in a variety of different meetings and activities across the life of the project. In addition, we would like to thank Heledd Owen Griffiths for her administrative support on the report.
Contributions of authors
Christopher R Burton (https://orcid.org/0000-0003-1159-1494) (Head of School, School of Allied and Public Health Professions) was the co-chief investigator, led the study, was involved in all aspects of the review process and is the joint lead author of this report.
Lynne Williams (https://orcid.org/0000-0003-2575-9710) (Interim Head of School, School of Health Sciences) was the co-chief investigator, led the study, was involved in all aspects of the review process and is the joint lead author of this report.
Tracey Bucknall (https://orcid.org/0000-0001-9089-3583) [Chairperson in Nursing (Alfred Health), School of Nursing and Midwifery] was a co-applicant on the project, was involved in all aspects of the review process and participated in the preparation of the final report.
Denise Fisher was a co-applicant on the project, was involved in all aspects of the review process and participated in the preparation of the final report.
Beth Hall (https://orcid.org/0000-0003-4980-3720) (Research Support Librarian and Academic Support Librarian) was a co-applicant on the project, was involved in all aspects of the review process and participated in the preparation of the final report.
Gill Harris (https://orcid.org/0000-0002-7658-8088) (Executive Director of Nursing and Midwifery) was a co-applicant on the project, was involved in all aspects of the review process and participated in the preparation of the final report.
Peter Jones (https://orcid.org/0000-0001-6958-193X) (Lecturer in Adult Nursing) was the research fellow on the project, was involved in all aspects of the review process and participated in the preparation of the final report.
Matthew Makin (https://orcid.org/0000-0002-4451-5562) (Medical Director and Honorary Professor Health and Behavioural Sciences) was a co-applicant on the project, was involved in study design, attended meetings, provided clinical expertise and participated in the preparation of the final report.
Anne Mcbride (https://orcid.org/0000-0003-1047-1319) was a co-applicant on the project, was involved in study design, attended meetings, provided clinical expertise and participated in the preparation of the final report.
Rachel Meacock (https://orcid.org/0000-0001-8933-5058) (Senior Lecturer in Health Economics) was a co-applicant on the project, was involved in study design, attended meetings, provided clinical expertise and participated in the preparation of the final report.
John Parkinson (https://orcid.org/0000-0002-5605-3115) (Head of School, School of Psychology) was a co-applicant on the project, was involved in all aspects of the review process and participated in the preparation of the final report.
Jo Rycroft-Malone (https://orcid.org/0000-0003-3858-5625) (Dean of the Faculty of Health and Medicine) was a co-applicant on the project, was involved in all aspects of the review process and participated in the preparation of the final report.
Justin Waring (https://orcid.org/0000-0003-1459-5896) (Professor of Medical Sociology and Healthcare Organisation) was a co-applicant on the project, was involved in all aspects of the review process and participated in the preparation of the final report.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Ellul I, Wolff J, Rutherford S. Developing the NHS Long Term Plan: Evidence Based Interventions. NHS England Official Board Paper PB.04.07.2018/04. London: NHS England; 2018.
- Day RT, Norman R, Robinson S. Challenges and opportunities for disinvestment in Australia. J Health Organ Manag 2016;30:1301-7. https://doi.org/10.1108/JHOM-10-2016-0189.
- The King’s Fund . Trusts in Deficit 2018. www.kingsfund.org.uk/projects/nhs-in-a-nutshell/trusts-deficit (accessed 10 March 2020).
- Van Bodegom-Vos L, Davidoff F, Marang-van de Mheen PJ. Implementation and de-implementation: two sides of the same coin?. BMJ Qual Saf 2017;26:495-501. https://doi.org/10.1136/bmjqs-2016-005473.
- NHS Scotland . Realistic Medicine. Chief Medical Officer’s Annual Report 2014–15 2016.
- Bevan Commission . A Prudent Approach to Health: Prudent Health Principles 2015.
- Rich N. The Bevan Commission Exemplar Programme Cohort 3 Evaluation Summary. Cardiff: Bevan Commission; 2019.
- Bevan Commission . Transformation from Within: Bevan Exemplar Projects 2017–2018 2019.
- GOV.UK . What Works Network 2019. www.gov.uk/guidance/what-works-network (accessed 10 March 2020).
- ABIM Foundation . Choosing Wisely 2012. http://abimfoundation.org/what-we-do/choosing-wisely (accessed 10 March 2020).
- Prasad V, Ioannidis JP. Evidence-based de-implementation for contradicted, unproven, and aspiring healthcare practices. Implement Sci 2014;9. https://doi.org/10.1186/1748-5908-9-1.
- Rooshenas L, Owen-Smith A, Hollingworth W, Badrinath P, Beynon C, Donovan JL. ‘I won’t call it rationing . . .’: an ethnographic study of healthcare disinvestment in theory and practice. Soc Sci Med 2015;128:273-81. https://doi.org/10.1016/j.socscimed.2015.01.020.
- Niven DJ, Mrklas KJ, Holodinsky JK, Straus SE, Hemmelgarn BR, Jeffs LP, et al. Towards understanding the de-adoption of low-value clinical practices: a scoping review. BMC Med 2015;13. https://doi.org/10.1186/s12916-015-0488-z.
- Hahn EE, Munoz-Plaza CE, Wand J, Delgadillo JG. Working towards de-implementation: a mixed-methods study in breast cancer surveillance care. J Patient Cent Res Rev 2016;3:177-8. https://doi.org/10.17294/2330-0698.1298.
- McKay VR, Morshed AB, Brownson RC, Proctor EK, Prusaczyk B. Letting go: conceptualizing intervention de-implementation in public health and social service settings. Am J Community Psychol 2018;62:189-202. https://doi.org/10.1002/ajcp.12258.
- Pierson P. Dismantling the Welfare State?: Reagan, Thatcher and the Politics of Retrenchment. Cambridge: Cambridge University Press; 1994.
- Montini T, Graham ID. ‘Entrenched practices and other biases’: unpacking the historical, economic, professional, and social resistance to de-implementation. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0211-7.
- Johns DM, Bayer R, Fairchild AL. Evidence and the politics of deimplementation: the rise and decline of the ‘counseling and testing’ paradigm for HIV prevention at the US Centers for Disease Control and Prevention. Milbank Q 2016;94:126-62. https://doi.org/10.1111/1468-0009.12183.
- Voorn VMA, Marang-van de Mheen PJ, van der Hout A, Hofstede SN, So-Osman C, van den Akker-van Marle ME, et al. The effectiveness of a de-implementation strategy to reduce low-value blood management techniques in primary hip and knee arthroplasty: a pragmatic cluster-randomized controlled trial. Implement Sci 2017;12. https://doi.org/10.1186/s13012-017-0601-0.
- Robert G, Harlock J, Williams I. Disentangling rhetoric and reality: an international Delphi study of factors and processes that facilitate the successful implementation of decisions to decommission healthcare services. Implement Sci 2014;9. https://doi.org/10.1186/s13012-014-0123-y.
- Robinson S, Glasby J, Allen K. ‘It ain’t what you do it’s the way that you do it’: lessons for health care from decommissioning of older people’s services. Health Soc Care Community 2013;21:614-22. https://doi.org/10.1111/hsc.12046.
- Williams I, Harlock J, Robert G, Mannion R, Brearley S, Hall K. Decommissioning health care: identifying best practice through primary and secondary research – a prospective mixed-methods study. Health Serv Deliv Res 2017;5. https://doi.org/10.3310/hsdr05220.
- Elshaug AG, Hiller JE, Moss JR. Exploring policy-makers’ perspectives on disinvestment from ineffective healthcare practices. Int J Technol Assess Health Care 2008;24:1-9. https://doi.org/10.1017/S0266462307080014.
- Haas M, Hall J, Viney R, Gallego G. Breaking up is hard to do: why disinvestment in medical technology is harder than investment. Aust Health Rev 2012;36:148-52. https://doi.org/10.1071/AH11032.
- Harris C, Allen K, Waller C, Green S, King R, Ramsey W, et al. Sustainability in Health care by Allocating Resources Effectively (SHARE) 5: developing a model for evidence-driven resource allocation in a local healthcare setting. BMC Health Serv Res 2017;17. https://doi.org/10.1186/s12913-017-2208-1.
- Paprica PA, Culyer AJ, Elshaug AG, Peffer J, Sandoval GA. From talk to action: policy stakeholders, appropriateness, and selective disinvestment. Int J Technol Assess Health Care 2015;31:236-40. https://doi.org/10.1017/S0266462315000392.
- Polisena J, Clifford T, Elshaug AG, Mitton C, Russell E, Skidmore B. Case studies that illustrate disinvestment and resource allocation decision-making processes in health care: a systematic review. Int J Technol Assess Health Care 2013;29:174-84. https://doi.org/10.1017/S0266462313000068.
- Scheunemann LP, White DB. The ethics and reality of rationing in medicine. Chest 2011;140:1625-32. https://doi.org/10.1378/chest.11-0622.
- Dickinson H, Freeman T, Robinson S, Williams I. Resource scarcity and priority setting: from management to leadership in the rationing of health care?. Public Money Manag 2011;21:363-70. https://doi.org/10.1080/09540962.2011.598352.
- Norton WE, Kennedy AE, Chambers DA. Studying de-implementation in health: an analysis of funded research grants. Implement Sci 2017;12. https://doi.org/10.1186/s13012-017-0655-z.
- Rycroft-Malone J, McCormack B, Hutchinson AM, DeCorby K, Bucknall TK, Kent B, et al. Realist synthesis: illustrating the method for implementation research. Implement Sci 2012;7. https://doi.org/10.1186/1748-5908-7-33.
- Williams L, Rycroft-Malone J, Burton CR, Edwards S, Fisher D, Hall B, et al. Improving skills and care standards in the support workforce for older people: a realist synthesis of workforce development interventions. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-011964.
- Burton CR, Rycroft-Malone J, Williams L, Davies S, McBride A, Hall B, et al. NHS managers’ use of nursing workforce planning and deployment technologies: a realist synthesis. Health Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06360.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11. https://doi.org/10.1186/1741-7015-11-21.
- Burton C, Williams L, Bucknall T, Edwards S, Fisher D, Hall B, et al. Understanding how and why de-implementation works in health and care: research protocol for a realist synthesis of evidence. Syst Rev 2019;8. https://doi.org/10.1186/s13643-019-1111-8.
- Pawson R, Tilley N. Realistic Evaluation. London: SAGE Publications Ltd; 1997.
- Wong G, Westhorp G, Greenhalgh J, Manzano A, Jagosh J, Greenhalgh T. Quality and reporting standards, resources, training materials and information for realist evaluation: the RAMESES II project. Health Serv Deliv Res 2017;5. https://doi.org/10.3310/hsdr05280.
- McEvoy P, Richards D. Critical realism: a way forward for evaluation research in nursing?. J Adv Nurs 2003;43:411-20. https://doi.org/10.1046/j.1365-2648.2003.02730.x.
- Wynn D, Williams CK. Principles for conducting critical realist case study research in information systems. MIS Q 2012;36:787-810. https://doi.org/10.2307/41703481.
- Pawson R. The Science of Evaluation. London: SAGE Publications Ltd; 2013.
- Pawson RD. ‘Nothing as Practical as a Good Theory’. Evaluation 2003;9:471-90. https://doi.org/10.1177/135638900300900407.
- Pawson RD. Evidence-Based Policy: A Realist Perspective. London: SAGE Publications Ltd; 2006.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist Synthesis: An Introduction. Manchester: ESRC Research Methods Programme, University of Manchester; 2004.
- Cegarra-Navarro JG, Wensley AK, Sánchez-Polo MT. An application of the Hospital-in-the-Home unlearning context. Soc Work Health Care 2010;49:895-918. https://doi.org/10.1080/00981389.2010.506410.
- Lester DL, Parnell JA, Carraher SM. Organisational life cycle: a five-stage empirical scale. Int J Organ Anal 2003;11:339-54. https://doi.org/10.1108/eb028979.
- Lally P, van Jaarsveld CHM, Potts HWW, Wardle J. How are habits formed: modelling habit formation in the real world. Eur J Soc Psychol 2010;40:998-1009. https://doi.org/10.1002/ejsp.674.
- Nilsen P, Roback K, Broström A, Ellström PE. Creatures of habit: accounting for the role of habit in implementing research on clinical behaviour change. Implement Sci 2012;7. https://doi.org/10.1186/1748-5908-7-53.
- Atkins MS, Rusch D, Mehta TG, Lakind D. Future directions for dissemination and implementation science: aligning ecological theory and public health to close the research to practice gap. J Clin Child Adolesc Psychol 2016;45:215-26. https://doi.org/10.1080/15374416.2015.1050724.
- Rogers EM. Diffusion of Innovations. New York, NY: Free Press; 2003.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581-629. https://doi.org/10.1111/j.0887-378X.2004.00325.x.
- Rycroft-Malone J, Harvey G, Seers K, Kitson A, McCormack B, Titchen A. An exploration of the factors that influence the implementation of evidence into practice. J Clin Nurs 2004;13:913-24. https://doi.org/10.1111/j.1365-2702.2004.01007.x.
- Ferlie E, Crilly T, Jashapara A, Peckham A. Knowledge mobilisation in healthcare: a critical review of health sector and generic management literature. Soc Sci Med 2012;74:1297-304. https://doi.org/10.1016/j.socscimed.2011.11.042.
- Oliveira A. A discussion of rational and psychological decision-making theories and models: the search for a cultural-ethical decision-making model. Electron J Bus Ethics Organ Stud 2007;12:12-7.
- Plsek PE, Wilson T. Complexity, leadership, and management in healthcare organisations. BMJ 2001;323:746-9. https://doi.org/10.1136/bmj.323.7315.746.
- Burton CR, Rycroft-Malone J. Resource based view of the firm as a theoretical lens on the organisational consequences of quality improvement. Int J Health Policy Manag 2014;3:113-15. https://doi.org/10.15171/ijhpm.2014.74.
- The King’s Fund . The Future of Leadership and Management in the NHS 2011.
- The King’s Fund . Leadership and Engagement for Improvement in the NHS 2012.
- The King’s Fund . Patient-Centred Leadership 2013.
- Tomlinson J. Exploration of transformational and distributed leadership. Nurs Manag 2012;19:30-4. https://doi.org/10.7748/nm2012.07.19.4.30.c9168.
- West M, Eckert R, Steward K, Pasmore B. Developing Collective Leadership for Health Care. London: The King’s Fund; 2014.
- Wong C, Cummings G. Authentic leadership: a new theory for nursing or back to basics?. J Health Organ Manag 2009;23:522-38. https://doi.org/10.1108/14777260910984014.
- Aylward M, Phillips C, Howson H. Simply Prudent Healthcare – Achieving Better Care and Value for Money in Wales – Discussion Paper. Cardiff: Bevan Commission; 2013.
- The King’s Fund . Better Value in the NHS: The Role of Changes in Clinical Practice 2015.
- Sunstein CR, Thaler R. Nudge: Improving Decisions About Health, Wealth, and Happiness. London: Penguin; 2008.
- Marteau TM, Hollands GJ, Fletcher PC. Changing human behavior to prevent disease: the importance of targeting automatic processes. Science 2012;337:1492-5. https://doi.org/10.1126/science.1226918.
- Evans JS, Stanovich KE. Dual-process theories of higher cognition: advancing the debate. Perspect Psychol Sci 2013;8:223-41. https://doi.org/10.1177/1745691612460685.
- Parkinson JA EK and GA . Positive impact by design: the Wales centre for behaviour change. J Posit Psychol 2014;9:517-22. https://doi.org/10.1080/17439760.2014.936965.
- Catchpole K. Spreading human factors expertise in healthcare: untangling the knots in people and systems. BMJ Qual Saf 2013;22:793-7. https://doi.org/10.1136/bmjqs-2013-002036.
- Agency for Healthcare Research and Quality (AHRQ) . Cognitive Task Analysis: Methods to Improve Patient-Centered Medical Home Models by Understanding and Leveraging Its Knowledge Work 2013.
- Rogers EM. Diffusion of Innovations. New York, NY: Free Press; 1995.
- Wood W. Attitude change. Persuasion and social influence. Annu Rev Psychol 2000;50:539-70. https://doi.org/10.1146/annurev.psych.51.1.539.
- Pettigrew AM, Whipp R. Managing Change for Competitive Success. Oxford: Blackwell Publishing; 1991.
- Gnjidic D, Elshaug AG. De-adoption and its 43 related terms: harmonizing low-value care terminology. BMC Med 2015;13. https://doi.org/10.1186/s12916-015-0511-4.
- Walker LO, Avant KC. Strategies for Theory Construction in Nursing. Upper Saddle River, NJ: Pearson Prentice Hall; 2005.
- Plüddemann A, Aronson JK, Onakpoya I, Heneghan C, Mahtani KR. Redefining rapid reviews: a flexible framework for restricted systematic reviews. BMJ Evid Based Med 2018;23:201-3. https://doi.org/10.1136/bmjebm-2018-110990.
- Wang V, Maciejewski ML, Helfrich CD, Weiner BJ. Working smarter not harder: coupling implementation to de-implementation. Healthcare 2017:1-3. https://doi.org/10.1016/j.hjdsi.2017.12.004.
- Prasad VK, Cifu AS. Ending Medical Reversal: Improving Outcomes, Saving Lives. Baltimore, MD: Johns Hopkins University Press; 2015.
- Schondelmeyer AC, Simmons JM, Statile AM, Hofacer KE, Smith R, Prine L, et al. Using quality improvement to reduce continuous pulse oximetry use in children with wheezing. Pediatrics 2015;135:e1044-51. https://doi.org/10.1542/peds.2014-2295.
- Kost A, Genao I, Lee JW, Smith SR. Clinical decisions made in primary care clinics before and after Choosing Wisely. J Am Board Fam Med 2015;28:471-4. https://doi.org/10.3122/jabfm.2015.05.140332.
- Chamberlain CA, Martin RM, Busby J, Gilbert R, Cahill DJ, Hollingworth W. Trends in procedures for infertility and caesarean sections: was NICE disinvestment guidance implemented? NICE recommendation reminders. BMC Public Health 2013;13. https://doi.org/10.1186/1471-2458-13-112.
- Ritchie J, Spencer L, Burgess RG, Bryman A. Analyzing Qualitative Data. New York, NY: Routledge; 1994.
- Davies H, Nutley S, Smith P, Davies HTO, Nutley SMN, Smith PC. What Works? Evidence-Based Policy and Practice in Public Service. Bristol: The Policy Press; 2000.
- American Board of Internal Medicine . Choosing Wisely 2012. http://abimfoundation.org/what-wedo/choosing-wisely (accessed 21 May 2019).
- Rycroft-Malone J, Burton CR, Williams L, Edwards S, Fisher D, Hall B, et al. Improving skills and care standards in the support workforce for older people: a realist synthesis of workforce development interventions. Health Serv Deliv Res 2016;4. https://doi.org/10.3310/hsdr04120.
- Meyer SB, Lunnay B. The application of abductive and retroductive inference for the design and analysis of theory-driven sociological research. Sociol Res Online 2013;18:1-11. https://doi.org/10.5153/sro.2819.
- Kahneman D. Thinking, Fast and Slow. New York, NY: Farrar, Straus & Giroux; 2011.
- Meeker D, Knight TK, Friedberg MW, Linder JA, Goldstein NJ, Fox CR, et al. Nudging guideline-concordant antibiotic prescribing: a randomized clinical trial. JAMA Intern Med 2014;174:425-31. https://doi.org/10.1001/jamainternmed.2013.14191.
- Kullgren JT, Krupka E, Schachter A, Linden A, Miller J, Acharya Y, et al. Precommitting to choose wisely about low-value services: a stepped wedge cluster randomised trial. BMJ Qual Saf 2018;27:355-64. https://doi.org/10.1136/bmjqs-2017-006699.
- Trumbo SP, Iams WT, Limper HM, Goggins K, Gibson J, Oliver L, et al. Deimplementation of routine chest x-rays in adult intensive care units. J Hosp Med 2019;14:83-9. https://doi.org/10.12788/jhm.3129.
- Meeker D, Linder JA, Fox CR, Friedberg MW, Persell SD, Goldstein NJ, et al. Effect of behavioral interventions on inappropriate antibiotic prescribing among primary care practices: a randomized clinical trial. JAMA 2016;315:562-70. https://doi.org/10.1001/jama.2016.0275.
- Ryskina K, Jessica Dine C, Gitelman Y, Leri D, Patel M, Kurtzman G, et al. Effect of social comparison feedback on laboratory test ordering for hospitalized patients: a randomized controlled trial. J Gen Intern Med 2018;33:1639-45. https://doi.org/10.1007/s11606-018-4482-y.
- Sacarny A, Barnett ML, Le J, Tetkoski F, Yokum D, Agrawal S. Effect of peer comparison letters for high-volume primary care prescribers of quetiapine in older and disabled adults: a randomized clinical trial. JAMA Psychiatry 2018;75:1003-11. https://doi.org/10.1001/jamapsychiatry.2018.1867.
- Gulla C, Flo E, Kjome RL, Husebo BS. Deprescribing antihypertensive treatment in nursing home patients and the effect on blood pressure. J Geriatr Cardiol 2018;15:275-83. https://doi.org/10.11909/j.issn.1671-5411.2018.04.011.
- Martins CM, da Costa Teixeira AS, de Azevedo LF, Sá LM, Santos PA, do Couto ML, et al. The effect of a test ordering software intervention on the prescription of unnecessary laboratory tests – a randomized controlled trial. BMC Med Inform Decis Mak 2017;17. https://doi.org/10.1186/s12911-017-0416-6.
- Soon J, Traeger A, Elshaug A, Cvejic E, Maher C, Doust J, et al. Effect of two behavioural ‘nudging’ interventions on management decisions for low back pain: a randomised vignette-based study in general practitioners. BMJ Qual Saf 2018:1-9. https://doi.org/10.1136/bmjqs-2018-008659.
- U.S. Preventive Services Task Force . The Guide to Clinical Preventive Services, 2014: Recommendations of the U.S. Preventive Services Task Force 2014. https://www.ahrq.gov/sites/default/files/publications/files/cpsguide.pdf (accessed 4 November 2020).
- Winchester DE, Schmalfuss C, Helfrich CD, Beyth RJ. A specialty-specific, multimodality educational quality improvement initiative to deimplement rarely appropriate myocardial perfusion imaging. Open Heart 2017;4. https://doi.org/10.1136/openhrt-2017-000589.
- Bregnhøj L, Thirstrup S, Kristensen MB, Bjerrum L, Sonne J. Combined intervention programme reduces inappropriate prescribing in elderly patients exposed to polypharmacy in primary care. Eur J Clin Pharmacol 2009;65:199-207. https://doi.org/10.1007/s00228-008-0558-7.
- Menegueti MG, Ciol MA, Bellissimo-Rodrigues F, Auxiliadora-Martins M, Gaspar GG, Canini SRMDS, et al. Long-term prevention of catheter-associated urinary tract infections among critically ill patients through the implementation of an educational program and a daily checklist for maintenance of indwelling urinary catheters: a quasi-experimental study. Medicine 2019;98. https://doi.org/10.1097/MD.0000000000014417.
- Juola AL, Bjorkman MP, Pylkkanen S, Finne-Soveri H, Soini H, Kautiainen H, et al. Nurse education to reduce harmful medication use in assisted living facilities: effects of a randomized controlled trial on falls and cognition. Drugs Aging 2015;32:947-55. https://doi.org/10.1007/s40266-015-0311-8.
- Fenton JJ, Kravitz RL, Jerant A, Paterniti DA, Bang H, Williams D, et al. Promoting patient-centered counseling to reduce use of low-value diagnostic tests: a randomized clinical trial. JAMA Intern Med 2016;176:191-7. https://doi.org/10.1001/jamainternmed.2015.6840.
- Keijzers G, Cullen L, Egerton-Warburton D, Fatovich DM. Don’t just do something, stand there! The value and art of deliberate clinical inertia. Emerg Med Australas 2018;30:273-8. https://doi.org/10.1111/1742-6723.12922.
- Foy AJ, Filippone EJ. The case for intervention bias in the practice of medicine. Yale J Biol Med 2013;86:271-80.
- May L, Franks P, Jerant A, Fenton J. Watchful waiting strategy may reduce low-value diagnostic testing. J Am Board Fam Med 2016;29:710-17. https://doi.org/10.3122/jabfm.2016.06.160056.
- Sun D, McCarthy TJ, Liberman DB. Cost-Effectiveness of watchful waiting in acute otitis media. Pediatrics 2017;139. https://doi.org/10.1542/peds.2016-3086.
- Little P, Gould C, Williamson I, Moore M, Warner G, Dunleavey J. Primary care strategies for childhood acute otitis media. Br Med J 2001;322:336-42. https://doi.org/10.1136/bmj.322.7282.336.
- MacGeorge EL, Caldes EP, Smith RA, Hackman NM, San Jose A. Reducing unwarranted antibiotic use for pediatric acute otitis media: the influence of physicians’ explanation and instruction on parent compliance with ‘watchful waiting’. J Appl Commun Res 2017;45:333-45. https://doi.org/10.1080/00909882.2017.1320575.
- Daniels L, Ünlü Ç, de Korte N, van Dieren S, Stockmann HB, Vrouenraets BC, . Randomized clinical trial of observational versus antibiotic treatment for a first episode of CT-proven uncomplicated acute diverticulitis. Br J Surg 2017;104:52-61. https://doi.org/10.1002/bjs.10309.
- Pradhan BB, Brox JI, Indahl A. Watchful Waiting and Brief Education. Maryland Heights, MO: Mosby Inc.; 2012.
- Meredith S, Feldman P, Frey D, Giammarco L, Hall K, Arnold K, et al. Improving medication use in newly admitted home healthcare patients: a randomized controlled trial. J Am Geriatr Soc 2002;50:1484-91. https://doi.org/10.1046/j.1532-5415.2002.50402.x.
- Tannenbaum C, Martin P, Tamblyn R, Benedetti A, Ahmed S. Reduction of inappropriate benzodiazepine prescriptions among older adults through direct patient education: the EMPOWER cluster randomized trial. JAMA Intern Med 2014;174:890-8. https://doi.org/10.1001/jamainternmed.2014.949.
- Martin P, Tannenbaum C. A realist evaluation of patients’ decisions to deprescribe in the EMPOWER trial. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-015959.
- Kozlowski D, Hutchinson M, Hurley J, Rowley J, Sutherland J. The role of emotion in clinical decision making: an integrative literature review. BMC Med Educ 2017;17. https://doi.org/10.1186/s12909-017-1089-7.
- Elshaug AG, Hiller JE, Tunis SR, Moss JR. Challenges in Australian policy processes for disinvestment from existing, ineffective health care practices. Aust New Zealand Health Policy 2007;4. https://doi.org/10.1186/1743-8462-4-23.
- Mitchel D, Bardoel A, Haines T, Mitchell D. Understanding health professional responses to service disinvestment: a qualitative study. Int J Heal Policy Manag 2019;2019:1-9. https://doi.org/10.15171/ijhpm.2019.20.
- Haines TP, Bowles KA, Mitchell D, O’Brien L, Markham D, Plumb S, et al. Impact of disinvestment from weekend allied health services across acute medical and surgical wards: 2 stepped-wedge cluster randomised controlled trials. PLOS Med 2017;14. https://doi.org/10.1371/journal.pmed.1002412.
- Kubler-Ross E. On Death and Dying: What the Dying Have to Teach Doctors, Nurses, Clergy and Their Own Families. Abingdon: Taylor & Francis; 2009.
- Soril LJJ, Niven DJ, Esmail R, Noseworthy TW, Clement FM. Untangling, unbundling, and moving forward: framing health technology reassessment in the changing conceptual landscape. Int J Technol Assess Health Care 2018;34:212-17. https://doi.org/10.1017/S0266462318000120.
- Daniels T, Williams I, Bryan S, Mitton C, Robinson S. Involving citizens in disinvestment decisions: what do health professionals think? Findings from a multi-method study in the English NHS. Health Econ Policy Law 2018;13:162-88. https://doi.org/10.1017/S1744133117000330.
- Hodgetts K, Hiller JE, Street JM, Carter D, Braunack-Mayer AJ, Watt AM, et al. Disinvestment policy and the public funding of assisted reproductive technologies: outcomes of deliberative engagements with three key stakeholder groups. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-204.
- Gupta R, Moriates C. Swimming upstream: creating a culture of high-value care. Acad Med 2017;92:598-601. https://doi.org/10.1097/ACM.0000000000001485.
- McPherson S, Reese C, Wendler MC. Methodology update: Delphi studies. Nurs Res 2018;67:404-10. https://doi.org/10.1097/NNR.0000000000000297.
- Richmond S, Morton V, Cross B, Chi Kei Wong I, Russell I, Philips Z, et al. Effectiveness of shared pharmaceutical care for older patients: RESPECT trial findings. Br J Gen Pract 2010;60:14-20. https://doi.org/10.3399/bjgp09X473295.
- Spinewine A, Swine C, Dhillon S, Lambert P, Nachega JB, Wilmotte L, et al. Effect of a collaborative approach on the quality of prescribing for geriatric inpatients: a randomized, controlled trial. J Am Geriatr Soc 2007;55:658-65. https://doi.org/10.1111/j.1532-5415.2007.01132.x.
- Wouters H, Scheper J, Koning H, Brouwer C, Twisk JW, van der Meer H, et al. Discontinuing inappropriate medication use in nursing home residents: a cluster randomized controlled trial. Ann Intern Med 2017;167:609-17. https://doi.org/10.7326/M16-2729.
- Crotty M, Halbert J, Rowett D, Giles L, Birks R, Williams H, et al. An outreach geriatric medication advisory service in residential aged care: a randomised controlled trial of case conferencing. Age Ageing 2004;33:612-17. https://doi.org/10.1093/ageing/afh213.
- Gray TA, Rhodes S, Atkinson RA, Rothwell K, Wilson P, Dumville JC, et al. Opportunities for better value wound care: a multiservice, cross-sectional survey of complex wounds and their care in a UK community population. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-019440.
- Peiro S. In healthcare, more or less, less is more: notes on healthcare disinvestment. Rev Esp Sanid Penit 2014;16:68-74. https://doi.org/10.4321/S1575-06202014000300002.
- Parchman ML, Henrikson NB, Blasi PR, Buist DS, Penfold R, Austin B, et al. Taking action on overuse: creating the culture for change. Healthcare 2017;5:199-203. https://doi.org/10.1016/j.hjdsi.2016.10.005.
- Mortimer D. Reorienting programme budgeting and marginal analysis (PBMA) towards disinvestment. BMC Health Serv Res 2010;10. https://doi.org/10.1186/1472-6963-10-288.
- Hollingworth W, Rooshenas L, Busby J, Hine CE, Badrinath P, Whiting PF, et al. Using clinical practice variations as a method for commissioners and clinicians to identify and prioritise opportunities for disinvestment in health care: a cross-sectional study, systematic reviews and qualitative study. Health Serv Deliv Res 2015;3. https://doi.org/10.3310/hsdr03130.
- Meredith LS, Cheng WJ, Hickey SC, Dwight-Johnson M. Factors associated with primary care clinicians’ choice of a watchful waiting approach to managing depression. Psychiatr Serv 2007;58:72-8. https://doi.org/10.1176/ps.2007.58.1.72.
- Perry C, Chhatralia K, Damesick D, Hobden S, Volpe L. Behavioural Insights in Health Care Nudging to Reduce Inefficiency and Waste. London: The Health Foundation; 2015.
- Davidoff F. On the undiffusion of established practices. JAMA Intern Med 2015;175:809-11. https://doi.org/10.1001/jamainternmed.2015.0167.
- Wang MT, Gamble G, Grey A. Responses of specialist societies to evidence for reversal of practice. JAMA Intern Med 2015;175:845-8. https://doi.org/10.1001/jamainternmed.2015.0153.
- Tatsioni A, Bonitsis NG, Ioannidis JP. Persistence of contradicted claims in the literature. JAMA 2007;298:2517-26. https://doi.org/10.1001/jama.298.21.2517.
- Hasson H, Nilsen P, Augustsson H, von Thiele Schwarz U. Empirical and conceptual investigation of de-implementation of low-value care from professional and health care system perspectives: a study protocol. Implement Sci 2018;13. https://doi.org/10.1186/s13012-018-0760-7.
- Baker DW, Qaseem A, Reynolds PP, Gardner LA, Schneider EC. American College of Physicians Performance Measurement Committee . Design and use of performance measures to decrease low-value services and achieve cost-conscious care. Ann Intern Med 2013;158:55-9.
- Gupta A, Tang Z, Agrawal D. Eliminating in-hospital fecal occult blood testing: our experience with disinvestment. Am J Med 2018;131:760-3.
- Selby K, Barnes GD. Learning to de-adopt ineffective healthcare practices. Am J Med 2018;131:721-2.
- Zikmund-Fisher BJ, Kullgren JT, Fagerlin A, Klamerus ML, Bernstein SJ, Kerr EA. Perceived barriers to implementing individual Choosing Wisely® recommendations in two national surveys of primary care providers. J Gen Intern Med 2017;32:210-17. https://doi.org/10.1007/s11606-016-3853-5.
- Rosenquist R, Weiner J. Issues at the heart of advancing the de-adoption of low-value care. LDI Issue Briefs 2017;21.
- Rosenberg A, Agiro A, Gottlieb M, Barron J, Brady P, Liu Y, et al. Early trends among seven recommendations from the Choosing Wisely campaign. JAMA Intern Med 2015;175:1913-20. https://doi.org/10.1001/jamainternmed.2015.5441.
- DeLeon P. Public policy termination: an end and a beginning. Policy Anal 1978;4:369-92.
- Brownson RC, Allen P, Jacob RR, Jenine K, Duggan K, Hipp PR, et al. Understanding mis-implementation in public health practice 2016;48:543-51. https://doi.org/10.1016/j.amepre.2014.11.015.
- Malhotra A, Bailey S. Ignorance Is Not Bliss: Why We Need More Empowered Patients 2018. www.pharmaceutical-journal.com/news-and-analysis/opinion/comment/ignorance-is-not-bliss-why-we-need-more-empowered-patients/20204970.article (accessed 9 September 2020).
- Mulley AG, Trimble C, Elwyn G. Stop the silent misdiagnosis: patients’ preferences matter. BMJ 2012;345. https://doi.org/10.1136/bmj.e6572.
- Silverstein W, Lass E, Born K, Morinville A, Levinson W, Tannenbaum C. A survey of primary care patients’ readiness to engage in the de-adoption practices recommended by Choosing Wisely Canada. BMC Res Notes 2016;9. https://doi.org/10.1186/s13104-016-2103-6.
Appendix 1 Project milestones
| Key work | Milestone |
|---|---|
| Phase 1 (months 1–6) | |
| Initial programme theory development | Identification of contexts, mechanisms and outcomes |
| Scoping review | Submission of the review protocol for publication |
| Theory building workshop | |
| Interviews with managers and leaders | |
| Phase 2 (months 3–13) | |
| Search literature, review and synthesis | Comprehensive evidence base related to de-implementation |
| Stakeholder involvement | Set of plausible hypotheses to be refined in Phase 3 |
| Monthly reports of retrieval | |
| Project Steering Group meeting 1 | |
| Phase 3 (months 13–16) | |
| Test and refine programme theory | Refined set of hypotheses with accompanying evidence-based narrative |
| Interviews with managers and leaders | Validation of work by Project Steering Group and PPI group |
| Project Steering Group meeting 2 | |
| Phase 4 (months 16–18) | |
| Actionable recommendations and write-up | Report of the review including relevant and actionable findings |
| Refining and confirming workshop | Open-access paper for publication |
| Knowledge mobilisation activities | |
| Project report for NIHR | |
| Open-access paper for publication | |
Appendix 2 Participant information sheet: telephone interviews
Appendix 3 Participant information sheet: workshop
Appendix 4 Example search strategy
MEDLINE via EBSCOhost
Date searched: 1 May 2018.
Date range searched: 2014 onwards.
Search strategy
-
((abandon* OR ‘choosing wisely’ OR deadopt* OR de-adopt* OR decommission* OR de-commission* OR ‘decrease use’ OR ‘decreased use’ OR deimplement* OR de-implement* OR delist* OR de-list* OR deprescri* OR de-prescri* OR dis-incent* OR disincent* OR disinvest* OR dis-invest* OR ‘evidence reversal’ OR ‘do not do’ OR exnovat* OR ‘health technology reassessment*” OR ‘inappropriate medication use’ OR ‘inappropriate prescribing’ OR ‘inappropriate testing’ OR ‘less is more’ OR low-value OR ‘medical reversal’ OR misimplement* OR mis-implement* OR obsole* OR rationing OR reassess* OR re-assess* OR ‘reduce prescribing’ OR undiffus* OR un-diffus* OR withdrawn) N5 (healthcare OR health OR technolog* OR device* OR intervention* OR health practice* OR health practise* OR medical OR medical practice* OR medical practise* OR procedur* OR drug OR drugs OR biotechnology* OR clinical OR prescrib* OR screening OR surgery OR treatment OR care OR medicine OR therap* OR program* OR funding OR service* OR strategy* OR scheme*)).ti,ab
-
((withdrawal OR withdrawn) N5 market).ti,ab
-
discontinuation N5 (program* OR funding OR service* OR strateg* OR scheme*).ti,ab
-
1 or 2 or 3
Appendix 5 Review flow chart
FIGURE 8.
Review flow chart. a, A second sift for de-prescribing papers was conducted when it was established that these were in scope; b, www.youtube.com (YouTube, LLC, San Bruno, CA, USA); and c, www.twitter.com (Twitter, Inc., San Francisco, CA, USA).
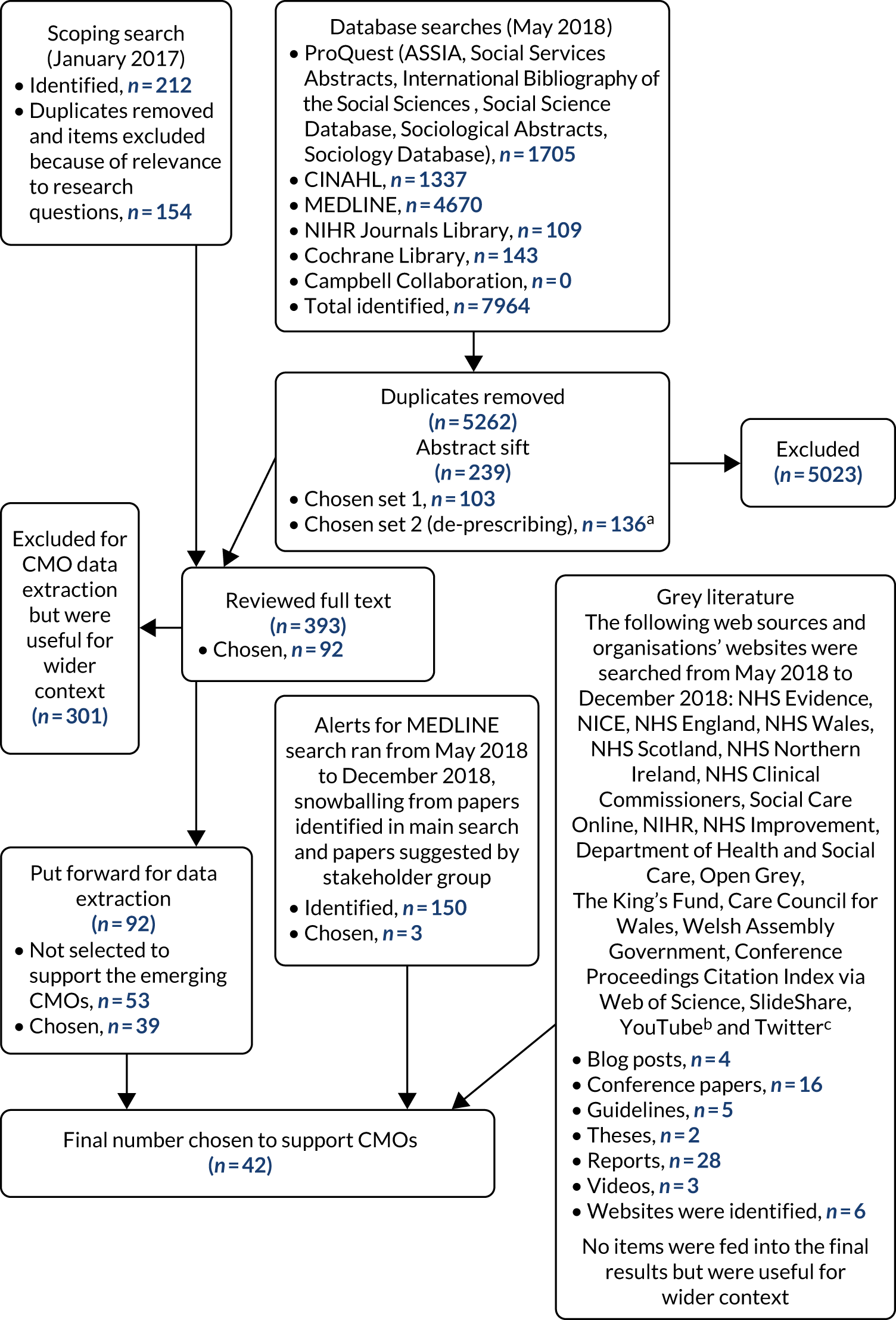
Appendix 6 Extraction table template
| Is the evidence good and relevant enough to be included in the review? | Yes – no – maybe |
|---|---|
| Q1: document ID/title | |
| Q2: authors/year published | |
| Q3: document type (e.g. research study/policy/local evidence/opinion) | |
| Q4: what is the study’s aim/purpose? | |
| Q5: what is the design/method used and was it appropriate for the aims/purpose of the study? | |
|
Q6: sample (type/size?) Factors relating to site, location, etc. |
|
| Q7: what data collection method was used, if applicable? | |
| Q8: were the data collected in a way that addressed the research issue? | |
| Q9: how did the authors define the concept of de-implementation? | Did the authors provide an explicit definition or was it implied? (If yes, what was it? Source of definition?) |
| Q10: what is being de-implemented? | This is the focus of change relating to one or more context areas, such as clinical behaviour change or organisational policy |
| Q11: driving force | Which factors are motivating the de-implementation process (e.g., lack of evidence of effectiveness, financial constraints, or safety issues)? |
| Q12: nature of the action | What is the continuum of the de-implementation process (from complete termination to replacement with another innovation)? |
| Q13: degree of Intentionality | To what extent is the de-implementation process intentional and planned or passive and opportunistic? |
| Q14: consequences of the de-implementation process | Were the outcomes as expected or were there unintended consequences that occurred over time and for different stakeholders? |
| Q15: any other explanatory theory | Theories that have already been identified within the project or other relevant theories |
| Q16: level of de-implementation process | Micro – meso – macro levels |
| Q17: other |
Appendix 7 Included studies
| CMO | Authors | Title | Source | Country | Practice setting | Citation |
|---|---|---|---|---|---|---|
| 3 | Bregnhøj et al. | Combined intervention programme reduces inappropriate prescribing in elderly patients exposed to polypharmacy in primary care | European Journal of Clinical Pharmacology | Denmark | Primary care – GP, Copenhagen | 98 |
| 6 | Crotty et al. | An outreach geriatric medication advisory service in residential aged care: a randomised controlled trial of case conferencing | Age and Ageing | Australia | Nursing homes | 126 |
| 4 | Daniels et al. | Randomized clinical trial of observational versus antibiotic treatment for a first episode of CT-proven uncomplicated acute diverticulitis | British Journal of Surgery | The Netherlands | Multicentre acute surgical wards | 108 |
| 5 | Daniels et al. | Involving citizens in disinvestment decisions: what do health professionals think? Findings from a multi-method study in the English NHS | Health Economics, Policy and Law | UK | Views of local health-care leaders in the English NHS | 119 |
| 5 | Day et al. | Challenges and opportunities for disinvestment in Australia | Health Economics, Policy and Law | Australia | Implementation of Choosing Wisely campaign | 2 |
| 3, 4 | Fenton et al. | Promoting patient-centered counseling to reduce use of low-value diagnostic tests: a randomized clinical trial | JAMA Internal Medicine | USA | One US general internal or family medicine service as part of the Choosing Wisely campaign | 101 |
| 6 | Gray et al. | Opportunities for better value wound care: a multiservice, cross-sectional survey of complex wounds and their care in a UK community population | BMJ Open | UK | Five northern England NHS trusts | 127 |
| 1, 3 | Gulla et al. | Deprescribing antihypertensive treatment in nursing home patients and the effect on blood pressure | Journal of Geriatric Cardiology | Norway | European long-term care settings | 93 |
| 5 | Gupta and Moriates | Swimming upstream: creating a culture of high-value care | Academic Medicine | USA | Current prevailing medical culture contributes to overtesting, overtreatment and health-care waste | 121 |
| 5 | Haines et al. | Impact of disinvestment from weekend allied health services across acute medical and surgical wards: 2 stepped-wedge cluster randomised controlled trials | PLOS Medicine | Australia | Twelve acute medical or surgical hospital wards across two hospitals | 116 |
| 5 | Hodgetts et al. | Disinvestment policy and the public funding of assisted reproductive technologies: outcomes of deliberative engagements with three key stakeholder groups | BMC Health Services Research | Australia | Deliberative engagements with a range of stakeholder groups were held on the topic of how best to structure the distribution of Australian public funding in this domain | 120 |
| Hollingworth et al. | Using clinical practice variations as a method for commissioners and clinicians to identify and prioritise opportunities for disinvestment in health care: a cross-sectional study, systematic reviews and qualitative study | Health Services and Delivery Research | UK | Two primary care trust Clinical Commissioning Groups | 131 | |
| 3 | Juola et al. | Nurse education to reduce harmful medication use in assisted living facilities: effects of a randomized controlled trial on falls and cognition | Drugs and Aging | Finland | Assisted-living facilities in Helsinki, Finland | 100 |
| 4 | Keijzers et al. | Don’t just do something, stand there! The value and art of deliberate clinical inertia | Emergency Medicine Australasia | Australia | Requesting investigations or providing treatment | 102 |
| 1 | Kullgren et al. | Precommitting to choose wisely about low-value services: a stepped wedge cluster randomised trial | BMJ Quality and Safety | USA | Forty-five primary care physicians in six adult primary care practices | 88 |
| 4 | Little et al. | Primary care strategies for childhood acute otitis media | British Medical Journal | UK | General practices in south-west England | 106 |
| 4 | MacGeorge et al. | Reducing unwarranted antibiotic use for pediatric acute otitis media: the influence of physicians’ explanation and instruction on parent compliance with ‘watchful waiting’ | Journal of Applied Communication Research | USA | An online survey of parents whose children took part in watchful waiting advice | 107 |
| 4 | Martin and Tannenbaum | A realist evaluation of patients’ decisions to deprescribe in the EMPOWER trial | BMJ Open | Canada | Community setting, Montréal | 112 |
| 2 | Martins et al. | The effect of a test ordering software intervention on the prescription of unnecessary laboratory tests – a randomized controlled trial | BMC Medical Informatics and Decision Making | Portugal | Primary care | 94 |
| 4 | May et al. | Watchful Waiting strategy may reduce low-value diagnostic testing | Journal of the American Board of Family Medicine | USA | One US general internal or family medicine service as part of the Choosing Wisely campaign | 104 |
| 3 | Menegueti et al. | Long-term prevention of catheter-associated urinary tract infections among critically ill patients through the implementation of an educational program and a daily checklist for maintenance of indwelling urinary catheters: a quasi-experimental study | Medicine (Baltimore) | USA | Intensive care unit of a tertiary care hospital | 99 |
| 1 | Meeker et al. | Nudging guideline-concordant antibiotic prescribing: a randomized clinical trial | JAMA Internal Medicine | USA | Primary care | 87 |
| 1 | Meeker et al. | Effect of behavioral interventions on inappropriate antibiotic prescribing among primary care practices: a randomized clinical trial | JAMA | USA | Primary care | 90 |
| 4 | Meredith et al. | Factors associated with primary care clinicians’ choice of a watchful waiting approach to managing depression | Psychiatric Services | USA | Primary care | 132 |
| 5 | Mitchel et al. | Understanding health professional responses to service disinvestment: a qualitative study | International Journal of Health Policy and Management | Australia | Aims to understand how health professionals react when confronted with a plan to disinvest from a health service they previously provided to their patients | 115 |
| 6 | Montini and Graham | ‘Entrenched practices and other biases’: unpacking the historical, economic, professional, and social resistance to de-implementation | Implementation Science | USA | 17 | |
| 6 | Mortimer | Reorienting programme budgeting and marginal analysis (PBMA) towards disinvestment | BMC Health Services Research | Australia | 130 | |
| 6 | Parchman et al. | Taking action on overuse: creating the culture for change | Healthcare | USA | Twenty-three health-care organisations across the USA | 129 |
| 6 | Peiro | [In healthcare, more or less, less is more: notes on healthcare disinvestment] (Spanish Article) | Revista Española de Sanidad Penitenciaria | Spain | Features of disinvestment and disinvestment strategies in several countries | 128 |
| 6 | Richmond et al. | Effectiveness of shared pharmaceutical care for older patients: RESPECT trial findings | British Journal of General Practice | UK | Evaluate the provision of pharmaceutical care by community pharmacists in primary care in England | 123 |
| 5 | Robert et al. | Disentangling rhetoric and reality: an international Delphi study of factors and processes that facilitate the successful implementation of decisions to decommission healthcare services | Implementation Science | UK | 20 | |
| 4 | Pradhan et al. | Watchful Waiting and Brief Education | Mosby, Inc. | USA | Management of acute low-back pain | 109 |
| 1 | Ryskina et al. | Effect of social comparison feedback on laboratory test ordering for hospitalized patients: a randomized controlled trial | Journal of General Internal Medicine | USA | Reduce ordering of routine laboratory tests for hospital patients | 91 |
| 1 | Sacarny et al. | Effect of peer comparison letters for high-volume primary care prescribers of quetiapine in older and disabled adults: a randomized clinical trial | JAMA Psychiatry | USA | Nationwide Medicare programme | 92 |
| 2 | Soon et al. | Effect of two behavioural ‘nudging’ interventions on management decisions for low back pain: a randomised vignette-based study in general practitioners | BMJ Quality and Safety | Australia | Primary care | 95 |
| 5 | Soril et al. | Untangling, unbundling, and moving forward: framing health technology reassessment in the changing conceptual landscape | International Journal of Technology Assessment in Health Care | USA | Health technology reassessment | 118 |
| 6 | Spinewine et al. | Effect of a collaborative approach on the quality of prescribing for geriatric inpatients: a randomized, controlled trial | Journal of the American Geriatrics Society | Belgium | Hospital setting at an acute geriatric evaluation and management unit | 124 |
| 4 | Sun et al. | Cost-effectiveness of watchful waiting in acute otitis media | Pediatrics | USA | Emergency department in children’s hospital | 105 |
| 4 | Tannenbaum et al. | Reduction of inappropriate benzodiazepine prescriptions among older adults through direct patient education: the EMPOWER cluster randomized trial | JAMA Internal Medicine | Canada | Community setting, Montréal | 111 |
| 1 | Trumbo et al. | Deimplementation of routine chest X-rays in adult intensive care units | Journal of Hospital Medicine | USA | Two intensive care units in one US medical centre. One unit was cardiovascular surgery and the other unit treated medical and pulmonary patients | 89 |
| 3 | Winchester et al. | A specialty-specific, multimodality educational quality improvement initiative to deimplement rarely appropriate myocardial perfusion imaging | Open Heart | USA | Unclear | 97 |
| 6 | Wouters et al. | Discontinuing inappropriate medication use in nursing home residents: a cluster randomized controlled trial | Annals of Internal Medicine | The Netherlands | Fifty-nine Dutch nursing home wards for long-term care | 125 |
Appendix 8 Set of plausible hypothesis
| ‘If–then’ statement | Derivation |
|---|---|
| If there is a clear focus as to what is being de-implemented (either policy, practice, behaviour, etc.), then the action (replacement, substitution, withdrawal, etc.) can be specified | Concept analysis model (V4) |
| If there is better alignment between the evidence (negative, new evidence, etc.) and professional and public expectations, then the outcomes of de-implementing the practice has a greater chance of success | Concept analysis model (V4) |
| If the indication for withdrawal of a practice or procedure is based on evidence that it inflicts harm to patients, then there is greater likelihood of the practice being de-implemented | Concept analysis model (V4) |
| If there is active facilitation of the de-implementation strategy, directed at the appropriate level (teams, organisation, etc.), then there is greater likelihood of the practice/process being reduced | Concept analysis model (V4) |
| If resources are allocated to the process of de-implementation, then there is greater likelihood of there being intended consequences, such as, stopping or reduction of the process | Concept analysis model (V4) |
| If the process of de-implementation is presented as a way of refining patient care, rather than allusion to practitioner competency, then abandonment of the practice is hastened | Davidoff134 |
| If the de-implementation process also targets the appropriate specialist professional societies (and journals) for supporting reduction in the low-value practice, then clinicians within the field are more likely abandon the practice | Wang et al.135 and Tatsioni et al.136 |
| If de-implementation is presented or framed as a ‘gain’ to the practitioner (and patient?), rather than a ‘loss’, then the chances of de-adoption will be boosted | Kahneman86 and Williams et al.22 |
| If professional stakeholders are encouraged to have a sense of ownership over the de-implementation process, then they feel more engaged, leading to greater success in de-adopting the practice | Johns et al.18 |
| If de-implementation is to be successful, then patient and public views, including media coverage, needs to be prioritised in the strategy | Williams et al.22 |
| If patient groups (PPI) are incorporated into the de-implementation process, then clinicians are more likely to de-adopt procedures | Hasson et al.137 |
| If clinicians and managers are provided with evidence-based alternative practice guidelines to follow during de-implementation process, then they will be more likely to de-adopt low-value procedures | Baker et al.138 |
| If de-implementation of low-value tests (screening) is to be successful, then engagement of local opinion leaders is required with targeted changes in the ability to order the test | Gupta et al.139 and Selby and Barnes140 |
| If clinicians provide clear evidence to patients of low-value interventions for their symptomatic conditions (e.g. X-ray low-back pain within 6 weeks), then de-adoption of the low-value procedure is improved | Zikmund-Fisher et al.141 |
| If commissioners create incentives (e.g. payment for de-implementation) for providers to identify and discard lower-value services in favour of higher-value, or evidence-based, procedures, then there is a greater chance of de-adoption of the low-value practice | Rosenquist and Weiner142 |
| If policy-makers highlight and focus on the de-adoption of frequently used low-value procedures, rather than those used infrequently, then the de-implementation strategy may have greater success | Rosenberg et al.143 |
| If de-implementation is re-framed as a positive, rather than envisaged as a negative strategy, then clinicians and managers are more likely to engage with the process | DeLeon144 |
| If de-adoption of practices or policies are to be improved, then engagement with national and local media (including social media) needs to be cultivated so that barriers to mis-information are limited | Brownson et al.145 |
| If clinicians adopt an authentic, shared decision-making approach with their patients that incorporates their preferences for treatment, then the possibility of overtreatment will be lessened | Malhotra and Baily146 and Mulley et al.147 |
| If de-adoption educational material is provided to patients in practice waiting rooms, etc., then there is improved patient knowledge that aids discussion with the clinician around unnecessary medications/treatments | Silverstein et al.148 |
| If the de-adoption is focused on clinicians’ perception of a treatment’s potential harm to patients, (appealing to ingrained instincts of nonmaleficence), rather than a lack of efficacy, then there is greater likelihood of it being stopped | Selby and Barnes140 |
Appendix 9 Interview schedule
Appendix 10 Participant role descriptors
| Role | Work environment | Number |
|---|---|---|
| Consultant physician/dentist | Primary care, secondary care, public health | 8 |
| General manager | Secondary care | 1 |
| Academic and director of postgraduate medicine | 2 | |
| Clinical medical director | Acute and primary care | 4 |
| Nurse and allied health professional director | Acute | 4 |
| Patient representative | 2 | |
| Total | 21 | |
Glossary
- Abductive analysis
- An approach in which something new is seen in evidence or observation and inference is made to the best explanation about the cause.
- Concept analysis
- An approach to examine the structure and function of a concept.
- Concept mining
- In realist synthesis, concept mining describes a process of searching through different bodies of evidence for information that could build theories.
- Context
- The conditions that influence the success or failure of different interventions or programmes.
- Cumulation
- The increase in understanding, through ongoing inquiry, of programme mechanisms, context and outcomes to increase the transferability of knowledge.
- De-implementation
- The idea and related processes of how managers and service leaders stop existing practices and interventions that are not evidence based, have marginal gain or, at worst, are harmful.
- Implementation
- Movement of evidence-based programmes from research to routine use.
- Mechanism
- What is the change? What influences the reasoning and behaviour of people? How the programme resources impinge on stakeholders’ reasoning, decision-making and responses.
- Mid-range theories
- Theories that explain phenomena that are located between grand theories and day-to-day working.
- Outcome
- Patterns resulting from the interplay between context and mechanism. The impact of the influence of context on mechanisms.
- Plausible hypotheses
- ‘If–then’ statements about what might work, for whom, how, why and in what circumstances.
- Professional judgement
- A process of reflection, integration and analysis of observable data to arrive at a decision.
- Programme theory
- The theory behind any given programme. The hypothesis of how an intervention may work.
- Realist And Meta-narrative Evidence Syntheses: Evolving Standards
- Specific publication standards for realist syntheses.
- Realist review
- The process of evidence review that follows the realist approach (also known as the realist synthesis).
- Realist synthesis
- The process of evidence review that follows the realist approach (also known as the realist review). A theory-driven evidence review that follows a realist approach.
- Retroductive analysis
- In realist approaches, an analytical approach to understanding the cause of an event.
- Scoping review
- A type of evidence review that aims to map the literature on a particular topic and provide an opportunity to identify key concepts.
- Soft systems methodology
- A systematic approach to addressing a real-world situation. An approach to understanding different perspectives and requirements from a real-world situation.
List of abbreviations
- 3MR
- Multidisciplinary Multistep Medication Review
- ART
- assisted reproductive technology
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CMO
- context–mechanism–outcome
- COSMOS
- COmmunication, Systematic assessment and treatment of pain, Medication review, Occupational therapy, Safety
- CPO
- continuous pulse oximetry
- CVICU
- cardiovascular intensive care unit
- GP
- general practitioner
- MAI
- Medication Appropriateness Index
- MICU
- medical intensive care unit
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- PPI
- patient and public involvement
- RCT
- randomised controlled trial
- USPSTF
- United States Preventive Services Task Force
