Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 16/01/79. The contractual start date was in October 2017. The final report began editorial review in March 2020 and was accepted for publication in November 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. This report has been published following a shortened production process and, therefore, did not undergo the usual number of proof stages and opportunities for correction. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2021. This work was produced by Brocklehurst et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2021 Queen’s Printer and Controller of HMSO
Chapter 1 Background to role substitution in dentistry
Role substitution in NHS dentistry in the UK
Workforce planning is an important policy objective in the NHS to ensure that ‘the right number of people with the right skills are in the right place at the right time to provide the right services to the right people’. 1 ‘Skill mix’ is a term that is used to describe a model of care in which the whole of the clinical team is utilised in delivering service activity. 2 It can be further subdivided into role substitution and role supplementation. In dentistry, the former means that different members of the dental team undertake clinical tasks instead of a general dental practitioner (GDP), while the latter means that team members augment the activity of a GDP. 3 The use of role substitution in NHS dentistry has been advocated for some time, but its implementation appears to have lagged behind that seen in medical specialties owing to a number of factors, including professional regulation, NHS regulations and financial incentives. 2 These, along with the current evidence from the literature, will be explored in this chapter.
Professional regulation of role substitution in NHS dentistry
In 1921, the Dentists Act4 created the Dental Board of the United Kingdom, which became the professional body for dentistry and oversaw its practice. In 1956, following amendments made to the Act, the Dental Board was superseded by the General Dental Council (GDC). 5 This reflected the recommendations in the Teviot Report,6 which argued that the dental profession had become sufficiently mature to self-govern. The Act also facilitated the training of ‘dental auxiliaries’ for the first time [referred to as dental care professionals (DCPs) in the remainder of this report]. The newly formed GDC subsequently developed the regulated titles of dental hygienist (DH) and dental therapist (DT). The duties of the former related to the provision of preventative and periodontal treatment, and the latter was permitted to provide a range of direct restorative procedures and extract deciduous teeth. In 1983, UK dental schools began to offer ‘dual’ integrated training over a period of 2 years. The new ‘hygiene–therapist’ qualification was able to offer the full range of clinical activities that both DHs and DTs could legally undertake, although only an individual title of DH or DT was registerable with the GDC. 7 In 2002, the Dentists Act was again amended and allowed DTs to practise in NHS dental practices. 8 Before this time, the DT’s role had been limited to the provision of care in NHS Community Dental Service settings only; the provision of care in NHS Community Dental Service settings had formerly been restricted to GDPs since 1948.
Despite this change, DCPs were not allowed to practice as ‘front-line’ clinicians in the NHS or in private practice. Instead, patients were required to see a GDP for an examination and treatment plan before being referred to DCPs for their NHS care (a condition in both the Dentists Act and the NHS regulations9). NHS regulations9 also prevented DCP services from being procured directly, with the ‘knock-on’ effect of DCPs not being able to receive a NHS pension (unlike their GDP counterparts). However, after a review of the available literature, a landmark decision by the GDC in 2013 allowed patients to have ‘direct access’ to dental care by DCPs without a referral from a GDP. 10 This was accompanied by an expansion of the DCPs’ Scope of Practice to incorporate undertaking examinations and developing treatments plans within their level of competence. 7 However, DCPs remained unable to contract directly with the NHS under NHS regulations9 and were also unable to prescribe dental radiographs or fluoride or administer local analgesia (owing to restrictions in the Ionising Radiations Regulations11 and the Medicines Act,12 respectively).
Policy recommendations on role substitution in NHS dentistry in the UK
Policy-makers have been interested in the potential of role substitution in NHS dentistry for some time. In 1993, the Nuffield report inquiry13 redefined the concept of the dental team through which dental care could be delivered and argued that the role of DCPs could be expanded. Subsequently, increasing attention has been paid to how role substitution can deliver the level of care in the NHS that is required to meet the population health need. This is now explicitly recognised in a number of policy documents that underpin NHS care. For example, both the Prudent Healthcare policy agenda in Wales14 and the NHS Long Term Plan15 call for greater use of role substitution.
In the UK, population oral health needs are changing. In the most recent epidemiological survey, 90% of young adults are expected to have > 21 teeth in 10 years’ time, and the levels of dental caries and periodontal disease have fallen dramatically. 16 By contrast, levels of dental caries in young children have remained relatively intransigent, despite the fact that dental caries, as a non-communicable disease, are entirely preventable. 17 As highlighted in the Child Dental Health Survey in 2013, ‘nearly a third (31%) of five-year olds and nearly a half (46%) of eight-year olds had obvious decay experience in their primary teeth. Untreated decay into dentine in primary teeth was found in 28% of five-year olds and 39% of 8 year olds’ (information from NHS Digital, licenced under the current version of the Open Government Licence). 17 This pattern of disease also follows a social gradient: ‘a fifth (21 per cent) of the five-year olds who were eligible for free school meals had severe or extensive tooth decay, compared to 11% of five-year olds who were not eligible for free school meals’ (information from NHS Digital, licenced under the current version of the Open Government Licence). 17
Equally, the increasing number of partially dentate older people with varying degrees of independence are giving rise to new health-care challenges. The oral health of care-home residents is much worse than their community-living peers (e.g. caries prevalence is 73% vs. 40%, respectively) and about half of all care-home residents now retain some of their natural teeth. 18,19 Poor oral health may also exacerbate a range of medical conditions, including pneumonia and delirium, which increases health-care costs and leads to poorer outcomes. 20 Despite this high level of need, dental service provision in residential care is poor, with little emphasis on prevention. 21,22 Access to domiciliary services is difficult and unscheduled care for dental problems (including hospital admissions) is common, complex to deliver and expensive. 20,23 The World Health Organization (WHO) argues that the design of long-term care systems that are fit for ageing populations should take priority,24 and the Royal College of Surgeons of England (RCS),25 Public Health England (PHE) and the National Institute for Health and Care Excellence (NICE)26 have all called for more high-quality research. The Care Quality Commission (CQC) also highlighted the paucity of dental care in care homes in its report of June 2019. 27
Along with these pressing and emerging population health needs, there is evidence that many who attend dental practices have good oral health. In the Adult Dental Health Survey,28 71% of all dentate adults reported that they attended their GDP at least once per year. A total of 6% reported that they attended once every 2 years and a further 10% attended less often than every 2 years. The remaining 13% of dentate adults reported that they attended only when they were having trouble with their teeth. Data from the Business Services Authority (the organisation responsible for paying GDPs in England and Wales) suggest that many of those who do attend do not require any further treatment. 29 In 2018/19, out of the 39.7 million courses of treatment delivered in 1 year in England, 23.3 million (58.7%) related to patients having check-ups with no further treatment. The figures for 2017/18 and 2016/17 were 58.0% and 57.0%, respectively. That many who attend do not need further treatment is further supported by data from the Assessment of Clinical Oral Risk and Needs (ACORN) in Wales, where GDPs collect ‘risk’ and ‘need’ data as part of the Welsh Dental Contract Reform programme. A total of 60.4% and 47.8% of adults in 2019 were classified as ‘green’, that is as having no active dental caries or periodontal disease, respectively, and many of these patients appear to return to their dental practice within a 9-month period (Colette Bridgman, Chief Dental Officer for Wales, 2020, personal communication). This suggests that a substantive level of the resource being invested into primary dental care in the NHS relates to managing low-risk dental patients. As a result, there are increasing calls for the development of a NHS dental workforce to meet these emerging population oral health needs, and the procurement of relevant NHS service provision, while freeing up resources to increase the capacity to provide care and reduce social inequalities in oral health. 3
Role substitution in NHS dentistry
Dental care professional utilisation by NHS dental practices appears to be heavily influenced by the financial incentives inherent in the NHS contract. 30 NHS GDPs run their practices as businesses to offset the cost of the capital risk of the premises and the equipment that they own while ensuring liquidity to cover their overheads. 31 In medicine, transaction costs can be offset by economies of scale, which enable a broader range of services to be made available. 32 This is more difficult in NHS dentistry because, historically, many practices have not been ‘purpose built’ and some remain ‘single handed’. 33 This limits the extent of role substitution and supplementation undertaken in the NHS.
Although DHs appear to be well-accepted members of the dental team in the UK,30,34 financial considerations appear to play a significant part in the decision to use a DT in the NHS. 35,36 In one of the few studies that examined the profitability of using role substitution,37 patient charges generated did not cover the cost associated with their use in the current remuneration system. As a result, many DTs have been employed in the NHS as DHs in England rather than being utilised across their full range of skills. 35 In addition, some patients expect to pay less for treatment provided by a DCP than by a GDP. 38
Dental practices operating in the NHS are acutely sensitive to the incentives in any given remuneration system. 39,40 This can influence the institutional logic of the dental practice (the culture in an organisation that shapes the collective behaviour and actions of those who work there) and whether or not role substitution is supported. 30,41,42 Retrospective payment systems, such as fee-for-service (FFS) (where a GDP submits a claim for every single item of completed treatment), have been shown to lead to overtreatment to maximise profit. 43,44 In these systems, the incentive for practices is to increase the amount of clinical activity delivered, which may not always suit the greater utilisation of role substitution. 30 In contrast, per-capita remuneration systems pay practices a fixed level of funding based on the number of registered patients. This breaks the link between treatment activity and practice income, giving practices greater autonomy on what to focus on. 45 This may lead some practices to place greater emphasis on prevention, which would favour role substitution and supplementation (to reduce staff costs and draw on the strengths of DCPs to deliver prevention). 30 However, per-capita systems can also lead to undertreatment and patient selection, that is, a preference for low-risk patients who require little treatment, given that funding for these practices is capped and unrelated to clinical activity. 46,47
Goodwin et al. 48 argue that institutional logics at any given NHS practice include not only dentistry as a business but also professional ethics and contextual factors based on where the practice is embedded. As highlighted by Watt et al. ,49 the most important factors influencing change in dentistry include concerns about financial risk, progressive practice environment, supportive organisational structure, supportive professional networks and opportunity for training. Therefore, the drive to maintain (and maximise) the viability of a NHS practice can also be tempered by a practice owner’s sense of duty to their patients and their ideas about how best to deliver care for their patients and community. 50 In our earlier study,30 the views of practice principles on the benefit of role substitution was found to be one of the most important factors, which could ameliorate concerns about the impact of using DCPs, in relation to the underlying NHS contract. Management of change is also a potential problem with role substitution because professionals seek to protect their clinical roles and maintain traditional clinical boundaries. 51,52 Managing a transition to role substitution takes time and good human resource skills. 53 McDonald et al. 54 found that the key factors that determined the acceptability of changes to role boundaries included the clarity around roles and responsibilities as well as personal relationships with colleagues, which raise issues of mutual trust and respect. Nevertheless, the influence of the underlying NHS contract remains substantive and warrants an understanding of the historical development of NHS funding and contractual reform across the UK.
The evolution of NHS dental contract in the UK
At the turn of the new millennium, Modernising NHS Dentistry55 set the agenda in England and subsequently gave primary care trusts (the organisations responsible for procuring NHS service provision at the time) powerful new commissioning tools to improve access to NHS dentistry and increase the provision of preventative services across England. This was further emphasised in Options for Change in 2002. 56
Prior to 2006, GDPs were paid on a FFS basis. This meant that GDPs claimed for every item of clinical activity that they undertook. As described in Role substitution in NHS dentistry, this payment mechanism can have a tendency to incentivise overtreatment because GDPs’ income is directly linked to the level of clinical activity undertaken on each patient. 43,45 It also had a negative impact on practices because many of the individual items of treatment were of a relatively low value and led to GDP complaints about being on a ‘treadmill’ (a high level of clinical activity on low-value items) to maintain the viability of their practices. 31 This was particularly relevant after 1990 because the Department of Health and Social Care (DHSC) had attempted to correct an overspend on the national dental budget and had placed a downwards pressure on the annual review process that controlled how individual items of treatment were costed. 57 In 2006, a new general dental services (GDS) NHS contract was introduced in England and Wales. 58 This contract collated NHS dental activity items into three broad bands in an attempt to lessen the number of individual items of treatment that GDPs would claim for on each patient:
-
band 1 – examination, radiographs and a simple scale and polish
-
band 2 – restorations, extractions and root canal treatments
-
band 3 – crowns, bridges and dentures.
These bands of treatment attracted 1, 3 and 12 units of dental activity (UDAs), respectively. The value of a UDA varied across NHS dental practices and was based on clinical activity and payments in a ‘reference year’ that were ‘earned’ under the previous FFS NHS dental contract in 2005. As a result, GDPs who had been undertaking significant levels of clinical activity in the reference year were rewarded with high UDA values, resulting in considerable heterogeneity and inequity across practices in England. For example, an examination (generating 1 UDA) in one practice could generate £18 whereas in another practice it could generate £30. Likewise, one or multiple fillings completed in a ‘course of treatment’ (generating 3 UDAs) would attract £54 or £90, respectively, for GDPs on the same NHS dental contract.
NHS dental contracts were raised with equity-owning GDPs in England and Wales (known as ‘providers’). They then subcontracted these contracts to non-equity-owning GDPs at their practices (known as ‘performers’). DCPs were provided with an income based on the proportion of clinical activity that they undertook, or were paid a salary. The former method of remuneration for DCPs led to a potential conflict of interest between performers (also known as ‘associate GDPs’) and DCPs, because both were funded based on the number of UDAs that they delivered. 30 Another important element of the 2006 contract was cost containment, which capped providers’ annual activity to an agreed number of UDAs per year, known as an annual contract value (ACV). 30 NHS GDPs were then paid one-twelfth of their ACV on a monthly basis. As a result, NHS GDPs’ outputs under the new contract in England were constrained and they were penalised if they underperformed (< 96% of their ACV) or overperformed (> 102% of their ACV).
The effect of this change to the NHS dental contract was significant changes in the types of treatments that were offered. For example, as providers and subcontracted performers were paid the same number of UDAs for endodontic treatment and extractions (which are often the two alternative treatment options for many teeth with advanced decay), the number of the former reduced in favour of the latter, given that the latter could be undertaken in one-quarter of the time in most cases. 39,40 Equally, one or multiple fillings completed within a course of treatment would generate the same level of revenue for a practice (3 UDAs). As a result, there was downwards pressure on the number of fillings undertaken in any one course of treatment, leading to multiple courses of treatment submitted for patients who required more than one restoration. 39,40 GDPs were also incentivised to make upper and lower partial or full dentures separately to claim two sets of band 3 payments. Preventative care was not remunerated separately and any preventative activity was expected to be undertaken in an existing course of treatment. 39,40
In addition to these unintended consequences at a regional and national level, the 2006 NHS dental contract proved unpopular with GDPs. 31 This was largely because of the loss of clinical autonomy and the need for practices to be accountable to local dental commissioners (DCs), who closely scrutinised providers’ ability to deliver to their ACV targets. GDPs argued that one form of treadmill had simply been replaced by another. As a result of this criticism, an independent review was undertaken in 2008/9 in England, which recommended the greater use of preventative care and a standardised approach to patient assessment, leading to patient care pathways. 59
This led to the development of a pilot programme in England in 2010, which was predominantly based on capitation. 60 It also required GDPs to undertake an oral health assessment that categorised patients into different risk categories (red, amber or green). However, the pilots in England were beset with a number of informatic problems, and based on concerns about the capitation payment system were relaunched in 2015 as ‘prototypes’. 61 Prototype practices were paid on the basis of a blended-funded system, drawing on features of the 2006 contract (a retrospective payment mechanism based on clinical activity) with capitation. This blended together the financial incentives to ‘care’ and prevent disease (associated with capitation payment mechanisms) with the incentives to undertake clinical activity (associated with FFS mechanisms). In similarity to the earlier pilots in England, the prototypes were based on establishing risk and then referring the patient to the appropriate patient care pathway.
An evaluation of the first year of prototyping was published in 2018. 62 Attendance marginally increased over the course of the evaluation period (3–6%). A total of 62% of prototype practices reported delivery of preventative care to adults according to evidence-based guidelines compared with 56% in the 2006 contract, with little change to the level of prevention offered to children (60% and 58%, respectively). The evaluation concluded:
. . . progress has been made in the first year of prototyping on the key issues of improving oral health, providing appropriate care and quality, and maintaining or increasing access to merit continuation of the programme.
The evolution of contractual reform followed a similar pattern in Wales, although the process was different under their devolved government. In 2011, eight dental practices took part in a pilot trial. 63 This process required these practices to deliver weighted ‘key performance indicators’ and a capitation target based on the number of unique patients treated in the practice within a defined time period. In 2012, the Quality and Outcome Pilot64 for adults was introduced, with the introduction of a dental care assessment and a risk-based preventative care plan. By 2016, all but two practices had reverted back to the 2006 UDA contract. The remaining practices continued as prototype practices to test new models of care and formed a ‘learning network’. An early evaluation of the Welsh pilots found a reduction in the number of patients attending NHS practices (7–10%) compared with baseline.
In 2017, the Welsh Government published Taking Oral Health Improvement and Dental Services Forward in Wales,65 which placed greater emphasis on incentivising needs-led care, role substitution/supplementation and prevention. This led to the development of a needs and risk assessment tool. In 2018 the Welsh Government increased the number of ‘contract reform’ practices to 23, and by late 2019 > 100 NHS practices had entered phase 1 of the process. This reduced ACV targets by 10% and raised all providers’ UDA values to a minimum of £25 to ensure greater parity across the nation. For this 10% reduction in their ACV, practices were required to undertake an ACORN at least once per year under the mantra ‘do it once, do it well’ (Colette Bridgman, personal communication). Phase 2 of the contract reform process saw further reductions in ACV targets (reduction to 70–80% of pre-reform levels) in exchange for greater emphasis on the provision of prevention, increasing the quality of care provided and greater utilisation of role substitution/supplementation. These policy objectives were further emphasised in The Oral Health and Dental Services Response to a Healthier Wales,66 published in 2018, and are being underpinned by a formal evaluation process undertaken by researchers at Bangor University. As of spring 2020, over one-quarter of the total NHS practice population was using ACORN and involved in the Dental Contract Reform programme in Wales.
In Northern Ireland, the predominant financial mechanism used to pay GDPs still resembles the pre-2006 contract in England and Wales, that is, the majority of funding draws on FFS and items of service as part of a retrospective payment system. An Oral Health Strategy for Northern Ireland67 was published in 2007 and reiterated the main themes identified by the Northern Ireland Primary Dental Care Strategy in 2006, namely a shift away from treatment in favour of prevention of disease while maintaining access to services. In 2014, the Northern Ireland Health and Social Care Board initiated a pilot NHS dental contract across the province, which involved > 30 GDPs. Similar to the English pilots, the chosen remuneration mechanism was prospective in nature, so reduced the incentive for GDPs to engage in unnecessary treatment. The underpinning policy intention was that practitioners would receive the equivalent gross income during the pilot period that they would have received under the GDS had they maintained their activity and list as per the baseline period. As highlighted in our evaluation of the pilot NHS contract led by Bangor University, we found ‘rapid changes in the patterns of care provided by GDPs to patients (compared with the control practices) when they moved from a FFS system to a capitation-based remuneration system’ and ‘there were statistically significant reductions in the volume of all treatments in the intervention practices during the capitation period’ (contains information licensed under the Non-Commercial Government Licence v2.0). 57 This highlighted the sensitivity that GDPs have to underlying incentives in the NHS dental contract.
In Scotland, the prevailing dental contract funding mechanism was similar to Northern Ireland’s model. After a consultation exercise in 2016, the Scottish Government published its Oral Health Improvement Plan68 in 2018 with a 41-point plan that focused on prevention, an oral health risk assessment and a personalised care plan. As highlighted by Brocklehurst et al. :57
. . . in contrast to the other three home nations, there were no plans for scrapping the item-of-service system of remuneration; instead there was an intention to ‘streamline’ items of service payments, which would be progressively introduced.
The proposed remuneration mechanism was based on a ‘mixed economy of item of service, capitation and continuing care payments’57 (contains public sector information licensed under the Open Government Licence v3.0).
Evidence base for the use of role substitution in dentistry
Proponents of role substitution argue that it has the potential to free resources, increase the capacity to care for high-need populations, improve access and reduce oral health inequalities. 69–71 In an international review, Nash et al. 72 concluded that ‘access to basic dental care will not be available without the utilization of dental therapists in the workforce’, and Johnson73 argued for a paradigm shift ‘from treatment to prevention, wellness and self care’.
Role substitution by DCPs has been established for some time in a number of European countries. 70,71 Sweden and the Netherlands legalised the independent use of DCPs in 1964 and 1978, respectively. 74 Finland, Denmark and Norway have allowed independent practice since 1994, 1996 and 2001, respectively. Similar practices are found in Switzerland, which started in 1997, and in Italy, where DHs have been able to work as independent practitioners since 1999. 74 In the USA and Canada, DH is a growing profession, and DHs can practice with varying degrees of independence in a number of US states, including California, Colorado, Montana, Nebraska, New Mexico, Oregon and Washington, and Canadian provinces, including British Columbia, Alberta, Saskatchewan and Manitoba, although some restrictions remain in terms of settings. 75 Tasmania has a liberal regulatory model in which DHs and DTs practice independently and can own their own practices. 74 DTs are also considered to be independent in New Zealand, although they are not able to treat adults. 74 In Samoa and Singapore, DTs must work under the supervision of a GDP. Fiji has allowed DTs to assume independent responsibility for managing clinics since 1985, and DTs have been allowed to practice independently in South Africa since 1994. 74
The research evidence for the greater use of DCPs is emerging. Despite suggestions from some elements of the dental professional that role substitution is unsafe, this is not borne out by the limited literature that is available. Two studies by Calache and Hopcraft,76,77 undertaken in Australia, found no evidence to question patient safety when adult patients were managed by DTs. No differences were found between DTs and graduating GDPs in infection control, local analgesia, cavity preparation, placement of restoration, occlusion and patient communication. 77 Knowledge and clinical skills were rated as good to high, and 80% of DTs were considered safe to treat adult patients. The potential of DCPs not to identify oral cancer is another frequently cited concern in terms of patient safety. However, in an in vitro study, Brocklehurst et al. 78 found that the diagnostic test accuracies of GDPs and DTs were similar when they were presented with a judgement task that required them to distinguish between malignant and benign diseases of the oral mucosa. Values of sensitivity and specificity were 81% and 73% for GDPs, compared with 77% and 69% for DTs, respectively. DTs also missed fewer frank carcinomas in the judgement task.
Although the social acceptability of DTs appears to be positive, public awareness of DTs as a professional group is not widespread. 38,79,80 In the UK, our earlier study found that the attitudes of practice owners were critical in the process of patients accepting treatment from DTs. 30 Despite this, it does appear that adults are willing to receive treatment from DCPs under the NHS and there is evidence of increased patient satisfaction. 80 In one of the Calache and Hopcraft studies,77 patients were very satisfied with the dental treatment that was provided. In another study conducted by the same team,81 356 direct coronal restorations were placed with high patient satisfaction. In Canada, 65.8% of respondents stated that they would visit an independent DH to maintain their oral health. In the USA, 98.0% of respondents strongly agreed or agreed that their care by DCPs was satisfactory (based on RAND criteria; RAND Europe UK, Cambridge, UK). 82 Perry et al. 83 reported 98.0% patient satisfaction. For DTs, the majority of adults and children’s caregivers receiving care in Alaska had a positive patient experience. 84 In the Netherlands, one-quarter of those surveyed (n = 1500) agreed that ‘simple dental treatments’ could be performed by a DH rather than by a GDP, and 15% agreed that a DH could undertake a check-up. 85,86 In another study, 85.0% of patients who received a simple restoration for the treatment of dental caries provided by a DCP claimed to be satisfied with the treatment provided. 87
In terms of efficacy, Wang and Riordan88 evaluated a population oral health programme undertaken in Norway that allowed DHs to undertake a check-up over a 3-year period. The quality of care provided was judged not to deteriorate over this time frame. 88,89 This is supported by Kwan et al. ,90 who compared the performance of DCPs with GDPs in an epidemiological programme. Sensitivity values for GDPs ranged from 0.54 to 1.00, and those for the DCPs from 0.80 to 0.94. The direction of effect in these studies has also been replicated by Patel et al. ,91 Kwan and Prendergast92 and Hopcraft et al. 93 In terms of restorative management by DCPs, Bader et al. 94 found that 74 out of the 84 direct amalgam restorations placed by DTs were considered to be completed to an adequate standard, compared with 32 out of 41 restorations provided by GDPs. This was not dissimilar to Wetterhall et al. ’s study,84 which found that 88.0% and 78.0% of amalgam restorations were rated as ‘satisfactory’ for DTs and GDPs, respectively. Calache et al. 81 evaluated 356 restorations placed by DTs in 115 patients. After 6 months, 95.0% were judged to be successful by blinded evaluators. This concurs with studies by Battrell et al. 95 and Freed et al. 82 Dyer et al. ’s Cochrane review96 identified four randomised controlled trials and one non-randomised controlled trial. Three found no evidence of a difference in retention rates of fissure sealants placed by DCPs compared with GDPs, and the study comparing the comparative effectiveness of ‘atraumatic restorative technique’ restorations found no difference in survival rates after 12 months. 96
These results concur with the findings of a number of studies97,98 led by our team that were undertaken with NHS clinicians. In 2012, we showed that both DTs and GDPs had comparable sensitivity and specificity in the recognition of occlusal caries in vitro. 97 In 2015, we tested the diagnostic test accuracy of DTs in vivo. 98 A total of 1899 adult NHS patients were screened by both a DT (index test) and a GDP (reference standard) prior to their routine NHS check-ups in 10 busy NHS practices. Both sets of clinicians made an assessment on the presence of dental caries and periodontal disease. The sensitivity and specificity values of DTs were 0.81 [95% confidence interval (CI) 0.74 to 0.87] and 0.87 (95% CI 0.78 to 0.92) for dental caries and 0.89 (95% CI 0.86 to 0.92) and 0.75 (95% CI 0.66 to 0.82) for periodontal disease, respectively. This suggests that DTs could recognise the two most common oral diseases. Brocklehurst et al. 78 found that the diagnostic test accuracies of GDPs and DTs were similar when they were presented with a judgement task that required them to distinguish between malignant and benign diseases of the oral mucosa. Values of sensitivity and specificity were 81% and 73% for GDPs, compared with 77% and 69% for DTs, respectively. DTs also missed fewer frank carcinomas in the judgement task.
Although diagnostic test accuracy is important as a measure of efficacy, a more important consideration is an assessment of the effect on health of using DTs in front-line roles. Given that precise estimates of effect, recruitment, retention and fidelity were unknown, we undertook a study to test whether or not a definitive trial could be feasible in the NHS. 99 Over a 15-month period, adult NHS patients were randomised into one of three arms in two NHS dental practices: patients who saw only a DT (arm 1), those who saw both a DT and a GDP (arm 2) and, finally, those who saw only a GDP (arm 3). The initial recruitment rate for the study was 33.7%. This figure increased to > 82.1% when telephone calls or face-to-face recruitment were utilised. The retention rates were 60% for the DT and DT/GDP arms and 70% for the GDP arm. The proportion of sites with bleeding on probing (BOP), a measure of gum inflammation, at the end of the 15-month period was 46.7%, 14.5% and 32.1% in arms 1, 2 and 3, respectively (44.6%, 17.2% and 26.5% at baseline, respectively). Similarly, plaque levels were found in 68.2%, 43.7% and 60.9% of patients, respectively (60.5%, 44.9% and 56.3% at baseline, respectively). Because these values did not differ significantly from baseline values, it suggested that oral health can be maintained by role substitution.
The majority of the studies examining the efficiency of DCP utilisation are from the UK. 100,101 Harris and Sun102 concluded that role substitution in the UK ‘may be limited to particular situations where conditions are conducive’. Patients with high levels of disease (many restorations) were thought less suitable for referral because GDPs would undertake care in fewer visits and there was a risk of complications necessitating referral back to a GDP. 99 In our earlier study30 we found that the extent of role substitution in NHS dental practices appears to be relatively limited and largely restricted to the use of DHs for routine periodontal treatment. This appears to be directly related to the incentives and disincentives in the NHS dental contract. This meant that ‘NHS dental practices that utilised fewer non-dentist team members were associated with higher levels of technical efficiency, that is as role substitution in NHS practices increased, their relative efficiency dropped’. 30 As highlighted in the report, ‘when UDAs were used as the output measure in England, NHS dental practices operated at a mean level of efficiency of 64.0%. This changed very little when the outputs were measured in terms of number of patients seen, or the number of treatment plans generated. NHS dental practices that did not use any form of role substitution had a higher mean level of efficiency (68.0%; n = 39)’ (contains public sector information licensed under the Open Government Licence v3.0). 30 Any use of DCPs was found to be associated with statistically significantly lower efficiency scores (14.0% lower for UDAs and 11.0% lower for treatment plans or patients seen) than no use of role substitution.
Discussion
As highlighted in this chapter, the potential use of role substitution in NHS dentistry is becoming increasingly recognised by policy-makers. Changes made by the GDC now make this more possible, but there remain regulatory barriers at this point in time: NHS general dental services regulations, the Medicines Act12 and the Ionising Radiations Regulations. 11 Financial incentives in NHS dental contracts also play a key role but can be mitigated by the institutional logics in a dental practice.
All dental contract reform programmes undertaken across the UK have placed an emphasis on increasing patient access and prevention while maintaining and improving the quality of service being delivered. In many cases, this is facilitated by the development of care pathways based on the risk status of the patient. In Wales, the use of role substitution is an explicit objective in the second stage of the contract reform process, and it is implicit in many other national programmes.
This means that it is timely to draw on the existing evidence base for the greater use of DCPs. However, the quality of the literature is relatively poor and, as Dyer et al. ’s Cochrane review96 highlighted, the number of trials empirically testing role substitution is limited. Although there have been a number of diagnostic test accuracy studies to demonstrate efficacy, no trials have examined the effectiveness of using DTs, instead of the GDP, to undertake the check-up. As highlighted by our feasibility study,99 there was some reservation about recruitment and retention rates in busy NHS dental practices. There were also specific design questions that remained unanswered. For example, what is the estimated size of effect of such an intervention and should the design be based on superiority or on the basis of non-inferiority (i.e. are DTs better than or no worse than a GDP in undertaking the check-up and any subsequent treatment that is required)? The latter question is a fundamental one and significantly influences the design of a definitive trial.
As a result, we proposed undertaking an individually randomised pilot study in the North West of England over a 15-month period based on the following population, intervention, control, outcome (PICO) format:
-
population – adult, asymptomatic, low-risk, routine dentate or partially dentate NHS patients
-
intervention – check-up and any subsequent treatment undertaken by a DT
-
control – check-up and subsequent treatment by a GDP (‘treatment as usual’)
-
outcome – proportion of sites that BOP (measured at six sites per tooth).
To facilitate the design of the definitive study, a realist-informed process evaluation was undertaken alongside the pilot study to explore the acceptability of using DTs as front-line clinicians, patient crossovers (from one arm to the other) and treatment fidelity. We also captured the contextual factors that shaped the intervention in NHS practices, mechanisms that sustained or potentiated effects, unexpected pathways and consequences and the contextual factors that shaped implementation. 103 This was framed from a realist perspective to understand ‘what is it about a programme that works for whom, in what circumstances, in what respects, over which duration’. 104 Realist methodology is becoming increasingly used in health services research because it recognises the complex and contingent nature that underpins the settings for new interventions and service delivery. This approach to process evaluation ‘supposes that regularities in the patterning of social activities are brought about by the underlying mechanism constituted by people’s reasoning and the resources they are able to summon in a particular context’. 105
Finally, we undertook a third workstream (WS) to develop and test the health economic data collection tool and rehearse the health economic analysis of the intervention compared with the current practice. We adopted the viewpoint of both the NHS and the patient, and collected resource use data that included the costs of dental consultation by GDPs and DTs, the use of primary and secondary NHS dental services, and participants’ out-of-pocket expenses relating to any dental problems during the pilot’s follow-up period.
Aims and objectives
The aim of this study was to inform the design for a definitive trial by undertaking a pilot study to determine whether or not DTs can maintain the oral health of low-risk routine NHS patients, who form the predominant proportion of the regularly attending practice population. The objectives of the research were to:
-
determine the most appropriate design of a definitive trial
-
determine whether or not BOP is the most appropriate primary outcome measure (POM) (and if not, determine the most appropriate measure)
-
confirm the appropriateness of the non-inferiority margin of the chosen outcome measure for the definitive trial (i.e. whether or not the effect estimate lies within an appropriate margin of non-inferiority)
-
further investigate recruitment, retention and fidelity rates
-
confirm willingness to be randomised among study participants
-
determine the potential for patient crossovers between arms (e.g. where the patient’s condition is considered too complex to be managed by the DT)
-
undertake a process evaluation underpinned by a realist framework to understand what works, for whom, why and in what circumstances
-
rehearse the health economic analysis and assess the health economic data collection tool, to inform the definitive trial design
-
explore patients’ preferences in a focus group setting, to inform a preference elicitation exercise [e.g. discrete choice experiment (DCE)] in the definitive trial.
Structure of the report
This report is arranged in chapters, as follows. Chapter 1 provides a review of the literature and describes the historical context of role substitution in dentistry. Chapter 2 describes the methods and results of the pilot study. Chapter 3 describes the realist-informed process evaluation and Chapter 4 details the health economic element of the study. Chapters 5 and 6 present the discussion and conclusions of the study.
Chapter 2 Pilot randomised controlled trial
Introduction
In 2013, the GDC expanded the Scope of Practice for both DHs and DTs following a review of the scientific evidence. 10 This allowed both DHs and DTs to see patients for the first time as the front-line health-care worker. This meant that they could now see patients directly without a referral from a GDP, undertake an examination, formulate a treatment plan and provide clinical treatment within their competence. For DHs, this amounted to the provision of preventative and periodontal care and for DTs this also included the provision of temporary and permanent restorations.
These changes formed the basis of this study and an opportunity to test an alternative care pathway using DTs to undertake the check-up on low-risk routine patients in the NHS. Two earlier NIHR grants investigated the efficacy and efficiency of using DTs in NHS practices [NIHR/CS/010/004 and Health Services and Delivery Research (HSDR) 11/1025/04]. The former demonstrated the diagnostic test accuracy and feasibility of using these groups to undertake check-ups and the latter found that dental practices using DTs in the NHS could be better organised. Pilot studies determine ‘whether something can be done, should we proceed with it, and if so, how’. 106 In WS1, we undertook such an approach to inform the design of a definitive trial.
Aims and objectives
The aim of this WS was to inform the design for a definitive trial by undertaking a pilot study over 15 months to determine whether or not DTs could maintain the oral health of low-risk routine NHS patients, who form a significant proportion of those who regularly attend NHS practices. The objectives of the research were to:
-
determine the most appropriate design of a definitive trial
-
determine whether or not BOP is the most appropriate POM (and, if not, determine the most appropriate measure)
-
confirm the appropriateness of the non-inferiority margin of the chosen outcome measure for the definitive trial (i.e. whether or not the effect estimate lies within an appropriate margin of non-inferiority)
-
further investigate recruitment, retention and fidelity rates
-
confirm willingness to be randomised among study participants
-
determine the potential for patient crossovers between arms (e.g. where the patient’s condition is considered too complex to be managed by the DT).
Methods
Workstream 1 was an individually randomised pilot study undertaken across the North West of England over a 15-month period:
-
population – adult, asymptomatic, low-risk, routine dentate or partially dentate NHS patients attending high-street dental practices
-
intervention – check-up and any subsequent treatment undertaken by a DT
-
control – check-up and subsequent treatment undertaken by a GDP (treatment as usual)
-
outcome – proportion of sites that had BOP.
Changes to design after pilot study commencement
The East Midlands (Nottingham 1) Research Ethics Committee provided a favourable ethics opinion on 9 November 2017 (Research Ethics Committee reference number 17/EM/0365). Subsequent to this approval, two substantial changes were made to the original protocol and these were approved by the East Midlands (Nottingham 1) Research Ethics Committee.
Amendment 1 (2 March 2018)
In the original protocol we stated in the participant inclusion criteria that the patient should not have presented with any active dental decay or required any dental fillings owing to caries within the previous 2 years. However, during the pre-trial training, consultation with the lead clinicians at participating practices suggested that this criterion was too strict. Therefore, this criterion was amended to read that the patient should present with no more than one active lesion in the last year or required no more than one dental filling owing to dental caries within the previous year.
Amendment 2 (16 March 2018)
In the original protocol we stated that we would recruit participants from up to six practices. However, early in the trial it became apparent that it would be difficult to fully recruit the number of participants that we required within the limited recruitment window. The decision was made to extend the number of practices to allow the study team to meet the recruitment target.
Amendments 1 and 2 mitigated any recruitment risks within the specified 5-month recruitment window and were also approved by the National Institute for Health Research (NIHR).
Eligibility criteria
High-street NHS dental practices were recruited across the North West of England. Initially, contact was made with the NHS practices through the NHS Local Area Teams in Greater Manchester and Cheshire and Merseyside (the latter including the Local Dental Network). Paul Brocklehurst ran a workshop to present the study to interested practices on 30 May 2017 and sent follow-up e-mails in June 2017 to confirm practice interest. NHS practices were provided with an overview of the pilot and the associated remuneration that was available to them to undertake the pilot trial:
-
£530 payment to each recruited NHS practice for attending the pre-trial training event to cover the loss of earnings.
-
£50 payment to each recruited NHS practice per participant recruited into the trial, split into £25 at the beginning and £25 at the end of the pilot trial.
-
£25 and £7 payment per patient in the intervention arm for band 1 courses of treatment and £75 and £26 for band 2 courses of treatment (for exempt and non-exempt patients, respectively). This was to cover the loss of NHS payments to the practice caused by the participant being treated by the DT rather than their GDP.
The eligibility criteria for the practices were as follows:
-
The practice should employ at least one DT with at least 2 years’ clinical experience.
-
The majority (> 50%) of adult service provision should be in the NHS.
-
The patient should be treated under the NHS.
-
The practice should have the support of a practice manager.
The following were the eligibility criteria for the individual participants:
-
Adult (aged > 18 years) NHS patient on the recall list of the participating NHS practice
-
no more than one active lesion in the last year or required no more than one dental filling owing to dental caries in the previous year
-
highest basic periodontal examination (BPE) score of ≤ 2
-
asymptomatic at time of the NHS check-up
-
no predisposing medical history elevating oral health risk status
-
seen for routine NHS check-up at least 6 months ago
-
dentate or partially dentate.
New patients, adult patients presenting in pain, patients requiring root fillings or extractions and patients who were edentate or receiving ongoing periodontal treatment were excluded. Patients with sites that had a BPE code of ≥ 3 were excluded (on the recommendation of the Local Dental Network).
Pilot study setting
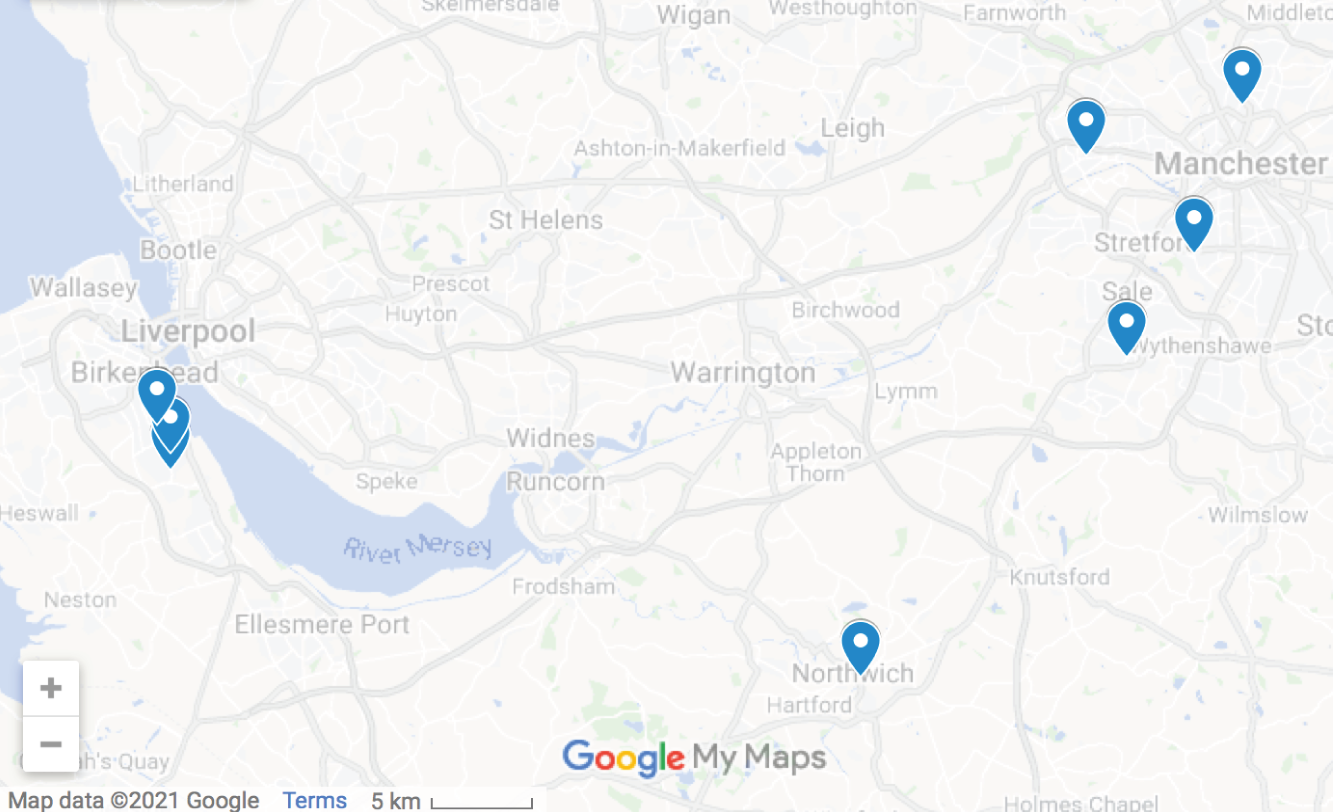
Eight high-street NHS dental practices were recruited across the North West of England. The geographic distribution of the practices is highlighted in Figure 1.
FIGURE 1.
Geographic distribution of participating practices.
Patient pathway
The patient pathway for the pilot study is provided in Figure 2.
FIGURE 2.
Participant pathway through the NHS practice.
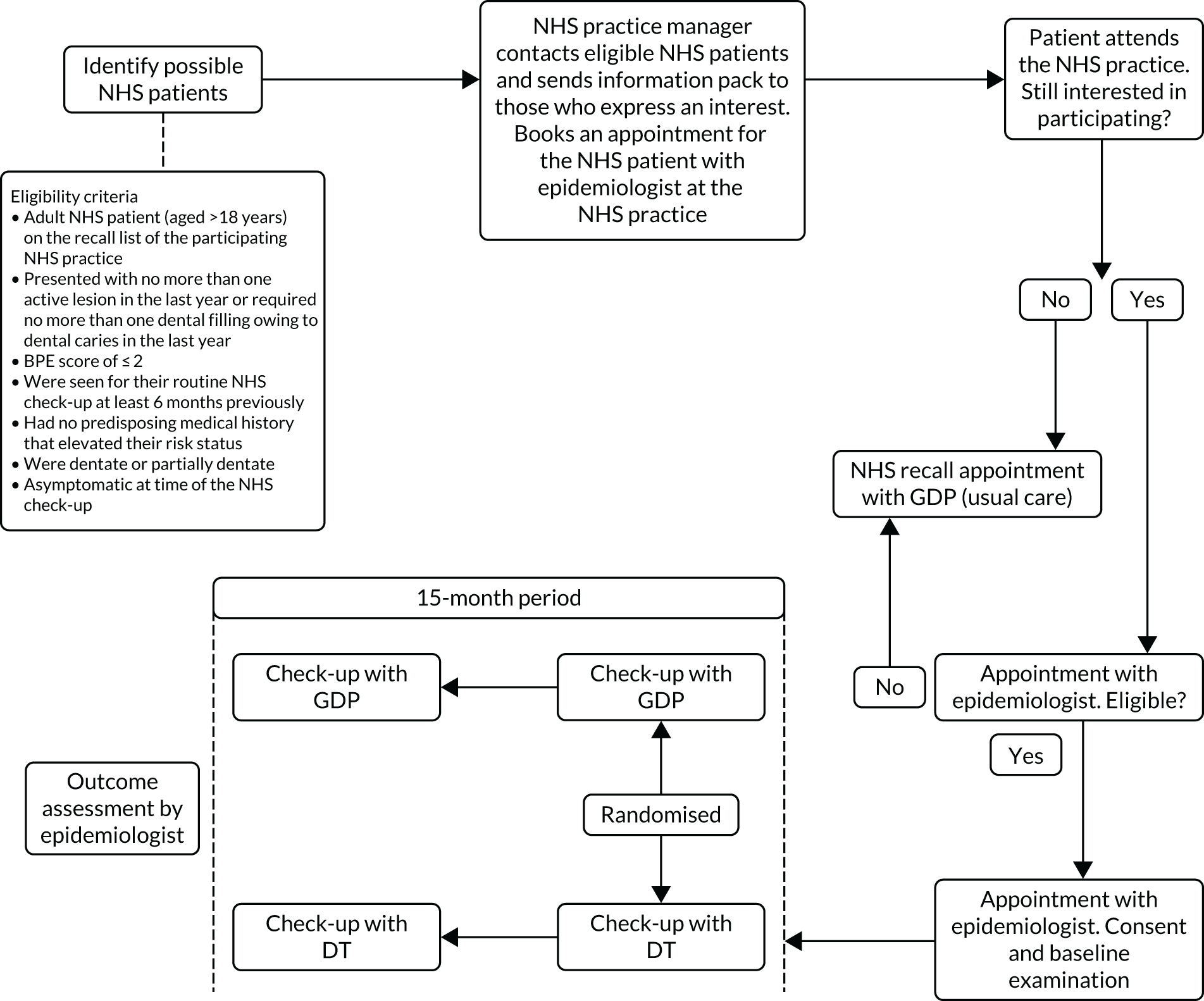
On arrival for their check-up, identified patients were asked by a member of the research team if they had any questions about the study and if they wished to participate. If they agreed, the participant was then asked to sign the consent form and a unique patient identifier was provided to ensure anonymity. A unique patient identifier reference sheet was kept throughout the study, which enabled the participants to be tracked, when necessary. The participants were examined by a trained epidemiologist, who first checked if the patient was eligible for the study and then undertook the baseline measurements for the case report form (CRF) (see Appendix 1). The baseline CRF recorded details that included:
-
age and gender
-
exemption status and employment type
-
ethnicity
-
number of teeth remaining and number of sites (six per tooth)
-
number of sites with BOP (to enable proportion to be calculated)
-
number of sites with visible plaque present
-
Oral Health Impact Profile-14 items (OHIP-14)107 score
-
reported levels of dental anxiety.
The participant was randomised, using the North Wales Organisation for Randomised Trials in Health (NWORTH) Clinical Trials Unit sequential dynamic adaptive randomisation algorithm, to see a DT (intervention arm) or their GDP (control arm). 108 After randomisation, each participant received a check-up in accordance with the arm that they were allocated.
Intervention arm
Under the National Health Service (GDS) Regulations 2005,109 the current care pathway for regular attenders is for NHS patients to see their GDP for their check-up. This reflects the regulatory environment at the time, where DTs could not see patients directly or undertake an examination or treatment plan (i.e. GDPs were the only clinician type entitled to see patients directly under the NHS regulations).
In the latest epidemiological survey (conducted every decade) (n = 11,380), half of all dentate adults reported that they attended their GDP at least once every 6 months and a further 21% indicated that they attended at least once per year. 28 This meant that approximately three-quarters of all the participants in the pilot study were likely to be seen twice in the 15-month period. This concurred with our experience in the feasibility study, where patients were seen for three check-ups during the study period. 99
The patient pathway in the pilot was based on the procedure detailed in the published feasibility study. 99 Given that half of the adult population does not require any further treatment after a check-up (based on national Business Services Authority data), the pilot study focused on low-risk patients. 28 High-risk, complex or symptomatic patients were excluded.
In the intervention arm, participants underwent a check-up by a DT and any subsequent treatment within the DT’s Scope of Practice. The GDC allows DTs to undertake all of the routine direct restorative treatment that GDPs can, except for root fillings. Subsequent visits and treatment were recorded in a separate CRF that recorded the following details:
-
clinical activity/advice provided
-
need for any additional input from the GDP
-
agreement on the subsequent treatment (DT’s plan took precedence)
-
need for the patient to be seen by the GDP (i.e. treatment required was beyond the DT’s Scope of Practice)
-
detail of the treatment undertaken by GDP (if required).
At the end of the study, the same measures that were undertaken at baseline were collected by the trained and blinded epidemiologist, in addition to the following information:
-
dental pain/problems over the study period (including detail)
-
number of new decayed and filled teeth
-
proportion of sites where the BPE exceeded a score of 2.
If participants in the intervention arm experienced pain or presented with problems during the study, they were initially seen by the DT and then offered appropriate treatment, depending on the presenting problem. All treatment information was entered onto the CRF (see Appendix 1), which recorded the type of treatment undertaken and the clinician type involved. After the check-up and/or the completion of any opened treatment plans, the patient was placed back on the recall list according to the recommendations of the DT.
In the feasibility study, no patient crossovers were seen among the 60 patients recruited. 99 Patients were willing to be randomised and recruitment and retention rates were 82% and 78%, respectively. To assess patient crossover, records were kept of those participants who started off in the DT arm but crossed over to the control arm because they were considered to be too complex for a DT to manage their care (this was not seen in the feasibility study). 99
Control arm
When participants were allocated to the control arm, they saw their usual GDP and had their check-up and any subsequent treatment. After the check-up and/or the completion of any treatment, the patient was placed back on the recall list according to the recommendations of the GDP. In similarity with the intervention arm, baseline and outcome assessments were recorded on the CRF by a trained and blinded epidemiologist. The GDPs also entered all check-ups and treatment data on the appropriate CRF.
Randomisation
Randomisation was at the individual level (patient) and performed by the NWORTH Clinical Trials Unit. Treatment allocation was on a 1 : 1 basis using a sequential dynamic randomised adaptive algorithm. 108 This meant that each participant’s allocation was recalculated and was based on the overall allocation level, within stratification variables and within stratum level. This enabled the research team to maintain adequate allocation ratios while maintaining the required balance across the two arms.
A number of potential prognostic factors were considered as stratification factors:
-
deprivation
-
previous history of disease
-
number of teeth remaining.
It was decided by the study team that the most appropriate strata to choose was a proxy measure for material deprivation (exemption status). This was recorded on the CRF.
Primary outcome measures for the pilot
In alignment with the aims of a pilot study, the following were assessed:
-
willingness to be randomised among study participants
-
appropriateness of BOP as the POM
-
appropriateness of the non-inferiority margin (i.e. whether or not the effect estimate lay within an appropriate margin of non-inferiority)
-
recruitment, retention and fidelity rates
-
numbers of participant crossovers between arms (e.g. where the patient’s condition is considered too complex to be managed by the DT).
Proposed primary outcome for the definitive trial
The proposed clinical POM for a future definitive trial was the proportion of sites with BOP. BOP is relevant to both clinicians and patients. It was considered by the research team as stable, measurable and had potential to change over the timescale of the project. This view was reinforced by the fact that BOP was used as the primary outcome in a number of recent NIHR Health Technology Assessment trials conducted in a primary dental care setting. 110,111 Other measures of periodontal health (e.g. pocket depths) were considered to be more sensitive to measurement bias, would take a long time to express and were likely to exhibit a smaller effect. 112
Bleeding on probing is routinely assessed in clinical practice to measure the degree of gingival and periodontal inflammation. Whereas the presence of BOP at isolated sites is not a particularly good indicator of risk for future disease progression, absence or minimal levels of BOP are a very good indicator of periodontal health and tissue stability. 113–115 It is also highly relevant to patients, who often complain of bleeding gums as a first sign of gingival and periodontal problems. This pragmatic end point was relevant to both patients and clinicians and has high generalisability to everyday clinical practice. Furthermore, in the context of the pilot, BOP was considered to be the most sensitive measure for detecting signs of developing gingival inflammation.
Secondary outcome measures collected were based on simple adaptations of indices that are used commonly in clinical practice:
-
proportion of sites that have visible plaque present (measure of oral cleanliness)
-
number of new decayed and filled teeth
-
unplanned visits between check-ups
-
oral health-related quality of life (OHIP-14 score)
-
patient-centred outcomes to explore dental anxiety.
Dental caries was chosen as a secondary rather than a potential POM because it has a relatively low prevalence and longer time to expression in routine low-risk NHS adult patients. This view was further supported by our feasibility study. 99
Sample size
A key issue for a definitive trial to evaluate role substitution is whether or not the design of the definitive study should be a non-inferiority or a superiority design, that is, whether DTs are equally good as GDPs at maintaining the oral health of low-risk routine NHS dental patients (but cheaper) or whether DTs provide superior/inferior care to GDPs. High-quality evidence from the literature is limited in terms of the direction of effect for detecting oral disease and undertaking direct restorations (see Chapter 1).
We decided to base our design on non-inferiority, because this aligned with our policy question about whether or not DTs were as good as GDPs. We also thought that it would provide a more robust estimate of the expected CIs should the results show that a superiority design is warranted. Had the research team undertaken a pilot study based on a superiority design, this would have led to broader estimates of the CIs for the definitive trial if no effect was found (given the smaller number of participants required for a superiority design).
As a result, we estimated that 216 (arm ratio of 108 : 108) low-risk routine dental patients should be recruited across eight NHS dental practices in the North West of England. This accounted for an attrition rate of 30% over the 15-month period, which was similar to the attrition rate seen in our feasibility study and other dental practice-based trials. 99,116 This was based on the CI approach described by Cocks and Torgerson,117 which considers the likelihood of the main study finding a relevant effect size (using the logic that if the observed difference between the arms in the pilot trial was zero, then the upper CI would exclude the estimate that is considered clinically significant in a future trial). Based on an 80% CI, this equated to 9% of the sample determined for the definitive trial. Assuming that BOP would be the POM in the definitive trial, taking a non-inferiority margin of 5% would require a sample of ≈ 1618; 9% of 1619 is ≈ 150 (which becomes 216 when attrition is accounted for).
Exploratory data analysis of clinical outcomes
From the perspective of potential effectiveness, the analysis was focused on the difference in means in relation to the width of the non-inferiority margin for the proposed POM, BOP, and the differences in means and proportions for the potential secondary outcome measures. The effect estimate was based on the difference in means between the two arms and was evaluated with respect to clinical significance over the 15-month period. The remaining clinical and patient-reported outcomes were analysed similarly and interpreted. Three different analysis models were employed. For outcome measures with a baseline measurement, mixed-effects analysis of covariance (ANCOVA) models were employed with the dental practice as a random effect and the following factors as fixed effects: exemption from dental charges (yes/no), number of teeth and the baseline measurement. For outcome measures without a baseline measurement, mixed-effects analysis of variance (ANOVA) models were employed with the dental practice as a random effect and exemption from dental charges and number of teeth as fixed effects. For the behavioural change outcome measures using a dichotomous response scale (yes/no), mixed-effects logistic regression models were employed. Analyses were made on an intention-to-treat (ITT) basis and a per-protocol basis, because per-protocol assessment is considered more conservative for non-inferiority designs. All statistical analyses were fully detailed in a statistical analysis plan that was developed and agreed before completion of data collection.
Ethics issues
Patient safety was paramount during the pilot study. Previous research undertaken by Brocklehurst et al. 78 has shown that DTs are safe as front-line health-care workers (in terms of detecting oral cancer and its precursors). Two large NIHR grants (led again by PB) have also shown that DTs are as good as GDPs in the detection of dental caries and periodontal disease. 97,98
Patient acceptability was another potential concern, but results from earlier studies suggest that this is positive (including a published feasibility study99 and a separate large NIHR project29). The purpose of the study was fully explained in the participant information sheet and patients had the opportunity to ask any questions to the dental team at the practice prior to being consented.
Patient confidentiality was also a key priority and CRFs from the study were anonymised. All forms and files were kept securely on a password-protected personal computer and any paper records kept in a locked drawer.
The protocol specified that all serious adverse events (SAEs) would be described and that we would compare SAEs between the intervention and the control arms. This was recorded on the SAE CRF and included the following details:
-
patient identification (ID)
-
details of SAE
-
severity of SAE (mild/moderate/severe)
-
date of SAE
-
location of SAE
-
consideration of whether or not the SAE was linked to trial participation.
Information on SAEs throughout the study was a standing item on the Trial Management Group, the Trial Steering Committee and the Data Monitoring Committee.
Study management
The study was managed in accordance with Good Clinical Practice (GCP) and overseen by NWORTH Clinical Trials Unit using a dedicated trial manager. The chief investigator is the director of the NWORTH Clinical Trials Unit, which is registered with the UK Clinical Research Collaboration (UKCRC) (#23) and has detailed standard operating procedures (SOPs). As a result, the pilot study adhered to NWORTH Clinical Trials Unit’s SOPs for all trial and data management and statistical and regulatory matters. GCP was employed throughout to ensure that the project was managed to the highest possible standard. Appropriate supervision and training of project-specific staff and training in GCP was ensured. Trial-specific training was provided to all practices at the start of the pilot and reviewed and reinforced throughout the study period. NWORTH Clinical Trials Unit’s quality assurance officer co-ordinated the oversight of monitoring, documentation and all aspects of quality management and regulatory issues. NWORTH Clinical Trials Unit’s senior trials manager provided advice to the management team on all aspects of the study.
The research was sponsored by Bangor University. The Trial Steering Committee consisted of an independent chairperson, independent members and PPI representatives. The group oversaw the running of the trial on behalf of the sponsor (Bangor) and funder (the NIHR Health Services and Delivery Research programme) and had overall responsibility for the continuation or termination of the trial. It ensured that the trial was conducted in accordance with the principles of GCP and the relevant regulations and provided advice on all aspects of the study.
Results
The outcome of the pilot trial and suitability of a definitive trial design were assessed using the following:
-
willingness to be randomised – quantified by considering the numbers approached and who subsequently consented (or refused based on not wanting to be randomised) (see Recruitment and retention)
-
recruitment, retention and fidelity rates – quantified throughout following the Consolidated Standards of Reporting Trials (CONSORT) flow chart process (see Recruitment and retention)
-
numbers of participant crossovers between arms (e.g. where the patient’s condition is considered too complex to be managed by the DT) – quantified from the logs kept by each dental practice (see Protocol deviations)
-
appropriateness of BOP as the POM – quantified by considering the potential effect size indicated by preliminary exploratory analysis (see Baseline measurements and Missing data)
-
appropriateness of the non-inferiority margin (i.e. whether or not the effect estimate lay within an appropriate margin of non-inferiority) – quantified by considering the outcome of the preliminary exploratory analysis (see Exploratory analysis of the primary outcome measure).
Recruitment and retention
A total of 546 NHS patients were invited to participate in the pilot trial. A total of 217 patients agreed to participate over a 5-month period (March 2018 to July 2018) and 328 stated that they were not interested in participating. This equated to a recruitment rate of 39.7% and a mean recruitment rate of 43.4 participants per month. The mean number of participants recruited per site was 27.1, across eight NHS dental practices over the 5-month recruitment period (Table 1). Out of the 217 patients who were randomised, 107 were randomised to the DT arm and 110 were randomised to the GDP arm. The arms appeared well balanced on stratification variables (see Table 1).
| Dental practice | Date first participant recruited | Date last participant recruited | DT arm (n) | GDP arm (n) | Overall, n (%) |
|---|---|---|---|---|---|
| 1 | 5 April 2018 | 3 May 2018 | 16 | 21 | 37 (17.1) |
| 2 | 17 July 2018 | 24 July 2018 | 9 | 9 | 18 (8.3) |
| 3 | 24 April 2018 | 29 May 2018 | 16 | 17 | 33 (15.2) |
| 4 | 2 May 2018 | 5 June 2018 | 18 | 18 | 36 (16.6) |
| 5 | 13 April 2018 | 9 July 2018 | 12 | 9 | 21 (9.7) |
| 6 | 15 March 2018 | 26 April 2018 | 6 | 4 | 10 (4.6) |
| 7 | 11 May 2018 | 22 June 2018 | 14 | 13 | 27 (12.4) |
| 8 | 12 March 2018 | 11 July 2018 | 16 | 9 | 35 (16.1) |
| Exempt | – | – | 10 | 13 | 23 |
| Non-exempt | – | – | 97 | 97 | 194 |
A total of 50 participants did not complete the follow-up assessment at 15 months. Among these 50 participants (23.0% of the total sample), nine participants withdrew from the trial and 41 were lost to follow-up. These 41 participants were lost because of the logistical difficulties of organising a follow-up appointment with an epidemiologist at the practice that the participant was attending. In some cases, participants could not be contacted (by mail, e-mail, telephone or text message), and other participants were unable to attend the practice on designated days owing to work or other commitments. The attrition rate was lower than the attrition rates obtained in previous dental-practice based trials. 99,115 This is represented in the CONSORT flow diagram (Figure 3).
FIGURE 3.
The CONSORT flow diagram for the pilot trial.
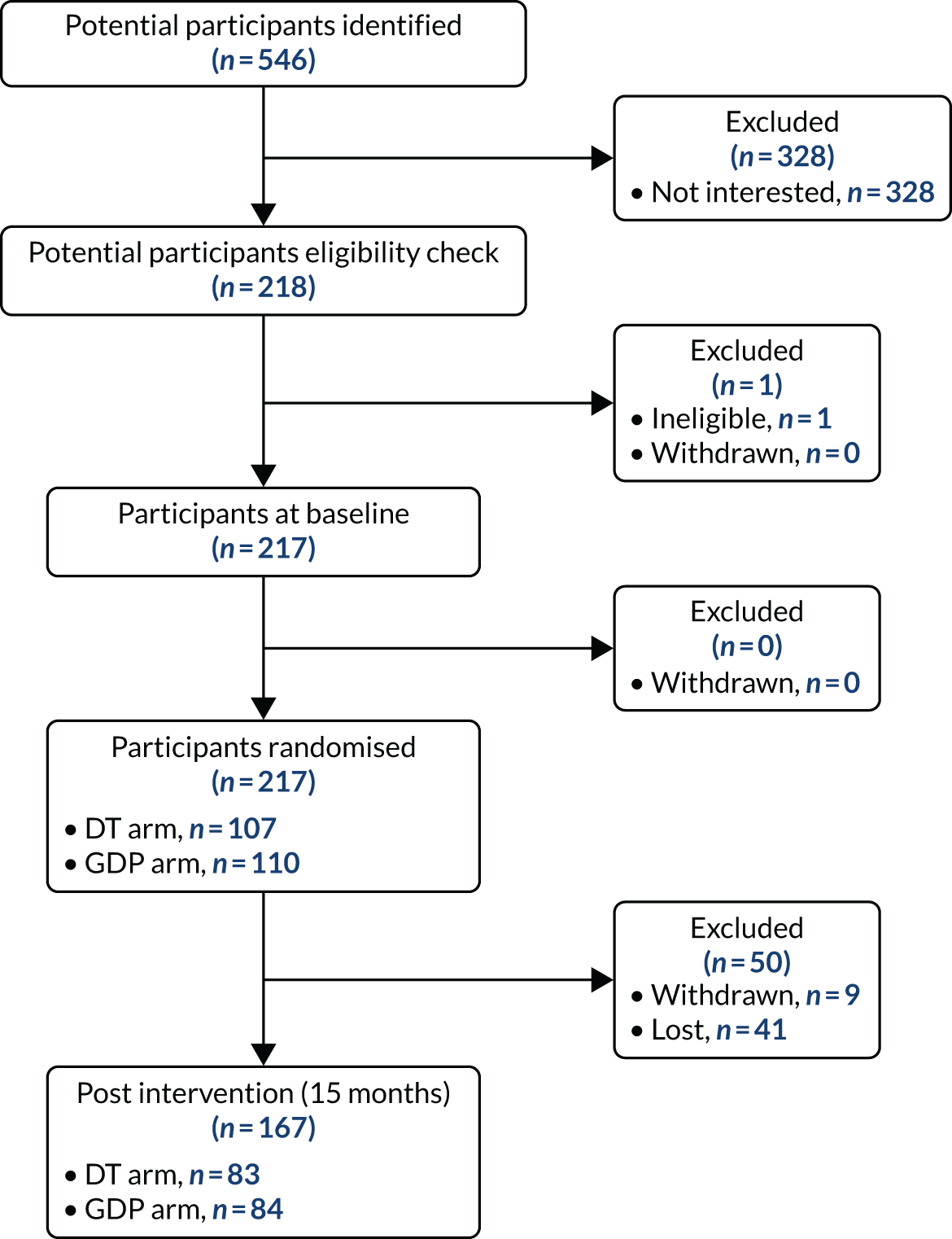
The attrition rates for the DT arm and the GDP arm were comparable (n = 24, 22.4%, vs. n = 26, 23.6%, respectively) over the 15-month period. There was no statistically significant difference in attrition across the randomisation stratification variables (arm, p = 0.873; dental practice, p = 0.676; number of teeth, p = 0.421; exempt from patient’s charge, p = 0.432).
Protocol deviations
There were 14 protocol deviations, all of which occurred in the DT arm. A total of 13 out of the 14 protocol deviations occurred because a participant was allocated to the DT arm but was seen once by the GDP in error, initially. The remaining protocol deviation occurred because a participant was allocated to an arm before being randomised. These 14 participants continued in the arm that they were allocated to but were excluded from the per-protocol analyses.
No participants permanently crossed over from the DT arm to the GDP arm, or vice versa. Therefore, there were no participants who were considered too complex to be managed by the DT. However, 20 participants from the DT arm were seen/treated by the GDP at interim visits, although two of these participants were seen by the GDP because the DT was unavailable. The treatment carried out by the GDPs during these visits included root canal treatment, extraction, crown fitting and restorations.
No adverse events were reported during the study.
Baseline measurements
Participants in the pilot trial were predominantly female (72.4%), non-smokers (92.2%) and white (93.1%) and were not exempt from patient charges (89.4%). The mean age of the participants was 46 years, with a standard deviation (SD) of 15.8 years and a range of 18–87 years. The participants’ occupations are summarised in Table 2.
| Occupation type | Percentage |
|---|---|
| Clerical and sales (e.g. administration, salesperson) | 12.0 |
| Professional and managerial (e.g. teacher, doctor, manager) | 35.5 |
| Semi-skilled and unskilled (e.g. factory worker, labourer) | 2.8 |
| Skilled blue collar (e.g. electrician, plumber, craftsperson) | 7.8 |
| Other | 40.6 |
| Prefer not to say | 1.4 |
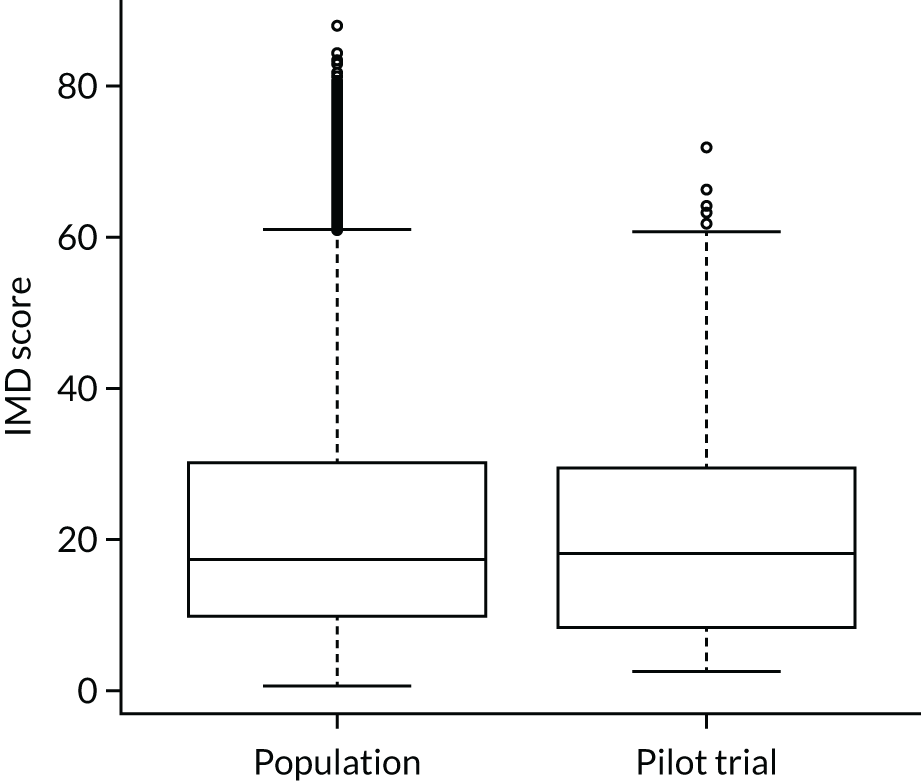
The mean participant Index of Multiple Deprivation (IMD) score was 22.49, with a SD of 17.02, and was comparable with the mean IMD score of the population (Figure 4).
FIGURE 4.
Distribution of IMD scores.
Descriptive statistics of the dental-related measures at baseline are provided in Tables 3–5.
| Measure | n | Mean | SD | 95% CI | Median | IQR | Range |
|---|---|---|---|---|---|---|---|
| Number of teeth | 217 | 25.51 | 2.89 | 25.12 to 25.90 | 26 | 24–28 | 11–28 |
| Number of sites | 217 | 153.04 | 17.32 | 150.72 to 155.36 | 156 | 144–168 | 66–168 |
| Number sites with BOP | 217 | 5.08 | 5.97 | 4.28 to 5.88 | 3 | 1–8 | 0–36 |
| Number sites with dental plaque | 217 | 3.30 | 4.95 | 2.64 to 3.96 | 2 | 0–5 | 0–30 |
| Number of dental caries lesions | 217 | 0.01 | 0.10 | 0.00 to 0.02 | 0 | 0–0 | 0–1 |
| Percentage of sites with BOP | 217 | 3.39 | 3.98 | 2.86 to 3.92 | 2 | 0.60–5.13 | 0–23 |
| Percentage of sites with dental plaque | 217 | 2.25 | 3.32 | 1.81 to 2.69 | 1.19 | 0.00–3.03 | 0–19 |
| OHIP-14 score (0–56 points) | 216 | 0.85 | 2.03 | 0.58 to 1.12 | 0 | 0–1 | 0–19 |
| Anxiety of GDP rating (1–10 points) | 217 | 2.10 | 1.77 | 1.86 to 2.34 | 1 | 1–3 | 1–10 |
| Anxiety of using DT rating (1–10 points) | 217 | 2.12 | 1.72 | 1.89 to 2.35 | 1 | 1–3 | 1–10 |
| Measure | n | Mean | SD | 95% CI | Median | IQR | Range |
|---|---|---|---|---|---|---|---|
| Number of teeth | 107 | 25.48 | 3.02 | 24.9 to 26.06 | 26 | 24–28 | 11–28 |
| Number of sites | 107 | 152.86 | 18.12 | 149.39 to 156.33 | 156 | 144–168 | 66–168 |
| Number sites with BOP | 107 | 5.60 | 6.20 | 4.41 to 6.79 | 3 | 1–9 | 0–28 |
| Number sites with dental plaque | 107 | 3.43 | 5.28 | 2.42 to 4.44 | 2 | 0–4 | 0–30 |
| Number of dental caries lesions | 107 | 0.02 | 0.14 | 0.01 to 0.05 | 0 | 0–0 | 0–1 |
| Percentage of sites with BOP | 107 | 3.79 | 4.24 | 2.98 to 4.60 | 2.08 | 0.60–5.95 | 0–17.95 |
| Percentage of sites with dental plaque | 107 | 2.36 | 3.61 | 1.67 to 3.05 | 1.19 | 0–2.88 | 0–19.33 |
| OHIP-14 score (0–56 points) | 107 | 1.07 | 2.43 | 0.60 to 1.54 | 0 | 0–2 | 0–19 |
| Anxiety of GDP rating (1–10 points) | 107 | 1.95 | 1.73 | 1.62 to 2.28 | 1 | 1–2 | 1–10 |
| Anxiety of using DT rating (1–10 points) | 107 | 1.98 | 1.7 | 1.65 to 2.31 | 1 | 1–2 | 1–10 |
| Measure | n | Mean | SD | 95% CI | Median | IQR | Range |
|---|---|---|---|---|---|---|---|
| Number of teeth | 110 | 25.54 | 2.77 | 25.02 to 26.06 | 26 | 24–28 | 14–28 |
| Number of sites | 110 | 153.22 | 16.59 | 150.08 to 156.36 | 156 | 144–168 | 84–168 |
| Number sites with BOP | 110 | 4.58 | 5.73 | 3.50 to 5.66 | 2.5 | 1–6 | 0–36 |
| Number sites with dental plaque | 110 | 3.17 | 4.63 | 2.30 to 4.04 | 1.5 | 0–5 | 0–25 |
| Number of dental caries lesions | 110 | 0.00 | 0.00 | 0.00 to 0.00 | 0 | 0–0 | 0–0 |
| Percentage of sites with BOP | 110 | 3.00 | 3.70 | 2.30 to 3.70 | 1.76 | 0.60–4.28 | 0–23 |
| Percentage of sites with dental plaque | 110 | 2.13 | 3.02 | 1.56 to 2.70 | 0.94 | 0–3.07 | 0–19 |
| OHIP-14 score (0–56 points) | 109 | 0.64 | 1.52 | 0.35 to 0.93 | 0 | 0–1 | 0–11 |
| Anxiety of GDP rating (1–10 points) | 110 | 2.24 | 1.80 | 1.90 to 2.58 | 1 | 1–3 | 1–8 |
| Anxiety of using DT rating (1–10 points) | 110 | 2.26 | 1.74 | 1.93 to 2.59 | 1.5 | 1–3 | 1–8 |
Missing data
There was an exceedingly low level of missing data in the pilot trial in participants attending baseline and follow-up appointments. There were < 1% missing data for the different primary and secondary outcome measures that were collected across the two time points (baseline and follow-up). The majority of the data points were able to be analysed (76.9%). A summary of the missing data is presented in Table 6.
| Measure | Missing data | |||
|---|---|---|---|---|
| Baseline | Follow-up | |||
| n | % | n | % | |
| Number of sites with BOP | 0 | 0 | 0 | 0 |
| Number of sites with dental plaque | 0 | 0 | 0 | 0 |
| Number of teeth with dental caries | 0 | 0 | 0 | 0 |
| OHIP-14 score (0–56 points) | 1 | 0.5 | 1 | 0.6 |
| Anxiety of GDP rating (1–10 points) | 0 | 0 | N/A | N/A |
| Anxiety of using DT rating (1–10 points) | 0 | 0 | N/A | N/A |
| Anxiety during pilot trial rating (1–10 points) | N/A | N/A | 0 | 0 |
| Total number of unplanned visits | N/A | N/A | 0 | 0 |
| Total time with GDP or DT (minutes) | N/A | N/A | 1 | 0.6 |
Exploratory analysis of the primary outcome measure
The difference between the percentage of sites with BOP in the DT arm and the GDP arm, based on a mixed-effect ANCOVA model, was 0.07% (95% CI –0.49% to 0.63%) over the 15-month period. This estimate is based on a mixed-effects ANCOVA model with the dental practice as a random effect and the following factors as fixed effects: exemption from dental charges (yes/no), number of teeth (≤ 26 teeth or > 26 teeth) and the proportion of sites with BOP measured at baseline.
This estimate did not cross the specified non-inferiority boundary of 5%. Hence, the proportion of sites with BOP for the DT arm could be considered non-inferior to the proportion of sites with BOP for the GDP arm when a 5% inferiority margin is assumed (Table 7). The adjusted mean difference and the 95% CI was replicated in the per-protocol analysis (adjusted mean difference 0.17%, 95% CI –0.41% to 0.75%).
| Measure | Adjusted mean | Adjusted mean difference (DT–GDP) | 95% CI for mean difference | |
|---|---|---|---|---|
| DT | GDP | |||
| Percentage of sites with BOP | 1.87 | 1.79 | 0.07 | –0.49 to 0.63 |
Exploratory analysis of the secondary outcome measures
For the secondary clinical outcome measures, analysis of the proportion of sites with dental plaque and the proportion of teeth with dental caries was based on a mixed-effects ANCOVA and the analysis of proportion of sites for which the BPE exceeded a score of 2 (collected at follow-up) as based on a mixed-effect ANOVA. For the patient-reported outcome measures, analysis of the OHIP-14 score was based on a mixed-effects ANCOVA and the analysis of the anxiety rating for trial check-ups was computed using a mixed-effects ANOVA. The analyses results are summarised in Table 8. The adjusted mean differences and associated 95% CIs from the per-protocol analyses for the proportion of sites with plaque (adjusted mean difference –0.26%, 95% CI –0.77% to 0.26%), the proportion of teeth with caries (adjusted mean difference –0.05%, 95% CI –0.15% to 0.07%) and the proportion of sites that BPE exceeded a score of 2 (adjusted mean difference 0.06%, 95% CI –0.09% to 0.22%) were not substantially different from the estimates obtained from the ITT analyses.
| Measure | Adjusted mean | Adjusted mean difference (DT–GDP) | 95% CI for mean difference | |
|---|---|---|---|---|
| DT | GDP | |||
| Percentage of sites with dental plaque | 1.36 | 1.65 | –0.29 | –0.77 to 0.19 |
| Percentage of teeth with dental caries | 0.12 | 0.18 | –0.05 | –0.16 to 0.05 |
| Percentage of sites where BPE score is > 2 | 0.06 | 0.01 | 0.05 | –0.09 to 0.19 |
| OHIP-14 score (0–56 points) | 0.63 | 1.16 | –0.53 | –1.39 to 0.32 |
| Anxiety rating (1–10 points) | 1.42 | 1.77 | –0.36 | –0.84 to 0.13 |
There were no discernible differences between DTs and GDPs for the clinical measures. The observed differences for patient-related outcome measures were also negligible: for the OHIP-14 score, a 0.5-point difference on a scale of 0–56 points and, for the anxiety rating, a 0.4-point difference on a scale of 1–10 points. Similar differences were also obtained in the per-protocol analysis: a difference of –0.45 points for the OHIP-14 score and a difference of –0.30 points for the anxiety ratings for trial check-ups.
The behaviour change outcome measures, which were based on a dichotomous response scale (yes/no), were modelled using a mixed-effects logistic regression (Table 9).
| Measure | Proportion | Proportion difference (DT–GDP) | 95% CI for proportion difference | Odds ratio | 95% CI for odds ratio | |
|---|---|---|---|---|---|---|
| DT | GDP | |||||
| Reported change in diet | 0.13 | 0.05 | 0.08 | 0.00 to 0.17 | 0.34 | 0.09–1.04 |
| Reported change in toothbrushing | 0.29 | 0.09 | 0.20 | 0.08 to 0.31 | 0.24 | 0.09–0.56 |
| Reported change in toothpaste use | 0.10 | 0.08 | 0.01 | –0.07 to 0.10 | 0.84 | 0.28–2.46 |
| Reported change in flossing | 0.20 | 0.18 | 0.02 | –0.10 to 0.14 | 0.88 | 0.40–1.92 |
| Reported change (other) | 0.19 | 0.09 | 0.10 | –0.01 to 0.20 | 0.44 | 0.17–1.07 |
The difference between the proportions for the DT and the GDP arms in the per-protocol analyses were not markedly different from those obtained in the ITT analyses: reported change in diet (0.08, 95% CI –0.01 to 0.17), reported change in toothbrushing (0.23, 95% CI 0.10 to 0.35), reported change in toothpaste use (0.02, 95% CI –0.07 to 0.11), reported change in flossing (0.01, 95% CI –0.11 to 0.14) and reported other changes (0.09, 95% CI –0.02 to 0.20). The most substantial difference to note is that 20% more participants in the DT arm changed their brushing behaviour. To understand the nature of the brushing behaviour change, a descriptive analysis of the open-ended responses associated with brushing behaviour change was conducted. It revealed that 60% (19/32) involved changing to an electric toothbrush, 16% (5/32) entailed use of interdental brushing and 25% (8/32) involved miscellaneous behavioural change including time spent brushing, thoroughness, technique and frequency of toothbrushing.
The visit-based outcome measure analyses were based on mixed-effect ANOVA models. The results are summarised in Table 10. The results from the per-protocol analyses were highly comparable with the results obtained from the ITT analyses: number of unplanned visits (adjusted mean difference 0.15, 95% CI –0.46 to 0.76) and clinical time with clinician (adjusted mean difference 13.65, 95% CI –6.49 to 33.78). In both cases, there were no substantial differences between the DT and the GDP arms.
| Measure | Adjusted mean | Adjusted mean difference (DT–GDP) | 95% CI for mean difference | |
|---|---|---|---|---|
| DT | GDP | |||
| Number of unplanned visits | 1.21 | 1.03 | 0.19 | –0.39 to 0.77 |
| Total time (minutes) with cliniciana | 68.48 | 53.20 | 15.28 | –3.72 to 34.29 |
Post hoc analysis of intraclass correlation coefficient and power
The interpretation of the statistical findings and the appropriateness of undertaking a post hoc analysis is discussed in Discussion. Intracluster correlation for the proportion of sites with BOP was 0.00 (95% CI –0.02 to 0.10). Therefore, a future trial employing the proportion of sites with BOP as the primary outcome could justify using a smaller estimate of cluster effect.
If we were to take the estimates directly generated from this pilot study to power a definitive study, then, to achieve 90% statistical power for a non-inferiority test for a full trial, assuming a non-inferiority margin of 0.05 and using a SD of 0.04 for the proportion of sites with BOP, we would require a sample size of 30. If we allowed for a 23% attrition rate, as observed in the pilot, we would require a total sample size of 40. If we adopted a more liberal estimate of a 30% attrition rate, we would require a sample size of 44. Note that the large discrepancy between the original pre-attrition sample size of 1618 is due to the SD estimate for the proportion of sites that BOP being vastly higher (0.31).
Discussion
The findings in this pilot trial appear to show that DTs were non-inferior to GDPs (within the non-inferiority boundary set a priori) over the 15-month time period. The point estimates were similar between the two arms in terms of the POM (BOP) and for the remaining clinical measures used the: proportion of sites with dental plaque and the number of new dental caries lesions. There were also no differences (within the non-inferiority boundary) between the two arms in terms of oral health-related quality of life (measured using the OHIP-14) or prospective anxiety about receiving treatment from a GDP or DT. For the process outcomes, there were also no differences between arms in any of the clinical measures. This would suggest that DTs are non-inferior to GDPs in their clinical management of low-risk NHS patients over the chosen timescale and using the selected POM. However, finding a ‘significant’ result in a pilot study should not be overinterpreted. 118,119 The estimates that we used may have still lacked precision, particularly the variability on our proposed primary outcome, and this may have influenced our ability to determine non-inferiority (owing to the reliance on the CI estimates for the parameters). In Results, we provided both ITT and per-protocol analyses, because the latter in this context is more conservative. However, it is also possible that the measures used for this study were exhibiting floor effects because of the low-risk patient population that we drew from (under-representing the variability).
The interpretation of these findings poses some interesting design questions. The purpose of this pilot trial was to determine the most appropriate design for a definitive trial, determine the appropriateness of the POM and the non-inferiority margin, and test recruitment, retention and fidelity rates. It would appear that any future definitive trial to determine the clinical effectiveness of role substitution in NHS dentistry should be based on non-inferiority. No differences were found in the oral health status of patients over the 15 months of the pilot. In addition, despite high retention and fidelity rates, recruitment rates were moderately low (39.7%) when based on the number of patients approached (mean recruitment rate of 43.4 participants per month). These two findings may have substantial implications for a definitive trial in this low-risk population group given the larger number of participants that would be required for a non-inferiority design. This could extend the duration of the definitive study to the point at which the value of information generated becomes questionable in this population group. Equally, there are challenges from a policy perspective, where the recommendations are to see low-risk patients every 2 years. 120
A further challenge is the type of POM that should be used. In this study, we considered BOP, which is routinely assessed in clinical practice to measure the degree of gingival and periodontal inflammation. Earlier studies suggest that the levels of BOP are a very good indicator of periodontal health and tissue stability. 112–114 As a pragmatic primary end point that is relevant to both patients and clinicians, BOP would also appear to be sensible and it was among the outcome measures used in our earlier feasibility study. 99 However, based on evidence from this 15-month pilot study, it could be argued that there are floor effects (i.e. the signal/event rate is so limited among low-risk patients that it makes differentiation between the two arms difficult). When compared with the Adult Dental Health Survey16 (a cross-sectional sample of the general population), the levels of both periodontal inflammation and plaque in this sample were much lower. Given that we used experienced epidemiologists in this pilot trial, this would suggest that NHS patients exhibit particularly low levels of need when only low-risk participants are included, which this only increases the potential for floor effects.
This is even more relevant for clinical measures, such as dental caries. Dental caries was chosen as a secondary outcome measure rather than a potential POM in this study because it has a low prevalence and longer time to expression in routine low-risk NHS adult patients. 16 This was supported by the data from this 15-month pilot, in which no new lesions developed, and by our feasibility study, in which the proportion of sites with active caries was between 1.19% and 2.60%. 99 Systems developed for the detection of small incremental changes in dental caries status, such as the International Caries Detection and Assessment System (ICDAS), have been advocated, but some argue that these suffer from measurement bias. 121,122 According to Frencken et al. ,122 ‘caries prevalence should not be based on the dmf/DMF [primary dentition decayed-missing-filled/permanent dentition decayed-missing-filled] index but on cavitated dentine carious lesions (d/D-component) as the M- and F- component do not refer to a disease stage’. Although it is acknowledged that these tools are used more in epidemiological surveys, signal/event definition, low event rate and slow progression of dental caries in low-risk patients remain problematic when marginal differences are being assessed in a clinical trial.
These issues are pertinent to the design of a definitive trial. In the recent NHS contract reform process undertaken in Wales, where need and risk where measured (using the ACORN), over two-thirds of NHS patients were judged to be low risk (Colette Bridgman, personal communication). As a result, even if we were to include a higher-risk patient population in the study sample for a definitive study, it is likely that any signal of effect would be drowned out by the proportion of low-risk NHS patients. It may be possible to consider analysing a ‘complete’ sample (including high- and low-risk patients) using an appropriate zero-inflated model, but this may not facilitate a full interpretation of effect or non-inferiority. The literature indicates that there are a number of ways of considering the development of various thresholds for a pilot study, but these should all be considered a priori. 118,119,123
It would appear that the types of clinical outcomes that would be used for a definitive trial on role substitution in dentistry may not be appropriate to test for non-inferiority. So, what would be an appropriate outcome measure? Patient-related outcome measures and patient-related experience measures may be two options, but their sensitivity and signal-to-noise ratios may, again, be problematic and appear to be further down the causal pathway to assess clinical effectiveness and/or non-inferiority. These issues are explored further in Chapter 6, Recommendations for further research.
Summary
The policy-relevant question that underpinned this pilot trial was whether or not role substitution is clinically effective in NHS dentistry. By virtue of the nature of the policy context for role substitution, it did appear that low-risk populations were the most relevant population to test a priori. The results from this study suggest that relaxing the eligibility criteria to include NHS patients with greater risk and greater clinical need may be more appropriate from a design perspective. However, the ratio of low to high risk remains problematic in a practice context, given the potential of the former diluting any effect seen in the latter. This does not mean that the results of this pilot lack any significance from a policy perspective. The results suggest that DTs could provide care for low-risk regular attenders in their own right or between longer recall frequencies with GDPs, although caution needs to be exercised in overinterpreting the findings from a statistical perspective. Given that the oral health of regular attenders is improving (see Chapter 1), the results of this study will help inform ongoing and future NHS dental reform programmes across the UK.
Chapter 3 Realist-informed process evaluation
Introduction
Workstream 2 was a theoretically-driven process evaluation that focused on the micro, meso and macro factors that influence implementation of role substitution in general dental practice. WS2 ran in parallel to the pilot trial using a realist-informed approach to understand ‘what is it about a programme that works for whom, in what circumstances, in what respects, over which duration’. 104 This built on the qualitative work undertaken alongside WS1, which explored operational factors that influenced the delivery of the pilot trial. Realist methodology is used extensively in health services research; the approach recognises the complex and contingent nature that underpins the settings for new interventions and service delivery. This approach alongside process evaluations ‘supposes that regularities in the patterning of social activities are brought about by the underlying mechanism constituted by people’s reasoning and the resources they are able to summon in a particular context’. 124
Aims and objectives
The aims and objectives of this WS were to undertake a process evaluation informed by realist methodology to understand what works, for whom, why and in what circumstances.
Methods
Moore et al. 103 argue that process evaluations should capture the contextual factors that shape the intervention, mechanisms that sustain or potentiate effects, unexpected pathways and consequences and the contextual factors that shape implementation. To aid the process, realist principles were used to develop an understanding of ‘what works about the intervention, why, how and under which circumstances’. 105,125 As Rycroft-Malone et al. 126 articulate, theories can capture how complex interventions and systems can interact, so a realist approach tends to combine the elements of both substantive theory and stakeholders’ own theories about how an intervention might work:
. . . rather than identifying linear cause and effect relationships through successionist logic (x causes y: often illustrated through logic models), realist enquiry is concerned with identifying the underlying generative mechanisms about how interventions work [or not].
Rycroft-Malone et al. 126
Although logic models are helpful for specifying intervention components as inputs and outputs, they can be less useful for developing contingent explanations between them. 126 As highlighted by Brand et al. ,127 ‘to build implementation and delivery knowledge it is helpful to understand how context (individual, social, cultural, organisational) interacts with intervention components and underpinning mechanisms to bring about desired outcomes’. In this sense, a mechanism is both the resource that an intervention provides and the recipients’ reasoning and response to it. 128 Dalkin et al. 128 argue that these mechanisms are not dichotomous in their action (on–off) but, rather, operate across a continuum, interacting in a context to produce a specific outcome. Realist methodology defines mechanisms as a reaction to ‘a resource that the intervention provides and the recipients’ reasoning about and response to that resource, and the context in which that mechanism will be activated’. 125 As highlighted in Chapter 1, this form of approach adds real value to our overarching research question about the use of role substitution, given the range of factors that can influence its utilisation in NHS dental practices.
In this chapter, we also use the idea of theories to refer to key stakeholders’ ideas about how an intervention works, which is derived from their experience. 129 Kislov et al. 130 argue for a ‘shift of focus from ‘theory’ as a relatively isolated, static, reified source guiding implementation, towards embracing ‘theorising’ as a set of processes that aim to use empirical data actively in developing, validating, modifying, and advancing conceptual knowledge in the field’. Theories in this sense are defined as ‘an ordered set of assertions about a generic behaviour or structure assumed to hold throughout a significantly broad range of specific instances’. 131 Kislov et al. 130 argue that mid-range theories (MRTs) are particularly helpful in understanding the factors that influence the implementation of new working practices. Here, the evaluation is focused on a narrow range of factors that could potentially influence adoption, as opposed to grand theories, which aim to ‘construct all-encompassing meta-narratives that span space and time’. 131 Realist methodologies commonly present these theories as a function of contexts (C) and mechanisms (M) that lead to a particular outcome or set of outcomes (O) [f(C,M,O)]. This can necessitate the apportioning of a specific factor to either a context or a mechanism, which can sometimes appear to stakeholders as a contorted process, particularly at the outset where initial programme theories (IPTs) are being developed. As a result, a number of realist researchers are now simplifying this process and using IF-THEN propositions capture a combination of f(C,M) that lead to any given outcome. 132,133
The process for this study is outlined in Figure 5. Initially, this involved working with a stakeholder group to develop IPTs, framed as IF-THEN statements. This was followed by a process of testing and refining the IPTs using semistructured interviews to develop ‘mid-level’ programme theories, to provide an explanatory framework for role substitution in NHS dentistry. 105 It then culminated in a final stakeholder group to ‘sense-check’ these theories and place them in order of priority. Ethics approval for the study was granted by the East Midlands NHS Research Ethics Committee (#17/EM/0365), as part of the larger study.
FIGURE 5.
Overview of a realist-informed process.

Initial programme theory development
Phase 1 of the realist-informed process evaluation aimed to develop an initial set of candidate IPTs. As highlighted by Randell et al. ,125 ‘theory elicitation can be carried out in a number of ways, such as interviewing stakeholders, reviewing the extant literature on the topic, identifying relevant theories from the literature, or some combination of these approaches’. In this study, we decided not to undertake a review of the literature or undertake a more formal realist synthesis, owing to the expertise of the group and the number of studies already known to the team (see Chapter 1) and/or undertaken by the chief investigator. This report builds on the work undertaken for a 5-year Clinician Scientist Award (reference number NIHR/CS/010/004) and two previous NIHR HSDR grants (reference numbers 11/1025/04 and 14/19/12). As a result, we used this and other evidence gleaned from the literature with key stakeholders as a starting point to elicit candidate IPTs, based on their experience of role substitution in general dental practice (Table 11).
| Factor | Detail |
|---|---|
| Financial | Dental practices have to maintain their profitability to survive as small- and medium-sized enterprises. Because of this, supplier-induced demand can prevail over health-care need. Remuneration structures should align with population need. The unit cost for DTs are higher than other DCPs because of their higher levels of skill. Coupled with the inability of DCPs to contract directly with the NHS, this makes it difficult for dental practices to financially capitalise on the promise of role substitution. Role substitution in medicine can reduce costs, but this occurs only where nurses release doctors’ time to undertake activities only they can perform |
| Estate | DTs and DHs require sufficient surgery space and clinical support and many practices have only one surgery in operation |
| Regulatory | Regulatory structures governing DCP practice limits the autonomy of DTs and DHs. GDPs are also liable for the acts of DCPs in a NHS contract. Changes to the GDC Scope of Practice have facilitated direct access to DTs and DHs, but the NHS GDS regulations still require a GDP to open a course of treatment. Transactional costs attributed to the time lost during a referral from GDPs to DTs and DHs can affect their use. DTs and DHs cannot prescribe medicines or radiographs, which further increases transactional costs |
| Institutional logics | Role substitution can challenge professional boundaries and lead to some resistance. Where GDPs support the use of role substitution, it is more effectively implemented. GDPs’ confidence in their DCPs also influences positive referral relationships |
| Patients | Social acceptability of DCPs is generally positive. However, public awareness of the Scope of Practice of DTs is lower than that of DHs and this may be a barrier to effective implementation |
| Training | Higher education institutions receive a lower tariff from the government for DT and DH training and DCPs do not attract ‘service increment for training’ payments (unlike doctors and dentists). Therefore, the incentive for higher education institutions to train a GDP is greater than for DTs and DHs. Updating workforce planning models and ensuring that demand and supply-side factors are accounted for is necessary to promote the training of DCPs |
Realist methodology proposes the use of ‘teacher–learner cycles’ in stakeholder interviews, where the researcher teaches back the theories to the interviewees. The researcher then invites the interviewees to comment, based on their particular experience and perspective, to teach the researcher. 104 Similar to the use of IF-THEN propositions, this type of approach allows greater circumspection in the theory-generating stage, ahead of refining into specific [f(C,M,O)] configurations. 134 As Nanninga and Glebbeek134 argue, ‘explication of what was rejected, modified and contextualized can help in the process of theoretical understanding’, facilitating the ‘insight that is needed to accumulate knowledge in the sense of families of context, mechanism and outcome (CMO) configurations (middle-range theories) that are more or less stable and (re)cognizable’. This was the approach that we adopted in the IPT development and refinement to generate the MRTs, using the information contained in Table 11 as a starting point and working with the stakeholders that we engaged with (Table 12).
| Stakeholder type | Reasoning |
|---|---|
| Chief dental officer for Wales | Senior policy-maker |
| Local Dental Network (Cheshire and Merseyside) | Active group of DCs and GDPs, with responsibility for regional commissioning (also included DCPs) |
| British Association of Dental Therapy (URL: www.badt.org.uk; accessed 8 December 2020) | One of the two professional groups for DCPs |
| DCP lead (Health Education and Improvement Wales) | Responsible for dental commissioning in Wales in relation to education and training for DCPs |
Given the range, geographic distribution and limited availability of the different stakeholders, the research team could not arrange a single focus group and so undertook semistructured interviews with representatives from each stakeholder type. In each interview, we focused on the current use of role substitution in general dental practice (informed by Table 11) and identified mechanisms that acted to facilitate or potentiate its use. We also sought to understand the unexpected pathways and consequences of using DTs to undertake the check-up and any subsequent treatment. Given the different types of stakeholders that we interviewed, we also focused on the contextual factors that shape implementation at a micro, meso and macro level. The emerging themes were then ‘sense checked’ by the chief dental officer and the DCP lead.
Semistructured interviews with the stakeholders were undertaken face to face and by telephone, audio-recorded and transcribed verbatim. A semistructured interview schedule ensured that the interviews focused on the views of the participants. In each interview, we presented the stakeholders with the evidence from the literature and asked them for comments based on their own experience of role substitution. Open-ended questions were also included to surface new areas for investigation. An iterative approach was taken to the data and a working document was used to record the emergent themes. These were reviewed after each interview. Interviews lasted no longer than 60 minutes.
Data analysis for phase 1 followed an inductive approach, guided by the literature, but also one that sought stakeholders’ experiences of role substitution in NHS dentistry. The researchers immersed themselves in the data by initially reading and re-reading the transcripts. Initial codes were then generated from the transcripts by each of the researchers independently (PB and CW). As part of this process, highlighted phrases were compared and a coding frame was developed to aid in the development of IF-THEN propositions. These statements captured the experience and thoughts of the stakeholders on role substitution, exploring the different conditional factors that were raised by the different groups (both barriers and enablers) and how this varied with the situational contexts at the micro, meso and macro level. 126 The results of the stakeholder analysis are provided below in Results, Initial programme theory development.
Theory testing
Phase 2 of the realist-informed process evaluation tested the IPTs developed from phase 1 (presented as IF-THEN propositions). This was undertaken using semistructured interviews with a broad range of stakeholders who had active and ongoing experience of role substitution (Table 13). To ensure that we could capture ‘mid-range’ theories, phase 2 focused initially on practice owners (n = 3) and DTs (n = 5). This enabled the research team to capture the perspective and experience at the micro level to test the emergent IPTs. 104
| Stakeholder type | Reasoning |
|---|---|
| DC | To understand the contextual factors that shape implementation in the supply of service provision at the meso and macro level |
| Dental practice owner | To understand the mechanisms that sustain or potentiate effects, unexpected pathways and consequences in the supply of service provision at the micro level from the perspective of the employer |
| DT | To understand the mechanisms that sustain or potentiate effects, unexpected pathways and consequences in the supply of service provision at the micro level from the perspective of the employee |
| Public | To understand the acceptability of role substitution at the micro level and the factors that may shape the demand of services |
Each participant was presented with a set of opening IF-THEN propositions (see Table 15) that had been developed from the literature and the research team in phase 1. They were divided into four main themes: contractual, institutional logics, regulatory and training. These were presented as initial thoughts to stimulate discussion, in accordance with the teacher–learner approach. As highlighted by Randell et al. ,125 ‘there is an infinite number of potential influences on the interactions between a complex intervention and its intended recipients, and an infinite number of potential impacts resulting from those interactions’.
Interviews were undertaken face to face and by telephone, audio-recorded and transcribed verbatim. After the participants were presented with the emergent IPTs (represented as IF-THEN statements), they were asked to reflect on whether or not, and in what ways, the emergent IPTs fitted with their own experiences. Open-ended questions were also included (Table 14) to elicit new areas for investigation. The teacher–learner approach enabled the research team to focus on the key issues that facilitate (or not) the use of role substitution in practice, testing the stakeholders’ responses to the different IPTs. Thus, the interviews were designed to support both ‘theory gleaning’ and ‘theory refinement’. 135
| Number | Question |
|---|---|
| 1 |
|
| 2 |
|
| 3 |
|
| 4 |
|
| 5 |
|
| 6 |
|
| 7 |
|
| 8 |
|
| 9 |
|
After each interview, the interview topic guide was reviewed and, where necessary, revisions were made to incorporate either new theory areas or refinements to the supplied IF-THEN propositions, in accordance with the teacher–learner approach. This enabled the research team to sense check with participants and explore emergent findings in subsequent interviews. An iterative approach was taken to the emerging data and a working document was maintained that recorded the emergent themes. These were reviewed after each interview (by PB, CW and LW). Any discrepancies were discussed (between PB, CW and LW) and were resolved through discussion and reference to the surrounding literature and the emerging data. The latter approach governed the analysis across the project, given the range of backgrounds of the different researchers. Chris Woods and Lynne Williams had no dental experience, whereas Paul Brocklehurst had previously undertaken research in this area. Given Lynne Williams’ experience in realist research, it was possible to ensure that multiple viewpoints were accommodated in a democratic manner.
A deductive approach was taken to the analysis of the interviews, where the IF-THEN propositions required refining. In parallel, an inductive thematic approach was taken to the emergent data, which provided fresh insight and new candidate IPTs. For the latter approach, the research team (PB, CW and LW) immersed itself in the data by initially reading and re-reading the transcripts. New IPTs were then generated from the transcripts, again expressed as IF-THEN statements, which were formed by collating common emergent themes and looking for patterns in these themes across different contexts, mechanisms and outcomes.
Observation can often be used alongside realist evaluation to enable IPTs to be ‘guided and informed by incidents arising from the[se] observations’. 135 As a result, our realist-informed process evaluation drew from observations that were made while running the pilot study. These took the form of field notes made before and after the semistructured interviews to allow for further theory testing. 136 We followed the approach adopted by Randell et al. 125 and ‘summarised the anticipated contextual factors from the theories (whether or not they were present), other contextual factors that appeared to exert influence, anticipated mechanisms from the theories (whether or not they appeared to be at play), other mechanisms that appeared to be at play, and anticipated and unanticipated outcomes’.
To develop new candidate IPT from the emergent data, coded extracts were first elicited from the transcripts and accompanying field notes. This was undertaken iteratively, indexing the earlier transcripts to test the applicability of the codes that were generated and to assess agreement across the research team undertaking the analysis. Where there was variation in the indexing, the codes were refined and definitions were clarified. Overarching themes were then developed from these codes by organising them into clusters based on the similarity of their meaning. These were then checked against the coded extracts and the raw data (by PB and CW) to ensure coherence and that they were representative of what the stakeholders were trying to convey.
As data collection continued, new interview transcripts were analysed and this enabled the research team to make across-stakeholder comparisons and develop a richer understanding and new perspectives on both the context and the mechanisms that led to specific outcomes. By presenting the stakeholder with the initial IF-THEN propositions, this allowed the team to explore the broad range of contexts and mechanisms (represented within the IF element of the IF-THEN statement) to outcomes (represented within the THEN element of the IF-THEN statement). The results of the stakeholder analysis are provided in Results, Theory testing.
Refinement of the initial programme theories
Phase 3 of the realist-informed approach involved refining the IPTs to prioritise and consolidate our understanding of pertinent and explanatory MRTs. Phase 3 of our realist-informed approach to the process evaluation involved interviews with dentists (n = 5), DTs (n = 8), DCs (n = 3) and patients (n = 6). Patient interviews were undertaken with a user researcher who had been trained in qualitative interviewing for this study. This strengthened patient voice in the interviews and ensured that the prioritisation and refinement process were grounded in patient experience. The six interviews equated to 32 hours of user researcher involvement and training.
Again, the interviews were undertaken face to face or by telephone according to the geographic location and the availability of the different stakeholders. Interviews were analysed deductively for the research team to prioritise and refine the IPTs. The results of the refinement of the IPTs are provided in Results, Refinement of the initial programme theories.
Feedback on the final programme theory
The final programme theory was presented to a key stakeholder meeting. The results of the refinement of the IPTs are provided in Results, Feedback on the final programme theory.
Results
The results of the different stages of the realist-informed process evaluation are provided in Initial programme theory development, Theory testing, Refinement of the initial programme theories and Feedback on the final programme theory.
Initial programme theory development
The IF-THEN propositions developed from the stakeholder group are given in Table 15. At this stage of the process, the focus of the discussions was on contractual, institutional logics, cultural, regulatory and training issues (informed by the literature presented in Chapter 1).
| Theme | Number | IF-THEN statement |
|---|---|---|
| Contractual | 1 | IF the NHS contract allowed DTs to open a NHS treatment plan THEN patients would have direct access to DTs without the need to see the DENTIST first, increasing the efficiency of the patient’s journey through the practice |
| 2 | IF the NHS contract allowed DTs to be put on the National Performers List THEN DTs could earn UDAs, thereby increasing the profitability of using DCPs in the practice | |
| Institutional logics | 3 | IF DTs are seen to be endorsed by the DENTISTs in the NHS practice THEN patients are more likely to trust being treated and managed by DTs |
| 4 | IF DTs are used to their full Scope of Practice THEN they can pose a threat to professional boundaries because of the overlap with GDPs, leading to a reluctance to delegate clinical tasks | |
| 5 | IF DHs are used in NHS practices THEN they can be used to upsell NHS courses of treatment, supplementing rather than substituting a GDP’s clinical activity | |
| 6 | IF DTs are used in NHS practices THEN they are commonly underutilised as DHs (for multiple reasons: DTs are a challenge to professional boundaries and DH skills are understood better and can be used to upsell NHS courses of treatment) | |
| Regulatory | 7 | IF DTs could prescribe medicines and radiographs THEN they could undertake NHS treatment without the need for the GDP to see the patient, which would improve the efficiency and profitability of the practice |
| Training | 8 | IF DTs have experience working to their full Scope of Practice THEN they can perform tasks as effectively as GDPs |
| 9 | IF GDPs were trained alongside DTs THEN they would become more aware of their Scope of Practice and clinical skills, leading to greater utilisation after they qualify | |
| 10 | IF there were incentives in the NHS contract to use DTs THEN more could be trained by dental schools |
Theory testing
In the theory-testing phase of the realist-informed process evaluation, we explored the IPTs that had been generated from the theory development phase. The results of this phase are detailed in this section, with representative quotations. The remaining data are presented in Report Supplementary Material 1.
Contractual
As highlighted in Chapter 1, NHS dental contracts can heavily influence the utilisation of role substitution. These were the first two IPTs that we sought to test. We gave some consideration to incorporating these into one ‘contractual’ theory area, but initially there appeared to be two separate issues that arose from the stakeholder workshops – one that related to access and efficiency and a separate (but related) issue on UDA generation:
-
IPT1 – IF the NHS contract allowed DTs to open a NHS treatment plan THEN patients would have direct access to DTs without the need to see the GDP first, increasing the efficiency of the patient’s journey through the practice.
-
IPT2 – IF the NHS contract allowed DTs to be put on the National Performers List THEN DTs could earn UDAs, thereby increasing the profitability of using DCPs in the practice.
For many of the stakeholders, these two theory areas were the most important. For DTs, there was frustration at the current NHS regulations, meaning that only a NHS GDP could open a course of treatment:
At the moment everything’s just . . . you have to have a dentist to open a course of treatment and for some of the simple examinations, especially that we’ve been doing on this [pilot] trial, there’s no reason why there needs to be a dentist to open a course of treatment.
DT 1.13
We should be able to open a course of treatment definitely. And, it would be easier for the patient because they have the periodontal treatment with you, and then they say, and I’m going to see you next time, because you say, I’d like to see you again in 3 months.
DT 3.138
I think that’s a good idea [therapists opening a course of treatment], because it just makes it easier, because obviously if they’re going to come in and see a therapist it’s better if they can manage things themselves rather than us having to do it for them.
GDP 5.62
This was also evidenced by all GDP responses, bar one:
Especially the therapists that I have for the last few years, I trust them, I trust their judgement; so yes, I will feel confident for them to treat or check the patient from day 1.
GDP 2.54
Assuming the therapist model goes ahead, I just feel that there is a role definitely and it’s just the system will need to adjust to it, to adapt to that role where if the patient comes in they can just see the therapist directly and they can open the form, manage and treat them, send the form off and do all the work that they need to do.
GDP 5.69
You always need a dentist on site. And it should be the dentist that is the main person, I would say, of the treatment, and the therapist supporting that.
GDP 2.378
One interesting element that was raised by the stakeholders was how the patient’s health status could mediate this. Opening a course of treatment for new or complex patients was seen to be more problematic for a DT than opening a course of treatment for low-risk patients who regularly visited the practice:
It would be difficult, I suppose, if it is a new patient, which is fair enough, that’s why they can’t always do that as well. But especially with the low-risk patients, easily they can open a course of treatment.
GDP 2.32
Maybe the initial appointment, I would say just probably the dentist. And then if it’s a long-established patient with really low risk, easily it can be treated and monitored by the therapist, and as soon as they’ve noticed something that is worrying, someone has changed medication, or habits, diet, all these things, obviously they just need to be involved.
GDP 2.43
Stakeholders also raised the issue of the management of emergency patients and here, unlike the management of new patients, the response was more nuanced:
From the patient’s point of view, to have better access to the practice for routine examination as well, instead of waiting for long appointments, or even for emergency appointments, if it’s a small fracture and something that the therapist can deal with, it’s definitely working much better to be able for the therapist to open the course of treatment.
GDP 2.105
It’s just the NHS have this rule where we can’t open our [own] courses [of treatment], as you probably know. So I sometimes think if you have a child in who’s in pain and there was no dentist that could open a course [of treatment] you could probably help that kid, you could take the tooth out or do a filling, but you can’t because you can’t open a course [of treatment].
DT 7.48
Stakeholders also highlighted how inefficient the current NHS contract was in relation to the use of role substitution (regarding opening a course of treatment):
They could see us in one appointment rather than having maybe several appointments, especially if the dentist is busy doing stuff that’s obviously outside my Scope of Practice.
DT 1.39
It’s not cost-effective either I don’t think for the practice. It would be much more effective if the patient just came once, especially if I’m free then I can see the patient and complete the treatment. The patient doesn’t have to come back.
DT 1.49
There are courses of treatment that, for example, periodontal treatments, where the therapist is more than capable of seeing the patient after 3 months for follow-up appointments without the dentists’ intervention. And, that would be easier for the patient then because they have to, at the moment they have an appointment with the dentist and then an appointment with the therapist and it’s not always possible to have that on the same day. So, it’s two journeys.
DT 3.59
The thing that the trial has sort of reinforced me is that the NHS restrictions and regulations are just so outdated and are restricting us to working as efficiently as we could.
GDP 6.832
The opinions of associate dentists were also referenced in relation to the transactional nature of internal referrals in the practice:
Sometimes they’re just like oh it’s more hassle to do it and some of the associates don’t necessarily want to refer some of the stuff to us because they’re like well we’re going to lose some of that.
DT 1.532
I know why they haven’t sent it through to me as well because they don’t want to pay for it. Because otherwise they’re not making any money on it, UDAs obviously just work out cost-efficient for them.
DT 4.98
Financially they think they can do it quicker or better. I think restorative, a lot of dentists do their treatment on the spot.
DT 4.123
In addition to the inability to open a course of treatment, the UDA system was constantly referred to by all of the stakeholders:
The number of UDAs and the holder of the contract, normally the practice owner or owners, have ultimate responsibility for that. And then there’s subcontracting, the self-employed [associate] dentists in a number of UDAs, and so if you did bring in a therapist, you can’t say, oh, I’ve got another member of the team now, we’ll just attract more UDAs. The NHS has stopped giving out more UDAs.
GDP 6.406
You’d have to work out a fair system. I don’t think the UDA system quite does it.
DT 3.542
Most of the work then that we’re going to do . . . say for example you’ve got your three UDAs, the dentist is still going to want that one UDA from you.
DT 1.420
In my practice what I’m trying to is that I’m mainly the only person that can refer the patient to the therapist, I don’t really involve my associates; so I don’t have this kind of argument whether to deduct UDAs or deduct . . .
GDP 2.423
I can’t just go down to them and be like, can you open it, because they won’t, because then it’s their UDAs, isn’t it, instead of the ones that it should be . . .
DT 4.69
If we could open a course of treatment then all the UDAs would then be allocated to the therapists . . . whereas at the moment the associate would get probably, one UDA and two UDAs would be allocated towards the therapist for doing umpteen fillings whatever . . .
DT 3.515
Institutional logics
The discussions around the NHS dental contract also related to four other IPTs that were tested within the domain of institutional logics:
-
IPT3 – IF DTs are seen to be endorsed by the GDPs in the practice THEN patients are more likely to trust being treated and managed by DTs.
-
IPT4 – IF DTs are used to their full Scope of Practice THEN they can pose a threat to professional boundaries because of the overlap with GDPs, leading to a reluctance to delegate clinical tasks.
-
IPT5 – IF DHs are used in practice THEN they can be used to upsell NHS courses of treatment, supplementing rather than substituting a GDP’s clinical activity.
-
IPT6 – IF DTs are used in practice THEN they are commonly underutilised as DHs.
Endorsement by key members of NHS dental practices was seen as a key area that strengthened the use of role substitution:
Because it’s been explained by the dentist who they’ve always seen . . . it does have to sometimes be then explained by me just to say what we do. But once they’ve seen you once they’re like OK, well yeah you do . . . you’re the person.
DT 1.207
You then find that a part of your career success or your capacity to earn money is your relationship with the dentist, because you’re relying on him so much.
DT 1.458
As soon as I mention to the patients, yes, it’s a restoration and a filling or something, that a treatment or scaling, that the therapist can do with a really good success rate, or they are qualified, the patient they are happy to go in to the therapist.
GDP 2.266
The [dentist] will say, and I’ll leave you in the capable hands of our therapist and that’s just adding those few little words in there.
DT 3.331
A lot of my experience where we send patients to the therapist we have to endorse them, we have to show that we’ve got faith in what they’re doing, just so the patient has the same faith as well.
GDP 5.200
It was apparent in this phase of the realist-informed process evaluation that the threat to professional boundaries was a consideration when using role substitution:
Some of the dentists are actually working as therapists anyway, so they find that that might be a little bit of a threat to their model.
DT 1.114
Historically dentists have always been at the top of the tree in the practice and they feel that the gap is closing. There is also that if the therapists are doing all the general dentistry then it’s only complicated stuff that’s left to them.
DT 3.467
I think the dentist needs to get over that. Their job is still secure, we are still going to be needing dentists, they have a broader Scope of Practice than therapists and they are going to be needed. I don’t think therapists are here to take over the dentist role.
DT 3.472
I think it’s only natural for anyone to feel threatened by someone else and to doubt their work, I think maybe dentists are this kind of breed of like humanity where it’s very professional, very conscientious of what they’re doing. And they go through university for 5 years where it’s very competitive as well to get into dental schools as well, I think maybe it’s just one of those traits that’s kind of within that profession.
DT 4.379
The IPT on professional boundaries was modified by the type of GDP, with equity-owning providers being more positive about the use of role substitution than non-equity owning performers:
I personally think practice owners will be all for it. Everyone who I know who is a practice owner are all using the skill mix where possible, are all using the therapists where possible.
GDP 5.338
Associate[s] feel a bit more threat because they have to pay for the therapist as well, so they can see their income less; and of course, they feel that it can replace their jobs.
GDP 2.400
The only slight conflict probably has been with the associates, and that’s probably just a financial way of how it works and how they’re rewarded and what the therapist costs. It’s a little bit different with me being practice-owner, because I . . . I think that’s the thought process the dentists will have to get their head round.
GDP 5.286
That they’ll panic about we’re possibly taking away the easier work from them, which is probably their bread and butter. I do get that, but for the NHS to survive in dentistry, we’re going to have to make it cheaper to do what we’re doing.
DT 8.327
Two of the IPTS from phase 1, IPT5 and IPT6, captured the idea that the role of DHs is more accepted than the role of DTs by GDPs. This appeared to relate to DHs’ non-threatening supplementary role (e.g. prevention and periodontal management) and the ability to upsell DH activity (e.g. scale and polishes) to increase the profitability of the practice:
They don’t want to see the dentist for the cleaning, I don’t know why, they just want to see the hygienist, so then they’ll come in expecting to see a hygienist. The person that they go through, that’s the hygienist, they’re going to do the cleaning, they’re going to pay for the cleaning, it’s going to be a private clean.
DT 1.555
But I think it might just be easier to employ a hygienist and do the restorative work yourself as a dentist. It’s more clearly defined, straightforward and the pay is straightforward.
DT 3.791
Mr [X] only works 3 days a week and an empty room, so that room will be doing nothing, if you then put a hygienist in, and all the patients who would have had a clean with the dentist will go next door and have the clean with the hygienist. Because it had an additional fee allocated to it, it was a viable model.
GDP 6.608
You can charge a lot for a hygienist visit, especially in London, half an hour you could charge 60 quid or something like that. So I think, at the end, it’s a good income stream for dentist practices.
DT 7.388
Hygienist will probably be paid more than the work of a therapist because most of the hygienist’s work, they’re done privately and they’re on a percentage.
DT 1.413
It’s just it’s new as well, like I said they’ve not seen a therapist before, they’re not sure what a therapist means. Everyone knows what a hygienist means. So it’s just a new situation for them.
GDP 5.270
I think it’s easier for a lot of therapists to get jobs as just hygiene, hygienist because it’s so difficult to face the rest of the barriers on the therapy side. And at least they know when they take a job under hygiene.
DT 4.619
I think they get bogged down with the NHS and they’ve got a tunnel vision and forget we’re here half the time. I think they push – oh, they don’t push – private hygiene probably pays more than a NHS therapist. I think that’s probably it. I think it’s cost.
DT 8.419
Nursing support was another issue that was raised:
Nurse support, so having a nurse and a therapist work without . . . they’re sometimes asked to work without a nurse.
DT 1.598
Totally think we should definitely have a nurse, it’s ridiculous to not have a nurse . . . to have someone in the room in case of medical emergencies or charting.
DT 4.784
They [the GDC] say it’s not right for us to work without a nurse and I personally would never work without a nurse because it’s not good for a patient, in my opinion, but some jobs out there, I had a look, they said without nurse support.
DT 7.450
It’s one rule for the dentists and a different rule for us, and it is totally wrong and I feel really strongly about that . . . It’s just wrong, dangerous, insulting.
DT 8.502
Regulatory
Regulation is another important factor that can affect the use of role substitution in NHS dentistry. The most important of these factors stem from the Radiation Protection Act,11 the Ionising Radiation (Medical Exposures) Regulations11 (in relation to prescribing radiographs) and the Medicines Act12 (relating to the professional use of fluoride and local analgesia):
-
IPT7 – IF DTs could prescribe medicines and radiographs THEN they could undertake treatment without the need for the GDP to see the patient, which would improve the efficiency and profitability of the practice.
This IPT was discussed at length in the theory-testing phase. For many, this reinforced some of the issues that were discussed in relation to improving efficiency in NHS practices:
How is it in the best interests of the patient that I then have to say to them, actually I’m sorry but I can’t do anything to you, I can’t prescribe you anything, I can’t do anything to your tooth in order to get you out of pain?
DT 1.380
Then the only thing that I wouldn’t be able to do then is apply the Duraphat® [Colgate-Palmolive Company, New York, NY, USA] varnish because that’s under a prescription of the dentist. So that could then obviously free up the dentist to be doing other things that are outside of my Scope of Practice and more complicated things that they need to do.
DT 1.139
Obviously they [GDPs]’re writing the prescription for it, because it’s a prescription medicine. But if we had an exemption or we were able to do an additional course to then enable us to prescribe these medicines it would just make much more sense.
DT 1.87
If I was to see a patient [under direct access] and they need a local anaesthetic I would then have to then leave the surgery or message the dentist to then add the prescription on, to wait for the prescription to come on to then administer the local anaesthetic.
DT 1.150
[If] they are able to provide fluoride, varnish, and even X-rays, and local anaesthetic, without our referral, I would say; and that will definitely work better again from the patient’s point of view, because sometimes the patient will need to come back just only for the referral or just for a review with a dentist.
GDP 2.131
It’s going to be 5 minutes before the messenger gets through to the right person, they look at the notes, or see the patient, and write that prescription, that referral form, to give the local anaesthetic.
DT 3.255
You’ll take longer in the appointment because you can’t always get a dentist [to prescribe] because they’ve got patients to see as well, like you’ve got to then sit around and wait for them to say yes or no. It just makes your day really difficult, you can’t just crack on and do your job.
DT 4.177
Unless everything is set up [for re-prescribing] and every dentist is on board and happy to just drop what they’re doing and come in. But even then, you still feel like a burden on the dentist as well when you’ve got to keep going into there and stopping their treatment, you feel like you’re being a pain and you’re incompetent almost.
DT 4.215
I think definitely like fluoride varnish, fissure sealants on the prevention side, perio[dontics] and things like that, I think they’re perfectly capable of prescribing it and managing it.
GDP 5.171
These are registered professionals who have a high level of responsibility and training to carry out the treatments that they’re carrying out. The thought that they can’t do the other things you just described [prescribing] is again just ridiculous.
GDP 6.166
I think that [prescribing]’s another massive barrier, as you’re aware, you can administer these things but you just can’t . . . it just doesn’t make sense.
DT 7.113
Training
We had proposed a number of IPTs in the domain of training:
-
IPT8 – IF DTs have experience working to their full Scope of Practice THEN they can perform tasks as effectively as GDPs.
-
IPT9 – IF GDPs were trained alongside DTs THEN they would become more aware of their Scope of Practice and clinical skills, leading to greater utilisation after they qualify.
-
IPT10 – IF there were incentives in the NHS contract to use DTs THEN more could be trained by dental schools.
These theory areas were not given as much credence in the theory-testing phase. Whereas a few of the stakeholders did comment on the importance of integrated training to increase awareness about what clinical duties DTs can undertake, others did not see this as the critical issue:
A lot of dentists don’t really know what we are or who we are, what we do.
DT 4.708
I trained at Manchester and I would say that we did work very closely with the dentists and they were fully aware of what we did. We did clinical skills together on the first year. We were very close . . . we worked very closely with them. So we had a great relationship with them and I’d hope that everyone who we graduated with fully understood what we did, because we were on clinical skills and we were also in the clinics with them.
DT 1.633
They should be trained together. It’s the same job, same cavity preparation, same bacteria, so they should train together in the parts, in the elements that cross over.
DT 3.889
There was also some unhappiness expressed about the inability of DTs to subsequently train as GDPs. There appeared to be no concessions to DTs, despite the level of training that they had, and this appeared to further highlight the disparity between the two roles:
If I wanted to go and do dentistry I’d have to go and either do a postgraduate for 4 years or another 5-years’ course. So there’s no kind of . . . if anyone ever wanted to upskill to something outside their Scope of Practice they can’t do it.
DT 1.656
If I want to be a dentist as well I have to go to uni[versity] again for the 4, 5 years which seems daft to me.
DT 7.664
Patients’ experience
A series of new theories were developed as a result of the theory testing, which related to the patients’ experience. Many of the stakeholders felt that role substitution was better for the patient:
From the patient’s point of view, to have better access to the practice for routine examination as well, instead of waiting for long appointments, or even for emergency appointments, if it’s a small fracture and something that the therapist can deal with, it’s definitely working much better to be able for the therapist to open the course of treatment.
GDP 2.105
But then some of them, who have been referred to see the therapist they see a different side of dentistry as well and they are quite open, they want to be seen by me for certain treatments and they ask to be referred.
DT 3.391
I think it’s what works for the patient. I think it’s just nice for them to come in, see the same person who’s going to look after them, manage and take care of them. It’s just a better way of doing it.
GDP 5.154
There’s a nice thing to that model, which is the patient gets a feeling of two people thinking about their care, and sometimes, potentially, a better outcome because two people have considered what each other think for that patient’s care.
GDP 6.63
Some stakeholders also argued that patients do not make the differentiation between a GDP and a DT:
Most of the time the patients don’t necessarily care who they get treated by, they just see you as the person.
DT 1.172
In similarity to the research highlighted in Chapter 1, many argued that patients do not understand what a DT is:
I mean people understand what a hygienist does and people understand what a dentist does, but not many people understand what a therapist does.
DT 1.189
Often they don’t even know what a therapist is. We haven’t got on the wall, dental therapist, this is the scope of a dental therapist, this is the scope of a nurse, this is what the dentist can do.
GDP 2.350
We don’t say therapist . . . but yeah, I’m going to refer you to the hygienist, but when it’s the therapist we try to avoid that as much as possible, so that they understand who they are actually going to see.
DT 3.425
And also it’s quite new to them. A lot of patients haven’t seen a therapist before, so they’re probably worried they’re going to get inferior treatment or not get the treatment by the right person.
GDP 5.222
So lots of patients are shocked when I tell them that I’m a therapist and what it is. So what we try and watch is we try and education patients what my role is, whether it’ll be on websites or there’s a TV screen upstairs that’s got rolling adverts on and stuff, and we’re just trying to ingrain it and tell you what I can do or what we can do as a workforce for patients.
DT 7.191
Logistics
Another new area that emerged from the theory-testing phase was the importance of having enough surgeries and ‘real estate’ in the practice to make the most of role substitution. A number of the DCs had views on this theory area:
Skill mix can be difficult if you’re limited with your surgery space and surgery chair time.
DC 9.173
If you trained your nurse to apply fluoride and you haven’t got another chair for them to do that in is that really that efficient?
DC 9.173
I can think of examples of practices where there is going to be a problem because they have only one or two surgeries, and the only way you can really move around without having building work undertaken is to expand the hours and for the performers within the practice to change their working practices . . . So even though they’re not actually doing more hours, the surgery is utilised for more hours.
DC 10.432
So yeah, you are quite restrained really, if you have a small practice, on how you’re able to change things going forward, unless you physically change the building.
DC 10.464
Refinement of the initial programme theories
As a result of our theory-testing phase, we prioritised and modified our IPTs (Table 16). These were then taken for further testing with a different set of stakeholders, as outlined in this section.
| Theme | Number | IF-THEN statement |
|---|---|---|
| Contractual | 1 | IF the NHS contract allowed DTs to be on the National Performers List THEN they could open and complete a NHS course of treatment, increasing the relative efficiency of role substitution (through UDA generation) and the patient’s journey through the practice |
| Institutional logics | 2 | IF DTs are seen to be endorsed by the GDPs in the NHS practice THEN patients are more likely to trust being treated and managed by DTs |
| 3 | IF DTs are used to their full Scope of Practice THEN they can pose a threat to some GDPs (e.g. associate dentists), leading to a reluctance to delegate clinical tasks | |
| 4 | IF DTs are used in NHS practices THEN they are commonly underutilised as DHs | |
| Regulatory | 5 | IF DTs could prescribe medicines and radiographs THEN they could undertake NHS treatment without the need for the GDP to see the patient, which would improve the relative efficiency of role substitution and the patient’s journey through the practice |
| Patients’ experience | 6 | IF patients were better educated about the DT role THEN they would accept treatment by DTs more readily |
| 7 | IF patients trust the DT THEN they are just as happy to be treated by a DT as they are a GDP | |
| Logistics | 8 | IF NHS dental practices had sufficient surgery space and/or time THEN role substitution is more likely to be utilised |
During this phase, attention was paid by the research team to the specific contexts and mechanisms that influenced the use of role substitution in NHS practices. In this section, we present the main findings in the different theory areas (transcripts are presented in Report Supplementary Material 2).
Contractual
General dental practitioner, DT and DC groups agreed that, under the current NHS contractual model, the use of role substitution can be difficult to implement. DTs work for NHS dental practice owners (providers) that are run as small businesses that seek to maximise profit while discharging their professional responsibility to their patients (context). NHS GDS regulations9 do not allow DTs to open a course of treatment (mechanism). This means that DTs cannot act as the front-line clinician, reducing practice efficiency (outcome) and causing disruption to the patient’s journey (outcome). All of the stakeholders agreed that this creates difficulties managing their ‘books’ if the GDP or DT have not synchronised their diaries, because any referrals from GDPs to DTs then require a separate appointment. Therefore, GDPs argued that the NHS dental contract does not support the use of a team-based approach (outcome). NHS GDS regulations9 require the claims for the number of UDAs undertaken to be split between those that opened a course of treatment and those that undertook the treatment. This creates an ‘internal market’ (mechanism) leading to competition in the practice between associate dentists and DTs and a disincentive for associate dentists to refer to DTs (outcome). In addition, GDPs argued that the target-driven nature of the current NHS contract to deliver to their ACVs (mechanism) does not allow the freedom or flexibility for GDPs to experiment with different models of care. Instead, GDPs argued that they have to be innovative, in spite of the current contract, to utilise role substitution.
One model that was suggested by the DTs was based on ‘upwards referral’ (akin to medicine), whereby a DT could triage patients and refer only if patients are seen to require treatment that is beyond their Scope of Practice. Although many DTs felt confident in recognising situations in which they were likely to encounter tasks that were beyond their Scope of Practice, some felt that additional training would be beneficial. As a professional group, DTs were highly frustrated by the time taken to refer a patient back to a GDP. At worst, the patient would need to be recalled to see the GDP for a check-up and then referred back to the DT, often taking months. This only served to confuse the patient and led to inefficient processes in NHS practice.
The DC group argued that there could be an option of using an intermediate performer level that would allow DTs to open preventative courses of treatment in the NHS, in a broader recall structure. This broader recall structure may include extended recall periods, DT fluoride application and GDP oversight for clinical safeguarding. The DC group also felt that the current NHS contract, based on UDAs, is not fit for purpose in contemporary dentistry. NHS GDS dental contract reform and other innovative initiatives were cited as opportunities to realign the remuneration system for DTs away from the reliance on UDAs. More broadly, it was suggested that the current contract did not sufficiently incentivise the level of access and the quality of care required by local populations.
Figure 6 presents contractual CMO configurations.
FIGURE 6.
Contractual CMO configurations.

Institutional logics
All stakeholders were in agreement that the use of DTs was strongly influenced by the prevailing culture in NHS practices and the equity-owner’s view(s) about role substitution and how best to deliver care for their patients and their community (context). Endorsement of ‘team dentistry’ and the provision of support and clinical leadership by the equity owner (provider) in an NHS practice (mechanisms) were seen as critical to help overcome some of the difficulties associated with role substitution in the current NHS contract. Examples provided by the stakeholders included their influence on securing additional surgery space (see Logistics), exploring different care pathways or internal payment systems for staff (performers) that work around current NHS service regulations. At its simplest, endorsement also related to the very practical task of providing reassurance for patients who are being referred from GDPs for treatment with DTs. There was unanimous agreement that a supportive team approach was required for effective use of role substitution. Endorsement of DTs through outward displays of trust, positive feedback and support were recognised as essential for effective implementation. There was also recognition that some GDPs require some experience of working with DTs. Overall, equity owners were seen to be supportive of role substitution in practice because ultimately it represented a mechanism for increasing profitability: meeting the needs of the local population using a less expensive workforce (outcome).
The GDP, DT and DC groups also recognised that DTs working to their full Scope of Practice can also be seen as a professional challenge (mechanism) to associate dentists and that this could influence the institutional logics in a NHS practice. This was for three reasons. The first mechanism, immediate conflicts in the ‘internal market’, was referred to above. The second related mechanism was the associate dentists’ perception that this added only complexity to intrapractice referrals. The third mechanism related to more medium-term concerns about DTs ‘taking over’ their future role.
Where role substitution was not working, a number of the stakeholders mentioned that DTs would often be undertaking DH roles (outcome). This was highlighted particularly by those in the DT stakeholder group, who stated that they’d often be asked to perform as DHs (outcome). Many DTs reported that there was a feeling of resignation among many in the profession and that they would be fortunate to work to their full Scope of Practice (outcome) in a typical NHS practice. Ultimately, this results in deskilling of the DTs workforce, leading to a loss of clinical confidence (outcome) and many DTs not returning to their full Scope of Practice (outcome).
Figure 7 presents institutional logics CMO configurations.
FIGURE 7.
Institutional logics CMO configurations.
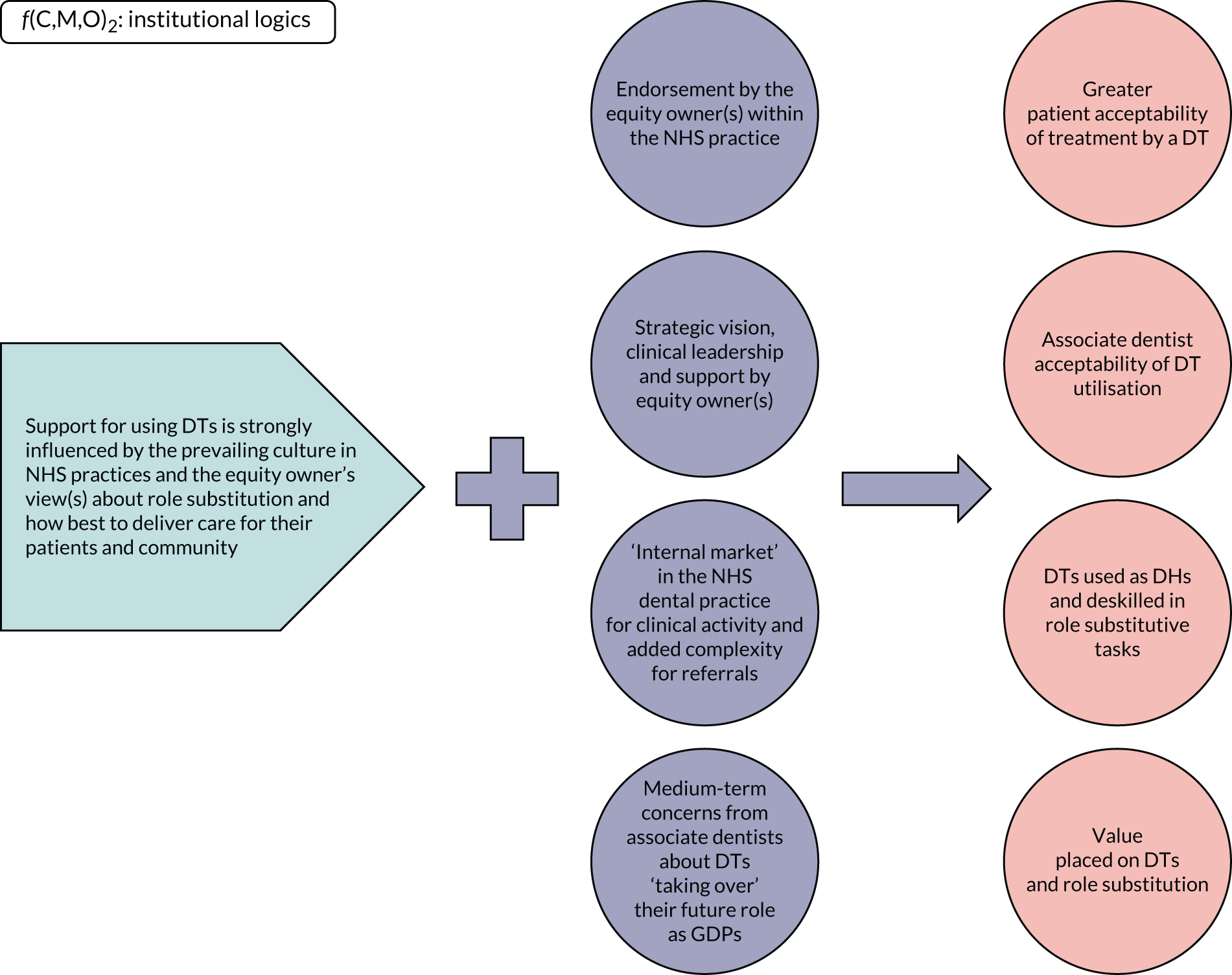
Regulatory
NHS dental practices and DTs are required to work to the Ionising Radiation Regulations Act, Ionising Radiation (Medical Exposure) Regulations11 and Medicines Act12 and the GDC’s Scope of Practice (context). The DTs inability to prescribe radiographs, fluoride varnish and local analgesia were all cited by the stakeholder groups as creating substantive inefficiencies (outcome) and practice disruption (outcome) when managing NHS patients. The DT group argued that this could manifest itself as the need to rebook the patient’s appointment, which had significant financial implications under the current NHS contract. Some DTs identified mechanisms for working around the inefficiencies of obtaining a prescription; these typically involved leaving some ambiguity in the treatment plan or GDPs issuing prescriptions post hoc, based on a trusting clinical relationship with the DT. The inability to prescribe for even basic treatments reduced the DTs’ sense of professional autonomy and was an addition burden for the referring GDP (outcomes).
All stakeholder groups agreed that the current Scope of Practice for DTs could present challenges in a NHS practice environment. Examples were given of how certain clinical presentations would initially appear to be within the DTs’ scope but later require a GDP to intervene (outcome). In these instances, the inefficiencies (outcome) caused by the need for a GDP intervention outweighed the efficiencies gained by referring to a DT. If DTs had a wider Scope of Practice (mechanism), it was thought that these instances would be less common. There was unanimous opinion that, when operating within their Scope of Practice, DTs could perform clinical tasks as well as GDPs.
Figure 8 presents regulatory CMO configurations.
FIGURE 8.
Regulatory CMO configurations.
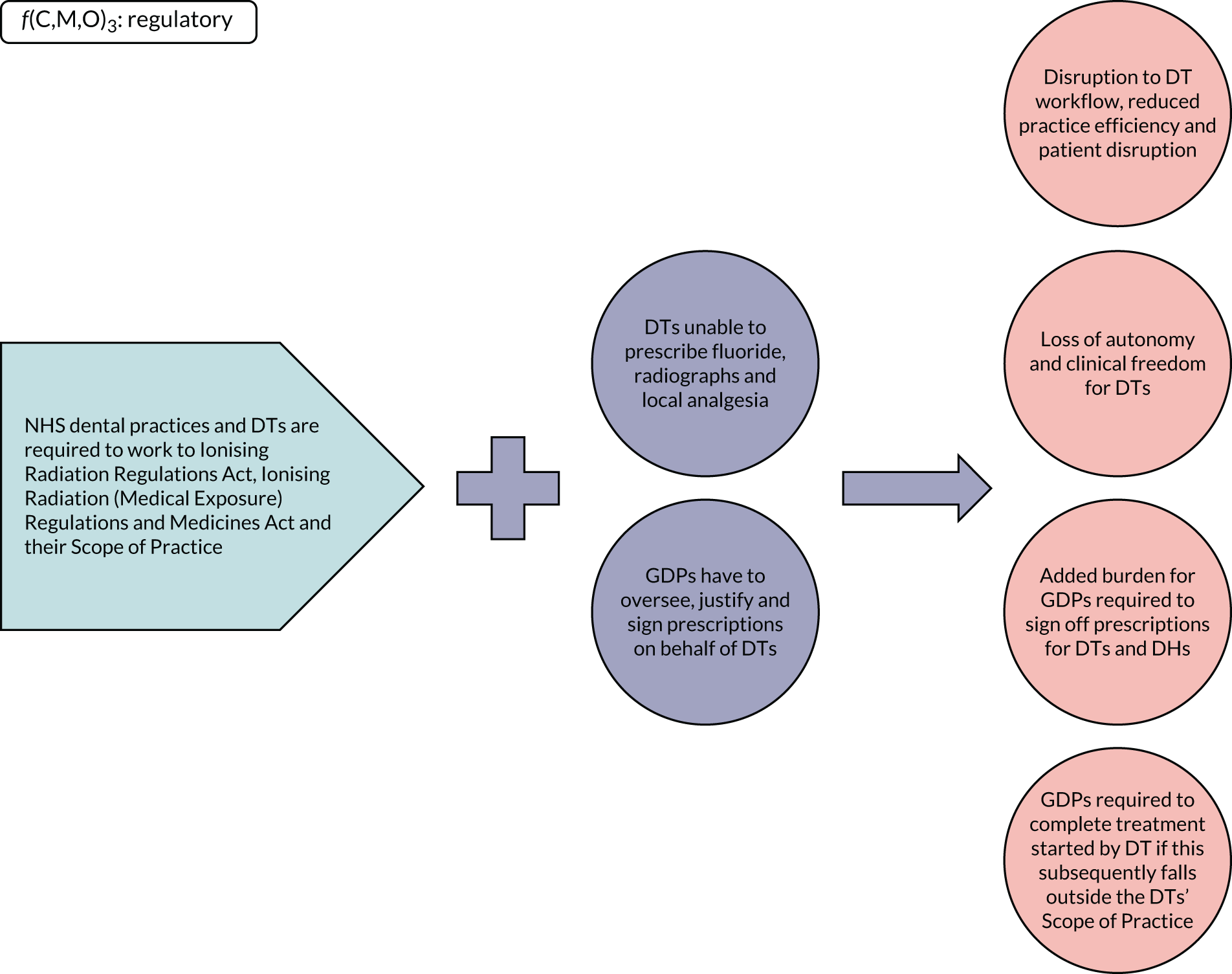
Patients’ experience
Patient acceptability was considered to be important at the theory-testing phase, but most patients who were interviewed in this phase argued that they would accept new ways of working. Given the importance of capturing the patient voice, key themes are supported by quotations from the patient group:
I probably wouldn’t be bothered who I saw in the first place, as long as you knew there was a structured approach.
22.33
But if I went somewhere else, I would accept the way they worked straightaway, almost certainly, and probably without question.
22.636
I would have faith in the profession, that they would do that. It’s not as if you just drag somebody off the street and say, fill this bloke’s teeth. They have been trained.
25.132
I would go there in expectation that I was going to be seen by the most appropriate person for my condition . . . I wouldn’t want to know, I’d just expect, it’s like if the car mechanic said, which of our mechanics would you like to do your car.
25.227
I would make the assumption that once you’d asked the question, they were qualified to deal with what was wrong, and off you go, give it a try.
27.459
Put our faith in the system. So, I would, unless the person that was treating me was very indecisive or didn’t look the part, or looked a bit rough or something, which gave me doubt as to their proficiency, then otherwise I’d accept that the dental practice knew what they were doing.
25.172
I’ve absolutely no preference who I see. I know some people are really adamant that they only want to see the person that’s the most specialised, but I think that’s just ignorance as to what that person can do really.
26.355
I don’t think it’s the job title or . . . it’s just the situation. You know, it’s fine, I don’t think it matters who’s doing it, as long as they can meet the needs, and that’s what’s happening . . . you know, they want to know they’ve seen the right person for it to be resolved.
27.268
Yes, so, yes I think in that situation. And also, if you’ve got a persistent problem, you really would want it fixed . . . So, I think that, you know, if it was really bothering you, you’d see whoever could solve it, you wouldn’t mind.
27.449
Some of the patient stakeholders also raised the issue of complexity as a factor:
You’re in a more complex situation, maybe having bridges . . . which, touch wood, you know, we’re not in, then I can understand why somebody might feel that they needed a particular person. But people like us, we wouldn’t mind at all, we wouldn’t be bothered. We’d be quite happy.
27.131
Others argued about the importance of consistency, in terms of the clinicians that they see in practice:
That’s probably one thing that will probably affect the changes more than anything else is that somebody my age probably for simplicity expects the same person because it’s stability, it’s a sense of comfort.
22.289
Perhaps older people who are more used to seeing, the dentist, you know, the authority figure, man, usually, traditionally, might be a bit wary, perhaps the other people, not so much.
25.423
They also emphasised the role of the whole of the dental team:
It’s the receptionist which is the first face that you meet, which is probably the person that can make the difference.
22.25
A key element was the need for the practice to communicate any process of change:
But as long as I was explained the benefits I would receive, and I think they’ve got to be, if that was projected that way, then I would probably see that.
22.785
Our user researcher provided her thoughts on the key context, mechanisms and outcomes that govern patients’ response to role substitution in NHS dentistry. Given that the public have no understanding of the current NHS system (context), a number of key mechanisms were identified:
-
A low level of patient awareness of what DTs can do (mechanism) means that patients are receptive to DT utilisation (outcome) only if they are explained the benefits (mechanism).
-
Patients want minimum disruption to their daily lives (mechanism).
-
Continuity and consistency are important (mechanism) to build trust.
-
Trust in the ‘system’ of NHS dentistry (mechanism) also reduces patient anxiety (outcomes).
Figure 9 presents patients’ experience CMO configurations.
FIGURE 9.
Patients’ experience CMO configurations.
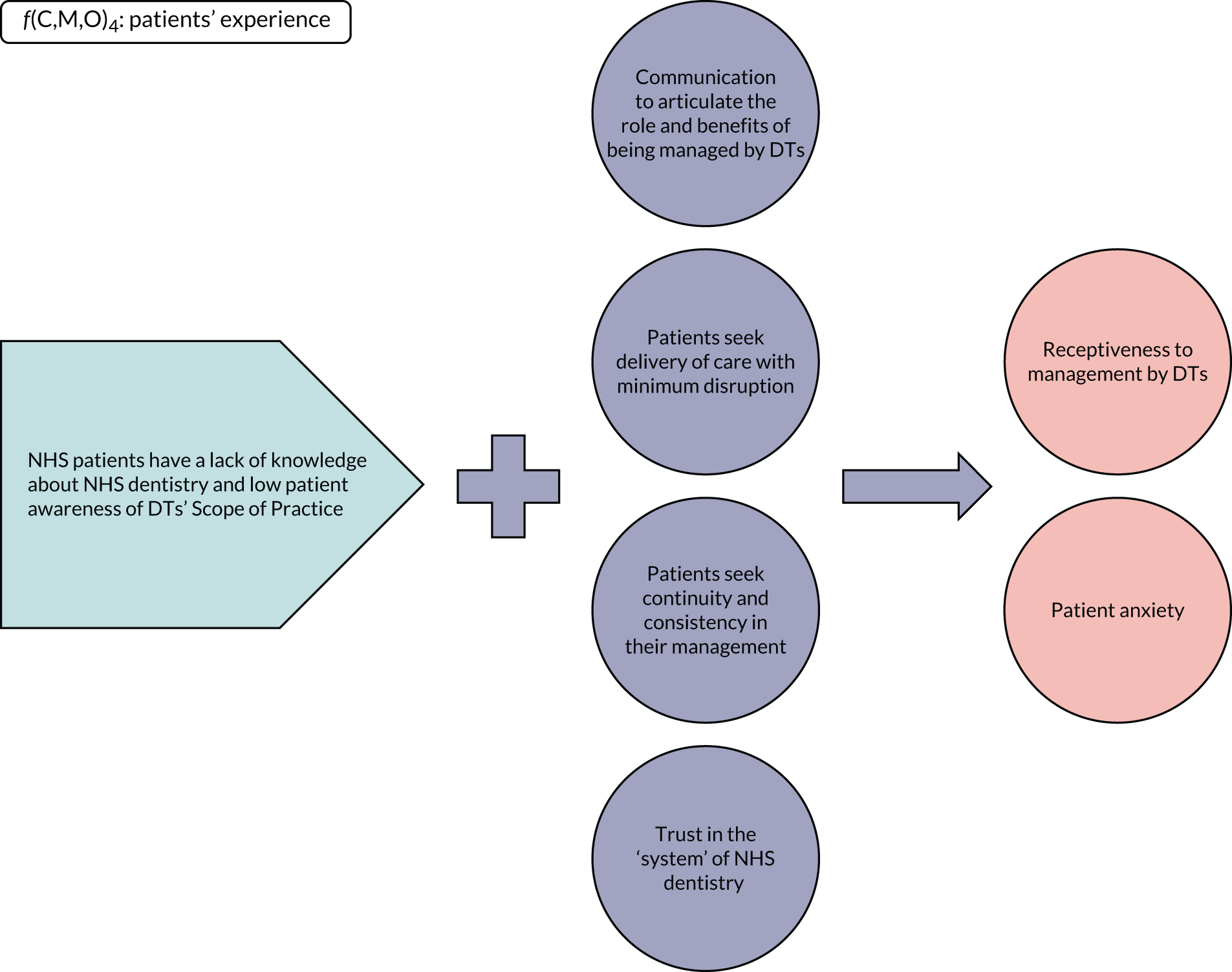
Logistics
Both the GDP and the DC groups argued that there were significant logistical barriers to the successful implementation of role substitution. Role substitution in NHS dentistry requires additional surgery space and/or surgery time to enable DTs to undertake patient management (context). The GDP and the DC groups argued that NHS dental practices that had only one or two chair practices would find it difficult to make role substitution work under the current NHS contract. Role substitution is predicated on NHS practices having sufficient clinical space to employ a DT. This was often difficult, because most high-street practices were not purpose built for team dentistry. Instead, their design had been strongly influenced by the incentives in previous NHS contracts that rewarded high levels of clinical activity undertaken by GDPs to maximise profitability (mechanisms). This ‘small business’ economic model was exacerbated further by the fact that NHS practices were essentially independent contractors with no structural investment from the NHS (mechanism). This meant that practice expansion was difficult (outcome) and that members of the dental team that could maximise profit (DHs) were preferred over DTs (outcome).
Some suggestions were made by the DCs about how best to counter this, including extended opening hours, building extensions and forming hubs for local health services in primary care, where capital resources would be pooled between providers to enable patients to access NHS dentistry, ophthalmology and pharmacy.
Figure 10 presents logistics CMO configurations.
FIGURE 10.
Logistics CMO configurations.
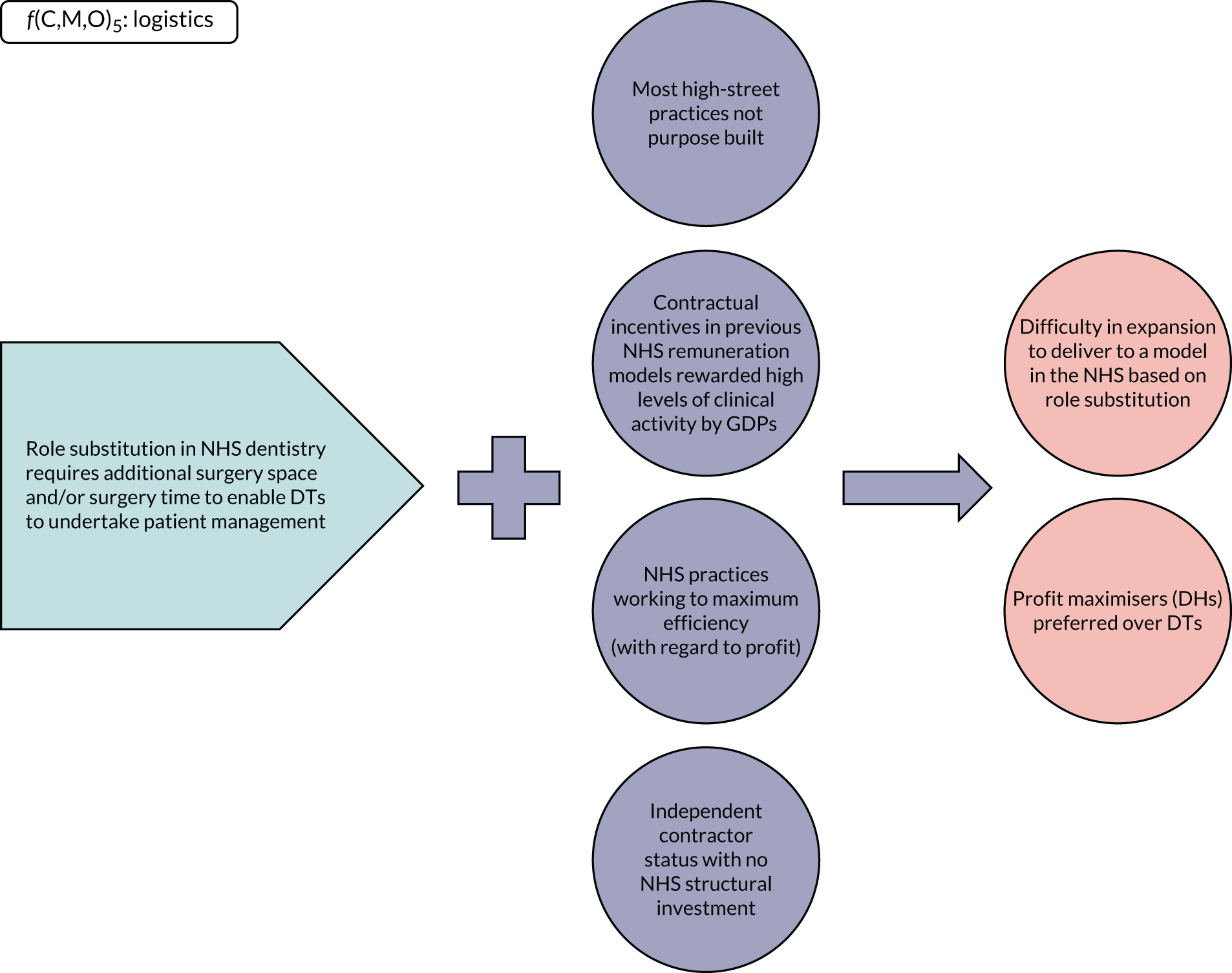
A common theme to these five areas of programme theory relates to the NHS dental contract. These five areas have been collated into one model (Figure 11) to highlight the different influences on role substitution in NHS dentistry. It highlights how contractual issues affect the business model in NHS dentistry and the institutional logic of the individual NHS dental practice. In turn, these can affect the logistics within the practice in terms of decisions around the numbers of surgeries needed and how much of the available clinical time is given to role substitution. It also highlights how regulatory issues affect the business model of the NHS dental practice while concomitantly directly affecting utilisation (given that DTs have a duty in their own right to discharge their Scope of Practice in accordance with the GDC regulations). Regulatory and contractual issues are seen to operate at a macro level and influence the business model and institutional logic at the micro level. These factors operate independently to the meso level, where there is little that DCs can do to facilitate role substitution (given the contractual and regulatory underpinning of the NHS system at the macro level), bar structural investment, which is difficult given the independent contractor status of NHS providers.
FIGURE 11.
Overarching model.
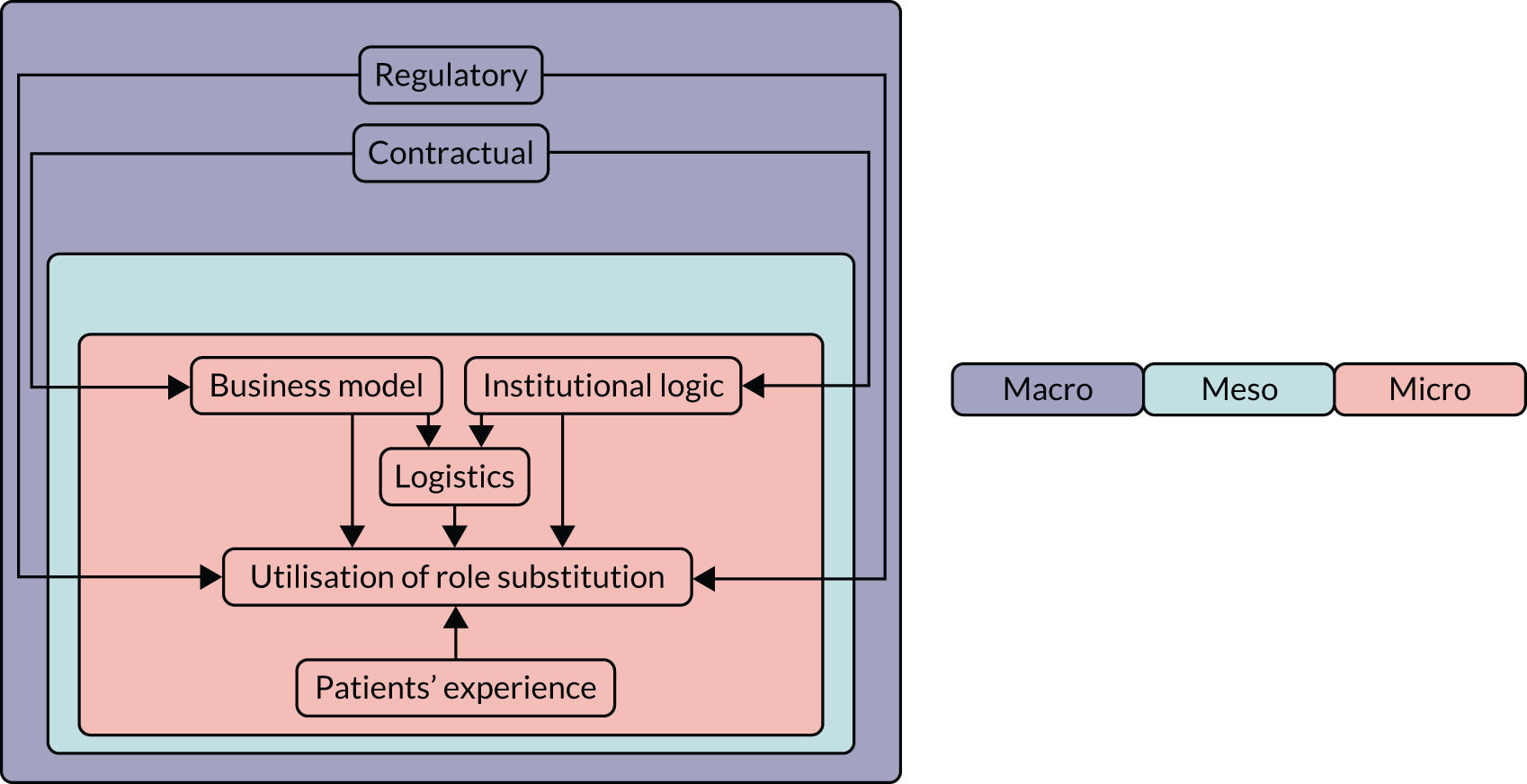
Feedback on the final programme theory
The final programme theories were presented to a key stakeholder meeting at the Cheshire and Merseyside Local Dental Network, with representation from the Local Dental Committee, consultants in dental public health, DCs and the postgraduate dental dean. The theory areas were presented sequentially, with stakeholders given the opportunity to feed back before moving on to subsequent theory areas.
Contractual
Stakeholders agreed that the NHS contract influences the utilisation of role substitution. As evidenced in the first f(C,M,O) configuration (see Figure 6), significant attention was paid to the professional strain that is placed on DTs and associates as a result of the UDA system. It was suggested that this conflict for resources is minimised when DTs are salaried, as is seen in Community Dental Services and some dental practices. However, the majority of stakeholders argued that there was no ideal model for practice owners should they try to implement role substitution in the current NHS dental contract. Many felt that it was difficult for established (compared with new) practices to adapt their business model to accommodate DTs without causing friction among their associates. It was suggested that clinical activity (UDAs) should form only part of an NHS dental contract model if role substitution was to be encouraged.
Institutional logics
Stakeholders agreed that the prevailing institutional logics in an NHS practice heavily influences the adoption of role substitution. They agreed that strong leadership was required to ‘sell’ the benefits of DTs to their dental teams. The stakeholders supported the second f(C,M,O) configuration (see Figure 7) and argued that the ‘internal market’ was an important factor that mediated the referral process within the practice and how this links back to the contractual issues highlighted in the first f[C,M,O] configuration (see Figure 6). This was thought to drive the underutilisation (and deskilling) of DTs in favour of DH use. The increasing feminisation of the dental workforce and the changing expectations of new dental graduates were also recognised as emerging drivers that could increase DT utilisation.
Regulatory
There was unanimous agreement on the disconnect between the DTs’ training, the Scope of Practice and the current regulatory framework in NHS dentistry (see Figure 8). Stakeholders expressed their frustration over the inability of DTs to prescribe fluoride, radiographs and local analgesia. They highlighted that DTs could prescribe in certain clinical settings (in Community Dental Services with Patient Group Directives) but that this was difficult in a GDS environment. The stakeholders agreed that regulatory barriers affected the efficiency of dental practices, given the need for GDP oversight. In addition, the stakeholders argued that there was a need for a review of current NHS contracts, alongside regulatory changes, to promote different referral models within the practice.
Patients’ experiences
The stakeholders agreed that most patients would be happy being treated by a DT providing certain criteria were met (see Figure 9). These criteria included appropriated patient education, trust and endorsement from the dental team. As highlighted by the fourth f(C,M,O) configuration, communication of the role and benefits of being managed by DTs was critical. It was also felt that this could be further facilitated by the education of the whole dental team. Moreover, the stakeholders suggested that members of the team, such as receptionists and dental nurses, were best positioned to deliver this education/information to patients.
Logistics
Stakeholders emphasised the importance of the final theory area (see Figure 10), arguing that many NHS dental practices are bound by the size/scope of their building and associated clinical space. Stakeholders agreed that, for most NHS dental practices in the current contractual framework, role substitution typically requires additional surgical space. The stakeholders also highlighted that practices often find it difficult to source capital investment from the NHS because of their status as independent contractors. The stakeholders did think that most NHS practices are ‘working to maximum efficiency’ within the current contractual and regulatory frameworks, but could become more efficient if the highlighted issues were addressed.
Overall
No new theory areas were suggested by the stakeholder group and no amendments were thought necessary to the mechanisms and outcomes that were presented.
Discussion
The realist-informed process evaluation added value to the study and captured many of the themes that were discussed in Chapter 1. Following a detailed and iterative process, it elicited five principle areas of programme theory: contractual, institutional logics, regulatory, patients’ experience and logistics. This enabled the research team to understand and capture the contextual factors that shaped the intervention, the mechanisms that sustained or potentiated effects, the unintended consequences and the contextual factors that shape the use of role substitution in NHS dentistry. 103 As highlighted by Rycroft-Malone et al. ,126 these theory areas were complex and to a large extent interdependent. The underlying generative mechanisms were largely at the macro and the micro level, with the latter being driven by the former and related to individual, social, cultural and organisational factors. 127 They were also seen to operate across a continuum and provided the research team with a rich explanatory narrative of the factors that potentially influence adoption. 128,130
The two most important elements that appear to shape the practice of NHS dentistry in the UK are contractual and regulatory factors. Despite the relaxation of the Scope of Practice from the regulator’s perspective, the requirements under the GDS contract for dentists to open a course of treatment appears to significantly limit the practice of role substitution in NHS dentistry. 9,10 This is further potentiated by the fact that DTs cannot contract directly with DCs, which appears to undermine strategic objectives at the level of the policy-maker to promote the use of the whole dental team. 9,14,15 The results from this WS also highlight how this appears to fundamentally affect the institutional logics of NHS practices. As highlighted by Goodwin et al. 48 and Watt et al. ,49 the institutional logics at any given NHS practice include not only dentistry as a business but also professional ethics and contextual factors, based on where the practice is embedded. The drive to maintain (and maximise) the viability of a NHS practice does appear to be tempered by a practice owner’s view about their sense of duty to their patients and their ideas about how best to deliver care for their patients and community. 50 However, contractual incentives remain a fundamental driver. Therefore, the results in this study concur with our earlier work, where the views of practice principals were found to be highly influential. 30 This is important, as promoting role substitution and any potentially disruptive transition caused by changes to local working practices takes time and good human resource skills. 53 In this study, most examples of successful implementation of role substitution in NHS dentistry appeared to be where the practice owners had found workarounds to the contractual and regulatory barriers.
The level of social acceptability of role substitution appeared to be high and patients appeared to trust the ‘system’ of NHS dentistry. Most suggested that they’d accept new ways of working but would want NHS practices to articulate the benefits of being managed by DTs. Equally, many highlighted the importance of continuity and consistency in their care and the need to keep disruption at a minimum. This appears key to the success of role substitution in NHS dentistry and was also raised by many dentists and DTs, who were frustrated at the difficulty of ensuring a smooth transition for patients, given the restrictions in the GDS contract.
From a dental public health perspective, these factors are critically important given the trend in future population health needs. 16,29 Oral health is improving overall and where there remains existing intransigent problems or new oral health challenges there will become a pressing need to better target the available resources in NHS dentistry. 17–19 All of the dental contract reform programmes undertaken across the UK place an emphasis on increasing patient access and prevention while maintaining and improving the quality of service being delivered. 59–68 It would appear that a key element in any reform programme would be to change the underlying contractual and regulatory incentives.
Summary
Substantial barriers exist to the practice of role substitution in NHS dentistry. The two most dominant factors were contractual and regulatory barriers. These appeared to drive the institutional logics at the micro level, with little influence exerted at the meso level by DCs. Where role substitution was successful, practice owners had found workarounds to the macro factors that dominated any potential implementation.
Chapter 4 Health economic analysis
Introduction
This chapter reports the methods and results of the within-trial economic evaluation (see Methods, Within-trial economic evaluation, and Results, Within-trial economic evaluation, respectively). This analysis developed and tested the health economic data collection tool. It also rehearsed the economic evaluation that would be conducted in the definitive trial of the intervention compared with current practice. Both pieces of work were designed to inform the definitive trial design. With regard to effects, we used the clinical measure BOP and oral health-related quality of life as measured using the OHIP-14 when estimating cost-effectiveness. The economic evaluation was conducted following best practice guidelines conforming to the Consolidated Health Economic Evaluation Reporting Standards (CHEERS). 137
The clinical measure BOP and the OHIP-14 are not ideal for use in an economic evaluation because it is unclear how important decision-makers consider a unit change in either measure to be. This means that any calculated incremental cost-effectiveness ratio (ICER) is difficult to interpret except in the sense that higher values for an ICER are less likely to be considered worthwhile than lower values. For this reason, preparatory work undertaking an investigation of patients’ preferences for being seen by DTs over being seen by GDPs is undertaken. Participant views were explored in the setting of focus groups and one-to-one interviews. The results of the qualitative work informed the development of a preference elicitation exercise (e.g. a DCE) that would be administered as part of the future definitive trial. The preference elicitation exercise in a definitive trial would be able to provide a metric to value the benefits of the intervention in monetary terms. This would extend the cost-effectiveness analysis into a cost–benefit analysis (in which both costs and benefits are measured in commensurate, normally monetary, units). The methods and results of this work are presented in this chapter (see Results, Discrete choice experiment: preparatory work, and Results, Discrete choice experiment: preparatory work, respectively).
This chapter finishes with a brief summary of the principal findings of the two elements of the health economics work (see Summary).
Aims and objectives
The aims of WS3 were to:
-
pilot the health economic data collection tool and rehearse the health economic analysis to inform the definitive trial design
-
explore patients’ preferences through focus groups to inform a DCE in a definitive trial.
Methods
Within-trial economic evaluation
Data collection
The following information was collected for WS3.
Clinical and quality-of-life data
The number of sites with BOP and OHIP-14 data was collected at baseline and at the end of study follow-up period at the epidemiologist visit as described in Chapter 2.
Dental treatment received
Case report forms were completed by health-care professionals at first and interim visits to dental practices, which captured the nature of the appointment (e.g. check-up, emergency), any treatment provided and the staff present.
Participant cost questionnaire
A self-completed questionnaire posted to patients at 12 months aimed to capture additional health service that was not recorded in the CRF as well as out-of-pocket costs. It also asked patients to provide time and travel information to dental appointments, details of usual activity if they were not attending the dental appointments and any lost earnings because of their dental appointments. Because the participant cost questionnaire (PCQ) referred to a 6-month time period, all costs were scaled to the 15-month study duration.
Costing methods (NHS costs and the use of health-care services)
In the main analysis, NHS costs were considered to primarily consist of UDA payments made to practices as part of their contract and incorporated prescription charges (these NHS costs were also estimated using a microcosting approach).
NHS unit of dental activity payments
Details on attendance and treatment provided at dental appointments were recorded by clinicians on the CRF. Treatment described was examined with reference to the NHS treatment band inclusion criteria and each treatment allocated a band. 138 NHS (and patient) costs were based on ‘courses of treatment’. Where appointments were classified as ‘emergency’ they were assumed to occur outside an existing course of treatment and were costed separately. 139 Each course of treatment was then assigned a corresponding number of UDAs (described in Appendix 2); where allocation to the appropriate band was unclear, a decision was made following discussion with clinical members of the research team. 138 Because UDA values can vary between geographic locations and practices and are dependent on the contract in place, earlier work was used to estimate a value of £25 per UDA for the primary analysis. 140 This was varied between £20 and £30 in a sensitivity analysis to reflect this potential variation. All treatment described in CRFs was considered to be received on the NHS unless explicitly stated otherwise or when that treatment was generally unavailable in NHS primary dental care (e.g. implants or Botox treatment). Where exclusively private treatment was described on CRFs, this was considered to occur outside NHS treatment costs. Where the CRF and the PCQ overlapped (e.g. attendance at secondary care dental visits and dental visits between check-ups), CRF data were used in preference to PCQ data to avoid costs being double counted and to avoid recall bias with the PCQ data.
Secondary care costs
In cases where a referral to secondary care was described in the CRF, a cost was applied based on the value of an outpatient attendance using the most up-to-date value available from the national schedule of reference costs. 140 This was considered more appropriate than costing the price of the treatment referred for because (1) it was not known if the treatment took place and (2) the treatment may have taken place outside the duration of the trial. Additional secondary care appointments reported in the PCQ were also included in this cost.
Prescription medication
The cost of any prescription medicine referred to in the CRF was taken into account. In the small number of prescriptions described, details were limited and assumptions of medication, dosages and durations were estimated based on details provided in the British National Formulary141 to estimate cost.
Costing methods (patient costs)
Patient costs comprised five categories:
-
NHS treatment charges – NHS treatment band charges were applied to courses of treatment, using NHS patient charges rather than UDA payments. No cost was applied to NHS treatment where a patient was exempt from charges.
-
Prescription costs – these were based on CRF data describing medications prescribed at the dental practice and costed at the standard NHS prescription charge rate.
-
Over-the-counter medication costs – these costs were reported in the PCQ. If patients did not complete this questionnaire it was assumed that they did not have associated out-of-pocket costs.
-
Private treatment – where private treatment was referred to in the CRF this was estimated using NHS information, practice price lists and a national survey of private dental charges.
-
Time and travel – this was based on time and travel data reported in the PCQ. A mean unit cost per appointment was calculated from patients providing complete time and travel information. This unit cost consisted of the following:
-
Travel costs – calculated as public transport cost to appointments or costs of mileage if a private car was used. Parking costs were included where reported.
-
Time costs – a time value per appointment was based on the combined travel and appointment time reported by patients. Time was costed based on the Department of Transport value for leisure time,142 where individuals reported not missing work to attend appointments. Where individuals reported unpaid absence from work, an average hourly pay rate was used to calculate this (see Appendix 2).
-
The same cost calculations were undertaken for any additional accompanying person to the patient, where participants reported that they were accompanied by a companion.
-
A mean cost was taken, which provided a time and travel unit cost. This was then applied to every appointment reported in the CRF data.
Inflation
Unit cost calculations were based on 2019 data where available,143 and where these were unavailable costs were inflated using the Consumer Price Index. 143
Discounting
Because the duration of the study extended beyond 12 months, all costs beyond 1 year from study entry were discounted at the recommended NICE rate. 144
Analysis of costs and benefits
Clinical outcomes used in this analysis were those used in the primary trial analysis:
-
BOP
-
OHIP-14 score.
The economic analysis used both of these clinical outcomes to rehearse the effectiveness measure that would be used in the definitive trial and was performed on the basis of ITT. The mean cost and effectiveness in each of the trial arms were used to estimate the adjusted incremental cost, incremental effectiveness and incremental cost per unit change in the effectiveness measure (i.e. ICER) as point estimates. Seemingly unrelated regression [using Stata® (StataCorp LP, College Station, TX, USA) command sureg] analysis, a recommended method when costs and effects are likely to be correlated, was used to generate the estimates of incremental costs and incremental effectiveness. 145 Both the the incremental costs and incremental effects were adjusted for age, sex, baseline proportion of sites with BOP, baseline OHIP-14 point, charge exemption status, number of teeth at baseline and dental practice. The point estimates for the ICER do not reflect the statistical imprecision surrounding estimates of costs, effects and cost-effectiveness. Therefore, the deterministic results alone are not sufficient to support decision-making. To assess the level of uncertainty around point estimates, a stochastic analysis was conducted with the application of the bootstrapping technique. The results of this stochastic analysis (1000 simulations) were presented as cost-effectiveness plane and as cost-effectiveness acceptability curves. A deterministic sensitivity analysis was used to explore the changes in the results with the variation in the value of UDA payments of (1) £20 and (2) £30 and when the analysis was based on patient costs alone. All of the analyses were performed in Stata version 15.1.
Treatment of missing data
Although CRF entries varied in the level of detail that they recorded and, therefore, the level of interpretation required, no data that were required to calculate costs were missing and, therefore, no imputation methods were required.
For the PCQ, patients who did not return a questionnaire or who provided no data for a particular question were assumed to have no costs associated with that category.
With regard to outcome measures and as described in Chapter 2, baseline and follow-up BOP data were present for all participants and only two participants were missing OHIP-14 data at baseline and follow-up, respectively. Given the extremely low level of missing data, no imputation was performed. The implication of this is that participants missing outcome data were excluded from the analysis.
Sensitivity analysis
As an alternative approach to basing NHS dental costs on UDA values, a microcosting approach was taken separately. This was undertaken to estimate actual staff time and materials associated with check-ups and treatments carried out in each arm. Capital costs were not considered because these were considered fixed and unaffected by the level of activity. The treatments costed in this way were those described in the CRF data collected at each appointment. These costs were not included in the cost-effectiveness analysis reported in Results.
Materials
Methods for calculating material costs for each treatment were based on previous dental microcosting work and other information (Tara Homer, Newcastle University, 2019, personal communication), with all costs updated to current values through reference to up-to-date costs of materials using a dental supplies website. 146 Where treatments not featured in this trial were described on the CRF, clinical input was provided to assemble and cost a list of likely consumable and reusable equipment. Laboratory costs were estimated through discussions with clinicians on the study team and reference to available published price lists. Resources were inflated by 20% to account for value-added tax. It was assumed that reusable items had a 3-year lifespan and were used six times per week for their duration. The total cost per item was converted into the equivalent annual cost, using a 3.5% discount rate, and combined with an autoclave cost where appropriate to estimate a per-use cost (see Appendix 2). 144
Staff costs
Staff costs included in the microcosting were based on estimates published by the Personal Social Sciences Research Unit (PSSRU) in 2019. 147 It was assumed that a dental nurse was present for appointments in addition to either a DT or a GDP (dependent on trial arm). It was assumed that participants saw the type of staff consistent with the arm that they were randomised to, unless it was indicated on the CRF that the participant saw another practitioner (e.g. in error, for an emergency appointment, through patient preference or for additional clinical input). In the DT arm, where GDP time was described as additional, this was costed in addition to the DT time. When clinical notes indicated that a treatment had been provided by the GDP, it was assumed that the DT was not present at this appointment.
The staff salaries provided by the PSSRU were adjusted to account for employer pension and national insurance contributions not included in the taxable income provided and a per-minute salary calculated.
Discrete choice experiment: preparatory work
Although there is potential for overlap with Chapter 3, the objectives were different for the preparatory work for a DCE. In this WS, we aimed to understand the acceptability of receiving check-ups from DTs (from the perspective of a health service user) to inform future preference elicitation work in the form of a DCE.
Two rounds of qualitative data collection were conducted. The first comprised focus group discussions held at practices participating in the pilot study. The second comprised one-to-one interviews with members of the public who were not connected to the pilot study or participating practices. This latter sample provided a more heterogeneous sample and a broader range of perspectives.
Recruitment
In round 1, focus group participants were approached by a member of staff at their practice and asked if they would be interested in taking part in a focus group discussion about the use of DTs in the management of low-risk patients. If interested, participants liaised with the practice and three focus groups were arranged on the practice premises. Written consent was taken by the group facilitator (MB) ahead of the focus group.
In round 2, this part of the study was advertised locally in a newspaper, a number of community centres and on a patient and public involvement (PPI) forum. Participants contacted the researcher (MB) directly or through a volunteer co-ordinator (in the case of the public involvement forum) if interested.
For those participants who contacted the volunteer co-ordinator, the researcher then made initial contact by telephone or e-mail and sent out an information sheet. For these interviews, we aimed to achieve a more heterogeneous sample, so we were flexible with regard to the format and setting of interviews, offering participants the choice of location and face-to-face or telephone interviews.
Prior to the interview a consent form was signed (or in the case of telephone interviews a signed form was returned in a freepost envelope). Because there were no clinical data regarding risk, unlike in round 1, three brief questions were asked at the start of the interview: (1) whether or not the participant was currently experiencing pain from their teeth, (2) whether or not the participant had received more than one filling in the past year and (3) whether or not the participant’s gums bleed during brushing. Answering any of these questions positively classified the patient as non-low risk for the purpose of this qualitative work. Participants in both rounds were given a £10 shopping voucher as a gratuity for taking part.
Data collection for the interviews
A flexible topic guide was used that contained questions on the following topics:
-
understanding of different dental professionals’ roles and the importance of level of training
-
relationship with existing dentist and views on seeing a different practitioner
-
confidence in DTs to carry out routine check-ups
-
factors influencing choice of dentist
-
attitudes towards cost
-
perception of individual risk.
Data were transcribed verbatim by an external transcription company. Although efforts were made in focus groups to identify participants (participants were asked to introduce themselves in addition to stating their name before speaking), this was later anonymised.
Data analysis of the interviews
Data analysis followed the principles of thematic analysis (see Chapter 3), and NVivo version 12 (QSR International, Warrington, UK) was used to manage the analysis process:
-
Familiarisation was achieved through reading transcripts multiple times in conjunction with listening to the interview recording. This also served as an opportunity to correct any transcription errors observed. Notes were made on initial thoughts using NVivo.
-
Data were initially coded using a mixture of inductive and deductive codes, referring back to the study objectives as well as emerging themes from the process evaluation.
-
Coded data were then examined to identify common themes.
-
Data were discussed regularly in the health economics and wider study team to inform subsequent versions of the topic guide.
Results
Within-trial economic evaluation
Completeness of data
A total of 167 participants were eligible for inclusion in the primary ITT sample and were included in the analysis of costs. At 6 months, 133 respondents returned the PCQ; however, owing to missing ID numbers, this could not be matched to individuals and is not included in this analysis. A total of 12 respondents (95 included in the ITT sample comprising 47 and 48 in the DT and GDP arms, respectively; 28 were subsequently lost to follow-up) returned the PCQ at 12 months, describing health-care appointments and out-of-pocket costs in the past 6 months. Among these respondents, 44 provided complete time and travel details of a health-care appointment in the past 6 months; these were used to generate a time and travel unit cost.
Estimates of resource use and cost
Table 17 describes resource use. No formal testing was conducted to explore difference between groups. Similar mean numbers of visits to dental practices were observed, with the average appointment duration being longer in the DT group (see Table 10). The number of band 1, 2 and 3 treatments were similar in both arms, as were the number of emergency appointments. The mean amount of time spent with a GDP in the DT group appeared to be large, although this is understandable, because the GDP would be undertaking more complex and time-consuming procedures given the nature of the study (where these were likely to be treatments that could not be undertaken by the DT). Notably, no participants reported use of other primary care services and this suggests that data collection might be simplified for the definitive trial. The number of people reporting additional DH visits in the PCQ was small (n = 2), as was the number of people referred to secondary care (n = 4) and the number of those reporting a visit to an emergency or out-of-hours dental service (n = 1).
| Resource use | Data source | DT arm (n = 83), mean (SD) | GDP arm (n = 84), mean (SD) |
|---|---|---|---|
| Number of visits to dental practice | CRF | 3.3 (2.3) | 3.0 (2.2) |
| Average recall appointment duration (minutes) | CRF | 18.4 (5.9) | 14.0 (6.2) |
| GDP time (minutes) in DT arm | CRF | 14.5 (39.0) | N/A |
| DT time (minutes) in GDP arm | CRF | N/A | 0.2 (2.2) |
| Number of visits to other primary care, mean (SD) | PCQ | 0 (0) | 0 (0) |
| Number of band 1 courses of treatments | CRF | 1.9 (0.9) | 1.8 (0.9) |
| Number of band 2 courses of treatments | CRF | 0.3 (0.7) | 0.2 (0.5) |
| Number of band 3 courses of treatmentsa | CRF | 0.1 (0.3) | 0.1 (0.4) |
| Number of emergency band treatments | CRF | 0.3 (0.8) | 0.2 (0.5) |
| Number of dental specialist visits | PCQ and CRF | 0.02 (0.15) | 0.02 (0.15) |
| Number of emergency visits (e.g. to A&E or dental emergency clinic) | PCQ | 0.1 (0.5) | 0 (0) |
| Number of additional hygienist appointments | PCQ | 0.09 (0.47) | 0 (0) |
Table 18 describes the average (mean) cost per patient for each cost category in each arm. As would be expected, the similar UDA payments reflect the similar number of bands described in Table 17. Prescription costs were low for both groups owing to a small number of prescriptions being reported in the CRF (5 in the DT arm and 4 in the GDP arm) and the relatively low unit cost of these medications. Given the minimum impact on cost estimates, this also suggests that data collection might be simplified for the definitive trial.
| Cost type | DT arm (n = 83), mean (SD) | GDP arm (n = 84), mean (SD) |
|---|---|---|
| NHS (£) | ||
| UDA payments | 126.50 (127.74) | 114.93 (130.10) |
| Prescription medicines cost | 0.15 (0.65) | 0.13 (0.63) |
| Secondary care costs | 4.66 (24.22) | 2.95 (19.03) |
| Total NHS costs | 131.31 (132.57) | 118.01 (131.26) |
| NHS costs minus patient contributions (prescription and dental charges) | 44.30 (70.29) | 36.75 (64.03) |
| Time/materials (£) | ||
| Reusable and consumables costs | 22.08 (30.41) | 24.53 (53.18) |
| Staff costs | 39.78 (42.80) | 44.70 (60.52) |
| Total | 61.86 (71.07) | 69.22 (111.67) |
| Patient (£) | ||
| NHS dental charges | 86.57 (93.40) | 80.73 (104.68) |
| Prescription charges | 0.43 (1.94) | 0.54 (2.14) |
| Over-the-counter medication charges | 0.16 (1.37) | 0.21 (1.45) |
| Private treatment | 21.00 (153.48) | 5.02 (40.38) |
| Time and travel costs | 12.06 (8.05) | 10.37 (7.48) |
| Total | 120.23 (176.62) | 96.86 (122.82) |
Although the cost of private care appears higher in the DT arm, it is worth noting that private treatment was recorded for a small number of patients (n = 6) and the private costs for one of these patients in the DT arm was nearly £1400. Thus, although infrequent, the use of private care would be important to capture in a definitive trial given its potentially high costs.
Figure 12 illustrates the distribution of costs in each of the two arms. This shows that the data are highly skewed (as expected), with a small number of participants incurring substantially higher costs and > 60% of participants in both arms having total NHS costs of < £50.
FIGURE 12.
Total NHS cost by arm: (a) GDP arm and (b) DT arm.
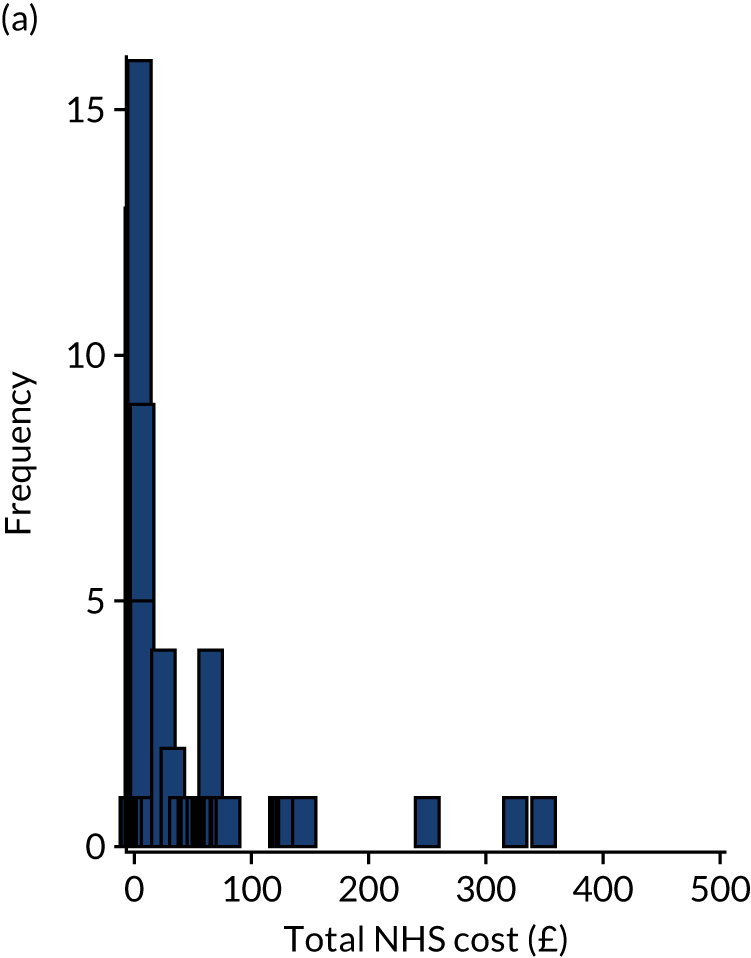
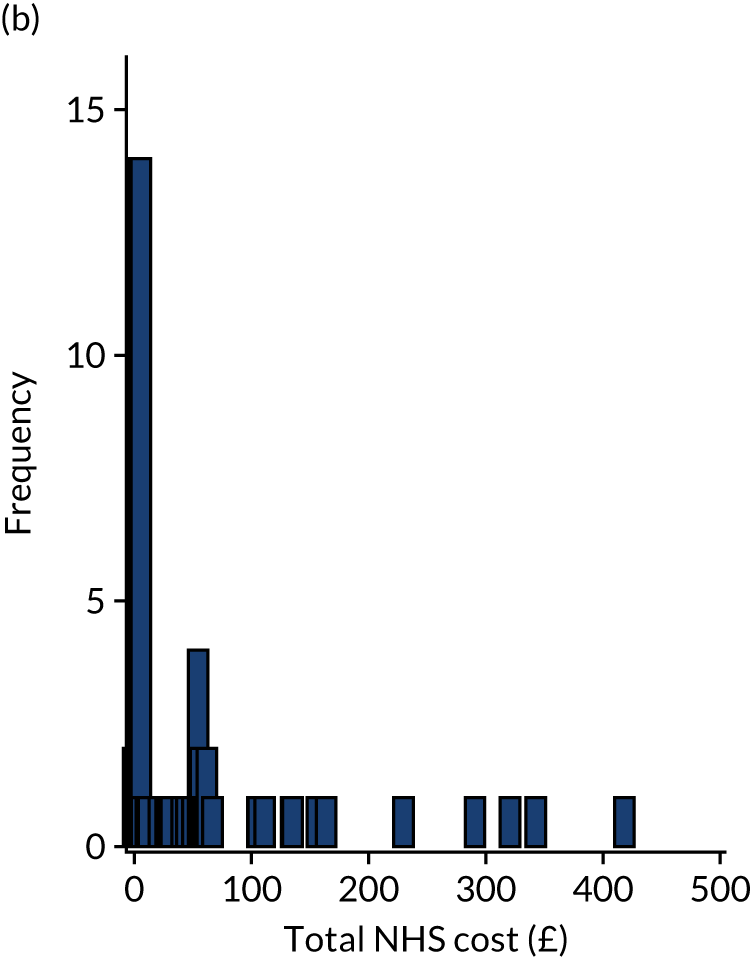
Clinical effectiveness data
The evidence on the impact of the intervention on both BOP and OHIP-14 scores are described in detail in Chapter 2. Figures 13 and 14 describe the distribution of scores in the study population. As Figure 13 illustrates, more participants in the GDP arm than in the DT arm had close to zero sites (where there was BOP). However, in both arms a small number of participants had BOP at 10% of sites. The low proportion of sites with BOP is to be expected given the selection criteria for the study, but it is possible that the distributions would change in a larger sample (should a definitive trial become available).
FIGURE 13.
Proportion of sites with BOP by arm: (a) GDP arm and (b) DT arm.
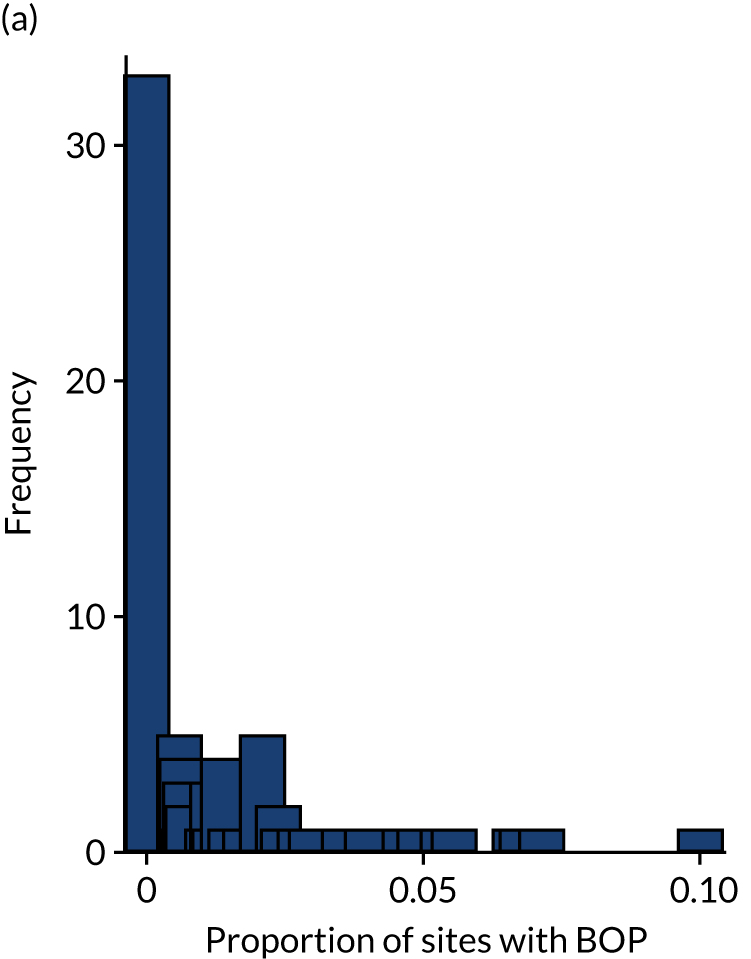

FIGURE 14.
Oral Health Impact Profile-14 items score by arm: (a) GDP arm and (b) DT arm.
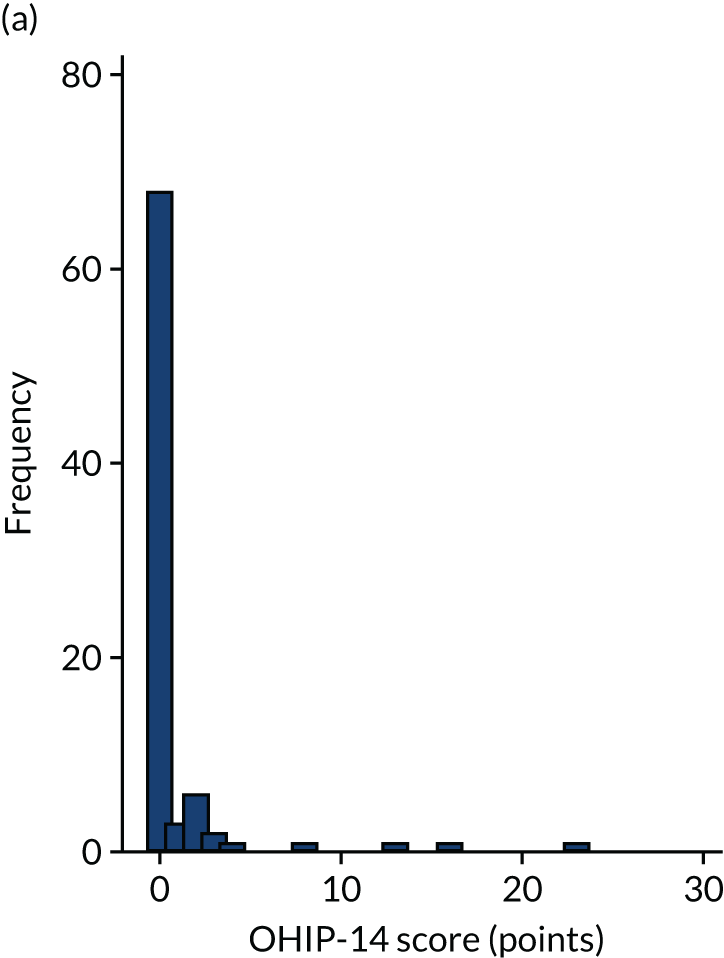
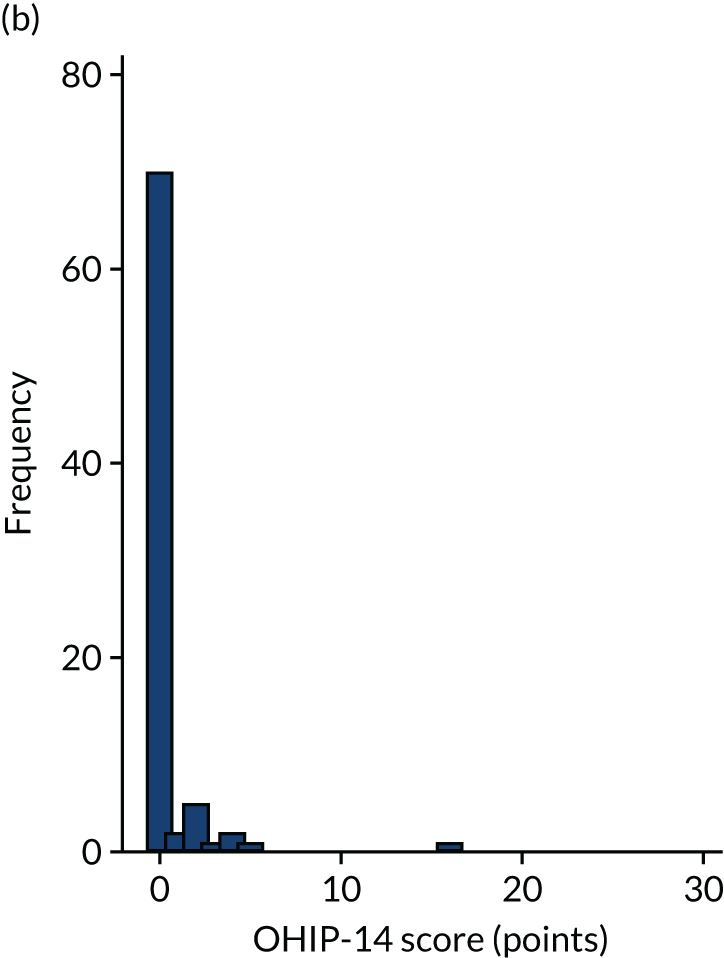
With respect to OHIP-14 scores, the majority of participants had a very low score (where low scores indicate better oral health) (see Figure 14). However, a small number of participants in both arms had higher scores. As with the other outcomes, it is possible that the distribution of scores would change if data from more a sufficiently large sample were available (e.g. from a definitive randomised controlled trial).
Incremental cost-effectiveness analysis
The adjusted cost-effectiveness analysis investigating BOP showed that the DT strategy was, on average, less effective (incremental proportion of sites with BOP 0.0006, 95% CI –0.005 to 0.006) and more costly (incremental cost £14.85, 95% CI –£8.50 to £38.20) than the GDP strategy. Therefore, in terms of BOP, the DT strategy is dominated by the GDP strategy and, thus, no ICER is calculated (Table 19).
| Intervention strategy | Mean NHS cost (£) (95% CI) | Mean proportion of sites with BOP (95% CI) | Incremental cost (£) (95% CI) | Incremental proportion of sites with BOP (95% CI) | ICER (£) | Probability (%) of the DT arm being considered cost-effective at different threshold values for society’s WTP per proportion of site with BOP avoided | ||
|---|---|---|---|---|---|---|---|---|
| £0 | £100 | £500 | ||||||
| Incremental cost per additional site with BOP avoided | ||||||||
| DT (n = 82)a | 55.66 (34.15 to 77.17) | 0.018 (0.013 to 0.023) | 14.85 (–8.5 to 38.20) | 0.0006 (–0.005 to 0.006) | Dominated | 9.3 | 9.0 | 9.2 |
| GDP (n = 84) | 36.75 (22.86 to 50.65) | 0.013 (0.009 to 0.017) | ||||||
| Intervention strategy | Mean NHS cost (£) (95% CI) | Mean OHIP-14 score, points (95% CI) | Incremental cost (£) (95% CI) | Incremental OHIP-14 point (95% CI) | ICER (£) | Probability (%) of the DT arm being considered cost-effective at different threshold values for society’s WTP for each OHIP-14 point reduced | ||
| £0 | £100 | £500 | ||||||
| Incremental cost per OHIP-14 point reducedb | ||||||||
| DT (n = 82)a | 55.66 (34.15 to 77.17) | 0.54 (0.09 to 0.97) | 14.85 (–8.5 to 38.20) | –0.64 (–1.51 to 0.23) | 23.20 per OHIP-14 point reduced | 9.3 | 84.4 | 92.3 |
| GDP (n = 84) | 36.75 (22.86 to 50.65) | 1.01 (0.26 to 1.76) | ||||||
When benefits were considered in terms of the OHIP-14 score, the DT strategy was, on average, more effective (incremental OHIP-14 score –0.64 points, 95% CI –1.51 to 0.23 points) but more costly (incremental cost £14.85, 95% CI –£8.50 to £38.20) than the GDP strategy (see Table 19). The incremental cost per unit reduction in OHIP-14 score was £23.20.
The cost-effectiveness plane (Figure 15) illustrates that, for the majority of the bootstrap iterations, the DT strategy is more likely to have more sites with BOP than the GDP strategy. Contrary to this, in terms of OHIP-14 score the majority of the bootstrap estimates show that the DT strategy provides better OHIP-14 scores than the GDP strategy. The DT strategy is also likely to be more costly than GDP (Figures 16 and 17).
FIGURE 15.
Cost-effectiveness plane showing the incremental proportion of sites with BOP and incremental cost (DT vs. GDP). Because the expected difference in BOP between arms is very small (over-the-threshold ranges of WTP considered), the decision is that the GDP arm is more likely to be cost-effective, primarily as a result of lower cost.
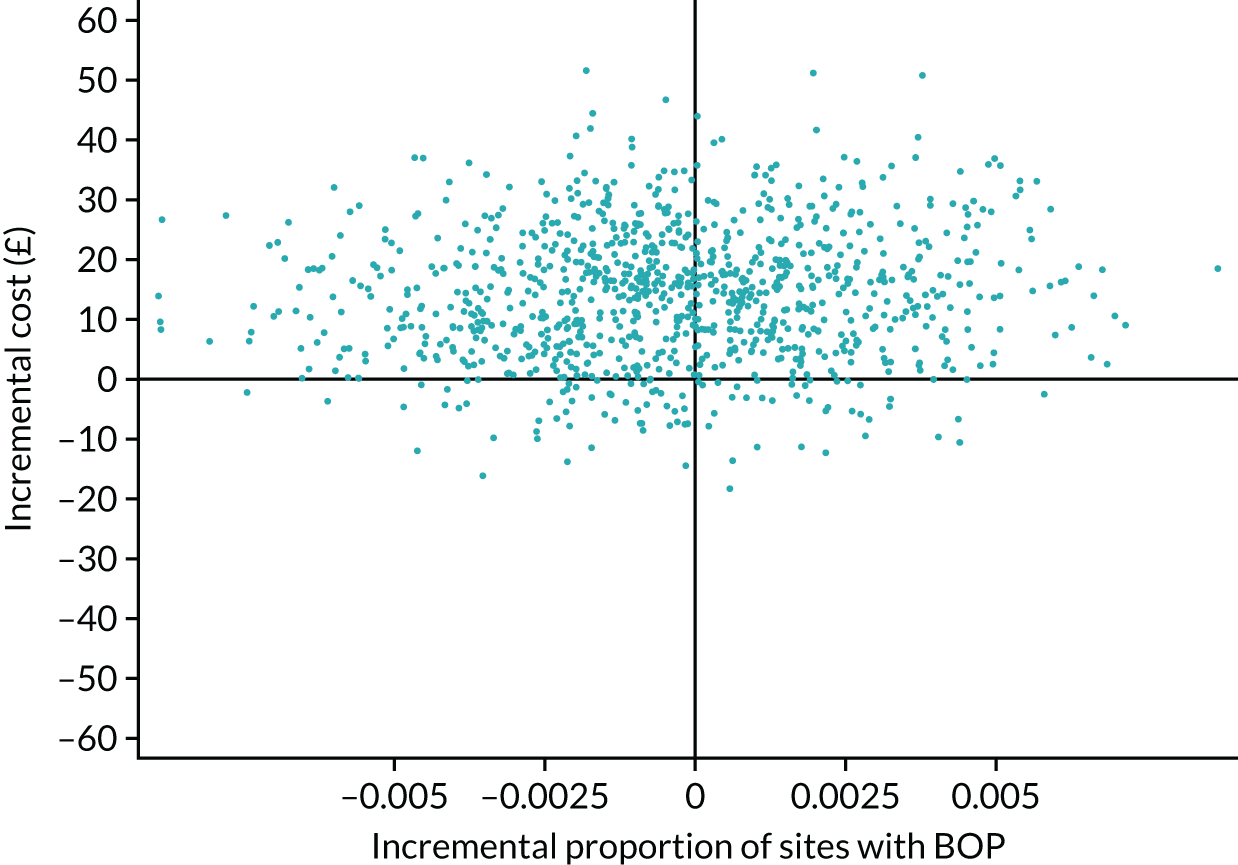
FIGURE 16.
Cost-effectiveness acceptability curve showing probability cost-effectiveness for a given WTP threshold per proportion of site with BOP avoided. A positive incremental OHIP-14 score means that the DT arm is associated with a higher quality of life than the GDP arm. WTP, willingness to pay.
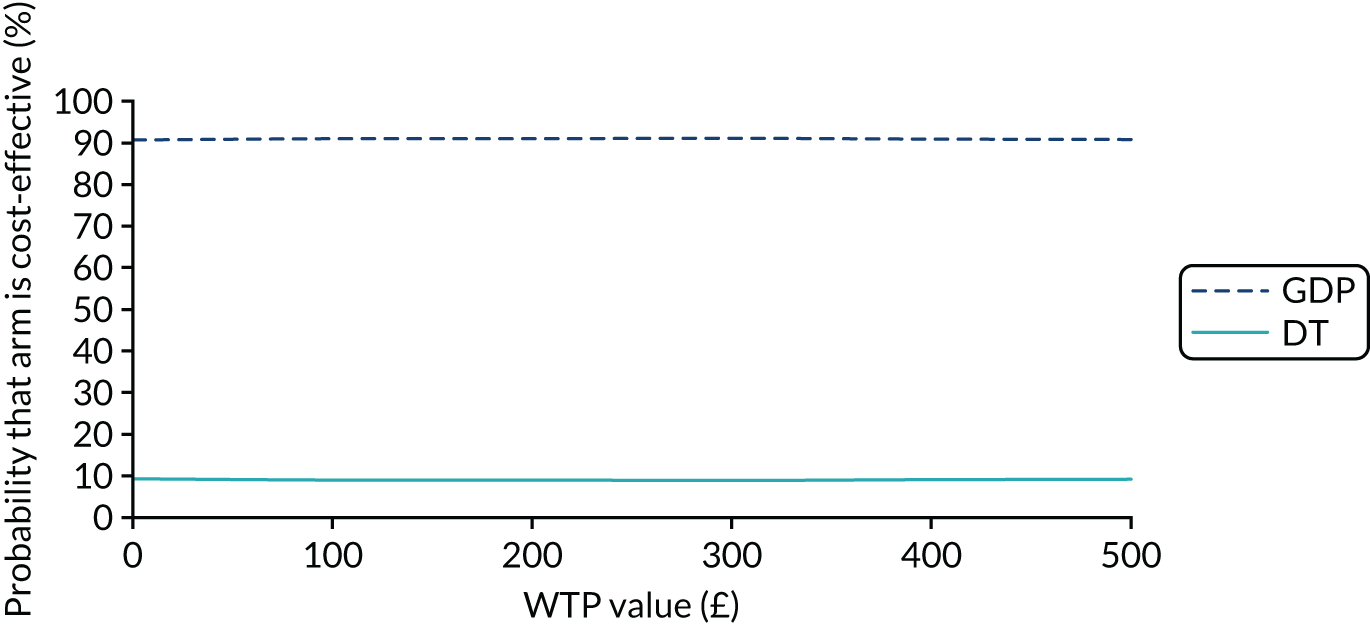
FIGURE 17.
Cost-effectiveness acceptability curve showing probability cost-effectiveness for a given WTP threshold per OHIP-14 point reduced. WTP, willingness to pay.
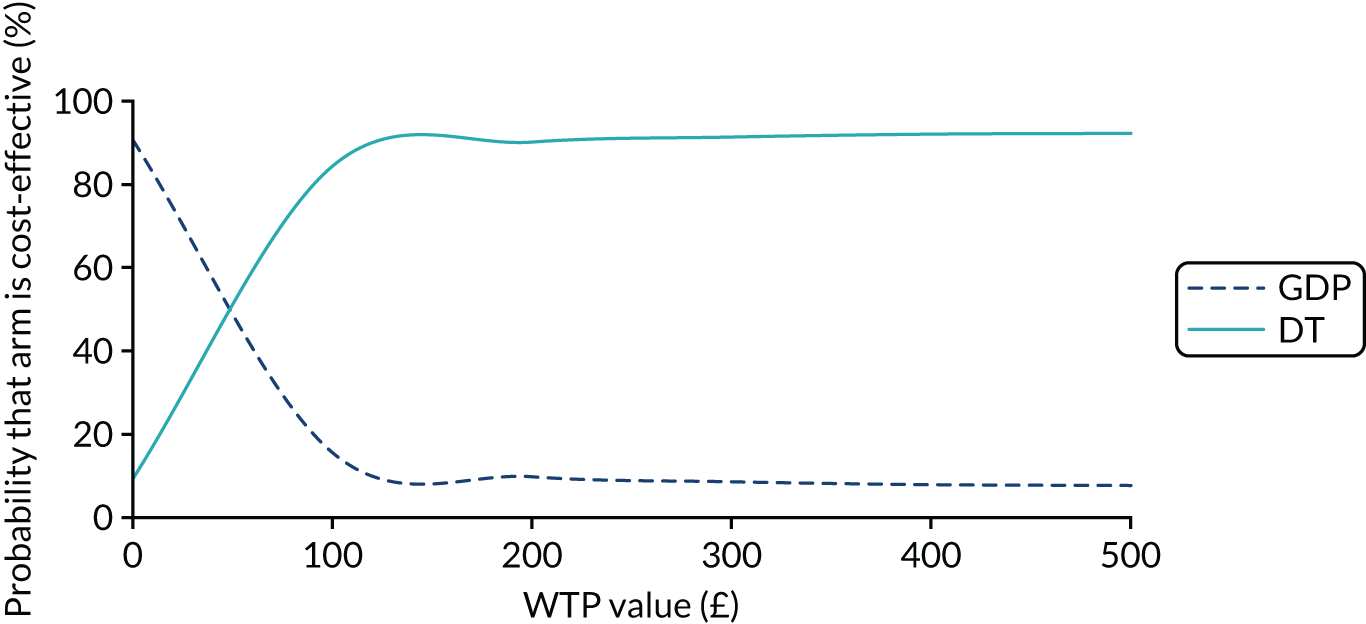
With respect to BOP, Figure 16 shows that there is a 91% chance that the current practice with GDPs would be a more cost-effective strategy than a DT strategy should society be willing to pay £100 per proportion of site with BOP avoided. With respect to OHIP-14, there is an 84.4% chance that the DT strategy would be a more cost-effective strategy than the current practice with GDPs, should society be willing to pay £100 for a 1-point improvement in OHIP-14 score (Figure 18).
FIGURE 18.
Cost-effectiveness plane showing incremental OHIP-14 score and incremental cost (DT vs. GDP). The GDP strategy is expected to be less costly, as it is for BOP, but for the OHIP-14 score, it is also expected to be less effective (although the CIs for a difference include ‘no difference’).
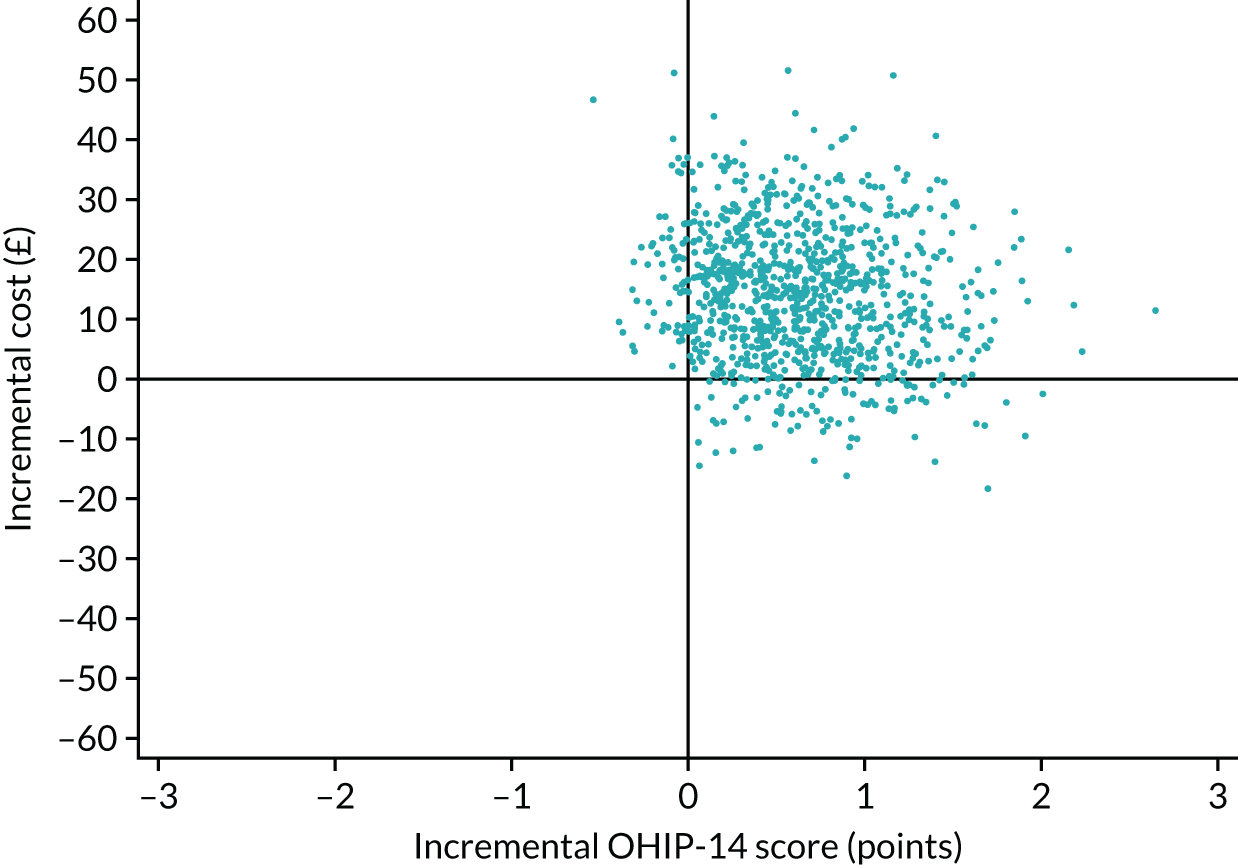
The evidence on costs and cost-effectiveness should be treated cautiously because the results reported are not conclusive given that they were derived from pilot data. Figures 12–14 illustrate that there was marked variability in both cost and clinical effectiveness parameters and it is likely that these results may change substantially, should data from more participants become available in a definitive trial.
Sensitivity analysis
The results of the sensitivity analyses for which high (Table 20) or low (Table 21) NHS costs are used are very similar to the base-case analysis, indicating that the results are not sensitive to the differing methods for costs that have been considered in this WS. Furthermore, the cost-effectiveness results that take into account the patient and carer perspective (derived from PCQ data) do not change the main findings either (Table 22).
| Intervention strategy | Mean NHS cost (£) (95% CI) | Mean proportion of sites with BOP (95% CI) | Incremental cost (£) (95% CI) | Incremental proportion of sites with BOP (95% CI) | ICER (£) | Probability (%) of the DT arm being considered cost-effective at different threshold values for society’s WTP per proportion of site with BOP avoided | ||
|---|---|---|---|---|---|---|---|---|
| £0 | £100 | £500 | ||||||
| Incremental cost per proportion of sites with BOP reduced | ||||||||
| DT (n = 82)a | 81.15 (55.77 to 106.53) | 0.018 (0.013 to 0.023) | 15.41 (–13.13 to 43.95) | 0.0006 (–0.005 to 0.006) | Dominated | 15.7 | 15.7 | 15.6 |
| GDP (n = 84) | 59.73 (41.94 to 77.53) | 0.013 (0.009 to 0.017) | ||||||
| Intervention strategy | Mean NHS cost (£) (95% CI) | Mean OHIP-14 score, points (95% CI) | Incremental cost (£) (95% CI) | Incremental OHIP-14 point (95% CI) | ICER (£) | Probability (%) of the DT arm being considered cost-effective at different threshold values for society’s WTP for each OHIP-14 point reduced | ||
| £0 | £100 | £500 | ||||||
| Incremental cost per OHIP-14 point reduced | ||||||||
| DT (n = 82)a | 81.15 (55.77 to 106.53) | 0.54 (0.1 to 0.97) | 15.41 (–13.13 to 43.95) | –0.64 (–1.51 to 0.23) | 24.08 per OHIP-14 point reduced | 15.7 | 84.0 | 92.3 |
| GDP (n = 84) | 59.73 (41.94 to 77.53) | 1.01 (0.26 to 1.76) | ||||||
| Intervention strategy | Mean NHS cost (£) (95% CI) | Mean proportion of sites with BOP (95% CI) | Incremental cost (£) (95% CI) | Incremental proportion of sites with BOP (95% CI) | ICER (£) | Probability (%) of the DT arm being considered cost-effective at different threshold values for society’s WTP per proportion of site with BOP avoided | ||
|---|---|---|---|---|---|---|---|---|
| £0 | £100 | £500 | ||||||
| Incremental cost per proportion of sites with BOP avoided | ||||||||
| DT (n = 82)a | 30.18 (11.60 to 48.75) | 0.018 (0.013 to 0.023) | 14.30 (–5.42 to 34.02) | 0.0006 (–0.005 to 0.006) | Dominated | 5.1 | 5.0 | 4.6 |
| GDP (n = 84) | 13.76 (2.22 to 25.31) | 0.013 (0.009 to 0.017) | ||||||
| Intervention strategy | Mean NHS cost (£) (95% CI) | Mean OHIP-14 score, points (95% CI) | Incremental cost (£) (95% CI) | Incremental OHIP-14 point (95% CI) | ICER (£) | Probability (%) of the DT arm being considered cost-effective at different threshold values for society’s WTP for each OHIP-14 point reduced | ||
| £0 | £100 | £500 | ||||||
| Incremental cost per OHIP-14 point reduced | ||||||||
| DT (n = 82)a | 30.18 (11.60 to 48.75) | 0.54 (0.1 to 0.97) | 14.30 (–5.42 to 34.02) | –0.64 (–1.51 to 0.23) | 22.34 per OHIP-14 point reduced | 5.1 | 85.3 | 92.5 |
| GDP (n = 84) | 13.76 (2.22 to 25.31) | 1.01 (0.26 to 1.76) | ||||||
| Intervention strategy | Mean patient cost (£) (95% CI) | Mean proportion of sites with BOP (95% CI) | Incremental cost (£) (95% CI) | Incremental proportion of sites with BOP (95% CI) | ICER (£) | Probability (%) of the DT arm being considered cost-effective at different threshold values for society’s WTP per proportion of site with BOP avoided | ||
|---|---|---|---|---|---|---|---|---|
| £0 | £100 | £500 | ||||||
| Incremental cost per proportion of sites with BOP avoided | ||||||||
| DT (n = 82)a | 121.06 (82.05 to 160.10) | 0.018 (0.013 to 0.023) | 17.00 (–29.15 to 63.14) | 0.0006 (–0.005 to 0.006) | Dominated | 28.9 | 29.1 | 28.3 |
| GDP (n = 84) | 96.86 (70.21 to 123.52) | 0.013 (0.009 to 0.017) | ||||||
| Intervention strategy | Mean patient cost (£) (95% CI) | Mean OHIP-14 score, points (95% CI) | Incremental cost (£) (95% CI) | Incremental OHIP-14 point (95% CI) | ICER (£) | Probability (%) of the DT arm being considered cost-effective at different threshold values for society’s WTP for each OHIP-14 point reduced | ||
| £0 | £100 | £500 | ||||||
| Incremental cost per OHIP-14 point reduced | ||||||||
| DT (n = 82)a | 121.06 (82.05 to 160.1) | 0.54 (0.1 to 0.97) | 17.00 (–29.15 to 63.14) | –0.64 (–1.51 to 0.23) | 25.60 per OHIP-14 point reduced | 28.9 | 79.6 | 91.6 |
| GDP (n = 84) | 96.86 (70.21 to 123.52) | 1.01 (0.26 to 1.76) | ||||||
Discrete choice experiment: preparatory work
In total, 32 people took part in the qualitative study. One focus group was held with non-low-risk patients who were not taking part in the study (n = 6) and two focus groups were held with low-risk patients who were taking part in the study (n = 7 and n = 6). A total of 13 patients took part in face-to-face interviews. Overall, the sample consisted of eight male and 24 female, and the mean age of the sample was 61 years (range 23–84 years). Seven participants were employed, four were not working, 19 were retired, one participant was a student and one participant did not answer this question. A total of 30 participants described themselves as ‘white British’, and the remaining two participants did not answer this question. A total of 17 participants were classed as low risk and two reported that they were exempt from charges (one did not answer this question).
Interview participants were asked to describe factors that were important in choosing which dental practice or dentist to attend. This raised a number of considerations, from simple practical factors to descriptions around relationships with health-care professionals.
Practical considerations
Location and convenience
Many participants described initially registering with a dental practice purely on the basis that it was local to them. In the absence of any other factors, this seemed to be the most likely primary reason to register with a particular GDP:
I saw the dentist at [previous employer] and then when I left in the ‘70s, then looking for another dentist and this was the nearest.
Focus group 1 (FG1) participant
Others agreed that distance was important but cited practical factors, such as parking, public transport and proximity to other services or shops.
Personal recommendation
Similarly, participants were likely to be guided by personal recommendations when choosing a dentist, whether this came from friends, their family or other health-care professionals:
So, the last time I was at a dentist, it was on a personal recommendation.
Interview 7
Participants also talked about other factors that affected how satisfied they were with their dental practice. These commonly focused on the ongoing relationship that they had with both the practice and the health-care professionals therein.
Availability
The availability of services was cited as an important factor by many participants. Although there may not have been as much importance placed on routine appointments (typically made months in advance), many stated that it was important that practices were able to deal promptly with emergency appointments. Some suggested that larger practices were more likely to have capacity and flexibility to meet these urgent needs:
And the appointments, you seem to be able to get one quite regular even in an emergency, but they seem to have quite a few staff.
Interview 7
Many argued that they would want to be seen quickly should they or their family have urgent medical needs. This appeared to affect the type of relationship that they had with a practice, because it highlighted the extent to which they were cared for:
If they can’t fit you in fair enough but they do seem to try and say, ‘Come along. You may have a half-an-hour wait or so but we’ll fit you in, even if it’s just a quick look and then we do another appointment,’ but they are willing to do for you.
FG1 participant
Trust and continuity of care
Continuity of care was a dominant topic at many interviews and occupied much of the discussions in the focus groups. This was more than simply seeing the same GDP; it also appeared to affect the perceived level of care that participants received and indicated that they were valued as a patient. This discussion drew parallels with access to care from named general medical practitioners:
I see the same dentist every time. And that is pleasing as opposed to doctors, for example, where if you want to see the same doctor the next appointment is about 5 years away, but you can see someone else tomorrow.
Interview 11
Some participants talked about continuity of care in an almost nostalgic manner, but acknowledged that role substitution may improve efficiency in larger practices, for example being able to get an appointment on the same day for an urgent issue:
Before it was more like a family house, you know, had goldfish in the waiting room, you know what I mean? And it has all been much enlarged and modernised and they take NHS and private patients. And I think a lot more people go. Mind, if it’s an emergency and you are in pain they will see you the same day. But of course you might not always get the dentist you always have, you might just have to take whoever is available.
Interview 4
Participants also spoke about the importance of continuity of care for people with complex medical histories or care needs:
She knows because I’ve had different things going on with my teeth. I prefer to see her because she knows my history without me going through everything again.
FG1 participant
My son is autistic and they are really calm with him and explain everything to him because he doesn’t like sudden noises or the environment, and they are lovely with him – they understand.
Interview 13
Another important element in this theme was the establishment of trust with health-care professionals. Participants commonly described a relationship with a GDP built up over time, which could help ameliorate dental anxiety and result in delivery of more tailored treatment according to their needs:
I don’t like to be flat when the treatment is done. And I said could he raise me up a bit and he didn’t mind doing that, so I was comfortable in the chair, which was important. And he said if I was nervous or worried to put my hand up and he would stop – I found him very reassuring actually.
Interview 4
Although the importance of trust was often inferred at the level of an individual practitioner, some participants also described being attached to a dental practice:
They are very nice. I haven’t met anyone who hasn’t inspired me, they’ve [the practice] actually got my interests at heart.
FG3 participant
NHS status
Although a minority of patients described using non-NHS services, the NHS status of a practice was of great importance to many participants. Some people described their choice of practice as being based on it being a NHS practice that was accepting new patients:
Obviously, I was aware that there are pressures on NHS lists, but in the town I like there were some available appointments and asking around they seemed like an OK type of dentist and I enrolled with them.
Interview 2
A change from NHS status was enough motivation for some patients to seek treatment elsewhere; several people reported changing practices when their existing NHS practice went private and some described how they did this despite being happy with their existing GDP. These participants spoke about an ‘NHS principle’ as well as financial motivation for not wishing to attend on a private basis:
I was with my dental practice for approximately 40-something years, and they were an NHS provider and they turned them totally private. So, my finances and principles said that I wanted to go to a NHS dentist.
Interview 2
This was not always the case, and one participant described how they preferred to stay with their GDP after they became private to ensure continuity of care. In this particular case, the participant described a previous negative experience with a GDP, which meant that they did not want to change GDP despite them having gone private:
About 10 or 15 years ago my dentist gave up the practice and I transferred to another one, and I didn’t have a very pleasant experience. And the guy I go to now I have a good relationship with – it’s about relationships for me, I really need to have trust in somebody who is doing anything inside my mouth.
Interview 6
Although NHS dentistry was highly valued, a minority of participants expressed the view that paying for NHS treatment was not in line with NHS principles:
I said to the receptionist the last time she gave me a bill, I said, ‘Nye Bevan would be turning in his grave’.
Interview 8
Although this is an extreme example, there were other criticisms of how NHS dentistry is funded, highlighting the strong attachment to the NHS held by many.
Acceptability of dental therapists
For the purpose of this study, we were interested in whether or not the introduction of a DT and the use of role substitution might be socially acceptable.
Understanding of dental therapist role
For most participants, the DT was a role that they had not heard of and this was frequently confused with the role of the DH. Exceptions to this were a number of low-risk participants who were in the DT arm of the study and a small number of people whose practice employed a DT. Confusion was perhaps exacerbated by the name ‘dental hygiene therapist’, which was similar to the more familiar term of DH:
What we’re getting slightly confused about is we’re still thinking hygienist because we don’t know what a hygiene therapist . . . you’ve told us now what their role is but we’ve not been used to that. We’re thinking hygienist who just cleans your teeth.
FG1 participant
This term was subsequently avoided during interviews, but this highlighted both the unfamiliarity of the role and the importance of an understanding the role for people to consider its acceptability:
If somebody had offered me to see a dental hygiene therapist, I would have been reluctant. Obviously, I’m unsure. I was thinking they were a hygienist.
FG2 participant
This perhaps highlighted the need for the patient to be well informed about roles and their Scope of Practice in order for them to make treatment decisions.
Efficiency
Some participants described seeing how the role of the DT could improve efficiency in dental practices, particularly for low-risk patients. Conversely, others felt that this could have the opposite effect, requiring more professional and patient time if the DT identified an issue but was unable to carry out the necessary treatment. The following focus group exchange illustrated both sides of this debate:
I can understand why they don’t, because out of every 100 people that come in, I’ve no idea how many of them need something doing but let’s say half of them. That means half the routine appointments are taken off the shoulders of the dentists, which to me is fine. If there’s anything wrong then you see a dentist. You may have to come back to see a dentist.
But that’s got implications, hasn’t it, because that’s extra time not only for you as the patient, it is extra time that they thought they’d save for the dentist. Where do the cost implications start to come in then?
FG13 participants
Cost
From the perspective of the patient and provider, some questioned whether or not a DT would cost less to see than a GDP, although some suggested that patients should pay less to see a DT than a GDP:
I think even if it was a couple of pounds, you know, people count their pennies these days.
Interview 12
In general, there was agreement that in the patient payment bands the cost of a check-up represented fairly good value for money and that it was the check-up itself that the value was attached to, rather than the type of health-care professional undertaking it:
Do you think you should pay the same amount to see somebody who has a different qualification?
If they done the same work, then probably, yeah.
Interview 6
Motivation for the introduction of DTs into practice was questioned, in some cases angrily by some participants, who questioned the rationale for introducing a less-qualified and lower-paid individual:
Well it smacks of cheapness, doesn’t it? That’s what it’s about, cost cutting, isn’t it?
FG1 participant
What are they freeing the dentist up to be doing? Are they going more towards cosmetic dentistry? Is that giving them more time to be doing that and the hygiene therapist is taking over a big role of what the dentist was doing in the first place?
FG1 participant
In this respect, some saw the introduction of a less-qualified professional as a reduction in the quality of a service that they were receiving:
At the time I didn’t realise when he said, and when I went I thought hmm, no. I go to see my dentist and I felt like I was being fobbed off.
Interview 3
This quotation came from a participant whose practice employed a DT and they had unknowingly been referred for an appointment with them. One participant also described leaving a former practice when they were referred to a DT for a filling because they felt that this should be carried out by a GDP.
A small group of participants believed that any change motivated by cost cutting would reduce the quality of the service they received. However, a number of participants countered this and argued that it was important to ensure NHS dentistry was run as efficiently as possible, given that it is publicly funded:
And then obviously reserve the dentists for the more highly intense jobs because they have had longer training, etc, etc. So, it’s like in the realm of making use of your resources to full efficiency.
Interview 10
Competence and risk
Interestingly, among those who saw advantages to seeing a DT, there appeared to be differences in how people saw this role. These were particularly apparent between low-risk and non-low-risk focus group participants. Some low-risk participants described being happy with a DT performing a check-up but reported that if they identified any problems then they would prefer treatment to be carried out by a GDP:
I’m quite happy to see the therapist, whatever. If she then says, ‘Right, well I think you actually now need a tooth out,’ I would then prefer to go to the dentist. But for routine things, I am quite happy and I would prefer to see her than I would the dentist.
FG3 participant
Conversely, the opposite was sometimes expressed in the non-low-risk focus group participants, with debate about continuity of care being important at dental check-ups:
I’d rather see the same dentist. I mean, as you say, for a filling or something in between, I wouldn’t mind seeing somebody else but the actual check-up, I’d rather see the same dentist.
FG1 participant
The question of Scope of Practice prompted a large amount of discussion of individual circumstances, with participants citing their medical and dental history as the rationale for their beliefs on the appropriateness of a DT to conduct their check-ups. People suggested that people with complex medical or dental histories were more likely to require a GDP because of the necessary additional precautions or considerations:
I wouldn’t expect my wife to be seen by one because she is on blood thinners and I wouldn’t expect someone to be poking in her mouth and making her bleed. I would expect them to be more trained, yeah.
Interview 11
These views appeared to be based on people’s perceptions of risk, with regard to not only their oral health but also other existing or past medical conditions. Participants seemed to agree that if someone was at low risk of dental problems then it would be appropriate for them to be seen by a DT. Equally, they felt that a stratified approach was a good one and that it would be reassuring for a patient to understand that they were being seen by a DT because of their low-risk status:
Yeah, I think that is a good way of doing it, because obviously if you are high risk you would feel that it’s better to see someone who has trained for a bit more because they should have knowledge on those kind of things, so I think that is fair. And if you are low risk why should you take up a dentist’s time instead of someone who is high risk, when you can just get the same service off a therapist?
Interview 5
Some questioned the appropriateness of a label of ‘risk’ and wondered whether or not their risk status could change. They argued that basing risk on the level of recent dental activity did not account for the dental treatment that they may require in the near future:
But my worry is am I always going to be a simple, straightforward patient with no issues?
FG3 participant
Part of the acceptance of the DT role may be derived from their level of faith in their training. Some emphasised that seeing someone who was ‘less qualified’ than a GDP was concerning:
I think it’s just being told that that person’s the therapist, it puts you off a little bit, doesn’t it? You would think then that they’re not qualified.
FG1 participant
However, others felt that a DT was appropriately qualified to carry out check-ups:
Absolutely yeah, obviously they have gone through the right training and qualifications to be qualified to do that.
Interview 13
Some participants suggested that this may be related to the existing relationship with the dental practice:
I just think if they, as a practice has decided that is the service that is suitable for me, then I would take that as a given that it’s fine and it doesn’t necessarily mean it’s a lesser service.
Interview 1
Some participants felt that there were advantages to seeing a DT over a GDP for routine care, particularly with regard to their expertise in oral hygiene and their appointments feeling less time-pressured:
Well, for me, she actually got a mirror and showed me all the back of my gums and showed me where I wasn’t brushing it right and how to brush there.
FG3 participant
Others felt that a DT would be an acceptable part of a dental team but were concerned about not seeing a GDP again, suggesting that a compromise would be to maintain some form of periodic review with a GDP:
Perhaps they should have a system which says you must see a dentist once every 2 years.
FG3 participant
Change
Ultimately, given the pros and cons of DTs raised at the interviews, the idea of seeing a different practitioner occupied much of the discussion, particularly among the focus groups. The idea of changing practitioner seemed almost unthinkable to some:
If I am going to see a dentist I want to see a dentist.
Interview 3
However, in many cases this did not appear to be a rejection of role substitution per se, but rather a concern at seeing someone other than their existing GDP who knew them (continuity of care) and who they had built a relationship with (trust):
As I say, he knows my mouth inside out as it were and he knows me and what have you so I really wouldn’t go to anybody else.
FG2 participant
Other participants argued that it was possible to establish a relationship and build trust with a different practitioner:
OK. So, it would be a personality thing?
Yeah. And because obviously she [current dentist] seems to know what I needed, but no, I would be fine, I think I would just make up a relationship with the next person.
Interview 13
By one participant’s own admission, people’s positions were influenced by emotion:
I mean, I know logically – I think it’s emotionally that I find difficulty with that having had 50 years of going to the dentist – because I have gone regularly since I was a child – it’s hard to actually accept that change, as much as my logical brain tells me it would be OK. [Laughter]
Interview 2
Those who expressed more resistance to the idea of DTs often had complex medical histories or high levels of anxiety, sometimes attributed to a past dental experience:
I mean I was anaesthetised too much and blinded in my eye by one dentist for 12 hours. That’s the reason I went to [current dentist]. He put faith back into me because it was a really bad experience and I had to pay for the job as well, mentioning no names. But that was terrifying in itself so to gain confidence again, he was really, really good.
FG2 participant
On the other hand, many participants described being happy with the idea of attending a DT for check-up appointments:
I would be fine with a dental therapist because they still know what they are doing – they have still gone through multiple years of training – so they can still provide adequate care and give advice.
Interview 10
These views expressed opposite ends of the spectrum and it was not the case that everyone was emphatically for or against the idea of being seen by a DT; there was also a group of people who might be a little disappointed at seeing someone other than their dentist but who ultimately felt that they would be accepting of a change of system:
So, yes, I suppose if I knew that my dentist was in charge – there was a team as it were – then I suppose I would be content, but I wouldn’t be happy with it, but I would be content with that, yes.
Interview 8
Discrete choice experiment design
These data have provided us with an understanding both of factors that people value and of how these might feature in a DCE. They have been useful not only in highlighting important potential attributes for a subsequent study but also in demonstrating important dimensions within these attributes that could inform levels in a DCE. The work also highlights the importance of including more subjective factors as attributes and levels. 148,149 These would help capture issues such as patient–practitioner relationships, continuity of care and trust, which were discussed at length in the qualitative interviews. From the results of the interviews, a long list of suggested attributes and levels describing each attribute can be identified:
-
distance/travel time (walking distance/short drive/long drive)
-
location (public transport/parking/town centre)
-
waiting time for routine appointment (days/weeks/months)
-
waiting time for urgent appointment (same day/same week)
-
cost (current payment bands/cheaper for DT/more expensive for GDP)
-
practice status (NHS/corporate/private/dental plan)
-
qualifications of health-care professional (GDP/DT)
-
length of time in practice (newly qualified/experienced)
-
continuity of care (same practitioner/different practitioners in same practice).
In line with good practice for the development of DCEs, this stage focused on the identification of potential attributes. 150,151 It would be followed by further design work to narrow down and clarify the precise attributes and levels for a definitive study. Part of this consideration would be the statistical design of the DCE, so that the chosen DCE design results in data that are analysable to inform an economic evaluation. Further work is also needed to consider who would complete the DCE. Having participants from the trial complete the DCE is likely to be more consistent with economic welfare theory, but consideration would need to be given about when the DCE is completed (e.g. at baseline or at the end of trial follow-up), because this will influence responses. There may also be concerns about response burden on participants because DCE questionnaires can be quite lengthy and cognitively demanding to complete. Administering a DCE at baseline in a definitive trial may reduce retention rates if it is seen as indicative of the burden of data collection to come. The alternative would be to administer the DCE in a sample of the general population and use the resultant analysis to score data for each trial participant on the level of each attribute being assessed.
Discussion
This WS has demonstrated that we can collect the data required for an economic evaluation using costs based on either UDAs or microcosting of dental care. The economic evaluation has been rehearsed and consistent results have been produced across the range of analyses conducted. On average, the DT strategy was more costly and less clinically effective in terms of BOP. Over the range of values for society’s WTP to get one less site of BOP, it is debatable whether or not DTs are cost-effective (although this may have been influenced by the floor effects of the BOP measure). In contrast, in terms of OHIP-14 scores, the DT strategy would be increasingly likely to be considered cost-effective as society’s WTP threshold for a 1-point reduction in OHIP-14 score. GDP care is estimated to be less costly but also less effective (although the CIs for a difference include ‘no difference’). Given that the measure of cost-effectiveness is incremental cost per 1-point improvement in OHIP score and the mean difference in OHIP score is likely to be approximately 0.5 points, the ICER is likely to be less than the WTP thresholds considered, especially when the WTP threshold increases.
Critical here is ‘what is society’s WTP for a unit change in each outcome measure?’, which is uncertain. It is for this reason that we undertook the preparatory work for a DCE to be developed. An alternative to a DCE would be a contingent valuation study. However, valuing a unit reduction in BOP or OHIP score would exclude people’s preferences over the way that care is provided. However, it is important to note that, although we have been able to use the data to estimate cost-effectiveness results, these may be unreliable because we do not have an accurate representation of costs and possible outcomes. For example, private costs are uncommon but very high. As the incidence of incurring private costs is quite low, we may not have an accurate estimate of the impact on total mean of private costs.
The interviews demonstrated that there are many issues that patients consider in relation to the use of DTs to conduct check-ups. The rationale for including a wider sample was to elicit a broad range of perspectives, but this also meant that we gathered data from a broader range of participants with disparate views. These data suggest that the social acceptability of using DTs is mixed. They also highlight the need for patient education in terms of how a new system might work, alleviating concerns about training and competence, and the referral process. This suggests that understanding patients’ information needs ahead of service change is vital, particularly because concerns about continuity of care and loss of long-held personal relationships with GDPs were raised a number of times.
The potential attributes and levels collected in the study primarily relate to process and organisational factors about the service. One of the proposed purposes of the DCE is to develop a tool that could be useful to gather information for NHS decision-makers. A potentially important element of this is the inclusion of a cost attribute, which appears appropriate, given the responses provided in the interviews.
Although we have demonstrated that we can collect data on the use of services, in the pilot study sample only low levels of service use were reported. Some of these data, such as on referrals to secondary care, were duplicated in the CRF. This raises questions about the value of a detailed PCQ. An alternative solution might be to ask participants about the use of services at their appointment at the same time as OHIP-14 data are collected. For the majority of participants a simple yes/no question would only be needed.
The estimation of the use of private treatment was also unclear. Some data were collected in the CRF but in the PCQ the question focused on ‘problems with face and mouth’. This blurred the line between dental services for maintaining or improving oral health and dental services for cosmetic services. Furthermore, although there were no significant differences in any cost category (NHS, patient and time/materials) observed between those who had not returned PCQs and those who had returned PCQs (p > 0.05), the assumptions of missing data in the PCQ meant that where patients did not return questionnaires describing additional costs these costs were potentially underestimated.
The data collection via the CRF facilitated a microcosting exercise. For the definitive trial, consideration needs to be given to the value of this exercise. The microcosting arguably identifies the ‘economic’ cost of care as opposed to the charges for care. Differences between the two illustrate potential inefficiencies caused by charges that do not reflect the economic costs. However, such data might not be considered of sufficient importance to NHS decision-makers given the costs of collecting such data.
With respect to the UDA costing, further information about treatment bands and patient charges could have been included. The precision of current estimates of cost may be improved by revisions to the CRF, which might be completed at the time of each appointment. However, this would be balanced against the increased time for busy staff to complete the CRF.
With respect to measures of cost-effectiveness, it is unclear what the value is of a unit change in either of the two measures used in the pilot. This limitation could be overcome by seeking to formally estimate the value of a unit change. However, the findings of the qualitative work reported in the second half of this chapter suggest that a broader range of impacts is worth consideration.
Summary
This WS has demonstrated that a meaningful economic evaluation could be conducted and has provided valuable information to inform a definitive trial. The qualitative component of this WS has elicited views from patients regarding the acceptability of management of low-risk patients by DTs and allowed us to compile a list of potential attributes and levels for inclusion in a preference elicitation exercise in a definitive trial.
Chapter 5 Discussion
Summary of main findings
The aim of this study was to inform the design for a definitive trial by undertaking a pilot study to determine whether or not DTs can maintain the oral health of low-risk routine NHS patients. WS1 was an individually randomised pilot study conducted over a 15-month period. Eight NHS practices from the North West of England recruited 217 NHS patients, who were randomised into one of two groups. One involved DTs undertaking the routine check-up and any treatment during the intervention period and the other was ‘treatment as usual’ (using GDPs to undertake the check-up and treatment). WS2 was a theoretically driven process evaluation that ran in parallel to the pilot to understand ‘what worked, for whom and under what circumstances’. 104 In WS3, we developed and tested a health economic data collection tool and rehearsed the health economic analysis of the proposed intervention. We also explored patients’ preferences to inform a preference elicitation exercise to inform the design of the definitive trial.
In WS1, we approached 546 patients and 217 were recruited over the 15-month period, equating to a mean recruitment rate of 43.4 participants per month. The attrition rates were comparable with our feasibility study. 99 These were 22.4% and 23.6% for the DT group and the GDP group, respectively, and there were no statistically significant differences in attrition across the randomisation stratification variables.
A total of 13 out of the 14 protocol deviations occurred because participants were allocated to the DT group but were seen once by the GDP in error. The remaining protocol deviation occurred because a participant was allocated to a group before being randomised. The recruited participants in WS1 were predominantly female (72.4%), non-smokers (92.2%), white (93.1%) and were not exempt from patient charges (89.4%). Deprivation scores across the two groups did not show any statistically significant differences.
We found no difference between the two groups in BOP over the 15-month period in the ITT analyses. Therefore, the performance of the DT group in this pilot study was non-inferior to the GDP group. This lack of difference between the two groups was also found across all of the secondary clinical, patient-related and process outcomes. The only substantial difference to note was that 20% more participants in the DT group changed their brushing behaviour. These results were also supported by the per-protocol analyses. Therefore, the findings appear to suggest that DTs were non-inferior to GDPs in the context of a pilot trial run over a 15-month period. However, it is important to be cautious and not overinterpret these findings. 118,119 As we highlighted in Chapter 2, it is possible that the estimates that we used may have still lacked precision, particularly the variability on our proposed primary outcome, and this may have influenced our ability to determine non-inferiority (because of the reliance on the CI estimates for the parameters). We explore these issues further in Chapter 6.
Despite high retention and fidelity rates, recruitment rates were moderately low (39.7%), which was lower than our earlier feasibility study. 99 This may have been caused by the broader range of practices recruited in the pilot study compared with the two practices recruited in our earlier study. To reduce self-selection bias, we deliberately targeted a wide range of NHS practices across the North West of England, which would need to be expanded further for a definitive study. The mean recruitment rate of 43.4 participants per month, along with the non-inferiority design, may have substantial implications for a definitive trial in a low-risk population group. The duration of the recruitment period could become extensive and this could be compounded by the time needed in the intervention period to detect enough of a signal to make comparison between the two groups meaningful.
In WS2, we elicited five areas of programme theory: contractual, institutional logics, regulatory, patients’ experience and logistics. These theory areas were largely interdependent and operated at both a macro and a micro level. It appears that the two most important elements that shape the use of role substitution in NHS dentistry are contractual and regulatory factors, which in turn drive institutional logics at a micro level. All stakeholders were in agreement that the current NHS contractual model makes it difficult to implement role substitution. Despite the relaxation of the Scope of Practice from the regulator’s perspective, the requirements under the GDS contract for GDPs to open a course of treatment appeared to limit the extent of role substitution in NHS dentistry. 9,10 DTs work for NHS dental practice owners (providers) that are largely run as small businesses. The inability of DTs to open courses of treatment means that DTs cannot easily act as the front-line clinician. This has knock-on effects in terms of reducing the efficiency of the practice and in many cases causes disruptions to the patient’s journey. The ‘provider’ and ‘performer’ split also tends to create an ‘internal market’ in NHS practices, leading to competition for work between associate GDPs and DTs. We also found that it acted as a disincentive for associate GDPs to refer to DTs.
Given the need for NHS dental practices to work to the Ionising Radiation Regulations Act, Ionising Radiation (Medical Exposure) Regulations and the Medicines Act, DTs were not allowed to prescribe radiographs or fluoride. These restrictions added to practice inefficiency and patient disruption.
Similar to our earlier research, there was also agreement that the views of the equity owner were highly influential. 30 They were seen as critical in setting the tone in the institutional logics of the NHS practice and overcoming the barriers associated with role substitution at the macro level (contractual and regulatory factors). As highlighted in Chapter 3, a positive attitude towards role substitution saw the equity owners actively seeking workarounds to facilitate different care pathways or internal payment systems for staff (performers). The extent to which their estate was partitioned (e.g. securing additional surgery space) could also influence the promotion of role substitution. This was often difficult in NHS dentistry because most practices were not purpose built for team dentistry.
Endorsement of DTs through outward displays of trust, positive feedback and support were recognised as essential for effective implementation. Although the social acceptability of role substitution was positive, patients did express the need for better communication for them to understand what a DT could do clinically. Most of the patients who were interviewed argued that they would accept new ways of working but that they were concerned about the potential disruption to their care and the need to potentially rebook their appointments.
Because NHS practices were essentially independent contractors, structural investment from the NHS was more difficult. This highlighted the limited number of mechanisms that were available at a meso level for DCs to facilitate the implementation of role substitution.
In WS3, we demonstrated that the data required for an economic evaluation can be reliably collected in terms of costs based on UDAs and/or microcosting of dental care. The pilot study has identified areas where data collection can be refined and simplified for a definitive trial (e.g. simplifying the data collection of use additional health services because these were rarely reported). The economic evaluation was rehearsed and estimates of cost-effectiveness made.
The findings of the qualitative work in preparation for a DCE identified a long list of potential attributes and levels that can form the basis of a future preference elicitation exercise. This could be used to combine the different clinical and process outcomes into a single metric so that the results of the study would be more useful to decision-makers. The attributes and levels identified relate primarily to process and organisational factors about the service (e.g. practice premises).
Qualitative data also highlighted how social acceptability of role substitution can be complex, with strongly held views on either side, and that these views were affected by factors including previous oral health and experience of dental care. This suggests that there may be a role for patient information and/or education ahead of any proposed service changes.
What have we added to the evidence base?
As highlighted by Barnes et al. ,152 ‘there is considerable scope to delegate routine examinations and restorations to DTs’. It is estimated that approaching one-third of restorative interventions could be undertaken by DTs, which would produce a knock-on reduction in the number of dentists required to undertake these routine tasks. 153,154 By conducting a pilot trial and rehearsing a health economic evaluation, we have thoroughly tested the feasibility of a future definitive trial to evaluate role substitution in NHS dentistry in a highly policy-relevant area of research.
The Cochrane Effective Practice and Organisation of Care review96 found a lack of experimental or quasi-experimental evidence for the expanded role of DTs, which concurred with the study by Brocklehurst et al. 155 In this study, we have confirmed recruitment and retention rates and found high levels of clinical fidelity to the intervention in NHS practices. We have also confirmed that a non-inferiority design is the most appropriate, but highlight further challenges to empirically testing role substitution using experimental studies. Of particular note is the challenge of determining the most appropriate primary and secondary outcome measures. As detailed in Chapter 2, even if the eligibility criteria were relaxed to include high-risk patients, there is still a high probability that the strength of any effect may remain undetected, given the large numbers of low-risk patients in NHS practices. To detect clinically meaningful changes, it is also possible that we would need to extend the duration of the trial (at least doubling the duration of the pilot study) and, even then, type II errors may still be possible because any potential signal may remain undetected.
Despite this, the direction of effect in this study (i.e. non-inferiority) is not dissimilar to the non-experimental studies we highlighted in Chapter 1. A number of studies have shown that GDPs and DTs perform to similar standards in terms of their efficacy and clinical effectiveness. The results presented in Chapter 2 concur with Wang,89 Wang and Riordan,88 Kwan et al. ,90 Patel et al. ,91 Kwan and Prendergast92 and Hopcraft. 93 DTs appeared to be able to diagnose and manage low-risk patients within their competency. They were also able to perform routine restorative tasks over the study period, which supports earlier studies by Calache et al. ,81 Freed et al. ,82 Wetherhall et al. ,84 Bader et al. ,94 Battrell et al. 95 and Dyer et al. 96
The realist-informed process evaluation has reinforced findings from our earlier research. 30
Barnes et al. 152 identified the following key mechanisms, which map well onto the results of Chapter 3:
-
a payment system that supports appropriate employment of DTs
-
appropriate referral systems to promote DTs utilisation
-
workplace values and culture*
-
good communication within the practice*
-
experience of working with DTs*
-
team training.*
[List items marked with an asterisk (*) were described in this study as institutional logics.]
Similar to our study, Barnes et al. 152 also contrast the position of the GDC (who allow direct access) with the contractual legislation in the GDS,9 which allows only a dentist to open a course of treatment. The dominance of the contractual theory area in our study is supported by our earlier Cochrane review57 on the effects of financial incentives and also the work of Robinson et al. ,156 who argue that contractual incentives appear to ‘determine dentists’ and patients’ perceptions of need, their behaviours, health outcomes and patient satisfaction’. It is also supported by the work of Harris and Sun,101,102 who explored the efficiency of NHS practices that employ DTs. Barnes et al. 152 contrasts this with other countries, where direct access has been facilitated by favourable regulatory frameworks. 157,158
As highlighted in our study, Barnes et al. 152 also found institutional logics, which are described as intrapersonal and interpersonal factors, to be critical, alongside a lack of knowledge of DTs’ role and their Scope of Practice. Again, this concurs with earlier studies. 158,159 Attitudes towards DTs were also a key factor in influencing the amount and type of work referred to them in practice. 160–162 Barnes et al. 152 also identified the conflict in the internal market between DTs and associate GDPs (because of the competition for UDAs). 152
Our findings also concur with Goodwin et al. 48 and the work of Harris et al. 42 in two large NIHR HSDR projects undertaken in NHS practices. Goodwin et al. 48 found that ‘general dental practitioners are affected by a number of competing interests and incentives and that this can influence their behaviour in a variety of ways’. As Harris et al. 42 argue, there appears to be differences in institutional logic between NHS dental practices and NHS medical practices; they describe the differences between these two groups of NHS practitioners in terms of ‘population health managerialism’ and ‘public health good’. These relate to the extent to which clinicians feel responsible and accountable to their immediate community and the extent to which practices operate to improve the health of their local community. Among general medical practitioners this appears to be prominent and explicitly stated. This contrasts with the prevailing institutional logic in dental practices, which relates to ‘ownership responsibility, professional clinical values and entrepreneurialism’. 42 This may have implications for role substitution in NHS practices, for which the decision to support DTs and/or increase surgery space appears to be driven by a ‘business model’ (linking to contractual incentives) rather than a logic driven by population health managerialism or public health good. This appears to be exacerbated in NHS dentistry by the relative lack of levers that DCs can apply at a meso level to promote role substitution.
As highlighted in Chapter 3, the institutional logic at NHS dental practices also affects our final theory area of logistics. Logistics was also found to be a substantive barrier to role substitution in the NHS by Barnes et al. (i.e. the need for NHS practice owners to invest in additional surgery space to promote role substitution). 152 International evidence also supports these findings. Where NHS dentists are working in larger multisurgery practices, they are more likely to support role substitution because of their capacity to optimise surgery space. 163,164
The social acceptability of role substitution found in this study concurs with earlier work referred to in Chapter 1. 30 It also supports the findings from a survey undertaken in 2018 by Barnes et al. ,165 who found that both patient satisfaction and patient confidence in dentists’ or DTs’ ability was uniformly high (97% and 99%, respectively). This concurs with the studies cited in Chapter 1 in which social acceptability was positive once patients had been educated about the role of the DT. 77,80–86,97 No questions around patient safety were raised in this study, in similarity to other studies cited in Chapter 1. 76–78
The study directly builds on a 5-year Clinician Scientist Award (NIHR/CS/010/004) and a HSDR grant (11/1025/04). 30 As highlighted in Chapter 1, to date, the research team has demonstrated that DTs can identify occlusal caries in vitro, can screen for dental caries and periodontal disease in vivo and are safe as front-line health-care workers. 78,97,98 In addition, the feasibility of undertaking a full trial has been tested as part of NIHR/CS/010/004 over a 15-month period. 99
Strengths and limitations of the research
This study has provided a wealth of information to design a definitive randomised controlled trial. WS1 was conducted in NHS dental practices and recruited a relatively large number of NHS patients. This means that the findings are grounded in the experience of NHS dentists and conducted in a manner that helps research teams understand the challenges of working in a NHS environment. The pilot study has confirmed that the recruitment and retention rates of NHS patients are sufficient to test role substitution in a definitive trial. Fidelity rates were also shown to be high. It also provided estimates of effect for a future definitive study and highlighted the challenges of determining the most appropriate primary and secondary outcome measures. In addition, it revealed the impact that study eligibility might have on the strength of the signal and the impact that including low-risk patients has on a study of this nature.
Four limitations of WS1 related to the exclusion of high-risk patients, the number of practices included in the study, the duration of the pilot and the number of patients lost to follow-up. The eligibility criteria of the study were amended to low-risk patients on the advice of the funding board. Budgetary constraints also required the research team to limit the number of practices and duration of the pilot, but we felt that the design provided enough data to test recruitment, retention and fidelity rates across the practices. The data also showed relatively limited variance, suggestive of a broadly representative sample of practices and patients. In addition, although we tried to be as flexible as possible with regards to the availability of epidemiologist, the fact that we could not schedule appointments with some participants owing to their prior commitments contributed to a number of participants being lost to follow-up. The information we have about the 41 participants who were lost to follow-up suggests that participants were lost primarily because of logistical difficulties. It is important to acknowledge the limitations of this assumption (i.e. that these data are missing at random and these participants did not represent a group with different clinical outcomes to those included in the ITT analysis).
Workstream 2 has provided a novel approach to conducting the process evaluation by using the principles of the realist approach to evaluation of complex social programmes to build on the qualitative component of the study. Realist approaches can help build an explanatory account of what works in any given situation, and places emphasis on stakeholders’ experiences and perspectives to identify and refine the underlying (unseen) mechanism of action. In this study, using the principles of realist methodology were important to articulate and explain the factors that underpin intervention success or failure.
As expected, there are limitations to using realist approaches in this way. Owing to the time frame, pragmatic decisions were made not to conduct a full systematic realist synthesis of evidence. In this instance, the team chose to rely on data derived from experts. As a result, it could be argued that other information is lost. Purposive and convenience sampling could have missed other opportunities to gain insight into theories driven by a wider catchment of different stakeholders. Finally, the theories articulated are at a particular level of abstraction. However, further additional cycles of testing and refining could have developed the theories towards more practice-level specification.
Workstream 3 has demonstrated the feasibility of collecting data required for an economic evaluation from multiple perspectives (health service and patient). We have successfully rehearsed the economic analysis, which produced consistent results across the range of analyses conducted in terms of cost-effectiveness. In addition, the qualitative component of this work has provided rich data regarding the acceptability of the use of DTs in the management of low-risk patients and provided us with a number of attributes and levels to take forward in a future preference elicitation exercise. We were able to recruit both low-risk and non-low-risk participants for qualitative work, which has provided us with a wide spectrum of views on DTs and role substitution.
As discussed in Chapter 4, there are some limitations to the health economics work. With regard to the data collection processes, the collection of service use data from both clinicians and patients meant that there was potential overlap or conflict between the two data sources. The importance of accurately capturing data, such as secondary care use, and patient costs, such as private treatment, should be taken into account in a definitive trial because these costs have the potential to be high and skew the data, and alternative methods to capturing these data should be investigated; for example, capturing these data during clinic visits or through follow-up telephone calls would be a quick way of collecting data, with the potential to reduce the level of missing data. The 6-month PCQ questionnaire data were missing by design and this meant that additional assumptions were made regarding participants having consistent costs over both of the 6-month periods covered by the questionnaires. In addition, our assumption that patients with missing PCQ data had no additional costs had the potential to underestimate cost categories covered in this questionnaire in both arms. Although our microcosting work was based on a previous study, the accuracy of our unit costs could be potentially improved by further exploring materials and methods used by participating practices in a future study.
In the qualitative work, although the inclusion of non-low-risk patients provided us with a range of perspectives, it could also be argued that prominent views were included by those who would be unlikely to be affected by changes in service provision.
Chapter 6 Conclusions
Possible considerations for future policy
The results of this study are important for policy, given the predicted trends in future population health needs. 16,29 There remain challenges in improving the oral health of young children, and providing adequate care for older people is an emerging public health challenge. As a result, there will be a pressing need to better target the available resources in NHS dentistry, which appear to be increasingly spent on low-risk NHS patients. 17–19
As highlighted in this report, the dental contract reform programmes undertaken across the UK place an emphasis on increasing patient access and prevention while maintaining and improving the quality of service being delivered. 59–68 Increasing the use of role substitution is an important consideration for policy-makers and explicitly stated as a strategic objective in Wales. 14,66
Although our pilot study confirmed the potential of using role substitution in NHS dentistry, our realist-informed process evaluation highlighted the barriers to its use. Contractual and regulatory factors were dominant and concurred with our earlier work30 and the international literature. 144 Given that the supply of NHS dentistry is provided by NHS practices operating to a ‘business model’, there is a need to align the financial incentives in NHS GDS contracts with the policy objective of greater use of role substitution. This is concomitant with recommendations from the WHO, which argues that there is an opportunity to think again about how we educate our future health workers. 166 Although amending the regulations to the use of medicines (local analgesia and fluoride) and radiographs may be more problematic, changing the GDS contract is within the scope of many dental policy-makers.
Implications for practice
Because this study was a pilot study, care needs to be exercised in the interpretation of the findings. As highlighted in Chapter 5, the direction of effect concurs with earlier non-experimental research and the same barriers and enablers were identified to the use of role substitution in NHS practices. Institutional logics at a micro level were found to be important but were largely secondary and dependent on the contractual and regulatory factors at a macro level. It appears that the social acceptability of role substitution is high if the DT role and its benefits are clearly articulated to NHS patients. Therefore, the implications for practice would appear secondary to the dominant factors that could be influenced at a policy-level. Because NHS practices largely operate as small businesses, financial incentives that promote role substitution appear key in shaping the response at the level of the practice.
From a patient perspective, the qualitative data collected as part of this study have highlighted that the acceptability of role substitution may vary greatly between patients, influenced by a number of factors including perceived risk, history of oral health, prior dental treatment and dental anxiety. A further understanding of these factors is of vital importance to understand how any changes to services may affect patients.
Recommendations for further research
As highlighted in Chapter 2, the interpretation of the findings of the pilot study poses some interesting design questions. The purpose of the pilot was to determine the most appropriate design for a definitive trial and determine the appropriateness of the primary and secondary outcome measures and the non-inferiority margin. It also tested recruitment, retention and fidelity rates.
It would appear that a future definitive trial, should one be warranted, should be based on non-inferiority. This would align with the findings in this study and the international literature but would require a large number of participants depending on the size of the non-inferiority margin. The relatively low recruitment rates also have practical implications for a future trial and may prolong the recruitment period to reach the desired number of participants in each arm. This could be compounded further by the length of time needed in the intervention period to detect enough of a signal (on the chosen POM) to make comparison between the two arms meaningful.
The nature of the POM is also problematic. It would appear that the inclusion of low-risk NHS patients in a future study would pose a number of design challenges in relation to the POM, yet this is the group of patients to whom role substitution would be the most relevant from a policy perspective. In this study, we used BOP as the POM. Earlier studies suggest that BOP is a good indicator of periodontal health and tissue stability and is well known to NHS practitioners. 112–114 However, it would appear that there are floor effects with this measure in low-risk patients. We anticipate the same kind of effects in clinical measures, such as dental caries, owing to low prevalence and longer times to expression. 16 As highlighted in Chapter 2, there are systems that measure incremental changes in dental caries status, but marginal changes in low-risk patients may create issues with measurement error. 121,122 As we argue, it may be possible to consider analysing a ‘complete’ sample (including high- and low-risk patients) using an appropriate zero-inflated model, but this may not facilitate a full interpretation of effect or non-inferiority. As a result, it would appear that the types of clinical outcomes that would be used for a definitive trial on role substitution in dentistry may not be appropriate to test for non-inferiority. Patient-related outcome measures and patient-related experience measures may be two options, but their signal-to-noise ratio may be problematic. They are also further down the causal pathway to assess clinical effectiveness and/or non-inferiority.
These issues highlight the challenge of designing a definitive randomised controlled trial to test role substitution in NHS dentistry. It would appear that measuring changes to health and/or care pose substantial design problems. This is further exacerbated by the length of time that may be needed to capture the effect of the intervention and the knock-on effect on the cost of the trial. This raises questions about the role of definitive studies in answering these types of important policy questions when they are undertaken on largely healthy participants.
Alternative methods to experimental designs may be advocated here. There is a developing argument about the need to embrace a broader range of research methods for policy-related and population health issues, rather than restricting the approach to randomised controlled trials. As argued by Brocklehurst et al. :167
We need to consider a broader range of conceptual and methodological approaches to increase the value of information generated. This should be undertaken either in parallel with empirical and experimental designs, or in some cases, instead of. This is important if we are going to understand the complexity and contextual knowledge of the ‘system’, within which interventions are implemented.
What is evident from Chapter 3 is that this ‘system’ is complex, with multiple interdependent elements that operate at different macro, meso and micro levels. As Braithwaite et al. 168 argue, accounting for this complexity is key; there are ‘no simple solutions, no single ingredient’. 169
There are alternatives to experimental designs and these may be warranted here to determine whether or not role substitution is both clinically effective and cost-effective. As highlighted by Brocklehurst et al. 170 and Listl et al. ,171 ‘ex-post techniques typically evaluate the impact of an already implemented health policy programme and include a range of quasi-experimental methods including Instrumental Variables, Difference-in-Difference, panel data analyses using fixed or random effects, and Regression-Discontinuity-Designs’170 and ‘ex-ante methods include structural modelling, agent-based modelling and micro-simulation’171 to help model the short-, mid- and long-term health effects of an intervention. For example, difference-in-difference designs have been used in other dental public health studies before. 57,172 In Northern Ireland, difference-in-difference design was used to assess the implementation of a NHS pilot based on capitation. 57 This enabled the research team to measure changes in activity levels during three time periods, and the coefficients were triangulated by an interrupted time series approach undertaken in parallel. Such methodologies can ‘provide very helpful information on the evaluation of policies and interventions that would otherwise not be rigorously evaluated as the standard [randomised controlled trial-]related methodologies are neither feasible nor suitable’. 170 They might also prove eminently more affordable when compared with a lengthy definitive trial based on non-inferiority. They would also allow multiple outcome measures to be followed over time, rather than selecting one single POM.
In addition to the empirical aspect of any future study, it would be important to undertake a parallel process evaluation to further explore the factors that influence the pathway to impact for role substitution. In this study, WS2 provided helpful insight to the barriers to and enablers of role substitution in NHS dentistry. This element of the study captured how complex interventions and systems can interact and identified the underlying generative mechanisms about how role substitution works. 126 This gave us a good understanding of ‘how context (individual, social, cultural, organisational) interacts with intervention components and underpinning mechanisms to bring about desired outcomes’. 127 This allowed the research team to develop a set of focused MRTs that enabled us to determine the range of factors that could potentially influence adoption. 130 As a result, we remained focused on the barriers and enablers that could make a difference at both a policy and a practice level as opposed to constructing ‘all-encompassing meta-narratives that span space and time’. 131 As a result, we commend the use of these types of approaches alongside future experimental and quasi-experimental study designs. Future teams could make use of the different CMO configurations that were generated in this study as a starting point for undertaking a further realist cycles.
Following this pilot study, there is an important role for economic evaluation work in any future study to establish cost-effectiveness of role substitution in the management of low-risk dental patients (WS3). As discussed in Chapter 4, recommendations from this WS include potentially revising data collection methods with regard to patient-reported data, possibly integrating these into the collection of clinical data at dental appointments, given that the routine nature of appointments has the potential to achieve higher levels of accuracy and completion. Telephone interviews have been used successfully in past studies to collect details of health service use and this may also offer a method of supplementing data collection. In addition, completion of clinical data has the potential to be simplified, therefore reducing burden on participating health-care professionals and standardising the data collected. In a future study there is potential to improve the accuracy of resource-based microcosting through further investigation into materials and methods. These methods could be incorporated into either an experimental or a quasi-experimental design.
The preparation work undertaken in this pilot demonstrated the importance of including a DCE to help further understand the relative importance of different attributes. These could provide valuable data for future service design. In addition, given the need to understand the impact of service changes on people using these services, there is an important role for future qualitative work to explore some of the questions to arise out of the qualitative component of the health economics work, such as patient information needs or exploring the experience of receiving care from different health-care professionals.
Acknowledgements
The research team would like to thank all of the key stakeholders who took part in WS2: Colette Bridgman, Kirstie Moons, Lesley Gough, Roger Hollins and Emma Hall-Scullin. We would like to thank Ivor Chestnut for chairing the Study Steering Committee, Richard Watt for chairing the Data Monitoring Committee and to our PPI members (Christine Barwood and Pat Foy). Finally, we would like to thank all of the committee members, the NHS practitioners who took part in this study and our PPI group, who were essential throughout the study (see Appendix 3).
Contributions of authors
Paul Brocklehurst (https://orcid.org/0000-0003-1878-9030) wrote the application to secure the research funds from the NIHR, led the project, provided dental public health input, undertook the analysis and oversaw the writing of the report.
Zoe Hoare (https://orcid.org/0000-0003-1803-5482) wrote the application to secure the research funds from the NIHR, provided statistical input throughout the study and made a substantive contribution to the design of the pilot study and the writing-up of Chapter 2.
Chris Woods (https://orcid.org/0000-0003-4546-3028) managed the pilot trial, conducted the interviews for the realist-informed process evaluation, undertook the analysis and co-wrote Chapter 3.
Lynne Williams (https://orcid.org/0000-0003-2575-9710) wrote the application to secure the research funds from the NIHR, undertook the analysis and co-wrote Chapter 3.
Andrew Brand (https://orcid.org/0000-0002-6942-0404) provided statistical input throughout the study and made a substantive contribution to the design of the pilot study and the writing-up of Chapter 2.
Jing Shen (https://orcid.org/0000-0001-8450-5003) wrote the application to secure the research funds from the NIHR, planned and conducted the DCE development work, planned and conducted the pilot health economic evaluation and co-wrote Chapter 4.
Matthew Breckons (https://orcid.org/0000-0003-3057-6767) planned and conducted the DCE development work, planned and conducted the pilot health economic evaluation and co-wrote Chapter 4.
James Ashley (https://orcid.org/0000-0003-0058-4889) wrote the application to secure the research funds from the NIHR and provided input to the study design from the perspective of a NHS GDP.
Alison Jenkins (https://orcid.org/0000-0003-1963-4903) managed the pilot trial.
Lesley Gough wrote the application to secure the research funds from NIHR and provided input to the study design from the perspective of a consultant in dental public health.
Philip Preshaw (https://orcid.org/0000-0002-7153-4865) wrote the application to secure the research funds from NIHR, provided valuable input at the design stage and proofread the iterations of the final report.
Christopher Burton (https://orcid.org/0000-0003-1159-1494) wrote the application to secure the research funds from NIHR and provided input in the writing of Chapter 3.
Karen Shepherd acted as our user researcher in WS2, co-wrote the Plain English summary and contributed to our dissemination strategy.
Nawaraj Bhattarai (https://orcid.org/0000-0002-1894-2499) planned and conducted the pilot health economic evaluation and co-wrote Chapter 4.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Birch S. Health human resource planning for the new millennium: inputs in the production of health, illness, and recovery in populations. Can J Nurs Res 2002;33:109-14.
- Gallagher JE, Wilson NHF. The future dental workforce?. Br Dent J 2009;206:195-200. https://doi.org/10.1038/sj.bdj.2009.114.
- Brocklehurst P, Macey R. Skill-mix in preventive dental practice – will it help address need in the future?. BMC Oral Health 2015;15. https://doi.org/10.1186/1472-6831-15-S1-S10.
- King NC. The new Dentists Act. Br Med J 1921;2. https://doi.org/10.1136/bmj.2.3164.302-b.
- Great Britain . The Dentists Act 1956 1956.
- Great Britain . Dentistry (Teviot Committee, Final Report) 1946.
- General Dental Council (GDC) . Scope of Practice 2013. www.gdc-uk.org/docs/default-source/scope-of-practice/scope-of-practice.pdf?sfvrsn=8f417ca8_4 (accessed 13 March 2020).
- Great Britain . Draft Dental Auxiliaries (Amendment) Regulations 2002 2002. https://publications.parliament.uk/pa/cm200102/cmstand/deleg4/st020508/20508s01.htm (accessed 13 March 2020).
- Great Britain . The National Health Service (General Dental Services Contracts) Regulations 2005 2005. www.legislation.gov.uk/uksi/2005/3361/pdfs/uksi_20053361_en.pdf (accessed 13 March 2020).
- General Dental Council (GDC) . Direct Access 2013. www.gdc-uk.org/information-standards-guidance/standards-and-guidance/direct-access (accessed 13 March 2020).
- Great Britain . The Ionising Radiations Regulations 2017 2017. www.legislation.gov.uk/uksi/2017/1075/pdfs/uksi_20171075_en.pdf (accessed 13 March 2020).
- Great Britain . Medicines Act 1968 1968. www.legislation.gov.uk/ukpga/1968/67 (accessed 13 March 2020).
- The Nuffield Institute . Nuffield Report: The Education and Training of Personnel Auxiliary to Dentistry 1993.
- Health in Wales . Making Prudent Healthcare Happen n.d. www.wales.nhs.uk/sitesplus/documents/866/PHW%20Prudent%20Healthcare%20Booklet%20Final%20English.pdf (accessed 13 March 2020).
- NHS . NHS Long Term Plan n.d. www.england.nhs.uk/long-term-plan/ (accessed 13 March 2020).
- NHS Digital . Adult Dental Health Survey: Summary 2009. https://digital.nhs.uk/data-and-information/publications/statistical/adult-dental-health-survey/adult-dental-health-survey-2009-summary-report-and-thematic-series (accessed 13 March 2020).
- NHS Digital . Child Dental Health Survey 2013, England, Wales and Northern Ireland 2013. https://digital.nhs.uk/data-and-information/publications/statistical/children-s-dental-health-survey/child-dental-health-survey-2013-england-wales-and-northern-ireland (accessed 13 March 2020).
- Morgan MZ, Johnson IG, Hitchings E, Monaghan NP, Karki AJ. Dentist skill and setting to address dental treatment needs of care home residents in Wales. Gerodontology 2016;33:461-69. https://doi.org/10.1111/ger.12185.
- Karki AJ, Monaghan N, Morgan M. Oral health status of older people living in care homes in Wales. Br Dent J 2015;219:331-4. https://doi.org/10.1038/sj.bdj.2015.756.
- Givens JL, Selby K, Goldfield KS, Mitchell SL. Hospital transfers of nursing home residents with advanced dementia. J Am Geriatr Soc 2012;60:905-9. https://doi.org/10.1111/j.1532-5415.2012.03919.x.
- Public Health England (PHE) . Dental Public Health Intelligence Programme: North West Oral Health Survey of Services for Dependent Older People, 2012–13 2013.
- Public Health England (PHE) . Commissioning Better Oral Health For Vulnerable Older People: An Evidence-Informed Toolkit for Local Authorities 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/738722/CBOH_VOP_V16_Final_WO_links.pdf (accessed 13 March 2020).
- Pretty IA. Special Issue: developing pathways for oral care in elders. Gerodontology 2014;31:1-8. https://doi.org/10.1111/ger.12092.
- World Health Organization (WHO) . World Report on Ageing and Health n.d. www.who.int/ageing/events/world-report-2015-launch/en/ (accessed 13 March 2020).
- Royal College of Surgeons of England (RCS) . Improving Older People’s Oral Health 2017.
- National Institute for Health and Care Excellence (NICE) . Oral Health for Adults in Care Homes. NICE Guideline [NG48] 2016. www.nice.org.uk/guidance/ng48 (accessed 25 November 2020).
- Care Quality Commission (CQC) . Smiling Matters: Oral Health Care in Care Homes 2019. www.cqc.org.uk/sites/default/files/20190624_smiling_matters_full_report.pdf (accessed 13 March 2020).
- NHS Digital . 6: Service Considerations – A Report from the Adult Dental Health Survey 2009 2011. https://files.digital.nhs.uk/publicationimport/pub01xxx/pub01086/adul-dent-heal-surv-summ-them-the6-2009-rep8.pdf (accessed 13 March 2020).
- NHS Digital . NHS Dental Statistics for England 2018–19, Annual Report [PAS] n.d. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-dental-statistics/2018-19-annual-report-pas (accessed 13 March 2020).
- Brocklehurst P, Birch S, McDonald R, Hill H, O’Malley L, Macey R, et al. Determining the optimal model for role substitution in NHS dental services in the UK: a mixed-methods study. Health Serv Deliv Res 2016;4. https://doi.org/10.3310/hsdr04220.
- House of Commons Health Select Committee . Dental Services – Fifth Report of Session 2007–08 2008.
- Adams A, Lugsden E, Chase J, Arber S, Bond S. Skill-mix changes and work intensification in nursing. Work Employ Soc 2000;14:541-55. https://doi.org/10.1177/09500170022118563.
- Burke FJT, Wilson NHF, Christensen GJ, Cheung SW, Brunton PA. Contemporary dental practice in the UK: demographic data and practising arrangements. Br Dent J 2005;198:39-43. https://doi.org/10.1038/sj.bdj.4811956.
- Gallagher JL, Wright DA. General dental practitioners’ knowledge of and attitudes towards the employment of dental therapists in general practice. Br Dent J 2003;194:37-41. https://doi.org/10.1038/sj.bdj.4802411.
- Godson JH, Williams SA, Csikar JI, Bradley S, Rowbotham JS. Dental therapy in the United Kingdom: part 2. A survey of reported working practices. Br Dent J 2009;207:417-23. https://doi.org/10.1038/sj.bdj.2009.962.
- Ross MK, Ibbetson RJ, Turner S. The acceptability of dually-qualified dental hygienist-therapists to general dental practitioners in South-East Scotland. Br Dent J 2007;202. https://doi.org/10.1038/bdj.2007.45.
- Harris R, Burnside G. The role of dental therapists working in four personal dental service pilots: type of patients seen, work undertaken and cost-effectiveness within the context of the dental practice. Br Dent J 2004;197:491-6. https://doi.org/10.1038/sj.bdj.4811749.
- Dyer TA, Humphris G, Robinson PG. Public awareness and social acceptability of dental therapists. Br Dent J 2010;208. https://doi.org/10.1038/sj.bdj.2010.1.
- McDonald R, Cheraghi-Sohi S, Sanders C, Tickle M. Changes to financial incentives in English dentistry 2006-2009: a qualitative study. Community Dent Oral Epidemiol 2012;40:468-73. https://doi.org/10.1111/j.1600-0528.2012.00687.x.
- Tickle M, McDonald R, Franklin J, Aggarwal VR, Milsom K, Reeves D. Paying for the wrong kind of performance? Financial incentives and behaviour changes in National Health Service dentistry 1992-2009. Community Dent Oral Epidemiol 2011;39:465-73. https://doi.org/10.1111/j.1600-0528.2011.00622.x.
- Harris R, Holt R. Interacting institutional logics in general dental practice. Soc Sci Med 2013;94:63-70. https://doi.org/10.1016/j.socscimed.2013.05.038.
- Harris R, Perkins E, Holt R, Brown S, Garner J, Mosedale S, et al. Contracting with general dental services: a mixed- methods study on factors influencing responses to contracts in English general dental practice. Health Serv Deliv Res 2015;3. https://doi.org/10.3310/hsdr03280.
- Birch S. The identification of supplier-inducement in a fixed price system of health care provision. The case of dentistry in the United Kingdom. J Health Econ 1988;7:129-50. https://doi.org/10.1016/0167-6296(88)90012-4.
- Chalkley M, Tilley C. Treatment intensity and provider remuneration: dentists in the British National Health Service. Health Econ 2006;15:933-46. https://doi.org/10.1002/hec.1162.
- Grytten J. Models for financing dental services: a review. Community Dental Health 2005;22:75-8.
- Gosden T, Forland F, Kristiansen IS, Sutton M, Leese B, Giuffrida A, et al. Capitation, salary, fee-for-service and mixed systems of payment: effects on the behaviour of primary care physicians. Cochrane Database Syst Rev 2000;3. https://doi.org/10.1002/14651858.CD002215.
- Ellis RP, McGuire TG. Supply-side and demand-side cost sharing in health care. J Econ Perspect 1993;7:135-51. https://doi.org/10.1257/jep.7.4.135.
- Goodwin TL, Brocklehurst PR, Hall E, McDonald R, Tickle M, Williams L. How, and why, does capitation affect general dental practitioners’ behaviour? A rapid realist review. Br J Healthcare Manag 2018;24:505-13. https://doi.org/10.12968/bjhc.2018.24.10.505.
- Watt R, McGlone P, Evans D, Boulton S, Jacobs J, Graham S, et al. The facilitating factors and barriers influencing change in dental practice in a sample of English general dental practitioners. Br Dent J 2004;197:485-9. https://doi.org/10.1038/sj.bdj.4811748.
- Bhaskar R. The Possibility of Naturalism: A Philosophical Critique of the Contemporary Human Sciences. London: Routledge; 2014.
- Wilson A, Pearson D, Hassey A. Barriers to developing the nurse practitioner role in primary care-the GP perspective. Fam Pract 2002;19:641-6. https://doi.org/10.1093/fampra/19.6.641.
- Charles-Jones H, Latimer J, May C. Transforming general practice: the redistribution of medical work in primary care. Sociol Health Illn 2003;25:71-92. https://doi.org/10.1111/1467-9566.t01-1-00325.
- Doyal L, Cameron A. Reshaping the NHS workforce: necessary changes are constrained by professional structures from the past. BMJ 2000;320. https://doi.org/10.1136/bmj.320.7241.1023.
- McDonald R, Cheraghi-Sohi S, Sanders C, Ashcroft D. Professional status in a changing world: the case of medicines use reviews in English community pharmacy. Soc Sci Med 2010;71:451-8. https://doi.org/10.1016/j.socscimed.2010.04.021.
- Department of Health and Social Care (DHSC) . Modernising NHS Dentistry – Implementing the NHS Plan 2000.
- Pitts NB. NHS Dentistry: Options for Change in context – a personal overview of a landmark document and what it could mean for the future of dental services. Br Dent J 2003;195:631-5. https://doi.org/10.1038/sj.bdj.4810779.
- Brocklehurst P, Tickle M, Birch S, McDonald R, Walsh T, Goodwin TL, et al. Impact of changing provider remuneration on NHS general dental practitioner services in Northern Ireland: a mixed-methods study. Health Serv Deliv Res 2020;8. https://doi.org/10.3310/hsdr08060.
- Great Britain . The National Health Service (General Dental Services Contracts) Regulations 2005 2005. www.legislation.gov.uk/uksi/2005/3361/contents/made (accessed 13 March 2020).
- Steele J. NHS Dental Services in England. London: Department of Health and Social Care; 2009.
- Department of Health and Social Care (DHSC) . NHS Dental Contract Pilots – Learning After First Two Years of Piloting 2014. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/282760/Dental_contract_pilots_evidence_and_learning_report.pdf (accessed 13 March 2020).
- Department of Health and Social Care (DHSC) . Dental Contract Reform: Prototypes 2015. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/395384/Reform_Document.pdf (accessed 13 March 2020).
- Department of Health and Social Care (DHSC) . Dental Contract Reform: Evaluation of the First Year of Prototyping 2016–17 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/709555/evaluation-report-2016-2017.pdf (accessed 13 March 2020).
- Public Health Wales (PHW) . Welsh Dental Pilots Programme 2017. www.wales.nhs.uk/sitesplus/888/page/66924 (accessed 13 March 2020).
- Public Health Wales (PHW) . Future Plans for the Continuation and Development of the Welsh Dental Pilot Programme 2017.
- Welsh Government . Taking Oral Health Improvement and Dental Services Forward in Wales 2017. https://gov.wales/sites/default/files/publications/2019-04/taking-oral-health-improvement-and-dental-services-forward-in-wales.pdf (accessed 13 March 2020).
- Welsh Government . The Oral Health and Dental Services Response to a Healthier Wales 2018. https://gov.wales/sites/default/files/publications/2019-03/the-oral-health-and-dental-services-response.pdf (accessed 13 March 2020).
- Department of Health, Social Services and Public Safety (DHSSPS) . An Oral Health Strategy for Northern Ireland 2007. www.health-ni.gov.uk/publications/oral-health-strategy-northern-ireland-june-2007 (accessed 13 March 2020).
- Scottish Government . Oral Health Improvement Plan 2018. www.gov.scot/Publications/2018/01/9275 (accessed 13 March 2020).
- Brocklehurst PR, Ashley JR, Tickle M. Patient assessment in general dental practice – risk assessment or clinical monitoring?. Br Dent J 2011;210:351-4. https://doi.org/10.1038/sj.bdj.2011.284.
- Mertz E, Glassman P. Alternative practice dental hygiene in California: past, present, and future. J Calif Dent Assoc 2011;39:37-46.
- Edelstein BL. Examining whether dental therapists constitute a disruptive innovation in US dentistry. Am J Public Health 2011;101:1831-5. https://doi.org/10.2105/AJPH.2011.300235.
- Nash DA, Friedman JW, Kardos TB, Kardos RL, Schwarz E, Satur J, et al. Dental therapists: a global perspective. Int Dent J 2008;58:61-70. https://doi.org/10.1111/j.1875-595x.2008.tb00177.x.
- Johnson PM. International profiles of dental hygiene 1987 to 2006: a 21-nation comparative study. Int Dent J 2009;59:63-77.
- Nash DA, Friedman JW, Mathu-Muju KR, Robinson PG, Satur J, Moffat S, et al. A review of the global literature on dental therapists. Community Dent Oral Epidemiol 2014;42:1-10. https://doi.org/10.1111/cdoe.12052.
- Kitchener M, Mertz E. Professional projects and institutional change in healthcare: the case of American dentistry. Soc Sci Med 2012;74:372-80. https://doi.org/10.1016/j.socscimed.2010.10.005.
- Calache H, Hopcraft MS. Evaluation of a pilot bridging program to enable Australian dental therapists to treat adult patients. J Dent Educ 2011;75:1208-17. https://doi.org/10.1002/j.0022-0337.2011.75.9.tb05164.x.
- Calache H, Hopcraft MS. Provision of oral health care to adult patients by dental therapists without the prescription of a dentist. J Public Health Dent 2012;72:19-27. https://doi.org/10.1111/j.1752-7325.2011.00279.x.
- Brocklehurst P, Pemberton MN, Macey R, Cotton C, Walsh T, Lewis M. Comparative accuracy of different members of the dental team in detecting malignant and non-malignant oral lesions. Br Dent J 2015;218:525-9. https://doi.org/10.1038/sj.bdj.2015.344.
- Dyer TA, Robinson PG. Exploring the social acceptability of skill-mix in dentistry. Int Dent J 2008;58:173-80.
- Sun N, Burnside G, Harris R. Patient satisfaction with care by dental therapists. Br Dent J 2010;208. https://doi.org/10.1038/sj.bdj.2010.209.
- Calache H, Shaw J, Groves V, Mariño R, Morgan M, Gussy M, et al. The capacity of dental therapists to provide direct restorative care to adults. Aust N Z J Public Health 2009;33:424-9. https://doi.org/10.1111/j.1753-6405.2009.00423.x.
- Freed JR, Perry DA, Kushman JE. Aspects of quality of dental hygiene care in supervised and unsupervised practices. J Public Health Dent 1997;57:68-75. https://doi.org/10.1111/j.1752-7325.1997.tb02476.x.
- Perry DA, Freed JR, Kushman JE. Characteristics of patients seeking care from independent dental hygienist practices. J Public Health Dent 1997;57:76-81. https://doi.org/10.1111/j.1752-7325.1997.tb02477.x.
- Wetterhall S, Burrus B, Shugars D, Bader J. Cultural context in the effort to improve oral health among Alaska Native people: the dental health aide therapist model. Am J Public Health 2011;101:1836-40. https://doi.org/10.2105/AJPH.2011.300356.
- Hansen J, van der Maat M, Batenburg R. De Eerstelijns Mondzorg Door Consumenten Bekeken. Utrecht: Netherlands Institute for Health Services Research; 2010.
- Van der Lee I, Batenburg RS. De Eerstelijns Mondzorg Doorconsumenten Opnieuw Bekeken. Utrecht: Netherlands Institute for Health Services Research; 2012.
- Jerkovic-Cosic K . The Relation Between Profession Development and Job (Re)design; The Case of Dental Hygiene in The Netherlands 2012.
- Wang NJ, Riordan PJ. Recall intervals, dental hygienists and quality in child dental care. Community Dent Oral Epidemiol 1995;23:8-14. https://doi.org/10.1111/j.1600-0528.1995.tb00190.x.
- Wang NJ. Variation in clinical time spent by dentist and dental hygienist in child dental care. Acta Odontol Scand 1994;52:280-9. https://doi.org/10.3109/00016359409029040.
- Kwan SY, Prendergast MJ, Williams SA. The diagnostic reliability of clinical dental auxillaries in caries prevalence surveys – a pilot study. Community Dent Health 1996;13:145-9.
- Patel RS, Sprod AJ, Harwood P, Drugan CS. The use of dental therapists as examiners in dental epidemiological surveys. Community Dent Health 2012;29:195-7.
- Kwan SY, Prendergast MJ. The use of clinical dental auxiliaries as examiners in caries prevalence surveys in the United Kingdom: a feasibility study. Community Dent Oral Epidemiol 1998;26:194-200. https://doi.org/10.1111/j.1600-0528.1998.tb01949.x.
- Hopcraft MS, Morgan MV, Satur JG, Wright FA. Utilizing dental hygienists to undertake dental examination and referral in residential aged care facilities. Community Dent Oral Epidemiol 2011;39:378-84. https://doi.org/10.1111/j.1600-0528.2010.00605.x.
- Bader JD, Lee JY, Shugars DA, Burrus BB, Wetterhall S. Clinical technical performance of dental therapists in Alaska. J Am Dent Assoc 2011;142:322-6. https://doi.org/10.14219/jada.archive.2011.0171.
- Battrell AM, Gadbury-Amyot CC, Overman PR. A qualitative study of limited access permit dental hygienists in Oregon. J Dent Educ 2008;72:329-43. https://doi.org/10.1002/j.0022-0337.2008.72.3.tb04499.x.
- Dyer TA, Brocklehurst PR, Glenny AM, Davies L, Tickle M, Issac A, et al. Dental auxiliaries for dental care traditionally provided by dentists. Cochrane Database Syst Rev 2014;8. https://doi.org/10.1002/14651858.CD010076.pub2.
- Brocklehurst P, Ashley J, Walsh T, Tickle M. Relative performance of different dental professional groups in screening for occlusal caries. Community Dent Oral Epidemiol 2012;40:239-46. https://doi.org/10.1111/j.1600-0528.2012.00671.x.
- Macey R, Glenny A, Walsh T, Tickle M, Worthington H, Ashley J, et al. The efficacy of screening for common dental diseases by hygiene-therapists: a diagnostic test accuracy study. J Dent Res 2015;94:70-8. https://doi.org/10.1177/0022034514567335.
- Macey R, Glenny A-M, Brocklehurst PR. Feasibility study: assessing the efficacy and social acceptability of using dental hygiene-therapists as front-line clinicians. Br Dent J 2016;221:717-21. https://doi.org/10.1038/sj.bdj.2016.913.
- Sun N, Harris RV. Models of practice organisation using dental therapists: English case studies. Br Dent J 2011;211. https://doi.org/10.1038/sj.bdj.2011.624.
- Harris RV, Sun N. Dental practitioner concepts of efficiency related to the use of dental therapists. Community Dent Oral Epidemiol 2012;40:247-56. https://doi.org/10.1111/j.1600-0528.2012.00670.x.
- Harris RV, Sun N. Translation of remuneration arrangements into incentives to delegate to English dental therapists. Health Policy 2012;104:253-9. https://doi.org/10.1016/j.healthpol.2011.11.013.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. https://doi.org/10.1136/bmj.h1258.
- Pawson R. The Science of Evaluation: A Realist Manifesto. London: SAGE Publications Ltd; 2013.
- Pawson R, Tilley N. Realistic Evaluation. London: SAGE Publications Ltd; 2017.
- Eldridge SM, Lancaster GA, Campbell MJ, Thabane L, Hopewell S, Coleman CL, et al. Defining feasibility and pilot studies in preparation for randomised controlled trials: development of a conceptual framework. PLOS One 2016;11. https://doi.org/10.1371/journal.pone.0150205.
- Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol 1997;25:284-90. https://doi.org/10.1111/j.1600-0528.1997.tb00941.x.
- Russell D, Hoare ZSJ, Whitaker R, Whitaker CJ, Russell IT. Generalised method for adaptive randomisation in clinical trials. Statistics in Medicine 2011;30:922-34. https://doi.org/10.1002/sim.4175.
- Great Britain . The National Health Service (General Dental Services Contracts) Regulations 2005 2005.
- Clarkson JE, Pitts NB, Bonetti D, Boyers D, Braid H, Elford R, et al. INTERVAL (investigation of NICE technologies for enabling risk-variable-adjusted-length) dental recalls trial: a multicentre randomised controlled trial investigating the best dental recall interval for optimum, cost-effective maintenance of oral health in dentate adults attending dental primary care. BMC Oral Health 2018;18. https://doi.org/10.1186/s12903-018-0587-2.
- Ramsay CR, Clarkson JE, Duncan A, Lamont TJ, Heasman PA, Boyers D, et al. Improving the Quality of Dentistry (IQuaD): a cluster factorial randomised controlled trial comparing the effectiveness and cost-benefit of oral hygiene advice and/or periodontal instrumentation with routine care for the prevention and management of periodontal disease in dentate adults attending dental primary care. Health Technol Assess 2018;22. https://doi.org/10.3310/hta22380.
- Imrey PB. Considerations in the statistical analysis of clinical trials in periodontitis. J Clin Periodontol 1986;13:517-32. https://doi.org/10.1111/j.1600-051x.1986.tb01500.x.
- Lang NP, Joss A, Orsanic T, Gusberti FA, Siegrist BE. Bleeding on probing: a predictor for the progression of periodontal disease?. J Clin Periodontol 1986;13:590-6. https://doi.org/10.1111/j.1600-051X.1986.tb00852.x.
- Lang NP, Adler R, Joss A, Nyman S. Absence of bleeding on probing. An indicator of periodontal stability. J Clin Periodontol 1990;17:714-21. https://doi.org/10.1111/j.1600-051x.1990.tb01059.x.
- Chapple IL. Periodontal disease diagnosis: current status and future developments. J Dent 1997;25:3-15. https://doi.org/10.1016/S0300-5712(95)00118-2.
- Jones CL, Milsom KM, Ratcliffe P, Wyllie A, Macfarlane TV, Tickle M. Clinical outcomes of single-visit oral prophylaxis: a practice-based randomised controlled trial. BMC Oral Health 2011;11. https://doi.org/10.1186/1472-6831-11-35.
- Cocks K, Torgerson DJ. Sample size calculations for pilot randomized trials: a confidence interval approach. J Clin Epidemiol 2013;66:197-201. https://doi.org/10.1016/j.jclinepi.2012.09.002.
- Lancaster GA, Dodd S, Williamson PR. Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Pract 2004;10:307-12. https://doi.org/10.1111/j.2002.384.doc.x.
- Lee EC, Whitehead AL, Jacques RM, Julious SA. The statistical interpretation of pilot trials: should significance thresholds be reconsidered?. BMC Med Res Methodol 2014;14. https://doi.org/10.1186/1471-2288-14-41.
- National Institute for Health and Care Excellence (NICE) . Dental Checks: Intervals Between Oral Health Reviews. Clinical Guideline [CG19] n.d. www.nice.org.uk/guidance/cg19 (accessed 31 March 2020).
- Ekstrand KR, Gimenez T, Ferreira FR, Mendes FM, Braga MM. The international caries detection and assessment system – ICDAS: a systematic review. Caries Res 2018;52:406-19. https://doi.org/10.1159/000486429.
- Frencken JE, Giacaman RA, Leal SC. An assessment of three contemporary dental caries epidemiological instruments: a critical review. Br Dent J 2020;228:25-31. https://doi.org/10.1038/s41415-019-1081-1.
- Walters SJ. Consultants’ forum: should post hoc sample size calculations be done?. Pharm Stat 2009;8:163-9. https://doi.org/10.1002/pst.334.
- Vaessen J, Leeuw FL. Mind the Gap: Perspectives on Policy Evaluation and the Social Sciences. London: Routledge; 2010.
- Randell R, Honey S, Hindmarsh J, Alvarado N, Greenhalgh J, Pearman A, et al. A realist process evaluation of robot-assisted surgery: integration into routine practice and impacts on communication, collaboration and decision-making. Health Serv Deliv Res 2017;5. https://doi.org/10.3310/hsdr05200.
- Rycroft-Malone J, Seers K, Eldh AC, Cox K, Crichton N, Harvey G, et al. A realist process evaluation within the Facilitating Implementation of Research Evidence (FIRE) cluster randomised controlled international trial: an exemplar. Implement Sci 2018;13. https://doi.org/10.1186/s13012-018-0811-0.
- Brand SL, Quinn C, Pearson M, Lennox C, Owens C, Kirkpatrick T, et al. Building programme theory to develop more adaptable and scalable complex interventions: realist formative process evaluation prior to full trial. Evaluation 2019;25:149-70. https://doi.org/10.1177/1356389018802134.
- Dalkin SM, Greenhalgh J, Jones D, Cunningham B, Lhussier M. What’s in a mechanism? Development of a key concept in realist evaluation. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0237-x.
- Davidoff F, Dixon-Woods M, Leviton L, Michie S. Demystifying theory and its use in improvement. BMJ Qual Saf 2015;24:228-38. https://doi.org/10.1136/bmjqs-2014-003627.
- Kislov R, Pope C, Martin GP, Wilson PM. Harnessing the power of theorising in implementation science. Implement Sci 2019;14. https://doi.org/10.1186/s13012-019-0957-4.
- Weick KE. Theory construction as disciplined imagination. Acad Manage Rev 1989;14:516-31. https://doi.org/10.5465/amr.1989.4308376.
- Rycroft-Malone J, Burton CR, Williams L, Edwards S, Fisher D, Hall B, et al. Improving skills and care standards in the support workforce for older people: a realist synthesis of workforce development interventions. Health Serv Deliv Res 2016;4. https://doi.org/10.3310/hsdr04120.
- Pearson M, Brand SL, Quinn C, Shaw J, Maguire M, Michie S, et al. Using realist review to inform intervention development: methodological illustration and conceptual platform for collaborative care in offender mental health. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0321-2.
- Nanninga M, Glebbeek A. Employing the teacher–learner cycle in realistic evaluation: a case study of the social benefits of young people’s playing fields. Evaluation 2011;17:73-87. https://doi.org/10.1177/1356389010393586.
- Manzano A. The craft of interviewing in realist evaluation. Evaluation 2016;22:342-60. https://doi.org/10.1177/1356389016638615.
- Burgess RG. In the Field: An Introduction to Field Research. London: Routledge; 2006.
- Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. Value Health 2013;16:e1-5. https://doi.org/10.1016/j.jval.2013.02.010.
- NHS . What Is Included in Each NHS Dental Band Charge? 2018. www.nhs.uk/common-health-questions/dental-health/what-is-included-in-each-nhs-dental-band-charge/ (accessed 13 March 2020).
- Watson M. What is a UDA?. Vital 2010;7. https://doi.org/10.1038/vital1131.
- Department of Health and Social Care (DHSC) . NHS Reference Costs 2017 18 2018.
- Joint Formulary Committee . British National Formulary n.d. www.medicinescomplete.com (accessed 13 March 2020).
- Department for Transport (DfT) . TAG Data Book 2019.
- Office for National Statistics (ONS) . CPIH ANNUAL RATE 00: ALL ITEMS 2015=100 2020. www.ons.gov.uk/economy/inflationandpriceindices/timeseries/l55o/mm23 (accessed 13 March 2020).
- National Institute for Health and Care Excellence (NICE) . Guide to the Methods of Technology Appraisal 2013. Process and Methods [PMG9] 2013. www.nice.org.uk/process/pmg9/chapter/foreword (accessed 13 March 2020).
- Nixon RM, Thompson SG. Methods for incorporating covariate adjustment, subgroup analysis and between-centre differences into cost-effectiveness evaluations. Health Econ 2005;14:1217-29. https://doi.org/10.1002/hec.1008.
- Homer T, Maguire A, Douglas GVA, Innes NP, Clarkson JE, Wilson N, et al. Cost-effectiveness of child caries management: a randomised controlled trial (FiCTION trial). BMC Oral Health 2020;20. https://doi.org/10.1186/s12903-020-1020-1.
- Personal Social Services Research Unit (PSSRU) . Unit Costs of Health and Social Care 2019 n.d. www.pssru.ac.uk/project-pages/unit-costs/unit-costs-2019/ (accessed 13 March 2020).
- Clark MD, Determann D, Petrou S, Moro D, de Bekker-Grob EW. Discrete choice experiments in health economics: a review of the literature. PharmacoEconomics 2014;32:883-902. https://doi.org/10.1007/s40273-014-0170-x.
- de Bekker-Grob EW, Ryan M, Gerard K. Discrete choice experiments in health economics: a review of the literature. Health Econ 2012;21:145-72. https://doi.org/10.1002/hec.1697.
- Bridges JF, Hauber AB, Marshall D, Lloyd A, Prosser LA, Regier DA, et al. Conjoint analysis applications in health – a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health 2011;14:403-13. https://doi.org/10.1016/j.jval.2010.11.013.
- Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making: a user’s guide. PharmacoEconomics 2008;26:661-77. https://doi.org/10.2165/00019053-200826080-00004.
- Barnes E, Bullock A, Chestnutt IG, Cowpe J, Moons K, Warren W. Dental therapists in general dental practice. A literature review and case-study analysis to determine what works, why, how and in what circumstances. Eur J Dent Educ 2020;24:109-20. https://doi.org/10.1111/eje.12474.
- Evans C, Chestnutt IG, Chadwick BL. The potential for delegation of clinical care in general dental practice. Br Dent J 2007;203:695-9. https://doi.org/10.1038/bdj.2007.1111.
- Wanyonyi KL, Radford DR, Harper PR, Gallagher JE. Alternative scenarios: harnessing mid-level providers and evidence-based practice in primary dental care in England through operational research. Hum Resour Health 2015;13. https://doi.org/10.1186/s12960-015-0072-9.
- Brocklehurst P, Mertz B, Jerković-Ćosić K, Littlewood A, Tickle M. Direct access to midlevel dental providers: an evidence synthesis. J Public Health Dent 2014;74:326-35. https://doi.org/10.1111/jphd.12062.
- Robinson PG, Douglas GVA, Gibson BJ, Godson J, Vinall-Collier K, Pavitt S, et al. Remuneration of primary dental care in England: a qualitative framework analysis of perspectives of a new service delivery model incorporating incentives for improved access, quality and health outcomes. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2019-031886.
- Bagnell S. DCP practice in the International context. Dent Health 2012;51:6-9.
- Moffat S, Coates D. Attitudes of New Zealand dentists, dental specialists and dental students towards employing dual trained Oral Health graduates. Br Dent J 2011;211:374-75. https://doi.org/10.1038/sj.bdj.2011.870.
- Farghaly MM, Lang WP, Woolfolk MW, Faja BW, Ziemiecki TL, Pritzel SJ. Factors associated with fissure sealant delegation: dentist characteristics and office staffing patterns. J Public Health Dent 1993;53:246-52. https://doi.org/10.1111/j.1752-7325.1993.tb02712.x.
- Nor NA, Murat NA, Yusof ZY, Gamboa AB. Senior dentists’ perceptions of dental therapists’ roles and education needs in Malaysia. Int J Dent Hyg 2013;11:280-6. https://doi.org/10.1111/idh.12038.
- Bolin KA. Assessment of treatment provided by dental health aide therapists in Alaska: a pilot study. J Am Dent Assoc 2008;139:1530-5. https://doi.org/10.14219/jada.archive.2008.0080.
- Darling BG, Kanellis MJ, McKernan SC, Damiano PC. Potential utilization of expanded function dental auxiliaries to place restoratives. J Public Health Dent 2015;75:163-8. https://doi.org/10.1111/jphd.12089.
- Kempster C, Luzzi L, Roberts-Thomson K. Australian dentists: characteristics of those who employ or are willing to employ oral health therapists. Aust Dent J 2015;60:154-62. https://doi.org/10.1111/adj.12317.
- Bruers JJ, van Rossum GM, Felling AJ, Truin GJ, van’t Hof MA. Business orientation and the willingness to distribute dental tasks of Dutch dentists. Int Dent J 2003;53:255-63. https://doi.org/10.1111/j.1875-595x.2003.tb00754.x.
- Barnes E, Bullock A, Cowpe J, Moons K, Warren W, Hannington D, et al. General dental practices with and without a dental therapist: a survey of appointment activities and patient satisfaction with their care. Br Dent J 2018;225:53-8. https://doi.org/10.1038/sj.bdj.2018.522.
- World Health Organization (WHO) . Framework for Action on Inter-Professional Education &Amp; Collaborative Practice 2010. http://whqlibdoc.who.int/hq/2010/WHO_HRH_HPN_10.3_eng.pdf?ua=1 (accessed 13 March 2020).
- Brocklehurst PR, Baker SR, Langley J. Context and the evidence-based paradigm: the potential for participatory research and systems thinking in oral health [published online ahead of print August 19 2020]. Community Dent Oral Epidemiol 2020. https://doi.org/10.1111/cdoe.12570.
- Braithwaite J, Churruca K, Long JC, Ellis LA, Herkes J. When complexity science meets implementation science: a theoretical and empirical analysis of systems change. BMC Med 2018;16. https://doi.org/10.1186/s12916-018-1057-z.
- Baker SR. Editorial: ‘No simple solutions, no single ingredient’: systems orientated approaches for addressing wicked problems in population oral health. Community Dent Health 2019;36:3-4. https://doi.org/10.1922/CDH_BakerMarch19editorial02.
- Brocklehurst PR, Baker SR, Peres MA, Tsakos G, Rycroft-Malone J. How should we evaluate and use evidence to improve population oral health?. Dent Clin N Am 2019;63:145-56. https://doi.org/10.1016/j.cden.2018.08.009.
- Listl S, Jurges H, Watt RG. Causal inference from observational data. Community Dent Oral Epidemiol 2016;44:409-15. https://doi.org/10.1111/cdoe.12231.
- Ikenwilo D. A difference-in-differences analysis of the effect of free dental check-ups in Scotland. Soc Sci Med 2013;83:10-8. https://doi.org/10.1016/j.socscimed.2013.01.027.
- Which?. Private and NHS Dental Charges n.d. www.which.co.uk/reviews/dentists/article/private-and-nhs-dental-charges (accessed 13 March 2020).
- NHS . Botox Injections 2019. www.nhs.uk/conditions/cosmetic-procedures/botox-injections (accessed 13 March 2020).
- Dental Care Plus . Cost of Dental Implants at DentalCarePlus 2020. www.dentalcareplus.org.uk/implant-costs (accessed 13 March 2020).
- NHS Business Services Authority . Help With NHS Prescription Costs 2020. www.nhsbsa.nhs.uk/help-nhs-prescription-costs (accessed 13 March 2020).
- NHS . How Much Will I Pay for NHS Dental Treatment? 2020. www.nhs.uk/common-health-questions/dental-health/how-much-will-i-pay-for-nhs-dental-treatment (accessed 13 March 2020).
- Gov.uk . Average Hourly Pay 2018. www.ethnicity-facts-figures.service.gov.uk/work-pay-and-benefits/pay-and-income/average-hourly-pay/latest (accessed 13 March 2020).
- Gov.uk . Travel – Mileage and Fuel Rates and Allowances 2019. www.gov.uk/government/publications/rates-and-allowances-travel-mileage-and-fuel-allowances/travel-mileage-and-fuel-rates-and-allowances (accessed 13 March 2020).
Appendix 1 Case report forms (baseline and outcome)
Case report form (baseline)
Case report form (outcome assessment)
Appendix 2 Unit costs
Table 23 highlights the costs used in Chapter 4.
| Detail | Resource | Unit | Cost (£) | Source |
|---|---|---|---|---|
| UDA payments | Band 1 | 1 UDA | 25 (varied between 20 and 30 in sensitivity analysis) | Brocklehurst et al.30 |
| Band 1 urgent | 1.2 UDAs | 30 (varied between 24 and 36 in sensitivity analysis) | ||
| Band 2 | 3 UDAs | 75 (varied between 60 and 90 in sensitivity analysis) | ||
| Band 3 | 12 UDAs | 300 (varied between 240 and 360 in sensitivity analysis) | ||
| Treatment provider | GDP | Cost per minute | 0.68 | PSSRU147 |
| DT | Cost per minute | 0.29 | ||
| DH | Cost per minute | 0.23 | ||
| Treatment costs: materials | Check-up cost | 1 (applied to all appointments) | 2.21 |
Materials informed by previous dental microcosting work: Homer et al. 146 Updated based on 2019 prices from dental supplies websites Dental Sky (URL: www.dentalsky.com; accessed 20 January 2020) and MediMatch Dental Laboratory Ltd (London, UK) (URL: www.medimatch.co.uk; accessed 20 January 2020) |
| Composite filling | 1; subsequent fillings |
18.66 12.01 |
||
| Glass Ionomer filling | 1; subsequent fillings |
11.21 4.56 |
||
| Amalgam filling | 1; subsequent fillings |
11.15 4.70 |
||
| Ultrasonic scaling cost | Per treatment | 0.64 | ||
| Hand scale cost | Per treatment | 0.48 | ||
| Periodontal treatment | Per treatment | 1.98 | ||
| Crown preparation | Per tooth | 20.48 | ||
| Crown fit | Per tooth | 48.65 | ||
| Crown and post fit | Per tooth | 61.37 | ||
| Temporary crown | Per tooth | 20.48 | ||
| Fluoride varnish | One tooth; subsequent teeth |
2.71 2.53 |
||
| Pulp extirpation | One tooth | 12.78 | ||
| Access and drainage/root canal appointment 1 | Per tooth | 10.75 | ||
| Chlorohexidine irrigation | Per treatment | 0.57 | ||
| Dental impression | Set of impressions | 1.93 | ||
| Bite raising appliance | Per appliance | 48.93 | ||
| Extraction | One extraction | 2.78 | ||
| Dry socket treatment | One site | 1.28 | ||
| Root canal treatment appointment 1 | Per single tooth | 10.75 | ||
| Root canal treatment appointment 2 | Per single tooth | 12.78 | ||
| Radiography unit cost | Two radiographs | 1.57 | ||
| Charting (BPE/6PPC) | Charting performed | 0.48 | ||
| Local anaesthetic | Per appointment | 1.23 | ||
| Filling adjust | Per appointment | 5.42 | ||
| Denture adjust | Per appointment | £3.21 | ||
| Private treatments | Scale and polish | One treatment | 55 | Which?173 |
| Crown | One crown | 715 | ||
| Botox | One treatment | 225 | NHS174 | |
| Implant consultation | One appointment | 125 | Dental Care Plus175 | |
| Prescription medicine | Penicillin | Course of treatment | 3.26 | British National Formulary 141 |
| Aciclovir | Course of treatment | 1.69 | ||
| Sodium fluoride (Duraphat®, Colgate) | Course of treatment | 3.26 | ||
| Prescription charges | Per prescription | 9.00 | NHS Business Services Authority176 | |
| Patient dental charges | Band 1 | Course of treatment | 22.70 | NHS177 |
| Band 2 | Course of treatment | 61.10 | ||
| Band 3 | Course of treatment | 269.30 | ||
| Emergency appointment | Course of treatment | 22.70 | ||
| Time and travel costs | Leisure time | Per hour | 4.23 | Department for Transport142 |
| Average salary | Per hour | 11.77a | Gov.uk178 | |
| Mileage rate | Per mile | 0.45 | Gov.uk179 | |
| Secondary care cost | A&E outpatient attendance | One attendance | 138.31a | DHSC140 |
| Dental medicine specialties outpatient attendance | One attendance | 124.07a |
Appendix 3 Patient and public involvement
Two PPI representatives supported the research team throughout the study and were active members of the Trial Steering Committee. A dedicated PPI user researcher (KS) also supported the research team in the patient-facing research elements of WS2. The user researcher had considerable experience as a PPI representative and was recruited from the PARC–Bangor network (see PARC-Bangor). However, this was their first experience in a user researcher role. As a result, the user researcher was provided with training by the research team to familiarise themselves with the context of the intervention (i.e. role substitution in NHS dentistry and the corresponding roles of the dental team). The training consisted of two 3-hour sessions over 2 weeks. Following this, the user researcher received 1-day specific training on semistructured interviews. This training was provided by an independent contractor (Social Research Association, London, UK).
The user researcher was employed to support the PPI element in the following ways:
-
To strengthen the patient voice in semistructured interviews. By using a user researcher the interviews naturally assumed a peer-to-peer dynamic, with topics and inputs supplied by the core research team and explored in detail between the user researcher and interviewee.
-
To guide the research team on appropriateness of language and communication. This included reviewing developing research documents ahead of patient involvement to ensure the appropriateness of topics and language.
-
Provide a patient voice in the realist research cycle. Specifically, to sense check during the analysis of research data and the development and understanding of theory areas to ensure that the interpretation was correct.
A PPI group was established to determine the impact of the intervention on the patient experience. This group consisted of six individuals from the PARC-Bangor network, all of whom had been registered with an NHS dental practice.
As highlighted in Chapter 3, clinical stakeholder groups had been used to understand the context for role substitution in NHS dentistry. From these discussions, it became apparent that the patient experience was influenced by the prevailing clinical model adopted at the level of the practice. Clinicians had indicated that issues such as institutional trust and dental team endorsement and stability were important factors in maintaining the patient experience and embedding role substitutive practices. The research team, in conjunction with the user researcher, used these data to develop an emerging theoretical framework for the ‘patient experience’ theory area as part of the broader programme theory development.
Individual semistructured interviews were held with members of the PPI group, the user researcher and a member of the research team. These interviews explored, among other things, patients’ experiences of NHS dentistry and their thoughts on role substitution. In addition, patients were guided towards specific topics determined from the emerging theoretical framework and associated coding document. Patients were encouraged to explore areas of personal interest and concern.
Where possible, the transcribed data from the PPI interviews were reviewed by the research team and user researcher before the subsequent interviews. In this way, the research team were able to reflect and update the programme theory in conjunction with the user researcher as the interviews progressed.
The emergent findings were compiled in a coding framework document. The document was copopulated with themes, codes and quotes from PPI focus groups held as part of the health economic analysis (see Chapter 4). Three focus groups were conducted, with a total of 19 PPI participants for WS3; this was later supplemented with a further 13 semistructured interviews. These data, coupled with the existing PPI findings, were reviewed in detail by two members of the research team (CW and PB) and the user researcher. This review formalised the f(C,M,O) contingency on patients experiences’ (see Figure 9).
In total, the project accrued > 70 hours of PPI activity during the realist-informed process evaluation (see Chapter 3), including > 32 hours of individual user researcher activity for WS3 (see Chapter 4).
The user researcher also read through the Plain English summary and will be a key member of the team during the dissemination phase of the project.
PARC-Bangor
PARC-Bangor is the public involvement and engagement group at the NWORTH Clinical Trials Unit at Bangor University (URL: https://nworth-ctu.bangor.ac.uk/parc-bangor.php.en; accessed 9 December 2020). Members of the public across North Wales can sign up to the PARC-Bangor database if they are interested in taking part in research or taking part in developing research ideas at NWORTH Clinical Trials Unit.
Members of the PARC-Bangor network meet four times per year to discuss new and ongoing studies. Some members of the PARC-Bangor network sit on Trial Steering Committees and others engage with projects as and when their input is required. The functions of PARC-Bangor are to:
-
provide insight and a public perspective to the development of research questions
-
ensure that documents and information associated with a study are easy to understand for patients and the public taking part in the research
-
discuss and comment on the research process described in funding applications to ensure patient perspectives are accounted for
-
provide a ‘patient voice’ to NWORTH’s executive.
Being a member of the PARC-Bangor network means that members of the public can:
-
learn about and influence health research in their area
-
use their experience as patients, service users, carers or family members to help others
-
influence study designs to make funding applications more successful
-
discuss the work with research teams via e-mail, in person, or over the telephone
-
access free training about health and social care research.
List of abbreviations
- ACORN
- Assessment of Clinical Oral Risk and Need
- ACV
- annual contract value
- ANCOVA
- analysis of covariance
- ANOVA
- analysis of variance
- BOP
- bleeding on probing
- BPE
- basic periodontal examination
- CI
- confidence interval
- CMO
- context, mechanism and outcome
- CONSORT
- Consolidated Standards of Reporting Trials
- CRF
- case report form
- DC
- dental commissioner
- DCE
- discrete choice experiment
- DCP
- dental care professional
- DH
- dental hygienist
- DHSC
- Department of Health and Social Care
- DT
- dental therapist
- FFS
- fee-for-service
- GCP
- Good Clinical Practice
- GDC
- General Dental Council
- GDP
- general dental practitioner
- GDS
- general dental service
- HSDR
- Health Services and Delivery Research
- ICER
- incremental cost-effectiveness ratio
- ID
- identification
- IMD
- Index of Multiple Deprivation
- IPT
- initial programme theory
- ITT
- intention to treat
- MRT
- mid-range theory
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NWORTH
- North Wales Organisation for Randomised Trials in Health
- OHIP-14
- Oral Health Impact Profile-14 items
- PCQ
- participant cost questionnaire
- PHE
- Public Health England
- PICO
- population, intervention, control, outcome
- POM
- primary outcome measure
- PPI
- patient and public involvement
- PSSRU
- Personal Social Sciences Research Unit
- RCS
- Royal College of Surgeons of England
- SAE
- serious adverse event
- SD
- standard deviation
- SOP
- standard operating procedure
- UDA
- unit of dental activity
- WHO
- World Health Organization
- WS
- workstream
Notes
-
Theory testing phase of the realist-informed process evaluation
-
Theory refinement phase of the realist-informed process evaluation
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/hsdr09030).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
