Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 16/115/17. The contractual start date was in February 2018. The final report began editorial review in March 2020 and was accepted for publication in October 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2021. This work was produced by Knighting et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2021 Queen’s Printer and Controller of HMSO
Chapter 1 Background and rationale
This mixed-methods systematic review focuses on young adults with complex health-care needs due to life-limiting and life-threatening conditions (LLCs) or complex physical disability.
Young adults with life-limiting or complex physical disability needs
Young adults with LLCs or complex physical disabilities are often regarded as distinct populations, but they share experiences of health-care services and a lack of available respite care services to meet their needs. They are often described as having complex health-care needs because of a single diagnosis or multiple diagnoses (e.g. illness, congenital conditions or trauma), and many individuals live with multimorbidities. They commonly need continuous health care, with support from similar services across a range of conditions and disabilities, but survival to adulthood and the consequent transfer from children to adult services has increased the demand for appropriate services to meet their complex health-care needs. There is therefore a clear rationale for combining the population of young adults with LLCs and those with complex physical disabilities for the purpose of exploring service provision for young adults with complex health-care needs to inform future research and service development. This section describes and defines the patient population included in the review.
Definition of life-limiting conditions
The population of children with LLCs who survive to adulthood is rising annually in England. Owing to medical advances, the number of 16- to 19-year-olds with palliative care needs has increased by 45% over the past decade to 1 in 10 young people, with approximately 55,721 young adults (aged 18–40 years) with complex needs living in England in 2010. 1,2 Their needs are diverse, involving complex life-long symptom and medication management, and palliative care. 3 Many of these children and young people die in infancy and childhood, but those surviving into adulthood tend to have degenerative and progressive conditions lasting for many years. This results in complex health-care needs and high dependency on care that is mainly provided by family members, with support from paid carers and health and social care professionals. The duration and frequency of care for these young adults differs from those of adults with terminal illness, who predominantly require care during the last 12 months of life. In contrast, the care needs of young adults with LLCs are longer term and are associated with higher costs that escalate as their condition deteriorates. The increasing proportion of young people surviving to adulthood has consequently placed increasing demands on commissioners and service providers to meet their complex needs as they transition to adult services. 1,3
Over 300 diagnoses are encapsulated within the population of children and young adults with LLCs, which can be grouped into the following four broad categories:4
-
Life-limiting conditions where a cure is possible but may fail (e.g. cancer or irreversible organ failure).
-
Conditions that, although treated intensively over a period of time, inevitably lead to early death (e.g. cystic fibrosis).
-
Progressive conditions where treatment is exclusively palliative and often extends over many years (e.g. muscular dystrophy).
-
Irreversible but non-progressive conditions that give rise to severe disability and sometimes premature death (e.g. disabilities following brain or spinal cord insult or severe cerebral palsy).
Drawing on key terms from the literature and the definition from Together for Short Lives (TfSL),1–4 the UK charity for children, young people and young adults who are expected to have short lives, we have defined a young adult with LLCs as follows:
Young adults with a life-limiting or life-threatening condition, where there is no reasonable hope of cure and from which they are expected to die.
Definition of complex physical disability
Over the last 13 years, the prevalence of children and young people with severe disability and complex needs has risen because of increasing survival rates. 4,5 In 2007, there were an estimated 100,000 disabled children with complex care needs in England, with a projected increase of 50% over the following decade. 4,6 There is therefore an urgent need to gather evidence on the life experiences of this rising population to explore their needs and assess implications for future service demand. 4
There is wide variation in the definitions of disability and severity, particularly compared with definitions used in the adult population. 6 The Equality Act 2010 defines ‘disability’ as a physical or mental impairment that has a ‘substantial’ and ‘long-term’ negative effect on a person’s ability to engage in normal daily activities. 7 Complex physical disability can be grouped into the following three broad categories:8
-
sudden onset conditions (e.g. acquired brain injury, spinal cord conditions, peripheral nervous system conditions, multiple trauma)
-
progressive and intermittent conditions (e.g. neurological and neuromuscular conditions, severe musculoskeletal or multiorgan disease or physical illness/injury)
-
stable conditions with or without degenerative change (e.g. congenital conditions, post-polio syndrome or other previous neurological injury).
Complex physical disability is sometimes referred to as ‘severe’ or ‘profound’ disability and may overlap with other health conditions, creating a complex patient profile. These profiles often include learning disability or cognitive impairment; however, this review has focused on health-care needs and the population was therefore restricted to young adults with complex health-care needs due to complex physical disability. Given the variance in definitions of disability between children and adults, we also included complex physical disability arising from cancer diagnosed as a young adult.
For the purpose of this review, we defined a young adult with complex physical disability as follows:
Young adults with impairments and/or physical disabilities due to congenital or acquired physical disability, or major neurological trauma, which require a complex level of physical management and support.
Definition of complex health-care needs
Defining the concept of ‘complex’ is challenging, as it may vary according to setting and perspective. 9 The health-care needs of a young adult population with LLCs or complex disability may range from complex to highly complex. For example, young adults who are dependent on long-term ventilation or have complex drug regimens are often considered too complex for many respite care services, leading to ineligibility for universal respite care and therefore requiring specially commissioned services. The variation in terminology, the spectrum of complexity and inflexibility of adult assessment processes may result in inequality of care and loss of funding for services, including respite care. Therefore, adoption of a broad definition facilitated the capture of all relevant evidence. There is no consensus-based definition of complex health-care needs,3 but it typically refers to physical, mental and/or health needs that vary across the population in different and often multidimensional ways. It has been argued that the term ‘complex’ relates more to the complexity of service provision rather than individual needs, and that the term ‘multifaceted condition’ may better describe the interconnectedness of an individual’s varied health and social care needs. 10 However, complex health-care needs is a term commonly used in the literature and variation between definitions suggest that complex needs can be considered both in terms of breadth (i.e. the wide range of needs) and depth (i.e. the high level of needs). 11 We have therefore defined complex health-care needs as follows:
Complex health-care needs that are substantial and ongoing that typically involve multiple health concerns and require a co-ordinated response from more than one service.
Definition of young adult
There is no universal consensus on the definition of a young adult in the UK. For example, the Ministry of Justice uses the age band of 18–20 years, the National Health Survey for England uses 16–24 years and the Crime Survey for England & Wales uses 18–25 years. 12 UK services do not tend to define respite services by age group and therefore it is important to use a sufficiently broad age range to capture our target population. Services for children with complex health-care needs may be extended beyond 18 years of age, but the upper limit varies by specific service and geographical location. For example, the upper limit is 23 years at Claire House Children’s Hospice (Wirral, UK), 35 years at St Elizabeth Hospice (Ipswich, UK) and 40 years at The J’s Hospice (Essex, UK), with the lower limit for many adult NHS services set at 16 or 18 years. The Care Quality Commission and the National Institute for Health and Care Excellence (NICE) recommend initiation of transition planning when the child is aged 13 or 14 years, although this may vary according to individual preferences. 13,14 Drawing on key definitions from the literature,2,15 feedback from stakeholders, and the profile of known UK service provision and TfSL, we adopted the following definition:
Young adults are defined as people aged 18–40 years.
Respite care and short breaks for young adults with complex health-care needs
Respite care and short breaks are an essential component of ongoing support for children, young people and young adults with complex health-care needs. 16,17 They provide relief from the caring environment, with multidimensional benefits for all members of the family. 18,19 TfSL defines three main functions of short break care: ‘1) to provide the child or young person with an opportunity to enjoy social interaction and leisure facilities; 2) to support the family in the care of their child in the home or an alternative community environment such as a children’s hospice; and 3) to provide opportunities for siblings to have fun and receive support in their own right’ (reproduced with permission from Together for Short Lives). 19 Typically, such provision includes residential hospice care or a similar service, day care, host family respite and home-based support, including sitting services and holiday cover. Respite care and short breaks are provided by both formal and informal carers. Formal carers are typically defined as registered professionals or care staff who work privately, for provider organisations or who receive payment for their services. Informal carers are often family members or friends who provide the same type of care on an unpaid basis, although some informal carers may receive payments through personal care budgets managed by families. This section summarises current respite care and short breaks services that helped shape our definition of the intervention.
Current service provision
There are clear differences between child and adult services in the way that respite care is conceptualised, funded and provided. 20 Typically, the term ‘short breaks’ is used in children’s services to encompass all levels of care, whether residential or in the home, and is a key service provided by children’s hospices and some specialist children’s services. 21 Planned respite care in adult services focuses on the need to give the carer a break from caring rather than providing opportunities for the person receiving care, and is typically referred to as ‘respite’ or ‘replacement’ care. The respite care and short breaks provided by children’s services may be inappropriate for young adults and the upper age limit for eligible access varies between providers and commissioners. On the other hand, typical adult services predominantly serve the needs of older people, those with cancer or other terminal diagnosis, and people requiring end-of-life care, rather than fluctuating health conditions and may be inappropriate respite care for young people with complex health-care needs due to a LLC or complex physical disability. 16,22–25 With notable exceptions such as cystic fibrosis and long-term ventilation, adult sector staff in the UK generally have little experience of paediatric conditions or of supporting young adults with complex needs. 3,13,24,26 Limited respite care, particularly for those with highly complex health needs, is available for planned short breaks or emergency family situations once young adults with complex health-care needs have transitioned to adult services. 3,13,27
The definition of ‘residential short breaks’ for young people with disabilities varies considerably between social care authorities, ranging from residential schools, sitting services and day care in the home or other settings, to flexible packages tailored to suit individuals. 6 This is an element of the wider problem of service model variation across health and social care in terms of service definition, commissioning, funding and delivery, even within the same authority. 5 However, estimates from local authorities suggest that only 8 in 10,000 disabled children aged 0–17 years receiving social care services, and 18% of children receiving a service from disabled children’s teams, had received residential short breaks. 6
The nature and costs of respite care may vary considerably, depending on the provider and level of complex health needs to be supported, and estimating costs may therefore be a complex process. Referral, assessment models and procedures may also vary between services and the care required by young adults with complex health-care needs is highly individual. Decision-making and care planning may be further complicated by legal and policy changes associated with the transition to adult services, including the transfer of parental to personal responsibility (unless there are capacity issues), and many families are ill-prepared for these changes. The changes associated with transition may also have an impact on the wider family, for example where housing and welfare support assessments move away from the whole ‘family’ (such as using parental income and other dependents to assess need) to assessment of the young adult alone, with their family largely disregarded in the assessment process. Consequently, young adults may face significant barriers to accessing appropriate care and support as they make the transition to adult services. 28,29 Parents have described the transition process as ‘like falling off a cliff’ when the support from children’s services ends and appropriate adult services are not in place, adding to the complex burden of living with complex health-care needs for young adults and their families. 30
Benefits of respite care and short breaks
The limited evidence indicates that respite care and short breaks may have a broad range of benefits, such as increasing family-carer resilience,27 improving the psychological well-being of parents,16,31 reducing the risk of carer breakdown23,27 and avoiding costly unplanned hospital admissions, a longer length of stay and social care intervention. 32,33
However, most of the evidence on the use and impact of respite care and short breaks relates to children’s services, such as hospices, rather than services for young adults with LLCs, partly because, until relatively recently, so few children survived into adulthood. However, more people with LLCs are now surviving beyond childhood and their needs may increase as they grow older, for example with the desire for independence and the need for support outside the family as ageing parents develop their own health problems. With a rapidly growing population of young adults making the transition from child to adult services, there is growing evidence of poor continuity of care, including respite care provision, that leads to the needs of the young adult and their family being unmet. The consequences of poor continuity of care may include adversely affected social, educational, vocational and spiritual outcomes; inadequate management of complex comorbidities; deterioration in the young adult’s physical and mental health; family-carer burnout; and inappropriate, costly hospital admissions. 24,34,35 Most disturbingly, earlier death may result from poor transition and loss of services. 35
Definition of respite care and short breaks
A systematic review of respite care provision for older people with dementia identified eight models of respite care and short breaks, and characterised services according to duration, pattern of use, location, response (e.g. planned or emergency care) and the characteristics of service users and staff. 36 The types of respite care included day care, home day care, clubs, interests or activity groups, home-based support, host family respite, overnight respite in specialist facilities, overnight respite in non-specialist facilities and holidays. 36 Other types of care, such as emergency residential respite and emergency home-based respite, are also described in the literature. These reflect many of the known service types for young people with LLCs and complex physical disability, illustrating variations in service configuration. It is also likely that other types of care will evolve in response to growing demand.
Following an initial scoping of evidence for the review protocol, we characterised nine service types (Figure 1), grouped into five overarching service categories. However, we note that some providers may offer more than one type of service.
FIGURE 1.
Preliminary types of respite care.
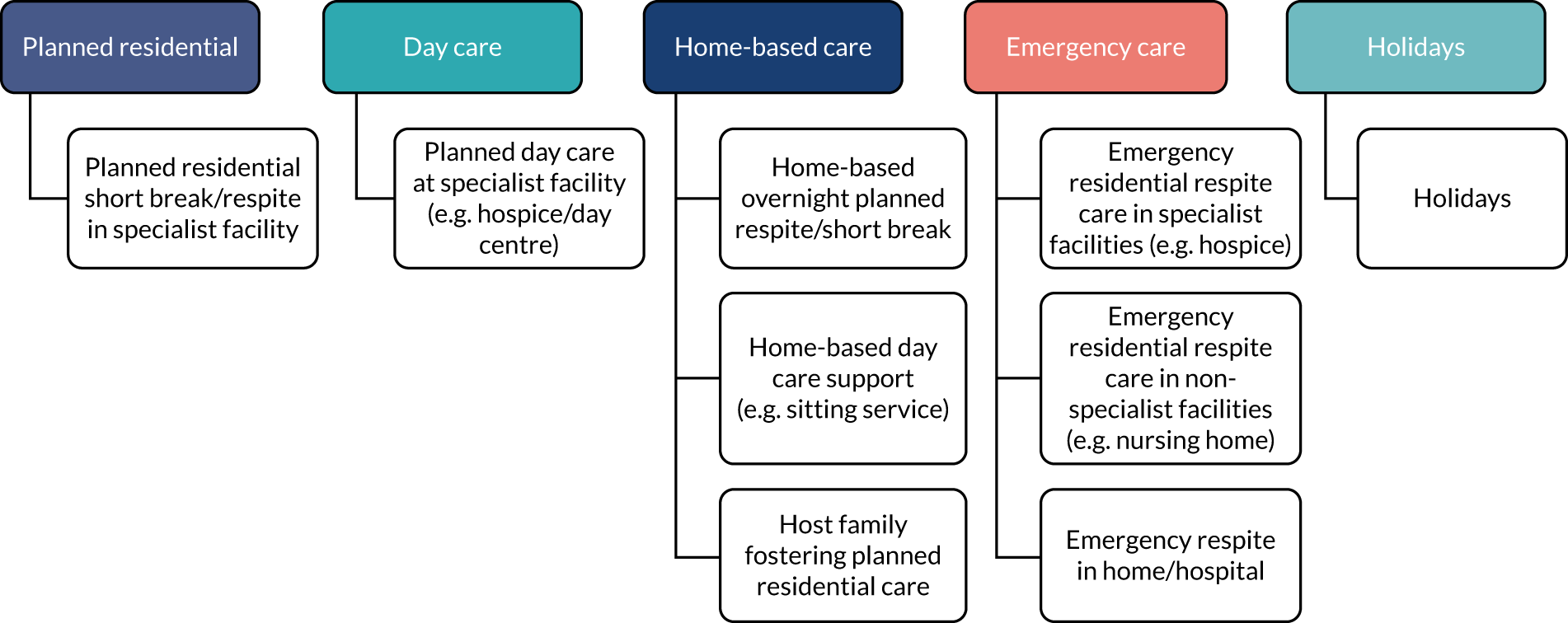
The definition of short breaks and respite care used by children and adult services differ by service type and intended outcomes. More information on the intended outcomes by service types can be found in the logic models that form the conceptual framework for the review in Appendices 8–20. This is partly attributable to the flexibility required to meet the needs of both service users and providers when developing services. Some of the factors that may influence service delivery include:33
-
location (e.g. in the person’s own home, at a carer’s home, residential or community setting)
-
duration (e.g. for a few hours, overnight, several days)
-
timing (e.g. weekdays, weekends, evenings)
-
provider (e.g. local authorities, health agencies, voluntary/independent agencies)
-
care funding (e.g. use of personal budget, care package, provider or charity funded).
Drawing on the literature and policy statements we used the following definition of respite care and short breaks:
Respite care and short breaks are the temporary provision of formal or informal physical, emotional, spiritual or social care for a dependent person.
Formal respite care is provided by organisations or individuals who receive financial payment, including family carers paid through management of personal care budgets.
Informal respite care does not involve financial payment.
Need for the review
Children, young people and young adults with complex health-care needs have multiple comorbidities and/or disabilities in addition to their primary diagnosis or condition. They are therefore at increased risk of other health-care problems. Care for these young people is an ongoing, complex process, with no simple care pathway and often multiple, unplanned episodes of illness. The Department of Education and Skills’ report Aiming High for Disabled Children: Supporting Families37 made a clear policy commitment to improving available data on disabled young people and their access to services, but further work is required to improve access to specialist services, such as short breaks/respite care. 38 Seven out of 10 families caring for someone with profound or multiple disabilities report having reached or come close to ‘breaking point’ because of a lack of short break services. 39
The Care Quality Commission found a significant shortfall between policy and practice during transition from child to adult services due to fragmentation of the system, which can be confusing and difficult to navigate for young adults with complex health-care needs, their families and staff caring for them. 13 This is supported by evidence showing that poor service provision following transition to adult services has a significant impact on both the life expectancy and quality of life for these young adults, including early death and increased psychosocial burden on families and carers. 20,24,34,35 Previously published research by the review team35,40 and a national survey of hospices and health-care professionals conducted by the team in 2015 identified significant gaps in the evidence base, challenges in providing respite care for young adults with complex health-care needs and the need for robust evidence to inform service development. 41
Commissioning of respite services is devolved in England, Scotland, Wales and Northern Ireland. Commissioners and service providers in England and Wales have a statutory duty under the Children and Families Act 201442 and the Care Act 201443 to ensure seamless provision of responsive, appropriately funded and integrated services for young adults with complex health-care needs as they transition to adult services. 1,13,22 Despite the rising number of young people with complex health-care needs surviving into early adulthood, and the consequent escalation in care service demand for themselves and their families, the current scale, cost and types of available respite care have not been collated and evaluated at a national level. Comprehensive data collation is challenging because of the range of public and private providers, fragmented development of independent services and the variability in funding practices, including commissioned care (NHS or social care), local authority, charity funded and use of personal budgets.
Evidence on the effectiveness and cost-effectiveness of respite care/short breaks and the views and experiences of service users is published in a variety of sources across the evidence spectrum. Given the uncertainties concerning types of available care and lack of clarity on the optimum types of service provision, it is essential to systematically review the plethora and diversity of sources, and to integrate these into a cohesive summary, highlighting gaps in evidence to inform future research.
Chapter 2 Aims and objectives
The aim of this mixed-methods review was to identify, appraise and synthesise evidence relating to the type and impact of respite care and short breaks provision for young adults (aged 18–40 years) with complex health-care needs. The review aimed to explore policy intentions, service intentions and service-user perspectives (i.e. factors that may inhibit or facilitate the delivery of such care) and cost-effectiveness to develop a conceptual framework for respite care, and to form the basis of recommendations for future service development and the need for new research.
To achieve the above aim, our objectives were as follows:
-
To explore current UK policy, not-for-profit organisation (NFPO) publications and guideline recommendations regarding respite care and short break provision for young adults (aged 18–40 years) with complex health-care needs due to a LLC or complex physical disability.
-
To identify and characterise the different types of formal and informal respite care and short break provision for young adults (aged 18–40 years) with complex health-care needs due to a LLC or complex physical disability.
-
To develop a series of logic models that embody the programme logic and programme theories of respite care and short break types for young adults (aged 18–40 years) with complex health-care needs due to a LLC or complex physical disability that will inform service planning and commissioning.
-
To determine the effectiveness and cost-effectiveness of different types of formal and informal respite care and short break provision for young adults (aged 18–40 years) with complex health-care needs due to a LLC or complex physical disability.
-
To better understand the impact, experiences and perceptions of respite care and short break provision from the perspectives of service users and providers.
-
To make recommendations for further empirical research to inform intervention development and evaluation.
Systematic review questions
For young adults (aged 18–40 years) with complex health-care needs due to a LLC or complex physical disability we considered the following:
-
What are the current UK policy and guidance recommendations for the provision of respite care and short breaks? (Objective 1.)
-
What types of respite care and short breaks are provided in the UK and similar global economies? (Objectives 2 and 3.)
-
What is the effectiveness and cost-effectiveness of different types of formal and informal respite care and short break provision? (Objective 4.)
-
What is the economic impact of respite care and short breaks? (Objective 4.)
-
What are service users’ and providers’ views of current respite care provision and the need for new services? (Objective 5.)
-
What are the facilitators of and barriers to providing, implementing, using and sustaining respite care and short breaks, taking into account the different perspectives of young adults, family members and providers? (Objectives 3–5.)
Chapter 3 Methods
This section describes in detail all aspects of the search strategy, screening and selection of evidence, data extraction and quality appraisal, methods of synthesis and the role of members of the Patient and Public Advisory Group (PAG) and Steering Group (SG). As anticipated, because of the complexity of the mixed-methods approach and the nature of the evidence, there were minor methodological departures from the published protocol. 44 A summary of the differences between the protocol and the review are described in Summary of deviations from the protocol.
Overview
To achieve the review objectives set out in Chapter 2, we conducted a two-stage mixed-methods systematic review, adopting a similar approach to that used in other mixed-methods systematic reviews. 45,46 Figure 2 depicts the planned flow of work through the two stages, incorporating the development of logic models as the conceptual framework for the review.
FIGURE 2.
Mixed-method systematic review flow chart.
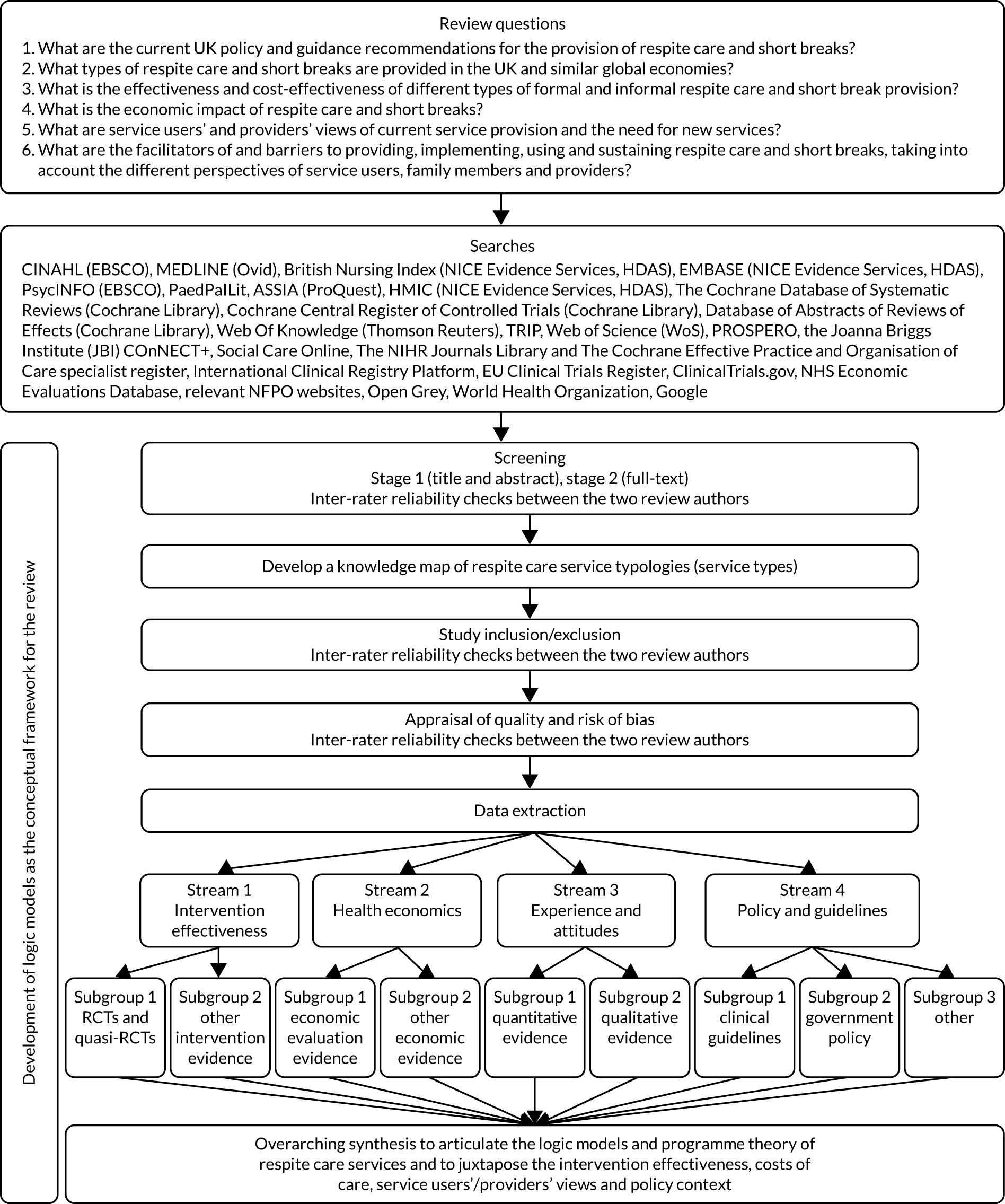
We conducted comprehensive literature searches of electronic databases and grey/unpublished literature. The results were independently assessed for inclusion through two screening stages and categorised as included in stage 1 and/or stage 2 as follows.
Stage 1: knowledge map of types of respite care services
We identified, catalogued and described different types of formal and informal respite care and short break services for young adults (aged 18–40 years) with complex health-care needs due to a LLC or complex physical disability. We developed an initial logic model for each type of service to illustrate the differences in context, service configuration, populations, implementation and intended outcomes for various stakeholders.
Stage 2: evidence review
We synthesised evidence in method-specific streams and grouped the evidence according to the types of service identified in stage 1, extracted key descriptive information from each source and evaluated methodological quality. Results and recommendations were extracted from each source and synthesised within each evidence stream. We also identified key policies and extracted the policy intent concerning respite care.
Further development and refining the logic models as a conceptual framework
Building on the knowledge map identified in stage 1 and the evidence synthesised in stage 2, we continued to further develop and refine a series of logic models that encapsulated the essential elements and intended outcomes of different types of respite care service provision, forming a conceptual framework for the review, which became a product of the review when fully developed(see Appendices 8–20).
Identifying the literature
Evidence selection criteria
We defined selection criteria using the SPICE (Setting, Perspective, Intervention/phenomenon of interest, Comparison, Evaluation) framework47 (Table 1).
| Criterion | Inclusion | Exclusion |
|---|---|---|
| Setting | Services and providers of formal respite care and short breaks, including hospices, residential care homes, adult day services, individual providers and paid carers/family carers working within young adults’ home settings, and informal care from unpaid family members |
Services and providers of care other than respite care and short breaks Services specifically commissioned for young adults with a learning disability or mental health needs |
| Perspective | Young adults (aged 18–40 years) with complex health-care needs due to a LLC or complex physical disability receiving respite care and/or short breaks, and their parents, families, carers and/or those involved in the commissioning or delivery of their care |
Young people aged < 18 years or people aged > 40 years Young adults who do not require respite care/short breaks |
| Intervention/phenomenon of interest | Formal (paid) and informal (unpaid) respite care/short breaks in relation to intervention effectiveness, cost-effectiveness, stakeholder experience and attitudes, UK policy and guidance | Care other than respite care and short breaks |
| Comparison | Any type of formal and informal respite care/short break | Care other than respite care and short breaks |
| Evaluation |
Evidence from 1 January 2002 to 18 September 2019 from the 35 OECD countries will be included Intervention effectiveness: any quantitative service user, family, carer and service provider outcomes, such as quality of life, well-being, health impact, stress and coping, family cohesion or satisfaction with care Cost-effectiveness: information on the costs and economic impact of care, such as incremental cost per QALY, cost per admission avoided, staff costs, equipment and transport Experience and attitudes: qualitative, quantitative and mixed methods information, such as concepts and themes arising from recognised methods (e.g. grounded theory analysis, thematic analysis, framework analysis), surveys or reports that capture attitudes, beliefs, preferences and opinions on the provision of respite care Policy and guidelines: recommendations, directives, actions or anticipated outcomes identified in UK policy statements or guidelines |
Streams 1 and 2: outcomes unrelated to effectiveness, experience or economic evidence Stream 3 (experience and attitudes): unconfirmed reports and anecdotal opinion (e.g. newspapers, social media, online blogs) Stream 4: non-UK policy or guidelines |
Search strategy
The investigative team and SG, led by our information specialist (MM), developed the search strategy to identify relevant published and unpublished evidence (e.g. primary studies, evaluations, policy documents). The search strategy was informed by the complexity of the SPICE framework and the need to identify all data from a diverse range of sources. 47 To minimise missing evidence, our overall strategy was to maximise sensitivity of the searches.
We developed an exploratory search using the MEDLINE database. The investigative team and SG identified an initial set of keywords to inform the search strategy and discussed the search structure. The review team also identified a set of key relevant studies and the full text of these studies was analysed to identify additional relevant keywords. The information specialist mapped the keywords to relevant thesaurus terms in MEDLINE. Analysis of the MEDLINE records of key relevant studies identified additional relevant thesaurus terms.
We conducted a sensitivity analysis on the search strategy by comparing the retrieval of different search techniques (e.g. proximity operators, phrase searching and field searching) to develop a search strategy that ensured the retrieval of all key relevant studies. The final version of the exploratory search was adapted for other search sources (see Appendix 1).
We limited the search to evidence available from January 2002 onwards because of significant changes in service demand [including an increase by 45% over the past decade to 1 in 10,1 changes in the law (e.g. Children and Families Act 2014,42 Care Act 201443) and new policy/guidance documents published during the last 17 years]. As the review is specifically concerned with the provision of respite care or short breaks in the UK, we also limited the search to the 35 Organisation for Economic Co-operation and Development (OECD) countries considered comparable, except for evidence relating to stream 4 (policy and guidelines), which focused entirely on domestic policy.
We searched the following sources from 1 January 2002 to 26 September 2018: Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCOhost), MEDLINE (Ovid), British Nursing Index (NICE Evidence Services, Healthcare Databases Advanced Search), EMBASE (NICE Evidence Services, Healthcare Databases Advanced Search), PsycINFO (EBSCOhost), Applied Social Sciences Index and Abstracts (ASSIA) (ProQuest), Health Management Information Consortium (HMIC) (NICE Evidence Services, Healthcare Databases Advanced Search), the Cochrane Database of Systematic Reviews (The Cochrane Library), Database of Abstracts of Reviews of Effects (to 31 March 2015) (Archived by Centre for Reviews and Dissemination), Web Of Science (Thomson Reuters), Trip, PROSPERO, Joanna Briggs Institute Systematic Reviews and Implementation Reports (Wolters Kluwer), Social Care Online and the National Institute for Health Research Journals Library.
To further identify evidence for each specific stream, the strategy was adapted and applied to the following databases:
-
Cochrane Central Register of Controlled Trials (The Cochrane Library), International Clinical Trials Registry Platform (URL: http://apps.who.int/trialsearch/), EU Clinical Trials Register (URL: www.clinicaltrialsregister.eu/ctr-search/search) and ClinicalTrials.gov (URL: https://clinicaltrials.gov/).
-
NHS Economic Evaluations Database and Health Technology Assessments (Centre for Reviews and Dissemination).
Additional evidence was identified through internet searches (Google and Google Scholar, Google Inc., Mountain View, CA, USA), relevant NFPO websites, hand-searching and consultation with the SG and PAG.
We also searched the International Journal of Paediatric Palliative Care (URL: www.worldcat.org/title/paedpallit-the-international-journal-of-paediatric-palliative-care/) for relevant evidence. All searches were updated in February 2019 and September 2019. For the update run on 18 September 2019, we modified the full search strategy to improve specificity by eliminating redundant terms (see Appendix 2). Sensitivity and specificity of the modified strategy was validated by comparing the new and existing strategies for the update in MEDLINE. Results screened by two reviewers confirmed the same list of included items and the modified strategy was therefore implemented across all databases for the full update search.
Grey and unpublished literature
Results from scoping searches suggested that relevant information was likely to be found within the grey literature (e.g. central and local government evaluations and impact assessments, or unpublished data produced by third-sector organisations). We conducted a broad search for grey and unpublished literature via Open Grey (formerly System for Information on Grey Literature in Europe, URL: www.opengrey.eu/), Grey Literature Report (URL: www.greylit.org), the World Health Organization (URL: www.who.int/en/) and Google. In addition, we:
-
asked SG and PAG members to identify relevant known literature
-
asked SG and PAG members to identify topic experts, useful websites and organisations to contact (see Appendix 3)
-
scanned relevant websites for potentially relevant literature
-
targeted topic experts, stakeholders and service providers through a ‘call for evidence’, which was shared through networks, direct e-mails and social media.
In addition to examining the reference lists of included evidence identified through database searching, a purposive and iterative approach to searching the literature was undertaken. The CLUSTER (Citations, Lead authors, Unpublished materials, Scholar search, Theories, Early examples, Related projects)48 approach aims to identify additional relevant outputs that may include a ‘sibling’ paper (i.e. papers from the same study, for example qualitative studies, economic evaluations or process evaluations associated with a randomised controlled trial) or ‘kinship’ studies that inform relevant theoretical or contextual elements. Table 2 shows the key details of this approach, which emphasised the need to adopt multiple search techniques (e.g. citation searching, ‘key pearl’ searching, ancestral searching) to supplement and enhance the main search, and to ensure identification of relevant evidence and grey literature. It aims to identify additional material associated with a study of interest, rather than those simply using the same terminology, therefore overcoming the limitation of selected terminology common to most search strategies.
| Element | Search procedure | Source |
|---|---|---|
| Citations | Identify at least one ‘key pearl’ through consensus with review team | Preliminary searches of databases and grey literature |
| Lead authors | Check reference list of ‘key pearl’ and conduct lead author search | Full text of ‘key pearl’, search of reference management collection, Google (e.g. institutional repository, author publication web page) |
| Unpublished materials | Make contact with lead author | |
| Scholar searches | Citation searches on ‘key pearl’ and other relevant studies and conduct search of ‘project name’ | Web of Science/Google Scholar |
| Theories | Follow up ‘key pearl’ and other cluster documents for citations of theory. Recheck for mention of theory in titles/abstracts/keywords and conduct iterative searches for theory in combination with condition of interest | Full text of ‘key pearl’, search of reference management collection and databases |
| Early examples | Follow up ‘key pearl’ citation and other cluster documents for citations to project antecedents and related projects | Full text of ‘key pearl’ |
| Related projects | Conduct named project and citation searches for relevant projects identified from cluster documents, seek cross-case comparisons by combining project name/identifier for cluster with project name/identifiers for other relevant projects | Web of Science/Google Scholar, databases |
Where possible, we implemented search alerts in source databases to identify additional relevant studies as the review progressed. Results from the searches of multiple electronic databases and other sources were combined and de-duplicated using EndNote reference management software [Clarivate Analytics, Philadelphia, PA, USA; URL: https://endnote.com (accessed 9 December 2020)] and then entered into Covidence, a web-based systematic review management platform [Veritas Health Innovation, Melbourne, VIC, Australia; URL: www.covidence.org (accessed 8 December 2020)]. The use of a single comprehensive search strategy enabled identification of all potential evidence for the knowledge map and review streams. Included sources were then filtered into the appropriate review stage and review stream.
Evidence selection
Multiple reviewers (MOB, LB, BJ, BR and JD) independently screened titles and abstracts for eligibility against review selection criteria for stage 1 (knowledge map) and/or stage 2 (evidence review). Additional reviewers (GP and KK) independently verified eligible evidence. The full texts of eligible records were retrieved and screened for inclusion in the review by multiple reviewers and independently verified as before. Reasons for exclusion of full-text records were recorded. Disagreements were resolved through discussion and consultation with separate reviewers (SS and JN), where necessary. We coded multiple publications from individual studies using a single core reference and source identifier. Owing to the high volume of search results and the need to streamline review processes, the selection of evidence for stages 1 and 2 of the review was undertaken concurrently (sequential stage 1 and 2 selection was planned in the review protocol).
Stage 1: knowledge map methods
One of the key review objectives was to identify and characterise the different types of formal and informal respite care and short break services provided for young adults (aged 18–40 years) with complex health-care needs due to a LLC or complex physical disability. The criteria for inclusion in the stage 1 knowledge map were less restrictive than selection criteria for inclusion in the evidence review because we were looking for examples of these services (Table 3). To enable inclusion of relevant respite services for our target population, evidence was included if it met the following three criteria: (1) it broadly met the perspective (population) element of the SPICE criteria; (2) it broadly met the intervention (respite care/short breaks) element of the SPICE criteria (see Table 1) and (3) it provided a sufficiently detailed specification of service provision to inform the stage 1 knowledge map. Evidence that did not provide a sufficiently detailed description of services to be included in stage 1 may nevertheless have met the following full SPICE criteria for stage 2.
| Criterion | Inclusion | Exclusion |
|---|---|---|
| Perspective | Young adults (aged 18–40 years) with complex health-care needs due to a LLC or complex physical disability (including those where no upper age limit is stated) |
Young people aged < 18 years or people aged > 40 years Young adults who do not require respite care/short breaks |
| Intervention/phenomenon of interest | Any type of evidence about respite care/short breaks in any setting |
Care other than respite care and short breaks Services specifically commissioned for young adults with learning disability or mental health needs |
This process presented some challenges because of the complexity of commissioned services. Many respite services are commissioned for people with a range of different needs and the population mix therefore includes people with other needs as well as our target population. To maximise sensitivity of the stage 1 search and to avoid missing relevant services, we retained a very broad selection strategy at this stage. Mixed populations were included when young adults aged 18–40 years were clearly part of the wider population. Similarly, services provided for populations with a range of needs were also included, providing that young adults with complex health-care needs were part of the wider service population. However, the review focuses on the provision of respite care for young people with complex health-care needs and evidence about services for people with solely educational or social care needs were therefore excluded.
The following information from evidence included in the stage 1 knowledge map (where available) was extracted and logged:
-
evidence bibliographic details
-
location (setting)
-
description of the intervention guided by the TIDieR (Template for Intervention Description and Replication) checklist49
-
information on service delivery processes required for programme theory and logic models.
Using preliminary categories published in the protocol as a starting point, and considering the population, timing, location and level of care provision, the evidence was used to categorise distinct service types that were validated following consultation from our PAG and the review SG.
Development of logic models
The information extracted from each item of evidence was synthesised to create a profile of each service type. The profiles catalogue the service aims and objectives, eligibility criteria, delivery components, implementation resources, user expectations and intended outcomes for various stakeholders. Some aspects of service specification, such as implementation resources and user expectations, had to be inferred because of a lack of information and this is noted in footnotes of the logic models, where appropriate.
The logic models evolved throughout the stage 1 knowledge map, the stage 2 evidence synthesis and the overarching synthesis. We developed logic models for the different types of respite care using Cochrane guidance50 and examples of good practice. 51,52 The logic models illustrate the programme theory for each type of respite care/short breaks service. Each model encapsulates the intended service aims, how the service is intended to work and for whom, the potential resources needed to deliver the service, and the anticipated outcomes and outputs from the service (i.e. how the services are conceptually designed to work). The models were continually updated and the completed logic models for each type of respite service were independently validated by the PAG and SG (see Appendices 8–20).
Stage 2: evidence review methods
Evidence was included in the stage 2 evidence synthesis only if it met all of the SPICE study selection criteria (see Table 1). This necessarily meant that some evidence was included in only one of the stages. The evidence included at each stage is reported in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram (see Figure 3). Sources included in stage 2 were categorised as one of the following four streams of evidence.
Evidence stream 1: intervention effectiveness (review question 3)
Quantitative evidence of the effectiveness of the intervention (i.e. respite care and short breaks), such as randomised, quasi-randomised controlled trials, before-and-after studies, observational cohort studies or other types of quantitative evidence of effectiveness.
Evidence stream 2: health economics (review questions 3 and 4)
Quantitative evidence relating to health economics, such as economic evaluations (e.g. cost–utility and cost-effectiveness analyses), reports of care costs and other economic evidence (e.g. cost of illness or burden of disease studies).
Evidence stream 3: experience and attitudes (review questions 2, 5 and 6)
Qualitative, quantitative and mixed-methods evidence exploring experience and attitudes relating to the provision of respite care or short breaks. Studies using recognised methods of data collection and analysis, such as surveys, interviews, focus groups, observational techniques, case studies, process and realist evaluations, and studies that include independent or components of a mixed-methods design.
Evidence stream 4: UK policy and guidelines (review question 1)
All relevant current UK government policy, clinical guidelines and NFPO literature.
Data extraction
Bespoke extraction forms were developed for each evidence stream, tailored to the type of evidence and the underlying review question. Where it was available, we extracted the following information on study characteristics and their results:
-
publication characteristics [e.g. type (peer reviewed), year, country of data collection, dates of study data collection, publication language, source of study funding]
-
aims, objectives and target audience (policy)
-
methods (e.g. study design, recruitment/selection, data collection methods, methods of analysis)
-
participant characteristics [e.g. type of complex health-care needs and/or carers, study inclusion/exclusion criteria, age (mean, range), sex proportion, ethnicity, number in each study group, baseline characteristics]
-
intervention characteristics (e.g. type of service, setting, duration of care)
-
a description of all outcomes, measurement frequency, duration of follow-up and results reported in any format
-
the authors interpretations/conclusions
-
study limitations.
Data were extracted by one reviewer from the team assigned to each stream (GP, LB, MOB, BJ, JD, JN or BR) and accuracy was independently verified by a second reviewer (KK, GP or CM). Disagreements were resolved through consensus or by a third reviewer allocated to each stream by expertise (SS, BR, JN or CM). Data from sources with multiple publications were extracted and reported using the core reference as a source identifier.
Knowledge map: evidence matrix
We categorised each item of evidence by type of respite care or short break (identified in stage 1) and one of the four types of evidence stream to create an evidence matrix. The nature, quantity and quality of evidence was summarised and reported for each evidence stream and for each type of respite care/short breaks service (see Appendix 23). The matrix template was included in the review protocol. 44
Quality assessment strategy
The methodological limitations of included evidence were assessed by two reviewers (GP and KK) and disagreements resolved through consensus or by a third reviewer (JN or SS). No evidence was excluded on the basis of methodological strengths and limitations. However, design limitations were taken into account during synthesis and are included in the discussion.
No studies were identified for streams 1 or 2, but the intended quality assessment methods are described in the published protocol. 44
We used the CASP (Critical Appraisal Skills Programme)53 appraisal tool to assess the methodological limitations of the qualitative studies included in stream 3. We did not use other appraisal tools described in the protocol, for example the Mixed Method Appraisal Tool for mixed-methods studies, as they were not applicable to any of the included evidence.
For stream 4, we intended to use the AGREE II (Appraisal of Guidelines, REsearch and Evaluation Version II) instrument to assess quality, but we did not identify any relevant practice guidelines. The quality of law and policy documents was not appraised.
Methods of data synthesis
Detailed methods are provided for streams 3 and 4, as no evidence was identified for inclusion in streams 1 and 2. Planned methods for all evidence streams are in the published protocol. 44 For reference, a detailed model of the review design and planned evidence syntheses are in Appendix 4.
Evidence stream 3: experience and attitudes
Framework synthesis was used to translate evidence from qualitative studies. Drawing on the planned review questions in the protocol and the logic models created in stage 1 of the review, we developed an iterative coding framework for the qualitative evidence (see Appendix 5). Each source was independently coded by two reviewers (LB, MOB, BJ or GP). Disagreements were resolved through consensus or by a third reviewer (KK). Evidence contributing to each code was collated and synthesised. The emergent themes are reported narratively and supported by tabulated summary of the evidence for each respite care type in the evidence matrix (see Appendix 23).
Evidence stream 4: UK policy and guidelines
We conducted content analysis of the evidence from UK policy using a documentary analysis informed approach54 to tabulate the evidence, based on an iterative coding framework (KK and GP). The content of each document was analysed using the eight-step process recommended for textual analysis. 55 This approach is an efficient and effective way of gathering, extracting and synthesising data from documents.
Overall synthesis
We planned to use the framework method for overall synthesis, advocated by the Evidence for Policy and Practice Information and Co-ordinating Centre. 56,57 The team planned to conduct within-service type and evidence stream integration of qualitative and quantitative data57 by juxtaposing evidence in an a priori framework, based on the review questions and policy intentions, and moving on to develop themes and subthemes to support further elicitation of the programme theory (i.e. types of service) and outcomes (i.e. benefits and harms), leading to further development and refinement of the logic models. Team members with expertise in quantitative and qualitative analysis and synthesis were assigned to each stream to ensure appropriate skills for synthesis of mixed-methods evidence. Arbitrators were also assigned to each evidence stream to mediate disagreements and uncertainties. However, as we did not identify any quantitative or mixed-methods evidence, the qualitative findings are reported according to each relevant review question [see Chapter 6, Experience and attitudes (evidence stream 3)]. This is supported by the evidence matrix described above (see Knowledge map: evidence matrix). Findings were then used to further develop the logical models as the overarching integration framework.
Overall assessment of the evidence
We used GRADE-CERQual (Grading of Recommendations Assessment, Development and Evaluation-Confidence in the Evidence from Reviews of Qualitative research) to assess the overall confidence of the synthesised qualitative findings against four domains: (1) methodological limitations, (2) relevance of evidence to the review question, (3) coherence of the finding and (4) adequacy of data supporting the finding. 58 Two reviewers from the team (KK and JN) independently made an overall assessment using the aforementioned domains to assign a level of confidence for each synthesised qualitative finding:
-
high confidence (i.e. it is highly likely that the finding is a reasonable representation of the phenomenon of interest)
-
moderate confidence (i.e. it is likely that the finding is a reasonable representation of the phenomenon of interest)
-
low confidence (i.e. it is possible that the finding is a reasonable representation of the phenomenon of interest)
-
very low confidence (i.e. it is not clear whether the finding is a reasonable representation of the phenomenon of interest).
Table 4 provides a GRADE-CERQual qualitative evidence profile.
| Review finding | GRADE-CERQual assessment of confidence in the evidence | Explanation of GRADE-CERQual assessment | Studies contributing to the review finding |
|---|---|---|---|
| Respite services facilitated the development of independence and empowerment of young adults through opportunities to make choices and engage in a range of different activities, share their views to plan and develop services, and spend time away from parents | High confidence | No concerns, all perspectives included | Five sources59–63 |
| A significant benefit of respite services was the opportunity for young adults to socialise with peers and to interact with different staff to prevent isolation, create a sense of camaraderie with others who faced similar challenges and to allow engagement in activities they may not be able to access at home | High confidence | Minor concerns for methodological limitations. No concerns for relevance or adequacy. All perspectives included | Five sources59,62,64–66 |
| Respite care provided a sense of hope and lifted the spirits of young adults by fostering a sense of belonging where people did not feel defined by their disability or health condition | Low confidence | Only two sources. Moderate concerns for methodological limitations, coherence and relevance. No parent and service-provider perspective | Two sources62,65 |
| Respite care provided parents with time to themselves to rest, recuperate and engage in personal hobbies or interests while having a break from their 24/7 caring responsibilities, which reduced their physical and psychological strain | High confidence | Minor concerns for methodological limitations, coherence and adequacy. No concerns for relevance. No service-provider perspective | Nine sources59,61,62,65–70 |
| Respite care is a support mechanism for parents and the wider family, helping to re-establish family cohesion through time with partners and other children, which builds resilience for the family to continue with the demands of providing care | High confidence | Minor concerns for methodological limitations. No concerns for coherence, adequacy or relevance. No service-provider perspective | Five sources27,60,61,71,72 |
| Practical barriers to accessing respite care were identified, including volume and complexity of paperwork; delay between referral and service provision; the distance between home and the service; limited access to condition-specific services; lack of physical space for equipment in the available setting; lack of appropriately trained staff and limited inclusion of BAME populations | High confidence | Minor concerns for methodological limitations, coherence and adequacy. No concerns for relevance. No young adult perspective | Seven sources27,35,59,61,65,67,71 |
| Barriers to respite care from both the ‘anticipated’ loss of services during transition planning and ‘actual’ loss of services were identified because of the lack of age-appropriate and developmentally appropriate adult services, and the lack of a knowledgeable and experienced staff to provide safe care for young adults with complex health-care needs. Despite the anticipated increase in service demand as both young adult service users and their parents age, there is a lack of suitable alternatives for planned and emergency respite, which could result in a range of potential harms for young adults, parents and the wider family, and for service providers supporting young adults through transition | High confidence | Minor concerns for methodological limitations. No concerns for coherence, adequacy or relevance. All perspectives included | 12 sources22,27,35,59,61,63,64,67,73–76 |
| Trusted relationships between young adults, their parents and providers is an essential element of an acceptable respite service. This trust was underpinned by confidence in appropriately trained staff, providing safe care to the young adults and enabling young adults’ decision-making, which enriched their experience of the service. Lack of trust and confidence would result in poor uptake of services | High confidence | No concerns, all perspectives included | Nine sources27,59–64,69,73 |
| Respite care is viewed as acceptable by young adults, parents and providers when services offer a degree of flexibility and adaptability to the individual needs and wishes of the young adult and parents, including the types of respite accessed and the choice and control of activities engaged in. Parents also expressed a preference for flexibility in their dealings with the services rather than rigid timetables | Moderate confidence | Moderate concerns for methodological limitation. Minor concerns for coherence. No concerns for adequacy or relevance. All perspectives included | Six sources35,61,63,65,67,73 |
| The lack of appropriate respite care services for young adults was identified across the evidence. All stakeholders acknowledged that for services to be acceptable and improve outcomes for young adults, they should be designed and developed with young adults’ interests, life course stage and needs in mind. Young adults valued spending time with peers and wanted staff to be of a similar age and sex to themselves. Respite care in residential homes for the elderly or adult hospices where activities did not align with the young adult’s interests or preferences was viewed as unacceptable. Involving young adults and parents in the development or planning of services was encouraged to improve the acceptability of the service to its users | High confidence | Minor concerns for methodological limitations and coherence. No concerns for adequacy or relevance. All perspectives included | 10 sources27,35,61–65,67,73,76 |
| The need for appropriately trained and experienced staff is acknowledged as a vital resource for the implementation and delivery of safe respite care services for young adults, and for their care to be considered comparable to the standard of care at children’s hospices | High confidence | No concerns, all perspectives included | Four sources60,61,64,75 |
| Funding, commissioning and capacity issues were identified as the key barriers to the development and provision of appropriate respite services for young adults. Providers spoke of inequalities in the funding and commissioning of services across the life span due to inconsistencies between requirements to pay for respite care in children and adult hospices in the third sector, and lack of understanding of the commissioning process among some providers that required encouragement to meet their assessment duties. The challenges of commissioning and delivering services were perceived to be exacerbated by the low volume but high cost of care for this population. Children and adult hospices lack the funding and capacity to provide all the care needed, requiring partnership working and funding with statutory and NHS support to meet current and future need. Parents felt under pressure to agree to short breaks that cost much less than those provided by services for those with individual care packages and continuing health-care funding | High confidence | No concerns. No young adult perspectives | Six sources35,59,61,62,67,76 |
The role of the Steering Group
The SG comprised individuals with an in-depth knowledge of care for young adults with complex health-care needs or the provision of respite care/short breaks, for example those with professional roles in commissioning or delivering services, clinical experts, and parent and young adult representatives from the PAG. The SG was chaired by the review manager (KK) and a young adult from the PAG. The group contributed to the review process electronically and met on four occasions to advise the review team on all aspects of the systematic review, including the scope of the searches, interpretation of results and dissemination of the research findings. The group specifically contributed to the following:
-
Development of the protocol (i.e. clarification of concepts and definitions, particularly in relation to inclusion criteria).
-
Identification of unpublished evidence.
-
Identification of ongoing and arising issues relevant to the review (e.g. current service provision, changes to local or national policies or best practice).
-
Summary of implications of the review findings, particularly in terms of service delivery or policy.
-
Validation of the knowledge map.
-
Validation of the logic models as the conceptual framework.
-
Review of drafts of the final report.
-
Planning and dissemination of the review findings to relevant audiences.
The role of the Patient and Public Advisory Group
The PAG comprised individuals who represented young people with complex health-care needs, carers and parents/guardians. A young adult and a parent from the initial PAG for the funding application remained involved throughout the study. Other original members of the PAG withdrew because of changes in health or life circumstances. Recruitment of additional members of the PAG through social media and our networks initially proved challenging. Some potential participants commented that they were not attracted to systematic reviews, while others were interested but were not able to participate owing to competing demands on their time or deterioration in the health status of the young adult. We continued to recruit members during the study, including for the development of a film and other media outputs, which was more successful in attracting young adults. During the study, five young adults, two parents and four carers were involved in the PAG.
We adopted an inclusive and flexible approach to working with members of the PAG in an effort to overcome challenges in meeting at a mutually agreed time and location. This included working together via telephone, Skype™ (Microsoft Corporation, Redmond, WA, USA) or e-mail to suit individual preferences and the needs of members for whom travel was challenging because of their complex health conditions. All PAG members received ongoing support and guidance throughout the study. A parent and young adult were members of the SG and attended meetings to enable representation and appropriate feedback between the two groups. There were between three and eight contacts with each member of the group, depending on their preferred level of involvement and length of time with the study. Some members engaged individually via telephone or Skype, some attended up to four meetings at the university and others took a combined approach, depending on the weather and their health. All members of the group said that they felt that their contribution to the study was meaningful and that they had enjoyed being part of the study.
The aim of the PAG was to ensure that the experiences of service users was included in the review processes. The PAG was invited to contribute to the following activities at appropriate points during the study:
-
finalising the protocol (e.g. clarifying concepts and definitions, co-writing the Plain English summary)
-
identifying unpublished evidence
-
identifying ongoing and arising issues relevant to the review (e.g. current service provision, changes to local or national policies or best practice)
-
interpreting the review findings
-
validating the knowledge map
-
validating the logic models as the conceptual framework
-
reviewing drafts of the final report
-
planning and developing materials to raise awareness of the review (e.g. audio clips, ‘talking head’ video clips, blogs, a short film).
Members of the PAG will continue to be involved in the dissemination of the review findings to relevant audiences, including ‘talking heads’ video clips and co-presenting at future conferences or regional events to share findings. A film workshop was held in December 2019 to plan the structure of the film and record ‘talking head’ videos of the young adults’ experience and why they feel respite care is important. A second workshop was planned to record ‘talking heads’ and plan an animation of the findings at the university; however, because of the coronavirus pandemic, this work was placed on hold and is now being arranged to take place remotely, when group members are available. The media outputs are planned for release in April 2021. All dissemination materials will be made available on the study website and social media, and will be included in any conference presentations.
Both the SG and PAG were vitally important in providing context from their lived experience of using and providing respite services during the study. This was particularly key when the knowledge map categories and types of respite care needed to be validated. It was reassuring that the types of respite care identified and the growth of certain types, such as the social activities, was reflected in the experience of our members. Their experience also supported and validated the themes identified in the qualitative evidence, particularly where there were areas of overlap or uncertainty about aspects of the provision. The views and experience of the SG and PAG members also enhanced the development of the recommendations for research, policy and practice to ensure that they are appropriate and will support the development of knowledge and the necessary service provision.
Summary of deviations from the protocol
We intended to conduct stages 1 and 2 sequentially but because of the volume of search results, and to improve efficiency, these stages were run concurrently.
We conducted two updates of the study searches, which used a modified version of the original search to improve sensitivity and specificity.
Owing to the nature of the evidence included in the review, some planned processes were not required. These instances are described in the relevant sections of the report.
Chapter 4 Search results
To support the transparent reporting of review methods, we have included an annotated PRISMA checklist. 77 A systematic search conducted in 2018 identified 126,267 records that, following de-duplication, resulted in 77,339 unique records that were entered into Covidence. Of these records, we considered 76,092 irrelevant following inspection of their titles and abstracts. The full texts for the remaining 1247 records were obtained and scrutinised for selection.
We formally excluded 1180 records, which are listed by exclusion category in Appendix 6. We excluded 530 records that did not include our review population, 374 records that did not relate to respite care or short breaks (i.e. the phenomena of interest), 12 records where there was insufficient information for selection, 84 unconfirmed reports or anecdotal opinions, two records not published in OECD countries, 52 duplicate records and 125 records for which the full text was unobtainable.
The remaining 67 records were selected for inclusion. We identified a further 8699 records following updated searches in February and September 2019 and four of these were selected for inclusion. A further eight records were included following CLUSTER searching (n = 4) and searches of reference lists (n = 4). A total of 78 unique records relating to 69 sources were selected for inclusion in the stage 1 knowledge map and/or the stage 2 evidence review. 22,26,27,30,35,41,59–76,78–131 The selection process is summarised in a flow diagram (Figure 3).
FIGURE 3.
A PRISMA flow diagram. a, Some sources are included in only the knowledge map or the evidence review and some are included in both.
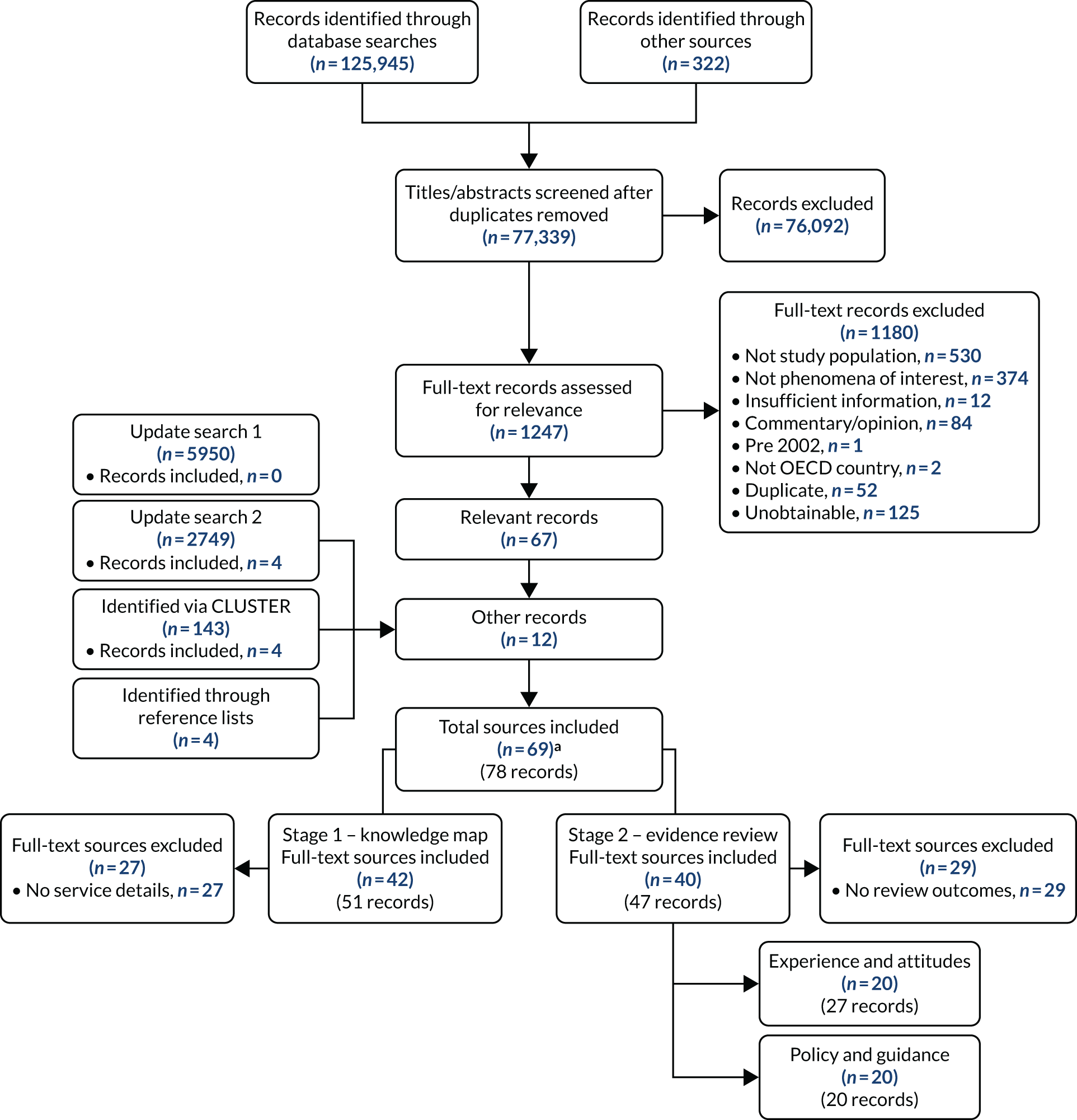
It is important to note that some sources are included in the knowledge map only, some in the evidence review only and some records were included in both. Brief reasons for exclusion from stages 1 or 2 are listed in Figure 3. Details of the records contributing to stages 1 and 2 are listed in Table 5.
| Source | Title | Knowledge map (n = 51 records from 42 sources) | Experience and attitudes (n = 27 records from 20 sources) | Policy and guidance (n = 20 sources) |
|---|---|---|---|---|
| Abbott and Carpenter73 | Becoming an Adult. Transition for Young Men with Muscular Dystrophy | No | Yes | No |
| Arnold and Godwin78 | The Shakespeare Hospice Transitional Care Service Innovation in Practice | Yes | No | No |
| The Asian Health Agency79 | Ashra Carers Project: Children & Young People with Special Needs | Yes | No | No |
| Barnet Country Council80 | Barnet Short Breaks Duty Statement 2017/2018 | Yes | No | No |
| Beresford et al.63 | My Life: Growing Up and Living with Ataxia-Telangiectasia: Young People’s and Young Adults’ Experiences | Yes | Yes | No |
| Bishop81 | Making The Most Of Life | Yes | No | No |
| Bona et al.82 | Massachusetts’ Pediatric Palliative Care Network: Successful Implementation of a Novel State-Funded Pediatric Palliative Care Program | Yes | No | No |
| Brighton and Hove City Council83 | Brighton & Hove City Council Short Breaks Statement 2017–18 | Yes | No | No |
| Brook84 | Jacksplace – A Hospice Dedicated to Teenagers and Young Adults in Hampshire | Yes | No | No |
| Care Quality Commission85 | Claire House Children’s Hospice Inspection Report | Yes | No | No |
| Care Quality Commission87 | Francis House Children’s Hospice Inspection Report | Yes | No | No |
| Claire House Children’s Hospice86 | Claire House Children’s Hospice Local Offer Statement | Yes | No | No |
| Dawson and Liddicoat62 | ‘Camp Gives Me Hope’: Exploring the Therapeutic Use of Community for Adults with Cerebral Palsy | Yes | Yes | No |
| Department of Education and Skills and DHSC89 | Commissioning Children and Young People’s Palliative Care Services: A Practical Guide for the NHS Commissioners | No | No | Yes |
| DHSC90 | Carers and Disabled Children Combined Policy Guidance Act 2000 and Carers (Equal Opportunities) Act 2004 | No | No | Yes |
| Department for Children, Schools and Families and DHSC91 | Aiming High for Disabled Children: Short Break Implementation Guidance | No | No | Yes |
| DHSC26 | Better Care, Better Lives. Improving Outcomes for Children Young People and Their Families Living with Life-Limiting and Life-Threatening Conditions | No | No | Yes |
| Department for Education92 | The Breaks for Carers of Disabled Children Regulations 2011 | No | No | Yes |
| Department for Education and DHSC88 | Special Educational Needs and Disability Code of Practice: 0 to 25 Years | No | No | Yes |
| DHSC93 | Care Act 2014 – Care and Support Statutory Guidance | No | No | Yes |
| East Anglia Children’s Palliative Care Managed Clinical Network94 | The East of England Children and Young People’s Palliative Care Service Directory | Yes | No | No |
| aGans et al.95 | Impact of a Pediatric Palliative Care Program on the Caregiver Experience | Yes | No | No |
| Gans et al.96 | Better Outcomes, Lower Costs: Palliative Care Program Reduces Stress, Costs of Care for Children with Life-Threatening Conditions | Yes | No | No |
| Grinyer et al.71 | Issues of Power, Control and Choice in Children’s Hospice Respite Care Services: A Qualitative Study | Yes | Yes | No |
| Hanrahan97 | A Host of Opportunities: Second NHSN Survey of Family Based Short Break Schemes for Children and Adults with Intellectual and Other Disabilities in the Republic of Ireland | Yes | No | No |
| Health Information and Quality Authority98 | Draft National Standards for Residential Centres for People with Disabilities (Consultation Document) | No | No | Yes |
| HM Treasury 200799 | Aiming High for Disabled Children: Better Support for Families | No | No | Yes |
| Hutcheson et al.59 | Evaluation of a Pilot Service to Help Young People with Life-Limiting Conditions Transition From Children’s Palliative Care Services | Yes | Yes | No |
| Institute of Public Care and National Commissioning Board Wales100 | Integrated Services for Children and Young People with a Disability in Conwy. A Case Study | Yes | No | No |
| Kerr et al.74 | A Cross-Sectional Survey of Services for Young Adults with Life-Limiting Conditions Making the Transition From Children’s to Adult Services in Ireland | No | Yes | No |
| Kirk and Fraser22 | Hospice Support and the Transition to Adult Services and Adulthood for Young People with Life-Limiting Conditions and Their Families: A Qualitative Study | No | Yes | No |
| Knighting et al.101 | An Evaluation of the Rachel House at Home Service for the Children’s Hospice Association Scotland (CHAS): Summary Public Report | Yes | No | No |
| aKnighting et al.67 | Meeting the Needs of Young Adults with Life-Limiting Conditions: A UK Survey of Current Provision and Future Challenges for Hospices | Yes | Yes | No |
| Knighting et al.41 | Children and adult Hospice Provision for Young Adults with Life-Limiting Conditions: A UK Survey (Poster at Hospice UK Conference) | Yes | Yes | No |
| Knighting et al.102 | Highlights From a UK Survey of Children and Adult Hospice Provision for Young Adults with life-Limiting Conditions | Yes | Yes | No |
| aKnighting et al.103 | Short Break Provision for Young Adults with Life-Limiting Conditions: A UK Survey with Young Adults and Parents | Yes | Yes | No |
| Knighting et al.75 | Family Respite Care Survey with Young Adults and Parents: Summary Findings Report | No | Yes | No |
| Knowsley Council104 | Knowsley Children and Family Services Short Breaks Statement | Yes | No | No |
| Leason105 | Let’s Face the Music and Dance | Yes | No | No |
| Luzinat et al.68 | The Experience of a Recreational Camp for Families with a Child or Young Person with Acquired Brain Injury | Yes | Yes | No |
| MacDonald and Greggans70 | ‘Cool Friends’: An Evaluation of a Community Befriending Programme for Young People with Cystic Fibrosis | Yes | Yes | No |
| Marsh et al.35 | Young People with Life-Limiting Conditions: Transition to Adulthood. ‘Small Numbers, Huge Needs, Cruel and Arbitrary Division of Services’. Executive Summary of Phase 1 Report for Marie Curie Cancer Care | No | Yes | No |
| Martin House Children’s Hospice60 | Supporting Children with Life-Limiting Conditions and Their Families – Research Examining Service Provision in Yorkshire and the Humber | Yes | Yes | No |
| Martin House Children’s Hospice106 | Professionals’ Booklet | Yes | No | No |
| aMitchell et al.27 | Short Break and Emergency Respite Care: What Options for Young People with Life-Limiting Conditions? | Yes | Yes | No |
| Mitchell et al.107 | ‘No Other Choice’ When Children’s Hospice Care is Unavailable: An Emergency Care Impact Assessment for Claire’s House Children’s Hospice | Yes | Yes | No |
| Mitchell et al.108 | Emergency Care Impact Assessment (ECIA) project: Claire House Children’s Hospice: Final Report | Yes | Yes | No |
| Murphy and Mackay109 | Will Anyone Listen to Us? What Matters to Young People with Complex and Exceptional Health Needs and Their Families During Health Transitions | No | Yes | No |
| Muscular Dystrophy Campaign65 | Give us a Break: Hospice and Respite Care for Young Disabled Adults in Scotland | No | Yes | No |
| NICE111 | Improving Outcomes in Children and Young People with Cancer | No | No | Yes |
| NICE110 | Supporting Adult Carers – Draft Guidance for Consultation | No | No | Yes |
| Rainbows Hospice for Children and Young People112 | Rainbows Quality Account 2017–2018 | Yes | No | No |
| Rochdale County Council113 | Rochdale Short Breaks Provision for Children and Young People with Disabilities | Yes | No | No |
| Social Care Institute for Excellence 2019114 | Carers’ Breaks: Guidance for Commissioners and Providers | No | No | Yes |
| Scottish Children and Young People’s Palliative Care Executive Group115 | A Framework for the Delivery of Palliative Care for Children and Young People in Scotland | No | No | Yes |
| Scottish Government116 | National Care Standards: Short Breaks and Respite Care Services for Adults | No | No | Yes |
| Scottish Government117 | Carers (Scotland) Bill 2015 | No | No | Yes |
| Scottish Government118 | Carers (Scotland) Act 2016: Statutory Guidance | No | No | Yes |
| Shared Care Scotland119 | Short Break Case Studies | Yes | No | No |
| Shared Care Scotland120 | It’s About Time: An Overview of Short Break (Respite Care) Planning and Provision in Scotland | Yes | No | No |
| Shared Care Scotland72 | Short Breaks Fund Evaluation of Round One Projects | Yes | Yes | No |
| Shared Care Scotland66 | Evaluation Report on Round Two of the Short Breaks Fund | Yes | Yes | No |
| Shared Care Scotland121 | Evaluation Report of CREATIVE breaks October 2012–September 2013 | Yes | No | No |
| aSt Elizabeth Hospice122 | Young Adult Short Break Pilot | Yes | No | No |
| St Elizabeth Hospice123 | Business Care for Short Stay Unit for Young Adults | Yes | No | No |
| St Elizabeth Hospice124 | Short Break Unit Procedure for Attending with Own Carers | Yes | No | No |
| St Joseph’s Hospice 2013125 | St Joseph’s Hospice Quality Account 2012/2013 | Yes | No | No |
| St Oswald’s Hospice126 | St Oswald’s Young Adult Service – Your Guide | Yes | No | No |
| Staley127 | Having a Break: Good Practice in Short Breaks for Families with Children Who Have Complex Health Needs and Disabilities | Yes | No | No |
| Stylianou69 | Mothers with Disabled Children in Cyprus: Experiences and Support | Yes | Yes | No |
| TfSL128 | Jointly Commissioning Palliative Care for Children and Young People Aged 0–25 Including Short Breaks: Guide for Local Areas in England | No | No | Yes |
| TfSL129 | Stepping Up: A Guide to Enabling a Good Transition to Adulthood for Young People with Life-Limiting and life-Threatening Conditions | No | No | Yes |
| TfSL30 | Transition: A Guide for Clinical Commissioning Groups | No | No | Yes |
| Urbanowicz et al.130 | Use of Equipment and Respite Services and Caregiver Health Among Australian Families Living with Rett Syndrome | Yes | No | No |
| Welsh Government131 | The Breaks for Carers of Disabled Children (Wales) Regulations 2012 | No | No | Yes |
| aYoung et al.61 | Qualitative Accounts of Young-People, Parents and Staff Involved with a Purpose-Designed, Pilot Short-Break Service for 18–24 Year Olds with Life-Limiting Conditions | Yes | Yes | No |
| Young and Cameron76 | Living Longer Than You Thought I Would. Working with Young People with Complex Health Needs and Life-Limiting Conditions to Meet the Challenges Facing Them as They Grow into Adulthood | Yes | Yes | No |
| Young et al.64 | Small Service, Big Impact. Evaluation of a New Short Break Service for Young Adults with Life Limiting Conditions at St Oswald’s Hospice | Yes | Yes | No |
Chapter 5 Stage 1: knowledge map
A total of 42 sources (51 records)27,41,59,60,61–64,66–72,76,78–87,94–97,100–108,112,113,119–127,130 were included in the knowledge map and the service categories are listed in Table 5. The knowledge map is not an exhaustive list of all services or sources of evidence about each service type. The map is a catalogue of the types of respite and short break services delivered to young adults with complex health-care needs due to LLCs and/or complex physical disability that are in the included literature and are described in sufficient detail to inform the logic models that formed the conceptual framework. Our review excluded services delivered solely to young adults with educational or social care needs, or to young people aged < 18 years.
Twenty-three sources related to services in England,27,60,61,64,71,78–80,83–87,94,104–106,112,113,122,125–127 seven to services in Scotland,66,70,72,101,119–121 two to services in Wales,81,100 one to services in Northern Ireland,59 three to services in the UK,41,63,67 one source to services in each of the Republic of Ireland97 and Cyprus,69 three sources to services in the USA62,82,95 and two to services in Australia. 68,130
Twenty-five sources were classified as research studies or reports,27,59–63,66–72,78,82,95,97,100,101,103,119–121,127,130 nine were classified as service directories or local offers of provision from local authorities,79,80,83,86,94,104,106,113,126 three were commentaries,81,84,105 four were inspection reports or quality accounts85,87,112,125 and one source was classed as grey literature. 122
Types of services
Service descriptions were extracted from each source and categorised as one of the following six overarching categories based on the published protocol for the review:44 (1) residential respite in a specialist facility, (2) home-based respite, (3) day-care respite at a specialist facility, (4) community, leisure and social provision, (5) funded holidays and (6) emergency respite (unplanned). The categories are based on where and when the services are delivered, taking service funding into account.
Within the six main categories, we identified 13 distinct service typologies (Figure 4) with varying levels of evidence (Table 6). Residential respite encompassed three service typologies. There were 21 examples of residential respite in specialist palliative care facilities (e.g. a hospice), six examples of residential breaks delivered in a specialist disability facility (such as condition-specific or adventure camps) where there is less focus on the nursing element of care (Australia, USA and UK based) and one example of residential respite care delivered to young adults in a nursing home.
FIGURE 4.
Respite care categories and types logic models. a, Paid carer, unpaid carer and respite as part of a hospital-led palliative care package, included in both categories. ‘Respite’ refers to respite care and short breaks. Specialist palliative care facilities refer to services where there is an element of nursing care or medical supervision. Specialist disability facilities refer to services that have been built or adapted to meet needs or have additional staff to supervise activities.

| Type of service | Number of examples (sourcesa) |
|---|---|
| Residential respite in specialist palliative care facility (e.g. a hospice) | 2127,59–61,64,67,71,84–87,94,100,104–106,112,120,123,125,126 |
| Residential respite in specialist disability facility (e.g. condition-specific or adventure camps) | 662,66,68,72,119 |
| Residential respite in a nursing home | 1120 |
| Home-based daytime respite | 1460,63,69,79,80,82,83,95,101,120,130 |
| Home-based overnight respite | 1160,63,69,79,80,82,83,95,101,120,130 |
| Host family/fostering respite | 483,97,120 |
| Day care at specialist facility | 463,67,78,120 |
| Organised recreational activities | 1559,60,66,72,80,83,106,113,120,127 |
| Befriending schemes | 560,70,104,113,120 |
| Funded holidays | 963,104,113,119–121 |
| Emergency respite in a specialist palliative care facility (e.g. a hospice) | 827,67,81,85,86,94,100,106 |
| Emergency respite provided in home or hospital | 285,120 |
| Host family emergency respite | 197 |
| Total | 101 |
Home-based respite included three main service typologies and we encountered many examples of overnight and daytime care. In these categories, we included paid carers,60,63,69,79,80,130 unpaid carers69,130 and components of palliative care packages82,95 (USA based) that were home based but unspecific about whether or not they provided daytime/overnight care. We also found four examples of host family (day and overnight) respite in three sources. 83,97,120
Day-care respite at a specialist facility was a single typology that included four examples in four sources. 63,67,78,120 Two examples were provided within a hospice that offered day activities or daytime respite to aid transition to adult services, but no other age-appropriate respite care provision was available. One example was an adult day centre that offered structured activities during the day and one example was an adult day centre that offered a drop-in service.
Community, leisure and social provision included two service typologies. We found 20 examples of social and recreational services for young adults (15 of these related to organised recreational activities59,60,66,72,80,83,113,120,127 and five related to befriending schemes60,70,104,113,120).
Funded holidays was a single service typology that covered nine services that organised or funded tailored breaks to suit the needs of young adults and their families, where nursing care was not necessarily included as part of the provision. 63,104,113,119–121
We also found three types of emergency respite care, eight examples of care provided by a specialist palliative care facility,27,67,81,85,86,94,100,106 two examples of services provided in the home or hospital85,120 and one example of emergency respite provided by a host family. 97
The 13 logic models for each individual service type are shown in Appendices 8–20. The logic models present a summary of the service components, service user expectations, and intended and reported outcomes available for each service type using the headings of service aim and objectives, eligibility criteria, resources needed to provide the service, programme logic, expectations of the young adults, parents and wider family, intended short-term outcomes (proximal) and intended mid- to long-term outcomes (distal). The programme logic summarises what the service does and how it is delivered (e.g. the frequency, location and activities provided). The service components, intended outcomes and service user expectations were populated from the knowledge map sources and engagement with the patient and public involvement (PPI) group. The service user experiences and actual outcomes were mainly completed from the evidence in the review, again with engagement with the PPI group.
Summary discussion
A broad range of respite care service types were identified during the knowledge map stage. These were refined into categories and types of respite care through several stages of discussion with the SG and PAG to facilitate consensus on the final categories and service types, and to ensure that they were validated by service users and providers. In the initial scoping of the evidence for the review protocol, we identified nine service types that were grouped into five overarching service categories (see Figure 1). During the knowledge map process, two additional service types [i.e. planned respite in a specialist disability facility (e.g. condition-specific or adventure camps) that are available in Australia, the USA and the UK, and emergency respite with a host family] and one new service category (i.e. community, leisure and social provision, which included organised recreational activities in the community and befriending schemes staffed by volunteers) were identified. No additional services were identified for home-based respite, day-care respite or holidays.
Chapter 6 Stage 2: evidence review
The evidence review is presented by stream below. The streams have been reordered to reflect the process of the review and revised order of the review questions, as the policy intentions identified provided a contextual frame for further interpretation of the evidence found.
UK policy and guidance (evidence stream 4)
This evidence stream summarises the information extracted from 20 sources,26,30,88–93,98,99,110,111,114–118,128,129,131 consisting of 16 policy documents and four NFPO guidance documents.
Description of sources
The aim of this stream was to capture the main intentions stated in policy and guideline documents for respite care and short break provision for young adults with complex health-care needs, with a focus on issues of access, acceptability, information provision, funding and commissioning of services, joint and integrated working and transition planning. In addition to the searches, sources were identified through consultation with stakeholders, including policy leads for national organisations. Sixty-one sources were screened using the inclusion criteria and then allocated as policy or NFPO guideline or guidance sources for extraction and synthesis [Figure 5 is a Consolidated Standards of Reporting Trials (CONSORT)-style flow chart].
FIGURE 5.
A CONSORT-style flow diagram for policy stream.
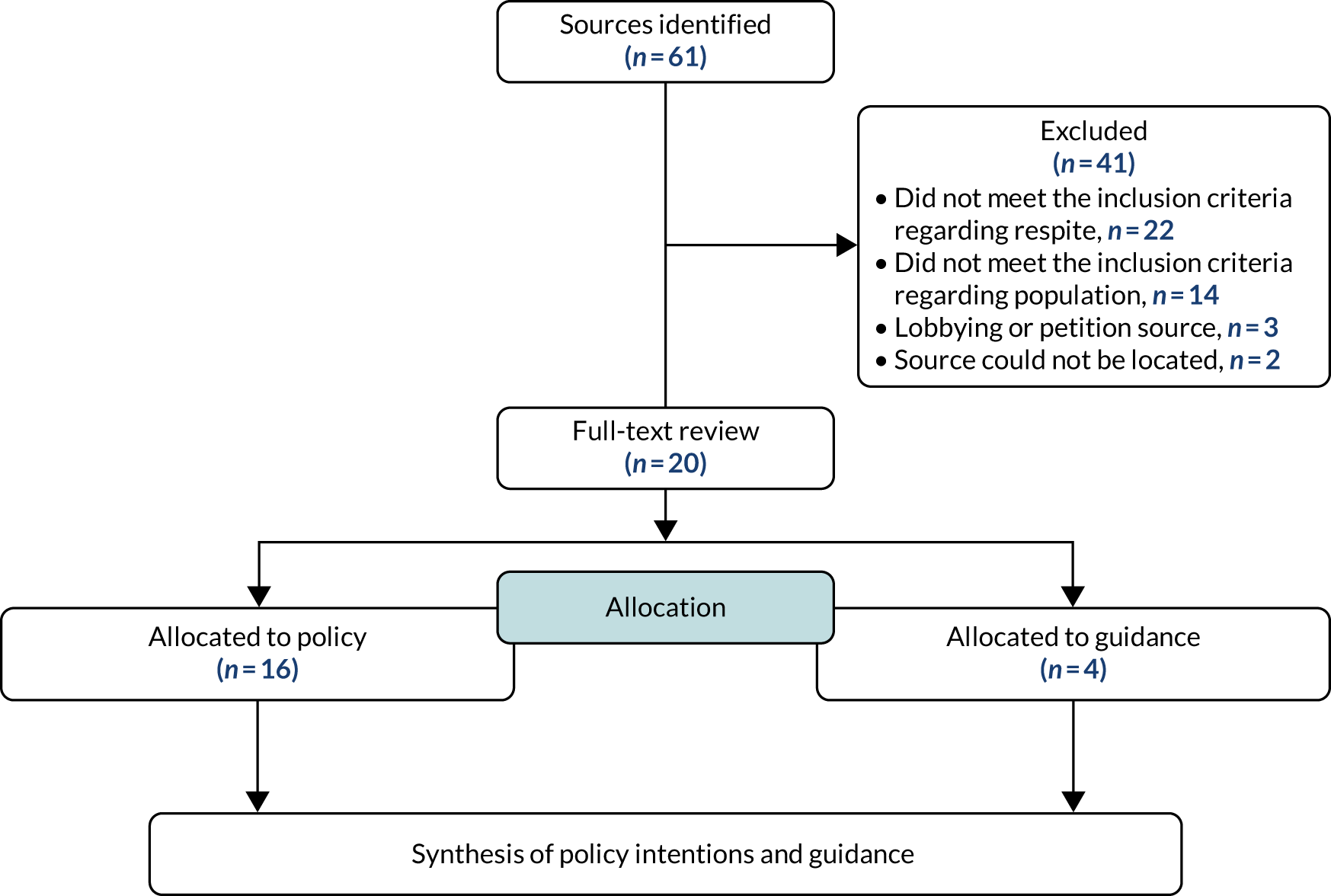
Some sources focused on the young person receiving care, typically from childhood up to age 19 or 25 years, whereas adult carer sources focused primarily on the needs of the parent or carer, and used different terms, such as ‘replacement care’ for the person receiving care while the adult carer has a ‘break’. The synthesis of policy intentions presented here does not claim to provide an exhaustive review of every policy change across all four nations that has affected young adults aged 18 to 40 years in the UK, but provides an account of the key policy intentions and implementation guidance, which subsequently informed the analysis in the other evidence streams.
The 20 sources26,30,88–93,98,99,110,111,114–118,128,129,131 comprised eight sources published by the UK Government,26,88–93,99 four sources published by the Scottish Government,115–118 one source published by the Welsh Government,131 one source published by the Health Information and Quality Authority98 (a statutory government-funded agency in Dublin, Ireland), two sources published by NICE110,111 (an executive non-departmental public body of the Department of Health and Social Care in the UK), three sources published by TfSL30,128,129 (a national charity for children, young people and young adults with LLCs in the UK) and one source published by the Social Care Institute for Excellence114 (a UK charity and improvement agency).
Quality appraisal
We had intended to use the AGREE II instrument to assess quality of practice guidelines, but none was identified. The policy and NFPO guidance documents were not appraised.
Findings
The policy included in the review was developed in the four nations of the UK (England, Scotland, Wales and Northern Ireland), although the overall intent is similar across the different nations. Findings from the UK policy and NFPO sources have been grouped by type of intention. Seven emergent areas of policy intention were identified: (1) accessibility, (2) acceptability, (3) outcome-focused services, (4) eligibility criteria and information provision, (5) multiagency and integrated working through and post transition, (6) funding and commissioning and (7) service user involvement.
Accessibility to appropriate respite care
Young adults and their parents/carers have the right to request a needs assessment should they wish to do so (also known as an adult carer support plan in Scotland). 116,117,128 The quality of carers’ assessments and Care Act 201443 compliance can be improved by:
-
including provision of information and advice about respite and carer breaks so carers can make informed choices
-
taking a whole-family approach to include outcomes and impacts holistically
-
taking a joined-up approach to all assessments that carers undertake
-
gathering and providing key information at transitions points
-
individually tailoring information and support to arrange breaks. 114
Although they do not have the same duty to provide short breaks for young adults as they do for children, under the Care Act 2014,43 local authorities must ensure the provision of preventative services that provide quality of care and support for carers. These services include a wide range of breaks that will meet carers’ specific needs and identified personal outcome, address diversity to meet racial, cultural, linguistic and religious needs, and are intended for all parents/carers and not just those who would be unable to continue to provide care without a break. 26,88,90–92,99,110,114,116–118,128,131
The term ‘replacement care’ is often used in policy documents that detail provision of respite for carers of adults. In all nations, under the Care Act 2014,43 replacement care is provided for the cared-for person, either on its own or alongside other services that the local authority can provide, such as assistive technology or short breaks for the carer. 118 Where a carer meets the eligibility criteria for a break from caring and replacement care is needed because there is no other alternative support from family or voluntary sector, the cared-for person may receive the replacement care from the local authority, regardless of their own eligibility for social care in their own right. 118 Therefore, replacement care can be provided by the local authority to the person being cared for if the carer or person needing care is entitled to support. 110 The Care Act 2014 does allow local authorities to charge carers for services, which can be a deterrent, and clear information about charges must be available. 114 Charges for replacement care cannot be made to the carer. These can be charged directly to the person receiving care only. 114
Policy from all nations states that children, young people and young adults with additional needs, such as complex health-care and disability needs, should have equitable access to short breaks as a core component of palliative care, with medical and nursing input as required. 26,88,91,92,111,115,128,131 The care should comply with national standards,98 be fit for purpose, be age appropriate91 and should be delivered as close to home as possible. 98 Where needed, creative solutions to transport challenges should be resolved by agencies working in partnership to ensure that transport is suitable and accessible to access respite and any activities while receiving the respite service. 26,91
Respite should enable the young person to participate in everyday activities, such as leisure and education, and should be supported by good-quality health-care provision. 91,98,131 There should be an equivalent level of service provision for young people who require both short-term and long-term respite stays,98 with care provided across a range of time periods (including day, night, at weekends and during the school/college holidays) and with capacity to respond to emergency requirements. 91,118,128,131
Young people with complex health needs should not experience an inequality of access to respite due to lack of appropriate provision as they approach transition, as this is often when young adults and their family require increased need for respite support. 30,91 Respite, including short breaks, should be included in proactive planning for transition, with consideration of the needs of young adults and their parents/carers and the most appropriate settings. 30,114 Young adult needs are different from those of young children and it is recommended that respite and hospice services be developed for them. 111
Acceptability
As part of palliative care, respite care should be safe, flexible, holistic, planned and person centred to ensure that it is acceptable to them and takes their complex needs into account. 89,98,115,116,128 The care should take account of the person’s physical, emotional, cultural, spiritual and practical needs and the needs of the family, and be appropriate for their age and/or developmental needs, so that each young person receives the optimum care and support in a way that promotes dignity, choice, independence, creativity and quality of life, as close to home as possible. 89,98,115,116 Where desired, breaks should enable parents/carers to care at home. 128 Services should promote engagement of young adults in daily activities that offer positive benefits, such as regular opportunities for play, leisure, recreation activities, training and employment. 98,116
In addition to the needs of the young adult receiving the respite care, some sources, which were aimed at adult carers, had parent-/carer-focused intentions. The intentions included that carer assessments should comprise a consideration of the carer’s needs, including their wish to work or engage in other education, training or social activities, so they have the same meaningful opportunities as those without caring responsibilities. 90,118 Local authorities should provide breaks tailored to the needs of individual carers as a mainstream form of support, and this should be provided in a reliable and consistent way and as part of a range of support. 110,114,118 Therefore, a ‘break from caring’ can be any form of support that enables a carer to have time away from their normal caring responsibilities. 110,114,118 Breaks can be provided on a regular or temporary basis, during the day or overnight,118 and can be taken with or without the cared-for person. 114,118 A broad range of breaks, with or without those being cared for, are recommended, including holidays, social and sport activities, and breaks at home during the day or overnight. 114,118 Although local authorities are required to consider if personal outcomes and needs for support can be met with a break from caring, there is currently no duty to provide a break for parents/carers in all cases. 118
Outcome-focused services
Palliative care services should be planned and delivered to achieve the best outcomes for individual young people, young adults and their families. 115,128 Outcomes are not clearly defined in the policy, but commissioning guidance documents defined outcomes as measurable benefits of an intervention that can be categorised at an individual, service or strategic level. 128 To have a positive impact, the Care Act 2014 guidance states that short breaks should be provided on a planned basis, rather than as a response to a crisis situation, so that carers have certainty of what will be provided and the opportunity to benefit from enhanced health, well-being and personal outcomes for themselves and the cared-for person. 118
Previous policy and implementation guidance to support development of short breaks for disabled children and young adults clearly states that having measurable outcomes and outputs can provide a measure of service effectiveness, including prevention of family breakdown, reduction of stress, identification of services that support transition between services, and identification of issues of workforce capacity and safe practice. 91 Development of local data through regular monitoring would allow for comparison and learning across areas, enabling services to demonstrate if their provision makes a difference. 26,114 Performance indicators should be outcome focused and meaningful in terms of measuring improvement in the young person’s outcomes, but they should not reduce flexibility to respond to the full range of needs, which include but are not limited to respite provision. 99
In the Care Act 2014, an important policy intention is to identify and support the personal outcomes of carers that enable them to provide, or continue to provide, care for the cared-for person. 117 In addition to traditional short breaks, there should be inclusion of flexible and innovative provision to provide respite from caring (e.g. a greenhouse to facilitate breaks in the garden while remaining close to the cared-for person). 117
Eligibility criteria and information provision
The need for fair, transparent, clear eligibility criteria and public information about the range of respite service available was a distinct intention in policy and guideline sources from all nations. 88,90–92,110,114–117,128,131 All local authorities are required to provide a short break service statement within their local offer provision, and this should provide information and details of the range of services provided90–92,116,117,128,131 (including palliative and respite care), other provision for young people with complex health needs and other services (such as emergency care provision and rehabilitation support). 88 It must also contain any criteria by which eligibility for those services will be assessed90–92,116,117,128,131 and how the range of services is designed to meet the needs of carers in their area. 92,110,114,117,131 Local authorities should have appropriate strategies in place to ensure that carers are being told of their rights and that ‘hidden’ carers who are not currently accessing services are reached. 90
It is recommended in the guidance that information and options for respite and carers’ breaks should be provided and discussed regularly with carers, preferably with health and social care professionals and those conducting carer assessments. 110,114 Assessors should be confident to discuss respite and short breaks with carers and be able to provide relevant information to them. 114 Peer support should be utilised to improve carers’ knowledge of the options available and to support them in making informed choices. 114 Young adults and their carers should have information in a language and format that they can understand, and they should have the opportunity to discuss the options with staff from the service. 116 The local offer information should also include information on the support for young people when moving between children and adult health-care services. 88,128 Information should be shared in a timely fashion between systems and services to ensure continuity of care in different settings. 98
Multiagency and integrated working through and post transition
Co-ordination of care based on need and integrated working by a range of agencies, including the NHS, children and adult hospices, the voluntary sector, social care and education, is required for high-quality palliative care to be available to all children, young people and young adults who need it,26,89,91,114,117,118 preferably with a lead professional or key worker to co-ordinate the care plan and transition care. 26,115 It is essential that commissioners engage with services from all sectors, including the voluntary sector. The commissioners should have a strong role in developing partnership-based service delivery and augmenting the available local statutory provision. 26,91,117 Clear communication between services and co-ordination of services available to meet the needs of the person receiving care is imperative to ensure that the available support has the best impact, and that carers do not have to navigate multiple assessment and access routes. 114 It is a requirement for public authorities to consider any request from the local authority for assistance in planning services for a carer. 90,114
The transition duties within the Care Act 2014 require local authorities to recognise the need for phased and timely transitions of young people. 26,128 This includes the need to assess the future social care, education and health needs of young people and their carers, provided the assessment is in the young person’s best interest and they consent to being assessed. 26,128 Innovative approaches that maximise the potential for voluntary and third-sector contribution and collaboration with the local authority are encouraged to extend the range and quality of short breaks to meet the needs of carers. 26,91,118 During childhood, young adults may have received short break provision from children’s hospices and other voluntary and statutory agencies. When these services can no longer be accessed, the needs of young adults should be reviewed to ensure that the most appropriate care setting is used for short breaks. 129 The guidance recognises that creative use of alternative settings may be needed to provide appropriate care for young adults, such as residential colleges with hospice or palliative care staff going in to provide nursing or medical care, or adult hospices making adjustments to their current provision to suit the needs of a younger population. 129 While planning for transition, it is important that the young person and family have realistic expectations of what is available and enough knowledge to have confidence that their care and support needs will be met. 26,129 While planning for young adults, the needs of parents, which may be significant, should also be identified to ensure that they are supported in caring for their young adult effectively. 88 It is important that children and adult services work together to ensure that needs are met. 26,88
Funding and commissioning
Effective commissioning and funding of services plays a vital role in enabling service provision that is cost-effective, addresses inequalities and achieves successful outcomes,26,91,128 such as supporting early discharge for young people from acute care settings through step-down care and reducing unplanned admissions of young people to acute care settings;30,128 care that includes the required clinical care for young people and adults with complex health-care needs;30 and commissioners acting as market managers by utilising providers that offer the appropriate and best combination of skills and experience to deliver a high-quality service to meet individual needs at the most efficient cost. 91 Good-quality data on the number of potential service users, the types and range of services available, who is using them and their needs, patterns of breaks and gaps in provision, along with transparent pricing, are required to support effective commissioning and attraction of new providers for a relatively small population. 26,91,99,111,114
Policy intentions include joint commissioning at local, subregional and regional levels across health, social care, education, third-sector and social enterprises to provide an integrated service that meets the complex needs of the young adult population;30,89,91,114,128 services can be specialist or through equal access to universal services;26,91 services should secure economies of scale, which will attract independent providers and increase the skilled workforce for those with complex health-care and disability needs;91 and provision should meet the needs of minority groups. 91 In addition, available grants should be used to provide additional practice support (e.g. housing adaptions);89 the NHS should be responsible for providing and commissioning short breaks where the ‘scale and type of nursing care’ is outside that which can be provided by the local authority;128 and short break vouchers or direct payments should be used, where appropriate, to increase choice of provider, but this should not reduce the onus on commissioners to follow the Care Act 2014 market shaping duties to provide access to a range of diverse, high-quality provision that supports development of the market and sufficient provision to meet independent demand. 90,91,93,114
Service user involvement
Co-production of services that is underpinned by the needs of the people who will use it improves outcomes by ensuring that provision is planned, shaped and delivered in the most appropriate way. 114 Policy intentions included engaging carers and families in the planning of carer services and short breaks to draw on their experiences and knowledge, and enhancing the young adult’s sense of control and independence for their future. 26,91,114,117,118,131
Summary discussion
There are many legal duties set out in existing policy regarding the commissioning, funding and delivery of respite care and short breaks by local authorities. All nations have similar stated intentions to meet the provision of respite care and short breaks for carers, as set out in the legal framework of acts (e.g. the Care Act 2014),43 although there is some variation by nation in their final documents and accompanying guidance. The legal duties and priorities change in focus between the children-focused policies, which are aimed at the holistic needs of the child and family, and policies that are more directed at provision of breaks for the adult carer. This change in focus is a factor that may affect the provision of appropriate respite for young adults, depending on their NHS continuing health-care status, and may also result in a lack of any support for siblings, unless they are identified as a young carer in their own right.
Since the Aiming High for Disabled Children91,99 programme in 2007/8, there has been little in the way of policy aspirations for young people and young adults that are specifically intended to improve respite care provision or to address the needs of the growing population of young adults with complex health-care needs who find themselves unable to access children’s services. Much of the relevant guidance on addressing these challenges for commissioning and transition has come from NFPOs, such as TfSL. 30,128,129
In England and Wales, the legal duties with the Care Act 2014 set out requirements for early transition planning and future care based on clear assessment and a care plan being agreed to ‘meet eligible needs’, as set out in the Care and Support (Eligibility Criteria) Regulations. 132 Although local authorities do not need to provide a list of services, they must assess and take into account the wishes and preferences of the young adult and make an agreed plan for future support following transition. When the young adult has complex health or disability needs and is eligible for NHS continuing care, there is a requirement for the NHS to provide respite for these young people and young adults and to work with the local authorities to provide appropriate care. When a young adult is not eligible for NHS continuing care, the updated national framework of 2018133 states that they may still be able to receive a joint package of health and social care. Therefore, the NHS is bound to support and fund respite health care if it is identified and agreed as part of an assessment and care plan. 133
The key policy intentions to shape the experience, implementation and delivery of respite care for young adults can be summarised separately for them and their parents, as well as intentions that apply generally. For young adults, good transition planning should start early, at approximately age 14 years, with early assessment and development of a care plan to meet the young adult needs, including respite care and short breaks. In addition, respite care should be provided in a range of services that are age-appropritate and developmentally appropriate and resourced with appropriately trained staff to ensure safe care. For the parents, a carer assessment should be conducted to identify and develop a care plan for their needs, including any personal outcomes that they wish to achieve. Intentions for all include the following:
-
Respite care and short breaks to be planned, rather than responsive to a crisis.
-
Clear eligibility criteria, charges and information about available services should be publicly available.
-
Assessors should know and be confident in discussing the available respite care available during assessments.
-
Care should be available at different times and on different days to suit the recipient.
-
A broad range of respite should be made available, including holidays, organised social and sport activities, and outings.
-
Performance indicators and outcomes should be monitored to identify gaps in provision, data on service use and impact for service users.
-
Services from all sectors should work together to develop partnership-based services.
-
Service user choice of provider should be supported by the use of short break vouchers or direct payments, where appropriate, but this should not limit effective commissioning, which shapes the market to meet the needs of local young adults and parents.
-
Young adults and parents should be involved in the development and delivery of services.
Effectiveness of respite care/short breaks (evidence stream 1)
We did not find any sources that formally quantified the effectiveness of respite care or short breaks for young people with complex health-care needs, either in comparison with no services or by comparing different types of services. A high proportion of the observational before-and-after studies in the screened evidence related to children with complex health-care needs but not young adults, or were based on populations not included in our review. The absence of evidence on effectiveness represents a gap in the knowledge base.
Health economics and the costs of care (evidence stream 2)
We did not find any sources that assessed the health economic or broader cost implications of providing respite care, either for a given service or the relative cost comparisons between services. As above, much of the screened evidence did not meet our review inclusion criteria and the included evidence that did meet our review inclusion criteria was either not focused on the costs of respite services or the attribution of cost was unclear and therefore it could not be included. Of the four sources97,134–136 that reached the full-text screening, one source was excluded because it presented information about the payments made to hosts providing respite care without supplying any evidence regarding the costs of actually delivering respite services. 97 The other three sources were excluded because (1) no costs were reported,134 (2) limited data were used to develop illustrative examples135 or (3) there was heterogeneity in the costs reported and lack of transparency on what was included in the costs presented. 136 Again, the absence of evidence on the absolute and relative costs of service provision represents an important gap in knowledge.
Experience and attitudes (evidence stream 3)
This evidence stream summarises qualitative information included from 20 sources (reported in 27 publications22,27,35,41,59–76,102,103,107–109) that explored experiences and attitudes relating to the provision of respite care or short breaks.
Description of sources
The sources included in this evidence stream are tabulated by respite type in Table 7, which details key sources and level of available evidence for the 13 respite care types identified in the knowledge map. There are several sources that relate to multiple sources or were generic, and so the two categories of ‘non-specific services’ and ‘multiple respite sources’ are also reported in the table. Where the evidence within the multiple services sources could be clearly identified for any of the 13 respite services, this has been noted in the table. Although the knowledge map identified examples of 13 respite care types, not all sources were eligible for inclusion in the in-depth stream 3 evidence review, either because they were not empirical studies or because we could not determine population eligibility because of a lack of information that would have enabled us to discern which evidence related to our population of interest. For example, not all the service types have evidence relating to views and experiences, and no clear evidence was found for three types of respite care (i.e. host family/fostering respite, emergency respite provided in home or hospital and host family emergency respite), highlighting gaps in the current evidence base. A matrix and gap analysis of evidence by respite care type is presented in Appendix 23.
| Type of service | Source |
|---|---|
| Residential respite in specialist palliative care facility (e.g. hospice) |
Grinyer et al. 71 Hutcheson et al. 59 Knighting et al. 75 Knighting et al. 67 Martin House Children’s Hospice60 Mitchell et al. 107 Young et al. 76 Young et al. 64 Young et al. 61 |
| Residential respite in specialist disability facility (e.g. condition-specific or adventure camps) |
Dawson and Liddicoat62 Luzinat et al. 68 |
| Residential respite in a nursing home | Young et al.61 |
| Home-based day care |
Beresford et al. 63 Martin House Children’s Hospice60 Stylianou69 |
| Home-based overnight care (planned short break or respite) |
Beresford et al. 63 Martin House Children’s Hospice60 Stylianou69 |
| Host family/fostering respite | No evidence found |
| Day-care respite at a specialist facility | Beresford et al.63 |
| Organised recreational activities |
Beresford et al. 63 Hutcheson et al. 59 Martin House Children’s Hospice60 Shared Care Scotland72 Shared Care Scotland66 |
| Befriending | Macdonald and Greggans70 |
| Funded holidays with friends/parents/carers |
Beresford et al. 63 Shared Care Scotland72 Shared Care Scotland66 |
| Emergency residential in specialist facilities (e.g. hospice) |
Mitchell et al. 107 Knighting et al. 67 |
| Emergency respite provided in home or hospital | No evidence found |
| Host family emergency respite | No evidence found |
| Non-specific service |
Abbott and Carpenter73 Kerr et al. 74 Kirk and Fraser22 Marsh et al. 35 Murphy and Mackay109 Muscular Dystrophy Campaign65 |
| Multiple respite services (sources that document/mention more than one service from those listed above) |
Beresford et al. 63 Knighting et a. 103 Knighting et al. 67 Martin House Children’s Hospice60 Mitchell et al. 107 Shared Care Scotland72 Shared Care Scotland66 |
Evidence from 20 sources included the views and experiences of young adults, parents, professionals and service providers on 10 specific types of service and respite services: (1) residential respite in a specialist palliative care facility (e.g. a hospice),27,59,61,67,71,103,106 (2) respite in a residential specialist disability facility (e.g. a camp),62,66,68,72 (3) residential respite in a nursing home,61 (4) home-based day care,60,63,69 (5) home-based overnight respite,60,63,69 (6) day care at a specialist facility,63 (7) organised recreational activities,59,60,66,72 (8) befriending,60,70 (9) funded holidays63,66,72 and (10) emergency residential respite in specialist palliative care facility (e.g. a hospice). 27,67 Six sources22,35,65,73,74,109 gathered information from young adults, parents, professionals and service providers on their views and experiences of respite services as a whole (i.e. a non-specific service).
Characteristics of the sources, including aims/objectives, location, population of interest, methodological information and study funding, are tabulated in Appendix 22.
Sixteen studies were conducted in the UK. Five studies22,35,61,67,103 were described as conducted in the UK, five27,60,61,71,73 were conducted in England, five65,66,70,72,109 were conducted in Scotland and one59 was conducted in Northern Ireland. One source74 covered Northern Ireland and the Republic of Ireland. Three studies62,68,69 were conducted outside the UK (in the USA,62 Australia68 and Cyprus69).
Six22,27,59–61,103 of the 20 sources included participants with a range of LLCs and five sources66,69,71,72,109 included participants with a range of complex health-care needs. Six studies62,63,65,68,70,73 included participants with specific conditions: two sources with Duchenne muscular dystrophy65,73 and one source each with cerebral palsy,62 cystic fibrosis,70 acquired brain injury68 and Ataxia–Telangiectasia. 63 Two sources67,74 focused solely on service providers rather than service users.
A total of 886 service users, parents or wider family members and professionals/service providers participated in 20 studies. The three largest studies were by Martin House Children’s Hospice60 (with 274 service users, parents, and service providers), Mitchell et al. 27 (with 135 participants, comprising service users, parents, siblings and service providers) and Abbott and Carpenter73 (with 109 participants, comprising young adults, siblings and service providers). Four sources22,64,72,94 included 27–100 participants, including service users, parents and wider family. Eight sources35,59,61,63,69–71,109 included the views and experiences of no more than 25 participants (ranging from 10 to 25 participants), including service users, parents and wider family. The number of participants was unclear in three sources. 65,66,72
Of the 886 participants clearly identified in 17 of the studies,22,35,59–63,67–71,73-75,107,109 472 were professionals/service providers (53%), three were volunteer befrienders, four were paid carers, 220 were parents or wider family members, such as grandparents (25%), 12 were siblings (1%) and 175 were young people/adults (20%).
Seventeen studies reported sources of funding. Five sources35,59,66,72,73 were funded by government bodies, four sources27,60,65,71 were funded by service providers, three sources61,63,109 were funded by charitable organisations, two sources69,74 were funded doctoral theses, two sources67,103 were funded by Clinical Commissioning Groups (CCGs) and one source22 reported that no funding was received. The remaining three studies62,68,70 did not report their source of funding.
Quality appraisal of sources
We assessed the quality of all included studies using the CASP tool53 (see Appendix 22). All of the sources used either a single data collection method or a combination of qualitative methods. Eleven sources22,35,59–61,63,65,68–70,109 used interviews or focus groups. Four sources27,62,71,73 used mixed qualitative methods, such as open-text surveys in combination with focus groups and interviews. Three sources67,74,103 used survey methods alone, which had open questions to gather qualitative data. Two sources66,72 used a range of methods to evaluate services.
Some sources did not report data collection methods, although this does not necessarily infer poor study design. Fourteen studies22,27,35,60–62,67–70,73,74,103,109 were considered valuable research sources. Seventeen sources22,35,59–63,67–71,73–75,107,109 clearly described the research aims and appropriateness of the chosen methods, although this was unclear in three sources. 65,66,72 In five sources,65,66,72,73,103 the participant recruitment strategy was not reported and we were therefore unable to judge its suitability for the research aims. We were unable to determine whether or not data collection was appropriate for the research question in three sources. 65,66,72 The relationship between researcher and participant was adequately addressed by three sources only59,61,74 and ethics issues were reported by 11 sources. 22,27,35,60,61,68–71,103,109 A clear statement of findings was provided by all but three sources. 65,66,72
Findings of the framework synthesis
The synthesis of evidence in the experience stream was guided by review questions 4 and 5 [i.e. ‘What are service users’ and providers’ views of current service provision and the need for new services?’ and ‘What are the facilitators of and barriers to providing, implementing, using and sustaining respite care and short breaks, taking into account the different perspectives of service users (young adults, family members) and providers?’, respectively]. To inform the logic models and to identify concerns of service users and providers, we focused on the optimisation, implementation and delivery of respite care in the context of outcomes. The evidence is presented in two sections (see Section 1: experience and benefits of respite care delivered to young adults and Section 2: facilitators of and barriers to the uptake, implementation and delivery of respite care to young adults). There was substantial consistency in the emergent themes between service types, and so to avoid repetition, the evidence is presented by theme rather than by type of respite care. A summary of the types of respite care services, service perspectives and any evidence on service inequalities that contributed to the theme are summarised at the beginning of each theme. Both first- and second-order constructs from the sources are included in the themes. Where direct quotes from participants are included in the theme narrative, the original participant identifier of the source has been used, if one was provided, and clarification of cohort has been added where needed. Other quoted text includes the authors interpretation of the evidence from the sources.
Section 1: experience and benefits of respite care delivered to young adults
This section brings together available evidence on the experience of respite care from the perspectives of young adults, parents and service providers, along with the short- and mid-range benefits and outcomes of respite care for young adults, parents and providers. There was no evidence that explicitly described longer-term benefits because of the lack of longitudinal studies in this area. The initial coding framework derived from the logic models sought to identify the key outcomes and associated benefits for the service user (i.e. the primary intended intervention outcomes and experienced outcomes by service recipients, and unintended consequences and harms) and secondary outcomes for those other than the service recipient (i.e. the secondary intended intervention outcomes and experienced outcomes, and unintended consequences and impacts). However, it was not always possible to discriminate in the evidence between service outcomes that were planned and intended, and service outcomes that were unintended. The benefits and outcomes of the service are reported from three perspectives (i.e. the experiences of young adults, parents and the wider family, and service providers).
Benefits and outcomes of respite care for young adults
The evidence in this theme was drawn from five respite care types (i.e. residential short breaks,59–62 residential respite in a specialist disability facility,62,68 day-care respite at a specialist facility,63 organised recreational activities60,63,66 and funded holidays63,66) and two generic categories (non-specific services65 and multiple respite services). 60,63,66 In this theme, we did not identify any evidence relating to service inequalities. The evidence was predominantly from young adult service users, who identified numerous and varied benefits as outcomes of respite care, encompassed by three main subthemes: (1) promoting independence and empowerment, (2) social interaction and (3) holistic well-being.
Promoting independence and empowerment in young adults
Many of the young adults felt that respite services facilitated the development of independence and empowerment. Some young adults with LLCs and complex needs have very limited opportunities to make their own decisions while spending time away from their families. Respite services that provided opportunities to develop and engage in independent daily activities and to spend time away from parents were highly valued. 63 This ‘freedom’ was enjoyed by young adults and it gave them ‘confidence’ [young person (YP)02]:59
When I was 16/17 and I was going, it was nice because I would go out shopping and I wasn’t with mum . . . They organise all sorts don’t they but it is just nice to do it sort of as independently as you can.
Debbie, age 21 years.
Respite services further enhance the development of independence by supporting young adults in ‘taking more control of decision-making about their health and living’, while at the same time ‘supporting parents to relinquish some of their control’. 61
Engaging young adults in the planning of services supported their sense of independence and empowerment, and may also have improved acceptability of the service. One source highlighted the experience of young adults contributing to the planning of a residential short break centre, for example ‘meeting with the architect when the new lounge area was being discussed’ and ‘being part of the consultation group for new policies and procedures’,61 and the difference this made to the final respite care services.
Parents felt that respite services improved their young adult’s self-esteem ‘as a result of being able to be with others and participating in activities she loves, such as swimming, climbing, crafts etc.’62 and young adults felt that it improved their confidence and empowerment:
. . . it has taught me to cope with life. People stare at me, but I can go anywhere. 62
Service providers also recognised the inherent value in supporting young adults to have ‘freedom of choice over daily routines and activities’ (reproduced with permission from Martin House Research Centre)60 and to ‘give them the opportunity [over a weekend] to have their own programme, self-determination – the whole lot’. 59
Social interaction
Young adults, their parents and service providers commented on the benefits of social interaction as an outcome for young adults and collectively as part of a wider community. The greatest perceived benefit of some respite services was the opportunity for young adults to socialise with peer groups, some of whom became friends, and to interact with staff. This was particularly beneficial for those accessing residential respite services:
[Beyond Horizon] also fulfils your social needs; getting out and away from your family and not be attached to one person, and that’s really important.
Young adult59
Young adults described how some short break respite services gave them the chance to ‘meet a lot of friends’,62 ‘interact with friends’62 and to socialise with their peers. 65 This was considered important for overcoming a sense of isolation {e.g. ‘. . . [feel] a bit isolated, so this really helps us’ (YP02)59} arising from limited opportunities to engage with peers in daily life (‘Here you get time to talk to people’61). For some young adults, it also offered an opportunity to sustain relationships established in the respite environment:
. . . it gives me a break from my routine and a chance to socialise and catch up with friends, some of whom I don’t see outside of respite breaks.
Young adult65
Social interaction also facilitated a sense of normality [‘Yes, we all have good laughs. What a normal teenager would do really’ (YP03)] through shared life experiences, being ‘around other people with my disability’65 and benefit from facing ‘the same issues and challenges that can only be resolved by coming together’ (YP01). 59
Parents’ views were largely consistent with those of the young adults expressed above. The benefits of social interaction were observed by watching their child ‘. . . enjoying himself with friends’ (parent)72 or having ‘. . . a few days of fun with friends’. 62 Parents also felt that attending a camp with similar young people enabled their child to feel less alone68 and this in turn had an impact on their social networks and interactions with their family:
They can go on Facebook [Facebook, Inc., Menlo Park, CA, USA] and discuss different things, whereas if they didn’t have it there isn’t anything to discuss and after being in a room with somebody for a full day, by the time it comes to the next day they’ve run out of conversation’.
P0159
Service providers spoke of how young adults benefited from becoming part of a like-minded community:
Campers benefit from the membership of community itself and from the growth the community fosters. 62
Services provided young adults with the opportunity to join in with physical and social activities they may not be able to engage in at home:
The young adults benefit by spending time with a peer group away from home (many for the first time) and are encouraged to plan and try out new activities. 66
Promoting holistic well-being
Young adults described some respite services as providing them with ‘hope’, which had a positive impact on well-being as an outcome62 and, again, this was particularly evident for planned residential respite services. These services fostered a sense of belonging and warmth ‘where everybody loves everybody’62 and where the young adult did not feel defined by their disability: ‘[I come to camp] just to meet people like me, I guess’. 62 These residential respite camps were described by a young adult as ‘lifting my spirits’. 62 A sense of well-being during respite was described as gained through ‘time away from home’ and ‘time to try new activities’. 65
We found no direct evidence from parents or service providers for this subtheme, although it is noted that the above subthemes are inter-related to young adult well-being.
Benefits of respite care for parents and the wider family
The benefits of respite services extended beyond the immediate impact on young adults to provide benefits for their parents and wider family. The underpinning evidence for this theme was drawn from seven respite care types (i.e. residential short breaks,27,59–61,66,71 residential respite in a specialist disability facility,62,68 home-based day care,69 home-based overnight care,69 organised recreational activities,59,60,66,72 befriending70 and funded holidays66,72) and two generic categories (i.e. non-specific service65 and multiple respite services27,66,67,72).
The evidence is predominantly from the parents and family, although some evidence is drawn from the perspective of the young adults. We did not find any evidence on service providers views or relating to service inequalities in this theme. The evidence of benefits of respite care for families is encapsulated by two subthemes: (1) rest and resilience and (2) time with family.
The main benefits for parents were to be able to rest and recuperate (which led to outcomes such as reduced stress and enhanced resilience), pursue their own interests, spend time with their partner and spend time with their other children. However, the benefits of respite for the family were tempered by the need for trust in the standard and quality of respite care provided.
Rest and resilience
Although respite services are primarily designed to benefit the young adult service users, a key intended, or sometimes unintended, benefit for their families was the respite from caring responsibilities. Young adults acknowledged the benefits of respite care for their parents in terms of the gain of personal time and as a relief from daily caring. One young adult regarded it as an opportunity for parents to ‘get some time to themselves’67 and another felt that a befriending service saved her ‘mum and dad having to do all that stuff’ (woman aged 18 years). 70
One of the most positive and frequently experienced outcomes for parents was the break from daily caring, ‘a chance to catch my breath and be able to go on another year’62 and a chance to ‘sleep without being awakened’,62 ‘for a whole night’. 67 In this way, respite care, particularly planned residential breaks, provided parents ‘with a break’,59 a chance to ‘relax and recharge batteries’65 and for parents to take ‘a break from being a full-time carer’ (parent):65
I kind of felt that it was as much a break for me as it was for [my son].
P04, parent59
Residential respite was seen as an opportunity for parents to have ‘time to themselves to rest and re-energise’66 and have the ‘opportunity to relinquish the caring role’61 while the young adult was in the service. For parents, the opportunity to have a break from their ‘24/7 caring responsibilities’ was vital in enabling them to build resilience and to ‘continue caring’ for their young adult. 65 The provision of home-based respite care also helped to ‘lower stress levels’ associated with their caring roles. 69
The potential benefits of residential respite for reducing psychological outcomes, such as the stresses and anxieties associated with a caring role, were tempered by the need to trust the quality of service provision so they could ‘leave [the young adult] and relax’. 59 The benefits of respite for the parents were dependent on knowing ‘that the specialist short break service met the needs and preferences of their child’. 61
However, some of the evidence identified that the service does not need to be highly technical or specialised to provide the intended outcome of respite. Befriending services can also achieve respite for parents and relieve the physical and emotional burden that continuous caring places on them:
Befriending helped relieve the burden on parents physically and emotionally and gave them some time out for themselves both at home and when their child was in hospital. 70
Another benefit that contributed to improved resilience of parents of young people with acquired brain injury who attended a family camp was ‘not feeling alone’, as they could share similar struggles and concerns with other parents while feeling accepted as part of a community. 68
Time with family
Young adults recognised the secondary benefits of their respite break for other members of their family:
It’s all me, you know, ’cause I’ve got a lot of appointments . . . and [sibling] misses out on a lot, so they [parents] try and give him a bit of time as well while they have the time to do it.
Young person27
Respite care was viewed as a support mechanism for the wider family, helping to re-establish family cohesion and facilitate a period of ‘normal’ family life, when wanting a ‘normal life’ was a key desired outcome of parents. It provided parents with personal time to ‘enjoy doing other activities for their own benefit’ and ‘to spend more time’ with their partner and other children. 61
Respite provision enabled parents to spend some time with other family members, for example to ‘give attention to their other children’, as siblings were acknowledged as ‘missing out on a lot’ (reproduced with permission from Martin House Research Centre). 60 For a brief amount of time at regular intervals, ‘the parents could live a more “normal” family life’:71
One mother said that as a result of her son being able to access short breaks, they [her and her son’s father] had been able to enjoy doing other activities for their own benefit. Another mother had returned to work and taken holidays with her husband. Those with more than one child appreciated the time they have been able to give to their other, healthy child. 61
Periods of respite care, especially those of a residential nature, also provided the opportunity for couples to pursue their own interests and ‘enjoy doing activities together’ or ‘take holidays’,61 which helped to sustain their relationship and build resilience to continue with the demands of caring.
Section 2: facilitators of and barriers to the uptake, implementation and delivery of respite care to young adults
This section summarises key factors that facilitate or act as barriers to the uptake, implementation and delivery of services. Barriers and facilitators are often opposite sides of the same coin, for example trust was perceived as a facilitator and lack of trust as a barrier, and so presenting all factors separately becomes repetitive. We have therefore summarised the key barriers identified in terms of accessibility and acceptability for service users, and for the implementation and delivery of respite services for service provides. The section has three main themes: (1) accessing respite care services, (2) acceptability of services and (3) implementation, delivery and reliability of services.
Accessing respite care services
Most of the evidence on accessibility related to the practical limitations of gaining access to services or accessing respite services after the transition from child to adult services. The evidence for this theme is drawn from five respite care types (i.e. residential short breaks,27,59,61,64,67,71,76,102 residential respite in a specialist disability facility,62 residential respite in a nursing home,61 organised recreational activities59 and funded holidays63) and two generic categories (i.e. non-specific service22,35,65,73,74 and multiple respite services27,67,102). The evidence for this theme has been grouped into two subthemes: (1) practical barriers to access and (2) barriers relating to transition from child to adult respite services.
Practical barriers to access
This subtheme includes the perspectives of parents and service providers. There was no direct evidence from young adults. There was some limited evidence of service inequalities of black, Asian and minority ethnic (BAME) groups in relation to service accessibility. Several practical barriers to access were identified in the evidence, including volume and complexity of paperwork, delay between referral and service provision, the distance between home and service, limited access to condition-specific services, age limits, lack of physical space for equipment, lack of appropriately trained staff and limited inclusion of BAME populations.
Many families reported challenges with accessing services, including high levels of paperwork and form filling, making respite ‘more hassle than it’s worth’71 or the lengthy time (e.g. ‘18 months’61) required to secure a place in a service. Families were keen that respite services were local and did not require extensive travel. 65,67,71 The perception that families need local services was also mentioned by one service provider who stated ‘they want local – not travelling miles – to access care’ (children’s hospice 10). 67 Variation in access by geographical location was also noted, with one family who were considering relocation advised ‘don’t do it, you will get much less here’ (reproduced with permission from Marsh et al.). 35
The level of work required to prepare for a break experienced by some parents could have a negative impact on the intended benefits:
. . . it might be more work . . . to get everything organised, to get your folders and your drugs, your feeds . . . and then I think by the time you get here sometimes . . . I find it’s nearly more tiring for me.
P04 parent59
Several factors contributed to inequalities of access to services, including specific LLC, age, ethnicity and geographical location. The mother of a 28-year-old man with Duchenne muscular dystrophy observed the following:
. . . there is no respite/hospice provision in our area or the whole of Scotland suitable for my son apart from CHAS’s [Children’s Hospice Association Scotland] services’. 65
The inability of services to accommodate bulky equipment or fully grown young adults was also cited as a barrier to access for some service users:
Barriers to accessing alternative respite care increase as the young person grows physically larger or requires bulky equipment that cannot easily be accommodated in other locations. These issues can make it difficult, if not impossible, to visit or stay with informal carers, such as extended family members, or to be cared for in other care settings, including the homes of foster carers. 27
Although limited evidence is available, service provider opinion from one source suggests that current respite care services may not be meeting the needs of particular BAME communities, as ‘the apparently low usage of services for particular ethnic minority communities indicates a potential problem of unmet need’ (reproduced with permission from Marsh et al.). 35
The lack of evidence from service users of BAME communities suggests that their respite care needs may be under-represented and that inequalities of access to respite care services needs further work:
‘We need ethnically diverse services, [they are] seen as a white service’. Commissioners and service planners have a duty to assess the needs of their populations and this will mean pushing them on this group that has low volume, high cost problems and needs closer scrutiny.
Barriers relating to transition from child to adult respite services
A key factor in achieving intended service outcomes that benefit users is provision of a service that is developmentally appropriate for the young adult:
Mothers said they benefited from time alone or with other family members in the knowledge that the specialist short break service met the needs and preferences of their child as they made the transition to adult services. 61
However, the transition from child to adult respite services may be traumatic for young adults and their parents, involving the stress of uncertain service provision and, in some cases, the total loss of services. This subtheme presents evidence relating to both the ‘anticipated’ loss of services during transition planning and ‘actual’ loss of services. The perspectives of young adults, parents and service providers are included. There was no evidence identified relating to inequalities for loss of service provision, although the inequality of access to appropriate services between children and adult services is highlighted by the experience of young adults and their families.
Anticipated loss of respite services
The fear of not having access to acceptable respite care and of ‘having nowhere to go once [children’s hospice] say he’s too old to go there’ (reproduced with permission from Abbott and Carpenter)73 was shared by parents, with some wondering how they would cope. 27,35,59,61,67,73,102 One parent expressed their concerns as follows:
Once my daughter leaves respite at 23 we have nothing else to transfer to as her needs are so complex. We will basically have no respite at all and I am my daughters full time carer I do not have a care package in place either.
Parent 275
Service providers also anticipated increasing service demand as both young adult service users and their parents age:
. . . as these children are getting older, the parents are getting older as well, and are maybe not fit to do what they could’ve when the young people were younger, so it’s almost they need more respite.
S02 staff59
Part of the fear of the loss of access to children’s hospice provision centred on the lack of suitable alternatives ‘as the equivalent service doesn’t really exist in the adult world’ (adult hospice 13)67 and being ‘offered an old people’s home’. 61 One source specifically focused on the challenges of providing emergency respite care and how ‘if a family phones today, no-one would be able to put care in tomorrow’ (hospice staff)27 outside of the children’s hospice because of the complexity of the medical condition of the young adult and the need for an appropriately educated workforce. This view was shared by parents, who were aware that the limited alternatives of hospital or residential care homes were not appropriate for young adults. One parent spoke of how this would not be optimal for their daughter:
It’s not appropriate for [young adult name] to go into a nursing home. Her anxiety – it would be detrimental to her health . . . and ours, ‘cause there’d be none of that continuity of care, they wouldn’t know her.
Parent27
The anticipated loss of services described above was of great concern to young adults, parents and service providers. Lack of access to a suitable replacement service was widely reported and identified as a significant barrier to young adults accessing respite care in the future. 22,27,35,59,61,64,73,75
Actual loss of respite services
Young adults who had experienced the actual loss of respite services described feeling bereft:
I didn’t have anywhere to go after I left the children’s hospice, just at home doing not a lot, feeling a bit isolated.
YP0259
This was mirrored in other evidence where young adults who had previously accessed services were keenly aware of what they had lost:
I valued my time in the children’s hospice so much and hate that there is not a suitable service for me now.
Young adult 175
For one young adult, transition to adult services resulted in them feeling trapped at home, accompanied by a perceived lack of understanding from their local commissioners:
I wish the CCG would see how vital it is for me to leave the house and enjoy days out, events and so on. The CCG say I never need to leave the house. I wish I had a more suitable care package and respite support to enable me to enjoy days out and things.
Young adult 275
For families, an integral part of transition into adult services had been this service loss. 22,35,59,63,64,73 One parent, whose child had lost service access, described the Beyond Horizon service as ‘a lifeline’ ‘when they had nobody to turn to – it’s like everything is just stopped!’ (P05 parent). 59
The sudden loss of health services and not being able to access respite when their child turned 18 years old was not uncommon:
We’ve gone from 28 nights a year respite . . . and four hours a week . . . now E’s turned 18 that has all stopped . . . we’ve no adult budget, . . . no care plan, . . . no support package, there’s just nothing . . . we’re just in the black hole of nowhere . . . everybody seems to be discharging her.
Parent participant 0622
One parent perceived the withdrawal of respite services as a clear sign of service inequality:
[Children’s hospice] is being taken away from us and there is absolutely nothing to replace it. We went overnight from having the perfect support system to absolutely nothing . . . If [our son] had cancer, it would be a totally different story but because he was born this way then it doesn’t pull at people’s heart strings. He can’t voice how he feels and show people what a special chap he is. The time in our lives when we need help and support – there is nothing available.
The loss of services for young adults also had an impact on the wider family, especially when a children’s hospice had previously provided holistic care for the whole family, including siblings. 27 Parents spoke of the loss of benefits that the whole family were no longer able to experience following transition and loss of respite care for their young adult:
Chance for him to socialise with other young people. We got a chance to do the same, get rest and recovery in our own home. His teenage sibling also had the opportunity to have friends around as he wouldn’t do so when his brother was present.
Parent 675
A parent who experienced loss of planned residential care for their young adult after they had transitioned spoke of the subsequent loss of any respite from the burden of their caring role for the rest of the family:
The adult hospice is setting up a young adult care service which includes social and emotional support, but which currently lacks funding for any non-emergency or end of life overnight care. We have no break as a family overnight, and our son needs frequent care at night.
Parent 1075
Loss of services was described by service providers as a ‘fall off the shelf’ (professional 14). 27 Staff working to support young adults through transition have reported the impact of a lack of services on families:
We have looked for a suitable place for [young man] to have short breaks for the three years since he was 18 and had to leave the children’s service. Unfortunately, this has meant that he has had no break in that time and neither have his parents boat trip was.
Care manager76
Key barriers that precipitated the actual loss of respite services for young adults following transition primarily related to the lack of age-appropriate and developmentally appropriate adult facilities, and a ‘lack of knowledgeable and experienced staff’ (manager, hospice, Northern Ireland). 74
Acceptability of services
The evidence in this theme relates to the expectations and preferences of young adults, parents and service providers’ views of an acceptable respite service. The evidence for this theme came from nine respite care types (i.e. residential short breaks,27,59–61,64,67 residential respite in a specialist disability facility,62 residential respite in a nursing home,61 home-based day care,69 home-based overnight care,69 day-care respite at a specialist facility,63 organised recreational activities,59,63 funded holidays63 and emergency respite in a specialist facility27) and two generic categories (i.e. non-specific service35,65,73 and multiple respite services27,60,63,67).
The perspectives of young adults, parents and service providers are presented separately within each subtheme, although there was a high degree of consistency between these groups. One account of service inequalities was identified, relating to the acceptability of services for young adults from BAME communities. The acceptability of services has three subthemes: (1) trust and relationships, (2) flexible and tailored services and (3) developmentally appropriate services.
Trust and relationships
Accounts from young adults, parents and service providers highlighted trust and good relationships as a core component of acceptable respite services. These values promoted confidence in safe, high-quality service provision. This trust and confidence in services was deemed necessary to mitigate negative outcomes, such as the worry, stress and anxiety associated with use of residential, short breaks and emergency respite services.
The development of trusted relationships between young adults, their parents and staff was considered an essential element of an acceptable respite service. This trust was influenced by confidence in there being appropriately trained staff providing care to the young adults:
I mean they do have people there who have obviously got a lot of knowledge on things and it is nice if you ever have any questions about something, like there is somebody there who is really good about gastrostomies and everything.
Andrew, age 19 years.
Young adults appreciated services that fostered a sense of normality and felt like ‘. . . a second home’. 62 Relationships developed during repeated short breaks and residential camps, which provided continuity and consistency of service, enabled young adults to feel valued and form strong bonds building trust and confidence in the service:
I just get so attached to seeing everybody and everything. 62
Respite services that could foster these meaningful relationships within a ‘home’ environment were perceived by young adults as ‘unique in what they do’ (YP01). 59
Close and trusted relationships that developed between service users and staff also supported the growing independence of young adults by enabling daily choices and decision-making, which in turn enriched their experience of the service. 63
Likewise, partnership working between parents and key workers fostered trust in respite staff and carers and was felt to be ‘the single most important enabler for ensuring that children and families are well supported’ (reproduced with permission from Martin House Research Centre)60 and that services were delivered in an acceptable way. Trust in short break and respite services was a ‘big thing’ for parents59 and this was facilitated by good relationships with staff that parents trusted. Medication was a vital area where parents needed confidence in the staff to support their young adult appropriately:
I wouldn’t even leave him for five minutes elsewhere. I don’t let nobody do his medication. But as I say when I bring him here [hospice], I never worry.
The impact of positive relationships with staff on parents’ trust and confidence in the quality of care provided was an important facilitator for respite care of young adults. 59–61,63 An example given by one mother was:
There’s a nurse there who would use their initiative if he needed to go to hospital. 61
Parents considered a lack of trust and perceived lack of clinical competence as a source of anxiety:
I would be too stressed in case they did not do the right thing. 69
Ultimately, this could result in the poor uptake of services:
Families rejected the possibility of using informal carers such as family, friends and neighbours, even in an emergency, due to them lacking the level of skill, experience, physical strength or confidence to provide high quality care for the young person. 27
The need for established and trusted relationships was also recognised by service providers, who acknowledged the need for young adults to ‘like the professionals and feel like it is reciprocated, to have someone on their side’ (reproduced with permission from Abbott and Carpenter). 73
Flexible and tailored services
Services were viewed as acceptable by young adults, parents and providers when they offered a degree of flexibility and adaptability to the individual needs and wishes of the young adult. Flexible services that are sensitive to the needs of individuals were seen to offer choice and control to young adults, which in turn supported the development of independence, as discussed in the above theme.
Young adults valued day centre respite services that could offer some flexibility and choice in the activities that they were involved in, so that they felt enabled to make decisions, rather than being ‘constrained by a structured activity programme’:63
. . . basically you get to do what you want really. Like you don’t have to do certain things, you can do anything you like.
Young adults also felt valued by having a degree of control or choice over their respite service provision, for example, as one young adult noted, by ‘employing people to help me and stuff, like when we go on holidays’63 or, as another noted, by having ‘support workers who can also drive my [adapted] van . . . so I can decide on the day where I’m going’. 61
There was limited evidence regarding parents’ perceptions of service flexibility, although there were positive reports of planned short break services that did not require parents to stick to strict timetables, for example ‘having to be in for [staff] handover time at 9.00 pm’. 61
Service providers acknowledged the need for a variety of services to meet the ‘growing cohort of young people’67 with life-limiting illnesses or complex needs and recognised that ‘what suits one young person will not always be appropriate for another’. 65 Therefore, a spectrum of opportunities was seen as required to provide flexible individually tailored respite care to meet young adult needs, including ‘short breaks, brokered breaks, specialist tourism services, building-based respite and adult hospice provision’ (adult hospice 22). 67 Young adults and their families would then be able to choose and control their support needs ‘adapted to their age and changing need from a new national pot’ (reproduced with permission from Marsh et al.). 35
Developmentally appropriate services
Young adults, parents and service providers all acknowledged that, for services to be acceptable, they should be designed and developed with young adults’ interests, life course stage and needs in mind. Involving young adults and families in the development or planning of services was encouraged to improve the acceptability of the service to its users. Owing to limited developmentally appropriate or age-appropriate options, young adults were being cared for alongside very young children or elderly adults.
Services that understood the needs of young adults according to their age and developmental stage were viewed positively by young adults:
As you grow up, they let you grow up and treat you your age, and you don’t get that anywhere else. 62
Young adults sought residential respite services that offered peer interaction, but also valued carers of a similar age and sex to themselves, with shared interests ‘such as watching sport and gaming’. 63
Age-inappropriate services were deemed unacceptable, such as respite care in residential homes for the elderly and activities that did not align with the young adult’s interests or preferences. These negative experiences typically resulted in cessation or reduction of service use:
Specialist day services tended to be geared towards much older people and/or those with learning disabilities. The activities offered in these settings did not align to the young person’s interests or preferences, and they had nothing in common with the others attending. This experience typically resulted in the young person stopping using a service, or reducing their use of it.
Attending respite in services designed for the elderly resulted in young adults being apprehensive about accessing the service:
I thought I was just going to end up in a really bad [elderly] care home, which I kind of did.
Young adult male aged 23 years61
Some of the experiences of respite in a care home were very poor:
Well, if I am being honest, it was like prison . . . it was just miserable. I didn’t look forward to going in. It was the fact I was shut in a room. The staff didn’t really have time to talk to me or anything.
Young adult male aged 19 years61
Adult hospices, generally, did not fare well when compared with children’s services. Young adults who had experienced services at adult hospices, when they were no longer eligible to access children’s hospices, described adult hospices as ‘not the same at all’ and said that they ‘just don’t like going there as much’ (reproduced with permission from Abbott and Carpenter). 73
Young adults could be inhibited socially as a result of a service being provided, which did not meet their needs for developmentally appropriate services:
In the worst scenarios, there were relationships with much less warmth or humanity: carers from an agency which required staff always to wear uniforms, thus inhibiting the young person from going out in public with them; and the carers who came to one young man’s home at 9 p.m. every night to, ‘put him to bed’ so that he did not have an evening social life.
Parents valued services that enabled their young adult to spend time away from home, as many young adults would at a similar stage of their life course:
He′s 22 and doesn’t want his mum and dad around him all the time.
Mother61
However, parents described challenges in finding services for their young adult that were developmentally appropriate. Placing a young adult aged 19 years in a residential nursing home for a short break was described as ‘not suitable’59 and ‘not appropriate’27 because of the lack of continuity of care and potential for staff not being experienced in the complex conditions of young adults. Elderly care homes or nursing homes were seen to be old-fashioned and did not facilitate age-appropriate short breaks:
. . . he needs to be around kids his own age, to be able to go out and not just sit in a chair and stare out of a window. 61
. . . no disrespect to the elderly but my son’s not an old person.
Parent65
Some young adults with complex needs were offered specialist day services or weekend breaks aimed at people with learning disabilities. 63
The focus on end-of-life care and ‘strong connotations of death’ (reproduced with permission from Abbott and Carpenter)73 associated with adult hospices was off-putting to families and ‘not age appropriate’. 65 There was a perceived ‘mismatch between families’ expectations of a service and what the adult hospice services primarily provided (end-of-life care, symptom management)’. 67
Additionally, a lack of resources, whether that be in staffing numbers or equipment provision, could result in a negative experience with a service:
I could not fault them as carers when he was in respite at [name of service] but he never got out on trips . . . if a nurse left the place there was no nurse left to care for the others. There would be maybe a couple of board games around the table . . . but they didn’t have a sensory room and things to stimulate him.
Mother61
Service providers were very aware of the preferences of young adults and parents for age-appropriate services and the challenges in being cared alongside elderly people:
Our families and young people say – they want a service – but they are often put off by the older persons accessing this type of care [adult hospice]. They are wanting a bespoke service often with children’s [hospices] extending their remit.
Children’s hospice 1067
The positive impact of age-appropriate and novel life experiences was noted by one member of staff and illustrates the need for activities outside the clinical care setting to overcome a sense of marginalisation and alienation from peer groups:
The boat trip was carefully risk assessed but no one bothered to tell us that once on the water the boatman would go as fast as the young adults wanted to go! The River Tyne is a very windy place. I was responsible for the risk assessment and watching from the river side as the boat skimmed the waves was an unforgettable experience! The young adults loved the whole thing. One of them said to me, ‘They don’t let people like us do this kind of thing’. 76
As highlighted in the independence and empowerment theme, the interest and value of service users being involved in the development of services to ensure that they are fit for purpose has merit for the young adults involved, as well as ensuring that services are designed to meet the needs of the users. When designing future services, working ‘with young people and families in co-producing changes’ to ensure that they are appropriate was considered essential (reproduced with permission from Marsh et al.). 35
Implementation, delivery and reliability of services
This theme relates to the implementation, delivery and the commissioning of respite care services for young adults. The evidence for this theme has been drawn from two respite service types (i.e. residential short breaks59–61,64,67,75,76 and residential respite in a specialist disability facility62) and two generic categories (i.e. non-specific services35 and multiple respite services60,67,75). The perspectives of young adults, parents and service providers are presented across the theme. There was no evidence found of service inequalities. The theme has two subthemes: (1) appropriately trained and experienced staff and (2) challenges for commissioning and delivering respite care for young adults.
Appropriately trained and experienced staff
The need for appropriately trained and experienced staff was acknowledged as a vital resource for the implementation and delivery of young adult respite care services by young adults, parents and service providers:64,67,75
Ensuring an appropriately trained and skilled workforce . . . there is a need for upskilling of their staff to ensure they can meet the needs of these young people who can present with a range of medical complexities.
Adult hospice 2267
However, young adults reported facing particular challenges in finding appropriately staffed respite care services to support their complex needs, often resulting in no service being provided:
There’s a distinct lack of respite services, especially for those like myself with complex needs. Many places cannot provide 1 : 1, enteral tube feeding/Hickman line/TPN [Total Parenteral Nutrition] trained nurses. The young adult hospice we fought to get funding for is great, but it was so far away and it’d take months of planning for up to 5 days respite . . . Because I have very complex and specialist needs, it’s hard to find places who can take me.
Young adult 275
Service providers also acknowledge the challenge of staff being equipped to provide care for young adults with complex needs, and the need for appropriate training and experience to support staff confidence with this population:
The ones who are dual trained like myself, who have looked after adults, it’s quite easy for them to do that. But the girls who have never looked after anybody over the age of, say 16/17, it’s hard for them to get into the mindset of being an adult looking after an adult.
Staff member.
Parents who have experienced children’s respite care want young adult services to be comparable to children's services. Being within a reasonable travelling distance of the same standard of care as children’s hospices and having appropriately trained and experienced staff are key facilitators of young adult services being viewed as acceptable:
Families expressed a desire for the quality of care provided at home and closer to home to be of the standard received from their children’s hospice.
Lack of appropriately trained staff can lead to a poor experience for the young adult and parents. Poor experiences such as ‘medication errors occurring and a lack of understanding about [the young adult’s] clinical condition’ may also serve to undermine confidence in services. 61
Challenges for commissioning and delivering respite care for young adults
This subtheme relates to the challenges of balancing demand and limited resources when commissioning and delivering respite care services for young adults. The perspectives of parents and service providers are included. No evidence from young adults was found on this topic.
The impact of funding and commissioning constraints on respite services was reported by families and service providers. 35,59,61,62,67 An exemplar of this was reduction in services. For example, the reduction of a residential camp service from the usual 2 weeks to only 1 week was a source of disappointment and frustration for young adult service users, as it reduced participation in a valued community. 62 Similarly, the influence of financial limitations on specific service choices was noted by parents, who reported having felt under pressure ‘to agree to short breaks that cost much less than those provided by the [individual care package] service’. 61
Service providers highlighted inequalities in the funding and commissioning of services across the lifespan due to ‘inconsistencies between requirements to pay for respite care in child, young person’s and adult hospices in 3rd sector’ (reproduced with permission from Marsh et al.). 35 These inequalities influenced the consistent delivery and sustainability of services, particularly when budget holders and commissioners were ‘unwilling to pay the actual costs, or even half the actual costs of a short break’ (children’s hospice 3). 67 The challenges of commissioning and delivering services were perceived to be exacerbated by the low volume but high cost of care for this population. Some professionals spoke of how they needed to encourage commissioners and services to meet their assessment duties for the needs of young adults and for the resources to meet those needs. 35
A lack of clarity and understanding of commissioning processes among the health-care community was also noted by one parent:
Funding issues are a bit of a mystery to doctors who find it difficult to understand that commissioners will only pay one third of the cost of care in the service, whilst paying the full cost in other settings.
Funding and capacity issues were identified as the key barriers to the development and provision of developmentally appropriate and age-appropriate respite services for young adults. 67 Owing to services being overstretched, many adult hospices did not have the capacity, finance or staff to extend their service to young adults or to make it a priority. 67 One of the respondents from an adult hospice stated:
Finance is the biggest challenge. Most young adults are 100% health funded and commissioners do not have enough young people with complex life limiting conditions in their area for this to be a priority before, or unless, there is a crisis.
Adult hospice 2367
Similar challenges were reported by the Marie Curie Hospice service, with one medical director commenting that the adult service was:
. . . not equipped or resourced to engage with young people who may have very high expectations of extended support to make the most of their lives, physically, psychologically and socially. Providing respite care for this group of people, for example, could have significant implications for our ability to look after other people who have more clearly defined needs for palliative care.
Section 3: harms identified in the evidence due to poor respite care provision
Although there were many benefits and key outcomes identified for young adults, their parents and wider family, several harms were also identified in the qualitative evidence. The harms described are a consequence of inappropriate settings and timing of the respite care, and of staff providing the respite care being viewed as lacking the appropriate training and experience for young adults with complex needs.
Parents experienced an increase in their level of stress or anxiety when a service was not viewed as being acceptable for a young adult because of inappropriateness or a lack of trust in the service and staff. This negative impact on their psychological well-being reduced their service use, even if it was the only service available, as it did not have the desired outcomes, and so the potential harms were perceived to outweigh the benefits.
For example, young adults who experienced care in settings designed for older people, such as day services or nursing homes, had a poor experience due to unmet needs, and negative psychological impact, and typically stopped or reduced their service use. Young people did not wish to be accompanied in public by staff in uniforms and this restricted their ability to socialise. Limited service schedules also had a negative impact on age-appropriate experiences of young adults, for example being ‘put to bed’ at 9 p.m. caused distress and limited opportunities to socialise.
A key outcome was for young adults to have the opportunity to spend time away from the family and, consequently, for the family to have quality time together without providing care. If respite was offered within the home only, it could lead to frustration and distress, as the service did not deliver the main outcomes wanted and so needs were not fulfilled.
Poor service experiences reported by parents and young adults have also included concerns about medication errors (a reportable harm) and lack of understanding of the young adult’s condition because of poor staff training, which is not a foundation for safe care and the prevention of harm.
The loss of trusted and reliable services, such as children’s hospices, particularly during transition to adult services, had a considerable detrimental impact on the well-being of young people and their families. The harms articulated by young adults included feeling trapped in their homes and despair at having nowhere to go. They also lost opportunities to socialise, develop independence, learn new skills and have time away from their family, which, again, affected their health and psychological well-being. Parents spoke of no longer being able to rest and recuperate and losing their ‘lifeline’59 at a time when the need for family support was most urgent. Loss of respite care also had an impact on siblings, who lost dedicated time to maintain family bonds, with the potential for similarly detrimental effects on the health and well-being of the wider family.
Summary discussion
The benefits and outcomes identified for young adults in the qualitative evidence were numerous and varied, including the promotion of independence and empowerment, increased opportunities for social interaction with peers and other staff, and the enhancement of their holistic well-being. The main benefits and outcomes experienced by parents included time to rest and recuperate to build resilience to continue providing care, spending time engaging in interests or hobbies, and time with partners and other children who are acknowledged as missing out when they have a sibling who has complex needs. The reported benefits of the respite were underpinned by the need for trust in the standard and quality of care that would be provided to the young adult by the respite care service.
The main facilitators of ensuring that a service was accessible and acceptable to young adults, parents and providers included a range of psychological and practical factors:
-
The building of trust and valued relationships between families and the respite care service to establish confidence in the care provided.
-
Enabling young adults to spend time with their peers away from home, with choice and control over their activities and routines.
-
For respite care services to be developmentally appropriate and age appropriate, providing suitable accommodation, activities and staff for the individual life course stages and abilities of young adults.
-
For the standard of care of adult respite care to be comparable to a children’s hospice and within a reasonable travelling distance.
It was highly desirable for young adults and families to be engaged in the planning of respite care services to ensure that respite care services are fit for purpose and delivered in a flexible and individualised way, and to ensure that a choice of respite care types can be accessed with a range of activities on offer.
The barriers to accessing and using a service as acceptable included many of the opposite psychological and practical factors. This included a lack of trust and clinical credibility between families and the respite care service if the standard of care was viewed as inadequate (especially around important areas of care such as medication) and the lack of respite care services available to young adults, which sometimes resulted in no respite care for the family. Likewise, lack of access to appropriate services could result in young adults being able to access respite only in settings that were not developmentally or age appropriate, such as care homes for the elderly or adult hospices, with activities that did not suit young adult interests, creating a mismatch between service users’ expectation and the actual service provision. The mismatch was more acute if the young adult had previously accessed a children’s hospice where their expectations were met. Service providers also highlighted the lack of service use by BAME communities, suggesting a level of unmet need and access barriers that need to be understood and addressed.
Several harms were identified in the evidence because of the lack of appropriate respite care services. Young adults and their parents and siblings experienced negative impact on their psychological well-being, including stress and anxiety due to concerns over safe care, frustration and distress at needs not being met appropriately, lack of opportunities for young adults to socialise and develop independence, exhaustion for parents, and, ultimately, the detrimental effects on the health and well-being of all the family due to the reduction or complete loss of any respite care service at a time when the young adult and family may have increasing need for it.
Chapter 7 Discussion
This two-stage mixed-methods review has made a substantial contribution to our knowledge and evidence on respite care for young adults. We created a knowledge map of respite care services, developed 13 logic models of different types of respite care from a broad range of sources, identified clear gaps in the evidence for effectiveness and cost-effectiveness of respite care, synthesised relevant policy and synthesised qualitative evidence (including barriers to and facilitators of implementation of respite care for young adults with complex health-care or disability needs). All stages and findings of the review have been informed and validated by young adults with complex health-care needs, parents and service providers of respite care through the SG and PAG. The discussion summarises the evidence by methodological stream and by type of respite care, identifying where it aligns with policy intentions, and concludes with the implications for policy and practice, and prioritised recommendations for future research.
Summary of evidence by stream
This section summarises the results from each of the four evidence streams.
UK policy and guidance (evidence stream 4)
Twenty sources26,30,88–93,98,99,110,111,114–118,128,129,131 of UK policy and NFPO guidance were included from all four nations in the UK and national organisations (e.g. TfSL). Guided by regulatory and statutory frameworks (e.g. the Care Act 201443) that stipulate the obligations of local authorities providing publicly funded care and support, the intention of service providers was similar across the UK. As children become adults, legal duties and priorities shift from child-focused policies aimed at the holistic needs of the child and their family26,88,90,131 to policies directed at the provision of breaks for carers. 43,93,118 This shift in focus may influence the appropriate provision of respite care for young adults, as it depends on continuing NHS health-care status and may result in lack of support for siblings, unless they are identified as young carers in their own right. We identified seven key features of respite care policy:
-
Accessibility to respite care through early planning and assessment (policy 1).
-
Provision of respite care acceptable to service users (policy 2).
-
The need for outcome-focused services with local data monitoring and performance indicators (policy 3).
-
Clear eligibility criteria and information about the provision of respite care (policy 4).
-
Multiagency and integrated working to support the transition to adult services (policy 5).
-
Equitable and planned funding and commissioning to shape the market and local service provision (policy 6).
-
Service user involvement in the planning and delivery of respite care services (policy 7).
Policy intentions have been mapped on to the main findings of the review to highlight alignment with the experience of service users and gaps in the evidence.
Effectiveness of respite care/short breaks (evidence stream 1)
There was an absence of evidence on the effectiveness of respite care for our population. The lack of quantitative evidence of effectiveness, for example from clinical trials and non-randomised studies, highlights the need for new research. Measuring effectiveness of an intervention such as respite care, which is multifaceted in its mode of delivery, range of stakeholder and beneficiaries, and broad-ranging outcomes, is complex. It is unlikely that one or two outcomes or performance indicators would fit all types of respite care services, and core outcomes may need to be tailored to the specific services. Respite care services should be evaluated in the context of a package of care and support that may include informal services (e.g. recreational activities) as well as formal services, which in turn may influence the impact of the individual components. A range of quantitative outcome measures to establish effectiveness/cost-effectiveness, along with qualitative indicators to characterise the service experiences of young adults and their families, and long-term service outputs to monitor service use and uptake for providers, would capture the impact of services from a number of perspectives. Establishing a set of core outcomes and performance indicators to gather data would allow for comparison and learning across areas, enabling services to demonstrate service impact (policy 3). 26,114 Studies comparing no services with current services or comparing different types of respite care services used by young adults would help to determine which services are meeting policy intentions, delivering their intended intervention outcomes and meeting the outcomes prioritised by young adults and their carers. Future studies should also include a broad age range of young adults, reflect relevant services and report the findings for different age groups and different needs to build the evidence of effectiveness for young adults. This will support the development of evidence to help optimise service provision responsive to the needs of this complex population, which also fulfils policy intentions.
Health economics and the costs of care (evidence stream 2)
There was an absence of evidence on the health economic or broader cost implications of providing respite care, either for a given service or the relative cost comparisons between services. The screened evidence did not meet our review inclusion criteria, as it did not focus on the costs of respite services or the attribution of cost was unclear and therefore the evidence could not be included.
The lack of evidence that met our inclusion criteria highlights the dearth of research in this area, despite previous research finding only a handful of studies of the economic impact of different models of care for children with complex needs, which did not include cost specifically for respite care. 136 Although we did not find any formal health economics studies that met our review criteria, we did find a limited amount of information on projected costs of care in response to our call for evidence. This young adult respite service has been piloted and evaluated, and so updated figures based on implementation will be available in due course [URL: www.stelizabethhospice.org.uk/how-we-can-help/hospice-care/young-adult-service/short-break-unit/ (accessed 9 December 2020)]. The business plan included provision of 47 residential three-night weekends over 12 months (i.e. Friday afternoon to Monday morning), based on two young adults aged 18–40 years sharing a room. The projected annual costs of £123,625 included registered nurses and health-care assistants, a multidisciplinary assessment, use of the day unit and facilities at the hospice, meals and 20 hours for a co-ordinator role. In addition, the business plan forecast £11,589 for annual training of 10 staff members. 123
Despite the lack of health economic evidence, it is worth noting that UK unit costs for respite care and short breaks for disabled children up to age 18 years are reported elsewhere. 137 The cost of providing a similar respite care service for young adults with similar complex care needs is unlikely to be significantly different from the reported unit costs for those aged < 18 years. This is because the service costs are mainly driven by the staffing ratios required to provide the appropriate care to someone with a complex health-care condition, rather than chronological age. Some illustrative unit costs of £35 per day for activity days, £420 per week for residential care and £1,000 per week for a longer break were also reported by the Welsh Government, although these figures are 10 years old and not for complex care. 135 The costs of respite care for children with congenital conditions and chromosomal disorders who have complex needs that require specialist care are higher than the average costs for short breaks for children with less complex conditions. 136 The costs of respite care for young adults with complex needs, due to comorbidities or the use of specialist technology, are also likely to be higher than average, and escalate according to the complexity of the young person’s needs, as a consequence of the requirement for specialist staff and increased staffing ratios.
Absence of evidence on the absolute and relative costs of different types of respite care for young adults highlights the need for studies that compare the economic costs of this service variation. This is particularly salient in view of the increasing prevalence of lower cost respite provision that can accommodate more people, such as organised recreational activities, but would be unsuitable for many of the young adults with complex health-care needs. Moreover, the benefits of respite services for young adults with complex needs may be multidimensional and involve a range of outcomes for the young person and the wider family. The economic implications of these wider benefits should not be disregarded. Comparative studies of different types of respite care that incorporate measures of cost-effectiveness are vital to ensure that the balance of costs, individual needs and experienced outcomes are reported to inform evidence-based commissioning and the provision of services.
Performance indicators and outcome measures that capture unintended consequences and harms, as well as benefits, are needed (policy 3). In addition, capturing unit and cost-effectiveness data would provide evidence for the socioeconomic argument for respite care as an intervention and to inform future commissioning (policy 6). Appropriate economic indicators would increase understanding of how cost-effective respite care can support quality of life for the young adult and their parents. This information could also support service planning and commissioning to prevent the breakdown of care that can result in crisis hospital admissions and the detrimental impact on the physical and mental health of family carers, including the impact on educational attainment of siblings. Quantifiable measures may include comparison of unit costs for different respite care services and comparison of the cost of regular respite care with health-care costs for emergency interventions (policies 3 and 6).
Experience and attitudes (evidence stream 3)
We searched for quantitative, qualitative and mixed-methods evidence reporting the experience of young adults, families and providers of respite care services and their attitudes towards the services provided. No quantitative or mixed-method evidence that met the inclusion criteria was found. Twenty qualitative sources across 27 records22,27,35,41,59–76,102,103,107–109 met the review inclusion criteria. These included peer-reviewed academic journal papers, NFPO reports and evaluation reports of funding schemes for respite care that included limited qualitative evidence, although methods were not reported. The quality of each source of evidence was assessed using the CASP checklist for qualitative research, and GRADE-CERQual was used to assess the confidence in synthesised qualitative findings (see Table 4). The key findings for each of the themes identified in the data were assessed, with a high confidence rating attributed to most findings. The evidence captured the perspectives of young adults, parents, wider family and service providers via professionals. However, it is worth noting that only 20% of participants were young adults (n = 175) and 1% were siblings (n = 12), highlighting the need for future work to include the views and experiences of young adults and siblings to ensure that their voice is heard about their access and experience of care, and wishes for future services (policies 1, 2, 5 and 7).
Evidence by respite type
Evidence for 10 of the 13 types of respite services identified in the knowledge map met the review inclusion criteria, ranging from one source12 for residential respite in a nursing home to nine sources27,41,59–61,64,67,71,76 for residential respite in a specialist palliative care facility (e.g. hospice). Much of the excluded literature on respite care for those with physical disabilities focused on children and young people up to the age of 18 years. However, some evidence captured in the knowledge map and review included respite care services with broad inclusion criteria for young adults with complex health-care needs due to life-limiting conditions and disability.
Given the prevalence of residential respite for young people in children’s hospices, with upper age limits of early 20s, it is not surprising that the largest volume of evidence was for this type of care. The largest number of benefits and reported outcomes for young adults, parents and wider family were for residential respite care because of the holistic nature and intensity of the respite provided. The evidence suggests that where young adults can access residential respite care that meets their needs it also meets the policy intention of providing accessible and acceptable care, with clear information about the service and eligibility criteria (policies 1, 2 and 4). Given that care needs continue or increase as children grow into adults, the benefits of respite care for young adults and their families will be similar. The whole family also benefited when the young adult attended residential respite in a specialist disability facility. 62,68
Although a range of different services were included in the knowledge map, there was limited evidence for respite care in nursing homes, home-based daytime and overnight care, day care at a specialist facility, befriending, holidays and emergency residential respite care in a specialist service. Although additional detail on service specification and the experience of these types of respite care would add to our current understanding, we should prioritise further evidence on services associated with harm. Only one source63 directly reported on young adults’ experiences of residential respite in a nursing home. It was considered an unacceptable service setting for young adults and this was indirectly supported by several other sources of evidence. 27,63,75
Adequate provision of emergency care is a source of anxiety and uncertainty for young adults, families and service providers, but our review included only two sources27,67 on the experience of emergency residential respite in a specialist facility, such as a hospice. For those who previously accessed respite care through children’s hospices, this emergency support was considered more valuable by parents, often above planned respite care, because of the lack of a safe and appropriate alternative. 27 The lack of evidence on emergency respite care suggests that more research is needed in this area. Lack of appropriate emergency respite care can result in unplanned hospital admissions or the provision of inappropriate care in a setting unfamiliar with these types of young adults and the care they require, such as residential care homes, which may be unsafe for this population. The need for confidence in emergency respite care is key to parents’ well-being, and the continuity and appropriateness of care is vital for young adults to receive safe care. Following discharge or transition from children’s hospices, planned respite care should include the provision of emergency respite. 3,27 More evidence is needed to evaluate how current planning and services meet the requirements of the Care Act 2014 for commissioning and provision of safe, acceptable, user-friendly and integrated services for young adults and their families (policies 1, 2, 5 and 6). There was a greater perceived risk of potential harms associated with inappropriate care settings compared with other service settings (such as the negative psychological and physical impact on young people and families), again highlighting the need for future research.
The evidence matrix and the logic models that form the conceptual framework illustrate the gaps in the evidence base and the need for new research (see Appendices 8–20). We did not find evidence for host family/fostering respite, emergency respite provided in the home or hospital, or host family emergency respite to complete the logic models, but the service aims, resources and intended outcomes in the model demonstrate the programme theory for these types of services. The gaps in the evidence for these three types of respite care may be because of the relative novelty of host family/fostering.
There was a lack of longitudinal evidence to facilitate exploration of long-term outcomes and achievement of planned, regular respite care for young adults. Much of the evidence was a cross-sectional snapshot of experiences, although the limited evidence from regular service users demonstrates the accrued benefits of planned, regular respite care, particularly residential care, for the whole family.
The review has two incomplete evidence streams because of the lack of effectiveness and cost-effectiveness data, but decision-makers also need information on the feasibility and acceptability of interventions to understand implementation factors and equity of service provision. 138 Qualitative research can be a key source of complementary evidence on these issues, along with benefits and harms, because of its holistic view of people’s experiences, values and preferences. Therefore, although we acknowledge that there are some limitations in the evidence, we discuss the key findings in terms of the review questions and prevailing policy landscape. Owing to the varying levels of evidence between the different types of respite care and the consistency of themes across services, the evidence synthesis focused on the main benefits, harms and outcomes experienced by service users or providers, and the main barriers to and facilitators of access to respite care.
Benefits of respite care for young adults and parents
The evidence suggests many positive outcomes of respite care for young adults, their parents and wider family. Respite care facilitated the development of independence and empowerment for young adults in a number of ways, all of which enhanced their overall well-being. This included the following:
-
Creating opportunities to make choices and engage in a range of different activities.
-
Increasing opportunities for social interaction with peers and other staff, which reduced isolation and reinforced peer groups.
-
Encouraging contribution to service development.
-
Enabling time away from parents.
The main benefits experienced by parents included time to rest and recuperate, time spent on personal interests and having a break from their 24 hours a day, 7 days a week (24/7), caring responsibilities, which reduced physical and psychological strain, and built resilience to continue providing care. Respite care also acts as a support mechanism for the wider family, helping to re-establish family cohesion with partners and other children, maintaining the family unit and building resilience within the family to meet the challenges of providing care.
The benefits reported by young adults, or by their parents as proxies, align with the stated intention of most respite services for young adults identified in the logic models. The outcomes for parents and the wider family are often not stated explicitly by services, but could be viewed as secondary to the benefits aimed at the young adults. Outcomes used to measured the successful delivery of services are often not clearly defined in policy documents, but commissioning guidance documents define outcomes as measurable benefits due to an intervention that can be categorised at an individual, service or strategic level. 128 The evidence suggests that this is partially fulfilled through service evaluations that include the experiences of service users (policies 1–3). Additional measures are needed to facilitate comparison and learning between different types of services, so that their effectiveness and impact can be assessed (policies 3, 5 and 6). 26,114 There was little evidence found on individual and carer assessments, despite this underpinning all policy intentions for accessibility of services (policy 1) or views on the provision of service information (policy 4), which is worthy of future exploration.
Facilitators of delivering and accessing respite care for young adults
The main facilitators for a service to be viewed as accessible and acceptable to young adults, parents and providers were the building of trust and valued relationships between families and respite care service to establish confidence;27,59,60,62–64,69,73 enabling young adults to spend time with their peers away from home with choice and control over their activities and routines;59–65 for respite care services to be developmentally appropriate and age appropriate, providing suitable accommodation, activities and staff;35,61–63,67 and for the standard of care of adult respite care to be comparable to a children’s hospice and within a reasonable travelling distance. 60,67 Engaging young adults and families in the planning of respite care services was considered key to ensuring that services were fit for purpose. 35,61 Parents also expressed a preference for flexible service working practices.
Policy from all nations states that children, young people and young adults with additional needs, such as complex health-care and disability needs, should have equitable access to short breaks as a core component of palliative care, with medical and nursing input as required. 26,88,91,92,111,115,128,131 The care should comply with national standards,98 be fit for purpose and age appropriate,91 and should be delivered as close to home as possible. 98 Many of the facilitators described by young adults and their families are consistent with policy intentions; however, service equity and consistency according to need was variable, with many needs not met following transition to adult services.
The policy intention for a range of services at different times to suit the needs of young adults and carers114,118 was supported to an extent for those who had access to respite care (policy 1). The availability of services varied both within and between different types of respite care (policies 1 and 2) and provision was patchy, often with an upper age limit not much above age 25 years. The knowledge map and evidence review revealed an increase in a range of organised activities, described as respite care, which was confirmed through consultation with review stakeholders. This type of respite care is viewed as a lower-cost service that can accommodate a large number of young adults, making it attractive to commissioners and providers. However, young adults with more complex health-care needs may not be able to access this type of care and it does not offer the opportunity for an overnight break, which may be a primary need for the wider family to rest and build resilience. The policy intention to draw on the experiences and knowledge of carers and families when planning services26,91,114,117,118,131 was supported by evidence from the development of a new service for young adults (policy 7).
Barriers to delivering and accessing respite care for young adults
For some families, there were practical barriers to accessing respite care that affected the quality of their experiences, including the volume and complexity of paperwork, a delay between referral and service provision, the distance between their home and the service, limited access to condition-specific services and lack of appropriately trained staff. 35,61,65,67,71 The lack of physical space for equipment in some services meant that respite care could not be offered to young adults who were dependent on specialist technology. 27 We found very little evidence on the uptake and experience of services by BAME populations, an area that requires further work to ensure that equitable access is provided for all young adults, including traditionally marginalised communities. 35 Service professionals also spoke of needing to encourage commissioners and services to meet the assessment needs of young adults so that respite care could be provided. 35 Likewise, parents felt under pressure to agree to short breaks that cost much less than those provided by individualised care package services. 61 These barriers represent a shortfall in the intention of policies to deliver an equitable, accessible and acceptable respite care service (policies 1 and 2). However, the most significant barrier to achieving a consistent and reliable respite care service for young adults was the transition from children to adult services.
Impact of service transition on the experience of respite care for young adults
Following transition to adult services, the picture of who can access appropriate respite care is less positive. Policy and guidance documents set out a range of expectations around transition, aligned with the transition duties within the Care Act 2014, which require local authorities to recognise the need for phased and timely transitions of young people. 26,128 This includes the need to assess the future adult social care, education and health needs of young people and their carers, provided the young person consents to assessment and it is in their best interests. 26,114,128
Respite, including short breaks, should be included in proactive planning for transition, with consideration of the needs of young adults and their parents/carers in the most appropriate settings. 114,129 A lead professional or key worker should co-ordinate the care plan and transition of care. 91,115 The intention is to avoid inequitable access to respite care for young adults with complex needs as they approach transition, particularly as this is a time when young adults and their families have an increased need for respite support. 91,129 This policy also acknowledges that the needs of young adults differ from those of young children and that tailored respite and hospice services are needed. 111
Despite these intentions, the evidence review captured many stories of young adults unable to access any respite care because of ineligibility for adult services, where the focus is primarily on symptom management and end-of-life care. Others could access respite in inappropriate settings only, such as nursing homes or adult hospices, which are not tailored to their interests or complex health-care needs. 59,61,63,75 These findings are not consistent with the policy intention for accessible or acceptable respite care (policies 1 and 2). Young adults and parents experienced both the ‘anticipated’ loss of services during transition planning and the ‘actual’ loss of services after transition. The main barriers to respite care after transition were the lack of developmentally appropriate and age-appropriate adult services and the lack of a knowledgeable and experienced staff to provide safe care for young adults with complex health-care needs. 60,64,67,75 Yet, despite the anticipated increased service demand as both young adults and their parents age, there are a lack of suitable alternatives for planned and emergency respite. This could result in a range of potential harms for young adults, parents and the wider family, and for service providers supporting young adults through transition. The recent Department of Health and Social Care-commissioned report on services for children and young adults requiring long-term ventilation (i.e. some of the most technically complex needs) also notes the disappearance of respite services for this specific group post transition. 139
The reduction in or complete loss of respite care services at a time of particular need had a negative impact on the psychological well-being of young adults, their parents and siblings, including stress and anxiety due to safety concerns, frustration and distress about unfulfilled needs, and detrimental effects on the health and well-being of the wider family.
Further work on service development and implementation is required to ensure that the policy intention of acceptable and safe respite care being available to all young adults who are assessed as requiring it can be met. 26,88,91,92,111,115,128,131 Equally, without appropriate respite care for the young adults, parents assessed as needing a break would be unable to do so, falling short of the policy intention to provide respite for all parents and not just those in a direct caring role (policies 1 and 2). 26,88,90–92,99,110,114,116–118,128,131 Most of the evidence focuses on residential respite, partly because of the provision by some children’s services to those aged over 18 years old. However, once young adults reach the maximum age for a particular children’s hospice, they have limited choices, if any. The majority of providers do not offer the whole-family-oriented residential respite offered by children’s hospices.
Young adults, parents and providers acknowledged that, for services to be acceptable and to improve outcomes for young adults, they should be designed and developed with young adults’ interests, life course stage and needs in mind. Young adults wish to spend time with peers and staff of a similar age and sex to themselves. Respite care should provide opportunities for the wider family to spend time together or engage in their own social activities with a break from care, including overnight services. Involving young adults and parents in the development or planning of services was encouraged to improve the acceptability of the service to service users.
Funding and commissioning of services
Funding, commissioning and capacity issues were identified as key barriers to the development and provision of appropriate respite services for young adults. Providers spoke of inequalities in the funding and commissioning of services across the lifespan because of inconsistencies between requirements to pay for respite care in hospices for children, young people and adults in third sector and lack of understanding of the commissioning process. 35,67 Service providers and commissioners face challenges in providing appropriate, safe and acceptable respite care and short break services to a population that is considered small and disparate. The small number but high needs of this population creates particular challenges for local funding and services to meet demand, particularly when young adults and parents have different respite care needs. Children and adult hospices lack the funding and capacity to provide all the care needed, requiring joined-up working with statutory and NHS support to meet current and future need. Partnership working to optimise use of physical and staff resources is key to the development and sustainability of respite care services for young adults, including emergency respite care, and requires service planning, commissioning and co-ordination on a regional scale. 67 Regional working is supported by policy recommendations for commissioners and services across all sectors to explore ways of working together, but we identified little evidence of these types of shared working practices (policies 5 and 6). We identified little evidence of service integration and innovation for the knowledge map (policy 5), but as services evolve in response to local demand this may become more prevalent, with a market-shaping steer from commissioners (policy 6).
Strengths and limitations of the review
We included a broad range of evidence in the review to address multiple and interrelated policy- and practice-related questions concerning the provision of respite care. The protocol was peer reviewed and published in PROSPERO. We used a comprehensive systematic search, conducted by a highly experienced information specialist, to identify potentially eligible studies. We searched multiple resources, including electronic databases, journals, conference proceedings, reference lists of included studies, citations of included studies, and trial registries, along with a call for evidence distributed internationally on social media and via team networks. We used the CLUSTER method to identify relevant studies and found four additional studies through key ‘pearl’ papers. 30,64,76,121 Policy evidence on respite care for young adults with life-limiting conditions is a small part of a broader set of policy documents relating to care. Our use of two topic experts enabled identification of relevant policy around respite care for young adults and led to the addition of another 10 sources to the policy stream. The team was deliberately diverse, covering a range of discipline and method expertise to ensure capture and appropriate scrutiny of all relevant material. Two review authors independently assessed all studies, and at least one review author verified study selection and data extraction to minimise potential conflict-of-interest bias arising from inclusion of sources from review authors.
Patient and public engagement was extensive at all stages of the review and met the new UK standards for PPI involvement in research. 140 In addition to the report and peer-reviewed publications, outputs from the collaborative process include a short film on the needs of young adults with complex health care, developed with young adults, parents and providers, which is currently in final stage of production. An animation and a range of blogs will also be available on the study website.
The review has several limitations. Evidence selection was challenging because of the variable definitions used by diverse services and activities that encompass the term respite care. We included all sources that described any type of respite care for young adults aged ≥ 18 years in the knowledge map, and all sources that reported outcomes or benefits and harms for young adults or families in the main evidence review. Therefore, sources that included the term respite care and our population may have been excluded from the knowledge map because of insufficient detail on service specification or may have been excluded from the evidence review because outcomes were not reported. Despite the broad inclusion criteria, we identified both an absence of evidence and gaps in the evidence.
We recognise that the review includes only one type of evidence and a full assessment is therefore incomplete. Some papers may have been misclassified as not eligible for inclusion in this review, but at least two review authors independently assessed all studies and at least one review author verified the selection and information extracted from each source. Therefore, we are confident that we assessed study exclusion on the basis of consistent and appropriate criteria. For some full-text reports, it is possible that we could have extracted relevant information incorrectly, although at least two reviewers checked all information extraction to minimise errors. We did not contact source authors to obtain further information because of resource constraints and this may have reduced the overall quality of the extracted information. Owing to the small number of included sources and the limited information they contained, we were unable to explore the impact of BAME subgroups on our findings.
Although caution is needed because of the quality of some evidence, the findings show the positive benefits and outcomes for the young adult, as well as their parents and wider family. However, to develop and deliver a respite service that meets the needs of young adults and their families in the best and most cost-effective way, evidence is required to better understand the costs and effectiveness of different respite care interventions and to explore how these benefits can be achieved for all young adults who require respite. To achieve this, future studies are needed with robust methods, embedded health economic measures, appropriate quantitative outcome measures and qualitative experience data to capture quality-of-life outcomes from larger samples. Gathering consistent evidence across service types would enable comparisons of the different types of respite care and support services and commissioners to ensure that the provision of respite care is based on high-quality evidence for the best outcomes at the best cost.
Chapter 8 Implications
The review identified several areas with implications for practice and policy, and provides recommendations for future research.
Implications for policy
Policy intentions are clearly stated in UK policy documents, but are more comprehensively applied to young people aged < 18 years, who can still access children’s services, and who appeared to be better served by respite services that meet policy intentions. After the age of 18 years, and especially for those with the most complex of needs, policy intentions are not consistently fulfilled, and this imbalance needs to be addressed.
Implications for practice
-
The findings suggest a lack of regular and local monitoring to support shared learning and comparison of services across regions, as recommended by policy. It would be beneficial to develop and agree a core set of outcomes measures to gather quantitative and qualitative measures for use across services. This would permit the collation of outcomes across a diverse and disparate population.
-
More research and routine service evaluation is required to inform the planning and commissioning of appropriate respite care services for young adults. This could include an exploration of international initiatives and good practice to serve as a model for future provision.
-
The evidence identified inequity of service provision before and after transition, and this needs to be understood and addressed by commissioners.
Recommendations for research
Several areas are recommended for future research to address gaps in the evidence (these are listed in order of priority).
-
To establish the effectiveness and cost-effectiveness of different types of respite care for young adults, larger comparative longitudinal studies using robust methods are required, using quantitative and health economic measures to determine whether or not services work, and qualitative data to assess implementation, uptake and service experience. These studies should include BAME subgroups.
-
Research on the uptake and impact of carer assessments on service provision to young adults and their parents is needed to improve the evidence base and inform practice.
-
Further research is required on the impact of transition from children to adult services on respite care provision for young adults and breaks for their parents.
-
Clearer reporting of populations and definitions in published research is needed to support capture of data from young adults with complex health-care needs included in mixed populations.
Acknowledgements
The team would like to acknowledge and thank the young adults, parents and professionals who have supported the review from inception to completion through the SG and PAG. Their continued support of the dissemination and development of media outputs, and the contribution of their expertise and lived experience have made a significant contribution throughout the review.
Contributions of authors
Katherine Knighting (https://orcid.org/0000-0002-6292-823X) (Senior Research Fellow/Senior Lecturer) was the review manager, contributed to the conceptualisation, design and methods of the review, finalised the protocol, supported running of the searches and retrieval of sources, data screening and extraction, quality appraisal, evidence synthesis and application of GRADE-CERQual, and drafting of the report.
Gerlinde Pilkington (https://orcid.org/0000-0003-0028-0746) (Research Fellow) contributed to the conceptualisation, design and methods of the review, finalised the protocol, supported running of the searches and retrieval of sources, data screening and extraction, quality appraisal, evidence synthesis and drafting of the report.
Jane Noyes (https://orcid.org/0000-0003-4238-5984) (Professor of Health and Social Services Research and Child Health) contributed to the conceptualisation, design and methods of the review, finalised the protocol, supported screening and data extraction, quality appraisal, evidence synthesis and application of GRADE-CERQual, and drafting of the report.
Brenda Roe (https://orcid.org/0000-0001-8227-0116) (Professor of Health Research) contributed to the conceptualisation, design and methods of the review, finalised the protocol, supported screening and data extraction, quality appraisal, evidence synthesis and drafting of the report.
Michelle Maden (https://orcid.org/0000-0003-4419-6343) (Information Specialist) contributed to the conceptualisation, design and methods of the review, finalised the protocol, led development and running of the searches and retrieval of sources, supported evidence synthesis and drafting of the report.
Lucy Bray (https://orcid.org/0000-0001-8414-3233) (Professor of Child Health Literacy) contributed to the conceptualisation, design and methods of the review, finalised the protocol, supported screening and data extraction, quality appraisal, evidence synthesis and drafting of the report.
Barbara Jack (https://orcid.org/0000-0001-6318-516X) (Professor of Palliative Care) contributed to the conceptualisation, design and methods of the review, finalised the protocol, supported screening and data extraction quality appraisal, evidence synthesis and drafting of the report.
Mary O’Brien (https://orcid.org/0000-0002-8509-3650) (Professor of Palliative and Supportive Care) contributed to the conceptualisation, design and methods of the review, finalised the protocol, supported screening and data extraction, quality appraisal, evidence synthesis and drafting of the report.
Julia Downing (https://orcid.org/0000-0002-3450-785X) (Chief Executive of International Children’s Palliative Care Network) contributed to the conceptualisation, design and methods of the review, finalised the protocol, supported screening and data extraction, quality appraisal, evidence synthesis and drafting of the report.
Céu Mateus (https://orcid.org/0000-0001-6219-219X) (Professor of Health Economics) contributed to the conceptualisation, design and methods of the review, finalised the protocol, supported screening and data extraction for the health economics stream, evidence synthesis and drafting of the report.
Sally Spencer (https://orcid.org/0000-0001-6330-7200) (Professor of Clinical Research) was chief investigator of the review, contributed to the conceptualisation, design and methods of the review, finalised the protocol, supported screening and data extraction, quality appraisal, evidence synthesis and drafting of the report.
Publications
Published protocol (gold open access)
Pilkington G, Knighting K, Bray L, Downing J, Jack BA, Maden M, et al. The specification, acceptability and effectiveness of respite care and short breaks for young adults with complex healthcare needs: protocol for a mixed-methods systematic review. BMJ Open 2019;9:e030470.
Poster conference presentations of the published protocol
Pilkington G, Knighting K, Noyes J, Roe B, Maden M, Bray L, et al. Deconstructing the Maze: Identifying and Categorising Models of Respite Care and Short Breaks for Young Adults with Complex Healthcare Needs (CHCNs). The Martin House Research Centre 1st Biennial Research conference. 21 September 2018, University of York. Poster presentation.
Pilkington G, Knighting K, Noyes J, Roe B, Maden M, Bray L, et al. Uncharted Territory: Mixed-Methods Systematic Review to Map, Characterise, and Evaluate Respite Care for Young Adults with Complex Healthcare Needs. Health Services Research UK. 2 and 3 July 2019, Manchester, UK. Spoken poster.
Invited talk on patient and public involvement in evidence synthesis
Knighting, K. Patient and Public Involvement in Evidence Synthesis. Invited speaker at an open seminar at Liverpool Reviews and Implementation Group, University of Liverpool, Liverpool, UK, November 2018.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Marie Curie Cancer Care . Don’t Let Me Down: Ensuring a Good Transition for People With Palliative Care 2012.
- Fraser L, Miller M, Aldridge J, McKinney PA, Parslow Roger C. Prevalence of Life-Limiting and Life-Threatening Conditions in Young Adults in England 2000–2010. Final Report for Together for Short Lives 2013. www.togetherforshortlives.org.uk/wp-content/uploads/2018/01/ExRes-Life-Limiting-and-Life-Threatening-Conditions-in-Young-Adults-Lorna-Fraser-Report.pdf (accessed 8 December 2020).
- Noyes J, Pritchard A, Rees S, Hastings R, Jones K, Mason H, et al. Bridging The Gap: Transition from Children’s to Adult Palliative Care 2014. www.england.nhs.uk/midlands/wp-content/uploads/sites/46/2019/05/bridging-the-gap-between-children-adult-palliative-care.pdf (accessed 26 November 2020).
- World Health Organization . Global Atlas of Palliative Care at the End of Life 2014.
- Gatehouse M, Ward H, Holmes L. Developing Definitions of Local Authority Services and Guidance for Future Development of the Children in Need Census 2008. https://figshare.com/articles/online_resource/Developing_definitions_of_local_authority_services_and_guidance_for_future_development_of_the_Children_in_Need_Census/9580310 (accessed 31 July 2020).
- Mooney A, Owen C, Statham J. Disabled Children: Numbers, Characteristics and Local Service Provision 2008. https://discovery.ucl.ac.uk/id/eprint/1482347/1/Numbers_and_characteristics_of_disabled_children.pdf (accessed 26 November 2020).
- Great Britain . Equality Act 2010 2010.
- NHS England . NHS Standard Contract for Specialised Rehabilitation for Patients With Highly Complex Needs (All Ages) 2014.
- Marchant R, Lefevre M, Jones M, Luckock B. SCIE Knowledge Review 18: ‘Necessary Stuff’ – The Social Care Needs of Children With Complex Health Care Needs and Their Families 2007. www.scie.org.uk/publications/knowledgereviews/kr18.asp (accessed 8 December 2020).
- Limbrick P. TAC for the 21st Century: Nine Essays on Team Around The Child. Interconnections; 2009.
- Rankin J, Regan S. Meeting complex needs: the future of social care meeting complex needs. Hous Care Support 2004;7:4-8. https://doi.org/10.1108/14608790200400016.
- Devitt K, Knighton L, Lowe K. Key Data on 16–25 Year-Olds Transitions, Disadvantage and Crime 2009. https://researchportal.port.ac.uk/portal/files/1587567/Young_People_in_Focus_Young_Adults_Today_2009.pdf (accessed 26 November 2020).
- Care Quality Commission . From the Pond into the Sea. Children’s Transition to Adult Health Services 2014.
- National Institute for Health and Care Excellence (NICE) . Transition from Children’s to Adults’ Services for Young People Using Health or Social Care Services (NG43) 2016.
- Fraser LK, Lidstone V, Miller M, Aldridge J, Norman P, McKinney PA, et al. Patterns of diagnoses among children and young adults with life-limiting conditions: a secondary analysis of a national dataset. Palliat Med 2014;28:513-20. https://doi.org/10.1177/0269216314528743.
- Remedios C, Willenberg L, Zordan R, Murphy A, Hessel G, Philip J. A pre-test and post-test study of the physical and psychological effects of out-of-home respite care on caregivers of children with life-threatening conditions. Palliat Med 2015;29:223-30. https://doi.org/10.1177/0269216314560008.
- Together for Short Lives . A Guide to the Development of Children’s Palliative Care Services 2009.
- Champagne M, Mongeau S. Effects of respite care services in a children’s hospice: the parents’ point of view. J Palliat Care 2012;28:245-51. https://doi.org/10.1177/082585971202800402.
- Together for Short Lives . Children’s Palliative Care Definitions n.d. www.togetherforshortlives.org.uk/get-support/supporting-you/family-resources/childrens-palliative-care-definitions/ (accessed 31 July 2020).
- NHS Choices . Carers’ Breaks and Respite Care 2019. www.nhs.uk/conditions/social-care-and-support-guide/support-and-benefits-for-carers/carer-breaks-and-respite-care/ (accessed 31 July 2020).
- World Health Organization . WHO Definition of Palliative Care 2012. www.who.int/cancer/palliative/definition/en/ (accessed 28 February 2018).
- Kirk S, Fraser C. Hospice support and the transition to adult services and adulthood for young people with life-limiting conditions and their families: a qualitative study. Palliat Med 2014;28:342-52. https://doi.org/10.1177/0269216313507626.
- Carter B, Edwards M, Hunt A. ‘Being a presence’: the ways in which family support workers encompass, embrace, befriend, accompany and endure with families of life-limited children. J Child Health Care 2015;19:304-19. https://doi.org/10.1177/1367493513516391.
- Doug M, Adi Y, Williams J, Paul M, Kelly D, Petchey R, et al. Transition to adult services for children and young people with palliative care needs: a systematic review. Arch Dis Child 2011;96:78-84. https://doi.org/10.1136/adc.2009.163931.
- Fraser LK, Aldridge J, Manning S, O’Leary S, Miller M, McCulloch R, et al. Hospice provision and usage amongst young people with neuromuscular disease in the United Kingdom. Eur J Paediatr Neurol 2011;15:326-30. https://doi.org/10.1016/j.ejpn.2011.02.003.
- Department of Health and Social Care (DHSC) . Better Care, Better Lives. Improving Outcomes for Children, Young People and Their Families Living With Life-Limiting and Life-Threatening Conditions 2008.
- Mitchell TK, Knighting K, O’Brien MR, Jack BA. Short break and emergency respite care: what options for young people with life-limiting conditions?. Int J Palliat Nurs 2016;22:57-65. https://doi.org/10.12968/ijpn.2016.22.2.57.
- Kelly D, Edwards J, Faull C, Carter YH, Daniels L. Handbook of Palliative Care. 2nd edn. Hoboken, NJ: Wiley; 2005.
- Knighting K, Mitchell T, O’Brien MR, Jack BA. Emergency Care Impact Assessment (ECIA) Project. Final Report 2014.
- Together For Short Lives . Transition: A Guide for Clinical Commissioning Groups 2015. www.togetherforshortlives.org.uk/wp-content/uploads/2018/01/ProRes-Transition-A-Guide-for-CCGs.pdf (accessed 31 July 2020).
- Whiting M. Support requirements of parents caring for a child with disability and complex health needs. Nurs Child Young People 2014;26:24-7. https://doi.org/10.7748/ncyp2014.05.26.4.24.e389.
- Ling J. Respite support for children with a life-limiting condition and their parents: a literature review. Int J Palliat Nurs 2012;18:129-34. https://doi.org/10.12968/ijpn.2012.18.3.129.
- Robertson J, Hatton C, Wells E, Collins M, Langer S, Welch V, et al. The impacts of short break provision on families with a disabled child: an international literature review. Health Soc Care Community 2011;19:337-71. https://doi.org/10.1111/j.1365-2524.2010.00977.x.
- National Collaboration for Integrated Care and Support . Integrated Care and Support: Our Shared Commitment 2013. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/198748/DEFINITIVE_FINAL_VERSION_Integrated_Care_and_Support_-_Our_Shared_Commitment_2013-05-13.pdf (accessed 26 November 2020).
- Marsh S, Cameron M, Duggan M, Rodrigues J, Eisenstadt N, Iskander R, et al. Young People With Life-Limiting Conditions: Transition to Adulthood. ‘Small Numbers, Huge Needs, Cruel and Arbitrary Division of Services’. Executive Summary of Phase 1 Report for Marie Curie Cancer Care 2011. www.mariecurie.org.uk/globalassets/media/documents/commissioning-our-services/past-initiatives/ypt/phase1_young-people-transition-exec-summary.pdf (accessed 26 November 2020).
- Bamford C, Arksey H, Poole M, Kirkley C, Hughes J, Corner L, et al. Person- and Carer-Centred Respite Care for People With Dementia: Developing Methods of Evaluating the Effectiveness of Different Models. Report for the National Institute for Health Research Service Delivery and Organisation Programme 2009. http://www.netscc.ac.uk/netscc/hsdr/files/project/SDO_FR_08-1511-113_V01.pdf (accessed 26 November 2020).
- Department for Education and Skills and HM Treasury . Aiming High for Children: Supporting Families 2007.
- Pinney A. Understanding the Needs of Disabled Children With Complex Needs or Life-Limiting Conditions: What Can We Learn From National Data? 2017. https://councilfordisabledchildren.org.uk/sites/default/files/field/attachemnt/Data%20Report.pdf (accessed 26 November 2020).
- Foundation for People with Learning Disabilities . Learning Disability Statistics: Effects of Being a Carer 2014.
- Malcolm C, Forbat L, Knighting K, Kearney N. Exploring the experiences and perspectives of families using a children’s hospice and professionals providing hospice care to identify future research priorities for children’s hospice care. Palliat Med 2008;22:921-8. https://doi.org/10.1177/0269216308098214.
- Knighting K, Bray L, Downing J, Kirkcaldy A. Children and adult hospice provision for young adults with life-limiting conditions: a UK survey. BMJ Support Palliat Care 2017;7:A94-A95. https://doi.org/10.1136/bmjspcare-2017-hospice.261.
- Great Britain . Children and Families Act 2014 2014.
- Great Britain . Care Act 2014 2014.
- Pilkington G, Knighting K, Bray L, Downing J, Jack BA, Maden M, et al. The specification, acceptability and effectiveness of respite care and short breaks for young adults with complex healthcare needs: protocol for a mixed-methods systematic review. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2019-030470.
- Thomas J, Sutclifee K, Harden A, Oakley A, Oliver S, Rees R. Children and Healthy Eating: A Systematic Review of Barriers and Facilitators. London: EPPI-Centre, Social Science Research Unit, Institute of Education, University of London; 2003.
- Whitaker R, Hendry M, Aslam R, Booth A, Carter B, Charles JM, et al. Intervention Now to Eliminate Repeat Unintended Pregnancy in Teenagers (INTERUPT): a systematic review of intervention effectiveness and cost-effectiveness, and qualitative and realist synthesis of implementation factors and user engagement. Health Technol Assess 2016;20. https://doi.org/10.3310/hta20160.
- Booth A. Clear and present questions: formulating questions for evidence based practice. Library Hi Tech 2006;24:355-68. https://doi.org/10.1108/07378830610692127.
- Booth A, Harris J, Croot E, Springett J, Campbell F, Wilkins E. Towards a methodology for cluster searching to provide conceptual and contextual “richness” for systematic reviews of complex interventions: case study (CLUSTER). BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-118.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: Template for Intervention Description and Replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Noyes J, Hendry M, Booth A, Chandler J, Lewin S, Glenton C, et al. Current use was established and Cochrane guidance on selection of social theories for systematic reviews of complex interventions was developed. J Clin Epidemiol 2016;75:78-92. https://doi.org/10.1016/j.jclinepi.2015.12.009.
- Anderson LM, Petticrew M, Rehfuess E, Armstrong R, Ueffing E, Baker P, et al. Using logic models to capture complexity in systematic reviews. Res Synth Methods 2011;2:33-42. https://doi.org/10.1002/jrsm.32.
- Kneale D, Thomas J, Harris K. Developing and optimising the use of logic models in systematic reviews: exploring practice and good practice in the use of programme theory in reviews. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0142187.
- Critical Appraisal Skills Programme . CASP Qualitative Checklist 2018.
- Bowen GA. Document analysis as a qualitative research method. Qual Res 2009;9:27-40. https://doi.org/10.3316/QRJ0902027.
- O’Leary Z. The Essential Guide to Doing your Research Project. Thousand Oaks, CA: Sage; 2014.
- EPPI-Centre . The Evidence for Policy and Practice Information, Social Science Research Unit n.d. https://eppi.ioe.ac.uk/cms/ (accessed 8 December 2020).
- Oliver S, Harden A, Rees R, Shepher J, Brunton G, Garcia J, et al. An emerging framework for including different types of evidence in systematic reviews for public policy. Evaluation 2005;11:428-46. https://doi.org/10.1177/1356389005059383.
- Lewin S, Glenton C, Munthe-Kaas H, Carlsen B, Colvin CJ, Gülmezoglu M, et al. Using qualitative evidence in decision making for health and social interventions: an approach to assess confidence in findings from qualitative evidence syntheses (GRADE-CERQual). PLOS Med 2015;12. https://doi.org/10.1371/journal.pmed.1001895.
- Hutcheson S, Maguire H, White C. Evaluation of a pilot service to help young people with life-limiting conditions transition from children’s palliative care services. Int J Palliat Nurs 2018;24:322-32. https://doi.org/10.12968/ijpn.2018.24.7.322.
- Martin House Children’s Hospice . Supporting Children With Life-Limiting Conditions and Their Families – Research Examining Service Provision in Yorkshire and the Humber 2013.
- Young L, Egdell A, Swallow V. Qualitative accounts of young-people, parents and staff involved with a purpose-designed, pilot short-break service for 18–24 year olds with life-limiting conditions. Child Youth Serv Rev 2018;86:142-50. https://doi.org/10.1016/j.childyouth.2018.01.016.
- Dawson S, Liddicoat K. ‘Camp gives me hope’: exploring the therapeutic use of community for adults with cerebral palsy. Ther Recreation J 2009;43.
- Beresford B, Moran N, Clarke S. My Life. Growing Up and Living With Ataxia-Telangiectasia: Young People’s and Young Adults’ Experiences 2013. www.york.ac.uk/inst/spru/research/pdf/ATMyLife.pdf (accessed 26 November 2020).
- Young L, Egdell A, MacFadyen A, Swallow V. Small Service, Big Impact. Evaluation of a New Short Break Service for Young Adults with Life Limiting Conditions at St Oswald’s Hospice. Manchester: St Oswald’s Hospice and University of Manchester; 2013.
- Muscular Dystrophy Campaign . Give Us a Break: Hospice and Respite Care for Young Disabled Adults in Scotland 2014. https://lx.iriss.org.uk/sites/default/files/resources/give_us_a_break.pdf (accessed 26 November 2020).
- Shared Care Scotland . Evaluation Report on Round Two of the Short Breaks Fund 2012.
- Knighting K, Bray L, Downing J, Kirkcaldy AJ, Mitchell TK, O’Brien MR, et al. Meeting the needs of young adults with life-limiting conditions: a UK survey of current provision and future challenges for hospices [published online ahead of print May 06 2018]. J Adv Nurs 2018. https://doi.org/10.1111/jan.13702.
- Luzinat KJ, Analytis P, Hicks AJ, Warren N, Ponsford JL. The experience of a recreational camp for families with a child or young person with acquired brain injury. Neuropsychol Rehabil 2020;30:233-48. https://doi.org/10.1080/09602011.2018.1461657.
- Stylianou A. Mothers With Disabled Children in Cyprus: Experiences and Support 2017. https://discovery.ucl.ac.uk/id/eprint/10023393/1/Stylianou_10023393_Thesis.pdf (accessed 31 July 2020).
- Macdonald K, Greggans A. ‘Cool friends’: an evaluation of a community befriending programme for young people with cystic fibrosis. J Clin Nurs 2010;19:2406-14. https://doi.org/10.1111/j.1365-2702.2010.03294.x.
- Grinyer A, Payne S, Barbarachild Z. Issues of power, control and choice in children’s hospice respite care services: a qualitative study. Int J Palliat Nurs 2010;16:505-10. https://doi.org/10.12968/ijpn.2010.16.10.79216.
- Shared Care Scotland . Short Breaks Fund Evaluation of Round One Projects 2011.
- Abbott D, Carpenter J. Becoming an Adult. Transition for Young Men With Muscular Dystrophy 2010. https://research-information.bris.ac.uk/ws/portalfiles/portal/187889043/Becoming_an_Adult_Transition_for_Young_Men_with_Duchenne_Muscular_Dystrophy_PDF_922kB_.pdf (accessed 31 July 2020).
- Kerr H, Price J, O’Halloran P. A cross-sectional survey of services for young adults with life-limiting conditions making the transition from children’s to adult services in Ireland. Ir J Med Sci 2020;189:33-42. https://doi.org/10.1007/s11845-019-02054-z.
- Knighting K. Family Respite Care Survey With Young Adults and Parents: Summary Findings Report 2017.
- Young L, Cameron M. Living Longer Than You Thought I Would. Working With Young People With Complex Health Needs and Life-Limiting Conditions to Meet the Challenges Facing Them As They Grow into Adulthood 2012. www.stoswaldsuk.org/media-new/1650/st-oswalds_living-longer.pdf (accessed 8 December 2020).
- Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med 2009;6. https://doi.org/10.1371/journal.pmed.1000097.
- Arnold A, Godwin H. The Shakespeare Hospice transitional care service innovation in practice. BMJ Support Palliat Care 2017;7. https://doi.org/10.1136/bmjspcare-2017-hospice.240.
- The Asian Health Agency . Ashra Carers Project: Children &Amp; Young People With Special Needs n.d. www.taha.org.uk/services/medical-escort/ (accessed 31 July 2020).
- Barnet County Council . Barnet Short Breaks Duty Statement 2017 2018 2017. www.barnet.gov.uk/sites/default/files/assets/citizenportal/documents/childrenyoungpeopleandfamilies/Childrenandyoungpeoplewithdisabilities/ShortBreakDutyStatementPDF.pdf (accessed 26 November 2020).
- Bishop L. Making the most of life. Nurs Stand 2008;23:24-5. https://doi.org/10.7748/ns.23.5.24.s27.
- Bona K, Bates J, Wolfe J. Massachusetts’ Pediatric Palliative Care Network: successful implementation of a novel state-funded pediatric palliative care program. J Palliat Med 2011;14:1217-23. https://doi.org/10.1089/jpm.2011.0070.
- Brighton and Hove City Council . Brighton &Amp; Hove City Council Short Breaks Statement 2017–18 2017. www.brighton-hove.gov.uk/sites/default/files/migrated/article/inline/Short%20breaks%20statement%202017.pdf (accessed 26 November 2020).
- Brook L. Jacksplace – a hospice dedicated to teenagers and young adults in Hampshire. Eur J Palliat Care 2013;20:277-9.
- Care Quality Commission . Claire House Children’s Hospice Inspection Report 2015.
- Claire House Children’s Hospice . Claire House Children’s Hospice Local Offer Statement 2019.
- Care Quality Commission . Francis House Children’s Hospice Inspection Report 2016.
- Department for Education, Department of Health and Social Care . Special Educational Needs and Disability Code of Practice: 0 to 25 Years 2015.
- Department of Education and Skills, Department of Health and Social Care . Commissioning Children and Young People’s Palliative Care Services: A Practical Guide for the NHS Commissioners 2005.
- Department of Health and Social Care . Carers and Disabled Children Combined Policy Guidance Act 2000 and Carers (Equal Opportunities) Act 2004 2005.
- Department for Children, Schools and Families, Department of Health and Social Care . Aiming High for Disabled Children: Short Break Implementation Guidance 2008.
- Department for Education . The Breaks for Carers of Disabled Children Regulations 2011 2011.
- Department of Health and Social Care . Care Act 2014 – Care and Support Statutory Guidance 2018.
- East Anglia Children’s Palliative Care Managed Clinical Network . The East of England Children and Young People’s Palliative Care Service Directory n.d. www.each.org.uk/docs/default-source/MCN/east-of-england-cyp-palliative-care-service-directory.pdf?sfvrsn=92f1410b_0 (accessed 8 December 2020).
- Gans D, Hadler M, Chen X, Wu S, Dimand R, Abramson JN, et al. Impact of a pediatric palliative care program on the caregiver experience. J Hosp Palliat Nurs 2015;17:559-65. https://doi.org/10.1097/NJH.0000000000000203.
- Gans D, Kominski GF, Roby DH, Diamant AL, Chen X, Lin W, et al. Better outcomes, lower costs: palliative care program reduces stress, costs of care for children with life-threatening conditions. Policy Brief UCLA Cent Health Policy Res 2012;PB2012–3:1-8.
- Hanrahan D. A Host of Opportunities: Second NHSN Survey of Family Based Short Break Schemes for Children and Adults With Intellectual and Other Disabilities in the Republic of Ireland 2010. http://nhsn.ie/downloads/A%20Host%20of%20Opportunities%20NHSN%202010.pdf (accessed 26 November 2020).
- Health Information and Quality Authority . Draft National Standards for Residential Centres for People With Disabilities (Consultation Document) 2012.
- HM Treasury . Aiming High for Disabled Children: Better Support for Families 2007.
- Institute of Public Care . National Commissioning Board Wales. Integrated Services for Children and Young People With a Disability in Conwy. A Case Study 2019.
- Knighting K, McCann L, Forbat L, Kearney N. An Evaluation of the Rachel House at Home Service for the Children’s Hospice Association Scotland: Summary Public Report 2007.
- Knighting K. Highlights from a UK Survey of Children and Adult Hospice Provision for Young Adults With Life-Limiting Conditions n.d. https://ehospice.com/inter_childrens_posts/highlights-from-a-uk-survey-of-children-and-adult-hospice-provision-for-young-adults-with-life-limiting-conditions/ (accessed 26 November 2020).
- Knighting K, Bray L, Downing J, Kirkcaldy A, Mitchell T, O’Brien MR, et al. Short Break Provision for Young Adults With Life-Limiting Conditions: A UK Survey With Young Adults and Parents n.d.
- Knowsley Council . Knowsley Children and Family Services Short Breaks Statement n.d. www.knowsley.gov.uk/knowsleycouncil/media/Documents/kmbc-short-breaks-statement.pdf (accessed 26 November 2020).
- Leason K. Let’s Face the Music and Dance 2003. www.communitycare.co.uk/2003/03/14/lets-face-the-music-and-dance/ (accessed 31 July 2020).
- Martin House Children’s Hospice . Professionals’ Booklet 2016.
- Mitchell TK, Knighting K, O’Brien MR, Jack BA, Sutherland-Oakes J. ‘No other choice’ when children’s hospice care is unavailable: an emergency care impact assessment for Claire’s House Children’s Hospice. J Palliat Med 2016;22:57-65.
- Mitchell T, Knighting K, O’Brien MR, Jack BA, Sutherland-Oakes J. Emergency Care Impact Assessment (ECIA) Project: Claire House Children’s Hospice: Final Report 2015.
- Murphy J, Mackay M. Will Anyone Listen to Us? What Matters to Young People with Complex and Exceptional Health Needs and Their Families During Health Transitions. Stirling: Talking Mats Ltd; 2015.
- National Institute for Health and Care Excellence (NICE) . Supporting Adult Carers – Draft Guidance for Consultation 2019.
- National Institute for Health and Clinical Excellence (NICE) . Improving Outcomes in Children and Young People With Cancer 2005.
- Rainbows Hospice for Children and Young People . Rainbows Quality Account 2017–2018 2018.
- Rochdale County Council . Rochdale Short Breaks Provision for Children and Young People With Disabilities 2013.
- Social Care Institute for Excellence . Carers’ Breaks: Guidance for Commissioners and Providers 2019. www.scie.org.uk/carers/breaks (accessed 31 July 2020).
- Scottish Children and Young People’s Palliative Care Executive Group . A Framework for the Delivery of Palliative Care for Children and Young People in Scotland 2012.
- Scottish Government . National Care Standards: Short Breaks and Respite Care Services for Adults 2005. www.gov.scot/Resource/Doc/349516/0116835.pdf (accessed 31 July 2020).
- Scottish Government . Carers (Scotland) Bill 2015 2015.
- Scottish Government . Carers (Scotland) Act 2016 Statutory Guidance 2018.
- Shared Care Scotland . Short Break Case Studies 2010.
- Shared Care Scotland . It’s About Time: An Overview of Short Break (Respite Care) Planning and Provision in Scotland 2010.
- Shared Care Scotland . Evaluation Report of Creative Breaks October 2012–September 2013 2013.
- St Elizabeth Hospice . Young Adult Short Break Pilot 2019.
- St Elizabeth Hospice . Business Care for Short Stay Unit for Young Adults 2019.
- St Elizabeth Hospice . Short Break Unit Procedure for Attending With Own Carers 2019.
- St Joseph’s Hospice . St Joesph’s Hospice Quality Accounts. 2012 2013 2013.
- St Oswald’s Hospice . St Oswald’s Young Adult Service – Your Guide 2018.
- Staley K. Having a Break: Good Practice in Short Breaks for Families With Children Who Have Complex Health Needs and Disabilities 2008. www.scie.org.uk/publications/guides/guide25/files/guide25.pdf (accessed 3 July 2020).
- Together for Short Lives . Jointly Commissioning Palliative Care for Children and Young People Aged 0–25 Including Short Breaks: Guide for Local Areas in England 2015.
- Together for Short Lives . Stepping Up: A Guide to Enabling a Good Transition to Adulthood for Young People With Life-Limiting and Life-Threatening Conditions 2015.
- Urbanowicz A, Downs J, Bebbington A, Jacoby P, Girdler S, Leonard H. Use of equipment and respite services and caregiver health among Australian families living with Rett syndrome. Res Autism Spectr Disord 2011;5:722-32. https://doi.org/10.1016/j.rasd.2010.08.006.
- Welsh Government . The Breaks for Carers of Disabled Children (Wales) Regulations 2012 2012.
- Great Britain . Care and Support (Eligibility Criteria) Regulations 2015.
- Department of Health and Social Care . National Framework for NHS Continuing Healthcare and NHS-Funded Nursing Care 2018.
- Lancaster B. Social Work Services for Disabled Children and Young People and Their Families: Assessment and Eligibility 2012. https://core.ac.uk/download/pdf/9589266.pdf (accessed 26 November 2020).
- LE Wales . Respite Care in Wales. Final Report to Welsh Assembly Government 2010. https://londoneconomics.co.uk/wp-content/uploads/2011/06/2-Review-of-respite-care-in-Wales.pdf (accessed 26 November 2020).
- Hunt A, Coad J, West E, Hex N, Staniszewska S, Hacking S, et al. The BiG Study for Life-Limited Children and Their Families. Final Research Report for Together for Short Lives 2013. www.togetherforshortlives.org.uk/wp-content/uploads/2018/01/ProRes-The-Big-Study-Final-Research-Report.pdf (accessed 31 July 2020).
- Curtis LA, Burns A. Unit Costs of Health and Social Care 2018. Canterbury: PSSRU, University of Kent; 2018.
- Lavis JN, Oxman AD, Lewin S, Fretheim A. SUPPORT Tools for evidence-informed health Policymaking (STP) 3: setting priorities for supporting evidence-informed policymaking. Health Res Policy Syst 2009;7. https://doi.org/10.1186/1478-4505-7-S1-S3.
- National Confidential Enquiry into Patient Outcome and Death (NCEPOD) . Long Term Ventilation: Balancing the Pressures 2020. www.ncepod.org.uk/2020ltv.html (accessed 26 November 2020).
- National Institute for Health Research (NIHR) . UK Standards for Public Involvement in Research 2018. https://sites.google.com/nihr.ac.uk/pi-standards/standards (accessed 8 October 2018).
Appendix 1 Respite review search strategies (all databases: September 2018)
MEDLINE
(Ovid) MEDLINE(R) ALL.
Date searched: September 2018.
Date range searched: 1 January 2002 to 26 September 2018.
Search strategy
-
exp Respite Care/
-
exp Hospice Care/
-
exp HOSPICES/
-
exp “Hospice and Palliative Care Nursing”/
-
exp Day Care, Medical/
-
exp Night Care/
-
exp Intermediate Care Facilities/
-
exp Terminal Care/
-
exp HOLIDAYS/
-
“day* away”.ti,ab.
-
“day care*”.ti,ab.
-
“day centre*”.ti,ab.
-
“day center*”.ti,ab.
-
“day program*”.ti,ab.
-
“day service*”.ti,ab.
-
holiday*.ti,ab.
-
“home support*”.ti,ab.
-
hospice*.ti,ab.
-
“intermediate care”.ti,ab.
-
“night care*”.ti,ab.
-
“night-time care*”.ti,ab.
-
“partial hospitalisation*”.ti,ab.
-
“partial hospitalization*”.ti,ab.
-
“relief care*”.ti,ab.
-
“relief support”.ti,ab.
-
“residential care*”.ti,ab.
-
“residential home*”.ti,ab.
-
“residential facilit*”.ti,ab.
-
respite*.ti,ab.
-
“short break*”.ti,ab.
-
“short stay*”.ti,ab.
-
“sitting service*”.ti,ab.
-
“support program*”.ti,ab.
-
“support scheme*”.ti,ab.
-
“support service*”.ti,ab.
-
“temporary admission*”.ti,ab.
-
“temporary break*”.ti,ab.
-
“temporary care*”.ti,ab.
-
“temporary relief”.ti,ab.
-
“temporary support*”.ti,ab.
-
“short-term admission*”.ti,ab.
-
“short-term break*”.ti,ab.
-
“short-term care*”.ti,ab.
-
“short-term relief”.ti,ab.
-
“short-term support*”.ti,ab.
-
“time off”.ti,ab.
-
vacation*.ti,ab.
-
“care service*”.ti,ab.
-
“overnight stay*”.ti,ab.
-
“home-based support*”.ti,ab.
-
“befriend* service*”.ti,ab.
-
“short-break foster*”.ti,ab.
-
“adult placement scheme*”.ti,ab.
-
“shared care”.ti,ab.
-
“replacement care”.ti,ab.
-
“family support”.ti,ab.
-
or/1-56
-
exp Palliative Care/
-
exp Palliative Medicine/
-
exp Terminally Ill/
-
exp Heart Failure/
-
exp MUSCULAR DYSTROPHY, DUCHENNE/
-
exp Neoplasms/
-
exp Muscular Dystrophies/
-
exp Cerebral Palsy/
-
exp Spinal Dysraphism/
-
exp Cystic Fibrosis/
-
exp Disabled Persons/
-
exp Disabled Children/
-
exp Neurodegenerative Diseases/
-
exp Multiple Trauma/
-
exp Genetic Diseases, Inborn/
-
exp Chromosome Disorders/
-
exp “CONGENITAL, HEREDITARY, AND NEONATAL DISEASES AND
-
ABNORMALITIES”/
-
(advanc* adj3 disease*).ti,ab.
-
(advanc* adj3 illness*).ti,ab.
-
(advanc* adj3 condition*).ti,ab.
-
(advanc* adj3 disorder*).ti,ab.
-
(advanc* adj3 abnormalit*).ti,ab.
-
(advanc* adj3 impairment*).ti,ab.
-
(advanc* adj3 handicap*).ti,ab.
-
(degenerative adj3 disease*).ti,ab.
-
(degenerative adj3 illness*).ti,ab.
-
(degenerative adj3 condition*).ti,ab.
-
(degenerative adj3 disorder*).ti,ab.
-
(degenerative adj3 abnormalit*).ti,ab.
-
(degenerative adj3 impairment*).ti,ab.
-
(degenerative adj3 handicap*).ti,ab.
-
(progressive adj3 disease*).ti,ab.
-
(progressive adj3 illness*).ti,ab.
-
(progressive adj3 condition*).ti,ab.
-
(progressive adj3 disorder*).ti,ab.
-
(progressive adj3 abnormalit*).ti,ab.
-
(progressive adj3 impairment*).ti,ab.
-
(progressive adj3 handicap*).ti,ab.
-
“diminished life expectancy”.ti,ab.
-
“limited life expectancy”.ti,ab.
-
cancer*.ti,ab.
-
duchenne.ti,ab.
-
dying.ti,ab.
-
“end of life”.ti,ab.
-
(“end stage renal failure” or “end stage liver failure”).ti,ab.
-
“heart failure”.ti,ab.
-
incurable.ti,ab.
-
life-limit*.ti,ab.
-
“life limit*”.ti,ab.
-
(life adj3 short*).ti,ab.
-
(live* adj3 short*).ti,ab.
-
“life threaten*”.ti,ab.
-
“limited life expectancy”.ti,ab.
-
LLC.ti,ab.
-
LLI.ti,ab.
-
“muscular dystroph*”.ti,ab.
-
neoplasm*.ti,ab.
-
“neurodegenerative condition*”.ti,ab.
-
“neurodegenerative disease*”.ti,ab.
-
“neurodegenerative illness*”.ti,ab.
-
“neurodegenerative disorder*”.ti,ab.
-
“neurodegenerative abnormalit*”.ti,ab.
-
“neurodegenerative impairment*”.ti,ab.
-
“neurodegenerative handicap*”.ti,ab.
-
oncology.ti,ab.
-
palliative.ti,ab.
-
“poor prognosis”.ti,ab.
-
(serious* adj3 ill*).ti,ab.
-
(terminal* adj3 ill*).ti,ab.
-
(terminal* adj3 care*).ti,ab.
-
(terminal* adj3 disease*).ti,ab.
-
(terminal* adj3 condition*).ti,ab.
-
(terminal* adj3 disorder*).ti,ab.
-
(terminal* adj3 abnormalit*).ti,ab.
-
(terminal* adj3 impairment*).ti,ab.
-
(terminal* adj3 handicap*).ti,ab.
-
(genetic adj3 disease*).ti,ab.
-
(genetic adj3 disorder*).ti,ab.
-
(genetic adj3 illness*).ti,ab.
-
(genetic adj3 condition*).ti,ab.
-
(genetic adj3 abnormalit*).ti,ab.
-
(genetic adj3 impairment*).ti,ab.
-
(genetic adj3 handicap*).ti,ab.
-
(chromosomal adj3 disease*).ti,ab.
-
(chromosomal adj3 illness*).ti,ab.
-
(chromosomal adj3 disorder*).ti,ab.
-
(chromosomal adj3 condition*).ti,ab.
-
(chromosomal adj3 abnormalit*).ti,ab.
-
(chromosomal adj3 impairment*).ti,ab.
-
(chromosomal adj3 handicap*).ti,ab.
-
(congenital adj3 disease*).ti,ab.
-
(congenital adj3 illness*).ti,ab.
-
(congenital adj3 disorder*).ti,ab.
-
(congenital adj3 condition*).ti,ab.
-
(congenital adj3 abnormalit*).ti,ab.
-
(congenital adj3 impairment*).ti,ab.
-
(congenital adj3 handicap*).ti,ab.
-
“complex health* need*”.ti,ab.
-
“early death*”.ti,ab.
-
“cerebral pals*”.ti,ab.
-
“spina bifida”.ti,ab.
-
“cystic fibrosis”.ti,ab.
-
encephalopath*.ti,ab.
-
disabilit*.ti,ab.
-
disabled.ti,ab.
-
handicap*.ti,ab.
-
spastic*.ti,ab.
-
“impaired motor skill*”.ti,ab.
-
“spinal cord condition*”.ti,ab.
-
“multiple trauma”.ti,ab.
-
“acquired brain injur*”.ti,ab.
-
“neurological condition*”.ti,ab.
-
“neuromuscular condition*”.ti,ab.
-
“multi-organ disease*”.ti,ab.
-
neurodisabilit*.ti,ab.
-
or/58-172
-
“young adult*”.ti,ab.
-
“young person”.ti,ab.
-
“young people”.ti,ab.
-
youth*.ti,ab.
-
“emerg* adult*”.ti,ab.
-
“early adult*”.ti,ab.
-
(child* adj3 transition adj3 adult*).ti,ab.
-
(adolescen* adj3 transition adj3 adult*).ti,ab.
-
(teenage* adj3 transition adj3 adult*).ti,ab.
-
(paediatric* adj3 transition adj3 adult*).ti,ab.
-
(pediatric* adj3 transition adj3 adult).ti,ab.
-
“college student*”.ti,ab.
-
“university student*”.ti,ab.
-
“post-secondary student*”.ti,ab.
-
undergraduate*.ti,ab.
-
postgraduate*.ti,ab.
-
exp Young Adult/
-
exp ADOLESCENT/
-
exp ADULT/
-
exp FAMILY/
-
exp CAREGIVERS/
-
exp PARENTS/
-
famil*.ti,ab.
-
carer*.ti,ab.
-
caregiver*.ti,ab.
-
parent*.ti,ab.
-
grandparent*.ti,ab.
-
relative*.ti,ab.
-
relation*.ti,ab.
-
sibling*.ti,ab.
-
or/174-203
-
57 and 173 and 204
-
limit 205 to yr = “2002 -Current”
Cumulative Index to Nursing and Allied Health Literature
EBSCOhost.
Date searched: September 2018.
Date range searched: 1 January 2002 to 26 September 2018.
Search strategy
-
S1 (MH “Respite Care”)
-
S2 (MH “Hospice Care”)
-
S3 (MH “Hospices”)
-
S4 (MH “Hospice and Palliative Nursing”)
-
S5 (MH “Day Care”)
-
S6 (MH “Child Day Care”)
-
S7 (MH “Night Care”)
-
S8 (MH “Terminal Care+”)
-
S9 (MH “Holidays”)
-
S10 TI “day* away”
-
S11 AB “day* away”
-
S12 TI “day care*”
-
S13 AB “day care*”
-
S14 TI “day centre*”
-
S15 AB “day centre*”
-
S16 TI “day center*”
-
S17 AB “day center*”
-
S18 TI “day program*”
-
S19 AB “day program*”
-
S20 TI “day service*”
-
S21 AB “day service*”
-
S22 TI holiday*
-
S23 AB holiday*
-
S24 TI “home support*”
-
S25 AB “home support*”
-
S26 TI hospice*
-
S27 AB hospice*
-
S28 TI “intermediate care”
-
S29 AB “intermediate care”
-
S30 TI “night care*”
-
S31 AB “night care*”
-
S32 TI “night-time care*”
-
S33 AB “night-time care*”
-
S34 TI “partial hospitalisation*”
-
S35 AB “partial hospitalisation*”
-
S36 TI “partial hospitalization*”
-
S37 AB “partial hospitalization*”
-
S38 TI “relief care*”
-
S39 AB “relief care*”
-
S40 TI “relief support”
-
S41 AB “relief support”
-
S42 TI “residential care*”
-
S43 AB “residential care*”
-
S44 TI “residential home*”
-
S45 AB “residential home*”
-
S46 TI “residential facilit*”
-
S47 AB “residential facilit*”
-
S48 TI respite*
-
S49 AB respite*
-
S50 TI “short break*”
-
S51 AB “short break*”
-
S52 TI “short stay*”
-
S53 AB “short stay*”
-
S54 TI “sitting service*”
-
S55 AB “sitting service*”
-
S56 TI “support program*”
-
S57 AB “support program*”
-
S58 TI “support scheme*”
-
S59 AB “support scheme*”
-
S60 TI “support service*”
-
S61 AB “support service*”
-
S62 TI “temporary admission*”
-
S63 AB “temporary admission*”
-
S64 TI “temporary break*”
-
S65 AB “temporary break*”
-
S66 TI “temporary care*”
-
S67 AB “temporary care*”
-
S68 TI “temporary relief”
-
S69 AB “temporary relief”
-
S70 TI “temporary support*”
-
S71 AB “temporary support*”
-
S72 TI “short-term admission*”
-
S73 AB “short-term admission*”
-
S74 TI “short-term break*”
-
S75 AB “short-term break*”
-
S76 TI “short-term care*”
-
S77 AB “short-term care*”
-
S78 TI “short-term relief”
-
S79 AB “short-term relief”
-
S80 TI “short-term support*”
-
S81 AB “short-term support*”
-
S82 TI “time off”
-
S83 AB “time off”
-
S84 TI vacation*
-
S85 AB vacation*
-
S86 TI “care service*”
-
S87 AB “care service*”
-
S88 TI “overnight stay*”
-
S89 AB “overnight stay*”
-
S90 TI “home-based support*”
-
S91 AB “home-based support*”
-
S92 TI “befriend* service*”
-
S93 AB “befriend* service*”
-
S94 TI “short-break foster*”
-
S95 AB “short-break foster*”
-
S96 TI “adult placement scheme*”
-
S97 AB “adult placement scheme*”
-
S98 TI “shared care”
-
S99 AB “shared care”
-
S100 TI “replacement care”
-
S101 AB “replacement care”
-
S102 TI “family support”
-
S103 AB “family support”
-
S104 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 OR S52 OR S53 OR S54 OR S55 OR S56 OR S57 OR S58 OR S59 OR S60 OR S61 OR S62 OR S63 OR S64 OR S65 OR S66 OR S67 OR S68 OR S69 OR S70 OR S71 OR S72 OR S73 OR S74 OR S75 OR S76 OR S77 OR S78 OR S79 OR S80 OR S81 OR S82 OR S83 OR S84 OR S85 OR S86 OR S87 OR S88 OR S89 OR S90 OR S91 OR S92 OR S93 OR S94 OR S95 OR S96 OR S97 OR S98 OR S99 OR S100 OR S101 OR S102 OR S103
-
S105 (MH “Palliative Care”)
-
S106 (MH “Terminally Ill Patients+”)
-
S107 (MH “Heart Failure”)
-
S108 (MH “Muscular Dystrophy+”)
-
S109 (MH “Muscular Dystrophy, Duchenne+”)
-
S110 (MH “Neoplasms+”)
-
S111 (MH “Cerebral Palsy”)
-
S112 (MH “Spina Bifida”)
-
S113 (MH “Cystic Fibrosis”)
-
S114 (MH “Disabled+”)
-
S115 (MH “Multiple Trauma”)
-
S116 (MH “Neurodegenerative Diseases+”)
-
S117 (MH “Chromosome Disorders”)
-
S118 TI cancer*
-
S119 AB cancer*
-
S120 TI advanc* N3 disease*
-
S121 AB advanc* N3 disease*
-
S122 TI advanc* N3 illness*
-
S123 AB advanc* N3 illness*
-
S124 TI advanc* N3 condition*
-
S125 AB advanc* N3 condition*
-
S126 TI advanc* N3 disorder*
-
S127 AB advanc* N3 disorder*
-
S128 TI advanc* adj3 abnormalit*
-
S129 AB advanc* N3 abnormalit*
-
S130 TI advanc* N3 impairment*
-
S131 AB advanc* N3 impairment*
-
S132 TI advanc* N3 handicap*
-
S133 AB advanc* N3 handicap*
-
S134 TI degenerative N3 disease*
-
S135 AB degenerative N3 disease*
-
S136 TI degenerative N3 illness*
-
S137 AB degenerative N3 illness*
-
S138 TI degenerative N3 condition*
-
S139 AB degenerative N3 condition*
-
S140 TI degenerative N3 disorder*
-
S141 AB degenerative N3 disorder*
-
S142 TI degenerative N3 abnormalit*
-
S143 AB degenerative N3 abnormalit*
-
S144 TI degenerative N3 impairment*
-
S145 AB degenerative N3 impairment*
-
S146 TI degenerative N3 handicap*
-
S147 AB degenerative N3 handicap*
-
S148 TI progressive N3 disease*
-
S149 AB progressive N3 disease*
-
S150 TI progressive N3 illness*
-
S151 AB progressive N3 illness*
-
S152 TI progressive N3 condition*
-
S153 AB progressive N3 condition*
-
S154 TI progressive N3 disorder*
-
S155 AB progressive N3 disorder*
-
S156 TI progressive N3 abnormalit*
-
S157 AB progressive N3 abnormalit*
-
S158 TI progressive N3 impairment*
-
S159 AB progressive N3 impairment*
-
S160 TI progressive N3 handicap*
-
S161 AB progressive N3 handicap*
-
S162 TI “diminished life expectancy”
-
S163 AB “diminished life expectancy”
-
S164 TI “limited life expectancy” OR AB “limited life expectancy”
-
S165 TI duchenne
-
S166 AB duchenne
-
S167 TI dying
-
S168 AB dying
-
S169 TI “end of life”
-
S170 AB “end of life”
-
S171 TI “end stage renal failure”
-
S172 AB “end stage renal failure”
-
S173 TI “end stage liver failure”
-
S174 AB “end stage liver failure”
-
S175 TI “heart failure”
-
S176 AB “heart failure”
-
S177 TI incurable
-
S178 AB incurable
-
S179 TI life-limit*
-
S180 AB life-limit*
-
S181 TI “life limit*”
-
S182 AB “life limit*”
-
S183 TI life N3 short*
-
S184 AB life N3 short*
-
S185 TI live* N3 short*
-
S186 AB live* N3 short*
-
S187 TI “life threaten*”
-
S188 AB “life threaten*”
-
S189 TI “limited life expectancy”
-
S190 AB “limited life expectancy”
-
S191 TI LLC
-
S192 AB LLC
-
S193 TI LLI
-
S194 AB LLI
-
S195 TI “muscular dystroph*”
-
S196 AB “muscular dystroph*”
-
S197 TI neoplasm*
-
S198 AB neoplasm*
-
S199 TI “neurodegenerative disease*”
-
S200 AB “neurodegenerative disease*”
-
S201 TI “neurodegenerative condition*”
-
S202 AB “neurodegenerative condition*”
-
S203 TI “neurodegenerative illness*”
-
S204 AB “neurodegenerative illness*”
-
S205 TI “neurodegenerative disorder*”
-
S206 AB “neurodegenerative disorder*”
-
S207 TI “neurodegenerative abnormalit*”
-
S208 AB “neurodegenerative abnormalit*”
-
S209 TI “neurodegenerative impairment*”
-
S210 AB “neurodegenerative impairment*”
-
S211 TI “neurodegenerative handicap*”
-
S212 AB “neurodegenerative handicap*”
-
S213 TI oncology
-
S214 AB oncology
-
S215 TI palliative
-
S216 AB palliative
-
S217 TI “poor prognosis”
-
S218 AB “poor prognosis”
-
S219 TI serious* N3 ill*
-
S220 AB serious* N3 ill*
-
S221 TI terminal* N3 ill*
-
S222 AB terminal* N3 ill*
-
S223 TI terminal* N3 care*
-
S224 AB terminal* N3 care*
-
S225 TI terminal* N3 disease*
-
S226 AB terminal* N3 disease*
-
S227 TI terminal* N3 condition*
-
S228 AB terminal* N3 condition*
-
S229 TI terminal* N3 disorder*
-
S230 AB terminal* N3 disorder*
-
S231 TI terminal* N3 abnormalit*
-
S232 AB terminal* N3 abnormalit*
-
S233 TI terminal* N3 impairment*
-
S234 AB terminal* N3 impairment*
-
S235 TI terminal* N3 handicap*
-
S236 AB terminal* N3 handicap*
-
S237 TI genetic N3 disease*
-
S238 AB genetic N3 disease*
-
S239 TI genetic N3 disorder*
-
S240 AB genetic N3 disorder*
-
S241 TI genetic N3 illness*
-
S242 AB genetic N3 illness*
-
S243 TI genetic N3 condition*
-
S244 AB genetic N3 condition*
-
S245 TI genetic N3 abnormalit*
-
S246 AB genetic N3 abnormalit*
-
S247 TI genetic N3 impairment*
-
S248 AB genetic N3 impairment*
-
S249 TI genetic N3 handicap*
-
S250 AB genetic N3 handicap*
-
S251 TI chromosomal N3 disease*
-
S252 AB chromosomal N3 disease*
-
S253 TI chromosomal N3 illness*
-
S254 AB chromosomal N3 illness*
-
S255 TI chromosomal N3 disorder*
-
S256 AB chromosomal N3 disorder*
-
S257 TI chromosomal N3 condition*
-
S258 AB chromosomal N3 condition*
-
S259 TI chromosomal N3 abnormalit*
-
S260 TI chromosomal N3 impairment*
-
S261 AB chromosomal N3 impairment*
-
S262 TI chromosomal N3 handicap*
-
S263 AB chromosomal N3 handicap*
-
S264 TI congenital N3 disease*
-
S265 AB congenital N3 disease*
-
S266 TI congenital N3 illness*
-
S267 AB congenital N3 illness*
-
S268 TI congenital N3 disorder*
-
S269 AB congenital N3 disorder*
-
S270 TI congenital N3 condition*
-
S271 AB congenital N3 condition*
-
S272 TI congenital N3 abnormalit*
-
S273 AB congenital N3 abnormalit*
-
S274 TI congenital N3 impairment*
-
S275 AB congenital N3 impairment*
-
S276 TI congenital N3 handicap*
-
S277 AB congenital N3 handicap*
-
S278 TI “complex health* need*”
-
S279 AB “complex health* need*”
-
S280 TI “early death*”
-
S281 AB “early death*”
-
S282 TI “cerebral pals*”
-
S283 AB “cerebral pals*”
-
S284 TI “spina bifida”
-
S285 AB “spina bifida”
-
S286 TI “cystic fibrosis”
-
S287 AB “cystic fibrosis”
-
S288 TI encephalopath*
-
S289 AB encephalopath*
-
S290 TI disabilit*
-
S291 AB disabilit*
-
S292 TI disabled
-
S293 AB disabled
-
S294 TI handicap*
-
S295 AB handicap*
-
S296 TI spastic*
-
S297 AB spastic*
-
S298 TI “impaired motor skill*”
-
S299 AB “impaired motor skill*”
-
S300 TI “spinal cord condition*”
-
S301 AB “spinal cord condition*”
-
S302 TI “multiple trauma”
-
S303 AB “multiple trauma”
-
S304 TI “acquired brain injur*”
-
S305 AB “acquired brain injur*”
-
S306 TI “neurological condition*”
-
S307 AB “neurological condition*”
-
S308 TI “neuromuscular condition*”
-
S309 AB “neuromuscular condition*”
-
S310 TI “multi-organ disease*”
-
S311 AB “multi-organ disease*”
-
S312 TI neurodisabilit*
-
S313 AB neurodisabilit*
-
S314 S105 OR S106 OR S107 OR S108 OR S109 OR S110 OR S111 OR S112 OR S113 OR S114 OR S115 OR S116 OR S117 OR S118 OR S119 OR S120 OR S121 OR S122 OR S123 OR S124 OR S125 OR S126 OR S127 OR S128 OR S129 OR S130 OR S131 OR S132 OR S133 OR S134 OR S135 OR S136 OR S137 OR S138 OR S139 OR S140 OR S141 OR S142 OR S143 OR S144 OR S145 OR S146 OR S147 OR S148 OR S149 OR S150 OR S151 OR S152 OR S153 OR S154 OR S155 OR S156 OR S157 OR S158 OR S159 OR S160 OR S161 OR S162 OR S163 OR S164 OR S165 OR S166 OR S167 OR S168 OR S169 OR S170 OR S171 OR S172 OR S173 OR S174 OR S175 OR S176 OR S177 OR S178 OR S179 OR S180 OR S181 OR S182 OR S183 OR S184 OR S185 OR S186 OR S187 OR S188 OR S189 OR S190 OR S191 OR S192 OR S193 OR S194 OR S195 OR S196 OR S197 OR S198 OR S199 OR S200 OR S201 OR S202 OR S203 OR S204 OR S205 OR S206 OR S207 OR S208 OR S209 OR S210 OR S211 OR S212 OR S213 OR S214 OR S215 OR S216 OR S217 OR S218 OR S219 OR S220 OR S221 OR S222 OR S223 OR S224 OR S225 OR S226 OR S227 OR S228 OR S229 OR S230 OR S231 OR S232 OR S233 OR S234 OR S235 OR S236 OR S237 OR S238 OR S239 OR S240 OR S241 OR S242 OR S243 OR S244 OR S245 OR S246 OR S247 OR S248 OR S249 OR S250 OR S251 OR S252 OR S253 OR S254 OR S255 OR S256 OR S257 OR S258 OR S259 OR S260 OR S261 OR S262 OR S263 OR S264 OR S265 OR S266 OR S267 OR S268 OR S269 OR S270 OR S271 OR S272 OR S273 OR S274 OR S275 OR S276 OR S277 OR S278 OR S279 OR S280 OR S281 OR S282 OR S283 OR S284 OR S285 OR S286 OR S287 OR S288 OR S289 OR S290 OR S291 OR S292 OR S293 OR S294 OR S295 OR S296 OR S297 OR S298 OR S299 OR S300 OR S301 OR S302 OR S303 OR S304 OR S305 OR S306 OR S307 OR S308 OR S309 OR S310 OR S311 OR S312 OR S313
-
S315 (MH “Young Adult”)
-
S316 (MH “Adolescence+”)
-
S317 (MH “Adult+”)
-
S318 (MH “Family+”)
-
S319 (MH “Caregivers”)
-
S320 (MH “Parents+”)
-
S321 (MH “Students, Graduate”)
-
S322 (MH “Students, Undergraduate”)
-
S323 (MH “Students, College”)
-
S324 (MH “Grandparents”)
-
S325 (MH “Siblings”)
-
S326 (MH “Extended Family”)
-
S327 TI “young adult*”
-
S328 AB “young adult*”
-
S329 TI “young person”
-
S330 TI “young person”
-
S331 TI “young people”
-
S332 AB “young people”
-
S333 TI youth*
-
S334 AB youth*
-
S335 TI “emerg* adult*”
-
S336 AB “emerg* adult*”
-
S337 TI “early adult*”
-
S338 AB “early adult*”
-
S339 TI child* N3 transition N3 adult*
-
S340 AB child* N3 transition N3 adult*
-
S341 TI adolescen* N3 transition N3 adult*
-
S342 AB adolescen* N3 transition N3 adult*
-
S343 TI teenage* N3 transition N3 adult*
-
S344 AB teenage* N3 transition N3 adult*
-
S345 TI paediatric* N3 transition N3 adult*
-
S346 AB paediatric* N3 transition N3 adult*
-
S347 TI pediatric* N3 transition N3 adult*
-
S348 AB pediatric* N3 transition N3 adult*
-
S349 TI “college student*”
-
S350 AB “college student*”
-
S351 TI “university student*”
-
S352 AB “university student*”
-
S353 TI “post-secondary student*”
-
S354 AB “post-secondary student*”
-
S355 TI undergraduate*
-
S356 AB undergraduate*
-
S357 TI postgraduate*
-
S358 AB postgraduate*
-
S359 TI famil*
-
S360 AB famil*
-
S361 TI carer*
-
S362 AB carer*
-
S363 TI caregiver*
-
S364 AB caregiver*
-
S365 TI parent*
-
S366 AB parent*
-
S367 TI grandparent*
-
S368 AB grandparent*
-
S369 TI relative*
-
S370 AB relative*
-
S371 TI relation*
-
S372 AB relation*
-
S373 TI sibling*
-
S374 AB sibling*
-
S375 S315 OR S316 OR S317 OR S318 OR S319 OR S320 OR S321 OR S322 OR S323 OR S324 OR S325 OR S326 OR S327 OR S328 OR S329 OR S330 OR S331 OR S332 OR S333 OR S334 OR S335 OR S336 OR S337 OR S338 OR S339 OR S340 OR S341 OR S342 OR S343 OR S344 OR S345 OR S346 OR S347 OR S348 OR S349 OR S350 OR S351 OR S352 OR S353 OR S354 OR S355 OR S356 OR S357 OR S358 OR S359 OR S360 OR S361 OR S362 OR S363 OR S364 OR S365 OR S366 OR S367 OR S368 OR S369 OR S370 OR S371 OR S372 OR S373 OR S374
-
S376 S104 AND S314 AND S375
-
S377 S104 AND S314 AND S375 Limit 2002-2018
EMBASE
Ovid.
Date searched:
Date range searched: 1996 to week 38 2018.
Search strategy
-
exp respite care/
-
exp hospice care/
-
exp hospice/
-
exp “HOSPICE AND PALLIATIVE CARE NURSING”/
-
exp “DAY CARE, MEDICAL”/
-
exp day care/
-
exp night care/
-
exp terminal care/
-
“day* away”.ti,ab.
-
“day care*”.ti,ab.
-
“day centre*”.ti,ab.
-
“day center*”.ti,ab.
-
“day program*”.ti,ab.
-
“day service*”.ti,ab.
-
holiday*.ti,ab.
-
“home support*”.ti,ab.
-
hospice*.ti,ab.
-
“intermediate care”.ti,ab.
-
“night care*”.ti,ab.
-
“night-time care*”.ti,ab.
-
“partial hospitalisation*”.ti,ab.
-
“partial hospitalization*”.ti,ab.
-
“relief care*”.ti,ab.
-
“relief support”.ti,ab.
-
exp “RESIDENTIAL CARE”/
-
“residential care*”.ti,ab.
-
exp “RESIDENTIAL HOME”/
-
“residential home*”.ti,ab.
-
“residential facilit*”.ti,ab.
-
respite*.ti,ab.
-
“short break*”.ti,ab.
-
“short stay*”.ti,ab.
-
“sitting service*”.ti,ab.
-
“support program*”.ti,ab.
-
“support scheme*”.ti,ab.
-
“support service*”.ti,ab.
-
“temporary admission*”.ti,ab.
-
“temporary break*”.ti,ab.
-
“temporary care*”.ti,ab.
-
“temporary relief”.ti,ab.
-
“temporary support*”.ti,ab.
-
“short-term admission*”.ti,ab.
-
“short-term break*”.ti,ab.
-
“short-term care*”.ti,ab.
-
“short-term relief”.ti,ab.
-
“short-term support*”.ti,ab.
-
“time off”.ti,ab.
-
vacation*.ti,ab.
-
“care service*”.ti,ab.
-
“overnight stay*”.ti,ab.
-
“home-based support*”.ti,ab.
-
“befriend* service*”.ti,ab.
-
“short-break foster*”.ti,ab.
-
“adult placement scheme*”.ti,ab.
-
“shared care”.ti,ab.
-
“replacement care”.ti,ab.
-
“family support”.ti,ab.
-
or/1-57
-
exp palliative therapy/
-
exp terminally ill patient/
-
exp heart failure/
-
exp muscular dystrophy/
-
exp duchenne muscular dystrophy/
-
exp neoplasm/
-
exp cerebral palsy/
-
exp spinal dysraphism/
-
exp cystic fibrosis/
-
exp disabled person/
-
exp handicapped child/
-
exp multiple trauma/
-
exp degenerative disease/
-
exp chromosome disorder/
-
exp congenital disorder/
-
exp genetic disorder/
-
(advanc* adj3 disease*).ti,ab.
-
(advanc* adj3 illness*).ti,ab.
-
(advanc* adj3 condition*).ti,ab.
-
(advanc* adj3 disorder*).ti,ab.
-
(advanc* adj3 abnormalit*).ti,ab.
-
(advanc* adj3 impairment*).ti,ab.
-
(advanc* adj3 handicap*).ti,ab.
-
(degenerative adj3 disease*).ti,ab.
-
(degenerative adj3 illness*).ti,ab.
-
(degenerative adj3 condition*).ti,ab.
-
(degenerative adj3 disorder*).ti,ab.
-
(degenerative adj3 abnormalit*).ti,ab.
-
(degenerative adj3 impairment*).ti,ab.
-
(degenerative adj3 handicap*).ti,ab.
-
(progressive adj3 disease*).ti,ab.
-
(progressive adj3 illness*).ti,ab.
-
(progressive adj3 condition*).ti,ab.
-
(progressive adj3 disorder*).ti,ab.
-
(progressive adj3 abnormalit*).ti,ab.
-
(progressive adj3 impairment*).ti,ab.
-
(progressive adj3 handicap*).ti,ab.
-
“diminished life expectancy”.ti,ab.
-
“limited life expectancy”.ti,ab.
-
cancer*.ti,ab.
-
duchenne.ti,ab.
-
dying.ti,ab.
-
“end of life”.ti,ab.
-
“end stage renal failure”.ti,ab.
-
“end stage liver failure”.ti,ab.
-
“heart failure”.ti,ab.
-
incurable.ti,ab.
-
life-limit*.ti,ab.
-
“life limit*”.ti,ab.
-
(life adj3 short*).ti,ab.
-
(live* adj3 short*).ti,ab.
-
“life threaten*”.ti,ab.
-
“limited life expectancy”.ti,ab.
-
LLC.ti,ab.
-
LLI.ti,ab.
-
“muscular dystroph*”.ti,ab.
-
neoplasm*.ti,ab.
-
“neurodegenerative disease*”.ti,ab.
-
“neurodegenerative condition*”.ti,ab.
-
“neurodegenerative illness*”.ti,ab.
-
“neurodegenerative disorder*”.ti,ab.
-
“neurodegenerative abnormalit*”.ti,ab.
-
“neurodegenerative impairment*”.ti,ab.
-
“neurodegenerative handicap*”.ti,ab.
-
oncology.ti,ab.
-
palliative.ti,ab.
-
“poor prognosis”.ti,ab.
-
(serious* adj3 ill*).ti,ab.
-
(terminal* adj3 ill*).ti,ab.
-
(terminal* adj3 care*).ti,ab.
-
(terminal* adj3 disease*).ti,ab.
-
(terminal* adj3 condition*).ti,ab.
-
(terminal* adj3 disorder*).ti,ab.
-
(terminal* adj3 abnormalit*).ti,ab.
-
(terminal* adj3 impairment*).ti,ab.
-
(terminal* adj3 handicap*).ti,ab.
-
(genetic adj3 disease*).ti,ab.
-
(genetic adj3 disorder*).ti,ab.
-
(genetic adj3 illness*).ti,ab.
-
(genetic adj3 condition*).ti,ab.
-
(genetic adj3 abnormalit*).ti,ab.
-
(genetic adj3 impairment*).ti,ab.
-
(genetic adj3 handicap*).ti,ab.
-
(chromosomal adj3 disease*).ti,ab.
-
(chromosomal adj3 illness*).ti,ab.
-
(chromosomal adj3 disorder*).ti,ab.
-
(chromosomal adj3 condition*).ti,ab.
-
(chromosomal adj3 abnormalit*).ti,ab.
-
(chromosomal adj3 impairment*).ti,ab.
-
(chromosomal adj3 handicap*).ti,ab.
-
(congenital adj3 disease*).ti,ab.
-
(congenital adj3 illness*).ti,ab.
-
(congenital adj3 disorder*).ti,ab.
-
(congenital adj3 condition*).ti,ab.
-
(congenital adj3 abnormalit*).ti,ab.
-
(congenital adj3 impairment*).ti,ab.
-
(congenital adj3 handicap*).ti,ab.
-
“complex health* need*”.ti,ab.
-
“early death*”.ti,ab.
-
“cerebral pals*”.ti,ab.
-
“spina bifida”.ti,ab.
-
“cystic fibrosis”.ti,ab.
-
encephalopath*.ti,ab.
-
disabilit*.ti,ab.
-
disabled.ti,ab.
-
handicap*.ti,ab.
-
spastic*.ti,ab.
-
“impaired motor skill*”.ti,ab.
-
“spinal cord condition*”.ti,ab.
-
“multiple trauma”.ti,ab.
-
“acquired brain injur*”.ti,ab.
-
“neurological condition*”.ti,ab.
-
“neuromuscular condition*”.ti,ab.
-
“multi-organ disease*”.ti,ab.
-
neurodisabilit*.ti,ab.
-
or/59-173
-
“young adult*”.ti,ab.
-
“young person”.ti,ab.
-
“young people”.ti,ab.
-
youth*.ti,ab.
-
“emerg* adult*”.ti,ab.
-
“early adult*”.ti,ab.
-
(child* adj3 transition adj3 adult*).ti,ab.
-
(adolescen* adj3 transition adj3 adult*).ti,ab.
-
(teenage* adj3 transition adj3 adult*).ti,ab.
-
(paediatric* adj3 transition adj3 adult*).ti,ab.
-
(pediatric* adj3 transition adj3 adult*).ti,ab.
-
“college student*”.ti,ab.
-
“university student*”.ti,ab.
-
“post-secondary student*”.ti,ab.
-
undergraduate*.ti,ab.
-
postgraduate*.ti,ab.
-
exp “YOUNG ADULT”/
-
exp ADULT/
-
exp ADOLESCENT/
-
exp FAMILY/
-
exp CAREGIVER/
-
exp PARENT/
-
famil*.ti,ab.
-
carer*.ti,ab.
-
caregiver*.ti,ab.
-
parent*.ti,ab.
-
grandparent*.ti,ab.
-
relative*.ti,ab.
-
relation*.ti,ab.
-
sibling*.ti,ab.
-
exp SIBLING/
-
exp GRANDPARENT/
-
exp RELATIVE/
-
exp UNIVERSITY STUDENT/
-
exp COLLEGE STUDENT/
-
or/175-209
-
58 and 174 and 210
-
limit 211 to yr = “2002 -Current”
PsycINFO
EBSCOhost.
Date searched: September 2018.
Date range searched: 1 January 2002 to 26 September 2018.
Search strategy
-
S1 DE “Respite Care”
-
S2 DE “Hospice”
-
S3 DE “Child Day Care”
-
S4 DE “Adult Day Care”
-
S5 DE “Day Care Centers”
-
S6 DE “Holidays”
-
S7 TI “day* away”
-
S8 AB “day* away”
-
S9 TI “day care*”
-
S10 AB “day care*”
-
S11 TI “day centre*”
-
S12 AB “day centre*”
-
S13 TI “day center*”
-
S14 AB “day center*”
-
S15 TI “day program*”
-
S16 AB “day program*”
-
S17 TI “day service*”
-
S18 AB “day service*”
-
S19 TI holiday*
-
S20 AB holiday*
-
S21 TI “home support*”
-
S22 AB “home support*”
-
S23 TI hospice*
-
S24 AB hospice*
-
S25 TI “intermediate care”
-
S26 AB “intermediate care”
-
S27 TI “night care*”
-
S28 AB “night care*”
-
S29 TI “night-time care*”
-
S30 AB “night-time care*”
-
S31 TI “partial hospitalisation*”
-
S32 AB “partial hospitalisation*”
-
S33 TI “partial hospitalization*”
-
S34 AB “partial hospitalization*”
-
S35 TI “relief care*”
-
S36 AB “relief care*”
-
S37 TI “relief support”
-
S38 AB “relief support”
-
S39 TI “residential care*”
-
S40 AB “residential care*”
-
S41 TI “residential home*”
-
S42 AB “residential home*”
-
S43 TI “residential facilit*”
-
S44 AB “residential facilit*”
-
S45 TI respite*
-
S46 AB respite*
-
S47 TI “short break*”
-
S48 AB “short break*”
-
S49 TI “short stay*”
-
S50 AB “short stay*”
-
S51 TI “sitting service*”
-
S52 AB “sitting service*”
-
S53 TI “support program*”
-
S54 AB “support program*”
-
S55 TI “support scheme*”
-
S56 AB “support scheme*”
-
S57 TI “support service*”
-
S58 AB “support service*”
-
S59 TI “temporary admission*”
-
S60 AB “temporary admission*”
-
S61 TI “temporary break*”
-
S62 AB “temporary break*”
-
S63 TI “temporary care*”
-
S64 AB “temporary care*”
-
S65 TI “temporary relief”
-
S66 AB “temporary relief”
-
S67 TI “temporary support*”
-
S68 AB “temporary support*”
-
S69 TI “short-term admission*”
-
S70 AB “short-term admission*”
-
S71 TI “short-term break*”
-
S72 AB “short-term break*”
-
S73 TI “short-term care*”
-
S74 AB “short-term care*”
-
S75 TI “short-term relief”
-
S76 AB “short-term relief”
-
S77 TI “short-term support*”
-
S78 AB “short-term support*”
-
S79 TI “time off”
-
S80 AB “time off”
-
S81 TI vacation*
-
S82 AB vacation*
-
S83 TI “care service*”
-
S84 AB “care service*”
-
S85 TI “overnight stay*”
-
S86 AB “overnight stay*”
-
S87 TI “home-based support*”
-
S88 AB “home-based support*”
-
S89 TI “befriend* service*”
-
S90 AB “befriend* service*”
-
S91 TI “short-break foster*”
-
S92 AB “short-break foster*”
-
S93 TI “adult placement scheme*”
-
S94 AB “adult placement scheme*”
-
S95 TI “shared care”
-
S96 AB “shared care”
-
S97 TI “replacement care”
-
S98 AB “replacement care”
-
S99 TI “family support”
-
S100 AB “family support”
-
S101 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 OR S52 OR S53 OR S54 OR S55 OR S56 OR S57 OR S58 OR S59 OR S60 OR S61 OR S62 OR S63 OR S64 OR S65 OR S66 OR S67 OR S68 OR S69 OR S70 OR S71 OR S72 OR S73 OR S74 OR S75 OR S76 OR S77 OR S78 OR S79 OR S80 OR S81 OR S82 OR S83 OR S84 OR S85 OR S86 OR S87 OR S88 OR S89 OR S90 OR S91 OR S92 OR S93 OR S94 OR S95 OR S96 OR S97 OR S98 OR S99 OR S100 OR S101
-
S102 DE “Palliative Care”
-
S103 DE “Terminally Ill Patients”
-
S104 DE “Muscular Dystrophy”
-
S105 DE “Neoplasms” OR DE “Benign Neoplasms” OR DE “Breast Neoplasms” OR DE “Endocrine Neoplasms” OR DE “Leukemias” OR DE “Melanoma” OR DE “Metastasis” OR DE “Nervous System Neoplasms” OR DE “Terminal Cancer”
-
S106 DE “Cerebral Palsy”
-
S107 DE “Spina Bifida”
-
S108 DE “Cystic Fibrosis”
-
S109 DE “Multiple Disabilities”
-
S110 DE “Neurodegenerative Diseases” OR DE “Alzheimer’s Disease” OR DE “Amyotrophic Lateral Sclerosis” OR DE “Corticobasal Degeneration” OR DE “Dementia with Lewy Bodies” OR DE “Multiple System Atrophy” OR DE “Parkinson’s Disease” OR DE “Semantic Dementia”
-
S111 DE “Genetic Disorders” OR DE “Albinism” OR DE “Charcot-Marie-Tooth Disease” OR DE “Chromosome Disorders” OR DE “Cornelia De Lange Syndrome” OR DE “Huntingtons Disease” OR DE “MELAS” OR DE “Neurofibromatosis” OR DE “Phenylketonuria” OR DE “Porphyria” OR DE “Rh Incompatibility” OR DE “Sex Linked Hereditary Disorders” OR DE “Sickle Cell Disease” OR DE “Tay Sachs Disease” OR DE “Williams Syndrome”
-
S112 DE “Chromosome Disorders” OR DE “Autosome Disorders” OR DE “Deletion (Chromosome)” OR DE “Sex Chromosome Disorders” OR DE “Translocation (Chromosome)” OR DE “Trisomy” OR DE “Williams Syndrome”
-
S113 DE “Congenital Disorders” OR DE “Agenesis” OR DE “Cleft Palate” OR DE “Drug Induced Congenital Disorders” OR DE “Hermaphroditism” OR DE “Microcephaly” OR DE “Prader Willi Syndrome” OR DE “Spina Bifida”
-
S114 DE “Encephalopathies” OR DE “Creutzfeldt Jakob Syndrome” OR DE “Leukoencephalopathy” OR DE “Toxic Encephalopathies” OR DE “Wernicke’s Syndrome”
-
S115 TI cancer*
-
S116 AB cancer*
-
S117 TI (advanc* N3 disease*)
-
S118 AB (advanc* N3 disease*)
-
S119 TI (advanc* N3 illness*)
-
S120 AB (advanc* N3 illness*)
-
S121 TI (advanc* N3 condition*)
-
S122 AB (advanc* N3 condition*)
-
S123 TI (advanc* N3 disorder*)
-
S124 AB (advanc* N3 disorder*)
-
S125 TI (advanc* adj3 abnormalit*)
-
S126 AB (advanc* adj3 abnormalit*)
-
S127 TI (advanc* N3 impairment*)
-
S128 TI (advanc* N3 impairment*)
-
S129 AB (advanc* N3 impairment*)
-
S130 TI (advanc* N3 handicap*)
-
S131 AB (advanc* N3 handicap*)
-
S132 TI (degenerative N3 disease*)
-
S133 AB (degenerative N3 disease*)
-
S134 TI (degenerative N3 illness*)
-
S135 AB (degenerative N3 illness*)
-
S136 TI (degenerative N3 condition*)
-
S137 AB (degenerative N3 condition*)
-
S138 TI (degenerative N3 disorder*)
-
S139 AB (degenerative N3 disorder*)
-
S140 TI (degenerative N3 abnormalit*)
-
S141 AB (degenerative N3 abnormalit*)
-
S142 TI (degenerative N3 impairment*)
-
S143 AB (degenerative N3 impairment*)
-
S144 TI (degenerative N3 handicap*)
-
S145 AB (degenerative N3 handicap*)
-
S146 TI (progressive N3 disease*)
-
S147 AB (progressive N3 disease*)
-
S148 TI (progressive N3 illness*)
-
S149 AB (progressive N3 illness*)
-
S150 TI (progressive N3 condition*)
-
S151 AB (progressive N3 condition*)
-
S152 TI (progressive N3 disorder*)
-
S153 AB (progressive N3 disorder*)
-
S154 TI (progressive N3 abnormalit*)
-
S155 AB (progressive N3 abnormalit*)
-
S156 TI (progressive N3 impairment*)
-
S157 AB (progressive N3 impairment*)
-
S158 TI (progressive N3 handicap*)
-
S159 AB (progressive N3 handicap*)
-
S160 TI (“diminished life expectancy”)
-
S161 AB (“diminished life expectancy”)
-
S162 TI (“limited life expectancy”)
-
S163 AB (“limited life expectancy”)
-
S164 TI duchenne
-
S165 AB duchenne
-
S166 TI dying
-
S167 AB dying
-
S168 TI (“end of life”)
-
S169 AB (“end of life”)
-
S170 TI “end stage liver failure”
-
S171 AB “end stage liver failure”
-
S172 TI “end stage renal failure”
-
S173 AB “end stage renal failure”
-
S174 TI “heart failure”
-
S175 AB “heart failure”
-
S176 TI incurable
-
S177 AB incurable
-
S178 TI life-limit*
-
S179 AB life-limit*
-
S180 TI “life limit*”
-
S181 AB “life limit*”
-
S182 TI (life N3 short*)
-
S183 AB (life N3 short*)
-
S184 TI (live* N3 short*)
-
S185 AB (live* N3 short*)
-
S186 TI (“life threaten*”)
-
S187 AB (“life threaten*”)
-
S188 TI “limited life expectancy”
-
S189 AB “limited life expectancy”
-
S190 TI (LLC)
-
S191 AB (LLC)
-
S192 TI (LLI)
-
S193 AB (LLI)
-
S194 TI “muscular dystroph*”
-
S195 AB “muscular dystroph*”
-
S196 TI neoplasm*
-
S197 AB neoplasm*
-
S198 TI (“neurodegenerative disease*”)
-
S199 AB (“neurodegenerative disease*”)
-
S200 TI (“neurodegenerative condition*”)
-
S201 TI (“neurodegenerative condition*”)
-
S202 AB (“neurodegenerative condition*”)
-
S203 TI (“neurodegenerative illness*”)
-
S204 AB (“neurodegenerative illness*”)
-
S205 TI “neurodegenerative disorder*”
-
S206 AB “neurodegenerative disorder*”
-
S207 TI “neurodegenerative abnormalit*”
-
S208 AB “neurodegenerative abnormalit*”
-
S209 TI “neurodegenerative impairment*”
-
S210 AB “neurodegenerative impairment*”
-
S211 TI “neurodegenerative handicap*”
-
S212 AB “neurodegenerative handicap*”
-
S213 TI oncology
-
S214 AB oncology
-
S215 TI palliative
-
S216 AB palliative
-
S217 TI “poor prognosis”
-
S218 AB “poor prognosis”
-
S219 TI (serious* N3 ill*)
-
S220 AB (serious* N3 ill*)
-
S221 TI (terminal* N3 ill*)
-
S222 AB (terminal* N3 ill*)
-
S223 TI (terminal* N3 care*)
-
S224 AB (terminal* N3 care*)
-
S225 TI (terminal* N3 disease*)
-
S226 AB (terminal* N3 disease*)
-
S227 TI (terminal* N3 condition*)
-
S228 AB (terminal* N3 condition*)
-
S229 TI (terminal* N3 disorder*)
-
S230 AB (terminal* N3 disorder*)
-
S231 TI (terminal* N3 abnormalit*)
-
S232 AB (terminal* N3 abnormalit*)
-
S233 TI (terminal* N3 impairment*)
-
S234 AB (terminal* N3 impairment*)
-
S235 TI (terminal* N3 handicap*)
-
S236 AB (terminal* N3 handicap*)
-
S237 TI (genetic N3 disease*)
-
S238 AB (genetic N3 disease*)
-
S239 TI (genetic N3 disorder*)
-
S240 AB (genetic N3 disorder*)
-
S241 TI (genetic N3 illness*)
-
S242 AB (genetic N3 illness*)
-
S243 TI (genetic N3 condition*)
-
S244 AB (genetic N3 condition*)
-
S245 TI (genetic N3 abnormalit*)
-
S246 AB (genetic N3 abnormalit*)
-
S247 TI (genetic N3 impairment*)
-
S248 AB (genetic N3 impairment*)
-
S249 TI (genetic N3 handicap*)
-
S250 AB (genetic N3 handicap*)
-
S251 TI (chromosomal N3 disease*)
-
S252 AB (chromosomal N3 disease*)
-
S253 TI (chromosomal N3 illness*)
-
S254 AB (chromosomal N3 illness*)
-
S255 TI (chromosomal N3 disorder*)
-
S256 AB (chromosomal N3 disorder*)
-
S257 TI (chromosomal N3 condition*)
-
S258 AB (chromosomal N3 condition*)
-
S259 TI (chromosomal N3 abnormalit*)
-
S260 AB (chromosomal N3 abnormalit*)
-
S261 TI (chromosomal N3 impairment*)
-
S262 AB (chromosomal N3 impairment*)
-
S263 TI (chromosomal N3 handicap*)
-
S264 AB (chromosomal N3 handicap*)
-
S265 TI (congenital N3 disease*)
-
S266 AB (congenital N3 disease*)
-
S267 TI (congenital N3 illness*)
-
S268 AB (congenital N3 illness*)
-
S269 TI (congenital N3 disorder*)
-
S270 AB (congenital N3 disorder*)
-
S271 TI (congenital N3 condition*)
-
S272 AB (congenital N3 condition*)
-
S273 TI (congenital N3 abnormalit*)
-
S274 AB (congenital N3 abnormalit*)
-
S275 TI (congenital N3 impairment*)
-
S276 AB (congenital N3 impairment*)
-
S277 TI (congenital N3 handicap*)
-
S278 AB (congenital N3 handicap*)
-
S279 TI (“complex health* need*”)
-
S280 AB (“complex health* need*”)
-
S281 TI “early death*”
-
S282 AB “early death*”
-
S283 TI “cerebral pals*”
-
S284 AB “cerebral pals*”
-
S285 TI “spina bifida”
-
S286 AB “spina bifida”
-
S287 TI “cystic fibrosis”
-
S288 AB “cystic fibrosis”
-
S289 TI encephalopath*
-
S290 AB encephalopath*
-
S291 TI disabilit*
-
S292 AB disabilit*
-
S293 TI disabled
-
S294 AB disabled
-
S295 TI handicap*
-
S296 AB handicap*
-
S297 TI spastic*
-
S298 AB spastic*
-
S299 TI “impaired motor skill*”
-
S300 AB “impaired motor skill*”
-
S301 TI “spinal cord condition*”
-
S302 AB “spinal cord condition*”
-
S303 TI “multiple trauma”
-
S304 AB “multiple trauma”
-
S305 TI “acquired brain injur*”
-
S306 AB “acquired brain injur*”
-
S307 TI “neurological condition*”
-
S308 AB “neurological condition*”
-
S309 TI “neuromuscular condition*”
-
S310 AB “neuromuscular condition*”
-
S311 TI “multi-organ disease*”
-
S312 AB “multi-organ disease*”
-
S313 TI neurodisabilit*
-
S314 AB neurodisabilit*
-
S315 S102 OR S103 OR S104 OR S105 OR S106 OR S107 OR S108 OR S109 OR S110 OR S111 OR S112 OR S113 OR S114 OR S115 OR S116 OR S117 OR S118 OR S119 OR S120 OR S121 OR S122 OR S123 OR S124 OR S125 OR S126 OR S127 OR S128 OR S129 OR S130 OR S131 OR S132 OR S133 OR S134 OR S135 OR S136 OR S137 OR S138 OR S139 OR S140 OR S141 OR S142 OR S143 OR S144 OR S145 OR S146 OR S147 OR S148 OR S149 OR S150 OR S151 OR S152 OR S153 OR S154 OR S155 OR S156 OR S157 OR S158 OR S159 OR S160 OR S161 OR S162 OR S163 OR S164 OR S165 OR S166 OR S167 OR S168 OR S169 OR S170 OR S171 OR S172 OR S173 OR S174 OR S175 OR S176 OR S177 OR S178 OR S179 OR S180 OR S181 OR S182 OR S183 OR S184 OR S185 OR S186 OR S187 OR S188 OR S189 OR S190 OR S191 OR S192 OR S193 OR S194 OR S195 OR S196 OR S197 OR S198 OR S199 OR S200 OR S201 OR S202 OR S203 OR S204 OR S205 OR S206 OR S207 OR S208 OR S209 OR S210 OR S211 OR S212 OR S213 OR S214 OR S215 OR S216 OR S217 OR S218 OR S219 OR S220 OR S221 OR S222 OR S223 OR S224 OR S225 OR S226 OR S227 OR S228 OR S229 OR S230 OR S231 OR S232 OR S233 OR S234 OR S235 OR S236 OR S237 OR S238 OR S239 OR S240 OR S241 OR S242 OR S243 OR S244 OR S245 OR S246 OR S247 OR S248 OR S249 OR S250 OR S251 OR S252 OR S253 OR S254 OR S255 OR S256 OR S257 OR S258 OR S259 OR S260 OR S261 OR S262 OR S263 OR S264 OR S265 OR S266 OR S267 OR S268 OR S269 OR S270 OR S271 OR S272 OR S273 OR S274 OR S275 OR S276 OR S277 OR S278 OR S279 OR S280 OR S281 OR S282 OR S283 OR S284 OR S285 OR S286 OR S287 OR S288 OR S289 OR S290 OR S291 OR S292 OR S293 OR S294 OR S295 OR S296 OR S297 OR S298 OR S299 OR S300 OR S301 OR S302 OR S303 OR S304 OR S305 OR S306 OR S307 OR S308 OR S309 OR S310 OR S311 OR S312 OR S313 OR S314
-
S316 S101 AND S315
-
S317 DE “Emerging Adulthood”
-
S318 TI “young adult*”
-
S319 AB “young adult*”
-
S320 TI “young person”
-
S321 AB “young person”
-
S322 TI “young people”
-
S323 AB “young people”
-
S324 TI youth*
-
S325 AB youth*
-
S326 TI “emerg* adult*”
-
S327 AB “emerg* adult*”
-
S328 TI “early adult*”
-
S329 AB “early adult*”
-
S330 TI child* N3 transition N3 adult*
-
S331 AB child* N3 transition N3 adult*
-
S332 TI adolescen* N3 transition N3 adult*
-
S333 AB adolescen* N3 transition N3 adult*
-
S334 TI teenage* N3 transition N3 adult*
-
S335 AB teenage* N3 transition N3 adult*
-
S336 TI paediatric* N3 transition N3 adult*
-
S337 AB paediatric* N3 transition N3 adult*
-
S338 TI pediatric* N3 transition N3 adult*
-
S339 AB pediatric* N3 transition N3 adult*
-
S340 TI “college student*”
-
S341 AB “college student*”
-
S342 TI “university student*”
-
S343 AB “university student*”
-
S344 TI “post-secondary student*”
-
S345 AB “post-secondary student*”
-
S346 TI undergraduate*
-
S347 AB undergraduate*
-
S348 TI postgraduate*
-
S349 AB postgraduate*
-
S350 TI famil*
-
S351 AB famil*
-
S352 TI carer*
-
S353 AB carer*
-
S354 TI caregiver*
-
S355 AB caregiver*
-
S356 TI parent*
-
S357 AB parent*
-
S358 TI grandparent*
-
S359 AB grandparent*
-
S360 TI relative*
-
S361 AB relative*
-
S362 TI relation*
-
S363 AB relation*
-
S364 TI sibling*
-
S365 AB sibling*
-
S366 DE “Family” OR DE “Biological Family” OR DE “Extended Family” OR DE “Family of Origin” OR DE “Interethnic Family” OR DE “Interracial Family” OR DE “Military Families” OR DE “Nuclear Family” OR DE “Schizophrenogenic Family” OR DE “Stepfamily”
-
S367 DE “Parents” OR DE “Adoptive Parents” OR DE “Fathers” OR DE “Foster Parents” OR DE “Homosexual Parents” OR DE “Mothers” OR DE “Single Parents” OR DE “Stepparents” OR DE “Surrogate Parents (Humans)”
-
S368 DE “Grandparents”
-
S369 DE “Siblings” OR DE “Brothers” OR DE “Multiple Births” OR DE “Sisters”
-
S370 DE “Caregivers”
-
S371 DE “College Students” OR DE “Postgraduate Students”
-
S372 S317 OR S318 OR S319 OR S320 OR S321 OR S322 OR S323 OR S324 OR S325 OR S326 OR S327 OR S328 OR S329 OR S330 OR S331 OR S332 OR S333 OR S334 OR S335 OR S336 OR S337 OR S338 OR S339 OR S340 OR S341 OR S342 OR S343 OR S344 OR S345 OR S346 OR S347 OR S348 OR S349 OR S350 OR S351 OR S352 OR S353 OR S354 OR S355 OR S356 OR S357 OR S358 OR S359 OR S360 OR S361 OR S362 OR S363 OR S364 OR S365 OR S366 OR S367 OR S368 OR S369 OR S370 OR S371
-
S373 S316 AND S372
-
S374 S316 AND S372
-
S375 S101 AND S315
-
S376 S101 AND S315
Applied Social Sciences Index and Abstracts
Date searched: September 2018.
Date range searched: 1 January 2002 to 26 September 2018.
Search strategy
[MAINSUBJECT.EXACT.EXPLODE(“Respite care”) OR MAINSUBJECT.EXACT.EXPLODE(“Hospices”) OR MAINSUBJECT.EXACT.EXPLODE(“Day care centres”) OR MAINSUBJECT.EXACT.EXPLODE(“Terminal care”) OR MAINSUBJECT.EXACT.EXPLODE(“Residential care”) OR MAINSUBJECT.EXACT.EXPLODE(“Holidays”) OR MAINSUBJECT.EXACT.EXPLODE(“Residential care”) OR MAINSUBJECT.EXACT.EXPLODE(“Short term care”) OR MAINSUBJECT.EXACT.EXPLODE(“Shared care”) OR MAINSUBJECT.EXACT.EXPLODE(“Family support”) OR [ti(“day* away” OR “day care*” OR “day centre*” OR “day center*” OR “day program*” OR “day service*” OR holiday* OR “home support*” OR hospice* OR “intermediate care” OR “night care*” OR “night-time care*” OR “partial hospitalisation*” OR “partial hospitalization*” OR “relief care*” OR “relief support” OR “residential care*” OR “residential home*” OR “residential facilit*” OR respite* OR “short break*” OR “short stay*” OR “sitting service*” OR “support program*” OR “support scheme*” OR “support service*” OR “temporary admission*” OR “temporary break*” OR “temporary care*” OR “temporary relief” OR “temporary support*” OR “short-term admission*” OR “short-term break*” OR “short-term care*” OR “short-term relief” OR “short-term support*” OR “time off” OR vacation* OR “care service*” OR “overnight stay*” OR “home-based support*” OR “befriend* service*” OR “short-break foster*” OR “adult placement scheme*” OR “shared care” OR “replacement care” OR “family support”) OR ab(“day* away” OR “day care*” OR “day centre*” OR “day center*” OR “day program*” OR “day service*” OR holiday* OR “home support*” OR hospice* OR “intermediate care” OR “night care*” OR “night-time care*” OR “partial hospitalisation*” OR “partial hospitalization*” OR “relief care*” OR “relief support” OR “residential care*” OR “residential home*” OR “residential facilit*” OR respite* OR “short break*” OR “short stay*” OR “sitting service*” OR “support program*” OR “support scheme*” OR “support service*” OR “temporary admission*” OR “temporary break*” OR “temporary care*” OR “temporary relief” OR “temporary support*” OR “short-term admission*” OR “short-term break*” OR “short-term care*” OR “short-term relief” OR “short-term support*” OR “time off” OR vacation* OR “care service*” OR “overnight stay*” OR “home-based support*” OR “befriend* service*” OR “short-break foster*” OR “adult placement scheme*” OR “shared care” OR “replacement care” OR “family support”)]
AND
[MAINSUBJECT.EXACT.EXPLODE(“Palliative care”) OR MAINSUBJECT.EXACT.EXPLODE(“Palliative medicine”) OR MAINSUBJECT.EXACT.EXPLODE(“Terminally ill people”) OR MAINSUBJECT.EXACT.EXPLODE(“Terminally ill young adults”) OR MAINSUBJECT.EXACT.EXPLODE(“Heart failure”) OR MAINSUBJECT.EXACT.EXPLODE(“Muscular dystrophy”) OR MAINSUBJECT.EXACT.EXPLODE(“Duchenne muscular dystrophy”) OR MAINSUBJECT.EXACT.EXPLODE(“Cancer”) OR MAINSUBJECT.EXACT.EXPLODE(“Cerebral palsy”) OR MAINSUBJECT.EXACT.EXPLODE(“Spina bifida”) OR MAINSUBJECT.EXACT.EXPLODE(“Cystic fibrosis”) OR MAINSUBJECT.EXACT(“Disabled people”) OR MAINSUBJECT.EXACT(“Disabled adolescent girls”) OR MAINSUBJECT.EXACT(“Disabled adolescents”) OR MAINSUBJECT.EXACT(“Disabled adolescent boys”) OR MAINSUBJECT.EXACT(“Disabled children”) OR MAINSUBJECT.EXACT(“Disabled young adults”) OR MAINSUBJECT.EXACT.EXPLODE(“Neurodegenerative diseases”) OR MAINSUBJECT.EXACT.EXPLODE(“Genetic disorders”) OR MAINSUBJECT.EXACT.EXPLODE(“Chromosome abnormalities”) OR MAINSUBJECT.EXACT.EXPLODE(“Congenital abnormality”) OR MAINSUBJECT.EXACT.EXPLODE(“Congenital disorders”) OR MAINSUBJECT.EXACT.EXPLODE(“Encephalopathy”) OR ti(“advanc* disease*” OR “advanc* illness*” OR “advanc* condition*” OR “advanc* disorder*” OR “advanc* abnormalit*” OR “advanc* impairment*” OR “advanc* handicap*” OR “degenerative disease*” OR “degenerative illness*” OR “degenerative condition*” OR “degenerative disorder*” OR “degenerative abnormalit*” OR “degenerative impairment*” OR “degenerative handicap*” OR “progressive disease*” OR “progressive illness*” OR “progressive condition*” OR “progressive disorder*” OR “progressive abnormalit*” OR “progressive impairment*” OR “progressive handicap*” OR “diminished life expectancy” OR “limited life expectancy” OR cancer* OR duchenne OR dying OR “end of life” OR “end stage renal failure” OR “end stage liver failure” OR “heart failure” OR incurable OR life-limit* OR “life limit*” OR “life short*” OR “live* short*” OR “life threaten*” OR “limited life expectancy” OR LLC OR LLI OR “muscular dystroph*” OR neoplasm*.ti,ab OR “neurodegenerative condition*” OR “neurodegenerative disease*” OR “neurodegenerative illness*” OR “neurodegenerative disorder*” OR “neurodegenerative abnormalit*” OR “neurodegenerative impairment*” OR “neurodegenerative handicap*” OR oncology OR palliative OR “poor prognosis” OR “serious* ill*” OR “terminal* ill*” OR “terminal* care*” OR “terminal* disease*” OR “terminal* condition*” OR “terminal* disorder*” OR “terminal* abnormalit*” OR “terminal* impairment*” OR “terminal* handicap*” OR “genetic disease*” OR “genetic disorder*” OR “genetic illness*” OR “genetic condition*” OR “genetic abnormalit*” OR “genetic impairment*” OR “genetic handicap*” OR “chromosomal disease*” OR “chromosomal illness*” OR “chromosomal disorder*” OR “chromosomal condition*” OR “chromosomal abnormalit*” OR “chromosomal impairment*” OR “chromosomal handicap*” OR “congenital disease*” OR “congenital illness*” OR “congenital disorder*” OR “congenital condition*” OR “congenital abnormalit*” OR “congenital impairment*” OR “congenital handicap*” OR “complex health* need*” OR “early death*” OR “cerebral pals*” OR “spina bifida” OR “cystic fibrosis” OR encephalopath* OR disabilit* OR disabled OR handicap* OR spastic* OR “impaired motor skill*” OR “spinal cord condition*” OR “multiple trauma” OR “acquired brain injur*” OR “neurological condition*” OR “neuromuscular condition*” OR “multi-organ disease*” OR neurodisabilit*) OR ab (“advanc* disease*” OR “advanc* illness*” OR “advanc* condition*” OR “advanc* disorder*” OR “advanc* abnormalit*” OR “advanc* impairment*” OR “advanc* handicap*” OR “degenerative disease*” OR “degenerative illness*” OR “degenerative condition*” OR “degenerative disorder*” OR “degenerative abnormalit*” OR “degenerative impairment*” OR “degenerative handicap*” OR “progressive disease*” OR “progressive illness*” OR “progressive condition*” OR “progressive disorder*” OR “progressive abnormalit*” OR “progressive impairment*” OR “progressive handicap*” OR “diminished life expectancy” OR “limited life expectancy” OR cancer* OR duchenne OR dying OR “end of life” OR “end stage renal failure” OR “end stage liver failure” OR “heart failure” OR incurable OR life-limit* OR “life limit*” OR “life short*” OR “live* short*” OR “life threaten*” OR “limited life expectancy” OR LLC OR LLI OR “muscular dystroph*” OR neoplasm*.ti,ab OR “neurodegenerative condition*” OR “neurodegenerative disease*” OR “neurodegenerative illness*” OR “neurodegenerative disorder*” OR “neurodegenerative abnormalit*” OR “neurodegenerative impairment*” OR “neurodegenerative handicap*” OR oncology OR palliative OR “poor prognosis” OR “serious* ill*” OR “terminal* ill*” OR “terminal* care*” OR “terminal* disease*” OR “terminal* condition*” OR “terminal* disorder*” OR “terminal* abnormalit*” OR “terminal* impairment*” OR “terminal* handicap*” OR “genetic disease*” OR “genetic disorder*” OR “genetic illness*” OR “genetic condition*” OR “genetic abnormalit*” OR “genetic impairment*” OR “genetic handicap*” OR “chromosomal disease*” OR “chromosomal illness*” OR “chromosomal disorder*” OR “chromosomal condition*” OR “chromosomal abnormalit*” OR “chromosomal impairment*” OR “chromosomal handicap*” OR “congenital disease*” OR “congenital illness*” OR “congenital disorder*” OR “congenital condition*” OR “congenital abnormalit*” OR “congenital impairment*” OR “congenital handicap*” OR “complex health* need*” OR “early death*” OR “cerebral pals*” OR “spina bifida” OR “cystic fibrosis” OR encephalopath* OR disabilit* OR disabled OR handicap* OR spastic* OR “impaired motor skill*” OR “spinal cord condition*” OR “multiple trauma” OR “acquired brain injur*” OR “neurological condition*” OR “neuromuscular condition*” OR “multi-organ disease*” OR neurodisabilit*)]
AND
[MAINSUBJECT.EXACT.EXPLODE(“Young adults”) OR MAINSUBJECT.EXACT.EXPLODE(“Young adulthood”) OR MAINSUBJECT.EXACT.EXPLODE(“Adolescents”) OR MAINSUBJECT.EXACT.EXPLODE(“Adults”) OR MAINSUBJECT.EXACT.EXPLODE(“Families”) OR MAINSUBJECT.EXACT.EXPLODE(“Carers”) OR MAINSUBJECT.EXACT.EXPLODE(“Parents”) OR MAINSUBJECT.EXACT.EXPLODE(“Grandparents”) OR MAINSUBJECT.EXACT.EXPLODE(“Siblings”) OR MAINSUBJECT.EXACT.EXPLODE(“Postgraduate students”) OR MAINSUBJECT.EXACT.EXPLODE(“Undergraduate students”) OR ti(“young adult*” OR “young person” OR “young people” OR youth* OR “emerg* adult*” OR “early adult*” OR (child* AND transition AND adult*) OR (adolescen* AND transition AND adult*) OR (teenage* AND transition AND adult*) OR (paediatric* AND transition AND adult*) OR (pediatric* AND transition AND adult) OR “college student*” OR “university student*” OR “post-secondary student*” OR undergraduate* OR postgraduate* OR famil* OR carer* OR caregiver* OR parent* OR grandparent* OR relative* OR relation* OR sibling*) OR ab(“young adult*” OR “young person” OR “young people” OR youth* OR “emerg* adult*” OR “early adult*” OR (child* AND transition AND adult*) OR (adolescen* AND transition AND adult*) OR (teenage* AND transition AND adult*) OR (paediatric* AND transition AND adult*) OR (pediatric* AND transition AND adult) OR “college student*” OR “university student*” OR “post-secondary student*” OR undergraduate* OR postgraduate* OR famil* OR carer* OR caregiver* OR parent* OR grandparent* OR relative* OR relation* OR sibling*)]
Limit 2002-2018
Cochrane (Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, Protocols)
Date searched: September 2018.
Date range searched: 1 January 2002 to 26 September 2018.
Search strategy
-
#1 MeSH descriptor: [Respite Care] explode all trees
-
#2 MeSH descriptor: [Hospice Care] explode all trees
-
#3 MeSH descriptor: [Hospices] explode all trees
-
#4 MeSH descriptor: [Hospice and Palliative Care Nursing] explode all trees
-
#5 MeSH descriptor: [Day Care, Medical] explode all trees
-
#6 MeSH descriptor: [Night Care] explode all trees
-
#7 MeSH descriptor: [Intermediate Care Facilities] explode all trees
-
#8 MeSH descriptor: [Terminal Care] explode all trees
-
#9 MeSH descriptor: [Holidays] explode all trees
-
#10 (day* next away):ti,ab
-
#11 (day next care*):ti,ab
-
#12 (day next centre*):ti,ab
-
#13 (day next center*):ti,ab
-
#14 (day next program*):ti,ab
-
#15 (day next service*):ti,ab
-
#16 holiday*:ti,ab
-
#17 (home next support*):ti,ab
-
#18 hospice*:ti,ab
-
#19 (“intermediate care”):ti,ab
-
#20 (night next care*):ti,ab
-
#21 (night-time next care*):ti,ab
-
#22 (partial next hospitalisation*):ti,ab
-
#23 (partial next hospitalization*):ti,ab
-
#24 (relief next care*):ti,ab
-
#25 (“relief support”):ti,ab
-
#26 (residential next care*):ti,ab
-
#27 (residential next home*):ti,ab
-
#28 (residential next facilit*):ti,ab
-
#29 respite*:ti,ab
-
#30 (short next break*):ti,ab
-
#31 (short next stay*):ti,ab
-
#32 (sitting next service*):ti,ab
-
#33 (support next program*):ti,ab
-
#34 (support next scheme*):ti,ab
-
#35 (support next service*):ti,ab
-
#36 (temporary next admission*):ti,ab
-
#37 (temporary next break*):ti,ab
-
#38 (temporary next care*):ti,ab
-
#39 (“temporary relief”):ti,ab
-
#40 (temporary next support*):ti,ab
-
#41 (short-term next admission*):ti,ab
-
#42 (short-term next break*):ti,ab
-
#43 (short-term next care*):ti,ab
-
#44 (short-term next relief*):ti,ab
-
#45 (short-term next support*):ti,ab
-
#46 (“time off”):ti,ab
-
#47 vacation*:ti,ab
-
#48 (care next service*):ti,ab
-
#49 (overnight next stay*):ti,ab
-
#50 (home-based next support*):ti,ab
-
#51 (befriend* next service*):ti,ab
-
#52 (short-break next foster*):ti,ab
-
#53 (adult next placement next scheme*):ti,ab
-
#54 (“shared care”):ti,ab
-
#55 (“replacement care”):ti,ab
-
#56 (“family support”):ti,ab
-
#57 {OR #1-#56}
-
#58 MeSH descriptor: [Palliative Care] explode all trees
-
#59 MeSH descriptor: [Palliative Medicine] explode all trees
-
#60 MeSH descriptor: [Terminally Ill] explode all trees
-
#61 MeSH descriptor: [Heart Failure] explode all trees
-
#62 MeSH descriptor: [Muscular Dystrophies] explode all trees
-
#63 MeSH descriptor: [Muscular Dystrophy, Duchenne] explode all trees
-
#64 MeSH descriptor: [Neoplasms] explode all trees
-
#65 MeSH descriptor: [Cerebral Palsy] explode all trees
-
#66 MeSH descriptor: [Spinal Dysraphism] explode all trees
-
#67 MeSH descriptor: [Cystic Fibrosis] explode all trees
-
#68 MeSH descriptor: [Disabled Persons] explode all trees
-
#69 MeSH descriptor: [Disabled Children] explode all trees
-
#70 MeSH descriptor: [Neurodegenerative Diseases] explode all trees
-
#71 MeSH descriptor: [Multiple Trauma] explode all trees
-
#72 MeSH descriptor: [Genetic Diseases, Inborn] explode all trees
-
#73 MeSH descriptor: [Chromosome Disorders] explode all trees
-
#74 MeSH descriptor: [Congenital, Hereditary, and Neonatal Diseases and Abnormalities] explode all trees
-
#75 (advanc* near/3 disease*):ti,ab
-
#76 (advanc* near/3 illness*):ti,ab
-
#77 (advanc* near/3 condition*):ti,ab
-
#78 (advanc* near/3 disorder*):ti,ab
-
#79 (advanc* near/3 abnormalit*):ti,ab
-
#80 (advanc* near/3 impairment*):ti,ab
-
#81 (advanc* near/3 handicap*):ti,ab
-
#82 (degenerative near/3 disease*):ti,ab
-
#83 (degenerative near/3 illness*):ti,ab
-
#84 (degenerative near/3 condition*):ti,ab
-
#85 (degenerative near/3 disorder*):ti,ab
-
#86 (degenerative near/3 abnormalit*):ti,ab
-
#87 (degenerative near/3 impairment*):ti,ab
-
#88 (degenerative near/3 handicap*):ti,ab
-
#89 (progressive near/3 disease*):ti,ab
-
#90 (progressive near/3 illness*):ti,ab
-
#91 (progressive near/3 condition*):ti,ab
-
#92 (progressive near/3 disorder*):ti,ab
-
#93 (progressive near/3 abnormalit*):ti,ab
-
#94 (progressive near/3 impairment*):ti,ab
-
#95 (progressive near/3 handicap*):ti,ab
-
#96 (“diminished life expectancy”):ti,ab
-
#97 (“limited life expectancy”):ti,ab
-
#98 cancer*:ti,ab
-
#99 duchenne:ti,ab
-
#100 dying:ti,ab
-
#101 (“end of life”):ti,ab
-
#102 (“end stage renal failure”):ti,ab
-
#103 (“end stage liver failure”):ti,ab
-
#104 “heart failure”:ti,ab
-
#105 incurable:ti,ab
-
#106 (life-limit*):ti,ab
-
#107 (life next limit*):ti,ab.
-
#108 (life near/3 short*):ti,ab
-
#109 (live* near/3 short*):ti,ab
-
#110 (life next threaten*):ti,ab
-
#111 (“limited life expectancy”):ti,ab
-
#112 LLC:ti,ab
-
#113 LLI:ti,ab
-
#114 (muscular next dystroph*):ti,ab
-
#115 neoplasm*:ti,ab
-
#116 (neurodegenerative next condition*):ti,ab
-
#117 (neurodegenerative next disease*):ti,ab
-
#118 (neurodegenerative next illness*):ti,ab
-
#119 (neurodegenerative next disorder*):ti,ab
-
#120 (neurodegenerative next abnormalit*):ti,ab
-
#121 (neurodegenerative next impairment*):ti,ab
-
#122 (neurodegenerative next handicap*):ti,ab
-
#123 oncology:ti,ab
-
#124 palliative:ti,ab
-
#125 (“poor prognosis”):ti,ab
-
#126 (serious* near/3 ill*):ti,ab
-
#127 (terminal* near/3 ill*):ti,ab
-
#128 (terminal* near/3 care*):ti,ab
-
#129 (terminal* near/3 disease*):ti,ab
-
#130 (terminal* near/3 condition*):ti,ab
-
#131 (terminal* near/3 disorder*):ti,ab
-
#132 (terminal* near/3 abnormalit*):ti,ab
-
#133 (terminal* near/3 impairment*):ti,ab
-
#134 (terminal* near/3 handicap*):ti,ab
-
#135 (genetic near/3 disease*):ti,ab
-
#136 (genetic near/3 disorder*):ti,ab
-
#137 (genetic near/3 illness*):ti,ab
-
#138 (genetic near/3 condition*):ti,ab
-
#139 (genetic near/3 abnormalit*):ti,ab
-
#140 (genetic near/3 impairment*):ti,ab
-
#141 (genetic near/3 handicap*):ti,ab
-
#142 (chromosomal near/3 disease*):ti,ab
-
#143 (chromosomal near/3 illness*):ti,ab
-
#144 (chromosomal near/3 disorder*):ti,ab
-
#145 (chromosomal near/3 condition*):ti,ab
-
#146 (chromosomal near/3 abnormalit*):ti,ab
-
#147 (chromosomal near/3 impairment*):ti,ab
-
#148 (chromosomal near/3 handicap*):ti,ab
-
#149 (congenital near/3 disease*):ti,ab
-
#150 (congenital near/3 condition*):ti,ab
-
#151 (congenital near/3 abnormalit*):ti,ab
-
#152 (congenital near/3 illness*):ti,ab
-
#153 (congenital near/3 impairment*):ti,ab
-
#154 (congenital near/3 disorder*):ti,ab
-
#155 (congenital near/3 handicap*):ti,ab
-
#156 (“complex health* need*”):ti,ab
-
#157 (early next death*):ti,ab
-
#158 (cerebral next pals*):ti,ab
-
#159 (“spina bifida”):ti,ab
-
#160 (“cystic fibrosis”):ti,ab
-
#161 encephalopath*:ti,ab
-
#162 disabilit*:ti,ab
-
#163 disabled:ti,ab
-
#164 handicap*:ti,ab
-
#165 spastic*:ti,ab
-
#166 (impaired next motor next skill*):ti,ab
-
#167 (spinal next cord next condition*):ti,ab
-
#168 (“multiple trauma”):ti,ab
-
#169 (acquired next brain next injur*):ti,ab
-
#170 (neurological next condition*):ti,ab
-
#171 (neuromuscular next condition*):ti,ab
-
#172 (multi-organ next disease*):ti,ab
-
#173 neurodisabilit*:ti,ab
-
#174 {OR #58-#173}
-
#175 MeSH descriptor: [Young Adult] explode all trees
-
#176 MeSH descriptor: [Adult] explode all trees
-
#177 MeSH descriptor: [Adolescent] explode all trees
-
#178 MeSH descriptor: [Family] explode all trees
-
#179 MeSH descriptor: [Caregivers] explode all trees
-
#180 MeSH descriptor: [Parents] explode all trees
-
#181 (young next adult*):ti,ab
-
#182 “young person”:ti,ab
-
#183 “young people”:ti,ab
-
#184 youth*:ti,ab
-
#185 (emerg* next adult*):ti,ab
-
#186 (early next adult*):ti,ab
-
#187 (child* near/3 transition near/3 adult*):ti,ab
-
#188 (adolescen* near/3 transition near/3 adult*):ti,ab
-
#189 (teenage* near/3 transition near/3 adult*):ti,ab
-
#190 (paediatric* near/3 transition near/3 adult*):ti,ab
-
#191 (pediatric* near/3 transition near/3 adult*):ti,ab
-
#192 (college next student*):ti,ab
-
#193 (university next student*):ti,ab
-
#194 (post-secondary student*):ti,ab
-
#195 undergraduate*:ti,ab
-
#196 postgraduate*:ti,ab
-
#197 famil*:ti,ab
-
#198 carer*:ti,ab
-
#199 caregiver*:ti,ab
-
#200 parent*:ti,ab
-
#201 grandparent*:ti,ab
-
#202 relative*:ti,ab
-
#203 relation*:ti,ab
-
#204 sibling*:ti,ab
-
#205 {OR #175-#204}
-
#206 #57 AND #174 AND #205
Centre for Reviews and Dissemination
Date searched: September 2018.
Date range searched: 1 January 2002 to 26 September 2018.
Search strategy
-
MeSH DESCRIPTOR Respite Care EXPLODE ALL TREES
-
MeSH DESCRIPTOR Hospice Care EXPLODE ALL TREES
-
MeSH DESCRIPTOR Hospices EXPLODE ALL TREES
-
MeSH DESCRIPTOR Hospice and Palliative Care Nursing EXPLODE ALL TREES
-
MeSH DESCRIPTOR Day Care, Medical EXPLODE ALL TREES
-
MeSH DESCRIPTOR Night Care EXPLODE ALL TREES
-
MeSH DESCRIPTOR Intermediate Care Facilities EXPLODE ALL TREES
-
MeSH DESCRIPTOR Terminal Care EXPLODE ALL TREES
-
MeSH DESCRIPTOR Holidays EXPLODE ALL TREES
-
(“day* away”) IN DARE, NHSEED, HTA
-
(“day care*”) IN DARE, NHSEED, HTA
-
(“day centre*”) IN DARE, NHSEED, HTA
-
(“day center*”) IN DARE, NHSEED, HTA
-
(“day program*”) IN DARE, NHSEED, HTA
-
(“day service*”) IN DARE, NHSEED, HTA
-
(holiday*) IN DARE, NHSEED, HTA
-
(“home support*”) IN DARE, NHSEED, HTA
-
(hospice*) IN DARE, NHSEED, HTA
-
(“intermediate care”) IN DARE, NHSEED, HTA
-
(“night care*”) IN DARE, NHSEED, HTA
-
(“night-time care*”) IN DARE, NHSEED, HTA
-
(“partial hospitalisation*”) IN DARE, NHSEED, HTA
-
(“partial hospitalization*”) IN DARE, NHSEED, HTA
-
(“relief care*”) IN DARE, NHSEED, HTA
-
(“relief support”) IN DARE, NHSEED, HTA
-
(“residential care*”) IN DARE, NHSEED, HTA
-
(“residential home*”) IN DARE, NHSEED, HTA
-
(“residential facilit*”) IN DARE, NHSEED, HTA
-
(respite*) IN DARE, NHSEED, HTA
-
(“short break*”) IN DARE, NHSEED, HTA
-
(“short stay*”) IN DARE, NHSEED, HTA
-
(“sitting service*”) IN DARE, NHSEED, HTA
-
(“support program*”) IN DARE, NHSEED, HTA
-
(“support scheme*”) IN DARE, NHSEED, HTA
-
(“support service*”) IN DARE, NHSEED, HTA
-
(“temporary admission*”) IN DARE, NHSEED, HTA
-
(“temporary break*”) IN DARE, NHSEED, HTA
-
(“temporary care*”) IN DARE, NHSEED, HTA
-
(“temporary relief”) IN DARE, NHSEED, HTA
-
(“temporary support*”) IN DARE, NHSEED, HTA
-
(“short-term admission*”) IN DARE, NHSEED, HTA
-
(“short-term break*”) IN DARE, NHSEED, HTA
-
(“short-term care*”) IN DARE, NHSEED, HTA
-
(“short-term relief”) IN DARE, NHSEED, HTA
-
(“short-term support*”) IN DARE, NHSEED, HTA
-
(“time off”) IN DARE, NHSEED, HTA
-
(vacation*) IN DARE, NHSEED, HTA
-
(“care service*”) IN DARE, NHSEED, HTA
-
(“overnight stay*”) IN DARE, NHSEED, HTA
-
(“home-based support*”) IN DARE, NHSEED, HTA
-
(“befriend* service*”) IN DARE, NHSEED, HTA
-
(“short-break foster*”) IN DARE, NHSEED, HTA
-
(“adult placement scheme*”) IN DARE, NHSEED, HTA
-
(“shared care”) IN DARE, NHSEED, HTA
-
(“replacement care”) IN DARE, NHSEED, HTA
-
(“family support”) IN DARE, NHSEED, HTA
-
#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35 OR #36 OR #37 OR #38 OR #39 OR #40 OR #41 OR #42 OR #43 OR #44 OR #45 OR #46 OR #47 OR #48 OR #49 OR #50 OR #51 OR #52 OR #53 OR #54 OR #55 OR #56
-
MeSH DESCRIPTOR Palliative Care EXPLODE ALL TREES
-
MeSH DESCRIPTOR Palliative Medicine EXPLODE ALL TREES
-
MeSH DESCRIPTOR Terminally Ill EXPLODE ALL TREES
-
MeSH DESCRIPTOR Heart Failure EXPLODE ALL TREES
-
MeSH DESCRIPTOR Muscular Dystrophies EXPLODE ALL TREES
-
MeSH DESCRIPTOR Muscular Dystrophy, Duchenne EXPLODE ALL TREES
-
MeSH DESCRIPTOR Neoplasms EXPLODE ALL TREES
-
MeSH DESCRIPTOR Cerebral Palsy EXPLODE ALL TREES
-
MeSH DESCRIPTOR Spinal Dysraphism EXPLODE ALL TREES
-
MeSH DESCRIPTOR Cystic Fibrosis EXPLODE ALL TREES
-
MeSH DESCRIPTOR Disabled Persons EXPLODE ALL TREES
-
MeSH DESCRIPTOR Disabled Children EXPLODE ALL TREES
-
MeSH DESCRIPTOR Neurodegenerative Diseases EXPLODE ALL TREES
-
MeSH DESCRIPTOR Multiple Trauma EXPLODE ALL TREES
-
MeSH DESCRIPTOR Genetic Diseases, Inborn EXPLODE ALL TREES
-
MeSH DESCRIPTOR Chromosome Disorders EXPLODE ALL TREES
-
MeSH DESCRIPTOR Congenital, Hereditary, and Neonatal Diseases and Abnormalities EXPLODE ALL TREES
-
(advanc* adj3 disease*) IN DARE, NHSEED, HTA
-
(advanc* adj3 illness*) IN DARE, NHSEED, HTA
-
(advanc* adj3 condition*) IN DARE, NHSEED, HTA
-
(advanc* adj3 disorder*) IN DARE, NHSEED, HTA
-
(advanc* adj3 abnormalit*) IN DARE, NHSEED, HTA
-
(advanc* adj3 impairment*) IN DARE, NHSEED, HTA
-
(advanc* adj3 handicap*) IN DARE, NHSEED, HTA
-
(degenerative adj3 disease*) IN DARE, NHSEED, HTA
-
(degenerative adj3 illness*) IN DARE, NHSEED, HTA
-
(degenerative adj3 condition*) IN DARE, NHSEED, HTA
-
(degenerative adj3 disorder*) IN DARE, NHSEED, HTA
-
(degenerative adj3 abnormalit*) IN DARE, NHSEED, HTA
-
(degenerative adj3 impairment*) IN DARE, NHSEED, HTA
-
(degenerative adj3 handicap*) IN DARE, NHSEED, HTA
-
(progressive adj3 disease*) IN DARE, NHSEED, HTA
-
(progressive adj3 illness*) IN DARE, NHSEED, HTA
-
(progressive adj3 condition*) IN DARE, NHSEED, HTA
-
(progressive adj3 disorder*) IN DARE, NHSEED, HTA
-
(progressive adj3 abnormalit*) IN DARE, NHSEED, HTA
-
(progressive adj3 impairment*) IN DARE, NHSEED, HTA
-
(progressive adj3 handicap*) IN DARE, NHSEED, HTA
-
(“diminished life expectancy”) IN DARE, NHSEED, HTA
-
(“limited life expectancy”) IN DARE, NHSEED, HTA
-
(cancer*) IN DARE, NHSEED, HTA
-
(duchenne) IN DARE, NHSEED, HTA
-
(dying) IN DARE, NHSEED, HTA
-
(“end of life”) IN DARE, NHSEED, HTA
-
(“end stage renal failure”) IN DARE, NHSEED, HTA
-
(“end stage liver failure”) IN DARE, NHSEED, HTA
-
(“heart failure”) IN DARE, NHSEED, HTA
-
(incurable) IN DARE, NHSEED, HTA
-
(life-limit*) IN DARE, NHSEED, HTA
-
(“life limit*”) IN DARE, NHSEED, HTA
-
(life adj3 short*) IN DARE, NHSEED, HTA
-
(live* adj3 short*) IN DARE, NHSEED, HTA
-
(“life threaten*”) IN DARE, NHSEED, HTA
-
(“limited life expectancy”) IN DARE, NHSEED, HTA
-
(LLC) IN DARE, NHSEED, HTA
-
(LLI) IN DARE, NHSEED, HTA
-
(“muscular dystroph*”) IN DARE, NHSEED, HTA
-
(neoplasm*) IN DARE, NHSEED, HTA
-
(“neurodegenerative condition*”) IN DARE, NHSEED, HTA
-
(“neurodegenerative disease*”) IN DARE, NHSEED, HTA
-
(“neurodegenerative illness*”) IN DARE, NHSEED, HTA
-
(“neurodegenerative disorder*”) IN DARE, NHSEED, HTA
-
(“neurodegenerative abnormalit*”) IN DARE, NHSEED, HTA
-
(“neurodegenerative impairment*”) IN DARE, NHSEED, HTA
-
(“neurodegenerative handicap*”) IN DARE, NHSEED, HTA
-
(oncology) IN DARE, NHSEED, HTA
-
(palliative) IN DARE, NHSEED, HTA
-
(“poor prognosis”) IN DARE, NHSEED, HTA
-
(serious* adj3 ill*) IN DARE, NHSEED, HTA
-
(terminal* adj3 ill*) IN DARE, NHSEED, HTA
-
(terminal* adj3 care*) IN DARE, NHSEED, HTA
-
(terminal* adj3 disease*) IN DARE, NHSEED, HTA
-
(terminal* adj3 condition*) IN DARE, NHSEED, HTA
-
(terminal* adj3 disorder*) IN DARE, NHSEED, HTA
-
(terminal* adj3 abnormalit*) IN DARE, NHSEED, HTA
-
(terminal* adj3 impairment*) IN DARE, NHSEED, HTA
-
(terminal* adj3 handicap*) IN DARE, NHSEED, HTA
-
(genetic adj3 disease*) IN DARE, NHSEED, HTA
-
(genetic adj3 disorder*) IN DARE, NHSEED, HTA
-
(genetic adj3 illness*) IN DARE, NHSEED, HTA
-
(genetic adj3 condition*) IN DARE, NHSEED, HTA
-
(genetic adj3 abnormalit*) IN DARE, NHSEED, HTA
-
(genetic adj3 impairment*) IN DARE, NHSEED, HTA
-
(genetic adj3 handicap*) IN DARE, NHSEED, HTA
-
(chromosomal adj3 disease*) IN DARE, NHSEED, HTA
-
(chromosomal adj3 illness*) IN DARE, NHSEED, HTA
-
(chromosomal adj3 disorder*) IN DARE, NHSEED, HTA
-
(chromosomal adj3 condition*) IN DARE, NHSEED, HTA
-
(chromosomal adj3 abnormalit*) IN DARE, NHSEED, HTA
-
(chromosomal adj3 impairment*) IN DARE, NHSEED, HTA
-
(chromosomal adj3 handicap*) IN DARE, NHSEED, HTA
-
(congenital adj3 disease*) IN DARE, NHSEED, HTA
-
(congenital adj3 illness*) IN DARE, NHSEED, HTA
-
(congenital adj3 disorder*) IN DARE, NHSEED, HTA
-
(congenital adj3 condition*) IN DARE, NHSEED, HTA
-
(congenital adj3 abnormalit*) IN DARE, NHSEED, HTA
-
(congenital adj3 impairment*) IN DARE, NHSEED, HTA
-
(congenital adj3 handicap*) IN DARE, NHSEED, HTA
-
(“complex health* need*”) IN DARE, NHSEED, HTA
-
(“early death*”) IN DARE, NHSEED, HTA
-
(“cerebral pals*”) IN DARE, NHSEED, HTA
-
(“spina bifida”) IN DARE, NHSEED, HTA
-
(“cystic fibrosis”) IN DARE, NHSEED, HTA
-
(encephalopath*) IN DARE, NHSEED, HTA
-
(disabilit*) IN DARE, NHSEED, HTA
-
(disabled) IN DARE, NHSEED, HTA
-
(handicap*) IN DARE, NHSEED, HTA
-
(spastic*) IN DARE, NHSEED, HTA
-
(“impaired motor skill*”) IN DARE, NHSEED, HTA
-
(“spinal cord condition*”) IN DARE, NHSEED, HTA
-
(“multiple trauma”) IN DARE, NHSEED, HTA
-
(“acquired brain injur*”) IN DARE, NHSEED, HTA
-
(“neurological condition*”) IN DARE, NHSEED, HTA
-
(“neuromuscular condition*”) IN DARE, NHSEED, HTA
-
(“multi-organ disease*”) IN DARE, NHSEED, HTA
-
(neurodisabilit*) IN DARE, NHSEED, HTA
-
#58 OR #59 OR #60 OR #61 OR #62 OR #63 OR #64 OR #65 OR #66 OR #67 OR #68 OR #69 OR #70 OR #71 OR #72 OR #73 OR #74 OR #75 OR #76 OR #77 OR #78 OR #79 OR #80 OR #81 OR #82 OR #83 OR #84 OR #85 OR #86 OR #87 OR #88 OR #89 OR #90 OR #91 OR #92 OR #93 OR #94 OR #95 OR #96 OR #97 OR #98 OR #99 OR #100 OR #101 OR #102 OR #103 OR #104 OR #105 OR #106 OR #107 OR #108 OR #109 OR #110 OR #111 OR #112 OR #113 OR #114 OR #115 OR #116 OR #117 OR #118 OR #119 OR #120 OR #121 OR #122 OR #123 OR #124 OR #125 OR #126 OR #127 OR #128 OR #129 OR #130 OR #131 OR #132 OR #133 OR #134 OR #135 OR #136 OR #137 OR #138 OR #139 OR #140 OR #141 OR #142 OR #143 OR #144 OR #145 OR #146 OR #147 OR #148 OR #149 OR #150 OR #151 OR #152 OR #153 OR #154 OR #155 OR #156 OR #157 OR #158 OR #159 OR #160 OR #161 OR #162 OR #163 OR #164 OR #165 OR #166 OR #167 OR #168 OR #169 OR #170 OR #171 OR #172 OR #173 22950 Delete
-
#57 AND #174
-
MeSH DESCRIPTOR Young Adult EXPLODE ALL TREES
-
MeSH DESCRIPTOR Adolescent EXPLODE ALL TREES
-
MeSH DESCRIPTOR Adult EXPLODE ALL TREES
-
MeSH DESCRIPTOR Family EXPLODE ALL TREES
-
MeSH DESCRIPTOR Caregivers EXPLODE ALL TREES
-
MeSH DESCRIPTOR Parents EXPLODE ALL TREES
-
(“young adult*”) IN DARE, NHSEED, HTA
-
(“young person”) IN DARE, NHSEED, HTA
-
(“young people”) IN DARE, NHSEED, HTA
-
(youth*) IN DARE, NHSEED, HTA
-
(“emerg* adult*”) IN DARE, NHSEED, HTA
-
(“early adult*”) IN DARE, NHSEED, HTA
-
((child* adj3 transition adj3 adult*)) IN DARE, NHSEED, HTA
-
((adolescen* adj3 transition adj3 adult*)) IN DARE, NHSEED, HTA
-
((teenage* adj3 transition adj3 adult*)) IN DARE, NHSEED, HTA
-
((paediatric* adj3 transition adj3 adult*)) IN DARE, NHSEED, HTA
-
((pediatric* adj3 transition adj3 adult)) IN DARE, NHSEED, HTA
-
(“college student*”) IN DARE, NHSEED, HTA
-
(“university student*”) IN DARE, NHSEED, HTA
-
(“post-secondary student*”) IN DARE, NHSEED, HTA
-
(undergraduate*) IN DARE, NHSEED, HTA
-
(postgraduate*) IN DARE, NHSEED, HTA
-
(famil*) IN DARE, NHSEED, HTA
-
(carer*) IN DARE, NHSEED, HTA
-
(caregiver*) IN DARE, NHSEED, HTA
-
(parent*) IN DARE, NHSEED, HTA
-
(grandparent*) IN DARE, NHSEED, HTA
-
(relative*) IN DARE, NHSEED, HTA
-
(relation*) IN DARE, NHSEED, HTA
-
(sibling*) IN DARE, NHSEED, HTA
-
#176 OR #177 OR #178 OR #179 OR #180 OR #181 OR #182 OR #183 OR #184 OR #185 OR #186 OR #187 OR #188 OR #189 OR #190 OR #191 OR #192 OR #193 OR #194 OR #195 OR #196 OR #197 OR #198 OR #199 OR #200 OR #201 OR #202 OR #203 OR #204 OR #205
-
#175 AND #206
-
(#207) IN DARE, NHSEED, HTA FROM 2002 TO 2018
Web of Science
Date searched: September 2018.
Date range searched: 1 January 2002 to 26 September 2018.
Search strategy
-
# 1 TOPIC: (“day* away” OR “day care*” OR “day centre*” OR “day center*” OR “day program*” OR “day service*” OR holiday* OR “home support*” OR hospice* OR “intermediate care” OR “night care*” OR “night-time care*” OR “partial hospitalisation*” OR “partial hospitalization*” OR “relief care*” OR “relief support” OR “residential care*” OR “residential home*” OR “residential facilit*” OR respite* OR “short break*” OR “short stay*” OR “sitting service*” OR “support program*” OR “support scheme*” OR “support service*” OR “temporary admission*” OR “temporary break*” OR “temporary care*” OR “temporary relief” OR “temporary support*” OR “short-term admission*” OR “short-term break*” OR “short-term care*” OR “short-term relief” OR “short-term support*” OR “time off” OR vacation* OR “care service*” OR “overnight stay*” OR “home-based support*” OR “befriend* service*” OR “short-break foster*” OR “adult placement scheme*” OR “shared care” OR “replacement care” OR “family support”)
-
# 2 TOPIC: (advanc* NEAR/3 disease* OR advanc* NEAR/3 illness* OR advanc* NEAR/3 condition* OR advanc* NEAR/3 disorder* OR advanc* NEAR/3 abnormalit* OR advanc* NEAR/3 impairment* OR advanc* NEAR/3 handicap* OR degenerative NEAR/3 disease* OR degenerative NEAR/3 illness* OR degenerative NEAR/3 condition* OR degenerative NEAR/3 disorder* OR degenerative NEAR/3 abnormalit* OR degenerative NEAR/3 impairment* OR degenerative NEAR/3 handicap* OR progressive NEAR/3 disease* OR progressive NEAR/3 illness* OR progressive NEAR/3 condition* OR progressive NEAR/3 disorder* OR progressive NEAR/3 abnormalit* OR progressive NEAR/3 impairment* OR progressive NEAR/3 handicap* OR “diminished life expectancy” OR “limited life expectancy” OR cancer* OR duchenne OR dying OR “end of life” OR “end stage renal failure” OR “end stage liver failure” OR “heart failure” OR incurable OR life-limit* OR “life limit*” OR life NEAR/3 short* OR live* NEAR/3 short* OR “life threaten*” OR “limited life expectancy” OR LLC OR LLI OR “muscular dystroph*” OR neoplasm*.ti,ab OR “neurodegenerative condition*” OR “neurodegenerative disease*” OR “neurodegenerative illness*” OR “neurodegenerative disorder*” OR “neurodegenerative abnormalit*” OR “neurodegenerative impairment*” OR “neurodegenerative handicap*” OR oncology OR palliative OR “poor prognosis” OR serious* NEAR/3 ill* OR terminal* NEAR/3 ill* OR terminal* NEAR/3 care* OR terminal* NEAR/3 disease* OR terminal* NEAR/3 condition* OR terminal* NEAR/3 disorder* OR terminal* NEAR/3 abnormalit* OR terminal* NEAR/3 impairment* OR terminal* NEAR/3 handicap* OR genetic NEAR/3 disease* OR genetic NEAR/3 disorder* OR genetic NEAR/3 illness* OR genetic NEAR/3 condition* OR genetic NEAR/3 abnormalit* OR genetic NEAR/3 impairment* OR genetic NEAR/3 handicap* OR chromosomal NEAR/3 disease* OR chromosomal NEAR/3 illness* OR chromosomal NEAR/3 disorder* OR chromosomal NEAR/3 condition* OR chromosomal NEAR/3 abnormalit* OR chromosomal NEAR/3 impairment* OR chromosomal NEAR/3 handicap* OR congenital NEAR/3 disease* OR congenital NEAR/3 illness* OR congenital NEAR/3 disorder* OR congenital NEAR/3 condition* OR congenital NEAR/3 abnormalit* OR congenital NEAR/3 impairment* OR congenital NEAR/3 handicap* OR complex NEAR/3 health* NEAR/3 need* OR “early death*” OR “cerebral pals*” OR “spina bifida” OR “cystic fibrosis” OR encephalopath* OR disabilit* OR disabled OR handicap* OR spastic* OR “impaired motor skill*” OR “spinal cord condition*” OR “multiple trauma” OR “acquired brain injur*” OR “neurological condition*” OR “neuromuscular condition*” OR “multi-organ disease*” OR neurodisabilit*)
-
# 3 #2 AND #1
-
# 4 TOPIC: (“young adult*” OR “young person” OR “young people” OR youth* OR “emerg* adult*” OR “early adult*” OR (child* NEAR/3 transition NEAR/3 adult*) OR (adolescen* NEAR/3 transition NEAR/3 adult*) OR (teenage* NEAR/3 transition NEAR/3 adult*) OR (paediatric* NEAR/3 transition NEAR/3 adult*) OR (pediatric* NEAR/3 transition NEAR/3 adult) OR “college student*” OR “university student*” OR “post-secondary student*” OR undergraduate* OR postgraduate* OR famil* OR carer* OR caregiver* OR parent* OR grandparent* OR relative* OR relation* OR sibling*)
-
# 5 #4 AND #3
Timespan = 2002–18
Social Care Online
Date searched: September 2018.
Date range searched: 1 January 2002 to 26 September 2018.
Search strategy
[SubjectTerms:’”short break care”‘ including this term only OR SubjectTerms:’”intermediate care”‘ including this term only OR SubjectTerms:’”hospices”‘ including this term only OR SubjectTerms:’”holidays”‘ including this term only OR AllFields:’respite* or “short break*” or hospice*’]
AND
[SubjectTerms:’”palliative care”‘ including this term only OR SubjectTerms:’”terminal illness”‘ including this term only OR SubjectTerms:’”muscular dystrophy”‘ including this term only OR SubjectTerms:’”cancer”‘ including this term only OR SubjectTerms:’”cerebral palsy”‘ including this term only OR SubjectTerms:’”spina bifida”‘ including this term only OR SubjectTerms:’”cystic fibrosis”‘ including this term only OR SubjectTerms:’”disabilities”‘ including this term only OR SubjectTerms:’”complex needs”‘ including this term only OR SubjectTerms:’”long term conditions”‘ including this term only OR AllFields:’”life limit*” OR “life-limit*” OR “life shorten*” OR “complex health* need*” or “complex need*” or disabilit* or disabled’]
AND
[SubjectTerms:’”young adults”‘ including this term only OR SubjectTerms:’”young people”‘ including this term only OR SubjectTerms:’”adults”‘ including this term only OR SubjectTerms:’”carers”‘ including this term only OR SubjectTerms:’”families”‘ including this term only OR SubjectTerms:’”parents”‘ including this term only OR SubjectTerms:’”siblings”‘ including this term only OR SubjectTerms:’”grandparents”‘ including this term only OR AllFields:’”young adult*” or “young person” or “young people” or famil* or carer* or caregiver* or parent*’]
Trip database
Date searched: September 2018.
Date range searched: 1 January 2002 to 26 September 2018.
Search strategy
((“day* away” OR “day care*” OR “day centre*” OR “day center*” OR “day program*” OR “day service*” OR holiday* OR “home support*” OR hospice* OR “intermediate care” OR “night care*” OR “night-time care*” OR “partial hospitalisation*” OR “partial hospitalization*” OR “relief care*” OR “relief support” OR “residential care*” OR “residential home*” OR “residential facilit*” OR respite* OR “short break*” OR “short stay*” OR “sitting service*” OR “support program*” OR “support scheme*” OR “support service*” OR “temporary admission*” OR “temporary break*” OR “temporary care*” OR “temporary relief” OR “temporary support*” OR “short-term admission*” OR “short-term break*” OR “short-term care*” OR “short-term relief” OR “short-term support*” OR “time off” OR vacation* OR “care service*” OR “overnight stay*” OR “home-based support*” OR “befriend* service*” OR “short-break foster*” OR “adult placement scheme*” OR “shared care” OR “replacement care” OR “family support”) AND (“life-limit*” OR “life limit*” OR “life shorten*” OR “complex health* need*” OR “complex need*” OR disab*) AND (“young adult*” or “young person” or “young people” or famil* or carer* or caregiver* or parent*)) (from:2002 to:2018)
NICE Evidence
Date searched: September 2018.
Date range searched: 1 January 2002 to 26 September 2018.
Search strategy
(respite* OR “short break*” OR hospice*) AND (“life-limit*” OR “life limit*” OR “life shorten*” OR “complex health* need*” OR “complex need*” OR disab*)
International Clinical Trials Registry Platform
URL: http://apps.who.int/trialsearch/AdvSearch.aspx
Date searched: September 2018.
Date range searched: 1 January 2002 to 26 September 2018.
Search strategy
(“day* away” OR “day care*” OR “day centre*” OR “day center*” OR “day program*” OR “day service*” OR holiday* OR “home support*” OR hospice* OR “intermediate care” OR “night care*” OR “night-time care*” OR “partial hospitalisation*” OR “partial hospitalization*” OR “relief care*” OR “relief support” OR “residential care*” OR “residential home*” OR “residential facilit*” OR respite* OR “short break*” OR “short stay*” OR “sitting service*” OR “support program*” OR “support scheme*” OR “support service*” OR “temporary admission*” OR “temporary break*” OR “temporary care*” OR “temporary relief” OR “temporary support*” OR “short-term admission*” OR “short-term break*” OR “short-term care*” OR “short-term relief” OR “short-term support*” OR “time off” OR vacation* OR “care service*” OR “overnight stay*” OR “home-based support*” OR “befriend* service*” OR “short-break foster*” OR “adult placement scheme*” OR “shared care” OR “replacement care” OR “family support”)
EU Clinical Trials Register
URL: www.clinicaltrialsregister.eu/ctr-search/search
Date searched: September 2018.
Date range searched: 1 January 2002 to 26 September 2018.
Search strategy
“day away” OR “day care” OR “day centre” OR “day center” OR “day program” OR “day service” OR holiday OR “home support” OR hospice OR “intermediate care” OR “night care” OR “night-time care” OR “partial hospitalisation” OR “partial hospitalization” OR “relief care” OR “relief support” OR “residential care” OR “residential home” OR “residential facility” OR respite OR “short break” OR “short stay” OR “sitting service” OR “support program” OR “support scheme” OR “support service” OR “temporary admission” OR “temporary break” OR “temporary care” OR “temporary relief” OR “temporary support” OR “short-term admission” OR “short-term break” OR “short-term care” OR “short-term relief” OR “short-term support” OR “time off” OR vacation OR “care service” OR “overnight stay” OR “home-based support” OR “befriending service” OR “short-break foster” OR “adult placement scheme” OR “shared care” OR “replacement care” OR “family support”
ClinicalTrials.gov
URL: https://clinicaltrials.gov/
Date searched: September 2018.
Date range searched: 1 January 2002 to 26 September 2018.
Search strategy
respite OR “short break” OR hospice | Child, Adult | Start date from 01/01/2002 to 01/09/2020
National Institute for Health Research Journals Library
Date searched: September 2018.
Date range searched: 1 January 2002 to 26 September 2018.
Search strategy
Search 1: respite* OR “short breaks” OR hospice*
Search 2: “life limiting” OR “life-limiting” OR “life shortening” OR “complex health needs” OR “complex healthcare needs” OR “complex needs” OR disabilities OR disability OR disabled
Grey Literature Report
URL: www.greylit.org
Date searched:
Date range searched:
Search strategy
Search 1: respite
Search 2: short break
Search 3: hospice
JBI Systematic Reviews and Implementation Reports
Date searched: September 2018.
Date range searched: 1 January 2002 to 26 September 2018.
Search strategy
(respite* OR “short break*” OR hospice*) AND (“life limit*” OR “life limit*” OR “life shorten*” OR “complex health* need*” OR “complex need*” OR disab*)
Google Scholar
Date searched: September 2018.
Date range searched: 1 January 2002 to 26 September 2018.
Search strategy
Respite life-limiting “young adult”
Respite life-limiting “young adults”
“short breaks” life-limiting “young adult”
“short breaks” life-limiting “young adults”
Respite “complex health needs” “young adult”
Respite “complex health needs” “young adults”
“short breaks” “complex health needs” “young adult”
“short breaks” “complex health needs” “young adults”
Respite “complex healthcare needs” “young adult”
Respite “complex healthcare needs” “young adults”
“short breaks” “complex healthcare needs” “young adult”
“short breaks” “complex healthcare needs” “young adults”
Respite life-limiting “young person”
Respite life-limiting “young people”
“short breaks” life-limiting “young person”
“short breaks” life-limiting “young people”
Respite “complex health needs” “young person”
Respite “complex health needs” “young people”
“short breaks” “complex health needs” “young person”
“short breaks” “complex health needs” “young people”
Respite “complex healthcare needs” “young person”
Respite “complex healthcare needs” “young people”
“short breaks” “complex healthcare needs” “young person”
“short breaks” “complex healthcare needs” “young people”
Appendix 2 Modified MEDLINE(R) ALL search strategy
Date searched: September 2019.
Date range searched: 1946 to 18 September 2019.
Search strategy
-
exp Respite Care/
-
exp Hospice Care/
-
exp HOSPICES/
-
exp Day Care, Medical/
-
exp Night Care/
-
exp Intermediate Care Facilities/
-
exp HOLIDAYS/
-
“day* away”.ti,ab.
-
“day care*”.ti,ab.
-
“day centre*”.ti,ab.
-
“day center*”.ti,ab.
-
“day program*”.ti,ab.
-
“day service*”.ti,ab.
-
holiday*.ti,ab.
-
“home support*”.ti,ab.
-
hospice*.ti,ab.
-
“intermediate care”.ti,ab.
-
“night care*”.ti,ab.
-
“night-time care*”.ti,ab.
-
“relief care*”.ti,ab.
-
“relief support”.ti,ab.
-
“residential care*”.ti,ab.
-
“residential home*”.ti,ab.
-
“residential facilit*”.ti,ab.
-
respite*.ti,ab.
-
“short break*”.ti,ab.
-
“short stay*”.ti,ab.
-
“sitting service*”.ti,ab.
-
“support program*”.ti,ab.
-
“support scheme*”.ti,ab.
-
“support service*”.ti,ab.
-
“temporary admission*”.ti,ab.
-
“temporary break*”.ti,ab.
-
“temporary care*”.ti,ab.
-
“temporary relief”.ti,ab.
-
“temporary support*”.ti,ab.
-
“short-term admission*”.ti,ab.
-
“short-term break*”.ti,ab.
-
“short-term care*”.ti,ab.
-
“short-term relief”.ti,ab.
-
“short-term support*”.ti,ab.
-
“time off”.ti,ab.
-
vacation*.ti,ab.
-
“care service*”.ti,ab.
-
“overnight stay*”.ti,ab.
-
“home-based support*”.ti,ab.
-
“befriend* service*”.ti,ab.
-
“short-break foster*”.ti,ab.
-
“adult placement scheme*”.ti,ab.
-
“shared care”.ti,ab.
-
“replacement care”.ti,ab.
-
“family support”.ti,ab.
-
or/1-52
-
exp MUSCULAR DYSTROPHY, DUCHENNE/
-
exp Neoplasms/
-
exp Muscular Dystrophies/
-
exp Cerebral Palsy/
-
exp Spinal Dysraphism/
-
exp Cystic Fibrosis/
-
exp Disabled Persons/
-
exp Disabled Children/
-
exp Neurodegenerative Diseases/
-
exp Multiple Trauma/
-
exp Genetic Diseases, Inborn/
-
exp Chromosome Disorders/
-
exp “CONGENITAL, HEREDITARY, AND NEONATAL DISEASES AND
-
ABNORMALITIES”/
-
(advanc* adj3 disease*).ti,ab.
-
(advanc* adj3 illness*).ti,ab.
-
(advanc* adj3 condition*).ti,ab.
-
(advanc* adj3 disorder*).ti,ab.
-
(advanc* adj3 abnormalit*).ti,ab.
-
(advanc* adj3 impairment*).ti,ab.
-
(advanc* adj3 handicap*).ti,ab.
-
(degenerative adj3 disease*).ti,ab.
-
(degenerative adj3 illness*).ti,ab.
-
(degenerative adj3 condition*).ti,ab.
-
(degenerative adj3 disorder*).ti,ab.
-
(degenerative adj3 abnormalit*).ti,ab.
-
(degenerative adj3 impairment*).ti,ab.
-
(degenerative adj3 handicap*).ti,ab.
-
(progressive adj3 disease*).ti,ab.
-
(progressive adj3 illness*).ti,ab.
-
(progressive adj3 condition*).ti,ab.
-
(progressive adj3 disorder*).ti,ab.
-
(progressive adj3 abnormalit*).ti,ab.
-
(progressive adj3 impairment*).ti,ab.
-
(progressive adj3 handicap*).ti,ab.
-
“diminished life expectancy”.ti,ab.
-
“limited life expectancy”.ti,ab.
-
cancer*.ti,ab.
-
duchenne.ti,ab.
-
incurable.ti,ab.
-
life-limit*.ti,ab.
-
“life limit*”.ti,ab.
-
(life adj3 short*).ti,ab.
-
(live* adj3 short*).ti,ab.
-
“life threaten*”.ti,ab.
-
“limited life expectancy”.ti,ab.
-
LLC.ti,ab.
-
LLI.ti,ab.
-
“muscular dystroph*”.ti,ab.
-
neoplasm*.ti,ab.
-
“neurodegenerative condition*”.ti,ab.
-
“neurodegenerative disease*”.ti,ab.
-
“neurodegenerative illness*”.ti,ab.
-
“neurodegenerative disorder*”.ti,ab.
-
“neurodegenerative abnormalit*”.ti,ab.
-
“neurodegenerative impairment*”.ti,ab.
-
“neurodegenerative handicap*”.ti,ab.
-
oncology.ti,ab.
-
“poor prognosis”.ti,ab.
-
(serious* adj3 ill*).ti,ab.
-
(genetic adj3 disease*).ti,ab.
-
(genetic adj3 disorder*).ti,ab.
-
(genetic adj3 illness*).ti,ab.
-
(genetic adj3 condition*).ti,ab.
-
(genetic adj3 abnormalit*).ti,ab.
-
(genetic adj3 impairment*).ti,ab.
-
(genetic adj3 handicap*).ti,ab.
-
(chromosomal adj3 disease*).ti,ab.
-
(chromosomal adj3 illness*).ti,ab.
-
(chromosomal adj3 disorder*).ti,ab.
-
(chromosomal adj3 condition*).ti,ab.
-
(chromosomal adj3 abnormalit*).ti,ab.
-
(chromosomal adj3 impairment*).ti,ab.
-
(chromosomal adj3 handicap*).ti,ab.
-
(congenital adj3 disease*).ti,ab.
-
(congenital adj3 illness*).ti,ab.
-
(congenital adj3 disorder*).ti,ab.
-
(congenital adj3 condition*).ti,ab.
-
(congenital adj3 abnormalit*).ti,ab.
-
(congenital adj3 impairment*).ti,ab.
-
(congenital adj3 handicap*).ti,ab.
-
“complex health* need*”.ti,ab.
-
“early death*”.ti,ab.
-
“cerebral pals*”.ti,ab.
-
“spina bifida”.ti,ab.
-
“cystic fibrosis”.ti,ab.
-
encephalopath*.ti,ab.
-
disabilit*.ti,ab.
-
disabled.ti,ab.
-
handicap*.ti,ab.
-
spastic*.ti,ab.
-
“impaired motor skill*”.ti,ab.
-
“spinal cord condition*”.ti,ab.
-
“multiple trauma”.ti,ab.
-
“acquired brain injur*”.ti,ab.
-
“neurological condition*”.ti,ab.
-
“neuromuscular condition*”.ti,ab.
-
“multi-organ disease*”.ti,ab.
-
neurodisabilit*.ti,ab.
-
or/54-151
-
“young adult*”.ti,ab.
-
“young person”.ti,ab.
-
“young people”.ti,ab.
-
youth*.ti,ab.
-
“emerg* adult*”.ti,ab.
-
“early adult*”.ti,ab.
-
(child* adj3 transition adj3 adult*).ti,ab.
-
(adolescen* adj3 transition adj3 adult*).ti,ab.
-
(teenage* adj3 transition adj3 adult*).ti,ab.
-
(paediatric* adj3 transition adj3 adult*).ti,ab.
-
(pediatric* adj3 transition adj3 adult).ti,ab.
-
“college student*”.ti,ab.
-
“university student*”.ti,ab.
-
“post-secondary student*”.ti,ab.
-
undergraduate*.ti,ab.
-
postgraduate*.ti,ab.
-
exp Young Adult/
-
exp ADOLESCENT/
-
exp ADULT/
-
exp FAMILY/
-
exp CAREGIVERS/
-
exp PARENTS/
-
famil*.ti,ab.
-
carer*.ti,ab.
-
caregiver*.ti,ab.
-
parent*.ti,ab.
-
grandparent*.ti,ab.
-
relative*.ti,ab.
-
relation*.ti,ab.
-
sibling*.ti,ab.
-
or/153-182
-
53 and 152 and 183
-
limit 184 to ed = 20190201-20190918.
Appendix 3 Organisations and charities (grey literature search)
Association for Palliative Medicine (Fareham, UK).
European Association for Palliative Care (Vilvoorde, Belgium).
International Children’s Palliative Care Network (Bristol, UK).
NICE (London, UK).
NHS CCGs in the UK, Wales, Scotland and Northern Ireland.
North West Clinical Commissioning Network (Halton, UK).
North West Coast Strategic Clinical Networks and Senate (Warrington, UK).
North West Coast Clinical Networks for Palliative and End of Life Care (composed of two networks: Cheshire and Merseyside, UK, and Lancashire and South Cumbria, UK).
Palliative Care Research Society (Southampton, UK).
Peninsula Childhood Disability Research Unit (Exeter, UK).
Parent Voices Count (Manchester, UK).
Royal College of Nursing (London, UK).
Royal College of Paediatrics and Child Health (London, UK).
Social Care Institute for Excellence (London, UK).
TfSL Regional Action Groups and Transition Taskforce (Bristol, UK).
The Collaboration for Leadership in Applied Health Research and Care, North West Coast (Liverpool, UK).
The Innovation Agency (Daresbury, UK).
UK local authority websites.
CharitiesAction Duchenne (London, UK, URL: www.actionduchenne.org/).
bibic (Somerset, UK, URL: https://bibic.org.uk/).
The Children’s Trust (Surrey, UK, URL: www.thechildrenstrust.org.uk/brain-injury-information).
British Heart Foundation (London, UK, URL: www.bhf.org.uk/).
Carers Trust (London, UK, URL: https://carers.org/).
Carers UK (London, UK, URL: www.carersuk.org/).
Cerebra (Carmarthen, UK) URL: www.cerebra.org.uk/).
Children’s Hospices Across Scotland (Edinburgh, UK, URL: www.chas.org.uk/).
Cystic Fibrosis Trust (London, UK, URL: www.cysticfibrosis.org.uk/).
Disability Rights UK (London, UK, URL: www.disabilityrightsuk.org/).
Down’s Syndrome Association (Middlesex, UK, URL: www.downs-syndrome.org.uk/).
Epilepsy Action (Leeds, UK, URL: www.epilepsy.org.uk/).
Genetic Disorders UK (Haywards Heath, UK, URL: www.geneticdisordersuk.org/).
Headway (Nottingham, UK, URL: www.headway.org.uk/).
Hospice UK (London, UK, URL: www.hospiceuk.org/).
Huntington’s Disease Association (Liverpool, UK, URL: www.hda.org.uk/).
Muscular Dystrophy Association (Chicago, IL, USA, URL: www.mda.org/).
Mencap (London, UK, URL: www.mencap.org.uk/).
Motor Neurone Disease Association (Northampton, UK, URL: www.mndassociation.org/).
Motor Neurone Disease Scotland (Glasgow, UK, URL: www.mndscotland.org.uk/).
MS Society (London, UK, URL: www.mssociety.org.uk/).
Muscular Dystrophy UK (London, UK, URL: www.musculardystrophyuk.org/).
My Life (Wigan, UK, URL: www.my-life.org.uk/).
Rainbow Trust (Surrey, UK, URL: https://rainbowtrust.org.uk/).
Reach (Tavistock, UK, URL: http://reach.org.uk/).
SCOPE (London, UK, URL: www.scope.org.uk/).
Shine (Peterborough, UK, URL: www.shinecharity.org.uk/).
Spinal Injuries Association (Milton Keynes, UK, URL: www.spinal.co.uk/).
SWAN UK (London, UK, URL: www.undiagnosed.org.uk/).
TfSL (Bristol, UK, URL: www.togetherforshortlives.org.uk/).
Appendix 4 Review design and synthesis methods model
| Review question | Stream | Study type | Selection of evidence for in-depth review data extraction | Synthesis of evidence according to type, using appropriate methods | Overarching narrative synthesis and programme logic models for interventions |
|---|---|---|---|---|---|
| What is the effectiveness and cost-effectiveness of different types of formal and informal respite care and short break provision? | Stream 1: intervention effectiveness | RCTs and quasi-RCTs |
↑ Searches Screening Study inclusion/exclusion Appraisal of quality or risk of bias Data extraction Confirm typology and different interventions (models of service)↑ |
Meta-analysis Narrative summary |
↑ Overarching narrative synthesis of qualitative and quantitative evidence, including articulation of programme theories Logic model development for interventions (models of service) to show the different designs, inputs, processes and intended outcomes for various stakeholders↑ |
| Other experimental or quasi-experimental studies | |||||
| What is the economic impact of respite care and short breaks? | Stream 2: health economics | Cost–utility, cost-effectiveness |
Meta-analysis Narrative summary |
||
| Other economic studies | |||||
|
What are service users’ and providers’ views of current service provision and the need for new services? What are the facilitators of and barriers to providing, implementing and using respite care and short breaks (taking into account the different perspectives of service users, family members and providers)? |
Stream 3: experience and attitudes | Quantitative (e.g. questionnaire surveys) |
Narrative summary (quantitative data) Thematic synthesis (qualitative data) Mixed-methods matrix for integration of quantitative and qualitative evidence |
||
| Qualitative studies and qualitative data (e.g. from open-ended survey questions) | |||||
| Mixed-methods studies (e.g. case studies and process evaluations) | |||||
| What are the current UK policy and guidance recommendations for the provision of respite care and short breaks? | Stream 4: policy and guidelines | Clinical guidelines | Framework synthesis | ||
| Government policy | |||||
| Other |
Appendix 5 Framework analysis codebook
| Theme | Description |
|---|---|
|
1. Acceptability of the service |
Evidence that relates to the acceptability of the service for all service user perspectives. This will include data on the expectations, preferences and values of service users through their views on the service, their preferred use and delivery of the service Is it what people want (young adults, parents, wider family)?Confirming case: look for and code evidence that confirms the service was acceptable Deviant (disconfirming) case: the counter pattern in the literature, where the service was not acceptable |
|
2. Implementation of the service |
Code evidence that looks at issues relating to service implementation and deliveryConfirming case Deviant (disconfirming) case |
|
3. Feasibility and accessibility of the service |
Code evidence that relates to service demand, service resources to meet demand and sustainability of the service Consider from the perspectives of the young adult, parent, wider family and service provider:Confirming case Deviant (disconfirming) case Note: feasibility and implementation may overlap |
|
4. Primary (intended) outcomes |
Code evidence that relates to all short-term and mid- to long-term intended outcomes and benefits for the person the intervention is intended for (typically this is the young adult, but could be other perspectives). This may include a broad range of areas:
|
|
5. Secondary (intended) outcomes |
As above, but code evidence that relates to any secondary outcomes (e.g. if service is delivered to the young adult, but there are also intended outcomes for others, such as a break for parents) |
|
6. Primary experienced outcomes |
Code evidence relating to any other outcomes or benefits that may not have been intended, but have been experienced by the person to whom the respite intervention was delivered |
|
7. Secondary experienced outcomes |
As above, but outcome is experienced by a secondary person (e.g. a parent). There may be unintentional consequences of service delivery [e.g. with the social activity model, the focus is on young adult (service user) and the secondary outcome could be from the parental perspective as they get time to spend with other family members] |
|
8. Negative experience/impact |
Evidence describing any negative impact for all perspectives, including service provider, young adult, parent, wider family [e.g. harms of respite (such as the young adult not wanting to go, service could not manage behaviour so sent them home, etc.)] |
|
9. Measurable outcomes |
Any evidence of measurable outcomes (e.g. quantitative reports of satisfaction) |
|
10. Miscellaneous |
Anything else that cannot be coded, using above framework for discussion in stream meetings |
|
11. Was respite achieved? |
Primary focus of analysis is whether or not the primary goal was achieved |
Appendix 6 Excluded studies with reasons for exclusion
Owing to limitations in the information retrieved from searches, not all of the excluded sources can be referenced in full.
Not study population (n = 530)
LE Wales. Respite Care in Wales Final Report to Welsh Assembly Government. Cardiff: LE Wales; 2010.
Leisure Activities and Short Breaks for Disabled Children. Solihull: Solihull Metropolitan Borough Council; 2019.
Thompson R. The Importance of Respite Care: A Parent’s Perspective. URL: www.togetherforshortlives.org.uk/resource/importance-respite-care-parents-perspective-rachel-thompson/ (accessed 3 December 2020).
Worcester County Council. Position Statement For Current Overnight Short Break Provision. Worcester: Worcestershire County Council.
Carlin J. What Contributes to Adult Children Carers’ Well-being? 2015. URL: www.nationalelfservice.net/populations-and-settings/caregivers/what-contributes-to-adult-children-carers-well-being/ (accessed 3 December 2020).
South Gloucestershire Council. Short Break Services Statement South Gloucestershire. Bristol: South Gloucestershire Council.
Support service will focus on the needs of young people. Cancer Nurs Pract 2015;14:6.
Welch V, Hatton C, Emerson E, Robertson J, Collins M, Langer S, Wells E. Do short break and respite services for families with a disabled child in England make a difference to siblings? A qualitative analysis of sibling and parent responses. Child Youth Serv Rev 2012;34:451–9.
Wood C. Personal Best: ‘Personal Budgets will Revolutionise Social Care Delivery, but Only if Local Authorities are Fully Prepared . . .’. New York, NY: Demos; 2010.
Improving palliative care for children and their families. J Psychosoc Nurs Ment Heal Serv. 2002;40:12.
Wiseman R. Impact of the Short Break Programme on the Prevention of Disabled Children Entering the Looked After System. London: Contact; 2011.
Welch V, Collins M, Hatton C, Emerson E, Robertson J, Wells E, Langer S. Short break and respite services for disabled children in England: comparing children’s and parents’ perspectives of their impact on children. Child Soc 2014;28:478–94.
Extending access to short breaks for disabled children from black families: a case study of research into practice. Soc Serv Res Gr. 2006.
Transition Care. St Joseph’s Hospice. Gap from child to adult palliative services ‘too large’. Br J Hosp Med 2014;75:608.
NEF Consulting. The Social and Economic Value of Short Breaks. London: NEF Consulting; 2009.
Shared Care Scotland. Shared Care Scotland Inspiring Breaks Programme. Dunfermline: Shared Care Scotland; 2011.
Gadsby EW. Personal Budgets and Health: A Review of the Evidence. London: Policy Research Unit in Commissioning and the Healthcare System; 2013.
Successful respite care needs consultation with children and their families. Nurs Child Young People 2012;24:11.
Payne J. Adult Community Care: Key Issues. Edinburgh: The Scottish Parliament; 2011.
Cornwall Council. Cornwall’s Short Break Statement. Truro: Cornwall Council; 2018.
Standards for pediatric patients offer support for community hospice. Hosp Manag Advis 2010;15:73–5.
Knowsley Council. Short Breaks for Children with Disabilities Duty Statement. Huyton: Knowsley Council; 2017.
Children’s palliative care is about living – not just dying: ACT emphasises differences from adult services. Paediatr Nurs 2007;19:5.
Respite needs still unmet: families face delays, lack of information and bureaucracy. Paediatr Nurs 2003;15:4.
Spending the New Money on Short Breaks Wisely. Brighton: Reed Business Information; 2010.
Services for Children and Young People. 2007.
Barnsley Council. Calderdale, Kirklees, Wakefeld and Barnsley (CKWB) Transforming Care Partnership Plan. Barnsley: Barnsley Council; 2016.
Selected abstracts from Social Care Online. Eur J Soc Work 2008;11:185–91.
Council pays out for failing to give respite. Learn Disabil Pract 2005;8:5.
Rest Assured? A Study of Unpaid Carers’ Experiences of Short Breaks. Glasgow: Institute for Research and Innovation in Social Services; 2012.
Aiming High for Disabled Children: Delivering Improved Health Services. The Voice of NHS Leadership.
Hospice. FPnotebook. 2015. URL: https://fpnotebook.com/hemeonc/Manage/Hspc.htm (accessed 3 December 2020).
Department for Education. TSD Workbook for Short Break Foster Carers. London: Department for Education; 2012.
Stevens M. Direct Payments in Residential Care: Ideas for Implementation and Some Concerns About Their Value. 2018. URL: www.nationalelfservice.net/social-care/personal-budgets-and-direct-payments/direct-payments-in-residential-care-ideas-for-implementation-and-some-concerns-about-their-value/ (accessed 3 December 2020).
NHS Education for Scotland. Local Delivery Plan 2016–17. Edinburgh: NHS Education for Scotland; 2016.
National Institute for Health and Care Excellence (NICE). End Of Life Care for Infants, Children and Young People with Life-Limiting Conditions: Planning and Management. NICE guideline NG61. London: NICE; 2016.
Russell C, Boelman V. Together We Can: Exploring Asset-Based Approaches and Complex Needs Service Transformation. London: The Young Foundation; 2013.
Adult day services relieve caregiver stress, boost outcomes. Hosp Manag Advis 2010;15:97–9.
Department of Health and Social Care (DHSC). Children and Young People’s Continuing Care Guidance. London: DHSC; 2012.
A Break from Caring for a Disabled Child: Parent Perceptions of the Uses and Benefits of Short Break Provision in England. Oxford: Oxford University Press; 2014.
Respite Care. Purchasing the Right Services – OpenGrey.
Shared Lives Plus. Personal Health Budgets 2018: What Every Voluntary, Community and Social Enterprise Needs to Know. Liverpool: Shared Lives Plus; 2018.
Carers Trust. Care Act for Carers: One Year On. London: Carers Trust; 2016.
Better support and more choice for families of disabled children. Paediatr Nurs 2007;19:5.
Helen H. Meeting the Needs of Disabled Children and Their Families: Some Messages From the Literature. Abingdon: Taylor & Francis; 2008.
End of Life Care for Infants, Children and Young People – Quality Standard (QS160). 2017.
Respite Care. Providing Services to Meet User and Carer Needs – OpenGrey.
What is the Future for Short Breaks in Wales for Disabled Children and Young People? Cardiff: Children in Wales; 2010.
Every Disabled Child Matters. Short Breaks Services Statements: Commitment and Transparency. London: Every Disabled Child Matters; 2012.
Youth Residential Treatment. St John’s, NL: Newfoundland and Labrador Centre for Health Information; 2010.
The Future of Disability. London: Demos; 2014.
Parker G, Spiers G, Gridley K, Atkin K, Cusworth L, Mukherjee S et al. Evaluating Models of Care Closer to Home for Children and Young People who are Ill. York: University of York; 2011.
Ruth Northway. High Cost Placements for People with Learning Disabilities and Complex and Challenging Needs. 2015. URL: www.nationalelfservice.net/learning-disabilities/challenging-behaviour/high-cost-placements-for-people-with-learning-disabilities-and-complex-and-challenging-needs/ (accessed 3 December 2020).
Department for Education. Short Break Care: How Local Authorities Should Provide It. London: Department for Education; 2011.
Respite Care. Merck Manuals. 19th edn. 2013.
Shared Care Network. A Job Worth Doing: A Guide to Setting Up and Running a Contract Carers Service to Provide Short Breaks for Disabled Children. Dunfermline: Shared Care Network; 2008.
The need for short breaks and how to run them. Community Care 2007:26.
Support Care Gives a Break to Families Under Pressure. London: Haymarket; 2011.
Don’t Let Me Down. Ensuring a Good Transition for Young People with Palliative Care Needs. 2012.
Charity highlights parents’ concerns over palliative care. Nurs Child Young People 2012;24:5.
Personal Health Budgets: A Revolution in Personalisation. London: 2020 health; 2013.
Bishop K. Young People’s Views on Responsive Social Services: What Makes a Difference? 2015. URL: www.nationalelfservice.net/populations-and-settings/child-and-adolescent/young-peoples-views-on-responsive-social-services-what-makes-a-difference/ (accessed 3 December 2020).
Children and Young Persons Bill [HL] Committee Stage Report. 2008.
Stepping Stones. 2004.
A Personal Account of Caring. Evidence-Based Nursing Blog. 2015.
World Health Organization. World Report on Disability. Geneva: World Health Organization; 2011.
Update plus. Update 2006;72:124–7.
Twycross A, Smith J. Perspectives on current child health issues. Evidence-Based Nurs 2016;19.
Every Disabled Child Matters. Short Breaks Tracking: Interim Report April 2009. London: Every Disabled Child Matters; 2009.
Gautheron V. Does the respite stay in a paediatric department of PRM meet a patient need? Ann Phys Rehabil Med 2012;55:e241.
Abbott D, Kotecha M, Scott S, Jessiman P, Kazimirski A, Read J, et al. Disabled Children’s Access to Childcare (DCATCH): A Qualitative Evaluation. 2011.
Abbott D, Watson D, Townsley R. The proof of the pudding: what difference does multi-agency working make to families with disabled children with complex health care needs? Child Fam Soc Work 2005;10:229–38.
Children with Disabilities Short Breaks Duty Statement (0–25 Disability Service). 2017.
Alaee N, Shahboulaghi FM, Khankeh H, Mohammad Khan Kermanshahi S. Psychosocial challenges for parents of children with cerebral palsy: a qualitative study. J Child Fam Stud 2015;24:2147–54.
Allen A, Allen T. The absolute perfect vacation. Except Parent 2006;36:92.
Great Britain. National Care Standards. Short Breaks and Respite Care Services for Adults. London: The Stationery Office; 2002.
Andrews F, Hood P. Shared care: hospital, hospice, home. Paediatr Nurs 2003;15:20–2. https://doi.org/10.7748/paed2003.07.15.6.20.c865
Andrews G, Steele R, Pek J, Siden H. Respite care for families of children with life-threatening conditions. J Pain Symptom Manage 2016;52:e135.
Anonymous. Royal College of Paediatrics and Child Health, abstracts of the annual conference jointly held with 6th Europaediatrics. Arch Dis Child Educ Pract Ed 2013;98.
Short Breaks Consultation – Findings, Graphs and Tables. pp. 1–30.
Aoun S, Kristjanson L, Oldham L. The challenges and unmet needs of people with neurodegenerative conditions and their carers. ACCNS J Community Nurses 2006;11:17–20.
Arango P, Anderson B, Wells N. Families, clinicians, and children and youth with special healthcare needs: a bright future. Pediatr Ann 2008;37:212–22. https://doi.org/10.3928/00904481-20080401-01
Archer KF. Audit of children’s palliative care services in the East Midlands and identification of the gaps in service provision. 2015;44:5.
Arens G. Support for siblings. Ther Today 2006;17:42–5.
Arno PS. Cost-savings due to respite. 2006;2004.
Davies B, Steele R, Collins JB, Cook K, Smith S. The impact on families of respite care in a children’s hospice program. J Palliat Care 2004;20:277–86.
Zebrack B, Bleyer A, Albritton K, Medearis S, Tang J. Assessing the health care needs of adolescent and young adult cancer patients and survivors. Cancer 2006;107:2915–23. https://doi.org/10.1002/cncr.22338
Barnsley Short Breaks Statement. Young People and Families.
Barrett M, Wheatland B, Haselby P, Larson A, Kristjanson L, Whyatt D. Palliative respite services using nursing staff reduces hospitalization of patients and improves acceptance among carers. Int J Palliat Nurs 2009;15:389–95. https://doi.org/10.12968/ijpn.2009.15.8.43798
Bath M, East N. Short Breaks Statement and How to Access Short Breaks and Activities for Disabled Children and Young people in Bath and North East Somerset Revised: February 2015. 2015.
Beecham J, Sloper P, Greco V, Webb R. The costs of key worker support for disabled children and their families. Child Care Health Dev 2007;33:611–18.
Behuniak SM. Free bird. Am J Hosp Palliat Care 2007;24:429.
Belmore J. Supportive Care of Children with Cancer. In Carachi R, Grosfeld JL, editors. The Surgery of Childhood Tumors. Berlin: Springer; 2016. pp. 641–55.
Benedict RE, Farel AM. Identifying children in need of ancillary and enabling services: a population approach. Soc Sci Med 2003;57:2035–47.
Bennett CA. A place for palliative care. Am J Nurs 2010;110:72. https://doi.org/10.1097/01.NAJ.0000370163.84802.8d
Beresford B, Cavet J. Transitions to Adult Services by Disabled Young People Leaving Out Authority Residential Schools. York: Social Policy Research Unit, University of York; 2009.
Beresford B, Clarke S, Sloper T. Integrating Services for Disabled Children, Young People and Their Families in York: Consultation Project. York: Social Policy Research Unit, University of York; 2005.
Bigham A, Cunningham J, Johnston K. Respite care for families of children with disabilities: a university/faith community model. J Christ Nurs 2017;34:52–8. https://doi.org/10.1097/CNJ.0000000000000337
Bishop C, Small N, Parslow R, Bowles D. Improving service coordination for children with complex needs. Br J Healthc Manag 2015;21:469–75.
Bishop L. Tŷ Hafan: ‘here to hold your hand’. Paediatr Nurs 2008;20:40. https://doi.org/10.7748/paed.20.8.40.s28
Bona K, Bates J, Wolfe J. Successful implementation of a novel state-funded pediatric palliative care program (413-B). J Pain Symptom Manage 2011;41:230.
Bowman J, Butcher R, Dolby S. Respite care needs for families of children with life-limiting conditions. Nurs Child Young People 2011;23:14.
Bradford Metropolitan District Council. Different Types of Fostering. 2008.
Braun S. Fried eggs and nursing. Nursing 2007;37:44–5.
Brawn E, Rogers C. Keep Us Close: Ensuring Good, Inclusive and Accessible Local Services for Disabled Children and Their Families. London: SCOPE; 2012.
Brennan EM, Rosenzweig JM, Jivanjee P, Stewart LM, Allen TD, Eby LT. Challenges and Supports for Employed Parents of Children and Youth with Special Needs. In Allen TD, Eby LT, editors. The Oxford Handbook of Work and Family. Oxford: Oxford University Press; 2016. pp. 165–81.
Brennan F. Silent. Am J Hosp Palliat Care. 2006;23:157.
Brenner M, Connolly M, Cawley D, Howlin F, Berry J, Quinn C. Family and healthcare professionals’ perceptions of a pilot hospice at home programme for children: a qualitative study. BMC Palliat Care 2016;15:89. https://doi.org/10.1186/s12904-016-0161-0
Brigend Short Breaks Statement. Support for the Whole Family for Carers of Disabled Children and Young People.
Bristol City Council. Short breaks for disabled children. Work 2011;117:8250.
Broberg M, Starke M. Everybody needs a break! The relation between need, availability and usage of respite-care and contextual, parental and child factors. J Intellect Disabil Res 2012;56:735.
Brodin J, Lindstrand P. Parents’ needs of respite care – a discussion based on a literature review. Eurorehab 2005;15:5.
Brown JD, Rodger S. Children with disabilities: problems faced by foster parents. Child Youth Serv Rev 2009;31:40–6.
Brown M, Trimbee O. Changing Perceptions. 2007.
Brown N. Evidence-based Care of Children with Complex Medical Needs. Paediatric Nursing in Australia: Principles for Practice. 2017.
Bumbalo J, Ustinich L, Ramcharran D, Schwalberg R. Economic impact on families caring for children with special health care needs in New Hampshire: the effect of socioeconomic and health-related factors. Matern Child Health J 2005;9:3–11. https://doi.org/10.1007/s10995-005-4350-3
Burke MM, Patton KA, Taylor JL. Family support: a review of the literature on families of adolescents with disabilities. J Fam Soc Work 2016;19:252–85.
Burton P, Phipps S. Economic costs of caring for children with disabilities in Canada. Can Public Policy 2009;35:269–90.
Burton-Smith R, McVilly KR, Yazbeck M, Parmenter TR, Tsutsui T. Service and support needs of Australian carers supporting a family member with disability at home. J Intellect Dev Disabil 2009;34:239–47.
Bužgová R, Páleníková A. Lived experience of parents of children with life-limiting and lifethreatening disease. Cent Eur J Nurs Midwifery 2015;6:209–17.
Bynum WE. A different kind of home. J Palliat Med 2014;17:1410–11. https://doi.org/10.1089/jpm.2014.0009
Ullrich C, Morrison RS. Pediatric palliative care research comes of age: what we stand to learn from children with life-threatening illness. J Palliat Med 2013;16:334–6. https://doi.org/10.1089/jpm.2013.9518
Caicedo C. Children with Special Health Care Needs: Comparison of the Effects of Home Care Setting, Prescribed Pediatric Extended Care Setting, and Long-Term Care Setting on Child and Family Health Outcomes and Health Care Service Use. PhD thesis. 2013.
Care P. Tourmaline House.
Ingleton C, Payne S, Nolan M, Carey I. Respite in palliative care: a review and discussion of the literature. Palliat Med 2003;17:567–75. https://doi.org/10.1191/0269216303pm803ra
Carey TA, Schouten K, Wakerman J, Humphreys JS, Miegel F, Murphy S, Arundell M. Improving the quality of life of palliative and chronic disease patients and carers in remote Australia with the establishment of a day respite facility. BMC Palliat Care 2016;15:62. https://doi.org/10.1186/s12904-016-0136-1
Carmichael A, Brown L. The future challenge for direct payments. Disabil Soc 2003;17:797–808.
Carmichael L. The Ayrshire hospice respite and response service – caring for the carers. Palliat Med 2016;30:S59.
Carruthers M, Stevens A-M. Palliative care and cystic fibrosis – the benefits of integrated working. Eur J Palliat Care 2014;21:277–81.
Carstairs A, Bowler E. ‘Man-made.’ An innovative male cooking group in a hospice day service. Palliat Med 2016;30:S102.
Carter B. ‘They’ve got to be as good as mum and dad’: children with complex health care needs and their siblings’ perceptions of a Diana community nursing service. Clin Eff Nurs 2005;9:49–61.
Carter KB, Mandrell BN. Development of a respite care program for caregivers of pediatric oncology patients and their siblings. J Pediatr Oncol Nurs 2013;30:109–14. https://doi.org/10.1177/1043454212473652
Castor C, Landgren K, Hansson H, Kristensson Hallström I. A possibility for strengthening family life and health: family members’ lived experience when a sick child receives home care in Sweden. Health Soc Care Community 2018;26:224–31. https://doi.org/10.1111/hsc.12512
Champagne M, Comeau E, Gervais A, De Varennes V, Tétreault C, Baril G, et al. Training volunteers who provide home respite for families for children with a life-threatening illness: the development of a program through action research. J Palliat Care 2006;22:214.
Champagne M, Mongeau S. Les retombées de séjours de répit dans une maison de soins palliatifs pédiatriques: le point de vue des parents. 18th International Congress on Palliative Care, October 5–8, 2010 – Palais Des Congres, Montreal, Canada. J Palliat Care 2010;26:245.
Chan J. What do people with acquired brain injury think about respite care and other support services? Int J Rehabil Res 2008;31:3–11. https://doi.org/10.1097/MRR.0b013e3282f45215
Chan L, Mehta A, Murray MA. How to best meet the needs of palliative patients and families in the 21st century: a question of evidence. J Palliat Care 2006;22:251–2.
Charlton P, Azar R, Luke A, Doucet S, Montelpare W, Nagel D, et al. Falling through the cracks: barriers to accessing services for children with complex health conditions and their families in New Brunswick. J New Brunswick Stud 2017;8.
Children and Young Persons Services Handbook. Big Stars, Little Stars. 2018.
Birmingham Disabled Children’s Directory. Family Information Service.
Chong PH, De Castro Molina JA, Teo K, Tan WS. Paediatric palliative care improves patient outcomes and reduces healthcare costs: evaluation of a home-based program. BMC Palliat Care 2018;17:11. https://doi.org/10.1186/s12904-017-0267-z
Chris H, Michelle C, Vicki W, Janet R, Eric E, Susanne L, et al. The Impact of Short Breaks on Families with a Disabled Child Over Time: The Second Report from the Quantitative Study.
Chum M, Schulz V, Watling C, Gofton T. The palliative care needs of patients living with life-limiting neurological illness. Neurology 2014;82.
Clark J. Inspection of Social Care Services for Disabled People: Dorset County Council: February 2002. Dorset: Dorset Council; 2002.
Clark M. A little respite: essential bundle. Perspect Infirm 2011;8:16.
Clarke H. Preventing Social Exclusion of Disabled Children and Their Families: Literature Review Paper Produced for the National Evaluation of the Children’s Fund. 2006.
Clarke S, Mitchell W, Sloper P. Psychosocial Support Services for Children and Young People with Cancer and Their Families. 2005.
Clay G. Community-based respite – reaching rural areas. Dementia 2002;1:256–9.
Cleary AS. Integrating palliative care into primary care for patients with chronic, life-limiting conditions. Nurse Pract 2016;41:42–8. https://doi.org/10.1097/01.NPR.0000480588.01667.58
Clemens KE, Klaschik E. State of the art 2007. 2007;42:280.
Coates-Dutton N. Syndrome Without a Name? The Experience of Living Without a Diagnosis for Parents of Disabled Children. 2015.
Cohen E, Berry JG, Camacho X, Anderson G, Wodchis W, Guttmann A. Patterns and costs of health care use of children with medical complexity. Pediatrics 2012;130:e1463–70. https://doi.org/10.1542/peds.2012-0175
Cohen E. Caring for the Family Caregiver: Lessons Learned in Child Health.
Cole E. ‘In palliative care we help children make memories’. Nurs Stand 2016;31:38–9.
Cole E. Sunflowers Care: ordinary lives in extraordinary circumstances. Nurs Child Young People 2017;29:16.
Coleman A, Kelly A, Leigh L, Gersch I, Dix A, Haythorne D. Beginning, middle, end, beginning: dramatherapy with children who have life-limiting conditions and with their siblings. 2012;117–25.
Collins A, Hennessy-Anderson N, Hosking S, Hynson J, Remedios C, Thomas K. Lived experiences of parents caring for a child with a life-limiting condition in Australia: a qualitative study. Palliat Med 2016;30:950–9.
Collins F. An evaluation of palliative care services in the community. Nurs Times 2004;100:34–7.
Conte T, Mitton C, Trenaman LM, Chavoshi N, Siden H. Effect of pediatric palliative care programs on health care resource utilization and costs among children with life-threatening conditions: a systematic review of comparative studies. CMAJ Open 2015;3:E68–75. https://doi.org/10.9778/cmajo.20140044
Conway Church J, Conway McCoin SE. A perspective on hospice reform and additional caregiver support. JAMA Intern Med 2016;176:1032. https://doi.org/10.1001/jamainternmed.2016.2734
Copps J, Heady L. What Price an Ordinary Life?: The Financial Costs and Benefits of Supporting Disabled Children and Their Families. London: New Philanthropy Capital; 2007.
Corkin D, Price J, Gillespie E. Respite care for children, young people and families: are their needs addressed? Int J Palliat Nurs 2006;12:422–7.
Costello J. Research roundup. Int J Palliat Nurs 2014;20:566–7.
Costello J. Research roundup. Int J Palliat Nurs 2018;24:204–5.
Courtney E, Kiernan G, Guerin S, Ryan K, McQuillan R. Mothers’ perspectives of the experience and impact of caring for their child with a life-limiting neurodevelopmental disability. Child Care Health Dev 2018;44:704–10. https://doi.org/10.1111/cch.12580
Cowen PS, Reed DA. Effects of respite care for children with developmental disabilities: evaluation of an intervention for at risk families. Public Health Nurs 2002;19:272–83.
Cox M, Feigin A, Napolitano B. Caregiver quality of life in Huntington’s disease. Neurotherapeutics 2010;7:138.
Cox S, Murtagh F, Tookman A, Gage A, Sykes N, McGinn M, et al. A review of specialist palliative care provision and access across London. Palliat Med 2016;30:S102–3.
Cramer H. Family-based short breaks (respite) for disabled children: results from the fourth national survey. Br J Soc Work 2008;38.
Craven DA. Letters to the editor. Ann Long-Term Care 2011;19:17.
Crettenden A, Wright A, Beilby E. Supporting families: outcomes of placement in voluntary out-of-home care for children and young people with disabilities and their families. Child Youth Serv Rev 2014;39:57–64.
Crews JE, Talley RC, Talley RC, Crews JE. Introduction: Multiple Dimensions of Caregiving and Disability. 2012. pp. 1–10.
Cross KL. The art of conversation through serious illness: lessons for caregivers. J Palliat Med 2011;14:375.
Curseen KA. Hospice and long term care partnership. ASBN Updat 2011;15:14–7.
Ferrell BR. Why isn’t all care ‘palliative care’? Am J Nurs 2004;104:11.
Meier DE, Beresford L. Preventing burnout. J Palliat Med 2006;9:1045–8. https://doi.org/10.1089/jpm.2006.9.1045
Damiani G, Rosenbaum P, Swinton M, Russell D. Frequency and determinants of formal respite service use among caregivers of children with cerebral palsy in Ontario. Child Care Health Dev 2004;30:77–86.
Dangel T. The status of pediatric palliative care in Europe. J Pain Symptom Manage 2002;24:160–5.
Darbyshire P. A Review of Palliative Care and Support Services in South Tyrol for Children and Young People Living with a Life-threatening or Life-limiting Illness and Their Families. 2013.
Davies B, Contro N, Larson J. Giving information to Latino and Chinese families in pediatric palliative care. 17th International Congress on Palliative Care, September 23–26, 2008, Palais Des Congres, Montreal, Canada. J Palliat Care 2008;24:214.
Davies B, Collins JB, Steele R, Cook K, Brenner A, Smith S. Children’s perspectives of a pediatric hospice program. J Palliat Care 2005;21:252–61.
Davies R. Establishing need for palliative care services for children/young people. Br J Nurs 2003;12:224–32. https://doi.org/10.12968/bjon.2003.12.4.11162
Davies R. Perspectives on palliative care for children and young people. Paediatr Nurs 2010;22:12.
Davies R, Harding Y. The first Diana Team in Wales: an update. Paediatr Nurs 2002;14:24–5. https://doi.org/10.7748/paed2002.03.14.2.24.c785
Davis K. ChiPPS E-Journal Pediatric Palliative and Hospice Care Issue #51, May 2018.
Day L, Gregory A, Read P. P127 Hospice respite: moving forwards not backwards. BMJ Support Palliat Care 2013;3:A55.
Araújo CA, Paz-Lourido B, Gelabert SV. Types of support to families of children with disabilities and their influence on family quality of life. Cien Saude Colet 2016;21:3121–30.
De Castilla EMR. Support, recreational and cultural program for adolescents and young adults with cancer and survivors. Pediatr Blood Cancer 2009;53:744.
Dean E. A refuge to lift the spirits. Nurs Stand 2012;26:18–19.
DeCourtney CA, Branch PK, Morgan KM. Eleanor McMullen’s story. J Palliat Care 2010;26:67.
Department for Education. Short Breaks: Statutory Guidance on How to Safeguard and Promote the Welfare of Disabled Children Using Short Breaks. London: Department for Education; 2010.
DiBello K, Coyne N. Palliative care hits a triple. Home Healthc Nurse 2014;32:183–90.
Dickson G. Succession planning in children’s palliative care services. Palliat Med 2016;30:S92–3.
Dixon J, Lee J, Ellison S, Hicks L. Supporting Adolescents on the Edge of Care: The Role of Short Term Stays in Residential Care: An Evidence Scope. 2015.
Doig JL, McLennan JD, Urichuk L. ‘Jumping through hoops’: parents’ experiences with seeking respite care for children with special needs. Child Care Health Dev 2009;35:234–42. https://doi.org/10.1111/j.1365-2214.2008.00922.x
Dolan P. A mother’s perspective: the power of holistic care for the terminally iii child. Holist Nurs Pract 2013;27:114–17.
Downing J, Knapp C, Muckaden MA, Fowler-Kerry S, Marston J, ICPCN Scientific Committee. Priorities for global research into children’s palliative care: results of an International Delphi Study. BMC Palliat Care 2015;14:36. https://doi.org/10.1186/s12904-015-0031-1
Downman TH. Hope and hopelessness: theory and reality. J R Soc Med 2008;101:428–30. https://doi.org/10.1258/jrsm.2008.080193
du Plessis J. Family Experiences and Viewpoints of Palliative and Supportive Care for Children with Cancer: Can We Do Better? Cape Town: University of Cape Town; 2017.
Dubois AC, Cuvelier S, Murinni C, Aujoulat I. Respite care: regards on decision making of the parents of a seriously ill child. Prat Psychol 2018;24:257–75.
Duff MA. The Child and Family Living with Complex Health Needs in the Community: Lived Experiences and Patterns of Coping and Relationship. 2012.
Dumont S, Jacobs P, Fassbender K, Anderson D, Turcotte V, Harel F. Palliative care in Canada: the economic perspective for families and health care system. Canadian Hospice Palliative Care Conference, Voyages in Care and Understanding, October 18–21, 2009, Winnipeg, Manitoba, Canada. J Palliat Care 2009;25:235.
Dumont S, Jacobs P, Turcotte V, Anderson D. Palliative care in Canada: the economic perspective for families and the health care system. 18th International Congress on Palliative Care, October 5–8, 2010 – Palais Des Congres, Montreal, Canada. J Palliat Care 2010;26:220.
Dumont S, Jacobs P. Palliative care in Canada: the economic perspective for families and the health care system. Canadian Hospice Palliative Care Conference: Navigating Safe Pathways to Quality Hospice Palliative Care, September 8–11, 2011, St John’s, Newfoundland, Canada. J Palliat Care 2011;27:256.
Dyke P, Mulroy S, Leonard H. Siblings of children with disabilities: challenges and opportunities. Acta Paediatr 2009;98:23–4. https://doi.org/10.1111/j.1651-2227.2008.01168.x
Eaton N. ‘I don’t know how we coped before’: a study of respite care for children in the home and hospice. J Clin Nurs 2008;17:3196–204. https://doi.org/10.1111/j.1365-2702.2008.02630.x
Eatough V, Santini H, Eiser C, Goller ML, Krysa W, de Nicola A, et al. The personal experience of parenting a child with juvenile Huntington’s disease: perceptions across Europe. Eur J Hum Genet 2013;21:1042–8. https://doi.org/10.1038/ejhg.2013.15
Edwards RT, Hounsome N, Noyes J, Bennett V, Hobson L, Spencer L. Children in North Wales: Current Provision. My Choices Project Report. 2010.
Ellis P. Research roundup. J Ren Nurs 2010;2:95–6.
Ens C, Chochinov H, Harlos M, Berard J, Stenekes S, Wowchuk S, et al. Canadian Virtual Hospice + children = a needs assessment. J Palliat Care 2006;22:233–4.
Etzioni S, Rosenfeld K, Bérubé M. Case study: deciding for the patient. Hastings Cent Rep 2004;34:12–3.
Faw MH. Supporting the supporter: social support and physiological stress among caregivers of children with severe disabilities. J Soc Pers Relat 2018;35:202–23.
Fellowes D, Goodman M, Wilkinson S, Low J, Harvey F. District nurses’ referrals to home-based palliative nursing services. Nurs Times 2003;99:34–7.
Ferris FD. Standards and guidelines: do they matter? J Palliat Med 2004;7:750–2. https://doi.org/10.1089/jpm.2004.7.750
Feyh JM. Perspectives of Close Relatives in Pediatric Palliative Care: A Grounded Theory Approach. 2011.
Fleming JW. Home Health Care for Children Who Are Technology Dependent. New York, NY: Springer Publishing; 2003.
Fleming P, Sawley L. The other side of life. Learn Disabil Pract 2003;6:16–21.
Flynn R. Short Breaks: Providing Better Access and More Choice for Black Disabled Children and Their Parents. Bristol: The Policy Press; 2002.
Flynn R, Patel P. Ensuring access to short breaks by black disabled children and their families. J Integr Care 2003;11:16–21.
Fountain R. What Factors Make for Successful Family-Based Short Breaks for Children with Complex Healthcare Needs?
Fowler-Kerry SE. Voices of Parents: The Lived Experience of Caring for a Child with a Life-Threatening and Life-Limiting Diagnosis Within Existing Social Policies. PhD thesis. 2008.
Franklin A, Lane M. Friendship Opportunities for Disabled Children and Young People. 2016.
Margolan H, Fraser J, Lenton S. Parental experience of services when their child requires long-term ventilation. Implications for commissioning and providing services. Child Care Health Dev 2004;30:257–64. https://doi.org/10.1111/j.1365-2214.2004.00414.x
Fraser LK, Miller M, McKinney PA, Parslow RC, Feltbower RG. Referral to a specialist paediatric palliative care service in oncology patients. Pediatr Blood Cancer 2011;56:677–80. https://doi.org/10.1002/pbc.22667
Freeman JM. On learning humility: a thirty-year journey. Hastings Cent Rep 2004;34:13–16.
Fringer A, Hechinger M, Schnepp W. Transitions as experienced by persons in palliative care circumstances and their families – a qualitative meta-synthesis. BMC Palliat Care 2018;17:22. https://doi.org/10.1186/s12904-018-0275-7
Frost N, Parton N. Understanding Children’s Social Care: Politics, Policy and Practice. Newbury Park, CA: Sage; 2009.
Fulda K., Johnson K., Hahn K, Lykens K. Do unmet needs differ geographically for children with special health care needs? Matern Child Health J 2013;17:505.
Fulton GB, Fins JJ. Removing the mask. Hastings Cent Rep 2003;33:12.
Gallagher R. Me and my job. Maggi Reading. Pract Nurse 2003;26:66.
Gardiner C, Ingleton C, Ryan T, Ward S, Gott M. Novel approaches for economic evaluations in palliative care: considering family caregivers. Palliat Med 2018;32:251–2.
Gaudette L, Dunbrack J. Through the looking glass: perspectives from the family caregiver at the hospital bedside. Hospice palliative care: at a crossroads. November 4–7, 2007, Westin Harbour Castle Hotel, Toronto, Ontario, Canada. J Palliat Care 2007;23:204–5.
Gelman CR, Sikes P, Hall M. The experience and needs of young children in younger-onset dementia families: a U.K.–U.S. comparison. Alzheimer’s Dement 2017;13:P1248.
Gerber GJ, Gargaro J. Participation in a social and recreational day programme increases community integration and reduces family burden of persons with acquired brain injury. Brain Inj 2015;29:722–9. https://doi.org/10.3109/02699052.2015.1004745
Gilligan P, Taylor J. Social Service Support for Disabled Children, Children with Complex Needs and Their Families. In Teare J, editor. Caring for Children with Complex Needs in the Community. Hoboken, NJ: Wiley; 2008. pp. 149–66.
Gilmore L. Supporting families of children with rare and unique chromosome disorders. Res Pract Intellect Dev Disabil 2018;5:8–16.
Glajchen M. The emerging role and needs of family caregivers in cancer care. J Support Oncol 2004;2:145–55.
Gonzalez-Alonso MY. The needs of families of aging people with cerebral palsy. Dev Med Child Neurol 2016;58(Suppl. 6):19.
Gothelf D, Cohen IJ, Himelstein BP, Hilden JM. Pediatric palliative care. N Engl J Med 2004;351:301–2.
Himelstein BP, Hilden JM, Boldt A, Weissman D. Pediatric palliative care. N Engl J Med 2004;350:1752-62.
Goudie A, Narcisse MR, Hall DE, Kuo DZ. Financial and psychological stressors associated with caring for children with disability. Fam Syst Health 2014;32:280–90. https://doi.org/10.1037/fsh0000027
Grant SO. Janet A. Phoenix, MD, MPH S. Orlene Grant, RN, BSN, MSN. Vienna, VA: The Grant Group, LLC; 2012.
Gravdal Kvarme L, Albertini-Früh E, Brekke I, Gardsjord R, Halvorsrud L, Liden H. On duty all the time: health and quality of life among immigrant parents caring for a child with complex health needs. J Clin Nurs 2016;25:362–71. https://doi.org/10.1111/jocn.13056
Gray C. Crossing cultural barriers: children’s views on the recuperative holiday experience. Eur Early Child Educ Res J 2017;25:321–39.
Greenbaum A. Louis Greenbaum. BMJ 2008;336:1025.
Greer J. Grove House. 2014.
Greig R. Short Breaks Pathfinder Evaluation: Interim Report: End of Phase One. London: Department for Education; 2010. URL: www.education.gov.uk/publications/standard/publicationdetail/page1/DCSF-RR223 (accessed 3 December 2020).
Greig R. Short Breaks Pathfinder Evaluation. London: Department for Education; 2010.
Gridley K, Brooks J, Glendinning C. Good practice in social care for disabled adults and older people with severe and complex needs: evidence from a scoping review. Health Soc Care Community 2014;22:234–48. https://doi.org/10.1111/hsc.12063
Hagena A, Stananought N, Greene M, Asiam E, Pybus L, Carroll F, et al. Motor neurone disease: what are the support needs of patients and carers? Eur J Palliat Care 2014;21:232–5.
Haidrani L. Royal Trinity Hospice. Vol. 31. London: RCNi; 2017.
Halamandaris VJ. Pediatric home care: continuing issues for the future. Caring 2005;24:6–11.
Hall WJ. The right care in the right place. JAMA Intern Med 2013;173:2053–4. https://doi.org/10.1001/jamainternmed.2013.8592
Hancock PJ, Jarvis JA, L’Veena T. Barriers to respite: a case study of a sub-group from an older carers program in Western Australia. Aust J Prim Health 2006;12:113–23.
Hanlon K. It’s not just a vacation, it’s an adventure. Except Parent 2009;39:34–5.
Hanlon K. Sometimes getting there is half the fun. Except Parent 2008;38:38–9.
Harding R. Informal caregivers in home palliative care. Prog Palliat Care 2013;21:229–31.
Harris MD. A home away from home: a unique hospice model. Home Healthc Nurse 2010;28:56. https://doi.org/10.1097/01.NHH.0000366800.00925.f8
Hart J. Music therapy for children and adults with cancer. Altern Complement Ther 2009;15:221–5.
Harwick RM. Transition to Adulthood for Young Adults with Disabilities that Experienced Foster Care. 2015.
Healthwatch CW. Identifying Gaps in Service Provision for Disabled Children Young People, their Families and Carers. 2016.
Heatley R. Carers’ Services Guide: Setting Up Support Services for Carers of the Terminally Ill. 2006.
Heatley R. Carers’ Services Guide: Setting Up Support Services for People with Life-limiting and Terminal Illnesses. 2008.
Henriksson A, Årestedt K, Benzein E, Ternestedt BM, Andershed B. Effects of a support group programme for patients with life-threatening illness during ongoing palliative care. Palliat Med 2013;27:257–64. https://doi.org/10.1177/0269216312446103
Hewitt-Taylor J. The impact of having a child with complex and continuing health needs on employment. J Child Young People’s Nurs 2007;1:219–24.
Hickie M. Respite Care or Short Breaks for Families of Children with Complex Needs. In Teare J, editor. Caring for Children with Complex Needs in the Community. Hoboken, NJ: Wiley; 2008. pp. 129–47.
Hill K. Respite services for children with life-limiting conditions and their families in Ireland. Nurs Child Young People 2016;28:30–5. https://doi.org/10.7748/ncyp.2016.e658
Hinds PS, Menard JC, Jacobs SS. The child’s voice in pediatric palliative and end-of-life care. Prog Palliat Care 2012;20:337–42.
Hobson L, Noyes J. Fatherhood and children with complex healthcare needs: qualitative study of fathering, caring and parenting. BMC Nurs 2011;10:5. https://doi.org/10.1186/1472-6955-10-5
Holland J, Chowdhury D, Hutchinson P. Respite care for children with complex health care needs: caregivers’ perspectives. Paediatr Child Health 2010;15:11A.
Holmes L, McDermid S, Sempik J. The Costs of Short Break Provision. London: Department for Education; 2010. URL: www.education.gov.uk/publications/RSG/publicationDetail/Page1/DCSF-RR224 (accessed 3 December 2020).
Houser AN. The State of Measurement of Respite Care. 2012.
Huang IC, Shenkman EA, Madden VL, Vadaparampil S, Quinn G, Knapp CA. Measuring quality of life in pediatric palliative care: challenges and potential solutions. Palliat Med 2010;24:175–82. https://doi.org/10.1177/0269216309352418
Hughes PM, Ingłeton MC, Noble B, Clark D. Providing cancer and palliative care in rural areas: a review of patient and carer needs. J Palliat Care 2004;20:44–9.
Hunter-Jones P. Young people, holiday-taking and cancer – an exploratory analysis. Tour Manag 2004;25:249–58.
Hurley F, Kiernan G, Nicholl H, Price J. Perspectives of parents caring for their child with a non-malignant life-limiting condition: the role of children’s palliative care services. Palliat Med 2016;30:NP370.
Hutton E, King A, Hamilton-West K, Hotham S. Understanding the Support Needs of Disabled Children and their Families in East Kent. 2016.
Isbister JC, Broadbent AM. Life did not stop at the doors to the palliative care ward. J Palliat Med 2009;12:643–4.
Jackson P, McTaggart I, McGirr D, Taylor J, McKenzie J, Picton-Howell Z, et al. Literature Review NMCN CEN on Topics Relating to the Care of Children with Exceptional Healthcare Needs. 2011.
Jagt CT. Improving Aspects of Palliative Care for Children. 2017.
James A, Mitchell E. ‘Can We Fix It?!’: Understanding the Impact of Children’s Hospice Short Breaks on Parental Relationships of Life-limited and Life-threatened Children and Young People.
Jenkins G. Letter to the editor. Ann Long-Term Care 2003;11:21.
Johnston K. Perspectives worth sharing – respite care camps: helping parents and children with special healthcare needs. CompassPoint 2017;27:10–13.
Jones DK. The gift. J Palliat Med 2018;21:1189.
Kamal AH, LeBlanc TW, Meier DE. Better palliative care for all: improving the lived experience with cancer. JAMA 2016;316:29–30. https://doi.org/10.1001/jama.2016.6491
Kamen BA. What I did on my summer vacation! J Pediatr Hematol Oncol 2011;33:483. https://doi.org/10.1097/MPH.0b013e3182357c76
Kaya E, Stajduhar K, Tayler C. Impact of a palliative approach for nursing – Canadian Hospice Palliative Care Conference: Navigating Safe Pathways to Quality Hospice Palliative Care, September 8–11, 2011, St John’s, Newfoundland, Canada. J Palliat Care 2011;27:251.
Keats K, Ham J, Miller T, Siden H. An outpatient pediatric palliative care clinic model to build local capacity: a 4-year experience and outreach expansion. Paediatr Child Health 2010;15:61A.
Kelly A, Kelly C. Unpaid Care. 2018.
Kersten C, Cameron MG, Oldenburg J. Truth in hope and hope in truth. J Palliat Med 2012;15:128–9. https://doi.org/10.1089/jpm.2011.0209
Khoo SY. When it hits close to home. J Palliat Med 2013;16:703. https://doi.org/10.1089/jpm.2012.0428
Kikuchi H, Narita Y, Abe M, Odachi K, Kitano K, Harada Y, et al. Nationwide survey of respite admission for incurable neurodegenerative diseases in Japan. J Neurol Sci 2017;381:561.
Kirk S, Glendinning C. Developing services to support parents caring for a technology-dependent child at home. Child Care Health Dev 2004;30:209–18. https://doi.org/10.1111/j.1365-2214.2004.00393.x
Kirk S. Legal Issues and Young People’s Children and Young People with Health Complex Healthcare Needs and Long-term Conditions. In Gelling L, editor. Public Health Practice and the School-Age Population. 2007.
Knapp CA, Contro N. Family support services in pediatric palliative care. Am J Hosp Palliat Care 2009;26:476–82. https://doi.org/10.1177/1049909109350205
Knapp CA, Madden VL, Curtis CM, Sloyer PJ, Huang IC, Thompson LA, Shenkman EA. Partners in care: together for kids: Florida’s model of pediatric palliative care. J Palliat Med 2008;11:1212–20. https://doi.org/10.1089/jpm.2008.0080
Knapp CA. Research in pediatric palliative care: closing the gap between what is and is not known. Am J Hosp Palliat Care. 2009;26:392.
Koch KD, Jones BL. Supporting parent caregivers of children with life-limiting illness. Children 2018;5:E85.
Kochanowski P. Why couldn’t you just tell us? Fla Nurse 2008;56:11.
Korones DN. Two hats. J Palliat Med 2010;13:1488.
Korver S, Kinghorn A, Negin J, Shea-Perry M, Martiniuk A. An exploration of parental social support: camp trillium’s pediatric oncology family program. Pediatr Blood Cancer 2013;60:178.
Kragerup KBK, Bisgaard AM, Larsen JL, Stahlhut M. Social counselling at the danish center for Rett syndrome. Wiener Medizinische Wochenschrift 2016;166:393.
Kristjanson L, Tandon A, Roderick E, Carmody S, Leigh A, Griffiths G, et al.Palliative Care in Western Australia: Final Report December 2005. 2006.
Kronberger-Vollnhofer M, Nemeth C. Hospice and palliative care for children, adolescents, and adults. Padiatr Padol 2016;51:249–52.
Kuo DZ, Berry JG, Glader L, Morin MJ, Johaningsmeir S, Gordon J. Health services and health care needs fulfilled by structured clinical programs for children with medical complexity. J Pediatr 2016;169:291–296e1.
Kuschner WG. Palliative care for pulmonary patients. Am J Respir Crit Care Med 2011;183:416.
Kvarme LG, Albertini-Fruh E, Liden H. How do immigrant parents of children with complex health needs manage to cope? Qual Life Res 2017;26:108–9.
Rallison LB, Raffin-Bouchal S. Living in the in-between: families caring for a child with a progressive neurodegenerative illness. Qual Health Res 2013;23:194–206. https://doi.org/10.1177/1049732312467232
Kristjanson LJ, Cousins K, White K, Andrews L, Lewin G, Tinnelly C, et al. Evaluation of a night respite community palliative care service. Int J Palliat Nurs 2004;10:84–90. https://doi.org/10.12968/ijpn.2004.10.2.12453
Lahtinen M, Joronen K. Parents’ Experiences of Caring for a Ventilator-Dependent Child: A Review of the Literature. In Kollak I, editor. Safe at Home with Assistive Technology. Basel: Springer International; 2017. pp. 137–51.
Laing CM. ‘It’s Not Just Camp’: Understanding the Meaning of Children’s Cancer Camps for Children and Families. PhD thesis. 2013.
Lambley E. ‘To Me, He’s Still My Brother’ – The Experience of Having a Brother or Sister with a Life-limiting or Life-threatening Condition. Sheffield: University of Sheffield; 2013.
Lancaster University Centre for Disability Research, National Development Team for Inclusion. Short Breaks for Disabled Children: Briefing Papers Pack. Lancaster: Lancaster University, Centre for Disability Research; 2011.
Lang D, Lim LC. Effects of art therapy for family caregivers of cancer patients: a systematic review protocol. JBI database Syst Rev Implement Reports 2013;11:64.
Langer S, Collins M, Welch V, Wells E, Hatton C, Robertson J, et al. A Report on Themes Emerging from Qualitative Research into the Impact of Short Break Provision on Families with Disabled Children. 2010.
Laverty D, Arber A, Faithfull S. Respite care for patients with neuro-degenerative diseases. A grounded theory study. Palliat Med 2014;28:563.
Laverty D, Arber A, Faithfull S. Respite for patients and carers in neurodegenerative disease: a grounded theory study. Eur J Palliat Care 2016;23:175–9.
Law M. Multi-Agency Care for Children with Complex Needs. In Teare J, editor. Caring for Children with Complex Needs in the Community. Hoboken, NJ: Wiley; 2008. pp. 93–111.
Lester PE. What to hope for? J Palliat Med 2011;14:786–7.
Levinson DR. Memorandum Report: Hospice Beneficiaries’ Use of Respite Care. 2008.
Leyshon M, Tverin T. Bridging the Generation Gap. Intergenerational Sp. 2015.
Life Care Strategy. Developing Respite Care at an Inner London Hospice. 2013.
Lindsey B. Therapeutic Camps and their Impact on the Family of Children with Special Health Care Needs: A Mixed Method Study. PhD thesis. 2014.
Ling J, Payne S, Connaire K, McCarron M. Parental decision-making on utilisation of out-of-home respite in children’s palliative care: findings of qualitative case study research – a proposed new model. Child Care Health Dev 2016;42:51–9. https://doi.org/10.1111/cch.12300
Ling J. An Exploration of the Respite Needs and Experiences of Parents Caring for a Child with a Life-limiting Condition Requiring Palliative Care. Dublin: Trinity College; 2013.
Ling J. First International Children’s Palliative Care Network Conference. Int J Palliat Nurs 2014;20:149. https://doi.org/10.12968/ijpn.2014.20.3.149
Ling J, O’Siorain L. Palliative Care in Ireland. London: McGraw-Hill Education; 2005.
Lockie S, Bottorff J, Robinson C, Pesut B. Like a bridge over troubled water: family caregivers commuting for palliative care. Canadian Hospice Palliative Care Conference, Voyages in Care and Understanding, October 18–21, 2009, Winnipeg, Manitoba, Canada. J Palliat Care 2009;25:237.
Lopatin S. Caring for the caregiver: TRICARE offers respite care and emotional support. Except Parent 2010;40:58–9.
Low J, Perry R, Wilkinson S. A qualitative evaluation of the impact of palliative care day services: the experiences of patients, informal carers, day unit managers and volunteer staff. Palliat Med 2005;19:65–70. https://doi.org/10.1191/0269216305pm942oa
Lundström S. Please, let us in. J Palliat Med 2012;15:1166. https://doi.org/10.1089/jpm.2012.9551
Lynn L. Respite Services for Children with Life-limiting Conditions and Their Families in Ireland; A National Needs Assessment. 2013.
Macaulay C, Powell P, Fertleman C. Learning from Paediatric Patient Journeys: What Children and Their Families Can Tell Us. Boca Raton, FL: CRC Press; 2016.
Macdonald H, Callery P. Parenting children requiring complex care: a journey through time. Child Care Health Dev 2008;34:207–13.
Macleod AM, Donald. A Review of Respite/Short Break Provision for Adult Carers of Adults in the Highland Partnership Area Key Findings and Main Recommendations. 2016.
Madden EE, Chanmugam A, McRoy RG, Kaufman L, Ayers-Lopez S, Boo M, et al. The impact of formal and informal respite care on foster, adoptive, and kinship parents caring for children involved in the child welfare system. Child Adolesc Soc Work J 2016;33:523–34.
Mahadevan J. Parents of Disabled Children Denied Short Breaks. London: Children & Young People Now; 2010.
Mahon MM. Children, Youth, and Families Receive Appropriate Palliative and/or Hospice Care. In Craft-Rosenberg, editor. Guidelines for Nursing Excellence in the Care of Children, Youth and Families. New York, NY: Springer Publishing; 2017.
Malcolm C, Forbat L, Knighting K, Kearney N. Exploring the experiences and perspectives of families using a children’s hospice and professionals providing hospice care to identify future research priorities for children’s hospice care. Palliat Med 2008;22:921–8. https://doi.org/10.1177/0269216308098214
Marsh S, Rodrigues J. How can helpful policy plus helpful professionals produce system failure? Exploring development interventions with active local professionals and active young people with life-limiting conditions. Evid Policy 2015;11:253–72.
McCaffrey N, Cassel JB, Coast J. Bringing the economic cost of informal caregiving into focus. Palliat Med 2015;29:866–7. https://doi.org/10.1177/0269216315612653
McClain BC, Kain ZN. Pediatric palliative care: a novel approach to children with sickle cell disease. Pediatrics 2007;119:612–14.
McConkey R, Truesdal M, Conliffe C. The features of short-break residential services valued by families who have children with multiple disabilities. J Soc Work 2004;4:61–75.
McDermid S. Evaluation of the Made to Measure Pilot: Pooling Personal Budgets First Interim Report. 2014.
McDermid S, Soper J, Lushey C, Lawson D. Evaluation of the Impact of Action for Children Short break Services on Outcomes for Children – Final Report. 2011.
McIntosh J, Runciman P. Exploring the role of partnership in the home care of children with special health needs: qualitative findings from two service evaluations. Int J Nurs Stud 2008;45:714–26.
McIntyre R, Lugton J. Supporting the Family and Carers. In Lugton J, McIntyre R, editors. Palliative Care: The Nursing Role. 2nd edn. 2005. pp. 261–301.
McKay T, Chung C, Orkin J, Adams S. Are children with medical complexity (CMC) meeting transition-related milestones before entering the adult healthcare system? A cross-sectional chart review. Paediatr Child Health 2018;23:e31.
McNamara-Goodger K. Together for short lives: uniting children’s palliative care services. Eur J Palliat Care 2012;19:46–8.
McNeill S, Wilson G. Use of direct payments in providing care and support to children with disabilities: opportunities and concerns. Br J Soc Work 2017;47:1903–22.
Medforth N, Huntingdon E. Found in transition. Compr child Adolesc Nurs 2017;1–18.
Mei Ling L, Saharudin SA, Behzadnia A. The needs of patients, and their caregivers, with non-malignant life-limiting illnesses. Eur J Palliat Care 2017;24:43–6.
Meltzer LJ, Suzanne Bennett J. Summer camps for chronically ill children: a source of respite care for mothers. J Child Health Care. 2004;33:317–31.
Miller M. Managing Transitions to Hospice Care: The Hospice Consultant’s Perspective. In Pfund R, Kerry-Folwer S, editors. Perspectives on Palliative Care for Children and Young People: A Global Discourse. Abingdon: Taylor & Francis; 2010.
Miller S. Respite care for children who have complex healthcare needs. Paediatr Nurs 2002;14:33–7. https://doi.org/10.7748/paed2002.06.14.5.33.c804
Mitchell W. Research review: the role of grandparents in intergenerational support for families with disabled children: a review of the literature. Child Fam Soc Work 2007;12:94–101.
Mitchell W. Quality indicators: disabled children’s parents’ prioritizations and experiences of quality criteria when using different types of support services. Br J Soc Work 2003;33.
Mohammadi D. Joan Marston: don’t forget the children. Lancet 2016;388:2733.
Mongeau S, Champagne M, Liben S. Participatory research in pediatric palliative care: benefits and challenges. J Palliat Care 2007;23:5–13.
Monterosso L. Palliative care and young people. Aust Nurs J 2008;15:35.
Monterosso L, Kristjanson L, Phillips M, Rowell S. Paediatric Palliative and Supportive Care: Caring for Life: The Needs of Children and Families in Western Australia. 2005.
Moore A, Carter B, Hunt A, Sheikh K. ‘I am closer to this place’ – space, place and notions of home in lived experiences of hospice day care. Health Place 2013;19:151–8. https://doi.org/10.1016/j.healthplace.2012.11.002
Morrison WE. ‘Is that all you got?’ J Palliat Med 2010;13:1384–5.
Murphy O, Delany A. A Designated Centre for People with Disabilities Operated by Enable Ireland Disability Services Limited, Wicklow.
Nadash P. Adult day centers: everything you wanted to know but were afraid to ask! Caring 2003;22:6–8.
Nageswaran S. Respite care for children with special health care needs. Arch Pediatr Adolesc Med 2009;163:49–54. https://doi.org/10.1001/archpediatrics.2008.504
Nakai M, Narita Y, Tomimoto H. An investigation of perspectives of respite admission among people living with amyotrophic lateral sclerosis and the hospitals that support them. J Prim Care Community Health 2017;8:163–8. https://doi.org/10.1177/2150131917696940
Nankervis K, Rosewarne A, Vassos M. Why do families relinquish care? An investigation of the factors that lead to relinquishment into out-of-home respite care. J Intellect Disabil Res 2011;55:422–33. https://doi.org/10.1111/j.1365-2788.2011.01389.x
Narita Y, Odachi K, Abe M, Nakai M, Harada Y, Kitano K, et al. Patient’s communication stage influences the usage of respite admission for the patients with ALS in Japan. Amyotroph Lateral Scler Front Degener 2016;17:302.
Narramore N. Meeting the emotional needs of parents who have a child with complex needs. J Child Young People’s Nurs 2008;2:103–7.
Nawaz S. Improving access to services for black and minority ethnic disabled children. Adopt Foster 2006;30:52–9.
Needs HJS. Children with Disabilities and Complex Health Needs.
Neff JM. Respite care: an essential yet unmet need for families with children with special health care needs. Arch Pediatr Adolesc Med 2009;163:89–90. https://doi.org/10.1001/archpediatrics.2008.527
Nenner F, Thompson K. A family’s struggle. J Palliat Med 2011;14:1264–5. https://doi.org/10.1089/jpm.2011.0141
Neri MT, Kroll T. Understanding the consequences of access barriers to health care: experiences of adults with disabilities. Disabil Rehabil 2003;25:85–96.
Nicholas DB, Beaune L, Barrera M, Blumberg J, Belletrutti M. Examining the experiences of fathers of children with a life-limiting illness. J Soc Work End Life Palliat Care 2016;12:126–44. https://doi.org/10.1080/15524256.2016.1156601
Nicholl H. ‘Going between worlds’: travelling with children with complex needs. J Child Health Care 2015;19:293–303. https://doi.org/10.1177/1367493513508233
Nicholl HM. An Exploration of Mothers’ Experiences in Caring for Children with Complex Needs. Dublin: Trinity College; 2008.
Nicholl HM, Begley CM. Explicating caregiving by mothers of children with complex needs in Ireland: a phenomenological study. J Pediatr Nurs 2012;27:642–51. https://doi.org/10.1016/j.pedn.2011.07.003
Nishigaki K, Yoneyama A, Ishii M, Kamibeppu K. An investigation of factors related to the use of respite care services for children with severe motor and intellectual disabilities (SMID) living at home in Japan. Health Soc Care Community 2017;25:678–89. https://doi.org/10.1111/hsc.12358
Nkosi B. Palliative care and children living with non-communicable diseases. Nurs Updat 2015;40:18–21.
Nolan K, Camfield CS, Camfield PR. Coping with a child with Dravet syndrome: insights from families. J Child Neurol 2008;23:690–4. https://doi.org/10.1177/0883073808314162
North Carolina Institute of Medicine. Short- and long-term solutions for co-location in adult and family care homes. N C Med J 2010;71:593.
Bath & North East Somerset Council. What You Need to Know About a Short Break . . . A Guide For Children And Young People. Bath: Bath & North East Somerset Council.
Norton M, Dyches TT, Harper JM, Roper SO, Caldarella P. Respite care, stress, uplifts, and marital quality in parents of children with Down syndrome. J Autism Dev Disord 2016;46:3700–11. https://doi.org/10.1007/s10803-016-2902-6
Nottinghamshire County Council. Improve the Effectiveness of Services for Disabled Children. Nottingham: Nottinghamshire County Council; 2011.
Noyes J, Godfrey C, Beecham J. Resource use and service costs for ventilator-dependent children and young people in the UK. Health Soc Care Community 2006;14:508–22.
Noyes J, Lewis M. From Hospital to Home: Guidance on Discharge Management and Community Support for Children Using Long-term Ventilation. Essex: Barnardo’s; 2005.
Oetting-Rob C. And than I said to my mum: take it easy! The perspective of children with life-limiting conditions in homecare settings. Palliat Med 2014;28:664.
Leeds Local Offer. The Leeds Local Offer: What do Families Think? What Have we Learned so far? Report at January 2014. Leeds: Leeds Local Offer; 2014.
Ofsted. Inspections of Residential Holiday Schemes for Disabled Children: Interim Evaluation Schedule and Grade Descriptors. Manchester: Ofsted; 2014.
Orloff SS. Respite care: an essential, not a luxury! Except Parent 2007;37:69.
Orloff SF. Pediatric Palliative Care in the United States of America. 2012. pp. 359–76.
Ouellet CM. Mothers’ Experiences of the Care Provided to their Child with a Life-Limiting Illness. 2009.
Owen E, Johnson M. A neurological respite programme in a specialist palliative care setting. Eur J Palliat Care 2005;12:194–7.
Oxfordshire County Council. Meeting of The Executive. 2 April 2003.
Clark P, Macarthur J. Children with physical disability: gaps in service provision, problems joining in. J Paediatr Child Health 2008;44:455–8. https://doi.org/10.1111/j.1440-1754.2008.01327.x
Parker G, Bhakta P, Lovett CA, Paisley S, Olsen R, Turner D, Young B. A systematic review of the costs and effectiveness of different models of paediatric home care. Health Technol Assess 2002;6(35). https://doi.org/10.3310/hta6350
Parker W, Gage H, Sterr A. Services for Families with Disabled Children A Scoping Study: Summary Report. 2011.
Parker W, Gage H, Sterr A, Williams P. Holiday play for children with disabilities in England: access, choice and parents’ views about integration. Int J Disabil Dev Educ 2017;64:573–95.
Pascuet E, Cowin L, Vaillancourt R, Splinter W, Vadeboncoeur C, Dumond LG, et al. A comparative cost-minimization analysis of providing paediatric palliative respite care before and after the opening of services at a paediatric hospice. Healthc Manage Forum 2010;23:63–6. https://doi.org/10.1016/j.hcmf.2010.04.009
Pathways N, Pathway N. Transition from Children’s to Adults’ Services. 2016. pp. 1–11.
Payne S, Ingleton C, Scott G, Steele K, Nolan M, Carey I. A survey of the perspectives of specialist palliative care providers in the UK of inpatient respite. Palliat Med 2004;18:692–7. https://doi.org/10.1191/0269216304pm951oa
Payne S, Hudson P, Grande G, Oliviere D, Tishelman C, Pleschberger S, et al. White Paper on improving support for family carers in palliative care: Part 2 – continued from the European Journal of Palliative Care (EJPC) 17.5. Eur J Palliat Care 2010;17:286–90.
Pearlman L. The Unique Needs of Children with Life-Limiting Illnesses. In Arnold C, editor. Understanding Child and Adolescent Grief. Abingdon: Taylor & Francis; 2017. pp. 112–26.
Periyakoil VS. Hole in one. J Palliat Med 2002;5:743.
Petrie P, Knight A, Zuurmond M, Potts P. On Holiday! Policy and Provision for Disabled Children and their Families. 2007.
Pickard L, Brimblecombe N, King D, Knapp M. ‘Replacement care’ for working carers? A longitudinal study in England, 2013–15. Soc Policy Adm 2018;52:690–709.
Plummer S, Hearnshaw C. Reviewing a new model for delivering short-term specialist palliative care at home. Int J Palliat Nurs 2006;12:183–8. https://doi.org/10.12968/ijpn.2006.12.4.21016
Porepa M, Hoffman A, Fellin M, Kublick L. Children with medical complexities: addressing the gaps in respite care during transition from paediatrics to adult health care in Ontario. Paediatr Child Health 2017;22:369–71. https://doi.org/10.1093/pch/pxx142
Pottie CG, Burch KA, Thomas LP, Irwin SA. Informal caregiving of hospice patients. J Palliat Med 2014;17:845–56. https://doi.org/10.1089/jpm.2013.0196
Poulter D, Carroll S, Jones G. Hospice Care: A Framework for the Future. 2011.
Prabhakar M. Individual Budgets for Families with Disabled Children: Scoping Study: Final Case Study Report. 2008.
Pudlo J. Hospice care. Home Healthc Now 2017;35:404.
Johnston LM. The effect of respite services on the emotional well-being of caregivers of children with cerebral palsy. Dev Med Child Neurol 2012;54:63.
Sebag-Lanoë R, Lefebvre-Chapiro S, Feteanu D, Trivalle C. Palliative care in a long-term care setting: a 25-year French experience. J Palliat Care 2003;19:209–13.
Steele R, Derman S, Cadell S, Davies B, Siden H, Straatman L. Families’ transition to a Canadian paediatric hospice. Part one: planning a pilot study. Int J Palliat Nurs 2008;14:248–56. https://doi.org/10.12968/ijpn.2008.14.5.29492
Steele R, Derman S, Cadell S, Davies B, Siden H, Straatman L. Families’ transition to a Canadian paediatric hospice. Part two: results of a pilot study. Int J Palliat Nurs 2008;14:287–95. https://doi.org/10.12968/ijpn.2008.14.6.30024
Welsh R, Dyer S, Evans D, Fereday J. Identifying benefits and barriers to respite for carers of children with complex health needs: a qualitative study. Contemp Nurse 2014;48:98–108. https://doi.org/10.5172/conu.2014.48.1.98
Rallison L. Living in the in-between: a hermeneutic study of families living with and caring for a child with a progressive neurodegenerative illness. Canadian Hospice Palliative Care Conference, Voyages in Care and Understanding, October 18–21, 2009, Winnipeg, Mani. J Palliat Care 2009;25:238.
Remedios C, Willenberg L, Zordan R, Murphy A, Hessel G, Philip J. A pre-test and post-test study of the physical and psychological effects of out-of-home respite care on caregivers of children with life-threatening conditions. Palliat Med 2015;29:223–30. https://doi.org/10.1177/0269216314560008
Reynolds MAH. Unique needs of terminally ill young and middle age adults. American Psychosocial Oncology Society (APOS) Third Annual Conference, Amelia Island, Florida, 16–19 February 2006. Psycho-Oncology 2006;15:S15–6.
Richards S. Promoting more accessible cancer care services. Br J Health Care Manag 2004;10:182–4.
Rigby P, Edwards P, McIntyre A. Halton Joint Strategic Needs Assessment 2016 Children with Special Educational Needs and Disabilities. 2016.
Ritchie B. Palliative care reaches out. World Irish Nurs Midwifery 2008;16:49–50.
Roberts L. Meeting children’s needs within a family focussed agenda: the case of support care. Child Youth Serv Rev 2015;53:105–12.
Roberts L. Time to change? Exploring the impact of time-limited service provision in a family support service. Child Fam Soc Work 2017;22:21–30.
Robinson-Lane SG. Accessing respite care for persons with a disability. Arch Phys Med Rehabil 2017;98:2103–5.
Robson A, Beattie A. Diana Children’s Community Service and service co-ordination. Child Care Health Dev 2004;30:233–9. https://doi.org/10.1111/j.1365-2214.2003.00401.x
Rodriguez A. We Are Here for a Good Time Not a Long Time: Being and Caring for a Child With a Life-Limiting Condition. Huddersfield: University of Huddersfield; 2009.
Romley JA, Shah AK, Chung PJ, Elliott MN, Vestal KD, Schuster MA. Family-provided health care for children with special health care needs. Pediatrics 2017;139:e20161287.
Rosenbaum JR. When you least expect it. Hastings Cent Rep 2010;40:7–8. https://doi.org/10.1353/hcr.0.0226
Rosengard A, Laing I, Ridley J, Hunter S. A Literature Review on Multiple and Complex Needs. Edinburgh: Scottish Executive; 2007.
Ross S, Robbins S, Daffern K, Salminen R, Rapoport A, Widger K. An evaluation of utilization of services and quality of respite care at Emily’s House children’s hospice. J Pain Symptom Manage 2016;52:e137.
Rosseau P. Hospice vignettes. Living in the present. Am J Hosp Palliat Med 2004;21:467–8.
Rousseau PC. Recent literature. J Palliat Med 2008;11:942–3.
Rousseau PC. Ten values. J Palliat Med 2009;12:561–2.
Rousseau PC. Recent literature. J Palliat Med 2010;13:621–2.
Rousseau P. Reflections on caring: watching a mother. Curr Probl Pediatr Adolesc Health Care 2016;46:251–2.
Rousseau P. The promise of presence. Am J Hosp Palliat Care 2011;28:435–6. https://doi.org/10.1177/1049909110397928
Rousseau P. Rocky. Palliat Support Care 2012;10:141–2.
Rousseau P. The mirror. Am J Hosp Palliat Med 2013;30:317.
Rousseau PC. Recent literature. J Palliat Med 2018;21:404–5.
Rutledge DN. Models of palliative care: moving beyond hospice. ONS News 2003;18:1, 4–6.
Kirk S, Pritchard E. An exploration of parents’ and young people’s perspectives of hospice support. Child Care Health Dev 2012;38:32–40. https://doi.org/10.1111/j.1365-2214.2011.01232.x
Talebreza S, Widera E. The hospice referral. Am Fam Physician 2014;89:745.
Smeets SM, van Heugten CM, Geboers JF, Visser-Meily JM, Schepers VP. Respite care after acquired brain injury: the well-being of caregivers and patients. Arch Phys Med Rehabil 2012;93:834–41. https://doi.org/10.1016/j.apmr.2011.10.029
Salladay SA. Relinquishing a burden. Nursing 2012;42:10.
Satoh K, Kamigaito M, Yokoyama H, Science AI. A snapshot of the impact Creative Breaks had during 2016–17. Macromolecules 2007;7433.
Satterley G. An audit of respite provision in a palliative care setting. Eur J Palliat Care 2007;14:68–9.
Schlicht J. Practical strength training for adults with disabilities. ACSMs Health Fit J 2011;15:31–2.
Schuyler D, Coker W. Hospice. Prim Care Companion J Clin Psychiatry 2014;16.
Schwantes S, O’Brien HW. Pediatric palliative care for children with complex chronic medical conditions. Pediatr Clin North Am 2014;61:797–821. https://doi.org/10.1016/j.pcl.2014.04.011
Schwehr B. Why did West Berkshire lose over its decision to cut funding for short breaks? Community Living 2016;30:20–1.
Seamark D, Seamark C, Hynson J. Life-limiting Illness: The Illness Experience. In Mitchell G, editor. Palliative Care: A Patient-Centred Approach. Abingdon: Oxford Radcliffe Publishing; 2008. pp. 47–78.
Bath & North East Somerset Council. Bath & North East Somerset Council Disabled Children Strategy Action Plan for 2011/2012. 2012. URL: www.bathnes.gov.uk/sites/default/files/dcsg_strategy_2011-2012.pdf (accessed 3 December 2020).
Shared Care Scotland. Occasional Papers Series: A Break in Communication. Dunfermline: Shared Care Scotland; 2009.
Shelton KJ, Witt PA. Therapeutic camps as respite care providers: benefits for families of children with disabilities. Ther Recreation J 2011;45:17–31.
Simkiss DE. Community care of children with complex health needs. Paediatr Child Health 2012;22:193–7.
Simon C, McNicholas N. Children living with chronic disability. InnovAiT 2014;7:502–8.
Skilbeck JK, Payne SA, Ingleton MC, Nolan M, Carey I, Hanson A. An exploration of family carers’ experience of respite services in one specialist palliative care unit. Palliat Med 2005;19:610–18. https://doi.org/10.1191/0269216305pm1087oa
Sloper T, Beresford B. Families with disabled children: social and economic needs are high but remain largely unmet. BMJ 2006;333:928.
Smith J, Cheater F, Bekker H. Parents’ experiences of living with a child with a long-term condition: a rapid structured review of the literature. Health Expect 2015;18:452–74. https://doi.org/10.1111/hex.12040
Smith S, Brick A, O’Hara S, Normand C. Evidence on the cost and cost-effectiveness of palliative care: a literature review. Palliat Med 2014;28:130–50. https://doi.org/10.1177/0269216313493466
Sonaike A. Respite. Except Parent 2018;48:34–6.
Soriani MH, Desnuelle C. Care management in amyotrophic lateral sclerosis. Rev Neurol 2017;173:288–99.
Soudrie B. Respite/rehabilitation hospital stays for rare neurological diseases and severe disabilities: reporting on the experience 2003–2011. Ann Phys Rehabil Med 2011;54:e74.
Spiers G, Allgar V, Richardson G, Thurland K, Hinde S, Birks Y, et al. Transforming community health services for children and young people who are ill: a quasi-experimental evaluation. Heal Serv Deliv Res 2016;4.
Spruin E, Abbott N, Holt N. Examining the experiences of a short break scheme amongst adolescents with disabilities (service users) and their parents. Int J Disabil Dev Educ 2018;65:148–62.
Stalker K, MacDonald C, King C, McFaul F, Young C, Hawthorn M. ‘We could kid on that this is going to benefit the kids but no, this is about funding’: cutbacks in services to disabled children and young people in Scotland. Child Care Pract 2015;21:6–21.
Stalker K, MacDonald C, King C, McFaul F, Young C, Hawthorn M, et al. ‘It Always Comes Down to Money’: Recent Changes in Service Provision to Disabled Children, Young People and Their Families in Scotland. 2013.
Statham J, Greenfields M. Part-time fostering: recruiting and supporting carers for short-break schemes. Adopt Foster 2005;29:33–41.
Stevens E. What role does palliative day care have in supporting family caregivers? J Palliat Care 2010;26:229.
Strawderman M. Caregiver fatigue and the importance of respite. Virginia Nurses Today 2015;23:8–11.
Strunk J. Respite care for families of special needs children: a systematic review. J Dev Phys Disabil 2010;22:615–30.
Studies H, Littlechild B, Fearns D, Smith R. Respite Care and Short Break Services for Children and Young People with Disabilities in Luton Borough. 2014.
Swallow V, Forrester T, Macfadyen A. Teenagers’ and parents’ views on a short-break service for children with life-limiting conditions: a qualitative study. Palliat Med 2012;26:257–67. https://doi.org/10.1177/0269216311401947
Tarleton B, Porter S. Transition in Suffolk. 2011.
Teare J. Caring for Children with Complex Needs in the Community. Hoboken, NJ: John Wiley & Sons; 2009.
Tétreault S, Blais-Michaud S, Marier Deschênes P, Beaupré P, Gascon H, Boucher N, et al. How to support families of children with disabilities? An exploratory study of social support services. Child Fam Soc Work 2014;19:272–81.
Kirklees Council. All Age Disability: Short Breaks and Respite Engagement: Feedback Received in Free Format Face to Face Engagement Sessions. URL: www.kirklees.gov.uk/involve/publisheddoc.aspx?ref=yhu1of14%26e=852 (accessed 3 December 2020).
Thiele P. A mother’s journey: choosing life with disability. Except Parent 2012;42:32–5.
Thomas S, Price M. Respite care in seven families with children with complex care needs. Nurs Child Young People 2012;24:24–7. https://doi.org/10.7748/ncyp2012.10.24.8.24.c9338
Thomé B, Dykes AK, Hallberg IR. Home care with regard to definition, care recipients, content and outcome: systematic literature review. J Clin Nurs 2003;12:860–72.
Thurgate C. Home from home: evaluation of a respite service in Kent. Paediatr Nurs 2004;16:20.
Thurgate C. Respite for children with complex health needs: issues from the literature. Paediatr Nurs 2005;17:14–18. https://doi.org/10.7748/paed2005.04.17.3.14.c974
Thurgate C. The importance of appropriate respite care. p. 129.
Thurgate C, Warner H. Living with disability: part 1. Paediatr Nurs 2005;17:37–44. https://doi.org/10.7748/paed2005.12.17.10.37.c983
Together for Short Lives. On the Brink: A Crisis in Children’s Palliative Care Funding in England: The Results of Together for Short Lives and Hospice UK’s Survey on Children’s Palliative Care Funding and Commissioning in England 2015/2016. Bristol: Together for Short Lives; 2016.
Torkildson C. ChiPPS Pediatric Palliative Care Newsletter Issue #23, May 2011.
Townsley R, Abbott D, Watson D. Making a Difference?: Exploring the Impact of Multi-agency Working on Disabled Children with Complex Health Care Needs, their Families and the Professionals Who Support Them. Bristol: Policy Press; 2004.
Trustam R. Holiday memories. Community Living 2015;29:26–7.
Ullrich CK, Wolfe J. Caring for children living with life-threatening illness: a growing relationship between pediatric hospital medicine and pediatric palliative care. Pediatr Clin North Am 2014;61:xxi–xxiii. https://doi.org/10.1016/j.pcl.2014.05.004
Boulton M. The context of respite care. Palliat Med 2010;24:S170.
Strang VR, Koop PM, Peden J. The experience of respite during home-based family caregiving for persons with advanced cancer. J Palliat Care 2002;18:97–104.
van Exel J, Morée M, Koopmanschap M, Goedheijt TS, Brouwer W. Respite care – an explorative study of demand and use in Dutch informal caregivers. Health Policy 2006;78:194–208.
Van Haren B, Fiedler CR. Support and empower families of children with disabilities. Interv Sch Clin 2008;43:231–5.
Vasileiou K, Barnett J, Barreto M, Vines J, Atkinson M, Lawson S, Wilson M. Experiences of loneliness associated with being an informal caregiver: a qualitative investigation. Front Psychol 2017;8:585. https://doi.org/10.3389/fpsyg.2017.00585
Victoria T, Kate F, Ian W, Bill H, Samantha B. The Palliative Care Needs of People with Motor Neurone Disease (MND) and Their Informal Carers. 2017.
Wallis L. In-hospital pediatric respite care. Am J Nurs 2013;113:18.
Ward C, Glass N, Ford R. Caring for Children with Serious Illness: a Partnership Model for the Future.
Warner HK. Meeting the Fundamental Needs of Children with Disabilities. 14–23.
Washio M, Yoshida H, Ura N, Togashi N, Sakauchi F, Arai, et al. Burden among family caregivers of patients on chronic hemodialysis in northern Japan. Int Med J 2012;19:221.
Watson D, Abbott D, Townsley R. Listen to me, too! Lessons from involving children with complex healthcare needs in research about multi-agency services. Child Care Health Dev 2007;33:90–5.
Watson D, Townsley R, Abbott D. Exploring multi-agency working in services to disabled children with complex healthcare needs and their families. J Clin Nurs 2002;11:367–75.
Weis JM. ‘Excuse me, but do you mind if I play through . . .’ J Palliat Med 2005;8:1289.
Weissman DE. Who is in control? J Palliat Med 2002;5:1.
Weissman DE, Quill TE, Arnold RM, Rosielle DA. The family meeting: starting the conversation #223. J Palliat Med 2010;13:204–5.
Welch V, Hatton C, Emerson E, Collins M, Robertson J, Langer S, Wells E. Using direct payments to fund short breaks for families with a disabled child. Child Care Health Dev 2012;38:900–9. https://doi.org/10.1111/j.1365-2214.2011.01339.x
West Sussex County Council. Carers Services – Strategic Commissioning Review – Public. Chichester: West Sussex County Council; 2013.
White L, Moola F, Kirsh J, Faulkner G. A therapeutic recreation camp for children with congenital heart disease: examining impact on the psychosocial well-being of parents. J Child Fam Stud 2016;25:3034–43.
Whiting M. Caring for children – ‘24-7’: the experience of WellChild Nurses and the families for whom they are providing care and support. J Child Health Care 2018;23:35–44.
Whiting M. Children with disability and complex health needs: the impact on family life. Nurs Child Young People 2014;26:26–30. https://doi.org/10.7748/ncyp2014.04.26.3.26.e388
Whiting M. Support requirements of parents caring for a child with disability and complex health needs. Nurs Child Young People 2014;26:24–7. https://doi.org/10.7748/ncyp2014.05.26.4.24.e389
Whitmore KE. The concept of respite care. Nurs Forum 2017;52:180–7. https://doi.org/10.1111/nuf.12179
Whitmore KE, Snethen J. Respite care services for children with special healthcare needs: parental perceptions. J Spec Pediatr Nurs 2018;23:e12217. https://doi.org/10.1111/jspn.12217
Wilcock SV. Children/Young People with Disabilities and Complex Health Care Needs. In Moyse K, editor. Promoting Health in Children and Young People: The Role of the Nurse. Hoboken, NJ: Wiley; 2009. p. 228.
Williams V, James N, Barclay M, Stalker K, Watson N, Hudson K. The Conversations Project: A Report to the Steering Group of the National Review of Services for Disabled Children and Young People. 2012.
Willis C, Girdler S, Thompson M, Rosenberg M, Reid S, Elliott C. Elements contributing to meaningful participation for children and youth with disabilities: a scoping review. Disabil Rehabil 2017;39:1771–84. https://doi.org/10.1080/09638288.2016.1207716
Winnett M. A piece of my mind: cries and whiskers. JAMA 2002;288:806.
Wirral Council. Fact Sheet 7: Paying for Your Support (Non-Residential). Wallasey: Wirral Council; 2014.
Wolkowski A, M Carr S, L Clarke C. What does respite care mean for palliative care service users and carers? Messages from a conceptual mapping. Int J Palliat Nurs 2010;16:388–92. https://doi.org/10.12968/ijpn.2010.16.8.388
Woodall HE, Dennis W. Comfort always. The Rainey Hospice House: South Carolina’s first inpatient hospice. J S C Med Assoc 2003;99:224–6.
Woodgate R. Effects of respite care services in a children’s hospice: the parents’ point of view. Am J Matern Child Nurs 2015;40:334.
Wu YP. Assessing experiences of children who attend a camp for children with cancer and their siblings: a preliminary study. Child Youth Care Forum 2011;40:121–33.
Wylde C. G519 (P) A study to investigate parental satisfaction with the allocation of respite care for their child by a children’s hospice. Archives of Disease in Childhood 2016;101:A306–7.
Yantzi NM, Rosenberg MW, McKeever P. Getting out of the house: the challenges mothers face when their children have long-term care needs. Health Soc Care Community 2007;15:45–55.
Not phenomena of interest (n = 373)
Oral Evidence: How the Government is Meeting its Commitment to Choice for Babies, Children and Young People Who Need Palliative Care Session 3: 21 February 2018. 2018.
Transition to adult services for young people with-limiting conditions. Nurs Child Young People 2014;26:13.
Abstracts of the 9th World Research Congress of the European Association for Palliative Care, EAPC 2016. Palliat Med 2016;30.
Delivering Support and Aspiration for disabled Young People. 2013.
Palliative and End of Life Care Delivery Plan – March 2017. 2017.
Scottish Government. Supporting Young People’s Health and Wellbeing: A Summary of Scottish Government Policy. Edinburgh: Scottish Government; 2013.
Smith S, Morgan S, Riley V, Soanes L. Priorities and challenges in the care of teenagers and young adults. Cancer Nurs Pract 2011;10:32–8.
El-Jawahri A, Greer JA, Temel JS. Does Palliative Care Improve Outcomes for Patients with Incurable Illness? A Review of the Evidence. York:Database of Abstracts of Reviews of Effects; 2011.
Audit Scotland. Report: Changing Models of Health and Social Care. Edinburgh: Audit Scotland; 2016.
Report into the Needs of Young People with Life Limiting Illnesses. Beyond breaking point? 2013.
Marie Curie. A Review of Specialist Palliative Care Provision and Access Across London. London: Marie Curie; 2015.
Social Care Institute for Excellence. Facts About FACS 2010: A Guide to Fair Access to Care Services. London: Social Care Institute for Excellence; 2010.
Improving care for children with complex needs. Clin Trials 2012.
Kim B, Whote K, Patterson P. Understanding the experiences of adolescents and young adults with cancer: a meta-synthesis. Eur J Oncol Nurs 2016;24:39–53.
Canadian Paediatric Society. Transition to Adult Care for Youth with Special Health Care Needs. Ottawa, ON: Canadian Paediatric Society; 2012.
Oral Evidence: How the Government is Meeting its Commitment to Choice for Babies, Children and Young People Who Need Palliative Care Session 5: 7 March 2018. 2018.
Growing Up Matters: Better Transition Planning for Young People with Complex Needs. 2007.
Film for young people with life-limiting conditions. Paediatr Nurs 2008;20:4.
Social Care Institute for Excellence. Changing Social Care: An Inclusive Approach. London: Social Care Institute for Excellence; 2009.
Discussing palliative care with pediatric patients and their families. AACN Bold Voices 2015;7:8.
Edworthy A, Donne H. The Availability and Intelligibility of Information for Carers of Children with a Brain Injury. Bingley: Emerald; 2010.
Disabled Children and Young People in Out-of-home-care: Summary Report. Belfast: Queens University Belfast; 2016.
10D – NHS Continuing Healthcare. 2017.
National Council for Palliative Care. Commissioning Guidance for Specialist Palliative Care: Helping to Deliver Commissioning Objectives. London: National Council for Palliative Care; 2012.
National Voices. My Life, My Support, My Choice: A Vision for Person Centred Coordinated Care and Support for Children and Young People with Complex Lives. London: National Voices; 2015.
Carers and families. Prog Palliat Care 2007;15:269–70.
Muscular Dystrophy Campaign. Access to Specialist Neuromuscular Care: The Walton Report. London: Muscular Dystrophy Campaign; 2009.
National Children’s Bureau. Turning the Tide: Reversing the Move to Late Intervention Spending in Children and Young People’s Services. London: National Children’s Bureau; 2017.
Office of the Children’s Commissioner. Public Spending on Children in England: 2000 to 2020. London: Office of the Children’s Commissioner; 2018.
Canadian Pediatric Society. A Model of Paediatrics: Rethinking Health Care for Children and Youth. Ottawa, ON: Canadian Paediatric Society; 2009.
Nankervis KL, Rosewarne AC, Vassos MV. Respite and parental relinquishment of care: a comprehensive review of the available literature. J Policy Pract Intellect Disabil 2011;8:150–162.
House of Commons Health Committee. End of Life Care: Fifth Report of Session 2014–15. London: House of Commons; 2015.
A National Framework and Preferred Practices for Palliative and Hospice Care Quality. 2006.
Grinyer A. Palliative and end of life care for children and young people. home, hospice, hospital. Int J Palliat Nurs 2012;18:307.
Social Services Research Group. Researching the Support Needs of Pakistani Families with Disabled Children in the UK. Social Services Research Group; 2007.
The State of the UK Children’s Hospice Nursing Workforce. 2017.
Children and Young Persons Bill HL. 2008.
Office of the Children’s Commissioner. ‘They Still Need to Listen More’: A Report About Disabled Children and Young People’s Rights in England. London: Office of the Children’s Commissioner; 2014.
Care and Support for Good Days, Difficult Days and Last Days. 2013.
A Good Life. Exploring What Matters to People Facing Multiple and Complex Needs (2015). 2015.
Carers Strategies (Wales) Measure 2010. 2012.
Maddison J, Beresford B. The development of satisfaction with service-related choices for disabled young people with degenerative conditions: evidence from parents’ accounts. Health Soc Care Community 2012;20:388–99.
Scottish Government. Home Care Services, Scotland, 2011. Edinburgh: Scottish Government; 2011.
Smyth L. How Stormont is Failing our Young Adults Who Need Respite Care. Belfast: Belfast Telegraph; 2012.
Chapter 35: Caring for the Child with a Chronic Condition or the Dying Child. 2009. pp. 1133–56.
Doka KJ. Caring for the carer: the lessons of research. Prog Palliat Care 2014;22:150–4.
Forder J, Caiels J, Harlock J, Wistow G, Malisauskaite G, Peters M, et al. A System-level Evaluation of the Better Care Fund: Final Report. Kent: Quality and Outcomes of Person-centred Care Policy Research Unit; 2018.
10G – Support for Families with Children. 2017.
Putting Families with Disabled Children at the Heart of the NHS Reforms. London: Contact; 2011.
3A – MND Care Centres and Networks. 2018.
Transition from Children’s to Adults’ Services: Draft Guidance. 2015.
Scottish Government. Statutory Guidance on Part 3 (Children’s Services Planning) of the Children and Young People (Scotland) Act 2014. Edinburgh: Scottish Government; 2016.
Social Care Institute for Excellence. Direct Payments: Answering Frequently Asked Questions. 2005. URL: www.scie.org.uk/publications/guides/guide10/questions/.
The King’s Fund. Case Management. London: The King’s Fund; 2011.
Lea S. Impact of Cancer in Children & Young People. Evidence-Based Nursing Blog. 2015. URL: https://blogs.bmj.com/ebn/2015/09/24/impact-of-cancer-in-children-young-people/.
Funding for MS Services in England: A Practical Guide. 2016.
Abbott D, Carpenter J. ‘Wasting precious time’: young men with Duchenne muscular dystrophy negotiate the transition to adulthood. Disabil Soc 2014;29:1192–205.
Ahlström G, Wadensten B. Family members’ experiences of personal assistance given to a relative with disabilities. Health Soc Care Community 2011;19:645–52. https://doi.org/10.1111/j.1365-2524.2011.01006.x
Ajayi TA, Edmonds KP. Palliative care answers the challenges of transitioning serious illness of childhood to adult medicine. J Palliat Med 2014;17:469–71. https://doi.org/10.1089/jpm.2013.0263
Aldridge J, Fraser L, Manning S, Miller M, O’leary S. Use of hospice services by children with a neuromuscular condition. Dev Med Child Neurol 2011;53:44.
Alvarelhao J, McLaughlin J, Brandao D, Pennington L. Perceptions of the impact of the environment on their societal participation by young adults with cerebral palsy. Dev Med Child Neurol 2016;58:18.
Alwell M, Cobb B. Social/communicative interventions and transition outcomes for youth with disabilities: a systematic review. Career Dev Except Individ 2009;32:94–107.
Amadoru S, McFerran K. The role of music therapy in children’s hospices. Eur J Palliat Care 2007;14:124–7.
Amin R, MacLusky I, Zielinski D, Adderley R, Carnevale F, Chiang J, et al. Transition from pediatric to adult health care for young adults with neurological disorders: parental perspectives. Can J Respir Crit Care Sleep Med 2017;1:7–36.
Apel L. Holiday fun for all. Except Parent 2007;37:23.
Appleton AL. A comment on ‘Douglas House: a ‘respice’ for young people’. Eur J Cancer 2004;40:1453. https://doi.org/10.1016/j.ejca.2004.02.012
Arias RA, Andrews J, Cunniff C, Meaney F, Davis M, Pandya S. Palliative care services in families of young men with Duchenne muscular dystrophy. J Investig Med 2008;56:250.
Arias R, Andrews J, Pandya S, Pettit K, Trout C, Apkon S, et al. Palliative care services in families of males with Duchenne muscular dystrophy. Muscle Nerve 2011;44:93–101. https://doi.org/10.1002/mus.22005
Armstrong D. ChiPPS E-Journal Pediatric Palliative and Hospice Care Issue #47, May 2017.
Bachmann MO, O’Brien M, Husbands C, Shreeve A, Jones N, Watson J, et al. Integrating children’s services in England: national evaluation of children’s trusts. Child Care Health Dev 2009;35:257–65. https://doi.org/10.1111/j.1365-2214.2008.00928.x
Barling JA. From Go to Woe: Family Member’s Stories of Adolescents and Young People Living with and Dying from Cancer. 2011.
Barton L, King M, Smith E. Integrated Disability Service.
Bellon M, Crocker R, Farnden J, Gardner J, Sando S, Peterson C. Family support needs following acquired brain injury across metropolitan and regional/remote South Australia. Brain Impair 2015;16:131–44.
Beresford B, Rabiee P, Sloper P. Priorities and Perceptions of Disabled Children and Young People and Their Parents Regarding Outcomes from Support Services. Vol. 15. York: University of York, Social Policy Research Unit York; 2007.
Betz CL, Nehring WM, Lobo ML. Transition needs of parents of adolescents and emerging adults with special health care needs and disabilities. J Fam Nurs 2015;21:362–412. https://doi.org/10.1177/1074840715595024
Bhatnagar S, Joshi S. Palliative care of young adults: an issue which needs higher and better awareness. Indian J Palliat Care 2011;17:173–4. https://doi.org/10.4103/0973-1075.92332
Bill S, Hodges B. Transitional care. Nurs Care Child Young People with Chronic Illn. 2007;234–55.
Palliativedrugs.com. Scope of Palliative Care.
Breneol S, Belliveau J, Cassidy C, Curran JA. Strategies to support transitions from hospital to home for children with medical complexity: a scoping review. Int J Nurs Stud 2017;72:91–104.
Brombley K. Supporting children living with life-limiting illnesses. Indep Nurse 2015;2015:31–4.
Brooks F, Bloomfield L, Offredy M, Shaughnessy P. Evaluation of services for children with complex needs: mapping service provision in one NHS Trust. Prim Health Care Res Dev 2013;14:52–62. https://doi.org/10.1017/S1463423612000217
Browne GB, Jack S, Thabane L. Experiences of Young Adults with Pediatric Life Threatening Conditions Transitioning from Pediatric to Adult Services: A Case Study. 2013.
Tilsley DWO. A qualitative focus group to investigate the psychosocial support needs of teenage young adult cancer patients undergoing radiotherapy in Wales. Support Care Cancer 2012;20:S34.
Friebert S. The concurrent care requirement for children with life-threatening illness: challenges and opportunities (TH318) Pediatric SIG. J Pain Symptom Manage 2013;45:346.
Mandic C, Johaningsmeir S, Corden T, Okun A, Earle A, Acevedo-Garcia D, Gordon J. Impact of caring for children with medical complexity and fragility due to multiple chronic conditions on family life. Dev Med Child Neurol 2013;55:74–75.
Cadell S, Wilson K, Hemsworth D, Davies B, Liben S, Steele R, et al. Factors that contribute to personal growth in parent caregivers of children with life-limiting illnesses: a structural equation model – 18th International Congress on Palliative Care, October 5–8, 2010 – Palais Des Congres, Montreal, Canada. J Palliat Care 2010;26:217–18.
Cadell S, Wilson K, Siden H, Steele R, Davies B, Straatman L, et al. Caregiving parents of children with life-limiting illnesses: beyond stress and coping to growth. Canadian Hospice Palliative Care Conference, Voyages in Care and Understanding, October 18–21, 2009 – Winnipeg, Manitoba, Canada. J Palliat Care 2009;25:240.
Cadell S, Wilson K, Siden H, Straatman L, Liben S, Davies B, et al. Caregiving parents of children with life-limiting illnesses: beyond stress and coping to growth – hospice palliative care: at a crossroads. November 4–7, 2007, Westin Harbour Castle Hotel, Toronto, Ontario, Canada. J Palliat Care 2007;23:227.
Campbell F, Biggs K, Aldiss SK, O’Neill PM, Clowes M, McDonagh J, et al. Transition of care for adolescents from paediatric services to adult health services. Cochrane Database Syst Rev 2016;4:CD009794. https://doi.org/10.1002/14651858.CD009794.pub2
Corr CA, Torkildson C, Horgan M. ChiPPS Pediatric Palliative Care Newsletter Issue #25. 2011. URL: https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.572.3272%26rep=rep1%26type=pdf (accessed 3 December 2020).
Health and Social Care Alliance Scotland, Scottish Government Directorate for Children and Families. Experiences of Transitions to Adult Years and Adult Services. 2017. URL: www.alliance-scotland.org.uk/wp-content/uploads/2017/11/ALLIANCE-GIRFEC-Experiences-of-Transitions-to-Adult-Years-and-Adult-Services-2017-1.pdf (accessed 3 December 2020).
Case L. Supportive care: what works for teenagers and young adults? Eur J Cancer 2011;47:S243.
Chakravarti U. Burden of caring: families of the disabled in urban India. Indian J Gend Stud 2008;15:341–63.
Chan J. Carers’ perspective on respite for persons with acquired brain injury. Int J Rehabil Res 2007;30:137–46. https://doi.org/10.1097/MRR.0b013e32813a2f11
Charles A, Ham C, Baird B, Alderwick H, Bennett L. Reimagining Community Services. 2018.
Danvers L, Freshwater D, Cheater F, Wilson A. Providing a seamless service for children with life-limiting illness: experiences and recommendations of professional staff at the Diana Princess of Wales Children’s Community Service. J Clin Nurs 2003;12:351–9.
Christ G, Blacker S. Editorial: the continuing quest for ‘better’. J Palliat Med 2006;9:773.
Christine M, Peter T, Vivian W, Amy H, Michelle P. A Systematic Review of Economic Evaluations of Palliative Care Models. 2016.
Ciccarelli MR, Gladstone EB, Armstrong Richardson EA. Implementation of a transdisciplinary team for the transition support of medically and socially complex youth. J Pediatr Nurs 2015;30:661–7. https://doi.org/10.1016/j.pedn.2015.07.003
Waldman HB, Perlman SP, Rader R. Hardships of raising children with special health care needs (a commentary). Soc Work Health Care 2010;49:618–29. https://doi.org/10.1080/00981381003635189
Cohen E, Kuo DZ, Agrawal R, Berry JG, Bhagat SK, Simon TD, Srivastava R. Children with medical complexity: an emerging population for clinical and research initiatives. Pediatrics 2011;127:529–38. https://doi.org/10.1542/peds.2010-0910
Cook K, Siden H, Jack S, Thabane L, Browne G. Up against the system: a case study of young adult perspectives transitioning from pediatric palliative care. Nurs Res Pract 2013;286751. https://doi.org/10.1155/2013/286751
Cooper R, Labour MP, Lancashire W, George A, Liberal MP, Ives S, et al. Health Committee Managing the Care of People with Long-term Conditions. 2014.
Cope D. Study finds that children do not receive necessary palliative care. Clin J Oncol Nurs 2003;7:506.
Corboy KJ. Crossing paths. J Palliat Med 2002;5:421–4. https://doi.org/10.1089/109662102320135333
Cox M. Quality of life among carers of people with Huntington’s disease. Br J Neurosci Nurs 2012;8:288–94.
Crane K. Pediatric palliative care gains recognition. J Natl Cancer Inst 2011;103:1432–3. https://doi.org/10.1093/jnci/djr401
Criteria E. Short Breaks: Small Grant Application.
Cross KL. We are all teachers. J Palliat Med 2016;19:688–9. https://doi.org/10.1089/jpm.2016.0190
Crusse EP, Messler T. Hospice care is. Nurs Made Incred Easy 2014;12:40–9.
Csikai EL. Editor’s introduction. J Soc Work End Life Palliat Care 2008;4:1–2.
Dabbs D, Butterworth L, Hall E. Tender mercies: increasing access to hospice services for children with life-threatening conditions. MCN Am J Matern Child Nurs 2007;32:311–19. https://doi.org/10.1097/01.NMC.0000288003.10500.00
Scarlett WG. For Xavier. J Palliat Med 2011;14:1068.
Oswald DP, Gilles DL, Cannady MS, Wenzel DB, Willis JH, Bodurtha JN. Youth with special health care needs: transition to adult health care services. Matern Child Health J 2013;17:1744–52. https://doi.org/10.1007/s10995-012-1192-7
Wells P. Pediatric palliative care program development: priorities from the perspective of bereaved family members. Support Care Cancer 2009;17:987.
Kuo DZ, Cohen E, Agrawal R, Berry JG, Casey PH. A national profile of caregiver challenges among more medically complex children with special health care needs. Arch Pediatr Adolesc Med 2011;165:1020–6. https://doi.org/10.1001/archpediatrics.2011.172
da Silva SC, Dessen MA, Perez-Lopez J. Evaluation of the care services for families of disabled children. Perspective of Brazilian family members and professionals. An Psicol 2012;28:866–74.
Dalkin S. The Realist Evaluation of a Palliative Integrated Care Pathway in Primary Care: What Works, for Whom and in What Circumstances? Newcastle upon Tyne: Northumbria University; 2014.
Darbyshire P. ‘Have a good weekend’. J Palliat Med 2015;18:716–17. https://doi.org/10.1089/jpm.2015.0047
Darlington AS, Heule F, Passchier J. Granting wishes: parents’ perception of a wish fulfilment for a child with a life-threatening illness. Acta Paediatr 2013;102:e480–2. https://doi.org/10.1111/apa.12345
Darnill S, Gamage B. The patient’s journey: palliative care – a parent’s view. BMJ 2006;332:1494–5.
Davies B, Larson J, Contro N. Giving information to Latino and Chinese families in pediatric palliative care – hospice palliative care: at a crossroads. November 4–7, 2007, Westin Harbour Castle Hotel, Toronto, Ontario, Canada. J Palliat Care 2007;23:227.
Davies H, Rennick J, Majnemer A. Transition from pediatric to adult health care for young adults with neurological disorders: parental perspectives. Can J Neurosci Nurs 2011;33:32–9.
Davies R. The potential of integrated multi-agency care pathways for children. Br J Nurs 2006;15:764–8. https://doi.org/10.12968/bjon.2006.15.14.21578
Davies R. Establishing need for palliative care services for children/young people. Br J Nurs 2003;12:224–32. https://doi.org/10.12968/bjon.2003.12.4.11162
Davis K. Extending the scope of pediatric palliative care. J Palliat Med 2011;14:A4.
Davis K. ChiPPS E-Journal Pediatric Palliative and Hospice Care Issue #48, August 2017. 2017.
Dew A, Llewellyn G, Balandin S. Exploring the later life relationship between adults with cerebral palsy and their non-disabled siblings. Disabil Rehabil 2014;36:756–64. https://doi.org/10.3109/09638288.2013.816786
Dickson G. Collecting evidence of nursing vacancies in voluntary children’s palliative care organisations. Palliat Med 2016;30:S93.
Doug M, Adi Y, Williams J, Paul M, Kelly D, Petchey R, Carter YH. Transition to adult services for children and young people with palliative care needs: a systematic review. Arch Dis Child 2011;96:78–84. https://doi.org/10.1136/adc.2009.163931
Doull I. Shared care – is it worth it for the patient? J R Soc Med 2012;105:S25–9.
Dow J. Continuing health care – the plot thickens. J Integr Care 2009;17:20–2.
Dowling S, Joughin C, Logan S, Laing G, Roberts H. Financial Benefits and Child Health. Essex: Barnardo’s; 2004.
Dowrick C. In this issue. Chronic Illn 2008;4:3.
Drew D. Developing palliative care for children globally. Int J Palliat Nurs 2015;21:263. https://doi.org/10.12968/ijpn.2015.21.6.263
Duffin C. Hospice’s family-centred focus gains ‘outstanding’ rating from regulator. Nurs Child Young People 2015;27:11. https://doi.org/10.7748/ncyp.27.2.11.s10
Dunbar HA. ‘Place Bonding’: Parents’ Journeys Towards a Sense of Rootedness in Children’s Hospice Care. 2016.
Mash E, Lloyd-Williams M. A survey of the services provided by children’s hospices in the United Kingdom. Support Care Cancer 2006;14:1169–72. https://doi.org/10.1007/s00520-006-0123-9
Eaves N. A Bohemian Rhapsody’: using music technology to fulfil the aspirations of teenage lads with muscular dystrophy. In Music Therapy in Children’s Hospices. 2005. pp. 95–109.
Ebeling S, Cowee D. P129 Equitable allocation in needs-led care: developing an assessment tool for respite allocation in a hospice for young adults. BMJ Support Palliat Care 2013;3:A55.
Eisenberg JS. Journal highlights. Caring Ages 2013;14:14–5.
Elias ER, Murphy NA, Council on Children with Disabilities. Home care of children and youth with complex health care needs and technology dependencies. Pediatrics 2012;129:996–1005. https://doi.org/10.1542/peds.2012-0606
Sheldon F, Speck P. Children’s hospices: organizational and staff issues. Palliat Med 2002;16:79.
Fahlberg B. Integrating supportive and palliative care for young adults with serious illnesses. Nursing 2016;46:12–14. https://doi.org/10.1097/01.NURSE.0000482877.08113.ab
Falvo D, Holland BE. Medical and Psychosocial Aspects of Chronic Illness and Disability. Burlington, MA: Jones & Bartlett Learning; 2017.
Fawcett TN, Baggaley SE, Wu C, Whyte DA, Martinson IM. Parental responses to health care services for children with chronic conditions and their families: a comparison between Hong Kong and Scotland. J Child Health Care 2005;9:8–19.
Feinstein JA. Comfort amidst the chaos. Contemp Pediatr 2010;27:60–3.
Feinstein R, Rabey C, Pilapil M. Evidence supporting the effectiveness of transition programs for youth with special health care needs. Curr Probl Pediatr Adolesc Health Care 2017;47:208–11.
Fern LA, Taylor RM, Whelan J, Pearce S, Grew T, Brooman K, et al. The art of age-appropriate care: reflecting on a conceptual model of the cancer experience for teenagers and young adults. Cancer Nurs 2013;36:E27–38. https://doi.org/10.1097/NCC.0b013e318288d3ce
Care Quality Commission (CQC). The J’s Hospice. Newcastle upon Tyne: CQC; 2014. URL: https://cqc.org.uk/sites/default/files/old_reports/1-350850907_The_Js_Hospice_INS1-966985130_Scheduled_13-02-2014.pdf (accessed 19 January 2020).
Flores Cano JC, Lizama Calvo M, Rodríguez Zamora N, Ávalos Anguita ME, Galanti De La Paz M, Barja Yañez S, et al. [Models of care and classification of ‘children with special health care needs – CSHCN’: recommendations from the CSHCN Committee, Chilean Paediatric Society.] Rev Chil Pediatr 2016;87:224–32. https://doi.org/10.1016/j.rchipe.2016.03.005
Floriani CA. Home-based palliative care: challenges in the care of technology-dependent children. J Pediatr 2010;86:15–20. https://doi.org/10.2223/JPED.1972
Forbat L, Haraldsdottir E, McManus E. Evaluating Family Support Needs of People Using Strathcarron Hospice Services. 2010.
Forbes A, While A, Ullman R, Lewis S, Mathes L, Griffiths P, et al. A Multi-Method Review to Identify Components of Practice Which May Promote Continuity in the Transition from Child to Adult Care for Young People with Chronic Illness or Disability.
Ford S. Clinical news summary: top nurse research and practice stories from January 2018. Nurs Times 2018;114:23.
Forrest Lucy C, Clare O, Denise G. Cultural considerations in the provision of paediatric palliative care music therapy services in Melbourne Australia. Palliat Med 2018;32:112.
Forrest L. Your song, my song, our song: developing music therapy programs for a culturally diverse community in home-based paediatric palliative care. Aust J Music Ther 2014;25:15–27.
Forrester AB, Barton-Gooden A, Pitter C, Lindo JL. The lived experiences of adolescents with sickle cell disease in Kingston, Jamaica. Int J Qual Stud Health Well-being 2015;10:28104. https://doi.org/10.3402/qhw.v10.28104
Foster TL. Pediatric palliative care revisited. J Hosp Palliat Nurs 2007;9:212–19.
Franklin J. Research roundup. Int J Palliat Nurs 2015;21:304–5.
Fraser L, Jarvis S, Moran N, Aldridge J, Parslow R, Beresford B. Children in Scotland Requiring Palliative Care: Identifying Numbers and Needs (The ChiSP Study). 2015. URL: https://york.ac.uk/media/spru/projectfiles/ProjectOutput_ChispReport.pdf (accessed 19 January 2020).
Freeborn D, Knafl K. Growing up with cerebral palsy: perceptions of the influence of family. Child Care Health Dev 2014;40:671–9. https://doi.org/10.1111/cch.12113
Friedel M, Brichard B, Renard M, Fonteyne C, Vandecruys E, Misson JP, et al. Hidden part of the iceberg: pediatric palliative care in Belgium. Palliat Med 2016;30:S12–S13.
Fuehrer M. The coordination centre for pediatric palliative medicine in Munich: a model for the future? J Palliat Care 2006;22:234.
Funk L, Stajduhar K, Cloutier-Fisher D. Family caregivers describe the non-use of formal services at the end of life – 18th International Congress on Palliative Care, October 5–8, 2010 – Palais Des Congres, Montreal, Canada. J Palliat Care 2010;26:230.
Dejong G, Palsbo SE, Beatty PW, Jones GC, Knoll T, Neri MT. The organization and financing of health services for persons with disabilities. Milbank Q 2002;80:261–301.
Gawne-Kelnar G. Listening. Palliat Support Care 2013;11:531–3.
Gessell P. Creating a lasting impression of a short life. Can Nurse 2011;107:24–6.
Gethins M. Pediatric palliative care in Europe expands. J Natl Cancer Inst 2012;104:10–11. https://doi.org/10.1093/jnci/djr537
Getter A. End-of-life vignette. Not ‘just the daughter.’ Am J Hosp Palliat Med 2008;25:72–3.
Gillies M. Scottish Public Health Network (ScotPHN) Palliative and End of Life Care in Scotland: The Rationale for a Public Health Approach. 2016.
Gillis J. ‘We want everything done’. Arch Dis Child 2008;93:192–3. https://doi.org/10.1136/adc.2007.120568
Gillmor L, Patel L, Thompson C. Rounding third: bringing pediatric palliative care home. J Palliat Med 2017;20:A32.
Goossens E, Bovijn L, Gewillig M, Budts W, Moons P. Predictors of Care Gaps in Adolescents With Complex Chronic Condition Transitioning to Adulthood. Pediatrics 2016;137:e20152413. https://doi.org/10.1542/peds.2015-2413
Gr C. Charity calls for review of family travel costs. Paediatr Nurs 2002;14.
Grady A, Travers E. Hospice at home 2: evaluating a crisis intervention service. Int J Palliat Nurs 2003;9:326–35. https://doi.org/10.12968/ijpn.2003.9.8.11522
Department for Education. Short Break Carers: Supplementary Guidance for Managers, Supervisors and Trainers. London: Department for Education; 2012. Available from: http://media.education.gov.uk/assets/files/pdf/s/short break carers supplementary guidance for managers supervisors and trainers.pdf (accessed 3 December 2020).
Green SE, Darling RB, Wilbers L. Has the parent experience changed over time? A meta-analysis of qualitative studies of parents of children with disabilities from 1960 to 2012. Res Soc Sci Disabil 2013;7:97–168.
Greene RR. Contemporary Issues of Care. Abingdon: Routledge; 2012.
Greffe B. The butterfly program: a partnership model for pediatric palliative care (S726). J Pain Symptom Manage 2013;45:432.
Grinyer A. Palliative and End of Life Care for Children and Young People: Home, Hospice and Hospital. 2013.
Grinyer A, Barbarachild Z. Teenage and Young Adult Palliative and End of Life Care Service Evaluation. 2011.
Guenther KD, Graham D, O’Donnell HK, Sellers DE, Sawicki GS, Robinson W, et al. Perceived social support predicts selfreported mental and physical health in adults with cystic fibrosis. Pediatr Pulmonol 2016;51:454.
Gwilym O, Sayers A, Hassan N, Prosser A, Speight L, Ketchell RI, et al. SPARC questionnaire: identifying needs in people with cystic fibrosis (CF) attending the All Wales Adult CF Centre (AWACFC). J Cyst Fibros 2017;16:S165.
Bourketaylor H. Social, recreation and leisure participation of families who have a child with a severe physical disability: parents’ perspectives. Dev Med Child Neurol 2012;54:73.
Koutsogiannopoulos S. Transition from pediatric to adult health care for young adults with significant cognitive impairments and epilepsy: parental perspectives. Epilepsia 2013;54:233.
Muenchberger H, Sunderland N, Kendall E, Quinn H. A long way to Tipperary? Young people with complex health conditions living in residential aged care: a metaphorical map for understanding the call for change. Disabil Rehabil 2011;33:1190–202. https://doi.org/10.3109/09638288.2010.524275
Hansson H, Hallström I, Kjaergaard H, Johansen C, Schmiegelow K. Hospital-based home care for children with cancer. Pediatr Blood Cancer 2011;57:369–77. https://doi.org/10.1002/pbc.23047
Harmon N. Understanding the experiences of family caregivers of individuals with acquired brain injury following discharge from rehabilitation. Brain Inj 2010;24:440.
Harper EK. A Review of Factors Contributing to the Shortage of Palliative Care Service for Adolescent and Young Adult Oncology Patients. Yellow Springs, OH: Antioch University; 2016.
has an H. Meeting the Needs of Children with Medical Complexity: A Framework for Building a Pediatric Complex Care Program. 2016.
Heath G, Farre A, Shaw K. Parenting a child with chronic illness as they transition into adulthood: a systematic review and thematic synthesis of parents’ experiences. Patient Educ Couns 2017;100:76–92.
Hebdon HM. Coping with deployment for the child with special needs and the entire family. Except Parent 2007;37:75–7.
Hefner JL. Children with Complex Special Health Care Needs and the Health Services System: Unmet Needs, Barriers to Care, and Coordination of Health Services. 2010.
Henwood M, Hudson B. Keeping it Personal: Supporting People with Multiple and Complex Needs: A Report to the Commission for Social Care Inspection. 2009.
Herbert A, Smith C, Graham C. Respite Needs Of Families Receiving Palliative Care.
Hewitt-Taylor J. Parents whose children have complex needs: experiences of hospitalization. J Child Young People’s Nurs 2008;2:13–19.
Hewitt-Taylor J. Children with Complex and Continuing Health Needs: The Experiences of Children, Families and Care Staff. London: Jessica Kingsley Publishers, Ltd.; 2007.
Hilliard RE. Music therapy in pediatric palliative care: complementing the interdisciplinary approach. J Palliat Care 2003;19:127–32.
Himelstein BP. Palliative care in pediatrics. Anesthesiol Clin North America 2005;23:837–56.
Homer CJ, Klatka K, Romm D, Kuhlthau K, Bloom S, Newacheck P, et al. A review of the evidence for the medical home for children with special health care needs. Pediatrics 2008;122:e922–37. https://doi.org/10.1542/peds.2007-3762
Horridge KA, Wolff T. Palliative care for disabled children and young people. Paediatr Child Health 2014;24:343–50.
Hunt A, Elston S, Galloway J. Voices for Change: Current Perception of Services for Children with Palliative Care Needs and Their Families. 2003.
Hunt A, Hacking S. The BiG Study for Life-Limited Children and Their Families. 2013.
Illhardt FJ. From Germany: helpful differentiation. Palliat Med 2003;17:130.
Billings J, Jenkins L, Black R. A learning and development strategy for children’s hospices across London. Int J Palliat Nurs 2011;17:483–91. https://doi.org/10.12968/ijpn.2011.17.10.483
De Man J. Living my life with day care with treatment. Clin Genet 2009;76:87.
Janisch M, Nolte-Buchholtz S, Von Der Hagen M. What kind of general and special palliative care do children, adolescents, and young adults with Duchenne muscular dystrophy need? Neuropediatrics 2016;47.
Jessup MM. Living with Cystic Fibrosis: A Phenomenological Study of Children, Adolescents, Young Adults and Their Parents. Hobart, Tas: University of Tasmania; 2004.
Johanna T, Lorna F, Bryony B, Bob P, Alison B, Kath W, et al. Specialist paediatric palliative care for children and young people with malignancies: a mixed methods systematic review. 2017.
John Duffy S, Murray P. Transition and integration – changing our starting point. J Integr Care 2013;21:306–14.
Johnson HL, DeLeon PH. Accessing care for children with special health care needs. Pract Innov 2016;1:105.
Jones BL. The challenge of quality care for family caregivers in pediatric cancer care. Semin Oncol Nurs 2012;28:213–20. https://doi.org/10.1016/j.soncn.2012.09.003
Jones D, Crawford A, Bearn S, Plant R. Mind the gap: rethinking community neurological rehabilitation services. Int J Ther Rehabil 2007;14:136–40.
Jones E, Thienprayoon R, Hidalgo M, Stapleton S. Quality in Pediatric Palliative Care. New York, NY: Springer Publishing; 2017.
Gridley K, Brooks J, Glendinning C. Good practice in social care for disabled adults and older people with severe and complex needs: evidence from a scoping review. Health Soc Care Community 2014;22:234–48. https://doi.org/10.1111/hsc.12063
Kamal AH, Bull JH, Swetz KM, Wolf SP, Shanafelt TD, Myers ER. Future of the palliative care workforce: preview to an impending crisis. Am J Med 2017;130:113–14.
Kassam A, Wolfe J. The ambiguities of free-standing pediatric hospices. J Palliat Med 2013;16:716–17. https://doi.org/10.1089/jpm.2013.9500
Kastenholz E, Eusébio C, Figueiredo E. Contributions of tourism to social inclusion of persons with disability. Disabil Soc 2015;30:1259–81.
Keim-Malpass J, Cohrs AC, Lindley LC, Leslie DL. An economic examination of private insurance claims among adolescents and young adults who were enrolled in hospice during the last year of life. Adolesc Health Med Ther 2018;9:117–20. https://doi.org/10.2147/AHMT.S168501
Kelly D. Developing new support services for young people with cancer. Eur J Oncol Nurs 2012;16:S8.
Kelly D. The challenge of caring for adolescents and young adults. Int J Palliat Nurs 2013;19:211. https://doi.org/10.12968/ijpn.2013.19.5.211
Kerr H, O’Halloran P. Transition from Children’s to Adult Services for Young Adults with Life-limiting Conditions in Ireland. 2017.
Kerr H, Price J, Nicholl H, O’Halloran P. Facilitating transition from children’s to adult services for young adults with life-limiting conditions (TASYL): programme theory developed from a mixed methods realist evaluation. Int J Nurs Stud 2018;86:125–38.
Kerr H, Price J, Nicholl H, O’Halloran P. Transition from children’s to adult services for young adults with life-limiting conditions: a realist review of the literature. Int J Nurs Stud 2017;76:1–27.
Kimberely W, Gregorio Zuniga V, Madeline T, Christina M, Jürg S. A systematic review of the impact of specialized paediatric palliative care for children with life-threatening/limiting conditions. 2017.
King N, Barclay B. Caring for young adults with rare neurological conditions. Eur J Palliat Care 2007;14:200–3.
Klikovac T, Steinhorn DM. Developing paediatric palliative care in Serbia: parents’ point of view. Eur J Palliat Care 2017;24:186–90.
Kmietowicz Z. Palliative care services should have higher priority, says NICE. BMJ 2004;328:725. https://doi.org/10.1136/bmj.328.7442.725
Knapp C, Madden V, Wang H, Curtis C, Sloyer P, Shenkman E. Music therapy in an integrated pediatric palliative care program. Am J Hosp Palliat Care 2009;26:449–55. https://doi.org/10.1177/1049909109341870
Knapp C, Quinn GP, Murphy D, Brown R, Madden V. Adolescents with life-threatening illnesses. Am J Hosp Palliat Care 2010;27:139–44. https://doi.org/10.1177/1049909109358310
Knapp C, Thompson L. Factors associated with perceived barriers to pediatric palliative care: a survey of pediatricians in Florida and California. Palliat Med 2012;26:268–74. https://doi.org/10.1177/0269216311409085
Knight A, Oliver CM. Providing Advocacy for Disabled Children, Including Children Without Speech. In Dalrymple J, Oliver C, editors. Developing Advocacy for Children and Young People: Current Issues in Research, Policy and Practice. London: Jessica Kingsley Publishers; 2008. p. 116.
Knight J. Happier endings. Nurs Stand 2010;25:24–5.
Kozlowski-Moreau O, Danze F, Pollez B, Brooks N, Johnson C, Line MC, et al. Long-term management of severe TBI in Europe – the value of a network. Brain Inj 2016;30:650.
P, et al. Palliative care for children and young people with progressive neuromuscular conditions. Dev Med Child Neurol 2011;53(Suppl. 1):47.
Fraser LK, Aldridge J, Manning S, O’Leary S, Miller M, McCulloch R, Childs AM. Hospice provision and usage amongst young people with neuromuscular disease in the United Kingdom. Eur J Paediatr Neurol 2011;15:326–30. https://doi.org/10.1016/j.ejpn.2011.02.003
Fraser LK, Miller M, Hain R, Norman P, Aldridge J, McKinney PA, Parslow RC. Rising national prevalence of life-limiting conditions in children in England. Pediatrics 2012;129:e923–9. https://doi.org/10.1542/peds.2011-2846
Fraser LK, van Laar M, Miller M, Aldridge J, McKinney PA, Parslow RC, Feltbower RG. Does referral to specialist paediatric palliative care services reduce hospital admissions in oncology patients at the end of life? Br J Cancer 2013;108:1273–9. https://doi.org/10.1038/bjc.2013.89
Fraser LK, Lidstone V, Miller M, Aldridge J, Norman P, McKinney PA, Parslow RC. Patterns of diagnoses among children and young adults with life-limiting conditions: a secondary analysis of a national dataset. Palliat Med 2014;28:513–20. https://doi.org/10.1177/0269216314528743
Laidlaw S, Carduff E. The ‘forgotten’ generation: quality of life in adults living with Duchenne muscular dystrophy. Palliat Med 2018;32:124–5.
Ngo C. Experiences of Pediatric Parenting Stress and Family Support for Caregivers of Children with Special Health Care Needs or Developmental Disabilities. 2017.
Lancaster B. Social Work Services for Disabled Children and Young People and Their Families: Assessment and Eligibility. 2012.
Lewis JM, DiGiacomo M, Luckett T, Davidson PM, Currow DC. A social capital framework for palliative care: supporting health and well-being for people with life-limiting illness and their carers through social relations and networks. J Pain Symptom Manage 2013;45:92–103. https://doi.org/10.1016/j.jpainsymman.2011.12.283
Liao S, Arnold RM. Editorial: caring for caregivers: the essence of palliative care. J Palliat Med 2006;9:1172–3. https://doi.org/10.1089/jpm.2006.9.1172
Liao S, Arnold RM. Editorial: supporting pediatric palliative care: helping ourselves. J Palliat Med 2006;9:161–2. https://doi.org/10.1089/jpm.2006.9.161
Lindley L, Mark B, Lee SY. Providing hospice care to children and young adults: a descriptive study of end-of-life organizations. J Hosp Palliat Nurs 2009;11:315–23. https://doi.org/10.1097/NJH.0b013e3181bcfd62
Lindley LC, Shih-Lung S. Who are the children using hospice care? J Spec PediatrNurs 2014;19:308.
Linebarger JS, Ajayi TA, Jones BL. Adolescents and young adults with life-threatening illness: special considerations, transitions in care, and the role of pediatric palliative care. Pediatr Clin North Am 2014;61:785–96. https://doi.org/10.1016/j.pcl.2014.05.001
Together for Short Lives. Together For Short Lives’ Report on Children’s Palliative Care Services Commissioned by NHS Clinical Commissioning Groups (CCGs) and Local Authorities in England November 2017. Bristol: Together for Short Lives; 2017.
Clairicia M, Poisson C, Levret M, Lenoir G, Scheinman P, Robert JJ. [Cystic fibrosis in home care services.] Soins Pediatr Pueric 2004;218:31–3.
Duff M, Giles B. Making the best of things: raising a child with complex health needs that include respiratory technology dependence. Chest 2013;144.
Duff M, Giles B. A constricted life: growing up with complex health needs that include respiratory technology dependence. Chest 2013;144.
Roebroeck ME, Jahnsen R, Carona C, Kent RM, Chamberlain MA. Adult outcomes and lifespan issues for people with childhood-onset physical disability. Dev Med Child Neurol 2009;51:670–8. https://doi.org/10.1111/j.1469-8749.2009.03322.x
Wilkins ML, Dallas RH, Fanone KE, Lyon ME. Pediatric palliative care for youth with HIV/AIDS: systematic review of the literature. HIV AIDS 2013;5:165–79. https://doi.org/10.2147/HIV.S44275
Maguire H, Smith M. Re-moving Mountains: an Exploration into the Respite Needs of Adolescents with Life-Limiting Conditions. BMJ Specialist Journals; 2009.
Major J, Stewart D, Amaria K, Canadian Foundation for Healthcare Improvement. Care in the Long Term for Youth and Young Adults with Complex Care Needs. Ottawa, ON: Canadian Foundation for Healthcare Improvement; 2014.
Malcolm C, Adams S, Anderson G, Gibson F, Hain R, Morley A, et al. The Symptom Profile and Experience of Children with Rare Life-Limiting Conditions: Perspectives of Their Families and Key Health Professionals. 2011.
Malcolm C, Gibson F, Adams S, Anderson G, Forbat L. A relational understanding of sibling experiences of children with rare life-limiting conditions: findings from a qualitative study. J Child Health Care 2014;18:230–40. https://doi.org/10.1177/1367493513485825
Mandic CG, Johaningsmeir S, Corden TE, Earle A, Acevedo-Garcia D, Gordon JB. Impact of caring for children with medical complexity on parents’ employment and time. Community Work Fam 2017;20:444–58.
Mao S, von Moreau D. [The state of implementation of music therapy in pediatric oncology: an online survey in German speaking countries.] Musik Umschau 2018;39:129–40.
Marie Curie Cancer Care. Young People with Life-limiting Conditions: Further Evidence Gathering: BME/Faith Issues. London: Marie Curie Cancer Care; 2011.
Maunder EZ. The challenge of transitional care for young people with life-limiting illness. Br J Nurs 2004;13:594–6. https://doi.org/10.12968/bjon.2004.13.10.13047
McDowell BC, Duffy C, Parkes J. Service use and family-centred care in young people with severe cerebral palsy: a population-based, cross-sectional clinical survey. Disabil Rehabil 2015;37:2324–9. https://doi.org/10.3109/09638288.2015.1019649
McGrath A, Yeowart C. Rights of Passage. London: New Philanthropy Capital; 2009.
McKenzie LM. Exploring and Developing Resources for Families of Children with a Life-limiting Illness. Regina, SK: Faculty of Social Work, University of Regina; 2016.
McNamara K. Government plan needed for children’s palliative care. Nurs Stand 2017;32:31.
McNamara-Goodger K, Cooke R. Children’s and young people’s palliative care: good practice guidelines. J Prim Health Care 2009;19:40–8.
McNamara-Goodger K. Transitional Care for Children and Young People with Life-threatening or Life-limiting Conditions. In Davies R, editor. Children and Young People’s Nursing Principles for Practice. Abingdon: Routledge; 2011.
Meaney F, Pandya S, Andrews J, Davis M. Palliative care services in families of males with Duchenne muscular dystrophy. Neuromuscul Disord 2007;17:866.
Medforth N, Huntingdon E. Real Lives. 2015.
Meier DE, Periyakoil VS. Finding my place. J Palliat Med 2009;12:331–5.
Michelle E, Susan A, Alan S, Jane C. Adolescents’ and Young People with Sickle Cell Anaemia Perspectives, Views and Experiences of Sickle Cell Services. 2018.
Mitchell S, Bennett K, Morris A, Dale J. Palliative care services for children and young people: realist review of the literature. Arch Dis Child 2016;101:A305–6.
Mitchell S, Dale J. Palliative care from diagnosis for all ages including children and young people. BMJ 2017;357:j2465. https://doi.org/10.1136/bmj.j2465
Mitchell S, Slowther A-M, Coad J, Dale J. The journey through care: study protocol for a longitudinal qualitative interview study to investigate the healthcare experiences and preferences of children and young people with life-limiting and life-threatening conditions and their families in the West Midlands, UK. BMJ Open 2018;8:e018266.
Mohammed TS, Awosoga O. Impacts of caring for youth with severe disabilities on parents’ quality of life. Qual Life Res 2017;26:18–19.
Mollidor C, Berridge D. Residential Care for Children and Young People. In Dolan P, Frost N, editors. The Routledge Handbook of Global Child Welfare. Abingdon: Routledge; 2017.
Mooney-Doyle K, Deatrick JA. Promoting Family participation in pediatric palliative care research. Nurs Outlook 2016;64:111.
Munford R, DeMichelis C, Ferrari M. Building Strengths and Resilience: Supporting Families and Disabled Children. In DeMichelis C, Farrari M, editors. Child and Adolescent Resilience Within Medical Contexts. New York, NY: Springer Publishing; 2016. pp. 227–45.
Myburgh D. Lived experiences of children with life threatening illnesses participating in ‘dream’ realization projects. Pediatr Blood Cancer 2016;63:S287.
Young NL, Barden WS, Mills WA, Burke TA, Law M, Boydell K. Transition to adult-oriented health care: perspectives of youth and adults with complex physical disabilities. Phys Occup Ther Pediatr 2009;29:345–61. https://doi.org/10.3109/01942630903245994
Natalie E, Laura H, Devon C, Megan B, Dio K, Michele K-F, et al. Specialty and non-specialty palliative care delivery: a systematic review and meta-analysis. 2017.
Neff J, Villareale N. Health institution of the month: the Center for Children with Special Needs: creating system changes through a collaborative, family-centered approach. Except Parent 2003;33:50–4.
Nehring I, Riedel C, Baghi L, Moshammer-Karb T, Schmid R, Kries R V. [Psychosocial situation of families with chronically ill children: a survey of parent initiatives.] Gesundheitswesen 2015;77:102.
Nelson L, Inglis S, Howell F, Gibbs M, Thorley J. Vulnerable Adults. In Wood I, Garner M, editors. Initial Management of Acute Medical Patients: A Guide for Nurses and Healthcare Practitioners. Hoboken, NJ: Wiley; 2012.
Ngwenya N, Kenten C, Jones L, Gibson F, Pearce S, Stirling C, et al. ‘hospice scares the life out of me’: breaking down barriers to communication with young adults with terminal cancer.’ J Pain Symptom Manage 2016;52:E62.
Nicholl H, Tracey C. Children’s palliative care – developing a service. World Irish Nurs Midwifery 2015;23:55–6.
Noyes J, Hastings RP, Lewis M, Hain R, Bennett V, Hobson L, et al. Planning ahead with children with life-limiting conditions and their families: development, implementation and evaluation of ‘My Choices’. BMC Palliat Care. 2013;12:5–21.
Noyes J, Pritchard A, Rees S, Hastings R, Jones K, Mason H, et al. Bridging the Gap: Transition from Children’s to Adult Palliative Care. 2014.
Nyatanga B. Transition from paediatric to adult palliative care: more than a physical change. Br J Community Nurs 2013;18:466. https://doi.org/10.12968/bjcn.2013.18.9.466
O’Connor J. The challenges faced when leaving a children’s hospice. Nurs Child Young People 2014;26:8–9. https://doi.org/10.7748/ncyp2014.02.26.1.8.s9
O’Donnell C. A simple gesture that meant so much. World Irish Nurs Midwifery 2007;15:60.
Olauson A. The Agrenska centre: a socioeconomic case study of rare diseases. PharmacoEconomics 2002;20:73–5.
Great Ormond Street Hospital. Making Choices: Information for Families of Children Who Have a Life-limiting or Life-threatening Condition. London: Great Ormond Street Hospital; 2010.
Linck P, Tunnage B, Hughes DA, Edwards RT. NHS and charitable funding for children and young people with cancer in England and Wales. J Child Health Care 2008;12:156–68. https://doi.org/10.1177/1367493508090173
Williams PD, Williams KA, Williams AR. Parental caregiving of children with cancer and family impact, economic burden: nursing perspectives. Issues Compr Pediatr Nurs 2014;37:39–60. https://doi.org/10.3109/01460862.2013.855843
Palliative WA, Gott M, Williams L, Moeke-Maxwell T. Chapter Nine the Paradoxes of ‘Home’.
Pan R, Fuller J, Gaines T, Hill J, Hueso B, Liu C, et al. Overview: Mapping Systems of Care for Children with Special Needs in the State of California. 2016. URL: www.senate.ca.gov/sites/senate.ca.gov/files/final_brief_overview-mapping_systems_of_care_for_children_with_special_needs_select_committee_march_2016.pdf (accessed 3 December 2020).
Park MJ, Adams SH, Irwin CE. Health care services and the transition to young adulthood: challenges and opportunities. Acad Pediatr 2011;11:115–22. https://doi.org/10.1016/j.acap.2010.11.010
Parker AE, Robb SA, Chambers J, Davidson AC, Evans K, O’Dowd J, et al. Analysis of an adult Duchenne muscular dystrophy population. QJM 2005;98:729–36.
Parker G, Spiers G, Gridley K, Atkin K, Birks Y, Lowson K, Light K. Systematic review of international evidence on the effectiveness and costs of paediatric home care for children and young people who are ill. Child Care Health Dev 2013;39:1–19. https://doi.org/10.1111/j.1365-2214.2011.01350.x
Peay HL, Meiser B, Kinnett K, Tibben A. Psychosocial needs and facilitators of mothers caring for children with Duchenne/Becker muscular dystrophy. J Genet Couns 2018;27:197–203. https://doi.org/10.1007/s10897-017-0141-4
Pfund R. The Path to Excellence. In Pfund R, Kerry-Folwer S, editors. Perspectives on Palliative Care for Children and Young People: A Global Discourse. Abingdon: Taylor & Francis; 2010. p. 314.
Pfund R, Boath E. Palliative Care Nursing of Children and Young People. Abingdon: Routledge; 2016.
Pinney A. Understanding the Needs of Disabled Children With Complex Needs or Life-limiting Conditions: What Can We Learn From National Data? Exploratory Analysis Commissioned by the Council for Disabled Children and the True Colours Trust. London: Council for Disabled Children; 2017.
Pravin RR, Xin SC. Of children and X-Men. Eur J Palliat Care 2015;22:46–8.
Pritchard AW, Rees SA. Challenges and ‘obstacles’: reframing our perspective on the transition into adulthood for young people with life-limiting and lifethreatening conditions. J R Coll Physicians Edinb 2016;46:223–7.
Proot C, Yorke M. Life to Be Lived: Challenges and Choices for Patients and Carers in Life-threatening Illnesses. Oxford: Oxford University Press; 2013.
Quick P. Palliative care and its benefits: a consultant’s viewpoint. J Nurse Pract 2007;3:566–8.
Barth R, Binnewitt N. [Palliative care in the pediatric and youth hospice. Living and laughing – dying and grieving.] Pflege Z 2014;67:656–9.
Pangalila RF, van den Bos GA, Stam HJ, van Exel NJ, Brouwer WB, Roebroeck ME. Subjective caregiver burden of parents of adults with Duchenne muscular dystrophy. Disabil Rehabil 2012;34:988–96. https://doi.org/10.3109/09638288.2011.628738
Tamburro RF, Shaffer ML, Hahnlen NC, Felker P, Ceneviva GD. Care goals and decisions for children referred to a pediatric palliative care program. J Palliat Med 2011;14:607–13. https://doi.org/10.1089/jpm.2010.0450
Read J, Kinali M, Muntoni F, Weaver T, Garralda ME. Siblings of young people with Duchenne muscular dystrophy – a qualitative study of impact and coping. Eur J Paediatr Neurol 2011;15:21–8. https://doi.org/10.1016/j.ejpn.2010.07.006
Remedi PP, Mello DF, Menossi MJ, Lima RA. [Palliative care to adolescents with cancer: a literature review.] Rev Bras Enferm 2009;62:107–12.
Report I. Making Every Day Count the True Impact. 2017.
Revill P, Ryan P, McNamara A, Normand C. A cost and outcomes analysis of alternative models of care for young children with severe disabilities in Ireland. EurJ Disabil Res 2013;7:260–74.
Rost M, De Clercq E, Wangmo T, Elger BS. The need for a shared understanding: domains of care and composition of team in pediatric palliative care guidelines. J Hosp Palliat Nurs 2017;19:556–64.
Rousseau PC. Palliative care: who is it for? J Palliat Med 2013;16:3.
Rousseau PC. Hospice vignettes. Lessons from Lisa. Am J Hosp Palliat Care 2003;20:155–6.
Rousseau PC. Hole in the Air. J Palliat Med 2018;21:725. https://doi.org/10.1089/jpm.2017.0563
Russell N. Management of multiple sclerosis and the role of respite and palliative care. Int J Palliat Nurs 2010;16:472, 474. https://doi.org/10.12968/ijpn.2010.16.10.79210
Russell P. ‘Access and achievement or social exclusion?’ Are the government’s policies working for disabled children and their families? Child Soc 2003;17:215–25.
Ryynänen O-P, Nousiainen P, Soini EJO, Tuominen S. Efficacy of a multicomponent support programme for caregivers of disabled persons: a randomised controlled study. Z Gerontol Geriatr 2013;46:449–55.
Daykin N. Music therapy in children’s hospices: an evaluative survey of provision. Arts Psychother 2014;41:570.
Coordination of paediatric palliative home care services. Palliat Med 2010;24:S22.
Lenton S, Franck L, Salt A. Children with complex health care needs: supporting the child and family in the community. Child Care Health Dev 2004;30:191–2. https://doi.org/10.1111/j.1365-2214.2004.00416.x
Positive and negative dimensions of social support: associations with quality-of-life outcomes among adults with cystic fibrosis. Pediatr Pulmonol 2013;48:441.
Rogers SK, Gomez CF, Carpenter P, Farley J, Holson D, Markowitz M, et al. Quality of life for children with life-limiting and life-threatening illnesses: description and evaluation of a regional, collaborative model for pediatric palliative care. Am J Hosp Palliat Care 2011;28:161–70. https://doi.org/10.1177/1049909110380594
Sætrang T, Bjørk IT, Capjon H, Rasmussen M. Parent–child communication and timing of interventions are challenges in the Duchenne muscular dystrophy care. Acta Paediatr 2019;108:535–40.
Sarah M, Andrew M, Karina B, Laiba S, Jeremy D. Specialist Paediatric Palliative Care Services: What Are the Benefits?
Sarah M, Mark B, Zechen M, Amir A-S. Strategies to Improve Quality of Life for Individuals with Childhood Onset Disabilities. 2018.
Sass B, Beresford P. Shaping our Lives.User-Driven Commissioning. London: Disability Rights UK; 2012.
Scott R. Transition and caring for young adults: are you part of the solution? Prog Palliat Care 2011;19:299.
Shchurovska IP, Andreychuk IP, Bojko YE. Palliative and hospice pediatric care. Emerg Med 2018:81–5.
Slade Z, Coulter A, Joyce L. Parental Experience of Services for Disabled Children: Qualitative Research. 2009.
Sloper P, Beecham J, Clarke S, Franklin A, Moran N, Cusworth L. Models of Multi-agency Services for Transition to Adult Services for Disabled Young People and Those with Complex Health Needs: Impact and Costs. 2010.
Smith L, Wylie F, Grant J. P-216 Adult and children’s palliative care services working together to transform transitions. BMJ Support Palliat Care 2017;7:A87.
Smith S, Case L, Waterhouse K, Pettitt N, Beddard L, Oldham J, et al. A Blueprint of Care for Teenagers and Young Adults with Cancer. London: Teenage Cancer Trust; 2012.
Smyth D. Web words. Support and services for adolescents affected by chronic and life-limiting illness. Int J Palliat Nurs 2005;11:210.
Soanes L. How do young adults (19–24 years) living with cancer experience supportive care? International Conference on Cancer Nursing (ICCN). July 8–11, 2015. Vancouver, Canada. Cancer Nurs 2015;38:S3–S4.
Stalker K, Green Lister P, Lerpiniere J, McArthur K. Child Protection and the Needs and Rights of Disabled Children and Young People: A Scoping Study. 2010.
Steele R, Davies B, Siden H, Straatman L, Cadell S, Fleming C. An exploration of families’ transition into a children’s hospice program. J Palliat Care 2006;22:209.
Wright K, Perman S, Brodie C. Westminster’s Joint Strategic Needs Assessment – Transition from Children’s to Adults’ Services for Young People Aged 14 to 25 in Westminster. 2011.
Sullins EM. Caregiver Role Strain. 2016.
Takahashi A. [Home medical care and respite care for children – from the viewpoint of the local medical office]. No to Hattatsu 2012;44:205.
Tarleton B. Committed to caring: family-based short-break carers’ views of their role. Adopt Foster 2003;27:36–46.
Theodosopoulos G. Accounting for the Hospice Business Model in England. 2016.
Thomas S, Davies A, Peel C. A mid-term review of the NSF for long-term neurological conditions. Br J Neurosci Nurs 2010;6:366–70.
van Dyck PC, Kogan MD, McPherson MG, Weissman GR, Newacheck PW. Prevalence and characteristics of children with special health care needs. Arch Pediatr Adolesc Med 2004;158:884–90. https://doi.org/10.1001/archpedi.158.9.884
van Staa A, Sattoe JN. Young adults’ experiences and satisfaction with the transfer of care. J Adolesc Health 2014;55:796–803. https://doi.org/10.1016/j.jadohealth.2014.06.008
Varela AM, Deal AM, Hanson LC, Blatt J, Gold S, Dellon EP. Barriers to hospice for children as perceived by hospice organizations in North Carolina. Am J Hosp Palliat Care 2012;29:171–6. https://doi.org/10.1177/1049909111412580
Varela AM, Deal A, Dellon E, Hanson L, Gold S, Blatt J. Current state of hospice care for children in North Carolina (754). J Pain Symptom Manage 2011;41:305.
Vecchio N. Understanding the use of respite services among informal carers. Aust Health Rev 2008;32:459–67.
Vlaskamp C, Hiemstra SJ, Wiersma LA, Zijlstra BJH. Extent, duration, and content of day services’ activities for persons with profound intellectual and multiple disabilities. J Policy Pract Intellect Disabil 2007;4:152–9.
Walker A, Alfonso ML, Colquitt G, Weeks K, Telfair J. ‘When everything changes:’ parent perspectives on the challenges of accessing care for a child with a disability. Disabil Health J 2016;9:157–61.
Walker C. Children’s palliative care needs are not being met. Nurs Child Young People 2018;30:5.
Ware J, Raval H. A qualitative investigation of fathers’ experiences of looking after a child with a life-limited illness, in process and in retrospect. Clin Child Psychol Psychiatry 2007;12:549–65.
Wazneh LM, Tsimicalis A, Loiselle CG. Young adults’ perceptions of the Venturing Out Pack program as a tangible cancer support service. Oncol Nurs Forum 2016;43:E34–42. https://doi.org/10.1188/16.ONF.E34-E42
Wenger B. Everyone wins: K.E.E.N. makes triumphs possible for children and young adults with special needs. Except Parent 2004;34:20–5.
Wilkins D. The impact of ‘being assessed’ by a disabled children’s team: a personal reflective account. Child Fam Soc Work 2015;20:10–18.
Winckler V. Fair Play for Disabled Children and Young People in Wales. Merthyr Tydfil: The Bevan Foundation; 2011.
Wiseman R. Towards a More Ordinary Life: A Report on the Progress of Parent Carer Participation and the Development of Short Breaks: 2008–2011: Summary Of Final Programme Report. Birmingham: Together for Disabled Children; 2011.
Woodgate RL, Edwards M, Ripat JD, Borton B, Rempel G. Intense parenting: a qualitative study detailing the experiences of parenting children with complex care needs. BMC Pediatr 2015;15:197. https://doi.org/10.1186/s12887-015-0514-5
Woodgate RL, Edwards M, Ripat JD, Rempel G, Johnson SF. Siblings of children with complex care needs: their perspectives and experiences of participating in everyday life. Child Care Health Dev 2016;42:504–12. https://doi.org/10.1111/cch.12345
Wu YP, McPhail J, Mooney R, Martiniuk A, Amylon MD. A multisite evaluation of summer camps for children with cancer and their siblings. J Psychosoc Oncol 2016;34:449–59. https://doi.org/10.1080/07347332.2016.1217963
Zhou H, Roberts P, Dhaliwal S, Della P. Transitioning adolescent and young adults with chronic disease and/or disabilities from paediatric to adult care services – an integrative review. J Clin Nurs 2016;25:3113–30. https://doi.org/10.1111/jocn.13326
Insufficient information (n = 12)
Colussa M, Badcock K, Conway M, Britto J, Boltong A. A break away from cancer: the impact of a short holiday. Support Care Cancer 2016;24:S222.
Court B. Noah’s Ark Children’s Hospice Inspection Report. 2017.
Derian House Children’s Hospice. Derian House Children’s Hospice. 2018. URL: www.derianhouse.co.uk (accessed 3 December 2020).
Finlins H. Exploration of adult hospices as a short break provider for young adults with palliative care needs. BMJ Support Palliat Care 2016;6:A40.
Hatton C, Welch V, Collins M, Wells E, Langer S, Robertson J, et al. Evaluating the impact of short breaks on families with a disabled child/young person: findings and questions. J Intellect Disabil Res 2012;56:735.
Lane N. Hope House Children’s Hospice Inspection Report. 2016.
Laverty D. Respite care reframed – a palliative care service for the future. BMJ Support Palliat Care 2013;3:A55.
Laverty D, Flatley M, Cain K, Crossland K. Establishing a nurse led respite ward within a hospice. FoNS Improv Insights 2013;8:1.
Lorton C, Davies C, Davies AC, Tamlyn P, Fear K, Davies S, et al. Access to respite and social care for young adults in Wales: please mind the gap. Palliat Med 2016;30:NP374.
McDermid S. The Cost of Short Break Provision: Resource Pack for Service Providers. 2010.
Noyes J, Pritchard S, Pritchard A, Bennett V, Rees S. Conflicting realities experienced by children with life-limiting and life-threatening conditions when transitioning to adult health services. J Adv Nurs 2018;74:2871–81. https://doi.org/10.1111/jan.13811
Teasdale D, Summers K, Ruston A. A Service Evaluation: Ellenor Lions Hospices Children and Young Peoples Service: Executive Summary. 2011.
Commentary/opinion (n = 84)
Oral Evidence: How the Government is Meeting its Commitment to Choice for Babies, Children and Young People Who Need Palliative Care Session 4: 21 February 2018. 2018.
Mathews S. Best Practice in Care and Rehab of Adults and Children with Disabilities.
Great Britain. Children and Young Persons, England: The Breaks for Carers of Disabled Children Regulations 2011: Statutory Instrument 2011 no. 707. London: Stationery Office; 2011.
Motor Neurone Disease Association. Caring and MND (Motor Neurone Disease): Support For You. Northampton: Motor Neurone Disease Association; 2016. URL: www.mndassociation.org/wp-content/uploads/carers-guide-2016-standard.pdf (accessed 3 December 2020).
10F – Your Rights to Social Care. 2017; URL: www.mndassociation.org/wp-content/uploads/10f-your-rights-to-social-care.pdf
Chambers L, Taylor V. A Family Companion. Together for Short Lives; 2014. URL: www.togetherforshortlives.org.uk/wp-content/uploads/2018/01/FamResFamilyCompanion.pdf (accessed 3 December 2020).
Representation from Together for Short Lives. Frankfurt. 2017.
Victor E. A Systematic Review of Interventions for Carers in the UK: Outcomes and Explanatory Evidence. Woodford Green: Princess Royal Trust for Carers; 2009.
Motor Neuron Disease Association. Caring and MND: Quick Guide. Northampton: Motor Neuron Disease Association; 2017. URL: www.mndassociation.org/wp-content/uploads/caring-and-mnd-quick-guide-for-web.pdf (accessed 3 December 2020).
Strategy and Projects Team. Carers Action Plan 2018 to 2020. London: Department of Health and Social Care; 2018. URL: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/713781/carers-action-plan-2018-2020.pdf (accessed 3 December 2020).
Stalker K, Moscardini L. A Critical Review and Analysis of Current Research and Policy Relating to Disabled Children and Young People in Scotland: A Report to Scotland’s Commissioner for Children and Young People. Edinburgh: Scotland’s Commissioner for Children and Young People; 2013.
Oral Evidence: How the Government is Meeting its Commitment to Choice for Babies, Children and Young People Who Need Palliative Care Session 6: 14 March 2018. 2018.
Gheera M. The Disabled Children (Family Support Bill); Bill 20 of 2006-07. London: House of Commons Library; 2007. URL: http://researchbriefings.files.parliament.uk/documents/RP07-15/RP07-15.pdf (accessed 3 December 2020).
National Care Standards: Hospice Care. Edinburgh: Scottish Government; 2005. Available from: http://www.gov.scot/Resource/Doc/46910/0025661.pdf.
Caring for the caregivers to individuals with disabilities or other special needs. Except Parent 2008;38:56–8.
Hodgson J. A Checklist to a Good Transition. Bristol: Together for Short Lives; 2018. URL: www.togetherforshortlives.org.uk/wp-content/uploads/2018/03/18-03-20-A-checklist-to-a-good-transition.pdf (accessed 3 December 2020).
Children’s Hospice Grant Consultation: Analysis of Responses and Together for Short Lives’ Recommendations Report Back to NHS England. 2017.
Edelstein H, Schippke J, Sheffe S, Kingsnorth S. Children with medical complexity: a scoping review of interventions to support caregiver stress. Child Care Health Dev 2017;43:323–333.
Adonis A, Lewis I. Aiming High for Disabled Children: Short Breaks for Disabled Children and Their Families. 2007.
Age UK. Advice for Carers: A Practical Guide. London: Age UK; 2012.
Anonymous. Children with life-shortening conditions are denied the support they need, says charity. Nurs Child Young People 2016;28:7.
Armstrong D, Florida N, County NY. ChiPPS Pediatric Palliative Care Newsletter Issue #33. ChiPPS,November 2013.
Barkin SL. Planning for the holidays with your special needs child. Except Parent 2010;40:29.
Sutton Centre for the Voluntary Sector. A-Z Directory of Voluntary Sector Services In the London Borough of Sutton for Children and Young people. Sutton: Sutton Centre for the Voluntary Sector.
Bradley N, Lloyd-Williams M, Dowrick C. Effectiveness of palliative care interventions offering social support to people with life-limiting illness – a systematic review. Eur J Cancer Care 2018;27:e12837. https://doi.org/10.1111/ecc.12837
Broach S. Short Breaks for Disabled Children: A Legal Guide for Local Authorities. London: Council for Disabled Children; 2017. URL: https://councilfordisabledchildren.org.uk/sites/default/files/field/attachemnt/Shortbreaks legal duty guide for LAs.pdf (accessed 3 December 2020).
Call for Evidence. Appendix Information on Education and Training Costs for 2019 Pilot.
Chan JB. A profile of respite service providers in New South Wales. Int J DisabilDev Educ 2008;55:289–302.
Chase SS. Transition in Surrey’s Children and Adult Hospices.
Clarke E. Short Breaks – Dudley Pathfinder Presentation.
Coyne PJ. The case of Mrs. A. J Palliat Med 2012;15:1396.
Craft A, Killen S. Palliative Care Services for Children and Young People in England. London: Department of Health and Social Care; 2007.
Craft A. Children with complex health care needs – supporting the child and family in the community. Child Care Health Dev 2004;30:193–4. https://doi.org/10.1111/j.1365-2214.2004.00423.x
David M, Kristina T, Peter H. A Systematic Review of Reviews of the Core Needs of Family Carers of Patients With Advanced Disease. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018088678 (accessed 3 December 2020).
Davis H. Magic moments. Nurs Stand 2010;25:18–19.
Dentzer S. ‘Swinging for the fences’ versus striking out on cancer. Health Aff (Millwood) 2012;31:662.
Dio K, Jennifer C, Natalie E, Lucas H, Michele K-F, Yael S, et al. Effectiveness of Palliative and Supportive Care: A Systematic Review. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42014013696 (accessed 3 December 2020).
Disability T, Service I, House FU, Street U. Holiday Services (P09).
Dominica FS. Douglas House: a ‘respite’ for young people. Eur J Cancer 2003;39:2669.
Downing J. Palliative care for infants, children and adolescents: a practical handbook. Int J Palliat Nurs 2012;18:254–5.
Edwards D, Carrier J, Gillen E, Hawker C, Sutton J, Kelly D. Factors influencing the provision of end of life care for adolescents and young adults with advanced cancer: a scoping review protocol. JBI Database Syst Rev Implement Rep 2013;11:386.
Finella C, Huijer H, Benini F, Kuttner L, Wood C, Ferraris P, et al. IMPaCCT. Standard pediatric palliative care in Europe. Monatsschr Kinderheilkd 2008;156:1114.
Hardiman O. A systematic review of ALS service users’ perceptions of services and decision making in care. Amyotroph Lateral Scler 2011;12(Suppl.):13.
Gaskin K. A Team Approach to Palliative and End of Life Care For Children and Young People. 2011.
George K, Sonja M, Felicity H, Joanne J, Kevin B, Louise J, et al. What is the Value of Attendance at Palliative Day Care? A Systematic Review. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42015024925 (accessed 3 December 2020).
Goodrich TJ. Trouble in paradise. Am J Hosp Palliat Care 2007;24:523.
Grossman BR, Magana S. Introduction to the special issue: family support of persons with disabilities across the life course. J Fam Soc Work 2016;19:237–51.
Hardwick R, Pearson M, Byng R, Anderson R. The effectiveness and cost-effectiveness of shared care: protocol for a realist review. Syst Rev 2013;2:12. https://doi.org/10.1186/2046-4053-2-12
Horsburgh M, Trenholme A, Huckle T. Paediatric respite care: a literature review from New Zealand. Palliat Med 2002;16:99.
Ryegate House. Ryegate House Emergency Care. 2018.
Isabelle A, Anne-Catherine D, Jean-Marie D, Marie F. How are the Outcomes of Paediatric Palliative Care Interventions Measured? A Systematic Review. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017080541 (accessed 3 December 2020).
James A. Short breaks: providing better access and more choice for black disabled children and their parents. Br J Soc Work 2003;33:575–6.
Janet D, Gunn G, Gail E, Susan K. The Support Needs of Parents of Children and Young People With Life-Limiting or Life-Threatening Conditions: A Systematic Integrative Review.: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018106034 (accessed 3 December 2020).
Joanne W, Victoria D, Katherine M, Gisella S, Agustin C, Daniel C, et al. A Systematic Review of Integrating Specialized Pediatric Palliative Care into the Care of Children with Complex Chronic Conditions and Effects on Quality of Life. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016049533 (accessed 3 December 2020).
Kirwan L. Student voice – Life is precious and we must cherish it. Nurs Child Young People 2015;27:17. https://doi.org/10.7748/ncyp.27.2.17.s22
Kyzar KB, Turnbull AP, Summers JA, Gómez VA. The relationship of family support to family outcomes: a synthesis of key findings from research on severe disability. Res Pract Pers with Sev Disabil 2012;37:31–44.
Lafond D, Perko K, Carpenter P, Jacobs S. Lions and tigers and bears, oh my! Caring for pediatric patients in an adult hospice. J Pain Symptom Manage 2014;47:382.
Laura H, Sonya P-N, Daniel J. Effectiveness of Interventions to Improve the Transition from Pediatric to Adult-Oriented Care: A Systematic Review of Systematic Reviews. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016046808 (accessed 3 December 2020).
Liisa P, Luciana N, Silvia D, Augusto C, Giovanni A, Nicole C, et al. Palliative care for patients with cancer: an overview of systematic review. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018084697 (accessed 3 December 2020).
Ling J. Respite support for children with a life-limiting condition and their parents: a literature review. Int J Palliat Nurs 2012;18:129–34. https://doi.org/10.12968/ijpn.2012.18.3.129
Luckett T, Phillips J, Agar M, Virdun C, Green A, Davidson PM. Elements of effective palliative care models: a rapid review. BMC Health Serv Res 2014;14:136. https://doi.org/10.1186/1472-6963-14-136
Margareta B, Joakim Ö, Ingela H, Anneli O, Susanna B, Hanan Hamdan A. Palliative care implementations: a systematic review. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018100663 (accessed 3 December 2020).
Martiniuk A, Silva M, Amylon M, Barr R. Camp programs for children with cancer and their families: review of research progress over the past decade. Pediatr Blood Cancer 2014;61:778–87. https://doi.org/10.1002/pbc.24912
McCann D, Bull R, Winzenberg T. Sleep deprivation in parents caring for children with complex needs at home: a mixed methods systematic review. J Fam Nurs 2015;21:86–118. https://doi.org/10.1177/1074840714562026
Mila P, Stephen B, Ian W, Isla K, Geoff W. Realist Review of Palliative and End of life Care Programmes in Primary Care and Community Settings: Underpinning Mechanisms, Programme Theories, and Differential Outcomes Across Patients Groups, Contexts, and Stages in the Patient Journey. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018097218 (accessed 3 December 2020).
National Development Team for Inclusion. Short Breaks for Disabled Children. Bath: National Development Team for Inclusion; 2011.
Nelson A. Special needs families: creating summer fun! Except Parent 2017;47:24–7.
Poulsen PB, Kolbye A, Rajani N, Hornamnn A. [Hospice Without Walls]. Copenhagen: Danish Centre for Evaluation and Health Technology Assessment; 2005.
Robertson J, Hatton C, Wells E, Collins M, Langer S, Welch V, Emerson E. The impacts of short break provision on families with a disabled child: an international literature review. Health Soc Care Community 2011;19:337–71. https://doi.org/10.1111/j.1365-2524.2010.00977.x
Robertson J. 15th Report, 2015 (Session 4): We Need to Talk About Palliative Care. 2015.
Robertson J. The Impacts of Short Break Provision on Disabled Children and Families: An International Literature Review. London: Department for Education; 2010.
Rykov M, Cohen R, Leis A, Macdonald ME, Pringle A, Cadrin L, et al. Palliative care music therapy: insights from patients, family and staff. 17th International Congress on Palliative Care, September 23–26, 2008/Palais Des Congres, Montreal, Canada. J Palliat Care 2008;24:199–200.
Satoh K, Kamigaito M, Yokoyama H, Science AI. A snapshot of the impact creative breaks had during 2016–17. Macromolecules 2007;7433.
Shared Care Scotland. Short Break Checklist – Planning for the Best Outcomes. Dunfermline: Shared Care Scotland; 2010.
Shared Care Network. Short Break Carers: Be the Big Difference. Bristol: Shared Care Network; 2010.
Sidey A, Bean D. Meeting the Palliative Care Needs of Children in the Community. In Sidley A, Widdas D, editors. Textbook of Community Children’s Nursing. Amsterdam: Elsevier; 2005. p. 261.
Social Care Institute for Excellence. Disabled Children and Young People: Improving Short Breaks. London: Social Care Institute for Excellence; 2010.
Blackburn With Darwen Short Breaks Statement. 2016.
Transitional Care. Stratford-upon-Avon: The Shakespeare Hospice; 2018.
Trueland J. Breakaway success. Nurs Stand 2012;27:18.
Virdun C, Brown N, Philips J, Luckett T, Agar M, Green A, et al. Elements of optimal paediatric palliative care for children and young people: an integrative review using a systematic approach. Collegian 2015;22:421–31.
Welsh L, Williamson D, McCulloch H. Occasional Papers Series: More Than a Break. Dunfermline: Shared Care Scotland; 2010.
Williams-Reade J. Palliative and end of life care for children and young people: home, hospice, and hospital. Fam Syst Health 2013;31:230–1.
Woodgate R. Toward evidence-based practice. Effects of respite care services in a children’s hospice: the parents’ point of view. Am J Matern Child Nurs 2015;40:334.
Pre 2002 (n = 1)
Hill D, Penso D. Opening Doors: Improving Access to Hospice and Specialist Palliative Care Services by Members of the Black and Ethnic Minority Communities. London: National Council for Hospice and Specialist Palliative Care Services; 1995.
Not an Organisation for Economic Co-operation and Development country (n = 2)
Keim-Malpass J, Hart TG, Miller JR. Coverage of palliative and hospice care for pediatric patients with a life-limiting illness: a policy brief. J Pediatr Health Care 2013;27:511–16. https://doi.org/10.1016/j.pedhc.2013.07.011
Birnkrant DJ, Bushby K, Bann CM, Apkon SD, Blackwell A, Colvin MK, et al. Diagnosis and management of Duchenne muscular dystrophy, part 3: primary care, emergency management, psychosocial care, and transitions of care across the lifespan. Lancet Neurol 2018;17:445–55.
Duplicate (n = 52)
Great Britain. Disabled Children (Family Support) Bill. London: The Stationery Office; 2007. URL: www.publications.parliament.uk/pa/cm200607/cmbills/020/2007020.pdf (accessed 3 December 2020).
Social Care Institute for Excellence. Having a Break: Good Practice in Short Breaks for Families With Children Who Have Complex Health Needs and Disabilities. London: Social Care Institute for Excellence; 2008.
Together for Disabled Children. Towards a More Ordinary Life . . . A Report on the Progress of Parent Carer Participation and the Development of Short Breaks: 2008–2011. Contact; 2011. URL: https://contact.org.uk/media/399529/research_and_reports_towards_a_more_ordinary_life._a_report_on_the_progress_of_parent_carer_participation_and_the_development_of_short_breaks_2008__2011..pdf (accessed 3 December 2020).
Rest Assured? 2012.
Better Care: Better Lives. 2009.
Better Care, Better Lives. Improving Outcomes and Experiences for Children. Bristol: University of the West of England; 2008.
Together for Short Lives. Commissioning Children’s Palliative Care in England: 2017 Edition. London: Together for Short Lives; 2017.
National Institute for Health and Care Excellence. End of Life Care for Infants, Children and Young People with Life-limiting Conditions: Planning and Management: Information for the Public. NICE; 2016. URL: www.nice.org.uk/guidance/ng61/informationforpublic (accessed 3 December 2020).
Department of Health and Social Care (DHSC). Commissioning Children’s and Young People’s Palliative Care Services: A Practical Guide for Primary Care Trusts and Practice-based Commissioners. London: DHSC; 2005.
Better Care: Better Lives. Framework. 2008.
Carers’ Services Guide. Help the Hospices; 2008. URL: www.helpthehospices.org.uk/hweb/get_Document.aspx?id=3430
Appleton AL. A comment on Douglas House: a ‘respice’ for young people 1. Eur J Cancer 2004;40:1453.
Payne S, Ingleton C, Scott G, Steele K, Nolan M, Carey I. A survey of the perspectives of specialist palliative care providers in the UK of inpatient respite. Palliat Med 2004;18:692–7.
Carter B, Edwards M, Hunt A. Being a presence. J Child Health Care 2015;19:304–19.
Castor C, Landgren K, Hansson H, Kristensson Hallström I. A possibility for strengthening family life and health: Family members’ lived experience when a sick child receives home care in Sweden. Health Soc Care Community 2018;26:224–31.
Champagne M, Comeau E, Gervais A, De Varennes V, Tétreault C, Baril G, et al. Training volunteers who provide home respite for families for children with a life-threatening illness: the development of a program through action research. J Palliat Care 2006;22:214.
Chugg R. Managed networks and integrated children’s services – case study of Devon. J Integr Care 2009;17:37–45.
Cohen E, Gandhi S, Toulany A, Moore C, Fu L, Orkin J, et al. Health care use during transfer to adult care among youth with chronic conditions. Pediatrics 2016;137:e20152734.
Damiani G, Rosenbaum P, Swinton M, Russell D. Frequency and determinants of formal respite service use among caregivers of children with cerebral palsy in Ontario. Child Care Health Dev 2004;30:77–86.
Faw MH. Supporting the supporter. J Soc Pers Relationships 2018;35:202–23.
Gridley K, Brooks J, Glendinning C. Good practice in social care: the views of people with severe and complex needs and those who support them. Health Soc Care Community 2014;22:588–97. https://doi.org/10.1111/hsc.12105
Grinyer A. Palliative and End of Life Care for Children and Young People: Home, Hospice and Hospital. 2012.
Hatton C, Collins M, Welch V, Robertson J, Emerson E, Langer S, Wells E. The impact of short breaks on families with a disabled child over time: the second report from the qualitative study. London: Department for Education; 2011. p. 8. URL: www.education.gov.uk/publications/eOrderingDownload/DFE-RBX-10-12.pdf
Hill K. Respite services for children with life-limiting conditions and their families in Ireland. Nurs Child Young People 2016;28:30–5. https://doi.org/10.7748/ncyp.2016.e658
Hilliard RE. Music therapy in pediatric palliative care: complementing the interdisciplinary approach. J Palliat Care 2003;19:127–32.
Hunt A, Elston S, Galloway J. Voices for Change.
Hunt L. Rainbow reasures. Community Care 2008:26–7.
Ingleton C, Payne S, Nolan M, Carey I. Respite in palliative care: a review and discussion of the literature. Palliat Med 2003;17:567–75.
James A. Short breaks: providing better access and more choice for black disabled children and their parents. Br J Soc Work 2003;33:575–6.
Knapp C, Quinn GP, Murphy D, Brown R, Madden V. Adolescents with life-threatening illnesses. Fourth in a series on pediatric palliative care. Am J Hosp Palliat Med 2010;27:139–44.
Laing CM. ‘It’s Not Just Camp’: Understanding the Meaning of Children’s Cancer Camps for Children and Families. PhD thesis. Calgary, AB: University of Calgary; 2013.
Marsh S, Cameron M, Duggan M, Rodrigues J. Young People With Life-Limiting Conditions: Transition to Adulthood. ‘Small Numbers, Huge Needs, Cruel and Arbitrary Division of Services’. Executive Summary of Phase 1 Report for Marie Curie Cancer Care. 2011. URL: www.mariecurie.org.uk/globalassets/media/documents/commissioning-our-services/past-initiatives/ypt/phase1
Meltzer LJ. Mothers of children with chronic illnesses: a caregiver burden model and summer camp as respite care. 2003;63:4915.
Mitchell S, Bennett K, Morris A, Dale J. Palliative care services for children and young people: realist review of the literature. Arch Dis Child 2016;101:A305–A306.
Ngo CL. Experiences of pediatric parenting stress and family support for caregivers of children with special health care needs or developmental disabilities. Psychology 2018;79.
Read J. Will the Carers and Disabled Children Act 2000 make a difference to the lives of disabled children and their carers? Editorial. Child Care Health Dev 2002;28:273–5.
Read J. Will the Carers and Disabled Children Act 2000 make a difference to the lives of disabled children and their carers? Child Care Health Dev 2002;28:273–5.
Stalker K, Charlotte M, King C, McFaul F, Young C, Hawthorn M, Patrizio L. It always comes down to money: recent changes in service provision to disabled children, young people and their families in Scotland. 2013.
Robertson J, Hatton C, Wells E, Collins M, Langer S, Welch V, Emerson E. The impacts of short break provision on families with a disabled child: an international literature review. Health Soc Care Community 2011;19:337–71. https://doi.org/10.1111/j.1365-2524.2010.00977.x
Rochdale Metropolitan Borough Council. Short Breaks for Children. Rochdale: Rochdale Metropolitan Borough Council; 2015.
Ruth Davies MA, Caerleon G. The first Diana Team in Wales: an update. Paediatr Nurs 2002;14.
Ryynänen OP. Efficacy of a multicomponent support programme for caregivers of disabled persons: a randomised controlled study. 2007.
Shared Care Network. Short Breaks Project Report: The Findings of a Viability Study to Explore the Possibility of Setting Up a National Network for Non-family Based Short Break Services. London: Shared Care Network; 2009.
Skilbeck JK, Payne SA, Ingleton MC, Nolan M, Carey I, Hanson A. An exploration of family carers’ experience of respite services in one specialist palliative care unit. Palliat Med 2005;19:610–18. https://doi.org/10.1191/0269216305pm1087oa
Steele R, Derman S, Cadell S, Davies B, Siden H, Straatman L. Families’ transition to a Canadian paediatric hospice. Part one: planning a pilot study. Int J Palliat Nurs 2008;14:248–56. https://doi.org/10.12968/ijpn.2008.14.5.29492
Swallow V, Forrester T, Macfadyen A. Teenagers’ and parents’ views on a short-break service for children with life-limiting conditions: a qualitative study. Palliat Med 2012;26:257–67. https://doi.org/10.1177/0269216311401947
Ware J, Raval H. A qualitative investigation of fathers’ experiences of looking after a child with a life-limiting illness, in process and in retrospect. Clin Child Psychol Psychiatry 2007;12:549–65. https://doi.org/10.1177/1359104507080981
Warner HK. Meeting the Fundamental Needs of Children with Disabilities.
Welch V, Hatton C, Wells E, Collins M, Langer S, Robertson J, Emerson E. The Impact of Short Breaks on Families with a Disabled Child: Report One of the Qualitative Phase. Department for Education; 2010. URL: www.education.gov.uk/publications/eOrderingDownload/DFE-RR063.pdf (accessed 3 December 2020).
Woodgate R. Toward evidence-based practice. Exploring the perceived met and unmet need of life-limited children, young people and families. Am J Matern Child Nurs 2015;40:334.
Wu Y, Prout K, Roberts M, Parikshak S, Amylon M. Assessing experiences of children who attended a camp for children with cancer and their siblings: a preliminary study. Child Youth Care Forum 2011;40:121–33.
Unobtainable (n = 126)
Every Disabled Child Matters. Short Breaks in 2015: An Uncertain Future. London: Every Disabled Child Matters; 2015. URL: www.scie-socialcareonline.org.uk/short-breaks-in-2015-an-uncertain-future/r/a11G000000752qWIAQ (accessed 3 December 2020).
Kelly B, Dowling S, Winter K. Profiling the Population of Disabled Children and Young People in Out-of-home Care in Northern Ireland. Queens University Belfast; 2015. URL: www.scie-socialcareonline.org.uk/profiling-the-population-of-disabled-children-and-young-people-in-out-of-home-care-in-northern-ireland/r/a11G0000009TJXuIAO (accessed 3 December 2020).
Respite care for children, young people and families: discovery service for IJsselland Ziekenhuis. Polres Hosp 2017:1–20.
New Legislation Proposed to Offer Breaks to Parents of Disabled Children. Care Health News. 2008.
Short Breaks Disabled Children ‘Me Time’.
Southend on Sea Borough Council Department of Children and Learning. Short Breaks for Children and Young People with Disabilities 2014–15. Friends and Fun at Just Ride Southend. Southend-on-Sea: Southend on Sea Borough Council; 2014.
NHS Choices. Respite Care. 2007. URL: www.nhs.uk/conditions/Respite-care
Parsons E. Pilots Aim High for Short Break Success. Reed Business Information; 2009. URL: www.scie-socialcareonline.org.uk/pilots-aim-high-for-short-break-success/r/a1CG0000000GUXXMA4 (accessed 3 December 2020).
Quick Guide to Children’s Hospices. London: Children & Young People Now; 2008.
Every Disabled Child Matters. No Going Back!: Parents’ Expectations of Short Breaks: Short Breaks Tracking Second Interim Report. Every Disabled Child Matters; 2010. URL: www.scie-socialcareonline.org.uk/no-going-back-parents-expectations-of-short-breaks-short-breaks-tracking-second-interim-report/r/a11G00000017vVGIAY (accessed 3 December 2020).
Local Offer in North East Lincolnshire. 2014.
Partners at Meals – Respite Care and Home (PAM) Status: Active, Not Recruiting.
Wessex Children‘s Hospice Trust Report and Financial Statements. 2014.
Together for Short Lives Commissioning and Funding Survey Report.
Children’s Palliative Care Networks: A Report on the Key Learning and Achievements of Children’s Palliative Care Networks in England. 2011.
Department of Health and Social Care (DHSC). A Practical Guide for Disabled People or Carers: Where to Find Information, Services and Equipment. London: DHSC; 2003.
Carers and Disabled Children Act 2000: Short Break Voucher Schemes: Policy Guidance. 2002.
Untitled. J Palliat Med 2018;21:1057.
Campaign for respite care moves to the courts. Community Living 2007;21:4.
Better Health Channel. Children with a Disability – Support for Parents. Winchester: Wessex Children’s Hospice Trust; 2016.
Morris J. Carers and Disabled Children Act 2000: Vouchers for Short Term Break: Practice Guidance. York: Joseph Rowntree Foundation; 2002.
Funding boost for respite care. Nurs Stand 2010;24:6.
Shared Care Network. Safe and Healthy: Health And Safety Good Practice Guide for Carers and Workers Providing Home and Community Based Short Breaks to Disabled Children and Young People. 2nd edn. Bristol: Short Breaks Network; 2011.
Directory of Services for Disabled Children and Young People in Wales.
Directory of Hospice and Palliative Care Services in the United Kingdom and Republic of Ireland. St Christopher’s Hospice Information Service.
Short Breaks Bureau Final Evaluation of Short Break Voucher Pilot Completed December 2011.
Together for Short Lives. Key Working: How to Embed Keyworking Approaches in the Care of Children with Wider Complex Health Needs. Bristol: Together for Short Lives; 2014.
Government Announces Funding Boost for Children’s Hospices: 27 Million Support for Palliative Care. 2006.
Short Breaks Guide. London: Council for Disabled Children; 2014.
Guidelines in Practice. SIGN Notes for Discussion with Patients and Carers. 2005. URL: www.guidelinesinpractice.co.uk/sign-notes-for-discussion-with-patients-and-carers/304804.article (accessed 3 December 2020).
The Transition Care Pathway: A Framework for the Development of Integrated Multi-Agency Care Pathways for Young People with Life-threatening and Life-limiting Conditions. 2007.
Leonard Cheshire Disability. Your Money or Your Life: Disabled People’s Experiences of the Loss of Social Care Services in England. London: Leonard Cheshire Disability; 2008.
Grumbach-Wendt M. Life-threatening illness of children and adolescent. Load factors of parents and siblings which are considered in paediatric palliative care. Padiatr Prax 2013;81:367.
Anonymous. 10th international congress on adolescent health. Turkish Arch Pediatr 2013;48:1.
Pediatric Nursing Associations of Europe Network. Palliative Nursing Care of Children and Young People Across Europe. London: Pediatric Nursing Associations of Europe Network; 2017.
Boland K. Voluntary out-of-home care: collaborative service provision for children, young people and their families. Dev Pract 2010:7–11.
Brasch S. Hospice Directory: Hospice and Palliative Care Services in the United Kingdom and Republic of Ireland. 2003. Hospice Information. 2003. URL: www.opengrey.eu/item/display/10068/411809 (accessed 3 December 2020).
Break S. Short Breaks for Children with Disabilities.
Burkhard AM. The Lived Experience of Mothers Caring for an Adolescent or Young Adult with Severe Cerebral Palsy. PhD thesis. 2011.
Campbell CL. Experiences and Processes used by Black People Living with a Life-Limiting Illness. PhD thesis. 2004.
Care C. Young Adults. Who Can We help? How Can I Help? 2018.
Carlin J, Cramer H. Creative Responses to Changing Needs?: Fourth national Survey of Short Break Services for Disabled Children in the UK. London: Shared Care Network; 2007.
Carter B. What Narratives Do Families and Nurses/Professionals Tell About the Life-Journeys of Children with Complex Needs and/or Life-Limiting Illness?
Chamberlain H. Safeguarding and supporting children and young people and their families. Dev Nurs Pract with Child Young People 2015;142–58.
Children T. Short Breaks Statement 2018 to 2019. 2019.
Cicero K. A vacation for everyone. Parents 2014;89:96–101.
Clark J. Independence Matters: An Overview of the Performance of Social Care Services for Physically and Sensory Disabled People: A Summary. Social Services Inspectorate; 2003.
Connole P, LaPorte M. NewsCurrents. Provider 2011;37:9–18.
Conway M. Residential Short Breaks Project Report: The Findings of a Viability Study to Explore the Possibility of Setting Up a National Network for Non-family Based Short Break Services. Shared Care Network. 2009. URL: www.sharedcarenetwork.org.uk/echo/modules/files/filedownload.jsp?action=dFile%26key=453436925601 (accessed 3 December 2020).
Cope C. Inspection of services for disabled people: Bolton Metropolitan Borough Council: October 2002. Bolton; Bolton Council: 2003.
Council BMD. Short Break Fostering Schemes. 2012.
Council BC. Inclusive Play Project. Work. 2011.
Council BC. Can you Provide a Short Break for a Disabled Child/Children? 2011.
Council DB. Support for Disabled Children and Young Adults. 2011.
Leicestershire County Council. Short Breaks. Leicester: Leicestershire County Council; 2011.
Currow DC, Burns CM, Abernethy AP. Palliative care services meet different needs for different Caregivers. Psychooncology 2008;17:S124.
Ausserhofer D, Mantovan F, Pirhofer R, Huber M, Them C. [The burden of parents caring for their children and adolescents with severe disabilities in South Tyrol.] Pflege 2009;22:184–92. https://doi.org/10.1024/1012-5302.22.3.184
Casey P. Caregiver burden and unmet needs of children who have complex and chronic medical care needs. Dev Med Child Neurol 2010;52:34.
D. I L. Most children receiving palliative care live for more than a year after beginning such treatment. AHRQ Res Act 2011:13.
Daoudi M. Oral evidence: how the government is meeting its commitment to choice for babies, children and young people who need palliative care. J Vis Lang Comput 2000;11:287.
Darvill J, Thomas K, Henry P. Children with Chronic Health Problems and Their Families. In Child, Youth and Family Health Strengthening Communities. Melbourne: Elsevier; 2013.
Dean E. NICE standards on end of life care for children [including commentary by Katrina McNamara]. Nurs Stand 2018;32:15.
Department for Education. Short Breaks for Carers of Disabled Children. Departmental Advice for Local Authorities. Manchester: Department for Education; 2011.
Department for Education. Local Offer. Manchester: Department for Education; 2014.
Dinkins H, Cernoch JM. Preventative care. Respite – a gift of time. Prem Outlook 2004;4:42–8.
Dunbar H, Carter B, Brown J. Place bonding in children’s hospice care: a qualitative study. BMJ Support Palliat Care 2020;10:e25.
Easton C. Short Break Grants. 2013.
Eiser C. Symposium: consequences of child cancer for families and health care services. Psychol Health 2009;24:30.
Fowler L. Rebranding to respond to community needs. Remingt Rep 2017;25:8–10.
Gaudette L, Dunbrack J. Through the looking glass: perspectives from the family caregiver at the hospital bedside. Hospice palliative care: at a crossroads. November 4–7, 2007, Westin Harbour Castle Hotel, Toronto, Ontario, Canada. J Palliat Care 2007;23:204–5.
Gelhaus L. Policies stress more freedom of choice for people with disabilities. Provider 2002;28:26–8, 31–2, 35–6.
Glasper EA. Why Policy is Important for Disabled Children. London: MA Healthcare London; 2007.
Gleason T. One more day. Am J Nurs. 2009;109:79.
Goldberg SS. Care that soothes patients and families. Provider 2002;28:51–3.
Grace J. Paying for Care Needed by Children with Life-Limiting Conditions. 2002.
Grant J, Davis C, Forsyth C. The case study masterclass. Case 24: managing a young woman with cystic fibrosis. Eur J Palliat Care 2006;13:13–14.
Department for Education. Induction Guide for the Short Break Workforce. London: Department for Education; 2012.
Hamlets T. Transition means change, such as when you are moving from you want to happen in your life, The Transition Service is a specialist community based service for teens and young adults with disabilities who live in Tower Hamlets. Transition planning begins.
Hartman RG. Noblesse oblige: states’ obligations to minors living with life-limiting conditions. Duq L Rev 2012;50:333.
Heslop P, Byford S, Weatherly H, Jones V. Better Rewards.
Homes I. Commissioners Handbook. 2018.
Hunt L. Rainbow reassures. Community Care 2008:26–7.
Integrated JN, Children C. This Report is Different\Family. 2013.
Jackson A, Eve A. Directory 2002: Hospice and Palliative Care Services in the United Kingdom and Republic of Ireland. Hospice Information. 2001.
James CJ. Handle with care. Vacations for persons with disabilities. Prem Outlook 2004;4:49–58.
Kissane C. Looking after Bob. Nurse2Nurse 2002;2:21–3.
Klein J. Special needs of dying children and their families not being met. Oncol Times 2003;25:13–14.
Kumar A, Stoll ST, Hensel K. Ehlers Danlos Syndrome: a case report. AAOJ 2007;17:26–8.
Lamott A. Caring for a child who has severe neurological impairment. A life with grace. 2013.
Langerman C, Worrall E. Ordinary Lives: Disabled Children and Their Families: A Guide for Donors and Funders. London: New Philanthropy Capital; 2005.
Letzing G. [Possibilities and limits of inpatient pediatric hospice care.] Kinderkrankenschwester 2006;25:281–3.
Lewis I, Adonis A. Investment to Improve Services for Disabled Children. 2007.
Lewis M. Children and Young People’s Palliative Care Networks. The Southwest Experience. 2007.
Life A. Strategy 2016–2021 It’s About Life. London: Nursing Children and Young People; 2016.
Lowson K, Duffy S, Lowson P. Independent review of palliative care services for children and young people: economic study: final report. 2007.
Macdonald D. Better days ahead: respite homes can help families stay together. Abilities 2007:15–16.
Mahadevan J. Short Breaks Inaccessible to Severely Disabled. Children & Young People Now, 2009. URL: www.cypnow.co.uk/other/article/short-breaks-inaccessible-to-severely-disabled (accessed 3 December 2020).
Mahadevan J. Services for Disabled Children to be Axed Despite 800m Investment. Children & Young People Now, 2011. URL: www.cypnow.co.uk/news/article/services-for-disabled-children-to-be-axed-despite-800m-investment (accessed 3 December 2020).
Malas S. From Cyprus. Palliat Med 2003;17:150.
Mather M, Burns C. Invisibility, disability and the problems of public care. 2009:15–27.
Messeri A, Caprilli S. Palliative care in children. 36.
Mitchell W, Clarke S, Sloper P. Psychosocial support services for children and young people with cancer and leukaemia and their parents: identifying and meeting different needs. Psychooncology 2004;13:S122.
Moore S. NI 54: Services for Disabled Children. Dartington: Research in Practice; 2010.
Niwa H. Directory of services. Development 2007;134:635.
Pandya S, Meaney J, Andrews J, Davis M, Palliative Care Grp Mdstarn. Palliative care services in families of patients with Duchenne muscular dystrophy. Neurology 2008;70:A219.
Rousseau P. Seven words. Ann Intern Med 2010;152:261.
Jennessen S, Bungenstock A, Schwarzenberg E, Kleinhempel J. [What is good pediatric hospice work?] Kinderkrankenschwester 2010;29:320.
Savage D. A review of palliative care for children and young adults in the Thames Valley. 2012.
Schmidt VM, Davidsen-Nielsen M. [Patient support focusing on life.] Ugeskr Laeger 2002;164:3001–4.
Sebego M. Family Caregiving Demands During Life-Threatening Illness in Botswana. PhD thesis. 2003.
Sharp PC. Fulfilling a Need: An Examination of Families’ Preferences for Pediatric Respite and Hospice Care in a Residential-Styled Facility. Nacogdoches, TX: Stephen F. Austin State University; 2015.
Short Breaks Network. Safe and Sound: Safeguarding and Safer Care Guidelines for Carers and Workers Providing Short Breaks to Disabled Children. Bristol: Short Breaks Network; 2011.
Simmons D. Charges for Community Care Services: A Guide for Disabled People and Carers in England and Wales. 2002.
Smith A. Caregivers’ corner. Help for the holidays: cancer and children. Cancer Updat Res Educ 2002;1:67–9.
Social Care Institute for Excellence. Short breaks for disabled children. Community Care 2009:26.
Stolarska M. Pediatric palliative care. Prz Pediatryczny 2010;40:201.
Sunderland C. Short Breaks Statement for Disabled Children – 2018. 2018.
Suplee PD. The Christmas that keeps on giving. Nurs Spectrum 2002;11:17.
Talvin J-M. [Day care, respite for the caregivers’ burden?] 2006:28.
Team FP. Can You Offer Short-term Care for a Disabled Child or Young Person?
Vesela J, Rehulka E. What Means Health to Parents of Handicapped Children. 2006.
Wanner F. [Holiday for the disabled – is later payment for holidays possible?] Schweiz Arch 2010;152:493–4.
Winter G. Research roundup: August 2015. Pract Nurs 2015;26:409–10.
Appendix 7 Sources included in knowledge map
| Source | Title | Type of source | Location | Types of respite |
|---|---|---|---|---|
| Arnold and Godwin78 | The Shakespeare Hospice Transitional Care Service Innovation in Practice | Study abstract | England |
|
| The Asian Health Agency79 | Ashra Carers Project: Children & Young People with Special Needs | Service description | England |
|
| Barnet County Council80 | Barnet Short Breaks Duty Statement 2017/2018 | Local offer | England |
|
| Beresford et al.63 | My Life. Growing Up and Living with Ataxia-Telangiectasia: Young People’s and Young Adults’ Experiences | Report | UK |
|
| Bishop81 | Making the Most of Life | Commentary | Wales |
|
| Bona et al.82 | Massachusetts’ Pediatric Palliative Care Network: Successful Implementation of a Novel State-Funded Pediatric Palliative Care Program | Study | USA |
|
| Brighton & Hove City Council83 | Brighton & Hove City Council Short Breaks Statement 2017–18 | Short breaks statement | England |
|
| Brook84 | Jacksplace – A Hospice Dedicated to Teenagers and Young Adults in Hampshire | Commentary | England |
|
| Care Quality Commission85 | Claire House Children’s Hospice Inspection Report | Local offer | England |
|
| Care Quality Commission87 | Francis House Children’s Hospice Inspection Report | Inspection report | England |
|
| Claire House Children’s Hospice86 | Claire House Children’s Hospice Local Offer Statement | Inspection report | England |
|
| Dawson and Liddicoat62 | ‘Camp Gives Me Hope’: Exploring the Therapeutic Use of Community for Adults with Cerebral Palsy | Study | USA |
|
| East Anglia Children’s Palliative Care Managed Clinical Network94 | TheEast of England Children and Young People’s Palliative Care Service Directory | Service directory | England |
|
| Gans et al.95 | Impact of a Pediatric Palliative Care Program on the Caregiver Experience | Study | USA |
|
| Grinyer et al.71 | Issues of Power, Control and Choice in Children’s Hospice Respite Care Services: A Qualitative Study | Study | England |
|
| Hanrahan97 | A Host of Opportunities: Second NHSN Survey of Family Based Short Break Schemes for Children and Adults with Intellectual and Other Disabilities in the Republic of Ireland | Report | Republic of Ireland |
|
| Hutcheson et al.59 | Evaluation of a Pilot Service to Help Young People with Life-Limiting Conditions Transition from Children’s Palliative Care Services | Study | Northern Ireland |
|
| Institute of Public Care100 | National Commissioning Board Wales. Integrated Services for Children and Young People with a Disability in Conwy. A Case Study | Case study | Wales |
|
| Knighting et al.101 | An Evaluation of the Rachel House at Home Service for the Children’s Hospice Association Scotland (CHAS): Summary Public Report | Evaluation | Scotland |
|
| Knighting et al.67 | Meeting the Needs of Young Adults with Life-Limiting Conditions: A UK Survey of Current Provision and Future Challenges for Hospices | Study | UK |
|
| Knighting et al.103 | Short Break Provision for Young Adults with Life-limiting Conditions: A UK Survey with Young Adults and Parents | Study | UK |
|
| Knowsley Council104 | Knowsley Children and Family Services Short Breaks Statement | Short breaks statement | England |
|
| Leason105 | Let’s Face the Music and Dance | Commentary | England |
|
| Luzinat et al.68 | The Experience of a Recreational Camp for Families with a Child or Young Person with Acquired Brain Injury | Study | Australia |
|
| MacDonald and Greggans70 | ‘Cool Friends’: An Evaluation of a Community Befriending Programme for Young People with Cystic Fibrosis | Study | Scotland |
|
| Martin House Children’s Hospice60 | Supporting Children with Life-Limiting Conditions and Their Families – Research Examining Service Provision in Yorkshire and the Humber | Study | England |
|
| Martin House Children’s Hospice106 | Professionals’ Booklet | Information leaflet | England |
|
| Mitchell et al.27 | Short Break and Emergency Respite Care: What Options for Young People with Life-Limiting Conditions? | Study | England |
|
| Rainbows Hospice for Children and Young People112 | Rainbows Quality Account 2017–2018 | Quality account | England |
|
| Rochdale County Council113 | Rochdale Short Breaks Provision for Children and Young People with Disabilities | Service directory | England |
|
| Shared Care Scotland119 | Short Break Case Studies | Case example | Scotland |
|
| Shared Care Scotland120 | It’s About Time: An Overview of Short Break (Respite Care) Planning and Provision in Scotland | Report | Scotland |
|
| Shared Care Scotland72 | Short Breaks Fund Evaluation of Round One Projects | Report | Scotland |
|
| Shared Care Scotland66 | Evaluation Report on Round Two of the Short Breaks Fund | Report | Scotland |
|
| Shared Care Scotland121 | Evaluation Report of Creative Breaks October 2012–September 2013 | Report | Scotland |
|
| St Elizabeth Hospice122 | Young Adult Short Break Pilot | Grey literature | England |
|
| St Joseph’s Hospice125 | St Joesph’s Hospice Quality Accounts. 2012/2013 | Grey literature | England |
|
| St Oswald’s Hospice126 | St Oswald’s Young Adult Service – Your Guide | Information leaflet | England |
|
| Staley127 | Having a Break: Good Practice in Short Breaks for Families with Children Who Have Complex Health Needs and Disabilities | Report | England |
|
| Stylianou69 | Mothers with Disabled Children in Cyprus: Experiences and Support | Study | Cyprus |
|
| Urbanowicz et al.130 | Use of Equipment and Respite Services and Caregiver Health Among Australian Families Living with Rett Syndrome | Study | Australia |
|
| Young et al.64 | Small Service, big impact. Evaluation of a New Short Break Service for Young Adults with Life Limiting Conditions at St Oswald’s Hospice | Report | England |
|
| Young et al.61 | Qualitative Accounts of Young-People, Parents and Staff Involved with a Purpose-Designed, Pilot Short-Break Service for 18–24 Year Olds with Life-Limiting Conditions | Study | England |
|
Appendix 8 Logic model: residential respite in specialist palliative care facility (e.g. hospice) (21 sources)
Logic model: planned residential respite at specialist palliative care facility (e.g. hospice) (21 services in 21 sources)
| Service aim/objective | Eligibility criterion | Resources (what is needed to provide the service) | Programme logic (what the service does/delivers): activities and frequency | Expectations of young adult/parent/wider family | Proximal: intended short-term outcomes/impacts | Distal: intended mid- to long-term outcomes/impacts |
|---|---|---|---|---|---|---|
|
Overall aim of this type of respite To provide young adults with access to regular residential respite services in specialist facilities and access to a range of age- and condition-appropriate amenities and activities, providing a break for young adults, parents/carers and support for the wider family Aims identified (different perspectives and identifiers) |
Eligibility and age range change depending on service provider Children’s hospice: babies, children, young people and young adults with life-threatening or life-limiting conditions Adult hospice: young people and young adults with life-threatening or life-limiting conditions Patients with the following specific conditions accessed the services: life-threatening or life-limiting conditions, physical disability Age range: zero to no upper limit Specific age cohorts for services included were 0–19 years, 0–23 years, 0–25 years, 0–30 years, 0–30 years, 18–24 years, 18–25 years, 16–40 years, 18 years to no upper limit (as move from young adult unit to main adult hospice ward), zero to no upper limit if referred < 16, (exceptional circumstances considered outside this criterion) |
Environmental StaffingFor example, Friday afternoon to Monday morning (three nights) based on two patients staying was costed at £4545.22. This included care from a registered nurse and a health-care assistant/multidisciplinary team assessment, full use of the day unit, meals and 20 hours of a co-ordinator post Staff training To ensure that staff have the necessary skills and experience to address the wide range of needs (e.g. equality, diversity and human rights, specialist feeding, medication, moving and handling, equipment use and care, such as suction and tracheostomy care, infection control and safeguarding) Transport Appropriate transport for equipment and services users Funding Funding to cover costs of external activities and running of transport |
Frequency Services varied in reporting number of visits or number of nights available, ranging from 12 to 16 nights per year over three or four visits Individual services reported the following frequency over a 12-month period Three visits; four visits; four visits; four visits; 16 nights; and 7–14 nights Location Children’s and adult hospices (specialist facility) What’s offered? Overnight respite care in a specialist facility with access to the following amenities and activities:‘Own carer’ modelIn addition to the traditional respite care model, there is an emerging ‘own carer’ model of respite for young adults: |
Young adults Increased socialisation outside service user’s immediate family network Development of peer support network To establish new relationships Reduction in social isolation/increase in social inclusion To experience positive and enriching social activities Improved access to social and leisure activities Increased freedom of choice over activities Gain life skills Gain confidence To experience safe and secure short breaks Improved access to appropriate breaks when needed Parents and wider family To have a break from caring responsibilities Have confidence in the service for the young adult |
Lack of longitudinal data to identify long-term outcomes and ongoing achievement of respite care that meets needs of young adults, parents/carers and support for the wider family. Indications from snapshot data of participants who had used services for several years indicates accruing benefits for the whole family of planned, regular residential respite care. Nine sources27,41,59–61,64,67,71,76 in the review Benefits Respite was achieved and expectations generally met when respite care was viewed as safe and acceptable and accessed when needed. Benefits included: Harms Lack of appropriate respite care or loss of respite following transition were reported to have negative impact on psychological well-being, including stress and anxiety due to concerns over safe care (parent/carer), frustration and distress at needs not being met appropriately (young adults and parent/carer), lack of opportunities for young adults to socialise and develop independence (young adults) and ultimately the detrimental effects on the health and well-being of all the family (young adults, parents/carers and the wider family including siblings) |
|
Appendix 9 Logic model: residential respite in a specialist disability facility (e.g. condition-specific or adventure camps)
Logic model: planned residential – residential respite in a specialist disability facility (e.g. condition-specific or adventure camps) (six services in five sources)
| Service aim/objective | Eligibility criterion | Resources (what is needed to provide the service) | Programme logic (what the service does/delivers): activities and frequency | Expectations of young adult/parent/wider family | Proximal: intended short-term outcomes/impacts | Distal: intended mid- to long-term outcomes/impacts |
|---|---|---|---|---|---|---|
|
Overall aim of this type of respite To provide young adults with access to residential respite services in specialist disability facilities and to provide access to a range of age-and condition-appropriate amenities and activities, providing a break for young adults, parents/carers and support the wider family Aims identified |
Young adults with a range of conditions, including ABI, cerebral palsy, complex disability and degenerative muscle disorders Patients with the following specific conditions accessed the services: cerebral palsy, ABI, muscular dystrophy, complex disabilities, degenerative muscle disorders and complex needs Age range: 0 to no upper limit Specific age cohorts for services included were 19–21 years, 19 years, up to 21 years, children and young adults, and young adults |
Staffing 1 : 1 staff for some campers, with a 1 : 2 average ratio Staff training Environmental (appropriate facilities) Funding |
Frequency One to three times per year, ranging from a weekend to a week Location Specialist disability facilities What’s offered? Condition-specific camps with organised activities |
Young adults To experience a residential break away from parents/carers and family members To experience an age-appropriate break To have an increase in choice and decision-making For parents and wider family To experience a break from routine caring responsibilities To have quality time with partners and other children For all To enjoy a break away with family members when family breaks available at the service To make new friends and socialise as part of a supportive community |
Lack of longitudinal data to identify long-term outcomes and ongoing achievement of respite care that meets needs of young adults, parents/carers and the wider family, including siblings. Indications from snapshot data of participants who had used services for several years indicates accruing benefits for the whole family of planned, regular residential respite care. Two sources62,68 in the review Benefits Respite was achieved and expectations generally met when respite care was viewed as safe and acceptable, and accessed when needed. Benefits included:Harms A reduction in the level of camp respite care was reported to have a negative impact on psychological well-being due to frustration and distress at needs not being appropriately met (young adults and parents/carers), lack of opportunities for young adults to socialise and develop independence (young adults) and ultimately the detrimental effects on the health and well-being of all the family (young adults, parents/carers and the wider family, including siblings) |
|
Appendix 10 Logic model: residential respite in a nursing home
Logic model: planned residential – residential respite in a nursing home (one service in one source)
| Service aim/objective | Eligibility criterion | Resources (what is needed to provide the service) | Programme logic (what the service does/delivers): activities and frequency | Expectations of young adult/parent/wider family | Proximal: intended short-term outcomes/impacts | Distal: intended mid- to long-term outcomes/impacts |
|---|---|---|---|---|---|---|
|
Overall aim of this type of respite To provide short-term respite care with separate facilities and appropriate planned activities Aims identified To offer separate facilities (‘more than a “spare bed” for short term guests’120) To offer carefully planned programme of activities for short-term guests to suit individual needs and interests |
The specific conditions of patients accessing services were not specified, but refers to adult and older people’s services, by default includes the review population Age range: young people with disabilities Specific age cohorts for services included were not specified |
No resources reported Staffing Staff training Transport Funding Environmental (appropriate facilities): |
Frequency Unclear Location Residential nursing home What’s offered? Breaks in residential care homes (with or without nursing) |
Young adults To experience a short-term break To have a break in separate facilities To experience appropriate planned activities Parents and wider family To experience a break from caring To have quality time with partners and other children |
Low evidence for respite care delivered in residential nursing homes identified in the review, as only one source61 identified Benefits Poor experience reported in only source. 120 Young adult experienced a break from home and their parents, and parents experienced a break from caring; however, it did not meet their expectations and had potential for harms Harms Negative impact on psychological well-being, including stress and anxiety due to concerns over safe care (parents/carers), frustration and distress at needs not being met appropriately (young adults and parents/carers), lack of opportunities for young adults to socialise and develop independence (young adults) and ultimately the detrimental effects on the health and well-being of all the family, which may lead to reduced uptake or withdrawal from the service without changes to service delivery and available opportunities (young adults, parents/carers and the wider family, including siblings) |
|
Appendix 11 Logic model: home-based daytime respite care
Logic model: home based – home-based daytime respite (14 services in 11 sources)
| Service aim/objective | Eligibility criterion | Resources (what is needed to provide the service) | Programme logic (what the service does/delivers): activities and frequency | Expectations of young adult/parent/wider family | Proximal: intended short-term outcomes/impacts | Distal: intended mid- to long-term outcomes/impacts |
|---|---|---|---|---|---|---|
|
Overall aim of this type of respite To provide young adults, carers and wider families with individual home-based respite Aims identified (different perspectives and identifiers) |
Children and young adults with a range of physical and learning disabilities and LLCs Patients with the following specific conditions accessed the services: severe learning/physical disability, progressive life-limiting condition, Rett syndrome, complex health-care needs, autistic spectrum condition, severe learning disabilities, speech and language difficulties, complex health needs and with a disability (including life-limiting conditions), palliative care, sensory impairment and those who have moving and handling needs, disabilities, A–T, LLCs and life-limiting illness Age range: 0–28 years Specific age cohorts for services included were 0–25 years, 0–18 years, unspecified, 2–28 years, 3–19 years, children and young adults, 6–22 years, 16–27 years, young people and young adults, 0–21 years and 0–19 years |
No resources reported Staffing Staff training Transport Funding |
Frequency Unclear, but typically a few hours during the day Location Service user’s home What’s offered? Different types of individual home-based day care: Members of extended family (e.g. parents/in-laws, other children, ‘relatives’) and friends offered respite, overnight stays and in-home support |
Young adults Increased independence Engagement with leisure and social activities Time spent away from main carer/parents A chance to experience and enjoy new activities To receive respite as part of a programme of comprehensive palliative care To have appropriate home-based respite services To experience fewer hospitalisations For parents and wider family To experience a break from caring To have quality time with partners and other children Time to spend on own pursuits For all An increase in quality of life |
Lack of longitudinal data to identify long-term outcomes and ongoing achievement of respite care that meets needs of young adults, parents/carers and the wider family, including siblings. Three sources60,63,69 in the review Benefits Limited depth of evidence on day respite in the home, but respite was achieved and expectations generally met, with respite care being viewed as safe and acceptable, and accessed when needed. Strength of benefits vary depending on the length of respite provided in the home and whether by formal or informal providers, but can include: Harms Limited depth of evidence to identify harms; however, because of the nature of the respite provision, some potential limitations can be experienced because of the lack of opportunities for young adults to socialise and develop independence and for parents and the wider family to have overnight rest |
|
Appendix 12 Logic model: home-based overnight respite
Logic model: home based – home-based overnight respite (11 services in 10 sources)
| Service aim/objective | Eligibility criterion | Resources (what is needed to provide the service) | Programme logic (what the service does/delivers): activities and frequency | Expectations of young adult/parent/wider family | Proximal: intended short-term outcomes/impacts | Distal: intended mid- to long-term outcomes/impacts |
|---|---|---|---|---|---|---|
|
Overall aim of this type of respite To provide respite for the parent/carer by enabling time away or time to sleep overnight Aims identified (different perspectives and identifiers) |
The specific conditions of patients accessing services were not specified Age range: not specified, but refers to adult and older people’s services Specific age cohorts for services included were not specified |
No resources reported Staffing Staff training |
Frequency Overnight Location In home What’s offered? Breaks provided at home through a care attendant or sitting service and individual support provided in the home of the cared-for person overnight |
Young adults Increased independence Time spent away from main carer/parents To receive respite as part of a programme of comprehensive palliative care To have appropriate home-based respite services To experience fewer hospitalisations For parents and wider family To experience a break from caring To have quality time with partners and other children To be able to sleep undisturbed For all An increase in quality of life |
Lack of longitudinal data to identify long-term outcomes and ongoing achievement of respite care that meets needs of young adults, parents/carers and the wider family, including siblings. Three sources60,63,69 in the review Benefits Limited depth of evidence on overnight respite in the home, but respite was achieved and expectations generally met when respite care was viewed as safe and acceptable, and accessed when needed. Benefits included: Harms Limited depth of evidence; however, if overnight respite is not experienced in some form from a trusted provider, potential harms were reported and these include negative impact on psychological well-being [such as stress and anxiety due to concerns over safe care (parents/carers and young adults)] and detrimental effects on the health and well-being of parents due to a lack or rest and recuperation (parents/carers) |
|
Appendix 13 Logic model: host family/fostering respite
Logic model: home based – host family/fostering respite (four services in three sources)
| Service aim/objective | Eligibility criterion | Resources (what is needed to provide the service) | Programme logic (what the service does/delivers): activities and frequency | Expectations of young adult/parent/wider family | Proximal: intended short-term outcomes/impacts | Distal: intended mid- to long-term outcomes/impacts |
|---|---|---|---|---|---|---|
|
Overall aim of this type of respite To provide young adults and their families with a break from normal routine and caring responsibilities Aims identified (different perspectives and identifiers) |
Children and adults with physical and intellectual disabilities Patients with the following specific conditions accessed the services: severe learning and/or physical disability, intellectual and other disability Age range: 0–25 years Specific age cohorts for services included were 0–25 years, and unspecified children and adults |
Staffing Volunteers who are paid expenses/allowance Staff training Specific training for host family Environmental Transport Funding |
Frequency Few hours to overnight, including weekends Location Host family’s home What’s offered Personalised sleepover, daytime visits, overnight stays and weekend breaks in the home of a host family |
Young adults To have a break from everyday routine To enjoy time away from family and carers Parents and wider family To have a period of respite and a break from caring responsibilities |
No evidence identified in the review for this type of respite to inform the logic model | |
Appendix 14 Logic model: day care at a specialist facility
Logic model: day care – day care at a specialist facility (4 services in 4 sources)
| Service aim/objective | Eligibility criterion | Resources (what is needed to provide the service) | Programme logic (what the service does/delivers): activities and frequency | Expectations of young adult/parent/wider family | Proximal: intended short-term outcomes/impacts | Distal: intended mid- to long-term outcomes/impacts |
|---|---|---|---|---|---|---|
|
Overall aim of this type of respite To provide young adults with appropriate support and respite at a specialist facility and to enable parents/carers to take a break from routine caring (It was noted in some of the service documents that day care is not generally provided for short break or respite purposes, but services that offer more flexible arrangements, designed around the needs of both the service user and carer, can achieve this purpose) Aims identified (different perspectives and identifiers) |
Young people and young adults with a range of disabilities and LLCs Patients with the following specific conditions accessed the services: LLCs, A–T Age range: 16–27 years Specific age cohorts for services included were 16–24 years, > 18 years, 16–27 years and not specified |
No resources reported Staffing Staff training Transport Funding Environmental (appropriate facilities) |
Frequency Unclear Location Hospice or community setting What’s offered? Planned respite as day care in a specialist facility, including: |
Young adults: To spend time away from carer for a few hours Parents and wider family To get a break from routine caring |
Lack of longitudinal data to identify long-term outcomes and ongoing achievement of respite day care that meets the needs of young adults, parents/carers and the wider family, including siblings. Limited evidence of one source in the review. 63 Other sources that included multiple services made reference to day care at a specialist facility within the generic narrative67,78,120 Benefits Respite was achieved and expectations generally met when respite care was viewed as safe and acceptable, and accessed when needed. Benefits included:Harms Loss of respite care following transition or inappropriate day care (e.g. for older people) was reported to have a negative impact on psychological well-being, including stress and anxiety due to concerns over safe care (parents/carers), frustration and distress at needs not being met appropriately (young adults and parents/carers), lack of opportunities for young adults to socialise and develop independence (young adults) and potential for detrimental effects for all the family when the young adult reduced attendance or completely withdrew from the service (young adults, parents/carers and the wider family, including siblings) |
|
Appendix 15 Logic model: organised recreational activities
Logic model: community, leisure and social provision – organised recreational activities (15 services in 10 sources)
| Service aim/objective | Eligibility criterion | Resources (what is needed to provide the service) | Programme logic (what the service does/delivers): activities and frequency | Expectations of young adult/parent/wider family | Proximal: intended short-term outcomes/impacts | Distal: intended mid- to long-term outcomes/impacts |
|---|---|---|---|---|---|---|
|
Overall aim of this type of respite To provide opportunities that support young adults to develop and maintain relationships and a peer network outside the home, develop skills, try new activities and to have a break from their carer Aims identified (different perspectives and identifiers) |
Teenagers and young people making the transition to adulthood and young adults with a range of complex, physical and life-limiting conditions (this also includes other disabilities, such as sensory, learning, and speech and language difficulties) Patients with the following specific conditions accessed the services: complex health-care needs, autistic spectrum condition, severe learning disabilities, speech and language difficulties, physical difficulties, young people with disabilities, children and young people with disabilities, sensory and other disabilities, young people with LLC who previously accessed children’s hospice services, young people/young adults with LLCs and complex learning and physical disabilities Age range: 0–26 years Specific age cohorts for services included were 14–19 years, 11–19 years, 13–19 years, 16–20 years, 14–20 years, 18–25 years, adults aged > 18 years, 0–19 years, young people making the transition to adulthood, 12–19 years, 5–25 years, 18–26 years and 18–25 years |
Staffing Appropriate staff to service user ratio Staff training Funding To cover costs of external activities Transport |
Frequency Ranges from a few hours to a full day, once/twice per week to once per month, taking place in evenings, at weekends and during school holidays Location Youth centres and out and about in the community What’s offered? |
Young adults Increased socialisation outside service user’s immediate family network To establish new relationships with the development of a peer support network Reduction in social isolation and an increase in social inclusion Improved access to social and leisure activities To gain independence into adulthood Increased freedom of choice over activities Gain life skills and confidence Improvement in quality of life/well-being Improved access to appropriate breaks when needed Parents and wider family To have a break from caring responsibilities Parental confidence in the service |
Lack of longitudinal data to identify long-term outcomes and ongoing achievement of respite day care that meets the needs of young adults, parents/carers and the wider family, including siblings. Five sources in the review59,60,63,66,72 Benefits Respite was achieved and expectations generally met when respite care was viewed as safe and acceptable, and accessed when needed. Benefits included: Harms No specific harms identified for organised activities, although the potential for harms is noted if this was the only respite care provision available to young adults. This type of respite care is not necessarily appropriate for young adults with the most complex needs, nor does it offer the opportunity for an overnight break for parents, which may result in the negative impacts reported for lack of respite care because of needs not being appropriately met (young adults, parents/carers and the wider family, including siblings) |
|
Appendix 16 Logic model: befriending schemes
Logic model: community leisure and social provision – befriending schemes (five services in five sources)
| Service aim/objective | Eligibility criterion | Resources (what is needed to provide the service) | Programme logic (what the service does/delivers): activities and frequency | Expectations of young adult/parent/wider family | Proximal: intended short-term outcomes/impacts | Distal: intended mid- to long-term outcomes/impacts |
|---|---|---|---|---|---|---|
|
Overall aim of this type of respite To provide support to access and experience a range of social and leisure activities with other young people without a parent/carer Aims identified (different perspectives and identifiers) To develop friendship and social skills through:To provide opportunities that improve/enhance quality of life/well-being through:To give parents/carers a break from routine caring (parents/carers and the wider family, including siblings) |
Children and young adults with disabilities and life-limiting conditions Patients with the following specific conditions accessed the services: cystic fibrosis, LLCs, disabilities Age range: 0–19 years Specific age cohorts for services included were 15–19 years, 0–19 years and 8–19 years |
Staffing Trained volunteer befrienders Transport Funding for activities |
Frequency 1–4 hours, ranging from weekly to every six weeks Location Various locations to suit befriendee/befriender What’s offered? Support to access social and leisure activities of young person’s choice, such as: |
Young adults Reduce boredom by increasing opportunities for fun activities Improvement in self-esteem Reduction in social isolation Parents and wider family Parents/carers given a break from caring responsibilities |
Lack of longitudinal data to identify long-term outcomes and ongoing achievement of respite day care that meets needs of young adults, parents/carers and the wider family, including siblings. One source70 in the review Benefits Respite was achieved and expectations generally met when respite care was viewed as safe and acceptable, and accessed when needed. Benefits included:Harms No specific harms identified for respite care through befriending, although the potential for harms is noted. If this was the only respite care provision available to young adults, it may not offer the same breadth of opportunities as other respite types and does not offer the opportunity for an overnight break for parents, which may result in negative impacts because of needs not being appropriately met (parents/carers and wider family, including siblings) |
|
Appendix 17 Logic model: funded holidays with friends, parents or carers
Logic model: holidays – funded holidays with friends, parents or carers (nine services in six sources)
| Service aim/objective | Eligibility criterion | Resources (what is needed to provide the service) | Programme logic (what the service does/delivers): activities and frequency | Expectations of young adult/parent/wider family | Proximal: intended short-term outcomes/impacts | Distal: intended mid- to long-term outcomes/impacts |
|---|---|---|---|---|---|---|
|
Overall aim of this type of respite To provide young adults with a residential break away from home and provide age-appropriate opportunities to engage in leisure and social activities with or without their parents/carer Aims identified (different perspectives and identifiers) To provide opportunities to experience a residential break away from parent/usual carers (young adults) |
Children and young adults aged 0–20 + years with a wide range of physical and learning disabilities, degenerative muscle disorders and complex needs Patients with the following specific conditions accessed the services: CP, significant physical and learning disabilities, A–T, substantive special needs and a range of care needs and disabilities Age range: 0–22 years; some services did not specify ages or an upper limit Specific age cohorts or non-specified descriptors for services included were 0–19 years, 5–19 years, 15–19 years, 19 years, 22 years, over 19 years with CP, up to 21 years with ABI, young people and young adults with A-T, young adults and adults |
Limited resources identifiedStaffing Staff training Transport Funding Environmental (appropriate facilities) |
Frequency Ranges from a weekend to 7 days Location Various holiday locations, including canal boats, caravans and adapted accommodation What’s offered? Funded holidays and tailored breaks with friends, family or paid carers |
Young adults To experience a residential break away from parents/carers and family members To experience an age-appropriate break Parents and wider family To experience a break from routine caring responsibilities For all To enjoy a break away as a family where desired |
Lack of longitudinal data to identify long-term outcomes and ongoing achievement of respite care that meets needs of young adults, parents/carers and the wider family, including siblings. Three sources63,66,72 in the review Benefits Respite was achieved and expectations generally met when respite care was viewed as safe and acceptable, and accessed when needed. Benefits included:In addition, when the young adult holidayed without family, parents had time to rest and recuperate, including:Other children experienced time with parents and a break from supporting parents with the caring role (the wider family, including siblings) Harms No specific harms were identified for holiday respite care, although the potential for harms is noted if this was the only respite care provision available to young adults and if it was limited to once a year, as the lack of regular, planned respite care may result in the negative impacts when needs are not being appropriately met (young adults, parents/carers and the wider family, including siblings) |
|
Appendix 18 Logic model: emergency respite in a specialist palliative care facility (e.g. hospice)
Logic model: emergency respite (unplanned) – emergency respite in specialist palliative care facility (e.g. hospice) (eight services in nine sources)
| Service aim/objective | Eligibility criterion | Resources (what is needed to provide the service) | Programme logic (what the service does/delivers): activities and frequency | Expectations of young adult/parent/wider family | Proximal: intended short-term outcomes/impacts | Distal: intended mid- to long-term outcomes/impacts |
|---|---|---|---|---|---|---|
|
Overall aim of this type of respite To provide unplanned respite care for young adults in specialist facilities in an emergency situation (e.g. parents called away urgently or ill) Aims identified (different perspectives and identifiers) To provide respite care during times of family crisis (service provider) To provide emergency respite due to a change in the child’s/young adult’s condition (service provider) |
Children and young adults with LLCs aged up to 30 years Patients with the following specific conditions accessed the services: LLCs Age range: 0–30 years Specific age cohorts for services included were 0–23 years, up to 19 years, up to 30 years, up to 23 years and > 18 years |
Staffing Sufficient hospice staff to deliver unplanned respite at short notice Standard resources for provision of hospice care, including trained staff for patient : staff ratios Staff training Funding Environmental (appropriate facilities)Transport |
Frequency When required Location Hospice What’s offered? A few nights of unplanned respite in a specialist facility |
Young adults To receive emergency respite during times of need in a safe, known environment Parents and wider family To be confident in the quality and continuity of care provided in an emergency |
Limited evidence to identify experience and achievement of emergency respite care, despite it being described as ‘invaluable’ by parents able to access children’s hospice services. Two sources27,67 in the review Benefits Respite was achieved and expectations generally met when respite care was viewed as safe and acceptable, and accessed when needed. Benefits included:Harms No harms were identified when respite was provided by a known provider. Lack of appropriate regular respite care due to complexity of care may result in families feeling that they have no back up in an emergency, or young adults being admitted to a nursing home or hospital when no alternative is available. Use of inappropriate emergency respite has the same reported negative impacts on psychological well-being, including stress and anxiety due to concerns over safe care (parents/carers), frustration and distress at needs not being appropriately met (young adults and parents/carers) and lack of opportunities for young adults to socialise and develop independence (young adults) |
|
Appendix 19 Logic model: emergency respite provided in home or hospital
Logic model: emergency (unplanned) – emergency respite provided in-home or hospital (two services in three sources)
| Service aim/objective | Eligibility criterion | Resources (what is needed to provide the service) | Programme logic (what the service does/delivers): activities and frequency | Expectations of young adult/parent/wider family | Proximal: intended short-term outcomes/impacts | Distal: intended mid- to long-term outcomes/impacts |
|---|---|---|---|---|---|---|
|
Overall aim of this type of respite To provide emergency care in the home or in hospital for young adults and to provide parents/carers with a break Aims identified To provide emergency care to the young adult at home because of an emergency situation (e.g. parents called away urgently or ill) To provide emergency supplementary care to young adults during a hospital stay to provide a break to parents/carers |
Predominantly children and young adults with complex medical needs Patients with the following specific conditions accessed the services: LLCs or not specified Age range: 0–23 years Specific age cohorts for services included were 0–23 years or not specified |
No resources reported Staffing Staff training Transport Funding |
Frequency Unclear Location Home based/hospital based What’s offered? Emergency respite in the home or hospital-based care for service users with complex health-care needs requiring medical supervision |
Young adults To receive appropriate care when their parents/main carer is not available Parents and wider family To receive a break from caring during emergency situations which require attention |
No evidence identified in the review for this type of respite to inform the logic model | |
Appendix 20 Logic model: host family emergency respite
Logic model: emergency – host family emergency respite (one service in one source)
| Service aim/objective | Eligibility criterion | Resources (what is needed to provide the service) | Programme logic (what the service does/delivers): activities and frequency | Expectations of young adult/parent/wider family | Proximal: intended short-term outcomes/impacts | Distal: intended mid- to long-term outcomes/impacts |
|---|---|---|---|---|---|---|
|
Overall aim of this type of respite To provide emergency or unplanned respite for a young adults with a host family No specific aims identified To provide emergency care to the young adult at the home of a host family in an emergency situation (e.g. parents called away urgently or ill) To provide a break from caring for parents/carers in urgent situations |
Children and adults with intellectual and other disabilities Patients with the following specific conditions accessed the services: not specified Age range was not specified Specific age cohorts for services included were not specified |
Staff training Training on moving and handling, invasive procedures and behaviour management Staffing Transport Funding |
Frequency For contract families 16 nights per month; for homeshare families a few nights to 7 days per week Location With host family What’s offered? Emergency or unplanned placement with host family |
Young adults To receive appropriate care when their parents/main carer is not available Parents and wider family To receive a break from caring during emergency situations which require attention |
No evidence identified in the review for this type of respite to inform the logic model | |
Appendix 21 Table of characteristics for studies included in stream 3 (experience and attitude)
| Source | Aim/objective | Location | Population | Study design and methods | Data collection period | Sample selection/recruitment | Funding |
|---|---|---|---|---|---|---|---|
| Abbott and Carpenter73 | To investigate, from their own perspectives, how the health and well-being of young men living with Duchenne muscular dystrophy and that of their parents can be maximised, particularly at the transition to adulthood. To consider the potential contribution of the national service framework for long-term neurological conditions for this group of people | England |
Young adults aged > 15 years with Duchenne muscular dystrophy (n = 40) Parents of young adults with Duchenne muscular dystrophy (n = 31) |
Qualitative methods, including postal surveys of parents and face-to-face interviews with young men | October 2007–November 2008 | Recruitment not detailed, sampling not clear | Department of Health and Social Care Policy Research Programme |
| Beresford et al.63 | The key purpose of the My Life Project was to hear and give a voice to the experiences of young people with A–T | England |
Young people and young adults with A–T aged 16–27 years (n = 11) Parents of young people and young adults with A–T (n = 10) |
Qualitative interviews | May and June 2012 | NR | AT Society (Harpenden, UK) |
| Dawson and Liddicoat62 | The study aimed to gather data on the therapeutic value of camp of individuals with disability and also attempted to understand what the mechanisms of the camp experience generate these benefits | USA |
Adults aged 19–76 years with cerebral palsy (n = 27) Parents also surveyed, but no numbers presented |
Qualitative methods, including questionnaire to young adults and parents, interviews (either by individual one to one or focus groups) and thematic analysis of interview data | NR | All camp participants invited to take part in questionnaire, purposeful sample of these invited to take part in the interviews | NR |
| Grinyer et al.71 |
To better understand how hospice services were experienced by the families who use them To discover how the children and young people and their families experienced the hospice services, what they found helpful and supportive, and what improvements they felt could be made |
England |
Service users with a range of conditions aged 10 months to 36 years (n = 3) Parents, siblings, wider family and paid carers (n = 21) |
Qualitative methods, including questionnaires, qualitative interviews and framework analysis | NR | Hospice staff distributed questionnaires to 76 families that had accessed the service, 26 families responded and of these 11 families volunteered for interview. Twenty-four interviews were conducted with family members from these 11 families | Commissioned by the hospice trustees and managers |
| Hutcheson et al.59 | To determine: the views of the young people, their families and staff towards the ‘Beyond Horizon’ pilot and whether or not it has met its aims in facilitating young people to live life to the fullest, whether or not the service has helped young people and their parents transition from children’s palliative care services and, if so, how this service could be developed and replicated in other areas | Northern Ireland | Young people aged 18–25 years with LLCs who previously accessed children’s hospice services (n = 14) | A qualitative focus group with young people, parents and health professionals, and thematic analysis | Commenced June 2015 | Total population sample of all young people who used the service | Office of First Minister and Deputy First Minister of Northern Ireland: Developing Social Change Programme |
| Kerr et al.74 | To obtain an overview of organisational approaches to transition on the island of Ireland, and to explore important organisational factors that may influence the effectiveness of the process | Republic of Ireland and Northern Ireland | Participants were 104 individual service providers from 29 statutory and non-statutory organisations providing transition services to young adults with life-limiting conditions | A cross-sectional questionnaire survey | April–October 2014 | All Ireland Institute of Hospice and Palliative Care (Dublin, Ireland) and Health and Social Care, Research and Development Division, Public Health Agency (Belfast, Northern Ireland) as part of a Doctoral Fellowship for Helen Kerr | |
| Kirk and Fraser22 |
To examine how young people with life-limiting conditions and their parents experience transition To identify families’ and hospice staff’s perceptions of family support needs during transition To identify the implications for children’s hospices |
UK |
Young people aged 16–31 years, not at an end-of-life stage, from one children’s hospice (n = 16) Parents (n = 16) |
Qualitative semistructured interviews and grounded theory approach | February–July 2012 | Young people and their parents were recruited from one children’s hospice. Hospice workers were recruited from a hospice staff list | No specific grant from any funding agency in the public, commercial or not-for-profit sectors |
| Knighting et al.67 | To answer the question what are views of staff working in children’s and adult hospices in the UK on the availability and challenges of providing services for young adults with LLCs aged ≥ 18 years? | UK | Respondents included children and adult hospices in England, Wales, Scotland and Northern Ireland (n = 76) | Cross-sectional online survey and open-text responses analysed using a content analysis approach | October 2015 to February 2016 | A convenience sample was recruited via an e-mail invitation, which was sent to all 221 hospice leads in the UK | Liverpool CCG (Liverpool, UK) |
| Knighting75 | To explore the views and experiences of transition planning, access to services and wishes for future services from young adults aged > 18 years and parents across the UK | UK |
Young adults aged 22–37 years who had accessed short break service at a hospice, hospital or other setting (n = 6) Parents (n = 38) |
Online survey | June and August 2017 | NR | Liverpool CCG |
| Luzinat et al.68 |
To explore parental perspectives of the benefits gained from HTC for individual family members and examine parental perspectives on how HTC influenced the family as a whole HTC aims to provide families with a fun experience where they can create new friendships, share experiences of ABI with other families, rebuild individual and family identity, and become part of a supportive community |
Australia | Parents of children and young adults aged 7–21 years with ABI who had attended HTC (n = 31) | Semistructured interviews and thematic analysis | May 2016 | Parents who attended HTC in May 2016 were approached | NR |
| MacDonald and Greggans70 | To evaluate the impact of a community youth-befriending programme on a group of young people with chronic illness and their carers | Scotland |
Children and young people with cystic fibrosis aged 8–18 years (n = 10) Professionals (n = 4) Befrienders (n = 3) |
A descriptive qualitative design, interviewing young people and their parents, including focus groups with befrienders and framework analysis | NR | All families that used the befriending programme were approached | NR |
| Marsh et al.35 | To answer the questions:
|
UK |
Groups: young people and young adults with LLCs aged 13–25 years (n = 15) Interviews: young people and young adults aged 13–25 years with LLCs (n = 7) |
Qualitative methods, including interviews, open-space multistakeholder events, individual and group interviews and social network analysis | January–March 2011 | Unclear | Marie Curie Cancer Care supported by funding from the Department of Health and Social Care |
| Martin House Children’s Hospice60 | This research aimed to further our understanding of the barriers to and facilitators of providing effective and appropriate palliative care and support to children and their families | England |
Young people and young adults aged ≥ 18 years with LLCs (n = 12) Parents (n = 12) Professionals (n = 53) Service providers (n = 181) |
Qualitative methods, including interviews, focus groups, consultation with advisory group, narrative review, mapping services, surveys, in-depth interviews and semistructured interviews | 2011–12 | Key informants identified through key individuals in the funding organisation, the mapping exercise identified organisations to send survey to and a random sample of referrals to Martin House Children’s Hospice | Martin House Children’s Hospice |
| Mitchell et al.27 | To explore the impact of the hospice planned and emergency respite care on children and young people with life-limiting conditions, their families and stakeholders to inform future service development | England |
Children and young adults aged ≥ 11 years with LLCs Phase 1 (n = 8) Carers phase 1 (n = 8) Professionals phase 1 (n = 39) Families phase 2 (n = 33) |
Mixed methods, including a survey, semistructured interviews and focus groups | December 2013 to June 2014 | Purposive sample identified in consultation with hospice staff, participants recruited via e-mail/letter | Claire House Children’s Hospice |
| Murphy and Mackay109 | To ascertain the views of young people with complex needs and the views of their parents about health services before transition, health services during transition, health services after transition and what could be improved | Scotland | Young people aged 14–30 years with complex health needs (n = 4):
|
Qualitative and interviews | NR | CEN team (Edinburgh, UK) agreed to contact families to explain the project and obtain consent. They then sent the contact details to the Talking Mats team (Stirling, UK) who arranged the visits, which were all conducted in the family’s home | Commissioned by CEN |
| Muscular Dystrophy Campaign65 | The Muscular Dystrophy Campaign began to compile evidence for this report on hospice and respite care for young adults following the announcement by the Children’s Hospice Association Scotland of its proposals to phase out its services for young adults | Scotland | Young people with Duchenne | Consultation with young people | NR | NR | Muscular Dystrophy Campaign |
| Shared Care Scotland72 | To consider what round 1 projects have achieved, to capture their challenges and, from this, to consider what learning can be taken forward into future funding allocations | Scotland | The report details a range of services for carers and cared-for individuals with a range of conditions, we have extrapolated those delivered to young adults with complex health-care needs only | Mixed methods, including analysis of End of Grant Reports, interviews with funded projects, meetings with key groups and telephone consultations | March–October 2011 | Scottish Government, managed by Shared Care Scotland | |
| Shared Care Scotland66 |
To review the individual projects and explore their achievements and challenges To consider how well round 2 projects have contributed towards delivery of the outcomes set for the Short Breaks Fund To consider how well round 2-funded projects delivered the principles of the Short Breaks Fund and to capture and highlight examples of innovation, good practice and learning To make recommendations for improving the reach and impact of the Short Breaks Fund in the future |
Scotland | The report details a range of services for carers and cared for individuals with a range of conditions, we have extrapolated those delivered to young adults with complex healthcare needs only | Evaluation methods, including case studies | October 2011 to October 2012 | Scottish Government, managed by Shared Care Scotland | |
| Stylianou69 | The study addresses four main research questions:
|
Cyprus | Parents of children and young adults with a range of disabilities (n = 25) | Qualitative semistructured interviews and thematic analysis | NR | Mothers were selected through purposive and snowball sampling techniques | This is a thesis submitted to University College London, (London, UK) for PhD |
| Young et al.61 | To build on previous research and explore the views and perspectives of young adults, parents/carers and professionals engaged with the service to determine how the service was delivered, how the service was experienced and what difference the service makes to the lives of young adults and carers | England |
Young adults with LLCs (n = 2) Parents (n = 4) Service staff (n = 15) |
Semistructured individual interviews or focus group interviews and framework analysis | 2012–13 | Young adults were identified using an opportunistic sampling approach. Parents and staff were then identified using snowball sampling | Big Lottery Fund (Now known as the National Lottery Community Fund) |
Appendix 22 Quality assessment of included sources in stream 3 (single source documents n = 20)
| Source | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| aAbbott and Carpenter73 | Yes | Yes | Yes | Cannot tell | Yes | No | Cannot tell | Cannot tell | Yes | Yes |
| aBeresford et al.63 | Yes | Yes | Yes | Yes | Yes | Cannot tell | Cannot tell | Cannot tell | Yes | Not very |
| Liddicoat and Dawson62 | Yes | Yes | Yes | Yes | Yes | No | Cannot tell | Cannot tell | Yes | Yes |
| Grinyer et al.71 | Yes | Yes | Yes | Yes | Yes | Cannot tell | Yes | Cannot tell | Yes | Not very |
| Hutcheson et al.59 | Yes | Yes | Yes | Yes | Yes | Yes | Cannot tell | Cannot tell | Yes | Not very |
| Kerr et al.74 | Yes | Yes | Yes | Yes | Yes | Yes | Cannot tell | Cannot tell | Yes | Yes |
| Kirk and Fraser22 | Yes | Yes | Yes | Yes | Yes | Cannot tell | Yes | Yes | Yes | Yes |
| bKnighting et al.67 | Yes | Yes | Yes | Yes | Yes | Cannot tell | Yes | Yes | Yes | Yes |
| a,bKnighting et al.75 | Yes | Yes | Yes | Cannot tell | Yes | Cannot tell | Cannot tell | Cannot tell | Yes | Yes |
| Luzinat et al.68 | Yes | Yes | Yes | Yes | Yes | Cannot tell | Yes | Yes | Yes | Yes |
| MacDonald and Greggans70 | Yes | Yes | Yes | Yes | Yes | Cannot tell | Yes | Yes | Yes | Yes |
| aMarsh et al.35 | Yes | Yes | Yes | Yes | Yes | Cannot tell | Yes | Yes | Yes | Yes |
| aMartin House Children’s Hospice60 | Yes | Yes | Yes | Yes | Yes | Cannot tell | Yes | Yes | Yes | Yes |
| bMitchell et al.107 | Yes | Yes | Yes | Yes | Yes | Cannot tell | Yes | Yes | Yes | Yes |
| aMurphy and Mackay109 | Yes | Yes | Yes | Yes | Yes | Cannot tell | Yes | Yes | Yes | Yes |
| aMuscular Dystrophy Campaign65 | Cannot tell | Cannot tell | Cannot tell | Cannot tell | Cannot tell | Cannot tell | Cannot tell | Cannot tell | Cannot tell | Cannot tell |
| aShared Care Scotland72 | Yes | Cannot tell | Cannot tell | Cannot tell | Cannot tell | Cannot tell | Cannot tell | Cannot tell | Cannot tell | Cannot tell |
| aShared Care Scotland66 | Cannot tell | Cannot tell | Cannot tell | Cannot tell | Cannot tell | Cannot tell | Cannot tell | Cannot tell | Cannot tell | Cannot tell |
| aStylianou69 | Yes | Yes | Yes | Yes | Yes | Cannot tell | Yes | Yes | Yes | Yes |
| bYoung et al.61 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
Appendix 23 Review evidence matrix
| Evidence stream | Knowledge map respite care classification | Gap analysis by type of evidence | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Residential respite (specialist facility) | Home-based respite | Day-care respite (specialist facility) | Community, leisure and social provision | Funded holidays with friends, parents/carers | Emergency respite (unplanned) | |||||||||
| Palliative care facility | Disability facility | Nursing home | Daytime | Overnight | Host family/fostering | Organised recreational activities | Befriending schemes | Palliative care facility | In home or hospital | Host family | ||||
| Intervention effectiveness | No evidence | No evidence | No evidence | No evidence | No evidence | No evidence | No evidence | No evidence | No evidence | No evidence | No evidence | No evidence | No evidence | No evidence identified |
| Health economics | No evidence | No evidence | No evidence | No evidence | No evidence | No evidence | No evidence | No evidence | No evidence | No evidence | No evidence | No evidence | No evidence |
No formal evidence identified Limited cost information from one knowledge map source included narratively in discussion123 |
| Experience and attitudes | Nine sources27,41,59–61,64,67,71,76 | Two sources62,68 | One source61 | Three sources60,63,69 | Three sources60,63,69 | No evidence | One source63 | Five sources59,60,63,66,72 | One source70 | Three sources63,66,72 | Two sources27,67 | No evidence | No evidence | Evidence from young adults, parents, wider family and service providers. Evidence of benefits and potential for harms identified. No evidence for host family/fostering, emergency respite in home or hospital, or emergency respite by host family. Some generic sources |
| UK policy and guidelines | Sixteen UK policy sources and four NFPO guidance sources26,30,88–93,98,99,110,111,114–118,128,129,131 | Statutory and regulatory sources, national standards/frameworks and NFPO guidance for commissioners and providers on services for young people with complex needs and transition between children and adult services | ||||||||||||
|
Gap analysis by type of respite service (See individual logic models in Appendices 8–20 for details) |
Respite type with most evidence was typically children’s hospices. Evidence from all perspectives. Benefits and potential harms identified. Lack of longitudinal data to identify long-term outcomes | Limited evidence. Further evidence needed of use and experience of day and overnight respite care. Perspectives from parents and service providers only. Benefits and potential harms identified. Lack of longitudinal data to identify long-term outcomes | Limited evidence. Further evidence needed of use and experience of day respite care. Benefits and potential harms identified | Limited evidence of befriending and low evidence of organised recreational activities. Further evidence needed of use and experience of befriending as a low-cost, potential high-benefit respite type. Benefits and potential harms identified | Limited evidence. Further evidence needed of use and experience of holidays taken with families and with carers. Some benefits identified | Limited evidence. Further evidence needed of use and experience of emergency respite care across all services. Perspectives from parents and service providers only |
Despite high confidence in most sources of evidence (see Table 4), there is low evidence for the majority of respite types, particularly emergency respite care Lack of longitudinal data to identify long-term outcomes for all types of respite care, and no comparison studies to compare types and costs with experience and outcomes |
|||||||
Glossary
- Complex care
- Substantial and ongoing health-care needs typically requiring a co-ordinated response from more than one sector or organisation. Complex care needs can be the result of chronic illness or disabilities or follow hospital treatment. Complex care is sometimes referred to as long-term care or continuing care.
- Complex physical disability
- Complex impairments and/or physical disabilities, often due to congenital or acquired disability, or major neurological trauma, requiring a high level of physical management and support. Sometimes referred to as severe or profound disability. May overlap and interlock with other health conditions or learning disabilities, creating a complex patient profile.
- Disability
- According to the Equality Act 2010, ‘a physical or mental impairment that has a “substantial” and “long-term” negative effect on a person’s ability to do normal daily activities’ (Great Britain. Equality Act 2010. Chapter 15. London: The Stationery Office; 2010).
- Formal respite care
- Care that is provided by organisations or individuals who receive financial payment, including family carers paid through management of personal care budgets.
- Informal respite care
- Respite care for which no financial payment is received.
- Life-limiting condition
- A condition of which there is no reasonable hope of cure and from which the person is expected to die.
- Respite care
- The temporary provision of formal (paid) or informal (unpaid) physical, emotional, spiritual or social care for a dependent person to promote well-being and independence and to reduce carer distress.
- Short breaks
- Care defined by Together for Short Lives as having three main functions: ‘(1) to provide the child or young person with an opportunity to enjoy social interaction and leisure facilities; (2) to support the family in the care of their child in the home or an alternative community environment such as a children’s hospice; and (3) to provide opportunities for siblings to have fun and receive support in their own right’ [Reproduced with permission from Together for Short Lives. Children’s Palliative Care Definitions. URL: www.togetherforshortlives.org.uk/get-support/supporting-you/family-resources/childrens-palliative-care-definitions/ (accessed 31 July 2020).].Reproduced with permission from Together for Short Lives2020Together for Short Lives
- Young adults
- Typically considered to be adults aged 19–25 years, although some definitions begin at 18 years and extend to 40–45 years. For the purposes of this protocol, the definition is 18–40 years of age.
List of abbreviations
- 24/7
- 24 hours a day, 7 days a week
- AGREE II
- Appraisal of Guidelines, REsearch and Evaluation Version II
- BAME
- black, Asian and minority ethnic
- CASP
- Critical Appraisal Skills Programme
- CCG
- Clinical Commissioning Group
- CLUSTER
- Citations, Lead authors, Unpublished materials, Scholar search, Theories, Early examples, Related projects
- GRADE-CERQual
- Grading of Recommendations Assessment, Development and Evaluation-Confidence in the Evidence from Reviews of Qualitative research
- LLC
- life-limiting and life-threatening condition
- NFPO
- not-for-profit organisation
- NICE
- National Institute for Health and Care Excellence
- OECD
- Organisation for Economic Co-operation and Development
- PAG
- Patient and Public Advisory Group
- PPI
- patient and public involvement
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- SG
- Steering Group
- SPICE
- Setting, Perspective, Intervention/phenomenon of interest, Comparison, Evaluation
- TfSL
- Together for Short Lives
