Notes
Article history
The research reported here is the product of an HS&DR Evidence Synthesis Centre, contracted to provide rapid evidence syntheses on issues of relevance to the health service, and to inform future HS&DR calls for new research around identified gaps in evidence. Other reviews by the Evidence Synthesis Centres are also available in the HS&DR journal.
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 17/06/04. The contractual start date was in April 2018. The final report began editorial review in January 2020 and was accepted for publication in July 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2021. This work was produced by Price et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2021 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Parts of this report are reproduced or adapted with permission from Price et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
When encountering a [doctor] who is not thriving, it is often difficult to figure out what is wrong and how to help. And when confronted with a serious violation of professional ethics or a repeated threat to patient safety, it is equally unclear what to do . . . Unfortunately, problems often become worse, and if uncorrected, result in harm to patients, disruption of the healthcare team, and occasional dismissal . . .
Kalet et al. 2
Proficient and safe doctors, operating efficiently within teams, are an essential part of the provision of high-quality and safe care for patients. If the performance of a doctor is lacking, patients may be at risk. 3 Performance issues can be experienced by doctors at any stage in their careers for a variety of reasons, including health/well-being, personal reasons, the environment of the workplace, and not keeping up to date and participating in continuing medical education. Performance concerns are often complex and multifactorial, and can involve issues relating to knowledge, skills and professionalism. 4–6 To ensure patient safety, it is vital that if there are questions about the performance of a doctor they are identified quickly and, where appropriate, addressed through remediation. 7
Remediation is the process by which a doctor’s poor performance is ‘remedied’ and the doctor returned to safe practice. 8 Remediation can be formally defined as ‘an intervention, or suite of interventions, required in response to assessment against threshold standards’. 9 Threshold standards are set by regulatory bodies [e.g. the General Medical Council (GMC)] to keep patients safe. What actually constitutes a remedial intervention ranges from informal arrangements to complete some reskilling, through to more formal programmes of remediation and rehabilitation. 10 It is generally agreed that there are three necessary components of remediation: (1) the identification of performance deficit, (2) remediation intervention and (3) reassessment of performance after intervention. 11
Remediation has been classified as a ‘wicked’ problem the medical profession has struggled with for decades. 12,13 One of the main difficulties relates to the fact that remediation has historically been conceptualised as a way of addressing a person’s lack of knowledge in a particular area. Although addressing knowledge is important, it is not enough to achieve behaviour change. 12,14,15 The performance of a doctor is shaped by a variety of different contextual factors, including the attributes and skills of colleagues, system resources and organisational culture. Viewing remediation as merely an educational exercise, ignoring the contextual factors influencing competence in individuals, is unlikely to be enough to address significant performance gaps. 12 In recent years, there has been an important shift in the conceptualisation of remediation towards being a behaviour change process (i.e. understanding what is necessary to produce lasting performance improvement for a particular doctor in a particular context). 7,12
Remediation interventions are widely used in health-care systems across the globe to address underperformance. When we use the term underperformance, we are referring to situations in which a doctor’s performance is below the standards required to ensure safe practice. It is estimated that approximately 6% of doctors (i.e. approximately 9400 doctors) in the hospital workforce in England may be underperforming at any time and that 2% (approximately 4100) of all practising doctors will be undergoing remediation. 10 These figures will have increased because of the process of revalidation, which is the UK’s relicensing system for practising doctors that is regulated by the GMC. 8 Medical revalidation was introduced in 2012 as a statutory requirement. It is the procedure by which all UK doctors evidence that they are up to date and fit to practise. This is achieved by collating supporting information as part of an annual appraisal. Then, usually every 5 years, a senior doctor called the ‘responsible officer’ within an associated organisation (known as the ‘designated body’) recommends a revalidation outcome decision to the GMC. If underperformance is identified through the revalidation process (or through any other route), the responsible officer has a statutory responsibility to ensure that the designated body offers ‘training or retraining’. 16 Specific guidelines for responding to a concern about a doctor’s practice have recently been published to support this process. 17 Data from research evaluating medical revalidation suggest that revalidation is helping to identify such poor performance. 18
It is difficult to quantify the real human cost of an underperforming doctor; however, approximately 12,000 patients die in England each year as a result of preventable medical errors. 19 There is also the corresponding financial cost of these errors to consider. The NHS paid out > £2227.5M in medical negligence claims in 2017/18 alone. 19 However, the true societal costs when things go wrong are unknown. The relatively few incompetent doctors need to be stopped from practising; however, there is a more widespread and difficult problem to solve that would improve the health of the public and patients in the NHS, and that is doctors who underperform. Remedying underperformance, where possible, is both a practical and a financial imperative, as doctors are in short supply and are expensive to train. 20 There are shortages of doctors in particular specialties and geographical areas. 21 The NHS in England, Northern Ireland, Scotland and Wales has been under extreme pressure to cut spending in recent years. 22 On average, it costs £485,390 to train a general practitioner (GP) and £726,551 to train a consultant. 23 Therefore, offering remediation to retain expensively trained but underperforming doctors is a logical financial solution.
Although offering remediation to underperforming doctors makes sense on a practical and financial level, there is another important reason related to the ‘duty of care to doctors’. 24 Rather than ‘striking off’ or ‘firing’ a doctor who is underperforming, providing the necessary support and remediation, and the opportunity to improve, is imperative in a caring workplace. The GMC states that its aim is to ‘protect patients and the reputation of the profession’ (Reproduced with permission from General Medical Council. 24 © 2015 General Medical Council). Once this has been achieved, the GMC says that it also has a parallel duty of care to the doctors to encourage and enable remediation in suitable circumstances. 24 Remediation is therefore important for a doctor’s personal and professional development, as well as their patients’ safety and well-being.
Despite the importance of remediation in the regulation of doctors and in ensuring patient safety, research on remediation is lacking. 12,25 Three systematic reviews and one thematic review have been conducted on remediation across the continuum of medical education. 11,25–27 All four reviews on the topic of remediating doctors identify a lack of research that would provide a firm theoretical base to guide remediation interventions. The reviews were also unable to identify why particular interventions work for some doctors and not for others (i.e. detailed analyses on important contexts were missing):
. . . we cannot delineate precisely what works, and why, in remedial interventions for medical students and doctors.
Cleland et al. 25
This issue was also highlighted by research recently commissioned by the GMC, which investigated the impact on doctors of undertakings (i.e. remediation measures agreed with the doctors), conditions (i.e. remediation imposed on the doctors) and official warnings. 24 The study had a small sample size; however, the outcomes suggested that stipulating remediation in some cases engendered more reflective and safer practice, but in other cases it engendered more defensive or unchanged practice. 24 In other words, the same interventions were producing different outcomes in different contexts and for different doctors. An important issue that has limited our deeper understanding of remediation interventions for doctors has been the way in which systematic reviews have been carried out. In particular, the previous systematic reviews on remediation use inclusion criteria that were too restrictive (e.g. by study design, intervention type) and, hence, were only able to draw on a narrow body of literature. In summary, ‘rigorous approaches to developing and evaluating remediation interventions are required’. 25
To design high-quality remediation interventions, it is fundamental to understand the theory of how remediation of doctors is supposed to work, for whom and the contexts that lead to different outcomes. Our review will make an empirical contribution to the existing body of knowledge by developing a programme theory of how remediation of doctors is supposed to work, for whom and in what contexts. The review will enable us to develop recommendations for the tailoring, design and implementation of remediation interventions for underperforming doctors. Finally, this research will produce new knowledge about a poorly understood area of health-care delivery that has a direct impact on the standard of care received by patients.
Review questions
Aim
The REalist SynThesis of dOctor REmediation (RESTORE) review aimed to identify why, how, in what contexts, for whom and to what extent remediation interventions work for practising doctors to restore patient safety. The review was structured around the following objectives and review questions.
Objectives
-
To conduct a realist review of the literature to ascertain why, how, in what contexts, for whom and to what extent remediation programmes for practising doctors work to restore patient safety.
-
To provide recommendations on tailoring, implementation and design strategies to improve remediation interventions for doctors.
Review questions
-
What are the mechanisms by which remediation interventions work to change the behaviour of practising doctors to produce their intended outcomes?
-
What are the contexts that determine whether or not remediation interventions produce their intended or unintended outcomes?
-
In what circumstances are these remediation interventions likely to be effective?
The next chapter provides a detailed description of the methods utilised in the review. Chapter 3 presents the results, followed by the discussion in Chapter 4. Finally, the conclusions and recommendations are presented in Chapter 5.
Chapter 2 Review methods
We followed a realist approach to evidence synthesis to understand the contexts in which remediation interventions are most effective. Realist review is a practical, methodological approach designed to inform policy and practice. The realist review approach is distinct from other types of literature reviews, as it is based on an interpretive and theory-driven approach, synthesising evidence from qualitative, quantitative and mixed-methods research. 28 The unique contribution of this approach is that it yields transferable findings that explain how and why context can affect outcomes. 28 It does so by developing programme theories that explain how, why, in what contexts, for whom and to what extent interventions ‘work’. 29,30
Realist review methods are particularly suited to research on the remediation of doctors, as they focus on the contextual factors that determine the outcomes of an intervention. 31 Like other interventions that seek to promote behavioural change, remediation is highly context dependent (i.e. the same intervention will vary in its success depending on, for example, who delivers it and how it is delivered, the characteristics of the learners, the circumstances surrounding it, and the tools and techniques used). Research designs that seek to ‘strip away’ this context limit an understanding of ‘how, when and for whom’ the intervention will be effective. 31 A realist review takes context as central to any explanation by exploring how an intervention manipulates context to trigger mechanisms that cause behavioural change.
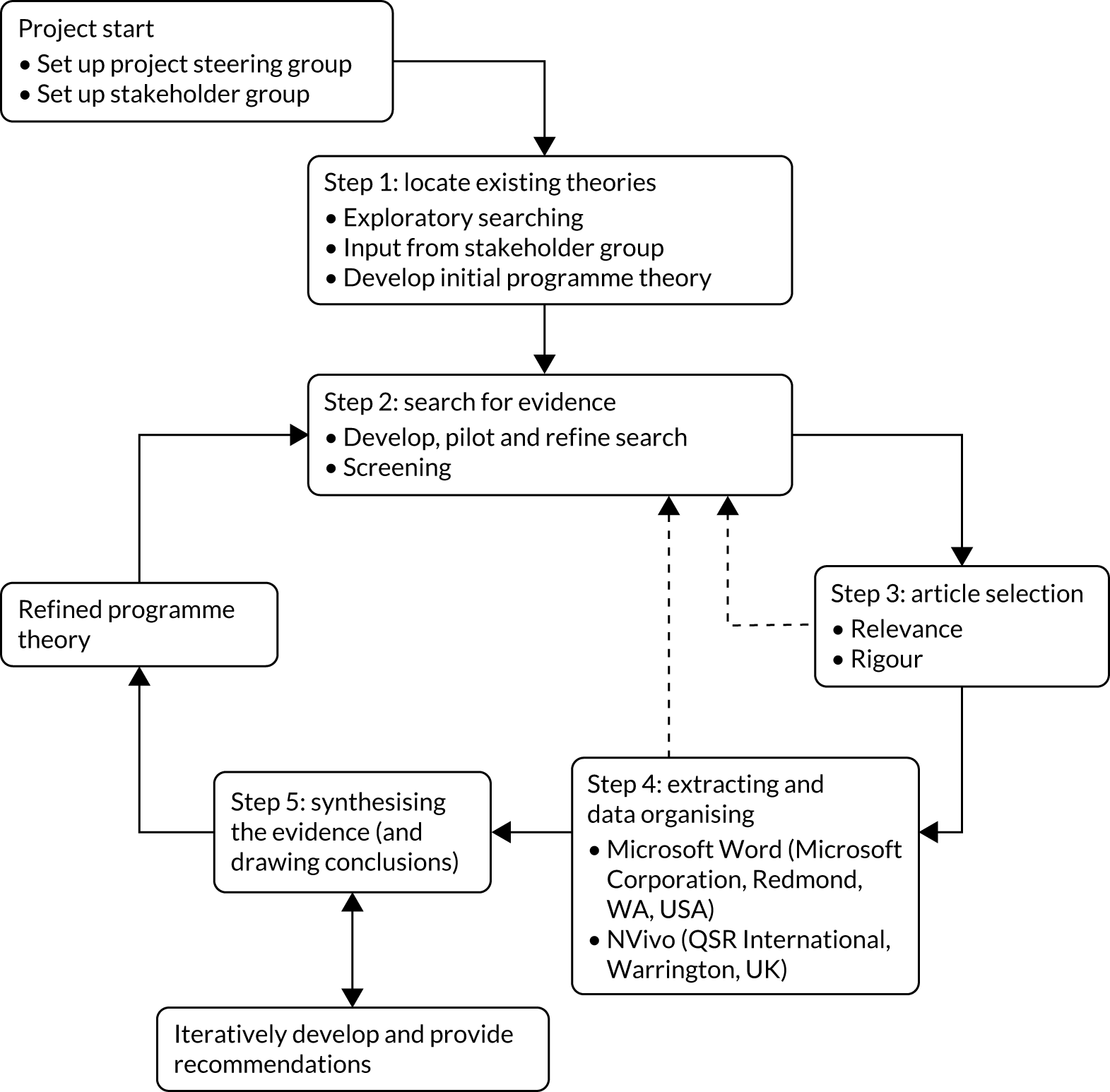
The research design is illustrated in Figure 1. 32 The plan of investigation followed a detailed protocol based on Pawson’s33 five iterative stages for realist reviews: (1) locating existing theories, (2) searching for evidence, (3) selecting articles, (4) extracting and organising data and (5) synthesising the evidence and drawing conclusions. The review ran for a 22-month period from April 2018 to January 2020. The review was registered with PROSPERO (CRD42018088779) and the protocol was published in BMJ Open. 34 The review was informed by the quality and publication standards and training materials for realist reviews that were developed by one of the core research team members (GW). 35 We were granted ethics clearance by the University of Plymouth, Faculty of Health and Human Sciences and Faculty of Medicine and Dentistry Research Ethics and Integrity Committee.
FIGURE 1.
Flow diagram of the project. Dashed arrows to indicate iteration where necessary. Reproduced with permission from Wong et al. 32 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.
Stakeholder group
A diverse stakeholder group was recruited for the RESTORE review to provide subject knowledge for programme theory refinement, to optimise dissemination plans and to aid the generation of feasible and practical recommendations. A total of 12 people were consulted throughout the review, including doctors who have undergone a remediation programme, personnel who identify underperforming doctors and initiate involvement in remediation programmes, personnel involved in the delivery of remediation programmes, responsible officers, remediation coaches, remediation researchers, patient and public representatives, and members of relevant medical bodies. Two-hour meetings with stakeholder group members took place at regular intervals throughout the project. Individual telephone calls were also held if stakeholders were not able to attend meetings (n = 4) and e-mail exchange was also used. A list of the meetings that took place is presented in Table 1. The table includes the number of participants who attended each meeting and the topics discussed. The review team members also attended stakeholder meetings.
| Date | Stakeholder group members | Key topics discussed |
|---|---|---|
| 26 June 2018 | Seven participants:
|
Explored definitions and conceptualisations of remediation, when remediation works and why, and definitions of a ‘practising doctor’ |
| 12 October 2018 | Eight participants:
|
Discussed aspects of the emerging programme theory, including the identification of underperforming doctors, intervention activities, processes engendering behaviour change and the concepts that might be important to CMOcs, and how these reflected stakeholders’ experiences of remediation |
| 16 May 2019 | Five participants:
|
Continued to discuss findings of the review, including remediating insight, autonomy and professional identity, goal-setting, triggers and consequences, and facilitating change |
| 13 November 2019 | Six participants:
|
Discussed and refined the recommendations of the review and the dissemination strategy |
In the early stages of the study, the review team struggled to recruit to the stakeholder group any doctor who had undergone remediation. Members of the review team and stakeholder group used existing contacts to try to recruit remediated doctors. The professional support unit at Health Education England South West (Bristol, UK) was also approached by NB and they e-mailed all of their trainees undergoing professional support to ask if they were interested in being involved in the stakeholder group. As undergoing remediation is a sensitive issue, we offered the remediating doctor the option of feeding into the stakeholder group via individual telephone calls. Finally, we recruited a remediated doctor to the group in January 2019. TP had two meetings with this stakeholder who provided valuable insight into the remediation process.
We organised stakeholder meetings to take place at the University of Exeter Medical School (Exeter, UK). At each meeting, a brief slide presentation was given by the review team at the start of the meeting to introduce stakeholders to the topic under discussion. The programme theory was presented to the group in the form of diagrams and statements in order to obtain stakeholders’ feedback. The final stakeholder group meeting focused on the dissemination of the findings. The meetings were facilitated in an inclusive way, providing everyone the opportunity to contribute and voice their opinion, whether or not they were in agreement.
All stakeholder meetings were audio-recorded. The recordings were not used as a form of data, but were used to enable the project team to focus on the meeting, as opposed to being distracted by note-taking. Stakeholders were informed of the purpose of the recording and verbal consent to audio-recording was gained at the start of each meeting. Detailed summaries of the meeting were produced by TP and shared with all members of the stakeholder group, regardless of whether or not they had attended the meeting. The meeting notes were used to orientate the review and to inform programme theory development, and were not used as primary data for analysis. The report does not include any direct quotations from these meetings.
The input of stakeholders in the review provided a reality check based on their ‘on the ground’ experiences of remediation. The use of realist review terms was kept to a minimum in the meetings to avoid discussions focusing too much on methodological concepts. Stakeholder involvement also contributed significantly to refinement of recommendations and dissemination of findings in accessible formats.
Patient and public involvement
The RESTORE review included strong patient and public involvement (PPI) throughout the project. LW, our PPI representative, was a co-applicant and a member of the review team and attended all of the team meetings, meaning that she had direct input into the management of the study from start to finish. As well as LW, we also had further PPI input in the stakeholder meetings from a representative from an existing PPI forum that we had established for two other studies on revalidation, funded by the GMC and the Department of Health and Social Care. In the stakeholder meetings, patients and members of the public provided significant input to programme theory development, often highlighting unique aspects of the remediation process.
Steering group
A steering group was set up for the project and comprised the review team plus representatives from the finance department and research and innovation department at the University of Plymouth. The steering group met four times throughout the study (June and October 2018, and May and November 2019). During these meetings, the steering group was updated about the progress of the study, provided scientific and budget oversight, and made sure that the project was delivered as proposed in the protocol. The steering group ratified all changes that were made during the study (e.g. the change of principal investigator and other staff changes).
Step 1: locate existing theories
The purpose of this step was to locate existing theories that explain why, how, in what contexts, for whom and to what extent remediation programmes for practising doctors work. This involved identifying the theories that explain how remediation interventions are supposed to work to bring about behavioural change in clinical settings. Having already established from previous systematic reviews on the topic25–27 that there is limited theory underlying existing remediation interventions, the realist review approach allowed for the literature net to be cast wider to include literature from other fields and other professions, where potentially similar mechanisms may be in operation.
An initial programme theory was devised by TP and NB during the funding application phase of the project (see Appendix 1). This initial programme theory included some early thoughts on the mechanisms that may interact with important contexts to produce certain outcomes. The elements incorporated in this programme theory were identified through literature included in the personal libraries of TP, NB and JA, which had been carefully and purposefully collected on the topic area. This initial programme theory was then shared with the review team and the stakeholder group for further refinement. The informal searches carried out in step 1 were different from the more formal searching that was carried out in step 2 (see Step 2: search strategy), as their purpose was to quickly identify the kinds of theory that may be relevant. Therefore, exploratory and informal search methods, including citation tracking and ‘snowballing’, were used. 36 We carried out these informal searches during April and May 2018. We used terms such as ‘remediation’ and ‘underperformance’ in Google Scholar (Google Inc., Mountain View, CA, USA) and MEDLINE databases. Once the theories had been identified, we built an initial programme theory to test in the review.
Step 2: search strategy
Formal search
In step 2, the goal was to find a body of relevant literature to further develop and refine the initial programme theory developed in step 1. The searches were designed, piloted and carried out by AW, an experienced information specialist with expertise in carrying out searches for realist reviews. AW used MEDLINE (via Ovid) to develop the search strategy. An iterative process was adopted, whereby search terms were added, removed and refined to achieve a balance of sensitivity and specificity in the results. The overall aim was to capture a broad range of relevant literature while minimising irrelevant literature.
As the search developed, sample sets of results were screened by TP and NB. This facilitated the selection of relevant search terms. In addition, highly relevant studies that had already been identified by the review team through their own personal libraries were used to test the search strategy (i.e. if these papers were returned in a particular search it confirmed the effectiveness of the search). The final search strategy used a range of search terms for the concepts ‘remediation’, ‘performance’ and ‘doctors’, which were combined using the AND Boolean operator (see Appendix 1).
The following databases were searched on 4 June 2018: MEDLINE (via Ovid), EMBASE (via Ovid), PsycINFO (via Ovid), Health Management Information Consortium (HMIC) (via Ovid), Cumulative Index to Nursing and Allied Health Literature (CINAHL) (via EBSCOhost), Education Resources Information Center (ERIC) (via EBSCOhost), Applied Social Sciences Index and Abstracts (ASSIA) (via ProQuest) and Database of Abstracts of Reviews of Effects (DARE) (via the Centre for Reviews and Dissemination). The search syntax and indexing terms were amended where needed from the original MEDLINE for use in these databases.
The search results were exported to EndNote X7 (Clarivate Analytics, Philadelphia, PA, USA) and deduplicated using the ‘find duplicates’ function. The search strategies for the main database search are reproduced in full in Appendix 1.
Inclusion criteria
The following inclusion criteria were applied.
-
Aspect of remediation, including all documents that focus on the remediation of practising doctors. We defined remediation as ‘an intervention, or suite of interventions, required in response to assessment against threshold standards’. 37
-
Study design, including all study designs.
-
Types of setting, including all documents about primary or secondary care settings.
-
Types of participant, including all practising doctors. A practising doctor can be defined as a licensed doctor who has graduated from medical school and is practising medicine. Studies about only medical students were excluded.
-
Outcome measures, including all remediation-related outcome measures.
-
Language, including studies published in the English language.
-
Publication date, including all studies published up until June 2018.
Additional searches
Although we conducted a grey literature search in the main search using HMIC, following a discussion with our third stakeholder group, where some of the stakeholders highlighted the relevance of some key grey literature, we decided to do a subsequent search specifically to identify grey literature. Searches for grey literature were conducted on 25 June 2019. The following databases/websites were searched: Google Scholar, OpenGrey, NHS England, North Grey Literature Collection, National Institute for Health and Care Excellence Evidence, Electronic Theses Online Service, Health Systems Evidence and Turning Research into Practice. The databases were searched with free-text keywords and controlled vocabulary where appropriate, using terms such as remedi*, reskilling, and retraining, combined with the concept of doctors.
Citation searching was undertaken, including searches of the reference list of all included documents and ‘cited by’ searches of certain papers that were particularly rich in terms of building the programme theory. The ‘cited by’ searches were undertaken using Google Scholar. Stakeholders were also asked to identify any literature they thought relevant. Any literature identified through grey literature searching, citation searching and via stakeholders that satisfied the inclusion criteria were included in the review.
The supplementary searches were purposive and undertaken on an ad hoc basis, as and when more data were needed on specific theories regarding different aspects of our programme theory of how remediation is supposed to work (e.g. insight, dissonance, psychological safety, feedback and behaviour change). Google Scholar was searched using topic keywords. Once relevant references were found, backwards and forwards citation searching techniques were used to identify further relevant papers.
Step 3: article selection
Documents were selected based on relevance (i.e. whether or not data can contribute to theory development and refinement). 38 We did not assess the rigour of the included studies, as we had already established from previous systematic reviews on remediation that existing literature was of poor quality. An initial random sample of 10% was assessed and discussed by TP and NB to ensure that selection decisions were made consistently. TP then screened all the remaining titles and abstracts to ensure that they matched the inclusion and exclusion criteria. A 10% random sample was reviewed independently by NB to ensure consistency around the application of the inclusion criteria. Very few inconsistencies were identified, and these were resolved through discussion. All of the screening was carried out in Rayyan. Rayyan is a free web application designed to help reviewers manage the screening process. If TP was uncertain over the relevance of an article, then it was initially discussed with NB. If it was still unresolved after discussion with NB, then it was discussed with the review team. The full texts of included articles were screened again using the inclusion and exclusion criteria. Again, a 10% random subsample was reviewed independently by NB to ensure consistency around the application of the inclusion criteria. No inconsistencies were identified. The results were screened in alphabetical order. TP read all of the included papers and ultimately included all documents or studies that contributed to the development of some part of the programme theory.
Grey literature searches were exported into a Microsoft Word document (Microsoft Corporation, Redmond, WA, USA) and screened in Word by TP. NB carried out a 10% check to ensure consistency in article selection.
Step 4: extracting and organising data
Once article selection was complete, TP uploaded the electronic versions of the included articles into NVivo 12 (QSR International, Warrington, UK) for further analysis. Articles were coded in alphabetical order. The coding concentrated on the conceptual level of the data, categorising content into analytical categories to enable these to be refined further. Therefore, we did not code the data in terms of context, mechanisms and outcomes at this stage, but approached coding with an open mind to understand what themes were emerging from the data. Initial coding categories included barriers to and facilitators of remediation, strategies employed by remediation programmes and processes engendering change. Coding was both inductive (i.e. the codes were identified from analysing the literature) and deductive (i.e. the codes generated were informed by the initial programme theory, stakeholder group discussions and exploratory literature searches). For example, insight was identified as an important theme in the first stakeholder meeting and was present in some of the literature. However, the way that insight was described by the stakeholder group covered a wider range of subthemes than used specifically in the literature under the term ‘insight’. We therefore went back to the literature to look for data on processes related to the way in which our stakeholder group had described the concept of insight.
When conceptual coding was complete, we began to consider whether or not the categories (or subcategories within them) contained data that could be identified as contexts, mechanisms and outcomes. In other words, we applied a realist logic of analysis to make sense of the data (see Step 5: synthesising evidence and drawing conclusions). Initially, we focused on the returned literature that was richest in terms of theoretical depth. This allowed us to build context–mechanism–outcome configurations (CMOcs) that could be tested with the data from the wider literature.
To develop and test (i.e. confirm, refute or refine) the CMOcs, TP presented the CMOcs in narrative form on a Word document, along with extracted data to support the CMOcs plus a descriptive explanation of each CMOc. These CMOcs were examined by the review team and further refined. CMOc development was conducted using a realist logic of analysis, whereby we first considered the outcomes (intermediate and/or final desired) that had been identified in the literature and by our stakeholder group, and then worked backwards (using retroduction where needed) to infer the mechanisms that might generate the outcome, and the contexts created by the remedial intervention that might trigger the mechanism. In most cases, although the mechanisms were sometimes alluded to, they were not directly referred to in the literature itself. In these cases, the review team would suggest mechanisms that offered a potential ‘fit’ with the data. At this point, we conducted further supplementary searches to examine the literature relating to these mechanisms and to test whether or not they offered a viable explanation in the CMOc. In some cases, mechanisms were derived from substantive theory (the role of which is described in Use of substantive theory).
Throughout this process of CMOc development, we compared the CMOcs with the evolving programme theory. The programme theory was updated periodically by TP, presented in diagrammatic form with accompanying narrative explanation and discussed at review team meetings. It was important to consider the relationship between the CMOcs and the programme theory. Although, for the main part, the CMOcs would inform the shape of the programme theory, its overall shape enabled us to consider other potentially important outcomes that required further investigation. It also enabled us to consider the linkage between CMOcs and the sequence of intermediate outcomes.
Throughout the review, the programme theory was iteratively refined based on our interpretations of the data included in the literature. The characteristics of the documents were extracted into a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheet separately for the results of the main search and the supplementary searches (see Appendices 2 and 3).
Step 5: synthesising evidence and drawing conclusions
A realist logic of analysis was used to interrogate the data and develop and test the initial programme theory, which we used to explain what it is about remediation of doctors that works and for whom, in what circumstances and respect, and why. To develop, refine and test the programme theory, we moved between the data (as extracted and coded in NVivo and Word documents) and the analysis, advice and feedback offered by the review team and the stakeholder group. To operationalise a realist logic of analysis, we asked these questions of our data (Box 1).
Are the contents of a section of text within an included article referring to data that might be relevant to programme theory development?
Judgements about trustworthiness and rigourAre these data sufficiently trustworthy to warrant making changes to the programme theory?
Interpretation of meaningIf the section of text is relevant and trustworthy enough, does its contents provide data that may be interpreted as being context, mechanism or outcome?
Interpretations and judgements about CMOcsWhat is the CMOc (partial or complete) for the data?
Are there data to inform CMOcs contained within this article or another included article? If so, which other article?
How does this CMOc relate to CMOcs that have already been developed?
Interpretations and judgements about programme theoryHow does this (full or partial) CMOc relate to the programme theory?
Within this same article, are there data that inform how the CMOc relates to the programme theory? If not, are there data in other articles? Which ones?
In the light of this CMOc and any supporting data, does the programme theory need to be changed?
Reproduced with permission from Papoutsi et al. 39 Contains information licensed under the Non-Commercial Government Licence v2.0.
Throughout the review, we moved iteratively between the analysis of examples, refinement of programme theory and further iterative searching for data to test specific parts of the programme theory. The final realist programme theory is presented in a diagram and through a narrative description of CMOcs.
As mechanisms were often hidden or not articulated very well, we used retroductive reasoning (see Glossary) to infer and elaborate on the mechanisms. Retroductive analyses are analytical processes that seek to identify the hidden causal processes that lie beneath identified patterns or changes in those patterns. 39 Therefore, our approach involved repeatedly going from data to theory, to refine explanations about the occurrence of certain behaviours. We tried to construct these explanations at a level of abstraction that would encompass a range of phenomena or patterns of behaviour.
We tried to identify relationships between contexts, mechanisms and outcomes within individual studies, but also across different sources (i.e. inferred mechanisms from one study could help explain the way contexts influenced outcomes in another study). The synthesis of data from different sources was often required to compile CMOcs, as not all parts of the configurations were always present in the same source.
In summary, the process of evidence synthesis was achieved by the following analytical processes:
-
juxtaposition of sources of evidence (i.e. where evidence about behaviour change in one source allows insights into evidence about outcomes in another source)
-
reconciling of sources of evidence (e.g. when results differ in similar situations, these are further examined to find explanations for these differences)
-
consolidation of sources of evidence (i.e. where different outcomes occur in similar contexts, reasons can be developed as to how and why these outcomes happen differently).
Use of substantive theory
In realist reviews, a substantive theory is an existing and established theory within a particular subject area that describes patterns of behaviours at a greater level of abstraction from the intervention than is the aim of a realist review. 35 A substantive theory can help to make sense of emerging CMOc patterns and, therefore, aid in their development and/or may be used to provide an analogy (i.e. situate the causal explanation provided by the CMOcs with what is already known from existing research).
In some cases, substantive theories, particularly related to behaviour change, were cited or alluded to in the returned papers. However, much of the literature was not very theoretically rich. In these instances, substantive theory drawn from outside the returned literature became an important component in CMOc development. Some of the theories that informed the development of the programme theory related to the way in which remediation was conceptualised. Early in the review, through discussions among the review team and the stakeholder group, we began to conceptualise remediation as practice change, rather than an educational process. This drew us to theories of behaviour change to help make sense of the intermediate outcomes in the remediation process. In other cases, substantive theory would be drawn from previous realist research that considered interventions with similar contexts.
Chapter 3 Results
Results of the review
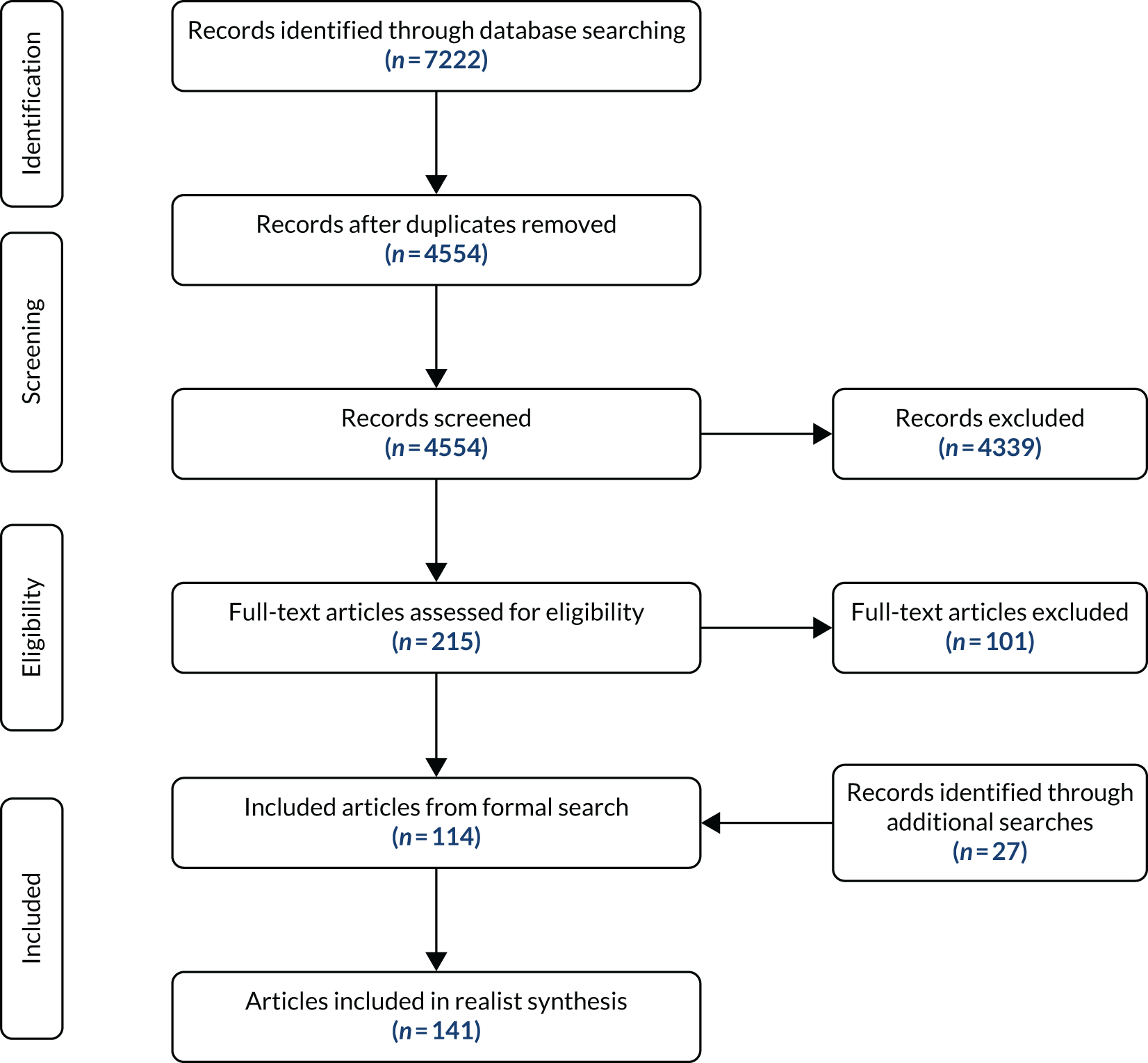
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram (Figure 2) reports the number of studies identified, included and excluded. A description of the characteristics of the included studies is available in Appendices 3–7. The main search returned 4554 articles. Of these articles, 114 were included in the review. A further 27 articles were returned from the additional searches (i.e. citation searches, grey literature searches, requests to stakeholders and supplementary searches).
FIGURE 2.
The PRISMA flow diagram. Reproduced with permission from Price et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.
Study characteristics
Of the 141 studies included in the review, 64% related to North America, with 14% coming from the UK. The majority of studies were published between 2008 and 2018 (72%). Forty per cent of the articles were commentaries, 37% were research papers and 31% were case studies. Of the research papers, 64% were quantitative, 19% were literature reviews and 14% were qualitative. Forty per cent of the articles were about junior doctors/residents and 31% were about practising physicians, whereas 17% were a mixture of both (with some including medical students). Forty per cent of studies focused on remediating all areas of clinical practice, including medical knowledge, clinical skills and professionalism. Twenty-seven per cent of studies focused on only professionalism and 19% focused on knowledge and/or clinical skills. Thirty-two per cent of studies described a remediation intervention, 16% outlined strategies for designing remediation programmes and 11% outlined remediation models. Appendices 3–7 provide a more in-depth overview of the characteristics of the included studies.
Conceptualisation of remediation and implication for the review
The purpose of this review is to gain a better understanding of what is working in remediation programmes to produce their effects. There is already an extensive literature on how doctors or trainees learn at different stages of their career, but remediation is a particular type of intervention, describing the process by which doctors are returned to safe levels of practice after having fallen below accepted standards. We decided in the early review meetings that the most useful approach to focus our review was to start to identify what was unique about remediation compared with, for example, medical education or, indeed, education more generally.
Remediation is, by definition, concerned with rectifying underperformance or poor behaviour. In the case of medicine, a remedial intervention is linked to a judgement on an individual’s fitness to practise medicine safely (i.e. relating to threshold standards of competence). This link between performance standards and patient safety associates remediation with failure, because the safe practice of medicine is the sine qua non of the medical profession. 8,40,41 However, at the same time, implicit in the term ‘remediation’ itself and the process it describes is the potential for remedy. 8 Therefore, remediation is conceptually nebulous. A study of stakeholders involved in remediation in Canada revealed that they held a dual conceptualisation of remediation (i.e. remediation was understood as both an educational and a regulatory intervention). 13 This latter conceptualisation directly links to the inherent association between remediation and the minimum standards required for practice. Remediation may be seen as a direct threat to professional practice, which is a particular challenge as it discourages doctors from self-identifying as needing help and engaging with remediation processes at an early stage.
In this sense, these interventions ‘work’ when they can create the opportunities and resources to overcome the barriers that are unique to remediation. Some of the more theoretically rich literature, combined with early discussions with stakeholders, led us to conceptualise remediation not so much as an educational intervention, but a change in practice and behaviours that would influence the learning experience. Reference to behaviour change theory early in the review, combined with stakeholder and review team discussions, enabled us to tease out the various outcomes that were relevant to CMOc building.
This conceptualisation has informed the development of the programme theory and, therefore, the structure of the way in which the results are reported here. Although remediation is by no means a linear process, there is a logical sequence whereby certain outcomes would precede others. Accordingly, the results are grouped into three categories, based around the kinds of outcome that occur at these stages in a remediation process: (1) insight, (2) motivation and (3) practice change. Within these three broad categories, the results are organised around the intervention strategies that are used to facilitate these outcomes.
Despite the logical sequence of the outcomes, it is important to emphasise that, early on, we identified remediation as a non-linear and an iterative process. For example, although a degree of insight into the nature of a problem may be an important outcome that precedes a remediating doctor from being motivated to change, insight can further develop all the way through a remediation programme.
The results are presented here in such a way as to ensure that they are both accessible and academically robust. Each section begins with a narrative explanation of how the different parts of the remediation process work to produce a particular outcome. This is then followed by a realist explanation in the form of a series of CMOcs, alongside a comprehensive explanation of the evidence base underpinning the CMOcs. The realist explanations for the CMOcs will include reference to substantive theory, where necessary. The purpose of structuring the findings in this way is so that the findings can be read and understood without having to read the realist explanations. The realist explanations of how we arrived at those findings are important for transparency. To provide a full and coherent explanation of our findings, there are elements of discussion in this chapter.
Summary of CMOcs
Table 2 provides a summary of the 29 CMOcs identified through our research in their three main clusters. This constitutes our final programme theory. The programme theory is also presented graphically in Figure 3.
| Cluster/CMOc | Summary |
|---|---|
| Insight | |
| Providing safe spaces and using advocacy to develop trust in the remediation process | |
| CMOc 1 | When a remediating doctor fears the consequences of remediation or does not trust the remediation process (C), an environment of trust will not develop (O) because they do not feel psychologically safe (M). An intervention strategy that can be used to change this context is the provision of a safe space where issues can be discussed in confidence |
| CMOc 2 | When a remediating doctor feels that their discussions are confidential and is able to express any negative emotions they feel (C), they will be more likely to feel psychologically safe (M), leading to an environment of trust (O) and a readiness to explore perceptions of their performance (O) |
| CMOc 3 | When a remediating doctor experiences empathy and positive regard (C), psychological safety is invoked (M), leading to a trusting relationship (O) and a readiness to explore perceptions of their performance (O). Advocacy may be used as an intervention strategy to provide opportunities for the remediating doctor to experience empathy and positive regard |
| CMOc 4 | If a remediating doctor has their motivations validated (C) then this may invoke psychological safety (M), leading to an environment of trust (O) and a readiness to explore others’ perceptions of their performance (O). An intervention strategy that may be used to provide validation is advocacy, where the advocate can acknowledge the motivations of the remediating doctor and their dedication. The role of an advocate may be most effective when the advocate has no role in the summative judgements about the remediating doctor |
| Framing feedback 1: juxtaposition | |
| CMOc 5 | When a remediating doctor’s perceptions of good practice/behaviour are juxtaposed against data on their actual practice/behaviour (C) then this may lead to an uncomfortable professional dissonance (M), which, in turn, invokes an acceptance of the need to change (O) |
| Framing feedback 2: specific data from different sources | |
| CMOc 6 | When feedback contains specific performance data and/or clear examples of reported behaviours, and is derived from a number of different sources (C), it is more likely to be validated by the remediating doctor (M), leading to an awareness of the discrepancy between perceived and actual performance or behaviours (O) |
| CMOc 7 | When a remediating doctor accepts that their perceptions of their performance or behaviours are not the same as their actual performance or behaviour (C), dissonance (M) leads to an acceptance of the need to change (O) |
| CMOc 8 | When feedback is perceived as a generalised judgement about an individual doctor, the remediating doctor is more likely to be defensive (C) and, therefore, go into denial (M), leading to rejection of the feedback (O) and/or rejection of the standards to which that feedback pertains (O) |
| Framing feedback 3: affirmation, normative frameworks and feedback standard discrepancy | |
| CMOc 9 | When a remediating doctor perceives remediation to be a threat to their career or their professional identity (C) then they may deny either the veracity of the feedback itself or the standard to which they are being held (M), leading to non-engagement in the programme (O) or superficial engagement (O) |
| CMOc 10 | If a coach or mentor is able to affirm a remediating doctor’s strengths and offer perspective (C) then the doctor is more likely to accept negative feedback (O) because they have received professional affirmation (M) |
| CMOc 11 | If feedback data are presented in a way that makes the problem seem manageable (C) then dissonance (M) may lead to the doctor accepting the need to change performance or behaviours (O). Intervention strategies that make issues seem manageable include affirming prior achievements, breaking up issues into manageable chunks and setting realistic goals |
| CMOc 12 | If feedback is framed in terms of a remediating doctor’s professional values (C) then a mechanism of normative enticement (M) may lead to accepting the need to change (O) |
| CMOc 13 | In the context of a remediating doctor who accepts that there is a performance issue but does not receive validation of their professional motives/unconditional positive regard/affirmation of their professional identity (C) then identity dissonance (M) may lead to rejection of medical professional identity (O) |
| Motivation | |
| Involving the remediating doctor in remediation planning | |
| CMOc 14 | If the remediating doctor has a role in planning aspects of the remediation process (C) then they may perceive that they have some control over the process (perceived agency) (M) and be intrinsically motivated to change (O) |
| CMOc 15 | When a remediating doctor rejects their professional identity (C) then they lack the motivation to change (O) because of normative rejection (M). Intervention strategies that can mitigate against a loss of professional identity include maintaining a degree of autonomy for the remediating doctor in the remediation programme |
| Correcting causal attribution | |
| CMOc 16 | When the remediating doctor is able to identify those aspects of their performance or behaviour that have caused problems that they can change (C) then they have more perceived control over the process (M), leading to greater motivation to engage (O) |
| CMOc 17 | When a remediating doctor is given specific strategies for learning or behaving (C) then, because of improved self-efficacy (M), they have greater motivation (O) |
| CMOc 18 | When a remediating doctor explores their own emotional triggers (C) then they are less likely to react to these triggers (O) because they are self-aware (M) |
| Goal-setting | |
| CMOc 19 | When the remediating doctor has a clear goal and a realistic sense that a goal is achievable (C) then they may have greater belief in their own ability to achieve these goals (self-efficacy) (M), which may lead to more motivation to change (O). Interventions that may create this context include SMART goal-setting strategies |
| Destigmatising remediation | |
| CMOc 20 | When the process of remediation is reframed in a more positive light (C) then the remediating doctor feels more psychologically safe (M), leading to greater motivation to engage in the programme (O) |
| CMOc 21 | When remediation is framed as punishment (C) and/or when a community of practice stigmatises those who have to be remediated (C) then the remediating doctor may feel alienated from their peers (M), leading to a sense of isolation (O) |
| CMOc 22 | When a doctor feels isolated from their peers (C) then normative rejection (M) may lead to a lack of motivation to change (O). Remediating in groups and/or networking with peers undergoing remediation may lessen the sense of isolation |
| Clarity of consequence | |
| CMOc 23 | When a remediating doctor understands the consequences of not changing their behaviour or improving performance (C) then they may be able to evaluate the costs and benefits of change (M), and may be motivated to engage with remediation (O) or change their goal (O) |
| Facilitating practice change | |
| Practising new behaviours/skills | |
| CMOc 24 | With repeated performance of correct behaviours or skills (C), performance or behaviour improves (O) because of repetition (i.e. practice) (M). This practice can be in situ if appropriate, but can be simulated if needed |
| CMOc 25 | When repeated performance is accompanied by appropriate feedback and guided reflection (C) then positive improvements are more likely (O) because the remediating doctor is able to integrate new knowledge and experiences into their learning (M) |
| Guided reflection | |
| CMOc 26 | When a remediating doctor has been guided through what the feedback means (C) then they are more likely to engage with the feedback (O) because it makes sense to them (M). Intervention strategies that may help to bring this about include regular face-to-face meetings and open reflective questioning from a trained coach |
| CMOc 27 | When feedback makes sense to a remediating doctor (C), dissonance is more likely to be invoked (M), leading to the remediating doctor gaining further insight into their performance or behaviours (O) |
| CMOc 28 | When the process of reflection is guided by someone from outside the remediating doctor’s employing organisation (C) then the feedback will be perceived as less threatening (M), leading to more meaningful reflection (O) |
| CMOc 29 | When a remediating doctor is allowed to develop and keep a reflective log that is meaningful to them (C), they have the opportunity to integrate their new learning and experiences (M), leading to insight into their own progress (O) and sustained changes in performance or behaviour (O). This may work best when the reflective logs are not assessed, but when their completion is nonetheless verified |
Facilitating remediation: developing insight
Based on our analysis and interpretation of the data, a remediating doctor must have insight for remediation to be successful. If they do not have insight going into remediation, then the remediation programme must work to help them develop insight. Insight is mentioned in a number of the returned papers,7,40,42–50 but two papers,42,43 in particular, have been useful in conceptualising insight in the context of remediation. Hays et al. 43 note that the term insight has been poorly defined in the setting of medical education, and that, in this setting, insight may be a combination of awareness of one’s own and others’ performance and the capacity to reflect. Brown et al. 42 discuss insight as a readiness to explore, intellectually and emotionally, our own and others’ thoughts and behaviours. Taken together, and considering the unique circumstances surrounding remediation, insight can be understood as comprising two different aspects, which we have used to help delineate some of the outcomes of the remediation processes in this review:
-
a readiness to explore others’ perceptions of one’s own behaviour or performance, and to validate those perceptions
-
acceptance that one’s own performance or behaviour is divergent from accepted standards.
Providing safe spaces and using advocacy to develop trust in the remediation process
As remediation is a threat to a doctor’s professional identity, and may also be perceived as a threat to their career, feelings such as anger and mistrust may prevent a doctor from even engaging with negative feedback on their performance or behaviour. 51 A recurring theme in the literature is that a remediating doctor is more likely to be ready to explore and to validate others’ perceptions of their behaviour or performance if they have trust in the people involved in remediation and trust in the process of remediation itself.
The actual word ‘trust’, although used on occasion,52,53 does not appear frequently in the returned literature. However, the idea of developing trusting relationships is implicit in a number of papers. 49,50,52,54–62 Trust also emerged as an important theme in the stakeholder meetings. To develop this relationship, the literature points to features of remediation programmes that might bring about trust. In particular, the literature noted the importance of developing safe spaces and using advocacy to engender trusting relationships.
The literature describes the need to create a ‘safe space’ in which a confidential discussion can take place, without fear of sanction or judgement. 49,52,54,55,57–62 A safe space is important because remediating doctors usually fear the consequences of being identified as needing remediation. One aspect of creating a safe space is to provide assurance of confidentiality. The literature refers to conversations in a remediation process that are not only confidential, but allow the remediating doctor the opportunity to express negative emotions, such as anger and shame, that might be invoked by being identified as needing remediation. 44,54 Our stakeholders suggested that this provision of confidentiality may also facilitate the remediating doctor to express any mental health issues that may not have come to light.
Trust can also be developed through building personal relationships during the process of remediation. Sometimes, such a relationship is described in the context of a coaching model53–56,59,60,63–66 and elsewhere in terms of a mentoring programme. 44,48,49,55,63,67–75 Regardless of the term used, a key focus in the literature is that someone in the remediation programme takes on the role of being an advocate for the remediating doctor.
Advocacy is described as offering ‘unconditional positive regard’76 in the context of a one-to-one relationship in a remediation programme. Empathy and validation are key to this role,75 which has been described as a ‘therapeutic relationship’. 77 In practice, this may mean empathising on specific issues, such as working conditions being very challenging, and acknowledging that others have similar struggles,55 or that behavioural norms have changed since the remediating doctor did their training. 76 Shapiro et al. 53 point to the importance of validating a doctor’s good motivations, even if the ultimate goal is to reach a point where the remediating doctor understands that they were not acting in a way that was compatible with this motive. 53
The person performing this advocacy role may be a senior doctor76 or a peer55,71 in a role labelled as either coach, mentor or other. A key point noted in a number of papers is that advocacy is deemed to be most effective when the individual fulfilling this function has no role in the summative evaluation of the remediating doctor or the final outcome of the process. 54,56,76 The advocate does not necessarily have to be intimately involved with the delivery of the remediation programme, but should be familiar with the case. 78 Our stakeholders suggested that this individual should be someone who is chosen by the doctor. Having this supportive relationship and non-judgemental encouragement allows for trust to develop, which, in turn, means that the remediating doctor is more likely to engage in the process and be ready to explore concerns about their performance or behaviour.
Realist analysis of providing safe spaces and using advocacy to develop trust in the remediation process
Extract 1 (Box 2) is typical of the way in which insight is addressed in the literature (i.e. a lack of insight is a barrier to remediation, but is potentially remediable). The emphasis on the importance of insight was mirrored in the stakeholder group discussions, in which a lack of insight was unequivocally associated with failure in remediation. The link between establishing safe spaces because of the reactions and vulnerability of the remediating doctor is drawn from data such as those in extracts 2–6 (see Box 2) and was verified explicitly in the stakeholder group discussions. The stakeholder group, both within meetings and in later e-mail exchanges, also emphasised the importance of trust as an important outcome when someone feels psychologically safe.
1. Paice:46
The question of insight is one that tends to come up whenever underperformance is discussed . . . studies on this phenomenon have shown that when offered extra training in the activity concerned the poor performers improve . . . This research suggests that lack of insight . . . [is] not an unsurmountable obstacle to remediation.
2. Egener:76
Confidentiality is critical to the physician/client’s honest disclosure of events and his or her personal reactions to those events.
3. Kalet et al. :54
It [coaching relationships] allows a safe space for a learner to express vulnerable emotions such as anger, shame, sadness, or to explain cultural issues that may have arisen. These issues generally must be recognized and validated before the majority of remediation can occur.
4. Kimatian and Lloyd:44
A compassionate and empathetic approach to the remediation process should include an opportunity for the resident to have a frank, honest, and private discussion with a trusted mentor, advisor, or objective coach or counselor.
5. Samenow et al. :79
The priority of the program’s first day is to create a safe environment conducive to transformative learning. Ground rules, including confidentiality, are established.
6. Shapiro et al. :53
In developing a system for reporting, evaluating, and responding to professionalism lapses, we created a process that is confidential, centralized, clear, and respectful.
7. Shapiro et al. :41
Denial is often based on a profound fear of the external and internal consequences of accepting the judgement of others. Thus it is important to create an environment that is as psychologically safe for the resident as possible.
8. Whiteman and Jamieson:49
We start by discussing their situation and exploring their narrative account, trying to harness the work done in their last GP appraisal – often viewed in a positive light as a piece of work done by a non-judgemental peer.
9. Papadakis et al. :58
The core message of this [first] meeting is: ‘We have important feedback that you need to hear . . . We value you, and we want to support you in your efforts to change’.
10. Paglia and Frishman:80
For a concerned programme director, denial that there is even a problem is often the major barrier to assisting a resident in the process of remediation. One way to circumvent denial is to provide a safe environment.
11. Egener:76
While the process is framed as education, in truth it is a therapeutic relationship, not unlike the patient–physician relationship. Empathy, genuineness, and unconditional positive regard are the most transformative elements of such relationships.
12. Mar et al. :71
The events leading to the decision for the need of and the conduct of a remediation plan are likely to involve some element of controversy. The resultant stress may be mitigated by the presence of an advocate at any meetings with the resident, by ensuring a fair process.
13. Smith et al. :78
The resident is under stress during this process and benefits from general encouragement in efforts to improve from the cheerleaders.
14. Sargeant et al. :55
To his surprise, as he talks with the facilitator and shares his dismay at these results and his frustration about not being able to do anything, he finds that the facilitator understands his perspectives and confirms that he is not alone – others feel this way, too.
15. Egener:76
The physician/consultant [person acting as coach or mentor] validated his sense of unfairness at having to change behavior that had previously been tolerated.
16. Kalet et al. :54
It is worth the effort to identify a ‘neutral party’ to conduct at least some of the remediation so that program leaders are freer to make difficult decisions if need be . . . it ensures that the learner can develop in a safe environment without threat of high stakes reprisal.
17. Warburton and Mahan:56
We advocate use of the term coaching to signify a process by which a struggling trainee receives individualized mentorship and guidance from an individual who is committed to his/her success and is not directly involved in his/her reassessment.
18. Egener:76
The consultant assumes the roles of coach, mentor, or teacher, but for several reasons the referring source must remain the sole evaluator of success.
19. Shearer et al. :47
Most institutions implemented some form of mentorship program for residents in remediation. It was commonly specified that a mentor . . . must be someone who would not play an evaluative role with the resident.
Therefore, CMOc 1 establishes the context that remediation is feared by those who engage in the process and that they will not engage if they do not feel psychologically safe (Table 3). CMOcs 2–4 refer to the role of psychological safety as a generative mechanism that leads to outcomes of trust and, because there is trust, a readiness to explore performance or behavioural concerns. Only one paper41 that was returned in the remediation literature search explicitly mentions psychological safety (see Box 2, extract 7). Psychological safety was examined as a concept at the suggestion of a member of the review team. We subsequently conducted a supplementary literature search to examine whether or not the concept was appropriate to help understand the causal mechanisms at work in building trusting relationships.
| CMOc | Description |
|---|---|
| 1 | When a remediating doctor fears the consequences of remediation or does not trust the remediation process (C), an environment of trust will not develop (O) because they do not feel psychologically safe (M). An intervention strategy that can be used to change this context is the provision of a safe space where issues can be discussed in confidence |
| 2 | When a remediating doctor feels that their discussions are confidential and is able to express any negative emotions they feel (C), they will be more likely to feel psychologically safe (M), leading to an environment of trust (O) and a readiness to explore perceptions of their performance (O) |
| 3 | When a remediating doctor experiences empathy and positive regard (C), psychological safety is invoked (M), leading to a trusting relationship (O) and a readiness to explore perceptions of their performance (O). Advocacy may be used as an intervention strategy to provide opportunities for the remediating doctor to experience empathy and positive regard |
| 4 | If a remediating doctor has their motivations validated (C) then this may invoke psychological safety (M), leading to an environment of trust (O) and a readiness to explore others’ perceptions of their performance (O). An intervention strategy that may be used to provide validation is advocacy, where the advocate can acknowledge the motivations of the remediating doctor and their dedication. The role of an advocate may be most effective when the advocate has no role in the summative judgements about the remediating doctor |
The literature returned in the supplementary search showed that psychological safety was specifically concerned with developing trust within the contexts where perceptions of risk and fear are prevalent. Extract 3 (Box 3), from the most recent study83 we could find on psychological safety in medical education, also discusses its importance in relation to building relationships of trust. This focus on overcoming perceptions of risk and threat is well suited to the environment of remediation and provides a credible explanation of how intervention strategies can create the contexts that lead to trusting relationships in a remediation programme, in turn leading to a readiness to explore a problem. As a mechanism, psychological safety describes a process in which the opportunities and resources provided by the programme (i.e. the provision of a safe space and the advocacy role) alter the reasoning of individuals, enabling them to take the psychological risk of exploring their performance or behaviour.
1. Newman et al. :81
[Psychological safety is] the degree to which people view the environment as conducive to interpersonally risky behaviours.
2. Edmondson et al. :82
Psychological safety today is seen as especially important for enabling learning and change in contexts characterized by high stakes, complexity, and essential human interactions, such as hospital operating rooms . . . psychological safety plays a vital role in helping people overcome barriers to learning and change in interpersonally challenging work environments.
3. Tsuei et al.:83
PS [psychological safety] appeared to free them to focus on learning in the present moment without considering the consequences for their image in the eyes of others. Feeling safe also seemed to facilitate relationship building with the mentors.
These CMOcs identify the different contexts that can facilitate psychological safety, including a confidential and safe space for discussion and support provided by advocacy. Some papers note that part of this advocacy role may be acknowledging a doctor’s intentions and professional motives. Extracts 8–15 (see Box 2) imply that a more psychologically safe environment can be created with such validation, and this has informed the contexts noted in CMOc 2.
For CMOcs 3 and 4, we assert that the advocacy role may be most effective when this individual has no role in summative judgements about the performance of the doctor, and this point is explicitly noted in the literature (see Box 2, extracts 16–19). Although not developed in the literature, the notion of trust here offers a reasonable explanation (i.e. if someone is feeling judged then it is likely to be more difficult for them to build a trusting relationship and feel that they are being validated). This was also noted in stakeholder group discussions.
If a remediating doctor is ready to explore a potential behavioural or performance concern, and there is enough trust to validate others’ perceptions and judgements, a further aspect of developing insight is to accept the need to improve performance or change behaviour. 84 The acceptance comes when a remediating doctor realises that their behaviours or performance do not meet the standards that they consider to be important to the practice of medicine. However, as noted above, the fear and anger that accompany remediation may mean that, rather than accept these standards, a remediating doctor may just reject them or reject the feedback itself. Therefore, the important question is how can feedback be delivered in such a way that a remediating doctor accepts that they must improve their performance or change their behaviour?
Framing feedback 1: juxtaposition
One strategy is to use the remediation process to elicit the remediating doctor’s own ideas about what makes a good doctor, and then compare their own behaviours to these standards. One ethics remediation programme in the USA starts by asking all participants on the first day of the programme to describe the ‘ideal healer’. On the second day of the programme the participants describe their own actions and are presented with their previous ideals. 85,86 The authors expressly stated that the purpose of these programmes is to create a ‘professional dissonance’ or ‘ethical discomfort’85 that can be reconciled through an acceptance that the remediating doctor’s behaviour does not conform to the expectations of either the profession or the remediating doctor’s idea of what constitutes a good doctor. As these values come from the remediating doctor, rather than an external source, they may be perceived as being more authentic and less challengeable.
Acceptance may also occur when a remediating doctor’s own perceptions of their performance or behaviours are juxtaposed with the perceptions of trusted colleagues. Samenow et al. 79 describe a university hospital’s professional behaviours remediation programme. The first part of the programme for a referred doctor involves collecting feedback on behaviour from different members of staff. Similar to the aforementioned ethics remediation programme, the express purpose is to create a ‘disorientating dilemma’ where the remediating doctor contrasts their own perceptions of their behaviour with that of their colleagues. Another version of the juxtaposition strategy is to use video simulations in which actors act out unprofessional behaviours. The remediating doctor views a number of simulations, the last of which (unbeknown to them) has been specifically devised to show behaviours similar to their own behaviours. 65 Again, the purpose here seems to be contrasting their views on professional behaviours with their own behaviours.
Realist analysis of framing feedback using juxtaposition
Dissonance as a mechanism appears quite explicitly in the literature. In Box 4, extracts 2 and 3 discuss this in almost realist terms. In describing the disorientating dilemma or ethics discomfort that is induced through the strategy of juxtaposition, the authors offer a causal explanation of the way in which change can occur. This is based on the premise that the remediating doctor must accept the need to change performance or behaviour, which is noted or implied throughout much of the literature. This was also a continuing theme in stakeholder group discussions. Similarly, in extract 4, a process of guided reflection is used to enable the remediating doctor to compare their own actions with how they were perceived by others.
1. Caldicott and d’Oronzio:85
If the goal of the Program is to revitalize a commitment to the profession and reinforce its ethical values . . . the first two modules provide the experiential basis, ethical discomfort, and emotional energy for the undertaking. The task of the remaining five modules is to . . . create professional dissonance.
2. d’Oronzio:86
The contrast between knowing the idealized virtues and behaving in ways judged to be unprofessional creates a dramatic, dynamic tension.
3. Samenow et al. :79
The survey serves two purposes: to give objective feedback to physicians on how they are perceived, which they can then compare with their self-perceptions, and to monitor progress post intervention for as long as necessary.
4. Rumack et al. :87
We have found that some residents recognize such [unprofessional] behaviors only when they are videotaped and given directed feedback.
Context–mechanism–outcome configuration 5 (Table 4) describes the process whereby strategies that create this juxtaposition invoke change through dissonance. The outcome created here is the acceptance of the discrepancy between their own and acceptable behaviours.
| CMOc | Description |
|---|---|
| 5 | When a remediating doctor’s perceptions of good practice/behaviour are juxtaposed against data on their actual practice/behaviour (C) then this may lead to an uncomfortable professional dissonance (M), which, in turn, invokes an acceptance of the need to change (O) |
Framing feedback 2: specific data from different sources
Gaining insight from accepting feedback is important at all stages of remediation. Initial presentation of feedback may be part of what Papadakis et al. 58 have termed the ‘feedback conversation’. 58 As remediation progresses, feedback and reflection on new skills and progress will create more insight and more progress. Trust may then link into feedback, in that the remediating doctor may react more readily to the feedback received if they have a trusting relationship.
A frequently identified barrier to successful remediation is the negative emotions of the remediating doctor throughout the remediation process. 49,51 In the remediation environment, therefore, providing feedback does not mean that feedback will automatically effect behaviour change. 55 Rejecting feedback may be likely throughout remediation. One of the contexts that may lead to a rejection of feedback is when a doctor perceives that accepting the feedback is a threat to their career or their professional identity. 51 There are a number of strategies within the literature that are used to manipulate the context within remediation programmes to mitigate or ameliorate these emotional barriers to engaging in remediation.
A relatively common argument in the literature (and one that also arose in the stakeholder group) is that feedback needs to be as clear and as specific as possible so that it might not be so easily dismissed or discredited. In particular, the feedback should be articulated in ways that are unambiguous and objective. 52,63,65,71,88,89
This is particularly challenging when the issue is a behavioural one, as specific and direct feedback is difficult to gather. However, it is also particularly important, as receiving feedback that is non-specific may be interpreted by the remediating doctor as being victimised by the organisation or specific individuals within it. This raises the issue of the role of soft intelligence (i.e. an ear to the ground) within remediation programmes. The literature suggests that soft intelligence may be particularly useful in gaining a better understanding of the nature of performance or behavioural concerns and, therefore, help tailor a remediation programme appropriately. 50,52,56,66,67,69,73,79,87,89–93 However, such data may be less useful in invoking behaviour change for the participant, given the importance attached to specific and unambiguous feedback.
In addition to having specific data, remediating doctors are more likely to validate feedback when it is derived from multiple sources. 42,46,52,58,79 Although the reason for this is not really described in the literature, it seems logical that feedback is much more difficult to deny if it comes from a range of sources. Patient feedback may be particularly useful, as provision of safe and effective care is central to medical professional identity (see Framing feedback 3: affirmation, normative frameworks and feedback standard discrepancy).
Realist analysis of how specific feedback from different sources can lead to acceptance
Context–mechanism–outcome configuration 6 is derived from a substantial body of literature that suggests that feedback is more effective when it is specific (Table 5). This is clearly supported in Box 5, extracts 1–3, whereas extract 7 notes that feedback in the absence of specific data may be unconvincing. The importance of a variety of sources of feedback is noted in a number of the extracts (see Box 5) and was strongly supported in stakeholder group meetings. Validation describes a simple but important mechanism whereby, once the feedback is recognised as a legitimate and accurate description of behaviour, the remediating doctor will logically recognise the discrepancy between their own perceptions of their performance or behaviour, and others’ perceptions.
| CMOc | Description |
|---|---|
| 6 | When feedback contains specific performance data and/or clear examples of reported behaviours, and is derived from a number of different sources (C), it is more likely to be validated by the remediating doctor (M), leading to an awareness of the discrepancy between perceived and actual performance or behaviours (O) |
| 7 | When a remediating doctor accepts that their perceptions of their performance or behaviours are not the same as their actual performance or behaviours (C), dissonance (M) leads to an acceptance of the need to change (O) |
| 8 | When feedback is perceived as a generalised judgement about an individual doctor, the remediating doctor is more likely to be defensive (C) and therefore go into denial (M), leading to rejection of the feedback (O) and/or rejection of the standards to which that feedback pertains (O) |
1. Mar et al. :71
Specific comments from supervisors may also be quoted, as they provide concrete examples of suboptimal clinical performance or behavior.
2. Rougas et al. :52
This data should be objective and multifaceted – all available avenues for gathering specific, observable behaviors should be sought from other health professionals (nurses, social workers, pharmacists, physicians, etc.).
3. Liu et al. :93
. . . instead of informing a resident that he or she is ‘underperforming,’ the more specific ‘you are reading an average of five CT scans a day while your peers are averaging 10 per day’ clearly conveys the issue . . .
4. Paice:46
The decision that remedial training is necessary should be based on objective evidence from more than one source.
5. Roberts et al. :59
Our research suggests that nearly two-thirds of individuals who have demonstrated patterns of disruptive behavior and who are provided reliable data delivered in a respectful, non-judgmental way will respond.
6. Rumack et al. :87
We have found that some residents recognize such [unprofessional] behaviors only when they are videotaped and given directed feedback.
7. Bhatti et al. :67
. . . more than half of the problematic residents were identified through personal communication between a faculty member and the PD. Because no documentation or objective evaluation is available in many such cases, it may be difficult to convince residents of their deficiencies, and litigation is a possible consequence.
8. Papadakis et al. :58
The core message of this [first] meeting is: ‘We have important feedback that you need to hear. We have data from many sources that we can present to you . . . in a de-identified fashion with specific behavioral issues that you will need to change . . .’
9. Samenow et al. :79
The physician receives standardized objective feedback from colleagues, staff, and administrators that can then be compared with his or her own responses . . .
10. Brown et al. :42
The basic data are obtained from historical information regarding the individual provided by their employer, MSF, including self-assessment, psychometric profiling and the results of a semi-structured interview.
CT, computed tomography; MSF, multi-source feedback; PD, programme director.
In CMOc 7, this outcome of the gap between the remediating doctor’s perceptions and the actual behaviours or performance becomes the new context that triggers the mechanism of dissonance. CMOc 8 describes what happens when feedback is not framed in this way and therefore becomes perceived as a generalised judgement on the remediating doctor as a person. Denial (discussed in more detail in Realist analysis of framing feedback: affirmation, normative frameworks and feedback standard discrepancy) is the remediating doctor’s way of reconciling the uncomfortable professional dissonance they experience.
Framing feedback 3: affirmation, normative frameworks and feedback standard discrepancy
Having specific feedback from multiple sources may be important for that feedback to be validated, but it may not be enough, given the emotional barriers associated with engaging in remediation. The literature points to a number of other framing strategies. If a doctor gets feedback that does not fit with their professional identity, a state of acute identity dissonance may be alleviated only through denial of the feedback itself. 57 Some intervention strategies appear specifically directed at framing feedback in such a way that it protects the professional identity of a doctor being remediated, namely affirming the remediating doctor’s strengths, framing discordant data in accordance with relatable normative frameworks, and presenting feedback in a way in which the gap between actual and perceived standards is neither too big nor too small.
Affirming a remediating doctor’s strengths may increase the chances that any corresponding negative feedback is validated. 50,94,95 Moreover, care should be taken to ensure that the feedback is delivered in a way that is not judgemental or demeaning. 50 The important point here, as noted above, is that feedback that undermines a doctor’s professional identity may result in rejection of that feedback.
It may also be important to frame feedback according to norms that a doctor can relate to and that are congruent with their professional identity. For example, respect for colleagues may be a difficult normative reference to grasp if the remediating doctor thinks that they are motivated by appropriate norms. However, doctors may find it easier to relate to normative frameworks around patient safety. 52 In other words, if possible, it may be useful to ‘honor the intent’ of the remediating doctor, while pointing out that the behaviour poses safety risks. 53
In our stakeholder meetings there was discussion on the importance of framing feedback so that it seems manageable. It may be important to deliver feedback in a way that encourages perspective, conveying to the doctor that the issue to be addressed is one part of their practice and not their practice in its entirety. The discussions included suggestions that effective coaching can be used to remind a doctor that they have already achieved a great deal by getting through medical school and have proven themself to be a capable practitioner.
Realist analysis of framing feedback: affirmation, normative frameworks and feedback standard discrepancy
The context for CMOc 9 is the fear that characterises remediation (Table 6). Denial functions here as the mechanism, as it is a way for the remediating doctor to reconcile what we previously described as uncomfortable professional dissonance without accepting the feedback on their performance or behaviour. Citation searching from one of the returned papers96 pointed to some of the wider literature on denial in the medical education literature. This suggests that denial may take different forms (i.e. denial of the feedback or denial of the standards to which they are being held). This fits with the remediation literature, which discusses situations where there may be denial of the veracity of the feedback itself (i.e. ‘I don’t believe this feedback reflects my performance or behaviour’)55 or a denial of the standard, or even the values, of the profession to which those standards pertain. 57,96,97 Denial has been posited as a mechanism that explains non-engagement or superficial engagement with remediation. Box 6, extracts 1–4 offer examples of the different types of denial that might take place in remediation.
| CMOc | Description |
|---|---|
| 9 | When a remediating doctor perceives remediation to be a threat to their career or their professional identity (C) then they may deny either the veracity of the feedback itself or the standard to which they are being held (M), leading to non-engagement in the programme (O) or superficial engagement (O) |
| 10 | If a coach or mentor is able affirm a remediating doctor’s strengths and offer perspective (C) then the doctor is more likely to accept negative feedback (O) because they have received professional affirmation (M) |
| 11 | If feedback data are presented in a way that makes the problem seem manageable (C) then dissonance (M) may lead to the doctor accepting the need to change performance or behaviours (O). Intervention strategies that make issues seem manageable include affirming prior achievements, breaking up issues into manageable chunks and setting realistic goals |
| 12 | If feedback is framed in terms of a remediating doctor’s professional values (C) then a mechanism of normative enticement (M) may lead to accepting the need to change (O) |
| 13 | In the context of a remediating doctor who accepts that there is a performance issue but does not receive validation of their professional motives/unconditional positive regard/affirmation of their professional identity (C) then identity dissonance (M) may lead to rejection of medical professional identity (O) |
1. Nelson:98
The process will likely provoke a disagreeable response in many physicians . . . They may conclude they have been unfairly evaluated . . . or even that other motives are at work in the peer review process . . . the physician may agree to remediation but remain emotionally and intellectually resistant.
2. Shapiro et al. :41
Denial is often based on a profound fear of the external and internal consequences of accepting the judgement of others.
3. Kimatian and Lloyd:44
This allows participants to accept parts of the evaluation that are consistent with ego preservation, while rejecting aspects that challenge their sense of self.
4. Arnold et al. :57
Identity dissonance is a mechanism that causes some individuals to restructure their identity, much like cognitive disequilibrium functions for constructivists. Others who experience identity dissonance may actively reject the professional identity being imposed by the community of practice.
Affirming strengths
5. Hickson et al. :99
Such encounters must be followed, if possible, by an expressed appreciation for the colleague’s contribution to the team. The colleague’s reaction to this discussion may include anger, denial, or rationalization.
6. Grant:100
There [should be] full acknowledgement of accomplishments and improvements.
7. Hanna et al. :95
Strengths and weaknesses were outlined, and all physicians were encouraged to undertake an ongoing program of self-study.
Relatable normative frameworks
8. Rougas et al. :52
In order to make feedback relevant to the learner’s context, medical educators often require innovative ways to connect lapses in professionalism to relevant issues such as patient safety, quality metrics, reimbursement, and promotion. This places the lapse within a context that learners can relate to.
9. Shapiro et al. :53
For example, if the discussion reveals that the FP [Dr. Jones] raises his voice and criticizes his team because he is trying to advocate for his patients, the feedback provider can honor that intent and point out that such behavior actually represents a risk to his patients.
FP, focus person.
Context–mechanism–outcome configuration 10 explains that affirmation, which has been identified as a mechanism in other realist research on doctor performance,101 may be a process that helps protect professional identity. This was discussed in the stakeholder group and is supported by Box 6, extracts 5–7, which suggest that some positive feedback, and affirmation of a remediating doctor’s strengths, can be helpful in remediation. This is a tentative CMOc, as the literature does not discuss this in much detail.
Context–mechanism–outcome configuration 11 concerns the degree of variance in feedback. This was informed by stakeholder group discussions on the need to make remediation seem ‘manageable’ and to deliver feedback in a way that did not make the process seem overwhelming. In the wider literature on feedback, the gap between the data provided in the feedback and the accepted standards is known as the ‘feedback-standard discrepancy’. 96 Again, the use of coaches and advocacy may be important in conveying this. This links to CMOc 6, where specific feedback is important because it is less likely to be seen as a generalised judgement about a doctor’s performance and more likely to allow for the identification of achievable improvements. If a remediating doctor feels that the remediation is manageable, then the mechanism of dissonance, rather than denial, is more likely to be triggered.
Context–mechanism–outcome configuration 12 develops a causal explanation for how a doctor can be motivated to align their performance or behaviours with those of the profession, when feedback is framed in such a way that aligns with their values. Pawson’s seminal work on realist synthesis draws on a number of broader substantive sociological theories that help understand the role of identity in behaviour change. One of these is Merton and Merton’s reference group theory,102 developed in the 1950s largely in relation to the behaviour of US soldiers who were situated either on the inside or on the margins of the established community of soldiers. 102 This theory posits that individuals will change attitudes and behaviours to assimilate with the reference group. More recently, Elder-Vass103,104 has developed the idea of norms circles which, like reference groups, invoke change through people assimilating to the norms of the group. Linking this to behaviour change theory, studies have shown that self-identification with the perceived norms of a reference group can significantly predict behavioural intention. 105 This is particularly relevant in the field of medical education, given the importance attached to the communities of practice model of learning. 106–109
The causal mechanism can be termed ‘normative enticement’, as it describes a situation in which an individual is enticed to the norms of a particular group. This mechanism could crudely but accurately be described as ‘I identify as being part of a particular group and therefore will accept the need to change my behaviour to retain membership of that group, to reaffirm to myself that I am a legitimate group member’. The normative enticement mechanism may run alongside the dissonance mechanism, feeding into it and facilitating its function at various stages throughout the remediation programme. This mechanism also bridges motivation and insight outcomes. The enticement to follow the norms of the profession may lead to acceptance that change is necessary (i.e. insight), but also intrinsic motivation to embark on that change. Motivation is discussed in the next section.
Context–mechanism–outcome configuration 13 suggests that being identified as needing remediation may, in the absence of efforts to frame feedback in a way that seeks to protect the remediating doctor’s professional identity, trigger a mechanism of identity dissonance. This type of dissonance, rather than invoking acceptance, may lead to a reconstruction or rejection of that identity to relieve this dissonance. Again, this is likely to have demotivating influence. This alluded to in Box 6, extract 4.
Motivation
The processes that occur to induce motivation are not divorced from those processes that lead to insight. However, it is worth distinguishing between insight and motivation, as, although there is a logical overlap, motivation arose as a clear and distinct theme in stakeholder group discussions and is addressed specifically in the literature. Moreover, although remediation is by no means a linear process, insight into a performance problem or behaviour logically precedes motivation in building a programme theory.
Although motivation is mentioned relatively frequently in the literature, it is not often presented as a specific outcome. In some of the literature, a lack of motivation is identified as a barrier to remediation (i.e. if the remediating doctor lacks motivation, remediation will be more difficult). 40,45,53,110 Other papers discuss, even if only briefly, some of the strategies in remediation programmes that bring about motivation. 7,44,48,50,55,57,91,97,111 There is a basic distinction between intrinsic motivation (i.e. linked in values and beliefs) and extrinsic motivation (i.e. ‘I do it because I want to avoid a punishment or earn a specific reward’) that features in the literature and was part of stakeholder group discussions. The distinction provides a useful starting point to begin to think about the intermediate outcomes related to motivation and its role in remediation.
Through examining the literature and through extensive stakeholder discussions, we were able to identify a number of strategies that facilitate intrinsic motivation in remediation programmes; for example, involving the remediating doctor in remediation programme planning to encourage perceptions of control, correcting causal attribution and effective goal-setting.
These are analysed in turn below to explain how and why they work for remediating doctors, in which contexts and to what extent they produce outcomes related to intrinsic motivation.
Involving the remediating doctor in remediation planning: perceived control
Involving a remediating doctor in planning a remediation programme may have a motivating influence. Facilitating a remediating doctor to maintain a degree of professional autonomy may have positive motivational consequences because it protects professional identity and engenders a sense of agency. Being involved in the remediation planning necessitates that the remediating doctor has an active, rather than a passive, role and they may perceive that they have more control over the outcome. In the literature, this is often framed in terms of developing ‘buy-in’ to the programme, suggesting that involving the doctor in the design of the programme may also give them more of an emotional investment. 44,48,50,55,57,91,97,111,112
Having input into remediation planning may also help protect professional identity. Autonomy is a key component of professional identity, especially in those doctors who have passed through training and become a consultant doctor (i.e. an attending physician). 12 As noted in Facilitating remediation: developing insight, professional identity is part of how doctors learn, and doctors may be intrinsically motivated by the desire to serve patients. 55 As highlighted above, invoking the remediating doctor’s own sense of professionalism and professional values may help create professional dissonance, leading to insight. This is because individuals can be intrinsically motivated to adopt certain behaviours or practices when these behaviours are associated with their own professional values, previously discussed in terms of the mechanism of normative enticement (see Table 6). 57 In other words, remediating doctors can be motivated because they want to be, or remain, part of the ‘in group’.
The amount of professional autonomy available in a remediation programme may be limited (remediation, by definition, means that the doctor has no choice but to remediate if they want to continue in their existing role or continue in their training pathway). However, reducing the inevitable loss of professional autonomy may be an important part of a successful remediation programme.
The important point here is that remediation necessitates a loss of autonomy, but if doctors have some input into the design of the programme then their professional identity will be less disrupted and the doctor will feel a greater degree of control over the process. Subsequently, they will have more intrinsic motivation.
Realist analysis for involving the doctor in remediation planning: perceived control
In CMOc 14 (Table 7), the extent to which a remediating doctor has input into the remediation programme functions as context. The input into the remediation programme increases the perception of control. Perceived control has been identified as a behaviour change mechanism in previous realist reviews. 113 This is consistent with behavioural change theories that have been used to understand and develop remediation programmes, and were identified through supplementary searching, which emphasise the importance of perceived control in motivation. 114 This provides a credible causal explanation for the substantial emphasis placed on creating remediating doctor involvement in remediation planning in a number of remediation programmes worldwide. This is illustrated in several of the extracts in Box 7.
| CMOc | Description |
|---|---|
| 14 | If the remediating doctor has a role in planning aspects of the remediation process (C) then they may perceive that they have some control over the process (perceived agency) (M) and be intrinsically motivated to change (O) |
| 15 | When a remediating doctor rejects their professional identity (C) then they lack the motivation to change (O) because of normative rejection (M). Intervention strategies that can mitigate against a loss of professional identity include maintaining a degree of autonomy for the remediating doctor in the remediation programme |
1. Arnold et al. :57
This conceptualization of remediation then transforms the goal of remediation as not only a matter of changing inappropriate behavior, but also of developing a professional identity accepted by the community of practice.
2. Sargeant et al. :55
Internal motivation can arise through a general recognition of the need to remain current and to be able to serve one’s patients as optimally as possible.
Buy-in
3. Kimatian and Lloyd:44
[T]he resident must be engaged affectively to meet the challenge presented by the remediation process. Successfully engaging the resident must take into consideration the resident’s personal goals, values and beliefs.
4. Katz et al. :91
The [remediation] plan should be discussed with the resident. When appropriate, plans can be further modified based on the resident’s input. Resident buy-in is critical in the success of any remediation plan. Some program directors have successfully solicited residents to develop their own remediation plans to use as a framework.
5. Shah et al. :111
The supervisors then meet the registrar. Opportunity is given firstly to the registrar to express their thoughts and feelings about the past month. Issues may be brought up which need to be incorporated into the final remediation plan.
6. Sullivan and Arnold:48
Motivational interviewing requires the individual to identify and mobilize values and intrinsic goals to change behaviour. It enables the individual to resolve his/her ambivalence regarding behaviors/perceptions and thereby promotes willingness for change.
7. Papadakis et al. :58
Resources such as personal coaching or educational programs are offered, but the individual decides how to best facilitate the behavioral changes. Explicit warnings are detailed regarding the dangers if the individual decides to retaliate.
8. Guevara et al. :115
The resident’s input is obtained in refining the IEP [individualised education plan].
Conversely, in CMOc 15, the loss of professional identity triggers normative rejection, which leads to a lack of motivation. This normative rejection is the converse of the CMOc of normative enticement in CMOc 12. The remediating doctor may be less likely to reject their professional identity if they maintain a degree of autonomy in the remediation programme.
Correcting causal attribution
If a remediating doctor does not believe that they have the ability to improve their performance or their behaviour then they will not be motivated. This is likely to happen when the remediating doctor incorrectly attributes the problem to something they cannot control. Durning et al. 116 use the example of a remediating doctor who attributes his poor performance to a lack of ability, which is demotivating because ability is perceived as an innate and immutable characteristic. However, after investigating the causes of the problem and finding that it is related to study techniques – something over which the remediating doctor has control – motivation is increased. 116
Similarly, for behaviour, literature points to the importance of doctors identifying particular emotional triggers. If a remediating doctor is able to recognise particular triggers for poor behaviour, they may become more aware of why they are behaving in this way and how they might seek to change their behaviour. In some papers the process of self-identification is part of an initial conversation, in which the remediating doctor is encouraged to explore their own perceptions of a particular problem. 90,117
This supports the strategies for post-referral assessment4,7,45,50,52,56,65,71,76,78,79,89–91,116–118 that examine not just the identified performance or behavioural problem, but also the possible causes of that problem. Accurate causal attribution will also enable the development of individualised and targeted remediation plans, a feature of a large number of remediation programmes. 7,11,47,73,100,118–123
This points to a further overlap between insight and motivation. Identifying the causes of a performance or behavioural issue is important in developing insight (i.e. the remediating doctor knows what is triggering a particular set of behaviours or performance and therefore has greater insight). This kind of insight leads directly to motivation, as it may enable doctors to overcome problems with causal attribution and therefore improve self-efficacy.
Realist analysis for correcting causal attribution
In CMOc 16 (Table 8), the causal mechanism is again a perception of control. In this case, the perception of control comes from correctly identifying the issue itself and through this process understanding that the problem is manageable. Again, this is supported by the wider literature on motivation and learning that highlights the motivational consequences of someone knowing what they are capable of and what they can control. 124
| CMOc | Description |
|---|---|
| 16 | When the remediating doctor is able to identify those aspects of their performance or behaviour that have caused problems that they can change (C) then they have more perceived control over the process (M), leading to greater motivation to engage (O) |
| 17 | When a remediating doctor is given specific strategies for learning or behaving (C), because of improved self-efficacy (M), they have greater motivation (O) |
| 18 | When a remediating doctor explores their own emotional triggers (C) then they are less likely to react to these triggers (O) because they are self-aware (M) |
When a remediating doctor can be coached through specific strategies to improve learning then they may also improve their self-efficacy, which in turn leads to more engagement. This process is explained in CMOc 17. Self-efficacy in the setting of remediation is about having the confidence that you can successfully remediate and achieve the goals that have been put in place. There are clear overlaps here with the perceived control mechanism, because having confidence to put knowledge into action implies a belief in control over the application of this knowledge. This is informed in Box 8, extract 3. Extract 4 informs the overall points about the relationship between self-efficacy and motivation.
1. Durning et al. :116
The supervisor wants to improve George’s self-efficacy beliefs, and an important first step is to challenge his attribution that his lack of success is due to his innate ability instead of his approach to learning.
2. Samenow et al. :79
Dr. Jones recognizes that his perfectionist drive and extreme work ethic have cost him dearly. He tells the group how, in his efforts to be self-sufficient and the ‘best’, he has pushed people away, including colleagues, family, and loved ones. He identifies this loneliness as a major contributor.
3. Liu et al. :93
It is also important to assess residents’ confidence in their knowledge, because actionable knowledge is only the knowledge the person is confident enough to use.
4. Prescott-Clements et al. :7
Similarly, a lack of self-efficacy or confidence can be encountered by individuals who are performing poorly (suggesting a degree of insight), which can also reduce intrinsic motivation to engage with remediation through negative feelings about ability, unless addressed quickly through support.
5. Swiggart et al. :89
Detailed inquiry of her social history focused upon her family, using a family genogram to depict individual family members, addiction issues, and relationships.
Literature returned through supplementary searching
6. Zimmerman:125
Self-efficacy beliefs also provide students with a sense of agency to motivate their learning.
The role of self-efficacy in enhancing motivation is noted in the wider literature on behaviour change that was uncovered through supplementary searching on the topic of self-efficacy and behaviour change (see Box 8, extract 6). 114,125 CMOc 18 explains how strategies that are related to identifying emotional triggers for behaviour work. Self-awareness here describes the process of identifying those triggers and becoming aware of when and how they operate to change behaviour.
Goal-setting
There are other features of interventions that may induce self-efficacy. One of these may be goal-setting. A number of interventions note the importance of having clear and achievable goals set out in the remediation programme. 52,55,71,87,91,118,126,127 There are various ways that this goal-setting is framed, but the basic premise is that goals should be both clear and achievable. Telling a doctor to ‘improve background radiology knowledge’ is not as helpful as ‘improve knowledge of chest radiography, anatomy and pathology’. 71 The clarity is not just about the goals themselves, but ensuring that the doctor understands how these goals are being assessed. 118
Although developing self-efficacy (i.e. the sense that the goals can be achieved) may be an important component of a remediation programme, it does not necessarily mean that very high self-efficacy will always facilitate effective remediation. Indeed, there may at times be an inverse relationship between levels of self-efficacy and successful remediation if the doctor’s self-efficacy is not based on insight. Studies on doctor performance, and professional performance more generally, have shown that poor performers tend to have the extra burden of being less likely than higher performers to judge their own performance level accurately. 128–132 If a remediating doctor has very high self-efficacy beliefs going into a remediation programme then this may suggest a lack of insight and may impede remediation. 93 The corollary to this is that low self-efficacy may be a sign of insight, as the remediating doctor is aware of their deficiencies, although this may also induce low intrinsic motivation. 7 Therefore, it seems that there is a fine line in remediation programmes. Feedback has to be direct enough to ensure that an individual is faced with credible evidence of the need to change (we called this juxtaposition; see Framing feedback 1: juxtaposition). However, careful goal-setting and support may be important in inducing the self-efficacy required to believe that goals are achievable. This relates to what was discussed in Facilitating remediation: developing insight, about framing feedback in manageable way.
Realist analysis of goal-setting
In CMOc 19 (Table 9), the extent to which the goal is perceived to be achievable functions as context and can be changed with specific, measurable, achievable, relevant, time-bound (SMART) goal-setting strategies and goals that are tailored to the individual being remediated. Again, the focus on self-efficacy as a mechanism fits with behaviour change models that underpinned some of the literature on remediation that were found through citation searching. This was also a point of discussion in the stakeholder group. Box 9 sets out the data that we have drawn on to develop this CMOc.
| CMOc | Description |
|---|---|
| 19 | When the remediating doctor has a clear goal and a realistic sense that a goal is achievable (C) then they may have greater belief in their own ability to achieve these goals (self-efficacy) (M), which may lead to more motivation to change (O). Interventions that may create this context include SMART goal-setting strategies |
1. Katz et al. :91
By setting concrete and achievable goals, and ensuring that residents understand and accept them, program directors define performance targets. Success or failure will be defined by whether or not these targets are eventually met.
2. Katz et al. :118
By making the criteria transparent, the resident was given every opportunity to target the goals and accomplish them in a reasonable timeframe. The time allowed was appropriate for the resident to succeed or fail on his own merits.
3. Mar et al. :71
A clear and comprehensive set of remedial objectives is then created directly from the issues identified in the background assessment. An example of . . . [a performance goal] ‘to improve the knowledge base of ultrasound physics and anatomy’, while a behavioral task may be ‘to improve attendance and punctuality’.
4. Rougas et al. :52
Several practical approaches have been utilized by educators across disciplines including frameworks such as the ‘SMART’ goals: specific, measurable, achievable, relevant, and timely (Day & Tosey 2011). This type of framework helps ensure that individual learners know what is expected of them in a defined time period with established consequences.
5. Rumack et al. :87
Regardless of how many deficits a resident may have, it is wise to choose one or two skills per competency to remediate first (6,8). Choosing too many may confuse the resident and weaken their response.
6. Sargeant et al. :55
The coaching conversation then moves to guiding the physician to set specific and realist goal(s) and to developing a plan for attaining the goals. Planning involves paying special consideration to the factors which may both impede and enable progress and success, setting timelines, and considering how success will be measured.
Destigmatising remediation
If professional identity is important for intrinsic motivation, then all efforts to mitigate the negative impact of remediation on a remediating doctor’s professional identity are potentially important. In this respect, a number of papers note that the stigma attached to remediation acts a barrier to engagement. 8,41,133 If a doctor feels stigmatised, then they will feel isolated from their colleagues and this can have negative implications for identity development. The importance of professional identity in remediation therefore brings into the focus some of the broader contextual issues around how remediation is conceptualised within the medical profession and the extent to which it stigmatises remediation. 12
A study in Canada considered the perception of remediating doctors from various stakeholders within the medical community. It found that those involved in remediation programmes often held ambivalent perceptions, describing remediating doctors as being both ‘one of us’ and ‘not like us’. 134 This is important as it suggests that negative perceptions exist and also that it may be possible to nurture more positive perceptions of remediation. This finding emphasises the relevance of in- and out-group dynamics that may impact professional identity for remediating doctors. Similarly, in the UK, it has been noted that policy developments have simultaneously sought to normalise remediation, while also creating a contradictory and unhelpful climate of fear around doctor performance. 8
One approach to mitigate this barrier is to seek to remove the stigma attached to remediation. This is noted as important in a number of papers. 8,40,84,91,117,135 However, the literature does not elaborate on what this looks like in practice beyond renaming the process itself,91 ensuring that the process is not framed as punishment84 and seeking to conduct remediation in such a way so that the remediating doctor is not easily identified as such by peers. 41
A further approach to lessen the sense of isolation and the stigma attached to remediation is to bring remediating doctors together. Group remediation is advocated in a number of papers. 4,51,73,74,85,89,95,120,121,136–138 The process of working in a group may help doctors feel less alone and the process of seeing colleagues progress through and complete a remediation programme may be motivating. 85 However, as noted in stakeholder group discussions, group work may in many situations be impractical. Other ways of networking with doctors undergoing remediation may be more pragmatic.
Realist analysis for destigmatising remediation
Context–mechanism–outcome configuration 20 provides a causal explanation for the emphasis placed on seeking to remove the stigma of remediation, which is discussed in a number of papers (Table 10 and Box 10, extracts 4–6). 41,84,135 Again, this is a plausible explanation because it is congruent with broader notions of the importance of professional identity and negative impacts of isolation on motivation. This was derived, in part, from the discussions with the stakeholders, including those undergoing remediation, which noted how doctors would often not disclose their remediation to friends or family, let alone other doctors, and the ensuing sense of loneliness experienced.
| CMOc | Description |
|---|---|
| 20 | When the process of remediation is reframed in a more positive light (C) then the remediating doctor feels more psychologically safe (M), leading to greater motivation to engage in the programme (O) |
| 21 | When remediation is framed as punishment (C) and/or when a community of practice stigmatises those who have to be remediated (C) then the remediating doctor may feel alienated from their peers (M), leading to a sense of isolation (O) |
| 22 | When a doctor feels isolated from their peers (C) then normative rejection (M) may lead to a lack of motivation to change (O). Remediating in groups and/or networking with peers undergoing remediation may lessen the sense of isolation |
1. Krzyzaniak et al. :133
Major themes identified as barriers to remediation were: (1) faculty concern about the premature labelling of residents as ‘struggling’ and the stigma that comes with remediation.
2. Price and Archer:8
This culture of fear is in part fuelled by the negative associations with remedial interventions; as recognised by the Steering Group on remediation, the term remediation has ‘negative connotations’.
3. Harthun et al. :117
Significant effort is expended to remove any hint of punishment in any aspect of the program. Also, we actively minimize stigma associated with poor scores and discuss this aspect of performance with the residents.
4. Gunderman and Rackson:135
One strategy for encouraging the prompt reporting of learning difficulties is to diminish the generally pejorative connotation of remediation. If there is any profession in which remediation should be widely understood, it is medicine.
5. Kalet et al. :84
Remediation should be reframed from a matter of punishment and stigma to a form of training that many, if not most, will need and benefit from at some point.
6. Shapiro et al. :41
The less the resident’s normal schedule is disrupted, the less he or she is distinguished and differentiated from peers and the less likely he or she will see the remediation as a punishment.
7. Caldicott and d’Oronzio:85
In a setting that features face-to-face peer communication and feedback, participants lose their feeling of isolation. Exchanging with other accomplished and dedicated healthcare professionals who have also acted unprofessionally . . . participants realize that committing a transgression and experiencing the consequences do not nullify their own professional accomplishments and dedication.
Context–mechanism–outcome configurations 21 and 22 offer a causal explanation of what happens when the framing of remediation creates isolation. In CMOc 21, the sense of alienation – broadly speaking, the process of detachment of things that belong together – can be understood as a causal mechanism, leading to isolation. Extract 7 (see Box 10) advocates the use of group remediation to lessen isolation. In CMOc 22, the corresponding sense of isolation invokes the mechanism of normative rejection, as discussed above. In this case, it is the sense of isolation that leads the remediating doctor to dissociate with the community of practice in which they work. These are not well substantiated in the literature and would benefit from further testing.
Although intrinsic motivation may be the ultimate goal of remediation, extrinsic motivation is widely used and deemed effective. One paper reports a survey of residency programme directors (n = 253) in the USA. The threat of termination or not progressing were reported in the survey as the most effective strategies of ensuring engagement with remediation programmes. 139 A number of papers noted the importance of having clear consequences for not improving performance or behaviour. 58,71,76,78,122,140 In the stakeholder group discussions, it was also suggested that understanding the consequences of engaging (or not) with a remediation programme may also be considered an aspect of insight (i.e. insight into the consequences of future actions).
The way in which extrinsic motivation works and interacts with other mechanisms within a remediation programme is not clearly expressed in the remediation literature. In a sense, it is presented as common sense logic (i.e. if a remediating doctor understands that non-engagement will be bad for their career, then they are more likely to engage). However, as our earlier findings and CMOcs have demonstrated, it is difficult to explain how extrinsic motivation alone could induce sustained changes to performance or behaviour. Even if a remediating doctor is sufficiently motivated by the potential consequences of not engaging, the engagement could be superficial or transitory if they are not intrinsically motivated to engage.
Clear consequences
However, outlining clear consequences in remediation may play a role in maintaining engagement throughout a remediation programme141 and, once engaged in a remediation process, this may provide extra motivation to keep a remediating doctor on board. The consequences can escalate if there is continued lack of improvement at specified intervals. 53 Inducing extrinsic motivation through clearly articulating the consequences of actions is not advocated as a standalone strategy, rather it works to support strategies aimed at stimulating a remediating doctor’s intrinsic motivation. Hanna et al. 95 report that mandatory engagement with a remediation programme encouraged attendance, but not necessarily engagement. 95 If a remediating doctor is not intrinsically motivated to change, then they may also re-evaluate their goal. In stakeholder group discussions it was suggested that older doctors, who are nearing retirement, may choose to accept restrictions on the scope of their practice.
The potential for external motivation may be contingent on the perceptions of self-efficacy and perceived control. If a remediating doctor understands that there will be consequences if they do not improve, but does not believe that the improvement is possible, they may change their goals or their commitment. A doctor may adapt their goals for other reasons, such as being near retirement, and, from a patient safety perspective, this may not be a bad thing. Doctors still in training may use the opportunity to reflect on their career and choose a different career path. A number of papers highlighted the importance of systems for ‘coaching out’ of a particular programme of study. 40,50,66,69,91,142
Realist analysis for clear consequences
Context–mechanism–outcome configuration 23 (Table 11) posits that a process of evaluating costs and benefits will be a causal factor in determining the level of motivation. However, the outcomes of this evaluation will be contingent on a number of factors. The processes overlap, so whether a remediating doctor engages in remediation or decides to change their goal may depend on processes present in some of the other CMOcs presented earlier (Box 11). For example, whether or not they experience affirmation and feel psychologically safe, perceive that they have some control over the outcome, and feel part of the medical profession with which they identify and wish to retain in-group status.
| CMOc | Description |
|---|---|
| 23 | When a remediating doctor understands the consequences of not changing their behaviour or improving performance (C) then they may be able to evaluate the costs and benefits of change (M), and may be motivated to engage with remediation (O) or change their goal (O) |
1. Sparks et al. :62
A formal performance review and written contract, with specifically identified problems and general themes, recommendations for time-based successful behaviors, and clearly identified consequences for unsuccessful behaviors, was initiated.
2. Krzyzaniak et al. :40
A resident cannot be indefinitely remediated . . . Thus, we must establish a time frame for the remediation goals to be accomplished.
3. Domen:69
The remediation plan should only target and address the specific issue(s) identified, should have clearly defined goals with defined measures/assessments . . . and clearly delineated consequences or next steps if the resident fails the remediation plan.
4. Kalet et al. :54
. . . learners should be required to participate in remediation and be held accountable to engage actively with the remediation team in developing an individualized remediation plan, to initiate and complete the remediation activities, and to successfully undertake whatever assessment is deemed appropriate.
Facilitating practice change/improving performance or behaviour
This section outlines our findings related to the way in which remediation works to improve performance or behaviour. Again, it is worth re-emphasising that we do not view remediation as a linear process, and insight and motivation would logically increase as performance or behaviour improves, with these processes working alongside each other. This section specifically focuses on the processes that occur to embed changes in behaviour or performance at the point at which someone has some insight into the problem and some degree of motivation to change.
Qualified doctors are high achievers who have proven to be competent learners. The way in which remediation programmes may work to improve performance and the specific strategies used will, in many ways, be similar to those used in medical education more broadly. We do not want to repeat tried and tested theories of education here. Rather, we seek to focus on the aspects of learning or behaviour change within a remediation programme that are specific to remediation and the particular challenges, such as the fear of engaging in remediation and its threat to professional identity development, that are associated with undergoing remediation.
Practising new behaviours/skills
Remediation may be most effective at changing behaviour or performance when remediating doctors get the opportunity to practise and master new behaviours or skills. Two papers70,143 in the returned literature explicitly discuss learning in a remediation programme in terms of an experiential learning cycle. Experiential learning theories posit that learning occurs most effectively when the learner gets the opportunity to move from abstract reasoning to concrete experience, and then reflect on that experience to develop learning. 70,143 Processes of guided reflection (discussed below) are likely to be integral to that process if the remediating doctor is practising new skills in the workplace.
Interestingly, some studies also noted the importance of practising behaviours in a professionalism remediation programme. 51,65 One paper51 notes that, during a course on boundary violations, it is not a lack of understanding of ethics issues that besets the referred doctors, but a lack of understanding of how these apply to clinical situations. Therefore, practising behaviours in a simulated environment is an important component of behavioural change. 51 Coaching may also be used to facilitate practising new behaviours. This links to reflection (see Table 2, CMOcs 10, 11, 25 and 26), in that the coach can discuss progress with a remediating doctor, help them rehearse correct behaviours59 and set proper boundaries. 76
Realist analysis for practising new behaviours and skills
Context–mechanism–outcome configuration 24 (Table 12) describes the repetition of performance or behaviours as contexts, as noted in Box 12, extracts 1 and 2. This seems fairly obvious, but practising new skills and behaviours is not always easy in remediation programmes. When simulation is not available, guided reflection on workplace interactions may be even more important. CMOc 25 links the repetition of skills/behaviours to guided reflection (see Box 12, extract 3). The process of guided reflection facilitates the remediating doctor to integrate the new knowledge and experience into their learning. Integration of new knowledge and experience is a mechanism that underpins learning theories such as the Kolb learning cycle, and so it is no surprise that it functions here. What is important is that, in remediation, the circumstances under which the intervention occurs can make this a more complicated process, especially if the problem is a behavioural one.
| CMOc | Description |
|---|---|
| 24 | With repeated performance of correct behaviours or skills (C), performance or behaviour improves (O) because of repetition (i.e. practice) (M). This practice can be in situ if appropriate, but can be simulated if needed |
| 25 | When repeated performance is accompanied by appropriate feedback and guided reflection (C) then positive improvements are more likely (O) because the remediating doctor is able to integrate new knowledge and experiences into their learning (M) |
1. Parran et al. :51
Boundary maintenance skills require practice. Therefore, each participant practices from both the physician and patient perspective the clinical skill of “Getting to ‘no.”’ The specific scenario that is focused on in this skill practice exercise involves practicing saying “no” when asked to prescribe controlled drugs . . .”
2. Roberts et al. :59
. . . a ‘coach’ – either a chief resident or junior faculty member, who could meet with the intern frequently (weekly to biweekly) to discuss specifics of the incidents that are troublesome, get him to ‘own’ the behaviors that are incorrect and work to rehearse and then reinforce the proper behaviors.
3. Egener:76
A series of visits [from a coach], 1–2 hours in duration, spread 2–8 weeks apart . . . Most often as they practice acknowledging others’ perspectives, their own view of what constitutes ‘the truth’ becomes less black and white.
4. Rumack et al. :87
When professionalism lapses present as poor interpersonal and communication skills – yelling, berating, being disrespectful, or poor team communication – training in a simulated environment can be useful. We have found that some residents recognize such behaviors only when they are videotaped and given directed feedback.
Guided reflection
As noted above, the literature suggests that the way in which feedback is delivered in a remediation programme is important in determining whether or not that feedback is accepted. In particular, we noted that feedback that is both specific and from multiple sources is more likely to induce dissonance rather than denial. Building on this, feedback works to enhance performance when a practitioner reflects on what that feedback means,56,65,87,115,126,144 and this process works best when it is a guided process (i.e. reflection will not automatically follow feedback, but with guidance from a coach or mentor, reflective practice can aid behaviour change). This is noted for both clinical skills and knowledge issues,63,87,126 as well as professionalism. 56,87 It seems that a key role of coaches or mentors is to guide the remediating doctor in reflection.
Guided reflection may be easier to facilitate with face-to-face meetings with a coach, mentor or supervisor. Our stakeholders suggested that in remediation coaching situations this guidance can start with an open question, inviting the remediating doctor to reflect in general on their experience throughout the remediation programme. If the meeting is face to face, then body language may be important in determining whether reflection is genuine or if they are just going through the motions. These meetings are also an opportunity to invite the remediating doctor to consider what they think the consequences, either positive or negative, are likely to be as a result of their efforts and progress so far.
Meetings with someone external to the organisation may be more effective than meetings with someone from within the organisation. This is because guided reflection will seem less threatening. For example, if someone is asked ‘what do you think the consequences might be if you do not engage in this programme?’ this may seem like an implied threat if it comes from someone senior within the organisation. If it comes from someone outside the organisation, or someone that is deemed impartial, it is much more likely to be perceived as a genuine question for reflection. This links back to the earlier points of receiving feedback in an environment that is perceived as being safe by the doctors involved (see Table 2, CMOcs 1 and 3).
In addition to face-to-face meetings, written reflective logs of experience and learning will help a remediating doctor to learn from their experiences. 49,51 The purpose of these logs is that they are meaningful to the remediating doctor and, therefore, should not form part of the assessment process. However, it may encourage engagement if a supervisor checks to ensure that reflections have been completed. 71 The idea that assessment of written reflections could diminish their effectiveness was also raised by stakeholders. Stakeholders were broadly agreed that such written reflections should not be summatively assessed, but noted that they might form part of a process of formative assessment that would enable remediating doctors to progress through the remediation process.
In general, the process of reflection may be most effective when divorced from the assessment of progress entirely. Like feedback presented initially, feedback on progress should also be as specific and objective as possible (see Table 2, CMOc 7). In our stakeholder group, it was suggested that multisource feedback, including feedback from patients, may be the most effective in engendering change, although clearly the optimum type of feedback would be dependent on the issues being remediated.
Realist analysis for guided reflection
Context–mechanism–outcome configuration 26 (Table 13) is derived from the importance attached to guided reflection through regular meetings, clearly evidenced in Box 13, extracts 1–6. This process of guidance functions as new context in a remediation programme. A common theme in these extracts is the notion that the process of regular guided reflection is used to ensure that remediating doctors are engaging with feedback and making sense of it, hence ‘making sense’ is a causal mechanism that helps change practice. The intervention strategies of face-to-face meetings and open questioning came from stakeholder group discussions. CMOc 27 illustrates how the mechanism of dissonance operates throughout a remediation programme, with the process of guided reflection facilitating the function of the dissonance mechanism at various points in the remediation journey.
| CMOc | Description |
|---|---|
| 26 | When a remediating doctor has been guided through what the feedback means (C) then they are more likely to engage with the feedback (O) because it makes sense to them (M). Intervention strategies that may help to bring this about include regular face-to-face meetings and open reflective questioning from a trained coach |
| 27 | When feedback makes sense to a remediating doctor (C), dissonance is more likely to be invoked (M), leading to the remediating doctor gaining further insight into their performance or behaviours (O) |
| 28 | When the process of reflection is guided by someone from outside the remediating doctor’s employing organisation (C) then the feedback will be perceived as less threatening (M), leading to more meaningful reflection (O) |
| 29 | When a remediating doctor is allowed to develop and keep a reflective log that is meaningful to them (C), they have the opportunity to integrate their new learning and experiences (M), leading to insight into their own progress (O) and sustained changes in performance or behaviour (O). This may work best when the reflective logs are not assessed, but when their completion is nonetheless verified |
1. Decoteau et al. :63
. . . one-on-one sessions [were used] to assess the learner in their abilities to review, analyze and learn . . . Based on the assessment, the teacher identified any particular deficits that the learner possessed and provided structured feedback to the learner to allow for a more refined approach in studying and completion of assigned SCORE.
2. Rumack et al. :87
Second, frequent feedback on the resident’s progress is essential for coaching to be effective. Third, the resident needs to take time to reflect on their actions with their mentor or coach to understand what progress or barriers are occurring.
3. Guerrasio et al. :65
After each scenario, the individual watched the video with the actors and remediation team, and was coached through self-reflection, receiving feedback and suggestions for change in an iterative fashion with goal setting for subsequent scenarios.
4. Warburton and Mahan:56
Coaching should focus on ensuring that the learner incorporates proper knowledge (virtues), attitudes (professional identify), and skills (professional behaviors) into practice through discussion, reflection, problem-solving scenarios, and ultimately, actions in real clinical settings.
5. Stirling et al. :145
Trainee receives feedback on their performance (30 minutes). On completing their self-assessment the trainee meets with the assessment panel. This constructive feedback focuses solely on the trainee’s performance during the PgWSE [Postgraduate Ward Simulation Exercise], and is structured using stages 1–6 of Pendleton’s guidelines, as follows.
6. Whiteman and Jamieson:49
We find that [written reflective logs] directly challenges the commonly encountered passivity of practitioners in this situation, which can originate from a practitioner’s perception of continuing education as a transfer of information from experts to passive learners.
7. Parran et al. :51
[Written reflective logs] provide physicians an opportunity to consider their strengths and weaknesses and help them to successfully integrate new learning into existing knowledge.
8. Mar et al. :71
These [reflective log] entries are for the resident’s use only, but their regular completion should be demonstrable.
Context–mechanism–outcome configuration 28 posits that the position of the individual providing the feedback is a context that determines how threatening the feedback is perceived to be. This links back to psychological safety, in that engagement and insight are more likely to follow when a remediating doctors feels safer. The idea that perceptions of safety will be enhanced if the person guiding the reflection is external to the employing organisation was derived from stakeholder group discussions.
Context–mechanism–outcome configuration 29 is based on the evidence (see extracts 6–8 in Box 13) that producing written reflections serves as contexts that trigger engagement. For example, extract 7 (see Box 13) describes this process as challenging ‘passivity’. This engagement allows the remediating doctor to integrate new knowledge and experiences, which is a mechanism that provides new insights and therefore more authentic learning and changes to performance or behaviour.
Programme theory
The complete programme theory of how remediation of doctors produces its effects is presented in Figure 3.
FIGURE 3.
Programme theory of remediation. Reproduced with permission from Price et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.
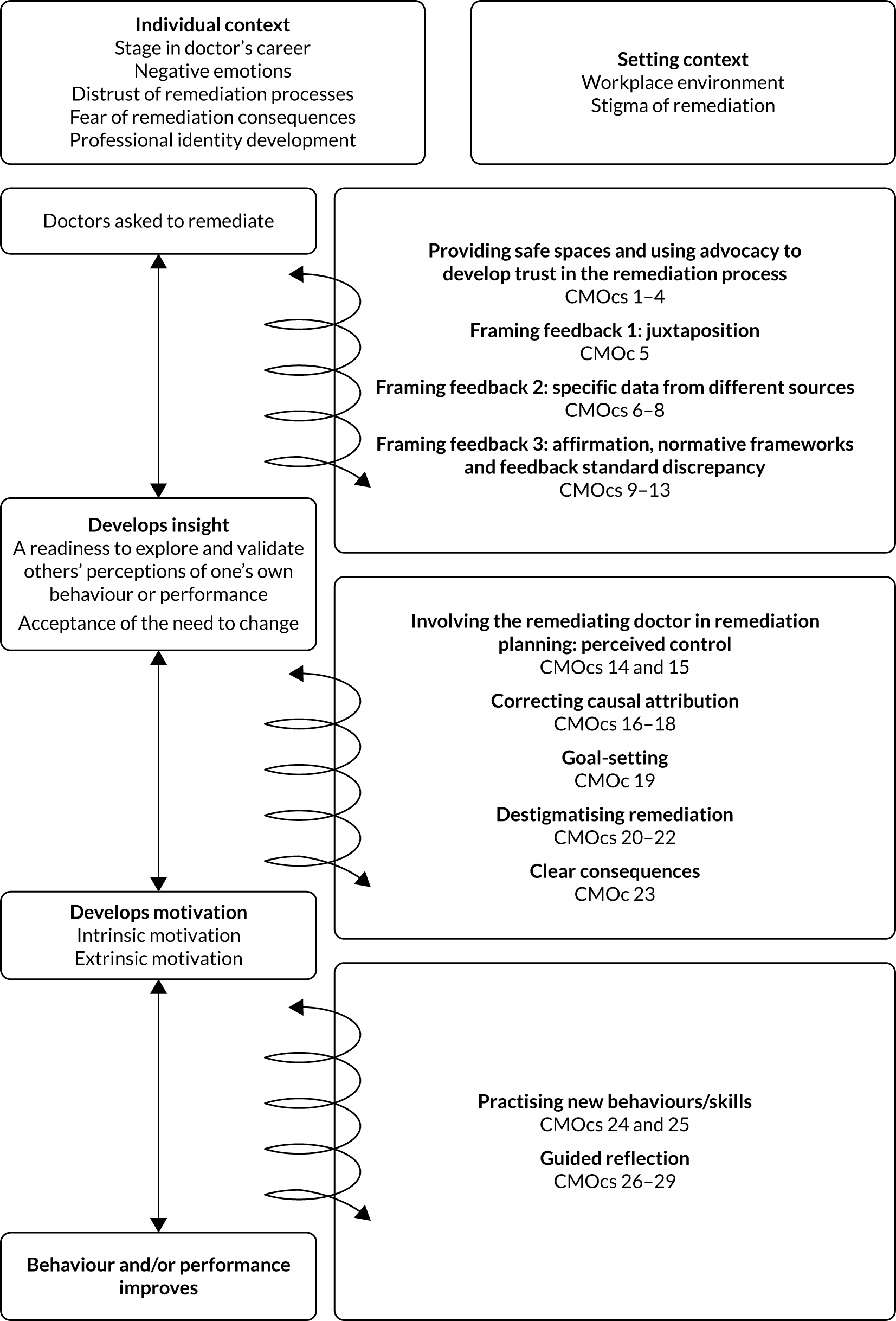
Chapter 4 Discussion
We have developed a programme theory of what is working in remediation to improve patient safety and reduce attrition of the medical workforce. As already noted, we did not seek to repeat what is already known about how doctors learn. Rather, we sought to understand what it is that makes remedial interventions unique, and to develop a model that helps us understand how improvements in performance or behaviour occur under these conditions. Indeed, the uniqueness of remediation has recently been characterised as a ‘wicked problem’, in the sense of the term used by design theorists Rittel and Weber. 146 In this sense, wicked problems are described as such because they are difficult or impossible to solve because of the many environmental factors involved and the interconnectedness of the many smaller problems of which they are comprised. 12 Others have described remediation as a ‘Gordian knot’ because of the difficulties associated with unravelling how it works. 147 Remediation suits such a characterisation, and a further challenge for conducting an evidence review of remediation is that, in large part because of its ‘wickedness’, there is a paucity of information on what is working when it works. 11,25
However, the realist review approach that we have employed has sought to tackle this issue head on. Rather than conduct a descriptive or narrative synthesis of existing evidence, which we know has thus far produced a limited understanding of remediation,25 the realist approach has allowed us to draw on a wider range of literature and the guidance of a stakeholder group. The process of building CMOcs is one of theory building, whereby causal explanations for what is working (or not working) are built, refined and tested. This has allowed us to go beyond a scant literature that is not theoretically rich to develop an explanation of what is happening in a remediation programme to produce its effects, for whom and in what contexts. The overall programme theory is presented in Figure 3.
Before providing a narrative explanation of our findings in relation to our programme theory, it is important to note what a programme theory is and what it is not. The word ‘theory’ can be used in different ways, and here we mean theory in the sense described by Klee:148
A theory is an attempt to organize the facts – some ‘proven’, some more conjectural – within a domain of inquiry into a structurally coherent system.
Klee148
Our programme theory is a ‘theory’ in the sense described by Klee,148 because the processes it describes were inferred through our analysis of the existing literature, subsequent discussions with the stakeholder group and through drawing on substantive theories to provide an abstracted description of the processes that occur in a programme to produce its effects. We propose that this is the best fit theory, at this time, based on the data available. Programme theories are never completely finished products to the extent that any subsequent data from new research should always be viewed as an opportunity to modify, develop and refine the programme theory.
The programme theory for remediation is the sum of the CMOcs that have been described in Chapter 3. Each CMOc represents an explanation of what is happening in different parts of the programme to create particular outcomes. The outcomes are not always, or even usually, the outcomes that are described in a particular study. Often, the outcomes described in a study will relate to quantifiable measures, such as subsequent examination performance or attrition rates from the programme. These measures are important, but they do not tell us much about how the intervention is working and what processes are happening along the way to get there. Rather, as described in the Chapter 3, Results of the review, in a realist review these more intermediate outcomes are deduced from developing an understanding of what it is that needs to happen at different stages for an intervention to produce its effects.
Summary of main findings
Conceptualising remediation
Remediation is not a straightforward educational intervention, as the issues being addressed can be wide-ranging, often related to behaviour rather than knowledge and skills, and because of the negative connotations that surround it. Moreover, remediation for practising doctors, as opposed to medical students, often occurs outside formal educational settings. Therefore, in line with Bourgeois-Law et al. ,12,13 we have conceptualised remediation for practising doctors as ‘supporting practice change’ as opposed to ‘redressing gaps in skills and knowledge’. 12,13
Although educational processes are clearly central to what is going on in remediation, in developing a programme theory of what is working, in what contexts, for whom and to what extent, we have focused on what is happening to create the environments where those educational processes can function. Doctors are, generally, academically able (i.e. high academic achievement is a prerequisite to enter medical school in the first place, and medical school curricula are stringent and assessment processes usually very robust). However, remediation often does not work, because of a number of identifiable barriers (i.e. lack of insight and motivation, negative emotions towards the process, isolation and denial). These barriers are more behavioural than educational. 7 In this sense, remediation works when the intervention is able to change the context to overcome these barriers and engage doctors in activities that facilitate a change in practice.
Therefore, this programme theory highlights the processes that occur to induce the behaviours that can create those learning opportunities. Theories of behaviour change, in particular the transtheoretical model, incorporate a temporal dimension that disaggregates the behaviour change process into contemplation, preparation and outcome phases. 149 This temporal disaggregation was useful in mapping outcomes as, although remediation is by no means a linear process, there are some outcomes related to insight that logically precede other aspects of changes in practice. Moreover, the focus on attitudes, subjective norms and perceived behavioural control in the theory of planned behaviour helped us to understand and tease out the mechanisms that operate to induce insight and motivation, and facilitate practice change. 150
How remediation programmes work to develop insight
As depicted in our programme theory, remediation works when it induces participants to develop insight. Insight here refers to those outcomes in which a doctor is ready to explore feedback on their performance and accept any highlighted divergence between their own perceptions of their performance and the feedback that is presented. The intervention strategies that help produce insight relate to the environment created and the framing of feedback. A supportive environment, with confidential discussions and someone who provides advocacy and emotional support, will help invoke psychological safety that may lead to trust and, subsequently, a readiness to explore feedback. If feedback is then framed in a supportive and effective way (i.e. juxtaposition, specific data from multiple sources, affirmation and relatable normative frameworks) then further mechanisms of affirmation, dissonance and normative enticement may be triggered, which may lead to the remediating doctor validating the feedback that is presented to them. This is because they feel safe enough to explore the feedback and because that feedback has been presented in a way that is not threatening, but in a way that highlights the problem effectively and shows the discrepancy between actual and perceived behaviours.
This process is not linear and may continue to operate throughout the remediation process, moving from intervention strategy, to mechanism, to intermediate outcome and back to intervention strategies. This is depicted in the programme theory by the spiral situated alongside the categories of outcomes (see Figure 3). At some point remediation may cease to work–perhaps if the doctor does not feel safe or if the remediation is not framed effectively. In such cases, the mechanisms of denial or rejecting the norms of the profession may lead to outcomes of distrust or isolation. In which case, if the remediation programme is to work again, more facilitative environments need to be created.
How remediation programmes work to motivate remediating doctors
In our programme theory, a remediating doctor must be motivated to engage with the process. Strategies aimed at developing intrinsic motivation include doctor involvement in remediation planning, correcting causal attribution, effective goal-setting and destigmatising remediation. When these strategies are employed, perceptions of control, self-efficacy and self-awareness may function as mechanisms to induce intrinsic motivation. Alongside this, clarity in terms of the potential outcomes of the process may trigger an evaluation of costs and benefits. Although insight logically precedes motivation, once some motivation has been induced, the processes may function alongside the insight mechanisms, with each process enforcing the other.
How remediation works to facilitate practice change
Remediating doctors need, at some point, to learn new skills and behaviours to effect behaviour or performance change. In many cases, this will relate to standard educational interventions and we have not sought to develop programme theories for such tried and tested educational models. However, the environment in which remediating doctors learn new behaviours and skills in a remediation programme may be much more restricted than general continuing medical education.
Practising new skills or behaviours in simulated environments may be an important aspect of a remediation programme. This applies to professionalism issues, such as boundary violations, as well as more straightforward educational processes. However, when simulated practice is not possible, then reflection on experiences in the workplace may serve the same purpose. A doctor may be tasked with specific behaviours to practise and, through a coaching process, can reflect on the success or otherwise of these processes when they meet with their coach.
Guided reflection is likely to be important at all stages of a remediation programme. Written reflections may be useful, but their value could be undermined if they are summatively assessed. Face-to-face meetings with a skilled coach will enable the coach to elicit reflection and ask probing questions. Guided reflection may also work better when it is facilitated by someone external to the organisation, so that difficult questions can be asked without the perception of any implied threat.
Other contexts that impact on remediation
In realist explanations of an intervention, the interventions work when they manipulate the context to create the opportunities and resources to induce change. Not all remediating doctors would need to engage with every intervention strategy for the same length of time. There will be individual contexts and contexts related to the setting that will impact on how remediation works.
The individual context includes the stage in a doctor’s career, as this will influence the extent to which undergoing remediation results in a loss of autonomy and the subsequent likely barriers to intervention. The other individual contexts here relate to the negative emotions and fear attached to a remediation process, which can lead a remediating doctor to deny that there is an issue to be addressed. Related to this is a doctor’s professional identity development, which will impact on their learning, and their motivation and engagement with remediation. The setting context relates to the work environment, which may determine how safe a doctor feels to engage in remediation and the stigma attached to remediation.
Comparison with existing literature
Bourgeois-Law et al. 12 have noted that conceptualisations of remediation have tended not to differentiate between trainees and those doctors who are consultant-level (i.e. attending-level) physicians. They argue that consultants and attending physicians operate in a more autonomous environment as opposed to the educational environment surrounding trainees. As such, remediation for consultants and attending physicians entails a much greater loss of professional autonomy, particularly if that remediation entails a return to supervised practice. 12
This review of the literature supports Bourgeois-Law et al. ’s12 assertion that in remediation studies little consideration is given to this difference. The majority of the literature uncovered in the formal search (66/114) focused on doctors in training, with only 11 studies focusing specifically on consultants, GPs and attending physicians. Out of the remaining 36 studies that included both categories, little or no consideration was given to the different contexts in which these doctors operate. Stakeholders strongly supported this assertion about the importance of autonomy (and the loss thereof) in a remediation process. However, in our review, we have also, in a number of ways, moved beyond this binary distinction and have developed a more nuanced understanding of the importance of a doctor’s operational autonomy in determining how remediation works. As noted by our stakeholders, a binary distinction between doctors practising independently and those in training may be an oversimplification. Autonomy increases incrementally throughout a medical career and, for example, the step from a senior trainee to a consultant may not be as great as that from a junior trainee to a senior trainee. We have therefore developed a programme theory that is sufficiently transferable to remediating doctors whatever the stage in their career, from medical school graduation to consultant level. We have identified that is not simply the stage of a doctor’s career that is either a barrier or a facilitator, but the loss of autonomy experienced (see Table 2, CMOcs 14 and 15).
The last systematic review to develop a model for remediation was conducted by Hauer et al. in 2009. 11 Broadly speaking, the model advocated by Hauer et al. 11 was akin to a medical model of treatment (i.e. assessment, diagnosis, intervention and follow-up) (Figure 4).
FIGURE 4.
Hauer et al. ’s11 model for remediation of physicians across the continuum of medical education.
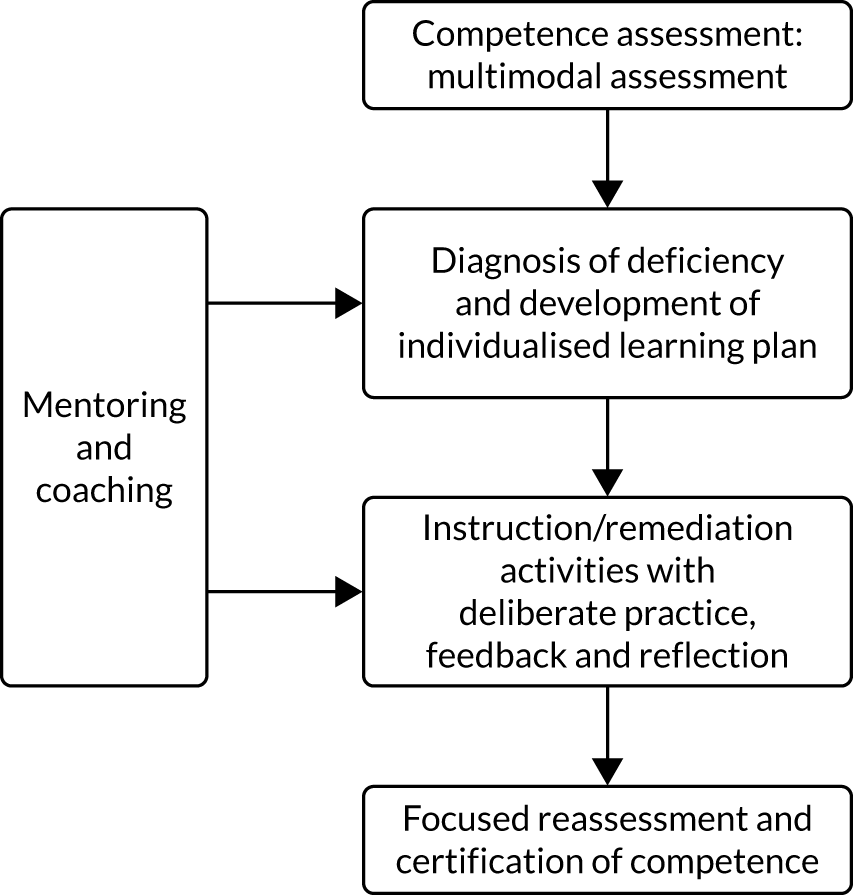
Our findings do not contradict Hauer et al. ’s11 model, but they develop considerably greater detail on what some of these processes might look like in a successful programme. The use of multimodal forms of assessment, highlighted by Hauer et al. ,11 is widely supported in the literature returned in this review. 47,62,115,119,144,151–153 This assessment serves a number of functions. As noted by Hauer et al. ,11 a central purpose of assessment in remediation is to aid the accurate diagnosis and understanding of the concern. However, we suggest that multimodal assessment should also be used to gather specific and direct feedback that is more likely to be validated by a remediating doctor. Our findings in relation to the stigma of remediation and influence on professional identity suggest that it is important to evaluate organisational issues that may have an effect on how a remediating doctor reacts in a particular work setting, and may point to the need to instigate organisational changes to facilitate a more effective remedial environment. The assessment of the workplace environment is not common in remediation assessment processes, with the UK’s Practitioner Performance and Advisory service (formerly the National Clinical Assessment Service) being a notable exception. 5 Importantly, research by the same organisation found that, although only a minority of referrals noted problems in the workplace environment, the majority of assessments found workplace to be an important contributing factor to performance or behavioural problems. 154 The need to consider the importance and impact of organisational problems in remediation has been highlighted in a number of papers, and our findings would support this approach. 155–157
Diagnosing a deficiency–the next stage in Hauer et al. ’s11 model–is central to remediation. Our research suggests that identifying the manifest problem itself may be a slightly different endeavour from identifying the cause of the problem. Identifying the cause of the problem, which will allow a remediating doctor to develop self-awareness and a sense of control, means that guided reflection with a coache/mentor can help engender insight and a sense of control and self-efficacy. Developing an individualised remediation plan should be, we suggest, an activity undertaken with the remediating doctor, if possible, affording the greatest opportunity to enable input into the process.
We would agree with Hauer et al. 11 that coaching and mentoring has an important role in a remediation process. What we have added via this realist review is how coaches and mentors are an integral part of the remediation process. The importance of developing insight is not really captured in Hauer et al. ’s11 linear model of remediation, and we have argued here that it is absolutely central to the remediation process. The way in which coaches or mentors frame feedback and whether or not they create an environment in which a remediating doctor is able to feel safe and be candid about their thoughts and feelings, is central to whether feedback is likely to be accepted or rejected, and whether or not that feedback will engender the self-efficacy and sense of control needed to motivate a doctor to complete a remediation programme. Coaches and mentors should be trained and focused on the provision of support and guiding reflections, and may be most effective when they have no role at all in any decisions on the progress of the remediating doctor. This accords with an increasing recognition of the importance of reflection in medical education. 158,159
Remediation is often viewed in terms of an educational model,12,25 and our focus here has been on the more behavioural aspects of change that are required for learning to take place. We are not the first to argue that remediation should be understood in this way. Prescott-Clements et al. 7 developed a model for assessment in remediation similarly rooted in concepts of behaviour change. We have used this same conceptualisation to build a more detailed theory about the processes that occur throughout a remediation programme to produce its effects.
Our programme theory addresses the questions of why, how, and in what contexts remediation works. Our answer to this aspect of the question uses a behaviour change approach to describe the way in which remediation interventions change the contexts to create insight, motivation and practice change–stages that we argue are essential to successful remediation. In terms of ‘for whom?’, we have noted that a doctor’s career stage may be an important factor, and that those who practise with more autonomy and away from educational cultures associated with training grades may find remediation more challenging. This fits with how we think remediation works, but the stage of a doctor’s career is only explicitly referred to in one scoping review paper. 12 Some studies have also pointed to the difficulties in remediating older doctors in particular,7,95,110,160,161 but there was not enough evidence in the literature to integrate this into the programme theory. Similarly, we acknowledge that gender, culture, or medical specialty may all be relevant factors, but, once again, because of the absence of data in the documents included in our review, we were unable to further elucidate these factors.
The aspect of the question ‘to what extent’ is not about producing a summative judgement of remediation programmes. Rather, in our review, it is meant to be much more explanatory than judgemental in its focus, and to develop an understanding of remediation in depth. In fact, we do not think it is possible from this literature to produce any kind of summative judgement, as there is too much variation in multiple aspects of the delivery of remediation, the setting and the characteristics of the remediating doctor. Indeed, this variation is the reason why we chose a realist review approach, so that we could start to understand the differential impacts (i.e. the ‘to what extents’) of remediating programmes. To do this, we picked apart the remediation process, as illustrated by our CMOcs.
Our programme theory and embedded CMOcs show that, although there is a final desired outcome, namely patient safety, there are also many other intermediate or more proximal outcomes that need to be ‘achieved’. Our CMOcs set out when (and in what contexts) these are likely to occur, but we cannot quantify the likelihoods, as the data needed to do so were not available in the included documents. This is not surprising, as none of the included documents had set out to measure these intermediate or more proximal outcomes. More primary research is needed to evaluate whether or not these intermediate or more proximal outcomes are achieved.
Chapter 5 Conclusions and recommendations
This realist review has developed a programme theory of how remediation works to produce outcomes that ensure patient safety. The key academic contributions of this review are listed below.
-
Remediation is most usefully conceptualised in terms of practice change because of the uniqueness of the environment in which remediation occurs and the subsequent nature of the barriers that arise in engaging doctors in successful remediation.
-
For remediation to be successful, remediating doctors must develop insight. Insight entails both a readiness to engage with and validate others’ perceptions of one’s own performance, and acceptance of the need for change. Insight can be developed when supportive and confidential environments are created, when advocacy can be used to enhance levels of emotional support and when feedback is carefully framed so that it creates dissonance leading to change, rather than denial or rejection (CMOcs 1–13).
-
Doctors must be motivated to engage with remediation. This is often challenging because being identified as needing remediation can be demotivating. Engaging doctors with remediation planning can foster motivation by mitigating the loss of autonomy that is inherent in undergoing remediation for practising doctors, and by enhancing perceptions of control. Similarly, setting realistic and incremental goals will help (CMOcs 14–23).
-
Remediation plans are effective when they afford the opportunities for remediating doctors to practise behaviours and skills in a simulated environment. Importantly, in terms of behaviour, understanding that behaviours are wrong may not be enough, and practising new behaviours may facilitate behavioural change (CMOcs 24 and 25).
-
Processes of reflection are central to facilitating remediation. However, despite the centrality of reflection to the process, assessing reflection itself may undermine its transformative potential. Written reflections on a remediation process may help give meaning to feedback received. Guided reflection with a skilled coach is an effective way of giving meaning to feedback and helping ensure that feedback helps to develop insight (CMOcs 26–29).
-
It is important to evaluate any organisational issues that may contribute to poor performance or behaviour. This will help determine whether or not the work environment is a contributory factor, and whether or not this environment will be suitable for undertaking remediation activities.
There are a number of significant implications related to the findings from our review. First, focusing remediation interventions on developing insight will be an important first step for a remediation programme. Insight is a necessary condition for successful remediation. Bringing about insightful practice may require remediation programmes to give significant attention to the way in which feedback is framed and the environments created for reflective practice. This is important because practising doctors are often not functioning within an educational environment in which making mistakes and learning from those mistakes is an integral part of the process. Rather, doctors function in an environment (more or less, depending on their stage of training and/or their role) in which a return to a more educational environment entails a loss of autonomy and is likely to invoke adverse reaction. This brings into focus a careful consideration of how the roles in remediation are structured, and how the remediation programme can create facilitative environments for feedback to be accepted.
If the important processes that function within a remediation programme relate to behavioural change, then it is important to acknowledge that the transformative learning that really matters may be some of the most difficult to measure. Intermediate outcomes essential to the remediation process, related to insight and motivation, may be assessed through the qualitative judgements of trained individuals who are able to identify, respond, frame feedback, challenge (in a supportive way) and recognise when reflection is a genuine rather than strategic endeavour. If programmes focus on only measurable outcomes, they may not be able to deliver sustainable practice change.
This in turn points to issues of resource allocation. We have not sought here to prescribe the exact structure of a remediation team. Our recommendations are designed to work with existing programmes and are subsequently broad in their scope. However, our findings do suggest that the training of individuals in coaching- and mentoring-type roles should be a priority for remediation programmes, rather than an optional extra.
RESTORE review recommendations
Based on our findings, we have developed a series of recommendations for those working to deliver remediation programmes, on tailoring, implementation and design strategies to improve remediation interventions for doctors (Table 14). Although this review did not include studies on other health-care professionals, these recommendations would also be relevant for other health-care professionals.
| Finding | Recommendation |
|---|---|
| 1. Remediation programmes work when they develop insight | |
| 1.1 Safe spaces for confidential discussion help a remediating doctor become ready to explore issues related to their performance or behaviour | Remediating doctors should have the opportunity for confidential discussion with someone in a supportive role |
| 1.2 Juxtaposing a remediating doctor’s own values with their actual behaviours help remediating doctors accept the need for change | Remediation programmes for issues related to conduct should include an opportunity for remediating doctors to reflect on their own professional values and contrast these with the feedback they receive on their own behaviours |
| 1.3 When a remediating doctor has the support of an advocate who has no role in summative judgements then they are more likely to develop trust in the remediation process | Remediating doctors should be supported by someone who has the role of advocate. This individual may be a coach or mentor, and should not have a role in making summative judgements throughout the remediation programme |
| 1.4 When feedback on performance/behaviour is specific and comes from multiple sources it is more likely to be validated by a remediating doctor |
Remediating doctors should be provided with specific feedback that details the reasons and provides examples of underperformance or poor conduct. If the feedback relates to behaviour, it should detail specific events with a date and time This feedback should ideally come from more than one source and include feedback from patients whenever possible Feedback will be needed throughout the remediation process, not just at the beginning. The appropriate feedback to determine progress, and the way that it is delivered, should be ascertained in the remediation planning stage |
| 1.5 When feedback is framed in a way that is sensitive to a doctor’s professional identity, they are less likely to reject that feedback and may accept the need to change performance or behaviour to align with their own professional values | Feedback may be more effective when in person and should be guided by someone who has been trained to deliver feedback. The feedback should be framed in such a way that it relates to the professional values of the doctor, is presented in a way that seems manageable and affirms any identified strengths |
| 1.6 Remediation is more likely to be successful when assessment is used to explore and identify the full range of possible causes for a ‘problem’ |
Multimodal assessment should be used to explore a full range of potential issues, including behavioural issues, even when the identified problem may appear to relate to knowledge and skills Assessment should also be used to determine any organisational issues that may contribute to poor performance or behaviour. This will help determine whether or not the work environment is a contributory factor, and whether or not this environment will be suitable for undertaking remediation activities. If there are problems with the work environment, then remediation may need to be conducted elsewhere |
| 1.7 When remediating doctors are facilitated to identify and reflect on the triggers of poor performance or unprofessional behaviour, they may be able to avoid these reactions in the future | Remediation programmes should offer the opportunity for the remediating doctor to reflect on the reasons for their referral and to identify the triggers for underperformance/poor conduct |
| 2. Remediation programmes work when they motivate practitioners to change | |
| 2.1 If a remediating doctor has input into the design of an individualised remediation programme then they are more likely to have buy-in to the programme and will be more motivated to engage | When possible, remediating doctors should collaborate in the design of the individualised remediation plan and help to shape it. The planning stage should include setting scheduled points for assessing progress and determining what kind of feedback will be appropriate for the assessment of this progress |
| 2.2 When part of the remediation planning process includes setting realistic and achievable goals, the remediating doctor may feel that they are more capable of achieving these goals | The remediating doctor should collaborate in the process of goal-setting, and the goals set should be achievable and measurable |
| 2.3 When remediating doctors are clear about what happens when targets are achieved or not achieved then they are more likely to choose to engage in the remediation programme | Remediation programmes should include an individualised plan that specifies the milestones, points for review of progress and the consequences of achieving or not achieving targets |
| 2.4 If efforts are made to destigmatise remediation, wherever possible, remediating doctors are more likely to engage with the process and be more motivated because there is less of a threat to their professional identity |
Remediation programmes should seek to destigmatise the process of undergoing remediation and frame it, as far as possible, in terms of positive professional development If relevant, remediation programmes could consider changing the name from remediation to professional support or similar. Positive framing may also include changing the language around the guidance for remediation to include terms that indicate support and development |
| 3. Remediation programmes work when changes to practice are facilitated | |
| 3.1 When there is an opportunity for remediating doctors to practise new performance or behaviours then these new performances or behaviours are more likely to be integrated into their practice | When appropriate, remediation programmes should offer an opportunity for remediating doctors to practise any new skills or behaviours they have developed. This may include rehearsing new behaviours in simulated settings. When this is not possible, guided reflection can offer an opportunity to reflect on in situ practice |
| 3.2 When there are scheduled points for guided reflection, remediating doctors have more opportunity to integrate new knowledge and skills and develop further insight | Remediation programmes should have scheduled points for reviewing progress with the remediating doctor. The remediating doctor should be involved in this process of review and reflections should be guided so that the remediating doctor continues to gain insight into their progress |
| 3.3 When the remediating doctor has an active role in reflecting on feedback then the feedback is more likely to be accepted and engender a change in performance |
Reflection should be built into the remediation programme and should be guided, but not form part of a final judgement on progress. Reflection may include one-to-one discussion of feedback or discussions of entries in reflective logs. The purpose of reflection is to have an interesting and meaningful conversation to embed new knowledge and behaviours and engender further insight Recent medico legal cases may have placed uncertainty over the confidentiality of reflective logs. The exact legal status of any written reflections should be established in advance |
Strengths and limitations
The main strengths of this report are the way that we have carried out a robust and thorough realist analysis, following Realist And Meta-narrative Evidence Syntheses: Evolving Standards (RAMESES) quality standards for realist synthesis. 35 This has allowed us to go beyond the explanations provided in the existing data to build theories about how remediation works in different circumstances. Although previous reviews have focused on outcomes related to only quantifiable measures, such as pass/fail tests scores or programme completion/attrition, we have been able to uncover a range of intermediate outcome measures that form important points in a remediation journey. This has allowed us to uncover what is working (or not) in remediation programmes.
We have had excellent input from a diverse range of stakeholders with various expertise in remediating doctors, as well as PPI input to ensure that a patient voice has been present in all discussions. The stakeholders have been central throughout all stages of the process, including sense-checking our findings against their real-world experience and directly contributing to aspects of the theory-building process. This has enabled us to develop findings that are relevant at the level of policy and practice. As realist reviewing develops theory at a level of abstraction that is transferable and above the level of the intervention itself, a further strength of the realist approach is that the findings do not provide just a single model of how a remediation programme should be structured; rather, our findings offer guidance for implementing strategies that work in certain contexts and that could be applied to a range of remedial intervention types. This enhances the versatility of our findings, maximising their relevance to the broad range of remediation programmes that exist across the NHS.
The main weakness of this review is that, as with any review of existing evidence, it is limited by the quality of the literature reviewed. In this case, the literature was generally of a low quality in terms of a lack of robust studies. Much of the more theoretically rich data for developing the programme theory were derived from reports of existing programmes, rather than studies or evaluations of programmes. The studies that we did find that were more robust were generally not theoretically rich (i.e. they did not tell us much about how the programme worked to produce its effects). To some extent, the iterative, theory-building approach used in realist reviews allowed us to transcend these limitations, as theories could be built and tested against the different types of relevant data drawn from across studies and related topic areas, as well as having a critical input from our stakeholder group. We also have to acknowledge that only a small proportion of the literature we reviewed came from the UK. Most of the literature was from North America and therefore the programmes covered in the literature were not always directly transferable to the UK context. Again, our stakeholder group was indispensable in helping to ensure that the findings made sense in the UK context. We managed to recruit only one doctor who had undergone remediation to the stakeholder group (albeit one of the stakeholders had undergone remediation during medical school). Having more doctors in the stakeholder group who had undergone remediation may have provided more of a variety of perspectives on the experience of undergoing remediation and how remediation produces its effect. As mentioned in the methods section in Chapter 2, we tried different ways to recruit more remediating doctors to the stakeholder group. For future research, contacting professional support units outside the south-west of the UK may be more fruitful.
A final potential weakness, relating to the realist review methodology, is that these findings are a result of our interpretation of the data. We accept that other researchers could interpret the data differently. However, we strongly believe that our explanations of the data are plausible and have been thoroughly tested through a robust, iterative process.
Future research
We propose three areas for future research.
-
Future research can build on the work presented here to evaluate and refine remediation interventional strategies that have been already implemented, or design, implement and evaluate new interventional strategies.
-
Although we have successfully identified why remediation programmes work in some contexts and not others, we also recognise that a greater understanding of the specific contexts relevant to real-world NHS settings is required. A high proportion of studies included in our review emanate from North America (64%), where the organisation of both health-care and remediation programmes is very different from the UK. Therefore, there is a need for better specification of our programme theory to NHS settings. Future research should focus on using our evidence-based recommendations to optimise the delivery of remediation programmes for doctors in the NHS and then evaluating these changes using a realist evaluation approach. This would result in an improvement of existing programmes in the NHS and would also enable us to further test, refine, confirm or refute our programme theory of remediation and to identify other potential mechanisms at work in the remediation process, as well as other important contexts specific to the NHS.
-
Another avenue for future research involves investigating the topic of remediation relating to other health-care professions, which lag behind medicine in terms of support structures for underperforming individuals. This could involve an extended realist review looking at literature from other health-care professionals.
Acknowledgements
We would like to express our sincere gratitude to the members of our stakeholder group, those who took part in the policy workshop and others who offered their perspective through individual meetings for their significant contributions to the programme theory and recommendations emerging from the review. These included (alphabetically by first name): Alex Haig, Alison Budd, Andrew Long, Anne Rothery, Danielle Carrieri, James Read, Joe Brett, Kal Winston, Karen Chummun, Lyndsey Withers, Richard Bishop, Sol Mead and Thandie Hara. We would also like to thank the members of our steering group (alphabetically by first name), Mark Godden and Sue Varley, for their excellent advice and guidance throughout.
Contributions of authors
Dr Tristan Price (https://orcid.org/0000-0002-2135-6212) (Research Fellow) developed the research project, carried out the exploratory literature search for the review, contributed to the formal search strategies, screened the resulting references, carried out the coding, applied a realist logic of analysis to the data, developed and refined the programme theory and CMOcs for the review, identified the theoretical ideas underpinning this analysis, facilitated the stakeholder meetings, and drafted and revised the final report.
Dr Nicola Brennan (https://orcid.org/0000-0002-2165-0155) (Senior Research Fellow, Medical Education) developed the research project, contributed to the formal search strategies, carried out consistency checks on the literature retrieved from the formal searches, as well as consistency checks on the screening, contributed to the development and refinement of the programme theory and CMOcs, contributed theoretical ideas underpinning this analysis, provided methodological and relevant content support and input, and drafted and revised the final report.
Dr Geoff Wong (https://orcid.org/0000-0002-5384-4157) (GP, Clinical Research Fellow, Realist Approaches) developed the research project, applied a realist logic of analysis to the data, developed and refined the programme theory and CMOcs for the review, provided methodological support and revised this report.
Dr Lyndsey Withers (https://orcid.org/0000-0002-0027-2626) (PPI representative) developed the research project, provided PPI input and revised the final report.
Professor Jennifer Cleland (https://orcid.org/0000-0003-1433-9323) [Director, Medical Education Research and Scholarship Unit (MERSU)] developed the research project, provided relevant content knowledge and revised the final report.
Ms. Amanda Wanner (https://orcid.org/0000-0002-7899-7651) (Information Specialist) developed and conducted the main and grey literature search strategies, and contributed to writing the literature search sections for the final report.
Professor Thomas Gale (https://orcid.org/0000-0003-4551-5860) (Clinical Associate Professor) provided relevant content knowledge and revised the final report.
Dr Linda Prescott-Clements (https://orcid.org/0000-0001-9748-3659) (Director of Education) developed the research project, provided content knowledge and revised the final report.
Professor Julian Archer (https://orcid.org/0000-0001-9983-9655) (Adjunct Professor) developed the research project and revised the final report.
Dr Marie Bryce (https://orcid.org/0000-0001-7876-2265) (Senior Research Fellow) revised the final report.
Publications
Price T, Brennan N, Cleland J, Prescott-Clements L, Wanner A, Withers L, et al. Remediating doctors’ performance to restore patient safety: a realist review protocol BMJ Open 2018;8:e025943.
Price T, Wong G, Withers L, Wanner A, Cleland J, Gale T, et al. Optimising the delivery of remediation programmes for doctors: a realist review. Med Ed Rev 2021;00:1–16.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Price T, Wong G, Withers L, Wanner A, Cleland J, Gale T, et al. Optimising the delivery of remediation programmes for doctors: a realist review. Med Ed Rev 2021;00:1-16. https://doi.org/10.1111/medu.14528.
- Kalet A, Tewksbury L, Ogilvie JB, Yingling S, Kalet A, Chou CL. Remediation in Medical Education. New York, NY: Springer; 2014.
- Leape LL, Woods DD, Hatlie MJ, Kizer KW, Schroeder SA, Lundberg GD. Promoting patient safety by preventing medical error. JAMA 1998;280:1444-7. https://doi.org/10.1001/jama.280.16.1444.
- Lillis S, Takai N, Francis S. Long-term outcomes of a remedial education program for doctors with clinical performance deficits. J Contin Educ Health Prof 2014;34:96-101. https://doi.org/10.1002/chp.21227.
- Humphrey C. Assessment and remediation for physicians with suspected performance problems: an international survey. J Contin Educ Health Prof 2010;30:26-3. https://doi.org/10.1002/chp.20053.
- Berrow D, Faw L, Jobanputra R. Analysis of the First 50 NCAS Assessment Cases: NCAS Evaluation, Research and Development. London: National Clinical Assessment Authority; 2005.
- Prescott-Clements L, Voller V, Bell M, Nestors N, van der Vleuten CPM. Rethinking remediation: a model to support the detailed diagnosis of clinicians’ performance problems and the development of effective remediation plans. J Contin Educ Health Prof 2017;37:245-54. https://doi.org/10.1097/CEH.0000000000000173.
- Price T, Archer J. UK policy on doctor remediation: trajectories and challenges. J Contin Educ Health Prof 2017;37:207-11. https://doi.org/10.1097/CEH.0000000000000167.
- Swanwick T, Whiteman J. Remediation: where does the responsibility lie?. Postgrad Med J 2013;89:1-3. https://doi.org/10.1136/postgradmedj-2012-131642.
- Department of Health and Social Care . Remediation Report: Report of the Steering Group on Remediation 2009. www.aomrc.org.uk/wp-content/uploads/2016/04/Remediation_report_0310.pdf (accessed 8 October 2020).
- Hauer KE, Ciccone A, Henzel TR, Katsufrakis P, Miller SH, Norcross WA, et al. Remediation of the deficiencies of physicians across the continuum from medical school to practice: a thematic review of the literature. Acad Med 2009;84:1822-32. https://doi.org/10.1097/ACM.0b013e3181bf3170.
- Bourgeois-Law G, Teunissen PW, Regehr G. Remediation in practicing physicians: current and alternative conceptualizations. Acad Med 2018;93:1638-44. https://doi.org/10.1097/ACM.0000000000002266.
- Bourgeois-Law G, Varpio L, Regehr G, Teunissen PW. Education or regulation? Exploring our underlying conceptualisations of remediation for practising physicians. Med Educ 2019;53:276-84. https://doi.org/10.1111/medu.13745.
- Kennedy T, Regehr G, Rosenfield J, Roberts SW, Lingard L. Exploring the gap between knowledge and behavior: a qualitative study of clinician action following an educational intervention. Acad Med 2004;79:386-93. https://doi.org/10.1097/00001888-200405000-00006.
- Mazmanian PE, Daffron SR, Johnson RE, Davis DA, Kantrowitz MP. Information about barriers to planned change: a randomized controlled trial involving continuing medical education lectures and commitment to change. Acad Med 1998;73:882-6. https://doi.org/10.1097/00001888-199808000-00013.
- legislation.gov.uk . The Medical Profession (Responsible Officers) Regulations 2010. www.legislation.gov.uk/uksi/2010/2841/contents/made (accessed 8 October 2020).
- Conlon M, Kirk J. A Practical Guide for Responding to Concerns About Medical Practice. London: NHS England; 2019.
- Walshe K, Boyd A, Bryce M, Luscombe K, Tazzyman A, Tredinnick-Rowe J, et al. Implementing medical revalidation in the United Kingdom: findings about organisational changes and impacts from a survey of Responsible Officers. J R Soc Med 2017;110:23-30. https://doi.org/10.1177/0141076816683556.
- NHS Litigation Authority . NHS Litigation Authority: Annual Report and Accounts 2015 16 2016. www.gov.uk/government/publications/nhs-litigation-authority-annual-report-and-accounts-2015-to-2016 (accessed 12 November 2020).
- Curtis L. Unit Costs of Health and Social Care 2012. Canterbury: PSSRU, University of Kent; 2012.
- British Medical Association . Staffing Crisis in NHS Laid Bare, As New BMA Analysis Shows That Three Quarters of Medical Specialities Face Shortage of Doctors 2018.
- Robertson R, Wenzel L, Thompson J, Charles A. Understanding NHS Financial Pressures: How Are They Affecting Patient Care?. London: The King’s Fund; 2017.
- Curtis L. Unit Costs of Health and Social Care 2014. Canterbury: PSSRU, University of Kent; 2014.
- General Medical Council . The State of Medical Education and Practice in the UK Report: 2015 n.d. www.gmc-uk.org/publications/somep2015.asp (accessed 8 October 2020).
- Cleland J, Leggett H, Sandars J, Costa MJ, Patel R, Moffat M. The remediation challenge: theoretical and methodological insights from a systematic review. Med Educ 2013;47:242-51. https://doi.org/10.1111/medu.12052.
- Brennan N, Price T, Archer J, Brett J. Remediating professionalism lapses in medical students and doctors: a systematic review. Med Educ 2019;54:196-204. https://doi.org/10.1111/medu.14016.
- Lacasse M, Audétat MC, Boileau É, Caire Fon N, Dufour MH, Laferrière MC, . Interventions for undergraduate and postgraduate medical learners with academic difficulties: a BEME systematic review: BEME guide no. 56. Med Teach 2019;41:981-1001. https://doi.org/10.1080/0142159X.2019.1596239.
- Wong G, Brennan N, Mattick K, Pearson M, Briscoe S, Papoutsi C. Interventions to improve antimicrobial prescribing of doctors in training: the IMPACT (IMProving Antimicrobial presCribing of doctors in Training) realist review. BMJ Open 2015;5.
- Pawson R. Evidence-based policy: the promise of ‘realist synthesis’. Evaluation 2002;8. https://doi.org/10.1177/135638902401462448.
- Merton RK. Social Theory and Social Structure. New York, NY: The Free Press; 1968.
- Wong G, Greenhalgh T, Westhorp G, Pawson R. Realist methods in medical education research: what are they and what can they contribute?. Med Educ 2012;46:89-96. https://doi.org/10.1111/j.1365-2923.2011.04045.x.
- Wong G, Brennan N, Mattick K, Pearson M, Briscoe S, Papoutsi C. Interventions to improve antimicrobial prescribing of doctors in training: the IMPACT (IMProving Antimicrobial presCribing of doctors in Training) realist review. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-009059.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review – a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10:21-34. https://doi.org/10.1258/1355819054308530.
- Price T, Brennan N, Cleland J, Prescott-Clements L, Wanner A, Withers L, et al. Remediating doctors’ performance to restore patient safety: a realist review protocol. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2018-025943.
- Wong G, Greenhalgh T, Westhorp G, Pawson R. Development of methodological guidance, publication standards and training materials for realist and meta-narrative reviews: the RAMESES (Realist And Meta-narrative Evidence Synthesis: Evolving Standards) project. Health Serv Deliv Res 2014;2. https://doi.org/10.3310/hsdr02300.
- Greenhalgh T, Peacock R. Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. BMJ 2005;331:1064-5. https://doi.org/10.1136/bmj.38636.593461.68.
- Swanwick T. Understanding Medical Education: Evidence, Theory and Practice. Hoboken, NJ: John Wiley & Sons; 2013.
- Pawson R. Evidence-Based Policy: A Realist Perspective. Thousand Oaks, CA: Sage; 2006.
- Papoutsi C, Mattick K, Pearson M, Brennan N, Briscoe M, Wong G. Interventions to improve antimicrobial prescribing of doctors in training (IMPACT): a realist review. Health Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06100.
- Krzyzaniak SM, Wolf SJ, Byyny R, Barker L, Kaplan B, Wall S, et al. A qualitative study of medical educators’ perspectives on remediation: adopting a holistic approach to struggling residents. Med Teach 2017;39:967-74. https://doi.org/10.1080/0142159X.2017.1332362.
- Shapiro J, Prislin MD, Larsen KM, Lenahan PM. Working with the resident in difficulty. Fam Med 1987;19:368-75.
- Brown N, McAvoy P, Joffe M. Defining insight: a challenge that matters. Clin Teach 2014;11:170-3. https://doi.org/10.1111/tct.12123.
- Hays RB, Jolly BC, Caldon LJ, McCrorie P, McAvoy PA, McManus IC, et al. Is insight important? Measuring capacity to change performance. Med Educ 2002;36:965-71. https://doi.org/10.1046/j.1365-2923.2002.01317.x.
- Kimatian SJ, Lloyd SH. Remediation and due process for trainees: setting the stage for future success. Int Anesthesiol Clin 2008;46:113-25. https://doi.org/10.1097/AIA.0b013e3181817b04.
- Leung FH, Ratnapalan S. A framework to teach self-reflection for the remedial resident. Med Teach 2011;33:e154-7. https://doi.org/10.3109/0142159X.2011.543199.
- Paice E. Identification and management of the underperforming surgical trainee. ANZ J Surg 2009;79:180-4. https://doi.org/10.1111/j.1445-2197.2008.04837.x.
- Shearer C, Bosma M, Bergin F, Sargeant J, Warren A. Remediation in Canadian medical residency programs: established and emerging best practices. Med Teach 2018:1-8. https://doi.org/10.1080/0142159X.2018.1436164.
- Sullivan CMD, Arnold LPD, Cruess RL, Cruess SR, Steinert Y. Teaching Medical Professionalism. Cambridge: Cambridge University Press; 2008.
- Whiteman J, Jamieson A. Remediation with trust, assurance and safety. Educ Prim Care 2007;18:665-73. https://doi.org/10.1080/14739879.2007.11493604.
- Wu JS, Siewert B, Boiselle PM. Resident evaluation and remediation: a comprehensive approach. J Grad Med Educ 2010;2:242-5. https://doi.org/10.4300/JGME-D-10-00031.1.
- Parran TV, Pisman AR, Youngner SJ, Levine SB. Evolution of a remedial CME course in professionalism: addressing learner needs, developing content, and evaluating outcomes. J Contin Educ Health Prof 2013;33:174-9. https://doi.org/10.1002/chp.21182.
- Rougas S, Gentilesco B, Green E, Flores L. Twelve tips for addressing medical student and resident physician lapses in professionalism. Med Teach 2015;37:901-7. https://doi.org/10.3109/0142159X.2014.1001730.
- Shapiro J, Whittemore A, Tsen LC. Instituting a culture of professionalism: the establishment of a center for professionalism and peer support. Jt Comm J Qual Patient Saf 2014;40:168-77. https://doi.org/10.1016/S1553-7250(14)40022-9.
- Kalet A, Guerrasio J, Chou CL. Twelve tips for developing and maintaining a remediation program in medical education. Med Teach 2016;38:787-92. https://doi.org/10.3109/0142159X.2016.1150983.
- Sargeant J, Bruce D, Campbell CM. Practicing physicians’ needs for assessment and feedback as part of professional development. J Contin Educ Health Prof 2013;33:54-62. https://doi.org/10.1002/chp.21202.
- Warburton KM, Mahan JD. Coaching nephrology trainees who struggle with clinical performance. Clin J Am Soc Nephrol 2018;13:172-4. https://doi.org/10.2215/CJN.07270717.
- Arnold L, Sullivan C, Quaintance J, Cruess RL, Cruess SR, Steinert Y. Teaching Medical Professionalism: Supporting the Development of Professional Identity. Cambridge: Cambridge University Press; 2016.
- Papadakis MA, Paauw DS, Hafferty FW, Shapiro J, Byyny RL. Alpha Omega Alpha Honor Medical Society Think Tank . Perspective: the education community must develop best practices informed by evidence-based research to remediate lapses of professionalism. Acad Med 2012;87:1694-8. https://doi.org/10.1097/ACM.0b013e318271bc0b.
- Roberts NK, Williams RG, Klingensmith M, Sullivan M, Boehler M, Hickson G, et al. The case of the entitled resident: a composite case study of a resident performance problem syndrome with interdisciplinary commentary. Med Teach 2012;34:1024-32. https://doi.org/10.3109/0142159X.2012.719654.
- Walsh LA, Davies SJ, Gallen DD. Model of service provision for performance related issues in Wales school of postgraduate medical education. Med Educ Suppl 2010;3.
- Mahmood T. Dealing with trainees in difficulty. Facts Views Vis Obgyn 2012;4:18-23.
- Sparks JW, Landrigan-Ossar M, Vinson A, Dearden J, Navedo AT, Waisel DB, et al. Individualized remediation during fellowship training. J Clin Anesth 2016;34:452-8. https://doi.org/10.1016/j.jclinane.2016.04.004.
- Decoteau MA, Rivera L, Umali K, Chan AD, Soballe P, Ignacio RC. A multimodal approach improves American Board of Surgery In-Training Examination scores. Am J Surg 2018;215:315-21. https://doi.org/10.1016/j.amjsurg.2017.10.039.
- Frankel RM, Hafferty FW, Denberg T, Feldman MD. Behavioral Medicine: A Guide for Clinical Practice. New York, NY: McGraw-Hill; 2014.
- Guerrasio J, Broadfoot KJ, Aagaard EM. Using simulation to remediate poor professional behaviors. J Gen Intern Med 2016;1:S853-4.
- Sanfey H, Williams R, Dunnington G. Recognizing residents with a deficiency in operative performance as a step closer to effective remediation. J Am Coll Surg 2013;216:114-22. https://doi.org/10.1016/j.jamcollsurg.2012.09.008.
- Bhatti NI, Ahmed A, Stewart MG, Miller RH, Choi SS. Remediation of problematic residents – a national survey. Laryngoscope 2016;126:834-8. https://doi.org/10.1002/lary.25599.
- Borman KR. Does academic intervention impact ABS qualifying examination results?. Curr Surg 2006;63:367-72. https://doi.org/10.1016/j.cursur.2006.06.007.
- Domen RE. Resident remediation, probation, and dismissal basic considerations for program directors. Am J Clin Pathol 2014;141:784-90. https://doi.org/10.1309/AJCPSNPAP5R5NHUS.
- Kosir MA, Fuller L, Tyburski J, Berant L, Yu M. The Kolb learning cycle in American Board of Surgery In-Training Exam remediation: the Accelerated Clinical Education in Surgery course. Am J Surg 2008;196:657-62. https://doi.org/10.1016/j.amjsurg.2008.07.004.
- Mar C, Chang S, Forster B. Remedial training for the radiology resident: a template for optimization of the learning plan. Acad Radiol 2015;22:240-6. https://doi.org/10.1016/j.acra.2014.10.005.
- Mugford B. Performance and remediation in general practice training. Aust Fam Physician 2003;32:544-6.
- Ratan RB, Pica AG, Berkowitz RL. A model for instituting a comprehensive program of remediation for at-risk residents. Obstet Gynecol 2008;112:1155-9. https://doi.org/10.1097/AOG.0b013e31818a6d61.
- Regan L, Hexom B, Nazario S, Chinai SA, Visconti A, Sullivan C. Remediation methods for milestones related to interpersonal and communication skills and professionalism. J Grad Med Educ 2016;8:18-23. https://doi.org/10.4300/JGME-D-15-00060.1.
- Rehm CG, Rowland PA. The remedial year in the general surgery board certification process: how effective is it?. Curr Surg 2005;62:644-50. https://doi.org/10.1016/j.cursur.2005.02.001.
- Egener B. Addressing physicians’ impaired communication skills. J Gen Intern Med 2008;23:1890-5. https://doi.org/10.1007/s11606-008-0778-7.
- Kern DE, Wright SM, Carrese JA, Lipkin M, Simmons JM, Novack DH, et al. Personal growth in medical faculty: a qualitative study. West J Med 2001;175:92-8. https://doi.org/10.1136/ewjm.175.2.92.
- Smith CS, Stevens NG, Servis M. A general framework for approaching residents in difficulty. Fam Med 2007;39:331-6.
- Samenow CP, Worley LL, Neufeld R, Fishel T, Swiggart WH. Transformative learning in a professional development course aimed at addressing disruptive physician behavior: a composite case study. Acad Med 2013;88:117-23. https://doi.org/10.1097/ACM.0b013e31827b4cc9.
- Paglia MJ, Frishman G. The trainee in difficulty: a viewpoint from the USA. Obstet Gynaecol 2011;13:247-51. https://doi.org/10.1576/toag.13.4.247.27690.
- Newman A, Donohue R, Eva N. Psychological safety: a systematic review of the literature. Hum Resour Manag Rev 2017;27:521-35. https://doi.org/10.1016/j.hrmr.2017.01.001.
- Edmondson AC, Higgins M, Singer S, Weiner J. Understanding psychological safety in health care and education organizations: a comparative perspective. Res Hum Dev 2016;13:65-83. https://doi.org/10.1080/15427609.2016.1141280.
- Hsiang-Te Tsuei S, Lee D, Ho C, Regehr G, Nimmon L. Exploring the construct of psychological safety in medical education. Acad Med 2019;94:S28-S35. https://doi.org/10.1097/ACM.0000000000002897.
- Kalet A, Chou CL, Ellaway RH. To fail is human: remediating remediation in medical education. Perspect Med Educ 2017;6:418-24. https://doi.org/10.1007/s40037-017-0385-6.
- Caldicott CV, d’Oronzio JC. Ethics remediation, rehabilitation, and recommitment to medical professionalism: a programmatic approach. Ethics Behav 2015;25:279-96. https://doi.org/10.1080/10508422.2014.930687.
- d’Oronzio JC. Remedial ethics programs for physicians and dentists. J Am Coll Dent 2009;76:41-5.
- Rumack CM, Guerrasio J, Christensen A, Aagaard EM. Academic remediation: why early identification and intervention matters. Acad Radiol 2017;24:730-3. https://doi.org/10.1016/j.acra.2016.12.022.
- Leung FH, Martin D, Batty H. A theory-based curriculum design for remediation of residents’ communication skills. Med Teach 2009;31:e555-9. https://doi.org/10.3109/01421590902849529.
- Swiggart WH, Dewey CM, Hickson GB, Finlayson AJ, Spickard WA. A plan for identification, treatment, and remediation of disruptive behaviors in physicians. Front Health Serv Manage 2009;25:3-11. https://doi.org/10.1097/01974520-200904000-00002.
- Boiselle PM. A remedy for resident evaluation and remediation. Acad Radiol 2005;12:894-900. https://doi.org/10.1016/j.acra.2005.03.056.
- Katz ED, Dahms R, Sadosty AT, Stahmer SA, Goyal D. CORD-EM Remediation Task Force . Guiding principles for resident remediation: recommendations of the CORD remediation task force. Acad Emerg Med 2010;17:95-103. https://doi.org/10.1111/j.1553-2712.2010.00881.x.
- Krzyzaniak S, Wolf S, Byyny R, Barker L, Kaplan B, Guerrasio J. A qualitative study of medical educators’ perspectives on resident remediation. West J Emerg Med 2016;17.
- Liu J, Yucel K, Bedi HS. Radiology resident remediation: five important questions to ask. AJR Am J Roentgenol 2016;206:1045-8. https://doi.org/10.2214/AJR.15.15551.
- Grant WD. Identification and restoration of lapsed skills for primary care providers. Int J Psychiatry Med 1998;28:147-57. https://doi.org/10.2190/Q2C0-9F11-FJYL-23H7.
- Hanna E, Premi J, Turnbull J. Results of remedial continuing medical education in dyscompetent physicians. Acad Med 2000;75:174-6. https://doi.org/10.1097/00001888-200002000-00017.
- Kluger AN, DeNisi A. The effects of feedback interventions on performance: a historical review, a meta-analysis, and a preliminary feedback intervention theory. Psychol Bull 1996;119.
- Arnold L. Responding to the professionalism of learners and faculty in orthopaedic surgery. Clin Orthop Relat Res 2006;449:205-13. https://doi.org/10.1097/01.blo.0000224034.00980.9e.
- Nelson R. Remediation through personalized CME (part II). Iowa Med 1993;83.
- Hickson GB, Pichert JW, Webb LE, Gabbe SG. A complementary approach to promoting professionalism: identifying, measuring, and addressing unprofessional behaviors. Acad Med 2007;82:1040-8. https://doi.org/10.1097/ACM.0b013e31815761ee.
- Grant WD. An individualized educational model for the remediation of physicians. Arch Fam Med 1995;4:767-72. https://doi.org/10.1001/archfami.4.9.767.
- Brennan N, Bryce M, Pearson M, Wong G, Cooper C, Archer J. Towards an understanding of how appraisal of doctors produces its effects: a realist review. Med Educ 2017;51:1002-13. https://doi.org/10.1111/medu.13348.
- Merton RK, Merton RC. Social Theory and Social Structure. New York, NY: Simon and Schuster; 1968.
- Archer MS, Elder-Vass D. Cultural system or norm circles? An exchange. Eur J Soc Theory 2012;15:93-115. https://doi.org/10.1177/1368431011423592.
- Elder-Vass D. The Causal Power of Social Structures: Emergence, Structure and Agency. Cambridge: Cambridge University Press; 2010.
- Terry DJ, Hogg MA, White KM. The theory of planned behaviour: self-identity, social identity and group norms. Br J Soc Psychol 1999;38:225-44. https://doi.org/10.1348/014466699164149.
- Cox A. What are communities of practice? A comparative review of four seminal works. Journal Inf Sci 2005;31:527-40. https://doi.org/10.1177/0165551505057016.
- Handley K, Sturdy A, Fincham R, Clark T. Within and beyond communities of practice: making sense of learning through participation, identity and practice. J Manag Stud 2006;43:641-53. https://doi.org/10.1111/j.1467-6486.2006.00605.x.
- Lave J, Wenger E, Clarke J, Hanson A, Harrison R, Reeve F. Supporting Lifelong Learning. Abingdon: Routledge; 2001.
- Parboosingh JT. Physician communities of practice: where learning and practice are inseparable. J Contin Educ Health Prof 2002;22:230-6. https://doi.org/10.1002/chp.1340220407.
- Goulet F, Gagnon R, Gingras ME. Influence of remedial professional development programs for poorly performing physicians. J Contin Educ Health Prof 2007;27:42-8. https://doi.org/10.1002/chp.93.
- Shah S, Knowlden S, Fisher R, Harris M, Yeo G. General practice trainees in the ‘borderline’ zone of competence: the experience of remediation at a regional general practice training and education centre. Educ Gen Pract 1997;8:102-11.
- Rhydderch M, Matthews P, Beech M. The advanced training practice network: providing prescribed further training for general practitioners in Wales. Educ Prim Care 2007;18:572-81. https://doi.org/10.1080/14739879.2007.11493590.
- Pittam G, Boyce M, Secker J, Lockett H, Samele C. Employment advice in primary care: a realistic evaluation. Health Soc Care Community 2010;18:598-606. https://doi.org/10.1111/j.1365-2524.2010.00929.x.
- Montano DE, Kasprzyk D, Glanz K, Rimer BK, Viswanath K. Health Behavior: Theory, Research and Practice. Hoboken, NJ: Wiley; 2015.
- Guevara M, Grewald Y, Hutchinson K, Amoateng-Adjepong Y, Manthous C. Individualized education plans in medical education. Conn Med 2011;75:537-40.
- Durning SJ, Cleary TJ, Sandars J, Hemmer P, Kokotailo P, Artino AR. Perspective: viewing ‘strugglers’ through a different lens: how a self-regulated learning perspective can help medical educators with assessment and remediation. Acad Med 2011;86:488-95. https://doi.org/10.1097/ACM.0b013e31820dc384.
- Harthun NL, Schirmer BD, Sanfey H. Remediation of low ABSITE scores. Curr Surg 2005;62:539-42. https://doi.org/10.1016/j.cursur.2005.04.020.
- Katz ED, Goyal DG, Char D, Coopersmith CM, Fried ED. A novel concept in residency education: case-based remediation. J Emerg Med 2013;44:493-8. https://doi.org/10.1016/j.jemermed.2012.09.031.
- Cerda JJ, Van Susteren TJ, Hatch R, Herkov M. Remedial education: can this doctor be saved?. Trans Am Clin Climatol Assoc 2000;111:188-96.
- Goulet F, Jacques A, Gagnon R. An innovative approach to remedial continuing medical education, 1992–2002. Acad Med 2005;80:533-40. https://doi.org/10.1097/00001888-200506000-00004.
- Guerrasio J, Garrity MJ, Aagaard EM. Learner deficits and academic outcomes of medical students, residents, fellows, and attending physicians referred to a remediation program, 2006–2012. Acad Med 2014;89:352-8. https://doi.org/10.1097/ACM.0000000000000122.
- Rosenblatt MA, Schartel SA. Evaluation, feedback and remediation in anesthesiology residency training: a survey of 124 United States programs. J Educ Perioper Med 1999;1. https://doi.org/10.1016/S0952-8180(99)00084-7.
- Visconti A, Gaeta T, Cabezon M, Briggs W, Pyle M. Focused board intervention (FBI): a remediation program for written board preparation and the medical knowledge core competency. J Grad Med Educ 2013;5:464-7. https://doi.org/10.4300/JGME-D-12-00229.1.
- Martiny-Huenger T, Martiny SE, Gollwitzer PM, Haggard P, Eitam B. The Sense of Agency. Oxford: Oxford University Press; 2015.
- Zimmerman BJ. Self-efficacy: an essential motive to learn. Contemp Educ Psychol 2000;25:82-91. https://doi.org/10.1006/ceps.1999.1016.
- Goldberg A, Samuelson S, Levine A, DeMaria S. High-stakes simulation-based assessment for retraining and returning physicians to practice. Int Anesthesiol Clin 2015;53:70-8. https://doi.org/10.1097/AIA.0000000000000079.
- Bulstrode C, Hunt V, Hamilton L, Briggs T, Hilton C. Retraining: can do, will do? A practical guide to process and pitfalls. Surg-J R Coll Surg E 2005;3:261-4. https://doi.org/10.1016/S1479-666X(05)80088-5.
- Ehrlinger J, Johnson K, Banner M, Dunning D, Kruger J. Why the unskilled are unaware: further explorations of (absent) self-insight among the incompetent. Organ Behav Hum Decis Process 2008;105:98-121. https://doi.org/10.1016/j.obhdp.2007.05.002.
- Hodges B, Regehr G, Martin D. Difficulties in recognizing one’s own incompetence: novice physicians who are unskilled and unaware of it. Acad Med 2001;76:S87-9. https://doi.org/10.1097/00001888-200110001-00029.
- Kruger J, Dunning D. Unskilled and unaware of it: how difficulties in recognizing one’s own incompetence lead to inflated self-assessments. J Pers Soc Psychol 1999;77. https://doi.org/10.1037/0022-3514.77.6.1121.
- Kruger J, Dunning D. Unskilled and unaware of it: how difficulties in recognizing one’s own incompetence lead to inflated self-assessments. J Psychol 2009;1:30-46.
- Schlösser T, Dunning D, Johnson KL, Kruger J. How unaware are the unskilled? Empirical tests of the ‘signal extraction’ counterexplanation for the Dunning–Kruger effect in self-evaluation of performance. J Econ Psychol 2013;39:85-100. https://doi.org/10.1016/j.joep.2013.07.004.
- Krzyzaniak S, Wolf S, Byyny R, Kaplan B, Barker L, Guerrasio J. Barriers to the remediation of struggling learners: a qualitative study. West J Emerg Med 2016;17.
- Bourgeois-Law G, Teunissen PW, Varpio L, Regehr G. Attitudes towards physicians requiring remediation: one-of-us or not-like-us?. Acad Med 2019;94:S36-S41. https://doi.org/10.1097/ACM.0000000000002896.
- Gunderman RB, Rackson M. Identifying and helping struggling residents. J Am Coll Radiol 2006;3:485-8. https://doi.org/10.1016/j.jacr.2006.02.016.
- Andrews M, Artino AR, Douglas KM, DeZee K. Self-regulated learning and standardized test performance in internal medicine residents. J Gen Intern Med 2015;2:S505-6.
- Grams GD, Longhurst MF, Whiteside CB. The faculty experience with the ‘troublesome’ family practice resident. Fam Med 1992;24:197-200.
- Jolly J, Bowie P, Price J, Mason M, Dinwoodie M. Qualitative evaluation of an educational intervention to reduce medicolegal risks for medical doctors experiencing significantly more cases than their peers in the UK and Ireland. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-020838.
- Torbeck L, Canal DF. Remediation practices for surgery residents. Am J Surg 2009;197:397-402. https://doi.org/10.1016/j.amjsurg.2008.10.008.
- Raman HS, Limbrick DD, Ray WZ, Coble DW, Church S, Dacey RG, et al. Prevalence, management, and outcome of problem residents among neurosurgical training programs in the United States. J Neurosurg 2018;130:322-6. https://doi.org/10.3171/2017.8.JNS171719.
- Sanfey H, Darosa DA, Hickson GB, Williams B, Sudan R, Boehler ML, et al. Pursuing professional accountability: an evidence-based approach to addressing residents with behavioral problems. Arch Surg 2012;147:642-7. https://doi.org/10.1001/archsurg.2012.832.
- Ellaway RH, Chou CL, Kalet AL. Situating remediation: accommodating success and failure in medical education systems. Acad Med 2018;93:391-8. https://doi.org/10.1097/ACM.0000000000001855.
- Boileau E, St-Onge C, Audétat MC. Is there a way for clinical teachers to assist struggling learners? A synthetic review of the literature. Adv Med Educ Pract 2017;8:89-97. https://doi.org/10.2147/AMEP.S123410.
- Warburton KM, Goren E, Dine CJ. Comprehensive assessment of struggling learners referred to a graduate medical education remediation program. J Grad Med Educ 2017;9:763-7. https://doi.org/10.4300/JGME-D-17-00175.1.
- Stirling K, Hogg G, Ker J, Anderson F, Hanslip J, Byrne D. Using simulation to support doctors in difficulty. Clin Teach 2012;9:285-9. https://doi.org/10.1111/j.1743-498X.2012.00541.x.
- Rittel HW, Webber MM. Dilemmas in a general theory of planning. Policy Sci 1973;4:155-69. https://doi.org/10.1007/BF01405730.
- Bennion LD, Durning SJ, LaRochelle J, Yoon M, Schreiber-Gregory D, Reamy BV, et al. Untying the Gordian knot: remediation problems in medical schools that need remediation. BMC Med Educ 2018;18. https://doi.org/10.1186/s12909-018-1219-x.
- Klee R. Introduction to the Philosophy of Science: Cutting Nature at its Seams. Oxford: Oxford University Press; 1997.
- Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot 1997;12:38-4. https://doi.org/10.4278/0890-1171-12.1.38.
- Ajzen I. The theory of planned behaviour: reactions and reflections. Psychol Health 2011;26:1113-27. https://doi.org/10.1080/08870446.2011.613995.
- Cosman BC, Alverson AD, Boal PA, Owens EL, Norcross WA. Assessment and remedial clinical education of surgeons in California. Arch Surg 2011;146:1411-15. https://doi.org/10.1001/archsurg.2011.208.
- Finan P. How to identify & deal with the unsafe or under performing surgeon. Colorectal Dis 2011;5.
- Norcross WA, Henzel TR, Freeman K, Milner-Mares J, Hawkins RE. Toward meeting the challenge of physician competence assessment: the University of California, San Diego physician assessment and clinical education (PACE) program. Acad Med 2009;84:1008-14. https://doi.org/10.1097/ACM.0b013e3181ad199c.
- Berrow D, Humphrey C, Field R, Jobanputra R, Faw L. Clarifying concerns about doctors’ clinical performance: what is the contribution of assessment by the national clinical assessment service?. J Health Organ Manag 2007;21:333-43. https://doi.org/10.1108/14777260710751780.
- Farmer EA, Beard JD, Dauphinee WD, LaDuca T, Mann KV. Assessing the performance of doctors in teams and systems. Med Educ 2002;36:942-8. https://doi.org/10.1046/j.1365-2923.2002.01311.x.
- Grol R. Changing physicians’ competence and performance: finding the balance between the individual and the organization. J Contin Educ Health Prof 2002;22:244-51. https://doi.org/10.1002/chp.1340220409.
- Leape LL, Fromson JA. Problem doctors: is there a system-level solution?. Ann Intern Med 2006;144:107-15. https://doi.org/10.7326/0003-4819-144-2-200601170-00008.
- Ng SL, Kinsella EA, Friesen F, Hodges B. Reclaiming a theoretical orientation to reflection in medical education research: a critical narrative review. Med Educ 2015;49:461-75. https://doi.org/10.1111/medu.12680.
- Sandars J. The use of reflection in medical education: AMEE guide no. 44. Med Teach 2009;31:685-95. https://doi.org/10.1080/01421590903050374.
- Remedial program good for those who can improve . Hosp Peer Rev 2001;26:119-21.
- Norton PG, Ginsburg LS, Dunn E, Beckett R, Faulkner D. Educational interventions to improve practice of nonspecialty physicians who are identified in need by peer review. J Contin Educ Health Prof 2004;24:244-52. https://doi.org/10.1002/chp.1340240408.
- Remediation Steering Group . Remediation Report: Report of the Steering Group on Remediation 2011.
- Adams KE, Emmons S, Romm J. How resident unprofessional behavior is identified and managed: a program director survey. Am J Obstet Gynecol 2008;198:692.e1-4. https://doi.org/10.1016/j.ajog.2008.03.023.
- Andrews MA, Kelly WF, DeZee KJ. Why does this learner perform poorly on tests? Using self-regulated learning theory to diagnose the problem and implement solutions. Acad Med 2016;1.
- Audetat MC, Voirol C, Beland N, Fernandez N, Sanche G. Remediation plans in family medicine residency. Can Fam Physician 2015;61:e425-34.
- Barrett A, Galvin R, Steinert Y, Scherpbier A, O’Shaughnessy A, Horgan M, et al. A BEME (best evidence in medical education) review of the use of workplace-based assessment in identifying and remediating underperformance among postgraduate medical trainees: BEME guide no. 43. Med Teach 2016;38:1188-98. https://doi.org/10.1080/0142159X.2016.1215413.
- Lee SM, Lee MC, Reed DA, Halvorsen AJ, Berbari EF, Mcdonald FS, et al. Success of a faculty development program for remediating clinical teachers. J Gen Intern Med 2014;1.
- Brooks R, Robb A, Tabak D. A remedial course on interviewing skills. Acad Med 1996;71. https://doi.org/10.1097/00001888-199605000-00090.
- Edeiken BS. Remedial program for diagnostic radiology residents. Invest Radiol 1993;28:269-74. https://doi.org/10.1097/00004424-199303000-00025.
- Gas BL, Buckarma EH, Mohan M, Pandian TK, Farley DR. Objective assessment of general surgery residents followed by remediation. J Surg Educ 2016;73:e71-6. https://doi.org/10.1016/j.jsurg.2016.07.002.
- Guerrasio J, Aagaard EM. Methods and outcomes for the remediation of clinical reasoning. J Gen Intern Med 2014;29:1607-14. https://doi.org/10.1007/s11606-014-2955-1.
- Hashimoto N. Report on retraining for physicians subject to administrative punishment. Jpn Med Assoc J 2005;48.
- Hatch DJ. Professional performance. Curr Anaesth Crit Care 1998;9:223-7. https://doi.org/10.1016/S0953-7112(98)80039-2.
- Kim RH, Tan TW. Interventions that affect resident performance on the American Board of Surgery in-training examination: a systematic review. J Surg Educ 2015;72:418-29. https://doi.org/10.1016/j.jsurg.2014.09.012.
- Larson CP, Steadman RH. An advanced specialty training program in anesthesiology: a special educational fellowship designed to return community anesthesiologists to clinical practice. Anesth Analg 2006;103:126-30. https://doi.org/10.1213/01.ane.0000220903.33100.15.
- Matthews P, Beech M, Rhydderch M, Lewis M. A new model of educational provision for GPs directed to undertake further training in Wales. Educ Prim Care 2007;18:316-27. https://doi.org/10.1080/14739879.2007.11493557.
- Murano T, Lypson M, Smith JL, Silverberg M, Weizberg M, Lukela M, et al. Creating clarity for the process of managing residents through remediation, probation and termination. West J Emerg Med 2015;16:S50-1.
- Silverberg M, Weizberg M, Murano T, Smith JL, Burkhardt JC, Santen SA. What is the prevalence and success of remediation of emergency medicine residents?. West J Emerg Med 2015;16:839-44. https://doi.org/10.5811/westjem.2015.9.27357.
- Spickard WA, Swiggart WH, Manley GT, Samenow CP, Dodd DT. A continuing medical education approach to improve sexual boundaries of physicians. Bull Menninger Clin 2008;72:38-53. https://doi.org/10.1521/bumc.2008.72.1.38.
- Swiggart W, Dewey C, Ghulyan M, Spickard A. Spanning a decade of physician boundary violations: are we improving?. HEC Forum 2016;28:129-40. https://doi.org/10.1007/s10730-015-9282-8.
- Tabby DS, Majeed MH, Schwartzman RJ. Problem neurology residents: a national survey. Neurology 2011;76:2119-23. https://doi.org/10.1212/WNL.0b013e31821f4636.
- Whiteman J, Morris P, Halpern H. Professional support, London: the professional development unit supporting practitioner well-being, refreshment, remediation and revalidation. BMJ Qual Improv Rep 2013;2. https://doi.org/10.1136/bmjquality.u201038.w720.
- Zbieranowski I, Takahashi SG, Verma S, Spadafora SM. Remediation of residents in difficulty: a retrospective 10-year review of the experience of a postgraduate board of examiners. Acad Med 2013;88:111-16. https://doi.org/10.1097/ACM.0b013e3182764cb6.
- Hardie Alvanzo A, Cohen GM, Nettleman M. Changing physician behavior: half-empty or half-full?. Clin Govern Int J 2003;8:69-78. https://doi.org/10.1108/14777270310459995.
- Spickard A, Swiggart WH, Manley G, Dodd D. A continuing education course for physicians who cross sexual boundaries. Sex Addict Compulsivity 2002;9:33-42. https://doi.org/10.1080/107201602317346629.
- Williamson K, Moreira M, Quattromani E, Smith JL. Remediation strategies for systems-based practice and practice-based learning and improvement milestones. J Grad Med Educ 2017;9:290-3. https://doi.org/10.4300/JGME-D-16-00334.1.
- Cavenagh P, Dewberry C, Jones P. Becoming professional: when and how does it start? A comparative study of first-year medical and law students in the UK. Med Educ 2000;34:897-902. https://doi.org/10.1046/j.1365-2923.2000.00680.x.
- Meyer SB, Lunnay B. The application of abductive and retroductive inference for the design and analysis of theory-driven sociological research. Sociol Res Online 2013;18:1-11. https://doi.org/10.5153/sro.2819.
- Prochaska JO. Decision making in the transtheoretical model of behavior change. Med Decis Making 2008;28:845-9. https://doi.org/10.1177/0272989X08327068.
Appendix 1 Initial programme theory
Reproduced with permission from Price et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original figure.
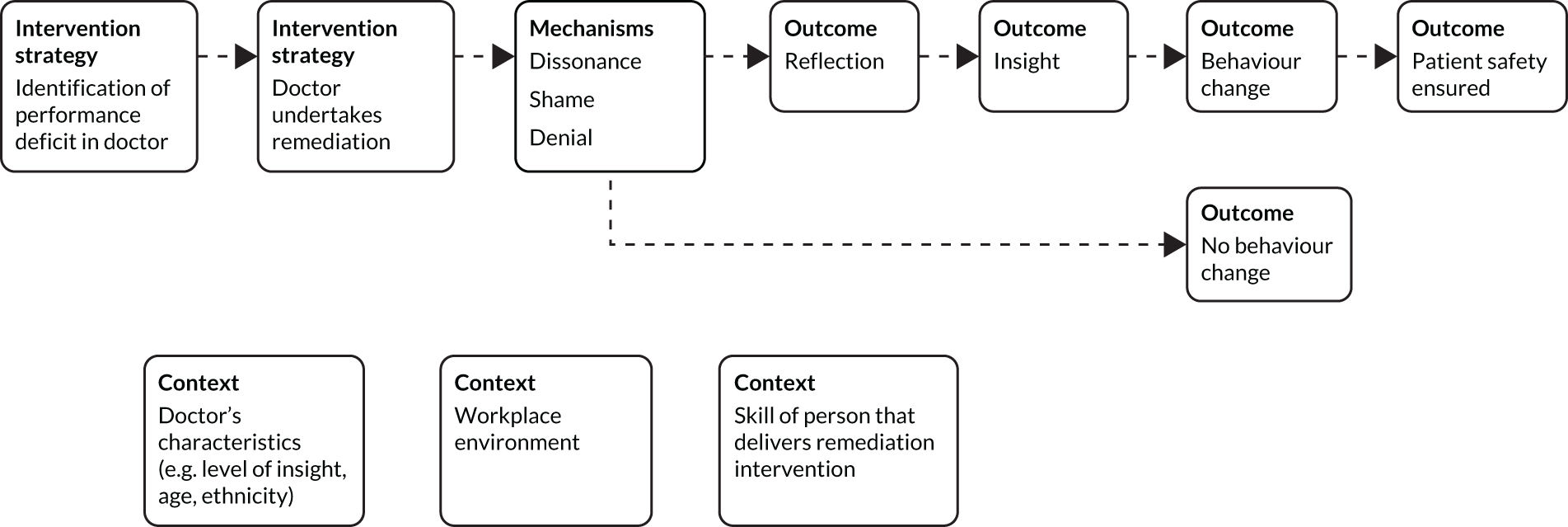
Appendix 2 Main search of databases results
| Database | Hits (n) |
|---|---|
| MEDLINE | 2000 |
| EMBASE | 2362 |
| PsycINFO | 1209 |
| HMIC | 113 |
| CINAHL | 718 |
| ERIC | 587 |
| ASSIA | 216 |
| DARE | 17 |
| Total | 7222 |
| Duplicates | 2668 |
| Total to screen at title/abstract stage | 4554 |
MEDLINE
Host: Ovid.
Data parameters: Ovid MEDLINE(R) Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R).
Date range searched: 1946 to week 3 2018.
Date searched: 4 June 2018.
Searcher: AW.
Hits: n = 2000.
Search strategy
| # | Searches | Results |
|---|---|---|
| 1 | remedia*.ti,ab,kw. | 21,621 |
| 2 | (reskilling or re-skilling or retraining or re-training).ti,ab,kw. | 3577 |
| 3 | remedial teaching/ | 1330 |
| 4 | or/1-3 | 25,960 |
| 5 | exp physicians/or “education, medical, continuing”/or “Practice Patterns, Physicians’”/or “Internship and Residency”/ | 224,220 |
| 6 | (physician* or doctor* or clinician* or practitioner* or allergist* or anaesthesiologist* or cardiologist* or dermatologist* or endocrinologist* or gastroenterologist* or GP or GPs or geriatrician* or hospitalist* or neonatologist* or nephrologist* or neurologist* or neurosurgeon* or oncologist* or ophthalmologist* or otolaryngologist* or pathologist* or paediatrician* or pediatrician* or physiatrist* or psychiatrist* or pulmonologist* or radiologist* or rheumatologist* or surgeon* or urologist*).ti,ab,kw. | 1,069,237 |
| 7 | ((residen* or trainee*) and (medic* or clinic* or hospital* or surger* or surgical or radiolog* or patient* or “primary care” or “general practice”)).ti,ab,kw. | 111,865 |
| 8 | continuing medical education.ti,ab,kw. | 5168 |
| 9 | or/5-8 | 1,231,580 |
| 10 | 4 and 9 | 2015 |
| 11 | remove duplicates from 10 | 2000 |
EMBASE
Host: Ovid.
Date range searched: 1996 to week 23 2018.
Date searched: 4 June 2018.
Searcher: AW.
Hits: n = 2362.
Search strategy
| # | Searches | Results |
|---|---|---|
| 1 | Remedia*.ti,ab,kw. | 24,632 |
| 2 | (reskilling or re-skilling or retraining or re-training).ti,ab,kw. | 3984 |
| 3 | or/1-2 | 28,542 |
| 4 | exp physician/or resident/ | 593,984 |
| 5 | (physician* or doctor* or clinician* or practitioner* or allergist* or anaesthesiologist* or cardiologist* or dermatologist* or endocrinologist* or gastroenterologist* or GP or GPs or geriatrician* or hospitalist* or neonatologist* or nephrologist* or neurologist* or neurosurgeon* or oncologist* or ophthalmologist* or otolaryngologist* or pathologist* or paediatrician* or pediatrician* or physiatrist* or psychiatrist* or pulmonologist* or radiologist* or rheumatologist* or surgeon* or urologist*).ti,ab,kw. | 1,298,687 |
| 6 | ((residen* or trainee*) and (medic* or clinic* or hospital* or surger* or surgical or radiolog* or patient* or “primary care” or “general practice”)).ti,ab,kw. | 141,396 |
| 7 | continuing medical education.ti,ab,kw. | 5616 |
| 8 | or/4-7 | 1,536,798 |
| 9 | 3 and 8 | 2430 |
| 10 | remove duplicates from 9 | 2362 |
PsycINFO
Host: Ovid.
Date range searched: 1806 to May week 4 2018.
Date searched: 4 June 2018.
Searcher: AW.
Hits: n = 1209.
Search strategy
| # | Searches | Results |
|---|---|---|
| 1 | Remedia*.ti,ab,id. | 12,899 |
| 2 | (“reskilling” or “re-skilling” or “retraining” or “re-training”).ti,ab,id. | 2312 |
| 3 | remedial education/ | 899 |
| 4 | or/1-3 | 15,250 |
| 5 | exp physicians/or medical residency/ | 44,402 |
| 6 | (physician* or doctor* or clinician* or practitioner* or allergist* or anaesthesiologist* or cardiologist* or dermatologist* or endocrinologist* or gastroenterologist* or GP or GPs or geriatrician* or hospitalist* or neonatologist* or nephrologist* or neurologist* or neurosurgeon* or oncologist* or ophthalmologist* or otolaryngologist* or pathologist* or paediatrician* or pediatrician* or physiatrist* or psychiatrist* or pulmonologist* or radiologist* or rheumatologist* or surgeon* or urologist*).ti,ab,id. | 285,078 |
| 7 | ((residen* or trainee*) and (medic* or clinic* or hospital* or surger* or surgical or radiolog* or patient* or “primary care” or “general practice”)).ti,ab,id. | 34,211 |
| 8 | “continuing medical education".ti,ab,id. | 724 |
| 9 | or/5-8 | 310,816 |
| 10 | 4 and 9 | 1212 |
| 11 | remove duplicates from 10 | 1209 |
Health Management Information Consortium
Host: Ovid.
Date range searched: 1979 to March 2018.
Date searched: 4 June 2018.
Searcher: AW.
Hits: n = 113.
Search strategy
| # | Searches | Results |
|---|---|---|
| 1 | remedia*.ti,ab. | 322 |
| 2 | remedial teaching/ | 2 |
| 3 | (reskilling or re-skilling or retraining or re-training).ti,ab. | 101 |
| 4 | or/1-3 | 424 |
| 5 | exp medical staff/ | 21,728 |
| 6 | (physician* or doctor* or clinician* or practitioner* or allergist* or anaesthesiologist* or cardiologist* or dermatologist* or endocrinologist* or gastroenterologist* or GP or GPs or geriatrician* or hospitalist* or neonatologist* or nephrologist* or neurologist* or neurosurgeon* or oncologist* or ophthalmologist* or otolaryngologist* or pathologist* or paediatrician* or pediatrician* or physiatrist* or psychiatrist* or pulmonologist* or radiologist* or rheumatologist* or surgeon* or urologist*).ti,ab. | 49,412 |
| 7 | ((residen* or trainee*) and (medic* or clinic* or hospital* or surger* or surgical or radiolog* or patient* or “primary care” or “general practice”)).ti,ab. | 4499 |
| 8 | "continuing medical education".ti,ab. | 284 |
| 9 | or/5-8 | 58,723 |
| 10 | 4 and 9 | 113 |
Cumulative Index to Nursing and Allied Health Literature
Host: EBSCOhost.
Date range searched: not available.
Date searched: 4 June 2018.
Searcher: AW.
Hits: n = 718.
Search strategy
| # | Query | Results |
|---|---|---|
| S10 | S4 AND S9 | 718 |
| S9 | S5 OR S6 OR S7 OR S8 | 420,167 |
| S8 | TI (“continuing medical education”) OR AB (“continuing medical education”) | 2193 |
| S7 | TI ((residen* or trainee*) and (medic* or clinic* or hospital* or surger* or surgical or radiolog* or patient* or “primary care” or “general practice”)) OR AB ((residen* or trainee*) and (medic* or clinic* or hospital* or surger* or surgical or radiolog* or patient* or “primary care” or “general practice”)) | 35,312 |
| S6 | TI (physician* or doctor* or clinician* or practitioner* or allergist* or anaesthesiologist* or cardiologist* or dermatologist* or endocrinologist* or gastroenterologist* or GP or GPs or geriatrician* or hospitalist* or neonatologist* or nephrologist* or neurologist* or neurosurgeon* or oncologist* or ophthalmologist* or otolaryngologist* or pathologist* or paediatrician* or pediatrician* or physiatrist* or psychiatrist* or pulmonologist* or radiologist* or rheumatologist* or surgeon* or urologist*) OR AB (physician* or doctor* or clinician* or practitioner* or allergist* or anaesthesiologist* or cardiologist* or dermatologist* or endocrinologist* or gastroenterologist* or GP or GPs or geriatrician* or hospitalist* or neonatologist* or nephrologist* or neurologist* or neurosurgeon* or oncologist* or ophthalmologist* or otolaryngologist* or pathologist* or paediatrician* or pediatrician* or physiatrist* or psychiatrist* or pulmonologist* or radiologist* or rheumatologist* or surgeon* or urologist*) | 346,873 |
| S5 | MH (“Physicians+” OR “Education, Medical, Continuing” OR “Interns and Residents”) | 96,816 |
| S4 | S1 OR S2 OR S3 | 4739 |
| S3 | MH (“Remedial Teaching”) | 361 |
| S2 | TI (“reskilling” or “re-skilling” or “retraining” or “re-training”) OR AB (“reskilling” or “re-skilling” or “retraining” or “re-training”) | 1450 |
| S1 | TI (“remedia*”) OR AB (“remedia*”) | 3135 |
Education Resources Information Center
Host: EBSCOhost.
Date range searched: not available.
Date searched: 4 June 2018.
Searcher: AW.
Hits: n = 587.
Search strategy
| # | Query | Results |
|---|---|---|
| S10 | S4 AND S9 | 587 |
| S9 | S5 OR S6 OR S7 OR S8 | 51,525 |
| S8 | TI (“continuing medical education”) OR AB (“continuing medical education”) | 472 |
| S7 | TI ((residen* or trainee*) and (medic* or clinic* or hospital* or surger* or surgical or radiolog* or patient* or “primary care” or “general practice”)) OR AB ((residen* or trainee*) and (medic* or clinic* or hospital* or surger* or surgical or radiolog* or patient* or “primary care” or “general practice”)) | 3856 |
| S6 | TI (physician* or doctor* or clinician* or practitioner* or allergist* or anaesthesiologist* or cardiologist* or dermatologist* or endocrinologist* or gastroenterologist* or GP or GPs or geriatrician* or hospitalist* or neonatologist* or nephrologist* or neurologist* or neurosurgeon* or oncologist* or ophthalmologist* or otolaryngologist* or pathologist* or paediatrician* or pediatrician* or physiatrist* or psychiatrist* or pulmonologist* or radiologist* or rheumatologist* or surgeon* or urologist*) OR AB (physician* or doctor* or clinician* or practitioner* or allergist* or anaesthesiologist* or cardiologist* or dermatologist* or endocrinologist* or gastroenterologist* or GP or GPs or geriatrician* or hospitalist* or neonatologist* or nephrologist* or neurologist* or neurosurgeon* or oncologist* or ophthalmologist* or otolaryngologist* or pathologist* or paediatrician* or pediatrician* or physiatrist* or psychiatrist* or pulmonologist* or radiologist* or rheumatologist* or surgeon* or urologist*) | 47,759 |
| S5 | DE “Physicians" | 4131 |
| S4 | S1 OR S2 OR S3 | 18,631 |
| S3 | DE (“Remedial Instruction” OR “Refresher Courses” OR “Remedial Programs”) | 7770 |
| S2 | TI (“reskilling” or “re-skilling” or “retraining” or “re-training”) OR AB (“reskilling” or “re-skilling” or “retraining” or “re-training”) | 2286 |
| S1 | TI (“remedia*”) OR AB (“remedia*”) | 13,000 |
Applied Social Sciences Index and Abstracts
Host: ProQuest.
Date range searched: not available.
Date searched: 4 June 2018.
Searcher: AW.
Hits: n = 216.
Search strategy
(MAINSUBJECT.EXACT(“Remedial teaching” OR “Remedial education”) OR TI(remedia* or “reskilling” or “re-skilling” or “retraining” or “re-training”) OR AB(remedia* or “reskilling” or “re-skilling” or “retraining” or “re-training”)) AND (MAINSUBJECT.EXACT.EXPLODE(“Doctors”) OR TI(physician* or doctor* or clinician* or practitioner* or allergist* or anaesthesiologist* or cardiologist* or dermatologist* or endocrinologist* or gastroenterologist* or GP or GPs or geriatrician* or hospitalist* or neonatologist* or nephrologist* or neurologist* or neurosurgeon* or oncologist* or ophthalmologist* or otolaryngologist* or pathologist* or paediatrician* or pediatrician* or physiatrist* or psychiatrist* or pulmonologist* or radiologist* or rheumatologist* or surgeon* or urologist*) OR AB(physician* or doctor* or clinician* or practitioner* or allergist* or anaesthesiologist* or cardiologist* or dermatologist* or endocrinologist* or gastroenterologist* or GP or GPs or geriatrician* or hospitalist* or neonatologist* or nephrologist* or neurologist* or neurosurgeon* or oncologist* or ophthalmologist* or otolaryngologist* or pathologist* or paediatrician* or pediatrician* or physiatrist* or psychiatrist* or pulmonologist* or radiologist* or rheumatologist* or surgeon* or urologist*) OR TI((residen* or trainee*) and (medic* or clinic* or hospital* or surger* or surgical or radiolog* or patient* or “primary care” or “general practice”)) OR AB((residen* or trainee*) and (medic* or clinic* or hospital* or surger* or surgical or radiolog* or patient* or “primary care” or “general practice”)) OR TI(“continuing medical education”) OR AB(“continuing medical education”)).
Database of Abstracts of Reviews of Effects
Host: Centre for Reviews and Dissemination.
Date range searched: not available.
Date searched: 4 June 2018.
Searcher: AW.
Hits: n = 17.
Search strategy
(remedia* OR reskilling OR re-skilling OR retraining OR re-training) AND (physician* or doctor* or clinician* or practitioner* or allergist* or anaesthesiologist* or cardiologist* or dermatologist* or endocrinologist* or gastroenterologist* or GP or GPs or geriatrician* or hospitalist* or neonatologist* or nephrologist* or neurologist* or neurosurgeon* or oncologist* or ophthalmologist* or otolaryngologist* or pathologist* or paediatrician* or pediatrician* or physiatrist* or psychiatrist* or pulmonologist* or radiologist* or rheumatologist* or surgeon* or urologist* or continuing medical education or ((residen* or trainee*) and (medic* or clinic* or hospital* or surger* or surgical or radiolog* or patient* or primary care or general practice)))
Appendix 3 Characteristics of studies identified by main search
| Author(s) | Year | Country | Type | Aim | Study design | Sample and setting | Population (targeted) | Aspect being remediated | Intervention/model/strategy | Findings |
|---|---|---|---|---|---|---|---|---|---|---|
| Department of Health and Social Care162 | 2011 | UK | Report | To consider remediation processes, focusing on competence and capability problems | N/A | N/A | Practising physicians and doctors in training | Knowledge, skills, conduct and health | N/A | N/A |
| Anonymous160 | 2001 | USA | Case study | To describe a remediation scheme for doctors in Colorado | N/A | N/A | Practising physicians | Knowledge, skills and professionalism | Intervention | N/A |
| Adams et al.163 | 2008 | USA | Research | To determine how unprofessional behaviour by residents is managed | Survey | Directors of obstetrics and gynaecology residency programmes | Resident physicians | Professionalism | N/A | One hundred and forty-one programme directors responded. Methods of addressing problems with unprofessional behaviour identified by respondents were expressing expectation of improvement (95%), psychological counselling (68%), probation (59%) and dismissal (30%). The majority of respondents felt that remediation was not completely successful |
| Andrews et al.164 | 2016 | USA | Research | To provide evidence and improve methods for remediating learners who underperform on standardised tests | Development of an assessment based on self-regulated learning | Twenty graduate medical students classed as ‘struggling learners’ in one academic institution | Graduate medical students | Knowledge | N/A | Use of learning plans based on the results of the self-regulated learning assessment tool in one institution resulted in improvements in examination scores |
| Arnold97 | 2006 | USA | Commentary | Discussing developments in assessing professionalism and remediating unprofessional behaviour | N/A | N/A | Professionalism | Strategy | N/A | |
| Arnold et al.57 | 2016 | N/A | Book chapter | Discussing remediation of unprofessional behaviour | N/A | N/A | Professionalism | Model | N/A | |
| Audetat et al.165 | 2015 | Canada | Research | To assess use of a remediation instrument implemented to support faculty to diagnose and remediate resident academic difficulties | Mixed methods | Family medicine residents in academic difficulty at training sites linked to one academic institution | Resident physicians | Knowledge, skills and professionalism | N/A | Twenty-three remediation plans produced by 10 teaching sites for 21 residents were analysed. All documented cognitive problems and implemented various remediation measures. Of the plans, 48% were assessed as being good quality. Implementation of a remediation plan was positively associated with success in subsequent rotations |
| Barrett et al.166 | 2016 | Multiple | Review | To examine the use of workplace-based assessment in identifying and remediating performance | Systematic review | N/A | Postgraduate trainees | Knowledge, skills and professionalism | N/A | Twenty studies included. The use of workplace-based assessment in the context of remediation was not found to be supported by the literature. Specific areas of underperformance may be identified by workplace-based assessment events. Multisource feedback may facilitate identification of underperformance |
| Lee et al.167 | 2014 | USA | Research | To determine whether or not a faculty development programme could improve the evaluations of underperforming clinical teachers | Quantitative | One hundred and twenty-three faculty members who had participated in the Mayo Clinic faculty enhancement and development programme from 2009 to 2012 | Clinical teachers | Knowledge and skills | N/A | For all faculty, MTE scores improved following completion of the faculty enhancement and education development programme. The bottom 20% of the faculty had a significantly greater improvement in scores than the top 80%. In multivariate analysis, there were significant associations between changes in scores after the intervention and the following variables: bottom 20% vs. top 80%; procedural vs. non-procedural specialty; academic rank; and receiving a teaching award |
| Bhatti et al.67 | 2016 | USA | Research | To gather information on performance evaluation and remediation strategies used by otolaryngology programmes | Survey | One hundred and six programme directors of otolaryngology residency programmes | Resident physicians | Knowledge, skills and professionalism | N/A | There was a 74.5% response rate with a 2% cumulative incidence of problematic residents during the past 10 years. The most frequently reported deficiencies were unprofessional behaviour with colleagues (38%), insufficient medical knowledge (37%) and poor clinical judgement (34%). Personal or professional stress was the most frequent underlying problem (73%). Remediation interventions included general counselling (78%), feedback sessions (73%), mentoring (58%) and extra teaching (47%). In 23% of the residents, these interventions failed to produce improvement |
| Boileau et al.143 | 2017 | Multiple | Review | To review and synthesise the empirical evidence and theory available to guide clinical teachers supervising struggling learners | Synthetic literature review | N/A | N/A | Knowledge, clinical skills and professionalism | N/A | Suggests that the SOAP clinical model could be used to structure approaches to learners with difficulties. Between 10% and 15% of learners will experience difficulties during medical training |
| Boiselle90 | 2005 | USA | Case study | N/A | N/A | N/A | Resident physicians | Attitudes, behaviours, knowledge and skills | Intervention | N/A |
| Borman68 | 2006 | USA | Research | To assess the impact of an academic support programme on examination scores and assessment outcomes | Quantitative | Residents (n = 8) in a mandatory intervention programme | Resident physicians | Knowledge | Intervention | Seven of eight residents returned ABSITE total test scores of > 30. Post-intervention scores on ABSITE tests were large compared with national peer group. Six of eight residents passed the qualifying examination on first attempt |
| Bourgeois-Law et al.12 | 2018 | Multiple | Review | To explore conceptualisations of remediation and of individuals being remediated, and how the culture of medicine influences these | Scoping review | N/A | Practising physicians | Clinical skills | N/A | Conceptualisations of remediation and the surrounding culture might affect the medical community’s ability to support physicians in need of remediation and also its willingness to engage in such processes. Reconceptualisaing remediation as supporting practice change rather than as redressing gaps in knowledge and skills may be beneficial |
| Brooks et al.168 | 1996 | Canada | Case study | To increase student understanding of patient-centred interviewing | Remediation intervention: 6-week programme focused on patient interviewing skills | Candidates who failed a simulated office oral at the College of Family Physicians of Canada | Resident physicians | Clinical skills | Intervention | Based on observations of faculty and standardised patient instructors, participation in the course improved residents’ understanding of patient-centred interviewing. Residents valued the course |
| Brown et al.42 | 2014 | UK | Review | To define the concept of insight | Narrative review | N/A | Practising physicians | Profesionalism | N/A | A working definition of insight, incorporating reflection, emotional intelligence, self-awareness and motivation |
| Bulstrode et al.127 | 2005 | UK | Commentary | To look at issues involved in carrying out and evaluating remediation interventions | N/A | N/A | Postgraduate trainees | Knowledge, clinical skills and professionalism | Strategy | N/A |
| Caldicott and d’Oronzio85 | 2015 | USA | Case study | Describes the development of the ProBE programme | N/A | N/A | Practising physicians and other health professionals | Professional ethics (e.g. boundaries, sexual boundaries, prescribing controlled substances, financial issues) | Intervention | N/A |
| Cerda et al.119 | 2000 | USA | Case study | Describes the University of Florida Comprehensive Assessment and Remedial Education Service programme | N/A | N/A | Practising physicians | Knowledge, clinical skills and professionalism | Intervention | N/A |
| Cleland et al.25 | 2013 | Multiple | Review | To synthesise available evidence to clarify how and why remediation interventions may have worked | Systematic review | N/A | Medical students and practising physicians | Knowledge and clinical skills | Intervention | Thirty-one studies were included for review and most published after 2000. Most studies focused on improving medical student exam performance. Study quality was often low. Few studies included long-term follow-up and those that did found that improvement was not sustained. Interventions were complex, but their design or reporting typically did not allow identification of the active elements of the remedial process |
| Cosman et al.151 | 2011 | USA | Research | To establish whether assessment and remedial clinical education of practising surgeons is feasible and possibly beneficial | Quantitative | Forty-seven general, general/vascular and colorectal surgeons | Practising physicians | Professionalism, interpersonal/communication skills, medical knowledge, patient care, practice-based learning and systems-based practice | Intervention | Twenty-three surgeons underwent a 2-day assessment, including a 1-hour mock oral board examination, which eight surgeons passed with no recommendations, six passed with minor recommendations, six passed with major recommendations, and three failed. Twenty-four surgeons also completed 26 5-day clinical education programmes, with 20 passes, one pass with a minor recommendation, three passes with major recommendations and two fails |
| Decoteau et al.63 | 2018 | USA | Research | To identify the optimal approach to remediate poor ABSITE scores | Quantitative | A total of 268 exam scores from 52 residents over a 15-year period | Resident physicians | Knowledge | Intervention | Mean scores for the ABSITE and first-time pass rates for the ABS QE increased following the establishment of the focused remediation programme. Scores of residents who undertook the remediation programme improved on the next ABSITE exam |
| Domen69 | 2014 | USA | Commentary | To suggest a new approach to remediation in pathology training programmes | N/A | N/A | Resident physicians | Knowledge, clinical skills and professionalism | Model | N/A |
| d’Oronzio86 | 2009 | USA | Commentary | To describe the ProBE programme | N/A | N/A | Practising physicians and other health professionals | Professional ethics (e.g. boundaries, sexual boundaries, prescribing controlled substances, financial issues) | Intervention | N/A |
| Durning et al.116 | 2011 | USA | Commentary | To propose a theory-based framework to assist medical trainees in difficulty | N/A | N/A | Medical students and resident physicians | Professionalism and self-regulated learning | Strategy | N/A |
| Edeiken169 | 1993 | USA | Case study | To describe a remediation intervention for radiology residents | N/A | Six radiology residents during an 8-year period | Resident physicians | Knowledge | Intervention | During the period of remediation, all six residents improved their performance in faculty evaluations from below average ratings to above average and superior ratings |
| Egener76 | 2008 | USA | Case study | To describe a coaching model to remediate poor communication skills | N/A | N/A | Practising physicians | Communication | Intervention | Participants and their supervisors rated the consultation highly for satisfaction |
| Ellaway et al.142 | 2018 | USA/Canada | Commentary | To provide a conceptual review of current remediation practices | N/A | N/A | Medical students and resident physicians | Knowledge, clinical skills and professionalism | Intervention | By linking remediation theory and practice with competency-based medical education, a more integrated approach to learners in difficulty can be developed |
| Finan152 | 2011 | UK | Abstract | To provide an approach to identifying and dealing with unsafe or underperforming surgeons | N/A | N/A | Practising physicians | Knowledge, clinical skills and professionalism | N/A | N/A |
| Frankel and Hafferty64 | 2014 | USA | Chapter | To define and illustrate challenges to professionalism and their institutional implications | N/A | N/A | Medical students and resident physicians | Professionalism | Strategy | N/A |
| Gas et al.170 | 2016 | USA | Research | To develop a novel assessment methodology and an efficient remediation system | Quantitative | Thirty-five surgical residents at an academic medical centre | Resident physicians | Clinical skills | Intervention | Of 35 residents, 31 had below-par scores on at least one OSCE station. Eighteen residents attempted remediation and all achieved a score of ≥ 4 on a subsequent OSCE attempt. It is feasible to objectively assess surgery trainees and offer opportunities to remediate where necessary |
| Goldberg et al.126 | 2015 | USA | Commentary | To discuss the use of simulation as a tool for physician re-entry to the workforce | N/A | N/A | Practising physicians | Knowledge, clinical skills and professionalism | N/A | N/A |
| Goulet et al.110 | 2007 | Canada | Research | To measure the influence of a remedial professional development programme | Quantitative | A total of 207 physicians | Practising physicians | Knowledge and clinical skills | Intervention | Statistically significant improvements were observed for 51 physicians with regard to record-keeping, clinical investigation plans, diagnostic accuracy, patient treatment and follow-up |
| Goulet et al.120 | 2005 | Canada | Case study | To describe remedial training programmes organised and planned by the Collège des médecins du Québec | N/A | N/A | Practising physicians | Clinical skills | Intervention | N/A |
| Grams et al.137 | 1992 | Canada | Research | To identify and conceptualise the characteristics of troublesome residents | Qualitative | Four family practice residents, from a total of 111, who had been identified as troublesome | Resident physicians | Professionalism | N/A | Comments in residents’ written evaluations were categorised into three categories. The first category was discomforting behaviours, including affronting, avoiding responsibility and lack of initiative. The second category was failure to meet faculty and programme expectations. The third category related to the process of recognising and addressing issues with residents |
| Grant100 | 1995 | USA | Research | To design and implement an individualised programme evaluation and education to remediate physicians | Quantitative | 28 physicians | Practising physicians | Professionalism | Intervention | Of 28 physicians referred to remediation evaluation, five had completed their educational programmes, five were participating in directed educational programmes, five had approved educational programmes and were awaiting placements, and 10 were awaiting acceptance of their programme |
| Grant94 | 1998 | USA | Research | To describe the Physician Prescribed Educational Program | Descriptive report | A total of 300 referrals about physicians | Practising physicians | Professionalism | Intervention | Of 300 referrals, 100 had received evaluations. A wide range of deficits were addressable. Carefully planned and executed remediation programmes can provide appropriate and successful experiences for participants |
| Guerrasio and Aagaard171 | 2014 | USA | Research | To assess the effectiveness of a standardised clinical reasoning remediation plan on medical learners at various stages of training | Quantitative | A total of 151 medical students, residents, fellows and physicians | Medical students, resident physicians and practising physicians | Medical knowledge, clinical skills, clinical reasoning, time management, interpersonal skills, communication skills, professionalism and mental well-being | Intervention | Fifty-three individuals were identified as having clinical reasoning deficits. Prevalence of clinical reasoning deficit did not differ by level of training. The mean amount of faculty time required for remediation was 29.6 hours. Fifty-one individuals passed the post-remediation assessment. Thirty-eight individuals either graduated or continued to practise in good standing. Four individuals were placed on probation and five who transferred to another programme subsequently graduated |
| Guerrasio et al.65 | 2016 | USA | Case study | To implement a consistent approach for the remediation of poor professional behaviours | Descriptive report | Fifteen resident physicians and six faculty members offered remediation | Resident physicians and practising physicians | Communication and interpersonal behaviours | Intervention | The remediation programme has a standardised format, with content tailored to the individual. Eleven residents and six faculty completed the remediation programme. Early feedback from individual participants and their departments or programmes was positive |
| Guerrasio et al.121 | 2014 | USA | Research | To identify deficit types and predictors of poor academic outcomes among students, residents, fellows and physicians referred to the University of Colorado School of Medicine’s remediation programme | Quantitative | A total of 151 students, residents, fellows and physicians referred to the remediation programme between 2006 and 2012 | Medical students, resident physicians and practising physicians | Medical knowledge, clinical skills, clinical reasoning, time management, interpersonal skills, communication skills, professionalism and mental well-being | Intervention | Most individuals had more than one deficit. Medical knowledge, clinical reasoning and professionalism were most common. Medical students were more likely to have mental well-being issues. Prevalence of professionalism issues increased as training increased. Men were more likely to have communication and mental well-being issues. Increased faculty face time reduced the odds of probation and of all negative outcomes |
| Guevara et al.115 | 2011 | USA | Research | To describe the use of IEPs to define and address student deficiencies in medical education | Quantitative | Ninety-two resident physicians between 2003 and 2010 | Resident physicians | Knowledge, professionalism and communication | Intervention | Of 92 residents, 16 received IEPs. Of these IEPs, 13 related to medical knowledge, four to professionalism and one to communication skills. Average age and time since graduation were greater for those requiring remediation than for those who did not. US MLE step 1 and American Board of Internal Medicine in-service scores were lower for those with IEP. Of the 16 with IEPs, 12 were successful |
| Gunderman and Rackson135 | 2006 | USA | Commentary | To discuss how residents having difficulties in training can be identified and helped | N/A | N/A | Resident physicians | Knowledge, clinical skills and professionalism | N/A | N/A |
| Hanna et al.95 | 2000 | Canada | Case study | To investigate the effects of an educational intervention on physicians with moderate to severe competence problems | N/A | N/A | Practising physicians | Knowledge and clinical skills | N/A | Of five physicians who completed the intervention, only one improved, one remained the same and three deteriorated. Successful remediation of severely incompetent physicians is uncertain at best. Alternative education techniques may be needed, or it may be that improvement is not possible |
| Harthun et al.117 | 2005 | USA | Case study | To describe a programme initiated to improve ABSITE scores | N/A | N/A | Resident physicians | Knowledge | Intervention | From 2000 to 2004, 12 ABSITE scores were below standard, which resulted in eight residents receiving programme support nine times. All but one programme encounter resulted in increased, above-standard scores the following year. Two residents later returned to substandard scores |
| Hashimoto172 | 2005 | Japan | Commentary | To describe retraining arrangements for physicians subject to administrative punishment | N/A | N/A | Practising physicians | Professionalism | N/A | N/A |
| Hatch173 | 1998 | UK | Commentary | To describe the GMC’s approach to performance assessment | N/A | N/A | Practising physicians | Knowledge, clinical skills and professionalism | N/A | N/A |
| Hauer et al.11 | 2009 | Multiple | Review | To describe the literature on remediation at undergraduate, graduate, and continuing medical education levels | Systematic review | N/A | Medical students, resident physicians and practising physicians | Knowledge, clinical skills and professionalism | Model | Thirteen studies were included for review. At undergraduate and graduate levels, deficits were largely identified through assessments. For practising physicians, deficits were identified by peer assessors and licensing organisations. Studies at undergraduate or graduate level described the remediation of knowledge deficits and clinical skills problems. Articles focused on practising physicians described remediation of multiple practice skills |
| Hays et al.43 | 2002 | Multiple | Commentary | To explore the nature of insight, its relationship to professional performance and its measurement | N/A | N/A | Practising physicians | Professionalism: insight | N/A | N/A |
| Humphrey5 | 2010 | Multiple | Research | To describe remediation programmes offered internationally | Survey | Fifteen organisations providing remediation programmes | Practising physicians | Knowledge, clinical skills and professionalism | N/A | Assessment and remediation programmes identified were small in scale. Their focus ranged from narrowly identifying and redressing specific knowledge and skill deficits to wider interest in the whole functioning of the physician. Less attention was paid to systemic or contextual factors that might impact physician performance. Progress through remediation was carefully monitored but no programmes undertook regular longer-term follow-up |
| Jolly et al.138 | 2018 | UK | Research | To understand doctors’ experiences of a risk education remediation process | Qualitative | Twenty GPs and hospital specialists | Practising physicians | Professionalism | Intervention | Three key themes in participant responses to the remediation intervention were (1) personal and professional impacts and actions, (2) the comprehension and validity of risk education interventions and (3) feedback |
| Kalet et al.84 | 2017 | Multiple | Commentary | To present a critical systems perspective on remediation | N/A | N/A | N/A | Knowledge, skills and professionalism | Model | N/A |
| Kalet et al.54 | 2016 | N/A | Commentary | To offer guidance for the development and maintenance of competency-based remediation programmes | N/A | N/A | N/A | Clinical skills | Strategy | N/A |
| Katz et al.91 | 2010 | USA | Case study | To describe recommendations made by a task force on remediation | N/A | N/A | Resident physicians | Knowledge, clinical skills and professionalism | Strategy | N/A |
| Katz et al.118 | 2013 | USA | Case study | To describe a remediation case and evaluate the processes for remediation | N/A | N/A | Resident physicians | Knowledge, clinical skills and professionalism | Intervention | N/A |
| Kim and Tan174 | 2015 | USA | Review | To systematically review published literature on the effectiveness of interventions intended to improve residents’ exam scores | Systematic review | N/A | Resident physicians | Knowledge | N/A | Twenty-six articles were included and there was heterogeneity in study designs and reporting. Structured reading programmes and clear expectations with mandatory remedial programmes were consistently effective in improving ABSITE scores. The effect of didactic teaching conferences and problem-based learning was mixed |
| Kimatian and Lloyd44 | 2008 | USA | Commentary | To discuss remediation as the elevation of feedback and education to a higher level, in support of a goal of helping doctors overcome perceived deficiencies | N/A | N/A | Resident physicians | Knowledge, clinical skills and professionalism | Strategy | N/A |
| Kosir et al.70 | 2008 | USA | Case study | To discuss impact on ABSITE scores of a course using Kolb’s learning cycle | N/A | N/A | Resident physicians | Knowledge | Intervention | Scores on ABSITE increased for 78.6% of residents who completed the course |
| Krzyzaniak et al.92 | 2017 | USA | Research | To characterise remediation experiences from the perspective of medical educators and propose a holistic framework | Qualitative | Nineteen medical educators | Resident physicians | Knowledge, clinical skills and professionalism | N/A | Thirteen themes were identified, some addressing practical components of remediation and others relating to barriers to remediation or the impacts of remediation. The themes were used to inform the development of a framework for remediation |
| Krzyzaniak et al.133 | 2016 | USA | Research | To characterise remediation experiences from the perspective of medical educators | Qualitative | Nineteen medical educators | Practising physicians/medical educators | Knowledge, clinical skills and professionalism | N/A | Fifteen themes were identified in the data, including eight that were not anticipated. Themes addressed both practical components of remediation and participants’ frustrations with delivering these processes |
| Krzyzaniak et al.40 | 2016 | USA | Research | To understand faculty perspectives on remediation, especially barriers to implementation | Qualitative | Regional stakeholders in medical education | Resident physicians | NS | N/A | Major barriers to implementation of remediation were concerns about premature labelling as ‘failing’ and associated stigma, limited resources, lack of faculty training and development, residents’ unwillingness to participate and a lack of honest documentation |
| Larson and Steadman175 | 2006 | USA | Case study | To describe a remediation programme for community anaesthesiologists | N/A | N/A | Practising physicians | Clinical Skills | Intervention | N/A |
| Leung et al.88 | 2009 | N/A | Commentary | To describe a remediation curriculum for communication skills | N/A | N/A | Resident physicians | Professionalism and communication skills | Model | N/A |
| Leung and Ratnapalan45 | 2011 | N/A | Commentary | To describe an approach for including self-reflection in a remediation curriculum | N/A | N/A | Resident physicians | Professionalism and self-reflection | Model | N/A |
| Lillis et al.4 | 2014 | New Zealand | Research | To describe a remediation programme and outcomes for doctors | Quantitative | Twenty-four doctors | Practising physicians | Knowledge and clinical skills | Intervention | Of 24 doctors, five failed to engage and stopped clinical work. The other 19 doctors completed a 12-month programme and 13 were deemed to be at an acceptable standard at the end. Six doctors required a second performance assessment, of whom only one was deemed to be at an acceptable standard. Health concerns were common among the doctors included in the study |
| Liu et al.93 | 2016 | USA | Commentary | To describe common signs that a doctor may need remediation | N/A | N/A | Resident physicians | Knowledge, skills and professionalism | Strategy | N/A |
| Mahmood61 | 2012 | UK | Commentary | To examine underlying factors to consider before planning remediation for trainees in obstetrics and gynaecology | N/A | N/A | Doctors in training | Knowledge, skills and professionalism | Strategy | N/A |
| Mar et al.71 | 2015 | USA | Commentary | To provide a template for a team-based approach to remediation of radiology residents | N/A | N/A | Resident physicians | Medical knowledge, clinical skills and professionalism | Intervention | N/A |
| Matthews et al.176 | 2007 | UK | Commentary | To describe the Wales Deanery remediation scheme for GPs | N/A | N/A | Practising physicians | Knowledge, clinical skills and professionalism | Intervention | N/A |
| Mugford72 | 2003 | Australia | Commentary | To discuss the development of strategies for performance review | N/A | N/A | Registrars | Knowledge, clinical skills and professionalism | Strategy | N/A |
| Murano et al.177 | 2015 | USA | Case study | To develop a framework for programme directors managing residents in need of remediation | N/A | N/A | Resident physicians | NS | Model | N/A |
| Nelson98 | 1993 | USA | Commentary | To discuss remediation through personalised continued medical education plans | N/A | N/A | Practising physicians | NS | Strategy | N/A |
| Norcross et al.153 | 2009 | USA | Case study | To describe the University of California, San Diego, PACE programme | N/A | N/A | Practising physicians | Knowledge, clinical skills and professionalism | Intervention | N/A |
| Norton et al.161 | 2004 | Canada | Case study | To describe the College of Physicians and Surgeons of Ontario’s (Ontario, Canada) peer review process, and educational programmes | N/A | N/A | Practising physicians | Knowledge and clinical skills | Intervention | N/A |
| Paice46 | 2009 | UK | Commentary | To discuss processes for identifying and supporting surgical trainees in need of remediation | N/A | N/A | Surgical trainees | Knowledge, clinical skills and professionalism | Strategy | N/A |
| Papadakis et al.58 | 2012 | USA | Commentary | To report recommendations from a think tank of experts on remediation | N/A | N/A | Practising physicians, resident physicians and medical students | Professionalism | Intervention | N/A |
| Parran et al.51 | 2013 | USA | Case study | To describe an intensive course in medical ethics at Case Western Reserve University School of Medicine, Cleveland, OH, USA | N/A | N/A | Practising physicians | Professionalism | Intervention | N/A |
| Prescott-Clements et al.7 | 2017 | UK | Case study | To describe a model for diagnosing physician performance problems | N/A | N/A | Practising physicians | Knowledge, clinical skills and professionalism | Model | N/A |
| Price8 | 2017 | UK | Commentary | To critique UK remediation policy from the 1990s onwards | N/A | N/A | Practising physicians | Knowledge, clinical skills and professionalism | N/A | N/A |
| Raman et al.140 | 2018 | USA | Research | To establish the prevalence of problem residents in US neurosurgical residency programmes and to identify predictive risk factors | Survey | A total of 108 neurosurgical training programmes | Resident physicians | Knowledge, clinical skills and professionalism | N/A | Thirty-six responses were received. Mean prevalence of problem residents was 18.1% (95% CI 14.7% to 21.6%). The most common problems identified were poor communication skills (59.9%), task inefficiency (40.1%) and poor medical knowledge (39.1%). The most common interventions were additional feedback meetings (93.9%), verbal warnings (78.7%) and formal written remediation plans (61.4%). Fifty per cent of identified problem residents left their training programme. Factors independently associated with departure were dishonesty, poor medical knowledge and poor technical skills |
| Ratan et al.73 | 2008 | USA | Case study | To offer a model for a programme to help residents overcome deficiencies | N/A | N/A | Resident physicians | Knowledge, skills and professionalism | Strategy | N/A |
| Regan et al.74 | 2016 | USA | Commentary | To discuss remediation strategies for interpersonal and communication skills and professionalism | N/A | N/A | Resident physicians | Professionalism | Strategy | N/A |
| Rehm and Rowland75 | 2005 | USA | Research | To investigate the effectiveness of the ABS’s remediation programme | Survey | Ten institutions rated ‘outstanding’ by the ABS | Resident physicians | Knowledge | Intervention | Nine institutions responded and identified the essential components of a successful remediation year, and emphasised that remediation has to be more than correcting knowledge deficits |
| Rhydderch et al.112 | 2007 | UK | Case study | To describe the activity of an advanced training practice network that undertakes further training for qualified GPs referred to its services | N/A | N/A | Practising physicians | Knowledge, clinical skills and professionalism | N/A | N/A |
| Roberts et al.59 | 2012 | USA | Research | To describe a frequently occurring performance problem in residents and to present approaches to addressing this type of case | Qualitative | Interviews with programme directors | Resident physicians | Professionalism | Strategy | The composite case study described a resident with attitudinal issues and unprofessional behaviour. Analysis of expert views on this type of case suggested that extra work was created for both other team members and faculty to address the issues. Analysis also highlighted the importance of the programme director’s role in addressing problems, but queried the cost–benefit ratio of work-intensive remediation |
| Rosenblatt and Schartel122 | 1999 | USA | Research | To review remediation methods in US anaesthesiology residency programmes in 1995–6 | Survey | Survey sent to directors of 145 anaesthesiology residency programmes | Resident physicians | Knowledge | N/A | The survey achieved an 85.5% response rate. Frequency of evaluations ranged from daily to quarterly. Evaluations used both narrative comments and rating scales in 89% of institutions. A total of 67.7% of programmes had a written policy on problem residents and 82.2% had a formal probation policy |
| Rougas et al.52 | 2015 | USA | Commentary | To offer a framework for educators addressing professionalism lapses | N/A | N/A | Resident physicians and medical students | Professionalism | Strategy | N/A |
| Rumack et al.87 | 2017 | USA | Case study | To describe a remediation programme covering 142 graduate medical education programmes | N/A | N/A | Resident physicians | Knowledge, clinical skills and professionalism | Strategy | N/A |
| Samenow et al.79 | 2013 | USA | Case study | To describe an approach to remediation centring on ideas of transformative learning | Composite case study | N/A | Practising physicians | Professionalism | Model | N/A |
| Sanfey et al.141 | 2012 | USA | Research | To develop an evidence-based approach to identifying, preventing and managing surgical residents with unprofessional behaviour | A 1-day think tank | Medical and nursing leaders in remediation and related fields, and surgical residents | Resident physicians | Professionalism | Strategy | Drawing on the literature and on the expert discussions, recommendations for the identification, remediation and performance assessment of problem residents are made. These include prompt notification and description of the problem and the expected standard. The importance of understanding the behaviour and the underlying factors shaping it is emphasised |
| Sanfey et al.66 | 2013 | USA | Commentary | To discuss best practice in identifying surgical residents with deficient operative skills | N/A | N/A | Resident physicians | Clinical skills | Strategy | N/A |
| Sargeant et al.55 | 2013 | N/A | Commentary | To propose a facilitated reflective process for supporting engagement with assessment data and feedback for learning | N/A | N/A | Practising physicians | Professionalism | Model | N/A |
| Shah et al.111 | 1997 | Australia | Commentary | To describe the remediation programme for trainees in general practice training | N/A | N/A | Registrars | Knowledge and clinical skills | Intervention | N/A |
| Shapiro et al.41 | 1987 | USA | Commentary | To explore definitions and means of identifying ‘the resident in difficulty’ and principles of effective intervention | N/A | N/A | Resident physicians | Professionalism | Strategy | N/A |
| Shapiro et al.53 | 2014 | USA | Case study | To describe the development of the Centre for Professionalism and Peer Support at Brigham and Women’s Hospital, Boston, MA, USA | N/A | N/A | Practising physicians | Professionalism | Intervention | N/A |
| Shearer et al.47 | 2018 | Canada | Review | To examine policies for remediation in postgraduate medical education in Canada | Literature review | N/A | Resident physicians | Knowledge, skills and professionalism | N/A | Most policies aligned with some but not all best practices in remediation. All schools tailored remediation programmes to individual needs, but few required the teaching of goal-setting, strategic planning, self-monitoring and self-awareness |
| Silverberg et al.178 | 2015 | USA | Research | To determine the prevalence of remediation, competency domains for remediation, length of remediation and success rates of remediation in emergency medicine | Survey | Emergency medicine programme directors | Resident physicians | Knowledge, clinical skills and professionalism | N/A | A total of 126 programme directors responded (126/158, 79.7%). The prevalence of remediation was 4.4%. The most common problems were with medical knowledge (63.1%), patient care (46.6%) and professionalism (31.5%). Mean length of remediation was 8 months. A total of 59.9% of residents were successfully remediated, 31.3% were in ongoing remediation and remediation was unsuccessful for 8.7%. Training year (PGY-1), longer time in remediation and problems with practice-based learning and professionalism were associated with unsuccessful remediation |
| Smith et al.78 | 2007 | USA | Commentary | To describe a general framework for managing residents in difficulty | N/A | N/A | Resident physicians | Knowledge, clinical skills and professionalism | Model | N/A |
| Sparks et al.62 | 2016 | USA | Case study | To describe remediation programme for anaesthesiology training fellows | N/A | N/A | Training fellows | Knowledge, clinical skills and professionalism | Intervention | N/A |
| Spickard et al.179 | 2008 | USA | Case study | To describe a course on professional sexual boundaries | N/A | N/A | Practising physicians | Professionalism: sexual boundaries | Intervention | N/A |
| Stirling et al.145 | 2012 | UK | Case study | To describe a ward simulation exercise for postgraduate trainees with performance concerns | N/A | N/A | Doctors in training | Knowledge and clinical skills | Intervention | N/A |
| Sullivan and Arnold48 | 2008 | USA | Book chapter | To discuss the process of remediation for unprofessional behaviour | N/A | N/A | Practising physicians and resident physicians | Professionalism | Strategy | N/A |
| Swanwick and Whiteman9 | 2013 | UK | Commentary | To discuss provisions for remediation | N/A | N/A | Doctors in training | Knowledge, clinical skills and professionalism | Model | N/A |
| Swiggart et al.180 | 2016 | USA | Research | To report on physicians referred to a professional development course following sexual misconduct | Mixed methods | Twenty-nine physicians from 2001 cohort interviewed; data analysed on 70 physicians from 2014 cohort | Practising physicians | Professionalism: boundary violations | Intervention | The majority of physicians in both cohorts were referred by their state board of medical examiners. Most attended the course because of disciplinary action following allegations of sexual misconduct. Participants were from 47 US states and Canada |
| Swiggart et al.89 | 2009 | USA | Commentary | To discuss a systems approach to identifying and reducing unprofessional behaviour | N/A | N/A | Practising physicians | Professionalism and disruptive behaviour | Intervention | N/A |
| Tabby et al.181 | 2011 | USA | Research | To explore the prevalence and causes of neurology residents in difficulty | Survey | A total of 126 US neurology residency programmes | Resident physicians | Knowledge, clinical skills and professionalism | N/A | Ninety-five programme directors responded. A total of 81% reported problem residents. Problems most commonly arose in the first year of residency. Increased supervision and assigning a faculty mentor were the most common responses. Eleven per cent of residents in difficulty needed a programme for impaired physicians and 16% were dismissed from their programmes |
| Torbeck and Canal139 | 2009 | USA | Research | To determine the extent and type of remediation used by surgery programmes | Survey | A total of 253 programme directors from US surgical residency programmes | Resident physicians | Knowledge, clinical skills and professionalism | N/A | The response rate was 35% (89/253). Programmes seemed to find remediating problems with professionalism and interpersonal skills more difficult than remediating medical knowledge and patient care deficits |
| Visconti et al.123 | 2013 | USA | Research | To determine if remediation for emergency medicine residents is associated with improved assessment outcomes | Quantitative | Twenty-six residents enrolled in the programme from 2000 to 2008 | Resident physicians | Knowledge | Intervention | Of the 26 eligible residents, 10 had a first-time pass rate of 100%. A control group, who either graduated before the introduction of the programme or did not complete it, had a pass rate of 44% (7/16) |
| Walsh et al.60 | 2010 | UK | Case study | To describe systems for responding to concerns about trainee doctors in Wales | N/A | N/A | Doctors in training | NS | Model | N/A |
| Warburton et al.144 | 2017 | USA | Case study | To describe a process for diagnosing deficits to support remediation | N/A | N/A | Resident physicians | Knowledge, clinical skills and professionalism | N/A | N/A |
| Warburton and Mahan56 | 2018 | USA | Commentary | To discuss approaches to coaching nephrology trainees identified as in difficulty | N/A | N/A | Training fellows | Knowledge, clinical skills and professionalism | Model | N/A |
| Whiteman and Jamieson49 | 2007 | UK | Case study | To describe the remediation approach used by the London Deanery, London, UK | N/A | N/A | Practising physicians | Knowledge, skills and professionalism | Intervention | N/A |
| Whiteman et al.182 | 2013 | UK | Case study | To describe the remediation approach of the Professional Support Unit, London Deanery | N/A | N/A | Practising physicians and doctors in training | Knowledge, clinical skills and professionalism | Intervention | N/A |
| Wu et al.50 | 2010 | USA | Case study | To describe evaluation and remediation of resident performance in a radiology programme | N/A | N/A | Resident physicians | Attitudes, behaviours, knowledge and skills | Intervention | N/A |
| Zbieranowski et al.183 | 2013 | Canada | Research | To determine the prevalence of residents in difficulty, their characteristics, problems, and remediation outcomes | Quantitative | Resident case files 1999–2009 at the University of Toronto, Toronto, ON, Canada | Resident physicians | Knowledge, clinical skills and professionalism | N/A | A total of 103 residents were referred for evaluation (3% of all enrolled residents). The annual prevalence was 0.2–1.5%. All 100 residents studied had medical expertise problems (85%), professionalism weaknesses (15%) or both. There were often multiple remediation periods, of an average of 6 months’ duration. Most residents were successfully remediated, with 78% completing residency education. Seventeen per cent were unsuccessful and 5% were still in training |
Appendix 4 Characteristics of studies identified by citation searches
| Author(s) | Year | Country | Type | Study design | Sample/setting | Population (targeted) | Aspect being remediated | Intervention/model/strategy | Findings |
|---|---|---|---|---|---|---|---|---|---|
| Bennion et al.147 | 2018 | Multiple | Commentary | N/A | N/A | Medical students and doctors in training | Knowledge and clinical skills | Strategy | Individual, institutional and systemic factors need to be considered to develop effective remediation programmes within a medical school/residency programme |
| Grol156 | 2002 | Multiple | Commentary | N/A | N/A | Practising physicians | Knowledge, clinical skills and professionalism | Strategy | Educational approaches to remediation alone are insufficient. Such approaches should be integrated with a focus on teams, organisations, or the political or economic context |
| Hardie Alvanzo et al.184 | 2002 | Multiple | Commentary | N/A | N/A | Practising physicians | Professionalism and behaviour | N/A | Behaviour change in physicians is akin to behaviour change in patients. The key elements affecting change are education, motivation and facilitation |
| Hickson et al.99 | 2007 | USA | Case study | N/A | N/A | Resident physicians and practising physicians | Professionalism and behaviour | Model | Addressing disruptive behaviour focuses on four graduated interventions: (1) informal conversations for single incidents, (2) non-punitive ‘awareness’ interventions when data reveal patterns, (3) leader-developed action plans if patterns persist and (4) imposition of disciplinary processes if the plans fail |
| Spickard et al.185 | 2002 | USA | Case study | To report on physicians referred to a professional development course following sexual misconduct | Thirty physicians who attended the course during 1999–2000 | Practising physicians | Professionalism: boundary violations | Model | Describes the course and screening process for physicians entering the programme. Concludes that screening may be an important part of remediating boundary violation. Also makes recommendations for medical schools and residency programmes in relation to their curricula and support |
Appendix 5 Characteristics of studies identified by grey literature search
| Author(s) | Year | Country | Type | Study design | Sample/setting | Population (targeted) | Aspect being remediated | Intervention/model/strategy | Findings |
|---|---|---|---|---|---|---|---|---|---|
| Paglia and Frishman80 | 2011 | USA | Commentary | N/A | N/A | Resident physicians | Professionalism and communication skills | N/A | A framework for assessing US medical residents should provide clearly defined goals and expectations. Residency remediation is a difficult process that requires a large investment of time and dedication from the programme director and faculty. All issues and meetings should be carefully documented to meet legal requirements |
| Williamson et al.186 | 2017 | USA | Commentary | N/A | N/A | Resident physicians | Knowledge and clinical skills | N/A | By aiding in the recognition and remediation of residents struggling to achieve proficiency in the SBP and PBLI subcompetencies, the instruments developed by this task force may improve resident training within the framework of the new accreditation system |
Appendix 6 Characteristics of studies identified by review team or stakeholder group
| Author(s) | Year | Country | Type | Study design | Sample/setting | Population (targeted) | Aspect being remediated | Intervention/model/strategy | Findings |
|---|---|---|---|---|---|---|---|---|---|
| Berrow et al.154 | 2007 | UK | Research | Case file review | Fifty UK doctors referred to NCAS | Practising physicians | Knowledge, clinical skills and professionalism/behaviours | N/A | Findings indicate that the NCAS assessment process provides a more accurate and comprehensive ‘diagnosis’ of performance issues, enabling more appropriate recommendations for ‘treatment’ and helping to differentiate between potentially remediable and more fundamental problems |
| Bourgeois-Law et al.134 | 2019 | Canada | Research | Qualitative | Seventeen remediation stakeholders | Practising physicians | Knowledge, clinical skills and professionalism/behaviours | N/A | The medical profession’s attitude towards those who struggle with clinical competency, as individuals and as a whole, is ambivalent at best. This ambivalence grows out of psychological and cultural factors and may be an undiscussed factor in the profession’s struggle to deal adequately with underperforming members. To contend with the challenge of remediating practising physicians, the profession needs to address this ambivalence and its underlying causes |
| Bourgeois-Law et al.13 | 2019 | Canada | Research | Qualitative | Seventeen remediation stakeholders | Practising physicians | Knowledge, clinical skills and professionalism/behaviours | N/A | Understanding that stakeholders frequently approach the complex issue of remediation with two different perspectives and without conscious awareness of doing so may help to explain several challenges in the field, including the issues of what falls under the umbrella of remediation and who should be responsible for offering remediation support |
Appendix 7 Characteristics of studies identified by supplementary searches
| Author(s) | Year | Country | Type | Study design | Sample/setting | Population (targeted) | Aspect being remediated | Intervention/model/strategy | Findings |
|---|---|---|---|---|---|---|---|---|---|
| Ajzen150 | 2011 | N/A | Commentary | N/A | N/A | N/A | N/A | N/A | Research on the TPB has made considerable progress since the theory was introduced some 2 dozen years ago. Initial studies were mostly attempts to test the theory’s predictive validity in various behavioural domains. The combined weight of much empirical evidence, perhaps best captured in such meta-analytic syntheses as the one included in the current set of articles, lends clear support to the theory |
| Brennan et al.101 | 2017 | Multiple | Literature review | Realist synthesis | N/A | Practising physicians | N/A | N/A | Three mechanisms were identified that explain how medical appraisal produces its effects: dissonance, denial and self-affirmation |
| Cavenagh et al.187 | 2000 | UK | Research | Questionnaire survey | A total of 162 law students and 195 medical students | N/A | N/A | N/A | The study shows a greater commitment of medical students than law students to their chosen career. This is demonstrated by medical students’ greater desire to pursue their career, their greater satisfaction with their choice of career and finding that more medical students would persist with reapplying for medicine than law students would in reapplying for law |
| Edmondson et al.82 | 2016 | USA | Research | Quantitative surveys | Approximately 20,000 New York City, NY, USA, teachers and 28,998 health-care personnel | N/A | N/A | N/A | Health-care and education organisations had different perspectives on psychological safety, but also some similarities. Psychological safety is one important dimension of the adult work environment (especially under conditions of high stakes, complexity, and uncertainty) that can enable human development, growth and learning, and that warrants additional research |
| Ehrlinger et al.128 | 2008 | USA | Research | Quantitative | A total of 124 psychology students | N/A | N/A | N/A | Poor performers show little insight into the depth of their deficiencies relative to their peers. They tend to think that they are doing just fine relative to their peers when, in fact, they are at the bottom of the performance distribution |
| Elder-Vass104 | 2010 | N/A | Book | N/A | N/A | N/A | N/A | N/A | The book examines the way in which interactions between individuals generate the causal powers of certain structures. One of these relates to the causal power of identity, specifically the social norms that can compel people to behave in certain ways when those norms form part of their identity |
| Handley et al.107 | 2006 | N/A | Commentary | N/A | N/A | N/A | N/A | N/A | The article examines situated learning theory in the context of learning in communities of practice. The important arguments here relate to the pull of identity in developing motivation and guiding learning |
| Hsiang-Te Tsuei et al.83 | 2019 | Canada | Research | Descriptive exploratory study | Eight students in a peer mentorship in a medical education programme | N/A | N/A | N/A | A sense of psychological safety appears to free learners from constantly being self-conscious about projecting an image of competence. This enables learners to be present in the moment and concentrate on engaging with the learning task at hand. The authors propose that the term ‘educational safety’ be used to describe a relational construct that can capture the essence of what constitutes PS for learners |
| Kluger and DeNisi96 | 1996 | N/A | Research | Meta-analysis | N/A | N/A | N/A | N/A | Feedback interventions can be more effective when certain criteria are met. Importantly, one of these criteria relates to the discrepancy between perceived performance and the feedback |
| Merton and Merton102 | 1968 | N/A | Book | N/A | N/A | N/A | N/A | N/A | The book explores a number of themes related to social structures and their impact on behaviour. The book argues that one such structure relates to the need to identify with a group, and how this can motivate certain actions |
| Meyer and Lunnay188 | 2013 | N/A | Commentary | N/A | N/A | N/A | N/A | N/A | Abductive and retroductive inferences can be used to build theories around how a programme or system works |
| Montano and Kasprzyk114 | 2015 | N/A | Book chapter | N/A | N/A | N/A | N/A | N/A | A book chapter that argues that there are key similarities between different theories of behaviour change and examines how they can be applied |
| Newman et al.81 | 2017 | N/A | Literature review | Systematic review | N/A | N/A | N/A | N/A | We need to advance our understanding of psychological safety through the integration of key theoretical perspectives to explain how psychological safety develops and influences work outcomes at different levels of analysis |
| Prochaska189 | 2008 | N/A | Commentary | N/A | N/A | N/A | N/A | N/A | Behaviour change models help gain an understanding of why people undertake particular health-related behaviours |
| Sandars159 | 2009 | N/A | Commentary | N/A | N/A | N/A | N/A | N/A | Guided reflection, with supportive challenge from a mentor or facilitator, is important so that underlying assumptions can be challenged and new perspectives considered. Feedback also has an important role to enhance reflection |
| Schlösser et al.132 | 2013 | N/A | Research | Quantitative | A total of 140 psychology and human development students, 414 psychology students and 103 participants recruited via a commercial crowd-sourcing platform | N/A | N/A | N/A | This research builds on the work of Kruger and Dunning130 on the relationship between poor performance and poor insight. In applying the Krajč–Ortmann model, it finds that the framework failed to anticipate self-evaluative misperceptions on the part of poor performers, but that it does much better at accounting for misperceptions among top performers. Paradoxically, the model suggests that Kruger and Dunning130 may have underestimated the accuracy of top performers, even though their account asserts such accuracy |
| Zimmerman125 | 2000 | N/A | Commentary | N/A | N/A | N/A | N/A | N/A | Levels of self-efficacy can be used in predicting common motivational outcomes, such as students’ activity choices, effort, persistence, and emotional reactions. Self-efficacy beliefs have been found to be sensitive to subtle changes in students’ performance context, to interact with self-regulated learning processes and to mediate students’ academic achievement |
Glossary
- Context
- Settings, structures, environments, conditions or circumstances that trigger behavioural and emotional responses (i.e. mechanisms) for those affected.
- Context–mechanism–outcome configurations
- Relationships between the building blocks of realist analysis (i.e. how mechanisms are triggered under specific contexts to cause particular outcomes).
- Mechanism
- The way in which individuals and groups respond to, and reason about, the resources, opportunities or challenges offered by a particular programme, intervention or process. Mechanisms are triggered in specific contexts and lead to changes in behaviour.
- Outcome
- The impacts or behaviours resulting from the interaction between mechanisms and contexts.
- Programme theory
- A set of theoretical explanations or assumptions about how a particular programme, process or intervention is expected to work.
- Rayyan QCRI
- A web application used to facilitate the screening process for a literature review.
- Retroductive analysis
- Analytical processes based on the identification of hidden causal processes that lie beneath identified patterns or changes in those patterns.
List of abbreviations
- ASSIA
- Applied Social Sciences Index and Abstracts
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CMOc
- context–mechanism–outcome configuration
- DARE
- Database of Abstracts of Reviews of Effects
- ERIC
- Education Resources Information Center
- GMC
- General Medical Council
- GP
- general practitioner
- HMIC
- Health Management Information Consortium
- PPI
- patient and public involvement
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RESTORE
- REalist SynThesis of dOctor REmediation
- SMART
- specific, measurable, achievable, relevant, time bound
