Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 15/70/101. The contractual start date was in March 2017. The final report began editorial review in April 2020 and was accepted for publication in February 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© 2021 Pollock et al. This work was produced by Pollock et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2021 Pollock et al.
Chapter 1 Context and introduction
This report presents findings of a 30-month study that was funded by the National Institute for Health Research Health Services and Delivery Research programme [URL: www.nets.nihr.ac.uk/programmes/hsdr (accessed 16 March 2021)]. The study investigates how patients, their social networks and the health-care professionals (HCPs) who support them engage in the tasks of managing complex medication regimens and routines of care in the domestic setting for patients with severe and terminal illness who are approaching the end of life. In recent decades, there has been a shift of care from hospital or institutional settings to the home for increasingly complex and serious illness. 1–5 This transition has been made possible by advances in treatment and technologies of care that enable patients to remain at home despite experiencing serious and debilitating conditions, which would previously have required institutional care. 6–8 Home as a place of care and death is widely regarded as the best and preferred option for most patients. 9 However, a consequence has been that patients and their family and friend caregivers (FCGs) are required to take on the responsibility for increasingly demanding programmes of care, including managing complex medicines regimens. 6,10–14 Managing the demands of serious illness and the health-care system that provides treatment is hard work. 15,16 Family caregivers are critical in enabling seriously ill patients to be cared for and die at home. 17,18 To date, however, there has been little professional acknowledgement or understanding of the nature of the tasks undertaken or the burden of care assumed by families. 13,19 There has also been little research into how patients and family caregivers manage the challenges of home health care or what they feel about the responsibilities involved in the tasks of medicines management for terminally ill and dying patients. The Managing Medicines study used qualitative methods to investigate these issues from the multiple perspectives of patients, FCGs and HCPs from a wide range of roles in community and specialist care.
Increasing need for palliative and end-of-life care
Worldwide, it is predicted that the number of people dying in need of palliative care will double in the next four decades, with the most rapid increases being among those aged > 70 years and those with dementia. 20,21 Indeed, it has been proposed that expertise in palliative care should be promoted among all HCPs as ‘everybody’s business’. 22,23
In the UK, most people die in late old age and after prolonged and increasing comorbidity and/or frailty. 24 The UK population of those aged > 85 years has increased by almost one-third in the last decade. 25 Demand for health care continues to rise, not just from the ageing population but because of the increasing number of people living with complex, multiple and chronic conditions. 26 Alongside this increased demand, there has also been a reduction in social care provision and a promotion of policy drivers to encourage death at home, which is presumed to be the preference of the majority of people. 27–29 Regardless of the place of death, patients usually spend much of their last year of life being cared for at home, where they and their FCGs are often required to manage complex medication regimens, often involving powerful medicines that have a high risk of adverse side effects. 6,7
Informal care
The UK health-care system is heavily indebted to the contribution of informal carers. 30,31 The UK Census of 2011 estimated that 6.5 million people provide informal care for a friend or relative. More recently, Age UK (London, UK)32 puts the figure at 9 million people, with 18% of the population helping friends and family members with increasingly complex care needs. In 2015, unpaid care work was estimated to have an economic value of £132B per year. 30,31,33 The number of carers continues to increase, as does the intensity and duration of the support that they provide. 30,34,35 Many carers (especially spouses) are themselves old and in poor health. 36 Recent polls suggest that over > 2,000,000 carers are aged > 65 years. 34 Carers UK (London, UK) reports evidence of the detrimental effects that caring can have on carers’ physical, mental, social and financial health and well-being. 37,38 The critical role of FCGs in supporting patients to remain at home and be cared for at the end of life has not been widely recognised. 39 Questions have been raised about whether or not we are reaching the practical limits of informal carer capacity. 35,40 Support for medicines management to control distressing symptoms is a core area of home health care in which FCGs are heavily involved. 41 However, little is known about the complex realities of managing medicines from the point of view of patients or carers or how they respond to the challenges involved. 42,43
Managing medicines
Medicines management is a socially situated activity that is carried out mainly within the domestic setting. 6,44 Its work is embedded into daily routines and organised in terms of space, as medicines are located in different places within the house, and time, as medicine-taking is scheduled alongside the goals and activities involved in carrying on with life. 17 Therefore, different medicines may be laid out daily in different parts of the house to correspond with the movement of people through their daily routines (e.g. some by the bedside table, some on the kitchen sideboard and others in the sitting room beside the television). Some people may prefer to keep medicines concealed in cupboards rather than on display, given their signification of compromised health. 45 However, this may prove difficult, if not impossible, where space is restricted and the number of medicines and the amount of associated equipment and medical paraphernalia becomes extensive. Some medicines must be taken with and some without food and some must be taken at specified times before or after meals. Others may be taken on an as-needed basis. Medicine-taking must be managed around ongoing activities, such as work, leisure and social arrangements, and, when necessary, medicines may need to be taken outside the private space of the home. The complexity of the relationships between patients, prescribers and family caregivers, and the practical and lifestyle issues that medications may impose on patients, are substantial and infrequently acknowledged or understood by HCPs. 7,18,41,46–49
Many people are reported to express ambivalence towards medicine-taking. Medicines may be valued as a means to sustain an active life or be resisted as toxic substances, signifying loss of health and personal agency. 50–52 Low adherence has been a long-standing professional concern. It is often stated that up to 50% of patients do not take their medicine as prescribed. 19,53 However, accounts of how patients and FCGs undertake the work of medicines management suggest that non-adherence is often unintentional rather than deliberate and a common by-product of attempts to integrate complex regimens of medicine-taking into the demands of everyday lives. 17–19,52,53
The tasks of managing medicines are complex and various, and include organising timely access and supply of medicines; ordering prescriptions; acquiring information and understanding the purpose, use, dose and side effects; monitoring the benefits and harms; taking as prescribed; and liaising effectively with a range of different HCPs and services. 18,42,43 In addition to the practical work of medicines management, many patients contend with a subjective and emotional burden resulting from concerns about loss of health, personal autonomy and the adverse effects and potential toxicity of taking powerful medicines over the long term. 50,54
Managing medicines at the end of life
The burden of care, including medicines management, increases with illness severity and complexity, and as patients approach the end of life. 55 The palliative care population is identified as being at high risk for experiencing inappropriate prescribing and medicine side effects. 56,57 Twenty per cent of patients take eight or more medicines at the point of referral to palliative care, and the number of prescribed medicines increases as death approaches. Some reduction in long-term medicines tends to be offset by prescribing of new medicines to control symptoms (such as pain, nausea and agitation) as the end of life approaches. 22,58,59 As patients become more ill and severely debilitated, the tasks of medicines management are increasingly delegated, most often to family caregivers. Increasingly complex tasks can be involved, including giving injections, changing syringe driver cartridges and managing peritoneal dialysis, chest drains and percutaneous endoscopic gastrostomy (PEG). 8,33,60
Our literature review of carers’ experience of managing medicines for patients dying at home identified that FCGs face increasing demands for care, but there was limited professional knowledge or understanding of the challenges that they face, how they cope with these challenges or how they can best be supported. 61 The literature reports widespread concerns among carers about managing end-of-life medication for the dying person in the home. 12,42,43,56,62–64 Patients and their FCGs report being inadequately informed and supported in medicines management. 42,43,62 They experience anxiety about administering powerful medicines, especially for pain relief. 65 Morphine carries a high symbolic load as being addictive, causing loss of consciousness and a signifier of impending death. 65,66 There are concerns about giving correct and timely doses and balancing the control of symptoms with the risk of overdosing or hastening death. Although FCGs can struggle to manage medications for someone who is seriously ill and dying at home, there is an expectation that they will take on these roles, and the performance of this is often judged by professional standards. 8,61 Conflict and disagreement between FCGs and professional staff have been widely reported. 12,42,43,62,63
Previous studies report a high incidence of pain and other distressing symptoms among dying patients. 62,66,67 The last days of life often involve aggravation of existing symptoms, including pain, or the sudden onset of nausea, vomiting, shortness of breath, agitation, confusion, retained respiratory secretions and weakness. 68 Patients may also become unable to swallow, requiring medicines to be administered in other forms, including patches, liquids, sublingually or subcutaneously. Pain is reported to be the greatest fear, and pain control is accorded a higher priority than place of death in public surveys. 69–72 However, evidence suggests that a high incidence of pain and distress is reported for patients dying at home62,66,67,72 and that pain is less well controlled in the home than in institutional settings. 29,73 In addition to the distress caused to patients and FCGs, failure to control symptoms at home leads to costly and unwanted use of health-care resources, including out-of-office hours (OOH) visits and unscheduled hospital admissions. 19,57,68
Burden of treatment theory
The work of managing medicines carried out by patients and FCGs, especially at the end of life, involves considerable burden and sometimes unwanted responsibility. 7,74 de Swaan’s75 characterisation of patients and carers as ‘proto-professionals’ is applicable in this context, where the home is annexed as an extension of the hospital and patients and FCGs are increasingly required to undertake the administration of complex regimens of care. These regimens also involve considerable effort, time and cost, which are required to attend appointments for routine tests and consultation with a wide range of different health professionals and services outside the home. The extent of work being carried out in the informal sector is not widely acknowledged by professionals, nor are the very considerable demands and associated burden placed on patients and FCGs confronting the considerable challenges and vulnerabilities of old age, serious illness, frailty and incapacity within a bewilderingly complex and bureaucratic system. 48,56
May et al. 7,74,76 have theorised burden of treatment relating to four main areas of work:
-
Coherence involves the unfolding process of making sense of illness and developing an understanding of treatment within a complex system of care.
-
Appraisal involves the work of assessing efficacy and quality of health care, and monitoring and adjusting treatments.
-
Relationship work refers to the effort required by patients and FCGs in negotiating support from others within informal and professional networks.
-
Enacting work is the effort put into operationalising treatment, including taking/administering medicines, monitoring supplies, ordering prescriptions, attending appointments and communicating with HCPs.
May et al. 7,74,76 propose that treatment burden should be a barometer of the quality of health care and that the goal should be to achieve ‘minimally disruptive medicine’. The question then becomes not how an overstretched health-care system can cope with the pressure of unrelenting demand from patients, but rather how do overburdened patients and FCGs cope with the pressure of the unrelenting demand imposed on them by a complex and bureaucratic system? The patient deficit model is rooted in a discourse of non-adherence, non-participation and a presumed lack of competence. By contrast, a professional deficit model can be proposed, which is rooted in poor communication and lack of organisational co-ordination.
Some patients have a more positive experience of health care than others. May et al. 7,74,76 highlight the extent to which individual responses are shaped by the opportunities afforded by their location within interconnected structures of socioeconomic advantage, environment, local infrastructures and health-care resources, and the resilience enabled by personal and professional networks of care through which information and material resources flow. 7 The acquisition and deployment of social capital is particularly difficult for people who are old, frail or lacking capacity or who have other challenges to contend with, such as belonging to a disadvantaged or underserved group. The burden of treatment theory proposes that care, and the capacity of patients to benefit from care, must take account of the wider context of social and structural constraints in which they are embedded. It highlights the extent to which personal agency is underpinned and enabled by the relationships that the individual has with others and how personal and professional networks may enable or disable access to key resources, including effective health care.
Diversity and disadvantage
Inequalities in access and provision persist in palliative care, particularly for patients affected by conditions other than cancer, from social and economic disadvantage and who come from ethnic minority groups. 77–81 Little research has been carried out into how terminally ill patients from socially and ethnically diverse backgrounds or patients who confront forms of social and personal disadvantage (e.g. homelessness, serious mental ill health, substance misuse or cognitive or sensory impairment or disability) manage medicines at home. 82,83 Ethnic and cultural differences can influence health-seeking behaviour, illness experiences and access and use of services and treatment. 84 The UK continues to be more ethnically diverse, with ethnic minority groups accounting for one-fifth of the population in England and Wales in 2018. 85 Ethnic minority populations are also ageing and increasingly experiencing life-limiting illnesses, which has considerable implications for the provision of palliative and end-of-life care. 86 Reduced access results, in part, from lack of information about the services that are available. Markham et al. ’s84 study to explore the reasons for low levels of hospice use among ethnic minority groups found that many had very limited or erroneous knowledge of palliative care services. A further barrier was that many key terms, such as ‘cancer’, ‘palliative care’ and ‘terminal care’, did not have direct translations into languages such as Hindi and Gujarati. Differing cultural approaches to death and dying meant that frameworks [e.g. advance care planning (ACP)] and decision-making could be problematic. 84 Little is known about how attitudes to medicines and medicines use, especially pain relief, are shaped by religious and cultural beliefs, or how HCPs respond to the consequences of these. 87–89
There has been very limited exploration of how people with disabilities manage medications, particularly at the end of life. In a study of the pharmacy needs of people with visual impairments in Scotland, Alhusein et al. 90,91 found that pharmacists had limited training and no policy to support them when dealing with patients with visual and hearing impairments. Patients reported that they did not always tell pharmacists about their impairment, but struggled to identify medications when the name, shape or colour of them changed. Patients also reported finding the layout of pharmacies to be challenging, not knowing if they had been seen or not hearing their name called when collecting medications. This led many to prefer to use the telephone or online ordering services, although these have communication challenges of their own. 90
Research is lacking into the needs of other underserved and marginalised groups, such as the homeless, asylum seekers, travellers and people affected by substance misuse and serious mental ill health. Symptom control and pain management can be a critical issue in end-of-life care for people with substance misuse. 92 Fractured relationships and family conflict can also make end-of-life care challenging. 81 Services for substance misuse often use a ‘recovery’-focused approach, which may not be useful as a patient shifts into palliative care because it restricts the dialogue that can be had around end-of-life care and ACP. 93
Optimising medicines management at the end of life
Good communication between patients and FCGs, between families and HCPs, and between HCPs, is fundamental to identifying and managing issues with medication in end-of-life care. 94,95 Timely access to medicines and support in understanding their purpose, dose and use are critical for patients and their FCGs in managing care at home. However, interprofessional communication and co-ordination of services is frequently reported to be poor, particularly in relation to securing patient and FCG access to medicines OOH. 12,42,62,96–98 Links between community and secondary care providers and between usual care and OOH providers are particularly unstable. 99,100
Community pharmacists
Although community pharmacists (CPs) evidently have relevant and specialist expertise in medicines management, historically they have predominantly occupied a medicine supply function in relation to community health-care teams. 57,101 Nevertheless, there is considerable scope for CPs to be involved in more direct and proactive advice giving to HCPs, patients and carers about the safe management, storage and disposal of medicines. Several initiatives have explored the extension of CP roles and clinical contact in community care, including Medicines Use Reviews, the New Medicine Service and non-medical prescribing. 57,101 However, it is not clear if, as a profession, pharmacists are keen to engage in greater involvement in supporting medicines management in palliative and end-of-life care or the logistical barriers that this would entail. 97 It is still rare for pharmacists (as well as other non-medical prescribers) to prescribe in palliative care. 102 A few schemes have indicated promise in developing greater involvement of CPs and greater integration of pharmacists within care pathways and integrated multidisciplinary teams (MDTs). 55,57,103–106 Lack of public and professional awareness of the existence or scope for such role development is one obstacle to greater CP involvement in medicines management. 107 However, CPs reportedly remain uncertain about their role in direct patient care and communication. 108 Indeed, Ziegler et al. 109 report that half of all qualified non-medical prescribers, including pharmacists, who work in palliative care do not prescribe. The current impact of non-medical prescribing in palliative care remains minimal.
Deprescribing
Polypharmacy is a major contributor to the burden of managing medicines for patients approaching the end of life, as well as increasing the risks of non-compliance and medicine incompatibility and side effects. 56,110 Evidence suggests that, far from reducing, the number of prescribed medications can increase, particularly for older patients. 110–113 Arevalo et al. 114 state the average number of medications taken in the last 7 days of life to be nine medications. Additional prescribing may often be required for the relief of symptoms, such as pain and nausea, occurring in the last days of life. However, in a Swedish cohort study of 58,415 decedents, Morin et al. 111,112 report that 32% of patients continued and 14% initiated at least one medicine of questionable clinical benefit in the last 3 months of life. Such ‘potentially inappropriate medications’ or ‘problematic polypharmacy’56 is common in palliative care. 59,115 Reasons for deprescribing not taking place include the reluctance of prescribers to broach difficult conversations about the significance of patients no longer needing to take medicines that were formerly prescribed to help keep them alive. 116,117 In addition, clinicians may want to avoid the additional workload of monitoring withdrawal or making changes to dosette boxes, as well as having concerns about creating conflict with the professional who originally prescribed the medication. 118,119 This example illustrates the continuing impact of professional hierarchy and deference, and the pitfalls that can occur when the professional network becomes overly complex. Different prescribers may become involved in individual patient cases without having a clear picture of the active care network or a sense that any one individual role should assume responsibility for undertaking an overview and rationalisation of what has been prescribed and is still needed. This is another area in which CPs could potentially play a greater role: in rationalising and simplifying the prescribed medicines with which patients and FCGs contend. Patient responses to deprescribing are unknown; however, given what is established about a widespread tendency to minimise medicines consumption, it is likely that many would be receptive. 50,54 Indeed, the tendency of many patients to undertake their own experiments to establish the efficacy and acceptability of particular medicines,120 often considered to be ‘non-compliance’ from a professional perspective, could alternatively be considered a form of patient-initiated ‘deprescribing’.
Anticipatory prescribing
The prescribing of anticipatory medicines (AMs) in end-of-life care has become widespread. 121,122 AMs presented in ‘just in case’ boxes comprise a small supply of injectable medicines and necessary equipment to treat the symptoms most likely to occur in the period shortly before death (e.g. pain, nausea, agitation, respiratory distress and excessive salivary secretions). 123 Most AMs continue to be prescribed by general practitioners (GPs), although other clinicians, including OOH doctors and non-medical nurses and CP prescribers, may also do so. The medicines are kept in the patient’s house in anticipation of future need. In most cases, the AMs are administered by community nurses (CNs), who undertake on-the-ground decisions about the appropriate time and dose of medicines to be used. 124 If regular or increased doses are required, a syringe driver is likely to be set up. In most cases, this would be prescribed by a GP but administered by CNs. Given the frequently reported problems of access to end-of-life care medicines,125 AMs have been widely welcomed as a means of ensuring that HCPs have a rapid and effective means of responding to an exacerbation of symptoms and distress in dying patients. However, the availability of AMs, especially in care homes, is also expected to reduce the demands and costs of OOH care and unscheduled patient hospital admissions. 68,121
Although AMs have become widely used and are recommended as good practice, they have been subject to little formal evaluation or research and their safety and efficacy have yet to be established. 121 Concerns have been raised about the increasingly early timing of prescribing AMs, the tendency for their use once prescribed and available in the home, and the potential risks keeping controlled drugs in patients’ homes for prolonged periods of time. 99 In addition, as most prescribed AMs are not actually used, there is a great deal of waste, with little supervision of their use or disposal. 121,126
Prescribers remain responsible for the use of AMs, but have little control over how and when they are administered. Lack of trust and communication between professionals and services can be a major obstacle to their timely and effective delivery. 12,62,99 There is evidence that CNs can struggle with administration, decision-making and ethics issues. 96 Appropriate use of AMs requires a reasonably accurate assessment of the likelihood of imminent death, which is notoriously hard to achieve. Wilson et al. 127 also found that district nurses (DNs) tend to err on the side of caution, adopting a conservative and parsimonious approach to the initiation and subsequent use of AMs, especially for pain relief.
In a situation of rising patient need and increased pressure on health-care resources, including a declining number of available professionals (e.g. CNs),128 questions have been raised about the scope for extending patient and FCG roles to directly administering medicines, including AMs, particularly to enable prompt relief of pain and other acute symptoms. The provision of such ‘emergency medication kits’ and the giving of subcutaneous injections for use by patients and relatives at home is well established in countries such as Australia129–131 and the USA. 132 Such practices remain uncommon in the UK, with only a small body of exploratory work and local policy having been developed to date. 133–136
The prescribing and subsequent use of AMs is a very significant moment in the patient’s dying trajectory. Little is known about what patients are told or understand about these or how they respond to such information, or about what FCGs would feel about taking a more active role in making decisions and using AMs directly. A few studies have reported that AMs are welcomed by families, who find their availability reassuring, especially when experiencing increasingly difficult circumstances of care at home,131 although these findings tend to be based on professional perceptions rather than patient and FCG testimony. 122,124 However, much more research needs to be undertaken to establish the understanding and acceptability of AMs for patients and FCGs, and the extent to which FCGs are willing to take a more proactive approach to managing medicines in end-of-life care.
Networks of care in a complex system
As health care has shifted from the institution to the home, domestic households are at the centre of complex networks of practice and health-care management that involve diverse health and social services and professionals, as well as wider informal networks of friends and family and technologies, including the internet and social media. 5,6,137 The consequences of colonising the private space of the home as a site of care for co-resident family members as well as patients have yet to be established. FCGs (co-resident or otherwise) are critical to enabling terminally ill patients to remain at home, increasingly often to the point of death. However, little is known about the experience of care, the nature of the tasks undertaken or how the labour of care, including medicines management, is distributed across the informal network. Cheraghi-Sohi et al. 17 found that chronically ill patients preferred to retain administrative and functional responsibility for medicines management and delegated relatively few tasks to family members. Medicine-taking was a moral practice and the capacity to self-manage care was bound up with patients’ sense of self and agency. However, patients confronting terminal illness often face extended periods of increasing dependency on others to support them with the tasks of care, including medicines management. We know little about the distribution of labour within the home, how FCGs feel about the practical and emotional responsibilities of managing complex regimens of care, or how their changing roles affect relationships within the home. Professional services and the relationships established between professionals and between professionals, patients and FCGs can be critical to the experience of end-of-life care and to enabling patients to remain at home. For patients approaching the end of life, the experience of great debility and vulnerability occurs in conjunction with increasing care needs from informal and professional networks and often an increase in the complexity of care. At a time of great physical effort and emotional distress, the family must adjust to increasing complexity of care and rapidly changing inputs from professional services. Effective medicines management is critical to the control of symptoms and to the experience of death and dying for patients and their FCGs.
In the Managing Medicines study, we wanted to explore the range of services and people involved in supporting patient care, particularly in relation to how the tasks of medicines management were distributed throughout the patient’s informal and professional networks. 17,138 Reflective accounts of bereaved family caregivers (BFCGs) provided insights into the entire trajectory of end-of-life care and the nature and impact of the experience of informal care provision. We also wanted to understand the experience of care of patients from disadvantaged and underserved groups, and how professional services identify and respond to the difficulties and concerns arising in medicines management for patients in these groups. 82,83
Aims and objectives
Aim
To explore how seriously ill patients, their FCGs and the HCPs who support them engage collaboratively in managing medicines prescribed for relief of symptoms towards the end of life, and to provide evidence from a detailed study of barriers to, facilitators of, and information about and training needs for the improved support at home of terminally ill people and their families.
Objectives
-
To explore how patients and FCGs, particularly from minority, underserved and hard-to-reach groups (e.g. ethnic minority groups, the economically disadvantaged, those affected by severe mental health problems or those affected by non-cancer disease) manage medicines prescribed for patients with serious and terminal illness being cared for and dying at home.
-
To compare and contrast the experience of symptom control and FCG involvement in medicines management for patients who have been referred to specialist palliative care (SPC) services and patients who have not been referred.
-
To establish what further support, information and training FCGs and HCPs need to feel confident in managing medicines, including those for end-of-life care, for patients being cared for and dying at home.
-
To explore lay and professional stakeholder perspectives (including those of GPs, CPs and nurses) about how CPs could be better integrated into the network of care and support for families and professionals in medicines management and end-of-life care.
-
To use the knowledge gained, from the perspective of all stakeholders, to make empirically founded recommendations for service development and effective commissioning in relation to medicines management to improve the care and experience of patients being cared for and dying at home and that of their FCGs.
Structure of the report
This chapter has provided a background to the study and considers the policy context in which it is set, alongside evidence available from previous studies. The next chapter outlines the design and methods of the study before five further chapters present a summary of patient and public involvement (PPI), participant demographics and the empirical findings from workstreams 1 and 2. Chapter 8 presents a summary of the stakeholder workshops that constitutes workstream 3 and the conclusions and recommendations resulting from these. Chapter 9 includes a discussion and critical appraisal of the findings in relation to the current literature and health-care policy. Finally, Chapter 10 provides a summary of the findings and their significance, and considers their implications for the development of policy and practice to optimise service development and professional support for patients and FCGs confronted by the challenges of managing medicines for serious and terminal illness within the home.
Chapter 2 Methodology
Study design
The Managing Medicines study explored how terminally ill people, their families and the HCPs who care for them engage in the tasks of managing complex medication regimens and routines of care at home.
A qualitative study design was employed to generate data in three workstreams:
-
HCP and BFCG interviews
-
family-centred case studies
-
stakeholder workshops.
Qualitative methods of data collection and analysis facilitate the in-depth exploration of participants’ experiences and their views. They are particularly suitable for use where little is known about the issue and in the study of sensitive and complex topics. Semistructured interviews allow participants and researchers to explore core topics, while simultaneously offering the flexibility to follow-up on new issues of interest and importance. 139–141 Case studies are eminently suited to the examination of complex real-world situations in which a variety of perspectives are at play. 142,143 The engagement of several participants within each case enables the comparison of different perspectives, and longitudinal follow-up allows for an exploration of processes and experiences developing over time, rather than the cross-sectional snapshot provided by one-off interviews. Interview data were supplemented by additional data sources, including observations, photographs and medical records. Each case was followed up, where possible, for a period of approximately 3 months.
Setting/context
The study was based in the East Midlands, UK, with participants recruited across the counties of Nottinghamshire and Leicestershire.
Ethics and governance approvals
NHS Research Ethics Committee approval was obtained in March 2017 (reference 17/EM/0091) and for two subsequent amendments to allow an increase the sample size for workstreams 1 and 2 and to include the option to seek consultee advice in relation to research involvement of patients lacking capacity. Permission was also sought, via the Health Research Authority, from the appropriate NHS trusts for their sites to act as patient identification centres in recruiting participants to the study.
Engaging severely ill patients and, recently, BFCGs in research projects presents challenges and requires flexibility and sensitivity throughout the process. Previous research has reported that participants find taking part in qualitative research to be a positive experience, even when they anticipate that this might involve discussion of distressing issues. Indeed, some people find the opportunity to reflect on their experience in the ‘neutral’ context of a research interview to be helpful and may value the opportunity to contribute to a research effort that may benefit others. 144,145 As a research team, we believe that not offering vulnerable people the opportunity to take part in research because of assumptions made about their experiences and preferences is discriminatory and exclusionary. 146,147 Prior to the decision take part, participants were asked to consider how they would feel about discussing their experience of illness and dying. They were assured that participation was voluntary and that they could withdraw from the study at any time. Some participants did become emotional during the interviews, but all clearly indicated their preference to continue the discussion.
Eligibility
Workstream 1: health-care practitioner and bereaved family caregiver interviews
Health-care professional interviews
The purpose of the HCP interviews was to explore participants’ experience of supporting medicines management for seriously ill patients being cared for and dying at home. HCPs with experience of providing care or prescribing, dispensing or administering medicines for such patients were eligible to participate.
Bereaved family and friend caregiver interviews
Interviews with BFCGs explored participants’ experiences of professional and informal support for medicines management in relation to the last months of care of their deceased relative or friend. These included the extent to which participants had undertaken different types of tasks and responsibility for medicines management, the support that they had received from their professional and informal networks, and how well they felt that the health-care system had co-ordinated this aspect of care. BFCGs of patients who had been cared for at home during a substantial part of the last 6 months of life were eligible to take part.
Workstream 2: case studies
Patients who were identified by a member of their clinical team as likely to be in the last 6 months of life and to be experiencing issues with medicines management were eligible to participate in workstream 2. Where a patient did not wish or was not able to take part directly in the study (e.g. because of poor health), the key participant was a FCG who might be a family member or a friend. HCPs were also invited to take part after being nominated by the patient as someone closely involved in their care. Each case was developed on its own terms. There was no standard configuration. Some cases lacked a FCG or nominated HCP (e.g. where the patient lived alone). More than one FCG or HCP could be recruited for each case. Participants had to be ≥ 18 years of age and with capacity to consent.
Workstream 3: stakeholder workshops
The purpose of the stakeholder workshops was to disseminate the study findings, identify priorities for implementation in education and practice, and promote collaboration in the development of education and training resources and research. Members of lay and professional stakeholder groups who had experience and/or expertise of medicines’ management for patients being cared for at home at the end of life were eligible to take part in the workshops.
Recruitment
The data collection period for all three workstreams ran from June 2017 to June 2019.
Workstream 1: health-care practitioner and bereaved family caregiver interviews
Eligible HCPs were identified through service managers and professional networks, or following presentations about the study given by members of the research team to local services and practices. Each HCP was given or e-mailed the information about the study and was invited to contact the research team if they wished to take part.
Bereaved family and friend caregivers were identified through general practices and palliative care registers, hospices, the caseloads of community and SPC professionals and through local community organisations. BFCGs were approached between 8 weeks and 6 months after the death of their relative by a HCP known to them. They were posted or given an information pack, which included a covering letter, the information sheet and a reply slip with return envelope, along with contact details for the research team. Individuals then made contact directly with the researchers if they were interested in taking part in the study.
Workstream 2: case studies
Family-centred case studies were established around the care of a patient who was likely to be in the last 6 months of life and who was in receipt of a complex medication regimen or experiencing issues with medicines management. Such complexity was associated, for example, with the number of medicines required, but could also be related to the need for different routes of administration or the use of technologies to support medicines’ use. Key HCPs were also invited to take part after being nominated by the key participant. In case studies where the patient was not recruited as a participant, a FCG was identified as the core participant.
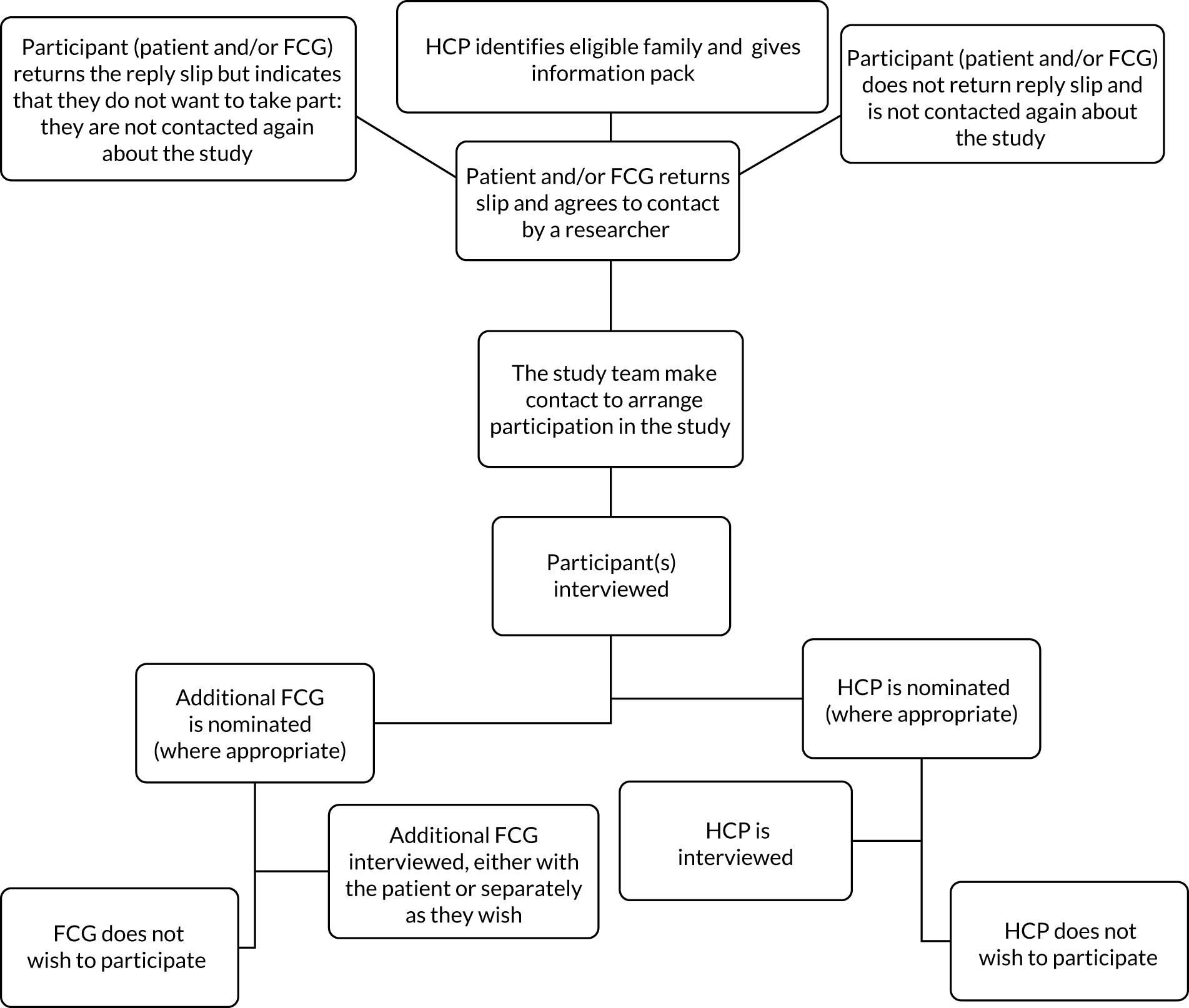
A purposive sampling strategy was employed to promote recruitment of a culturally and socially diverse sample of patients and FCGs. This included individuals from communities underserved by palliative care services, such as those from ethnic minority groups, those with learning disabilities and those with experience of conditions other than cancer [e.g. chronic obstructive pulmonary disorder (COPD) and renal failure]. In addition, we aimed to recruit approximately equal numbers of participants from SPC services and generalist community services; Figure 1 shows the recruitment flow chart.
FIGURE 1.
Flow chart of participant recruitment to the study.
Workstream 3: stakeholder workshops
Members of stakeholder groups who had experience and/or expertise of medicines management for patients being cared for at home at the end of life were invited to take part in one of two workshops, which were held in Nottingham and Leicester in June 2019. Invitations were sent to all of the HCPs who had participated in the study, all key professional links to the study and our professional networks, the University of Nottingham Dementia, Frail Older and Palliative Care Patient and Public Involvement Advisory Group (Nottingham, UK) and the Marie Curie Research Voices PPI Group (London, UK). We also asked all invitees to disseminate to their own networks and promoted these events on Twitter (Twitter, Inc., San Francisco, CA, USA; URL: www.twitter.com) and ResearchGate (ResearchGate, Berlin, Germany; URL: www.researchgate.net). The workshops took place in Nottingham and Leicester to make them as accessible as possible to the local teams who had engaged with the study throughout.
Data collection
Workstream 1: health-care practitioner and bereaved family caregiver interviews
A single semistructured interview was carried out with BFCGs to explore their experiences and perspectives of looking after their deceased relative and the management of their medicines. HCPs were also interviewed once about their experience of supporting patients towards the end of life with medicines management.
Workstream 2: case studies
The key participant in each case study was interviewed at least once and, in most cases, also on at least one further occasion over a period of 3–4 months. This could be the patient or the FCG and, in some cases, both, where interviews were undertaken jointly. Where appropriate, participants (i.e. the patients and/or FCGs) were invited to nominate a HCP who they considered to play a significant part in patient care to take part in an interview. Each case was singular and established in its own terms and could be composed of patients, FCGs and key HCPs. In addition to semistructured interviews, participants were invited to construct simple ecograms to represent their support networks. Where participants had given written consent to consider photographs being taken of medicine storage and equipment used in the home, verbal consent was confirmed prior to these being recorded. Care was taken not to include identifying information or images of people. With the permission of all of those involved, observations were carried out of some consultations with professionals and medicine-taking. The patient consent form also included an option to allow permission to review medical notes. In cases where the patient was not a participant, their medical notes were not reviewed. These data were collected via general practices and one of the participating hospices. Figure 2 shows the potential types of data generated as part of a ‘case’. A narrative summary and composite ecogram for each case is given in Appendix 1.
FIGURE 2.
Types of data generated from each type of participant within the cases.

All interviews were recorded with permission. We experienced one failed recording in the BFCG data set and one participant requested not to be recorded. Comprehensive field notes were made after each interview.
Workstream 3: stakeholder workshops
The purpose of the workshops was twofold. First, they were dissemination events for representatives from a wide range of stakeholder groups, including HCPs, managers, commissioners, educators and PPI representatives. Workshop participants were, in turn, encouraged to disseminate awareness of the study findings and its implications for practice through their wider networks. Second, they were a forum to identify priorities for implementation and to initiate collaboration with members of the research team to develop further research proposals, training and information resources, and strategies to implement the findings in education and practice at regional and national levels and for lay and professional audiences.
During the first part of the session, data were presented on three key topic areas. For the second element, participants were allocated to a table for a small group discussion based on one of the three topics. Each table was provided with a topic sheet, which included three questions central to that issue to be used as guidance for the discussions. With permission, each discussion was audio-recorded and used as a form of group interview data. Each group was led and guided by a researcher, who also asked participants to make a note of what they considered to be three key points or issues raised as part of their discussion group. The workshops were half-day events held in Nottingham and Leicester. The findings and recommendations arising from the workshops are presented in Chapter 8.
Patient and public involvement
Patient and public involvement was a key element of this study from the outset. The Dementia, Frail Older and Palliative Care Patient and Public Involvement Advisory Group gave feedback on the developing proposal, were involved in two engagement sessions to discuss the issues raised by one of the cases, and co-designed a patient poster to encourage greater consultation with CPs about medication issues. Several members of the group, including Alan Caswell, have reviewed and commented on sections of this report. Alan Caswell was a co-applicant on the grant application and has been very actively involved from the outset as a key member of the project team. He has been involved in a wide range of activities, including study design, ethics review, data analysis and dissemination. PPI involvement is discussed further in Chapter 3, including Alan Caswell’s reflections on his role throughout the study.
Analysis
Workstream 1: health-care practitioner and bereaved family caregiver interviews
The qualitative software program NVivo 12 (QSR International, Warrington, UK) was used to facilitate a thematic analysis of the data set based on the principle of constant comparison. 139 The analysis was carried out through an initial process of open coding, when segments of interview transcripts were allocated to one or more broad ‘nodes’ within NVivo to capture all text relating to an idea or topic. The coding frame was then developed through an iterative process of reading coding and discussion of the data to identify, compare and link ‘themes’ occurring within and across the two data sets involved in workstream 1. After open coding was complete, a more refined and selective process of coding of individual nodes was undertaken to explore, differentiate, reorganise and relate the themes identified as of greatest relevance to the study objectives. These were grouped hierarchically within broad categories that represented key themes identified in each data set. Further exploration was undertaken by comparing themes between each series of interviews to enable an understanding of the key issues relating to medicines management for BFCGs and HCPs, and the degree of difference, overlap and mutual understanding that exists between them.
Workstream 2: case studies
Case study analysis combined different data sources, including baseline and follow-up interviews with patients, FCGs and HCPs, observations, medicines lists, photographs, reviews of clinical records and analysis of ecograms (Figure 3). 142 Individual case narratives (see Appendix 1) synthesised the entire body of data for each case to provide a clearer view of the key elements in participants’ living situation, care input, support, medications and changes over time. These were the basis for within- and between-case comparison, using matrix charting. Follow-up interview data went beyond cross-sectional and static accounts of specific participants and groups of stakeholders to enable an understanding of how medicines at the end of life are managed over time within a complex network of care. 142 In addition, each parallel data set within the case studies (i.e. patients, FCGs and HCPs) was subject to a separate and comparative thematic analysis. 139
FIGURE 3.
Sources of data within each case.
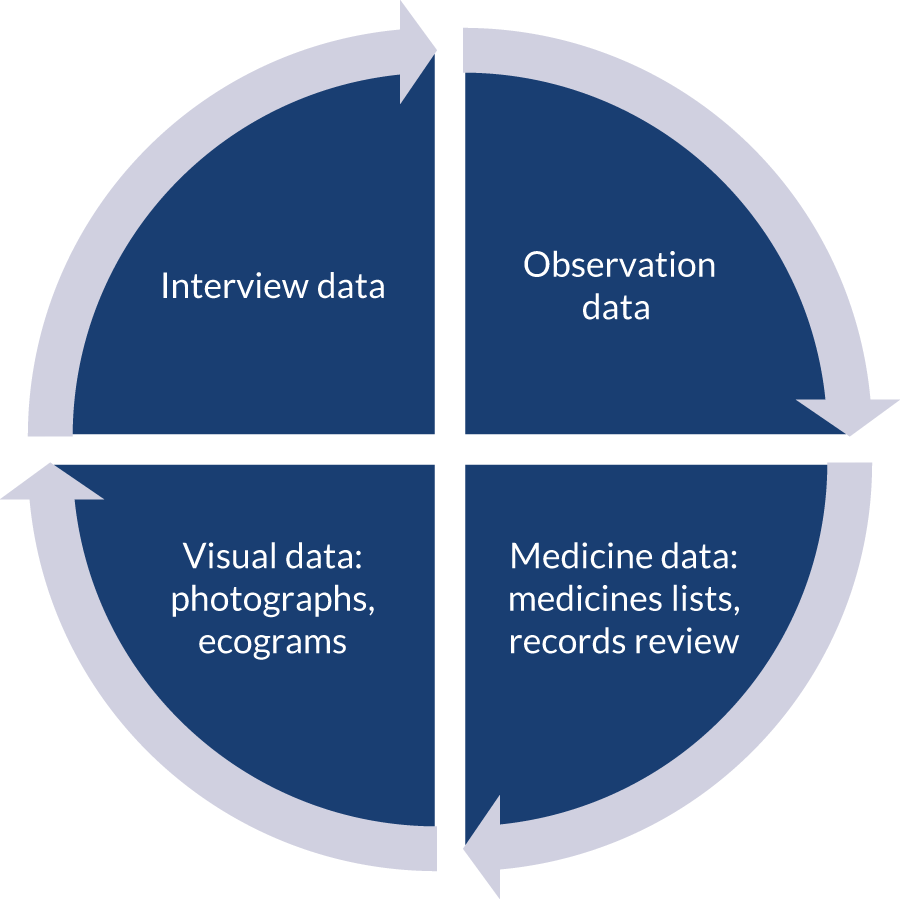
The ecograms were used to generate context and perspective on how the work of medicines management is undertaken within the patient’s home and through professional communication and inter-relations within the wider network of services and family involved in each case. 17,44,148–150 When obtained from the patient or FCG, medicines lists were compared with data generated from record reviews. These provided greater detail around prescribing choices, information about the prescriber and the most up-to-date list of current medications. Photographic data could also be compared across the cases to identify similarities and be specific examples to use as visual illustrations. Such cross- and within-case analytical formats allow for complexity of themes to be explored without losing the context of each case.
Analysis of social networks
The ecograms constructed during interviews with case study participants were intended to provide a diagrammatic representation to support the researchers’ understanding of the network of people and organisations involved in supporting the patient’s care, particularly in relation to medicines management. The process of completing the ecograms provided a prompt for participants to think through and reflect on the nature and significance of the different kinds and sources of support that they received, including those that were negative or absent. We wanted to identify key contacts within the network and get some idea of the extent to which these were linked or independent. However, participants reacted very differently to the task of drawing an ecogram, with variable levels of detail and criteria for inclusion. In most cases, it became clear that these omitted many sources of support and information mentioned throughout the interviews and other sources of data. In addition, ecograms drawn by different participants showed some variation in the links identified and how these were assessed. As we wished to gain an idea of the range of individual networks and the resources to which participants had access, we opted to draw on all relevant information available throughout the case, rather than confine analysis to the more limited content of ecograms drawn by individual participants. Moreover, participant ecograms were generated at different points in the illness trajectory. For example, some included information relating to a late stage in the patient’s illness, including after death, and may, therefore, be considered more comprehensive than others. The diagrams included in each case summary (see Appendix 1) indicate which links were included in the initial ecograms drawn by participants and which were subsequently added by the researchers. The ecograms include, in addition to informal and professional caregivers, a range of services and institutions (e.g. hospice, hospital and pharmacy) where these were referred to generically, as well as other links identified by participants as important resources. We have been careful not to overinterpret the comprehensiveness or significance of an interpretive exercise in reconstruction. However, taken together with the wider data we have about each case, we have found the ecograms valuable as a means of visualising the network of care, including informal and professional links, and the range and nature of contacts as a way of aiding analysis of each case. They also provide a simple way of exploring the range and distribution of informal and formal contacts and their significance within each case (see Appendix 1).
Workstream 3: stakeholder workshops
The researcher facilitating each group made detailed notes of the discussion. Further notes were made from listening to the audio-recordings from each of the workshop table discussions and key passages were transcribed verbatim. The recorded discussions echoed and reinforced many of the themes identified in the study data. These notes were amalgamated with the written notes provided by the participants. Already grouped into the three broad topics presented on the day, these notes were then further examined using a thematic approach to identify additional themes within and across the three topics, with a particular focus on potential areas of implementation and learning for practice (see Chapter 8).
Reflexivity
The researcher carrying out social research inevitably has an impact on, and is impacted by, the research. During this project, three researchers carried out recruitment, data collection and analysis and here we reflect briefly on our positionality and its impact. We are white female social scientists from non-clinical backgrounds. Our experience in terms of research into medicines and their use varies: the principal investigator has a substantial track record in the field, but we are all experienced qualitative end-of-life researchers. We utilised several techniques to enhance the quality of the data we generated and the analysis that we carried out. First, for each instance of data collection we wrote field notes, enabling reflection on the content, process and outcome of each interview and observation. Second, we consulted regularly with our PPI team member, the project team and the project oversight group to share findings and our developing analysis of them. In this way, we were able to access input from a range of relevant professions, including pharmacists, nurses and doctors. Third, we worked together on the analysis, with regular discussions of the ongoing process, ensuring that each transcript was coded by at least two researchers. We believe that, as non-clinicians, we are well placed to explore processes of medicines management for people approaching the end of life, but that our analysis is enhanced by input from our clinical colleagues.
Chapter 3 Patient and public involvement
Introduction
The Managing Medicines project team has been fortunate to work with the established University of Nottingham Dementia, Frail Older and Palliative Care, Patient and Public Involvement Advisory Group (Nottingham, UK). The group supports a wide range of research projects undertaken in the Schools of Health Sciences and Medicine. Members advise on every stage of the research process, including early discussion of topic, design, ethics issues, content of information sheets and interview schedules. They also contribute to data collection, data analysis and publications, including review of the final project reports. The Managing Medicines study has benefited from the inclusion of group member Alan Caswell as co-applicant on the grant. This has enabled greater integration and continuity of PPI involvement from the outset and has enabled Alan Caswell to develop a deep understanding of the study and its challenges. As researchers, we have benefited from Alan Caswell’s involvement in many ways. His perspective as a public advocate has allowed us to see the study from a different perspective, and this has improved the way in which the study was planned and delivered. He has embraced working with clinicians, researchers and academics and has been considered by the team to bring considerable expertise, as well as collegial support. From the outset, we agreed with Alan Caswell that he should take on elements of study engagement only to the extent that he felt comfortable in doing so. However, his involvement has been considerable and has extended throughout all stages of the research. Alan Caswell has taken on active roles in data analysis, dissemination and public engagement. We have welcomed Alan Caswell’s support as a very level-headed ‘critical friend’, as well as his encouragement and ongoing support through all stages of the study. Alan Caswell’s account of his involvement in the study is given below (see Box 1).
At the outset, members of the PPI group endorsed the value of the research and its resonance with their personal experience, as well as the research priorities identified by the James Lind Alliance (Southampton, UK). The group has commented on participant materials, including information sheets and consent forms. Group members have discussed and commented on the study design, ethics issues and findings. They have contributed to the co-produced patient poster workshop and to the two end-of-project stakeholder workshops. Members expressed concern about the sensitive nature of the topic, the need for skilled interviewing and the risk of the interviews causing distress to participants at a very challenging and vulnerable period of their lives. It was also suggested that FCG participants might, in reflecting on their experience, become aware of shortcomings in the care received by their relatives. The researchers have been mindful of these concerns throughout the process of data collection for the project. Illustrative extracts from the PPI member reviews of the final report are given below.
Case study: Mr Conner
The case study in its depth and quality of narration was brought to life for us. It brought back our memories of our different experiences of managing medicines but also our lived pain of coping as carers in end-of-life situations.
The detail was its strength, its authenticity. It read as though the researcher was walking alongside Mr and Mrs Connor and knew their path. The journey showed the professional strengths and unspoken underlying compassion of health-care staff. It also realistically showed the gaps in end-of-life care provision which pointed to how hard joined-up care can be when so many are involved.
Demographics
I found this section difficult to read. Could more of the figures be presented in diagrammatic or tabulated form, as is done later in this section? I appreciate from a research point of view for future reference it is valuable to know the uptake achieved from each source but is it necessary for this project?
Findings
Initially I had reservations about the photographs, however I now consider they graphically show the intrusion and medicalisation of the family home and are integral to understanding how the participant and carer had to make space and adjust to the burden of storing and administering medicines and aids placed on them. It shows a home changed to a medical storeroom. It highlights the narrative, showing the distress of illness, the responsibility of managing so many medicines and acknowledges the inevitability of the outcome of the following months.
Conclusions: consequences of managing medicines at home
Experience of a loved one dying at home can be a nightmare and one which lives with the FCG for ever. Sitting with a dying loved one unsure/unable to administer medication, without support of a HCP and not knowing what to expect; death is not always peaceful. Accessibility of HCP 24/7 [24 hours per day, 7 days per week] needs to be alongside managing medicines at home. FCGs are not only managing medicines at home but managing daily life – cooking, cleaning, changing beds, sometimes dealing with highly charged stressful situations. It cannot be assumed that FCGs have a good relationship with the terminally ill patient.
Overarching comment
This research has exposed the complexity of how we live and how we die. How do the many disciplines of health care, pharmacists, consultants, GPs, physiotherapists, occupational therapists, community nurses of all types, social care workers, social workers interact with each other and with their patients and their families and friends when people become ill?
Patient and public involvement group members have identified with the problems reported by study participants in relation to decisions about when to use medicines, getting the dose right, problems of access and supply, and, especially, effectively managing pain. Their own experience of problems resulting from poor communication between members of the MDT, particularly GPs and nurses, were shared and also the value of carers having 24-hour access to advice and information. They anticipated that provision of such a service would result in saving NHS costs by reducing unscheduled hospital admissions and achieving more rational and effective prescribing. PPI group members highlighted the importance of considering diversity and the problems of minority and disadvantaged groups in medicines management at the end of life, and of maintaining focus on the lived experience of families caring for a dying relative at home. All of these issues feature in the report of the study findings, which are detailed in the following chapters.
In addition to Alan Caswell, we thank four members of the PPI group, Kate Sartain, Maureen Godfrey, Margaret Kerr and Marianne Dunlop, for their reviews and detailed feedback on the draft final report. They provided reassurance about the depth of detail included in reporting the study findings, particularly in the extended case study presented in Chapter 5, and identified priority areas for further research. Reviewers also pointed out parts of the draft chapters that were unclear or difficult to read, overly detailed and unnecessarily complex. These comments have been extremely helpful in revising and improving the text of the final report.
The PPI reviewers highlighted the importance of further research into the following areas:
-
the prescribing and use of AMs, in particular the emotional and psychological as well as practical issues that these entailed for patients and FCGs
-
the great variation in patient and FCGs’ experience of treatment and input from different HCPs and services, particularly the lack of co-ordination, structural barriers and bureaucracy that they encounter
-
the lack of communication between HCPs involved in patient care and the apparent unwillingness of individual HCPs to take on a ‘liaison’ role in helping patients and HCPs navigate the health-care system
-
the role of domiciliary home health-care workers (HCWs) in supporting families and the much greater recognition that should be awarded to training and development of staff in this role in future
-
the variability in FCG capacity and willingness to engage with managing medicines at home
-
the role of GPs and their expectations of their role in supporting patients at the end of life
-
the consequences of COVID-19 for changing norms in patient and public attitudes and discussion of death and dying, and how recently configured primary care networks will impact on social care and its integration with health-care services.
Box 1 gives an account by Alan Caswell, our PPI co-applicant, of his involvement in the Managing Medicines study and collaborative working with the research team. This is followed by a summary of the extension work undertaken for the project, which resulted in a learning article and positional paper about extending pharmacist involvement in supporting medicines management for seriously ill patients and a co-produced patient-facing poster for display in pharmacies, general practices and other community settings. The extension work was led by Asam Latif.
In 2015, at the University of Nottingham, at a meeting of the Dementia, Frail Older and Palliative Care, Patient and Public Involvement Advisory Group, Professor Kristian Pollock spoke to the group about a proposed research project titled ‘Managing medicines at the end-of-life: supporting patients, carers, and professionals in community care settings’. During this discussion she suggested that if a member of the Patient and Public Involvement Group (PPI) felt that they wanted to be involved with this research as a PPI representative, they should contact her.
A couple of days later after giving this proposed research project some thought I contacted Professor Pollock and said that I would like the opportunity to discuss this further with her. The following week we met and during a couple of hours’ discussion, we explored both personal and work experience in this area. I agreed to be involved and most importantly, from my point of view, Professor Pollock felt that I would have something to offer to the research working group.
Before making the application for funding to the National Institute for Health Research (NIHR) there was a lot of work to do to prepare the proposal and all the necessary documentation. During this time the research title changed to ‘Managing medicines for patients with serious illness being cared for at home’ (MM@H). I became a study co-applicant, contributed to, and approved, the ‘Plain English summary’ section of the application and undertook to review and comment on the protocol and associated documents.
During this period, it was agreed that my PPI involvement would be in the following areas:
Once NHIR approved funding, I was next involved with the preparation of documents so that we could apply for ethical approval through National Health Service National Research Committee (NRES). I contributed to, and reviewed, all patient-facing materials, such as patient information sheets, consent forms and letters. I also went with Professor Pollock to the NRES committee meeting at which our application was reviewed, and even answered a question. We received a favourable opinion, so enabling MM@H to start.
My ongoing involvement in the project has been in the following areas:
At all the project team meetings I was an active participant and was, on occasion, directly asked what my thoughts were on any given subject. I always felt that my views were listened to and given due consideration by all the other members of the team. The discussions covered many aspects of the study and we often had to consider ethics dilemmas. On one occasion we even went back to the NRES committee on a particularly vexing issue, and we were given ethics approval to go ahead with it.
At the end of the study, MM@H was given a no-cost extension of 6 months, during this time work was ongoing around the area of pharmacy data, and a 1-day workshop was arranged to look at the possibility of producing a poster for use at pharmacies to explain their role in advising about medication. As a PPI member I was involved with that workshop, again greeting people, giving out information packs, ensuring the participants received vouchers for attending. I also participated in the workshop and we produced a poster at the end of the day.
I was approached by Katie Porter, Assistant Research Manager NIHR, and asked if I would be willing to speak at a workshop about my experiences as a PPI co-applicant in MM@H. On 6 February 2020 I attended a PPI workshop at NIHR Southampton and along with Doreen Tembo, Patient and Public Involvement and External Review, Senor Research Manager NIHR, gave a joint presentation which lasted 2 hours. My involvement was:
It is hoped that a paper I am writing with Dr Eleanor Wilson on PPI involvement with MM@H will eventually be published.
From being involved with this project I have become more informed on how patients, relatives and friends view the support they are given at a very difficult point in their lives; the experiences varied from good to pretty poor. Likewise, I gained a better understanding about how differing staff views on risk could lead to disagreements. For example, in one case professionals differed in their views as to the acceptability of just in case pain relief medication being given by relatives or friends, which could lead to an accidental overdose. This is a serious area and one where both relatives and professionals need support.
I also developed a better understanding of how the researchers approached the subject and at times had to develop strategies to achieve the goals of the research.
Overall, I am pleased I took the opportunity to be involved with this research project, and I would encourage other PPI members to become involved with research projects that they would have an interest in.
Co-produced pharmacist learning article, positional paper and co-produced patient-facing poster: Asam Latif
The findings of this study151 revealed considerable scope for better co-ordination and streamlining of the processes of medicines prescribing, supply and access, and greater involvement of CPs in providing support for patients and FCGs, as well as to other HCPs. The findings particularly exposed opportunities for HCPs to better engage patients and carers. An educational learning article aimed at front-line CPs was written to illustrate the practical ways that pharmacists could help patients manage their medicines at the end of life. The learning article covers the following areas:
-
What is palliative and end-of-life care?
-
A holistic approach to palliative care.
-
The case for greater involvement of CPs in palliative care.
-
Opportunities for pharmaceutical care.
-
Medicine optimisation.
-
Understanding the work that patients do to manage their medications.
-
Diversity and disadvantage.
-
Appreciating the system and the complexity from the lay perspective.
-
New palliative care models.
-
Pharmaceutical care after the death.
A positional paper aimed at pharmacy professional bodies, commissioners and policy-makers is currently under review. This aims to provide clarity and vision for future medicines management for palliative and end-of-life patients. Through this, we intend to spark a debate and illustrate the need for pharmacists to take on new roles, as well as provide guidance for educators on how best to support them.
Poster workshop
One significant finding was that patients/FCGs were often unaware of the support available from the CP. It was decided that a co-produced patient-facing poster displayed in CPs and general practices could be a simple way to raise patient and carer awareness of ways to access much needed help with medicines from their CP.
Twelve participants were recruited to a 3-hour mixed patient and professional workshop to discuss the findings and co-produce a poster. There was a range of participants, all of whom had personal experience as a FCG or an interest in palliative care. They included three patients/PPI representatives, two FCGs, three pharmacy support staff (two pharmacy dispensers and one accredited checking technician), three pharmacists and one GP. A £25 goodwill voucher was given to each participant as a token of appreciation.
Prior to the workshop, a draft patient poster was developed by the study team based on the findings of the study (Figure 4). It was intended that this would not be revealed to workshop participants until after they had co-produced their poster. The workshop began with an overview presentation of the study findings. Participants were then divided into two groups, each comprising a mix of patients and professionals. Each group formed ideas for the poster, which were then produced onto an A4 flip chart. Finally, the study team draft poster (see Figure 4) was then compared with the workshop participant poster and a composite version was produced. The new poster was subsequently circulated after the workshop to participants via e-mail for further editing, minor revision and refinement for producing a final version (Figure 5).
FIGURE 4.
Poster 1: pre-workshop poster designed by the study team.

FIGURE 5.
Poster 2: post-workshop co-produced poster.

Conclusion
Patient and public involvement has played a very significant part in the Managing Medicines study, and we are grateful to group members for their continuing support throughout the project. We have been encouraged by members’ endorsement of the topic and its importance, and their response to the study findings, which resonated with their own experience. At the outset, members expressed concern that the study should be conducted in such a way as to minimise the risk of distress or burden to participants. Throughout, they have stressed the importance of incorporating diversity in recruitment and representation of diversity within the findings, as well as staying close to the lived experience of participants in managing medicines at home. Although we have not managed to incorporate every point raised by the PPI reviewers, the comments and concerns they have expressed throughout the study have made a significant contribution to its focus and reporting of the findings.
Chapter 4 Findings: participant demographics
This chapter presents demographic information about participants in workstreams 1 and 2. Details of participants in workstream 3 are given in Chapter 8.
Recruitment
Workstream 1
Twenty-one BFCGs were recruited over a 15-month period between August 2017 and November 2018. Although we do not know how many information packs were subsequently given or sent to BFCGs, we have recorded that at least 94 information packs were given to 16 different HCP teams to distribute. Over half (12/21) of the participating BFCGs were referred via two hospices engaged with the study. Five were recruited through hospital teams across three hospitals. Two more were recruited via community nursing teams and the final two via community organisations.
Forty HCPs were recruited through a variety of routes over a 16-month period between June 2017 and October 2018. Information about the study was sent directly to key professional contacts, primarily via e-mail, and they were asked to distribute this to their networks. We also employed a snowball sampling technique by asking those interviewed to suggest other suitable HCPs or pass on information packs to colleagues. The Clinical Research Network representative supported engagement with general practices and several were visited to explain the study and leave information packs for both workstreams. We particularly targeted SPC teams, GPs, pharmacists and community nursing teams to obtain a range of perspectives from different professional roles.
Workstream 2
Over 136 patient information packs and 103 FCG information packs were provided to 16 different HCP sources. We do not know how many of these were given out. Twenty-two patient cases were recruited over a 15-month period between August 2017 and November 2018. Two patients were subsequently withdrawn: one died before sufficient data could be collected and it emerged, during interview, that the other did not meet the eligibility criteria for the study. Twenty patient case studies were completed. Nine further patients or FCGs expressed an interest in the study, but subsequently died or became too ill to take part. In addition, we are aware of 26 potential patients identified by HCPs and discussed with the research team for eligibility who did not go on to engage with the study. In some instances, the HCP subsequently decided that it was not appropriate to discuss the study, often because of a deterioration in the patient’s condition or family circumstances. In other instances, the patients or FCGs who received information packs decided against taking part and did not contact the researchers.
The 20 completed case study participants were recruited through one of three hospices (9/20), a hospital team such as respiratory (5/20), their GP (3/20), a CN (2/20) or a community organisation (1/20). The central participant in the case could be a patient or FCG, who could then go on to nominate other key people. Nominated individuals were then given information about the study and were asked to take part. We utilised a range of key contacts to recruit patients with conditions other than cancer and, where possible, from diverse or disadvantaged groups.
Study participation
Workstream 1: bereaved family caregiver interviews
Twenty-one BFCGs were interviewed (15 women and six men). All were single interviews conducted face to face. Nineteen took place in the participant’s own home and two took place at the university. In relation to the patient, 11 identified as a wife, three as husbands, six as sons or daughters (including two in-laws) speaking about a mother, one was a father and one was a friend. The patients referred to in the BFCG interviews were 12 males and nine females and had a range of diagnoses (Table 1), with many having multiple comorbidities. Of the 13 patients with cancer, there was considerable variety in the types of the disease, and for one patient cancer was not the primary diagnosis. Reflecting the high prevalence of cancer in this group, the majority (n = 16) of patients in the BFCG accounts had been in receipt of SPC.
| Diagnosisa | Participants (n) |
|---|---|
| Cancer | 13b |
| Heart failure/disease | 6 |
| Dementia | 3 |
| Diabetes (type 1 or type 2) | 3 |
| Kidney disease | 2 |
| Parkinson’s disease | 2 |
| Falls | 1 |
| Hydrocephalus | 1 |
| Stroke | 1 |
| COPD | 1 |
| Rheumatism | 1 |
| Osteoporosis | 1 |
Workstream 1: health-care practitioner interviews
We completed 27 interviews with HCPs, including one joint interview and three group interviews, with a total of 40 different participants from different professional roles (Table 2). These were single interviews, usually taking place face to face at participants’ place of work, with four conducted by telephone.
| Role | Participants (n) |
|---|---|
| SPCN | 9 |
| CNa | 8 |
| Hospice at home nurse | 7 |
| GP | 7 |
| Pharmacist | 4 |
| CNSb | 3 |
| Consultant | 2 |
| Total | 40 |
Workstream 2: case studies
The workstream 2 case studies included several different data sources (Table 3).
| Data source | Number of data |
|---|---|
| Interview | 53 |
| Ecogram | 15 (5 joint) |
| Photo | 14 sets |
| Observation | 11 |
| Records review | 8 |
Fifteen of the 20 cases had patient participants who took part to a variable extent, depending on their health and abilities. Each of the 20 cases had between one and five participants, involving 48 separate participants (Table 4). In four cases, the patient was the only participant, and in two other cases the FCG was the only participant. Fourteen HCPs were involved in 11 cases, with 11 of those participating in interviews and three in observations. Patients and FCGs reported that patients often had a number of conditions and it was not always possible to identify their primary diagnosis (Table 5).
| Participant (n = 20 cases) | Number of participants |
|---|---|
| Patients | 15 participated to some extent (male, n = 9; female, n = 6) |
| FCGs | 19 as participants (male, n = 3; female, n = 16) |
| HCPs | 14 (11 in interviews and a further three in observations)a |
| Diagnosisa | Participants (n) |
|---|---|
| Heart failure | 5 |
| Respiratory disease | 4 |
| Diabetes (type 1 and type 2) | 5 |
| Cancer | 4 |
| MND | 3 |
| Renal failure | 2 |
| Parkinson’s disease | 2 |
Across all 20 case studies, a total of 54 interviews were conducted with patients, family members, friends and HCPs. FCGs were predominantly wives, but also husbands, siblings, sons, daughters and, in one case, a friend. HCP participation in the case studies included six HCWs/support workers, four consultants, two GPs, two clinical nurse specialists (CNSs) and one specialist palliative care nurse (SPCN). All interviews with case patients and FCGs took place at their home. Fifteen interviews were conducted as joint interviews with the patient and FCG (four with two FCGs present). In one interview, a HCW was also present. One patient chose to participate solely by telephone throughout their engagement with the study. Two follow-up FCG interviews were conducted by telephone. Three of the 11 interviews with HCPs were carried out by telephone. All others took place at the participants’ place of work. The average duration of data collection for each case, excluding review of medical records, was just under 4 months.
Observations
Over the period of case study data collection, 11 observations were carried out with 10 case participants. The specific length of time spent on each observation was not recorded, but ranged from a few minutes to almost 2 hours. Observations were predominantly undertaken during visits to interview participants. Two were undertaken at outpatient appointments. These included observations of:
-
general care and feeding via a PEG
-
storage and management of medications in the home
-
pain management consultation
-
renal clinic outpatient appointment observation
-
support worker administering medications
-
a specialist nurse visit to discuss injections and ACP documents
-
the delivery of medications from the pharmacy
-
equipment (including hospital bed, hoist, lift, wheelchairs, walking aids, non-invasive ventilation, oxygen machine and wheelchair adaptation for digital tablet use).
Photographs
With consent, photographs were taken as part of data collection in 13 of the cases. Participants gave an overarching written consent to allow photographs to be taken, and verbal consent was then used to check for each individual photograph once an item of interest was identified. Where a participant expressed an interest, they were also shown the photograph to check that they were happy with the content. These were visual ways to document medication storage, medication devices and equipment and to illustrate their impact on the space and environment of the home. They include pictures of dosette boxes, blister packs, personal storage boxes, locations of medication storage (e.g. kitchen cupboard), mobile telephone applications, alarms, non-invasive ventilation and oxygen machines, and equipment such as hospital beds, hoists and a lift installed in a living room. All photographs (see Figures 7–17 and Box 2) used in this report have been anonymised to remove both patient- and pharmacy-identifying data and each has been reproduced with permission from copyright holders Eleanor Wilson and Glenys Caswell (University of Nottingham, 21 January 2021).
Ecograms
Case study participant ecograms were completed during interviews, where appropriate, and subsequently included in diagrammatic summaries of each case compiled by the researchers on the basis of all data available within each case (see Appendix 1).
The largest network included 32 links and the smallest network included nine links (mean, n = 22 links; median, n = 20 links). Key caregivers or links were identified as individuals or services of particular emotional and/or practical importance to the case participants (indicated by dark colours in the ecograms in each case summary in Code Key – for case summaries). The number of key informal caregivers within each network was between zero and two, with two cases recording no informal caregivers as ‘key’. Key formal caregivers ranged from zero to four, with seven cases considered to have no key formal caregivers. Thirteen out of 20 cases had accessed SPC by the end of the study. In five cases, SPC links featured as key caregivers eight times. The most frequent formal caregiver link was with GPs (n = 7) and the most cited informal caregiver link was a wife (n = 10). Spouses in total were the most common key informal caregivers (13/20). Where HCWs were in place, they were always seen as key to care (four cases). Disease-specific CNSs were identified as key in three cases and DNs in two.
Records review
Given the considerable time that sometimes elapsed between the completion of case interviews and the records review, we felt that it was appropriate to check consent given by patient participants at the start of the study. In five of the cases, there was no patient participant and in one other case the patient had refused consent. We deemed three further patient cases unsuitable to contact, either because we were aware that the patient had died or because the research team felt that it was inappropriate to make further contact. This left 11 cases for which consent had originally been given that needed to be checked. We endeavoured to follow up on each of these cases and to establish GP contact details to undertake reviews. Where the patient had died (in three cases), we discussed this with their FCG and each wanted to support the patient’s initial decision. One patient decided to revoke his initial consent. In two further cases, we were not able to contact the participant to confirm consent. This left eight participants with records that to review, two of whom also had hospice records that we were able to access (Figure 6).
FIGURE 6.
Process of reviewing patient records.
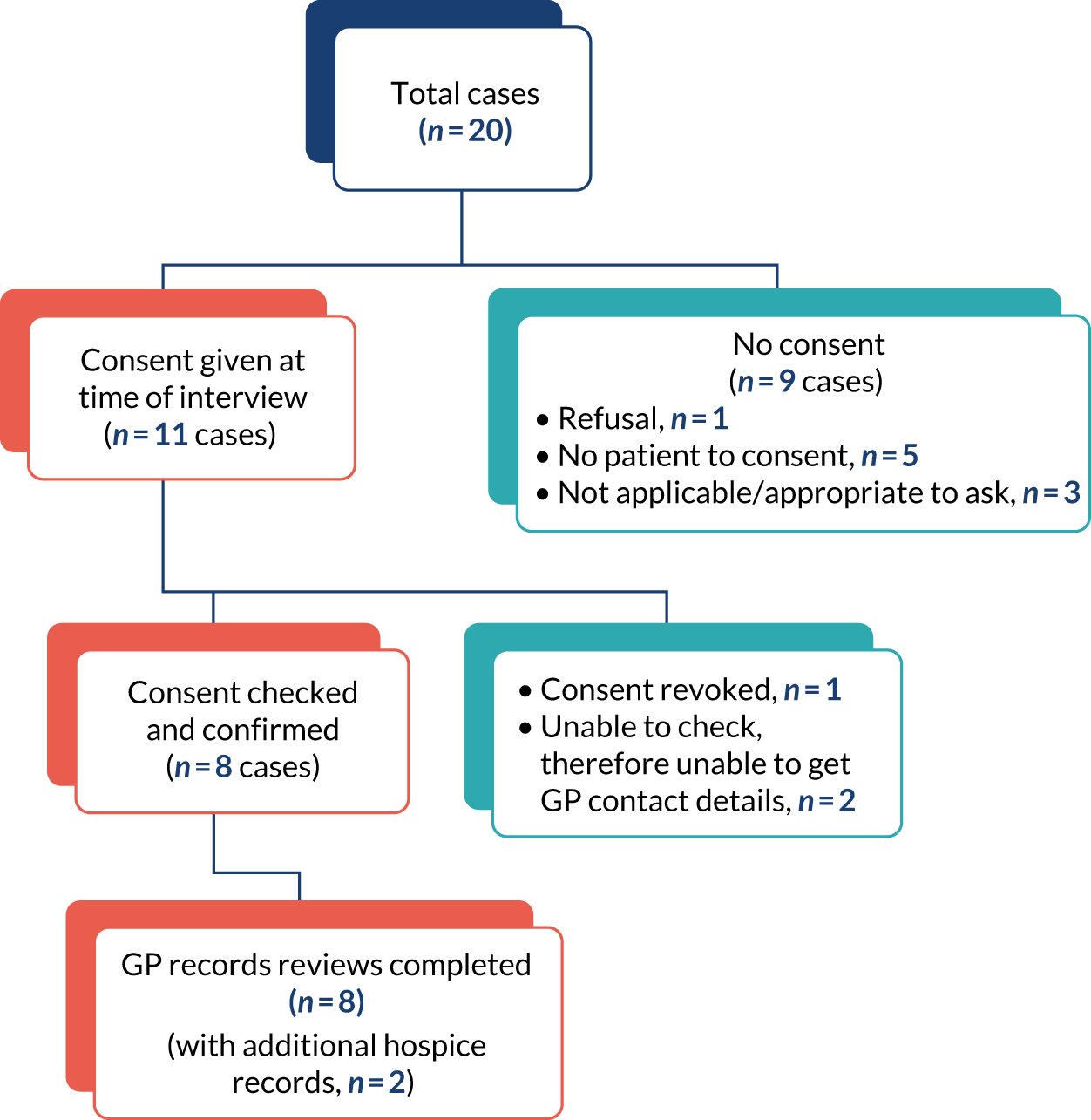
Specialist palliative care
Initially, we had intended to search for differences in the experience of care between patients who had and patients who had not been referred to SPC. For the purposes of the study, the term SPC covers access to SPCNs, consultants and hospices. In practice, however, we found that this distinction was not particularly useful. In part, this was because of the very diverse conditions affecting patients, as well as the different stages of their illness and natural variation between these. All but three of the patient cases survived past the end of the study and would likely be referred for palliative care at a later stage of their illness. Consequently, we have not considered quality or experience of care in terms of a contrast between ‘specialist’ and ‘generalist’. All patients in workstreams 1 and 2 who were affected by cancer and half of those with other conditions had been referred for SPC. Some patients without cancer reported having prolonged input from specialist teams, including those dealing with long-term conditions, respiratory specialists and disease-specific nurses who had considerable experience and expertise in palliative and end-of-life care [e.g. nurses specialising in Parkinson’s disease, COPD, renal disease and motor neuron disease (MND)]. The most significant resource available to patients was the establishment of a key caregiver relationship with a particular HCP, and this resource was drawn from a wide range of general and specialist roles.
However, the established association between cancer and palliative care was apparent in the study data. Based on primary diagnosis, all four cancer patients in the case studies had prolonged hospice stays, outpatient appointments and SPC nursing at home. In comparison, for respiratory disease (e.g. COPD and emphysema), only one of four patients reported access to SPC. Several of these patients described a pattern of bypassing community professionals and contacting emergency and ambulance services directly when they recognised onset of an acute exacerbation of their condition that they anticipated from past experience would require hospitalisation. Three patients with MND had some access to SPC. The experiences of those with conditions such as heart failure, progressive supranuclear palsy (PSP), renal failure or multiple comorbidities all varied. In total, 13 out of our 20 cases reported accessing SPC at some level during their involvement in the study. The majority of BFCGs reported SPC input for their relatives prior to death in a group in which most patients were affected by cancer. The care of some patients in both workstreams had been predominantly managed by GP and DN teams.
Do not attempt cardiopulmonary resuscitation
Do not attempt cardiopulmonary resuscitation (DNACPR) status was not routinely discussed during the interviews and it was not often mentioned in the BFCG interviews (6/21). However, from the cases for which we have been able to draw on multiple sources of data, we know that 12 patients had a DNACPR in place and two had some form of advanced directive (one with and one without a DNACPR).
Anticipatory medications
Thirteen of the BFCGs reported that the patient had been prescribed AMs. In six instances, these were reported to have been used. Six of the case study participants also reported that AMs were in place. This number is likely to have increased as more of the participating case patients reached the end of life. A further four case study patients held a prescription for ‘just in case’ or ‘rescue’ antibiotics for chest infections. Across both groups, there did not appear to be any association between having anticipatory medications in place and having access to SPC.
Syringe drivers
Ten of the patients described in the BFCG interviews had a syringe driver put in place for symptom management at the end of life. All but two of these patients had a diagnosis of cancer. Three of the case study patients also had syringe drivers in place. Two of these patients had cancer and one had renal failure. Across both groups, all of the patients recorded to have syringe drivers also had SPC input.
Medications
Patient case studies
Within the 20 patient cases a total of 222 prescribed items were identified. Appendix 2 provides a list of all of the medication prescribed, as reported by participants or found in medical notes. We were able to review the medical notes of eight patients and in the other 12 we relied on participants’ accounts. Supporting information was also obtained in some interviews with HCPs who had immediate access to medical notes. On average, case patients had just under 12 prescribed medications and this ranged from 6 to 20. These include equipment and machines, such as oxygen concentrators, non-invasive ventilation and nebulisers, creams, eye drops, supplements (e.g. vitamins and fortifying drinks), laxatives and anticoagulants. There were a range of formulations prescribed, including tablets, liquids, injections, inhalers and patches. Complementary medicines were mentioned by participants, but not often and we did not enquire specifically about their use.
The aim of Appendix 2 is to illustrate the number, complexity and range of prescribed items across a relatively small cohort of 20 patients. The data show that participants frequently had more than one medication prescribed from a certain group of medications. Opioid analgesics were the most frequently prescribed medications, followed by proton pump inhibitors, which reduce acid in the stomach and are often prescribed to manage the side effects of other medications in palliative care.
Bereaved family caregiver interviews
We do not have extensive knowledge of the medications used by the relatives of BFCG participants and we have not attempted to collate this. Information was accessed during a single interview and based on participants’ recall of past events. However, some BFCGs gave very detailed accounts based on meticulous records maintained during the patient’s illness. The researchers were sometimes shown prescription and medicine lists. We cannot, of course, know how medications were taken by patients and whether or not they were taken as prescribed.
Conclusion
This chapter has presented background information on the participants who took part in the study and the different sources and extent of data collected. It includes a summary of the process of recruitment, characteristics of participants in workstreams 1 and 2, their involvement with SPC and the medications prescribed for case study patients. The next chapter gives a detailed account of a single case as a way of understanding the experience of treatment and decision-making at the end of life and to provide context for the key themes and issues presented in the chapters that follow.
Chapter 5 Findings: case study
Mr Connor
We begin the presentation of the study findings with a detailed account of a single case study. This is intended to convey something of the lived experience of patients and family caregivers confronting the challenges of terminal illness, the work involved in managing medicines and how this work is an integral component of a wider regimen of care involving visits to clinics and hospitals, communication with HCPs and maintaining records, alongside managing the demands and aspirations of ongoing daily life. None of the case studies included in the study can be considered ‘typical’. However, we have selected Mr Connor’s case to illustrate an experience that was neither particularly good nor particularly bad, and about which we have information extending from the start of his participation in the study to his subsequent death several months later.
Mr Connor and his wife participated in the study over a period of 3 months. They took part in two interviews and guided the researcher to draw an ecogram illustrating the support that they had in place in terms of managing medicines. The data for this case study also included photographs of Mr Connor’s dosette box, his medicines’ storage and the syringes used to give him his weekly injections, plus a list of his medicines. Seven months after the second research interview, Mr Connor died at home and his GP records were reviewed 3 weeks later.
Mr Connor was in his late 70s and had been retired for about 15 years. He had end-stage kidney disease, having suffered with renal problems for about 20 years. Several years previously, Mr Connor had experienced a stroke, which had left him with no feeling in his dominant hand and a tremor in the other, and this had an impact on many of his daily activities and meant that he was unable to write. He also had type 2 diabetes and diverticulitis. He lived with his wife, who was his carer, particularly in relation to his medicines. Mrs Connor also had health issues. She had a heart condition and blocked arteries, which caused a problem with one of her legs. This meant that she could not walk very far and found driving difficult.
Health
Mr Connor’s main health problem was end-stage kidney disease. He had known for about 20 years that he had kidney problems and thought that his kidney function was ‘49%’. Although this was a serious matter, he was not too troubled about it because as he said ‘people live with one kidney, 49% is OK’. As far as Mr Connor was aware, his level of kidney function had not altered in about 10 years. During a period when Mr Connor’s diverticulitis was causing him a great deal of pain, his GP referred him to a consultant, who would have liked Mr Connor to undergo a computerised tomography (CT) scan. However:
. . . and well he said, ‘Can’t do a CT scan because it will kill you’. And we sort of sat there and went, he [Mr Connor] said . . . ‘Well how do you mean it will kill me?’. And he [consultant] said, ‘Well, you’re stage four kidney failure!’ . . . So I said to him, ‘I’m sorry but I don’t understand stage four kidney failure, what’s that?’. So, he said, ‘Well, stage five you’re on dialysis’.
Mrs Connor
About 1 year before taking part in the study, Mr and Mrs Connor learned that his kidney function was down to 18%, which came as a great shock to them both as did the fact that ‘nobody bothered to tell me’ (Mr Connor).
Mr Connor was referred to the renal team, which meant outpatient appointments with the consultant and occasional meetings with a CNS. His kidney function continued to decrease and he kept an eye on its progression. Dialysis was suggested as a treatment option, but Mr Connor decided against this with the agreement of his wife.
Mr Connor understood that his condition was terminal:
I said, ‘How long am I going to last now?’. And because my results have fallen and he says, ‘Well, I don’t expect to see you this time next year’. And that’s the only thing that come out of it, wasn’t it? . . . Well, I’ve come to terms with it. The only thing is it’s like living with a time bomb, you don’t know when it’s going to go off.
Mr Connor
At the time that Mr Connor took part in the research he was experiencing a number of symptoms, including fatigue and itching. He was advised by his renal consultant that the fatigue would increase and he would gradually sleep more until eventually he would not wake up.
Medicines
Mr Connor was taking a range of medicines, although the medication for his type 2 diabetes had been stopped. He had lost weight because of his kidney problems, Mrs Connor thought, and his blood sugar levels were well maintained and so it seemed he no longer needed the medication, although he did continue to monitor his levels. He had an inhaler for asthma, medicines to help manage the tremor resulting from his stroke plus medication to reduce the risk of a future stroke.
Managing medicines day to day
When Mr Connor came out of hospital after his stroke, he brought his discharge medicines home with him in a dosette box. This seemed like a good idea:
[When] he came out of hospital, they gave him his medication in a dosette box. Prior to him going in, I’d noticed that he was suddenly ordering a lot of one thing or not enough of something else, so it was a bit erratic. So, I thought if I asked them at the local chemist if they could do the same thing, the dosette boxes, it would solve the problem of me having to give him medication because he wasn’t well, and it would also solve the problem of having to order things at a particular time because it all just came together. So, we approached the chemist and they agreed to do that . . . So, we’ve been having dosette boxes ever since. So, the only things that he needs to order are things like for his asthma, you know, inhalers and things that they can’t actually put in the dosette box.
Mrs Connor
This worked well. The pharmacy ensured that they had the necessary prescription from the general practice, dispensed the medicines and placed them in the dosette box (Figure 7). The pharmacy then delivered 4 weeks’ worth of medicines to the couple’s home.
FIGURE 7.
Mr Conner’s dosette box. Reproduced with permission from Eleanor Wilson (University of Nottingham, 2021, personal communication).

It is easy to see from looking at the box which medicines have or have not been taken:
They send you a month’s supply and you know you’ve got a month’s supply of all the drugs that you need really.
Mrs Connor
However, there were drawbacks. Although the boxes came with a list of medicines that were included, the couple did not always know which one was which. When his blood pressure medication was changed, Mr Connor said ‘I had to take it [dosette box] into the pharmacy one day to find out . . . what they were’. It could also be problematic if a change was made to the medication part way through the 4-week period. For example, on one occasion, Mr Connor’s prescription for alfacalcidol was doubled. Sorting this out and accessing the extra medicine necessitated Mrs Connor to make four or five trips to the pharmacy. Mr Connor requested other medicines, such as his asthma medication and creams, from the general practice online.
Mr Connor’s medicines were mainly stored in the kitchen cupboard, with his erythropoietin and asthma medication kept in the fridge. The dosette box in use was kept in the kitchen, with the stock of boxes stored upstairs in the bathroom cabinet. When it was time for Mr Connor to take his medicines, his wife would put them in a small cup to make it easier for him. She had taken on this task when Mr Connor started to drop some of his pills on the floor but did not notice.
Injections
Given that he was anaemic, Mr Connor was given ‘. . . an infusion of red blood cells – which did a fair job’ (Mr Connor), and this was followed up with weekly injections of erythropoietin, which was intended to increase the production of haemoglobin in his body. They were shown a DVD (digital versatile disc) about the process and Mrs Connor was given the job of doing the injections (Figure 8). A DN came to the house to demonstrate how to do it. Mrs Connor said ‘No I’m not really squeamish. I’m not thrilled about having to inject him, but it’s fine’. She described the process:
The syringes are such that you stick the needle into the flesh, and it releases the contents of the syringe and then it just disappears up itself, so there’s no messing about with syringes. It comes fully loaded . . .
Mrs Connor
FIGURE 8.
Injectable medication. Reproduced with permission from Eleanor Wilson (personal communication).

Support
Although there were a number of HCPs involved in the care and support of Mr Connor as well as his adult children and grandchildren, Mr and Mrs Connor were committed to remaining independent and, as far as possible, self-sufficient, and said that they supported themselves:
We support ourselves. We don’t have any support do we?
Mr Connor
No, we don’t really need any, do we? If we really need something we’ll ask, but we don’t ask very often, do we?
Mrs Connor
Mr and Mrs Connor took part in joint research interviews. Although Mr Connor was the person with the terminal illness and the one whose medicines were the focus of the interviews, they both spoke in an inclusive way. This is demonstrated by their use of the first-person plural, talking about how ‘we’ are supported or visited by ‘our’ kidney nurse, highlighting the relational nature of managing medicines and the practice of care in a domestic setting.
Professional support
A number of different HCPs worked with Mr Connor at different times. His GP was regularly involved and occasionally made home visits, particularly towards the end of Mr Connor’s life. DNs tended to visit when there was a specific task for them to carry out, such as demonstrating how to give the weekly injections. The local pharmacy dispensed and delivered the prescriptions.
Mr Connor was also under the care of the renal team, with outpatient appointments every couple of months. The couple was unsure how useful these appointments were:
All we’ve heard from the hospital appointments are things like, you’ve got to decide whether you’re going to have dialysis or whether you’re just going to manage your condition as best you can . . . and really every appointment has been, you’ve got to make a decision as to how you’re going to die really, and it’s not been very pleasant to go to the hospital, to say the least, and sometimes you’ve come away a bit shell-shocked from it and sometimes a bit resigned to it.
Mrs Connor
Mr Connor had a renal CNS allocated to him and his wife said that if they encountered any kidney-related problems they would get in touch with her:
Yes she would be the first port of call, because she is our designated kidney nurse.
Mrs Connor
During a home visit, the renal CNS began to write a care plan, laying out Mr Connor’s wishes for his future care. She asked if he had completed a DNACPR order and said that she would check with his GP. She did so and later:
He [GP] came back really to make sure that that’s what [Mr Connor] wanted and the nicest thing that anybody’s said to us in a year, he sat where you’re sat now and he said, ‘Of course, it’s not going to happen any time soon’.
Mrs Connor
The DNACPR identified Mr Connor’s preferred place of death as a hospice. There were reasons for this:
But the issue of not wanting to die here was more it’s a very small house, we’ve got no room in the bedrooms really . . . So, if he needs equipment, like if he’s very weak and he can’t get in and out of bed and has to be hoisted and things, we haven’t got room for those sorts of things.
Mrs Connor
The couple anticipated further difficulties that might arise if people they knew wished to visit Mr Connor when there was not room in the house for people to sit round the bed. In addition, Mrs Connor felt that she would be unable to cope with an influx of visitors in the house at this time. In addition:
You see, what worries me is if one morning she [my wife] gets up and goes down, makes a cup of tea and comes back with the cup of tea and I’ve been dead for about 4 hours.
Mr Connor
Mr Connor had been referred to a counsellor. He stopped attending after three sessions because, as Mrs Connor explained, he felt that they were not helping him. She, herself, felt that they could have been beneficial, but that the sessions were misdirected:
I felt that she could have helped him more. I don’t really know. She’d got him saying, ‘Oh, I want to do this and I want to do that, and I’d like to go here and I’d like to go there, and I just sit at home and I don’t do anything’. Well, none of these things are practicalities and yet she was trying to tell him that, ‘Yes, you can do this!’, and actually he can, provided he can get somebody to take him or go with him, because I can’t walk round these places and do these things.
Mrs Connor
This raised another concern for Mrs Connor: that there were certain aspects of caring for her husband that she was not physically able to undertake.
Work of being a carer
Mr Connor handed responsibility over to his wife for his medication, except for his inhaler, which he kept in his pocket ready for use. Mrs Connor felt the responsibility involved in looking after her husband and ensuring that he took his medicines. She had her own health issues, including heart disease. She had been offered surgery to clear blocked arteries, which should improve her quality of life. However, she said:
. . . well I can’t take the risk, because who knows what’s going to happen and I can’t go and have another cardiac arrest, can I, at the moment?
Mrs Connor
Mrs Connor was concerned about who would look after her husband should she become unable to do so:
[My wife] does a fantastic job looking after me. I wouldn’t want anyone else to do it, but it’s not that fair on her really.
Mr Connor
Although the couple had stated that they supported each other and needed little support from others, Mrs Connor did acknowledge that they sometimes felt isolated and unsure who they might turn to in case of a query or an emergency, saying ‘we feel a bit left alone here, who do we go to? The GP?’. Mrs Connor was told by a friend about the single point of access (SPA) service that was designed to co-ordinate referrals and to provide one telephone number that patients and their families could ring when in need of assistance. She took the initiative and contacted their GP to ask about this and a referral was made to the SPA service. Thereafter, Mr and Mrs Connor had a single telephone number to call if they needed help. From this (late) point onwards, Mrs Connor felt that she had access to a ‘very valuable’ service.
Last week of life: from the review of Mr Connor’s medical records
Six months before Mr Connor took part in the first research interview, and 15 months before he died, Mr Connor’s GP placed him on the practice’s Gold Standards Framework (GSF) register. He was then classified as green, that is with unstable/advanced disease and a likely prognosis of months. Twelve months later, Mr Connor was reclassified as yellow, with his condition deteriorating and a prognosis assessed at weeks.
During the month before Mr Connor died, he became increasingly unwell, with several GP home visits and a hospital admission with a suspected gastrointestinal bleed. The GP noted that Mr Connor was probably entering the terminal phase. The original DNACPR had been lost and so a new one was completed, with this one noting Mr Connor’s preferred place of death to be home. The next day the GP stopped most of Mr Connor’s medicines and prescribed morphine (Oramorph®, Boehringer Ingelheim Ltd). The palliative care nurse (PCN) visited and carried out an assessment. A DN arranged for the delivery of a hospital bed and a referral to Marie Curie (London, UK) for sitters for three nights per week over the following 4 weeks. This was to allow Mrs Connor to have some nights of good sleep. Mr Connor also had carers twice per week to help with his personal care. He was not keen on this, but agreed to it to help his wife. The DN noted that end-of-life medicines (i.e. AMs) were in place and signed for. A few days before he died, the DN delivered a syringe driver and set it up with morphine, midazolam, levomepromazine and glycopyrronium. A PCN visited later in the morning, showing Mrs Connor how to carry out mouth care and noting that the couple both realised that Mr Connor was dying.
Two days later, Mr Connor was visited by a DN, an OOH doctor and a PCN. Marie Curie Care rang to say that they would be sending a sitter for that night. When two DNs visited the next morning, Mrs Connor told them that her husband had died. They recorded that this had happened shortly before their arrival. They stopped the syringe driver and took it away with them. Mrs Connor said that she wished to be left alone to wait for her son to arrive. The GP called and confirmed death 1 hour later.
Conclusion
Managing medicines was one aspect of dealing with life in the face of terminal illness for Mr and Mrs Connor. Their approach was relational, in that the decisions that they made took into account the perceived impact on each other. One of Mr Connor’s reasons for wishing to die in a hospice, for example, was that he was concerned about the effect on his wife of finding him dead in bed. Mrs Connor felt the responsibility involved in helping her husband to manage his medicines, alongside the other tasks she carried out in her role as carer, such as accessing help when needed and supporting her husband in his interactions with HCPs. In addition to monitoring and arranging access and supply, this case illustrates the extent to which managing medicines was a joint endeavour and also how the responsibilities of providing care could have a negative impact on the FCG’s well-being and health. Although clearly committed to supporting her husband, Mrs Connor acknowledged the responsibility and effort involved, as well as the need to prioritise his health-care needs over her own. She was also concerned about his dependence on her in relation to the restrictions imposed by her own poor health and limited mobility. The couple saw themselves as self-contained and neither needing nor wanting support from others. This was portrayed in their ecogram, which was unusual in excluding family members or friends and included HCPs in terms of their roles rather than as individuals. It appears that, despite quite extensive involvement with different HCPs and services, neither partner had established a relationship with an individual HCP who could be identified as a key worker to be a first point of contact if they needed help and assist in co-ordinating care. Despite their stance of independence and self-sufficiency, both partners were aware of Mr Connor’s limited prognosis and inevitable decline. They expressed uncertainty about how they would manage this. Mrs Connor was pleased to have found out about the SPA service during a meeting with a friend (who is not included in their ecogram). Although there is no record of them having used this service, knowledge that they could access a dedicated helpline 24 hours per day was very reassuring.
The medical records review indicates that Mr Connor’s care during the last days of his life was well organised and that the system responded well in co-ordinating care, although, at this point, we have no knowledge of the couple’s experience and assessment. The GP recognised Mr Connor’s approaching death and ensured support from DNs and PCNs. A few days before he died, a new DNACPR was put in place, as it appeared the original one had been misplaced. It was not possible to tell from the medical notes if Mr and Mrs Connor had changed their minds about preferred place of death, which had previously been hospice, or if home was assumed to be his inevitable place of death given that there had been no hospice referral. However, Mr Connor achieved his wish of not dying in the night while his wife slept beside him.
The Connors’ experiences prefigure issues explored in the following findings chapters, which cover the themes of the work of medicines management, diversity and disadvantage, and systems and complexity.
Chapter 6 Findings: the work of medicines management
When someone is seriously ill and dying at home, the burdens of care can be considerable for patients and their FCGs. In this study, issues such as washing, dressing, moving the patient, toileting, cooking, laundry, cleaning, prompting eating and medicine-taking, being ‘on call’, providing emotional support, liaising with HCPs, attending appointments and encouraging social interaction were just some of the activities that were undertaken alongside the diverse tasks involved in medicines management. These tasks intensify this workload and further deplete the already limited physical and emotional resources of many patients and their FCGs, who may themselves be old and in poor health, or juggling complex obligations of care, family and work. A few HCPs acknowledged the difficulties that the debilitating effects of illness combined with the complexity of medicines management routines could pose, and the adverse consequences, intentional or otherwise, for patient compliance:
It was a bit of an ongoing issue of trying to convince him to take the medicines that were appropriate and necessary, at the same time as him wanting to not be on them at all . . . So, he was weak, weary, tired, had no appetite and then on top of that, I was trying to get him to take a concoction of medication.
SPCN, HCP15
As patients’ health deteriorates, FCGs increasingly bear the brunt of this wider workload, taking on the substantial practical, physical, emotional and knowledge-based aspects of managing medications. All but three of the patient cases in our study lived with a FCG who supported their care and medicine needs (see Box 2 for a focus on some of the issues for patients). BFCGs had experienced the entire trajectory of care preceding their relative’s death and were able to reflect on their experiences throughout. For FCGs, the work of managing medicines occurred in the context of increasing exhaustion, poor health, emotional distress and sometimes the experience of inadequate support and social isolation:
Everything I have to do, and I have to be here, and have to make sure that he’s safe if I go out and make sure he eats, because he doesn’t want to eat half the time these days and, so it’s all onerous, being a carer is onerous. But it’s no good thinking like that or you’ll just go under. So, I just try and just deal with what needs doing on a day to day basis and . . . you know, I just get on with it, really, no choice.
Mrs Crump, FCG, Int1
Mrs Crane was a 69-year-old woman living alone. She had a diagnosis of heart failure, but also suffered with advanced arthritis in her knees, asthma, considerable sleep apnoea and depression (for further details see Appendix 1, Case summary: Mrs Crane).
Mrs Crane managed her own medications (Figure 9), with prompting from her friend in the evening when she was tired. Her medications were delivered in blister packs from the pharmacist (each cell containing 12 tablets), with a further five additional medications and an inhaler. Mrs Crane appeared to be very well organised and reported knowing what each of the medications were for, if not their names:
The dosette box are made up with the regular tablets. If there’s a new tablet they bring it in either a small box or similar. There’s some of the medication that don’t go in the dosette boxes because it can vary the amount I take . . . I’ve got a routine, between eight and nine I take my first lot. Dinnertime I take one or two. I’ve got my inhalers as well. You just get yourself in a routine.
Int1
FIGURE 9.
Patient focus: Mrs Crane. Reproduced with permission from Glenys Caswell (University of Nottingham, 2021, personal communication).
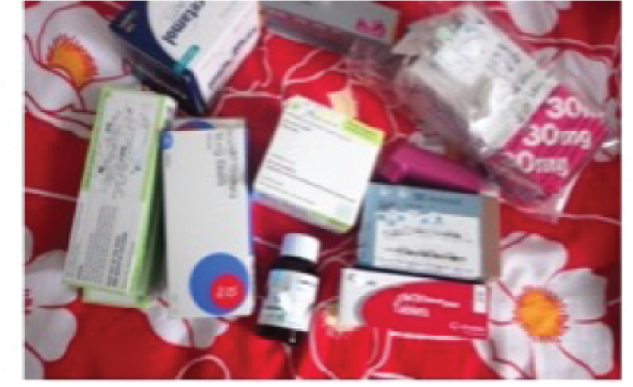

Mrs Crane reported finding the blister packs from the pharmacy to be helpful and was reassured to know that these were organised and consistently delivered to her as she needed them. This had taken a lot of the work out of managing her medications and supported her by keeping her organised when her depression clouded her thinking:
They deliver them. It’s done automatically every month . . . last time I was at [the hospice] they changed one of the medications. They get in touch with the doctor, the doctor gets in touch with the chemist and they’re delivered . . . main thing, there is times when I get depressed that I can’t remember whether I took my tablets or not. So, then I know looking in my boxes whether I’ve took them or not.
Int1
However, Mrs Crane reported frustration at finding changes in the size, shape or colour of her medications that she had not been informed about and suggested that this was because of pressure to cut costs. These changes created additional work to investigate and clarify these issues:
It’s confusing because you could have the same tablet but under a different name. A cheaper version. I mean that’s another problem they don’t inform you. You’re ringing back, I’ve not got so and so. Oh, you have, it’s under another name. Well please let me know!
Int1
. . . last time I sent my carer all the way back to say you sent the wrong tablets . . . So she took the tablets back up there and they said, ‘Oh no, it’s just another name for them . . . They’re different colours’. That’s how I knew it. . . . That’s what worries me, things like that.
Int2
Mrs Crane recognised that she was starting to struggle and was putting plans in place for additional help and support at home (by the time of her records review the HCW was attending daily):
I don’t feel so confident as I used to . . . That’s why I’m asking for extra care . . . if I have a really bad day you don’t always focus.
Int1
Mrs Crane’s hospice notes indicated that she had, on at least two occasions, asked her family to remove medications from her house for her own safety. In relation to her medications, Mrs Crane’s ecogram depicts a small network of support, including her friend, occasionally her daughters, her HCW and the hospice. Latterly, the long-term conditions team had been added. GP records documented two instances when Mrs Crane had telephoned the SPA line with medication queries. Her call had been referred to, returned and advice given by the long-term conditions team.
Regimens can be complex, with patients prescribed multiple medications to be administered through different routes and at different times throughout the day and night. Some medicines need to be taken at a specified period before or after meals. Others should be taken with food. Many also had medications to be taken ‘as needed’ or pro re nata (p.r.n.):
Eventually, we ended up on a buprenorphine sublingual. Which he had as a p.r.n. He had paracetamol as a regular, trying to think of the one he had at night, gabapentin, he used to have gabapentin at night which used to help him through the night. And then, there were his renal medications, I can’t remember them all now, but one of them was a calcium, which he hated. And then he was on supplement drinks, went from Fortijuce to Fortisip, back to Fortijuce, but coming up to the last 4 to 5 weeks, before his death, we were struggling to get medications down him, he wouldn’t swallow them, so we did end up changing to syrup form, and the syrup form we was having to syringe. He wouldn’t take it off the spoon. But he’d suck on the syringe. Some of his medications weren’t available in syrups. So, them medications were then omitted from his treatment plan. But he did have the subcut hyoscine bromide, because he had chest infection after chest infection after chest infection. He’d got a lot of secretions, unable to cough because he hadn’t got the strength, so I was delivering the subcut hyoscine until 5 days before he passed away and they put the syringe driver on. But I used to do the top-up if he needed a top-up with the hyoscine.
Mrs Brown
Practical work
Patients and FCGs engaged in many aspects of practical medicines work, such as reordering, collecting and checking medications (Box 3), keeping track of their use and organising their storage (Figures 10–12). Given that there is little guidance or information on how best to manage medications in the home, patients and family caregivers often worked out their own ways to organise and store medications. Many described keeping these in different locations in the house to access them as needed. For example, most might be stored in a kitchen cupboard, with night-time medications kept by the bed and those needed throughout the day on a table by a lounge chair.
Mrs Crawford (FCG) explained not only the practical issues with monitoring, reordering and collection of medications, but also the sheer effort it takes to keep track of them all, in this case 10 (Table 6):
I find this quite onerous, to be honest, because I put them into daily . . . boxes, that you buy yourself. But, of course, because we’ve had such varying amounts and different drugs, nothing finishes at the same time. So, you’ve got to keep a constant tally of what you’ve got, so I tried to make up two boxes, so I’ve got a week in advance, and I know how short I’m going to be of medication. Then I have to make sure, see how many I have left over, because, by the time I’ve got a prescription down to the surgery, it takes them 2 days to actually get a doctor to write the prescription. Now we have this wretched system that’s been introduced, whereby it’s sent online, but some things aren’t sent online. If they’re controlled [drugs], you have to then go and get your prescription, so you don’t know what’s going to be sent to this pharmacy online and what’s you have to go and collect. So that can be a week, so you’ve got to think to yourself, it might be a week before I can get more medication, so you have to always be thinking, ‘What do I, what am I going to need?’. And I’ve got to get, obviously, I have to make sure that I have sufficient tablets, so, it’s not particularly a system. It’s just, I make them up weeks in advance so I know where I am with it.
Mrs Crawford, FCG, Int1
| Drug | Prescription |
|---|---|
| Hyoscine patch | Change every 72 hours |
| Liquid morphine | As needed |
| Lorazepam | Up to every 2 hours (maximum four tablets over 24 hours) |
| Mirtazapine | Orodispersible at night |
| Beclomethasone | Nasal spray |
| Rivaroxaban | Once per day |
| Ipratropium bromide | Inhaler |
| Propranolol | Once per day |
| Amantadine | Once per day |
| Clonazepam | At night |
FIGURE 10.
Storage: kitchen cupboard. Reproduced with permission from Eleanor Wilson (personal communication).

FIGURE 11.
Storage: portable box. Reproduced with permission from Glenys Caswell (personal communication).

FIGURE 12.
Storage: easy daytime access. Reproduced with permission from Eleanor Wilson (personal communication).

Some patients reported a dislike of having their medication visible and cited a lack of storage options as problematic. This was particularly an issue for larger items, such as boxes of continence pads, convenes, fortifying drinks, oxygen cylinders and PEG feeds. Medications could also add to already overcrowded living quarters when a hospital bed, hoist, specific chair or lift might be in situ in the home. Examples can been seen in Figures 13–17.
FIGURE 13.
Space limitations. Reproduced with permission from Glenys Caswell (personal communication).

FIGURE 14.
Specialist bed in the living room. Reproduced with permission from Eleanor Wilson (personal communication).

FIGURE 15.
Multiple sizes and types of medications. Reproduced with permission from Eleanor Wilson (personal communication).

FIGURE 16.
Storage alongside other household items. Reproduced with permission from Eleanor Wilson (personal communication).

FIGURE 17.
Bulky items, such as oxygen machines. Reproduced with permission from Eleanor Wilson (personal communication).

We had boxes of stuff and we had all the boxes and bags that the carers were using, all upstairs in the bedroom. Couldn’t get in the bedroom and then I had a wheelie commode up there in the bedroom. We had this all singing all dancing bed.
Mrs Bruce
When you’re in a drugs regime, it ties you down almost as much as this [oxygen] machine. I always have to eat first thing in the morning if I want to or not, simply because I’m taking the rivaroxaban . . . So it gets complicated. You have to think about it all the time.
Mr Campbell, Int1
Some participants kept detailed records of the dose and time that each medicine was taken every day. A few had been encouraged to undertake this by HCPs, but the majority who had undertaken some form of written log did so of their own accord (Box 4).
Did somebody at the hospice sit down with you and go through what it all was and what it was for?
No . . . No. Because it’s, because I started to ask about it, and she said, ‘Everything is down on paper. Everything you need to know, what time of day, what dosage, and what it’s for’. So, I was quite happy with that. Because, if she was to tell me, verbally, I’d more than likely forget half of it, but it’s all written down, so I just have to look, it’s not a problem.
Mr Cramer, FCG, Int1
The sheet below was devised by Mrs Blakemore (Figure 18). It shows eight different medications, along with supportive supplements, such as folic acid and calcium carbonate (Adcal, Kyowa Kirin Ltd), and monitoring of bowel movements. The chart shows that these elements could be tracked up to six times per day and included a log of the dosage given for pain medications.
So, when he was sort of taking this quite extensive list of medications, how was that, did he manage that himself or were you?
No. No. I did it.
OK. So how did you sort of work out what he needed when and all of those kind of things?
Oh, I drew up a drugs chart.
OK, so you would tick these off when they were given?
Yes, yeah, yeah. Filled them in at the time, whatever time it was. Like paracetamol, it had to be 4-hourly so, I would write in the time and . . . I did that sort of thing for whatever I was doing, because you can’t remember, you can’t remember, and I didn’t want to be writing out a list every day. So I thought, Well, that’s the easiest way to manage it . . . I’m very pragmatic.
FIGURE 18.
Mrs Blakemore’s chart. BO, bowel movement. Reproduced with permission from Eleanor Wilson (personal communication).

Monitoring medicine-taking and keeping track of stocks became more challenging for FCGs when they did not live with the patient, as in the case of adult children who were supporting a parent. In some cases, participants reported that it was a medication incident that compelled them to become more involved in supporting medicines management for their relative. Most of these caregivers used dosette boxes to manage medications and undertook the task of filling these each week and subsequently monitoring their use (Figure 19 shows an example of a dosette box).
FIGURE 19.
Self-fill dosette box. Reproduced with permission from Eleanor Wilson (personal communication).

Mum would usually look after her own medication. Initially she would deal with it by herself. But there came a point in time when there was so much medication she was taking clearly she was getting confused . . . And from that point on, I bought mum a pillbox and then we’d sort out her medication . . . And then I took over and started doing it so I knew what was what.
Mr Bhuta
Physical work
Medicines management sits within the wider physical work of care, including cleaning, food preparation, laundry, attending clinical consultations, supporting someone to wash and dress, and supporting someone with moving and handling tasks, such as getting upstairs or in and out of the car. Dropping tablets, shaking and being unable to pick up small pills were reported to be problematic. Mrs Bruce, an 80-year-old BFCG, described some of the challenges that she faced when supporting her husband’s mobility as his Parkinson’s disease progressed:
He’d dropped a tablet . . . he tried to get it himself, and he fell off the chair. Fortunately, he fell that way, so I was able to get my arms underneath his. Although he was thin, he was heavy, and I managed to lift him on to this chair . . . And that was difficult to move him, especially when he wanted to go to the loo . . . because eventually we did have commodes, but at first we didn’t, [I] managed to get him upstairs . . . I used to lift his feet, like that, on one stair, then the other. And then push him up with my head.
Mrs Bruce
Medicines can add to this workload when there are additional visits to collect prescriptions. This may involve travelling considerable distances or visiting different pharmacies on multiple occasions when specific items are not available or kept in stock:
So, I had to go to the doctor’s first, get the charts changed by them. And then, go into the chemist with the new prescription. And as soon as you went into the chemist for a new prescription, they’d go, ‘Well, we haven’t got that much morphine in, you’ll have to come back tomorrow’, or, ‘We’ll get it in for you later this afternoon’.
Mr Berger
Emotional work
The emotional work of medicines management can involve prompting, providing reassurance in terms of supporting reasons for medicines-taking and being vigilant about when medication is required and the potential side effects. Box 5 provides a FCG focus. This is embedded in the emotional work of managing loss, personality changes and the patient’s reduced abilities and capacity. In addition, there is a strong sense of responsibility and anxiety about administering medications correctly and not causing harm. Family caregivers reported finding medicines work stressful and, at times, frightening:
It was hard and stressful. It was like the enoxaparin, he was on 7 mls but the things are 8 mls, that you get, so I think, ‘Hang on a minute, he’s on 0.7. This says 0.8’. So, it’s Monday morning, I’m thinking, ‘What do I do here?’ . . . I’ve got squirt a bit out, obviously. I don’t know how much to squirt out, and that was quite traumatic for me, that day. I’m thinking, ‘Is it dangerous?’ ‘Could I be giving him too much or too little?’ ‘Is he going to collapse now because I’ve given him 0.7 and a bit, rather than nought point?’.
Mrs Baker
Mrs Baker’s partner was diagnosed with a very rare form of soft tissue sarcoma. He was told that his condition was palliative from diagnosis. The couple were given very little information, and the rarity of Mr Baker’s cancer made it difficult to find any information for themselves. Mr Baker had started with paracetamol to relieve the pain in his leg, but was reluctant to take it or anything stronger, leaving Mrs Baker to take on the emotional work of prompting him to take his medication:
It was hard to get [him] to take them because from a man who never took anything . . . so I, it was my [job] – I prompted him throughout the day . . . I kind of turned into a bit of a carer quite quickly.
About 9 months after his diagnosis, Mr Baker’s pain had increased and the introduction of a SPCN resulted in a significant change in his medication regimen; he was prescribed a number of different pain medications. Mrs Baker expressed concern and fear in managing these new medications and conveyed the strain that this placed on her to acquire knowledge about administering these medications:
I was terrified because I’d never done anything like this before, I was terrified of overdosing [him], because I knew nothing about nothing . . . I read all the bottles and I was very sort of, as good as I could be so there was not much explaining, at that point . . . you’re not instructed how to give it and everything. It’s just, you get it and you look at the leaflet and the instructions on the box and hope that’s how it goes.
Mr Baker continued to struggle with pain and underwent a course of palliative radiotherapy. He was also prescribed steroids for the swelling in his leg, which caused severe side effects. Mrs Baker reported his behaviour becoming extremely out of character. He barely slept, became disagreeable and argumentative, and expressed strange ideas. After a number of telephone calls and requests for help, the consultant from the hospital instructed Mrs Baker to take him off the steroids. From this time onwards, Mrs Baker felt that she had to constantly battle with HCPs to make sure he was not prescribed steroids again. This meant that she had to undertake administration and information work, alongside the emotionally taxing work of having to liaise, inform and, potentially, dispute with multiple HCPs:
And every time he was admitted to the hospital . . . at 12 at night, 2 in the morning, or whatever . . . I had to be with him, ‘What, what medication are you on?’. Because I always had a sheet in my bag or, because I knew what they had on the computer wasn’t what [he] was on at that point. It was always different. And every time, ‘We’re going to put him on steroids’. ‘No. No, please don’t put him on steroids’ . . . [the adverse reaction was noted in his notes] . . . but they always prescribed them, and they just seemed to ignore it . . . I had to hammer that point home. To every doctor . . . So, every time I’d go through this with everybody – every doctor, nurse . . .
As his illness progressed, her husband’s medication needs became more complex and Mrs Baker expressed feeling quite isolated, not only managing his care by herself but not knowing who to contact for support when needed. This lack of knowledge is expressed as stressful and emotionally draining:
I did feel very, I did feel a bit lonely and concerned . . . and I did all of [his] care myself, and it was just me, I did everything . . . I’d got all his medications, and his needs are very complex at this time . . . He got a sore on his anklebone, and that’s when they [DNs] started coming every couple of days . . . which I found reassuring. Just somebody coming round. Because I was a bit paranoid: ‘Am I looking after him properly, am I giving his meds?’. You really are, the responsibility is enormous.
Managing someone else’s medications was felt as a considerable responsibility, and FCGs were keen to do it to the best of their abilities. They were often also advocates for the patient and needed to draw on emotional resources to be assertive, insistent and sometimes prepared to argue with HCPs to make sure that the patient received the medications needed:
So, then we went to the hospital pharmacy to pick it up, and they didn’t stock it. So, we had a prescription but no supply. So, at that point I then rang the GP pharmacy . . . I remember having to be extraordinarily assertive to say ‘No you can do this, you must do this, she is in pain, you can’t leave a cancer patient who’s on regular painkillers in pain’ . . . And it sounds simple, a very low dose of co-codamol . . . she could have spent the whole weekend in pain without painkillers.
Mrs Best
In taking on such considerable responsibilities, FCGs are also open to the emotional consequences of making a mistake that could have an impact on their loved one’s health as well as the emotional work involved in having to persuade the patient to take their medication when they were reluctant to do so. In some instances, patients felt that the medication was not helping them in any way, whereas others did not like the taste or struggled to swallow the drug. In other cases, their illness caused confusion and resistant behaviour. This role as a persuader could be an added emotional burden, jarring with the FCGs’ perceptions of caring, and could cause conflict in relationships in the family:
It is her father who gets the meds out of the pack and adds any additional items . . . and encourages his wife to take them. [Mrs Creasy] has told him that is all he can do – if her mother will not take the tablets he can’t make her . . . [she] describes the relationship between her parents as increasingly strained – sometimes they don’t speak for weeks. She feels very bad about the firm stand she tries to take with her mother – but says that she has to support her father [as he is] the main carer for her mother.
Mrs Creasy, FCG, interview notes
Knowledge and emotional work were closely linked because it was often lack of knowledge and/or limited access to information that caused concern, distress and fear.
Knowledge work
Knowledge work must be undertaken to establish information and understanding about what each medication is for, when and how much to take, and what kind of adverse effects to be aware of. Patients and FCGs also needed to have knowledge about identifying who to call for assistance and in what circumstances:
But it was also the knowing what your maximums were . . . knowing I wasn’t going to poison him, because it’s at what level am I going to kill him basically? That was the scary part. You know, when am I physically overdosing him?
Mrs Bailey
Control and knowledge of medicines management varied across the case and BFCG data. Sometimes the patient retained full or partial control of their medications while delegating some tasks. Other cases involved a collaborative effort, and in others FCGs assumed all responsibility. The complexity of some regimens required FCGs to learn new skills, such as giving injections (e.g. Mrs Connor) or dialysis (e.g. Mrs Brown). FCGs needed to have a good working knowledge of what each medication was for and when to give it. Even when efforts had been made to simplify this through pharmacy-prepared blister packs or dosette boxes, as patients deteriorated these systems were often no longer suitable. Mrs Crump describes how she deals with two sets of blister packs and three additional medications, one of which was to be given three times per week and another given at different times:
We have blister packs from [pharmacy] for the medication provided by the GP. And then I have another blister pack which is delivered for medications provided by the renal clinic. And there is also a particular medication . . . I have to incorporate that into the rest . . . And then, they’ve just added another separate one . . . he has that three times a week, and I have to pop that into the mix. And he also has warfarin which again, because it’s variable, I just have them in the packets, and I have to put them into the packs.
Mrs Crump, FCG, Int1
Although pharmacy-prepared blister packs were reportedly beneficial for some patients and FCGs, others found that the pace of change could quickly make them redundant.
Most patients and families reported being given at least some information about their medications. However, even when this was reinforced and checked, verbal information alone was considered to be insufficient. Mr Butcher had recently cared for both his mother with Alzheimer’s disease and his wife who had died of cancer. He explained that he was given information and why he was unable to process it:
Yes, it was processing it. And, the problem is that, when you’re dealing with your stress, you are really running on adrenalin constantly. So, you’re not thinking completely clearly. You’re adrenalin based, and your stress levels are high, and your sleep hours are low. Because you’re constantly, when you’re sleeping, you’re waiting for her to shout or be sick or something like that, so you are at the absolute top point of your stress levels. So yes, you’re given the information, but, sometimes, I had to think, ‘Now, what did she say?’.
Mr Butcher
Despite often feeling that they did not understand the complexities of many medications, some FCGs displayed detailed knowledge of the medications and kept excellent track of what had been given and when, so that HCPs could work from this information. Some patients were not able or willing to take an active role in managing medicines. Others remained involved in decision-making, at least for as long as they could, requesting certain drugs and deciding what to taken, as in Mr Butcher’s account of close collaborative working between himself, his wife and different HCPs providing care (Box 6). Another key element of Mr Butcher’s narrative is an insightful recognition of the difference between pain and agitation. He also describes the types of support that he and his wife received and the ways in which they accessed and utilised input from SPC nurses, DNs and their GP.
And the nurses were working very carefully with me on what I’d given, as against, what they were about to give, and we kept very close records. If I’d given her a sort of full lorazepam, they would not give a full dose of midazolam . . . If I called them and sort of said, ‘We need something here’, they would say, ‘OK, what’s happened now?’. I said, ‘Well, I gave her at 2 o’clock a lorazepam or, about two or three strange named ones, [laughs]’ and they would say, ‘Well, we can’t give the midazolam now, but what we can do, we can give her morphine’. And, and they, we balanced it very carefully between us . . . [with the patient’s input] . . . She was, even though, in late stages, she would say, ‘I would like a lorazepam’ and would say, ‘Well, are we going to go for a half or a full?’. And she was quite conscious of, look, ‘I’ll just go for a half’. And then if it isn’t working, we can either put another half in, or we can go and call a district nurse and get something a little bit stronger. We just worked through on a, on a level of, sort of, orange, red, and crimson. [laughs] Whether it was pain or just pure distress and anxiety. The anxiety was probably, more so than the pain was sometimes. You know, so long as you know what’s going on . . . And we, again, we used to make decisions ourselves, and then sometimes, I would actually say ‘Well, OK, well, let’s just give the nurses a call’, or ‘let’s just give the GP surgery a call’. And get a call back and say, ‘Look, this is the situation, we’re thinking about doing this, what would you say? Would you think we should get someone for midazolam or something else?’, or, and, you know, they would then sort of say, ‘Yeah, let’s go with, let’s try this one, but if [wife]’s no different, do please call back’. So, there was a lot of support and guidance a helluva a lot.
Managing pain
The challenges involved in effectively managing pain were raised by patients, their FCGs and the HCPs across all data sets. Sometimes unwanted side effects, such as nausea or drowsiness, could be an important issue:
So, we didn’t really have problems until, real problems, until the end, really. The last couple of weeks at home, were probably the worst at persuading him to take things and him refusing to take things . . . Oramorph was, just persuading him to take it really, because he knew that it could make him drowsy, and he wanted to be in complete control, all the time.
Mrs Becker
Some patients were considered sensitive to certain medications, resulting in particularly disturbing side effects, such as altered personality and behaviour and generally feeling out of control or disorientated:
You know, when they get on to morphine, quite a bit, they completely change . . . Mentally, they change . . . Everything. Everything. Everything. It seems to change them, they’re not the person you know. And, he lost patience, with everything you were doing, you were just a damned nuisance to him. You know what I mean? I knew it was the morphine because we could see [it] in, gradually increased the dose.
Mrs Brooks
Experimentation with different drugs, different doses and different routes of administration could be tried to balance pain management and side effects:
She’s on pregabalin, which she takes different doses different times of the day . . . And we jiggled around with those, because they tried her with, because she was in pain, 100 in the morning, but then, she was just asleep so they’ve jiggled it and worked it through, and they’ve got that on her.
Mr Carter, FCG, Int1
Health-care practitioners acknowledged the prescribing challenges that they faced when adverse reactions to standard drugs significantly limited their options for supporting pain control for their patients. Cases in which it proved impossible to achieve adequate pain control were described by HCPs and FCGs:
. . . It’s been a bit complex really . . . because he’s not tolerated a lot of opioids. As they’ve increased in dose he’s become quite symptomatic of side effects, confusion mainly . . . He has got complex needs, because whatever we’ve increased it to has helped a bit, but it’s never got rid of the pain. And I don’t know whether we’ll ever get on top of [his] pain. And we’re running out of pharmacology to do that.
Mr Cole’s HCP2, Int1
So, when they put up the syringe driver, was that simply because of the amount of drugs she was needing to have?
Yes. They were hoping to control the pain. It never happened. They never, because . . . every time they upped it, it needed going up again, they were always two steps behind the actual pain threshold so the illness just, that’s the rapid rate it was going at, so.
The consequences of pain control had great significance for the emotional and practical burden of care; for example, when the prescribing decision was made to introduce patches as an alternative delivery mechanism for pain medication or when swallowing tablets became problematic:
She had quite a lot of nausea from morphine, a certain type of morphine, and they changed it to a patch, and that, the nausea went away with the patch, so it was a big help. And, the constipation-type side effects of the morphine as well were massively reduced with a patch. So, there was definitely a lot of, you know, shunting things around to try and get to the best possible set of drugs that would help.
Mrs Booth
The management of medications for pain relief caused considerable anxiety for FCGs. Many reported taking meticulous care in their monitoring, recording and use of pain medications. They felt great responsibility for getting the management of pain right. This led to concerns about wanting to relieve the symptoms, but not to ‘overdose’ the patient. FCGs could feel intimidated by their responsibility for administering powerful medications and the limitations of their knowledge about their use and side effects:
I wasn’t quite sure about these Oxy [Oxycodone hydrochloride] [. . .] this short, Shortec®, Longtec®, because the hospitals are always that busy that they don’t give you a lot of information . . . I just was constantly worried that I’d overdose him with the [laughs] with the Oxy, you know, with the Longtec and the . . . but I never did. Well, I don’t know, I may have done.
Mrs Bristow
Prescribed pain relief, particularly opioids, could have complex meanings and significance. For some participants, however, being prescribed these drugs was a powerful indicator of the severity of their illness:
. . . we had paracetamols and they were effective . . . [but then the pain got worse] . . . Oh, you can try this, and he brought the bottle [of Oramorph] home . . . And he didn’t really touch it. Just sat there for a long time . . . he was putting it off going down that route. I know, latterly, he always did avoid it, because I, it was like acknowledging, you know, what was happening to him, maybe, a bit.
Mrs Baker
The management of pain at home forced families to engage with all of the elements of medicines work. FCGs, in particular, took on considerable responsibility in supporting someone to manage their pain. They were often tasked with keeping track of the type, frequency and dosage of pain medication administered and in providing emotional support. All participants wanted to help in this way, but some were anxious about the limitations of their knowledge about how to manage controlled drugs safely and effectively, make judgements about when and how much to give, and who and when to contact for advice and support. Opiates and morphine, in particular, held negative connotations for patients, often signalling disease progression and ‘things getting worse’.
Specialist palliative care
Specialist palliative care was often introduced when generalists required additional support to manage pain. Contact with SPC through outpatient appointments and hospice inpatient stays meant that patients, such as Mrs Clarke and Mrs Cramer, had tailored packages of care in place at home, including medications and syringe drivers to manage their pain:
It [syringe driver] definitely helped the pain. She slept a lot better when they put that in, because she wasn’t having to, there wasn’t that cycle of take a tablet, or take some morphine, feel a bit better, and then the pain’s set in again, so you have to wake up and start it all again, overnight, because the syringe driver was in, she just was much more settled.
Mrs Booth
Mr Bryman reports how the introduction of the hospital SPC team resulted in positive adjustments to his mother’s care:
They pretty quickly switched her from oral medication to a syringe driver . . . So, I think it was, watching them in action, watching them discuss things with her and sort things out, I think they were quite impressive. And so, she was having a laugh and a joke with them about things. But we could see in that last period, that last 24 hours when her pain was better controlled and her breathlessness was better managed. I think they were the best 24 hours in the 6 weeks.
Mr Bryman
As these extracts illustrate, referral to SPC, which occurred close to the patient’s death, could bring about a reprieve for the family and enable the experience of a (relatively) ‘good death’ at home. However, it was clear from participants’ accounts throughout the study that families often experienced a period of weeks, or even months, of very difficult and distressing emotional and practical ‘work’ in managing the patient’s care, especially where deteriorating symptoms were not adequately controlled. The nature and intensity of the burden of care during this period are rarely acknowledged in conventional discourses about dying at home as a prerequisite for a ‘good death’.
Conclusion
This chapter has explored aspects of the extensive ‘work’ with which patients and FCGs engage in managing medicines at home. ‘Focus boxes’ have been included to provide detailed context and illuminate key areas. Participants varied in the extent to which they felt supported by professional services. Instances of collaborative working between patients, their FCGs and the HCPs were described. More often, however, patients and FCGs described the effort and anxiety involved in taking on responsibility for managing complex medication regimens and making judgements about administration dosage, when the limits to their coping strategies had been reached and when they needed to call for additional help and support. Professional awareness of the nature and extent of the practical, physical, emotional and knowledge-based work being undertaken by patients and FCGs was not common. Control of pain was a frequent concern and not always achieved.
Chapter 7 Findings: system and complexity
Introduction
The previous chapter has considered the different kinds of work of managing medicines and the considerable effort involved for both patients and their FCGs (Box 7). Despite the very great demands imposed by the patient’s illness, most lay participants were positive about professional services and care. Complex judgements were based on mixed and diverse experiences of care. Some BFCG participants expressed praise and appreciation for professionals, even when the patient’s illness and death had been very difficult and distressing. They were also prepared to make allowances for a system that they recognised to be overstretched, with staff trying to do their best. Nevertheless, most participants described occasions when they felt inadequately supported and, in some cases, when their difficulties were prolonged. A strong theme throughout the data was frustration with a complex system that was experienced as fragmented and poorly integrated. Even those who felt that they had established good and supportive relationships with key services and personnel reported that their knowledge of the system and how to work it had been built up over time, and that they had, effectively, been ‘left to figure things out’.
So it’s made me more conscious of, as the regime of tablets starts to get more and more complicated, so the network of people around that patient needs to be broadened so that the responsibility for that can’t rest with – I don’t think we can leave it to a patient to manage a complicated medication regime without there being support in place. And some people will be absolutely fine, but I think what it taught me is if people just tip over the edge a little bit, how quickly things can go wrong. How easy it is for a simple regime, well, within the space of a couple of weeks how easy it is for a simple regime that you’re managing with to somehow become a very complex regime that at your best you could probably just about manage, but add in a little bit of confusion and it just goes out of the window.
Mr Bryman
As described in Chapter 6, many participants reported developing considerable expertise in evolving their own systems and detailed procedures for organising, accessing, administering and recording medicines into relatively stable routines. However, these networks of care were dynamic systems and vulnerable to change. This applied especially during the later stages of the patient’s illness when deterioration could be rapid and frequent changes were made to the nature and dose of medicines prescribed. A particularly distressing consequence of this stage of the illness was the difficulty in accessing help, particularly in a crisis. In this chapter, we present issues relating to participants’ experience within a complex system of care and how this constrains or enables their capacity to manage medicines and effectively access professional support.
Networks of care
In the Managing Medicines study, we were interested to explore how the work of medicines management was distributed across patients’ informal and professional networks and if it was possible to determine structural features that had a bearing on the support available to patients. Cases differed in terms of the specific disease and comorbidities and the stage or severity experienced by the patient at the point that they engaged with the study. These factors had a major bearing on the input of services and the family’s experience of care, and make it difficult to establish patterns within the small number of patient cases included in the study. Nevertheless, we have found the construction of the ecograms in Appendix 1 to be a useful way of informing and visualising our analysis of the dynamics of each case, viewed from the perspective of the researchers and constructed from all data generated with the study.
Networks were made up of informal and professional links (i.e. individuals and services) and included electronic systems of prescribing, sharing records and accessing information in the media and internet. Networks ranged in size from 9 to 32 links (mean 22 links; median 20 links) (see Chapter 4). Most ecograms included a small number of informal links and usually contained one or two key individuals (lay and/or professional) who were involved in supporting medicines management. Most patients had retained control over the process of ordering, organising and taking medicines for as long as they could, perhaps with practical tasks, such as collecting medicines from the pharmacy or storing these in different parts of the house, delegated to FCGs. As their health deteriorated, however, patients gradually relinquished responsibility for all aspects of medicines management, even to the point of requiring physical assistance with administration (e.g. swallowing liquid medicines from a syringe). With little formal training or support, key FCGs tended to assume and maintain responsibility for most of the work. This work was not widely distributed across the patient’s network. However, informal links, within and outside the family, were valued for other kinds of practical and emotional support:
Family were at the top of the tree though, because we had four children . . . grown up, and they were there constantly, on the phone, visiting every weekend, taking it in turns, setting a rota up, and they were there all the way, and they were grieving, they still are.
Mr Butcher
Mrs Best describes a striking case of the extent to which a local community rallied to the support of a dying neighbour who lived alone and without nearby kin. For several months, a network of neighbours had taken on the care of this woman who was dying of cancer. This involved providing practical care, including extensive engagement with the tasks of medicines management, liaising with services and HCPs, accompanying the woman to many hospital appointments, organising a rota to provide company and division of tasks, and, eventually, keeping an extended vigil at her bedside in the days prior to her death.
In the course of managing the patient’s medicines, FCGs undertook a great deal of work liaising with different parts of the system, including a wide range of HCPs and services. There is great contrast in the range and complexity of professional links within the ecograms. The degree of complexity could fluctuate over time and there was not a unilateral tendency for this to increase. For example, participants described complex interactions with different services and personnel during the sometimes protracted period of obtaining a diagnosis and then a reduction during the more stable process of treatment. Discharge from active specialist treatment was a significant transition for some patients, mainly those affected by cancer, and could be followed by a reduction in active professional links. However, as they approached the end of life, patients were often subject to a cascade of care, which FCGs described as burdensome if not overwhelming.
Networks were dynamic and potentially vulnerable. Families took time to build stability in the connecting links, but these could be jeopardised quickly by changes in the system of professional or informal care. Some patients were dependent on the support of relatives, often elderly spouses, who were themselves in poor health. Several FCGs reported putting off treatment that required hospitalisation for themselves because they felt that they could not leave their relative alone at home.
Feeling supported by the system
Participants varied widely in the extent to which they felt supported by the system. This was often experienced as fragmented and bureaucratic. The quality of relationships established with individual professionals was often key to confidence in managing the patient’s care, a large part of which was bound up with medication. What we term key professionals could be drawn from any service (e.g. GP, consultant, DN, CN or SPCN) and appeared to result from the serendipitous development of good relationships rather than from a designated role. Indeed, several respondents referred to having been allocated a ‘key worker’ with whom they had failed to establish any engagement or rapport, and in one case had never seen. Key professionals were identified as the ‘go to’ people whenever difficulties arose and took a proactive role in fixing a wide range of issues, often related to symptom management and medicines use:
It would have been either [SPCN] or the doctor’s surgery . . . But, definitely in the first instance, [SPCN]. You know, because she was always available on the phone so yeah.
Mrs Bristow
Ease of access and rapid response were critical to the sense of security that participants derived from these relationships. This could become of great significance during the period before the patient’s death, during an experience of great emotional distress and vulnerability throughout which FCGs had to deal with rapid changes in prescribing, treatment and professional service input. It is worth noting that the availability of a key professional was not necessarily sufficient for participants to report feeling supported by the system overall, but it was certainly a powerful buffer against the difficulties and frustrations with which they had to contend. Some participants described having good relationships with two or three particular individuals or services, which, again, were a source of confidence in navigating a complex system. However, patients and FCGs who had not been able to establish any close or supportive relationships within this described a much more difficult and frustrating experience of care (e.g. Mrs Creasy).
It was also clear that the quality of relations and communication between professionals could have a critical impact on families’ experience. Hospices sometimes provided a nexus of care in which patients might attend outpatient consultations, attend day care services and receive home visits from specialist nursing staff. The availability of a 24-hour hospice-based advice line was also highly valued by the few participants who knew about it or had access to it. The existence of an efficient relationship between the GP and the pharmacist was an important determinant of family experience of accessing medicines. Pharmacies co-located with a general practice were considered very convenient and tended (although not always) to be associated with a positive experience of co-ordinated care. Mrs Blakemore described having a good relationship with her CP and considered them her first port of call for medication-related issues. She found that the pharmacist was more easily accessible than her GP, especially as she could walk to the pharmacy and speak to someone who was able to spend time explaining medications and their side effects. This reassurance boosted Mrs Blakemore’s confidence in dealing with her husband’s medication at home:
Couple of times, there was major problems with prescriptions, you know, where they’d been changed and the, they’re weren’t updating the records, and everything, I would just go and have a word with [the pharmacist] and she’d say ‘Oh, leave it, I’ll sort it out for you’. She was really, really good.
Mrs Blakemore
More generally, however, pharmacists were considered by lay and professional participants to be primarily suppliers of medicines, with little wider involvement in providing advice about medicines use or prescribing. When processes of prescribing and dispensing worked well, care was experienced as seamless and largely invisible, especially when medicines were delivered directly to the patient’s door. One or two participants described personal contact with a pharmacist and a sense of being known when they visited the pharmacy:
So, you got, big bag. So, he, the pharmacist knew what was needed. And if there was a change, the GP would let the pharmacist know. And the pharmacist would alter what he was sending . . . himself, so we’d just get it, we didn’t have to do anything about that.
Mrs Bishop
One area in which the lack of a joined-up system was experienced concerned delays in interprofessional communication about prescribing changes, particularly the transfer of information from hospital and outpatient services to GPs. The transition from home to hospital was particularly associated with delays in updating records, which were reported sometimes to be ≥ 2 weeks. Mrs Bristow described how she had taken the initiative in circumventing this blockage by taking her husband’s copy of the hospital discharge letter directly to the general practice to make the information immediately available and enable the GP to amend the prescription. Even when participants described having a good relationship with an individual GP, the difficulty in getting direct access, by telephone or by appointment, and the unresponsiveness of practice staff caused great frustration.
Establishing a personal relationship with a GP was difficult for some patients because of the lack of continuity of care. In some cases, the patient’s referral to specialist treatment seemed to marginalise the GP’s input, as the family then looked to hospital consultants and their teams as the key figures in managing treatment. Especially when the relationship between the GP and the patient had not been close, there was a risk that it would be difficult for this to be re-established subsequently, following the patient’s discharge back to community care. Several participants commented that they experienced long delays in seeing the GP of their choice and usually saw different doctors with whom they had no relationship. Most importantly, unfamiliar professionals, in any role, were recognised to have no knowledge of the patient or the details of the case. The feeling of ‘being known’ was important. Study participants expressed a range of views about their GPs. Taking a personal interest and, particularly, being willing to undertake home visits to dying patients were much appreciated. The following account is unusual, but also illustrates what is possible:
Our doctor’s surgery, everybody at the surgery, and the office staff knew me. And I could just phone up and they would put it straight through to our GP, one of my doctors, and he’d come straight out, he was brilliant, absolutely brilliant.
Mrs Brooks
Good relationships with individual HCPs, especially key professionals, were intrinsically vulnerable to change, for example if individual staff moved to different roles and services, if individual staff went on leave or if changes were made to the services to which the patient was referred. Mrs Brown described having a key professional relationship with a community matron that ended when this role was abolished, and she did not establish such good relations with the SPCN who succeeded her and whose working hours and accessibility were more restricted. Subsequently, Mrs Brown did not feel confident or well supported by the system beyond good relationships with the three HCWs who provided a daily package of intensive personal care for her husband but did not provide a point of access or liaison with other HCPs or services. She reported difficulty accessing help OOH, specifically about medication issues. When her husband was dying, Mrs Brett wanted him to remain in the hospice to which he had been admitted so that medication to control his pain could be sorted out. However, she felt that the hospice put pressure on her to move her husband to a nursing home. Eventually, Mrs Brett decided to take him home, where she had a difficult experience of his death. She felt that there had been no consultation with her or her husband or consideration of the best place of death for him. Rather, she felt that this had been determined by the system on grounds of cost. Therefore, patients and FCGs have little leverage on the system. Even during the experience of dying, there was a sense of the system making disposals and arrangements without consultation or consideration of family circumstances and preferences.
Some key professionals were valued, even if they were not always accessible (e.g. during office hours only or because they worked part time). In this case, the ability to contact a wider team or a 24-hour service, such as the hospice or SPA helplines, could be invaluable. However, these were mentioned by a minority of participants. Several of those who were aware of extended services reported that they had found out by chance and at a relatively late stage in the patient’s illness. Mrs Connor, for example, was alerted to the existence of the SPA through a chance encounter with a friend.
Although participants valued good and long-term relationships with individual professionals and wider service teams, it was not always the case that frequent contact resulted in positive or productive experiences. As in Mrs Creasy’s case, negative relationships could simply be perpetuated with mutual frustration all round:
But the problem is I actually have to go. If I ring, I get nowhere. So, when I deal with something over the phone with them it takes 2 weeks to sort. So, I have to go down [to GP surgery], I have to ask for J. Usually, I have to make a special trip and go down and try and sort it [prescription] out. I have got to the stage where I’d just stand outside [the GP’s] door and wait until he’s done, because it was getting that bad. But we haven’t seen [that GP] in a while. We just can’t get in to see him.
Mrs Creasy
Communication
Complexity, especially when care involved many professionals from different services, was confusing to professionals, as well as patients and FCGs. It increased the risk of poor communication between all members of the care network, as well as inconsistency between the professional opinions and the advice received by families:
So sometimes, it’s around communication. So sometimes, the patients and relatives, they find it, you know, one person will advise them something, another health-care professional might tell them something else, and then they see a third one, so there’s that lack of continuity sometimes they find difficult. Particularly if they’re being told different things by different people. I suppose, that can happen if they’re under multiple different specialities. That can be quite challenging. So sometimes, it’s better to be under one key kind of key point of contact, particularly in the late stages.
CNS, HCP19
And I got more information from the pain specialist nurse at the hospital, who explained to me about the excretion of the opiates. And which were best for [patient]. She did actually have a discussion with my GP and they did have a debate at one point. But I felt like I was better informed from her than the palliative care nurse and the GP and the district nursing team. And then, the renal nurse, I used to phone her and say ‘They’ve prescribed such and such’, and then she [said], ‘Oh no, oh no, no, we can’t have that, they need to liaise with [the consultant]’. So, then I used to have to ring them back.’ You need to liaise with the hospital, we need to get this sorted out’. And I always felt like I was the driver of it.
Mrs Brown
Professionals (especially nurses) described discussing medicines with patients and FCGs following prescribing, and sometimes expressed awareness of the demands involved for families in managing medicines. Some also described taking on the task of reviewing medicines currently prescribed, often following referral or first contact with the patient. However, there was little apparent monitoring or supervision of what patients actually did with the medicines prescribed. It was noted that patients often did not raise queries because they did not know what questions to ask, who to ask or that they even have something to ask about. HCPs, often nurses, who visited patients at home had the advantage of being able to observe the settings in which patients were receiving care. Some noted incidents when their explanations had been insufficient for the patient or FCG to fully understand and, therefore, a different approach might be required:
So, there’s a lady that I wanted to increase her Parkinson’s tablets . . . And so I wrote it all out for her, and I said ‘Right so on Thursday you’re going to do this’ . . . And I had a phone call, she phoned my secretary about 2 hours later and just went ‘I don’t get it’. And I’m like, ‘Oh no, I thought I’d written it down really clear’. She’s like, ‘So, what am I doing on Friday and Saturday?’. I’m like, ‘Well, you stick with whatever’s happened before’ . . . So I think that was a learning point for me that actually . . . I assumed that she’d followed my logic, and she very clearly didn’t.
Consultant, HCP27
Although the communication in this case had not been effective, it was unusual as an example of a professional offering personally written, tailored information for the patient. Most professional accounts of providing information focused on direct discussion and the time that was invested in this, as if duration was the significant factor rather than effectiveness. Despite being effective, even the time required to provide individually written guidance was clearly a disincentive:
. . . And you said you’d typed it all out for her [patient] so that she knew what to take when? And does she use that, does she use it?
Yeah, it seems to have enabled her not to worry about stuff. I don’t know if I’d type it out again if we changed the doses of things or timings of things . . .
I was thinking it’s quite time consuming to type it out, isn’t it, really? . . . I can’t really see myself doing this, because of such a time . . .
Well, it took a long time, it took, because she’s . . .
Because she’s on multiple medications, it’s not just one medication and you just type it quickly out.
The nature and function of small-world networks seemed to be a key determinant of the quality of experience of communication and care by patients and their families, rather than organisational properties of the system. However, the efficiency of transfer of information between staff and services was also crucial. Several bottlenecks were described, including delays in specialist clinicians communicating with GPs, a lack of integration between systems of electronic records [e.g. EMIS Web (EMIS Health, Leeds, UK) and SystmOne (The Phoenix Partnership, Leeds, UK)] used by different parts of the system and a lack of information available to OOH clinicians and CPs:
It would be really helpful on a discharge summary if they said, you know, someone is managing the medications. Because you get this discharge summary of quite ill patients, maybe never met, your colleague’s on holiday. There’s 10 new drugs which are quite dangerous. You don’t know is someone managing those, do I need to arrange a dosette? All of a sudden, you know, in the afternoon, there’s no information about who’s managing this.
GP, HCP26
Alongside the systems that families worked out for themselves, some HCPs described taking the initiative to implement simple strategies and aids that would help patients and FCGs to manage medicines more easily. The emphasis here is on simple, and virtually cost-free, measures, such as providing laminated sheets or simple charts with information about drug, dose and frequency, or writing directly instructions directly on the boxes:
I feel like maybe people need, I don’t know whether they’d read it, but need information or flash cards or something, about each medication. So, obviously, if you’re getting the medication in a box, and you’ve got that leaflet, it is huge, isn’t it? Whereas I’ll often, on boxes, write for people, ‘This is for’, and will write, big, ‘Muscle cramping’. You know.
CNS, HCP06
Provision of such simple, tailored information would take less time than lengthy discussion, which, as indicated above, may not result in mutual understanding. Although by no means a substitute for direct communication about medicines, this is a task that could be undertaken by the pharmacist when dispensing medicines. Within the study, however, there is only a single reference to a pharmacist engaging in this kind of initiative. Mrs Baker described a hospital nurse printing off an information leaflet from the internet, but only after she had specifically requested information about her husband’s medicine and how to use it. However, there were no other references to professionals using the internet or signposting patients and FCGs to this as resource for information about their illness or prescribed medication.
Language, culture and translation
The provision of effective and tailored care to patients from diverse social and cultural backgrounds is a test of capacity and quality of systems of care. The study included two BFCGs and one patient case from an Asian background. None of the three patients involved spoke fluent English. In addition, HCPs spoke about working with patients and carers from ethnic minority backgrounds. They tended to focus on issues around language and how this can act as a barrier to care. Although available, translation services were not often used in practice, and reliance on a relative to translate was the more common option in such circumstances:
I’ve never had to use LanguageLine Solutions for those discussions in general practice, to be fair, the end-of-life discussions. In reality, it’s usually through a relative.
GP, HCP11
The potential impact of language difficulties is not confined to consultations that take place between patients and HCPs. The labels on medicines and the instruction leaflets, re-order slips for requesting prescriptions from the GP and instructions about how to use re-ordering services from both general practices and pharmacies are in English, which can be problematic for any patients with limited literacy and, especially, for older patients from ethnic minority communities who do not read English:
The person could speak really good English, but they had very poor, it was actually the writing of it, and most surgeries, they request that you put something [controlled drugs] in writing to the surgery.
SPCN, HCP14
The fact that Mrs Choudhury, Mr Bhutan and Mr Bhatt’s mothers could speak little English did not appear to be a significant issue. The general practices that the families used were staffed by Gujarati-speaking doctors, who were their key professional contacts. FCGs mediated contacts with other services. Mrs Chowdhury was frail and elderly and the GP made house calls to see her. Her medicines came from the pharmacy in dosette boxes and were administered and monitored by her daughter-in-law. Mrs Choudhury relied on a few key individuals within a small but effective informal and local professional network. Her FCGs were able to advocate for her regarding issues arising, for example in obtaining agreement for the DNs, rather than family members, to administer her daily insulin injections. Mr Bhuta described a very different experience in relation to his mother’s interaction with secondary care services. The family had supported her decision to refuse dialysis; however, during a hospital admission, Mr Bhuta reported the following:
I asked could I speak to them to see what had been discussed. And he [doctor] came back to me and he said, ‘Oh yeah, I’ve managed to persuade your mum to have dialysis’. And I said,’ There’s actually no way on earth mum has agreed to that’. And he goes, ‘Yeah. I had an interpreter here and she explained everything to mum and she wants to have dialysis’. And I said, ‘I’m sorry. I just don’t buy it’. And it’s very easy for mum to misunderstand things even if there’s an interpreter there. Very easy, I know, she’s my mum.
Mr Bhuta
Language issues clearly compound the difficulties of establishing the nature of patient preference and the problems of translation. However, this case also illustrates the way that such preferences may be subject to framing by family members as well as HCPs, regardless of ethnic and cultural background. This is not to say, in this case, that Mr Bhuta was not representing his mother’s position as she would have wished. However, her voice is effectively absent from the discussion.
Problems with prescribing and accessing medicines
A minority of patients and FCGs described an experience of GPs and pharmacists having systems in place to make prescribing and accessing medications a smooth process. This seemed to involve a good understanding of palliative care and shows what can be achieved when the system manages to produce joined-up care:
They [pharmacy] was absolutely brilliant. And even some of the problems with some of the medications, when they were prescribed, they would go and sort it out with the GP’s practice without me having to get involved.
Mrs Brown
However, difficulties in accessing help and advice from their GP, and delay and confusion over prescriptions, often attributed to ineffective communication between GPs and pharmacists, was widely reported as a source of considerable frustration. Even when they expressed overall satisfaction with care, all lay participants described at least one problematic incident that caused substantial difficulty and distress:
So, it was kind of a backwards and forwards. And eventually I managed to get it sorted and I said to both the sides, I said, ‘Look, don’t treat me like this because you are telling me to go there and these people are telling me to go there. I’m caught in between. This is where we come and this is the pharmacy we use, so why don’t you communicate between two of you and sort it out for us, then I don’t have this issue at all?’. Eventually they got it, but that kind of a breakdown of communication.
Mr Bhatt
Home delivery of medicines was undoubtedly appreciated as a valuable and convenient service. However, a downside is the extent to which it can undermine the extent and opportunity for personal contact with pharmacists and their potential as a source of medicines advice for patients. Not all pharmacists provided home delivery and controlled drugs had to be signed for and collected directly from the pharmacy. In most cases, this was not experienced as a problem, at least in relation to routine prescriptions. It became more of an issue when drugs were prescribed by different sources and dispensed at different times. This could involve participants having to make quite lengthy journeys to collect medicines from the different pharmacies or hospital dispensaries. Mr Crispin, for example, continued to receive a prescription from the MND clinic after his condition deteriorated to such an extent that he could no longer attend as an outpatient. This meant that a member of his family had to travel to the hospital to collect the prescription. This became difficult to manage in view of Mr Crispin’s deteriorating health and the heightened level of care that he needed at home.
Difficulty in accessing medicines urgently, especially OOH, is a recurring theme in professional and lay accounts. Professionals expressed concerns about timely anticipation of need and then effectively planning for the supply of medicines in good time. The process could be complex. The first task was to find someone who could and would prescribe the medicines, then there could be a search for an open pharmacy that stocked the drugs and could dispense them. Mrs Bates described how she had to set out in the middle of the night to obtain a prescription prescribed for her husband by an OOH doctor. Fortunately, some friends who had come to provide support during her vigil for her husband’s death were able to remain with him while she tried to find a pharmacy that both was open and could fill the prescription:
I didn’t know where [OOH pharmacy] were and I had to drive, on my own, in a fairly distressed state, leaving two people in the house, thinking, ‘Oh dear, well, I’ve got to go and get this’.
Mrs Bates
As described in Chapter 6, some nurses were aware of the practical difficulties that families could experience in accessing medicines and were willing to help proactively in checking supplies with local pharmacists or even going to collect the medicines to take directly to the home. However, others considered that this task was part of the family responsibility, even in the case of families caring for a dying relative and at a time when the demands of care in addition to responding to rapid changes in prescribing could become intense:
There are times where the community nurse will say to the family, ‘We’re running short of this, will you order it through the GP surgery?’. That’s quite difficult for a family member to actually do to be quite honest. They’ve got enough to do at the end of life, to actually be supporting the patient, not to be having to run around, to ring, wait on, because some surgeries have got like a call system where you’re actually probably 17th on-line [sic] or something to actually do a prescription. You can’t order prescriptions over the phone for many of my surgeries now, you have to physically go in. So that means leaving the patient to actually go and do it.
SPCN, HCP17
Nurses commented that they preferred to work with smaller pharmacies, rather than big chains, because they tended to be more responsive and there was greater continuity of staff. Nevertheless, the spectre of not having adequate supplies of drugs, especially during the night or over weekends and bank holidays, was frequently raised by professional respondents. Only one pharmacist in the study reported having access to patient records, which he considered to contribute greatly to the quality of the service that he could provide. This illustrates the scope that there may be for greater pharmacist involvement in end-of-life care.
Navigating the system and maintaining vigilance
Lay participants described a process of growing awareness that a lot of help was available, but finding out about what was on offer, and knowing how to access it, particularly at the right time, was a difficult and protracted process, especially as needs changed. Many reported an experience of learning on the job and figuring out how the system worked as they went along, with few professionals signposting to resources. Lack of information and guidance about how to use medicines was a recurring concern. Simple, direct information given at an appropriate time was a clear requirement that was rarely met. Some reported being told things at a time when they were not able to take it in or found that the information was not delivered in a comprehensible way:
I had no help with chemo [chemotherapy], when he, he literally had chemo in hospital, and they sent him home. And I said to the nurse, ‘Can I have a leaflet or something? [laughs] I don’t know what to do. What do I do when I get him home?’. And she went on the internet and she printed off a leaflet which was off the Macmillan website. That’s all I had.
Mrs Baker
Even relatively expert caregivers, such as Mrs Bates, reported finding out by chance, and late in the day, that certain resources, such as home visits from psychiatrists or liquid formulations of medicines, were available. Mrs Bates was very proactive in managing her husband’s care and liaising with services. She was quite positive about their experience of care and broadly trusted services and professionals to give her good advice. She was willing to take the initiative in making suggestions about discontinuing medicines that her husband no longer needed. When his ability to swallow was impaired, she asked if it was possible to have these made up in a liquid form to be administered by syringe rather than a tablet, which made things much easier. This was her initiative and not a suggestion that had been made by HCPs. Although acknowledging that she was carrying a heavy care load as her husband’s needs intensified, Mrs Bates was confident in managing this, including his medicines, and was extremely committed to doing so. She was determined that he should die at home. Mrs Bates was comfortable with making decisions about stopping some drugs and when to administer anticipatory antibiotics, as well as when to stop using these altogether. She was articulate and confident in her dealings with HCPs, with whom she described having good relations. However, she also described the considerable effort required to learn how the system worked and how to work the system, and how the process of figuring this out unfolded in a piecemeal fashion.
Family caregivers often found themselves in an ambiguous position. On the one hand, they desperately sought clarity and confidence in managing medicines, and ready access to help when critical situations arose. On the other hand, they felt frustrated when professionals failed to acknowledge their expertise, particularly their knowledge of the patient, the nature and severity of their symptoms and how they responded to specific drugs:
Pain-wise, we had lots of different medications. Some made him delirious, so he was labelled with a label of dementia, vascular dementia, which I, I still debate. Once them medications were changed, you’d got the old person back. So, I had, every time, they had to do a change in pain medication along an opiate route, I had to battle for them not to put him back on them.
Mrs Brown
In addition, FCGs had to negotiate a fragmented system in which they found that different services and HCPs were never up to date and lacked understanding of the patient’s illness and treatment and the input that other services were making to this. Consequently, many participants reported maintaining constant vigilance regarding the patient’s care, for which they effectively took on the role of case manager. Meticulous details were maintained about the patient’s medicines, what had been prescribed and what had been taken. Often, it was the FCG who mediated the gaps in professional knowledge of awareness of recent developments in their relative’s treatment:
If you get the call-out doctor at night, theirs [records] were never accurate. They were always out, so I had to be on it, all the time, definitely. And it’s not their fault, it’s, you know, because you could be on something on Monday, go and see the doctor on Tuesday and you’re on a different, you know, medication on Wednesday, aren’t you? You know, the hospital, they’re not going to know that the doctor at [town] is giving him an increased dose of gabapentin, say, for example, they won’t know. Not until I go back, and he has his meeting, and they have this chat with the consultant, and I’ll say, ‘By the way, I need to tell you that he’s doing this, he’s taking this’. And, he used to call me administrator, the doctor.
Mrs Baker
At the same time, FCGs did not always feel that their testimony was accepted and struggled to find a voice within the professional system:
I think they need to listen to people that have actually lived with these people for years and know exactly what’s going to happen. She never listened to what I said.
Mrs Bristow
Relatives commented that HCPs who spent a few minutes visiting patients at home had no insight into the wider picture or how the patient’s condition could change rapidly over the day and, especially, the night. This was extremely frustrating if FCGs felt that drugs had been inappropriately prescribed or mistakes had been made. Another cause of dissatisfaction was professionals or services that stuck to a narrow task-based remit, unwilling or unable to see the bigger picture from the family’s point of view or take ownership of a problem that remained unresolved.
The input of DNs was sometimes assessed in very positive terms. Some participants valued continuity in establishing a relationship with an individual nurse. Others said that they did not mind being visited by different nurses, provided that the care and communication they experienced was good:
No. They [DNs] were absolutely first class. And 24/7 [24 hours per day, 7 days per week] [laughs] you know . . . Oh yeah . . . we were calling them sort of, probably every other night during the last 2 to 3 weeks.
Mr Butcher
However, other participants described the very limited and sometimes task-based focus of individual nurses, attending to only a narrow brief, such as wound dressing, and being unresponsive to the bigger picture and other issues and concerns that the family may have had. Mrs Brand described her frustration when she called the DNs because her husband urgently needed pain relief, but they insisted on laboriously checking how much had been used prior to administering this to her husband:
They would come in, and they would count all the medication which could take 20 minutes because there was a lot of medication. And then they’d give him the medication. And I kept saying to the nurses, ‘Why can’t you – ?’, ‘Well, we need to count it’. I says, ‘Well, what if it’s not there, what do you do?’ Says, ‘Well, we’ll still give him it’, I says, ‘Why don’t you give it him now then?’ So, we did have a few heated arguments because I could see him in so much pain. But it was their policy that they have to count before they give.
Mrs Brand
Exasperation at being referred on from one professional role to another was frequently expressed. Several participants expressed their frustration when nurses had to contact the GP for a prescription, given the delay that they often experienced in establishing contact with the surgery, followed by the time taken for the prescription to be issued. In this connection, the wider ability of CNs to prescribe could be helpful, especially in expediting the process of obtaining medicines.
Relatives who had been helping patients manage their medicines for years could find it difficult to hand over responsibility to professionals, on whom they nevertheless depended for critical care. Even when they felt annoyed that their expertise and knowledge was ignored, and when they felt that they were not kept adequately informed about changes to the patient’s medicines, FCGs expressed awareness of the need to position themselves appropriately in relation to the services on which they depended. They tried to present as ‘good’ patients and as ‘reasonable’ relatives, to be not too demanding or difficult, and to make sensible and considerate demands on a system of health care that they recognised to be overstretched and under-resourced.
The hazard of change
Families confronting the challenges of caring for a dying relative struggled to maintain a sense of order and coherence in the face of dynamic instability. Alterations to prescribed medicines were common and were usually made because symptoms, especially pain, had changed or because the patient was struggling to take the medication in the form in which it had been prescribed. Sometimes medications were changed multiple times to find the right drug or dose to control symptoms effectively and with minimal side effects for the patient. Changes to routes of administration were helpful (e.g. syringes or liquid formulations to support deteriorating swallow, or the move from tablets/liquids to pain relief patches or syringe driver). However, in these circumstances, change was often experienced as a hazard. Delays in transferring details of changed prescriptions between different services have been described above. Even very small changes could have substantial consequences.
Patients and FCGs frequently found that the brand and, consequently, the shape and colour of medicines were changed by the pharmacist without notice or explanation:
. . . because the prescription hasn’t changed, but obviously the thing the patient recognises is the tablet, the colour, the shape . . . so there’s a disconnect there and we’re not involved with any of that . . . That’s just whatever stock the pharmacy can get and that can change quite, speaking to B, our pharmacist, because stuff, new producers come and go and things come and things still change, oh well, that new producer can make things cheaper. So, there’s this continual chasing of cheaper meds for NHS costings.
GP group, HCP25
Lay participants understood that brand changes arose through issues with suppliers and from the effort by GPs and pharmacies to contain costs through effective ‘shopping around’ for the cheapest deal. However, this made it difficult for them to identify specific drugs or link tablets to function, especially if they arrived made up in blister packs, potentially undermining agency in reducing responsibility for self-management of care. For Mrs Creasy, a patient who had allergies to common ingredients of many drugs, the consequences of changing brands could be onerous and distressing for her and her FCGs.
Family caregivers had to adapt quickly to deal with new drugs and increased doses to control pain and symptoms arising as the end of life approached. This was a period of great anxiety and concern, even for FCGs who had reported being previously confident in managing care. The introduction of controlled drugs, such as morphine, was often met with apprehension. These were issued on paper prescriptions, rather than electronically, and had to be collected and signed for at the pharmacy:
I’d never done it before, and it’s a whole new rather scary . . . [laughs] way of administering things. It’s one thing to give something, a tablet which we’re familiar with but, you know, measuring it out with a syringe and everything.
Mrs Bates
This introduced a further task at a time when FCGs faced increasing care responsibilities and difficulty in leaving patients unattended at home. In addition, it was often these drugs that were urgently required, which caused problems of access and supply at local pharmacies, particularly when they were prescribed OOH. Several participants expressed their discomfort, at least initially, at having controlled drugs in the house. FCGs felt that they were left in charge of powerful medicines, often in different formulations, which they lacked confidence in administering. This was quite apart from the practical difficulties that could arise from a patient’s inability or unwillingness to take their medicines. Responsibility for managing medicines, especially making decisions about p.r.n. doses of morphine or other powerful drugs, was stressful. FCGs feared making mistakes, getting the dose wrong and making bad judgements about what was required. The cascade of care that frequently characterised the last days of life could be particularly distressing for FCGs, as they struggled to keep up with rapid changes in the patients’ condition, the medicines prescribed to relieve new and distressing symptoms, and the personnel and services brought in to administer and monitor care:
But she did have quite a lot of side effects from quite a lot of the medication, so we did have to keep changing it a lot. I think where it got really stressful was more when she was much more poorly, she wasn’t as able to understand herself, obviously, at that, what she was taking, and we were also having to have a lot more people come to the house. So, it might have been an on-call doctor, or the palliative care nurse, or the nurses that just come to the home on-call. And, at that point, then, obviously, all of those people were able to prescribe or change her medication, which is where it got quite difficult, I think, and overwhelming, because she sort of, I, I think I know where I am, and then the next day, it was something else would change.
Mrs Booth
Transitions to and from hospital
Many FCGs describe episodes of unscheduled hospitalisation of their relative. In some cases, these were repeated or frequent. Hospitalisation was sometimes episodic for acute developments and relapses. However, some admissions were subsequently realised to mark the divide between managing illness and acknowledging the end of life. This heralded an escalation in the intensity of care and the responsibility required from lay participants, as well as from health and social services. This abrupt transition could be quite challenging, as FCGs struggled to cope with the practical as well as the emotional challenges involved.
Hospital admissions were usually described negatively by lay participants. They called for continuing vigilance. Staff were described as lacking knowledge or understanding of the patient, ignoring family advice or concerns, and sometimes as providing poor care in failing to check that the patient was actually taking the medicines provided. Participants experienced confusion when the advice of hospital staff contradicted what they had been told by community professionals, and when they became aware that staff from different hospital specialties were giving conflicting opinions and advice. FCGs reported difficulty in getting hospital staff to listen to their concerns or acknowledge their expertise and experience in relation to the patient’s care. There are also accounts of poorly co-ordinated administration, including discharging frail older patients late at night, of not checking that there was adequate support at home, and of needless delays and protracted stays in hospital that were not necessary and effectively wasted time that the patient and family could not afford.
Hospital admissions often involved difficult and risky transitions. Stable systems of managing medicines that families had painstakingly developed over time could be dismantled in an instant and were difficult to re-establish after the patient’s discharge home with a large bag of unfamiliar drugs:
And then he’d get discharged, and I bring him home, and I got that discharge sheet with what you’re taking away and, you know, and, they weren’t always right, I learned in the end, to check those, they weren’t always correct . . . There was an occasion when he was having chemotherapy, and I said to this nurse, I was given these tablets to give him when he got home but I’ve never seen them before. And she says, Oh, don’t have those if you’re having cyclizine, I mean, I don’t know, this is what they’re giving you, they don’t tell you, you know, as well as they could.
Mrs Baker
Participants felt inadequately informed about changes that had been made or what new medicines were for. Some reported feeling at a loss about what to do. As described above, hospital prescribing was often problematic, as it did not tally with community records and was not always supported by the GP, and so did not transfer smoothly into community care.
Participants reported that some drugs needed to be prescribed by the hospital because they could not be prescribed by GPs or covered by their budgets. This could involve FCGs needing special trips to the hospital pharmacy. One pharmacist observed that hospitalisation could result in a review and reduction in prescribed drugs. This could be a telling indication that the end of life was approaching (i.e. ‘the slide downhill’). Pointing to an apparently rare example of good and effective practice, he said that in this case the hospital would call him directly to advise him of the changes that had to be made to the patient’s drugs and blister packs. However, more commonly, community HCPs, especially nurses, were disparaging about the disruption caused by hospitalisation and discharge, after which families could be left struggling to know how to manage new medicines and also how to integrate drugs prescribed by the hospital with those they had been using before.
Getting help in a crisis
Most patients and FCGs shouldered the burden of illness and the responsibility for care with great forbearance and resilience. They acknowledged the constraints of an overstretched system of health care and were broadly positive in their assessment of the care that the patient had received. However, difficulty in getting help, particularly in a crisis, was a frequently reported cause of frustration and distress. It was precisely at the time when lay participants most valued the continuity of staff and consistency of service that they found themselves confronting a bureaucratic and unresponsive system, in which the patient was ‘not known’. Participants reported difficulties in getting through to a general practice, of waiting for DNs to arrive to administer pain relief, of summoning help OOH or of having to continually repeat the details of the case to anonymous staff on the end of 111 calls:
I kept having, you know, to have to call the doctor quite a lot and be like, ‘Well, was I still supposed to give her this one?’. Or not, and, you know, we were never quite sure. Or if we ran out of one, how much of a problem is that? You know, and, so yeah, quite a lot to kind of do in that period of time when she was really poorly. And I think the, the continuity of the help at that point was not very good, really. Like it just, it was just sort of, and I completely understand why, but it was, you know, it’s whoever’s available on the end of a phone, or, which meant I found myself phoning that 111 number quite a bit.
Mrs Booth
Home could be a very lonely place when FCGs found themselves struggling to cope with patients in extreme pain or agitation, especially when this occurred at night:
You can ring [the hospital ward]. And I think I did actually ring them at one point and say, ‘Look, you’re going to have to tell me what I can do because otherwise I’m putting him in the car and I’m bringing him down’. Because I daren’t go to sleep because if I go to sleep – I mean I had to hide the drugs because I had such a fear that he was just going to get hold of them and just take them himself.
Mrs Bailey
Having direct access to a 24-hour helpline of some kind was a critical resource. However, most families did not have this or discovered it only late on. Some participants had access to a hospital ward or a 24-hour hospice helpline and a couple had been told or found out about a local SPA service. Regardless of whether or not they needed to use it, the knowledge that accessible help was always available was greatly reassuring. The general 111 service was the advice line most frequently mentioned. However, participants commented on their frustration at having to start again with each contact and provide details of the patient’s illness, as well as their sense of interacting with a formulaic and anonymous service:
And like I say, phoning all these different numbers. I was probably phoning three times a day at that point, to get help on whatever it was, you know, new symptom or the thing you’ve just tried isn’t helping so what else can we do? Or, you know, the syringe driver’s beeping and not working, can you come and change it? And, you know, it was just those sorts of things, constantly. For that period of time, and that, yeah, we did say, just got to the point where we couldn’t have carried on.
Mrs Booth
Lay participants described difficult judgements involved in decisions about when and who to ask for help, especially in what they felt to be a crisis. On the one hand, they desperately needed advice and reassurance. On the other hand, they were reluctant to make unnecessary or inappropriate demands on a system that they perceived to be overstretched and struggling to cope. Wrong judgements on their part were taken to signify a lack of competence, which was strongly resisted. This could go either way. FCGs could fail to call for help when it was needed or make needless demands on the system when it was not:
Because, you say, ‘Is this serious enough to call the doctor, what do you think?’. I mean, luckily, throughout the whole time I was caring for [patient] I got it right every time. And I, and I used to really beat myself up about it, but I know, looking back, now, I was fortunate I’d got each decision right, because sometimes, it’s, ‘Do I give him some more medicine? Do I ring the doctor? Do I call the ambulance? Is it 111?’. You know, you’re thinking, all the time, ‘Which one is it? Which one is it? Because you got so many options, got too many options. Do I ring the Macmillan nurse? Do I ring the community nurse? Do I ring the consultant?’.
Mrs Baker
Deprescribing
Deprescribing of unnecessary medicines is widely advocated for clinical and cost-saving reasons. Patients approaching the end of life are unlikely to benefit from continuing to take medicines previously prescribed for the prevention of disease. Simplifying medication regimens is clearly desirable for FCGs, especially when additional items to control pain and other symptoms arising during dying are likely to be prescribed. Professional participants from a range of roles talked about their involvement in deprescribing, but FCGs did not often refer to awareness of professional intervention of this kind. Some professionals expressed discomfort about raising the issue of deprescribing with patients because of its clear significance in intimating a limited prognosis. They anticipated that this would be distressing for patients and found these conversations to be difficult encounters. Having spent many years encouraging patients to continue taking drugs, such as statins or antihypertensives, to prevent or control illness to protect the patient’s health and prolong life, it was difficult to subsequently suggest that these drugs were no longer needed. Although such conversations would benefit from the application of good communication skills, some HCPs described an approach that was quite direct:
So, we rationalised her medication so we would limit the stuff that she didn’t really need, down to the minimal amount that she needed. I would go through all her medication saying, ‘If you don’t take this one, then this could happen. Do you want to take it? No’.
Community nurse, HCP05
Some tablets she should have had because she had thyroid trouble, so she was on, technically, she was on a 125 mg of thyroxine. But the consultant said, ‘ What’s the point? Don’t bother taking it, it didn’t matter now’.
Mr Berger
Patients and their FCGs were often receptive to reducing the medicine load and discontinuing drugs when it was appropriate to do so. They describe instances where they had themselves taken the initiative in asking for a medicines review, querying why particular medicines were still being prescribed or if they needed to be continued. For example, Mr Crispin described repeatedly asking his GP to undertake a medicine use review for his father. One issue with deprescribing is that within a complex system in which individual patient care was provided by many different services and professional roles, it was not clear which of these should be allocated responsibility for undertaking specific tasks. Consequently, it was quite likely that no one did. Pharmacists were rarely referred to in the context of deprescribing, although this is one area in which they could have a considerable contribution to make.
Anticipatory medicines
Anticipatory medicines or just-in-case drugs are injectable medicines to treat commonly occurring symptoms (e.g. pain, nausea, secretions and agitation) in the last days of life, which are prescribed in advance of, and just in case of, future need (Box 8 gives a focus on AMs). Once prescribed, these drugs are kept in the patient’s house to be immediately available for DNs or other HCPs to administer should the need arise. Thirteen of the BFCGs reported that the patient had been prescribed AMs; in six instances these had been used. Six of the case study participants also reported that AMs were in place. In practice, professionals in the study tended to favour prescribing AMs quite well in advance of anticipated need or, indeed, even when there was not a strong likelihood that they would be needed. Mrs Crawford described asking the DNs to remove the drugs from her house 1 year after they had been prescribed but not used. This was partly because she did not like having them in the house, but also because she found the monthly visits made by the DNs to check the drugs to be irksome. Mrs Bates described how her mother, whom she had also cared for, as well as her husband had been prescribed AMs for over 1 year before they had been withdrawn by the nurses providing care. Prescribing AMs so far in advance of the patient’s anticipated death is to ensure that they are available and to pre-empt the anticipated delays in getting drugs prescribed and prescriptions filled when the need does arise. This ‘just-in-case’ argument was reported by HCPs to be a way of softening the import of the discussion about AMs:
One of the things that I always say to patients or to carers, to families, I always call them the just-in-case meds [medications]. These are just in case, or we’re not asking you, on a Saturday or a Sunday, to go and find a chemist to go and get these medicines in because we’ve got, relatives spend so much time trying to find a chemist . . . And then getting to a chemist, then the chemist hasn’t got it. We get that scenario time and time again . . .
Community nurse, HCP09
Bereaved family caregivers described their experience of the entire process of anticipatory prescribing, from collection and storage to medicines use and disposal. Getting the medication in place so that they could be used was not always straightforward. In one instance, it was reported that the authorisation had not been correctly written and so the DN was unable to give the medications, despite them being available. In another instance, the prescription was written by the GP just an hour before the patient died. Other participants reported AMs being in place in good time and stored them out of sight to keep them safe so that they were not reminded of their purpose:
I mean, basically, I picked up the bag of stuff, I looked in it, I thought, I hope we’re not going to need that . . . we certainly didn’t need it at the time, this was months, months before, I rolled it up and put it in a lockable cupboard, told the carers where it was, in case something happened when I wasn’t around . . . In fact, one of the things in it went out of date before we needed it, and the carer . . . spotted this and she caused it to be updated.
Mrs Butler
It was the emergency district nurse . . . ‘We’re going to come but we think, for the weekend, we ought to have the grey box’ . . . I can remember having to go and get the prescription from the emergency place and then finding a pharmacist who would do it late on a Friday night . . . that wasn’t easy actually. I had to get a friend to come and stay here. And obviously, it was quite distressing. Because I knew . . . I knew what it meant.
Mrs Bates
But [he] didn’t want them on show. You know. Because he knew what they were. He says, ‘Yeah, just put them in that bottom cupboard in the kitchen’, and we never really touched them again, until after he’d died, and I took them back to the chemist again.
Mrs Becker
Although BFCGs eventually realised the purpose of AMs, this was rarely explained directly to them at the point of prescribing. As Mrs Best describes, HCPs tended to be vague and avoided opportunities for providing explicit information:
When they were picked up from the pharmacy there was no description by the pharmacy about this is what they’re for or anything like that . . . There was never any written information. And then when the nurses started coming in they said, ‘Oh have you got any of these medicines in the house?’. So, there’s no communication with them either . . . We just, we knew what they were and we had them in a particular place.
Mrs Best
However, BFCGs valued the availability of AMs when they were needed.
When we needed it, both with [my wife] and my mother, the district nurses were literally there, normally within about 20 minutes.
Mr Butcher
There was a point when a couple of days before he passed away, his breathing was very laboured and . . . the district nurse came and she put this butterfly in and she used something that was in the box, and . . . it did calm him down.
Mrs Bates
However, a consequence of there being a number of professional roles able to prescribe AMs, alongside the tendency for these to be prescribed far in advance of need, meant that it could be difficult for individuals to keep track of what had been prescribed previously. It might not be remembered that AMs were already in the house or that they had been prescribed by another service:
I visited the gentleman and then I think he took quite a . . . sort of nosedive . . . he’d stopped swallowing. And I hadn’t been in contact and by the time I’d noticed on his notes that the GP had been out and recommended that he start on some subcut injections, which incidentally, [FCG] sort of forgot she’d got in the house, because we put them in pre-emptively. Well, that can be, you know, could be a couple of months before the person needs them. And I think sometimes people put them away very safely, and then actually forget that they’ve got them, so, you know, that can be a tricky one.
SPCN, HCP14
The prescribing of AMs is a significant event for patients and their families, clearly signifying the imminence of death. It calls for skilled and sensitive communication. This might be one reason why prescribers avoid discussion or explanation of AMs and why they had been prescribed. Several FCGs reported that they had been unaware that medicines taken home after hospital discharge included AMs. Others reported AMs being prescribed without accompanying explanation or discussion:
And, I get a call . . . from the surgery, to say there’s a prescription for you . . . So, I went down, got this prescription, and the nurse had left a message asking me to phone. So, I phoned back, ‘Oh, there’s these drugs, and you must keep them on one side’ . . . And it still didn’t click. So I then went to get the prescription, and I took it and got the medication, ‘You should have it on one side, you know, it shouldn’t be touched, it’s got to be on one side’. So, I said, OK . . . [a different nurse who was doing a home visit] said, ‘Oh, they call them anticipation, anticipatory drugs’. And then I thought, ‘Oh . . . it’s for if he gets really agitated, and of course, it’s morphine, nobody had told me, I’d picked them up, not realising’.
Mrs Crawford
Our participants did not express overt concern about this issue, rather they were more anxious and uncomfortable about the nature and status of the drugs. They felt vulnerable about having controlled drugs stored in the house:
Having never handled any controlled drugs at all, it was actually quite scary when the chemist is making you sign for things, and they talk about words like morphine, [laughs] and dangerous drugs. And you do actually feel quite sort of, ‘OK, I’ve got these in the house, am I going to be burgled?’ [laughs]. And, you do feel sort of rather reticent to ever use them.
Mr Butcher
Risk and responsibility
The limits to family responsibility
The experience of FCGs varied widely in terms of the duration and complexity of their role in supporting medicines management. Individuals differed, also, in the resources of time, energy and confidence that they brought to this task. Some embraced the responsibility, even for complex tasks and administration of controlled drugs, keen to provide any support that they could and to enable the patient to remain at home for as long as possible, even if this did not always extend to death. Others described the burden of care to be difficult and were apprehensive about assuming responsibility that they did not feel confident or competent in:
I think a lot of family members are very, very, very eager to kind of . . . It’s their way of feeling that they can do something . . . and are very, very happy to administer medication and will contact us with absolutely any concerns . . . We also need to kind of identify if it is too much of a responsibility for some family members and being able to pick up on that and making sure that the carers aren’t feeling totally overwhelmed and feeling that it’s expected of them and they are struggling to do it.
SPCN, HCP23
Especially as the patient’s condition deteriorated towards the end, home could be experienced as a very vulnerable and lonely place when faced with the responsibility of having to make judgements about care. In some cases, this was manifestly unwelcome:
The other thing I found was people would ask me, ‘Well, what do I want to do? Or What do you think?’. And I’d feel like saying, ‘I don’t know, I’m not a doctor, why don’t you tell me?’. Like, ‘Do you think she needs to go to the hospice now, or do you think she needs to be in hospital, or do you think that just a doctor will be OK?’, ‘Well, that’s why I’m ringing you’. You know? I just don’t know. I’m in a panic and I need help from somebody . . . Yeah, just ask you, just, yeah, felt like sometimes, you were being, you were having to make all the calls?
Mrs Booth
Participants who had previously worked out relatively stable regimens of managing medicines could find themselves knocked off balance and overwhelmed by the escalation of care that commonly occurred in the period prior to death. This could be the point at which the patient was admitted to the hospice or hospital. The decision to abandon the goal of caring for the patient at home could be deeply felt as a betrayal and failure, especially where families had started out with a strong commitment to do this:
It was horrible admitting that she’d have to go to the hospice and my brother and I were sort of feeling guilty that we couldn’t keep, you know, keep her at home. But, it just did get to the point where I was like, ‘Oh, I can’t, I don’t think I can do this anymore’. I just felt so stressed and so panicked and so helpless.
Mrs Booth
Health-care practitioners and FCGs varied in their assessment of the safety and feasibility of technical tasks that family carers could reasonably and appropriately to take on. For example, some FCGs gave injections, managed dialysis and were willing to take on additional tasks, such as changing cartridges in syringe drivers or calibrating doses of morphine. Mr Berger said that he would have been happy to give his wife injections of morphine for breakthrough pain. He had been in the process of being trained to do this prior to her death because it took so long for the DNs to arrive after a call-out. Some HCPs were receptive to extending the role of FCGs, given appropriate support and training. They acknowledged the advantages in enabling patients to receive faster and more tailored control of symptoms, cutting out the wait for professionals to make home visits:
I think in terms of end-of-life medication, when somebody’s very end of life, I think managing that at home is ad hoc to say the least. I think there ought to be some sort of scope for assessment with a relative should they want to, to be able to administer something themselves. Because to sit and watch somebody who can’t breathe or is in huge pain, or is so terminally agitated, and you ring up a nurse and they can’t come for four hours, is just horrendous. And they have the injectable medicines there that they cannot touch and they can’t give them, so I don’t see how, I mean it would be difficult but I don’t see. You send people home with their dalteparin and you teach them how to give the dalteparin and the insulin and injectable drugs, could we not have some way of assessing and empowering somebody to be able to do that?
SPCN, HCP16
Professionals also recognised a trend towards increasing the range of tasks that FCGs could be trained to do:
I think it’s something we need to explore, because we’re heading towards a lot of self-care models, aren’t we? We’ve got to do something different. And we’ve got patients and carers who do numerous, bowel care, continence care, their own leg dressings, [why can’t], if they’re geared up and they’ve got the right support systems in place and the right knowledge and education, and support to say, ‘Do you know what, they’re in pain, or, [. . .] [vomiting], and we can support them through that’, and we’re heading towards self-care for every other thing, why not, because they can wait hours.
Community nurse, HCP09
The advantages of greater FCG input in relieving strain on an overburdened health service were acknowledged. However, some HCPs and FCGs also recognised that family members may feel intimidated and even overwhelmed by the prospect of taking on greater responsibility for care:
You also get, and I’ve always encouraged families to be open and honest, you’ve got a patient who wishes to die at home, no matter what, and you’ve got a family member who’s very nervous about being responsible for administering controlled drugs.
SPCN, HCP08
Concerns were also expressed over safety issues resulting from the delegation of more care to FCGs, especially around administration of controlled drugs and about the allocation of responsibility and blame when mishaps occurred:
You end up making somebody [feel] responsible for killing their [relative] because they gave the last dose of whatever, and they died 10 minutes later. And, what you need to balance that against is, waiting 2 hours for a harassed nurse who comes and then says, ‘Oh, I haven’t got the right bit of paperwork and I can’t . . . ’, you know, which sometimes happens. And so, I think it’s about managing risk.
Consultant, HCP03
In addition to doubts about the commitment and competence of FCGs to shoulder the burden of care, there is also the issue of capacity. As the population ages, the primary caregiver of dying patients is often an elderly spouse, likely themselves to be affected by the limitations imposed by frailty and comorbidity:
If the person can’t manage themselves, it does fall onto the relatives and where, how can we expect them to suddenly have the knowledge of when to give them [medicines]? I had a referral yesterday for a lady who was in hospital but wants to come home to die very soon. Her husband’s 87. You know, how can we expect this man to look after his wife? And be able to provide her with medication?
SPCN, HCP02
The proposal that some relatives could be trained and trusted to take on greater responsibilities for care is strengthened by the number of FCGs who are also HCPs within the wider population, as well as within the study. Several study participants were, or had been, HCPs. Their experience could give confidence about managing care but could also bring additional difficulties. Personal and emotional involvement could override professional detachment and judgement. Some found the system to be bureaucratic and unresponsive and reported similar difficulties to those experienced by participants with no professional training. Some participants described their uncertainty about how to present themselves in dealing with professionals and services, including whether or not to reveal their expertise. They also felt frustrated when, on occasion, professionals providing care did not acknowledge this. Alternatively, it could be the case that other HCPs assumed too much, and participants with a dual role as HCPs received less information and support than they felt other FCGs would have received.
Vulnerability and disadvantage
Risk management, especially of powerful medicines for pain relief, generated concern among both lay and professional participants. These risks were compounded in patients who experienced one or more kinds of additional disadvantage. It is important to know how the system responds to the needs of terminally ill patients who experience homelessness, substance misuse or dependency and serious mental illness. Although we were unable to recruit such patients directly, we gained some insight into the issues arising in their care from the accounts of HCPs who took part in the study. Practitioners spoke of their experience in working with people from diverse or disadvantaged backgrounds and the ways in which they adapted their practice to provide good care.
Homelessness
Several HCP participants had experience of caring for homeless patients, including two who worked in practices that specialised in the provision of services to this group. These included a GP who said of this patient group that ‘the average age of death is 46 in our population’ and then went on to say that ‘when we do have a terminally ill patient, they tend to be an exception’ (HCP22_GP). However, the GP felt that the homeless population is a vulnerable one:GP, HCP22
When you ask, one standard question is would you be surprised if the person died in the next 6 months? To tell the truth we wouldn’t be surprised if any of our population died in the next 6 months.
Managing medicines and prescriptions could be difficult for homeless people and controlling pain posed particular challenges. A CN who worked regularly with homeless people linked some of the difficulties that she encountered in providing good care to this group of patients to their relative youth and the way in which services did not want ‘to admit that it’s end of life’ (Community nurse, HCP24). Her preference would always be to develop a care plan, although this was not straightforward:
I tend to do a care plan but there’s no like DNRs [do-not-resuscitate orders] and it’s very, there’s a lot of pain issues and there’s a lot of fear because those people are young. So sometimes I find it very difficult to manage their pain and to actually give them dignity sometimes.
Community nurse, HCP24
The lives of people who are homeless can be chaotic, making it difficult for them to keep track of when and where appointments are scheduled. HCPs described management strategies for issuing prescriptions and the need for responsive tailoring of services. For example, a palliative care specialist nurse described one case in which a patient who was approaching the end of his life lived in a car. She worked with the GP to schedule joint appointments to reduce the effort of making and keeping appointments for the patient so that they could more easily co-ordinate his care. The GP was the only person who prescribed in this case so that the professionals could keep track of what was going on with his medicines. There was a perceived risk that prescriptions or medicines could be lost, stolen or sold on to other users. These were consequently issued in small amounts:SPCN, HCP14
I cover one of the homeless practices in [city] and that’s always a big challenge because obviously, they don’t want to be walking [around], that’s when the local pharmacies come in . . . They’ll give it to them in stages rather than give them a whole supply of one lot of medication at a time. Because they lose it, sell it.
Options available to homeless people who were dying were limited. Sometimes the local authority could find accommodation, but not everyone would wish for this because ‘Some people haven’t got anybody to support them out there and they’d feel very lonely’ (Community nurse, HCP24). Some homeless people would opt to stay in a hostel as they were dying, which the team did their best to facilitate, but often a hospital was the final place of care and death.
Substance misuse and dependency
Providing end-of-life care for people with substance misuse issues could also present challenges for practitioners, particularly in relation to ensuring that pain is managed while keeping medicines secure from misuse (Box 9). Issues could arise when it was not patients themselves, but another family member, who had the problem. A GP spoke about a patient for whom she was caring who had end-stage COPD and was experiencing pain that was increasingly difficult to manage. The patient required ‘whopping doses, of morphine, midazolam for her symptoms to be controlled’ (GP, HCP10), but there was a potential problem in that her son was a drug addict and, although he did not live with his mother, he did visit her on a regular basis. The patient was keen to remain at home and the local hospice at home service was brought in to support her in doing so. Her drugs were kept in a locked cupboard and her son did not know where the key was kept. All HCPs involved in the patient’s care were informed of the situation and the success of the procedure was helped by the fact the son ‘was very open about his abuse’ (GP, HCP10).
A SPCN described a patient who was approaching the end of life and was experiencing increasing pain. He was a heroin addict, as was his partner, and their house was frequented by other drug users:
At the moment, because of his heroin addiction and his partner’s heroin addiction, and there’s frequent other users going in and out of the property, we have to have restricted the amount of medication that’s actually in the house. So, the majority of his medication is kept here [hospice], and he just has a very small supply of Oramorph, at the property at one time . . . His pain is changing and his pain is increasing, so we’ve had to increase the amount of visits . . . he’s also started on a patch. Because, obviously, people coming in and out can’t see that, hopefully. And can manage it better.
SPCN, HCP07
The patient’s medicine was collected from the pharmacy by the HCP, rather than the FCG, and taken in small quantities to the house, where the patient’s partner undertook to keep his medication out of sight of visitors. The HCP was aware that the patient continued to take non-prescribed drugs that had an impact on the effectiveness of his prescribed medicines and increased the difficulty of appropriately calibrating the required dose:
It’s about managing the relationship with him, because if you, you know, he’s going to buy things anyway, he’s going to continue to use heroin . . . at the beginning I said to him, ‘I’m not here to tell you what to do, but if you tell me what you’re buying, it helps me to manage your symptoms better.’
SPCN, HCP07
The HCP believed that the patient was honest with her about what else he was taking besides the prescription medicines because she was open with him and had taken time to build up a relationship effectively as the keyworker involved in his case. She remained non-judgemental about the patient’s lifestyle or addiction and expressed a strong commitment to supporting his autonomy and choices for end-of-life care (i.e. to remain at home), despite the additional demands and difficulties this imposed. However, she was also aware that her colleagues took a very different view and some were not willing to undertake home visits where they felt vulnerable and at risk.
Balancing risks in relation to safety and potential misuse of controlled drugs with effective control of pain and other symptoms called for fine judgement and innovative practice, based on the ability to establish strong and trusting relationships with patients and their families. The case outlined in Box 9 illustrates the potential for attentive and individualised care, and the importance of strong relationships in which HCPs effectively act as keyworkers mediating the vagaries and complexities of the system and using professional knowledge and expertise to adapt this flexibly to the singular needs of individual patients.
The role of home health-care workers
The role of HCWs in supporting families to cope with care, including medicines management, and so enabling patients to remain at home is not widely acknowledged. Home care was sourced from different agencies and a mixture of social and hospice services and private care. There was considerable variation in the tasks and responsibilities HCWs were reported to undertake and the intensity of care provided, although this tended to increase as the patient neared the end of life. Accounts varied regarding the extent to which HCWs could and should be involved in medicines management. At one extreme, HCWs were described as being able to only oversee and prompt patients to take their medicines:
They can’t physically put the tablet in their mouth. They can get them out and they can put them in the patient’s hand. But they can’t physically put it in their mouth, because then that’s administering it. So, they can prompt it, but they can’t administer it. If the patient gets to the point where it needs putting in their mouth for them, then the medication would have to be reviewed.
CNS, HCP18
In other cases the HCWs’ input was more proactive, although their training in medicines management varied widely and seemed sometimes to be ad hoc. The HCW who provided regular support for both Mr and Mrs Cole described the training that she had received on starting work for the company that employed her: ‘It’s 4 days, your first lot of training when you first start with the company, and 1 day is specifically medication’. Mrs Cole received her medicines and food through a PEG tube, which were both administered by the HCW, who said that she received on-site training for this from the company nurse who ‘has to sign us off to say that we’re competent. So, she has to watch us get the medications ready, put the medications in, put the pump on’. The HCW found this ‘quite a daunting thing’ to undertake. For Mr Cole, the HCW put the medicines he needed to take into a small cup and handed it to him so that he could take them himself. She did, however, change his fentanyl patches for pain relief.
Home health-care workers who were involved in supporting patients with their medicines spoke of receiving some training. The HCW who worked with Mr Crispin, for example, said ‘We do have specific medication training. So, we have the induction. It touches on every subject but then there’s alternate training for medications’. However, it was not clear what the training covered nor how extensive it was. The HCW went on to describe being able to handle controlled drugs, such as morphine, but not being permitted to use needles to administer medicines.
The HCW supporting Mr Cooper described being able to place pills into a patient’s mouth, but in certain circumstances only, such as when the patient consented, as Mr Cooper had:
We actually place it in his mouth and then he takes water via a straw . . . His consent – like his tablet and then it’s, B, OK to have them, and he says, yeah, go ahead.
Mr Cooper, HCP02
The role that HCWs took in supporting the people under their care in relation to the management of medicines varied, as did the training they received to do so. It seemed clear, however, that they played a key role in helping people to remain at home:
One gentleman who has passed away, now, and that kept him at home for a long time. When I first got involved, he was bouncing back and forward to hospital, and actually, when we got that medication in place, we trained all of the carers in how to use it, they were using it really well, at the appropriate times and it meant that patient, for his last 6 months, was at home.
CNS, HCP06
As this case illustrates, HCWs could have an important role in supporting medicines management, which enabled patients to remain and to die at home.
A few patients with very complex and severe health problems received intensive packages of care. Mrs Brown’s husband had undergone bilateral amputation below the knee as a result of poorly controlled diabetes. He required daily home peritoneal dialysis for renal failure. Towards the end of his life, two HCWs came 24 hours per day and supported his wife to manage his medicines and dialysis. This enabled Mr Brown to remain at home and his wife to continue to work outside the home. In this case, HCWs took an active role in monitoring and administering medicines. When patient needs were less intense, even a modest amount of HCW input could be critical to the patient and FCG’s ability to cope at home. Other patients would clearly have benefited from some HCW input, especially those, such as Mrs Carter, who lived alone and lacked the dexterity to open packets or pick up tablets and transfer these to her mouth. The system seemed to respond to patients with self-evidently intense care needs, including escalation at the end of life. However, those with less intense or clearly visible impairments, or whose difficulties gradually intensified over time, were more likely to slip below the radar of professional surveillance and intervention.
After the death
Despite the security measures put in place for access and storage of controlled drugs while the patient was alive, following his death, family members were surprised to find that they were handed the responsibility of returning these and other unused medicines to the pharmacist. This was an additional and unwelcome task occurring at a difficult time:
When a patient has passed away, we give the responsibility to the family to take the medication back to the pharmacy.
SPCN group, HCP01
It was not clear what happened in most cases, as the disposal of medicines after a patient’s death seems to be unmonitored. However, FCGs were not comfortable with the responsibility for managing this risk. Some families described how they responded quickly and were glad to get rid of the controlled drugs as soon as they could:
One of the first things we did [laughs] was to get all the end-of-life meds [medications] out of the house. Because we just thought, I mean, they’re, you know, they’re obviously very potent things and we just wanted to get, we just took them up to the pharmacy that morning . . . I mean, presumably, one of the things about them is they’re the kind of medications that people want to get hold of for less desirable reasons . . . So, we just, we wanted to get them out, for all sorts of reasons really.
Mrs Butler
I had all sorts of stuff like bottles of morphine, and I kind of just felt a bit uncomfortable that I’d been left with all this stuff . . . You know, and, kind of thought, Well, luckily, I, didn’t feel in any way suicidal, and I’ve got my family but I thought, ‘[Gosh], some people must feel like that, in those situations’. And, and then you got a houseful of drugs, and I thought that point was a bit, it was left to us to dispose of that . . . But again, it was left to us to work out.
Mrs Booth
The enormous waste of unused medicines was sharply exposed after the patient’s death, as boxes of unused drugs were gathered together. This was a subject of regret on the part of HCPs and FCGs:
And the sad thing is that all the medications we had, many were not opened. They all had to be rubbished and scrapped. What a waste. You know, if they’re still sealed, why did they have to be destroyed?
Mr Butcher
Several HCPs observed that the waste of medicines might continue after the patient’s death in the case of automated repeat prescriptions. If the patient’s family did not let them know directly, there was no mechanism within the system to alert the pharmacist to the need to stop delivering supplies.
What could have been better
Participants were asked how their experience of care could have been improved and put forward a range of suggestions. These were often accompanied by statements acknowledging that HCPs were very busy and that services were overstretched. Indeed, concerns about making inappropriate use of these services and struggling to decide whether or not in fact a request for urgent help was justified recurred throughout the data. Nevertheless, participants described the anxiety and distress that they experienced when finding themselves unable to access effective help in a crisis and the frustration caused by their experience of a system that could be unresponsive and bureaucratic. A more responsive service was considered important, both in picking up on the fact that families were struggling and needed more proactive professional engagement and, particularly, in enabling rapid access to help in a crisis. The idea that dying patients merited recognition and special consideration from services throughout the system was strongly expressed. A dedicated telephone line and systems for better communication of this status throughout the services and professionals involved in care were frequently suggested. The perceived unresponsiveness of some general practice staff was underlined by the suggestion of several participants that the medical records of dying patients should be clearly flagged so that the need for a sensitive and rapid response would be immediately apparent:
I would have, it would have been really helpful if the district nurse, or someone, had recognised the fact that we were starting to struggle.
Mrs Becker
One thing, I think GP surgeries should do is, anyone caring for a terminally ill person, it should be noted on their record.
Mrs Blakemore
Being given more appropriate and timely information about medicines, their purpose, their side effects and how they should be used, especially when they were first prescribed, was also considered to be important. The provision, without having to ask, of simple reference information about the drugs was one of the most frequent responses:
It could have been a lot better. I do think that the GP practice actually lacks the knowledge on how best to prescribe palliative care medications, well, for the ones we’ve got anyway . . . I think they could have explained things better to me. About the medications.
Mrs Brown
Having access to a quick and reliable source of help and information about medicines was one of the most important things:
Just one point of contact, where I could say, ‘I’m not sure about these tablets, I’m not sure about this, that and the other’.
Mrs Baker
The scope for greater pharmacist involvement in providing advice and help with medicines was rarely recognised by lay or professional participants, including pharmacists.
Conclusion
This chapter has considered how patients and family caregivers experienced interactions with HCPs and services within a complex system of care in relation to medicine-related issues. Frustration with the experience of a fragmented and bureaucratic system was frequently reported. Poor communication with and between HCPs and services and a lack of adequate information and support to families were recurring themes. Many FCGs assumed a pivotal role in patient case management, including undertaking surveillance of professional care and monitoring of medicines management. Even small changes in medicines or relationships with key staff could have far-reaching consequences for families working to maintain a stable network of care. These were particularly likely to rupture during crises occurring in the last weeks or days of the patient’s life. Problems with prescribing and accessing medicines were common, especially of controlled drugs and when required OOH. Pharmacists were considered primarily as suppliers of medicines, and there was little recognition of the scope for extending their role in medicines optimisation and support. Variation in family resources and responses to extending responsibility for administration of medicines in the home raise questions about the limits of what FCGs could and should be asked to do, and how professional support can be tailored to individual preferences and circumstances. In this context, the largely unacknowledged role of HCWs in supporting medicines management at home, especially for patients living alone, will become increasingly critical in future.
Chapter 8 Findings: stakeholder workshops
In June 2019, we held two dissemination and discussion stakeholder workshops. Both events were structured in a similar way, starting with lunch and an opportunity for informal discussion. After a welcome and an introduction, the research team presented data based on three key themes identified from the study findings: (1) the work of managing medications, (2) diversity and disadvantage, and (3) system and complexity. All participants were then allocated to a table of approximately four to six people to discuss one of these selected themes using the prompt questions provided in Boxes 10–12. With permission, discussions were recorded and facilitated by a research team member. We had pre-assigned participants to groups to ensure that each group was interprofessional and had a PPI representative. This worked well, and the groups engaged in conversations not only about their allocated theme, but also about the other themes and wider issues raised by the study findings. Forty-five minutes were allocated for each group discussion, after which we asked participants to anonymously make a note of three key issues relating to their primary discussion topic. Many identified more than three and some responded to more than one topic. We received 52 sets of notes across the three topic themes. The group recordings were not transcribed in full, but listened to repeatedly by the researchers, who made detailed notes and verbatim transcripts of selected extracts. These notes were compared with the written notes made by participants and amalgamated. The final part of the workshop sessions was a presentation from a team at Southampton who are undertaking a National Institute for Health Research-funded study, ‘Accessing Medicines at End-of-life (ActMed)’ [URL: www.journalslibrary.nihr.ac.uk/programmes/hsdr/165223/#/ (accessed 19 March 2021)].
A total of 48 stakeholders attended the two workshops (Nottingham, n = 29; Leicester, n = 19]. A wide range of professional and PPI representatives with interests in SPC, community service provision, pharmacy, research and education were included. Table 7 shows the breakdown of attendees by professional grouping. The largest overall group of stakeholders was the 10 people engaged through PPI. We also had representation from 11 nurses working either in hospices or working in the community as CNSs in palliative care. Alongside two consultants in palliative medicine and a further two hospice community liaison personnel, we had considerable engagement from SPC services. We were also pleased to see participants from our university education teams who were keen to incorporate the findings into evidence-based teaching, particularly for the non-medical prescribing course.
| Role | Nottingham (n = 29) | Leicester (n = 19) | Total (n = 48) |
|---|---|---|---|
| SPCNs | 4 | 7 | 11 |
| Consultant in palliative medicine | 1 | 1 | 2 |
| Community hospice teams | 1 | 1 | 2 |
| Community clinical nurse specialists (HF and PD) | 1 | 2 | 3 |
| Research nurses | 1 | 1 | 2 |
| Pharmacy | 5 | 1 | 6 |
| PPI | 7 | 3 | 10 |
| Academic: lecturers | 3 | 1 | 4 |
| PhD students | 2 | 0 | 2 |
| Researchers | 4 | 2 | 6 |
| Dual roles |
1 (PhDa student and nurse) 1 (PPIa and PhD student) |
1 (pharmacista and lecturer) |
Participants were provided with three questions to consider within their allocated theme. These provided a degree of uniformity between the groups and acted as a starting point for discussion (Box 10). Participant identifiers have not been added to the direct quotations included in this chapter. Some are example of written feedback on notes that participants left anonymously at the end of workshops. Others are taken from recorded round-table discussions in which it was not possible to identify individual speakers.
-
How should we balance the issues of risk and responsibility for patients and FCGs managing medicines in the home at the end of life?
-
How can we set up better processes to enable patients and FCGs to access responsive help in a crisis?
-
What could and should be the role of the pharmacist in supporting patients and FCGs to achieve optimal medicines management at the end of life?
System and complexity
Participants acknowledged that health and social care systems were complex and that the different parts did not always intersect well:
The system does not support people dying at home, especially re [regarding] availability of medicines when needed suddenly, despite policy push for death at home.
Some also recognised that constant changes to services and their titles, based on funding availability, meant that even as HCPs they were not always knowledgeable about what was available for patients in their area. Reflecting the findings from the HCP interviews in workstream 1, it became apparent that, although interdisciplinary discussions were considered important, most of the HCPs attending expressed limited understanding of roles outside their own. The system and complexity discussions focused on issues around communication, information and advice, and the difficulties for different HCPs and sectors in responding to patient need.
Participants noted communication as a core issue within all systems, citing the need for better communication between HCPs and families and between different HCPs, especially GPs and pharmacists. Issues around the sharing of patients’ medical records were raised several times. Sharing these between HCPs was considered to facilitate communication, but it was often not considered possible to share records, such as across primary and secondary care and with community pharmacy. ‘360-degree patient-held records’ in the home along with the promotion and implementation of ACP were suggested as ways to support improved communication between HCPs and between HCPs and families.
Participants felt that it was important that patients and families should be given numbers to call for ready access to help and advice, including OOH:
I think the problem with when you’ve got a lot of people involved is that it does end up going back to the relatives or carers or the patient themselves and that’s where it does tend to fall down . . . it’s very disjointed and unfortunately it’s the patient and carer who get left to deal with it.
However, they acknowledged that our data demonstrated that this clearly did not always happen. Who should be responsible for giving out this information was less clear, particularly when services, such as district nursing or SPC teams, were not in place. Key/case workers who could function as a central point of contact and care co-ordination were considered beneficial for patients. However, there was no agreement about who might take on this role or how this could be accommodated within current health or social care systems. Participants voiced the need to empower patients to self-manage and have strategies in place to avoid and respond to crises. They also acknowledged the difficulties involved when patients lacked necessary information or knowledge of where to seek advice and support. SPA lines that offer a 24 hours per day, 7 days per week (24/7), telephone helpline were considered a good resource. Again, it was acknowledged that knowledge of this service was not widespread and most workshop participants felt that they did not cater for medication-specific queries.
Participants recognised that, in relation to medications, the complexity of the system and its multiple parts could mean that there were many points at which things could go wrong:
System of medicines’ management is flawed, there’s overprescribing, stockpiling, waste, etc., sometimes you lose sight of that actual person.
Participating HCPs reported considerable issues with lack of staffing, increased caseloads and systemic problems leading to staff burnout. Some also felt that systems and policies had made HCPs overly risk averse, with too few taking the time to assess individual risk against the level of responsibility that families were willing and able to take on. Discussion led participants to agree that systems at the end of life needed to be streamlined, with fewer professionals involved and an emphasis on simplifying medications. Again, a designated key worker or case manager was considered an asset in ensuring that systems were updated and communication between professionals was optimised.
Pharmacists were judged to be underutilised, particularly in reviewing medications usage and potentially expanding their role in the removal of medications from a patient’s home after death:
Pharmacists well placed – given increasing placement alongside GPs.
. . . pharmacists going to be key moving forward for managing medicines for all patients, but particularly for patients that are disadvantaged or struggling.
However, with representation from a pharmacy in most groups, the limitations of the role of pharmacists were clarified. Participants emphasised that pharmacists’ lack of access to shared information and reduced budgets would hinder them taking on additional roles:
Pharmacists ‘are completely blind’: don’t have access to patient records, nor to other pharmacists’ records, so only know of the prescriptions a patient has dispensed from their pharmacy. Summary record meant to address some of the issues, but doesn’t, it’s ‘just a snapshot in time’ and pharmacists are not part of a joined-up system.
Some participants also felt that pharmacists had an ‘image problem’ in that patients and families and, indeed, HCPs were not aware of the roles that they could play in advising medication use. HCPs expressed concerns that even if pharmacists did take on this wider role, patients may prioritise information from their GP over advice given by a pharmacist, particularly in relation to stopping unnecessary medications at the end of life. Deprescribing or rationalising medications could be a more active role for pharmacists. However, some discussion was had about how this may lead to ‘difficult conversations’ about why preventative medications, such as statins, were no longer necessary and whether or not pharmacists would have the necessary skills to undertake, and potentially initiate, such end-of-life conversations.
The work of managing medicines
The importance of the methodological design of the workshops to provide both dissemination of findings and interdisciplinary conversations was confirmed when one group discussion was started by a nurse who characterised the comments of many of the HCPs across the 2 days:
I work as a nurse in the community and I didn’t realise the responsibility we put on the patients’ relatives, on medication, until this workshop. I didn’t realise we put a lot of responsibility on them and some of things we expect them to know . . . [this patient] was taking the medication the wrong way, because of her condition she got confused, every visit I had to go and explain, no you should be taking this at that time, this at that time. I ended up writing a simple format . . . for them to understand it, [to] do it correctly and today I just realised we just put so much on them.
As part of exploring how the ‘work’ being undertaken by patients and families could be reduced, discussions centred on communication, co-ordination, information and prescribing medications (Box 11). As noted in System and complexity, good-quality communication between HCPs, between HCPs and families, between primary and secondary care, and between HCPs and pharmacists was considered the foundation of delivering good end-of-life care. One PPI participant suggested that the default starting point should be to ‘assume patient and family know nothing’. Again, a key co-ordinator or key worker was noted as important, but there was debate about whose responsibility that could and should be, and acknowledgement that ultimately this often fell to the family caregiver. Consequently, family caregivers need to be included in discussions about medication and care and should have their insights, knowledge, reports and concerns listened to:
Listen to patients/carers about what they have noticed. Often key information is overlooked because we think we have the answers [as clinicians] without knowing full context of situation.
-
How can HCPs reduce the ‘work’ for patients and families?
-
What do you find works well in practice?
-
What do you find to be the biggest challenge?
Increasing the number of regular home visits was also considered to improve rapport, understanding of the patients’ needs and to avert crises.
Clearer, tailored information was considered essential in not only reducing workload but also anxiety and stress for families. Although all considered verbal information to be essential, backing this up with written information and ways to support families to instigate their own medication charts was featured as a central issue. As the nurse quoted above demonstrates, reiterating information verbally over and over may not work. As shown in Chapter 6, listening and retaining complex information is extremely difficult for patients and FCGs during a time of considerable strain and exhaustion. This was also considered important when regimens were changed, such as when patients were discharged from hospital. PPI participants emphasised the need for clearer information about who families could contact for help and support. Echoing findings from the case studies and BFCG interviews, participants acknowledged that information and training about the use of medication and equipment often fell through the gaps, with no one taking responsibility for this.
Discussions about prescribing and medicines use centred on ways to simplify regimens and to make medicine-taking easier. It was suggested that a simple planner could be provided to include the dose, time that it should be taken and what the medication looks like. Medication no longer needed should be removed, both from repeat prescriptions and physically from the home. Patients should not have to wait for their medicines to be ready when they were discharged from hospital, and a member of staff should go through the medications with the patient and FCG before the patient leaves. Pre-emptive prescribing of AMs was reported to be essential and reassuring for HCP and families.
Within the groups, some of the biggest challenges were reported to be not just a lack of co-ordination but uncertainty about who should assume responsibility for undertaking this role (i.e. ‘there are a number of fingers in the pie with only the FCG, a rookie, trying to co-ordinate’). Many HCPs felt that delays were often caused by a lack of access to records and the limitations of written records owing to time constraints. Nurses highlighted an issue with delays in their ability to administer prescribed AMs when there was a lack of written authorisation for them to do so:
Use of electronic records can be problematic, in that there is nothing in the patient’s home to indicate what is happening/why; number of patients live alone and depend upon HCWs coming in and all they have is the MAR [medicines administration record] charts; need paper, patient-held record in home.
A lack of paper records in the home was also seen as problematic by CNs, as it restricts their knowledge of who is coming into the home and what they might be doing or prescribing.
Alongside the problems, some participants identified things that worked well:
What works well in practice? Every aspect – somewhere – but not consistently everywhere, e.g. 24-hour line.
These included systems that enabled effective sharing of electronic records, medication reviews being undertaken and electronic repeat prescriptions. Good communication, especially between key HCPs, was thought to be facilitated by involvement of palliative care services and GSF registers that promoted interdisciplinary discussion. Patient-held records or communication books in the home were simple but effective ways of co-ordinating care. The importance of HCWs as a source of support for FCGs as well as patients was emphasised, particularly as a means of enabling patients to remain at home despite intensive care needs.
Diversity and disadvantage
Discussion groups that focused on the diversity and disadvantage theme deliberated a number of the same issues raised in the other two themes, but with greater emphasis on advocacy, holistic care planning, capacity issues and a system that facilitates a joint health and social care approach (Box 12). A dedicated person or advocate was considered key to supporting people with additional needs. This person built a relationship of trust and was able to co-ordinate care by providing a case management approach. For ethnic minority communities, this would be a person who could mediate cultural differences and potentially provide support through translation. Language barriers were recognised to be a specific issue for medicines management when patients and FCGs did not read or write English:
When there is a language barrier we quite often get people to write on the [medicines] box in their own language.
-
In your experience, what are the key issues in medicines management for patients from culturally diverse and/or socially disadvantaged groups?
-
What measures do you put in place to support patients in these groups?
-
How could support for managing medicines in these groups be improved:
-
at an immediate and practical level
-
at a policy or health services level?
-
There was a call for care planning that addresses needs more holistically to include mental and physical health, as well as end-of-life care wishes. A disconnect between physical and mental health services, as well as between health and social care services, often left gaps in provision and responsibility for patient welfare:
The care available [informal/formal] is much more vulnerable to being inadequate to provide the help the person needs. E.g. if someone is seen as being ‘inappropriate’ or there are ‘safety risks’, care is reduced/removed to protect the carers. Then the person who needed the help with meds is even more vulnerable.
General practitioner registration was reported as a barrier for some (e.g. the homeless). In general, the discussion groups recognised the need to ‘look at the individual’ and ‘stop trying to fit people into groups’.
Participants in the discussion groups cited a range of experiences, identifying key issues from culturally diverse and disadvantaged groups:
At point of discharge home from hospital – takes some time to set up an [interpreter] and we have them for an hour, so we have to get everyone within that hour; complexity can be disincentive, but good service to have; having interpreter can take the anxiety out of the situation, knowing patient understands; resource limited, and where does it go from there.
In particular, some individuals had experience of patients and family members with mental health issues, illustrating issues around risk assessment in the home being based on the assessor standards and how advance statements of patients’ wishes can be useful if professionals are confident in carrying them out:
In mental health [we] have a lot of advance statements, saying these are the people I want to deal with if I lose capacity, I give you permission to talk to them and like that, so . . . they’re more and more common; professionals need to be confident that they hold legal weight if they are to follow them, and this probably includes at the end of life.
A particular example of the intersection, or its lack, between mental and physical health was highlighted by one professional as they recounted a recent patient’s circumstances. The professional explains how both the patient and the FCG had mental health issues, with the patient having an additional diagnosis of advanced cancer:
Two individuals who were being managed by psychiatric services who said well we don’t know anything about cancer and then when you try to, we got support from specialist services in palliative care but not a bed because her behaviour was very chaotic . . . so we tried to manage it as best we could, but . . . the carer was giving not only her medication to the patient but the patient’s medication and the dog’s tablets. It resulted in the GP going out at 8 o’clock in the morning, the Macmillan nurse out at 7.30 in the morning to give medication to sort things out and then we had to safeguard the whole situation because the patient was vulnerable . . . it was almost like they had been invisible and unseen until this happened, they had been muddling along . . . until this physical manifestation of illness came into play . . . it kind of showed the cracks.
Conclusion
The workshops were an important way of disseminating the study findings and creating a wider interdisciplinary discussion about the issues these raised. These were very well-attended events and attracted a wide range of professionals, students, teaching staff and PPI representatives, although the absence of GPs was unfortunate. We tailored the group discussions to narrow the focus within the time constraints of the day, and this has helped to consolidate our analysis of the data from the previous two workstreams and to shape the chapters of this report. The themes clearly resonated with participants and they engaged extremely well with each of them, providing detailed discussions and comprehensive written notes.
Chapter 9 Discussion
Introduction
The study findings have documented the considerable effort required by patients and their FCGs in carrying out the complex work of medicines management for serious illness. This tended to intensify as the patient’s illness progressed, especially in the last months and weeks of life. This progression was depicted in the BFCG interviews and two patient case bereavement interviews in which participants looked back and reflected on the death of their relative. Families varied in terms of their circumstances and composition and in relation to the resources that they could mobilise through their informal and professional networks. Patients gradually relinquished responsibility for managing medicines to FCGs, usually to one key individual, with some tasks delegated to others (e.g. collecting prescriptions from the pharmacy). The key FCG was usually a spouse, in the case of couples, and an adult son or daughter, in the case of patients who lived alone. Where the patient was affected by progressive, long-term chronic illness, FCGs had gradually adopted the role of carer. Where onset was unexpected and deterioration rapid, FCGs could find themselves making a much more hurried transition to the role. Primary FCGs who were spouses tended themselves to be old and affected by frailty and poor health. Problems with prescribing and accessing medicines were frequently reported, by lay and professional participants, especially in critical situations and those arising OOH.
Families developed more or less elaborate and personally effective systems for managing medicines and recording use. The onus was on the patient and FCG to find out how to navigate a complex system of care. This could take a great deal of time and involved a considerable amount of luck, as well as effort. Patients and FCGs varied in the extent to which they felt supported by the professionals and services with which they interacted. The development of a strong relationship with a key professional was an important (but not sufficient) determinant of a positive experience of care. 15 Lay participants remained vulnerable to changes in a system over which they had little understanding or control. Although broadly appreciative of the care that they received from an NHS that they perceived to be under-resourced and under strain, lay participants described an experience of services that were often bureaucratic, task focused and poorly co-ordinated. Patients and FCGs described taking on the role of care co-ordinator, maintaining vigilance in their dealings with professional services and the medicines that could be prescribed, and changed, by different HCPs. They maintained and communicated up-to-date information about the patient’s medicines and tried to fill in the gaps in interprofessional co-ordination and communication. FCGs were frustrated when professionals failed to recognise their expertise and lived experiences, on the one hand, and their concerns and apprehension about managing complex and potent medication regimens, on the other. 15,152 Lay participants were overburdened with responsibility and did not feel that enough information had been provided to give them confidence, especially in relation to administering controlled drugs. FCGs described feeling that they were left alone to work things out for themselves. They came to realise that information and resources were available within the system, but these were effectively hidden because they were not made aware of their existence and often discovered only by chance.
Lay participants appreciated and worked to establish stable systems of care within informal and professional networks. Patients and FCGs valued continuity, particularly if they had established good relationships with individual HCPs. However, consistency of service rather than individual staff members was generally accepted. Problems and delays in accessing services, and problems of communication between and with professionals and services, were frequently encountered and criticised. Changes to personnel – either because of arbitrary shifts in the system or because of changes in the patient’s illness and circumstances – were out of participants’ control, but could have significant consequences for their well-being. Discharge from or transfer between services could rupture established relationships and routines and disrupt carefully established regimens of medicines management. Families could be overwhelmed by rapid changes in the patient’s condition and in the medicines prescribed to control distressing symptoms in the last stage of life, especially when a cascade of care and different prescribers entered the fray, as well as new and different services. In the intensely charged period during which the patient was dying, families could find themselves dealing with professionals who had no knowledge of the person, but assumed responsibility for making very significant decisions about their care. This applied particularly to urgent home visits, especially made during OOH, and contacts to emergency services and helplines. BFCGs described widely different experiences of their relative’s death and the period leading up to it. In some cases, symptoms were well controlled. Others described the experience of their relative dying as intensely distressing, with poorly controlled symptoms, especially pain, and lack of access to prompt or effective professional input.
Health-care practitioners acknowledged the work of patients and FCGs in managing medicines and sometimes expressed awareness of the demands and burdens that this could impose. However, they tended to assume the willingness of FCGs to shoulder the responsibility for home care and do whatever they could to support their relative, particularly to remain at home, without being fully aware of what this personally entailed for the individual within the domestic setting. 152,153 Professional participants, particularly nurses, described giving patients and FCGs explanations about how to use their medicines and sometimes undertook a review of what had been prescribed. Beyond that, they did not often follow this up and enquire about how these were being managed or proactively investigate whether or not any practical problems were arising. The pharmacist’s role was usually confined to supplying prescribed medicines and participants found their home delivery service valuable. However, both professional and lay participants identified problems of supply and access to medicines, especially controlled drugs and OOH.
The burden of treatment
May et al. 7,74,154,155 have called attention to the excessive burden that health-care services impose on patients and FCGs in complying with complex treatment regimens, and the need for these to be streamlined and simplified to realise the goal of ‘minimally disruptive medicine’. Co-opted family caregivers have become an essential resource that underpin the system of professional health care, as the boundaries between private and professional spaces become increasingly blurred. 2,4,5,8,33,131,156,157 Patients and FCGs are being asked to undertake tasks formerly carried out by professionals, but with little, if any, training or supervision. 14,31,60,158 The shift in cost and responsibility for care from institutional to domestic settings is spearheaded by an ideology of ‘responsible citizenship’, a consumerist model of health care that valorises personal autonomy and patient ‘choice’ and the expectation that most people wish to age and die at home. 9 However, little attention has been paid to the experience of patients and FCGs confronting death at home or the challenges involved in providing intensive care. 157,159–162 The Managing Medicines study has highlighted that dying at home is difficult and that FCGs require a degree of professional accessibility and support, which is not always forthcoming. 15 Failure to control pain and other symptoms caused great anxiety and distress for patients and FCGs. 8,33,42,46,163–165 HCPs in the present study rarely conveyed a high level of awareness or insight into the difficulties families confronted in handling either the responsibility or the sheer work of managing medicines, and the amount of scarce time and energy that had to be expended on basic tasks. These included ordering, obtaining, calibrating, administering, recording and storing medicines in the home, and liaising with professionals about changes, errors and problems with prescribed medication. 41,42,60,165 Patients and FCGs often took on the role of care co-ordinator, maintaining ‘hypervigilance’39 in their dealings with services and HCPs and filling in gaps in information and co-ordination between these. O’Hara et al. 166 refer to the proactive work of patients and FCGs as ‘reaching in’ to create a ‘scaffold’ to support the quality and safety of care and compensate for system complexity. HCPs did not often attend proactively to the details of how patients and FCGs felt about managing medicines in the home, as well as the practical difficulties and concerns they confronted while doing so and the tensions and conflicting interests arising between patients and family members. 14,19,167 The challenges involved in managing medicines in the home can be intense, if not overwhelming, especially in the last weeks and days of life. 7,14,16,39,74 However, the realities of care remain overlooked in the policy and public166 perpetuation of an idealised depiction of care at home as a prerequisite for accomplishing ‘a good death’. 3,4,9
Navigating care in a complex and fragmented system
It is disappointing that patients and FCGs continue to report an experience of fragmented and poorly co-ordinated care,19,39,126,131,155,157,159,168,169 especially in view of policy goals of seamless service delivery following the End-of-Life Care Strategy in 200827 and resulting tools and processes such as the GSF and End-of-life Care Pathway. 170 More recently, there has been a great emphasis on the work of Sustainability and Transformation Partnerships as a means of integrating and simplifying care. 171 However, the National Audit Office reports limited progress172 and a lack of robust evidence that these schemes have delivered the expected benefits in reducing costs and hospital admissions and in improving patient experience of care. 173 Many local initiatives and commissioning bodies focus on horizontal rather than vertical integration of services, especially in relation to social care. Expectations of the benefits to be achieved through integrated care tend to outstrip evidence of their effectiveness, particularly in relation to patient experience of treatment, possibly because the service developments involved appeal more to the goals and values of professionals rather than the public. 173,174 Notably, moves to achieve greater integration of care have not yet succeeded in reducing the trend towards increased hospitalisation, particularly of frail and terminally ill patients. 175 Going forward, the NHS Long Term Plan176 aims to improve the efficiency and convenience for patients by putting an even greater focus on integrated care systems, including increased use of digital technologies and the creation of primary care networks to achieve greater integration of services at a local level.,177 Whatever benefits the NHS Long Term Plan176 may deliver, it contains virtually no reference to palliative and end-of-life care. Rather, it perpetuates a rhetoric of patient empowerment, responsible citizenship and ‘transformation’, which has questionable relevance to the reality of dying, particularly following the prolonged experience of comorbidity and frailty, which characterises the epidemiological transition of the current century. 1
Participant experience reported in the Managing Medicines study showed that current levels of integration between the primary and the secondary care interface was largely insufficient during transfer to and from home to hospital. Families’ experience of care was shaped not just by the relationships established with individual HCPs, but by how these professionals inter-related with each other. 15,98,99,178,179 Consequently, the lack of timely and effective communication between hospital and community HCPs resulted in confusion and delays for patients’ access to medicines. Patient and FCGs described the considerable time and effort required to resolve these issues. The dysfunctional consequences of complex, bureaucratic and poorly co-ordinated systems of health care affect HCPs as well as patients and FCGs. For example, DNs described being subject to the same difficulties as patients in telephoning through to GPs or practice receptionists when seeking advice about changes to use or prescribing of medicines. Professionals, as well as lay participants, found the health-care system hard to navigate, having access to only a partial knowledge of its component elements. HCPs tended to have little knowledge or understanding of the functions and roles of specialist services and professionals with whom they did not regularly interact. The hospital–community divide was a case in point. In our construction of patient case ecograms, it became quickly apparent that much of an individual’s network (lay or professional) is invisible to others. Keeping track of rapidly changing developments involving different services and personnel was challenging, especially when information sharing was impeded by use of different electronic systems. Professionals who had no knowledge of the patient could be charged with making significant decisions about care and treatment.
Patients’ and FCGs’ partial understanding of how the health-care system worked, alongside its lack of responsiveness, was one reason for making direct use of hospital accident and emergency services. 180 However, this could also result from familiarity, as participants had worked out the most effective ways of accessing the help that they needed. A cluster of patients affected by COPD bypassed community staff and their GP and called an ambulance directly to take them straight to hospital when they realised a relapse in their condition was imminent. 180 These individuals had a good understanding of their illness and felt confident about managing this within a simple network with few active professional links. There is not necessarily a direct connection between complexity and a negative experience of uncoordinated care, although this is suggested by our analysis and is a question worth exploring in further research. Moreover, patients with complex networks tended to engage directly with a small number of professional contacts, with many other links being episodic, marginal or negative. For example, in contrast to the simple networks of the patients with COPD, the patient cases with the most complex ecograms tended to the least functional. For example, although aware that he was included in the PRISM (Pathway and Referral Implementation SysteM) scheme, an integrated care system or ‘professional hub’, Mr Crispin had no idea what this involved and did not perceive any benefit. His GP, in contrast, was enthusiastic about a scheme that he felt had potential for linking-up multiple services and sources of professional expertise on which he could draw. However, it is precisely this multiplicity that can prove problematic for patients. It is possible that schemes, such as PRISM, may be more attractive as a resource for professionals than for patients and their families who value consistency and simplicity, rather than change and diversity in their dealings with the health-care system. 154 An alternative model is based on the development of self-governing Buurtzorg nursing teams developed in the Netherlands and trialled elsewhere, including in the UK. Rather than work on mechanisms to integrate a complex array of specialist professional services, this model is based on ‘integrating simplicity’. Small teams of CNs work together within a flat organisational structure to provide all aspects of health and social care and organise referral to additional specialist services as required. 181–184
Feeling supported by the system: the role of the key professional
The availability of a HCP who took on the role of a key professional (or key worker) was highly valued by the families who had managed to establish such a relationship. In a few cases, participants characterised staff at a particular clinic or hospice day service collectively as their key contacts. A key professional relationship helped participants to feel safe and, also, to ‘feel known’ within the system. 39,153 This was the ‘go-to’ person when problems or queries arose, who had an in-depth knowledge and understanding of their case and could proactively help in navigating the system. The benefit of a single point of contact has been reported in other studies. 39,131,185,186 In the Managing Medicines study, key professional relationships were established with HCPs from community, hospital and hospice settings, and tended to be with someone in a nursing role, occasionally a GP or consultant. These relationships seemed to develop serendipitously from an elective affinity between the parties involved (agency), rather than the result of deliberate allocation or organisational properties of the system (structure). There is considerable scope for this role to be routinely formalised and developed further. The role of the key professional could be flexible and wide ranging, including, for example, co-ordinating and liaising with services and other HCPs to simplify and streamline care and mitigate the negative impact of change. It could include providing and sourcing information about medicines, reviewing and optimising medicines prescribed and used, identifying and explaining changes that needed to be made, as well as providing training and support to FCGs in taking on the responsibility for more challenging aspects of medicines management, such as administering subcutaneous injections and judging dose and frequency of pain relief. The key professional could play an important role in liaising directly with prescribers regarding medicines-related issues, regardless of whether or not they were themselves prescribers. 126 Key professionals could also help families make appropriate judgements about when and where to access help – reportedly a widespread concern – and support FCGs to achieve credibility and a voice within the wider system of professional health care. 8,39,180 Although the role of the key professional or key worker has been widely advocated as a quality marker and means of co-ordinating end-of-life care,185,187 these did not feature in cases reported in the study. The one participant who mentioned having specifically been allocated a key worker had never met or had any contact with the individual concerned.
One of the most frequently expressed shortcomings of patient and FCG experience of the health-care system was that, from their perspective, the system was insufficiently responsive to the needs of patients when they were dying. Participants felt that this circumstance merited special consideration and that there should be a co-ordinated way for the system to acknowledge and share information to expedite effective help. It may well be that professional recognition of the patient’s prognosis had been logged and shared, for example, through general practice GSF meetings, but this information, and subsequent decisions about care, was not communicated to families. 188 Families who had been coping well could quickly feel out of their depth as the patient’s symptoms changed or worsened in the days or weeks prior to death. At this point, having rapid access to responsive sources of help that are available 24/7 was critical to their capacity to cope. This was another point at which ‘being known’ within the system was significant. Having repeatedly to tell and retell one’s story to different and frequently anonymous 111 telephone service staff was alienating and frustrating. Only a few participants had access to a SPA telephone number. This was helpful, particularly in providing a sense of security, regardless of whether or not the service was used. However, it was likely to have been discovered by a chance encounter, rather than a systemic process of information provision. Contact with helpline services was frequently medicines related. At the time of the study, neither 111 nor the SPA services were specifically equipped to deal with medication-related issues. The introduction (November 2019) of an NHS Community Pharmacist Consultation Service within the 111 service is welcome. However, it is not clear from the current specification that this service could resolve many of the urgent queries and concerns reported by participants in the study, particularly around use and access to controlled drugs for patients receiving palliative care. Moreover, access is through referral from a GP or the 111 service, rather than direct. Cancer patients were more likely than others to have access to 24/7 helplines provided by local palliative care and hospice services, but this was by no means always the case. Provision appeared to be idiosyncratic and patchy. Nationally, the provision of specialist 24/7 helplines for patients approaching the end of life is reported to be available in a relatively small number of areas,189 despite being recognised as a priority. 23,168,190
Communication and complexity
Poor communication between patients and HCPs is a frequently cited source of dissatisfaction and experience of poor end-of-life care. 168,191 The nature and function of small-world networks seemed to be a key determinant of the quality of experience of communication and care by patients and families, including whether or not the GP and pharmacist had an efficient system of co-ordinating medicine prescriptions and supply (and ironing out problems arising from these), and whether or not the GP had confidence in the judgement of DNs about use of AMs. 124 The efficiency of transfer of information between staff and services was crucial. HCPs greatly appreciated the efficiency of communication when the same information technology system was used by different services and enabled full access to patient records. Where this was not the case, bottlenecks were described, including delays in specialist clinicians communicating with GPs, lack of integration between systems of electronic records (e.g. EMIS and SystmOne) used by different parts of the system and lack of information available to OOH clinicians and CPs. 192 Lack of access to patient medical records has been cited as a particular barrier to effective medicines management,19 including use of AMs,99 and greater engagement of pharmacists within palliative and end-of-life care. 22,55,57,97
Specialist versus generalist care
We were interested to see if there was a discernible difference between the care experiences of patients affected by cancer as a primary diagnosis compared with those with diagnoses other than cancer, and among patients who had received SPC and those who had not. All patient cases and the deceased relatives of BFCGs who had been affected by cancer had been referred for SPC, as had most of the others, although cancer patients evidently had more extended input. Some participants who had not received SPC input had long-term support from disease-specific CNSs who were experienced at caring for patients at the end of life. However, too many individual factors relating to the type and stage of illness, the point at which referral was made and the extent and duration of SPC input made it difficult to systematically compare this aspect of care across the relatively small number of participants included in the study. The same applies to patient and FCG experience of hospice care. Most participants were positive about this, especially those who had long, established relations with staff and services. However, participants who were not referred to hospice did not report less satisfactory care. It should be noted, in either case, that there was no clear correlation between participants’ assessment of the care they had received and whether they felt that good symptom control had been maintained or ‘a good death’ achieved. Participant experiences – and their assessment of these – were variable and complex.
Diversity and disadvantage
The intrinsic disadvantage affecting all patients experiencing terminal illness is compounded through additional sources of vulnerability, such as living alone, having physical or sensory impairment, or experiencing social or economic disadvantage. 189,193–195 The study sought to incorporate diversity in participant experience and to include patients and FCGs from minority and hard-to-reach groups that are medically underserved and not well represented in mainstream research. 79,82,83 In this context, diversity referred to patients affected by conditions other than cancer, from ethnic minority groups, or to patients who were affected by the often interlinked factors of socioeconomic disadvantage, sensory or physical impairment, severe mental illness, living alone, homelessness or substance abuse. The small amount of research into end-of-life care for disadvantaged groups has focused primarily on issues relating to inequality and access to services, rather than the challenges of symptom control and medicines management. 82,196–199
We achieved inclusion of diversity in illness condition, particularly in the patient cases, and in incorporating the experience of patients with additional disadvantage, such as living alone, being affected by sensory or physical impairment, dementia and learning difficulties. The sample included limited representation of the experience of ethnic minority participants, all three of whom were from Asian backgrounds. We were not able to directly recruit participants affected by serious mental illness, homelessness or substance dependency. Recruitment of all participants to the Managing Medicines study was challenging, particularly those from diverse or particularly vulnerable groups. We depended on clinical gatekeepers to identify eligible participants and provide them with information and an invitation to take part in the study. Understandably, clinicians were protective of patients whom they perceived to be particularly vulnerable and with whom they felt it was not appropriate to broach participation in the study. However, we did obtain some insight into the particular issues of medicines management with patients affected by serious mental illness, substance dependency and homelessness from the detailed accounts of specific cases given in the HCP interviews. The key issues reported related to problems with prescribing, safe storage and disposal of controlled drugs, problems in symptom control, especially pain, when medicines were not easily accessible, and maintaining contact with individuals, particularly those without safe accommodation or access to FCG support. 199
Several HCPs described their proactive and innovative responses to such problems and the considerable effort they were willing to make to support patients and FCGs affected by homelessness or substance dependency, particularly their commitment to respecting individual preferences, even when these were very much at odds with the mainstream. Overall, however, HCP accounts did not strongly feature care of patients from diverse or minority disadvantaged groups as a significant aspect of their work. The need for, or use of, translation services was not common. The Asian patients included in the study described being enclosed within small but effective networks of family and community services, within which their relationship with the GP who could converse in their native language was particularly significant. Older patients may still rely on younger members of their family to communicate with HCPs and for knowledge and understanding of their medicines and options available for health care. Lack of awareness of services, including hospice and palliative care, has been widely attributed as a cause of reduced use among ethnic minority groups. 84 It may be significant that none of the three Asian patients had been referred to SPC. Their experience highlights issues of communication and literacy, which affect more than individuals from ethnically and linguistically diverse groups. Beyond the domain of community care, their FCGs reported similar problems in dealing with a complex and poorly co-ordinated system to those described by other participants, and more widely in the literature. 193,196
Reduced and late access to SPC is widely reported in the literature for all patients with diagnoses other than cancer. 193,194 However, patients from marginalised and vulnerable groups are less likely to receive palliative care, and when they do this is likely to happen at a late stage of their illness. 79,198,200 People who are homeless and/or affected by additional difficulties, such as serious mental illness or substance dependency, die at a considerably younger age than the rest of the population. 197 HCPs are less likely to recognise that younger people are approaching the end of life. 189,196 Accessing effective pain and symptom management is difficult, particularly when professionals lack experience with addiction or if patients are unwilling to disclose their drug use. 201 Vulnerability on the streets, substance misuse and limited access to pharmacy makes the management of medications an additional complexity when someone is terminally ill. The storage and administration of medications in hostels is also reported to be problematic, as staff have no training in this area. 196,202 The challenges resulting from system complexity and poorly co-ordinated services affect all patients, but are compounded for those who are vulnerable and marginalised within mainstream health care. 189,196 The results of this study support wider calls for the need for further research among diverse vulnerable and disadvantaged patient groups, specifically with reference to how medicines management is undertaken as individuals approach the end of life. The experience of patients experiencing severe mental illness should be a priority, as these have been a particularly neglected group. 198
Risk and responsibility
The challenges of meeting the increased demands of home care, including medicines management, have not been adequately acknowledged. The strongly promoted policy preference for dying at home has created normative expectations of FCG support for dying relatives. Many families may be strongly committed to this outcome, but by no means all. 203 Patients may lack available family members or other sources of informal support, especially those who have outlived their spouses and are living alone. Notwithstanding the desire, families may lack the resources or capacity to provide home care, particularly if FCGs are themselves old and in poor health or living far away. 3 Lay and professional attitudes to risk involved in medicines management, including use of controlled drugs in the home, vary widely. Some families felt that they were handed more responsibility than they felt comfortable with managing. They felt intimidated by the task of storing and administering controlled drugs, which outstripped their capacity to cope. 3,8,42,126 Participants in the Managing Medicines study, as in others, have commented on concerns about causing harm by giving relatives the wrong dose of medicine, particularly pain relief, and about making the wrong judgement about when and how much medicine to give. 42,61 Their anxiety is compounded if support and advice is not readily available round the clock. Other participants were willing – sometimes keen – to extend their role in managing medicines and learn techniques of administration, such as giving injections, administering AMs, replacing syringe driver cartridges or managing dialysis. 112,133 Taking a proactive role could be valued as a means of providing rapid pain relief and reducing dependence on HCPs. FCGs could be frustrated when professionals did not acknowledge their competence and expertise. 131
Professionals varied, also, in their personal thresholds of risk acceptance or aversion and how they assess the competence of families and the suitability of the home environment. Some families were willing to assume greater responsibility for patient care than HCPs are willing to delegate. 131 The question is how should considerations of risk and responsibility be balanced, and in such a way as to take account of the consequences of changes in the patient’s illness trajectory? This applies especially when the work involved in medicines management is conflated with intense emotional engagement and distress arising from deterioration in the patient’s condition and the anticipation of death being imminent. In the Managing Medicines study, we found that some FCGs who had developed confidence in managing medicines regimens during relatively stable stages of the patient’s illness found their equilibrium disintegrated with the changes in symptoms and prescribing occurring in the last weeks or days of the patient’s life.
These findings raise issues about what it is reasonable to ask families to do, and how the limits to family engagement can be acknowledged and tailored to individual resources and situations and the changes occurring over time. 131 Schemes extending family involvement in managing medicines for dying relatives have proved successful, especially in Australia, where the logistics of distance and geography prompt innovative solutions regarding access to professional help. 57,129,131 Local schemes or research projects have been undertaken in the UK, but are not widespread. 133 Regardless of the role that patients and families wish to take in medicines management, it is important that this should be explicitly discussed, agreed and kept under review throughout different stages of the patient’s illness. All patients and FCGs should have round-the-clock access to responsive, expert help and advice about medicines management and symptom control. 23,61 There is considerable scope for use of telemedicine-related technologies to facilitate this access, and it is likely that these will remain more widely used following the COVID-19 pandemic. 204–208
The widespread practice of anticipatory prescribing has increased the amount of controlled drugs stored in patients’ homes, often for an extended period of time. 68,124,209,210 Many of these are not used, raising concerns about the risk of misuse or criminal diversion and waste. 99,126,211 Beyond the observation that relatives should be informed that they should return controlled drugs and other unused medicines to the pharmacy after the patient’s death, there do not seem to be any procedures for monitoring how such drugs are disposed of in the home. 212 HCP participants monitored the supply, storage and use of controlled drugs while the patient was alive, but appeared to pay little attention to their fate afterwards. FCGs expressed concern about storage of controlled drugs in the house and about their role in administering these to patients. They were keen to remove them from the house following the patient’s death, and several expressed concern and resistance to being allocated responsibility to return them to the pharmacy (see Chapter 7). It seems that little is known about the disposal of AMs in the community and that it would be helpful to have clearer procedures for these. However, FCGs and some HCPs felt strongly that family members should not be handed responsibility for this task.
The role of the community pharmacist
Historically, the CP role has been marginalised from the mainstream MDT, with a focus limited largely to medicines dispensing and supply. 101,213 More recently, professional and policy initiatives have provided opportunities for CPs to substantially extend their role and to engage directly in patient care. This includes services such as new medicines reviews and providing vaccinations, blood pressure checks and non-medical prescribing. 102,214–218 The public are encouraged to consult CPs for advice about treatment of minor ailments as a means of reducing the load on general practice and community health-care services. 216 This is in the context of a continuing anticipated decrease in the number of GPs, DNs and community matrons. 219,220 The recently introduced NHS Community Pharmacist Consultation Service provides access to pharmacists through referrals from GPs and the NHS 111 telephone service. This is intended to reduce the pressure on acute emergency services. 177
To date, however, CPs have played little part in supporting medicines management at home for patients receiving palliative and end-of-life care. 221 In the Managing Medicines study, CPs were considered primarily suppliers of medicine, with little acknowledgement of potential for greater involvement. Pharmacists and other HCPs, including GPs, rarely reported that other HCPs asked CPs for advice about drug choice and prescribing issues. Where discussion occurred, it tended to be about what the CP could/did stock and possibly alternative brands/products if a prescribed drug was not in stock. There were no references to CP involvement in non-medical prescribing by any participants within the study. This is in accordance with wider findings that the practice of non-medical prescribing among CPs and other HCPs who have completed training is low, especially in palliative and end-of-life care. 102,109
Patients and FCGs preferred independently owned or smaller-branch community pharmacies, as well as those attached to general practices, which were more convenient. Home deliveries were valued by most participants who received these, particularly when access would otherwise have been difficult. However, one consequence of this service was the reduced face-to-face contact with patients and FCGs, hindering the scope for more direct involvement in care. Indeed, when the process of prescription and supply was running smoothly, the pharmacist’s input to the process tended to go largely unnoticed and unremarked. Several patients or FCG participants observed that they preferred to collect their prescriptions directly because they welcomed the personal contact with pharmacy staff and the opportunity to discuss their medicines and ask questions. This also contributed to the sense of ‘being known’ by staff and services within the system, which was an important component of a positive experience of care. The study findings illustrated the impact that a more proactive stance on the part of pharmacists could have in optimising patients’ experience of using medicines. Examples include pharmacists taking the initiative to streamline or automate the process of accessing medicines, in contacting the GP to resolve prescribing issues and in suggesting alternative formulations (e.g. liquids rather than tablets) that would be easier for patients to take.
In relation to end-of-life care, CPs remain an underused resource. 55,101,221 Recent initiatives within the UK have shown the potential contribution that pharmacists could make in supporting medicines management for palliative care patients in the community, but these remain episodic, limited in scope or disease specific. 104 A number of barriers to greater integration of CPs within palliative and end-of-life care remain hard to resolve. 222–224 This is despite the long-standing commitment of greater integration of community services within the NHS. 219 This was most recently set out in the NHS Five Year Forward View and subsequent initiatives,171,225–227 alongside the development and increased used of digital technologies to improve access and communication between patients, HCPs and services within the community and across the primary–secondary care interface. However, it is acknowledged that progress has been slow. Most patients are not feeling the benefits of better co-ordinated care. 181,226
The nature of the relationship between GPs and pharmacists was an important determinant of patients’ and FCGs’ experience of medicines access and supply. Where communication and organisation were good, and a well-worked-out collaboration established, the process of medicines supply went smoothly and problems that did arise could be promptly resolved. When it was not, participants described experiencing delays or errors in their prescription and having themselves to make the effort to intervene and get the issue sorted out. Although access to summary care records is now established, lack of access to full patient medical records has been frequently cited as a major barrier to greater CP involvement in patient care. 178,192,228 This contrasts with the situation in other European countries where shared access has been long established. 228 Pharmacists reported that without knowledge of the patient’s medical record, they had no way of knowing that he or she had been flagged as end of life, although eventually they may deduce this from the drugs prescribed. It is not just CPs who are affected by problems of information sharing, separate information technology systems also make it hard for HCPs from different services to communicate and co-ordinate care. 227
The Royal Pharmaceutical Society (London, UK) has estimated that CPs could prevent 10% of GP consultations and 5% of accident and emergency attendances. 104 However, barriers to greater involvement of CPs in patient care are long-standing. Apart from issues of professional hierarchy and marginalisation, there are problems of cost, payment time and other resources. Some local schemes have enabled CP access to patient medical records. However, as was evident in the Managing Medicines study, patients receive prescriptions from different prescribing sources and may have to access them from more than one pharmacy, which makes access to records more difficult. It also remains to be established whether many CPs actively wish to engage in end-of-life care or prefer other forms of service development and diversification. 229
The contribution of domiciliary home health-care workers
The study findings highlight the important and hitherto neglected contribution made by domiciliary HCWs in supporting dying patients at home, including managing and administering medicines. This support is particularly important for older people living alone who wish to remain at home. 36 Some patients in the study had long-term support and intensive packages of care. In other cases, domiciliary care was in place only to cover a critical period of days or weeks prior to death. HCWs undertake a wide range of tasks, not least of which is providing companionship and emotional support for patients and their FCGs. 230 In relation to medicines management, a wide variation was reported in the tasks and responsibility undertaken by HCWs, from prompting patients to take medicines to directly administering controlled drugs. This reflected diversity in provider organisations and training. 231 However, families reported the very significant contribution HCWs made to their ability to cope with care at home. The scope for greater training and involvement of HCWs in supporting medicines management in end-of-life care for patients dying at home is an important area for further research.
Strengths and limitations of the study
The substantial body of qualitative data collected by the Managing Medicines study enabled a very detailed account and comparison of the experience and perspectives of patients, FCGs and HCPs about the work of managing medicines for seriously ill patients being cared for and dying at home. The interviews with BFCGs provided complete narratives of the experience of illness and process of care through the last months of life and the patient’s death. The professional interviews provided comparative perspectives from a wide range of different roles and highlighted the limited understanding of the difficulties and demands of medicines management frequently experienced by patients and family caregivers, as well as concerns about the difficulties of giving as well as receiving care in a complex system, within which communication and co-ordination of services was often difficult and inefficient. The patient case studies gave insight into how patients and FCGs adjusted to the process of care, as symptoms and medicines changed over a period of several months and enabled us to triangulate data from a range of different sources (i.e. patients, FCGs, HCPs, photographs, observations and review of medical records). A longer period of follow-up would have deepened our understanding of families’ experience of managing medicines in end-of-life care, but was beyond the resources available to the project. The cases included patients with very different conditions and circumstances. Alongside the singularity and diversity of individual experience, our analysis also identified recurring themes relating to the two broad issues of the work of medicines management and the impact of a complex system of care on patient experience, resilience and access to resources. It was not the aim that the study findings be directly generalised to other settings, but rather to provide in-depth insight into patients’ experience and practice. However, they are supported by findings from the limited number of previous studies from the UK and wider international literature.
It is the nature of qualitative research that the focus of investigation develops in its own terms as the study progresses. Lines of enquiry and topics of interest that were not initially envisaged may become apparent, as do the practical limits of realising original objectives in complex real-world settings. We had intended to recruit a substantial number of participants from diverse patient groups and minority, underserved and disadvantaged communities; however, we found recruitment of these participants to be particularly challenging. In part, this was likely due to issues such as language barriers and cultural differences around talking about death and dying. We were, however, successful in recruiting patients with conditions other than cancer, those with disabilities or dementia and those from a range of rural and urban, affluent and economically disadvantaged areas. The three ethnic minority families recruited to the study were Gujarati, and we did not manage to include participants from a wider range of ethnic backgrounds. Nor did we succeed in directly recruiting patients affected by substance dependency, serious mental illness, homelessness or other forms of social disadvantage. Some insight into the particular difficulties of managing medicines in end-of-life care for patients as well as HCPs was provided by the accounts of professional participants who had experience of supporting individuals experiencing different forms of disadvantage.
Diversity of diagnosis was achieved in the sample by recruiting through different services that were sometimes approached directly or on other occasions through referral from someone with whom the research team already had a working relationship. The latter process was most productive. Recruiting diversity in terms of ethnic minority participants was harder to achieve. The research team did not start with established connections within relevant communities, which take time to build. This reflects the fact that this aspect of the study was a late addition, requested by the funders, rather than an integral part of the study design. The team made efforts to recruit through five different community groups operating in Nottingham and Leicester. However, this resulted in recruitment of only one BFCG. It was not appropriate to attempt to recruit patients to take part in case studies through community groups, given the sensitive nature of the research. For this, we were dependent on our clinical gatekeepers, who reported that patients from diverse and underserved groups made up a small part of their caseload.
At the outset, we were interested to see if there was a discernible difference in the care experiences of patients affected by cancer as a primary diagnosis compared with those who were not, and among patients who had received SPC and those who had not. This distinction turned out not to be relevant, however. All patients affected by cancer and some of those who were not had received input from palliative care services. Most patients who had not been referred to SPC had long-term support from disease-specific specialist CNs who were themselves experienced at caring for patients at the end of life. In addition, it was not feasible to compare the experience of patients at different stages of their illness in relation to the extent and duration of palliative care. Too many individual factors made it difficult to systematically compare this aspect of care across the cases. A comparative focus on groups of patients affected by specific conditions would be required to explore this question.
A further intention, at the start of the study, was to undertake a simple qualitative analysis of how the work of medicines management was distributed across patients’ social networks, including both informal and professional sources of care. The process of completing the ecograms provided a prompt for participants to think through and reflect on the nature and significance of the different kinds and sources of support they received, including those that were negative or absent. However, the elusive nature of the social network and their representation quickly became apparent. Participants approached the task of drawing an ecogram with widely different perspectives and commitment. Ecograms drawn by different participants in each case varied in the links identified and how these were assessed. They were often very selective and contained many omissions. The study revealed the extent to which individual ecograms are a construction, or artefact, of the interview and setting in which they are produced. As we wished to gain an idea of the range of individual networks and the resources to which participants had access, we opted to draw on all relevant information available throughout the case. Consequently, the ecograms reproduced in Appendix 1 are quite deliberately a composite, or construction of the researchers rather than the individual participants. We have been careful not to overinterpret the comprehensiveness or significance of an interpretive exercise in reconstruction. However, taken together with the wider data we have about each case, the ecograms have enabled us to easily visualise and compare the network of care, including informal and professional links and the range and nature of contacts, as a way of aiding analysis of each case. They also provide a simple way of exploring the range and distribution of informal and formal contacts and their significance within each case, particularly the importance of relationships and communication between HCPs and professional services, as well as between patients and professionals.
Finally, we have omitted consideration of the fifth objective as stated in the study protocol. This referred to the formulation of empirically founded recommendations for service development and effective commissioning to improve the care and experience of patients dying at home, and that of their FCGs. However, it is a condition of Health Service and Delivery Research programme funding that project reports should not make recommendations for policy or practice. Consequently, we have framed our implications for practice in terms of topics and priorities for future research.
Conclusion
The Managing Medicines study has documented the work involved in managing medicines at home for patients approaching the end of life as a core part of a considerable burden of care. In this respect, it adds considerably to the available literature on this topic, particularly through the case study triangulation of professional, patient and FCG perspectives, and the narratives of BFCG’s experiences of the period leading up to the patient’s death. The findings reveal the resourcefulness of many participants in developing routines and schedules of medicines management and the process of gradually working things out as they grappled with the confusion and impenetrability of a complex, fragmented and bureaucratic system of care. They also highlight the extent to which families struggled with different tasks and stages of illness, particularly in the weeks and days prior to the patient’s death. The difficulties caused by complexity, the need for 24/7 SPC help for dying patients and their families, and the value of a key professional to help families navigate the system have been widely reported over a considerable time. NHS policy has been directed towards developing effective solutions and a clear vision of streamlined, supportive and co-ordinated care. Integrated care remains a long-term goal and the commitment to providing 24/7 access to support for terminally ill patients is well established. Translating this vision into reality remains elusive, but must surely be based on an understanding of patient and FCG experiences and perspectives of illness and what is most valued in the provision of excellent health care.
Chapter 10 Conclusions
The Managing Medicines study identified two key and inter-related areas in which patient and FCG experience of managing medicines at home in end-of-life care could be improved: (1) reducing the work of medicines management and (2) improving co-ordination and communication in health care. The complexity of the health-care system and requirements for patients to access multiple parts meant that there were many points at which things could go wrong. The burden of treatment theory proposes that improvements to patient and FCG experience of care require an understanding and modification of the structurally dysfunctional elements of health-care systems, rather than focus entirely on intervening at the level of individual practices, such as improving communication skills. Access to support, resilience and coping capacity is mediated through the resources available to patients, the relationships that they have with people in their personal and professional networks, and beyond that through the wider connections – or disconnections – that these links have with others.
The NHS has struggled to achieve systems of user-friendly integrated care that centre on the patient. NHS costs and unscheduled hospital admissions continue to rise despite ongoing efforts to reduce them. Despite a rhetoric of patient choice and patient-centred care, there is little evidence that such initiatives start from an understanding and receptiveness to patient and FCG experience or perspectives about care, and the changes required to improve this. The Managing Medicines study collected a detailed body of qualitative evidence that we hope will increase professional awareness and understanding of the substantial challenges faced by patients and FCGs managing medicines in the home at the end of life and how they may be better supported in this endeavour.
The detail and complexity of the case study data provide a sense of the everyday work that families undertake in managing medicines and the associated demands incurred over time. The BFCG interviews provide accounts of the process of caring for a dying relative in its entirety, in which participants reflected on their experiences throughout a process that was usually very challenging and intrinsically distressing. The triangulation of professional, patient and FCG perspectives in the longitudinal case studies provided insights into the problems confronting different stakeholders over time and how they attempt to resolve these. The quality of the connections between HCPs and services have a direct impact on patient and FCG experience of prescribing and access to medicines. They also affect if and when the patient is recognised to be dying and the treatment and prescribing decisions that follow. The patient case studies and BFCG interviews enabled an analysis of what patients and FCGs valued in their dealings with health services and professionals and how they worked to navigate a complex, bureaucratic system of care. They also expose areas of concern, including lack of access to rapid and effective support when problems arose, especially in the weeks and days prior to the patient’s death. The professional interviews revealed the considerable efforts and resourcefulness that HCPs could bring to bear in addressing issues of medicines management for terminally ill patients, especially those affected by disadvantage. They also reveal the extent to which professionals often had a limited awareness of the burden of treatment confronting families and the difficulties that they encountered, particularly in accessing help during a crisis.
The study aimed to explore the different perspectives of key stakeholders in the context of medicines management as a collaborative effort between families and professionals. Within a complex system of care, which many participants (professional as well as lay) experienced as fragmented and uncoordinated, effective collaboration was often lacking. Where many professionals and services were involved in an individual case, lack of communication and joined-up care increased the burden of treatment, as everyone ‘gave’ but no one ‘took away’ accumulating tasks and medicines for the patient and their family to deal with. The scope for improving patient and FCG experience of care is considerable, as was illustrated by participants’ accounts of positive experiences. These included effective sharing of medical records and information about the patient, the scheduling of pharmacist medication reviews, efficient systems of electronic prescriptions, good communication between key professionals (particularly between hospital consultants and GPs, and between GPs and CPs) and active management of GSF registers. The role of the key professional (or key worker) could include supporting and co-ordinating the patient’s care, checking understanding and use of medicines, calibrating capacity and preferences for undertaking specialist tasks relating to medicines administration, and judgement about administering pain relief to dying patients. However, these examples of good practice were patchy, operating at a local level and dependent largely on interpersonal relations between agents, rather than being an outcome of the wider integrated or co-ordinated system.
It was often the patient or, especially as illness progressed, the FCG who assumed the role of care manager, trying to co-ordinate care and maintaining ‘hypervigilance’ about the impact of professional input, especially to prescribing changes. Initiatives to develop integrated care tend towards proliferation of services and linking professionals from different specialist areas and expertise. However, families can find the resulting increase in inputs and visits bewildering and demanding. Moreover, it was evident from the patient case ecograms that complex networks usually contain obsolete, vestigial and negative links. Families valued simplicity and a reduction in the number of services, people and visits to contend with. Those who had established a relationship with a key professional benefited from their ability to act as intermediary between a wide range of additional services, reducing the need for patients and FCGs to maintain vigilance and themselves take on the role of care co-ordinator. An important aspect of the key professional role was to promote transitivity to ensure that different parts of the system were connected and communicating effectively with each other. It also engendered a feeling for patients and FCGs of ‘being known’, buffering the impersonality of the system and offering protection against the hazard of change, especially during the cascade of care occurring often in the period prior to the patient’s death.
The involvement of a key professional was highly valued by families, but was not in itself enough to optimise the experience of care. Key professional roles developed in an ad hoc manner during contact with families and the personal relationships that developed as a result of this. However, the evidence of this study indicates the need for a reorientation of palliative and end-of-life care services to more closely correspond with the needs and lived experience of the patients and FCGs providing care at home, including medicines management. The availability of key professionals and necessary information should not be left to ad hoc, chance discovery. With increasing specialisation, service delivery has developed in such a way as to fragment care and contribute to a complex system. However, patients and FCGs, especially when they are old, severely ill and frail, find it difficult to understand or navigate and are unable to cope with the demands of this complexity. Current policy aims to resolve the problem of complexity through the strategy of integration of services and the development of professional ‘hubs’ that will bring together practitioners from a wide range of different services and specialties. However, although this may improve efficiency for professionals, it does not engage directly with patient perspectives and needs, nor does it necessarily reduce complexity for the patient. By contrast, the Buurtzorg model aims explicitly to achieve simplicity through small teams of community nursing teams undertaking all aspects of health and social care and co-ordinating involvement of additional services as and when these may be required. This model incorporates a vision of the organisation of end-of-life care as a community or public enterprise. However, the goal of integrated care or of health care as a genuinely collective endeavour will not be realised until the patient perspective is placed truly at the starting point of health-care organisation.
We complete this report of the Managing Medicines project at a time when the world is struggling to overcome the effects of the COVID-19 pandemic. Rapid guidance from the National Institute for Health and Care Excellence has already been issued, prompting changes in how AMs are prescribed and used. To cope with the pressures of rising demand for end-of-life care drugs, and on professional time, it is suggested that prescribers use long-acting formulations that can be administered by subcutaneous injection, buccally, sublingually or rectally, and that these may need to be administered by family members. This proposal will likely result in extending the role and responsibility of FCGs, where they may take on extra responsibility in administering end-of-life care medicines in relation to the type of drug and method of delivery. It is unclear how the pandemic will change the experience and practice of palliative and end-of-life care. However, it is likely that changes to practices that have been made will not be easily be undone and that increased FCG involvement in administering AMs may become the norm. This is asking a great deal of FCGs at a time of great anxiety and distress. It highlights the urgent need for research into family experience of medicines management for seriously ill patients during the pandemic, especially in relation to how AMs were prescribed and used, as well as after. It is important to be mindful of the need for transparency and open discussion about the extent to which patients and FCGs can and should be co-opted as proto-professionals in the technically and emotionally demanding tasks of managing medicines at the end of life.
Implications for future research
The study findings indicate the following priority areas for future research:
-
Studies should explore the role of the key professional as a means of (1) integrating and co-ordinating care and prescribing, (2) supporting the family in optimising medicines management, (3) acting as patient advocate in negotiating a complex system, particularly the interface between primary and secondary care, and (4) negotiating the role that individual patients and FCGs are willing and able to accept in managing medicines at home at the end of life.
-
Studies should evaluate current initiatives to integrate care, including the extent to which these (1) improve the communication nexus and incorporate a genuine understanding of and insight into patient experience and perspectives of medicines management, especially at the end of life, and (2) overcome traditional barriers to interprofessional working, particularly those preventing the integration of CPs as members of the health-care team.
-
Studies should explore the scope for extending the role of the CP into supporting patients and FCGs with managing medicines in the home at the end of life. Research is needed into patient, public and professional attitudes towards greater CP involvement and the kinds of support that would be most useful.
-
Studies should explore the effectiveness and value of radically different models of community care that aim specifically at ‘integrating simplification’ rather than complexity (e.g. the Buurtzorg model).
-
Studies should explore the current role of domiciliary HCWs in supporting medicines management for seriously ill patients in the home, the scope for expanding this role in future and the training and support needed to enable HCWs to undertake extended responsibility with confidence and competence.
-
Studies should explore the understanding, experience and attitudes of patients and FCGs towards the prescribing and use of AMs, their preferred and actual role in decision-making relating to prescribing and use, and how professionals initiate and conduct discussions about AMs with patients and FCGs.
-
Studies should investigate the experience of medicines management during terminal illness among diverse vulnerable and disadvantaged patient groups, including ethnic minority groups, the homeless and those with serious mental illness and/or substance dependency. The experience of patients affected by serious mental illness should be a priority.
-
Studies should explore the feasibility and effectiveness of a patient-held prescribing record and medicines chart available for all prescribers to review and record changes made during consultations and in the patient’s home.
-
Studies should develop and evaluate use of digital technologies as a means of supporting palliative care patients with medicines management at home, including access to help 24/7.
-
Studies should investigate the COVID-19 legacy, how this affected anticipatory prescribing during and after the pandemic, and changes in the way families engage in, and respond to, discussions and decisions about, and administration of, end-of-life care drugs.
Acknowledgements
The University of Nottingham acknowledges the support of the National Institute for Health Research, through the Primary Care Research Network, in carrying out this study.
We thank the patients and family caregivers for their generosity in taking part in the study during a very difficult period in their lives when their time was so valuable. Without their contributions, this study would not have been possible. We also acknowledge the input of the HCPs who took part as interviewees and also in recruiting patients and FCGs to the case studies and interviews. Thanks also go to the practice staff who made reviewing patients records possible.
We are grateful to Nicola Turner for her contribution to data collection and the systematic review paper while Elli Wilson was on maternity leave.
Throughout the study, we have benefited from the support and involvement of the Nottingham University Dementia, Frail Older People and Palliative Care Patient and Public Involvement Advisory Panel. Members have been involved in the project from the outset, commenting on the study design, ethics and participant materials. They have also contributed to several workshops held to discuss the findings and develop the patient poster, as well as the two end-of-project stakeholder workshops. We would like to thank the following members of the panel for reviewing and giving detailed comments on a draft of the final report: Maureen Godfrey, Kate Sartain, Marianne Dunlop and Margaret Kerr. We are grateful for the substantial and collegial input of Alan Caswell who is a co-applicant on the grant and has worked on all aspects of the study as an integral member of the project team. We thank you all.
Where patient and public involvement is acknowledged
| Section and topic | Item | Reported on page number |
|---|---|---|
| Aim | Report the aim of PPI in the study | 13 |
| Methods | Provide a clear description of the methods used for PPI in the study | 12, 13 |
| Study results | Outcomes: report the results of PPI in the study, including both positive and negative outcomes | 17–22; 81–7 |
| Discussion and conclusions | Outcomes: comment on the extent to which PPI influenced the study overall. Describe positive and negative effects | 17–22 |
| Reflections/critical perspective | Comment critically on PPI input in the study, reflecting on the things that went well and those that did not, so others can learn from this experience | 15, 17–22 |
Contribution of authors
Kristian Pollock (https://orcid.org/0000-0002-6836-8595) (Professor of Medical Sociology, School of Health Sciences, University of Nottingham) was the principal investigator and was involved in study conception, design and delivery, data collection and analysis, and writing of the final report.
Eleanor Wilson (https://orcid.org/0000-0003-0419-5901) (Senior Research Fellow, School of Health Sciences, University of Nottingham) was involved in project management, design, data collection and analysis, and writing of the final report.
Glenys Caswell (https://orcid.org/0000-0002-8246-8189) (Senior Research Fellow, School of Health Sciences, University of Nottingham) was involved in project management, design, data collection and analysis, and writing of the final report.
Asam Latif (https://orcid.org/0000-0003-0730-7120) (Senior Research Fellow, School of Health Sciences, University of Nottingham) was involved in project design and oversight, was the lead on extension work relating to the role of CPs in palliative and end-of-life care and the patient poster co-production, and was involved in writing of the final report.
Alan Caswell (https://orcid.org/0000-0001-8059-2648) (PPI representative, Dementia, Frail Older and Palliative Care, Patient and Public Involvement Advisory Group, University of Nottingham) provided advisory support, and was involved in project oversight, data analysis and dissemination, and writing of the final report.
Anthony Avery (https://orcid.org/0000-0001-7591-4438) (Professor of Primary Health Care, Faculty of Medicine and Health Sciences, University of Nottingham) provided clinical expertise and advisory support, and was involved in project oversight, facilitation of recruitment and liaison with HCPs and services, and review of the findings and final report.
Claire Anderson (https://orcid.org/0000-0002-5406-2296) (Professor of Social Pharmacy, University of Nottingham) provided clinical expertise and advisory support, and was involved in project oversight and review of the findings and final report.
Vincent Crosby (https://orcid.org/0000-0002-7070-9600) (Consultant in Palliative Medicine, Nottingham University Hospitals NHS Trust) provided clinical expertise and advisory support, and was involved in project oversight, facilitation of recruitment and liaison with HCPs and services, and review of the findings and final report.
Christina Faull (https://orcid.org/0000-0002-0064-8056) (Consultant in Palliative Medicine, LOROS Hospice, Leicester) provided clinical expertise and advisory support, and was involved in project oversight, facilitation of recruitment and liaison with HCPs and services, and review of the findings and final report.
Publications
Wilson E, Caswell G, Pollock K. The ‘work’ of managing medications when someone is seriously ill and dying at home: A longitudinal qualitative case study of patient and family perspectives’ [published online ahead of print July 12 2021]. Pall Med 2021.
Literature review paper
Wilson E, Caswell G, Turner N, Pollock K. Managing medicines for patients dying at home: a review of family caregivers’ experiences. J Pain Symptom Manage 2018;56:962–74.
Health professional perspectives paper
Wilson E, Caswell G, Latif A, Anderson C, Faull C, Pollock K. An exploration of the experiences of professionals supporting patients approaching the end-of-life in medicines management at home. A qualitative study. BMC Palliat Care 2020;19:66.
Community pharmacy article
Latif A, Faull C, Ali A, Wilson E, Caswell G, Anderson C, Pollock K. Caring for palliative care patients at home: medicines management principles and considerations [published online ahead of print 9 June 2020]. Pharm J 2020.
Pharmacy position paper
Latif A, Faull C, Waring J, Wilson E, Anderson C, Avery A, Pollock K. The management of medicines for patients with serious illness being cared for at home: a positional paper for healthcare policy and practice. J Health Organ Manag 2021; in press.
Posters and presentations
Pollock K, Caswell G, Wilson E. Thinking Outside the (Dosette) Box: Health Professionals’ Experiences of Supporting Medicines Management in the Home Environment for Patients who are Seriously Ill. HSRUK Conference 2019, Manchester, UK, 2 and 3 July 2019.
Latter S, Campling N. Accessing Medicines at End-of-life (ActMed). University of Southampton, Southampton, UK, 20 and 26 June 2019.
Pollock K, Wilson E, Caswell G. Managing Medicines for Patients with Serious Illness Being Cared for at Home. University of Nottingham, Nottingham, UK, 20 and 26 June 2019.
Latif A, Anderson C, Pollock K. Managing Medicines: A Qualitative Study of the Community Pharmacist's Role in Supporting Patients with Serious Illness and Family Caregivers. Special Issue: Abstracts from The Royal Pharmaceutical Society Science and Research Summit, 19 June 2020, London, UK.
Data-sharing statement
This is a qualitative study and therefore the data generated is not suitable for sharing beyond that contained within the report. Further information can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Pollock K, Seymour J. Reappraising ‘the good death’ for populations in the age of ageing. Age Ageing 2018;47:328-30. https://doi.org/10.1093/ageing/afy008.
- Imison C, Curry N, Holder H, Castle-Clarke S, Nimmons D, Appleby J, et al. Shifting the Balance of Care: Great Expectations. London: Nuffield Trust; 2017.
- Exley C, Allen D. A critical examination of home care: end of life care as an illustrative case. Soc Sci Med 2007;65:2317-27. https://doi.org/10.1016/j.socscimed.2007.07.006.
- Allen D, Ceci C, Bjornsdottir K, Purkis ME. Perspective on Care at Home for Older People. London: Routledge; 2012.
- Milligan C. There’s No Place Like Home: Place and Care In An Ageing Society. Abingdon: Routledge; 2016.
- Dew K, Chamberlain K, Hodgetts D, Norris P, Radley A, Gabe J. Home as a hybrid centre of medication practice. Sociol Health Illn 2014;36:28-43. https://doi.org/10.1111/1467-9566.12041.
- May CR, Eton DT, Boehmer K, Gallacher K, Hunt K, MacDonald S, et al. Rethinking the patient: using burden of treatment theory to understand the changing dynamics of illness. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-281.
- Reinhard SC, Levine C, Samis S. Home Alone: Family Caregivers Providing Complex Chronic Care. Washington, DC: AARP Public Policy Institute; 2012.
- Pollock K. Is home always the best and preferred place of death?. BMJ 2015;351. https://doi.org/10.1136/bmj.h4855.
- Ward-Griffin C, McKeever P. Relationships between nurses and family caregivers: partners in care?. Adv Nurs Sci 2000;22:89-103. https://doi.org/10.1097/00012272-200003000-00008.
- Langstrup H. Chronic care infrastructures and the home. Sociol Health Illn 2013;35:1008-22. https://doi.org/10.1111/1467-9566.12013.
- Sheehy-Skeffington B, McLean S, Bramwell M, O’Leary N, O’Gorman A. Caregivers experiences of managing medications for palliative care patients at the end of life: a qualitative study. Am J Hosp Palliat Care 2014;31:148-54. https://doi.org/10.1177/1049909113482514.
- Reinhard SC, Choula R. Meeting the Needs of Diverse Family Caregivers. Washington, DC: AARP Public Policy Institute; 2012.
- Ullgren H, Tsitsi T, Papastavrou E, Charalambous A. How family caregivers of cancer patients manage symptoms at home: a systematic review. Int J Nurs Stud 2018;85:68-79. https://doi.org/10.1016/j.ijnurstu.2018.05.004.
- Rosenberg JP, Horsfall D, Leonard R, Noonan K. Informal care networks’ views of palliative care services: help or hindrance?. Death Stud 2018;42:362-70. https://doi.org/10.1080/07481187.2017.1350216.
- McCoy L. Time, self and the medication day: a closer look at the everyday work of ‘adherence’. Sociol Health Illn 2009;31:128-46. https://doi.org/10.1111/j.1467-9566.2008.01120.x.
- Cheraghi-Sohi S, Jeffries M, Stevenson F, Ashcroft DM, Carr M, Oliver K, et al. The influence of personal communities on the self-management of medication taking: a wider exploration of medicine work. Chronic Illn 2015;11:77-92. https://doi.org/10.1177/1742395314537841.
- Reid M, Clark A, Murdoch DL, Morrison C, Capewell S, McMurray J. Patients strategies for managing medication for chronic heart failure. Int J Cardiol 2006;109:66-73. https://doi.org/10.1016/j.ijcard.2005.05.051.
- Brown MT, Bussell JK. Medication adherence: WHO cares?. Mayo Clin Proc 2011;86:304-14. https://doi.org/10.4065/mcp.2010.0575.
- Sleeman KE, de Brito M, Etkind S, Nkhoma K, Guo P, Higginson IJ, et al. The escalating global burden of serious health-related suffering: projections to 2060 by world regions, age groups, and health conditions. Lancet Glob Health 2019;7:e883-92. https://doi.org/10.1016/S2214-109X(19)30172-X.
- Etkind S, Bone A, Gomes B, Lovell N, Evans C, Higginson I, et al. How many people will need palliative care in 2040? Past trends, future predictions and implications for services. BMC Med 2017;15. https://doi.org/10.1186/s12916-017-0860-2.
- Cortis LJ, McKinnon RA, Anderson C. Palliative care is everyone’s business, including pharmacists. Am J Pharm Educ 2013;77:1-3. https://doi.org/10.5688/ajpe77221.
- National Palliative and End-of-life Care Partnership . Ambitions for Palliative and End-of-Life Care: A National Framework for Local Action 2015–2020 2015. http://endoflifecareambitions.org.uk/wp-content/uploads/2015/09/Ambitions-for-Palliative-and-End-of-Life-Care.pdf (accessed 14 December 2020).
- Organisation for Economic Co-operation and Development . Ageing Societies. OECD Factbook 2009: Economic, Environmental and Social Statistics 2009.
- Age UK . Health and Care of Older People in England 2017 2017. www.ageuk.org.uk/documents/EN-GB/For-professionals/Research/The_Health_and_Care_of_Older_People_in_England_2016.pdf?epslanguage=en-GB?dtrk=true (accessed 14 December 2020).
- Care Quality Commission . The State of Health Care and Adult Social Care in England 2017 18 2018.
- Department of Health and Social Care (DHSC) . End-of-Life Care Strategy – Promoting High Quality Care for All Adults at End-of-Life 2008.
- Gomes B, Calanzani N, Higginson I. Local Preferences and Place of Death in Regions Within England 2010. London: Cicely Saunders Institute of Palliative Care, Policy & Rehabilition; 2011.
- Office for National Statistics . Statistical Bulletin: National Survey of Bereaved People (VOICES): England, 2015: Quality of Care Delivered in the Last 3 Months of Life for Adults Who Died in England 2015.
- Buckner L, Yeandle S. Valuing Carers 2015 – The Rising Value of Carers’ Support. Leeds: University of Leeds; 2015.
- Rowland C, Hanratty B, Pilling M, van den Berg B, Grande G. The contributions of family care-givers at end of life: a national post-bereavement census survey of cancer carers’ hours of care and expenditures. Palliat Med 2017;31:346-55. https://doi.org/10.1177/0269216317690479.
- Age UK . Briefing: Health and Care of Older People in England 2017 2017.
- Look KA, Stone JA. Medication management activities performed by informal caregivers of older adults. Res Social Adm Pharm 2018;14:418-26. https://doi.org/10.1016/j.sapharm.2017.05.005.
- Carers UK . Facts About Carers, Policy Briefing August 2019 2019.
- Oliver D. David Oliver: Taking carers for granted. BMJ 2017;357. https://doi.org/10.1136/bmj.j1523.
- Age UK . Briefing: Health and Care of Older People in England 2019 2019.
- Carers UK . The State of Caring Report 2017. Annual Survey Report 2017.
- Carers UK . The Cost of Caring. How Money Worries Are Pushing Carers to Breaking Point 2011.
- Totman J, Pistrang N, Smith S, Hennessey S, Martin J. ‘You only have one chance to get it right’: a qualitative study of relatives’ experiences of caring at home for a family member with terminal cancer. Palliat Med 2015;29:496-507. https://doi.org/10.1177/0269216314566840.
- Age UK . Later Life in the United Kingdom 2015.
- Noureldin M, Plake KS. Correlates of caregivers’ involvement in the management of older adults’ medications. Res Social Adm Pharm 2017;13:840-8. https://doi.org/10.1016/j.sapharm.2016.09.009.
- Payne S, Turner M, Seamark D, Thomas C, Brearley S, Wang X, et al. Managing end-of-life medications at home – accounts of bereaved family carers: a qualitative interview study. BMJ Support Palliat Care 2014:1-18. https://doi.org/10.1136/bmjspcare-2014-000658.
- Joyce BT, Berman R, Lau DT. Formal and informal support of family caregivers managing medications for patients who receive end-of-life care at home: a cross-sectional survey of caregivers. Palliat Med 2014;28:1146-55. https://doi.org/10.1177/0269216314535963.
- Vassilev I, Rogers A, Blickem C, Brooks H, Kapadia D, Kennedy A, et al. Social networks, the ‘work’ and work force of chronic illness self-management: a survey analysis of personal communities. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0059723.
- Palen L, Aalokke S. Of Pill Boxes and Piano Benches: ‘Home-made’ Methods for Managing Medication n.d. https://doi.org/10.1145/1180875.1180888.
- Notenboom K, Beers E, van Riet-Nales DA, Egberts TC, Leufkens HG, Jansen PA, et al. Practical problems with medication use that older people experience: a qualitative study. J Am Geriatr Soc 2014;62:2339-44. https://doi.org/10.1111/jgs.13126.
- Orlu-Gul M, Raimi-Abraham B, Jamieson E, Wei L, Murray M, Stawarz K, et al. Public engagement workshop: how to improve medicines for older people?. Int J Pharm 2014;459:65-9. https://doi.org/10.1016/j.ijpharm.2013.11.024.
- Maidment ID, Aston L, Moutela T, Fox CG, Hilton A. A qualitative study exploring medication management in people with dementia living in the community and the potential role of the community pharmacist. Health Expect 2017;20:929-42. https://doi.org/10.1111/hex.12534.
- While C, Duane F, Beanland C, Koch S. Medication management: the perspectives of people with dementia and family carers. Dementia 2013;12:734-50. https://doi.org/10.1177/1471301212444056.
- Pound P, Britten N, Morgan M, Yardley L, Pope C, Daker-White G, et al. Resisting medicines: a synthesis of qualitative studies of medicine taking. Soc Sci Med 2005;61:133-55. https://doi.org/10.1016/j.socscimed.2004.11.063.
- Townsend A, Hunt K, Wyke S. Managing multiple morbidity in mid-life: a qualitative study of attitudes to drug use. BMJ 2003;327. https://doi.org/10.1136/bmj.327.7419.837.
- Haslebeck JW, Schaeffer D. Routines in medication management: the perspective of people with chronic conditions. Chronic Illn 2009;5:184-96. https://doi.org/10.1177/1742395309339873.
- Furniss D, Barber N, Lyons I, Eliasson L, Blandford A. Unintentional non-adherence: can a spoon full of resilience help the medicine go down?. BMJ Qual Saf 2013;23:95-8. https://doi.org/10.1136/bmjqs-2013-002276.
- Fallsberg M. Reflections on Medicines and Medication: A Qualitative Analysis Among People on Long Term Drug Regiments. Stockholm: Swedish Pharmaceutical Press; 1991.
- Tait P, Swetenham K. Forging an advanced practice role for pharmacists in palliative care. Pharm Pract Res 2014;44:120-4. https://doi.org/10.1002/jppr.1008.
- Duerden M, Avery T, Payne R. Polypharmacy and Medicines Optimisation: Making It Safe and Sound. London: The King’s Fund; 2013.
- Hussainy SY, Box M, Scholes S. Piloting the role of a pharmacist in a community palliative care multidisciplinary team: an Australian experience. BMC Palliat Care 2011;10. https://doi.org/10.1186/1472-684X-10-16.
- Currow DC, Stevenson JP, Abernethy AP, Plummer J, Shelby-James TM. Prescribing in palliative care as death approaches. J Am Geriatr Soc 2007;55:590-5. https://doi.org/10.1111/j.1532-5415.2007.01124.x.
- Paque K, De Schreye R, Elseviers M, Vander Stichele R, Pardon K, Dilles T, et al. Discontinuation of medications at the end of life: a population study in Belgium, based on linked administrative databases. Br J Clin Pharmacol 2019;85:827-37. https://doi.org/10.1111/bcp.13874.
- Baillie J, Lankshear A. Patient and family perspectives on peritoneal dialysis at home: findings from an ethnographic study. J Clin Nurs 2015;24:222-34. https://doi.org/10.1111/jocn.12663.
- Wilson E, Caswell G, Turner N, Pollock K. Managing medicines for patients dying at home: a review of family caregivers’ experiences. J Pain Symptom Manage 2018;56:962-74. https://doi.org/10.1016/j.jpainsymman.2018.08.019.
- Oliver DP, Wittenberg-Lyles E, Washington K, Kruse RL, Albright DL, Baldwin PK, et al. Hospice caregivers’ experiences with pain management: ‘I’m not a doctor, and I don’t know if I helped her go faster or slower’. J Pain Symptom Manage 2013;46:846-58. https://doi.org/10.1016/j.jpainsymman.2013.02.011.
- Lau DT, Berman R, Halpern L, Pickard AS, Schrauf R, Witt W. Exploring factors that influence informal caregiving in medication management for home hospice patients. J Palliat Med 2010;13:1085-90. https://doi.org/10.1089/jpm.2010.0082.
- Tjia J, Ellington L, Clayton MF, Lemay C, Reblin M. Managing medications during home hospice cancer care: the needs of family caregivers. J Pain Symptom Manage 2015;50:630-41. https://doi.org/10.1016/j.jpainsymman.2015.06.005.
- Parker Oliver D, Demiris G, Wittenberg-Lyles E, Porock D, Collier J, Arthur A. Caregiver participation in hospice interdisciplinary team meetings via videophone technology: a pilot study to improve pain management. Am J Hosp Palliat Care 2010;27:465-73. https://doi.org/10.1177/1049909110362402.
- Hackett J, Godfrey M, Bennett MI. Patient and caregiver perspectives on managing pain in advanced cancer: a qualitative longitudinal study. Palliat Med 2016;30:711-19. https://doi.org/10.1177/0269216316628407.
- Lau DT, Kasper JD, Hauser JM, Berdes C, Chang CH, Berman RL, et al. Family caregiver skills in medication management for hospice patients: a qualitative study to define a construct. J Gerontol B Psychol Sci Soc Sci 2009;64:799-807. https://doi.org/10.1093/geronb/gbp033.
- Wowchuk SM, Wilson EA, Embleton L, Garcia M, Harlos M, Chochinov HM. The palliative medication kit: an effective way of extending care in the home for patients nearing death. J Palliat Med 2009;12:797-803. https://doi.org/10.1089/jpm.2009.0048.
- Wood C, Salter J. A Time and a Place. London: Sue Ryder; 2013.
- Waghorn M, Young H, Davies A. Opinions of patients with cancer on the relative importance of place of death in the context of a ‘good death’. BMJ Support Palliat Care 2011;1:310-14. https://doi.org/10.1136/bmjspcare-2011-000041.
- Robinson J, Gott M, Ingleton C. Patient and family experiences of palliative care in hospital: what do we know? An integrative review. Palliat Med 2014;28:18-33. https://doi.org/10.1177/0269216313487568.
- National Council for Palliative Care . Dying Matters Coalition – Public Opinion on Death and Dying 2016.
- ElMokhallalati Y, Woodhouse N, Farragher T, Bennett MI. Specialist palliative care support is associated with improved pain relief at home during the last 3 months of life in patients with advanced disease: analysis of 5-year data from the national survey of bereaved people (VOICES). BMC Med 2019;17. https://doi.org/10.1186/s12916-019-1287-8.
- Mair FS, May C. Thinking about the burden of treatment. Should it be regarded as an indicator of the quality of care?. BMJ 2014;349. https://doi.org/10.1136/bmj.g6680.
- de Swaan A. The Management of Normality: Critical Essays in Health and Welfare. London: Routledge; 1990.
- May CR, Cummings A, Myall M, Harvey J, Pope C, Griffiths P, et al. Experiences of long-term life-limiting conditions among patients and carers: what can we learn from a meta-review of systematic reviews of qualitative studies of chronic heart failure, chronic obstructive pulmonary disease and chronic kidney disease?. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-011694.
- Care Quality Commission . Dementia Care Update: Issue 2 2013.
- Dixon J, King D, Matosevic T, Clark M, Knapp M. Equity in the Provision of Palliative Care in the UK: Review of Evidence. London: London School of Economic and Political Science; 2015.
- Calanzani N, Koffman J, Higginson IJ. Palliative Care and End-of-life Care for Black, Asian and Minority Ethnic Groups in the UK. London: King’s College London; 2013.
- Thomas B. Homelessness Kills: An Analysis of the Mortality of Homeless People in Early Twenty-First Century England. Sheffield: University of Sheffield; 2012.
- Mundt-Leach R. End-of-life and palliative care of patients with drug and alcohol addiction. Ment Health Pract 2016;20:17-21. https://doi.org/10.7748/mhp.2016.e1148.
- Latif A, Tariq S, Abbasi N, Mandane B. Giving voice to the medically under-served: a qualitative co-production approach to explore patient medicine experiences and improve services to marginalized communities. Pharmacy 2018;6. https://doi.org/10.3390/pharmacy6010013.
- Latif A, Pollock K, Anderson C, Waring J, Solomon J, Chen L-C, et al. Supporting underserved patients with their medicines: a study protocol fora patient/professional coproduced education intervention for community pharmacy staff to improve the provision and delivery of medicine use reviews (MURs). BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-013500.
- Markham S, Islam Z, Faull C. I never knew that! Why do people from Black and Asian Minority Ethnic groups in Leicester access hospice services less than other groups? A discussion with community groups. Divers Equal Health Care 2014;11:23-745. https://doi.org/10.21767/2049-5471.100016.
- Office for National Statistics . United Kingdom Census 2011.
- Suleman M, Asaria M, Haque E, Safdar M, Shafi S, Sherif J. Elderly and End-of-life Care for Muslims in the UK. Cambridge: Muslim Council of Britain; 2019.
- Wilkie DJ, Ezenwa MO. Pain and symptom management in palliative care and at end of life. Nurs Outlook 2012;60:357-64. https://doi.org/10.1016/j.outlook.2012.08.002.
- Kwok W, Bhuvanakakrishna T. The relationship between ethnicity and the pain experience of cancer patients: a systematic review. Indian J Palliat Care 2014;20:194-200. https://doi.org/10.4103/0973-1075.138391.
- Horne R, Graupner L, Frost S, Weinman J, Wright SM, Hankins M. Medicine in a multi-cultural society: the effect of cultural background on beliefs about medications. Soc Sci Med 2004;59:1307-13. https://doi.org/10.1016/j.socscimed.2004.01.009.
- Alhusein N, Macaden L, Smith A, Stoddart KM, Taylor AJ, Killick K, et al. ‘Has she seen me?’: a multiple methods study of the pharmaceutical care needs of older people with sensory impairment in Scotland. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2018-023198.
- Alhusein N, Killick K, Macaden L, Smith A, Stoddart K, Taylor A, et al. ‘We’re really not ready for this’: a qualitative exploration of community pharmacy personnel’s perspectives on the pharmaceutical care of older people with sensory impairment. Disabil Health J 2019;12:242-8. https://doi.org/10.1016/j.dhjo.2018.10.006.
- Ebenau A, Dijkstra B, Stal-Klapwijk M, Ter Huurne C, Blom A, Vissers K, et al. Palliative care for patients with a substance use disorder and multiple problems: a study protocol. BMC Palliat Care 2018;17. https://doi.org/10.1186/s12904-018-0351-z.
- Hudson BF, Shulman C, Low J, Hewett N, Daley J, Davis S, et al. Challenges to discussing palliative care with people experiencing homelessness: a qualitative study. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-017502.
- Archer W, Latif A, Faull C. Communicating with palliative care patients nearing the end-of-life, their families and carers. Pharm J 2017;298.
- Wilson E, Seymour J. The importance of interdisciplinary communication in the process of anticipatory prescribing. Int J Palliat Nurs 2017;23:129-35. https://doi.org/10.12968/ijpn.2017.23.3.129.
- Wilson E, Morbey H, Brown J, Payne S, Seale C, Seymour J. Administering anticipatory medications in end-of-life care: a qualitative study of nursing practice in the community and in nursing homes. Palliat Med 2015;29:60-7. https://doi.org/10.1177/0269216314543042.
- O’Connor M, Pugh J, Moyez J, Hughes J, Fisher C. The palliative care interdisciplinary team: where is the community pharmacist?. J Palliat Med 2011;14:7-11. https://doi.org/10.1089/jpm.2010.0369.
- Lucey M, McQuillan R, MacCallion A, Corrigan M, Flynn J, Connaire K. Access to medications in the community by patients in a palliative setting. A systems analysis. Palliat Med 2008;22:185-9. https://doi.org/10.1177/0269216307085722.
- Faull C, Windridge K, Ockleford E, Hudson M. Anticipatory prescribing in terminal care at home: what challenges do community health professionals encounter?. BMJ Support Palliat Care 2012;3:91-7. https://doi.org/10.1136/bmjspcare-2012-000193.
- Taubert M, Nelson A. Out-of-hours GPs and palliative care-a qualitative study exploring information exchange and communication issues. BMC Palliat Care 2010;9. https://doi.org/10.1186/1472-684X-9-18.
- Smith J, Catherine P, Dayan M. Now or Never. Shaping Pharmacy for the Future. London: Royal Pharmaceutical Society; 2013.
- Robinson J. The trials and triumphs of pharmacist independent prescribers. Pharm J 2018;1.
- Clifford S, Barber N, Elliott R, Hartley E, Horne R. Patient-centred advice is effective in improving adherence to medicines. Pharm World Sci 2006;28:165-70. https://doi.org/10.1007/s11096-006-9026-6.
- McCusker K. Macmillan Pharmacy Service Year 3 Final Report 2016.
- Macmillan Cancer Support . Macmillan Pharmacist Facilitator Project Final Evaluation Report 2012.
- Macmillan Cancer Support . Macmillan Rural Palliative Care Pharmacist Practitioner Project Final Report 2016.
- General Pharmaceutical Council . Prescribers Survey Report 2016.
- Salter C. Compliance and concordance during domiciliary medication review involving pharmacists and older people. Sociol Health Illn 2010;32:21-36. https://doi.org/10.1111/j.1467-9566.2009.01193.x.
- Ziegler L, Bennet MI, Mulvey M, Hamilton T, Blenkinsopp A. Characterising the growth in palliative care prescribing 2011–15: analysis of national medical and non-medical activity. Palliat Med 2017:1-8. https://doi.org/10.1177/0269216317739805.
- McNeil MJ, Kamal AH, Kutner JS, Ritchie CS, Abernethy AP. The burden of polypharmacy in patients near the end of life. J Pain Symptom Manage 2016;51:178-83.e2. https://doi.org/10.1016/j.jpainsymman.2015.09.003.
- Morin L, Vetrano DL, Rizzuto D, Calderón-Larrañaga A, Fastbom J, Johnell K. Choosing wisely? Measuring the burden of medications in older adults near the end of life: nationwide, longitudinal cohort study. Am J Med 2017;130:927-36.e9. https://doi.org/10.1016/j.amjmed.2017.02.028.
- Morin L, Wastes son JW, Laroche ML, Fastbom J, Johnell K. How many older adults receive drugs of questionable clinical benefit near the end of life? A cohort study. Palliat Med 2019;33:1080-90. https://doi.org/10.1177/0269216319854013.
- LeBlanc TW, McNeil MJ, Kamal AH, Currow DC, Abernethy AP. Polypharmacy in patients with advanced cancer and the role of medication discontinuation. Lancet Oncol 2015;16:e333-41. https://doi.org/10.1016/S1470-2045(15)00080-7.
- Arevalo JJ, Gateman ECT, Huisman BAA, Dees MK, Surmont WWA, van Kuylen L, et al. Medication use in the last days of life in hospital, hospice, and home settings in the Netherlands. J Palliat Med 2018;21:149-55. https://doi.org/10.1089/jpm.2017.0179.
- Pipe P, Mertens F, Halewood F, Duster B, De Sutter A. Potentially inappropriate medication in primary care at the end of life: a mixed-method study. Acta Clin Beg 2018;73:213-19. https://doi.org/10.1080/17843286.2017.1410606.
- Morin L, Laroche ML, Vetrano DL, Fastbom J, Johnell K. Adequate, questionable, and inadequate drug prescribing for older adults at the end of life: a European expert consensus. Eur J Clin Pharmacol 2018;74:1333-42. https://doi.org/10.1007/s00228-018-2507-4.
- Dees MK, Gateman ECT, Dekkers WJM, Huisman BAA, Perez RSGM, van Kuylen L, et al. Perspectives of patients, close relatives, nurses, and physicians on end-of-life medication management. Palliat Support Care 2018;16:580-9. https://doi.org/10.1017/S1478951517000761.
- Duncan P, Duerden M, Payne RA. Deprescribing: a primary care perspective. Eur J Hosp Pharm 2017;24:37-42. https://doi.org/10.1136/ejhpharm-2016-000967.
- Avery AJ, Bell BG. Rationalising medications through deprescribing. BMJ 2019;364. https://doi.org/10.1136/bmj.l570.
- Donovan J, Blake D. Patient non-compliance: deviance or reasoned decision-making?. Soc Sci Med 1992;34:507-13. https://doi.org/10.1016/0277-9536(92)90206-6.
- Bowers B, Ryan R, Kuhn I, Barclay S. Anticipatory prescribing of injectable medications for adults at the end of life in the community: a systematic literature review and narrative synthesis. Palliat Med 2019;33:160-77. https://doi.org/10.1177/0269216318815796.
- Wilson E, Seymour J, Seale C. Anticipatory prescribing for end-of-life care: a survey of community nurses in England. J Prim Health Care 2016;26:22-7. https://doi.org/10.7748/phc.2016.e1151.
- Bullen T, Rosenberg JP, Smith B, Maher K. The use of emergency medication kits in community palliative care: an exploratory survey of views of current practice in Australian home-based palliative care services. Am J Hosp Palliat Care 2015;32:581-7. https://doi.org/10.1177/1049909114536922.
- Bowers B, Redsell SA. A qualitative study of community nurses’ decision-making around the anticipatory prescribing of end-of-life medications. J Adv Nurs 2017;73:2385-94. https://doi.org/10.1111/jan.13319.
- Miller EJ, Morgan JD, Blenkinsopp A. How timely is access to palliative care medicines in the community? A mixed methods study in a UK city. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2019-029016.
- National Institute for Health and Care Excellence (NICE) . Care of Dying Adults in the Last Days of Life. 2015.
- Wilson E, Seymour J, Morbey H, Payne S, Brown J, Seale C. Anticipatory prescribing in end-of-life care. Nurs Times 2014;110:24-5.
- Buchan J, Chalesworth A, Gershlick B, Seccombe I. A Critical Moment: NHS Staffing Trends, Retention and Attrition. London: The Health Foundation; 2019.
- Anderson BA, Kralik D. Palliative care at home: carers and medication management. Palliat Support Care 2008;6:349-56. https://doi.org/10.1017/S1478951508000552.
- Israel F, Reymond L, Slade G, Menadue S, Charles MA. Lay caregivers’ perspectives on injecting subcutaneous medications at home. Int J Palliat Nurs 2008;14:390-5. https://doi.org/10.12968/ijpn.2008.14.8.30774.
- Rosenberg JP, Bullen T, Maher K. Supporting family caregivers with palliative symptom management: a qualitative analysis of the provision of an emergency medication kit in the home setting. Am J Hosp Palliat Care 2015;32:484-9. https://doi.org/10.1177/1049909114531326.
- Bishop MF, Stephens L, Goodrich M, Byock I. Medication kits for managing symptomatic emergencies in the home: a survey of common hospice practice. J Palliat Med 2009;12:37-44. https://doi.org/10.1089/jpm.2008.0193.
- Poolman M, Roberts J, Byrne A, Perkins P, Hoare Z, Nelson A, et al. CARer-ADministration of as-needed subcutaneous medication for breakthrough symptoms in homebased dying patients (CARiAD): study protocol for a UK-based open randomised pilot trial. Trials 2019;20. https://doi.org/10.1186/s13063-019-3179-9.
- Lee L, Headland C. Administration of as required subcutaneous medications by lay carers: developing a procedure and leaflet. Int J Palliat Nurs 2003;9:142-9. https://doi.org/10.12968/ijpn.2003.9.4.11504.
- Lee L, Howard K, Wilkinson L, Kern C, Hall S. Developing a policy to empower informal carers to administer subcutaneous medication in community palliative care; a feasibility project. Int J Palliat Nurs 2016;22:369-78. https://doi.org/10.12968/ijpn.2016.22.8.369.
- Lincolnshire Community Health Service St . Barnabas Lincolnshire Hospice. The Lincolnshire Policy for Informal Carer’s Administration of As Required Subcutaneous Injections in Community Palliative Care 2013.
- Milligan C, Turner M, Blake S, Brearley S, Seamark D, Thomas C, et al. Unpacking the impact of older adults’ home death on family care-givers’ experiences of home. Health Place 2016;38:103-11. https://doi.org/10.1016/j.healthplace.2016.01.005.
- Jarrett N, Porter K, Davis C, Addington-Hall J, Duke S, Corner J, et al. The networks of care surrounding cancer palliative care patients. BMJ Support Palliat Care 2015;5:435-42. https://doi.org/10.1136/bmjspcare-2014-000782.
- Charmaz K. Constructing Grounded Theory: A Practical Guide Through Qualitative Analysis. London: SAGE Publications Ltd; 2006.
- Rubin H, Rubin I. Qualitative Interviewing: The Art of Hearing Data. London: SAGE Publications Ltd; 2005.
- Bazeley P. Qualitative Data Analysis, Practical Strategies. London: SAGE Publications Ltd; 2013.
- Yin R. Case Study Research, Design and Method. London: SAGE Publications Ltd; 2008.
- Stake RE. Multiple Case Study Analysis. London: Guildford Press; 2006.
- Cook AS. Ethical issues in bereavement research: an overview. Death Stud 1995;19:103-22. https://doi.org/10.1080/07481189508252719.
- Lowes L, Paul G. Participants’ experiences of being interviewed about an emotive topic. J Adv Nurs 2006;55:587-95. https://doi.org/10.1111/j.1365-2648.2006.03950.x.
- Addington-Hall J. Research sensitivities to palliative care patients. Eur J Cancer Care 2002;11:220-4. https://doi.org/10.1046/j.1365-2354.2002.00343.x.
- Adshead G. Studying the mind: ethical issues and guidance in mental health research. Clin Ethics 2008;3:141-4. https://doi.org/10.1258/ce.2008.008026.
- Early BP, Smith ED, Todd L, Beem T. The needs and supportive networks of the dying: an assessment instrument and mapping procedure for hospice patients. Am J Hosp Palliat Care 2000;17:87-96. https://doi.org/10.1177/104990910001700208.
- Ray RA, Street AF. Ecomapping: an innovative research tool for nurses. J Adv Nurs 2005;50:545-52. https://doi.org/10.1111/j.1365-2648.2005.03434.x.
- Ray RA, Street AF. Who’s there and who cares: age as an indicator of social support networks for caregivers among people living with motor neurone disease. Health Soc Care Community 2005;13:542-52. https://doi.org/10.1111/j.1365-2524.2005.00586.x.
- Latif A, Faull C, Ali A, Wilson E, Caswell G, Anderson C, et al. Caring for palliative care patients at home: medicines management principles and considerations. Pharm J 2020.
- Tarberg AS, Kvangarsnes M, Hole T, Thronæs M, Madssen TS, Landstad BJ. Silent voices: family caregivers’ narratives of involvement in palliative care. Nurs Open 2019;6:1446-54. https://doi.org/10.1002/nop2.344.
- Røen I, Stifoss-Hanssen H, Grande G, Brenne AT, Kaasa S, Sand K, et al. Resilience for family carers of advanced cancer patients-how can health care providers contribute? A qualitative interview study with carers. Palliat Med 2018;32:1410-18. https://doi.org/10.1177/0269216318777656.
- Allen D, Griffiths L, Lyne P. Understanding complex trajectories in health and social care provision. Sociol Health Illn 2004;26:1008-30. https://doi.org/10.1111/j.0141-9889.2004.00426.x.
- Funk LM, Dansereau L, Novek S. Carers as system navigators: exploring sources, processes and outcomes of structural burden. Gerontologist 2019;59:426-35. https://doi.org/10.1093/geront/gnx175.
- Turner M, King C, Milligan C, Thomas C, Brearley SG, Seamark D, et al. Caring for a dying spouse at the end of life: ‘It’s one of the things you volunteer for when you get married’: a qualitative study of the oldest carers’ experiences. Age Ageing 2016;45:421-6. https://doi.org/10.1093/ageing/afw047.
- Robinson CA, Bottorff JL, McFee E, Bissell LJ, Fyles G. Caring at home until death: enabled determination. Support Care Cancer 2017;25:1229-36. https://doi.org/10.1007/s00520-016-3515-5.
- McDonald J, McKinlay E, Keeling S, Levack W. Becoming an expert carer: the process of family carers learning to manage technical health procedures at home. J Adv Nurs 2016;72:2173-84. https://doi.org/10.1111/jan.12984.
- Mohammed S, Swami N, Pope A, Rodin G, Hannon B, Nissim R, et al. ‘I didn’t want to be in charge and yet I was’: bereaved caregivers’ accounts of providing home care for family members with advanced cancer. Psychooncology 2018;27:1229-36. https://doi.org/10.1002/pon.4657.
- Proot IM, Abu-Saad HH, Crebolder HF, Goldsteen M, Luker KA, Widdershoven GA. Vulnerability of family caregivers in terminal palliative care at home; balancing between burden and capacity. Scand J Caring Sci 2003;17:113-21.
- Woodman C, Baillie J, Sivell S. The preferences and perspectives of family caregivers towards place of care for their relatives at the end-of-life. A systematic review and thematic synthesis of the qualitative evidence. BMJ Support Palliat Care 2016;6:418-29. https://doi.org/10.1136/bmjspcare-2014-000794.
- Payne S. EAPC Task Force on family carers. White paper on improving support for family carers in palliative care: part 1. Eur J Palliat Care 2010;17:238-45.
- Latter S, Hopkinson JB, Lowson E, Hughes JA, Hughes J, Duke S, et al. Supporting carers to manage pain medication in cancer patients at the end-of-life: a feasibility trial. Palliat Med 2017:1-11. https://doi.org/10.1177/0269216317715197.
- Baillie J, Anagnostou D, Sivell S, Van Godwin J, Byrne A, Nelson A. Symptom management, nutrition and hydration at end-of-life: a qualitative exploration of patients’, carers’ and health professionals’ experiences and further research questions. BMC Palliat Care 2018;17. https://doi.org/10.1186/s12904-018-0314-4.
- Sluggett JK, Stasinopoulos J, Bell JS. Medication management by informal caregivers – under-recognized and under-supported. Res Social Adm Pharm 2018;14:215-17. https://doi.org/10.1016/j.sapharm.2017.11.002.
- O’Hara JK, Aase K, Waring J. Scaffolding our systems? Patients and families ‘reaching in’ as a source of healthcare resilience. BMJ Qual Saf 2019;28:3-6. https://doi.org/10.1136/bmjqs-2018-008216.
- Pottle J, Hiscock J, Neal RD, Poolman M. Dying at home of cancer: whose needs are being met? The experience of family carers and healthcare professionals (a multiperspective qualitative study). BMJ Support Palliat Care 2020;10. https://doi.org/10.1136/bmjspcare-2016-001145.
- Parliamentary and Health Service Ombudsman . Dying Without Dignity 2015. www.ombudsman.org.uk/sites/default/files/Dying_without_dignity.pdf (accessed 14 December 2020).
- Seamark D, Blake S, Brearley SG, Milligan C, Thomas C, Turner M, et al. Dying at home: a qualitative study of family carers’ views of support provided by GPs community staff. Br J Gen Pract 2014;64:e796-803. https://doi.org/10.3399/bjgp14X682885.
- Hansford P, Meehan H. Gold Standards Framework: improving community care. End Life Care 2007;1:56-61.
- NHS . NHS Five Year Forward View 2014. www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf (accessed 14 December 2020).
- National Audit Office . Health and Social Care Integration. 2017.
- Baxter S, Johnson M, Chambers D, Sutton A, Goyder E, Booth A. The effects of integrated care: a systematic review of UK and international evidence. BMC Health Serv Res 2018;18. https://doi.org/10.1186/s12913-018-3161-3.
- Rand Europe, Ernst and Young . National Evaluation of the Department of Health’s Integrated Care Pilots 2012.
- Bardsley M, Steventon A, Smith J, Dixon J. Evaluating Integrated and Community-Based Care. How Do We Know What Works?. London: Nuffield Trust; 2013.
- NHS . NHS Long Term Plan 2019.
- Anderson C, Sharma R. Primary health care policy and vision for community pharmacy and pharmacists in England. Pharm Pract 2020;18. https://doi.org/10.18549/PharmPract.2020.1.1870.
- Savage I, Blenkinsopp A, Closs SJ, Bennett MI. ‘Like doing a jigsaw with half the parts missing’: community pharmacists and the management of cancer pain in the community. Int J Pharm Pract 2013;21:151-60. https://doi.org/10.1111/j.2042-7174.2012.00245.x.
- Mason B, Epiphaniou E, Nanton V, Donaldson A, Shipman C, Daveson BA, et al. Coordination of care for individuals with advanced progressive conditions: a multi-site ethnographic and serial interview study. Br J Gen Pract 2013;63:e580-8. https://doi.org/10.3399/bjgp13X670714.
- Green E, Shaw SE, Harris T. ‘They shouldn’t be coming to the ED, should they?’ A qualitative study of why patients with palliative care needs present to the emergency department. BMJ Support Palliat Care 2019;9. https://doi.org/10.1136/bmjspcare-2015-000999.
- Gray B, Sarnak DO, Burgers J. Home Care by Self-Governing Nursing Teams: The Netherlands’ Buurtzorg Model. New York, NY: The Commonwealth Fund; 2018.
- Drenna VM, Calestani M, Ross F, Saunders M, West P. Tackling the workforce crisis in district nursing: can the Dutch Buurtzorg model offer a solution and a better patient experience? A mixed methods case study. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2018-021931.
- Kreitzer MJ, Monsen KA, Nandram S, de Blok J. Buurtzorg Nederland: a global model of social innovation, change, and whole-systems healing. Glob Adv Health Med 2015;4:40-4. https://doi.org/10.7453/gahmj.2014.030.
- Maybin J, Honeyman M, Williams E, Perks-Baker S. A Review of the West Suffolk Buurtzorg Test-and-Learn in 2017–18. London: The King’s Fund; 2019.
- Brogaard T, Jensen AB, Sokolowski I, Olesen F, Neergaard MA. Who is the key worker in palliative home care?. Scand J Prim Health Care 2011;29:150-6. https://doi.org/10.3109/02813432.2011.603282.
- Marie Curie Cancer Care . Difficult Conversations With Dying Patients and Their Families 2014.
- National Institute for Health and Care Excellence (NICE) . End-of-Life Care for Adults. Quality Standard 2017.
- Pollock K, Wilson E. Care and communication between health professionals and patients affected by severe or chronic illness in community care settings: a qualitative study of care at the end-of-life. Health Serv Deliv Res 2015;3. https://doi.org/10.3310/hsdr03310.
- Care Quality Commission . A Second Class Ending 2017.
- Leadership Alliance for the Care of Dying People . One Chance to Get It Right: Improving People’s Experience of Care in the Last Few Days and Hours of Life 2014.
- Caswell G, Pollock K, Harwood R, Porock D. Communication between family carers and health professionals about end-of-life care for older people in the acute hospital setting: a qualitative study. BMC Palliat Care 2015;14. https://doi.org/10.1186/s12904-015-0032-0.
- Royal Pharmaceutical Society . Pharmacist Access to the Patient Health Record 2015.
- Care Quality Commission . A Different Ending. Addressing Inequalities in End-of-Life Care 2016.
- Buck J, Webb L, Moth L, Morgan L, Barclay S. Persistent inequalities in hospice at home provision. BMJ Support Palliat Care 2020;10. https://doi.org/10.1136/bmjspcare-2017-001367.
- NHS England . Avoiding Unplanned Admissions Enhanced Service: Proactive Case Funding and Care Review for Vulnerable People. Guide and Audit Requirements 2014.
- Shulman C, Hudson BF, Low J, Hewett N, Daley J, Kennedy P, et al. End-of-life care for homeless people: a qualitative analysis exploring the challenges to access and provision of palliative care. Palliat Med 2018;32:36-45. https://doi.org/10.1177/0269216317717101.
- Klop HT, de Veer AJ, van Dongen SL, Francke AL, Rietjens J, Onwuteaka-Philipsen BD. Palliative care for homeless people: a systematic review of the concerns, care needs and preferences, and the barriers and facilitators for providing palliative care. BMC Palliat Care 2018;17. https://doi.org/10.1186/s12904-018-0320-6.
- McNamara B, Anne S, Rosenwax L, Kelly B. Palliative care for people with schizophrenia: a qualitative study of an under-serviced group in need. BMC Palliat Care 2018;17. https://doi.org/10.1186/s12904-018-0309-1.
- Ebenau A, Dijkstra B, Ter Huurne C, Hasselaar J, Vissers K, Groot M. Palliative care for patients with substance use disorder and multiple problems: a qualitative study on experiences of healthcare professionals, volunteers and experts-by-experience. BMC Palliat Care 2020;19. https://doi.org/10.1186/s12904-019-0502-x.
- McNeil R, Guirguis-Younger M, Dilley LB. Recommendations for improving the end-of-life care system for homeless populations: a qualitative study of the views of Canadian health and social services professionals. BMC Palliat Care 2012;11. https://doi.org/10.1186/1472-684X-11-14.
- McNeil R, Guirguis-Younger M. Illicit drug use as a challenge to the delivery of end-of-life care services to homeless persons: perceptions of health and social services professionals. Palliat Med 2012;26:350-9. https://doi.org/10.1177/0269216311402713.
- Webb W. When dying at home is not an option: exploration of hostel staff views on palliative care for homeless people. Int J Palliat Nurs 2015;21:23-644. https://doi.org/10.12968/ijpn.2015.21.5.236.
- Wittenberg Y, Kwekkeboom R, Staaks J, Verhoeff A, de Boer A. Informal caregivers’ views on the division of responsibilities between themselves and professionals: a scoping review. Health Soc Care Community 2018;26:e460-e473. https://doi.org/10.1111/hsc.12529.
- Stern A, Valaitis R, Weir R, Jadad AR. Use of home telehealth in palliative cancer care: a case study. J Telemed Telecare 2012;18:297-300. https://doi.org/10.1258/jtt.2012.111201.
- Kidd L, Cayless S, Johnston B, Wengstrom Y. Telehealth in palliative care in the UK: a review of the evidence. J Telemed Telecare 2010;16:39-4402. https://doi.org/10.1258/jtt.2010.091108.
- Watanabe SM, Fairchild A, Pituskin E, Borgersen P, Hanson J, Fassbender K. Improving access to specialist multidisciplinary palliative care consultation for rural cancer patients by videoconferencing: report of a pilot project. Support Care Cancer 2013;21:1201-7. https://doi.org/10.1007/s00520-012-1649-7.
- Greenhalgh T, Koh GCH, Car J. COVID-19: a remote assessment in primary care. BMJ 2020;368. https://doi.org/10.1136/bmj.m1182.
- Greenhalgh T, Shaw S, Wherton J, Vijayaraghavan S, Morris J, Bhattacharya S, et al. Real-world implementation of video outpatient consultations at macro, meso, and micro levels: mixed-method study. J Med Internet Res 2018;20. https://doi.org/10.2196/jmir.9897.
- Healy S, Israel F, Charles MA, Reymond L. An educational package that supports laycarers to safely manage breakthrough subcutaneous injections for home-based palliative care patients: development and evaluation of a service quality improvement. Palliat Med 2013;27:562-70. https://doi.org/10.1177/0269216312464262.
- General Practitioners Committee . Focus on Anticipatory Prescribing for End-of-Life Care 2012.
- Johnstone L. Facilitating anticipatory prescribing in end-of-life care. Pharm J 2017;298.
- National Institute for Health and Care Excellence (NICE) . Controlled Drugs: Safe Use and Management 2016.
- Blenkinsopp A, Tann J, Evans A, Grime J. Opportunity or threat? General practitioner perceptions of pharmacist prescribing. Int J Pharm Pract 2008;16:29-34. https://doi.org/10.1211/ijpp.16.1.0006.
- Bush J. Let’s be honest about the new medicine service. Pharm J 2018;301.
- Elliott RA, Boyd MJ, Salema NE, Davies J, Barber N, Mehta RL, et al. Supporting adherence for people starting a new medication for a long-term condition through community pharmacies: a pragmatic randomised controlled trial of the New Medicine Service. BMJ Qual Saf 2016;25:747-58. https://doi.org/10.1136/bmjqs-2015-004400.
- NHS England . Quick Guide: Extending the Role of Community Pharmacy in Urgent Care 2015.
- Graham-Clarke E, Rushton A, Noblet T, Marriott J. Facilitators and barriers to non-medical prescribing – a systematic review and thematic synthesis. PLOS ONE 2018;13. https://doi.org/10.1371/journal.pone.0196471.
- Weeks G, Ceorge J, McLure K, Stewart D. Non-medical prescribing versus medical prescribing for acute and chronic disease management in primary and secondary care (review). Cochrane Database Syst Rev 2016;11.
- The King’s Fund . Workforce Planning in the NHS 2015. www.kingsfund.org.uk/sites/default/files/field/field_publication_file/Workforce-planning-NHS-Kings-Fund-Apr-15.pdf (accessed 14 December 2020).
- Palmer W. Is the Number of GPs Falling Across the UK?. Nuffield Trust; 2019.
- Presland M. Case-based learning: palliative and end-of-life care in community pharmacy. Pharm J 2019.
- Hughes CM, McCann S. Perceived interprofessional barriers between community pharmacists and general practitioners: a qualitative assessment. Br J Gen Pract 2003;53:600-6.
- Jorgenson D, Laubscher T, Lyons B, Palmer R. Integrating pharmacists into primary care teams: barriers and facilitators. Int J Pharm Pract 2014;22:292-9. https://doi.org/10.1111/ijpp.12080.
- Bradley C. Learning to say no to requests for prescriptions. Prescriber 1995:5-35.
- Charles A, Ham C, Baird B, Alderwick H, Bennett L. Reimagining Community Services. Making the Most of our Assets. London: The King’s Fund; 2018.
- Ham C. Making Sense of Integrated Care Systems, Integrated Care Partnerships and Accountable Care Organisations in the NHS in England. London: The King’s Fund; 2018.
- The King’s Fund . Integrated Care: Our Position 2019. www.kingsfund.org.uk/projects/positions/integrated-care (accessed 14 December 2020).
- Torjesen I. Access to patient records: Britain lags behind other countries. Pharm J 2018;300.
- Wickware C. New pharmacist consultation service could provide just £35 per month for pharmacies. Pharm J 2019;303.
- Pollock K, Wilkinson S, Perry Young L, Turner N, Schneider J. What do family care-givers want from domiciliary care for relatives living with dementia? A qualitative study. Ageing Soc 2020:1-14. https://doi.org/10.1017/S0144686X20000185.
- Royal Pharmaceutical Society . The Handling of Medicines in Social Care 2007.
Appendix 1 Case summaries
Code key for case summaries
FIGURE 20.
Ecogram code key.
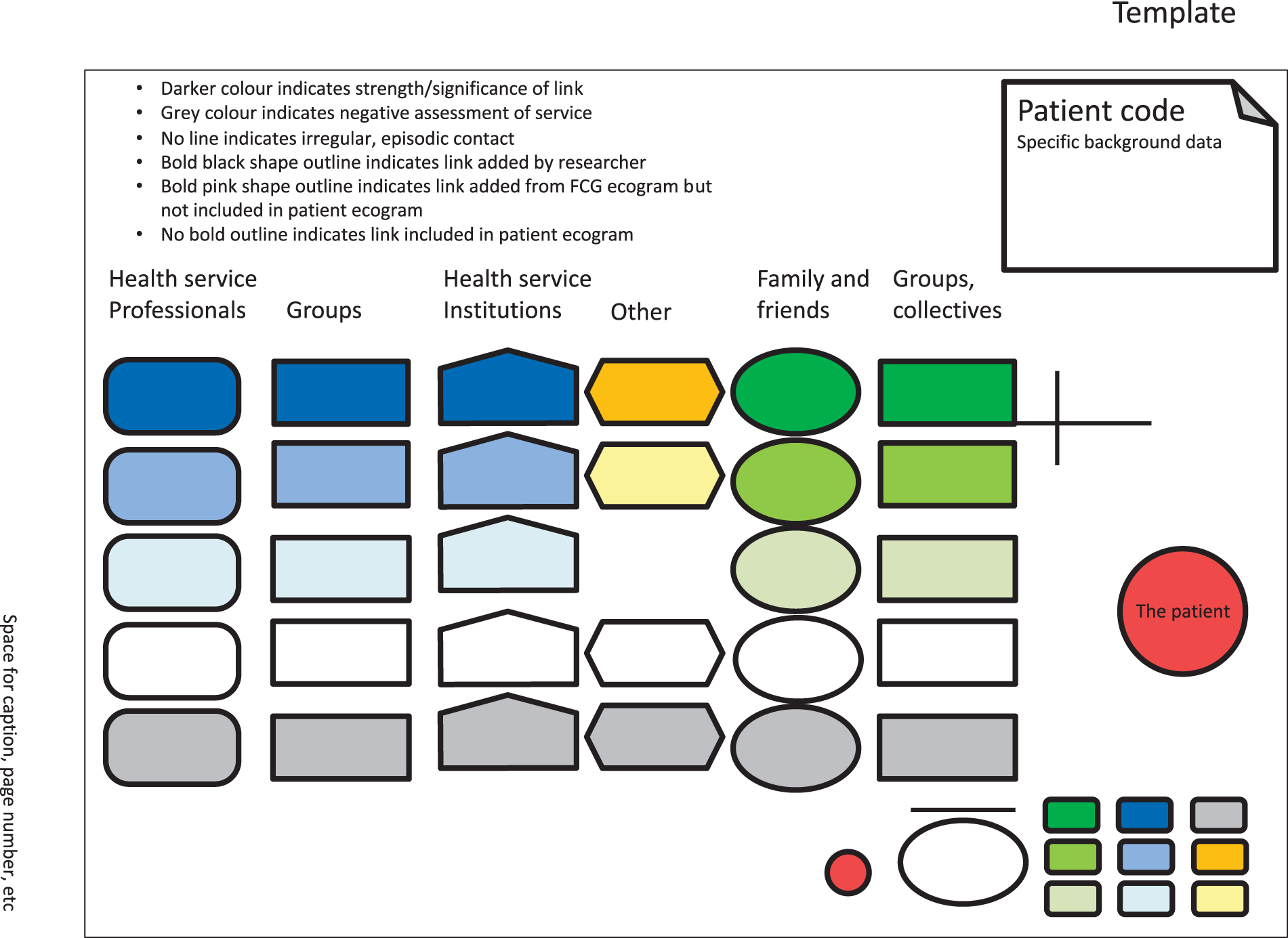
Case summary: Mrs Clark
Family and living arrangements
Mrs Clark was a woman in her 40s, married and living at home with her husband and teenage daughter. She retained responsibility for managing her medication during the period of interview data collection, with support from her informal network (Table 8).
| Participant | Data collection |
|---|---|
| Patient stage 4 ovarian cancer | Two interviews |
| Friend (FCG) | One interview |
| Palliative care consultant (HCP) | One interview |
| Patient, friend | Two ecograms |
| Six photographs | |
| Medicines list | |
| Medical record review |
Background
Mrs Clark had been diagnosed with stage 4 ovarian cancer and within 9 months she had been told that her condition was terminal and referred to hospice for SPC. In the last few weeks of life, she had considerable pain that became increasingly difficult to manage and she subsequently died in the hospice < 2 years after her diagnosis.
Managing medications
Mrs Clark took responsibility for ordering prescriptions using an application on her telephone, which she also used to show her hospice consultant her GP record. She also organised the storage and taking of her medicines at home. A weekly dosette box was used to organise her pills and an alarm was set on her telephone to remind her of the times at which she should be taking medication. She also had a file for letters and information regarding treatment and appointments, plus a notebook that she used to keep track of the five oral medicines that she was taking at the time of interview (i.e. when she had taken them and what kind of effects they had). Mrs Carter’s husband sometimes reminded her to take her medication and had also learned to give injections. Her friend, who also took part in a research interview, had provided extensive practical and emotional support, administered a daily anticoagulation injection over an extended period, attended consultations and surgery with Mrs Clark and her husband, helped her to organise and document her medicines and her reactions to them, and provided moral support. Her sister collected her medication, including morphine, from the local pharmacy.
Mrs Clark felt well supported by the palliative care consultant at the hospice and regarded him as her main point of contact (i.e. key professional) should she have any queries or worries.
Last days of life
Record reviews from her general practice and the hospice recorded Mrs Clark’s preferred place of death as the hospice. Two weeks prior to her death, Mrs Clark was admitted to hospital after suffering with increased nausea and vomiting, and several days later she was discharged directly to the hospice for symptom management and end-of-life care. The hospice records indicate that symptom control continued to be difficult. However, the GP records that Mrs Clark died 'fairly peacefully’.
Ecogram
Mrs Clark’s active network is quite compact and effective (Figure 21). She remained in charge of ordering and administering her medications, even when she sometimes needed physical help to do so (e.g. injections administered by her friend). Her key informal links were her husband and her friend, who had had an unusual amount of involvement over an extended period of time. She had been actively involved with an internet forum and made contact with another contributor whom she corresponded with directly. The GP is a marginal figure in this network. The hospice consultant was her key professional and she was also close to the SPC nurse and DNs, who had been regular attenders to change her syringe driver earlier in her illness. Overall, Mrs Clark remained in charge of managing her medications and was content with a system she experienced as being quite flexible and supportive through her experience of rapidly progressing illness and ongoing issues with drug administration and symptom control. There was no reported change in her network between interviews and no additional services recorded in the period prior to death, rather an intensification of input.
FIGURE 21.
Ecogram: Mrs Clark.
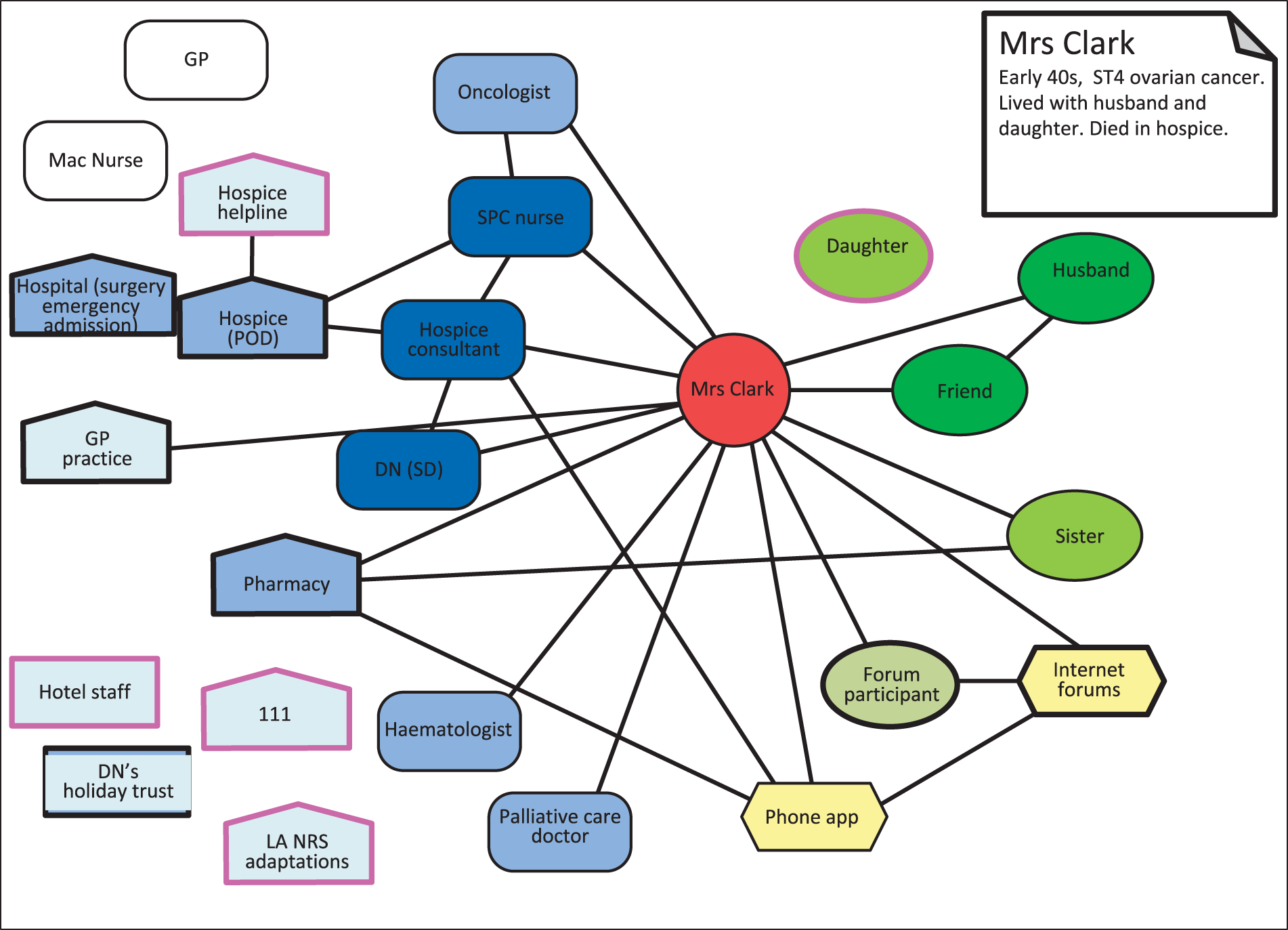
Case summary: Mrs Carter
Family and living status
Mrs Carter was a widow in her late 70s who lived alone. She had a daughter and granddaughter who did not live locally, plus siblings and their spouses who lived nearby. She retained responsibility for managing her medication during the period of interview data collection, with support from her informal network (Table 9).
| Participant | Data collection |
|---|---|
| Patient metastatic breast cancer, type 2 diabetes, impaired kidney function | Two interviews |
| Sister-in-law (FCG) | One interview |
| Palliative care consultant (HCP) | One interview |
| Patient, sister-in-law | Three ecograms |
| Three photographs | |
| Medicines list |
Background
Mrs Carter was diagnosed with metastatic breast cancer and was affected by lymphoedema, which made her left arm unusable while mobility in her right arm was decreasing. This made handling medicines difficult as she struggled to undo bottles, pick up small pills or co-ordinate the pouring of liquid medicines. Mrs Carter was under SPC from the hospice and enjoyed attending for day care. The main issue in terms of medicines for Mrs Carter was to manage her pain while taking account of her diabetes and impaired kidney function.
Managing medications
Mrs Carter took responsibility for ordering prescriptions by ringing the general practice when she needed a refill. She organised the storage and taking of her medicines at home. This was difficult at times because of her lack of manual dexterity. She used plastic containers to store her pills, which remained in their packaging. Mrs Carter was able to remember what she should take and when, saying that she placed the medicines in the box in a certain order, which aided her memory. She understood what her medicines were for, although she struggled with the physical processes necessary for taking her pills and to co-ordinate pouring medicine on a spoon. She managed small pills by licking her finger to pick them up and transfer to her mouth. She had discussed this difficulty with her palliative care consultant and they had agreed that they would leave things as they were for the time being.
Mrs Carter’s sister-in-law collected her medicines from the local pharmacy. As she was taking a controlled drug, the prescription had to be on paper and signed for on collection from the pharmacy.
Mrs Clark felt well supported by the staff at the hospice, particularly the consultant who oversaw her care and the PCN. She regarded the hospice as her main point of contact should she have any queries or worries.
Issues with medicines
Pain was an ongoing problem for Mrs Carter and the pills that she was prescribed made her drowsy so that she would fall asleep during the daytime. Her consultant had considered a bisphosphonate drip, but a blood test had revealed that Mrs Carter’s kidney function was too poor to make this a safe option. Instead, Mrs Carter was given a patch for pain relief and found that she was more alert than when she was taking the pain relief pills.
A further issue for Mrs Carter was that her diabetes was not well controlled, as she was not physically able to test her blood sugar levels herself. It appeared that no one was able to do this for her on a regular basis and the DNs could not visit for this purpose. Staff at the hospice checked her blood sugar levels when she went to the day hospice. Her consultant acknowledged this as a gap in care.
Ecogram
Mrs Carter had a relatively compact and simple network, which seemed not to be densely interconnected (Figure 22). Key informal contacts were her daughter and her sister-in-law who did quite a lot for her, including collecting her medicines. Several other family members and neighbours provided at least social support. Mrs Carter had eight informal links (two of which were core) and 12 professional links (eight of which were active). One of these links (a hospice bereavement counsellor) was added in between interviews. Four professional links were episodic, including the GP who features in the sister-in-law’s ecogram, but not Mrs Carter’s. Her most significant professional contacts were through the interconnected links of hospice day care, PCN and consultant.
FIGURE 22.
Ecogram: Mrs Carter.
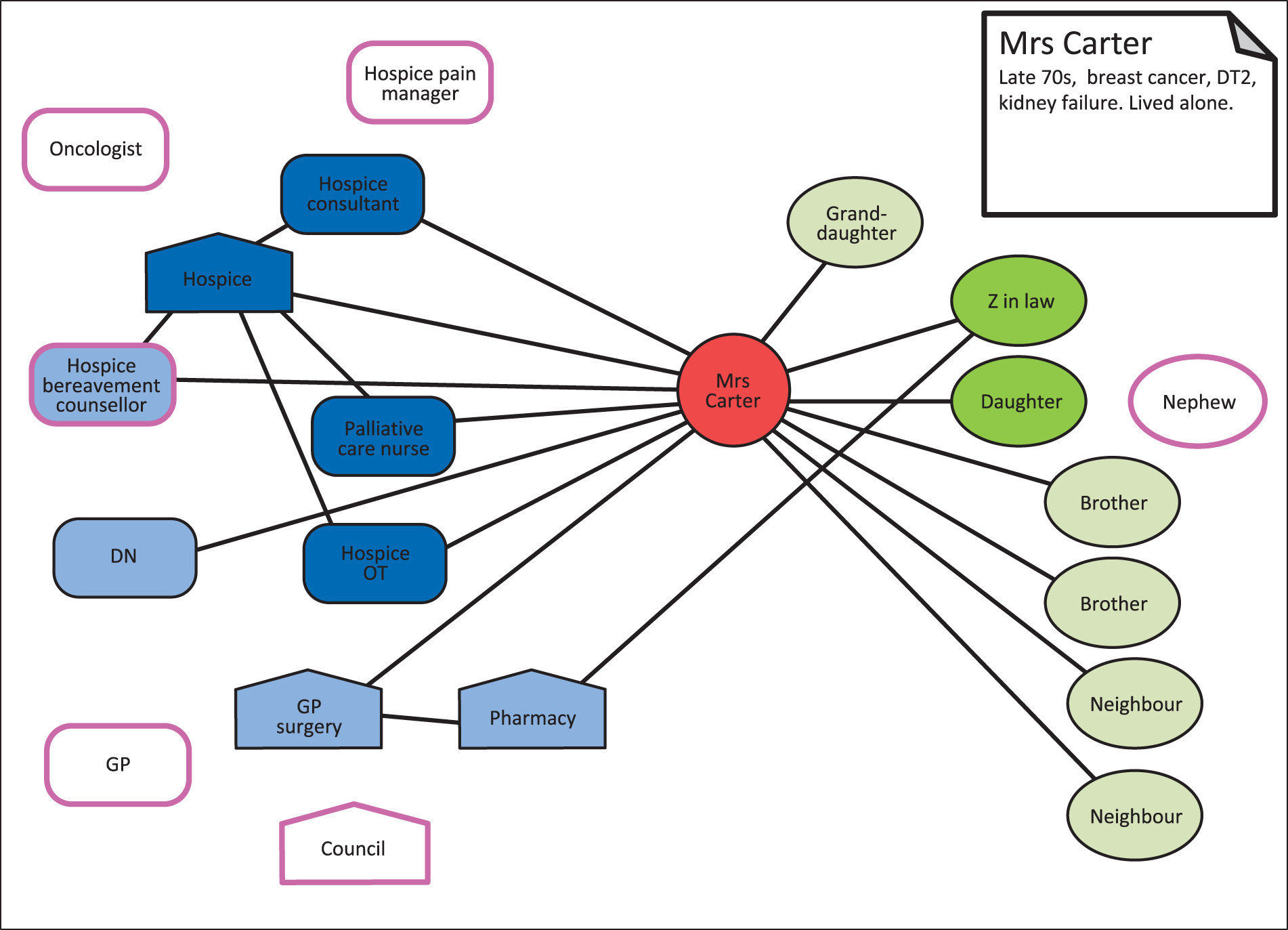
Case summary: Mr Crump
Family and living arrangements
Mr Crump, the patient, was in his 80s and lived with his wife, his main carer, who was in her 60s. Both Mr and Mrs Crump have adult children from previous relationships and Mrs Crump has a sister and two friends who offer some support (Table 10).
| Participant | Data collection |
|---|---|
| Renal failure, dementia, type 2 diabetes | |
| Patient’s wife (FCG, key respondent) | Two interviews |
| Patient, patient’s wife, renal specialist nurse | Observation of outpatient appointment |
| Patient’s wife | Ecogram |
| Medicines list |
Background
Mr Crump had a kidney transplant some years previously and was still taking medication to support his immune system. He also had vascular dementia, for which he was not taking medication, and type 2 diabetes. Until about 4 years before the couple joined the study, Mr Crump had managed his own medicines. Gradually, his wife had taken over responsibility for these as her husband’s dementia had got worse.
The couple had reduced their social activities over recent years and Mrs Crump was building up a new support network through a dementia carers’ group of which she was a member. At the time that Mr and Mrs Crump took part in the research, Mrs Crump still felt that it was safe to leave her husband alone for a few hours, but believed that this was likely to change in the near future. The implications of this worried her. Mrs Crump accompanied her husband to all his clinic appointments, GP consultations and for any blood tests he needed to have. Mrs Crump found her GP very supportive.
Managing medications
Most of Mr Crump’s medicines were provided in two separate blister packs: one put together by the GP and the other, which contained his immunosuppressant drugs, by the hospital pharmacist. Mrs Crump managed this by combining the medicines into a weekly dosette box and adding in the additional medicines that did not form part of either blister pack. Mrs Crump appeared to have a good understanding of her husband’s medicines and what they were for. However, she acknowledged that if there were a change and she needed to remove one of the tablets from the dosette box she would struggle to identify it away from its packaging.
Issues with medicines
In addition to the two blister packs provided through the GP and the renal clinic, Mr Crump was taking some drugs with variable doses, such as warfarin, which the pharmacist was unable to include in the blister packs. This combined to make the process of managing her husband’s medicines challenging for Mrs Crump. She set an alert on her telephone as a reminder of when he was due to take his medication, but if she was occupied when the alarm went off she would defer giving him his pills and would sometimes forget. Mrs Crump was then presented with the quandary as to whether or not to give him the missed dose when the next dose was almost due. She also sometimes woke in the night to the sudden memory that she had not given her husband his evening tablets. The schedule of medicine-taking was difficult to fit within the schedule of their other activities and commitments, such as being ready for the ambulance to take Mr Crump to a day centre on several days each week.
Ecogram
Mr Crump depended on his wife for all aspects of medicines management and administration, and to remind and encourage him to take his medicines or he would ignore/forget them. This was quite a committment, which, although shouldered resolutely, she nevertheless experienced as a burden. Mrs Crump tried to retain some time for her own activities and interests, but expressed concern that this would become increasingly difficult as her husband’s condition deteriorated. Mrs Crump was very outgoing and enterprising in many ways, in engaging both with the system (social services and benefits) and with informal support services, such as a local dementia support group, through which she extended her social contacts and network (Figure 23). However, her main source of informal support was one of her sisters, to whom she was becoming increasingly close, and also two friends. Her sister and friends came to stay and they would go out on jaunts. Her husband went to a respite home when she was away. For shorter stays, her sister and a friend had come to stay at the house to look after her husband and give him his medicines. Mrs Crump’s key HCP was their GP whom she described as being emotionally supportive and understanding. Mrs Crump had quite a wide informal network, although most links seemed fairly weak. Despite moral and practical support from her friend and sister, on a day-to-day basis Mrs Crump felt rather isolated and on her own. No SPC referral had been made.
FIGURE 23.
Ecogram: Mr Crump.
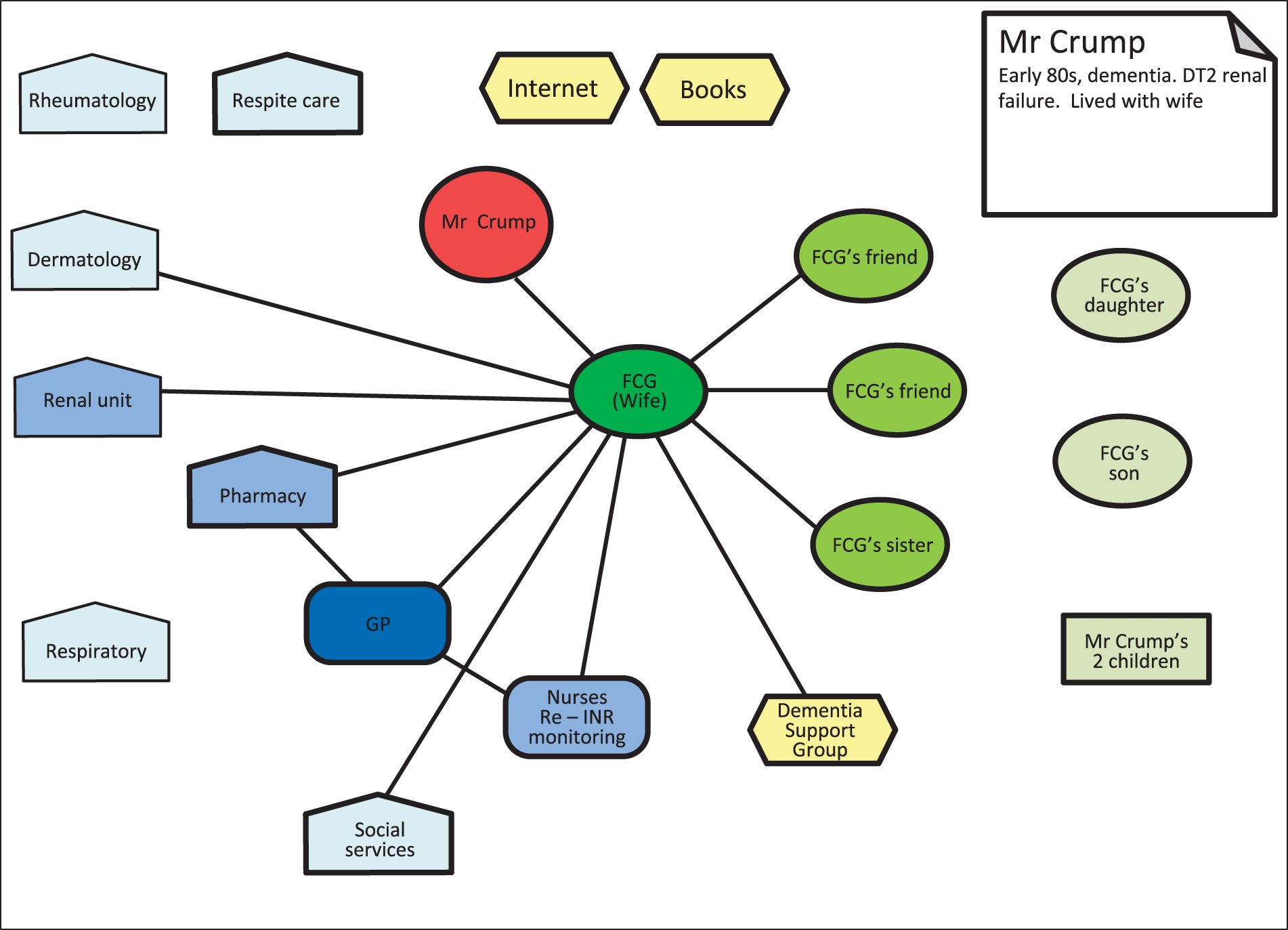
Case summary: Mr Crawford
Family and living status
Mr Crawford was a retired man who lived with his wife, who was his main carer, and his daughter (Table 11).
| Participant | Data collection |
|---|---|
| Patient: PSP | No formal participation in study |
| Wife (FCG, key respondent) | One interview |
| Specialist Parkinson’s nurse (HCP) | One interview |
| Wife | Ecogram |
| Medicines list |
Background
About 7 years before Mrs Crawford joined the study, her husband became unwell, initially becoming forgetful and struggling to find the right words to use. It took 4–5 years and disagreements between HCPs to obtain a diagnosis. One possible diagnosis was dementia and treatment was prescribed for that. PSP was then mooted as a possibility, as Mr Crawford had a number of falls in addition to memory difficulties. However, consultants disagreed and no specific diagnosis was offered, although the focus was on PSP, and Mr Crawford was referred to a specialist Parkinson's disease nurse.
Mr Crawford attended a day hospice, and for some time they had support from night sitters, carers and occasional respite care.
Managing medications
Mr Crawford was prescribed different drugs by different HCPs at different times. Mrs Crawford took full responsibility for the management and administration of these, although she found it difficult to keep on top of the changing drug regimen. Initially, they had received blister packs from the pharmacist, but the constant changes created waste, which was unacceptable to Mrs Crawford. She, therefore, moved to a system whereby she filled a weekly dosette box, which she purchased herself, and created a written record of the drugs her husband was taking. Their general practice had moved to an online system for ordering repeat prescriptions, which Mrs Crawford did not like, although this was not possible for controlled drugs. If Mrs Crawford had any queries she would contact the specialist Parkinson’s nurse.
Issues with medicines
Mrs Crawford worked hard to manage her husband’s care and medicines. She reported poor communication with HCPs, exacerbated by the uncertainty created by the lack of diagnosis and disagreement between professionals. On one occasion, Mrs Crawford received a telephone call from the general practice asking her to pick up a prescription for medicines, which she later realised were AMs. The specialist Parkinson’s nurse had discussed placing her husband on fast track, but no one had discussed AMs with either her or her husband. Mrs Crawford felt that it was a matter of trial and error in relation to her husband’s medicines. She also reported some errors that had been made, such as night sitters calling a DN to give Mr Crawford morphine, when she had already given him Oramorph. She described maintaining vigilance over her husband’s medicines and the prescribing decisions made by different professionals.
Last days of life
The specialist Parkinson’s nurse was interviewed after Mr Crawford’s death. He died at home, with a syringe driver having been installed 2 days earlier. The nurse was uncertain whether or not any of Mr Crawford’s medicines had been withdrawn as he was dying because she was unable to access GP records.
Ecogram
Mr Crawford’s network was complicated (Figure 24), reflecting a large number of contacts over about 7 years, which was difficult in terms of working the system and coping with the increasing severity of his illness, an unusual form of Parkinson’s disease. Perhaps the difficulties of diagnosis and treatment set the scene for the family’s struggle and dissatisfaction with a number of elements of the system. Mrs Crawford, her husband’s carer, was relatively isolated, with only a little help from her sister, but no other informal links of help or support. There was a very complex array of professional links, a significant number of which she expressed dissatisfaction with, including their GP and even elements of the hospice and associated services. The ecogram had 28 links, including four informal links (one was the PSP association), 24 professionals, no key informal supporter and nine negative links. There was no key HCP. Mrs Crawford reported that caring for her husband and managing his medicines was an ongoing struggle, in which they both felt all at sea.
FIGURE 24.
Ecogram: Mr Crawford.
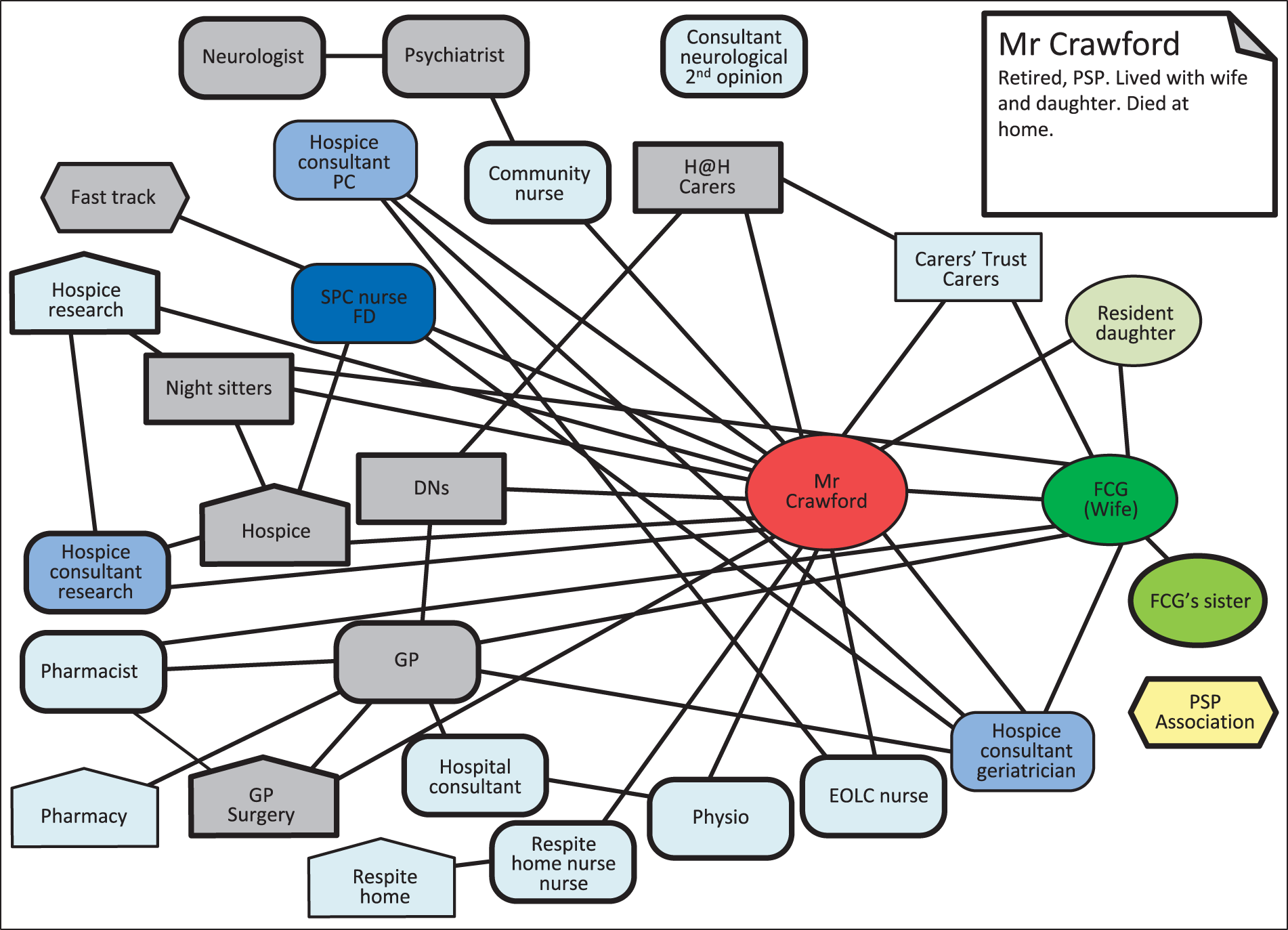
Case summary: Mr Cole
Family and living status
Mr Cole, a man in his late 60s, lived with his wife who was in her late 50s. Mr Cole had a brother, a sister and a niece living locally, and Mrs Cole had a son who was not local. They had a supportive neighbour who would call to see them regularly and sometimes bring a meal for Mr Cole (Table 12).
| Participant | Data collection |
|---|---|
| Patient: complex co-morbidities including heart disease, type 2 diabetes, kidney failure and prostate cancer | Three interviews (joint with wife) |
| Wife: blind, type 1 diabetes, PEG fed | Three interviews (joint with husband) |
| SPCN (HCP) | One interview |
| HCW | One interview |
| Patient, wife | Ecogram |
| Six photographs | |
| Medicines list | |
| Wife, HCW | Observation of administration of PEG feed |
| Patient | Medical record review |
Background
Mr Cole had multiple comorbidities for which he was taking a large number of medicines in different forms, including tablets, patches and liquids. He had limited mobility and occasional confusion, perhaps caused by the pain medication that he took. Pain was a big issue for Mr Cole. He was under the care of a hospice and had experienced more than one admission in an attempt to manage his pain. He had been discharged from hospice on a previous occasion on fast track, which had subsequently been removed.
Mrs Cole had become blind as a complication of diabetes and was unable to eat or drink, being fed through a PEG tube, with her medicines also being administered in this way, except for her insulin. Mr and Mrs Cole described themselves as supporting each other.
Managing medications
Mr Cole, in particular, was on a complex drug regimen (daily), involving several different modes of administration, which were handled by a HCW who came four times per day. The HCW also set up Mrs Cole’s PEG. Mr Cole’s medicines were delivered routinely by the pharmacy in a blister pack, without him needing to make a request or contact the GP. The pharmacy also sometimes rang to check that everything was OK. Mrs Cole was impressed that after changes to her husband’s medicines the system still worked well. The HCW put Mr Cole’s pills in a plastic cup and handed them to him to take, applied/changed his fentanyl patch and handed him the insulin pen for him to inject himself.
Mrs Cole was able to manage checking her blood sugar levels with a talking device and injected herself with insulin. In the early evening, a HCW administered Mrs Cole’s medicines through the PEG tube, before connecting it to the food, which was administered overnight.
Mr Cole was well supported by the hospice and his PCN was the first point of contact in case of any concern about medicines. Mr and Mrs Cole described their relationship with one of the HCWs who came regularly to visit them as being ‘more of a friend’ than a professional.
Issues with medicines
The system by which Mr and Mrs Cole both received their medicines seemed to work efficiently on the whole. However, Mr Cole was sent home from the hospice with a bag of AMs, although he was not told that this was what they were. On at least one occasion, Mrs Cole’s GP prescribed medication that could not be fully dissolved, which was unsuitable for her. It is notable that the couple were completely dependent on the support of professionals in their day-to-day management of their medicines and were in receipt of an extensive package of care.
Ecogram
Mr and Mrs Cole had complex health problems requiring intensive input from health and social services (Figure 25). They reported having a good relationship with the HCW and the SPCN from the hospice, who was their key contact. Different parts of their care system seemed to communicate quite well: the SPCN and GP communicated to sort out issues, the GP and pharmacist liaised with each other and Mr and Mrs Cole could communicate with the pharmacist about any problems with prescriptions, which the pharmacist sorted out directly. Ordering and supply of medicines was handled smoothly by the pharmacy. The couple did not have to put in a request for repeat prescriptions. The system even worked when Mr Cole was discharged from hospice with a new drug regimen, although they later discovered that this included AMs, which they had not been told about. The SPCN reported being ‘disgusted’ about this. The couple had one close and supportive neighbour. Mr Cole’s brother-in-law and also Mrs Cole’s son who lived at some distance were accessible and involved if and when necessary. However, the couple maintained a stance of independence and self-sufficiency, despite increasing involvement of active help with the organisation and administration of their medicines. The HCW had sorted out the considerable muddle in which their medicines were kept and set up a good system of storage and administration. The HCW had considerable responsibility for supporting medicines management, and also a very good relationship with the couple.
FIGURE 25.
Ecogram: Mr Cole.

Case summary: Mr Collins
Family and living status
Mr Collins was in his 60s and lived with his wife, also in her 60s, who was his main carer. Adult children and other family members lived locally (Table 13).
| Participant | Data collection |
|---|---|
| Patient: PSP | No formal study participation |
| Wife (FCG, key respondent) | Two interviews |
| Specialist Parkinson’s nurse (HCP) | One interview |
| Wife | Ecogram |
| Six photographs | |
| Medicines list | |
| Observation of medication storage |
Background
Mr Collins had been ill for about 8 years, although was diagnosed with PSP only 2.5 years before joining the study. It was originally thought that he had Parkinson’s disease and the diagnosis of PSP was made following a brain scan. Although professionals were aware of this diagnosis, Mr and Mrs Collins were not aware of this and discovered it only when Mr Collins was assessed by a surgeon for a hip replacement operation and informed that the surgery could not take place because of the PSP.
Mr Collins attended hospice day care twice per week. Mrs Collins said that her husband experienced incontinence, a level of confusion and restricted vision. He was also increasingly weak, to the degree that his mobility was affected and he used a walking frame indoors and a wheelchair outside. He had difficulty controlling his saliva, although a Botox (botulinum toxin) injection had helped. Mrs Collins provided most of his care, believing that she knew him best and could understand his speech.
Managing medications
Mrs Collins managed her husband’s medicines effectively, although pain in her hands made physically managing bottles and pill packets difficult. She kept a list of medicines and stored them in a tin, which was kept in a cupboard with a list on it. Once per week, Mrs Collins made up a dosette box containing the week’s medicines. Both Mr and Mrs Collins had an alarm on their telephones that was set to go off when Mr Collins needed to take the next dose of medicine. Mr Collins carried his day’s pills with him and knew that the alarm signalled when it was time to take his pills. Family members were aware of this, as were the nurses at hospice day care.
Mr Collins experienced a number of infections and had prophylactic antibiotics on hand, in case of recurrence. However, Mrs Collins took an active role in deciding how to handle a developing infection and believed that sometimes the key was to ensure that he drank plenty of fluids. Mr Collins’ medication regimen was stable over the course of Mrs Collins’ study participation, although he had experienced one hospital admission and received two courses of antibiotics.
The specialist Parkinson’s disease nurse was a key professional and the person to whom Mrs Collins would go with any queries about medicines.
Issues with medicines
Mrs Collins reported that they had few issues with medicines. She found it difficult that she needed to tell their story every time they met a HCP, particularly early on in the disease experience. The main difficulty that they experienced was related to Mr Collins’ incontinence and the infections that developed because of this. In addition, Mrs Collins was concerned about the impact of her husband’s deteriorating swallow on his ability to take his (currently 14) medicines in future.
Ecogram
Mrs and Mrs Collins received good support from informal and professional members of their network (Figure 26). Their key professional contact was a Parkinson’s disease specialist care nurse and they also positioned the GP in a strong position in the chart, as well as the nurses at the hospice day centre. In addition to available local family and community support, the couple was in touch with support organisations such as the Carers Trust (Essex, UK) and PSP Association (Milton Keynes, UK). Mrs Collins reported experiencing a marked improvement in care following the Parkinson’s disease specialist care nurse’s suggestion that they agree to sharing their electronic medical records between HCPs involved in Mr Collins’s care. This removed the need to continually retell their story.
FIGURE 26.
Ecogram: Mr Collins.
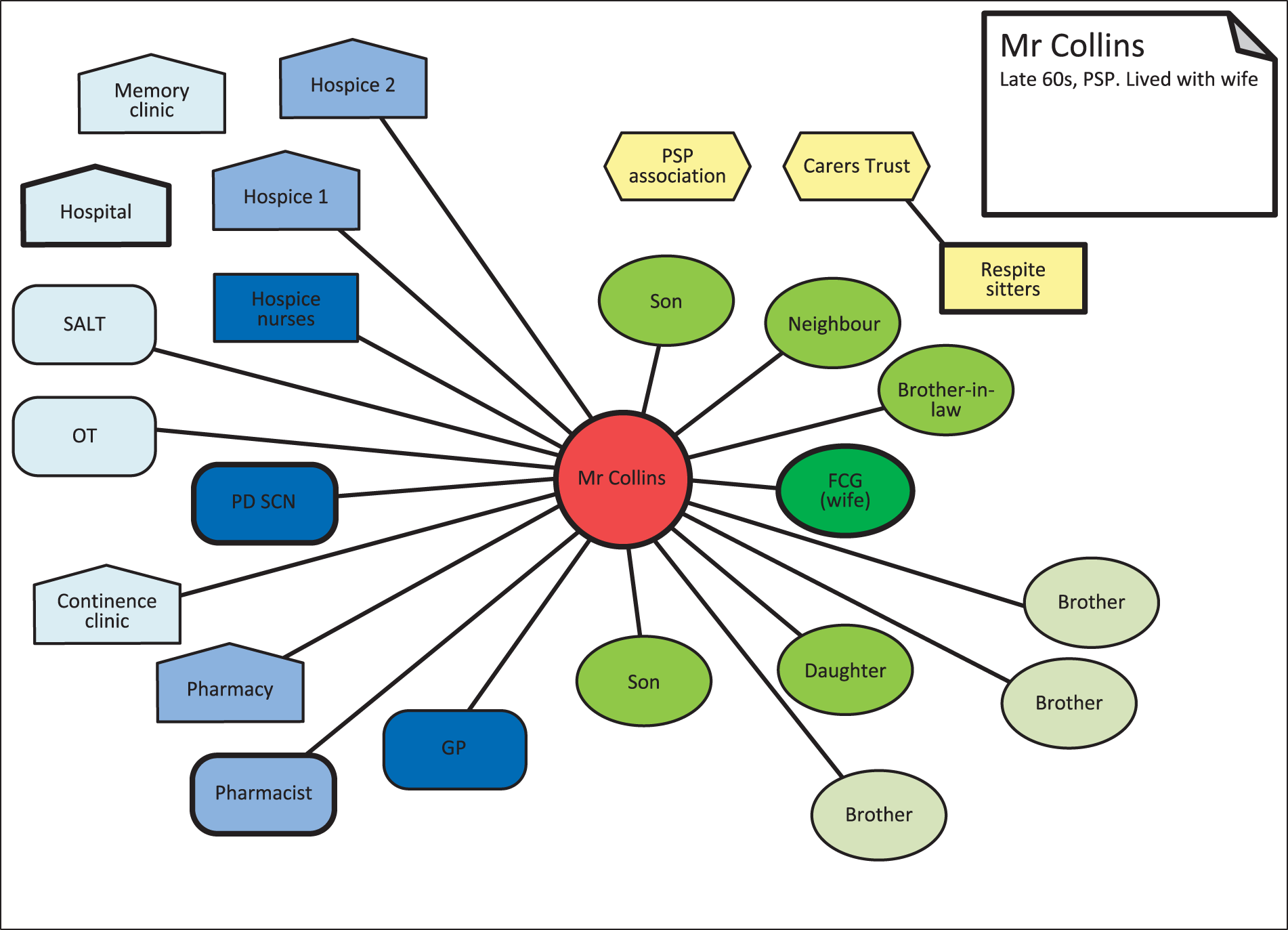
Case summary: Mrs Creasy
Family and living status
Mrs Creasy was a woman in her 80s who lived with her husband, who was her main carer. Mr Creasy also had complex health problems (including cancer, diabetes and deafness). One of her daughters, Ms Creasy, who lived nearby, also took an active role in caring for her mother, spending 1 day per week with her parents. Her siblings, a sister and three brothers, were less actively involved in providing support (Table 14).
| Participant | Data collection (March) |
|---|---|
| Patient: heart failure, husband (FCG 2), daughter (FCG 1) | Two interviews (joint) |
| Daughter (FCG 1) | One interview |
| Daughter (FCG 1) | Ecogram |
| Medicines list |
Background
Mrs Creasy had a heart attack in her 30s, which was misdiagnosed and untreated. A second heart attack in her 70s left her with heart failure, for which she was treated. Mrs Creasy was attending a 12-week course at the hospice, which she enjoyed. She had been taught some techniques by the hospice to help her manage anxiety when she was feeling unwell and could not catch her breath. She also used a fan to help her with her breathing.
Managing medications
Mr Creasy took responsibility for administering his wife’s medicines on a day-to-day basis, and the couple’s daughter took charge of collecting the medicines and liaising with HCPs. Most medicines were received from the pharmacy in a blister pack, which the family collected. Ms Creasy reported that she felt alone and unsupported by services and that she had been unable to get social services support for her parents. She also reported that her parents’ relationship was deteriorating and that her own relationship with her mother was under strain.
Issues with medicines
Mrs Creasy had an allergy to a substance present in a number of medicines, and it was very difficult to maintain a supply of medicines that did not contain this. Her daughter spent quite a lot of time on the internet searching for information about medications and liaising with services and HCPs. Despite her hard work, Ms Creasy had little satisfaction from her dealings with professional services. She reported having to be quite vocal in her protests that medicines needed to be free from this allergen. Her mother always needed to keep loratadine to counteract the allergy. Pharmacies tended to change brands according to cost and manufacturing deals, which played havoc with their system, as new medicines were likely to contain the allergen and apparently no one gave the family any warning. Ms Creasy worked hard at reading the information sheets and trying to track down pharmacies that stocked appropriate medicines, with variable success. Her father had to periodically make a trip to a distant pharmacy to get one medicine. Other medicines were supplied by the practice pharmacy and also other pharmacies according to supply and availability, which kept changing.
Ms Creasy also reported that her mother did not take her medicines as they were prescribed. Her husband would take them out of the pack and hand them to her, but Mrs Creasy had told them that she did not wish to continue taking some of her medicines and her husband had seen her throwing them away.
Ecogram
Mrs Creasy had an extensive network of professional contacts, but reported no supportive contact or relationships with any individual or service. The family liked one GP at their local practice, but did not see him often and he did not seem to be proactive in managing Mrs Creasy’s health issues. Care seemed to be distributed across a disparate and rather ad hoc network (Figure 27), frequently involving OOH calls and paramedics, resulting in several past hospital admissions. Different professionals tended to change/add to Mrs Creasy’s prescriptions, which caused difficulties in getting these entered on the system and in locating a source of medicines without allergens. There are a number of grey cells in the network because of the struggle to get medicines and also services that were started and then stopped. There are no real key professional contacts, which may be part of the problem. Despite Ms Creasy being very proactive and engaged, she did not seem to have got the system to work for them. There was a hospice day care referral, but it seems no active specialist nursing care (although a heart failure nurse was included in the chart).
FIGURE 27.
Ecogram: Mrs Creasy.
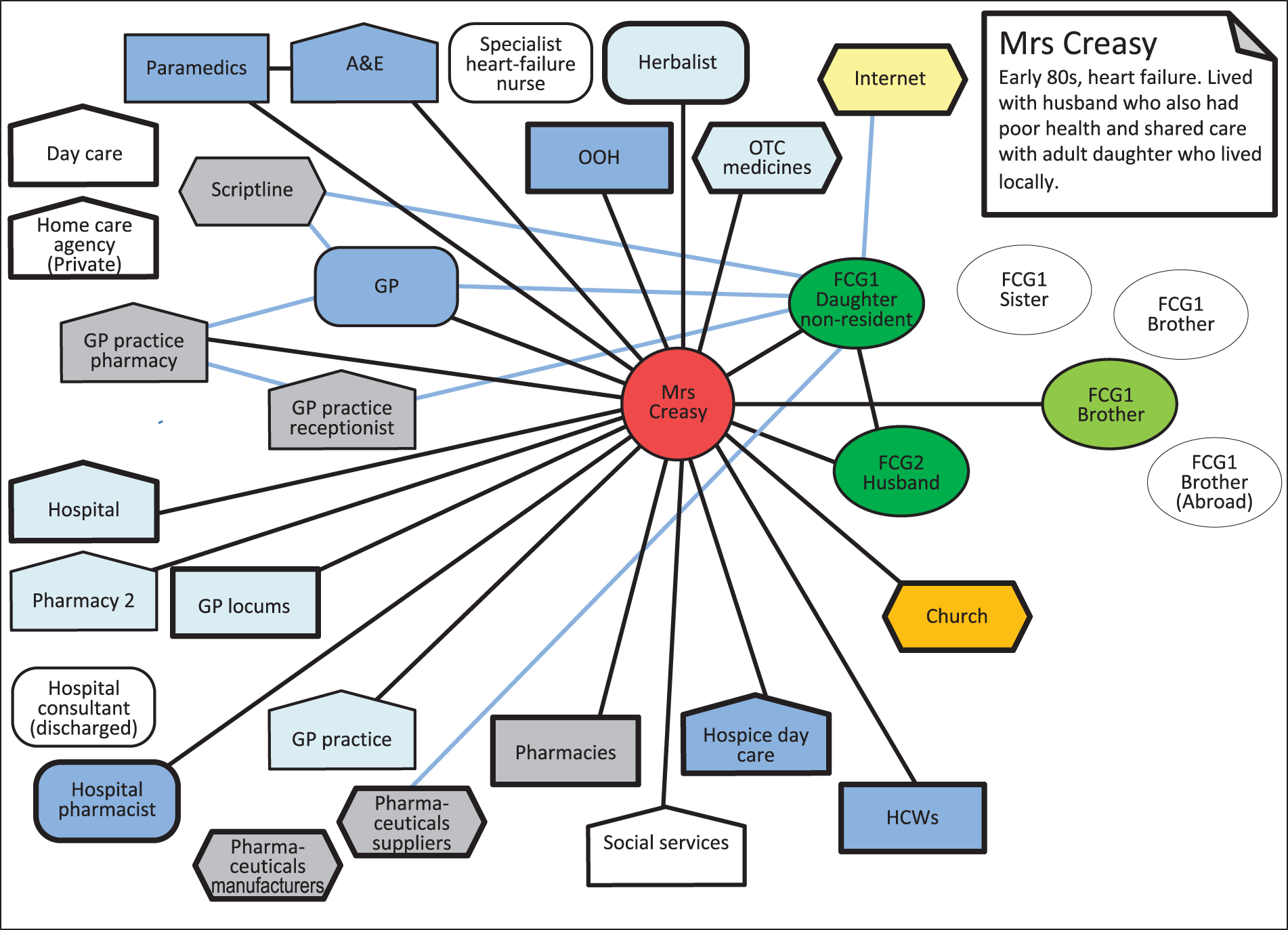
Case summary: Mr Cooper
Family and living status
Mr Cooper lived with his partner and both were in their 70s. They each had adult children from previous relationships. Mr Cooper’s children lived at some distance and visited rarely. Mrs Cooper’s children lived locally and visited quite often (Table 15).
| Participant | Data collection |
|---|---|
| Patient, MND, partner (FCG) and HCW (HCP 1) | One interview |
| Patient and partner (FCG) | One interview |
| HCW (HCP 2) | One interview |
| Patient (FCG) | Two ecograms |
| Medicines list | |
| Photographs | |
| Medical records review | |
| Observation of medication storage, NIV and tablet use |
Background
Mr Cooper’s main health issues were MND and type 2 diabetes. He was confined to a wheelchair and had only a little movement in his hands, although he had devised his own technologies that enabled him to steer his wheelchair and hold his tablet. Mr Cooper received 24-hour non-invasive ventilation. He felt that his voice and swallow had deteriorated between the first and the second interviews, although he was still able to eat and take oral medications if he timed this well with his ventilator. Mr Cooper had an extensive package of care from a private agency, with HCWs in attendance most of the day. The care agency had a nurse whom they could contact in case of queries. A DN visited twice per month, but was perceived by Mr Cooper to be able to offer little help. He was in contact with an occupational therapist, attended the lung function clinic and saw a MND nurse during hospital visits. Mr Cooper attended hospice day care and felt supported by the nurses who worked there. He appreciated the equipment that the British Red Cross (London, UK) had provided.
Managing medications
Mrs Cooper took responsibility for keeping track of medicine supplies, ordering prescriptions online and collecting medicines. Mr Cooper was prescribed nine oral medicines to take each day, one spray and two others p.r.n. These were administered by HCWs and recorded on a medicines administration record. Medicines were stored in plastic boxes on a work surface in the kitchen. This was not ideal, but there was no other place that they could be kept. Mr Cooper felt that his GP would be his first port of call in case of queries, including emergencies relating to medicines.
Issues with medicines
Mr Cooper’s partner had originally ordered prescriptions by ringing the general practice, but moved to ordering medicines online and collecting them from the pharmacy. She preferred this system, which she felt gave her more control over what was ordered. She did not wish to use the pharmacy delivery service as she considered this to be unreliable. Mr Cooper was critical of his contact with and poor support from the orthotics department and the supply and maintenance of his ventilation equipment. This was critical because Mr Cooper depended on his ventilation machine to support his breathing.
Last days of life
Mr Cooper was given rescue medicines when he experienced breathing difficulties, but these did not help. When Mrs Cooper called for an ambulance, the operator suggested moving her husband to the floor to start cardiopulmonary resuscitation (CPR). When the ambulance crew arrived they enquired about a DNACPR, which Mrs Cooper found and so the resuscitation attempt was stopped. GP notes state that the patient died peacefully at home.
Ecogram
Mrs Cooper was her husband’s key carer. Despite Mr Cooper’s disabilities and her own health problems, they seemed to be quite a self-sufficient couple in the sense of being emotionally contained. Some family members lived nearby, but they did not seem to be involved. They also had contact with their neighbours, although these neighbours do not feature in the interviews. Some support was provided by non-statutory agencies and services (Figure 28). Mr Cooper seemed quite proactive in finding and using information. He had a moderate-sized professional network, but about one-third were specified as free-standing rather than interconnected. No key professional was identified, although the GP was specified as their first port of call. The intensive personal support provided by the HCWs was the nearest to a key resource. Although they were positive about the staff and what they did, neither Mr Cooper nor his partner seemed to engage with these individuals on a personal level.
FIGURE 28.
Ecogram: Mr Cooper.
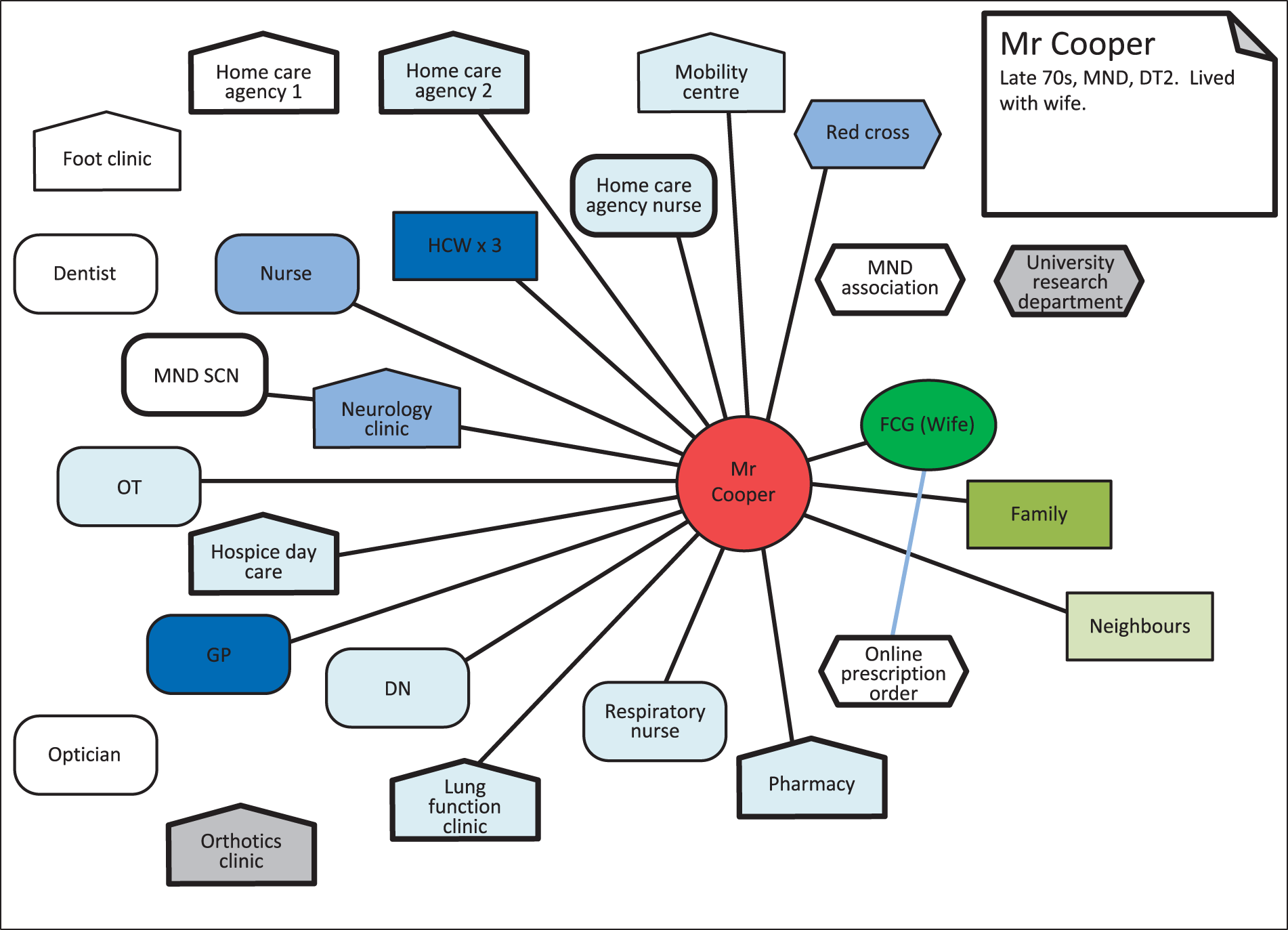
Case summary: Mrs Crane
Family and living status
Mrs Crane was a widow in her 60s who lived alone in what had been the family home. She had two daughters who visited but were not involved in the management of her medicines, and a friend who visited 6 days per week and was a valuable source of support. A couple of neighbours also provided support (Table 16).
| Participant | Data collection |
|---|---|
| Patient: heart failure, arthritis, asthma, depression, sleep apnoea | Two interviews |
| Patient and consultant in anaesthesiology and pain management (HCP) | Observation of pain management consultation |
| Patient | Ecogram |
| Fifteen photographs | |
| Medicines list | |
| Medical record review |
Background
Mrs Crane had heart failure as well as arthritis in her knees, which caused her considerable pain and sleep apnoea. She struggled to get upstairs in her home and had a lift installed to facilitate access to the bathroom. She had a hospital bed in her living room, leaving just enough space for two armchairs and a small television. She was visited twice per week by a HCW whom she considered a friend. Her friend who visited regularly cooked meals for her and reminded her to take her evening medicines, which sometimes Mrs Crane would forget when she was tired. Pain was a big issue for Mrs Crane, as was tiredness because of her apnoea. At the time of taking part in the research, she recognised that she was starting to need more support and was trying to secure further visits from the HCW.
Mrs Crane attended day care at the hospice, which she enjoyed very much. When her time there came to an end she was matched up with a hospice home visitor instead. Her HCW was a key professional contact, as was the heart failure nurse whom she contacted via the SPA in case of concerns about medicines or her health. Mrs Crane also regarded the hospice as an important place for support. She had a DNACPR in place, which she had initiated herself about 1 year prior to the interview.
Managing medications
Mrs Crane managed her own medicines. She received a blister pack from the pharmacist, as well as several other medicines and inhalers. She was organised and knew what each of the medicines were, if not their names, so that she could identify if something was missing or had changed, although she found it frustrating that the pharmacist would change the brand without informing her. Mrs Crane had attended the sleep clinic where she was given a continuous positive airway pressure machine that she wore overnight, which helped her to breathe while asleep. This had improved the quality of her sleep so that she was less tired.
Ecogram
Mrs Crane lived alone and was mainly housebound. She received a good deal of help from one friend and a couple of neighbours. She also had some home help and extensive support from the hospice (Figure 29). Mrs Crane took a lot of medicines (quite a complex regimen), which she was absolutely on top of in terms of ordering arranging and sorting (some come in blister pack from pharmacy). However, she relied on her friend, who visited every evening and prompted her to take these when she was tired. She acknowledged feeling apprehensive about needing more organised help soon. Mrs Crane disliked the pharmacist changing the brand of her medicines without giving notification. However, she was willing to contact the pharmacy and her GP directly regarding any problems arising and other staff through the SPA, if necessary.
FIGURE 29.
Ecogram: Mrs Crane.
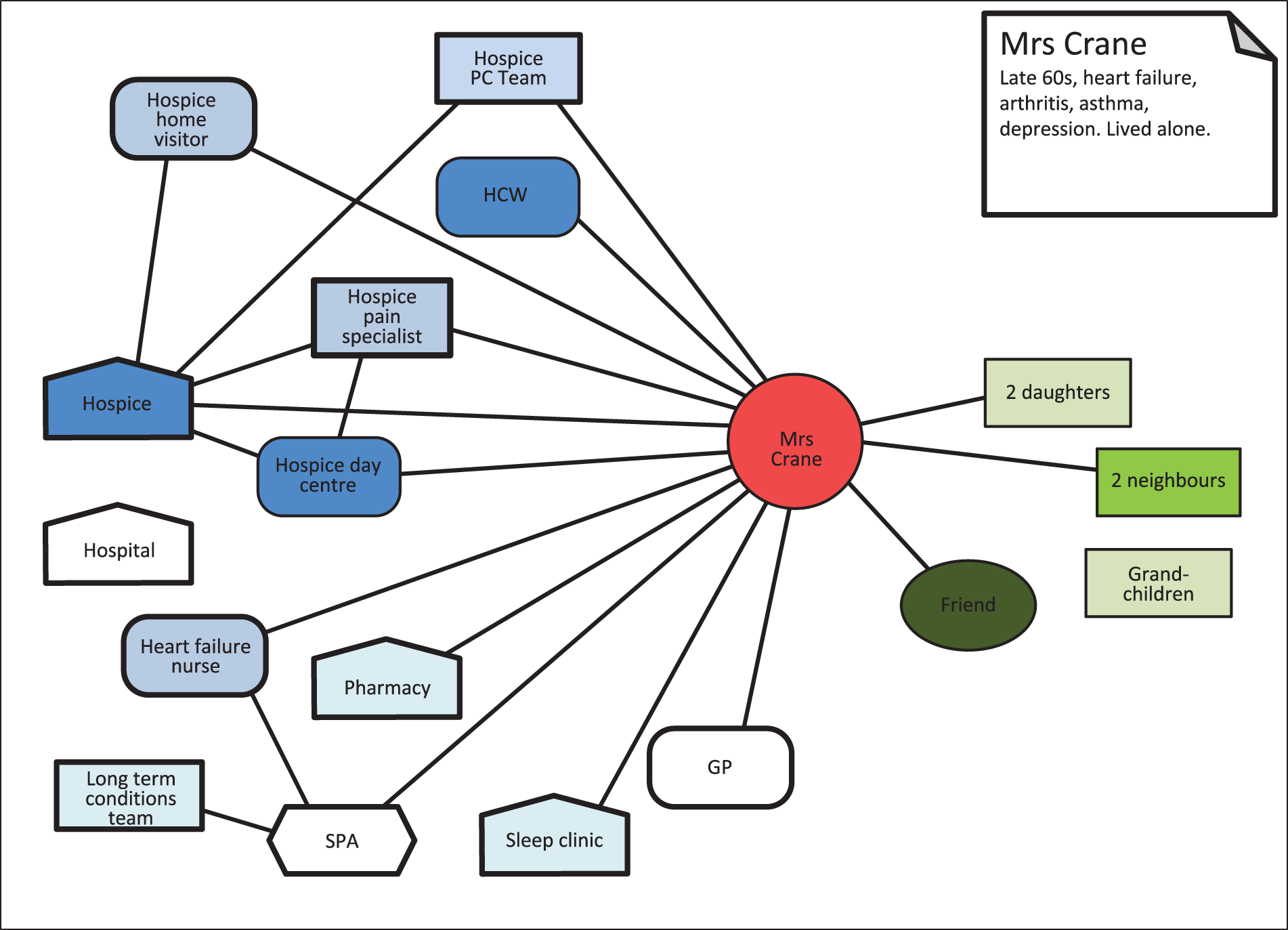
Case summary: Mrs Choudhury
Family and living status
Mrs Choudhury was a widow in her 80s who lived with her son and daughter-in-law and one of their three adult children. The family were originally from India and spoke Guajarati. Mrs Choudhury spoke very little English, although younger generations of the family spoke this fluently (Table 17).
| Participant | Data collection |
|---|---|
| Patient: angina, diabetes, arthritis, vertigo | No formal study participation |
| Daughter-in-law (FCG, main respondent) | Two interviews |
| Two photographs | |
| Medicines list |
Background
Mrs Choudhury had angina, diabetes, arthritis and vertigo. She was unable to stand for very long and required someone to be with her at all times. Her daughter-in-law was her main carer and the person who undertook all of the household tasks. She also took part in the research interviews. Mrs Choudhury was present during the interviews, but she did not contribute.
In the past, Mrs Choudhury had a number of previous hospital admissions, but she was no longer under hospital care. The family were told to come back to clinic if they needed to. The main source of HCP support was the general practice at which there were two Guajarati-speaking GPs who were considered by Mrs Choudhury’s daughter-in-law to provide excellent care.
Managing medications
Mrs Choudhury’s daughter-in-law took responsibility for administering medicines at the right time and for monitoring her mother-in-law’s blood sugar levels. The medicines came automatically from the pharmacy on a 4-weekly basis in blister packs. On occasion, Mrs Choudhury would have difficulty breathing or experience a tight chest from the angina. She had a spray to use for this, but her daughter-in-law reported that often it would be caused by something such as the room being overheated, and this was easily remedied without recourse to medication. Mrs Choudhury’s daughter-in-law’s first port of call in case of queries about medicines or her mother-in-law’s health was always the general practice. The GPs were willing to do home visits, and when there was any need to make changes to her mother-in-law’s medicines they would ensure that her daughter-in-law knew about it and understood what it was for.
Ecogram
Mrs Choudhury’s daughter-in-law provided intensive support for her and managed all aspects of her medicines, which she was confident about and happy to do. The family had good relations with two Gujarati GPs at their local practice, who liaised efficiently with the pharmacy if any drugs needed changing. The network was small and self-contained (Figure 30). No other services were mentioned, although Mrs Choudhury had had contact with the hospital in past. Staff there told her to come back if she needed further attention, which seems not to have been the case.
FIGURE 30.
Ecogram: Mrs Choudhury.
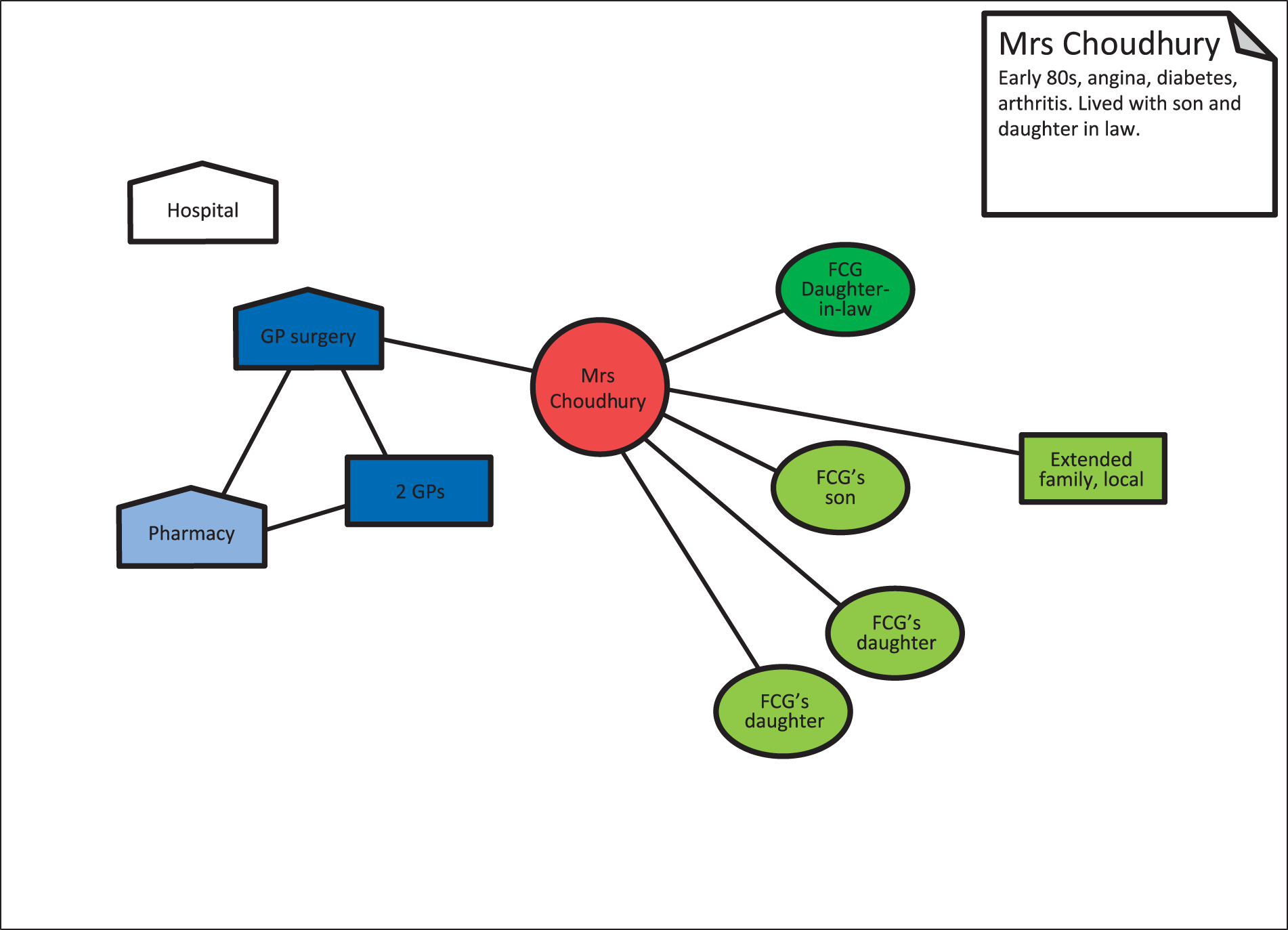
Case summary: Mr Connor
Family and living status
Mr Connor was in his late 70s and lived at home with his wife. They had adult children but appeared not to rely on them for support (Table 18).
| Participant | Data collection |
|---|---|
| Patient: end-stage kidney disease, stroke, diverticulitis, type 2 diabetes | Two interviews (joint with wife) |
| Wife (FCG) | Three interviews (two joint with husband) |
| Patient and wife (FCG) | Ecogram |
| Five photographs | |
| Medicines list | |
| Medical record review | |
| Observation of CNS visit and storage of medication |
Background
The couple had known that Mr Connor had kidney disease, but discovered that it was stage 4 only when Mr Connor was told that he could not have a CT scan for his diverticulitis because it would kill him. Mr and Mrs Connor had visited the renal dialysis unit, but Mr Connor had decided against undergoing kidney dialysis. In addition, Mr Connor had type 2 diabetes and had experienced a stroke. Mrs Connor also had health problems, including a heart condition and a problem with one of her legs, which made walking difficult.
Managing medications
Mr Connor was discharged from hospital after his stroke, with his medicines in a dosette box. At Mrs Connor’s request, their local pharmacy continued to supply his medicines in a dosette box and also delivered them to the house. The couple found this helpful, although it did mean that they did not necessarily know which tablet was which. It could also cause complications if the consultant made changes to the medicines during a clinic appointment. On one occasion, for example, Mrs Connor went backwards and forwards to the general practice and pharmacy five times to sort out an increase in the dose of Mr Connor’s tablets. Mrs Connor supported her husband to take his medicines by putting the pills into a small cup for him to take, morning and evening. She had also been trained to give her husband erythropoietin injections into his stomach once per week.
If Mr and Mrs Connor thought that something was missing from the dosette box or prescription then they would talk to either the pharmacist or the general practice. If they had a problem, however, they would talk to the renal nurse specialist (CNS), although they said that they encountered very few difficulties that they could not handle themselves. They both found the renal CNS approachable.
Last days of life
Records review from the general practice indicated that there appeared to be good support during the last month of Mr Connor’s life, when the GP visited regularly without being asked. Mr Connor was on the GSF register. He had a DNACPR order in place, giving his preferred place of death as the hospice. This DNACPR could not be found and a new one was signed in the last week of Mr Connor’s life, giving his preferred place of death as home. Mr Connor was visited by a palliative care CNS and DNs as required. Approximately 1 week before Mr Connor died, his GP stopped most of his medication, and 4 days before his death a hospital bed was delivered to the family home and a syringe driver set up. Marie Curie sitters were in place the night before Mr Connor died and the intention had been to allow Mrs Connor to sleep without being disturbed. Mr Connor died in the morning, with his wife and the Marie Curie sitter present. Two DNs visited and called the GP to visit and verify death. Mrs Connor asked to be left alone with her husband to wait for their son to arrive.
Ecogram
Mr Connor and Mrs Connor were an unusually self-contained couple. They did not include any informal links in a very sparse ecogram (Figure 31) and referred only in passing to having obtained information about the SPA from a friend. They had not used this, but appreciated knowing that it was available. After Mr Connor’s death, his wife opted to wait for their son to arrive to help and this was the first reference to their children’s involvement in the entire data set. They said that they did not have any sources of support and would not have liked to ask anyone for help. This was in spite of quite a large range of professional services and contacts being mentioned throughout the interviews. The only significant links, from the couple’s perspective, were the renal CNS and the GP, who became increasingly important as time went by, making several home visits, which were appreciated by the couple. They had some past and episodic links and contacts, and good ongoing relations with the pharmacy, the renal clinic and the consultant. There was an escalation in home services and equipment in the last days of Mr Connor’s life. He died at home with his wife and Marie Curie sitters present. They had 23 links (three weak informal links and 20 professional links, including the GSF register) and two close links with the GP (increasingly towards end of life) and the renal CNS.
FIGURE 31.
Ecogram: Mr Connor.
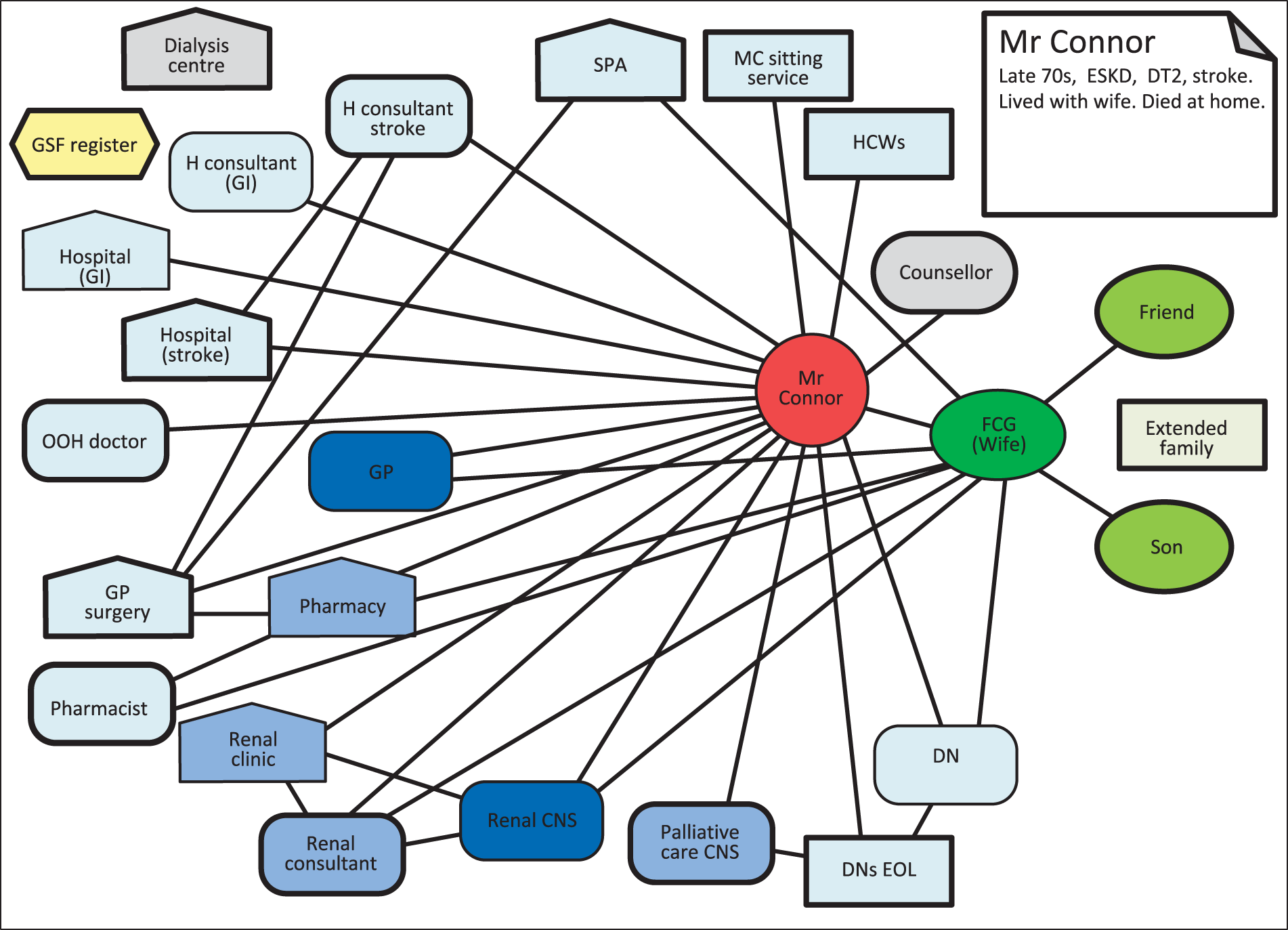
Case summary: Mrs Cramer
Family and living status
Mrs Cramer was in her 70s and lived at home with her husband (Table 19).
| Participant | Data collection |
|---|---|
| Patient: cholangiocarcinoma (bile duct cancer) | No formal study participation |
| Husband (FCG) | One interview |
| Ecogram | |
| Medicines list |
Background
Mrs Cramer was diagnosed with a rare form of cancer. She had been admitted to the hospice in an effort to bring her pain under control. This was successful and she was discharged home, as she wished, for the last days of her life. Mr Cramer assessed his wife as being too ill to take part in the research, but did so himself as he knew this was her wish. Mrs Cramer was discharged with a care package, which included HCW visits four times per day to assist with her personal care.
Managing medications
On discharge from the hospice, Mrs Cramer and her husband were given a chart listing all of her medicines, what they were for and when they were to be given. Mr Cramer found this very helpful. By this stage, as his wife was unable to take charge of her own medicines, Mr Cramer took on this role. Mrs Cramer was set up with a syringe driver and a DN visited every day to replenish this and to keep an eye on how she was. Mrs Cramer had liquid medicine for pain relief, extra to the syringe driver, in case of breakthrough pain and her husband would administer this if needed. The DN monitored supplies of medication for the driver and reordered if necessary. They were also willing to reorder other medicines if Mr Cramer asked them to. Prescriptions were generally delivered by the pharmacy, but it was not a problem for Mr Cramer to collect them if necessary. Mr Cramer felt well supported by professionals. He had a telephone number for the district nursing service and was also able to ring the hospice in the event of any problems. He believed that his wife was given good care and was pleased with this and the organisation of her medicines.
Last days of life
Mrs Cramer’s preferred place of death was her home and this was achieved as she died a few days after her husband took part in the research interview.
Ecogram
At the end of her life, Mrs Cramer (and Mr Cramer) were supported by small informal and professional networks that worked well (Figure 32). Their professional network was set up and co-ordinated by the hospice. The DNs came daily to manage the syringe driver and Mr Cramer managed other medicines. DNs were key contacts for medicines management. Mrs Cramer had an intensive care package of HCWs who came daily but took no part in managing her medicines. The GP was the other significant contact. Care was simplified after Mrs Cramer’s hospice admission and prior to her discharge home to die. This put an end to aggressive treatments and confusing and effortful journeys to hospital. Over half of the professional links mentioned in Mr Cramer’s account were no longer active.
FIGURE 32.
Ecogram: Mrs Cramer.
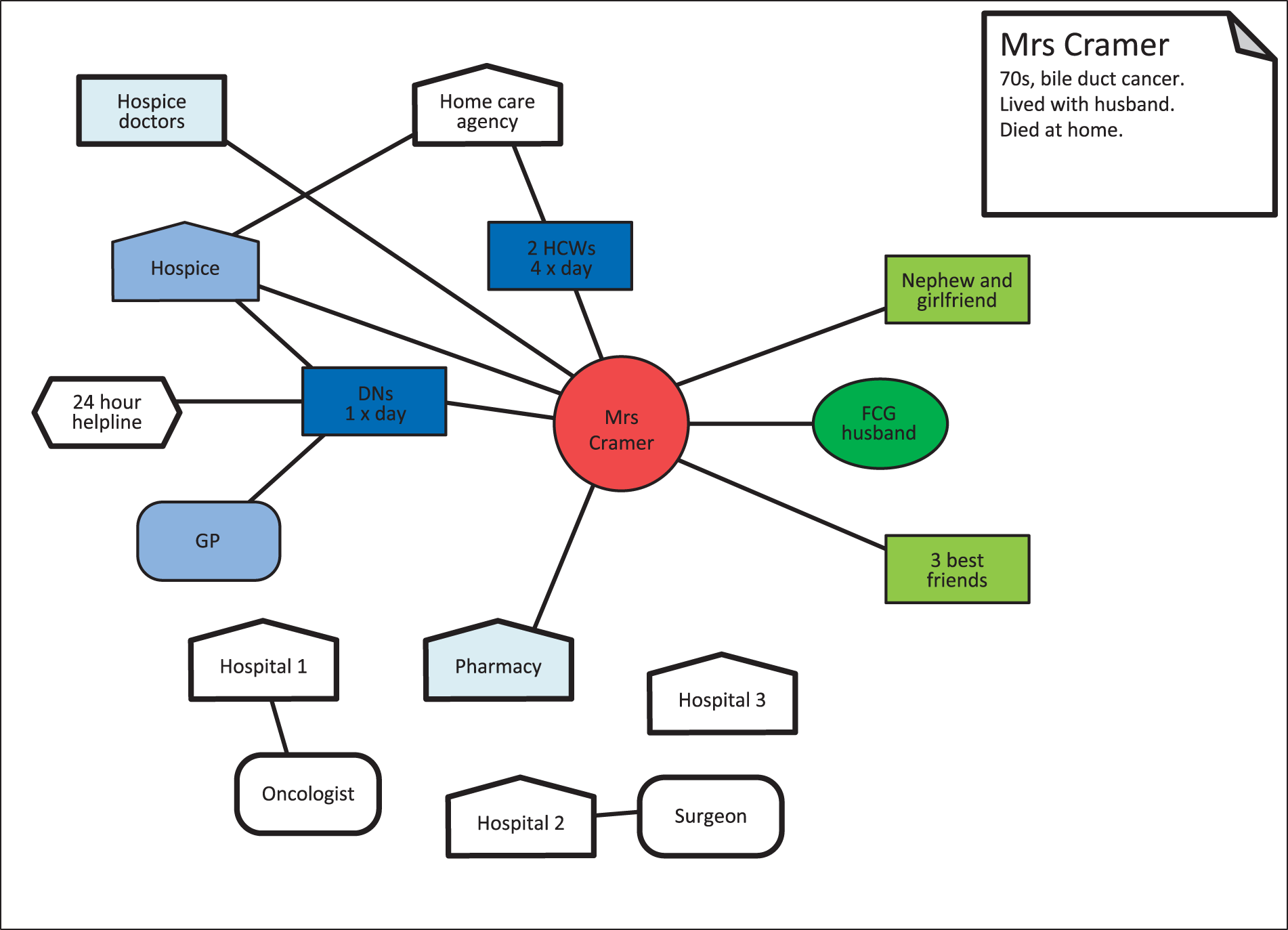
Case summary: Mr Crispin
Family and living status
Mr Crispin was in his 70s and lived with his wife. One of their sons, who lived some distance away, was active in supporting his parents, whereas his siblings lived further away and were less involved (Table 20).
| Participant | Data collection |
|---|---|
| Patient: MND, son (FCG1), wife (FCG2) | One interview (joint) |
| HCW (HCP 1) | One interview |
| Son (FCG 1) | One interview |
| Three e-mails | |
| GP (HCP 2) | One interview |
| Two photographs | |
| Medicines list | |
| Observation of medication storage and equipment |
Background
Mr Crispin received a diagnosis of MND and experienced a rapid deterioration in his condition, such that he died 6 months later. He retained full mental capacity, but by the time he participated in the study he was severely disabled and unable to use his limbs, or to drink, eat or use the toilet independently.
Managing medications
Mrs Crispin obtained, stored and administered her husband’s medicines as required. These were stored all over the house in a system that made sense to Mrs Crispin. Although she occasionally became confused about his medicines, Mr Crispin monitored what he was taking and was able to help her sort it out. One of their sons visited often and provided regular support. He was very proactive in managing his father’s medicines and chasing up the system to get the best that he could for his father, especially with the GP. He had a power of attorney for each of his parents. Mr Crispin’s diagnosis was made privately, and the consultant had prescribed riluzole. Mr Crispin experienced a delay in obtaining subsequent prescriptions and his care through the NHS. Mr Crispin had two carers, who attended four times per day, and a night sitter. The family had AMs in the house ready, with pain relief and injections, in case Mr Crispin became unable to swallow his medicines.
Mr Crispin’s son took an active approach to managing his father’s medicines and dealing with HCPs. More than once, he initiated a review of his father’s medicines, which led to the stopping of something non-essential. He believed that there was poor co-ordination and inconsistency between professionals and services and felt the need to monitor his father’s situation. He felt that there was little communication between professionals and little co-ordination of medicines prescribed. On one occasion, for example, a GP added a drug to control secretions but did not remove the existing one, and it was the DN who noticed that these two drugs should not be taken together.
A wide range of professionals and services were involved in Mr Crispin’s care. However, it was difficult for both the family and the system to respond appropriately, given the rapidity of his physical deterioration. The family felt, overall, that they had been left very much on their own to ensure timely access to medicines and to work out a regimen of organising and administering these. A hospice referral was made for Mr Crispin and he was visited three or four times by hospice staff.
Last days of life
Mr Crispin died a few days after he lost the ability to swallow. He asked for the DNs to be called out to give him pain relief and then died peacefully later that same evening, with his wife by his side and the HCWs present.
Ecogram
Mr Crispin’s large network included 25 contacts with people and services [four core family members, 23 professional and two ‘schemes’ (i.e. PRISM and Electronic Palliative Care Coordination Systems)] (Figure 33). Of these, nine were significant/ongoing relationships with individuals or services, but three (the GP, general practice and pharmacy services) were considered as unsatisfactory. HCWs were a core resource. Other contacts were individuals or services that were used regularly but infrequently and/or to supply equipment, specialist appraisal and assessment, such as the British Red Cross or speech and language therapists. Specialist services, including the hospice/SPC nurse, MND nurse and community matron, formed a cluster and the GP and DNs were connected, but not always positively. As Mr Crispin became quickly and progressively more ill, a cascade of interventions seemed to have been directed to his care. His son was particularly critical of the GP–pharmacy axis, which he felt lacked organisation and continuity. There was no single key professional contact, although the HCWs were a very important source of support as the illness progressed. The family maintained good enough working relationships with a lot of regular services, including the MND nurse, community matron, hospice staff, DN and continence nurse. However, they did not seem to have established close relationships with any of these. A confusing cascade of care occurred close to the end of Mr Crispin’s life, including prescribing from different HCPs, which the family found difficult to cope with.
FIGURE 33.
Ecogram: Mr Crispin.
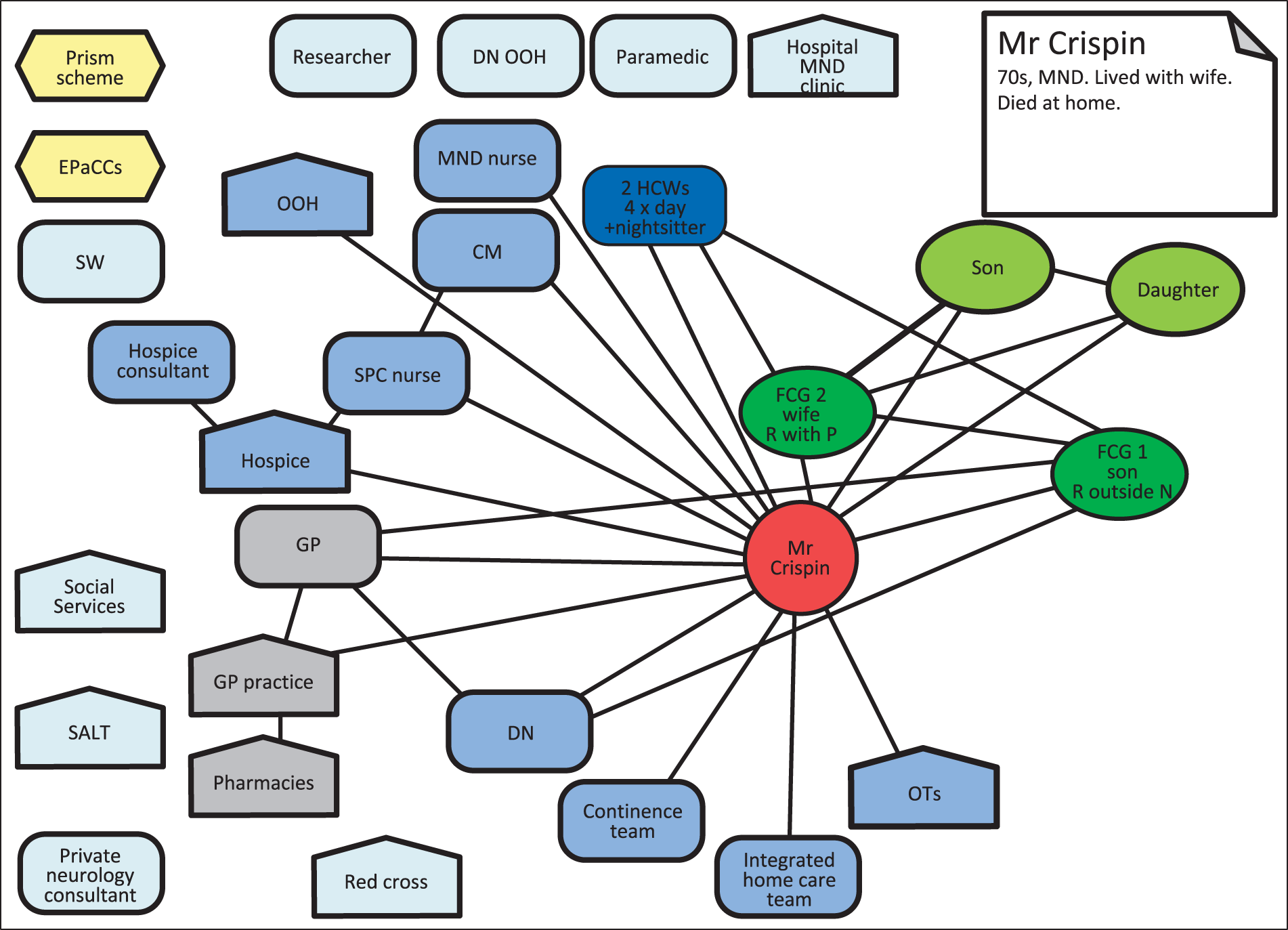
Case summary: Mrs Chambers
Family and living status
Mrs Chambers was a woman in her 70s who lived alone. She had a daughter and son-in-law and a son living locally, plus five grandchildren (Table 21).
| Participant | Data collection |
|---|---|
| Patient: vascular disease, diabetes, hypertension, cardiac cirrhosis, bilateral amputation below knee (phantom limb pain) | Four interviews |
Background
Mrs Chambers experienced a range of health problems. Both her legs were amputated below the knee and she was vulnerable to falls. She also suffered from phantom limb pain and had vascular disease, diabetes, hypertension and cardiac cirrhosis. Pain was a big issue, which she tried to address with the use of oxycodone hydrochloride (OxyNorm®, Napp Pharmaceuticals Ltd) taken as needed.
Managing medications
Mrs Chambers appeared to have a difficult relationship with her medicines. She received blister packs that contained paracetamol from the pharmacy, but she said that she removed these because she had no wish to take any more paracetamol. Mrs Chambers said that she had been told that she should take her medicines on time, but also said that she had decided for herself what that time would be. Although she received her pills in a blister pack, she then placed them in a dosette box on a daily basis. She did not find the blister packs helpful because she struggled to get the pills out of them and sometimes dropped the pills on the floor because her hands shook. This worried her because her grandchildren visited and she did not want them finding and eating her pills. Mrs Chambers did not ask for her medicines to be dispensed in this way, but thought that her GP and her daughter between them came up with the idea.
Mrs Chambers was determined to retain her independence and was concerned that she would come under pressure to move to supported living. However, she acknowledged that she sometimes got confused over her medicines and it was not clear how reliably she took them. Although her GP had provided her with a chart, it seemed that Mrs Chambers stuck to her own regimen of medicine-taking, which involved splitting her tablets into morning and evening batches, with liquid morphine as needed in between, quite a lot of this with variable effects.
Mrs Chambers’ daughter collected the medicines from the pharmacy. At the first interview, Mrs Chambers expressed herself as content with the support that she received from her GP, who had gone through her medicines with her and written out a list of them and when they should be taken. Mrs Chambers had also had a consultation with a pain specialist at the local hospice. She said they had considered putting her on ketamine, but had decided against it because she lived on her own.
Ecogram
Mrs Chambers’ complex health conditions and limited mobility left her in a very vulnerable position, although she was adamant in wishing to maintain her independence and to continue living alone at home. She received support from her family, particularly her daughter and son-in-law, and probably more than she acknowledged. Her daughter fetched her prescriptions and it seems also liaised, to some extent, with her GP and possibly others. A small professional network was described, with the main contacts being her GP and the pain specialist whom she saw at the hospice (Figure 34). A few other HCPs were involved on a regular basis (e.g. DN), but Mrs Chambers did not seem to have a close relationship with these HCPs. On a day-to-day basis, there was no one to help her monitor or manage her medicine-taking, which seemed fairly erratic.
FIGURE 34.
Ecogram: Mrs Chambers.

Case summary: Mr Church
Family and living status
Mr Church was in his 70s and lived with his wife in the family home in a small rural village. The couple had made adaptations to their house to make it easier for Mr Church to maintain his independence. They had two adult children and a grandchild living locally (Table 22).
| Participant | Data collection |
|---|---|
| Patient: MND, asthma, high blood pressure, previous transient ischaemic attack | Two interviews (joint with wife) |
| Wife (FCG) | |
| GP (HCP) | One interview |
| Patient, wife | Ecogram |
| Four photographs | |
| Medicines list | |
| Medical record review |
Background
Mr Church was diagnosed with MND 2 years before joining the research study. Despite severely restricted mobility, he still drove an adapted car and ran his own business. He also had asthma and high blood pressure, and had previously experienced a transient ischaemic attack.
Managing medications
Mr Church was affected by complex comorbidities, including severe pain from arthritis. He assumed overall management of his medicines, although his wife helped with organisation, fetching and storage. His two children and a business employee sometimes collected his prescriptions. Mr Church had a lot of trouble finding medicines without bad side effects, but was willing to experiment with different drugs and dosage, apparently with his GP’s agreement. He was determined to maintain his independence despite very restricted mobility and attempted to maintain work and normal activities as far as possible while keeping health-care staff and services at a distance. His GP liaised with the hospice on his behalf for advice on how to manage his pain and had tried most of the standard options. Mr Church’s GP had also referred him to the hospice for day care and consultant input. He had declined this option, but his wife made use of some of the services for carers.
Mr Church had been referred to a specialist MND nurse, but did not find this particularly helpful. Referrals had also been made to occupational therapy and physiotherapy services, but he did not feel that they could meet his needs. Mr Church’s relationship with HCPs was not always an easy one.
It appeared from the records review that Mrs Church was finding her husband’s physical deterioration difficult to manage and that she felt tied to the house looking after him. Mr Church’s key health professional was his GP, who rang him every 3 or 4 weeks and made occasional home visits. Both Mr and Mrs Church felt that they could approach their GP with any issues about medicines or health. Mrs Church also reported a good relationship with their local pharmacist. At the time of the research, Mr Church did not have any AMs in place nor a DNACPR order. He was, however, flagged as being on the GSF and as being at risk of dementia.
Ecogram
Mr and Mrs Church were well integrated into a rural village community. He had a supportive informal network that involved family and neighbours. Their informal network was of greater significance than his contact with quite a complex network of professional services, from which he deliberately maintained a distance (Figure 35). Mr Church was particularly resistant to hospice day care involvement, although his wife found some of their alternative therapies useful. He had a good relationship with his GP, with whom he maintained regular contact, but considered most other services and HCPs as not helpful. Many professional services are greyed out on his ecogram as being either declined or unsatisfactory.
FIGURE 35.
Ecogram: Mr Church.
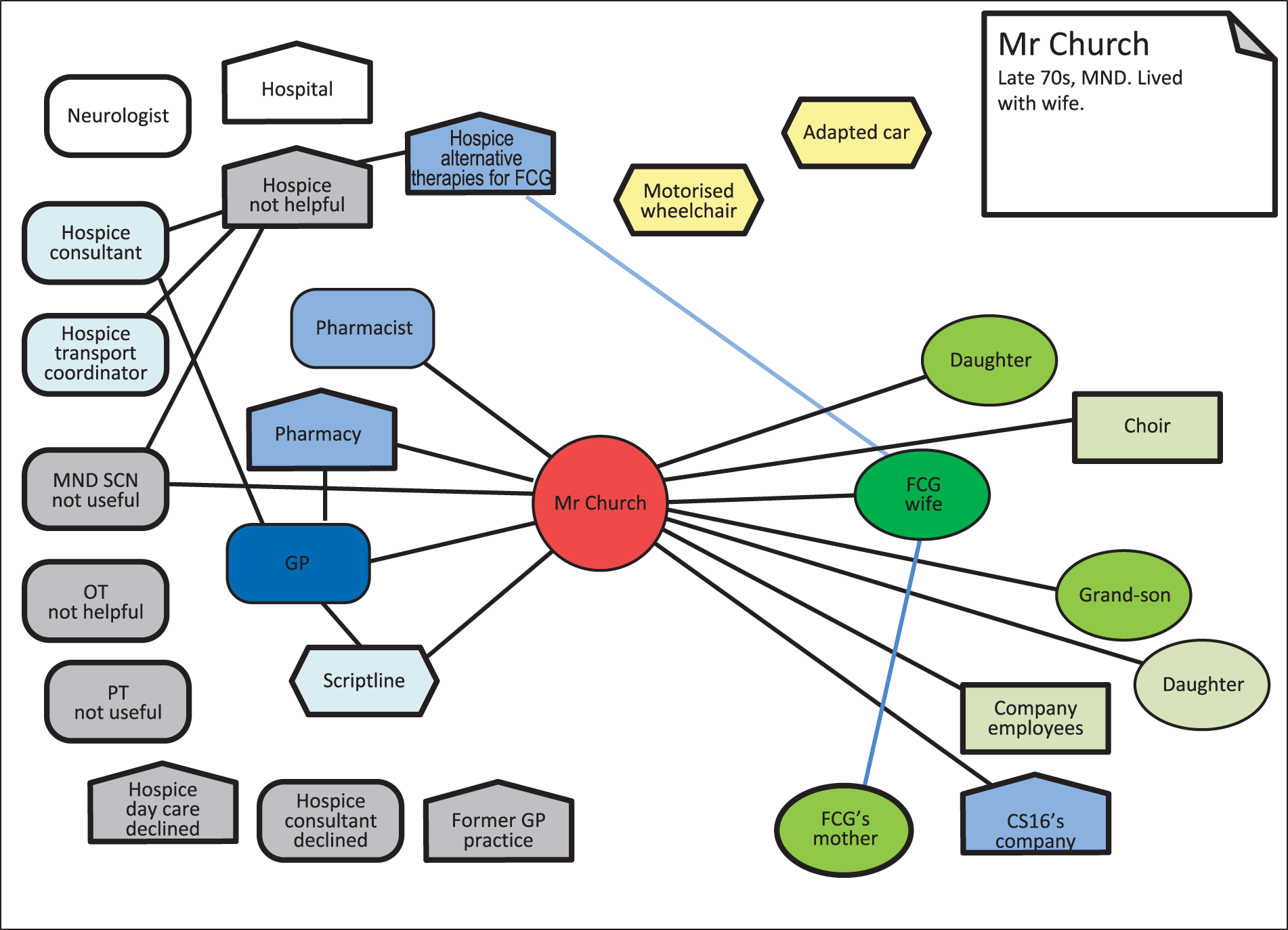
Case summary: Mr Campbell
Family and living status
Mr Campbell was in his mid-60s and lived with his younger sister, having lost his previous home through inability to pay the rent. Mr Campbell also had two older sisters, but had no contact with them (Table 23).
| Participant | Data collection |
|---|---|
| Patient: emphysema, pulmonary hypertension | One interview |
| Two photographs | |
| Medicines list | |
| Ecogram compiled from interview data |
Background
Mr Campbell was severely affected by long-standing emphysema and pulmonary hypertension. He was oxygen dependent and struggled to go out, as exhaustion made it difficult for him to walk up and down the stairs to the flat and there was no lift. Mr Campbell felt socially isolated because he could not go out, although he had some friends who visited him occasionally. Mr Campbell was aware that he was terminally ill and spoke about this during the research interview. He had a good understanding of his illness and how it affected his body.
Managing medications
Mr Campbell experienced some difficulties with his prescriptions, either being given the wrong things or being given too much of something. He viewed this as an unnecessary cost to the NHS. It appeared that the general practice and the pharmacy blamed each other for this. Mr Campbell was keen to take as little medication as possible. He was proactive in managing his medicines and tried to keep on top of what he was taking, what supplies he had, what they were for and how effective they were. This was an ongoing job, particularly given that his prescription included controlled drugs. Mr Campbell had effectively deprescribed some of his medicines himself by deciding not to take them. He was on continuous oxygen and used a nebuliser.
Mr Campbell was frustrated by the continuing inability of the hospital, GP and pharmacy to co-ordinate his medicines. They often got this wrong, gave him the wrong medicines or failed to respond to his notification that he did not need/want specific drugs. As a result, he had stockpiled morphine. He preferred to keep medicine-taking to a minimum and initially was inclined to ‘tough it out’ and keep morphine at bay, but he later decided that he had too little time left to spend it in pain.
Mr Campbell said that he rarely saw the same HCP twice on clinic visits, which meant that he had to repeat his story every time he attended. They gave him advice about how to take his medicines, but he believed that often it is a case of finding out how they can be most effective through personal experience.
Mr Campbell found the best HCPs to be the palliative care team at the hospital. He felt that the consultant there saw the whole picture and pulled things together for him. She recommended antidepressants, but he was cautious about taking these. Overall, the palliative care professional was the key HCP for Mr Campbell. His sister, with whom he lived, usually drove him to appointments at the hospice.
Ecogram
Mr Campbell had become homeless as a result of his inability to pay rent and moved to live with his younger sister. He continued to do so after his financial situation improved. Mr Campbell was very aware that he was dying and reflected a lot on this. His struggle to cope with his symptoms left him pretty much housebound and socially isolated. A significant professional was his hospital palliative care consultant and the team (Figure 36). More recently, he had been referred to hospice day care unit and as an inpatient. He liked the hospice because everyone was in the same boat, but he did not seem to have established significant relationships with staff there.
FIGURE 36.
Ecogram: Mr Campbell.
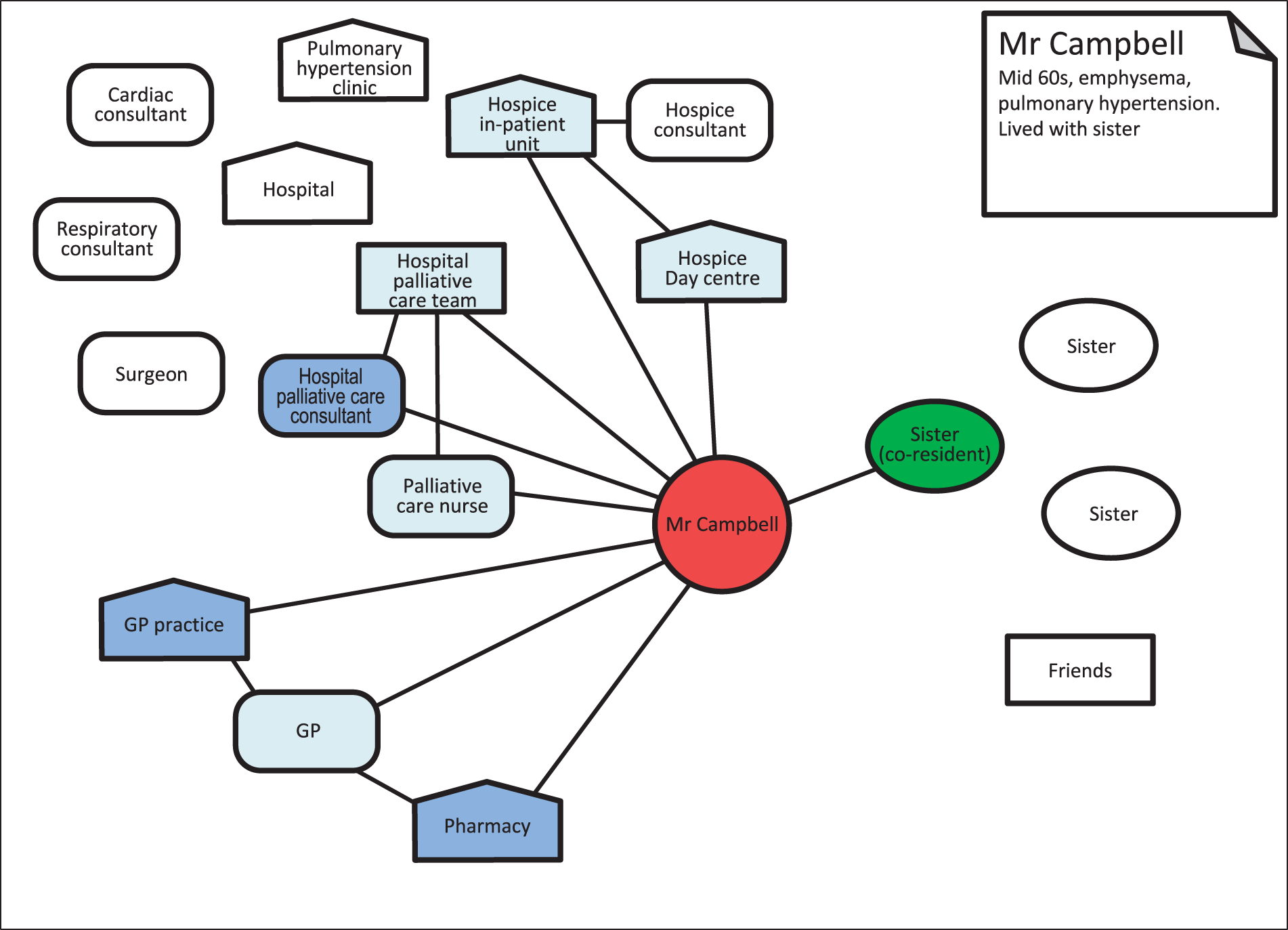
Case summary: Mr Cormack
Family and living status
Mr Cormack was in his 40s and lived in a flat in an assisted living complex, with residential support workers. He had a learning disability and had lived for 4 years in the complex. He had regular contact with his mother and sister (Table 24).
| Participant | Data collection |
|---|---|
| Patient: oesophageal cancer | One interview (joint with sister and mother) |
| Sister (FCG 1) | |
| Mother (FCG 2) | |
| Patient | |
| Support worker (HCP 2) | One interview |
| Medicines list | |
| Ecogram | |
| Observation of medicines administration |
Background
Mr Cormack had oesophageal cancer, which, he had been told, was terminal. His sister had always considered his learning disability to be a mild one, but she found that he did not understand the nature of his diagnosis and its implications and that it took weeks before he was able to grasp the fact that he was dying. Support workers in the complex in which Mr Cormack lived provided help with daily living activities and a member of staff slept in overnight in case of need. Mr Cormack often visited his mother, who lived nearby.
Managing medications
Prior to his cancer diagnosis, Mr Cormack managed all aspects of his medicines with some support, including a dosette box. Since a crisis admission to hospital and then hospice, he had gradually handed over this responsibility to the support staff, who ordered and collected his medicines and stored and administered his controlled drugs. They said that he asked them to do this. During these admissions, his medicines were rationalised, with the focus on pain management and the reduction in the number of tablets he needed to take, as swallowing was becoming increasingly difficult. His medication administration at the time of participation in the study consisted of a patch, liquids and soluble tablets.
Support workers were key to supporting Mr Cormack in managing his medicines. Another key professional was the PCN, who provided advice and information to both Mr Cormack and the support workers. AMs had been prescribed and these were kept in a locked cupboard in a locked office in the supported living complex office. Should the time come when these were needed, the DN would be called to come and administer them.
Mr Cormack’s sister took a key role in advocating and supporting her brother, and placed herself as the one who asked questions and challenged the HCPs when necessary.
Issues with medicines
Mr Cormack had liquid morphine for pain. This was kept in a locked cupboard in his kitchen and was administered by a member of support staff at predefined times. This made it harder for Mr Cormack to access breakthrough pain relief. He was reluctant to ask and would have to make a specific trip to the staff office to do so. His sister felt that the support staff were not good at recognising the signs that he was in pain. This situation improved once a SPCN prescribed patches.
Ecogram
One of Mr Cormack’s sisters played a key role in advocating for her brother and monitoring all aspects of his care, liaising with staff and services. He also had a close relationship with his mother and one of his sister’s friends. On a day-to-day basis, Mr Cormack’s support workers assumed responsibility for all aspects of managing and administering his medicines (Figure 37). His key professional was a SPCN from the hospice who was very proactive in managing his care and liaising with support staff and other services, including hospice resources. Mr Cormack’s sister appreciated this input, but commented that the SPCN was not experienced in dealing with patients with learning disabilities.
FIGURE 37.
Ecogram: Mr Cormack.
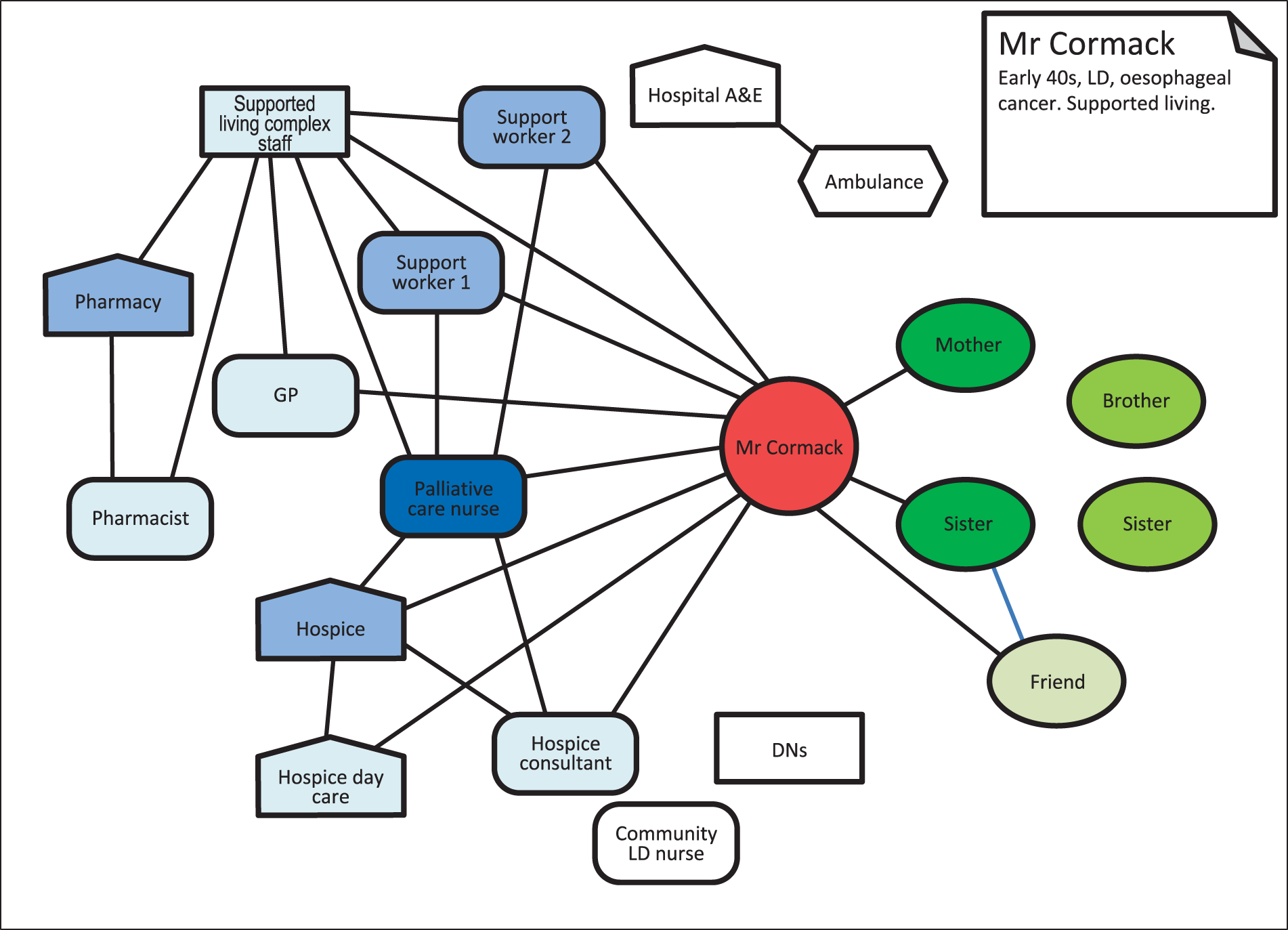
Case summary: Mr Carpenter
Family and living status
Mr Carpenter was in his 70s and lived at home with his wife (Table 25).
| Participant | Data collection |
|---|---|
| Patient: COPD/tuberculosis, wife (FCG) | One interview (joint with wife) |
| Wife (FCG) | One bereavement interview |
| Patient, wife | Ecogram |
| Medicines list | |
| Medical record review |
Background
Mr Carpenter had COPD and a non-virulent strain of tuberculosis for 10–14 years, with increasing oxygen use for the last 9 years. At the time of interview, he was oxygen dependent, using it for about 20 hours per day. Mr Carpenter died after the first research interview and his widow later took part in a bereavement interview. She had a small group of friends and a sister who offered mutual support.
Managing medications
Mr Carpenter managed his own medicines, reordering prescriptions online and collecting the medicines from the pharmacy himself. He kept an emergency kit of antibiotics upstairs in the house in case of exacerbations. His 14 daily medicines were kept in the kitchen. His wife was not involved at all and said that she was confused by his medicines. Although his medicines could have been delivered, Mr Carpenter preferred to collect them directly. This was partly because he liked the human contact with the pharmacist, with whom he had a good relationship and who was happy to help with any queries. The couple also had a good relationship with their GP, whom they found accessible and willing to do home visits. Their other key resource was the hospital respiratory ward and outpatient clinic and the consultant and nurses there (Figure 38). The consultant’s receptionist was also a key figure as they could telephone her any time and she would liaise with the consultant and call them back directly. Mr Carpenter had been using oxygen for a number of years and found the system whereby tanks were delivered and renewed to be straightforward.
FIGURE 38.
Ecogram: Mr Carpenter.
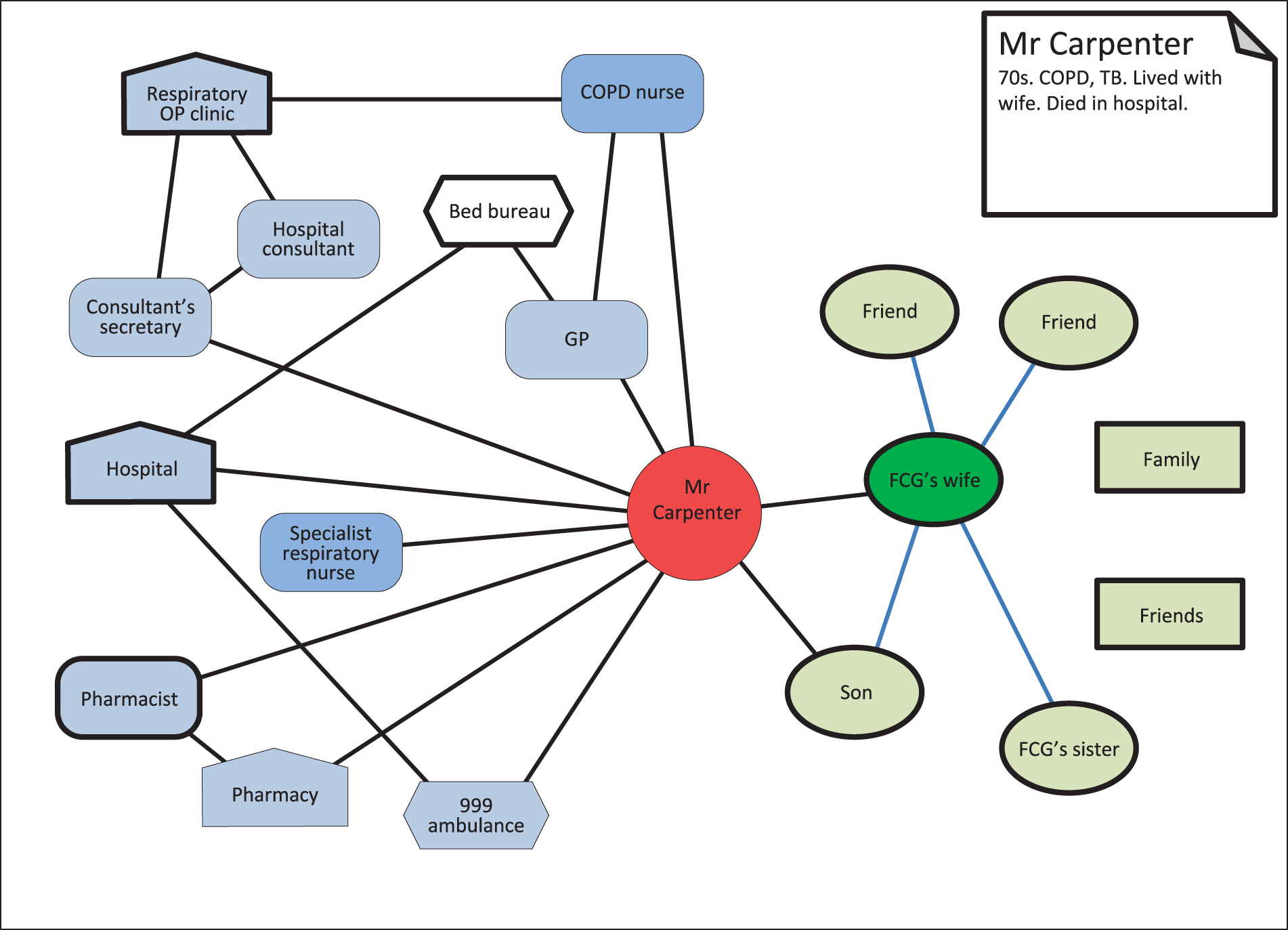
Mr Carpenter required little support in the management of his medicines. He described one instance when antibiotics made him feel very ill and so he stopped taking them. The hospital consultant reintroduced them more slowly along with antisickness medicines, which were effective. Mr Carpenter had attended the same respiratory clinic at the hospital for a number of years, and experienced good continuity of care. He also reported a good relationship with the general practice and the pharmacy. He had been seen by a COPD specialist nurse at the general practice and a respiratory specialist nurse from the hospital, but did not feel that he needed to receive regular visits from either of them. If he needed advice or had a query, Mr Carpenter would contact the respiratory clinic at the hospital.
Last days of life
Mr Carpenter died 2 months after the first interview. The day before this happened, his wife had called the GP for a home visit. She was aware that her husband probably needed hospital admission, but was wary of the ambulance men taking him to the accident and emergency department and possible admission to a hospital other than his usual one. The GP agreed that he needed to go to hospital and arranged through the Bed Bureau for the ambulance to take Mr Carpenter directly to his usual respiratory unit, where he died the next day. This was their preferred place of death, although it was not recorded anywhere (and neither was a DNACPR). He and his wife had been quite clear that he did not wish to die at home, as she was worried about waking up to find him dead beside her. Overall, despite very poor health, Mr Carpenter and his wife took a very pragmatic and independent approach to his problems and their management of them. They just got on with things but were confident and appreciative of the professional support they had available.
Ecogram
Mr Carpenter’s professional network was relatively compact, with interlinked clusters characterised by a few key services and considerable continuity of staff and place. Mr Carpenter felt known by the people in the network and had confidence in them, despite his poor health. Two specialist nurses for respiratory conditions and COPD are on the periphery and were felt not to be needed. Mr Carpenter’s ecogram (see Figure 38) is unusual in that it contains no reference to informal links, and neither did his interview. However, during the bereavement interview, Mrs Carpenter mentioned that she has support from friends and family members and mentioned a few individuals in particular; however, these individuals relate to her rather than her husband, apart from one reference to their son, who was present at the hospital when her husband died.
Case summary: Mr Clunes
Family and living status
Mr Clunes was in his 70s and lived at home with his wife. This was a second marriage for them both and they each had adult children from previous relationships, plus grandchildren and great grandchildren (Table 26).
| Participant | Data collection |
|---|---|
| Patient: COPD/emphysema, type 2 diabetes, angina, arthritis | One interview (joint with wife) |
| Wife (FCG) | |
| Patient, wife | Ecogram |
| Two photographs | |
| Patient | Medicines list |
| Medical record review | |
| Observation of medication storage and equipment |
Background
Mr Clunes had emphysema, which restricted his mobility quite severely, although he was still able to drive. He had a number of health problems, including type 2 diabetes, angina, an enlarged prostate and arthritis. His wife was in her 80s and also had complex health problems that restricted the physical activities that she could undertake.
Managing medications
Mr Clunes was prescribed a large number of medicines that he managed himself with some prompting from his wife. He was able to keep track of a complex regimen, he said, because he had been on most of the medicines for a long time. He was a little concerned about the effects that the medicines might have on each other, but took them anyway.
Mr Clunes had an annual review of his medicines at the pharmacy, but only if he asked for it, and his GP occasionally called him in to review his medicines. The pharmacy the couple used did not deliver, but this was not a problem as they preferred not to have to wait in for the medicines to be delivered. Mr Clunes’ son would take the repeat prescription request to the pharmacy and then collect the medicines a couple of days later. If he was unable to do so, Mrs Clunes would collect the medicines.
Mr Clunes had monthly visits from the COPD specialist nurse and he could ring her if he had any problems. He also attended the COPD clinic at the hospital. DNs would visit if required, and during general practice opening hours Mr Clunes felt he could always contact the GP. However, if he needed help it was likely to be necessary to call an ambulance, which he would do.
Ecogram
Initially, the couple both said that they had no support. It emerged, however, that Mr Clunes received considerable support from members of his extended local family and friends/neighbours (Figure 39). This was more extensive and significant than that received from professional services, from which Mr Clunes seemed slightly distant. No key professional was identified. His son fetched his prescriptions and helped with shopping and gardening, and a granddaughter helped him with personal care a couple of times per week. One good friend assisted with the housework and another with the (small) garden. Mrs Clunes also had health problems that limited her activity a lot, and so they both needed practical help in the house. However, the couple did not want HCWs from social services because they did not want to be tied to someone else’s agenda in terms of what time people arrive and what they think should be carried out. A COPD nurse visited once per month and Mr Clunes felt that he could ring her if he needed to. The DNs called if needed. His GP would be his first contact if he needed help, but they felt that this did not happen often. Mr Clunes related mainly to the hospital and if help was needed it would be to call an ambulance to take him there, although it was not clear if he had actually done this.
FIGURE 39.
Ecogram: Mr Clunes.
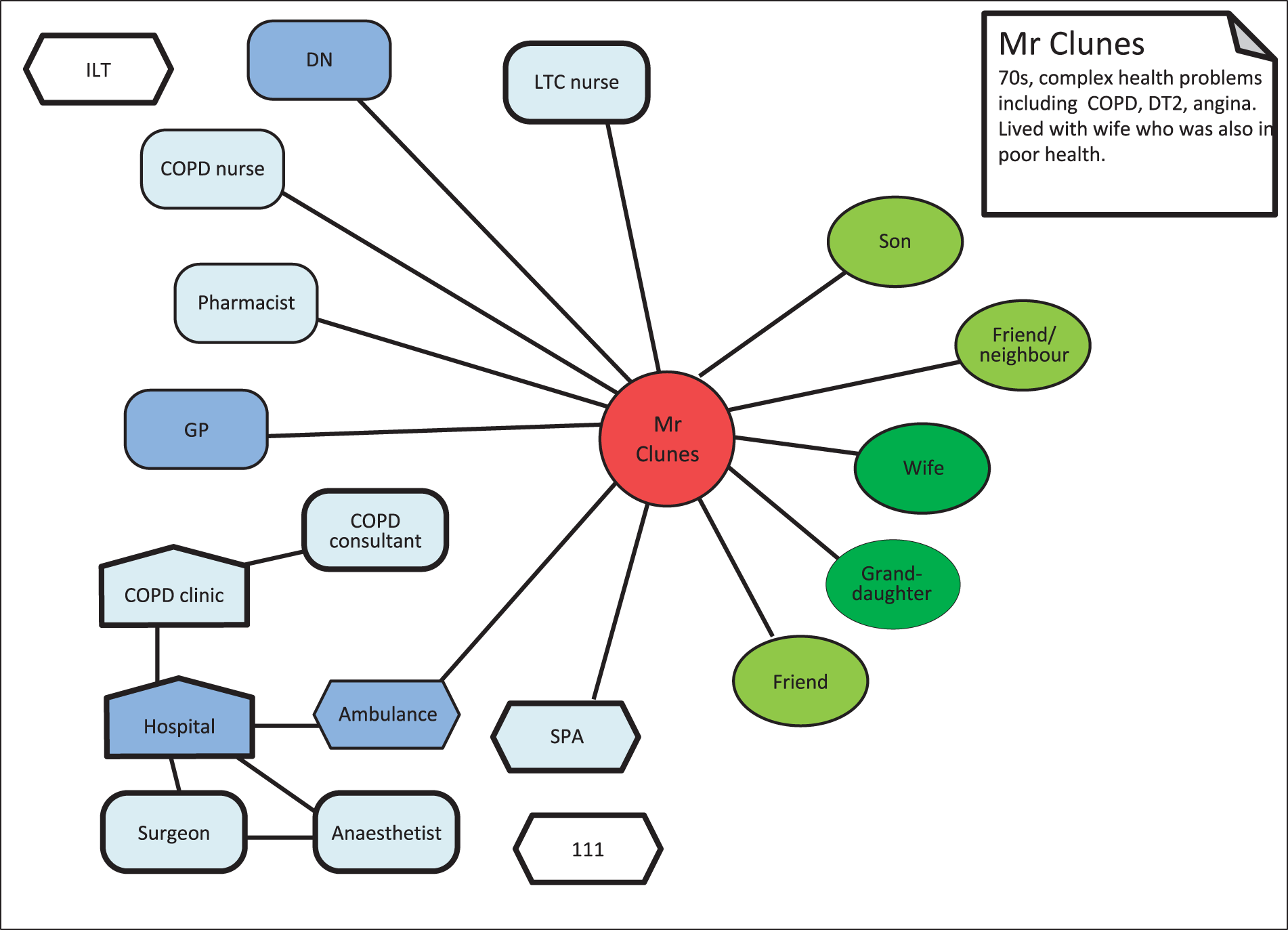
Case summary: Mr Corner
Family and living status
Mr Corner was in his 70s and lived with his daughter and her family (Table 27).
| Participant | Data collection |
|---|---|
| Patient: COPD | Two interviews |
| Patient | Ecogram |
| Seven photographs | |
| Medicines list | |
| Observation of medication storage |
Background
At the start of his study participation, Mr Corner was just out of hospital after an admission for pneumonia and a heart attack. He was on oxygen 24 hours per day and found it very difficult to go out. By the time of the second interview, he was looking much better and, although still requiring oxygen, he was able to get out and about a bit more using an oxygen cylinder.
Managing medications
Mr Corner described himself as self-sufficient in managing his own medicines and oxygen, and as understanding what they were all for. When discharged from hospital he had 11 items on his prescription, with medicines to be taken in different forms, including pills, inhalers, liquid Oramorph, sublingual and oxygen. His medicines were re-issued automatically and, when able, he collected them himself from the pharmacy. When he was unable to do this, his daughter collected them for him. Each week either Mr Corner or his daughter would dispense his medicines into a dosette box, which he found a useful tool as it simplified the process of taking his medicines. Mr Corner’s oxygen machines were serviced twice per year by an external company and in between times he cleaned the filters himself.
Issues with medicines
Mr Corner did not feel that he had any issues with his medicines nor with his oxygen. Although stating at the first interview that he knew what his medicines were for, he acknowledged during the second interview that he did not know what all of the medicines were for or why he was taking them. He noted that the pharmacist would write on the medicine packet how many tablets he needed to take and when. He had never needed to make any enquiries about his medicines from either the GP or the pharmacist. He attended outpatient appointments with the respiratory team every 3–6 months and rarely saw his GP. If necessary, he would ring the GP and request ‘rescue antibiotics’ and a prescription would be issued without the need for an appointment.
Ecogram
Overall, Mr Corner had quite a small network, which worked reasonably well (Figure 40). Despite being in poor health, Mr Corner wished to maintain his independence, including control of managing medicines. He received some help from his daughter and her family. When he felt that he was becoming ill from an acute attack of COPD, his preferred response was to call 111 and get an ambulance to take him directly to hospital, bypassing his daughter and his GP. He saw no point in involving the GP who would, he felt, simply call the ambulance, resulting in an unnecessary delay. Mr Corner said that the paramedics and the hospital were familiar with his case and he kept a card to show them his details, of which they were aware. Thinking to the future, Mr Corner said that he wanted to train both his granddaughter and his nephew in making up his dosette boxes so that he will have additional back up. He was happy that his daughter was able to do this and felt that he had resources available when others were able to provide this care.
FIGURE 40.
Ecogram: Mr Corner.
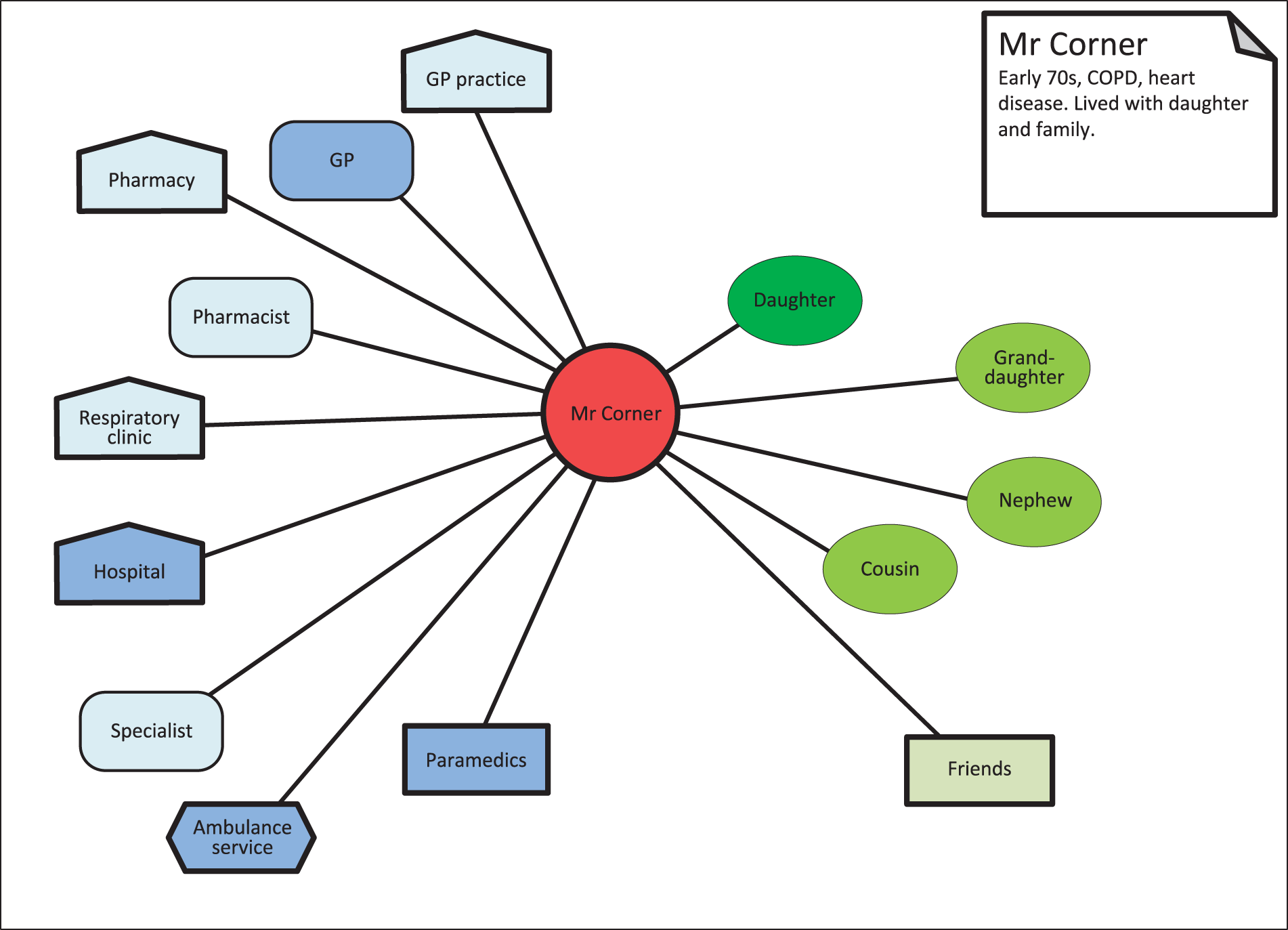
Appendix 2 Frequency of prescribed medication by case
Medications are listed by frequency of prescription, rather than alphabetically, to illustrate which classifications of medications were most frequently prescribed. The table includes both brand and generic names for medications, as reported by participants and their record reviews. Some cases had more than one drug prescribed from the same group.
| Medicine classification | Number of cases in which these medicines were prescribed |
|---|---|
| Opioid analgesics | 18 |
| Proton pump inhibitors/H2-receptor antagonists | 11 |
| Diuretics | 10 |
| Antibacterials, antifungals | 9 |
| Benzodiazepines | 8 |
| Corticosteroid inhalers (with beta2 agonists) | 8 |
| Antiplatelets | 7 |
| Statins | 7 |
| Non-opioid analgesics | 7 |
| Calcium and vitamin D analogues | 6 |
| Beta2 agonists | 6 |
| Emollient creams and ointments | 6 |
| Nitrates | 6 |
| Angiotensin I/II receptor antagonists; ACE inhibitors | 6 |
| Anticholinergics/antimuscarinics | 6 |
| Antiepileptics | 6 |
| Mucolytics | 6 |
| Laxatives | 5 |
| Tricyclic/tetracyclic antidepressants | 5 |
| Antipsychotics | 5 |
| Corticosteroids | 5 |
| Selective serotonin re-uptake inhibitors | 5 |
| Alpha-adrenoceptor blockers | 4 |
| Beta-adrenoceptor blocker | 3 |
| Biguanides | 3 |
| Cardiac glycosides | 3 |
| Factor Xa inhibitors | 3 |
| Neuroprotectives | 3 |
| Non-steroidal anti-inflammatory drugs | 3 |
| Antihistamines | 2 |
| Antimalarials | 2 |
| Antispasmodics | 2 |
| Aromatase inhibitors | 2 |
| Bisphosphonates | 2 |
| Calcium channel blockers | 2 |
| Corticosteroid creams | 2 |
| Dopamine receptor agonists | 2 |
| Gliptin | 2 |
| Iron, oral | 2 |
| Non-benzodiazepine hypnotics and sedatives | 2 |
| Non-sedating antihistamines | 2 |
| Ocular lubricants | 2 |
| Oxygen | 2 |
| Penicillin | 2 |
| Serotonin (5-HT3) receptor antagonists | 2 |
| Sulfonylureas | 2 |
| Vitamin K antagonists | 2 |
| Xanthine oxidase inhibitors | 1 |
| 5α-reductase inhibitors | 1 |
| Anaesthetics, local | 1 |
| Antiandrogens | 1 |
| Antimetabolites | 1 |
| Antipropulsives | 1 |
| Antiseptic mouthwash | 1 |
| Antivertigo preparation | 1 |
| Corticosteroid nasal spray | 1 |
| Dopamine precursors | 1 |
| Gonadotropin-releasing hormones | 1 |
| Heparin | 1 |
| Hyperpolarisation-activated cyclic nucleotide-gated channel blockers | 1 |
| Immunosuppressants | 1 |
| Muscle relaxants | 1 |
| Nebuliser | 1 |
| Non-invasive ventilation | 1 |
| Oral rehydration salts | 1 |
| Pancreatin | 1 |
| Somatostatin analogues | 1 |
| Thyroid hormone | 1 |
| Bone resorption inhibitors | 1 |
Glossary
- Adherence
- The extent to which a patient takes medication as intended by the health-care professional who prescribed them.
- Advance care planning
- A process of planning for future care, particularly within the context of end of life. This includes discussing and, if the patient wishes, documenting preferences regarding place of death, decisions about resuscitation and the limits of future treatment.
- Anticipatory medicines
- Medicines to control common symptoms occurring at the end of life that are prescribed in advance and kept in the home ‘just in case’ they are needed.
- Comorbidity
- The coexistence of two or more long-term health conditions (also known as multimorbidity).
- Controlled drugs
- Medicines that are subject to additional legal controls.
- Dosette box
- A box with small compartments that allow the medicines needed for a day or a week to be organised and set out in advance to assist with taking them as prescribed.
- End-of-life care
- A part of palliative care concerned with supporting patients identified as likely to be within their last year of life. In addition to providing excellent symptom control and emotional support, end-of-life care provides an opportunity for patients and family members to anticipate and express their preferences for future care (see Advance care planning).
- Family caregiver
- A family member, friend or neighbour providing care and/or support for the patient.
- Life-limiting illness
- An illness that may be treated but cannot be cured and is likely to result in death. Examples include advanced cancer and progressive neurological conditions, such as motor neuron disease and dementia.
- Palliative and supportive care
- Care takes a holistic approach to treatment and provides support to people affected by life-limiting illness, including family and friends, as well as individual patients. Palliative care aims to help support physical and emotional well-being and support excellent control of symptoms, including those that occur at the end of life.
- Percutaneous endoscopic gastrostomy
- A tube that is inserted into the stomach to allow delivery of nutrition, hydration and medicines when a patient cannot take these orally.
- Polypharmacy
- When a patient takes two or more medicines.
- Social care
- Care that provides help, care and protection from harm for people with a range of requirements, including people at the end of life.
- UK Census
- A count of the populations of the UK nations, which takes place once every 10 years.
List of abbreviations
- 24/7
- 24 hours per day, 7 days per week
- ACP
- advance care planning
- AM
- anticipatory medicine
- BFCG
- bereaved family caregiver
- CN
- community nurse
- CNS
- clinical nurse specialist
- COPD
- chronic obstructive pulmonary disorder
- CP
- community pharmacist
- CT
- computerised tomography
- DN
- district nurse
- DNACPR
- do not attempt cardiopulmonary resuscitation
- FCG
- family and friend caregiver
- GP
- general practitioner
- GSF
- Gold Standards Framework
- HCP
- health-care professional
- HCW
- home health-care worker
- MDT
- multidisciplinary team
- MND
- motor neurone disease
- OOH
- out-of-office hours
- PCN
- palliative care nurse
- PEG
- percutaneous endoscopic gastrostomy
- PPI
- patient and public involvement
- PRISM
- Pathway and Referral Implementation SysteM
- p.r.n.
- pro re nata
- PSP
- progressive supranuclear palsy
- SPA
- single point of access
- SPC
- specialist palliative care
- SPCN
- specialist palliative care nurse
