Notes
Article history
The research reported here is the product of an HS&DR Evidence Synthesis Centre, contracted to provide rapid evidence syntheses on issues of relevance to the health service, and to inform future HS&DR calls for new research around identified gaps in evidence. Other reviews by the Evidence Synthesis Centres are also available in the HS&DR journal.
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number NIHR127257. The contractual start date was in June 2019. The final report began editorial review in January 2021 and was accepted for publication in July 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2021 Chadborn et al. This work was produced by Chadborn et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2021 Chadborn et al.
Chapter 1 Background
Parts of this chapter are reproduced with permission from Gordon et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Care home context
Around 420,000 people, most of whom are aged > 85 years, live in UK care homes. Care homes are primarily a social care setting and yet many residents have long-term health conditions, frailty and dementia. 2 These complex conditions can generate a diversity of care needs that, in turn, require input from number of different professionals and carers. 3 Most care homes rely on general practitioners (GPs) to co-ordinate and deliver medical care and to access specialty community and hospital services for their residents. How GPs work with care homes is variable and is determined by local custom and practice, as well as the availability of other health-care services to augment or replace some aspects of the GP role. Previous research and evaluation has suggested that differences in provision result in undesirable variation in care delivery and health outcomes, and are likely to contribute to increased unscheduled use of NHS resources. 4,5 As care homes are just one of many responsibilities for GPs, they must compete for attention and resource with other commitments. Parts of the British Medical Association (London, UK) have suggested that it is not sustainable for GPs to continue to support the complex needs of care home residents in addition to their other work. 6 Some improvement initiatives have sought to remove part of the responsibility for routine health-care provision to care homes from GPs, whereas others have sought to encourage GPs to become more engaged with care homes via specific commissioning arrangements and incentive payments. 7,8
The Optimal study9–11 found that health-care services for care homes achieved better outcomes when NHS staff were given time and space to develop relationships with care home staff and residents, and their work with care homes was legitimised through role specification and valued by their employer. Specific expertise in care of older people, particularly in the management of dementia, supported these relationships with care home staff. A further enabling feature was where multiple services were commissioned to work together and link with care home staff. This provided ‘wrap-around’ support for care homes that was less reliant on single practitioners, such as the GP, as the main clinician. Interactions with GPs were, however, identified as being integral to how residents interpreted the quality of their health care, particularly around medication management and the role that the GP played in this. The Optimal study9–11 reported that the way services were organised around, and with, GPs influenced the willingness of GPs to engage and be proactive with care homes and their residents.
Quality improvement and other types of advancing practice
The ProactivE heAlthcare for older people living in Care Homes (PEACH) study12 looked at how a quality improvement (QI) collaborative could be used to improve health care for older people living in care homes. It found that GPs could play a role in broader improvement initiatives that extended beyond their specific duty of care as doctors because they were powerful and well connected within local health and social care economies. However, when GPs sought to play a central role, their limited capacity (owing to conflicting commitments) could limit progress. 12
In many countries, developing and improving care in long-term care institutions is not the responsibility of generalist medical practitioners. In the USA, medical directors have specific obligations to support the quality of health-care delivery in nursing homes. These medical directors undergo training in leadership and management competencies to support their role in service development and QI. 13,14 In the Netherlands, the specialty of elderly care medicine is separate from geriatric medicine and is a primary care specialty based in nursing homes. Doctors are expected to play an explicit role in institutional leadership, with a focus on quality assurance and improvement, in addition to their specialist clinical input. 15
The NHS England framework for Enhanced Health in Care Homes (EHCH), published in 2016, was proposed as the basis for a national improvement programme around health care in care homes. 16 EHCH laid out an approach to health care in care homes that favoured enhanced primary care support, access to multidisciplinary services, access to rehabilitation, high-quality end-of-life and dementia care, workforce development, collaborative approaches to commissioning health and social care, and effective use of data. NHS England has stated the ambition to have every area in England develop a plan to implement the EHCH model by 2024. 17 Early evaluations of pilot sites using this approach have demonstrated better resident outcomes than sites without this approach. 5,18 Modifications to EHCH, announced during the COVID-19 pandemic in 2020, led to the allocation of NHS-employed professionals as ‘clinical leads’ for care homes. 19 These roles lacked detailed specification, but were intended to enable engagement between health-care and care home staff, with a focus around the organisation and delivery of health care. Although there are similarities between the ‘clinical lead’ role and the role of medical directors in the USA, the lines of responsibility and accountability for ‘clinical leads’ remain unclear. Clinical leads are not required to be doctors and they do not take over the role of primary health-care practitioner from a resident’s GP. 20 There is a danger that these recently implemented changes could compound longstanding problems with accountability and responsibility, which have confounded previous attempts to improve care delivery in the sector. 21 Given the lack of clarity about the role of the GP in these recent changes, constraints on the capacity of GPs, and the continued centrality of the GP to primary care delivery more generally, we need to know when and where GP engagement or support is an important requirement for improvement work around health care in care homes. This is particularly important if the improvements envisaged as part of EHCH are to be delivered consistently, at scale and pace.
What we mean by ‘quality’ and ‘quality improvement’
The Institute of Medicine defined quality health care as being safe, effective, patient centred, timely, efficient and equitable. 22
Health care is, of course, only one part of what care homes are supposed to offer. Much of the literature focused on quality in long-term care has stressed the importance of a broader, more holistic, approach to health and well-being, with emphasis on capturing what is important to residents and their families, adhering to principles of person- and relationship-centred care. 23–25 The Care Quality Commission (i.e. the regulator for all care providers in England) has attempted to capture these principles for care homes by specifications within a regulatory framework organised under the same headings it uses for health-care providers. 26
An iteration of these principles was developed to define quality in social care through the ‘Quality Matters’ programme27 led by the UK Department of Health and Social Care, with input from 24 organisations, including representatives of patient groups, social and health-care providers and commissioners, the care home sector, the nursing and social work professions, and regulators. This programme defined quality as having three service user-centred domains and two service provider domains. User domains of quality comprised a positive and safe experience, as well as an effective service, whereas provider domains comprised services that are committed to improvement and learning, and services that are sustainable and equitable. 27
The Quality Matters board suggested four action areas that could help to drive up quality in social care. Actions included effective use of data, enabling improvement and use of feedback. 27
Quality improvement is defined as any activity that might drive up quality in one or more of the domains described. The Institute of Healthcare Improvement (Boston, MA, USA) describes this as being delivered by iterative activities defined by planning, implementation, measurement and reflection. 28 Although QI infrastructure in long-term care is relatively underdeveloped,29 these processes have been shown to deliver improvement in care homes30 where the complexity of care delivery demands that improvement is delivered by teams comprising professionals from multiple disciplines and sectors. GPs have, in numerous recent initiatives, been expected to become involved in such approaches where they apply to health-care delivery for care home residents. 30
The General Practitioners’ Role in Advancing Practice in Care Homes study
Aim
-
To understand the roles that GPs have played in the development and improvement of health care in care homes.
-
To inform ongoing and future improvement work within the sector.
Objectives
-
To develop a programme theory describing contexts in which GPs can improve care in UK care homes and in international settings similar to UK care homes.
-
To describe the causative mechanisms whereby GP involvement with care homes results in outcomes of service development, implementation of evidence and improved quality of care.
A realist review was chosen by the project team as a suitable method with which to address the complex nature of QI that occurs at the interface between medical and social care sectors. Key to developing this understanding, as described earlier, is the ability to take account of varying care home and primary care contexts around the country and how these are likely to have an impact on the role required of, and played by, GPs. Localism has previously been identified as a long-standing, persistent and legitimate approach to care delivery in care homes. This subtends the agendas of multiple and diverse care home provider organisations and other issues, such as availability of NHS staff to support care homes, to mean that variation is, and will continue to be, the rule so far as the care home sector is concerned. 4 A context-sensitive approach was required to describe and make sense of this situation and this was the rationale for using realist review.
Chapter 2 Methods
Realist review is a theory-driven approach to evidence review often used to address complex issues of health service delivery. Realist approaches recognise that context always influences a social programme’s outcomes. By testing different plausible explanations of how particular contexts trigger responses or mechanisms to achieve (or not) certain outcomes, it provides an evidence-based narrative of what is most likely to work, how and when. 31,32 Realist theories are often expressed as a statement of (1) context (i.e. social and environmental factors), (2) mechanism (i.e. the causal powers that lead to patterns of behaviour or choices) and (3) outcome (i.e. the change in process, relationships or empirical measure). 33 Several contexts–mechanisms–outcomes (CMOs) may be linked together into a programme theory that describes the key attributes and or activities of an intervention necessary for it to achieve the desired outcomes. The realist review method is iterative and revisits, reinterprets and tests the evidence against the programme theory as it evolves. These core concepts are further described in Box 1.
Context can be broadly understood as any condition that triggers and/or modifies the behaviour of a mechanism, that is, the ‘backdrop’ conditions (which may change over time). For example, education and qualifications of care home staff and residents’ functional abilities.
Mechanism (M)A mechanism is the generative force that leads to outcomes. Often denotes the reasoning (cognitive or emotional) of the various ‘actors’, that is, care home staff, residents, relatives and visiting HCPs. Identifying the mechanisms goes beyond describing ‘what happened’ to theorising ‘why it happened, for whom and under what circumstances’.
Outcomes (O)Outcomes are the result of mechanisms and may be processes or empirical observations. These may be the expected outcomes and address the aim of the programme, or there may be unexpected outcomes. If the context does not sufficiently support the mechanism, there may be a lack of outcome. For health systems, outcomes could include quality of life of residents, a reduction in episodes of unplanned hospital admissions and improvement in medication management or staff confidence.
Programme theoryProgramme theory specifies what mechanisms are associated with which outcomes and what features of the context will affect whether or not those mechanisms operate. The programme theory encapsulates ideas about what needs to be changed or improved in how NHS services work with care home staff, and what needs to be in place to achieve an improvement in residents’ health and organisations’ use of resources.
HCP, health-care professional.
Reproduced from Goodman et al. 9 Contains information licensed under the Non-Commercial Government Licence v2.0.
Here, the social programme that we are describing relates to the role played by GPs, or primary care doctors, in service development, implementation of evidence and improvement in care homes. The scope of the project was purposefully broad to explore how GPs engage with a range of improvement approaches and topic areas. Although we include QI, we acknowledge that this term is used differently and, therefore, have not constrained our search to this term. The diversity of QI initiatives, together with diversity of GPs and care homes, prompted the project team to select realist review because the method is capable of synthesising complex systems. Furthermore, our review proceeded with a primary search followed by secondary iterative searches to enable flexibility and refinement of scope and to enable greater focus on emergent themes.
Protocol, registration and ethics approval
A protocol for the General Practitioners’ Role in Advancing Practice in Care Homes (GRAPE) study has been published1 and the work has been registered with PROSPERO (CRD42019137090). 34 Following scoping searches and discussion with the project team, the decision was made to amend the protocol by focusing on studies based within UK. This was because the context of general practice is distinct within the UK’s NHS and, therefore, international literature will be based within different contexts that may elicit different mechanisms.
This review conforms to the RAMESES (Realist And Meta-narrative Evidence Syntheses: Evolving Standards) quality standards for realist reviews35,36 and follows the outline of necessary processes as set out by Pawson31 (see Appendix 6 for details).
Ethics approval was given by University of Nottingham Research Ethics Committee (reference 354-1907). Subsequent discussion with the project team indicated that a modification of the recruitment of participants would require a minor amendment to the ethics approval. Approval of the minor amendment was granted on 20 October 2019.
Co-applicant Group: the project team
The authors are the project team. All authors were co-applicants on the initial grant proposal except for Neil H Chadborn. We have a patient and public involvement (PPI) representative (KS) as both a co-applicant and a team member. Our PPI member attended all project meetings, contributed extensively to theory generation and is a co-author of this report. Kathleen Sartain referred back to a PPI group based in the Division of Rehabilitation and Ageing at the University of Nottingham, which meets four times per year. We will share findings, including the final version of this report, with this group and will seek their advice about dissemination plans and future research proposals.
Stakeholder Group: Context Expert Group
The Context Expert Group was recruited through professional networks and comprised GPs, a care home manager, a pharmacist and a care home nurse. Participants of the interviews were also invited to join the group. The group met twice (once during step 3 to discuss programme theory 1 of the realist review and again during step 3 to discuss programme theory 2) for half a day each time. These meetings were conducted using videoconferencing technology because of COVID-19 lockdown restrictions during the period that the research was conducted. A presentation was given about the background and progress of the review, including putative programme theories, and members were asked to reflect on these (see Report Supplementary Material 1 and 2). Members were asked if CMO configurations resonated with their experience or if their views differed from our interpretation and if they could add or amend to improve our interpretation. Members were asked to highlight any further documents that may have been missed from our searches. Individual members of the group were also consulted before, between and after meetings to consult on emerging programme theories. Notes were taken during meetings, but the discussion was a stakeholder consultation and was not treated as research data.
Steps of the realist review
The review followed a four-step approach:
-
locating existing theories and developing putative programme theories (i.e. if/then statements)
-
searching for evidence
-
extracting and organising data
-
synthesising the evidence and drawing conclusions.
Although described as discrete, these steps were an iterative approach that moved between the literature, stakeholder interviews and our Context Expert Group to develop a robust and evidenced programme theory that addressed the aims and objectives. This is summarised in Figure 1.
FIGURE 1.
Flow diagram summarising iterative review process.

Step 1: locating existing theories
This initial step explored what has worked well when GPs work with care homes, how the different elements of GP working are thought to have made this happen and what is needed to be in place for it to occur. The scope included service development, delivery and improvement in care homes. Our starting point was the theories developed within two realist studies: the Optimal study9,10 and the PEACH study. 12,37 These studies had identified key principles of working across health and social care, with the former focusing on design, provision and delivery of statutory services and the latter focusing on bottom-up QI initiatives driven by practitioners in response to the needs of residents. Both studies9,10,12,37 identified the issues of how GPs work with care homes to be a particular issue for further study. Examples from the Optimal study9,10 included how incentive payments to GPs could have both anticipated and unanticipated effects on practice, depending on how GPs integrated specified activities into existing models of working. The PEACH study,12,37 meanwhile, identified GPs as prominent leaders within primary and community health care who could influence the success or failure of an initiative by virtue of their level of engagement and the ‘permission’ they gave, either implicitly or explicitly, for improvement to proceed. The reference lists from these studies, alongside initial scoping reviews of the literature, using broad search terms around care homes and general practice, enabled us to structure a series of theory-gleaning interviews with GP leaders and practitioners. We describe the ways in which these findings led to the stakeholder interviews in Chapter 3 and we provide a schedule for these interviews in Appendix 1 as a way of making transparent how previous research informed and shaped interviews. Interviews, in turn, informed further scoping reviews (see Figure 1). This work enabled us to iterate towards a definitive search strategy for step 2.
For the interviews, we recruited a purposive sample of GPs through professional networks from different parts of England. Participants had experience of QI work in care homes or had senior leadership roles. Participants were given participant information sheets and asked to give written consent. Interviews were semistructured and took place by telephone or videoconference. Themes for the interview schedule were developed from the scoping literature and discussions within the project team (see Appendix 1). Themes included the range of approaches used by GPs working with care homes to achieve health-care improvement. In addition, interviewees were asked about the extent to which the achievement of improvement objectives were influenced by the support and involvement of GPs, and the ways in which this operated through engagement with other professional groups. We asked how the GP contribution was affected by the presence or absence of other care professionals. Furthermore, we explored aspects of context identified in the literature as important for QI and improved resident outcomes. Interviews were transcribed and coded in qualitative data analysis software (NVivo 12; QSR International, Warrington, UK). From analyses of GP interviews, and scoping literature, as well as the expert knowledge of the project team, we built an initial programme theory that shaped our literature searches during step 2.
Step 2: searching for evidence
We used our initial programme theories (from the literature scoping and theory-gleaning interviews with GPs) to structure the evidence search terms and review parameters. There were specific topics that had been the focus of improvement interventions in care homes and were particularly relevant to the role of the GPs, namely medication optimisation through medication review and end-of-life care. Our stakeholder interviews and Context Expert Group suggested that the ways in which GPs worked with and for QI in these areas could provide case studies to inform more general programme theories about the how GPs participate in improvement in care homes. Discussions with the project team about the context raised the concern that international literature may not be informative because of the distinct context of the GP within the NHS in UK. Therefore, searches were limited to UK literature.
Three searches, in addition to citation searches, were conducted across five academic databases [MEDLINE, EMBASE™ (Elsevier, Amsterdam, the Netherlands), Cumulative Index to Nursing and Allied Health Literature (CINAHL), Web of Science™ (Clarivate Analytics, Philadelphia, PA, USA) and PsycInfo® (American Psychological Association, Washington, DC, USA)] and also the Cochrane Library. In consultation with information specialists, we decided to use Web of Science rather than the Applied Social Sciences Index and Abstracts (ASSIA), as had been proposed in the protocol,1 because initial searches indicated that the social science focus of ASSIA would result in relatively low yield. In summary, the searches were as follows:
-
primary search – GP and care homes, limited to UK, 2000 to April 2020 (see Appendix 2)
-
secondary search – medication review or pharmacy optimisation and care homes (but not specifying GP), limited to UK, 2010 to April 2020
-
secondary search – end-of-life care or palliative care and care homes (but not specifying GP), limited to UK, 2010 to April 2020
-
citation searches of key authors and key articles.
We chose different date ranges for these searches based on criteria of relevance and rigour. 36 Relevance relates to whether or not data within a document can contribute to theory building and/or testing, and rigour describes the extent to which the methods used to generate the relevant data are credible and trustworthy. We found that, when focusing on GPs and care homes, much of the literature before 2000 did not describe QI and was less relevant to current models of clinical practice because of changes in how primary care has been configured in relation to care homes over the intervening period. Arrangements such as GPs charging retainer fees to care homes and a focus on care delivery at the individual resident level were prevalent in papers from the early 2000s. 38–40 These arrangements were less of a focus from 2010 onwards, when articles shifted to focus on structured interaction between GPs and care homes at an organisational level, and on contractual arrangements. In topic-specific searches, we did not specify ‘GP’ and searches were intentionally broader; however, screening to investigate GP involvement in each article was more time-consuming and, therefore, we focused on more recent literature (from 2010 to April 2020) that would be more reflective of current contexts.
As improvement and other types of development work undertaken in care homes are frequently discussed outside academic literature, we searched for grey literature using web searches (Google; Google Inc., Mountain View, CA, USA) to look for outputs from royal colleges, specialist societies and other professional bodies, such as the British Medical Association (including local medical councils), the National Association of Primary Care (London, UK) and the Social Care Institute of Excellence (London, UK). Websites of charities, such as the Nuffield Foundation (London, UK) and the Health Foundation (London, UK), were also searched. We made enquiries via the Health Foundation ‘Q Community’, which is a national network of practitioners, leaders, managers and academics that is focused on health-care improvement, and through the community geriatrics and general practice special interest groups of the British Geriatrics Society (London, UK) to further source relevant grey literature.
Step 3: extracting and organising data
The initial programme theories informed the design of a bespoke data extraction tool that included details about the study type, the intervention, the improvement approach and the number of care homes, staff, residents and GPs (see Appendix 4).
Evidence reviewed included a description of the involvement of GPs in the implementation of a new service or service model, or evidence that described an intervention to improve the quality of existing health care. Articles were excluded if they described routine health-care provision outside the context of service development, implementation or improvement, if they described social care in isolation from health care or if the role of GPs was not explicitly considered. Screening at all stages of the inclusion/exclusion steps was conducted by one reviewer (NHC). Relevant data from studies were extracted onto a bespoke data extraction form by two reviewers (NHC and RD). The list of included/excluded articles, the text of included articles and how these articles were used to populate the data extraction form, were reviewed and discussed by all team members at regular project meetings.
Qualitative synthesis was undertaken in qualitative analysis software (NVivo 12). All interview transcripts, selected articles and selected grey literature were imported into the software. Nodes were created based on the putative programme theories described in step 2.
Step 4: synthesising the evidence and drawing conclusions
In step 4, analysis focused on how the evidence built on, refuted or provided alternative explanations for key aspects of GP work in care homes, where outcomes may be at the level of the organisation or the resident.
We looked for outcomes in articles that mapped to our outcomes in our emergent CMO patterns. These outcomes largely related to improved partnership working or improved co-ordination of care processes. For each CMO, we visited our collated literature, first to look for evidence that supported our theory and then for evidence that contradicted or required us to adjust it. We focused on CMOs in which there was evidence from more than one paper that there was some replication of the way in which contexts triggered mechanisms to achieve outcomes (i.e. demi-regularities).
Chapter 3 Findings
Step 1: locating existing theories – theory-gleaning interviews and a scoping literature review
In step 1 of the review, we explored three sources to develop our putative programme theories that would be the basis of the literature search strategy. These comprised (1) the views and expertise of the project team (i.e. the authors), (2) theory-gleaning interviews with senior GPs and (3) scoping of literature and grey literature.
Views from project team
The project team met regularly throughout the review and discussed key findings from previous research projects, QI initiatives and clinical experiences. The following is a summary of the topics raised.
The Optimal study9,10
-
Improvement initiatives could not leave GPs out of health-care delivery, even if systems aimed to substitute for GP tasks.
-
Initiatives did not always recognise the work of GPs.
-
Referrals of residents with multiple health problems to multiple services could be problematic. There was co-ordination and triage of referrals that could introduce bottlenecks and direct access that was quick but could lead to duplication. These tensions featured in discussions about the role of GPs.
The PEACH study12
-
Improvement initiatives struggled to ‘get off the ground’ without GP input.
-
In some instances, teams started initiating plans on the basis of what could be achieved in the absence of GPs because, in these instances, the engagement of GP colleagues was unpredictable or uncertain.
-
When GPs did engage, they were found to play an essential role in brokering relationships and legitimising improvement initiatives across the broader health and social care community.
Views of patient and public involvement based on experience of several research projects
-
There had been limited focus on what resources GPs need to support care home initiatives.
-
GPs do not consistently have topic expertise in the care of older people, which our PPI member argued was essential to care delivery in care homes.
-
The role of the GP as gatekeeper for referrals in the NHS was important to their role in improvement initiatives.
-
GPs are busy and have an area of specific expertise and, therefore, should not be expected to do ‘non-GP’ tasks.
Clinical experience from general practitioner and geriatrician team members
-
The GP–care home relationship is often overlooked.
-
This should be considered at the level of local systems, as well as at the patient level.
-
We should consider how QI initiatives influences GP–care home relationships.
-
General practitioner stakeholder interviews
Seven participants took part in telephone interviews that lasted between 28 and 50 minutes. Backgrounds and experience of participants are summarised in Table 1.
| ID | Category | Area of England |
|---|---|---|
| #02 | Clinical academic | Midlands |
| #06 | Clinical academic | Midlands |
| #10 | Practising | Midlands |
| #11 | Clinical academic (retired) | London |
| #16 | Commissioner | South West |
| #19 | Practising | London |
| #21 | Practising | London |
Emergent themes are summarised in Box 2 and are discussed in greater detail below.
-
Diversity of ways of working among GPs.
-
Recognising relationships with care homes.
-
Capacity and skill in QI.
-
Specialist expertise in medicine for older people.
-
Medication review.
-
End-of-life care.
Diversity of ways of working
The diversity of ways of working ranged from a single general practice working exclusively with a single care home to GPs as ‘care home specialists or leaders’ and making improvements at a system level across multiple care homes. It was noted, although this is not typical, that some care homes are GP owned.
The usual contractual relationship between a GP and care home residents is the same as for patients living in their own home and is outlined in the General Medical Services contract. Additional or alternative contractual arrangements have made available additional financial resource for general practice staff to attend care homes, including Personal Medical Services and Local Enhanced Service contracts. 41,42
There was a concern that national policy discourses and local commissioning may not fully acknowledge GPs’ concerns about the day-to-day practice of delivering care within care homes, and a sense that GPs had latitude in how they prioritised their care home work. Several respondents indicated that they were part of a minority of GPs who had an interest in care homes and highlighted that the majority were not similarly inclined. The implication is that the majority of GPs tend to regard residents on an individual basis and do not always consider the contribution to care delivery from care home staff.
The Royal College of General Practitioners’ (London, UK) curriculum learning outcomes on older adults, identified through our scoping review, highlights five complex roles required of GPs. 43 One of these roles is to co-ordinate with other organisations and professionals, including care homes, and that the GP should be an advocate for residents. 43 Care homes are framed as locations and not as partners in care delivery. Care homes are identified as one of several organisations with which GPs must liaise. This supports the views expressed in the stakeholder interviews that the organisational importance of care homes in the delivery of relationship-centred care is not widely recognised in general practice. Within these roles, medication review and end-of-life care planning are included and described as areas of particular focus, highlighting that these could be a lens through which to better understand GP involvement with care homes. 43
Recognising relationships with care home
The Optimal study9 and the PEACH study,12 our starting points for this work, had highlighted the importance of relational working to achieve effective partnership between GPs and care homes. This was endorsed by participants who cited a key context as GPs not recognising care homes as partners in care delivery. Attempts to change GP alignment with care homes as part of EHCH was an example of an attempt to change the patterns of working, creating continuity and fostering closer working relationships between one general practice and a care home. 16 Therefore, implementation of alignment through additional contract arrangements triggered a closer alignment and relationship between GPs and care homes. Some respondents felt this meant that GPs, simply because of increased frequency of contact and familiarity, were given the opportunity to acquire a greater awareness of care home organisations:
Because they were in care homes so often and could see how things weren’t working . . .
Participant #16
The recent reconfiguration of general practices into primary care networks also had the potential for constructive working with care homes because it organised GPs at a regional, rather than practice, level. This was seen as offering more consistent and co-ordinated approaches to GPs working with care homes:
. . . so we might see a shift in commitment and involvement and responsibility for care home residents maybe.
Participant #11
There was a recognition, as well, that the onus was not exclusively on GPs when it came to building meaningful relationships for QI. One participant described how the heterogeneity of care home types affected what was carried out and who engaged. The care homes that belonged to large corporate provider chains would carry out their own QI projects led by the organisations’ directors of quality, but GPs were often not engaged in these corporate initiatives. In contrast, small independent care homes struggled to find resource or capacity for co-ordinated QI activity.
The impact of the regulator on how care homes worked with GPs was also seen as important. Inspections require evidence of access to health care and appropriate procedures, but one interview participant did not think that the Care Quality Commission inspections asked for evidence or recognised the importance of ongoing QI work or partnering with local NHS providers:
. . . this is a real problem with CQC [Care Quality Commission], they are not very proactive about understanding about QI methodology.
Participant #16
Capacity and skill in quality improvement
One participant reflected on QI projects and the expertise that they had seen in other parts of the NHS, and suggested that there was a relative paucity of experience and training in QI among GPs. This participant described a recent improvement workshop that they had led:
. . . realise how little training is done in primary care around QI methodology . . . we had maybe 60 GPs and ANPs [advanced nurse practitioners] in the room and we asked them, for example do you know what a PDSA [Plan Do Study Act] cycle is, and they didn’t, maybe two hands went up.
Participant #16
This was seen as a fundamental reason that could explain why GPs would struggle to engage with improvement in care homes:
I don’t think you’ll ever have GP-led QI programme in care homes because they don’t know enough, don’t understand enough . . .
Participant #06
This was at odds with earlier statements about GPs being well placed to build relationships with care homes and to identify foci for improvement, suggesting a tension between QI competencies (which were regarded to be lacking) and clinical competencies and the ability to carry out day-to-day care (which were more evident).
Many of the improvement projects that participants had seen undertaken around care homes had been led by non-GP health-care professionals. This was attributed to work pressures, how clinical work was prioritised and the limited capacity of GPs to take on these kind of roles. Some respondents felt, however, that this left GPs exposed to risks associated with improvement projects and without any control over their content or progress. This respondent described an experience of working with pharmacist-led improvement, and felt that GPs had been left to ‘pick up the pieces’:
Unless the pharmacist is working at the highest level of their competency, then either they are unsafe, or the workload falls back on primary care anyway.
Participant #16
This lack of time and training in QI, coupled with worries about responsibility or accountability, were seen as significant barriers to GPs engaging in QI more generally and in care homes in particular.
Tension between developing specialism and maintaining generalism
Multiple respondents described how health care in care homes was complex and challenging and required subspecialist skills or knowledge. Some respondents felt exposed by the lack of expert multidisciplinary support in the community:
. . . somebody’s diabetes had gone really off and it just didn’t feel like we’d got the resources in the care home to manage this and that he needed to go in the hospital.
Participant #02
One respondent went as far as to suggest that specialists in acute medicine or care of older people, rather than GPs, should be attending to older people in care homes, with support from a multidisciplinary team (MDT):
Care home residents are some of the most medically complex patients . . . a group of people that need that expertise of the internist with a multidisciplinary team.
Participant #06
This group of hospital-based specialists, however, have limited or no experience of community working. One respondent described the development of a special interest group for GPs as part of the British Geriatrics Society. The group wanted to develop a GP with special interest model, in which some GPs would step away from their other responsibilities to focus on care of older people, including in care homes. The group expressed frustration that training and accreditation mechanisms did not currently enable them to fully pursue this approach in their working:
. . . we’ve had challenges about whether or not, in order to remain accredited, we have to do what is seen as standard general practice or Geri-GP [GP with extended role in geriatrics] work, and there is inconsistency across the country. So some appraisers are saying that GPs have to do sessions in normal primary care and other assessors are saying we don’t.
Participant #16
General practitioners’ relationship with pharmacists
General practitioner participants described the value of pharmacists conducting medication reviews of care home residents, particularly for residents with complex medication regimes that may have been adjusted following hospital admission:
. . . in 6 weeks’ time when I have got the notes, have I got the time then to do the medication review properly? So, they are all potential areas of error.
Participant #21
There were concerns about limited capacity for pharmacists to conduct follow-up consultations. Another participant questioned whether or not pharmacists would have the broader knowledge of care of older people, such as mental capacity legislation. Therefore, GPs considered that risks arising from pharmacists changing medication could increase the workload of the GP. When there was an established and trusting relationship between GP and pharmacist, however, the GP could see the advantages provided by the pharmacist’s skills and expertise:
. . . if you’ve got a very good pharmacist, I think GPs are only too happy for them to do some of the work . . .
Participant #16
General practitioners supporting end-of-life care
General practitioner participants discussed advance care plans (ACPs) and end-of-life care. Two participants had been involved in implementing a data-sharing system (electronic palliative care system) to improve continuity of care for people with end-of-life care plans:
. . . if you can get into a good system of making advance care planning routine on admission [to the care home] . . . the conversation is had, wishes and preferences are gathered. That information is then stored but then is shared, so obviously we are lucky that we are able to do that with [electronic palliative care system].
Participant #21
One participant mentioned that there could be a problem if care home staff did not approve of implementing advance directives, possibly because of a lack of confidence or resources:
Problem of staff member who doesn’t approve of providing high level of care and refuses to deliver an ACP.
Participant #11
Therefore, GP participants recognised the importance of palliative care and advance care planning in care homes. They also described how good end-of-life care is dependent on good communication, not only between the GP and the care home, but also with the resident, family members and other health practitioners (e.g. paramedics).
Scoping the literature
The interviews described variability in practice driven by variable GP interest in, and engagement with, the care home sector, lack of training in specialist care of older people, lack of training and experience in QI, and nervousness about working with other disciplines around improvement projects for fear that it may generate additional work. The improvement work involving GPs that had taken place had focused on integrated working between GPs and care homes, medication management and end-of-life care. The scoping review focused on evidence to support these findings and inform the programme theory development.
Patterns of general practitioner working with care homes
To gain understanding of multiple and varied contexts, scoping searches aimed to identify the challenges or problems of GPs delivering care within care home settings that had been described in observational studies (i.e. surveys, cohort studies, descriptive studies or qualitative studies). A qualitative study of English GPs in 200344 explored views on continuity of care and the challenges of maintaining people’s GP as they move into a care home (as opposed to changing to a GP assigned to the care home). The study44 concluded that if one practice cared for all residents within a care home, then interactions could be more efficient because the GP could establish working relationships with the care home staff, which, in turn, could lead to improvements in resident care. The benefits and additional workload of regular clinics at the care home were acknowledged but not resolved. Reviewing contractual arrangements for GPs was described as one possible one way of addressing increased workload.
In two consecutive studies45,46 surveying GPs in Ireland, experiences, training needs and workload issues around care home practice were explored. The studies found that GPs with small numbers of care home residents on their lists had low confidence in care home practice, particularly around ethically complex issues, such as decision-making around end-of-life care. A proportion of GPs felt that their training in geriatric medicine could be improved. The majority of respondents felt uncertain about how to handle safeguarding issues in partnership with care home staff. 45 Approximately three-quarters of respondents indicated that they conducted medication reviews at least annually, with the authors suggesting that a national quality standard (i.e. Health Information and Quality Authority standard number 15) was a major driver behind this high level of compliance. 46
Two recent reviews47,48 give a broad perspective on the topic of improving health care in care homes. In the first review, Barker et al. 47 conducted a systematic review of primary care in care homes. The selection criteria for this review included a comparator group (e.g. controlled trials) and reporting quantitative outcomes. Only 9 out of 24 studies in this review included GPs (family physician) as playing a role within the intervention. In five of these studies, a geriatrician contributed medical expertise, whereas in another three studies the intervention was led by a specialist nurse. One small study,49 based in Australia, described a multidisciplinary intervention led by the GP.
The second review was a scoping review of QI in care homes48 with broad inclusion criteria selected 65 international studies. A striking finding was the absence of evidence or discussion about how GPs were involved, although a few studies referenced the involvement of specialists in gerontology/geriatric medicine. However, only one article,50 based in Canada, included a family physician as part of the intervention.
Foci of improvement programmes
We searched for current or recent programmes in grey literature. The ‘Primary Care Home’ project in England is a GP improvement project, running across 248 sites in England, and is supported by the National Association of Primary Care. 51,52 Only 15 projects mention care homes and, of these, only 11 had commenced. Four projects describe MDTs providing care in place of regular GP visits. Three projects involve medication review and proactive care planning. One project, Health 1000, is a GP partnership that specialises in care of older people and includes four nursing homes. 53
The Scottish General Medical Services contract54 described the following: pharmacist-led medication reviews in care homes, with this replacing work previously undertaken by GPs, and advanced clinical practitioners assessing and treating care home residents to release GP time to focus on complex cases in care homes.
The findings of the scoping review identified recurring topics of interest as the focus of improvement projects that involved GPs (Box 3).
-
End-of-life care.
-
Polypharmacy/pharmacist/medication review.
-
Urgent care and out-of-hours care (i.e. information transfer).
-
Training GPs.
-
GPs facilitating learning.
-
MDT case conference or virtual conference.
-
Voice of patient and/or family.
-
Dementia diagnosis/behaviour psychotropic de-prescribing.
The most commonly described interventions are highlighted in bold.
Conclusions and development of putative programme theories
At the end of this step (i.e. locating existing theories) we had evidence of the following:
-
Variability in practice between GPs.
-
Variability in how GPs prioritise and relate to care homes, and the extent to which they recognise care homes as partner organisations.
-
Conflict between traditional training and remuneration structures, which supported variability in practice, and more recent innovations (e.g. EHCH and primary care networks), which were seen as providing opportunities for more standardisation of approach.
-
Limited capacity, training and experience that would enable GPs to lead QI.
-
Limited engagement with the complex care of older people in care homes by GPs and uncertainty in how to work with care homes as social care organisations.
-
Many improvement projects with care homes were led by specialists other than GPs, and a recognition that limited GP involvement could have unintended consequences for GP workload and sustaining improvements.
-
Improvement projects had focused predominantly around end-of-life care, de-prescribing (including psychotropic de-prescribing) and integration of health care around care homes.
We developed a series of ‘if/then’ statements based on initial interviews and the scoping of the literature. These are summarised below and related to:
-
polypharmacy and review of medications
-
developing ACPs
-
the extended role of GPs and expertise in care of older people.
Polypharmacy and review of medications
Inappropriate polypharmacy is associated with adverse outcomes in people with multimorbidity and frailty. 55 Medication review can address these concerns, with a balancing of risk and benefit of multiple drugs. This can potentially be achieved through multiprofessional working, involving a pharmacist, doctor and the care home staff to explore where drugs may no longer be necessary, especially where side effects can be problematic, where drug interactions could be avoided or where non-pharmacological interventions could be substituted56 (Box 4).
If the GP reviews prescriptions together with a pharmacist, then they may find opportunities to alter prescription or regimens to reduce the ‘burden’ of medication and adverse outcomes, improving the quality of care.
Developing advance care plans
Developing an ACP has been shown to improve outcomes for older people living in care homes as they approach the end of life, and doctors have been reported to have a key role within this process, which is, nevertheless, multidisciplinary. 57,58 The role of the GP in this process is to provide diagnostic and care planning expertise, and to support and clarify the documentation process of residents’ preferred priorities of care for professionals and care staff. 59 It is an area of QI that can support future continuity of care and confidence that resident wishes, and those of their representatives, will be observed60,61 (Box 5).
If GPs are involved in documenting and implementing ACPs, then it will ensure that all those involved in providing and receiving care will be able to review medical diagnoses in a way that reflects residents’ priorities and inform care provision and ongoing decision-making.
The extended role of general practitioners and expertise in care of older people
The interviews had identified different views about whether or not GPs were qualified or sufficiently supported to be the clinician responsible for care home residents. Specialism could lead to specific GPs having confidence, skills and expertise to participate or lead QI projects, but not all GPs were thought to have time or motivation. GP specialism would, therefore, be an important context of other programme theories.
The interviews with GPs suggested that to ensure effective medication review there was the need for a trusting relationship and recognition of GP and pharmacist skills. When the GP is confident in their own pharmacy knowledge and had the capacity, then there was commitment to medication review.
Another interview discussed the additional skill level required to effectively deliver acute care in care homes, which may be required for ‘hospital at home’ or step-up care (hospital avoidance), supported discharge from hospital and end-of-life care.
General practitioners may be motivated to develop special interests or extended roles for a number of reasons (over and above financial reward), such as career development, the opportunity to focus on a topic of interest and to lead or develop a service area. 62–64 Owing to the increased engagement, this may be a route by which GPs would engage in QI (Box 6).
If support, training or professional networks are available, then GP may develop special interests and expertise in care homes, leading to fuller engagement with QI and resident outcomes.
Step 2: search strategy, PRISMA flow diagram and included articles
We developed an iterative search strategy based on the putative programme theories developed in step 1 to capture the GP role in improvements under these headings to provide case studies that would inform programme theory development. We have summarised this search strategy in Chapter 2 and in Appendix 2.
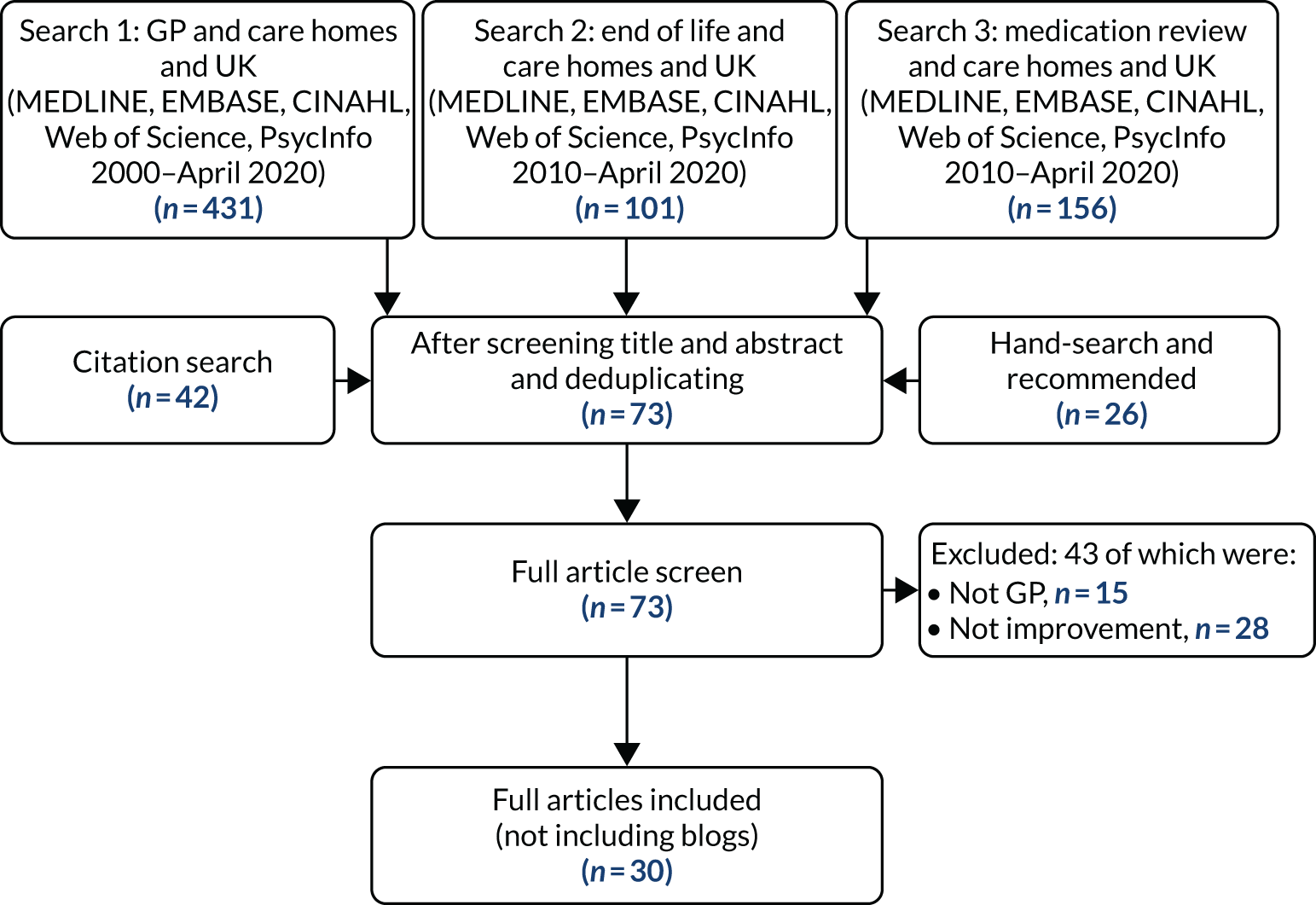
A PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram is shown in Figure 2. The primary search for UK articles including care homes and GPs (with a publication date range of 2000 to April 2020) retrieved 431 articles (see Appendix 3, Table 8). Secondary iterative searches were performed for end-of-life care and medication review (both with care homes, but GP was not specified in search terms), with the aim of identifying articles that may have been missed by the primary search. These searches (with a publication date range of 2010 to April 2020) retrieved 101 and 156 articles, respectively (see Appendix 3, Tables 9 and 10). Citation searches were conducted, as well as hand-searches of selected journals and follow-up of recommendations from the project team and interview participants. After removing duplicates and screening, 73 articles were included in a full-text screen. Twenty-eight articles were excluded following the screen of the full text because the studies were observational (e.g. qualitative, cross-sectional survey or database analyses), rather than studying an intervention, QI or other type of change management process. Fifteen articles were excluded because they were found to not describe GP involvement (e.g. GP records may have been used to identify participants or extract data as an outcome, but the GP was not specifically involved in the intervention). Thirty articles were finally selected for data extraction and synthesis, as listed in Table 2.
FIGURE 2.
A PRISMA flow diagram.
| Programme theory | Study keyword | Date | First author surname | Title | Journal | Study type | Key findings | Reference |
|---|---|---|---|---|---|---|---|---|
| 1 | New care models | 2018 | Elvey | Implementing new care models: learning from the Greater Manchester demonstrator pilot experience | BMC Family Practice | Qualitative observation of pilot projects | Challenges identified were trust to enable collaboration, especially relating to data-sharing | 65 |
| 1 | Palliative care | 2016 | Iliffe | Improving palliative care in selected settings in England using quality indicators: a realist evaluation | BMC Palliative Care | Realist evaluation | GPs could not be recruited. Care homes could not be retained. The quality indicators set were not motivating for GPs or care homes (they may have been too specialist) | 66 |
| 1 | EVIDEM-EoL | 2016 | Amador | Evaluation of an organisational intervention to promote integrated working between health services and care homes in the delivery of end-of-life care for people with dementia: understanding the change process using a social identity approach | International Journal of Integrated Care | Qualitative appreciative inquiry |
The intervention supported integrated working due to shared goals and recognition of different expertise Bottom-up process of implementing context-specific practice innovations and tools The approach accommodates diversity |
67 |
| 1 | End-of-life care | 2011 | Evans | Factors influencing emergency hospital admissions from nursing and residential homes: positive results from a practice-based audit | Journal of Evaluation in Clinical Practice | QI: audit | Initial audit showed that 55% of deaths occurred in the care home, whereas this had increased to 75.5% in the second audit. GP visits to nursing home patients increased by 10.3%, but visits to residential home patients decreased by 5.4%. There was a 43% reduction in emergency admissions with a 45% decrease in deaths in hospital | 68 |
| 1 | Vanguard | 2018 | Stocker | Care home services at the vanguard: a qualitative study exploring stakeholder views on the development and evaluation of novel, integrated approaches to enhancing healthcare in care homes | BMJ Open | Qualitative study of planned implementation | There was a moral imperative for proposed change to services. However, integrated working was not clearly understood. There was a perception of the programme being ‘top-down’ and imposed by the health service. Trust within the system was valued | 69 |
| 1 | Antipsychotic de-prescribing | 2016 | Szczepura | Antipsychotic prescribing in care homes before and after launch of a national dementia strategy: an observational study in English institutions over a 4-year period | BMJ Open | Quantitative retrospective analysis | Prescribing rates did not change following implementation of the policy, nor was there a shift to second-generation antipsychotics. Duration of prescribing was excessive in 69.7% of cases. There was an association between high prescribing and deprivation of the area of the care home. There was an association between low prescribing and single general practice | 70 |
| 1 | Medication review | 2011 | Patterson | A cluster randomized controlled trial of an adapted U.S. model of pharmaceutical care for nursing home residents in Northern Ireland (Fleetwood Northern Ireland study): a cost-effectiveness analysis | Journal of the American Geriatrics Society | Cluster randomised controlled trial | Psychoactive drugs were taken by fewer residents after 12 months of the intervention (19.5%) compared with control (50%). No differences in falls rates were observed | 71 |
| 1 | Medication review | 2003 | Hughes | Information is care: the need for data to assess the quality of care in UK nursing and residential homes | Expert opinion on drug safety | Expert opinion | There is a lack of data on prescribing | 72 |
| 1 | Neuroleptic de-prescribing | 2002 | Ballard | Can psychiatric liaison reduce neuroleptic use and reduce health service utilization for dementia patients residing in care facilities | International Journal of Geriatric Psychiatry | Non-randomised controlled trial | Liaison service was associated with a reduction in use of neuroleptics and a decrease in deterioration of expressive language skills, but no change in well-being. There were fewer GP contacts | 73 |
| 1 | Medication review | 2000 | Khunti | Effect of systematic review of medication by general practitioner on drug consumption among nursing-home residents | Age & Ageing | Evaluation | A total of 51% of patients had a medication stopped and 26% of patients changed to a cheaper alternative or reduced dosage | 74 |
| 1 | WHELD | 2016 | Ballard | Impact of WHELD intervention on neuropsychiatric symptoms, antipsychotic use and quality of life in people with dementia living in nursing homes: a cluster randomized trial | American Journal of Psychiatry | Factorial cluster randomised controlled trial | There was a reduction of antipsychotic prescription by 50% with a reduced mortality. Social interaction and exercise mitigated the detrimental impact of de-prescribing antipsychotics on neuropsychiatric symptoms | 75 |
| 1 | WHELD | 2018 | Ballard | Impact of person-centred care training and person-centred activities on quality of life, agitation, and antipsychotic use in people with dementia living in nursing homes: a cluster-randomised controlled trial | PLOS Medicine | Cluster randomised controlled trial | Improvement in quality of life, agitation and neuropsychiatric symptoms. Rates of prescribing of antipsychotic were low and did not change | 76 |
| 1 | WHELD | 2020 | Ballard | Improving mental health and reducing antipsychotic use in people with dementia in care homes: the WHELD research programme including two RCTs | Programme Grants for Applied Research | Programme report | A systematic review found four training manuals with randomised controlled trial evidence. Meta-synthesis identified four key elements, including antipsychotic review by GPs. A factorial randomised controlled trial showed a reduction in drug use, and exercise and social interaction were needed to mitigate detriment of drug withdrawal. Focus groups indicated need for a whole-home approach, including sustained relationships. A 9-month randomised controlled trial showed improvement in quality of life, agitation and neuropsychiatric symptoms. Health and social care costs were reduced. Delivering the intervention required a flexible approach. An e-learning module was developed for GPs | 77 |
| 1 | Shine | ND | Baqir | Blogs | Health Foundation | QI | Various aspects of a QI initiative are described, including responding to diversity of GP working practices | 78–80 |
| 1 | Shine | 2014 | Northumbria Healthcare NHS Foundation Trust | Shine 2012 final report. A clinico-ethical framework for multidisciplinary review of medication in nursing homes | Health Foundation | QI | Similar to Baqir 2013 | 81 |
| 1 | Shine | 2014 | Baqir | A clinico-ethical framework for multidisciplinary review of medication in nursing homes | BMJ Open Quality | QI | Similar to Baqir 2013 (see below) | 82 |
| 1 | Shine | 2013 | Baqir | A clinico-ethical framework for multidisciplinary review of medication in nursing homes: a Health Foundation Shine project | International Journal of Pharmacy Practice | QI | A total of 422 residents were reviewed and 17.4% of medicines were stopped (6% were stopped because of safety concerns). A total of 2.1% of residents had potential adverse events, but these were reversed. One-hour nursing time was released per day because of fewer medications. Care home nurses and GPs were supportive and allowed access to records | 83 |
| 1 | Shine | 2017 | Baqir | Impact of medication review, within a shared decision-making framework, on de-prescribing in people living in care homes | European Journal of Hospital Pharmacy | QI | A total of 70.6% of patients had at least one medicine stopped. No significant difference in medicines stopped between pharmacists alone or pharmacist plus GP | 84 |
| 1 | Medication review | 2006 | Zermansky | Clinical medication review by a pharmacist of elderly people living in care homes – randomised controlled trial | Age & Ageing | Randomised controlled trial | Pharmacist recommended to GP 3.1 drug changes whereas GP alone made 2.4 changes per patient. There was a lower rate of falls in pharmacist-attended residents (0.8 vs. 1.3 falls per patient for the GP group). A total of 75.6% of pharmacist recommendations were accepted and, of these, 76.6% were implemented | 85 |
| 1 | Independent prescribers | 2016 | Bond | GP views on the potential role for pharmacist independent prescribers within care homes: Care Homes Independent Pharmacist Prescribing Study (CHIPPS): ‘there has to be something in it for me’ | International Journal of Pharmacy Practice | Qualitative interview study | GPs welcomed the pharmacist service. Some concerns about pharmacist initiating medicines. Issues raised: trust, governance and knowledge of older people’s medicine | 86 |
| 1 | Independent prescribers | 2019 | Inch | The Care Home Independent Prescribing Pharmacist Study (CHIPPS) – a non-randomised feasibility study of independent pharmacist prescribing in care homes | Pilot and Feasibility Studies | Non-randomised feasibility study | A total of 44 general practices and 16 pharmacists were recruited and were retained. Forty residents were recruited and were retained. Outcomes selected were number of falls, Drug Burden Index score, hospitalisations, mortality, activities of daily living and quality of life. The service was well received by care homes and GPs | 87 |
| 2 | Difficult Conversations | 2018 | Brighton | ‘Difficult Conversations’: evaluation of multiprofessional training | BMJ Supportive & Palliative Care | Evaluation | A total of 655 participants, including GPs, nurses, social care staff, allied health professionals and care home staff. All groups showed increased self-confidence, knowledge and skills. They appreciated interprofessional learning | 60 |
| 2 | GSF-CH | 2009 | Badger | An evaluation of the implementation of a programme to improve end-of-life care in nursing homes | Palliative Medicine | Evaluation | Significant improvements in end-of-life care, increase in proportion of residents who had an ACP and increase in proportion of residents who died in the care home. Crisis admissions to hospital were reduced | 88 |
| 2 | GSF-CH | 2011 | Hall | Implementing a quality improvement programme in palliative care in care homes: a qualitative study | BMC Geriatrics | Qualitative study of QI |
Benefits included improved symptom control, team communication, external support (including GP), staff confidence, residents’ choice, reputation of home Barriers included increased paperwork, lack of knowledge, costs, problems with lack of co-operation of GPs |
89 |
| 2 | GSF-CH | 2012 | Badger | An evaluation of the impact of the Gold Standards Framework on collaboration in end-of-life care in nursing homes. A qualitative and quantitative evaluation | International Journal of Nursing Studies | Qualitative and quantitative evaluation | Challenges to collaboration: working with many GPs and poor access to out-of-hours and specialist services. Improved collaboration was identified by 33% of managers. Staff reported increased knowledge and confidence, and discussing care with GP and palliative specialists | 61 |
| 2 | GSF-CH | 2014 | Kinley | The provision of care for residents dying in U.K. nursing care homes | Age & Ageing | Review of deceased care records | Dependency of residents increased, with 56% dying within 1 year of admission. Within the last 6 months of life, support from health-care specialists was variable | 90 |
| 1 | CMHT | 2018 | Stewart | Provision and perceived quality of mental health services for older care home residents in England: a national survey | International Journal of Geriatric Psychiatry | Survey | Only 18% of CMHTs for older people allocated staff for care homes and services varied. Forty per cent of teams provided training to care homes staff. Service manager was likely to report their service as good if the service had a systematic process for reviewing mental health and antipsychotic prescriptions, including contact with a GP | 91 |
| NA | Nutrition review | 2014 | Madigan | A cluster randomised controlled trial of a nutrition education intervention in the community | Journal of Human Nutrition & Dietetics | Cluster randomised controlled trial | GPs and nurses who attended an educational intervention about supporting patients following discharge from hospital showed greater knowledge than the control, although this was not sustained at 6 months | 92 |
| NA | Stroke | 2017 | Sadler | Shaping innovations in long-term care for stroke survivors with multimorbidity through stakeholder engagement | PLOS ONE | Qualitative study | Thirty-seven participants, including GPs, selected the following purposes as priorities for data improvement: continuity of care, mental health, access to health and social care, and multiple risk factors. From this consultation, a decision support tool was co-designed | 93 |
| NA | Quality and Outcomes Framework | 2011 | Shah | Quality of chronic disease care for older people in care homes and the community in a primary care pay for performance system: retrospective study | British Medical Journal | Quantitative retrospective | Quality indicators of chronic disease care were lower for residents of care homes than for the community over 14 out of 16 indicators (after adjustment). Residents of care homes were more likely to be excluded by GPs from targets within the Quality and Outcomes Framework | 94 |
| NA | Fracture prevention | 2008 | Cox | Educating nursing home staff on fracture prevention: a cluster randomised trial | Age & Ageing | Cluster randomised trial | There were no differences between the intervention and control in primary outcomes, incidence of total fractures or total hip fractures. No differences were found for falls or hip protector use. An increase in prescription of bisphosphonate, calcium and vitamin D was observed in the intervention group | 95 |
These articles and grey literature are arranged according to the programme theory for which they provide evidence. Four articles did not provide in-depth description of the role of the GP and were not consistent with either programme theories 1 or 2 and are, therefore, noted as not assigned.
Steps 3 and 4: extracting and organising data, synthesising evidence and drawing conclusions
Owing to the iterative and cyclical nature of steps 3 and 4, as outlined in Figure 1, we have presented these steps together. Across the 30 articles found and included in the review, there was often only superficial or passing mention of GP involvement in improvement. From these 30 articles, we were able to piece together two main programme theories: one relating to negotiated working with GPs around local improvement initiatives and one outlining the role of GPs in a national improvement programme. Table 3 lists the main articles used to develop the programme theories. In addition, Table 3 lists articles that did not contribute to theory development and provides the reason for exclusion.
| Programme theory | CMO | Main study used | Articles limited in relevance or rigour | Rationale for exclusion |
|---|---|---|---|---|
| Programme theory 1: negotiated working with GPs on local improvement initiatives | CMO 1: pharmacist-led medication review | CMR,83 CHIPPS85,87 | Data for quality72 | Rigour: commentary without empirical evidence |
| RCT: pharmaceutical care71 | Relevance: limited involvement of GP | |||
| Shine84 | Pharmacist independent prescribers86 | Richness: limited description of change | ||
| Evaluation of Vanguard69 | Relevance: described future improvements | |||
| CMO 2: de-prescribing, working with care home staff | WHELD77 | Evaluation of national policy70 | Relevance: no description of change | |
| Medication review by GP74 | Richness: limited description of change | |||
| CMO 3: collaborating for end-of-life care | EVIDEM-EoL67 | Quality indicators for end-of-life care66 | Relevance: could not engage GPs in improvement | |
| Implementing new care model 65 | Relevance: unable to attribute change to care home | |||
| Programme theory 2: role of GPs in supporting national improvement programmes | CMO 4: GP-led end-of-life care | GSF-CH61,89,96 | Critique of GSF-CH study97 | Rigour: opinion piece |
| Response to critique98 | Rigour: opinion piece | |||
| Difficult Conversations60 |
Programme theory 1: negotiated working with general practitioners around local improvement initiatives
We found only a small number of articles about local or regional improvement initiatives that were primarily led by GPs. We found no articles describing how GPs became involved in initiatives, what role they played, what resources were involved or how projects could be sustained or replicated. We did, however, find evidence of initiatives that were led by other professionals where GPs formed part of the mechanism by which outcomes were realised. These are summarised in Figure 3.
FIGURE 3.
Programme theory 1: negotiated involvement of GPs in local improvement initiatives.
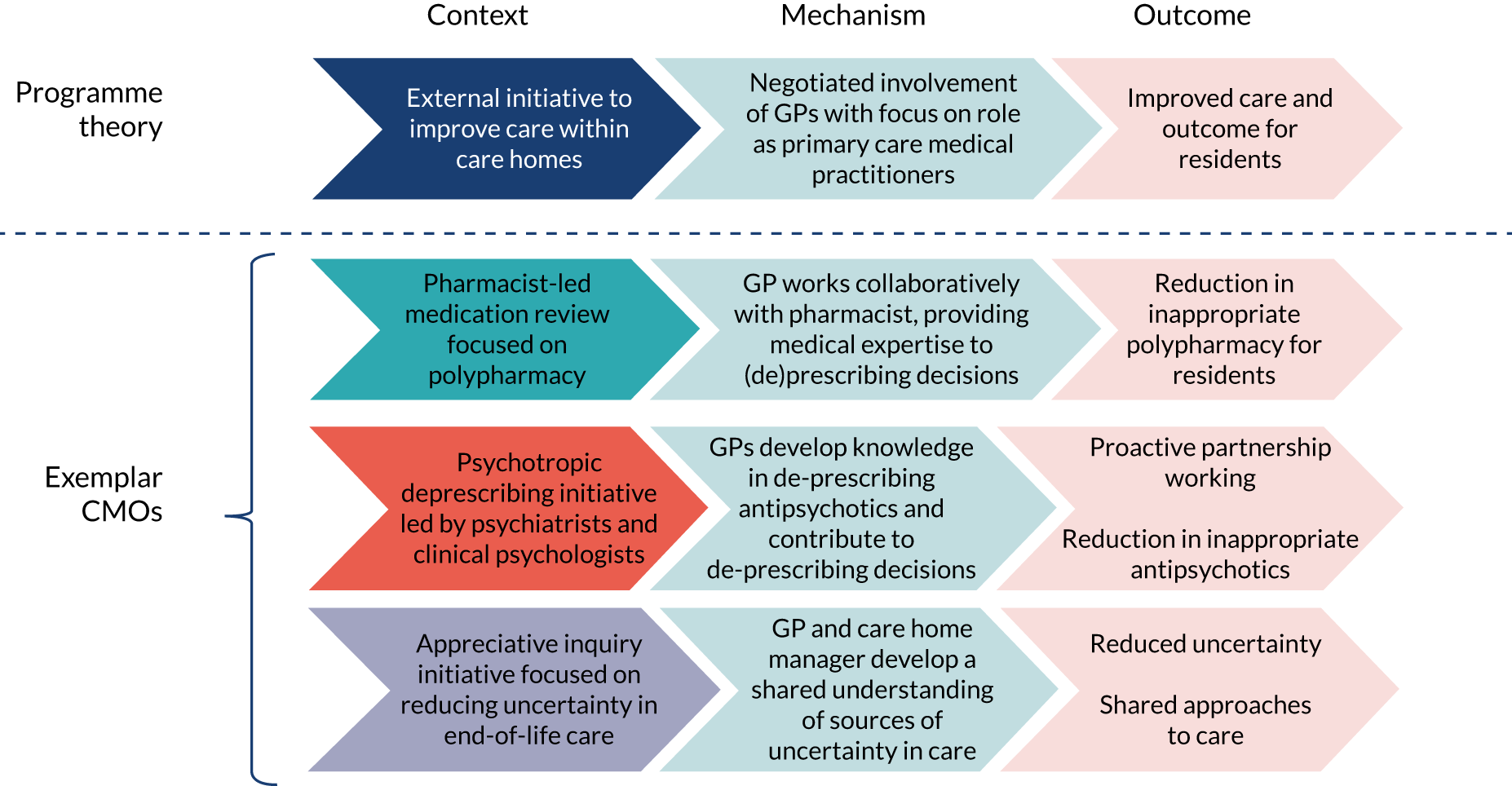
In each of the examples found, an initiative that commenced outside general practice was deliverable only through the direct involvement of GPs. To each initiative, GPs brought technical medical expertise, their understanding and an overview of how health-care delivery in the community operates. In addition, GPs also provided a legitimising function by virtue of their role as the doctor, with overall responsibility for co-ordinating patient care in the community. Their role within the improvement initiative had to be negotiated and worked out. The professionals, or external practitioners, had neither the expertise nor authority to specify the role that GPs should play within the improvement programme and this had to be worked out in conjunction with GPs, alongside their competing responsibilities outside the care home setting.
We present here three exemplar CMOs where similar principles played out. These relate to:
-
pharmacist-led medication review (CMO 1)
-
psychotropic de-prescribing led by psychiatrists and clinical psychologists (CMO 2)
-
teamwork focused on reducing uncertainty in end-of-life care (CMO 3).
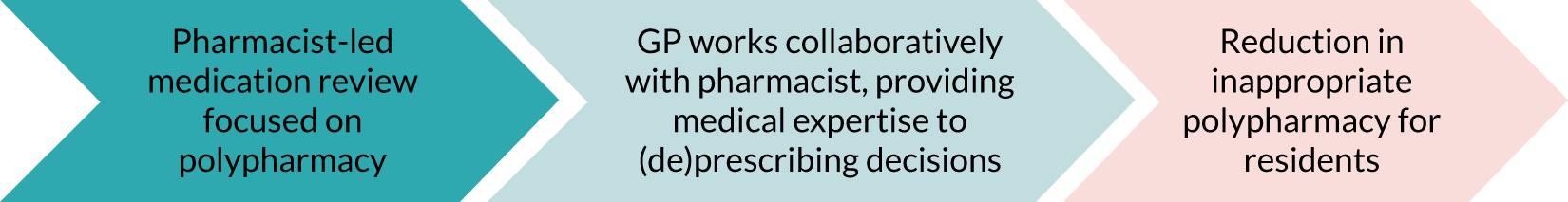
Exemplar CMO 1: pharmacist-led medication reviews
The schematic outlining this CMO is provided in Figure 4 and details of supporting evidence for each component is provided in Table 4.
FIGURE 4.
Schematic of exemplar CMO 1: pharmacist-led medication review.
| Context | Mechanism | Outcome |
|---|---|---|
| Medication review is challenging and complex (interview #16)84 | Trusted relationship between GP and pharmacist develops within framework of consultations (interview #19)84,85,87 | Reduction in inappropriate polypharmacy, reduced costs, reduced falls and reduced hospitalisation84,85 |
| Multidisciplinary meetings with a focus, including prescribing9,84 | Negotiated adaptation of implementation to take account of diverse ways of working, enabling GP to engage in a way that is consistent with their working practice81,84 |
Where GP attended a MDT there were greater numbers of prescription changes per resident84 Resident input into meetings78 |
| GP fear of adverse events and responsibility for these81 | GP authorises the process, but does not contribute to individual resident reviews81,85 | Fewer medication changes may be implemented |
Table 4 identifies key references or quotations from interview transcripts and greater detail of analysis is given in Appendix 5. Qualitative analysis software (NVivo 12) was used to create codes that detailed aspects of context across all sources of evidence for pharmacist-led medication review. This coding is summarised in Table 4, column 1. In a similar way, mechanisms were coded and summarised in Table 4 to match the context described in those sources. Finally, where outcomes were measured or observed, these were also extracted (see Appendix 5), summarised and aligned with the contexts and mechanisms (see Table 4). Some sources indicated a lack of outcome (see Table 4, bottom row) and for these problems or deficiencies in the context were identified that explain the lack of firing of mechanisms (see Appendix 5). Our interpretation of a synthesis of CMO across multiple evidence sources is represented in the schematic (see Figure 4).
The medication review projects, which have been described in several programmes82,87 in England, introduce an intervention that modifies the context. The intervention involves new personnel to supplement the GP input (e.g. a pharmacist-independent prescriber) and the additional process of collecting information about the individual. 85 The latter includes extracting information from the GP records, as well as care home records (e.g. to identify any falls). This provisional step requires GP approval. 86
The mechanism of the polypharmacy medication review initiative is the trusting relationship between the pharmacist and GP. In a feasibility study, the Care Home Independent Prescribing Pharmacist Study (CHIPPS),87 all GPs recruited to the study (44 practices in total) remained throughout the study, and success of recruitment and retention was attributed to selecting those with existing relationships with prescribing pharmacists. A quotation from our theory-gleaning interviews with GPs illustrates the importance of communication within relationships:
. . . someone comes out of hospital, there has been a medication change that hasn’t gone on a discharge summary. So, to me having the care home pharmacist liaising with the home, liaises with the manager . . . does a review when someone has been discharged from hospital to reconcile the meds [medications].
GP#21
Another medication review initiative was a QI project called ‘Shine’. GPs were involved in several cycles of QI, during which the model of interaction with GPs varied. 81 The project team recognised that the diversity of GPs’ working routines meant that there needed to be flexibility in how the pharmacist interacted with them. The preferred way of working was when the GP attended the multidisciplinary meeting with the pharmacist and the care home staff, and this occurred for 38% of resident participants. When the GP was not able to attend the multidisciplinary meeting, the pharmacist was able to meet with the GP after the meeting to discuss cases, and this happened for 30% of residents. For the remaining 27% of residents, the pharmacist carried out the medication review with only occasional discussions with the GP about changes in medication. 78,81 Within these models, patients could also be referred to an old age psychiatry service, enabling access to further expertise around the particularly challenging prescribing and de-prescribing decisions for psychotropic medications. A key role was identified for GPs in facilitating shared decision-making with the resident, involving family or advocate when possible, and further discussing decisions with care home managers and staff. 78,81
A key context is the complexity of prescribing for care home residents, particularly the cumulative impact for those living with multimorbidity. The policy context for this comes from national (England) clinical guidance99 and the policy framework for primary care networks,100 which specify the need for regular medication review in care homes. Although there is broad agreement on the importance of medication review, the resources required to complete medication review for care home residents mean that they are time-consuming, require a level of health literacy not always present with residents and their representatives, and exceed the available resource in general practices:
. . . there is little support for practitioners who wish to stop medicines. Solutions to support de-prescribing include tools which identify potentially inappropriate medication, such as the STOPP-START tool and Beers criteria.
Baqir et al. 84
The outcome in CMO 1 is that the individual resident benefits from multidisciplinary expertise and is consulted on proposed changes to medications. Outcomes from the ‘Shine’ project indicate benefits in terms of direct cost saving, reduced falls and reduced hospitalisation. 84,85 The cost saving was greatest for the model in which the GP played a permissive role, rather than contributing directly to the MDT (because GP time did not have to be included in costs). However, the model in which the GP attended the MDT meeting led to a larger number of changes of medication, which may indicate a more thorough, or person-centred, review. 84 Overall, the GP supports and approves the medication review and integrates the intervention into broader care planning, for example taking account of prognosis and likely clinical trajectory. This was supported by one of our theory-gleaning interviews with a GP who outlined that medical input, provided by GPs, was required to contextualise prescribing decisions in wider plans for medical management:
We then set aside an hour where we will go through the ones where she is considering stopping, or this person has got this illness and they haven’t got this drug. And so, she doesn’t make any of the decisions on her own, those decisions are made with me with my clinical knowledge of the patient.
GP#21
The GP may also be best placed to interact with residents and family members to facilitate shared decision-making, a key role identified within the ‘Shine’ QI project:82
. . . decisions are based on having conversations around context and I don’t know many pharmacists who are sighted on being like the Mental Capacity Act and how we should be making decisions based on a person’s wishes and preferences or who is the legal decision maker authority is and then having a conversation.
GP#19
The interviews highlighted that GPs remain the accountable professional for patient care during and after medication reviews, and that any problems arising from review would return to the GP. Building trust with the pharmacist and the broader MDT was necessary for GPs to permit medication reviews to proceed. The limitations placed on implementation if GPs were not reassured about its safety were noted in one study by Zermansky et al. 85 as follows:
The low implementation rate might have been higher if the pharmacist had been allowed to implement agreed changes. 85
In summary, when a QI project reviews medication of care home residents using a structured process that seeks input from resident and care home staff (context), then a trusting relationship between pharmacist and GP can facilitate the procedure, enabling combination of the structured approach and specialist knowledge of the pharmacist with the medical expertise of the GP (mechanism). This results in successful reduction of inappropriate polypharmacy with measurable improvement in care and cost savings (outcomes).
Exemplar CMO 2: psychotropic de-prescribing led by psychiatrists and clinical psychologists
This second CMO focused on how a QI prescribing innovation linked to a specific goal of reducing antipsychotic prescribing relied on working with GPs. It refines the earlier evidence and draws on a rigorous programme of research that specifically engaged with the care home staff and how they worked. The schematic outlining of this CMO is shown in Figure 5 and a detailed explanation of the components of the CMO with supporting evidence is provided in Table 5.
FIGURE 5.
Schematic of exemplar CMO 2: de-prescribing antipsychotics.
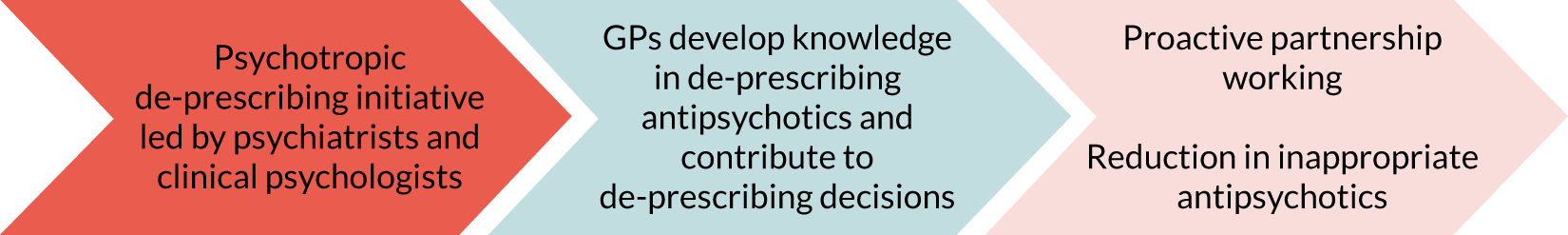
| Context | Mechanism | Outcome |
|---|---|---|
| GP co-designed training for GPs | GP gains confidence in ability of care home manager | Proactive working to de-prescribe |
| Care home delivers social intervention and nudges GP to de-prescribe | GP feels reassured that alternative therapy to antipsychotic is being provided | De-prescribing of antipsychotics, leading to cost savings and reduced side effects of antipsychotics |
People with dementia can exhibit behavioural or psychological symptoms of dementia that staff find challenging and difficult to manage. The causes of these behaviours are often a communication of a particular issue, for example undiagnosed pain or environmental factors. Prescribing antipsychotics for these symptoms is increasingly recognised as associated with adverse outcomes. National policies have encouraged a reduction in the frequency antipsychotic prescriptions. 102
Ballard et al. 77,101 led a programme of research to develop multifactorial approaches to behavioural and psychological symptoms of dementia that could reduce the need for antipsychotic medication. This programme of research was called Wellbeing and Health for People with Dementia (WHELD). 77,103 The research team included psychiatrists and clinical psychologists who developed a psychosocial intervention. The intervention had four components: (1) person-centred care training for staff, (2) review of antipsychotic medication by the resident’s GP, (3) a social interaction component and (4) an exercise component. The programme developed training and resources to support GPs in carrying out de-prescribing:
Physicians were invited to an interactive seminar and/or practice meeting, provided with a toolkit or best practice guide, and given an opportunity for detailed discussion, including scenarios with individual patients.
Ballard et al. 101
Therefore, the context of this CMO was the improvement project that was led by psychiatrists and clinical psychologists. Care home staff were trained to provide social interaction as a non-pharmacological alternative to antipsychotic medication. Alongside this, staff were encouraged to support GPs in reviewing medication. 77,101 Similar to the previous mechanism (i.e. CMO 1), the relationship of the GP with other members of the care team is important, but, here, the care staff are responsible for the initiative. Therefore, the training and activity in the care home to identify alternative non-pharmacological interventions and greater awareness of the harms of antipsychotics among the team provided the context in which the GP de-prescribed. The initiative was supported by additional training that was co-designed with GPs and developed into a digital learning package. The opportunity and increased confidence afforded GPs (i.e. that care home staff were equipped to offer alternative approaches to care) represented a mechanism whereby de-prescribing could occur, delivering key outcomes around reduction of polypharmacy and harm.
Exemplar CMO 3: general practitioner integral within change initiative to improve end-of-life care
The schematic outlining this CMO is provided in Figure 6 and details of supporting evidence for each component is provided in Table 6.
FIGURE 6.
Schematic of exemplar CMO 3: delivery of end-of-life care using appreciative inquiry.
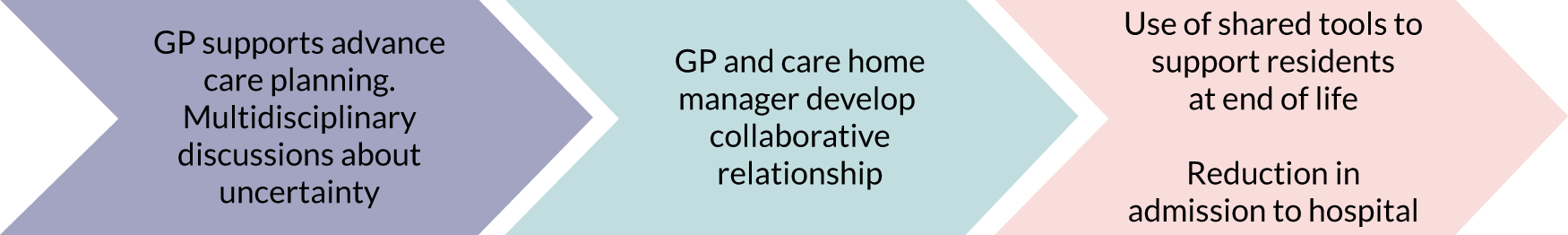
| Context | Mechanism | Outcome |
|---|---|---|
| Different perspectives were held by the GP and the care home manager. The usual routine of GP care may not suit residents with complex needs67 | Appreciative inquiry identified shared opportunities. GP taking a collaborator role rather than leader (GP interviews #11 and #21)67 | Implementation of tools and processes improves consistency of care67 |
| GPs reflect on visiting frequency and co-ordination with out-of-hours teams and district nurse to support care home68 | Collaborative support to enable end-of-life care to be provided in care home and to implement ACPs68 | More frequent visits reduce need for emergency care68 |
A care home improvement project about end-of-life care used an appreciative inquiry method to bring together the care team. The project had identified areas of uncertainty within teams when decisions had to be made about end-of-life care and this could lead to conveyance to hospital towards the end of life. 67 A series of three workshops brought together the care home manager, GP and district nurse, from three care homes. Appreciative inquiry enabled issues to surface, including who should lead care decisions, communication and care routines. This approach engaged GPs in how changes were planned and elicited the commitment to deliver the agreed change. Discussions explored different perspectives that members of the team may bring to care of individual residents. Tools and frameworks were implemented through the project67 and these, together with the above issues, may be considered as context within CMO 3.
Reflecting on our theory-gleaning interviews, we can add greater depth to our understanding of context. GP participants mentioned that communication could be a challenge, with care home staff at times feeling ‘isolated, unsupported and unheard’ (GP#21). Communication difficulties may be linked to different approaches between GPs and care home staff, with one participant indicating that the ward-round approach, which may be the approach favoured by GPs, was not optimal for patients with complex needs (GP#11).
Further evidence for this CMO can be drawn from a project that used audit and feedback to improve GP involvement in end-of-life care and urgent care. 68 Case notes of residents of six care homes, all registered with one general practice, were audited, and data were presented at a multidisciplinary study day with care home managers and staff, GPs, out-of-hours staff and district nurses. A follow-up audit showed changes in GP attendance at care homes and reductions in emergency admissions to hospital. The different contexts of the residential and the nursing home were analysed. Although the number of residents admitted to hospital by GPs attending residential and nursing homes decreased, for residential homes there was an increase in the number of residents admitted to hospital following the care home staff calling for an ambulance, but this did not increase for nursing homes. One aspect of the improvement work was to encourage discussions about preferred place of care and death between residents and family, care home staff and GPs. The outcome was an increase in deaths within both residential and nursing homes and an equivalent decrease in deaths in hospital. GPs reflected that they had spent more time with residents and that this enabled better advance care planning. The audit data showed an increase in visits for nursing home residents. 68 Finally, it should be noted that a GP conducted this study and, although it is not explicitly stated, the GP led the improvement initiative.
Context–mechanism–outcome 3 may be summarised as follows: GPs and care home managers may hold different perspectives and approaches to complex care and end-of-life care, and these can lead to uncertainties (i.e. treatment uncertainty and service uncertainty) (context). When a resident is deteriorating there may be different views about capacity of the home to provide care or, alternatively, if the resident needs to be transferred to hospital, and this will be influenced by availability of GP (or out-of-hours team) and if there is on-site nursing or access to a district nurse for residential homes (context). Appreciative inquiry and audit and feedback methods have been used to develop collaborative relationships between GPs and care home managers. A GP interview participant described the relationship as a ‘whole team’ (GP#21). This mechanism identified shared opportunities and approaches to end-of-life care (mechanism). The outcome was implementation of care planning tools that addressed uncertainty and delivered co-ordinated care, leading to fewer residents being admitted to hospital and more residents dying in the care home (outcome). 67,68
Programme theory 2: role of general practitioners in supporting national improvement programmes
We found limited evidence of national initiatives for which GPs were involved in improvement programmes in care homes around the country in a consistent way. Although under way as we conducted the research, the EHCH programme of NHS England had hitherto conducted its work as part of local pilot initiatives known as ‘Vanguards’. 9
There were two examples of nationally co-ordinated care home improvement initiatives focused on end-of-life care that had evidence of GP involvement: (1) a series of studies describing the development and evaluation of the Gold Standards Framework for Care Homes (GSF-CH), which is a structured way to prognosticate and deliver appropriate care to people as they approach the end of their lives,61 and (2) a study that described the development and implementation of a programme called ‘Difficult Conversations’. 60 The schematic for this programme theory is illustrated in Figure 7 and supporting evidence is outlined in Table 7.
FIGURE 7.
Schematic of programme theory 2.
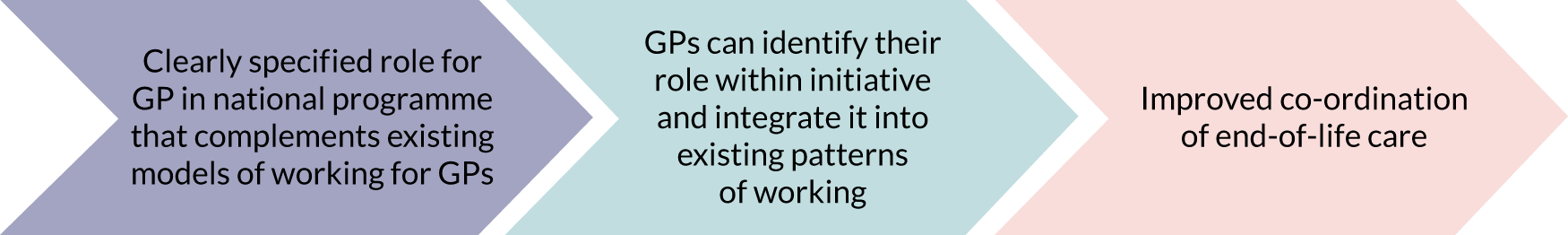
| Context | Mechanism | Outcome |
|---|---|---|
| Programme aligns with existing initiatives in place in general practice61 | GPs can integrate improvement with existing models of working61 | Improved confidence in individual and team decisions, and clearer understanding of roles and responsibilities between GP and care home61,89 |
| Training provides care home staff with a structured way to communicate with GP61 | GPs and care home staff have a shared framework for understanding end-of-life care decisions89 | Improved use of shared documentation and communication of care around dying residents61 |
| Specific GP-focused learning outcomes and training delivered as part of a multidisciplinary training programme60 | GPs can understand and feel confident in their role in the team60 | Improved multidisciplinary working around end-of-life care60 |
There is some overlap between this CMO and the exemplar CMOs used in support of programme theory 1. We separated this CMO because of an observation that impetus for national roll-out of each of these programmes came from an influential leader who was also a GP. We looked for evidence that their status as a GP was, in some way, integral to the success of these programmes at a national level, but we were unable to find this. Nevertheless, we have separated this CMO into a programme theory to illustrate that the impetus for change came from within, rather than outside, general practice, which is a key distinction from the exemplars given in support of programme theory 1.
The Gold Standards Framework (GSF) was developed to support GPs delivering end-of-life care to people in their own homes and, more recently, this has been adapted into the GSF-CH. The main part of the implementation of the GSF-CH is about training care home staff and accrediting care homes. There seems to be an assumption that the GP for the care home is also GSF accredited and, therefore, enabling the care home and GP to collaborate using the same framework for end-of-life care. The many reports and evaluations61,88,89 of GSF-CH describe the care homes’ role and their communication with their GP, but do not explicitly state the role of the GP in implementing GSF-CH or how this has changed (improved) the GP’s care of the individual.
As the GSF programme was well established in general practice and the framework deployed in care homes was largely similar to that used in the community (context), this made it easier for GPs to integrate it into existing models of working (mechanism). In addition, the shared framework between GPs and care home staff led to a shared understanding of end-of-life care decisions (mechanism). There was evidence that care homes accredited with GSF-CH experienced more respectful communication with GPs. 61 The outcomes were better understanding of the roles and contributions of care home staff and GPs, improved use of shared documentation and improved communication of care around dying residents, with the results that the team (i.e. the GP and care home) made decisions more confidently and had greater confidence in their decisions (outcome). The framework (i.e. the process, accreditation and the documentation) could be considered to act as a boundary spanner between the GP profession and the care home sector:
The focus is on organising and improving the quality of care for care home residents in the last year of life in collaboration with GPs, primary care and specialist palliative care teams.
Hall et al. 89
The ‘Difficult Conversations’ programme was evaluated by Brighton et al. 60 This was an evaluation of delivery of multiprofessional training, including GPs and care home staff. The supplementary appendix of the article60 states that a GP was involved in developing the intervention. Furthermore, GPs were trained to be champions to deliver the training (i.e. a train-the-trainer model). 60 Participants who received training completed a self-report questionnaire on their confidence, knowledge and skills in communicating about end-of-life care with patients and carers. Neither the training nor the evaluation were specific to the care home setting, but participants included care home staff (6% of participants), as well as community nurses and allied health professionals. GP participants showed a small but significant increase in self-reported confidence and skills about end-of-life care. Other staff groups showed a greater increase, although this appeared to be partly due to the GPs starting at a higher baseline score. In response to open questions, participants said that they valued the interprofessional learning:
They praised the expertise of the workshop facilitators (n = 64), noted the benefits of interprofessional learning (n = 36). 60
This evaluation indicates that the course may have given increased confidence, not only of the GPs ability, but also confidence in the ability of the multidisciplinary care team.
The founder of the GSF programme is a national leader for general practice, Dame Professor Keri Thomas:
The GSF was developed by generalist practitioners to address their own needs for support and education related to end-of-life care. 61
The ‘Difficult Conversations’ programme was led by Dr Catherine Millington-Sanders, who is a clinical champion for end-of-life care for the Royal College of General Practitioners and the Marie Curie Foundation (London, UK). The website for the programme states that it is endorsed by the Royal College of General Practitioners, General Medical Council (London, UK) and British Medical Association. Whether senior GP leadership for these initiatives, or the sponsorship of national umbrella organisations, confers credibility in the eyes of GPs or increases the likelihood that they will engage with the programme is not clear. It is, however, a potentially important structural difference from the initiatives described by programme theory 1. GPs did play a more direct role in the implementation of ‘Difficult Conversations’ than in all of the other programmes described, at least by design. However, the precise detail of the work undertaken by individual GPs as part of either of these national initiatives was not well reported in the literature.
Programmes in which the evidence was too thin to describe mechanisms
We identified programmes that did not fit the above programme theories; however, the evidence was too thin to describe realist mechanisms. One article74 describing medication review was authored by GPs and, by implication, the project had been led by the GP authors; however, there was no description of how the GP carried out the review and, therefore, it was not possible to describe mechanism or CMO configuration. Another programme53 described a general practice that had been set up to provide specifically for care homes, but, again, there was insufficient evidence to describe a CMO.
General practitioner carrying out medication review
One early study,74 which claims to be the first report of medication review in care homes, was conducted by two GPs, rather than pharmacists. The authors conducted the medication reviews with nursing homes where patients were registered with their own practice. The number of prescriptions was reduced (from mean of 4.3 repeat prescriptions to a mean of 3.5 repeat prescriptions) in residents reviewed. 74 There was a lack of depth of description about the process of the medication review. It may be that the GPs had capacity within a specific role (e.g. research) to carry out reviews. The care homes were local to the general practice and, therefore, they may have well-established relationships with the care home managers, which would be part of the context. This GP-led medication review project74 is consistent with some aspects of CMOs 1 and 2, but there is no evidence of resources required for the initiative, how it was established and if it could be sustained or replicated. 74
General practitioner specialising in care homes
Our understanding of recent policy in England led to drafting a putative programme theory about general practices that cared for care home residents only. We considered that if this were the case, or if policy was developing in this direction, it would support the development of GPs with special interests (or extended role) in older people’s care and care homes. Therefore, we conducted further scoping searches for these topics. We received an informal report about one care home-specific general practice and found a brief mention of another example (Dr Louise Butler, Salford Royal NHS Foundation Trust, 2020, personal communication). However, we were unable to identify any further literature and, therefore, the evidence was insufficient to be able to elaborate this putative programme theory.
Chapter 4 Discussion
The starting point for this realist review was findings from our own research studies9,37,104 and experience from our own improvement practice30 that suggested that GPs are integral to service delivery in care homes. As the source of medical support and access to specialist care for care home residents, GPs hold a position of significant power and influence over residents’ care and health-care improvement in these settings. We had expected to find within the QI literature accounts of how GPs had been involved, descriptions of how they negotiated their role in relation to other visiting health-care professionals and information on what supported the development of relationships over time. We were particularly interested to identify patterns of GP involvement that led to improved staff outcomes and systems of working at the interface between health and social care. The review, however, demonstrated that this is an unexamined role in contrast to work on the specialist contribution to care homes. 47 The paradox is that the GPs are central to recent policy for enhancing health-care provision to care homes, despite questions about GP capacity to fulfil this, and the relative effectiveness of core activities and practices that GPs fulfil when working with care homes, such as medication management, end-of-life care and working with others, remain neither tested nor compared with the input of other visiting health-care professionals. The interviews and scoping confirmed the central role of the GP as the provider of medical care to residents, but without agreement about the responsibilities and role. How the GP role enabled QI to occur (or not) relied on how working relationships were negotiated. Specifically, it depended on the presence of the following factors: the GP role as facilitator and endorser of change, GP involvement in co-designing innovations, ability of GPs to prioritise this work against the larger caseload and, finally, GPs having the resources and expertise to support the work.
There is a growing literature on care home innovation and sophistication in understanding how contextual factors affect uptake and engagement. 105,106 GPs’ input is acknowledged as part of this, but, to the best of our knowledge, how they co-ordinate or integrate with care homes has not been explained or discussed in detail. 48 The fact that GPs have not featured significantly in descriptions of care home improvement work to date could mean that their role has been taken for granted as core, but not described. Alternatively, it could be that the need for QI is a reflection of the absence of GP involvement in particular aspects of care delivery in care homes. If the level of GP engagement in care home work has historically been discretionary or dependent on the quality of working relationships, are studies of QI recognising gaps in provision that could or should be GP-led work? Are they compensating for limited medical engagement or limited access to specialist care that can deliver improved outcomes? The literature about the role of GPs in improvement in care homes raised questions about the capacity of GPs to deliver and what system-based expectations existed as to what is, and is not, the role of the GP. 61,65–95,101 This resulted in the following:
-
GPs were not the instigators or leaders of improvement initiatives in the setting.
-
The role of GPs was always negotiated to take account of their likely contribution as primary care doctors and the ways in which they could use their unique skills and competencies as part of a MDT to deliver improvement goals.
-
What was generalist (GP) work, and appropriate to expect GPs to fulfil, was unclear. Often QI required additional training to orientate GPs to technical components of an intervention, for example around behavioural and psychological symptoms of dementia and antipsychotics. In the contexts described these activities went beyond core GP work. They were represented as new skills. It was not clear from the articles included in our review, our interviews, or subsequent consultations whether or not being able to respond to needs commonly experienced by care home residents was core or specialist GP work.
-
Training about frameworks (e.g. around structured approaches to polypharmacy or end-of-life care) that could inform interactions between GPs and care home staff, or other professionals, such as pharmacists, was negotiated, was not core and could not be assumed as in place for improvement work.
-
Building trust through communication and shared understanding of roles and responsibilities was a recurrent mechanism by which GP support could be enlisted for improvement initiatives. This was particularly the case when reassuring GPs about mitigating risk of adverse events for which they were nervous about assuming subsequent responsibility.
For each of the initiatives described (around polypharmacy, antipsychotic de-prescribing and end-of-life care) the improved outcomes identified could be achieved through GP involvement only. In polypharmacy, this related to the unique ability of GPs to balance prognosis and diagnosis alongside consideration of drug–drug and drug–patient interactions. For antipsychotic de-prescribing, it related to the GPs’ role as the first-line provider of health care and the usual prescriber in care home settings. Finally, for end-of-life care, it related to the role of GPs as a specialist medical contributors to a MDT, which enabled that team to make decisions with confidence, avoiding uncertainty and indecision that could lead to adverse outcomes for care home residents. In each of these instances, although GPs did not lead change, they were instrumental to its delivery. They could not have been ‘written out’ of any of the programmes described.
A recurring context necessary to lead on to GP engagement was identifying and agreeing the unique contribution of GPs within the QI initiative, either from the outset or as an integral part of the work. This worked best when the QI initiative focused on what it was that GPs, and GPs alone, could provide, and structured the approach accordingly to facilitate the input of GPs. GPs then had an active role in iterative development of medication reviews, in co-designing training aimed at GPs around behavioural and psychological symptoms of dementia and antipsychotic de-prescribing, and in designing care home-specific approaches to end-of-life care. In each instance, however, GPs helped determine how the intervention would interdigitate with general practice, rather than taking a more overarching leadership role. Innovation was required to design ways of making improvement initiatives fit in, or adapt to, existing systems so that what was asked of GPs was recognised as part of their core role and complemented the wider caseload. Examples included two national initiatives – the GSF-CH and the ‘Difficult Conversations’ programme – in which GPs played a central role. These examples provide evidence that GPs can, and have, led QI initiatives in the care home sector; however, there remains an absence of description of the different ways that GPs were able to initiate and sustain change. It also was not clear, despite such initiatives being framed in a way that complemented and accounted for GP ways of working, the role that GPs actually played in delivering improvements on the ground. These findings add to a growing literature on QI in care homes. Innovation and improvement are not new to care homes. Indeed, there is a rich tradition in the nursing literature of participatory approaches to research and improvement within care homes. These approaches include action research- and appreciative inquiry-based approaches to innovation and improvement. 107 Structured approaches to QI, of the sort that are now widely established among health-care providers, are, however, new to care homes. 37 Managers and staff have shown that they can adopt and adapt such approaches, and that they can use them to improve outcomes for residents,29 but without links to the surrounding systems of care, sustaining improvement is difficult. Care homes are not universally equipped to engage with improvement and a number of organisational factors can influence their ability to support and adapt to change. 105 How to enable care homes to prepare effectively for change is relatively unexplored. The data maturation of the UK care home sector, although substantially accelerated during the COVID-19 pandemic, is still considerably behind that of other long-term care sectors internationally. 108,109 Although regional pilots of benchmarking data for improvement have shown some promise,110 and, although ongoing National Institute for Health Research projects promise to develop a minimum data set for UK care homes,111 further development and implementation will be required to enable data to be readily available for measuring improvement initiatives. 111 There is clearly a role for GPs in this growing programme of work and this review has demonstrated the need to articulate what needs to be in place to achieve meaningful engagement.
All of the programmes discussed in this paper were contingent on GP involvement for some, or all, of their reported outcomes. The EHCH framework roll-out,16 discussed in Chapter 1, Quality improvement and other types of advancing practice, calls for closer working of GPs with care homes. The appointment of clinical leads in the midst of the COVID-19 pandemic is a further indicator of the NHS’s intent to take more direct responsibility for structured health-care delivery to care home residents. However, it could potentially be a mistake to expect GPs to assume a leadership role in QI in care homes when, in fact, other professional groups are arguably better placed to lead such work if they engage directly with GPs to consult and co-design where they will add value.
The strengths of the study were that we took a systematic approach to searching academic and grey literature databases. We followed the RAMESES guidelines for realist review (see Appendix 6). We were able to bring a disparate and diverse literature together to inform our theory development. We used stakeholder interviews and a Context Expert Group, which included GPs, a care home manager, a nurse and a pharmacist, to sense-check emerging programme theories and ensure that they reflected real-world experience. Our expert consultation group also helped our approach to the grey literature to ensure that we did not miss key publications that were relevant to the scope of our review.
Our findings are limited by the paucity of description or discussion in the literature on the role of GPs in QI in UK care homes to date. Although our programme theories are evidenced, and evidence-based, they are based upon a relatively small body of work. To answer the questions of ‘what works, when and in what circumstances’, our findings point to the importance of articulating from the outset what the expected role of the GP is and what resources are required. How relationships between other disciplines and care home staff are negotiated is important and the review found that these are ‘soft skills’ that are built up over time or incorporated into the QI initiative. Focusing on how the QI initiative takes account of the GP as ultimately responsible for the residents’ health care may explain why GPs are cautious to lead and collaborate. If GPs were peripheral or not involved, then this also raised questions about the additional workload generated and the sustainability of the programme.
Much of the international literature failed the relevance test by virtue of the relatively unique role played by GPs within the UK health-care system. This meant that findings from long-term care sectors, in the Netherlands and USA for example, with more evolved approaches to QI in long-term care, were difficult to incorporate. We were also limited to publications in English, which may have excluded significant chunks of literature from the Netherlands in particular. It is possible that our decision to look for case studies in prescribing, end-of-life care and extended role general practice could have excluded important segments of the literature that could have further developed our theoretical understanding. There are initiatives that have changed the organisation of care delivery (e.g. care home-based ‘ward rounds’, asking staff to triage residents by need for GP care, online consultations and use of early warning scores), but we found limited accounts or evidence on how the GP role was negotiated and the impact on the service. We did, however, consult regularly with members of our Context Expert Group expert who were unable to direct us to other sources.
Even taking account of the grey literature, it is possible that the type of QI initiatives that are reported in articles, or on the internet, are externally commissioned and funded formal QI initiatives, and are of the type that are likely to be externally led and highly structured. QI should be a bottom-up approach and integrated into daily working, and we may not have captured smaller, less formal QI initiatives led by GPs. This could have biased our findings. This review made some effort to overcome this by the use of stakeholder interviews and an expert consensus group, which took discussions beyond what was published in the literature. Nevertheless, smaller, bottom-up QI initiatives may have been out of sight to such contributors.
One methodological limitation related to the use of a single reviewer to screen abstracts. This could have been a problem if it led to articles that could have provided important evidence being excluded. This was a consequence of limitations on the availability of team members, several of whom are clinicians, as a result of the COVID-19 pandemic, which coincided with this work. We did, however, conduct multiple secondary searches and regularly checked with our Context Expert Group to ensure that we had not missed key references as a consequence of this. In addition, we were driven by the paucity of evidence retrieved to continually return to the literature in search of more and, if anything, we sought to be inclusive and expand the relevant evidence, reducing the risk that we will have missed important papers.
Chapter 5 Conclusions and implications for practice
Based on our findings, we recommend that for GPs to work as part of QI initiatives in care homes it is important to address, from the outset, their role in the initiative, how they complement the work of other disciplines and the opportunities for them to engage in approaches that support a care home focus (and not just individual patients) when working with care home staff. There is a persistent narrative of conflicting commitments, and the nature of their largely medical expertise, that they are not always the best-placed professional group to lead QI initiatives. 6 GPs do, however, frequently lie on the critical path to success for QI initiatives undertaken in the sector and they are responsible for medical care and referral to other specialist services.
We recommend the following steps for stakeholders involved in QI:
-
Meet early with GPs to identify how and when they might contribute to QI initiatives, focusing on their role as medical practitioners and the specific contributions that can be made only by GPs and not by other community-based health or social care professionals.
-
Recognise that GPs exist on a continuum of expertise and interest in relation to care homes, and care of older people more generally, and ensure that improvement models allow for likely variability in practice.
-
Consider what specialist training, either clinical or QI oriented, GPs might need to engage with the improvement initiative. When possible, co-design this with GPs.
-
Consider what adaptations to policies, procedures, documentations and schedules might be required to make best use of GPs as part of an improvement initiative. Recognise that the GPs, care home staff and other professionals may need to train, or work side by side, for a period of time to develop the shared trust and understanding required to build the necessary confidence as a team to deliver improvement outcomes.
-
Recognise the impact of QI on longer-term GP working and develop outcome measures to capture this. Demonstrating this impact will enable sustained and repeated engagement with GP colleagues.
For GPs, we recommend the following:
-
Be receptive to local QI projects that approach you to support their initiative. Try to have early conversations about the unique input you could contribute and the limits of your capacity.
-
Reflect on the working relationship between your general practice and local care homes. Can you concisely convey this working pattern to the QI team? (Other GPs or care homes may work in different ways.)
-
Are you confident that you have the specialist skills to support the GP role within the improvement initiative? Within your general practice or network, does one of your colleagues have a special interest in older people’s care, or could you commit to developing your own interest or extended role? Convey and negotiate the necessary training to deliver the GP role in initiative to the improvement team. Be prepared to help design this, and, if you do, it will likely better reflect your needs and those of colleagues.
-
Consider how the QI initiative may develop in future. If the general practice has limited capacity or resource at the time, can you make a limited commitment at this stage, but aim to explore future contributions as the project develops?
-
Consider how the improvement team can show you, and others, that the project had improved quality, or added value, to care. Be prepared to describe this to the project team so that they can design process and outcome measures that can illustrate this for you and others.
Although this realist review has focused primarily on the role of GPs in improvement, it is important that this is not seen in isolation. We have written elsewhere about the need to engage early and often with care home staff during improvement and innovation in care homes,9,30,37 and the need to build structures to minimise traditional hierarchies and organisational boundaries that serve to disempower care home staff during improvement initiatives. The need to carefully delineate and work to accommodate the unique contribution of GPs does not conflict with, but rather complements, this. Improving outcomes through shared understanding of roles and responsibilities was a recurrent pattern identified during the work undertaken in this review and building opportunities to work together as a team to develop such understanding should be seen as core to good QI in this sector.
Future research
We have identified five priorities for future research.
Further defining what ‘care home medicine’ should look like in the UK
This review has identified no research that has systematically mapped what GPs do in care homes. Some of the work described (around minimisation of polypharmacy or end-of-life care planning) is arguably ‘core’ primary care for a population that is older, affected by frailty and multiple long-term conditions and many of whom are approaching the end of life. Nonetheless, GP involvement initiatives that developed these core functions needed to be carefully negotiated because of competing demands on doctors’ expertise and time. Good care of older people in the care home setting is likely to be multidisciplinary and there is no expectation that it should be provided by GPs in its entirety. However, in our interviews and in the reviewed literature,61,65–95,101 we encountered time and time again evidence that issues commonly encountered in clinical practice within care homes (e.g. the need for regular review of antipsychotic prescribing) required for many GPs to undergo specialist clinical training. As mentioned at the outset, other countries have specialist training programmes for doctors who support settings similar to care homes. There are now, across Europe, specifications of what might comprise a set of minimum standards for care home medicine, although these exist as an outline only. However, in the UK, care home medicine remains underspecified and something that GPs must juggle alongside their other, manifold, roles. Future research should consider what a set of core competencies for care home medicine in the UK should look like and how doctors, whether from general practice or from other disciplines, can incorporate these into established or new ways of working.
Better understanding what effective multidisciplinary working looks like in care homes
Regardless of these debates about care home medicine, the evidence reported here adds to what we already know from our previous work about the emergence of a community-based MDT that supports care homes. The parameters of this remain ill-defined and it may be that some of the uncertainty about the role of GPs reflects wider uncertainty about, and variability in, the professional groupings that support care homes and how these interact with each other. In the PEACH study,12 we described how comprehensive geriatric assessment could be reframed to describe a model of multidisciplinary working that could meet the needs of care home residents, but then went on to describe how this model landed poorly with community-based teams that struggled to reconcile it with existing ways of working. This realist review has shown that GPs are part of this MDT, interdigitating with other team members, such as pharmacists or mental health teams, to deliver clinical care. Future research needs to further, and better, describe what effective multidisciplinary working looks like in this setting, and to find a way to frame this such that it can be consistently adopted across health-care delivery to care homes.
How to enable leadership by care home nurses and care staff, taking account of organisational and cultural barriers
We specifically considered the role of GPs in this project because previous research4,9–12 has shown it to be important. In our discussion, we drew contrast between the underdeveloped literature on medical leadership for the sector and the much more substantial body of work around nursing leadership. However, within this, the role of care home-employed carers and nurses as leaders remains underdeveloped. The challenges of negotiated working across the health and social care interface are well described and have tended to disenfranchise nurses working in social care. Efforts to develop core competencies for care home nurses and to move towards formal recognition of expertise in care home nursing and leadership may go some way to improve this. However, if the potential of care home nurses and carers to lead change in the sector is to be harnessed, then the longstanding organisational and cultural boundaries to relational working across the health and social care, and public and private, interfaces will need to be taken into account. Future research should explore how these can be consistently taken account of to deliver more efficient and effective integrated working.
How to frame quality improvement in a way that is useful for general practitioners and to build quality improvement infrastructure that will work across the interface of health and social care
The issues of change leadership and of QI expertise came up at multiple points during this review. There was a sense from interviewees that many GPs did not hold such expertise, nor were they inclined to prioritise it against competing demands, many of which drew on skills and competencies that they already held in abundance. Which parts of QI are core to the GP role, and which parts they need when working with care homes, may to an extent be context dependent (i.e. GPs will need different parts of the skillset at different times). Further research is required to work out how to deliver QI competencies in a modular way that will enable GPs to access the components most relevant to them and when they need them. In addition, it remains unclear how to provide QI infrastructure in the community, which straddles the boundary between health and social care. Future research should consider this.
Paying more attention to describing the role that general practitioners play in quality improvement initiatives
There is a paucity of research on how and why GPs get involved in QI in care homes as work extra to their core responsibilities. It may be that GPs have not been involved much, that initiatives involving them are under-reported, or that their involvement is taken for granted or overlooked. It is clear that with the EHCH programme, and with other health-care initiatives necessary to help the care homes sector find its feet again after the COVID-19 pandemic, there will be plenty of opportunities to study the role that GPs play in supporting improvement in care homes. It could be that the findings presented here are more driven by absence of evidence than evidence of absence. Regardless, the programme theories established here are an important starting point and can be tested and refined through data from ongoing and future initiatives. Specific research will need to be undertaken to capture the specific roles that GPs play and to consider these against a theoretical framework of the sort presented here. The potential to overlook the role played by GPs is writ large in this. Future research into improvement in the care home sector should explicitly explore what it is that GPs do when new practice is developed in care homes.
Acknowledgements
We would like to thank information scientists Deirdre Andre and Sally Dalton, University of Leeds (Leeds, UK), who constructed search strategies and conducted searches of academic databases.
We would like to thank all interview participants and members of the Context Expert Group for their time and valuable input.
Contributions of authors
Neil H Chadborn (https://orcid.org/0000-0003-1368-7983) (Research Fellow, University of Nottingham) contributed to protocol development, led scoping searches, conducted interviews, contributed to literature search design, conducted screening, conducted data extraction alongside Reena Devi, led theory development, co-ordinated the Context Expert Group and drafted the report.
Reena Devi (https://orcid.org/0000-0003-2834-8597) (Research Fellow, University of Leeds) co-led research proposal development; contributed to scoping searches, literature search design and screening; conducted data extraction alongside Neil H Chadborn; contributed to theory development; and drafted the report.
Christopher Williams (https://orcid.org/0000-0001-6036-5157) (GP, Lecturer, University of Leicester) contributed to research proposal development, scoping searches and theory development, and drafted the report.
Kathleen Sartain (https://orcid.org/0000-0002-5080-7190) (PPI lead, PPI group, University of Nottingham) contributed to research proposal development, scoping searches and theory development, and drafted the report.
Claire Goodman (https://orcid.org/0000-0002-8938-4893) (Professor of Health Care Research, University of Hertfordshire) contributed to research proposal development, scoping searches and theory development, and drafted the report.
Adam L Gordon (https://orcid.org/0000-0003-1676-9853) (Professor in Medicine of Older People, University of Nottingham) was principal investigator, co-led research proposal development, contributed to scoping searches and theory development, and drafted the report.
Data-sharing statement
All data are available for sharing. Please contact corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Gordon AL, Devi R, Williams C, Goodman C, Sartain K, Chadborn NH. Protocol for a realist review of General Practitioners’ Role in Advancing Practice in Care Homes (GRAPE study). BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2019-036221.
- Gordon AL, Franklin M, Bradshaw L, Logan P, Elliott R, Gladman JR. Health status of UK care home residents: a cohort study. Age Ageing 2014;43:97-103. https://doi.org/10.1093/ageing/aft077.
- Gordon AL. What is the case for care home medicine? The geriatrician’s perspective. J R Coll Physicians Edinb 2015;45. https://doi.org/10.4997/JRCPE.2015.213.
- Iliffe S, Davies SL, Gordon AL, Schneider J, Dening T, Bowman C, et al. Provision of NHS generalist and specialist services to care homes in England: review of surveys. Prim Health Care Res Dev 2016;17:122-37. https://doi.org/10.1017/S1463423615000250.
- Wolters A, Santos F, Lloyd T, Lilburne C, Steventon A. Emergency Admissions to Hospital From Care Homes: How Often and What For?. London: The Health Foundation; 2019.
- British Medical Association . Government Needs to Address Problems Facing Care Home Services, Warn GP Leaders 2016.
- Donald IP, Gladman J, Conroy S, Vernon M, Kendrick E, Burns E. Care home medicine in the UK – in from the cold. Age Ageing 2008;37:618-20. https://doi.org/10.1093/ageing/afn207.
- Goodman C, Davies SL, Gordon AL, Meyer J, Dening T, Gladman JR, et al. Relationships, expertise, incentives, and governance: supporting care home residents’ access to health care. An interview study from England. J Am Med Dir Assoc 2015;16:427-32. https://doi.org/10.1016/j.jamda.2015.01.072.
- Goodman C, Davies S, Gordon A, Dening T, Gage H, Meyer J, et al. Optimal NHS service delivery to care homes: a realist evaluation of the features and mechanisms that support effective working for the continuing care of older people in residential settings. Health Serv Deliv Res 2017;5. https://doi.org/10.3310/hsdr05290.
- Gordon AL, Goodman C, Davies SL, Dening T, Gage H, Meyer J, et al. Optimal healthcare delivery to care homes in the UK: a realist evaluation of what supports effective working to improve healthcare outcomes. Age Ageing 2018;47:595-603. https://doi.org/10.1093/ageing/afx195.
- Goodman C, Dening T, Gordon AL, Davies SL, Meyer J, Martin FC, et al. Effective health care for older people living and dying in care homes: a realist review. BMC Health Serv Res 2016;16. https://doi.org/10.1186/s12913-016-1493-4.
- Devi R, Meyer J, Banerjee J, Goodman C, Gladman JRF, Dening T, et al. Quality improvement collaborative aiming for Proactive HEAlthcare of Older People in Care Homes (PEACH): a realist evaluation protocol. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2018-023287.
- Dimant J. Roles and responsibilities of attending physicians in skilled nursing facilities. J Am Med Dir Assoc 2003;4:231-43. https://doi.org/10.1097/01.JAM.0000075915.15039.B1.
- White HK, Buhr G, McConnell E, Sullivan RJ, Twersky J, Colon-Emeric C, et al. An advanced course in long term care for geriatric medicine fellows. J Am Med Dir Assoc 2013;14:499-506. https://doi.org/10.1016/j.jamda.2013.02.012.
- Koopmans RT, Lavrijsen JC, Hoek JF, Went PB, Schols JM. Dutch elderly care physician: a new generation of nursing home physician specialists. J Am Geriatr Soc 2010;58:1807-9. https://doi.org/10.1111/j.1532-5415.2010.03043.x.
- NHS England . New Care Models: The Framework For Enhanced Health in Care Homes 2016.
- NHS England . NHS Long Term Plan 2019.
- Lloyd T, Conti S, Santos F, Steventon A. Effect on secondary care of providing enhanced support to residential and nursing home residents: a subgroup analysis of a retrospective matched cohort study. BMJ Qual Saf 2019;28:534-46. https://doi.org/10.1136/bmjqs-2018-009130.
- NHS England and Improvement . COVID-19 Response: Identifying a Clinical Lead For All Care Homes 2020.
- Pulse . Care Home ‘Clinical Leads’ Will Not Be Held ‘Medically Responsible’ For Residents 2020. www.pulsetoday.co.uk/news/uncategorised/care-home-clinical-leads-will-not-be-held-medically-responsible-for-residents/ (accessed 25 August 2021).
- Robbins I, Gordon A, Dyas J, Logan P, Gladman J. Explaining the barriers to and tensions in delivering effective healthcare in UK care homes: a qualitative study. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-003178.
- Institute of Medicine . Crossing the Quality Chasm: A New Health System For the 21st Century 2001.
- Wilberforce M, Challis D, Davies L, Kelly MP, Roberts C, Loynes N. Person-centredness in the care of older adults: a systematic review of questionnaire-based scales and their measurement properties. BMC Geriatr 2016;16. https://doi.org/10.1186/s12877-016-0229-y.
- Nolan M, Davies S, Brown J. Transitions in care homes: towards relationship-centred care using the ‘Senses Framework’. Qual Ageing Older Adult 2006;7. https://doi.org/10.1108/14717794200600015.
- Corazzini KN, Anderson RA, Bowers BJ, Chu CH, Edvardsson D, Fagertun A, et al. Toward common data elements for international research in long-term care homes: advancing person-centered care. J Am Med Dir Assoc 2019;20:598-603. https://doi.org/10.1016/j.jamda.2019.01.123.
- Care Quality Commission . Guidance for Providers 2020. www.cqc.org.uk/guidance-providers (accessed 11 January 2021).
- Department of Health and Social Care . Quality Matters Summary Action Plan: Second Edition 2019. www.gov.uk/government/publications/adult-social-care-quality-matters-action-plan-for-year-2/quality-matters-summary-action-plan-second-edition (accessed 19 May 2020).
- Langley GL, Moen R, Nolan KM, Nolan TW, Norman CL, Lloyd P. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. San Francisco, CA: Jossey-Bass Publishers; 2009.
- Marshall M, de Silva D, Cruickshank L, Shand J, Wei L, Anderson J. What we know about designing an effective improvement intervention (but too often fail to put into practice). BMJ Qual Saf 2017;26:578-82. https://doi.org/10.1136/bmjqs-2016-006143.
- Devi R, Martin G, Banerjee J, Butler L, Pattison T, Cruickshank L, et al. Improving the quality of care in care homes using the quality improvement collaborative approach: lessons learnt from six projects conducted in the UK and the Netherlands. Int J Environ Res Public Health 2020;17. https://doi.org/10.3390/ijerph17207601.
- Pawson R. The Science of Evaluation: A Realist Manifesto/Ray Pawson. London: Sage Publications Ltd; 2013.
- Dalkin SM, Greenhalgh J, Jones D, Cunningham B, Lhussier M. What’s in a mechanism? Development of a key concept in realist evaluation. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0237-x.
- Lacouture A, Breton E, Guichard A, Ridde V. The concept of mechanism from a realist approach: a scoping review to facilitate its operationalization in public health program evaluation. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0345-7.
- Gordon AL, Devi R, Williams C, Goodman C, Sartain K, Chadborn NH. Engaging General Practitioners in Service Development and Quality Improvement for Healthcare in Care Homes: A Realist Synthesis of the Published Evidence. York: University of York; 2019.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11. https://doi.org/10.1186/1741-7015-11-21.
- Wong G, Westhorp G, Manzano A, Greenhalgh J, Jagosh J, Greenhalgh T. RAMESES II reporting standards for realist evaluations. BMC Med 2016;14. https://doi.org/10.1186/s12916-016-0643-1.
- Devi R, Chadborn NH, Meyer J, Banerjee J, Goodman C, Dening T, et al. How quality improvement collaboratives work to improve healthcare in care homes: a realist evaluation. Age Ageing 2021;50:1371-81. https://doi.org/10.1093/ageing/afab007.
- Balbes J. The Practice of GPs Charging Retainers to Care Homes. London: Care England; 2014.
- Social Care Institute for Excellence . GP Services for Older People: A Guide for Care Home Managers 2013. www.scie.org.uk/publications/guides/guide52/entitlements-and-requirements/access.asp (accessed 2 January 2021).
- Pulse Today . Care Homes ‘to Stop Paying Retainer Payments to GP Practices’ 2015. www.pulsetoday.co.uk/news/clinical-areas/prescribing/care-homes-to-stop-paying-retainer-payments-to-gp-practices/ (accessed 2 January 2021).
- Riley AJ, Harding G, Meads G, Underwood MR, Carter YH. An evaluation of personal medical services: the times they are a changin’. J Interprof Care 2003;17:127-39. https://doi.org/10.1080/1356182031000081731.
- Sheaff R, Lloyd-Kendall A. Principal-agent relationships in general practice: the first wave of English Personal Medical Services pilot contracts. J Health Serv Res Policy 2000;5:156-63. https://doi.org/10.1177/135581960000500306.
- Royal College of General Practitioners . The Curriculum Topic Guides 2019.
- Jacobs S. Addressing the problems associated with general practitioners’ workload in nursing and residential homes: findings from a qualitative study. Br J Gen Pract 2003;53:113-19.
- Corroon-Sweeney E, Murphy C, Collins DR. Caring for nursing home patients – a primary care perspective. Ir Med J 2009;102:317-20.
- Gleeson LE, Jennings S, Gavin R, McConaghy D, Collins DR. Primary care in nursing homes revisited: survey of the experiences of primary care physicians. Ir Med J 2014;107:234-6.
- Barker RO, Craig D, Spiers G, Kunonga P, Hanratty B. Who should deliver primary care in long-term care facilities to optimize resident outcomes? A systematic review. J Am Med Dir Assoc 2018;19:1069-79. https://doi.org/10.1016/j.jamda.2018.07.006.
- Chadborn NH, Devi R, Hinsliff-Smith K, Banerjee J, Gordon AL. Quality improvement in long-term care settings: a scoping review of effective strategies used in care homes. Eur Geriatr Med 2021;12:17-26. https://doi.org/10.1007/s41999-020-00389-w.
- Crotty M, Halbert J, Rowett D, Giles L, Birks R, Williams H, et al. An outreach geriatric medication advisory service in residential aged care: a randomised controlled trial of case conferencing. Age Ageing 2004;33:612-17. https://doi.org/10.1093/ageing/afh213.
- Kezirian AC, McGregor MJ, Stead U, Sakaluk T, Spring B, Turgeon S, et al. Advance care planning in the nursing home setting: a practice improvement evaluation. J Soc Work End Life Palliat Care 2018;14:328-45. https://doi.org/10.1080/15524256.2018.1547673.
- National Association of Primary Care, Association of Directors of Adult Social Services . Primary Care Home and Social Care: Working Together 2018.
- National Association of Primary Care . Primary Care Home 2020 2019.
- Sherlaw-Johnson C, Crump H, Curry N, Paddison C, Meaker R. Transforming Health Care in Nursing Homes. An Evaluation of a Dedicated Primary Care Service in Outer East London. London: Nuffield Trust; 2018.
- Scottish Government . General Medical Services Contract in Scotland 2017.
- Jokanovic N, Jamsen KM, Tan ECK, Dooley MJ, Kirkpatrick CM, Bell JS. Prevalence and variability in medications contributing to polypharmacy in long-term care facilities. Drugs Real World Outcomes 2017;4:235-45. https://doi.org/10.1007/s40801-017-0121-x.
- Patterson SM, Hughes CM, Crealey G, Cardwell C, Lapane KL. An evaluation of an adapted U.S. model of pharmaceutical care to improve psychoactive prescribing for nursing home residents in Northern Ireland (Fleetwood Northern Ireland Study). J Am Geriatr Soc 2010;58:44-53. https://doi.org/10.1111/j.1532-5415.2009.02617.x.
- Molloy DW, Guyatt GH, Russo R, Goeree R, O’Brien BJ, Bédard M, et al. Systematic implementation of an advance directive program in nursing homes: a randomized controlled trial. JAMA 2000;283:1437-44. https://doi.org/10.1001/jama.283.11.1437.
- Garden G, Green S, Pieniak S, Gladman J. The Bromhead Care Home Service: the impact of a service for care home residents with dementia on hospital admission and dying in preferred place of care. Clin Med 2016;16:114-18. https://doi.org/10.7861/clinmedicine.16-2-114.
- Sharp T, Malyon A, Barclay S. GPs’ perceptions of advance care planning with frail and older people: a qualitative study. Br J Gen Pract 2018;68:e44-53. https://doi.org/10.3399/bjgp17X694145.
- Brighton LJ, Selman LE, Gough N, Nadicksbernd JJ, Bristowe K, Millington-Sanders C, et al. ‘Difficult Conversations’: evaluation of multiprofessional training. BMJ Support Palliat Care 2018;8:45-8. https://doi.org/10.1136/bmjspcare-2017-001447.
- Badger F, Plumridge G, Hewison A, Shaw KL, Thomas K, Clifford C. An evaluation of the impact of the Gold Standards Framework on collaboration in end-of-life care in nursing homes. A qualitative and quantitative evaluation. Int J Nurs Stud 2012;49:586-95. https://doi.org/10.1016/j.ijnurstu.2011.10.021.
- Royal College of General Practitioners (RCGP) . RCGP Framework to Support the Governance of General Practitioners With Extended Roles 2020.
- Gérvas J, Starfield B, Violán C, Minué S. GPs with special interests: unanswered questions. Br J Gen Pract 2007;57:912-17. https://doi.org/10.3399/096016407782317865.
- Fisher RF, Croxson CH, Ashdown HF, Hobbs FR. GP views on strategies to cope with increasing workload: a qualitative interview study. Br J Gen Pract 2017;67:e148-156. https://doi.org/10.3399/bjgp17X688861.
- Elvey R, Bailey S, Checkland K, McBride A, Parkin S, Rothwell K, et al. Implementing new care models: learning from the Greater Manchester demonstrator pilot experience. BMC Fam Pract 2018;19. https://doi.org/10.1186/s12875-018-0773-y.
- Iliffe S, Davies N, Manthorpe J, Crome P, Ahmedzai SH, Vernooij-Dassen M, et al. Improving palliative care in selected settings in England using quality indicators: a realist evaluation. BMC Palliat Care 2016;15. https://doi.org/10.1186/s12904-016-0144-1.
- Amador S, Goodman C, Mathie E, Nicholson C. Evaluation of an organisational intervention to promote integrated working between health services and care homes in the delivery of end-of-life care for people with dementia: understanding the change process using a social identity approach. Int J Integr Care 2016;16. https://doi.org/10.5334/ijic.2426.
- Evans G. Factors influencing emergency hospital admissions from nursing and residential homes: positive results from a practice-based audit. J Eval Clin Pract 2011;17:1045-9. https://doi.org/10.1111/j.1365-2753.2010.01471.x.
- Stocker R, Bamford C, Brittain K, Duncan R, Moffatt S, Robinson L, et al. Care home services at the vanguard: a qualitative study exploring stakeholder views on the development and evaluation of novel, integrated approaches to enhancing healthcare in care homes. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-017419.
- Szczepura A, Wild D, Khan AJ, Owen DW, Palmer T, Muhammad T, et al. Antipsychotic prescribing in care homes before and after launch of a national dementia strategy: an observational study in English institutions over a 4-year period. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-009882.
- Patterson SM, Hughes CM, Cardwell C, Lapane KL, Murray AM, Crealey GE. A cluster randomized controlled trial of an adapted U.S. model of pharmaceutical care for nursing home residents in Northern Ireland (Fleetwood Northern Ireland study): a cost-effectiveness analysis. J Am Geriatr Soc 2011;59:586-93. https://doi.org/10.1111/j.1532-5415.2011.03354.x.
- Hughes CM, Patterson S, Schweizer A. Information is care: the need for data to assess the quality of care in UK nursing and residential homes. Expert Opin Drug Saf 2003;2:523-7. https://doi.org/10.1517/14740338.2.6.523.
- Ballard C, Powell I, James I, Reichelt K, Myint P, Potkins D, et al. Can psychiatric liaison reduce neuroleptic use and reduce health service utilization for dementia patients residing in care facilities. Int J Geriatr Psychiatry 2002;17:140-5. https://doi.org/10.1002/gps.543.
- Khunti K, Kinsella B. Effect of systematic review of medication by general practitioner on drug consumption among nursing-home residents. Age Ageing 2000;29:451-3. https://doi.org/10.1093/ageing/29.5.451.
- Ballard C, Orrell M, YongZhong S, Moniz-Cook E, Stafford J, Whittaker R, et al. Impact of antipsychotic review and nonpharmacological intervention on antipsychotic use, neuropsychiatric symptoms, and mortality in people with dementia living in nursing homes: a factorial cluster-randomized controlled trial by the Well-Being and Health for People With Dementia (WHELD) Program. Am J Psychiatry 2016;173:252-62. https://doi.org/10.1176/appi.ajp.2015.15010130.
- Ballard C, Corbett A, Orrell M, Williams G, Moniz-Cook E, Romeo R, et al. Impact of person-centred care training and person-centred activities on quality of life, agitation, and antipsychotic use in people with dementia living in nursing homes: a cluster-randomised controlled trial. PLOS Med 2018;15. https://doi.org/10.1371/journal.pmed.1002500.
- Ballard C, Orrell M, Moniz-Cook M, Woods R, Whitaker R, Corbett A, et al. Improving mental health and reducing antipsychotic use in people with dementia in care homes: the WHELD research programme including two RCTs. Programme Grants Appl Res 2020;8. https://doi.org/10.3310/pgfar08060.
- The Health Foundation . Medication Review Project: An Interview With Project Lead, Dr Wasim Baqir n.d. www.health.org.uk/article/medication-review-project-an-interview-with-project-lead-dr-wasim-baqir (accessed 25 August 2021).
- Baqir W. Improving Medicine Prescribing in Care Homes. London: The Health Foundation; 2013.
- Baqir W. Multidisciplinary Review of Medication in Nursing Homes: A Clinico-Ethical Framework. London: The Health Foundation; 2018.
- Northumbria Healthcare NHS Foundation Trust . Shine 2012 Final Report. A Clinico-Ethical Framework For Multidisciplinary Review of Medication in Nursing Homes 2014. www.health.org.uk/sites/default/files/Shine2012_NorthumbriaHealthcareNHSFoundationTrust_report.pdf (accessed 25 August 2021).
- Baqir W, Barrett S, Desai N, Copeland R, Hughs J. A clinico-ethical framework for multidisciplinary review of medication in nursing homes. BMJ Qual Improv Rep 2014;3. https://doi.org/10.1136/bmjquality.u203261.w2538.
- Baqir W, Barrett S, Hughes J, Desai N, Riddle J, Laverty A, et al. A clinico-ethical framework for multidisciplinary review of medication in nursing homes: a Health Foundation Shine project. Int J Pharm Pract 2013;21. https://doi.org/10.1111/ijpp.12064.
- Baqir W, Hughes J, Jones T, Barrett S, Desai N, Copeland R, et al. Impact of medication review, within a shared decision-making framework, on deprescribing in people living in care homes. Eur J Hosp Pharm 2017;24:30-3. https://doi.org/10.1136/ejhpharm-2016-000900.
- Zermansky AG, Alldred DP, Petty DR, Raynor DK, Freemantle N, Eastaugh J, et al. Clinical medication review by a pharmacist of elderly people living in care homes – randomised controlled trial. Age Ageing 2006;35:586-91. https://doi.org/10.1093/ageing/afl075.
- Bond C, Lane K, Poland F, Maskrey V, Blyth A, Desborough J, et al. GP views on the potential role for pharmacist independent prescribers within care homes: Care Homes Independent Pharmacist Prescribing Study (CHIPPS): ‘There has to be something in it for me’. Int J Pharm Pract 2016;24. https://doi.org/10.1111/ijpp.12258.
- Inch J, Notman F, Bond CM, Alldred DP, Arthur A, Blyth A, et al. The Care Home Independent Prescribing Pharmacist Study (CHIPPS) – a non-randomised feasibility study of independent pharmacist prescribing in care homes. Pilot Feasibility Stud 2019;5. https://doi.org/10.1186/s40814-019-0465-y.
- Badger F, Clifford C, Hewison A, Thomas K. An evaluation of the implementation of a programme to improve end-of-life care in nursing homes. Palliat Med 2009;23:502-11. https://doi.org/10.1177/0269216309105893.
- Hall S, Goddard C, Stewart F, Higginson IJ. Implementing a quality improvement programme in palliative care in care homes: a qualitative study. BMC Geriatr 2011;11. https://doi.org/10.1186/1471-2318-11-31.
- Kinley J, Hockley J, Stone L, Dewey M, Hansford P, Stewart R, et al. The provision of care for residents dying in UK nursing care homes. Age Ageing 2014;43:375-9. https://doi.org/10.1093/ageing/aft158.
- Stewart K, Hargreaves C, Jasper R, Challis D, Tucker S, Wilberforce M. Provision and perceived quality of mental health services for older care home residents in England: a national survey. Int J Geriatr Psychiatry 2018;33:364-70. https://doi.org/10.1002/gps.4753.
- Madigan SM, Fleming P, Wright ME, Stevenson M, Macauley D. A cluster randomised controlled trial of a nutrition education intervention in the community. J Hum Nutr Diet 2014;27:12-20. https://doi.org/10.1111/jhn.12079.
- Sadler E, Porat T, Marshall I, Hoang U, Curcin V, Wolfe CDA, et al. Shaping innovations in long-term care for stroke survivors with multimorbidity through stakeholder engagement. PLOS ONE 2017;12. https://doi.org/10.1371/journal.pone.0177102.
- Shah SM, Carey IM, Harris T, Dewilde S, Cook DG. Quality of chronic disease care for older people in care homes and the community in a primary care pay for performance system: retrospective study. BMJ 2011;342. https://doi.org/10.1136/bmj.d912.
- Cox H, Puffer S, Morton V, Cooper C, Hodson J, Masud T, et al. Educating nursing home staff on fracture prevention: a cluster randomised trial. Age Ageing 2008;37:167-72. https://doi.org/10.1093/ageing/afm168.
- Kinley J, Stone L, Dewey M, Levy J, Stewart R, McCrone P, et al. The effect of using high facilitation when implementing the Gold Standards Framework in Care Homes programme: a cluster randomised controlled trial. Palliat Med 2014;28:1099-109. https://doi.org/10.1177/0269216314539785.
- Killick S, Pharaoh A, Randall F. Advance care planning in care homes. Palliat Med 2010;24:445-6. https://doi.org/10.1177/0269216310366748.
- Badger FJ, Shaw KL, Hewison A, Clifford C, Thomas K. Gold Standards Framework in Care Homes and advance care planning. Palliat Med 2010;24. https://doi.org/10.1177/0269216310366606.
- National Institute for Health and Care Excellence . Medicines Management in Care Homes. Quality Standard [QS85] 2015. www.nice.org.uk/guidance/qs85 (accessed 24 August 2021).
- Coleman A, Croke S, Checkland K. Improving care in care homes: what can primary care networks learn from the vanguards?. J Integr Care 2020;29:85-96. https://doi.org/10.1108/JICA-06-2020-0037.
- Ballard C, Orrell M, Sun Y, Moniz-Cook E, Stafford J, Whitaker R, et al. Impact of antipsychotic review and non-pharmacological intervention on health-related quality of life in people with dementia living in care homes: WHELD – a factorial cluster randomised controlled trial. Int J Geriatr Psychiatry 2017;32:1094-103. https://doi.org/10.1002/gps.4572.
- National Institute for Health and Care Excellence (NICE) . Antipsychotics in People Living With Dementia 2015.
- Ballard C, Corbett A. Reducing psychotropic drug use in people with dementia living in nursing homes. Int Psychogeriatr 2020;32:291-4. https://doi.org/10.1017/S1041610219001455.
- Chadborn NH, Goodman C, Zubair M, Sousa L, Gladman JRF, Dening T, et al. Role of comprehensive geriatric assessment in healthcare of older people in UK care homes: realist review. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-026921.
- Bunn F, Goodman C, Corazzini K, Sharpe R, Handley M, Lynch J, et al. Setting priorities to inform assessment of care homes’ readiness to participate in healthcare innovation: a systematic mapping review and consensus process. Int J Environ Res Public Health 2020;17. https://doi.org/10.3390/ijerph17030987.
- Keenan J, Poland F, Manthorpe J, Hart C, Moniz-Cook E. Implementing e-learning and e-tools for care home staff supporting residents with dementia and challenging behaviour: a process evaluation of the ResCare study using normalisation process theory. Dementia 2020;19:1604-20. https://doi.org/10.1177/1471301218803195.
- Owen T, Meyer J. My Home Life: Promoting Quality of Life in Care Homes. York: Joseph Rowntree Foundation; 2012.
- Hanratty B, Burton JK, Goodman C, Gordon AL, Spilsbury K. Covid-19 and lack of linked datasets for care homes: the pandemic has shed harsh light on the need for a live minimum dataset. BMJ 2020;369. https://doi.org/10.1136/bmj.m2463.
- Burton JK, Goodman C, Guthrie B, Gordon AL, Hanratty B, Quinn TJ. Closing the UK care home data gap – methodological challenges and solutions. Int J Popul Data Sci 2021;5. https://doi.org/10.23889/ijpds.v5i4.1391.
- Darby J, Horne J, Lewin J, Crocker C, Coates E, McEwan K, et al. Benchmarking the Prevalence of Care Problems in UK Care Homes Using the LPZ-I: A Feasibility Study 2017. https://nottingham-repository.worktribe.com/output/853694/benchmarking-the-prevalence-of-care-problems-in-uk-care-homes-using-the-lpz-i-a-feasibility-study (accessed 25 August 2021).
- Musa MK, Akdur G, Hanratty B, Kelly S, Gordon A, Peryer G, et al. Uptake and use of a minimum data set (MDS) for older people living and dying in care homes in England: a realist review protocol. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2020-040397.
- The Health Foundation, Northumbria Healthcare NHS Foundation Trust . Shine – Multidisciplinary Review of Medication in Nursing Homes 2018. www.sps.nhs.uk/articles/shine-multidisciplinary-review-of-medication-in-nursing-homes-christine-randall/ (accessed 25 August 2021).
Appendix 1 Theory-gleaning interview schedule
-
Describe the variety of general practice and care home structures.
-
Can you describe the GP–care home ‘link’ [i.e. the working relationship and communication between GP and care home (manager)]?
-
Is it helpful to characterise or categorise different care homes or different types of partnership (GP/care home)?
-
-
How do GPs work with teams outside their jurisdiction? For example, out-of-hours care?
-
Is it similar to the working relationship and communication with the care home, but this time with another team delivering care to the GP’s patients?
-
-
How do GPs support ‘holistic care’ when aspects may be outside the medical remit of the GP?
-
Within person-centred care or multidisciplinary care, are there aspects that the GP may leave to other practitioners or providers (e.g. social or occupational care) or does the GP take an interest in the oversight of all aspects of care?
-
-
Please describe medical teaching or training.
-
How are trainee GPs supported in learning how to deliver high-quality care for care home residents?
-
Are there particular aspects where additional training is available or recommended for GPs?
-
-
Please describe cross-cutting resources and capacity.
-
Is lack of resource a constraint in the above topics?
-
-
What outcomes are expected or assessed?
-
Well-being, quality of life?
-
Service use, such as hospital admissions?
-
-
What information technology systems are used?
-
Are these integral to projects or additional ‘extras’?
-
-
Is there anything that I’ve missed or do you have any additional comments?
Appendix 2 Search strategies
Primary search
Ovid® (Wolters Kluwer, Alphen aan den Rijn, the Netherlands) MEDLINE® and Epub Ahead of Print, MEDLINE In-Process & Other Non-Indexed Citations and Daily
Date searched: April 2020.
Date range searched: 1946 to 18 October 2019 and updated to include up to April 2020.
Search strategy
-
Nursing home/ (8490)
-
nursing home*.tw. (28,672)
-
homes for the aged/ (13,479)
-
care home*.tw. (3640)
-
or/1-4 [care homes] (47,826)
-
Long-Term Care/ (25,324)
-
Residential facilities/ (5332)
-
((long-term or longterm or retir*) adj5 (facility or facilities or institution* or resident*)).tw. (10,445)
-
or/6-8 [long term care or residential facility terms] (36,831)
-
exp aged/ (3,005,375)
-
Geriatrics/ (29,509)
-
Geriatric Nursing/ (13,480)
-
health services for the aged/ (17,340)
-
((older or elder*) adj (person or people or adult* or patient* or inpatient* or resident* or men or women)).tw. (237,237)
-
(geriatric* or elderly or seniors or senior citizen* or pensioner* or oldest old or very old).tw. (275,140)
-
or/10-15 [old people] (3,140,511)
-
9 and 16 [long term or residential facilities for older people] (17,408)
-
5 or 17 [all care home or long term care or residential facilities for older people] (60,893)
-
(general adj (practice* or medical practitioner* or practitioner*)).ti. (33,662)
-
(general adj (practice* or medical practitioner* or practitioner*)).ab./freq = 2 (18,266)
-
(family adj (medicine or practice* or doctor* or physician* or practitioner*)).ti. (14,762)
-
(family adj (medicine or practice* or doctor* or physician* or practitioner*)).ab./freq = 2 (9570)
-
Family Practice/ (64,754)
-
physicians, Family/ (16,156)
-
Physicians, Primary Care/ (3134)
-
GP.ti. (4505)
-
GP.ab./freq = 2 (22,927)
-
(elderly adj2 physician*).ti. (52)
-
(elderly adj2 physician*).ab./freq = 2 (20)
-
Physician Executives/ (4198)
-
medical director*.ti. (706)
-
medical director*.ab./freq = 2 (409)
-
(primary adj1 care doctor*).ti. (195)
-
(primary adj1 care doctor*).ab./freq = 2 (143)
-
or/19-24 [gps or care home doctors] (102,790)
-
exp Great Britain/ (357,312)
-
(national health service* or nhs*).ti,ab,in. (179,827)
-
(english not ((published or publication* or translat* or written or language* or speak* or literature or citation*) adj5 english)).ti,ab. (92,722)
-
(gb or “g.b.” or britain* or (british* not “british columbia”) or uk or “u.k.” or united kingdom* or (england* not “new england”) or northern ireland* or northern irish* or scotland* or scottish* or ((wales or “south wales”) not “new south wales”) or welsh*).ti,ab,jw,in. (1,973,824)
-
(bath or “bath’s” or ((birmingham not alabama*) or (“birmingham’s” not alabama*) or bradford or “bradford’s” or brighton or “brighton’s” or bristol or “bristol’s” or carlisle* or “carlisle’s” or (cambridge not (massachusetts* or boston* or harvard*)) or (“cambridge’s” not (massachusetts* or boston* or harvard*)) or (canterbury not zealand*) or (“canterbury’s” not zealand*) or chelmsford or “chelmsford’s” or chester or “chester’s” or chichester or “chichester’s” or coventry or “coventry’s” or derby or “derby’s” or (durham not (carolina* or nc)) or (“durham’s” not (carolina* or nc)) or ely or “ely’s” or exeter or “exeter’s” or gloucester or “gloucester’s” or hereford or “hereford’s” or hull or “hull’s” or lancaster or “lancaster’s” or leeds* or leicester or “leicester’s” or (lincoln not nebraska*) or (“lincoln’s” not nebraska*) or (liverpool not (new south wales* or nsw)) or (“liverpool’s” not (new south wales* or nsw)) or ((london not (ontario* or ont or toronto*)) or (“london’s” not (ontario* or ont or toronto*)) or manchester or “manchester’s” or (newcastle not (new south wales* or nsw)) or (“newcastle’s” not (new south wales* or nsw)) or norwich or “norwich’s” or nottingham or “nottingham’s” or oxford or “oxford’s” or peterborough or “peterborough’s” or plymouth or “plymouth’s” or portsmouth or “portsmouth’s” or preston or “preston’s” or ripon or “ripon’s” or salford or “salford’s” or salisbury or “salisbury’s” or sheffield or “sheffield’s” or southampton or “southampton’s” or st albans or stoke or “stoke’s” or sunderland or “sunderland’s” or truro or “truro’s” or wakefield or “wakefield’s” or wells or westminster or “westminster’s” or winchester or “winchester’s” or wolverhampton or “wolverhampton’s” or (worcester not (massachusetts* or boston* or harvard*)) or (“worcester’s” not (massachusetts* or boston* or harvard*)) or (york not (“new york*” or ny or ontario* or ont or toronto*)) or (“york’s” not (“new york*” or ny or ontario* or ont or toronto*))))).ti,ab,in. (1,327,221)
-
(bangor or “bangor’s” or cardiff or “cardiff’s” or newport or “newport’s” or st asaph or “st asaph’s” or st davids or swansea or “swansea’s”).ti,ab,in. (51,805)
-
(aberdeen or “aberdeen’s” or dundee or “dundee’s” or edinburgh or “edinburgh’s” or glasgow or “glasgow’s” or inverness or (perth not australia*) or (“perth’s” not australia*) or stirling or “stirling’s”).ti,ab,in. (197,789)
-
(armagh or “armagh’s” or belfast or “belfast’s” or lisburn or “lisburn’s” or londonderry or “londonderry’s” or derry or “derry’s” or newry or “newry’s”).ti,ab,in. (24,417)
-
or/36-43 (2,542,613)
-
(exp africa/or exp americas/or exp antarctic regions/or exp arctic regions/or exp asia/or exp australia/or exp oceania/) not (exp great britain/or europe/) (2,763,442)
-
44 not 45 [UK publications search filter] (2,403,187)
-
18 and 35 and 46 (201)
Secondary searches
Medication review
Ovid MEDLINE®
Date searched: April 2020.
Date range searched: 1996 to April week 3 2020.
Search strategy
-
(medication* adj2 review).tw. (1550)
-
(medication* management or medication* therapy management or medication* strateg*).tw. (3066)
-
“Drug Utilization Review”/ (3465)
-
Medication Therapy Management/ (2056)
-
(drug utili?ation adj2 (review* or evaluat*)).tw. (237)
-
((multi-drug* or multidrug*) adj2 (therapy or therapies or prescribing or treatment or regime?)).tw. (3142)
-
polypharm*.tw. (5788)
-
polypharmacy/ (4780)
-
(beer* adj1 criter*).tw. (503)
-
((appropriate or optim* or inappropriat* or suboptim* or sub-optim* or unnecessary or incorrect* or in-correct* or excessive or multiple or concurrent*) adj2 (medicine? or medication* or prescription* or drug*)).tw. (22,716)
-
((over adj1 prescript*) or (overprescrib* or overprescript*)).tw. (1033)
-
((under adj prescript*) or (underprescrib* or underprescript*)).tw. (326)
-
Inappropriate Prescribing/ (3134)
-
medication appropriateness index.tw. (103)
-
((prescribing or prescription*) adj2 pattern*).tw. (3478)
-
Drug Prescriptions/ (20,426)
-
exp Medication Errors/ (14,508)
-
(quality adj (prescribing or prescription* or medication*)).tw. (109)
-
(improv* adj (prescrib* or prescription* or pharmaco*)).tw. (2641)
-
case conferencing.tw. (55)
-
drug regimen review*.tw. (34)
-
pharmacy review.tw. (15)
-
Prescription Drugs/ (5789)
-
pharmacotherap*.tw. (26,202)
-
Pharmacists/ (12,465)
-
Potentially Inappropriate Medication List/ (432)
-
Medical Overuse/ (1469)
-
or/1-27 [medication review] (112,713)
-
Homes for the Aged/or “home* for the aged”.tw. (9412)
-
exp Nursing Homes/or nursing home*.tw. (30,294)
-
“care home*”.tw. (2765)
-
Long-Term Care/ (14,976)
-
((long-term or longterm or long-stay or longstay or retir*) adj5 (facilit* or institution* or setting* or resident*)).tw. (12,296)
-
Residential Facilities/ (2795)
-
or/29-34 [care homes] (53,906)
-
28 and 35 (2338)
-
limit 36 to yr = “2010 -Current” (1426)
End-of-life care
Ovid MEDLINE®
Date searched: April 2020.
Date range searched: 1996 to April week 2 2020.
Search strategy
-
end of life.tw. (18,018)
-
Terminal Care/ (19,827)
-
terminally ill.tw. (3536)
-
Terminally Ill/ (5067)
-
end stage.tw. (50,023)
-
dying.tw. (22,037)
-
palliat*.tw. (51,567)
-
Palliative Care/ (41,024)
-
terminal care.tw. (721)
-
Attitude to Death/ (10,421)
-
or/1-10 [End of life care] (152,986)
-
Homes for the Aged/or “home* for the aged”.tw. (9399)
-
exp Nursing Homes/or nursing home*.tw. (30,257)
-
“care home*”.tw. (2759)
-
Long-Term Care/ (14,957)
-
((long-term or longterm or long-stay or longstay or retir*) adj5 (facilit* or institution* or setting* or resident*)).tw. (12,271)
-
Residential Facilities/ (2791)
-
or/12-17 [care homes] (53,826)
-
11 and 18 (3071)
-
limit 19 to yr = “2010 -Current” (1744)
Appendix 3 Search results
| Database | Platform | Year searched from | Number of results |
|---|---|---|---|
| MEDLINE® and Epub Ahead of Print, MEDLINE In-Process & Other Non-Indexed Citations and Daily | Ovid | 1948 | 201 |
| CINAHL | EBSCOhost | 1982 | 437 |
| Total before deduplication | 638 | ||
| Total after deduplication | 586 | ||
| Set limit on year of publication from 2000 | 2000 | 431 | |
| Database | Platform | Year searched from | Number of results |
|---|---|---|---|
| MEDLINE® and Epub Ahead of Print, MEDLINE In-Process & Other Non-Indexed Citations and Daily | Ovid | 2010 | 1751 |
| EMBASE | Ovid | 2010 | 4228 |
| CINAHL | EBSCOhost | 2010 | 1749 |
| Web of Science (SCIE, SSCI, CPCI-S, CPCI-SSH) | Clarivate Analytics | 2010 | 1604 |
| PsycInfo | Ovid | 2010 | 350 |
| Scopus | Clarivate Analytics | 2010 | 1149 |
| Total before deduplication | 10,831 | ||
| Total after deduplication | 6287 | ||
| Articles with authors with UK addresses | 156 | ||
| Database | Platform | Year searched from | Number of results |
|---|---|---|---|
| MEDLINE | Ovid | 2010 | 1754 |
| EMBASE | Ovid | 2010 | 3529 |
| CINAHL | EBSCOhost | 2010 | 2675 |
| Web of Science | Clarivate Analytics | 2010 | 572 |
| PsycInfo | Ovid | 2010 | 849 |
| Scopus | Clarivate Analytics | 2010 | 872 |
| Total before deduplication | 10,251 | ||
| Total after deduplication | 5680 | ||
| Articles with authors with UK addresses | 101 | ||
Appendix 4 Data extraction fields
Extraction within Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) before importing into NVivo 12
-
Authors.
-
Year of publication.
-
Publication details.
-
Country: address of main authors.
-
Screening criteria: GP, care homes, improvement.
-
Contains information about intervention types: medication review, end-of-life care, GP special interests.
-
Intervention: description.
-
Improvement type: categorisation (e.g. QI Collaborative, plan–do–study–act).
-
Number of care homes recruited.
-
Number of residents covered (maybe ‘number of beds’).
-
Number of resident participants recruited.
-
Number of general practices.
-
Number of GPs covered (i.e. total number in all general practices).
-
Number of GP participants recruited.
-
Name of other professions involved in intervention.
-
Name other professions involved.
-
Number of nurse participants.
-
Number of manager participants.
-
Number of care home assistant participants.
-
Number of family carer participants.
-
Number of administrative staff participants.
-
Number of pharmacist participants.
-
Notes about the article quality, identification of bias.
-
Quotations or key points.
Appendix 5 Analysis of excerpts from references and quotations from interviews
| CMO | Description | Excerpt or quotation | Reference or interview |
|---|---|---|---|
| CMO 1 | Context: problem of inappropriate prescribing | Seventy percent of care home residents experience at least one medication error. In addition 50% of medicines are not taken as prescribed, with adverse drug reactions contributing to 17% of all hospital admissions | 112 |
| CMO 1 | Context: problem of inappropriate prescribing | . . . excess medicines (sometimes inappropriate), lack of structured review of medicines, communication issues: many residents were unaware of what treatment they are on, long medication rounds and timing of rounds not resident-centred | 84 |
| CMO 1 | Context: problem of inappropriate prescribing | Whilst there are clear guidelines for starting medicines; there is less guidance for stopping medicines. The issues can be summarised as: Prescribers face a number of ethical, legal and professional challenges when considering stopping medicines. Residents are usually not involved in decisions about medicines prescribed to them | 84 |
| CMO 1 | Context: problem of inappropriate prescribing | . . . in 6 weeks time when I have got the notes, have I got the time then to do the medication review properly. So, they are all potential areas of error. And then they go into hospital, and you know someone comes out of hospital there has been a medication change that hasn’t gone on a discharge summary. So, to me having the care home pharmacist who liaising with the home, liaises with the manager | Participant #21 |
| CMO 1 | Context: problem of inappropriate prescribing | . . . general practitioners do not review most care home patients’ medication | 85 |
| CMO 1 | Context: problem of inappropriate prescribing | Our pre-baseline annual review rate was 24%, which is lower than in our previous study in older people living in their own homes (44%). Three-quarters of this vulnerable group are not having their medication reviewed | 85 |
| CMO 1 | Context: complexities | . . . decisions are based on having conversations around context and I don’t know many pharmacists who are sighted on being like the Mental Capacity Act and how we should be making decisions based on a person’s wishes and preferences or who is the legal decision-maker authority is and then having a conversation | Participant #16 |
| CMO 1 | Context: complexities | . . . they are so thin on the ground, they haven’t got the capacity to go back into review. So actually, a GP will say, they are asking me to stop that but actually I don’t know why they’re on it, it may cause symptoms, they may be worse off of it, so actually I’m going to leave them on it. But so, unless the pharmacist is working at their highest level of their competency, then either they are unsafe or the workload falls back on primary care anyway | Participant #16 |
| CMO 1 | Context: complexities | De-prescribing is difficult with few tools, guidelines and little evidence to support practitioners | 84 |
| CMO 1 | Context: multidisciplinary work | . . . the approach they tested involved getting people together to discuss treatment and make decisions. Where possible, the group included the care home resident, a family member, a nurse from the care home, a GP and a pharmacist© The Health Foundation, 20212021© The Health Foundation | 78 |
| CMO 1 | Context: multidisciplinary work | Getting the right team together was important. The team included health professionals or managers from GP practices and care homes, experts in psychiatry, Age UK, and the executive management team© The Health Foundation, 20212021© The Health Foundation | 78 |
| CMO 1 | Context: multidisciplinary work | The medication reviews were conducted by clinical pharmacists, with the findings discussed by multidisciplinary teams which included care home nurses and GPs as well as patients, families and carers where this was possible© The Health Foundation, 20182018© The Health Foundation | 80 |
| CMO 1 | Context: multidisciplinary work | A pharmacist undertook detailed medication reviews using primary care records and the results were discussed at a multidisciplinary team (MDT) meeting involving the care home nurse and the resident’s general practitioner (GP), with input from the local psychiatry of old age service (POAS) where appropriate | 112 |
| CMO 1 | Context: multidisciplinary work | . . . followed by a MDT meeting involving pharmacists and care home nurses, with other professionals (e.g., general medical practitioners and mental health professionals) joining when required. At the MDT, the information from the pharmacist-led review was discussed and an action plan was formulated | 84 |
| CMO 1 | Context: multidisciplinary work | One of the key concerns practices had was the capacity to release GPs to attend the MDT. However, our differential analysis of the models showed that GP involvement in the MDT resulted in the greatest interventions© The Health Foundation, 20142014© The Health Foundation | 81 |
| CMO 1 | Context: multidisciplinary work | . . . we will set aside an hour to go through . . . out of the 40-bedded home, that she will do a medication review round maybe twice a year . . . We then set aside an hour where we will go through the ones where she is considering stopping, or this person has got this illness and they haven’t got this drug. And so, she doesn’t make any of the decisions on her own, those decisions are made with me with my clinical knowledge of the patient | Participant #21 |
| CMO 1 | Context: policy | The National Service Framework for Older People proposed (without citing evidence of its value) regular review of care home residents and their treatment | 85 |
| CMO 1 | Context where mechanism may not fire: risk of complaints | . . . the risk is that people say well, living with significant frailty, they are over 85, we’re going to stop their statins. Now some people would say that, some people would defend that but then if you haven’t had that conversation with a family member and then they have a stroke the next week because you’ve stopped their statins, then that opens up all sorts of avenues for complaints | Participant #16 |
| CMO 1 | Context: structured processa | We collected clinical data from GP records. The criterion for a medication review having occurred was if the term ‘medication review’ or ‘drug review’ or a similar phrase was recorded | 85 |
| CMO 1 | Context: structured processa | She obtained the number of falls from the homes’ official accident book. The details of medication were from GP records | 85 |
| CMO 1 | Context: structured processa | . . . review of the GP clinical record and a consultation with the patient and carer. The pharmacist formulated recommendations with the patient and carer and passed them on a written proforma to the GP for acceptance and implementation. GP acceptance was signified by ticking a box on the proforma | 85 |
| CMO 1 | Mechanism: trusted relationship | . . . if you’ve got a very good pharmacist, I think GPs are only too happy for them to do some of the work | Participant #16 |
| CMO 1 | Mechanism: trusted relationship | . . . clinical pharmacists involved were experienced independent prescribers competent to make autonomous decisions | 112 |
| CMO 1 | Mechanism: trusted relationship | . . . the biggest legacy of our Shine award has been the positive relationships that we have built with a number of health professionals, social services and patient advocates. It became apparent very quickly that, for our proposal to work, we needed care homes, GPs and patients to start working together when making decisions about medicines – the project has really brought these groups together . . . Better relationships have meant better care for patients in care homes© The Health Foundation, 20132013© The Health Foundation | 79 |
| CMO 1 | Mechanism: trusted relationship | . . . that model has the potential to be excellent, provided that those AHP’s are well aligned, trained by, trusted by their teams. I’ve worked with some brilliant AHP’s, but where it works well is when they’re really well embedded into an organisation and they really know each other’s skills and strengths and weaknesses. In particular they know what they don’t know | Participant #19 |
| CMO 1 | Mechanism: trusted relationship | . . . having the care home pharmacist who liaising with the home, liaises with the manager does the first review on a new patient, and then also does a review when someone has been discharged from hospital to reconcile the meds [medications]. Who then involves me, so does the research, does the . . . you know has been . . . it was my one area that as a committed GP I previously felt I wasn’t doing to the standard I wanted to do it. So, having that extra support, but it is still a team, you know and obviously the pharmacist won’t be there all the time | Participant #21 |
| CMO 1 | Mechanism: trusted relationship | An existing arrangement with a PIP [pharmacist-independent prescriber] . . . was preferred . . . final selection prioritised practices that had an established working relationship with a PIP | 87 |
| CMO 1 | Mechanism: trusted relationship | We also created better links between experts in old age psychiatry and general practice, so decisions that ordinarily wouldn’t have been made (e.g. stopping ‘specialist’ medicines such as antipsychotics in dementia patients) could be openly discussed. Better relationships have meant better care for patients in care homes© The Health Foundation, 20132013© The Health Foundation | 79 |
| CMO 1 | Mechanism: tailoring to diverse GP working practices | The care homes were enthusiastic about their residents having detailed medication reviews. Working with GPs was a bit more challenging‘We were naïve in thinking we could come up with a model and apply it across the whole health economy. Every practice was different,’ Wasim says. To overcome this, the team came up with several different ways of involving GPs, so that GPs could be part of every review© The Health Foundation, 20212021© The Health Foundation | 78 |
| CMO 1 | Mechanism: tailoring to diverse GP working practices | Over several cycles four potential models of working with GPs were developed: 1) GP attended the MDT, joint decisions made with the care home nurse and pharmacist, 2) Interventions discussed with the GP after pharmacist review and prior to the MDT, 3) Interventions discussed with the GP following the MDT but prior to resident involvement, 4) No GP involvement, prescribing pharmacist leads the process. Interventions recorded in the general practice electronic notes, GPs could challenge the interventions | 112 |
| CMO 1 | Mechanism: tailoring to diverse GP working practices | Individual medical practices work differently with regard to care home reviews and we learned that our model of having the GP at the MDT would not work across all the practices we were planning to work with. Through consultation with lead GPs and practice managers we identified four models of GP involvement© The Health Foundation, 20142014© The Health Foundation | 81 |
| CMO 1 | Mechanism: tailoring to diverse GP working practices | . . . some GP practices won’t take on a care home, you know they won’t do it for love nor money. And you will get other GP practices that might look after six or eight, and we have got those two extremes within [our locality] | Participant #21 |
| CMO 1 | Outcome: prescriptions changed | The patient’s GP accepted 75.6% (565/747) of the pharmacist recommendations. Of the accepted recommendations, 76.6% (433/565) were acted upon | 85 |
| CMO 1 | Lack of outcome: recommendations rejected by GP | The GP did not implement 23.4% (132/565) of the accepted recommendations, however. Over 7% (52/747) recommendations were rejected by the patient’s doctor. The overall implementation rate of recommendations was therefore 58% (433/747). The low implementation rate might have been higher if the pharmacist had been allowed to implement agreed changes | 84 |
| CMO 1 | Outcome: cost saving | The net cost savings are £21,705 or £206 per patient reviewed© The Health Foundation, 20132013© The Health Foundation | 79 |
| CMO 1 | Outcome: reduction in falls | There was a large and significant reduction in the number of falls (0.8 falls per patient in the intervention group, compared with 1.3 in the control group) | 85 |
| CMO 1 | Outcome: safety monitoring | There were nine adverse effects reported thought to be related to the cessation of a medicine during the study. The events were discussed with GP colleagues and not deemed serious and they were identified and appropriately rectified by either monitoring the patient or reinstating the drug or an alternative . . . | 84 |
| CMO 1 | Outcome: safety monitoring | Of the intervention patients, 42% (139/331) required a test to monitor their condition and/or their medicines. For 24% (161/672) of medicine-related interventions, a test was recommended, 13.7% (23/161) of these resulting in a change in medication | 85 |
| CMO 1 | Neutral outcome of number of medicines prescribed | . . . two models of delivery for the service (pharmacist actioning decisions or pharmacist and GP actioning decisions), there was no statistical difference in number of medicines de-prescribed between the two methods | 84 |
| CMO 1 | Outcome: reduction in hospital admissions | We found a statistical reduction in hospital admissions – people were actually less likely to go into hospital after having one of our interventions© The Health Foundation, 20212021© The Health Foundation | 78 |
| CMO 1 | Neutral outcome of hospitalisation | There is no significant change in consultations, hospitalisation, mortality, SMMSE or Barthel scores | 85 |
| CMO 2 | Context: evidence-based guidelines | Antipsychotic review focused specifically on the review of antipsychotic prescriptions by primary care physicians or psychiatry specialists, based on the National Institute for Health and Clinical Excellence dementia guidelines and facilitated by antipsychotics guidance developed by the Alzheimer’s Society in partnership with the U.K. Department of Health | 75 |
| CMO 2 | Context: evidence-based guidelines | The guidelines emphasized careful medical assessment of underlying causes of neuropsychiatric symptoms such as pain and factors leading to delirium, the use of monitoring and/or nonpharmacological interventions as a first-line approach before considering pharmacotherapy . . .A trial discontinuation was recommended as the preferred practice for patients who had had antipsychotic prescriptions for more than 3 months, but on the basis of evidence from a previous randomized controlled trial, caution was recommended in people with baseline Neuropsychiatric Inventory scores above 14 | 75 |
| CMO 2 | Context: training for care home staff | Seminars were conducted for care staff regarding safe antipsychotic prescribing, monitoring, and review | 75 |
| CMO 2 | Context: seminar for GP | Physicians were invited to an interactive seminar and/or practice meeting, provided with a toolkit or best practice guide, and given an opportunity for detailed discussion, including scenarios with individual patients | 75 |
| CMO 2 | Context: MDT meetinga | Therapists also worked with physicians and staff to augment person-centered care during antipsychotic withdrawal | 75 |
| CMO 2 | Context: structured processa | WHELD therapists worked with the champions and other staff to develop processes to prompt physician review according to best practice guidelines | 75 |
| CMO 2 | Mechanism: GP as decision-maker | Prescribing decisions were still made entirely by the participants’ own physician. In the majority of cases this was the primary care physician | 75 |
| CMO 2 | Outcome: antipsychotic review reduced use | The main factorial study demonstrated that antipsychotic review significantly reduced antipsychotic use by 50% (OR 0.17, 95% CI 0.05 to 0.60). The intervention of antipsychotic review plus social interaction significantly reduced mortality (OR 0.26, 95% CI 0.13 to 0.51) compared with the group receiving neither antipsychotic review nor social interaction | 77 |
| CMO 3 | Context: national policy – enabling dignified and peaceful death | [Aim of QI] to reduce emergency admissions and enable a dignified and peaceful death in the care home setting, as envisaged in both the National Dementia Strategy [reference] and the End of Life Care Strategy [reference] | 68 |
| CMO 3 | Context: continuity diminishing | . . . when I first started in general practice, I really knew all my patients and their families and there was continuity of care and currently continuity of care is diminishing rapidly and that in itself is a potential real problem | Participant #19 |
| CMO 3 | Context: recognising the dying phase | . . . when you’re dealing with COPD, heart failure, diabetes, dementia and all of those things and then I think there’s that final, the dying phase, so the last weeks to days, hours of life where it’s then clear that the person isn’t going to recover and is dying and you’re looking at managing those final days | Participant #19 |
| CMO 3 | Context: co-operation and confidence | . . . prerequisites for the successful implementation of end-of-life tools and frameworks in these settings. These include the cooperation of GPs with care homes and the confidence of GPs in care home staff, . . . | 67 |
| CMO 3 | Context where mechanism may not fire: different attitudes | Difficulties arise between care home staff, GPs, multidisciplinary team members and families when there are competing accounts of who should lead care decisions at the end-of-life, misunderstandings, communication difficulties and different attitudes towards death and dying | 67 |
| CMO 3 | Mechanism: involving a MDT in QI (audit) | The results of the 05/6 audit, and the implications for patients, were also presented to the staff of all six care homes during a multidisciplinary study day to which GPs, District Nurses, OOH staff, care home managers and staff were invited | 68 |
| CMO 3 | Mechanism: GP discusses ACP with resident, family and care home staff | One facet of anticipatory planning is discussion about preferred place of care and death. This involves not only providing patients and families with the opportunity to express their wishes but also understanding the views of nursing and care staff | 68 |
| CMO 3 | Outcome: more visits and a more active role in ACP | The 10% rise in visits by GPs to nursing homes in 08/9 reflects a greater workload which on discussion with the partners is seen to reflect a more active role in anticipatory planning and end of life care | 68 |
| CMO 4 | Context: variability in care homes | Additionally homes vary in terms of resident type, size, management style and culture, which may all influence collaboration | 61 |
| CMO 4 | Context: variability in services | Practitioners working with nursing homes include general practitioners, district nurses and nursing and medical specialists in palliative care (SPC). However there is little research into collaboration between homes and these services [citations]. This requires investigation, because the various health care sectors have different cultures which may impact upon care [citations] | 61 |
| CMO 4 | Context: variability in services | GP services remain disjointed and variable. (Home 29, survey) | 61 |
| CMO 4 | Context: GP with interest in frailty | if you do get a GP that has got an interest in, you know frailty, end of like care, you know holistic approach to medicine. Then I think, you know it’s a win, win if they are your care home lead | Participant #21 |
| CMO 4 | Context: collaboration | The focus is on organising and improving the quality of care for care home residents in the last year of life in collaboration with GPs, primary care and specialist palliative care teams | 89 |
| CMO 4 | Context: collaboration | . . . our evaluation also revealed that improved collaboration was not a universal outcome, and it appeared that a minimum level of collaboration at baseline helped support GSF-CH implementation, and retention in the programme | 61 |
| CMO 4 | Context: GP delivering training (as part of interprofessional group) | Workshops are taught by trained facilitators from a variety of backgrounds in health and social care (e.g. GPs, palliative care specialists, social workers, nurses) | 60 |
| CMO 4 | Context: GP leading the national programme | The GSF was developed by generalist practitioners to address their own needs for support and education related to end-of-life care | 61 |
| CMO 4 | Context: GP leading the national programme | Keri Thomas led the team which devised the Gold Standards Framework in care homes | 61 |
| CMO 4 | Mechanism: GP as leader | . . . leadership; galvanising change, being catalytic, is something that lots of people can do; it can be the visiting nurse, it can be your dietitian who decides to do something. At least, going about improving all health and hygiene in a resident population. So lots of people can do the bright new things. I guess the task is to challenge them and say: can you sustain it and can you see this happening on a repeated basis over a long period of time . . . it doesn’t have to be general practitioners who do this, although they may be quite well positioned in some ways . . . | Participant #11 |
| CMO 4 | Mechanism: facilitating trusted relationship | . . . the GSF-CH programme helped to address a number of limiters to collaborative working, including some perceptions of unequal status and lack of trust between practitioners. This was achieved by providing nursing homes with frameworks for considering end-of-life care, relevant training, networking and support | 61 |
| CMO 4 | Outcome: interprofessional learning | They praised the expertise of the workshop facilitators (n = 64), noted the benefits of interprofessional learning (n = 36) | 60 |
| CMO 4 | Context where mechanism does not fire: lack of support from GP | Concerns included GPs who respondents felt did not understand the GSFCH or palliative care, were slow to appreciate the benefits of GSFCH, were not pro-active, who lacked trust in nurses, or who were reluctant to prescribe anticipatory medicationComments from homes included . . . ‘GPs have been reluctant to participate . . . and I have had received little co-operation’. (Home 61, survey) ‘. . . we still don’t seem to have a brilliant communication with the actual GP that works with us’. (Manager 84) | 61 |
| CMO 4 | Context where mechanism may not fire: lack of support from GP | . . . you need a GP that’s cooperating. So the GP needs to take it as their responsibility. Because we needed to involve them – that was the difficulty, you know, because of their time. There was the lazy response and things like that | 89 |
| CMO 4 | Context where mechanism may not fire: lack of action by care home | Problem of staff member who doesn’t approve of providing high level of care and refuses to deliver ACP | Participant #11 |
Appendix 6 The RAMESES checklist
| Section | Description | Page number | |
|---|---|---|---|
| 1 | Title | i | |
| 2 | Abstract | v | |
| Introduction | |||
| 3 | Rationale | There is a gap in the literature about how GPs get involved in improvement within care homes. There is variability in practice and, therefore, we sought to identify and synthesise reports where low-quality care was identified and addressed, or where best practice was shared and implemented | 6 |
| 4 | Objectives |
Describe contexts where GPs can improve care in care homes Describe mechanisms that involve GPs and lead to service change or implementation of evidence-based practice |
6 |
| Methods | |||
| 5 | Changes | Changes from initially planned: Web of Science was searched, rather than ASSIA | 6 |
| 6 | Rationale for realist | GP involvement in improvement in care homes is complex because it involves different professional groups and two institutions: primary health care and care homes (social care sector) | 6 |
| 7 | Scoping | Grey literature was searched and also key literature from the database searches. Interviews with GPs helped to shape the scoping | 8 and Figure 1 |
| 8 | Search |
A broad initial search strategy was used across five academic databases. UK literature was identified and the most common interventions were selected to develop iterative searches focusing on the intervention rather than the profession (GP) Citation searches were performed for key authors and for all articles selected from the searches above Other articles were identified by hand-searching key journals and websites of professional organisations |
8 |
| 9 | Selection and appraisal | Articles were screened by title and abstract by one reviewer (NHC). Full-text articles were screened by three reviewers (NHC, RD and ALG). Articles were judged on the basis of relevance and rigour. If there were disagreements, then typically the article would be included | 9 |
| 10 | Extraction | Key aspects of each article were extracted, such as the type of intervention, a description of the change management process, type of study and details about participants and outcomes. Key claims made within the article were coded in NVivo for qualitative analysis | 9 |
| 11 | Analysis and synthesis | Articles that described a common intervention were explored for commonalities in causative mechanisms. Analysis aimed to identify key reasons why contexts described along with the intervention delivered could result in outcomes. Mechanisms were sought with greater leverage (i.e. explanatory power) in terms of generating outcomes described. We aimed to build programme theory from synthesising commonalities across similar CMO configurations | 9 |
| Results | |||
| 12 | Flow diagram |
A PRISMA-style flow diagram Iterative searches focused on UK literature and searched for terms related to end-of-life care and medication review. A citation search and hand-searching of relevant journals was also performed. Searches were carried out in five academic databases |
19 and Figure 2 |
| 13 | Document characteristics | Selected documents are listed and range from randomised controlled trials to evaluations of QI initiatives | 20 and Table 2 |
| 14 | Main findings | Step 1 brought together the project team’s own published research and citations together with scoping work within database search results. Findings described a scoping of the experience and challenges of general practice in care homes, and identification of categories of interventions that had been implemented in care homes | 11 |
| In step 2, iterative searches focused on three categories of intervention: end-of-life care, medication review and GPs with special interests. Grey literature for care homes and for general practice was searched for QI projects. In addition, GPs were interviewed | 19 | ||
| In step 3, NVivo was used to synthesise extracts from published literature, grey literature reports and blogs, and GP interviews. We collated literature into three areas: medication review, end-of-life care and care home specialised practice. However, there were too few articles describing the latter to develop theory | 28, 33 | ||
| In step 4, we developed two overarching theories. Programme theory 1 was about the embedded relationship and benefits of multidisciplinary, and programme theory 2 was about GP leadership at regional or national level | 28, 33 | ||
| Discussion and conclusion | |||
| 15 | Summary |
GPs can support improvement in care homes by building relationships within the MDT. In turn, the care home manager and other practitioners, such as pharmacists, should consider the need to be flexible to work with GPs with different routines of working with care homes Some authors of articles were GPs and had led improvement projects. This is likely to build buy-in of the profession. However, studies had not shown a GP-specific outcome |
37 |
| 16 | Strengths and weaknesses |
Strengths of the review were its systematic literature search and iterative-focused searches. GP interviews and a Context Expert Group helped to shape the study and test for resonance of our theories among practitioners and stakeholders The main limitation was difficulty finding literature specific to improvement in care homes that involved GP. Some studies describe a range of different interventions (not just GP) or a number of settings, making it difficult to attribute outcomes to GP involvement |
39 |
| 17 | Comparison | There is a lack of previous work on this topic | 39 |
| 18 | Conclusion |
GPs working in partnership with care home manager and pharmacists can bring about improvements to care of care home residents The relationship between GP and the care home manager should be negotiated and is context dependent Ownership of the agenda by the profession or leadership from the profession could facilitate GPs getting involved in improvement |
41 |
| 19 | Funding | National Institute for Health Research Health Services and Delivery Research programme | iii |
Glossary
- Advance care plan
- A document describing an individual’s wishes and priorities for treatment as they approach the end of life.
- British Medical Association
- A professional body for general practitioners.
- Care home
- Care home includes both residential and care homes with on-site nursing (international terms include long-term care facility, residential care facility and skilled nursing facility).
- Care Quality Commission
- The regulator for health care and social care services in England.
- Clinical Commissioning Group
- A NHS organisation with responsibility for a local population that plans, arranges and funds health services. Individual general practitioners are also members of these organisations.
- Context–mechanism–outcome
- A summary statement of realist programme theory.
- Direct Enhanced Services contract
- A national contract for general practitioners to provide services in addition to a General Medical Services contract.
- Enhanced Health in Care Homes
- A NHS England framework that sets out requirements for the co-ordination of health care with care homes.
- General Medical Services contract
- The standard contract for general practitioners to deliver care to all their registered patients.
- Gold Standard Framework for Care Homes
- A programme of training and accreditation in end-of-life care for care home staff, which was built on the established Gold Standard Framework in general practice.
- Locally Enhanced Services contract
- A local contract for general practitioners to provide services in addition to the General Medical Services contract (e.g. additional services to care homes).
- Optimal
- A realist evaluation involving realist review and case studies of the different ways primary care services worked with care homes to build a theory of what supports integrated working between NHS and long-term care.
- Personal Medical Services
- A voluntary option for general practitioners to enter into locally negotiated contracts. The scheme applies to general practices in England only. It enables innovative and flexible ways of working in primary care, a greater skill mix and a team-based approach to managing patients, and can provide a general practitioner-salaried option contract.
- ProactivE heAlthcare for older people living in Care Homes
- A research programme in which quality improvement collaboratives were studies in care homes across four sites.
- Quality and Outcomes Framework
- A performance management and payment system of general practitioners (part of the General Medical Services contract in April 2004).
- Quality improvement
- A set of techniques of change management within a broader concept of ‘improvement’.
- Realist And Meta-narrative Evidence Syntheses: Evolving Standards
- Reporting guidelines for realist reviews.
- Royal College of General Practitioners
- A professional body for general practitioners.
- Shine
- A programme of quality improvement funded by The Health Foundation (London, UK), including a pharmacist-led medication review quality-improvement programme in Northumbria, UK.
- Vanguard
- A NHS England programme piloting integrated care or new models of care. One element of the scheme involved care homes.
- Wellbeing and Health for People with Dementia
- A programme of research to develop and test a social interaction intervention to support de-prescribing of antipsychotic medication in care homes.
List of abbreviations
- ACP
- advance care plan
- ASSIA
- Applied Social Sciences Index and Abstracts
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CMO
- context–mechanism–outcome
- EHCH
- Enhanced Health in Care Homes
- GP
- general practitioner
- GSF
- Gold Standards Framework
- GSF-CH
- Gold Standard Framework for Care Homes
- MDT
- multidisciplinary team
- PEACH
- ProactivE heAlthcare for older people living in Care Homes
- PPI
- patient and public involvement
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- QI
- quality improvement
- RAMESES
- Realist And Meta-narrative Evidence Syntheses: Evolving Standards
- WHELD
- Wellbeing and Health for People with Dementia
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/hsdr09200).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
