Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 16/01/17. The contractual start date was in September 2017. The final report began editorial review in February 2021 and was accepted for publication in June 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
Copyright © 2021 Fisher et al. This work was produced by Fisher et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2021 Fisher et al.
Chapter 1 Background and introduction
Parts of this chapter have been adapted with permission from Fisher et al. 1,2 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
The NHS landscape
Stroke has a devastating and lasting impact on people’s lives and on the nation’s health and economy. Stroke is one of the top four causes of death and one of the largest causes of adult disability. 3 Recovery can continue for many years after an individual has a stroke; therefore, it is important that consideration is given to how to provide stroke rehabilitation services. The NHS Long Term Plan4 recommends increased investment in community health-care services. The provision of rehabilitation for stroke survivors following hospital discharge has also been highlighted as a national priority.
In England, the National Clinical Guidelines from the Royal College of Physicians5 and the National Institute for Health and Care Excellence6 recommend the provision of early supported discharge (ESD) as part of an evidence-based stroke care pathway. ESD is a multidisciplinary team (MDT) intervention that facilitates discharge from hospital and the delivery of stroke-specialist rehabilitation at home and at an intensity equivalent to that provided in an acute stroke unit. There is currently widespread implementation of stroke ESD services in the UK. However, despite research and policy drivers, national audit reports showed that the type of ESD services that stroke patients receive is variable and, in some regions, ESD is still not offered at all. 7 Alternative models of operation have been adopted, but it is not known how close they are to the evidence-based models that have demonstrated effectiveness in clinical trial settings. It remains unclear whether or not health and cost benefits of the ESD intervention are achieved when services are implemented in practice.
This report presents findings from a multimethod study investigating what, why and how ESD services are implemented and operate in real-world settings. The study responds to the second translation gap between clinical trials and clinical practice, with the view to facilitate further implementation of ESD nationally and internationally. We drew on realist evaluation (RE) principles to unpick the interplay between ESD services and the context within which they operate, and to determine whether or not and how they are effective and in what conditions. 8
Existing evidence
There is strong research evidence to show that the provision of stroke-specialist rehabilitation enhances recovery. 9,10 Service delivery models that offer home-based stroke rehabilitation have gained increasing interest, particularly as health-care services face the challenges of cost reduction and integrated care provision. 4,11 Cumulative evidence from clinical trials has shown that ESD can reduce the length of hospital stay and the risk of dependency of stroke survivors. 10
Our research to date, together with national clinical guidelines, has defined core evidence-based components of ESD,12,13 essential characteristics that theory suggests need to be implemented for the intervention to remain effective in practice. These include that ESD should be delivered by a stroke-specialist MDT, and consist of co-ordinated discharge from hospital and rehabilitation provided to eligible patients in their own home. 5,6,12–14 Findings so far have informed the successful implementation of a number of evidence-based ESD services in areas across the East Midlands. 12 What remains to be investigated is the impact of ESD in other geographical areas, given that these areas may differ in the ways that may influence how ESD operates.
In most other high-income countries, ESD has not been well developed in practice, resulting in some locally established services but a lack of large-scale implementation. 15 In many countries it is unclear what provision of rehabilitation there is for stroke survivors beyond the hospital setting, with the majority of national audits or registries focusing on acute stroke care. 16 There are also unanswered questions relating to the implementation of ESD in rural settings, with the original clinical trials mainly conducted in urban sites. 10,13 It has been reported that the role of ESD services in more dispersed rural communities has not really been adequately addressed. 17
In England, with outcome-based commissioning being a priority in the NHS, it is important to investigate whether or not ESD services are still effective in real-life clinical settings. Distinguishing between effective and ineffective implementation is crucial to addressing inequities in service provision and plan service improvements. 18 It is also vital with regard to informing the implementation of sustainable evidence-based service models.
Study aims
-
To investigate the effectiveness of ESD services when implemented at scale, in practice.
-
To understand how the context within which they operate influences the implementation and effectiveness of ESD schemes.
-
To identify transferable lessons to drive effective implementation of stroke ESD in clinical practice.
Research questions
-
What adopted models of ESD exist and how do these relate to evidence-based recommendations?
-
Can realised benefits of implementing ESD be quantified by defined measures of effectiveness: reduction in length of hospital stay, responsiveness of the service, amount of rehabilitation delivered and changes in patient dependency?
-
What site, model and patient-level characteristics influence the effectiveness of ESD services?
-
What are the cost consequences of adopted ESD models?
-
What contextual elements influence whether or not ESD is implemented in the first place and how do they shape the model of the service adopted?
-
What are the perceived outcomes of implementing ESD from the perspective of service users, clinicians, managers and commissioners, and how are these achieved in practice?
-
What are the conditions that contribute to the successful implementation and sustainability of ESD in practice?
Theoretical implications
Large-scale implementation of ESD needs to be considered in the light of the complexity inherent in the delivery of this type of intervention. ESD is a multidisciplinary and multicomponent health-care intervention that involves a critical mass of stakeholders working across different organisation settings along the stroke care pathway. It is acknowledged that successful community-based care requires not only a shift in budget investment from acute to community services but also dissolving traditional occupation and organisational boundaries. 4,19
Early supported discharge services do not operate in the controlled environments of experimental settings but in a complex and multilevel system, such as the NHS. They are, therefore, exposed to a range of contextual influences at different levels of the health-care system that act synergistically or antagonistically to evidence-based implementation. Decoding the observed variability requires distinguishing between receptive and non-receptive contexts, as well as understanding the interplay between these environments and the programme’s ‘active ingredients’. 14 This process of inquiry permits a better understanding of why the programme works in certain settings and not in others, what mechanisms underlie the programme’s success and what steps we need to make to achieve the desired outcomes. Findings can then inform future implementation, reconfiguration and improvement of ESD services to facilitate provision of evidence-based stroke care.
Implications for the NHS
This research was designed to benefit patients affected by stroke by investigating the effectiveness of services that they experience and to identify ways to improve the provision of care. The research focuses on provision of care at a particularly distressing time: when stroke survivors leave the hospital and face the consequences of stroke back at home. By investigating models of community service in practice and identifying the consequences of adopting different ESD models in variable contexts, we hope to provide clear guidance to commissioners with regard to the outcomes and impact of their decision-making, and, hence, to influence the commissioning of stroke services and address inequity in service provision.
Patient and public involvement
The Nottingham Stroke Partnership group is a group of stroke survivors and caregivers who meet bimonthly to provide a patient and public perspective to stroke research at the University of Nottingham (Nottingham, UK). This group is co-chaired by stroke survivors and Dr Rebecca J Fisher. This group have provided guidance and support throughout this study. Their concerns about inequitable access to stroke care in the community, particularly in rural areas, informed the study protocol. Trevor Gard and Frances Cameron have been members of our steering group, offering guidance on interpretation of findings, approaches to patient interviews and lay summaries of our results. They advised us on our approach to sending a feedback package to our patient participants, in which we summarised our findings and offered our thanks.
Chapter 2 Study design and methods
Overview of the study
Work package 1: how effective is early supported discharge when implemented at scale in practice?
This work package (WP) addresses research questions 1–3 (see Chapter 1, Research questions).
Work package 2: how do contextual factors influence the implementation and effectiveness of early supported discharge in practice?
This WP addresses research questions 4–7 (see Chapter 1, Research questions).
Methodology
Conceptual framework
To address our research questions, we drew on a RE approach. 8 RE is a theory-driven research evaluation that attempts to unpack the black box between complex health-care programmes and the generated outcomes (i.e. it attempts to explain the processes through which complex health-care programmes generate outcomes). Health-care programmes are perceived to be the manifestation of explicit or implicit theories that embody the developers’ and implementers’ assumptions about how the programme works. 8,20
The evaluation starts by eliciting these key theories and mapping them into context–mechanisms–outcome (CMO) configurations. CMO configurations are essentially hypotheses that explain what works, for whom, under what circumstances and how. In the process of data collection, realist hypotheses are put to the test, revised and refined, leading to a better understanding of how programmes achieve their outcomes and in what settings. 21 We started our inquiry, as advocated by the evidence base and RAMESES standards, by surfacing the core ‘formal programme theory’ about how ESD schemes work. 8,20–22 Our previous research and national clinical guidelines have shed light on the ‘active ingredients’ that make an ESD service effective by defining evidence-based core components; these are the proposed essential characteristics that theory suggests need to be implemented for the programme to work in clinical practice. 12,13
Formulated as a CMO proposition, this evidence suggests that in urban settings (context), the provision of timely hospital discharge and intensive home rehabilitation (mechanism) by co-ordinated, stroke specialist multidisciplinary ESD teams (mechanism), reduces length of in-hospital stay and improves long-term functional outcomes (outcomes).
Articulated in RE terms, it becomes apparent that the formal theory only partially explains how and in what contexts the programme works. In addition to patient-level factors (i.e. stroke severity), previous research suggests that contextual elements operating at the levels of the team and the organisation, as well as features of location, need to be considered as part of an investigation of ESD services. 12,13,23 This fits well with current implementation research frameworks that highlight the importance of considering the characteristics of context at the meso- and macro-levels. 14,24
Given that ESD is delivered to patients in their own home, thus necessitating the delivery of rehabilitation over potentially large geographical areas, the influence of the geographical location within which the service operates also needs to be understood. The question of how ESD schemes might operate in rural settings has been raised, given that most of the original trials were conducted in urban settings. What needs to be stressed, however, is that the mere description of context does not explain why a different context generates different outcomes. 25 Examining the interaction between contexts and programme mechanisms is also required to understand how the conditions within which the programme works to activate and shape these mechanisms.
Regarding the underlying mechanisms, formal theory implies a causal relationship between the core components of the intervention and its outcomes. 14 We tested this with quantitative analyses in WP1. However, according to the realist understanding of causation, interventions cannot directly cause outcomes, but they provide (or take away) resources. 21 Programme mechanisms are understood to be an interaction between the opportunities offered by the interventions and the stakeholders’ reasoning and responses to these resources. Realists’ definition of mechanisms highlights the importance of human reasoning and interpretation as vital to understanding how an intervention works. 20 Evidence suggests that the behaviour of individual ESD team members, particularly across organisational boundaries, might influence the adoption and delivery of ESD services. 23 This also resonates with current implementation theory, which acknowledges the importance of actors involved in implementation, as well as the context in which they are operating. 24 To fulfil the study’s aim, the formal theory needs to be refined and preliminary realist hypotheses developed, codified into CMO conjectures, and tested through data collection.
We drew on the work of Dalkin et al. ,26 who suggested that explicitly disaggregating mechanisms into resources and responses highlights the difference between the intervention and the generative mechanisms, and facilitates the formulation of CMO configurations. We conceptualised the evidence-based core components of ESD services as the programme resources and we sought to surface the perspectives and behaviours of actors and stakeholders (staff and patients) who are making ESD happen on the ground. As intended outcomes, we used the process and patient outcomes examined by clinical trials and the national stroke audit, but we also allowed for exploration of unintended outcomes, mainly through the qualitative component of the study.
Study design
We adopted a mixed-methods design to draw information from multiple complementary sources. Our previous research and quantitative data analysis informed mainly the ‘Context’, ‘Mechanisms-resources’ and ‘Intended Outcomes’ and qualitative data used to elicit ‘Mechanisms-responses’ and ‘Unintended outcomes’. 12,13,23 The study was conducted in stages corresponding to two interlinking WPs undertaken sequentially (Figure 1).
FIGURE 1.
Flow chart of the study, including WPs 1 and 2.
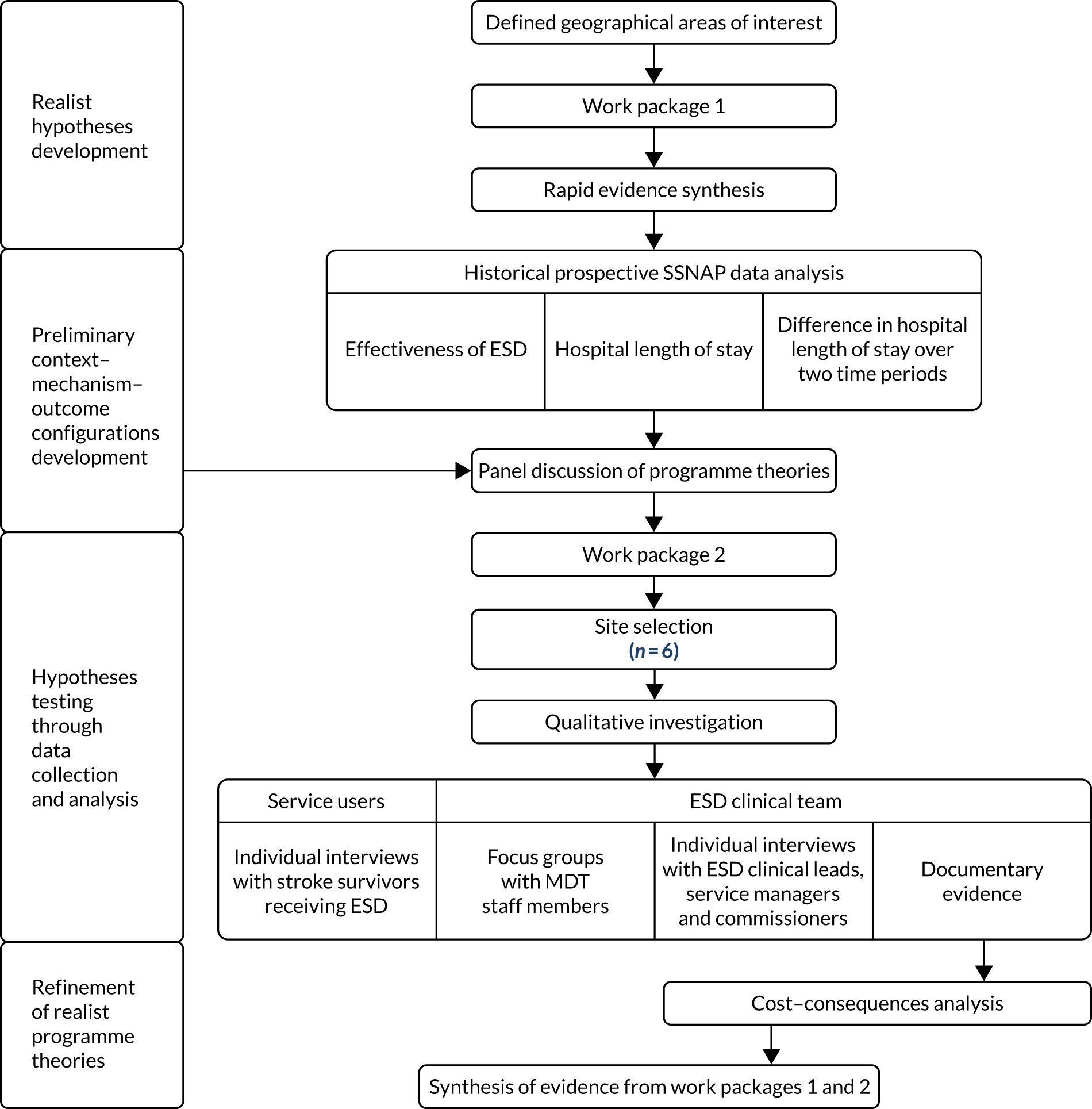
Work package 1 began with a literature review that aimed to identify key contextual determinants to the implementation of ESD services and elicit potential mechanisms. Quantitative analyses of historical prospective Sentinel Stroke National Audit Programme (SSNAP) data were then performed. The nature of the statistical modelling approaches used meant that context was explored in terms of defined and measurable variables, some of which were treated as ‘confounding’ (or ‘controlled for’) factors. We recognise that this is somewhat at odds with the philosophy of RE. However, the decision was made to use this quantitative analysis primarily to test the causal relationship between the core components of the intervention and the outcomes and, hence, findings were written up in line with recognised statistical convention.
These analyses did enable an investigation of the predictor variables of interest (as mechanisms-resources) in terms of our measure of adoption of evidence-based core components. By investigating the relationships between context, mechanisms-resources and outcomes as measurable ‘factors’, we were able to test our preliminary programme theories from a quantitative perspective. Findings informed the development of CMO hypotheses, which were tested through WP2.
Work package 2 generated insights from the perspectives of actors and stakeholders who make ESD happen in the real world, enabling mechanism-responses to be explored. An exploratory, multiple-case study design allowed ESD sites featured in WP1 to be investigated qualitatively, drawing information from individual interviews, focus groups and documentary evidence. A cost–consequences analysis (CCA) was performed to investigate the costs associated with ESD implementation, drawing information from interviews and documentary evidence. Finally, data from each WP were synthesised in relation to programme theories (with underpinning CMOs) that address the study’s questions.
Work package 1: how effective is early supported discharge when implemented at scale in practice?
Rapid evidence synthesis (see Chapter 3)
Given that context is a ‘slippery’ notion, identifying the salient contextual conditions relevant to the operation of ESD services was an important step with regard to developing and testing realist hypotheses. A rapid evidence synthesis (RES) was conducted to identify contextual features that have the potential to facilitate or impede the implementation of services providing home-based stroke rehabilitation. 27 RES is gaining popularity because it provides a robust and pragmatic approach to conducting a literature review to address specific questions. Key contextual determinants to the implementation of ESD services identified by the RES informed the development of CMO configurations to be tested through data collection and analysis.
Site selection
This study was designed to investigate the impact of different models of ESD operating over defined geographical regions of the East Midlands, West Midlands, East of England and North of England (clinical network boundaries). This allowed an investigation of the consequences of a Midlands and East initiative to implement ESD, which began in 2012,28 compared with a region (North of England) that has been slower to implement ESD based on SSNAP post-acute organisational audit data. 7 Sites in each of the four regions were defined according to Clinical Commissioning Group (CCG) and local authority boundaries. All individual ESD teams in each site that participate in the SSNAP clinical audit were included.
Data collection and analysis
Work package 1 involved the analysis of historical prospectively collected SSNAP data from hospital and community providers across the East Midlands, West Midlands, East of England and North of England Strategic Clinical Networks. In line with our programme theories, a key aim of WP1 was to investigate whether or not the degree to which an ESD service had adopted an evidence-based model (mechanism-resources) was related to better outcomes. The influence of rurality of the ESD service location, as a key contextual factor of interest, was also investigated.
The effectiveness of ESD was measured with evidence-based metrics, as defined by national clinical guidelines for stroke and that reflect outcome measures used in the original ESD trials. 10 Outcomes of interest were process measures (ESD responsiveness and rehabilitation delivered) and patient dependency (modified Rankin Scale)29 and effects of ESD on length of hospital stay.
To conduct these analyses, we employed multilevel modelling. This is an appropriate technique for analysing outcome variables that are generated from a clustered/nested structure, whereby the outcome under consideration is produced by patients in different ESD team/hospital settings. Measuring the effects that ESD teams have on their patients was a necessary first step to learning how ESD practices combine to generate differences between teams. Combining SSNAP clinical audit data at the patient level with post-acute organisational audit data at the ESD team level, we measured the ‘true’ effects that ESD teams have on their patients. This was carried out by fitting two-level patients nested within teams multilevel models to patient and process outcomes, in which covariate adjustments were made for a range of patient and ESD team characteristics.
Evaluating the effectiveness of early supported discharge service provision (see Chapter 4)
To investigate our study hypotheses, information about each ESD service, collected by SSNAP in the 2015 post-acute organisational audit, was collated by the research team. ESD team models were then analysed by comparing ESD service information with ESD consensus statements and national clinical guideline recommendations. 5,6,13 An ESD consensus score was then applied to each ESD team. Multilevel modelling enabled us to appreciate the variation in outcomes as a mixture of patient variability nested within ESD service provision variability. This approach is displayed graphically in Figure 2.
FIGURE 2.
Schematic representation of the WISE (What is the Impact of Stroke Early supported discharge?) study multilevel modelling approach. The triangle represents the fact that many patients are nested within fewer ESD/hospital units in a multilevel structure.

Additional ‘contextual’ variables at the patient level in the model, obtained from the 2016 SSNAP clinical data, included age at admission, sex, pre-stroke independence, comorbidities, National Institutes of Health Stroke Scale (NIHSS) score on admission, type of stroke and modified Rankin Scale score at discharge from hospital. 29,30 These reflect previously validated stroke case-mix models. 31,32 A key factor of interest at the ESD team level (in addition to the ESD consensus score) was the level of rurality. 33 Effectiveness of ESD service provision was measured with the following outcome variables: responsiveness (time from hospital discharge to first contact), rehabilitation intensity (total number of treatment days/total days with ESD) and stroke survivor outcome (modified Rankin Scale score after ESD delivered).
Early supported discharge impact on patient length of hospital stay (see Chapter 5)
A key benefit of ESD that was identified in the original randomised controlled trials was a reduction in the length of hospital stay. 10 Using our multilevel modelling framework and controlling for our covariates, this analysis examined how patient length of hospital stay was influenced by the presence or absence of an ESD service on their care pathway.
Independent of the ESD team data, 2015–16 hospital SSNAP data were analysed to determine if patients from admitting hospitals who had ESD available as part of their care pathway differ in their total length of inpatient stay from patients from admitting hospitals who do not have ESD available, while controlling for confounding variables (e.g. patient-level characteristics highlighted above). For this analysis, patients were nested within admitting hospitals rather than ESD teams and, hence, different data sets were used. The outcome variable for these analyses was hospital length of stay at the patient level. A repeated cross-sectional analysis using two sets of SSNAP data (2013–14 and 2015–16) was also used to establish whether or not the length of hospital stay changed over time and whether or not any change was attributable to ESD. The implementation of ESD was measured in terms of ESD being offered as part of the patients’ care pathway from their admitting hospital and across the two time periods.
Work package 2: how do contextual factors influence the implementation and effectiveness of early supported discharge in practice?
Site selection
Using a purposive sampling approach, case study sites from WP1 were selected based on the level to which evidence-based ESD had been implemented (contrasting ESD models) and the influence of rurality on ESD effectiveness (urban vs. rural sites). Table 1 displays the site characteristics that we focused on to select our six study sites.
| Site | ESD consensus score in 2015 | Staff in 2015 (n) | Total WTE staff in 2015 | New referrals in 2015 (n) | Rural population in 2011 (%) | Stroke patients from December 2017 to March 2018 (n) |
|---|---|---|---|---|---|---|
| Aa | 7 | 20 | 5.1 | 214 | 0.08 | 27 |
| Ba | 14 | 14 | 6.7 | 125 | 4.53 | 42 |
| C | 11 | 26 | 22.1 | 558 | 33.88 | 92 |
| D | 12 | 14 | 12.4 | 209 | 49.95 | 71 |
| E | 12 | 27 | 23.9 | 424 | 66.16 | 95 |
| F | 10 | 42 | 41.4 | 639 | 70.90 | 194 |
Service descriptions (see Chapter 6)
To investigate the contextual factors that stakeholders may not readily articulate and to understand the operation costs of each service, we also gathered documentary evidence. This comprised service specifications, monthly and annual reports, meeting notes and paperwork used by the teams as part of their day-to-day operational activities. Costs were explored using forms that were developed to be completed by service managers. Other information to inform service descriptions was obtained from staff interviews (see Appendix 2).
Cost–consequences analysis (see Chapter 7)
Cost implications are likely to be an important consideration with regard to successful adoption and implementation of interventions, such as ESD. Economic evaluation methods for complex interventions, such as ESD, should ideally consider the wider costs and benefits associated with the intervention. It has been argued that generic outcomes, such as quality-adjusted life-years (QALYs), may not be suitable to capture these wider effects. 34 In addition, standard cost-effectiveness measures have poor recognition of the importance of context, lacking interest in links between causal mechanisms and relevant contexts that are thought to produce expected outcomes. Resources associated with the delivery of a complex intervention are likely to equate to different costs in different places. 35
Given these issues, a CCA was deployed. This form of analysis has been recommended for complex interventions that have multiple effects because it offers a more flexible approach to presenting costs and benefits alongside each other rather than combining these into a single measure. 34 This approach also fits with the realist approach of the study, in that costs associated with ESD-related mechanisms were considered in the light of the context in which they are operating and the outcomes or benefits that are achieved.
To obtain the cost data necessary for an analysis of this kind, contrasting ESD model types represented by the six teams selected for inclusion in WP2 were used. SSNAP post-acute organisational audit data were supplemented by more detailed information gathered from the teams directly (e.g. service specifications). The MDT composition and workload [whole-time equivalent (WTE)] information was used to calculate the associated NHS costs. Staff training budgets were considered (given the importance of stroke-specific expertise). Travel costs associated with the delivery of rehabilitation were estimated by defining the geographical area over which the ESD service operates, determining the average distances travelled and the number of patient visits made. Using patient caseload information, direct costs per patient were also calculated. Consequences were expressed as the total ESD consensus score obtained (out of 17). This measure (developed in WP1) was used as a consequence to indicate the level by which each service had adopted an evidence-based service model.
Staff and patient interviews (see Chapters 8 and 9)
Staff interviews
Semistructured, one-to-one interviews were conducted at each ESD site with up to eight NHS staff informants at the senior management, service lead and commissioning levels. Stakeholders (e.g. commissioners and ESD team leads) were identified through collaboration with the national audit team and stroke clinical leads operating in each region.
Semistructured interviews allowed us to explore the individual stakeholder perceptions on a one-to-one basis, using a topic guide and prompts informed by our programme theories. These ‘realist’ interviews were designed to expose individual stakeholder perspectives on the mechanisms involved in the implementation, delivery and effectiveness of ESD, and how these relate to contextual factors and desired outcomes.
Early supported discharge team interviews
We also conducted two group interview sessions at each site. Two sessions ensured a representative sample of the ESD team [e.g. physician, nurses, therapists and rehabilitation assistants (RAs)]. The aim was to facilitate group discussion to uncover shared group perspectives on how and why the ESD service operated as a whole and how this related to performance and sustainability. Teams were given the opportunity to reflect on contextual conditions and processes that they perceived contributed to service effectiveness and to consider how this related to their environment and team make up. These were then discussed in relation to their perspectives on effectiveness and the outcomes that the service achieves.
Stroke survivor interviews
Interviews were also conducted with purposively selected ESD patients from each ESD site. Patients were recruited by the ESD teams in consultation with the research team, selecting patients currently on their caseload. Purposive sampling ensured that the sample included patients with a variety of experiences. Semistructured interviews focused on areas such as experience of rehabilitation at home, staff interaction and what aspects of ESD mattered most to patients. Interviews also explored what stroke survivors believed the purpose of ESD to be and how services could be improved and why. A realist interviewing approach did not prove feasible because patient interviews required a more informal conversational style.
Qualitative analysis
Staff interview data were analysed iteratively, following a retroductive approach. 21 Predefined programme theories and related CMO configurations were used as a framework to guide the analysis (deductive approach). However, as data collection and analysis progressed the framework was revised and refined to reflect the cumulation of new insights (inductive approach) (see Chapter 8 for further information on the analysis of staff interviews). Given that realist standards were not enforced, patient interview data were analysed using a thematic analysis approach. 36
Synthesis of findings from work packages 1 and 2 (see Chapter 10)
A synthesis of findings from WP1 and WP2 was conducted when data sets had been analysed separately. This allowed consideration of CMO configurations relating to outcomes perceived to be important by stakeholders on the ground and how this related to the implementation and effectiveness of ESD, as measured by the national audit. Findings were also considered in relation to existing implementation frameworks. 14,24
Ethics approval
Ethics approval for WP1 was obtained from the University of Nottingham (28 July 2017; ethics reference number 86-1707) because it involved the analysis of national stroke audit data. Governance approvals for data access were obtained by application to Healthcare Quality Improvement Partnership (HQIP) and a data-sharing agreement was signed between HQIP (data controller), the Royal College of Physicians (data provider) and the University of Nottingham (October 2017; application number HQIP 189). The study protocol, including the statistical analysis plan, is available online. 37 Ethics approval for WP2 was granted by the Nottingham 1 Research Ethics Committee (IRAS ID 243066; 18/EM/0160) and the Health Research Authority on 23 July 2018.
Chapter 3 Work package 1: programme theories and rapid evidence synthesis
This chapter presents the initial programme theories and how these were informed through conducting a RES before data collection and analysis. The three overarching programme theories were defined a priori from the proposal stage of this project informed by our previous research and national clinical and policy guidelines on ESD operation. 12–14,23,38 This chapter begins with a description of the content and origins of each programme theory.
Description of overarching programme theories
Programme theory 1
Our first programme theory hypothesised that the adoption of evidence-based ‘core components’ of ESD is important for the intervention to be effective in practice. 13 Our previous research12,13,23,38,39 and national clinical guidelines5,6 have shed light on the ‘active ingredients’ that make an ESD service effective by defining evidence-based core components; these are the proposed essential characteristics that theory suggests need to be implemented for the programme to work in clinical practice. 14 The core components include that ESD is delivered by stroke-specialist staff operating as a co-ordinated MDT [e.g. physician, physiotherapist, occupational therapist (OT), and speech and language therapist (SLT)]; that the ESD team has weekly MDT meetings and regular meetings with stroke unit hospital staff; and that an effective ESD intervention consists of co-ordinated, facilitated discharge from hospital and the provision of timely rehabilitation for eligible (mild to moderate) stroke patients at home. 13 We have previously shown that the adoption of these identified core components of ESD, by two services in urban areas of Nottinghamshire, led to a reduction in the length of hospital stay and accelerated patient recovery. 12
Framed in realist teams, the formal theory implied by the evidence base would suggest that in urban settings (context), the provision of timely hospital discharge and intensive home rehabilitation (mechanism) by co-ordinated, stroke specialist multidisciplinary ESD teams (mechanism), reduces length of in-hospital stay and improves long-term functional outcomes (outcomes). What this theory fails to consider, however, is how these components operate in contexts other than urban environments and how they are influenced by known and unknown contextual determinants. As with every complex intervention, a causal relationship between the intervention characteristics and the intervention outcomes cannot be assumed, but there is a need to understand the effect of human agency, the perspectives and behaviour of actors involved with the implementation of the intervention. Under a RE approach, we conceptualised the evidence-based core components of ESD services as the programme resources, and the stakeholders’ (staff and patients) reasoning and responses to these resources as the underlying mechanisms that interact with the context to produce intended and unintended outcomes. As intended outcomes, we used the process and patient outcomes examined by clinical trials and the national stroke audit (WP1) and we allowed for exploration of unintended outcomes, mainly through the qualitative component of the study (WP2).
Programme theory 2
Given that ESD is delivered to patients in their own home, thus necessitating the delivery of rehabilitation over potentially large geographical areas, the influence of the geographical location within which the service operates also needs to be understood. The second programme theory suggested that core components of ESD will operate differently in urban and rural settings. The question of how ESD might operate in rural settings has been raised given that the majority of randomised controlled trials were conducted in urban settings. 10 ESD services will typically deal with fewer patients dispersed over greater distances, which can have implications for how these services are resourced. 13 However, the delivery of ESD services in dispersed, rural communities has not yet been adequately assessed. 13
Programme theory 3
Our third programme theory suggested that the quality of the communication processes between key stakeholders and services in the pathway will influence the implementation of an evidence-based service. Evidence suggests that the behaviour of individual ESD team members, particularly across organisational boundaries, might influence the adoption and delivery of ESD services. 40 Our previous research12,13,23,38,39 has highlighted the need to consider the broader organisation and the value of strong links with other health-care and social care providers on the stroke care pathway. The importance of effective communication and liaison between inpatient services, ESD teams, community services and commissioners was identified as a key factor to successful outcomes for ESD. 13,23 Preliminary evidence suggests that effective cross-service communication might be promoted through processes such as staff rotations, boundary-spanning roles and data-sharing practices. 23 The role of ongoing communication and the provision of information to patients and carers has also been identified as important for providing a patient-centred rehabilitation, responsive to service users’ needs. 38
Table 2 depicts our conceptualisation of the interaction between contextual influences, evidence-based intervention components and staff and service users’ reasoning and responses, and how this interaction leads to intended and unintended outcomes. This framework underpins our three programme theories and it was used to guide the development of specific hypotheses in the form of CMO configurations to be tested through data collection and analysis. The table also presents an example of CMO development concerning the influence of rurality. More specifically, the CMO explores how the rurality of the location of the ESD service may lead to a facilitatory or countervailing interaction with mechanisms to generate intended or unintended outcomes.
| Context | Mechanisms | Outcomes | |
|---|---|---|---|
| Resources | Responses | ||
| Capacity | Eligibility criteria | Accelerated transfer of care from hospital to home | |
| Geography | Team composition | ||
| Commissioning and financial arrangements | WTE | Staff perspectives/behaviour | Rehabilitation delivery: responsiveness |
| ESD provider organisation | Staff-to-patient ratio | Patient perspectives/behaviour | Rehabilitation delivery: intensity of rehabilitation |
| Stroke specialism and staff training | |||
| Referring services characteristics and locations | MDT co-ordination (e.g. meetings) | Patient outcomes: recovery | |
In conceptualising ‘context’, it became apparent that we needed to focus our exploration of contextual features linked to the delivery of ESD. Identifying the salient contextual conditions relevant to the operation of ESD services was a necessary first step towards the development of realist hypotheses. We conducted a RES41 to identify contextual determinants with the potential to facilitate or impede the implementation and routine delivery of services providing home-based stroke rehabilitation.
Rapid evidence synthesis
Aims and objectives
The synthesis aimed to identify evidence on barriers to and facilitators of influencing the delivery of home-based stroke rehabilitation. We were also interested in factors influencing the discharge process and the transition from hospital to home. We intended to use our findings to clarify key determinants that we needed to consider in our exploration of context and to inform the development of specific CMO hypotheses to be tested through data collection and analysis.
Methods
Although there are no established standards for conducting and reporting RES, there is agreement that the process involves summarising and synthesising evidence from quantitative and/or qualitative studies to address specific research questions. 27 We adopted an integrated mixed-research synthesis approach,42 where both qualitative and quantitative studies were considered for inclusion by their relevance to the research aims and were grouped based on their findings rather than their methods.
The RES was conducted between May and September 2018. Database searches were carried out in the MEDLINE (via Ovid), Cumulative Index to Nursing and Allied Health Literature (CINAHL) and EMBASE™ (Elsevier, Amsterdam, the Netherlands) databases for articles published between January 2000 and June 2018. Search terms included ‘stroke/cerebrovascular accident’, ‘community based/home rehabilitation’, ‘early supported discharge/ESD’, ‘early/earlier/prompt/accelerated/supported discharge’, ‘early/earlier/prompt/accelerated/supported return home’, ‘reduce duration or length of hospital stay’, ‘organised/multidisciplinary discharge team’, ‘intermediate care/community care’, ‘barriers/facilitators/enablers’, ‘health services/implementation research’ and ‘community healthcare and service delivery/organisation’. The search strategy and inclusion and exclusion criteria are presented in Appendix 1.
Abstracts were independently assessed by two authors (NC and AB) who read all titles and abstracts. Differences in opinion were discussed between reviewers until consensus was reached.
We used the Critical Appraisal Skills Programme43 as a structured approach to understand the quality of available evidence; this checklist is a frequently used instrument that is recommended by the Cochrane Collaboration. 44 However, studies were not excluded on the basis of quality appraisal, but inclusion was decided based on the study’s ability to address the research aims. As suggested by Pawson,45 even methodologically weak studies may contain potentially valuable ‘nuggets’ of information relevant to the review. A data extraction form was created that included studies’ aims, methods and key findings. Identified studies were also coded in relation to the type/level of contextual determinants that they described. This categorisation process was informed by the Consolidated Framework for Implementation Research (CFIR) model of contextual determinants influencing implementation. 14 Following the initial coding, and where adequate information was available, data were synthesised into emerging CMO patterns that informed data collection and testing (Table 3; see Appendix 2 for the accompanying interview schedules).
| Type/level of contextual influences | Context | Mechanisms | Outcomes | Interview schedule group of questions | |||
|---|---|---|---|---|---|---|---|
| Positive influences | Negative influences | Resources | Reasoning | Intended | Unintended | ||
| Characteristic of the intervention (adaptability) | Flexibility of the ESD service’s model of operation | Lack of appropriate follow-up on services; disjointed transition between ESD and future services | Staff members adopting a flexible approach around the length of the intervention | To account for local context/patients’ individual needs | Patients receiving patient-centred care/rehabilitation services tailored to their needs | Failure to meet targets and demonstrate effectiveness | Staff interview schedule: factors influencing model of operation (see Appendix 2, section 3) |
| Intervention (team composition) | Access to social worker | Disjointed transfers between services on the stroke care pathway | Improved communication and co-ordination between health-care and social care services | Successful discharge planning and timely care transition | Improved ESD responsiveness |
Assessed through WP1 and WP2 Staff interview schedule: factors influencing model of operation (see Appendix 2, section 3) Team-level factors (see Appendix 2, section 5.2) |
|
| Characteristics of individuals (patients’ and carers’ expectations) | Home is perceived as a comforting place in which patients can reclaim autonomy supported by family members | Patients having unrealistic expectations of recovery | Ongoing communication and collaborative working between ESD, patients and carers | Patients and carers feeling safe at home | Effective management of expectations and successful adjustment to life after stroke |
Staff interview schedule: patient-level factors (see Appendix 2, section 4) Patient interview schedule: patients’ experience of ESD (see Appendix 2, section 2) Outcomes of the service (see Appendix 2, section 3) |
|
| Networks and communications (stakeholder engagement in implementation) | Developing formal implementation plan; initial consultation with other services, commissioners | Services implemented against background of cultural and organisational divides | Active involvement of multiple stakeholders in the development of the service | Promoting a shared sense of ownership | Ensuring that services fit with the pathway | Service responsive to local needs | Team leads and managers’ interview schedule: factors influencing the adoption and model of ESD (see Appendix 2, section 2) |
Results
A total of 33 papers that met the inclusion criteria were identified for full-text review and 20 publications were included in the final evidence synthesis based on whether or not they could address the research aims. The papers were published between 2000 and 2017, with two studies conducted in Australia,46,47 six in Sweden48–53 and the rest in the UK. 13,19,23,38,39,54–60 Ten studies focused on stroke ESD services,13,19,23,38,46,47,49,50,54,58 four investigated community stroke rehabilitation services39,57,59,60 and six examined stroke patients’ transition from hospital to home. 48,51–53,55,56 Data collection methods mainly involved qualitative interviews; two studies conducted surveys,46,56 two undertook observations,19,59 two used consensus methods and one provided insights from a service development project. 60 Eleven studies examined health-care professionals’ perspectives13,19,23,39,46–48,56,57,59,60 and six studies captured carers’ opinions. 19,38,49,54,55,57
The following section provides a summary of key findings, organised thematically based on the level and type of determinant that they described. The categorisation and definition of concepts were informed by the CFIR model. 14
The intervention
Relative advantage
This theme refers to stakeholders’ perception of the advantage of implementing ESD. 14 Studies reported differing views among health-care professionals regarding the relative advantage of ESD. In the studies by Chouliara et al. 23 and McGinnes et al. ,60 the provision of specialist rehabilitation in the patient’s home was positively regarded by staff members. Kraut et al. 46,47 investigated referrers’ beliefs and attitudes towards ESD and captured their concerns about the capability of ESD to provide an intensive stroke-specialist service. Staff reported more disadvantages and fewer benefits than patient participants, although the authors did not find any evidence suggesting that staff’s beliefs had a negative impact on patient views of ESD. 47 They also noted that concerns were mainly voiced by less experienced staff, which, according to the authors, highlighted the need for ongoing education of referrers and communication of evidence-based ESD outcomes.
The idea of home-based rehabilitation was highly valued by stroke survivors and was a consistent finding across the qualitative studies investigating patients’ beliefs of ESD. 38,47,49–51 Benefits included being in a familiar environment and supported by family members;38 becoming autonomous and having control over daily routines;50 and developing a more equal relationship with health-care professionals than in a hospital setting. 49
Adaptability
This theme concerns the degree to which ‘periphery components’ of the intervention can be adapted and tailored to meet local needs. 14 In addition to defining core components, two consensus documents13,39 commented on the need to adjust certain elements of the intervention, such as its time limitation, in response to the local context and clinical needs. In the study by Fisher et al. ,13 ESD triallists agreed that the length of ESD interventions should be adapted to patient need and the existence and type of other community-based stroke services in the area. It was also suggested that clinical judgement should be exercised in relation to how patients were admitted to ESD, an opinion shared by staff members interviewed by Chouliara et al. 23 The study by Cowles et al. 54 further reiterated the need to tailor ESD to patients’ needs and preferences.
Composition of the multidisciplinary team
The role of certain professions in shifting barriers to the operation of ESD was discussed in some of the included studies. Geddes and Chamberlain59 suggested that ESD teams need medical support from a consultant, who would have a ‘product champion’ and a boundary-spanning role between acute services, general practitioners (GPs) and service managers. The need for access to a stroke physician, although not necessarily as part of the team, was further stressed by Fisher et al. 13 Their findings also supported the need to liaise with a social worker and SLT, and provided some evidence on the benefits of including RAs as part of the team. The contribution of RAs in promoting the sustainability of the service was further discussed by Chouliara et al. 23 Cowles et al. 54 noted that having psychology input overseen by a clinical neuropsychologist promoted psychological thinking in the team and contributed to the effective management of mood issues for service users.
Characteristics of individuals
Patients’ and carers’ knowledge and beliefs about the intervention
Patients’ experiences of care through their hospital stay and transfer home appeared to influence their expectations of ESD. Lou et al. 49 noted that patients’ and carers’ feelings of security about going home related to their confidence in the judgement of hospital staff. Ellis-Hill et al. 55 commented on how a positive relationship between staff members and patients during their hospital stay set the tone for their perception of a trusting relationship with health-care professionals in the community. By contrast, when patients felt abandoned and unsupported during discharge, they felt that their return home was accelerated owing to pragmatic reasons, for example the hospital needing beds, rather than clinical reasons. In the study by Wottrich et al. ,48 MDT professionals thought that introducing home visits during the hospital stay helped alleviate both staff and patient concerns and anxiety about returning home. Having a positive experience of ESD staff streamlining their transfers into and out of the service contributed to patients feeling that they were safe and supported. 54
Patients’ and carers’ expectations of recovery
Patients’ and carers’ perceptions of ESD were also influenced by their own expectations of recovery,52 which were shaped by life experiences as well as previous interactions with health-care professionals. 55 For example, Lou et al. 49 discussed differences in expectations between retired stroke survivors and younger patients of working age. In the study by Kraut et al. ,47 patient opinion regarding the level of mobility required for discharge with ESD was influenced by their expectations of recovery along with the level of support available at home. Patients and carers may have unrealistic beliefs, anticipating fast recovery or even complete dependency on their relatives; it was suggested that effective management of these expectations by the ESD team promoted engagement with the rehabilitation process. 50,52
Networks and communications
Communication and co-ordination with other services
The importance of good communication and co-ordination between services on the stroke care pathway was a prevalent theme in the reviewed literature. In their qualitative investigation of a stroke community rehabilitation team (CRT), Ryan-Woolley et al. 57 found that lack of clarity about the service’s remit and inadequacies in communication with other services were factors undermining the successful implementation of the service. The need for ongoing education and improved communication and information exchange were shown to be important for the timely transfer of appropriate patients to ESD services. 23,46,53 Close working relationships with the acute service were particularly emphasised, as was ongoing communication with commissioners. 13,23,39 Co-ordination with social workers during discharge was described as problematic, leading to unnecessary delays and disjointed transfers. 23,56 Cross-service communication was deemed particularly important during the early stages of the service development. 23,57,59 Studies highlighted the need to invest time in consultation with local health and social services to clarify service remit and local relevance in the pathway and alleviate concerns. Strategic leadership and the development of a network with service representation from across health, social and voluntary sectors were identified as key for achieving partnership working and integration along the local pathway. 39,59 It was noted that the availability and use of information communication technologies had a role to play in facilitating communication and discharge planning,19 as well as promoting service integration. 23
Communication with patients and carers
The need to establish processes that promote communication and information provision with patients and carers was a consistent finding in the literature. Interviews with patients and carers highlighted the importance of having access to stroke-specialist information in appropriate formats. 38,49,55,58 Managing endings through timely and constant communication was identified as one of the factors contributing to a positive patient experience in a study by Cowles et al. 54
Conclusion
The RES was a first step in assessing our initial programme theories and informing the development of CMO hypotheses to be tested through data collection and analysis. In line with our third programme theory, findings further supported the need to consider the services’ wider networks and communication processes. They also identified certain patient-level factors that deserve further exploration, including patients’ beliefs and expectations of their own recovery and how ESD could contribute to their recovery process. One of the included studies suggested that certain features of physical geography (i.e. hilly terrain) were a common patient-reported barrier to outdoor physical activity. 53 We did not identify any other studies investigating the impact of rurality on ESD, highlighting a paucity of research in relation to the influence of geographical factors.
We are aware that this synthesis was pragmatically tailored to resources and time constraints and, therefore, very focused. As a result, it did not consider findings from a wider body of evidence (e.g. different population groups, grey literature) that could have further enriched insights from this review. Although our intention was to include quantitative studies, very few studies contained any description of contextual factors relevant to the purpose of this study. The decision to include studies based on their relevance to our research question, rather than their scientific quality, was a pragmatic one, considering the small sample size of relevant studies. Although this decision could have introduced bias, we need to note that in the context of the wider project this synthesis was a starting point to further data collection and hypotheses testing. Although we attempted to configure findings across studies into CMO hypotheses, this study was not a realist synthesis and, therefore, we did not engage in the process of distinguishing between contextual features and underlying mechanisms. None of the included studies had attempted to make these links, reiterating the need to better understand the interaction between contextual influences and the evidence-based active ingredients of the intervention.
Chapter 4 Work package 1: evaluating the effectiveness of early supported discharge service provision
Parts of this chapter are adapted with permission from Fisher et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Introduction
The SSNAP is the national stroke register of England, Wales and Northern Ireland in which all acute admitting hospitals and post-acute stroke teams are mandated to participate. 61 SSNAP has played a key role in monitoring the performance and improving the provision of acute stroke care. The collection of SSNAP data from community stroke services now offers a unique opportunity to investigate the large-scale impact of ESD.
Clinical guidelines recommend that ESD services should provide responsive and intensive rehabilitation (with treatment at home beginning within 24 hours of hospital discharge), with the aim to promote stroke survivor recovery. 5,6,62–65 By investigating if and how these aspects of an effective ESD service can be realised in practice, this study aims to inform the provision of evidence-based care for stroke survivors.
Our previous research has hypothesised that the active ingredients of ESD can be defined with evidence-based core components,13 and that these core components are essential characteristics that need to be implemented for the ESD intervention to be effective in practice. 12 The aim of this study was to determine if such core components had been adopted by ESD teams in real-world settings in England and whether or not these related to realised benefits of ESD.
Methods
Study design
We present results from this observational cohort study (Figure 3), which was conducted as part of the larger mixed-methods study. 37 We determined a priori a sample size of 4750 patients for a study power of 80% to detect standardised effect sizes of 0.25 for each outcome.
FIGURE 3.
The ESD study design flow chart. WISE, What is the Impact of Stroke Early supported discharge?
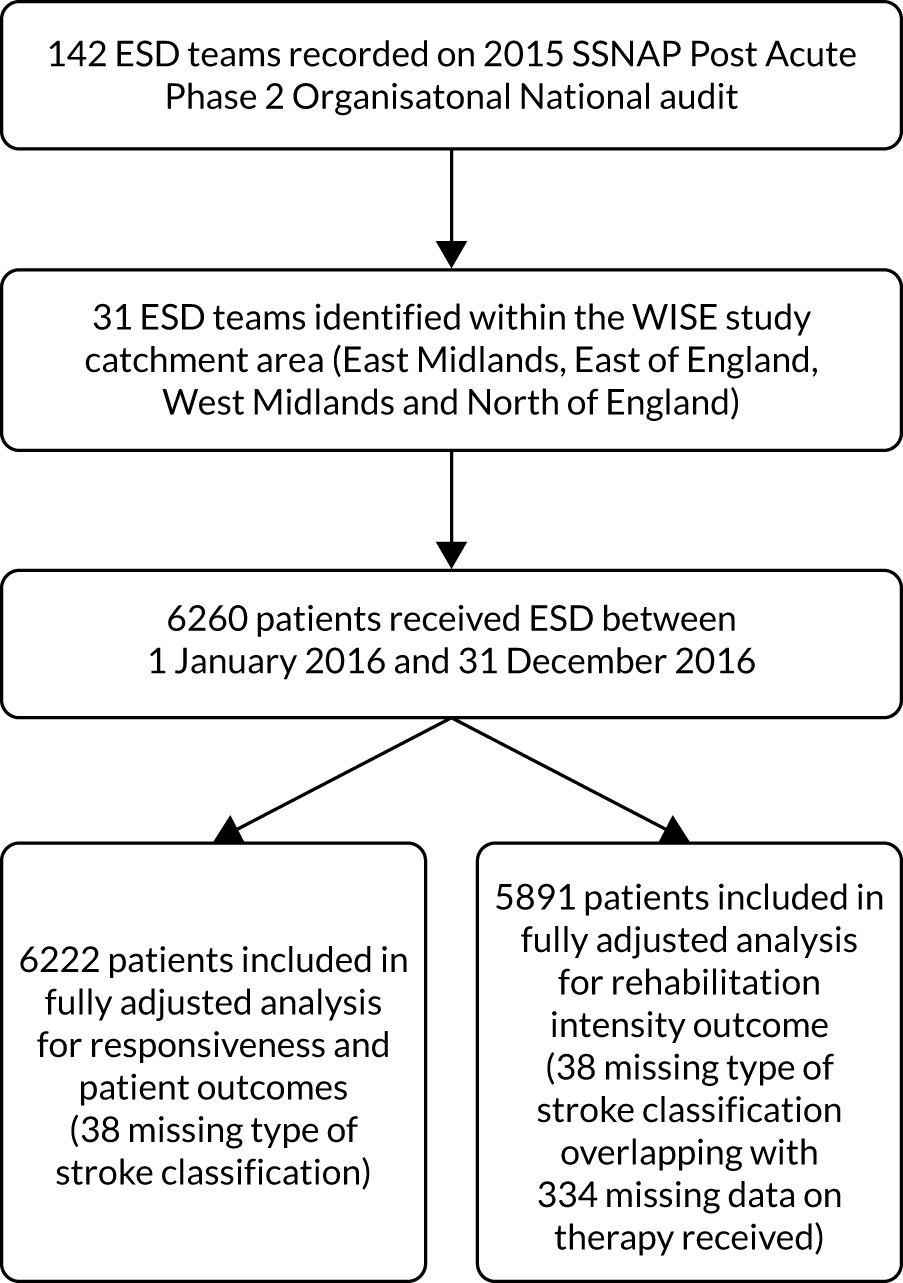
Setting
Early supported discharge services were sampled across a large geographical area of England. The sampling strategy was devised in accordance with the overall mixed-methods study design and included all ESD services in specific regions of England. 37 Here we report the findings from the quantitative investigation of ESD effectiveness across the West and East Midlands and East of England (across which a specific initiative to promote ESD was initiated in 2010), and the North of England, a region with a defined lack of ESD. 7,28
Data sources and participants
The aim of this study was to examine the association between ESD service models and process and patient outcome measures of ESD effectiveness. Information about ESD service models included in the study was obtained from SSNAP post-acute organisational audit data, which were published freely in the public domain in 2015. 7 ESD teams had participated in the 2015 post-acute organisational audit by completing questionnaires that investigated the organisational characteristics of their service in relation to evidence-based standards, which were distributed and collated by SSNAP. 7
Patient-level SSNAP data are entered by clinical teams onto a secure webtool with real-time data validations to ensure data quality. 61 Historical, prospective, clinical (patient-level) SSNAP data from all SSNAP-participating ESD teams in the geographical area of interest (n = 31) were obtained with permission from HQIP.
Key predictor: early supported discharge consensus score
We hypothesised that the adoption of evidence-based core components of ESD was important for the ESD intervention to be effective in practice. An ESD consensus score was developed using defined evidence-based core components of ESD, as outlined in an international consensus document and evidence-based post-acute organisational audit criteria utilised by SSNAP in the post-acute audit (Table 4). 7,13 Statements defining core components of ESD from the consensus document (derived using an international panel and modified Delphi process) were compared with items from the post-acute organisational audit questionnaire that was used previously by SSNAP. Using this process, a 17-item ESD consensus score was designed by the study team to measure the adoption of core components of an ESD service model, for example team composition (core team and others), staff training, team meetings and service specificity (Table 5). This 17-item ESD consensus scoring system was then applied to organisational audit questionnaire data (categorical data previously collected by SSNAP) for each of the 31 ESD teams involved in the study. The adoption of evidence-based core components was measured by calculating an ESD consensus score for each of the 31 teams.
| ESD consensus score component | Yes | No |
|---|---|---|
| Core team members meeting or exceeding recommended WTE level per 100 stroke patientsa | ||
| Doctors: ≥ 0.1 | 1 | 0 |
| Nurses: ≥ 0.4 | 1 | 0 |
| Occupational therapists: ≥ 1 | 1 | 0 |
| Physiotherapists: ≥ 1 | 1 | 0 |
| Speech and language therapists: ≥ 0.3 | 1 | 0 |
| Access to other team members | ||
| Clinical psychologists | 1 | 0 |
| Social workers | 1 | 0 |
| Rehabilitation assistants | 1 | 0 |
| Training opportunities | ||
| Nurses | 1 | 0 |
| Therapists | 1 | 0 |
| Rehabilitation assistants | 1 | 0 |
| MDT meetings | ||
| Weekly meetings | 1 | 0 |
| Core team attend | 1 | 0 |
| ESD member attends acute meeting | 1 | 0 |
| Service | ||
| Stroke specific | 1 | 0 |
| Median waiting time between referral and ESD of ≤ 1 day | 1 | 0 |
| Weekly service of > 5 days | 1 | 0 |
| ESD consensus score component | ESD teams, n (%) |
|---|---|
| Core team members meeting or exceeding recommended WTE level per 100 stroke patientsa | |
| Doctors: ≥ 0.1 | 3 (9.7) |
| Nurses: ≥ 0.4 | 15 (48.4) |
| Occupational therapists: ≥ 1 | 15 (48.4) |
| Physiotherapists: ≥ 1 | 15 (48.4) |
| Speech and language therapists: ≥ 0.3 | 22 (71.0) |
| Access to other team members | |
| Clinical psychologists | 15 (48.4) |
| Social workers | 4 (12.9) |
| Rehabilitation assistants | 31 (100) |
| Training opportunities | |
| Nurses | 21 (67.7) |
| Therapists | 30 (96.8) |
| Rehabilitation assistants | 30 (96.8) |
| MDT meetings | |
| Weekly meetings | 30 (96.8) |
| Core team attend | 7 (22.6) |
| ESD member attends acute meeting | 22 (71.0) |
| Other service characteristics | |
| Stroke specific | 31 (100) |
| Median waiting time between referral and ESD of ≤ 1 day | 20 (64.5) |
| Weekly service of > 5 days | 14 (45.2) |
To evaluate the level of service provided by the ESD teams, we proposed a scoring system, as set out in Table 4, that relates ESD organisational audit data directly to evidence-based core components. Based on our proposed scoring system, an ESD team can score a maximum of 17 points: a maximum of 5 points for core team members meeting or exceeding the recommended WTE level per 100 stroke patients, and a maximum of 3 points each for access to other team members, training opportunities, MDT meetings and level of service provided.
Process and patient outcome measures
The measures of the effectiveness of ESD were based on clinical guidelines and ESD systematic review recommendations, and were dependent on what patient-level SSNAP data variables were collected routinely. 5,10 Using historical prospective SSNAP clinical data (1 January 2016 to 31 December 2016), measures of ESD effectiveness were ‘days to ESD’ (number of days from hospital discharge to first face-to-face contact; number of patients, n = 6222), ‘rehabilitation intensity’ (total number of treatment days/total days with ESD; n = 5891) and stroke survivor outcome (modified Rankin Scale score at discharge from ESD; n = 6222). The measure of rehabilitation intensity was based on established approaches used by SSNAP. 66 The modified Rankin Scale score, routinely collected at discharge from the ESD service, was used as the stroke survivor outcome and in analysis was controlled for by modified Rankin Scale score at discharge from hospital.
‘Days to ESD’ was a binary variable (0 = ESD team sees the patient within 1 day; 1 = ESD team sees patient after ≥ 1 day) and ‘rehabilitation intensity’ was a natural log-transformed continuous measure (the results presented in the text have been back transformed to give the per cent change per unit). The stroke survivor outcome measure of modified Rankin Scale (at ESD discharge) was treated as an ordinal categorical variable with the following categories of increasing dependency: 0, 1, 2, 3 and 4–5 (combined owing to small patient numbers).
Other variables
To investigate the effect of ESD consensus score on the process and patient outcomes, we controlled for a number of covariates, which were measured at the ESD team level (level 2 in our multivariate model described in Statistical analyses) or the patient level (level 1).
We identified a need to control for the effect of preceding hospital care and geographical context of delivery of rehabilitation. At the site (or ESD team) level, we included two confounding variables: a rurality score and a hospital SSNAP rating score. The rurality score was based on the rural–urban classification reported for the geographical area associated with the NHS CCG who had procured each ESD team. 67 Each CCG in England has a geographical area over which it operates to procure NHS services. Where an ESD team included in this study was managed by multiple commissioning groups, the weighted average level of rurality was calculated based on the prevalence of stroke and transient ischaemic attack in that commissioning area (figures obtained from NHS Quality and Outcomes Framework68).
The hospital rating scores used in this study were an overall quality rating for each hospital obtained from SSNAP (total key indicator score derived across 10 domains of stroke care, with adjustments made for case ascertainment levels and the quality of data submitted to SSNAP). The score for each referring hospital (associated with each ESD team of interest) was used as an indication of the overall standard of inpatient care prior to ESD referral. 69 For ESD teams with multiple discharging hospitals, a weighted average SSNAP rating score was calculated based on the number of patients being discharged to those ESD teams.
To account for differing patient characteristics between ESD teams, we also included variables at the patient level. These were stroke patient characteristics, reflecting validated stroke case-mix models and collected as part of the SSNAP data set, and included age, sex, pre-stroke independence, comorbidities, NIHSS score on admission, type of stroke and modified Rankin Scale score at discharge from hospital. 31,32
Statistical analyses
Multilevel modelling was used to investigate the relationships between ESD model and process and patient outcomes in an approach consistent with previous observational studies of this type. 31,32,70,71 By combining SSNAP post-acute organisational audit data at the site (ESD team) level with SSNAP clinical audit data at the patient level, we fitted generalised linear mixed models on two levels, ESD team (level 2) and patient nested within an ESD team (level 1), to process and patient outcome variables. Covariate adjustments were made for site (ESD team) (level 2) and patient (level 1) variables. Models were fitted for ‘days to ESD’, ‘rehabilitation intensity’ and modified Rankin Scale score at ESD discharge using multilevel logistic, linear logistic and ordinal logistic models, respectively.
The ESD consensus score was used in three different ways: total score, disaggregated by component and, where appropriate, as an individual item. We began by assessing the significance of the total score in relation to our outcomes of interest (both unadjusted and adjusted). If a significant association was found, further analyses by components and then by individual items were conducted to uncover the key driver(s) behind the significant association(s). Any statistically significant components were tested for linearity (using likelihood ratio tests) to assist with substantive inference. Where possible, variables were interpreted in a continuous fashion, otherwise they were treated as categorical if any variable could not be interpreted in a linear way.
We chose multilevel modelling to evaluate the effectiveness of ESD service provision because it can accommodate and appreciate the variation that may exist within and between different ESD teams. Furthermore, the intraclass correlation coefficient was calculated as a measure of the proportion of the total variance in outcomes that is attributable to variance within ESD services as opposed to between services.
The adequacy of different statistical models was compared using the log-likelihood, Akaike information criterion and Bayesian information criterion values from single-level and multilevel regression models for each outcome variable, with multilevel preferable on each occasion. Multicollinearity was investigated by examining variance inflation factor scores of all predictor variable sets and was found not to be an issue. Covariate linearity was examined by checking the consistency of a linear trend in relation to each outcome variable. To explore the impact of missing data, we conducted a sensitivity analysis excluding any teams that had missing outcome data; no substantial differences were found. A two-tailed significance level of 0.05 was used in all hypothesis tests. We carried out all analyses using Stata/SE® 15.1 (StataCorp LP, College Station, TX, USA).
Results
Figure 4 shows the variation of ESD consensus scores across the 31 ESD teams and four English regions. The total ESD consensus scores across the 31 teams varied between 5 and 15 {mean 10.6 [standard deviation (SD) 2.4]}, with no team achieving 100% adherence, reflecting that a range of ESD models had been adopted. In terms of the English regions, adherence to the core components of ESD service delivery was greatest in the East of England.
FIGURE 4.
Distribution of ESD consensus score by (a) study team; and (b) region.

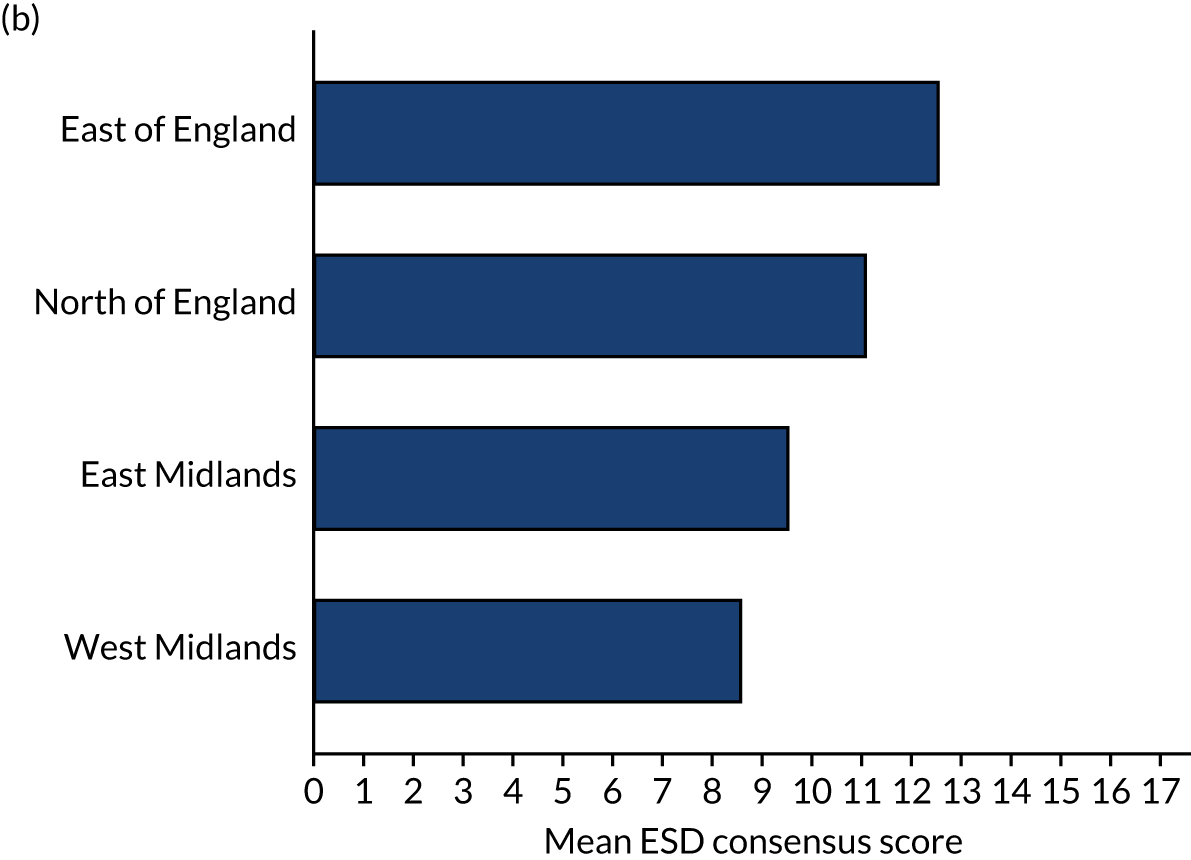
All 31 ESD teams included in this study reported that they provided a stroke-specific service (see Table 5). Only three teams reported having at least the recommended level of input from doctors and only four teams said that they had access to social workers. For the range of ESD models, there was a mixture of urban and rural settings [mean level of rurality 35.6 (SD 21.8)], as well as varying performance of associated referring hospitals [mean SSNAP hospital rating score 72.2 (SD 12.1)].
Data from 6260 patients with a completed NIHSS score were included in the primary analysis, and their characteristics are shown in Table 6. The majority of patients (91.9%) had a mild or moderate stroke (NIHSS score of < 15). The most common age group was 70–79 years (30.8%) and 4151 (66.3%) patients were functionally independent prior to their stroke (modified Rankin Scale score of 0).
| Patient characteristic | Number of patients (N = 6260) (%) |
|---|---|
| Age (years) | |
| < 60 | 1058 (16.9) |
| 60–69 | 1181 (18.9) |
| 70–79 | 1926 (30.8) |
| 80–89 | 1708 (27.3) |
| > 89 | 387 (6.2) |
| Sex: male | 3530 (56.4) |
| Already inpatient at time of stroke: yes | 197 (3.2) |
| Congestive heart failure prior to admission: yes | 241 (3.9) |
| Hypertension prior to admission: yes | 3410 (54.5) |
| Atrial fibrillation prior to admission: yes | 970 (15.5) |
| Diabetes prior to admission: yes | 1281 (20.5) |
| Stroke/transient ischaemic attack prior to admission: yes | 1487 (23.8) |
| Modified Rankin Scale score before stroke | |
| 0 | 4151 (66.3) |
| ≥ 1 | 2109 (33.7) |
| NIHSS score on arrival | |
| 0 | 746 (11.9) |
| 1–5 | 3407 (54.4) |
| 6–14 | 1597 (25.5) |
| 15–24 | 452 (7.2) |
| > 24 | 58 (0.9) |
| Type of stroke | |
| Ischaemic | 5648 (90.8) |
| Intracerebral haemorrhage | 574 (9.2) |
| Modified Rankin Scale score at inpatient discharge | |
| 0 | 790 (12.6) |
| 1 | 1703 (27.2) |
| 2 | 1376 (22.0) |
| 3 | 1570 (25.1) |
| 4–5 | 821 (13.1) |
In terms of the outcomes, 69% of the sampled patients were seen after ≥ 1 day, with 31% of patients seen within 1 day for the ‘days to ESD’ variable. The median rehabilitation intensity value of the sampled patients was 0.38 treatment days for every day with the ESD team, with the 25th percentile being 0.19 and the 75th percentile being 0.59. For the stroke survivor outcome measure, 9% of sampled patients were classified as moderate to severe at ESD discharge (modified Rankin Scale score of 4–5), with the percentages of patients with a modified Rankin Scale score of 0, 1, 2 and 3 being 9%, 31%, 31% and 20%, respectively.
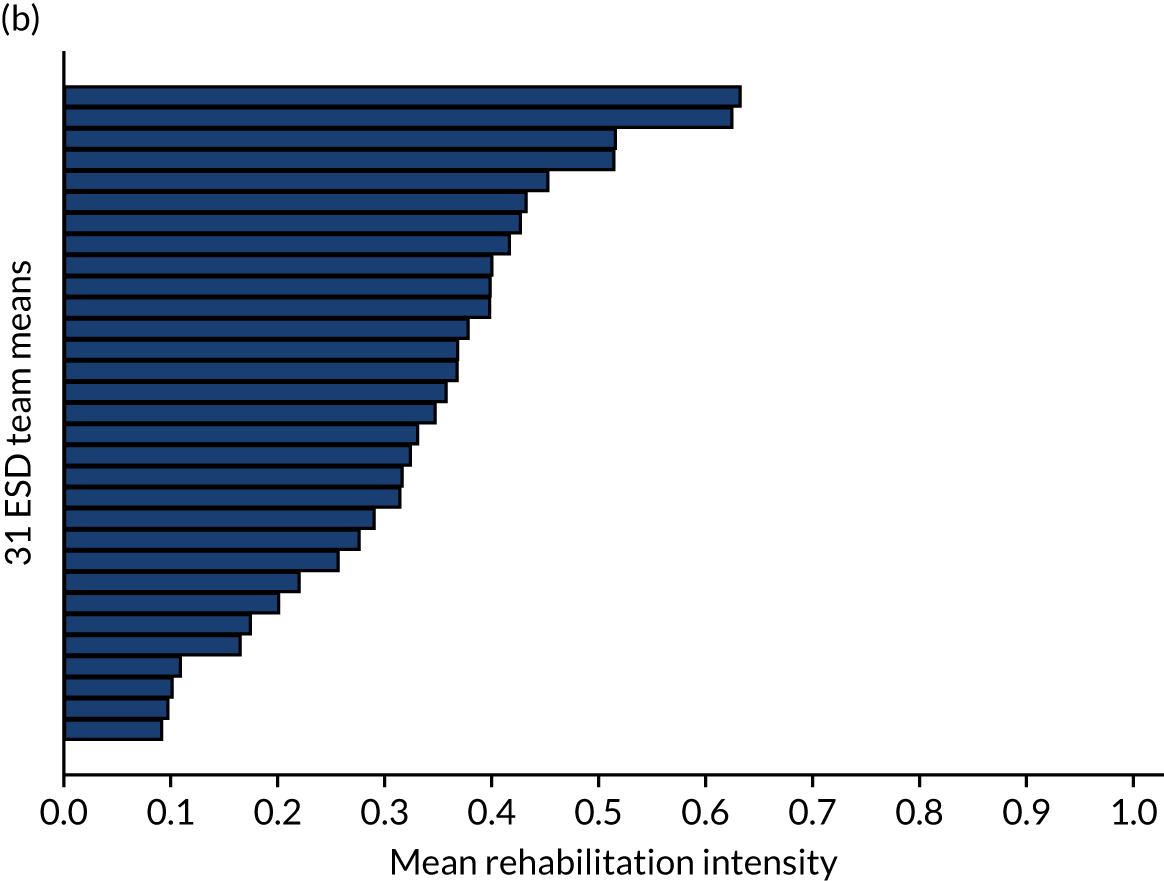
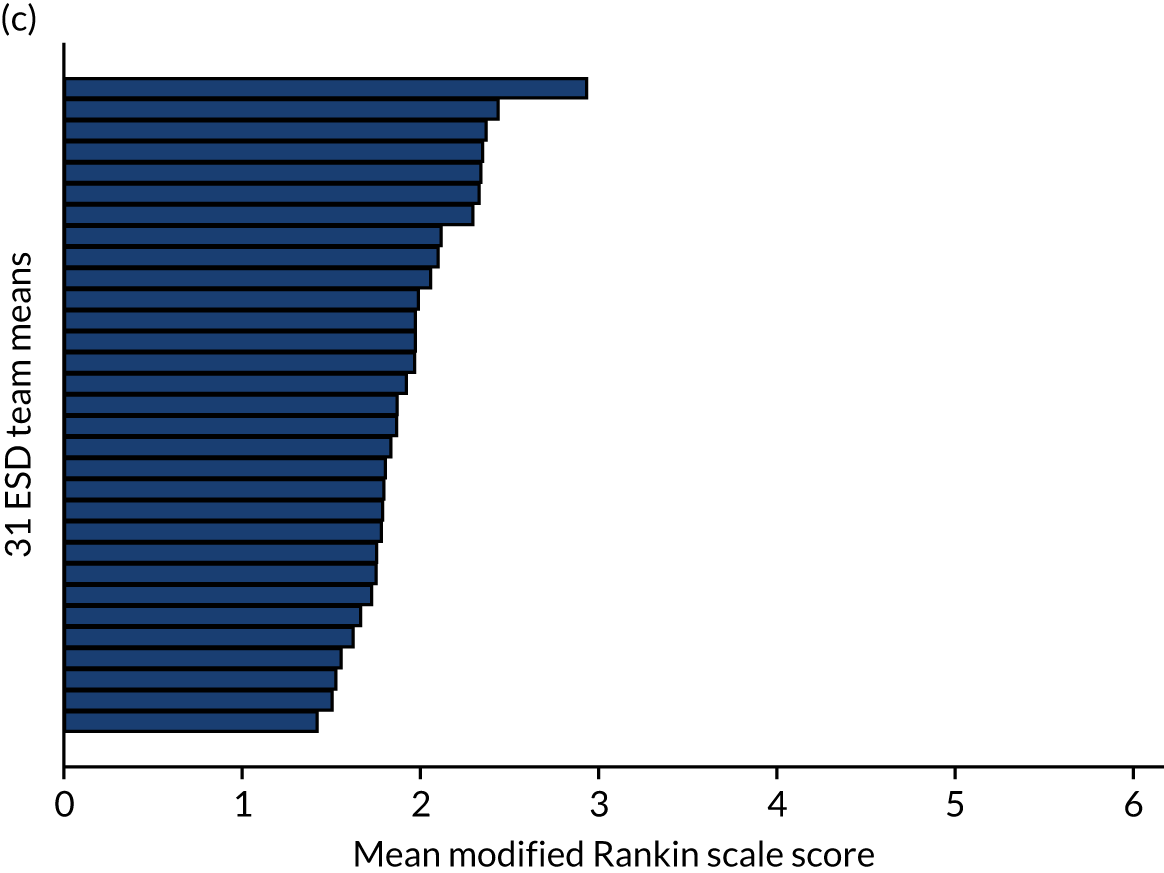
Results of the multilevel modelling are presented below. The degree of clustering was greater for the process measures ‘days to ESD’ and ‘rehabilitation intensity’ than that for the patient outcome measure of modified Rankin Scale score (adjusted intraclass correlation coefficients: 0.56, 0.26 and 0.08, respectively). Figure 5 shows the amount of variation among the 31 ESD teams in relation to the outcomes of this study.
FIGURE 5.
Distribution of study outcome variables across study teams. (a) Proportion of EDS teams that make patient contact within 24 hours; (b) mean rehabilitation intensity; and (c) mean modified Rankin Scale score.
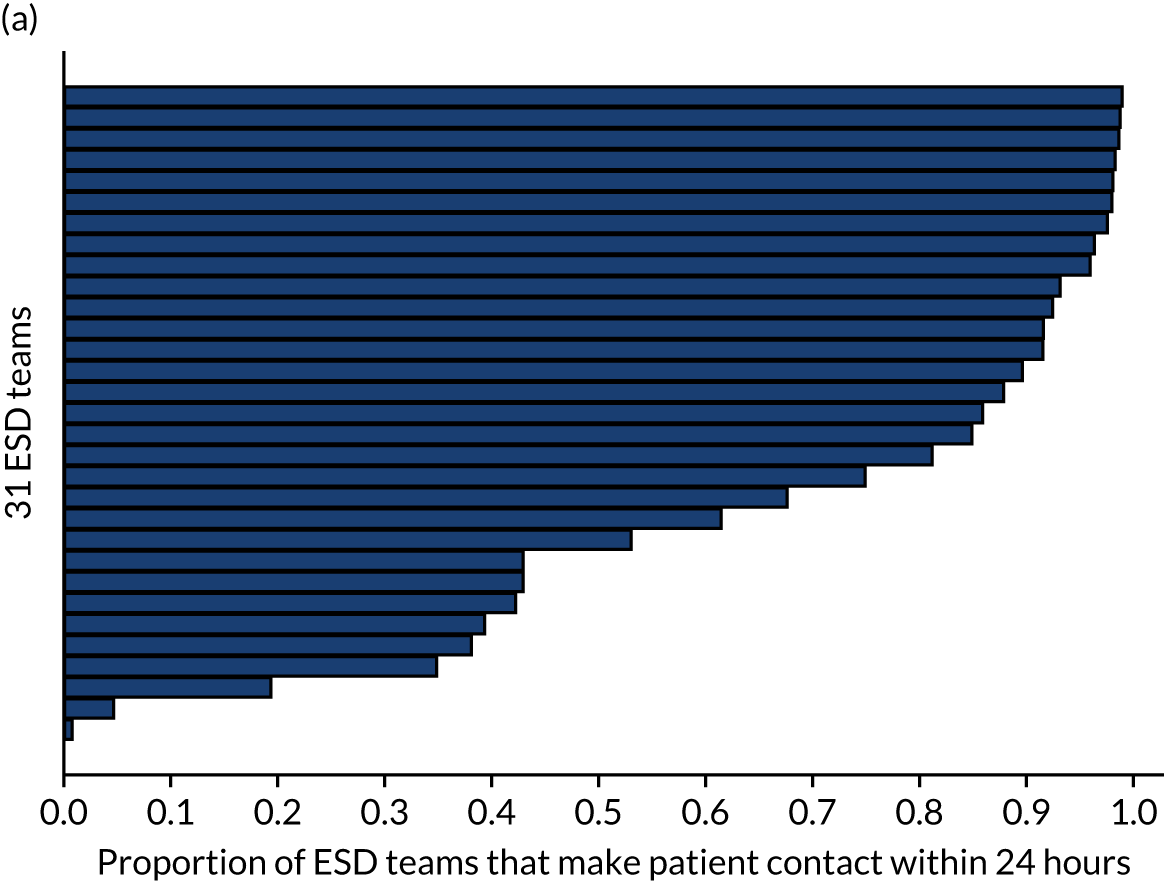
Results for the association between the total ESD consensus score and the ‘days to ESD’ variable are shown in Table 7, which are unadjusted and adjusted for all patient characteristics, the level of rurality and weighted average SSNAP hospital score. Odds ratios are also presented in Table 7, with percentage odds reported here. From the adjusted results, a 1-unit increase in the ESD score was associated with an odds ratio of 0.71 [95% confidence interval (CI) 0.51 to 0.99] or, in other words, with a reduced odds (by 29%) of the ESD team seeing the patient after ≥ 1 day following hospital discharge. Hence, an increase in ESD consensus score was associated with a more responsive ESD service. Exploring the effect of components, this association appeared to be driven by having more core team members meeting or exceeding the recommended WTE level per 100 stroke patients [a 1-unit increase was significantly associated with a 47% reduction in the odds of the ESD team seeing the patient after ≥ 1 day (95% CI 14% to 67%)]. There was some evidence at borderline significance of an effect of access to other team members (reduced odds of 70%, 95% CI –8% to 92%). Further investigation at an individual item level showed that having access to a social worker was associated with more responsive ESD service, with a 97% reduced odds of the ESD team seeing the patient after ≥ 1 day (95% CI 61% to 99%).
| Unadjusted | Adjusteda | |
|---|---|---|
| ESD models | ||
| Patients | 6260 | 6222 |
| ESD teams | 31 | 31 |
| Patients per ESD team | ||
| Minimum | 32 | 32 |
| Mean | 201.9 | 200.7 |
| Maximum | 481 | 479 |
| Intraclass correlation coefficient | 0.56 | 0.56 |
| ESD core components, odds ratio (95% CI); p-value | ||
| ESD consensus score | 0.69 (0.52 to 0.92); 0.011 | 0.71 (0.51 to 0.99); 0.041 |
| Core staff (WTE per 100 patients) | 0.52 (0.32 to 0.83); 0.006 | 0.53 (0.33 to 0.86); 0.010 |
| Access to other team members | 0.31 (0.11 to 0.86); 0.025 | 0.30 (0.08 to 1.08); 0.066 |
| Training opportunities | 0.51 (0.13 to 2.01); 0.335 | 0.54 (0.14 to 2.15); 0.386 |
| MDT meetings | 1.48 (0.48 to 4.52); 0.491 | 2.94 (0.85 to 10.16); 0.089 |
| Other service characteristics | 0.71 (0.28 to 1.80); 0.467 | 0.84 (0.31 to 2.30); 0.739 |
Table 8 presents the linear multilevel model results for the rehabilitation intensity outcome measure, which are unadjusted and adjusted for all patient characteristics, the weighted level of rurality, the average SSNAP hospital score and the total ESD consensus score. Focusing on the adjusted results and coefficients (presented as percentages here), the ESD consensus score was significantly associated with treatment intensity, such that a 1-unit increase in ESD consensus score increased treatment intensity (total number of treatment days/total days with ESD) by 2% (95% CI 0.3% to 4%). With respect to this significant association, holding weekly MDT meetings with the core team attending (see Table 5) and a member of the ESD team attending the acute meetings were all positively associated with increased rehabilitation intensity: specifically an average of 8% (95% CI 0.9% to 16%) improvement in rehabilitation intensity.
| Unadjusted | Adjusteda | |
|---|---|---|
| ESD models | ||
| Patients | 5926 | 5891 |
| ESD teams | 31 | 31 |
| Patients per ESD team | ||
| Minimum | 26 | 26 |
| Mean | 191.2 | 190.0 |
| Maximum | 457 | 457 |
| Intraclass correlation coefficient | 0.28 | 0.26 |
| ESD core components, odds ratio (95% CI); p-value | ||
| ESD consensus score | 0.03 (0.01 to 0.04); 0.002 | 0.02 (0.00 to 0.04); 0.019 |
| Core staff (WTE per 100 patients) | 0.03 (–0.00 to 0.06); 0.066 | 0.02 (–0.00 to 0.05); 0.101 |
| Access to other team members | 0.04 (–0.02 to 0.11); 0.209 | 0.01 (–0.07 to 0.08); 0.884 |
| Training opportunities | 0.07 (–0.02 to 0.15); 0.138 | 0.06 (–0.02 to 0.14); 0.124 |
| MDT meetings | 0.09 (0.03 to 0.16); 0.004 | 0.08 (0.01 to 0.15); 0.026 |
| Other service characteristics | 0.03 (–0.03 to 0.09); 0.369 | 0.01 (–0.04 to 0.07); 0.655 |
Table 9 presents the ordinal logistic multilevel model results for the patient outcome measure, which are unadjusted and adjusted for all patient characteristics, weighted average SSNAP hospital score and level of rurality. There was no significant association between the ESD consensus score and the stroke survivor outcome measured by the modified Rankin Scale score at ESD discharge. Site-level control variables, namely percentage rurality and hospital SSNAP rating score, had no statistically significant relationship with any of the outcomes.
| Unadjusted | Adjusteda | |
|---|---|---|
| ESD models | ||
| Patients | 6260 | 6222 |
| ESD teams | 31 | 31 |
| Patients per ESD team | ||
| Minimum | 32 | 32 |
| Mean | 201.9 | 200.7 |
| Maximum | 481 | 479 |
| Intraclass correlation coefficient | 0.06 | 0.08 |
| ESD core components, odds ratio (95% CI); p-value | ||
| ESD consensus score | 1.04 (0.97 to 1.11); 0.288 | 1.01 (0.92 to 1.11); 0.783 |
| Core staff (WTE per 100 patients) | 1.08 (0.96 to 1.22); 0.187 | 1.05 (0.92 to 1.21); 0.449 |
| Access to other team members | 1.06 (0.82 to 1.37); 0.654 | 0.95 (0.67 to 1.36); 0.789 |
| Training opportunities | 1.33 (0.97 to 1.83); 0.075 | 1.34 (0.93 to 1.93); 0.119 |
| MDT meetings | 0.95 (0.72 to 1.24); 0.685 | 0.79 (0.56 to 1.11); 0.170 |
| Other service characteristics | 0.96 (0.77 to 1.20); 0.723 | 0.93 (0.71 to 1.22); 0.611 |
Discussion
This study was designed to inform the large-scale implementation of ESD by evaluating its effectiveness in real-world conditions, at scale, using recommended methodology. 71 This addresses recent recommendations for investment in stroke rehabilitation made in NHS England’s Long Term Plan4 and the lack of large-scale development of ESD worldwide. 15 The study found that a variety of ESD service models have been adopted in regions of interest, as reflected by the variability in the ESD consensus score. The ESD consensus score was significantly associated with a more responsive ESD service (reduced odds of patient being seen after ≥ 1 day) and increased rehabilitation intensity when controlling for patient characteristics and other confounding variables, but no effect on stroke survivor outcome, as measured by the modified Rankin Scale, was demonstrated. We conclude that adopting defined core components of ESD was associated with providing a more responsive and intensive ESD service, suggesting that adherence to evidence-based criteria is likely to result in more effective services in practice. This builds on methods used to investigate the organisation of stroke unit care, bringing a much needed focus on community-based stroke care. 70
There are limitations inherent to observational data that we aimed to address with the study design. Although the study used a large sample of stroke patient data, it must be acknowledged that data from a relatively small sample of ESD services were used in this study; further research would be required to confirm wider transferability, particularly beyond England. A key feature of this study was the development of the ESD consensus score. Although we acknowledge that more in-depth investigation of ESD model features is required to make definitive conclusions, this approach offered a useful way to quantify the adoption of core components for quantitative analytical purposes. 37 It provided a simple means by which to evaluate services based on international consensus and clinical guidelines relating to ESD. 5,6,13 We attempted to control for a number of confounders, however we cannot rule out the possible influence of unobserved variables. Outcomes of interest were reliant on a relatively small SSNAP data set, which was entered by community stroke service staff. Findings are reliant on accurate reporting and the possibility of bias cannot be excluded. It should also be noted that previous studies have suggested that ESD reduces length of hospital stay; investigation of this, using hospital SSNAP data, is reported in Chapter 5. 37
Clinical guidelines emphasise the importance of seamless transfers of care and previous studies have reported the negative impact of delayed or un-coordinated transfers on patients. 23,38 In addition to teams with higher total ESD consensus scores being more likely to see patients sooner, findings highlighted the importance of the ratio of staff to patients. Hence, teams that met (or exceeded) consensus-recommended WTE levels of staff per 100 stroke patients were more likely to be responsive, emphasising the need for ESD services to be appropriately resourced. 13 Previous studies have also highlighted the transfer problems relating to lack of joint working between health care and social care. 23,38,72 This study adds to this debate by highlighting the importance of access to a social worker as part of the ESD team.
Early supported discharge has been recommended as a high-intensity rehabilitation intervention, with guidelines and systematic reviews referring to daily visits or four or five visits per week. 5,6,10 In this study, the intensity of rehabilitation delivery was measured by calculating the percentage of treatment days in relation to the patients’ total time with the ESD service. In addition to the total ESD score, the MDT working component was associated with increased intensity of rehabilitation delivery. This resonates with previous studies emphasising the importance of MDT working in the delivery of stroke care and, in particular, MDT meetings. 73–75
Routine collection of patient outcomes in SSNAP is currently limited to the use of the modified Rankin Scale. Findings could be interpreted such that the model of ESD adopted did not influence patient outcomes, as measured by the modified Rankin Scale; however, caution is required. Robust modified Rankin Scale data were available only at discharge from the ESD service (instead of at a later follow-up stage) and, therefore, it is possible that there was not sufficient time to investigate ESD effects. There was also a lack of variability of this outcome measure in the study, possibly reflecting a focus of ESD services on treatment of mild to moderate stroke survivors. There have also been concerns from teams about the reliability of the use of this score across the stroke care pathway. 76 We suggest that routine collection of additional validated patient outcome measures (e.g. measuring activities of daily living, general health/mood and quality of life) at longer follow-up periods in national stroke audits or registries is required. 10,12,13
Finally, at the site level, the lack of effect of rurality was surprising. It is encouraging that we found examples of evidence-based ESD models in rural regions; however, reported challenges with health-care provision in these settings cannot be overlooked. 77,78 Further investigation of the impact of geographical location on implementation of ESD is required.
Conclusion
Original clinical trials of ESD were conducted across the world and implementation of ESD is recommended in many countries’ stroke guidelines. 5,6,62–65 This study supports the use of an international ESD consensus document as a means to guide the implementation of effective, evidence-based ESD in practice. 13 We suggest that the extension of national stroke registries with the inclusion of community stroke data could offer important opportunities to evaluate stroke service delivery beyond the hospital setting. 16 This could go some way towards addressing the current gaps in the provision of stroke rehabilitation that exist globally, moving towards the goal of ensuring that stroke survivors receive the evidence-based care that they deserve.
Chapter 5 Work package 1: early supported discharge impact on patient length of hospital stay
Parts of this chapter are reproduced from Fisher et al. 2 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Introduction
One of the attractive features of the ESD intervention, as reported in clinical trials, has been the reduction in length of hospital stay, with the most recent Cochrane systematic review suggesting a reduction of 6 days. 10 This reduction has contributed to the reported cost-effectiveness of combined stroke unit care and ESD. 11 Small-scale evaluation of ESD operating in localised areas has suggested smaller, but significant, reductions in length of acute hospital stay, but it remains unknown what impact ESD is having over a larger scale. 79 The average length of hospital stay for all stroke patients who survived fell from 40 days in 2001 to 20 days in 2013, and has remained around this length since then. 80 This trend over time has meant that more stroke unit beds are available for new patients, but it has also increased the demand for patient care in the community post hospital discharge.
The study reported here, similar to that reported in Chapter 4, explored the effectiveness of ESD service models. We investigated if trial-based benefits of ESD are realised in practice, with the focus here on the impact of ESD on the length of hospital stay.
Methods
Study design
We present the results from an observational cohort study (Figure 6), which was conducted as part of an overall mixed-methods study. 37 We determined a priori a sample size of 21,760 patients for a study power of 80% to detect standardised effect sizes of 0.25 for each outcome.
FIGURE 6.
Length of hospital stay study design flow chart. WISE What is the Impact of Stroke Early supported discharge?
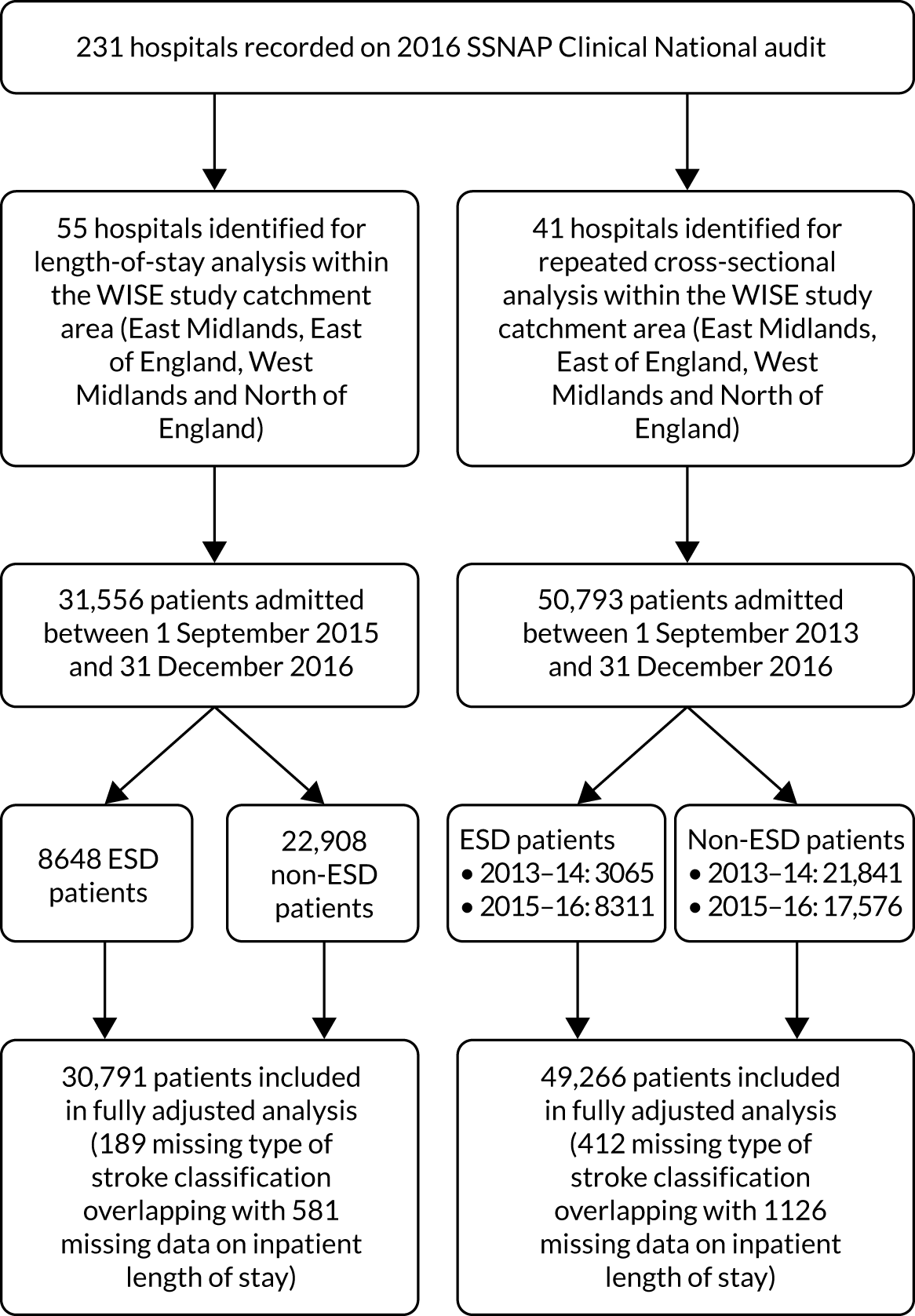
In this chapter, we have used two different study designs: (1) a cross-sectional analysis (using SSNAP data from 2015–16) comparing the length of hospital stay between patients who did and patients who did not have ESD on their care pathway, with adjustment for hospital and individual confounding factors; (2) repeated cross-sectional analysis using two sets of SSNAP data (2013–14 and 2015–16) to establish whether or not length of hospital stay changed over time and whether or not any change was attributable to ESD.
Setting
Hospitals (and associated ESD services) were sampled across a large geographical area of England. The sampling strategy was devised in accordance with the overall mixed-methods study design and included all ESD services in specific regions of England. 37 Here we report findings from the quantitative investigation of the effect of ESD on length of hospital stay across the West and East Midlands and the East of England (across which a specific initiative to promote ESD was initiated in 2010), and the North of England, a region with a defined lack of ESD. 7,28 We have included all main referring hospitals within the defined geographical area, as well as referring hospitals where patients did (or did not) go on to receive ESD along their care pathway within the catchment area.
Data sources and participants
Patient-level SSNAP data were entered by clinical teams onto a secure webtool with real-time data validations to ensure data quality. 61 Historical, prospective, clinical (patient-level) SSNAP data were obtained from the SSNAP team with permission from HQIP. The first study design involved 55 admitting hospitals and SSNAP data for all patients admitted from 1 September 2015 to 31 December 2016 (31,556 stroke patients). The second study design included 41 admitting hospitals, which were those of the 55 hospitals for which we could obtain SSNAP data for all patients admitted during two time periods: 1 September 2013 to 31 December 2014 and 1 September 2015 to 31 December 2016 (50,793 stroke patients).
Outcomes
The length of hospital stay was defined as the total length of hospital stay per patient (as an inpatient) from the arrival at the admitting hospital (or time of stroke onset, if already an inpatient) to the time of discharge from the last inpatient setting, including the time spent at any other inpatient setting. Owing to the positive skewness of the underlying distribution, the length of hospital stay was natural log-transformed before undertaking the statistical modelling and all effect sizes were exponentiated afterwards to aid interpretation.
Confounding factors
To investigate the effect of ESD on length of hospital stay, we identified a need to control for the overall standard of hospital care and the influence of the provision of social care. At the hospital level, we included two confounding variables: a hospital SSNAP rating score and a measure of delayed transfers of care from hospital, derived from the Adult Social Care Outcomes Framework (ASCOF).
The hospital rating scores used in this study were an overall quality rating for each hospital obtained from SSNAP (total key indicator score derived across 10 domains of stroke care, with adjustments made for case ascertainment levels and the quality of data submitted to SSNAP). 66 SSNAP produced performance-rating scores for admitting hospitals during the periods of interest and we used the score produced during the latter part of the period of interest for each analysis. 69 This score for each admitting hospital was used as an indication of the overall standard of inpatient care after the onset of stroke. The ASCOF data report the average daily rate of delayed transfers of care per 100,000 population aged ≥ 18 years at the local authority level. Data were aggregated to NHS trust level, using averages where multiple local authorities were associated with one NHS trust. Again we focused on the scores produced during the latter part of the period of interest, in line with the SSNAP hospital performance ratings. 81
To account for comparison between different groups of individual patients, we also included variables at the patient level. These were stroke patient characteristics, reflecting validated stroke case-mix models and collected as part of the SSNAP data set. These were age at admission, sex, pre-stroke independence, cardiovascular comorbidities, NIHSS score on admission, type of stroke and modified Rankin Scale score at discharge from hospital. 31,32
Statistical analyses
We employed a linear multilevel model framework for both study designs whereby patients (level 1) were clustered within admitting hospitals (level 2) in an approach consistent with previous observational studies of this type. 1,31,32,70,71 Within our multilevel models, we adjusted for a range of patient and hospital characteristics as covariates. We chose multilevel modelling to evaluate the effect of ESD on length of hospital stay because it could accommodate and appreciate the variation that existed within and between different admitting hospitals. Furthermore, the intraclass correlation coefficient was calculated as a measure of the proportion of the total variance in length of hospital stay, which was attributable to variance within admitting hospitals instead of between admitting hospitals.
The adequacy of different statistical models was compared using the log-likelihood, Akaike information criterion and Bayesian information criterion values from single-level and multilevel regression models, with multilevel preferable on each occasion. Multicollinearity was investigated by examining the variance inflation factor scores of all predictor variable sets and was found not to be an issue. Covariate linearity was examined by checking the consistency of a linear trend in relation to each outcome variable. Regarding the impact of missing data, we assessed the mean change in the outcome variable between the ESD and the non-ESD groups in relation to missing predictor data (which amounted to a loss of 0.6% of the total sample size); no substantial differences were found because we observed a mean difference of < 0.3%.
Analysis of cross-sectional data from 2015 to 2016
A quasi-experimental cross-sectional design was used in which patients who received ESD on their care pathway were compared with patients who had not (non-ESD). Hence, across 55 admitting hospitals covering the data period from 1 September 2015 to 31 December 2016, we investigated the effect of ESD being on the care pathway (yes/no) for stroke patients on their total length of hospital stay from admitting hospital to being discharged from the last inpatient setting.
Analysis of repeated cross-sectional data from 2013 to 2014 and from 2015 to 2016
This analysis studied whether or not the length of hospital stay changed over time, that is between the earlier (1 September 2013 to 31 December 2014) and the later (1 September 2015 to 31 December 2016) time periods, and whether or not any change was attributable to ESD, given that ESD provision was higher in the later time period. 7 The patients formed distinct groups over the two time periods because they were admitted in either the 2013–14 time period or the 2015–16 time period, with no patient covering both time periods. 82 The same multilevel model approach was used as in the cross-sectional analysis, but also incorporated an effect of time (2013/14 or 2015/16) and an interaction between time and the effect of ESD, which modelled whether or not the effect of ESD was similar in the two time periods. The main effect of receiving ESD (with adjustment for time) indicated the effect of ESD on the length of hospital stay in the first time period. An interaction between time and ESD would indicate whether or not there was any difference in the effect of ESD on length of hospital stay between the first and the second time periods.
Sensitivity analysis using propensity score matching
Given that it was important to ensure that the effects of ESD were not the result of potential confounding factors, we also used an alternative method of controlling for confounders, propensity score matching, as a sensitivity analysis. Propensity score matching involved matching patients with ESD on their pathway with similar patients who did not, based on their patient characteristics. In this case, we explored two alternative approaches to propensity score matching. In the first approach, we matched patients with ESD to patients without ESD in the same hospital, that is within-admitting hospital matching. 83 This resulted in a truncated sample size as only hospitals with both ESD and non-ESD patients could contribute to this first matching analysis.
Second, we then allowed the matching to occur with similar patients without ESD in different hospitals, that is between-admitting hospital matching. 84 This second approach enabled us to use a larger sample size because all hospitals could contribute to the probability estimate of whether or not a patient received ESD regardless of what their patients actually received. To ensure greater accuracy in the latter analysis, we used a stratified matching process so that patients were matched only to patients in a hospital with a similar proportion of patients having access to ESD.
A two-tailed significance level of 0.05 was used in all hypothesis tests. We carried out the majority of analyses using Stata/SE® 15.1 and the R (The R Foundation for Statistical Computing, Vienna, Austria) package Matching was used to undertake the between-admitting hospital propensity score matching.
Results
Analysis of cross-sectional data from 2015–16
Table 10 presents descriptive statistics of the patient- and admitting hospital-level variables and the median number of days spent as an inpatient disaggregated by patients who received ESD (ESD, n = 8648) or did not receive ESD (non-ESD, n = 22,908) on the care pathway. Compared with patients who did not receive ESD, those who did were younger and more likely to be independent (lower pre-morbid modified Rankin Scale score) before stroke, and were more independent at inpatient discharge (lower post-morbid modified Rankin Scale score). ESD patients were also more likely to have been admitted to a hospital with a higher SSNAP score rating and higher rate of delayed transfers than non-ESD patients.
| Patient characteristic | ESD (N = 8648) | Non-ESD (N = 22,908) |
|---|---|---|
| Age (years), n (%) | ||
| < 60 | 1422 (16.4) | 3674 (16.0) |
| 60–69 | 1692 (19.6) | 3932 (17.2) |
| 70–79 | 2646 (30.6) | 6080 (26.5) |
| 80–89 | 2373 (27.4) | 6873 (30.0) |
| > 89 | 515 (6.0) | 2349 (10.3) |
| Sex: male, n (%) | 4869 (56.3) | 11,785 (51.4) |
| Already inpatient at time of stroke: yes, n (%) | 264 (3.1) | 995 (4.3) |
| Congestive heart failure prior to admission: yes, n (%) | 348 (4.0) | 994 (4.3) |
| Hypertension prior to admission: yes, n (%) | 4743 (54.9) | 12,299 (53.7) |
| Atrial fibrillation prior to admission: yes, n (%) | 1370 (15.8) | 4016 (17.5) |
| Diabetes prior to admission: yes, n (%) | 1770 (20.5) | 4834 (21.1) |
| Stroke/transient ischaemic attack prior to admission: yes, n (%) | 2075 (24.0) | 6100 (26.6) |
| Modified Rankin Scale score before stroke, n (%) | ||
| 0 | 5688 (65.8) | 12,796 (55.9) |
| > 0 | 2960 (34.2) | 10,112 (44.1) |
| NIHSS score on arrival, n (%) | ||
| 0 | 1041 (12.0) | 3267 (14.3) |
| 1–5 | 4640 (53.7) | 11,252 (49.1) |
| 6–14 | 2253 (26.1) | 5596 (24.4) |
| 15–24 | 636 (7.4) | 2322 (10.1) |
| > 24 | 78 (0.9) | 471 (2.1) |
| Type of stroke, n (%) | ||
| Infarction | 7804 (90.8) | 20,772 (91.2) |
| Primary intracerebral haemorrhage | 789 (9.2) | 2002 (8.8) |
| Modified Rankin Scale score at inpatient discharge, n (%) | ||
| 0 | 1046 (12.1) | 4016 (17.5) |
| 1 | 2259 (26.1) | 5024 (21.9) |
| 2 | 1928 (22.3) | 3420 (14.9) |
| 3 | 2189 (25.3) | 3838 (16.8) |
| 4 | 1118 (12.9) | 4154 (18.1) |
| 5 | 108 (1.3) | 2456 (10.7) |
| Total length of hospital stay (days), median (IQR) | 6.9 (2.9–18.8) | 6.0 (2.2–24.8) |
Figure 7 shows the amount of variation among the 55 admitting hospitals in relation to their average inpatient length of stay and the variation in the proportion of stroke patients who received ESD on their care pathway. In this study, almost one-quarter of stroke survivors attended admitting hospitals with no ESD on their care pathway and more than three-quarters of the stroke survivors attended admitting hospitals with less than a 40/60 split of ESD/non-ESD being available on the care pathway.
FIGURE 7.
Distribution of (a) mean inpatient length of stay; and (b) the proportion of patients who received ESD across admitting hospitals.
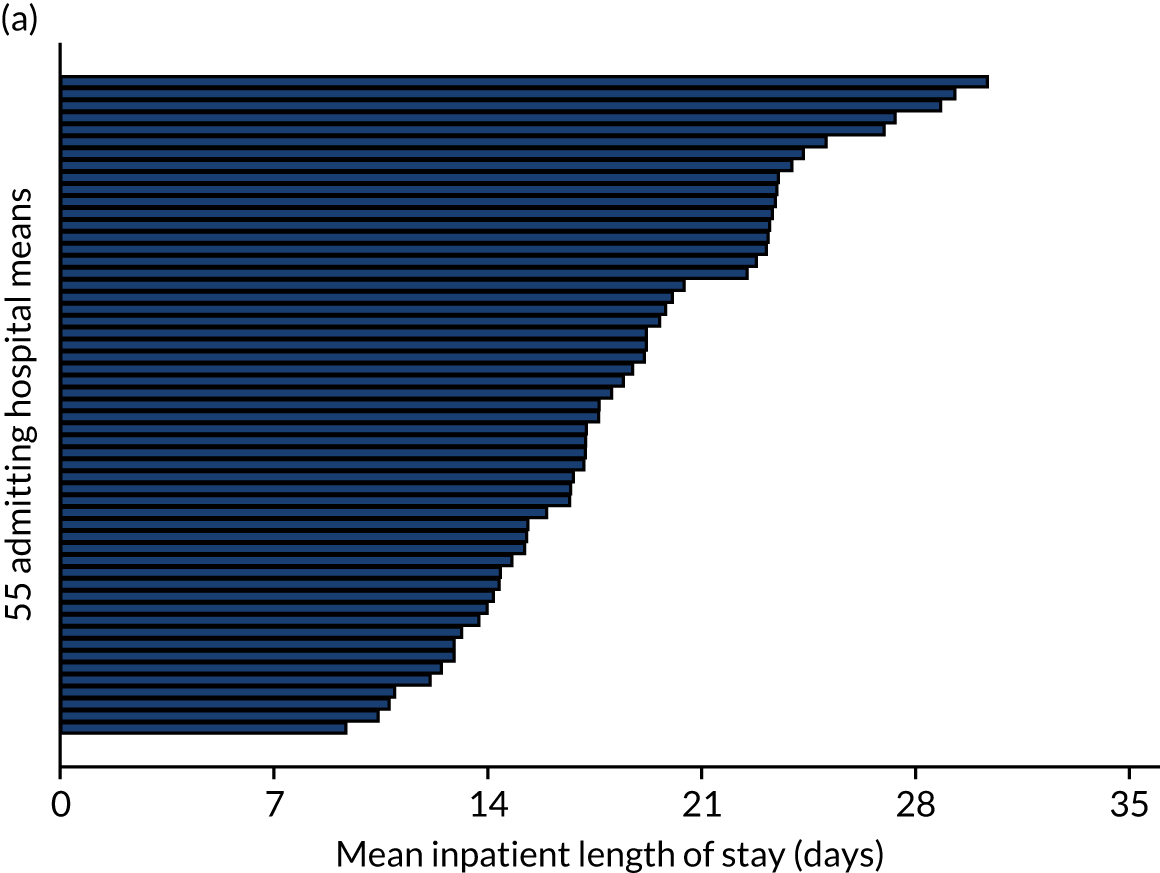

Before adjustment, ESD patients had a longer length of hospital stay than non-ESD patients: median 6.9 days [interquartile range (IQR) 2.9–18.8 days] compared with median 6.0 days (IQR 2.2–24.8 days), respectively. Following multilevel model analysis, after controlling for patient- and hospital-level characteristics, the mean length of stay for patients who received ESD along their care pathway compared with those who did not remained significantly longer by 15.8% (95% CI 12.3% to 19.4%) (Table 11). Similarly, from the sensitivity analysis using propensity score matching, patients who received ESD on their care pathway, on average, stayed in hospital longer than patients who did not receive ESD (when controlling for all other patient characteristics and hospital SSNAP and ASCOF scores) (Table 12). The within admitting hospital propensity score-matching process (n = 10,449) suggested that ESD patients stayed in hospital longer than non-ESD patients by an average of 8.7% (95% CI 4.8% to 12.6%). The between-admitting hospital propensity score matching process (n = 30,791) found that ESD patients stayed in hospital longer by an average of 7.3% (95% CI 3.0% to 11.8%).
| Inpatient length of stay models | ESD model | |
|---|---|---|
| Unadjusted | Adjusteda | |
| Patients (n) | 30,975 | 30,791 |
| Admitting hospitals (n) | 55 | 55 |
| Patients per admitting hospital (n) | ||
| Minimum | 27 | 26 |
| Mean | 563.2 | 559.8 |
| Maximum | 1331 | 1310 |
| Intraclass correlation coefficient | 0.05 | 0.08 |
| ESD on the care pathway, coefficient (95% CI); p-value | ||
| Received ESD | 0.08 (0.04 to 0.12); < 0.001 | 0.15 (0.12 to 0.18); < 0.001 |
| Inpatient matching models | Betweenb,c | Withinc,d |
|---|---|---|
| Patients (n) | 30,791 (ESD 8593; non-ESD 22,198) | 10,449 (ESD 4572; non-ESD 5877) |
| Admitting hospitals (n) | 55 | 14 |
| ESD on the care pathway, coefficient (95% CI); p-value | ||
| Received ESD | 0.07 (0.03 to 0.11); < 0.001 | 0.08 (0.05 to 0.12); < 0.001 |
Analysis of repeated cross-sectional data from 2013 to 2014 and 2015 to 2016
Table 13 presents descriptive statistics of the patient- and admitting hospital-level variables used in the repeated cross-sectional analysis, as well as the median number of days spent as an inpatient disaggregated by patients who received ESD (n = 11,376) or did not receive ESD (n = 39,417) on the care pathway across the two time periods. This descriptive, repeated, cross-sectional analysis showed that the number of patients who received ESD significantly increased over the two time periods. Moreover, across the two time periods, ESD patients were younger, more likely to be male and more likely to have pre-morbid independence, as evidenced by a lower modified Rankin Scale score. Before adjustment, ESD patients were recorded as having a longer length of stay in hospital than non-ESD patients [median 7.7 days (IQR 3.2–23.8 days) vs. median 6.3 days (IQR 2.5–22.1 days) in 2013–14, respectively; median 6.8 days (IQR 2.9–18.5 days) vs. median 5.7 days (IQR 2.1–24.6 days) in 2015–16, respectively].
| Patient characteristic | ESD (N = 11,376) | Non-ESD (N = 39,417) |
|---|---|---|
| Age (years), n (%) | ||
| < 60 | 1847 (16.2) | 6212 (15.8) |
| 60–69 | 2239 (19.7) | 6647 (16.9) |
| 70–79 | 3467 (30.5) | 10,543 (26.8) |
| 80–89 | 3126 (27.5) | 12,087 (30.7) |
| > 89 | 697 (6.1) | 3928 (10) |
| Sex: male, n (%) | 6352 (55.8) | 19,959 (50.6) |
| Already inpatient at time of stroke: yes, n (%) | 361 (3.2) | 1766 (4.5) |
| Congestive heart failure prior to admission: yes, n (%) | 481 (4.2) | 1558 (4) |
| Hypertension prior to admission: yes, n (%) | 6261 (55) | 21,313 (54.1) |
| Atrial fibrillation prior to admission: yes, n (%) | 1840 (16.2) | 7299 (18.5) |
| Diabetes prior to admission: yes, n (%) | 2345 (20.6) | 8074 (20.5) |
| Stroke/transient ischaemic attack prior to admission: yes, n (%) | 2740 (24.1) | 10,482 (26.6) |
| Modified Rankin Scale score before stroke, n (%) | ||
| 0 | 7389 (65) | 22,847 (58) |
| > 0 | 3987 (35.1) | 16,570 (42) |
| NIHSS score on arrival, n (%) | ||
| 0 | 1430 (12.6) | 6884 (17.5) |
| 1–5 | 6020 (52.9) | 18,802 (47.7) |
| 6–14 | 2955 (26) | 9162 (23.2) |
| 15–24 | 861 (7.6) | 3833 (9.7) |
| > 24 | 110 (1) | 736 (1.9) |
| Type of stroke, n (%) | ||
| Infarction | 10,315 (91.2) | 35,989 (92.1) |
| Primary intracerebral haemorrhage | 998 (8.8) | 3079 (7.9) |
| Modified Rankin Scale score at inpatient discharge, n (%) | ||
| 0 | 1440 (12.7) | 8474 (21.5) |
| 1 | 2928 (25.7) | 8649 (21.9) |
| 2 | 2562 (22.5) | 5456 (13.8) |
| 3 | 2817 (24.8) | 6090 (15.5) |
| 4 | 1471 (12.9) | 6733 (17.1) |
| 5 | 158 (1.4) | 4015 (10.2) |
| Time period, n (%) | ||
| 2013–14 | 3065 (26.9) | 21,841 (55.4) |
| 2015–16 | 8311 (73.1) | 17,576 (44.6) |
| Total length of hospital stay (days), median (IQR) | ||
| 2013–14 | 7.7 (3.2–23.8) | 6.3 (2.5–22.1) |
| 2015–16 | 6.8 (2.9–18.5) | 5.7 (2.1–24.6) |
Figure 8 shows the amount of variation across the two time periods in relation to their average inpatient length of stay, as well as the variation in the proportion of stroke patients who received ESD on their care pathway. Although the mean inpatient length of stay fell only slightly between the two time periods, the prevalence of ESD availability more than doubled across the 41 admitting hospitals in this study.
FIGURE 8.
Distribution of (a) the mean inpatient length of stay; and (b) the proportion of patients who received ESD across time periods.
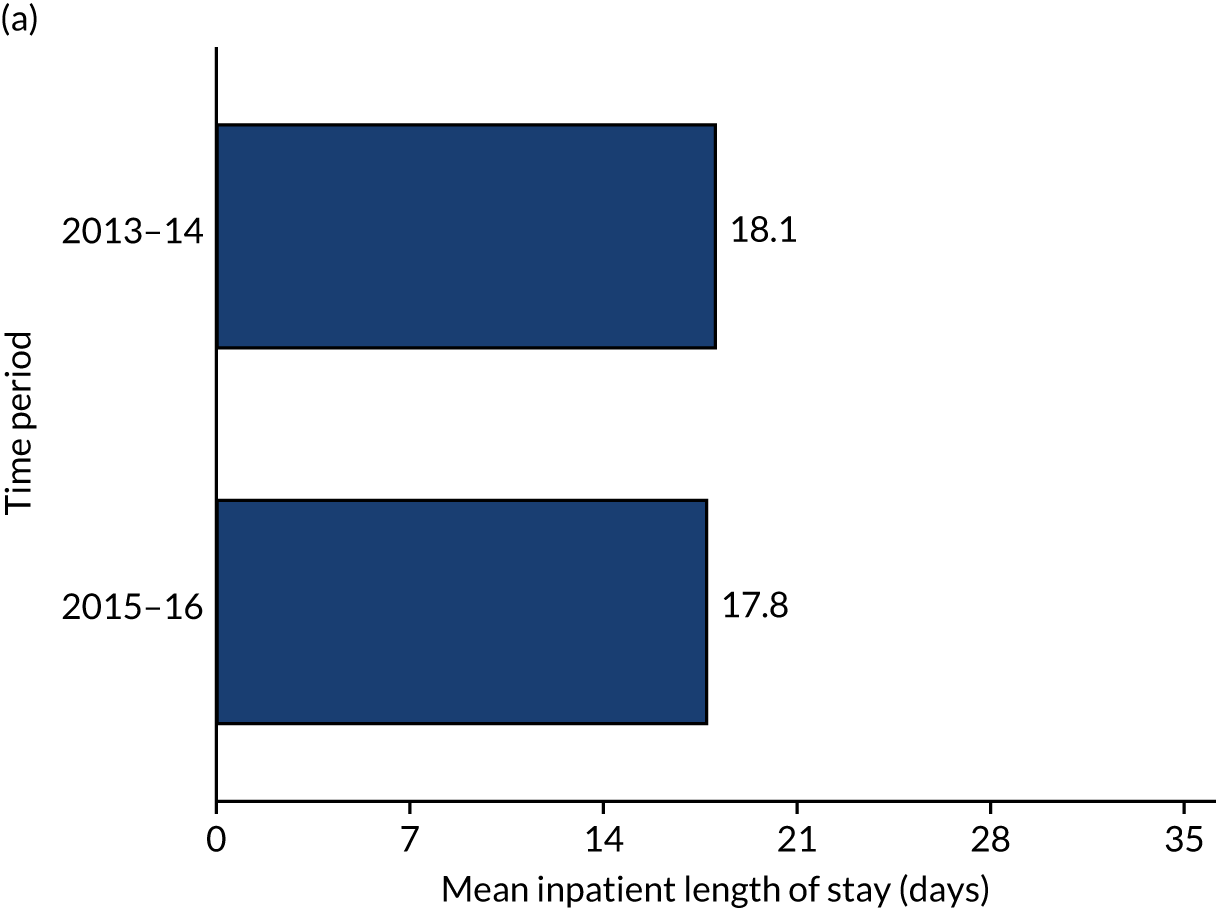

Table 14 presents the results from the linear multilevel model. Again, we controlled for patient characteristics, SSNAP admitting hospital score and average ASCOF rates for each admitting hospital. There was no significant interaction between receiving ESD and time period (p = 0.79); therefore, the effect of ESD was similar in both time periods, despite more patients accessing ESD over time. Therefore, the main effect of ESD across both time periods was estimated to be an increase in the length of hospital stay by an average of 18.8% (95% CI 13.9% to 24.0%) compared with patients who did not receive ESD on their care pathway. Furthermore, the main effect of the 2015–16 time period compared with the 2013–14 time period was found to significantly reduce the length of hospital stay by an average of 14.0% (95% CI 12.2% to 15.9%).
| Inpatient length of stay models | Unadjusted | Adjusteda |
|---|---|---|
| Patients (n) | 49,667 | 49,266 |
| Admitting hospitals (n) | 41 | 41 |
| Patients per admitting hospital (n) | ||
| Minimum | 115 | 106 |
| Mean | 1211.4 | 1201.6 |
| Maximum | 2512 | 2446 |
| Intraclass correlation coefficient | 0.04 | 0.08 |
| ESD on the care pathway, coefficient (95% CI); p-value | ||
| Received ESD | 0.14 (0.09 to 0.20); < 0.001 | 0.17 (0.13 to 0.22); < 0.001 |
| 2015–16 time period | –0.06 (–0.09 to –0.04); < 0.001 | –0.15 (–0.17 to –0.13); < 0.001 |
| Received ESD × (2015–16 time period) | –0.05 (–0.11 to 0.02); 0.162 | 0.01 (–0.04 to 0.06); 0.790 |
Using the parameter estimates from the adjusted multilevel model results in Table 14, we calculated the predicted average length of hospital stay for patients who did and patients who did not receive ESD in both time periods. We exponentiated the predictions to convert the unit back to days and present the results in Figure 9. This visual representation highlights our main findings from this repeated cross-sectional analysis, which is a reduction in average length of hospital stay for both ESD and non-ESD patients and that the ESD patients stayed in hospital longer than non-ESD patients by about 1 day on average across the two time periods.
FIGURE 9.
Predicted mean length of hospital stay by time period and whether or not patients received ESD.

The degree of clustering was low in both adjusted multilevel models (adjusted intraclass correlation coefficients 0.08 and 0.08, respectively) implying that the total variance that we observed in the length of hospital stay data was more greatly accounted for by the patients than by the admitting hospitals.
Discussion
This study has investigated the effect of ESD on length of hospital stay in real-world settings, with the aim to inform evidence-based improvements in stroke care. Unadjusted findings indicated that stroke patients who received ESD spent approximately 1 day longer in hospital than all other patients; however, those who received ESD differed from those who did not in their characteristics. With adjustment using two different designs and alternative analyses for the differing case mix, the length of hospital stay remained longer for those who received ESD on their care pathway. This contrasts with findings from original ESD randomised controlled trials, in which a reduction in length of hospital stay was reported. 10
This is an important finding, particularly when considering the implementation of ESD in practice. The promise of reducing the length of hospital stay made ESD attractive with regard to cost savings and is likely to have contributed to the widespread implementation in England. 7,11 The economic implications of ESD in the real world have previously been investigated through simulation modelling (informed by SSNAP data similar to data used here). 85 The authors reported an estimated mean length of hospital stay for ESD patients that was 8 days less than that for non-ESD patients and, thereby, derived cost savings associated with modelling the increased use of ESD.
However, an important difference with that economic analysis and the study reported here relates to the fact that we used actual and total inpatient length of stay data combining different inpatient settings where applicable on a per-patient basis. Analysis showed that ESD patients were younger and more likely to have a lower modified Rankin Scale score at inpatient discharge. The simulation modelling findings drew on sample statistics derived from patient distributions for each separate inpatient setting, stratified by age category and modified Rankin Scale score, and their results were driven by assuming that more severe stroke survivors received ESD. What our study adds is that when comparing ESD with non-ESD patient groups matched for important patient characteristics, receiving ESD does not relate to a reduction in length of hospital stay.
Another important consideration is that the average length of hospital stay for stroke survivors overall has reduced dramatically over the last 20 years, from 40 days to 20 days, the latter decade of which our study captures between the two cohorts in this chapter (i.e. 2013–14 and 2015–16). 80 This makes it less likely for an intervention like ESD to have an effect (than the years 1997–2004 when the original UK clinical trials were conducted). 10 That ESD in this study was associated with an average increase in length of stay of 1 day could be interpreted as the need for additional time to facilitate the transfer of care to the ESD team, rather than stroke survivors simply leaving hospital without support (if ESD was not available). Previous studies have also highlighted transfer problems relating to lack of joint working between health care and social care. 23,38,72 Chapter 4 added to this debate by highlighting the importance of access to a social worker as part of the ESD team. 1
What was not possible to investigate in this study was whether or not access to ESD (despite an additional day in hospital) was associated with improved patient outcomes over the longer term. Recent observational studies in Sweden suggest patient and care-giver benefits related to the provision of ESD in regular clinical practice, in line with our previous study findings from England. 86,87 We suggest that the routine collection of additional validated patient outcome measures (e.g. measuring activities of daily living, general health/mood and quality of life) at longer follow-up periods in national stroke audits or registries is required. 10,12,13
Like other observational studies, this study had its limitations. Although the numbers of patients were sufficient for the analysis undertaken, by focusing on specific regions of England the transferability of findings could be questioned, particularly outside England. Other limitations include the potential sources of residual confounding and the reliance on SSNAP data being accurately reported by hospital teams. Length of hospital stay data are inherently variable and, although we tried to include a proxy measure for other sources of delays in discharge, analysis would have benefited from social care-related patient-level variables. 85,86 Patients also experienced a series of hospital stays (e.g. transfer between acute and rehabilitation wards), relying on accurate transfer of SSNAP records between hospitals and resulting in us focusing on total length of hospital stay and ESD provision on a care pathway. 88 What this means is that the impact of ESD on a particular hospital may not be apparent, which may be of more interest to providers of hospital services.
Conclusion
Original clinical trials of ESD were conducted across the world and implementation of ESD is recommended in many countries’ stroke guidelines. 5,6,62–65 This study investigated the impact of ESD in real-world settings and focused on the length of hospital stay. ESD was not associated with a reduction in length of hospital stay as previously reported in clinical trials, although the increased average length of stay was just 1 day. This highlights the importance of investigating whether or not trial-based outcomes of interventions are realised in the real world. What remains to be investigated and reported are the benefits of accessing ESD over the longer term. In addition, by focusing the analysis on patients who would have been eligible but did not receive ESD, we have highlighted an important gap in service provision.
Chapter 6 Work package 2: service descriptions
Introduction
Findings from WP1 (see Chapter 4) suggested that a range of ESD models had been adopted. In WP2, our aim was to gain a deeper understanding of the types of model in operation. Using a purposive sampling approach, case study sites from WP1 were selected based on the level to which evidence-based ESD was implemented (contrasting ESD models) and the influence of rurality on ESD effectiveness (urban vs. rural sites). To create service descriptions of each ESD model in operation, we collected documentary evidence from the six purposively selected sites. We also collected data about staffing and adopted models of care from each team leader using a questionnaire (also used in Chapter 7). These data were complemented and validated by qualitative data collected in ESD team interviews (details in Chapter 8).
This chapter provides a brief overview of the six services that participated in our WP2 fieldwork research.
More detailed information about each individual service is provided in Appendix 3. Service descriptions are based on data collected during WP2, information gathered at meetings with services during site visits, documentary material and interviews with staff and commissioners within the data collection process.
Site summary
The sites were labelled A–F, with site A being the most urban through to site F being the most rural. Sites A and B were clearly distinguished as hybrid services providing both an ESD service and a community rehabilitation service. The more rural services were not providing a clearly defined hybrid service but they did offer additional time and service to their patients based on need beyond the level of a strict ESD service.
The individual service descriptions in Appendix 3 highlight variation in the way that services had been developed and configured to meet the needs of the local stroke pathways and geography. Some had been established for a much longer period of time than others, and had gradually adapted over time to meet the changing needs of their population and wider health services.
Models of operation were tailored to each service, with some teams taking referrals widely, including from GPs and by self-referral, whereas other teams adhered rigidly to acute trust referrals only. Some teams in-reached to the acute trusts and others did not. Eligibility criteria also varied depending on the way that services were configured and again were related to the wider stroke pathway, capacity and resources (Table 15) in the team, and the availability of other services to take patients with more severe disability. Patient length of stay varied from the recommended average of 6 weeks to 20 weeks.
| Discipline | Site | |||||
|---|---|---|---|---|---|---|
| Aa | Ba | C | D | E | F | |
| Occupational therapist | ||||||
| Grade 7 | 0.21 (0.83) | 0.8 (1.6) | 1 | 0.5 | 0.64 | 0.92 |
| Grade 6 | 0.24 (0.94) | 0.9 (1.8) | 1.8 | 1 | 1.4 | 6.71 |
| Grade 5 | N/A (N/A) | N/A (N/A) | 2 | 0.5 | 1 | 1 |
| Physiotherapist | ||||||
| Grade 7 | 0.16 (0.65) | 0.8 (2.29) | 0.81 | 0.6 | 0.64 | 2.64 |
| Grade 6 | 0.68 (2.71) | 0.75 (1.5) | 1.8 | 1 | 1.64 | 6.59 |
| Grade 5 | N/A (N/A) | N/A (N/A) | 2 | 1 | 1 | 6.49 |
| Speech and language therapist | ||||||
| Grade 7 | 0.15 (0.6) | 0.32 (0.64) | N/A | N/A | 0.6 | 0.8 |
| Grade 6 | 0.13 (0.5) | N/A (N/A) | 1 | 1 | 1 | 2.1 |
| Grade 5 | N/A (N/A) | 0.2 (0.4) | 0.6 | 0.5 | N/A | 1 |
| APs at grade 4 | 0.91 (3.64) | 0.5 (1) | N/A | N/A | 2.6 | 7.8 |
| RAs at grade 3 | 0.35 (1.39) | 0.92 (1.84) | 7.55 | 1.9 | 5.71 | 9.9 |
| CSWs at grade 2 | 0.11 (0.43) | N/A (N/A) | N/A | 0.05 | N/A | N/A |
| Nurses | Access to | 0.5 (1) | 1.32 | N/A | 5.05 | Access to |
| Psychologists | Access to | Access to (0.8) | Access to | 0.1 | 1.6 | N/A |
| Social workers | Access to | N/A (N/A) | N/A | 0.1 | N/A | Access to |
| Dietitians | 0.25 (1) | N/A (N/A) | N/A | N/A | N/A | N/A |
| Administration | 0.53 (2.12) | 0.8 (1.6) | 0.62 | 1 | 1 | N/A |
| Manager | 0.06 (0.23) | N/A (N/A) | N/A | 1 | N/A | N/A |
| Total | 3.76 (15.03) | 6.49 (14.47) | 20.5 | 10 | 23.88 | 45.95 |
| Patient caseload | 183 (696) | 312 (551) | 440 | 268 | 509 | 874 |
There were some commonalities between the teams, including stated responsiveness times driven by national SSNAP targets. Systems, processes and ways of working were configured to ensure that patients were seen within 24 hours and had a therapy assessment within 72 hours of admission to the team, although mechanisms for achieving these targets varied widely. All teams held weekly MDT meetings and routinely collected data for audit and evaluation purposes over and above the nationally mandated SSNAP data set.
Team compositions
Table 15 displays the MDT compositions for the six sites in terms of WTE units for all of the main job types and grades. Only two services had a stated manager as part of the team and the most rural service in this study was operating without administrative support or a manager at the time of our data collection. The total WTE units for each service appear to increase as the patient caseload increases, but on closer inspection the two stated hybrid services see approximately double the number of patients per WTE unit than the ESD-only services. It is important to note that the hybrid services in this study operate in the most urban areas, therefore, are dealing with more densely populated areas than the more rural ESD-only services in this study.
As can be seen from Table 15, the variation in the models is considerable and has consequences for the effectiveness of the team and monetary costs associated with providing the service. These costs and consequences are explored and discussed in greater detail in Chapter 7.
Chapter 7 Work package 2: evaluating stroke early supported discharge using cost–consequences analysis
Parts of this chapter have been adapted from Fisher et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Introduction
Cost implications are likely to be an important consideration with regard to successful adoption and implementation of interventions, such as ESD. There is a drive for cost-effective, evidence-based practice that seeks to ensure that limited health-care resources are used to their maximum benefit. 89,90
Some of the more technical forms of economic evaluation (including cost-effectiveness, cost–utility and cost–benefit analyses) have caused concern in relation to the lack of impact on the practice of service development. 91–93 The use of QALYs (used in cost–utility analyses), a utility-based index measure of health benefit, presents particular interpretation problems in a policy-making context. Complex interventions, such as ESD, have multiple health- and non-health-related outcomes, and it is neither feasible nor meaningful to combine the costs and outcomes into a single measure, such as an incremental cost-effectiveness ratio, as is undertaken in cost-effectiveness or cost–utility analysis.
The CCA is advocated, which presents information about costs and outcomes (clinical and other) in the form of a balance sheet. 94 Outcomes or consequences are shown in their natural units (some of which may be monetary), and costs and outcomes are not combined into a single measure. This economic evaluation approach is very versatile and practical. 95 CCA allows the decision-maker to determine whether or not, overall, the treatment or intervention or service is worth carrying out or commissioning. 96 The CCA approach helps to refine economic methods, identifying relevant costs and outcomes, and helps to generate hypotheses for definitive cost-effectiveness studies. It provides a broad and rich source of economic information, which is increasingly needed by NHS decision-makers. 97
Given our overall realist approach and the recognised importance of context, the wider costs and benefits associated with the intervention need to be acknowledged. 34 Moreover, the resources associated with the delivery of a complex intervention, such as ESD, are likely to equate to different costs in different places. 35 Hence, we undertook a CCA in which the costs associated with different models of ESD service provision were considered in the light of the geographical context in which they were operating and the outcomes or benefits that were achieved.
Materials and methods
Sampling
Six stroke services offering ESD were included in the study. These services were purposively selected as part of a wider research study in which services were qualitatively evaluated. The purposive sampling frame was designed to compare different models of ESD provision, operating in areas of differing levels of rurality. 37 The six services have been anonymised in this chapter and are represented by the first six letters of the alphabet.
The level of rurality measure was based on the rural–urban classification reported for the geographical area associated with the NHS CCG that had procured each ESD service. 67 Each CCG in England has a geographical area over which it operates to procure NHS services. Where an ESD service included in this study was managed by multiple CCGs the weighted average level of rurality was calculated based on the prevalence of stroke and transient ischaemic attack in that commissioning area (figures obtained from the NHS Quality and Outcomes Framework). 68
Data capture
Data regarding staffing and adopted models of care were collected from each team leader using a questionnaire that was designed by the authors. The models of care questions were based on the 2015 SSNAP post-acute phase 2 audit. 98 The staffing questions asked about each team member’s role, the WTE hours of work per week, the grade, the cost at the middle of the band and the associated overhead costs for each team member. This information enabled the authors to calculate the number of staff within each service, as well as the total staff cost. The number of patients admitted to the service over a 1-year period between 2018 and 2019 was also captured from the same questionnaire. The questionnaire asked about any other staff who were funded elsewhere that the patients had access to, as well as all non-staff costs, including travel, training and equipment. Service specifications from each service were also collected to supplement the data.
Costs
Information regarding MDT composition and the workforce (WTE) was used to calculate the total staff costs. Staff training, equipment and travel costs associated with delivery of rehabilitation were used to calculate total non-staff costs. Using patient caseload information, direct costs per patient were calculated for the 2018–19 time period.
Consequences
The main outcome or consequence of focus in this chapter was each service’s adherence to the ESD core components, which was measured using an ESD consensus score. The ESD consensus score has been previously developed using defined evidence-based core components of ESD, as outlined in an international consensus document and evidence-based criteria utilised by the SSNAP in the UK. 13,98 This 17-item ESD consensus score was used to measure the adoption of core components by each of the six services’ ESD models, for example service composition (core service and others), staff training, service meetings and service specificity. Each item was awarded a binary yes (1 point) or no (0 points) response in relation to each service meeting that particular criterion. This 17-item ESD consensus score was calculated based on questionnaire data for each of the six ESD services. The variability observed in ESD consensus scores was used to indicate the different models of service delivery and whether or not these adhered to evidence-based core components.
Analysis
We tabulated each service’s ESD core components (Table 16) to show how the consensus score was obtained. Descriptive statistics were used to quantify different characteristics across the six ESD services. Costs and consequences for all six services were then collated in a cost–consequences balance sheet. The services were ordered by the percentage of rurality and the total (including staff and travel) costs were presented in aggregate and on a per-patient basis. Consequences were expressed as the total ESD consensus score obtained (out of 17). This measure was used as a consequence to indicate the level by which each service had adopted an evidence-based service model. Pairwise linear correlations of the variables contained in the balance sheet were conducted to assist with understanding the associations observed, and statistical significance was determined at the 5% level for the accompanying p-values. Given that the size of a team may be directly related to the cost of that team, the number of staff per service was added as a comparator variable in the correlation analysis to help appreciate any differences between the aggregate costs and the costs disaggregated by the number of patients seen by each service.
| ESD consensus score component | Site | |||||
|---|---|---|---|---|---|---|
| Aa | Ba | C | D | E | F | |
| Core team members meeting or exceeding recommended WTE level per 100 stroke patients | ||||||
| Doctors: ≥ 0.1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Nurses: ≥ 0.4 | 0 | 0 | 0 | 0 | 1 | 0 |
| Occupational therapists: ≥ 1 | 0 | 0 | 1 | 0 | 0 | 0 |
| Physiotherapists: ≥ 1 | 0 | 0 | 1 | 0 | 0 | 1 |
| Speech and language therapists: ≥ 0.3 | 0 | 0 | 1 | 1 | 1 | 1 |
| Access to other team members | ||||||
| Clinical psychologists | 1 | 1 | 1 | 1 | 1 | 0 |
| Social workers | 1 | 1 | 0 | 1 | 0 | 1 |
| Rehabilitation assistants | 1 | 1 | 1 | 1 | 1 | 1 |
| Training opportunities | ||||||
| Nurses | 0 | 0 | 1 | 0 | 1 | 0 |
| Therapists | 1 | 1 | 1 | 1 | 1 | 1 |
| Rehabilitation assistants | 1 | 1 | 1 | 1 | 1 | 1 |
| MDT meetings | ||||||
| Weekly meetings | 1 | 1 | 1 | 1 | 1 | 1 |
| Core team attend | 0 | 0 | 1 | 0 | 0 | 0 |
| ESD member attends acute meeting | 0 | 1 | 0 | 1 | 1 | 1 |
| Service | ||||||
| Stroke specific | 1 | 1 | 1 | 1 | 1 | 1 |
| Median waiting time between referral and ESD of ≤ 1 day | 0 | 1 | 1 | 1 | 1 | 1 |
| Weekly service of > 5 days | 0 | 1 | 0 | 0 | 1 | 1 |
| Total ESD consensus score | 7 | 10 | 12 | 10 | 12 | 11 |
Results
Table 16 shows the 17-item ESD consensus score for each of the six ESD services and represents the level of adherence to the core components of ESD service delivery. The information presented indicates that no two services are configured in the same way even if they achieved the same consensus score, thereby underlining the variability in models of service delivery. In addition, the two services that provide both ESD and community rehabilitation did not meet or exceed the recommended WTE level of core staff per 100 patients.
Table 17 provides an overview of the six services involved in this study. The services varied in terms of the percentage of rurality of their location, which is in line with our purposive sampling strategy. There were also differences in the patient caseload and number of staff. We also noted some variability in their ESD consensus scores, which indicated different levels of adherence to an evidence-based service model.
| Site | Location: rurality (%) | Patient caseload (2018–19) (n) | Staff (n) | ESD consensus score |
|---|---|---|---|---|
| Aa | 0 | 183 (696) | 28 (28) | 7 |
| Ba | 5 | 312 (551) | 11 (19) | 10 |
| C | 34 | 440 | 24 | 12 |
| D | 50 | 268 | 13 | 10 |
| E | 66 | 509 | 28 | 12 |
| F | 71 | 874 | 50 | 11 |
The cost–consequences balance sheet is shown in Table 18. The services with the highest overall costs were located in the most rural areas. The largest element of any ESD service cost was pay. As the level of rurality increased, the travel cost on a per-patient basis also increased.
| Costs and consequences | Site (% rurality) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A (0)a | B (5)a | C (34) | D (50) | E (66) | F (71) | |||||||
| Total | Per patient | Total | Per patient | Total | Per patient | Total | Per patient | Total | Per patient | Total | Per patient | |
| Cost (£) | ||||||||||||
| Overall | 108,777 (446,679) | 594 (641) | 258,333 (688,261) | 827 (1249) | 700,424 | 1591 | 383,844 | 1432 | 856,725 | 1683 | 1,679,273 | 1921 |
| Staff | 106,849 (427,397) | 583 (614) | 243,040 (660,638) | 778 (1198) | 666,185 | 1514 | 356,144 | 1328 | 820,334 | 1611 | 1,558,385 | 1783 |
| Travel | 1333 (13,331) | 7 (19) | 12,180 (22,000) | 39 (39) | 32,799 | 74 | 20,000 | 74 | 40,569 | 79 | 70,932 | 81 |
| Consequence | ||||||||||||
| ESD consensus score | 7 | 10 | 12 | 10 | 12 | 11 | ||||||
The pairwise linear correlation matrix is presented in Table 19. This analysis confirmed that higher costs per patient (overall, staff and travel costs considered separately) were significantly and positively associated with ESD services in areas of higher rurality, as well as higher ESD consensus scores. The aggregate costs (not on a per-patient basis) were not associated with ESD consensus scores. By contrast, the aggregate overall and staff service-level costs were significantly and positively associated with the number of staff in each service, that is the size of team but not on a per-patient basis. This contrast showcased how per-patient costs relate to the adherence to evidence-based core components of ESD service delivery, whereas aggregate costs relate to the size of team.
| Measure | Rurality (%), R (p-value) | Staff (n), R (p-value) | ESD consensus score, R (p-value) |
|---|---|---|---|
| Staff (n) | 0.53 (0.28) | ||
| ESD consensus score | 0.70 (0.12) | 0.14 (0.79) | |
| Overall cost per patient (£) | 0.95 (0.00) | 0.53 (0.28) | 0.83 (0.04) |
| Staff cost per patient (£) | 0.94 (0.00) | 0.53 (0.28) | 0.84 (0.04) |
| Travel cost per patient (£) | 0.90 (0.02) | 0.26 (0.62) | 0.89 (0.02) |
| Overall cost (£) | 0.81 (0.05) | 0.84 (0.04) | 0.59 (0.22) |
| Staff cost (£) | 0.82 (0.05) | 0.83 (0.04) | 0.60 (0.21) |
| Travel cost (£) | 0.86 (0.03) | 0.78 (0.07) | 0.67 (0.14) |
Discussion
This chapter has evaluated different stroke ESD service models in different geographical settings according to their operational costs and adherence to core components of service delivery using CCA. We present an analysis of the costs, consequences and their associations using data collected directly from six purposively sampled ESD services. This study has provided evidence of variability in terms of the adopted model, which was measured as the level of adherence to ESD core components using an ESD consensus score. No two services proved to be the same in terms of the ESD consensus score, level of rurality and size of team in terms of the number of staff and patients, as well as the overall, staff and travel costs.
This study has shown that higher ESD service costs per patient were significantly associated with the level of rurality in which the ESD service operated. It is known that health-care service provision in rural areas is more costly than in urban areas for a similar level of service provision. 99,100 Higher costs have been attributed to difficulties in staff recruitment and retention, higher travel costs and non-productive staff time when travelling, as well as difficulties in realising economies of scale while adequately serving sparsely populated areas. 100
In terms of consequences, higher service costs on a per-patient basis were associated with greater adherence to the evidence-based core components, as measured by our ESD consensus score. One important aspect of the ESD consensus score was to determine if a service meets the recommended WTE level of core staff per 100 patients. 1 Therefore, services that were resourced appropriately and had the adequate number of staff per patients were awarded a higher ESD consensus score. In this study, we found that it was the lower WTE amount of core staff per 100 patients within the most urban service, as displayed in Table 16, that contributed to this service having the lowest ESD consensus score. Furthermore, our correlation analysis in Table 19 showed how these staff to patient ratios were detected by the significant positive association between service costs per patient and the ESD consensus score. Therefore, resourcing a service that adheres to the core components of ESD service delivery requires costs to be appreciated on a per-patient basis rather than just in aggregate.
This study does suffer from some limitations. A major limitation is the small sample size. There were 142 ESD services in operation in the UK in 2015, but data from only six services (4%) were used in this study. Therefore, our findings are suggestive and the associations reported would benefit from being tested in a larger sample, including further exploration of different ESD and community stroke rehabilitation models. 98 Another limitation pertains to our use of CCA. This CCA provides a snapshot in time, which suffers from being unable to capture all of the consequences, especially indirect effects arising from ESD service provision, as well as failing to capture consequences that occur at other points in time. This limitation hinders decision-makers, who may still encounter difficulties in drawing unambiguous conclusions for service delivery. 94
The evidence relating to the cost implications of ESD is mixed, with previous studies reporting reductions, increases and no differences compared with treatment as usual. 10,79 Teng et al. 101 postulate that any reductions in hospital length of stay associated with ESD translate into negligible cost savings, as any beds made available are then used by other patients. From this perspective, the authors suggest that ESD can be viewed as an additional cost. In this chapter, we have looked at the cost of providing ESD across six services and presented evidence to show how this cost differs across the level of rurality, size of team and adherence to ESD core components of service delivery.
Conclusion
We conclude that additional resource and the associated costs were required by rural services to meet evidence-based standards (and appropriate staff to patient ratios). Our previous findings would suggest that additional cost implications may be associated with additional patient benefit via the ESD service’s ability to deliver a more responsive and intensive service. 1 We recommend further research to evaluate observed cost differences, across different geographical areas, from a patient outcome perspective.
Chapter 8 Work package 2: staff perspectives
Introduction
This chapter presents a qualitative interview study with staff members involved in the delivery of stroke ESD services. A realist approach was used to guide both data collection and data analysis, which was informed by three a priori-defined programme theories (see Chapter 3). The results section presents key CMO configurations identified for each of the programme theories. Key messages are discussed in the light of previous literature, including methodological strengths and limitations.
Aims and objectives
The aim of this qualitative study was to obtain a better understanding of the interaction between contextual influences, core intervention components and the reasoning and actions of staff members involved with ESD delivery. Through the process of interview collection and analysis we assessed and refined the three programme theories that we developed at an earlier stage:
-
Programme theory 1 – ‘The adoption of evidence-based core components is important for the intervention to be effective in practice’.
-
Programme theory 2 – ‘Core evidence-based components of ESD will operate differently in urban versus rural settings’.
-
Programme theory 3 – ‘The quality of communication processes between key stakeholders and services in the pathway will influence the implementation of an evidence-based service’.
Data collection
The site selection process is described in Chapter 2. Information was collected through both one-to-one and group interviews with up to 20 NHS staff participants who were associated with each ESD service. Purposive and snowball sampling was employed to recruit a cross-section of key informants for each of the participating services.
Participants had to meet the following eligibility criteria:
-
adults (aged ≥ 18 years)
-
NHS clinical staff participants involved in the clinical delivery of the ESD service (i.e. consultants, OTs, RAs, physiotherapists, social workers, nursing staff and psychologists)
-
NHS non-clinical staff participants involved in managing the delivery of the ESD service (i.e. office managers and administrators)
-
stroke service commissioners (i.e. members of a CCG involved in the commissioning of ESD services).
Recruitment to the study started in September 2018 and data collection continued until August 2019. The initial approach to ESD staff members was through their line manager, who gave permission for their staff to be approached to participate in the study. The service leads were approached by the research team (RF, NC and AB) and were invited to participate in the study using an e-mail introduction in which we included the participant information sheet. Researchers also offered to visit the sites and present the study to clinical teams to give them the opportunity to have their questions answered. All participants provided written informed consent and were given a unique ID number to ensure anonymity and confidentiality.
Data analysis
Data were analysed following an iterative, retroductive process moving between deductive and inductive phases. 21 We started our analysis using a top-down approach, the starting point being three key programme theories and related CMO configurations. Staff participants’ narratives and documentary data from each site were examined to identify connections between contexts, mechanisms and outcomes, which were coded into CMO strings. 102 These were then further developed and refined through new insights from participants’ narratives during the early stage of data collection. The three programme theories formed the overarching framework that guided the types of hypotheses that we investigated through the interview data and, therefore, what we coded in participants’ narratives. However, we also looked for examples that both confirmed or disconfirmed the theory or pre-existing CMOs or led to further refinements, allowing for an inductive process to take place. The coding process of the interviews took place in the following stages:
-
Participant-level data.
At this stage, the units of analysis were individual interviews and focus groups. The same coding and analysis processes were followed for both of these types of interview. Analysis started by reading through each transcript to map out where different topics and theories were being introduced and identify potential connections between CMOs. Service descriptions synthesised from interviews and documentary evidence served to provide background information on the operation of each service. Coding was guided by the overarching framework of the key programme theories. Only text relevant to one of the three areas described by each programme theory was considered for coding. Text extracts were coded as candidate CMO strings under the relevant core programme theory/theories, where the connections between these elements could be discerned from participants’ narratives. CMO configurations were coded as either triads (where all three elements are present) or dyads (e.g. C–M, M–O combinations). 102 At this stage of preliminary coding, it was not always clear whether certain processes operated as contexts or mechanisms. We were conscious that these initial configurations may need to be revisited/refined at a later stage of analysis as the connections between these features became better understood. Where it was not possible to identify dyads or triads but the inclusion of a text extract was considered important, the extract was coded as referring to distinct CMO processes. Information coded this way was retained only if it provided insights towards the development of CMO patterns when combined with information from other interviews within the same site.
-
Site-level data.
Once the analysis of interviews from each site was completed and insights from both one-to-one and group interviews were brought together to identify key CMOs, cross-site comparisons were conducted to identify confirming and disconfirming cases and explore how pertinent mechanisms interact with site-specific contextual conditions to generate variation in outcomes. The identified CMO configurations were related back to the original programme theories and further refinements were made.
The analysis was conducted by two members of the research team (NC and TC). They initially coded data independently, producing tables of CMO configurations related to each overarching programme theory. They then discussed and compared their analysis and insights with the rest of the research group until agreement was reached that no further revisions and refinements were required.
Results
As shown in Table 20, we spoke to 117 staff members in total, through either one-to-one or focus group interviews. In the following section, we present our CMO configurations and provide supporting interview quotes. Within each programme theory, subsections describe key CMOs organised thematically under relevant headings. To facilitate the reader, descriptions corresponding to context, mechanism and outcome elements are indicated in the text in brackets. The narrative is complemented by figures showing how the interaction of identified contexts and mechanisms leads to intended (in coral boxes) or unintended outcomes (dark purple boxes). The participants are identified in the following quotations by the letter denoting the site that they came from, an ‘S’ for staff and a number showing the order of interview at that site. Focus group quotations are prefixed with an ‘FG’ and include an ‘R’ plus a number to indicate the initial responder order where required.
| Site | Individual interviews (n) | Focus group attendees (n) | Total staff participants (n) |
|---|---|---|---|
| Aa | 5 | 12 | 17 |
| Ba | 5 | 15 | 20 |
| C | 8 | 9 | 17 |
| D | 2 | 13 | 15 |
| E | 9 | 16 | 25 |
| F | 6 | 17 | 23 |
| Total | 35 | 82 | 117 |
Programme theory 1: ‘the adoption of evidence-based core components is important for the intervention to be effective in practice’
This programme theory investigated how participants responded to the adoption of evidence-based intervention characteristics that they identified as key to the operation of the service. We remind the readers that, according to research13 and clinical guidelines,5 core components include the provision of a responsive stroke-specialist rehabilitation service to eligible stroke survivors (mild to moderate disability) and at an intensity similar to what they would receive at hospital. The intervention is delivered by a co-ordinated MDT (e.g. physician, physiotherapist, OT and SLT) that has regular weekly MDT meetings and regular meetings with stroke unit hospital staff. Each of the components is described in a separate section through relevant hypotheses (CMOs) about how prominent contextual factors interact with intervention resources and staff’s reasoning to lead to intended and unintended outcomes.
Patient eligibility criteria
These CMOs concerned how teams responded to clinical guideline recommendations for admitting patients with mild to moderate disability. Services had differing approaches in relation to adherence to selection criteria. CMOs described in Adhering to eligibility criteria reflect staff’s responses to the adoption of eligibility criteria regarding disability levels. In Flexibility in applying eligibility criteria, CMOs concern the flexibility demonstrated by some services in the application of selection criteria in response to pressures posed by certain contextual characteristics, such as the availability of community stroke rehabilitation in the local stroke care pathway.
Adhering to eligibility criteria
Most respondents agreed that adhering to selection criteria regarding disability levels (M) helped the services to manage capacity and promote responsiveness (O) (Figure 10). Services struggled to offer the therapeutic intensity that is required to address the needs of more severe patients (C), and attempting to cater for their needs could dilute the intensity of the service for the rest of the patients or reduce the flow of new patients into the service:
We need to be targeted to be able to take new patients – to have capacity to take on new patients. Once upon a time, they would have seen patients for up to a year within this team. They would just be on the books.
BS20
Yes we are very strict with eligibility.
Even though you want to change it and you want to make exceptions, the moment you start doing it the more you’ll do it, you’ve just got to be cruel sometimes and say no to people.
Yeah. And I think not forgetting the fact that it’s supposed to be a virtual ward and it should be an intense service. So being able to provide that intense service by not offering too many slots depending on how many staff you have.
FGCS1
FIGURE 10.
Adhering to eligibility criteria CMOs.

One of the team leads (ES1) explained that focusing on the mild to moderate patients meant that hospital discharge became a less complex process (O); reasons included this patient group not requiring care packages and, therefore, avoiding delays in having to put these systems in place before returning home. Applying selection criteria was also identified as key to timely admissions to ESD (O). One team explained how they changed their model of service to improve responsiveness and further reduce hospital length of stay. Introducing two streams in the service allowed them to distinguish between mild to moderate patients with a straightforward discharge process and patients requiring more complex discharge planning. As a result, they managed to maintain the flow of patients from the hospital and free therapy time:
We honed our model to that under 15 days, over 15 days because prior to that, we all saw – all the patients that came in were referred and ready to go home, but what we found was everybody was getting caught up in very complex discharge planning and what have you, that actually to respond and keep the length of stay down for the more mild to moderate, higher level patients, became quite difficult. [. . .] So to keep this flow going, we developed this, so that we’re able to respond much quicker and that some of the therapists are able to free themselves up and keep themselves more flexible and not have a full caseload of very complex people.
FGBS2
Patients with mild to moderate disability levels were also considered more likely to be safe at home (O). Ensuring the safety of patients who had more severe disability was an important concern. One team questioned whether or not they would be able to provide the right equipment to support these patients at home (C). Relying on relatives to support patients with severe disability was risky (C) and respondents highlighted the need to consider the willingness and readiness of patients’ spouses and families to assume caring responsibilities. One team also noted the potential implications of admitting patients with more severe disability on staff well-being (O). After a trialling period of accepting more complex strokes, staff observed that staff sickness rates increased dramatically. Staff working harder to maintain the quality of the service at the expense of their own health was suggested as a potential explanation:
They get home and it’s actually the carers that really struggle and they just can’t cope, and that’s when accidents happen and they end up back in hospital, or infections and that sort of thing come on quite quickly.
FGES1
The context of an ageing population called for the management of increasingly complex patients with multiple health-care needs (C). Cognition was mentioned as an important comorbidity that could influence outcomes; however, this was mediated by other factors, such as a supportive home environment, social isolation and mood (C). Adding cognition to the eligibility criteria, however, was not considered the way forward because it could lead to the exclusion of patients who could benefit from the service, despite their cognitive problems. Teams also discussed how medical advances, such as the introduction of thrombolysis and thrombectomy, successfully addressed physical impairment but left other potentially hidden issues, including cognition, fatigue and mood, creating a ‘new type’ of patients: the ‘walking wounded’. Given that the services’ eligibility criteria focused on physical function, it was common for teams to admit patients who had retained some motor ability while having very complex needs (M). For instance, it was suggested that thrombolysis patients tended to be of working age and required additional support, such as vocational rehabilitation. The teams felt the pressure to respond to the needs of these patients without, however, always having the resources to do so (O):
At the minute because of thrombolysis and thrombectomy, we’re starting to see some new trends [. . .]. So the thrombectomy, thrombolysis as well, we’re seeing that they’re coming out a bit shocked, you know, that they’re physically fine but there’s a lot of quite unusual cognitive deficits coming out of thrombectomy and so I think in that there’s probably going to be another shift again of the kinds of patients we’re seeing in working age people, as well. From a vocational rehab point of view, we’re not funded to provide vocational rehab but again, we’ll do it. We’ll support people in it and the numbers of working age patients are going up as well.
FGBS1
I feel that some bed managers don’t understand what is a stroke. They think that if you’re medically stable, you can go home. But apart from being medically stable, you should be rehabilitation stable as well. Cognitively, if the patient is not able to function, can’t remember how to make a cup of tea, turn off the faucet, take his or her medication, it’s not going to be safe. We had one patient who was sent home, medically stable but cognitively not. The following week, the patient was cooking at 1 o’clock in the morning and all the medications went all over the floor. We had to phone the GP and send her back to the hospital because she doesn’t have capacity with her safety. If patients will go back to the hospital, it’s a failed discharge.
FS1
Flexibility in applying eligibility criteria
The availability and quality of community rehabilitation services in the catchment area (C) was a key factor influencing the level of flexibility demonstrated by the teams in the use of eligibility criteria (Figure 11). In some sites, patients who did not meet the criteria for ESD could have to wait for weeks or months to be admitted to a community rehabilitation service. The linearity of stroke care pathways also meant that patients who could not handle the intensity of ESD (e.g. owing to infection or fatigue) at the point of discharge could lose the opportunity for specialist rehabilitation (C). In response, some ESD teams felt under pressure to use criteria flexibly and provide short-term support to patients who fell through the net or were deemed to be too complex for ESD (M). ES16 explained that, although their managers knew about these patients, they were not included in the official caseload nor reported on the SSNAP:
We may get somebody that, for example, has come out of a specialist neuro rehab unit who really should be going into community therapy, they won’t; they’ll come to ESD. Or somebody that’s needing less-intensive therapy who under different circumstances would go through community therapy but because they’re going to wait for 18 weeks they won’t, they’ll come through ESD. So we take anybody that’s had a new stroke and has got rehabilitation potential.
DS14
The difficulty at the moment is you might have someone who, in the early stages, it takes a long time to rehab but say in 3 months time they start to make some progress, but unfortunately they’re then out of the stroke pathway that we have, so it’s then very difficult to think, well this patient wasn’t ready at that time but now they may benefit from a period of rehabilitation and whether there’s a pathway that we can bring them back in when maybe rehab is more beneficial for them.
FGES1
FIGURE 11.
Flexibility in applying eligibility criteria CMOs.

Within the context of a fragmented pathway (C), it was not uncommon for hospital staff to upgrade a patient to make them eligible for ESD or delay a patient’s discharge until they met the selection criteria (M). According to ESD staff, these practices led to preventable hospital re-admissions or hindered ESD services’ potential to achieve a demonstrable reduction in hospital length of stay (O):
Some of the patients are, sort of heavier, more kind of on the cusp of whether we would accept them or not, and sometimes they will tell us that they hold patients in, because they think that they can get them to a level where they’re suitable for ESD. Because then they know that they’re getting really good rehab maybe.
CS1&2
As noted by one of the team leads, accepting patients with more severe disability would call for a more integrated stroke care pathway in which health-care and social services co-ordinate to support these patients at home:
If you had the resources could be extended to more severe patients?
Big question. You definitely have to have your care packages to deal with that.
It would require more integrated systems?
I definitely think so. It couldn’t just be picked up by health, so there would have to be very clear integrated working with people that are going to be ring fenced for that, and that’s the difficulty, isn’t it? Why would you take someone who was more dependent home, when you are going to have to rely on many more agencies to make sure that they get out there in a timely manner. You’ve got an ambulance crew that are prepared to take someone into the house because we have huge issues with transferring patients from the ambulance, to get them in to their homes again. So, that’s not just a decision that can be made by an ESD team providing it. It’s also about whether ambulance would support it, whether social services would support that, whether the carer’s want it.
ES1
In response to acute trust pressures, three teams saw higher-intensity patients in care homes to teach the staff positioning, mouth care and communication. This was considered important because care home staff had a high turnover and needed this support to effectively handle these patients. Although the service’s input would be short term, there was an impact on caseload and resources because double visits could be required. The aim was to prevent re-admissions and later complications rather than achieve improvements on disability:
However, if we’ve got somebody that’s going into a nursing home or a care home, particularly if they’re really quite impaired so if they’re bed bound or if they’ve got a new communication impairment, we will put two people into the care home for a short period of time just to make sure that the care home know how to move somebody, and also so the family are aware, because there’s such a high turnover in the care home staff.
DS14
Admitting more complex patients also related to how flexible the services could be around extending patients’ length of stay to spread treatments over a longer period of time (C). Most services did not have the capacity to significantly extend patients’ length of stay and called for a combined service that would provide both ESD and community stroke team components, tailored around patients’ needs. One service (site B) operated a case management system that involved bursts of treatment followed by breaks and scheduled reviews. Patients would be seen for a long time but not with the same intensity, which allowed services to maximise capacity while considering the medium- and long-term patient needs:
I think it’s a huge issue, I think the fact that we have an ESD team and then we have a CST [community stroke team] is a really, really big issue. Because I think the fact that you don’t just get your 6 weeks and then you are discharged is just so important because we know everybody won’t rehabilitate in 6 weeks, no matter how much you try and how skilled your team is. So for me, to think about the kind of long, you know, the medium-term and long-term support is crucial for people because the problems that they encounter post stroke carry on very often.
BS19
Responsiveness
These CMOs concerned how teams responded to clinical guideline recommendations for provision of responsive rehabilitation, with treatment beginning within 24 hours of hospital discharge (Figure 12). Teams had different approaches to managing the tension between capacity issues (C) and meeting responsiveness targets. In some sites, patients could be held in the acute trust until a slot became available (M), which unnecessarily prolonged their hospital length of stay (O). When caseloads were full (C), some teams refused admissions completely (M) and patients were discharged to the care of a non-specialised rehabilitation service, for which waits could be long. Where other services did not exist, patients did not receive any rehabilitation at all (O):
The difficulty for us is when we have far too many people coming out and it’s not possible to get around to see everyone within 24 hours [. . .] I think from a point of view of trying to get the message through to commissioning, the business plan that we put forward was focusing on the impact of having a higher number of patients, meant that the length of stay was increased. So, if you really want this snappy service, where you get people through quickly, you’re not going to achieve that. If you’ve got far too many patients coming out there, you can’t get around to seeing them.
ES1
We couldn’t accept that patient, because that day we didn’t have slots available and that patient couldn’t stay in the hospital for any longer because they’d allocated a package of care for her. So that patient didn’t receive ESD when she really, really did need it.
FGCS1
FIGURE 12.
The CMOs on ESD service responsiveness.
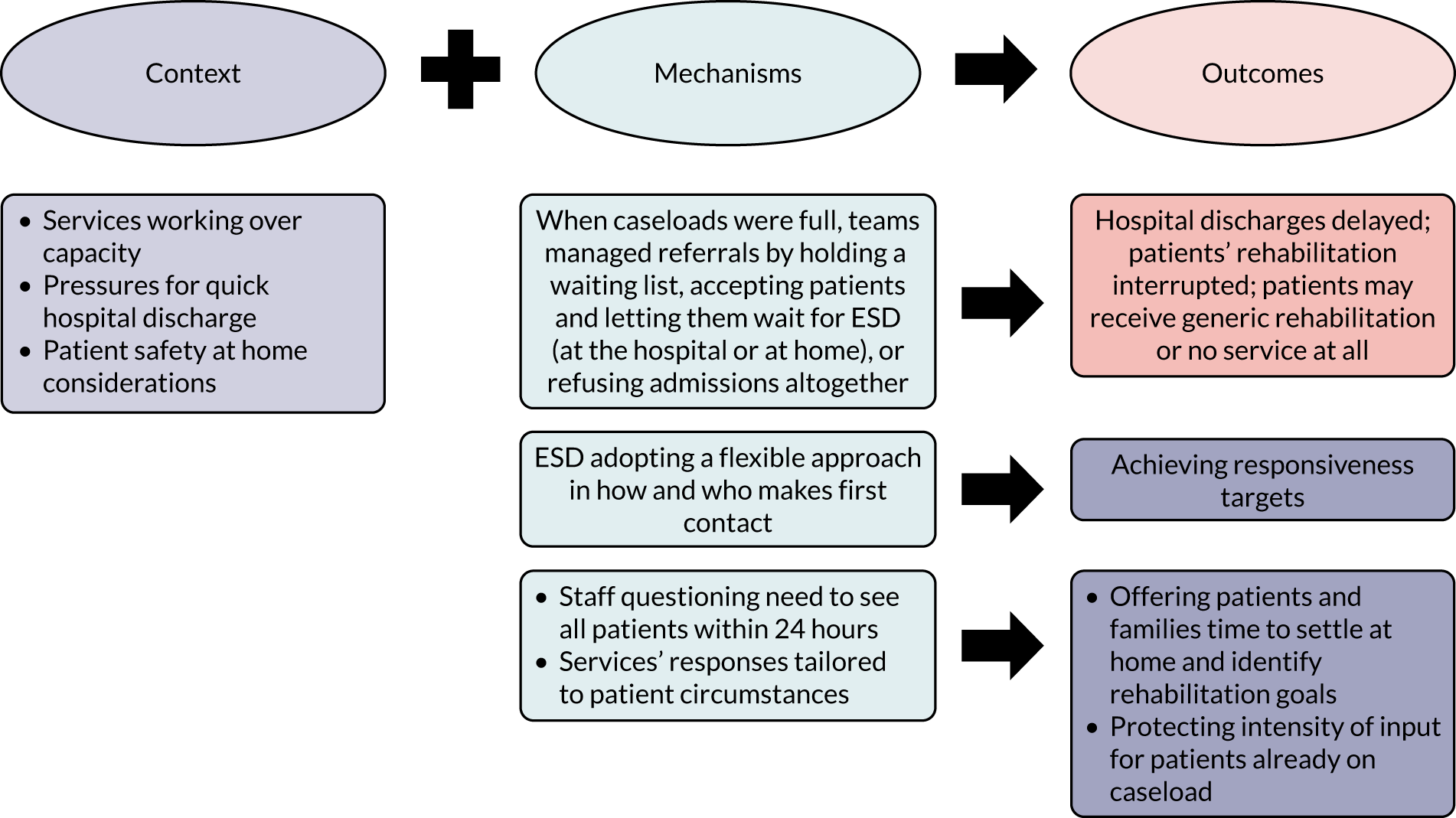
When patients were deemed safe at home (C), patients’ timely discharge from the hospital would be prioritised even if they had to wait at home for an ESD slot to become available (M). This approach resulted in interruptions to patients’ rehabilitation at a critical point for their recovery time (O). In these cases, the focus of the team shifted towards managing patients’ expectations while they were waiting to be seen. Referrers did not always relay this information to patients and in-reaching to the hospital allowed ESD staff to ensure that patients knew what to expect. To minimise the break in rehabilitation provision, two ESD teams would ask their respective acute trust to send therapy plans for the assistants to start work before a formal therapeutic assessment could be completed in the community:
So at the point of referring, we’re saying how long, roughly, it’s going to take us to get in. So we say, is the patient safe to wait for the week and then if that is the case, generally we’re in there quicker, but it sets their expectation that the referrer is ensuring that they’re safe and that we’re not promising to be in quicker than we possibly can be.
FGDS1
The urgency to see all patients within 24 hours was questioned by some respondents (M), who felt that stroke survivors and their families could use more time at home to settle and identify their rehabilitation goals (O). In the context of capacity issues (C), some teams suggested that, in line with their overarching patient-centred rehabilitation approach, patients’ individual circumstances should dictate how quickly they were seen:
I think you’ve got those people on one end of the scale who haven’t processed that they’ve had the stroke really, don’t feel that they’ve got a lot of deficits. And when you go out very quick to say ‘I don’t need anything’, my feeling is if we were to leave them, they know we’re there, but leave them for a week or two to process some of that or just be in the background, I think they might identify things that are more of a problem. [. . .]. Does that person need to be seen in 24 hours over that person who’s got a therapy visit and should we cancel it? So we’ll make contact within that time. We’re working a bit more with the hospitals to say ‘can you let us know whether they’re that urgent really?’. In theory, based on the criteria, nobody should be coming out needing us to go that rapidly.
FS12
Quite often they may have been discharged the night before so we’re seeing them on the morning. All they’ve done is go home, probably not even unpacked and they’ve gone to bed and then they’ve woken up and they’re seeing a therapist. Some of the feedback I’ve had personally is that ‘Well, I haven’t had a chance to try anything so I can’t really say how I’m managing because I only came out of hospital last night’.
AS16
Adopting a flexible approach in how and who makes the first contact with patients (M) was used strategically to improve responsiveness (O). Telephone contact was used by some teams at weekends to complete initial holistic assessments, enabling them to extend the service to 7 days. One service trained experienced RAs to complete initial holistic assessments, which helped the service to work across a large rural geographical area and meet their responsiveness targets:
You need the therapy in there as quickly as possible but at the same time we need to make sure that it’s a safe discharge. So I would say there’s benefits to all the staff doing it, but some of the band 3’s and 4’s, their initial assessments are far superior really, making sure they’ve covered everything. I would get distracted by the OT part of it and lose your focus slightly. So, yeah, they would see them at the weekends as well so if we know someone’s coming on a Friday, that’s booked in for Saturday.
FS12
Rehabilitation intensity
The NICE clinical guideline6 suggests that an ESD team should provide rehabilitation and care at the same intensity as they would if the person were to remain on a stroke unit, that is 45 minutes of each appropriate therapy every day (Figure 13). Against a background of staff shortages and reduced resources, teams were struggling to strike a balance between responding to an expanding list of referrals and offering the intensity required to achieve improvements in patient outcomes (C). For instance, staff at site D reported that they could offer the recommended intensity to a maximum of 19 patients, but there were 30 patients in their caseload at the time of the interviews:
It would be lovely to be able to offer the intensity that each patient needs and deserves. I think at the moment we offer the best service that we possibly can, and I think patients really acknowledge and are grateful for that [. . .]. We either follow the guidelines and see a few patients or we see more patients but we’re really struggling to get the outcomes. So where is the balance?
(DS7)
FIGURE 13.
The CMOs on rehabilitation intensity.

In this context, guideline recommendations on intensity were treated with scepticism. Most respondents thought that they were logistically unrealistic or even inappropriate for their patient group and highlighted the need to provide rehabilitation intensity tailored to people’s needs (M). It was suggested that patients received a bespoke service while services made an efficient use of resources as a result (O). According to respondents, patient feedback often substantiated this view, with patients requesting the time and space to ‘feel at home’ and resume some of their activities:
And we do all the other referrals, like psychology, or if they need extra equipment, that can all get started and you can support them because they may be thinking about their finances and, you know, returning to work and feeling very depressed, and actually you couldn’t then really get started straight away and say ‘I know you’re depressed and you’re thinking about your money and there’s loads of things wrong with the house and the family, but we’re going to have to get stuck in because we’ve got this limited period’.
FGAS1
Some of the feedback we had from people was that sometimes it got a bit too much because they might have reablement coming in three or four times a day to support them with their care, and then we were going in three times a day and it was like, ‘Oh, I’m at home’. [. . .] They were at home. They wanted to be pottering and doing things that they wanted to be doing.
DS14
Gaps in the local stroke care pathway and slow response from other services (C), such as GPs, resulted in staff having to work with many different hats on to try and cater for patients’ needs (M). Addressing unmet information needs was a common issue, as was ensuring that patients received the right medication, which could take hours of work for staff to clarify. Although rehabilitation intensity was diluted (O), staff saw it as part of their role to support their patients with reaching out to other services, especially when their physical and cognitive issues meant that they relied on ESD services for help:
The other end of therapy is sorting out things with them, like an emergency, if something happened to them. We don’t just stay there 45 minutes. Sometimes we stay there for 1 hour and 30 minutes because of other issues. Sometimes a patient’s partner or wife has had an emotional breakdown, and we talk to them and phone the Stroke Association [London, UK] to provide carer support. Those things that we’re dealing, it’s not just the therapy. It’s about the whole, because our approach is holistic.
FS1
Discharge letters themselves can be quite confusing, so I had to sit and study a discharge letter the other week that said a certain drug had to be stopped. I’ve phoned up the consultants in the past just to get clarification so that the patient knows what they’re doing.
FGES2
The impact of care arrangements on rehabilitation provision was stressed by respondents (C). They explained that if the care package was not working well and the amount of support that the family received was inadequate, then the priority of the therapy could become addressing personal care needs rather than providing active rehabilitation. Teams were required to liaise and co-ordinate with multiple services to provide emergency cover for patients until a care package was put in place. They were often put under pressure to problem solve beyond their services’ remit (M), moving the focus away from hands-on therapy and diluting the intensity of rehabilitation (O):
If a patient is just staying in hospital, got a bed, taking up a bed and they can go home but we’re waiting for care, we can sometimes offer the morning. We’ll offer like a morning call.
So instead of waiting for the social care to sort things out you can . . .
We can be that stop-gap.
FGFS1
All of the services sought strategies to enhance the intensity of rehabilitation practice without further stretching their capacity (C). To achieve this, they offered relevant training to family members and care providers, implemented telerehabilitation and promoted a self-management ethos (M). They envisaged to promote rehabilitation practice between sessions and empower patients and carers to effectively manage their recovery after discharge from the service (O):
We have a whole load of iPads [Apple Inc., Cupertino, CA, USA] that we can leave there and they can work, they love doing that. So that gives them the opportunity to practise between sessions.
DS7
We also recruit some of the family members as well.
They might help with therapy, so just similar to how a rehab assistant would do if there’s a relative that can help.
Do you show them how to do things?
Yes, because sometimes they don’t want somebody else coming in. They say they’ll just do it themselves if we show them.
FGBS1
In one site, staff were discouraged from seeing patients daily for 6 weeks; it was thought that this intensity could create psychological dependency and result in people feeling abandoned when discharged. In most sites, visits were the most intense initially and then tailed off, with patients being directed towards self-care in preparation for discharge:
I think the other reason why it’s highly performing is it was set up so that people could have frequent, quite intense input, and that’s something we’ve moved away from a bit. So, people aren’t seen every day like they used to be, but we’ve moved away from it very consciously – we’ve not done it because we were forced to, because we can’t fill vacancies, or the demands are too high. We’ve done it because it’s the right thing to do for the patients and some of the outcomes are better if you give people that self-efficacy to do things themselves. In other services, that self-care element has been forced upon them rather than choosing it. So, I think that’s helped us to be a highly performing service.
FS4
Capacity issues often meant that services relied on staff ‘walking the extra mile’ and maintaining momentum despite the difficulties (M) to meet intensity targets. To quote one of the respondents, teams strived to ‘offer a champagne service on beer money’ (FGCS2). Although their hard work helped them to meet patients’ needs, it also meant that services could become victims of their own success because senior managers and commissioners could maintain an unrealistic picture of the service’s capacity. As a result, resources remained unchanged and both rehabilitation intensity and staff’s well-being were compromised (O). One team had started documenting unmet visits, hoping to collect the evidence to make a case about the need for more staff. Although it was frustrating to accept that they did not meet their intensity targets, they also felt that it was necessary to acknowledge that working overtime to keep up with demand was not sustainable (site E):
I love my laptop, it comes home with me. I can do referrals, but I do it when the children are in bed. [. . .]. So time at work becomes so precious and so little because it’s consumed, so all those other tasks, we probably give a lot of hours in our own time without realising it – which is fine. We work for the NHS so I think it comes with the package.
AS17
We’ve been over our capacity for a while now and to the commissioners, I can imagine they’re sitting there and going, ‘Yeah, but you’re managing’. [. . .]. I can spread out a patient to have one visit every 3 weeks and they only get visited twice but it still looks good on paper that we’ve got that many people going through the service. But then – you know, ‘Who’s [patient name]? I’ve only seen her once’.
And the thing is once they’ve been discharged with us because they’ve got their timeline– they’re having to put more money into community for them to pick up what we couldn’t achieve, so at the end of the day it’s costing them more money because they’re having to get another service involved.
Or re-admissions.
FGDS2
Team composition
Respondents endorsed recommendations by clinical guidelines and the ESD consensus that ESD is delivered by a fully resourced and well-co-ordinated MDT. Particular emphasis was placed on the role of nurses, social workers and RAs, and relevant CMOs are presented in the following sections. Configurations relevant to other disciplines are presented and discussed in Appendix 4.
Access to nurses
With ESD services being the first point of call post hospital, staff felt tasked with ensuring that patients were doing well medically (C) (Figure 14). Having a stroke-specialist nurse in the team (M) allowed them to respond in a timely fashion to patients’ medication queries and address information gaps around medical issues (O). As noted by respondents, nurses were in a better position to identify when liaison with a stroke consultant or the GP was required:
We sometimes get patients that are really struggling with administering diabetes med[ication]s, insulin and things, and we’ve had to involve the nurses in that. I had a patient last week that had got a really high pulse rate [. . .] so it was a conversation with the stroke nurse, who then spoke to the stroke consultant and had a conversation with the GP to tweak some of the medication to try and bring that down. So there was a bit of MDT work with that.
CS3&4
FIGURE 14.
Access to nurses CMOs.

In one site, nurses had assumed the role of the ‘gatekeeper’ of the service by conducting the in-reaching and initial screening of the patients (C). Their thorough medical assessment (M) helped ensure that patients who fit the criteria were admitted to the service as opposed to patients with increased risk of re-admission (O). Respondents also noted that registered nurses had a more holistic approach (M) with their initial assessment of patients, touching effectively on sensitive issues, such as mood and incontinence:
I think that’s part of the in-reaching role is to make sure that they are medically OK. So possibly one of the strengths is two nurses who do the in-reaching; we might be a little bit more forensic in terms of the medical side than maybe our therapy colleagues. So we’ll be looking at blood pressure, continence, medication, those sorts of things maybe and whether they’ve had all the correct investigations and sort of maybe a little bit more detail than maybe the therapists might be looking – have a different angle on it.
ES16
In addition to providing advice and reassurance to the MDT around medical issues (O), nurses’ presence in the team was perceived as a factor contributing to the development of an interdisciplinary skillset across the team, facilitating in this way the provision of holistic care and improving the efficiency of activities (O). In one site, participants described how the lack of a nurse in their team meant that they had to spend a lot of their time trying to secure nursing input from external services, such as district nurses, and the support that they would receive would not always be stroke specific.
A frequently raised issue was that nurses’ contribution was not captured by SSNAP, leading to a big loss of information on ESD input:
The nurses spend an awful lot of time with our patients and none of their data is captured on SSNAP. I know how hard the team works and it’s just so, so frustrating when you see – because we get data sheets out from our SystmOne and our information team whenever the patient is discharged, and you see 2000, 3000 minutes and you think – and that’s effectively worthless because we can’t record it anywhere.
ES17
Access to rehabilitation assistants
Respondents agreed that under the supervision of specialist staff, RAs had a key role in freeing time for therapy staff and maximising the service capacity and cost-effectiveness (O) (Figure 15). As noted by two teams, the success of this process depended on effective delegation (M). This related to registered staff’s experience and ability to effectively manage increased workload. Less-experienced staff could be risk averse or lacked the confidence to judge the right time to hand over therapy tasks to RAs (C); as a result, patients’ length of stay in ESD could increase:
The level of caution, or that ability to let a person do something takes longer, so the length of stay takes longer. That person who isn’t as experienced and isn’t on the higher banding, tends to – you can see that their length of stay with the patient is longer and they need more support. It’s fine, you can pass that to the rehab assistant now and you can take on a new patient.
BS20
FIGURE 15.
The CMOs concerning access to RAs.
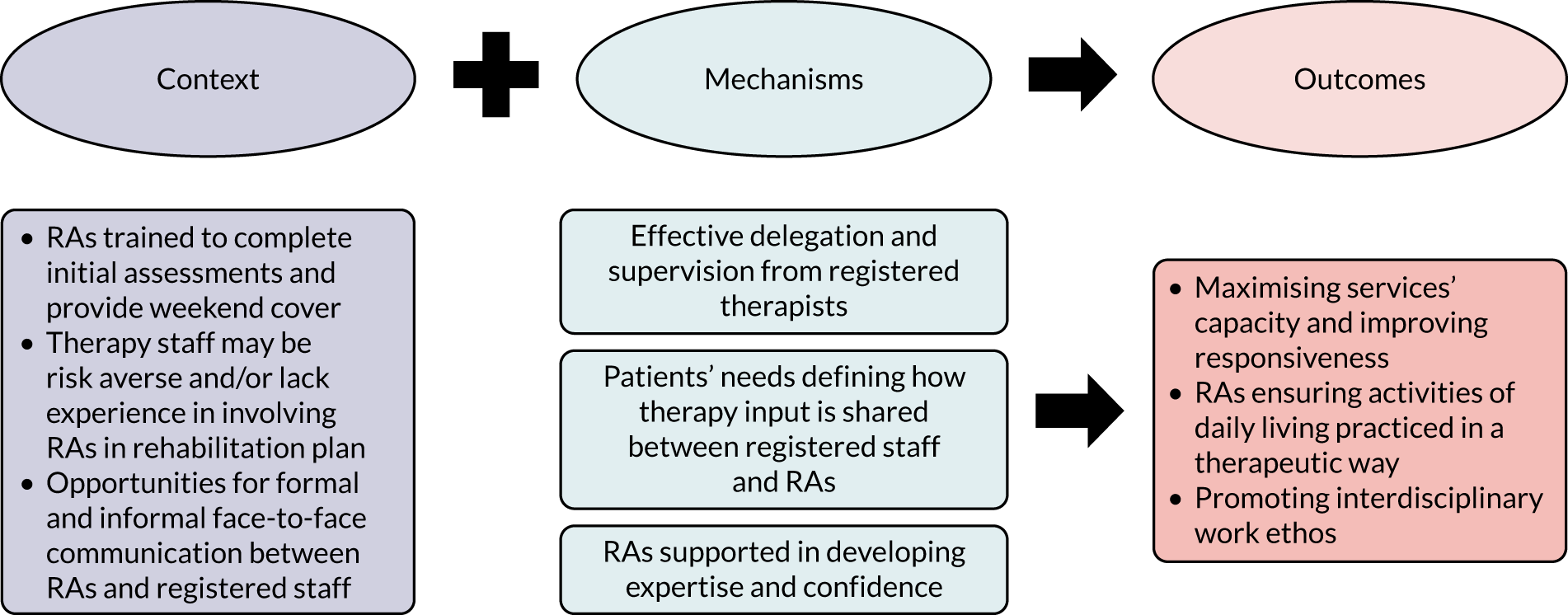
Therapy input was shared between registered staff and RAs based on patient need (M). One team lead stressed the need to empower experienced RAs to handle difficult situations, escalating when they judged necessary, and encourage them to bring in new ideas that would benefit their patients (M). Face-to-face daily communication with registered therapists at their office base (C) was thought to allow RAs to address any concerns and receive guidance and reassurance (M):
To be honest, if patients really needed a physiotherapist every single day for the whole of the 6 weeks, that would be hard to do. But actually, we’ve upskilled our assistants to a level now where once we’ve got our plan and we’re happy with that plan and to deploy them, and they can go. It depends on their need.
FS2
Research assistants’ daily contact with patients could ensure that simple care activities, such as washing and dressing, were carried out in a rehabilitative way as part of their therapy plan (O). Having generic RAs with an interdisciplinary skillset in the team was thought to further promote a holistic and interdisciplinary rehabilitation ethos:
I think having generic assistants helps because they are, they do cover all disciplines. So they are by their nature kind of able to go in and do different things and not be very set on just having one side of things.
ES3
Access to a social worker
Delays in social care arrangements could prolong hospital length of stay or lead to unsafe discharges (C) (Figure 16). ESD services admitting complex and more dependent stroke cases were the ones mainly affected. The problem was accentuated when effective communication channels between the ESD services and the referring teams were not in place and, as a result, ESD teams were not informed about the delays in a timely way (C). Slots were unnecessarily reserved, limiting the capacity of the ESD service for new patients. Having a social worker embedded in the pathway and liaising with both the acute and the ESD services (M) streamlined discharge, as it permitted the allocation of targeted admission slots, ensuring that the patient was seen soon after their return home (O). One team contrasted between referring wards with and referring wards without social workers:
Ward [X] have their own social worker, so they’re much more precise with what date their patients are discharged from the hospital, and that makes it much easier for them to refer a week early, and line it up with one of our dischargers and the process is really smooth.
And [Hospital X] don’t have that, so we ask them to give us 3 days’ notice but very often they get a last minute notice, the care package has changed, or it’s suddenly arrived, and patients will go out without them ringing us and it makes it a little bit more difficult. [. . .]. The main problem is the late notice discharges. If we get a lot of them, it makes it really challenging for us.
CS1 &2
FIGURE 16.
The CMOs concerning access to a social worker.
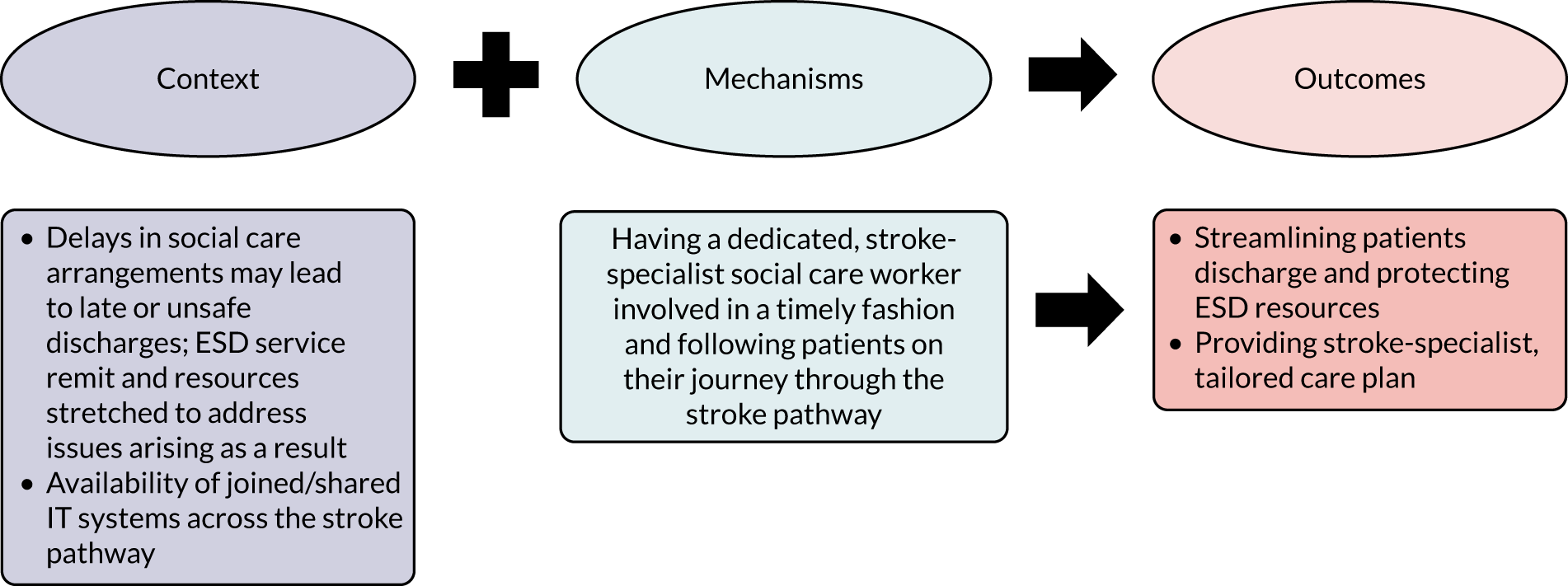
Following discharge home, ESD services could be called to address issues arising from delays in social care input to prevent hospital re-admissions. However, as noted by a social worker, it would be difficult for them to provide a quick and effective response to premature and unsafe discharges if they were not already familiar with the cases. They highlighted the importance of the timely involvement of a dedicated social worker who would follow patients and their families in their journey from the stroke unit into the community (M). Having access to the same electronic note systems (i.e. SystmOne) was emphasised (C), especially in the context of the peripatetic nature of the ESD team. Being able to draw the right information would allow the social worker to identify areas of concern, develop a personalised and detailed care plan and observe patients’ progress (O):
We went to visit and she told us that morning and then when we saw her walking, we realised she wasn’t going to be able manage, so we arranged for care but then care wasn’t available that night, so we did it between the team this morning. We’ve prevented hospital admissions, we’ve prevented them having to into respite and things like that, just by doing that one extra thing. By me doing that lady’s tea when I put her to bed, and then the band 7 went and got her up It was just, we all had to one little thing out of our normal day, but it stopped that lady going into hospital.
FGES1
I said this could have been an unsafe discharge and then people expect me to jump into things like that and I would be very reluctant to do that, because I do not know if it’s a mental health issue or what issue, if the person is not known to us.
CMS15
Seven-day service
These CMOs concern participants’ responses to recommendations about the provision of a 7-day service (Figure 17). Most teams did not provide a 7-day service, mainly because of capacity issues (C). Concerns were voiced that 7-day working reduced therapists’ time during the week, which, in turn, impeded communication with the MDT or other services and could negatively affect responsiveness. Where the service was provided, this was done either with reduced therapist input or with non-registered staff doing the home visits or providing telephone cover (C). Running the service without the presence of experienced therapists, however, meant that non-registered staff could be put under pressure to handle complex cases without the required support and expert input (M). Regarding the benefits of covering weekends, opinions were divided. Some respondents considered 7-day working as instrumental to the provision of responsive ESD (O), especially for patients discharged on a Friday or over the weekend:
I think it’s a good idea to have a 7-day service because what you’re doing is that early supported discharge and that can be any day of the week. If you weren’t functioning on a Saturday or Sunday, I think you would hold up discharges. But that’s a very basic – it’s absolutely got to happen. I think there will be more therapists that work on Saturdays and Sundays, but we need to have more staff to do it. And more money in the budget to pay them weekend rate.
FS2
Originally, when we were first up we did cover weekends as well on a rota, but we found that it wasn’t a very useful thing of our time, really.
Why was that?
I think it’s hard to, as a team, communicate. If you needed to speak to someone, sometimes in the week they weren’t there and then you’d have to wait for them, so it was kind of delaying things.
FGES1
FIGURE 17.
The CMOs on provision of weekly service > 5 days.
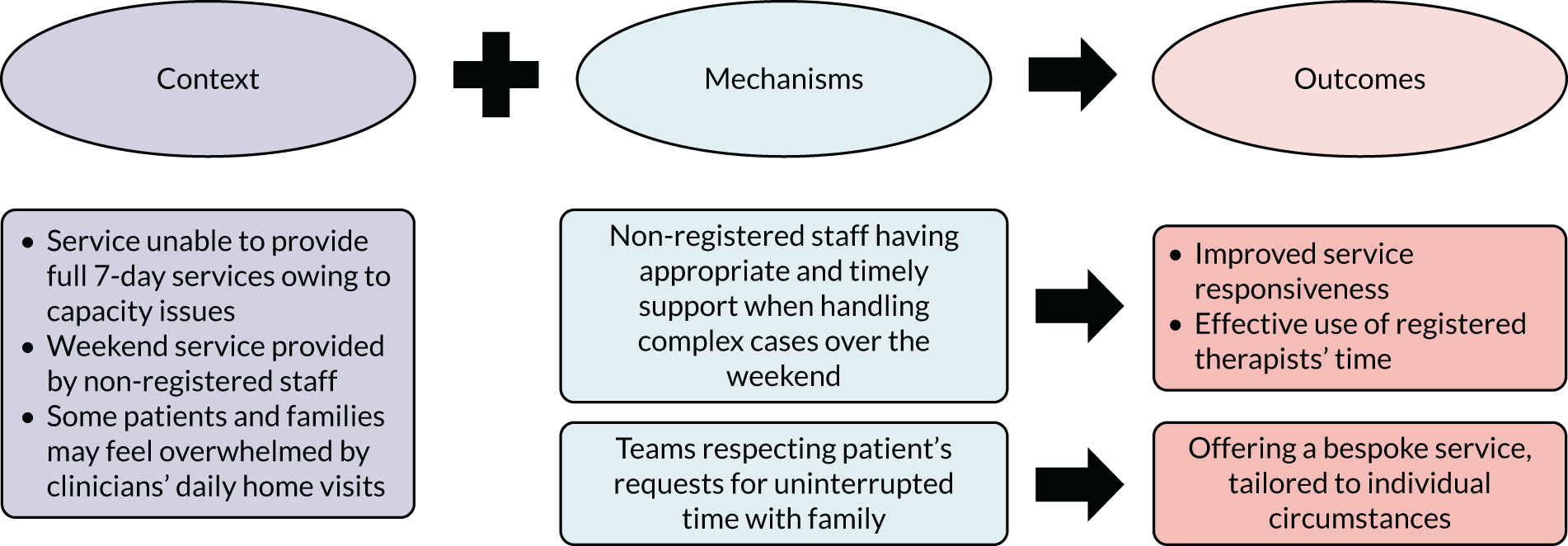
Weekend visits were discussed as an opportunity to meet family members and capture important information regarding patients’ adjustment at home. Seven-day working allowed for flexibility on when to see patients, however, it was also acknowledged that not everyone wished to be seen at weekends, especially the high-functioning patients. Respondents referred to patients’ feedback, which suggested that some of them found daily home visits by health-care professionals overwhelming, preferring some downtime and quality, uninterrupted time with family and friends (C). The need to consider and respect these requests was stressed (M) with the view to providing a patient-centred service, tailored to individual circumstances (O):
Sometimes the patients find it quite invasive having somebody from our team come every day, and then even sometimes two people will turn up at the same time, and then if they’ve got carers coming in as well, which they might have for a short amount of time, it can be really overwhelming, you know, this constant stream of people coming through your house. So I think sometimes they like a bit of a day off.
CS1&2
At the end of the day there’s very few patients that can tolerate seven visits per week from us with a therapy plan of an hour and a half. [. . .]. They often ask actually and say, ‘No, please don’t come’.
FS2
Multidisciplinary team working
Clinical guidelines and the ESD consensus have identified the delivery of ESD by a co-ordinated MDT that meet regularly and offer training opportunities as key to the delivery of an effective evidence-based service. Participants’ accounts further highlighted the importance of good multidisciplinary teamwork as a core component of a successful ESD service. They also identified processes and mechanisms through which effective multidisciplinary teamwork was achieved, which mainly included (1) formal and informal communication processes, such MDT meetings; (2) interdisciplinary working; and (3) collegiality and good leadership. CMOs concerning each of these mechanisms are described in separate sections below.
Team meetings
Regular MDT meetings with good attendance were thought to remediate breakdowns in team communication caused by increased workload and travelling (Figure 18). Despite the challenges of getting everyone physically together in times of high pressure (C), all teams agreed on the importance of safeguarding these meetings (M) as essential to achieving clear communication between staff members and ensuring that staff were well informed about patients’ progress (O). MDTs were forums for discussing goal-setting, sharing expertise and learning from each other. Complex cases could be approached collaboratively, drawing on the pool of experience in the team (M). Ensuring that every discipline was part of the decision-making process was seen as a key function of the MDT (M), serving a holistic approach to rehabilitation. Team leads viewed MDT meetings as a time investment that was necessary for their staff to ‘gel’ as a team, promote trusting relationships and avoid silo working (O). Staff members from all disciplines and bandings should feel empowered to actively participate and contribute ideas to these meetings:
That’s the power of the MDT, it’s not a single person seeing one person. It is a shared responsibility, it’s a shared kind of understanding across the team.
FGDS1
It’s the one time in the week when everybody should come together to discuss the patient’s needs and their plans. So primarily it’s to ensure that everybody is clear about what’s happening with that patient and if there are going to be changes to their stay with the service, perhaps we are going to bring their discharge date forward if they are progressing well and they are achieving their goals, then that is discussed with everybody involved, it’s not just one of us making that decision because most patients have more than one discipline going in to see them.
CS5
FIGURE 18.
The CMOs concerning team meetings.
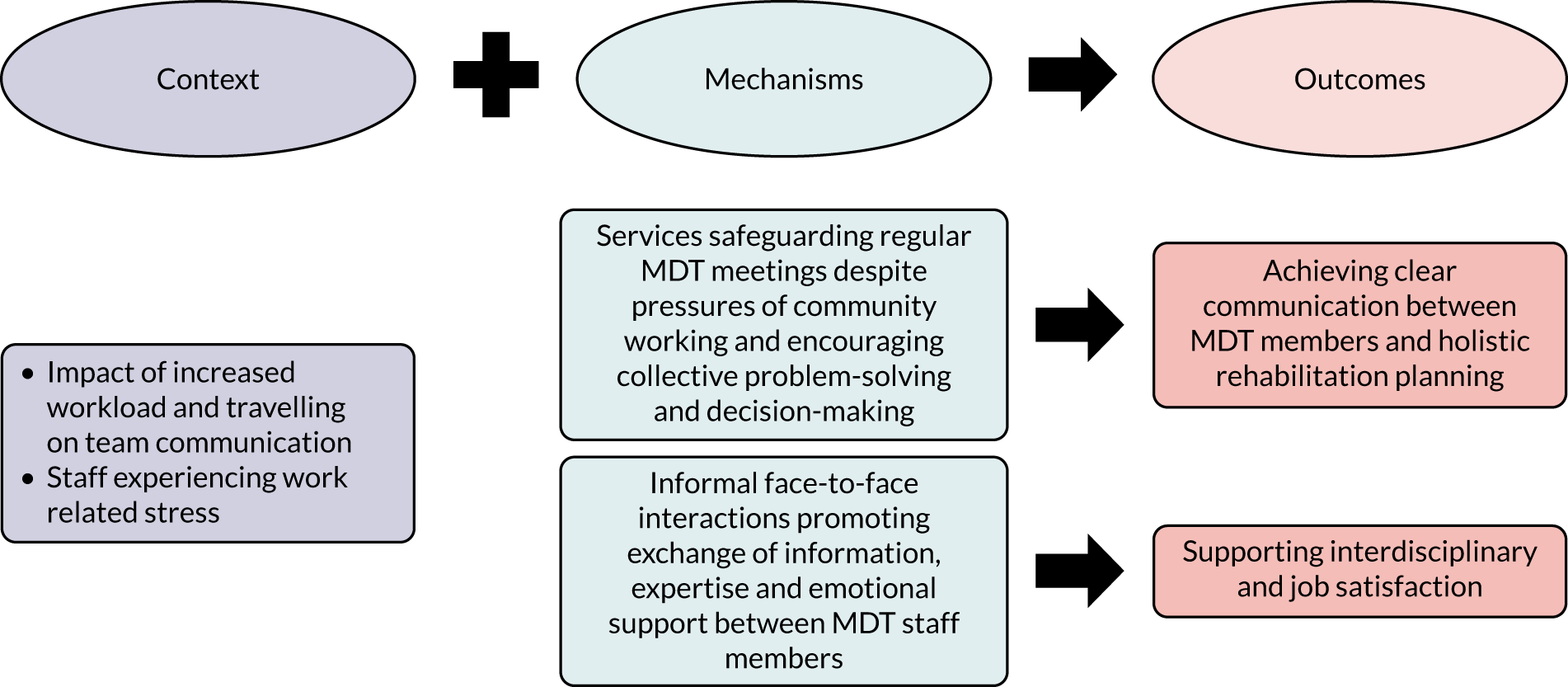
In addition to formal meetings, most teams emphasised the value of opportunistic face-to-face interactions (M) not only for maintaining communication channels but also for promoting staff well-being (O). In one site, team leads talked about how they would have ad hoc face-to-face conversations with their therapists about treatment approaches and clinical reasoning. The nature of community working required staff to handle difficult and stressful situations in people’s homes (C). One team described how having an office base meant that they could ring in and the whole team in the office would get involved in problem-solving. Meeting colleagues at the end of the day helped staff combat feelings of isolation and loneliness that were related to being on the road most of the day, and presented opportunities for mutual support (O). It was also suggested that physical proximity helped socialising across bandings and professions, promoting an interdisciplinary ethos (O). According to a service manager, the lack of frequent face-to-face interactions in their site did not allow them to fully appreciate staff’s workload and slowed down their reflexes in relation to staff who struggled or underperformed:
I’m much more reliant on other members of the team coming to me and saying, ‘Something is not quite right with that member of staff’. Whether that’s around performance or well-being.
DS14
And because the office is so small we’re all sitting together, we’re always having lunch all together. There’s no allocated physio area or allocated OT area, or speech area.
FGCS1
You could work remotely. But a lot of what our handover is, is verbal. Observational, subjective, the handover that you give. Also, some of the therapeutic things that you’re doing, and you actually demonstrate what you – how you want that exercise performing. Or they want to come and show you what they’ve observed; you know, the posture that they’re sitting in or whatever. So, I don’t think that once a week would work. I think they need to be within that team environment more often than that. Not necessarily daily but maybe twice a week, three times a week, just being in that office. It’s important.
FS2
Interdisciplinary working
Respondents agreed that effective multidisciplinary working was enhanced by the blurring of professional divides and an interdisciplinary approach to the rehabilitation provision (M) (Figure 19). The challenges of community working (C) called for cross-boundary working to provide intensive input in an efficient way (O). Holistic goal-setting meant that staff needed to work closely together to help patients to consider and practice different aspects of activities (C). In the context of a time-limited service (C), quick adjustments in the therapy plan could be necessary to better meet patients’ needs (O), a process facilitated by the development of an interdisciplinary skillset across the team (M):
You play every role. You play an occupational therapist, you play a speech and language therapist, you play physio, don’t you, you don’t just go in and do one thing that is physio. You talk about how they’re feeling, what appetite, sleep is like, how they’re managing their everyday tasks, how their speech is. You cover all bases.
FGCS1
That’s where the MDT works, it’s just really natural and really in sync. The OT’s in this service they’ll have OK physio skills, and the physios will have OK OT skills. I think part of that as well is the therapy assistants are all generic. So, you’ve got the qualified therapists and the unregistered staff, and they’ll do all three elements of the treatment, whereas in some other services, you have OT assistants and physio assistants. So, you’re siloing your workforce the whole time.
FS4
FIGURE 19.
The CMOs concerning interdisciplinary working.

Training was used to nurture interdisciplinary working (M) because it helped staff understand each other’s work and feel comfortable with providing aspects of different roles (O). Some respondents noted that, in addition to the development of awareness of other disciplines, the development of an interdisciplinary skillset promoted trust and respect for all professions in the team (O). One team lead saw it as part of their role to nurture this climate; they thought that staff could only treat their patients with respect if they felt respected within their team:
I think if you’re in somebody’s house and there’s a medication issue or a mobility issue, as an occupational therapist, you can’t, in somebody’s house, say that’s not my job. I’ll go back and I’ll – you just deal with what you’ve got to deal with in that person’s house on the day.
You mentioned earlier that you do change hats a bit, so is it something – does it come through training or does it come through experience of learning to work with each other?
I think both, really. We get a level of training. You know, from a blood pressure point of view, the team lead will do a level of training with every new member of staff, but again because we talk a lot in the MDTs, there’s a lot of learning done in MDTs as well, from that point of view and we deal a lot with lifestyle, anxiety and fatigue, which really are something that we all deal with. It’s not profession specific.
FGBS1
One team introduced the term ‘nerapists’ as a reference to their nurses’ and therapists’ shared skillset and approach to rehabilitation. Despite this, they emphasised the need to strike a balance between specialism and interdisciplinarity (M) to avoid duplication and ensure that people are comfortable and confident with what they do without feeling ‘threatened’ by other disciplines (O):
A ‘nerapist’ is a nurse therapist. So they come and are like, ‘Oh my God, I can’t test urine, I can’t do a BP’. So everybody has to have the basics, nobody should freak out. A nurse shouldn’t freak out at a stick. An OT shouldn’t freak out about a blood pressure. [. . .] So the physios we’ve got to trust each other and we’ve got to respect that we can do those basics. The bigger the team has got and the busier we’ve got. I see we’re separating off into our houses again, which we need to watch. But it’s hard because people feel secure in their professional thing. [. . .]. Sometimes I look through a system and I’m like, ‘Well the OT has been out and talked about the bungalow, the physio’s been and talked about the bungalow, the nurse has talked about the bungalow. Stop with the bungalow, you know it’s a bungalow – just do your specialist bit’.
NRS4
Leadership
The importance of leadership in driving effective MDT working was emphasised in the interviews (Figure 20). Reflecting on the qualities of a good leader, respondents noted the importance of acknowledging the link between staff well-being and staff performance. This was particularly in the context of the impact that travelling and handling stressful situations in the community could have on staff well-being and job satisfaction (C). For one of the team leads, good teamwork was synonymous to ensuring that staff were happy and proactive:
It sounds corny but if you come in and your team look happy and they’re proactive and they’re getting out and doing what they need to do, then that’s good for me.
BS20
FIGURE 20.
The CMOs concerning leadership.
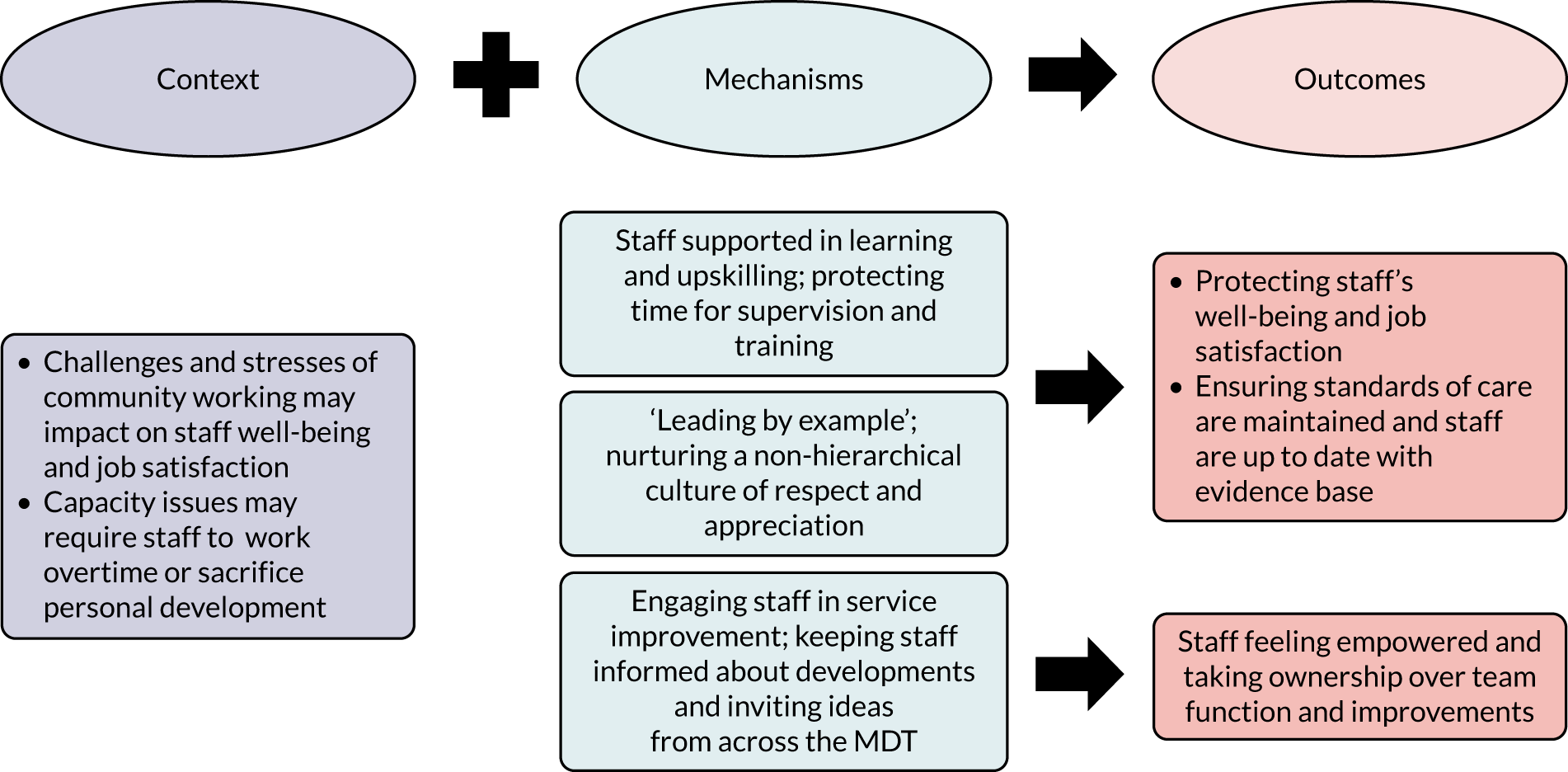
Supporting their staff in learning and upskilling (M) was thought to contribute to achieving high job satisfaction and maintaining the team’s momentum (O). Clinical leads and managers were praised by their teams for creating a safe environment for staff to reflect on and acknowledge their limitations, while providing the opportunities to address knowledge gaps through further training. Despite capacity issues (C), time for supervision and training was protected in most teams (M); it was a way to promote staff retention and well-being and cascade knowledge of evidence-based standards through the team (O):
How can we deliver quality, effective, treatment approach if half of my team don’t have the training? So that’s what I’ve always been asking my manager, and that’s the agreement. Training wise, my manager is very supportive with that. The trust is very supportive because we said we can’t see patients effectively if we don’t have knowledge and skills.
FS1
I think staff support must work because the retention here is very good [. . .]. The training aspect makes people feel that they are constantly learning and being able to manage things. And the supervision aspect of people being able to explore what they are doing with people, where the blocks are with people and how they are dealing with things themselves as well keeps the system quite efficient really and effective.
BS19
In addition to encouraging reflexivity and striving to develop and grow, good leadership was linked to enabling staff members to engage in the running and development of the team (M). It was suggested that people perform better when they have ownership over aspects of the team function (O). Part of the leaders’ role was to keep the team informed about developments, share their vision and invite ideas. When introducing changes, some team leads stressed the importance of securing the team’s buy in and support to take things forward. Successful improvements happened collectively, with staff working in partnership to develop and implement a plan of action:
What would you like to see from good leadership?
Well, it’s asking you for an idea or suggestion and then taking that on board if you suggest something and then kind of running with it or showing their appreciation if you suggested something. It’s not kind of dismissing it. You know, I’m valued as a band 3 as much as everybody else, no matter what band in the team. Our managers are fantastic.
FGCS2
As discussed in previous sections, capacity issues meant that staff were often required to work over time to provide the best care for their patients (C). Feeling respected and appreciated (O) by their colleagues and managers was highly valued by respondents. Some leaders took active steps to develop a non-hierarchical ‘culture of kindness’ and collegiality by adopting an open-door policy and encouraging simple day-to-day acts of appreciation and reciprocity (M). The aim was to bring out the best in each staff member so that everyone benefited from each other’s strengths. ‘Leading by example’ (M) was identified by some respondents as key in inspiring dedication and setting the tone for the relationships between team members and towards patients (O):
For them to see that you’re a good leader, that you’re doing what you ask them to do, you have to show them that you’re willing to do it as well, I think you have to empathise, patients wise and to your colleagues, but also instil in them the importance of ‘How would you feel if that was your relative?’. And also, appreciation of the staff. I think dedication as well. I always try to be honest and transparent. That’s my principle; you have to be honest. You can’t tell them, yes we will do that, and then we can’t do that. So, we are trying our best, we will do it, this is the plan.
FS1
Summary of programme theory 1 findings
Despite differences in contexts and models of service operation and contextual influences, all teams identified core evidence-based components as central to the intervention effectiveness. Most respondents agreed that adhering to selection criteria regarding disability levels helped the services to manage capacity and promote responsiveness. However, the lack of or slow response of community rehabilitation services in the local pathways put ESD and/or referring teams under pressure to use eligibility criteria flexibly to respond to the needs of more complex patients. Most services were unable to offer the therapeutic intensity required to address the needs of patients with more severe disability, and attempting to do so could dilute the intensity of service for the rest of the patients. Research and clinical recommendations around intensity and responsiveness were treated with scepticism, and respondents called for flexibility in their implementation to account for capacity issues and to respond to patients’ individual needs and circumstances. Involving carers in the rehabilitation plan, promoting a self-management ethos and implementing telerehabilitation approaches were thought to increase practise between sessions and improve adherence. Mechanisms thought to streamline discharge and help teams to meet their responsiveness targets included having access to a social worker, adopting a flexible approach in terms of who conducts the initial assessment and establishing ongoing communication and a trusting relationship with hospital staff. The role of RAs in facilitating the delivery of an intensive and responsive service was highlighted, as was the need for appropriate supervision and upskilling. Effective MDT working with frequent formal and informal meetings was key to the services’ successful operation. Key mechanisms to enhancing MDT working were identified, and included interdisciplinary working and leadership.
Programme theory 2: ‘core evidence-based components of ESD will operate differently in urban versus rural settings’
Investigating how participating services achieved their targets unveiled subtle but important differences between urban and rural settings, especially regarding the delivery of an intensive service tailored to patients’ needs. Staff interviews supported the programme theory; however, they also highlighted the need to consider service capacity and the time spent travelling to further disentangle the influence of geography. Teams covering a large catchment area experienced similar challenges to rural services, although to a lesser extent. Findings are presented in two sections: (1) the first section describes how rurality and other important contextual influences interacted with staff’s efforts to offer an equitable and intensive service across their catchment areas; and (2) the second section focuses on travel time as a prevalent contextual challenge and how teams adapted MDT structures and processes to mitigate its impact.
Providing an equitable service
The time required to reach their patients (C) was identified by respondents as an important contextual influence, which could affect the number of patients they could see per day and the intensity of service that they could offer, especially against a background of reduced resources and stretched capacity (C) (Figure 21). Although all teams perceived travel times to be an issue that had to be considered and managed, the impact was more pronounced in services covering rural and/or large catchment areas, for which teams spent a big part of their day on the road, leaving less time for hands-on therapy. In rural areas, further delays were caused by poor road infrastructure and poor connectivity for mobility phones and satellite navigation systems. When coupled with capacity issues, achieving the recommended intensity targets was especially challenging for services covering rural/large geographical areas (C). Some participants from these sites voiced concerns about whether or not patients living at distal points of the catchment area received the same rehabilitation intensity as those living closer to the service:
I think if you live up on the north you’re probably not going to get as many visits as if you live around the corner. And it’s very hard to be equitable when you’re looking at patients and the geography and the number of visits they need and the staff you’ve got to make sure – so of course, if they live around the corner I would say, I don’t think we’ve ever actually done a piece of work looking at that, but I would say anecdotally that probably if you live up on the north you may not get as intense a service.
ES16
FIGURE 21.
The CMOs concerning an equitable service.
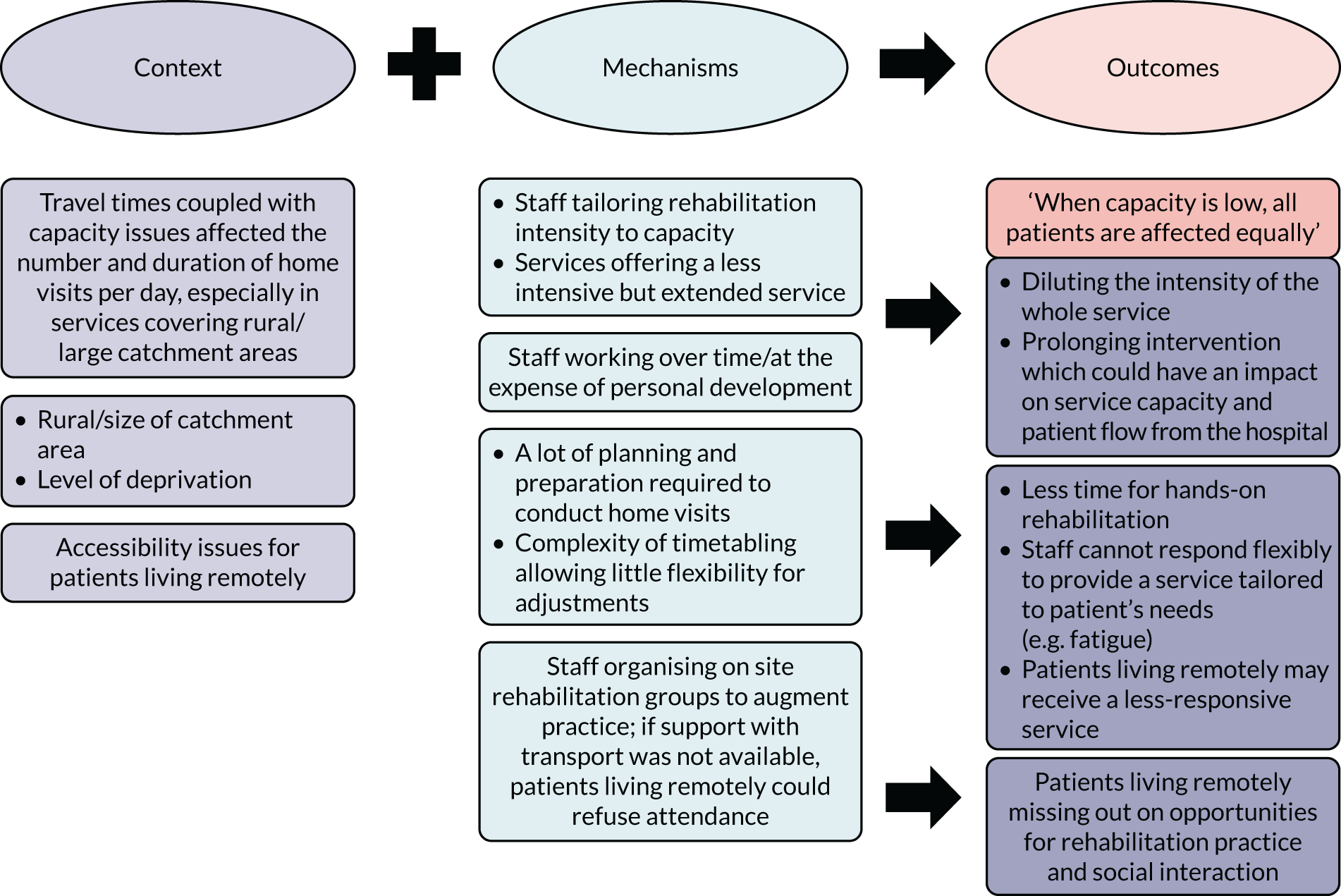
To try and cater for patients based on their needs and not where they lived (O), rurally based teams would often have to work overtime or cancel training activities, ‘putting their patients first’ (FGES1) (M), to increase their capacity. They also spread the number of visits permitted by their capacity evenly across their patients to give the opportunity to those living remotely to access the same amount of therapy as those living closer to the service (M). However, when capacity was low (C), this strategy could mean that all patients on the caseload received a less-intensive service over a longer period of time (O). Staff at one of the rural sites explained that, with intensity being diluted, the service had to be prolonged to allow patients the time to achieve benefits before discharge. This in turn had a knock-on effect on patients’ flow from the hospital and the service’s capacity (O):
It really is about what patients’ need is and that’s where you get this conflict, because actually, they would benefit from this, but the reality is we can only give this. Then the outcome is that they’re sat there longer than they should be and we’re not seeing them as quickly and not progressing as quickly and they’re getting bored because they’ve got exercise plans which are too easy and they’re not feeling challenged.
ES1
In rural and/or large geographical areas (C), a lot of time and effort was invested in timetabling and planning home visits. The same was reported in a site with a high level of deprivation and a recent increase in patients with a history of alcohol abuse (C). Staff visited in pairs for safety or to obtain a holistic assessment while saving on mileage and costs. However, the complexity and resources required to organise these visits (M) often had an impact on the time available for hands-on therapy (O), especially when the team did not include a dedicated administrator:
[Distance] cuts down the number of patients that you see if you are sending two staff out at a time and we do have a few complex ones like that.
FGSF1
If anyone’s got a history of alcoholism we have to go out in twos because we just can’t predict it. That then makes it so much more complicated because we all manage our own diaries and just getting the right person at the right time to be able to double up with you is difficult.
AS1
Respondents from services covering rural/large geographical areas (C) noted that the complexity of their timetabling allowed little flexibility when arranging home visits for patients living remotely (M). This could mean reduced opportunities for rehabilitation provision tailored to patients’ needs (O), for instance arranging shorter and more frequent visits to manage patients’ fatigue. It was also suggested that patients living closer to the service might benefit from cancellations and opportunistic visits, or even experience a more responsive service (O). One team explained that when capacity was low and patients had to be put on a waiting list, patients living closer to the location of staff members would be prioritised once a slot became available:
It does make a difference, though, because if there’s someone just down the road and someone’s had a cancellation and they’re in the office, they could quickly nip out to see them in their afternoon where they’ve got a slot, whereas if they’re right at the top of north of the county then they can’t just nip out to see them.
FGES1
We’ve got people that are on the real outer borders. And if there’s nobody else out there, I’m just thinking the border which might take you over an hour to get to, if you’ve got nobody else out in that direction, I suspect the clinicians are thinking carefully about how frequently they need to go out there. I’d like to think it’s not impacting on – but I think that would be – that’s kind of human nature really, isn’t it?
DS14
All of the teams were set to encourage functionally oriented rehabilitation practice. In urban and inner-city areas, goal-setting could involve using local facilities, such as catching public transport or visiting a shop or café. Some teams organised on-site rehabilitation groups to augment practice and achieve the recommended intensity. However, patients living remotely, especially those living in rural areas, had a disadvantage in terms of being able to access such services because they often relied on poor or non-existent public transport, while fatigue and physical disabilities made travelling even less desirable (C). If support with transport could not be arranged by the service, patients often refused participation (M) and, therefore, missed out on opportunities for rehabilitation practice and socialisation (O):
And what would be the reasons why they couldn’t attend?
Some decide it’s too far too travel so we only have this location to work from so some live in the peripheries of the county so they would travel for an hour, you know, they don’t want to do that.
Do they just miss out then?
Yes.
There is no alternative that will replace that opportunity?
No, the resources in that workshop we can’t take out of the workshop so the equipment we can’t take from there to the patient’s home even though some of it is mobile. Patients that attend that group are the ones that have transport or want to come.
CS5
I have got a patient this afternoon who is very remote and that’s one of the things we are going to be talking about, would you like to be socialising more, to do that would you like to travel? So we would be mindful of it and offer it and see if we could link in with social services who can provide transport so that those patients could potentially get picked up, taken to a group and brought back. I think, we are kind of aware of possible things that effect their rehabilitation and try and offer things around it.
ES18
Managing the impact of travel time
Although services covering rural and/or large geographical areas were particularly affected by the time spent on the road, all teams took active steps to mitigate the impact of travelling on the operation of their services. The following two sections describe CMOs related to services’ efforts to reduce travel times and use resources efficiently (O) through (1) the adaptation and management of MDT structures and processes (M) (see Adapting multidisciplinary team structures and processes), and (2) flexible working arrangements (M) (see Flexible working arrangements).
Adapting multidisciplinary team structures and processes
The CMOs described in this section concerned how teams adjusted the way that their MDTs were organised and operated (M) to mitigate the impact of travel time on the operation of the service (O) and staff’s well-being (O) (Figure 22). All of the teams organised patients geographically and most sites implemented ‘patch working’: dividing their MDTs into subteams that covered different geographical areas (M). This strategy was thought to allow services to meet responsiveness targets and deliver the greatest intensity of service possible. In one site, the MDT was split into five subteams; it was envisaged that this would ensure that patients across the catchment area had equal access to senior therapists:
Because we work geographically we do reduce the amount of travelling we have to do and we can plan our own diary so we have that flexibility to say, ‘OK. I’m seeing that person, they live here. So I’ll see that person this time and then I’ll come back to here, or I’ll finish where I can just go straight home so I’ll do all of these at the end of my day’. So we have that flexibility with our diaries.
AS16
FIGURE 22.
Adapting MDT structures and processes CMOs.
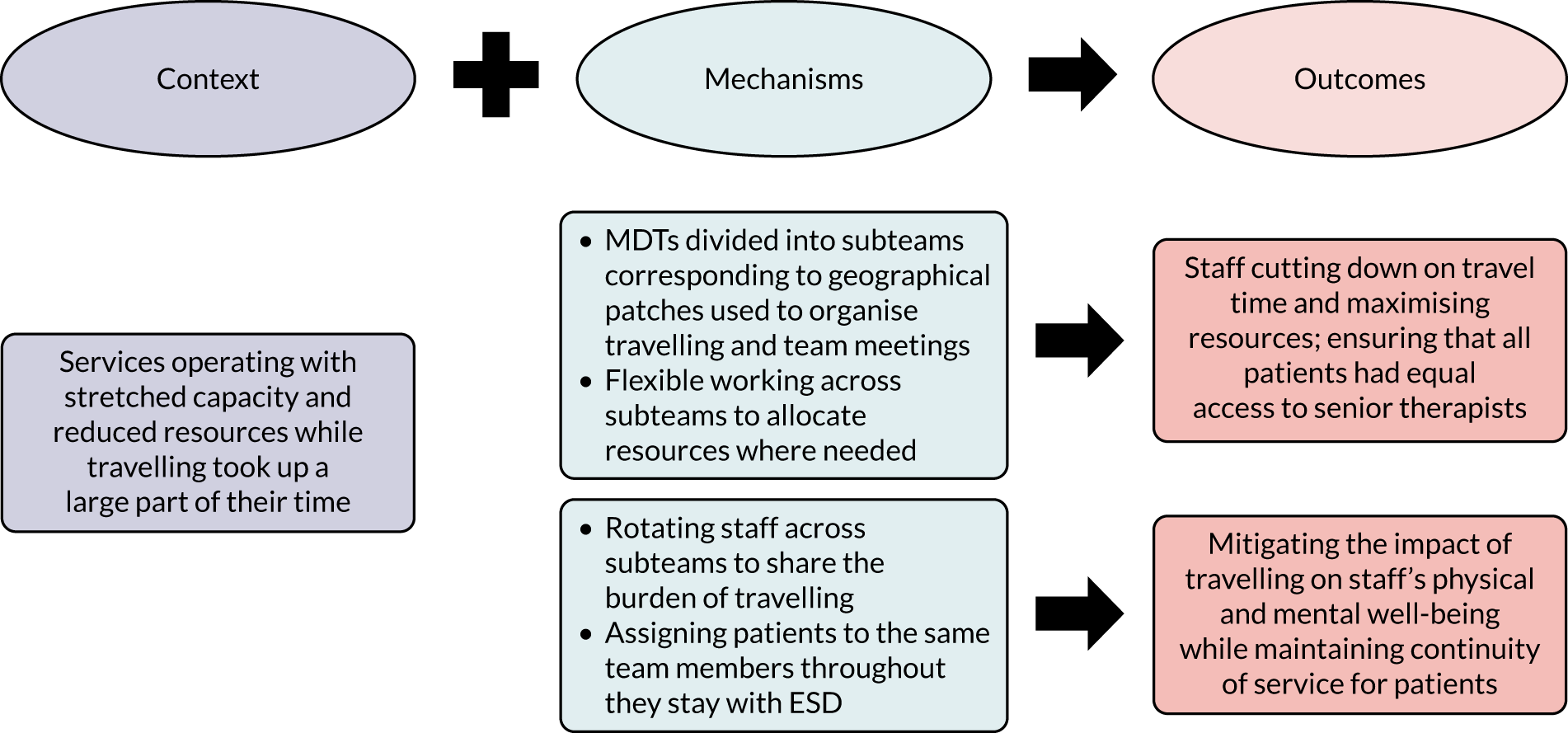
Site C divided the weekly MDT meetings into two patches to make the best use of staff’s time, reducing the length of the main MDT meeting. In addition to the weekly MDT and wider meetings, some teams had introduced separate patch meetings to plan the visits for the following week. During these meetings, staff would collectively do their timetabling for the week to ensure that every patient was seen daily and that there were no overlaps. This process was thought to encourage communication between staff members and allowed subteams to discuss cases in more detail:
We’ve just fairly recently introduced patch meetings, so that we can just sort diaries for the week, so just making sure that patients get a visit on each day, and nobody clashing with anyone else. We just do it together, standing in front of the roll with their diaries, and go, right who’s going what day, and then they can say, they’re off on annual leave and can you cover that day instead of that day and switch it all round.
CS3&4
Good planning and co-ordination across subteams was key. When the service capacity was stretched, subteams would work flexibly and support each other to keep caseloads evenly spread and allocate resources where they were most needed (M). The latter was not always easy to achieve, especially in the context of wide/rural geographical catchment areas; the complexity associated with travelling in these areas made it difficult to plan the capacity of each subteam. As discussed in one of the focus groups (FGDS1), patches tended to continually shift as the caseload from each geographical area fluctuated. Despite the challenges, patch-working was thought to allow the teams to respond faster to changing circumstances:
Because you realistically see one in the morning and one in the afternoon. And there are times that if they all happen to live within a 5-mile radius, which has happened, then you can see four of them quite comfortably in a day. And it’s really variable to then say OK yes we can have this number of patients or this capacity because it’s not really a straight forward figure.
ES3
From my point of view, the patch-working is essential in a team, when you cover a huge area because it allows you that flexibility to sort of say right, OK, we’re not getting as many referrals from [area X] so you shift your patch up a little bit and we can work from there.
FGDS1
In sites that covered large geographical areas with high levels of rurality, when possible, staff treated patients who were based near their homes. However, despite the steps taken to reduce the burden of travelling, many respondents from across the six sites talked about how spending a big part of their day on the road affected their work–life balance and their physical and mental well-being (C). Respondents also felt that the way that the national rates for mileage and car wear and tear were calculated placed staff who travelled a lot, and especially those in lower bandings, at a disadvantage. These issues affected staff morale and led to occasional resistance to work in areas that required a lot of travelling (C). Team leads tried to manage the situation by having staff or subteams rotate in covering geographical patches (M) to share the burden of travelling and promote job satisfaction (O):
People will sit in the area that’s closest to their home generally speaking. So, we kind of allow half an hour travel per patient, as an average.
DS14
It’s quite a long way and we have had to ask the other existing support workers to cover that area. There is some of them that are saying, I won’t do it and we have had to try and say to that person, everybody is going to have to take a turn doing that area. One of the new ladies that we have recruited will have to go there permanently and she has been told that at interview.
CS5
To maintain continuity of care despite staff rotations (O), one team explained that, once staff were assigned to a patient, they would stay with them until they were discharged (M):
Once you’ve got that patient in your team, we’ll be their stroke nurse for the whole journey that they’re with us; so they know your stroke nurse, you can ring her on this number, and the same with the therapists. Generally, they’ll see the same people, so once they’ve got to know us all and they’ve got to meet us, they’ve got a bit of continuity of care, so we get to know the patients really well.
FGES1
Flexible working arrangements
Where good information technology (IT) facilities were in place (C), flexible working arrangements that allowed staff to return to the office only when necessary (M) could further help to manage travel time and optimise resources (O) (Figure 23). Staff were encouraged to start and finish their day with patients rather than in the office, which, for some teams, meant that they could be visiting the base only once per week:
If I had a space in the morning and my first patient was down south, I might come here just to maybe get some resources or do my e-mails quickly, but I certainly wouldn’t come here if a patient wasn’t on the way. And I might use it as a base to come back for lunch or something, but only if I was close otherwise it’s a layby or wherever.
DS7
You tend to have to be quite resourceful in your day as well. Some of us use the live SystmOne, which is where we do our notes. So we might choose to do notes in between visits to help speed things—
So you don’t have to travel back to the base and do your notes.
We’ve got the new mobile app that we download everything onto before we leave the office, then you can do your notes and you can access it.
FGES2
FIGURE 23.
Flexible working CMOs.

Remote working helped to reduce travel time, but it could also mean that there were less opportunities for interaction and for the exchange of information, expertise and emotional support (O), all of which were deemed by respondents as particularly important in community working. Teams highlighted the value of developing and sharing good local knowledge on a team level (C) to maximise efficiency. These exchanges were put at risk by a lack of face-to-face communication between team members. Although technology facilitated flexible working arrangements, it did not address all of the issues arising from the lack of face-to-face interactions. As noted by respondents, one had to be an excellent communicator to ensure that staff and patients knew when patients were seen and by whom merely through mobile telephones and texting:
Parts of the city where you can’t park because you’ll be clamped, things like that. Don’t park there because you think you can park there but you’ll get a ticket. This is where you need to park. All that knowledge you do build up as a team.
ES1
I think there’s a really strong argument for actually having physical contact with people. We can see if a member of staff is struggling. You can just pick up on a whole load more if you’re actually seeing the team. And it is hard, you know, it’s not easy working out in the community without coming back and touching base I think you lose that sense of team. And yes, we’re very good at using e-mail on our phones but it’s not the same. And I know that members of the team who don’t attend MDT because of their working structure, they battle. They don’t like not being a part of it, they want to come back into it. And we do telephone handovers but nothing replaces actually being in MDT, actually seeing each other otherwise it’s really lonely being out there [laughs] all week. So just having that one contact I think is really valuable.
DS7
Summary of programme theory 2 findings
The findings suggested that rurality, especially when coupled with capacity issues, could influence (1) the intensity of rehabilitation provision, (2) teams’ flexibility to adjust the frequency and duration of the visits to people’s needs, and (3) patients’ access to facilities that would promote rehabilitation practice and socialisation. Staff responded by working overtime or extending the length of the service, which, however, could have a knock-on effect on service capacity and patient flow from the hospital. The time required to travel to patients was a key contextual influence, which meant that services covering large catchment areas were also affected, albeit to a lesser extent than rural services. Therefore, the results support the initial programme theory but also highlight the importance of considering travel times and service capacity in interpreting the intended and unintended outcomes. To mitigate the impact of travel times on their operation, services organised their MDTs around local geography and encouraged flexible working arrangements. When good IT facilities were in place, returning to the office only when necessary contributed to the efficient use of resources; however, unless frequent face-to-face communication was safeguarded, working remotely minimised the opportunities for the exchange of information, expertise and emotional support between staff members.
Programme theory 3: ‘the quality of communication processes between key stakeholders and services in the local stroke care pathway will influence the provision of a seamless, patient-centred pathway’
The initial programme theory concerning communication was developed during the preliminary analysis of staff interviews while data collection was ongoing. It suggested that the quality of the communication processes between key stakeholders and services in the pathway would influence the implementation of an evidence-based service. As data collection and analysis progressed, new insights required this programme theory to be revised to better reflect the staff accounts. The refined programme theory focused on patient experience and the provision of a seamless stroke care pathway as the key areas influenced by the quality of communications between services and stakeholders. Findings are structured in three sections corresponding to CMOs concerning communication between ESD and (1) patients and carers, (2) stroke units and (3) services across the stroke care pathway.
Communication with patients and carers
Unrealistic expectations of ESD were common, and often reflected gaps in information provision prior to discharge or even referrers’ lack of clarity around the intensity and length of the service (C) (Figure 24). All teams recognised the need for timely, clear and constant information provision to both patients and families (M). This was important for addressing concerns about returning home and misconceptions about their recovery (O):
I don’t think referrers know us as well, so they probably don’t know exactly what we can provide. So in terms of patient expectations sometimes you get ‘Well I was told I was going to be seen every day’ or they’re not happy with being discharged at 6 weeks or they’re just in a bad place because they’ve just had a stroke and they’re low in mood.
FGES1
FIGURE 24.
The CMOs on communication between ESD teams, patients and carers.
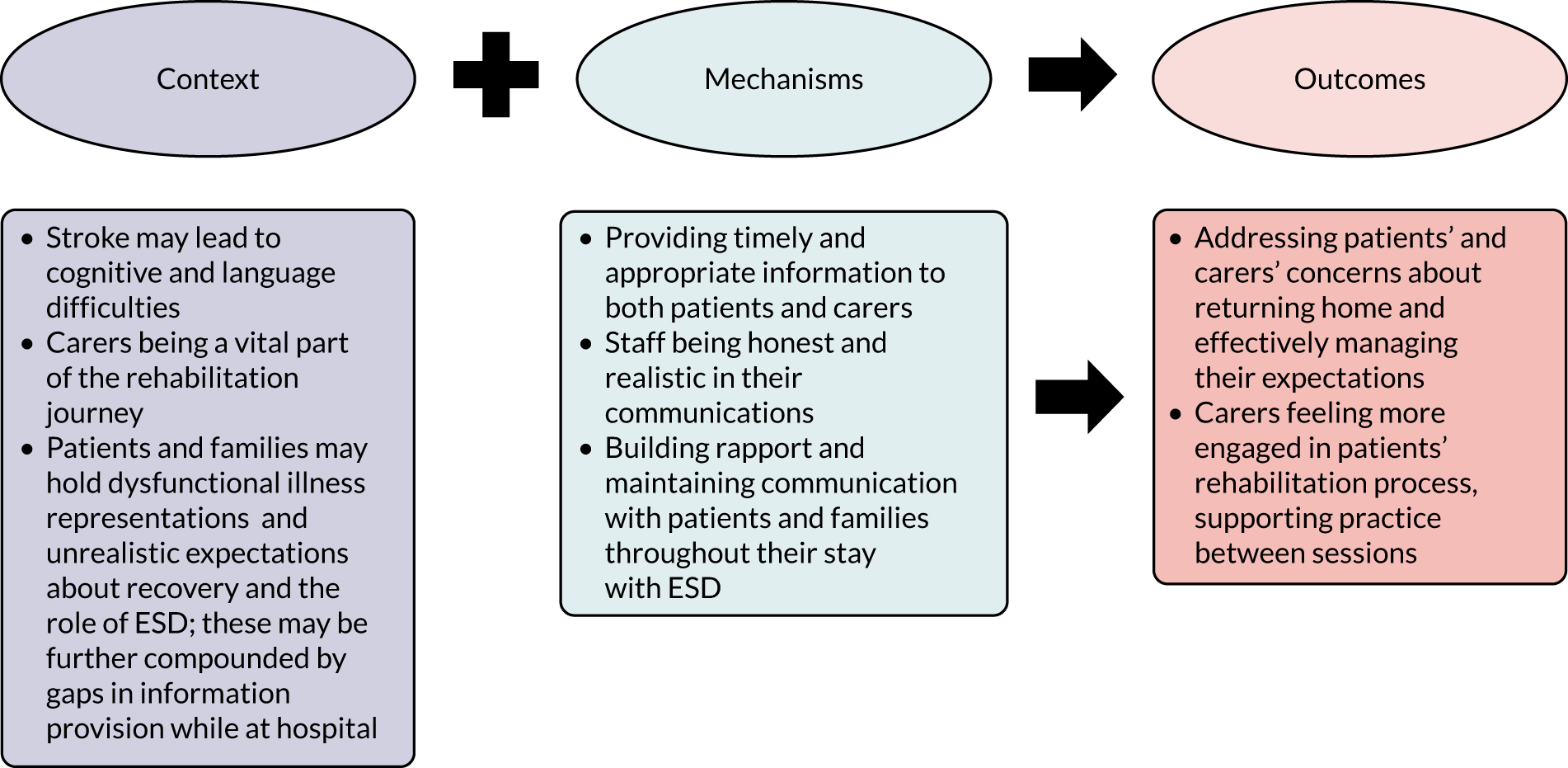
Families occasionally held cultural expectations that therapists would ‘do it for’ the patient rather than patients taking responsibility for their own rehabilitation and recovery (C). Being honest and realistic in their communication (M) was identified as key in managing expectations and improving adherence to rehabilitation (O). Striking a balance in relation to information provision was also considered necessary to ensure that patients were not overwhelmed. Some teams discussed how they developed their information material to consider stroke-related cognitive and language difficulties (C). In response to patient feedback, one service adapted their discharge letters (M) to make them more accessible (O):
I think they do come with some expectations and the people that in-reach on the ward will go and introduce themselves to the patient and give them a bit of an explanation anyway. So, they do have some idea of what’s likely to happen. But I think they’re often still quite surprised at how much we see them and how much they get and how much they improve. I don’t think they expect to get as much as they do actually. But some people want lots of therapy and some people don’t, and we try to have that negotiation with them earlier on. I think sometimes people want to keep us a bit longer but that’s always going to be the case isn’t it, no matter how long we see people for.
FS3
According to respondents, patients would often feedback that their discharge from ESD came too soon; this observation was common across all sites (C). As noted by a team lead, discharge from ESD services should be actively managed to avoid leaving patients and their families with a sense of ‘abandonment’ and to avoid an abrupt ending of the service. Timely communication (M) was key to effectively preparing patients practically and emotionally for their discharge from ESD services (O):
The ending bit used to be a problem about saying to patients, ‘We think – there’s that awful thing that’s used – you’ve maximised your rehabilitation capacity now so we’re going to say goodbye’. It’s not very helpful for patients to hear that, as in I’m going to have a meeting with the patient today to tell them I’m not going back next week. You should have done it long before that. The patient should be aware and ready that this the process they’re on.
BS20
Carers were acknowledged to be a vital component of the rehabilitation journey (C). Establishing and maintaining communication with the carers (M) was required to manage the delicate family dynamics that come as part of home-based rehabilitation and to help carers to feel engaged in the rehabilitation process (O). Staff worked to acknowledge carers’ presence and role in the rehabilitation plan, honour their own wishes and emotions, and provide support. Early goal-setting that involved the carers allowed patients and their families to have a clear understanding of what they were working towards and start the process of adjustment. This, in turn, helped to engage everybody in optimising the amount of time spent on functional therapy practice between formal therapy sessions:
Occasionally, the carer might find it as an intrusion because you’re going in someone’s house and it’s a very different dynamic to being in hospital. [. . .] They come as a package quite often I think, your family dynamics. But I will go out and talk to the carer. So, I’ll actually say ‘I’ve come out today but perhaps we can go and have a cup of tea just to see how you are as well’. Some of that is about acknowledging that they’re part of the picture, but they’re also going through a lot. It’s about giving them the forum to talk through those things as well. Some people didn’t like each other in the first place as well, which is always very difficult. So, you get people dynamics where they were living very separate lives to start with. [. . .] The big thing is to acknowledge that person that’s living with somebody has something to say. Nobody is a passive recipient of anything.
B20
Communication between early supported discharge services and stroke units
Good communication with teams from the referring stroke units (M) was described as a key enabling factor to a patient’s smooth discharge process (O) (Figure 25). Respondents emphasised the need to be proactive, especially in the early days of the services’ development, as referrers may not fully understand the screening and referral process nor appreciate the quality of the service that patients would receive at home (C). In one site, the service manager had engaged in a lot of preparatory work to establish good communication with referrers, visiting the stroke unit daily for about 1 year before the service’s full operation. Communication and rapport-building efforts were a vehicle to educating about the service’s role and remit, shifting attitudinal barriers and promoting a trusting relationship with the referring team (O):
Developing communication and rapport and I suppose trust as well, communication and trust. Because if the therapists don’t trust the community team then they are reticent to let that patient out so you have to develop that and that’s developed over time.
FGBS2
FIGURE 25.
The CMOs on communication between ESD teams and stroke units.
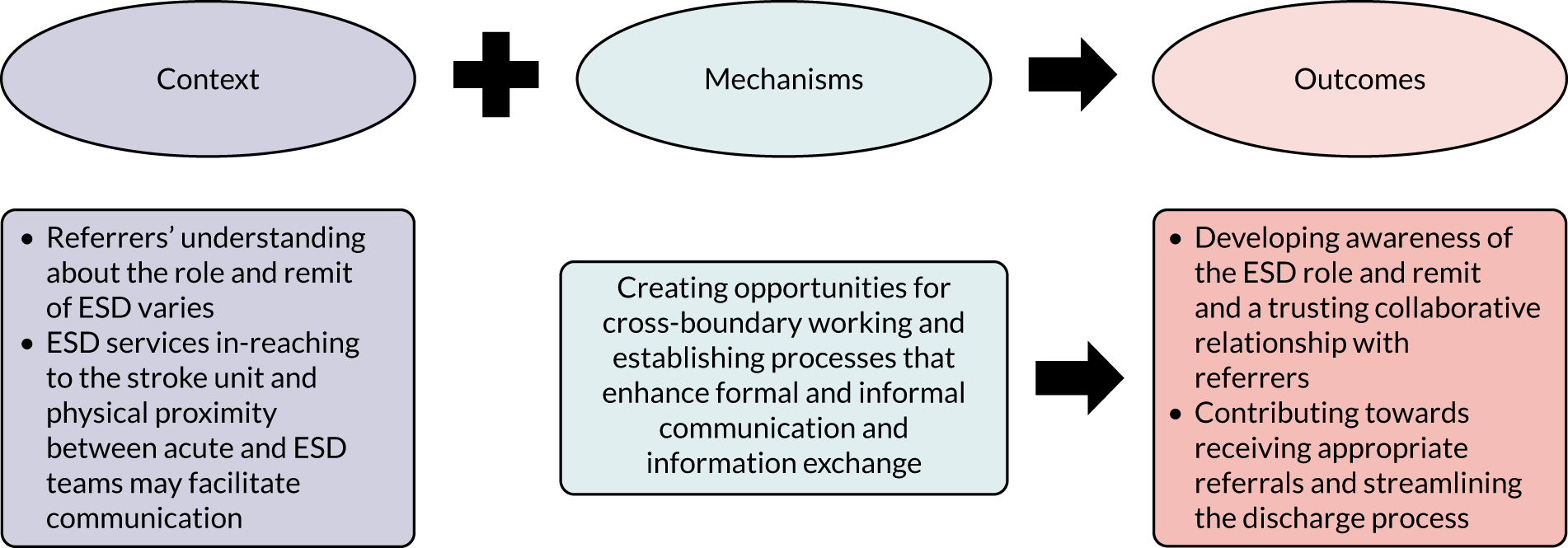
Four teams in-reached to the acute trust and perceived this process as a central feature of their services’ models, enhancing relationships and formal and informal communication (C). Two teams were embedded in the acute trust, and attended ward rounds, were involved in assessment and assisted with discharge planning. Not everyone agreed on the benefits of in-reaching. Some teams had trialled and dismissed in-reach as a model, deciding that it was not an efficient use of their resources. To mitigate the lack of direct communication about patients, they had put other processes in place. These processes included designing their own referral forms to provide detailed information about patients, which, however, were often poorly completed by the referring teams; as a result, ESD teams would have to either screen all referrals and telephone for missing information or search the trust’s databases. They also made periodic visits to the stroke unit to refresh ward staff on their role and the referral criteria, a process further necessitated by the high turnover of acute staff:
I think the communication’s strong and because we pitch up at their MDTs frequently, we can ask the questions and prompt that because obviously when there’s a turnover of staff at the hospital end or our end, we do need to keep revisiting the criteria, so yes we do that. I think trying to get night-time charts from nursing staff and things, so that we know we can help form our risk assessment. So it’s a very MDT approach, asking the nurses for their thoughts on the ward as well about the patient because they see them throughout the night. Often their behaviour and their needs can be quite different.
Do you see yourselves then as – do you see them as part of the team?
Yes, and I think that’s another reason why the speed of getting the ESD patients out has become better over time, because they trust us.
I think as you say, we have a quite trusting relationship, I think it works both ways. They know they can send people home earlier than maybe if they were elsewhere because of us.
They know us and we know them, so we work with them.
FGBS2
We did trial in-reaching for a short period of time but it just didn’t quite work and we didn’t feel it was a good use of our time, sitting in a meeting where you’re discussing lots and lots of people and then we’re just coming back with a list of names when actually, we could be out there treating patients. Sometimes the dates that they propose weren’t necessarily the date they were discharged either.
AS16
In one site, senior management encouraged meetings between the managers of ESD and stroke unit teams (M); it was envisaged that if they could understand each other’s pressures and needs they would be more supportive and collaborative (O). Other commonly practised communication processes included staff rotations, where teams were employed by the same organisation, and hosting visits by acute trust staff to shadow ESD team members where they were not from the same organisation. Respondents agreed that cross-boundary working (M) promoted an understanding of the ESD role and assisted in achieving appropriate and timely referrals (O):
What I say to them is ‘Oh, I’m from ESD, do you know what we do?’. And I give them a leaflet and I say, ‘Come and spend some time with us’, but it’s about good relationships, communicating. I usually try and grab any new nurse that I don’t know and sometimes if they’ve got a good mentor the mentor will send them down. So yeah I always ask people to come and be here.
ES4
There were differing opinions of the value of physical proximity with the stroke unit (C). For one ESD service, co-location with the acute team meant face-to-face interactions, shared IT and training events, or even supporting each other when at overcapacity. By contrast, communication with other referring hospitals was more strenuous because, other than speaking over the telephone, they did not have many opportunities to build up rapport in the same way:
I think one of the things that really helps is that the stroke rehab unit and the early supported discharge team are effectively the same team. You know, we’re the same organisation and we’re on the same site, so it’s much more seamless than other referral routes. We communicate quite closely with the ward team here. Some of the staff have worked in both environments, which helps with that as well. [. . .].
Another advantage with some of the staff who are on the ward, who have worked in ESD, they appreciate what it’s like to work in ESD, so when they’re making their referrals to us, they consider that. You’re not just doing it to this other team, that you have no idea of their working processes.
Yes, and also when I’m with board round, I’ve got both hats on. ‘What about this patient, what about that patient?’. You get a really good handover. So it’s those personal relationships that we’ve built up as well, that make a difference.
FGDS1
Communication across the stroke care pathway
Community-based care was characterised as one of the riskiest parts of the patient’s journey through the pathway owing to the difficulty in predicting how families or systems are going to cope or manage (Figure 26). ESD service staff often assumed a case worker/key worker role, liaising with other services (as for instance GP and social care) and signposting patients to ongoing services (C). Teams reported that they had to contact multiple organisations both statutory and voluntary and much time could be spent in identifying which service was appropriate based on the patients’ GP and their postcode. At the same time, the frequent restructuring and decommissioning of services was not communicated effectively, leading to staff not knowing what was available for their patients (C). Meetings across the entire pathway, as regular service management meetings, quality improvement meetings or whole pathway service redesign meetings, promoted clarity on the availability and role of each service and awareness of the pressure points in the pathway (M). Communication was streamlined as a result, leading to smoother and safer handover between services (O):
If you have a very clear pathway from acute to the community, where everyone knows their role and doing that, then less time is wasted and it’s a more streamlined process, and timely, and also safer, hopefully, as well. Everyone takes part in developing the pathway, which is I think what happened here.
FGBS2
FIGURE 26.
The CMOs concerning communication across the stroke care pathway.
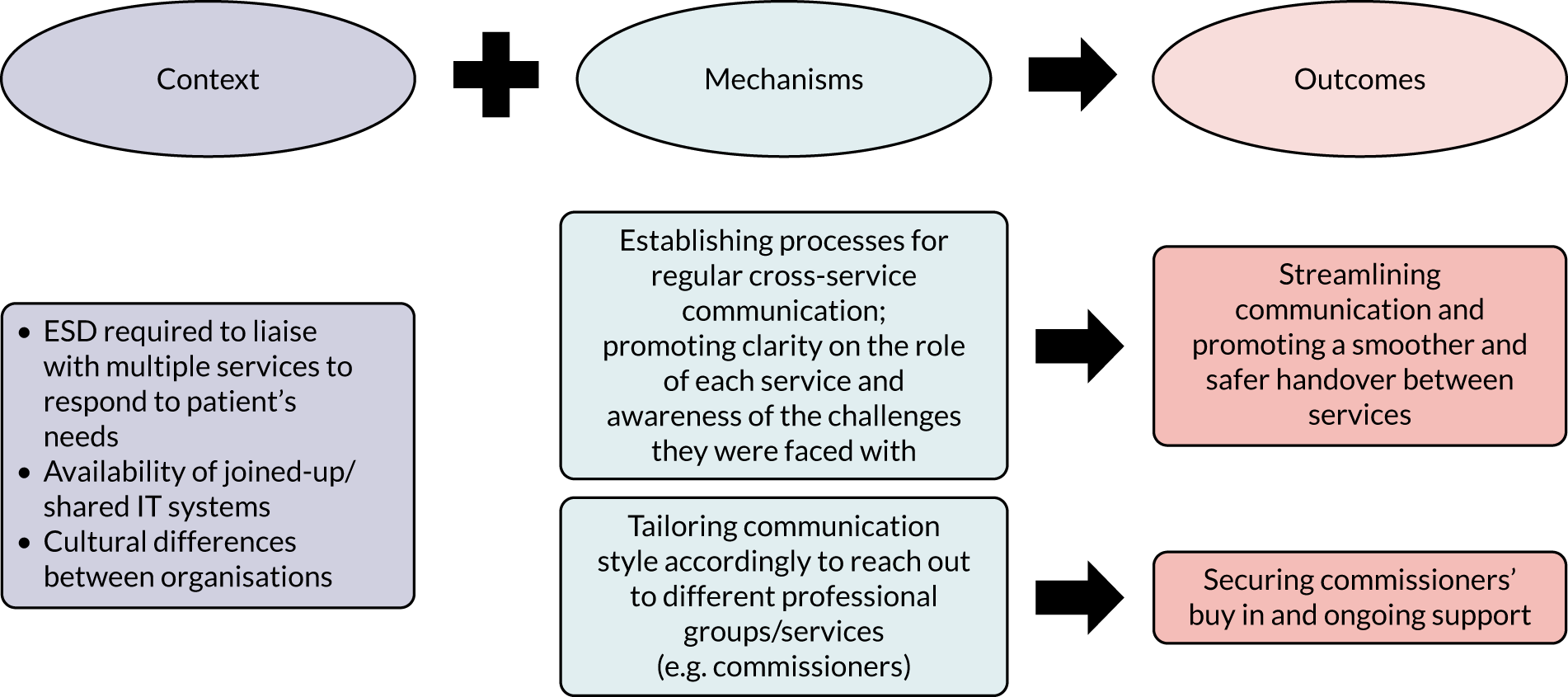
Liaison between teams was hindered by a lack of joined-up or shared IT systems in many areas (C). Acute trusts and ESD services were rarely able to share electronic records, scan results or test results, which hampered the sharing of information about patients. Different therapies were sometimes employed by different organisations and, therefore, had separate electronic notes or even paper-based notes. In one team, SystmOne contained standardised templates across all four patches (C), which meant that teams could access each other’s caseloads and notes (M). This meant that they could cover for each other in busy periods (O):
I think SystmOne is really working well, because we can see what other people have put on the system, and providing we’re all on SystmOne we can see what the care plans are. So that doesn’t hinder if we’re working across team, that’s a fantastic facility. Where it falls down is when we’ve got patients coming in from say some of the hospitals and we can’t see what’s happened to the patient before they come to us. So particularly for speech therapy, I don’t know whether it happens in the other therapies quite so much, but they might be complex, they might’ve had a lot of assessment and we have no knowledge.
I think from a hospital point of view we have that frustration as well, and with the absolute kind of utopia would be, we’re all on the same system, so that you can see scans, if they’ve had a stroke prior to that and we can see what’s happened and where – that would be the absolute ideal, wouldn’t it, if we were all on the same system.
I mean to be fair we can access the care portal, but it’s still not the same as what we can access on SystmOne, so while we can see the big things on the care portal we can’t see some of the . . .
Therapy notes.
. . . details. We can’t access those.
FGFS2
Achieving and maintaining good communication with commissioners was identified as an important parameter in developing an ESD service and establishing its position in the stroke care pathway (O). One team described liaising with commissioners as a time-consuming and stressful exercise that could end fruitless as ‘they don’t speak the same language’; it resulted in ESD leads disengaging from the process because they felt that they had to prioritise their clinical work. As noted by a service manager, cultural differences between organisations reflected differences in their communication style (C); they thought that this characterised communication efforts between commissioners and clinicians and stressed the importance of ESD services tailoring their networking approach (M) to effectively reach out to different stakeholders (O):
I think there are very, very many competing priorities for funding other than commissioners, what you have to do is make sure that you get the ear of the commissioner, establish your relationships and networks and never miss an opportunity and that’s very much an individual thing.
CS6
Summary of programme theory 3 findings
Findings highlighted the importance of good communication in developing collaborative trusting relationships between key stakeholders and promoting the provision of a seamless patient-centred pathway. In their communications with service users, participants stressed the need to be honest and pragmatic and ensure the ongoing provision of tailored information to both patients and carers. Building rapport and a two-way communication with carers as well as patients was considered key to effectively managing expectations and engaging carers in the rehabilitation process. Creating opportunities for formal and informal communication with the stroke unit was identified as a mechanism driving the development of a trusting and collaborative relationship with hospital referrers, and contributed to improving the referral and discharge process. Establishing processes for regular cross-service communication emerged as a facilitatory mechanism to ESD teams’ efforts to liaise with multiple stakeholders across the pathway to ensure smooth and safe handovers for their patients. Against a background of cultural differences between organisations, the need to tailor communication style to engage stakeholders, such as commissioners, was important in securing their buy-in and ongoing support.
Discussion
Overall findings supported our programme theories by (1) indicating the value of core evidence-based components to successfully deliver the intervention in different settings; (2) demonstrating how features of geography and particularly the time required to travel to patients shaped the delivery of certain intervention components; and (3) demonstrating why and how effective communication across the pathway can influence the provision of a seamless and patient-centred pathway.
In line with our first programme theory, findings supported the need for the adoption of core evidence-based components in achieving effective ESD. Despite considerable variations in their model of operation, services identified key characteristics and processes that reflect research and clinical recommendations and, when in place, were believed to facilitate the delivery of evidence-based practice. These included the provision of an intensive and responsive service to eligible individuals by a co-ordinated MDT that met frequently. For instance, the application of eligibility criteria allowed services to manage capacity, promote responsiveness and ensure patient safety at home, although it was accepted that relying on physical disability scores to decide eligibility may not provide the full picture.
To deliver these components, however, services had to respond and manage countervailing conditions of specific contexts within which they operated. This reflects the Damschroder’s conceptualisation of a complex intervention as consisting of core active ingredients and an adaptable periphery that can be modified to account for contextual influences without compromising the intervention integrity. 14 For instance, services safeguarded their MDT meetings but adjusted the way that their MDT was organised, dividing the team into smaller subgroups corresponding to geographical locations with the view to reduce travel time and use resources efficiently.
Respondents recognised the need for intensive and responsive ESD; however, they disagreed with the prescriptive nature of the clinical guidelines,5 arguing that clinical judgement is required to ensure that individual patient circumstances are considered and the service best meets people’s needs. Participants did not recognise a dose-dependent relationship between intensity of practice and patient outcomes. They emphasised that the need to provide a holistic service addressing the multifaceted impact of stroke might take time away from hands-on practice. For instance, teams could be called to address mood problems or issues related to returning to work. The analysis also showed that intensity and responsiveness targets were sensitive to certain contextual characteristics, including the fragmentation of the local care pathway with lack of slow response of other services.
Service intensity and responsiveness were also influenced by the delicate balance between service capacity and the time that the team spent travelling to patients, as suggested by the analysis of the second programme theory. The impact was more prominent in rural services, but those covering large catchment areas were also affected. Distinguishing between remoteness and rurality103 might help to explain the impact of travelling times in these contexts and frame it in relation to geography. Barriers associated with rurality and travelling times stretched the capacity of these teams; when staffing levels were low, services often relied on staff commitment and hard work to sustain optimal levels of care. Roots et al. ’s104 study on rural rehabilitation practice in Canada found that OTs and physiotherapists ‘stretched their role’ beyond the normal expectation of the professions as a strategy to overcome resource shortages. In the study by Adams et al. ,105 workforce, including staffing levels, was identified as a key factor in delivering and sustaining a rural physiotherapy service.
Qualitative feedback included in the ESD consensus document13 also suggested that travelling times might reduce face-to-face contact and stretch service capacity. Supported by previous research, our findings suggest that the pressures posed by travel times and rurality make sustaining the quality of service provision a resource-intensive task. These teams may require higher staffing levels than similar-sized teams operating in urban contexts to meet their targets and deliver evidence-based care, which needs to be highlighted at a commissioning level and be taken into account in developing service specifications.
Good communication and the development of trusting, collaborative relationships was a consistent theme across the three programme theories. Findings related to the first programme theory focused on ‘inner setting’14 communication within the MDT. Although MDT meetings were recognised as the main forum for supporting communication and collective decision-making, the importance of informal face-to-face interactions was also stressed as key to exchanging expertise and practical and emotional support. The value of regular informal communication has been previously highlighted in the literature. 19,106 Waring et al. 19 found that informal interactions enable the development of trust and collaboration, and may contribute to improved hospital discharges. Episodes of opportunistic dialogue, facilitated by physical proximity, contributed to mutual learning and achieving interdisciplinary working in stroke rehabilitation settings, according to Clarke. 107 In this study, we found that efforts to reduce travelling times, through flexible working arrangements, could have a negative impact on face-to-face communication. Although the use of digital technologies supported communication and information exchange, they could not substitute face-to-face interactions. At a time when telerehabilitation approaches gain ground, our findings highlight the need to protect opportunistic communications and encourage face-to-face meetings.
Building on existing guidelines, this study examined staff’s perspectives on why and how certain evidence-based components influence outcomes, allowing a deeper exploration of certain elements of the intervention. With regard to team composition, the study clarified the role of RAs, for which agreement was not achieved on the consensus document. Based on our findings, a recommendation could be made for RAs being a core member of an ESD team. Findings also stress the need to address certain contextual elements that enhance the role of RAs, such as delegation from registered therapists and the need to empower and promote the autonomy of support staff through appropriate supervision and upskilling.
The access to nurses, psychologists, doctors and social workers offering stroke-specialist input was essential to promoting an interdisciplinary skillset and enabling a holistic approach to rehabilitation provision. The timely involvement of social workers who understand the needs of stroke survivors and who are embedded in the pathway was perceived as an important facilitatory mechanism, streamlining the discharge process and ensuring that stroke survivors received a tailored care plan. Social carers were called to play a boundary-spanning role,19 working across social care and health-care organisational boundaries to identify and address unmet needs in a timely fashion. The need for partnership working with social care has been a consistent finding in the ESD literature23,39,56,108 but the issue remains pertinent.
In addition to further supporting the value of certain MDT processes, such as formal meetings, the research design surfaced nuanced, qualitative features of MDT working, including interdisciplinary working and leadership. Across the six sites, respondents agreed on the need to invest in developing an interdisciplinary skillset and work ethos across the MDT. It was suggested that the nature of community working and the efficiency of activities required collaborative working and blurring of professional boundaries. As noted by Baillie et al. ,108 skills transfer permits a better management of resources in community working because it reduces the need to have more than one staff member at home visits. Baillie et al. 108 identified trust and confidence in colleagues’ expertise as a context facilitating the development of an interdisciplinary skillset. In this study, we found that interdisciplinary working further promoted trust and respect in other disciplines. Our conceptualisation of interdisciplinary working as a mechanism overlaps with the ‘role blurring’ construct identified by Sims et al. ,109 which enabled carryover of skills by other disciplines, enhancing the continuity of care and helping staff professional development. Interestingly, and in line with our findings, both Baillie et al. 108 and Sims et al. 109 stressed the need to protect expertise and specialism and ensure that staff did not feel professionally threatened.
The role of effective leadership in maintaining standards of care and protecting staff well-being and job satisfaction was highlighted in the findings. Key mechanisms for effective leadership included the provision of training and support, and the development of a non-hierarchical culture of respect and appreciation. Staff across disciplines and bandings were encouraged to participate in collective decision-making and were empowered to contribute to service improvements. In a study investigating rural physiotherapy service provision, Adams et al. 105 highlighted the importance of staff engagement in decision-making and the provision of professional development and upskilling as important workforce factors contributing to staff retention in rural areas. Motivation, empowerment and feeling supported and valued were key mechanisms of leadership identified by De Brún and McAuliffe,110 which were linked with staff and patient satisfaction and enhanced team working. A review of relevant evidence in health care by West et al. 111 stressed the importance of leadership in shaping organisational culture and influencing the success of service improvement efforts. Our results on the importance of MDT working resonate with realist research in stroke care by Harris et al. 112 Taken together, our findings further emphasise the need for services to invest in enhancing effective multidisciplinary teamwork. However, similar to Harris et al. ,112 our identified outcomes operated at a team and not at a patient level, which implies an indirect relationship between effective teamwork and patient outcomes. Future research could develop specific interventions targeted to elements of effective team working, focusing on clarifying their relationship with patient-level outcomes.
The complex and multifaceted impact of stroke requires that ESD services work across occupational and organisation boundaries, often championing patients’ needs, to ensure that they receive comprehensive, integrated care. As demonstrated by the analysis of programme theory 3, effective communication with other services was key but not easy to achieve, especially against a background of cultural divides and lack of integrated communication systems. The relationship with inpatient services was perceived to be a particularly important one in streamlining the discharge process and ensuring the appropriateness of referrals. Despite that most participating sites had a well-established position in the local pathways, ongoing efforts to clarify the ESD role and build a trusting relationship with referrers were considered necessary. The need to address knowledge gaps among hospital staff regarding the ESD remit and benefits has been stressed in the literature. 23,46,108,113 This study identified opportunities for formal and informal communication and cross-boundary working arrangements to be key mechanisms for building a collaborative relationship. In-reaching and physical proximity appeared to provide a facilitatory context, although not everyone shared this view.
Findings from across the three programme theories highlight the interdependency between the ESD services and the local stroke care pathways. The quality of communication and transitions across services had a direct impact on the operation of the service, including its ability to achieve its responsiveness and intensity targets. Supported by previous studies,13 our findings stress the importance of a more integrated and comprehensive stroke service provision. As noted by our participants, the lack of an integrated stroke care pathway was especially obvious when they attempted to address the needs of more complex patients who did not fall within the mild to moderate eligibility criteria. Integration may take different shapes or forms. 114 Although organisational integration may not be feasible, virtual integration may be achieved through the development of networks and alliances. 114 In this study, we found examples of services establishing cross-service communication processes to promote information-sharing and collaboration; these efforts need to be protected and further enhanced. Our findings also have implications for evaluating context in implementation research. Damschroder et al. ’s14 and Rogers et al. ’s115 conceptualisation of ‘Cosmopolitanism’ as an organisation’s networking efforts through, for instance, boundary-spanning roles, is consistent with our findings. Future studies should include representation of stakeholders from across the stroke care pathway to investigate these system-level factors in greater depth and identify further strategies to promote integration.
The RE methodology allowed us to address the complexity of ESD delivery in clinical practice and obtain a better understanding of how intervention resources and stakeholders’ reasoning interact with contextual conditions to generate intended and unintended outcomes. Findings reiterated the importance of context for successful implementation of large-scale interventions and highlighted contextual features and mechanisms that need to be either addressed or capitalised on to improve effectiveness. By distinguishing between intervention components, which need to be safeguarded and adaptable elements, this study could effectively inform customisation efforts and interventions aimed to maximise success in local contexts.
The analytical task of linking CMO chains is suggested to help unpack causation, increase the explanatory power of findings and improve the external validity of case studies. 8,20 Although the iterative analytic process required considerable investment of time and resources, we also found that the theory-informed approach and the application of the CMO heuristic facilitated the analysis of a very large and information-rich data set. The lack of prescriptive guidance on ‘how to’ configure CMOs makes the process an interpretative task that requires ongoing reflection and negotiation between researchers. In this study, having data independently analysed by two researchers helped to reduce ambiguity and increased the confidence in the trustworthiness of our findings. Disaggregating mechanisms between intervention resources and stakeholder reasoning was a particularly helpful approach, and we think that it allowed us to achieve a clearer delineation of mechanisms and contexts. We took a pragmatic position to configure our CMOs at a level of abstraction that would allow us to draw take-home messages relevant to clinical practice. However, we are conscious that this approach has led to a large number of CMOs and theoretical nuggets rather than an overarching higher-level theory. Although the exact replication of the identified CMOs in other settings is unlikely, the accumulation of insights from further testing of these programme theories in different geographical and organisational contexts could help to develop an evidence-informed theory base for the large-scale implementation of rehabilitation services in the community.
Conclusion
The findings supported our overarching programme theories and shed light on the key contextual features and underlying mechanisms driving the successful delivery of evidence-based ESD. The adoption of core evidence-based components was identified as central to the effectiveness of the intervention. Mechanisms facilitating patient discharge and ESD responsiveness included (1) the application of eligibility criteria, (2) having access to a social worker, (3) adopting a flexible approach in who conducts the initial assessment and (4) establishing ongoing communication with hospital staff. Rehabilitation assistants had a key role to play in supporting the delivery of an intensive and responsive service. Involving carers in the rehabilitation plan, promoting a self-management ethos and implementing telerehabilitation approaches may contribute to augmenting practise between sessions and improving adherence. Service intensity and responsiveness were influenced by the interaction between service capacity and the time spent travelling to patients. Rural services and those covering large catchment areas may require higher staffing levels than similar-sized teams operating in urban contexts to meet their targets and deliver evidence-based care. Across all settings, effective MDT working was perceived as key to ESD success. The need for good communication both within ESD and across services in the stroke care pathway was emphasised as a mechanism driving the development of collaborative trusting relationships between stakeholders and streamlining patient experience of care transitions.
Chapter 9 Work package 2: patient perspectives
Introduction
The previous chapter qualitatively explored how staff attitudes and behaviours influenced the way that stroke ESD services were configured and run. It also explored the way in which community-wide stroke pathway development and contingent structures and processes shaped service delivery. This chapter focuses on the views and lived experiences of stroke survivors and their families. The purpose is to provide additional depth of understanding on how the variation in operation and delivery of services, as described in Chapter 6, affect and are experienced by service users in the real world. The findings could help inform future service planning, including what may and may not add value from a service user’s perspective.
Aims and objectives
Patients were interviewed as part of WP2 to explore their views and experiences of ESD services. The purpose was to contribute to the pool of data informing how the proposed mechanisms identified from the RES actually operate in real-world settings and the outcomes, as perceived and experienced by the patients.
Methods
Five purposively selected ESD patients from each of the six ESD sites (n = 30) were invited to participate in semistructured interviews. Patients who were actively on caseloads were recruited by the ESD teams in consultation with the research team to ensure that the sample included patients with a variety of characteristics (e.g. sex, age and stroke severity). Interview guides were informed by the three programme theories described in Chapter 3. 116–118 However, a realist interviewing approach did not prove feasible because patient interviews required a more informal conversational style.
Procedures
Potential participants were approached by the clinical teams during a routine visit to establish their interest in the study, provide participant information sheets and gain consent to pass their contact details to the research team. If consent was given, contact details were transferred to the research team via a password-protected encrypted spreadsheet. The research team contacted potential participants to explain the study further and to establish whether or not they wished to participate. Patients with mild aphasia were not excluded and, if patients wished, their relatives were able to join the interview to support them. Interviews were arranged at a time convenient for the patient. Information sheets were again provided and explained at the beginning of each interview before written informed consent was gained. Interviews were audio-recorded and transcribed verbatim. All audio-recordings and transcripts were password protected and stored securely on the university server.
Analysis
The interview schedule spanned five overarching topics that were designed to capture the patients’ experiences of ESD: the experience of rehabilitation at home, staff interaction, aspects of ESD that mattered most to them, what patients believe the purpose of ESD to be, and how services could be improved and why. The semistructured design meant that participants could also discuss what mattered most to them about ESD outside the constraints of this schedule.
Data were analysed using the six stages of reflexive thematic analysis recommended by Braun and Clarke. 36 In line with conventional practice for this type of analysis, a combination of deductive and inductive analysis was undertaken, with a greater emphasis on deductive analysis in view of the overarching programme theories.
Pen and paper and computer-assisted software QSR NVivo (version 12) (QSR International, Warrington, UK) for Windows (Microsoft Corporation, Redmond, WA, USA) were used to store, sort and retrieve the data to assist with the analysis.
Inclusion and exclusion criteria
The following inclusion criteria were applied:
-
having sustained first or recurrent stroke
-
medically stable
-
ability to give informed consent
-
aged between 16 and 100 years
-
having received ESD within the past 3 months from the beginning of recruitment at each site.
The following exclusion criteria were applied:
-
stroke patients who are not eligible for ESD
-
patients who do not have adequate understanding of the English language to participate in the interviews (translators may not be available in community-based services).
Results
Data were collected from 30 patients between November 2018 and November 2019. Interviews lasted between 24 and 70 minutes (mean 45 minutes, median 45 minutes), excluding consent time. All interviews were conducted in the patient’s home.
Patient characteristics
Overall, patient ages ranged from 32 to 88 years, with a mean of 65.9 years (median 68.5 years). There were 10 females and 20 males. The disability scores at admission to the ESD teams ranged from 8 to 20 (mean 15.7, median 16) on the Barthel scale, with lower scores indicating a greater disability out of a maximum score of 20. The length of stay with the ESD teams ranged from 15 to 107 days, with a mean of 48 days (median 42 days). Patient characteristics by site can be seen in the Table 21.
| Characteristic | Site | |||||
|---|---|---|---|---|---|---|
| A | B | C | D | E | F | |
| Male (n) | 3 | 3 | 2 | 4 | 4 | 4 |
| Female (n) | 2 | 2 | 3 | 1 | 1 | 1 |
| Age (years) (range) | 53–86 | 53–78 | 47–86 | 32–74 | 38–79 | 57–88 |
| ESD length of stay (days) (range) | 15–45 | 42–42 | 27–46 | 34–107 | 56–83 | 36–74 |
| Barthel score at start of ESD (range) | 15–20 | 11–19 | 13–20 | 14–20 | 10–19 | 8–18 |
Sites A–C had the shortest length of stay, indicating closer adherence to the ESD model of an average stay of 6 weeks. Sites A and B provided both ESD and community stroke rehabilitation services; therefore, some patients could be transferred from the ESD pathway to the community pathway, but only the ESD pathway is captured for our length-of-stay comparison. Sites D–F were the most rural services in our study and each service had the flexibility to extend the length of stay of their patients if they deemed it appropriate, hence why we recorded longer length of stays among these services.
Thematic analysis
Three overarching themes were identified, with nine subthemes, and are presented in Table 22.
| Theme | Subtheme |
|---|---|
| Theme A: the role of ESD in post-stroke recovery | Lack of prior knowledge and understanding of the service |
| Satisfaction with the service | |
| Rehabilitation dose | |
| Trust in clinician’s expertise | |
| Theme B: the desire to recover quickly | Goal-oriented rehabilitation and support |
| Taking control | |
| Importance of the home environment in recovery | |
| Theme C: the psychological impact and importance of support | Loss of identity |
| Family support |
In the following sections, participants are identified in the quotations by the letter denoting the site that they came from, a ‘P’ for patient and a number showing the order of interview at that site.
Theme A: the role of early supported discharge in post-stroke recovery
Lack of prior knowledge and understanding of the service
Most patients had been informed that they would be referred to the ESD team after discharge (n = 24 out of 30 patients). However, half of the patients did not understand what that meant or what services the ESD team would be providing for them and, therefore, were confused about which services were delivering different parts of their care:
I was in hospital when it was mentioned that this discharge team would come in and see me at home.
BP3
I don’t think I have heard of ESD, except when you made me the phone call.
FP1
So what part of the treatment that we have received so far comes under ESD . . . the early thing. Is it the support like dressing and washing or is it the occupational . . . occupational therapist? Or the voice.
Clinical psychologist (CP)2
The lack of prior knowledge of the purpose of the service created low expectations for the majority of patients, who expected just to receive physiotherapy. Most patients were surprised and delighted with the amount and breadth of support that the therapists offered:
No. I didn’t know anything about it at all. So I was amazed and pleased that it did, especially . . . I had as I said such a lot of problems coming and people really putting and helping me out. I was astounded at that. So I’m delighted with it.
EP2
Satisfaction with the service
All participants were very positive about the service. They particularly valued the rapid start of the service after discharge, which provided continuity of therapy, support and assistance with immediate problems encountered in the early days post discharge:
It’s . . . it’s a good service because when you come out, you . . . I think you need some form of . . . otherwise you’ll be straight to the doctor probably. So it is a good . . . good idea.
Assistant practitioner (AP)3
The main benefit I think is the fact that it’s immediate. There’s not this gap between hospital and coming out. It’s immediate.
CP1
And I think as well if you come straight out of hospital home and there’s nothing, that’s such a big change isn’t it? I mean that was difficult anyway, wasn’t it getting used to not having people around twenty-four seven.
EP5
Participants reported that they thought that the service was playing a vital role in their recovery. Many participants could already see rapid and important improvements in their physical recovery, which was helping to rebuild their confidence. They attributed this to the therapists’ motivational working style and did not think that they would have carried on with exercises without their input:
I couldn’t even sit up, so physio’s have, well, they have made a massive improvement in me really. And I can see that. Yeah.
EP3
Which is I think as much the point as the benefit. I’ve enjoyed them being here. I’ve enjoyed them pushing me, because if they hadn’t pushed me I wouldn’t have done it.
DP4
The service was valued by all participants. They stated that they would highly recommend the service to all new stroke survivors to assist with navigating the changes that were needed to adjust to their new disabilities and required changes to ways of living:
Yeah. And they’re good. They’re very good. Yeah. I’d recommend them to anybody.
AP2
In fact, the service was valued so much by the stroke survivors that they worried about new stroke survivors who may not have access to an ESD service:
I think it’s a very good service. And I think, you know, they should give it to everybody when they come out from hospital if they need it. You know. Because I did need it. I was at a point, but I wasn’t at a very good point when they discharged me from hospital. You know there was a lot more to do.
CP3
However, there was a downside to the extreme satisfaction and benefits that patients experienced from the service, which was expressed as a concern by more than half of the participants: what was going to happen after the initial 6 weeks of the service ended:
I don’t know. I . . . I was just worried after this 6 weeks. What happens after this 6 weeks. Because you know you have these people come four times a week and then all of a sudden . . . what’s going to happen? And they said there is another plan [inaudible] . . . but it could take time.
CP5
Rehabilitation dose
The majority of participants felt that they received a sufficient number of sessions at the right frequency. They further acknowledged that it was as much as they could cope with time wise and energy wise:
I think it’s been just the right amount.
AP1
I think it’s probably to a certain degree as much as I could probably take.
DP4
Some wanted more or longer input from the service, but did not want to deprive other people who may have needed the service more:
I wouldn’t want to take it . . . I wouldn’t like to take it away from people who need it more than me if you know what I mean. I think, you know, selfishly I think . . . I think it’s enough you know.
DP1
Patients seemed to be happy with whatever service they were offered. Those receiving a 7-day service had made adjustments to accommodate having visits at the weekend, while those receiving a 5-day service valued the space at weekends to rest and recover and spend time with family and friends:
I only need 2 days. Or I only . . . I could only manage 2 days. I couldn’t manage more than 2 days.
BP3
The reason for that, when they come every day you spend quite a significant time preparing for them to come. So in some ways, it’s a chore. Do you know what I mean? You know, having a shave or brushing your hair, or getting dressed. There is that you know . . . they’re coming so I’d better be ready . . . And I think if I did a 7-day week I’d go barmy. You know, on a Saturday . . . on a Saturday I want to watch the football. So if I don’t have a shave, to hell with it, you know what I mean. So that break on a Saturday and Sunday is nice.
CP1
And you said they came five or six times a week. Was that just during the weekdays? Monday to Friday or did they come on the weekend?
Saturdays and Sundays as well.
OK. And did you . . . were you happy with that?
Yeah. Suits us.
EP5
A few higher-functioning patients felt that they did not really need the service and were happy to be discharged quickly:
No. Because I’ve . . . you know for some people I’m sure it’s very good, but I just don’t . . . don’t really feel as though I really needed it.
AP5
Trust in clinician’s expertise
Patients held clinicians in high regard and looked up to them as authority figures. For this reason, they were unwilling to challenge or criticise them. They were happy to do whatever the clinicians directed them to do:
I’ll leave up to . . . I’ll leave it up to the early discharge team of when they think it’s best for me, because let’s face it, I could say, well I don’t want you’s anymore.
BP2
So . . . is . . . is that because you’re very grateful to be getting the service, that you’re just happy to accept whatever they . . . whatever the visit is, yeah?
Probably. Yeah. Probably. Yeah.
EP3
Patients also valued the therapists’ expertise and knowledge of the wider stroke pathway and health community, and relied on them to signpost to other agencies for support:
And . . . and I do Pilates. And she . . . we were on about trying to get back to that. And she was going to try and find out whether there was a Pilates class at the [hospital] for stroke people, so . . . she was trying to organise that for me.
AP3
Theme B: the desire to recover quickly
For all participants, the need to recover as fully and quickly as possible was key.
Goal-oriented rehabilitation and support
The majority of participants felt that the goal-oriented therapy plans were highly valuable and contributed significantly to their recovery. The time that the therapists spent with the participants to understand their life styles, needs and goals was a fundamental part of this process and very much appreciated:
What I found with the ESD team was that they would come . . . there was no . . . there was no sort of timetable . . . they would stay here as long as I needed them, you know what I mean? There was never a case of ‘I’ve got to go’ . . . I know they’ve got other patients to look after, but this was a very personal experience for me. And certainly I wouldn’t be where I am now as far as improvement if it wasn’t for the ESD team.
CP1
The team established personal rehabilitation goals with the patients, and then planned bespoke exercise and therapy programmes to help patients move forward. Patients practised in between sessions, engendering a sense of agency and involvement in their own recovery and providing a sense of moving forward:
She set a plan in place of things to do to increase mobility and again we started talking task, because that seemed to be one way of trying to get what I needed and what I wanted to be able to do. And then behind her, there is a team of either physios or I think assistant physios who then come out and work through the plan with you. And when things are too easy they make it harder and add things in so . . . and they brought with them quite a lot of equipment to enable me to do these things . . . If there’s something that’s important in your life that you’ve always done and you want to continue doing then they are the enablers of that. They can make that happen.
FP5
The rapid provision of specialised equipment to support the different stages of recovery was particularly valued for comfort and safety and to promote independence and confidence. Equipment could be rapidly changed to meet the differing stages of progression in the recovery:
They’ve given me a . . . stuff for the stairs and everything, haven’t they? Like handrails for the bathroom and things like that. Which have helped.
BP5
Taking control
All participants commented on the restrictions that stroke had brought to their lives in terms of their independence, activities of daily living and leisure activities. They felt the need to be able to challenge themselves to speed up the rate of recovery:
I mean I’ll do what . . . like I say, I’ll do whatever it takes to . . . to improve. Just because I’m so determined and I . . . I want to get back on my feet as quickly as I can really.
DP3
Many were keen to explore additional sources of support, such as support groups at which they could share their experiences with others in a similar situation:
There is . . . there is like a stroke club isn’t there? [Rehab assistant] runs one at [local centre] just up the road here. I would go. Yeah. Just to talk to like other survivors I suppose.
BP5
The majority of participants had recognised and embraced the need to carry on and take charge of their rehabilitation and subsequent recovery:
But it is about your own determination. It’s about making use of what’s there. It’s about making sure you get everything that is available to you.
FP5
The importance of the home environment in recovery
Most patients were happy to have moved to their own homes and felt that they were more empowered to actively participate in their own rehabilitation and recovery. They also felt that the rehabilitation was more tailored to their lives and needs:
They always thought ahead in that respect, you know. If I wanted . . . if they knew that I needed to walk from there to the kitchen, they would leave that place clear. You know what I mean? It’s almost like thinking out the box.
CP1
Receiving therapy at home was also easier to manage from an energy perspective and financially. Given that most of the participants were unable to drive at the time of the interviews, the cost and feasibility of travelling to the hospital daily or even several times per week for rehabilitation would not have been a viable option. This was even more pertinent to patients living in rural areas where public transport was not available even if the patient had been well enough to travel:
They said ‘oh you’d probably have to go there for physio’. And I thought, God how am I going to get there? You know, I’d have to have a taxi every day. And I thought, God I can’t afford that. And then when they said about these coming in, I was like ‘oh that’s brilliant’. You know, because it’s like £6 each way in a taxi. I wouldn’t be able to afford that every . . . four times a week.
CP5
Theme C: the psychosocial impact and importance of support
Loss of identity
All of the participants were having to come to terms with their new lives, altered abilities and routines. Many found it psychologically challenging and were shocked at their own reactions to the situation that they now found themselves in:
I have broke down quite a lot . . . which has shocked me. Since I’ve had my stroke in the hospital I think . . . well since coming out, I’ve cried a couple of times of being home, since I’ve been home. But I’m . . . I was really shocked about that side of things and I . . . well I don’t know where it’s come from if that makes sense.
CP4
Participants described how they worried about being a burden for partners and families:
It’s . . . it’s being a burden to my wife, because she’s having to do everything for me.
AP4
Participants really needed someone to listen to them and to help them to work through some of their feelings, worries and frustrations. Dealing with the emotional and financial impact of their stroke, and being uncertain about their future recovery, was overwhelming. Participants really appreciated the flexibility and the skills that the ESD team had to respond to their emotional and psychological needs when it was needed the most:
I think they were . . . certain times, especially when . . . when I was upset about not being able to go to the [best friend’s] funeral . . . I spoke to . . . [occupational therapist] and we literally spent most of the . . . the hour chatting about it. Because he knew it was something that I needed to get off my chest when you actually think that, you know they’ve come with a training . . . planned and yet they can just totally stop it and listen. And it was fantastic because I just wanted to get it off my chest and . . . and . . . And I think it was more needing than any training I could have been given. I thought it was fantastic what they’d done.
DP1
Although some ESD teams were able to refer patients to psychological support services, not all teams had access to this. Sometimes issues were just surfacing and the new reality was becoming more apparent just as the ESD team were preparing to discharge the patients, leaving some patients with unresolved problems and potentially no specialist support.
Family support
Most of the participants described how the support of significant others was a vital part of their recovery plan. ESD teams involved families in goal-planning and extending therapy sessions by motivating and supporting stroke survivors to continue to practice their rehabilitation in between formal sessions. Partners and spouses appreciated being involved and having the support of the ESD team:
They have involved my wife, but yeah. Yeah, they said that she can walk me round the block and my wife’s quite strict. She makes sure I do my exercise. Yeah.
EP3
Because they’re coming in virtually every day, if I’ve got any problems, you know, I can talk to them about it and if they can’t answer it, they’ll take it back to the team.
EP4
Discussion
Semistructured interviews with patients aimed to explore their views and lived experiences of receiving ESD services to help to augment the understanding of the three study programme theories relating to the adoption of evidence-based core components, geography and communications.
Patients were very satisfied with the ESD service, as has been found previously. 38,119 They also reported that it was the main conduit and catalyst for their recovery. Most patients had been told to expect a service after hospital discharge, but did not know or understand what the service was going to be. Several patients expected just to receive physiotherapy and, therefore, were delighted and surprised at the flexibility of the team to work holistically and support their psychological issues, as well as work towards meeting their physical needs. The teams’ ability to signpost and refer to wider community support services were also vital to assist with reintegration into family and community life. Patient expectations are important to manage because the evidence base suggests that positive expectations can increase patient engagement and motivation, and positively influence functional outcomes. 120,121
The responsiveness of the team in terms of the early first contact and visit was particularly important. It helped patients and families to feel safe in the transition from hospital, where they were heavily supervised, to home, where there was no immediate professional help and support. They particularly valued the team’s interventions on their behalf to sort out immediate problems and gaps in services. Previous studies have demonstrated that this transfer of care can be a traumatic time for patients and carers, and can increase stress and burden if not supported appropriately. 38,49,122,123
Patients especially appreciated that the service was delivered at home. This made the service more accessible and affordable, and meant that rehabilitation could be tailored to real lives, empowering patients to be more involved in their recovery. 49 These findings were replicated by Cobley et al. 38 in a study of ESD patients who reported that services delivered at home were more cost-effective and less demanding. It also enabled family members to be more involved in the delivery of therapy. Furthermore, research has shown that rehabilitation delivered in the home can improve high-level activities of daily living, such as walking and managing stairs, above that delivered in hospital settings,124 and other functional outcomes. 10,122,123
The person-centred approach afforded by the ESD teams with personalised goal-setting was a key component in their recovery by targeting what was most important to patients. This has been evidenced previously. 125 This helped with patient and carer motivation to extend therapy outside formal therapy sessions and helped to progress recovery at a more rapid rate. This included rapid assessments and the provision of access to aids and equipment, which was updated and changed as patients moved forward in their recovery. This is important because patient and family motivation and engagement are associated with good rehabilitation outcomes. 9 In addition, patients reported that this forward progression helped them to feel more positive and improved their mood.
Patients, overall, wanted to recover as quickly as possible, but recognised that ESD services were stretched and had to be shared out equally across the stroke pathway. They adapted their expectations of the service to the model of service in place in their area. They accepted that the number of visits and the length of service that they received was driven by the capacity in the team, and were happy to receive less than they ideally would like to make sure that those in greatest need also received a service.
Conclusion
Overall, patient experience of ESD was very positive. Patients reported that it was the main conduit and catalyst for their recovery. Early contact from the ESD team was critical to help patients and families in the transition from hospital to home. It was also the mechanism by which immediate problems were de-escalated and resolved, avoiding potential unplanned re-admission to hospital or transfer to residential care.
The delivery of the service at home enabled patients to engage and participate in their recovery more fully. This would not have been achievable if travel to a treating centre had been required. This was particularly relevant in rural and remote areas.
The person-centred, goal-oriented approach of the teams was highly regarded by patients. They reported that this optimised their engagement in the therapy and provided them with a locus of control, which they felt resulted in a more rapid and fuller recovery.
Patients accepted and were grateful for the dose and intensity of the therapy that they received. Although some would have preferred more frequent visits to speed-up their recovery, they were cognisant of the constraints that the teams were working under. Patients were satisfied with either the 5- or the 7-day service model, dependent on what was on offer to them.
Early supported discharge services delivered by experienced specialist stroke teams enhanced patient experience and optimised their potential recovery.
Chapter 10 Work packages 1 and 2: synthesis of findings
In this report, we have presented how our programme theories have been formalised, tested and refined. We conceptualised the evidence-based core components of ESD services as programme resources, and sought to surface the perspectives and behaviours of actors and stakeholders (staff and patients) who were making ESD happen on the ground. Using a mixed-methods approach, we were able to explore how these resources operated in different contexts (with a particular focus on urban and rural settings) and uncover important stakeholder responses necessary to achieve intended outcomes.
Here, we present an overall synthesis of findings and discuss how collectively these support or contrast with our programme theories. Theoretical implications and contributions to the wider literature will be discussed in Chapter 11.
Programme theory 1: ‘The adoption of evidence-based core components is important for the intervention to be effective in practice’
A 17-item ESD consensus score was used successfully to quantitatively measure the adoption of core components of an ESD service model, for example team composition (core team and others), staff training, team meetings and service specificity (see Chapter 4).
Responsiveness
We showed that adopting defined core components of ESD was associated with providing a more responsive ESD service, with responsiveness positively associated with meeting or exceeding recommended WTE levels of core team members per 100 stroke patients (see Chapter 4). There was also some evidence that access to a social worker was associated with a more responsive ESD service.
The findings in Chapter 8 further emphasised the need for teams to be appropriately resourced to meet the demand of increasing patient caseloads. Having a social worker embedded in the pathway and liaising with both the acute and the ESD services was reported to streamline hospital discharge because it permitted the allocation of targeted admission slots, ensuring that the patient was seen soon after their return home.
Chapter 8 revealed that adopting a flexible approach in how and who makes first contact with patients was used strategically to improve responsiveness. Targeting appropriate patients was identified as key to timely admissions. Introducing two streams in the service and adhering to the selection criteria regarding disability levels helped the services to manage capacity and promote responsiveness, which supports our programme theory.
Responsiveness was also an outcome that was particularly important to patients (see Chapter 9). The first visit helped patients and families to feel safe in the transition from hospital, where they were heavily supervised, to home, where there was no immediate professional help and support.
Intensity
The ESD consensus score was also significantly associated with treatment intensity, with significant association between features of MDT working and intensity (see Chapter 4). More specifically, treatment intensity was positively associated with holding weekly MDT meetings and a member of the ESD team attending acute stroke unit meetings.
Findings in Chapter 8 provided more insight into the importance of MDT meetings and good leadership. The need for interdisciplinary team working and the blurring of professional divides was highlighted. The important role of RAs to maximise capacity was also reported.
Contrasting findings
Chapter 8 suggested that rehabilitation intensity might be dictated by service capacity rather than patient needs. Against a background of staff shortages and reduced resources, guideline recommendations on intensity were treated with scepticism and most respondents thought that they were logistically unrealistic. Staff felt that recommendations were rigid and prescriptive, whereas they needed to respond flexibly to tailor rehabilitation intensity to patients’ needs and address the multifaceted impact of stroke.
Insight from a patient perspective showed that, in terms of intensity of treatment (or dose), many participants felt that they received a sufficient number and the right frequency of sessions. They further acknowledged that it was as much as they could cope with time wise and energy wise (see Chapter 9).
Length of hospital stay
The length of hospital stay was chosen as a measure of effectiveness of ESD in Chapter 5, based on previous clinical trial findings. Findings showed that when comparing ESD with non-ESD, patient groups matched for important patient characteristics and receiving ESD resulted in a 1-day increase in length of hospital stay. This suggests that not all benefits of ESD are realised in the real world and highlights the importance of investigating whether or not trial-based outcomes of interventions are achieved. However, the large reduction in length of hospital stay overall since original trials were conducted may explain why a reduction was not observed.
This was supported by staff participants’ accounts in Chapter 8, who did not expect ESD to lead to further reductions in length of hospital stay, which they felt was already short. Staff also suggested that ESD capacity issues meant that patients were kept in the hospital until a slot became available. In addition, patients could be kept in hospital for longer by hospital staff until they met the criteria for ESD, which related to gaps in the pathway for more complex stroke patients.
Programme theory 2: ‘Core evidence-based components of ESD will operate differently in urban versus rural settings’
Chapters 4 and 6 provided evidence of variability in the types of ESD model adopted across both urban and rural sites. In Chapter 7, the CCA found that rural services were associated with higher costs per patient, which, in turn, were associated with adherence to evidence-based core components of the ESD model. This suggests that additional resources and costs are required for rural services to meet evidence-based criteria.
This was supported by findings in Chapter 8, in which the time required to travel to patients was highlighted. In the context of wide/rural geographical catchment areas, allocating resources was a challenge, particularly when there were capacity issues. Teams adjusted the way that their MDT meetings were organised and operated to respond to challenges posed by travelling. All teams organised patients geographically to improve efficiency and most sites implemented ‘patch working’, dividing their MDTs into subteams covering different geographical areas. It was through staff commitment and hard work that the impact of travelling times was mitigated, so that intensity and responsiveness targets could be met. Good planning and co-ordination across subteams was key.
Many respondents talked about how spending a big part of their day on the road affected their work–life balance and physical and mental well-being. Again, relating to this programme theory, the impact was more pronounced in teams covering rural and wide geographical areas.
Contrasting findings
In Chapter 4, the level of rurality, as an ESD team-level variable, had no statistically significant relationship with any of the outcomes. This could be interpreted to say that the effects of adopting core components were similar for rural and urban sites. Although it is encouraging that we found examples of evidence-based ESD models in rural regions, reported challenges with health-care provision in these settings cannot be overlooked. It may be that the investigation of rurality at an individual patient level (which was not possible with the data provided), rather than the level of rurality across the site as a whole, will provide better insight into the impact of geographical location on implementation of ESD. Findings from Chapter 8 also support this suggestion, in that it could be geographical influences relating to travelling to individual patients’ homes that influenced service operation (rather than level of rurality per se).
Programme theory 3: ‘The quality of communication processes between key stakeholders and services will influence provision of a seamless stroke care pathway to patients’
All teams recognised the need for timely, clear and constant information provision to both patients and families. Being honest and realistic in their communication was identified as key in managing expectations and improving adherence to rehabilitation (see Chapter 8).
Findings from Chapter 9 showed that more could be undertaken to improve this, particularly with regard to the transition across hospital and community settings. Most patients had been told to expect a service after hospital discharge, but did not know or understand what the service was going to be. However, patient expectations were exceeded and, overall, patients were satisfied. The teams’ ability to signpost and refer to wider community support services was vital for patients to assist with reintegration into family and community life.
Timely communication was identified by staff as key to effectively preparing patients practically and emotionally for their discharge from ESD services. Staff reported that discharge from ESD services should be actively managed to avoid leaving patients and their families with a sense of ‘abandonment’ and to avoid an abrupt ending of the service. This stemmed from an observation common across all sites, which was that patients felt that their discharge from ESD services came too soon (see Chapter 8). This was confirmed by patients themselves, as reported in Chapter 9, in which more than half of the participants were concerned about what was going to happen after the initial 6 weeks of the service ended.
Good communication with teams from the referring stroke units was described as a key enabling factor to patients’ smooth discharge process. Communication and rapport-building efforts were a vehicle to educating about the service’s role and remit, shifting attitudinal barriers and promoting a trusting relationship with the referring team. In one site, senior management encouraged meetings between the managers of ESD and stroke unit teams; it was envisaged that if they could understand each other’s pressures and needs they would be more supportive and collaborative (see Chapter 8).
This aligns with findings from Chapter 4, in which attendance to the acute MDT meetings was a component of the ESD consensus score, which, overall, related to the responsiveness of ESD service delivery.
The implications of these findings for research and clinical practice are discussed in the next chapter.
Chapter 11 Summary and implications for research and practice
This report presents findings from a mixed-methods study using a RE approach, conducted in two interlinking WPs:
-
WP1 – how effective is ESD when implemented at scale, in practice?
-
WP2 – how do contextual factors influence the implementation and effectiveness of ESD in practice?
This study was designed to inform large-scale implementation of ESD by evaluating its effectiveness in real-world conditions, at scale. Our methodological approach was informed by recommendations for health service evaluation. 126,127 Overall, our findings have extended the literature relating to the implementation of ESD, fulfilling our overall aim to guide implementation of effective, evidence-based ESD in practice. This addresses recent recommendations for the investment in stroke rehabilitation that were made in NHS England’s Long Term Plan and the lack of large-scale development of ESD worldwide. 1,4,15
We started this research with a hypothesis about the ‘active ingredients’ that would make an ESD service effective. Our previous research, including an international ESD consensus document, has defined evidence-based core components. 12,13 Based on the CFIR, these core components were proposed to be essential characteristics that need to be implemented for ESD to be effective in clinical practice. 14
A RE approach allowed us to test hypotheses about how these active ingredients achieve outcomes and, importantly, in what contexts. To the best of our knowledge, this was the first study to use a RE approach to investigate ESD, building on research investigating interprofessional teamwork in stroke care. 112 We began with programme theory 1: the adoption of evidence-based core components is important for the intervention to be effective in practice.
Our second programme theory was based on the need to investigate the implementation of ESD in rural settings, given that original trials were conducted in urban sites, and the potential impact of the delivery of home-based rehabilitation over large geographical areas. 10,13 This and a RES generated programme theory 2: core evidence-based components of ESD will operate differently in urban versus rural settings.
Our third programme theory was initially based on previous qualitative findings, which highlighted the importance of strong links with collaborating services through boundary-spanning working arrangements. 23 Programme theory 3 initially stated: the quality of communication processes between key stakeholders and services in the local stroke care pathway will influence the implementation of an evidence-based service.
In WP1, we investigated the adoption of evidence-based core components by conducting, to the best of our knowledge, the first large-scale observational study using national registry data to investigate the effectiveness of ESD in a real-world setting. This maximised the availability of national registry data to conduct health services research and built on previous approaches to evaluate effectiveness of stroke unit care. 31,61,70,128
We developed an ESD consensus score based on our international consensus paper. This was successfully used to determine the degree to which evidence-based core components had been adopted in models of ESD operating in the real world. The findings showed that adopting an evidence-based ESD model, in both urban and rural sites, was significantly related to the responsiveness and intensity of the rehabilitation delivered.
Qualitative investigation in WP2 then enabled us to move beyond the assumption of a causal relationship between the core components of the intervention and its outcomes, regardless of context. 37 By examining the interaction between contexts, mechanisms and outcomes from stakeholder perspectives, we were able to understand how and in what circumstances adopting core components resulted in effective ESD. Critically, this approach acknowledged the importance of human reasoning and interpretation as vital to understanding how ESD works. 37 This also resonates with current implementation theory, which acknowledges the importance of actors involved in implementation as well as the context in which they are operating. 37
In WP2, we were able to further investigate programme theories 1 and 2. We uncovered examples of how operating in rural settings, especially when coupled with capacity issues, could influence the intensity of rehabilitation provision and teams’ flexibility to adjust the frequency and duration of the visits to people’s needs. These relate to challenges reported in other countries and confirm workforce as a key factor in delivering and sustaining a rural therapy service. 104,105
We were also able to refine programme theory 3: the quality of communication processes between key stakeholders and services will influence provision of a seamless stroke care pathway to patients.
This emphasised the importance of good communication strategies and the need for collaborative trusting relationships between ESD staff and patients and carers, stroke unit staff and across the wider stroke care pathway. This builds on other study findings emphasising the importance of regular communication and opportunistic dialogue across disciplinary and organisational boundaries. 19,106,107 We also found examples of how interdisciplinary working further promoted trust and respect in other disciplines, resonating with previous reports of ‘role blurring’, which enabled carry-over of skills by other disciplines enhancing continuity of care. 109 An example of this was the crucial role of RAs, which, with appropriate supervision and upskilling, was said to maximise service capacity.
The RE methodology allowed us to address the complexity of ESD delivery in clinical practice and obtain a better understanding of how intervention resources and stakeholders’ reasoning interact with contextual conditions to generate intended and unintended outcomes. The cumulation of insights from further testing of these programme theories in different geographical and organisational settings could help develop an evidence-informed theory base for the large-scale implementation of rehabilitation services in the community.
Robustness of the results and limitations
We adopted a mixed-methods design that allowed us to draw information from multiple complementary sources using methodological guidance on the conduct of RE. 8
The study responded to the call for evaluation designs that consider the complexity of the large-scale service innovations in health care. 71 To achieve rigour in developing and reporting the study, the RE quality standards were applied. 37 Quantitative aspects of our methodological approach meant some deviation away from realist practice, including reporting standards. 21 To conduct robust quantitative analyses, context, mechanisms (resources)26 and outcomes were instead reflected in defined and measurable variables, the relationships between which were investigated with statistical modelling.
Work package 1: use of national registry data
Work package 1 involved the use of the SSNAP, with established data quality. 61 The use of data sets obtained from SSNAP enabled large sample sizes of 30,791 and 49,266 patients to be included in quantitative analysis. Multilevel modelling was used to investigate the relationships between the adopted ESD model and process and patient outcomes in an approach consistent with previous observational studies of this type. 31,32,70,71 Although numbers of patients were sufficient for the analysis undertaken, by focusing on specific regions of England, the transferability of the findings could be questioned, particularly outside England. In addition, although we attempted to control for a number of confounders, we cannot rule out the possible influence of unobserved variables. Findings are also reliant on accurate reporting in SSNAP and the possibility of bias cannot be excluded.
Although we identified a significant relationship between ESD consensus score and process measures, there was no relationship with the modified Rankin Scale. This finding was interpreted with caution, based on the lack of sensitivity of this scale and its collection immediately at ESD discharge. It emphasises the need for the routine collection of a wider range of validated patient outcome measures to appreciate the effectiveness of ESD with regard to patient recovery. We also acknowledge that our 17-item ESD consensus score included equal weighting across components in line with our analytical approaches. Given the simple and pragmatic nature of this scoring system, we would recommend complementary collection of descriptive qualitative data (e.g. service mapping) for routine service evaluation.
Work package 2: cost–consequences analysis
In WP2, validity was enhanced through the selection of six purposively selected case study sites, maximising variability and a good understanding and description of each context. Although it is accepted that the context-specific nature of the findings in realist and case study research limits their quantitative generalisability,129,130 the theory-driven nature of the enquiry enhances the transferability of the refined programme theories to other settings with similar characteristics. 131,132
Cost implications are an important consideration with regard to successful adoption and implementation of interventions, such as ESD. We adopted a recommended CCA approach, presenting information about costs and outcomes in the form of a balance sheet. 34 CCA allows the decision-maker to determine whether or not, overall, the treatment or intervention or service is worth carrying out or commissioning. 96 Although a cost-effectiveness analysis may be regarded as more rigorous, it has poor recognition of the importance of context. 34 The resources associated with the delivery of a complex intervention, such as ESD, are also likely to equate to different costs in different places. 35
Given that QALYs were not calculated, cost-effectiveness cannot be directly compared with other interventions. Other limitations of the CCA approach were that it was unable to capture all of the consequences, especially indirect effects arising from ESD service provision, as well as failing to capture consequences that occur at other points in time. Again, relating to the lack of routinely collected patient outcomes, we were also unable to infer what cost consequences there might have been from a patient perspective. In addition, we were able to conduct the CCA only with our six selected case study sites, limiting the transferability of the findings.
Work package 2: staff and patient perspectives
The qualitative component of the study sought to include a large and diverse sample of purposively selected stakeholders to ensure that varied and contrasting perspectives were captured. 116 Staff interview schedules were devised to explore our defined programme theories. In an iterative process, emerging themes and issues identified from these interviews were explored and checked out in subsequent focus groups and individual interviews. 116 This contributed to ensuring the accuracy and robustness of the data collected, and to a rich and detailed account of ESD pathways, staff experiences and service delivery.
In total, 117 staff were interviewed in focus groups and individual interviews who came from a range of staff groups, professions and parts of the stroke pathway. This provided a varied sample from which detailed perspectives were obtained, enabling an in-depth investigation of the context within which ESD services operate in the real world. Data were analysed by two experienced qualitative researchers using a detailed analysis plan. This involved analysis at an individual participant level using a retroductive approach to identify confirmatory and disconfirmatory examples to support or refute programme theories. Findings were then compared and any variations or inconsistencies were discussed and resolved before moving to the second and third stages of analysis.
The analytical task of linking context, mechanisms and outcome chains is suggested to help unpack causation, increase the explaining power of findings and improve the external validity of case studies. 8,20 We took a pragmatic position to configure our CMOs at a level of abstraction that would allow us to draw take-home messages relevant to clinical practice. However, we are conscious that this approach has led to a large number of CMOs and ‘theoretical nuggets’ rather than an overarching higher-level theory.
Implications for health care and policy
There were two findings of this study that were perhaps surprising based on previous research and require further comment in relation to health-care delivery and policy.
First, higher ESD consensus scores were not significantly associated with patient outcomes, as measured by the modified Rankin Scale. Although this could be interpreted as adopting evidence-based core components of ESD does not result in improved patient outcomes, we would emphasise caution at coming to this conclusion. Previous research has shown that ESD is associated with improved outcomes. 10,12 What our findings suggest is that the modified Rankin Scale is an insensitive measure of the effect of ESD on patient outcomes. This is in line with concerns from teams themselves about the reliability of the use of this score across the stroke care pathway. 76 We suggest routine use of other validated patient outcome measures, over time, to monitor the longer-term impact of ESD on patient recovery.
Our findings also showed that stroke patients who received ESD spent, on average, approximately 1-day longer in hospital. This is in contrast with previous clinical trials. 10 ESD patients were younger and more likely to have a lower modified Rankin Scale score at their final inpatient discharge. It was, therefore, important to compare their total inpatient length of stay with that of a group of patients matched for these (and other) important patient characteristics. It should also be emphasised that we used total inpatient length of stay data (combining different inpatient settings). Previous modelling appears to have been driven by assuming that patients with a higher modified Rankin Scale score receive ESD. 85 Although it is tempting to conclude that patients with more severe disabilities should be able to access ESD, previous research and our current findings suggest caution with this because without an appropriately resourced service, this may be detrimental to stroke patient recovery (and unsafe) over the longer term. 10
As reported in Chapter 5, the average length of hospital stay for stroke survivors overall has reduced dramatically over the last 20 years, from 40 days to 20 days, and, hence, all patients are being discharged much sooner. 80 Based on our qualitative findings, ESD patients spending, on average, 1-day longer in hospital could relate to the delays associated with the capacity of the ESD teams to accept patients (emphasising the importance of appropriate staffing). We also suggest that the additional day could be required to facilitate and co-ordinate the appropriate transfer of care to the ESD team (i.e. required administration) and to liaise with social care.
Here, we summarise other take-home messages with the aim to guide implementation and evaluation of ESD in practice.
The adoption of evidence-based core components is important for the intervention to be effective in practice
-
We have developed an ESD consensus score that can be used as a simple quantitative measure to determine if evidence-based core components of ESD have been adopted by a service.
-
Services that adopted evidence-based core components were more responsive and delivered a more intensive service.
-
Rehabilitation assistants should be considered core members of an ESD team because they help to maximise capacity.
-
Nurses are also important members of the ESD team and their contribution should be captured in national audits (e.g. in SSNAP).
-
The timely involvement of social workers embedded in the pathway ensures that unmet needs can be quickly identified and streamlines the hospital discharge process.
-
Effective ESD provision is dependent on other parts of the stroke care pathway. Specifically, the availability of further community rehabilitation services for stroke survivors with rehabilitation needs beyond ESD. Collaborative working with stroke unit staff is also key.
-
ESD needs to be appropriately resourced so that services have sufficient capacity to provide the appropriate level of intensity of stroke rehabilitation to patients.
-
Adhering to eligibility criteria to determine which patients access ESD allows services to manage capacity, promote responsiveness and ensure patient safety at home. However, flexibility is required to allow for clinical judgement and holistic assessment on an individual patient basis, where appropriate.
-
There was concern for patients deemed inappropriate for ESD, particularly if there was a lack of alternative community stroke services. ESD teams felt under pressure to use criteria flexibly and provide short-term support to patients who fell through the net or were deemed too complex for ESD, which stretched resources.
-
A model of service combining ESD and community stroke rehabilitation could reduce handover delays, protect capacity and provide a more streamlined experience for patients. This requires improved integration of community stroke services and fostering of independence and self-management to adequately support patients and carers over the longer term.
-
Stroke pathways need to be configured to address the needs of patients with more severe disability. Attempting to cater for their needs without appropriate resource diluted the intensity of the service for the rest of the patients or reduced the flow of new patients into the service.
-
Introducing two streams in community stroke services can allow staff to distinguish between mild or moderate patients who require a straightforward discharge process and patients who require more complex discharge planning. Using criteria based on disability levels to determine two pathways for patients can help services to manage capacity, manage patient flow and promote responsiveness.
-
Adopting a flexible approach relating to length of stay with the service allows services to be more responsive to specific patients’ needs and to manage problems, such as fatigue and emotional issues.
Core evidence-based components of early supported discharge will operate differently in urban compared with rural settings
-
Dividing the MDT into subteams corresponding to geographical patches might help teams reduce travel times and use resources efficiently, especially when covering a large/rural geographical area. Working flexibly across these boundaries when required and seeking opportunities for formal and informal meetings is essential to safeguard MDT working and to allow the team to ‘pool’ their expertise and knowledge of their local context, and provide mutual practical and emotional support.
-
Additional resources (and associated costs) may be required for rural services to meet evidence-based criteria.
The quality of communication processes between key stakeholders and services in the local stroke care pathway will influence the provision of a seamless, patient-centred pathway
-
Rapport-building between ESD teams, patients and carers at the earliest stage in the stroke pathway builds trust, helps to manage expectations and engages patients and carers in the rehabilitation process. This can be facilitated by in-reaching to patients during their hospital stay. Engaging with service users at this early stage helps to dispel any mistaken belief that ESD teams will ‘do it for’ the patients and encourages the whole family’s active involvement in recovery planning and implementation.
-
The engagement of carers is vital to support meaningful goal-planning and facilitate functional rehabilitation practice in between formal therapy sessions.
-
Maintenance and facilitation of good relationships and communication between referring stroke units and ESD is essential to ensure that the patients are referred into the correct pathway. This ensures smooth and safe discharges.
-
In-reach by ESD teams to the acute trust is facilitatory, where it is feasible. In the absence of in-reach other mechanisms are key, such as regular telephone contact regarding individual referrals; robust regularly reviewed and reinforced referral pathways; routine service planning meetings between service managers; secondments; and joint training sessions.
-
The tailored management of information flow and timing to patients and carers is vital to ensure that the right information is delivered at the right time and in the right format. This helps to build trust and confidence and avoids overwhelming patients with too much information at any one time.
Recommendations for future research
Observational studies in Sweden suggest patient and caregiver benefits related to the provision of ESD in regular clinical practice, in line with our previous study findings from England. 86,87 Here, we showed the modified Rankin Scale to be of limited use in assessing ESD in terms of influencing patient outcomes. We suggest that further research using validated patient outcome measures (e.g. measuring activities of daily living, general health/mood and quality of life) at longer follow-up periods is required to enable the investigation of the impact of ESD on patients over the longer term. 10,12,87
The extension of national stroke registries with the inclusion of community stroke data, including measures of activities of daily living (e.g. Barthel index score or Nottingham Extended Activities of Daily Living score) and impairment, activity, participation and well-being (e.g. Therapy Outcome measure), could offer important opportunities to evaluate stroke service delivery beyond the hospital setting. 1,16
The evidence relating to the cost implications of ESD is mixed, with previous studies reporting reductions, increases and no differences in cost compared with treatment as usual. 10,79 An original attraction of ESD from a commissioning perspective was a reduction in length of hospital stay. 11 However, Teng et al. 101 postulated that any reductions in hospital length of stay associated with ESD translate into negligible cost savings because empty beds are then used by other patients. Our findings suggested that the benefits of ESD relate more to the provision of a responsive and intensive intervention when patients leave hospital, rather than shortening their overall length of hospital stay. The cost implications of integrating ESD and community stroke rehabilitation models and the consequences with regard to patient outcomes over the longer term need to be investigated.
We conclude that the adoption of defined evidence-based components are necessary for both urban and rural sites, and it is encouraging that we found examples of evidence-based ESD models in rural regions. Rural services were more costly but they also resourced larger numbers of staff on a per-patient basis, which ensured that they delivered an evidence-based service. We suggest evaluating these observed cost differences from a patient outcome perspective. More research is also required to identify what interventions could help services to manage logistical challenges associated with delivering effective home-based stroke rehabilitation in different geographical contexts.
Impact
We conducted virtual engagement events with representatives from each of the ESD services who had participated in this research to share our findings and discuss implications for practice. We facilitated sharing of perspectives on providing evidence-based community stroke care and encouraged staff to build on our recommendations and support each other as a community of practice. We also provided our stroke survivor participants with a feedback package, which included a lay summary of findings and a thank you for being involved.
In April 2020, Rebecca J Fisher was appointed the National Rehabilitation and Life After Stroke Workstream lead, with NHS England and NHS Improvement Clinical Policy Unit. This was in recognition of our team’s research in informing national commissioning guidance, clinical guidelines,133–136 and national and regional stroke care improvement. 137 Further details of national activities, informed by this research, can be found in Appendix 5.
Acknowledgements
The authors acknowledge and thank Kristina Koller for her assistance with the patient interview analysis; the NHS staff and stroke survivors who participated in this study; and members of the SSNAP collaboration. We also thank Trevor Gard and Frances Cameron, stroke survivors who were members of our study steering group.
Contributions of authors
Rebecca J Fisher (https://orcid.org/0000-0001-6866-6341) (Stroke Association Senior Lecturer, University of Nottingham) was the principal investigator and budget holder, and was involved in all aspects of the research.
Niki Chouliara (https://orcid.org/0000-0001-8294-0722) (Research Fellow, University of Nottingham) managed the day-to-day delivery of studies, led the use of realist methodology, conducted the rapid evidence synthesis, collected and analysed staff interview and focus group data, contributed to the interpretation of the results, wrote the report and disseminated the results.
Adrian Byrne (https://orcid.org/0000-0003-4887-2572) (Research Fellow, University of Nottingham) managed the day-to-day delivery of studies, led the design of the statistical plan, obtained data from SSNAP, undertook statistical analyses, conducted the CCA, managed stroke patient interviews, contributed to the interpretation of the results, wrote the report and disseminated the results.
Trudi Cameron (https://orcid.org/0000-0002-4273-3611) (Research Fellow, University of Nottingham) managed the day-to-day delivery of studies, collected and analysed staff interview and focus group data, analysed patient interview data, contributed to the interpretation of the results, wrote the report and disseminated the results.
Sarah Lewis (https://orcid.org/0000-0001-5308-6619) (Professor of Medical Statistics, University of Nottingham) contributed to the conceptualisation of the research, the development of the grant application, the development of the statistical plan, data analysis and interpretation, production of the report and disseminated the results.
Peter Langhorne (https://orcid.org/0000-0001-8185-2659) (Professor of Stroke Care/Geriatric Medicine, University of Glasgow) contributed to the conceptualisation of the research, the development of the grant application, the development of the statistical plan, the interpretation of results and the production of the report, and disseminated the results.
Thompson Robinson (https://orcid.org/0000-0003-2144-2468) (Professor of Stroke Medicine, University of Leicester) contributed to the conceptualisation of the research, the development of the grant application, the development of the statistical plan, the interpretation of results and the production of the report, and disseminated the results.
Justin Waring (https://orcid.org/0000-0003-1459-5896) (Professor of Organisational Sociology, University of Birmingham) contributed to the conceptualisation of the research, the development of the grant application, the interpretation of results and the production of the report, and disseminated the results.
Claudia Geue (https://orcid.org/0000-0003-2243-0733) (Health Economics Lecturer, University of Glasgow) contributed to the conceptualisation of the research and the development of the grant application, advised on cost–consequences analysis, contributed to the interpretation of results and the production of the report, and disseminated the results.
Lizz Paley (https://orcid.org/0000-0002-3879-5377) (Intelligence Manager, SSNAP at the time of the study) contributed to the preparation of the data, the interpretation of results and the production of the report, and disseminated the results.
Anthony Rudd (https://orcid.org/0000-0002-5738-2703) (Clinical Director of SSNAP at the time of the study) contributed to the development of the grant application, the interpretation of results and the production of the report, and disseminated the results.
Marion F Walker (https://orcid.org/0000-0002-3534-591X) (Professor in Stroke Rehabilitation, University of Nottingham) contributed to the conceptualisation of the research, the development of the grant application, the interpretation of results and the production of the report, and disseminated the results.
Publications
Fisher R, Chouliara N, Byrne A, Lewis S, Langhorne P, Robinson T, et al. What is the impact of large-scale implementation of stroke early supported discharge? A mixed methods realist evaluation study protocol. Implement Sci 2019;14:61.
Fisher R, Byrne A, Chouliara N, Lewis S, Paley L, Hoffman A, et al. Effectiveness of stroke early supported discharge: analysis from a National Stroke Registry. Circ Cardiovasc Qual Outcomes 2020;13:e006395.
Fisher R, Byrne A, Chouliara N, Lewis S, Paley L, Hoffman A, et al. Effect of stroke early supported discharge on length of hospital stay: analysis from a National Stroke Registry. BMJ Open 2021;11:e043480.
Data-sharing statement
This project involved secondary analysis of anonymised, routinely collected clinical data. The data were made available under a data-sharing agreement between the University of Nottingham, SSNAP and the HQIP. A condition of that agreement was that all the data would be destroyed at the end of the project. Therefore, we are unable to make them available to others. Further information can be obtained from the corresponding author.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data are vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Fisher RJ, Byrne A, Chouliara N, Lewis S, Paley L, Hoffman A, et al. Effectiveness of stroke early supported discharge: analysis from a national stroke registry. Circ Cardiovasc Qual Outcomes 2020;13. https://doi.org/10.1161/CIRCOUTCOMES.119.006395.
- Fisher RJ, Byrne A, Chouliara N, Lewis S, Paley L, Hoffman A, et al. Effect of stroke early supported discharge on length of hospital stay: analysis from a national stroke registry. BMJ Open 2021;11. https://doi.org/10.1136/bmjopen-2020-043480.
- Stroke Association . State of the Nation: Stroke Statistics 2018.
- NHS England . The NHS Long Term Plan 2019. www.longtermplan.nhs.uk/ (accessed 28 September 2021).
- Intercollegiate Stroke Working Party . National Clinical Guideline for Stroke 2016.
- National Institute for Health and Care Excellence (NICE) . Stroke Rehabilitation in Adults 2013.
- Royal College of Physicians, Care Quality Improvement Department on behalf of the Intercollegiate Stroke Working Party . Sentinel Stroke National Audit Programme (SSNAP). Post-Acute Organisational Audit; Phase 2: Organisational Audit of Post-Acute Stroke Service Providers 2015.
- Pawson R, Tilley N. Realistic Evaluation. Thousand Oaks, CA: SAGE Publications Ltd; 1997.
- Langhorne P, Bernhardt J, Kwakkel G. Stroke rehabilitation. Lancet 2011;377:1693-702. https://doi.org/10.1016/S0140-6736(11)60325-5.
- Langhorne P, Baylan S. Early Supported Discharge Trialists. Early supported discharge services for people with acute stroke. Cochrane Database Syst Rev 2017;7. https://doi.org/10.1002/14651858.CD000443.pub4.
- Saka O, Serra V, Samyshkin Y, McGuire A, Wolfe CC. Cost-effectiveness of stroke unit care followed by early supported discharge. Stroke 2009;40:24-9. https://doi.org/10.1161/STROKEAHA.108.518043.
- Fisher RJ, Cobley CS, Potgieter I, Moody A, Nouri F, Gaynor C, et al. Is stroke early supported discharge still effective in practice? A prospective comparative study. Clin Rehabil 2016;30:268-76. https://doi.org/10.1177/0269215515578697.
- Fisher RJ, Gaynor C, Kerr M, Langhorne P, Anderson C, Bautz-Holter E, et al. A consensus on stroke: early supported discharge. Stroke 2011;42:1392-7. https://doi.org/10.1161/STROKEAHA.110.606285.
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-50.
- Stevens E, Emmett E, Wang Y, McKevitt C, Wolfe C. The Burden of Stroke in Europe, Report. King’s College London for The Stroke Alliance For Europe (SAFE) 2017.
- Cadilhac DA, Kim J, Lannin NA, Kapral MK, Schwamm LH, Dennis MS, et al. National stroke registries for monitoring and improving the quality of hospital care: a systematic review. Int J Stroke 2016;11:28-40. https://doi.org/10.1177/1747493015607523.
- Brewer L, Williams D. A review of early supported discharge after stroke. Rev Clin Gerontol 2010;20. https://doi.org/10.1017/S0959259810000249.
- Pawson R, Manzano-Santaella A. A realist diagnostic workshop. Evaluation 2012;18:176-91. https://doi.org/10.1177/1356389012440912.
- Waring J, Marshall F, Bishop S. Understanding the occupational and organizational boundaries to safe hospital discharge. J Health Serv Res Policy 2015;20:35-44. https://doi.org/10.1177/1355819614552512.
- Pawson R, Sridharan S, Killoran A, Kelly MP. Evidence-based Public Health: Effectiveness and Efficiency. Oxford: Oxford University Press; 2010.
- Wong G, Westhorp G, Greenhalgh J, Manzano A, Jagosh J, Greenhalgh T. Quality and reporting standards, resources, training materials and information for realist evaluation: the RAMESES II project. Health Serv Deliv Res 2017;5. https://doi.org/10.3310/hsdr05280.
- Wong G, Westhorp G, Manzano A, Greenhalgh J, Jagosh J, Greenhalgh T. RAMESES II reporting standards for realist evaluations. BMC Med 2016;14. https://doi.org/10.1186/s12916-016-0643-1.
- Chouliara N, Fisher RJ, Kerr M, Walker MF. Implementing evidence-based stroke early supported discharge services: a qualitative study of challenges, facilitators and impact. Clin Rehabil 2014;28:370-7. https://doi.org/10.1177/0269215513502212.
- Harvey G, Kitson A. PARIHS revisited: from heuristic to integrated framework for the successful implementation of knowledge into practice. Implement Sci 2016;11. https://doi.org/10.1186/s13012-016-0398-2.
- Westhorp G, Emmel N, Greenhalgh J, Manzano A, Monaghan M, Dalkin S. Doing Realist Research. London: SAGE Publications Ltd; 2018.
- Dalkin SM, Greenhalgh J, Jones D, Cunningham B, Lhussier M. What’s in a mechanism? Development of a key concept in realist evaluation. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0237-x.
- Clarke D, Jones F, Harris R, Robert G. Collaborative Rehabilitation Environments in Acute Stroke (CREATE) team . What outcomes are associated with developing and implementing co-produced interventions in acute healthcare settings? A rapid evidence synthesis. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-014650.
- NHS Midlands and East . NHS Midlands and East. Stroke Services Specification 2012. www.england.nhs.uk/mids-east/wp-content/uploads/sites/7/2018/03/final-stroke-spec.pdf (accessed 28 September 2021).
- van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke 1988;19:604-7. https://doi.org/10.1161/01.str.19.5.604.
- Brott T, Adams HP, Olinger CP, Marler JR, Barsan WG, Biller J, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke 1989;20:864-70. https://doi.org/10.1161/01.STR.20.7.864.
- Turner M, Barber M, Dodds H, Murphy D, Dennis M, Langhorne P, et al. Implementing a simple care bundle is associated with improved outcomes in a national cohort of patients with ischemic stroke. Stroke 2015;46:1065-70. https://doi.org/10.1161/STROKEAHA.114.007608.
- Teale EA, Forster A, Munyombwe T, Young JB. A systematic review of case-mix adjustment models for stroke. Clin Rehabil 2012;26:771-86. https://doi.org/10.1177/0269215511433068.
- Department of Health and Social Care (DHSC) . The Adult Social Care Outcomes Framework 2016 17. Handbook Of Definitions 2017.
- Craig LE, Wu O, Bernhardt J, Langhorne P. Approaches to economic evaluations of stroke rehabilitation. Int J Stroke 2014;9:88-100. https://doi.org/10.1111/ijs.12041.
- Anderson R, Hardwick R. Realism and resources: towards more explanatory economic evaluation. Evaluation 2016;22:323-41. https://doi.org/10.1177/1356389016652742.
- Braun V, Clarke V. One size fits all? What counts as quality practice in (reflexive) thematic analysis?. Qual Res Psychol 2020;18:1-25. https://doi.org/10.1080/14780887.2020.1769238.
- Fisher R, Chouliara N, Byrne A, Lewis S, Langhorne P, Robinson T, et al. What is the impact of large-scale implementation of stroke early supported discharge? A mixed methods realist evaluation study protocol. Implement Sci 2019;14. https://doi.org/10.1186/s13012-019-0908-0.
- Cobley CS, Fisher RJ, Chouliara N, Kerr M, Walker MF. A qualitative study exploring patients’ and carers’ experiences of early supported discharge services after stroke. Clin Rehabil 2013;27:750-7. https://doi.org/10.1177/0269215512474030.
- Fisher RJ, Walker MF, Golton I, Jenkinson D. The implementation of evidence-based rehabilitation services for stroke survivors living in the community: the results of a Delphi consensus process. Clin Rehabil 2013;27:741-9. https://doi.org/10.1177/0269215512473312.
- Bate P, Robert G, Fulop N, Øvretveit J, Dixon-Woods M. Perspectives on Context. London: The Health Foundation; 2014.
- Featherstone RM, Dryden DM, Foisy M, Guise JM, Mitchell MD, Paynter RA, et al. Advancing knowledge of rapid reviews: an analysis of results, conclusions and recommendations from published review articles examining rapid reviews. Syst Rev 2015;4. https://doi.org/10.1186/s13643-015-0040-4.
- Sandelowski M, Voils CI, Barroso J. Defining and designing mixed research synthesis studies. Res Sch 2006;13.
- Critical Appraisal Skills Programme (CASP) . CASP Qualitative Checklist 2018.
- Noyes J, Popay J, Pearson A, Hannes K, Booth A, Higgins JPT, et al. Cochrane Handbook for Systematic Reviews of Interventions. London: The Cochrane Collaboration; 2008.
- Pawson R. Digging for nuggets: how ‘bad’ research can yield ‘good’ evidence. Int J Soc Res Methodol 2006;9:127-42. https://doi.org/10.1080/13645570600595314.
- Kraut JC, Singer BJ, Singer KP. Referrer and service provider beliefs and attitudes towards rehabilitation in the home; factors related to utilisation of early supported discharge. Disabil Rehabil 2014;36:2178-86. https://doi.org/10.3109/09638288.2014.893373.
- Kraut J, Singer B, Singer K. Clinician and client views of utilising early supported discharge services. Int J Ther Rehabil 2016;23:464-71. https://doi.org/10.12968/ijtr.2016.23.10.464.
- Wottrich AW, von Koch L, Tham K. The meaning of rehabilitation in the home environment after acute stroke from the perspective of a multiprofessional team. Phys Ther 2007;87:778-88. https://doi.org/10.2522/ptj.20060152.
- Lou S, Carstensen K, Møldrup M, Shahla S, Zakharia E, Nielsen CP. Early supported discharge following mild stroke: a qualitative study of patients’ and their partners’ experiences of rehabilitation at home. Scand J Caring Sci 2017;31:302-11. https://doi.org/10.1111/scs.12347.
- Nordin Å, Sunnerhagen KS, Axelsson ÅB. Patients’ expectations of coming home with very early supported discharge and home rehabilitation after stroke - an interview study. BMC Neurol 2015;15. https://doi.org/10.1186/s12883-015-0492-0.
- Olofsson A, Andersson SO, Carlberg B. ‘If only I manage to get home I’ll get better’ – interviews with stroke patients after emergency stay in hospital on their experiences and needs. Clin Rehabil 2005;19:433-40. https://doi.org/10.1191/0269215505cr788oa.
- Wottrich AW, Aström K, Löfgren M. On parallel tracks: newly home from hospital – people with stroke describe their expectations. Disabil Rehabil 2012;34:1218-24. https://doi.org/10.3109/09638288.2011.640381.
- Algurén B, Lundgren-Nilsson A, Sunnerhagen KS. Facilitators and barriers of stroke survivors in the early post-stroke phase. Disabil Rehabil 2009;31:1584-91. https://doi.org/10.1080/09638280802639004.
- Cowles M, Dysch L, Perry E, Randle-Phillips C. How stroke patients and carers experience early supported discharge services: a qualitative study with recommendations for service development. Neuropsychologist 2017;3:46-53.
- Ellis-Hill C, Robison J, Wiles R, McPherson K, Hyndman D, Ashburn A. Going home to get on with life: patients and carers experiences of being discharged from hospital following a stroke. Disabil Rehabil 2009;31:61-72. https://doi.org/10.1080/09638280701775289.
- Tyson S, Turner G. Discharge and follow-up for people with stroke: what happens and why. Clin Rehabil 2000;14:381-92. https://doi.org/10.1191/0269215500cr331oa.
- Ryan-Woolley B, Wilson K, Caress A. The implementation and evaluation of a community rehabilitation team: a case study. Disabil Rehabil 2004;26:817-26. https://doi.org/10.1080/09638280410001696737.
- Collins G, Breen C, Walsh T, McGrath M. An exploration of the experience of early supported discharge from the perspective of stroke survivors. Int J Ther Rehabil 2015;23:207-14. https://doi.org/10.12968/ijtr.2016.23.5.207.
- Geddes JML, Chamberlain MA. Improving community rehabilitation teams for people with stroke. Br J Ther Rehabil 2001;8:92-5. https://doi.org/10.12968/bjtr.2001.8.3.13740.
- McGinnes A, Easton S, Williams J, Neville J. The role of the community stroke rehabilitation nurse. Br J Nurs 2010;19:1033-8. https://doi.org/10.12968/bjon.2010.19.16.78193.
- Rudd AG, Hoffman A, Paley L, Bray B. 20 years of researching stroke through audit. Clin Rehabil 2018;32:997-1006. https://doi.org/10.1177/0269215518784645.
- European Stroke Organisation Executive Committee, ESO Writing Committee . Guidelines for management of ischaemic stroke and transient ischaemic attack. Cerebrovasc Dis 2008;25:457-50. https://doi.org/10.1159/000131083.
- Adeoye O, Nyström KV, Yavagal DR, Luciano J, Nogueira RG, Zorowitz RD, et al. Recommendations for the establishment of stroke systems of care: a 2019 update: a policy statement from the American Stroke Association. Stroke 2019;50:e187-e210. https://doi.org/10.1161/STR.0000000000000173.
- Hebert D, Lindsay MP, McIntyre A, Kirton A, Rumney PG, Bagg S, et al. Canadian stroke best practice recommendations: stroke rehabilitation practice guidelines, update 2015. Int J Stroke 2016;11:459-84. https://doi.org/10.1177/1747493016643553.
- Stroke Foundation . Clinical Guidelines for Stroke Management 2017.
- Sentinel Stroke National Audit Programme (SSNAP) helpdesk . Therapy Report 2017. https://ssnap.zendesk.com/hc/en-us/articles/360001955854-Download-fullpack-of-Therapy-Report (accessed 6 March 2019).
- Office for National Statistics . RuralUrban Classification 2011.
- NHS Digital . Quality and Outcomes Framework (QOF) – 2015–16 2016.
- Royal College of Physicians . Sentinel Stroke National Audit Programme (SSNAP) Clinical Audit December 2016–March 2017 Public Report 2017.
- Morris S, Hunter RM, Ramsay AI, Boaden R, McKevitt C, Perry C, et al. Impact of centralising acute stroke services in English metropolitan areas on mortality and length of hospital stay: difference-in-differences analysis. BMJ 2014;349. https://doi.org/10.1136/bmj.g4757.
- Barratt H, Campbell M, Moore L, Zwarenstein M, Bower P. Challenges, solutions and future directions in the evaluation of service innovations in health care and public health. Health Serv Deliv Res 2016;4. https://doi.org/10.3310/hsdr04160.
- Swinkels A, Mitchell T. Delayed transfer from hospital to community settings: the older person’s perspective. Health Soc Care Community 2009;17:45-53. https://doi.org/10.1111/j.1365-2524.2008.00796.x.
- Clarke DJ. The role of multidisciplinary team care in stroke rehabilitation. Prog Neurol Psychiatry 2013;17:5-8. https://doi.org/10.1002/pnp.288.
- Hewitt G, Sims S, Greenwood N, Jones F, Ross F, Harris R. Interprofessional teamwork in stroke care: is it visible or important to patients and carers?. J Interprof Care 2015;29:331-9. https://doi.org/10.3109/13561820.2014.950727.
- Tyson SF, Burton L, McGovern A. Multi-disciplinary team meetings in stroke rehabilitation: an observation study and conceptual framework. Clin Rehabil 2014;28:1237-47. https://doi.org/10.1177/0269215514535942.
- Holpin L. Does inter-rater variability occur in modified Rankin Scale (mRS) scoring? An audit within an early supported discharge (ESD) service. Int J Stroke 2018;13.
- Dwyer M, Rehman S, Ottavi T, Stankovich J, Gall S, Peterson G, et al. Urban-rural differences in the care and outcomes of acute stroke patients: systematic review. J Neurol Sci 2019;397:63-74. https://doi.org/10.1016/j.jns.2018.12.021.
- Koifman J, Hall R, Li S, Stamplecoski M, Fang J, Saltman AP, et al. The association between rural residence and stroke care and outcomes. J Neurol Sci 2016;363:16-20. https://doi.org/10.1016/j.jns.2016.02.019.
- Neale S, Leach K, Steinfort S, Hitch D. Costs and length of stay associated with early supported discharge for moderate and severe stroke survivors. J Stroke Cerebrovasc Dis 2020;29. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.104996.
- King’s College London . Sentinel Stroke National Audit Programme (SSNAP) Clinical Audit April 2018–March 2019 Public Report 2020.
- NHS Digital . Measures from the Adult Social Care Outcomes Framework, England (2016–17) 2017.
- Rafferty A, Walthery P, King-Hele S. Analysing Change Over Time: Repeated Crosssectional and Longitudinal Survey Data 2015.
- StataCorp LP. Stata Treatment-Effects Reference Manual. College Station, TX: StataCorp LP; 2015.
- Sekhon JS. Multivariate and propensity score matching software with automated balance optimization: the matching package for R. J Stat Softw 2011;42:1-52. https://doi.org/10.18637/jss.v042.i07.
- Royal College of Physicians . Sentinel Stroke National Audit Programme Cost and Cost-Effectiveness Analysis 2016.
- Tistad M, von Koch L. Usual clinical practice for early supported discharge after stroke with continued rehabilitation at home: an observational comparative study. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0133536.
- Bråndal A, Eriksson M, Glader EL, Wester P. Effect of early supported discharge after stroke on patient reported outcome based on the Swedish Riksstroke registry. BMC Neurol 2019;19. https://doi.org/10.1186/s12883-019-1268-8.
- Gittins M, Lugo-Palacios DG, Paley L, Bray B, Bowen A, Vail A, et al. How do patients pass through stroke services? Identifying stroke care pathways using national audit data. Clin Rehabil 2020;34:698-709. https://doi.org/10.1177/0269215520907654.
- Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2015.
- Drummond M. Economic analysis alongside clinical trials: problems and potential. J Rheumatol 1995;22:1403-7.
- Donaldson C, Currie G, Mitton C. Cost effectiveness analysis in health care: contraindications. BMJ 2002;325:891-4. https://doi.org/10.1136/bmj.325.7369.891.
- Coast J, Hensher M, Mulligan JA, Shepperd S, Jones J. Conceptual and practical difficulties with the economic evaluation of health services developments. J Health Serv Res Policy 2000;5:42-8. https://doi.org/10.1177/135581960000500110.
- Byford S, Sefton T. First aid: lessons from health economics for economic evaluation in social welfare [Health and Social Care Discussion Paper]. London: London School of Economics and Political Science; 2002.
- Gage H, Kaye J, Owen C, Trend P, Wade D. Evaluating rehabilitation using cost-consequences analysis: an example in Parkinson’s disease. Clin Rehabil 2006;20:232-8. https://doi.org/10.1191/0269215506cr936oa.
- Coast J. Is economic evaluation in touch with society’s health values?. BMJ 2004;329:1233-6. https://doi.org/10.1136/bmj.329.7476.1233.
- Optimity Advisors . Community Engagement–Approaches to Improve Health and Reduce Health Inequalities. Cost–Consequence Analysis 2016.
- Hunter R, Shearer J. Cost-Consequences Analysis - An Underused Method of Economic Evaluation. Southampton: National Institute for Health Research; 2014.
- Royal College of Physicians . Sentinel Stroke National Audit Programme (SSNAP) 2015.
- Organisation for Economic Co-operation and Development (OECD) . Strategies to Improve Rural Service Delivery, OECD Rural Policy Reviews 2010.
- Palmer B, Appleby J, Spencer J. Rural Health Care: A Rapid Review of the Impact of Rurality on the Costs of Delivering Health Care. London: Nuffield Trust; 2019.
- Teng J, Mayo NE, Latimer E, Hanley J, Wood-Dauphinee S, Côté R, et al. Costs and caregiver consequences of early supported discharge for stroke patients. Stroke 2003;34:528-36. https://doi.org/10.1161/01.str.0000049767.14156.2c.
- Jackson SF, Kolla G. A new realistic evaluation analysis method: linked coding of context, mechanism, and outcome relationships. Am J Eval 2012;33:339-49. https://doi.org/10.1177/1098214012440030.
- Farmer J, Philip L, King G, Farrington J, Macleod M. Territorial tensions: misaligned management and community perspectives on health services for older people in remote rural areas. Health Place 2010;16:275-83. https://doi.org/10.1016/j.healthplace.2009.10.010.
- Roots RK, Brown H, Bainbridge L, Li LC. Rural rehabilitation practice: perspectives of occupational therapists and physical therapists in British Columbia, Canada. Rural Remote Health 2014;14. https://doi.org/10.22605/RRH2506.
- Adams R, Jones A, Lefmann S, Sheppard L. Decision making about rural physiotherapy service provision varies with sector, size and rurality. Internet J Allied Health Sci Pract 2015;13. https://doi.org/10.46743/1540-580X/2015.1525.
- Luker JA, Craig LE, Bennett L, Ellery F, Langhorne P, Wu O, et al. Implementing a complex rehabilitation intervention in a stroke trial: a qualitative process evaluation of AVERT. BMC Med Res Methodol 2016;16. https://doi.org/10.1186/s12874-016-0156-9.
- Clarke DJ. Achieving teamwork in stroke units: the contribution of opportunistic dialogue. J Interprof Care 2010;24:285-97. https://doi.org/10.3109/13561820903163645.
- Baillie L, Gallini A, Corser R, Elworthy G, Scotcher A, Barrand A. Care transitions for frail, older people from acute hospital wards within an integrated healthcare system in England: a qualitative case study. Int J Integr Care 2014;14. https://doi.org/10.5334/ijic.1175.
- Sims S, Hewitt G, Harris R. Evidence of collaboration, pooling of resources, learning and role blurring in interprofessional healthcare teams: a realist synthesis. J Interprof Care 2015;29:20-5. https://doi.org/10.3109/13561820.2014.939745.
- De Brún A, McAuliffe E. Identifying the context, mechanisms and outcomes underlying collective leadership in teams: building a realist programme theory. BMC Health Serv Res 2020;20. https://doi.org/10.1186/s12913-020-05129-1.
- West M, Armit K, Loewenthal L, Eckert R, West T, Lee A. Leadership and Leadership Development in Health Care: The Evidence Base. London: The King’s Fund; 2015.
- Harris R, Sims S, Hewitt G, Joy M, Brearley S, Cloud G, et al. Interprofessional Teamwork Across Stroke Care Pathways: Outcomes and Patient and Carer Experience. Southampton: NIHR Service Delivery and Organisation programme; 2013.
- Siemonsma P, Döpp C, Alpay L, Tak E, van Meeteren N, Chorus A. Determinants influencing the implementation of home-based stroke rehabilitation: a systematic review. Disabil Rehabil 2014;36:2019-30. https://doi.org/10.3109/09638288.2014.885091.
- Ham C, Curry N. Integrated Care. What Is It? Does It Work? What Does It Mean for the NHS? 2011. www.kingsfund.org.uk/sites/default/files/field/field_publication_file/integrated-care-summary-chris-ham-sep11.pdf (accessed 28 September 2021).
- Rogers L, De Brún A, McAuliffe E. Development of an integrative coding framework for evaluating context within implementation science. BMC Med Res Methodol 2020;20. https://doi.org/10.1186/s12874-020-01044-5.
- Manzano A. The craft of interviewing in realist evaluation. Evaluation 2016;22:342-60. https://doi.org/10.1177/1356389016638615.
- Pawson R. Theorizing the interview. Br J Sociol 1996;47:295-314. https://doi.org/10.2307/591728.
- Mukumbang FC, Marchal B, Van Belle S, van Wyk B. Using the realist interview approach to maintain theoretical awareness in realist studies. Qual Res 2019;20:485-51. https://doi.org/10.1177/1468794119881985.
- Bautz-Holter E, Sveen U, Rygh J, Rodgers H, Wyller TB. Early supported discharge of patients with acute stroke: a randomized controlled trial. Disabil Rehabil 2002;24:348-55. https://doi.org/10.1080/09638280110093677.
- McDevitt AW, Mintken PE, Cleland JA, Bishop MD. Impact of expectations on functional recovery in individuals with chronic shoulder pain. J Man Manip Ther 2018;26:136-46. https://doi.org/10.1080/10669817.2018.1432541.
- Thompson AG, Suñol R. Expectations as determinants of patient satisfaction: concepts, theory and evidence. Int J Qual Health Care 1995;7:127-41. https://doi.org/10.1093/intqhc/7.2.127.
- Indredavik B, Fjaertoft H, Ekeberg G, Løge AD, Mørch B. Benefit of an extended stroke unit service with early supported discharge: a randomized, controlled trial. Stroke 2000;31:2989-94. https://doi.org/10.1161/01.str.31.12.2989.
- Mayo NE, Wood-Dauphinee S, Côté R, Gayton D, Carlton J, Buttery J, et al. There’s no place like home: an evaluation of early supported discharge for stroke. Stroke 2000;31:1016-23. https://doi.org/10.1161/01.str.31.5.1016.
- Mayo NE. Stroke rehabilitation at home. Stroke 2016;47:1685-91. https://doi.org/10.1161/STROKEAHA.116.011309.
- Langhorne P, Holmqvist LW. Early Supported Discharge T. Early supported discharge after stroke. J Rehabil Med 2007;39:103-8. https://doi.org/10.2340/16501977-0042.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. https://doi.org/10.1136/bmj.h1258.
- Raine R, Fitzpatrick R, Barratt H, Bevan G, Black N, Boaden R, et al. Challenges, solutions and future directions in the evaluation of service innovations in health care and public health. Health Serv Deliv Res 2016;4. https://doi.org/10.3310/hsdr04160.
- Cadilhac DA, Fisher R, Bernhardt J. How to do health services research in stroke: a focus on performance measurement and quality improvement. Int J Stroke 2018;13:166-74. https://doi.org/10.1177/1747493017750924.
- Tremblay D, Touati N, Roberge D, Denis JL, Turcotte A, Samson B. Conditions for production of interdisciplinary teamwork outcomes in oncology teams: protocol for a realist evaluation. Implement Sci 2014;9. https://doi.org/10.1186/1748-5908-9-76.
- Dixon-Woods M, Bosk CL, Aveling EL, Goeschel CA, Pronovost PJ. Explaining Michigan: developing an ex post theory of a quality improvement program. Milbank Q 2011;89:167-205. https://doi.org/10.1111/j.1468-0009.2011.00625.x.
- Turner S, Goulding L, Denis J-L, McDonald R, Fulop NJ, Raine R, et al. Challenges, solutions and future directions in the evaluation of service innovations in health care and public health. Health Serv Deliv Res 2016;4. https://doi.org/10.3310/hsdr04160.
- Rycroft-Malone J, Wilkinson JE, Burton CR, Andrews G, Ariss S, Baker R, et al. Implementing health research through academic and clinical partnerships: a realistic evaluation of the Collaborations for Leadership in Applied Health Research and Care (CLAHRC). Implement Sci 2011;6. https://doi.org/10.1186/1748-5908-6-74.
- NHS RightCare, Stroke Association . RightCare Pathway: Stroke 2017. www.england.nhs.uk/rightcare/wp-content/uploads/sites/40/2017/09/stroke-pathway.pdf (accessed 25 January 2021).
- NHS England . Commissioning Guidance for Rehabilitation 2016. www.england.nhs.uk/wp-content/uploads/2016/04/rehabilitation-comms-guid-16-17.pdf (accessed 25 January 2021).
- National Institute for Health and Care Excellence . Transition Between Inpatient Hospital Settings and Community or Care Home Settings for Adults With Social Care Needs 2015. www.nice.org.uk/guidance/ng27/evidence/full-guideline-pdf-2185185565 (accessed 25 January 2021).
- National Institute for Health Research . Roads to Recovery: Organisation and Quality of Stroke Services 2017. www.arc-swp.nihr.ac.uk/uploads/attachments/PenCHORD/Roads-to-recovery-final.pdf (accessed 25 January 2021).
- East Midlands Academic Health Science Network . Stroke Rehabilitation Resources 2016. https://emahsn.org.uk/our-work/previous-projects/503-stroke-rehabilitation-resources/966-stroke-rehabilitation-resources (accessed 25 January 2021).
Appendix 1 Rapid evidence synthesis
Search strategy (MEDLINE example)
Database: MEDLINE(R) (via Ovid).
Date of search: July 2018.
Date range searched: January 2000 to June 2018.
| # | Search terms | Results |
|---|---|---|
| 1 | Patient Discharge/and Stroke Rehabilitation/ | 421 |
| 2 | (stroke or cerebrovasc*or brain vasc* or cerebral vasc* or cva* or apoplex*).tw. | 147,029 |
| 3 | (early supported discharge or accelerated discharge).mp. [mp = title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] | 116 |
| 4 | accelerated discharge.tw. | 18 |
| 5 | (community stroke rehabilitation adj5 (based or services)).tw. | 4 |
| 6 | early supported discharge.tw. | 97 |
| 7 | (reduce*adj5 duration adj5 (stay or hospital)).tw. | 0 |
| 8 | (reduce*adj5 length adj5 (stay or hospital)).tw. | 0 |
| 9 | ((early or earlier or accelerate* or supported) adj5 discharge).tw. | 3650 |
| 10 | ((early or earlier or accelerate* or supported) adj5 (discharge or return) adj3 home).tw. | 221 |
| 11 | (qualitative adj2 (research or study)).tw. | 32,557 |
| 12 | ((qualitative or interview) adj2 (research or study)).tw. | 34,509 |
| 13 | (research adj3 (health services or implementation)).tw. | 4538 |
| 14 | ((post-discharge or home rehabilitation) adj5 (support* or care)).tw. | 365 |
| 15 | ((early or earlier or post-discharge) adj5 (community or domiciliary or home or home-based) adj5 (rehabilitation or support* or care)).tw. | 356 |
| 16 | 2 and 3 | 75 |
| 17 | ((qualitative or interview*) adj3 (research or stud*)).tw. | 47,414 |
| 18 | 2 and 3 and 17 | 6 |
| 19 | 2 and 5 and 17 | 1 |
| 20 | 2 and 4 and 17 | 0 |
| 21 | 2 and 3 and 13 | 0 |
| 22 | 2 and 15 and 17 | 4 |
| 23 | 2 and 9 and 17 | 10 |
| 24 | 2 and 14 and 17 | 3 |
| 25 | 2 and 8 and 17 | 0 |
| 26 | 2 and 7 and 17 | 0 |
| 27 | 2 and 10 and 17 | 3 |
| 28 | 2 and 9 and 13 | 0 |
| 29 | 2 and 13 | 48 |
| 30 | “COMMISSION ON PROFESSIONAL AND HOSPITAL ACTIVITIES”/ | 138 |
| 31 | 2 and 30 | 2 |
| 32 | (barriers adj3 (facilitators or enablers)).mp. [mp = title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] | 4721 |
| 33 | 2 and 32 | 97 |
| 34 | (evidence-based or clinical guidelin*).mp. [mp = title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] | 127,367 |
| 35 | 2 and 34 | 2778 |
| 36 | 2 and 3 and 34 | 12 |
| 37 | RURAL HEALTH/or HOSPITALS, RURAL/or RURAL HEALTH SERVICES/ | 23,352 |
| 38 | 1 and 37 | 1 |
| 39 | 3 and 37 | 0 |
| 40 | 15 and 37 | 3 |
| 41 | Intermediate Care.tw. | 877 |
| 42 | 13 and 41 | 2 |
| 43 | 17 and 41 | 23 |
Publications were eligible for inclusion in the review if the following criteria were met.
Inclusion criteria
-
Evidence published in peer-reviewed journals.
-
Published in English.
-
The title or abstract reported research on ESD/community stroke rehabilitation services.
-
The title or abstract reported research on stroke survivors’ or carers’ experiences of receiving rehabilitation at home.
-
The title or abstract reported research on stroke survivors’ and carers’ experiences in the early post discharge phase (up to 6 months post stroke).
-
The title or abstract reported research on health-care professionals’ views on home-based rehabilitation.
-
The results section described contextual factors that might facilitate or impede the implementation and delivery of home-based rehabilitation services.
Exclusion criteria
-
No full-text paper available online or via The British Library.
-
Publication did not report on factors influencing the process of discharge from hospital/transition to community rehabilitation/delivery of home rehabilitation.
Appendix 2 Interview schedules
Appendix 3 Individual site service descriptions
Site A
Development of the service
The stroke-specific service at site A started in 2005, with the ESD component being added in 2011. In 2013, community teams were merged into one umbrella service, that is site A has three pathways for stroke, neurological and general rehabilitation patients. Both the ESD and the stroke CRT components are staffed by the same team who provide a specialist stroke service to stroke patients. The stroke service forms part of a larger community rehabilitation service, with resources spread more widely than just dedicated to providing ESD. Furthermore, one-third of the overall team are dedicated to stroke care, which excludes neurological and general rehabilitation as of December 2019. Teams are divided into north and south localities, with a further subdivision of two teams within each locality.
Model of operation
Referrals
The referrals to the service can be made by GPs, hospital staff, nursing homes, other health-care professionals, the Stroke Association and social services. Patients who have previously received therapy from the team can contact them directly (self-referral). Referrals from the acute trust to ESD are electronic and booked straight into ring-fenced new patient slots by administration. CRT patients are triaged by a clinician.
Eligibility
-
Within 6 weeks of the stroke.
-
Clinical or radiological diagnosis of a stroke.
-
Registered with a site A GP.
-
Barthel Index Score of > 11.
-
Low-level cognitive and behavioural difficulties.
-
Transfer independently or with assistance of one other person.
-
Clinically stable and fit for discharge from hospital or step down.
-
Requires and would benefit from intensive rehabilitation.
-
Able to meet their own nutritional needs and manage their continence (although accepting referrals for residential or nursing home patients since May 2019).
-
Transfer with assistance of two patients are placed on the community service pathway (but seen by the same staff).
-
The following should also be in place when clinically indicated: continence medication, nutrition and hydration, and skin-care management plans; and mental health, mood and emotion, and cognition and communication screens. Social, patient and carer needs assessed and care package in place prior to discharge to ESD.
Intervention
-
Stroke-specific multidisciplinary ESD team (within community rehabilitation service). The ESD and CRT are one service and are provided by the same team. The only difference between the two relates to the initial assessment target times.
-
Five-day service.
-
Initial assessment within 1 working day for ESD and within 3 working days for community rehabilitation services. Slots are scheduled each day for new ESD patients to be booked into, but if the slot is not filled with an ESD patient then it may be used for a new CRT patient. Thus, some CRT patients will be seen within 1 working day.
-
Either an OT or a physiotherapist undertake the initial assessment.
-
Input lasts for 6 weeks (but can be transferred to the community service to receive similar therapy from the same staff by admin transfer of code depending on clinical need). Transfer from ESD to CRT is strictly at 6 weeks and is an administrative transfer. Patients are unaware as the same team continues to provide the care.
-
The intensity of the service is dependent on patient need and capacity within the team.
-
Weekly MDT meetings (psychology attendance monthly).
Challenges
A challenge for site A is the number of part-time team members.
Auditing/evaluation processes
The team internally monitor how many patients achieve their rehabilitation-specific goals. The team have a response target of 95% of patients seen within 1 working day. Every breach of the 24-hour responsiveness target has to be exception reported and investigated for the commissioners. The team attend a monthly quality development practice team meeting with the acute trust, and SSNAP data are fed back to team leaders at monthly meetings.
A total of 90% of patients and carers report a positive experience collated from a patient experience questionnaire at discharge. The team also collect the number of referrals by month, length of stay and number of patients who received an appropriate intensity of treatment. Further outcome measures include the Friends and Family Test and that 80% of patients should experience an improvement in patient-reported outcome measures, such as the Family Quality Of Life and Stroke and Aphasia Quality of Life scales.
Site B
Development of the service
Site B has been operating for > 20 years. Site B comprises two subteams providing ESD < 15 days post stroke and ESD > 15 days post stroke. They are co-ordinated operationally as two MDTs, although some staff rotate between both teams. Both teams also offer a community stroke service for patients > 8 weeks and who may be referred back for further top-up of rehabilitation. The teams are based within the same offices in a health centre. The office base is not central and journey times are affected (owing to traffic congestion).
Model of operation
Referrals
Patients can be referred to the community team by GPs, hospital services, health-care and social care professionals and voluntary organisations. The team also accept self-referrals from carers or people who have had a stroke.
Referrals to the < 15-day team are by e-mail. Allocations to therapists are made twice per week at the allocation meeting or the MDT meeting. The first contact to triage the patient is by telephone and may be by the most relevant therapist for the greatest identified need or by anyone with capacity within the team.
Referrals to the > 15-day team are made by the ward, who request a screening visit. Not all screening visits will be provided. The ESD team make the final judgement and may refer the patient to an e-mail discharge that can be effected more quickly.
Patients requiring a reablement package receive a screening visit on the ward by the ESD team. The team can refer patients directly without a social work referral for a care package and the patient can be discharged within 48 hours.
More complex patients are referred to the MDT as an e-mail referral and the team may attend a home visit with the ward therapists and will then visit on the day of discharge or the next day.
Eligibility
-
Confirmed diagnosis of stroke and medically stable.
-
Continent (or a suitable management plan implemented).
-
Able to transfer with one or a suitable plan in place.
-
Medication concordance or a plan in place.
-
Mild to moderate patients are seen by the ESD team while patients with more complex needs are seen by the community team.
-
Registered with a site B GP and site B resident.
-
Live in their own home.
-
Aged ≥ 18 years.
Intervention
-
In-reach handover and attendance at ward MDT meetings.
-
Close interdisciplinary working with joint goal-setting and multidisciplinary case notes, plus patient-held records.
-
Joint working across health care and social care.
-
Joint environmental visits as well as joint home visits.
-
Stroke-specific multidisciplinary ESD team (within community stroke services).
-
The team operate a < 15 days (ESD) and > 15 days (community) patient process based on the date of stroke, which means that the service is divided into two teams.
-
Initial telephone contact is made within 24 hours of receipt of referral and is conducted by a therapist.
-
Intensity based on patient’s needs and caseload capacity.
-
Patients seen by the < 15-days team can be with the service up to 6–8 weeks (this can be extended up to another 12 weeks by transferring to the > 15-days team).
-
Weekly MDT meetings with patients discussed on alternate weeks to manage time.
-
Despite being a 5-day service, the team provide a telephone service over the weekend for those late-week/Friday discharges to check if care/medication has been put in place.
-
The team can undertake the secondary prevention as well (i.e. taking blood pressure and checking that the patient is alright in terms of dealing with fatigue, anxiety and adhering to their medication schedule).
-
Patients can return to the service (i.e. re-referrals) for short bursts of goal-led treatment/further rehabilitation for non-urgent stroke-specific issues.
-
The team do not cover residential/nursing/care homes.
Challenges
Speech and language therapists plus RAs work across both teams, whereas OTs and physiotherapists focus on a specific team. Most of the team work part time. Other challenges include:
-
Increasing number of survivors/clients.
-
Trends in stroke severity are documenting increasing numbers of patients more moderately affected.
-
Increasing demands on rehabilitation.
-
Duration of rehabilitation.
-
Delivery models.
-
Data collection.
-
Centralisation.
-
Stroke education/research.
-
Commissioning for stroke intervention into care homes.
-
Sustainability.
Auditing/evaluation processes
The information generated from patient surveys at discharge and the biennial listening event contributes to service redesign. The team also have a biannual staff planning event to review trends and review service development action plans:
-
biannual data collection and data reporting
-
data reporting to the stroke pathway
-
patient and carer feedback sheets
-
annual patient and carer listening event
-
annual review of trends and service redesign/development
-
team action plan annual
-
SSNAP.
Site C
Development of the service
The site C service was set up in 2010/11. The service is split into north and south patches covering the county. Each county team will also cover patients in the city area. Because there are fewer SLTs, they must work across both north and south teams.
Model of operation
Referrals
The discharge decision is made on the stroke wards and the referral form is faxed or e-mailed to the team. Each referral is screened for patient eligibility and team capacity before deciding to accept the referral or not. The team have a fixed caseload and will not accept new patients if they are full. Patients who cannot be taken owing to capacity issues either remain in hospital or are referred to the community stroke service team and receive less-intensive rehabilitation.
Eligibility
-
Confirmed diagnosis of stroke.
-
Have not been discharged home before a referral is made and accepted.
-
Barthel Scale score of ≥ 9.
-
Registered with a site C GP and site C resident
-
Able to transfer with one unless they have their own care organised.
-
Able to manage their own continence in their home environment.
-
Safe to be alone if they are living alone.
Intervention
-
Stroke-specific multidisciplinary ESD team.
-
Five-day outreaching service.
-
Caseload capacity is 40 patients at any given time.
-
Initial assessment within 1 working day.
-
By way of guidance for rotational and/or new staff, patients are triaged at the first assessment to levels 1–3 depending on the intensity required to meet patient needs. Level one patients who are almost back to baseline will receive a telephone follow-up. However, this guidance is not considered an integrated aspect of the whole service.
-
If patients are re-admitted to hospital, the space is kept for 48 hours, after which the patient is discharged and can be re-referred only if they have a new stroke.
-
Input lasts for a maximum of 6 weeks and is strictly applied. Patients requiring a review appointment can be moved from the main capacity and contacted for a review beyond their discharge date if appropriate.
-
Weekly MDT meeting for the north and south patches for all patients, organised in time slots for time efficiency.
Challenges
Team members do not attend MDT meetings at local acute hospitals to discuss stroke patients currently receiving acute care.
Resources are very tight and the team have to make many of their own rehabilitation aids, such as fasteners and buttons in their own time, or rely on gifts from people.
Auditing/evaluation processes
The team produce a report every month on data that come from their internal data system, that is how many patients are seen, how quickly are patients seen, what the response was for all of the services, how many new patients there were, how many follow-up sessions were carried out, whether or not each patient had outcome measures carried out, whether or not the patients had their goals discussed with them, etc. These reports are made available for management and commissioners who allocate funding to the site C budget and oversee the site C operation. The team also collect monthly data relevant to their key performance indicators and feed back directly to management and commissioners.
There are also monthly team meetings whereby the team discuss issues relating to working (e.g. recording patient data) rather than patient care as they do during their weekly MDT meetings. Furthermore, all staff have regular one-to-one meetings with the therapy leads and team manager, plus they have appraisals.
Site D
Development of the service
The site D team have been in operation since November 2011. The team covers a wide geographical area with long distances and rural communities.
Model of operation
Referrals
All patients must be referred by a health-care or social care professional, such as a GP or social worker.
Eligibility
-
Confirmed diagnosis of stroke.
-
Barthel Scale score of ≥ 10.
-
Registered with a site D GP and be a resident in the team’s catchment area.
-
Able to engage in rehabilitation.
-
Able to transfer with assistance of one.
-
Able to call for help.
-
Able to access toilet facilities/manage continence at home/have care needs met at home either independently or with carer support.
-
Aged ≥ 18 years.
Intervention
-
Stroke-specific multidisciplinary ESD team (within therapy stroke rehabilitation team, which also supports a 12-bedded inpatient unit).
-
Five-day in-reaching service.
-
Deliver care in people’s homes and are commissioned to take 17 patients per month (but typically run at 22 patients).
-
Input lasts for 6 weeks (but can be extended for up to 12 weeks with CCG agreement depending on clinical need or if the team reduce rehabilitation intensity owing to influx of new referrals/increased caseload).
-
Members of the ESD team attend acute ward rounds twice weekly to identify patients suitable for discharge to the team.
-
Weekly MDT meetings.
-
The team sometimes help the patient with their hospital discharge.
-
The team also see patients who have not been admitted to hospital, for example A&E, GP and community transient ischaemic attack patients.
-
Initial assessment is usually within 1 working day, unless there are capacity issues.
-
The therapy assistants can provide health advice, conduct initial assessments, order required equipment and book in the 6-month reviews.
-
The team operate a waiting list if their caseloads are full.
Challenges
The team’s capacity constraint has grown in recent times owing to there being more patients to see with the same number of staff in the team.
Onward referral/follow-up
The team provide a self-managed programme for the patient to carry on with their own rehabilitation, plus the team carry out 6-month post-discharge patient reviews with patients who have accessed stroke rehabilitation services (i.e. ESD or stroke rehabilitation unit). The team also have to access to a social worker and a neurological navigator who acts as a gateway to specialist rehabilitation.
Auditing/evaluation processes
A quarterly report is produced on the number of hours of face-to-face contacts, length of stay and whether or not there is an improvement based on the outcome measures of Barthel scale, modified Rankin Scale, Nottingham Extended Activities of Daily Living scale and Stroke Impact Scale. In total, 80% of patients should have an improvement in their outcome measures from admission to discharge.
Site E
Development of the service
The site E team started recruiting staff in May 2009 and began operating its service in July 2009. Given the rurality of the area covered, the team is subdivided into three smaller teams to reduce the travel burden.
Model of operation
Eligibility
-
Registered with a site E GP.
-
Mild to moderate stroke severity.
-
Able to transfer with a piece of equipment or one person.
-
Able to make an emergency call.
-
The patient can be safely discharged home.
-
Usually aged ≥ 18 years.
Intervention
-
Stroke-specific multidisciplinary ESD team.
-
In-reaching service to the acute hospital on weekdays.
-
Caseload capacity up to 80 patients (no patients are turned down but some may have to wait at home after discharge or wait in hospital before beginning treatment).
-
Seven-day service (reduced basis at weekends: nurses work Saturdays and band-4 assistants cover Sundays and newly discharged patient contacts on Sundays may be by telephone).
-
The initial assessment is by a nurse within 1 working day and by a therapist within 3 days.
-
Input lasts for 6 weeks (but can be longer depending on clinical need).
-
Weekly MDT meetings.
Challenges
There are fewer SLTs than OTs and physiotherapists, so they work across the regional ESD teams.
Onward referral/follow-up
A 6-month follow-up appointment is offered to all stroke patients who were on the site E caseload.
Auditing/evaluation processes
The ESD team leads have a monthly performance meeting to discuss performance data, which include SSNAP data and key performance indicators.
Site F
Development of the service
The service was commissioned and commenced in November 2009 based on the numbers of strokes, geography of the county and available bases. It was decided that an ESD model would not work and that a broader supported discharge model taking a wider spectrum of strokes was deemed more appropriate. The site F service is divided into four hubs across the county: north-west area, north-east area, south-west area and south-east area.
Model of operation
Referrals
The team also access ‘nhs.net’ referrals because a lot of the hospitals are putting the referral straight into the nhs.net e-mail.
Eligibility
-
Confirmed diagnosis of a stroke.
-
Registered with a site F GP.
-
Able to transfer with one, can transfer with one within 1 week or so or can transfer with one and a hoist or steady.
-
Able to be safe in-between visits.
-
Have clear goals.
Intervention
-
Stroke-specific multidisciplinary ESD team.
-
The team have an in-reach model that is implemented differently for each referring trust according to the distance from the base and the number of referrals usually received. Some in-reaching is carried out in person and some by telephone.
-
The service in-reaches twice per week to the main referring hospital.
-
Seven days per week rehabilitation service, with therapists working Monday to Friday and assistant practitioners and RAs working Monday to Sunday.
-
Initial assessment usually within 48 hours post hospital discharge can be undertaken by a RA or assistant practitioner.
-
A holistic assessment is completed within 24 hours of discharge. This can be completed by a trained RA, assistant practitioner or therapist.
-
The therapy assessment is conducted by a therapist within the first 72 hours of discharge.
-
Commissioned to provide ESD rehabilitation for up to 6 weeks (but can be extended up to 10 weeks based on clinical need).
-
Weekly MDT meetings.
Challenges
The county borders with eight counties, which creates challenges in identifying whether or not patients have a site F GP and are, therefore, eligible for the service. Trusts do refer patients who are not eligible. Each hub has different challenges created by differing demographics and geographical challenges. Further complexity is added by many patients living within one hub but being registered with a GP in a different hub.
The team do not have access to a clinical psychologist within their NHS trust, so they can make only an onward referral for psychology. In addition, the team face a large and varied Eastern European community and some patients from those communities require interpreters for the team to do their job.
Follow-up
The team provide the patients with a set of activities on discharge from the service so that they can continue to manage their own recovery.
Auditing/evaluation processes
The four teams use standardised assessment and outcome measures, as well as the number of patients referred and the number of patient contacts. The overall team also look at more general team indicators, such as long-term absences, complaints and outcomes from patient questionnaires, as well as the Friends and Family Test.
Appendix 4 Access to doctors and clinical psychologists
Access to doctors: context, mechanisms and outcomes
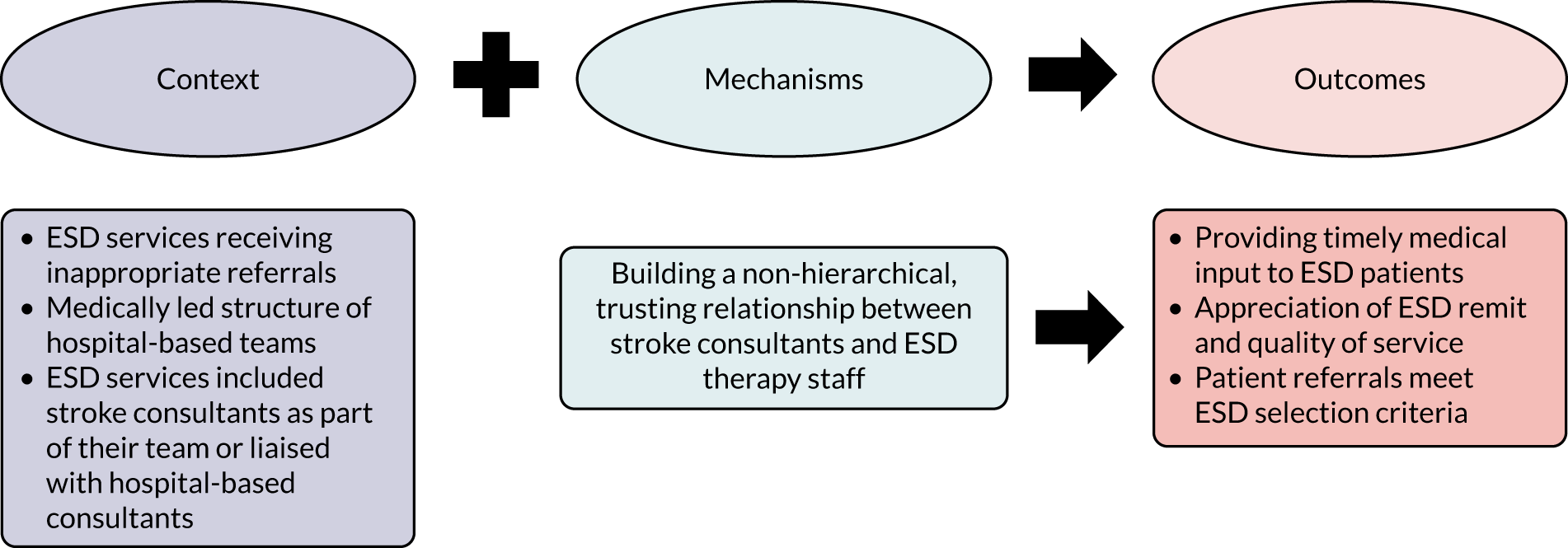
Being well-supported medically was perceived by the teams with access to stroke consultants as an important component of their services’ success. Respondents valued the opportunity to access timely specialist medical input via telephone or e-mail when they were concerned about a patient (O). One team explained that liaising with a stroke consultant permitted the assessment of any missed cases and reintroduction to the stroke pathway (O). A stroke consultant noted that, although they did not have paid time in the ESD service, the development of a trusting relationship with the team over the years and their own experience and expertise in handling issues pertinent to ESD patients (M) accelerated the process of providing input and advice:
I don’t have any time in my job plan to provide input to this service. It’s usually people you can trust most because you know they’ve worked in it for a long time. You know if they’re asking you something which is a problem, then you can trust the information provided is going to be reasonably appropriate and you can – because we’re experienced, we’ve dealt with this a long time, most of the problems or some of the problems you’ve encountered before. So the answers are usually quite easy to provide advice on. So no it’s not an onerous problem. It could be very onerous if you start another service and they don’t know each other, and people are referring a lot of things and you don’t have experience. So in the beginning it might be very difficult to do and time consuming until people get used to it and build up those experiences.
BS8
In two sites, respondents contrasted between the medically and consultant-led ethos of hospital-based teams and their therapy-led hierarchical structure (C). They thought that these differences between the community and the acute context could influence doctors’ attitudes towards the service and their confidence that ESD would be the best discharge destination for their patients. Having an established, non-hierarchical relationship with stroke consultants (M) improved referrers’ understanding of the remit and quality of the service and helped to ensure that referred patients met ESD selection criteria (O). In the extract below, a therapist talked about how the consultant attached to their service respected their way of working and offered a much-needed objective perspective:
I think on the acute ward the consultant will have the final say, you may make a recommendation about a patient, you may think that a patient isn’t safe to go home for A, B, C reason but the consultant may still make a decision about that patient being discharged or something happening to that patient. Here, I feel like we are more – our opinions are more respected, and the consultant will always take on board our feedback and consider that in relation to the patient’s needs. And sometimes it’s quite good for somebody else to make that observation if you are in there with that patient you can’t always see perhaps that maybe they are not making as much progress as you would hope or would expect, so it’s good to have that objective viewpoint. On a ward, often the pace of the turnover, the nature of the role in which you are providing treatment is very different to ESD.
CS5
He [consultant] and I had some really robust conversations, because he was really struggling to see the benefit of assisted discharge at the time. The biggest area of discord was the fact that we didn’t put in a medical component. So it was a therapy-led service, and that caused quite a furore in the medic within our consultant body, I have to day; and hence some of our rigorous conversations.
FS13
Access to clinical psychologists: context, mechanisms and outcomes
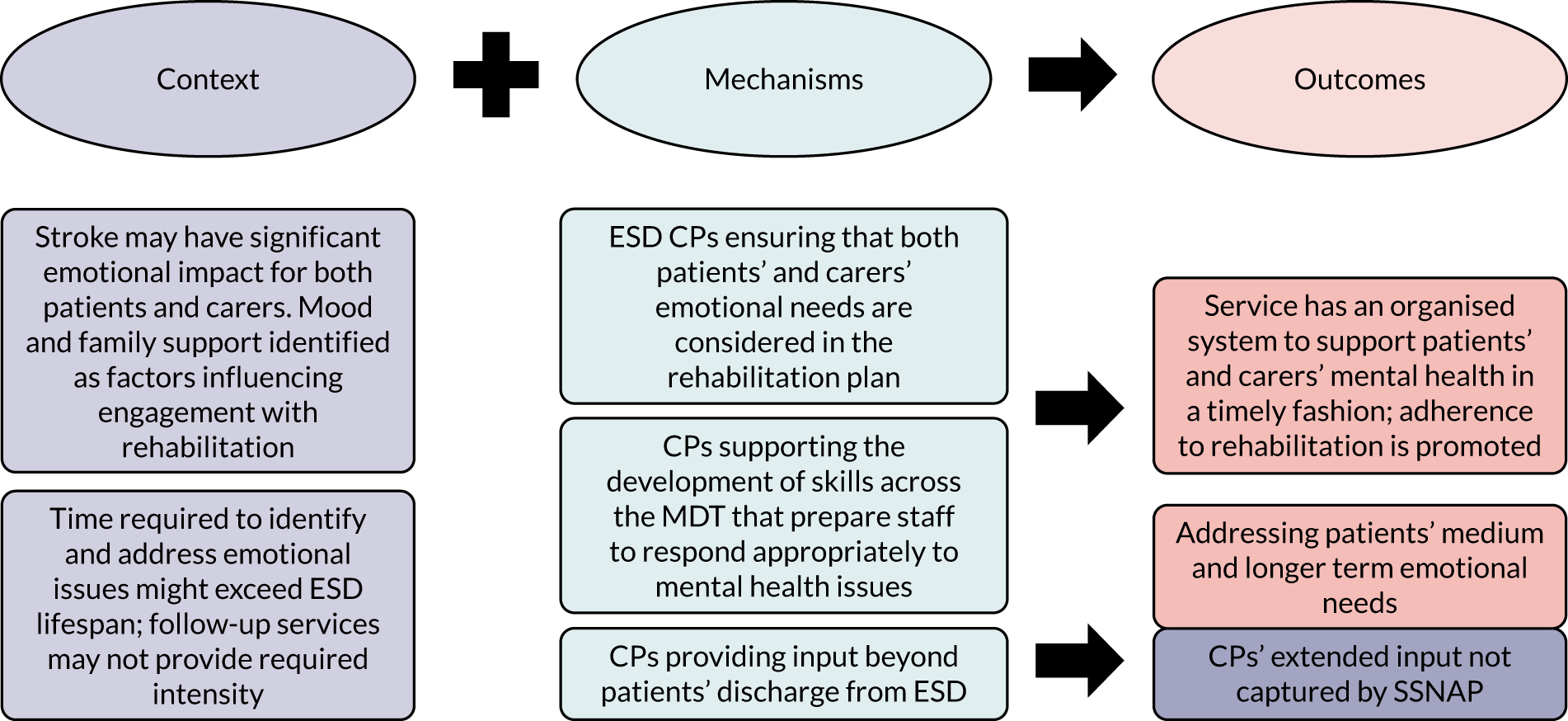
Where available, access to clinical psychologists and neuropsychologists was perceived by staff as one of the strong aspects of their service model, enabling the provision of a holistic rehabilitation approach. For most patients, their return home was marked by the emergence of mood issues in response to the losses and restrictions brought on by stroke (C). Acknowledging the psychological impact of stroke for patients and their carers and providing timely intervention (M) was seen as a key factor influencing patients’ readiness and adherence to physical and cognitive rehabilitation interventions (O). The provision of mental health training and support to staff members was considered to be equally important (M). Respondents described how clinical psychologists taught them the basic skills that enabled them to effectively talk about adjustment, anxiety and depression (O):
We’ve had a lot of training from psychology about how to deal with difficult situations as well, so I think we do a lot of psychology ourselves, with the patients and a lot of the carers. Sometimes it’s not the patient that needs it. You sit with the relative because they’re the one that’s struggling to adjust.
FGBS1
The neuropsychologist we have in the team does training for everyone who starts with the team, and gets us ready to do distress checklists, the outcome measure for mood, and have those nice awkward conversations that sometimes you need to have with patients.
I remember when I was a band 5 physio if a patient in the hospital was crying you would just autopilot, I need to make you happy again, whereas there’s less of that approach and more of a, let’s have a conversation about this, and let’s get something written down, and then we can have a conversation with the neuropsychologist.
CS1&2
A commonly reported concern related to the time required to identify and address psychological issues, which could well exceed the short lifespan of the ESD service (C). The problem was accentuated when emotional struggles did not become apparent until a later stage of patients’ recovery. By the time that staff had the chance to build the rapport required to identify the problem and the referral to a psychologist was made, patients could be close to their discharge date. Where available, follow-up services could take over but they would not offer the required intensity to make a difference (C). In these cases, psychologists from two sites suggested that they could consider extending their intervention long after patients’ discharge from ESD (M). In this way, clinical psychologists attempted to respond to patients’ medium- and longer-term emotional needs; their input, however, would not be captured by SSNAP (O):
It’s very difficult to capture the psychologist, because SSNAP again, very naïve, they think the psychology is all done and dusted by the time they’re discharged from ESD and we fed back to SSNAP and said no, that’s not the case because a lot of the patients aren’t ready for psychology interventions until the end of ESD. So, there’s a whole raft of data that SSNAP are potentially missing because I don’t think we’ll ever get a true picture of the impact or the psychological and emotional problems of stroke, because of the way that data set is. It’s far too early. It’s not just the patient, sometimes it’s the carer’s.
ES1
What’s the longest you have seen a patient for?
I think the longest would be probably 3 years.
And that would be you personally or supervising other team members to provide that support?
That would probably be me personally, but it wouldn’t be weekly because we have got to have a throughput.
BS19
Appendix 5 Further impact
Rebecca J Fisher was appointed the National Rehabilitation and Life After Stroke Workstream lead in April 2020, with NHS England and NHS Improvement Clinical Policy Unit. Rebecca J Fisher now chairs a fortnightly national community stroke call, in which regional representatives of community stroke services share best practice guided by evidence-based policy.
Prior to this, Rebecca J Fisher and Marion F Walker led a task and finish group to produce a National Integrated Community Stroke Rehabilitation service model, detailing team composition, intervention delivery and performance monitoring informed by our research. 1,12,13,23 This model outlines integration of ESD and community stroke rehabilitation as recommended in this report. The Integrated Community Stroke Rehabilitation service model was circulated in August 2020 to 20 new Integrated Stroke Delivery Networks covering all CCGs in England. Rebecca J Fisher is now working with the NHS England and NHS Improvement Clinical Policy Unit to support implementation of this model across England. In October 2020, Rebecca J Fisher was appointed Associate Director of the Stroke Audit Programme to implement improved national performance monitoring, including addition of patient outcome measures, informed by our research.
List of abbreviations
- ASCOF
- Adult Social Care Outcomes Framework
- CCA
- cost–consequences analysis
- CCG
- Clinical Commissioning Group
- CFIR
- Consolidated Framework for Implementation Research
- CI
- confidence interval
- CMO
- context–mechanism–outcome
- CRT
- community rehabilitation team
- ESD
- early supported discharge
- GP
- general practitioner
- HQIP
- Healthcare Quality Improvement Partnership
- IQR
- interquartile range
- IT
- information technology
- MDT
- multidisciplinary team
- NIHSS
- National Institutes of Health Stroke Scale
- OT
- occupational therapist
- QALY
- quality-adjusted life-year
- RA
- rehabilitation assistant
- RE
- realist evaluation
- RES
- rapid evidence synthesis
- SD
- standard deviation
- SLT
- speech and language therapist
- SSNAP
- Sentinel Stroke National Audit Programme
- WISE
- What is the Impact of Stroke Early supported discharge?
- WP
- work package
- WTE
- whole-time equivalent
