Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number NIHR128268. The contractual start date was in June 2020. The draft manuscript began editorial review in February 2023 and was accepted for publication in July 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Abel et al. This work was produced by Abel et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Abel et al.
Chapter 1 Introduction
Background and rationale
The move to online primary health care services
The National Health Service (NHS) is under pressure due to the increasing demands of a growing and ageing population, technological progress and changing expectations among the public. Successive governments have viewed technology as part of a solution in addressing the pressures facing primary care, and policy for delivery of general practice has reflected this thinking. 1
Recent years have seen a push towards the adoption of online services in primary care, ranging from booking appointments and ordering repeat prescriptions through to the use of alternatives to face-to-face consultation with a patient (e.g. e-mail, video). By 2022, the reach of such services had extended to 22 million users. 2 Current NHS policy in England emphasises use of digital services in primary health care, and to date 28 million people have downloaded the NHS app, and 40 million people have acquired an NHS login. 2 Drivers behind the move to online primary care provision include the assumption that online services lead to improved choice, convenience, and ease of access for users, improved triage systems and streamlining of service delivery. 3
Context of this research: the COVID pandemic
In March 2020, the UK recognised the global health emergency of a pandemic associated with rapidly spreading COVID virus. In the UK, COVID led to widespread changes in society and within the healthcare system. From the perspective of this research, some relevant policy initiatives4 are summarised in Box 1. Overall, the pandemic was associated with increasing and substantial pressure for many staff in primary care, and for primary care within the healthcare system. The British Medical Association has estimated that numbers of full-time equivalent general practitioners (GPs) fell by nearly 6% between 2015 and 2021. 5 Moreover, the telephone first consultation, which was available pre-pandemic and widely adopted during the COVID pandemic, initially generated a 33% increase in the mean number of GP contacts per patient per 28 days,6 and during the pandemic increased telephone consultations from 39% to 51%. 7
-
Introduction of COVID alert status.
-
Travel restrictions and various public health measures (e.g. social distancing, advice on personal hygiene) 25 February 2020.
-
Introduction of national lockdown on 23 March 2020.
-
Initial restrictions to online booking of appointments 23 March 2020, and associated with a rapid reduction in the number of GP face-to-face appointments from 15.9 million per month (March 2020) to 7.5 million (April 2020). 8
-
Rapid introduction and procurement of telephone, web-based and video technologies and consulting platforms in primary care. Detailed guidance and updates were produced for primary care clinicians and practices, for example, in respect of the implementation of total triage systems aimed at managing and reducing total footfall in primary care facilities. 9 Around three-fifths of UK adults who used the NHS during the early phase of the pandemic said that in doing so they used technology either in a new way or more than before. 10
-
Widespread use of apps and devices to facilitate home-working by NHS staff. 10
-
Escalation in remote linkages between practices and pharmacy suppliers.
-
Widespread promotion of the NHS app.
-
Introduction of large-scale vaccination programme (8 December 2020) utilising many health resources, including GP facilities and personnel, and primary care resources.
General practice settings moved to using remote methods of consultation to enable safe delivery of care. The shift was dramatic, with a rapid change to 90% remote GP consulting (46% for nurses) by April 2020. 11 The researchers in that study noted a universal consensus that remote consulting was necessary. Telephone consulting was sufficient for many patient problems, video consulting was used more rarely, and appeared less essential as lockdown eased. Short message service (SMS)-messaging increased more than threefold. 11,12
Figures from 2022 for use of technology and online primary care services show an increasing use of NHS online services13 (increased from 44% of respondents reporting that they had ‘recently used’ such services, to 55% in the year to July 2022) – covering areas such as ordering repeat prescriptions online (26–31%), having an online consultation or appointment (18–22%), booking appointments online (19–21%) or accessing personal health records (7–17%). Geographical variation across England is evident in the application of online general practice services (GP services) by integrated care systems (ICS), with usage ranging from 46% of patients using an online GP service in the past 12 months to a maximum of 70% across 42 systems. Increases were evident in the proportion of patients reporting use of their GP practice’s website (from 36% in 2018 to 60% in 2022) with around 66% of respondents reporting the practice’s website being ‘easy to use’ in 2022.
Prior to the pandemic, research studies had established that for patients a face-to-face consultation is seen as the ‘gold standard’ and was the most used type of consultation. 13 The rapid change occurring in general practice means that digital services are now more widely available to all patients, and they may be expected to use them, regardless of digital confidence, proficiency and ease of access to the required technology and connectivity. For some patients, this change in patterns of access has been beneficial, for others it has been more challenging. 14
Moving to online provision – impacts and sequelae
The introduction of digital services and the move to a digital-first health service envisaged at the time this research was commissioned, raises important questions about digital access in the population. The research reported here has taken place in a changing policy environment – from the early days of a ‘digital-first’ vision for access to primary care services, through the ‘total triage’ model encouraged by NHS England during the COVID-19 pandemic to reduce footfall in general practices and to protect staff and patients, and, more recently, to a refined and nuanced vision of GP access, encompassing a range of modes of access, responding to the needs and ambitions of the NHS and of local patients and populations. In order for GP practices and patients to gain the potential benefits that technological innovation can bring to primary care,15 patients must be able to, and wish to, access and use online services. Digital inequalities tend to adversely affect certain groups of people. In this context, individuals from older age groups, non-white ethnicities, those in lower socioeconomic groups, those in poorer health and individuals in rural settings are recognised as vulnerable groups who may struggle to access digital services. 16–19 As online delivery of primary care is a key priority for policy-makers,2,20–23 it is important to understand how barriers to uptake might be overcome and inequality avoided. In attempting to mitigate the potential for digital inequalities, the research literature suggests that meaningfully involving users, tailoring services and interventions to target groups’ contexts, delivering credible messages and having a clear understanding of how services using technology improve health are key elements in developing relevant interventions. 24 One way to combat these potential inequalities is via digital facilitation (DF) – actively supporting patients and carers in using practice-based online services.
Value of online services
Financial investment in online health services is enormous. In the USA, for example, digital health doubled between 2019 and 2020, being seen as a ‘quarter trillion dollar opportunity’, and investment in online and digital health being described as ‘skyrocketing’ in recent years. 25 The number of health apps available globally is rapidly increasing, and was estimated at around 318,000 by 2017. 26 Such substantial investment and development activity highlights the need to estimate the value of such services to the population being served – does the investment yield significant returns in terms of health and well-being or patient experience of care, and is it cost-effective?
These are reasonable questions to ask, but challenging questions to answer. UK investment in online healthcare provision is comparable to that from other advanced economies, all of whom have moved to increasing online provision of health services; in 2021 it was estimated that around US$40 billion was invested in digital health globally with around US$5 billion being invested in Europe/Switzerland, and a further US$4 billion being invested in the UK alone. 27 Capital investments within this sector support a variety of facilities and provision. These range from providing core infrastructure through to developing support for accessing services, and the development and delivery of necessary software to support online delivery of care to whole populations, or to those with specific health needs28,29 – such as the development of applications to provide support and care to people living with mental health conditions. 29
At a national level the NHS in England has described a range of sequelae associated with increasing digital health provision – seen as important for the NHS in its ability to achieve strategic health and social care priorities, and with potential benefits for patients and carers, and the wider healthcare system (Box 2). 30 Specifically, the introduction of a major NHS-funded programme aimed at widening digital healthcare participation amongst individuals with low digital health literacy was associated with substantial increases (59%) in confidence regarding use of online health information, substantial reductions (52%) in a sense of loneliness or isolation, a 21% reduction in visits to the GP for minor ailments, increased use (by around 20%) in booking GP appointments online and in ordering prescriptions online, and an apparent substantial saving in time through carrying out health transactions online. 31 A recent evaluation of that programme estimated a return on investment of £6.40 for every £1.00 spent by the NHS on digital inclusion support. 30 Earlier research32 calculated the social return on investment of digital inclusion for individuals and for workers. For individuals, getting online for general purposes was estimated to be worth £1064 a year due to increased confidence, less social isolation, financial savings and opportunities in employment and leisure. For workers, getting online was estimated to be worth £3568 a year due to opportunities for remote working and increased earnings opportunities. In England, digital transformation of health and social care services is seen as a top priority for the Department of Health and Social Care and National Health Service England (NHSE) with estimates of many billion GBP investment – for example, the anticipation of £2 billion of funding (against a commissioning budget of £153 billion)33 to support electronic patient records to be in all NHS trusts, and additional help for over 500,000 people to use digital tools to manage their long-term health conditions in their own homes. 2 A fully integrated, digitally based health and social care system covering primary and secondary care sectors is seen as the goal to be achieved. The stakes are high to ensure implementation of a nationally co-ordinated plan ensuring that all individuals, including those most vulnerable in society, are given opportunity to benefit from these dramatic and costly changes.
Proposed benefits to patients and carers:
-
improved self-care for minor ailments
-
improved self-management of long-term conditions
-
improved take-up of digital health tools and services
-
time saved through accessing services digitally
-
cost saved through accessing services digitally
-
reduced loneliness and isolation.
Proposed benefits for the health and care system:
-
lower cost of delivering services digitally
-
more appropriate use of services, including primary care and urgent care
-
better patient adherence to medicines and treatments.
a Reused in line with the Open Government Licence for public sector information. 34
Patients: inequality
Although there is a clear drive towards the development, promotion and use of online GP services, the impact for patients and for GP practices remains unclear. There is potential for NHS patients and primary care staff to benefit through reduced administrative burden for staff, better communication between patients and practices, expanded health knowledge for patients and improved access to care services. 35 But there is also the danger that such initiatives create or exacerbate inequalities in access to healthcare information and services. 36
Medically underserved and vulnerable populations are less likely, than other patient groups, to engage with online services. 37 For example, indices of deprivation were one of the strongest determinants of non-use of patient portals among patients with chronic kidney disease attending renal clinics in the UK, with patients from postcode areas with the lowest levels of deprivation being 2.4 times more likely to register for portals than patients from postcodes with the highest level of deprivation in England and Wales, and 3.2 times more likely in Scotland. 38 Underserved and vulnerable population groups span those captured by the PROGRESS Plus39 and NHSE40 criteria and include groups classified as vulnerable due to issues of race, ethnicity, culture or language; occupation; gender/sex; religion; education; socioeconomic status; social capital; age; disability; homelessness or migration status.
Engaging ‘harder to reach’ patients and reluctant users of online services may offer potential to reduce inequality of access, but also to improve patient health and potentially reduce GP and/or other NHS costs. Other sectors of health, commerce and business have developed initiatives to support clients in using online services, for example, Barclays ‘Digital Eagles’, where selected individuals acted as champions to encourage confidence and improve skills in use of digital services. 41
Patients: digital literacy
The concept of digital literacy, first proposed in 1997,42 is highly relevant where the health of individuals and populations and the uptake of online health services are at stake. Rowlands has proposed a definition of digital health literacy as ‘the ability to seek, and understand, and appraise health information from electronic sources and apply the knowledge gained to preventing, addressing or solving a health problem’. 43 Encompassing both technical skills and sociocultural domains, digital health literacy is recognised to vary widely across the population, to be measurable using standard instruments,44 and to be a key driver of the digital divide – the health inequality experienced by ‘populations able to benefit from access to and use of health information and services online and populations unable to take up such opportunities’. 45 Low digital health literacy is associated with low health literacy, and with poorer health outcomes, an effect seen, especially amongst poorer, more vulnerable sections of the population. 44 In planning their scoping review of digital health focused interventions, Hamilton and colleagues helpfully identify the need to address the digital health divide by targeting both the acquisition of necessary skills, especially in vulnerable individuals, and also to target health systems and healthcare practitioners and their need to be responsive to the digital health needs of the individuals and populations they serve. 45 Finally, Kim and Xie44 note that interventions aimed at addressing poor health literacy should not just offer online health services tailored to individual’s health literacy levels, but ‘should include education about how to access online resources for health information and disease management, how to search for information effectively, and how to evaluate the quality of online health information’.
Challenges to staff engagement with online services
The digital competence of healthcare professionals and their acceptance of online service provision are also important for successful implementation of online patient services. Konttila et al. 46 argue that healthcare professionals are more accepting of digital technologies when they perceive the technology as helpful for patients and supportive of the practice’s workflow, but that factors such as a lack of comfort or perceived issues of competence with using the technology can decrease acceptance and uptake. Healthcare professionals were found to be less accepting of digital technologies when they misunderstood the purpose of the technology, or found it difficult or uncomfortable to use, or when it was not seen as part of their principal work. Others47 have identified the potential loss of ‘valuable non-verbal communication’ in remote consultations as a specific concern. Israeli qualitative research48 identified the potential for better quality care resulting from integration of medical expertise – recognising the phenomenon of the patient, empowered with e-knowledge and challenging traditional boundaries of medical care. Konttila and colleagues’46 systematic review also found that healthcare professionals often experienced IT education for themselves as pointless, under-resourced, time-consuming and with poorly understood benefits. However, supportive organisations and managers were found to facilitate support for staff education and acceptance of digital technologies. It thus appears that support for practice staff in using and supporting patients in using digital health technologies is crucial, and must be carried out in a sensitive and constructive manner.
System: inverted investment
Concern has been expressed at the limited investment by healthcare planners and governments in addressing gaps identified around the uptake and use of services and innovations underpinning effective medical care. In system terms, NHS online services may be judged as potentially ‘effective’ and therefore potentially subject to implementation delays and delays in uptake. 49 In addition, the decision to introduce digital care on a widespread scale came before consideration of how that rollout might be achieved. This inverted approach to supporting implementation is exemplified by the introduction of toolkits to support practices delivering online consultations sometime after, and not alongside or before, the relevant policy and funding statements. 50
Challenges to patient engagement with online services
The reasons for the lower engagement of some sections of the population with digital and online health services are complex and include factors that limit access to technologies as well as factors affecting motivations to use the technologies. Specific barriers to engagement with online services for these groups include a lack of experience with using the internet,37,51 lower health literacy37,52 and a lack of trust towards the information being provided through online interfaces. 37,53 Issues relating to ‘usability’ can also impede older users from accessing information through patient portals. For example, when older users lost required access codes after registering on patient portals, they became discouraged in their use of the service. 37 Research in Scotland has identified technical and practical considerations (poor connection, ‘frozen’ images, poor sound quality, slow broadband) in adopting IT innovations,54,55 including amongst rural populations, who may have limited access to good quality broadband services. In research undertaken in homeless populations,56 qualitative research findings have highlighted the importance of addressing practical and technological barriers as well as supporting communication and choice for mode of consultation. In their reviews of the literature, Irizarry et al. 52 and others23 have concluded that the ability of patients to access online health services is strongly influenced by combinations of personal factors such as health literacy, health status, age, ethnicity, education level and whether individuals have caring responsibilities. 57 Likewise, in a systematic review of qualitative studies examining the factors affecting patient recruitment to digital health interventions, O’Connor et al. 58 concluded that greater investment is required to improve computer literacy to ensure that technologies are accessible and affordable. Cognisant of these issues, we have been involved in research examining the unintended consequences of providing some online services in primary care,59,60 and investigating patient use and experience of online booking in general practice.
Supporting the move to online services
For the purposes of this research, our focus is on services accessed via a primary care practice website (e.g. booking appointments, access to records) and via online platforms provided by general practices. From 1 November 2022, patients were due to have online access to new entries in their personal medical records,61 although this initiative has been delayed in implementation at the time of writing.
Digital facilitation
In this research, we address ‘digital facilitation’, a unique term defined as ‘that range of processes, procedures and personnel which seeks to support NHS patients in their uptake and use of online services’. The specific focus of this study relates to those processes, procedures and personnel provided by or on behalf of GP practices to support access by their registered patients, and carers of those patients, to NHS online primary care services. Support in accessing and using services is required at all stages, from supporting registration with practices, downloading and using the NHS app, and supporting patients in navigating NHS online provision and accessing the wide range of health resources and information of relevance to NHS patients.
At the inception of this project we were connected to Lea Valley Health Federation (9 GP practices, 86,000 patients), who took early steps to support patients to use digital services by employing a local digital facilitator officer to support patients’ and staff engagement with their online services. 62 In Lea Valley, implementation was driven by a ‘Primary Care Demand and Capacity Audit’. 63 The appointment of a digital facilitator was undertaken with the ambition of engaging patients and staff who might otherwise not engage, for personal or economic reasons or because they might lack the digital skills, with online GP services. Appointment of such an individual represents one approach to supporting and facilitating patient and user access. There is, however, no existing evidence as to the nature and scope, effectiveness, or cost impact of appointing such an individual. Other routes to achieve those aims, such as using volunteers to provide support or referring patients to community programme, may be of potential value, but the nature and extent of innovative approaches offered by practices are currently unknown.
Although research on the use of DF is relatively limited to date, there is evidence to support its use and its ability to reduce inequalities in access to digital resources amongst ‘harder to reach’ and vulnerable groups. One approach to facilitation identified by O’Connor et al. involved the use of ‘direct engagement’, including ‘consultations with health professionals, employers, personal recommendations from family or friends or being spoken to by research or management staff’. 58 Personal recommendations from family or peers, or the endorsement of digital resources by practice staff were found to increase enrolment in digital health technologies. This is further supported by evidence from systematic reviews which find that patients more generally, including comparatively less well-served populations, are more likely to engage with digital health resources when they have the encouragement of friends or family members. 51,64,65 Evidence also suggests that people with lower education levels and older people require more support than other patient groups in order to use digital health applications. We have not identified any evaluations of such engagement approaches in practice, although we have identified that poor understanding of service provision may be a barrier to service uptake,66 and that staff have expressed concerns regarding adverse workload implications which might ensue. There is also evidence showing that introducing the NHS App was associated with improved digital access during its pilot testing phase with 64% (out of 3192) of users of the App reporting that they had previously not used online services to access GP services. 67 Feedback from practice staff during the pilot testing of the NHS App identified that some practice staff wanted additional training and support in order to effectively communicate with patients about the app.
Other interventions designed to target direct engagement with digital technologies have been identified, for example, the use of staff ‘champions’ for GP online services,68 as well as specific interventions to improve people’s online health literacy. 69 Cowie et al. evaluated the implementation of an online tool providing advice to support self-management and the opportunity to digitally consult with a GP, concluding that the presence of a champion within the practice was a significant factor in ensuring successful integration of the tool. 68 Amongst some patients, who had no previous computer experience, training on computer and internet use, development of effective search skills and interpretation of online information was associated with greater health information seeking and interpretation skills, and with increased self-management.
It is thus important to understand the extent to which digital facilitators or other approaches to DF are being used, how they are being used, what impact they are having on uptake of online services, and how such uptake may be impacting patient health and access to healthcare information and services, GP practices and the wider NHS.
Aims, objectives and study structure
The overarching aims for the research study were to:
-
Identify, characterise and explore the potential benefits and challenges associated with different models of DF currently in use in general practice which are aimed at improving patient access to online services in general practice in England.
-
Use the resulting intelligence to design a framework for future evaluations of the effectiveness and cost effectiveness of such interventions.
-
Explore how patients with mental health conditions experience DF and to gauge their need for this support.
To address these aims, we have conducted a series of interlinked research work packages (WPs) (Figure 1). The objectives of the WPs were to:
FIGURE 1.
Flow diagram of study showing work stage flow.
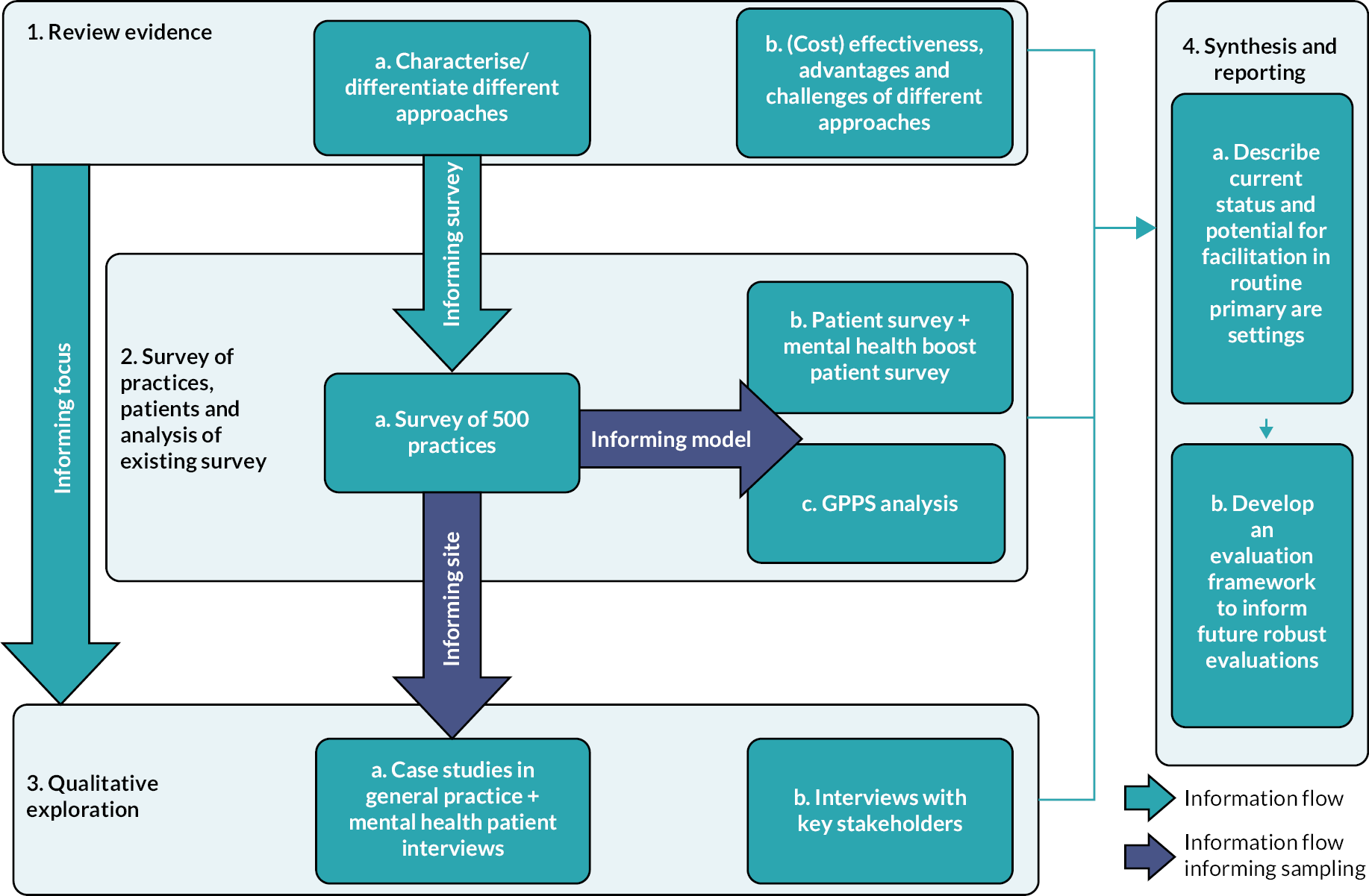
-
review published literature to understand and characterise the range, effectiveness and cost effectiveness of models of DF for improving access to online services within health and other sectors, and to develop a typology of DF (WP1)
-
undertake a practice staff survey to investigate the range of DF services currently offered in a sample of English primary care practices and relating this to patient experience of care in those practices as measured by the national General Practice Patient Survey (GPPS) (WP2A)
-
undertake a patient survey to investigate patient views of DF in a sample of English primary care practices and relating this to different modes of DF identified in the practice survey and to explore how patient factors predict awareness and uptake of DF (WP2B)
-
conduct a qualitative exploration seeking to understand in-depth and from the perspective of practice staff, patients and other stakeholders the potential benefits and challenges associated with different models of DF (WP3).
Synthesise learning from these elements and develop a framework for future evaluations of effectiveness and cost effectiveness of models of DF (WP4).
During the course of the project, we successfully responded to a NIHR commissioning brief to apply for further project funding to extend the scope of the project to perform additional work focusing on patients living with mental health conditions. In doing so, a further objective was added to the project:
-
Explore the experiences of patients living with mental health conditions by (1) augmenting our existing patient survey with a boost sample of patients with mental health conditions (added to WP2B) and (2) conducting additional qualitative interviews with patients with mental health conditions (added to WP3). In both cases, findings will be integrated with those from the original patient survey and patient interviews.
Outcome
The ultimate outcome of the project is a summary of the current status of DF as presently implemented within primary care. This includes what is known about the likely effectiveness, cost and equity of access implications of the approaches identified, and an indication of the prevalence of various approaches in four regions of England (East of England and North London; South-West; West Midlands;). We have provided recommendations for future development and implementation of promising approaches to DF, and a framework for future evaluations to assess the effectiveness, cost effectiveness and impact on inequalities of access to the online services, of relevant facilitation approaches within primary care settings.
Theoretical framework
We have used Weiss’s theory-based evaluation as our theoretical framework to understand how, and in what ways, different models of DF bring benefits and challenges to general practice. 70 Weiss distinguishes between ‘programme theory’, which specifies the mechanism of change, and ‘implementation theory’, which describes how the intervention is carried out.
We have done this by drawing on the findings of the evidence synthesis, surveys and case studies to develop the ‘programme theory’ and ‘the implementation theory’.
To develop the ‘programme theory’ we used a realist approach to describe provision of DF. A realist approach asks ‘What works for whom, in what circumstances, in what respects, and how?’71
We explored this in terms of:
-
context (e.g. characteristics of the general practice, the target patient population, the policy framework, and the IT infrastructure)
-
the theory and assumptions underlying the intervention (how and why DF might lead to benefits)
-
the flow of activities that comprise the intervention (the key processes that occur when patients make use of DF)
-
intended benefits/outcomes (those deemed important to patients and practitioners).
The ‘implementation theory’ explored moderating factors which influence the extent to which the process and outcomes were achieved, such as factors acting as barriers and facilitators to practices offering DF or to different groups of patients using them.
Patient and public involvement and engagement
This research is underpinned by recognition that patient and public involvement and engagement (PPIE) is an integral part of research practice. Patients’ voices should be reflected and addressed in the design and delivery of health research in order to ensure that research outputs are meaningful and relevant to them. As a research team we have followed the UK standards framework for public involvement in research including: inclusive opportunities, working together, support and learning, governance, communications and impact. 72
From the outset we have worked with patients to shape the scope and objectives of this research and continued to work collaboratively with patients throughout the research. Patients and carers have been active partners and included at all stages of the research process, including in setting the research agenda and analysing data. 73 The approach to involvement, the impact on the research and reflections on how it worked are included throughout the report.
Chapter 2 Literature review (work package 1)
Sections of this chapter have been reproduced from Leach et al. 74 under licence CC-BY-4.0. 75
Aims of literature review
The aims of this scoping review, conducted in autumn 2020, were to: identify, characterise and differentiate between different approaches to DF in primary care; and establish what is known about their effectiveness and cost effectiveness, perceived advantages and challenges, and how they affect inequalities of access to online services. We also sought early indications of the extent to which the COVID pandemic may be associated with changing approaches to DF. Our particular focus is on DF within general practice in England, but we also consider DF in other geographical areas and sectors where there is clear relevance to primary care.
In the following sections, we describe our review methods and document and discuss our results, including outlining a typology of DF, providing evidence on the efficacy of DF and reporting factors that enable successful DF. We highlight implications of our findings for medically underserved and vulnerable populations, and the potential role of DF in reducing inequalities in access to and use of online services for health purposes.
Methods
We conducted a systematic scoping review of the literature, as the basis for the remainder of the research. We sought to understand the current landscape of DF in primary care. Scoping reviews are appropriate for clarifying conceptual boundaries on topics, such as DF, where a concept is new and poorly defined. 76 By including multiple searches, the scoping review method allows the search strategy to evolve as conceptual boundaries are clarified through screening activities. Our protocol was based on guidelines from the PROSPERO international register of systematic reviews77 and was prospectively registered with that website. 78
The scoping review was conducted in stages as shown in Figure 2 to allow learning from earlier stages to feed into later stages. 78 All searches were restricted to English-language publications. Details of all stages’ search strings and numbers of results by database are available in Appendix 1, Tables 20–27.
FIGURE 2.
Overview of literature review process. This figure74 was originally published in the Journal of Medical Internet Research (www.jmir.org), 14 July 2022 and licensed under CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/). For further details, see Publications.
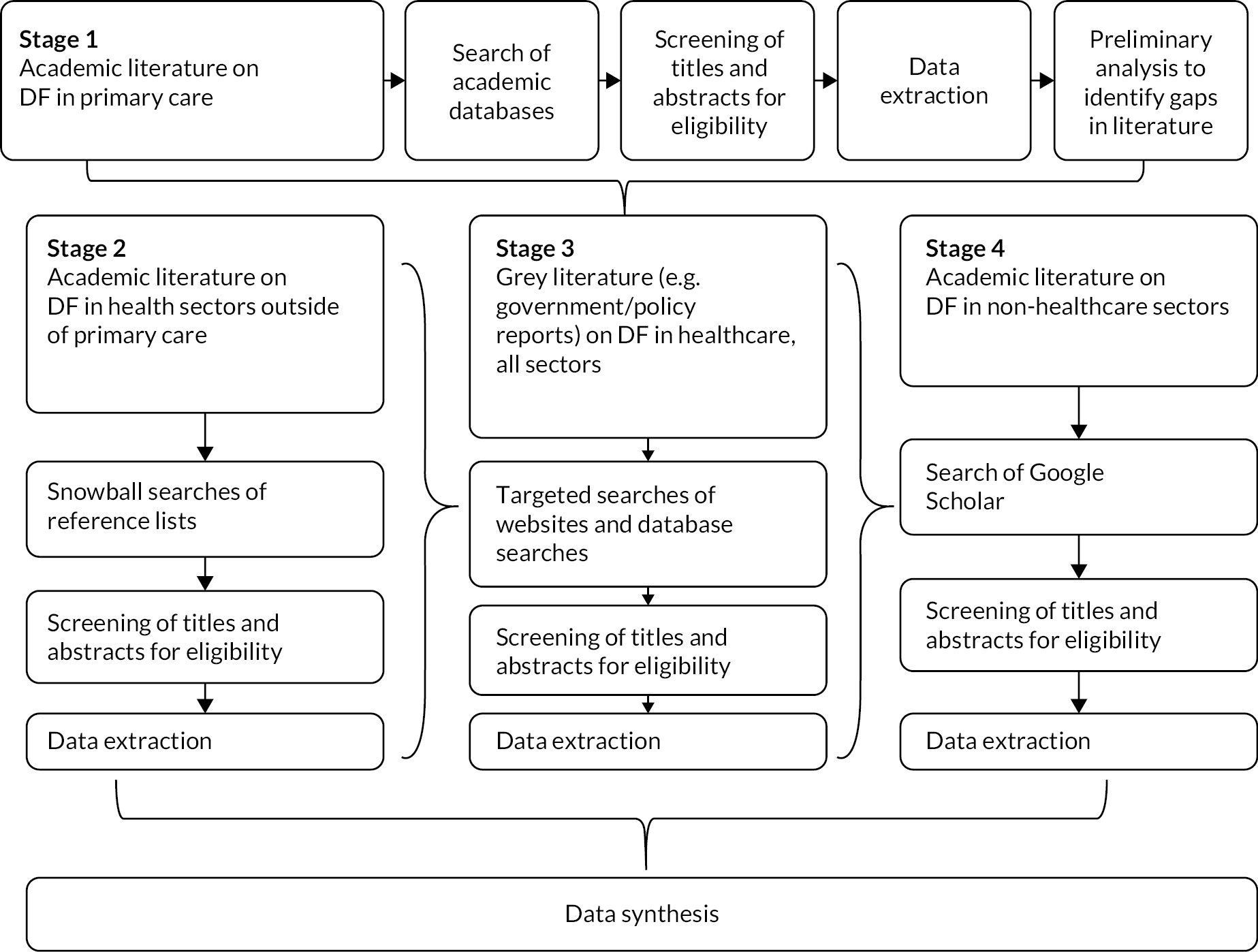
Searches
Stage 1: academic literature on digital facilitation in primary care
We searched the databases: PubMed, EMBASE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Web of Science and the Cochrane Library (we did not search the Global Health database as specified in our PROSPERO protocol78 because we did not have access to the database except at additional cost). The search strategy focused on three concepts: (1) online services; (2) DF and (3) primary care settings. Members of the Patient Advisory Group (PAG) contributed to the development of the search strategy and operationalisation of key terms, including ‘digital facilitation’. We restricted the searches to European economic area (EEA) and Organisation for Economic Cooperation and Development (OECD) countries as likely to be most relevant to primary care practice in England. We restricted the time period for the Stage 1 search to literature published in 2015 or later (up to June 2020, when the Stage 1 searches were conducted).
Stage 2: snowball searches to identify literature on digital facilitation in health sectors outside of primary care but relevant to primary care
Stage 2 consisted of snowball-type searches whereby we screened the reference lists of articles identified during Stage 1 for non-primary care health sector studies on DF that might nevertheless have relevance for DF in primary care (see Table 1 for eligibility criteria). We first screened the reference lists of studies included for full-text extraction from Stage 1. Next, we screened the reference lists of articles that we identified during Stage 1 as not fitting the inclusion criteria due to article type restrictions (e.g. protocols or editorials) but which were otherwise relevant. We searched for snowballed literature from 2010 onwards, on the grounds that although predating 2015 it was still evidently considered of some significance in 2015 or later. We did not search for snowballed literature earlier than 2010 due to the rapid change in the extent of online services since then.
| Stage of process | Criteria | Include | Exclude |
|---|---|---|---|
| All stages | Scale and spread of intervention | All scales and geographic levels from individual site to national coverage | None |
| Country | EEA or OECD countries | Countries not in the EEA or OECD | |
| Language | English | Languages other than English | |
| Availability | Full-text availability | Title and/or abstract only Conference proceedings with no full text article |
|
| Stages 1, 3 and 4 | Year of publication | 2015–January 2020 | 2014 or earlier |
| Stage 2 | Year of publication | 2010–January 2020 | 2009 or earlier |
| Stage 1 only Screening of academic literature on DF in primary care |
Topic relevance | Digital facilitation of online services in primary health care settings where DF was implemented in some form:
|
Where there is no reference to facilitation being implemented by or on behalf of primary care practices. Thus, solely theoretical papers are excluded |
| Article type | Original research |
|
|
| Stage 2 only Screening of literature on DF in health sectors outside of primary care |
Topic relevance | Digital facilitation of online services in non-primary care health sectors where DF was implemented in some form:
|
Where no reference to facilitation being implemented by or on behalf of healthcare providers. Thus, solely theoretical papers are excluded Articles that address aspects of DF already covered included articles identified in Stage 1 |
Articles that address aspects of DF found not to be covered by articles identified in Stage 1. Key gaps include:
|
|||
| Article type | Original research |
|
|
| Stage 3 only Screening of grey literature on DF in health care, all sectors |
Topic relevance | Digital facilitation of online services in health care, all sectors | Where there is no reference to facilitation being implemented by or on behalf of healthcare providers. Thus, solely theoretical papers are excluded Articles that address aspects of DF already covered by included articles identified in Stage 1 |
Articles that address aspects of DF found not to be covered by articles identified in Stage 1. Key gaps include:
|
|||
| Article type | Grey literature (i.e. literature produced in electronic and print formats outside of commercial publishing). To include, but not limited to:
|
Trial registrations (i.e. articles registered on ClinicalTrials.gov or the WHO ICTRP registry) | |
| Article type | Original research |
|
Stage 3: grey literature on digital facilitation in health care
In Stage 3 we searched grey literature from January 2015 to June 2020 to identify policy reports on DF in health care. The search had two main components: targeted searches of four health policy and professional association websites [The Health Foundation, The King’s Fund, The Nuffield Trust and The Royal College of General Practitioners (RCGP)}; and a general search of the Health Management Information Consortium (HMIC) database. The targeted searches of websites used combinations of terms such as ‘online services’, ‘digital’, ‘access’ and ‘patients’, using Boolean operators where website search functions allowed. The HMIC database allowed more complex searches, so we adopted a search strategy capturing concepts related to online (e.g. online, digital, virtual, technology) and facilitation (e.g. uptake, encourage, increased use). Full details of the grey literature search strategy are given in Appendix 1 (see Table 25).
Stage 4: academic literature on digital facilitation in non-healthcare sectors
We also looked, in Stage 4, for relevant academic literature from January 2015 to June 2020 on DF in non-healthcare sectors on Google Scholar. The searches were aimed at two sectors that the study team identified as potentially relevant based on their business models, which incorporate both online and offline customer services, namely: the tourism and travel sector, and the retail banking sector. Full details of the search strategy for these non-healthcare sectors are in Appendix 1 (see Table 27).
Screening
Publications for Stages 1, 3 and 4 were restricted to English-language articles published since 2015. We initially included articles from 2010 to January 2020; however, the resulting number of included publications from Stage 1 (n = 154) exceeded the scope of the project. We therefore then restricted to publications published since 2015, with the understanding that DF and widespread use of online services in primary care are relatively recent phenomena and therefore the most relevant literature was still likely to be captured by our revised inclusion criteria. For Stage 2, where publications were identified through snowball-type searches of reference lists, we expanded the eligibility to 2010–20 so as not to omit references still evidently deemed important post 2015.
A key inclusion criterion for all publications was that they addressed facilitation of online services. We operationalised this criterion as detailed in Table 2. Further eligibility criteria were tailored to the stage of the screening process (e.g. primary care literature, non-healthcare sector literature). The detailed inclusion and exclusion criteria for each stage of the screening process are presented in Table 1.
| Concept | Inclusion | Exclusion |
|---|---|---|
| Digital facilitation | Papers including reference to what is done to help patients to access and use online services, including (but not limited to):
|
Papers without information on what was done to help patients to access and use online services |
| Online services | Online services accessed through a website or app, such as
|
|
Prior to full screening, we undertook a pilot exercise examining 2% of the 11,853 publications from Stage 1 (n = 237), during which publications were jointly screened by two reviewers (EG and SP). The reviewers compared and discussed their results, and amended the inclusion and exclusion criteria, raising any points of concern with the members of an internal advisory group convened to advise on the scoping review. This group comprised members of the research team who were not directly involved in the literature search and screening process, but who have expertise in literature reviews (see Acknowledgements).
Data extraction and preliminary analysis
Data from eligible studies were extracted independently by two reviewers (EG and SP) using a data-charting form developed for this study. The form was piloted to ensure data extraction was consistent across reviewers. We extracted data relevant to DF (digital technology type, facilitation purpose, method, mode of delivery, target population, setting) and study details (study type, outcomes, size, setting), aiming to capture health outcomes; staff and patient/carer experience; impact on service use, cost and equity of access to healthcare services and information; and the nature and extent of other reported outcomes. Studies were not formally assessed for quality as this was a scoping review and furthermore, the breadth of study and article types included makes the use of formal quality tools impractical. However, reviewers noted the quality of the evidence source, clarity of aims, quality and comprehensiveness of the work, and any conflicts of interest from the authors (see Appendix 1, Table 28 for details) to assist with judging the quality of the overall evidence base for DF. A list of all data fields captured in the form is available in Appendix 1 (see Table 28).
During data extraction the team met frequently to discuss emerging findings, resolve uncertainties regarding the boundaries of DF activities and clarify eligibility criteria.
Before conducting further searches (see Figure 2), we undertook preliminary analysis of the extracted Stage 1 data, including in a study team workshop (attended by EG, BL, SP and JS) to identify themes emerging and gaps in the literature that might indicate a need to expand or alter the scope of our search during later stages.
We then discussed the identified themes and gaps at a second workshop with seven members of the PAG. The PAG members suggested that a barrier to DF could be the use of locums. This was an important gap in our preliminary analysis and one that was under-represented in the Stage 1 literature. The use of locums, and high staff turnover more generally, is an important potential barrier to DF because these staff might not have the proper training or buy-in for DF programmes. The PAG members at the workshop also confirmed the legitimacy of some themes we identified in the literature, including that awareness of online services by GP practices and training for staff members may be important enablers of DF, and that data privacy or security concerns by GPs or patients might hamper DF efforts. The PAG participants highlighted that although it can be challenging for members of some vulnerable patient groups to access or use online services, for others, such as those with limited mobility, online services might improve access to health care. These discussions aided in the identification of themes in the literature and later data synthesis.
Data synthesis
Data analysis followed the principles of narrative descriptive synthesis. 79 We began by identifying key themes captured during charting, which were then refined and expanded upon during preliminary synthesis. We did this through a process of study team discussions, analysis and writing. Preliminary synthesis was followed by further refinement of themes through a workshop including members of the wider study team, including a PPIE representative. The narrative synthesis further aimed to characterise and differentiate between different types of facilitation and to synthesise evidence relating to effectiveness or cost effectiveness, inequalities of access to online services, or potential advantages and challenges of different approaches.
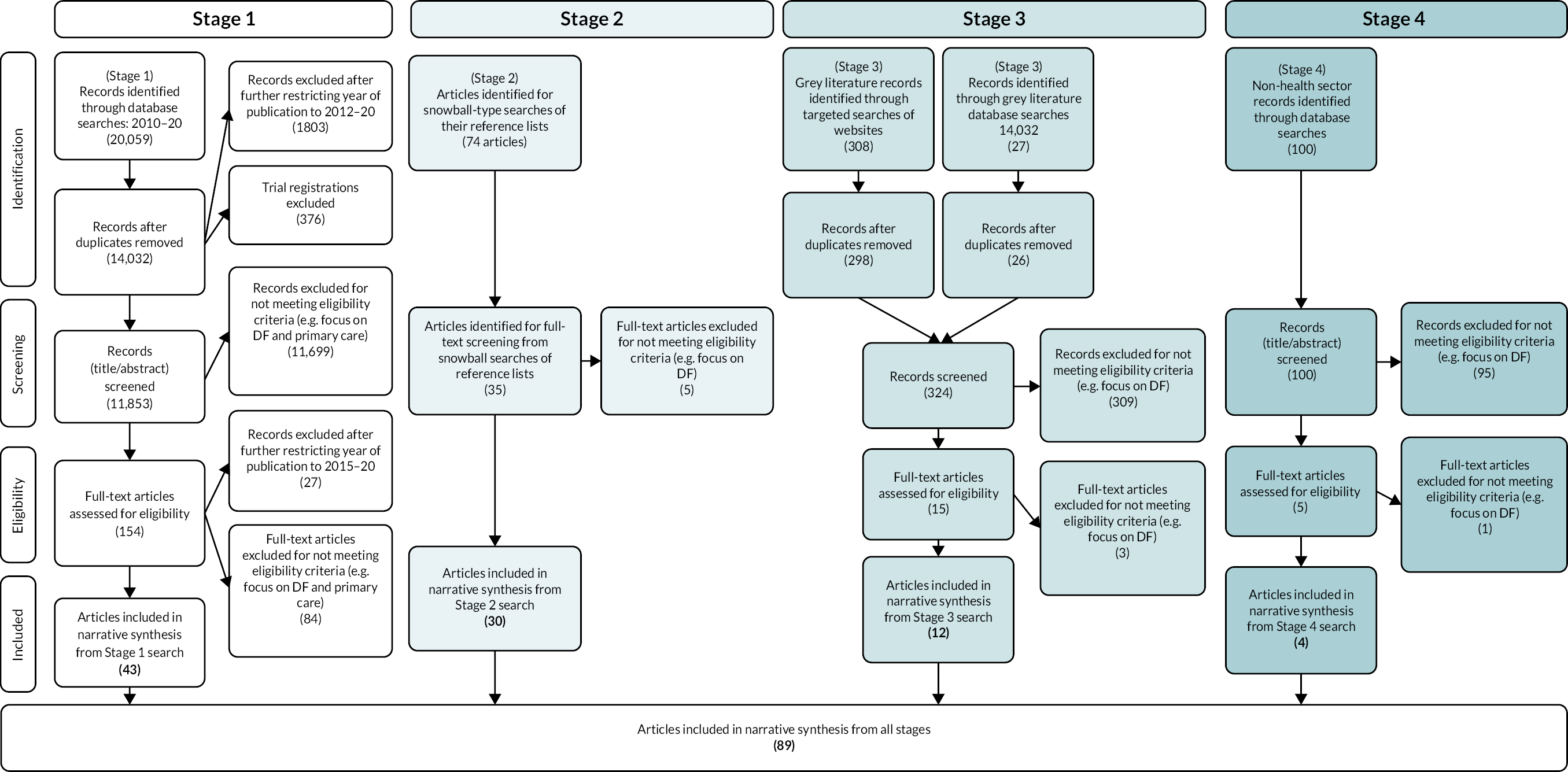
Results
Figure 3 shows the process of the literature search through a Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram. In Stage 1, we screened 11,853 records of which 43 met the criteria for inclusion. Later stages identified an additional 46 publications eligible for inclusion, for a total of 89 full-text publications included in the review. These are listed in Appendix 1 (see Table 29), along with information about the types of interventions and study designs.
FIGURE 3.
PRISMA flow diagram of search and screening process for scoping review, by stages. This figure74,78 was originally published in the Journal of Medical Internet Research (www.jmir.org), 14 July 2022 and licensed under CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/). For further details, see Publications.
Typology of digital facilitation
There are a wide variety of DF efforts discussed in the literature. Table 3 illustrates the typology we developed based on our findings. Although DF efforts are usually directed at patients, some are aimed at primary care staff to enable them to better support patients in using digital services. The DF efforts discussed in the literature review include those that are part of routine service delivery, and those that were introduced as part of an experimental study where facilitation was implemented for research purposes.
| Typology of DF | Definition | Examples of facilitation approaches | |
|---|---|---|---|
| Digital facilitation aimed at patients | Promotion | Broad category that captures ways of raising awareness of and knowledge about digital services, endorsements of specific digital services to patients, and methods of encouraging patients to use them. | Recommendation and prescription of digital services and other communication-centred interventions; e-mails and written reminders; video introductions to digital services. |
| Training and education | Education or training to help patients acquire technical skills to use digital services or to help patients understand what features of a digital service can be helpful to them. | Initial assistance with use of digital services. | |
| Guidance and support | Ongoing help provided by clinicians or other primary care staff to patients to use digital services. | Coaching and ongoing guidance from clinicians and other staff. | |
| Digital facilitation aimed at primary care staff | Interventions to increase staff’s knowledge of digital services so that they can better support patients in their use of the services, or to increase their trust in services. | Certified list of apps and websites (for staff to recommend to patients); practice champions (to increase buy-in); training to generate awareness of online services and how to use them. | |
Digital facilitation aimed at patients
Most efforts to facilitate uptake and continued use of online services are aimed directly at patients. Within the literature we reviewed, DF was usually delivered by primary care staff such as GPs and nurses, although other staff such as receptionists were also sometimes involved. It is important to note that the literature likely under-represents unplanned or ad hoc DF activities such as promotion of online services by receptionists. The types of facilitation aimed at patients that we identified can be grouped into three categories: (1) promotion, (2) training and (3) guidance and support.
Promotion
Promotion refers to ways of raising awareness of, and knowledge about, digital services; staff endorsing specific digital services to patients; and encouraging patients to use them. A lack of knowledge by patients of available online services is a barrier that primary care staff can help overcome. 80 Promotion can be via a range of media, including online, in-person during appointments, and in less personalised forms such as placing posters or promotional material in waiting rooms. Promotion efforts for digital services also vary in terms of how active providers and other primary care staff need to be. Some DF efforts require that providers actively raise the topic of digital services during consultations or that receptionists send e-mails to patients,81 while others do not require much action by staff, for example, posters or brochures in waiting rooms. 82
Examples of online promotion include practices: featuring links on their website to promote an e-consultation and self-help web service,83 sending reminders or links to online services via e-mail or SMS and using online promotional videos. Engaging patients by providing a tablet for use in the practice waiting room, rather than simply relying on verbal recommendations, has also been explored in a feasibility study as a way of motivating patients to keep using an online self-regulation programme once they return home. 84
There have been various types of offline promotion within UK primary care practices, such as leaflets, posters and television screens with information about online services. 83 Verbal recommendation by staff is one of the most widespread routinely used methods of DF. General practitioners were willing to recommend online services if they knew they could trust the service, or if they had been involved in its design.
Training and education
Training and education may also promote uptake and use of digital services, both by helping patients to acquire technical skills to use online services and by helping patients to understand what features of an online service can be most helpful. 85 In the literature we reviewed, training was delivered online through videos,86 or offline through presentations or seminars,87 and was delivered either in one session86 or over several. 87
Guidance and support
Guidance and support refers to ongoing help provided by clinicians or other primary care staff, through in-person meetings or phone calls. It can be focused on technical aspects of using digital services, similar to training, but appears to most often focus on interventions that help patients set goals, keep track of progress, improve adherence and other less technical aspects of digital services.
Practice champions88 have been used in primary care to increase the use of online services. As experts in a particular online service, they provide assistance and ongoing support to patients, with the potential to increase both initial uptake and continued use thereafter. An evaluation of 11 primary care practices in the UK concluded that practice champions could promote appropriate use by patients of a web-based consultation system, as well as encourage engagement of staff. 68
Clinician support was discussed in the literature as a way to provide ongoing guidance and support to patients, for example, a US study of an app to help military veterans manage symptoms of post-traumatic stress disorder (PTSD) concluded that adding clinician support improved access and utilisation of the app. 89 A study of an internet platform for cardiovascular self-management in the Netherlands, where patients had the option of contacting health coaches (e.g. practice nurses), concluded that human support was crucial to initial and sustained engagement with the platform. 90 Another evaluation found that patients overwhelmingly wanted online or face-to-face technical support, such as a helpdesk. 91
Digital facilitation aimed at primary care staff
For primary care staff to be able to help patients use online services, they must first be aware of what services are available, how they work, why they are useful and trustworthy, and how they can benefit specific patient groups. 68 Healthcare professionals also need to be clear about their role in endorsing and facilitating online services. 92 There is evidence of some GPs being opposed to the use of online services by patients. 93 Efforts have been made to train primary care staff and increase their knowledge, understanding and confidence in online services.
In the UK, researchers held practice-level discussions with GPs with the aim of tackling the strong views held by some GPs against prescribing online information, albeit with limited effect. 93 In Spain, an experimental study examined the effects of doctors prescribing apps that had been certified by public health authorities, on patient uptake and use of digital services. Since staff buy-in is an important enabler to DF, having a list of trusted apps can be valuable. 94
Other studies show that healthcare practitioners may benefit from training to acquire the technical skills to use online services;95 or to improve their communication strategy and relationship building skills, so that patients or their families are more likely to follow advice to use digital services. 96,97 Such training may be delivered through online meetings, face-to-face sessions, presentations or by sending explanatory videos to staff. 98
Is digital facilitation associated with increased uptake and use of digital services?
The evidence relating to whether different DF approaches increase uptake and use of digital services is summarised in Table 4 and described below.
| Typology | Digital facilitation effort | Evidence on increasing uptake and use |
|---|---|---|
| Promotion | Recommendation or prescription of digital service to patient | Staff recommendation/endorsement of a digital service was shown to be one of the most effective ways to increase patient uptake and use in two literature reviews on the topic.52,99 Qualitative evidence from primary studies also supports staff recommendation/endorsement as an effective way to boost use of digital services.100–102 |
| Strong evidence from RCTs that prescription and referral pads for digital services are effective in increasing patient uptake,98,103 along with evidence from a review on the topic.104 | ||
| Some evidence that a list of certified apps and websites (approved by a regulating body) may help providers to prescribe apps and websites to patients.94 But a study in the UK NHS found a similar approach ineffective in encouraging the use of high-quality online services.105 | ||
| Multiple mixed-methods studies suggest that recommendation/endorsement may be more effective when staff focus on specific aspects of a digital service that will be useful to particular patients, and gradually introduce patients to digital services based on their individual needs at that time.105–109 | ||
| Communication-centred interventions | Qualitative evidence and a RCT suggest that recommendation/endorsement of digital services may be more effective when staff are trained in how to best engage patients using specific communication strategies and shared messaging around the service.83,90,96,97,107,110 | |
| Strong evidence from three RCTs that interventions that help patients form specific ‘if–then’ plans are effective in increasing continued use of digital services.111 | ||
| E-mail and written reminders | Several mixed-methods and qualitative studies have shown that written materials such as brochures, leaflets and advertisements may increase patient use of digital services, and they require little effort from providers.83,106,112 | |
| Reminders (e.g. SMS messages and push notifications) have been implemented in some areas,110,113 and feedback from patients and service users suggests they may help to increase uptake and use.90,114 | ||
| Video introductions to digital services | Mixed evidence from RCTs on whether video introductions are effective in increasing uptake of digital services. No evidence that they are effective in increasing sustained use of digital services.86,115–117 | |
| Public information campaigns | In the UK, a public information campaign and personalised invitations to patients to use an electronic health record system were found to be ineffective in encouraging enrolment.82 | |
| Training | Initial assistance with use of digital services | Mixed evidence from RCTs and quantitative studies on whether initial assistance in registering and logging into digital services is effective in increasing uptake and use.38,87,118,119 Qualitative evidence suggests patients and providers feel this type of assistance would be useful,120,121 but the weight of the evidence suggests that it is likely ineffective, and that additional continued support is needed to encourage continued use of digital services. |
| Qualitative evidence suggests that allowing patients to log into and use digital services in primary care practices (e.g. in the waiting room on tablets) may encourage patients to continue using a service outside the practice.84,122 This intervention has been implemented within studies with some success.110 | ||
| Technical training support | There is a body of literature (including strong evidence from a systematic review and a RCT) emphasising the importance of technical support to patients using digital services and wider support around digital literacy and digital health literacy in encouraging patient use of digital services,81,107,114,115,123,124 particularly for older patients, patients from ethnic and racial minority groups and patients in low-income settings. At least one RCT found that simply providing information on using the internet was not effective in increasing use of digital health services.93 | |
| Guidance and support | Coaching and ongoing guidance for patients | Mixed evidence from RCTs and non-randomised trials on whether ongoing coaching and support increases uptake and sustained use of digital services.89,125–128 The weight of evidence suggests that certain forms of ongoing support are likely effective (see below). |
| Strong evidence from three RCTs and qualitative studies suggesting that ongoing guidance focused on adherence, content of digital services and goal setting is likely more effective than ongoing guidance on technical aspects alone in increasing use of digital services.111,120 | ||
| Qualitative evidence suggests that both face-to-face and telephone support are likely important in encouraging patients to continue to use digital services.90,91,94,129,130 |
Promotion
Recommendation and prescription of digital services and other communication-centred interventions
Studies suggest that promotion may increase the initial uptake and subsequent use of digital services. We explore factors that make DF efforts successful in What makes digital facilitation successful?.
A literature review of ways to promote engagement with patient portals suggested that endorsement by healthcare staff is one of the most influential factors for patient uptake and use. 52 Interviews with staff, patients and families indicate that staff recommending digital services to patients may be effective at increasing uptake of those services,100–102 especially when staff focus on specific features of a digital service that will be useful to individual patients,106,107,131 where staff are trained in how to best engage patients97 and where staff have a shared understanding of the messaging around digital services. 83,110
Other promotion-based DF strategies that appear to increase patient uptake of digital services include the use of written prescription or referral pads,98,104 and having a list of certified apps and websites that have been approved by a regulating body and to which practice staff can refer patients or issue prescriptions. 94,103 However, an NHS accreditation scheme in 2009 to certify online information so as to increase use of high-quality sources by patients was not very effective. 105
Certain communication strategies may be particularly effective. In a randomised controlled trial (RCT) examining the use of an online depression prevention programme for adolescents, intervention sites that were assessed as more completely implementing communication and relationship building techniques to help develop and maintain trust, authenticity and sincerity with adolescent patients were more effective in encouraging enrolment. 96 The literature also points to the effectiveness of gradually introducing patients to digital services and to new features rather than explaining all functions at one time. 108,109 Interviewing and conversational techniques such as motivational interviewing,90 and discussing patients’ ideas, concerns and expectations to help address patients’ misconceptions,107 have been shown to increase uptake of digital services. Helping patients form specific plans around the use of digital services was shown to be one of the strongest predictors of adherence in a RCT of an internet-based intervention for depression. 111
E-mails and written reminders
Written material that healthcare staff can give to patients about digital services may also be useful in encouraging uptake, with minimal staff time and effort. 106,112 In a study in the UK where an e-consultation and self-help web service were promoted through posters, leaflets and advertisements on television screens in waiting rooms and on practice websites, 79% of those who used the web service reported that they found out about the service through these promotion efforts. 83 Reminders for participants can also be helpful,90,114 for example, through SMS messages sent by receptionists with links to online tools,110 or sent to patients at key times, such as when healthcare staff upload new notes to patient portals, which in one quasi-experimental study resulted in over 85% of patients viewing at least one note on the patient portal. 113 However, a RCT of an internet-based therapy programme for depressive symptoms among high school students found that neither tailored nor standardised e-mails increased adherence. 132
Training and education
Initial assistance with and education on use of digital services
The evidence is mixed about whether initial assistance with, and education on, the use of digital services are effective in increasing uptake and continued use, and the weight of evidence from quantitative studies suggests that more support to patients is likely to be needed after initial introduction sessions to promote long-term use of digital services.
For example, a quantitative study of uptake and use of patient portals for patients with chronic kidney disease found that patients of renal clinics who were helped with initial login and registration to the portal were 20% more likely to be continued users of the portal after 3 years than in other clinics. 38 But there is contradicting evidence from a study on use of patient portals indicating that initial training/introductory educational sessions have little impact on actual use after initial sign-up. 119
A RCT of an initial 10-minute standardised personal information session on internet-based depression interventions found that these sessions were ineffective in increasing adherence in an inpatient and outpatient rehabilitation setting for diabetes care. 118 Similarly, a RCT from the Netherlands showed that initial group education sessions for patients with type 2 diabetes to help them use online platforms did not increase use of the service. 87
An interview-based study suggests that letting patients use tablet devices or computers in practice waiting rooms may encourage later use at home. 84 Both healthcare staff and patients expressed enthusiasm about the potential to access health information122 and complete digital screening tests110 on tablets while waiting for appointments. Other studies of initial educational sessions for patients where staff help patients sign up, install apps, provide pamphlets and answer questions on how to use online services have found that these may increase uptake and use of patient portals. 38,120,121
Video introductions to digital services
Four RCTs evaluated the effectiveness of video introductions on patient uptake and use of digital services. Two studies found that online video-based trainings increased patient uptake compared with people who received no form of training or introduction,115 although sustained use after 6 months was still very low in one of the studies. 116 The two remaining RCTs found contradictory results. One RCT found that a 3-minute video did not increase uptake or use of an online intervention for chronic pain,117 but another RCT found that a 7-minute video was effective in increasing acceptance of internet-based interventions for depression, although actual use was not measured. 86
Guidance and support
Coaching and ongoing guidance from clinicians and other staff
There is some evidence that ongoing support from clinicians and other staff is effective in increasing the use of digital services. Although some quantitative studies found that these interventions were ineffective, the weight of the evidence suggests that certain forms of ongoing support are effective.
Several RCTs evaluated the effectiveness of having clinicians or other staff guide patients in the use of digital services as compared to self-directed services. One study found that patients using online therapy for chronic pain who were guided by a psychologist completed more modules than unguided groups and had lower attrition rates. 125 But two other RCTs showed either mixed126 or no evidence127 for the effectiveness of guides and coaches to increase patient uptake and use of digital services. A series of RCTs in Germany133 found that both content-focused (personalised written feedback, reminders) and adherence-focused guidance (reminders, and ability to request feedback) were equally effective in increasing adherence as compared to administrative guidance (technical support). 133
Several quantitative studies with non-randomised control groups also tested the effectiveness of coaching sessions to help patients engage with app content. Interventions such as sessions with health coaches,89 hands-on and telephone assistance from nurses, and an intensive course for patients,128 may increase uptake and use of digital services.
Qualitative evidence also suggests that face-to-face support for patients along with ongoing web support may facilitate the uptake and use of digital services. 91,94,129,130 For example, incorporating digital services into regular care and providing patients with a way to message providers for support may encourage sustained engagement. 90 In addition, ongoing training in the use of particular digital services or more generally to increase digital literacy skills may encourage uptake and use. 91,107,114 However, a quasi-randomised control trial in the UK found that providing patients with general information about using the internet for health purposes did not increase patients’ readiness to use electronic health services. 93
Evidence relating to inequality between different population groups
A few studies identified strategies that may be effective at increasing uptake and use of digital services in specific patient populations. A systematic review found that technical training and assistance programmes have the best evidence for increasing portal use for vulnerable populations (elderly people; racial minorities; individuals with low socioeconomic status, low health literacy, chronic illness or disabilities), and that other interventions lack sufficient evidence. 81 A US study found qualitative evidence that ongoing training, both in the use of a particular service and more generally to increase digital and health literacy skills, can help address barriers to receiving care faced by African American and Latino patients134 and patients in low-income areas. 124
Ongoing training and support may also be helpful in encouraging uptake and use of digital services amongst older people. 114 Despite concerns about older groups being less able or willing to use technology,92,101 evidence suggests they are often willing to use tablets,122 patient portals,52 remote video consultations108 and health-related apps. 135 Some studies showed that older patients were more likely to use digital services after facilitation efforts115 or point to the importance for older patients of ongoing human support90 and training on both technical aspects of digital services and on general digital literacy skills. 114 Several studies include subgroup analyses, which revealed that patients with lower health literacy136 or with disabilities are less likely than others to use digital services even after facilitation efforts. 87,99,115
Cost effectiveness
No studies in the literature we found assessed the costs of DF efforts.
Evidence of disadvantages and risks from digital facilitation efforts
The literature identifies some disadvantages and risks associated with DF efforts. For example, communication-based facilitation efforts that require high levels of emotional engagement may contribute to distress and fatigue among staff. 96 Approved app lists may risk being biased in the sample of apps considered when the onus is on app developers to apply to be included on approved lists. 135 Reference is also made to some patients worrying whether the ongoing engagement to get involved with digital services meant they would replace valued in-person contact. 90 E-mail reminders can irritate some patients to the extent that they avoid certain online services. 130 Lastly, facilitation efforts that involved providing patients with tablets or computers to use digital services in waiting rooms may compromise patient confidentiality. 110
Evidence also suggests that healthcare staff’s perceptions of harms from digital services, such as negative impacts on the patient–provider relationship, increased workload and patients misinterpreting online health information, may negatively affect their willingness to recommend digital services to patients. 106
There is some evidence that providers may be more willing and able to engage in DF efforts with patients who are already confident users of digital services, including the ‘worried well’, potentially exacerbating inequalities in access to digital health resources. 105,137 A review found that providers are more likely to recommend digital services to patients they perceive as more technologically knowledgeable, and these perceptions may be based on age, socioeconomic status, education level and ethnic group. 106,116,138
Non-health literature in the area of banking focuses on digital exclusion, with concerns that financial institutions will market digital services more among high-income groups that are already more likely to use online banking. This literature points to the role of regulators in protecting vulnerable populations which may otherwise be digitally excluded. For example, regulators may enact inclusion objectives and they may address security concerns that deter people from participating in digital finance. 139
What makes digital facilitation successful?
The success of DF is influenced by the following factors.
Perceptions of usefulness of the digital service
One of the most important factors in the success of DF efforts is the perception, both from the patients and the healthcare staff, that the digital service will be useful. 85,92,94,95,109,140 Qualitative evidence suggests that healthcare staff’s likelihood of recommending a digital service to patients may be influenced by the alignment of information within apps and websites with the health information and recommendations that doctors commonly provide to patients,85 and by the existence of rigorous evaluations of digital services that demonstrate patient benefit. 80,107 Patients are more likely to use services that have been recommended by healthcare staff if they see the information and functionality as novel,82 if they are able to customise the service to their own needs and preferences,52,130 and if the service is specific enough to fit their needs. 141
Time and capacity in primary care
Challenges in terms of staff having enough time to implement DF efforts were commonly identified in the literature. 80,84,94,96,100,108,110,129,131,142,143 However, the literature also indicated ways to help address this issue. E-mail templates, protocols and scripts can help staff to automate some aspects of patient engagement. 104 Passive facilitation efforts such as posters and brochures can also help to mitigate time pressures in primary care. 112 In some studies, it was found helpful to have non-GPs engage with patients in DF efforts, due to time constraints for physicians,110,112,120,131 or to use the time that patients spend in waiting rooms as an opportunity to facilitate access to online services. 84,110,122 One study suggested that facilitation efforts may be more feasible during certain kinds of appointments where patients may have less pressing concerns (e.g. vaccination, contraception, nutritional and physical activity-focused appointments). 84
Staff buy-in
Staff buy-in and motivation were important enablers of successful facilitation efforts in many of the studies we found,38,96,135,144–146 and negative staff attitudes or a lack of motivation towards an intervention were often barriers to facilitation efforts. 93,94,97,143 In several studies, buy-in was encouraged through: early engagement of staff when developing an intervention, initial education or training sessions in practices to introduce staff to new online services or interventions, ongoing communication with staff and incorporation of digital services into discussions at staff meetings. 68,80,97,100,120 Early engagement of GPs and other primary care staff may also help by addressing anticipated barriers early in the implementation process. 68,80,84,147 Ongoing education and training for healthcare staff in how to use digital services has also been indicated as important in helping them to engage in DF. 104,106,107,148 Practice champions, that is, designated staff responsible for promoting digital interventions among other staff and patients, could also help. 68,112,120,143
Re-shaping roles may also be important in securing staff buy-in. 99,108,149 This not only applies to GPs and nurses, but also to wider primary care support teams. Seeing DF as part of their role rather than something added onto their existing job was important in increasing buy-in among practice receptionists. 110
Trust in, and knowledge of, digital services
Qualitative studies have shown that patients’ lack of trust in online services can be a barrier to using them,122,134,150 and this is an issue reported by older patients in particular. 151 Concerns about security and loss of confidentiality may also impact staff willingness to recommend digital services to patients. 106,134 Efforts to increase the perceived security of websites were described in the literature, such as the use of third-party seals on patient portal websites. 134
Trust in websites was also much discussed in the non-health literature we found, particularly that which looked at how to encourage people to buy travel and tourism services online. Perceived risk and trust were positively influenced by providing an explanation of security measures (e.g. non-disclosure of credit card details, encryption technology) and how information will be used, and by having a well-designed website. 152 The use of third-party seals which assure consumers that a website follows particular operating procedures and/or privacy standards, along with time stamps to indicate that information is up to date, have been found to encourage trust in online vendors in the travel industry. 153
Healthcare staff may be less likely to engage in facilitation efforts when they are uncertain which services are most trustworthy. 80,104,142 A review suggests that frameworks that help providers to identify high-quality apps, categorise them based on topics and intervention strategies, and match them to individual patient preferences, needs and motivations, may assist healthcare staff in recommending services to patients. 154
Guidelines for recommending digital services to patients and the role of regulators
Guidelines that help providers to recommend digital services to patients may also be helpful. 108,145 Evidence from qualitative studies highlights the importance of simple recruitment criteria, referral guides and specific triggers that prompt the recommendation of digital services to patients. 68,97,104,117,131 In some cases, mandates to recommend services have also been helpful. 148 In the UK, it has been suggested that setting targets for GPs to encourage the use of digital services could potentially be effective. 99 Policy that makes funding available for training, organisational development and infrastructure, and technology that allows providers to facilitate the use and uptake of digital services, will also be important in increasing use among patients. 99,108,135,145,149
A review of digital first consultations in England identified a concern among clinicians of ‘medical-legal’ issues around digital services, for instance through litigation and claims of medical negligence due to the inappropriate recommendation and use of digital services. 108 Guidelines and regulation may help address such issues.
Trust in healthcare staff
Trust, perhaps promoted by long-term relationships with healthcare staff, may be important in patients’ use of digital services that are recommended by those staff. 101,155 Where providers have given ongoing support to patients in using a digital service, trusting relationships and a positive, personal tone may boost patients’ motivation to participate in digital interventions. 90
Box 3 describes how PPIE influenced WP1.
The PAG gave us additional contextual understanding and examples of some themes that we found in the literature:
-
Awareness/lack of awareness by practices of online services is an important first step to any facilitation effort and training for staff is important if patients are to be supported to use online services.
-
Data privacy/security concerns by GPs or patients can hamper efforts.
-
That it can be particularly challenging for members of some vulnerable patient groups to access or use some online services.
PAG members contributed to the development of the search strategy and operationalisation of key terms, including ‘digital facilitation’.
What PPIE brought to the interpretation of the resultsWe discussed themes arising from the literature review, and any gaps they revealed, at a second workshop with seven members of the PAG. PAG members identified the following gaps:
-
An important point that was absent from the emerging findings of the literature review was the use of locums, which happens frequently and is a potential barrier to GP practices’ DF efforts. It is related to issues of high staff turnover, a point raised by both PAG break-out groups, and one that is under-represented in the literature.
-
PAG members made clear the importance of GP practices offering patients help/support to turn to when use of online services proves problematic. Providing the reassurance that such back-up exists, and then providing help when needed, could be an important way to facilitate use of online services, and was not one that we had identified clearly from the literature review.
Discussion
Our scoping review has revealed much information about ways in which healthcare staff in primary care settings can facilitate patients’ use of digital services. The range of approaches to DF is wide: to help thinking about them we have developed the typology shown in Table 3. Overall, we found that promotion of digital services through recommendation by practice staff, prescription of digital services, or e-mail and written reminders may be effective in increasing initial uptake of services. But few promotional efforts appear to contribute to sustaining use of digital services after initial sign-up, except for some communication-centred interventions that focus on helping patients to form specific plans to use digital services. Training and education on use of a digital service, such as providing initial assistance with registering for it, also appears to encourage initial uptake of digital services. But evidence suggests that patients likely require additional support beyond the initial introductory training or education session to promote long-term use of digital services. Hands-on facilitation approaches, in the form of promotion, guidance and support by staff, have some of the most consistently positive evidence of effectiveness, and may be especially important for elderly people.
Deviations from the original proposal
There were no deviations from the original proposal.
Strengths and limitations of the current literature review
We conducted a scoping review. This was appropriate given the exploratory nature of the study and our aim to capture the breadth of DF in primary care. We employed an iterative approach to identify literature relevant to DF in primary health care, including literature about health care more widely and, indeed, about non-healthcare sectors where that may have useful implications for DF in primary health care. Our focus was on the DF discussed, rather than on the quality of the study. Our approach was strengthened by PPIE inputs.
The limitations of our approach are evident from the inclusion and exclusion criteria presented earlier. In addition, by limiting the review mostly to articles published since 2015 we may have omitted earlier documents of interest. However, given the acceleration in recent years of the availability of online services for patients, we expect to have captured the large majority of relevant literature. The last few months of our literature review period overlapped with the first few months of the global COVID pandemic, but due to publication lags, we found very little literature that reflected the impact of the pandemic on the use of online services.
Gaps in the evidence base
We identified a number of areas that were not well addressed. We found few formal evaluations of DF effectiveness. While some studies examined the effects of particular DF efforts, most did not evaluate the benefits or costs of existing facilitation efforts; rather, their main focus was on ways of overcoming barriers to the uptake and/or sustained use of online services.
There were nevertheless a few formal evaluations of DF in the literature we reviewed, including some RCTs. Due to short time horizons, these studies concentrated on initial access to a service, such as registering with an online portal. There is little evidence available on how DF affects ongoing use of services, such as estimating how many more patients would routinely book their GP appointments online.
We found little comparative evidence on which types of facilitation are most effective, in what context, or for whom. Evidence of the effectiveness of DF in routine use in primary care settings is also thin, since most of the articles in our review reported on DF efforts introduced as part of research studies.
A key aim of the scoping review was to identify evidence about which, if any, models of DF are effective at reducing inequalities in the use of online services. But we found little evidence regarding the impact of DF with vulnerable groups. Just one article directly addressed the topic and a handful of other studies discussed differences in outcomes between population subgroups. Given the potential for online services to increase inequalities in access to health resources, this represents an important weakness the evidence base.
We found no studies that evaluated the cost effectiveness of a DF method, or even that quantified the costs. Some articles described time constraints in GP practices as a barrier to undertaking DF, which is presumably related to costs as well as workforce demands. However, a clearer understanding of the costs associated with different facilitation approaches, along with their effectiveness, would be important for assisting primary care practices in decision-making around implementing DF approaches.
Finally, evidence on the impact of COVID on DF is still emerging. Understanding the pandemic’s impact on the provision of digital services in primary care and how practices facilitate access to those services is a current challenge.
Suggestions for future research
Based on what we did not find, there is scope for more, and more formal, evaluations of approaches to DF. The emphasis in these evaluations could usefully be on the comparative effectiveness of different approaches, and with particular attention to the ability to sustain patients’ use of online services beyond initial sign-up. Given the push by the NHS for primary care practices to move services online,156,157 the lack of evidence about how best to facilitate patient access to these services is a significant gap to fill through future research.
The absence of economic evaluations of DF approaches is striking. There is a clear need for assessment of the costs of facilitation and the impact on the costs borne by health services, practices and patients as a result. Assessments of the cost effectiveness of DF and of different approaches in comparison with one another are much needed, to guide the use of scarce primary care resources.
Finally, although the literature we reviewed contains some examples of consideration of the differential effects of examples of DF on various subgroups of the population, the evidence overall about impact on (in-)equality of access to health care, particularly for vulnerable groups, is weak. It falls well short of providing clear guidance on how to avoid worsening inequalities, let alone reduce them, by means of DF. Starting to rectify that lack of guiding evidence is an important priority for future research.
Chapter 3 Practice and patient surveys (work package 2)
Aims and objectives
The overall aims of WP2 were to investigate the range of DF currently offered in a sample of primary care practices and to examine how this related to patient awareness and experiences of DF, and patient awareness and use of online services. We also wanted to understand how patient characteristics influenced their awareness and use of both DF and use of online services. Work package 2 comprised four interconnected elements:
-
a survey of general practices, with the primary objective of mapping the range of DF services currently offered in a sample of English primary care. Secondary objectives included understanding the impact of the COVID pandemic on digital service provision and the drivers influencing DF efforts
-
a survey of patients with the objectives of exploring patients’ views and experiences of different modes of DF identified through the practice survey, and identifying what patient factors predict awareness and uptake of DF
-
a patient survey boost sample of patients living with mental health conditions with the primary objective of exploring the experiences of DF in this population and potentially identifying any particular needs for these patients
-
analysis of national GPPS data with the objectives of examining, on a large scale, the factors associated with patients’ awareness and use of online services, and how that awareness and use varied according to the modes of DF identified in the practice survey.
Methods
Practice survey instrument
A questionnaire was designed to be completed in approximately 10 minutes by either practice managers or GPs and was produced in paper (postal) and online (using SmartSurvey Online Software and Questionnaire Tool) formats.
The practice survey questionnaire (see additional files www.fundingawards.nihr.ac.uk/award/NIHR128268; accessed 3 April 2024) was developed by a subgroup of the research team, with input and feedback from the PAG, the wider research team and additional GPs. The questions were developed using an iterative process, informed by the findings of the Di-Facto literature review (see Results). The questionnaire included questions addressing the range of online services offered to patients (currently and prior to the COVID pandemic), the activities used to promote online services or to support patients in using them, the staff involved in the provision of any support to patients and whether specific groups were targeted with that support. The questionnaire also sought the respondent’s views on responsibility for support, the influence of various factors on service provision and the rationale behind providing online services. There was also one question which gave the opportunity for a free-text response, inviting comment on anything else that the respondent saw as relevant.
Practice survey sample and distribution
The online version of the practice survey was piloted in 24 practices (November–December 2020) in Cambridgeshire and Peterborough Clinical Commissioning Group (CCG), and East and North Hertfordshire CCG. No changes to the questionnaire were required, but the recruitment process was refined after feedback (e.g. online survey formatting, improving the visibility of the online link). Subsequently, using the latest available NHS Digital data on General Practices,158 a sampling frame was defined comprising 610 practices from 8 CCGs (Devon, Birmingham and Solihull, South Warwickshire, Coventry and Rugby, Cambridgeshire and Peterborough, East and North Hertfordshire, Enfield, and Haringey CCGs with the latter 2 CCGs subsequently forming part of the North Central London CCG) from 4 Clinical Research Networks (CRNs) covering 4 geographical locations (South West England, West Midlands and East England and North London). Five hundred practices were randomly selected to form the sample, in anticipation of receiving one or more responses from 60% of practices. Pilot practices included in the final sample were not asked to complete the questionnaire again and the pilot data were retained. The research team searched www.nhs.uk to find practice e-mail addresses or websites for all 500 practices, and subsequently searched practice websites for e-mail addresses or contact forms. A sequential mixed mode was used, starting in mid-January 2021, whereby practices were contacted by e-mail or practice website contact form (where available) initially to alert them that a questionnaire would be soon sent, followed by the questionnaire itself, and up to three e-mail reminders (over 4 months). Paper versions of the questionnaire were also mailed to the practice manager, and subsequently to up to four named GPs identified from NHS Digital data on GP practitioners. 158 When a response was received by a practice no further mailings (electronic or postal) were sent to that practice. Where multiple responses were received, the first complete response per practice was used for analysis. Finally, CRNs were requested to follow-up practices who had not responded. Full details of the recruitment process are provided in (see additional files www.fundingawards.nihr.ac.uk/award/NIHR128268; accessed 3 April 2024). The practice survey was closed to responses in May 2021. Practices that responded and provided contact details were entered into a prize draw for 1 of 10 £250 vouchers.
Patient survey questionnaire
Patient survey questionnaire development commenced with a scoping meeting with the PAG, followed by a series of iterative workshops with the patient survey team. The questionnaire (see additional files www.fundingawards.nihr.ac.uk/award/NIHR128268; accessed 3 April 2024) drew on the literature review findings and adopted (revised) wording from existing questionnaires on eHealth literacy,159 the GPPS and the Get Digital basic skills assessment. Where possible, the patient survey content mirrored the practice survey questions (tailoring wording for patients with PAG input) to allow for direct comparison. It included sections exploring patients’ digital confidence, their awareness and uptake of online services and experience of the support provided by the practice to use online services. The questionnaire was piloted by volunteers. Feedback was that it was straightforward to complete; however, some words and layouts were subsequently changed for clarity.
For the Mental Health Boost sample, the questionnaire was identical to the main part of the patient survey. We consulted with a wider PAG, who had experience of mental health conditions, to identify acceptable language for the patient invitation letter and information sheet, to explain to patients how they would be identified, and to explore how to safeguard privacy when opening the invitations. The researchers involved with the mental health survey were experienced in and acutely aware of mental health issues and dealt very cautiously and sympathetically to the few patients where any concerns were raised.
Patient survey sample and distribution
We aimed to distribute the survey to 12,000 patients across 60 practices, in anticipation of a response rate of 35% (4200 responses). All practices returning at least one practice survey were invited to take part; however, additional practices, outside the original sample, serving deprived populations were later invited to participate to reach our target and to ensure that patients from deprived communities were included. The additional practices were selected with the support of the CRN. Practices were given instructions to run a patient record search and to produce a random sample of adult patients aged 16 and over. To ensure that patients from practices with more deprived populations had fair representation, practices with higher levels of deprivation were asked to identify more patients (320) than those with medium (240 patients) or low deprivation (170 patients). Practices were invited to review their list to exclude those experiencing severe mental illness, recently bereaved, under 16 years old, or incapable of giving informed consent to participate (all as defined by their GP). After exclusions, practices were asked to select the first 285, 220 and 150 reviewed patients, respectively, and to transfer the patient details onto an Excel file (with usernames and passwords added). The Excel file was then securely uploaded by the practice to the mailing company, CFH Docmail. The practice was instructed to initiate three patient mail outs. Each patient should have received an invitation letter, information sheet, patient survey and reply envelope for the first two mail outs and a postcard for the third. Patients were invited to provide contact details solely for the purpose of entering them into a prize draw for 1 of 10 £25 gift cards. Patients returning a survey either by post or online were deemed to have provided consent to participate in the study. Where paper copies were received data were entered by the study team using the same online survey platform. Double data entry was performed for four surveys per practice by a different member of the study team.
For the Mental Health Boost sample, we aimed to distribute 3000 questionnaires across 15 practices (200 each) to patients aged 16 years and over identified as living with anxiety or depression, in anticipation of a response rate of 20% (600 responses). A search was developed to identify a random selection of 220 patients who either had a code for anxiety or depression in their medical records (in the past 2 years) and/or received a recent anxiolytic or antidepressant drug prescription (in the previous 12 months) for anxiety or depression in their medical records. Patients taking Amitriptyline at < 50 mg/day were excluded since such doses may be commonly given for chronic pain management or for other non-mental health conditions. Practice staff were requested to screen the list to ensure patients fulfilled the eligibility criteria and excluded patients for the same reasons as for the main patient survey, but also for those who were known to be actively suicidal, or who were receiving diazepam for back pain or muscle spasm (with no history of anxiety).
General Practice Patient Survey
The GPPS is a national postal questionnaire that is sent to 2.3 million patients annually on behalf of NHS England. Further details of the survey and its development can be found elsewhere. 13,160,161 Data from the 2019, 2020, 2021 and 2022 GPPS162 were analysed both on their own and in relation to the practice survey. 160,163–166 We restricted the data to those who reported attempting to make a general practice appointment in the last 12 months to ensure that responders had the opportunity to use online services. We made use of two questions about the awareness and use of online services:
-
As far as you know, which of the following online services does your GP practice offer? Booking appointments online, ordering repeat prescriptions online, accessing my medical records online, none of these, don’t know.
-
Which of the following general practice online services have you used in the past 12 months? Booking appointments online, ordering repeat prescriptions online, accessing my medical records online, had an online consultation or appointment (e.g. completed an online form or had a video call).
The question on awareness of online services was removed from the questionnaire in 2021 and so responses from 2019 to 2020 were used for this question, while data from 2021 to 2022 were used for the analysis concerning use of online services. In addition, we used responses to questions addressing ease of getting through on the phone, helpfulness of practice receptionists, patients having a preferred GP and ease of using the GP practice website, as well as patient reported demographics, health status and the Index of Multiple Deprivation (IMD) based on the patient postcode of residence.
Data analysis
Descriptive statistics
Practices that took part in the practice survey were compared with other practices in England considering deprivation, rurality, list size and the percentages of registered patients over the age of 65 and (separately) with a non-white ethnicity. Deprivation and ethnicity data were obtained from the Public Health England Fingertips website167 based on 2021 data; list size and patients over 65 were obtained from NHS Digital December 2020 data, and rurality was based on practice postcodes as used in the 2019 GPPS. Descriptive statistics were produced for responses for the practice and two patient surveys. Following factor analysis indicating a single construct underlying the responses to Q2–Q6 of the patient survey (see Appendix 2, Tables 30–32 and Figure 17), a composite measure of digital confidence was formed from these questions. For each question, a response of ‘Not very confident/I can’t do this’ scored 0, ‘Quite confident’ scored 1 and ‘Very confident’ scored 2. Scores for the five questions were summed giving a score between 0 and 10. This was further split into three categories of 0–3 (not confident), 4–7 (quite confident) and 8–10 (very confident). For the subsample of responses to the patient surveys where double data entry was performed, the number and percentage of data items where there was disagreement between the primary and double data entry were recorded overall and by question.
Comparisons of the percentage of patients reporting being aware of and using different modes of facilitation in the main patient survey were made between practices who reported using the corresponding mode of facilitation in the practice survey. Similar comparisons were made for patients being aware of, and of using, any mode of facilitation between practices who reported undertaking ad hoc promotion or support and those who did not, and between those who reported employing a practice champion with specific responsibility for supporting or facilitating online services and those who did not. Finally, comparisons were made of awareness and use of any modes of facilitation between patients registered at practices that reported targeting older adults (65 years or older), people with physical health conditions, mental health conditions, limited or no internet access, non-English speakers/English as a second language, ethnic minorities and carers, restricting comparisons to patient respondents reporting that they belonged to that group.
Frequencies and percentages of awareness and use of online services by patient groups were calculated using national GPPS data using weights supplied with the data which accounted for sampling design and non-response bias.
Regression analyses
Main patient survey
Four binary outcomes were created from patient survey responses: (1) awareness of DF; (2) use of DF; (3) being told by someone from the practice about online services and (4) being helped by someone from the practice to use online services. Awareness/use of DF was based on the patient respondent endorsing one or more of the following modes of facilitation in the appropriate question: displays in the practice, leaflets, e-mail/text messages, practice website, social media, workshops/events and making IT equipment available to access online services.
Mixed-effects logistic regression models, with a random effect for practice, were used to examine variability in these outcomes by patient factors. For each of the binary outcomes, univariable associations were calculated along with a multivariable model adjusting for age, gender, deafness/hard of hearing, parental status, ethnicity, physical or mental long-term health condition, working status, first language and whether they had repeat prescriptions (adjusted Model 1). A second model (adjusted Model 2) augmented adjusted Model 1 with the digital confidence variable. A further regression was run using a binary version of the digital confidence scale (confident vs. quite or not confident) as the outcome and the same covariates as adjusted Model 1.
Sensitivity analyses were performed excluding respondents who reported having helped to complete the survey, and for the digital confidence model, using an alternative cut-point of confident or quite confident versus not confident.
Patient survey: mental health boost sample
The regression models performed on the data from the main patient survey were repeated on data from the mental health boost sample survey combined with data from responders to the main patient survey registered at those practices that took part in the mental health boost sample survey. These models were augmented with an additional variable indicating if responders were part of the main sample or the boost sample.
General Practice Patient Survey
Mixed-effects logistic regression models were applied to GPPS data with awareness and use of each of the services as binary outcomes (seven outcomes in total). Models included patient reported age, gender, ethnicity, the presence of long-term condition, not working due to long-term sickness/disability, hearing impairment with use of sign language, as well as deprivation based on national quintiles of IMD. All models included a random intercept to quantify variation between practices. 168
Another series of models extended the previous models to include other factors reported in the GPPS and to examine their influence on awareness and use of the online services. These other factors were: ease of getting through on the phone, helpfulness of practice receptionists, patients having a preferred GP and ease of using the GP practice website. The latter was chosen as a proxy for facilitation/enabling efforts of online services. To account for the fact that individuals’ general capacity to use websites in general may influence their response to the question about ease of use of practice websites, we repeated these models using a categorical practice-level version of the question on ease of use of practice website. This was obtained through the quintiles of the random effects of a mixed-effects logistic regression model with the question (Q6) as a binary outcome and adjusted for all known and available confounding factors with awareness and use of online services.
Finally, we explored the potential for DF to impact health inequalities, introducing pairwise interaction terms of ease of use of practice website with each of the demographic and health status variables. These models aimed to indicate whether there was evidence for different levels of association between the proxy for facilitating online services and different patient groups.
National GPPS data from those practices who responded to the practice survey were analysed to ascertain the extent to which the use of DF is associated with patients’ experiences (awareness and use) of online services and the ease of use of the GP website. Comparisons were made between practices using different approaches. Mixed-effects logistic regression models similar to those used to explore variation in awareness and use of online services were augmented with indicator variables derived from the practice survey and restricted responses of patients registered at practices responding to the practice survey.
Complete-case analysis was used throughout. All analyses were performed in Stata v17.0.
Analysis of free-text responses in the patient survey
We examined all the free-text responses for the main patient survey (i.e. not mental health boost sample) to the following questions:
-
Q16: What can the practice do to help you access the online services?
-
Q17: Is there anything else you would like to add about online services and the support of the practice to help you use them? If so, please tell us about it here.
We conducted a text-based analysis to reflect the topics emerging from the data. One researcher (NK) initially read and re-read all of the responses to familiarise herself with the data. The data were then coded to capture key concepts from the free-text responses. A second researcher (EP) independently read and re-read and double coded the responses. Both researchers met to discuss the initial coding to compare and contrast their findings and to resolve discrepancies. Codes were then organised into higher level themes based on the content and relationship between the codes. We used NVivo 12 (QSR International, Warrington, UK) qualitative analysis software to manage the data.
Findings
Practice survey
Of the 499 practices invited (2 were latterly found to have merged at the time of invitation), 156 (31%) sent back one or more questionnaires (in total 168 questionnaires were returned). This included 19 practices who had participated in the pilot version of the survey. Compared with other practices in England, participating practices were more likely to serve less deprived populations (26% in the least deprived quintile vs. 20% in other practices), to be in rural areas (30% vs. 15% in other practices) and have over 12,000 registered patients (35% vs. 23%). Smaller differences were seen in the age profile and ethnicity of the registered populations (see Appendix 2, Table 33).
Summaries of the responses to the practice survey are shown below (full details Appendix 3, Tables 34–43). Figure 4 and Table 34 show the online services that practices reported offering relative to the current COVID pandemic. All services were currently offered by over 80% of practices with the exception of online access to test results (77%) and online appointment booking (51%). There was a substantial reduction in online appointment booking provision associated with the pandemic (44% of practices offering the service pre-pandemic, but not at the time of the survey, due to temporary suspension). All other services had seen an increase in provision with between 25% (online access to test results) and 86% (video consultations) of practices providing a service that was not available pre-pandemic.
FIGURE 4.
Online services offered by practices responding to the practice survey pre coronavirus and at the time of the survey.
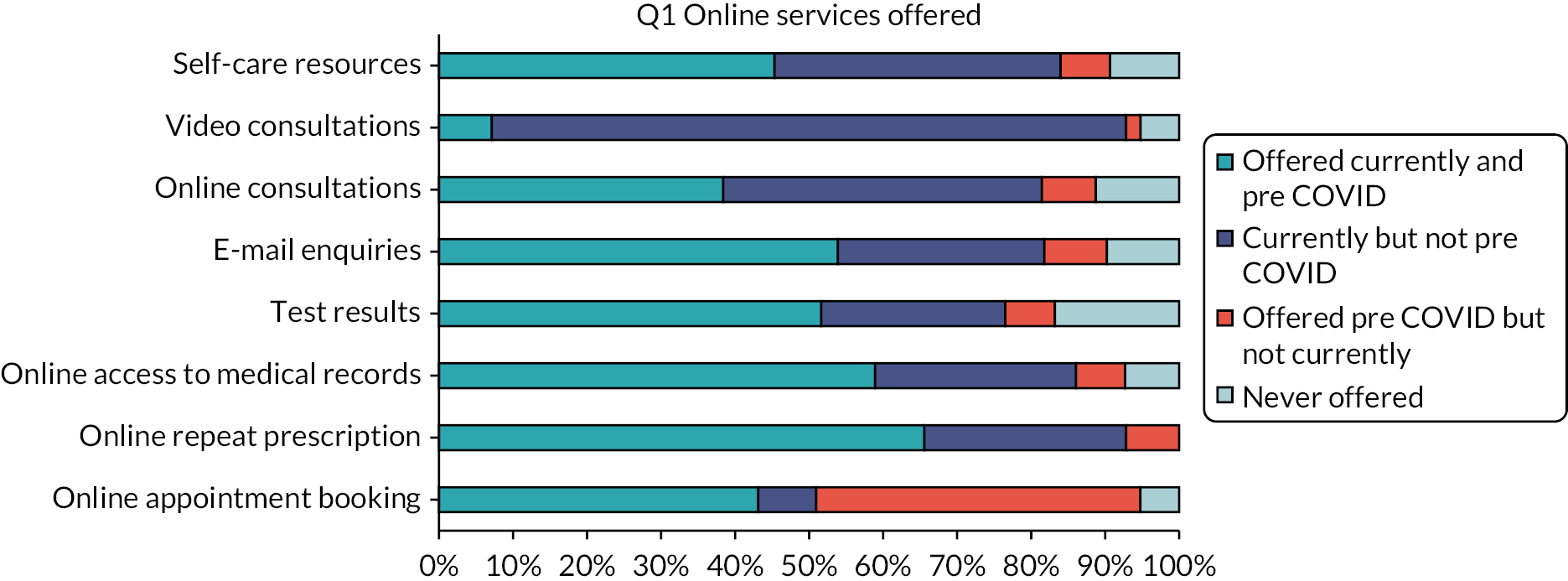
There was a clear division in the survey between the endorsement of modes of DF that might be described as passive (displays, leaflets, text messages, e-mails, social media and material on practice websites) and those that might be described as active (ad hoc support, employing a practice champion, holding workshops/events and the provision of tablets/computers). Passive modes of facilitation were reportedly used for either promotion of online services and/or supporting patients to use them in a majority of practices (see Figure 5, also Appendix 3, Table 35). In contrast, most active modes of facilitation (employing a practice champion, holding workshops/events and the provision of tablets/computers) were reported by only a minority of practices. An exception to this observation was the provision of ad hoc support which was reported in 91% of practices. Most practices reported using DF across a wide range of online services with 97% reporting using it to promote or support online repeat prescription ordering (see Appendix 3, Table 36).
FIGURE 5.
Digital facilitation activities used to promote online services and support patients to use them.
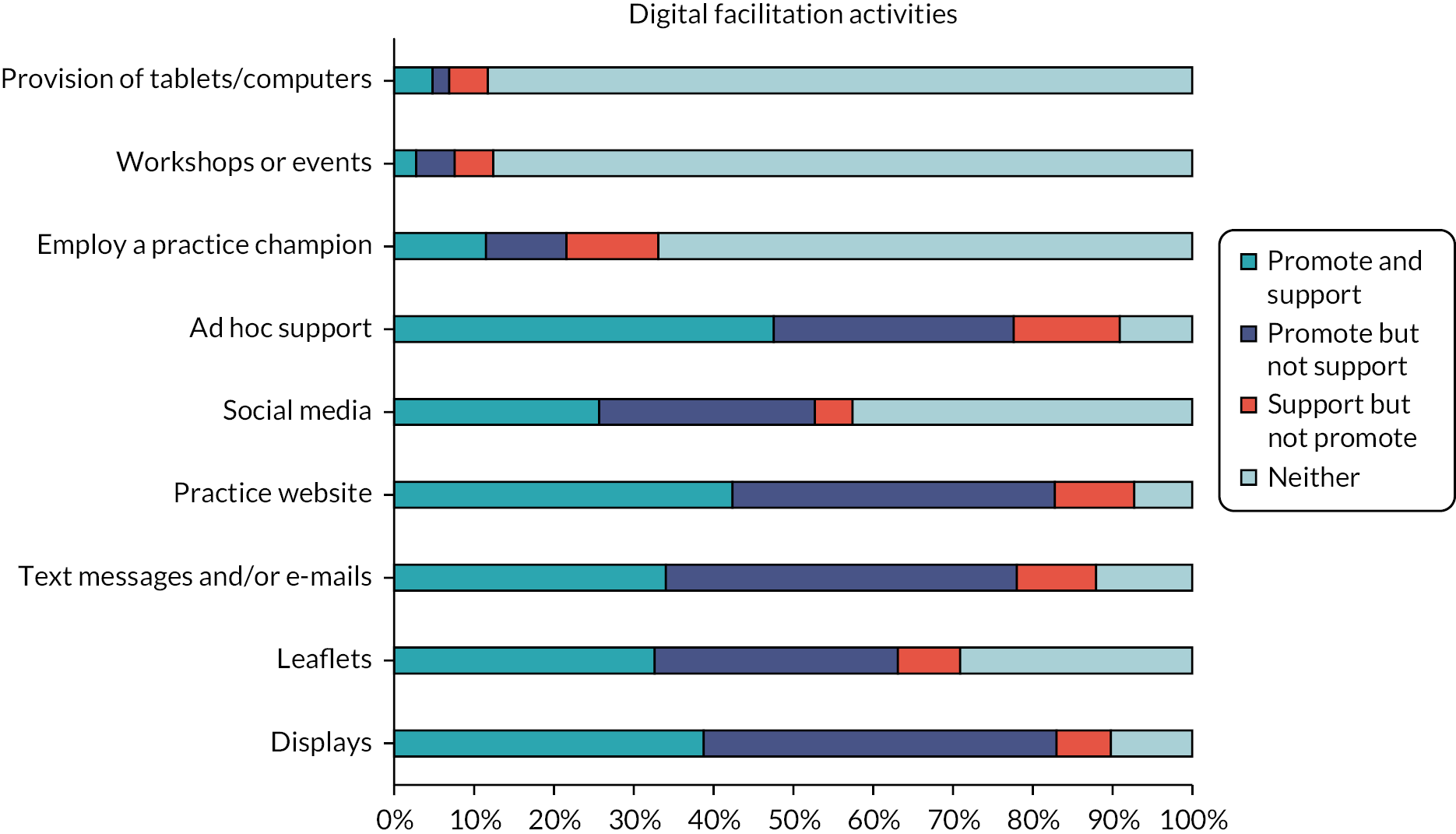
The vast majority of practices reported DF being carried out by administrative (86%) and reception (86%) staff, with doctors (62%), nurses (53%) and other healthcare professionals (42%) also frequently reported as being involved. IT staff (28%) volunteers (20%), external contractors (4%) and those with specific responsibilities around DF were reported less often (see Appendix 3, Table 37). Around 22% of practices reported targeting their facilitation activities at every patient group considered, with most practices reporting targeting multiple groups. However, the only specific group targeted by most practices were older adults (56% of practices) (Table 5).
| Patient group | N (%) | Patient group | N (%) |
|---|---|---|---|
| Older adults | 87 (55.8) | Non-English speakers or those for whom English is a second language | 49 (31.4) |
| People with physical health conditions | 68 (43.6) | People from ethnic minority communities | 45 (28.9) |
| People with mental health conditions | 64 (41.0) | Lower-income populations | 38 (24.4) |
| People with limited or no internet access | 45 (28.9) | People with low literacy levels | 37 (23.7) |
| People with limited computer skills | 50 (32.1) | Socially isolated individuals | 53 (34.0) |
| People living in rural communities | 35 (22.4) | Patients with caring responsibilities or patient carers | 67 (43.0) |
| Other | 22 (14.1) |
Most practices reported either reducing or removing in person access to services (including the provision of paper prescriptions) following the national lockdown starting 23 March 2020 (see Appendix 3, Tables 38 and 39). However, although most practices had not changed phone access, 10% of practices reduced access to booking appointments by phone, and 28% reported removing (13%) or reducing (15%) access to ordering repeat prescriptions on the phone.
FIGURE 6.
Level of agreement with statements about DF by practices responding to the practice survey. (continued)
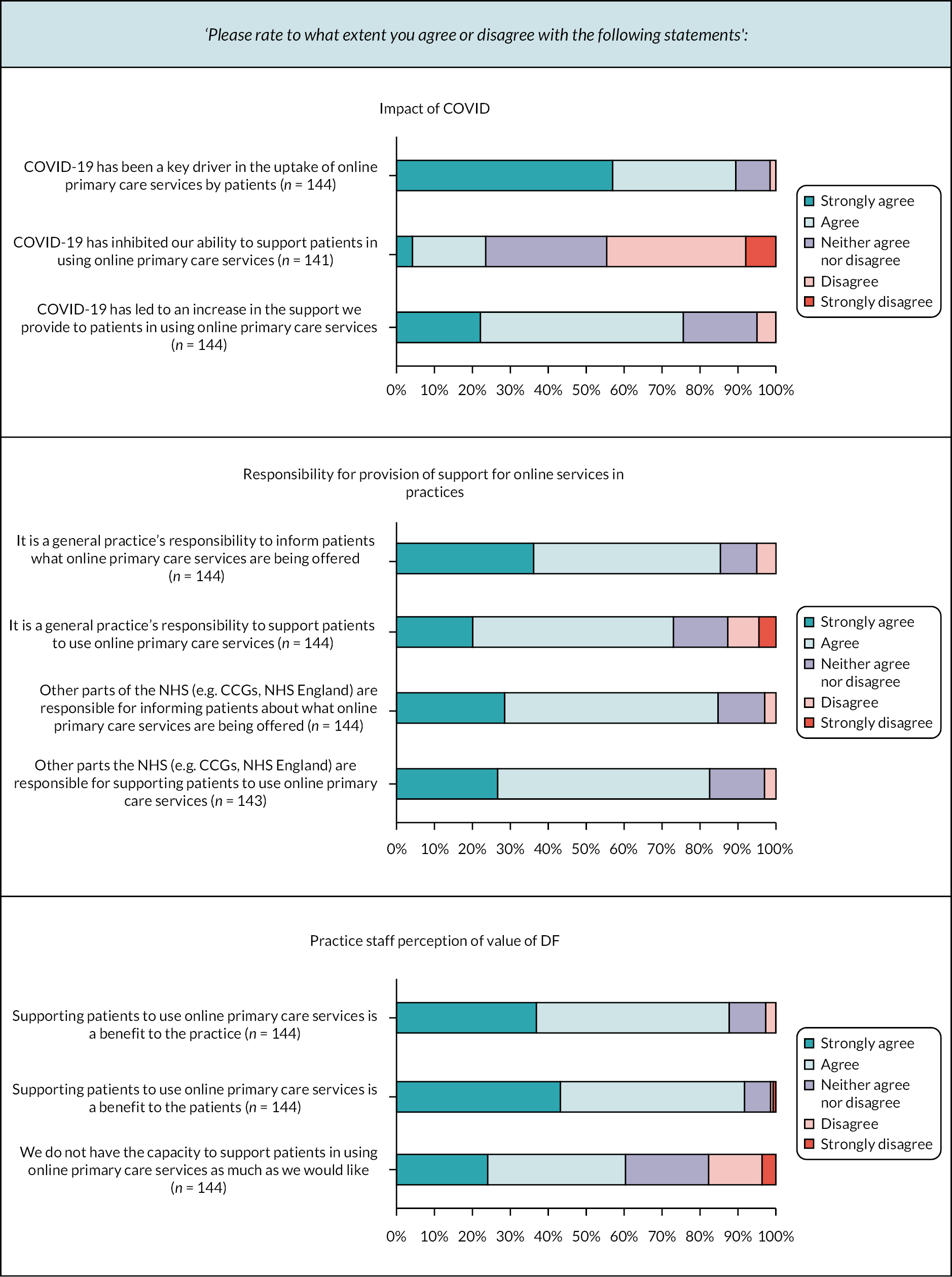

Most practices agreed in the survey (selecting ‘either agree’ or ‘strongly disagree’ when asked if they agreed with a statement) (see Figure 6, also Appendix 3, Tables 40–42) that:
-
COVID had been a crucial driver in the uptake of online services by patients
-
COVID had led to an increase in the support they gave to patients to use online services
-
it is the practices’ and NHS’s responsibility to inform patients about online services and provide support
-
support provided to patients was in response to patient demand rather than from the CCG, practice staff or monetary incentives
-
supporting patients to use online services benefited the practice and patients
-
they lacked the adequate capacity to provide this support
-
they had increased the uptake of online services by supporting patients to use them and that they hoped to further increase uptake through support
-
some patients were unlikely to use online services regardless of the support provided
-
some patient groups required more support than others
-
increased patient uptake of online services led to operational efficiencies for the practice
-
online access to primary care services was complementary to traditional forms of access.
Analysis of free-text comments made by (staff) responders throughout the practice survey identified two main themes which illustrated issues reported:
-
COVID had had an impact on digital services: many services made a shift to being mainly online. However, COVID also curtailed a few attempts to provide support (e.g. provision of workshops prior to COVID).
-
There was a relatively negative attitude to implementing digital services in terms of limited practice capacity, finances and motivation:
GP practices do not have the capacity or resources to facilitate online access.
Practice 1455, GP
-
There was a recognition that guidance, support and funding from CCGs or at the national level was required in order to provide more help to patients:
[F]unding would be useful to provide tablets/pc for waiting rooms where patients could access online/self- help/information/advice.
Practice 1451, Nurse
It makes sense for support to be delivered at a national level and outside of GP practice, as is the case with the NHS App.
Practice 1385, GP
Patient survey
Sixty-two practices participated in the patient survey, sending invitations to 12,822 patients, of whom 3051 (23.8%) responded (see Appendix 5, Table 49). Analysis of double data entry detected a difference of 0.4% in data points entered which was deemed acceptable. Response rates were lower in practices serving deprived populations; however, due to the approach to sampling we adopted, responses were reasonably representative in terms of deprivation (Figure 7).
FIGURE 7.
Main patient survey: invitations and response by deprivation quintile.
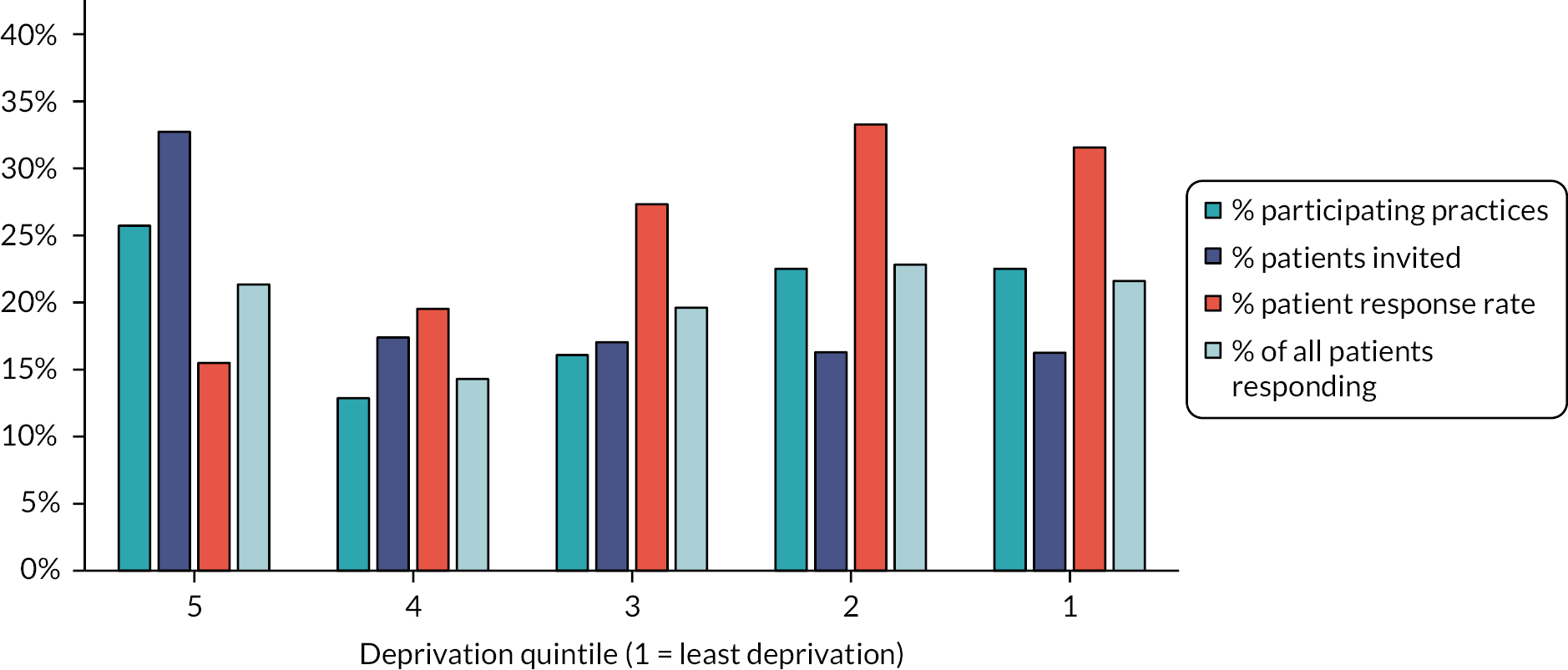
Of responders to the main patient survey, slightly more were female than male, 45% were 65 or older, the vast majority were white (93%), 9% reported that English was not their first language, 44% were working either full-time or part-time, and 43% were retired (Table 6).
| Demographic | Total (%) (n = 3051) |
Demographic | Total (%) (n = 3051) |
||
|---|---|---|---|---|---|
| Gender | Male | 1312 (43.4) | Working status | Full-time paid | 906 (31.2) |
| Female | 1710 (56.6) | Part-time paid | 363 (12.5) | ||
| Age (years) | 16–24 | 140 (4.6) | Full-time education | 75 (2.6) | |
| 25–34 | 195 (6.4) | Unemployed | 59 (2.0) | ||
| 35–44 | 262 (8.7) | Permanently sick | 72 (2.5) | ||
| 45–54 | 436 (14.4) | Fully retired | 1244 (42.8) | ||
| 55–64 | 619 (20.5) | Looking after family | 104 (3.6) | ||
| 65–74 | 727 (24.0) | Doing something else | 75 (2.6) | ||
| 75–84 | 515 (17.0) | Furloughed | 6 (0.2) | ||
| ≥ 85 | 131 (4.3) | ||||
| Deaf/hearing impediment | Yes | 358 (12.0) | English as first language | Yes | 2705 (91.2) |
| No | 2631 (88.0) | No | 261 (8.8) | ||
| Blind/partially sighted | Yes | 54 (1.8) | Carer | Yes | 700 (23.8) |
| No | 2909 (98.2) | No | 2237 (76.2) | ||
| Ethnicity | White | 2741 (92.7) | Parent | Yes | 420 (14.2) |
| Mixed | 31 (1.1) | No | 2536 (85.8) | ||
| Asian/Asian British | 107 (3.6) | ||||
| Black/African/Caribbean/black British | 57 (2.0) | Repeat prescriptions | Yes | 1957 (65.7) | |
| No | 1021 (34.3) | ||||
| Help to complete the survey | Yes | 183 (6.2) | |||
| Other | 22 (0.7) | No | 2780 (93.8) | ||
| Mental health condition/disabilities | Yes | 472 (16.4) | Physical health condition/disabilities | Yes | 1046 (36.1) |
| No | 2281 (79.3) | No | 1737 (60.0) | ||
| Don’t know | 72 (2.5) | Don’t know | 74 (2.6) | ||
| Prefer not to say | 51 (1.8) | Prefer not to say | 43 (1.5) |
Nine per cent of responders reported not having access to the internet at home, and nearly all of these completed a paper version of the survey (see Appendix 5, Table 50). The percentage of responders not confident or unable to complete digital tasks ranged from 17% for using search engines to 31% for installing apps (see Appendix 5, Table 50). The lack of confidence was strongly associated with response mode, with at most 4% of online responders lacking confidence in these tasks.
Figure 8 shows a clear bimodal distribution in the digital confidence score constructed from responses to questions 2–6. Almost 40% of responders scored 10, implying they feel very confident in undertaking all of the tasks considered, while around 12% of responders scored zero, implying that they are not very confident/cannot complete any of the tasks considered.
FIGURE 8.
Distribution of digital confidence score for responders to the patient survey.
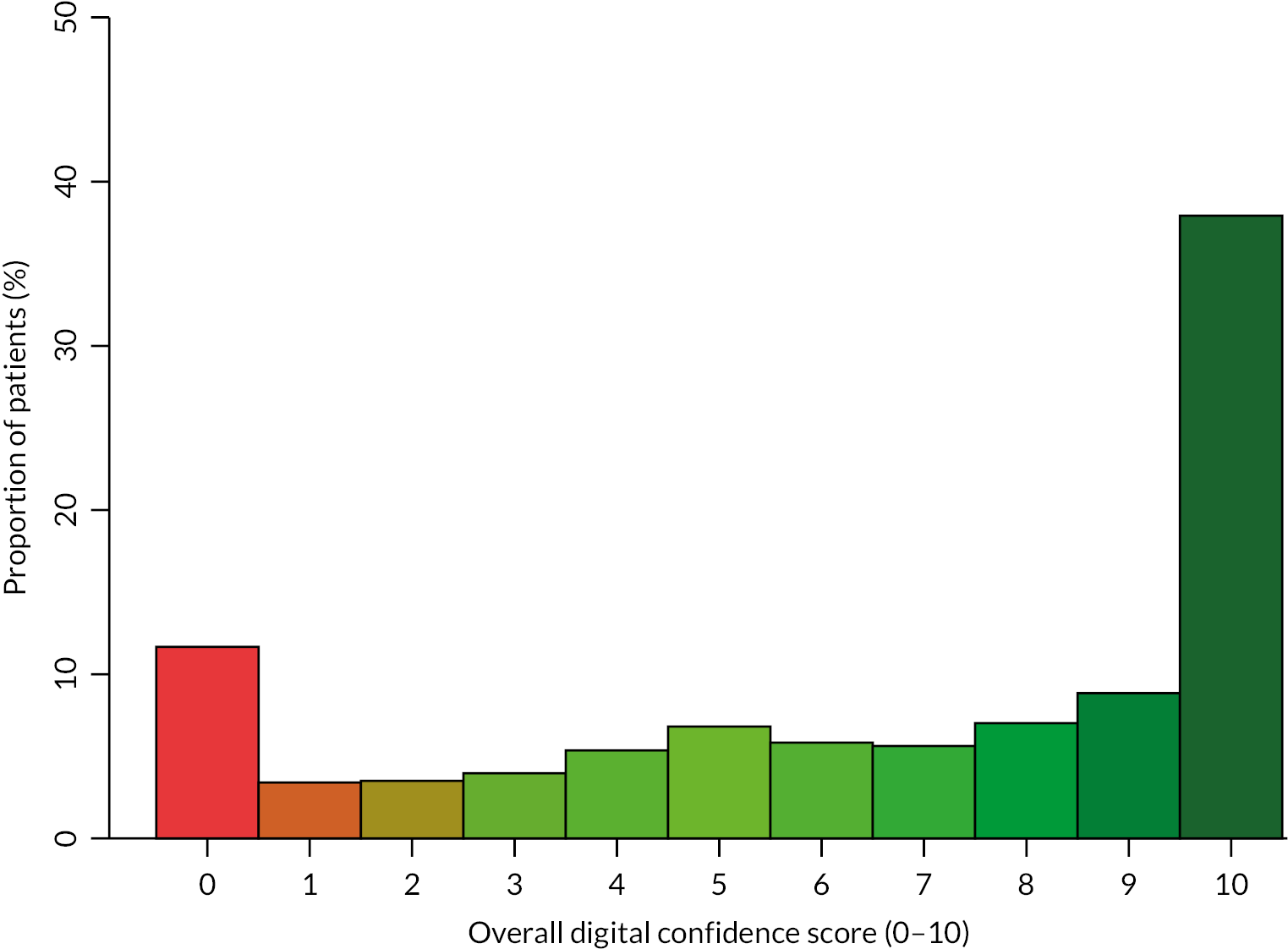
Table 7 provides a summary of responses to the core patient survey questions (i.e. not those concerning digital confidence or patient characteristics). Over a third of responders (37%) had not tried to use their general practice’s website, though most of those that had done so found it easy to use. Awareness of online services was generally low (≤ 37% of respondents were aware) for all online services apart from booking appointments and ordering repeat prescriptions online (55% and 64% respectively) and use of online services was universally low with at most 33% of patients reporting having ordered repeat prescriptions online. Awareness of DF efforts was low, with 17% or less being aware of any modes apart from texts or e-mails for which 39% of responders were aware of their use. The use of those facilitation efforts was even lower, with < 10% of patients making use of any mode apart from e-mail or text messages (28%).
| Questions | Total (%) (n = 3051) | Questions | Total (%) (n = 3051) |
|---|---|---|---|
| Q7. Ease of practice website use | Q10. Awareness of facilitation | ||
| Very easy | 541 (18.0) | Displays | 522 (17.1) |
| Fairly easy | 920 (30.7) | Leaflets | 178 (6.0) |
| Not very easy | 286 (9.5) | Text/e-mails | 1205 (39.4) |
| Not at all easy | 145 (4.8) | Web content | 229 (7.5) |
| Haven’t tried | 1106 (37.0) | Social media | 118 (4.0) |
| Q8. Awareness of online services | Workshop/events | 17 (0.6) | |
| Appointment booking | 1675 (55.0) | Tablets/computers | 16 (0.5) |
| Repeat prescriptions | 1944 (63.7) | Q11. Use of facilitation | |
| Access records | 945 (31.0) | Displays | 291 (9.5) |
| Access test results | 663 (21.7) | Leaflets | 93 (3.0) |
| E-mail enquiries | 1126 (37.0) | Text/e-mails | 860 (28.2) |
| eConsults | 945 (31.0) | Web content | 152 (5.0) |
| Video consults | 458 (15.0) | Social media | 79 (2.6) |
| Q9. Use of online services | Workshop/events | 15 (0.5) | |
| Appointment booking | 469 (15.4) | Tablets/computers | 15 (0.5) |
| Repeat prescriptions | 1003 (33.0) | Q12. Told about online services | |
| Access records | 393 (13.0) | Yes | 883 (29.8) |
| Access test results | 260 (8.5) | No | 2801 (70.2) |
| 457 (15.0) | Q13. Helped to use online services | ||
| eConsults | 501 (16.4) | Yes | 392 (13.4) |
| Video consults | 118 (3.8) | No | 2543 (86.6) |
| Q14. Usefulness of help | Q14. Usefulness of help | ||
| 14_1. Booking appointments online | 196 (6.4) | 14_7. Online video consultations | 81 (2.7) |
| Not helpful | 40 (20.4) | Not helpful | 28 (34.6) |
| Quite helpful | 77 (39.3) | Quite helpful | 19 (23.5) |
| Very helpful | 79 (40.3) | Very helpful | 34 (42.0) |
| 14_2. Ordering repeat prescriptions online | 211 (7.0) | 14_8. Other | 33 (1.1) |
| Not helpful | 22 (10.4) | Not helpful | 10 (30.3) |
| Quite helpful | 66 (31.3) | Quite helpful | 8 (24.2) |
| Very helpful | 123 (58.3) | Very helpful | 15 (45.5) |
| 14_3. Accessing medical records online | 121 (4.0) | Q15. Reasons why not using online services | |
| Not helpful | 24 (19.8) | No internet access | 247 (8.1) |
| Quite helpful | 42 (34.7) | Security concern | 228 (7.5) |
| Very helpful | 55 (45.5) | Confidentiality | 145 (4.8) |
| 14_4. Accessing test results online | 111 (3.6) | Not knowing how to register | 440 (14.4) |
| Not helpful | 23 (20.7) | Registration too difficult | 175 (5.7) |
| Quite helpful | 34 (30.6) | Not knowing how to get support | 259 (8.5) |
| Very helpful | 54 (48.6) | Practice too busy to help | 262 (8.6) |
| 14_5. E-mail enquiries to the practice | 154 (5.0) | Prefer to speak to person | 1432 (47.0) |
| Not helpful | 27 (17.5) | Other (with comments): | 811 (27.1) |
| Quite helpful | 53 (34.4) |
|
73 (2.4) |
| Very helpful | 74 (48.1) |
|
60 (2.0) |
| 14_6. Help from GP using online form | 171 (5.6) | ||
| Not helpful | 28 (16.4) | 55 (1.8) | |
| Quite helpful | 59 (34.5) | ||
| Very helpful | 84 (49.1) | ||
Only 30% of patients reported that they had been told about online services by someone at their general practice and only 13% reported being helped to use them. However, of those that did have help, they generally rated it as helpful (90% said ‘quite’ or ‘very helpful’ for repeat prescriptions, and 65% said ‘quite’ or ‘very helpful’ for video consultations). Various reasons were selected for not using online services, but most common was preferring to speak to a person (47%) with 20% either not knowing how to register (14%) or finding registration too difficult (6%).
The adjusted (Model 1) logistic regression analyses are shown in Table 8 with unadjusted results shown in Appendix 4 (see Table 44). Age was positively associated with a lower likelihood of all four outcomes (p < 0.05 for all), particularly for being helped to use online services (adjusted OR for ≥ 85 vs. 55- to 65-year-olds 0.08, 95% CI 0.02 to 0.36; p = 0.006). Patients in receipt of repeat prescriptions were more likely to have experienced all four facilitation outcomes (p < 0.05), for example, the adjusted odds ratio (OR) for being told about online services was 1.70 when compared with those not in receipt of repeat prescriptions (95% CI 1.36 to 2.13; p < 0.001). Patients of non-white ethnicity were more likely than those patients describing themselves as white to be aware of DF, have made use of DF and been helped to use online services, but no difference was seen between white and non-white patients for being told about online services (adjusted OR = 0.91, 95% CI 0.61 to 1.36; p = 0.651). Similarly, people for whom English was not their first language were more likely to use DF and be told about online services, and with very weak evidence (p < 0.1) of similar differences for the other two outcomes. Gender, being deaf or having a hearing impairment, and working status were not associated with any of the four outcomes (p > 0.1). Including the digital confidence measure in the models (see Appendix 4, Table 45) showed that lower digital confidence was associated with lower awareness and use of facilitation, and a lower chance of being told about, or being helped to use, online services. Comparing Model 1 with 2 we found that digital confidence explained some of the difference attributable to older age for awareness and use of facilitation and being told about online services. However, the reductions in odds ratios were fairly small (e.g. OR for 85 + awareness of facilitation reduced from 0.32 to 0.59). In contrast, digital confidence hid some difference attributable to older age in being given help indicated by ORs becoming larger when adjustment for digital confidence was made. Digital confidence also masked some differences in the four outcomes between those who spoke English as a first language and those who did not. Sensitivity analyses excluding those who reported having helped to complete the questionnaire did not lead to materially different findings (see Appendix 4, Tables 46 and 47).
| Awareness of any facilitation effortsa | Use of any facilitation effortsb | Being told about online services | Being helped to use online services | |||||
|---|---|---|---|---|---|---|---|---|
| Adjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value | |
| Q18. Gender | ||||||||
| Male | Reference | |||||||
| Female | 0.92 (0.78 to 1.09) | 0.342 | 0.90 (0.76 to 1.07) | 0.226 | 1.14 (0.95 to 1.36) | 0.161 | 0.86 (0.68 to 1.10) | 0.237 |
| Q19. Age | ||||||||
| 16–24 | 0.84 (0.50 to 1.42) | < 0.001 | 0.64 (0.37 to 1.09) | < 0.001 | 1.58 (0.93 to 2.70) | 0.043 | 1.00 (0.47 to 2.17) | 0.006 |
| 25–34 | 1.08 (0.73 to 1.58) | 1.07 (0.74 to 1.56) | 1.14 (0.77 to 1.69) | 1.11 (0.65 to 1.91) | ||||
| 35–44 | 0.98 (0.67 to 1.43) | 1.01 (0.70 to 1.46) | 1.08 (0.73 to 1.60) | 1.42 (0.85 to 2.37) | ||||
| 45–54 | 0.94 (0.70 to 1.27) | 0.94 (0.70 to 1.26) | 1.01 (0.74 to 1.38) | 1.31 (0.87 to 1.98) | ||||
| 55–64 | Reference | |||||||
| 65–74 | 0.71 (0.53 to 0.95) | 0.88 (0.66 to 1.17) | 0.77 (0.56 to 1.05) | 0.81 (0.52 to 1.24) | ||||
| 75–84 | 0.43 (0.30 to 0.60) | 0.62 (0.44 to 0.87) | 0.66 (0.45 to 0.95) | 0.50 (0.30 to 0.84) | ||||
| ≥ 85 | 0.32 (0.19 to 0.54) | 0.27 (0.15 to 0.49) | 0.38 (0.20 to 0.71) | 0.08 (0.02 to 0.36) | ||||
| Q20. Deaf/hearing impairment | ||||||||
| No | Reference | |||||||
| Yes | 0.93 (0.70 to 1.22) | 0.595 | 1.16 (0.87 to 1.53) | 0.314 | 0.82 (0.60 to 1.13) | 0.229 | 1.32 (0.88 to 2.00) | 0.184 |
| Q22. Parent | ||||||||
| No | Reference | |||||||
| Yes | 1.28 (0.96 to 1.72) | 0.095 | 1.03 (0.78 to 1.37) | 0.831 | 1.28 (0.95 to 1.73) | 0.105 | 1.03 (0.70 to 1.52) | 0.880 |
| Q23. Ethnicity | ||||||||
| White | Reference | |||||||
| Other | 1.48 (1.00 to 2.20) | 0.050 | 1.48 (1.03 to 2.15) | 0.036 | 0.91 (0.61 to 1.36) | 0.651 | 1.80 (1.14 to 2.86) | 0.012 |
| Q24–25. Long-term physical or mental health condition | ||||||||
| No | Reference | |||||||
| Yes | 1.25 (1.03 to 1.50) | 0.021 | 1.17 (0.97 to 1.41) | 0.092 | 1.07 (0.88 to 1.31) | 0.478 | 1.29 (0.98 to 1.70) | 0.069 |
| Q26. Working status | ||||||||
| Work | Reference | |||||||
| Education | 0.73 (0.38 to 1.41) | 0.118 | 1.05 (0.54 to 2.04) | 0.186 | 1.09 (0.56 to 2.12) | 0.978 | 1.23 (0.49 to 3.10) | 0.623 |
| Other | 0.72 (0.54 to 0.95) | 0.78 (0.59 to 1.04) | 0.95 (0.70 to 1.28) | 1.23 (0.83 to 1.82) | ||||
| Retired | 0.96 (0.72 to 1.26) | 0.77 (0.59 to 1.02) | 1.00 (0.74 to 1.35) | 1.24 (0.82 to 1.89) | ||||
| Q27. First language | ||||||||
| English | Reference | |||||||
| Other | 1.38 (0.96 to 1.96) | 0.078 | 1.79 (1.28 to 2.52) | 0.001 | 1.61 (1.12 to 2.32) | 0.010 | 1.52 (0.97 to 2.37) | 0.068 |
| Q29. Repeat prescription | ||||||||
| No | Reference | |||||||
| Yes | 1.28 (1.04 to 1.56) | 0.019 | 1.46 (1.19 to 1.79) | < 0.001 | 1.70 (1.36 to 2.13) | < 0.001 | 1.45 (1.06 to 1.97) | 0.018 |
-
Awareness of any facilitation efforts includes respondents who ticked any of the first seven options of Q10.
-
Use of any facilitation efforts includes respondents who ticked any of the first seven options of Q11.
Considering digital confidence as an outcome (see Appendix 4, Table 48), we found a strong age gradient, with over 85-year-olds much less likely to be very confident than 55- to 64-year-olds (adjusted OR = 0.04, 95% CI 0.01 to 0.11; p < 0.001). We also found that parents were much more likely to be digitally confident than non-parents. People with long-term health problems, whose first language is not English, who are retired, or not in work/education were less likely to be digitally confident.
Patient survey free text
A total of 2246 responses were provided to the free-text questions 16 and 17 (Table 9).
| Q16 free-text responses | Q17 free-text responses | Total | |
|---|---|---|---|
| Paper survey | 905 | 695 | 1600 |
| Online survey | 396 | 250 | 646 |
| Total | 1301 | 945 | 2246 |
Respondents highlighted the following six areas of importance relating to DF in primary care:
-
Personal barriers to accessing digital services
-
Respondents described barriers including age, poor eyesight, learning difficulties, lack of internet literacy and poor access to computers or smartphones as limiting their ability to access digital services.
-
Practice barriers to accessing digital services
-
Several respondents felt that their practice was not supportive of online services or discouraged patients from using them. Other respondents felt that they needed help from practice staff to help with getting access to and using the digital services but commented that this help was not routinely offered.
-
How concerns about data security impacted their views on digital services
-
Some participants raised concerns about data confidentiality, data security and fears about online ‘scams’ and how this impacted their trust in the digital services offered by the practice.
-
How technology design impacted on access
-
Several respondents described that they found practice websites and mobile applications confusing and difficult to navigate, and this limited the use of the services.
-
Barriers in getting the right online credentials to access digital services
-
Several respondents found the process of getting access to online services difficult, especially in terms of verifying their identity with the practice and getting the correct login codes.
-
Potential facilitators to adopting digital technology
Respondents wanted to have more visibility about what was on offer from their practice, and also described unmet training needs about how to access and use online services.
The themes are described in more detail in Appendix 5.
Combined analyses of the practice survey and main patient survey
We found only limited evidence of differences between the reported awareness, and use of, different modes of DF (as reported in the patient survey) by patients registered at practices who reported using the corresponding mode for either promotion of, or supporting patients to use, online services (as reported in the practice survey – Table 10). There was strong evidence (p = 0.004) that patients registered at practices who reported using in-practice displays to support DF were more likely to be aware of such displays (18% vs. 11% of patients). Similarly, awareness and use of social media for DF were higher in those practices that reported using it (6% vs. 1% for awareness and 4% vs. 1% for use) and awareness and use of DF workshops/events were higher in those practices that reported using them (1.5% vs. 0.5% for awareness and 1.5% vs. 0.4% for use). No evidence of differences in patient awareness and use was seen between practices reporting using leaflets, text messages/e-mails, putting content on practice websites and providing tablets or computers, and those that did not. There was no evidence of differences in the patient awareness and use of any mode of DF between those practices that reported using ad hoc support for DF and those that did not (see Appendix 6, Table 51). Employing a practice champion was associated with higher patient use of facilitation but no greater awareness of that form of facilitation. Furthermore, there was no evidence of differences in the patient awareness and use of any mode of DF within any particular patient groups where practices reported targeting that group (see Appendix 6, Table 52).
| Mode of facilitation | % patients aware in practices using mode of facilitation | % patients aware in practices not using mode of facilitation | p-value | % patients using in practices using mode of facilitation | % patients using in practices not using mode of facilitation | p-value |
|---|---|---|---|---|---|---|
| Displays (N = 2935) | 17.55% (466/2655) | 10.71% (30/280) | 0.004 | 9.64% (256/2655) | 7.50% (21/280) | 0.244 |
| Leaflets (N = 2776) | 5.39% (92/1707) | 6.27% (67/1069) | 0.333 | 2.75% (47/1707) | 3.18% (34/1069) | 0.515 |
| Text/e-mails (N = 2828) | 39.14% (1068/2729) | 43.43% (43/99) | 0.390 | 28.22% (770/2729) | 25.25% (25/99) | 0.519 |
| Web content (N = 3032) | 7.43% (197/2650) | 8.38% (32/382) | 0.514 | 5.09% (135/2650) | 4.45% (17/382) | 0.590 |
| Social media (N = 2975) | 6.06% (105/1733) | 0.97% (12/1242) | < 0.001 | 3.64% (63/1733) | 1.21% (15/1242) | < 0.001 |
| Workshops/events (N = 2874) | 1.50% (4/267) | 0.46% (12/2607) | 0.030 | 1.50% (4/267) | 0.38% (10/2607) | 0.013 |
| Tablets/computers (N = 2921) | 0.65% (2/306) | 0.54% (14/2615) | 0.791 | 0.98% (3/306) | 0.42% (11/2615) | 0.180 |
Mental health boost sample
Of the 26 practices (who had already participated in the main patient survey) invited to participate in the mental health boost sample element of the patient survey, 18 agreed to take part (3 serving deprived populations). In total, 3456 patients were sent questionnaires (maximum of 200 per practice) of which 756 (21.85%) responded (see Appendix 7, Table 53). Analysis of double data entry detected a difference of 0.4% in data points entered.
Table 11 shows the demographics of responders to the patient survey mental health boost sample along with the responders to the main survey registered at the same general practices. Sixty-one per cent of those responding to the mental health boost sample survey reported that they had a long-term mental health condition. A higher percentage of responders to the mental health boost sample survey were female, aged 25–64, reported a long-term physical health condition and were much more likely to be in receipt of repeat prescriptions (94% vs. 66% in the main survey).
| Characteristics | Main patient survey (n = 944) total (%) | Mental health survey (n = 756) total (%) | |
|---|---|---|---|
| Gender | Male | 388 (41.4) | 231 (30.8) |
| Female | 550 (58.6) | 519 (69.2) | |
| Age | 16–24 | 45 (4.8) | 30 (4.0) |
| 25–34 | 49 (5.2) | 49 (6.5) | |
| 35–44 | 78 (8.3) | 83 (11.1) | |
| 45–54 | 136 (14.5) | 134 (18.0) | |
| 55–64 | 205 (22.0) | 174 (23.2) | |
| 65–74 | 228 (24.3) | 154 (20.5) | |
| 75–84 | 159 (17.0) | 98 (13.0) | |
| ≥85 | 38 (4.1) | 29 (4.0) | |
| Deaf/hearing impairment | Yes | 99 (10.7) | 100 (13.5) |
| No | 829 (89.3) | 642 (86.5) | |
| Blind/partially sighted | Yes | 21 (2.3) | 23 (3.1) |
| No | 899 (97.7) | 717(96.9) | |
| Parent | Yes | 120 (13.0) | 104 (14.1) |
| No | 800 (87.0) | 636 (85.9) | |
| Ethnicity | White | 892 (97.4) | 732 (98.3) |
| Other | 24 (2.6) | 13 (1.7) | |
| Mental health condition | Yes | 148 (17.5) | 402 (60.5) |
| No | 698 (82.5) | 262 (39.4) | |
| Physical health condition | Yes | 346 (39.8) | 371 (54.0) |
| No | 523 (60.2) | 317 (46.1) | |
| Working status | Work | 396 (44.0) | 312 (43.6) |
| Education | 22 (2.4) | 13 (1.8) | |
| Retired | 399 (44.3) | 249 (34.8) | |
| Other | 83 (9.2) | 141 (19.7) | |
| English as first language | Yes | 857 (93.7) | 721 (97.0) |
| No | 55 (6.3) | 22 (3.0) | |
| Carer | Yes | 205 (22.8) | 204 (27.7) |
| No | 695 (77.2) | 532 (72.3) | |
| Repeat prescriptions | Yes | 603 (65.6) | 703 (94.1) |
| No | 316 (34.4) | 44 (5.9) | |
| Help to complete survey | Yes | 47 (5.1) | 68 (9.1) |
| No | 871 (94.9) | 678 (90.9) | |
A summary of responses given by respondents to the patient survey mental health boost sample are shown in Table 12. Responders to the mental health boost sample survey reported higher levels of digital confidence, and they were considerably more likely to have used practice websites than responders to the main survey. Reported awareness and use of online services were generally higher for those responding to the mental health boost sample survey compared with those responding to the main survey (with the exception of awareness of booking appointments online) as was awareness and use of DF efforts (with the notable exception of social media). Responders to the mental health boost sample survey were also more likely to have been told about online services and helped to use them. Finally, a higher percentage of responders to the mental health boost sample survey endorsed all reasons for not using online services, with the exception of not having internet access.
| Characteristics | Main patient survey (n = 944) total (%) | Mental health survey (n = 756) total (%) |
|---|---|---|
| Digital confidence | ||
| Very confident | 488 (53.0) | 416 (56.0) |
| Quite confident | 219 (23.7) | 163 (22.0) |
| Not confident | 215 (23.3) | 165 (22.1) |
| Ease of practice website use | ||
| Very easy | 156 (16.8) | 167 (22.1) |
| Fairly easy | 291 (31.3) | 251 (33.3) |
| Not very easy | 89 (9.6) | 91 (12.1) |
| Not at all easy | 34 (3.7) | 52 (6.9) |
| Haven’t tried | 359 (38.6) | 193 (25.6) |
| Awareness of online services | ||
| Appointment booking | 518 (55.0) | 398 (52.6) |
| Repeat prescriptions | 621 (65.8) | 560 (74.1) |
| Access records | 280 (29.7) | 286 (37.8) |
| Access test results | 205 (21.7) | 215 (28.4) |
| E-mail enquiries | 340 (36.0) | 342 (45.2) |
| eConsults | 272 (28.8) | 302 (40.0) |
| Video consults | 124 (13.1) | 116 (15.3) |
| Use of online services | ||
| Appointment booking | 125 (13.2) | 131 (17.3) |
| Repeat prescriptions | 301 (32.0) | 380 (50.3) |
| Access records | 109 (11.5) | 137 (18.1) |
| Access test results | 71 (7.5) | 109 (14.4) |
| E-mail enquiries | 152 (16.1) | 152 (20.1) |
| eConsults | 167 (17.7) | 187 (24.7) |
| Video consults | 29 (3.1) | 32 (4.2) |
| Awareness of facilitation | ||
| Displays in the practice | 163 (17.3) | 193 (25.5) |
| Leaflets | 53 (5.6) | 64 (8.5) |
| Text/e-mails | 336 (35.6) | 324 (43.0) |
| Web content | 65 (7.0) | 74 (9.8) |
| Social media | 28 (3.0) | 21 (2.8) |
| Workshop/events | 5 (0.5) | 13 (1.7) |
| Tablets/computers | 5 (0.5) | 8 (1.1) |
| Use of facilitation | ||
| Displays in the practice | 89 (9.4) | 85 (11.2) |
| Leaflets | 28 (3.0) | 24 (3.2) |
| Text/e-mails | 238 (25.2) | 224 (29.6) |
| Web content | 41 (4.3) | 46 (6.1) |
| Social media | 23 (2.4) | 12 (1.5) |
| Workshop/events | 5 (0.5) | 4 (0.5) |
| Tablets/computers | 6 (0.6) | 3 (0.4) |
| Told about online services | ||
| Yes | 286 (31.2) | 285 (38.6) |
| No | 631 (68.8) | 453 (61.4) |
| Helped to use online services | ||
| Yes | 123 (13.6) | 112 (15.1) |
| No | 784 (86.4) | 626 (84.8) |
| Usefulness of online help | ||
| Booking appointments | 66 (7.0) | 60 (8.1) |
| Not helpful | 12 (18.2) | 14 (23.3) |
| Quite helpful | 25 (38.8) | 24 (40.0) |
| Very helpful | 29 (44.0) | 22 (36.7) |
| Ordering repeat prescriptions | 70 (7.4) | 66 (9.0) |
| Not helpful | 5 (7.1) | 5 (7.6) |
| Quite helpful | 18 (25.7) | 16 (24.2) |
| Very helpful | 47 (67.1) | 45 (68.2) |
| Accessing medical records | 43 (4.6) | 45 (4.0) |
| Not helpful | 10 (23.3) | 12 (26.7) |
| Quite helpful | 14 (32.6) | 9 (20.0) |
| Very helpful | 19 (44.2) | 24 (53.3) |
| Accessing test results online | 38 (4.0) | 39 (6.1) |
| Not helpful | 12 (31.6) | 10 (25.6) |
| Quite helpful | 9 (23.7) | 12 (30.8) |
| Very helpful | 17 (44.7) | 17 (43.6) |
| E-mail enquiries to the practice | 44 (4.7) | 59 (8.0) |
| Not helpful | 11 (25) | 13 (22.0) |
| Quite helpful | 15 (34.1) | 14 (23.7) |
| Very helpful | 18 (41.0) | 32 (54.2) |
| Help from GP using online form | 56 (6.0) | 58 (7.8) |
| Not helpful | 10 (17.8) | 11 (19.0) |
| Quite helpful | 18 (32.1) | 17 (29.3) |
| Very helpful | 28 (50.0) | 30 (51.7) |
| Online video consultations | 23 (2.4) | 23 (3.1) |
| Not helpful | 11 (47.8) | 8 (34.8) |
| Quite helpful | 4 (17.4) | 2 (8.7) |
| Very helpful | 8 (34.8) | 13 (56.5) |
| Reasons why not using online services | ||
| No internet access | 76 (8.1) | 52 (7.0) |
| Security concern | 60 (6.4) | 61 (8.1) |
| Confidentiality | 44 (4.7) | 50 (6.6) |
| Not knowing how to register | 136 (14.4) | 100 (13.2) |
| Registration too difficult | 45 (4.8) | 56 (7.4) |
| Not knowing how to get support | 61 (6.5) | 77 (10.2) |
| Practice too busy to help | 82 (8.7) | 97 (12.8) |
| Prefer to speak to person | 439 (46.5) | 379 (50.1) |
The higher awareness and use of facilitation efforts by responders to the mental health boost sample survey, along with increased likelihood of being told about online services, were confirmed by univariable logistic regression (see Appendix 7, Table 53), but the difference in terms of being helped to use online services was not statistically significant. In adjusted models the only difference between responders to the mental health boost sample survey and the main survey that remained statistically significant was awareness of facilitation (see Appendix 7, Tables 54 and 55) indicating that observed differences in use of facilitation and being told about digital services may be related to differences in the demographics of the samples.
Findings from analysis of national General Practitioner Patient Survey data
Of the 1,510,149 responders to the 2019 and 2020 national GPPSs and the 1,569,343 responders to the 2021 and 2022 national GPPSs, 1,212,801 (77.3%) and 1,304,574 (86.4%) reported trying to make an appointment at their GP practice in the 12 months prior to responding to the survey, respectively.
Among this subset of responders, awareness of online appointment booking and ordering repeat prescriptions online was moderate (2019–20 percentages weighted for non-response = 49% and 45%, respectively), but awareness of the ability to access medical records online was low (2019–20 weighted percentage = 18%). Use of all three services (based on 2021–2 data) was lower at 23%, 32% and 13%, respectively. Around a quarter (25% in 2021–2) of responders reported use of online consultations.
The results of the adjusted logistic regression models are shown in Figures 9–13 and in Table 56, Appendix 8. There was a strong decrease in the awareness and use of all services (making appointments online, ordering repeat prescriptions online, accessing medical records online, and online consultations) with older age; individuals aged over 85 years were much less likely to be aware of, or to report using, online services than younger people (see Figure 9). For ordering repeat prescriptions online, there was a smaller reduction in awareness and use in younger responders than in 55- to 64-year-olds, but for the other services awareness plateaued, and use increased, in all but the youngest responders. Similarly, there were very strong deprivation gradients in the awareness and use of all online services (see Figure 10). Females were more likely to be aware of all three services considered (appointment booking, repeat prescriptions and access to medical records) and more likely to use online consultations and order repeat prescriptions online, but less likely to actually book appointments online or access medical records online (see Figure 11). All non-white ethnic groups were less aware of all three online services that were considered than white responders and were generally less likely to actually use the services, with the exception of booking appointments online where higher use among ethnic minorities was seen (see Figure 12). Those with long-term conditions were more likely to be aware of and use all online services, particularly ordering repeat prescriptions (see Figure 13). Finally, we found that the practice in which a patient was registered was, by far, the strongest predictor of awareness and use of online services (Table 13). For example, the OR comparing the practice with the highest awareness of online booking with the lowest among the middle 95% of practices (i.e. ignoring the most extreme) was 16.2 (95% CI 15.2 to 17.0).
FIGURE 9.
Variation of awareness (red) and use (blue) of online services by age obtained from adjusted logistic regression models (odds ratios and 95% CIs).
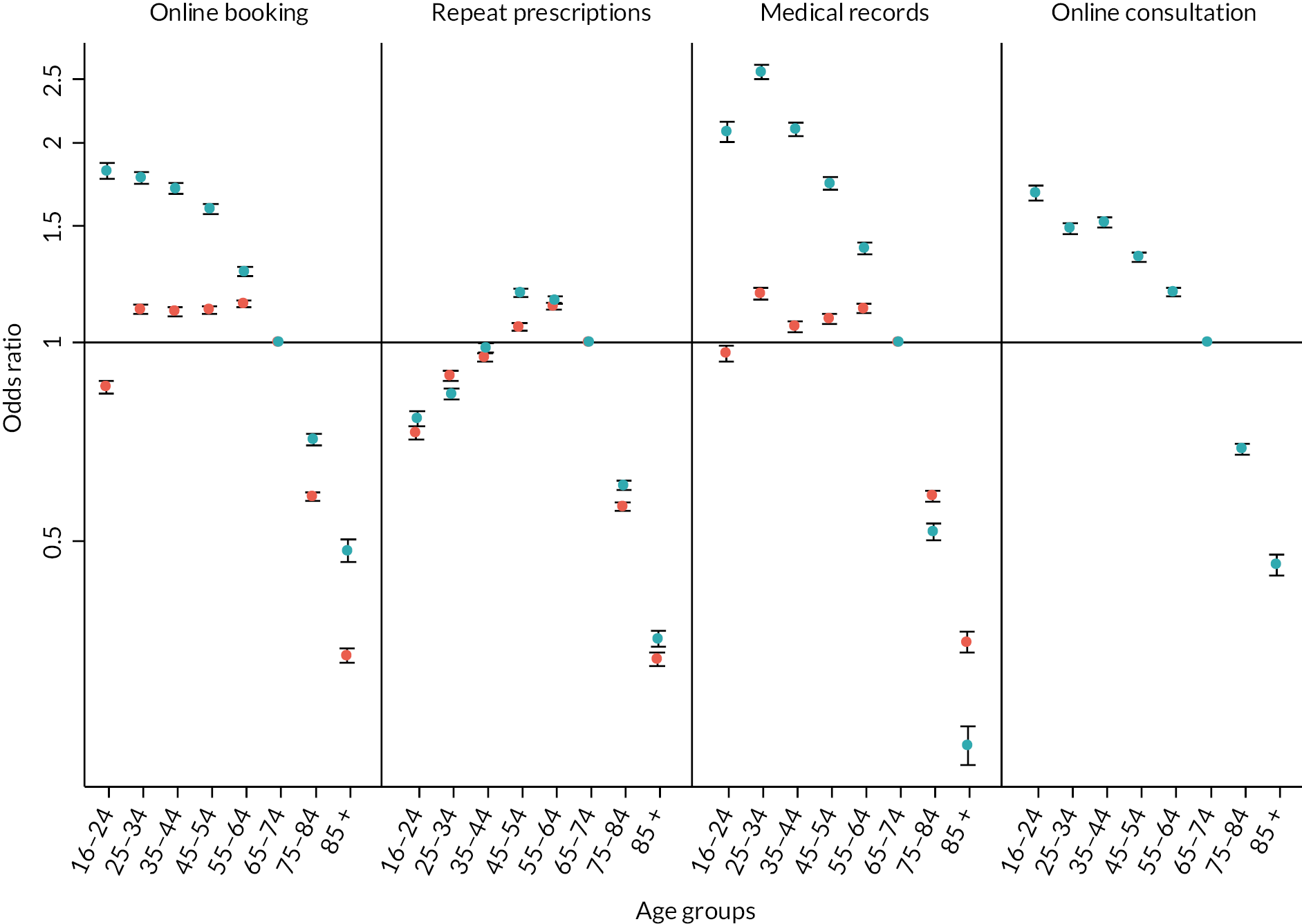
FIGURE 10.
Variation of awareness (red) and use (blue) of online services by deprivation obtained from adjusted logistic regression models (odds ratios and 95% CIs).
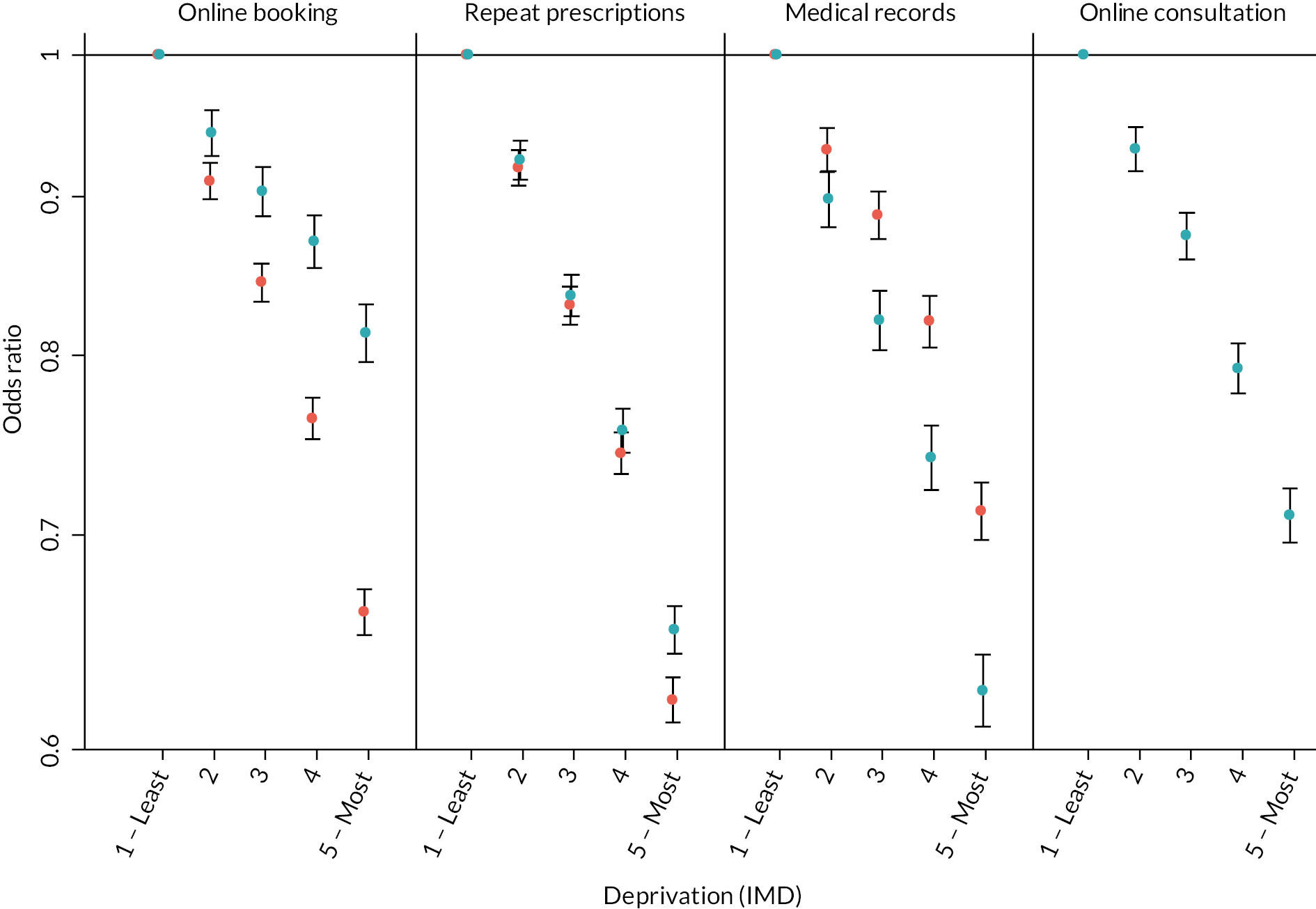
FIGURE 11.
Variation of awareness (red) and use (blue) of online services by gender obtained from adjusted logistic regression models (odds ratios and 95% CIs).
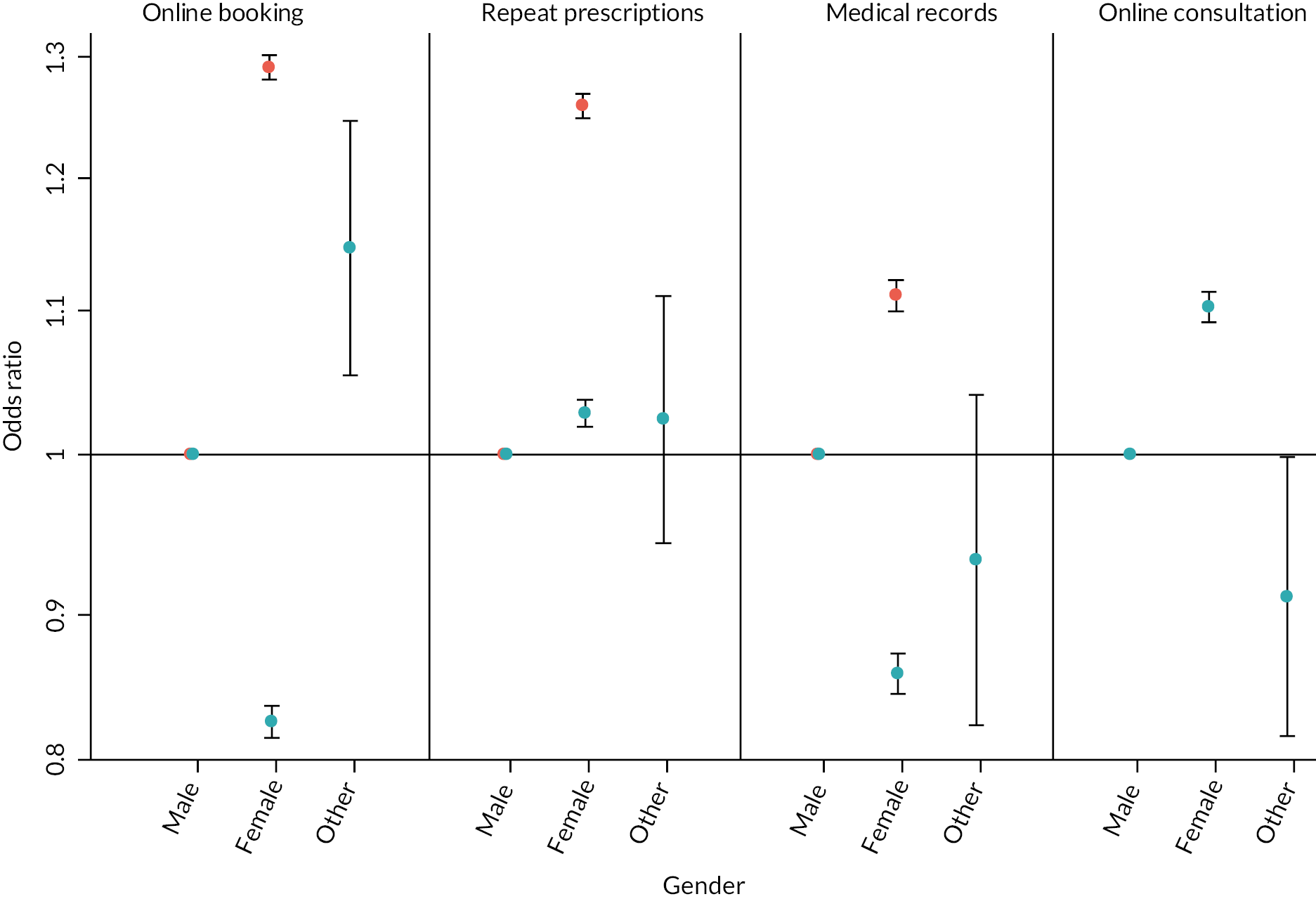
FIGURE 12.
Variation of awareness (red) and use (blue) online services by ethnicity obtained from adjusted logistic regression models (odds ratios and 95% CIs).
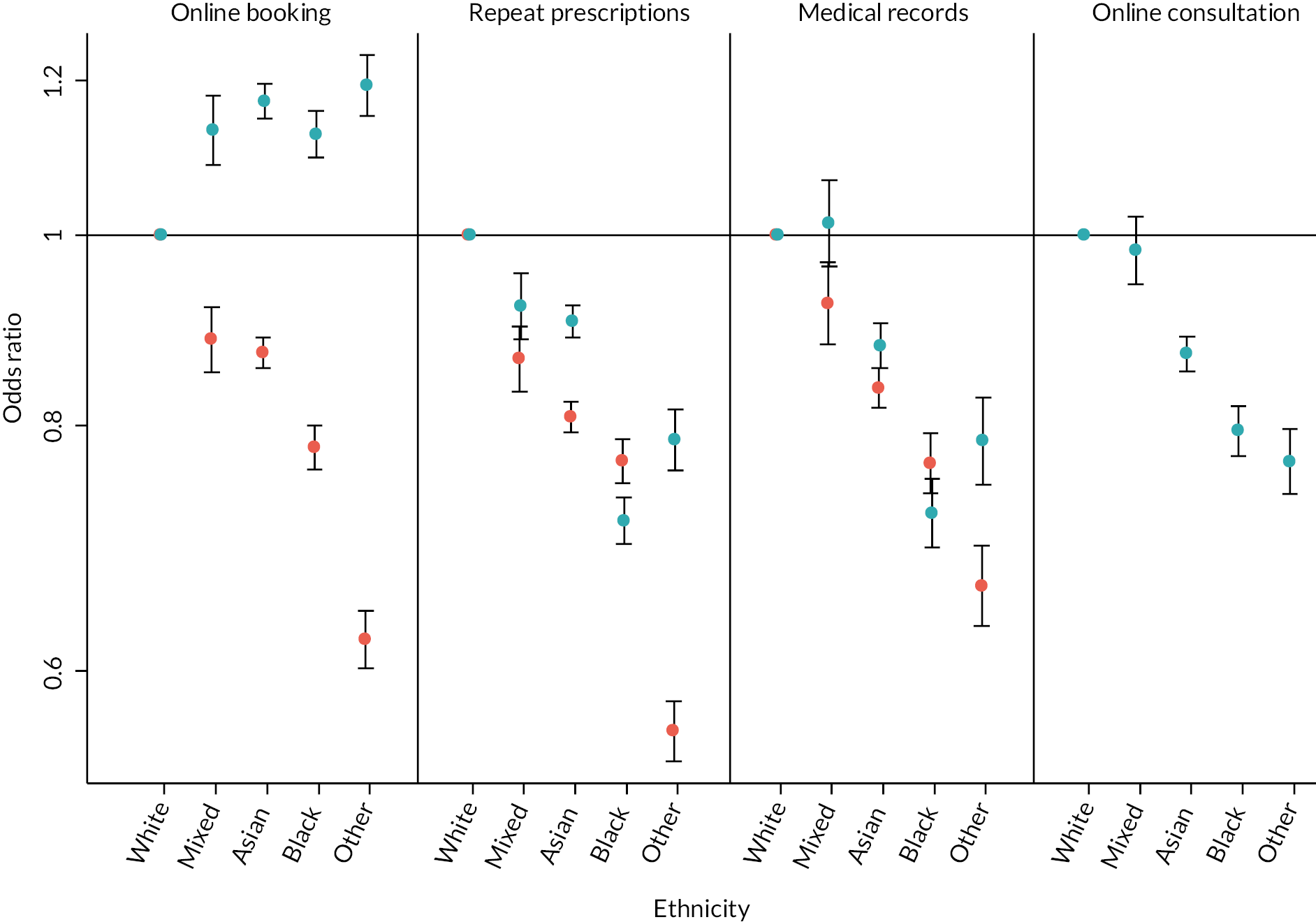
FIGURE 13.
Variation of awareness (red) and use (blue) of online services by long-term condition status obtained from adjusted logistic regression models (odds ratios and 95% CIs).
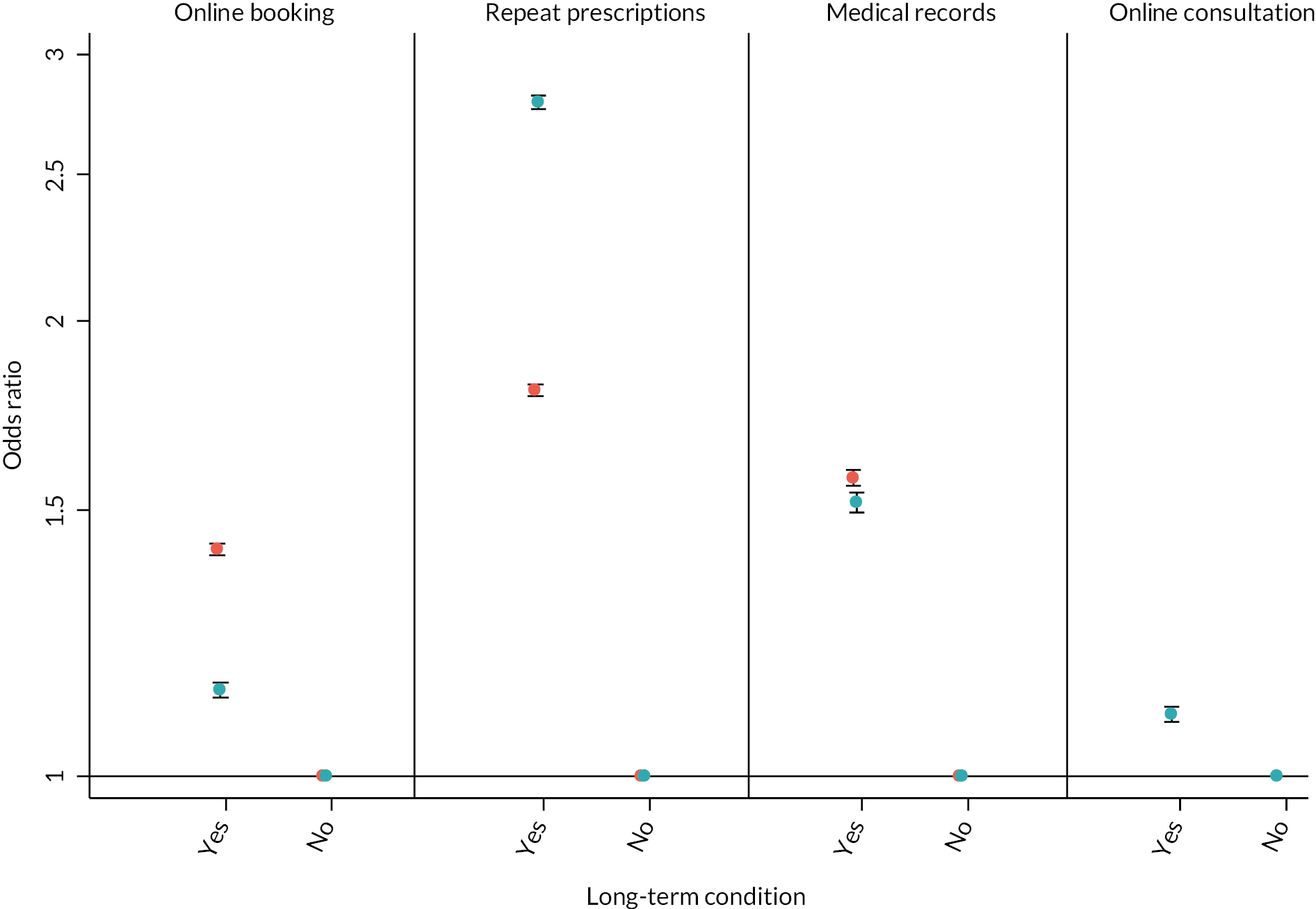
| Online booking appointment | Online repeat prescriptions | Online medical records | Online consultations | |||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Awareness | 16.18 | (15.34 to 17.02) | 8.40 | (8.07 to 8.75) | 12.32 | (11.7 to 12.95) | N/A | N/A |
| Use | 11.85 | (11.30 to 12.44) | 5.80 | (5.60 to 6.02) | 8.47 | (8.08 to 8.89) | 7.03 | (6.76 to 7.32) |
Augmenting the regression models with patients’ experiences of other aspects of the practice (see Appendix 8, Table 57) found that:
-
Patients who say it is easy to get through on the phone tend to have lower awareness and use of online services than those who say it is not at all easy.
-
Patients who report receptionists being helpful tend to have higher awareness but lower use of online services, than those who report receptionists being not at all helpful.
-
Awareness and use of all online services is most often reported for patients who have a preferred GP for some appointments. With the exception of online consultation use, this is followed by those who report a preferred GP for all appointments, with those who do not have a preferred GP least likely to report awareness or use of online services.
-
Patients who say the practice website is easy to use are much more likely to report awareness and use of online services.
The effect of ease of use of practice websites was particularly strong within the models of awareness and use of online provision; the ORs comparing those who rated practice websites as ‘very easy’ to use compared with those who said it was ‘not easy at all’ being 5.29 (5.12, 5.48), 5.73 (5.54, 5.93) and 4.07 (3.92, 4.24) for awareness of online appointment booking, ordering repeat prescriptions and accessing medical records online, respectively. Because these ORs may reflect individuals’ general difficulty with using websites we also repeated models replacing person-level responses with a practice score for ease of website use. In that case the odds ratios were more modest, but still substantial at 1.40 (95% CI 1.32 to 1.47), 1.51 (95% CI 1.45 to 1.58) and 1.45 (95% CI 1.38 to 1.52), respectively.
In the final set of models examining GPPS data in isolation (see Appendix 8, Table 58) we looked at whether reported ease of use of practice websites modified the effect of sociodemographic factors. We found evidence of interactions between age, deprivation, gender, having a long-term condition, rurality and one or more of awareness of online appointment booking, use of online appointment booking, or awareness of repeat prescriptions. In all cases good websites were associated with higher awareness and use and the direction of demographic associations did not change for when practices had good or poor websites, though the magnitude of the associations did change, but only to a modest extent. Age, ethnicity, long-term condition and rurality differences were slightly larger when websites were rated as good compared with when they were rated poorly. In contrast, gender and deprivation differences were slightly smaller when websites were rated as good compared with when they were rated poorly.
The results of the analysis of GPPS data from practices who participated in the WP2 practice survey are shown in Appendix 8, Table 59. After adjustment for patient characteristics, we find that 7 out of 63 associations examined are statistically significant at the p < 0.05 level and as such care must be taken with the interpretation of these findings. However, we do see a consistent effect whereby patients registered at practices who report the use of leaflets for DF are less likely to report being aware of online services (appointment booking, medical record access and repeat prescriptions) than those registered at practices that did not report use of leaflets.
Patient and public involvement and engagement
Box 4 describes how the PAG influenced WP2.
-
Some of the feedback for both practice and patient surveys provided the research team with a reminder of the wider picture of, for example, patient frustrations with trying to access practices, especially when moving to online services in practices.
-
The PAG made suggestions for changes to the contents of practice and patient surveys which were added or amended as a result:
Practice survey:
-
Adding in or amending response options (e.g. use of e-mails to/from practices as a further response choice).
-
Offered examples to add into the survey (e.g. use of smart phone apps).
-
Helped to reword some DF options (e.g. include TV display in surgeries).
-
Put forward the suggestion of including those with carer responsibilities as a potential group that practices might target with DF.
-
Generated discussion on whether to include or how to include points in the surveys.
Patient surveys:
-
Involvement in an initial brain-storming session for the survey helped to consider which minority groups may need targeted support when using online services (e.g. those with learning difficulties, older adults, isolated rural communities, and carers).
-
The PAG helped to identify words that might cause a barrier to understanding the questionnaire (e.g. ‘activities’, ‘facilitation’ and ‘engage with’), which were removed.
-
The group provided feedback on completion and on the length of the survey.
-
Further explanation of acronyms and abbreviations were requested in the patient invitation letter.
-
References to a mental health survey were changed in footnotes of patient facing documents and in the reminder postcard.
-
The PAG have been involved in meetings where results are presented and have contributed to discussions on interpretation of these from the perspective of their experiences as patients.
Practice survey:
-
Put forward suggestions to explore how the role of the member of staff completing the questionnaire may influence responses.
-
Suggested looking at whether the use of a practice champion or volunteers to provide digital support (practice survey) in practices affected patient’s experiences (patient survey).
Patient surveys:
-
The PAG met with researchers who presented the findings of both the patient survey and mental health boost sample survey. The findings reflected their own experiences of use of online services, access to primary care services and lack of support for their use, one commenting that to get access to ask for ad hoc support at their practice reception had been challenging.
Summary of main findings: work package 2
Practice survey
Most practices reported offering a range of online services. With the notable exception of online appointment booking (which was withdrawn nationally in response to the COVID pandemic), the number of practices offering them had substantially increased during the COVID pandemic (particularly video consultations). While most practices reported using passive modes of DF to promote or support patients’ use of online services (social media), more active modes of DF (e.g. employing a practice champion), were rarely reported. In the vast majority of practices, administrative and reception staff conducted DF efforts, with clinical staff contributing in more than half of practices. Most practices reported targeting their facilitation efforts at older adults. While most practices were generally positive about DF, many of them felt that they lacked the capacity to deliver it.
Patient survey
Among responders to the main survey there was bimodal distribution in digital confidence, with many patients indicating very high confidence, but a substantial number indicating very low confidence – highlighting a group of patients who lack the capability to use digital tools unaided. Furthermore, around a third of patients had not used their general practice’s website. While more than half of the patients were aware of online appointment booking and potential for ordering repeat prescriptions online, awareness of other online services (e.g. accessing test results) was much lower, and use of online services was low apart from online appointment booking. Patients endorsed a range of reasons for not engaging with online services, in particular reporting their preference to speak to someone and also reporting having difficulties registering to use online services. Such difficulties indicate the potential lack of effective DF. Older patients, and patients with lower digital confidence, were less likely to be aware of or to use DF efforts offered by practices, or to have been informed about or helped to use online services. However, it was encouraging to find that those of non-white ethnicity and those for whom English was not their first language were more likely to report experiences consistent with engagement with or being engaged in DF. Being in receipt of repeat prescriptions was also a factor associated with such engagement. Free-text responses indicated a range of barriers when accessing online services. These included personal barriers (e.g. access to resources), concerns about data security, difficulties with technology design, practice-level barriers and difficulties with credentials. Broadly similar findings were found in responders to the mental health boost sample survey, although these patients generally had higher awareness and use of online services, higher awareness and use of DF efforts, while also reporting more barriers to using online services. While there were some associations between the DF efforts reported in practice and patient survey responses, they were not always present, indicating a potential lack of effectiveness.
Responders to the mental health boost sample survey were more likely to be digitally confident, were more likely to have used general practice websites and were more likely to be aware of and use online services than responders to the main survey (though this may in part reflect the fact that responders to the mental health boost sample survey were younger, on average, than responders to the main survey). Responders from the mental health boost sample were also generally more likely to report that they were aware of, and made use of, DF undertaken by their practice. However, these associations (except for awareness of facilitation) did not persist once adjustments were made for the demographic composition of responders indicating that differences between responders to the main survey and the mental health boost sample survey were largely attributable to factors other than their mental health status.
General Practice Patient Survey
Of patients who recently tried to make an appointment, just under half were aware of online appointment booking and ordering repeat prescriptions. Considerably fewer were aware of the potential to access medical records online, which was consistent with the findings of our patient survey. Between 13% and 32% of these patients reported use of these online services, with around a quarter reporting the use of online consultations. Older patients, those from deprived areas and those from non-white ethnic groups were generally less likely to be aware of and use all online services. In contrast, those with long-term conditions were more likely to be aware of or to use all online services. While differences between patient groups were substantial, the practice with which a patient was registered was, by far, the strongest predictor of patient awareness and use of online services. Some of this between-practice variation may be attributed to the ease of use of the practice website, indicating the potential for DF.
Deviations from the original proposal
Our original proposal stated that we would aim for 60% of general practice responding to the practice survey. In reality, only 31% did so. This deficit can largely be attributed to the COVID pandemic which placed demand on practice staff, reducing the capacity to take part. Furthermore, we had planned for CRN staff to make phone calls to non-responding practices to encourage participation. However, at the time this research was undertaken, CRN staff were prioritising COVID-related studies and some CRN staff were redeployed to other duties resulting in relatively few practices actually being contacted by CRNs. In light of the smaller than anticipated number of practices participating in the practice survey, with the agreement of NIHR, we reduced the target number of practices participating in the patient survey from 120 to 60. In tandem the target number of patient surveys mailed from each practice was increased from an average of 100 to 200. To ensure representativeness, the number of patients mailed a survey was higher in practices serving deprived populations than those serving less deprived populations. Despite these changes, we were unable to recruit 60 practices to undertake the patient survey from within those practices who had responded to the practice survey. Consequently, we invited practices from outside of our original practice survey sample in order to achieve our target. When doing so we focused on practices in deprived areas to ensure representativeness overall. To facilitate comparisons between patient and practice responses, these additional practices completed a practice survey questionnaire, but were not included in the main practice survey data analysis (as they were not part of the original random sample).
A difference occurred with the analysis of data from the GPPS. One of the questions we had intended to analyse was removed from the questionnaire in 2021. So instead of using the most recent data, analysis of responses in relation to awareness of online services related to data from 2019 to 2020.
Strengths and limitations
There are a number of strengths to this quantitative work. First, we achieved a broadly similar number of responses from patients across all deprivation quintiles by over-sampling patients in deprived areas. Second, we adopted a multimodal approach, collecting data at the practice and patient levels and using national GPPS data, and combining data from the different sources. Third, we refined the survey procedures by piloting the survey and obtained extensive PPIE input. Finally, this work was undertaken as part of a large-scale research project commenced at the start of the COVID pandemic which presented multiple challenges. However, our agile approach allowed us to deliver the WP despite the challenges faced.
There were also some limitations. We had a low response rate from the patient and practice surveys. The response rate could have been an artefact of our efforts to target patients in more deprived areas where the response rate is typically lower. However, our patient survey response rate (24%) is comparable to other primary care-based surveys169–172 and should be considered credible considering the challenges presented by the COVID pandemic.
Furthermore, we did not have information on the socioeconomic status (e.g. deprivation) of patients or the rurality classification of where they lived. This was largely due to not having access to patient addresses which would allow linkage to data sets containing this information.
Chapter 4 Qualitative exploration (work package 3): methodology and sample
Aims and objectives of the qualitative exploration
The qualitative exploration was conducted to investigate in-depth, and from the perspective of practice staff, patients/carers and other stakeholders, the potential benefits and challenges associated with different models of DF. The study was informed by the research undertaken in earlier phases of the Di-Facto study, reported in previous chapters of this report.
The qualitative exploration comprised two elements:
-
Focused ethnographic case studies in general practices:
Focused ethnography was used to explore in-depth the use of DF in general practices. General practitioner practice case study sites were selected and through non-participant observation, semistructured interviews of staff and patients and secondary analysis of documentation, the researchers sought to build up a detailed picture of DF.
-
Interview study with key stakeholders:
In addition to the in-depth understanding of experiences of DF within individual practices, we sought to locate this study within a broader context and understanding what influences DF in primary care as a setting. We conducted semistructured interviews with stakeholders who may have critical oversight at a level beyond individual practices, for example, policy-makers, commissioners and third-sector organisations.
COVID pandemic
The study was designed prior to the COVID pandemic. COVID led to significant changes in the provision of primary care with an increase in remote consultations and use of digital services. It was necessary to adjust our approach in light of both the changes in primary care due to COVID and national COVID guidance. Fieldwork was conducted between September 2021 and July 2022. During this time, on 8 December 2021, England moved to ‘Plan B’ for Omicron which affected the fieldwork and recruitment, and the ‘living with COVID’ guidance was published on 24 February 2022. 173 The case studies focused on DF reported at the time of the research and within the context of the COVID pandemic, the research explored how general practice made changes to service delivery in light of COVID.
Rationale for the methodological approach
Rationale for the methodological approach
The study required an approach which would enable the research team to explore in-depth how DF occurred within general practice. As noted by Reeves et al. 174 ‘the central aim of ethnography is to provide rich, holistic insights into people’s views and actions, as well as the nature (that is, sights, sounds) of the location they inhabit, through the collection of detailed observations and interviews’. A focused ethnographic approach was selected. Unlike traditional ethnographic approaches, focused ethnography enables shorter and more focused periods of ethnography and focus on a predetermined topic. The approach had also been successfully used by researchers on this project (HA) in previous work. 175 Interviews were used to explore the views of stakeholders on DF and complement the general practice-based research.
Qualitative exploration team
Team composition
The core qualitative exploration team comprised nine members (see Contributions of authors).
Communication
Throughout the study the qualitative exploration team met monthly to ensure communication between team members. In early 2022 two whole-team face-to-face meetings occurred to discuss and develop analysis plans. In addition, the case study team met fortnightly during the data collection and analysis phase to ensure consistency of approach and discuss any issues arising. Researchers conducting the focused ethnography met weekly during the data collection phase. Stakeholder interview study researchers and mental health interview study researchers also met regularly during the relevant parts of the study.
Focused ethnographic case studies
The focused ethnographic case studies involved a researcher spending 6–8 weeks conducting fieldwork in each practice. The intensity of attendance varied according to the extent and types of DF activities within the practice, the size of the practice and COVID restrictions in place. We sought to understand the practice context (i.e. patient demographics, location, ways of working), how and why the model of facilitation in use might lead to benefits, the key processes involved in DF, and identify outcomes of importance to patients/carers and staff. We also investigated factors that may act as barriers and facilitators both to the practice being able to offer DF and to patients or carers using online services.
Case study recruitment
Sampling of general practices
Our aim was to include a varied sample of eight practices that would provide findings that are relevant across a range of primary care settings. Sampling of general practices focused on seeking variation according to two factors.
Experience of and/or delivery of digital facilitation using different approaches
As outlined in the protocol we aimed for variation according to the types and level of DF in use within practices. Individual practices were identified via the practice survey responses (see Practice survey) and where needed by obtaining information from practices directly about the types of DF in use.
Practice characteristics considered to inform sampling (illustrated in Figure 14)
FIGURE 14.
Illustration of sampling considerations for the selection of case study sites.

We selected practices for variation according to range of characteristics:
-
Practice setting (rural/semi-rural/urban) appears to be systematically associated with variation in access to general practice, for example, older people in rural areas have poorer access to GP services176 and face digital exclusion due to poor availability of broadband internet. 177
-
A range of IMD scores at practice level, as socioeconomic status appears to mediate health disparities via reduced health literacy. 167
-
Number of patients aged ≥ 65 years in the general practice, as although levels of use are increasing, older adults (≥ 75) are less likely to use the internet, and the 16–34 age group are the highest users of the internet.
-
List size of the practice [from a range across small (< 6000) to large (> 12,000) registered patients]. 167
Recruitment of practices
The results of the practice survey conducted in WP2 (see Practice survey) were used to identify general practices for potential participation. The sampling considerations indicated in Figure 14 were used to identify a range of potential sites via a sampling matrix. Where this was not possible, the researchers worked with local CRNs to support the initial approach to practices. Where this was not possible the researchers contacted general practices directly. Some CRNs also approached or provided contact details for practices that had not completed the survey but matched the matrix criteria. An eighth practice was recruited to ensure greater diversity in the study sample.
Practices were sent an introductory e-mail which was followed up with a phone call or e-mail up to two times with a week between each contact. In the case of no response, it was assumed that the practice did not wish to take part and they were not contacted again.
Interested practices were given written information about the study to share with staff members. For practices agreeing to participate, an online site visit was arranged where the research team, and where appropriate the CRN, explained the study and answered any questions. Sampling was continuously reviewed and further recruitment was tailored to ensure the intended range and variation in participating practices.
Data collection and management
Data collection approaches included in each case study site are given below.
Non-participant observation
Observations focused on DF occurring within the general practice, specifically, what was involved in the process of DF and how practice staff and patients/carers interact with different types of DF. We did not directly observe consultations with patients but did ask about DF in clinical consultations during interviews with both clinicians and patients. Observations and informal conversations were recorded in extensive handwritten fieldnotes, without use of identifiers or names. Where possible, fieldnotes were made at the time of observation but if not, were written up as soon as possible afterwards. Each participating practice was allocated a letter (i.e. Practice A, Practice B, etc.) so that any information stored about the practice was de-identified.
Posters were put on noticeboards in both public and staff-only areas of the practice, and, where possible, on the practice website. The poster included a photograph of the researcher and the researcher’s contact details, along with an explanation of the study and the dates that the researcher was to be in the practice. Staff members and patients had the right to decline to be observed; however, this did not occur.
The researchers were sensitive to situations where their presence could cause any issue. Researchers were trained in observation techniques and had the support of an experienced qualitative researcher (HA).
Attending practice meetings
Researchers explored whether there were any relevant practice-level meetings to attend. These meetings would include those where DF or related issues were discussed. When attending such meetings, the researcher ensured that all participants were aware of who they were and why they were there. Fieldnotes were maintained both during and after meetings and, with permission, relevant documentation collated.
Collection of relevant data and documentation
Researchers collected documentation pertaining to digital services or facilitation within the practice. Staff were asked to provide these with any identifiable information removed. The researcher discussed with the practice staff member the relevance of the documents and why they were important in relation to DF.
Semistructured interviews
Semistructured interviews were conducted with patients/carers and practice staff within case study practices.
Sampling and recruitment of practice staff
We sought to interview three to four staff at each practice during the fieldwork, based on their role and involvement in DF activities, and invited to participate in an interview but were free to decline without providing a reason.
Sampling and recruitment of patients/carers
We sought to recruit three to four patient/carer participants per practice, sampling to include a mix of characteristics in terms of age, ethnicity and experience (or not) of DF. Patients were identified by practice staff who also checked the suitability of those selected (aged 18 years and over) to ensure that they had capacity to consent and that there was no other reason why they should not be approached. The practice sent patients an invitation (by post, e-mail or given in person) to participate along with an information sheet about the study. Recipients were invited to reply to the study team (using an enclosed reply slip or e-mailing the researcher directly via contact information on the reply slip) to indicate that they were willing to participate in the study.
Interview procedure
Topic guides for staff and patient/carer interviews were informed by the review and practice survey. The topic guide for staff covered the drivers for facilitation in the practice, the type of facilitation in use (resources, processes, valued outputs), the perceived success of the facilitation model and barriers or facilitators to implementation (see additional files www.fundingawards.nihr.ac.uk/award/NIHR128268; accessed 3 April 2024). The topic guide for patients/carers explored their use of online services outside of health, experiences of DF with the practice and barriers and facilitators to using online GP services (see additional files www.fundingawards.nihr.ac.uk/award/NIHR128268; accessed 3 April 2024).
Interviews were conducted either in person, by online video conferencing or telephone according to participant preference. With permission, all interviews were audio-recorded with the use of encrypted recorders. Consent was obtained prior to all interviews. Interviews were transcribed verbatim by a professional transcription service. Patient/carer participants were given a £10 shopping voucher to thank them for their time.
Data management
Data files were stored on secure servers and only accessible to the study team after being anonymised. Recordings were stored until transcribed and checked then deleted from servers.
Vulnerable groups
In the context of digital inequalities, individuals from older age groups, those in minority ethnic groups, those in lower socioeconomic groups, those in poorer health and individuals in rural settings are recognised as vulnerable groups. 16–19 Throughout the qualitative exploration, researchers sought to include participants from these groups. This approach was embedded throughout the study and something researchers were conscious of in the design, conduct and writing up the research. For example, in the focused ethnographic work the research team sought to include a range of general practices from diverse areas to include vulnerable groups.
Stakeholder interview study
Figure 15 indicates the design of the stakeholder interview approach.
FIGURE 15.
Design of stakeholder interview approach.
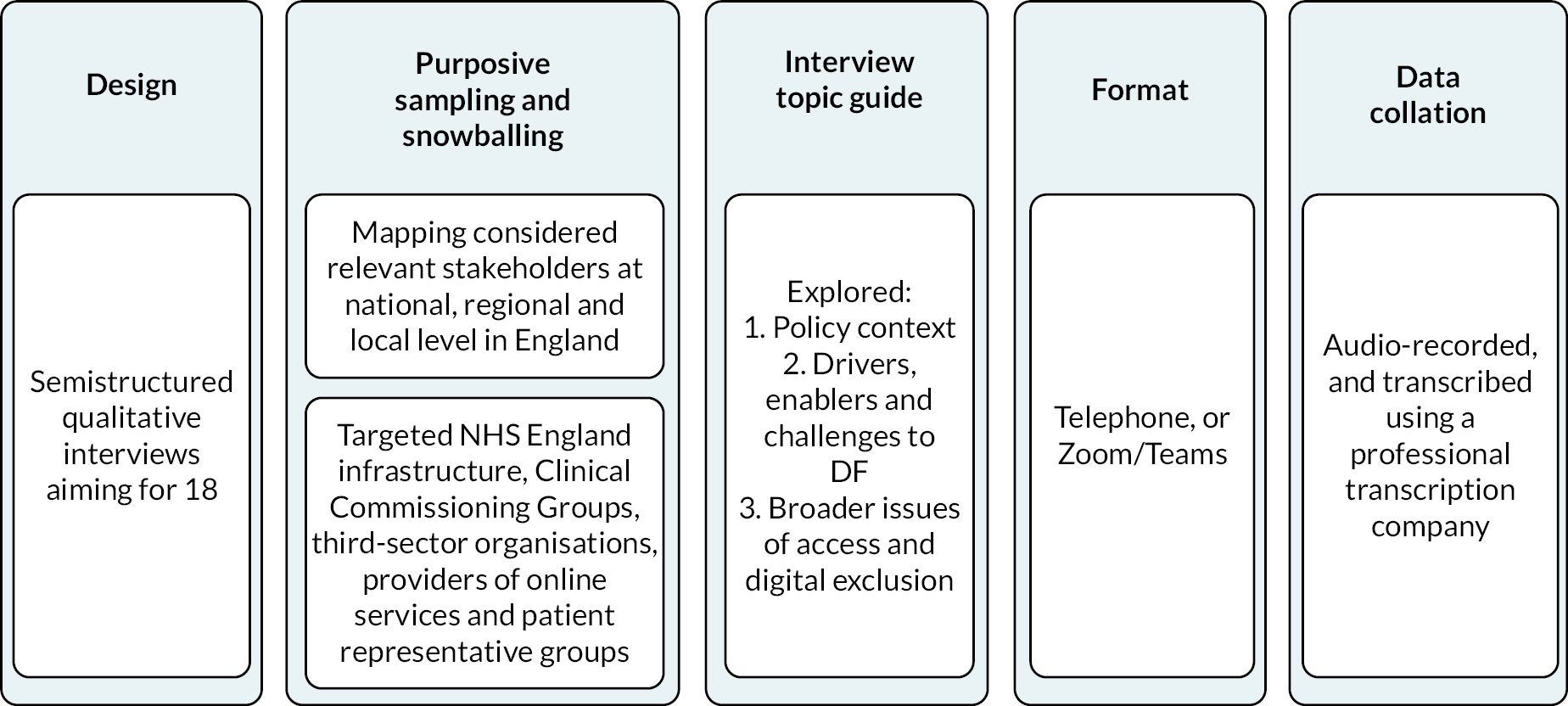
Stakeholder sampling and recruitment
This element sought to recruit 12–20 stakeholders relevant to the provision or impact of DF beyond the level of individual practices. This included stakeholders who may have critical oversight of DF in primary care or those representing patient groups at local, regional and national levels, including those from CCGs and ICSs, NHS England and third-sector organisations.
Identification of stakeholders was informed initially by integrating policy reviews, knowledge of the health system and patient and professional bodies, networks of the wider research team and internet searches. Snowball sampling was then used to identify further stakeholders and to respond to emerging findings from the study, including recruitment of representatives of organisations which focused on DF or digital primary care for potentially vulnerable populations.
Interview procedure
Individuals were invited for interview by e-mail and sent an information leaflet about the study. Recipients were asked to reply to the e-mail to indicate if they were willing to participate. The topic guide (see additional files www.fundingawards.nihr.ac.uk/award/NIHR128268; accessed 3 April 2024) explored the key drivers of DF, how stakeholders thought DF worked and the intended consequences of its application, both positive and negative. Interview procedures were followed as outlined for staff interviews.
The experience of patients living with mental health conditions
The project was extended to include an additional focus on patients with an experience of a mental health condition. The aim was to explore within case study practices how patients living with mental health conditions experience DF.
Practice sampling
This element of the study aimed to include four of the case study practices, seeking practices from each geographical area (Southwest, East of England, West Midlands, East of England and the North West).
Patient sampling and recruitment
Interviews with four to five patients with mental health conditions were sought per practice. We focused on patients with anxiety, depression, or severe enduring mental illness, identified from diagnoses or from recent prescriptions recorded in the patient record.
Searches of electronic records were run at participating practices to identify potential participants. Practice staff checked the suitability of patients, including capacity to consent, before sending them a postal invitation along with an information sheet about the study.
Patients were informed that they had been invited to take part because they had been identified by the practice as living with a mental health condition. Invitees were reassured that the invitation had come directly from the general practice therefore researchers were not aware of their details and health condition and would not be unless they chose to take part in an interview.
Interested participants responded by returning a reply slip to the research team.
Interview procedure
The topic guide was an adapted version of that used for the main study. Changes were made in conjunction with members of the PAG with specific lived experience of mental health conditions, set up to support this element of the study. The topic guide was adapted to focus on the specific experience of this group of patients (see additional files www.fundingawards.nihr.ac.uk/award/NIHR128268; accessed 3 April 2024). Interviews were handled as in the main study (see above).
Data analysis
Data from the focused ethnographic case studies and stakeholder interviews were analysed together using reflexive thematic analysis. 178 Analysis of the mental health interviews was conducted later using the same coding framework.
Reflexive thematic analysis178 was applied through the following steps:
-
Reading transcripts and developing the coding frames; transcripts were read, anonymised and accuracy checked by the researcher who conducted the interviewer. A selection of transcripts were read by the wider qualitative team. Coding frames were developed in a series of team meetings. A patient coding frame, a practice and staff coding frame (to include fieldnotes and interview data) and a stakeholder coding frame were developed. Analysis of relevant data and documentation obtained from each case study site was used to provide context.
-
Agreeing a final coding frame at an analysis meeting; we held an in-person meeting to finalise the coding frames and ensure that they captured data across all sources and of all types.
-
Gathering-related sections of transcripts, fieldnotes and documents under thematic codes; researchers coded the data using Microsoft Word templates for each code.
-
Applying thematic analysis to each line of argument in the text, looking for outliers and negative accounts; we used the ‘one sheet of paper’179 method to support the collation of the coded data into initial themes. The one sheet of paper approach is iterative and involves reading through the data under each code and creating a summary of the different issues. The issues for each code were then grouped into initial broad themes, or axial codes. This approach allows all of the issues raised by the data to be explained and not just those that are most commonly appearing. These axial codes were then compared across the one sheet of paper summaries and themes were derived and summarised.
The summaries of each theme were discussed refined at team meetings until the final themes were agreed.
-
Finally, sharing findings with the wider research team to finalise interpretation.
Patient and public involvement and engagement
Box 5 provides information about the PAG and how PPIE influenced the qualitative explorations.
-
The PAG were sent draft observation posters and patient information leaflets for the qualitative exploration element of the study. The research team incorporated their comments, particularly about language and made appropriate changes. In particular, they indicated where more or less information was required.
-
Six members of the PAG took part in a meeting (November 2020) to share their views on how the research (in particular the observations and interviews) could be conducted in general practice. The discussion led to useful suggestions about what would be acceptable to patients with regard to researchers being in the practice during the COVID pandemic. The group also made suggestions about how the researchers could approach the research within the practice.
-
The PAG and the research team discussed how to adapt the research design given the COVID restrictions. The research team found it useful to hear what the group felt would be acceptable.
-
The fieldwork was timed to coincide with reductions in COVID restrictions.
-
Chris Marriott (CM), a PAG member, was an integral member of the team during the analysis of the case study data. Chris Marriott read interview transcripts from patients and staff and drew out what she felt were the most salient points, adding to our interpretation. Chris Marriott also read a selection of the one-page summary documents and themes. Taking a selection of all the material collected and reflecting on the interviews previously reviewed, CM contributed to the interpretation of the data, attending relevant meetings to discuss the analysis. This was repeated for the mental health element with CM contributing to that team’s analysis.
Chapter 5 Qualitative exploration (work package 3): findings
As outlined in the previous chapter, the qualitative exploration comprised focused ethnographic case studies in general practices, an interview study with stakeholders and an interview study with patients who have a mental health condition. The data and findings are considered as an integrated whole, not as individual components. No critical incidents occurred during the data collection phase in this work package.
Description of the case study sites
Eight practices were recruited representing a broad variation across locations, ethnic diversity, practice size, the proportion of patients aged ≥ 65 years and level of deprivation (Table 14). Reasons for declining participation included COVID pressures, staffing challenges and site relocations.
| Practice ID | Size (small < 6000, medium 6000–12,000, large ≥ 12,000) |
Location | Percentage of ethnic minority patients (%) | Percentage of patient, ≥ 65 years (%) | Deprivation (1 = high, 10 = low) |
Example of DF offered | Taking part in mental health patient interviews |
|---|---|---|---|---|---|---|---|
| A | Large | Semi-rural | 4.2 | 23.4 | Low (score = 10) | Since COVID – Deputy practice manager with responsibility for supporting patients to use digital services. | No |
| B | Small | Urban | 85.7 | 7.3 | High (score = 1) | Active DF pre-pandemic via iPads and more recently leafleting local community about online services. | Yes |
| C | Medium | Urban | 40 | 9.4 | High (score = 3) | Devised new online consultation system tailored to population with high levels of English as a second language and promote this over other routes. | Yes |
| D | Large | Urban | 1.5 | 23.9 | Low (score = 9) | Promote and support a practice champion. | No |
| E | Large | Rural | 1.8 | 8.3 | Medium (score = 5) | ‘Super practice’ with active DF pre pandemic via iPads. Reception staff known as access support workers. | Yes |
| F | Large | Rural | 1.2 | 33.4 | Medium (score = 6) | Two IT officers providing support via e-mail, pre pandemic ran workshops. | No |
| G | Large | Urban | 6.4 | 19.6 | Low (score = 8) | Pre pandemic held a DF event. Have unofficial digital champion, ad hoc support for patients. | Yes |
| H | Small | Urban | 1 | 14.7 | High (score = 2) | March 2020 programme put in place to promote and support use of digital services and online for health in general. | Yes |
Participating practices were located in four geographical areas and five were classed as large practices, one as medium and two as small. Two were in rural areas, one in semi-rural and five in urban areas. Percentage of ethnic minority patients ranged from 1.2% to 85.7%. Deprivation scores ranged from 1 to 10, with two practices classed as being in an area of high deprivation according to their IMD score. The percentage of patients aged ≥ 65 years ranged from 7.3% to 33.8%. Types of DF ranged from ad hoc provision of support when needed to designing platforms targeted to specific patient groups. See practice summaries for details (see additional files www.fundingawards.nihr.ac.uk/award/NIHR128268; accessed 3 April 2024).
There were few examples identified of documentation relevant to policies and procedures for DF. New staff members were generally shown what to do rather than having any documentation as a reference guide. Across the case study practices there was just one meeting that was considered relevant to DF, and this was in the context of a patient participation group. It appeared that DF was not something that was routinely considered by general practice teams.
Researchers conducted fieldwork in practices from September 2021 to July 2022 and were in each practice for 2–6 weeks. Two researchers (BT, CB) collected data from three practices each, and one researcher from two practices (SS).
Description of case study interview participants
Practice staff
The majority of staff participants were female. We interviewed 36 staff from a range of roles and age groups (Table 15).
| Characteristics | Number of participants (total = 36) | |
|---|---|---|
| Gender | Female | 23 |
| Male | 13 | |
| Age group | 18–24 | 3 |
| 25–34 | 10 | |
| 35–44 | 7 | |
| 45–54 | 7 | |
| 55–64 | 4 | |
| ≥ 65 years | 1 | |
| Unknown | 4 | |
| Role in practice | Practice manager | 8 |
| Receptionist/admin | 9 | |
| Data/IT/quality control (QC)/Business manager | 4 | |
| GP | 8 | |
| Nurse/Healthcare assistant (HCA) | 3 | |
| Paramedic | 1 | |
| Clinical pharmacist | 2 | |
| Social prescriber | 1 |
Interview lengths ranged from 8 minutes to 1 hour. Interviews were conducted in person, via video conferencing or telephone.
Patients
Patients had a variety of self-reported experiences of using GP online services ranging from not at all to being frequent users. They had varied experiences with DF. We interviewed 33 patients across 8 practices, 7 were carers (Table 16).
| Characteristics | Number of participants (total = 33) | |
|---|---|---|
| Gender | Female | 18 |
| Male | 15 | |
| Age group | 18–24 | 2 |
| 25–34 | 3 | |
| 35–44 | 4 | |
| 45–54 | 5 | |
| 55–64 | 6 | |
| 65–74 | 6 | |
| 75–84 | 4 | |
| ≥ 85 years | 2 | |
| Undisclosed | 1 | |
| Ethnicity | White British | 26 |
| Asian | 6 | |
| Black Caribbean | 1 | |
| Health | Long-term condition(s) | 13 |
| Disability | 1 | |
| Carer | Yes | 7 |
| No | 26 | |
Interview lengths ranged from 14 minutes to 50 minutes. We achieved a maximally variable sample in relation to patient population demographics.
Description of participants with a mental health condition
We recruited 10 patients with a mental health condition, falling short of the intended 15 patients. These were from five of the eight case studies practices. We had intended to recruit three to four case study practices to this additional study element.
Only one participant was male (Table 17). All but one patient had a diagnosis of anxiety and/or depression and eight were White British.
| Practice | Gender | Age | Ethnicity | Mental health condition |
|---|---|---|---|---|
| Practice B | Female | 54 | British Pakistani | Depression |
| Practice C | Female | 42 | African | Depression |
| Practice C | Female | 42 | White British | Anxiety and depression |
| Practice E | Male | 39 | White British | Anxiety |
| Practice G | Female | 63 | White British | Bipolar disorder |
| Practice H | Female | 28 | White British | Anxiety and obsessive–compulsive disorder (OCD) |
| Practice H | Female | 65 | White British | Anxiety and depression |
| Practice H | Female | 67 | White British | Anxiety |
| Practice H | Female | 48 | White British | Anxiety and depression |
| Practice H | Female | 60 | White British | Anxiety and depression |
Description of stakeholder interview participants
Nineteen stakeholders participated in interviews between October 2021 and May 2022. Interviewees, including males and females, held one of the following roles, although many were also GPs and/or members of advisory groups relating to digital primary care (see Box 6).
-
Senior roles within the NHS infrastructure
-
Senior roles with digital focus within patient group charity
-
Senior roles within local CCGs or ICSs
-
Senior roles within primary care online consultation platform
-
Senior academic roles
To maintain confidentiality, we provided only limited information about roles. Interview lengths ranged from 22 to 62 minutes. Interviews were conducted via video conferencing and one by telephone.
Types of digital facilitation
Using the data from the focused ethnographic case studies, we outline the types of DF that we observed. The types of DF could be proactive, reactive, or a mixture of both.
Proactive forms of DF involved prior identification of the need for DF and a planned response to this perceived need. Reactive forms of DF involved responding to a real time need for DF without any planning. Sometimes DF had reactive and proactive aspects. The COVID pandemic was an important context for this as it had led to rapid change that necessitated both proactive planning as digital services were introduced and reactive responses to the changes faced by patients. The types of DF were not mutually exclusive, and more than one type of DF was used in each practice.
We identified six types of DF across the eight practices:
-
DF focused solely on an individual digital platform
-
patient facing DF being the responsibility of administrative staff
-
DF via passive paperwork
-
DF via workarounds
-
family/social network led DF
-
‘tablet computer in the drawer’ DF.
Digital facilitation focused solely on individual digital platforms
Proactive, reactive
This occurred where DF was focused on helping the patient population to use an individual digital platform at the general practice, for example, the online consultation platform. This type of DF was focused solely on assisting the patient population to take up and use the platform and does not go beyond that into supporting their use of online services in general. Here an example is given as observed by a researcher in the field.
Overheard call advising patient to use eConsult. Sent link by text. Or they could call at 8 am in the morning. Conversation with staff member after revealed the reason they sent the link by text is because sometimes it’s easier for the patient, and another thing is that they think it’s better to give them something than nothing – it satisfies the patient.
Practice H, fieldnote
Patient and carer facing digital facilitation as the responsibility of administrative staff
Reactive
This describes the situation in practices where providing patients with DF was deemed to be the responsibility of the administrative staff, particularly reception staff. This DF was provided on an 'as needed’ basis. Assisting patients in this way was seen as an ongoing administrative responsibility. Whether and how this kind of DF was delivered was very dependent on the attitudes of administrative staff towards digital services and their confidence in using these. Here is an example of older staff members on the administrative team being less confident in DF relative to younger staff.
we’re a bit older now, our work force downstairs, but we have the youngsters who are really good, you know, you’d say, ‘Oh, can you sort this out?’
Practice E, Care advisor (receptionist), Female
Digital facilitation via passive ‘paperwork’
Proactive
This type of DF was focused on awareness. General practices would place posters on the wall in the waiting room or put information on the practice website. Some left recorded messages on the general practice telephone lines for patients to listen to. Bulk text messages were used to inform patients about the availability of a particular digital service. In one example practice staff posted leaflets through the letterboxes of patients’ homes. This was a practice where the patient population lived in close proximity to the practice. In the example below, a staff member describes using text messages and posters to invite interest from patients in digital services.
So, it’s just the main thing of telling them, you know, setting up, I’ve set up some templates that you just send patients an easy text message, let them know that this is going on. Putting up posters so they can read it in their own time and, you know, a lot of the time it does get their attention and they’ll, they will come to the desk and they will ask more details.
Practice B, HCA/Reception Manager, Female
Digital facilitation via workarounds
Reactive
This was the application of DF to assist where patients were having particular issues with specific digital services across the spectrum of services available. This was something observed as being associated with the NHS App. For example, proxy access for parents and carers was difficult to use and led to staff formulating temporary ‘workarounds’ to enable patients to access services there and then. This reflected in part the NHS App being run and controlled centrally by NHS England but proxy access being the responsibility of the general practice.
Patient came in face-to-face as they had issues with patient access app access. They can see their child’s (8 yrs old) account on the app but not their own and need to order their medication. The receptionist unconfidently tried a couple of things to resolve the problem that did not work. Then the receptionist tried unlinking and re-linking the patient’s account. Patient said they could now see their account but that they (the parent) were under the proxy access of their child, rather than the child being under the parent.
Practice H, fieldnote
Family/social network led digital facilitation
Proactive, reactive
This kind of DF was provided to patients by family members, friends or carers. Carers were usually informal family carers. We observed some patients preferring to be supported in their use of digital services by family members, sometimes for cultural reasons because they routinely would seek family support for activity in their day-to-day lives. This was sometimes the case where the patient spoke English as a second language, or not at all. Grandchildren and children were mentioned as being supportive of parents and grandparents who needed to use digital services. General practice staff saw this as an acceptable way to ensure access to digital services for patients.
In the example below, a member of practice staff refers to adult children supporting older patients to use services by providing their mobile telephone number. This raises questions for the health service about confidentiality for patients where family members can access their health information as informal proxies.
And we have done in the past where we’ve had an elder member of the family who can’t fill in but it’s been the son’s mobile number and the son’s received it, he’s been with them and he’s completed the form.
Practice C, Practice Manager, Male
‘Tablet computer in the drawer’ digital facilitation
Proactive
We encountered practices that had, pre pandemic, actively supported patients to take up digital services, by using tablets in the waiting room to sign them up, or by running sessions to help patients. These initiatives had been put on hold for various reasons:
-
the rapid introduction of digital services in 2020 meant that the pre-2020 need for support was seen to have passed;
-
ongoing concerns about infection control limiting what could be done;
-
no clear reason, with plans outlined or intended but not acted upon.
In the example given here a member of practice staff talks about what the practice has considered doing, but not gone ahead with.
… perhaps we run a technology evening, so we could get somebody from the college down the road, that’s doing IT and get them to talk to the older generations … he or she could do a presentation on how to use technology … And that’s something that the PCN and I were going to look at …
Practice G, Quality and Performance Manager, Female
The types presented here are based on empirical data from the focused ethnographic case studies and they provide depth alongside the complementary quantitative approaches that are used in the wider study. Stakeholders taking part in the interview study described models of DF that were in place in general practices prior to the COVID pandemic. These were often programmes delivered by external organisations. We were not able to identify practices doing this type of DF at the time we recruited to this study.
Themes
We identified six themes, categorised into two groups; scene-setting themes that consider the background context within which digital services sit in general practice, and themes relating directly to DF.
Scene-setting themes
We identified three ‘scene-setting themes’, as being integral to our understanding of the potential benefits and challenges of DF. These were ‘COVID’, ‘the value and purpose of digital services in general practice’ and ‘conflation of access with digital routes to an appointment or contact’.
COVID
The delivery of digital services in general practice was impacted by changes brought about by the COVID pandemic.
Uptake of digital services by individual general practices and patients was low before the COVID pandemic169 and many practices were at the point of considering or planning the implementation of digital services. This was disrupted when uptake of digital services by general practices increased rapidly because of the COVID pandemic.
This was particularly the case at the height of the pandemic when face-to-face appointments were limited to avoid physical proximity. One practice described only offering a face-to-face appointment when:
There is a medical need for a face-to-face appointment
Practice G, Practice Manager, Male
Another described the scenario caused by multiple lockdowns and changing government guidance:
Crisis, solution, crisis, solution … the advantage for that method of it working is you have rapid change. But it’s not always without consequence.
Stakeholder D
The COVID pandemic was observed as a ‘catalyst’ for change by leading to the introduction of digital services within general practices, but general practices were not necessarily equipped for this change:
And then it, it was almost like we were just moving slowly towards, you know, some remote working and getting laptops and eConsults [mentioned as discussing training for eConsult]. And then all of a sudden, the pandemic just accelerated all of that through, through the need to manage it that way.
Practice A, GP Partner, Female
Where general practices had set up initiatives pre pandemic to support patients in using digital services these were paused due to COVID. Examples included asking patients to bring in their devices to obtain support or running advertising campaigns for video consultation use.
so [before the pandemic] the IT guys, in reception for, sort of, a couple of hours in the morning, a couple of hours in the afternoon, helping people if they were struggling to get online. Even if you’re … ‘Bring your device with you if it’s a, a laptop or a tablet, or, or even your phone. Bring it in, we’ll help you. They’ll sort it out.’ Again, a lot of that all stopped because of lockdown.
Practice F, Receptionist, Female
The rapid implementation of digital services was felt by those involved in organising services at a high level, with one stakeholder remarking that the COVID pandemic:
punched a hole in our timeline.
Stakeholder M
On the ground, experiences at this time were mixed. There were perceived benefits to this rapid change, with digital services being time saving, or fitting in with their lives better. The patient in the following example felt positive about the change:
I think that has helped to improve things. Because I think that’s encouraged people down the route of finding other ways other than just walking into a GP practice to access medical services. And I, I personally thought, when, sort of, telephone calls and WhatsApp calls took off with doctors, I thought it was great. Cause I’m a busy person.
Practice D, Patient, Female, aged 35–44
However, there was acknowledgement that the introduction of digital services was associated with difficulties for some. Patients felt digital services could reduce their ability to express themselves clearly or they felt rushed. Both staff and patients in older age groups were reported as struggling the most with the introduction of digital services. Some staff, particularly older GPs, and some stakeholders, expressed dissatisfaction with the move to digital services.
In this example a staff member describes the unfamiliarity of digital services:
And then language, not being able to read or what it says, where to touch and where to do these things.
Practice B, Assistant Practitioner, Female
Any requirement by staff and patients for support in using digital services had not necessarily been considered and resource limitations meant general practice did not have time to make strategic plans for supporting patients.
After the initial changes to the use of digital services that were required because of the COVID pandemic and need to deliver care at a distance, there were reflections on what would happen next:
But what is actually happening is that we’re, we’re channelling the work down the routes of maximum efficiency whilst trying to keep staff and patients safe at the time of the pandemic. But even outside of the pandemic it’s, it’s balancing the benefits of online services, to face-to-face, and some of them we need both, like the booking of an appointment for instance.
Practice A, Practice Manager, Female
While general practices regarded changes made as permanent, patients questioned whether services could return to the pre-pandemic approach. Acceleration of digital services was not uniform, with some services stalling, such as online appointment booking, as a result of the COVID pandemic when it was put on pause by NHSE, and others such as obtaining a repeat prescription online becoming more popular.
Value and purpose of digital services
We identified context relating to the value and purpose of digital services within general practice and the subsequent impact on the need for DF.
Rationale for digital services
Beyond the changes made in response to the pandemic, the rationale for using digital services in the first place was not always clear. There was a noted contrast between the views of stakeholders who were hugely engaged in the concept of digital services, and some staff and patients who struggled to understand the rationale for their introduction:
So, there are a number of different ways in which actually technology can be incredibly empowering and enabling for people with impairments and people of all ages.
Stakeholder C
I can’t be bothered going through all that sort of thing and then to be told at the end that no one can see her for a couple of days, you know. I like to know exactly what I am with it.
Practice G, Carer, Male, aged 65–74
There was a lack of shared understanding about what digital services should achieve and who was responsible for them. Stakeholders viewed digital services as a tool to manage patient demand on practices. Patients reported the view that the drive to use digital services was an attempt to reduce the burden on GP practices, while conversely staff reported that digital systems have created an uncapped demand, making general practice too available.
All participant groups reflected on the move from paper to digital in wider society as context for the changes happening in general practice. Stakeholders described the need for patients to build digital literacy and confidence across a lot of systems, not just health, and that it is not the responsibility of health care to address this:
So, they know that it’s an issue but there’s a big question mark about actually whose responsibility it is to really take this forward, hold this, make sure that digital inclusion is a core part of policies and programs and strategies. So, we are making, you know, we’re taking that message to the UK government.
Stakeholder C
On a practical level, CCGs were described by staff and stakeholders as being influential as to what services the practices would offer; they were responsible for determining which digital service or product was used and issued local directives for example, targets for use of particular digital services.
It was perceived by staff and stakeholders that there was no formal guidance or support from government to encourage the use of digital services by practices and patients. Two of the practice managers interviewed felt that the GP contract should have greater specificity about digital provision:
And at the same time practices have just got to buy into it and get it done. How you do that, I don’t know. I mean, I know they’ve tried to incentivise financially in practices. You know, NHS Digital have in terms of access to records and stuff like that. So, to me, they should just make it a contractual requirement that you, you know, you, you, you’ve got to do these online services.
Practice G, Practice Manager, Male
Good digital services
Staff and stakeholders acknowledged the importance of services ‘working’ for patients:
So, I think the, the task here onwards is to try and make the digital access acceptable for practices from a workload point of view, acceptable for patients from a convenience point of view but, obviously, still retaining all the benefits of that, that it can offer.
Stakeholder D
This was not the reality as the reported experiences were mixed; some patients reported difficulties with new digital approaches and others embraced them. This example outlines a positive view:
I mean, it’s just so much easier to have it. As somebody that does use their phone, has apps, it’s so easy to hit the app, load it up, book an appointment. It’s done in ten seconds.
Practice D, Patient, Male, aged 45–54
Contrasted by a negative view from a patient whose first language was a spoken language and therefore would not translate easily into text. In the example the patient talks about digital platforms being translated into non-English languages:
Some people … because what it is with our languages, people don’t, it’s not written. Some languages are just spoken. So, if it was written, they probably wouldn’t understand anyway. And it’s just spoken. So, you’ll, you’ll need like a voiceover. But how many languages would you have a voiceover for? So, it’s going to be really, really difficult.
Practice B, Patient, Female, aged 45–54
For staff and patients, named digital platforms are the point of reference, for example, ‘the eConsult’, ‘the NHS App’. Some practices did have written documents with policies/guidance on digital service use but often staff did not know that these existed or assumed more guidance existed than did, or guidance was seldom updated so often became out of date.
At practice level there was not necessarily a shared vision about what ‘good’ digital services looked like. The online repeat prescription ordering service was widely acknowledged as beneficial by both patients and staff and was routinely given as an exemplar of a good digital service illustrating that some digital services were a ‘good fit’:
Male member of staff thinks prescription requests done by e-mail are easier for the patients and the reply to say it has been done feels more personal (even though it is a template message).
Practice H, fieldnote
Digital services are difficult to deliver if patients do not want what is being offered and some practice staff perceived this to be the main barrier to use of digital services:
I think, I think getting them online, like, isn’t necessarily a problem. I think it’s more whether they want to is more of a problem, like, cause we do, we do, I mean, I think, feel like every other phone call is, ‘You can go online and do eConsults’, or, we’re pushing online all the time.
Practice G, Receptionist, Female
It appeared that a patient’s past experience of the NHS could influence their perceptions of using digital services in primary care, in either a positive or negative way. Previous experiences of using digital systems and communication outside of primary care also appeared to influence patients’ perceptions:
I like technology and I’m up to date with a, a telephone, or a mobile phone that allows me to do everything, that it, it appears that is required of me through online services. [ … ] I have found everything to be very simplistic but also in a very human way.
Practice E, Patient, Female, aged 55–64
On the whole, practices had reflected on the changes they had made to digital services and what this meant for different patient groups but had not yet considered how patients might start using online services and what support would be needed to enable this. Staff and stakeholders emphasised that the movement from paper to digital would take time and the experience for patients and staff can be complex and time and resource intensive.
Conflation of access with digital routes to an appointment/contact
Digital services are viewed by patients as a route to access the practice. Any kind of remote access, including the telephone, is regarded under the digital umbrella. Despite the research project being clearly focused on digital services, stakeholders and practice staff referred to telephone triage and increased use of the telephone for consultations and they were a key part of the recent changes to service delivery in general practice:
I think actually some of that [increased reliance on digital services] is just as much about telephone, frankly even more about telephone than about digital.
Stakeholder N
This reflected the crossover between the two when certain digital platforms were used, for example, those that required an online contact to be followed up by a telephone call from the general practice, or that used a mixture of approaches as outlined in this example:
With their online access they can order their medication so that is an online service because they can either phone and speak to somebody or they can text a message to somebody at the [system] and they call them back and speak to them, or they go online and order their medications.
Practice C, Lead Practice Nurse, Female
For patients, digital services are often viewed and treated purely as a gateway to access the general practice.
The patient priority is to successfully navigate the system to achieve access. For many, access is the key concept, not digital:
I wouldn’t even start to try and book an online appointment with my GP. Because if I did that, I would probably be offered something in four to five weeks’ time. And my only choice, if I want to see a doctor, urgent or not, is to phone up at 8.30 on the morning and fight with everybody else for an appointment on the phone, for a that-day appointment. So yeah, that, that facility is rubbish, to be honest. And it’s symptomatic of a much bigger problem that GP services have, to my mind.
Practice D, Patient, Female, aged 35–44
Overall, patients seem open to different consultation modes, with their priority being to be seen as quickly as possible in whichever way that access was achieved. Digital services were seen to increase accessibility of appointments for patients who were travelling, away for work or those where working commitments made traditional appointment booking methods difficult. In these situations, digital services overcome obstacles in attending healthcare appointments for some patients:
It’s much easier to just look at the screen and put an answer on there than actually physically talk to people. [ … ] it just saves time going down there. That’s all, really. It’s just convenient.
Practice G, Carer, Male, aged 65–74
Where general practices used a digital gateway for access this creates problems for those who are unable to use it, with those able to use it being able to get to the front of the queue for access:
Spoke to Patient Care Advisor about eConsult recommendations. She said that the only appointments available in the next 48 hrs are for eConsults. The patients can only have them if they complete an eConsult. She told the patient to complete one and that she would look out for their eConsult so that she could then give them an appointment for the next day. Otherwise they would have to phone back the next day and wait in line or wait over a month for a pre-bookable appointment.
Practice H, fieldnote
The onus is on patients to adopt digital services and understand their use if they wish to be able to access their health care.
Digital facilitation themes
We identified three themes relating directly to DF. These were comprised of subthemes: ‘the operationalisation of digital facilitation – making digital facilitation happen’, ‘usability of digital services in practice and the consequent need for digital facilitation’ and ‘assumptions and stereotypes’.
The operationalisation of digital facilitation – making digital facilitation happen
Digital facilitation as a concept
For the purposes of this research study, we developed and applied a definition for DF: The range of processes, procedures and personnel which seeks to support NHS patients (or their carers) in their uptake and use of online services.
When explained to staff, patient and stakeholder participants, DF is perceived to be conceptually valuable and regarded in the positive. However, it is not used or understood as a term in practice:
I, I don’t understand what that means, I don’t think other people would, not everyone … I wouldn’t understand what that means? … I don’t want to pigeonhole anyone, but if you said it to my mum, she would have no idea what you’re talking about … Yeah, I don’t, I just don’t, yeah, like, the, like, patient care and digital facilitation don’t sound like they go together, do they
Stakeholder U
It is regarded as difficult to have a working definition or usable term for something (DF) that is movable and relative to a person’s circumstance. We observed that it was difficult for participants to ‘grasp’ it as a concept, being mixed up with the digital services themselves.
Sometimes exemplars are used by stakeholders and general practice staff to illustrate the concept of DF, and these link to specific digital platforms (e.g. using iPads to support registration with the NHS App) or organisations (Barclays Bank and their Eagles programme to support people in accessing the internet). Stakeholders felt this was helpful in communicating examples of DF to the public:
And Barclays have done some great work on this with their Digital Eagles … work I don’t know if you’ve come across. But it’s definitely worth looking at. So during the pandemic Barclays Bank, they’ve got something called Digital Eagles. And we did get them doing some work with patients. And they would, like, get them, sort of, sorted out with iPads and … this is obviously when loads of people had nothing to do during the pandemic.
Stakeholder E
While the different participant groups (stakeholder, staff and patients) varied in their understanding and experience of DF, they were united in understanding it as a way to achieve the perceived end point; that being the successful use of digital services to access health care. It is not seen as anything more complex than this. Stakeholders felt that DF would improve access, and subsequently improve health care:
I suppose, so, you know, if you’ve gotta, gotta wait on a telephone for, for 25 minutes on a morning then actually we need to redirect them to the website and they need to be using online services, you know, that will then will free up the time of the wait for those who don’t want to use that system and need to speak to somebody.
Stakeholder B
The interpretation of DF as a means to achieve successful use of digital services to access health care assumes that digital services are desirable and positive. In this example the staff member refers to patients being asked to have belief in ‘eConsults’:
Yeah I’ve told them that they can use it yeah I have told them that they can use it and, and, and the benefits of using eConsults, they don’t always believe me.
Practice E, Lead Practice Nurse, Female
Engaging with the concept of DF requires some cognitive dissonance between what it is perceived that digital services can deliver (the positive elements) and the challenges and reality of how they work in day-to-day general practice.
Responsibility for delivery of digital facilitation
There was lack of clarity on the responsibility for delivering DF. There is a ‘bystander effect’ with patients, different staff groups and stakeholders assuming responsibility for DF to lie elsewhere.
Some participating stakeholders and also some patients expressed that the responsibility for DF should lie with the general practice, including reception staff, administrators and clinical staff:
for me I think it should be the GP practice’s responsibility to show their patients how to use their service ‘cause it is in their best interests. The more people they get using the automated services theoretically, the less, again, through on the phone every day.
Stakeholder C
General practice staff believe that patients bear some responsibility for being able to access their own health care and that support can be sought from friends and families:
a lot of people will get help from family members.
Practice C, GP Partner, Male
Within the general practice team, clinical staff were observed to pass responsibility for delivering DF onto reception staff and administrators:
… Online medication request system as well that patients can use, I’m not entirely familiar with but often I have perhaps direct patients to our admin staff or our receptionists if they needed to get set up with that. […] I guess use of online services that would be more for admin or reception staff.
Practice H, GP (salaried), Female
Patients stated that the responsibility for providing DF lay with the wider health system and regional or government level organisations as well as being a societal issue (described in ‘value and purpose of digital services’ theme). This may relate to how DF was viewed by patients, as being a means to use digital services so that they can achieve access:
It’s difficult, isn’t it? I, I don’t see the role of the practice to be educating us in, in how to adopt technology. I think it’s just too much. I think the remit of the NHS is so wide.
Practice D, Patient, Male, aged 45–54
There was an additional view from some patients that they themselves had some responsibility for trying to use digital services if they wanted to achieve access:
I think it’s like going to school again, isn’t it? You’ve got to practice and do it and learn it and, and remember. And, yes, yes, absolutely, you’ve gotta be a bit disciplined and do it.
Practice A, Patient, Female, aged 75–84
See Figure 16 for a visual representation of how different groups view responsibility for delivering DF.
FIGURE 16.
Perception of responsibility for delivering DF in different groups.
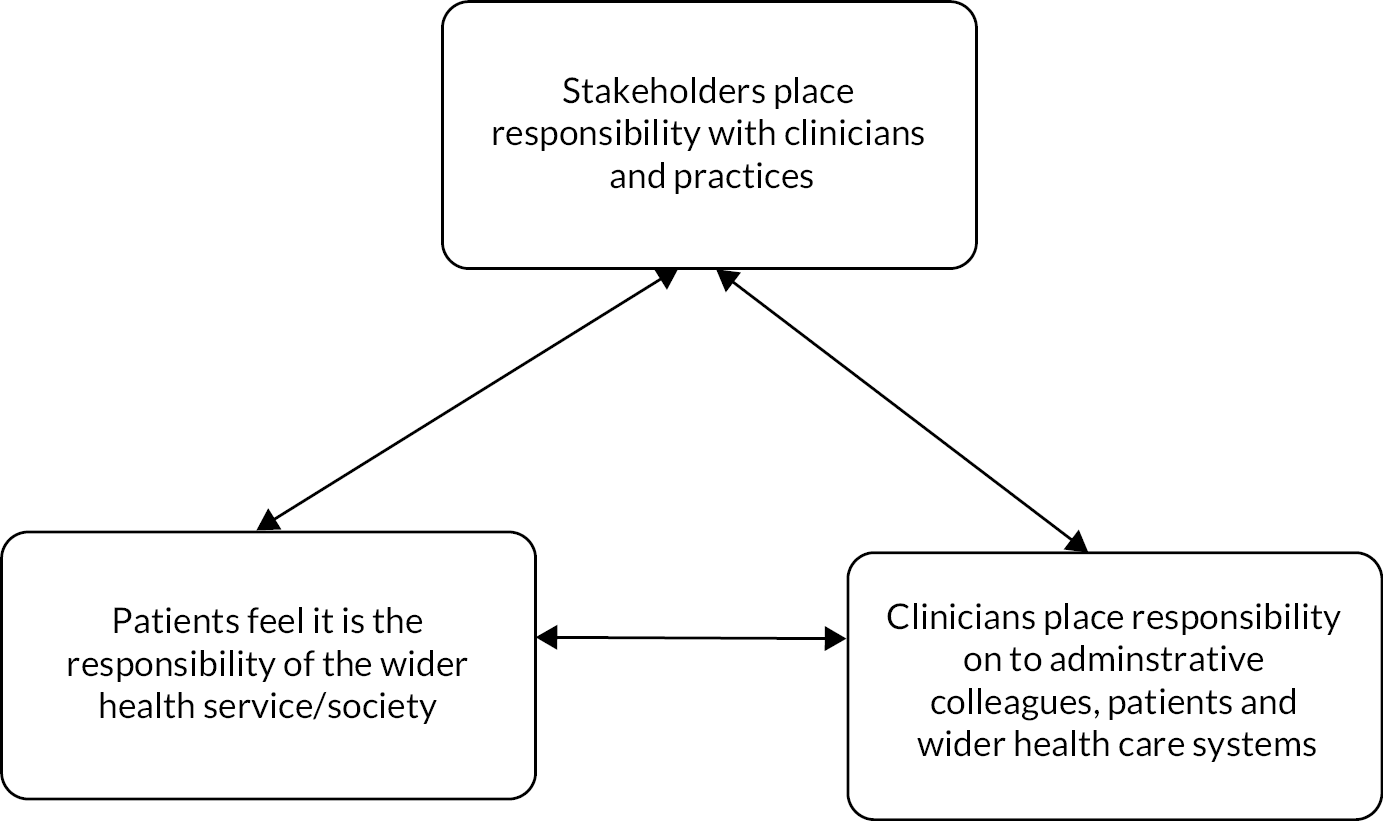
What is consistent across staff, patients and stakeholders is that, in practical terms, the responsibility for any facilitation in relation to digital access currently falls to reception staff.
Logistics of digital facilitation
There are day-to-day logistics underpinning the delivery of DF. Regardless of how DF is delivered and at what level there was awareness amongst participants that well-developed approaches to DF require organisation, planning, time, financial input and training resources:
Then it has to come from the NHS and government as well at the same time. Well, what provision have you put into place? Or what funding have you put into place that we can give time to patients say, this is how to do it.
Practice C, GP Partner, Male
At present, DF is largely occurring in an ad hoc fashion, without external support and with a lack of training or systematic approaches. As a result, organising DF is beyond the capability of most general practices.
The usability of digital services in practice and the consequent need for digital facilitation
Barriers and enablers created by individual digital platforms and the need for digital facilitation
There is a variation between digital platforms with some being easier to use than others for both patients and staff. Initial registration for the specific digital platforms created a barrier to digital services for patients before they had even managed to use them, creating a need for DF. Certain platforms require complex registration processes such as usernames, passwords and e-mail links. Complex registration processes lead patients to seek support from staff:
Because I kept doing it and it wasn’t accepting it and it wasn’t registering. And it was frustrating because I couldn’t do. And I was there forever, and my battery was dying, and I’m thinking, ‘I need to get this done but I can’t do it.’
Practice B, Patient, Female, aged 45–54
Patients also seek support when navigating the use of digital platforms, and staff are aware that certain platforms are likely to cause more need for DF than others:
I do think the patients need educating on it, and I do think the eConsult itself is, is clunky, because I’ve looked at it from a patient perspective on our eConsults, and it, you just get caught in a mine field of information
Practice G, Quality and Performance Manager, Female
There were digital platforms that were easier to use and did not create a need for DF. As mentioned earlier, some digital services (e.g. online repeat prescriptions) are a ‘good fit’ and tend not to be associated with a need for DF beyond any initial registration. This suggests that the choice of and purpose of the digital platform impact how much DF is required, and therefore the amount of DF that the general practice will need to deliver:
As long as I follow the instructions they’re, they’re quite easy.
Practice C, Patient, Male, aged 65–74
In other cases, where digital systems were designed and operated from outside of the general practice, as is the case for the NHS App, general practice staff felt unable to offer support to patients in their use of these platforms even though it concerned their use of digital services:
So, it’s a bit difficult because the NHS App is a third party app there is obviously only so much we can do our end which you can do.
Practice G, Receptionist, Female
Where these interoperability issues occurred, it could bring the patients’ digital journey to a halt.
Negative impact of mixing digital services and platforms: a fractured digital landscape
It can be challenging for patients and staff to navigate the range of different platforms and services used within a single practice. There could be multiple platforms all working in different ways and for different purposes and sometimes general practices used them interchangeably, as demonstrated in this example:
Or, like, on the phone, I’ve advised people how they can … so if you can’t manage the text message, I’ve talked people through how to go online and do an eConsult and upload the photographs that way.
Practice A, GP Partner, Female
While for some patients there are issues of digital skills and digital access, even for patients who were digitally literate this could cause issues with their access to digital services.
Some general practices attempted to manage changes to how the digital platforms were accessed limiting their use to certain times of day, or turning them on and off without warning and changing the digital platforms available, but without communicating this to patients or offering patient education:
The advisors explained that when the practice shuts down eConsult, it just shows an error message to patients, not anything like ‘eConsult will be available again tomorrow morning at 8 am’, so lots of patients ring up saying that their eConsult isn’t working. The care advisors said it would be good to add a message to the blurb at the start of the practice’s telephone call too when they’ve taken down eConsult.
Practice E, fieldnote
General practice staff had to contend with incompatible systems, old computers and remembering which platform was used for which purpose. This was the context in which they were supporting patients to use digital services.
Accessibility for different groups
Individual circumstances matter when it comes to having a need for DF to use digital services; especially to those vulnerable groups such as the homeless, those with learning disabilities, those with hearing or sight impairment, those experiencing an acute state of illness and those in lower socioeconomic groups. In this example, a patient talked about the costs associated with using digital services:
They’ve got to watch their data, you know, and if they’re not on Wi-Fi they can use a lot of data, especially homeless people, you know, who haven’t got access to Wi-Fi perhaps, and they, they all generally afford about a tenner a month for the phone. But the data for that online, they might not do it.
Practice H, Carer, Male, aged 55–64
There are some groups where circumstances influence their need for DF. For example, those with no access to technology or internet, those living in rural areas with poor internet connection, those with poor literacy, those with no third-party support, those with poor manual dexterity and those who do not speak English or speak it as a second language.
And again, with language barriers as well, because they don’t really understand what’s being asked of them and what they need to do.
Practice A, Receptionist, Female
General practices took steps to accommodate these patients in relation to their use of digital services as part of their attempts to provide DF. What was unclear was whether this was enough, given the complexity of adapting services for patients with very different needs:
Also, we are advertising, if people are unable to read stuff on the website or struggling with the online, that we can actually print larger print or we can make it accessible for anyone. And also, we can translate it. I think our website actually has got a option to translate in different language the page.
Practice F, IT Administrator/Officer, Female
Individual circumstances applied not only to patients but also to staff. Digital confidence in staff could be observed through how staff interacted with patients and in this example a staff member expressed uncertainty about their skills:
I think I’ve just sent you a link – I hope anyway.
Practice G, fieldnote
Age was perceived to have an impact on both staff and patients’ digital knowledge, understanding, experience and confidence. Patients and staff understood that for older patients, use of online service was partly a feature of having access and ability to use them but also an issue of trust in the use of online services, particularly for personal transactions. For example, patients drew parallels in the use of online banking services, which some were not comfortable with:
For banking, for ordering prescriptions, but I’m beginning to … oh, also filing my tax return … But I’m beginning to use it less and less … Security issues, basically, and the fact that people like Google are just so powerful and so invasive nowadays.
Practice F, Patient, Male, aged 65–74
Digital facilitation was required to be about more than practical digital skills for these patients and served a social function.
While there is a shared vision that all digital services should be designed to eventually work with ease for all groups of patients without extra efforts and support, at present, there is little consideration for how marginalised and vulnerable groups can be supported to use these services:
And then everybody’s talking about digital inclusion now. So, loads of people are talking about it. But how many people actually understand what it really means
Stakeholder E
It is not clear if patients who are not able to contact their practice are the ones in greatest need of DF and least able to navigate the digital processes involved, which makes planning for DF difficult.
Assumptions and stereotypes
We observed embedded attitudes about who needs DF. Assumptions were made about who may or may not be able to use digital services, and these are not necessarily grounded in evidence. There is a risk of stereotyping patients.
Patients and practice staff often categorise themselves or others around their digital abilities, for example, staff referring to patients as ‘tech savvy’ or ‘technophobes’ reflecting societal perceptions about who does or does not use digital services:
Yeah, I, I would say, so. I mean, we use it constantly, so we use Teams at work, Outlook, as well sort of Excel. I’m an, an accountant so I use finance systems and things like that at work as well. So, yeah, I guess compared to a lot of people who might not use the computer much at all, then, yeah, I’m reasonably tech savvy.
Practice D, Patient, Female, aged 45–54
There were cases of ‘othering’ with assumptions made about who needs help, or that there was little value in offering DF to help certain groups, this was particularly the case for assumptions made about age where younger people were deemed more competent and confident in using digital services than older people:
Yeah. It’s getting better, and obviously it depends on the demographics of the patient, because, you know, obviously the elderly and, and ones that aren’t so computer-literate, you know, can’t do it or aren’t interested in doing it.
Practice D, Senior Receptionist, Female
The youngsters, once they get, the younger people, once they tend to get up on it, there’s no real issues.
Practice G, Practice Manager, Male
When assumptions are made about patients with certain characteristics, for example, of a certain age, having a disability, low literacy or education level, those living what are deemed to be precarious lifestyles etc. it inevitably affects the range of choice of services offered or indeed supported, and this sometimes means that staff may not offer access to digital services at all.
We observed an assumption being made that those unable to use digital services would have some form of ‘proxy access’ either in the form of a family helper or carer who can support their online access. Reliance by practices on this form of input potentially excludes patients where family or carer support is not available:
She feels that different skills are needed for using online technology so if a person is not IT literate, they will ask them to get a family member or grandchildren involved to help them.
Practice B, fieldnote
Assumptions extend to staff and this impacts on who within the general practice team are expected to provide DF. Younger staff are often asked to deliver DF because of the assumption that they ‘understand’ digital services better, despite receiving the same training, if any.
… if anyone else needs IT help, it’s usually, ‘[youngest staff member name], can you help this …’ sort of like, ‘… patient out with this?’ sort of thing, and it’s usually me.
Practice G, Receptionist, Female
As outlined in the previous theme, it was the case that staff who are confident with digital services offered more support to patients, indicating that confidence is important rather than competence.
Patients with mental health conditions
The themes identified in the mental health interviews were closely aligned to most of the findings in the main sample. As with the main sample, patients conflated digital with access, referring to experiences in using the telephone to contact the practice alongside their reflections on digital services.
In contrast with the main sample, patients shared their experiences of how their condition impacted on their contact with the general practice. Many of the participants reported a cycle of infrequent GP visits during periods where their condition is well controlled, and frequent use of the general practice during periods of instability:
Yeah, I think it’s because I see the GP a lot … more than normal people … So sometimes I can see the GP for three, four days. I call today, I call tomorrow, I call the day after
Practice C, Patient, Female, aged 40–44
This impacted on their use of digital services and their need for DF. As frequent attenders, they were familiar with the practice’s digital services therefore did not require DF. As in the main sample, services were a good fit for patients and this meant they did not require DF.
There were participants who reported struggling with digital services and they were generally less familiar with technology and more likely to rely on family and friends, rather than the practice, for support:
I can’t say I have, really, but as I say, I’ve not been with this doctors’ that long, and I, obviously everything’s online, isn’t it … so if I do have any difficulty, [daughter’s name], will sort it out for me.
Practice H, Patient, Female, aged 45–49
This mirrored the situation for patients in the main sample where family support was used by patients.
There were experiences of using digital services that were specific to patients living with a mental health condition. There were patients who experienced digital services to be advantageous in relation to their condition by allowing them to avoid using the telephone:
Well, the advantages, I suppose, is it can be quick and convenient. And for some, for my personal reasons with my anxiety, I can get stressed knowing … I have to ring, you know, and ring round and try and sort things out, whereas if, if I can just use the app, and, you know, on my own phone in my own home … and I can do it, that, that works for me.
Practice C, Patient, Female, aged 40–44
Examples given included reduction in the anxiety caused by queuing on the telephone, or not having to telephone first thing in the morning when medication for their mental health condition made getting up difficult. Patients noted that because the telephone could cause anxiety, this meant that seeking DF if needed would be likely to be difficult as this would have to be via the only other access route, the telephone.
Some of the patients found digital services less acceptable because of a lack of trust in digital services or because using them caused increased anxiety. This was not attributed to a lack of DF or the nature of the services themselves:
It doesn’t help at all if you have to look at a screen … It, it makes you more anxious, and the only thing I can think of is actually talking to somebody on the telephone.
Practice H, Patient, Female, aged 60–64
On the whole, achieving access was the most important factor to these patients, with DF secondary to this, if needed at all.
Discussion
Summary of key findings
We identified different types of facilitation occurring in practices, and these were often reactive and in response to individual patient need. Context was important, with the value and purpose of digital services not always well understood by either patients or staff, and with access to an appointment often conflated with digital routes to an appointment or service. COVID had influenced how services were delivered with an increase in digital platforms used by practices.
Digital facilitation was seen as valuable but was poorly conceptualised within general practice. It was unclear where the responsibility for DF lay and there was a tendency to assume it was the responsibility of someone else. Well-developed DF requires support, resources and training and these were not available.
The usability of digital services influenced whether DF was needed. Where multiple digital platforms were used, this required support for patients to understand which to use and how to use them. General practices often made changes without informing patients and patients did not know what would be available to them.
We observed assumptions being made by both patients and practice staff about who could use digital services and who could not, including stereotypes about age that were applied to both staff and patients. When it came to who needed DF, individual circumstances mattered, with needs being movable in line with personal circumstances. Vulnerable populations were particularly in need but were also least likely to be considered when services are designed.
Deviations from the original proposal
We expanded from three to four geographical areas.
This allowed us to recruit a practice in an area of high deprivation and with a varied population profile relative to our other practices. This in turn ensured our sample was maximally variable.
We sampled practices according to their experience of and/or delivery of DF using different approaches. We had anticipated at the design stage of the study that we would be able to identify discrete approaches to DF, based on what we knew to be happening in general practice, and from the literature review. By the time we were recruiting general practices, the COVID pandemic had changed how GP services were delivered. To counter this, we ensured that we were fully appraised of DF activity at the point of recruitment rather than relying on the practice survey data or prior reports. We were alert to the possibility of changes due to the COVID pandemic while we conducted fieldwork.
Strengths and limitations
We were able to recruit a varied sample of general practices during the COVID pandemic and conduct ethnographic fieldwork as intended over the period from September 2021 to July 2022. During this time there were various levels of lockdown and restrictions which the team successfully negotiated to ensure the fieldwork was completed. We were conducting the fieldwork at a key time for general practice, with the COVID pandemic leading to an increased use of digital services. This allowed us to capture how practices responded to an increased need for DF in real time, and our sample included populations with high numbers of patients in ethnic minority groups, and in areas of high deprivation. We recruited a broad range of 19 key stakeholders at a time when those in professional roles were under extreme pressure.
The COVID pandemic has impacted the ways in which general practices were operating and in their relationships with their patients. There was little patient footfall in the practices’ premises, and this changed the nature of the non-participant observation, which was focused on staff. Because fewer patients were attending the practice in person, the main recruitment tool to access patients was a letter sent via the practices. In some practices, initial responses were very limited which resulted in second mail outs being necessary. However, we did recruit and interview a wide range of patients with varied characteristics.
Recognition of the need for and subsequent funding of the additional interviews was a strength in ensuring inclusion of this under researched group. However, in line with the broader challenges associated with conducting research in this area, recruitment of practices and patients for the study of patients with mental health conditions was challenging. We aimed to recruit the case study practices to this additional interview study but two declined for capacity reasons and a further declined due to sensitivities about the patient group. In the practices that were recruited, workforce capacity was an issue which delayed mail outs.
We were able to recruit patients in groups that are vulnerable to digital inequalities, which included individuals from older age groups, those in minority ethnic groups, those in poorer health, and individuals in rural settings. Several participants intersected these characteristics. We were not successful in recruiting patients who were in marginalised groups. This reflected the additional and substantial challenges in recruiting general practices and patients during the pandemic.
The response rate to the invitations to take part in an interview was lower amongst individuals living with a mental health condition than for the main study; and the majority of participants in this group were female and aged in their 40s. This may reflect the timing, with some invites sent over the summer period. However, it may also be due, in part, to the stigma associated with having a mental health condition, or a lack of recognition amongst some patients of their diagnosis. Even some participants that took part in interviews did not consider themselves to be ‘diagnosed’ with a condition but instead felt they had ‘a touch of anxiety’, or ‘a bit of low mood’. This suggests difficulties with the labelling of a mental health diagnosis for some patients. The approach may not have been appropriate for this cohort of patients and another strategy may have been more successful. The findings should be viewed in this light.
In conclusion, the qualitative exploration allowed an in-depth analysis of how DF is realised in general practices in England. It highlights areas that could be targeted in developing DF as a concept and in applying it to the delivery of care to patients.
Chapter 6 Synthesis (work package 4)
Introduction
The aims of the research reported here were to:
-
identify, characterise and explore the potential benefits and challenges associated with DF in general practice in England
-
design a framework for future evaluations of the effectiveness and cost effectiveness of DF interventions.
This chapter sets out the synthesis of the four major sources of evidence that we have produced in order to meet those objectives and which are presented in the preceding chapters: review of literature (WP1), survey of GP practices (WP2A), survey of patients (WP2B) and the qualitative exploration (WP3) that combined case studies in GP practices with stakeholder interviews. In this study, we are using Weiss’s approach to theory-based evaluation as our theoretical framework. 70 After describing our approach to the synthesis of the findings from all parts of the study, and the role of PPIE within that, the themes identified from the research are specified and a matrix is presented summarising the corresponding data. Following the approach defined by Weiss we use our findings to create a programme theory, which specifies the mechanism of change, and an implementation theory, which describes how DF is carried out and the associated barriers and enablers. We conclude the chapter by proposing a framework for future evaluations of approaches to DF in primary care.
Synthesis methods
We have applied a pragmatic, iterative and cumulative approach to synthesising the findings from all WPs and to developing the programme and implementation theories. The underlying approach has been to triangulate what we have found in each WP, summarising the results in a triangulation matrix,180 which has evolved as the study progressed and as different WPs’ evidence became available. The analyses within, and findings of, each WP have been detailed in earlier chapters. Those findings were brought together in a series of three workshop meetings of researchers and the PAG as each WP in turn was completed. Two team members who work in GP practices (one GP and one administrative) participated in all three synthesis workshops. Thus, all three workshops had PAG members and primary care staff inputs in addition to researcher inputs. Box 7 briefly summarises the PAG contributions.
Based on the PAG’s lived experiences:
-
Prompted clarification of researchers’ presentation of findings.
-
Provided reassurance that the themes identified by the research team from the research were genuine and not missing anything obvious.
-
Indicated findings from any of the WPs that appeared surprising.
-
Illustrated individual points with examples from their own, and their acquaintances’ reported experiences.
-
Overall, their comments complemented findings from the research, adding depth that helped the research team to develop its thinking.
In November 2021, the findings of the survey of practices (WP2A) were combined and compared with those from the literature review (WP1) in an online workshop with researchers from both WPs (nine researchers in all) and three PAG members. Briefing material had been circulated to all participants in advance of the workshop, which included plenty of time for clarification and further explanation as well as for identification of themes and discussion of the extent to which different evidence sources reinforced, added to, or differed from each other in their implications.
In July 2022 the emerging findings from the ethnographic case studies at GP practices and the stakeholder interviews (WP3) were analysed alongside the previous synthesis of WP1 and WP2A (practice survey). The participants at this online workshop were 12 researchers, including from all 3 WPs and 3 PAG members. The approach to this workshop mirrored the previous synthesis workshop, with pre-workshop briefing and time for clarification and further explanation of the material from all three WPs being considered, as well as for the synthesis work itself.
The final synthesis workshop, adding the findings of the patient survey (WP2B) and including the fully finalised WP3 findings, took place at an in-person meeting of the research team in London in September 2022, including 15 researchers and 3 PAG members. The approach to the third workshop was the same as for the two prior workshops. The following paragraphs describe the themes that were agreed after detailed discussion to represent the sum of triangulated findings from all WPs.
The synthesis process concluded in early December 2022 following an online discussion with national and regional stakeholders – from NHS Digital, NHS England and from NHS Devon Integrated Care Board (ICB) – at which the overall synthesis results were discussed, probed and, as a consequence, further clarified.
Themes after triangulation
The process of triangulating our findings from the different WPs has enabled us to build a detailed and balanced understanding of a range of approaches to DF, and patients’ experiences of it, in NHS primary care in England. After the cumulative synthesis of the findings from all WPs, the research team identified three scene-setting themes from the evidence, which relate to the context in which DF takes place (when it happens), and eight themes related to types of DF, their implementation and effectiveness.
Scene-setting themes (Table 18)
-
Value and purpose of digital services. The usefulness of DF depends on the value of the digital services whose use might be facilitated.
-
Digital is conflated with other routes to accessing care. Patients desire access to care, and digital is only one type of route to accessing NHS primary care services, along with face to face and telephone.
-
COVID. The onset of the pandemic, and of the response of primary care to the pandemic, was associated with a shift away from patients attending GP premises and towards remote transactions. Combined, these had a major impact on the need for, and provision of, DF.
| Theme | WP1 findings: literature review | WP2A findings: survey of GP practices | WP2B findings: survey of patients | WP3 findings: qualitative exploration |
|---|---|---|---|---|
| 1. Value and purpose of digital services | Not addressed | Not addressed | Not addressed | Need for, and of value of, digital services are not always clear and there is a lack of shared understanding or belief about what digital services should achieve. |
| 2. Digital conflated with other routes to access | Not addressed | Not addressed | Not addressed | Digital is a means to access the practice and anything delivered remotely is often seen as digital, for example use of telephone, SMS messaging. Digital can enable access and be a barrier to access. Patient priority is to navigate the system to access health care, making access a more important concept than DF to many. |
| 3. COVID | Not addressed | Found various services were reduced, including face-to-face consultations, ordering of prescriptions via paper or person, and appointment booking in person. | Not addressed | Pandemic stopped initiatives that have not resumed. Rationale for not reinstating pre-pandemic initiatives unclear. Change was necessarily sudden, poorly planned and implemented, and forced for all parties – staff, practices, patients. |
Digital facilitation themes (Table 19)
-
Defining and identifying DF can be difficult. There is lack of clarity among some practice staff and patients about what comprises DF.
-
Types of DF. It can be provided actively (e.g. practice staff recommending to patients that they use an online service and telling them how to do so) or passively (e.g. a poster in the waiting room, a recorded telephone message played to callers to the practice number); and DF can be reactive (helping patients when they ask for assistance) or proactive (without waiting to be asked).
-
Supporting initial sign-up or sustained use over time. When an online service is being introduced or rolled out, facilitation may focus on supporting patients to register for a service. But once they are registered, they may need support (e.g. problem solving) to continue using the service.
-
Who delivers DF. There is no clear consensus over whose responsibility it is and who should be expected to fund the resources needed to provide DF.
-
Enablers of DF, including the usability, or ‘user-friendliness’ of digital platforms.
-
Barriers to DF, including staff attitudes towards digital services and stereotyped assumptions about the capabilities of some patients.
-
Digital access and DF for different subgroups in the population. There is evidence in the literature that some groups are relatively disadvantaged when using online services and they might benefit from targeted DF efforts to support them.
-
Effectiveness. Is DF effective at supporting patients to access and use online services; and which types of facilitation are more effective than others.
| Theme | WP1 findings: literature review | WP2A findings: survey of GP practices | WP2B findings: survey of patients | WP3 findings: qualitative exploration |
|---|---|---|---|---|
| 4. Defining and identifying DF | DF defined by study team, so concept clearly defined as ‘that range of processes, procedures and personnel which seeks to support NHS patients in their uptake and use of online services’. | Survey asked GP practices to identify DF in their practices and it is unclear if they define DF in the same way as the study team did in WP1. For example, it seems likely that ad hoc facilitation efforts are not recognised as DF by all practices. | Patients conflate digital access with DF. Patients identify additional modes of DF including text messages and recorded messages on practice phone lines. Patients see phones as a digital service. |
Difficult to have a working definition or usable term for something (DF) that is movable and relative to a person’s circumstance. It is difficult for participants to ‘grasp’ as a concept, being conflated with the digital services themselves. Engaging with the concept of DF requires some cognitive dissonance between what it is perceived that digital services can deliver (the positive elements) and the challenges and reality of how they work in practice. |
| 5. Types of DF: active/passive/reactive/proactive and any combinations of those | Focus of literature is on active interventions that require GP practices to actively support patients as opposed to passive interventions (e.g. posting information on their website). | GP practices are more likely to report they facilitate in ways that are passive and reactive (i.e. responding to direct patient requests for support) rather than active and proactive (i.e. providing support before issues arise). | Awareness and use of all DF are low apart from the use of e-mail and text messages (a passive mode) which are noted by a substantial minority of patients. Free text suggests a demand for training and proactive updates that is not being met. |
Found that DF tends to be reactive rather than proactive. At least one practice tried to schedule training (proactive), but it was so poorly attended that they no longer do this. |
| 6. DF supporting initial sign-up vs. sustained use over time | Literature suggests that most DF focuses on supporting initial sign-up to digital services with less support for sustained use. | Not addressed | Survey showed that registering for digital services is a substantial barrier for patients, supporting the need for DF around registration and initial sign-up. | DF typically concerns getting people signed up to digital services, but this is still reactive in that staff respond to patients needing help signing up. Getting patients set up does not mean DF ends there but some practices felt that was their only role. |
| 7. Who delivers DF? | Not a key focus of the literature. Limited evidence suggests that GPs and nurses do much of the DF reported in the literature. |
Survey found that reception and administrative staff provide most DF support, but that GPs and nurses are also involved. Practices view responsibility for DF as being shared between GP practices and other parts of the NHS (e.g. CCGs, NHS England) |
Not addressed | There is a ‘bystander effect’ with patients, different staff groups and stakeholders assuming that responsibility for DF lies elsewhere.
|
| Where digital systems are designed and operated from outside of the general practice. For example, NHS App, general practice staff feel unable to support patients in their use of these platforms even though it concerns their use of digital services. Where these interoperability issues occur, it can bring the patients’ digital journey to a halt. |
||||
| 8. Enablers of DF (including usability of the digital platform) |
|
Majority of practices report that the COVID pandemic increased the support that practices provide to patients to use digital services and increased uptake of digital services by patients. Majority of practices support the view that uptake of digital services leads to operational efficiencies. |
Only 13% of patients report having been given help to use online services, but when this help is given, it is generally useful. | Findings suggest enablers of DF include:
|
Patients made helpful suggestions:
|
||||
| 9. Barriers to DF (including multiple platforms and staff assumptions/stereotyping of patients) | Active facilitation that requires high levels of emotional engagement may contribute to stress and fatigue amongst staff. Lack of staff capacity and time to deliver DF are noted barriers. |
Most practices agree that they ‘do not have the capacity to support patients in using online primary care services as much as we would like’, and 94% of practices agree that ‘Some patients are unlikely to use online primary care services no matter how much we support them’. |
Survey shows low levels of awareness of DF. Survey also suggests that some patients are unhappy about the shift to digital services and so do not want to engage. There is a desire for human interaction. |
Findings suggest multiple barriers to DF:
|
| 10. Digital access and DF for different subgroups in population | Little information available in the literature about how DF can support different subgroups in the population. Some evidence suggests that older people benefit from direct, human support. Some evidence suggests that technical training and assistance are effective for increasing uptake amongst vulnerable populations. Literature also highlights the risk of ‘selective DF’ whereby practice staff engage in facilitation efforts with most digitally savvy patients, excluding those seen as not having sufficient digital literacy. |
Practices report that they most frequently targeted DF efforts at older adults; however, many practices report targeting all groups listed as an option on the survey (e.g. people with physical or mental health conditions, digitally excluded people, lower income populations, those in rural areas, ethnic minority populations, and non-English speakers). This calls into question what practices mean by ‘targeting’. | Older patients less likely to be aware of or use DF. They are also less likely to be told about online services or helped to use them. Ethnic minorities, those with long-term health conditions, not speaking English as a first language and having repeat prescriptions are all associated with higher awareness of, and use of (passive) facilitation; but these groups are also less likely to be told about online services or helped to use them (i.e. less exposure to active DF). We found no evidence that practices who report targeting different groups have higher awareness of use of DF in those groups than other practices. |
Age is an important dimension in regard to both patients and staff members. The age of the individual is perceived to have an impact on both staff and patients’ digital knowledge, understanding, experience and confidence. This is sometimes assumed (stakeholders, staff, patients talking about other patients) and sometimes realised (patient and staff experiences). Younger staff and patients are perceived to be more competent and confident at digital use than those who are older. Digital platforms are not shaped around marginalised and vulnerable populations. Individual circumstances matter: those already in vulnerable groups such as the homeless, older people with less trust in the online world, and people with issues with literacy, require an individual approach to DF. Some patients are unable to use digital services at all and it is not clear to them where to go to get help. |
| 11. Effectiveness – Is DF effective and what kinds of facilitation are more effective than others? | Some evidence that promotion, including GP and other practice staff recommendations, and written reminders, can be effective in increasing initial patient uptake of digital services. Introductory sessions on how to use digital services that include assistance signing up or having questions answered can be effective in increasing initial patient uptake. It is unclear if promotion or introductory sessions lead to sustained use. Ongoing guidance and support that is incorporated into primary care consultations may be effective in increasing patient uptake and sustained use. |
Not addressed | Findings show that practices that report using displays, social media, workshops or events for DF are more likely to have patients that are aware of/use that mode of facilitation. We found no difference in awareness for practices that use leaflets, e-mail/text, or computer provision of DF. This implies that displays, social media, workshops or events are more effective forms of DF than leaflets, e-mail/text, or computer provision. Practices that report employing a practice champion have more people report being told about online services, but we found no difference seen for practices who report ad hoc support. |
Some practices highlight how many patients are signed up to a service as evidence of effectiveness, but this does not reflect actual use or the difference made by the DF activities. The key end point of interest for the practices is whether patients achieve access/obtain what they need. |
Mapping of findings to theoretical framework
We used Weiss’s theory-based evaluation as our theoretical framework. 70 Weiss distinguishes between ‘programme theory’, which specifies the mechanism of change, and ‘implementation theory’, which describes how the intervention is carried out. We used the theory-based evaluation approach to understand how, and in what ways, different models of DF bring benefits and challenges to general practice and patients. We did this by drawing on the findings of the evidence synthesis, surveys and case studies to develop the programme theory and the implementation theory.
To develop the ‘programme theory’ we used a realist approach to describe provision of DF in terms of:
-
context
-
the flow of activities that comprise the intervention
-
the theory and assumptions underlying the intervention, including the intended benefits/outcomes.
The ‘implementation theory’ explored moderating factors which influenced the extent to which the process and outcomes were achieved, including factors acting as barriers and facilitators to practices offering DF or to different groups of patients using them.
Programme theory
Context
Digital facilitation needs to be understood within the context of current NHS policy, which seeks to encourage greater use of digital services across the NHS, and with technology viewed by policy-makers as addressing some of the demands facing health care,181 including streamlining of service delivery, improved triage systems and improved access for patients. 3 Our focused ethnography found, however, that at the practice level there was a lack of shared understanding about what digital services should achieve, and that the need for and value of digital services was not always clear to practices themselves. This was also true for patients who sometimes saw methods of digital access to primary care services as a barrier to receiving care rather than as a method for expanding or improving their access to care. Supporting the uptake and use of digital services by patients is challenging when the value of those services is unclear to practices and patients.
Within primary care, practices are mandated to provide online access to services such as appointment booking, prescription ordering and access to medical records. However, practices individually determine which platforms or providers they will use to deliver them, and if and how they will support patients to use them. General practices in England have long been incentivised to introduce online consultation platforms, with particular commercial platforms being market leaders. 182 Provision of an online route of access to patients is now part of the GP contract in England. 183 These platforms have been promoted to general practice as tools for demand management while also fulfilling the need to provide patients with another access option. While practices can and do collaborate through various organisations such as primary care networks (PCNs) and ICBs, the responsibility for providing digital services and supporting patients to use those services rests with individual practices or groups of practices. The result is a patchwork of systems and approaches shaped according to the resources available to and choices made by practices in a context where commercial suppliers and other NHS organisations, such as local ICBs, may be influencing the decisions made. This might prioritise various (sometimes competing) aims including managing demand, enabling access or improving patient experiences of care. On the ground, this looks like a complex and varied collection of digital services at each practice that might change as the needs of the practice change or new providers and services are developed.
Digital facilitation should also be understood within the context of the pandemic. Our survey of GP practices showed that the pandemic led to the rapid introduction of remote ways of accessing and delivering primary care including online booking of appointments, online prescription ordering and remote consultation. Implemented alongside reductions in face-to-face services such as in-person appointment booking and repeat prescription requests, the rapid introduction of digital services during the pandemic accelerated the digital agenda set out by NHSE181 that patients will use digital services to access care, regardless of their ability to do so. 12
Our focused ethnography found that some practices that had provided proactive DF to support patients prior to the pandemic stopped those activities during the pandemic due to pandemic-related pressures on the practice or because the facilitation required face-to-face activities that were unsuitable given the social distancing requirements, for example, by using tablet computers to sign patients up to digital services as they sat in the waiting room. These facilitation activities were not resumed after the pandemic, and in some practices it was perceived that the need for support had passed. In others the capacity to do this under COVID restrictions was limited.
The pandemic also placed further strain on a primary care system that was already facing high levels of demand from a growing and ageing population. The national vaccination programme during the pandemic relied on GP facilities (among others) and personnel to deliver much of the work, drawing extensively on primary care resources. The primary care workforce is also facing declining numbers of GPs and primary care nurses, with many practices struggling to recruit and retain staff. 5,184 A recurring finding in our research was how competing demands on staff time make it challenging to provide DF.
Flow of activities comprising digital facilitation
Digital facilitation can take a wide variety of forms, encompassing active forms of facilitation such as practice champions, training and workshops, and passive forms such as informational leaflets, text messages and recorded messages on practice phone lines. Facilitation is reactive when it is responding to direct patient requests for support, and proactive when practices provide support before issues arise. We found that in practice, most facilitation efforts are reactive, and that many could be further described as ‘ad hoc’ in that they were seemingly applied anew each time an issue arose, relying on the digital skills of practice staff to respond to the immediate needs of the patient. This reflects the tendency of general practices (and patients) to conflate DF with the digital services themselves, and therefore to see facilitation efforts as troubleshooting activities to enable access to the services rather than as part of a wider effort to enable participation in a digitised, and digitally prioritised, healthcare economy.
Determining the ownership of and the responsibility for developing and delivering DF are not straightforward. In practice, most DF is delivered by general practice reception and administrative staff. This is consistent with reactive approaches to facilitation that view it as troubleshooting or enabling access to services, in that patient facing roles are given responsibility for helping patients resolve issues with access. Proactive DF requires planning and resources to develop and deliver it, that may be beyond practices’ capabilities. Our research found that practices and patients saw a role for ‘other parts’ of the NHS (e.g. CCGs, NHSE), in addition to a role for individual practices, in supporting patients to use digital services. Practices noted the need for wider patient education efforts about the benefits of booking appointments online, for example.
The release of the NHS App, which gives patients in England access to many digital healthcare services including appointment booking, prescription ordering and access to medical records through their smartphone, has added to the confusion over who has responsibility for supporting patients to use digital services. Practices were not able to support patients in their use of the NHS App as it sat outside of the practice with separate digital support via an NHS helpline and web page. Patients tended to view the NHS App as just another way to access the practice’s services and therefore turned to the practice for help. This contributed to confusion over who has responsibility for supporting patients with using services.
Theory and assumptions underlying digital facilitation
Digital facilitation has the potential to support the move to digital primary care services. It could do so through direct and indirect pathways. Digital facilitation directly supports the move to digital services when patients are helped to access or use specific digital services to meet their current or future healthcare needs, for example, when they are helped to order a prescription through an online platform. Indirect support occurs when facilitation helps patients to become more confident users of digital services through, for example, enhancing their digital literacy. Both pathways have the potential to lead to more people using digital services more often when accessing primary care, in theory leading to benefits such as efficiencies for practices and enhanced access for patients.
In our research we found that the pathways linking DF to anticipated beneficial outcomes are more complex than the version theorised above and that tensions over the concept and goals of DF contribute to this complexity. Firstly, our focused ethnographic case studies found that practices and patients conflated digital services with access to an appointment. This means that although DF is theoretically valuable to practices, they may not see themselves as providing facilitation to digital services more generally, but instead as just facilitating access to an appointment. Patients see themselves as seeking help with accessing practice services rather than as receiving support with digital services. It is unsurprising then that most DF provided by practices is ad hoc and reactive, resolving immediate issues of patient access rather than seeking to build patients’ capacity to access digital services more broadly.
Which raises the question: what does it mean for DF to be effective? The move to online primary care provision assumes that it can help address some of the pressures facing primary care while improving patient choice, convenience and ease of access. 3 Current government plans for digital health emphasise the importance of registering patients for services such as the NHS App. 181 Much of the DF that we identified in our research also focused on registering patients for digital services, with less effort directed at ensuring that patients remain engaged with those services and continued to use them. But if the path from DF to the theorised benefits it brings requires more than this, for example, if patients need to be supported to build their digital confidence so that they can engage with multiple or changing digital services, then DF approaches will need to evolve to meet these needs if they are to be effective. In our discussion with national and regional stakeholders, the point was made that patients need to be encouraged to see digital channels as part of their relationship with their GPs, rather than as substitutes for that relationship.
Digital facilitation has a role in combatting potential inequalities in accessing health care in an NHS with enhanced digital opportunities and enhanced digital access to primary care services. Our survey of GP practices suggests that practices are aware of the need particularly to support groups such as older age groups, non-white ethnicities, those in lower socioeconomic groups, those in poorer health, and individuals in rural settings who may struggle to access digital services. However, our findings also suggest that DF efforts to support potentially vulnerable groups of patients fall short. Specifically, our surveys found that although older patients were frequently mentioned by GP practices as a target of DF efforts, in practice older patients were less likely to be aware of or use DF and were less likely to be told about digital services or helped to use them. Evidence from the literature review and focused ethnography suggests that assumptions and stereotypes about older patients being less digitally competent might make practice staff less likely to engage in facilitation efforts with them.
Implementation theory
Contextual factors affecting implementation
Our findings highlight the variation between general practices in terms of capacity for, and approaches to, DF. The populations served by general practice also differ. In our case studies we observed that a practice serving a young population of predominantly minority ethnic groups had very different requirements to a practice serving an older white British population where digital uptake was lower and health needs were different. To date, approaches to digitising general practice have been broadly uniform in their approach, without apparent tailoring for the individual needs and requirements of populations.
Moderating factors affecting implementation, barriers and facilitators
Our findings suggest, unsurprisingly, that constraints on the resources available to GP practices to engage in DF affect implementation. Most practices that we surveyed agreed that they did not have sufficient capacity to support patients in using online primary care services to the extent they might wish. The literature review highlights how automating some aspects of patient engagement through e-mail templates, protocols or scripts can help mitigate staff capacity pressures, but we saw only limited evidence of these types of tools being used in practice. Passive facilitation efforts such as posters and leaflets use less staff time than more active approaches, and there was some evidence from our survey that passive approaches are used more often by GP practices. In the ethnographic fieldwork, there were examples of posters on the wall in practices and information provided on practice websites, but these were not widely publicised or updated.
Findings from the ethnography suggest that DF benefits from having someone in the practice with specific responsibility for it. This person may be chosen because they are perceived to be the most knowledgeable digitally rather than for any formal reason. Approaches such as practice champions, where a dedicated staff member acts as a cheerleader and source of information for DF, can be challenging to put in place for capacity constrained practices.
The quality and usefulness of digital services also affect approaches to DF. Some digital platforms are more difficult to navigate or register with and may not be seen by patients or practice staff as bringing added value. Other platforms can be considered a good fit, being easy to use and bringing tangible benefits to patients and staff. Services that are a good fit require less DF, for example, online repeat prescription ordering, was found to be relatively well used across the survey and focused ethnographic case studies. Findings from the ethnography suggest that issues with more difficult-to-use services are seen by practice staff as being a problem with the digital service itself, and outside the ability or responsibility of staff members to resolve. Findings from the patient survey show that patients are less willing to engage with digital services for which they see little value. For DF to be successful, practices would therefore need to devote more resource to supporting and encouraging patients to use digital services that are a poorer fit.
This highlights some related barriers to DF. First, practice staff need to understand how to use the digital services themselves in order to provide support to patients to do so. In some practices visited for our ethnography, it seemed to just be assumed that younger members of staff would know how to navigate digital technologies, but this was not always true. Practices have a range of digital platforms, which sometimes change, in addition to the NHS App, which is outside of practices’ control. This diverse and changing mix of services can create barriers for staff in maintaining the requisite skills to provide facilitation. It can also present challenges for patients in understanding what services are available and for which support might be available.
Unclear lines of responsibility for DF also present a barrier to implementation, with practice staff, patients and other stakeholders (e.g. other NHS organisations, suppliers of digital technology) all assuming that at least a portion of the responsibility for facilitation lies with the others. This contributes to the reactive, single-issue style approach to DF we observed in our ethnographic research. When no one is responsible for supporting patients with broader issues of digital access such as digital confidence and literacy, then the limited resources available for support will be targeted at addressing immediate needs. Resources to develop thoughtful, potentially cross-practice or cross-platform, support for patients are unlikely to be invested in by practices or other stakeholders without clearer lines of responsibility.
Implementation could be supported by having a clear understanding of what DF the practice population needs, and how best to deliver it, and for this to be understood by all members of staff in the general practice. Conversely, a barrier to implementing DF is that (as evidenced by our literature review and focused ethnography) practice staff may make assumptions and stereotypes about older patients being less digitally competent and not worth engaging with in facilitation efforts.
Digital facilitation seemed to be functioning well where practices had allocated a specific role for DF and provided resource to support this. The literature review showed the importance of having buy-in from staff about the purpose of digital services and facilitation efforts, including ensuring that staff trust and understand the specific technologies being supported. Although the ethnography found that practices often lacked this clear rationale at a general level, conflating digital services with access to practice services, it found that when digital services were a good fit for practice and patient needs it was then easier to support patients to use those services. Clarifying the purpose and value of digital services is therefore a critical aspect of DF.
Evaluation framework
The aim of the study was to ‘identify, characterise and explore the potential benefits and challenges associated with different models of digital facilitation currently in use in general practice in England’ and to subsequently ‘design a framework for future evaluations of the effectiveness and cost effectiveness of such interventions’.
Our research has enabled us to understand the following:
-
the concept of DF and how it is understood (or not) by all involved parties (patients, general practice staff, wider stakeholders)
-
the types of DF currently in use
-
to what extent DF is implemented and for what purposes
-
the outcomes that are important to practices and their patients and what they expect DF to achieve, if anything
-
the groups of patients who seek or have experienced DF
-
the types of research methodology that are likely to be suitable to further investigate DF.
The level of understanding obtained via our research has allowed us to devise a framework to help to structure future research into DF. This is based on the synthesised findings of the study and theoretical framework findings.
The latest version of the Medical Research Council (MRC) framework for evaluation of complex interventions185 defines evaluation as ‘going beyond asking whether an intervention works’ and suggests a broader approach is taken that includes factors such as ‘theorising whether it works’ and ‘how it contributes to system change’. In line with these methodological developments, our framework takes a correspondingly broad approach to assessing effectiveness and cost effectiveness.
We begin by outlining how DF may be considered an intervention, who is responsible for DF, the key patient groups that should be considered in any future evaluation, the potential outcome measures for evaluation including those related to cost, and the possible different types of future evaluation including key areas of focus.
Digital facilitation as an intervention
Our findings have highlighted the amorphous nature of DF and indicate that DF is part of the complex processes involved in delivering access to care for patients in general practice. This has implications for the future evaluation of DF. DF is flexible and adaptable, functioning as a complex intervention. The end point, achieving access, is the important factor for all parties. Therefore, DF may be defined as the support required and provided to enable patients to achieve access digitally. DF is one or more of numerous possible, mutually non-exclusive interventions.
Where an intervention is used, consideration should be made for the understanding of the intervention by all involved parties with our evidence indicating that DF is not a concept that is easily grasped and may be better linked to how patients access and receive health services rather than being a standalone intervention. There should be clear rationale for introducing it.
Responsibility for digital facilitation
We observed that understanding about who delivers DF was key to whether it happened at all. Any future evaluation of effort at DF as an intervention should consider who is responsible for it. This would include:
-
Who has overall responsibility for the success or failure of DF?
-
What are the responsibilities of general practices and their staff with regard to ensuring safe and appropriate delivery of DF?
-
Which staff groups are involved in delivering it? What does this involve and how does it fit with their current role?
-
What are patient responsibilities when engaging with DF?
-
If DF is delivered by an external party, how will they interface with the practice staff and patients and what responsibilities does this bring?
-
How does DF fit into the wider health community beyond general practice?
-
Will there be support from regional or national or other external organisations? This might include commercial suppliers of digital platforms, and charities to boost digital literacy in certain population groups.
Patient groups and potential for inequalities
A key element of this study has been to explore how different patient groups engage with and are affected by DF. This has had a particular focus on the potential for inequalities. Future evaluations should consider:
-
where DF is most needed and most likely to be successful (there is little point in focusing DF in primary care on people without internet access, for example)
-
differences in incidence of benefits and costs/savings to patients, for example, burden on patients and likelihood that it will lead to them being able to achieve access to health care in the way intended
-
weight of importance for patients, which may be low relative to importance for practices and other interested parties.
Potential outcome measures for future evaluation
Potential outcome measures for use in future studies should aim to capture quantifiable impacts where possible, and also to explore qualitative aspects of DF. They should consider both intended (e.g. increase in levels of use of online services) and unintended consequences (e.g. staff finding themselves expected by some patients to act as a help desk for IT problems). Here we outline potential outcomes, but these are not exhaustive. The outcomes can be collected for subpopulations within the overall population so as to permit evaluation of inequalities, or their mitigation, between different groups within the population.
Service use and delivery-related outcomes
We have shown that access is an important outcome for practices and patients, and that DF plays a role in achieving it. The interface between access and digital is an important consideration when choosing outcome measures related to service use and delivery:
-
awareness of digital services (where DF is positioned to change this)
-
levels of registrations with digital services, levels of use
-
change in use of online services at practice level and individual patient level. Specifically, levels of use after registration and attrition rate
-
measures of access within the general practice: numbers of consultations, speed of access, rates of digital access versus other routes.
Patient and healthcare professional-related outcomes
Patient and healthcare professional outcomes are likely to be best assessed using both quantitative and qualitative approaches to allow triangulation of data. The exact nature of outcomes needed would depend on the composition of the intervention and extent of patient and healthcare professional engagement:
-
Patient experiences with engaging in DF and with use of services facilitated. This could include existing patient-reported experience measures of satisfaction or specific intervention focused factors, for example, helpfulness of specific approach, reassurance gained by engaging with DF.
-
Perceptions about whether DF has worked for them, for example, was it effective in helping them reach their desired end point?
-
Patient confidence in using digital services.
-
Practice staff reported experiences with facilitation, for example, ease of delivery, impact on workload. Views on patients’ use of services facilitated, for example, do staff think DF works?
-
Perceptions about whether DF has worked for them, for example, does it provide a mechanism for staff to support patients in the way expected?
Cost outcomes
Any assessment of cost should take a societal perspective, moving beyond NHS and personal social services perspectives. Significant areas of costs and/or of likely cost savings that should be examined in future studies include:
-
costs of DF to practices (training, staff time, materials and equipment)
-
costs/savings to practices from increased use of online services by patients
-
costs/savings to the rest of the NHS
-
savings/costs to patients from using online services – for example, time savings from not attending a GP practice in person.
Different types of future evaluation including areas of focus
Given the difficulties in defining DF as an intervention and the many involved parties, measuring effectiveness would need to take a holistic approach. This fits with the latest MRC guidance on complex interventions which suggests that evaluation goes beyond whether an intervention works.
Our exploratory research has identified areas for focus that were previously unconsidered:
-
the role of general practice administrative staff in supporting digital services and the appropriate ways to support this
-
understanding how different approaches to DF work for population subgroups
-
supporting sustained patient use of digital services, moving the focus beyond registration
-
understanding the factors that need to be addressed to achieve a certain baseline of digital services use, and how service use can then be developed to support specific patient groups with particular needs
-
understanding the extent of patient demand for digital services to access and use general practice and thus the level of DF needed to achieve this.
This is not an exhaustive list but highlights the complexity of this area and some appropriate areas of focus to ensure benefit from future research.
Deviations from the original proposal
There were no deviations in methods for WP4 to report from the original proposal.
Chapter 7 Discussion
This report presents the work carried out across the four WPs of the Di-Facto project, including the additional work specifically undertaken with patients living with mental health conditions. The key results have been brought together and synthesised in Chapter 6. Here we suggest the key implications of the work for policy, practice and research. We also reflect on the contribution of PPIE throughout the research process, and on issues relating to equality, diversity and inclusion. Digital facilitation is a concept that the research team defined when developing this study. As such it does not yet have a widely accepted meaning, nor will it necessarily be recognised as a coherent concept by those not exposed to this research. However, the research has demonstrated the need for, and the potential value of, DF.
Implications for policy
The current policy direction for Primary Care in the UK highlights the continued implementation and use of digital services. If this change in service configuration is to happen, then there is a clear role for DF in providing relevant support. However, our research has shown that there is a disconnect between the perceptions and expectations of some key national and regional stakeholders and what DF efforts are actually occurring at practice level, where the reality is messier and often falling short of expectations. This disconnect needs to be recognised, as do the reasons why these expectations are not met. Our work provides some relevant insight, including the observations that many practices would like to support patients in their use digital service, but do not have the resources to do so. To realise the NHS vision of increasing use of general practice digital services, targeted investment looks certain to be required in terms of staff time and training.
In order for DF to happen effectively, there needs to be clarity provided around the responsibility for its delivery. Currently, responsibility is often assumed to be the role of ‘others’, and thus little action follows. Those ‘others’ are primarily the reception and administrative staff in individual general practices, who rarely have training or skills in DF. Responsibility for DF in the future may lie with several parties across health systems, rather than being the remit of an individual part of the health system. In addition, developing a specific facilitator role might benefit from involvement of a range of individuals such as community link workers, social prescribers alongside other, already recognised staff such as practice based administrators, IT, or other support staff roles such as Digital and Transformation Lead Roles reimbursable via the Additional Roles Reimbursement Scheme. 186 Some DF may well fall outside the health sector entirely, recognising the benefits of digital enablement at a societal level. An example of such societal investment in the USA has been linked to potential benefits in terms of health equity. 187 Educating patients on the benefits of digital services, and how to use them effectively, could well be performed at a national level. However, the variation in which digital services are implemented across England means that detailed, targeted, support for individual patients will be hard to achieve. This difficulty is reflected in current NHS patient facing materials, such as the ‘How to access your GP practice’ video,188 which makes multiple mentions of digital tools but provides only generic information about how these might work. We know from our research that the reality is each general practice offering a different range of tools. Where consistent digital tools are available at a national level (e.g. the NHS App, or the NHS website) there is the potential to provide specific patient support for these tools. Such support could include promotion activities, as well as user support that is either passive (e.g. ‘how to’ guides, such as the user directions for use of the NHS App provided on the national NHS website189,190) or reactive (e.g. support helpline). While the evaluation of this material fell outside the scope of our research, we note that the material provided is often generic and lacking specific details, reflecting the fact that different practices may utilise different functionality within the NHS App, and that often the specific tools used (e.g. for online consultations) will affect the appearance of those services within the app. How a tool functions is also user dependent and in reality will be influenced by the characteristics of the individual staff member and the individual patient using it, within a specific general practice.
Responsibility for providing support for patients to use specific platforms, commonly falls to general practice staff. However, this risks an inconsistent and inefficient approach whereby potentially thousands of practices are individually developing support for any given platform. There is a case to be made that the platform providers could be encouraged, or mandated, to provide patient facing support either directly to patients or to general practices to help them support their patients. Some platform providers do have passive guidance available that could be made available to patients, but these do not appear to be widely used. 191 Ultimately, general practices will be the point of first contact for many patients and so some responsibility for supporting patients will always fall to general practice staff. ICSs are being championed as having a ‘vital role to play in developing a more coherent approach to digital transformation in primary care’. 192 The extent to which ICSs will achieve this remains to be seen. Furthermore, DF activities inevitably face needs that vary across different groups in the population. We have found that GP practices are aware in principle of different needs for different groups, but we have found little evidence of targeted facilitation in practice for particular groups. In this context, we suggest there may be a role for national support to the provision of DF in primary care aimed at, for example, the less digitally literate in the population or those hindered by particular disabilities.
Our research has shown that DF is often more effective when the parties involved see worth in the digital tools that are being supported. Other research shows that doctors’ willingness to recommend digital tools depends on their own attitudes and beliefs around digital services. 193,194 There is a policy need to articulate to service users and staff the motivation for, purpose and potential benefits of, various online tools. Prior to the COVID pandemic, use of certain online tools by general practices was linked to remuneration or was mandated within the GP contract. 195 While this results in the provision of digital services, it does not necessarily lead to the effective use of them. During the COVID pandemic, the need for digital services was acknowledged by most healthcare providers and patients. However, as the restrictions associated with COVID have receded, the benefits of, and need for, all digital services are not universally agreed upon by providers or patients. There is anecdotal evidence emerging, along with some more formal sources of evidence, that the availability of online consultations may lead to rising patient demand. 196–199
It is not possible to consider DF entirely in isolation from the digital tools being implemented. Digital tools that are easier to use, easier to access and whose purpose is easier to understand will, by definition, require less DF. NHS policy could focus on improving the usability of different digital tools, and ensuring that the development of digital platforms is undertaken considering both the functionality from a clinical point of view, as well as the patient users’ perspectives. 199,200 The necessary rush to implement digital services is now passed. There is time for considered reflection on the impact of digital services, particularly on groups that cannot access them, or do not wish to.
Implications for practice
Our research indicates the potential for DF to help patients and practices make the most of various digital tools and platforms used in general practice. However, to capitalise on this potential will require substantial investment, in and by, general practices. Practices wishing to engage in effective DF will also have to ensure there is clear understanding of the responsibility for delivery. Since commonly the day-to-day responsibility for delivering DF falls to receptionists and administrative staff, care needs to be taken to ensure the staff are equipped to deliver this support and that assumptions are not made about which staff members can and cannot deliver the support based on age or gender stereotypes. Practice leadership and management will need to take responsibility for the overall DF strategy and will need to carefully monitor that what is being delivered does reflect expectations. Similarly, other research has found that adopting digital innovation is complex and will be improved by building consensus between stakeholders and developing dedicated implementation teams. 201,202
Our research also highlighted that patients are often supported in the use of online services by friends and family. While this overcomes barriers and enables patients to access online services, it may lead to challenges around patient confidentiality. Digital channels also make it more challenging for staff to ascertain if responses have come directly from a patient or from a carer or family member. Practices should be aware of this and ensure policies to ensure patient confidentiality are in place for use of digital services as they have been historically used for a third party joining a face-to-face consultation.
Practices may need to recognise that DF can take many forms, active and passive, proactive and reactive. It is likely to be important that all types of facilitation are conducted within a practice, though the balance of efforts may need to change depending on the needs of the registered population. Until more evidence emerges about DF, practices would be best served by focusing on understanding and responding to the needs of their specific patient population. This may include paying particular attention to vulnerable populations within their practice who may have specific needs which require more tailored help and support. Vulnerable populations are the least likely to be considered when services are designed which can severely impact on their ability to access and interact with primary care services.
Practices need to recognise that increasing awareness of, and sign up to, digital services do not inevitably lead to increased use. Monitoring continued use of services is at least as important as monitoring initial registration. Whatever form DF takes, it is important that part of this support involves making the purpose and benefits of using digital tools clear to patients and to practice staff. Relatedly, it might be that practices need to make the expectations of digital services use clear to patients. A shared agenda between practices and patients is likely to be important in ensuring effective facilitation, with both parties understanding the reasons for using digital services.
When implementing digital services, practices should ensure that they choose platforms and tools that are as patient-centred and easy to use as possible. In doing so, the need for facilitation will be minimised allowing efforts to be focused on those that need it most. Using digital services that function well together and collectively present a coherent service to patients is likely to be an effective facilitation approach in its own right. Alongside presenting a coherent package of services, there will likely need to be a recognition that digital services will not work for all patients all of the time, and that they may not work in all circumstances, and that some patients may never be able or willing to use them. Traditional, non-digital access to care will inevitably need to remain an option regardless of how developed and applied DF becomes.
Implications for research
The research deficit in this area is large, and the potential for useful research great. The primary care system is under pressure from increasing service demand, especially in the aftermath of the pandemic,192,203 and changing, for example, following the introduction of new professional roles and opportunities in primary care under the new reimbursement for additional roles scheme. 186 In these circumstances, the research recommendations highlighted in bold here would usefully be the subject of a priority setting exercise by relevant research funding bodies.
Future research on digital facilitation
We found only limited associations between the DF efforts described by practices and either the patient awareness and use of online services in those practices or the perception of DF efforts by patients. This is not surprising given the observations from the ethnographic case studies that facilitation efforts were often reactive rather than proactive, and that efforts to perform effective DF were hampered by lack of resources. Future research might therefore further explore the association between awareness by (potential) users of digital primary care and actual use of those same services, especially within the context of the introduction of specific efforts to support the awareness and use of such services.
In Evaluation framework we have laid out a framework for a future evaluation of DF in primary care, and while we set out some of the key facets that such an intervention might encompass, we do not specify exactly what form such an intervention might take. Our intention with the Di-Facto project was to explore DF that was already underway, with the potential of identifying good practice which could be either developed further as an intervention for testing or shared more widely for immediate implementation. However, we did not find an example of what might be considered ‘text book’ DF, and certainly nothing that would form a complete, practical intervention package. Any intervention development could build on our research, but given the findings around the need for digital technologies to be a ‘good fit’, it would be essential to co-develop any intervention both with patients, and with general practice staff who would be delivering it to ensure a responsive and adaptive approach.
Related to the development of DF interventions is the development of patient facing digital tools. Currently, these tools are generally developed by commercial providers, but research into what facets of digital platforms make them easier to use and understand by patients is warranted. The context in which these digital tools are presented to patients, usually a general practice website, also warrants consideration. A study in Scotland showed that 77% of practice websites featured information that exceeded the recommended 9–14 reading age for online content, while 81% scored below the recommended Flesch Reading Ease score for ‘plain English’. 204 Research into optimising the presentation of practice websites for patient engagement may lead to increased usage of digital tools and reduce the need for DF.
While it is clear that DF is likely to need to be tailored to different patient groups, there is currently a lack of evidence about what this should look like. Future research is needed to address this gap along with identifying which patient groups are most in need of DF. DF and the use of digital services have the potential to both introduce new and extend existing health inequalities, while addressing others (e.g. in groups who experience stigma). 205 Any future research on DF also needs to ensure that associated digital exclusion of certain groups, including, but not limited to, older patients, is investigated. 206 In addition to the observation that older patients were much less likely to be digitally confident, we have also found that people with long-term health problems, whose first language is not English, who are retired, or not in work/education had lower digital confidence. Care needs to be taken to remember that these findings represent an average picture, and any targeted support should not automatically stereotype patients into being digitally able or not. We found limited evidence that people living with mental health problems were particularly in need of DF, though they had varying views on the use of digital services. The newly developed framework for digital health equity may help to minimise any negative impacts on certain patient groups. 207
Finally, we would recommend that any research into DF monitors sustained use of online services, rather than the current focus on initial sign-up. Such sustained use will be required if the perceived benefits of digital service use are to be realised.
Research conduct
Taken at face value and in isolation, the findings from the practice survey might have implied that proactive, effective, DF was being carried out at scale across the country. However, comparisons of the practice survey responses with patient responses, and with the ethnographic observations, suggested a rather different picture. This has major implications for the isolated use of organisational-level surveys to examine how services are being delivered. Only by using a mixed-methods approach and synthesising the evidence from different research methods as we have done here, can a reliable and full picture be gained.
In studies of health service delivery as it is happening in everyday practice, it is important to examine a wide range of service providers to obtain findings that will be generalisable to the wider population. In conducting this study, we made efforts to include practices that were not ‘research active’ in order to make our results as generalisable as possible. However, the NIHR CRN, which was set up to support the delivery of NIHR funded research, has a strong focus on ‘research active’ practices. We found that CRNs were not set up to approach non-research active practices, and along with capacity issues, this posed a challenge to the delivery of the research. We would recommend a widening of the CRN remit to encourage contact with all general practices, especially for the conduct of health services research.
Equality, diversity and inclusion
Participant representation
Several steps have been taken in this research to ensure that the participants were representative of the wider population. Given the scope of this research, the population of interest is all users of GP services in England. The areas of the country where our research was conducted were selected to cover a diverse population, including a mix of city, urban and rural areas, a range of deprivation levels, and areas with high numbers of ethnic minorities.
Within WP2 we used a random sample of practices across our research area to ensure our findings were generalisable. Despite efforts to engage with all practices, the eventual practice survey respondent sample was somewhat less likely to include practices serving more deprived populations but was reasonably representative in terms of the age profile, and proportion from ethnic minorities, of the registered population.
The responders to the WP2B patient survey were skewed towards those of older age (over 65). However, this is reflective of the differential use of primary care services by older patients, and may denote improved representativeness of the sample relative to the people that exert most demand for primary care services. 208 Only 8% of responders described themselves as having a non-white ethnicity, which is below the national average (18%). This may in part reflect the age profile of responders but is still less than ideal. The respondent209 sample included participants with a wide range of working statuses as well good representation of carers and parents. There was also good representation of people with long-term physical and mental health conditions, with the latter group particularly focused on in the mental health boost sample. There were 358 patients who were deaf or had a hearing impediment, but only a small number describing themselves as blind, or partially sighted, a potentially important group for this study. Crucially, the patient survey was accessible in both paper and online formats to enable patients unable to engage with digital platforms to participate. We worked with our PAG to ensure the survey materials were accessible to as many potential responders as possible, although unfortunately resources did not allow for translations or large print versions. The steps taken to target more deprived populations in the patient survey resulted in an even spread of responders across the range of practice deprivation scores.
The analysis of GPPS data included data from across the country to maximise generalisability. Furthermore, due to the very large sample size of the GPPS survey, it was possible to examine awareness and use of online services in relatively small groups, something that would not have been possible with primary data collection. The GPPS is offered for patients to complete online, or over the phone, in 14 languages other than English as well as British Sign Language. However, given the paper version of the GPPS questionnaire is only available in English, and the strong relationship between response mode (paper/online) and digital confidence in our patient survey, it is likely that responders to the GPPS may be biased towards more digitally confident patients particularly among ethnic minorities.
Within WP3 the participating practices were purposefully sampled to include those serving populations with a range of deprivation levels, and varying proportions of both ethnic minority and older (aged over 65) patients. Practice staff participating in interviews covered a range of ages, and more than half were female, which probably reflects the gender balance in the staff roles included. Similarly, patient interview participants covered a range of ages, and again more than half were female. Around a third of patient participants described themselves as having a non-white ethnicity, all but one of whom described themselves as Asian.
The research team and wider involvement
There was no formal monitoring of the characteristics of the research team, as this was deemed inappropriate on the basis of potential disclosure. However, the research team included researchers and co-applicants across a range of ages, with a mix of genders and ethnicities. By the nature of being employed, none of the research team was over the age of 65 (a key population in this research). There was an even split of genders across the co-investigator team. The remaining research team was predominantly female. The team included researchers with a very wide range of experience and expertise, from undergraduate student interns to newly qualified post-doctoral researchers, more senior researchers, and the principal investigator with 35 years of experience.
Various development opportunities were provided to more junior members of the research team. Junior team members have presented work from the project at conferences and will continue to do so over the months following the end of the project as we continue to disseminate the findings. Furthermore, junior members of the team are taking leadership positions in many of the planned publications arising from this work. Informal training has been provided to those team members undertaking statistical analysis, and formal training was provided for conducting ethnographic fieldwork.
As with the research team, we did not formally monitor diversity within the PAG. However, its membership was predominantly white and had members aged over 50. While this is broadly representative of service users in one of our research areas (Southwest England), more could potentially have been done to make the PAG composition more representative of the broader areas covered. We took care to expand this group to inform the work focused on patients living with mental health, reflecting the importance of including relevant patients in the advice received.
Patient and public involvement and engagement
Patient and public involvement and engagement has been fully integrated within this project from the inception to completion. Due to the integrated nature of the PPIE we have reported the influence of integrated PPIE in each chapter of the report rather than describing it separately here. The project has benefited from a patient co-applicant, and a dedicated PPIE co-ordinator throughout the project. The PAG has been involved in every WP. In particular, three members of the PAG have been involved in each of the synthesis workshops in WP4 ensuring that the patient voice was at the heart of bringing the different research strands together.
Conclusion
Digital facilitation, while not a widely recognised concept, is important in the context of the move to an NHS with enhanced digital opportunities and enhanced digital access, and general practice staff are spending time and effort to provide it in general practices in England. It is viewed to have value and potential to increase the uptake of online services. DF can take many forms, though much of that is reactive and passive. As such there is clear scope to develop a more proactive approach to facilitation that actively engages patients. There is currently a disconnect between the expectations and perceptions of what DF is happening and its potential effectiveness, and the reality seen in everyday practice. This is related to a lack of clarity over the responsibility for delivering DF and resulting pressures on the time of general practice staff teams. Patients, practice staff members and national policy makers often perceive that the responsibility lies elsewhere. The establishment of clear lines of responsibility, and the development of digital tools and platforms that work well for patients and practice staff, will both be needed, alongside investment in staff time and training, if DF is to deliver on its promise.
Additional information
Acknowledgements
Steering Group Committee: Amrit Takhar, David Parkes, and Jeremy Horwood.
Patient Advisory Group (PAG): Laiya Bailey, Julie Harvey, Diana Lewis-Frost, Ben Marshall, Penny Thompson, Malcolm Turner, Lynn Tatnell, Andrea Shelly.
Sponsors: Vivienne Shaw (Lead), Pam Baxter (Co-Sponsor).
Sponsor team: Alexander Philips, Sarah Hider.
Administrator: Ellie Kingsland.
Survey support: Jodie Button, Mayam Gomez-Cano, Sine MacDonald, Isabelle Mayne, Charlotte Reburn, Claire Wright.
Project development: Richard Moore.
Clinical Research Networks (CRNs): East of England, North Thames, South West Peninsula, West Midlands, North West Coast.
All patients, general practices and general practice staff who supported and participated in the study.
Contributions of authors
Gary Abel (https://orcid.org/0000-0003-2231-5161) (Associate Professor of Primary Care, Study Coordinator) co-applicant, responsible for overall study design and co-ordination of work packages, led on work package 2, final report writing and review.
Helen Atherton (https://orcid.org/0000-0002-7072-1925) (Associate Professor of Primary Care Research) co-applicant, responsible for overall study design, and design of work package 3, led work package 3, conducted qualitative data analysis and synthesis, final report writing and review.
Jon Sussex (https://orcid.org/0000-0001-8970-4546) (Chief Economist) co-applicant, conceived the original research idea, contributed to overall study design, led work packages 1 and 4, conducted synthesis, final report writing and review.
Nurunnahar Akter (https://orcid.org/0000-0002-8802-9080) (Statistician, Data Analyst) conducted data analysis, modelling and synthesis for work package 2, final report writing and review.
Abodunrin Q Aminu (https://orcid.org/0000-0002-2349-407X) (Statistician, Data Analyst) conducted data analysis, modelling and synthesis for work package 2, final report writing and review.
Wiktoria Bak (https://orcid.org/0000-0002-5125-521X) (Medical Research Intern) analysis of the work package 2A practice survey, qualitative analysis of free-text responses and final report review.
Carol Bryce (https://orcid.org/0000-0003-1484-9032) (Assistant Professor) acquisition, analysis and interpretation of data for work package 3 and focused ethnography case studies, development of patient survey for work package 2B. Contributed to final report writing and review.
Christopher E Clark (https://orcid.org/0000-0002-7526-3038) (Clinical Senior Lecturer) co-applicant, supported conduct, analysis and writing up of literature review. Supported development and dissemination of surveys. Contributed throughout to all work packages and to final report writing and review.
Emma Cockcroft (https://orcid.org/0000-0003-3798-9492) (Research Fellow, PPIE) co-applicant, co-ordinated and led PPIE throughout all work packages, final report writing and review.
Hamish Evans (https://orcid.org/0000-0001-5941-4708) (Analyst) conducted work package 2A – practice survey and final report review.
Evangelos Gkousis (https://orcid.org/0000-0002-8560-8650) (Analyst) conducted work package 1, analysed and synthesised data, contributed to writing work package 1 chapter of final report.
Georgia Jenkins (https://orcid.org/0000-0003-2018-9974) (Research Assistant, PPIE) co-ordinated and led PPIE throughout the work packages, final report writing and review.
Caroline Jenkinson (https://orcid.org/0000-0002-9978-185X) (Research Fellow, Mental Health Patient Survey) conducted the mental health patient survey in work package 2B, final report writing and review.
Nada Khan (https://orcid.org/0000-0002-4014-5525) (NIHR Academic Clinical Fellow) qualitative data analysis work package 2, final report writing and review.
Jeffrey Lambert (https://orcid.org/0000-0003-4774-9054) (Lecturer) co-applicant, supported development and dissemination, analysis and interpretation of surveys and contributed to final report writing and review.
Brandi Leach (https://orcid.org/0000-0003-3262-1541) (Senior Analyst) conducted work package 1, analysed and synthesised data; conducted work package 2A – practice survey; conducted work package 4, synthesised data; final report writing and review.
Christine Marriott (https://orcid.org/0000-0002-8450-6222) (Patient Representative, PPIE contributions) co-applicant, contributed to all work packages and final report review.
Jennifer Newbould (https://orcid.org/0000-0002-2602-6984) (Research Leader) co-applicant, led the ethnographic element of work package 3. Conducted data analysis and synthesis, final report writing and review.
Sarah Parkinson (https://orcid.org/0000-0002-2858-1842) (Senior Analyst) conducted work package 1, analysed and synthesised data, contributed to writing work package 1 chapter of final report and review.
Jo Parsons (https://orcid.org/0000-0002-6542-8492) (Research Fellow) conducted and analysed mental health patient interviews, work package 3, final report writing and review.
Emma Pitchforth (https://orcid.org/0000-0001-9055-9331) (Senior Lecturer and Senior Research Fellow) co-applicant, contributed to overall study design, led on stakeholder interviews, conducted qualitative data collection and analysis for work package 3, final report writing and review.
Laura Sheard (https://orcid.org/0000-0002-9241-8361) (Associate Professor of Health Sciences) co-applicant, advised on work package 3 and conducted qualitative analysis, final report review.
Stephanie Stockwell (https://orcid.org/0000-0001-7828-3758) (Analyst) conducted qualitative data collection, analysis and synthesis for work package 3, final report writing and review.
Chloe Thomas (https://orcid.org/0000-0002-8881-3393) (Research Assistant and Administrator) provided administration support throughout the work packages, organised and minuted all meetings, assisted with survey data processing, final report review.
Bethan Treadgold (https://orcid.org/0000-0002-0255-7422) (Research Fellow) conducted qualitative data collection, analysis and synthesis for work package 3, final report writing and review.
Rachel Winder (https://orcid.org/0000-0002-9926-1280) (Research Fellow, Project Manager) responsible for the overall project management, conducted work package 2 including design and conduct of the surveys, conducted qualitative data collection (stakeholder interviews) and analysis for work package 3, involved in work package 4 synthesis, final report writing and review.
John L Campbell (https://orcid.org/0000-0002-6752-3493) (Professor of General Practice and Primary Care, Chief Investigator) co-applicant, responsible for overall study design and co-ordination of work packages. Contributed throughout to all work packages final report writing and review.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, or available in the tool kit on the NIHR journals Library report publication page at https://doi.org/10.3310/JKYT5803.
Primary conflicts of interest: All authors were funded by NIHR for their role in the project. Gary Abel serves on a Technical Expert Panel for the Agency for Healthcare Research and Quality (AHRQ), USA Safety Program for Telemedicine. An honoraria has been offered for taking part, which as yet has not been claimed. He has received funding as co-applicant for evaluating video and hybrid group consultations in general practice: mixed-methods, participatory study National Institute for Health and Care Research (NIHR) Health Services and Delivery Research (HS&DR) programme (NIHR133895). Helen Atherton declares relevant financial activities outside the submitted work: University of Warwick/eConsult Ltd: Warwick Industrial Fellowship funding a PhD Student, half the funding comes from eConsult Ltd. Paid to institution for purpose of funding studentship; NIHR 200778: Staff time and research costs paid to institution; NIHR PB-PG-1217-20033: Staff time and research costs paid to institution; NIHR 133620: Staff time and research costs paid to institution; University of Warwick/Advanced Ltd: Warwick Industrial Fellowship funding a PhD Student, half the funding comes from Advanced Ltd. Paid to institution for purpose of funding studentship; Medicspot Ltd: Analysed data provided by Medicspot Ltd. £1000 to institution to cover transcript costs for interviews conducted as part of study. She also received payment or honoraria for a lecture on e-mail consultation given to academic group at Aarhus University in 2020 – 500 Euro honorarium paid to her institution. She received support for attending meetings and/or travel: Royal College of General Practitioners Conference invited speaker October 2021: Registration fees paid for, one night of accommodation paid for, travel reimbursed directly to me. Royal College of General Practitioners Scientific Foundation Board meeting attendance December 2022 – Travel expenses reimbursed to her. She is an Advisory Board Member for NIHR128285 (no payments at all and the topic is relevant to the manuscript) and Digital-First Primary Care evaluation steering group NHS England and Improvement (no payments at all, content is relevant to the project). John L Campbell has received funding as co-applicant for evaluating video and hybrid group consultations in general practice: mixed-methods, participatory study National Institute for Health and Care Research (NIHR) Health Services and Delivery Research (HS&DR) programme (NIHR133895). He is also a member of the HTA National Stakeholder Advisory Group. Christopher E Clark is a board member of the HTA Prioritisation Committee: Primary and Community Based Care (A). He has received honoraria from ReCor Medical and Bayer UK for hypertension work unrelated to the topics discussed in this report. He is also Chair of the RCGP Rural Forum Steering Group. Christine Marriott has received payments for attending Di-Facto meetings and reviewing documents. Jennifer Newbould has received funding as co-applicant on another NIHR grant: 16/138/31 – NIHR HS&DR Rapid Service Evaluation Research Team – BRACE Centre. Payment was made to their employing institution: RAND Europe Community Interest Company. Jon Sussex has received funding as co-applicant on another NIHR grant: 16/138/31 – NIHR HS&DR Rapid Service Evaluation Research Team – BRACE Centre. Payment was made to his employing institution: RAND Europe Community Interest Company. Rachel Winder is a co-applicant on another NIHR grant – NIHR201070. Funding was provided to her employing institution. She also works in a GP practice which has participated in the Di-Facto surveys.
Patient data statement
This work used data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it is important that there are safeguards to make sure that they are stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation
Data-sharing statement
General Practice Patient Survey data were obtained under a data sharing agreement with NHS England. Study data may be made available to appropriate individuals on a case-by-case basis following an application to the Chief Investigator.
Ethics statement
Ethical approval was obtained for the patient survey and ethnographic case studies from the North East – Newcastle and North Tyneside 2 Research Ethics Committee on 27 April 2021, Health Research Authority approval was obtained in July 2021 (Integrated Research Application System number: 289425, protocol number: L01886).
During the course of the study, two minor and one major amendment were approved by the ethics committee, which included the inclusion of the mental health element of the study (approved 10 April 2022). All researchers conducting the fieldwork within practices obtained a research passport. Current protocol number: V1.3
Information governance statement
University of Exeter is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, University of Exeter is the Data Controller and the data processor and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here: www.exeter.ac.uk/about/oursite/dataprotection/dpo/
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the Health and Social Care Delivery Research programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Declaration of transparency
The lead author* affirms that this manuscript is an honest, accurate and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
* The manuscript’s guarantor:
Signatory:

Publications
Leach B, Parkinson S, Gkousis E, Abel G, Atherton H, Campbell J, Clark C, et al. Digital facilitation to support patient access to web-based primary care services: scoping literature review. J Med Internet Res 2022;24(7):e33911. https://doi.org/10.2196/33911
Khan N, Pitchforth E, Winder R, Abel G, Clark CE, Cockcroft E, Campbell J. What helps patients access web-based services in primary care? Free-text analysis of patient responses to the Di-Facto questionnaire. BMC Primary Care 2024;25:20. https://doi.org/10.1186/s12875-023-02257-5
List of potential journal publications:
| Date | Planned title and lead author | Journal for submission | Current status | |
|---|---|---|---|---|
| 1 | 25 May 2023 | Winder, R et al: How are patients supported to use online services in primary care in England? Exploring digital facilitation through practice and patient surveys as part of the Di-Facto study | JMIR | Draft |
| 2 | 25 May 2023 | Atker, N et al: Use of digital facilities in primary care and patients’ confidence | PLOS Digital Health | Draft |
| 3 | 25 May 2023 | Aminu, A et al: Variations in awareness and use of online services in England: analysis of the patient GPPS survey | BJGP | Draft |
| 4 | 25 May 2023 | Jenkinson, C et al: Effect of demographic characteristics on use and awareness of primary care digital services and digital facilitation in people with mental health conditions: a cross-sectional study | Lancet Psychiatry | Draft |
| 5 | Treadgold, B et al: Exploring the drivers, priorities and evolving policy context influencing digital facilitation in NHS primary care in England: qualitative interviews with stakeholders | Journal of Health Services Research and Policy | Draft | |
| 6 | 25 May 2023 | Stockwell, S et al: Going digital: evolution of the general practice receptionist role | BJGP | Draft |
| 7 | 25 May 2023 | Atherton, H et al: The hidden work of engaging with online services: ethnographic case study on digital facilitation | Social Science and Medicine | Draft |
| 8 | 25 May 2023 | Newbould, J et al: Digital Facilitation in General Practice: Focused Ethnographic case studies | BJGP | Draft |
| 9 | 25 May 2023 | Parsons, J et al: How do patients with a mental health diagnosis interact with online general services at the general practice? A qualitative study | Qualitative Health Communication | Draft |
| 10 | 6 September 2023 | Sussex, J et al: Helping primary care patients to use online services: synthesising the evidence from the DiFacto study | JMIR | Draft |
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- NHS England . GP Contract 2019 n.d. www.england.nhs.uk/gp/gpfv/investment/gp-contract/ (accessed 3 May 2019).
- UK Department of Health and Social Care . A Plan for Digital Health and Social Care. Appendix A: Our Action Plan for Delivering a Digital Future 2022 n.d. www.gov.uk/government/publications/a-plan-for-digital-health-and-social-care/a-plan-for-digital-health-and-social-care (accessed 17 January 2023).
- Clarke G, Dias A, Wolters A. Access to and Delivery of General Practice Services: A Study of Patients at Practices Using Digital and Online Tools. London: The Health Foundation; 2022.
- Wikipedia . British Government Response to the COVID-19 Pandemic: Wikipedia 2022. https://en.wikipedia.org/wiki/British_government_response_to_the_COVID-19_pandemic#Initial_response (accessed 17 January 2023).
- British Medical Association . Pressures in General Practice Data Analysis 2022. www.bma.org.uk/advice-and-support/nhs-delivery-and-workforce/pressures/pressures-in-general-practice-data-analysis (accessed 23 January 2023).
- Campbell JL, Fletcher E, Britten N, Green C, Holt TA, Lattimer V, et al. Telephone triage for management of same-day consultation requests in general practice (the ESTEEM trial): a cluster-randomised controlled trial and cost-consequence analysis. Lancet 2014;384:1859-68. https://doi.org/10.1016/S0140-6736(14)61058-8.
- Clarke G, Pariza P, Wolters A. How Has COVID-19 Affected Service Delivery in GP Practices that Offered Remote Consultations before the Pandemic?. The Health Foundation; 2020.
- Nuffield Trust, The Health Foundation . QualityWatch: The Remote Care Revolution During COVID-19 2020. www.nuffieldtrust.org.uk/resource/the-remote-care-revolution-in-the-nhs-understanding-impacts-and-attitudes (accessed 17 January 2023).
- NHS England . Updates and Guidance for General Practice 2020. www.england.nhs.uk/coronavirus/publication/preparedness-letters-for-general-practice/ (accessed 24 January 2023).
- Horton T, Hardie T, Mahadeva S, Warburton W. Securing a Positive Health Care Technology Legacy from COVID-19. London; 2021.
- Hutchings R. The Impact of COVID-19 on the Use of Digital Technology in the NHS. Nuffield Trust; 2020.
- Murphy M, Scott LJ, Salisbury C, Turner A, Scott A, Denholm R, et al. Implementation of remote consulting in UK primary care following the COVID-19 pandemic: a mixed-methods longitudinal study. Br J Gener Pract 2021;71:e166-77. https://doi.org/10.3399/bjgp.2020.0948.
- Ipsos MORI . GP Patient Survey: National Report – 2022 Survey 2022. www.gp-patient.co.uk/downloads/2022/GPPS_2022_National_report_PUBLIC.pdf (accessed 5 August 2022).
- Litchfield I, Shukla D, Greenfield S. Impact of COVID-19 on the digital divide: a rapid review. BMJ Open 2021;11. https://doi.org/10.1136/bmjopen-2021-053440.
- Marjanovic S, Sim M, Dubow T, Corbett J, Harte E, Parks S, et al. Innovation as a Driver of Quality and Productivity in UK Healthcare: Creating and Connecting Receptive Places: Emerging Insights Report. Santa Monica, CA: RAND Corporation; 2017.
- Mold F, de Lusignan S, Sheikh A, Majeed A, Wyatt JC, Quinn T, et al. Patients’ online access to their electronic health records and linked online services: a systematic review in primary care. Br J Gen Pract 2015;65:e141-51. https://doi.org/10.3399/bjgp15X683941.
- Mold F, de Lusignan S. Patients’ online access to their primary care electronic health records and linked online services: implications for research and practice. J Personal Med 2015;5:452-69. https://doi.org/10.3390/jpm5040452.
- Zhang M, Zhang C, Sun Q, Cai Q, Yang H, Zhang Y. Questionnaire survey about use of an online appointment booking system in one large tertiary public hospital outpatient service center in China. BMC Med Inform Decis Mak 2014;14. https://doi.org/10.1186/1472-6947-14-49.
- Green A, Bramley G, Annibal I, Sellick J. Rural Workforce Issues in Health and Care. Birmingham; 2018.
- NHS England . GP Online Services: What GP Practices Need to Do. 2022. www.england.nhs.uk/gp-online-services/about-the-prog/gp-practices/ (accessed 17 January 2023).
- UK Government Central Digital and Data Office . Transforming for a Digital Future: 2022 to 2025 Roadmap for Digital and Data 2022. www.gov.uk/government/publications/roadmap-for-digital-and-data-2022-to-2025/transforming-for-a-digital-future-2022-to-2025-roadmap-for-digital-and-data (accessed 17 January 2023).
- NHS England . GP Five Year Forward View 2016. www.kingsfund.org.uk/projects/nhs-five-year-forward-view (accessed 17 January 2023).
- Imison C, Castle-Clarke S, Watson RE, Edwards N. Delivering the Benefits of Digital Health Care. London: Nuffield Trust; 2017.
- Public Health Wales, King’s Fund . Digital Technology and Health Inequalities: A Scoping Review 2022. https://kingsfund.blogs.com/health_management/2020/12/digital-technology-and-health-inequalities-a-scoping-review.html (accessed 24 January 2023).
- McKinsey and Company . Telehealth: A Quarter-Trillion-Dollar Post-COVID-19 Reality? 2021. www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality (accessed 17 January 2023).
- IQVIA Institute . The Growing Value of Digital Health n.d. www.iqvia.com/insights/the-iqvia-institute/reports/the-growing-value-of-digital-health (accessed 24 January 2023).
- Buttlar M. The State of European Digital Health Investments. n.d. https://medium.com/birds-view/the-state-of-european-digital-health-investments-9f4e4d01b075 (accessed 24 January 2023).
- Kwasnicka D, Keller J, Perski O, Potthoff S, Ten Hoor GA, Ainsworth B, et al. White paper: open digital health – accelerating transparent and scalable health promotion and treatment. Health Psychol Rev 2022;16:475-91. https://doi.org/10.1080/17437199.2022.2046482.
- Lambert JD, Elliott LR, Taylor AH, Farrand P, Haase AM, Greaves CJ. A novel method for assessing design fidelity in web-based behavioral interventions. Health Psychol 2021;40:217-25. https://doi.org/10.1037/hea0001046.
- NHS Digital . Why Digital Inclusion Matters to Health and Social Care 2022. https://digital.nhs.uk/about-nhs-digital/corporate-information-and-documents/digital-inclusion/digital-inclusion-in-health-and-social-care (accessed 23 January 2023).
- Good Things Foundation . Widening Digital Participation Programme 2022. www.goodthingsfoundation.org/what-we-do/our-partnerships/health-and-wellbeing/widening-digital-participation/ (accessed 23 January 2023).
- Justeconomics . Digital Inclusion: The Social Return on Investment 2016. www.justeconomics.co.uk/uploads/reports/Just-Economics-BT-Digital-Inclusion-SROI.pdf (accessed 28 February 2023).
- NHS England . Our Funding 2022. www.england.nhs.uk/publications/business-plan/our-2022-23-business-plan/our-funding/ (accessed 24 January 2023).
- Open Government Licence . Open Government Licence for Public Sector Information 2017. www.nationalarchives.gov.uk/doc/open-government-licence/version/3/ (accessed 28 February 2023).
- NHS England . GP Online Services: The Key Benefits 2018. www.england.nhs.uk/gp-online-services/learning-so-far/key-benefits/ (accessed 17 January 2023).
- Atherton H, Ziebland S. What do we need to consider when planning, implementing and researching the use of alternatives to face-to-face consultations in primary healthcare?. Digit Health 2016;2. http://doi.org/10.1177/2055207616675559.
- Huh J, Koola J, Contreras A, Castillo AK, Ruiz M, Tedone KG, et al. Consumer health informatics adoption among underserved populations: thinking beyond the digital divide. Yearb Med Inform 2018;27:146-55. http://doi.org/10.1055/s-0038-1641217.
- Phelps RG, Taylor J, Simpson K, Samuel J, Turner AN. Patients’ continuing use of an online health record: a quantitative evaluation of 14,000 patient years of access data. J Med Internet Res 2014;16. http://doi.org/10.2196/jmir.3371.
- Cochrane Methods Equity . PROGRESS-Plus: Cochrane 2021. https://methods.cochrane.org/equity/projects/evidence-equity/progress-plus (accessed 17 January 2023).
- NHS England . Definitions for Health Inequalities (Archived 01-11-2021) 2021. https://webarchive.nationalarchives.gov.uk/ukgwa/20211101142006/https://www.england.nhs.uk/ltphimenu/definitions-for-health-inequalities/#inclusion-health-groups (accessed 17 January 2023).
- Barclays Bank Ltd . Barclays Digital Eagles 2018. www.barclays.co.uk/digital-confidence/eagles/ (accessed 17 January 2023).
- Lankshear C, Knobel M. Digital Literacies. New York: Peter Lang; 2022.
- Rowlands G. Health Literacy and Digital Literacy: Importance and Next Steps. University of Newcastle, UK; 2020.
- Kim H, Xie B. Health literacy in the eHealth era: a systematic review of the literature. Patient Educ Couns 2017;100:1073-82. https://doi.org/10.1016/j.pec.2017.01.015.
- Jenkins CL, Imran S, Mahmood A, Bradbury K, Murray E, Stevenson F, et al. Digital health intervention design and deployment for engaging demographic groups likely to be affected by the digital divide: protocol for a systematic scoping review. JMIR Res Protoc 2022;11. https://doi.org/10.2196/32538.
- Konttila J, Siira H, Kyngäs H, Lahtinen M, Elo S, Kääriäinen M, et al. Healthcare professionals’ competence in digitalisation: a systematic review. J Clin Nurs 2019;28:745-61. https://doi.org/10.1111/jocn.14710.
- Verma P, Kerrison R. Patients’ and physicians’ experiences with remote consultations in primary care during the COVID-19 pandemic: a multi-method rapid review of the literature. BJGP Open 2022;6. https://doi.org/10.3399/BJGPO.2021.0192.
- Shachar L. ‘You become a slightly better doctor’: doctors adopting integrated medical expertise through interactions with E-patients. Soc Sci Med 2022;305. https://doi.org/10.1016/j.socscimed.2022.115038.
- Glasziou P, Straus S, Brownlee S, Trevena L, Dans L, Guyatt G, et al. Evidence for underuse of effective medical services around the world. Lancet 2017;390:169-77. https://doi.org/10.1016/S0140-6736(16)30946-1.
- NHS England . Using Online Consultations in Primary Care: Implementation Toolkit 2020. www.england.nhs.uk/publication/using-online-consultations-in-primary-care-implementation-toolkit/ (accessed 17 January 2023).
- Reiners F, Sturm J, Bouw LJ, Wouters EJ. Sociodemographic factors influencing the use of eHealth in people with chronic diseases. Int J Environ Res Public Health 2019;16. https://doi.org/10.3390/ijerph16040645.
- Irizarry T, Dabbs AD, Curran CR. Patient portals and patient engagement: a state of the science review. J Med Internet Res 2015;17. https://doi.org/10.2196/jmir.4255.
- Xiao N, Sharman R, Rao HR, Upadhyaya S. Factors influencing online health information search: an empirical analysis of a national cancer-related survey. Decis Support Syst 2014;57:417-27. https://doi.org/10.1016/j.dss.2012.10.047.
- McKinstry B. ViCo (Video Conferencing) Study. Edinburgh: University of Edinburgh; 2021.
- Donaghy E, Atherton H, Hammersley V, Mcneilly H, Bikker A, Robbins L, et al. The benefits, challenges, and acceptability of video consultation with patients via the internet in general practice. BJGP 2019;69:e586-e94. https://doi.org/10.3399/bjgp19X704141.
- Howells K, Amp M, Burrows M, Brown J, Brennan R, Dickinson J, et al. Remote primary care during the COVID-19 pandemic for people experiencing homelessness: a qualitative study. Br J Gener Pract: J Royal Coll Gener Pract 2022;72:e492-500. https://doi.org/10.3399/BJGP.2021.0596.
- Beacom AM, Newman SJ. Communicating health information to disadvantaged populations. Fam Commun Health 2010;33:152-62. www.jstor.org/stable/44954183.
- O’Connor S, Hanlon P, O’Donnell CA, Garcia S, Glanville J, Mair FS. Understanding factors affecting patient and public engagement and recruitment to digital health interventions: a systematic review of qualitative studies. BMC Med Inform Decis Mak 2016;16:1-15. https://doi.org/10.1186/s12911-016-0359-3.
- Horwood J. Investigating the Unintended Consequences of the Use of Digital Health Tools in Primary Care. London: NIHR School for Primary Care Research; 2018.
- Seguin M, Hall L, Atherton H, Barnes R, Leydon G, Murray E, et al. Protocol paper for the ‘Harnessing resources from the internet to maximise outcomes from GP consultations (HaRI)’ study: a mixed qualitative methods study. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2018-024188.
- NHS England . Getting Ready for Patients to Have Access to Their Future Information 2022. www.events.england.nhs.uk/getting-ready-for-all-patients-to-have-access-to-their-future-data (accessed 17 January 2023).
- Yang M, Pollard J, Garrod B, Marjanovic S, Sussex J. Evaluating the impact of the Eastern Academic Health Science Network Transformation Support Unit (Product Page). RANDeurope; 2018.
- Primary Care Projects Associates Ltd . Primary Care Demand and Capacity Audit: Analysis of Survey Information Collected from Lower Lea Valley Locality GP Practices, Minor Injury Unit (MIU) and Community Pharmacy 2016.
- Sakaguchi-Tang DK, Bosold AL, Choi YK, Turner AM. Patient portal use and experience among older adults: systematic review. JMIR Med Inform 2017;5. https://doi.org/10.2196/medinform.8092.
- Amante DJ, Hogan TP, Pagoto SL, English TM. A systematic review of electronic portal usage among patients with diabetes. Diabet Technol Therap 2014;16:784-93. https://doi.org/10.1089/dia.2014.0078.
- Jenkinson CE, Asprey A, Clark CE, Richards SH. Patients’ willingness to attend the NHS cardiovascular health checks in primary care: a qualitative interview study. BMC Fam Pract 2015;16. https://doi.org/10.1186/s12875-015-0244-7.
- NHS Digital . NHS App Pilot Research Findings 2019 n.d. https://digital.nhs.uk/services/nhs-app/nhs-app-pilot-research-report#document-content (accessed 17 January 2023).
- Cowie J, Calveley E, Bowers G, Bowers J. Evaluation of a digital consultation and self-care advice tool in primary care: a multi-methods study. Int J Environ Res Public Health 2018;15. https://doi.org/10.3390/ijerph15050896.
- Kalichman SC, Cherry C, Cain D, Pope H, Kalichman M, Eaton L, et al. Internet-based health information consumer skills intervention for people living with HIV/AIDS. J Consult Clin Psychol 2006;74:545-54. https://doi.org/10.1037/0022-006X.74.3.545.
- Weiss C. Progress and Future Directions in Evaluation: Perspectives on Theory, Practice and Methods New Directions for Evaluation. San Francisco: Jossey-Bass; 1997.
- Pawson R, Tilley N. Realistic Evaluation. London: Sage; 1997.
- The UK Public Involvement Standards Development Partnership . UK Standards for Public Involvement 2019. https://sites.google.com/nihr.ac.uk/pi-standards/home (accessed 2 February 2023).
- Liabo K, Boddy K, Burchmore H, Cockcroft E, Britten N. Clarifying the roles of patients in research. Br J Sports Med 2019;53. https://doi.org/10.1136/bjsports-2018-k1463rep.
- Leach B, Parkinson S, Gkousis E, Abel G, Atherton H, Campbell J, et al. Facilitation to support patient access to web-based primary care services: scoping literature review. J Med Internet Res 2022;24. https://doi.org/10.2196/33911.
- Creative Commons . Attribution 4.0 International (CC BY 4.0) 2020. https://creativecommons.org/licenses/by/4.0/ (accessed 28 February 2023).
- Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid-Based Healthc 2015;13:141-6. https://doi.org/10.1097/XEB.0000000000000050.
- University of York Centre for Reviews and Dissemination . PROSPERO: Registering a Review on PROSPERO 2020. www.crd.york.ac.uk/prospero/#guidancenotes (accessed 17 January 2023).
- Leach B, Evangelos G, Parkinson S, Newbould J, Sussex J. Digital Facilitation to Support Patient Access to Online Primary Care Services. National Institute for Health Research; University of York, Centre for Reviews and Dissemination; 2020.
- Ryan R. Cochrane Consumers and Communication Review Group: Data Synthesis and Analysis. Cochrane Consumers and Communication Review Group; 2013.
- Nguyen AD, Frensham LJ, Baysari MT, Carland JE, Day RO. Patients’ use of mobile health applications: what general practitioners think. Fam Pract 2019;36:214-8. https://doi.org/10.1093/fampra/cmy052.
- Grossman LV, Creber RM, Benda NC, Wright D, Vawdrey DK, Ancker JS. Interventions to increase patient portal use in vulnerable populations: a systematic review. J Am Med Inf Assoc 2019;26:855-70. https://doi.org/10.1093/jamia/ocz023.
- Greenhalgh T, Hinder S, Stramer K, Bratan T, Russell J. Adoption, non-adoption, and abandonment of a personal electronic health record: case study of HealthSpace. Br Med J 2010;341. https://doi.org/10.1136/bmj.c5814.
- Carter M, Fletcher E, Sansom A, Warren FC, Campbell JL. Feasibility, acceptability and effectiveness of an online alternative to face-to-face consultation in general practice: a mixed-methods study of webGP in six Devon practices. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-018688.
- Plaete J, Crombez G, DeSmet A, Deveugele M, Verloigne M, De Bourdeaudhuij I. What do general practitioners think about an online self-regulation programme for health promotion? Focus group interviews. BMC Fam Pract 2015;16. https://doi.org/10.1186/s12875-014-0214-5.
- Hjelmager DM, Vinther LD, Poulsen SH, Petersen LS, Jensen MB, Riis A. Requirements for implementing online information material for patients with low back pain in general practice: an interview study. Scand J Prim Health Care 2019;37:60-8. https://doi.org/10.1080/02813432.2019.1569413.
- Ebert DD, Berking M, Cuijpers P, Lehr D, Pörtner M, Baumeister H. Increasing the acceptance of internet-based mental health interventions in primary care patients with depressive symptoms: a randomized controlled trial. J Affect Disord 2015;176:9-17. https://doi.org/10.1016/j.jad.2015.01.056.
- du Pon E, Kleefstra N, Cleveringa F, van Dooren A, Heerdink ER, van Dulmen S. Effects of the proactive interdisciplinary self-management (PRISMA) program on online care platform usage in patients with type 2 diabetes in primary care: a randomized controlled trial. J Diabetes Res 2020;2020. https://doi.org/10.1155/2020/5013142.
- Shaw EK, Howard J, West DR, Crabtree BF, Nease DE, Tutt B, et al. The role of the champion in primary care change efforts: from the State Networks of Colorado Ambulatory Practices and Partners (SNOCAP). J Am Board Fam Med 2012;25:676-85. https://doi.org/10.3122/jabfm.2012.05.110281.
- Possemato K, Kuhn E, Johnson E, Hoffman JE, Owen JE, Kanuri N, et al. Using PTSD Coach in primary care with and without clinician support: a pilot randomized controlled trial. Gen Hosp Psychiatry 2016;38:94-8. https://doi.org/10.1016/j.genhosppsych.2015.09.005.
- van Middelaar T, Beishuizen CRL, Guillemont J, Barbera M, Richard E, Moll van Charante EP. HATICE Consortium . Engaging older people in an internet platform for cardiovascular risk self-management: a qualitative study among Dutch HATICE participants. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-019683.
- Abidi S, Vallis M, Piccinini-Vallis H, Imran SA, Abidi SSR. Diabetes-related behavior change knowledge transfer to primary care practitioners and patients: implementation and evaluation of a digital health platform. JMIR Med Inform 2018;6. https://doi.org/10.2196/medinform.9629.
- Hardiker NR, Grant MJ. Barriers and facilitators that affect public engagement with eHealth services. Stud Health Technol Inform 2010;160:13-7. https://doi.org/10.3233/978-1-60750-588-4-13.
- Abbott-Garner P, Richardson J, Jones RB. The impact of superfast broadband, tailored booklets for households, and discussions with general practitioners on personal electronic health readiness: cluster factorial quasi-randomized control trial. J Med Internet Res 2019;21. https://doi.org/10.2196/11386.
- Lopez Segui F, Pratdepadua Bufill C, Abdon Gimenez N, Martinez Roldan J, Garcia Cuyas F. The prescription of mobile apps by primary care teams: a pilot project in Catalonia. JMIR Mhealth Uhealth 2018;6. https://doi.org/10.2196/10701.
- Bernhard G, Mahler C, Seidling HM, Stützle M, Ose D, Baudendistel I, et al. Developing a shared patient-centered, web-based medication platform for type 2 diabetes patients and their health care providers: qualitative study on user requirements. J Med Internet Res 2018;20. https://doi.org/10.2196/jmir.8666.
- Mahoney N, Gladstone T, DeFrino D, Stinson A, Nidetz J, Canel J, et al. Prevention of adolescent depression in primary care: barriers and relational work solutions. Calif J Health Promot 2017;15:1-12. www.ncbi.nlm.nih.gov/pmc/articles/PMC6214481/pdf/nihms-990620.pdf (accessed 17 January 2023).
- Molleda L, Bahamon M, St George SM, Perrino T, Estrada Y, Correa Herrera D, et al. Clinic personnel, facilitator, and parent perspectives of eHealth Familias Unidas in primary care. J Pediatr Health Care 2017;31:350-61. https://doi.org/10.1016/j.pedhc.2016.11.001.
- Byambasuren O, Beller E, Hoffmann T, Glasziou P. mHealth app prescription in Australian general practice: pre-post study. JMIR Mhealth Uhealth 2020;8. https://doi.org/10.2196/16497.
- Castle-Clarke S, Imison C. The Digital Patient: Transforming Primary Care?. London: Nuffield Trust; 2016.
- Aarts JW, Faber MJ, Cohlen BJ, Van Oers A, Nelen WL, Kremer JA. Lessons learned from the implementation of an online infertility community into an IVF clinic’s daily practice. Hum Fertil (Camb) 2015;18:238-47. https://doi.org/10.3109/14647273.2015.1057901.
- Hoffmann M, Hartmann M, Wensing M, Friederich HC, Haun MW. Potential for integrating mental health specialist video consultations in office-based routine primary care: cross-sectional qualitative study among family physicians. J Med Internet Res 2019;21. https://doi.org/10.2196/13382.
- Lipschitz J, Miller CJ, Hogan TP, Burdick KE, Lippin-Foster R, Simon SR, et al. Adoption of mobile apps for depression and anxiety: cross-sectional survey study on patient interest and barriers to engagement. JMIR Ment Health 2019;6. https://doi.org/10.2196/11334.
- Hassett L, van den Berg M, Lindley RI, Crotty M, McCluskey A, van der Ploeg HP, et al. Digitally enabled aged care and neurological rehabilitation to enhance outcomes with Activity and MObility UsiNg Technology (AMOUNT) in Australia: a randomised controlled trial. PLOS Med 2020;17. https://doi.org/10.1371/journal.pmed.1003029.
- Reynolds J, Griffiths KM, Cunningham JA, Bennett K, Bennett A. Clinical practice models for the use of e-mental health resources in primary health care by health professionals and peer workers: a conceptual framework. JMIR Ment Health 2015;2. https://doi.org/10.2196/mental.4200.
- Coulter A, Mearns B. Developing Care for a Changing Population: Patient Engagement and Health Information Technology. London: Nuffield Trust; 2016.
- Ronda MCM, Dijkhorst-Oei LT, Vos RC, Rutten G. Diabetes care providers’ opinions and working methods after four years of experience with a diabetes patient web portal; a survey among health care providers in general practices and an outpatient clinic. BMC Fam Pract 2018;19. https://doi.org/10.1186/s12875-018-0781-y.
- Slevin P, Kessie T, Cullen J, Butler MW, Donnelly SC, Caulfield B. Exploring the barriers and facilitators for the use of digital health technologies for the management of COPD: a qualitative study of clinician perceptions. QJM 2020;113:163-72. https://doi.org/10.1093/qjmed/hcz241.
- Rodgers M, Raine G, Thomas S, Harden M, Eastwood A. Informing NHS policy in ‘digital-first primary care’: a rapid evidence synthesis. Health Soc Care Deliv Res 2019;7:1-124. https://doi.org/10.3310/hsdr07410.
- Longacre M, Grande S, Hager A, Montan M, Bergquist RP, Martensson M, et al. Clinical adoption of mHealth technology to support pediatric cystic fibrosis care in Sweden: qualitative case study. JMIR Pediatr Parent 2018;1. https://doi.org/10.2196/11080.
- Webb MJ, Wadley G, Sanci LA. Experiences of general practitioners and practice support staff using a health and lifestyle screening app in primary health care: implementation case study. JMIR MHealth UHealth 2018;6. https://doi.org/10.2196/mhealth.8778.
- Zarski AC, Berking M, Reis D, Lehr D, Buntrock C, Schwarzer R, et al. Turning good intentions into actions by using the health action process approach to predict adherence to internet-based depression prevention: secondary analysis of a randomized controlled trial. J Med Internet Res 2018;20. https://doi.org/10.2196/jmir.8814.
- Radovic A, Odenthal K, Flores AT, Miller E, Stein BD. Prescribing technology to increase uptake of depression treatment in primary care: a pre-implementation focus group study of SOVA (Supporting Our Valued Adolescents). J Clin Psychol Med Settings 2019;27:766-82. https://doi.org/10.1007/s10880-019-09669-5.
- Delbanco T, Walker J, Bell SK, Darer JD, Elmore JG, Farag N, et al. Inviting patients to read their doctors’ notes: a quasi-experimental study and a look ahead. Ann Intern Med 2012;157:461-70. https://doi.org/10.7326/0003-4819-157-7-201210020-00002.
- Nijland N, van Gemert-Pijnen JE, Kelders SM, Brandenburg BJ, Seydel ER. Factors influencing the use of a Web-based application for supporting the self-care of patients with type 2 diabetes: a longitudinal study. J Med Internet Res 2011;13. https://doi.org/10.2196/jmir.1603.
- Lyles CR, Tieu L, Sarkar U, Kiyoi S, Sadasivaiah S, Hoskote M, et al. A randomized trial to train vulnerable primary care patients to use a patient portal. J Am Board Fam Med 2019;32:248-58. https://doi.org/10.3122/jabfm.2019.02.180263.
- North F, Hanna BK, Crane SJ, Smith SA, Tulledge-Scheitel SM, Stroebel RJ. Patient portal doldrums: does an exam room promotional video during an office visit increase patient portal registrations and portal use?. J Am Med Inform Assoc 2011;18:i24-7. https://doi.org/10.1136/amiajnl-2011-000381.
- Lin JX, Faust B, Ebert DD, Kramer L, Baumeister H. A web-based acceptance-facilitating intervention for identifying patients’ acceptance, uptake, and adherence of internet and mobile-based pain interventions: randomized controlled trial. J Med Internet Res 2018;20. https://doi.org/10.2196/jmir.9925.
- Baumeister H, Seifferth H, Lin J, Nowoczin L, Lüking M, Ebert D. Impact of an acceptance facilitating intervention on patients’ acceptance of internet-based pain interventions: A randomized controlled trial. Clin J Pain 2015;31:528-35. https://doi.org/10.1097/AJP.0000000000000118.
- Ramsey A, Lanzo E, Huston-Paterson H, Tomaszewski K, Trent M. Increasing patient portal usage: preliminary outcomes from the MyChart Genius project. J Adolesc Health 2018;62:29-35. https://doi.org/10.1016/j.jadohealth.2017.08.029.
- Ford JH, Alagoz E, Dinauer S, Johnson KA, Pe-Romashko K, Gustafson DH. Successful organizational strategies to sustain use of A-CHESS: a mobile intervention for individuals with alcohol use disorders. J Med Internet Res 2015;17. https://doi.org/10.2196/jmir.3965.
- Sieck CJ, Hefner JL, Schnierle J, Florian H, Agarwal A, Rundell K, et al. The rules of engagement: perspectives on secure messaging from experienced ambulatory patient portal users. JMIR Med Inform 2017;5. https://doi.org/10.2196/medinform.7516.
- Patel V, Hale TM, Palakodeti S, Kvedar JC, Jethwani K. Prescription tablets in the digital age: a cross-sectional study exploring patient and physician attitudes toward the use of tablets for clinic-based personalized health care information exchange. JMIR Res Protoc 2015;4. https://doi.org/10.2196/resprot.3806.
- Abidi S, Vallis M, Piccinini-Vallis H, Imran SA, Abidi SS. A decision support environment to design personalized behavior modification plans for diabetes self-management. Eur J Epidemiol 2016;31. https://doi.org/10.1007/s10654-016-0183-1.
- Tieu L, Sarkar U, Schillinger D, Ralston JD, Ratanawongsa N, Pasick R, et al. Barriers and facilitators to online portal use among patients and caregivers in a safety net health care system: a qualitative study. J Med Internet Res 2015;17. https://doi.org/10.2196/jmir.4847.
- Lin J, Paganini S, Sander L, Lüking M, Ebert DD, Buhrman M, et al. An internet-based intervention for chronic pain. Dtsch Arztebl Int 2017;114:681-8. https://doi.org/10.3238/arztebl.2017.0681.
- Ma J, Xiao L, Blonstein AC. Measurement of self-monitoring web technology acceptance and use in an e-health weight-loss trial. Telemed J E Health 2013;19:739-45. https://doi.org/10.1089/tmj.2013.0009.
- Apter AJ, Localio AR, Morales KH, Han XY, Perez L, Mullen AN, et al. Home visits for uncontrolled asthma among low-income adults with patient portal access. J Allergy Clin Immunol 2019;144:846-53. https://doi.org/10.1016/j.jaci.2019.05.030.
- Talboom-Kamp EP, Verdijk NA, Kasteleyn MJ, Harmans LM, Talboom IJ, Numans ME, et al. High level of integration in integrated disease management leads to higher usage in the e-Vita Study: self-management of chronic obstructive pulmonary disease with web-based platforms in a parallel cohort design. J Med Internet Res 2017;19. https://doi.org/10.2196/jmir.7037.
- Littlewood E, Duarte A, Hewitt C, Knowles S, Palmer S, Walker S, et al. REEACT Team . A randomised controlled trial of computerised cognitive behaviour therapy for the treatment of depression in primary care: the Randomised Evaluation of the Effectiveness and Acceptability of Computerised Therapy (REEACT) trial. Health Technol Assess 2015;19:viii-171. https://doi.org/10.3310/hta191010.
- van Beurden SB, Simmons SI, Tang JCH, Mewse AJ, Abraham C, Greaves CJ. Informing the development of online weight management interventions: a qualitative investigation of primary care patient perceptions. BMC Obes 2018;5. https://doi.org/10.1186/s40608-018-0184-6.
- Mares ML, Gustafson DH, Glass JE, Quanbeck A, McDowell H, McTavish F, et al. Implementing an mHealth system for substance use disorders in primary care: a mixed methods study of clinicians’ initial expectations and first year experiences. BMC Med Inform Decis Mak 2016;16. https://doi.org/10.1186/s12911-016-0365-5.
- Lillevoll KR, Vangberg HCB, Griffiths KM, Waterloo K, Eisemann MR. Uptake and adherence of a self-directed internet-based mental health intervention with tailored e-mail reminders in senior high schools in Norway. BMC Psychiatry 2014;14. https://doi.org/10.1186/1471-244X-14-14.
- Zarski AC, Lehr D, Berking M, Riper H, Cuijpers P, Ebert DD. Adherence to internet-based mobile-supported stress management: a pooled analysis of individual participant data from three randomized controlled trials. J Med Internet Res 2016;18. https://doi.org/10.2196/jmir.4493.
- Lyles CR, Allen JY, Poole D, Tieu L, Kanter MH, Garrido T. ‘I want to keep the personal relationship with my doctor’: understanding barriers to portal use among African Americans and Latinos. J Med Internet Res 2016;18. https://doi.org/10.2196/jmir.5910.
- Castle-Clarke S. What Will New Technology Mean for the NHS and Its Patients?: Four Big Technological Trends. London: The Health Foundation, Nuffield Trust, Institute for Fiscal Studies and The King’s Fund; 2018.
- Ancker JS, Grossman L, Benda NC. Health literacy 2030: is it time to redefine the term?. J Gen Intern Med 2019;35:2427-30. https://doi.org/10.1007/s11606-019-05472-y.
- Cameron G, Alderwick H, Bowers A, Dixon J. Shaping Health Futures: Preparing for Tomorrow’s Possibilities Today. London: The Health Foundation; 2019.
- Ayre J, Bonner C, Bramwell S, McClelland S, Jayaballa R, Maberly G, et al. Implications for GP endorsement of a diabetes app with patients from culturally diverse backgrounds: a qualitative study. Austr J Prim Health 2020;26:52-7. https://doi.org/10.1071/PY19062.
- Ozili PK. Impact of digital finance on financial inclusion and stability. Borsa Istanbul Rev 2018;18:329-40. https://doi.org/10.1016/j.bir.2017.12.003.
- Sprenger M, Mettler T, Osma J. Health professionals’ perspective on the promotion of e-mental health apps in the context of maternal depression. PLOS ONE 2017;12. https://doi.org/10.1371/journal.pone.0180867.
- Greenhalgh T, Wherton J, Papoutsi C, Lynch J, Hughes G, A’Court C, et al. Beyond adoption: a new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. J Med Internet Res 2017;19. https://doi.org/10.2196/jmir.8775.
- Miller KE, Kuhn E, Yu J, Owen JE, Jaworski BK, Taylor K, et al. Use and perceptions of mobile apps for patients among VA primary care mental and behavioral health providers. Profess Psychol: Res Pract 2019;50:204-9. https://doi.org/10.1037/pro0000229.
- Careyva B, Shaak K, Mills G, Johnson M, Goodrich S, Stello B, et al. Implementation of technology-based patient engagement strategies within practice-based research networks. J Am Board Fam Med 2016;29:581-91. https://doi.org/10.3122/jabfm.2016.05.160044.
- O’Cathain A, Drabble SJ, Foster A, Horspool K, Edwards L, Thomas C, et al. Being human: a qualitative interview study exploring why a telehealth intervention for management of chronic conditions had a modest effect. J Med Internet Res 2016;18. https://doi.org/10.2196/jmir.5879.
- Oliveira Hasiguchi TC. Bringing Health Care to the Patient: An Overview of the Use of Telemedicine in OECD Countries. OECD; 2020.
- Weppner WG, Ralston JD, Koepsell TD, Grothaus LC, Reid RJ, Jordan L, et al. Use of a shared medical record with secure messaging by older patients with diabetes. Diabetes Care 2010;33:2314-9. https://doi.org/10.2337/dc10-1124.
- Maguire D, Evans H, Honeyman M, Omojomolo D. Digital Change in Health and Social Care. London: The King’s Fund; 2018.
- Raza Khan U, Zia TA, Pearce C, Perera K. The MyHealthRecord system impacts on patient workflow in general practices. Stud Health Technol Inform 2019;266:162-7. https://doi.org/10.3233/shti190789.
- Rosen R. Delivering General Practice with Too Few GPs. London: Nuffield Trust; 2019.
- Ricciardi L, Mostashari F, Murphy J, Daniel JG, Siminerio EP. A national action plan to support consumer engagement via e-health. Health Aff 2013;32:376-84. https://doi.org/10.1377/hlthaff.2012.1216.
- Moult A, Burroughs H, Kingstone T, Chew-Graham CA. How older adults self-manage distress: does the internet have a role? A qualitative study. BMC Fam Pract 2018;19. https://doi.org/10.1186/s12875-018-0874-7.
- Amaro S, Duarte P. An integrative model of consumers’ intentions to purchase travel online. Tour Manag 2015;46:64-79. https://doi.org/10.1016/j.tourman.2014.06.006.
- Bonsón Ponte E, Carvajal-Trujillo E, Escobar-Rodríguez T. Influence of trust and perceived value on the intention to purchase travel online: integrating the effects of assurance on trust antecedents. Tour Manag 2015;47:286-302. https://doi.org/10.1016/j.tourman.2014.10.009.
- Hale K, Capra S, Bauer J. A framework to assist health professionals in recommending high-quality apps for supporting chronic disease self-management: illustrative assessment of type 2 diabetes apps. JMIR MHealth UHealth 2015;3. https://doi.org/10.2196/mhealth.4532.
- Lyles CR, Sarkar U, Ralston JD, Adler N, Schillinger D, Moffet HH, et al. Patient-provider communication and trust in relation to use of an online patient portal among diabetes patients: the Diabetes and Aging Study. J Am Med Inform Assoc 2013;20:1128-31. https://doi.org/10.1136/amiajnl-2012-001567.
- NHS England . Five Year Forward View 2014. www.england.nhs.uk/publication/nhs-five-year-forward-view/ (accessed 18 January 2023).
- Primary Care Strategy and NHS Contracts Group . 2019/20/General/Medical/Services/(GMS)/Contract:/Guidance/and/Audit/Requirements/for/GMS/Contract/[Version/1] 2019. www.england.nhs.uk/wp-content/uploads/2019/08/19-20-gms-contract-guidance-audit-requirements-v2.pdf (accessed 18 January 2023).
- NHS Digital . GP and GP Practice Related Data 2020 n.d. https://digital.nhs.uk/services/organisation-data-service/file-downloads/gp-and-gp-practice-related-data (accessed 18 January 2023).
- Karnoe A, Furstrand D, Christensen K, Norgaard O, Kayser L. Assessing competencies needed to engage with digital health services: development of the eHealth literacy assessment toolkit. J Med Internet Res 2018;20. https://doi.org/10.2196/jmir.8347.
- Campbell J, Smith P, Nissen S, Bower P, Elliott M, Roland M. The GP Patient Survey for use in primary care in the National Health Service in the UK: development and psychometric characteristics. BMC Fam Pract 2009;10. https://doi.org/10.1186/1471-2296-10-57.
- GP Patient Survey . GP Patient Survey: FAQ n.d. https://gp-patient.co.uk/faq (accessed 18 January 2023).
- GP Patient Survey . GP Patient Survey: See How Your GP Practice Is Doing or Compare Practices 2022. www.gp-patient.co.uk/ (accessed 2022).
- Ipsos MORI . GP Patient Survey 2021: Technical Annex 2021. https://gp-patient.co.uk/downloads/2021/GPPS_2021_Technical_Annex_PUBLIC.pdf (accessed 18 January 2023).
- Ipsos MORI . GP Patient Survey 2022: Technical Annex 2022. https://gp-patient.co.uk/downloads/2022/GPPS_2022_Technical_Annex_PUBLIC.pdf (accessed 18 January 2023).
- Ipsos MORI Social Research Institute . GP Patient Survey 2019: Technical Annex 2019. https://gp-patient.co.uk/downloads/archive/2019/GPPS_2019_Technical_Annex_PUBLIC.pdf (accessed 18 January 2023).
- Ipsos MORI Social Research Institute . GP Patient Survey 2020: Technical Annex 2020. https://gp-patient.co.uk/downloads/2020/GPPS_2020_Technical_Annex_PUBLIC.pdf (accessed 18 January 2023).
- Public Health England . Fingertips: Public Health Profiles 2022. https://fingertips.phe.org.uk/ (accessed 18 January 2023).
- Abel G, Elliott MN. Identifying and quantifying variation between healthcare organisations and geographical regions: using mixed-effects models. BMJ Qual Safe 2018;28. https://doi.org/10.1136/bmjqs-2018-009165.
- Bryce C, O’Connell MDL, Dale J, Underwood M, Atherton H. Online and telephone access to general practice: a cross-sectional patient survey. BJGP 2021;5. https://doi.org/10.3399/BJGPO.2020.0179.
- Sinclair M, O’Toole J, Malawaraarachchi M, Leder K. Comparison of response rates and cost-effectiveness for a community-based survey: postal, internet and telephone modes with generic or personalised recruitment approaches. BMC Med Res Methodol 2012;12. https://doi.org/10.1186/1471-2288-12-132.
- Peeters JM, Krijgsman JW, Brabers AE, Jong JDD, Friele RD. Use and uptake of eHealth in general practice: a cross-sectional survey and focus group study among health care users and general practitioners. JMIR Med Inform 2016;4. https://doi.org/10.2196/medinform.4515.
- Newbould J, Abel G, Ball S, Corbett J, Elliott M, Exley J, et al. Evaluation of telephone first approach to demand management in English general practice: observational study. BMJ 2017;258. https://doi.org/10.1136/bmj.j4197.
- Gov.UK . COVID-19 Response: Living With COVID-19 2022. www.gov.uk/government/publications/covid-19-response-living-with-covid-19/covid-19-response-living-with-covid-19 (accessed 11 January 2023).
- Reeves S, Kuper A, Hodges BD. Qualitative research methodologies: ethnography. BMJ 2008;337. https://doi.org/10.1136/bmj.a1020.
- Atherton H, Brant H, Ziebland S, Bikker A, Campbell J, Gibson A, et al. The potential of alternatives to face-to-face consultation in general practice, and the impact on different patient groups: a mixed-methods case study. NIHR Health Serv Deliv Res 2018;6:1-200. https://doi.org/10.3310/hsdr06200.
- Ford JA, Wong G, Jones AP, Steel N. Access to primary care for socioeconomically disadvantaged older people in rural areas: a realist review. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010652.
- Public Health England Local Government Association . Health and Wellbeing in Rural Areas 2017. www.local.gov.uk/sites/default/files/documents/1.39_Health%20in%20rural%20areas_WEB.pdf (accessed 18 January 2023).
- Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exerc Health 2019;11:589-97. https://doi.org/10.1080/2159676X.2019.1628806.
- Ziebland S, McPherson A. Making sense of qualitative data analysis: an introduction with illustrations from DIPEx (personal experiences of health and illness). Med Educ 2006;40:405-14. https://doi.org/10.1111/j.1365-2929.2006.02467.x.
- O’Cathain A, Murphy E, Nicholl J. Three techniques for integrating data in mixed methods studies. Br Med J 2010;341. https://doi.org/10.1136/bmj.c4587.
- Gov.UK . Policy Paper: A Plan for Digital Health and Social Care. 2022. www.gov.uk/government/publications/a-plan-for-digital-health-and-social-care/a-plan-for-digital-health-and-social-care (accessed 18 January 2023).
- NHS England . General Practice: Forward View 2016. www.england.nhs.uk/wp-content/uploads/2016/04/gpfv.pdf (accessed 18 January 2023).
- NHS England . Standard General Medical Services Contract 2022. www.england.nhs.uk/wp-content/uploads/2022/11/B1990i-standard-general-medical-services-contract-november-2022.pdf (accessed 18 January 2023).
- The Health Foundation . Projections: General Practice Workforce in England Summary of Findings 2022. www.health.org.uk/publications/reports/projections-general-practice-workforce-in-england (accessed 18 January 2023).
- Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ 2021;374. https://doi.org/10.1136/bmj.n2061.
- NHS England . Network Contract Directed Enhanced Service: Additional Roles Reimbursement Scheme Guidance 2019. www.england.nhs.uk/publication/network-contract-directed-enhanced-service-additional-roles-reimbursement-scheme-guidance/ (accessed 21 May 2023).
- Rodriguez JA, Shachar C, Bates DW. Digital inclusion as health care: supporting health care equity with digital-infrastructure initiatives. N Engl J Med 2022;386:1101-3. https://doi.org/10.1056/NEJMp2115646.
- NHS England . How to Access Your GP Practice 2020. www.youtube.com/watch?v=gXHPWbEmp5s (accessed 18 January 2023).
- NHS.UK . NHS Account Help and Support 2022. www.nhs.uk/nhs-app/nhs-app-help-and-support/ (accessed 18 January 2023).
- NHS Digital . NHS App – View and Share Your NHS COVID Pass: Step by Step Instructions 2022. https://digital.nhs.uk/services/nhs-app/nhs-app-guidance-for-gp-practices/tell-your-patients-about-the-nhs-app/view-and-share-your-nhs-covid-pass (accessed 11 January 2023).
- eConsult . How to Use EConsult 2023. https://econsult.net/nhs-patients/how-to-use-econsult (accessed 11 January 2023).
- NHS England . Next Steps for Integrating Primary Care: Fuller Stocktake Report 2022 2022. www.england.nhs.uk/wp-content/uploads/2022/05/next-steps-for-integrating-primary-care-fuller-stocktake-report.pdf (accessed 18 January 2023).
- Kong T, Scott MM, Li Y, Wichelman C. Physician attitudes towards-and adoption of-mobile health. Digit Health 2020;20. https://doi.org/10.1177/2055207620907187.
- Hu X, Fang H, Wang P. Factors affecting doctor’s recommendation for mobile health services. Digital Health 2022;8. https://doi.org/10.1177/20552076221125976.
- NHS England . Investment and Evolution: A Five-Year Framework for GP Contract Reform to Implement the NHS Long Term Plan 2019. www.bma.org.uk/media/1461/bma-investment-and-evolution-five-year-framework-gp-contract-jan-2019.pdf (accessed 28 February 2023).
- Llan Healthcare . Changes to EConsult System 2022. www.llanhealthcare.co.uk/changes-to-econsult-system/ (accessed 12 December 2022).
- The Doctors @ Dr Newman’s Surgery . A Note about Demand 2021. www.doctornewman.co.uk/wp-content/uploads/2021/05/A-note-about-demand.pdf (accessed 25 November 2022).
- Meng D, Palen TE, Tsai J, McLeod M, Garrido T, Qian H. Association between secure patient–clinician email and clinical services utilisation in a US integrated health system: a retrospective cohort study. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-009557.
- Kristiansen E, Atherton H, Austad B, Bergmo T, Norberg BL, Zanaboni P. Older patients’ experiences of access to and use of e-consultations with the general practitioner in Norway: an interview study. Scand J Prim Health Care 2022;41:33-42. https://doi.org/10.1080/02813432.2022.2161307.
- Otte-Trojel T, de Bont A, Rundall TG, van de Klundert J. What do we know about developing patient portals? A systematic literature review. J Am Med Inf Assoc 2015;23:e162-8. https://doi.org/10.1093/jamia/ocv114.
- Hammerton M, Benson T, Sibley A. Readiness for five digital technologies in general practice: perceptions of staff in one part of southern England. BMJ Open Qual 2022;11. https://doi.org/10.1136/bmjoq-2022-001865.
- Antonio MG, Petrovskaya O, Lau F. Is research on patient portals attuned to health equity? A scoping review. JAMIA 2019;26:871-83. https://doi.org/10.1093/jamia/ocz054.
- UK Government . The Hewitt Review: An Independent Review of Integrated Care Systems 2023. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1148568/the-hewitt-review.pdf (accessed 21 May 2023).
- Rughani G, Hanlon P, Corcoran N, Mair FS. The readability of general practice websites: a cross-sectional analysis of all general practice websites in Scotland. Br J Gener Pract 2021;71:e391-8. https://doi.org/10.3399/bjgp.2020.0820.
- Honeyman M, Evans H, Davies A. Digital Technology and Health Inequalities: A Scoping Review. Cardiff; 2020.
- Heponiemi T, Kaihlanen AM, Kouvonen A, Leemann L, Taipale S, Gluschkoff K. The role of age and digital competence on the use of online health and social care services: a cross-sectional population-based survey. Digit Health 2022;8. https://doi.org/10.1177/20552076221074485.
- Richardson S, Lawrence K, Schoenthaler AM, Mann D. A framework for digital health equity. NPJ Digital Med 2022;5. https://doi.org/10.1038/s41746-022-00663-0.
- Hobbs FDR, Bankhead C, Mukhtar T, Stevens S, Perera-Salazar R, Holt T, et al. National Institute for Health Research School for Primary Care Research . Clinical workload in UK primary care: a retrospective analysis of 100 million consultations in England, 2007–14. Lancet 2016;387:2323-30. https://doi.org/10.1016/S0140-6736(16)00620-6.
- Office of National Statistics . Ethnic Group, England and Wales: Census 2021 2022. www.ons.gov.uk/peoplepopulationandcommunity/culturalidentity/ethnicity/bulletins/ethnicgroupenglandandwales/census2021 (accessed 12 January 2023).
- Byczkowski TL, Munafo JK, Britto MT. Variation in use of Internet-based patient portals by parents of children with chronic disease. Archiv Pediatr Adoles Med 2011;165:405-11. https://doi.org/10.1001/archpediatrics.2011.55.
- Mafi JN, Mejilla R, Feldman H, Ngo L, Delbanco T, Darer J, et al. Patients learning to read their doctors’ notes: the importance of reminders. J Am Med Inform Assoc 2016;23:951-5. https://doi.org/10.1093/jamia/ocv167.
- Masterson Creber RM, Grossman LV, Ryan B, Qian M, Polubriaginof FC, Restaino S, et al. J Am Med Inf Assoc 2019;26:115-23. https://doi.org/10.1093/jamia/ocy146.
- Chan B, Lyles C, Kaplan C, Lam R, Karliner L. A comparison of electronic patient-portal use among patients with resident and attending primary care providers. J Gen Intern Med 2018;33:2085-91. https://doi.org/10.1007/s11606-018-4637-x.
- Collins B. Technology and Innovation for Long-Term Health Conditions. London: The King’s Fund; 2020.
- Lyles CR, Sarkar U, Tieu L, Schillinger D, Handley MA, Gourley GI, et al. Searching for meaning in meaningful use in the safety net: an implementation case study of 5 community health centers in California. J Gen Intern Med 2016;31.
- Cafazzo JA, Casselman M, Hamming N, Katzman DK, Palmert MR. Design of an mHealth app for the self-management of adolescent type 1 diabetes: a pilot study. J Med Internet Res 2012;14. https://doi.org/10.2196/jmir.2058.
- Ray JM, Kemp LL, Hubbard A, Cucciare MA. Developing a peer support protocol for improving veterans’ engagement to computer-delivered cognitive behavioural therapy. Behav Cogn Psychother 2017;45:253-65. https://doi.org/10.1017/S1352465816000539.
- Richardson CR, Buis LR, Janney AW, Goodrich DE, Sen A, Hess ML, et al. An online community improves adherence in an internet-mediated walking program. Part 1: results of a randomized controlled trial. J Med Internet Res 2010;12. https://doi.org/10.2196/jmir.1338.
- Honeyman M, Dunn P, McKenna H. A Digital NHS? An Introduction to the Digital Agenda and Plans for Implementation. London: The King’s Fund; 2016.
- Venkatesh V, Thong JY, Xu X. Consumer acceptance and use of information technology: extending the unified theory of acceptance and use of technology. MIS Quart 2012;36:157-78. https://doi.org/10.2307/41410412.
- Yamin CK, Emani S, Williams DH, Lipsitz SR, Karson AS, Wald JS, et al. The digital divide in adoption and use of a personal health record. Arch Intern Med 2011;171:568-74. https://doi.org/10.1001/archinternmed.2011.34.
Appendix 1 Literature searches
Stage 1: searches of the academic literature on digital facilitation in primary care
| Limits: English; 2010–present Search run: 18 June 2020 |
|---|
| ((online[tw] OR on-line[tw] OR web[tw] OR website[tw] OR internet[tw] OR network[tw] OR digital[tw] OR smartphone*[tw] or “smart phone*”[tw] OR app[tw] OR computer*[tw] OR “mobile phone*”[tw]) AND (consult*[tw] OR service*[tw] OR therap*[tw] OR treatment*[tw] OR counsel*[tw] OR appointment[tw] OR prescri*[tw] OR service*[tw] OR platform*[tw] OR portal*[tw])) OR “Internet-Based Intervention”[MeSH] OR “Patient Portals”[Mesh] |
| AND |
| Support*[tw] OR encourag*[tw] OR incentiv*[tw] OR “increase use”[tw] OR teach*[tw] OR train*[tw] OR help*[tw] OR assist*[tw] OR engag*[tw] OR facilitat*[tw] OR promot*[tw] OR expedit*[tw] |
| AND |
| “primary care” [tw] OR “community-based provider*”[tw] OR “general practitioner*”[tw] OR GP[tiab] OR “family doctor”[tw] OR “Physicians, Primary Care”[MeSH] OR “General Practice”[MeSH] OR “General Practitioners”[MeSH] OR “Family Practice”[MeSH] OR “Primary Health Care”[MeSH] OR “ambulatory care”[MeSH] |
| AND |
| “national health service”[tiab] OR “national health service”[affiliation] OR nhs[tiab] OR nhs[Affiliation] OR Britain[tiab] OR Britain[Affiliation] OR British[tiab] OR GB[tiab] OR G.B.[tiab] OR GB[affiliation] OR G.B.[affiliation] OR “united kingdom”[tiab] OR “united kingdom”[affiliation] OR UK[tiab] OR U.K.[tiab] OR UK[affiliation] OR U.K.[affiliation] OR England[tiab] OR England[affiliation] OR London[Affiliation] OR London[tiab] OR “northern Ireland”[tiab] OR “northern ireland”[affiliation] OR “northern irish*”[tiab] OR Scotland[tiab] OR Scotland[affiliation] OR Scottish*[tiab] OR wales[tiab] OR wales[affiliation] OR welsh[tiab] OR United Kingdom[MeSH] OR Australia[MeSH] OR Australia[Affiliation] OR Australia*[tiab] OR Austria[MeSH] OR Austria*[tiab] OR Austria[affiliation] OR Belgium[MeSH] OR Belgium[affiliation] OR Belgium[tiab] OR Belgian[tiab] OR Czech Republic[MeSH] OR Czech[tiab] OR Czech[Affiliation] OR Denmark[MeSH] OR Denmark[tiab] OR Denmark[affiliation] OR Dane[tiab] OR Danish[tiab] OR Estonia[MeSH] OR Estonia[Affiliation] OR Estonia*[tiab] OR Finland[MeSH] OR Finland[Affiliation] OR Finland[tiab] OR Finnish[tiab] OR France[MeSH] OR France[Affiliation] OR France[tiab] OR French[tiab] OR Germany[MeSH] OR Germany[tiab] OR Germany[Affiliation] OR German*[tiab] OR Greece[MeSH] OR Greece[Affiliation] OR Greece[tiab] OR Greek[tiab] OR Hungary[MeSH] OR Hungary[tiab] OR Hungary[affiliation] OR Hungarian[tiab] OR Iceland[MeSH] OR Iceland[Affiliation] OR Iceland[tiab] OR Ireland[MeSH] OR Ireland[Affiliation] OR Ireland[tiab] OR Italy[MeSH] OR Italy[Affiliation] OR Italy[tiab] OR Italian[tiab] OR Latvia[MeSH] OR Latvia[Affiliation] OR Latvia*[tiab] OR Luxembourg[MeSH] OR Luxembourg[Affiliation] OR Luxembourg[tiab] OR Netherlands[MeSH] OR Netherlands[Affiliation] OR Netherlands[tiab] OR Dutch[tiab] OR Norway[MeSH] OR Norway[Affiliation] OR Norway[tiab] OR Norwegian[tiab] OR Poland[MeSH] OR Poland[Affiliation] OR Poland[tiab] OR Polish[tiab] OR Portugal[MeSH] OR Portugal[Affiliation] OR Portugal[tiab] OR Portuguese[tiab] OR Slovakia[MeSH] OR Slovakia[Affiliation] OR Slovak[tiab] OR “Slovak Republic”[Affiliation] OR Slovenia[MeSH] OR Slovenia[Affiliation] OR Slovenia*[tiab] OR Spain[MeSH] OR Spain[Affiliation] OR Spain*[tiab] OR Sweden[MeSH] OR Sweden[Affiliation] OR Sweden[tiab] OR Swedish[tiab] OR Switzerland[MeSH] OR Switzerland[Affiliation] OR Switzerland[tiab] OR Swiss[tiab] OR Canada[MeSH] OR Canada[Affiliation] OR Canada[tiab] OR Canadian[tiab] OR Chile[MeSH] OR Chile[Affiliation] OR Chile[tiab] OR Chilean[tiab] OR Colombia[MeSH] OR Columbia[Affiliation] OR Columbia*[tiab] OR Israel[MeSH] OR Israel[Affiliation] OR Israel*[tiab] OR Japan[MeSH] OR Japan[Affiliation] OR Japan*[tiab] OR Korea[MeSH] OR Korea[Affiliation] OR Korea*[tiab] OR Mexico[MeSH] OR Mexico[affiliation] OR Mexico[tiab] OR Mexican*[tiab] OR New Zealand[MeSH] OR New Zealand[Affiliation] OR New Zealand*[tiab] OR Turkey[MeSH] OR Turkey[Affiliation] OR Turkey[tiab] OR Turkish[tiab] OR United States[MeSH] OR United States[Affiliation] OR USA[Affiliation] OR US[Affiliation] OR New York[tiab] OR New York[Affiliation] OR Paris[affiliation] OR Paris[tiab] OR Dublin[affiliation] OR Dublin[tiab] OR Rome[affiliation] OR Rome[tiab] OR Berlin[affiliation] OR Berlin[tiab] OR united states[tiab] |
| Results: 7682 – 4 internal duplicates = 7678 |
| Limits: English; 2010–present Search run: 18 June 2020 |
|---|
| ((online:ti,ab,kw OR on-line:ti,ab,kw OR web:ti,ab,kw OR website:ti,ab,kw OR internet:ti,ab,kw OR network:ti,ab,kw OR digital:ti,ab,kw OR smartphone*:ti,ab,kw or “smart phone*”:ti,ab,kw OR app:ti,ab,kw OR computer*:ti,ab,kw OR “mobile phone*”:ti,ab,kw) AND (consult*:ti,ab,kw OR service*:ti,ab,kw OR therap*:ti,ab,kw OR treatment*:ti,ab,kw OR counsel*:ti,ab,kw OR appointment:ti,ab,kw OR prescri*:ti,ab,kw OR service*:ti,ab,kw OR platform*:ti,ab,kw OR portal*:ti,ab,kw)) OR ‘web-based intervention’/exp |
| AND |
| Support*:ti,ab,kw OR encourag*:ti,ab,kw OR incentiv*:ti,ab,kw OR”increase use”:ti,ab,kw OR teach*:ti,ab,kw OR train*:ti,ab,kw OR help*:ti,ab,kw OR assist*:ti,ab,kw OR engag*:ti,ab,kw OR facilitat*:ti,ab,kw OR promot*:ti,ab,kw OR expedit*:ti,ab,kw |
| AND |
| “primary care”:ti,ab,kw OR “community-based provider*”:ti,ab,kw OR “general practitioner*”:ti,ab,kw OR GP:ti,ab,kw OR “family doctor”:ti,ab,kw OR ‘general practitioner’/exp OR ‘general practice’/exp OR ‘primary health care’/exp OR ‘ambulatory care’/exp |
| AND |
| “national health service”:ti,ab OR “national health service”:ff OR nhs:ti,ab OR nhs:ff OR Britain:ti,ab OR Britain:ff OR British:ti,ab OR GB:ti,ab OR G.B.:ti,ab OR GB:ff OR G.B.:ff OR “united kingdom”:ti,ab OR “united kingdom”:ff OR UK:ti,ab OR U.K.:ti,ab OR UK:ff OR U.K.:ff OR England:ti,ab OR England:ff OR London:ff OR London:ti,ab OR “northern Ireland”:ti,ab OR “northern ireland”:ff OR “northern irish*”:ti,ab OR Scotland:ti,ab OR Scotland:ff OR Scottish*:ti,ab OR wales:ti,ab OR wales:ff OR welsh:ti,ab OR ‘united kingdom’/exp OR ‘Australia’/exp OR Australia:ff OR Australia*:ti,ab OR ‘austria’/exp OR Austria*:ti,ab OR Austria:ff OR ‘Belgium’/exp OR Belgium:ff OR Belgium:ti,ab OR Belgian:ti,ab OR ‘Czech Republic’/exp OR Czech:ti,ab OR Czech:ff OR ‘Denmark’/exp OR Denmark:ti,ab OR Denmark:ff OR Dane:ti,ab OR Danish:ti,ab OR ‘Estonia’/exp OR Estonia:ff OR Estonia*:ti,ab OR ‘Finland’/exp OR Finland:ff OR Finland:ti,ab OR Finnish:ti,ab OR ‘France’/exp OR France:ff OR France:ti,ab OR French:ti,ab OR ‘Germany’/exp OR Germany:ti,ab OR Germany:ff OR German*:ti,ab OR ‘Greece’/exp OR Greece:ff OR Greece:ti,ab OR Greek:ti,ab OR ‘Hungary’/exp OR Hungary:ti,ab OR Hungary:ff OR Hungarian:ti,ab OR ‘Iceland’/exp OR Iceland:ff OR Iceland:ti,ab OR ‘Ireland’/exp OR Ireland:ff OR Ireland:ti,ab OR ‘Italy’/exp OR Italy:ff OR Italy:ti,ab OR Italian:ti,ab OR ‘Latvia’/exp OR Latvia:ff OR Latvia*:ti,ab OR ‘Luxembourg’/exp OR Luxembourg:ff OR Luxembourg:ti,ab OR ‘Netherlands’/exp OR Netherlands:ff OR Netherlands:ti,ab OR Dutch:ti,ab OR ‘Norway’/exp OR Norway:ff OR Norway:ti,ab OR Norwegian:ti,ab OR ‘Poland’/exp OR Poland:ff OR Poland:ti,ab OR Polish:ti,ab OR ‘Portugal’/exp OR Portugal:ff OR Portugal:ti,ab OR Portuguese:ti,ab OR ‘Slovakia’/exp OR Slovakia:ff OR Slovak:ti,ab OR “Slovak Republic”:ff OR ‘Slovenia’/exp OR Slovenia:ff OR Slovenia*:ti,ab OR ‘Spain’/exp OR Spain:ff OR Spain*:ti,ab OR ‘Sweden’/exp OR Sweden:ff OR Sweden:ti,ab OR Swedish:ti,ab OR ‘Switzerland’/exp OR Switzerland:ff OR Switzerland:ti,ab OR Swiss:ti,ab OR ‘Canada’/exp OR Canada:ff OR Canada:ti,ab OR Canadian:ti,ab OR ‘Chile’/exp OR Chile:ff OR Chile:ti,ab OR Chilean:ti,ab OR ‘Colombia’/exp OR Columbia:ff OR Columbia*:ti,ab OR ‘Israel’/exp OR Israel:ff OR Israel*:ti,ab OR ‘Japan’/exp OR Japan:ff OR Japan*:ti,ab OR ‘Korea’/exp OR Korea:ff OR Korea*:ti,ab OR ‘Mexico’/exp OR Mexico:ff OR Mexico:ti,ab OR Mexican*:ti,ab OR ‘New Zealand’/exp OR “New Zealand”:ff OR “New Zealand*”:ti,ab OR ‘Turkey’/exp OR Turkey:ff OR Turkey:ti,ab OR Turkish:ti,ab OR ‘United States’/exp OR “United States”:ff OR USA:ff OR US:ff OR “New York”:ti,ab OR “New York”:ff OR Paris:ff OR Paris:ti,ab OR Dublin:ff OR Dublin:ti,ab OR Rome:ff OR Rome:ti,ab OR Berlin:ff OR Berlin:ti,ab OR “United States”:ti,ab |
| Results: 5635 – duplicates = 2983 |
| Limits: English; 2010–present; academic journals Search run: 18 June 2020 |
|---|
| (TI(online OR on-line OR web OR website OR internet OR network OR digital OR smartphone* or “smart phone*” OR app OR computer* OR “mobile phone*”) AND TI(consult* OR service* OR therap* OR treatment* OR counsel* OR appointment OR prescri* OR service* OR platform* OR portal*)) OR (TI(online OR on-line OR web OR website OR internet OR network OR digital OR smartphone* or “smart phone*” OR app OR computer* OR “mobile phone*”) AND AB(consult* OR service* OR therap* OR treatment* OR counsel* OR appointment OR prescri* OR service* OR platform* OR portal*)) OR (AB(online OR on-line OR web OR website OR internet OR network OR digital OR smartphone* or “smart phone*” OR app OR computer* OR “mobile phone*”) AND AB(consult* OR service* OR therap* OR treatment* OR counsel* OR appointment OR prescri* OR service* OR platform* OR portal*)) OR (AB(online OR on-line OR web OR website OR internet OR network OR digital OR smartphone* or “smart phone*” OR app OR computer* OR “mobile phone*”) AND TI(consult* OR service* OR therap* OR treatment* OR counsel* OR appointment OR prescri* OR service* OR platform* OR portal*)) OR (MH “Patient Portals”) |
| AND |
| TI(Support* OR encourag* OR incentiv* OR “increase use” OR teach* OR train* OR help* OR assist* OR engag* OR facilitat* OR promot* OR expedit*) OR AB(Support* OR encourag* OR incentiv* OR “increase use” OR teach* OR train* OR help* OR assist* OR engag* OR facilitat* OR promot* OR expedit*) |
| AND |
| (TI(“primary care” OR “community-based provider*” OR “general practitioner*” OR GP OR “family doctor”) OR AB(“primary care” OR “community-based provider*” OR “general practitioner*” OR GP OR “family doctor”)) OR (MH “Physicians, Family”) OR (MH “Primary Health Care”) OR (MH “Family Practice”) OR (MH “Ambulatory Care”) |
| AND |
| TI(“national health service”) OR AB(“national health service”) OR AF(“national health service”) OR TI(nhs) OR AB(nhs) OR AF(nhs) OR TI(Britain) OR AB(Britain) OR AF(Britain) OR TI(British) OR AB(British) OR TI(U.K.) OR AB(U.K.) OR AF(U.K.) OR TI(UK) OR AB(UK) OR AF(UK) OR TI(England) OR AB(England) OR AF(England) OR AF(London) OR TI(London) OR AB(London) OR TI(“Northern Ireland”) OR AB(“Northern Ireland”) OR TI(“Northern Irish*”) OR AB(“Northern Irish*”) OR TI(Scotland) OR AB(Scotland) OR AF(Scotland) OR TI(Scottish*) OR AB(Scottish) OR TI(Wales) OR AB(Wales) OR AF(Wales) OR TI(Welsh) OR AB(Welsh) OR (MH “United Kingdom+”) OR (MH “Australia+”) OR AF(Australia) OR TI(Australia) OR AB(Australia) OR (MH “Austria”) OR TI(Austria) OR AB(Austria) OR AF(Austria) OR (MH “Belgium+”) OR AF(Belgium) OR TI(Belgium) OR AB(Belgium) OR TI(Belgian) OR AB(Belgian) OR (MH “Czech Republic+”) OR TI(Czech) OR AB(Czech) OR AF(Czech) OR (MH “Denmark”) OR TI(Denmark) OR AB(Denmark) OR AF(Denmark) OR TI(Dane) OR AB(Dane) OR TI(Danish) OR AB(Danish) OR (MH “Estonia+”) OR TI(Estonia) OR AB(Estonia) OR AF(Estonia) OR (MH “Finland+”) OR TI(Finland) OR AB(Finland) OR AF(Finland) OR TI(Finnish) OR AB(Finnish) OR (MH “France+”) OR TI(France) OR AB(France) OR AF(France) OR TI(French) OR AB(French) OR (MH “Germany+”) OR TI(German*) OR AB(German*) OR AF(Germany) OR (MH “Greece+”) OR TI(Greece) OR AB(Greece) OR AF(Greece) OR TI(Greek) OR AB(Greek) OR (MH “Hungary+”) OR AF(Hungary) OR TI(Hungary) OR AB(Hungary) OR TI(Hungarian) OR AB(Hungarian) OR (MH “Iceland+”) OR TI(Iceland) OR AB(Iceland) OR AF(Iceland) OR (MH “Ireland+”) OR TI(Ireland) OR AB(Ireland) OR AF(Ireland) OR (MH “Italy+”) OR TI(Italy) OR AB(Italy) OR AF(Italy) OR TI(Italian) OR AB(Italian) OR (MH “Latvia+”) OR TI(Latvia) OR AB(Latvia) OR AF(Latvia) OR (MH “Luxembourg+”) OR AF(Luxembourg) OR TI(Luxembourg) OR AB(Luxembourg) OR (MH “Netherlands+”) OR TI(Netherlands) OR AB(Netherlands) OR AF(Netherlands) OR TI(Dutch) OR AB(Dutch) OR (MH “Norway+”) OR TI(Norway) OR AB(Norway) OR AF(Norway) OR TI(Norwegian) OR AB(Norwegian) OR (MH “Poland+”) OR TI(Poland) OR AB(Poland) OR TI(Polish) OR AB(Polish) OR (MH “Portugal+”) OR TI(Portugal) OR AB(Portugal) OR AF(Portugal) OR TI(Portuguese) OR AB(Portuguese) OR (MH “Slovakia+”) OR TI(Slovakia) OR AB(Slovakia) OR AF(Slovakia) OR TI(“Slovak Republic”) OR AB(“Slovak republic”) OR AF(“Slovak Republic”) OR (MH “Slovenia+”) OR TI(Slovenia) OR AB(Slovenia) OR AF(Slovenia) OR (MH “Spain+”) OR TI(Spain*) OR AB(Spain*) OR AF(Spain) OR (MH “Sweden+”) OR TI(Sweden) OR AB(Sweden) OR AF(Sweden) OR TI(Swedish) OR AB(Swedish) OR (MH “Switzerland+”) OR TI(Switzerland) OR AB(Switzerland) OR AF(Switzerland) OR TI(Swiss) OR AB(Swiss) OR (MH “Canada+”) OR TI(Canada) OR AB(Canada) OR AF(Canada) OR TI(Canadian) OR AB(Canadian) OR (MH “Chile+”) OR TI(Chile) OR AB(Chile) OR AF(Chile) OR TI(Chilean) OR AB(Chilean) OR (MH “Colombia+”) OR AF(Colombia) OR TI(Colombia*) OR AB(Colombia*) OR (MH “Israel+”) OR TI(Israel*) OR AB(Israel*) OR AF(Israel) OR (MH “Japan+”) OR TI(Japan*) OR AB(Japan*) OR (MH “Korea+”) OR TI(Korea*) OR AB(Korea*) OR (MH “Mexico+”) OR TI(Mexico) OR AB(Mexico) OR AF(Mexico) OR TI(Mexican*) OR AB(Mexican*) OR (MH “New Zealand”) OR TI(“New Zealand”) OR AB(“New Zealand”) OR AF(“New Zealand”) OR (MH “Turkey+”) OR TI(Turkey) OR AB(Turkey) OR AF(Turkey) OR TI(Turkish) OR AB(Turkish) OR (MH “United States+”) OR TI(“United States”) OR AB(“United States”) OR AF(“United States”) OR AF(USA) OR AF(US) OR TI(“New York) OR AB(“New York) OR AF(“New York) OR AF(Paris) OR TI(Paris) OR AB(Paris) OR TI(Dublin) OR AB(Dublin) OR AF(Dublin) OR TI(Rome) OR AB(Rome) OR AF(Rome) OR AF(Berlin) OR AB(Berlin) OR TI(Berlin) OR TI(“united states”) OR AB(“united states”) |
| Results: 2899 – duplicates = 949 |
| Limits: English, 2010–present; article, review, early access Refined by: COUNTRIES/REGIONS: (will choose the countries on list) Search run: 18 June 2020 |
|---|
| (TS=(online OR on-line OR web OR website OR internet OR network OR digital OR smartphone* or “smart phone*” OR app OR computer* OR “mobile phone*”) AND TS=(consult* OR service* OR therap* OR treatment* OR counsel* OR appointment OR prescri* OR service* OR platform* OR portal*)) OR (TS=(“Internet-Based Intervention*”) OR TS=(“Patient Portal*”)) |
| AND |
| TS=(Support* OR encourag* OR incentiv* OR “increase use” OR teach* OR train* OR help* OR assist* OR engag* OR facilitat* OR promot* OR expedit*) |
| AND |
| TS=(“primary care” OR “community-based provider*” OR “general practitioner*” OR “family doctor” OR “General Practice” OR “Family Practice” OR “Primary Health Care” OR “ambulatory care”) |
| Results: 5147 – duplicates = 1966 |
| Limits: English, Added to Cochrane 2010–present – then published from 2010 to 2020; Search run: 18 June 2020 |
|---|
| ((online OR on-line OR web OR website OR internet OR network OR digital OR smartphone* or “smart phone*” OR app OR computer* OR “mobile phone*”):ti,ab,kw AND (consult* OR service* OR therap* OR treatment* OR counsel* OR appointment OR prescri* OR service* OR platform* OR portal*):ti,ab,kw) OR [mh “internet-based intervention”] OR [mh “patient portals”] |
| AND |
| (Support* OR encourag* OR incentiv* OR “increase use” OR teach* OR train* OR help* OR assist* OR engag* OR facilitat* OR promot* OR expedit*):ti,ab,kw |
| AND |
| (“primary care” OR “community-based provider*” OR “general practitioner*” OR GP OR “family doctor”):ti,ab,kw OR [mh “Physicians, Primary Care”] OR [mh “General Practice”] OR [mh “General Practitioners”] OR [mh “Family Practice”] OR [mh “Primary Health Care”] OR [mh “ambulatory care”] |
| AND |
| “national health service”:ti,ab OR nhs:ti,ab OR Britain:ti,ab OR British:ti,ab OR GB:ti,ab OR G.B.:ti,ab OR “united kingdom”:ti,ab OR UK:ti,ab OR U.K.:ti,ab OR England:ti,ab OR London:ti,ab OR “northern Ireland”:ti,ab OR “northern irish*”:ti,ab OR Scotland:ti,ab OR Scottish*:ti,ab OR wales:ti,ab OR welsh:ti,ab OR [mh “United Kingdom”} OR [mh Australia] OR Australia*:ti,ab OR [mh Austria] OR Austria*:ti,ab OR [mh Belgium] OR Belgium:ti,ab OR Belgian:ti,ab OR [mh “Czech Republic”] OR Czech:ti,ab OR [mh Denmark] OR Denmark:ti,ab OR Dane:ti,ab OR Danish:ti,ab OR [mh Estonia] OR Estonia*:ti,ab OR [mh Finland] OR Finland:ti,ab OR Finnish:ti,ab OR [mh France] OR France:ti,ab OR French:ti,ab OR [mh Germany] OR German*:ti,ab OR [mh Greece] OR Greece:ti,ab OR Greek:ti,ab OR [mh Hungary] OR Hungary:ti,ab OR Hungarian:ti,ab OR [mh Iceland] OR Iceland:ti,ab OR [mh Ireland] OR Ireland:ti,ab OR [mh Italy] OR Italy:ti,ab OR Italian:ti,ab OR [mh Latvia] OR Latvia*:ti,ab OR [mh Luxembourg] OR Luxembourg:ti,ab OR [mh Netherlands] OR Netherlands:ti,ab OR Dutch:ti,ab OR [mh Norway] OR Norway:ti,ab OR Norwegian:ti,ab OR [mh Poland] OR Poland:ti,ab OR Polish:ti,ab OR [mh Portugal] OR Portugal:ti,ab OR Portuguese:ti,ab OR [mh Slovakia] OR Slovak:ti,ab OR [mh Slovenia] OR Slovenia*:ti,ab OR [mh Spain] OR Spain*:ti,ab OR [mh Sweden] OR Sweden:ti,ab OR Swedish:ti,ab OR [mh Switzerland] OR Switzerland:ti,ab OR Swiss:ti,ab OR [mh Canada] OR Canada:ti,ab OR Canadian:ti,ab OR [mh Chile] OR Chile:ti,ab OR Chilean:ti,ab OR [mh Colombia] OR Columbia*:ti,ab OR [mh Israel] OR Israel*:ti,ab OR [mh Japan] OR Japan*:ti,ab OR [mh Korea] OR Korea*:ti,ab OR [mh Mexico] OR Mexico:ti,ab OR Mexican*:ti,ab OR [mh “New Zealand”] New Zealand*:ti,ab OR [mh Turkey] OR Turkey:ti,ab OR Turkish:ti,ab OR [mh “United States”] OR “united states”:ti,ab OR “New York”:ti,ab OR Paris:ti,ab OR Dublin:ti,ab OR Rome:ti,ab OR Berlin:ti,ab |
| Results: 1208 (33 Reviews/1175 Trials) – duplicates = 456 (13 Reviews/443 Trials) (of the trials: 212 CT.gov and 164 ICTRP) |
Stage 2: search of grey literature on digital facilitation in health care, all sectors
Targeted searches of websites
| Website | Search number | Search terms | Search results | Removal of duplicates |
|---|---|---|---|---|
| King’s fund | 1 | Online services | 35 | |
| 2 | Digital online services | 12 | –2 | |
| 3 | Digital facilitation | 10 | ||
| 4 | Online AND patients | 33 | –1 | |
| 5 | Digital AND patients | 44 | –2 | |
| 6 | Online access | 26 | –1 | |
| 7 | Technology access | 54 | –4 | |
| Royal College of GPs | 1 | Online services | 24 | |
| 2 | Online AND patients | 3 | ||
| 3 | Digital access | 3 | ||
| Nuffield Trust | 1 | Online digital technology (filtered for Primary Care) | 8 | |
| 2 | Online digital technology (no filter) | 41 | ||
| Health Foundation | 1 | Online | 4 | |
| 2 | Digital | 1 | ||
| 3 | Technology | 10 | ||
| Totals | 308 | –10 | ||
| Total after removing duplicates | 298 | |||
All searches limited to English, 2015–present.
Search of HMIC database
We searched the HMIC database using the following terms:
| Ltimits: English, 2015–present |
|---|
| ((online OR digital OR virtual OR technolog*3) AND (uptake OR encourage OR ‘increase use’ OR adopt*3 OR facilitat*3)).ti,ab [DT 2015-2020] |
| Results = 27 |
Search of academic literature on DF in non-healthcare sectors
We searched the literature on non-healthcare sectors via Google Scholar using the following search terms:
| Limits: English, 2015–present | ||
|---|---|---|
| Sector | Search terms | Search results |
| Tourism/Travel | (digital OR online OR smartphone OR “smart phone” OR application OR app) AND (airline OR flight OR travel OR accommodation OR tourism OR hotel) AND (uptake OR “increase use” OR facilitate) | 881,000 > Reviewed first 100 (sorted by relevance) for eligibility of which 2 were included for full-text extraction |
| Banking | (digital OR online OR smartphone OR “smart phone” OR application OR app) AND (banking OR banks OR finance) AND (uptake OR “increase use” OR facilitate) | 719,000 > Reviewed first 100 (sorted by relevance) for eligibility of which 3 were included for full-text extraction |
Data extraction chart
| Field | Instructions to reviewer |
|---|---|
| Study # | |
| Full citation | |
| Reviewer initials | |
| Article type | |
| Geographic focus of article | |
| Article topic | Briefly describe the main topic of the article. |
| Research question(s) (if applicable) | |
| Research method(s) used (if applicable) | |
| Study population | For example, number of practices, patients, etc. |
| Disease area/focus | |
| What online service is the article about? | Brief description. |
| What is the DF approach/activity? | Please describe what the DF approach/activity is. Please include a description of its size, scope, length of time in use/stage of development, if mentioned in the article. |
| Has the facilitation approach been implemented? | Routine use; experimental use; not implemented. |
| Why was the DF effort undertaken? | Please describe why the facilitation effort was undertaken (e.g. any drivers). This could include factors related to COVID. |
| How does the DF happen? | Please describe how the DF happens. |
| Who delivers the DF approach? | Please describe who is involved in the facilitation process. Please include any staff training activities as well as direct interactions with patients/members of the public. |
| Who is receiving the activity (population targeted)? | Please describe the target population. Mention any vulnerable groups that are targeted by the DF efforts, and describe how they were targeted. Examples of vulnerable groups include older adults, non-native/non-English speakers, low-income populations, people with low literacy levels, ethnic minority communities and rural populations. |
| Vulnerable group (Y/N) | (Examples of vulnerable groups include older adults, non-native/non-English speakers, low-income populations, people with low literacy levels, ethnic minority communities and rural populations). |
| Barriers to DF | Please describe any barriers to the facilitation effort. This could include factors related to COVID. |
| Enablers for DF | Please describe anything that enabled or helped the DF effort. This could include factors related to COVID. |
| Evidence of effectiveness | Was any form of evaluation conducted? Please describe any evidence cited in the article to support the efficacy (or lack of efficacy) of the facilitation approach. |
| Evidence of cost/resource use | What costs/resources were used to deliver the facilitation programme? |
| Evidence of cost effectiveness | Was a cost-effectiveness evaluation conducted? Please describe any evidence related to the cost effectiveness of the approach. |
| Evidence related to COVID | Did the article mention any other factors/responses to COVID related to the DF effort that have not already been captured in the template? |
| Any evidence of harm from the facilitation effort? | |
| Any other relevant information | |
| Quality of the research | |
| Quality of evidence source | Has the DF effort been evaluated? If so, how? If the evidence presented in the article is not from an evaluation, please describe the source of the evidence, noting any comments on quality. |
| Clarity of aims | Is the question(s) the paper seeks to answer clear and well described? |
| Clarity of methods | Are the method(s) the paper uses clear and well described? For example, if it is a survey, do they cite their sampling strategy and response rate? |
| Quality and comprehensiveness of work | How comprehensive is the publication? Does it draw on or at least seems to be informed by a robust evidence base? |
| Conflicts of interest | Are there any potential conflicts of interest amongst authors that could have influenced findings? |
| Other comments on quality: Please note any other reflections on the article’s quality. | |
| Notes for additional searches | Please note any additional terms or comments that you feel might be useful for snowballing or grey literature searches. |
Publications included in review
Articles from the non-primary care literature or from outside the health sector did not always include a method of DF, but were included in the review because they contained relevant learning for DF in primary care [see Chapter 2: Literature review (work package 1) for an explanation of our approach to screening the literature]. Consequently, some articles contain not applicable ‘N/A’ for the type of online service and/or DF.
Table 29 presents a full list of publications included in the scoping review of the literature. We defined a typology of online services supported by DF. These include: (1) websites (e.g. to access online health records or health information); (2) patient portals and personalised practice tools (e.g. to order repeat prescriptions or book appointments online); (3) health apps (e.g. for self-management of health conditions, or to access online health information or patient portals) and (4) screening programmes and customised health information on tablets.
We also developed a typology of DF approaches. The approaches are most frequently aimed at patients but may also target primary care staff. The approaches include:
-
Promotion: a broad category of DF that captures ways of raising awareness of and knowledge about digital services, endorsements of specific digital services to patients and methods of encouraging patients to use them.
-
Training and education: education or training to help patients acquire technical skills to use digital services or to help patients understand what features of a digital service can be most helpful to them.
-
Guidance and support: ongoing help in using digital services provided by clinicians or other primary care staff to patients.
Articles from the non-primary care literature or from outside the health sector did not always include a method of DF, but were included in the review because the contained relevant learning for DF in primary care [see Chapter 2: Literature review (work package 1) for an explanation of our approach to screening the literature]. Consequently, some articles contain ‘N/A’ for the type of online service and/or DF.
| Digital facilitation type | Reference | Study design | Study population | Disease area/focus | Online service supported |
|---|---|---|---|---|---|
| Promotion | Aarts et al. (2015)100 | Qualitative study | N = 1 practice site: interviews with N = 6 Healthcare professionals and N = 7 patients | Infertility | Website |
| Promotion | Abbott-Garner et al. (2019)93 | Prospective cohort study | N = 1388 households; from 78 postcodes served by 78 different GP practices | N/A | Patient portal |
| Promotion | Ayre et al. (2020)138 | Qualitative study | N = 25 GPs | Diabetes | Health app |
| Promotion | Baumeister et al. (2015)118 | RCT | N = 104; patients treated in pain centres | Pain | Website |
| Promotion | Byambasuren et al. (2020)98 | Pre/post study | N = 40, GPs | N/A | Health app |
| Promotion | Byczkowski et al. (2011)210 | Retrospective observational study | N = 1960; children with chronic diseases (1900 families) | Diabetes mellitus, juvenile idiopathic arthritis, cystic fibrosis | Patient portal |
| Promotion | Carter et al. (2018)83 | Mixed methods: qualitative and retrospective case series | N = 6 practices; N = 81 patients; N = 10 interviews (5 GPs, 5 administrators); N = 20 GPs completing case reports | N/A | Patient portal |
| Promotion | Castle-Clarke (2018)135 | Narrative review | N/A | N/A | Health app |
| Promotion | Delbanco et al. (2012)113 | Prospective cohort study | N = 13,669; 105 primary care providers and 13,564 patients | N/A | Patient portal |
| Promotion | Greenhalgh et al. (2010)82 | Mixed-method case study | N = 216 (for interviews); 56 patients and 160 policy-makers, project managers and clinical staff | N/A | Patient portal |
| Promotion | Hassett et al. (2020)103 | RCT | N = 300 patients | Mobility limitation | Health app |
| Promotion | Hoffmann (2019)101 | Qualitative study | N = 19 GPs | Mental health | Website |
| Promotion | Irizarry et al. (Jun 2015)52 | Narrative review | N/A | N/A | Patient portals |
| Promotion | Lillevoll et al. (2014)132 | RCT | N = 707; students in senior high school | Mental health; depressive symptoms | Website |
| Promotion | Lin et al. (2018)117 | RCT | N = 115; patients with chronic pain | Chronic pain | Website; Health app |
| Promotion | Lopez Segui et al. (2018)94 | Mixed methods; qualitative, prospective case study | N = 47 (Questionnaire); 17 doctors and 30 patients | Asthma; chronic illness; alcohol consumption | Health app |
| Promotion | Mafi et al. (2016)211 | Prospective cohort study | N = 15,360 patients | N/A | Patient portal |
| Promotion | Mahoney et al. (2017)96 | RCT | N = 369; adolescents | Depression | Website |
| Promotion | Mares et al. (2016)131 | Mixed methods; prospective case studies | N = 53; clinicians | Substance use disorder | Health app |
| Promotion | Masterson Creber et al. (2019)212 | RCT | N = 426 patients | N/A | Patient portal |
| Promotion | Nguyen et al. (2019)80 | Qualitative study | N = 10; GPs | Chronic conditions | Health app |
| Promotion | Ozili (2018)139 | Narrative review | N/A | N/A | N/A |
| Promotion | Patel et al. (2015)122 | Cross-sectional study | N = 89; 84 patients and 5 healthcare providers | N/A | Screening programmes and customised health information on tablets |
| Promotion | Plaete et al. (2015)84 | Qualitative study | N = 62; GPs | Chronic conditions | Screening programmes and customised health information on tablets |
| Promotion | Radovic et al. (2019)112 | Qualitative study | N = 14 +; primary care providers and adolescent patients with depression | Depression and anxiety | Website |
| Promotion | Ricciardi et al. (2013)150 | Narrative review | N/A | N/A | Website |
| Promotion | Ronda et al. (2018)106 | Cross-sectional study | N = 128; physicians and nurses from general practice and outpatient clinics | Diabetes | Patient portal |
| Promotion | Sprenger et al. (2017)140 | Cross-sectional study | N = 131; healthcare professionals working in maternity care | Maternal mental health | Health app |
| Promotion; training | Coulter and Mearns (2016)105 | Narrative review | N/A | N/A | Patient portal; Website |
| Promotion; training | du Pon et al. (2020)87 | RCT | N = 203 patients | Type-2 diabetes | Website |
| Promotion; training | Ebert et al. (2015)86 | RCT | N = 128 patients | Depression | Website |
| Promotion; training | Slevin et al. (2020)107 | Qualitative study | N = 32; providers (GPs and respiratory therapists) | Chronic obstructive pulmonary disease (COPD) | Health app |
| Promotion; training (for providers) | Raza Khan et al. (2019)148 | Case study | N = 10; primary care staff | N/A | Patient portal |
| Promotion; training; guidance and support | Castle-Clarke and Imison (2016)99 | Case studies | N/A | N/A | Health app; Website; patient portal |
| Promotion (for patient); training; ongoing support (for providers) | Molleda et al. (2017)97 | Qualitative study | N = 48; Hispanic adolescents and their parents | Behavioural health (drug use, sexual health) | Website |
| Promotion (for patients); training (for provider) | Webb et al. (2018)110 | Case study | N = 99; 4 GPs, 10 support staff and 85 young people aged 14–25 | N/A | Screening programmes and customised health information on tablets |
| Promotion; guidance and support | Lipschitz et al. (2019)102 | Cross-sectional study | N = 149; patients with mental health conditions in facility that treats veterans | Mental health; unipolar depression; anxiety disorders; PTSD | Health app |
| Promotion; guidance and support | O’Cathain et al. (2016)144 | Qualitative study | N = 53; 21 primary care staff, 8 NHS direct staff and 24 patients | Depression and cardiovascular risk | Website |
| Promotion; guidance and support | Reynolds et al. (2015)104 | Narrative review | N/A | Mental health | Websites |
| Promotion; guidance and support; training | Longacre et al. (2018)109 | Retrospective qualitative case study | Unclear | Paediatric cystic fibrosis | Health app |
| Promotion; guidance and support; training | Miller et al. (2019)142 | Cross-sectional study | N = 220; primary care mental health providers | Mental health | Health app |
| Training | Abidi et al. (2018)91 | Qualitative study | N = 21; 10 primary care providers, 11 patients | Diabetes | Website |
| Training | Bernhard et al. (2018)95 | Qualitative study | N = 48; 25 patients, 13 GPs, 10 health care assistants | Diabetes | Patient portal |
| Training | Chan et al. (2018)213 | Cross-sectional study | N = 17,699 patient records | N/A | Patient portal |
| Training | Collins (2020)214 | Case studies | N = 4 case study sites | N/A | Screening programme and customised health information on tablet |
| Training | Hjelmager (2019)85 | Qualitative study | N = 8 GPs | Low back pain | Website |
| Training | Lyles et al. (2016)215 | Qualitative study | N = 87; English-speaking Latino and African American patients | N/A | Patient portal; Health app |
| Training | Lyles et al. (2019)115 | RCT | N = 93; patients with chronic disease | Chronic diseases | Patient portal |
| Training | Moult et al. (2018)151 | Qualitative study | N = 18; adults 65 or older | Anxiety and depression; distress | Website |
| Training | Rodgers et al. (2019)108 | Rapid evidence assessment | N/A | N/A | Patient portal |
| Training | Tieu et al. (2015)124 | Qualitative study | N = 16; patients in safety net hospital with chronic diseases and carers | Chronic diseases | Patient portal |
| Training (both for patient and provider); promotion (for patient) | Ramsey et al. (2018)119 | Cross-sectional study | N = 96; patients 13–25 years old in urban clinic | N/A | Patient portal |
| Training (for patients); guidance and support (for patients and providers) | Ford et al. (2015)120 | Qualitative study | N = 44; clinicians and administrators providing drug and alcohol treatment | Addiction | Health app |
| Training (for providers and patients) | Sieck et al. (2017)121 | Qualitative study | N = 42; 29 patients and 13 primary care providers | Cardiopulmonary conditions | Patient portal |
| Training; guidance and support | Apter et al. (2019)127 | RCT | N = 300 | Asthma | Patient portal |
| Training; guidance and support | Talboom-Kamp et al. (2017)128 | Prospective cohort study | N = 215; patients with COPD | COPD | Website |
| Training; promotion | Grossman et al. (2019)81 | Systematic literature review | N/A – systematic review | N/A | Patient portals |
| Training; promotion | North et al. (2011)116 | RCT | N = 12,050 (office appointments) | N/A | Patient portal |
| Training; promotion | Phelps et al. (2014)38 | Longitudinal observational study | N = 11,352; patients with chronic kidney disease | Chronic kidney disease | Patient portal |
| Guidance and support | Baumeister et al. (2014)118 | RCT | N = 141; diabetes patients in inpatient and outpatient rehabilitation clinics | Diabetes; depression | Website |
| Guidance and support | Cafazzo et al. (2012)216 | Qualitative study | N = 20; adolescents with type 1 diabetes and their parents (12 interviewed) | Adolescent type 1 diabetes | Health app |
| Guidance and support | Careyva et al. (2016)143 | Cross-sectional study | N = 102, practice-based research network directors | N/A | Patient portals |
| Guidance and support | Lin et al. (2017)125 | RCT | N = 302 | Chronic pain | Website |
| Guidance and support | Littlewood et al. (2015)129 | Qualitative study | N = 11; GPs | Depression | Website |
| Guidance and support | Ma et al. (2013)126 | Secondary analysis of data from RCTs | N = 64; overweight adults with pre-diabetes | Weight loss; pre-diabetes | Website |
| Guidance and support | Possemato et al. (2016)89 | RCT | N = 20; veterans with PTSD from military-related trauma | PTSD | Health app |
| Guidance and support | Ray et al. (2017)217 | Qualitative study | N = 24; veterans with anxiety and depression | Depression and anxiety | Website |
| Guidance and support | Richardson et al. (2010)218 | RCT | N = 324 patients | Obesity | Website |
| Guidance and support | van Middelaar et al. (2018)90 | Qualitative study | N = 20; patients over 65 with risk of cardiovascular disease | Cardiovascular disease | Website |
| Guidance and support | Zarski et al. (2018)111 | Secondary analysis of data from RCTs | N = 101; patients with subclinical depression | Subclinical depression | Website |
| Guidance and support | Zarski et al. (2016)133 | Secondary analysis of data from RCTs | N = 395; employed adults with stress | Stress | Website |
| Guidance and support (for providers) | Hale et al. (2015)154 | Narrative review | N/A | Type 2 diabetes and other chronic conditions | Health app |
| Guidance and support; promotion | Cowie et al. (2018)68 | Mixed method: qualitative and retrospective case series | N = 11 GP practices and their patients | N/A | Patient portal |
| Guidance and support; Promotion | van Beurden et al. (2018)130 | Qualitative study | N = 20; patients that are overweight and want to lose weight | Overweight/obesity | Website |
| Guidance and support; training | Nijland et al. (2011)114 | Mixed methods: qualitative, prospective case study | N = 50; patients with diabetes enrolled to use app | Type 2 diabetes | Website |
| N/A | Amaro and Duarte (2015)152 | Mixed method: narrative review; cross-sectional study | N = 1732 | N/A | Website |
| N/A | Bonsón Ponte et al. (2015)153 | Mixed method: narrative review; cross-sectional study | N = 451 | N/A | Website |
| N/A | Cameron et al. (2019)137 | Narrative review | N/A | N/A | N/A |
| N/A | Castle-Clarke et al. (2016)99 | Qualitative study; case studies | N/A | N/A | Patient portal; Website |
| N/A | Oliveira Hashiguchi (2020)145 | Mixed method: qualitative, narrative review, cross-sectional study | N/A | N/A | Health app |
| N/A | Greenhalgh (2017)141 | Case study | N = 6 case studies | N/A | Various |
| N/A | Hardiker and Grant (2010)92 | Rapid evidence assessment | N/A | N/A | Website; patient portal; health app |
| N/A | Honeyman et al. (2016)219 | Narrative review | N/A | N/A | Various |
| N/A | Hutchings (2020)11 | Narrative review | N/A | N/A | Health app; patient portal |
| N/A | Maguire et al. (2018)147 | Case studies | N/A | N/A | Various |
| N/A | Rosen (2019)149 | Qualitative study | N/A | N/A | Patient portal; health app |
| N/A | Venkatesh (2012)220 | Mixed method: cross-sectional study; theoretical model development | N = 1521 online consumers | N/A | Website |
| N/A | Weppner et al. (2010)146 | Retrospective cohort study | N = 6185; older adults with diabetes | Diabetes | Patient portal |
| N/A | Yamin (2011)221 | Cross-sectional study | N = 75,056 patients | N/A | Patient portal |
Appendix 2 Practice, patient and general practice patient survey analyses
Factor analysis and scale development
Factor analysis of digital confidence scale
Question two through six of the main patient survey asked patients about their confidence levels in performing various digital task commonly performed in everyday life (see additional files www.fundingawards.nihr.ac.uk/award/NIHR128268; accessed 3 April 2024). Each question had three response options (‘Very confident’, ‘Quite confident’, and ‘Not confident’). Polychoric correlation coefficients were calculated for these five categorical variables. To determine the number of factors explaining the variability in responses to these questions, an unrestricted exploratory factor analysis (EFA) was performed. The eigenvalues from the polychoric correlation matrix were calculated and plotted against each factor. Both Kaiser rule and the Scree plot were used to determine the number of factors. Kaiser rules suggest retaining factors whose eigenvalues are > 1. The scree plot of eigenvalues was used to visually determine the number of factors to retain in the model based on the point of levelling off (the ‘elbow’).
Internal consistency reliability coefficients (Cronbach’s alpha) were calculated from the variance–covariance matrix of digital confidence. The range of Cronbach’s alpha coefficients in each factor when questions were sequentially omitted and reintroduced was also calculated. Polychoric correlation coefficients matrix was computed using the ‘psych’ package, and Cronbach’s alphas were computed using ‘MASS’ and ‘ltm’ packages in R.
Results
There were 1.7% missing values, all of which were among patients who submitted their response by post. The polychoric correlation coefficients presented in Table 30 indicate very strong correlations between each pair of variables. Only the first factor had an eigenvalue > 1, suggesting there is a single factor underlying the responses. The scree plot in Figure 17 for an unrestricted EFA confirms a single underlying factor. The value of Cronbach’s alpha was 0.936 indicating very high internal consistency and possible potential for item-redundancy. Cronbach’s alpha ranged from 0.916 to 0.933 when one question was left out at a time, and it ranged from 0.879 to 0.902 when two questions were left out at a time (Table 31). A restricted EFA model with a single factor resulted in factor loadings > 0.8 for the five questions (Table 32).
FIGURE 17.
Scree plot for the EFA applied to the responses to the five questions addressing digital confidence.

| Use of search engines | Completing online forms | Sending personal messages via e-mail | Installing apps | Sending personal messages via apps | |
|---|---|---|---|---|---|
| Use of search engines | 1.000 | 0.943 | 0.919 | 0.908 | 0.856 |
| Completing online forms | 1.000 | 0.923 | 0.891 | 0.841 | |
| Sending personal messages via e-mail | 1.000 | 0.848 | 0.855 | ||
| Installing apps | 1.000 | 0.880 | |||
| Sending personal messages via apps | 1.000 | ||||
| Digital confidence questions removed | Cronbach’s alpha coefficient |
|---|---|
| Q2 Q3 Q4 Q5 Q6 |
0.917 0.916 0.926 0.926 0.933 |
| Q2 and Q3 Q2 and Q4 Q2 and Q5 Q2 and Q6 Q3 and Q4 Q3 and Q5 Q3 and Q6 Q4 and Q5 Q4 and Q6 Q5 and Q6 |
0.879 0.898 0.889 0.902 0.897 0.893 0.898 0.9 0.921 0.931 |
| Question number | Factor loading |
|---|---|
| Q2 | 0.919 |
| Q3 | 0.919 |
| Q4 | 0.864 |
| Q5 | 0.844 |
| Q6 | 0.793 |
| Survey practices | Other practices | |
|---|---|---|
| Deprivation quintile N (%) according to patient postcode | ||
| 1 (least deprived) | 40 (25.6) | 1341 (19.9) |
| 2 | 43 (27.6) | 1337 (19.8) |
| 3 | 28 (17.9) | 1352 (20.1) |
| 4 | 24 (15.4) | 1356 (20.1) |
| 5 (most deprived) | 21 (13.5) | 1359 (20.1) |
| Total | 155 (100) | 6745 (100) |
| Rurality: % of urban and rural practices N (%) | ||
| Urban | 110 (70.5) | 5839 (85.3) |
| Rural | 46 (29.5) | 1004 (14.7) |
| Total | 156 (100) | 6843 (100) |
| Age: % of patients aged over 65 years (%) | ||
| Practices (N) | 155 | 6425 |
| Median | 20.3% | 17.7% |
| Mean | 20.1% | 17.6% |
| Standard deviation | 7.3% | 7.2% |
| Range | 4.5% to 41.7% | 0% to 98.5% |
| List size: % of practices with low, medium or high list sizes | ||
| ≤ 6000 patients | 36 (23.2) | 2130 (33) |
| > 6000 and ≤ 12,000 | 65 (41.9) | 2854 (44.2) |
| > 12,000 | 54 (34.8) | 1477 (22.8) |
| Total | 155 (100) | 6461 (100) |
| Ethnicity: % of non-white patients in practices in England | ||
| Practices (n) | 155 | 6468 |
| Median | 4.8% | 7.5% |
| Mean | 12.5% | 17.0% |
| Standard deviation | 15.7% | 19.8% |
| Range | 1.0 to 86.8% | 0.0 to 90.5% |
Appendix 3 Full details of practice survey responses
| Currently offered, n (%) | Offered pre COVID, n (%) | Offered currently and pre COVID, n (%) | Offered currently but not pre COVID, n (%) | Offered pre COVID but not currently, n (%) | Never offered, n (%) | |
|---|---|---|---|---|---|---|
| Online appointment booking (n = 153) | 78 (50.98) | 133 (86.93) | 66 (43.14) | 12 (7.84) | 67 (43.79) | 8 (5.23) |
| Online repeat prescriptions (n = 154) | 143 (92.86) | 112 (72.73) | 101 (65.58) | 42 (27.27) | 11 (7.14) | 0 (0.00) |
| Online access to medical records (n = 151) | 130 (86.09) | 99 (65.56) | 89 (58.94) | 41 (27.15) | 10 (6.62) | 11 (7.28) |
| Test results (n = 149) | 114 (76.51) | 87 (58.39) | 77 (51.68) | 37 (24.83) | 10 (6.71) | 25 (16.78) |
| E-mail enquiries (n = 154) | 126 (81.82) | 96 (62.34) | 83 (53.90) | 43 (27.92) | 13 (8.44) | 15 (9.74) |
| Online consultations (n = 151) | 123 (81.46) | 69 (45.70) | 58 (38.41) | 65 (43.05) | 11 (7.28) | 17 (11.92) |
| Video consultations (n = 154) | 143 (92.86) | 14 (9.09) | 11 (7.14) | 132 (85.71) | 3 (1.95) | 8 (5.84) |
| Self-care resources (n = 150) | 126 (84.00) | 78 (52.00) | 68 (45.33) | 58 (38.67) | 10 (6.67) | 14 (9.33) |
| Other (n = 13) | 11 (84.62) | 4 (30.77) | 3 (23.08) | 8 (61.54) | 1 (7.69) | 1 (7.69) |
| Promote, n (%) | Support, n (%) | Promote and support, n (%) | Promote but not support, n (%) | Support but not promote, n (%) | Neither, n (%) | |
|---|---|---|---|---|---|---|
| Display (n = 147) | 122 (82.99) | 67 (45.58) | 57 (38.78) | 65 (44.22) | 10 (6.80) | 15 (10.20) |
| Leaflet (n = 141) | 89 (63.12) | 57 (40.43) | 46 (32.62) | 43 (30.50) | 11 (7.80) | 41 (29.08) |
| Text messages and/or e-mails (n = 141) | 110 (78.01) | 62 (43.97) | 48 (34.04) | 62 (43.97) | 14 (9.93) | 17 (12.06) |
| Practice website (n = 141) | 125 (82.78) | 79 (52.32) | 64 (42.38) | 61 (40.40) | 15 (9.93) | 11 (7.28) |
| Social media (n = 148) | 78 (52.70) | 45 (30.41) | 38 (25.68) | 40 (27.03) | 7 (4.73) | 63 (42.57) |
| Ad hoc (n = 143) | 111 (77.62) | 87 (60.84) | 68 (47.55) | 43 (30.07) | 19 (13.29) | 13 (9.09) |
| Practice champion (n = 139) | 30 (21.58) | 32 (23.02) | 16 (11.51) | 14 (10.07) | 16 (11.51) | 93 (66.91) |
| Workshops or events (n = 145) | 11 (7.59) | 11 (7.59) | 4 (2.76) | 7 (4.83) | 7 (4.83) | 127 (87.59) |
| Provision of tablets/computers (n = 145) | 10 (6.90) | 14 (9.66) | 7 (4.83) | 3 (2.07) | 7 (4.83) | 129 (88.97) |
| Other (n = 14) | 1 (7.14) | 2 (14.29) | 1 (7.14) | 0 (0.00) | 1 (7.14) | 12 (85.71) |
| Promote, n (%) | Support, n (%) | Promote and support, n (%) | Promote but not support, n (%) | Support but not promote, n (%) | Neither, n (%) | |
|---|---|---|---|---|---|---|
| Online appointment booking (n = 144) | 106 (73.61) | 70 (48.61) | 53 (36.81) | 53 (36.81) | 17 (11.81) | 22 (15.28) |
| Online repeat prescriptions (n = 144) | 118 (81.94) | 77 (53.47) | 56 (38.89) | 62 (43.06) | 21 (14.58) | 5 (3.47) |
| Online access to medical records (n = 144) | 83 (59.29) | 57 (40.71) | 34 (24.29) | 49 (35.00) | 23 (16.43) | 34 (24.29) |
| Test results (n = 138) | 83 (60.14) | 54 (39.13) | 31 (22.46) | 52 (37.68) | 23 (16.67) | 33 (23.91) |
| E-mail enquiries (n = 142) | 73 (51.41) | 55 (38.73) | 32 (22.54) | 41 (28.87) | 23 (16.20) | 46 (32.39) |
| eConsult (n = 139) | 98 (70.50) | 64 (46.04) | 48 (34.53) | 50 (35.97) | 16 (11.51) | 25 (17.99) |
| Video consultations (n = 142) | 68 (47.89) | 69 (48.59) | 33 (23.24) | 35 (24.65) | 36 (25.35) | 38 (26.76) |
| Self-care resources (n = 142) | 94 (66.20) | 69 (48.59) | 43 (30.28) | 51 (35.92) | 26 (18.31) | 22 (15.49) |
| Other (n = 12) | 2 (16.67) | 3 (25.00) | 1 (8.33) | 1 (8.33) | 2 (16.67) | 8 (66.67) |
| Staff role | n (%) |
|---|---|
| Doctors | 96 (61.54) |
| Nurses | 83 (53.21) |
| Other healthcare professionals | 65 (41.67) |
| Reception staff | 134 (85.90) |
| Admin | 134 (85.90) |
| IT staff | 44 (28.21) |
| External contractors | 6 (3.85) |
| Specific | 16 (10.26) |
| Volunteer | 31 (19.87) |
| Other | 6 (3.85) |
| Access remained unchanged, n (%) | Access was reduced, n (%) | Access was removed, n (%) | |
|---|---|---|---|
| Booking appointments in person (n = 146) | 23 (15.75) | 51 (34.93) | 72 (49.32) |
| Booking appointments on the phone (n = 146) | 131 (89.73) | 14 (9.59) | 1 (0.69) |
| Face-to-face consultations with a GP at the practice (n = 146) | 19 (13.01) | 115 (78.77) | 12 (8.22) |
| Face-to-face consultations with a nurse at the practice (n = 147) | 48 (32.65) | 98 (66.67) | 1 (0.68) |
| Provision of paper prescriptions (n = 146) | 40 (27.40) | 77 (52.74) | 29 (19.86) |
| Ordering repeat prescriptions in person (n = 147) | 40 (27.21) | 69 (46.94) | 38 (25.85) |
| Ordering repeat prescriptions by phone (n = 135) | 97 (71.85) | 20 (14.82) | 18 (13.33) |
| Other (n = 13) | 13 (100.00) | 0 (0.00) | 0 (0.00) |
| Access remained unchanged, n (%) | Access was reduced, n (%) | Access was removed, n (%) | |
|---|---|---|---|
| Booking appointments in person (n = 144) | 103 (71.53) | 23 (15.97) | 18 (12.50) |
| Booking appointments on the phone (n = 145) | 135 (93.10) | 9 (6.21) | 1 (0.69) |
| Face-to-face consultations with a GP at the practice (n = 145) | 102 (70.34) | 39 (26.90) | 4 (2.76) |
| Face-to-face consultations with a nurse at the practice (n = 145) | 119 (82.07) | 25 (17.24) | 1 (0.69) |
| Provision of paper prescriptions (n = 145) | 80 (55.17) | 56 (38.62) | 9 (6.21) |
| Ordering repeat prescriptions in person (n = 144) | 96 (66.67) | 35 (24.31) | 13 (9.03) |
| Ordering repeat prescriptions by phone (n = 141) | 78 (55.32) | 34 (24.11) | 29 (20.57) |
| Other (n = 9) | 6 (66.67) | 1 (11.11) | 2 (22.22) |
| Strongly agree, n (%) | Agree, n (%) | Neither agree nor disagree, n (%) | Disagree, n (%) | Strongly disagree, n (%) | |
|---|---|---|---|---|---|
| It is a general practice’s responsibility to inform patients what online primary care services are being offered (n = 144) | 52 (36.11) | 71 (49.31) | 14 (9.72) | 7 (4.86) | 0 (0.00) |
| It is a general practice’s responsibility to support patients to use online primary care services (n = 144) | 29 (20.14) | 76 (52.78) | 21 (14.58) | 12 (8.33) | 6 (4.17) |
| Other parts of the NHS (e.g. CCGs, NHS England) are responsible for informing patients about what online primary care services are being offered (n = 144) | 41 (28.47) | 81 (56.25) | 18 (12.50) | 4 (2.78) | 0 (0.00) |
| Other parts of the NHS (e.g. CCGs, NHS England) are responsible for supporting patients to use online primary care services (n = 143) | 38 (26.57) | 80 (55.94) | 21 (14.69) | 4 (2.80) | 0 (0.00) |
| COVID-19 has been a key driver in the uptake of online primary care services by patients (n = 144) | 82 (56.94) | 47 (32.64) | 13 (9.03) | 2 (1.39) | 0 (0.00) |
| COVID-19 has inhibited our ability to support patients in using online primary care services (n = 141) | 6 (4.26) | 27 (19.15) | 45 (31.91) | 52 (36.88) | 11 (7.80) |
| COVID-19 has led to an increase in the support we provide to patients in using online primary care services (n = 144) | 32 (22.22) | 77 (53.47) | 28 (19.44) | 7 (4.86) | 0 (0.00) |
| Strongly agree, n (%) | Agree, n (%) | Neither agree nor disagree, n (%) | Disagree, n (%) | Strongly disagree, n (%) | |
|---|---|---|---|---|---|
| The support we provide to patients to use online primary care services is in response to patient demand/need (n = 142) | 25 (17.61) | 94 (66.20) | 18 (12.68) | 5 (3.52) | 0 (0.00) |
| The support we provide to patients to use online primary care services is in response to demand from practice staff (n = 142) | 9 (6.34) | 52 (36.62) | 54 (38.03) | 22 (15.49) | 5 (3.52) |
| The support we provide to patients to use online primary care services is in response to demand from the CCG (n = 142) | 8 (5.63) | 39 (27.46) | 60 (42.25) | 31 (21.83) | 4 (2.82) |
| Supporting patients to use online primary care services is a benefit to the practice (n = 144) | 53 (36.81) | 73 (50.69) | 14 (9.72) | 4 (2.78) | 0 (0.00) |
| Supporting patients to use online primary care services is a benefit to the patients (n = 144) | 62 (43.06) | 70 (48.61) | 10 (6.94) | 1 (0.69) | 1 (0.69) |
| We do not have the capacity to support patients in using online primary care services as much as we would like (n = 141) | 34 (24.11) | 51 (36.17) | 31 (21.99) | 20 (14.18) | 5 (3.55) |
| Strongly agree (%) | Agree (%) | Neither agree nor disagree (%) | Disagree (%) | Strongly disagree (%) | |
|---|---|---|---|---|---|
| Some patients are unlikely to use online primary care services no matter how much we support them (n = 143) | 70 (48.95) | 65 (45.45) | 5 (3.50) | 3 (2.10) | 0 (0.00) |
| Some patient groups (e.g. older or more deprived patients) require more support in using online primary care services than others (n = 143) | 59 (41.26) | 72 (50.35) | 12 (8.39) | 0 (0.00) | 0 (0.00) |
| We hope to increase uptake of online primary care services by supporting our patients to use them (n = 143) | 27 (18.88) | 77 (53.85) | 33 (23.08) | 6 (4.20) | 0 (0.00) |
| We have managed to increase uptake of online primary care services by supporting our patients to use them (n = 139) | 31 (22.30) | 78 (56.12) | 26 (18.71) | 3 (2.16) | 1 (0.72) |
| Financial incentives received by the practice influenced our decision to increase the support we provide to patients to use online primary care (n = 135) | 5 (3.70) | 15 (11.11) | 53 (39.26) | 43 (31.85) | 19 (14.07) |
| Increased patient uptake of online primary care services leads to operational efficiencies for the practice (n = 142) | 29 (20.42) | 66 (46.48) | 33 (23.24) | 11 (7.75) | 3 (2.11) |
| Online primary care services are complementary to traditional forms of access (n = 143) | 26 (18.18) | 95 (66.43) | 14 (9.79) | 6 (4.20) | 2 (1.40) |
| Online primary care services will ultimately replace traditional forms of access (n = 142) | 11 (7.75) | 41 (28.87) | 31 (21.83) | 46 (32.39) | 13 (9.15) |
| Aware of the toolkit, n (%) | Have used the toolkit, n (%) | Aware and used, n (%) | Aware but not used, n (%) | Not aware but used, n (%) | Not aware and not used, n (%) | |
|---|---|---|---|---|---|---|
| RCGP Patient Online toolkit (n = 136) | 66 (48.53) | 13 (9.56) | 8 (5.88) | 58 (42.65) | 5 (3.68) | 50 (36.76) |
| NHSE online consultations in primary care toolkit (n = 137) | 55 (41.04) | 12 (8.96) | 6 (4.48) | 49 (36.57) | 6 (4.48) | 57 (42.54) |
Appendix 4 Logistic regression analyses
| Unadjusted logistic regression analyses (Model 1) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Awareness of any facilitation effortsa | Use of any facilitation effortsb | Being told about online services | Being helped to use online services | |||||
| Unadjusted OR (95% CI) | p-value | Unadjusted OR (95% CI) | p-value | Unadjusted OR (95% CI) | p-value | Unadjusted OR (95% CI) | p-value | |
| Digital Confidence (Q2–6) | ||||||||
| Very confident | Ref | |||||||
| Quite confident | 0.84 (0.70 to 1.02) | < 0.001 | 1.02 (0.85 to 1.22) | < 0.001 | 0.84 (0.69 to 1.03) | < 0.001 | 0.86 (0.66 to 1.11) | < 0.001 |
| Not confident | 0.31 (0.26 to 0.38) | 0.40 (0.32 to 0.49) | 0.51 (0.41 to 0.64) | 0.32 (0.22 to 0.46) | ||||
| Q18. Gender | ||||||||
| Male | Ref | |||||||
| Female | 0.93 (0.80 to 1.08) | 0.337 | 0.95 (0.82 to 1.11) | 0.542 | 1.24 (1.06 to 1.47) | 0.009 | 0.96 (0.77 to 1.19) | 0.710 |
| Q19. Age | ||||||||
| 16–24 | 0.82 (0.56 to 1.21) | < 0.001 | 0.71 (0.48 to 1.05) | < 0.001 | 1.32 (0.89 to 1.96) | < 0.001 | 1.11 (0.65 to 1.88) | 0.005 |
| 25–34 | 1.22 (0.86 to 1.72) | 1.20 (0.86 to 1.68) | 1.27 (0.90 to 1.80) | 1.05 (0.65 to 1.69) | ||||
| 35–44 | 1.08 (0.79 to 1.46) | 1.02 (0.76 to 1.38) | 1.25 (0.91 to 1.71) | 1.35 (0.91 to 2.02) | ||||
| 45–54 | 1.03 (0.79 to 1.33) | 1.01 (0.78 to 1.30) | 1.13 (0.86 to 1.48) | 1.34 (0.95 to 1.90) | ||||
| 55–64 | Ref | |||||||
| 65–74 | 0.72 (0.58 to 0.90) | 0.75 (0.60 to 0.94) | 0.84 (0.66 to 1.07) | 0.91 (0.65 to 1.26) | ||||
| 75–84 | 0.44 (0.34 to 0.56) | 0.57 (0.44 to 0.73) | 0.70 (0.53 to 0.93) | 0.72 (0.49 to 1.05) | ||||
| ≥ 85 | 0.35 (0.24 to 0.53) | 0.32 (0.20 to 0.51) | 0.39 (0.23 to 0.66) | 0.37 (0.17 to 0.83) | ||||
| Q20. Deaf/hearing impairment | ||||||||
| No | Ref | |||||||
| Yes | 0.70 (0.55 to 0.87) | 0.002 | 0.85 (0.67 to 1.08) | 0.183 | 0.64 (0.49 to 0.84) | 0.001 | 1.00 (0.71 to 1.39) | 0.985 |
| Q22. Parent | ||||||||
| No | Ref | |||||||
| Yes | 1.59 (1.28 to 1.99) | < 0.001 | 1.32 (1.06 to 1.63) | 0.012 | 1.41 (1.13 to 1.77) | 0.003 | 1.43 (1.07 to 1.91) | 0.015 |
| Q23. Ethnicity | ||||||||
| White | Ref | |||||||
| Other | 1.71 (1.24 to 2.36) | 0.001 | 1.91 (1.41 to 2.59) | < 0.001 | 1.15 (0.84 to 1.59) | 0.386 | 2.20 (1.54 to 3.14) | < 0.001 |
| Q24–25. Long-term physical or mental health condition | ||||||||
| No | Ref | |||||||
| Yes | 1.04 (0.90 to 1.22) | 0.573 | 1.09 (0.93 to 1.27) | 0.282 | 1.15 (0.97 to 1.35) | 0.105 | 1.28 (1.02 to 1.60) | 0.033 |
| Q26. Working status | ||||||||
| Work | Ref | |||||||
| Education | 0.62 (0.38 to 1.02) | < 0.001 | 0.70 (0.43 to 1.15) | < 0.001 | 1.23 (0.75 to 2.02) | < 0.001 | 1.10 (0.57 to 2.11) | 0.101 |
| Other | 0.75 (0.58 to 0.97) | 0.90 (0.69 to 1.16) | 0.93 (0.71 to 1.23) | 1.26 (0.89 to 1.78) | ||||
| Retired | 0.55 (0.47 to 0.65) | 0.61 (0.52 to 0.72) | 0.70 (0.58 to 0.84) | 0.82 (0.64 to 1.05) | ||||
| Q27. First language | ||||||||
| English | Ref | |||||||
| Other | 1.64 (1.23 to 2.19) | 0.001 | 2.07 (1.57 to 2.72) | < 0.001 | 1.44 (1.08 to 1.92) | 0.013 | 2.00 (1.43 to 2.81) | < 0.001 |
| Q29. Repeat prescription | ||||||||
| No | Ref | |||||||
| Yes | 0.97 (0.83 to 1.14) | 0.737 | 1.16 (0.98 to 1.36) | 0.079 | 1.29 (1.09 to 1.54) | 0.004 | 1.24 (0.98 to 1.57) | 0.072 |
| Adjusted logistic regression analyses (Model 2) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Awareness of any facilitation effortsa | Use of any facilitation effortsb | Being told about online services | Being helped to use online services | |||||
| Adjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value | |
| Digital confidence (Q2–6) | ||||||||
| Very confident | Reference | |||||||
| Quite confident | 0.85 (0.69 to 1.06) | < 0.001 | 1.04 (0.84 to 1.28) | < 0.001 | 0.87 (0.69 to 1.09) | 0.005 | 0.93 (0.69 to 1.25) | < 0.001 |
| Not confident | 0.35 (0.27 to 0.46) | 0.39 (0.29 to 0.51) | 0.61 (0.46 to 0.83) | 0.32 (0.20 to 0.51) | ||||
| Q18. Gender | ||||||||
| Male | Reference | |||||||
| Female | 0.95 (0.80 to 1.13) | 0.581 | 0.92 (0.78 to 1.09) | 0.333 | 1.14 (0.95 to 1.37) | 0.147 | 0.86 (0.67 to 1.10) | 0.220 |
| Q19. Age | ||||||||
| 16–24 | 0.75 (0.44 to 1.27) | 0.181 | 0.60 (0.35 to 1.03) | 0.159 | 1.51 (0.88 to 2.58) | 0.478 | 0.93 (0.43 to 2.03) | 0.176 |
| 25–34 | 0.94 (0.64 to 1.40) | 0.99 (0.68 to 1.45) | 1.06 (0.71 to 1.59) | 1.06 (0.61 to 1.84) | ||||
| 35–44 | 0.91(0.62 to 1.33) | 0.97 (0.66 to 1.41) | 1.05 (0.71 to 1.57) | 1.37 (0.82 to 2.30) | ||||
| 45–54 | 0.88 (0.65 to 1.19) | 0.92 (0.68 to 1.23) | 1.01 (0.73 to 1.38) | 1.30 (0.86 to 1.98) | ||||
| 55–64 | Reference | |||||||
| 65–74 | 0.82 (0.61 to 1.11) | 1.00 (0.74 to 1.34) | 0.83 (0.61 to 1.15) | 0.90 (0.58 to 1.38) | ||||
| 75–84 | 0.60 (0.42 to 0.86) | 0.83 (0.58 to 1.19) | 0.79 (0.54 to 1.16) | 0.69 (0.40 to 1.17) | ||||
| ≥ 85 | 0.59 (0.34 to 1.02) | 0.48 (0.26 to 0.90) | 0.52 (0.27 to 1.01) | 0.15 (0.03 to 0.67) | ||||
| Q20. Deaf/hearing impairment | ||||||||
| No | Reference | |||||||
| Yes | 1.00 (0.75 to 1.33) | 0.994 | 1.24 (0.93 to 1.66) | 0.146 | 0.86 (0.62 to 1.18) | 0.352 | 1.45 (0.95 to 2.20) | 0.084 |
| Q22. Parent | ||||||||
| No | Reference | |||||||
| Yes | 1.19 (0.88 to 1.59) | 0.255 | 0.98 (0.73 to 1.30) | 0.875 | 1.22 (0.90 to 1.65) | 0.204 | 0.99 (0.67 to 1.47) | 0.967 |
| Q23. Ethnicity | ||||||||
| White | Reference | |||||||
| Other | 1.49 (0.99 to 2.22) | 0.053 | 1.50 (1.03 to 2.18) | 0.035 | 0.95 (0.64 to 1.41) | 0.793 | 1.83 (1.15 to 2.91) | 0.011 |
| Q24–25. Long-term physical or mental health condition | ||||||||
| No | Reference | |||||||
| Yes | 1.26 (1.04 to 1.53) | 0.017 | 1.18 (0.98 to 1.43) | 0.089 | 1.07 (0.87 to 1.31) | 0.526 | 1.30 (0.98 to 1.71) | 0.068 |
| Q26. Working status | ||||||||
| Work | Reference | |||||||
| Education | 0.74 (0.38 to 1.44) | 0.301 | 1.06 (0.54 to 2.07) | 0.514 | 1.11 (0.57 to 2.18) | 0.972 | 1.26 (0.50 to 3.16) | 0.271 |
| Other | 0.78 (0.58 to 1.05) | 0.85 (0.64 to 1.15) | 0.97 (0.72 to 1.33) | 1.40 (0.94 to 2.08) | ||||
| Retired | 1.02 (0.77 to 1.36) | 0.83 (0.62 to 1.10) | 1.04 (0.77 to 1.41) | 1.37 (0.90 to 2.08) | ||||
| Q27. First language | ||||||||
| English | Reference | |||||||
| Other | 1.56 (1.08 to 2.26) | 0.017 | 2.00 (1.41 to 2.84) | < 0.001 | 1.62 (1.12 to 2.34) | 0.011 | 1.71 (1.09 to 2.70) | 0.021 |
| Q29. Repeat prescription | ||||||||
| No | Reference | |||||||
| Yes | 1.28 (1.04 to 1.57) | 0.022 | 1.46 (1.18 to 1.80) | < 0.001 | 1.71 (1.36 to 2.14) | < 0.001 | 1.46 (1.07 to 2.00) | 0.016 |
| Adjusted Model 1 (excluding ‘yes’ group from Q30) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Awareness of any facilitation effortsa | Use of any facilitation effortsb | Being told about online services | Being helped to use online services | |||||
| Adjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value | |
| Q18. Gender | ||||||||
| Male | Reference | |||||||
| Female | 0.90 (0.76 to 1.07) | 0.221 | 0.89 (0.75 to 1.05) | 0.175 | 1.12 (0.93 to 1.34) | 0.236 | 0.87 (0.68 to 1.11) | 0.258 |
| Q19. Age | ||||||||
| 16–24 | 0.87 (0.51 to 1.47) | < 0.001 | 0.65 (0.38 to 1.12) | < 0.001 | 1.63 (0.95 to 2.81) | 0.105 | 1.01 (0.47 to 2.21) | 0.015 |
| 25–34 | 1.06 (0.72 to 1.58) | 1.06 (0.73 to 1.56) | 1.13 (0.76 to 1.70) | 0.97 (0.55 to 1.71) | ||||
| 35–44 | 0.91 (0.62 to 1.34) | 0.98 (0.67 to 1.44) | 1.08 (0.72 to 1.62) | 1.40 (0.83 to 2.36) | ||||
| 45–54 | 0.92 (0.68 to 1.25) | 0.95 (0.70 to 1.28) | 1.03 (0.75 to 1.42) | 1.30 (0.86 to 1.98) | ||||
| 55–64 | Reference | |||||||
| 65–74 | 0.70 (0.52 to 0.95) | 0.91 (0.68 to 1.22) | 0.80 (0.58 to 1.10) | 0.87 (0.57 to 1.35) | ||||
| 75–84 | 0.42 (0.30 to 0.59) | 0.63 (0.44 to 0.89) | 0.68 (0.46 to 0.99) | 0.52 (0.31 to 0.89) | ||||
| ≥85 | 0.34 (0.20 to 0.60) | 0.29 (0.16 to 0.55) | 0.42 (0.21 to 0.83) | 0.11 (0.02 to 0.47) | ||||
| Q20. Deaf/hearing impairment | ||||||||
| No | Reference | |||||||
| Yes | 1.09 (0.81 to 1.45) | 0.583 | 1.30 (0.97 to 1.75) | 0.079 | 0.81 (0.58 to 1.13) | 0.210 | 1.36 (0.89 to 2.08) | 0.153 |
| Q22. Parent | ||||||||
| No | Reference | |||||||
| Yes | 1.27 (0.94 to 1.71) | 0.120 | 1.01 (0.75 to 1.35) | 0.954 | 1.29 (0.95 to 1.75) | 0.107 | 1.05 (0.70 to 1.57) | 0.816 |
| Q23. Ethnicity | ||||||||
| White | Reference | |||||||
| Other | 1.48 (0.97 to 2.25) | 0.070 | 1.46 (0.99 to 2.16) | 0.057 | 1.01 (0.67 to 1.53) | 0.946 | 1.97 (1.23 to 3.15) | 0.005 |
| Q24–25. Long-term physical or mental health condition | ||||||||
| No | Reference | |||||||
| Yes | 1.25 (1.04 to 1.52) | 0.020 | 1.18 (0.98 to 1.43) | 0.081 | 1.10 (0.90 to 1.35) | 0.363 | 1.27 (0.97 to 1.68) | 0.087 |
| Q26. Working status | ||||||||
| Work | Reference | |||||||
| Education | 0.75 (0.38 to 1.48) | 0.670 | 1.06 (0.54 to 2.09) | 0.446 | 1.04 (0.53 to 2.06) | 0.919 | 1.32 (0.52 to 3.34) | 0.368 |
| Other | 0.86 (0.63 to 1.16) | 0.89 (0.66 to 1.20) | 1.12 (0.82 to 1.53) | 1.37 (0.92 to 2.05) | ||||
| Retired | 0.97 (0.73 to 1.29) | 0.80 (0.60 to 1.06) | 1.02 (0.75 to 1.38) | 1.28 (0.84 to 1.95) | ||||
| Q27. First language | ||||||||
| English | Reference | |||||||
| Other | 1.38 (0.94 to 2.02) | 0.103 | 1.81 (1.25 to 2.61) | 0.002 | 1.60 (1.08 to 2.36) | 0.018 | 1.80 (1.13 to 2.87) | 0.013 |
| Q29. Repeat prescription | ||||||||
| No | Reference | |||||||
| Yes | 1.28 (1.04 to 1.58) | 0.019 | 1.47 (1.19 to 1.81) | < 0.001 | 1.71 (1.36 to 2.14) | < 0.001 | 1.49 (1.09 to 2.03) | 0.013 |
| Adjusted Model 2 (excluding ‘yes’ group from Q30) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Awareness of any facilitation effortsa | Use of any facilitation effortsb | Being told about online services | Being helped to use online services | |||||
| Adjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value | |
| Digital confidence (Q2–6) | ||||||||
| Very confident | Reference | |||||||
| Quite confident | 0.84 (0.68 to 1.05) | < 0.001 | 1.05 (0.85 to 1.31) | < 0.001 | 0.86 (0.68 to 1.09) | 0.031 | 0.97 (0.72 to 1.32) | < 0.001 |
| Not confident | 0.40 (0.30 to 0.53) | 0.44 (0.33 to 0.60) | 0.66 (0.48 to 0.90) | 0.33 (0.20 to 0.55) | ||||
| Q18. Gender | ||||||||
| Male | Reference | |||||||
| Female | 0.94 (0.79 to 1.11) | 0.457 | 0.91 (0.76 to 1.08) | 0.280 | 1.13 (0.93 to 1.36) | 0.215 | 0.86 (0.67 to 1.11) | 0.242 |
| Q19. Age | ||||||||
| 16–24 | 0.78 (0.46 to 1.34) | 0.163 | 0.63 (0.36 to 1.09) | 0.189 | 1.56 (0.90 to 2.70) | 0.574 | 0.97 (0.44 to 2.13) | 0.207 |
| 25–34 | 0.95 (0.64,1.43) | 1.01 (0.68 to 1.49) | 1.07 (0.71 to 1.62) | 0.95 (0.53 to 1.69) | ||||
| 35–44 | 0.87 (0.59 to 1.29) | 0.97 (0.66 to 1.42) | 1.08 (0.72 to 1.62) | 1.41 (0.83 to 2.39) | ||||
| 45–54 | 0.88 (0.64 to 1.19) | 0.94 (0.70 to 1.28) | 1.03 (0.75 to 1.42) | 1.33 (0.87 to 2.04) | ||||
| 55–64 | Reference | |||||||
| 65–74 | 0.80 (0.59 to 1.08) | 1.01 (0.75 to 1.36) | 0.85 (0.62 to 1.18) | 0.95 (0.62 to 1.48) | ||||
| 75–84 | 0.56 (0.39 to 0.81) | 0.80 (0.55 to 1.15) | 0.80 (0.54 to 1.19) | 0.70 (0.41 to 1.20) | ||||
| ≥ 85 | 0.58 (0.32 to 1.05) | 0.49 (0.25 to 0.94) | 0.56 (0.28 to 1.15) | 0.19 (0.04 to 0.87) | ||||
| Q20. Deaf/hearing impairment | ||||||||
| No | Reference | |||||||
| Yes | 1.14 (0.84 to 1.54) | 0.395 | 1.36 (1.00 to 1.84) | 0.047 | 0.83 (0.59 to 1.17) | 0.286 | 1.46 (0.95 to 2.25) | 0.083 |
| Q22. Parent | ||||||||
| No | Reference | |||||||
| Yes | 1.18 (0.87 to 1.60) | 0.284 | 0.96 (0.72 to 1.29) | 0.797 | 1.22 (0.90 to 1.66) | 0.204 | 1.01 (0.68 to 1.51) | 0.957 |
| Q23. Ethnicity | ||||||||
| White | Reference | |||||||
| Other | 1.46 (0.95 to 2.24) | 0.081 | 1.46 (0.98 to 2.17) | 0.060 | 1.05 (0.69 to 1.58) | 0.830 | 1.99 (1.24 to 3.20) | 0.005 |
| Q24–25. Long-term physical or mental health condition | ||||||||
| No | Reference | |||||||
| Yes | 1.26 (1.04 to 1.53) | 0.021 | 1.18 (0.97 to 1.43) | 0.099 | 1.09 (0.89 to 1.34) | 0.424 | 1.27 (0.96 to 1.68) | 0.098 |
| Q26. Working status | ||||||||
| Work | Reference | |||||||
| Education | 0.77 (0.39 to 1.52) | 0.741 | 1.07 (0.54 to 2.13) | 0.683 | 1.07 (0.54 to 2.13) | 0.924 | 1.35 (0.53 to 3.41) | 0.184 |
| Other | 0.89 (0.65 to 1.21) | 0.91 (0.67 to 1.24) | 1.11 (0.81 to 1.53) | 1.47 (0.98 to 2.21) | ||||
| Retired | 1.03 (0.77 to 1.37) | 0.84 (0.63 to 1.12) | 1.05 (0.77 to 1.43) | 1.40 (0.91 to 2.13) | ||||
| Q27. First language | ||||||||
| English | Reference | |||||||
| Other | 1.46 (0.98 to 2.17) | 0.060 | 1.89 (1.30 to 2.76) | < 0.001 | 1.54 (1.04 to 2.29) | 0.032 | 1.89 (1.18 to 3.02) | 0.008 |
| Q29. Repeat prescription | ||||||||
| No | Reference | |||||||
| Yes | 1.28 (1.03 to 1.58) | 0.024 | 1.46 (1.18 to 1.80) | < 0.001 | 1.71 (1.36 to 2.15) | < 0.001 | 1.49 (1.08 to 2.04) | 0.014 |
| Outcome: digital confidence | ||
|---|---|---|
| Adjusted OR (95% CI) | p-value | |
| Q18. (Gender) | ||
| Male | Reference | |
| Female | 0.83 (0.68 to 1.01) | 0.057 |
| Q19. (Age) | ||
| 16–24 | 8.05 (3.39 to 19.11) | < 0.001 |
| 25–34 | 5.09 (2.96 to 8.75) | |
| 35–44 | 2.71 (1.69 to 4.35) | |
| 45–54 | 2.31 (1.64 to 3.25) | |
| 55–64 | Reference | |
| 65–74 | 0.53 (0.39 to 0.71) | |
| 75–84 | 0.18 (0.12 to 0.26) | |
| ≥ 85 | 0.04 (0.01 to 0.11) | |
| Q20. Deaf/hearing impairment | ||
| No | Reference | |
| Yes | 0.81 (0.58 to 1.13) | 0.205 |
| Q22. Parent | ||
| No | Reference | |
| Yes | 1.81 (1.23 to 2.67) | 0.002 |
| Q23. Ethnicity | ||
| White | Reference | |
| Other | 0.88 (0.55 to 1.39) | 0.578 |
| Q24–25. Disabilities (physical/mental) | ||
| No | Reference | |
| Yes | 0.79 (0.63 to 0.98) | 0.030 |
| Q26. Working status | ||
| Work | Reference | |
| Education | 1.12 (0.37 to 3.34) | 0.005 |
| Other | 0.56 (0.40 to 0.78) | |
| Retired | 0.76 (0.57 to 1.02) | |
| Q27. First language | ||
| English | Reference | |
| Other | 0.40 (0.26 to 0.62) | < 0.001 |
| Q29. Repeat prescription | ||
| No | Reference | |
| Yes | 1.04 (0.82 to 1.32) | 0.726 |
Appendix 5 Patient survey
| Main patient survey | Mental health boost sample survey | ||
|---|---|---|---|
| Practice invitation | Invited | 179 | 26 |
| Declined | 31 | 2 | |
| Practice response | Interest expressed | 74 | 20 |
| Agreement signed | 68 | 18 | |
| Mail out | Completed | 62 | 18 |
| Patients invited | 12,822 | 3456 | |
| Patient response | Paper | 2448 | 607 |
| Online | 603 | 149 | |
| Total | 3051 (23.8%) | 756 (21.9%) |
| Questionnaires | Online (%) (n = 598) | Paper (%) (n = 2453) | Total (%) (n = 3051) |
|---|---|---|---|
| Q1. Internet at home | |||
| Yes | 594 (99.3) | 2153 (88.6) | 2747 (90.7) |
| No | 4 (0.7) | 276 (11.4) | 280 (9.2) |
| Q2. Confidence using search engines | |||
| Very confident | 523 (87.5) | 1237 (51.2) | 1760 (58.4) |
| Quite confident | 67 (11.2) | 664 (27.5) | 731 (24.3) |
| Not very/can’t | 8 (1.3) | 513 (21.3) | 521 (17.3) |
| Q3. Confidence in completing online forms | |||
| Very confident | 486 (81.3) | 984 (41.0) | 1470 (49.0) |
| Quite confident | 97 (16.2) | 730 (30.4) | 827 (27.5) |
| Not very/can’t | 15 (2.5) | 691 (28.7) | 706 (23.5) |
| Q4. Confidence in sending personal messages via e-mail | |||
| Very confident | 519 (86.8) | 1347 (56.2) | 1866 (62.3) |
| Quite confident | 60 (10.0) | 524 (21.8) | 584 (19.5) |
| Not very/can’t | 19 (3.2) | 524 (21.8) | 543 (18.1) |
| Q5. Confidence in installing apps | |||
| Very confident | 476 (79.6) | 894 (37.2) | 1370 (45.7) |
| Quite confident | 98 (16.4) | 615 (25.6) | 713 (23.8) |
| Not very/can’t | 24 (4.0) | 893 (37.2) | 917 (30.6) |
| Q6. Confidence in sending personal messages via apps | |||
| Very confident | 505 (84.5) | 1272 (53.1) | 1777 (59.3) |
| Quite confident | 74 (12.4) | 493 (20.6) | 567 (19.0) |
| Not very/can’t | 19 (3.2) | 632 (26.4) | 651 (21.7) |
Analysis of responses to free-text questions from the main patient survey (Q16 and Q17)
Description of themes
| Personal barriers
Respondents described several personal barriers to using digital services, and described how the online access models in their practice disadvantaged digitally excluded patients, often the elderly. Poor access to web-based services was viewed as isolating by some respondents, such as this respondent: ‘as an 88-year-old technophobe I feel more and more isolated by “progress” in the NHS as so many of my generation’. (Female, aged ≥ 85, paper survey response) Respondents also highlighted that access to resources, such as computers, internet or phones was a barrier to using digital services. Personal health issues such as poor eyesight, learning disabilities and anxiety were also cited as barriers by some to using digital services. This respondent noted: ‘My sight is very poor and I have no PC, Laptop. Tablet or Smartphone. I do not want to be forced into learning new tricks at my age’. (Female, aged ≥ 85, paper survey response) |
| Concerns about data security
Several respondents highlighted that concerns about sensitive clinical data made them wary of using digital services. Specifically, the concerns revolved around data confidentiality, data security and concerns about NHS e-mails being a ‘scam’ or fraudulent. This respondent highlighted the importance of confidentiality and trust in having information online: ‘confidentiality is versus important – would need to feel more secure about my information online’. (Female, aged 45–54, paper survey response) |
| Technology design
Technology design played a part in how respondents were able to access digital services at their practices. Several respondents commented that the practice website was difficult and confusing to navigate, and it was difficult to find information about which digital services were available. A clearly organised website was viewed as especially important for people who were less confident using online services: ‘It needs to be a tad more user friendly as there is a lot of info, icons and links everywhere which can make it confusing to know where to search for things. Especially if you are trying to teach someone who is less fluent in technology’. (Female, aged 25–34, online response) Respondents suggested updating the practice website to make it more ‘user-friendly’, ‘accessible’, ‘clearer’ and ‘simpler’ to improve navigation and improve visibility of online services. Others were able to access the digital services, but found the services too complex to navigate, or it was unclear what the service offered (for instance, advice or results). Some respondents mentioned that mobile apps were not well designed, this being identified as a barrier to use. |
| Practice-level barriers
Respondents sometimes highlighted that their practice was not supportive of online services, describing them as ‘old fashioned’ and not wanting to embrace new technology. Some practices had withdrawn specific services, such as online appointment booking and access to medical records. In these instances, the respondents were willing to use digital services such as booking appointments online or view test results but were unable to do so due to a perception that their practice did not offer these services. This respondent reflected on how online services could be beneficial for the practice and its patients: ‘I am 60 + years of age and I welcome new technology; however, I feel our practice does not have the desire to use online services. I am sure if they embrace new technology, they will see many benefits; both for the patients and the practice management and staff. Of course, not all patients are going to be able to use all online facilities, but should be made available to the majority who can use these facilities’. (Male, aged 55–64, online survey response) Relating to the findings on facilitators to accessing digital services, some respondents felt that the practice staff were unable to offer help and advice when setting up access to online services, and viewed this as a barrier. |
| Access credentials for online services
Some patients described the registration process as ‘difficult’, and in general, patients wanted the registration process to be simpler and quicker. Patients wanted online login codes sent to them electronically or by post. A few patients described receiving codes that did not work, or not having the right access credentials when attempting to use online services. Several patients wanted to be able to access online credentials without having to come into the practice to show identification or to get passwords. Having to attend the practice was especially challenging during the COVID pandemic lockdowns. This respondent noted that she wanted the practice to simplify the registration process: ‘make the registration process easier – it involved in person documentation of multiple addresses and that kind of defeated the point of wanting online access’. (Female, aged 25–34, online survey response) |
| Facilitators to adopting digital technology
Respondents described the facilitators to accessing online services. Several respondents highlighted that they wanted to know more about what online services were on offer, and that these services needed to be made more visible either through direct contact from the practice (e-mails, posted leaflets) or signage within the practice. For instance, this respondent noted: ‘I think the practice can help by sending out e-mails or messages that inform patients of the online services available to them as I did not know of these online services until I received this research letter’. (Male, aged 16–24, online survey response) Other respondents described that they had unmet training needs relating to digital services, and suggested that the practice should offer workshops, online demonstration videos, step-by-step instruction videos, leaflets and instructions on how to use online services. Some respondents also described how eConsults, a service which allows patients to submit a clinical query to the practice, were not available on the practice website at certain times (for instance outside of practice opening hours) which was inconvenient for some, especially those who were in full-time employment. This respondent described how the time windows for submitting eConsultations meant that the service was not accessible for those who work full time: ‘They only open the eConsult during opening hours, which doesn’t work if you work full time and have weekend off. This makes online services inaccessible for some’. (Female, aged 16–24, online response) |
Appendix 6 Combined analyses of practice and patient surveys
| Mode of facilitation | % patients informed of any facilitation in practices using mode of facilitation | % patients informed of any facilitation in practices not using mode of facilitation | p-value | % patients using any support in practices using mode of facilitation | % patients using any support in practices not using mode of facilitation | p-value |
|---|---|---|---|---|---|---|
| Ad hoc promotion/ support by practice staff |
30.01% (696/2319) | 31.41% (120/382) | 0.581 | 13.12% (301/2294) | 15.00% (57/380) | 0.319 |
| Employ or train a ‘practice champion’ with specific responsibility in this area | 36.34% (149/410) | 29.04% (669/2304) | 0.003 | 16.01% (65/406) | 13.07% (298/2280) | 0.110 |
| Mode of facilitation | % of patient group informed of any facilitation in practices targeting this group | % of patient group informed of any facilitation in practices not targeting this group | p-value | % of patient group using any facilitation in practices targeting this group | % of patient group using any facilitation in practices not targeting this group | p-value |
|---|---|---|---|---|---|---|
| Older adults (65 years or older) (N = 1371) | 47.44% (343/723) | 43.98% (285/648) | 0.199 | 34.58% (250/723) | 31.02% (201/648) | 0.161 |
| People with physical health conditions (e.g. sight loss, mobility impairments, multimorbidity (N = 1044) | 52.35% (256/489) | 55.32% (307/555) | 0.338 | 38.04% (186/489) | 41.98% (233/555) | 0.194 |
| People with mental health conditions (e.g. depression, psychosis) (N = 470) | 59.32% (105/177) | 50.85% (149/293) | 0.074 | 40.11% (71/177) | 41.98% (123/293) | 0.690 |
| People with limited or no internet access (N = 279) | 25.56% (23/90) | 22.75% (43/189) | 0.606 | 13.33% (12/90) | 18.52% (35/189) | 0.279 |
| Non-English speakers or those for whom English is a second language (N = 246) | 59.55% (53/89) | 65.61% (103/157) | 0.343 | 48.31% (43/89) | 59.24% (93/157) | 0.098 |
| People from ethnic minority communities (N = 206) | 63.04% (58/92) | 66.67% (76/114) | 0.588 | 53.26% (49/92) | 55.26% (63/114) | 0.774 |
| Patients with caring responsibilities or patient carers (N = 696) | 52.11% (148/284) | 54.61% (225/412) | 0.516 | 38.73% (110/284) | 39.32% (162/412) | 0.876 |
Appendix 7 Mental health boost sample
| Unadjusted Model 1 | ||||||||
|---|---|---|---|---|---|---|---|---|
| Awareness of any facilitation effortsa | Use of any facilitation effortsb | Being told about online services | Being helped to use online services | |||||
| Unadjusted OR (95% CI) | p-value | Unadjusted OR (95% CI) | p-value | Unadjusted OR (95% CI) | p-value | Unadjusted OR (95% CI) | p-value | |
| Digital confidence (Q2–6) | ||||||||
| Very confident | Reference | |||||||
| Quite confident | 0.72 (0.55 to 0.90) | < 0.001 | 0.77 (0.60 to 0.99) | < 0.001 | 0.63 (0.47 to 0.81) | < 0.001 | 0.54 (0.37 to 0.78) | < 0.001 |
| Not confident | 0.29 (0.22 to 0.39) | 0.32 (0.25 to 0.44) | 0.49 (0.37 to 0.65) | 0.24 (0.14 to 0.39) | ||||
| Q18. (Gender) | ||||||||
| Male | Reference | |||||||
| Female | 0.93 (0.76 to 1.15) | 0.522 | 0.81 (0.65 to 1.00) | 0.051 | 1.30 (1.04 to 1.63) | 0.018 | 0.80 (0.60 to 1.07) | 0.145 |
| Q19. (Age) | ||||||||
| 16–24 | 0.96 (0.56 to 1.63) | < 0.001 | 0.90 (0.53 to 1.52) | < 0.001 | 1.37 (0.80 to 2.34) | < 0.001 | 1.18 (0.59 to 2.36) | 0.043 |
| 25–34 | 1.66 (1.01 to 2.72) | 1.17 (0.74 to 1.86) | 1.35 (0.83 to 2.17) | 1.65 (0.91 to 2.97) | ||||
| 35–44 | 1.19 (0.80 to 1.78) | 1.00 (0.68 to 1.47) | 1.94 (1.30 to 2.89) | 1.10 (0.64 to 1.87) | ||||
| 45–54 | 0.83 (0.59 to 1.15) | 0.98 (0.71 to 1.36) | 1.37 (0.98 to 1.93) | 1.39 (0.89 to 2.16) | ||||
| 55–64 | Reference | |||||||
| 65–74 | 0.88 (0.65 to 1.18) | 0.81 (0.60 to 1.10) | 1.05 (0.77 to 1.45) | 1.09 (0.71 to 1.66) | ||||
| 75–84 | 0.40 (0.29 to 0.56) | 0.50 (0.35 to 0.72) | 0.61 (0.41 to 0.90) | 0.66 (0.38 to 1.14) | ||||
| ≥ 85 | 0.26 (0.14 to 0.47) | 0.24 (0.12 to 0.48) | 0.48 (0.24 to 0.96) | 0.30 (0.11 to 1.02) | ||||
| Q20. Deaf/hearing impairment | ||||||||
| No | Reference | |||||||
| Yes | 0.68 (0.50 to 0.93) | 0.016 | 0.91 (0.66 to 1.24) | 0.560 | 0.74 (0.53 to 1.05) | 0.097 | 0.63 (0.38 to 1.05) | 0.078 |
| Q22. Parent | ||||||||
| No | Reference | |||||||
| Yes | 1.51 (1.21 to 2.05) | 0.007 | 1.17 (0.87 to 1.58) | 0.288 | 1.47 (1.08 to 1.99) | 0.013 | 1.26 (0.85 to 1.86) | 0.256 |
| Q23. Ethnicity | ||||||||
| White | Reference | |||||||
| Other | 2.03 (0.97 to 4.23) | 0.058 | 2.07 (1.05 to 4.10) | 0.035 | 1.76 (0.88 to 3.47) | 0.106 | 2.34 (1.08 to 5.06) | 0.030 |
| Q24–25. Long-term physical or mental health condition | ||||||||
| No | Reference | |||||||
| Yes | 0.99 (0.79 to 1.23) | 0.943 | 1.05 (0.85 to 1.32) | 0.615 | 1.21 (0.96 to 1.53) | 0.100 | 1.04 (0.77 to 1.42) | 0.774 |
| Q26. Working status | ||||||||
| Work | Reference | |||||||
| Education | 0.75 (0.35 to 1.59) | < 0.001 | 1.12 (0.55 to 2.28) | 0.001 | 1.08 (0.52 to 2.26) | 0.005 | 0.84 (0.32 to 2.18) | 0.225 |
| Other | 0.62 (0.45 to 0.85) | 0.76 (0.55 to 1.05) | 0.95 (0.69 to 1.32) | 0.86 (0.55 to 1.34) | ||||
| Retired | 0.55 (0.44 to 0.70) | 0.64 (0.51 to 0.80) | 0.65 (0.51 to 0.84) | 0.70 (0.51 to 0.98) | ||||
| Q27. First language | ||||||||
| English | Reference | |||||||
| Other | 1.28 (0.78 to 2.08) | 0.318 | 1.14 (0.70 to 1.84) | 0.601 | 1.29 (0.78 to 2.13) | 0.320 | 1.46 (0.78 to 2.71) | 0.231 |
| Q29. Repeat prescription | ||||||||
| No | Reference | |||||||
| Yes | 1.00 (0.78 to 1.29) | 0.960 | 0.98 (0.76 to 1.27) | 0.900 | 1.31 (1.05 to 1.72) | 0.020 | 1.44 (0.98 to 2.11) | 0.059 |
| Mental health patient | ||||||||
| No | Reference | |||||||
| Yes | 1.38 (0.13 to 1.69) | 0.001 | 1.23 (1.01 to 1.51) | 0.039 | 1.31 (1.05 to 1.64) | 0.007 | 1.10 (0.83 to 1.46) | 0.479 |
| Adjusted Model 1 | ||||||||
|---|---|---|---|---|---|---|---|---|
| Awareness of any facilitation effortsa | Use of any facilitation effortsb | Being told about online services | Being helped to use online services | |||||
| Adjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value | |
| Q18. (Gender) | ||||||||
| Male | Reference | |||||||
| Female | 0.89 (0.70 to 1.11) | 0.287 | 0.79 (0.62 to 0.98) | 0.042 | 1.27 (0.98 to 1.35) | 0.092 | 0.77 (0.62 to 0.95) | 0.016 |
| Q19. (Age) | ||||||||
| 16–24 | 1.01 (0.55 to 1.41) | < 0.001 | 0.67 (0.42 to 1.07) | 0.002 | 1.71 (1.06 to 2.73) | 0.072 | 1.45 (0.62 to 3.51) | 0.101 |
| 25–34 | 1.14 (0.80 to 1.60) | 1.07 (0.77 to 1.48) | 1.19 (0.84 to 1.69) | 1.50 (0.77 to 2.90) | ||||
| 35–44 | 1.06 (0.76 to 1.49) | 1.01 (0.73 to 1.39) | 1.41 (1.00 to 1.98) | 1.00 (0.51 to 1.91) | ||||
| 45–54 | 0.89 (0.69 to 1.15) | 0.93 (0.72 to 1.20) | 1.15 (0.88 to 1.50) | 1.46 (0.87 to 2.41) | ||||
| 55–64 | Reference | |||||||
| 65–74 | 0.73 (0.56 to 0.95) | 0.84 (0.56 to 1.24) | 0.82 (0.62 to 1.08) | 1.12 (0.50 to 1.07) | ||||
| 75–84 | 0.40 (0.29 to 0.55) | 0.47 (0.28 to 0.76) | 0.62 (0.44 to 0.87) | 0.48 (0.22 to 1.04) | ||||
| ≥ 85 | 0.26 (0.16 to 0.42) | 0.18 (0.10 to 0.43) | 0.43 (0.25 to 0.74) | |||||
| Q20. Deaf/hearing impairment | ||||||||
| No | Reference | |||||||
| Yes | 0.99 (0.78 to 1.27) | 0.963 | 1.26 (0.98 to 1.62) | 0.067 | 0.91 (0.69 to 1.21) | 0.527 | 1.11 (0.76 to 1.62) | 0.593 |
| Q22. Parent | ||||||||
| No | Reference | |||||||
| Yes | 1.24 (0.95 to 1.61) | 0.107 | 0.95 (0.65 to 1.30) | 0.932 | 1.17 (0.90 to 1.52) | 0.241 | 0.99 (0.70 to 1.39) | 0.953 |
| Q23. Ethnicity | ||||||||
| White | Reference | |||||||
| Other | 2.35 (0.89 to 1.51) | 0.065 | 1.80 (0.81 to 3.98) | 0.146 | 0.92 (0.63 to 1.35) | 0.685 | 1.77 (1.15 to 2.73) | 0.010 |
| Q24–25. Long-term physical or mental health condition | ||||||||
| No | Reference | |||||||
| Yes | 1.16 (1.04 to 1.46) | 0.017 | 1.15 (0.97 to 1.36) | 0.103 | 1.12 (0.93 to 1.34) | 0.220 | 1.14 (0.89 to 1.46) | 0.308 |
| Q26. Working status | ||||||||
| Work | Reference | |||||||
| Education | 0.83 (0.31 to 2.19) | 0.060 | 1.79 (0.64 to 2.14) | 0.124 | 1.11 (0.60 to 2.03) | 0.978 | 0.85 (0.25 to 2.35) | 0.937 |
| Other | 0.63 (0.45 to 0.89) | 0.76 (0.60 to 0.97) | 0.99 (0.77 to 1.27) | 0.89 (0.54 to 1.62) | ||||
| Retired | 1.03 (0.64 to 1.41) | 0.93 (0.63 to 1.04) | 1.00 (0.76 to 1.31) | 0.86 (0.50 to 1.52) | ||||
| Q27. First language | ||||||||
| English | Reference | |||||||
| Other | 1.14 (0.62 to 2.10) | 0.058 | 1.22 (0.68 to 2.18) | 0.498 | 1.31 (0.71 to 2.41) | 0.385 | 1.53 (0.91 to 2.13) | 0.123 |
| Q29. Repeat prescription | ||||||||
| No | Reference | |||||||
| Yes | 1.26 (0.92 to 1.72) | 0.026 | 1.15 (0.84 to 1.58) | 0.378 | 1.53 (1.09 to 2.15) | 0.013 | 1.52 (1.14 to 2.03) | 0.005 |
| Mental health patient | ||||||||
| No | Reference | |||||||
| Yes | 1.37 (1.07 to 1.75) | 0.012 | 1.17 (0.91 to 1.44) | 0.200 | 1.11 (0.86 to 1.43) | 0.131 | 1.02 (0.74 to 1.42) | 0.894 |
| Adjusted Model 2 | ||||||||
|---|---|---|---|---|---|---|---|---|
| Awareness of any facilitation effortsa | Use of any facilitation effortsb | Being told about online services | Being helped to use online services | |||||
| Adjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value | |
| Digital confidence (Q2–6) | ||||||||
| Very confident | Reference | |||||||
| Quite confident | 0.79 (0.59 to 1.06) | < 0.001 | 0.89 (0.67 to 1.18) | < 0.001 | 0.69 (0.51 to 0.94) | 0.030 | 0.55 (0.35 to 0.84) | < 0.001 |
| Not confident | 0.40 (0.28 to 0.56) | 0.37 (0.26 to 0.54) | 0.68 (0.47 to 0.99) | 0.28 (0.15 to 0.53) | ||||
| Q18. (Gender) | ||||||||
| Male | Reference | |||||||
| Female | 0.89 (0.71 to 1.13) | 0.340 | 0.81 (0.64 to 1.02) | 0.068 | 1.27 (0.99 to 1.62) | 0.055 | 0.70 (0.51 to 0.98) | 0.036 |
| Q19. (Age) | ||||||||
| 16–24 | 0.86 (0.43 to 1.73) | 0.007 | 0.67 (0.34 to 1.33) | 0.198 | 1.05 (0.52 to 2.14) | 0.228 | 1.17 (0.48 to 2.85) | 0.576 |
| 25–34 | 1.23 (0.71 to 2.12) | 0.96 (0.58 to 1.60) | 1.04 (0.61 to 1.77) | 1.29 (0.66 to 2.51) | ||||
| 35–44 | 1.00 (0.61 to 1.63) | 0.99 (0.62 to 1.59) | 1.63 (0.99 to 2.68) | 0.87 (0.44 to 1.74) | ||||
| 45–54 | 0.69 (0.48 to 1.00) | 0.91 (0.63 to 1.31) | 1.27 (0.86 to 1.86) | 1.32 (0.80 to 2.19) | ||||
| 55–64 | Reference | |||||||
| 65–74 | 1.03 (0.69 to 1.55) | 0.99 (0.67 to 1.47) | 1.17 (0.77 to 1.78) | 1.31 (0.74 to 2.30) | ||||
| 75–84 | 0.57 (0.34 to 0.93) | 0.69 (0.42 to 1.15) | 0.74 (0.43 to 1.26) | 0.80 (0.37 to 1.75) | ||||
| ≥ 85 | 0.40 (0.19 to 0.88) | 0.33 (0.14 to 0.81) | 0.64 (0.27 to 1.51) | |||||
| Q20. Deaf/hearing impairment | ||||||||
| No | Reference | |||||||
| Yes | 1.04 (0.70 to 1.53) | 0.854 | 1.48 (1.00 to 2.19) | 0.050 | 1.05 (0.70 to 1.58) | 0.821 | 0.78 (0.41 to 1.48) | 0.455 |
| Q22. Parent | ||||||||
| No | Reference | |||||||
| Yes | 1.15 (0.78 to 1.69) | 0.479 | 0.87 (0.60 to 1.26) | 0.466 | 1.05 (0.71 to 1.54) | 0.825 | 0.89 (0.54 to 1.48) | 0.659 |
| Q23. Ethnicity | ||||||||
| White | Reference | |||||||
| Other | 2.23 (0.89 to 5.61) | 0.089 | 1.72 (0.78 to 3.80) | 0.177 | 1.33 (0.59 to 2.97) | 0.494 | 1.76 (0.72 to 4.33) | 0.218 |
| Q24–25. Long-term physical or mental health condition | ||||||||
| No | Reference | |||||||
| Yes | 1.17 (0.90 to 1.53) | 0.234 | 1.19 (0.92 to 1.55) | 0.190 | 1.20 (0.91 to 1.59) | 0.188 | 1.04 (0.71 to 1.51) | 0.857 |
| Q26. Working status | ||||||||
| Work | Reference | |||||||
| Education | 0.84 (0.32 to 2.22) | 0.358 | 1.74 (0.68 to 4.46) | 0.405 | 1.18 (0.45 to 3.10) | 0.987 | 0.86 (0.26 to 2.88) | 0.971 |
| Other | 0.74 (0.52 to 1.05) | 0.81 (0.57 to 1.15) | 1.01 (0.71 to 1.45) | 1.06 (0.65 to 1.73) | ||||
| Retired | 1.00 (0.67 to 1.50) | 0.94 (0.63 to 1.39) | 0.97 (0.65 to 1.47) | 0.93 (0.53 to 1.63) | ||||
| Q27. First language | ||||||||
| English | Reference | |||||||
| Other | 1.27 (0.69 to 2.34) | 0.442 | 1.33 (0.74 to 2.38) | 0.336 | 1.40 (0.76 to 2.60) | 0.285 | 1.69 (0.80 to 3.58) | 0.169 |
| Q29. Repeat prescription | ||||||||
| No | Reference | |||||||
| Yes | 1.23 (0.90 to 1.68) | 0.203 | 1.11 (0.81 to 1.52) | 0.516 | 1.53 (1.09 to 2.15) | 0.014 | 1.64 (1.02 to 2.62) | 0.040 |
| Mental health patient | ||||||||
| No | Reference | |||||||
| Yes | 1.39 (1.08 to 1.78) | 0.010 | 1.18 (0.92 to 1.51) | 0.192 | 1.10 (0.85 to 1.43) | 0.458 | 0.98 (0.69 to 1.40) | 0.930 |
Appendix 8 Regression analyses
| Awareness | Use | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Totala | n b | %c | ORd | 95% CId | Totala | n b | %c | ORd | 95% CId | ||
| Gender | Male | 574,027 | 261,738 | 46 | Reference | 510,357 | 124,222 | 24 | Reference | ||
| Female | 663,795 | 347,173 | 52 | 1.29 | (1.28 to 1.30) | 654,607 | 148,097 | 23 | 0.84 | (0.83 to 0.85) | |
| Othere | 5332 | 1778 | 33 | 1.15 | (1.05 to 1.25) | ||||||
| Age group | 16–24 | 118,428 | 53,576 | 45 | 0.85 | (0.84 to 0.87) | 101,725 | 28,561 | 28 | 1.81 | (1.76 to 1.87) |
| 25–34 | 204,268 | 102,518 | 50 | 1.12 | (1.10 to 1.14) | 197,195 | 55,897 | 28 | 1.77 | (1.74 to 1.81) | |
| 35–44 | 210,372 | 105,224 | 50 | 1.11 | (1.09 to 1.13) | 210,151 | 57,173 | 27 | 1.71 | (1.68 to 1.74) | |
| 45–54 | 221,749 | 114,069 | 51 | 1.11 | (1.10 to 1.13) | 210,363 | 53,302 | 25 | 1.59 | (1.56 to 1.62) | |
| 55–64 | 200,772 | 106,226 | 53 | 1.14 | (1.13 to 1.16) | 193,918 | 41,631 | 22 | 1.28 | (1.26 to 1.30) | |
| 65–74 | 163,971 | 84,810 | 52 | Reference | 146,111 | 25,809 | 18 | Reference | |||
| 75–84 | 94,964 | 37,874 | 40 | 0.58 | (0.58 to 0.59) | 91,090 | 11,960 | 13 | 0.71 | (0.69 to 0.73) | |
| 85 + | 33,884 | 9615 | 28 | 0.33 | (0.33 to 0.34) | 31,498 | 2976 | 10 | 0.48 | (0.46 to 0.50) | |
| IMD quintile | 1 – least deprived | 244,001 | 134,716 | 55 | Reference | 225,876 | 55,816 | 24 | Reference | ||
| 2 | 249,058 | 129,532 | 52 | 0.91 | (0.90 to 0.92) | 232,206 | 54,129 | 23 | 0.94 | (0.93 to 0.96) | |
| 3 | 254,142 | 126,410 | 50 | 0.84 | (0.83 to 0.86) | 239,308 | 55,554 | 23 | 0.90 | (0.89 to 0.92) | |
| 4 | 259,604 | 122,422 | 47 | 0.76 | (0.75 to 0.78) | 246,793 | 59,952 | 24 | 0.87 | (0.85 to 0.89) | |
| 5 – most deprived | 258,444 | 107,972 | 42 | 0.66 | (0.65 to 0.67) | 246,956 | 53,714 | 22 | 0.81 | (0.80 to 0.83) | |
| Rurality | Urban | 1,091,449 | 537,212 | 49 | Reference | 959,843 | 230,340 | 24 | Reference | ||
| Rural | 174,715 | 84,298 | 48 | 0.99 | (0.94 to 1.03) | 226,502 | 47,522 | 21 | 1.00 | (0.98 to 1.02) | |
| Ethnic group | White | 1,047,821 | 526,017 | 50 | Reference | 963,921 | 214,591 | 22 | Reference | ||
| Mixed | 20,062 | 9673 | 48 | 0.88 | (0.85 to 0.92) | 22,213 | 6706 | 30 | 1.13 | (1.07 to 1.18) | |
| Asian | 107,930 | 49,059 | 45 | 0.87 | (0.86 to 0.89) | 116,074 | 33,852 | 29 | 1.17 | (1.15 to 1.19) | |
| Black | 41,533 | 17,654 | 43 | 0.78 | (0.76 to 0.80) | 44,894 | 12,425 | 28 | 1.13 | (1.10 to 1.16) | |
| Other | 25,703 | 9420 | 37 | 0.62 | (0.60 to 0.64) | 6,411 | 7840 | 30 | 1.19 | (1.15 to 1.24) | |
| Long-term condition | Yes | 689,896 | 328,180 | 48 | 1.41 | (1.40 to 1.43 | 657,037 | 148,104 | 23 | 1.14 | (1.13 to 1.15) |
| No | 531,919 | 228,690 | 43 | Reference | 444,061 | 111,125 | 25 | Reference | |||
| Awareness | Use | ||||||||||
| Totala | N b | %c | ORd | 95% CId | Totala | N b | %c | ORd | 95% CId | ||
| Working status | Other | 1,164,993 | 577,025 | 45 | Reference | 1,099,681 | 261,526 | 24 | Reference | ||
| Sick/disabled | 48,587 | 22,040 | 42 | 0.79 | (0.77 to 0.80) | 53,418 | 10,330 | 19 | 0.84 | (0.81 to 0.86) | |
| Deafness and sign language | Yes | 5274 | 2030 | 39 | 0.69 | (0.65 to 0.74) | 4,814 | 1595 | 33 | 1.50 | (1.39 to 1.63) |
| No | 1,240,109 | 610,827 | 49 | Reference | 1,169,679 | 274,431 | 24 | Reference | |||
| Period | 2019–21f | 647,932 | 304,268 | 47 | Reference | 621,194 | 140,800 | 23 | Reference | ||
| 2020–22f | 618,232 | 317,242 | 51 | 1.23 | (1.22 to 1.24) | 570,415 | 138,453 | 24 | 1.03 | (1.02 to 1.04) | |
| Total | 1,266,164 | 621,510 | 49 | 1,191,608 | 279,253 | 23 | |||||
| Awareness of online service | Use of online service | |||||||
|---|---|---|---|---|---|---|---|---|
| Appointment booking OR (95% CI)* |
Ordering repeat prescriptions OR (95% CI)* |
Access to medical records OR (95% CI)* |
Appointment booking OR (95% CI)* |
Ordering repeat prescriptions OR (95% CI)* |
Access to medical records OR (95% CI)* |
Online Consultations OR (95% CI)* |
||
| How easy is it to get through to someone at your GP practice on the phone? | Very easy | 0.81 (0.79 to 0.84) |
0.89 (0.86 to 0.92) |
0.93 (0.90 to 0.96) |
0.90 (0.88 to 0.93) |
0.73 (0.71 to 0.75) |
0.83 (0.80 to 0.86) |
0.83 (0.81 to 0.85) |
| Fairly easy | 0.96 (0.93 to 0.99) |
1.04 (1.01 to 1.07) |
0.98 (0.96 to 1.01) |
0.89 (0.87 to 0.92) |
0.86 (0.84 to 0.87) |
0.92 (0.90 to 0.94) |
0.86 (0.84 to 0.87) | |
| Not very easy | 0.98 (0.95 to 1.00) |
0.99 (0.96 to 1.01) |
0.97 (0.94 to 1.00) |
0.9 (0.88 to 0.92) |
0.90 (0.88 to 0.91) |
0.92 (0.89 to 0.94) |
0.90 (0.88 to 0.92) | |
| Not at all easy | Reference | |||||||
| How helpful do you find the receptionist at your GP practice? | Very helpful | 1.12 (1.06 to 1.18) |
1.15 (1.09 to 1.21) |
1.21 (1.14 to 1.28) |
0.88 (0.84 to 0.91) |
0.91 (0.88 to 0.94) |
0.92 (0.88 to 0.96) |
0.97 (0.94 to 1.01) |
| Fairly helpful | 1.09 (1.03 to 1.14) |
1.12 (1.06 to 1.17) |
1.14 (1.08 to 1.20) |
0.85 (0.82 to 0.88) |
0.93 (0.90 to 0.97) |
0.94 (0.90 to 0.97) |
0.91 (0.88 to 0.94) | |
| Not very helpful | 1.01 (0.96 to 1.06) |
1.03 (0.98 to 1.08) |
1.05 (0.99 to 1.12) |
0.94 (0.90 to 0.97) |
0.95 (0.91 to 0.98) |
0.98 (0.93 to 1.02) |
0.92 (0.89 to 0.96) | |
| Not at all helpful | Reference | |||||||
| Is there a particular GP you usually prefer to see or speak to? | Yes, for all appointment | 1.19 (1.16 to 1.21) |
1.05 (1.04 to 1.08) |
1.08 (1.06 to 1.10) |
1.24 (1.23 to 1.27) |
1.15 (1.13 to 1.17) |
1.11 (1.09 to 1.14) |
0.93 (0.91 to 0.94) |
| Yes, for some appointments | 1.32 (1.30 to 1.35) |
1.29 (1.26 to 1.31) |
1.17 (1.15 to 1.19) |
1.25 (1.22 to 1.26) |
1.25 (1.24 to 1.27) |
1.24 (1.21 to 1.26) |
1.11 (1.10 to 1.13) | |
| No | Reference | |||||||
| How easy is to use your GP practice website? | Very easy | 5.29 (5.12 to 5.48) |
5.73 (5.54 to 5.93) |
4.07 (3.92 to 4.24) |
2.73 (2.65 to 2.82) |
3.98 (3.87 to 4.10) |
2.49 (2.40 to 2.59) |
1.77 (1.72 to 182) |
| Fairly easy | 3.27 (3.18 to 3.38) |
4.00 (3.88 to 4.12) |
2.64 (2.54 to 2.74) |
1.85 (1.79 to 1.90) |
3.00 (2.92 to 3.07) |
1.91 (1.84 to 1.98) | 1.52 (1.48 to 1.56) | |
| Not very easy | 1.68 (1.62 to 1.73) |
1.91 (1.85 to 1.98) |
1.45 (1.39 to 1.52) |
1.27 (1.24 to 1.31) |
1.68 (1.64 to 1.73) |
1.31 (1.26 to 2.36) |
1.25 (1.22 to 1.28) | |
| Not easy at all | Reference | |||||||
| Practice website ratinga | Awareness of online service | Use of online service | ||||||
|---|---|---|---|---|---|---|---|---|
| Appointment booking, OR (95% CI) | Ordering repeat prescriptions, OR (95% CI) | Access to medical records, OR (95% CI) | Appointment booking, OR (95% CI) | Ordering repeat prescriptions, OR (95% CI) | Access to medical records, OR (95% CI) | Online Consultations, OR (95% CI) | ||
| Effect of age 85 + vs. 65–74 years old |
Best quintile | 0.35 (0.33 to 0.37) |
0.34 (0.32 to 0.36) |
0.47 (0.43 to 0.52) |
0.38 (0.35 to 0.41) | 0.30 (0.25 to 0.35) |
0.49 (0.45 to 0.54) |
|
| Worst quintile | 0.31 (0.29 to 0.33) |
0.30 (0.29 to 0.32) |
0.45 (0.41 to 0.49) |
0.34 (0.32 to 0.36) | 0.21 (0.18 to 0.24) |
0.46 (0.42 to 0.49) |
||
| Effect of gender Female vs. male |
Best quintile | 0.86 (0.84 to 0.89) |
1.15 (1.12 to 1.17) |
|||||
| Worst quintile | 0.79 (0.77 to 0.81) |
1.04 (1.02 to 1.06) |
||||||
| Effect of deprivation Least deprived vs. most deprived |
Best quintile | 0.63 (0.61 to 0.66) |
0.57 (0.54 to 0.61) |
0.68 (0.64 to 0.71) |
||||
| Worst quintile | 0.64 (0.61 to 0.66) |
0.68 (0.64 to 0.71) |
0.74 (0.71 to 0.78) |
|||||
| Effect of ethnicity Non-white vs. white |
Best quintile | 0.79 (0.73 to 0.86) |
||||||
| Worst quintile | 0.77 (0.69 to 0.87) |
|||||||
| Rurality Rural vs. urban |
Best quintile | 1.02 (0.97 to 1.07) | ||||||
| Worst quintile | 0.94 (0.90 to 0.98) | |||||||
| Long-term condition Present vs. absent |
Best quintile | 1.30 (1.28 to 1.33) |
1.71 (1.67 to 1.74) |
1.48 (1.44 to 1.52) | 1.03 (1.00 to 1.05) |
1.44 (1.39 to 1.49) |
1.07 (1.05 to 1.10) |
|
| Worst quintile | 1.45 (1.42 to 1.48) |
1.81 (1.78 to 1.85) |
1.56 (1.52 to 1.60) | 1.22 (1.19 to 1.25) |
1.55 (1.50 to 1.60) |
1.14 (1.11 to 1.16) |
||
| Digital facilitation mode | Awareness of online service | Use of online service | |||||
|---|---|---|---|---|---|---|---|
| Appointment booking, OR (95% CI), p-value | Ordering repeat prescriptions, OR (95% CI), p-value | Access to medical records, OR (95% CI), p-value | Appointment booking, OR (95% CI), p-value | Ordering repeat prescriptions, OR (95% CI), p-value | Access to medical records, OR (95% CI), p-value | Online Consultations, OR (95% CI), p-value | |
| Displays | 0.90 (0.65 to 1.26) p = 0.552 |
0.84 (0.60 to 1.18) p = 0.314 |
0.79 (0.61 to 1.03) p = 0.083 |
0.95 (0.71 to 1.27) p = 0.720 |
0.92 (0.69 to 1.23) p = 0.590 |
0.79 (0.63 to 1.00) p = 0.048 |
0.96 (0.74 to 1.26) p = 0.780 |
| Leaflets | 0.70 (0.55,0.87) p = 0.002 |
0.71 (0.57 to 0.89) p = 0.003 |
0.72 (0.61 to 0.86) p = 0.000 |
0.87 (0 to 71 to 1.06) p = 0.163 |
0.79 (0.65 to 0.96) p = 0.017 |
1.12 (0.89 to 1.40) p = 0.340 |
0.99 (0.83 to 1.19) p = 0.926 |
| Texts/e-mails | 1.44 (1.04 to 1.98) p = 0.026 |
1.22 (0.87 to 1.70) p = 0.252 |
1.27 (0.99 to 1.62) p = 0.062 |
1.13 (0.85 to 1.50) p = 0.388 |
1.09 (0.82 to 1.44) p = 0.543 |
1.12 (0.89 to 1.40) p = 0.163 |
1.02 (0.79 to 1.31) p = 0.891 |
| Practice website content | 0.84 (0.57 to 1.22) p = 0.362 |
1.10 (0.75 to 1.63) p = 0.627 |
0.75 (0.56 to 1.01) p = 0.061 |
1.10 (O.79 to 1.53) p = 0.576 |
1.42 (1.01 to 1.99) p = 0.041 |
0.96 (0.73 to 1.25) p = 0.749 |
1.10 (0.81 to 1.49) p = 0.531 |
| Social media | 1.06 (0.86 to 1.32) p = 0.576 |
1.08 (0.87 to 1.34) p = 0.474 |
1.18 (1.00 to 1.39) p = 0.052 |
0.80 (0.67 to 0.95) p = 0.012 |
0.98 (0.82 to 1.17) p = 0.821 |
1.00 (0.86 to 1.16) p = 0.993 |
0.93 (0.79 to 1.09) p = 0.353 |
| Ad hoc support | 1.04 (0.73 to 1.48) p = 0.840 |
1.37 (0.97 to 1.95) p = 0.077 |
1.07 (0.81 to 1.41) p = 0.652 |
1.06 (0.77 to 1.46) p = 0.724 |
1.12 (0.81 to 1.54) p = 0.506 |
0.95 (0.73 to 1.24) p = 0.704 |
1.06 (0.79 to 1.43) p = 0.698 |
| Employ a practice champion | 1.18 (0.95 to 1.47) p = 0.138 |
1.10 (0.87.1.37) p = 0.428 |
1.02 (0.85 to 1.21) p = 0.840 |
1.02 (0.84 to 1.24) p = 0.831 |
0.90 (0.74 to 1.09) p = 0.273 |
0.95 (0.81 to 1.11) p = 0.552 |
0.96 (0.80 to 1.15) p = 0.647 |
| Workshops or events | 1.37 (1.00 to 1.86) p = 0.050 |
1.32 (0.97 to 1.71) p = 0.082 |
1.26 (0.99 to 1.61) p = 0.064 |
1.10 (0.84 to 1.45) p = 0.496 |
1.06 (0.80 to 1.39) p = 0.700 |
1.03 (0.83 to 1.29) p = 0.763 |
1.04 (0.81 to 1.34) p = 0.760 |
| Provision of tablets/computers | 1.08 (0.77 to 1.51) p = 0.650 |
1.14 (0.82 to 1.51) p = 0.430 |
1.02 (0.78 to 1.33) p = 0.889 |
1.05 (0.78 to 1.41) p = 0.765 |
0.89 (0.62 to 1.20) p = 0.705 |
1.05 (0.82 to 1.33) p = 0.705 |
1.19 (0.91 to 1.56) p = 0.195 |
Glossary
eConsult A digital triage platform that allows patients to make medical or administrative requests to their National Health Service general practitioner.
PROGRESS Plus An acronym used to identify characteristics that stratify health opportunities and outcomes (Place of Residence, Race/ethnicity, Occupation, Gender, Religion/culture, Education, Socio-economic status, Social capital/networks and Plus incorporates personal characteristics associated with discrimination, features of relationships and time-dependent relationships).
PROSPERO An international database of prospectively registered systematic reviews in health and social care.
SARSCov2 Severe acute respiratory syndrome virus causing COVID.
SMS-messaging Short message service-messaging (text messages between phones).
List of abbreviations
- CCG
- Clinical Commissioning Group
- CRN
- Clinical Research Network
- DF
- digital facilitation
- EEA
- European economic area
- EFA
- exploratory factor analysis
- GP
- general practitioner
- GPPS
- General Practice Patient Survey
- GP services
- general practice services
- HCA
- healthcare assistant
- HMIC
- Health Management Information Consortium
- ICB
- Integrated Care Board
- ICS
- integrated care system
- IMD
- Index of Multiple Deprivation
- IT
- information technology
- MRC
- Medical Research Council
- N/A
- not applicable
- NHSE
- National Health Service England
- NIHR
- National Institute for Health and Care Research
- OECD
- Organisation for Economic Cooperation and Development
- PAG
- Patient Advisory Group
- PPIE
- patient and public involvement and engagement
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PTSD
- post-traumatic stress disorder
- RCGP
- Royal College of General Practitioners
- RCT
- randomised controlled trial
- WP
- work package (WP1, WP2, WP3, WP4)
