Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number 17/05/30. The contractual start date was in November 2018. The final report began editorial review in December 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Islam et al. This work was produced by Islam et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Islam et al.
Chapter 1 Context and introduction
This report presents the findings of a 35-month study funded by the National Institute for Health and Care Research (NIHR) Health and Social Care Delivery Research programme. The study explored how terminally ill patients with advanced illness from ethnically diverse backgrounds and their family caregivers (FCGs) thought ahead about preferences related to anticipated deterioration and dying, and whether or not, and how, they engaged with health-care professionals (HCPs) in end-of-life care planning (EOLCP). In this study we have used the term ‘ethnically diverse’ to describe individuals who are diverse in terms of language, culture and ethnic background. It should be noted that when using the term ‘ethnically diverse’, we are referring to all ethnic minority groups except the white British group. Throughout this report, the term ‘ethnically diverse’ also refers to white ethnic minorities, such as European, Gypsy, Roma and Irish Traveller groups. 1
When someone has an illness that is very advanced, progressive and terminal, a shift in the approach of care may be considered in the last months of their life that integrates a focus on symptom management, quality of life and preparation for dying. For some people this approach may be integrated alongside treatments aimed at prolonging life; for others this palliative approach may be the main focus of care to help people to live as comfortably as possible. Advance care planning (ACP) provides an opportunity for people to express their wishes about many things, including care and treatment in the future, should they subsequently lose capacity to do so: these principles are embedded in the Mental Capacity Act 2005 and national UK end-of-life care (EOLC) policy. 2,3 Offering the opportunity to patients with advanced disease to have discussions about their illness and future care planning is identified as good practice by the General Medical Council, the National Institute for Health and Care Excellence (NICE) and the NHS. 4–7 Throughout this report, we use ‘EOLCP’ as an umbrella term for the processes of discussion and documentation (including ACP) that aim to achieve the best outcomes for people with advanced disease who are at risk of deterioration and dying in the coming months.
End-of-life care planning enables the supportive and palliative care needs of both the patient and family to be identified and met during the last phase of life and into bereavement. It includes consideration of physical care; management of pain and other symptoms; provision of social care; and psychological, spiritual and practical support. 3 It is regarded as key to improving experiences and outcomes for patients and families, and to aligning care and treatment to a patient’s wishes. Furthermore, it optimises the use of health-care resources, including acute hospital care; emergency services; and drug, surgical and other treatments. 5–11
Evidence regarding the effectiveness of EOLCP is limited, but suggests that patients who have engaged in EOLCP are more likely to die at home; receive less invasive treatment in the period preceding death; and report a better experience of care, along with their relatives. 12,13 There is limited evidence that EOLCP alters outcomes such as number of hospital admissions and use of health-care resources, but there is some evidence of increased patient satisfaction; higher-quality EOLC; and reduced stress, anxiety and depression among surviving relatives. 12–19 There is low-level evidence that EOLCP is also potentially associated with lower health-care costs. 20
It is apparent that EOLCP remains uncommon in most areas of professional practice, and patients and professionals tend to avoid discussions they find difficult. 7–13,20–22 Patient and family responses to EOLCP outcomes remain poorly understood. Very significantly, much of the research about the approach to and benefits of EOLCP excludes patients from ethnically diverse groups, most especially those who cannot speak English. 19,22 There is a small body of work that suggests that ethnically diverse patients value what palliative and end-of-life care (PEOLC) would offer them, and our local research and preliminary patient and public involvement (PPI) work and clinical experience echoed this.
Evidence, mainly from outside the UK, highlights disparities and inequality of access to PEOLC by ethnically diverse patients. 23 They are less likely to access palliative services and are more likely to die in hospital and to receive more intensive treatments at the end of life. 24,25 Little is known about the nature of ethnically diverse patients’ preferences for EOLC or how current UK EOLCP policy and practice ‘fit’ with diverse cultural values and beliefs. There is the possibility that development of more culturally sensitive EOLC, based on evidence, may prompt a revision of the current model and norms of the EOLCP approach.
This study contributes to the currently limited knowledge regarding how ethnically diverse patients and their families live with advanced illness and consider the prospect of deterioration and dying. Using qualitative methodology, this study also makes a substantial contribution to understanding the barriers to and facilitators of EOLCP with ethnically diverse patients.
End-of-life care planning and policy
Every year, approximately 40 million people are in need of palliative care services worldwide, and only 14% of these people gain access to these services. 26 In England and Wales in 2008, the Department of Health and Social Care published an EOLC strategy to ‘bring about a step change in access to high quality care for all people approaching the end of life . . . irrespective of age, gender, ethnicity, religious belief, disability, sexual orientation, diagnosis or socioeconomic status’3 in all care settings. EOLCP is a major feature of this strategy. The first step of the care pathway set out in the End of Life Care Strategy is ‘discussions as the end of life approaches’ involving ‘open, honest communication’ and ‘identifying triggers for discussion’. 3
End-of-life care planning is in line with the provisions of the Mental Capacity Act 2005,2 which provides a legal framework to promote and safeguard decision-making by an individual. It empowers and enables people to plan ahead and communicate their wishes for a time when they might lose capacity and protects their place in the decision-making process. EOLCP may benefit patients by increasing their autonomy in deciding about their future care and choice of place of death. EOLCP is intended to align care to patient preferences before their health and decision-making ability deteriorate as a result of progression of illness and to reduce uncertainty about care decisions; thus, EOLCP may help ease the grieving process for families and result in more effective use of health-care resources. 27–29 A patient may refuse treatments, but cannot insist on treatments that are not clinically appropriate.
End-of-life care planning should be an ongoing process whereby patients, their families and health-care providers discuss the patient’s goals and values and how these should inform their current and future medical care. 30 These discussions help promote a shared understanding of what might happen, help make decisions about life-sustaining treatments and provide an opportunity to discuss potential preferences for care with patients and their families. 31,32
End-of-life care planning conversations aim to inform and empower patients to have a say about their current and future treatment in consultation with HCPs, family members and other important people in their lives. 3,33 From the patient’s perspective, there is evidence that the purpose of EOLCP is not only preparing for potential incapacity, but also preparing for dying. 34 For patients, the focus of EOLCP appears to be less on completing written advance directive forms or advance statements of wishes and more on the social processes that are enabled by discussions about dying. As a result, EOLCP is not based solely on autonomy and the exercise of control, but also on personal relationships and consideration of the impact of advanced disease and relieving burdens placed on others. With this perspective, EOLCP does not occur solely within the context of the physician/HCP–patient relationship, but also within relationships with close loved ones. 35
We have very little insight on a population-wide basis in how current EOLCP policy and practice ‘fits’ with the cultural values and beliefs of ethnically diverse patients and their end-of-life experiences. National satisfaction surveys such as the Views of Informal Carers – Evaluation of Services (VOICES)36 post bereavement and Quality Health37 have a low representation of patients from ethnically diverse communities (2.9% and 5%, respectively). However, ethnically diverse patients appear to use specialist palliative care services later and less often than white British patients. 3,38,39 There is a limited evidence base for the possible reasons for this, as discussed in the following sections: Resuscitation decisions, Communication and knowing the patient and family, Health literacy and inequalities, Cultural mores and religious beliefs and Embracing diversity in end-of life care planning.
Resuscitation decisions
Do not attempt cardiopulmonary resuscitation (DNACPR) is a recording of an advance medical decision to not attempt cardiopulmonary resuscitation when someone’s heart stops. Without a recorded decision, however, the default policy for health and care professionals is to initiate resuscitation, which may be distressing to all and may not be aligned with the preferences of the patient. The heart stopping is the last part of the dying process and is a certainty for all dying patients. In this situation, resuscitation will not work. For a few patients, who are not thought to be dying imminently, their heart may stop in a sudden and unexpected context.
Discussions of DNACPR are complex. From the perspective of the health professional, resuscitation is a key aspect of EOLCP discussions because the default position is to resuscitate and because it will not work as a treatment when someone has died from their illness, and may increase and prolong suffering for people with advanced illness. In England and Wales, the legal basis for DNACPR decisions are provided by the Human Rights Act 199840 and the Mental Capacity Act 20052 and interpreted in case law. There are nationally agreed professional guidelines that interpret this law and provide standards of practice for professionals when a decision about offering resuscitation is, first, a clinical decision about whether or not it can be offered. 7,28
In addition, a documented DNACPR decision may help a patient who is dying to avoid an emergency admission to hospital, enabling them to spend the last hours of their life in their preferred place of care. 7 These facts and the context of the need for such discussions are seldom known or understood by the public, or by patients, and little has been explored about the perspective of the public. 7
Our previous work explored, with HCPs, the nuances of discussing resuscitation and, more specifically, DNACPR discussions with ethnically diverse patients and relatives in the UK. 41 This work highlighted that HCPs recognised that these conversations were sensitive, and occurred at a challenging time for the patient and their families. They were also aware that both patients and their relatives had beliefs, expectations and emotions that influenced resuscitation discussions. These expectations related to both resuscitation specifically and to death and dying more broadly. Participants also understood that their own beliefs and expectations, alongside their understanding of laws and policies regarding DNACPR orders and the clinical circumstances of the patient, influenced these conversations. However, in general, there was a lack of understanding by HCPs of how forms of intersectionality, such as class, ethnicity, sexual orientation, age, religion, disability, gender, education and life experiences, are interwoven and affect patients’ and their families’ perceptions of EOLCP discussions and related resuscitation decisions. 42
Like other studies, our earlier work has found that challenges in communication between HCPs and ethnically diverse patients and their families are key barriers to resuscitation discussions. 24,41,43 Overcoming communication issues was regarded as a key enabler of DNACPR discussions, helping build rapport, particularly when patients and their families appeared to have limited understanding of their prognosis. At a practical level, certain words may not be translatable, and more exploration of the understanding of the procedures of cardiopulmonary resuscitation, the possible harms and the evidence of success rates, was required in such discussions.
Although the themes of language, family and religious beliefs are well documented within discussions of transcultural clinical practice, our findings identified how these cause uncertainty and considerable heart-searching for professionals when patients are so sick that they might die and the discussion of DNACPR might falsely appear to be a discussion about choosing whether to live or to die. Like Kai et al.,43 findings from our previous work41 show how this uncertainty within a highly emotive context can lead to disempowerment and a search for more ‘knowledge’ to become skilled and empowered.
Health-care professionals in our previous work felt more confident in having DNACPR discussions when they had existing knowledge about patients’ religious, spiritual and cultural values, and their confidence in initiating these conversations was developed through experience. However, our findings highlighted the need and desire of HCPs for further training to develop ‘cultural intelligence’ to navigate the cultural and individual beliefs about death and to deliver culturally sensitive EOLC, including discussing deterioration and decisions about resuscitation. 24,41
Communication and knowing the patient and family
The principles of good palliative care (patient centred, holistic, founded on listening to the patient’s needs and guided by their wishes) can be undermined when communication is difficult. 42 Clinicians are encouraged to actively seek to explore a patient’s cultural preferences and choices on a case-by-case basis to understand how best to approach different contexts of EOLC, such as family choices in decision-making and sharing information about their diagnosis and prognosis. 44 Knowing the patient and their family is an essential ingredient to good EOLC, yet attaining this can be challenging, especially for HCPs working with patients from culturally and linguistically diverse communities. HCPs have, for example, reported that, when trying to manage pain, they may encounter confusing messages from patients who believe in the importance of stoicism when experiencing physical pain. 45–47 Such patients downplay the extent of their pain, making it more difficult for clinicians to understand the patient experience and effectively manage pain. 48 On the other hand, patients who cannot articulate their needs to clinicians about their pain may find the experience distressing and isolating, may feel disempowered and may feel discriminated against because of their inability to competently communicate in English. 48–50 In addition, ethnically diverse patients may not want to initiate discussions even when they experience intolerable pain in late stages of life, but may later communicate a desire to engage in EOLCP discussions with HCPs once they have accomplished all their wishes with their family. 50–53
In their small UK-based study, Owens and Randhawa54 point out that staff seemed concerned that they frequently did not have the linguistic skills or sufficient understanding of a patient’s cultural background to ‘make them comfortable’. 54 Doctors in Karim et al.’s55 study highlight these issues as being major obstacles and key to the under-referral of ethnic minority patients to palliative care. The majority of the 27 doctors interviewed in this small UK study felt that palliative care services need to be sensitive to religion and culture and that this could not be achieved unless staff from black and Asian communities, fluent in the language spoken by the patient, were present in the workforce. 55
Effective communication between health-care providers and patients is complex. Patients describe having a positive care experience when knowing their needs were listened to and understood. 56 Interpreters can assist in mutual understanding between HCPs and patients and their families; however, this is not without challenges. As in other studies, HCPs in our previous work acknowledged their lack of understanding of the training and quality assurance of professional interpreters and the absence of training for HCPs on working effectively and safely with these essential team members. 41 Using professional interpreters becomes difficult when family members are not in support of this, sometimes because of concerns of confidentiality. When interpreting services are not available or not used, this can result in reduced access to services and not receiving information. There are often concerns about the accuracy and quality of information exchanged with patients, particularly those involving a family member as interpreter,55–58 with HCPs often left questioning if the information iterated to and from the patient has been verbatim. 41
Health literacy and inequalities
Patients’ and their families’ lack of understanding of the concepts used in health care, such as the palliative care approach, can affect care preferences. As an Australian study highlights,48 ethnically diverse communities confused a patient returning home as indicative of the onset of the dying process, in contrast to remaining in hospital, thought to indicate hope for recovery regardless of the illness progression. In addition, having no equivalent term for ‘palliative care’ in many languages has caused challenges in understanding and explaining this concept. 48,59 Equally, the concept of EOLCP can be foreign to some ethnically diverse groups, as one Canadian study exploring the perspectives of the South Asian community highlights:60 EOLCP was often associated with other end-of-life issues, such as organ donation and estate planning. 60
Many migrant communities have experience of health-care systems that are limited and require payments. Understanding of the NHS, hospice services and care homes may be limited and has considerable potential for misperceptions. 23,61 For example, both UK and international studies highlight that, among the Chinese community, lack of knowledge of and exposure to palliative services from their ‘home’ country is attributed to struggles in understanding the concept of palliative care services in their ‘host’ country. 49–51 For some, palliative care services never existed in their country of origin (at least by the time they migrated), and this influences their uptake for this kind of service in their new place of residence. 49 In addition, many are not clear about what palliative care services offer regarding pain control, and misunderstanding and misconceptions of the effects of drugs to manage pain results in fear of developing opioid addiction. 51 It seems that immigrants who are able to speak English have a better understanding of palliative care and palliative care services than others, but, even so, may still be reluctant to use these services, highlighting the role of other factors such as cultural, religious or personal beliefs, which are further explored in the following section. 41
In the UK, navigating the health-care system for patients and families from ethnically diverse communities is associated with level of health illiteracy, characterised by lack of accessible information about illnesses and possible prognoses and available services. 62,63 Evidence, mainly from the USA, documents a disproportionate gap in knowledge about palliative care among minority older adults.
Cultural mores and religious beliefs
Research, predominantly from outside the UK, provides some insights into some of the issues that relate to the nuances of how minoritised culture and religious beliefs may affect discussions, care and outcomes at the end of life. For example, among some African Americans, spiritual and religious beliefs may conflict with the goals of palliative care, and they may mistrust the health-care system because of past injustices in research. 64,65 Cultural mores that may present a barrier to the use of palliative care include an apparent attitude of non-disclosure of terminal illness among some Asian and Hispanic patients in the USA. 66 Cultural norms can significantly influence the perspectives of some South Asians of EOLCP, with some expressing the belief that planning ahead is not necessary because of close family ties, predefined roles within the family and trust in shared decision-making within the family. 60
Other challenges among ethnically diverse communities to a palliative care approach and anticipatory discussions about deterioration include cultural ‘taboos’ and fears of harm; believing that death is more likely to happen, or possibly be hastened, if openly acknowledged, verbalised or discussed; and strongly held ways of living whereby only their god knows the timing of death. 60,67–69 In such cultural and religious contexts, there is a strong desire to remain hopeful and, consequently, avoid discussing subjects such as cancer and end of life. People may avoid talking about the prospect of dying as it is viewed as not only demoralising but also inappropriate, upsetting and harmful. 48,60
Although striving to remain hopeful is not exclusive to families from minoritised ethnic communities, there is undeniably a complex interplay between culture, religion and care in the everyday experience of HCPs in the transition from active treatment to a palliative approach when dealing with patients and families from ethnically diverse communities. 48,70 Faith and religion can play a prominent role in many people’s lives and may become even more important when coping with illness and the end of life. However, the practice of faith and religion, linked perhaps to the philosophy and mores discussed previously, has sometimes been found to be in tension and conflict with medical treatment plans when patients ignore their doctor’s advice in the belief that the moment of death is divinely determined, and this negates discussion about the benefits or harms of treatments. 48
Yet there is also tension within religious philosophy. A report commissioned by the charity Compassion in Dying highlights the hesitancy among Muslims around the extent to which they can or should engage in an EOLCP. A hesitancy that is rooted in notions of divine will or god’s purpose that yields a mindset of ‘what is to happen, will happen’ is in tension with other instructions found in faith that endorse planning ahead, and, in fact, strongly encourage committing to such plans. Recommendations from this report stress that there is considerable support for the notion of EOLCP in theological terms, but little is known about this among health-care services specialising in EOLCP.
The inability to accurately translate terms used and equating the meaning of palliative care with being close to dying prompted some families to request clinicians to consciously refrain from using this term when talking to their ailing loved one in one Australian study48 exploring patient and caregiver perspectives across cultures and linguistic groups, and provider perspectives. Some families reported needing to do some kind of homework to aid their understanding of the subject of palliative care; others preferred to avoid discussions regarding terminal prognoses and planning for end of life altogether; and others recalled an explanation by a clinician, but not in a way they could understand. 48
There is great diversity within ethnically diverse groups, as well as between them. Ethnically diverse patients are indeed diverse, with the existence of ‘micro-cultures’. 71 In a small study (four participants) regarding the views of ethnically diverse patients attending a day-care centre in the UK,71 the participants involved showed a distinct lack of culturally specific needs. Instead, the authors found that ‘acculturation emerged as a strong theme’, and, moreover, that ‘regardless of a particular participant’s cultural group, their needs can be highly individual’. 71 This highlights both the significance of providing person-centred, holistic care and the need to embrace diversity and complexity and work competently in the context of uncertainty.
Our previous work, alongside a wider body of work, has identified that HCPs feel disempowered by the uncertainty that arises because of sociocultural and religious complexity and that staff training needs to respond to this. 41,72 Some cultural groups predominantly share familial responsibility for decision-making, in tension with the emphasis on autonomy and individual choice within UK policy. 23,41,72–76 Some groups predominantly prefer non-disclosure of diagnosis and prognosis, and discussing deterioration and planning for preferences related to dying is, potentially, unacceptable. Our work in cancer highlighted that professionals were concerned about offending or expressing culturally insensitive practices. 43,58,77,78 As a consequence of this uncertainty, professional disempowerment and reticence resulted in inequalities and lower-quality care, with poorer outcomes for patients and families. Patient ethnicity can influence the behaviour of HCPs, resulting in disparities in care. 24,58,79
Considering ethnic diversity in policy
In the UK, contemporary policy is directed at trying to increase the proportions of death that occur at home (or usual place of residence), both because this is seen by the majority of patients and the public as their ‘ideal’ environment in which to die and because cost savings are anticipated once a shift occurs from hospital to community care. 80 There is some evidence that this ‘ideal’ is not met for people from minority ethnic groups, who die at home less often than the ethnic majority in the USA and in Canada. 3,23,81–86 In the UK, it has been found that those of Caribbean origin were less likely to say that caregivers or patients were given sufficient choice about the location of death. 87 There also appears to be little support for Gypsies and Travellers to die at home (which also appears to be their wish). 23,84 It is, however, difficult to compare this evidence of place of death with the preferences for place of death because evidence of such preferences for ethnically diverse groups is not available. 23
Seymour et al. 88 suggest that this policy is largely based on ‘ethnocentric assumptions about the preferences of dying people and their informal caregivers for place of care and also for being somewhat blind to the problems (and household costs) with which older people and their informal carers may be confronted in accessing help and support during a final illness’. 88 In their research comparing findings from two linked studies of white (n = 77) and Chinese (n = 92) older adults living in the UK, in which they sought views about EOLC, they focused on experiences and expectations in relation to the provision of EOLC at home and in hospices. Concerns about dying at home were shared by both groups, and related to the demands on family that may arise from having to manage pain, suffering and the dying body within the domestic space. Among the white elders, these concerns appeared to be based on largely practical considerations, but were expressed by Chinese elders in terms of explanatory cultural beliefs about ‘contamination’ of the domestic home (and, by implication, of the family) by the dying and dead body. 88
In addition, they found that white elders perceived hospices in idealised terms, which resonate with a ‘revivalist’ discourse of the ‘good death’, and would choose this if home were not possible. In marked comparison, for those Chinese elders who had heard of them, hospices were regarded as repositories of ‘inauspicious’ care in which opportunities for achieving an appropriate or good death were limited. 89–91 They instead expressed preferences for the medicalised environment of the hospital and actively rejected death at home, because of the contamination and inauspiciousness this entailed.
Although having family present during death is perceived as a measure of the good quality of end of life, some patients may not want to die at home to avoid imposing on the family and burdening them with caring responsibilities and with having to witness the deterioration and death of a loved one. 49,57,92 Even when there is an expectation to receive care from family members out of familial bonding and personal sense of duty, this may sometimes be complicated by factors such as cultural beliefs that, if a patient is allowed to die at home, they ruin the chances of selling the house in future. 50,93,94 Evidence also suggests that some ethnically diverse patients and their families may require more support with symptom management, decision-making and communication, as they may interpret palliative care specialists’ support as an effort to stop curative treatment and focus on end of life, and hence continue to underuse hospice services. 81,95,96
Some people prefer to care for their loved ones at home, especially if they doubt the competence of the doctor and their ability to make decisions and judgements that fully consider the best interests of the patient, and also to avoid draining family resources in paying for nursing home charges. 72,97 Other studies have found that certain ethnically diverse groups express a strong ‘preference’ for death at home. 98,99 This preference is often unmet for all patients, but even more so for ethnically diverse patients. Koffman and Higginson’s87 survey of the family and friends of deceased first-generation black Caribbean and UK-born white patients with advanced disease found that the greatest single preference for location of death was at home and that twice as many Caribbean as white patients sought this location.
Only one-fifth of all these patients had died in their own home, with 61% dying in hospital, 12% in a hospice and 6% in a residential/nursing home. Although similar proportions of patients in both ethnic groups who wanted to die at home did so, the family members and friends of deceased black Caribbean patients felt that more could have been done to involve both the patient and themselves in decision-making about location of death. This points to a need to improve training in discussing care and treatment choices, including location of death, and a deeper qualitative understanding of the cultural and other factors that may facilitate or prevent home deaths, including the intersectionality of socioeconomic and cultural factors. 87
In Frearson et al.’s99 study exploring preferences for place of care and death among the British Hindu community, participants expressed an overwhelming wish to die at home. One reason for the preference for home was the central role of family members in providing care and sense of filial responsibility ‘with the wish to care being accompanied by a need to be seen to do so’. 99 This view also influences decision-making by professionals; for instance, the doctors in the study by Karim et al. 55 believed that black/minority ethnic families prefer to provide palliative care for ill members themselves. Despite having no empirical basis, doctors believed that sending elders to die in an unknown place and in the hands of unknown people ‘would be indicative of failure on the family’s part and a decision worthy of shame from within the particular ethnic community’. 55 Doctors in this study also believed that the extended family of patients from ethnic minority communities had the ‘resources to cope with this kind of demand’ more adequately than the ‘White community for whom the extended family is close to becoming a thing of the past’. 55
However, although home death was indicated as the ‘ideal’ in the Frearson et al. 99 study, it was also recognised by participants as not feasible for all and that care should ‘only be at home if the family was able to cope’. This study went on to consider the practicalities and the true reality of caring for a relative at home. 99 Similarly, Somerville’s57 study exploring Bangladeshi bereaved carers’ experiences highlights the numerous challenges faced by carers, including the demands and stresses of caring, which can leave carers isolated. These practical concerns are similar to those expressed by white elders in Seymour et al.’s88 study discussed previously, all of which highlight the shift between the ‘ideal’ place of death and the pragmatic choices that determine the actual place of death.
Embracing diversity in end-of-life care planning
The research considered throughout this chapter has highlighted the complexity of undertaking EOLCP in general and the additional complexity of navigating such discussions with ethnically diverse patients and their families when HCPs have limited understanding of the impact cultural mores and religious beliefs have on thinking ahead, deterioration and dying. 24,43,69 Evidence presented in the sections above can be summarised as follows:
Professionals should be sensitive to individual variations in perspectives and avoid stereotyping patients and their families, for example, by assuming a patient would or would not want to be told bad news, or have particular styles of coping or use of denial.[100,101] They should seek, as far as possible, to explore each patient and family’s wishes and attitudes to sharing of information and decision-making as a generic principle.
Reproduced from Kai et al. 58 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 3.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/3.0/
The need for consideration of individual needs, to provide ‘person-centred’ holistic care and to avoid cultural assumptions, coupled with the anxieties about cultural competence among HCPs and the consequences of such anxieties, are of great significance in providing EOLC to patients and families from ethnically diverse communities.
An appreciation of general cultural influences, as well as of the diversity of individual preferences, is essential for sensitive and effective EOLCP and to enable patients and families to understand and appraise the options open to them. 102,103 The importance of such an understanding is articulated in formally derived international consensus recommendations from the European Association for Palliative Care. 9 Most participants in this consensus recognised (at least within the context of ethnically ‘other’) that a diversity of preferences exist for how decisions are made and who makes them, but understanding was very limited as to how to work with this when the dominant ethic and duty of care is that of patient autonomy.
Models of decision-making and how this is shared between the patient and the clinician and with a wider stakeholder group are beginning to be more widely explored in the literature. Acculturation to Western Christian medical–ethical frameworks appears to be a dominant factor in the development of autonomous decision-making104 This should, however, be integrated in practice with consideration of a patient’s desire for varying family involvement and their own desired level of self-involvement in decisions, which has been shown to vary within ethnicities, including that of white British. 105 Findings from our previous work suggest that supporting clinicians in how to assess these factors and develop skills in wider ‘stakeholder’ decision-making would be valuable. 41,72,97 In this work, doctors and nurses discussed the interventions that they perceive have improved their confidence, knowledge and skills in these situations. It was clear that training was limited and failed to address the impact of such nuances between and within different communities. This is reiterated in Calanzani et al.’s23 seminal report in which they appraise the evidence from 45 literature reviews to describe the current state of PEOLC provision for ethnically diverse populations living in the UK and in other English-speaking countries.
Envisaged ‘solutions’ for working in such uncertainty and in such emotionally challenging scenarios are often to increase confidence through the provision and assimilation of more factual ‘knowledge’. However, HCP participants in our previous study (which focused on the experiences of HCPs in one aspect of EOLCP: decision-making about resuscitation with ethnically diverse patients and families) sought to access reflective support, sharing of practices with colleagues and learning through simulated scenarios. 41 In addition, our work using Q methodology (a structured way of eliciting and prioritising preferences) to explore the views of ethnically diverse public participants about resuscitation discussions in advanced, terminal illness indicates both a receptiveness (in terms of both desire and acceptability) to engage in the topic of end of life and the value to participants of receiving such information. The actions participants indicated that they would take as a result of the information and the decisions that they would make were diverse and reflective of the intersectionality of their beliefs, culture, experiences, circumstances and other factors. 41,97
The evidence from our own work and from Calanzani et al.’s23 report highlighted the need for further research with ethnically diverse patients and families, exploring how these factors influence end-of-life decision-making to inform evidence-based training. This could, in turn, support HCPs in developing ‘cultural intelligence’ when discussing the value of medical interventions with patients who are at risk of deterioration and dying.
Study justification
The evidence discussed previously, along with that presented in the work of Calanzani et al.,23 points to considerable gaps in knowledge, specifically in the existence of microcultures and in the experiences of, preferences for and goals of care of ethnically diverse patients with advanced illness, and those of their families. 23,71 We also know that ethnically diverse patients are disadvantaged in terms of access to palliative care services, especially those who cannot speak English confidently. 106
Despite UK policy prioritisation of EOLCP, 2015 work by Pollock and Wilson72 (funded by the Health and Social Care Delivery Research programme) found that EOLCP remains generally uncommon and problematic. Although this work added much to the body of knowledge about the real-world practice of EOLCP, it did not include patients or carers from ethnically diverse backgrounds. Nonetheless, Pollock and Wilson’s72 work alluded to the additional complexity perceived by HCPs in EOLCP with ethnically diverse patients and their families.
This evidence, along with emergent findings from our previous work, indicated considerable challenges in this area of practice and the desire from HCPs for evidence-based training. 41 The paucity of evidence about how culture affects the experience and anticipation of death and dying highlights the urgent need for this study. This study contributes to the currently limited knowledge regarding how patients from ethnically diverse backgrounds and their families live with an advanced illness and consider the prospect of deterioration and dying. Using qualitative methodology, this study also makes a substantial contribution to understanding the barriers to and facilitators of EOLCP with ethnically diverse patients. The design employed three approaches to exploring people’s experiences:
-
workstream (WS) 1: longitudinal cases studies with patients, FCGs and HCPs
-
WS2: individual interviews with bereaved family caregivers (BFCGs) who have experienced the loss of someone due to an advanced illness
-
WS3: findings from WSs 1 and 2 discussed with members of the public and professionals via virtual workshops and workbooks.
Aims and research question
The study aims to improve the quality and experience of EOLC for ethnically diverse patients and their families by addressing the research question: what are the barriers to and enablers of ethnically diverse patients, FCGs and HCPs engaging in EOLCP?
Objectives
-
To explore how terminally ill patients from ethnically diverse backgrounds, their FCGs and the HCPs who support them think ahead about deterioration and dying, to explore whether or not and how they engage in EOLCP, and to identify barriers to and enablers of this engagement.
-
To explore the experiences and reflections of BFCGs on EOLC, and the role and value of thinking ahead and of engagement with HCPs in EOLCP.
-
To identify information and training needs to support best practices in EOLCP and to produce an e-learning module with guidance notes available free to NHS staff and hospice providers.
Structure of the report
This chapter has provided a background to the study and considers the policy context in which it is set, alongside evidence available from previous studies. The next chapter outlines the design and methods of the study before subsequent chapters present a summary of PPI, followed by participant demographics. Findings are then presented and discussed for WSs 1 and 2. The response to these findings as introduced in WS3 are then deliberated. The conclusion provides a summary of the findings and their significance, and considers their implications for the development of policy and practice. This also includes implications of, and recommendations arising from, the study. The final chapter discusses outputs from the project, early dissemination and impact.
Chapter 2 Methodology
Study design
This was an exploratory study, which was carried out within a constructivist qualitative tradition of research. Qualitative research is concerned with eliciting how participants understand and experience the world through the cultural filters internalised through developmental processes of socialisation and through interaction with others in real-world situations and contexts. 107 Constructivism seeks to ‘see what happens’ in real-world settings and to illuminate the relevance of social context and processes for resilience, self-reliance, and the opportunities and constraints that govern access to resources for individuals and connected groups. This research approach aims to elicit and understand how research participants construct, negotiate and share meanings around the phenomenon of interest. In this study the phenomenon is deterioration, dying and medical treatments at the end of life.
The study was designed to undertake an in-depth exploration of the diversity and complexity of experience within a limited number of cases. There were three WSs:
-
WS1: longitudinal patient-centred case studies comprising an ethnically diverse patient with advanced illness, one or two of their FCGs and a HCP nominated by the patient
-
WS2: single interviews with bereaved FCGs who have experienced the loss of an ethnically diverse family member due to advanced illness
-
WS3: public and professional stakeholder virtual workshops to discuss fictionalised, EOLCP scenarios, derived from real-life experiences reported by participants.
Qualitative methods of data collection and analysis are particularly suitable for use when little is known about the issue and in the study of sensitive and complex topics. Semistructured interviews enable the exploration of key topics, while concurrently allowing the flexibility to follow up on new issues of interest and importance. 107–109 Recruiting severely ill patients to take part in research projects presents challenges, which required flexibility and sensitivity in engaging FCGs and patients in a way and at a level that they could comfortably accommodate. We adopted the case study approach because the issues are socially and culturally complex. Case studies aim to explore complexity through an intensive, holistic focus on the components of each case, rather than obtain limited data from a larger number of single types of unconnected respondents. 110–112 Case studies are suited to the investigation of complex real-world situations in which a diversity of perspectives are at play. 113,114 Engaging different participants within each case across longitudinal follow-up enables the comparison of different perspectives and the exploration of processes and experiences emerging over time, rather than the cross-sectional snapshot provided by one-off interviews. Interview data were supplemented when possible by additional data from a focused review of medical records. Each case was followed up, when possible, for a period of approximately 6 months.
Setting/context
The geographical setting for the study was the East Midlands across Leicester, Leicestershire, Nottingham and Nottinghamshire. Throughout the report, we shall refer to the settings as ‘Leicester’ and ‘Nottingham’. Patient participants were under the care of services in these areas and health professionals for WS1 and WS2 worked in these areas. FCGs for WS1 and WS2 did not have to be resident in these areas. Participants for WS3 were largely from these areas, but some key stakeholders worked elsewhere in the midlands or UK.
All research activity took place in this geographical area, and Leicestershire and Rutland Organisation for the Relief of Suffering (LOROS) Hospice was the single recruiting research site. For WS1 and WS2, interviews with FCGs who were not resident in these areas took place in a venue within a reasonable distance of LOROS Hospice or, after a protocol amendment in relation to COVID-19, virtually, as highlighted in the following section.
Ethics and governance approval
NHS Research Ethics Committee approval was obtained in December 2018 (reference number 18/WM/0310), and then two substantial amendments followed. Substantial amendment 1 (1 May 2019): we did not give copies of audio-recorded consent to the participants. This related to potential difficulties with participants having access to appropriate technology to listen to it. When interpreters were used, we informed participants that consent would be audio-recorded. The recording was then retained as source data. Paper copies of the consent forms were filed and a copy given to the participant. For practical and resource reasons, copies of audio-recordings were not distributed to participants. To enable greater flexibility for patient participation, we increased the time of maximum involvement from 4 months to 6 months, to enable our engagement with them to be at a slower pace should patients need this.
In the light of government and NIHR guidance on COVID-19, substantial amendment 2 (9 March 2020) was made to the study protocol to ensure the safe delivery of the remainder of the study. The first priority was the safety of participants, many of whom were very vulnerable to the virus. The second consideration was to minimise the burden on health services and professionals. In WS1, we completed the remaining interviews for existing participants by telephone, and also amended the timeline for these in the protocol from 6 months to 6–9 months. We recognised that, in these challenging times, it was not possible for us to review all medical records as originally planned, so we amended the relevant text in the protocol to capture this. In WS2, we obtained consent by telephone for the remaining participants and completed the single interview for these participants by telephone. In WS3, we amended the protocol to allow the workshops to be conducted face to face, via webinar or by individually completing a workbook via e-mail.
Although COVID-19 did not unduly affect the scientific quality of the project, it affected the progress of analysis and development of WS3. The chief investigator (CI) was redeployed clinically for 5 months from April to the end of August 2020. This had a knock-on effect on the timeline for study outputs. Hence, a case was put forward, and subsequently granted, for a 5-month costed extension.
As a research team, we believe that not offering vulnerable people the choice to take part in research because of assumptions made about their experiences and preferences is inequitable and exclusionary. 111–114 We also recognise that any research engaging with severely ill patients and bereaved FCGs presents challenges and needs to be broached with sensitivity and flexibility throughout the research process.
Prior to the decision to take part, participants were asked to contemplate how they would feel about deliberating their experience of illness and dying. They were assured that participation was voluntary and that they could withdraw from the study at any time. To further mitigate the potential risks for participants and researchers, an information sheet with contacts for further information or support was provided, and a follow-up telephone call with the study CI, if desired, was also offered. We developed a ‘pyramid of support needs’ to manage distress within the study, which comprised assessment by the interviewer, resulting in (1) no support required, (2) signposting to a general practitioner (GP), (3) written information provided about local third-sector organisations or (4) formal referral initiated for counselling (via study CI). Patients’ GPs were also informed that the patients were participants in this study to enable the GP to document this in their medical records as evidence of participation.
Eligibility
Workstream 1: longitudinal patient case studies
Patients were aged ≥ 18 years and from diverse ethnic backgrounds. This included patients from ethnic minority groups (i.e. not white British) and white minorities, such as European, Gypsy, Roma and Irish Traveller groups, who were identified by their treating health professional as being at risk of deteriorating and dying in the next year (note that the participant information leaflet addressed the question of why a patient has been identified using the phrase ‘because you are living with a serious illness that may get worse over the next year’). 1 Patients needed to agree to the use of an interpreter to translate on their behalf, if required.
Family caregivers were aged ≥ 18 years, had capacity to consent to take part and were nominated by the patient participant. If a patient lacked capacity to consent, the FCG who was closely involved in the care of the patient was nominated by the consultee. See Recruitment, Workstream 1: longitudinal patient case studies, for further details.
A HCP was nominated by each patient participant as currently significant to their care. They may have been drawn from a wide range of staff (including doctors, nurses and health-care assistants) in services within the community and in secondary care. For patients who lacked capacity, the consultee was asked to nominate the HCP.
Workstream 2: experiences of bereaved relatives
Bereaved FCGs were aged ≥ 18 years and had cared for a close adult family member from a diverse ethnic background. This included people from ethnic minority groups (except the white British) and white minorities, such as European, Gypsy, Roma and Irish Traveller groups, who had died within the preceding 3–12 months from a progressive illness.
Workstream 3: public and professional virtual workshops
The potential participants included the following:
-
public stakeholders, including faith and community figureheads, across Leicester and Nottingham
-
commissioners of health, social care and health education across the East Midlands
-
health-care educators in nursing and medical schools across acute and community trusts and hospices
-
health and social care professionals
-
academics focusing on end-of life issues.
Sample size and structure
There are no hard and fast criteria for establishing the sample size required in qualitative research. 115 Rather, this is determined by the circumstances and context of each study. Morse116 and Malterud et al. 110 propose that the number of participants required depends on the range and depth of information collected about each participant or case (information power): the greater this is, the fewer participants required. A qualitative sample size of between 20 and 40 participants is likely to include the majority of views and experiences to be found within the target population and is in line with previous longitudinal studies in EOLC adopting a similar design and method. 72,106,115,117
Purposive sampling, which involves participant selection being guided by strategic choices regarding the individuals who or groups that can yield the most valuable and relevant information for the study, is a strategy that can optimise the depth and breadth of data in a sample and reduce the sample size required to achieve thematic saturation (i.e. when no additional themes about the research topic are emerging from the participant interviews). Stake113 cautions against increasing the number of cases much beyond 15 because the number of qualitative data generated by a larger number of cases will become unmanageable. However, a guiding principle of qualitative research is that the nature and adequacy of the final sample must be kept continuously under review, and adjustments made if necessary, to enable the study to achieve its aims. 110 Above all, it is the relevance of the participants and the quality of the data that are important, rather than the number of participants per se.
In WS1 and WS2, we purposively sampled participants across three elements of diversity:
-
religious/faith group
-
ethnic backgrounds (ethnically diverse groups)
-
disease/illness group.
Findings from our previous work suggested that cultural–religious customs and mores are one of the key factors that increases the complexity of navigating EOLC and achieving patient preferences. 41,97 It was our intention that we achieve the greatest heterogeneity of religion/faith and ethnicity in the samples of WS1 and WS2.
This concern with cultural–religious diversity was complemented by selection criteria for recruitment across illness contexts and we also purposively sampled to achieve heterogeneity across a number of disease groups (including cancer, frailty in old age, and heart and renal disease).
In addition, demographic data were recorded, including gender, age and migration generation, and we aimed to include a diversity of these characteristics in the sample.
A sampling frame was utilised to target recruitment to achieve these purposive sampling aims and to construct a matrix that may be important for attribution of themes/subthemes and in our search for examples of variance within the data. The nationally agreed guidelines to characterise self-reported ethnicity into a set of 16 codes were used. 118
Recruitment
Taking on board best practice in recruitment for research involving ethnically diverse participants, an extensive programme of awareness-raising about the project took place within community groups and organisations. 119,120 This work was informed by the networks and experiences of our PPI lead (IM) and PPI consultees [named public, carers and bereaved relatives (PCBR) research consultees] and of the co-applicants and advisors to the project. The work involved communicating the project objectives and the opportunity to be involved in research through social and traditional media; the placement of flyers in organisations and services including, but not limited to, general practices, hospice services, patient and carer support groups, community and faith groups, and libraries; and attendance at meetings and events of patient and carer support groups and community and faith groups by members of the project team.
Workstream 1: longitudinal patient case studies
The Clinical Research Network East Midlands (in which co-applicant Simon Royal and the CI have clinical leadership roles); Clinical Commissioning Group research networks and the well-established clinical and research links of the CI and co-applicants Simon Royal, Simon Conroy and Alison Pilsworth; and collaborators including specialist nurses and research nurses within participant identification centre site services were engaged to promote awareness among HCPs of the study, to promote understanding of the criteria of case eligibility and to seek identification of patients within the participant identification centre sites, which were as follows:
-
five general practices with a substantial population of ethnically diverse patients and the linked community nursing services
-
community and primary health-care services that support a population with particularly harder-to-reach ethnically diverse communities (e.g. Somali)
-
palliative care services in community, hospice and hospital sectors
-
community and secondary care services for heart failure, elderly and psychogeriatric care, renal medicine and oncology.
In total we engaged with 110 community groups in Leicester and 67 community groups in Nottingham and attended 15 community events. Our engagement with a variety of community groups provided a platform to discuss the study and how it aimed to explore experiences and improve EOLC, thus achieving a high level of community engagement in the study. In small part this was about widening recruitment; in large part it was about underpinning dissemination of findings in the future and maximising the potential for impact on patient and family care, and outcomes.
We liaised and worked with research and EOLC leads, practice managers, nurses and other workers and primary care patient participation groups to promote understanding of the study. Presentations were delivered by the CI, the principal investigator (PI), a research fellow and a research associate at a number of meetings, including those of cardiology and renal teams, general practices and local hospices within the area, and at a number of community events in which the recruitment process was discussed (see Figure 1).
FIGURE 1.
Workstream 1: patient recruitment flow chart.
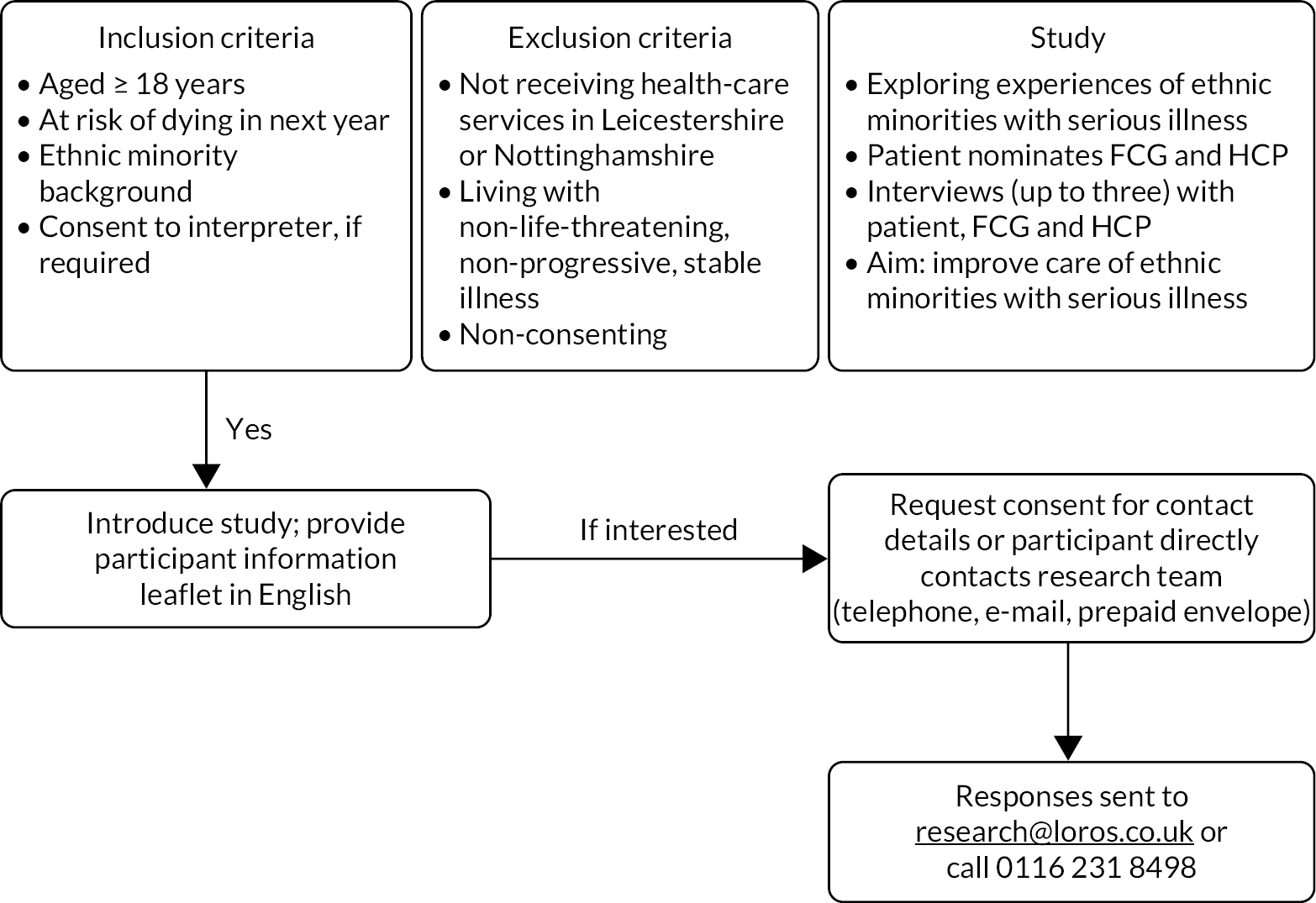
Health-care professionals were asked to identify eligible patients through a variety of means, depending on their role and the systems in place within their service. HCPs were provided with the Supportive and Palliative Care Indicators Tool (SPICT™, University of Edinburgh, Edinburgh, UK)121 as a means of identifying patients at risk of deteriorating and dying with one or more advanced, progressive and life-threatening conditions and the Gold Standards Framework ‘surprise’ question: ‘would you be surprised if this patient were to die in the next 12 months?’. 80,122
A HCP known to the patient was the first to approach a patient and provide them with the participant information leaflets for patients and FCGs. Patients, or someone acting on their behalf, then contacted the research team directly about their interest in the study by telephone, e-mail or returning a reply slip in a freepost envelope given to them by the HCP. Alternatively, if they preferred, they could give permission to the HCP who first approached them to pass their contact details to the research team, requesting that the team contact them.
If a patient did not speak English, the HCP would direct the patient (or FCG, if they were interpreting on their behalf) to the appropriate information video on the LOROS project website and/or ask if a researcher with shared language skills may contact them.
If potential patient participants lacked the capacity to give any or full consent owing to the nature of their illness (e.g. dementia), the study was introduced to them and to their FCG by a known HCP. If the FCG considered that the patient would want to consider involvement, then information about the study was shared with both parties in the ways described previously. For such patients, their involvement could be limited to permission to review their medical records and to approach a FCG and a HCP to seek their involvement. However, patients were not excluded from contributing to the study through interviews if the consultee considered that this would be appropriate and acceptable.
The research team contacted patients, or their consultees, who indicated that they were interested in the study and provided them with full participant information, including in audio/video format in their first language if needed. This was available in Gujarati and Hindi translations via the LOROS website link to the study. Audio-/video-recorded methods of facilitating informed consent are regarded as acceptable alternatives to written consent for study populations in which literacy skills are variable. 123
Workstream 2: interviews with bereaved family caregivers
Bereaved FCGs of ethnically diverse patients deceased from an advanced illness in the preceding 3–12 months were identified by HCPs in the services described in WS1. The HCPs identified and then contacted the BFCGs if they met the inclusion criteria in the first instance in the same way as described in WS1. BFCGs were also identified through the community networks of our PPI lead; through networks developed in our previous work, which included community groups and organisations; and through the awareness-raising work described previously. We also allowed participants to come forward themselves to engage in the research, provided they met the recruitment criteria. In such instances, potential participants could directly contact the research team via contact information provided in the study flyer. A member of the research team would then contact them and provide them with the study information sheet. Participants were purposely sampled in a way similar to that described in WS1. The recruitment and consenting of participants who did not speak English was facilitated in the same way as described in WS1.
Workstreams 1 and 2: consent
The process for obtaining participant-informed consent at the outset was undertaken with Research Ethics Committee guidance, and in accordance with good clinical practice and General Data Protection Regulation (2018)124 regulatory requirements.
The participants in WS1 and WS2 were given a copy of the original signed and dated consent form. The original signed and dated consent form was retained in the trial master file.
For patients who lacked capacity, a consultee was asked to complete the consultee declaration form in accordance with the process of the Mental Capacity Act 20052 and the Health Research Authority guidance.
The decision regarding participation in the study was entirely voluntary. The researcher emphasised to all participants that consent regarding study participation could be withdrawn at any time without penalty, without affecting the quality or quantity of their future medical care, and without loss of benefits to which the participant was otherwise entitled.
-
Written consent was taken.
-
If the participant’s first language was a language other than English, consent was taken verbally via a digital recorder, as well as the participant completing a written consent form in English. The interpreter was also asked to sign the written consent form under ‘witness signature’.
-
Informed consent took place at least 24 hours after the participant had been given the full participant information, or as long as they required to decide.
Consent from patients and FCGs (WS1) and BFCGS (WS2) was undertaken face to face, and via a professional interpreter accompanying the researcher when needed. Patients were seen in the LOROS Hospice, in their own home or at a suitable location of their choice. For those individuals thought not to have capacity to give fully informed consent, we used the provisions of the Mental Capacity Act 20052 and the consultee provided information regarding the patient’s wishes about participation in research.
For HCPs, consent was taken immediately before the interview. For telephone interviews, consent was taken verbally via a digital recorder and consent forms were sent to the HCP and they signed and sent the original back to the researcher by post, fax or e-mail. Further details of the consent process are detailed in Ethics and governance approval.
Data collection
Case studies: workstream 1
Longitudinal case studies comprised sequential interviews over a period of up to 9 months with a patient, FCGs and a HCP nominated by the patient. Participants took part in a semistructured, audio-recorded interview arranged at their convenience. Interviews with the patient and FCG participants were mostly face to face, but, post COVID-19, some were via telephone. If a patient died during the follow-up period, a bereavement interview was requested with each FCG at a minimum of 8 weeks after the death. When possible a review of each patient’s medical records was also undertaken.
We intended to be as inclusive as possible and each case study was explored on its own terms. It is not necessary for case studies to conform to a ‘standard’ composition and patients were given flexibility and options in how they wanted to be part of the study. Consequently, the data set includes the following:
-
patients who lacked FCGs or who were unwilling/unable to nominate specific FCGs or a HCP
-
patients who nominated more than one FCG to take part in their case study.
In some case studies, the greater part of the interview data were drawn from interviews with FCGs and HCPs. This occurred in the following situations:
-
Patients did not wish to participate in some or all interviews, but were willing for their nominated FCG(s) and HCP to do so and to have their notes reviewed.
-
Patients lacked capacity to give full consent from the start (e.g. patients with dementia or a brain tumour).
The number of interviews conducted with each participant was determined by the circumstances of each case study. A minimum of two interviews was needed for each case study. A maximum of two follow-up interviews over 6–9 months were undertaken with each patient and FCG. Interviews were with patients and FCGs separately, jointly or a combination, according to participant preferences and convenience.
A nominated HCP was invited to take part in at least one interview, and, at most, two interviews, to discuss their involvement in the case (see Figure 2).
FIGURE 2.
Patient case study composition.

Experienced researchers conducted all interviews. The same researcher conducted all the interviews with each participant in the patient’s case study.
The content discussed in each interview developed over time, but, in general, interviews with patients and FCGs included exploration of the following themes:
-
experience of living with serious illness
-
understanding of the illness and the prognosis
-
goals and values with regard to their future care
-
anticipation of and thinking about the future, about decision-making and treatment preferences, and the significant factors influencing these
-
preferences in how such decisions are made
-
expectations and experiences of professional support and communication about deterioration, EOLC and EOLCP.
We were mindful that the experience of taking part in the interviews may have had an influence on the individuals. 125 Participation in research has the potential to change the nature of the patient and their family’s way of living and coping with their illness and their future, and this was to be incorporated as a topic in the interviews. The potential impact would be beneficial in that the patient/carer may communicate more effectively with care providers. The listening skills of the researcher and the facilitation of reflection and discussion may potentially change things for the participant.
In subsequent interviews, we asked the following questions:
-
How are things?
-
What’s changed in the illness?
-
Have they been thinking about the future?
-
Have they had any conversations with family/HCPs about their illness/wishes and future death (if the patient brings this into the conversation)?
-
Do they think that they have done anything differently as a result of having these conversations/being part of the study?
Such actions were explored as an outcome of the research; importantly, such observations may provide information about potential facilitators of EOLCP, as discussed in the findings and discussion in Chapter 5.
The interview with HCPs also included the following themes:
-
their experience of providing care and support for the patient and family
-
barriers to and enablers of their care of the patient and family in:
-
understanding the illness and prognosis
-
thinking about the future
-
decision-making
-
EOLCP.
-
Health-care professionals were also asked for their assessment of whether or not they felt that being part of this study (either they themselves or the patient or FCG) had an impact on their relationship with the patient/carer or any other research-related outcomes. This will be further discussed in Chapter 5.
Medical record review
Patients were asked to give permission for access to relevant parts of their medical records and related documents recording future care preferences.
At the end of patient involvement in the study (after 6–9 months or at death), when possible, the medical records, including nursing and allied health professional records, were sourced. These included palliative care services, primary care, community services and hospital services. The records were scrutinised for data concerning the following:
-
discussions and information-sharing about prognosis, deterioration, dying, EOLC and EOLCP
-
records relevant to recording patient views and wishes, and EOLCP, including advance care plan and DNACPR documentation
-
preferences regarding place of death.
Data from electronic and paper case notes were extracted verbatim and entered into the electronic case report form for subsequent analysis. The date, place of discussion and role of the HCP were noted for each data extracted. The researcher also added an explanation of the circumstances of the discussion to provide context for the narrative.
Completed case report forms were incorporated within the project database and form part of the data set relating to each case. This is discussed further in Chapter 5.
Workstream 2: data collection
Interviews with recently bereaved FCGs of ethnically diverse patients who died following a period of advanced disease and deterioration were conducted, either face to face or by telephone, by experienced researchers in a participant’s primary language (using translation strategies described in WS1). The interviews explored participants’ perspectives of the following:
-
living with serious illness and EOLC
-
thinking ahead about deterioration and dying
-
information-sharing, communication and decision-making in illness deterioration with the patient, family members and HCPs involved in providing care
-
the role and value of EOLCP
-
the role of the HCP in helping patients and families prepare for deterioration and dying.
Interpreters and transcription of interviews
Our research team have considerable language skills to conduct interviews in the language preferred by a participant, and one of the BFCG interviews was conducted by the bilingual PI (ZI) in Punjabi. Zoebia Islam translated the audio-recorded interview into an English-recorded version before a professional transcriber transcribed the interview. This method has previously been employed by Zoebia Islam. 126 Professional interpreters were used for patient participants in four of the case studies.
There is limited guidance available for how to appropriately brief and debrief interpreters before/after each interview. Therefore, the research team developed its own to ensure that the interpreters felt suitably prepared for the types of questions that would be posed and the sensitive nature of these. Zoebia Islam also checked that each interpreter was able to pose the questions and obtain responses in debrief meetings, especially when there may not have been any literal translations for certain words. The debrief meeting also added further explanation and understanding to the data collected. This was particularly pertinent in one case for which the interpreter was able to explain the reasoning behind certain cultural beliefs as they held the same beliefs as the participant.
All interviews were audio-recorded. Interviews in English were transcribed verbatim. Interviews in other languages recorded Zoebia Islam asking the question in English and the interpreter then repeating this in the participant’s first language. After the participant responded in their first language, the interpreter would then repeat the response in English. The English parts of the audio-recording were transcribed verbatim. Again, this method has previously been employed by Zoebia Islam. 126
All transcripts were checked for accuracy against the audio file and anonymised. Turns of phrase, idioms and metaphors were sometimes complex to translate and a note was made on the transcript of literal translation, as well as the meaning constructed by the translation during the interviews conducted by Zoebia Islam. These notes were an important aspect of quality assurance and data accuracy.
Workstream 3: public and professional virtual workshops
Workstream 3 involved conducting virtual stakeholder workshops, with participants joining a virtual workshop or participants completing a workbook. Based on the findings from WS1 and WS2, we developed topic guides for workshops and workbooks. These had commonalities, but also included materials that were specific to each of the different participant groups; they iteratively evolved during the course of the workshops. Stakeholders were categorised as members of the public from diverse ethnic backgrounds (lay), community and faith leaders, academics, educators or HCPs.
Workstream 3: sampling and recruitment
For WS3, we purposively recruited and sampled across the range of stakeholders. The recruitment of stakeholder participants was via a process of snowballing. The study team and all collaborators, including members of the PCBR group, identified potential participants via local small-world networks. Study flyers and e-mails were circulated. Through this process, > 140 potential participants were contacted. Potential participants were contacted by e-mail, were sent a participant information leaflet and reply slip, and were offered the opportunity to attend a workshop or compete a workbook in their own time.
Workstream 3: data collection
Based on the findings from WS1 and WS2, eight fictionalised stories were developed for use in the workshops. Each of the stories highlighted key themes identified in WS1 and WS2. A topic guide for workshops and workbooks for those unable to attend workshops was drafted for each of the different stakeholder groups. These draft stories, topic guides and accompanying workbooks were piloted with the PPI lead (IM) and members of the PCBR group, and were refined based on their comments and after further discussion within the core research team. The HCP topic guide and accompanying stories were also piloted with professionals, with subsequent refinement.
The workbooks and topic guides had some commonalities; for instance, all participants were asked to identify challenges within each story and best practice for HCPs in supporting patients in EOLC discussions and planning, and to comment on the implication of these best practices for training and for service delivery. Key questions were as follows: what are the ‘generic’ issues? Are there any specific ethnically diverse issues? How do ethnically diverse backgrounds overlay/increase complexity of the generic issues? How do professionals make ‘best-interests’ decisions in the cross-cultural context?
Each stakeholder workshop also included material that was tailored to each of the different groups and that iteratively evolved during the course of the workshops. The stories and the key themes highlighted in each will be further discussed in Chapter 6 and are presented in Appendix 1.
Each virtual workshop had a maximum of five participants. Data resulting from the workbook tasks, contemporaneous field notes, audio-recordings of workshop interactions and semistructured questionnaires captured the participants’ views and are discussed in Chapter 6. Demographic information was also gathered, together with feedback on the workshop or workbook materials to inform the iterative development of WS3 and the educational outputs from the study.
Workstream 3: process and consent
On the day of the workshop, the chairperson of the session, the CI (CF), welcomed everyone joining the workshop; led the introduction of the team; and went through each item on the consent form, asking participants to initial and sign accordingly and return by post or e-mail. On receipt of a signed participant consent form, the study research associate (MH) also signed and dated the form and allocated each participant an identity number before returning a copy to the participant. Participants completing workbooks were also required to read the information leaflet before completing their consent form and the workbooks. On receipt of a completed and signed participant consent form and completed workbooks, for both participants who attended virtual workshops and participants who completed individual workbooks, Matilda Hanjari sent each participant thank-you vouchers.
Analysis of workstreams 1, 2 and 3: multiple datasets
There were several data sets for analysis.
-
WS1: 18 patient-based case studies comprising 93 interviews across three stakeholder groups (i.e. patients, FCGs and HCPs). Review of medical records for 13 cases.
-
WS2: 19 interviews with BFCGs.
-
WS3: workshop reflection notes, recordings and workbook responses.
In WS1, each data set was subjected to both separate and integrated thematic analysis through constant comparison. 108,127 The qualitative software program NVivo (QSR International, Warrington, UK) facilitated the management and coding of data sets and allowed for cross-stakeholder and cross-WS coding and queries. Analysis proceeded through a process of open coding of initial manuscripts by at least two researchers independently, and then development of the coding framework through discussion of the themes between core research team members (AP, MH, ZI, CF and KP). Coding has involved ‘coding’ segments of interview transcripts to one or more broad ‘nodes’ (or themes) within NVivo to capture all text relating to an idea or topic. The coding framework was developed through an iterative process of reading, coding and discussing data elements within the research team to identify, compare and link ‘themes’ occurring within and across the interviews. A more refined and selective process of coding from individual nodes was undertaken largely by Anne Patterson and by Kristian Pollock (co-applicant) to explore, differentiate, reorganise and relate the themes identified as of greatest relevance to the study objectives.
In WS1, patient-centred narrative case studies were developed for each of the 18 cases individually by the researcher undertaking the interviews in each case and one other core researcher, and then further refined after discussion between core researchers. These triangulate different stakeholder perspectives and data sources, including a review of medical records. Each case study involved a holistic in-depth analysis of each case to enable an understanding of how ‘thinking ahead’ and EOLCP evolve over time, and also a systematic cross-case comparison to discover patterns in the characteristics of the cases and to identify and examine any relationship between themes within a co-ordinated explanatory model of study findings. 113,127 Serial follow-up interview data go beyond cross-sectional and static accounts of specific participants and groups of stakeholders and enable an understanding of how EOLCP is managed and experienced over time within a complex network of care. The additional comparative dimension afforded by thematic analysis of the interviews of each participant group completed the triangulation of the different data sets. 114
Analysis of interview data for WS2 was similar to that for WS1: this was coded in terms of overall themes and subthemes occurring in the data through filtering in NVivo. Further exploration, by comparing themes between WS1 and WS2 and triangulating findings, was undertaken to enable an understanding of the key issues relating to EOLCP when bereaved relatives reflect on their experiences, and the degree of difference, overlap and mutual understanding that exists between them and FCGs involved in current, active care of a patient with advanced illness; patients; and HCPs.
In NVivo, data were initially coded for each of the stakeholder groups using a coding framework developed by (at least) double-coding of a range of interviews from each data set. Common threads were then drawn together from across the stakeholder groups. Relevant ‘nodes’ in NVivo were then drawn together around these common threads (e.g. communication, professional support). These were then interrogated further, for example enablers of and barriers to good communication; enablers of and barriers to effectively ‘knowing’ a patient and family. These were further coded to arrive at enablers and barriers for several aspects. For other sets of data, it was more appropriate to interrogate and code these further, using categories of ‘what worked’ and ‘what did not work’ (e.g. when scrutinising positive experiences and negative experiences of receiving health-care support). In this way, the coding framework looked both within and across stakeholder groups, which facilitated all stakeholders’ perspectives on particular emerging themes/issues.
Workstream 3: analysis
Analysis of WS3 involved a separate pragmatic thematic analysis of each workshop’s field notes (by ZI and MH). Field notes from each of the workshops were coded to themes and subthemes through a process of constant comparison, similar to that employed in WS1 and WS2. 108,127 In this, researchers focused on identifying themes and subthemes relating to the specific questions addressed in each workshop. Emerging themes were compared and grouped in relation to each category of stakeholder workshop and workbook (by ZI and MH), and then further refined after discussion with the rest of the core research team. The qualitative software program NVivo facilitated the management of this pragmatic thematic approach.
One of the co-applicants (LW) undertook separate analyses of the HCP workshop field notes. Analyses used two implementation science approaches. The first used a psychological approach to identify behaviour change techniques (BCTs) in the discussion of behaviour change by practitioners and family members. A BCT is an observable, replicable and irreducible component of an intervention designed to alter or redirect causal processes that regulate behaviour, that is a technique is proposed to be an ‘active ingredient’. 128 The 91-item taxonomy was applied to the transcripts of the workshops. The second is an organisation-level approach based in sociology: normalisation process theory (NPT). 129 It is a mid-range theory of the implementation, embedding and integration of organisational innovations, as result of individual and collective agency. This agency is developed through four processes: sense-making (coherence) work, engagement work (cognitive participation), enacting a practice (collective action) and how the intervention has an impact and on whom (reflexive action). Each of these four processes has four further components, making a 16-item framework applicable to any complex intervention or innovative practice involving the adoption of new practices. This approach was used to ascertain how the HCPs discussed the practices around ‘thinking ahead’ and EOLCP as applied to the stories and discussions in the workshops. These analyses informed the content of the learning resource.
Chapter 3 Patient and public involvement
Introduction
Patient and public involvement was a central characteristic of this project in ensuring that it was grounded in the concerns and experience of patients and FCGs and that it was conducted in an appropriate and sensitive manner. The project team included a PPI co-applicant, Irfhan Mururajani. We are greatly appreciative of the invaluable contribution and considerable work of members of the PCBR group and of Irfhan Mururajani to this work and thank them greatly for this.
Pre-award engagement
Prior to proposal submission, we obtained a public involvement funding award from Research Design Service East Midlands to develop a PCBR research consultation group. This group identified key areas of concern and discussed the proposed research topic and its significance to them and their loved ones. This group prioritised the research related to interdependence of professionals, patients and families in successfully navigating the end of life. They also highlighted the importance of professionals acting as guides and supports in this. Some of these group members were part of the Broadening Horizons project, which commenced in 2011; our PPI engagement builds on and is informed by this extensive earlier involvement with PPI. 61 In Broadening Horizons, we held 10 informal discussion groups (n = 135 participants) with users of 10 local voluntary and community organisations, to gain understanding of why the local ethnic minority communities were not using hospice services, the perceived barriers to using these, and the information they would welcome about EOLC and services. The project then recruited and trained volunteers from the communities to engage locally, raise awareness of services, and provide a mechanism to hear of unmet needs and dissatisfaction with care. The work of the Broadening Horizons project and the ongoing work of the Broadening Horizons volunteers with their communities was fundamental to generating the research questions for the Thinking Ahead project.
The public, carers and bereaved relatives group
The public involvement funding award enabled us to develop the PCBR group of 10 people from diverse ethnic and faith backgrounds, including:
-
Broadening Horizons volunteers
-
family of those in receipt of a palliative care service within Leicestershire and Rutland
-
members of ethnically diverse communities from the local interfaith group130
-
members of local user and carer groups listed in the Research Design Service East Midlands directory of local groups
-
volunteers at LOROS.
Two meetings were held with our PCBR group prior to submission of the full proposal for Thinking Ahead:
-
Meeting one: the PCBR group members were presented with lay summary and research questions. The lay summary, research questions and design were revised as a result of this initial meeting by the research team.
-
Meeting two: pior to the second meeting, participants were given the option of reading and advising on the lay summary. Thoughts were discussed and further revisions were made in the light of this second meeting.
Patient and public involvement was evaluated by a feedback questionnaire at the end of each meeting. This was a simple tick-box questionnaire with the option of expanding on certain responses if respondents wanted to do so. Their thoughts were collated with repsect to communication and organisation of the meeting before the meeting, how they felt the meeting went and how this could be improved. Participants were also asked to comment on any other concerns they may have had with regard to the research or other areas of importance to them in relation to EOLC.
The PCBR group supported the delivery of the research throughout the project, as detailed below. In pre-COVID-19 times, this was done via four face-to-face meetings; during the COVID-19 pandemic, a fifth meeting took place virtually using video. Some members also wished to contribute via one-to-one video meetings, and for those less technically oriented, we spoke via telephone calls. There has also been ongoing consultation with members of the whole group via e-mail. This mix of communication methods has enabled members to stay safe, but remain closely involved, throughout the whole project, even during periods of lockdown.
Irfhan Mururajani convened and facilitated the PCBR group meetings, with support from the research team, and acted as PPI representative at project management and steering group meetings. Irfhan Mururajani provided informal mentoring and support for each of the PCBR group members. In line with INVOLVE guidance, each of the group members was gifted £50 as a ‘thank you’ for attending each group meeting. Members were also invited to attend a research methods course run by the project PI. 131
Preparation of project materials
Members of the PCBR group were involved in discussing the protocol, methodology and materials for recruitment and data collection, ensuring that they were developed and implemented in an acceptable and feasible way.
The group also offered their diverse language skills in aiding the piloting of interviews in both English and in other languages (i.e. Gujarati and Hindi). They advised on the language use in the topic guides in WS1 and WS2 to ensure sensitivity, cultural appropriateness and clarity for a lay audience. They have supported the translation of information sheets to ensure that the written and spoken versions of the participant information leaflets in WS1 and project flyers in both WS1 and WS2 were translated to a standard that was understandable to lay participants who speak Gujarati.
Enhancing interpretations of findings
The PCBR group supported us with analysis through commenting on and discussing an excerpt provided from WS1 data (see Box 1). Their thoughts and interpretation were in line with those of the researchers, which was important in our quality assurance process. This discussion also promoted sharing examples of how their own beliefs/cultural beliefs influence behaviour during the life course and at key life events including birth, dying and death, which allowed for deeper discussion around the data collected and the interpretation of these data.
The text below comes from a patient interview conducted as part of the project WS1 (interviews with patients, FCGs and HCPs).
But I – personally it has not been easy to talk about death in our communities because over 70 per cent of the black population in one sense were Christian, and by Christian I don’t just mean Catholic or Methodist, I mean Pentecostal Christians, who believe in the power of the holy spirit and direct divine healing. And actually even when my mother was ill, because that’s what she solely depended upon, there was a point where I was thinking she just needs to get to the hospital and get some help. And my father tried, actually the church tried. We know nowadays that it’s not necessarily the church leaders that are encouraging people not to have treatments, some, some will even say to you, I have had it said to me a couple of times because we have a family history, ‘oh you need to deal with that generational curse’. Now this is happening not just in black churches, it’s happening in many Pentecostal churches where there is a body of movement that believes that if more than one family member is affected or you are ill, that it’s a spiritual curse. It’s not something that my family believes, though I have met individuals who are on the outskirts of the family who have been to certain services or read certain books where they do believe this. Or they can’t say certain words because it means that you will be inviting that to happen to you. So, for example, people will say to you, if you say, because you do sometimes say because you are living with it, and it happened in one of the support groups where I did invite somebody in to speak and one of the members said ‘my cancer’ and this person was from the faith group and she said ‘don’t say “my cancer”, don’t own it’. Well actually she can own it and counsellors will tell you that you need to allow people to express where they are.
We would appreciate it if you could please briefly note anything that is of interest in the context of the project’s aim of identifying the barriers and enablers in EOLCP with patients and families from black, Asian and minority ethnic backgrounds. We will discuss this together at the meeting.
Discussion with the PCBR group on the above activity was very fruitful in identifying a number of themes that contributed to answering our research questions regarding enablers of and barriers to thinking ahead about treatments towards end of life. In particular, they spoke of ‘taboos’ in talking of death in their own communities and the terminology around death and dying that was either helpful or problematic. Discussion also included how people bring to bear their own ‘superstitions’ and beliefs that influence their degree of willingness to engage in talk about illness, treatment and possible health deterioration, and indeed to engage in medical treatments at certain times and in certain ways. This directly informed the ideas that we went on to unpack further in our analysis and in our eventual write-up of findings.
Workstream 3: development of narratives and workbooks
The PCBR group provided considerable input into the production of materials for WS3. The group commented on both the narratives we had developed for discussion in the workshops and the questions that were to be asked of workshop participants, again bringing diverse personal insights to the discussion and the use of the study’s findings.
Providing additional cultural contextualisation for all aspects of the study
The members of the PCBR group were very forthcoming in adding their own experiences and understandings that were rooted in their varying faiths, for example talking about particular observances in their faith that would directly affect whether or not and how they would wish to receive treatment. They displayed frankness and candour in talking about being, for example, a Hindu accessing the hospital system, about the food they would need to have and whether or not they would actually avoid certain days/dates for treatment in accordance with their faith; or for example, being a Muslim and considering the sensitive issue of maintaining modesty while receiving personal care. These insights added to our appreciation of the diverse lens through which we needed to scrutinise the data and the sensitivity with which we report it.
Community engagement, recruitment, dissemination and outputs
The PCBR group enabled appropriate and sensitive recruitment throughout local ethnically diverse communities and via small world networks. This laid excellent groundwork for the subsequent dissemination of findings and project impact.
Irfhan Mururajani connected us to potential participants through his community and personal networks. A lay representative on the Study Steering Committee also supported us in the same way. Irfhan Mururajani helped to organise a community presentation and open evening at City Retreat in Leicester on 29 September 2019. This enabled a group of community members and faith and community leaders from a variety of faiths to discuss EOLC in a familiar space, and enabled the team to present the project and make requests for support for the project (particularly with WS3 in mind). Irfhan Mururajani also presented a Ramadan Special show on EAVA FM 102.5 FM, a local Leicester community radio station in June 2019. Both the CI and PI were invited to come and discuss the study. This allowed the team to raise awareness of the study and palliative care services. Irfhan Mururajani also arranged and took part in radio shows alongside a PCBR group member and the research team from 5–10 July 2021 on EAVA FM. The shows were entitled ‘LOROS Takeover Week. Let’s Talk! Opening the Conversation about End of Life’. The detail and content of these is further discussed in Chapter 8.
One of the PCBR group members (Gurpreet Grewal-Santini) was also employed on the study as a Community Network Liaison Worker (CNLW) between 6 July and 15 September 2021. Gurpreet Grewal-Santini was able to use her community links and language skills to undertake a number of events with ethnically diverse groups to discuss study findings and gain an understanding of how we can make services and EOLCP more accessible, appropriate and acceptable for all. This is discussed further in Chapter 8.
Irfhan Mururajani and PCBR group members also agreed to be the readers for stories in the audio-recordings that are to be used as part of the educational resource (see Chapter 8).
Final report and future research
The PCBR group has commented on aspects of clarity in this report and provided reassurance about the depth of detail included in reporting the study findings. In many discussions, the group members have identified priority areas for further research.
The PPI lead and PCBR group members also supported development of a follow-on study proposal (they advised on title and abstract), which was submitted for Health Foundation funding in September 2020, but was unsuccessful. This proposal aims to understand and improve the quality and experience of EOLC for ethnically diverse patients and their families in the crisis situation of COVID-19 by addressing the following research questions:
-
What are the barriers to and enablers of engaging in EOLC discussions with ethnically diverse patients and their family in the context of COVID-19?
-
How has EOLC been addressed with people from ethnically diverse backgrounds who have experienced COVID-19 and with their families?
Chapter 4 Participant recruitment and demographics
This chapter presents further information about the recruitment of participants in the three WSs of the study. Details about participants’ key demographics and the composition of case studies for WS1 are also presented.
Workstream 1: patient-centred case studies
Eighteen case studies were completed over 14 months between the end of February 2019 and the end of April 2020. Figure 3 describes the cumulative recruitment, showing when each case study was initiated by recruitment of a patient and when case studies reached completion. As discussed in Chapter 2, the length of time taken to complete each case study was up to 6 months. Before the start of the COVID-19 pandemic, we had recruited 18 of the maximum plan of 20 cases; further recruitment stopped at this time point. Although some interviews did take place after the national lockdown in March 2020, with the generosity of participants already recruited, the decision was made not to undertake any more interviews with HCPs.
FIGURE 3.
Cumulative case study commencement and completion.
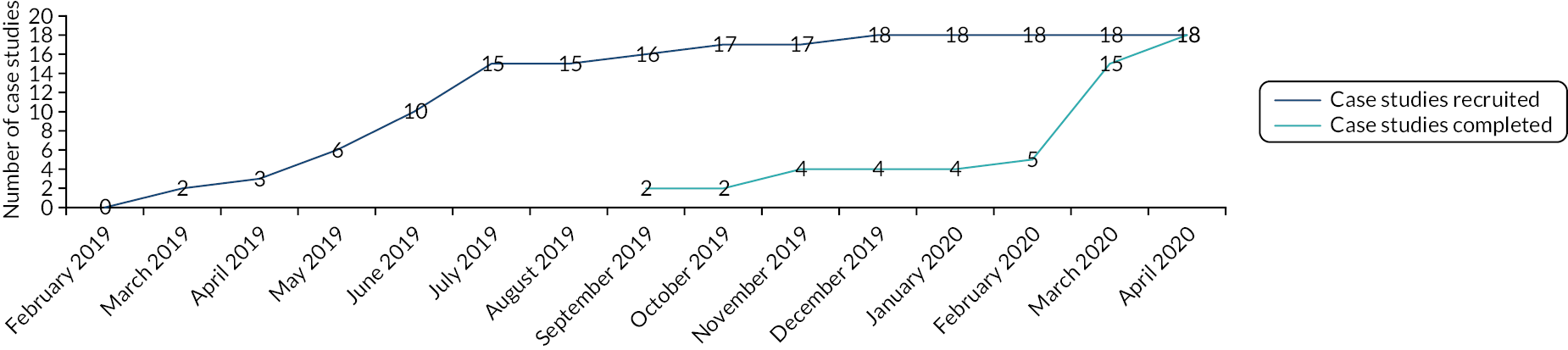
Each of the patients in the cases was given a pseudonym beginning with ‘C’. The details of the composition of each of the 18 case studies, including the number of interviews completed with each participant, are described in Table 1.
| Pseudonym | Interviews (n) | Case details | Medical notes reviewed? | ||
|---|---|---|---|---|---|
| Patients | FCGs | HCPs | |||
| Mrs Caprice | 3 | 3 | 2 | Case completed September 2019 HCP: specialist palliative care nurse FCG: husband |
Yes |
| Mr Chahine | 3 | 3 3 |
2 | Case completed November 2019 HCP: specialist MND nurse FCG1: wife; FCG2: son (adult) |
Yes |
| Mr Chaganti | 2 | 2 | 1 | Case completed September 2019 HCP: specialist cancer nurse FCG: wife |
Yes |
| Mrs Campbell | 3 | 3 | 1 | Case completed November 2019 HCP: specialist haematology nurse FCG: daughter (adult) |
Yes |
| Mr Chandhary | 1 | 2 3 |
1 | Case completed March 2020 HCP: specialist palliative care nurse FCG1: daughter (adult); FCG2: wife |
Yes |
| Mrs Challa | 2 | 2 | – | Case completed February 2020 FCG: husband |
Yes |
| Mr Chakraborty | 2 | 2 | 1 | Case completed February 2020 HCP: specialist MND nurse FCG: wife |
Yes |
| Mrs Cachalia | 2 | 1 1 |
– | Case completed November 2019 FGC1: daughter-in-law; FGC2: son (adult) Patient died in November 2019. No post-bereavement interviews |
No |
| Mrs Chawla | 1 | 2 | – | Case completed November 2019 FCG: daughter (adult) |
No |
| Mrs Cheng | 2 | 2 | – | Case completed December 2019 FCG: husband Patient died in February 2020. No post-bereavement interviews |
Yes |
| Mrs Chandyo | – | 2 2 |
– | Case completed February 2020 Includes two interviews with FCGs post bereavement FCG1: daughter; FCG2: daughter (adults) Patient died in September 2019 |
No |
| Mr Chitnis | 2 | – | 1 | Case completed March 2020 HCP: specialist cardiology nurse No FCGs identified |
No |
| Mrs Chadha | 3 | 3 | 1 | Case completed March 2020 HCP: specialist cardiology nurse FCG: daughter (adult) |
Yes |
| Ms Chapman | 3 | – | 1 | Case completed January 2020 HCP: specialist cancer nurse No FCG identified |
No |
| Mr Chifamba | 2 | 2 1 |
– | Case completed November 2019 FCG1: mother; FCG2: sister (adult) |
Yes |
| Mr Cobbina | 3 | – | 1 | Case completed March 2020 HCP: specialist cancer nurse No FCG identified |
Yes |
| Mrs Curkovic | – | 2 3 |
1 | Case completed April 2020 HCP: specialist nurse in primary care FCG1: daughter; FCG2: daughter (adults) |
Yes |
| Mrs Chavara | 1 | 1 | – | Case completed December 2019 FCG: husband Patient died in 2020. No post-bereavement interview |
Yes |
Sixteen cases involved patient participants and seven of these 16 cases comprised interviews with patients, their FCGs and their HCPs. Three of these 16 cases comprised interviews just with patients and their HCP and six out of the 16 cases were composed of interviews with patients and their FCGs. Two case studies did not include interviews with the patient, but comprised interviews with two FCGs and a HCP. In these two cases, the research team discussed with the FCGs the provisions of the Mental Capacity Act 20052 with regard to research and identified with the FCGs whether their relative had appointed an attorney for health and welfare or had a court-appointed deputy. In these two cases, a FCG agreed to be the consultee for the study.
Four patients died during the study. We were able to carry out post-bereavement interviews with two FCGs from the same case.
We interviewed HCPs nominated by 11 patients, all of whom were nurses. We were able to review the medical notes of 13 patient participants. A total of 93 interviews were conducted.
The 18 patients were recruited via a diversity of care providers: three hospices (10/18), acute trusts (2/18), primary care (1/18), one community trust (3/18) and self-referral through a community organisation (2/18). A detailed breakdown of the patient participant demographic characteristics is given in Table 2. In summary, the age of the participants ranged between 40 and 96 years. The majority (n = 11) had cancer. Eleven of the participants were female and seven were male. Ten participants described their ethnicity as Indian, three as Caribbean, two as African. The remaining three participants described themselves as Pakistani, former Yugoslavian and Chinese. Just over one-third of the participants described their faith as Christian (n = 7), with a further one-third describing themselves as Hindu (n = 6). Other participants were Muslim (n = 3), Jain (n = 1) and Buddhist (n = 1). Their living and social circumstances were quite diverse. The majority (n = 8) lived with a spouse, three lived alone as a sole adult and four had dependent children. Two lived with their adult children. Four of the case studies required at least one participant to be interviewed with the assistance of an interpreter.
| Pseudonym | Religion/faith | Self-identified ethnicity | Disease/illness | Language of interview | Age (years) | Lives with: other support |
|---|---|---|---|---|---|---|
| Mrs Caprice | Christian | Caribbean | Breast cancer | English | 64 | Spouse; dependent children |
| Mr Chahine | Muslim | Indian | MND | Gujarati | 86 | Spouse; adult children support nearby and at distance |
| Mr Chaganti | Hindu | Indian (from Kenya) | Cancer | English | 82 | Spouse; son supports at distance |
| Mrs Campbell | Christian | Caribbean | Bone cancer | English | 82 | Son (with mental health issues); daughter supports locally |
| Mr Chandhary | Hindu | Indian (from Tanzania) | Cancer | English | Not known | Spouse, daughter, grandson; other adult children at distance |
| Mrs Challa | Hindu | Indian | Cancer | Gujarati | 60 | Spouse; local support from son, daughter-in-law; grandson |
| Mr Chakraborty | Hindu | Indian/Ugandan | MND | English | 67 | Spouse; support from local adult children |
| Mrs Cachalla | Hindu | Indian | Kidney failure | Gujarati | 85 | Son and daughter-in-law in their home |
| Mrs Chawla | Muslim | Pakistani | Heart and kidney disease. Diabetes | Pashto | 72 | Son, in daughter’s home; other family members support regularly |
| Mrs Cheng | Christian | Chinese | Cancer | English | 48 | Spouse |
| Mrs Chandyo | Muslim | Indian | Dementia | English | 76 (approximately) | Alone with local adult children support |
| Mr Chitnis | Hindu | Indian/Kenyan | Heart failure | English | 70 | Alone: estranged from partner and children |
| Mrs Chadha | Jainism | Indian/Ugandan | Heart failure | English | 77 | Daughter moved in to support |
| Ms Chapman | Christian: Anglican | Caribbean | Breast cancer | English | 54 | Teenage daughter; parents local but no direct support |
| Mr Chifamba | Christian: New Apostolic | Zimbabwean | Brain cancer | English | 40 | Alone; mother visited from abroad when had visa |
| Mr Cobbina | Buddhist | Ghanaian | Prostate cancer | English | 59 | Teenage daughter and son. Widower. No direct support |
| Mrs Curkovic | Serbian Orthodox | Former Yugoslavian | Cancer Dementia | English | 96 | Alternates: own and daughter’s home. Two daughters share care |
| Mrs Chavara | Roman Catholic | Indian | Breast cancer and metastasis | English | 64 | Spouse; support from one son in UK, one abroad |
Workstream 2: bereaved family caregivers
Nineteen individual interviews were completed with BFCGs between February 2019 and May 2020. Figure 4 illustrates the recruitment of participants over the course of the study.
FIGURE 4.
Workstream 2: recruitment of BFCGs.
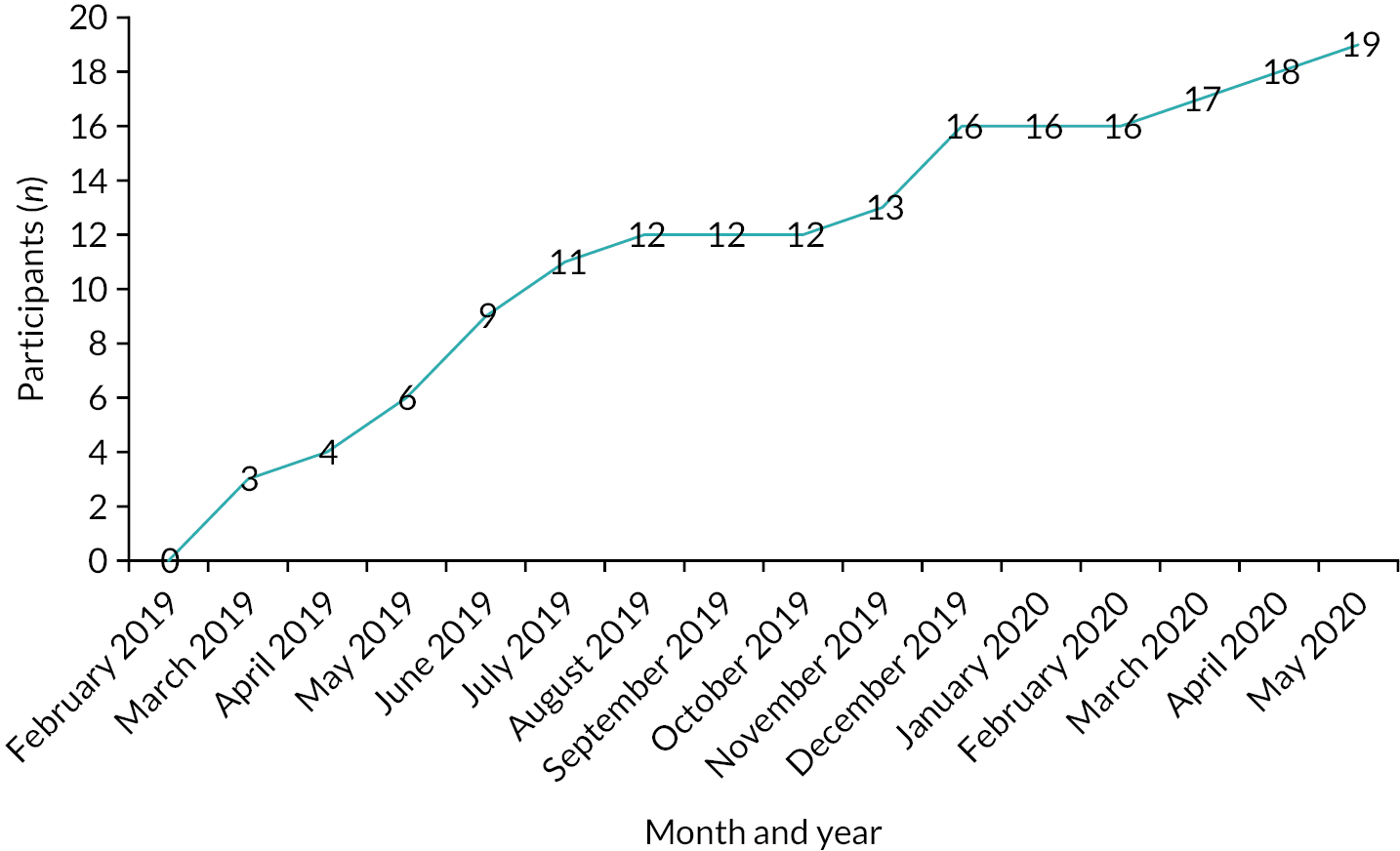
The 19 participants were recruited from two hospices (10/19), a community trust (1/19), two community groups (5/19) and an acute trust (1/19), and by self-referral (2/19). The demographic details of the BFCG participants are described in Table 3. Each of the BFCGs is identified by the pseudonym of the deceased patient, who have all been given pseudonyms that begin with ‘B’. In summary, the majority of the BFCGs described their ethnicity as Indian (n = 11), four as African Caribbean, two as Pakistani, and one each as British Indian and British Asian. Thirteen were female and six were male. Seven were spouses and eight were children, with others being siblings (n = 2), a grandchild (n = 1) and a daughter-in-law (n = 1). One participant was interviewed in Punjabi by a bilingual member of the research team.
| Pseudonym of deceased patient | Religion/faith of BFCG | Ethnicity of BFCG | Relationship to patient |
|---|---|---|---|
| Mr Bashir | Muslim | Indian | Daughter |
| Mrs BajPai | Hindu | Indian | Granddaughter |
| Hindu | Indian | Son | |
| Mr Beshara | Muslim | Pakistani | Son |
| Mrs Bailey | Christian | African Caribbean | Sister |
| Mr Bryan | Church of England | African Caribbean | Wife |
| Mrs Bhajwar | Muslim | Indian | Husband |
| Mr Blake | Christian | African Caribbean | Brother |
| Mr Barratt | Methodist | African Caribbean | Partner (female) |
| Mrs Badawi | Muslim | Indian | Daughter |
| Mr Bangura | Muslim | Indian | Son |
| Mr Bal | Sikh | Indian | Wife (interview conducted in Punjabi) |
| Mr Bharti | Hindu | British Indian | Wife |
| Mr Bedi | Muslim | Pakistani | Wife |
| Mr Bagri | Hindu | Indian | Wife |
| Mrs Banerjee | Hindu | Indian | Son |
| Mrs Bansal | Hindu | Indian | Daughter-in-law |
| Mrs Bhagat | Hindu | Indian | Daughter |
| Mrs Bakshi | Hindu | British Asian | Daughter |
The deceased relatives’ demographic characteristics, as described by the BFCGs, are detailed in Table 4. In summary, the majority of the deceased had cancer [n = 11 (58%)]. Eleven were female and eight were male. Their ethnicity was described as Indian or Indian and African (n = 12), African Caribbean (n = 4) and Pakistani (n = 1), and their faith was described as Hindu (n = 8), Muslim (n = 6), Christian (n = 4) and Sikh (n = 1).
| Pseudonym of deceased patient | Religion/faith | Ethnicity | Disease/illness | Language interview conducted in (if not English) | Sex |
|---|---|---|---|---|---|
| Mr Bashir | Muslim | Indian | Cancer | Gujarati | Male |
| Mrs BajPai | Hindu | Indian (from Kenya) | Dementia | Gujarati | Female |
| Mr Beshara | Muslim | Pakistani | Dementia | Male | |
| Mrs Bailey | Christian | African Caribbean | Pancreatic cancer | Female | |
| Mr Bryan | Christian | African Caribbean | Dementia | Male | |
| Mrs Bhajwar | Muslim | Indian | Ewing sarcoma (cancer) | Female | |
| Mr Blake | Christian | African Caribbean | Lung cancer | Male | |
| Mr Barratt | Christian | African Caribbean | Stroke | Male | |
| Mrs Badawi | Muslim | Indian | Cervical cancer | Female | |
| Mr Bangura | Muslim | Indian | Comorbidity | Male | |
| Mr Bal | Sikh | Indian | Cancer | Punjabi | Male |
| Mr Bharti | Hindu | Indian–Ugandan | Multimorbidity (diabetes, lymphoma, stoma) | Male | |
| Mr Bedi | Muslim | Pakistani | Brain cancer | Male | |
| Mr Bagri | Hindu | Indian–Kenyan | Parkinson’s disease and multiple system atrophy | Male | |
| Mrs Banerjee | Hindu | Indian | Pancreatic cancer | Gujarati | Male |
| Mrs Bansal | Hindu | Indian | Pancreatic cancer | Gujarati | Female |
| Mrs Bhagat | Hindu | Indian | Cervical cancer | Female | |
| Mrs Bakshi | Hindu | Indian | Kidney cancer and comorbidities | Gujarati | Female |
Workstream 3: stakeholder workshops
Between October 2020 and the end of April 2021, through a process of snowballing, > 140 potential participants were contacted (see details in Chapter 2). This resulted in a total of 11 virtual discussion workshops being held with 37 stakeholders between December 2020 and the end of April 2021. Another 13 participants completed workbooks. This resulted in a total of 50 participants in WS3, which comprised 18 laypeople or community and faith leaders, 19 HCPs, seven academics and six educators.
Most of the 18 laypeople and community or faith leaders described their ethnicity as Indian (n = 5); other ethnicities given were white (n = 3), Bangladeshi (n = 2), Pakistani (n = 1), Indian and Pakistani (n = 1), British Sikh (n = 1), Asian (n = 1), England (n = 1), white and Asian (n = 1), English (n = 1) and African (n = 1). Eleven were female. The key characteristics of the laypeople and community or faith leaders are detailed in Table 5.
| Participant | Workshop or Workbook | Age (years) | Sex | Ethnicity | Participant country of birth | Parents’ country/ies of birth | Religion | Education level |
|---|---|---|---|---|---|---|---|---|
| Layperson | Workshop | 31 | Female | Indian Pakistani | England | Pakistan and Kenya | Muslim | Degree |
| Layperson | Workshop | 63 | Female | Indian | Uganda | Both India | Hindu | Degree |
| Layperson | Workshop | 36 | Female | Pakistani | UK | Africa and Pakistan | Muslim | A Level |
| Layperson | Workshop | 64 | Male | White | Netherlands | Netherlands | Hare Krishna | College |
| Layperson | Workshop | 54 | Female | Indian | Uganda | Uganda and India | Hindu | Degree |
| Layperson | Workshop | – | Female | British Sikh | – | – | Sikh | Diploma |
| Layperson | Workshop | 66 | Female | White | Italy | Italy | Catholic | Teacher training |
| Layperson | Workbook | 66 | Male | Indian | India | India and India | Hindu | GCSE/O Level |
| Layperson | Workbook | 63 | Female | Asian | Kenya | India and Kenya | Muslim | Diploma |
| Layperson | Workbook | 58 | Female | Bangladeshi | Bangladesh | Bangladesh | Muslim | Other |
| Layperson | Workbook | 70 | Male | Bangladeshi | Bangladesh | Bangladesh | Muslim | Degree |
| Layperson | Workbook | 36 | Female | England | Kenya | Kenya | Hindu | Degree |
| Layperson | Workbook | 59 | Male | Indian | – | – | Muslim | Degree |
| Community/faith leader | Workshop | 37 | Male | White and Asian | UK | UK and Africa | Muslim | A Level |
| Community/faith leader | Workshop | 68 | Male | Indian | Malawi | India | Muslim | GCSE/O Level |
| Community/faith leader | Workbook | 46 | Female | African | Nigeria | Nigeria | Other Christian denomination | Degree |
| Community/faith leader | Workbook | 82.5 | Male | English | England | England | Muslim | Degree |
| Community/faith leader | Workbook | 58 | Female | White | – | – | Church of England | Degree |
The majority of the 19 HCP participants were nurses (n = 9); the others were doctors (including GPs) (n = 8), a care home manger (n = 1) and a public health programme manager (n = 1). Most described their ethnicity as white (this includes white British) (n = 13), with the rest describing themselves as African (n = 3), Indian (n = 2) and Pakistani (n = 1). Thirteen were female. Their detailed characteristics are described in Table 6.
| Participant group and specialty | Age (years) | Sex | Ethnicity | Religion |
|---|---|---|---|---|
| Doctor in training, palliative care | 36 | Female | White | Other Christian |
| GP, palliative care | 38 | Male | African | Other Christian |
| Nurse, renal | 57 | Female | White British | Other Christian |
| Nurse, primary care research | 61 | Male | White | Jewish |
| GP | – | Male | Pakistani | Muslim |
| Doctor in training, foundation programme | 25 | Female | White | No religion |
| GP, palliative care | – | Male | Indian | Sikh |
| Nurse, cancer | 55 | Female | White British | Church of England |
| Nurse, clinical educator | 59 | Female | White British | Other Christian |
| Manager, extra care scheme | 34 | Female | White British | No religion |
| Doctor in training, palliative care | 29 | Male | White British | No religion |
| Nurse, palliative care | 56 | Female | African | – |
| Consultant, palliative care | 44 | Female | Indian | Other Christian |
| Nurse, advanced nurse practitioner, community hospital | – | Female | White British | Other Christian |
| Nurse, palliative care | – | Female | White British | – |
| Nurse, palliative care | 61 | Female | White British | No religion |
| Consultant, palliative care | 43 | Female | African | Church of England |
| Nurse, EOLCP | 53 | Female | White British | Church of England |
| Manager, public health programme | 36 | Male | White British | Church of England |
The majority of the seven academics described themselves as having an interest in end-of-life issues (n = 4). They described their ethnicity as white (n = 5), white and Asian (n = 1) and Sri Lankan British (n = 1). Six were female. Their detailed characteristics as they provided are described in Table 7.
| Participant group and specialty | Workshop or workbook | Age (years) | Sex | Ethnicity | Religion |
|---|---|---|---|---|---|
| Social scientist, academic focusing on end-of-life issues, university employee | Workshop | 63 | Female | White | No religion |
| Clinician and educationalist | Workshop | 53 | Female | White and Asian | Church of England |
| Social scientist | Workshop | 58 | Female | Sri Lankan British | No religion |
| Social scientist, academic focusing on end-of-life issues, university employee | Workbook | 51 | Female | White | No religion |
| Academic focusing on end-of-life issues | Workbook | 68 | Female | White | Buddhist |
| Social scientist, academic focusing on end-of-life issues, educationalist and university employee | Workbook | 54 | Male | White | No religion |
| _ | Workbook | 53 | Female | White | – |
Two of the six educators described themselves as higher education lecturers; there was also a clinical educator, a GP, an educator, and a health and social care worker (n = 1). They described their ethnicity as white British (n = 5) and Indian (n = 1). Four were female. Their detailed characteristics as they provided them are described in Table 8.
| Participant group | Age (years) | Sex | Ethnicity | Religion |
|---|---|---|---|---|
| GP | – | Male | White British | – |
| Educator | 57 | Female | Indian | Hindu |
| Health and social care worker | 56 | Female | White British | Church of England |
| Clinical educator | 39 | Male | White British | – |
| Higher education lecturer | 46 | Female | White British | Buddhist |
| Nurse, higher education lecturer | 51 | Female | White British | No religion |
Conclusion
This chapter has presented background information on the 115 individual participants who took part in the study and the different sources and extent of data collected. It includes a brief summary of the process of recruitment and detailed characteristics of participants in WSs 1, 2 and 3. The next chapter gives a detailed account of the findings of WS1 and WS2.
Chapter 5 Workstreams 1 and 2: findings
Introduction
This chapter presents the findings from the Thinking Ahead study’s first two WSs, during which researchers sought insights from patients, FCGs, HCPs and BFCGs regarding whether or not and how terminally ill patients from ethnic minority groups and their FCGs think ahead about deterioration and dying. Data were derived from qualitative interviews with bereaved FCGs, and from longitudinal patient-centred case studies based on serial interviews with patients, family members and HCPs (see Chapter 2 for further details). In particular, we sought insights into approaches to discussing the future and perceptions of patients’ and families’ receptiveness to considering future health deterioration and the treatment decisions arising from this. In the following extracts, pseudonyms beginning with ‘B’ denote BFCGs and those beginning with ‘C’ refer to patient cases.
Patient and family caregivers’ perspectives of end-of-life care planning
When talking about dying, the accounts of patient and FCG participants in the case studies tended to orient to matters to do with funerals and wills (i.e. things that happen after death), rather than what might be anticipated during the process of dying. These broader considerations were more likely to occur in the interviews with BFCGs, who could reflect back on the entire process of the patient’s illness and experience of dying, whereas the accounts of participants’ who were living with the experiences of advancing illness tended to focus on the present rather than an uncertain future, preferring to confront issues as and when they arose:
I don’t think I need to talk to anybody right now; when I need to, at that time I will.
Mr Chahine, third interview
There are so many ifs, if, if, but for now I am not thinking of those ifs. I am thinking what has been done by the doctors now.
Mr Chifamba’s mother, second interview
In addition to the perceived pointlessness of trying to predict the future, participants also wished to preserve hope, particularly for the patient, which was felt to be incompatible with too much information or scrutiny of the likely course of the illness and deterioration. Maintaining a stance to protect hope, particularly for the patient, was felt to be a priority:
I told the doctor as well, ‘OK don’t discuss anything to any family member or to . . . my wife that’s going to happen sooner or later’, and they agreed as well. So, she [wife] was giving me the option to not to talk anything about that. She was keeping positive to the last minute: ‘No matter if you give me treatment or not, I might get better’.
Mrs Bhajwar’s husband
Health-care professionals also observed that there was a clear orientation by patients to live and focus on the present and deal with the future when it happened:
The patient has not wanted to have end-of-life discussions because he wants to concentrate on the now. He said he will deal with that when it comes to it.
Mr Chaganti’s HCP
Some patients and families maintained such a stance of therapeutic optimism, either because they did not know or accept how ill the patient was, or because this was a preferred coping strategy. The tendency towards optimism, to assuming that the illness was not too advanced, that treatment might contain its progression, that there was a lot of time left, made thinking ahead irrelevant for many. Indeed, for some, death (from their illness) was not necessarily considered inevitable:
And the reason we have not had that conversation is because I believe we can have that conversation if the time comes when that’s the case. But we have not really had that conversation, we don’t see, in a sense we don’t see cancer as a threat, we don’t see cancer as it’s a threat and it’s a ‘oh gosh, it’s inevitable that she is going to die from cancer’ in that sense.
Mrs Caprice’s husband, third interview
Health-care professionals gave accounts to support the idea that patients and families orient to the now rather than the future:
Sometimes . . . I am talking about haematology as a whole here . . . sometimes, yes the patients perhaps say, ‘Well, I am still having treatment’, and it’s still there in the back of their minds, they are still having treatment. And in some ways that potentially, I suppose, can allow a degree of, it’s a strong word isn’t it, a denial of what the outcome is going to be. Because as long as they keep coming to haematology for their blood products and their outpatient appointments, the finality perhaps is pushed away.
Mrs Campbell’s HCP
Several respondents from both WSs could justify their therapeutic optimism in the light of past experience of the patient having pulled through acute crises apparently against all odds, particularly when this outcome had confounded negative professional prognostication that death was imminent:
. . . given that we only had a couple of weeks to 2 months from her diagnosis and prognosis . . . we have had her . . . it’s 5 months in now.
Mrs Chandyo’s daughter, second interview
In other cases, participants pointed to the effectiveness of treatment and the apparent stability of the patient’s condition. This gave grounds for optimism and discouraged anticipation of a negative and threatening future, which was regarded as detrimental to the patient’s well-being:
I am not quite sure when would be the best time for that. Because if her condition is stable and I don’t think she needs to concentrate any more on the afterlife than she is now.
Mrs Cheng’s husband, first interview
Religious belief and culture played important roles in the lives and values of most families in the study, and participants from different faiths held strong convictions regarding divine determination of the moment and manner of their death. From this perspective, it was pointless, as well as presumptuous, to anticipate, plan for, or attempt to determine how and when one’s life will end:
I said, ‘Who I am to ask my god?’ That would be presumptuous. So, I said I don’t ask God questions. He is my god, why should I question him? He is the one who made me, I shouldn’t question him.
Mrs Campbell, first interview
Researcher: So you are not thinking about the care you might get as time . . .?
Mrs Challa, first interview: No, whatever happens, it’s in God’s hands.
Religious belief in divine intervention was one reason for families to express a preference for active treatment to maintain the patient’s life at all costs, although this stance was not limited to those with a strong religious affiliation.
Researcher: I guess what I want to know is, has anybody talked to you about end-of-life care planning?
Mrs Challa’s husband, first interview (via interpreter): So, they believe, they have got faith in god so whatever comes, comes and has to be accepted and faced. No one has talked to them about this end-of-life care plan and the question about I don’t want this to happen. So that question relating it to the chemotherapy he says ‘no they would like right to the very end for her to be having this treatment’.
I think it’s hard to let go, that’s what it is, it’s hard to let go. I just don’t think, especially my sister, she was very close to my dad really, really close to him so it’s very difficult for her to let go. She was very adamant no, let him keep going, let him keep going, keep him alive as long as possible sort of thing.
Mr Beshara’s son
Although a tendency for therapeutic optimism was common, if the family had lacked awareness of how gravely ill the patient was, the occurrence of unexpected deterioration and death could be a devastating experience, following which participants could feel regret that they had been denied the chance to prepare and to make the best use of the time they had remaining:
Obviously, we used those last moments in the best way that you can. It wasn’t always accurate though because, you know, she tended to go over the time limit that they gave. But at least it was mentally preparing everybody, it’s important for the family to be able to kind of reach the stage where they have acceptance and they are able to let go. . . . Because if they are not told then they will just carry on with life as usual and then maybe in the last moments the people around them are not there and they need to be there.
Mrs Chandyo’s daughter, post-bereavement interview
I feel they didn’t make it clear to me, they just needed to say clearly, ‘Your mum is at end of life and there is nothing we can do for her medically. We can make her comfortable and ease her pain, but we can’t make her better’. If they had said that to me in those words, I would know exactly where I would have been with Mum. As a family we would have known what do to. . . .
Mrs Bakshi’s daughter
The pace of illness, slow, fast, variable, cyclical, uneven, shaped family expectations for the future. Participants were sometimes taken by surprise at the speed with which the final decline and death occurred. Even when people were ‘aware’ that death was, or could be, imminent, they were still shocked when it came.
It also appeared that quite a lot of vague language was used in communication between patients, FCGs and HCPs. In some cases, HCPs described talking about treatment not being curative, but apparently left open the question of when, and if, it might eventually fail:
So, we kind of had a lot of talks around, you know, this isn’t something that we are going to be able to, sort of, cure and he knows he has got to live with it until such time as it isn’t going to be manageable.
Mr Chitnis’ HCP, first interview
Although vague and indeterminate language may have been the preferred mode of discourse for many families, it made it difficult for individuals who did want guidance about what to anticipate in future to obtain this. Several patients and/or FCGs were critical of what they considered to be professional evasion or unwillingness to provide a definite prognosis or information about their future treatment options:
I saw him [hospital doctor] last week and my cancer is growing, I have got . . . aggressive cancer and it’s growing very rapidly now, it seems to be moving along. And I said to him, ‘Where is it then?’. No answer. And now they are saying . . . there is a specialist scan and I said, ‘Is that going to show up where the cancer [is]?’, and he said, ‘Well, I don’t know much about . . .’. He has to find out. And, you know, I said, ‘Why wasn’t this done before we went through the radiotherapy so that we know exactly where it is so that we know when I have the radiotherapy it’s going to work?’. No answer.
Mr Cobbina, second interview
Patient and FCG accounts of professional vagueness and prevarication were corroborated in some HCP accounts:
Mr Cobbina’s HCP: . . . the conversations . . . with this patient have more been about planning for the future as opposed to thinking about when his future, when it’s going to end . . . we have talked about what if the cancer kills him. . . . But as far as I am aware, at the moment we don’t see that happening in the future, certainly not the near future . . . he is quite pessimistic and so for me to go in and start talking about end-of-life care with a patient who isn’t end of life yet would, for him in particular, would be awful, I feel, because, you know, he needs to try and be more positive. . . .
Researcher: But you did say you have had some sort of planning discussions . . .?
Mr Cobbina’s HCP: Yes, only because he has talked about it, he has said to me, you know, ‘But what will happen in the future?’, and I said, ‘Well, we don’t know that yet, we don’t know what is going to happen in the future. But when that time comes or if that time comes then that’s when we will need to talk about what needs to happen and where you want to be and that sort of thing’. But, I haven’t had, I can’t, because he is not at that stage. I wouldn’t talk to, I didn’t discuss end of life with him because I am not aware that he is dying from his prostate cancer.
Thus, accounts from both patients and HCPs indicated that patients’ efforts to raise the topic of future deterioration could be evaded or rebuffed. Professional accounts often aligned with those of patients and FCGs who considered that it would be inappropriate, and possibly damaging, to engage in discussion of EOLC progression and options substantially in advance of their occurrence.
Health-care professional perspectives
Most of the HCPs nominated by the patient participants to take part in the case studies were nurses from a range of acute specialist or community roles. They varied in the extent to which they knew the patient or details of the patient’s personal and family circumstances. Some HCPs were surprised to have been nominated by patients to participate in the study because of what they considered to be a brief or low-level involvement with the patient. Many did not see EOLCP discussions as falling within their remit. Specialist nurses, for example, engaged with patients, potentially for a long time, in providing active treatment, which was the focus of their interaction. When treatment options ran out, the patient was discharged and referred to palliative or community care services, which were considered responsible for having such conversations. Thus, even those HCPs who had a long-term relationship with patients did not necessarily consider that it was appropriate for them to raise the topic of future deterioration and care. This could depend on the configuration of services around specific illnesses. HCPs caring for patients receiving long-term treatment did not consider that it was relevant or appropriate to raise EOLC topics when the patient was still receiving active treatment and was not close to death. They felt that this would cause needless alarm and undermine the patient’s hope. They were also concerned that such a change of tack would damage their relationship with the patient and the patient’s family.
In these contexts, thinking ahead became relevant only when the end of life was close. In the preceding extracts, such discussions were not perceived to be staff responsibility. However, it appeared that the nature of the illness [e.g. motor neurone disease (MND) and myeloma] and how different services were organised to provide treatment could shape the duration and quality of relationships between patients and staff, and whether or not HCPs considered discussion of EOLC to fall within their remit. One specialist MND nurse described how patients remained within the care of the service from diagnosis right through to the end of life. In this context, she and her colleagues considered initiation of future planning discussions to be part of their role:
I act like a key worker for them so I can refer people to other health-care professionals that they may need to see. . . . We can refer them to any of the aspects of care that [hospice name] offer right from diagnosis . . . then they are followed up . . . supporting them in any way we can . . . whether its emotionally, physically, psychologically, practically. For both the person with the MND and their family. And we will see them right to the end of their journey, until they die. . . . If I felt it was important to talk to him [case patient] about it [end of life] I would. And . . . if something cropped up in conversation, you know, and I had that moment . . . to open up discussions I would. . . .
Mr Chakraborty’s HCP
In cases in which the patient suffered complex morbidities and/or treatment and had been referred to many different services, it was difficult for individual HCPs to know if and when future planning had been discussed:
So, I think, particularly in the acute setting, if you come in with . . . an immediate illness . . . you deal with that because that’s the emergency part. And then, you know, it might be that the teams swap over or they go to a different ward and when the patient is . . . medically fit . . . they go home. But then if they come back into hospital they are not going to be under the same team. So, it’s almost seen as another acute episode rather than a progression of the previous problem.
Mrs Chadha’s HCP
There was a congruence between professional and lay perspectives about discussion of thinking ahead, and in many cases professional (non-)responses may have been well tuned to patient preferences. However, for those individuals, a minority in our study, who did want to know a clear prognosis and to discuss their future options, the lack of professional awareness and responsiveness could be deeply frustrating and damaging:
. . . you know I found it very strange when he [doctor] is saying, oh he doesn’t know what to do and oh they have found something on the scan but he doesn’t know what it is. And I found it very strange because he is supposed to be a consultant; he is supposed to be the top man and they should know these things because they come across it day in and day out. I started doing my research online and I said could it be this or could it be that then he snapped at me to say, ‘Oh, we are the experts, you should listen to us, there is no need for you to do research’.
Mr Cobbina, third interview
And the doctors are not being, they are not giving me a, how can I put it, a prognosis. It’s a wait-and-see approach so they are not sure, it’s just monitoring. . . . And the doctors are unwilling to say you have got X amount of, I don’t know, a year or 5 years to live or, so I don’t know.
Mr Chifamba, second interview
Professionals may convey mixed messages about prognosis, which may be intrinsically uncertain, and also inadvertently mislead by not being explicit, in which case the family may persist with unrealistic aspirations, for example that the patient may even recover (which is not entirely unreasonable when the patient has made heroic recoveries from illness episodes in the past).
Initiation of end-of-life care planning discussions
Regardless of role and experience, HCPs felt that it was important that end-of-life discussions should not be initiated before the patient was ‘ready’. They tended to wait for patient cues that this was the case, and capitalised on opportunities as they arose, rather than initiate discussion pre-emptively. If the topic was raised, HCPs were prepared to withdraw quickly if they encountered resistance. It was important to respect the patient’s agenda, rather than risk causing distress and damaging relationships with patients and families that may have taken considerable time to establish:
Some patients are very open about wanting to talk about the future and, you know, give you many cues and you can sort of, you know, have conversations very easily. Certainly, when I first met him [Mr Chitnis], he was definitely not that patient, he did not want to discuss, he was very fearful . . . getting better that was his absolute priority.
Mr Chitnis’ HCP
Even when community and palliative care staff acknowledged discussion of EOLCP as part of their role, they too were cautious about introducing the topic before the patient was ‘ready’. Around two-thirds of HCPs nominated by patients in the case studies had not (yet) explicitly raised the topic of death and dying with the patients or their families. HCPs considered that it was important to elicit and address patient concerns and fears at any point, but this did not necessarily end up in a discussion of death and dying. Alongside this was an indication that some patients did express fears and concerns for the future, something they found hard to articulate, and that HCPs may not have recognised. Patient concerns and preferences can shift and be volatile. Several HCPs observed that, although they generally try to avoid a direct approach if patients are not inviting discussion, sometimes situations arise (e.g. rapid deterioration) whereby the subject of EOLC has to be broached, regardless of patient readiness or ‘good’ relationships being in place:
. . . you get people who don’t want to talk about it at all, people who want to talk about it every time you see them and then there are people in the middle.
Mr Chakraborty’s HCP
. . . quite often I will sort of say if people are absolutely, they do not want to talk about it, then I will say, ‘That’s absolutely fine, you know, just bear in mind that you know I am here to have those conversations should you change your mind. And I may come back to you again in a few months’ time and bring it up again. But you know if you don’t want to talk about it that’s fine’.
Mr Chitnis’ HCP
Setting for end-of-life care discussions
The location or setting in which EOLC discussions occurred was an important factor determining family experience and response. One of the key ‘sites’ for such discussions was in the acute setting following the patient’s admission for a health crisis when staff routinely raised the issue of resuscitation. Exchanges were often described as fraught in these settings. Relatives described being suddenly confronted by the gravity of the patient’s illness and being put under pressure to make momentous decisions about resuscitation and other treatments by staff working under pressure who lacked empathy and time to communicate with care and consideration:
. . . he was quite dismissive in his manner; he was quite harsh. And my sister at one time had to say to him ‘I am not discussing this anymore because you are upsetting me’. He was quite brutal. He wasn’t saying what was involved, he was, ‘Well what is your decision going to be? what is your decision going to be?’. Repeating the same thing . . . in the hospital he seemed to think we had got the medical knowledge and we knew exactly what was involved . . . just having been told that your mother has now got a mass of cancer . . . and you are expected within seconds to be able to attempt to instruct them on what then needs to happen, I just think was completely unrealistic.
Mrs Curkovic’s daughter-consultee, first interview
Much more positive experiences were described when EOLCP was discussed in the patient’s home or in a community health-care setting. Several patients and HCPs described having been invited by their GP to make an appointment to complete an advance care plan, and there were some accounts of specialist community and hospice nurses raising EOLC issues in the patient’s home for families to consider and discuss over time, before reaching their decision:
. . . it was very painful, but yes, we had her [patient’s] daughters and my daughter and everybody round and then she explained, but it was really, really helpful. Without that I think we would still be guessing what would happen next, what medication would she have or what would she do . . . they have a lot of time to support . . . and yeah to reassure. . . .
Mrs Bansal’s daughter-in-law
It was reportedly common for family members to be present when professionals raised the topic of EOLC with patients. Indeed, in some cases the patient never spoke to a HCP alone, especially if translators were required. Professionals sometimes spoke to family members first, before discussing issues with the patient:
When the GP wanted to do . . . an end-of-life care plan he called me in first and he is like, ‘Right, you need to talk to your dad about this’, and I was like, ‘How am I supposed to tell my dad about this?’.
Mr Chandhary’s daughter, second interview
Discussion between family members and professionals could happen because the patient was acutely ill or unconscious (e.g. during an acute admission), or because they lacked cognitive capacity, but was also described in situations in which the family had become the established interlocutor in the case, rather than the patient. Some patients seemed to be content for their relatives to lead in discussion and decision-making with HCPs, and in liaising with services. However, especially when there was a need for professional or family translators, there was a significant risk that the patient’s voice was over-ridden or not heard.
End-of-life care topics
One issue that arose in interviews with all participants (professionals, patients and FCGs) was the indeterminacy of what constituted discussion of ‘EOLCP’. A few participants described being prompted to make an appointment with a GP or nurse to discuss and document the patient’s care plan. However, in most cases, professionals did not articulate a specific agenda to ‘have an EOLCP discussion’ and patients and FCGs were not familiar with this term or what it involved. Indeed, the criteria for determining what should be included, whether an EOLCP discussion had taken place or what needed to be considered to establish that it had taken place were unclear. Consequently, some patients and FCGs reported not having engaged in EOLCP, but later described episodes in which aspects of this (e.g. decisions about DNACPR or preferred place of death) had been considered. Regardless of whether patients and families identified specific topics as relating to thinking ahead, a number of key topics recurred in their accounts.
Do not attempt cardiopulmonary resuscitation
In a majority of case studies and half of the bereaved FCG interviews, DNACPR was the most frequently and extensively referenced issue. It was often described as a very difficult and sometimes protracted decision for the patient and, commonly, their family. Patients and families tended to be more willing to continue active treatment, at all costs, than HCPs thought was appropriate. For some families, agreeing to a DNACPR instruction was described as tantamount to ‘signing a death warrant’ and ‘saying, “Right, Mum, your life is finished now”.’ (Mrs Curkovic’s daughter, first interview).
Some participants had been misinformed or misunderstood the nature of resuscitation and what DNACPR meant. One concern was that once an order was in place, the patient would not receive any further active treatment:
We have agreed to the form where it says do not resuscitate, when [HCP] came out to see us again she explained again clearly that it’s not a case of if Mum got a chest infection they would say, ‘Oh, we are not doing anything’. Or, heaven forbid, she was choking at home on a piece of food that they will turn round and say ‘no, do not resuscitate’ – it wasn’t that.
Mrs Curkovic’s daughter–consultee, second interview
In such cases, the role of the HCP in taking time to understand and discuss the family’s concerns and provide accurate information about DNACPR was critical in supporting patients and, especially, relatives to eventually accept, however painful, the decision that resuscitation would not work if the person had died or would not be appropriate as the patient would be damaged by the treatment and would, at best, not recover to a meaningful quality of life. This was not always the case, however, and some families held out, even in the face of professional opinion. When families had experienced the patient recovering after a severe health crisis in the past, this became a strong reason for rejecting such an instruction:
I would say no straight away [to DNACPR] because, like I said . . . when she went into a coma and they literally wrote her off with the sepsis, she pulled through.
Mrs Chawla’s daughter, first interview
Several FCGs described having sought advice from a faith leader regarding the acceptability of refusing resuscitation. In each case it was confirmed that there was no religious objection. Discussion within families was sometimes protracted, and the locus of decision-making was quite varied. In some cases, the patient was described as the sole or main decision-maker. In others, although the matter might be discussed collectively, one or two family members were recognised to have responsibility for the decision. An additional pattern involved core family members seeking to reach consensus:
I am the eldest, but I don’t like to make any decisions on my own. I don’t want the other brothers thinking I am taking over and doing what I think is right for me and keeping them out of the situation. I wouldn’t do anything without having a discussion between us. So we all agree on something and we are all happy with what is to be done. . . . So, we would, all of us would be aware of everything that is going to go on.
Mr Chahine’s son, second interview
In several case studies, participants described the patient’s initial agreement to accept DNACPR being overturned following a period of reflection and, particularly, discussion with family members. This seemed more likely in the case of older patients who required a translator to communicate with HCPs. The extent to which the patient’s change of mind had resulted from genuine reflection and discussion within the family or had been determined by family preferences was unclear. These cases also illustrate the significant role that HCPs played, albeit inadvertently, to seek to secure an agreement to DNACPR. Participants’ accounts of such discussions highlight the importance of insightful professional recognition of ‘readiness’ to broach the topic, and a good knowledge of family dynamics. It also raises concerns about the risk of the patient’s voice being unduly influenced by HCP and FCG influences, especially if an interpreter is required to mediate communication.
Preferred place of care or death
Of those who reported a conversation about preferences for place of care or death, around one-third of patients in the case studies expressed a wish to receive care and die at home. Over half of BFCGs reported having preferences for home as a preferred place of care/death. In two cases, patients acknowledged that, although their currently desired place of care and death would be home, their illness might dictate a hospital admission and they would reconsider or accept that. Individuals were often pragmatic in their appraisal, being prepared to accept an alternative such as hospice or hospital if this should become necessary, particularly if their FCGs became unable to cope with looking after them at home. Some patients were also content to delegate this decision to family members:
Yes, they did ask me. . . . I said maybe in hospital if I am not very well. But I don’t know how long, you ask me maybe I change my mind, maybe I want to be at home. . . . When I am not feeling well, if I am not feeling well normally, I will go to hospital, probably end up going to hospital, I don’t know. Or go to hospice home, but I don’t know what the hospice home is like, so I don’t know.
Mrs Cheng, second interview
She did ask us about that, and I said ‘No’, I said, ‘I want to keep him at home for as long as possible as long as I could look after him’. If I couldn’t do it any more, [if] I was completely ill, then he would have to go to hospital.
Mr Bal’s wife
So, I was just trying to care for her at home but it was quite, it is difficult. You don’t realise how difficult it is because you don’t have all the necessary tools to be able to do that yourself.
Mrs Bhagat’s daughter
Ceiling of care
Some patients and their families had set limits to future care, including cessation or rejection of treatment, such as dialysis or pain relief. Others were clear that they wished to receive all available treatment for as long as possible, and for professionals to make every effort to prolong life. Participants’ responses were strongly influenced by past experience and observation of others. Mrs Chadha expressed her resistance to being given morphine following the distressing death of her sister. She felt that morphine had caused some serious and undesired side effects and suspected that it might also have hastened her sister’s death. Some patients were selective in the treatments they were prepared to accept or reject. Mrs Cachalia had declined dialysis, having witnessed the great pain a relative had endured, which was attributed to this intervention. She was prepared to accept oral medication. Mrs Cheng had rejected any further intravenous chemotherapy, but was willing to take antihormone treatment for cancer. In a few cases, a patient had declared that they wanted no further, or at least any additional, treatment or efforts made to prolong their life:
He says, ‘I don’t want to extend my life span’. In that sense, he goes, ‘I want to be able to do things. I want to be able to just live my life. I don’t want to try . . .’. Because one of the things they said was that there could be a possibility that they could do a small surgery and he said, ‘No, if it’s a case of a surgery, I don’t want a single incision in my body’. He goes, ‘I just want it left the way, I don’t want any more surgery’.
Mr Chandhary’s daughter, first interview
Several older patients felt that they had lived a full and complete life and accepted that this was coming to an end:
Yes, we did ask our mum as well whether, we did ask her, ‘This [is] what the doctors are saying, and they are saying you are on the last stage whether you want treatment it will not be effective’. Mum says, ‘No, I don’t want to suffer more’, So we just left it at that point.
Mrs Banerjee’s son
In other cases, regardless of age and poor state of health, patients and FCGs persisted in the desire to maintain life at all costs:
Personal choice of my Mum, ‘I want you to do all that you can’.
Mrs Chawla’s daughter, second interview
Several participants expressed a concern that certain treatments would be either administered or withheld in a deliberate attempt to shorten life:
I believe that when you go in a hospice or certain places, they tend to feed you, give you more medication, to the point where you are drowsy, you don’t know what’s happening. And the medication slowly, slowly I think makes you worse and ends your life.
Mrs Chawla, first interview
The desire for active treatment was attributed in some cases to religious beliefs about divine intervention, but was also expressed by patients who had no religious convictions. It seemed that one reason for continuing active treatment was that the patient and family lacked awareness of how ill the patient was. Another was the hope that it might be possible to extend the patient’s life long enough for new and more effective treatments to become available:
[Translated by professional interpreter] . . . the world is constantly evolving, science is constantly finding out new stuff and new things, so why does it have to stop here? Why can’t they discover something more effective to treat this?
Mrs Challa’s husband, second interview
Indeed, a strong faith in divine determination was not necessarily incompatible with acceptance of prolonged and active treatment. Patients accepted all efforts to prolong their lives alongside a calm acceptance that the duration was entirely a matter of divine will. Given that life was a gift from god, it was incumbent on the individual to live this to the full:
You know treatment, I am so happy with the treatment, they are really, really good to me. But whatever happens to me in the future, I left it to the God’s hands . . . No I don’t think about what may happen.
Mrs Challa’s husband
I just leave it to God and see what happens. But I say to myself, ‘Oh, God will sort it out’, you know. . . . You just say, ‘Oh, I will leave it to God. He will decide what to do for us’. But really and truly . . . you have got to do it as well.
Mr Chakraboty’s wife
Documented care plans
Only a handful of patients and families clearly reported having documented care plans, with a copy kept in the patient’s house to be shown to attending HCPs and paramedics. A similar number made some mention of a plan being made, but not taken up, and the rest did not refer to a plan having been discussed, at least with HCPs. Discussions of plans with the patient and family members, including for care of the patient prior to and after death, were described by a few participants. For some families, it was the religious and cultural preparation for death that was of significance, rather than professional agendas regarding EOLC. Indeed, several patients and FCGs commented that planning for end of life was not something to be discussed with professionals. This was a family matter, not the business of strangers:
Researcher: Right now, when you look at your mum and her condition, do you think what is going to happen to her in the next however long?
Mrs Chandyo’s daughter: Yeah, it’s a thought that crosses our mind that we need to be prepared to be able to look after her in her final moments and making sure that the ending is good, that she has a good funeral. That we are able to cater for things to come after.
Researcher: When you say the ending is good, what does that look like?
Mrs Chandyo’s daughter: Like, for example, she is spiritually connected to her creator is the most important one for us. That she is comfortable in herself, that she is not suffering. And she is happy with the people that are supporting her and helping her and the ones that are around her.
Researcher: And in terms of operationalising that towards her last moments what would that involve?
Mrs Chandyo’s daughter: Yeah so if she was in her last stages, I think it would be a requirement that she has the, we have similar to the bible, but it’s a scripture that she can listen to. So, it’s very calming its . . . so we would have that playing in the background. She would have to be ritually cleaned and everything, the sheets have to be clean, be in a clean state, and just have people reminding her of her goal of where she is heading. Just reminding her, because she passes away it’s a requirement for us that she says then we call it the testification of faith, which is to say that she believes in one god and the Prophet Muhammad is the last messenger. And now that is fundamental to end-of-life care, so having people around that can encourage her to be reminded of that and to be able to say it or reflect and ponder if it’s really important.
Even so, and despite a strong desire for the family to provide her mother’s EOLC, and an aversion to this being handed over to ‘strangers’, Mrs Chandyo’s daughter–consultee accepted that, if it became no longer possible to achieve her comfort at home, then the family would consider her admission to hospice.
In other cases, participants indicated that they had concerns that had not been discussed with HCPs because they fell outside the limited agenda of professional EOLCP. Mrs Challa’s husband described how someone had come from the general practice surgery to speak to the family about the patient’s future wishes. It was not clear if this had been documented, but they had made it clear that, in addition to dying at home, the family wished Mrs Challa to be resuscitated in the event that her heart stopped and to have all possible treatment to prolong her life, the determination of which they believed to be in god’s hands. However, a critical issue for Mrs Challa’s husband was how to arrange for his wife’s funeral to be held in India, rather than the UK. He had not so far felt able to talk to the GP about this, but following a discussion in the interview, he resolved to do so in the near future.
Several bereaved carers recalled situations in which speedy deterioration had made plans redundant. They described being in a rather responsive mode of planning, although, in retrospect, they appreciated the value of such planning had they had the chance to do so:
I mean, I think had the situation been different, I think, yes she could have been a lot more involved in that decision-making process itself. But also . . . what’s potentially ahead of them if someone does broach the subject to say, ‘Well, OK you know, we are at a stage where, at some point in the future, we are going to be end of life, and we need to try and think about how that would work best for you as a family and for her as a patient’. And if, you know, if those discussions happen earlier on, I think it helps the family prepare in a better way.
Mrs Bhagat’s daughter
One BFCG described how useful having a care plan in place had been in ‘standing their ground’ when their relative deteriorated and the initial professional reaction was to admit them to hospital. The availability of the plan enabled her to question whether or not this was indeed the right option. In the event, the patient was admitted to hospital where he subsequently died. However, the BFCG felt that the documented plan had enabled her voice to be heard and contributed to a soundly decided outcome. She perceived great benefit in having thought ahead and felt empowered by having a documented plan:
Yes, I would say to people that . . . plan ahead, if you know there is progressive illness in the family, plan ahead. Go to your GP, make a plan as to what you want to do, how you want it done. Rather than the professionals pushing to say ‘you have to do this, you have to do that’. It’s your and your person’s decisions as to how they want to die and where they want to die. . . . And to be looked after by family at the end, which we did. Which is what [patient] would have liked. . . . So I was very fortunate that, you know, all this thing was in place.
Mr Bagri’s wife
Documented plans, or even informal discussion, of future care decisions were described as occurring in the community, during a scheduled visit to the GP or a domiciliary visit from a nurse. Hospital was a difficult setting in which to engage in extended talk. Participants described hospital admissions as being the site of stressful and upsetting encounters, often centring on single issues such as decisions about DNACPR or ceilings of care. These also seem to have been occasions when patients and family members were given information about a limited prognosis in rather brusque and insensitive terms. The distressing nature of this information was compounded when it was also the family’s confrontation with the severity of the patient’s illness and how close they were to the end of life:
Researcher: There has been no communication about . . . so they had the end-of-life care plan, they had that discussion with you when your mum had sepsis in the hospital?
Mrs Chawla’s daughter: Yes they had the do not resuscitate and everything like that, they had that discussion with us and they had the prepare for the worst and you need to get a funeral plan. But there was no real end-of-life care discussion, no.
Aspects of advance planning were quite common in relation to preparation for future events that were inevitable, but distant, for example making wills, completing lasting power of attorney, arranging and paying for funerals and collecting items for ritual ceremonies such as funeral shrouds. Discussion of such matters was easier to have far in advance of need. Mrs Chandyo’s daughter described having talked with her mother about the formalities to be observed before and after her death, including the shroud that the family had bought for her while she was still relatively well. However, in her mother’s present stage of fragile health, it would be inappropriate to raise such matters and, indeed, might be actively harmful, in prompting loss of hope, which would cause her body to ‘shut down’.
The difficulty of prognostication
For families that had engaged in discussion of EOLCP, prognosis was often described as a difficult issue. Accounts of professional estimation of the patient’s life expectancy were common, as was the experience of their inaccuracy:
I think a lot of people feel, maybe they are trying to cover their backs, I don’t know why they say that. Maybe they just want you to have realistic expectations, a minimum of how long your parent is alive. But we didn’t actually take it, it is upsetting, but as a family we have had an experience like this with my dad where they said he only had 24 hours to live, and he lived another 12 years.
Mrs Chandyo’s daughter
Where there was a discrepancy, most patients were reported to have outlived the prognosis, sometimes by a considerable period. This provided a robust justification for relatives to ignore professional invitations to engage in subsequent discussion of EOLCP. In some cases, however, participants expressed regret. Just as not realising how close the patient was to the end of life could deny family members the chance to savour the last days or weeks remaining, so the false anticipation of imminent death could prompt decisions that relatives later came to question or regret. Mrs Chandyo’s daughter–consultee described how the family had accepted a professional decision to cease active treatment and aim simply to make her mother comfortable, because she was judged to be close to death. Consequently, the family refused the offer of a blood transfusion, which, it was suggested, might make her mother feel better, apparently on the suggestion of a nurse.
Mrs Chandyo’s daughter–consultee: It is a different pathway, because they are not treating her any more. We are just trying to make her comfortable.
Researcher: What does that mean to you, they are not treating her any more, they are trying to keep her comfortable?
Mrs Chandyo’s daughter–consultee: It means they have, in terms of, for example, we didn’t expect her to live so long, we were expecting her maybe a couple of months and I think that was the expectation from the health-care professionals as well. At the time she was . . . they said if the family agreed, Mum could have another transfusion because that would perk her up, it would help her a lot. But because of the timescale we were looking at end of life, looking at her it might benefit her. And now I think that, and I think I had made that decision to go ahead with it, because that was 4 months ago.
Researcher: You think that would have helped her?
Mrs Chandyo’s daughter–consultee: I think it would have helped her yeah, not in terms of making her life better, just making her more comfortable. Because now she is, she goes blue, if it could help her even a little that would have been a help but that’s not there any more.
Researcher: Is that a decision you needed to make?
Mrs Chandyo’s daughter–consultee: It was, but we were swayed to saying well no because she might not have that long and it’s not going to benefit her. But she has actually been here about, I think, 4 months.
Several relatives described being told that there was no further treatment available for their relative, who was scheduled for comfort care only. This was a cause of some uncertainty, misunderstanding and distress, especially when participants felt that professionals were withholding treatment that might have been of benefit. Mrs Chadha’s daughter described how her mother had been told several times that the aim was simply to keep her comfortable because there was no more effective treatment available. She had also been told during an admission to accident and emergency (A&E) that she did not need to call an ambulance in future if she became unwell at home. Mrs Chadha’s daughter felt that this attitude was extremely unhelpful as her mother had several times experienced infections that were easily treatable with antibiotics. Consequently, she had endured a serious lung infection for an extended period of time, rather than ask for medical assessment and treatment. When Mrs Chadha had finally been admitted again to A&E in a state of serious ill health, Mrs Chadha’s daughter had told the consultant there that the reason her mother had not rung for an ambulance was because A&E staff had told her not to call one:
Mrs Chadha’s daughter: The only thing they keep on saying is that, you know, ‘There is no further treatment available for you. You know that you are on maximum medication, there isn’t anything else that we can do for you. And we just need to talk about making yourself comfortable rather than treating you any more because there is no treatments’.
Researcher: How does your mum take all that kind of discussion?
Mrs Chadha’s daughter: I think . . . I think she knows that she is unwell, very unwell . . . but things like, you know, things like chest infection, water infection that is minor, I would say that can be treatable with antibiotics. And Mum was really suffering months and months with it because somebody told in A&E to Mum that she doesn’t need to call an ambulance because there is no further treatment available for her. And when I said the same thing to the consultant there, when she was treated in the hospital with the chest infection and I said to them that, ‘This is the reason she didn’t ring for an ambulance, because she was told not to by one of your staff in A&E that why are you calling, you are on advanced you know’.
Researcher: So if you are in advanced whatever you don’t deserve to get any treatment?
Mrs Chadha’s daughter: Well that’s what the nurse would have thought and told Mum. Because when I spoke to the consultant and when I said to them, ‘That’s why Mum didn’t ring you’, he said, ‘But these are minor illnesses, like chest infection, we will be able to treat that. So I don’t know why they said that to your mum’.
Researcher: Hmm and you say that’s one of the nurses?
Mrs Chadha’s daughter: That’s one of the nurses in A&E yes. Who was checking Mum in.
At the same time as her mother was being told that there was no further active treatment available, and repeatedly raised the prospect of her being close to the end of life, Mrs Chadha’s daughter also reported that, when she had raised the issue of EOLC with her mother’s hospice consultant, she had been advised that it was not time to consider this yet, as her mother was not sufficiently ill:
Mrs Chadha’s daughter: I spoke to the consultant at the hospice when we went to see her.
Researcher: Was that after we spoke last?
Mrs Chadha’s daughter: Yes, I mentioned end-of [-life] care and she said, ‘Not yet’, she said, ‘It’s not, Mum’s not there yet’.
Researcher: So you initiated it with a consultant at the hospice?
Mrs Chadha’s daughter: Yes because they all keep mentioning advance care, so I said does that mean end of life. . . . So, I don’t know when does that kick in. Because at the moment it is still advance care plan.
Researcher: OK so the consultant said not yet.
Mrs Chadha’s daughter: Not yet. And that’s all.
A similar experience was described by Mrs Curkovic’s daughter. An advance care plan had been completed during a consultation with her mother’s GP, following a distressing emergency hospital admission. Staff had ‘gone on and on’ about a resuscitation decision and told the family that there was nothing more to be done for Mrs Curkovic, that a care plan had to be put in place and that she had only a few more weeks to live. However, this prognosis was subsequently over-ridden by a consultant who estimated that her mother had a life expectancy of 10–12 months:
And we said, we told her [hospital consultant] everything that had happened on the ward and [Mrs Curkovic’s daughter] then interrupted and said, ‘Can you please tell us, we know that nobody can tell us for definite how long Mum has got left, but some idea from weeks to not months, that’s what we were told, weeks not months’. And she said, ‘Well, they are not the specialist’, something to those effects, ‘They are not the specialist. Mum has got approximately between 10 to 12 months but I can’t guarantee that’. And I said, ‘But why, if they are not specialists in that field, did they even mention her life expectancy?’. If they had just left it and said an appointment will be made for you and you will be able to discuss this in further depth and hopefully the consultant might be able to tell you some sort of guidance as to how long Mum has got. But it tell us she has got weeks, not months; that was on the same day they told us they had found the cancer. I will be honest with you, I started looking at undertakers and things like that and oh my goodness all I could think of was funeral, funeral and it was horrible, it was just horrible.
Mrs Curkovic’s daughter
Mrs Curkovic’s consultant had continued to prescribe some treatment to stabilise her condition. Despite some kind of documented care plan having been drawn up while Mrs Curkovic was in hospital, apparently regarding the situations and conditions for which treatment would be given, Mrs Curkovic’s daughter said that the family had still not made a decision about DNACPR, even though they had been asked about this on a number of occasions:
I know that at some point, because they said they can take that decision out of our hands and I don’t want that decision to be taken out of our hands. I feel that I want to make that decision and I know that at some point we will sign the paperwork. But at this moment in time and I see that Mum is still strong and still well, I don’t want to sign it. You might think this is the wrong thing for me to say or a silly thing to say . . . but I just can’t do that at the moment. But as soon as I see Mum that she is getting . . . weaker and weaker and weaker, then I will say to (name), ‘I feel this is the time: are you agreeing with me?’.
Mrs Curkovic’s daughter
Their experience of the inaccuracy of professional prognostication was one reason for relatives to discount the forecasts they were given. This was also an area in which family members seemed confident in making their own assessments of their relative’s state of health and how near they were to death, based on their appearance and behaviour. This was one reason for reluctance to sign DNACPR forms before irreversible deterioration was beyond doubt; advance decisions about resuscitation were not considered to be appropriate or beneficial. Participants described feeling under pressure from hospital staff to make critical decisions about their relative’s future care, and also to accept professional judgements about the futility of resuscitation and continuing active care. These were distressing experiences, causing considerable doubt and uncertainty, especially when, as described previously, the patient subsequently outlived their prognosis. Although some participants resisted these professional judgements, others, including older patients, accepted them on the grounds that clinical expertise must be accurate and trustworthy.
Communication and language
Although acknowledging the uncertainty that characterises serious and prolonged illness, some patients expressed frustration that their concerns were not being addressed and that they were therefore ill-informed to consider what the future might hold. Poor communication and vague language, including what was perceived to be professional evasiveness and equivocation, contributed to uncertainty about diagnosis, illness progression, treatment options and prognosis:
. . . when he went in for his cancer appointment, if we asked him [doctor] ‘what is the stage, where are we, what are we looking at now?’. ‘Oh no, no, he is not at that stage now; you will know when he is at that stage . . .’. But how do you know when he is at that stage?
Mr Bashir’s daughter
Mr Cobbina had formed a much more negative assessment of his illness than was actually the case:
And then the consultant said to me, ‘Oh, yes that’s it, that will be it now, that will be all gone’, and it hasn’t. So, you know, you just don’t know what is in store for you and nobody knows how much time that we have. And, you know, it would be a good idea for consultants really to say, you know, to say it as it is. That, ‘Look, all the treatments have failed, I have got an aggressive cancer, we don’t know how long you are going to have’ or whatever. Then at least you know, and you can start preparing and be ready. But if they give you false sense of hope and say, ‘Oh yes, have this done and that should be it’. And because you rely on the consultants and the surgeons and what have you, thinking that’s their job, they do that day in day out, they know what they are talking about. So, we are relying on them and when it doesn’t work and then they tell you something different, you just don’t know where you are.
Mr Cobbina, third interview
However, the specialist nurse who had been involved in his care for a considerable time, and who described knowing the patient well, had no awareness of the nature and extent of his concerns:
We have always managed to discuss everything quite openly. And there has never been any barriers to communication I have not felt, between us. And he is a very, yeah a very intelligent gentleman that understands, you know, what everything is about.
Mr Cobbina’s HCP
Indeterminacy and professional equivocation, however motivated (e.g. whether due to genuine clinical uncertainty or from a concern not to undermine the patient’s hope and optimism), can thus serve to undermine patients’ confidence in clinicians and their relationships with them.
Some patients and FCGs felt that there were times when their ethnicity may have resulted in differential treatment and/or communication, although this was not a strong theme throughout the data:
I mean they are not overtly racist, but it’s their behaviour because they are not treating my mum the same as the English women that, the two English women next to her and opposite her.
Mrs Chandyo’s daughter, second interview
. . . probably because I am a single black male. . . . I look around when I am in the waiting room, how they are talking to other patients and what have you. It is totally different to what I am being treated.
Mr Cobbina, second interview
Some of the differential treatment noted by participants related to more practical aspects of care that held great import in whether they felt a sense of discrimination or acknowledgement of their particular needs:
. . . for BME [black and minority ethnic] people in particular, if there is no information, for example if you speak another language, there is no choice; you can’t make informed choices if you are not given the information.
Mrs Caprice, first interview
One FCG observed that professionals filter their dealings with patients and families through their own personal perspectives (‘cognitive screens’), and therefore may not fully appreciate their unique concerns, emotions and the like. The lack of close connection with the patient and their situation manifests in (mis)communication:
. . . the common factor is this, you are dealing with people whose cognitive screen is not in alignment with yours. And you may be saying the same thing, but somehow it’s not registering because there is something . . . it doesn’t match a particular profile of a person that screen is actually showing up. That’s my observation anyway.
Mrs Caprice’s husband, first interview
Most HCPs did not describe extensive experience of caring for ethnically diverse patients or the need to use interpreters. However, one participant observed that the professional team she worked in was itself ethnically diverse:
Really our team is quite diverse anyway, so we have got an Asian head of the team and so I think the patients that are Asian that come from a similar background kind of gravitate towards her, perhaps because . . . there is a less of a language barrier.
Mrs Campbell’s HCP
Several patients and FCG participants described effective communication with HCPs who could converse directly with the patient in their first language. Whereas patients may have long-standing relations with their GPs, in the secondary sector there was little chance of encountering the same individual during subsequent visits.
Translation issues
Most patients were routinely accompanied to medical appointments by at least one family member. Those who spoke little English were likely never to attend such consultations on their own. FCGs in the study indicated that offers to make professional translators available were either rejected or were not feasible within the time constraints, particularly in acute settings. Consequently, almost all translation reported to take place in health-care settings was completed by FCGs, and this was a strong preference. In a few cases, patients had access to a HCP, usually a GP, who spoke their first language and was able to explain and discuss options directly. This was felt to be particularly reassuring and made for better understanding of EOLC choices, in particular decisions about DNACPR. In addition to language challenges, two patients required assistance as a result of dementia, and two others needed help because of hearing and speaking challenges, as well as language challenges, compounding the efforts required from FCGs in providing translation in health-care discussions.
The discussion of EOLCP is intrinsically difficult, and may be more so through translators (whoever these may be). There is a risk of increasing what may already be a poor understanding of the meaning and significance of such critical issues. There is also the potential, when relying on family members to translate, for families to shape patient understanding and responses. It is clear that both HCPs and family can exert a strong influence on patient ‘choices’ if matters are filtered during, or become lost in, translation:
Mr Chahine’s HCP (second interview): So, we left the home that day having thought we’d had the conversation that [patient] agreed that he should have a DNACPR in situ. None of his care would change in any other way but [son] quite rightly wanted to discuss it with his other siblings. So obviously I wasn’t privy to the conversation he had with them, but he rang me and said actually they didn’t want the DNAR [do not attempt resuscitation] to be put in place. His father had misunderstood and he thought we were talking about him being on intensive care unit on a ventilator, on an invasive ventilator, that’s what he thought we were talking about and that’s what he wouldn’t want.
Researcher: So a complete misunderstanding?
Mr Chahine’s HCP: Well, I don’t know. I don’t know whether it’s the brothers, because I wasn’t there. I wasn’t privy to that conversation. It’s hard, isn’t it? I don’t know whether he – I don’t know.
Especially when translation is needed, it may be hard to establish the patient’s preference as they may be exposed to persuasion from both professionals and family. Accounts of both FCGs and HCPs indicated a strong professional orientation to family rather than the patient, particularly when translation was required. Mrs Curkovic had cancer and was also living with dementia, the result of which was the loss of English-language skills acquired over many years of living in the UK. Her daughters acted as translators and advocates and were purposely very selective about what they disclosed about her diagnosis to protect her from extra distress. In this case, in which FCGs were the sole source of translation, it was felt by HCPs that the FCGs were gatekeeping and that the patient’s autonomy was not fully facilitated.
Mrs Curkovic’s HCP described taking extra time and effort to try to prepare the family for the patient’s death. She was pragmatic and acknowledged the concerns of the family as legitimate areas for support while trying to empower the patient, in what appeared a delicate balancing act. The FCGs, however, felt much pressure and upset, when (acting as translators) they were asked to disclose details of her diagnosis to the patient, in front of HCPs, as this was counter to what they had decided was appropriate for their parent. Most patients, especially those who were older and communicated through translators, never saw HCPs in private and were always accompanied by at least one other relative. Although this could be seen as supportive and reassuring for the patient, it also potentially influenced what was discussed and decided on, and ultimately has the potential to sideline patient preferences for EOLC.
Some family members described feeling aggrieved that HCPs had handed them the task of undertaking translation and communication of bad news, including the responsibility for discussing DNACPR and other difficult issues with their relative. They questioned the appropriateness of this, given their own emotional involvement and personal responses to the sensitive matters being discussed:
So he [HCP] said, ‘Look, you guys need to take a decision as a family, you want to decide, we need to put a care plan in place for your dad, put a DNR [do not resuscitate] in place and things like that’. That was the hardest pill for me to swallow because I was like, I am going to have to talk to my dad about putting an end-of-life plan in place. I am going to have to talk to my dad about whether he wants to, if his heart stops, whether he wants to be resuscitated or not. And that was really, really difficult and I was driving home and I just rang my brother and I just broke down.
Mr Chandhary’s daughter, first interview
Family support
To engage with, and provide appropriate EOLC to, patients and families, HCPs need to understand the family support that is operating around the patient (see Table 2). Families displayed great diversity in composition, and availability and engagement of support. At one extreme, Mr Chitnis lived alone, estranged from his wife and family, with little contact or support from family members. At the other, Mrs Chawla lived with her eldest son in her daughter’s home, with many other family members visiting and providing support. Most cases occupied a middle ground between these extremes. Eight patients lived with spouses and sometimes other family members. Several cases included regular input from family living locally and some networks extended to virtual advice and involvement from members living at some distance, including those who lived abroad. Several patients mentioned receiving support from close friends in their community and from members of faith communities to which they belonged. Families varied also in their awareness and use of health and social services. One-third of the case study families reported accepting some sort of formal help. At least two others had turned this down. Older couples tended to be resistant to accepting outside help, even when the patient’s care needs were extensive and anticipated to increase, and despite their children’s encouragement to do so:
But, unfortunately, my mum is very reluctant to get any help and call anybody in. . . . We know that the offer is there . . . [but] as long as she can manage she wants to continue caring for my dad. And when the time comes, because she is in her 80s herself, and if the time comes she no longer is able to manage and care for him, then obviously we will have to get somebody to come in and help her along with the caring.
Mr Chahine’s son, first interview (providing care for both parents at home)
In terms of having professional carers in or having her go into a care home, it’s an alien concept to my mother. My mother’s culture is, and her background is, the family look after you. Is a bit different if she had been a lady with no offspring, with no children or no close family to look after her, that’s completely different. But when you have your own children or you have, say, close nieces or nephews, it’s expected and anticipated you look after your family.
Mrs Curkovic’s daughter–consultee, first interview (providing care for widowed parent at home)
Some families were open to the idea that they may need extra (outside) help in the future, although most wished to manage with family support until such time. Strong emotional bonds resulted in carers’ desire to provide all the patient’s support by themselves. Wives, especially, but also adult children, expressed concerns about being subject to censure for failing to show sufficient commitment to care for family members, especially parents and spouses, which would be demonstrated by acceptance of outside help. Several participants, usually wives or daughters, were fiercely possessive about ministering to patient’s needs because this discharge of family obligation was believed to be a way of acquiring religious merit:
Part of our faith is that we should be . . . be caring for the parents because that’s our door to paradise, our parents are our door to paradise. . . . If I want to get to paradise, I have got to, my way is through them. So you see the gravity and responsibility here, we wouldn’t feel comfortable handing that to somebody else.
Mrs Chandyo’s daughter–consultee
Some families had also experienced or anticipated that outside support might compromise patient dignity during personal care. Expressed concerns included the gender of carers or that timing of carer visits might not accommodate very specific religious and/or cultural requirements (e.g. for prayer or ritual preparation):
I just think she [mother] feels that somebody coming in and doing personal care with my dad, she maybe doesn’t feel quite comfortable about that . . . although she won’t come out and admit it, but I think that’s most probably at the back of her mind and that’s why she feels it’s better she does it herself.
Mr Chahine’s son, second interview (supporting parents in their own home)
. . . because we are vegetarian, strict vegetarians, and me personally, I wouldn’t like someone who is going to call and deal with someone doing meat stuff. I know they wear gloves and that, but I wouldn’t like that to touch my food and my fridge . . . I wouldn’t like it all mixed . . . I would prefer a like for like. Someone else like an Indian carer who understands and appreciates vegetarian people. . . . So, like very strict on the vegetarian; we don’t have any eggs or fish or anything like that. So, we would be worried about that, that would be a big issue for us.
Mr Chaganti’s wife, first interview (supporting husband in their own home)
This commitment to containing care within the family could foster a ‘self-sufficiency’ that potentially precluded looking outside the close family for support. It also intensified concerns about care that the patient received during hospital admission. Some families tried to replicate a home care model when in hospital, especially if translation might be needed or specific cultural requirements regarding food may exist.
Carer burden was often evident regardless of how care was organised: a range of experiences on this was shared. People were more or less willing, able, motivated or under pressure to provide care, which varied in their capacity and resources to provide. Patients often expressed a desire not to burden others, especially adult children who they felt had their own lives to lead, with many of their own family commitments. The input from some adult children was considerable, including cases in which the patient, and possibly their spouse, was co-resident with them. In other cases, there was much less support and some patients and/or their spouses clearly struggled.
Like case participants, BFCG responses regarding family care varied. Responses did, however, include accounts of the intensifying difficulties of providing EOLC as the patient’s illness progressed. These represent quite distinctive, reflective perspectives having ‘worked through’ the caring situation to its conclusion. Many bereaved carers, as with carers among the case participants, expressed a preference for family-centric care. However, there was, for some bereaved families, a realisation that their established and preferred model of caring was not necessarily the best fit for the situation they found themselves in prior to the patient’s death. This illustrated the evolving nature of caring models and also the eclectic model of caring that might result:
When my mother was diagnosed with dementia, I remember the consultant I spoke to at the beginning. . . . She said to me, ‘There will be a time when you have to consider putting her into a home’. And I said, ‘I don’t know about that’. And she said, ‘Well, it will affect your own family and your personal life’. I said, ‘We will just cross the bridge when we get to that’. And it did affect our life completely. My routine was when I come back from work at 6 a.m. I would freshen up a bit and drop my wife off to work, wait for the carers to come in . . . at the beginning we didn’t have the carers. . . . I had to find them to help Mum . . . then we had to get ready and drop my daughters off to school . . . and come back and get her ready for the day centre. That was a big relief for us . . . from 9 until about 4 she was at the day centre.
Mrs Bajpai’s son
This example encapsulates the commitment to maintain family-centric care, an acknowledgement that family life became very busy as a result (this actually included a change in work patterns to work night shifts so as to be available for the patient in the day), an eventual need for and acceptance of additional help from outside carers alongside accessing day care outside the home. These changes occurred over a prolonged period in this example, highlighting the evolving nature of each caring situation.
There are many factors that govern the way families organise support and that, ultimately, may affect support at end of life. Indeed, there appear to be complex, mixed motivations affecting choices made, as well as factors that are outside individual family control. The study findings also suggest that some families may have desired, or even been desperate for, much more help in supporting their relatives. However, they were hampered by lack of knowledge of the system and how it works, and by cultural constraints about the inappropriateness of accepting outside help:
We would try and persevere as much as possible . . . that’s generally what we would do unless, if it’s affecting our health. Recently my brother, he had sciatica . . . so we had to all pull in together, rather than saying actually we can’t, approaching some authority and saying we can’t cope and we need extra help. Instead we had to pull together and give him [rest] so he had his time to recover. So, it’s more that you have to persevere, there is no end.
Mrs Chandyo’s daughter–consultee, first interview
I can’t just leave her with any XYZ to look after her. Because I don’t think any XYZ will look after her the way I will. If that means that I will give up my job, I will have to; if that means I have to take unpaid leave I will do. But I can’t leave my mum with any XYZ person and rely on them. Because I have always had more to deal with when I have left my family member, whether it’s in hospital, whether it’s in the nursing home. I have always had more pressure, I have always had more stress. Because I can’t rely on that person doing the right thing.
Mrs Chadha’s daughter, second interview
As Mrs Chadha’s daughter illustrates, another constraint on accepting care and support outside the family was lack of confidence and trust in staff and services to provide appropriately skilled, tailored and culturally appropriate care. The result was that, far from providing relief and respite, accepting such help could cause family carers additional stress and anxiety.
Decision-making
Patient and FCG participants had diverse perspectives on the locus of decision-making and the extent to which patients and family members wanted to engage in decisions. This was shaped by the nature and severity of the patient’s illness, whether or not the patient had retained capacity, and by the availability and configuration of family support. Some patients, including those who were older and those with strong religious or cultural traditions, were described as being in charge of their own decisions. These were respected by their family members, who might also have been involved in shared decision-making and discussion:
Dad makes the decisions. We have not taken a single decision for him because the thing is, although he was, for some time he was physically impaired, he wasn’t mentally impaired. . . . He is that traditional Indian man where he is the head of the family, he is the person who supports everyone, not the one who gets supported. And he has been like that all our life, for us he has been that pillar of strength . . . I think that’s overall his family and his religion like his faith make the certain choices that he does.
Mr Chandhary’s daughter, first interview
At the other extreme, some patients, although respected for their age and position in their family, devolved decisions to particular members of their family in the knowledge that they could trust them to make decisions in their best interests:
Yes, they [sons] were doing the communications. But with my mother-in-law, because I think, because she was older and . . . they respected the sons so much as well and they never really wanted to, she never even spoke to her sons about . . . her illness . . . or what she should do . . . she just left it to them to make the decisions and everything and she just relied on them, you know. And she knew that they would make the right decision and that’s why she just left it to them and never spoke about it. And they all respected her . . . that’s how it was, you know.
Mrs Bansal’s daughter-in-law
Another type of arrangement involved wider family discussion and involvement, even if one or two individuals took on the major role in liaising with services and HCPs. It was notable too that, within some families, even if one or two FCGs took the lead in making decisions and liaising with HCPs, there was a wider forum of family involvement, and a very deliberate discussion and sharing of information about the patient’s illness and the decisions that were made about treatment:
Mrs Chawla’s daughter (first interview): At that stage Mum is unconscious, so it’s a family decision; whenever we have been asked, she has been out of it.
Researcher: So, if the doctor were to broach those discussions [DNACPR] with you . . .
Mrs Chawla’s daughter: I would say no, the whole family would say no.
Researcher: So, what I am trying to get at is it would very much be the whole family would be involved in that decision-making process?
Mrs Chawla’s daughter: The last time they approached about it to my eldest brother, he was on the phone straight away to me to say, ‘They are talking about DNACPR’, and I am like, ‘No, it’s not happening’. And they were all happy with that decision that it’s not happening.
Most patients had at least one supportive family member who provided care and who often became the spokesperson for that patient, although, in a few cases, little FCG support was available. Spouses tended to be heavily involved, except if they had severe health problems of their own. The local availability and involvement of supportive informal caregivers shaped the way they typically communicated and allocated responsibility for decisions:
Mr Chahine’s son (second interview): I am the eldest but I don’t like to make any decisions on my own, I don’t want the other brothers thinking I am taking over and doing what I think is right for me and keeping them out of the situation. I wouldn’t do anything without having a discussion between us. So we all agree on something and we are all happy with what is to be done. . . . So, we would, all of us would be aware of everything that is going to go on.
Researcher: So it is very much a joint decision?
Mr Chahine’s son: It is a joint decision.
Researcher: And then you would speak to your parents as well?
Mr Chahine’s son: Yes.
I prefer everything to share with my family; they are very, very helpful. I have not hidden anything from my son and because . . . I can’t use my hands . . . can’t do something, banking . . . then my son does it for me and I trust them there. And anything, it’s all written on the papers that they are authorised to take the decision; if I am in the hospital, my wife or my children individually can take decisions themselves without asking me because I know they will do the right things for me.
Mr Chahine, second interview
Preferences varied regarding disclosure and discussion between patient, family and HCPs. This resulted in some patients and/or families feeling that HCPs had little or no place in any decision-making for EOLC:
You don’t tell a stranger, like a doctor, he is a stranger. I wouldn’t tell him my business. No, I wouldn’t . . . I would say, ‘I am sorry, but that’s my family and my business so I can’t tell you’.
Mrs Campbell, third interview
As mentioned previously, there were instances when either patient or family members wished to restrict information about certain aspects of prognosis and any decisions arising from these. This was largely to protect others from the impact and the distress this would cause (e.g. as in Mrs Curkovic’s case). However, a consequence of selective disclosure was that when older patients relied on family members to translate and mediate communication with HCPs, the extent to which the patient’s voice in key decisions was heard and accurately represented was often unclear.
Religious beliefs and influence on end-of-life care planning
Several patient and FCG participants considered that advance discussion or decisions about treatment or EOLC were irrelevant and even inappropriate because they believed that the timing and manner of their death would be determined by their god:
. . . when they said end-of-life palliative care, a lot of people think, ‘Oh, they are giving my mum such and such a time’. But then the only thing that went in my head is they are not God; that’s the only thing that went in my head, they are not God, they don’t know when anyone is going to die.
Mrs Campbell’s daughter, first interview
Most HCP accounts indicated that they did not employ greatly different approaches to communication and care of patients on the basis of their religious or cultural beliefs. Several professionals noted that there could be a discrepancy between the stated commitment to accept or reject treatment on the grounds of religious belief and the subsequent decisions made by the patient and family:
And you can talk to them about how their breathing will just fade and fade until they can’t breathe any more and then they will die. And there is nothing . . . resuscitation isn’t a treatment that will work. So, it will be really nice for him or her to stay at home surrounded by his family. And sometimes they understand that. Sometimes they surprise you and say even though they have been saying, ‘leave it to Allah’, they will then have interventions.
Mr Chahine’s HCP
There were concerns about death in hospital in relation to the need to manage dying in accordance with religious observances. FCGs reported that attendance of a large numbers of visitors was extremely important in some faiths in ensuring a ‘good passage’ when someone was close to death. Positioning of the bed towards Mecca was cited as a further example of practical steps that may be needed to support religious affiliation. Diet, as mentioned previously, was also a source of some concern. These were all concerns raised by some patients/FCGs, but little or no mention of these came from HCPs.
One area of concern for Muslim families was the need for a death certificate to be issued very quickly to enable burial to take place within 24 hours:
As soon as we understood that this was my dad’s last time we had, we basically got everything in place before he passed away. Because with Muslim funerals they are so fast, but we did our own research; we found out that if our GP wasn’t around to sign off his death certificate that a Macmillan nurse could do that or somebody from Macmillan could do that. But that wasn’t made clear to us, we had to find out, we had to say to the doctors, ‘Right what happens?’.
Mr Bashir’s daughter
Participants described the need to remain vigilant, especially during their relative’s hospital admissions, to ensure that care did not transgress cultural and religious practices, and the need to be proactive in ensuring that these practices could be observed as far as possible.
Interaction with professionals and services
Participants’ accounts revealed a very wide range of experiences of contact with health professionals and services. This was shaped by the nature and duration of a patient’s illness and by the organisation of services. It was also determined by wider experience of illness and care received by family members in the past. Patients and families varied greatly in their understanding and the ease with which they navigated a complex system of health care and succeeded in establishing good and enduring relationships with HCPs. Older patients often relied on adult children as translators and systems navigators, some of whom were clearly very skilled advocates for their parents. When this was not the case, it could be hard to ascertain whether or not patients had a clear understanding and awareness of the content of medical consultations.
Most patients and family members expressed overall satisfaction with treatment, and some were extremely positive, notwithstanding specific instances of dissatisfaction and bad experiences. A few were deeply critical. Some families adopted a general attitude of trust in professional expertise, whereas others were more critical and questioning. Inadequate or confusing information was a common source of complaint, especially when participants felt that they had not been adequately informed or had received conflicting information from different staff or services. Frustration about what was perceived to be professional evasion or inability to give clear and definite information about a patient’s illness progression has been described previously. However, some participants described distressing experiences when precise prognoses had been given, but subsequently proved to be inaccurate and misleading.
In addition to this, patients and FCGs were critical of the bureaucratic appropriation of their time, especially when they knew this was precious and short. Relatives were involved in the extensive work of supporting the patient. They accompanied their relatives to appointments, often a long and arduous process, involving complex journeys and reliance on others to provide transport, perhaps with young children in tow. This might be followed by a long wait to see a clinician or undergo tests, learning the results of which might necessitate another visit. This was especially frustrating when such visits seemed to serve no obvious or productive purpose and the family felt that they learned nothing valuable as a result. Meanwhile, participants had to juggle medical appointments with many other work and family commitments:
So I have to take her [patient], or my husband if he is off on his 4 days off. . . . I am a little bit struggling when you talk about appointments, because if the NHS has decided that there is no further treatment for Mum, yet they still keep giving her appointments and drag her out of the home without any reason, because they are not treating her, they just want to know how she is getting on. But I haven’t got time to waste like that; neither has Mum because she just feels very strongly, ‘Why don’t they want to treat me?’.
Mrs Chadha’s daughter, second interview
A strong theme running through the data was participants’ frustration over not ‘being known’ within the system, of interacting with a large number of different individuals and services, and constantly having to tell and retell their story to individuals who displayed no knowledge of the case and were likely never to be seen again:
I think they need to get their act together, look at the notes and see where best to move forward. And have that information before I come to the appointment . . . Not saying, ‘Oh, I don’t know, I don’t know, I don’t know’. You know, what I find is they are looking at the notes when I arrive there and they haven’t really got much information . . . they really need to look at the notes, find the information have a meeting how we can progress forward. You know, have a small group of people that know about me and know about your circumstances, know about what treatment we can give you and what the outcome could be, with all the side effects so that we can make a decision.
Mr Cobbina, second interview
The biggest stress for me is having to repeat myself over and over again with Mum’s medical condition. But whether she is 999 going to A&E, whether she is going to the doctors, whether she is going to the consultant they should have Mum’s record. NHS should keep a record on the system: why am I repeating myself everywhere? . . . I am saying those words over and over again to so many NHS staff and it hurts as a family to repeat that because it’s just reminding me that she is going. It’s not nice. . . . I struggle to do that more than looking after Mum to be honest . . . that’s really annoying for me.
Mrs Chadha’s daughter, second interview
Another source of dissatisfaction was the experience of poorly integrated care. Some participants expressed a sense of falling through the cracks between services that were not joined up or well co-ordinated. This was a particular problem for cancer patients following discharge from active treatment. They felt a sense of being left in limbo after contact with HCPs came to an end, unless they had needs, such as control of pain, that occasioned referral to palliative care. However, several HCPs reported that, even after referral, patients were not always accepted by the service:
So, we were trying to contact the specialist nurse who, when you see them the first time at the cancer unit, they say to you, ‘This is your nurse’s number. Ring her any time and she will get back to you’. Well, no they don’t get back to you . . . and you are trying to find answers; you are trying to say, ‘Is this end of life . . . should we call family? We don’t know what is happening’. To get an answer from anybody was absolutely mind-numbingly not possible.
Mr Bashir’s daughter
The challenges from when a patient gets treated in hospital to when they die, there seems to be a gap in between where there is no cancer treatment available. I think they sometimes feel like they don’t know where to go to. There is nobody that sees them in between. . . . When we try to refer to palliative nursing in the community, they won’t just go and see them. Even though they could be 2 weeks away from passing away. . . . I find that difficult because they don’t have pain or they don’t have the typical palliative care needs . . . and I feel like they are missing out on the really good palliative care end.
Mr Chaganti’s HCP
Participants described a lack of information about services that were available to them. Their ability to navigate the system was often dependent on chance encounters, outside as well as within the system, and also the learning acquired through prior experience:
Yes, no one ever mentioned that to me. I found that out by a complete chance that there is such a thing for paraplegic people, there is such a thing called NHS Complete Care.
Mr Chaganti, second interview
Yes, because we didn’t really think about grants and whatever, we didn’t even really know anything, all we knew was that Dad was unwell. So, Mum has actually got quite a lot of the privileges, well not the privileges, she is like . . . Dad was first run at it so we were totally clueless on what sort of grants, what benefits, anything like that you could provide. We just thought ‘Dad is unwell; we will look after him, do what we can’. And it turns out we lost out on a lot of things because they just don’t tell you.
Mrs Chawla’s daughter, second interview
Alongside the struggle to get to grips with the intricacies of the system and find out about services and benefits that were available, participants described their need to exercise vigilance over a patient’s care. This was especially necessary in relation to religious and cultural requirements relating to ritual, diet and personal care. Concern about such matters was one reason why participants perceived hospital admission to be undesirable and even risky:
And then this blood sugar thing that was difficult to get the, to the point where even the cook was not made aware that he had diabetes, she was giving him puddings. It was only when my daughter went and said, ‘You do realise my father has got diabetes?’ . . . It’s like there wasn’t that awareness from the whole thing. I mean, we had, as a family, to make them aware at the hospital.
Mr Bharti’s wife
Generally she [patient] shies away from men and would prefer females to be responsible for her care. I think when we went onto the ward it was quite a traumatic experience for her there because we weren’t allowed to choose . . . [who] was able to change her. We didn’t know what our rights were and she felt her modesty was encroached and we weren’t able to do anything about it.
Mrs Chandyo’s daughter, first interview
The value of a key worker to help families navigate the system and think forward to future developments and decisions was considerable, but the availability of these was very variable and seemed largely determined by the nature of the illness. As indicated previously, continuity of care and specialist nurse support were well established for MND and haemophilia and some other areas, but notably not for cancer, for which patients were usually seen by a variety of different services and personnel that lacked effective interagency co-ordination or communication:
We help them find their way round the system sometimes because sometimes it’s easier for carers to ring in to us rather than think who they need to see. Because there can be at least 10 health-care professionals involved with somebody with MND, so it’s a very complicated system if you don’t know it, if you can’t navigate round. So, we help them a lot with that.
Mr Chakraborty’s HCP
Health-care professionals varied in their awareness of the difficulties patients and FCGs experienced in navigating health care and finding out about available support. However, they rarely, if ever, spontaneously commented on ethnic or cultural diversity as a relevant factor influencing their practice or the patient’s experience of care. Even when this was raised as a topic for discussion in the interview, few professional participants acknowledged this as a significant factor in the delivery or experience of care, in comparison to patients from a white British background:
I don’t really make any distinction between patients of different communities. I am sorry, I can’t really tell you from one community over another. . . . Yes, I can’t give you any specifics about BAME [black, Asian and minority ethnic].
Mrs Campbell’s HCP
Generally, I have found it harder to talk about advance care planning . . . I have found over the years that people of an Asian background or minority background are less inclined to want it in place.
Mr Chahine’s HCP
Several patients and FCGs did express concerns, or at least suspicion, that ethnicity had been a negative factor affecting the treatment they received. However, complaints more often concerned dissatisfaction with what was perceived to be poor treatment, poor communication or medical incompetence, which were not explicitly linked to the patient’s ethnicity:
And it was a minefield to find out who’s responsible for what. . . . Luckily, I was able to pin down the doctor and say, ‘Now, if he is a, if it’s a pre-existing condition like the blood pressure, low blood pressure, or the diabetes or whatever it is, who is responsible?’. Then they told me this bit is the hospital’s responsibility, this bit is the . . . responsibility of the doctors. I had to almost make a case to fight to make sure they knew that; they were not always communicating with one another, that was very difficult. Because the hospitals were not communicating with the doctors on the ongoing things. . . .
Mr Bharti’s wife
So, the next morning I got there and the sight of him really disgusted me. He was in a pool of urine sleeping on the bed and he hadn’t eaten anything. . . . He was so angry . . . he was very, very upset and to see him like that, because I have never ever known, because I used to give him shower every morning and he used to wear fresh clothes every day. And I said, ‘This is not on’. I said, ‘I am going to take him right away’. So, I said, ‘No, I am not waiting for anybody. I am just going to take him’. The nurses came running. I said, ‘No. I am not taking, I am not going to accept this’. I said, ‘This is, I am going to make a complaint and I am not going to let this go.’ I said, ‘He hasn’t even had his breakfast. He is diabetic and he has not had his breakfast. It’s 10.30 now’.
Mr Bagri’s wife
These extracts illustrate the very proactive role of some relatives in acting as advocates for the patient. However, patients who lacked access to the social and cultural capital required to exercise such vigilance experienced greater difficulties in successfully navigating a complex system of care that they experienced as bureaucratic and confusing.
Reflexivity
During case study interviews, most participants were asked if the experience of taking part in the research had influenced them in any way. In three cases, participants explicitly said that they had been prompted to reflect and to think a little more about what the future might entail (this included the idea of thinking ahead about end of life). In five cases, people described some therapeutic benefits of taking part in the research, including having a chance to air their feelings about their experiences to date. These included feelings of being quite isolated as a patient or carer or about the burden of caring generally. Others felt that they had benefited from a chance to vent frustrations at their situation and sometimes with services. In a couple of cases, participants’ reflections had led them to considering further practical help they might go on to seek. At least two HCPs expressed possible changes in their practice, in particular related to knowing more about their patients and their potentially diverse needs. One HCP indicated that they had further reflected on opportunities that might arise to introduce the idea of thinking ahead to patients, with reference to interactions with a former patient. Another reflected further on an instance when an opportunity had arisen and was taken up by the HCP: a plan loosely agreed, but then this was subsequently over-ridden by family members.
Conclusion
This chapter has reported the key findings from this qualitative, exploratory study of the lived experiences of patients and their families. The patients and FCGs who took part in the research represent a wide range of ethnically diverse groups and the inclusion of nominated HCPs in the case studies has enabled a triangulation of different stakeholder perspectives. The cultural and illness diversity of participants was paralleled by a very wide range of reported views and experiences of EOLC. Most participants were broadly satisfied with the care they had received, notwithstanding some negative experiences. A few were extremely critical. Reported shortcomings most often focused on poor communication, lack of information and unco-ordinated care, which have been widely reported elsewhere. 23,72 A few participants felt that they had experienced discrimination or experienced poorer quality care because of their ethnicity, but this was not a strong theme throughout the data. The findings will be further discussed in Chapter 7 and integrated with those of the following chapter related to WS3.
Chapter 6 Workstream 3: findings from public and professional stakeholder workshops
In this WS, we facilitated public and professional stakeholder discussions about the findings from exploring the experiences of patients, their families (FCGs) and professionals (HCPs), derived from findings considered in Chapter 5 (WS1 and WS2), and the implications of these findings for HCP practices. We explored the views of participants on the barriers to and enablers of discussing deterioration, dying and EOLCP with ethnically diverse patients, FCGs and HCPs and sought to identify information and training needs to support best practices.
Between December 2020 and the end of April 2021, we held 11 virtual, 1-hour discussion workshops with 37 participants. Another 13 participants completed workbooks. Each workshop and workbook was tailored for the stakeholder group [individuals from an ethnic minority community (laypeople), community or faith leader, academic, HCP and educator], but all included discussion of fictionalised stories that were developed, as discussed in Chapter 2. Although these stories were fictionalised, they were based around the real-life case studies, and the narrative themes that they incorporated were mapped to the findings from WS1 and WS2.
Details of the stakeholder participants in the workshops are shown in Table 9, and of those completing workbooks are described in Table 10. The generic and potential ethnically diverse themes of the stories used in the workshops and workbooks are described in Table 11 and the stories are presented in Appendix 1, Boxes 3–11.
| Stakeholder role | Workshops (n) | Participants (n) | Stories discusseda |
|---|---|---|---|
| Layperson | 2 | 8 | 1, 2 and 5 |
| Community or faith leader | 1 | 2 | 1 and 7 |
| Academic | 1 | 3 | 1 and 6 |
| HCP | 5 | 18 | 2, 4 and 8 |
| Educator | 2 | 6 | 8 |
| Total | 11 | 37 | – |
| Stakeholder role | Number completing workbooks | Stories discusseda |
|---|---|---|
| Layperson | 6 | 2 and 4 |
| Community or faith leader | 3 | 3, 4, 6 and 7 |
| Academic | 4 | 1, 3, 4, 6 and 7 |
| HCP | 0 | – |
| Educator | 0 | – |
| Total | 13 | – |
| Story name | Generic themes | Ethnically diverse themes | Other themes/keywords |
|---|---|---|---|
| Story 1: Jay (patient) | It’s not the right time yet The future is not in my hands I don’t want to think about that Fear of deterioration Maintenance of hope |
Activist Multiple family deaths Delayed diagnosis Mistrust of health systems: have to fight to get help/equality Faith-based approach to future: miracles will happen Role of eldest son Sense of duty |
Formidable Intellectual Frightened Autonomy: strong sense of who he is and what he wants State of readiness |
| Story 2: Ibrahim (patient) | Resuscitation decision-making Advanced non-malignant comorbidities |
Decisions take time to think about Duty: to god, to family Duty of care by family Religion and how life is lived Health literacy: understanding DNACPR Concept/clinical: what will happen in his illness/decisions he will face Collaborative decision-making Language barriers/interpreters/EOLCP discussions through family members |
I don’t want to talk about it Is it allowed in Islam? Social pressures and stigma Carer’s burden Expectation that HCP to make the decisions in time of crisis Ambiguity of views on decision-making and wanting to talk about it |
| Story 3: Patience (patient) | Ready and waiting Autonomy and choice, including desired but impossible choices Too early/prognosis uncertain/treatment ongoing Conflicting perspectives of patient and HCPs: missed opportunities Very little knowledge of patient and their home situation Carer burden Lack of information about support Perceived harsh and cold discussion of dying in crisis situation |
Patient’s opinions conflict with cultural ‘taboos’ (serves to isolate from even ‘close’ family who could help) Are HCPs treating this patient just like any other (i.e. equality and diversity means treating everyone the same, but thereby there is inequity)? No-one knows much about her family situation, so may not even think about ethnicity being important Access to services: generally, later maybe because of less information in their networks EOLCP is about funerals/after-death preparations. Social persona based on need to integrate into expected UK cultural norms |
Individual/independent response alongside cultural affiliation Equality and equity |
| Story 4: Adamma (patient) | Poor record systems Late diagnosis Previous poor health experiences Misconceptions/miscommunication Non-malignant illness |
Such discussions are a family matter Delayed diagnosis Mistrust of health-care systems Bad karma/evil forces Faith-based approach/thoughts Spiritual preparation for life after death |
– |
| Story 5: Delun (patient, but told by son) | Misconceptions/miscommunication Multiple family losses Carer burden: needing to take leave |
Isolation of someone who does not have English as a first language, within health-care systems and within his neighbourhood Language problems affecting ability and confidence to attend for treatment Mistrust of health-care systems Burden of responsibility on a young adult’s shoulders: missing work, affecting family economics possibly/carer’s burden Emotional burden for the FCG as interpreter, brings back previous sad memories Poor provision of interpreters, using who is available, unreliable system Misunderstandings arising from poor interpretation in very important areas of discussion Mistrust and lack of confidence in the system from patient as a result of previous misunderstandings Possible indignity that results in not being able to communicate what you need for personal care |
|
| Story 6: Shimbira (BFCG) | Missed opportunities Positive experiences of how information is delivered and communicated |
Strong faith Close family Delayed diagnosis Positive and negative experiences of HCPs and hospital Food is important in a spiritual way Family trust gained by HCP. Makes for easier EOLCP/EOLC discussions |
Gaining trust; peer support |
| Story 7: Kozal (patient) | The future is not in my hands Carer struggling Fear of morphine |
Such discussions are a family matter Delayed diagnosis Mistrust of health-care systems Faith-based approach to future Beliefs about use of morphine Evil and its reality in people’s lives as a force Spiritual preparation for life after death |
A battle to be known Not afraid of death Less common religion/community |
| Story 8: Mufaro (patient) | Stay positive Fight, don’t give up Selective listening/only positive interpretation Differing family approaches to the situation |
Expectation of strength owing to migration experiences Faith-based approach to future: miracles will happen Prayer In god’s hands Wrong to talk about dying Attitude to HCP Unrealistic expectations |
Chinks in his coping strategy Tension in family/community Openness/lack of openness |
Participants were asked to consider one or two stories and asked questions around the following key areas:
-
What are the ‘generic’ issues?
-
Are there any specific issues related to ethnicity, culture or faith?
-
How does an ethnically minoritised background overlay/increase the complexity of the generic issues?
-
How can professionals effectively engage with patients and families in EOLCP discussions in the cross-cultural context?
Stakeholders were also asked to discuss key themes presented in the stories. This included, but was not limited to the following:
-
Trust and mistrust: how do we help HCPs develop the skills to gain a patient’s trust?
-
Talking about dying: how do we help HCPs learn how to explore state of readiness and acceptability of having EOL discussions?
-
Being known: how do we equip HCPs to ‘get to know’ patients?
Table 11 presents the generic and potential ethnically diverse themes of the stories used in the workshops and workbooks.
As described in Chapter 2, the findings have been collated and analysed using a pragmatic approach to thematic analysis and are presented below under the two key areas of stakeholders’ views, first on the barriers and second on the enablers to ethnically diverse patients, FCGs and HCPs engaging in EOLCP. Key themes are also italicised below, and illustrative examples that participants shared about their experiences and that supported their views are discussed.
Barriers to engaging in end-of-life care planning
Religious beliefs, community pressure and cultural expectations
The key barriers to EOLCP suggested by laypeople and community and faith leaders were religious fundamentalism, community pressure and cultural expectations. Story 1 was viewed as an example of religious beliefs preventing EOLCP. Participants discussed how the story highlighted that the patient was ‘holding onto miracle’, which suggested that it would be difficult to break through such beliefs. They acknowledged that, although the patient in the story was terminal, he had not accepted that himself, ‘so he will make it difficult’. There was also the suggestion that community pressure and cultural expectations had an impact on a patient’s ability to accept a terminal diagnosis. There was also a strong sense of duty that the male has to look after the family, which was viewed as a reason why the patient, as the male figurehead, was not accepting his terminal diagnosis, ‘as he thinks he has to be strong for everyone’.
Lack of trust
Laypeople and community and faith leaders also acknowledged that previous negative health-care experiences meant that a patient was reluctant to have treatment, which had an impact on trust, or more significantly, lack of trust. Lack of trust of professionals and organisations was viewed as a key barrier to EOLCP by laypeople, community and faith leaders and HCPs. One of the participants in the community and faith leaders stakeholder workshop talked about his own experiences and stressed that doctors took decisions without permission from patients and merely asked patients as a formality with reference to the decision about resuscitation. Academic participants also recognised that past experiences could lead to misconceptions about medications for pain based on witnessing the end-of-life experiences of relatives. Time taken to have EOLCP discussions, along with effort to get to know the patient and continuity of care, all had an impact on ‘lack of trust’.
Communication needs and inaccessibility of language
Inability to address communication needs and the inaccessibility of language were highlighted as key barriers in EOLCP by all stakeholders. All recognised that ethnically diverse patients may have additional communication needs linked to both the challenges of a language that is not shared by the patient and the professional and mutual understanding of terminologies and concepts that need to be addressed. Participants discussed how the patient in story 2 could not speak for himself to the professionals because of language barriers and was reliant on his family to speak and interpret on his behalf. One community and faith leader stakeholder stressed that there is a lack of understanding from HCPs for people who cannot speak English. He went on to stress how, when people go through trauma, they revert to their first language. HCPs recognised the need to move away from using family members to interpret. However, using other avenues, such as NHS language line services, was viewed as being difficult and time-consuming. A HCP participant suggested taking a team member along with you who had the relevant language skills, but acknowledged that this was not always feasible because of other work pressures.
Stakeholders also recognised that inaccessibility of language, use of terminologies such as ‘end of life’ or ‘advance care planning’ may not be appropriate or comprehensible for patients or their families. Lay stakeholders stressed that many people may feel overwhelmed with options, stressing that it could be very hard to try to process all relevant information.
Lack of cultural and religious literacy
Lay participants also talked about the need for HCPs to have cultural awareness and sensitivity, stressing that in ‘our culture we don’t talk of death’. An example given was that, for Asians, talking about death is seen as a bad omen. One community and faith participant talked about HCPs as having lack of cultural and religious literacy, referring to his own personal experiences as a Shia Muslim. He stressed that his beliefs meant that he or his family ‘do not take DNACPR decisions’ and the hospital found it difficult to understand this. He went on to state how the moment he started talking about religion, the doctor was ‘put off’. Both community and faith leader stakeholders stated that HCPs should apply cultural sensitivity and humility in supporting patients:
HCPs look at life from a Western lens, which conflicts with some cultures, such as some Asian communities who would try their best and give the patient water even to the point of death, which is considered good for quality of life. Whilst in a Western culture the patient is alone to die in peace: let’s leave her in a corner – she will starve and die; that is peaceful.
Preconceived stereotypes and own agenda
Health-care professionals recognised that they often have their own preconceived stereotypes and own agenda, with one participant stating ‘you have to make yourself stop and listen’, and others recognised the need to take every opportunity to hear the patient. As one participant emphasised, despite there being a whole crowd in the room (family members), it was important not to forget the patient. The patient may still have capacity and it was important to have a one-to-one discussion. Community and faith leader stakeholders stressed that it was important to understand individual family background and dynamics, as some patients may be intimidated by other people and fail to express their personal wishes and beliefs. The view was that organisations needed to take time to understand patient and family attitudes, faith dynamics, and the pressure patients and their families are going through. Equally, it was important to respect patient and family wishes and dignity, as one community and faith participant stated it ‘is not upon any individual to decide when someone is dying; instead HCPs should consider individual dignity and respect’.
Lack of training, opportunities and time
In general, HCPs recognised the importance of family dynamics, but they also needed more resources and training. They stressed that they were not taught about how to deal with family dynamics. As one participant stated, ‘In advance care planning it’s about dealing with the patient, not family’. Lack of time along with lack of opportunities were key challenges discussed by HCPs concerning attempting to approach the subject of EOLCP and any patient or family misgivings, with some HCPs recalling better opportunities to discuss EOLCP planning than others. Whether or not all opportunities to engage with EOLCP were always recognised was dependent on a HCP’s experience and confidence to broach the subject. One participant stated that their confidence and experience prompted them to ask, ‘Do you have a belief system?’, finding that this ‘opens up a new door’ in dialogue. Furthermore, they stated that ‘while HCPs are reluctant to ask, in my experience patients are OK being asked about religious beliefs’. HCPs also questioned whether ‘end of life’ was the best term, as there is a need to make language more positive. One HCP talked about the need to change language and move away from ‘end-of-life’ drugs and paperwork as these ‘can make people fearful’, a suggestion being to change to ‘anticipatory’ drugs.
Enablers to engaging in end-of-life care planning
Trust
Educator and academic stakeholder participants considered HCPs developing the trust of the patient and their family or more significantly ‘enabling trust’ as key in enabling EOLCP. Academics stressed that time, effort, continuity and knowing the patient were key factors in developing this. They also stated that relatability, which is ‘how HCPs make person-to-person connections’, supported their ability to build trust. Getting to know the patient, to understand what a good death meant to them, was key. Otherwise, as a HCP, ‘you can have good intentions but still provide suboptimal care’. Educator stakeholders stressed that humility in building relationships was a key enabler of trust, stating that HCPs needed to accept that they may get it wrong, so they should be reflexive, learn from mistakes and develop their own approach.
Effective communication
Health-care professional participants recognised that building trust was also based on their ability to establish rapport by developing effective communication. An example was given of taking visual cues: ‘If there are shoes in hallway, then I take my shoes off’. HCP participants also recognised that they needed to embrace opportunities to establish shared understanding. As one participant stated, they needed to ‘make sure everyone’s singing from the same hymn sheet’. Hence it was important to explore patient and family understanding of prognosis, both long and short term, thereby setting realistic expectations ‘about what we can offer’. Effective communication was key, and all HCPs and lay participants agreed that there was a need to use professional interpreters to achieve this goal, as opposed to family members.
Developing a personalised approach to end-of-life care planning
Academic and HCP participants stated that there was no one ‘best’ time for having discussions about the illness getting worse and dying. Instead, taking a staged or staggered approach was viewed as the most favoured approach to EOLCP. Lay participants acknowledged that HCPs should be honest about prognosis to patient and family, but also stressed that it is important for HCPs to respect patients’ and families’ wishes, preferences and decisions. As one lay participant acknowledged, ‘EOLCP is a constant back and forth and you will not have an answer straight away and it is about building a trusting relationship’. This was reiterated by academic participants who stated that the timing of end-of-life discussions is personal. Furthermore, academic participants indicated that evidence suggests that HCPs need to take an individualised approach to EOLCP, avoid acting on stereotypes and assumptions, establish the right person to liaise with and establish a patient’s choice list.
The fact that not everyone wants to have the EOLC conversation was also something that HCPs needed to accept, as quality of life means different things for different people. Lay participants stressed that it was important to understand what is quality of life to individual people. Some patients will go to any length to stay alive, whereas others will evaluate whether or not it is worth it and choose to be comfortable and to have time with family and friends. HCPs need to establish what is acceptable for each individual. They need to establish a patient’s limit and ‘discuss what he is comfortable with when it comes to his EOLCP’. Hope is also interpreted differently. For some people, hope means to stay alive at all costs; for others, hope is ‘to be able or allowed and supported to peacefully pass away’.
Knowing the patient
Knowing the patient or having a shared understanding or commonality in cultural background was viewed as an enabler, but, equally, being self-aware and reflexive was regarded as key, thereby acknowledging that one’s own belief system may be different (regardless of any presumed commonality) and not approaching patients with preconceived ideas. A person-centred approach was viewed by all stakeholders as key in terms of knowing the patient and understating what matters to them. One community and faith leader stakeholder suggested that this was particularly important with older ethnically diverse patients: ‘Most people of their age are afraid to speak in English, but actually can understand, the other thing is his faith: so focus on his needs and how we can help him with those needs’. The community and faith leader stakeholders also stressed that HCPs need to know a patient’s daily routine and need to ask key questions about this: Did they meditate? Rest? Did they have any contact with family? What was their environment like at home? These factors were seen as playing an important role in patients’ EOLC preferences. As with academic stakeholder participants, lay participants stressed that it was important to establish the patients’ choice list, indicating that this was key in opening up discussion about EOLCP. Instead of HCPs doing a checkbox exercise with own checklist, HCPs need to establish what really mattered to patients and their families.
Working with a patient and their families
There was also a sense in discussions of the need to work with the family carers as opposed to against them. Hence, it was important to validate the carer’s role. This was viewed as being particularly important when there is an element of mistrust of health services from the patient due to past experiences and it was important for the HCP to establish family carer support.
Empowering patients and being an advocate for the patient by giving patients control are key in helping to build trust both with the patient and with the family: demonstrating a commonality of intent to do the best for the patient/loved one. It is also key to empower a patient by giving them ownership to direct what is discussed with them and what is discussed with the family or other designated person. However, lay stakeholders stressed that it is important not to assume that family share the same beliefs. Hence, recognise that, even when people share the same faith, they are likely to have different views regarding their health and treatment.
It is important to establish the key contact person for the individual patient and family. Community and faith leader stakeholders acknowledged that it is important to know who the right person is to liaise with, and not to assume that the next of kin is the person consulted for all matters. As one stakeholder stated ‘Healthcare setting should have someone who is a link between hospital and patient to give knowledge of patient background. Different family members will serve different things. Don’t assume “next of kin” is the person to be consulted with health and everything because that person may not be comfortable with that’.
Raising awareness
Both lay and HCP participants agreed that there was a need to ‘start the conversation’ and have more awareness-raising in society so that talking about death, dying and EOLCP was less of a taboo. A HCP participant also acknowledged that the ‘Majority of people would cling to life, reinforcing treatments, medicalising death, instead of starting a conversation for patient’s families and communities and make work easier for HCPs [to discuss this] so that [it] is not a taboo’. Lay stakeholders stressed that it was important to engage community and religious leaders ‘to take this discussion to the community’.
Further training
All HCPs agreed that the way forward is training that will help to build HCP confidence to ask about faith or cultural beliefs. Educators also stated that HCPs need more teaching tools or best-approach guidance for having EOLCP discussions with ethnically diverse patients. This would support them in developing confidence in understanding nuances and verbal and non-verbal cues. One way of doing this is using simulated patients. It is also key that HCPs are taught the significance of cultural humility as an approach to care. Educator participants also suggested that developing as a practitioner is an iterative process, and HCPs need to adopt a reflexive approach to practice.
Lay stakeholders suggested that HCPs engage with interfaith forums to learn about different religions and cultures. One lay stakeholder participant stated that HCPs were welcome to interfaith forums to learn and understand how to work with people of minority and religious communities. HCPs also acknowledged that there were benefits to having discussions with faith leaders and/or community leaders: ‘If we can have faith, community and HCPs in the same room there would be a good place for HCPs to learn’. Lay stakeholders acknowledged that it is important to raise discussions about faith and beliefs with patients. They acknowledged that this is sensitive, but it still needs to be introduced. HCPs acknowledged that some guidance about the best way to phrase the questions would be useful. An example of how to introduce the discussion about spiritual beliefs was given by one HCP stakeholder: ‘This is obviously a difficult time for you; do you have any faith background or spiritual beliefs that support you at a time like this?’.
Developing training materials
All stakeholders found the stories to be a powerful tool to open the discussion in the workshop, and also in training and learning. The preference for all stakeholders was to reveal the stories in stages, slowly adding layers to complexity and diversity. Academics in workshops suggested that, if the stories were to be used in training materials, there should be specific questions to accompany stories. Stories should perhaps be produced as audio or film and have accompanying questions specific to each case.
Academic participants stressed that stories needed to address generational differences and take an intersectional approach as patients’ behaviours and needs are ‘not just about race, it’s also about poverty, class, ethnicity and faith, etc.’, so the stories should not be overly dominated by stereotypical cultural signifiers that represent diversity, such as language needs and food restrictions. This was seen as important to avoid learners reaching for the certainty of a checklist approach to culture (e.g. Muslims do this, Jews do that) and enable practitioners to work within the realities of the context of uncertainty and of the nuances of individuality, particularity and the layering of life experiences, heritage, culture and faith. This potential for overculturalisation of stories was in some tension with other participants, suggesting that people need to have some understanding of core components of cultural diversity. There was mostly agreement, however, that stories as a learning tool need to show that cultural hybridity exists, and promote understanding that differences exist between generations, classes, cultures and faiths.
Educators stated that using a story as a teaching tool was positive. Stories needed to be complex and interesting and, at the same time, feel authentic and engender sparks of empathy, which was the case with the stories used in the workshops. They also viewed as positive that the stories had no ‘rounding-off’ ending, that what happened was left open. As one educator stakeholder stated ‘there is an opportunity that we can support people without fixing. It’s nice sometimes to not have a solution’.
Academics also talked about the value of creating a forum of researchers and faith leaders to expand knowledge and evidence about ethnic diversity and PEOLC and addressing inequalities and inequities.
Behaviour change techniques and the use of concepts from NPT (as described in Chapter 2) were applied to the data gathered in the discussions in workshops and the workbooks. The potential learning mechanism to promote BCTs and enact the new behaviours in their practice are shown in Table 12. These mechanisms inform the learning resources developed in this study.
| BCT | How a HCP might learn this | Behaviour in practice |
|---|---|---|
| Instruction on how to perform | Description of technique in practice by HCP focusing on stepwise approach to discussing culturally sensitive approach for elements of care, such as medications, treatment decisions, place of care | Introducing EOLC discussions in stages |
| Prompts and cues | Checklists that map to best practice | |
| Anticipated regret (for not raising EOLC) Identity (that is culturally sensitive) Information about emotional consequences (how people feel when it goes well) |
Cultural humility approach Storytelling |
Personalising care |
| Prompts and cues | Pictograms to initiate exploration of family and social context and get to ‘know’ the patient and their background | Building trust and rapport |
| Instruction on how to perform the behaviour | Potential phrases and exemplars to use in practice to offer the opportunity to discuss sensitive subjects that a HCP feel uncertain about, such as deterioration and dying, faith and health beliefs, working with families | Understanding patient preferences and approaches to decision-making |
| Prompts and cues | Checklists that map to best practice | |
| General social support (of colleagues in same circumstances) Feedback (on how EOLC discussions were received) Focus on past success (of successful EOLC discussions) Comparison of outcome (comparing how it works for different patients/families) |
Sharing experiences and practices with peers and trusted expert colleagues | |
| General social support Feedback Focus on past success Comparison of outcomes |
Sharing experiences and practices with peers and trusted expert colleagues | Working with carers in EOLC discussions |
| Prompts Instruction on how to perform Feedback |
Good-practice checklist (working with interpreters) Demonstration (video of working with interpreters) Post-session debrief (with interpreter) |
Working with interpreters in EOLC discussions |
| Rehearsal and feedback Framing/reframing |
Simulated training with formative feedback for complex situations of uncertainty | All of the above Reduce discomfort with working outside a comfort zone |
The field notes of the five workshops involving HCPs, in which the behaviours discussed were those involving ‘thinking ahead’ discussions with patients, were scrutinised for mention of BCTs. HCPs described behaviours that they thought were important to use in how thinking ahead was discussed with the family and also described ways of promoting these behaviours in practice through learning resources that included BCTs. HCPs described thinking-ahead discussions as a type of the goal-setting BCT that they employed in their work with patients and families, suggesting that HCPs should ‘set a staged approach, so that you break it down into pieces’. Another participant stated, ‘I try to make sure they understand that I am a support for them and that they make SMART [specific, measurable, achievable, relevant, time-bound] goals’. The BCT of general social support was twice mentioned by two people (and did not specifically apply to the BCTs related to emotional social support or practical social support): ‘I check with family what structures are there to support them’ and ‘I try to engage properly with the family and try and make sure they understand that I am a support for them . . . and also, as a HCP to respect family and culture of the family’.
In relation to influencing the behaviours of HCPs, a participant stated, ‘So maybe give HCP some guidance in the best way to phrase the questions’ about deterioration and dying in the context of ‘understanding their cultural belief systems’, which is an example of the BCT instruction on how to perform the behaviour. The BCTs of using prompts or cues was mentioned by three participants: two emphasised the need to take the cue from the patient to know if or when to progress a conversation ‘and exploring how far patients want to go’; another gave the example of ‘When patients say “I want to leave it to God”, you need to discuss whether to complete a DNACPR form to enable HCPs to know and respect her wishes’. A third professional said, ‘Sometimes HCPs have to tell themselves that they will need to deal with the crisis when it presents, as not all patients will take this conversation to the next level. It is important that HCPs don’t force these conversations’.
There was evidence for six of the NPT concepts in the HCP workshop discussions. Collective action is defined as the operational work that people do to enact a set of practices. This was implied in the statement related to working together to support HCPs talking with the patient and family about thinking ahead. It was stated in the context of understanding cultural differences that they ‘ensure they work together with, say, the GP, consultant, nurses and other stakeholders, so then all HCPs are singing from the same hymn sheet’. People also noted that being able to take the action together can depend on people having clearly understood roles (which is a component of collective action known as interactional workability): ‘So, making sure that they see HCP to be part of the family or friend so at least this helps to ease this process [of family involvement in thinking-ahead conversations]’. Learning resources that support the use of pictograms (described previously) to initiate exploration of family and social context and get to ‘know’ the patient and their background, and that are shared and updated within the practitioner and family ‘team’, are relevant to these practices.
In relation to the educational resources, a participant suggested a commonly used approach in adult learning, that of a collective forum of learners of differing perspectives and lived experiences. Having HCPs, public, and possibly patients in the same room with diversity of faith and ethnic community backgrounds was suggested to be a good place for HCPs to learn: ‘It is very powerful and makes you think about your responses.’ This suggests they want a common sense of coherence, defined as the ‘sense-making work’ that people do individually and collectively when they are faced with the problem of operationalising some set of practices. Sense-making relies on people working together to build a shared understanding of the aims, objectives and expected benefits of a set of practices. In the context of professional uncertainty, this is a powerful antidote to the paralysis that may otherwise arise. 43
There are four components of coherence, which are relevant to what HCPs want to achieve by their sense-making. First, the sense-making could be from discussing how and why these cases differ from their usual practice, which would be the concept of differentiation. Second, it could be about understanding their role and the tasks to undertake, defined as communal specification. Third, it can also be about individuals needing to do things that will help them understand their specific tasks and responsibilities around a set of practices, which is the NPT concept of individual specification. Fourth, it could also be sense-making to gain a collective understanding of the value and importance of new practices, defined as internalisation. So a forum could potentially support all four components of the concept of coherence.
Conclusions
The 50 participants in this WS came from a very broad diversity of backgrounds and the discussions have shed further light and depth from a breadth of stakeholder perspectives on the issues and themes that emerged from our interviews with patients, family members and some health professionals supporting them.
The perspectives of public participants have affirmed the themes in the experiences of participants in WS1 and WS2. The perspectives of academics have placed our findings in the literature and current ways of thinking about ethnic health and addressing inequalities and inequities.
Participants have discussed what these themes mean for the practice required of HCPs, what the key issues might be in achieving good practice and what training would be useful to develop this. The discussions of HCPs have provided insights into the behaviours that need to be integrated into practice and how these might be developed through training and learning resources and inform the e-learning output of this project. As an example, an interactive forum was not part of the specification of final learning resources as it is resource intensive, but could be used with groups of leaners using the same resource and sharing their learning experience, such as through a closed Facebook (Meta Platforms, Inc., Menlo Park, CA, USA) group.
The use of narratives and the story format was universally welcomed as a powerful tool to engage people and, through this emotional response to a patient’s story, promote the motivation to learn and to embed changes in practice. E-learning is usually an independent, solitary activity and a strong message from the findings is that HCP and other stakeholders regard collective working and coherence as key processes in achieving normalisation of greater competence in supporting patients and their families from diverse ethnic backgrounds.
Chapter 7 Discussion and conclusions
Introduction
Our learning over 35 months from patients and families from a diversity of ethnic, faith and sociocultural backgrounds who were living with advanced disease and with the likelihood of deterioration and dying over the coming months has been described in the previous chapters. These accounts paint a rich and diverse picture of how people live with the prospect of their death and whether or not and how they consider their future.
We acknowledge the difficulties in summarising participant experiences and perspectives because these relate to many clinical encounters in many different settings and are characterised by great diversity. 132 However, despite specific areas of dissatisfaction, most participants were broadly positive about their experience of care for the patient. A few had serious complaints and some were extremely satisfied. Dissatisfaction tended to relate to general shortcomings in care and communication, which have been widely reported previously. 24,72 A few complaints were specific to a patient’s ethnicity and culture, but, overall, this was not a strong theme in the data.
Our findings highlight the unique nature of every patient and family, and the differences between individuals within the same family and ethnic group, as well as between them. The findings also reveal many similarities in the experiences of EOLC and communication between patients and FCGs from ethnically diverse groups and from the wider UK population, as well as patient and FCG responses to EOLC and communication. 69,88 Previous work by co-applicant Kristian Pollock with white British participants concerning ACP discussions has found that prognostic uncertainties made such discussions challenging and that many HCPs found it difficult to raise the topic and recognise when patients were ready to talk about the future. Most patients preferred to leave such discussions until they had become severely unwell, and the findings challenged the policy assumptions about ACP that all patients wish for, or would benefit from, an open discussion about death. 72
Furthermore, a systematic review of the ACP experiences of patients with life-limiting illnesses identified diversity of experiences and individual preferences in engaging in discussions that aligned to three themes, which can be seen as a continuum along which patient receptiveness and desire for ACP rest, but which may also fluctuate, bidirectionally, during their illness: ambivalence to the balance of benefits and burdens of thinking ahead about future deterioration, ‘readiness’ as a prerequisite for the benefits, and a degree of openness or comfort in discussing preferences for the future. 133 These themes interlink as ‘two sides of the coin’ with respect to barriers to and enablers of both discussions about future deterioration and the development of personalised advance care plans that seek to enable self-determined preferences in that future.
Our findings affirm that these underpinning themes present barriers and facilitators for people from a diversity of ethnic and religious backgrounds. In addition, they indicate that there are distinctive and highly nuanced aspects of the experience and circumstances of patients and FCGs from ethnically diverse communities that compound the complexities alluded to in other studies of ethnically diverse and palliative care the UK. 23,134,135 The specific issues on which we focus here relate to the findings concerning understanding and engaging with EOLCP; prognosis; awareness of dying and thinking ahead; language, communication and decision-making; models of care; and navigating a complex system of health care.
Understanding and engaging with end-of-life care planning
Our findings indicate that there is some confusion, especially among patients and FCGs, about what constitutes EOLC and when discussions concerning this should be triggered. This serves to confound the current policy that it is valuable for people to have such discussions if they are to be enabled to express preferences and plan future care and obtain appropriate services at the end of life. 136 What constituted discussion about ‘thinking ahead’ and whether EOLCP had occurred was often ambiguous and hard to recognise.
In their accounts of thinking ahead, participants tended to focus their attention on death and what happened afterwards, such as funerals and wills, rather than the preceding and uncertain process of dying. 136,137 Some patient participants described their efforts to make arrangements in advance to help relatives cope with loss and administrative burden, to leave a legacy of care and support after their death. Several participants had completed lasting power of attorney documents, for financial affairs, and a few expressed a wish for their ashes to be repatriated to their native countries. Concern with funerals and disposal of the body reflects what was of most immediate importance to people and was how they tended to interpret questions about EOLCP.
Decision-making around EOLC was not so pertinent to participants, perhaps because they concerned experiences that were unknown, unwelcome and could not be easily imagined. 136–138 Consequently, reference in the accounts of participants to anticipatory questions about, or discussion of, what was likely to happen during the process of dying was unusual. 137 There was little detailed consideration in the data of the content and formal documentation of EOLC plans, although they were valued by the few families who reported having completed them. However, participants did often recognise specific topics that were mentioned by researchers during the interview (e.g. resuscitation, preferred place of care and death, limits to care and treatment) and described their experiences of talking about these. Although ACP should involve a holistic discussion of ‘what matters to me’ at the end of life, our participants’ experiences highlight the extent to which this consisted largely of a simplified, disaggregated, task-based focus on specific, documentable items such as decisions about DNACPR, and place of death. 3,10,33,72,139
Offering opportunity for conversations with people in the last year of life about future deterioration is supposed to fall within the remit of all HCPs, regardless of role. 140,141 However, in the Thinking Ahead study, many HCPs did not consider discussion of EOLCP to be their responsibility, suggesting this was the remit of palliative care services. They did not consider that it was relevant or appropriate to raise EOLC topics when the patient was still receiving active treatment and was not perceived to be close to death. They reported rarely initiating discussion of the topic, and not before the patient was clearly gravely ill. 142,143 Some positive accounts were given of consultations being scheduled to discuss EOLCP within the context of an established relationship with the patient’s GP. As widely reported in other studies, HCPs were concerned that talk about end of life, especially if mistimed, risked damaging their relationship with patients, and the trust they had established, as well as destroying hope. 72,143–145 Thus, there was often an alignment of motivation between patients, FCGs and HCPs to maintain a positive recovery orientation and avoid the topic of end of life. 72,146 Not knowing too much about the prognosis could be a prerequisite for maintaining hope, optimism and engagement.
Professionals emphasised the importance of identifying ‘readiness’ in patients and family members and the need to be alert to cues that they were receptive to discussion of future planning. 72,144,147 Policy drivers towards open and transparent communication between patients and professionals, and the encouragement of partnership and shared decision-making in medical consultations, have been promoted for decades. 148,149 In the face of this, the persistent entrenchment of patterns of communication in which ambiguity, and even denial, may be preferred over clarity points to the functional and adaptive capacity of the positive recovery orientation for many patients. 69,148 Although a positive recovery orientation may suit many patients and FCGs, there are some, a minority in our study, who have a strong desire to be fully informed about their illness, prognosis and future care to be aware of their ending and prepare for it. 150,151 In these cases, the positive recovery orientation might work to their disadvantage, much as previous studies have reported over a period of more than half a century. 148,152–154
Individuals who sought to know the details of their illness and prognosis became extremely frustrated by what they perceived to be professional reluctance to address these issues, and by their evasion and indeterminacy, whether this stemmed from deliberate evasion or lack of expertise. Some participants appreciated that professionals themselves were subject to the intrinsic uncertainty of prognosis. Their experience evokes the distinction originally made between ‘clinical’ and ‘functional’ uncertainty. 155 ‘Clinical’ uncertainty refers to the real unpredictability of illness progression and outcome, whereas ‘functional’ uncertainty is a strategy professionals adopt to manage their engagement with patients and families and avoid being drawn into difficult and protracted conversations. Some family members in the study adopted a similar strategy in withholding information from relatives, especially patients, to avoid distress and maintain hope. 69 This effort to protect patients from awareness of their poor prognosis has been widely reported among ethnically diverse populations. 99,136,156–158
In contrast to the circumspection with which professionals often approached EOLC discussion during scheduled or routine encounters, FCGs described a much blunter approach prompted by patients’ urgent hospital admissions following a crisis or rapid deterioration in their condition. The families described distressing experiences when professionals sought rapid answers to questions, notably about resuscitation, for which they were not prepared. These often occurred during times of great distress, when the patient was acutely ill, and relatives were struggling to come to terms with the gravity of the situation and the uncertainty of recovery. Consequently, the setting and context within which discussion of advance decisions occurred was an important determinant of patient and FCG experience and willingness to engage with the topic. 148
It might be proposed that it is precisely the purpose of advance discussion and documentation of wishes to pre-empt the occurrence of such situations. However, as Mol138 and others136,159–162 have argued, decisions by patients and FCGs are always hampered by the intrinsic uncertainty and incomplete nature of the information they have at their disposal about what is going to happen in the future and what is the best way to respond. Patients and FCGs (from any culture) tend to adopt a cautious, provisional and pragmatic approach to preferences for, and anticipation of, their future end of life, anticipating that these may change, as their illness progresses and their circumstances decline. 162 The current focus on ACP in the UK and other Western nations is underpinned by an ideological commitment to freedom of choice as a condition of individual autonomy. 154 However, the relevance of individual autonomy to the way most people live their lives, and in particular in isolation of their relationships with other people, is being called into question: the consumerist notion of autonomous ‘choice’ has limited relevance, particularly in relation to patients from ethnically diverse groups for whom individual autonomy may not be the predominant underpinning to decisions. 72,136,138,156,158,163,164
The limited and ethnocentric stance of current policy is underlined by consideration of the alternative approaches that have been identified in research from ethnically and culturally diverse groups. Respect for persons is manifest in the desire to protect the patient from an unwelcome truth, in the desire for the family or elders to assume responsibility for making decisions about treatment and in the commitment to care by family members, particularly of adult children for their parents. 99,106,136,156–158,165 A natural orientation to such approaches was apparent among many of the study cases. Alongside this was a strong preference by many patients to protect their family members from the burden of care and for their choices for treatment and care to be considered carefully in relation to their anticipated consequences for others. 72,138
Patient desire to reduce the burden their illness and death imposed on their significant others was a recurring theme, and was one reason for the very specific focus on making preparatory arrangements for after their death, especially the funeral. Thus, some patients expressed a preference to move from home to hospice once the demands of home care had become excessive, and to withhold information about their illness to protect individuals from distress. Just as HCPs search for a window of opportunity and assess the ‘readiness’ of patients to discuss EOLCP, patients and FCGs also exercise judgement and caution about what information about their future they wish to share and discuss with others, including HCPs. This prioritising of the interests of others can be viewed as a manifestation of agency and is also a reciprocation of the love, care and support bestowed by others on the patient.
Who to talk to about illness and when was influenced by perceptions of an individual’s situation. Information might be deliberately not shared with people who were themselves ill, who had experienced bereavement or who were thought to be in some way vulnerable. Patient awareness of the family suffering as a result of their illness was itself a source of suffering for the patient. The selection and management of information could be a means of patients asserting personal agency through protecting others from the distress and anxiety caused by terminal illness. Within informal networks it could be considered a form of reciprocal gift exchange, cementing ties of affection, obligation and responsibility. It could also be a source of conflict and tension, whereby individuals disagreed in their views about what information should be shared, especially with and by the patient.
In some families, EOLCP may not be something that members wish to discuss with HCPs. The family, or specific individuals within the family, may be considered the natural locus of discussion and decision-making in such matters. Thus, it is important for HCPs to be aware, and take account of, the nexus of relationships within which the patient is embedded, and to involve family members, as well as the patient, in planning and undertaking EOLC discussions. 166 In tension with this preference for fostering of optimism present in the majority of our case studies is the testimony of some bereaved FCG participants who, in retrospect, expressed regret that they had missed the significance of the final days or weeks of the patient’s life and perhaps even the chance to say goodbye. Regardless of what they had been told or understood, participants often seemed to have been taken by surprise by the speed with which the patient’s final decline and death occurred.
Prognosis, awareness of dying and reluctance to think ahead
Staff from disease specialist services such as oncology and cardiology largely expected colleagues from district nursing and palliative care services to initiate discussion of EOLCP with patients once they had exhausted all active treatment options and been referred to community services for ongoing care. However, prognostication, especially in relation to patients affected by conditions other than cancer, is notoriously difficult and prone to error. 167–170 The positive recovery orientation encouraged patients and families to maintain hope in the possibility of an extended future and to distance themselves from the imminence of death. 154,159,171–173 Having pulled through against the odds, on past occasions, FCGs proposed that the patient was likely to do so again, or at least they should be treated as if this was likely to be the case. There could be a lot of ambivalence about prognosis and how much people wanted to know about this and their future options. Moreover, preferences were not necessarily linear or stable. 138,162 Many participants preferred to maintain an overtly positive stance and to focus on making the most of the present, rather than an uncertain and probably unpleasant future. 72,164 Patients, FCGs and HCPs in many of the case studies converged in their view that there was no benefit, and could be a risk, in thinking too far ahead until the patient had become so gravely ill that death was clearly imminent.
Health-care professionals rarely expressed any awareness, or curiosity, about patients’ religious or other beliefs, their significance for EOLCP, how they should be factored into the discussion or how they might influence decisions about treatment and future goals of care. Patients and FCGs who held strong religious convictions about divine intervention regarded EOLCP as irrelevant and inappropriate. Indeed, when all matters of life and death were believed to be determined by a god, future planning could be considered presumptuous and indicative of insufficient faith. However, there was considerable variation and individuality in attitudes towards EOLCP and how participants positioned themselves in relation to religious or cultural affiliation. Preferences for resuscitation and continuation of active treatment, for example, could not be reliably predicted from knowledge of an individual’s religion or ethnic identity. Some families rejected DNACPR as being incompatible with religious faith, specifically the belief that life and death are subject to divine determination. Others had a purely secular desire to continue living for as long as possible, because of a hopefulness about the future and what this might deliver in terms of natural recovery or advances in treatment.
Language, communication and decision-making
Previously, we suggested that the optimistic recovery orientation often involved a degree of collusion between patients, FCGs and HCPs. This was an important mechanism for protecting others from damaging revelations and confrontation with unpleasant alternative truths, but it could also result in misunderstanding and false optimism among patients and family members, who failed to realise how seriously ill the patient was and how close to the end of life. Although this approach suited many participants, at least for a time, this vagueness and indeterminacy was regarded as highly unsatisfactory and intensified anxiety among patients and families who wished for clear and specific information about their illness and prognosis. Faced with very uncertain patient futures, HCPs were unable, and possibly reluctant, to pin down exactly when treatment might fail or deterioration might occur. However, HCPs had considerable power to frame information to influence patient awareness of the illness and the ‘choices’ with which they were confronted. 72,160,174 This was a much more general phenomenon than the blunt imperative for decisions to be made during acute hospital admissions, as described previously.
Regardless of the setting, HCPs raising the topic of resuscitation was a powerful signifier of the gravity of a patient’s illness and anticipated mortality: after discussion of DNACPR, the future abruptly felt shorter. It was clear that participants often did not have a clear or accurate idea of what resuscitation involved or the circumstances under which it would be attempted, or that it did not mean that treatment would be withheld for treatable or reversible conditions. However, several FCGs described situations when they felt that hospital staff had indicated that no further treatment of any kind would be given to their relative.
In discussions of resuscitation, professional input can be critical, in giving information, time, space, and repeated opportunities for patients and family members to reflect and discuss. Accounts of participants in this study identified their confusion and inconsistency in professional judgement and advice that had been distressing and, they felt, had resulted in poor care. It was evident, also, that some families disputed professional judgements about a patient’s quality of life being necessarily unacceptable following a resuscitation attempt, and disputed their capacity to predict prognosis. Others found the decision about resuscitation to be extremely difficult and one they were reluctant to accept.
Several participants described feeling under pressure from HCPs to agree to DNACPR orders and both lay and professional participants gave accounts of patients and FCGs changing their minds. It was not clear if this was following the chance for reflection and to obtain greater information and understanding, or if patients may have come under professional, family or other pressures to accept or make specific decisions. Especially when translators were required, it was not clear how much patients understood about future planning and decisions. Accounts of patient involvement in decision-making varied widely, from being actively in charge, through shared discussion, to family members taking full responsibility.
Some patients, especially those who lacked fluency in English, were reported never to see a HCP on their own, but always accompanied by at least one relative. Patients valued being able to communicate with HCPs directly in the patient’s first language. There were a few accounts of consultations in secondary care involving a HCP who could converse in the patient’s first language. These were off-chance encounters, following which it was unlikely that the same HCP would be seen again. If they cannot communicate directly with the patient, there is the potential that professionals may wrongly assume the locus of decision-making to be the family, especially in the case of older patients who rely on family members as translators and advocates.
Translators may act as gatekeepers, whether these are family members or professionals, framing and shaping patient understanding and choice. 56–58 Thus, patients who require translation may struggle to have their voice heard and HCPs may feel uneasy about a decision being in keeping with the patient’s wishes and best interests. Disclosing bad news requires skilled, empathetic communication, which is particularly difficult to achieve through third-party translation. Some relatives felt that HCPs had put on them the responsibility of translating on behalf of their parents, and recoiled from the decision-making responsibility, particularly about difficult decisions such as resuscitation, which they felt amounted to ‘signing a death warrant’ for their loved one. Thus, for some FCGs, being asked to act as an interpreter added to their emotional distress and burden of care.
Previous studies have reported that HCPs are dissatisfied with family members acting as translators because they suspect that they may be selective in filtering information given to the patient, and also will also find it difficult to explain technical details of illness and treatment options about which they lack knowledge and understanding. However, relatives are often reluctant to use translation services, from a desire to control information being conveyed to the patient, and also a concern about disclosing confidential information to strangers. It is evident that the need for translation continues to constitute a barrier to skilled and sensitive EOLC, particularly in a context of complex, challenging and difficult experiences relating to end of life in which, effectively, communication is care. 175 Wilkinson et al. 175 reported that understanding and effective communication were enabled by the availability of staff who could converse in a patient’s first language. The use of bilingual HCPs should be sought whenever possible. 56–58
However, even when consultations are conducted in English, it may be that patients and FCGs lack the fluency or cultural acclimatisation required to understand technical terms or pick up on the nuances of professional communication. In consultations involving participants from ethnically diverse communities, it is particularly important that professionals exhibit curiosity about patient and FCG understanding of the situation and interpretation of what they have been told, and elicit their concerns and expectations of illness progression and options for future care. This information must be placed within the context of the wider ecology of professional and informal care within which the patient is embedded and within which care is enacted. 166,176
Uncertainty is intrinsic to the experience and treatment of serious illness, and is a fundamental existential issue for patients and their family members. 138,150,162,177 Communication and decision-making occur against a backdrop of uncertainty through evolving prognosis linked to trial of treatments and progression of illness over time. 138 The centrality of uncertainty needs to be factored into all contacts and communication in health service consultations. The management of uncertainty has a powerful impact on patient and FCG experiences of illness and orientation to planning future care. For some patients, uncertainty can provide a justification for optimism and they can embrace the positive recovery orientation. For others, however, uncertainty can be profoundly unsettling. 150 The complex relationship between hope and uncertainty is dynamic. 128,162,178
A key message of the study findings is for staff to be aware of and responsive to patient and family experiences of uncertainty and to use this awareness as the basis for engaging in discussion of patient goals and values, rather than to evade the issue or seek to impose a formulaic agenda relating to ACP that derives from a narrow stratum of Western values centring on personal autonomy and decision-making. The findings also point to the importance of professional understanding of a patient’s informal network of support and awareness of the relational nature of decision-making.
Effective communication is pivotal to good care, and its centrality is reflected in the summary of our findings, ‘being known’ (termed with the Zulu word ‘sawubona’ in our key study outputs), presented in Figure 5. There is much evidence about what constitutes effective communication with patients about future illness progress and end of life and, specifically, in engaging people in an ‘end-of-life talk’. 179,180 However, there is scant literature on the additional attributes of such conversations with people when English is not their first language, when translation is required and when there may be disparities in conceptual understanding of health, illness and care provision. This study has highlighted the importance of professional awareness of these elements as an area for further research.
FIGURE 5.
Enablers of ‘knowing’ ethnically diverse patients and families to optimise EOLC.

Models of care
UK health policy is based on the idea of the patient as an autonomous decision-maker. The realisation of individual choice in EOLC, especially regarding place of death and preferences for or against treatment, is regarded as a marker of quality care. 10,158,161,181 However, recent research and associated critiques have cast doubt on the extent to which these policy assumptions represent the lived experience and concerns of many patients in the general population. 182–184 Instead, patients are understood to operate within a field of relational autonomy, where the decisions and choices are made with reference to, and mindful of the effects on, significant others within a social network. 137,138,159,185–187 This collectivist model of decision-making is recognised to be particularly relevant to patients from culturally and ethnically diverse backgrounds. 60,132,136,156–158,163 In these contexts, the locus of decision-making is often a joint responsibility, vested in the family group, and sometimes requiring concurrence from elders or respected non-family community or faith leaders, rather than the individual.
Degrees of individual family commitment to patient care very much affect their attitude and receptivity to accepting support from sources outside the family. In the Thinking Ahead study, varying levels of commitment appeared to be driven by profound personal attachment and close family ties, as well as by a sense of family, cultural and religious duty, and responsibility. This may include, for some individuals, a desire to accrue religious merit in line with their faith beliefs and a desire to avoid censure from the wider family or community. In some cases, adult children expressed concern about being criticised by their wider family or community if they were seen to fall short of expected commitment to care for their parents. This consequential stigma appears to be an important determinant of the family’s willingness to seek out and accept external help, especially regarding personal care and social support or care in a hospice or care home.
There was considerable variation between individuals and families in relation to closed or open awareness of a patient’s illness and prognosis and the extent of discussion and sharing of information between the patient, FCG and other relatives. 148,154,188 Preferences varied widely regarding what individuals wanted to know about illness and prognosis, even within the same family, generation and cultural or religious group. 189 The extent and composition of individual family networks also shaped how and with whom information was shared. There was also uncertainty about what different family members and the patient knew about the illness prognosis, who had talked to different professionals about this, and whether or not and how information had been relayed to others, within professional and informal networks. Some decisions were prolonged and distributed, seeming to require consensus among patient and family members, but the locus of decision-making could be configured differently across cases. This was largely determined by individual circumstances, of family composition; location; personality; religion; and cultural norms about family responsibility, engagement and authority. It was not the case that all patients had access to extended family support, and even when they did, some families struggled to provide this. Small, dense networks tended to be self-contained and seemed less likely to have established extensive contacts with health and social services.
This accords with Granovetter’s190 thesis that ‘weak’ ties connecting individuals within a network to external persons and agencies are more likely to provide access to information and resources than a strongly embedded tie. 191 Thus, although our data can be suggestive only, it may be that families that are insular, including those who have access to a GP who speaks their first language, and typically with elderly parents who do not want to accept outside help, are more likely to be disadvantaged in terms of the information and support they could effectively access. Conversely, within families that include a strong advocate, typically an adult child, who takes an active stance in relation to contacts with health and social services, and is willing and able to challenge these and follow through requests for support and information (e.g. through direct contact with different HCPs and services, who/which themselves are linked to wider points of contact and referral within the professional network), that advocate is an agent for extending the network of care around the patient.
Navigating a complex system of health care
Patients and families confronting the end of life enter an alien world, full of uncertainty and the need to engage with, usually, many different professionals and services. 138,150,177 May et al. 192 and Mair and May193 have drawn attention to the ‘burden of care’ imposed on patients and their families in the course of receiving treatment and services from a complex system of care. Several FCGs were exasperated by the demands imposed by an ongoing series of referrals and appointments for which they could identify no purpose or helpful outcome. Other participants described confusion, misunderstanding and lack of information during their experience of care. The difficulties posed by system complexity have been widely reported in the literature. 194 Stacey et al. 148 highlight the significance of institutional and organisational factors in shaping how resources such as time, expertise and resources are able to flow through complex systems of care. They identify the increased specialisation of professional roles and the consequent fragmentation of patient care as important factors contributing to the lack of effective communication and awareness of patient prognosis and future illness trajectories.
In the Thinking Ahead study, some patients and, more usually, their family members were skilled and effective mediators and advocates, with the ability and resources to find the information they needed. These skills developed with experience, sometimes in relation to the illness and death of more than one relative. In addition, some participants were, or had been, employed within the NHS in some capacity. However, the situation was very different for patients and FCGs who were unfamiliar with the system and lacked the confidence or fluency in English to communicate effectively with staff or achieve an understanding of their entitlements, especially if they lacked family support and translation.
A few patients described long-term relationships with specialist nurses, but the nurses, by their own admission, rarely engaged in discussion of planning of EOLC and did not, from the accounts available in the study, have a deep knowledge or understanding of the patients’ wider circumstances and concerns. Several HCP participants expressed surprise that they had been nominated to take part in the study because they had only brief or superficial contact with the patient. Few participants described a relationship with a HCP who could be described as occupying the role of ‘key worker’, a ‘go-to’ person who helped them navigate the complexities of care and whose sense of being available enabled the patient and FCGs to feel ‘safe’ within the system. 194 The experience of uncertainty, unfamiliarity and lack of information prompted a stance of vigilance on the part of relatives. A particular issue was the concern to ensure that cultural and religious practices relating to diet, hygiene, ritual purity and dignity should be observed during interactions with health and social care staff. For some families this was a motivation for refusing or limiting outside help. Hospitalisation was a particularly challenging experience, especially for older patients and those who were not fluent in speaking English. This is a known issue within the research and policy literature and should be on the agenda of things to address of all services.
Participants’ experiences of EOLC was shaped by the organisation of services relating to a patient’s illness and treatment needs and how these related to each other. This created subtle forms of disadvantage. Many different services and HCPs could be involved in each case and as the patient’s needs changed over time. However, some services, notably those for patients with MND, enabled a degree of continuity of care that was not available to most patients with cancer and other illnesses. In relation to other conditions, particularly cancer, patients tended to move through a process of referrals and to be seen by many different services and HCPs. 148 Participants described complex processes of referral to different types of test and treatment, and discontinuity of care and poor communication between staff from different services. It was not clear to individual patients, FCGs or HCPs what different individuals knew or had been told and had discussed with others. In addition, the boundaries of responsibility for discussing EOLCP were not clearly demarcated.
These are likely to be contributory factors underlying the reported vagueness of professional communication. In addition, patients and FCGs described their frustration at constantly having to tell and retell their story to the different HCPs they encountered during consultations and their sense of not ‘being known’ within the system, or the system ‘not knowing’ where patients were at any point in their process of care and referral. A great deal could hinge on chance encounters with individual HCPs, at any point in the treatment process, who proved to be particularly forthcoming and effective communicators. However, patients had no means of maintaining contact with such helpful individuals, who were likely to be replaced by other colleagues during subsequent appointments and consultations.
The centrality of effective care co-ordination in easing the experience of families negotiating their way through a complex system of health care was evident in the specialist MND nurse’s account of her role as a key worker accompanying patients from the moment of referral after diagnosis to the end of life. The study findings also highlighted the variability and ambiguity of the FCG’s role as advocate and decision-maker for the patient, especially when they also take on, or are co-opted into, the role of translators in medical consultations.
Being known: summary of the findings of workstreams 1 and 2
Family caregivers and HCPs often oriented to a positive recovery orientation unless and until the patient’s condition deteriorated to an extent that the imminence of death was clearly apparent. For some patients, not knowing their poor prognosis was a prerequisite for maintaining hope, optimism and engagement. Even in specialist community and hospice settings, professionals described not raising discussion of future goals of care or EOLCP until the illness was at an advanced stage. However, it could be hard for the minority of patients who did want to be fully informed about their illness to establish a clear prognosis. Moreover, there is a risk that, in leaving discussion of EOLC until patients are ‘ready’, or at least very close to death, professionals may never initiate a conversation that would have been of value, as some BFCGs subsequently reflected to be the case. Thus, there is a tension between the need to respect patient preferences, the negative consequences of revealing information about the future for which the patient and FCGs may not be ready, and the adverse consequences of families being confronted by crisis situations for which they are not prepared.
The clinical setting had a significant impact on the experience and content of thinking-ahead discussions. Families found being put under pressure to make decisions about whether or not their acutely ill relatives should undergo resuscitation following the stress of unscheduled hospital admission very difficult, and described professionals being brusque and lacking empathy. In contrast, when professionals in community settings, GPs or nurses took on board the need for the patient and family to engage in EOLCP and made time specifically for this purpose, participants reported a more positive experience.
A key issue is the very varying experiences of care reported within a complex system, including the type of illness, the services referred to, the relationship with individual professionals, experience of continuity or fragmentation of care, and the nature and availability of family support. In the absence of any clear demarcation of responsibility for staff to raise the topic of EOLCP, including in community and palliative care services and hospice, staff may be wary of raising the issue. This is possibly for good reason, since their judgement seems to be in accord with the preferences of many patients. However, some individuals were frustrated or felt disadvantaged by not being able to find a professional who would tell them what they wanted to know. The outcome may be (a possibly needless) anxiety or being misled into a false sense of security.
Many participants oriented to a collectivist or shared model of decision-making and responsibility regarding EOLC. This gave rise to tensions within some families and highlights the different agendas and values with which patients and family members may be operating. It contrasts with the foregrounding of individual autonomy and best interests embedded in consent and decision-making processes in health care, including EOLCP. Patients’ primary motivation in thinking ahead was often to protect their significant others by lessening the burden of care and responsibility resulting from their illness. These responses apply to all sections of the population, but have been highlighted in this study of patients and FCGs from ethnically diverse populations.
In contrast to ‘the logic of choice’, Mol138 has proposed that health care be informed by ‘the logic of care’. This underlines the limitations and precarity of forward planning based on formulaic tasks and oversimplified decisions. Instead, professionals need to engage with uncertainty, their own as well as that of patients’, and to exercise curiosity about patient agendas and their perspectives and goals regarding knowledge of their prognosis and future care. 138 Decisions may be pragmatic, provisional, tentative and changing, as patients learn how they respond to situations that may have been beyond their imagination previously. The professional’s role is to accompany the family in the moment and support their readiness to deal with challenges and the decisions that need to be made as these arise. 72,195
However, the current configuration of services makes it difficult for patients to experience sufficient continuity and consistency of care and for professionals to develop sufficient knowledge of the person to generate the trust required for patients to feel confident in their support. ‘Being known’ and ‘being seen’ are key desires of patients and are enablers of good care, including personalisation of discussions about deterioration and planning care for the end of life. Our model of the determinants of ‘being known’, and the enablers of this, is derived from the study data (see Figure 5).
We have suggested that an allocated key worker could be a valuable resource in providing continuity and helping patients, especially those experiencing additional vulnerabilities and inequities; navigating the complexities of health care; and translating between language and culture. It turns out, unsurprisingly, that, at a macro level, good care looks largely the same, regardless of ethnicity: personalised, compassionate, holistic and safe. Understanding participants’ experiences and aspirations for care in the Thinking Ahead study provides a powerful lens through which to view and calibrate these components and the nuances of care for all patients confronting the end of life.
Stakeholders’ views on the barriers to and enablers of ethnically diverse patients, family caregivers and health-care professionals engaging in end-of-life care planning
Key barriers
Lay and community and faith leader stakeholders in WS3 identified that the key barriers to EOLCP were religious fundamentalism, community pressure and cultural expectations. The religious or cultural perspective of a patient and family might be so averse to the concept of thinking and planning ahead for deterioration and dying that it negates the predominant policy and practice paradigm of ACP achieving the best end of life. The strong sense of familial and sometimes religious duty to provide care at home was seen by stakeholders as compounded for some ethnically diverse families by community pressure and the stigma and other consequences that can arise when care is supplemented by ‘outsiders’ or when a patient is moved to a care home or hospice. Hospital care appears to have more legitimacy for families who seek active treatment to prolong a patient’s life as long as possible. However, periods of admission were considered to carry risk of breaches in cultural and religious observances (e.g. not being able to perform daily prayers/rituals, instances of being given prohibited food), which called for increased vigilance from FCGs.
Cultural and religious literacy of organisations and of individual professionals was seen as lacking by community and faith leader stakeholders. This was born out in WS1 and WS2 data by the lack of curiosity and awareness of religious and cultural diversity expressed by HCPs, although this was not a shortcoming explicitly identified by patients and FCGs. Previous negative health-care experiences were also thought to contribute to a lack of trust of professionals and organisations. All stakeholder participant groups also identified that there was a lack of awareness and accurate understanding in communities about EOLC services.
Key enablers
Effective communication was seen by stakeholders in WS3 as the key enabler both in the translation between English and other languages and in the use and accessible explanations of concepts and terminologies related to future planning. In addition, information shared by trusted sources was seen as an important element to enhance care. Personalising care required additional ways of getting to ‘know’ the person (their sociocultural–spiritual context) and an openness to seeing and doing things differently.
Development of professional confidence and skills in supporting people when the ‘usual’ way of doing things is not adequate is needed; evidence-based stories were seen as a powerful component of training to this end. A number of BCTs were identified pertinent to enhancing practice in the context of professional uncertainty and to focus on enhancing trust and rapport and gaining an understanding of how to personalise care by exploring a patient’s ‘world’. A strong message from the findings is that HCP and other stakeholders regard collective working and coherence as key processes in achieving normalisation of greater competence in supporting patients and their families from diverse ethnic backgrounds.
Strengths and limitations of the study
The diversity of participants in the study is both a strength (in terms of including a wide range of experiences and perspectives) and a limitation. We have tried to include a broad ethnic diversity in the sample, but acknowledge that we could not include all groups; for example, Jewish, Gypsy, Roma and Irish Traveller communities were not included. Alongside ethnicity and faith, our sample included diversity in family and social circumstances, and in illness type, including two case studies of patients who lacked capacity; five participants were enabled to contribute through a professional interpreter and one by a bilingual researcher. The intention of the sampling frame was to explore the broadest diversity of experiences in the constraints of the project. However, this inevitably compromises, to some extent, the depth of understanding of specific experiences and issues related to discrete groupings of faith, ethnicity or culture. The study was pragmatically limited in its geographical recruitment to include two areas of the East Midlands. Each has somewhat differing ethnic demographics.
Most participants were recruited via three hospice services, which means their accounts may reflect experiences of a distinctive type of specialist care, available to a minority of terminally ill patients. 150 The majority of cases were identified and first approached by HCPs with whom the researchers had discussed the study eligibility criteria. However, several patients did not seem to consider themselves, nor were they considered by their nominated HCP, as being close to the end of life. Although these data may be outside the study’s original remit, they serve to highlight the variable and uncertain nature of prognosis in relation to terminal illness and the real-world challenges in integrating discussions about potential future deterioration alongside care of patients in stable and active treatment contexts.
Serial interviews by the same researcher in WS1 built rapport with patients and FCGs, allowing increasing depth of disclosure about participants’ experiences and feelings, and allowing a view, over a period of time, of the unfolding nature of their lived experience. We were also able to triangulate different perspectives from patients, FCGs and HCPs relating to experience and involvement in the same case. The richness of the data and the range of themes that emerged are strengths. The ‘messiness’ of life and the considerable labour in living with advanced illness is reflected in the accounts and in the logistical arrangements of undertaking the interviews. These are not sanitised accounts and give confidence in the veracity of the data, providing insight into the participants’ reality.
Many patients and families found it quite difficult to identify a HCP to nominate who they felt was to be closely involved in their care. All 11 of the nominated HCPs in WS1 were nurses. Consequently, the data do not encompass the perspectives of the wider clinical care team for an individual patient, including those of professionals, especially doctors, who may have a different approach to offering conversations about preparing for future deterioration and end of life. The need to stop data collection involving HCPs from March 2020 because of the COVID-19 pandemic meant that seven out of 18 cases did not contain HCP perspectives. Similarly, clinical notes were available for only 13 out of 18 patients. However, there were only three cases for which there was little or no additional information or representation of health-care perspectives outside the family.
The setting in which participant accounts were elicited is an important factor influencing their content, for example whether the interview was held in private or with one or more individuals, including an interpreter. Patient and FCG interviews were mostly held in the participant’s home. The use of translators enabled recruitment of patients who are normally excluded from research, which is a strength of the study. Issues with translation (in four case studies and one BFCG interview) and how these were handled are discussed in Chapter 2, Workstream 1: longitudinal patient case studies. However, as discussed previously in relation to clinical consultations, some degree of detail and nuanced meaning is inevitably lost in translation.
During case study interviews, most participants were asked if the experience of taking part in the research had influenced them in any way. In three cases, participants explicitly said that they had been prompted to reflect and to think a little more about what the future might entail (this included the idea of thinking ahead about end of life). In a couple of cases, participants’ reflections had led them to consideration of further practical help they might seek. At least two HCPs expressed possible changes in their practice, in particular related to knowing more about their patients and their potentially diverse needs. Some participants described interviews as being emotionally burdensome, causing anxiety, whereas others reported them as positive or even cathartic. Distress management of participants required careful consideration, particularly when using interpreters. Researchers also found interviews to be emotionally challenging. A pyramid of support needs for participants was in place, and preparatory and reflective resilience work, alongside regular support meetings, were provided for researchers.
Implications for health professional practice and training
Health professionals in the case studies and stakeholder workshops described approaches to the complexities and uncertainties involved in initiating EOLC discussions with patients and FCGs from ethnically diverse groups. HCPs have the advantage, but also the responsibility, of anticipation, from past experience and the literature, as to what may lie ahead for patients and the imperative as the expert guide to balance the present well-being of the patient and family with the potential regret in future. There was considerable reflection on the need to recognise and wait for when a patient may be ready for ‘end-of-life talk’ as their illness worsened. There was scant detail, however, on what the skills and attributes of this required and looked like in practice.
End-of-life care planning documentation is seen in policy as the predominant vehicle for enabling good EOLC, but this may be in tension with the preferences and values of patients. In particular, collectivist models or responsibility for care and decision-making is directly at odds with the commitment to patient autonomy and choice that underpins professional policy and practice. How HCPs assess and navigate the potential for harm in this policy context needs to be widely discussed and clarified. There is currently a risk that emphasising difference results in marginalising and stereotyping patients and overlooking both the heterogeneity of individuals within diverse groups and what is common to the experience of good EOLC for all patients, regardless of ethnicity. Good practice currently orients to encouraging patients to conform to UK policy and practice, so that diversity is seen to constitute a barrier, rather than a manifestation of alternative values and preferences. In addition, the predominant stance of patients was one of hopefulness, and for some it was against their religion to engage in planning for the end of their lives. Current policy aims for patients and FCGs to change their perspective, and reluctance to plan ahead is constituted as a problem. Within cultures oriented to a collectivist and relational approach to decision-making, or religious beliefs about the absolute nature of divine intervention, it is the assertion of autonomy that may be considered unsatisfactory.
The findings from the Thinking Ahead study are supported by those of previous research in reporting that many HCPs do not perceive engaging in EOLCP to be within the remit of their role. Among those who do, there is often a reluctance to raise the issue. Professionals wait for an indication of patient ‘readiness’ and tend to postpone discussion until the patient’s health has deteriorated to the point that death is clearly imminent. Our findings suggest that this approach is broadly aligned to the preferences of many patients. The desirability of otherwise routinely initiating such discussions pre-emptively, at a much earlier stage of a patient’s illness, may be debated. However, a significant minority of patients want to be informed and aware of their prognosis and are disadvantaged by the deferment of discussion about their options for future care and how this will affect the plans they make for the life they have remaining. A key task of HCPs involved in supporting patients through serious and terminal illness is to elicit patient preferences for future planning and respond appropriately.
Thus, professionals require high-level skills to navigate complex, sensitive communication and interpersonal relationships that foster appropriate discussions and planning for anticipated deterioration, when patients and FCGs wish to discuss this. In relation to ethnically diverse patients, this could be fostered by an integrated team approach that includes members with skills in language and cultural bridging or advocacy. Enabling patients to communicate confidently in their preferred language is an important means of reducing disadvantage. However, systemic support needs to be more effectively attuned to the values and sociocultural contexts of patients and families regardless of ethnicity, and to provide relational and service continuity to deliver sensitive and personalised care.
It is important to provide HCPs with the training they need to support skilled and appropriate discussion of EOLCP, including through translators. However, it is also important to acknowledge the systemic barriers to such discussions. These include the ways that health care is organised and staffed, particularly the fragmented nature of services, which block the transfer of information and co-ordination of care across a complex network. In addition, the intractable nature and pervasive influence of prognostic uncertainty and the influence of spiritual values on hope and value of life should be acknowledged as major barriers to the discussion of EOLC and as existential issues with which patients and professionals have to engage.
Implications for research
Our findings suggest prioritising the following research questions to benefit patients. Such research must include participants from ethnically diverse communities, including those who would want to contribute in a language other than English.
-
How can health professionals identify if/when a patient is ‘ready’ for anticipatory discussions of deterioration and dying?
-
How can discussions about uncertain recovery and the need for decisions about ceilings of care, especially resuscitation, be most effectively conducted in a crisis?
-
How can professionals recognise and respond both to the diversity of faith and cultural practices among different ethnic groups and to the heterogeneity of beliefs and preferences relating to EOLC between individuals from different ethnic groups?
-
What are the implications of an understanding of collectivist, relational and faith-led models of care and decision-making for current UK health policy and practice and their focus on individual choice, autonomy and anticipatory planning?
-
How can conversations be most effectively conducted when translation is required to enhance patient understanding?
Conclusion
The findings highlight the unique nature and experiences of every patient and family and the differences between individuals within the same family and ethnic group, as well as between ethnic and faith groupings. The overwhelming impression of these accounts is their diversity and real-world complexities, the ‘messiness’ and challenges of life when someone is progressively approaching death. For each individual patient and family, the specific details of how, when and if they want to engage in thinking about the future and develop anticipatory plans are singular and emergent. They are rooted in uncertainty and coloured by past experiences of the deaths of family and friends; by the intersectionality of ethnicity, educational attainment, socioeconomic status, available health care and other factors; by values and beliefs; by information and understanding; by trust in organisations and individual professionals; and by experiences of an often unco-ordinated and complex health-care system.
The data reveal many similarities in the experiences of EOLC and communication between patients and FCGs from ethnically diverse groups and those from the wider UK population, and in their responses to EOLC and communication. People from ethnically diverse backgrounds want compassionate care that is personal to them. This is no different from people from white British backgrounds, as is well described in the literature, and supports the use of physical, social, spiritual and psychological care frameworks used in palliative care to address the individual needs of patients and families. However, HCPs need additional skills to navigate complex, sensitive communication and enquire about spiritual values and aspects of people’s lives that may be unfamiliar. The data show that there are clearly distinctive aspects of the experiences and circumstances of patients and FCGs from ethnically diverse communities that compound their difficulties in achieving good care. Deficits in communication, especially involving translation, misunderstanding and lack of information result in patients falling through the cracks in services and suboptimal experiences of EOLC.
Personalising care requires HCPs to get to ‘know’ the person, and the development of confidence and skills in discussing EOLC with persons from ethnically diverse backgrounds is vital for enabling tailored responsive discussions that are of real value to patients and their families. Training resources, using stories based on our interviews, were seen as an effective way to support this.
Finally, the data reveal the rather marginal position of professional input in people’s lives. Most of our participants orientated their lives to getting on with the challenges of living in the present, rather than dwelling on the future: being positive, holding to the essence of faith and all things being in god’s hands, and fear and avoidance of future talk. A minority did seek to think and plan ahead and sought information and discussion to support them in this. Participants had difficulty in nominating a HCP who they considered had a significant role or any sense of accompaniment in their illness. HCPs came into their lives at times, but there was little sense of continuity of care or of professional support to accompany and think with them as their health deteriorated towards the end of life. Patient and FCG participants described an experience of care that was often fragmented and unco-ordinated. Workshop stakeholders proposed more effective sharing of information between multidisciplinary professional teams as a prerequisite to enabling more tailored and effective care. Effective communication and trusted individuals sharing information in an easier way was seen by stakeholders as important in providing better care.
Chapter 8 Outputs, dissemination and impact
The findings from the three WSs of this study, described in Chapters 5 and 6, have identified key areas in which patients and their families require compassionate competence from health and social care professionals. The findings also highlight the need for the empowerment of service users from diverse ethnic and faith communities. Our dissemination work is informed by the recent work of Lamont196 and the ‘steps to impact’ that she describes. Although our dissemination work is, of course, far from complete, we report here on three key aspects of this as important outputs from this project:
-
work with local communities to raise awareness to continue conversations about end of life and further develop collaboration to reduce inequalities and improve experiences
-
supporting the practice of health and social care professionals through learning resources, including a nationally adopted NHS e-Learning for Healthcare module available to all health and social care staff
-
a high-level national ‘think tank’ about education and training in PEOLC for HCPs.
Working with diverse ethnic and faith communities
Throughout the project, working collaboratively with the PCBR group and the PPI co-applicant (described in Chapter 3) and working with the LOROS Hospice community outreach team, we have continuously built engagement with the diverse ethnic communities of Leicester and Nottingham. Building trusting, collaborative relationships takes a great deal of time, especially with communities that are more recently established and have less developed engagement with systems and organisations. Successful community engagement requires collaboration with people of the community, taking an assets-based approach and that activities take place within the community: to go to where people are, alongside those they trust and respect. 119,120
In the first 2 years of the project, we sought to build awareness about the work and to enable the broadest diversity of recruitment (described in Chapter 2, Recruitment). As discussed in Chapter 2, we contacted 177 community groups and community and faith leaders, and the research team was invited to 15 events. This engagement formed a good platform for our dissemination work in the last year of the project, when we sought to share the key messages and to increase collaborative working so that the project may lead to real change for people in their experiences in the last months of their life, when they are dying, and for their families and communities in bereavement.
One impactful aspect of our engagement and dissemination work has been through community radio based in Leicester, Ramadan FM (a pop-up radio station)197,198 and EAVA FM. Both have a social media presence promoting access beyond the live broadcast.
EAVA FM ‘take over’, July 2021
EAVA FM is a multilingual radio station broadcasting programmes to meet the needs of all, including new migrant communities. Its objective is to socially develop, inform and entertain, which comprises a combination of local news, enterprise, music, information, and cultural, faith and educational programmes, all supported by community members and local stakeholders.
Collaboration between the PPI co-investigator (IM) and the station manager led to a daily broadcast for 6 days in July 2021, discussing the research, and end-of-life experiences and services. The programme host focused on Somali, African Caribbean, Polish, Hindi-speaking, Gujarati-speaking and other Asian communities. The interviews can be viewed online. 199
Community radio engagement enables layers of impact. First, there is the broadcast itself, which is listened to live or on-demand on the radio or via social media channels. Engagement with the live show through viewer comments online and through ‘call-ins’ were very few (two or three per show), but indicated a very meaningful impact on listeners in some of their comments. For example, people connected the need for more awareness of PEOLC issues with barriers and stigma within their communities that needed to change. Metrics, beyond ‘views’ and ‘likes’ on YouTube (YouTube, LLC, San Bruno, CA, USA), uploads and tweets, of the reach and impact are difficult to obtain, especially in such a sensitive topic considered as taboo by many. We know from the radio hosts that many conversations were stimulated and that people, although hesitant, wanted to explore the topic further, but we cannot measure these in number or impact.
Second, the hosts of the radio shows are trusted and respected members of their communities with a high profile, some with national awards for services to their communities. They are highly motivated to reduce hardship and inequalities in their communities. Their feedback to us after the week of EAVA FM broadcasts showed that, despite, for some, their own discomfort with the topic, they held a deep commitment to achieving change and a desire to engage and collaborate further on initiatives. One such collaboration on a proposal for community-based bereavement support has already been submitted for consideration.
Third, through the trusted radio show hosts, new networks can be built. Such new networks have been used as part of our dissemination and impact strategy by the CNLWs, whose activities and impact are detailed below. This endeavour goes beyond what was anticipated in the project plan and illustrates how impactful dissemination must be flexible enough to be pertinent to the target audiences.
The work with community radio is ongoing, with open invitations to return to share more activities and messages for the communities that the station serves, and we continue to build on these relationships.
Community Network Liaison Workers
In June 2021, when the possibility of more face-to-face activities opened up, we recruited three part-time CNLWs. We were fortunate to find three bilingual/multilingual people with the availability, experience and drive to reach out to the communities in Leicester and Nottingham, to go where they are, to discuss the findings of the study and to build collaborative relationships to take forward future work to achieve real change. We needed to develop their skills in this research role, their understanding of the findings, their confidence in discussing end of life and dying, and their knowledge about services that can be accessed, including myth-busting about hospice and palliative care services.
Between 23 July and 13 September 2021, the CNLWs facilitated discussions at 16 events with 106 people. The events were diverse and included selective and open groupings: groups at places of worship, women’s groups, a diabetes self-help group, a Bangladeshi community bus trip, picnics, a cultural festival and a young person’s group. The majority of people were from Asian communities, but there has also been contact with Jewish communities. Other communities were not able to be reached in this very short time frame.
The CNLWs used a number of resources to promote discussion and share information, including some of the evidence-based narratives described below.
The CNLWs focused discussions on:
-
understanding of what a hospice is and the services they provide
-
understanding of end of life and services that might be useful
-
EOLCP and the use of the Recommended Summary Plan for Emergency Care and Treatment (ReSPECT)200
-
discussing planning ahead about their own/their family member’s end of life.
When possible, Likert scales were completed at the beginning and end of each event assessing people’s views on these four areas.
Key findings so far
The events had a considerable impact on what people indicated about their understanding and likelihood of thinking ahead and planning about their own end of life, as shown in Figure 6.
FIGURE 6.
Mean score of participants at the beginning and end of a community event.
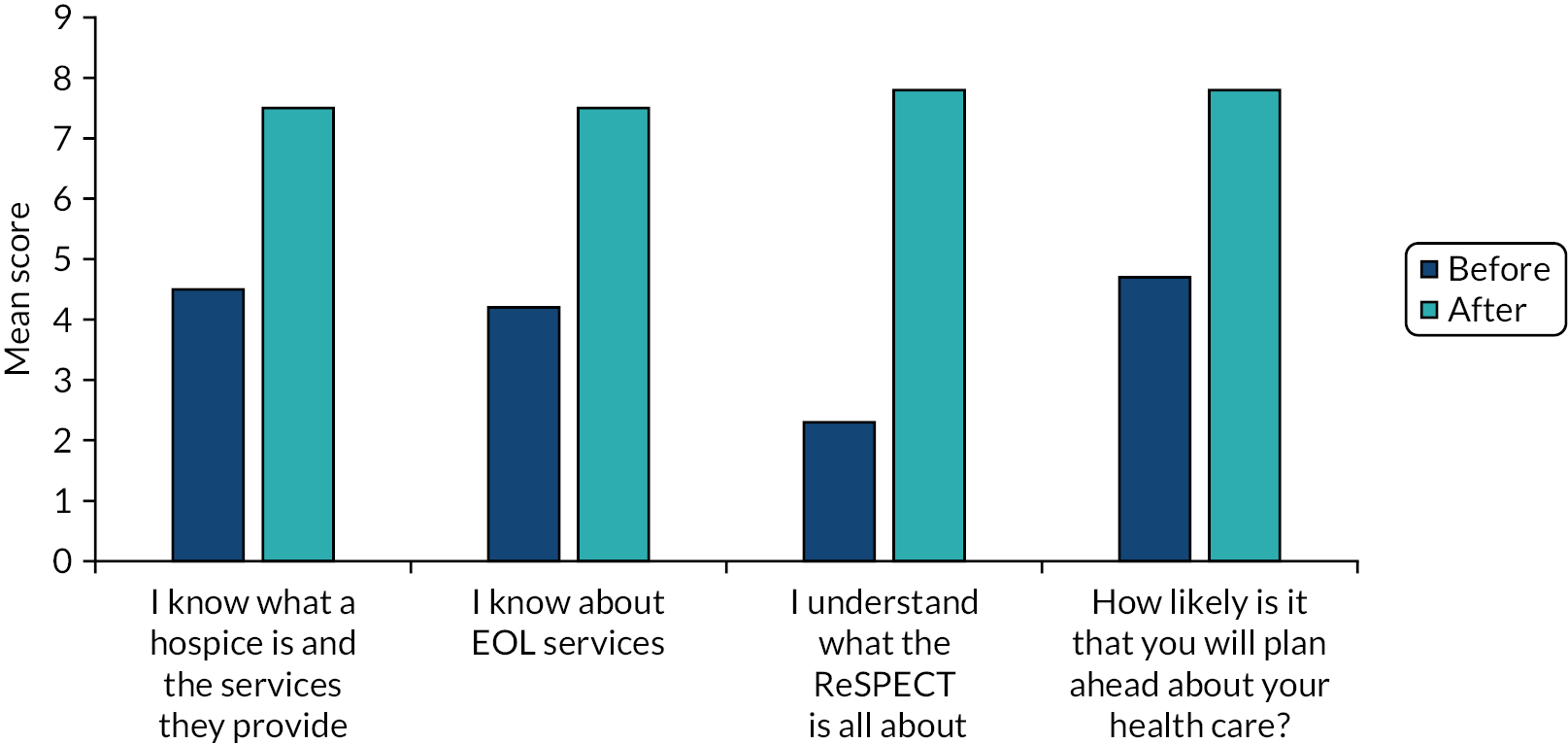
It was evident that most people had little knowledge of this area. The majority knew very little about what a hospice is or EOLCP, unless they had direct experience of a relative being terminally ill. Views about hospices were shared and misunderstandings and ‘myths’ (such as thinking hospices were a place where you will be left to die without any food or water) were discussed and corrected. Discussions about trust in health services and HCPs were especially layered in the context of COVID-19 and vaccines. It was also evident that there was an appetite for knowledge and sharing and that such discussions were welcome: ‘Yes, you need to go to communities to engage them on this topic so that it becomes less taboo’, ‘It has been quite therapeutic; we don’t talk about these things and today we have all shared our personal feelings’.
The key messages so far are that people:
-
want to know more and also want an opportunity to visit a hospice
-
wanted to know more about the ReSPECT.
Their suggestions as to what would be useful are as follows:
-
more discussion groups in the communities in different languages
-
most welcomed more discussion face to face
-
to put leaflets in the doctors’ surgery, library
-
talks on the radio and places of worship
-
it should be taught in schools
-
the information should be made available online and on social media for young people
-
they wondered if there could be information accessible via an app.
Training for professionals
Fictionalised evidence-based narratives
There is evidence to suggest that sharing key messages through stories has a greater potential than other methodologies for changing attitudes and having an impact on behaviours. A story is distinct from a series of sentences in its activation of affective, cognitive and belief changes in the story receivers. 201 Stories are often used with the public as interventions to influence health behaviours. 202,203 Narrative-based medicine has been shown to enhance and sustain the development of empathic practice of clinicians. 204
Research on the ability of narratives to transport their audience and thereby open them to new ideas and different ways of thinking and acting suggests that empathy with characters, identification with characters and vivid imagery change the usual way of thinking and acting of the person ‘hearing’ the narratives.
In addition to the summary narratives for each of the 18 case studies, for which three examples are presented in Appendix 2 (see Tables 14–16), we developed fictionalised narratives and stories based on the experiences of the 103 interview participants that convey the findings of this project in a number of outputs:
-
third-person narratives
-
first-person narratives (scripts)
-
audio-recordings of first-person narratives in long (circa 5 minutes) and short (circa 2 minutes) formats.
These narratives have evolved and developed iteratively, informed extensively by PCBR group members’ comments, researcher field notes from WS3 following their use in online group workshops and offline workbooks, and from their use in conference talks and teaching.
We worked with a professional writer/storyteller and producer to develop the narratives and the output typologies, including the development of the reading performances and the recording and editing of the audio stories. The stories were performed by four professional actors and four volunteers.
The narratives have been designed to reflect a diversity of demographic characteristics and contexts and to focus on specific themes arising in the data; Table 13 describes the characteristics of the eight stories that are used in the project dissemination and outputs. The audio-recordings and supporting materials, including a guide for educators, are available online (https://loros.co.uk/research-at-loros/thinking-ahead) and the scripts are included in Appendix 3.
| Fictional character | Sex | Age(s) (years) | Role | Ethnicity, faith | Main location | Stage of end of life | Illness | Key themes |
|---|---|---|---|---|---|---|---|---|
| Tawande | Male | 38 | Patient | African, Christian | Home | Post treatment and at start of end of life | Cancer | Ambivalence in discussing/relevance of planning to life approach Faith: god’s will, not mine Sustaining hope/collusion. Community pressure |
| Lanfen | Female | 65 | Patient | Chinese, Buddhist | Hospice | Early on in end of life | Diabetes/kidney failure | Being seen/known: don’t make assumptions about heritage and actions/preferences |
| Krushan | Male | 59 | Patient | Indian, Hindu | Home | Towards the later end of his life | Unspoken | Pressures of community/family judgement |
| Hafsa | Female | 80 | Patient | Pakistani, Muslim | Home | Later stages | Heart disease | Autonomy and decision-making complexities of family culture. Knowing the patient Communication |
| Dave | Male | 70 | Patient | Afro-Caribbean, agnostic | Home | In early to middle stages | Cancer | Lack of trust/misunderstanding |
| Balwinder | Female | 60/90 | Daughter/carer | Indian, Sikh | Hospital | At end of life | Unspoken | Carer’s duty and burdens. Language/communication barriers What’s going on below the surface |
| Emilija | Female | 80 | Patient | Latvian, Catholic | Hospice | Towards the later stages | Unspoken | Offering the opportunity to discuss deterioration and dying at a time of readiness Aligning care to priorities of patient |
| Sharmarke | Male | 25/50 | Son/carer | African, Muslim | Hospital | Middle to later stages | Unspoken | Complex life circumstances of migrants: what lies beneath the surface. Duty and misunderstandings Taboos and fears. Knowing the systems |
Open-access e-learning
A key objective of this project is to produce resources to be used in training and self-directed learning by health and social care professionals. With NHS e-Learning for Healthcare, we have developed an e-learning module within the End-of-Life Care for All e-learning programme. The content of this module integrated findings from WSs 1 and 2 with the thematic analysis of the data from professional participants in WS3, informed by NPT and the use of BCTs. The module has also been shaped at various stages of development by feedback from professionals.
The module is available free to health and social care staff online (www.e-lfh.org.uk/programmes/end-of-life-care/).
National Palliative and End-of-life care Education Think Tank
All staff are prepared to care
Wherever I am, health and care staff bring empathy, skills and expertise and give me competent, confident and compassionate care.
Our impact plan for the project included the development of a new initiative to bring together high-level professionals across a diversity of stakeholder organisations that plan, commission, deliver and monitor training for HCPs and their competence in delivering patient care. We worked with the NHS England and Professor Bee Wee (NHS Improvement National Clinical Director for End-of-life Care), and Anita Hayes (the Hospice UK Head of Learning and Workforce), to host two events. The first event was face to face and was before the COVID-19 restrictions; the second, in November 2021, was virtual to meet COVID-19 restrictions. The organisations represented are shown in Box 2.
NHS England
General Medical Council
Foundation Programme
Nursing and Midwifery Council
Macmillan Cancer Support
Hospice UK
Sue Ryder
South East Coast Ambulance Service NHS Foundation Trust
National Association of Clinical Tutors
British Islamic Medical Association
Cicely Saunders Institute
Medical Schools Council
Care Quality Commission
NHS e-Learning for Healthcare
Association for Palliative Medicine of Great Britain and Ireland
NHS England and NHS Improvement
Health Education England
NICE
Walsall Healthcare NHS Trust
LOROS Hospice
Derbyshire Community Health Services NHS Foundation Trust
University Hospitals of Leicester NHS Trust
Together for Short Lives
College of Paramedics, Royal College of Physicians, Royal College of Nursing, Royal College of General Practitioners
University of Hertfordshire
University of Leicester
University of Nottingham
University of York
The first event discussed what each organisation was doing to ensuring workforce competence to achieve the pertinent stated ambitions endorsed by NHS England (see Figures 7 and 8) and competence in personalised PEOLC as described in the NHS Long Term Plan,205 which focuses especially on increasing the percentage of people who have been offered personalised care and support planning at the end of life. 141
FIGURE 7.
The six ambitions for PEOLC, National Palliative and End of Life Care Partnership.
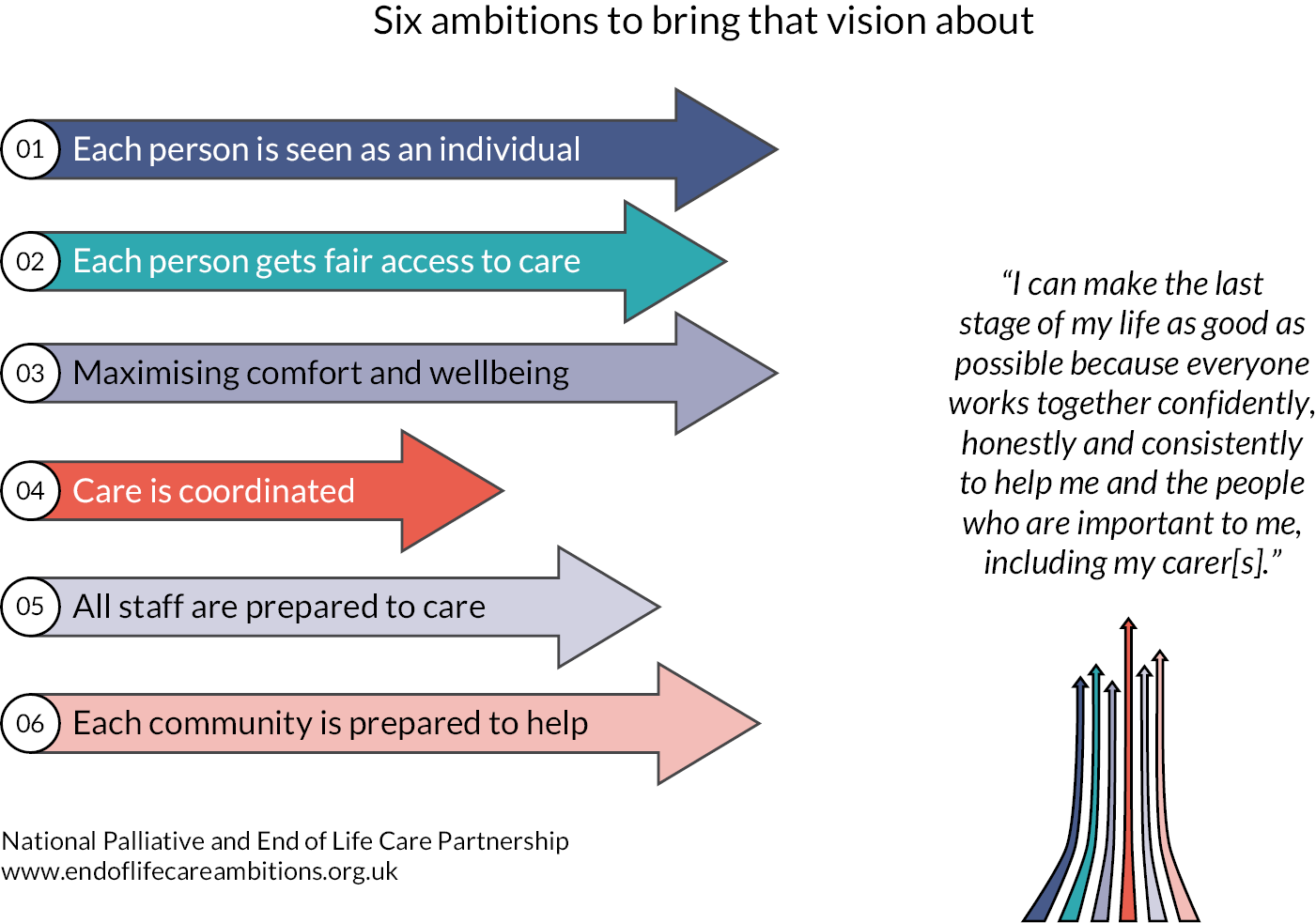
FIGURE 8.
The building blocks for ambitions: all staff are prepared to care.
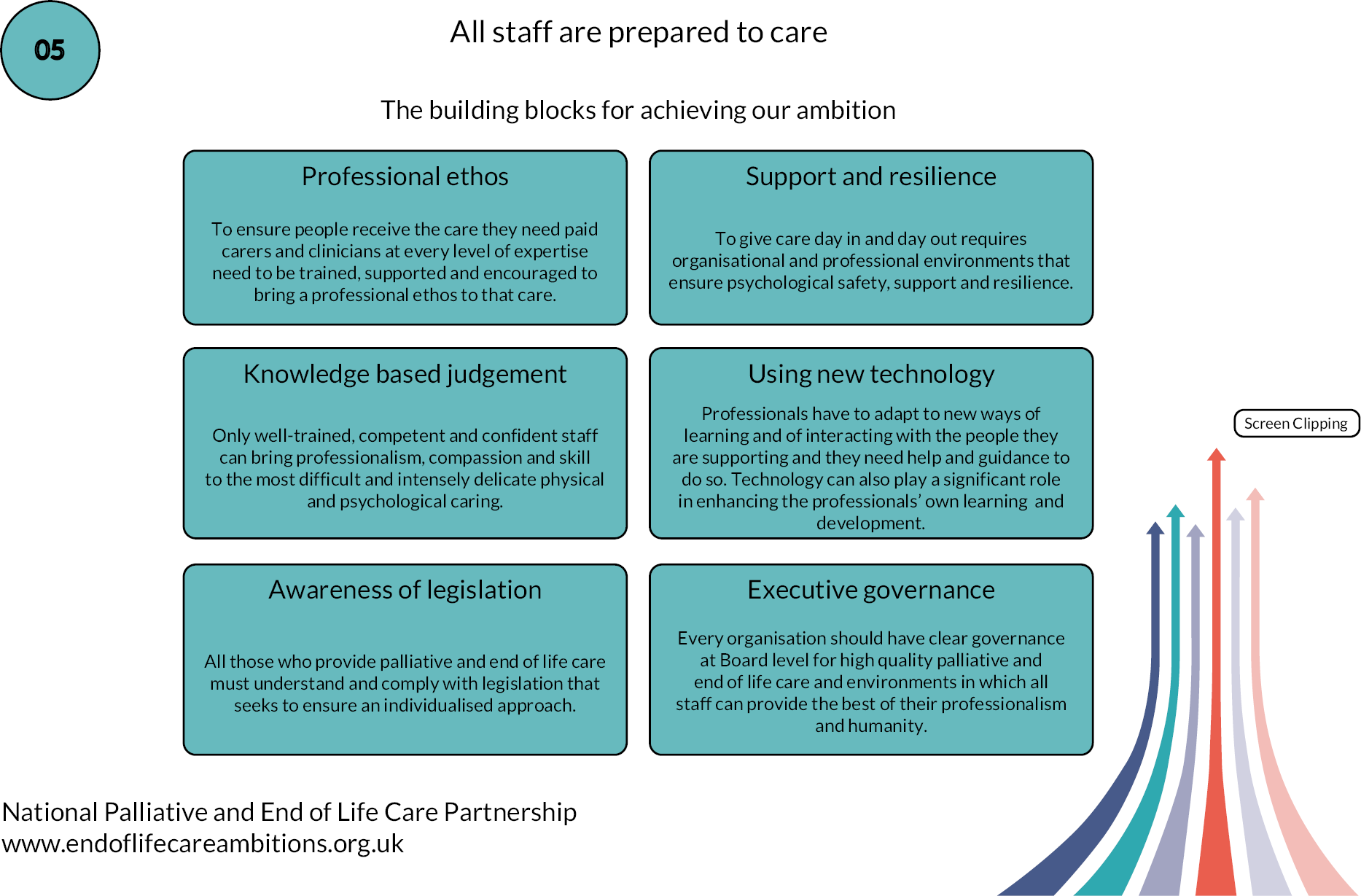
The following themes were discussed:
-
barriers to and enablers of preparing staff to care
-
the NHS culture for staff learning about EOLC and using their skills effectively
-
developing competence in honest conversations
-
using technologies in learning and assessment
-
implementation of standards and guidance in practice.
The group agreed that the meeting had been very useful, that there was a real need to improve education and training, and that there is value in doing this in a collaborative way.
A common focus was desired, and this was agreed as enhancing the workforce delivery of skilled honest and open conversations, including about deterioration and dying, to prepare staff to achieve ambition 1, each person is seen as an individual: everybody should have the opportunity for honest and well-informed conversations about dying, death and bereavement, and the NHS plans for personalised EOLC.
The importance of the competence of the health-care workforce in having open and honest conversations with patients and their families about deterioration and dying, and offering opportunities for personalised care planning, was dramatically foregrounded by the COVID-19 pandemic. The number of patients who were at risk of deterioration, the forced remote consultations and the diversity of staff who were caring for dying or very vulnerable patients meant that gaining skills and confidence in such conversations became a priority and greatly accelerated the development of resources and training.
The second event, delayed because of the impacts of the COVID-19 pandemic, was held in November 2021 and focused on supporting people from diverse ethnic and faith backgrounds.
Acknowledgements
We thank the patients and FCGs for their generosity in taking part in the study during a very difficult period in their lives, especially when their time was so precious. Without their contributions, this study would not have been possible. We also want to thank those members of the public and of community and faith organisations who participated in workshops or completed workbooks.
We acknowledge with thanks the input of the health professionals who took part as interviewees, those in organisations in Leicestershire and Nottinghamshire who recruited patients and FCGs, and those who took part in workshops to share their views.
Throughout the study, we have benefited from the invaluable support, wisdom and involvement of members of the public, carers and bereaved relatives PPI group. The members have been involved in the project from the outset, commenting on the study design, ethics and participant materials, including those for the workshop. They have also contributed to the interpretation of the data and the development of the narrative outputs.
We are grateful for the substantial and creative input of Irfhan Mururajani, who is a co-applicant on the grant and has worked on all aspects of the study as an integral member of the project team, and has been instrumental in the sharing of findings and building further dialogue with diverse ethnic communities. We are also grateful to our CNLWs for their support in disseminating the findings to local communities.
We are grateful for the support of the members of the Study Steering Committee, especially the chairperson Dr Jonathan Koffman. We have also benefited from the support of the study advisors and want to express our thanks to them all.
The audio-recorded stories were written and produced by Andy Barrett for Excavate (Nottingham, UK; www.excavate.org.uk). They were read by Sokari Erekosima, Jim Findley, Gurpreet Grewal-Santini, Violet Hais, Mufaro Makubika, Irfhan Ali Mururajani, Dipti Patel and Ling Peng. We are grateful for the collaboration with Andy and we would like to applaud and thank the readers of the stories.
The work would not have been possible without the research team at LOROS Hospice; we would like to thank Emma Bowler, Wendy Gamble, Natalie Ayton, Caroline Cupit and Penny Smith for their hard work. We would also like to thank co-applicants Alison Pilsworth and Simon Royal for their expertise and input. We would also like to acknowledge the board of trustees, the senior management team and the many departments in LOROS Hospice that have given enthusiastic support to the delivery of this huge endeavour.
Governance and approvals
The University Hospitals of Leicester NHS Trust was the study sponsor (reference number: IRAS 251664 Edge111248). NHS Research Ethics Committee approval was obtained in December 2018 (reference number: 18/WM/0310), with two subsequent substantial amendments (May 2019 and March 2020). Health Research Authority approval was obtained on 4 December 2018.
Contributions of authors
Zoebia Islam (https://orcid.org/0000-0001-9274-694X) (Senior Research Fellow) was responsible for study conception, project management, design, data collection, analysis and writing of the final report.
Kristian Pollock (https://orcid.org/0000-0002-6836-8595) (Professor of Medical Sociology) was responsible for study conception, design and delivery, data analysis and writing of the final report.
Anne Patterson (https://orcid.org/0000-0002-9105-9248) (Research Fellow) was responsible for data collection, analysis and writing of the final report.
Matilda Hanjari (https://orcid.org/0000-0003-0001-0797) (Research Associate) was responsible for community engagement, data collection, analysis and writing of the final report.
Louise Wallace (https://orcid.org/0000-0003-3770-0580) (Professor of Psychology and Health) was responsible for project oversight and advisory support, data analysis and writing of the final report.
Irfhan Mururajani (https://orcid.org/0000-0002-2624-9301) (PPI representative) was responsible for project oversight and advisory support, data analysis and dissemination, and writing of the final report.
Simon Conroy (https://orcid.org/0000-0002-4306-6064) (Professor of Primary Health Care, Faculty of Medicine and Health Sciences, University of Nottingham; Professor of Geriatric Medicine, University of Leicester) was responsible for project oversight, clinical expertise and advisory support, facilitation of recruitment and liaison with health professionals and services, and reviews of the findings and of the final report.
Christina Faull (https://orcid.org/0000-0002-0064-8056) (Consultant in Palliative Medicine, LOROS Hospice, and University Hospitals, Leicester): Study conception, design, data collection, data analysis, clinical expertise and writing of final report.
Ethics statement
NHS Research Ethics Committee approval was obtained in December 2018 (reference number: 18/WM/0310) from West Midlands – Coventry and Warwickshire Research Ethics Committee.
Data-sharing statement
This is a qualitative study; therefore the data generated are not suitable for sharing beyond those contained in the report. Further information can be obtained from the corresponding author.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
Appendix 1 Workshop stories
Jay has prostate cancer and strong family history of the disease. His father died when he was 19 from prostate cancer and, since then, as the eldest son, he has supported his mother. He has also taken over the care of his brother’s children and grandchildren after he died ‘because that’s what we do in our community’. The cancer has spread to his bones.
Jay has a strong sense of duty about helping and supporting people from his community affected by cancer. He talks about his own negative experiences, first in delayed diagnosis and, subsequently, in battling an unresponsive, ignorant and insensitive health service. For example, he describes how he found his brother was given meat in hospital meals, which went against his beliefs as a devout Rastafarian.
Jay told us that he does not think it is helpful to discuss the future or what it holds; they will respond when they need to, when that time is reached. He wants to avoid adding to family trauma resulting from the many deaths they have experienced. His wife says that she prefers to focus on the present rather than the future. Her husband might talk about the future with their youngest son who lives with them, but many of his family refuse to talk about this and strongly believe that he won’t die. He and his wife have both planned their funerals.
Jay and his wife have a very strong faith. Jay considers that he has many years to live and that a miracle may yet happen.
Jay has just started going to a hospice day centre. He finds being at the hospice difficult because seeing people who he considers to be less well than himself ‘point[s] to the future’. Health professionals feel that they have offered Jay the opportunity to discuss the future but that he is not yet ready; he does not see himself as dying, so feels he does not need to talk about dying. Professionals identify that the transition from who he is (advocate and campaigner) to who he is becoming (in his eyes a patient) is painful.
Jay has been having chemotherapy and is attending an appointment with the medical oncologist today. Although he is less well and in more pain, he does not anticipate that he will need to discuss anything other than treatments that will make him better.
Ibrahim is in his late 70s and has multiple sclerosis, a condition that affects his muscle strength, making him progressively weaker and more disabled. He left school in Pakistan at age 13. He has lived in the UK for 60 years, but needs an interpreter for conversations in English, which is usually his eldest son, Arshad. He is a devout Muslim and a hafiza who has memorised the Qur’an. Arshad is the person he turns to for help and he expects that decisions will be made jointly with him, his wife and his son Arshad. He does not want to think about what will happen as his illness gets worse, but if health professionals advise he will listen, and in crisis circumstances he would leave decisions to them.
Ibrahim’s illness is affecting his abilities. He needs help for many activities, including preparing for his salat (prayers) five times a day. Islamic and personal duties are very important in the way he and his wife conduct their lives. His wife is the main carer for her husband and stresses that this duty is important for her as a good wife and Muslim. They are both increasingly frail but have declined social care, in part because of the need to time visits around the sunrise and sunset prayers, but also because of other factors related to duty, cultural acceptability, community expectations and not wanting to be a burden to others.
The specialist nurse has spoken with his son Arshad about the need to decide on Ibrahim’s ‘resuscitation status’. Arshad has a good understanding of his father’s illness and has taken advice about Islamic acceptability of a ‘do not resuscitate’ decision and is consulting his siblings. Arshad feels scrutinised and judged by the community with pressure to always ‘do the right things’ that are acceptable for his parents, but also the community.
As Ibrahim’s disease progresses, he is likely to experience problems with swallowing and breathing, with life-threatening consequences. His nurse is coming today. He and his wife are worried that he is coughing more and that he may need some treatment for this.
a Hafiz and hafizah are men and women who preserve the purity of the Qur’an. It is believed that someone who memorises the Qur’an will enter Jannah (paradise) along with 10 others without question on the day of judgement. During Ramadan, huffaz (plural) give those who cannot read the Qur’an the opportunity to listen to the entire Qur’an over the 30 nights and gain many rewards as a result.
Ibrahim is a Pakistani man in his late 70s who has advanced multiple sclerosis, a condition that affects his muscle strength, making him progressively weaker and more disabled. Owing to his disability from the multiple sclerosis, he needs help for many activities of daily living, including personal care. His wife is the main carer for her husband. They are both increasingly frail, but they have declined social care.
As Ibrahim’s disease progresses, he is likely to experience problems with swallowing and chest infections, with life-threatening consequences. He and his wife are worried that he is coughing more.
The specialist nurse has spoken with his son Arshad about the need to decide on Ibrahim’s resuscitation status. Arshad feels that this is a very difficult decision to make.
His nurse/doctor is coming today to take discussions further about what to do if a crisis arises.
Patience used to be a school head teacher in Ghana and then in the UK until her retirement at age 63, just 2 years ago. At face value, she presents a carefree spirit, who is willing to engage and talk about her recent change in mobility on one side of her body, as a result of the removal of one of the cancerous tumours from her spine, for which she is receiving ongoing treatment. Her main concern is for her husband at the moment, and the fact that she was the main carer for him before being diagnosed with her own illness. Her ongoing episodes of treatment mean that her ability to take care of him fluctuates accordingly. She has already made sure plans are in place for her funeral and her husband’s ongoing care needs, should she deteriorate rapidly at some point. She has two adult children, but talks about her lack of support from any extended family.
Patience wants to be in control of her life and her death. She feels that HCPs have not initiated any discussion about deterioration, dying and her preferences for care and treatment, and that she and her husband would welcome such a conversation. She mentions how her cousin Dorah disagrees with her. Dorah has recently arrived in the UK from Ghana to look after her terminally ill daughter. Dorah has shared with Patience that she was tormented after the GP started discussing dying. She was also appalled when, during a recent emergency visit to A&E with her daughter, Dorah was asked ‘point blank’ if there was an instruction not to resuscitate her daughter if her heart should fail. Dorah felt that discussing death and dying so openly and so coldly was unheard of in her culture. Patience feels very differently. She and her husband are strongly ‘for’ assisted dying at a time of their choice.
Despite Patience’s stated willingness to discuss dying, a health professional whom she sees for regular check-ups feels that she has not raised any questions for them to respond to, and senses that Patience wants to focus on the now, rather than the future. This might be influenced by the uncertainty of whether or not treatment will work, whether or not her illness will change and how long she has left to live.
Patience is critical of services that have been unco-ordinated for her and her husband, and based on saving money and getting people out of hospital. She has struggled to secure support for adaptations to her home, which would enable them to stay at home for as long as possible, having only found out by chance after talking to an old colleague that they could apply for such support.
Today she is going for her third visit to a hospital clinic this month. She will be going alone, as it is difficult for her husband to access the building in which these appointments take place. Her own physical mobility is compromised, and although Dorah has offered to accompany her, Patience doesn’t want to trouble her as she has her daughter to care for.
Adamma is a frail 78-year-old woman with heart failure who spends most of the day in bed. She lives with her daughter Ada, who is her main carer.
Adamma recently refused to take morphine when it was prescribed for her pain relief. Adamma is growing more distant and closed off to others.
Adamma and Ada are seeing the GP/nurse today to discuss the flu jab.
Adamma was born in Nigeria and migrated to the UK in the 1970s.
She blames the health-care system for her delayed diagnosis and subsequent ill health. When her health started deteriorating, doctors took a long time to identify a faulty heart valve causing her heart failure. The operation to correct this resulted in Adamma requiring further corrective surgery. Adamma feels that the first operation was a disaster. Even though she regularly attended the hospital, Ada described it as a ‘battle’ to locate her mother’s records for insurance purposes.
Adamma is not afraid of dying; she feels she has had a good life. She has talked to her family about her wishes at end of life, but has not shared these with HCPs as she feels this is an intimate family matter in which HCPs should have no involvement.
Adamma has said that, apart from spiritual preparation for life after death, no one has the power to change anything. Ada feels that some spiritual preparation may be helping her mother to cope, but she is concerned that, in focusing more on life after death, her mother is not engaging with matters of this life.
Adamma’s preference is to die at home, but the memory of her sister Fumnanya’s death from cancer makes it difficult for her to trust health-care advice about end of life. Adamma and Fumnanya had many similar experiences of health care; what was especially painful was that each time they were referred to a new health service, they were asked to retell their story. Talking about the illness brings bad feelings and is not right. Fumnanya received palliative care for 2 years and Adamma felt that her death was hastened by the drugs she was given, after coming home from a hospital admission. Adamma knows these drugs were called end-of-life drugs, but her sister died a day after taking them. As a consequence, she believes that morphine is lethal and works only to hasten a patient’s death.
Adamma was close to her sister, but they had different beliefs: Adamma believes everything happens for a reason, whereas her sister saw things differently. Fumnanya struggled to see beyond her present life and believed that evil forces were at work and that these originated from previous, negative life experiences to do with her marriage and family relationships.
Ada struggles with administering her mother’s medication and also her own mental health issues.
Ada is worried about how Adamma will react if the GP wants to discuss pain relief.
My grandfather Delun is an 86-year-old Chinese gentleman and has lived with diabetes for many years. More recently, he has been diagnosed as having very advanced kidney disease. His wife, my grandmother, died a few years ago and Delun now lives alone, although not far away from me and my wife.
A few days ago he awoke to find himself in A&E, having collapsed while taking a short walk outside his home. A neighbour had called an ambulance, and then called me. The neighbour knew that I was now Delun’s main carer, since my father, my grandfather’s only son, died some years before. The neighbour also knew that I interpret for my grandfather. Delun has never fully learned English, having only ever worked in the family business until his retirement. Delun’s neighbour has never held a direct conversation with him, despite having been neighbours for many years! My mum is English and although she helps me care for Delun, she is unable to understand him fully.
At the hospital, dazed and confused, Delun had managed to answer a few questions with the help of a Cantonese-speaking porter at the hospital until an interpreter could be tracked down, although the interpreter never arrived. My mum arrived at the hospital just ahead of me and told me that when she arrived, Delun had been in a very distressed state as he had been unable to explain that he needed to visit the toilet.
When I got there, I was immediately questioned by the duty doctor, enquiring whether a DNACPR was in place, as they could have done with knowing this when he was admitted earlier that day. I explained that nothing was in place at present, as Delun had become very agitated during an earlier hospital admission when I was not there, and an interpreter had explained to him that they were seeking Delun’s permission to withhold care if he should become too poorly. This had disturbed Delun greatly and was upsetting to me because it meant that this was a conversation that I was going to have with my grandfather. It was also upsetting for me because it took me back to emotional conversations I had had with my father before his death.
Delun was now very wary of hospital visits and sometimes missed dialysis sessions when I was occasionally unable to accompany him due to my work commitments. I’ve now used up most of my annual leave entitlement. I’m the only one my grandfather trusts to make decisions about treatment.
I’ve now managed to re-register Delun with a Chinese-speaking GP at a local surgery. I do think that some important discussions need to be held sooner rather than later, and the best chance of hearing my grandfather’s true feelings about the future rests in the hands of this new GP. I’ll need to take leave, of course, to go with Delun.
Shimbira is a 66-year-old woman who lost her husband to a brain tumour 2 years ago. Her husband Abdul was a very committed family man who enjoyed having family dinners. Abdul was born in Zambia and came to the UK in the 1960s. They were married for 40 years and have two grown up children, a girl and a boy, and eight grandchildren. Abdul was a committed Muslim and very independent and had owned and managed his own business for more than 30 years. Shimbira recounts the events leading to Abdul’s illness, saying it was very sudden.
Abdul felt weak when he returned from his pilgrimage to Mecca and complained of a headache, so he went to the GP. The GP could not find anything wrong so he gave him painkillers, which did not work. Abdul then returned to the GP on two separate occasions, complaining of the same symptoms before he was referred to the hospital for further assessments. Eventually, a MRI scan found he had a brain tumour. Abdul had to have brain surgery.
Shimbira describes her experience at hospital as being offensive. She recalls the time when she walked in to Abdul’s ward and found her husband about to eat pork sausages, something he would never eat as a devout Muslim. She contrasted this experience with another at a different hospital where Abdul was referred to for further surgery. In Shimbira’s opinion, the doctors and nurses there were very good. For example, because of Abdul’s speech difficulties, caused by the tumour, they were keen to involve the family and make sure they got things right for him. Shimbira explained that whenever the doctor or nurse was unable to understand her husband, they always phoned her to explain or clarify things and to ask them for their input on all decisions, even his dietary requirements and preferences. Although this was a very difficult period in Shimbira’s life, she is grateful for the support she received from the hospital staff.
Shimbira described how, after Abdul was discharged from hospital, nurses continued to support her as his health deteriorated. She recalls the nurse, Judy, who used to come every Tuesday to check on them and provide support. To her, what made this support outstanding is the fact that Judy managed to win their trust as a family. Each time Judy would visit, she would make an effort to interact with Abdul and this assured them that she always had his best interests at heart. Judy guided them about changes in Abdul’s medications. She was also accessible and when they could not speak to her over the phone, she would always return their calls within a reasonable time. Judy also updated Shimbira and Abdul on what to expect as he deteriorated and this helped Shimbira and the family prepare for the eventuality of Abdul’s death. In that sense, Shimbira considers herself lucky, even though her husband is no longer here.
Shimbira compares her experience with her neighbour Prudence’s experience. She explains Prudence has just learned that her mother has liver cancer, and does not have long to live. The consultant has advised Prudence to take her mother home to die. Shimbira is helping Prudence access guidance and support for her mother at home and they are speaking to the doctor later today.
MRI, magnetic resonance imaging.
Kozal is a frail 78-year-old Asian woman, born in India, who migrated to the UK in the 1970s. She spends most days in bed, and lives with her daughter, Sunita. Sunita is the main carer and struggles with administering her mother’s medication and also her own mental health issues. Kozal blames the health-care system for her delayed diagnosis and subsequent ill health. When Kozal’s health started deteriorating, doctors took a long time to identify a faulty heart valve causing her heart failure. The operation to correct this resulted in Kozal requiring further corrective surgery. Kozal feels that the first operation was a disaster. Even though Kozal regularly attended the hospital, Sunita described it as a ‘battle’ to locate her mother’s records for insurance purposes.
Kozal is a Jain and believes that everyone’s soul is considered equal and should be treated with respect and compassion. She is not afraid of dying; she feels she has had a good life. She has talked to her family about her wishes at end of life, but has not shared these with HCPs as she feels this is an intimate family matter in which HCPs should have no involvement. Kozal’s preference is to die at home, but the memory of her sister Aarti’s death from cancer makes it difficult for her to trust health-care advice about end of life. Kozal and Aarti had many similar experiences of health care; what was especially painful was that each time they were referred to a new health service, they were asked to retell their story. Talking about the illness brings bad feelings and is not right. Aarti received palliative care for 2 years and Kozal felt that her death was hastened by the drugs she was given, after coming home from a hospital admission. Kozal knows these drugs were called end-of-life drugs, but her sister died a day after taking them. As a result, Kozal recently refused to take morphine when it was prescribed for her pain relief, as she believes it is lethal and works only to hasten a patient’s death.
Kozal was close to her sister, but they had different faith beliefs. Although Kozal is a committed Jain, reading scripture, praying regularly and believing everything happens for a reason, her sister saw things differently. Aarti struggled to see beyond her present life and believed that evil forces were at work and that these originated from previous, negative life experiences to do with her marriage and family relationships. Throughout her illness, she regretted not accepting offers of a priest to pray for her and cleanse her of these problems and misfortune. She believed that then her health might not have taken a turn for the worse.
Kozal’s daughter is concerned that, in focusing more on life after death, her mother is not engaging with matters of this life. Kozal has said that, apart from spiritual preparation for life after death, no one has the power to change anything. Sunita feels that, although some spiritual preparation may be helping her mother to cope, Kozal is growing more distant and closed off to others. Kozal and Sunita are seeing the GP today to discuss the flu jab. Sunita is worried about how Kozal will react if the GP wants to discuss pain relief.
Mufaro is a keen football player and football fan who is suffering from cancer; he is no longer receiving treatment at the hospital, having been told that they are unsure, at this stage, if there is any more treatment available. Although the pain has been getting worse, Mufaro is confident that he will pull through and that god will help him to recover. As long as he stays strong and does not start to doubt. As long as he does not give up. But he knows that he won’t. Everyone has always known that Mufaro is a fighter. Ever since arriving here as a young boy with his aunt, he has had to stand on his own two feet.
Furthermore, the fact that he has not received any news from the hospital suggests to him that he has a good chance of recovery, because they always treated him well and he is confident that if they think of a new treatment that might work, they will let him know. However, his wife, Chibuzo, has told him that she overheard a nurse saying that there was nothing more that they could do, and it was now just a matter of time. Chibuzo was shocked by this, and even more by the fact that she heard the nurse use the word ‘dying’, a term she cannot bring herself to use, for it is only god who knows whether or not somebody is dying. Mufaro has tried to console her, and anyway the nurse is not a proper doctor and doesn’t know what the doctor knows.
Mufaro respects his doctor; he has always encouraged his positive attitude. There was one time when he was going to talk about things with him; about what might happen to his wife if the treatment didn’t work; but he could see that the doctor was being positive, and he didn’t want to let him down. Everyone must all believe in the same thing and fight together. That’s the way that you win. Through teamwork.
Today some friends from the football team he used to play for are coming round to watch a big match with him on the television and he is willing himself to be in as good a shape as possible. He is worried that he may let himself and them down a little. He feels that he has let down some of the congregation at church who have been praying for his recovery, which has not yet started to materialise. But it will. He is sure of it. He knows he will never play football again, but he can still offer advice from the sidelines once his body has started to recover or if a new cure is found. And the doctors are always finding these new treatments and will contact him when they have found something that they think will work.
Mufaro also knows that he needs to apologise to one of his friends, Darren, who will be coming; someone he played with at the heart of defence the year they won the league. During a visit last week, Darren suggested to his wife, Chibuzo, that Mufaro was not dealing with the reality of the situation, that he could see that he was getting weaker and that perhaps they should talk to the doctor about what they could do to make the end of his life easier for them both when that moment arose. This confused and worried Chibuzo, like the time she overheard the nurse, because Chibuzo knows that such things shouldn’t be talked about like this. That to start to think about such things is the start of a slippery slope. Mufaro was very angry; it was wrong to do this to his wife. If Darren wanted to say anything, he should have spoken to him and not her. And anyway the doctor is the one who will decide when the right time is to talk about such things.
Mufaro is aware that Chibuzo is tired and can sometimes become very emotional with the work of looking after him. He jokingly calls her his trainer because she has become an expert on the peaks and troughs of his energy levels and mental well-being. Yet this moment of confusion for Chibuzo, because of Darren’s thoughtlessness, also threw Mufaro and, in a moment of weakness, he wrote down everything that he wanted to happen if he did die. Not just the funeral and what happens afterwards, but the actual days leading up to his dying. Not that he will.
He hasn’t given this to Chibuzo, and he hasn’t told her about it. But he has kept it. Just in case. Now that he’s written it, it would be stupid to throw it away. He has also decided that Chibuzo should let his organs be donated. That maybe he can help a young person who is unwell. That maybe this will help them run around a football field or engage in some other kind of sport as he would like to. He is not sure about the religious teachings considering this, but it is something that he has decided on. And he is pleased that he has done that.
He rang Darren and told him never to say things like that to his wife again. That although he was a good footballer, he never had the same level of commitment as Mufaro, and never understood his faith. That the rest of the team who have come to his house have known better. Even though some are non-believers, and the others are of a different faith to him, they know the importance of a positive mindset. That you never win anything if you go into a game fearing defeat.
But it is not just all about his inner strength; he knows that. It is ultimately in god’s hands. It is he who gives life and he who determines it will be taken away. Mufaro’s job is to stay positive and to keep praying. And he has forgiven Darren, as he knows he should. It is a time to embrace one’s love of friends.
He just hopes the match won’t go to extra time.
Appendix 2 Brief case narrative summaries
Mr Chahine
| Participant | Data collection: March 2019–July 2019 |
|---|---|
| Mr Chahine | 3 interviews |
| Mr Chahine’s wife | 3 interviews |
| Mr Chahine’s son | 3 interviews |
| HCP: specialist nurse for MND | 2 interviews |
Background
This is an elderly Muslim gentleman with MND. He left formal schooling at 13. Mr Chahine is a first-generation migrant; he came here from Gujurat, India and became an Islamic religious teacher (imam). He speaks Gujarati as a first language and has been interviewed via an interpreter. He has an Indian wife and three sons and a daughter, the eldest son being the one to whom the parents turn in the first instance for support in any health-related matters (e.g. speaking to HCPs).
Living arrangements
Mr Chahine and his wife live independently in a bungalow. They moved when Mr Chahine could no longer manage stairs well and now live a little further out of their community. Their elder son, who is their first point of contact if needed, lives on the other side of the city.
Understanding of end-of-life care planning
Mr Chahine has never spoken to any HCPs about his future care or EOLCP. He did not want to broach the subject of the future and what will happen as his health deteriorates. He is not ready to talk about EOLCP yet.
Experience and expectations of treatment
Treatment appears to be around management of his condition and the limits to his mobility.
Expectations for the future/goals/values
Mr Chahine wishes to stay in his house for as long as possible, although he has not communicated this to anyone other than his wife.
Health-care professional’s perspective
Mr Chahine’s nominated HCP is a specialist nurse for people with MND. She only sees him every 3 months as his illness is progressing slowly. The HCP had discussed DNACPR with Mr Chahine and tried to talk to the eldest son about this, especially as Mr Chahine had more or less come round to the idea of having a DNACPR instruction in place; however, the eldest son felt that he should consult his siblings to check this. They seemed to see the logic of having this though. The HCP, however, feels that the discussion came up only because Mr Chahine had a chest infection; it may not have been discussed otherwise.
Key observations and emerging issues
Knowledge of illness and prognosis
Mr Chahine does not know the name of his illness, but can talk about its effects on his mobility and the care that he needs. He is also aware that in time he may also experience problems with his throat, which by the third visit with him, had become apparent as he was struggling with swallowing. Although he stated that his health was deteriorating over the course of the interviews, he did not want to think about what will happen as he gets worse.
Choice and decision-making (who is involved?)
Mr Chahine stated that any decisions made about treatment and future care would be based on a joint decision between him, his wife and son. Mr Chahine’s son stated that, ultimately, any decisions made were his dad’s decisions, but that he himself would also speak to his siblings before anything final was in place.
Discussing end-of-life care planning with others (do not attempt cardiopulmonary resuscitation)
Mr Chahine’s HCP had discussed DNACPR with the him and tried to talk to the eldest son about this, especially as Mr Chahine had more or less come round to the idea of having a DNACPR instruction in place; however, the eldest son felt that he should consult his siblings to check this. Mr Chahine’s son explained that his dad had been confused about what DNACPR meant and, once he had explained this to his father, he had decided against this. Mr Chahine’s son also said that he had checked if DNACPR was actually feasible Islamically with a scholar who was an educated mufti (a Muslim legal expert who is empowered to give rulings on religious matters) and the mufti had confirmed that there was no reason Islamically why his father could not have a DNACPR instruction in place in the future. Mr Chahine decided not to sign a DNACPR form.
Faith/spirituality and culture
Mr Chahine is a hafiz (i.e. he has memorised the Qur’an). Faith appears to have been a part of Mr Chahine’s career and remains a big part of his prayer life. He prays five times a day. His wife helps him with ablutions. Mr Chahine’s wife’s desire to care for her husband herself is also, to some extent, rooted in faith. Mr Chahine does not feel that faith necessarily guides his treatment decisions; however, he does refer several times to how god is helping them (with good neighbours, helpful people in shops, etc.). Although nothing (regarding accepting treatment and care) has been completely ruled out on the basis of culture/religion, it is possible that any future outside personal care support given to Mr Chahine may also need to reflect appropriate timings (carers to arrive at sunrise and sunset because of prayer times) and methods (of correct washing to prepare for prayer) that are in line with religious requirements.
Family support (duty)/extent of family support
Mr Chahine’s wife feels a sense of duty to care for her husband: as her wifely duty, religiously, it is better if she cares for her husband rather than passing this over to others. She has struggled to handle him physically and also wheel him around in the wheelchair, but she is determined to care for him. Another reason given for not wanting carer support was because she wanted to do it herself, as it gave her a ‘sense of purpose’, she would not have anything to do if she did not care for her husband; she would become unwell if she did not keep active.
Ethnicity-specific issues (community pressure)
Mr Chahine’s son mentioned that he and his brothers have been judged by the wider community (namely his mum’s and dad’s friends) who question how much they do for their parents; he gave an example of his parents’ friends asking him if he had got the correct walking frame for his mother and also why they had not got personal care for his parents. This added ‘societal pressure’ to be seen as doing everything you can seems to add to the carers’ burden.
Personal reactions and stances (independence and dignity)
Independence and dignity are key for both Mr Chahine and his wife. Mr Chahine’s son stated that culture was a key reason in his parents not wanting to seek support outside the family. Both want to remain independent for as long as possible, and are sometimes reluctant to seek help. Particularly with personal care, Mr Chahine’s wife feels that she should do it and that is her ‘personal’ choice and also duty (see above). Mr Chahine’s HCP suggested that this seems to be frequently the case with other families, not just for this family or based on cultural norms.
Mr Chifamba
| Participants | Data collection: July 2019–November 2019 |
|---|---|
| Mr Chifamba | 2 interviews |
| Mr Chifamba’s mother | 2 interviews |
| Mr Chifamba’s sister | 1 interview |
Background
Mr Chifamba is a middle-aged man with cancer who came to UK from Zimbabwe to study and then to work as a mental health nurse. Before the illness, Mr Chifamba lived on his own. Mr Chifamba’s mother came to look after him, but after the 6-month compassionate visa expired, she had to return to Africa as immigration refused to renew it, even though her son still required care.
Living arrangements
At the time of the interviews, Mr Chifamba was living with his mother in his house. During the follow-up interview, the patient stated that his mother’s compassionate visa had expired and she had been asked to leave the country. She was planning to go back to Africa.
Understanding of end-of-life care planning
Mr Chifamba appears to understand EOLCP, but does not necessarily engage with it. In the interviews, when Mr Chifamba was asked about this, he mostly talked about his post-death wishes and financial preparations.
Experience and expectations of treatment
Mr Chifamba had mixed experiences when it came to treatment. It took HCPs a long time to determine what was wrong with him. For a long time he kept visiting the hospital; they would check him and say they could not see anything wrong with him. He feels disappointed and frustrated that it took so long to diagnose him with end-stage cancer. All this experience made Mr Chifamba lose trust in hospitals and also question whether or not they had his best interests at heart. He decided to put in a formal complaint about the way he was treated.
Expectations for the future/goals/values
Mr Chifamba has trouble seeing past his present situation when he talks of cancer not being in the agenda of his life. He expresses further frustration that he was told he was no longer fit to continue working. His narrative implies a life invaded by cancer and unfulfilled potential and promise. He says one of the hardest things to cope with is his own expectation of life and struggling to figure out the future in his present condition. Mr Chifamba’s mother made it clear that death, dying and EOLCP are topics he would refuse to discuss. In her opinion, she does not want to entertain any negative thinking by engaging in EOLCP discussions.
Key observations and emerging issues
Resistance to end-of-life care planning discussions
Mr Chifamba’s mother prefers not to talk about EOLCP, as she sees it as having a constant reminder of your ‘death penalty’. She says it is common sense for someone to be prepared about any eventuality in life. She says it is normal that people are born and die; thus, it is automatic that people have learnt and will be prepared when someone dies. She says things to do with death come automatically and people do not have to be reminded all the time about the death penalty. If this happens, people are wired to be able to handle this automatically and it need not be a topic for discussion.
Lack of trust
Mr Chifamba does not trust HCPs because of his past experiences and delay in diagnosis.
Ancestral roots
Mr Chifamba was born in Zimbabwe and wants to be buried there.
Culturally inappropriate
Mr Chifamba’s mother does not think it is culturally appropriate to discuss dying and death, as it may then happen sooner. Such discussions in her culture are not done and she views it as a Western style to discuss such things. Talking about death and dying takes away her morale and hope.
Religion and spirituality
Mr Chifamba’s mother talks a lot about her Christian values, saying that it is god who determines things, implying decisions should be made in consultation with him, following his guidance.
Immigration issues
Mr Chifamba’s mother was planning to return to Africa even though her son still required care.
Mrs Curkovic
| Participant | Data collection: October 2019–April 2020 |
|---|---|
| Mrs Curkovic’s daughter and consultee | 2 interviews |
| Mrs Curkovic’s daughter | 3 interviews |
| HCP: general practice nurse specialist (responsible for ACP) | 1 interview |
Background
Mrs Curkovic is an elderly Serbian lady who has a diagnosis of cancer. She also lives with dementia, so her youngest daughter was the consultee for Mrs Curkovic’s participation in the study. Mrs Curkovic is Serbian, was born in Croatia (formerly Yugoslavia) and migrated to the UK with her husband. Her husband died some years ago, rather suddenly. Her religion is Serbian Orthodox; Mrs Curkovic was able to speak English and had worked in several roles until retirement, but with the onset of dementia and less socialisation when she ceased working, she reverted back to her mother tongue. Her daughters interpret for her in all situations, even staying in hospital with her to do this.
Living arrangements
Mrs Curkovic is cared for by two British-born daughters. One of her daughters gave up work in January 2019 to care for Mrs Curkovic and the other reduced her working hours to share the care. Mrs Curkovic’s daughters see it very much as part of their culture that they care for their mother; being placed in care elsewhere would be countercultural and the last thing their mother would want. Mrs Curkovic is cared for at her own home and also at her youngest daughter’s home. This daughter also acts as a consultee for Mrs Curkovic.
Understanding of end-of-life care planning
The family have spoken repeatedly of home as their preferred place of care/dying. They acknowledge that things may deteriorate and that other care may become necessary, although they are determined that will not be in hospital, because of previous poor experiences of care there. The daughters have now signed a DNACPR form, although they agonised over this, feeling that they were signing their mum’s ‘death warrant’. It is hard to know whether or not Mrs Curkovic understands EOLCP except as far as her daughters try to ask their mum’s opinions on matters such as where she wishes to be cared for. It is not clear whether or not Mrs Curkovic would wish or be able to consider elements of her EOLC to plan DNACPR and place of care. Initially, Mrs Curkovic’s daughters feared that signing a DNACPR form meant that no care would be delivered to their mum in the event that she deteriorated. This was wrapped up with the emotional aspects they felt about ‘giving up’ on their mum. After being given time and space, they felt able to embrace the notion of having a DNACPR instruction in place.
Experience and expectations of treatment
The family (and possibly Mrs Curkovic) accept that there will be no further treatment for cancer except medication to manage symptoms. Mrs Curkovic is also seen in a primary care setting regarding dementia, and her daughters speak very positively of care received from the GP/practice nurse. The family’s experience in an acute/hospital setting has, however, been a cause of upset (harsh explanation of her illness in a very public area, abrupt questioning about DNACPR status). This has framed their future care expectations: they hope it will be possible to deliver future care at home or in a hospice.
Expectations for the future/goals/values
Care at home for Mrs Curkovic is desirable for as long as possible, with hospice a second-choice alternative; they hope to avoid hospital care indefinitely. This is partly related to poor previous experiences, but it is also derived from their cultural outlook to care for Mrs Curkovic within the family. Mrs Curkovic’s daughter explains that, as her mother has close family, it is ‘an alien concept’ to have outside carers to help, as culturally it is anticipated that, if you have family, the family will look after you. The wider family agree wholeheartedly with this and support Mrs Curkovic’s daughters in taking care of their mother themselves. Mrs Curkovic’s daughters are keen to have all the medical input possible to keep Mrs Curkovic going for as long as possible and palliative care to keep her comfortable and pain-free in later stages. They believe that this is what Mrs Curkovic wants, although she does not say this directly owing to her living with dementia.
Health-care professional’s perspective
There were two key aspects to Mrs Curkovic’s HCP’s account of supporting this family. First of all, she oriented to the fact that she had built a good relationship with them by taking the time to get to know them and, of course, to know Mrs Curkovic. She felt that building that rapport was very important to be able to introduce and discuss other things, namely EOLCP. So, for this HCP, knowing Mrs Curkovic was paramount and it paved the way for potentially tricky/sensitive conversations. Mrs Curkovic’s HCP felt that she needed to wait until the family was in the right space for this to be broached, giving them space to think it through, and she felt that that preparation work paid off. Second, Mrs Curkovic’s HCP expressed some concern about whether or not the patient’s voice had been fully heard. Although she knew that Mrs Curkovic’s daughters had their mother’s best interests at heart, she expressed concern that, as they always interpreted for her, HCPs could not be absolutely sure that any messages or discussions were being passed on verbatim or if they were being changed in translation. Mrs Curkovic’s HCP described the daughters as ‘gatekeepers’ to what Mrs Curkovic was being told, and, again, although she had little doubt they felt that they were doing the best for their mum, the HCP could not be sure whether or not the patient’s voice was being heard. This was quite tricky to navigate for Mrs Curkovic’s HCP.
Key observations and emerging issues
Case uses a consultee
We do not hear from Mrs Curkovic directly. Her family are the only interpreters, which concerns HCPs as they cannot be sure that they are hearing the patient’s voice.
Patient autonomy
Mrs Curkovic’s diagnosis is intentionally being kept from her, as her family believe it to be in her best interests. HCPs are concerned as to whether or not they are reaching their patient, which produces some very uncomfortable situations for all involved.
Compromised communication
Owing to dementia and language barriers, there are issues around Mrs Curkovic’s daughters as interpreters and as ‘gatekeepers’.
Daughters as experts
Fluctuating capacity affects decision-making, which is completed mainly by Mrs Curkovic’s daughters. Mrs Curkovic’s daughters claim to know their mother completely and want the best for their mum (even seeking guidance from older generation relatives); still, their opinions about what is best are brought into question.
Family takes care of their own
This is what is culturally expected, but can lead to carer burden.
Examples of good practice from primary care health-care professionals
Based very much on principles of building relationship and knowing the patient.
Examples of poor practice
In the hospital setting, Mrs Curkovic’s daughters were almost ‘hounded’ about DNACPR status; the daughters were delivered shocking, unknown news in a very public place and way.
Cultural/religious aspects
The family follows cultural norms of taking care of family; they see it as a natural part of their culture. Mrs Curkovic would anticipate this care and they are happy to provide it. Certain observances of the Serbian Orthodox tradition are important to Mrs Curkovic’s EOLC/EOLCP. The family have a great deal of respect for previous/older generations’ ‘wisdom’ about what is right to do. They have sought advice from Mrs Curkovic’s relatives abroad to support/guide their decision-making in Mrs Curkovic’s best interests.
Ethnicity-specific issues
Mrs Curkovic’s daughters have tended to keep a lot to themselves about their mum’s illness; some of this is explained as being because, in some cultures, dementia/illness is frowned on. This explains, in part, their wanting things to be kept private and why they do their own interpreting. This exposes something of a tension: the family interpreting is desirable for privacy, but can possibly create a gatekeeping effect for HCPs to access the patient voice.
Appendix 3 Fictionalised evidence-based narratives
Hafsa
Hafsa is an elderly Indian Muslim woman who has had a stroke. Her daughter has moved into her house to provide her care.
Key themes: autonomy and decision-making complexities of family culture. Knowing the patient. Communication.
The photograph has arrived of my cousin’s baby daughter, in a pretty pink frame too, ready to be put on the wall with the others. It’s what Doctor Lakhani talked to me about on her first visit, before anything else. Who all these people were, my very large family, from near and far. I could see my son was becoming annoyed, even then, wondering why she was spending time concerning herself with these photographs when there were far more important things to discuss.
She’ll be here later today, and it’s always nice to see her, even though I can’t talk to her anymore since the stroke. I miss it. All those conversations over several months. It was always so interesting, not what you’d expect from a doctor. She reminds me of myself a little when I was that age, although she’s far cleverer and kinder than I could ever have hoped to be. And she’s the last new friend I will make; although I’m not stupid, I know that I’m just one of her many patients. But I enjoy her company and she’s in my house so if I want to call her a friend then I can.
I’m not afraid of what’s coming. I know that I’m very ill. The last 2 years have been spent with the doctors and surgeons prodding and poking, but I’ve had a good life and now my son and daughter look after me, which is all that a mother could want. When I came back from the hospital, the room was newly painted with a vase of roses on the bedside table. It was strange at first, sleeping in the bed which had been moved so that now I look towards Mecca, though it’s not so easy to see the neighbour’s cherry tree, which will soon come into blossom.
My daughter stays here and cares for me and my son comes every day to help me perform my ablutions and recite Ya Seen Surah to me, now that I cannot speak the words of Shahadah, nor even mumble La ilaha illal-lah.
My son is such a devout young man. When Doctor Lakhani said that we might want to consider some help with home care if things became difficult, I could see he wasn’t pleased, although he is very polite and would never say what he thought until she left. That Allah will turn his face from those who do not care for their dying parents, that carers could not fit their schedule around prayers. That there are so many little things that he and his sister do every day that need to be learnt. How to cut up my food so that I can swallow it easily. How to move me gently into my wheelchair for my favourite walk around the park. The jewellery I like to wear on certain days.
I told them that the doctor is a good woman who is thinking of what is best for all of us and that, in this case, perhaps having a carer come to visit might be acceptable. Especially with my daughter looking so tired. But none have come, and I have to accept that it’s up to my children now to decide how things should be. And not being able to talk means it’s easier if I just accept everything that they do.
I think they might be seeking guidance though because during the last visit, Doctor Lakhani suggested bringing medicines to the house in case things became very difficult. And later the imam came round, and my son closed the door so that I couldn’t hear what they were talking about.
Sometimes I would like to be alone with the doctor even if I can’t tell her the things that I want to. I can sense her trying to hear the words that are in my mind but not inside my mouth. Looking right into my eyes, which is where we do most of our talking now. But my son is always here, standing by the window, watching carefully. She talks to him too of course, when there are things that she says we all need to discuss as a family. And then he always just nods quietly.
I wish my children knew that I feel blessed by having such a woman help me through these final days. I think I’d like a photograph of her on the wall too. I could just about fit her in. Or at least know that one day my son will thank her for all that she’s done. What she did.
Dave
Dave is an African Caribbean man who attends a community cancer support group. His wife believes in dietary approaches to cure his cancer.
Key themes: lack of trust and misunderstandings.
I’ve been having everything. As much as I can eat. I deserve it after all this fennel tea and tasteless veg my wife’s been putting down in front of me. And I need to get something good out of this trip to the hospital. I know the doctor is going to try and twist my arm, but I’m no fool. And when my old mate Biant and I stop off for my secret little treat on the way home, I will toast my fortitude with a bloody great milkshake.
‘You need to think about what you want to happen over the next few months, Dave, so we can put the proper plans in place’. That’s what they told me he’s going to say, down at the dominoes group, where they’re all going through the same thing as me. And that I need to be prepared. Well I am. ‘That’s right, doctor; now that the chemo’s not working, you want me to sign on the dotted line so that I don’t hang around too long. Well I’m not signing anything’.
They’re a good bunch, been helpful too. If Biant had told me what it really was when he first took me, I would never have walked through that door. And now I’m glad that he did. Who would have thought it would take prostate cancer to get me playing dominoes, like my old man. It’s getting harder though, to be honest. This bloody pain. But what you going to do?
Dad died of cancer, his father too. He was buried in his back yard in Portmore and I was lifted up, 4 years old, and passed over the coffin while they said my name so that he wouldn’t come back and haunt me. It was like the whole world came to visit for days afterwards, all dressed up with food and drink and music.
My dad always said that, like so many things in England, death is hidden away. Made me promise that his funeral would be a thing of joy. ‘The people here, son, they don’t know how to die and when they do, the way they are so quickly dispensed with and forgotten should be a warning of the way that they will treat us. So never forget, we have to stand up for our rights, every single day’.
And he was right. As soon as the treatment stopped working, they just washed their hands of me. And now, of course, when things are properly on the downward slope, they have to appear to make an effort. But I know what’s really going on. My cousin came out of hospital last month with some kind of dressing all over her hands and arms and they couldn’t even find something that was the same colour as her skin.
And, of course, I’ve been thinking about it. Of what I want to happen. And Biant knows. He’s the one I’ve told it all too. A cardboard coffin for starters. These funerals cost a fortune and I need to make sure my wife has something left after it all.
Maybe I should have asked her to come with me. She’s obviously worried and wants to know why I have to see the doctor today, but I’ve told her it’s nothing important, just some forms I’ve been asked to sign. And I don’t want her there, getting upset and confusing everything. It’s simple. I just need to stand my ground, tell him I know that things aren’t good, that we all step off the boat at some point, but they’re not going to get rid of me that easily.
And if she was there they would talk her into things, just like her sister does, with all this diet mumbo jumbo. I’ve told them both that my taste buds are shot, that everyone who has ever eaten my wife’s mutton and dumplings always ends up sneaking back round the kitchen table the first chance they get. That I need to have food in front of me that looks delicious, that reminds me of what it was like to enjoy eating. But there’s no listening. ‘If the doctors can’t cure you with all their mighty science and technology, Dave, then my sister is right, and it’s up to us to take charge and do what needs to be done’.
I keep quiet about it. On Biant’s advice. ‘If there’s one person you need to keep sweet at a time like this, mate, it’s your missus’. So I thank my sister-in-law for praying so hard for me, agree that it is all in God’s hands now, and nod my head to whatever my wife suggests.
She can come next time, because they’ll keep trying to talk me into what they want me to do to make things easier for them. That’s for certain. But not today. No chance. Today is for me and Biant to put the world to rights over some proper food, if he gets his car to start. Ah! I nearly forgot, the mints. Just so my loving wife doesn’t get a sniff of what we’ve been up to. You see! I think of everything. Nobody gets the better of me.
Balwinder
Balwinder and her sister Gurpreet care for their mother who is currently in hospital. They are preparing for the Sikh New Year, Vaisakhi.
Key themes: carer’s duty and burdens. Language/communication barriers. What’s going on below the surface.
We’re going to need a catering trolley from the hospital to take in all this food that Gurpreet’s making. I’ve told her it’ll be too much, but she won’t listen. ‘The food there is terrible, Balwinder; we must keep her strength up’. And of course, she wants everything to be perfect tomorrow. ‘It’s probably our last Vaisakhi together’.
Ajeet arrives tonight from Berlin, with his wife, which will delight Mum, who tells us over and over that we’re not to worry him, that our brother is a very busy man, and that the women can look after things on their own, thank you very much. I should be looking forward to it, all of us being together, but I’ve hardly slept all week. Why is it me, the youngest, that’s been put in this position?
The hospital said they’d provide someone to help Mum understand what the doctor was saying, but no one ever seemed to be there for her when it was really needed. And now she’s decided that she only wants her children to tell her what the doctor has said. That she doesn’t want strangers that might turn up every now and again being told things about her that she doesn’t want anybody else to know. And I’m the one that’s ended up having to translate everything for Mum, to try and make sense of all this medical information, while Gurpreet buries herself in her chapattis and saagwala.
And she’s in worse shape than we thought. Four days ago, a doctor told me we should make a decision about something called a DNACPR order. And quickly. I’ve written it down very carefully. Do Not Attempt Cardio-Pulmonary Resuscitation. I should have said something to Gurpreet straight away, and rung Ajeet as soon as I got home. But I was just so shocked. And then I thought I should wait until after Vaishaki to tell them. I don’t know why. I was flustered; I didn’t know the right thing to do. And to make it worse, I’ve lied to the doctors, telling them that I’ve explained everything, and that Mum understood and wanted to talk about it when we were all together. And we would tell them our decision then, straight away. Which of course I don’t want us to do. Not tomorrow. Not ever.
Why has nobody ever mentioned this thing before? About having to sign my mum’s death warrant. Why has our family doctor never mentioned anything about this, about these decisions? Always telling us not to worry, everything is in good hands. No help at all, which is no surprise really; we’ve been stuck with him ever since he became Dad’s badminton partner and of course Mum wouldn’t think of having anyone else once Dad died. But why has nobody else stepped up? Why has nobody warned me about this?
Gurpreet and Ajeet still think we might be able to bring Mum home, to this house. Maybe I did too until now. But it’s not suitable; anyone can see that. My brother is bound to start throwing his weight around; he’s never had a good word to say about the hospital since Mum was offered a halal dinner and is always asking if there are still male nurses helping her. But she keeps telling me that everyone is so nice to her, that everyone is so helpful. That we shouldn’t worry so much.
But now I have to talk to her about this other thing; so of course I’m worried.
Hopefully, the doctors won’t have mentioned anything about it to her. Hopefully, they’ll understand that tomorrow is the Sikh New Year, and they’ll have the sense not to talk to us about this horrible decision. So I just need to put it out of my mind for now, let Gurpreet take the lead for once, and do as she says. Try and embrace the day.
I’ll tell Gurpreet and Ajeet afterwards. We’ll come back here, and I’ll tell them that, however much Mum may have rallied for Vaishaki, and I pray she will, that she won’t be coming home. That she is dying, and we have decisions to make, and we must sit by her bed and ask her about this order before Ajeet goes back to Germany. And that he should probably stay here for the time being.
Yes. That is what is going to happen. And tonight I am going to sleep. And tomorrow I am going to dress up as brightly as possible and maybe sing a Shabad. And when we look at the piles of food that are left, I will help to share it out to everyone, just like we always do at this time of year. That’s it. It must be shared out. All of it.
Krushan
Krushan, a middle-aged British Asian Hindu, is largely bedbound and cared for at home by his wife, Dhanashree. He is awaiting a visit from his older brother, Abhijeet.
Key themes: pressures of community/family judgement.
Abhijeet is coming so the house is spotless; my pillows have been plumped and our snacks are plentiful. You would think he was the one we should all be worried about.
He’s not been here since our son’s wedding. Where the numbers of guests were less than he expected. ‘And the invitations, brother, if you don’t mind me saying, perhaps a little shabby’. Not since the changes have been made to the house, which have helped me move around more easily. It’s impressive, how much help is available if you know how to get it. I just wish I’d known earlier, that there was someone who had told me all of this. Everything has somehow seemed like a challenge, where life can only be made easier if you put the work in first.
I think my brother will be surprised when he sees me. I should have been more honest about how things are. Maybe Dhanashree has told Padma the truth, our wives have always got on well together, but it’s not easy to admit what’s happening to me. The pain comes in waves, I want everything to end, and then it washes away and I think all will be well. Even though the endless stream of visitors, all very sympathetic, is a sign that nobody thinks I will last too long.
I know that Dhanashree has asked that nobody come today, including my carers. I heard her whispering to them as they left last night. It’s not easy for her. She gets upset about some of the things that are said by the neighbours and at the temple. About my children not doing all that should be done by the children of sick fathers. About all of the help that we’re getting. When the ramp was put in, half the street seemed to come out to watch. And I know my dear wife doesn’t want her brother-in-law to see carers here in our house.
I tell her that there are always those looking to pass judgement, from whatever community you’re from. That after spending months getting flustered trying to keep track of all the different appointments and the endless telephone conversations, always looking for a pen to write down this appointment and that appointment, and this doctor and that doctor, she deserves some assistance now that I’m settled at home. And she does look less tired. Even with all the guests.
But still she insists that we shouldn’t tell Abhijeet. That he will say, as he will, that this is something that the family must take care of. ‘Don’t you understand, brother, that if your energies and forces are out of balance, then you need to address this rather than lying down and accepting their death warrant. How can these people do what is required so that you can attend the temple with peace of mind? Do they understand Ayurvedic medicine? Are they providing you with it?’ He will remind us how it reflects on the family. That it will soon be time to find our daughter, Garima, a husband. That people talk.
It angers me that Dhanashree is worried about his judgement. Maybe it’s because he is older. Maybe it’s because he is the successful one and somehow that means we must listen to him, like I have always had to listen to him. Of course, now that he’s in Mumbai making piles of money, he will pass his judgements about the way things should be with even greater certainty. Even though it is my daughter who is the Kathak dancer and my son who plays the sarangi alongside her, whilst his kids are as westernised as they come.
And why should I spend my last months watching my son and my daughter giving up their lives for me? I want to see them thrive. I want to imagine them doing well when I have gone.
With Garima, there are moments when I can see her trying to ask what she should do, what I want to happen if . . . when . . . I am reaching the end of the road. But she’s young, and it’s not right that she should have to confront such things, even though Dhanashree will never ask such questions. So it’s down to me to get these things all straight, although I’m not quite sure how.
Perhaps Abhijeet will surprise me. Maybe he won’t tell me about a friend in Mumbai who only had a week to live, but is now playing in the slips for his local cricket team through sheer force of will.
Maybe if my carers did come, he would embrace them and thank them for the work they were doing, the care they are giving.
Maybe he will come to the hospice with me when I go there next week for the first time. I think that is what I really want right now. For him to come with me. For my brother to be there with me.
Lanfen
Lanfen is a Chinese musician who is at a hospice day centre where she has unexpectedly made friends with Jim.
Key themes: being seen/known. Do not make assumptions about heritage and actions/preferences.
I know what Jim is going to say when I see him. ‘Have you been playing, Lanfen? You know that if we don’t keep playing, we may as well give up the ghost’.
We have promised each other that we will do a duet at the hospice. But we still haven’t done it and Jim is not looking too good. I was telling him that he needed to get better so we could start practising, but I’ve stopped doing that.
I thought I was too young to go there. That I didn’t want to be sitting with the kinds of people that found themselves trapped in a place like that. That there wouldn’t be anybody there like me to talk to. That just because you’re alone it doesn’t mean you’re lonely.
But if you don’t have any children at a time like this, or anyone at home to keep an eye on things, then they worry. So I did. Just so I could say ‘yes, doctor; I tried it, but I’m not sure I’ll go back’.
And within half an hour I met Jim, and we found out we were both musicians and we hit it off. And I did go back.
There was a week or two when he didn’t show up. I was more worried about him than I’ve ever been about myself. I played the erhu a lot then. And although I didn’t really enjoy it when he wasn’t there, I had to keep going to make sure he would come back. And he did. He looked terrible. We all do.
I’ve told my doctor I don’t want to know what they think is going to happen to me. I don’t trust them anyway. My sister died 2 weeks after an operation she was told would add years to her life.
And everybody knows the health system is a mess. But I know I’m not an easy patient. It took me months to agree to having help at the flat. Who needs strangers coming in and telling you what you should or shouldn’t be doing? It doesn’t matter if a habit is good or bad, it’s staying and that’s that.
They come now though. After so many visits to the hospital, some of which might have been avoided if I hadn’t been so stubborn, I finally agreed. But they know not to judge, and they never tell me what to do. They tried once and learnt.
My mother was a Buddhist who spent her last days breathing and meditating through her illness, but that’s not for me. I have decided to just carry on living as best as I can, for as long as possible. Anyway I’m not dying yet, I’m just very ill. I can still get a tune out of myself some days.
I need to be able to keep taking risks, that’s what Jim understands and nobody else does. It’s not some stupid Chinese thing, ‘oh you know how they love their gambling!’, it’s a musician thing.
All good musicians know you have to take risks to discover anything; it’s in those discoveries, however small they are, where life is lived.
But I’m not sure what risks I can take any more. It’s all so confusing. All I do know is that Jim is right, you have to keep playing. I know we’re not going to do a concert together; I’m not stupid. I know it won’t be long before he doesn’t show up and never returns, however much I hope he will. But I don’t know when he’s gone who is going to keep me going, rather than smothering me with all these things that are here to help me. I don’t know where I’ll find the space to breathe.
You look at all the pills and you wonder. Are they keeping you alive or are they stopping you living?
Maybe I should take my erhu in today and play something for him, however awful it might sound. But it wouldn’t. I would rise to the challenge. I always do.
Tawanda
Tawanda, a Zimbabwean man with a strong Christian faith and great love of football, is dying from cancer. He lives with his wife, Chibuzo.
Key themes: ambivalence in discussing/relevance of planning to life approach. Faith: god’s will, not mine. Sustaining hope/collusion. Community pressure.
Look at this. Chibuzo has found my shirt so that I can wear it when the boys come around later for the big game. When you’re in this much pain, it’s important to have moments to look forward to.
Number 5, ‘The Chief’. My nickname, borrowed from Lucas Radebe, the great South African defender. A gift from the team when I had to stop playing. And of course, she will help me put it on; reaching up with her little arms to pull it over my great big head. I’m a lucky man.
So many people are on our side that it’s humbling. And there are times when I feel responsible. When Chibuzo tells me how much they’re praying for us at our church, then I feel it’s even more important that I don’t succumb. And God is with me and provides me with the strength to carry on. And strength for my wife Chibuzo too. I’ve started to call her ‘boss’ because she’s as much my trainer as my wife now. She knows when my energy is low and when it’s a little better. When my mood is dark and when I’m able to smile and need some help to do so. She’s better than any doctor.
But she is worried. It started when she overheard a nurse at the hospital saying that if I was being sent home, it was only a matter of time. I’ve told her that a nurse is not a doctor. That we must remain positive. ‘With the right approach we can navigate a way through this; let’s see how things progress over the next few weeks before we start to worry, Tawanda’. These are the things my doctor says. He’s like a good manager shouting advice from the sidelines.
There was one time when I really didn’t feel too good, and I wanted to talk to him about what might happen if things were not to go so well. But I could see that he wanted to focus on the positive, so I didn’t. I think about that sometimes, if I should have stuck to my guns and said what I’d planned to. But the most important thing is that everyone must believe and fight together. That’s the way you win. Through teamwork.
Nobody could get past us those three seasons when we won just about every game. Which is why I was so confused and angry that it was my partner in central defence that said those things to Chibuzo. That it looked like I was getting weaker. That maybe somebody should talk to the doctor about what they could do to make things easier for both of us if it seemed unlikely that things would improve.
Chibuzo cried for days after that. And I rang Darren and told him that if he wanted to say anything, he should have spoken to me. It’s the doctor who will decide when it’s the right time to talk about such things. That if you go into a game fearing defeat, it’s the start of a slippery slope. He should know that. He was letting me down. I told him that I wasn’t stupid. That I didn’t expect to play football again, although maybe God will decree that I can. But I want to go back and stand on the sidelines. There are new cures all the time and the doctor has not contacted me for a while, which must be a good sign.
But since then I’ve been thinking. Not just about my funeral, but about what happens before then too, if . . . you know. I’ve written it down to give to Chibuzo when the time is right. And I feel better for doing this, a little lighter somehow. I’m going to thank Darren when he comes around and tell him that it was good that somebody finally had the courage to say something.
And anyway today is going to be one of those good days. I’m going to put on my shirt, summon up my strength and enjoy my friends’ company. I just hope the match won’t go into extra time.
Emilija
Emilija is a Lithuanian Catholic who is in a hospice and very near the end of her life. She is planning a special traditional celebration of Easter with her daughter Camilla and friends.
Key themes: offering the opportunity to discuss deterioration and dying at a time of readiness. Aligning care to the priorities of the patient.
They’re putting out a table for us. They think we’re going to make a mess so they’re putting something down on the floor in case we spill dye on the carpet.
I hope Camilla doesn’t mind that I’ve asked my friends to join in. She’s probably expecting it to be just the two of us, like usual. But it’s such fun and she always makes such a good job of it, and I want my friends to see how beautiful the eggs look when they’re finished. And anyway, I have to join in with all of their traditions so it’s about time they took part in something Lithuanian. And this is what we do on Holy Saturday. I think she was 3 when she did her first ones, and we’ve only missed one year since in all that time. And this will be the last time. Maybe I shouldn’t have asked the others to join in.
I mustn’t say that though. That these are probably our last eggs that we will paint together. Camilla still thinks that some kind of cure may appear out of the blue, some kind of Easter miracle, when I know that’s not going to happen. But I couldn’t have asked for things to be better than they are. All these lovely people here helping me to wash and dress and sometimes to eat and all so kind.
It’s not what you want really, people having to do all this for you, but it is what it is.
And everything is prepared, that’s the thing. Not like with my husband, which was terrible. I remember saying to Camilla ‘never let that happen to me’, and she said of course she wouldn’t. But when it came to it, of telling the doctor exactly what I wanted, what they should and shouldn’t do, it was Camilla who was unsure and trying to hold me back. After all that we both saw.
The doctor was very good. I think she knew I was ready to have that conversation. I was a little stronger after my operation and she approached it all very calmly and kindly, asking how she could be of most help in supporting me in what I cared for most going forward.
And I had thought of this. Of painting eggs on Holy Saturday with my daughter. Tracing patterns with wax and dipping them in dye; beetroot and onion skins. Red for life, yellow for a plentiful harvest. The doctor could see how upset Camilla was and had to console her and said that my decision would only ever be acted on if the doctors were absolutely convinced that it was for the best.
I’m determined that she won’t go through what we both did with her father. That really was terrible. The delayed diagnosis, all those days in hospital when nobody seemed to be able to explain anything properly and having all those questions being asked of me that I couldn’t really understand. It’s not a nice place to die, with everyone rushing around and a lack of space and privacy to grieve. It’s a shame that you have to learn about these things through experience, but sometimes that’s the only way we ever really understand anything properly.
That was the one year we missed painting the eggs, and the year when I started going to the church again, even though I’m not much of a religious person. But it’s been important, and I’ve enjoyed coming back to some of my roots and traditions and rituals, which I’d begun to forget. But not this of course. You never forget this.
And some of those I made friends with there come to visit, which is kind of them. And they tell me that everyone is praying that one day I may still be able to return to the village I moved away from as a little girl. I know that I won’t, but I can feel their belief and it comforts me very much. I’m very thankful for it. Between the doctors and God, I seem to be in very good hands. If only Camilla would understand I’m sure she would stop feeling so guilty about not having me at home with her.
Anyway, today is going to be fun. And I hope these hands of mine don’t shake too much because I want to show off my patterns to everyone here, so that they understand why it’s such a lovely thing to do. And when it’s over I’m not going to let the staff talk me into washing them, my hands, at least not for a while. I always remember how fascinated I was by the way the tips of my fingers used to change colour when I painted eggs with my mother when I was a tiny little girl. And I want to remember that too today. And to tell Camilla all about it. Like I do every year.
Sharmarke
Sharmake, a young Somali Muslim, is standing at a bus stop waiting to get to hospital to visit his father. He was angry on his last visit and the staff asked him to leave. A community worker, Warsan, has been helping him.
Key themes: complex life circumstances of migrants. What lies beneath the surface. Duty and misunderstandings. Taboos and fears. Knowing the system.
Remember what Warsan keeps telling me. Breathe. And count to 10 if I start to get anxious. Which I will. But it’s going to be alright. I can give my father this phone and now he’ll be able to listen to the verses from the Qur’an and that will soothe him. Keep calm. That’s the thing. Don’t let my father down again. Don’t get angry again. Try not to be scared again. But he can always see when I am hiding things. ‘What is it, Sharmarke? What is it you are not telling me?’
I should be at his bedside looking after him, doing my duty as a good son. But instead I make him worry. And what can I say to him? That I am being called up in the middle of the night to be told to come to work. That they pay so little. That I worry that somebody will report me; that I will be sent back, and he’ll be left here all alone.
And he is always apologising to me. Over and over. ‘I am so sorry. Why has this happened to me? What will happen to you, with no one by your side? How can I fight it?’ And again I will try and calm him. ‘Listen abo, the letter will be arriving soon saying that we can both stay here’.
But you never know when you get to the hospital how things have been. If he’s had a bad night or is confused again. Maybe he hasn’t been able to explain to anyone that he needs the toilet or that he can’t eat the food they’ve given him. And what happens if he’s no better? What happens if he never gets better? What will happen to his body? How can I bury him in the proper way?
I know I was wrong to react like that, but I was so tired, and he looked so weak, and I didn’t know why the doctor was asking those things of me. How could he use those words? These things are in Allah’s hands! Why were they giving up on my father? So quickly, so easily. Did they need the bed for someone else, someone who comes from this country? I was wrong to shout, to lash out, but why was there nobody there to help me understand what they meant?
I was sure the police would be sent to find me because of what happened. I didn’t dare go back. I didn’t even go to the mosque and pray for my father because I had to work. It was Warsan who came to look for me and took me to the community centre to get some advice. But nobody was really able to explain to me what is happening and what I am supposed to do.
Walaahi, I’ve never felt so frightened. Thinking that his bed would be empty when I finally went back to the hospital. But there he was, sitting up, waiting and worried. What kind of person can do that to their own father? He looked terrible. And the nurse who I pushed over said they could see that I was struggling, that all they wanted was to help us both deal with the situation as best as we could. And the doctor needed to ask us some difficult questions as soon as possible. Not now I said. Tomorrow. Please.
And now it is tomorrow, and I will listen to the doctor and I will breathe. And father can now listen to the Qur’an. And maybe Allah will be looking down on us and listening to our prayers. The letter will be waiting for us when I get back. With good news. And whatever happens today, in sha’Allah, will be for the best.
These stories were written by Andy Barrett from Excavate, June 2021.
List of abbreviations
- ACP
- advance care planning
- A&E
- accident and emergency
- BCT
- behaviour change technique
- BFCG
- bereaved family caregiver
- CI
- chief investigator
- CNLW
- Community Network Liaison Worker
- DNACPR
- do not attempt cardiopulmonary resuscitation
- EOLC
- end-of-life care
- EOLCP
- end-of-life care planning
- FCG
- family caregiver
- GP
- general practitioner
- HCP
- health-care professional
- LOROS
- Leicestershire and Rutland Organisation for the Relief of Suffering
- MND
- motor neurone disease
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health and Care Research
- NPT
- normalisation process theory
- PCBR
- public, carers and bereaved relatives
- PEOLC
- palliative and end-of-life care
- PI
- principal investigator
- PPI
- patient and public involvement
- ReSPECT
- Recommended Summary Plan for Emergency Care and Treatment
- WS
- workstream
