Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number NIHR133641. The contractual start date was in November 2020. The final report began editorial review in June 2022 and was accepted for publication in October 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Appleby et al. This work was produced by Appleby et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Appleby et al.
Chapter 1 Context
Background
There are rising levels of knife crime and other serious injuries among young people in London and elsewhere in the UK. The Office for National Statistics1 showed that, excluding homicides and threats to kill, figures for violence-related crime offences involving a knife or sharp object rose by 46% to 45,863 offences between 2010 and 2020 in England and Wales (Figure 1). The drop in offences between April 2020 and March 2021 is almost certainly related to COVID-19 and, in particular, measures introduced to combat the pandemic such as lockdowns and school closures.
FIGURE 1.
Number of police recorded offences involving a knife or sharp instrument, year ending March 2011 to year ending March 2020: England and Wales.
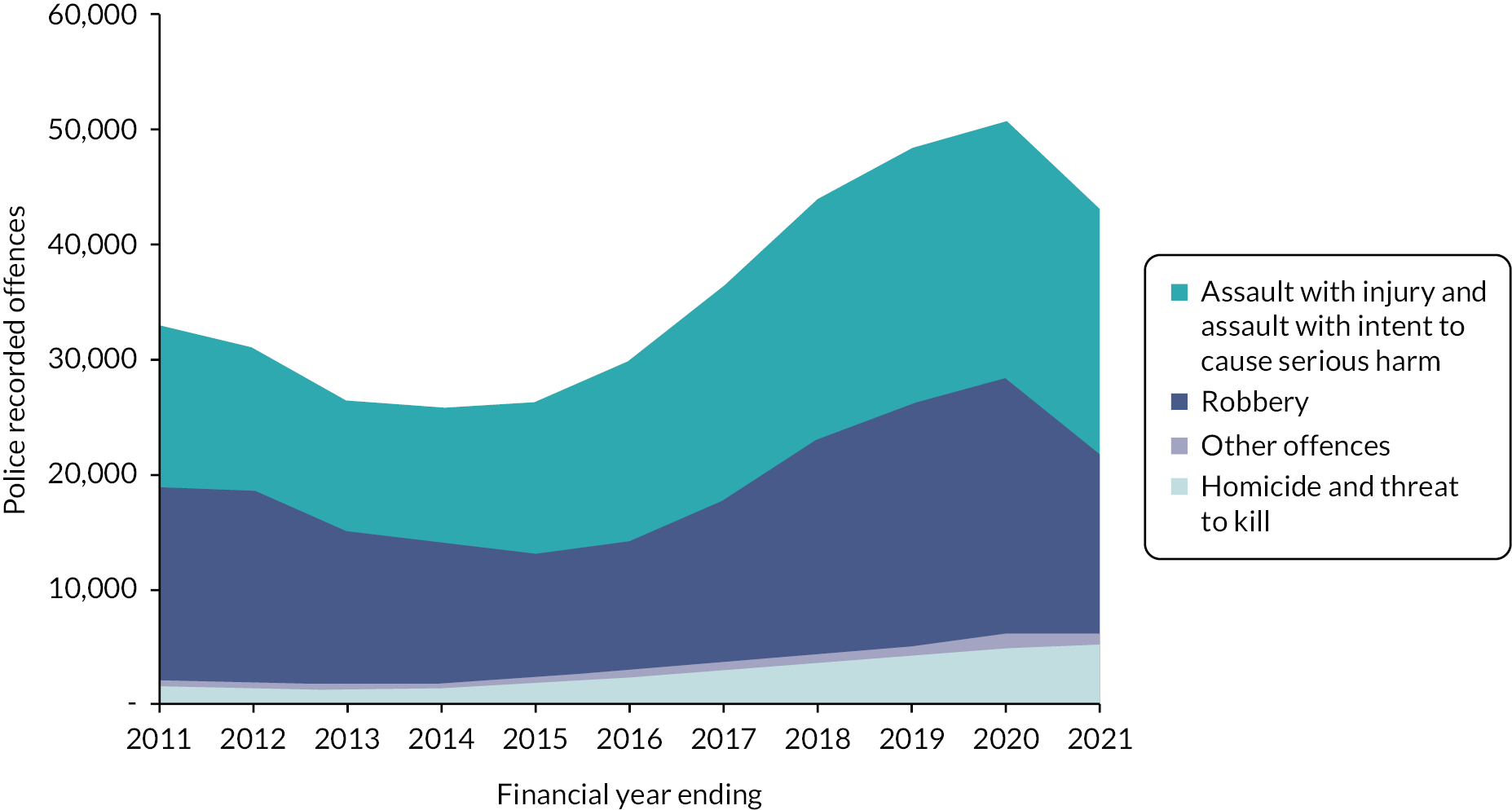
Assault with injury and assault with intent to cause serious harm rose by 58% between 2010 and 2021. Meanwhile, the number of hospital episodes with a classification of assault by a sharp object (including, but not limited to, knives) has fluctuated over the past 10 years, falling between 2010/11 and 2014/15, then rising to 2018/19 and dipping in 2019/20 and 2020/21 (Figure 2). 2 As with violent offences, the dip in 2020/21 is almost certainly associated with COVID-19 and measures taken to deal with the pandemic.
FIGURE 2.
Finished consultant episodes for assault by sharp instrument (clinical code X99 in ICD-10): England 2010/11 to 2020/21.

In addition, assault-injured young people are at significant risk of repeat injury. 3 The rate of repeat visits to the emergency department (ED) for violence-related injuries may be as high as 44%, and the risk of recurrent injury may be 80 times that of ‘unexposed’ individuals. 4,5
When assessed in the ED, the majority of injured young people and their parents believe that their injuries were preventable, and over one-third also believe that a similar violence-related injury is likely to occur in the future. 3 Moreover, youth assault injuries are often related to repeated disagreements and retaliatory behaviour that fuels repeated violence. 6 Interrupting this cycle of reactive decision-making has the potential to significantly reduce the burden of injury to young people in the UK.
The causes of these recent trends in violent assaults are multiple and varied and include factors related to deprivation and childhood poverty,7,8 and suggest multi-agency approaches to tackle the problem. Scotland, for example, has pioneered a public health approach to violence as advocated by the World Health Organization,8 including knife crime. 9 This has included educational programmes, multi-agency working and interventions such as the Navigator programme based in EDs and designed to support people who have suffered injury from violence. 10
As we discuss in Chapter 3, there is a literature base going back to the late 1990s and early 2000s describing violence prevention strategies that target vulnerable younger people and aim to reduce physical and emotional harm from peer violence. 6,11,12 ED youth violence prevention programmes have been studied more extensively in the United States than in the UK, including using randomised controlled trial (RCT) and comparative study designs. These programmes vary in their implementation and approach, and may be supported by specialist youth workers, social workers, community mentors and wider interdisciplinary teams of experts. There is also a literature about ‘brief interventions’,13 which are also delivered in emergency care settings and involve screening young people for safety risks and providing structured, short-term support. Common to all these interventions is engaging with a young person in an urgent care hospital setting and trying to reduce that patient’s exposure to harm in the community by encouraging positive behaviour change following discharge.
Research suggests that injuries serious enough to require medical intervention may make young people and their parents uniquely susceptible to behavioural intervention. 3 As Wortley and Hagell (p. 6)14 observe, ‘The incident bringing the young person to the ED may provide a hook for change’. Consequently, ED-based interventions that provide a ‘teachable moment’ offer a unique opportunity to identify and reach young victims of violence, inform individuals of the benefits of lifestyle changes and link them with supportive treatment programmes and agencies that can function in their daily life beyond the hospital, such as in education. However, as we discuss in this report, the evidence base about the implementation and impact of these programmes in the UK health system is still small (albeit growing) because these programmes are relatively new to the NHS.
Youth violence intervention programmes in the UK
Youth violence intervention programmes (YVIPs) and, in particular, those based in EDs, are part of a broader strategy and policies to tackle violence in general at national and local levels and involving many agencies, including local authorities, the police, the NHS and third-sector organisations. For example, in London, the Mayor’s Office set up the Violence Reduction Unit15 in 2019 with a 10-point plan16 that includes reducing the prevalence and impact of violence through a variety of interventions; notably, a public health approach, and involving NHS organisations and others such as specialist youth worker groups. As part of this approach, the NHS in London established a violence reduction clinical network in 2019,17 part of whose aim is to define best practice standards for in-hospital violence reduction services currently embedded in EDs.
Out of a total of 38 such services across England, Wales and Scotland, currently across London, 15 trusts have ED-embedded YVIPs involving a number of organisations providing such services in partnership with the NHS18 (Table 1).
| Trust | Service provider |
|---|---|
| King’s College Hospital | Redthread |
| St George’s Hospital | |
| St Mary’s Hospital | |
| Homerton University Hospital | |
| Croydon University Hospital | |
| University Hospital Lewisham | |
| Queen Elizabeth Hospital, Woolwich | |
| University College London Hospital | |
| Royal London Hospital | St Giles |
| Newham Hospital | |
| Northwick Park Hospital | |
| Whittington Hospital | |
| Whipps Cross Hospital | |
| North Middlesex University Hospital | Oasis |
| St Thomas’ Hospital |
Redthread
One provider – Redthread – currently operates in eight hospitals in London and five hospitals in the Midlands. Redthread is a charity set up in 1995 with the aim of involving young people in community activities. It developed interventions to improve young people’s access to health care, originally in general practices and, more recently, in hospitals. Its YVIP was designed to support young victims of violence. 19 The programmes embed trauma-informed, crisis intervention specialist youth workers into existing health systems, capitalising on ‘teachable moments’ to engage young people and encourage positive change (Box 1).
As the Behavioural Insights Team noted in their 2020 report20 for the London Violence Reduction Unit, there are currently hundreds of violence prevention interventions and approaches (not just those based in the NHS) being delivered across London, of which the vast majority are not being rigorously evaluated. This is reflected in the relative paucity of studies and economic evaluations of YVIPs and limited knowledge about their implementation processes and mechanisms, leading to repeated recommendations for further research and evaluation. Prior attempts to demonstrate the efficacy of ED-based programmes have also been underpowered and, although promising, results have been largely equivocal. 5
With the opening of the Redthread service at University College London Hospital (UCLH) and in consultation with Redthread and UCLH clinical colleagues, an evaluation of the service as part of the work of the National Institute for Health and Care Research (NIHR) Rapid Service Evaluation Team (RSET) was originally planned and scoped in 2019/20 with a start date in April 2020. However, the impact of COVID-19 on services required a delay in some aspects of the evaluation (although some desk-based work was possible), and a final protocol was published in May 2021 with the evaluation planned for one year. 21
A team of Redthread’s specialist crisis intervention youth workers is embedded in the ED at the participating hospital.
-
The team aims to meet every young person aged between 11 and 24 years who attends the ED as a victim of violence, assault or exploitation, or where there are concerns around undisclosed vulnerabilities.
-
The team uses the ‘teachable moment’ of arriving at hospital as a foundation from which to build a beneficial, trusting relationship with young people.
-
The team completes safety planning and risk assessments – identifying risk indicators and mapping personal and professional support networks for each young person.
-
The team creates a bespoke package of support for each young person according to their needs and goals, prioritising the building and scaffolding of robust professional networks. They:
-
Support (re-)engagement with professional agencies for young people who are known to statutory services and already engage.
-
Advocate on behalf of young people and co-ordinate networks of professionals across disciplines and locations.
-
Support other agencies and scaffold key professional relationships.
-
Make ‘relational referrals’ to new key worker, inviting professionals into the hospital or accompanying young people to initial meetings – for young people who do not have any current input from statutory agencies.
-
Complete intensive casework with young people, including goal setting for the future or discussions around self-esteem, safety or healthy relationships.
-
-
Supports and trains medical staff and other professionals to increase their confidence in working with young people and identifying those who may be at risk.
Study aims and research questions
Using quantitative and qualitative research methods, the overall aim of the study for both phases of the evaluation was to evaluate the implementation and local impact of the Redthread intervention at UCLH, including a cost-effectiveness analysis (CEA) of the intervention, and identify wider lessons and insights for similar initiatives drawing on published literature and the analysis of secondary data. The main objectives were as follows:
-
To conduct a scoping review of peer-reviewed evidence and grey literature about hospital-based violent crime interventions that focus on young people and behaviour change, identifying lessons for researchers, health professionals and policy makers.
-
To review and summarise existing and current evaluation(s) of Redthread interventions/services, in particular evaluation methods and main findings to identify lessons for Redthread, evaluators and NHS trusts.
-
To evaluate processes of local implementation and capture perceptions of UCLH staff and relevant local stakeholders concerning the intervention and its impact.
-
To assess the feasibility of using routine secondary care data such as national Hospital Episode Statistics (HES), local UCLH records to evaluate the impact of Redthread intervention through the comparison of appropriate control and intervention groups.
-
To conduct a CEA of the Redthread intervention at UCLH from the perspective of the NHS and personal social services.
-
To draw conclusions about the types of evaluation approaches and methodological designs that appear well suited and feasible for evaluations of the Redthread service and similar youth-based interventions in the NHS.
Key research questions were as follows:
-
What measurable impacts on the use of NHS services and wider benefits does implementation of the Redthread YVIP have at UCLH for both staff and patients?
-
What evidence exists in the published research and grey literature about the effectiveness, benefits and impact of interventions in urgent care and hospital settings that focus on violent crime and young people? What lessons can be learned from UK and international studies to help NHS trusts implementing such interventions?
-
How can a combination of routine secondary care and Redthread data inform an evaluation of the impact of the Redthread service on the use of NHS hospital services?
-
What are the views of UCLH NHS staff (e.g. paediatric consultants, ED nurses, service managers) of the Redthread intervention, its feasibility, service-level impacts and overall effectiveness?
-
What organisational factors, processes, resources and staff training are necessary for the successful implementation and delivery of the Redthread service?
-
How cost-effective is the implementation of the Redthread service at UCLH?
-
What evaluation approaches and methodological designs appear particularly well suited and feasible for evaluations of the Redthread service and similar services in the NHS?
Structure of the report
The rest of this report covers the methods used to evaluate the Redthread service (see Chapter 2, further elaborated in following chapters where appropriate); the review of the international published evidence on interventions similar to Redthread (see Chapter 3); findings from the qualitative research examining the programme theory and implementation of Redthread at UCLH (see Chapter 4); a description and review of data used to manage Redthread’s services at UCLH (see Chapter 5); an analysis of the costs and consequences of Redthread (see Chapter 6), a feasibility assessment of options to evaluate the impact of Redthread (see Chapter 7); and finally, a discussion of the evaluation and some conclusions.
Chapter 2 Methods
Design
The evaluation was designed as a mixed-methods multiphased study, including an in-depth process evaluation case study and quantitative and economic analyses. The project was undertaken in different stages over two years, starting with desk-based research and an exploratory phase suitable for remote working while COVID-19 was affecting NHS services. During the second stage we gathered more in-depth insights about the effectiveness of the intervention, including processes of implementation, staff perceptions and economic evaluation. We also conducted quantitative analyses to ascertain suitable measures of impact to inform stakeholders and future evaluations.
Phase 1
Phase 1 was the feasibility and scoping stage of the study, including a literature review of published evidence. Our activities in this phase were:
-
An evidence review of the literature including a review of other Redthread evaluations.
-
Documentary analysis alongside qualitative scoping interviews (conducted remotely) with the Redthread team and youth workers to confirm the interpretation of Redthread’s programme theory and the intervention at UCLH. This included any recent adaptations due to COVID-19.
-
An investigation into the feasibility of a quantitative evaluation of the service by studying local data flows and processes and analysing routine hospital data.
-
A desk-based review of available Redthread and UCLH documents to inform the economic analysis.
-
Setting up an advisory group for the project.
Evidence review
The evidence review was conducted in two parts and focused on youth interventions delivered in hospital settings to reduce or prevent violent crime and harm to young people (e.g. from criminal and gang exploitation) and involving professionals such as social workers, trauma experts and youth specialists who work alongside clinicians. We followed recommendations on conducting systematic scoping reviews22 (e.g. predefined eligibility criteria and research questions) to map out the topic and to identify recent evidence available on this topic and any theories or conceptual frameworks that have been applied. We used a two-phased search process – one exploratory, one targeted – focusing on the medical literature to understand what was currently known about youth-orientated violence reduction services delivered in hospital settings, specifically their impact and outcomes monitored, and to determine whether there are gaps in knowledge such as, for example, cost-effectiveness. We also looked for evidence of factors that either support or hinder the implementation of such services and identified any conceptual or theoretical lenses applied in this area, such as behavioural concepts applied to evaluate ‘teachable moments’ and drawn from social science subdisciplines, such as cognitive psychology. Our searches looked for evidence about these interventions from both within the UK and internationally.
Further details on the methods used in the review including the search methodology are described in Chapter 3.
Qualitative scoping interviews and documentary analysis
Qualitative data collection was conducted in two phases, and involved semistructured interviews, observations of staff meetings and review of Redthread documents and materials. Phase 1 was an exploratory stage which aimed to understand the Redthread programme theory and the background to the introduction of the charity at UCLH. Phase 2 (described below) consisted of a single-site, process case study to understand implementation of the Redthread intervention at UCLH as well as staff perceptions of Redthread’s impact and progress.
All interviews were conducted from April 2021 once Redthread youth workers were back on site at UCLH. Recruitment used a mixture of purposive and snowball sampling to capture the views of a range of respondents, both those close to the Redthread intervention (e.g. youth workers), subject experts and those who might be less familiar with Redthread (e.g. junior doctors/nurses working in emergency care). The main criteria for UCLH staff respondents to take part was being directly involved in the care of young people at risk of harm and in a position to refer young people to the Redthread service. Staff were identified with the support of UCLH clinical collaborators and all respondents were emailed an information sheet prior to taking part and given the opportunity to ask questions about the evaluation and interview process.
During phase 1, available Redthread documents were supplied to the evaluation team to map out referral pathways into the service and analyse the programme theory; that is, what the intervention aimed to do and how, and its main component parts. Programme theory can be defined as describing ‘how an intervention is expected to lead to its effects and under what conditions’. 23 We sought to understand Redthread’s programme theory (what they call their ‘theory of change’) to explore how the service was being implemented and was understood by staff at UCLH and to identify any contextual adaptations. We did not attempt to further develop or revise the Redthread logic model but were aware that the charity regularly reviews and updates its own materials.
This work was supplemented by exploratory discussions with key stakeholders at UCLH and members of the evaluation advisory group. We also examined the findings of previous Redthread evaluations undertaken at other trusts to see how they interpreted the Redthread programme.
During phase 1, we conducted nine scoping qualitative interviews with key stakeholders. Respondents were: two hospital consultants working in children and young people’s services at UCLH, six Redthread youth workers and other staff (e.g. managers, programme co-ordinators) and one senior NHS director involved with youth violence reduction interventions with knowledge of similar programmes at other NHS trusts. The aim of these interviews, which were semistructured, was to capture insights about the early introduction of the Redthread service at UCLH and the wider context. In particular, the early interviews aimed to understand what meaningful success looked like to those involved in delivering the intervention at UCLH (e.g. reduction in admissions, onward referrals to other services, positive case work with an individual) and to explore any skills and training required to deliver the intervention. Finally, we noted any novel service components that were new to the UCLH setting or arising because of COVID-19 (e.g. virtual delivery). Further details of our methods are described in Chapter 4.
Feasibility study of a quantitative evaluation
The aim of the quantitative component of phase 1 was to explore the feasibility of evaluating the impact of the Redthread service given the available data. The results of this investigation would then inform the nature of any quantitative analysis that would be undertaken in phase 2.
For a measure of impact, we focused on the use of hospital services, specifically, future hospital attendance either at ED or as an inpatient relating to assault, mental health, substance abuse as well as those who were perceived to be at risk of harm. We developed a set of options for evaluating impact that covered different perspectives:
-
the perspective of someone using the service
-
the perspective of the acute trust where the service is based (UCLH)
-
the perspective of the local communities where people using Redthread’s service live.
These perspectives were assessed by investigating the data requirements of each option, including any access to individual person-level data, the linking of their records, the identification of comparators and necessary sample sizes. We also identified possible barriers to accessing the necessary data such as patient consent, information governance approvals and time to obtain these approvals in relation to the duration of the project. Our analysis was informed by an investigation of HES admitted patient care and ED datasets and the Emergency Care Dataset (ECDS) alongside discussions with Redthread, UCLH, NHS Digital and our expert advisory group. Further details on the methods used in this feasibility analysis are described in Chapter 6 and Appendices 3–5.
Preliminary economic assessment
During phase 1 we conducted a documentary analysis of the Redthread evaluations that had already taken place since 2021. We collected information on the evaluation aims, their main components and their results, to identify the existing gaps in the evidence. This informed the assumption and parameters we adopted in our economic analysis.
Set-up of an evaluation advisory group
During phase 1 we also set up an evaluation advisory group to meet up to three times during the course of the evaluation (virtually or in person) and involving representatives from the NHS, health-care and relevant public agencies. Terms of reference were drafted with the aim of each meeting to provide helpful challenge and advice to the evaluation team from stakeholders more external to the programme.
Phase 2
Phase 2 involved a more in-depth study of the service at UCLH and included:
-
A qualitative process evaluation with interviews with staff at Redthread and UCLH, to understand the perceived impact and effectiveness of the service as well as identifying factors that enable the successful delivery of YVIPs.
-
Analysis of data collected by Redthread over the course of the project to understand more about the delivery of the service and what it tells us about who engages with it.
-
A cost–consequence analysis (CCA) using local data on the costs of the Redthread service and relevant hospital interventions.
We had intended to include a quantitative evaluation of the service as part of phase 2, but our phase 1 work established that this would not be feasible.
Process evaluation – qualitative case study
For phase 2 of the qualitative data collection, we completed a process evaluation, where the unit of analysis was emergency and specialist children’s and adolescent services at UCLH. A process evaluation was considered suitable because the Redthread service is a complex intervention and randomisation was not feasible in this study. What was required were insights about delivery and overall impact to inform future implementation. 24 Process evaluations aim to understand how a programme or intervention is implemented, including any important decisions that influence how it operates in practice, any important adaptations, and the contextual factors that influence the intervention and its implementation. 25 We were therefore particularly interested in understanding:
-
the different processes and mechanisms at work locally, such as different referral pathways to access the Redthread service
-
any adaptations made to the service over time (e.g. due to COVID-19)
-
the reach of the service (e.g. the extent to which it had spread across different hospital departments)
-
critical implementation factors (e.g. what was reported to help youth workers to deliver the programme, or hospital staff to refer young people to it).
This part of the study involved additional qualitative data collection (13 further semistructured interviews and three observations of staff meetings) and focused on the mechanisms and emergent themes identified in phase 1, including any linkages between them, and any features of the hospital setting and its environment that were shaping delivery of the Redthread programme. Examples of the factors that we explored in this phase included:
-
Internal context: departmental leadership and cross-departmental working; professional buy-in (especially by emergency, trauma and paediatric staff); hospital data sharing and governance policies; senior/executive team support for the intervention; staff training; perceptions of need; communication of information about the intervention.
-
External context: demands on hospital services (e.g. young people presenting at UCLH and their needs); any trust collaboration with external public agencies; lines of accountability within the area (e.g. responsibility for youth crime prevention and safeguarding for children and young adults).
The additional semistructured interviews were with clinical and non-clinical UCLH employees and Redthread staff. They included hospital social workers, Redthread youth workers and managers, a paediatric nurse, consultants (children and young people’s services, child and adolescent psychiatry) and a junior doctor. Of the interview respondents, a small number of individuals were interviewed twice (in phases 1 and 2) because of their close involvement with implementing the Redthread service. All interviews and observations were conducted remotely via Microsoft Teams® (due to COVID-19) following consent to participate. Interviews were digitally recorded and transcribed verbatim. Three observations of staff meetings were completed [e.g. an adolescent ward psychosocial multidisciplinary team (MDT) meeting] alongside review of essential Redthread documents. Anonymised field notes taken during staff meetings.
To support analysis and interpretation of the qualitative findings, the qualitative researcher and wider evaluation team held discussions with the evaluation advisory group, and held meetings with other researchers involved in Redthread evaluations at different NHS trusts, plus meetings with Redthread staff and UCLH clinical collaborators. For the final analysis, all interview transcripts (n = 22) and observational field notes were read by the lead researcher for data familiarisation, alongside key materials such as the Redthread planning and implementation guidance, and other relevant documents (e.g. the Redthread youth worker manual). Findings were analysed thematically with a specific focus on answering the evaluation questions (see Chapter 4 for further details of the themes).
Unfortunately, it was not possible to conduct interviews with young people who had experienced the Redthread service at UCLH or at other NHS trusts for ethical and practical reasons (e.g. identifying young people would have data sharing and confidentiality implications), although this possibility was explored with Redthread. Further details on the methods employed are described in Chapter 4.
Analysis of local Redthread data
Over the course of the project, we obtained data from Redthread that included the characteristics and reasons for hospital presentation of individuals who engaged with the service and of those who declined to take part. Using univariate analyses, we compared these characteristics to identify any differences between those who chose to engage and those who did not. All the data were provided at an aggregated level for each characteristic separately, which precluded more complex multivariate approaches. Further details of the methods employed are described in Chapter 5.
Economic evaluation
Based on the outcomes of phase 1 of the evaluation and documentary analysis, we conducted a CCA of the Redthread service at UCLH. Consequences were derived from Redthread’s risk assessment tool, which measures changes in perceived risks faced by young people before and after intervention. Costs of delivering the service were obtained from Redthread, and these were compared with the costs of hospital ED attendances and admissions for reasons that might suggest eligibility for Redthread, over the three-year period 2018–2021. Hospital costs were obtained from UCLH. Further details of the methods are described in Chapter 6.
Patient and public involvement
We involved patients and the public in this evaluation in a number of ways. During the RSET patient and public involvement panel meeting in November 2021, we asked our patient representatives for suggestions on how to effectively disseminate study findings to various stakeholders. While writing up this report, we worked with our patient representatives (Raj Mehta, Fola Tayo, Jenny Negus and Nathan Davies) to ensure that the plain English summary was clear and accessible. In line with the RSET patient and public involvement strategy, our patient representatives were paid for their support in the development and write-up of this evaluation. We will also involve our patient representatives in producing accessible output to share the study findings.
We wanted to involve young people who had received support from Redthread or who had similar lived experience in the planning and delivery of the evaluation. However, as the study progressed, a number of barriers to engaging with young people became evident (as described in Chapter 4) and it was decided that this approach would not be pursued.
Ethical and local research and development permissions
On the basis of the NHS Health Research Authority’s online decision tools, the study was classified as a service evaluation. We undertook local data collection after obtaining permission from clinical leads at UCLH (e.g. consultant paediatricians) and a formal letter of support from the clinical director of emergency services.
Chapter 3 Evidence reviews
What was already known?
-
Hospital-based violence intervention programmes (HVIPs) have been adopted since the late 1990s and early 2000s in the United States following high rates of gun crime and mortality rates among young people across American cities. A number of these HVIPs have been studied using RCTs and experimental designs to estimate efficacy, although often with relatively small follow-up time period (e.g. 12 months).
What this chapter adds
-
An up-to-date review of evidence about hospital-based (ED/trauma centre) youth interventions and programmes that aim to bring about behaviour change in young people and reduce their overall level of risk to harm found:
-
a limited evidence base in the UK; specifically, a lack of empirical studies
-
a lack of studies that focused on ways to increase referrals or reasons for low uptake by young people
-
studies reporting a variety of outcomes for both case management and brief interventions instigated in EDs: depressive and post-traumatic stress disorder (PTSD) symptoms; decreased feelings of aggression and involvement in peer violence; varying effects on victimisation; outcomes related to service uptake and use; mortality and morbidity outcomes; recidivism
-
two literature review studies confirming our findings that there are few studies following long-term outcomes, which limits conclusions about impact, as do the small sample sizes in studies
-
studies from the United States which suggest that there may be positive benefits with respect to recidivism and patient reported involvement in violence from interventions in ED settings
-
a small, recent and emerging grey literature consisting of evaluations evidencing the impact of programmes in the UK, such as Oasis and Redthread
-
-
Suggestions for future research and evaluation (e.g. multisite, longitudinal comparative studies, and more qualitative research with staff and young people, especially to understand reasons why some engage and some choose not to engage).
Background
Offences classified as assault with injury and assault with intent to cause serious harm have risen by 46% between 2011 and 2020 in England and Wales. 1 The number of repeat violent offenders is also rising. The majority of cases are concentrated within metropolitan areas, and most offenders, as well as victims, are male (55–74%). Also of note, in 2018, 37% of homicides in London were gang related, and just 14% of all violent incidents in England were linked to alcohol use. 1,26 Risk factors for involvement in violent crime are complicated and multi-factorial. Offenders and victims often have a history of childhood maltreatment, and strong evidence links future violence with having suffered violent experiences or abuse as a child. 27 There is some limited evidence to suggest that school exclusion and undiagnosed mental health issues are also contributors to youth violence. 28,29 Other well-accepted risk factors are linked to environmental exposures and include living in areas of socioeconomic deprivation and where damaged community relations with law enforcement exist. 30,31
Research evidence indicates that assault-injured youths are at significant risk of repeat injury. 3 While estimates vary, the risk of recurrent injury may be 80 times that of an ‘unexposed’ individual. 4,5 When assessed in the ED, the majority of injured youths believe their injuries are preventable, although over one-third also believe that a similar violence-related injury will occur in the future. Patients face significant obstacles after discharge (such as access to follow-up care, safe housing, return to work/school, or managing post-traumatic stress). Such hurdles often lead to continued engagement in high-risk behaviours that lead to repeat injury. Moreover, youth assault injuries are often related to repeated disagreements, and retaliatory feelings fuel repeated violence. 6 Over time, the victims and perpetrators become interchangeable. The goal of ED-based interventions is to interrupt the cycle of reactive decision-making.
Prior studies further suggest that trauma serious enough to require medical intervention may make youths uniquely susceptible to behavioural intervention and change. Consequently, ED-based interventions may provide a ‘teachable moment’ and a special opportunity to identify and reach youth victims of violence, as well as inform them of the benefits of intervention and link them with supportive treatment programmes that can function beyond the hospital.
Aims and methods
The evidence review aimed to answer the following overarching questions:
-
What evidence exists in the published research and grey literature about the effectiveness, benefits and impact of interventions in urgent care and hospital settings that focus on violent crime and young people?
-
What lessons can be learned from UK and international studies to help NHS trusts implementing such interventions?
In addition, the review aimed to:
-
identify existing gaps in the knowledge base, such as the cost-effectiveness and any economic evaluation of youth-orientated services based in hospital settings
-
identify factors that support or hinder the implementation and impact of youth-focused behavioural and preventative interventions delivered in hospital settings, particularly those that involve collaboration between secondary care professionals and youth workers/specialists
-
identify any conceptual or theoretical lenses applied in this area, such as behavioural concepts applied to evaluate ‘teachable moments’ with young people.
The review was organised into two phases, one conducted early into the evaluation project to inform data collection and provide a clearer understanding of the topic, and a scoping review conducted later into the project to ensure any recent, peer-reviewed evidence was captured.
Phase 1: exploratory search
Phase 1 consisted of an initial scoping review focused on youth-focused interventions delivered in emergency and hospital settings to reduce violent crime and address safeguarding risks (e.g. from knife crime, assault). It was led by one researcher (JF) with input from another researcher (JL). The review was intended to be broad in scope, with the aim of better understanding the topic and confirming the types of key terms that could be employed in a more targeted search to be conducted later. It was conducted in the earliest stages of the project, prior to empirical data collection.
A population, intervention, control/comparison, outcome framework was used to define the search terms:
-
population: youth patients 10–24 years of age, victims of interpersonal violence (excluding victims of self-harm, sexual violence, and child abuse)
-
intervention: youth or social worker hospital-based interventions
-
comparison: standard of care, no treatment, or differential treatment of a control group
-
outcome: recidivism, readmission, social services use, feasibility or patient self-reported outcomes.
The exploratory search was conducted in January 2020 and limited to English text sources but with no date restriction as the review was intended to be exploratory, as part of an initial search for available papers. The databases searched were PubMed, MEDLINE, the Cochrane Library and Embase databases. The a priori decision was made to limit screening to the first 200 hits (as sorted by best match) to provide a manageable number of initial sources of evidence; thereafter, further inclusions were determined based on reviewing cited literature for its relevance. Conference abstracts, editorials and commentaries were excluded. Fourteen studies were identified for inclusion due to their relevance to the evaluation, namely, studies that could help the researchers to understand the wider context of youth violence hospital interventions and programmes, and the types of prevention strategies commonly found in health care settings. These findings are presented in this chapter.
Phase 2: structured scoping review
A rapid scoping review was deemed appropriate due to the complexity of the topic, the emerging nature of the knowledge in this field, a need to understand the nature of the evidence base quickly and any knowledge gaps. In short, we needed a quick overview of the latest evidence related to hospital-based, youth-focused emergency care interventions such as Redthread. The findings of the phase 1 exploratory search informed drafting a review plan (not published) to guide a more systematic search of the medical and health care literature databases, which received team input (e.g. listing key words). The phase 2 scoping search also took into account early empirical findings from the qualitative interviews to understand the Redthread programme at UCLH (see Chapter 4).
This review was open to capturing a range of potential benefits of youth violence prevention services and youth worker programmes in hospital settings and followed a modified version of the PICO structure used in phase 1. As per guidelines for scoping reviews, we were chiefly focused on the population, concept (e.g. ‘teachable moment’, youth intervention following admission for trauma) and context (e.g. EDs) due to the wide range of possible outcomes of YVIPs. In terms of types of evidence, we were interested in identifying peer-reviewed published studies using a variety of study designs and any other evidence reviews (e.g. systematic and scoping).
The guiding questions and aims of the review remained the same, as outlined above, and the review inclusion criteria was as follows:
-
Population: young people, adolescents and children (aged up to age 30 years, to capture a wider literature), specifically groups at risk from gang-related exploitation, physical assault and injury (e.g. from knife attacks, shootings), sexual exploitation, human trafficking and other forms of violence (e.g. from peers and fighting).
-
Intervention: youth or social worker (or equivalent roles) hospital-based interventions aimed at risk management and prevention, and initiated within EDs/major trauma centres (MTCs).
-
Context: hospital-based interventions.
Inclusion parameters:
-
Study type: any [e.g. feasibility study/pilot, RCT, qualitative, evaluation, mixed-methods, cost–benefit analysis (CBA)] and literature reviews (narrative, scoping, systematic).
-
English language.
-
Peer-reviewed (i.e. no conference proceedings or abstracts).
-
Publication period: 2012–2022.
Searches were carried out on two medical databases (Medline and Embase) in February 2022 to focus on the health literature using key words and medical subject headings terms (see Appendix 1).
Results from Medline and Embase were imported into EndNote for deduplication and then exported to Rayyan.ai software for screening. Two researchers (JL and JF) independently assessed the retrieved sources using the inclusion criteria and considering relevance for answering the aims of the review. Papers were discussed and selected against the inclusion criteria and in light of their quality (e.g. an explication of the study design, nature of the intervention, intervention context and any limitations). Excluded papers included crisis interventions that did not feature a hospital-based youth or social worker’s input or equivalent role (e.g. sexual health crisis teams), conference and meeting abstracts and clinical case reports. A large number of studies were found to focus on community-based youth interventions, where young people are recruited to external programmes via EDs and seen by community youth workers or mentors, and this required further discussion and accessing full papers. It was decided that these studies should also be excluded. However, the boundary between hospital and community interventions was sometimes difficult to discern. Finally, mental health crisis interventions and any programmes designed to educate health professionals about youth violence (e.g. e-learning modules) were also excluded. The results for phase 2 are provided in the Preferred Reporting Items for Systematic Reviews and Meta-Analysis diagram below (Figure 3).
FIGURE 3.
Phase 2 search results.
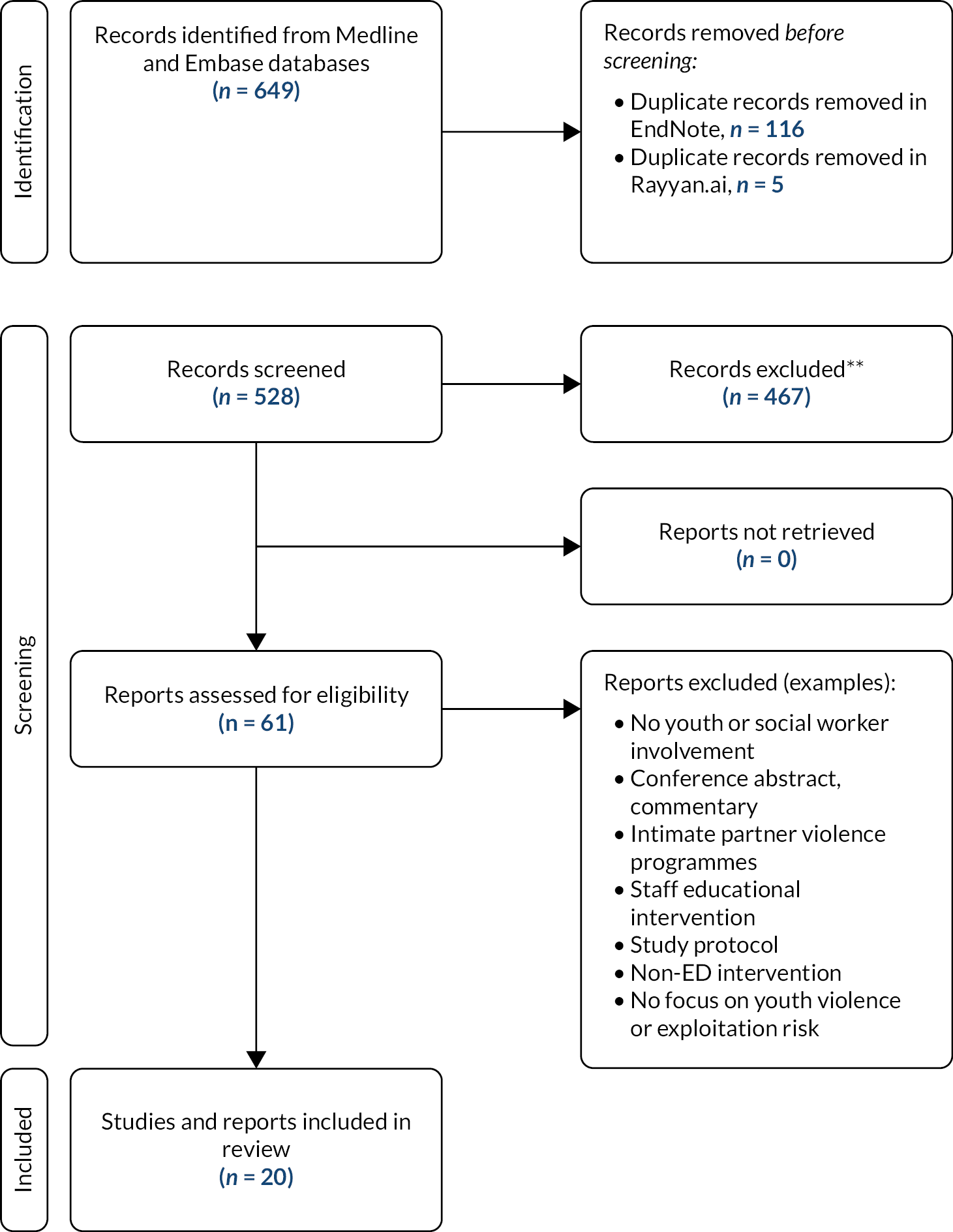
As we were following guidance for scoping reviews and conducting the search under resource and time restrictions, the focus was on mapping the evidence base in the literature rapidly, with the aim of describing the types of studies available according to our predefined eligibility criteria and analysing any knowledge or research gaps in light of this rapid evaluation. The evidence search was not intended to be a systematic review, and no meta-analysis of the results was performed. Results were limited to two databases and we summarised the findings in a table detailing the study type and main findings. Extracted data focused on study location, intervention characteristics/components, population; setting/context, outcomes and key findings.
In the final phase, we performed Google search for grey literature using key terms (e.g. ‘youth hospital violence programme’, ‘Redthread evaluation’, ‘violence prevention and hospital’) to see if there was any additional evidence arising from the UK. We also engaged with the Redthread charity about past or current service evaluations with which they were involved. In this way, we identified some evidence scans and evaluation reports that had not been picked up in our search of health-care databases, as well as published evaluations of youth violence prevention programmes. We discuss these at the end of this chapter. All sources were assessed for their relevance to the evaluation, namely, a focus on youth violence prevention and hospital-based interventions (i.e. programmes such as Redthread or similar).
Principal findings
Phase 1: exploratory review
Approaches to the prevention of violence in children and young people
Early intervention programmes aim to improve parenting skills and early child–parent relationships. They are often home-based and targeted at vulnerable parents whose children are at risk of poor outcomes. There is a solid base of literature supporting their efficacy and long-term cost savings. 33,34 More specifically, such programmes are designed to improve parenting practices and reduce child maltreatment, leading to less down-the-line behavioural problems and mental health issues that would otherwise increase the likelihood of a youth being involved with violence. The Nurse Family Partnership (United States and UK), Early Start (New Zealand) and Triple P (Australia) are well-known examples of such programmes. An economic evaluation of the Nurse Family Partnership found that the programme generated a saving of US$2.88 for every $1.00 invested; and by 15 years of age, youths whose parents participated in the programme ran away from home less, had fewer arrests or criminal convictions and fewer behavioural problems or substance abuse issues. An evaluation of Triple P suggested that the programme could reduce conduct disorder by 25–48%. 34,35 Furthermore, assessment of a similar intervention in the UK for parents of five-year-old children with conduct disorder estimated that a saving of £9288 per child could be generated over a 25-year period, when accounting for future potential NHS, social service and criminal justice system costs. 36
Prevention strategies for older (e.g. aged between 18 and 24 years) at-risk youths, in the form of substance-use deterrence, after-school enrichment programmes or social media campaigns have been less effective at reducing violence than early-life prevention programmes. Although promising, such interventions, including those to deter alcohol use (shown to strongly correlate with violence in some environments), have proved especially difficult to evaluate. 37–39 After-school enrichment programmes offer academic support and recreational activities to at-risk youths. Evaluation of such programmes in the United States and UK have demonstrated mixed and even negative effects on violence deterrence, especially when interventions single out high-risk youths. 34,40,41 Little evidence also exists to support the effectiveness of challenging social norms through mass media campaigns. Such programmes have demonstrated effects on changing social perceptions, but not on changing actual behaviour or violent outcomes, although social campaigns do serve to drive social debate and support other prevention work. 42,43 For example, the ‘#KnifeFree’ campaign in the UK uses real-life stories of youths involved in violence to encourage more positive alternative choices. 44
Other interventions, most of which come from outside the UK, consist of ‘therapy’ based and behavioural programmes to break the cycle of repeated youth violence. 45 Comprehensive meta-analytical studies have found that ‘skill’ building-based interventions are strongly correlated with recidivism reduction, measured as repeat contact, probation violation or incarceration, and self-reported ‘delinquency’. 46 The most successful ‘skill’ building programmes for young people are designed around cognitive behavioural therapy (CBT) techniques and aim to develop adaptive behaviour and social skills. Effective programmes, beyond providing counselling or mentoring, also include multiple co-ordinated community services and are restorative in nature, involving the participation of family members. This combination of efforts is collectively referred to as ‘multisystemic therapy’. 47,48
Criminal justice system-based interventions, such as increased use of ‘stop and search’ techniques or installing weapon detection systems in schools, are rarely effective in isolation, although they may have merit as part of larger, multisystemic interventions when thoughtfully implemented. There are data to suggest that such strategies may work as effective short-term deterrents, make some youths feel more secure in their environment and increase school attendance. 49,50 However, this type of policing also has the potential to stigmatise, induce anxiety and cause resentment among those who might be searched or caught, as well as damage police–community relationships when used more often against members of ethnic minority groups. 39,50 The Offensive Weapons Bill, which was passed by Parliament in May 2019, further limits youths’ ability to purchase bladed weapons, firearms and corrosive substances. Little is known, however, regarding the effectiveness of such policies and prior similar legislative efforts, such as knife amnesty or longer prison sentences for possession, have had no lasting effect on youth violent crime deterrence. 34,51 Finally, ‘zero tolerance’ or fear-based police enforcement of laws has been shown to either have no effect on or exacerbate violence. 52
Hospital-based youth violence prevention programmes
There have been a number of studies going back to the late 1990s and early 2000s describing HVIPs, some of which compare these interventions to outcomes arising from standard to care.
One RCT was conducted in Baltimore, MD, by Cheng et al. from 2000 to 2001 at a large urban level-1 trauma centre. 53 Eighty-eight youth victims of violence were enrolled who were aged 12–17 years. Patients were identified by records review and enrolled within two weeks over the phone. A 14-point standardised assessment was performed during the initial interview to assess needs and then prioritise services. The treatment group were assigned master’s-trained youth workers who oversaw their case. The case workers offered intense weekly services by telephone and in person for a period of four months, as well as facilitating the use of community resources and programmes by the patient and the family as deemed appropriate. The control group received referrals to further services as appropriate at time of enrolment alone. Follow-up interviews were assessed at six months. There was no significant difference between the study groups on social service use; there was also no difference in reported fighting, fight injury or weapon carrying. Limiting factors were a low overall follow-up rate (57%) and an average time from ED visit to enrolment of 19.5 days, more than two weeks after the violent event and potentially missing the ‘teachable moment’.
A larger follow-up RCT was performed by the same group (Cheng et al.) in the Washington DC–Baltimore metropolitan area from 2001 to 2004 at two large level-1 trauma centres, where 166 youth victims of violence aged 10–15 years were included. 11 Patients were enrolled either in hospital or by phone just after admission, and the initial needs assessment was conducted at the home residence of the patient through a standardised process. The treatment group received an assigned youth worker ‘mentor,’ recruited from the community, who met with them at least six times over a six-month period. Mentors spent time with the participants in an activity at either their home or in the community, while also completing a standardised violence prevention curriculum based on the Centers for Disease Control and Prevention’s Best Practices in Youth Violence Prevention. The curriculum was based on social cognitive theory and included constructive skill-ascertainment focused sessions on conflict management, problem-solving and decision-making. Parents of participants also received three home visits by licensed health educators who went over topics covered in the youth curriculum and conducted sessions on parental monitoring and involvement. The control group received case management in the hospital setting and two follow-up telephone calls, and tailored referrals were made for patients to appropriate community services and programmes. Follow-up assessments were conducted at six months. More than 90% of treatment group participants were satisfied with their experience, 71% completed follow-up interviews, and 54% completed the entire programme. A trend toward significance was found for self-reported ‘misdemeanour activity’, aggression scores and general ‘self-efficacy’ (increased conflict avoidance). No differences were found among youths regarding self-reported or parental-reported aggression, attitudes about retaliation or weapon carrying. Low study power, despite a higher number of participants, remained a limiting factor in detecting differences between study groups.
In a retrospective study, Marcelle and Melzer-Lange conducted chart analysis of youth victims of violence were who treated in an urban ED in Milwaukee, WI, in 1998. 54 Patients were aged 10–18 years; 218 of 394 received the intervention and were included in the analysis. Those in the treatment group were assigned an experienced youth worker during the initial ED visit who then arranged further programme services, such as home visitation counselling, mental health services and youth activities. Referral to additional community services was also provided on an ongoing basis. Only three youths returned to the ED with a new injury within 12 months of study enrolment. This was the only outcome measure reported. Outcomes of control youths and attendance to other EDs in the area were not tracked, and no comparison was made between study groups.
‘Caught in the Crossfire’ is another example of a hospital-based YVIP, based in Oakland, CA. Youth victims of violence were tended to in the hospital by experienced youth workers, called ‘intervention specialists’, who were themselves prior victims of violence. These interventionalists provided case management and mentorship, and connected both the patient and family to further community services for up to 12 months following the violent event. Two separate retrospective reviews of the programme have been performed. The first analysis was conducted by Becker et al. in 2004. 55 They evaluated 138 patients admitted to a large urban hospital who received the intervention aged 12–20 years between 1999 and 2000. Matched controls were over-selected from violently injured youths admitted in 1998 to the same hospital who had not received the intervention. Follow-up was assessed at six months, and 43 of 69 patients (62%) in the intervention group completed the treatment and were included in the analysis. There was no significant difference in subsequent arrests or any criminal involvement between treatment or control groups.
A larger retrospective evaluation of Caught in the Crossfire was carried out by Shibru et al. in 2007. 56 They evaluated 158 victims of youth violence aged 12–20 years who received the intervention and were admitted to the same hospital between 1998 and 2003. Follow-up was assessed at 18 months in this study and criminal justice data were also obtained by the Oakland Police Department for review. Those eligible for inclusion in the treatment group were required to have had a minimum of five interactions with programme services outside of the hospital. Matched controls were selected, similar to the first evaluation. There was no difference between study groups regarding reinjury or rehospitalisation. The treatment group did demonstrate a statistically significant lower risk of subsequent criminal justice involvement at 18 months (relative risk reduction of 0.67). The authors estimated US$750,000 to $1.5 million in annual societal savings based on county juvenile detention system costs and number-needed-to-treat analysis. It was not clear, however, given the requirements for treatment group inclusion, whether some of the controls started in the treatment group. Moreover, the choice at the onset to limit ‘non-users’ of programme services from inclusion in the treatment group affects the broader validity of the findings. Small cohort sizes also limited statistical power.
Summary: phase 1
Our exploratory review found evidence regarding different types of interventions to reduce youth violence recidivism, dating from the early 1990s onwards. This suggests that: (1) successful programmes are generally long term, restorative in nature, and based on CBT techniques designed to help victims identify cognitive distortions and develop adaptive social skills, (2) successful interventions often include active participation of family members and coordinated community services, and (3) hospital-based youth worker programmes may increase social services use, decrease self-reported peer violence, and lower hospital recidivism rates. However, most of the available literature is limited by reporting outcomes over a period of less than one year, and the long-term durability of self-reported effects and recidivism rates is unknown. Moreover, recidivism rates are often described at single institutions, potentially limiting their validity as an outcome measure. Long-term, multicentre longitudinal studies are necessary to better understand the effect of hospital-based youth violence interventions.
Phase 2
The phase 2 structured search identified 20 academic articles and more recent studies. The search focused on papers published post-2012 to bring the first review up-to-date. The findings below are organised thematically around our evaluation questions and lines of enquiry. Table 2 outlines the 20 studies, 15 of which involved young people directly. Studies were predominately from the USA, plus one study from Canada and one from the UK. Programmes covered a wide age range (6–30 year olds), included males and females and different ethnic groups (Black, White, Asian, Turkish, Mixed, Hispanic).
| No. | Study type | Reference | Location | Intervention characteristics/components | Target population | Setting | Outcome(s) monitored | Key findings |
|---|---|---|---|---|---|---|---|---|
| 1 | Case series (no control group) | Bell et al. 201857 | Indianapolis, IN | HVIP: Prescription for Hope | 328 patients (aged 15–30 years) | Hospital trauma centre (urban, public hospital) | Violent-injury recidivism in state-level data (ED visits for new injuries) in 328 patients enrolled in the programme between 2009 and 2016 | Only 15 patients (4.4%) were found to have recidivated due to physical assault, firearm or stabbing injuries. Of the cohort experiencing new injuries, more than half were treated at different hospitals (access to multiple hospital datasets is key for evaluation). Range of medical problems associated with violent injury – for example, pain and chronic pain (patients re-present in ED for issues from the original injury) |
| 2 | Cross-sectional study | Bernardin, Moen and Schnadower (2021)58 | Missouri, USA | HVIP: social workers assess all ED paediatric presentations for violence and firearm injury and offer enrolment in the programme | 407 patients (aged 6–19 years) | Hospital ED | Service uptake/enrolment | 104 (25.6%) of those offered the HVIP were enrolled. Average age of enrolled young people was 14 years. Those least likely to enrol in the programme were older adolescents, on probation or had illicit substance misuse. No significant difference in enrolment between injury type, physical assault or firearm |
| 3 | Descriptive Single-Site Case Study | Bernstein et al. (2017)13 | Boston, MD | HPA screen young people for risky behaviours using a survey (e.g. substance misuse, violence, safety concerns). Structured conversation (brief intervention) resulting in a plan to address behaviours, and referral to community/other relevant services if needed. Gun and knife crime victims are referred to the hospital-based trauma programme | 2149 eligible patients (aged 14–21 years) | Paediatric ED department | Engagement and implementation | HPA programme went beyond drug and alcohol issues to assessing young people’s level of risk. HPA role required integration into clinical teams so that staff would use the service and to ensure staff bought into the preventative approach. HPA role had to be distinguished from other professional roles, for example, hospital social workers. Administrative and budgetary issues a challenge for the service. 636/785 screened at risk for drug or alcohol use and received the brief intervention. Numbers on those receiving support for violence not reported |
| 4 | Retrospective review (firearm injuries) | Borthwell et al. (2021)59 | Los Angeles, CA | BAs for individuals with firearm injuries; history taking around social, medical, behavioural, educational factors, and violence and gang exposure. Hospital introduced a HVIP | 115 young people (aged under 18 years) | Hospital trauma centre | Use of inpatient BAs (specialist trauma consultations, post-discharge services (e.g. financial advice) and HVIP service | 57% of young people were ‘bystanders’ injured by crossfire. 21% were reported to be gang-related assaults. 43% completed BAs. 17 patients enrolled in the HVIP service (implemented for last two years of the study). HVIP integration with trauma approach and BAs. Need to link inpatient and outpatient care for patients at risk |
| 5 | Quasi-experimental study | Carter et al. (2016)60 | Michigan, USA | One aspect of a violence prevention programme: a 30-minute behavioural intervention based on motivation interviewing techniques. Standardised, computer-assisted counselling delivered by a therapist to a young person about their involvement in violence | 618 eligible patients (aged 14–20 years) | Hospital ED | Physical aggression, victimisation, and self-efficacy for avoiding fighting (intervention group and comparator) | Only 17.9% of young people refused the intervention. Self-reported data at 2 months suggested a significant decrease in violent aggression and self-efficacy for avoiding fighting. There were no significant changes for victimisation. 86% of participating young people rated the intervention as ‘very’ or ‘extremely helpful’ |
| 6 | RCT | Cunningham et al. (2012)61 | Michigan, USA | SafERteens intervention: BI delivered by TBI or CBI, plus control group. Intervention aimed at adolescents who screened positive for violence and alcohol use | 4296 eligible patients (aged 14–18 years) | Hospital ED | Alcohol and aggression: self-reported survey data at 12 months | 829 individuals met the study criteria and 726 completed the baseline survey, with 607 completing the 12-month follow-up survey. Mean number of participants was 16.8. The main reason for ED presentation was injury (26.8%) or a medical condition (65.7%). Participants receiving TBI were less likely to report severe peer aggression and peer victimisation at 12 months compared to the control arm. Effects were better for TBI than CBI. Empathy from a therapist may be a factor in explaining the findings |
| 7 | Retrospective study | Cunningham et al. (2013)62 | Michigan, USA | SafERteens: secondary data analysis focused on dating violence subgroup of the study above (Cunningham et al. 2012). Intervention content tailored to dating violence prevention strategies (e.g. a role play). Delivered as a stand-alone CBI or T+CBI | 397 individuals who endorsed dating violence when surveyed (aged 14–18 years), a subgroup of 726 in the programme | Hospital ED | Dating victimisation and aggression self-reporting at 3, 6 and 12 months | Effects seen for dating victimisation with CBI at 6 months. CBI+T was effective at 12 months for those with a more severe history of dating violence. CBI is effective at reducing dating violence within ED settings |
| 8 | RCT | Ehrlich et al. (2016)63 | Michigan, USA | ‘U-Connect’ study: BI delivered by a computer or therapist for young people screening positive for risky drinking, and admitted for any reason | 4389 eligible patients screened (14–20 years), 836 of whom were enrolled in the intervention – one-third of whom had presented with injury (intentional or unintentional) | Hospital ED | Alcohol consumption and consequences follow-up at three months | Those with injury more likely to be male; injured patients more likely to have higher alcohol consumption at 3-month follow-up than other medical patients. CBI or TBI can reduce alcohol consequences and consumption among young people, and a computer BI was found to be effective for those presenting with an injury |
| 9 | Single-site service evaluation | Jacob et al. (2020)64 | England, UK | Hospital-based youth worker prevention service aimed at young people suspected of involvement (victim, perpetrator or neither) in gang-related violence. 12 sessions working with a youth worker was the minimum for completing the programme. Based around concept of ‘teachable moment’ | 496 young people (aged under 25 years) referred to the service | Hospital ED | Self-reported risk screening tools: Strengths and Difficulties Questionnaire; Asset: What Do You Think questionnaire; feedback from young people | The mean age of referrals in the study was 14. 9 years (range 7–26). Most were seen on the weekends having been caught up in violence, and nearly 25% had involved a weapon; 17% engaged with youth workers and 18% completed the programme; 31% declined the service, 29% could not be contacted and 22% were ineligible (e.g. out of area). Of those that completed, 93% showed reduced or no change in their criminality and emotional disturbance scores. Young people interviewed welcomed the programme |
| 11 | Prospective, randomised pilot study and retrospective data analysis | Lumba-Brown et al. (2020)65 | St. Louis, MI | EYIPP, 2012–2015: social workers are based in emergency services for timely engagement with young people. Patients enrolled in EYIPP received mentoring and advocacy support by specially trained social workers who deliver individual and group therapy, and family training. These mentors are described as being both therapists and advocates and help with a range of activities (e.g. court appearances, education) | Young people aged <19 years who presented for interpersonal violence in the ED (family or any type of assault) | Paediatric ED | Morbidity (ED visits with injury) and mortality (secondary to interpersonal violence), recidivism (self-reported or police reported) | Following pilot, programme was rolled out as standard care. 160 were approached in ED to take part. 16 were ineligible and 78/135 eligible young people declined the intervention. 57 received the intervention, with a median age of 14.5 years. Most were black males. Participants spent 25–40 hours over 1 year receiving mentorship. Morbidity and recidivism rate 3.5%. There were no mortalities. Co-location of social workers deemed critical for feasibility of the intervention due to some eligible victims of violence not being admitted as patients. High numbers of eligible young people decline to take part (e.g. nearly 60% in the standard programme) |
| 12 | Integrative systematic review | Mikhail et al. (2016)12 | N/A | Youth violence interventions based in trauma centres | N/A | N/A | N/A | 10 studies included, published between 1970 and 2013, and limited to interventions in the USA. Authors applied a social ecological model to their analysis. Outcome measures were variable across all included studies (e.g. self-reported, referrals, ‘needs met’, re-arrest, conviction, reinjury and trauma recidivism). Case management that leverages community resources more likely to be associated with violence reduction than BIs |
| 13 | CBA simulation | Purtle et al. (2015)66 | N/A | HVIPs using data from 2012, with calculations for different effect sizes | Hypothetical patient population of 180 individuals violently injured – half of whom are allocated to the HVIP, and half who are not | N/A | Health-care costs, intervention costs, criminal justice costs, and ‘lost productivity’ costs, calculated over 5 years | Savings US$82,765–4,055. HYIPs can produce cost-savings for hospital and society (e.g. criminal justice costs), although their estimates are more conservative than those identified in other studies |
| 14 | Feasibility study and pilot RCT | Ranney et al. (2018)67 | USA | iDOVE: a BI instigated in the ED (in person, computer assisted), followed by an eight-week programme of automated text messaging based around CBT. Participants are screened by research assistants. Those included were deemed at risk for violence (victimisation or perpetration) and depression | 1190 patients presenting in ED, aged 13–17 years | Paediatric ED | Changes in peer violence and depressive symptoms at eight and 16 weeks (self-reported) from screening, baseline and follow-up, retention rates and enrolment. Ratings by service users | 1063 patients were screened, 142 were eligible and 116 eligible patients consented to take part in the trial. The mean for the ED intervention was 22 minutes. All participants rated the programme as ‘excellent’ or ‘good’. High participation rates (86%) and retention (91% at 16-week follow-up). Study unable to prove efficacy of the intervention to reduce peer violence and depression symptoms |
| 15 | Cost-Effectiveness Study (based on a prior RCT) | Sharp et al. (2014)68 | USA | SafERteens study: BI for adolescents presenting in ED and screened positive for aggression and alcohol consumption in past 12 months. Intervention is social worker-delivered, computer assisted, and based around motivation interviewing techniques | N/A | ED | Peer aggression, peer victimisation, and violence consequences as cost estimates; intervention costs | Implementation costs of the intervention were estimated to be US$70,000. Intervention estimated to avoid 4208 violent events per year among adolescents at $17 per episode. Downstream benefits of violence reduction were not calculated (e.g. additional use of mental health and criminal justice services) |
| 16 | Feasibility and pilot RCT | Snider et al. (2020)69 | Winnipeg, MB | EDVIP based on the ‘Circle of Courage’ framework. Support workers who have direct experience of violence contacts the young person in hospital, and then conducts assessments with a social worker to set goals for a programme of support lasting up to 1 year, and engaging with community resources | 130 eligible young people aged 14–24 year presenting with a violence-related injury | ED | Recruitment, fidelity, adherence, safety, hospital visits for repeat injury, mental health and substance use | 452 screened patients were deemed eligible. Uptake was low: 36% of eligible youth consented to take part in the cohort study. 68 participants were randomised to the EDVIP and 65 to a control arm. 74% of participants were still engaged in the intervention at six months and 57% at 1 year. Non-significant decrease in violence-related injuries among the intervention group (10.4%) and injury from a weapon. Participants were also more likely to present earlier to ED for repeat violence-related injury |
| 17 | Quality improvement project | Watkins et al. (2021)70 | Wisconsin, USA | Project Ukima – a HVIP: young people receive case management support and crisis intervention, with links to community support | 7–18-year-olds presenting with injuries related to violence assault | ED/TC | Referrals | Staff sought to increase referrals to the HVIP from 32.5% to 70% within 1 year. They did this through educating staff regarding eligibility requirements and other staff-based interventions. Referrals increased from 32.5% to 61.1%, but the improvement was not maintained |
| 18 | Scoping review | Wortley and Hagell (2021)14 | N/A | Youth violence interventions involving youth workers and ‘teachable moments’ | N/A | N/A | N/A | 13 papers identified, published between 2004 and 2018. No evidence that these interventions cause harm. Study sample sizes tend to be small. Results about overall impact are inconclusive, although there are positive indications of success (e.g. feedback from young people) |
| 19 | RCT | Zatzick et al. (2014)71 | Washington, USA | Stepped collaborative care intervention focused on risk behaviours and symptoms: young people received screening and an intervention based around motivational interviewing techniques, delivered by a social workers and nurse practitioner | Patients aged 12–18 years admitted with intentional or unintentional physical injury and admitted for 24 hours or more | ED | Risk scores for violence, alcohol and drug use, and symptom scores for PTSD and depression – all at 2, 5 and 12 months | Of 598 admitted patients, 493 were eligible for participation and 120 were randomised to the intervention or standard care. One-third of engaged young people that participated had scored for carrying a weapon; significant reductions found in weapon carrying at 12 months after hospitalisation found among the intervention group |
| 20 | Qualitative | James et al. (2014)72 | Boston, USA | Violence Intervention Advocacy Program: advocacy, case, needs assessment, management and onward referral to other relevant services | Victims of penetrating trauma aged over 15 and under 30 years | ED | Client experiences and perceptions | 10 interviews with English-speaking ED patients aged 18 years or over and enrolled in the programme. Key themes among patients were fear and safety; trust (or rather, lack of trust); isolation; bitterness; PTSD symptoms and mental health aspects of violent injury. The intervention can provide positive life-changing experiences through mentorship and support, helping to build trust in clients |
What is the evidence of effectiveness, benefits and impact of youth violence interventions in hospital settings?
The majority of studies of ED youth violence prevention programmes originate from the USA due to the high number of gun-related deaths and injuries affecting young people, a large proportion of which may simply be ‘bystanders’ harmed by gun crossfire. 59
Some hospitals have introduced hospital-based YVIPs aimed at lowering a young person’s risk of harm with a focus on physical injury and gun-related hospital attendances, supported by youth and social workers. There are also ‘brief interventions’ delivered in EDs which involve screening and assessing young people’s safety risks, such as harm resulting from substance misuse, fights and aggression, and involving shorter, structured interventions focused on motivating young people to make changes. Common to these interventions is approaching a young person in an ED and using a young person’s clinical presentation as an opportunity to conduct a risk assessment, reduce the individual’s exposure to risk in the community, engage the young person in positive behaviour change, and to refer the engaged young person to other types of support following discharge, such as charities or services based in the community.
As found in the initial exploratory review, hospital-based youth violence interventions involve specialist social and youth workers working alongside health professionals to support young people. A primary outcome of these interventions is a reduction in re-admissions to EDs for injury. For example, Bell et al. 2018 describe the ‘Prescription for Hope’ HVIP in Indiana, USA. 57 The programme was set up in 2009 and treats young people aged 15 to 30 presenting in EDs and ‘admitted to the trauma centre for treatment of injuries that were inflicted by another person and resulted from assault, a firearm, or stabbing’. The intervention provides multidisciplinary and holistic support to young people via social workers, youth violence specialists and advocates. Through enrolment in the programme, young people obtain assistance with securing a health insurance plan, primary care access, full-time employment/a return to education and help with meeting other needs (e.g. legal, housing).
To assess the impact of ‘Prescription for Hope’, the researchers looked at injury recidivism using state-level ED hospital data. They found a 4.4% recidivism rate for new violent injuries in a cohort of 328 patients engaged in the HVIP over an eight-year period. While there was no control group in the study, the authors concluded that the programme was able to reduce injury recidivism rates among this group of younger patients and maintained positive benefits over time. As well as providing evidence to support the use of HVIPs, the study authors stress that obtaining access to hospital data across different geographies is essential for the evaluation of HVIPs because young people present at different hospitals, often as a result of pain or complications arising from an initial violent injury.
One of the few UK studies64 was a service evaluation of a youth violence prevention service which placed youth workers in a district hospital ED (rather than a MTC). The evaluation team looked at self-reported outcomes (criminality and emotional disturbance scores) using questionnaire-based screening tools, and feedback from young people engaged with the programme. A total of 496 young people were referred to youth workers during the study period (all aged under 25 years) and were eligible if they were suspected of involvement in gang-related youth violence. The authors found that engagement and completion rates were disappointing: 85 engaged (17%) and of these, 15 (17%) were engaged in the longer-term programme, defined as 12 sessions with a youth worker. However, 155 (31%) declined to engage, 110 (22%) were ineligible, and 146 (29%) could not be contacted. Of those that did complete the programme, 14/15 (93%) did not reattend ED during the study (2014–2017), and the majority had no change or reduction in their risk scores. Feedback from young people engaged with the services suggested they appreciated ‘the opportunity to talk openly, ease of access, having reliable and credible mentors, and the chance to develop effective strategies’.
In terms of detail about the perceptions of young people engaged in these programmes, rich qualitative evidence is particularly limited. One study,72 involved interviews with 20 young people who had been engaged in the Boston Violence Intervention Advocacy Program, which was established in 2006. This programme attends to young people who present with gun and stabbing penetrating injuries in ED and uses a ‘peer advocate model and trauma-informed care approach’. Residents of the Boston community are trained as violence prevention advocates and employed by the hospital and provide case management, mentoring and onward referrals. Advocates also have access to hospital electronic health records and can screen for admissions and eligible young people. All those who present to ED with a penetrating injury from violence and aged over 15 are eligible for support. In addition, those young people who may be at risk of emotional distress arising from their injury are referred to trauma mental health specialists. The advocates foster relationships with young people within the hospital setting, and maintain this contact following discharge, in ways similar to the Redthread model.
The researchers found from interviews with programme participants – all of whom were aged 18–30 and English-speaking – that: (1) these group were at risk of isolation due to feeling unsafe, (2) had feelings of distrust (e.g. towards the legal system), (3) expressed emotions consistent with symptoms of PTSD, (4) described changing attitudes towards programme advocates over time and valued being listened to (a trusting relationship developed), and (5) through advocates, the programme was able to provide a service that was otherwise not available, ‘a caring and understanding adult that went beyond the scope of physical recovery from injury’ (Ibid.). Even if the impact of an advocate on a person’s day-to-day life was fairly minimal, as was reported by a minority of respondents, advocates were still viewed in a positive light. This research underscores how youth violence ED programmes can address a gap in existing service provision and how mental health and support needs intersect with young people at risk of harm in the community.
Lumba-Brown et al. (2017)65 present a study of the Empowering Youth Through Interpersonal Violence Prevention Program, based in St. Louis, USA. This developed specially trained social workers in youth violence prevention and co-located them in the hospital’s paediatric ED, with the service adopting a mentoring and advocacy approach for young people presenting with violent injuries. Following a RCT pilot study to assess the service’s feasibility and impact between 2012 and2014, the programme was rolled out and a retrospective analysis conducted in 2014–2015 to review outcomes. Participants would have at least six mentorship lessons with a social worker who had made contact with them in ED, and were followed up for a year with ongoing tailored support as required. Some 135 young people were eligible, of which 78 declined to take part in the programme and 57 accepted and became engaged. The primary outcomes for the participating group were mortality, ED visits with reinjury (for violence) and recidivism (based on reports of involvement in violence). While there was a high rate of decliners from young people to engage with the programme, the authors found evidence that the intervention reduced violence and recidivism and emphasise the importance of having specially trained social workers working alongside medical staff.
It was notable that to measure the impact of these programmes, a number of centres had attempted to pilot RCT and quasi-experimental study designs alongside feasibility analyses to determine whether a programme could be integrated with existing emergency services. Another example, this time from Canada, is Snider et al. (2020). 69 They enrolled young people aged 14 to 24 who had suffered a violent injury and presented to ED. Support workers with personal experience of violence engage with the young person – and possibly their family – during their hospital visit and address risks of further violence. Following discharge, support is provided with social worker input and may involve other community resources. Outcomes for a cohort of 68 young people randomised to the intervention were analysed, the majority of which were still having regular, weekly contact after six months with the programme. While not statistically significant, decreases were found among participants for violence-related injury. However, overall uptake of young people in the study was relatively low resulting in a small sample size.
Most studies found in this review report on levels of engagement with youth violence prevention services in ED and there is evidence that a young person’s age and other life circumstances impact on the likelihood of engagement with a youth violence prevention service based in a hospital. Bernardin et al. (2021) completed a cross-sectional study to understand the ‘demographic, psychosocial and behavioural factors’ associated with presentation to hospital for physical assault or firearm injury and the willingness of young people to join a HVIP in the USA. 58 The children’s hospital provides a service for 6–19-year-olds which also involves social workers assessing and enrolling eligible patients that have presented to ED with a firearm or physical assault injury. The authors found that 104 of 407 (25.6%) patients enrolled in the programme and younger patients were significantly more likely to enrol. Older adolescents, those on probation and those involved in illegal substance misuse were least likely to enrol. The authors suggest their work has implications for HVIP programmes that should focus on more ‘targeted recruitment’ to reach ‘high-risk’ individuals and younger patients not yet displaying the main risk factors associated with firearm and physical assault injuries.
Watkins et al. (2021) conducted a quality improvement project over one year to increase the number of patients referred to a HVIP – ‘Project Ujima’ which was introduced to the paediatric department. 70 Eligible young people for the programme were aged 7 to 18 years old and presented at ED for physical assault, stabbing, or gunshot wounds. The primary outcome measure was the number of young people referred to the service over the study period. The team delivered staff education about eligibility to increase referrals, such as to nurses and social workers. The researchers were able to increase the number of patients referred to the programme from 32.5% to 61.1%. However, this improvement was not sustained. The researchers largely attributed this to staff turnover, particularly among social workers, and the fact that key social worker roles were often part-time.
Another intervention involving social workers (Zatzick et al. 2014) was studied using a RCT. A total of 120 patients aged 12–18 years were randomised (59 to the intervention) having been randomly sampled after presenting to the hospital trauma centre with a traumatic physical injury. 71 The intervention was delivered by a social worker and nurse practitioner for 12 months within a trauma team and involved motivational interviewing and CBT techniques. The researchers found that patients in the intervention group had ‘clinically and statistically significant reductions in self-reports of carrying a weapon during the year after injury compared with controls’.
Economic evidence
Two cost analyses were identified in the review. Purtle et al. (2015) completed a CBA simulation and estimated savings of a HVIP over five years. 66 In a hypothetical situation of 90 patients who had received the HVIP, the team estimated that savings would be in the range of $82,000 to $4 million (approximate values) based on an effect estimate of 25%. They concluded that costs savings are likely to arise from HVIPs.
Sharp et al. (2014)68 conducted a CBA based on Walton et al. (2010)73 and the SafERteen – a brief intervention in the ED aimed at reducing peer aggression and violence in young people aged 14–18 years (see below). They demonstrated cost estimates in the range of $4–55 for every violent event averted. Implementation costs (fixed and variable annual costs) were estimated to be $71,000. The authors conclude that if the brief intervention avoids a single gun-related hospital admission each year, this can cover the cost of implementing the intervention.
Brief emergency department interventions
Similar to Mikhail et al. (2016)12, our review identified shorter brief interventions delivered in EDs, yet we found more evidence of impact, suggesting that research on brief interventions is growing. These shorter interventions may be delivered in hospitals by an advocate, social or youth worker or similar professional role. They may or may not be computer assisted to encourage standardisation in delivery. Brief interventions typically target a wider range of risky behaviour among the younger population, such as drug and alcohol use or aggression, which can result in ED presentations for injury.
Two further articles refer to the SafERteens intervention at a hospital in Missouri and researched by the University of Michigan. 61,62 These studies examined a brief intervention delivered to young people typically within 30 minutes in a hospital ED. In one study,61 the brief intervention was delivered either by a therapist with computer assistance (TBI) or by computer alone (CBI) and compared with a control group. The intervention was aimed at adolescents that had screened positive for violence and alcohol use. The researchers followed a cohort of 829 individuals who met the study criteria, of whom 607 completed the intervention and a follow-up survey at 12 months. The researchers found that young people that received the therapist and computer-assisted version of the intervention were less likely to self-report peer aggression and victimisation compared with the control group. A second, retrospective study focused on dating violence among a subgroup of 397 people aged 14–18 years. 62 This study found outcomes for dating victimisation were positive using a CBI at six months, although for young people with a severe history of dating violence, a therapist and computer-assisted intervention was more effective for reducing dating violence at 12 months.
Other brief interventions found in this review focused on screening young people for alcohol use, some of whom present with injury,63 violence,60 or both13, and use similar approaches that incorporate therapists or advocates, structured motivational conversations with young people, and may or may not be computer assisted. Some of these studies report positive outcomes, although these may be for shorter follow-up periods of three months or less.
The use of technology was an interesting finding of this review, with several studies reporting interventions that integrate computer-based tools. Ranney et al. (2018) conducted a pilot RCT of iDOVE, a ‘technology-augmented violence and depression prevention intervention’ aimed at high-risk adolescents aged 13–17 years seen in the ED. 67 The intervention comprises a brief computer-guided session (lasting around 15–20 minutes), which in the pilot was delivered by research assistants, followed by an eight-week programme of automated text messaging (e.g. with crisis information and support in the form of daily check-ins). Like other brief interventions, the content was grounded in motivational interviewing and CBT techniques. A control group received a technological intervention not based on these techniques, which provided healthy lifestyle information only. The intervention was rated positively by those engaged in the trial and engagement rates were high over the eight weeks. However, the trial was not able to demonstrate efficacy between the control and intervention groups for depression and violence, although the analysis suggested that a cohort of young people with higher baseline scores for violence and depression might benefit most from this text-based intervention.
Relevant literature reviews
Our search identified two relevant literature reviews about the impact of ED-based youth violence prevention programmes and interventions. The first, a scoping review by Wortley and Hagell (2021), specifically examined the evidence base on ‘teachable moments’ delivered by youth workers in EDs and whether there was any evidence about the outcomes arising from this type of intervention. 14 Their review used only a handful of key search terms: ‘teachable moment’, synonyms for ‘young person’, ‘youth worker’ and ‘ED’, and found that while the term ‘teachable moment’ was used variably in the literature, it was clearly associated with behaviour change models and theory. The authors identified 13 studies and found that they could not be conclusive about the overall impact of youth workers embedded in EDs because evidence on young people’s reattendance rates was mixed. They did suggest that the evidence exists that young people are positive about ED youth worker interventions overall. Interestingly, given that the ‘teachable moment’ is a core component of the Redthread service (which is presented in their paper as a case study example) the authors were unable to locate comparative or quasi-experimental studies that have contrasted the ‘teachable moment of ED admission against other intervention methods’. They conclude there is a lack of evidence to guide the implementation of these services within the UK health sector, despite positive findings of similar programmes in the United States, and also note the ongoing challenges to evaluation.
A systematic integrative review by Mikhail et al. (2016) looked at youth violence prevention programmes based in trauma (tertiary) health centres, targeting their search at identifying RCTs or observational studies published between 1970 and 2013, and applying a theoretical framework: the social ecological model that ‘asserts that an individual’s behaviour is affected by both personal characteristics and the social environment’. 12 The authors located 10 studies eligible for inclusion. In these studies, the main interventions consisted of either brief interventions or case management with young people, which started in EDs and extended to inpatient units. The studies reported on 9 violence prevention programmes across 10 urban centres in the United States (the review excluded interventions delivered outside of the United States). The age profile of those engaging in the programmes covered adults (up to 50 years of age in some cases), however, the majority of studies (80%) focused on children, adolescents and younger adults aged under 30 years. Studies tended to rely on a mixture of ‘indirect’ outcomes measures, such as self-reported questionnaires (e.g. attitudes towards aggression or retaliation, injury, substance use) and referral rates, and ‘direct’ outcome measures, such as re-arrests, convictions, reinjury and ‘trauma recidivism’. Although the programmes varied widely, case management approaches were ‘positively associated with a reduction of violence outcome measures’, and the majority of studies demonstrated improvements in at least one outcome measure. Based on their review, the authors suggest that brief interventions alone are insufficient for reducing trauma recidivism and that ‘case management programs allow trauma centers to move beyond that of providing physical care only, to that of addressing the social determinants of violence by addressing upstream inequities that promote downstream injury’ (p. 514).
While this review only included studies up to 2013, it does underscore the potential positive impact of case management youth violence programmes that link into community resources and promote in-depth support for young people that extends beyond the hospital setting.
Summary: phase 2
Our updated phase 2 search found new studies published after 2012, which had not been discussed in previous reviews due to our search terms and more recent date range. In particular, we found two new economic studies, new RCT and feasibility studies and a UK service evaluation. We observed that factors described in the literature that support or hinder the implementation of youth violence interventions in hospital settings include:
-
staff training and awareness to make referrals
-
characteristics of young people who may decline to engage with programmes (e.g. older adolescents)
-
staff turnover
-
co-location of specially trained social and youth workers in EDs.
Lessons are primarily drawn from North America, however, where case management approaches and brief interventions to youth violence prevention typically apply motivational interviewing techniques and cognitive behavioural approaches. Notably, some brief interventions now employ technology to standardise delivery, such as automated messaging to young people.
The evidence for efficacy and effectiveness across different interventions is mixed, owing to variations in study design, the professionals involved in delivery (youth workers, trauma nurses, social workers, researchers, mentors), relatively small sample sizes (given the numbers of young people presenting to EDs clinically with violent injuries and from exploitation), the nature of the interventions themselves, variable follow-up time periods, and differences in the primary and secondary outcomes reported.
Many studies rely on self-reported measures using questionnaires and only one study had attempted to examine reinjury and admission rates across more than one hospital setting. The theoretical lens we found applied was a social ecological model while the concept of the ‘teachable moment’ was discussed widely in the literature.
Our review found very limited qualitative evidence exploring the perceptions of young people and staff who had implemented the interventions, and reasons for engagement (or lack thereof). Any evidence that was presented tended to be positive and represented the views of those that had chosen to take part in these programmes.
Grey literature: additional reviews and evidence from the UK
One evidence summary report for the Scottish Violence Reduction Unit published in 2021 discussed the effectiveness of school-based programmes, such as on preventing violence in intimate partner and dating relationships; however, hospital-based interventions were out of the scope of the review. 74 The report suggests that it is ‘not yet possible to draw reliable conclusions on the effectiveness of programmes that specifically aim to prevent gang involvement and subsequent gang violence’ (p. 7).
A mapping review and horizon scanning on ‘good practice in youth violence prevention’ was completed in 2020 for the violence prevention unit in South Wales, drawing on over 100 sources of information. 75 The report describes how mentoring for high-risk young people is delivered across a variety of settings, such as hospitals, although most mentoring schemes are based in the community and the evidence base for their effectiveness is mixed. The report draws attention to the Cardiff Model, a data-driven approach to violence prevention, as having a strong evidence base;3 here hospital data about violent injuries is combined with police information to prevent further violence. 76,77 The report does mention hospital-based YVIPs in the UK (Redthread and Oasis specifically) both of which it says report positive outcomes. The authors suggest that the evidence base is ‘promising’ but cautions against drawing conclusions due to risks of selection bias and limited follow-up times.
Several ‘tertiary prevention’ hospital-based programmes were picked in a review for a public health team based in Lambeth, London. 78 These were Oasis, Redthread, SafeERteens, Project Sync and Caught in the Crossfire, as well as brief interventions in EDs (these findings are similar to our own review). While there is no detailed discussion of these programmes and their underpinning evidence, the report suggests that a general indicator of success across different types of tertiary prevention interventions, such as counselling approaches with young people, is ‘high quality implementation with fidelity to original specification’ (p. 38). 78
It is important to note that a number of evaluations of the Redthread service have already been undertaken and that these findings were shared with the NIHR RSET evaluation team. However, not all findings from these evaluations and final reports are publicly available. We identified six completed evaluations and two in progress, plus our own evaluation. Below we summarise information about Redthread evaluations and provide references where information is publicly available (the information below was reviewed and confirmed by the charity):
-
Redthread in the Midlands and wider programme: three evaluations funded by the Health Foundation: qualitative and quantitative focused evaluations on the Midlands sites and the feasibility of scaling up the intervention to other areas (Nottingham University Hospitals NHS Trust, 2019–2020) and a CBA for Redthread’s YVIP across all areas. Positive findings include that young people engaged in Redthread’s YVIP were 51% less likely to reattend EDs than those who did not engage; YVIPs fill a crucial gap in support in the NHS; and economic and social benefit valued at £4.90 for every £1 spent. 79,80
-
Redthread, St Mary’s Hospital, London: three-year evaluation by NPC Associates (2015–2018) using qualitative and quantitative data. Positive feedback from stakeholders about Redthread’s work, with hospital reattendance rates falling and the risk of harm and involvement in violence being reduced among young people who engaged in the YVIP. Collaborative working and sharing of data between relevant agencies were said to have improved, as well as emergency staff confidence, understanding and awareness of violence-related and exploitation issues affecting young people. 81
Evaluations in progress
-
Redthread in the Midlands: a service evaluation funded by NHS England Midlands (2020–22) was being undertaken by Liverpool John Moores University and nearing completion.
-
Redthread: a quasi-experimental design evaluation funded by the Youth Endowment Fund (2021–23) involving the University of Birmingham. This is an initial one-year pilot from April 2022 to March 2023 focused on 10- to 17-year-olds as part of the Another Chance – Diversion from the Criminal Justice System round. 82
Finally, a six-year, mixed-methods evaluation of the Oasis hospital-based violence prevention programme at St. Thomas’ Hospital, London, by researchers at Middlesex University was published in 2016. This evaluation found positive findings in terms of efficiency, implementation and impact on young people who had engaged with the service, some of whom were followed up after at least one year. 6 Benefits also included high staff satisfaction with the services and fewer reattendances among those had received the intervention.
Conclusions
The majority of peer-reviewed studies found in both phases of this review originate from the United States. Only a small number of studies have focused on how to increase referrals or reasons for low uptake by young people. We found studies reporting a variety of outcomes for both case management and brief interventions instigated in EDs: depressive and PTSD symptoms; decreased feelings of aggression and involvement in peer violence; varying effects on victimisation; outcomes related to service uptake and use; mortality and morbidity outcomes; recidivism; and one study exploring the perceptions of engaged young people; plus cost analyses. Other literature review studies confirmed our findings that there are few studies following long-term outcomes with young people, which limits conclusions about impact, as do the small sample sizes on studies (this being due to limited uptake among eligible patients).
Nevertheless, studies from the United States do suggest there may be positive benefits with respect to recidivism and patient reported involvement in violence from interventions in ED settings, with growing evidence that brief interventions may also have a positive impact (e.g. on weapon carrying). There are also promising economic assessments about the value of these interventions, yet these assessments must be read in the context of high-treatment costs in the United States. The extent to which these findings translate to other countries and tax-funded systems, like the NHS, is thus limited.
Overall, there is a paucity of studies from the UK health-care system context, as well as a lack of qualitative studies exploring, in depth, the perspectives or staff and young people involved in these programmes. Rather, engagement or enrolment in a programme is often taken as a positive outcome, and there are risks that engagement could be relatively low in programmes studied and the factors for this underexplored. There is, however, some promising evidence emerging from evaluations of programmes such as Redthread and Oasis, suggesting potential benefits alongside positive feedback from staff and patients. Overall, this evidence review suggests a need for more multisite studies (e.g. using hospital records) to track re-admissions and reinjury across different hospitals and geographies, longitudinal studies with longer follow-up times, studies with control groups and in-depth qualitative research (e.g. ethnographic, participatory or comparative case studies) to provide more rounded insights about effectiveness, implementation factors and young people’s lived experiences and their reasons for engaging (or not engaging) in hospital based violence reduction programmes.
Limitations of this review are, first, formally searching only two databases in the phase 2 scoping review and only Google for the grey literature, due to time limits, which means that some studies may have been missed; and second, not performing a meta-analysis of the results of the empirical studies included in phase 2. The review was intended to provide the team with a snapshot of the topic and available evidence rather than being a rigorous or comprehensive systematic review. While the phase 2 search was conducted in a transparent manner across the two databases using an explicit inclusion and exclusion criteria, with more key terms used than in some other available reviews on this topic, and screening and data extraction being conducted by two researchers, pragmatic choices had to be made to save time.
Chapter 4 Qualitative findings: programme theory and service implementation at UCLH
What was already known?
-
Redthread is a youthwork charity that provides a range of services within health-care settings. The charity aims to support young people as they navigate the transition to adulthood with a focus on prevention (e.g. injury from violence).
-
Redthread’s flagship programme is a hospital-based YVIP which has been adopted at 13 NHS organisations across London, Birmingham and Nottinghamshire (within seven local trauma units and six MTCs). A number of these services have had local evaluations.
-
Other charities provide similar services to Redthread within London (Oasis, St. Giles Trust).
-
NHS organisations may choose to adopt hospital-based youth violence reduction services due to the number of adolescents they see presenting (and reattending) in EDs and trauma services due to violent assault (e.g. stabbings) and criminal exploitation.
-
There has been growing attention on a public health approach to reducing youth violence in recent years; for example, NHS England has a violence reduction programme.
What this chapter adds
-
Evidence about the types of clinical presentations to a local adult and children’s ED in London that flag safeguarding concerns among health-care staff.
-
Evidence that hospital staff, both clinical and non-clinical, were receptive to working alongside youth workers in the hospital setting.
-
Understanding of the organisational enablers to implementing the Redthread YVIP in a London hospital; for example, physical space for youth workers located near the ED and electronic health record integration.
-
Understanding of the organisational barriers to implementation, such as high staff turnover.
-
Insights about service-level impacts and adaptations during the COVID-19 pandemic. specifically, how COVID-19 affected early implementation (qualitative data collection was conducted during COVID-19) and influenced the development of referral pathways into the service.
-
Views of clinical staff at UCLH about the potential benefits of placing youth workers within MDTs to help safeguard young people, including encouraging young people to engage in their care and treatment as both inpatients and outpatients.
-
Insights about why young adults aged over 18 years might be less likely to engage with the Redthread service or be referred, such as challenges around consent and follow-up.
-
Suggestions, based on empirical findings, to help the Redthread service continue to embed successfully at UCLH and across other NHS hospitals, and reach young people eligible for the service.
Introduction
In this chapter, we present background information about how the Redthread service came to be implemented at UCLH NHS Foundation Trust and data illustrating how the service is perceived by front-line NHS staff and Redthread youth workers. The chapter draws on a variety of qualitative data sources to answer the following evaluation questions:
-
RQ4: What are the views of UCLH NHS staff of the Redthread intervention, its feasibility, service-level impacts and overall effectiveness?
-
RQ5: What organisational factors, processes, resources and staff training are necessary for the successful implementation and delivery of the Redthread service?
This chapter covers in detail the nature of the Redthread intervention at UCLH, including the components of the intervention and programme theory, early and later implementation phases at UCLH, and staff and youth worker perceptions of the challenges and opportunities associated with introducing the service locally. Finally, the chapter briefly describes how the Redthread service at UCLH was affected by the COVID-19 pandemic.
It should be noted that qualitative data were collected following the redirection of patients aged under 18 years away from the UCLH site in the period 2020–21. We provide a brief account of how the Redthread service and clinical staff responded to these challenges.
Methods
This chapter is based on qualitative data collection at UCLH, which was conducted in two phases. Phase 1 was an exploratory stage aimed at understanding the Redthread programme and the background to its introduction at UCLH. This phase involved speaking with those closest to the service and its early implementation. During phase 1, available Redthread and UCLH documents were supplied to the NIHR RSET evaluation team and reviewed to confirm what the service aims to do, and how, and its core components.
As part of phase 1, nine qualitative interviews were conducted between April and July 2021 with Redthread staff and a small number of senior NHS clinicians closely involved in the treatment and care of young people (Table 3). Data collection was instigated once Redthread youth workers were back on site at UCLH, following disruption to the service on account of the COVID-19 pandemic. All data were collected remotely. Phase 1 data helped to situate the Redthread service at UCLH within a wider London context and uncover what meaningful success looked like to those closely involved in introducing the service to UCLH (e.g. reduction in admissions, onward referrals to other services, positive case work with an individual). Redthread documents were useful for understanding how the service intended to operate (e.g. the UCLH proposal for the service) and recording the changes wrought by COVID-19. This initial qualitative work was accompanied by discussions with members of the study evaluation advisory group and meetings with researchers involved in other Redthread evaluations at different NHS trusts to understand how the Redthread service had been introduced elsewhere.
| Interviews | Respondent type | Example of job roles | Combined total | ||
|---|---|---|---|---|---|
| Redthread | UCLH staff | External stakeholdera | |||
| Phase 1: exploratory | 6 | 2 | 1 | Consultant in children and young people’s services; Redthread youth worker/manager/team leader; NHS clinical director | 9 |
| Phase 2: implementation | 4 | 9 | 0 | Social worker; paediatric nurse; consultant in children and young people’s services; junior doctor; paediatrician; child and adolescent psychiatrist; Redthread youth worker/team leader/manager | 13 |
| Total | 10 | 11 | 1 | 22 | |
| Observations | |||||
| Phase 2: non-participant observations of staff meetings | Paediatric ED safeguarding meeting; adolescent ward psychosocial MDT meeting; level 3 child safeguarding training with Redthread presentation | 3 | |||
Phase 2 consisted of a single-site, process case study informed by qualitative data collection and followed directly on from the data collection above. The organisational unit of analysis was UCLH, specifically, the children and young people’s services and the adult ED within the hospital. The aim was to understand, in greater depth, the processes that were supporting the implementation of the Redthread intervention at UCLH and staff perceptions of Redthread’s impact and progress thus far. Data were collected between October 2021 and January 2022 to allow time for the service to embed following the phased reintroduction of Redthread youth workers to the UCLH site from summer 2020. This was important because UCLH paediatric patients had been redirected to the Whittington Hospital during the COVID-19 pandemic. The paediatric ED only fully returned to UCLH in April 2021.
Three observations of staff meetings were conducted and an additional 13 qualitative interviews (see Table 3) for phase 2. During this phase of data collection, the NIHR RSET evaluation team was interested in identifying any complicated or novel aspects of the Redthread intervention at UCLH, such as differentiated referral pathways, and any contextual factors that either supported – or made challenging – implementation of the service.
Interview data collection and analysis
A mixture of purposive and snowball sampling was used to identify UCLH staff that were both central and more peripheral to the Redthread intervention to take part in the evaluation. Interviews took place with a range of clinical health-care staff (e.g. nurses, junior doctors, senior psychiatrists and paediatricians) and non-clinical staff (safeguarding teams, Redthread youth workers and hospital social workers). The primary objective was to speak with staff involved in the care of young people at risk of harm at UCLH who either knew about the Redthread service and/or might refer young people to it. Phase 1 interviewees were identified through scoping work, while phase 2 interviewees were largely recommended by UCLH and Redthread staff involved with the service. The team were able to capture the views of both service ‘champions’ and staff with lower levels of awareness of Redthread service (e.g. junior doctors who worked across different EDs and wards). All respondents were individually emailed a study information sheet, consent form and given the opportunity to ask questions about the evaluation to a qualitative researcher before taking part. Some clinicians emailed their colleagues on behalf of the researcher to inform them about the study and encourage their participation.
Due to the impact of COVID-19, recruitment of front-line staff from the adult ED was particularly challenging, with some staff declining to take part because they felt they did not know enough about the Redthread service. This confirmed a finding from the case study: that the intervention had not fully embedded outside of children’s and adolescent services at the time of this evaluation and that Redthread’s awareness-raising activities had been severely disrupted by the pandemic.
One lead qualitative researcher (JL) conducted all the interviews, with a NIHR RSET colleague present in some instances where quantitative aspects (e.g. hospital and Redthread data flows) were being explored. Interviews were conducted remotely and on a confidential basis by telephone/MS Teams®. Interviews were digitally recorded with explicit written and/or verbal consent and were transcribed verbatim. A total of 22 interviews were completed across phases 1 and 2, with a small number of individuals interviewed twice because of their close involvement with the service. Different topic guides were used for interviews with hospital and Redthread staff but explored similar themes. Each topic was piloted to ensure that the questions resonated and were clear to respondents and then finalised (for topic guides, see Appendix 2).
Compared with phase 1 interviews, which were more exploratory, phase 2 interviews had a focus on the perceived impact and effectiveness of the service. Staff were asked to provide anonymised clinical case examples to explain how a young person had been referred to Redthread, why the young person had presented at UCLH, and how they had been supported by Redthread youth workers. This allowed two anonymised clinical case vignettes to be included in the findings, helping to elucidate how the Redthread service operates in practice and connections between the Redthread service and other organisations, especially those within the community. Finally, the phase 2 interviews explored factors that appeared especially important for the successful delivery of the Redthread programme in the hospital (enablers and barriers).
It was not possible to conduct interviews with young people who had experienced the Redthread service at UCLH or at other NHS trusts for ethical and practical reasons (e.g. identifying young people would have data sharing implications), although this possibility was explored with Redthread.
Observations
A qualitative researcher conducted a total of three non-participant observations of staff meetings to understand the implementation of the service, and to explain the purpose of the NIHR RSET evaluation to hospital staff at UCLH. This proved to be particularly helpful for phase 2 interview recruitment, especially given that hospitals were dealing with the ongoing effects of COVID-19. Meeting observations were undertaken between October and December 2021 with explicit permission from UCLH clinical collaborators and attending staff. Two virtual MDT meetings were observed during which Redthread youth workers worked alongside clinicians, helping to identify young people potentially eligible for their support. A staff safeguarding training session was also observed in which Redthread discussed their service. All meetings were held via MS Teams on account of the COVID-19 pandemic. The researcher took carefully anonymised field notes which were typed up and then securely saved electronically in UCL folders only accessible to the evaluation team.
Analysis
Interview transcripts and observational field notes were read by the lead researcher for data familiarisation and triangulated with the Redthread planning and implementation guidance gathered in phase 1 and other relevant documents (e.g. the Redthread youth worker manual). Emergent findings were discussed in team meetings and with clinical collaborators to confirm initial interpretations. The final qualitative data set (integrated phases 1 and 2 findings) were analysed with a specific focus on answering the evaluation questions. Interview transcripts (transcribed verbatim), Redthread documents and field notes were reviewed by the qualitative researcher and data extracted and organised according to following themes:
-
Redthread history and background; theory of change (e.g. ‘teachable moment’); key components of the intervention and associated processes (e.g. eligibility, consent model); data capture and monitoring; implementation context at UCLH (services and population); adaptations due to COVID-19; youth worker perceptions (e.g. implementation journey, impact, successes and challenges); staff perceptions (awareness of Redthread, impact, fit with existing services; successes and challenges); staff training; enablers and barriers to implementation; timeline and key events (e.g. Redthread introduction to UCLH).
Line-by-line coding of transcripts was not performed, but qualitative findings were compared in an iterative process with those arising from the economic and quantitative aspects of the evaluation. In addition, validation of findings was supported by providing draft chapters to Redthread for review; this was important to confirm a correct interpretation of the history of the charity, the local adaptations of the service offer at UCLH during COVID-19 and any sensitive issues regarding the presentation of qualitative findings (e.g. clinical vignettes to ensure patient anonymity).
Main findings
In this main section, we draw on the qualitative data sources described above (interview transcripts, documents and observations) to describe how the Redthread service was first introduced to UCLH and its early implementation, and how staff responded to the service following a longer period of embedding the service across paediatric, adolescent and adult departments admitting young people over 18 years.
Background to the Redthread intervention at UCLH
At the time of the evaluation, Redthread staff confirmed that the organisation (a registered charity) was established in 1995, in south-east London, initially as a group set up by parishioners from a number of local churches in Herne Hill, Dulwich and the surrounding area. Researchers were informed that, in the early days of the charity, it was felt that local children and young people could be more involved in the community if provided with the facilities and activities to do so. This led to a Redthread youth club being set up, providing a range of regular activities for young people.
Later in 2002, the senior manager of the charity started to move its youth work into health-care settings, realising that there was an opportunity to engage with young people (in particular, higher-risk groups) at the point when they accessed health care services. One Redthread interviewee described how the charity had been attentive to ‘high-risk’ young people who were falling outside of public services, such as social care, and often had a deep mistrust of authorities. Redthread started a young people’s clinic in partnership with a local general practice, which was run after school for 13- to 19-year-olds, regardless of whether or not they were registered. In primary care, it had been observed that young people could be missed and unknown to general practices while being frequent attenders at local EDs or other health services, such as child and adolescent mental health services (CAMHS) or sexual health clinics. Young people also risked being missed on account of silos existing between statutory services, and a lack of a joined-up preventative health approach for young people at risk of violence and exploitation at the pan-London level.
Against this backdrop, the first Redthread site was founded in 2006 at King’s College Hospital in south-east London. Later, the charity scaled up its activities with additional MTCs coming on board (at St. Mary’s Hospital in north-west London in 2014, and St. George’s Hospital in south-west London in 2015). This was enabled by funding from the Mayor’s Office for Policing and Crime and other funders. A senior Redthread manager explained how youth workers and clinicians were noticing patterns of injury affecting young people presenting in the EDs of MTCs. Injuries ranged from knife and gunshot wounds to attacks from broken bottles that a young person would present as an ‘accidental’ injury, even if the wound was likely to have been caused by a violent assault. By running audits on hospital data at the adopting MTCs for the cohort aged 11–24 years, evidence about who attended for violent injuries and later reattended in EDs was identified: ‘there was this sort of propensity for reinjury and this escalation of injury’ (Redthread manager, RED004).
Redthread gradually moved into local EDs across London, such as Homerton University Hospital and later UCLH, as well as to other hospitals based in the Midlands. This was viewed as a way of ‘joining the dots’ and not only focusing the charity’s work in MTCs.
The introduction of Redthread youth workers to hospital EDs coincided with growing policy attention on a holistic ‘public health’ approach to preventing youth violence in England,83 and the introduction of violence reduction services within the NHS, both in and outside London. 18 Redthread is one of a number of charities providing hospital-based interventions in London at the present time. For example, the St. Giles Trust, which is located at the Royal London Hospital (an MTC, part of Barts Health NHS Trust),84 Newham University Hospital, the Whittington Hospital and Northwick Park’s ED (part of London North West University Healthcare NHS Trust). 85 Oasis, another charity, has youth workers based in the ED of St. Thomas’ Hospital (part of Guy’s and St Thomas’ NHS Foundation Trust) and North Middlesex University Hospital.
Introduction of the Redthread service to UCLH
In the London Borough of Camden, where UCLH is located, the Camden Youth Safety Taskforce had been established in 2017 and published a report making recommendations to treat ‘youth violence as a broad public health issue rather than simply a law and order issue’, with better collaboration between public services. 83 The report encouraged the early identification of young people at risk of youth violence as a preventative measure, stressing the need for ‘appropriate referrals’ from public agencies and professionals, such as youth workers. 83 In 2018, two young men from Camden estates died from stab wounds drawing attention to a high number of violent incidences occurring within the borough, and highlighting the ongoing risks of violence facing young people in the local community. 83 It was in this context that two hospital consultants who were involved in safeguarding initiatives in the borough and aware of the work of the Camden Youth Safety Taskforce, began to consider the introduction of a violence reduction service at UCLH, around the same time that Redthread was starting to move into local hospital EDs. As one consultant closely involved in the service noted: ‘Redthread originally started in the community and it almost feels like it started out, it’s come into hospitals and we are almost going out again a bit, and so that’s our motivation’.
Clinicians involved in the introduction of Redthread’s service to UCLH spoke of their interest in providing ‘age-appropriate’ services for young people most at risk of harm in the community. Their review of hospital data at UCLH suggested that there was a cohort of vulnerable young people presenting with suspicious injuries and being discharged into the community, meaning this was a missed opportunity to engage with and protect young people at risk of harm:
we did an audit … although this was quite a while ago, that demonstrated that, although we don’t have major trauma here, a good twenty-five per cent of the young people coming through – say 13- to 18-year-olds – with soft-tissue injuries, or minor breaks, they would get patched up and sent out without anybody asking anything other than their tetanus status, actually had a worrying back-story.
Therefore, consultants working in paediatric and adolescent services at the trust played a key role in supporting Redthread service adoption at UCLH and brokering initial discussions between hospital managers and the UCLH Charity in the period 2017–18. Paediatric and adolescent clinical staff were interested in linking up with the Redthread charity to learn more about young people’s reattendances for violent injuries and were motivated by the opportunity for skilled youth workers to interact with young people within the hospital setting in a holistic way. They observed that, while a multidisciplinary approach to adolescent and child health care was already employed at UCLH (e.g. with a hospital-based social worker and play worker already part of the team), the youth worker element was still missing:
Because older teenagers when they come in tend to not be that medically unwell, nobody really asks them who they are having sex with, or how they got a broken bone in their hand. They just go, ‘Okay, you’re fine. You can go’. It was increasingly becoming clear to me that that wasn’t good enough and that we needed to do things differently.
Following discussions between Redthread and UCLH, it was agreed that the service would be introduced, supported by a three-year grant agreement from UCLH (with the funding being provided by UCLH Charity), with additional contributions from the London boroughs of Camden and Islington’s public health directorate in year 1 to make the service fully funded during its mobilisation period and first year of operations. Clinicians favoured such a funding model because it was distinctive from ‘policing money’ (associated with prosecution) and meant that a hospital-based violence reduction service would predominantly be funded by health resources and viewed as a health community initiative. Redthread relies on different sources of funding at each hospital site. This can include money from hospital charities, Redthread’s own fundraising activities, external government sources (e.g. the Mayor of London’s Office) as well as local authorities. Therefore, each hospital adopting the Redthread service will have its own funding arrangement to cover Redthread’s operating costs.
In early 2020, the Redthread service formally launched at UCLH, a few weeks before the COVID-19 pandemic struck.
UCLH: the hospital context
At UCLH, there is a dedicated children and young person’s ED (referred to by staff as ‘paeds ED’) which sees patients up to the age of 17 years. There are also two inpatient wards: an adolescent inpatient ward which treats patients from 13 years upwards and a children’s ward treating children aged under 13 years. A multidisciplinary approach is taken to providing care across these services, in particular the adolescent unit, which encourages ‘contextual safeguarding’ and ‘psychosocial’ support.
In addition, there is a separate adult ED at UCLH which sees patients aged 18 years and over. This is significant, given that Redthread covers patients up to their 25th birthday (11–24 years); thus, the Redthread service at UCLH had presence across two EDs to cater to patients aged 11–24 years.
UCLH is located near Euston and King’s Cross rail stations, both major transport hubs in central London. Staff at UCLH pointed out the significance of the hospital’s location for the population it served: vulnerable young people often present from out of area and it was felt that other local EDs in London might serve a more borough-based patient population (e.g. at Homerton University Hospital in Hackney).
displaced children that would just come from Euston, or from King’s Cross and either be found by the police or just be found, vulnerably, in the street. It just made me think about how can we serve this population better.
Vulnerable young people are sometimes brought to UCLH by emergency services and the police if they are experiencing a severe mental health crisis requiring urgent treatment. The hospital also serves a university population, refugees and young people caught up in drug trafficking and other forms of criminal exploitation. While staff had less experience of serious knife-crime injuries presenting, since these are typically directed to MTCs, soft-tissue injuries and wounds that raised safeguarding concerns about a young person at risk were reported to be common, along with severe mental health issues (such as suicidal ideation and suicide attempts), sexual assault, domestic violence, attacks/fights with peers, and problems related to substance misuse. Some clinical staff saw clear links between urgent clinical presentations among young people and potential gang involvement or sexual exploitation. Other staff felt that gang violence was not the main driver for young people presenting at UCLH:
We see quite a lot of young people that are either on the cusp or involved in gang culture, gang crime.
(Nurse, RED0012)
We have lots of young people coming in with self-harm. Sometimes that will link to violence that’s happening to them or around them. We have a small but clear group of young people who will come in having been assaulted or at risk of gun violence or involved with the gangs, particularly where we’re located.
(Consultant, RED0014)
I think what you’d find is that it’s mostly alcohol, drugs, child mental health.
(Non-clinical staff, RED0010)
When asked whether case presentations had shifted as a result of the COVID-19 pandemic, staff were unanimous in their perception that they were seeing a greater number of young people suffering from severe mental health crises associated with problems within the community or family home (e.g. isolation, unemployment, domestic abuse, housing instability).
The Redthread intervention at UCLH: programme theory
Guiding principles and theory of change
As described in Chapter 1, the Redthread intervention follows on from a young person experiencing a traumatic event that has led to a hospital presentation. The ‘classic’ Redthread intervention consists of youth workers engaging with young people aged between 11 and 24 years attending EDs as a victim of violence, assault or exploitation, with youth workers placed directly within hospitals to work ‘shoulder to shoulder’ with clinicians. This model is most familiar with the London MTCs, which receive higher numbers of young people presenting due to violent assault from knife crime. However, as is explained in more detail below, the Redthread service at UCLH was found to employ a number of referral pathways to the service, covering direct referrals from staff and active searching by youth workers for eligible patients.
The Redthread model draws on a range of research and academic influences: behaviour change theory (e.g. smoking cessation research), concepts such as the ‘teachable moment’ and ‘contextual safeguarding’, and frameworks such as the Anna Freud Centre’s AMBIT (adaptive mentalization based integrative treatment) model. 86 According to the Anna Freud website, AMBIT is:
a collaborative project that involves feedback from practitioners, clients and evidence-based treatment designers. It has been designed by and for community teams from mental health, social care, youth work, or that may be purposefully multidisciplinary/multiagency. It emphasises the need to strengthen integration in the complex networks that tend to gather around such clients, minimising the likelihood of an experience of care that is aversive.
Redthread’s youth worker manual describes the ‘teachable moment’ as comprising three essential parts:87
-
dialogue that links a young person’s concerns to the health risk
-
youth worker dialogue that fosters the young person’s motivation to change
-
the young person’s response that shows a willingness to engage and commit to change the specific behaviour(s).
One Redthread interviewee described this concept as going beyond a ‘reachable moment’ to a ‘teachable moment’. This means that youth workers interact with a young person within the hospital setting and involve them in decision-making and learning to empower them to identify where support is available, a task that clinical staff do not have time to do due to other priorities:
The job of the Redthread worker is to help the young person identify who their network of professionals is. And then look to scaffold that teachable moment out to the appropriate key worker, the one that the young person identifies. Don’t assume that you are going to be the key worker for the long term.
(Redthread manager, RED004)
Redthread shared their ‘theory of change and assessment process’ document, which is outlined in Figure 4 (see Appendix 6 for the most recent version). 88 Youth workers discussed Redthread’s role at UCLH as having a rather broad remit, yet ultimately being focused on taking a sensitive and holistic approach to caring for traumatised young people who had come to harm through violence, criminal or sexual exploitation, or who were affected by other safeguarding issues:
FIGURE 4.
Redthread theory of change (2018).
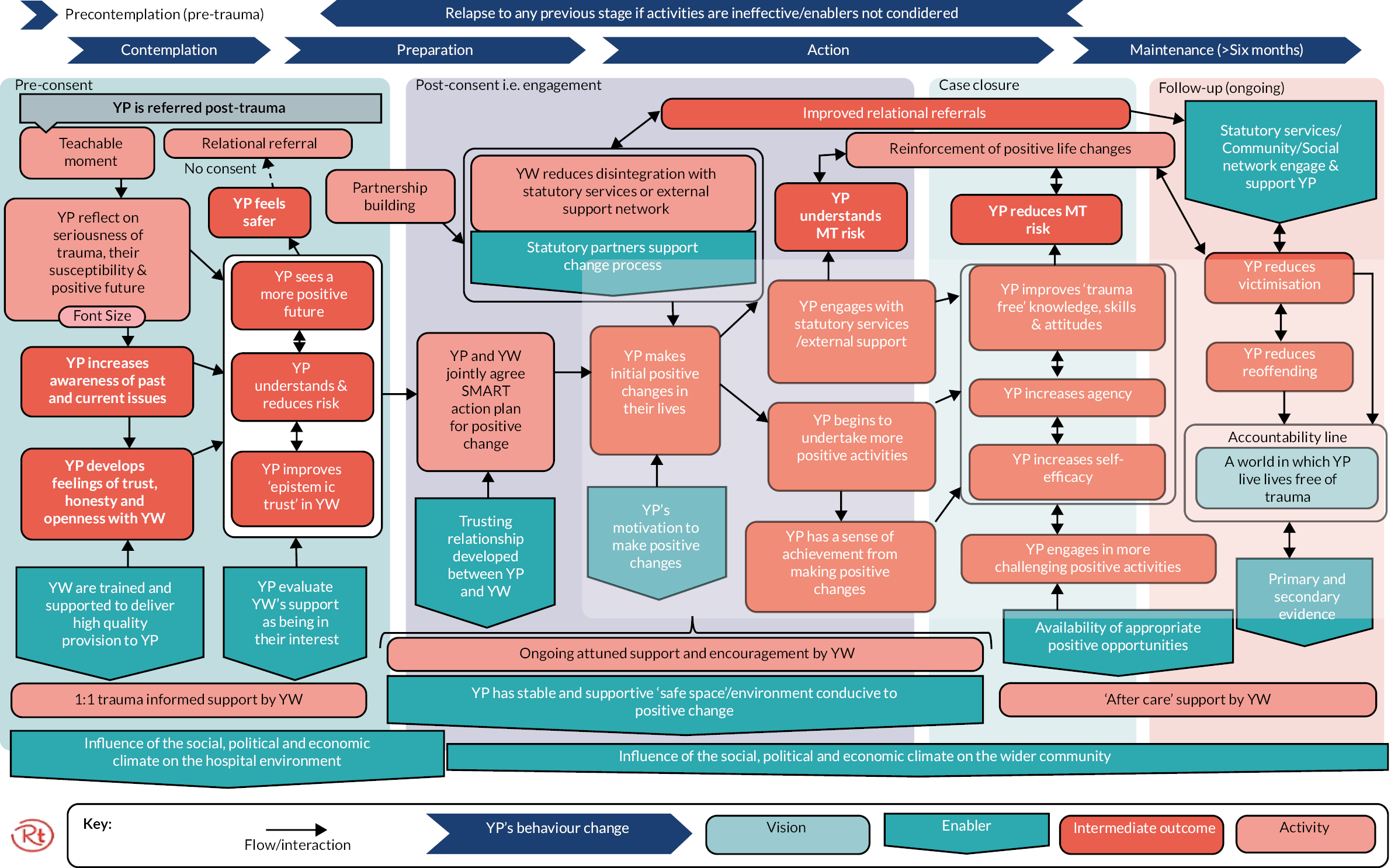
the main aims overarchingly are to contribute to the health, safety and happiness of young people. Obviously, we talk a lot about violence and harm but it actually exists more broadly just to make sure young people are well from a broader perspective as part of this whole public health approach to youth issues and to violence specifically.
(Redthread staff, RED009)
young people who come in really scared, anxious, unsure about what’s happening, and we can be that really comforting and compassionate presence for them in a time of kind of trauma … providing a very compassionate and trauma-informed approach to working with them, advocating for them, and ensuring that they are at the centre of their care, where sometimes things are done to young people rather than with young people.
(Redthread staff, RED003)
Intervention components
Redthread-employed youth workers become embedded within local hospital EDs and work alongside clinicians as part of the Redthread service offer. Youth worker engagement with a young person – the ‘teachable moment’ – can only occur if consent is received from the patient (see below for further details) following their presentation at hospital. The service provides a referral pathway for clinicians in EDs who can identify young people at risk, obtain consent, and refer them to youth workers for engagement and support.
Youth workers work with young people on a case-by-case basis providing tailored support (see the two clinical vignettes below for illustrative examples). The charity also delivers a wider set of services to the hospital once a Redthread team is on site, therefore the intervention has a number of interacting components. Table 4 outlines these components drawing on the qualitative data collected at UCLH. Interviews with Redthread staff, both managers and youth workers, indicated that the service was underpinned by a strong commitment to a voluntary consent model. This was deemed to be significant because Redthread is not a statutory service and young people have a choice to use the service.
| Intervention components | Examples | Objective(s) |
|---|---|---|
| Building relationships with hospital staff | Redthread youth workers and co-ordinators engage with hospital safeguarding teams clinical staff (e.g. paediatric and ED consultants, nurses and junior doctors in ED, paediatric and adolescent ward staff, safeguarding teams and in-house social workers) | Raise awareness so that staff know to refer eligible young people to the service and how to do so; support a holistic approach to care of young people |
| Awareness-raising events and communications for staff | Attend safeguarding meetings, deliver service launch events, posters displayed around the hospital, visible Redthread branding (e.g. youth worker T-shirts) | Service promotion; raise awareness so that staff know to refer eligible young people to the service and how to do so |
| Enabling referral pathways | The charity aims to ensure that the service receives referrals from clinicians; youth workers also search hospital electronic health records for eligible young people who can be referred to the service (i.e. those that have presented in the last 7 days) to ensure they are not missed | Ensure that vulnerable young people eligible for support are referred by clinicians and avoid ‘missed’ referrals following patient discharge from ED |
| Advocacy | Engage with the young person to help represent their needs in the hospital setting | Youth workers explain medical terms provided in language young people understand to ensure they are involved in decisions about their care Support young people to access other services they need outside of the hospital |
| Staff training and upskilling | Deliver content to hospital staff (e.g. safeguarding level 3), support continuing professional development, run training sessions on youth violence prevention both internally and externally (e.g. across social care, probation) | Raise awareness and skills for staff to effectively work with traumatised young people and safeguarding referrals; identify those most at risk in the population of violence and exploitation |
| Case management: internal and external to the hospital setting | Trained, trauma-informed youth workers support a caseload of young people with a tailored offer based on their needs, circumstances and preferences. This can be within ED, on hospital wards in outpatients, or continue within the community. The charity uses a case management log tool to record activity, with weekly case management meetings and fortnightly oversight meetings | Establish a trusting relationship between a youth worker and a young person, initially within the hospital setting, or shortly after patient discharge, and support a young person’s engagement with other services in the community to achieve positive change |
| External engagement and collaboration with public agencies and other voluntary sector organisations | Local authorities (e.g. integrated gangs teams), social care, domestic and sexual violence services, CAMHS, counselling services, education and training providers, employment organisations; courts; refugees groups; housing associations; victims support services | Work with other agencies to support young people, raise awareness of those at high-risk and safeguard young people within the community |
Individual consent is therefore sought from young people because the charity’s focus is on empowering young people and putting them at the centre of decision-making about the support they receive and their care in hospital. Redthread’s distance from entities such as social care and the police was believed to be critical because young people often distrust ‘authoritative’ bodies and situations where they sense they ‘have no choice about whether they can engage or not’ (RED009). By being a voluntary service and charity, it was felt that young people could be more open about sharing personal (and relevant clinical or social) information with Redthread youth workers:
we’re trying to make other organisations realise that young people will simply disengage, will be dishonest, if we come in authoritatively and we have to recognise their agency and have to empower them as opposed to force them through procedures that are now archaic.
(RED009)
Indeed, Redthread youth workers attributed high value to ensuring that young people consented to use their service, and that consent was obtained in a language that they would understand. ‘Staged consent’ was a term used to describe the process of obtaining consent for different activities that youth workers undertook as part of their ongoing engagement and support, with one stressing the need for ‘continual negotiation of a young person’s autonomy’ to secure willing participation and, at the same time, recognising that young people could at any time withdraw their consent or disengage.
Redthread staff confirmed that interventions are based on assessment of the needs of an individual, so the duration of support provided to a young person could vary from a few days to a number of months. The case management aspect of the Redthread service was typically an intervention of 6–12 weeks, although longer support was sometimes needed to have ‘meaningful impact’ depending on the specific circumstances and needs of a young person. Youth workers confirmed that trying to get a young person to engage could also take a lot of ‘persistence’ before they could begin to work meaningfully with an individual. Young people might initially decline support then later accept it following a subsequent traumatic incident and reattendance at hospital.
If a young person consents to receiving help from Redthread, youth workers begin by developing a ‘safety plan’ for the individual and understanding their support needs. Youth workers undertake different types of activities within the hospital setting, such as explaining medical terms, liaising between the young person and health professionals, getting a young person food, and generally trying to improve their overall experience of the hospital setting, and allaying any fears and concerns they might have. Support activities are therefore far ranging; for example, safety planning, completing safeguarding referrals, providing emotional support/containment, signposting young people –(or their families) to statutory and non-statutory services (e.g. Victim Support, drug and alcohol services), organising safe transport home, providing food vouchers, helping with clothing, and assisting a young person with accessing follow-up medical treatment/prescriptions.
Two main modes of youth worker engagement were therefore apparent: short-term crisis support and engaged, longer-term support. In the former category, a young person consents to talk with Redthread, such as when they are an inpatient on an adolescent ward or in the ED, yet no further support work takes place following discharge from the hospital. For example, because the young person did not wish to work further with youth workers, was not eligible for the service, or was unable to make an informed decision about the service while in hospital (i.e. due to intoxication). Even if a young person declines initially, if they are eligible for additional support, they will be informed that they can contact Redthread at a later date, should they wish to self-refer to the service. There is therefore a cohort of patients typically provided with short-term assistance in the hospital (e.g. access to food, safety planning, information about other services, help with onward travel) and recorded in the Redthread referral log as having received this type of intervention. Discussions with Redthread staff confirmed their observations that even short-term interactions with young people and short-term crisis support modes of engagement could have a positive impact (e.g. by helping a young person to feel comfortable and assured in the unfamiliar hospital setting and better engage in their care).
The second more ‘engaged’ group become part of Redthread’s formal case management work. This group of young people provide consent to work with a youth worker and a risk assessment is completed, along with a plan for tailored support. Youth workers engage with this cohort over a number of weeks, or even months, and enter information into the Redthread Lamplight system which records youth worker case notes and information regarding which other professionals are working with the young person (e.g. probation, social care). Indeed, Redthread staff emphasised the commitment of the charity to working closely with relevant hospital-based services, such as hospital social workers and safeguarding teams (adult and child), and external services, both statutory and non-statutory, to ensure that continuing support was provided to a young person following hospital discharge. Indeed, part of the set-up phase for the service at each hospital involved scoping work to establish ‘key partners’ and to ensure that Redthread avoided overlapping in ways unhelpful with other ‘jurisdictions’ and voluntary organisations. This meant that Redthread could easily refer young people to other local services where appropriate.
Implementation at UCLH
Identifying and referring young people eligible for support from the Redthread service
A relevant finding of this evaluation was that the context for Redthread service adoption at UCLH went beyond a single ED to a cluster of specialised services for children, adolescents and young adults at UCLH, including outpatient departments, fracture clinic and adolescent wards. This has implications for how young people are identified and referred to the Redthread service.
Staff and youth workers discussed how young people present to the hospital with a range of clinical and psychological problems that trigger safeguarding concerns and can indicate that a young person is vulnerable within their community. Examples included young people assaulted with an implement or sharp object (e.g. glass or knife), which they might report as happening ‘accidentally’, substance misuse, suicidal ideation and suicide attempts, sexual assault, and severe mental health crises requiring urgent treatment. A group of vulnerable young people are also reported to experience problems with managing a long-term condition such as diabetes, asthma, or a rare condition sometimes requiring urgent care. Redthread youth workers were therefore actively engaged in multiple processes to identify eligible young people for the service at UCLH, and this went beyond victims of violent injuries from gun or knife attacks. Indeed, hospital staff noted that because the hospital was not a London MTC, knife injuries were less frequent:
our major trauma centres, they get predominantly very violent assaults, whereas I think at local hospitals Redthread are known to receive a lot more varied referrals.
(RED005)
young people who come in with mundane or seemingly mundane presentations around asthma during the course of their care will divulge that the trigger might have been them being chased for example by a gang, which then makes them eligible for us or young people having seizures and then they divulge that it’s stress-related because they’re being targeted by certain groups.
(RED009)
the demographic of patients that present to A&E at UCH [sic], there’s very few knife crime directly related, but there tends to be more kind of either self-harm and that type of presentation, particularly in younger people 17 to 21, 23, 24.
(Doctor, RED0022)
At UCLH, staff suggested there was a cohort of young people, particularly those aged 18–24 years, who present ‘with less physically traumatic injuries’ (Redthread youth worker, RED009) and from ‘assaults without a weapon’ (Redthread staff, RED0020). These young people are less likely to be admitted to hospital for longer periods of time, are often seen outside of daytime hours, and can be especially difficult to follow up due to different processes of consent for those aged under 18 years and those aged over 18 years. For example, young adults over 18 years might sometimes give a false name or contact number or leave without providing any contact details, in which case, Redthread engagement and consent cannot happen (‘the pre-engagement stage’) within the hospital setting. Other young people were reported to engage more easily on site, particularly in the paediatric ED, emphasising the importance of Redthread youth workers having high visibility across EDs:
If the young person is in the A&E and we have a chance to see them face-to-face we don’t have to have consent per se to speak to them, but what we will ask the clinician to say is, ‘I’ve got a youth worker here do you mind if they come and talk to you?’, just so that they’re not a professional walking in and they have no idea who we are.
(RED003)
Clinicians close to the service with direct experience of engaging with Redthread youth workers, or making a referral to the service, also recognised the importance of timely identification of young people eligible for support by Redthread, especially once aged 18 years and over and beyond child safeguarding protections:
once they cross that magic line of age, if they are not consented in real time, it’s very hard to reach them if they don’t want to be reached, or if they are difficult to reach, which they often are.
(UCLH Clinician 1)
There were different referral processes that Redthread instigated at UCLH to ensure that no young person eligible for their service was missed (see Chapter 5). One important activity in this regard for Redthread was screening the electronic hospital electronic record (Epic) for admissions among 18- to 24-year-olds in the last seven days (e.g. from violent or sexual assault) since this group was most likely to be missed. In addition, youth workers attended MDT meetings (e.g. safeguarding) to identify young people and received direct referrals from staff. Youth workers also monitored patient admissions in real time (e.g. ED ‘track boards’) to identify young people that they could approach before they were discharged and who might respond to a ‘teachable moment’.
Redthread staff observed that while most referrals they received were from the paediatrics ED, their proactive screening of Epic suggested there was an equal proportion of patients eligible for the service across paediatrics and adult EDs, and that the ‘missed referrals are almost entirely concentrated in people aged 18 and over’ (Redthread staff, RED0020).
Interviews confirmed that the weekly paediatric ED safeguarding meetings at UCLH had become a central point of referral to the service with youth workers now fully embedded within them. This had been especially useful for the identification of young people prior to the integration of a Redthread referral form into Epic, enabling clinicians to make direct referrals via the hospital system. Redthread staff spoke of the need to ‘diversify referral pathways’ during early implementation of the service at UCLH due to impact of COVID-19 and the redirection of UCLH patients to other hospital sites (i.e. the Whittington and Great Ormond Street Children’s Hospital). This had resulted in both the closure of the paediatric ED, and led to discussions with outpatient and other specialist departments (e.g. rheumatology, diabetes) about staff referring young people to Redthread as an additional route. As one youth worker observed, ‘that left a legacy for our service’ and ‘represented a bit of a pivot’ in the type of patients they were now engaging with.
Use of data and service monitoring
To work optimally in the hospital setting, youth workers required an honorary contract to access Epic. Access to this system was introduced early into implementation of the service and enabled Redthread staff to proactively search for young people eligible for youth worker support who may been missed, and to log youth worker interactions with young people (e.g. at bedside) in the electronic health record. Epic further enabled direct staff referrals to the service through an integrated form. Youth workers would then liaise with clinical staff responsible for the young person’s care, and the clinician who had made the referral, and confirm whether it was appropriate to engage and offer this patient the Redthread service:
We had a young person who was stabbed with a bottle last week and they absconded before they were seen. They attended with police, I don’t know how they managed to slip away … So that’s why having access to the [Epic hospital electronic health record] system is good because you can see if there are any follow-up appointments and we’ll put it in our calendar and visit the hospital on that day because we know that if we see them in person it increases the likelihood of engagement.
(RED009)
Staff involved with safeguarding and monitoring patient records appeared most likely to make referrals via the Redthread referral form integrated with Epic. This was also the case for clinicians providing overnight care when youth workers were not available on site.
Redthread staff use a referral log template to capture information about young people referred to the service at UCLH, including who is not eligible for or declines support. This log (which is only available to view by Redthread staff) contains details such as the name of patient, their hospital number, sociodemographic details (e.g. age, gender and ethnicity), the arrival date and time, referral type, reason for hospital presentation and, where applicable, notes about the incident and any previous attendances for assault. The log is used to record who has made the referral (e.g. clinical staff) and whether there is consent for Redthread to contact the young person. Finally, the log details the type of support engaged and consented young people receive.
Data are only transferred to Redthread’s Lamplight system, which researchers/evaluators do not have permission to access or use, if a person is engaged for longer-term support and risk assessed. This system allows for the recording of more person-level sensitive information, such as case notes and the names of key statutory professionals in the young person’s network. The case management tool is used to record and monitor the allocation of young people to youth workers, ongoing contact, the duration of the support provided and date of case closure.
Redthread staff described a number of issues regarding data capture, flows and processes in interviews:
-
Missing useful information in Epic, the hospital record system, to flag when a young person is eligible for support, meaning young people can be missed (e.g. clinicians too busy to provide detail in the electronic health record, or unsure about the type of information that would be most useful to record, e.g. risk indicators).
-
The Redthread referral form within the Epic form being under-used (as mentioned, staff tended to make referral to Redthread directly via in-person contact, phone or email).
-
On the other hand, youth workers entering too much detail in the hospital record that could potentially lead to changes in how the individual is perceived and/or treated by clinicians (e.g. if the young person is involved in gang violence or has been a victim of sexual exploitation). Youth workers were especially concerned about notes by social care services and the language used to describe a young person and their needs.
-
A lack of information sharing between hospitals to identify where young people have been admitted before for violent injury or assault.
As one member of Redthread staff observed: ‘it would also just be incredibly helpful if there was essentially a button when anybody was logging a patient if they could just say this person is eligible for Redthread’ (Redthread staff, RED0020).
The Health Information Exchange portal was deemed to be useful because youth workers could review discharge summaries from other participating NHS trusts, and UCLH’s own Epic system was therefore found to be useful by staff for flagging the number of times a person had attended the hospital within a given period. Overall, however, issues remained during the evaluation regarding the lack of formal and systematic recording of Redthread referrals and markers in Epic to flag young people potentially eligible for the service. For more information about data processes and flows, please see Chapter 5.
Impact of COVID-19 and redirection of services COVID-19 service-level impacts early implementation (February 2020 to March 2021)
The Redthread service was introduced to UCLH in January 2020, shortly before the COVID-19 pandemic started and severely affected health systems and societies internationally. This led to the four main impacts in terms of implementing the Redthread service at UCLH, as outlined below:
-
Paediatric patients of UCLH were temporarily redirected to the Whittington Hospital (a provisional arrangement until March 2021) and referral processes were regularly reviewed by UCLH and neighbouring NHS trusts.
-
Redthread youth workers adapted to provide a virtual youth work service offer during the height of the pandemic and were not physically back ‘on site’ at UCLH until August 2020, and worked remotely for an interim period. Youth workers returned to fully working on site in April 2021. The service therefore continued to operate as usual, but for certain periods in a remote capacity. Youth workers received referrals from UCLH staff, including live referrals presenting within ED. Redthread youth workers also continued to work with young people once they were discharged from hospital.
-
Clinical presentations: UCLH staff observed that there were fewer cases of violent injury during lockdowns, yet more severe mental health and other types of safeguarding concerns presenting among young people during the pandemic (e.g. domestic violence and sexual assault).
-
There was significant disruption of Redthread’s launch and staff-awareness activities because youth workers and paediatric services were not on site and many staff at UCLH were focused on treating COVID-19 patients.
Interview respondents, both Redthread and UCLH staff, highlighted that the pandemic had not only influenced the types of clinical cases presenting at UCLH, it had also severely disrupted the service offer. Nevertheless, youth workers perceived that a remote support offer had been well received by many young people who were comfortable interacting via mobile phones: ‘we’ve probably engaged some young people that wouldn’t have engaged at bedside because remote conversation is better for them’ (Redthread staff, RED003).
Staff awareness and perceptions of the Redthread intervention
Several clinical staff interviewed had prior awareness of the Redthread service from its implementation at other London hospitals and MTCs. Staff viewed the charity as a youth violence service targeting young people caught up in gangs.
Staff spoke of Redthread youth workers as having a complementary and beneficial presence for both clinicians and young people, especially when young people were suddenly confronted with an unfamiliar and daunting hospital environment. The service was seen to align well with UCLH’s specialist services (e.g. adolescent wards and paediatric ED), with the result that youth workers had been enthusiastically welcomed and staff reported being ‘excited’ and ‘passionate’ about Redthread. The quotes below illustrate the value respondents placed on the service locally. In particular, staff praised the comforting and neutral presence of youth workers when working with young people and their ability to provide support to young people following their discharge from hospital:
I think it’s reassuring for the nursing staff if you’ve got a young person that’s obviously really unhappy and they can have somebody that’s there that can chat with them on their level.
(RED0012)
In terms of the intervention that they’ve been able to provide through our young people, it’s been absolutely invaluable. I think they essentially deliver a very assertive youth working intervention. They will meet young people on the ward, they will follow them up into the community… They tend to be very good at engaging young people who, which traditional services such as CAMHS or social care, often find it quite hard to reach.
(Consultant, RED0021)
that one kind of familiar face is very worthwhile.
(Doctor, RED0022)
it’s massively strengthened our offer of holistic care to young people … I think it has been a really instrumental part of facilitating that care. Particularly in those presenting in the greatest distress.
(Consultant, RED0015)
it’s helpful to share the burden around ensuring the safe plan for when young people are discharged. I think the team, they’re really positive to have around.
(RED0011)
Hospital consultant specialists (e.g. paediatric, adolescent, psychiatry) were particularly clear about Redthread youth workers filling a ‘gap’ as a non-statutory organisation able to connect with internal and external services to assist a young person, as well as hospital safeguarding processes:
the potential safeguarding connections and networking and linking in around trying to prevent someone at risk of violence, let alone someone who’s actually already experienced violence, I think puts Redthread in this meta position.
(RED0014, Consultant)
I would quite happily have a youth worker for every young person we saw in the rust, quite frankly.
(UCLH Clinician 2)
Staff were eager to refer young people to the Redthread service and would usually do so during the day via telephone, email or by approaching youth workers directly. Within paediatrics and adolescent services, attempts had been made to embed Redthread youth workers as part of different MDTs, rather than simply have the charity ‘co-located’ without proper involvement with standard care processes. Respondents were, however, aware that the UCLH’s dedicated adolescent services were unique and that staff are very ‘adolescent focused’ and receptive to youth workers, meaning the paediatrics ED was a highly conducive context for the Redthread service as a whole. By contrast, it was observed by both clinical staff and Redthread youth workers that embedding the service in adult emergency services covering the cohort aged 18–24 years had proven far more challenging:
the adult A&E is really very separate. That’s not to say that there aren’t fantastic medics and nurses around there, but I would say that as a paediatrician, I’ve got quite limited influence over them. I’m not really sure how much they know about it, how much they engage with it.
(Consultant, RED0015)
I think if you were predominantly interested in adult A&E, I think it’s probably a service that wouldn’t come to mind.
(Doctor, RED0022)
those of us who work in children and adolescents we got it much earlier on that it was a really good preventative way of working with young people.
(RED0010)
Staff also struggled to say whether Redthread had resulted in specific clinical or quantifiable outcomes and questioned whether hospital reattendances were an appropriate measure of the impact of the Redthread service. Staff discussed general positive benefits and impacts based on their observations of youth worker interactions with individuals and youth worker involvement within a multidisciplinary approach towards caring for adolescents and young people at risk of exploitation, gang crime and the most vulnerable within their local communities (see anonymised clinical case vignettes (Box 2 and Box 3) for examples).
A young person presents at UCLH with suicidal ideation. Staff become aware, through clinical assessment, that the young person is vulnerable because the family is ‘in crisis’ with aggression occurring in the home which is affecting the young person’s mental health. The young person is however ‘very suspicious’ of mental health services (i.e. CAMHS). Redthread youth workers visit the young person on the ward and interact with the family, and then continue to support the young person in the community by engaging with other public agencies.
UCLH staff perspective on the case: ‘So they [Redthread] are incredibly valuable, incredibly useful in reaching out and engaging that young person to make sure they got the right support they need to keep them safe.’
A young person is admitted to UCLH having been raped in a particularly violent incident. A large part of the youth worker role is ensuring that the patient can access statutory and support services within the area where the young person resides, with the youth worker liaising across service boundaries and helping the young person to re-engage in education. They ensure the young person can access appropriate local support given the level of trauma experienced.
Redthread youth worker perspective: despite feeling frustration because they were limited in what they could do with, ‘So many emails flying between different services’, they were able to mediate across services and provide emotional support to the young person and their family, ‘just offering a contained space for [the young person] to share [their] emotional experiences of those events’.
Some UCLH staff wanted to receive more feedback from Redthread about what happened to supported young people given that reattendance for knife injury, for example, was not necessarily a useful indicator about their impact:
I want to hear some narratives about how the work had shifted something for a young person. To hear their story and what they’re doing differently, because I think that can be much more powerful. The readmission might be a good thing, you see. It isn’t necessarily a bad thing.
(RED0014, Consultant)
Enablers and barriers
The qualitative data were used to identify the organisational factors, processes, resources, and staff training necessary for the successful implementation and delivery of the Redthread service. Table 5 lists the enablers and barriers that were raised in interviews with both Redthread youth workers and UCLH staff with regards to service implementation.
| Organisational | Example(s) | Presence at UCLH |
|---|---|---|
| Enablers | ||
| ‘Invested’ clinical champions and service advocates with influence among colleagues | Senior doctors act as brokers for hospital-based youth workers, supporting their attendance at MDT meetings, encouraging direct staff referrals, and liaising between hospital management and the charity; this is particularly important during early service implementation | Yes |
| Physical space for youth workers near EDs, office space | Rooms for having confidential conversations with young people, integration of youth workers as part of hospital staff – space to work | No |
| Endorsement and support from hospital managers – specifically, heads of EDs | Spread information about the service to ED staff, encourage referrals | Mixed: yes within the paediatric ED; less evidence of engagement and awareness in the adult ED |
| Electronic health care record integration | Form and potential reminder/prompt can encourage referrals among eligible population; supports timely information sharing about a young person at risk across professional groups (e.g. doctors, nurses, psychiatry, outpatients, social workers) | Yes, although tendency for referrals to come through via the telephone |
| Clear SOP agreed between hospital and Redthread | Sets out expectations for how the service will operate in practice, including the support and facilities needed to promote the service to staff; enables governance | Yes, although ongoing discussions about eligibility criteria for the service |
| Funding, dedicated resources | Fund longer-term involvement to allow time for youth workers to embed within a hospital | Yes |
| Staff training integration | Youth workers present at safeguarding training (e.g. level 3), hospital inductions and staff away days (e.g. for specialist nurses) | Mixed: while Redthread has provided a lot of training, staff observed further opportunities to raise awareness across the trust |
| Barriers | ||
| Service disruptions | COVID-19 redirecting patients to neighbouring hospitals, youth workers unable to work on hospital site | Yes, until March 2021 |
| Low staff awareness and/or engagement | Less awareness of the Redthread service in adult ED, consequences for missing eligible young people aged 18–24 years, missed opportunities to consent young people before discharged to the community | Mixed: high awareness in adolescent and paediatric departments; lower awareness and engagement in adult ED |
| Missing or inaccurate information in electronic health records | Changes in Epic or lack of information/human errors can make it more difficult to find out a young person’s reason for presentation or other factors psychosocially that might make them eligible for support | Mixed: Epic integration achieved, although limited integration with other London trusts |
| High numbers of hospital staff | Requires regular staff retraining by Redthread to ensure all staff are aware of the service and know how to refer young people to it (includes junior doctor rotations) | Yes |
| Pressures on clinical staff in EDs | Lack of time for clinicians to complete Epic referrals, send Redthread email or obtain consent and discuss Redthread with a young person if ‘hectic’ in ED; those over 18 years may be missed | Yes, reported to be difficult to gain traction within adult ED |
Discussion
Drawing on Nolte’s (2018) description of the ‘determinants of the adoption, implementation and sustaining of innovation in health service delivery and organization’,89 the Redthread service at UCLH can be viewed as having high compatibility with the local context and this supported adoption of the service. In particular, the ethos of a YVIP and Redthread’s ‘contextual safeguarding’ approach tailored to the vulnerable young person fitted with a multidisciplinary and holistic approach to care found in adolescent and paediatric services at UCLH.
Local clinical and non-clinical staff also perceived a need for youth workers, rather than duplicating other professional roles at the trust, such as social workers, or child safeguarding or play worker roles. Youth workers were viewed as complementing existing services, assisting with clinical care, and providing essential reassurance to young people on the wards and in EDs. Redthread’s independent status was viewed as encouraging young people to speak openly with youth workers, this in turn provided clinicians with important social and contextual information about a young person in the hospital, which could facilitate their care planning and treatment. Within paediatrics and adolescent services at UCLH specifically, staff were motivated to engage with Redthread youth workers and discuss cases with them, resulting in a receptive local context for the service. The service was also deemed to be feasible to implement once staff knew enough about how Redthread functioned, how to refer to youth workers, and the types of support the charity could provide.
UCLH had the resources available to implement the service and had already recognised a service ‘gap’ that youth workers might fill within the hospital environment, prior to implementation. While it was not clear during this evaluation what type of youth violence prevention or youth worker model was ultimately the most appropriate for the long term, especially given the trust’s transient patient population, clinicians nevertheless remained convinced of the value of youth workers being embedded within young people’s services at UCLH. Senior consultants played a critical role in advocating for youth worker service integration and presence at the trust, making the case for Redthread service adoption and finding the resources to both fund and evaluate the intervention locally (i.e. making links with the NIHR RSET evaluation team prior to full service implementation). In addition, the wider public health and community context in Camden (i.e. a high number of incidences leading to the premature deaths of young people in the local area) had made a youth violence intervention a timely service offer for UCLH. Clinicians were concerned that, while they could fix medical concerns and issues for young people, there was often little they could do once young people were discharged from their care.
Nevertheless, implementation challenges were reported and the Redthread service was yet to become more integrated in the adult ED. UCLH staff and youth workers were also poignantly aware that young people might not perceive themselves as at risk or vulnerable within their community and therefore choose not to engage with the Redthread service, especially if aged over 18 years and briefly visiting the adult ED. Recommendations for the future were that Redthread increase their promotional activities across the trust, such as by having presence at hospital inductions, more staff training events and nursing away days. This was deemed to be especially valuable given doctor rotations and changes in emergency staff.
Overall, there remain questions about the most appropriate youth worker service model for UCLH given that young people present for a variety of reasons (violence in the community, but also other types of risk such as those resulting in criminal and sexual exploitation, and domestic violence) and these can all have physical and mental health consequences for a young person. Different from many other EDs at other NHS trusts, at UCLH, specialist paediatric and adolescent services exist alongside an adult ED.
Staff therefore wondered how to place the Redthread service on a sustainable footing given limited resources, especially if referrals to youth workers increased (i.e. on account of more staff awareness-raising activities). The youth violence prevention approach in the trust also appeared to have wider repercussions for the management of long-term conditions among vulnerable young people presenting at UCLH, thus extending the charity’s reach beyond the ‘teachable moment’ in EDs to youth workers helping young people to positively engage in self-care management of long-term conditions (in cases where clinicians were concerned about safety risks to these patients, e.g. from exploitation or violence).
For the reasons outlined in this chapter, the service was going beyond a ‘teachable moment’ in adult EDs. Redthread has traditionally operated in MTCs via a service model highly dependent on youth workers’ physical presence in EDs and this approach was hugely disrupted during COVID-19, resulting in adaptations at UCLH. There was a virtual support offer to young people and more diverse referral pathways opened up involving direct staff referrals via outpatients’ departments, fracture clinics and MDT meetings. Later data collection (i.e. autumn/winter 2021–22) confirmed that the service had become well embedded in paediatric ED and adolescent services as a result (including on specialist wards). It was nevertheless still reported by staff and youth workers to be a struggle to embed Redthread in the adult ED.
To conclude, at UCLH, the Redthread service had been welcomed by staff working in UCLH paediatrics ED and adolescent wards; with some clinicians functioning as Redthread service advocates. Among UCLH staff interviewees, there was a perceived need for youth workers within the hospital setting to support clinical care and safeguarding functions. Overall, Redthread was viewed positively, not as duplicating other services or roles at UCLH (e.g. that of the hospital social worker).
Limitations
The team wanted to capture the views of young people that had received support from the charity and ask them about the impact Redthread had made on them and their lives as service users. However, as the study progressed, a number of barriers to engaging with young people who had used the Redthread service at UCLH and during the time period of the evaluation became evident, which we describe below.
First, interviews with staff revealed that there were a number of sensitivities and ethical issues given the types of complex cases presenting at UCLH (e.g. young victims of sexual exploitation, family abuse, mental health problems) as illustrated in this chapter. Indeed, a number of clinical cases where Redthread was supporting young people were associated with child and adolescent safeguarding processes in the hospital. Second, some of the young people who were likely to be benefitting from youth worker support would find it very difficult to discuss their recent experiences and reasons for attending UCLH with an unfamiliar outside researcher. Third, young people were often still receiving active support from youth workers and UCLH services (e.g. as outpatients), as well as other support agencies, and their issues around breaching patient confidentiality to identify and approach them. It was therefore agreed with Redthread that because of confidentiality and anonymity issues, it would be better to talk to young people who had worked with the charity for some time, and where personal risks to them had since decreased. From an evaluation perspective, it was also felt that to conduct meaningful interviews, where the young person felt comfortable, a decent amount of time would be required following hospital discharge, plus a carefully coordinated process of ‘high-risk’ ethical review, additional researcher education and training with Redthread and clinicians (e.g. about the specific cases and any safeguarding issues they raised), and that this was not feasible within the timeline of a rapid evaluation.
Due to these practical and ethical challenges, discussions were instigated between the lead qualitative researcher and Redthread managers about the possibility of conducting interviews or a focus group with up to five Redthread youth ambassadors with the support of the charity and using a co-designed topic guide. Ambassadors are young people who share their experience of receiving Redthread support and how it has impacted upon them. While the charity was supportive of this approach, further discussions revealed that the group was at risk of being ‘over-researched’ at the time, given a number of other evaluation teams and researchers also engaging with them, and this might induce some reluctant to engage. Furthermore, the group was based in the Midlands and Redthread staff suggested that their perspective would be quite different from young people living in London. Given the absence at the time of the evaluation of a less ‘over-researched’ group of youth ambassadors based in London, it was decided that this avenue would not be pursued.
In addition, data collection was performed remotely (using MS Teams) due to COVID-19, therefore no clinician–patient interactions were able to be observed (e.g. in the ED) to minimise the risks of spreading disease. When taken together, these factors meant that at the particular time point of this rapid evaluation, it was very difficult to engage with Redthread service users at UCLH or from across other London NHS trusts during this evaluation, or to directly observe youth workers engaging with young people in the ED.
The findings in this chapter also represent staff that were supporters of the service and volunteered to be interviewed about the Redthread service. Engagement with staff from the adult ED was difficult and some staff from the adult ED felt they did not know enough about Redthread to take part in an interview. This confirmed the case study findings that Redthread’s awareness-raising activities had been significantly disrupted by COVID-19 and the service was not yet fully embedded within UCLH’s adult ED. Finally, we did not take a theory-based approach (e.g. realist evaluation) or attempt to develop or revise Redthread’s own programme theory, although we noted that the charity updates and refines its own ‘theory of change’ and logic models described in this chapter. We were, however, in ongoing discussions with Redthread and clinical collaborators to ensure that the findings were accurate findings and could inform future implementation of the service at UCLH and the charity’s service offer across other local EDs which have different case presentations when compared to large MTCs.
Chapter 5 Description and review of data used to manage the Redthread service at UCLH
What this chapter adds
-
Between February 2020 and December 2021, 397 young people were referred to the Redthread service. Of these, 59 (15%) engaged with the full longer-term programme and 110 (28%) received shorter-term crisis support.
-
A total of 59% (124/210) of 11- to 17-year-olds who were referred to the service engaged with it, compared with 23% (42/181) of 18- to 24-year-olds. This difference would have been influenced by the safeguarding mechanisms in place for children, with it being more difficult to follow up 18- to 24-year-olds in the community.
-
Individuals eligible for Redthread may be identified by clinicians in the ED, on the wards or within outpatient clinics. They may also be identified by Redthread staff themselves within ED or by searching through patient notes.
-
Data on individuals referred to and engaging with the service is recorded in different systems depending on its purpose.
-
These databases are not formally linked to routine hospital data, and this can limit the ability of Redthread to view attendance histories of their service users and of UCLH staff to identify who has been referred to and is using the service. It also influences the chances of carrying out a robust quantitative evaluation of impact.
-
The absence of data linkage and the challenges of collecting service user consent retrospectively to analyse individual-level data has limited what we have been able to find out about the levels of engagement among different population groups because, in particular, we were not able to analyse the data by multiple characteristics at the same time.
-
We recommend that:
-
UCLH integrates the mandatory data collection Information Sharing to Tackle Violence with the ECDS or reporting a routine clinical code indicating a referral to a violence intervention scheme. This would help accurate identification of this cohort within routine data.
-
UCLH and Redthread populate key performance indicators developed by NHS England for effective implementation of in-hospital violence reduction programmes.
-
Introduction
In this chapter, we describe the data flows and data collected to manage Redthread’s service at UCLH to provide context for the subsequent chapter on the feasibility of quantitative evaluation. We describe what we have learned from the available data about the people who were referred to and engaged with the service and provide recommendations for improving data flows to help understand and monitor the impact of Redthread on hospital activity.
Use, collection and flow of data to manage referrals to Redthread’s youth violence intervention programme
The process of identifying young people eligible for Redthread’s YVIP in UCLH comes from two main data sources (Figure 5). This is either from a referral from a clinician who has seen an individual face-to-face (either from an emergency admission, an emergency attendance or an outpatient appointment), or through a Redthread member of staff screening hospital data for those that are potentially eligible to receive Redthread services.
FIGURE 5.
Process to identify young people eligible for Redthread services attending UCLH.
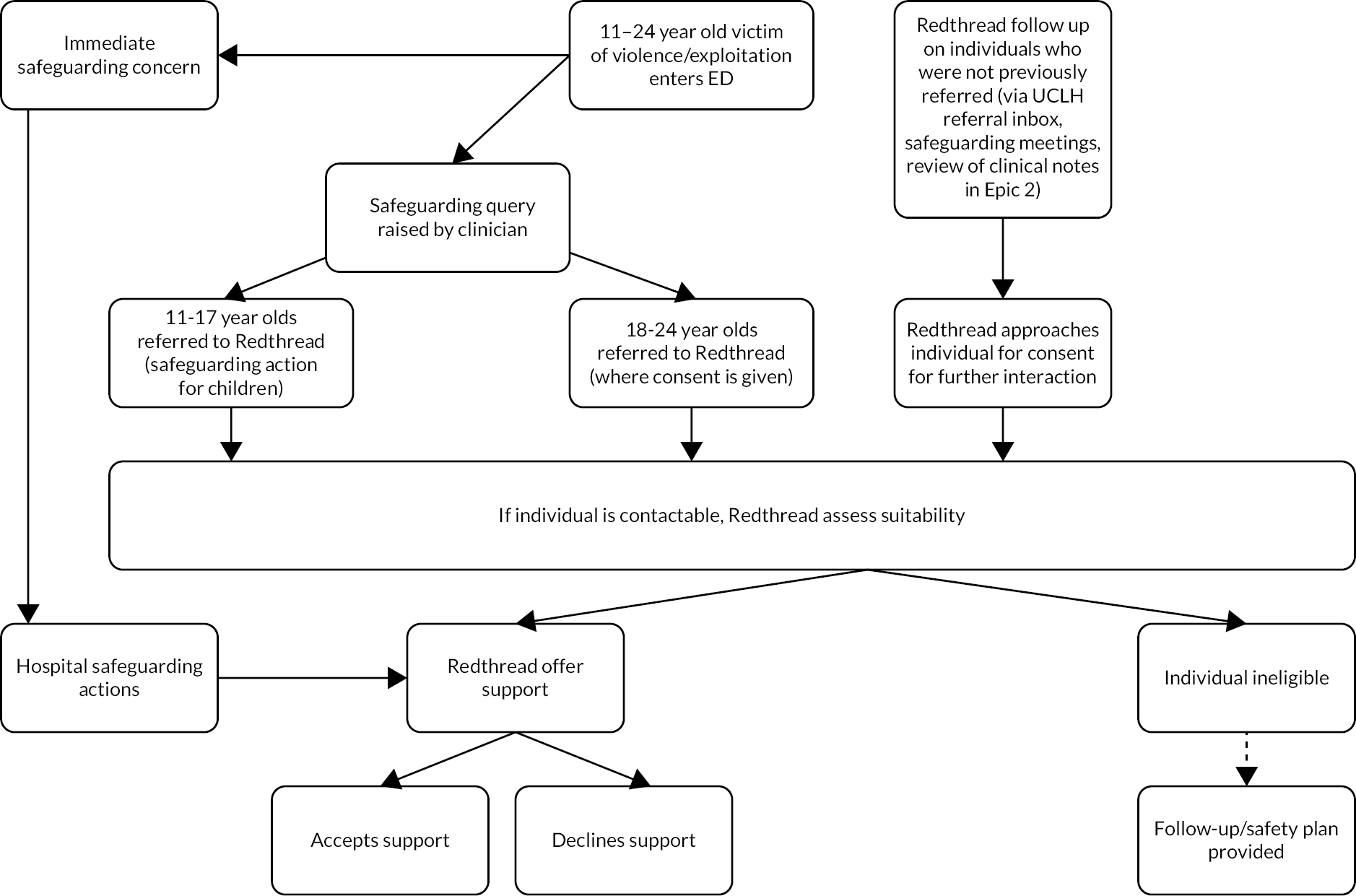
As well as clinicians making in-person referrals to Redthread services, a Redthread member of staff may occasionally be involved in ED through using the live track board within the department. This enables them to see all young people in the department at that time, checking the age and reason for presentation as well as free text comments when a young person presenting in ED appears to be eligible for Redthread services. After gaining approval from a clinician, Redthread staff may approach the young person to offer their support.
The latter process is carried out by Redthread on site at UCLH, where the Redthread team monitor UCLH’s referral email inbox. Redthread also implemented an additional process for referrals that entailed screening the hospital’s patient administration system, EPIC, for those who attended ED in the past seven days. This involves a detailed search of clinical notes, where a young person may appear eligible based on the details of their previous hospital attendance, such as whether they are victims of physical assault. However, this approach has its limitations. Since this is looking at previous hospital attendance, there is less clarity about the nature of the presentation due to limited information recorded on the system, whereas attendances happening at that moment would enable staff to pick up additional observations made by the responsible clinician.
Referrals can be received by Redthread via in-person conversations with a clinician, email, telephone, through the hospital database or through safeguarding meetings involving clinicians at UCLH. During the peaks of the COVID-19 pandemic, the vast majority of referrals were handled remotely, which differed from Redthread’s typical set-up of being based on site in a hospital’s ED. As lockdown restrictions eased, this enabled more in-person referrals to be made.
Once a referral is made by a clinician, Redthread then assess the eligibility of the referred young person for the service. A young person is considered eligible if they are within the target age range, if they present at UCLH and they are a victim or at risk of violence and exploitation. However, even if an individual is ineligible, Redthread can draw up a safety plan if they consent to receiving support.
When referrals are received by Redthread, details of referrals, data on the initial hospital presentation and attempts to contact individuals are recorded in Redthread’s referral log. Consent is also collected from young people referred to Redthread if they agree to receive support from the service, which can include consent to gather and store information on the individual to draw up a safety plan to provide short-term crisis support or can involve a young person consenting to engage longer-term with the programme. Young people are also reassured prior to consenting that appropriate measures are in place to uphold individuals’ confidentiality. This information is also captured in the referral log, which is maintained by and only accessible to Redthread (see Table 6 for a breakdown of information collected across the different systems).
| Redthread data collection | Included information | Key data fields |
|---|---|---|
| Referral log | All referrals | Details of hospital attendance (arrival date/day/time/reason for presentation/mode of arrival), discharge outcome, location of incident, name, date of birth, address, details of referral (method/date/time), age, consent for Redthread to contact (if given), signposted to other services, other support given (emotional, transport, food, clothing, prescription or further treatment) |
| Case management tool | All referrals | Name, date of birth, gender, initial hospital attendance and referral, reason for referral, responsible borough |
| Ongoing cases | Total referrals made, contact attempts (individual and professional network), case allocated to youth worker, contact successful/unsuccessful, ongoing/upcoming actions, risk level | |
| Open cases | Ongoing actions/engagement with the young person (support plan, risk assessment, action plan and end assessment) | |
| Closed cases | Contact attempts (individual and professional network), six-month follow-up, review status against initial risk assessment | |
| Lamplight | Long-term engaged young people | Age, MRN, gender, ethnicity, address, main language, referral route into Redthread, first contact point, 6-month follow-up completed, risk assessment, date of consent, contact details, preferred method of contact, family circumstances, accommodation, known to statutory services |
| UCLH data management system (Epic) | Clinical notes for all patients attending UCLH | MRN, free text (may include Redthread mentions or interactions Redthread workers had with the young people in hospital) |
| UCLH live track board | Live tracking of all patients in the ED attending UCLH | Age, reason for presentation |
If a young person has consented to longer-term engagement with the service, Redthread uses a more in-depth case management database, Lamplight, which enables the team to track all interactions with youth workers, the status of engagement and stores the safety plan, young person’s risk assessment and end assessment following completion of the intervention. All interactions and work done with young people is stored on this system for both record-keeping and safeguarding purposes.
A summary of all ongoing, open and closed cases is logged by Redthread in their case management tool. This provides an overview of the status of each referral that they receive, and it is updated weekly for use in case management meetings. Information on the number of referrals and young people engaged in long- or short-term crisis support with Redthread is also used in their newsletter, which is published quarterly. Redthread are seeking to implement a new case management tool and will be evaluating their risk assessment framework in the near future.
Reattendance data for violence-related reasons are collected by Redthread, though this only includes attendances at UCLH, rather than hospital activity elsewhere. This is done through matching the young person’s medical record number in Epic (an identifier specific to UCLH) to the one held in Redthread data.
While there is a wealth of information collected by Redthread, much of it is not linked to hospital record systems, even though linkage is technically possible as medical record numbers are held both by Redthread and UCLH. However, retrospective consent from Redthread service users would be needed to use individual-level data for the evaluation, and this is challenging to obtain. Acquiring consent from a young person in the first place can require building a trusted relationship with the individual, so the need to put appropriate confidentiality agreements in place aligns with the basic principle of the service: supporting and empowering the young person and ensuring that they feel safe to open up and work with Redthread. While this poses a challenge for the purposes of quantitative evaluation, the consent model for this service is an appropriate one due to the sensitivity of the information that Redthread hold on service users.
In addition, linking Redthread data to hospital data may mean that Redthread could get sight of additional hospital attendances that a young person has not disclosed to them, which could be particularly sensitive. There were also limitations to the data collected by UCLH, namely, an absence of codes specifying whether an individual was referred to or approached by Redthread. Rather, much of this information appeared in free text fields, if indeed it was recorded at all. This made it difficult to establish how many young people who were eligible to receive Redthread services were passing through UCLH. More reliable identification could be achieved, by, for example, using a clinical code indicating a referral to violence reduction services has been made (see Chapter 7).
One of our options for data analysis was to link data held by Redthread to routine hospital data. This would have allowed us to make a comprehensive assessment of past hospital attendances for Redthread service users and enable us to use matched controls to understand whether engagement with the service had any influence on hospital reattendance. However, UCLH do not record injury intent in emergency care records, which would have indicated whether the attendance was as a result of assault or self-harm. Integrating the mandatory data collection information sharing to tackle violence with ECDS,90 or reporting of a routine clinical code indicating a referral to a violence intervention scheme, would help with more accurate identification of this cohort from routine data. It should be noted that this still may not pick up instances where it is not immediately obvious that a young person is at risk, as they may be reluctant to reveal their real reason for requiring hospital treatment. In addition, the initial reason for hospital attendance may not always be the reason that a young person is referred, so this approach would also miss out these instances.
A guide for effective implementation of in-hospital violence reduction programmes, developed by NHS England, highlights key performance indicators and how they would be measured. This includes capturing data on exact numbers of eligible young people attending ED, and establishing a baseline of how many young people were referred and engaged compared to total numbers. 18 Quantitative data requirements for evaluation should be established at the outset, so that sufficient information is collected at the start of the study period for robust data analysis to take place.
Descriptive information about young people referred to Redthread’s youth violence intervention programme
Redthread shared aggregated information on age, gender, reason for hospital presentation, reason for referral, and who it was that made the referral, split by those who received short-term crisis support, longer-term support and by those who were not supported by Redthread services. Additional data on ethnicity was shared, but this was only collected for those who were engaged in long-term support from the Redthread programme.
Since the introduction of Redthread to UCLH in February 2020 to the end of the study period (December 2021), 397 eligible referrals were made to Redthread. Of these, 169 (43%) young people received some form of support from the service. This compares with engagement rates from previous studies ranging between 28% and 54%,91–93 although it was not clear how much the level of support that young people were receiving in these studies differed with the support received for this research. It should also be noted that a significant part of the study period was impacted by the COVID-19 pandemic, which may have impacted uptake.
In the first few months, the number of referrals to Redthread were low (Figure 6), coinciding with the first COVID-19 lockdown, where the overall number of hospital attendances decreased. 94 In addition, alternative methods to referring young people in person, such as via telephone, may have been less successful at reaching those who were being targeted to receive an offer of the service. However, the low referral numbers can also be attributed to paediatric services being redirected to the Whittington Hospital during the lockdown periods, with normal services for paediatrics in UCLH resuming in April 2021. Conversely, increases in the number of referrals nearer the end of the reporting period were largely due to the Redthread team being able to have more of a presence in ED.
FIGURE 6.
Number of eligible referrals to Redthread by level of engagement and by month.
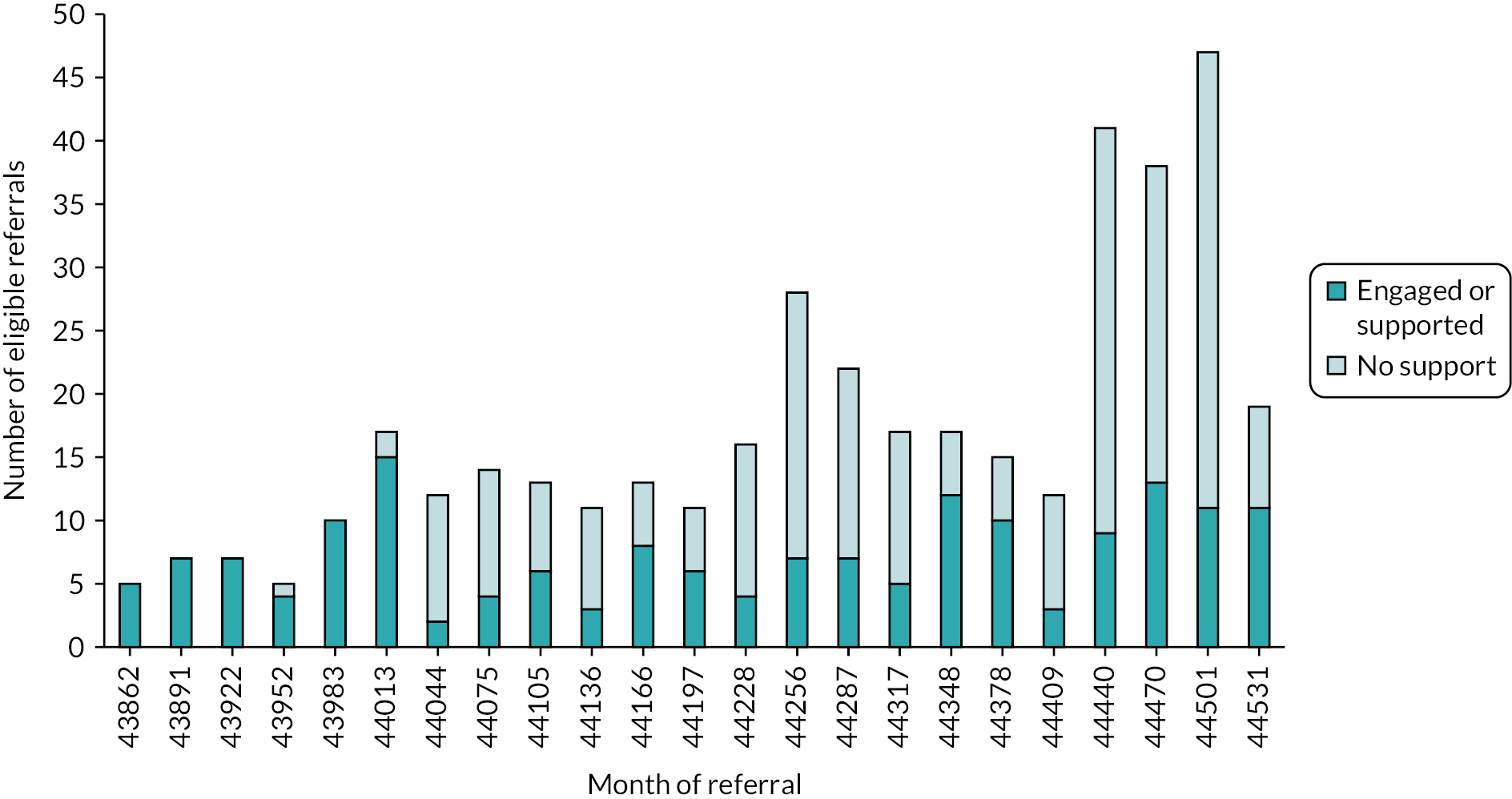
There were differences in the characteristics of young people who were supported by the service compared to those who were not supported (Table 7). For example, 77% of young people aged 18–24 years did not receive any support from Redthread services compared with 41% with no support in the 11–17 years age group. The lower proportion of engaged over-18s may partly be because hospital attendances that are retrospectively followed up as a referral cannot be done without consent for this age group. However, action can be taken for those aged under 18 years, due to safeguarding reasons, and the referral process within paediatrics has been reported to be more embedded than the process in place for young adults (see Chapter 4).
| Longer-term engagement | Short-term crisis support | No support | ||||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | Referrals by characteristic | Referrals (n)a | (n) | (%) | (n) | (%) | (n) | (%) |
| Total | 397 | 59 | (15) | 110 | (28) | 228 | (57) | |
| Age (years) | 11–17 | 210 | 40 | (19) | 84 | (40) | 86 | (41) |
| 18–24 | 181 | 17 | (9) | 25 | (14) | 139 | (77) | |
| Gender | Female | 152 | 29 | (19) | 39 | (26) | 84 | (55) |
| Male | 244 | 30 | (12) | 71 | (29) | 143 | (59) | |
| Ethnicityb | Asian | 11 | (19) | |||||
| Black | 16 | (27) | ||||||
| Mixed/other | 8 | (14) | ||||||
| White | 18 | (31) | ||||||
| Unknown | 6 | (10) | ||||||
Sixty-one per cent of referrals to Redthread were male. This proportion was lower than previous studies evaluating violence intervention programmes,56 although the Redthread service at UCLH includes young people supported for other reasons, such as mental health or substance abuse, which was not always the case in the existing literature. Looking at engagement by gender, a higher proportion of females engaged with Redthread compared with males (45% and 41% respectively).
Ethnicity data were only available for those who consented to longer-term engagement with the Redthread service, therefore it was not clear if there were differences in the likelihood of uptake between different ethnic groups. Of those who received longer-term support, nearly one-third (31%) were white; the second largest group were of black ethnicity (27%).
We also looked at the data by reason for referral and by reason for hospital presentation (Table 8). When breaking the data down by reason for hospital attendance, the group that had the highest engagement rate (60%) were those who attended hospital due to ‘illness’ but it was not clear what sort of illness this category referred to. The most common reason for hospital presentation of those referred was assault (44%). This was partly because referrals followed up retrospectively were identified through Epic, and were limited in detail, but those that had an assault recorded in their hospital record were likely to be eligible for Redthread. However, this group had an engagement rate of 34%, which was lower than other reasons given for hospital attendance.
| Longer-term engagement | Short-term crisis support | No support | ||||||
|---|---|---|---|---|---|---|---|---|
| Reason for hospital presentation or referral | Referrals by reason | Referrals (n) | (n) | (%) | (n) | (%) | (n) | (%) |
| Reason for hospital presentation | Accident | 59 | a | (a) | 17 | (29) | 39 | (66) |
| Assault | 175 | 22 | (13) | 36 | (21) | 117 | (67) | |
| Mental health/substance abuse | 102 | 18 | (18) | 34 | (33) | 50 | (49) | |
| Illness | 38 | 10 | (26) | 13 | (34) | 15 | (39) | |
| Other | 23 | 6 | (26) | 10 | (43) | 7 | (30) | |
| Reason for referralb | Risk of harm | 177 | 22 | (12) | 58 | (33) | 97 | (55) |
| Assault or history of assault | 173 | 21 | (12) | 35 | (20) | 117 | (68) | |
| Domestic or sexual violence | 42 | 7 | (17) | 10 | (24) | 25 | (60) | |
| Child criminal exploitation or child sexual exploitation | 18 | a | (a) | 8 | (44) | 7 | (39) | |
| Other | 14 | 6 | (43) | a | (a) | a | (a) | |
As with reasons for hospital presentation, assault (or history of assault) made up a large proportion of referral reasons. Rates of uptake were similar, with around one in three (32%) receiving longer-term or short-term support from Redthread. However, while there may be overlap with reasons for referral and reasons for hospital attendance, initial presentations to hospital may not record the underlying reason for a Redthread referral. Support from Redthread was also received by 45% of those who were referred due to risk of harm. While we are unable to conclude why the rates of uptake vary between different reasons for referral, there could be cases where certain presentations to hospital that are followed up retrospectively in hospital data (such as assault) are less ambiguous in whether the young person would be eligible for Redthread. These retrospective cases would be followed up remotely, which may have impacted on the likelihood of engaging.
Key findings
-
A total of 59% of referred young people aged 11–17 years engaged with the service, compared with 23% of those aged 18–24 years. This will, in part, have been influenced by the safeguarding mechanisms in place for children, with more challenges in following up 18- to 24-year-olds in the community.
-
Looking at engagement by gender, a higher proportion of females engaged with Redthread compared with males (45% and 41%, respectively), although this difference was not statistically significant. Previous literature typically focused on violence-related injury, where the proportion of males sustaining such injuries was typically higher.
-
There are limitations to what we can feasibly analyse and conclude from Redthread’s data in isolation without linkage to routine health data, given that Redthread’s consent model does not allow individual-level information to be shared outside their organisation. These limitations include:
-
Data that are captured on hospital activity relate to UCLH only, rather than hospital activity more widely.
-
We were not able to analyse levels of engagement by multiple characteristics, and so cannot reflect on whether there are combinations of age, gender and ethnic groups that are less likely to engage with the service.
-
-
There are also drawbacks to simply using data from UCLH’s patient administration system, as Redthread referrals are not consistently flagged. Where referrals are recorded, they are only done so in free text rather than within a dedicated coded data field, and there is no information beyond indicating that an initial referral has been made. Recording referrals consistently in a dedicated data field would help to readily draw more information out (such as demographics and retrospective hospital attendance) on those who were referred.
-
We found that UCLH did not make use of the injury intent field in their emergency care data systems. Completing this field would help more accurately identify whether an attendance was due to an assault or because of self-harm, which may be a helpful indicator of young people who are eligible for Redthread services.
-
Being able to link Redthread data to national routine datasets, such as HES and ECDS, would provide richer information pertaining to demographics, as well as an indication of retrospective hospital use and the reason for attendance where a referral to Redthread was given. This would allow for establishing what the impact of Redthread on hospital services would be, but sufficient time prior to service roll-out must be given to setting out data requirements and ascertaining the feasibility of each option.
Chapter 6 Cost–consequence analysis of Redthread’s youth violence intervention project at UCLH
What was already known?
-
The YVIP has helped in reducing hospital reattendance rates from 4.8% to 2.9% for at-risk young people attending St Mary’s hospital during a three-year period.
-
A comprehensive CBA evaluating Redthread’s YVIP found a £4.90 economic and social benefit per each £1 spent on the programme.
What this chapter adds
-
The mean Rethread cost per person engaging with the programme was estimated to be £1865.
-
The mean NHS cost for an ‘artificial’ group fulfilling eligibility criteria of Redthread and treated at UCLH was estimated to be £5789 for an emergency inpatient admission and £203 per attendance at the ED.
-
The costs of the Redthread service at UCLH would be offset by savings if around a third of the engagements with Redthread led to at least one avoided emergency inpatient admission.
-
Assessed risks for young people engaging with the Redthread programme decreased after the intervention for the risk of experiencing further harm and for not maintaining positive relationships with family. No statistically significant change was found for eight further aspects of risk and three overall measures of risk (harm from others, harm to others and harm to self).
Background
Knife-related incidents are a significant public and political concern in the UK. It has been estimated that violence-related care constitutes around 12.9% of trauma teams’ workload95 and that it costs the NHS £2.9 billion a year. 33,96 Violence-related trauma primarily affects young men and incurs substantial costs, not only in terms of the direct costs of medical care, but also the societal losses related directly to permanent disability and premature death. 97 Indirect costs, although not often quantified in the literature, can be much higher, including loss of psychological and social function to the individual, diminished community cohesion and loss of economic productivity.
The initial aim of the economic analysis was to conduct a CEA of the Redthread YVIP at UCLH from the perspective of the NHS and personal social services, answering the research question ‘How cost-effective is the implementation of the Redthread service at UCLH?’21 However, for reasons described in Chapter 7, we established that it was not going to be feasible to evaluate the quantitative impact of the service within the timeframe of the project so we focused on a CCA approach.
The aim of the CCA approach was to quantify the costs and consequences (or effects) of implementing the Redthread YVIP at UCLH. The analysis of costs comprised the costs of: (1) implementing and running the Redthread YVIP at UCLH; and (2) treating patients in the ED and/or inpatient settings at UCLH. The measures of consequences were based on the risk assessment outcomes of the young people engaging with the Redthread YVIP.
The specific research questions that this analysis aimed to address were:
-
What were the mean per person costs of engaging with the Redthread YVIP during the period February 2020 to December 2021, considering both the implementation costs for Redthread and the treatment costs at UCLH?
-
How do the mean costs per young person under the YVIP compare with the main consequences as identified in the individual risk assessment for those engaging with the Redthread YVIP?
Methods
A CCA is a type of economic evaluation in which all costs, both direct and indirect, and a catalogue of different consequences of all alternatives are computed and listed separately without aggregating these results into a cost-effectiveness ratio. 98,99 This approach allows quantification of findings and process measures and compares them with the costs of particular interventions. This form of economic evaluation is distinct from both CEA and CBA, which tend to focus on a single outcome measure and aggregate costs and the outcome into a single summary measure. 100,101 CCA is the appropriate form of economic analysis to use in the present study given the range of possible outcome measures for the Redthread intervention.
Measuring consequences based on the Redthread risk assessment
In total, 14 quantifiable measures of the consequences of the Redthread intervention were included. These were derived from Redthread’s own risk assessment tool which is completed by Redthread staff before young people were engaged with the intervention and reviewed when a case closes and again on a six-month follow-up. Data from these risk assessments covered the period April 2020 to November 2021 for 36 young people engaged with the Redthread programme. The risk assessment process is a specifically designed tool used by the Redthread youth workers to capture information on key outcomes and provides an overview of the risks faced by young people. The risk assessment is carried out by youth workers using their professional judgement and interpretation on what the young people using the YVIP service say and think (e.g. about their safety score on the safety plan).
Some 13 of the 14 risk dimensions used were based on an exclusive risk indicator varying from 1 to 3 (measuring low, medium or high risk) for engaging or experiencing: further harm, exploitation, engaging in criminal behaviour, risky lifestyle, not engaging in education, employment, not maintaining positive relationships with family, not engaging with other (provided) services and the risk of not being able to identify an escalating problem. While three of these were based on an overall risk assessment (risk of harm to others; risk of harm from others; risk of harm to self). The last referred to the level of safety perceived by the young people using a 10-point Likert scale where 1 equalled ‘very unsafe’ and 10 ‘very safe’ (see Appendix 5, Table 13 for the full list of risk indicators).
Statistical analysis
The mean score for each risk dimension was reported separately and statistical tests of the differences in risks ‘before’ and ‘after/during’ the follow-up were carried out using McNemar–Bowker and paired Student’s t-test. McNemar–Bowker tests were then conducted within subject to look at young people’s feelings of safety at the initial risk assessment compared with the ‘after’ risk assessment. Paired samples t-test were conducted to identify whether there was any statistically significant change in safety ratings pre- and post-intervention.
Measuring costs
The analysis of costs focused on the cost of Redthread YVIP and the cost of the young people treated at UCLH. The costs of the Redthread intervention were analysed from the perspective of: (1) the Redthread YVIP; and (2) the health-care provider (accounting for costs of UCLH hospital treatment). The YVIP costs were calculated as mean costs per young person for the study period (February 2020 to December 2021).
The information provided by Redthread covered expenditures for the fiscal year April 2020 to March 2021 and the budgeted expenditures for the fiscal year April 2021 to March 2022. Our period of analysis was limited to the 21 months (April 2020 to December 2021), for which we were provided with information on the numbers of young people receiving support. We assumed a constant rate of the expenditures over these months.
The main activities provided by Redthread team consisted of: (1) the front-line work, (2) programme development, (3) training provided to the medical staff, and (4) administrative work (Box 4). The information used to calculate the mean cost per young people included: (1) costs of staff that were involved in running the service (one team leader, two youth workers and one programme co-ordinator), (2) the operating costs, and (3) other administrative costs. No distinction was made between the mean costs per engaged in the longer-term programme compared with short-term crisis supported young people due to the lack of disaggregated information on the time and resources used for each category by Redthread.
Front-line work included all work undertaken for young people whether they are engaged in a longer-term programme or short-term crisis supported and included all bedside work and interventions, liaising with professional networks, any and all intervention work with young people, referrals and signposting for young people. Besides this, the front-line work also included any work that contributes to receiving referrals and engagement such as attending hospital-based safeguarding meetings or MDT meetings, screening the hospital system for referrals, attending handovers on site in ED and managing the referral phone and referral inbox.
Programme development covered any work done to support the delivery, evaluation, reporting or growth of the service. This included quarterly operations meetings, attending quarterly safeguarding committee meetings to provide updates on service delivery, partnership working, as well as all the data collection and information logging done by the programme co-ordinator. Partnership meetings were held across the team and were important in creating referral pathways through the service.
Training was related to the delivery of training sessions to clinical team, external partners, national conferences and clinical champions.
Administrative work covered anything that was supportive for the individual worker. This included clinical supervision spaces, supervision with manager, appraisals, case management meetings, individual case management oversight and continued professional development.
Source: Redthread, personal communication.
As the information collected by Redthread was not linked, or easily linkable, to UCLH’s patient administrative system (see Chapter 7), it was not possible to measure directly the cost of hospital treatment for young people using Redthread services. An ‘artificial’ treatment group was therefore created from HES admitted patient care data. This group was defined with reference to Redthread’s eligibility criteria: aged 11–24 years, admitted to UCLH as an emergency between February 2020 and November 2021, with recorded diagnosis codes that broadly matched reasons for referral to Redthread YVIP (for more information see Chapter 7 and/or Appendix 3). All the relevant Healthcare Resource Group (HRG) codes were then identified for each relevant admission spell using this artificial treatment group. UCLH provided the HRG codes for all the 11- to 24-year-olds admitted to the hospital through the ED for the three-year period 2018–21. For each relevant admission spell, the relevant HRG code was selected to extract UCLH cost information for each of the admitted patients for the three-year period. The mean cost per inpatient and for those attending the ED were averaged over the three years, given variations between years. All prices were inflated to 2020 prices.
Results
Consequences
The information on the initial (before) risk assessment for young people using YVIP for the period April 2020 to November 2021 is shown in Figure 7 (and in Appendix 5, Table 13). Young people were identified as facing a number of potential risks, particularly in relation to experiencing and participating in further harm, experiencing and participating in criminal behaviour, engaging in education, employment or training, not willing to engage with other services and not maintaining positive relationships with family.
FIGURE 7.
Risk factors in the initial risk assessment for young people who used the Redthread service in the period April 2020 to November 2021.

Figure 7 shows that, among all the assessed risks, the higher proportions of young people were identified as ‘high risk’ for (1) not maintaining positive relationships with family (22%) and, (2) not engaging in education, training or employment (19%). Figure 8 shows the range of assessed risks post-engagement. Broadly, the proportion of young people assessed to be facing high risks decreased or remained the same for all categories except for the risk of not willing to engage with other services, which rose from 2.8% to 5.6%.
FIGURE 8.
Risk factors in the end risk assessment for young beneficiaries who used the Redthread service in the period April 2020 to November 2021.
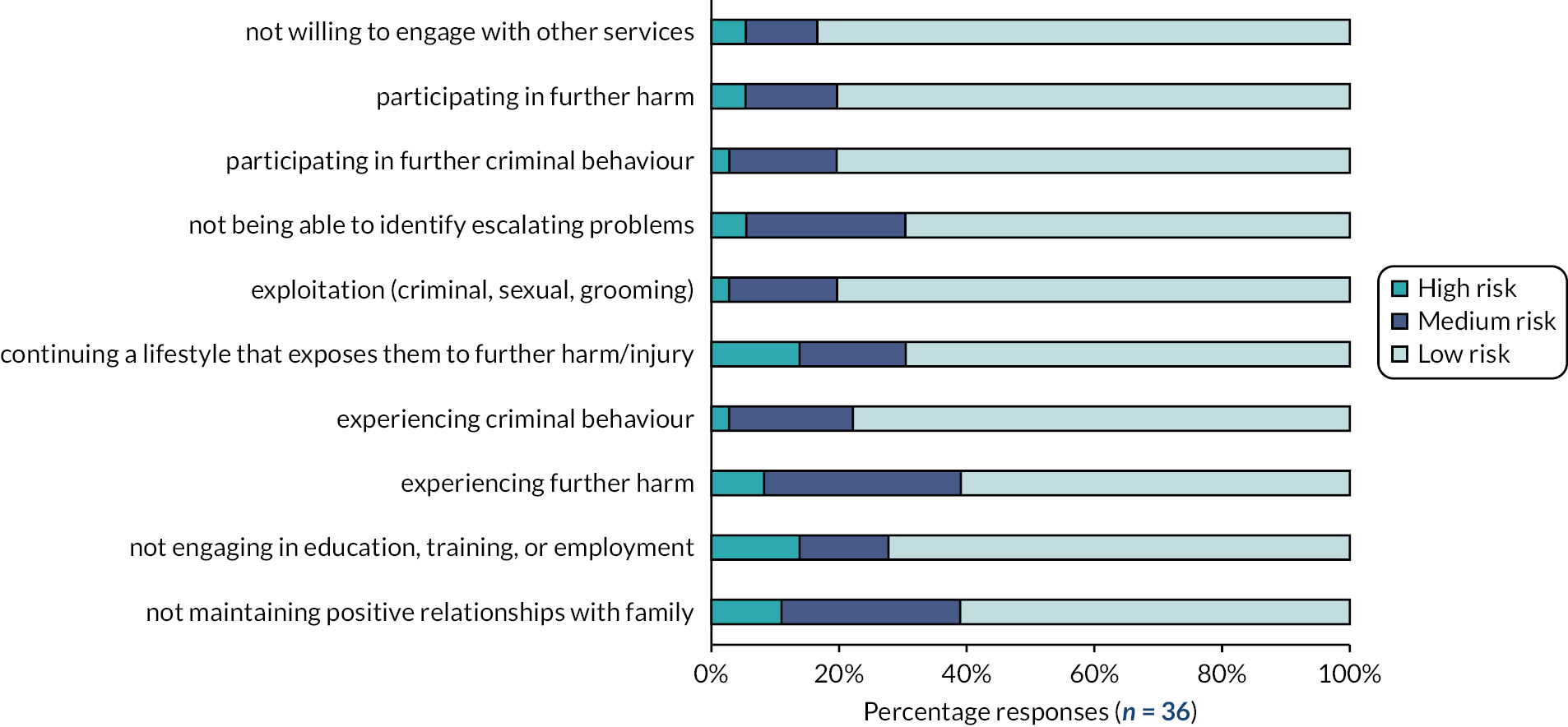
McNemar–Bowker tests of symmetry were then carried out to identify whether there were significant changes in risk factor ratings from the initial assessment to the end assessment (Table 9). The test revealed that the reduction in risks pre- and post-intervention were statistically significant for just two of the risk categories: risk of experiencing further harm (χ2(3) = 8.40, p = 0.0384) as well as for risk of young people not maintaining positive relationships with family (χ2(3) = 5.77, p = 0.050). The results show that the majority of the young people remained in the low-risk category and that changes from high to medium risk were more usual than remaining in the high-risk category.
| Initial risk assessment | End assessment | χ2 | p-value | |||
|---|---|---|---|---|---|---|
| Low risk | Medium risk | High risk | Total | |||
| Risk of young person of experiencing further harm | ||||||
| Low | 11 | 1 | 0 | 12 | 8.40 | 0.0384 |
| Medium | 9 | 8 | 2 | 19 | ||
| High | 2 | 2 | 1 | 5 | ||
| Total | 22 | 11 | 3 | 36 | ||
| Risk of young person participating in further harm | ||||||
| Low | 24 | 2 | 0 | 26 | 2.67 | 0.4459 |
| Medium | 4 | 3 | 1 | 8 | ||
| High | 1 | 0 | 1 | 2 | ||
| Total | 29 | 5 | 2 | 36 | ||
| Risk of exploitation (criminal, sexual, grooming) | ||||||
| Low | 25 | 1 | 0 | 26 | 4.00 | 0.2615 |
| Medium | 3 | 3 | 0 | 6 | ||
| High | 1 | 2 | 1 | 4 | ||
| Total | 29 | 6 | 1 | 36 | ||
| Risk of young person experiencing criminal behaviour | ||||||
| Low | 22 | 3 | 0 | 25 | 4.5 | 0.2123 |
| Medium | 5 | 1 | 0 | 6 | ||
| High | 1 | 3 | 1 | 5 | ||
| Total | 28 | 7 | 1 | 36 | ||
| Risk of young person participating in further criminal behaviour | ||||||
| Low | 28 | 2 | 0 | 30 | 1.33 | 0.5134 |
| Medium | 1 | 1 | 1 | 3 | ||
| High | 0 | 3 | 0 | 3 | ||
| Total | 29 | 6 | 1 | 36 | ||
| Risk of young person continuing a lifestyle that exposes them to further harm/injury | ||||||
| Low | 17 | 2 | 1 | 20 | 2.67 | 0.4459 |
| Medium | 6 | 3 | 2 | 11 | ||
| High | 2 | 1 | 2 | 5 | ||
| Total | 25 | 6 | 5 | 36 | ||
| Risk of young person not engaging in education, training, or employment | ||||||
| Low | 16 | 1 | 2 | 19 | 5.03 | 0.1694 |
| Medium | 7 | 2 | 1 | 10 | ||
| High | 3 | 2 | 2 | 7 | ||
| Total | 26 | 5 | 5 | 36 | ||
| Risk of young person not maintaining positive relationships with family | ||||||
| Low | 13 | 2 | 0 | 15 | 5.77 | 0.050 |
| Medium | 7 | 5 | 1 | 13 | ||
| High | 2 | 3 | 3 | 8 | ||
| Total | 22 | 10 | 4 | 36 | ||
| Risk of young person not willing to engage with other services | ||||||
| Low | 24 | 4 | 0 | 28 | 3.11 | 0.3748 |
| Medium | 5 | 0 | 2 | 7 | ||
| High | 1 | 0 | 0 | 1 | ||
| Total | 30 | 4 | 2 | 36 | ||
| Risk of young person not being able to identify escalating problems | ||||||
| Low | 20 | 4 | 0 | 24 | 2.11 | 0.3480 |
| Medium risk | 5 | 3 | 0 | 8 | ||
| High risk | 0 | 2 | 2 | 4 | ||
| Total | 25 | 9 | 2 | 36 | ||
| Overall scoring: risk of harm to others | ||||||
| Low | 28 | 3 | 0 | 31 | 3.3101 | 0.069 |
| Medium | 3 | 2 | 0 | 5 | ||
| High | 0 | 0 | 0 | 0 | ||
| Total | 31 | 5 | 0 | 36 | ||
| Overall scoring: risk of harm from others | ||||||
| Low | 16 | 1 | 0 | 17 | 5.90 | 0.1163 |
| Medium | 6 | 7 | 2 | 15 | ||
| High | 2 | 1 | 1 | 4 | ||
| Total | 24 | 9 | 3 | 36 | ||
| Overall scoring: risk of harm to self | ||||||
| Low | 20 | 1 | 0 | 21 | 4.57 | 0.2060 |
| Medium | 6 | 4 | 1 | 11 | ||
| High | 1 | 1 | 2 | 4 | ||
| Total | 27 | 6 | 3 | 36 | ||
A paired samples t-test was also conducted to identify whether there was a significant change in the overall score on how safe the young person felt right now. While there was a slight improvement on this overall measure (before: M = 7.11, standard deviation 2.18; after: M = 7.77, standard deviation 1.90), this change was not statistically significant.
Costs
Table 10 provides information on the mean costs for those engaging with the Redthread programme. Those engaged in a longer-term programme and short-term crisis supported young people combined and the mean costs per finished consultant episode for a group of patients matched to two characteristics of potential Redthread users: age (11–24 years) and HRG codes for inpatient stays selected on the basis of a range of possible treatments actual Redthread users may undergo at UCLH. ED costs were based on those reported by UCLH for 11- to 24-year-olds across all 12 HRG codes collected for EDs.
| Cost item | Total costs (£) | Mean cost (£) | Sample size (n) |
|---|---|---|---|
| Redthread YVIP costs (for the period April 2020 to December 2021) | |||
| Front-line activity (50% of the total budget/expenditure) | 157,599 | 933 | 169 |
| Service development (26%) | 81,951 | 485 | |
| Administration (14%) | 44,128 | 261 | |
| Training activity to medical staff (10%) | 31,520 | 187 | |
| Total Redthread YVIP costs | 315,197 | 1865 | |
| UCLH costs for inpatients and ED attendances | |||
| Inpatient (FCE) | 688,934 | 5789 | 119 |
| ED (attendance) | 3,364,863 | 203 | 19,501 |
The mean costs per young person (n = 169) for the Redthread intervention were calculated using information provided by Redthread for the 21-month period April 2020 to December 2021. Consumer price index inflation rate for 2020–21 was applied to 2020 prices. 102 All the resources used by Redthread were assumed to be spent on delivering the YVIP services for all the four activities (front line, service development, training to the medical staff and administration). All the costs are reported separately between these activities based on time Redthread staff spent on each activity (provided by Redthread).
Table 10 shows that the main cost for the Redthread service was for front-line services (50% of total costs), followed by service development (26%), administration (14%) and training activities (10%). The total mean cost per supported young person was £1865. Table 10 also provides the mean costs for the constructed group of actual patients treated at UCLH. For the inpatient costs, based on a set of diagnosis codes relevant to Redthread referral reasons (see Appendix 3, Table 12), between February 2020 and August 2021, 161 11- to 24-year-olds were anonymously identified as having a nonelective admission at UCLH. UCLH’s patient level information and costing system data were used to specify unit costs, which were then applied to each of the 161 patient spells via the spell HRG code. In practice, this reduced the sample to 119, as 42 had a ‘null/unknown’ HRG code. Based on this sample, the mean cost per patient was £5789 (range £473–73,837). The mean cost for an ED attendance was £203 (range £82–455) and was based on an average number of attendances of patients aged 11–24years of 19,501 per year across all types of coded attendance.
| Reasons for presentation | Reasons for referral to Redthread | ICD10 diagnosis codes in HES inpatient data | Chief complaint codes in ECDS |
|---|---|---|---|
| Assault (includes stabbing, other bladed or sharp object, gunshot, vehicle used as weapon, blunt object, bottle, glassed, burns, chemical substance used, combination of body parts used as weapon, explosive used, feet/fist/head/other body part used as weapon, physical assault but threatened with weapon, pushed, strangulation, rape); police-related injury; wound care | Assault | Contact with knife, sword or dagger (W26). Hit, struck, kicked, twisted, bitten, scratched by another person (W50). Striking against or bumped into by another person (W51). Crushed, pushed, or stepped on by crowd or human stampede (W52). Other fall on same level due to collision with, or pushing by, another person (W03). Assault (X85-Y05, Y08–Y09). Sequelae of assault (Y871) | Bleeding from nose, burn, chest injury, disturbance of consciousness, dizziness, dressing change/wound surveillance, injuries, laceration, light-headedness, nonfatal submersion, puncture wound, traumatic amputation, wound care |
| Mental health (includes overdose, self-harm, suicidality) or substance misuse (alcohol, drugs) | Symptoms and signs involving emotional state, including nervousness, agitation and restlessness, irritability and anger, hostility, physical violence (R45). Intentional self-harm (X60–X84) | Alcohol intoxication delirium, alcohol withdrawal syndrome, anxiety, bizarre behaviour, feeling depressed, delusions, drug withdrawal, poisoning, self-injurious behaviour, substance misuse, suicidal, suicidal thoughts | |
| Domestic violence, history of assault, sexual violence, child sexual exploitation | Physical, sexual or psychological abuse and other maltreatment syndromes (T74). Neglect and abandonment (Y06). Other maltreatment including mental cruelty, physical/sexual abuse, torture (Y07). Problems related to alleged sexual or physical abuse (Z614–Z616). Sequelae of events of undetermined intent (Y872) | Physical aggression, social problem, traumatic injury, unusual change in behaviour, victim of sexual aggression | |
| Accident: fall or accidental injury (third party or self-inflicted), road traffic accident | Falls (W00-W19) | Falls | |
| Illness; maternity appointment; threatened with a weapon; no hospital appointment; outpatient appointment; other | Risk of harm, child criminal exploitation, affected by gang activity, gang affiliation, witnessing violence, other | Unmatched | Unmatched |
Discussion
Principal findings
The analysis of assessed risks for young people engaged with the Redthread YVIP for the period April 2020 to November 2021 showed that the only risks for which we observed a statistically significant decrease after the intervention were the risk of ‘experiencing further harm’ and the risk of ‘not maintaining positive relationships with family’. Our results may be on the conservative side when compared with other studies evaluating YVIP in London. For example, one has reported that improvements in 6 of the 13 risk factors were statistically significant. 101
The average Redthread costs for Redthread cases was estimated to be £1865. However, following the reasons described in Chapters 5 and 7, it was not readily possible to link Redthread cases with their corresponding hospital records to track activity and, hence, their actual hospital costs. The costs of hospital treatment were therefore based on an artificial group that mirrored as best as possible Redthread cases in terms of age and diagnosis groups.
The mean cost for the emergency inpatient treatment of an artificially constructed group, similar to those likely to be referred to Redthread in UCLH were as estimated to be £5789, while the mean cost per attendance at the ED was £203. The estimated average costs of Redthread YVIP are around one-third of the costs of inpatient treatment for a similar group and around nine times larger than the mean ED attendance cost. Based on the 169 young people involved in Redthread as part of this analysis, and total Redthread costs of £315,197, this suggests that the Redthread programme would break even if, for every three people engaging with the service, at least one emergency inpatient admission was avoided.
Another important economic aspect related to programmes targeting youth violence is that some, and possibly the most significant part, of the costs and benefits materialise outside of health and social care. These include costs associated with the criminal justice system, as well as education, the welfare system in general and costs associated with disability or lost productivity as opposed to the generation of income from employment and tax. Other studies that have tried to quantify the costs of crime have estimated that the total unit costs from homicide amount to more than £3.2 million, for violence with injury £14,100, rape £39,400 and other sexual offences £6500. 103 Health-care services have been estimated to be only a small fraction of the total costs (especially in relation to lifetime effects of physical and emotional harm) amounting to just 0.03% of total costs for homicide or 3–6% for crimes with injuries, rape or sexual offences. 103
Overall, our evaluation showed that the Redthread YVIP intervention has the potential to reduce some risks of harm for young people and to be potentially self-financing if the intervention could avoid future use of health care. However, our research was limited by the small sample of patients, lack of a control group, inability to evaluate effectiveness and the subjective assessment of risks based on Redthread personnel (see also the limitations of the study).
Comparison with other studies
Global research on violence has identified the burden and costs that violence places on health and social prospects across the life course. 104 Violence affects not only health outcomes, quality of life and social choices that people make, but also has wider consequences on families, communities and society. 105 The acute treatment costs of penetrating trauma injury in England and Wales vary by patient, cause and body region of injury and treatment characteristics. The reported median cost of index admission for 532 patients aged 16+ years admitted to a MTC following knife-related injuries in a major UK city in 2018 was £4375. 95 This was lower than the costs reported previously for England and Wales, which were estimated at £7983 in 2008 by a Trauma Audit Research Network study, which focused on more severely injured patients and also included cost of prehospital care. 106 An earlier study, reviewing the cost of 187 gunshot injuries treated at a teaching hospital in Manchester, reported a mean cost of £2698 for patients admitted for inpatient care. 107 A study by Christensen et al. (2008),106 which examined the acute treatment costs of penetrating trauma injury in England and Wales, estimated average hospital costs of £7196 per penetrating injury due to stabbing. 106 In most of the studies, the ED costs are not identified separately from the total health-care costs. A study conducted in South Wales estimated that about 30.0% of assaults resulted in a visit to ED at a cost of £200 per attendance in 2019. 105
Our findings are consistent with other studies in England and Wales, showing that inpatient health-care costs are considerable and much higher than the costs of youth violence interventions. In fact, a 2020 study of the service, which looked at both health and social costs and benefits of Redthread’s YVIP,108 concluded that the programme may have a positive net economic and social benefit that was calculated at up to £4.90 economic and social benefit per £1 spent.
Strengths and limitations
While this study provides some insights on the main costs and risk reductions resulting from Redthread YVIP, it also has limitations which need to be taken into account. One limitation was that the information on costs from Redthread could not be directly linked with hospital data, and therefore we had to rely on an artificially constructed group of potentially similar patients to provide indicative, plausible inpatient costs for young people using the Redthread services. A second limitation was that findings from our analysis were based on a relatively small group of individuals (an impact of COVID-19 on hospital services) and were also limited from the lack of a comparable group with assault-related injuries.
The analysis of consequences was based on Redthread’s own risk assessment process. The answers to the risk assessment involved professional judgements of youth workers and their interpretation and therefore should be considered in this context.
Implications
Our analysis showed that young people attending Redthread YVIP report lower risk of experiencing further harm and a lower risk of not maintaining positive relationships with their family after completing the intervention programme. The cost of delivering the Rethread intervention per young person is considerably lower than the estimated inpatient costs for a comparable group.
Future studies need to collect detailed information on the costs of intervention, costs of the health-care treatment as well as the wider cost for society. Linking the data gathered on the young people attending the Redthread YVIP with hospital data and identifying a suitable control group will help to complete a full economic evaluation of the Redthread YVIP.
Chapter 7 Evaluating the quantitative impact of Redthread’s youth violence intervention programme: a feasibility assessment
What this chapter adds
-
For evaluating the benefits of the Redthread service, the impact on hospital reattendance rates is probably the easiest to quantify because of data availability.
-
After investigating a range of options for evaluating such impact, we found that none would be feasible within the timeframe of the project due to combinations of:
-
our inability to access individual person-level data for Redthread users due to lack of consent
-
relatively small numbers of young people who had so far engaged in the longer-term programme with Redthread at UCLH, leading to likely insufficiently powered analyses of the impact of that particular programme over the period of the research project
-
a difficulty in finding a representative control group from routine hospital data to match people engaging with Redthread
-
our inability to link national hospital inpatient and emergency care records due to the lack of linkable patient identifiers across the datasets
-
the difficulty in detecting the impact of the service among wider cohorts, such as people attending EDs with potentially eligible presentations
-
a lack of sufficient information in the ED data recorded by UCLH.
-
-
To enable the service to be evaluable, we recommend the following:
-
for Redthread to consider how to enable appropriate sharing of individual-level data on people who choose to engage and who choose not to engage with the service
-
for analysts to maintain reattendance as one measure of impact and work with clinicians and Redthread to develop criteria from routine hospital records that can be used to identify which attendances are potentially avoidable
-
similarly, if option 1 (see below) is the preferred evaluation model, then to develop criteria for identifying groups of patients attending other hospitals from which control groups can be selected
-
for clinicians to routinely record when a Redthread referral has been made by using the relevant code, rather than relying on free text
-
for UCLH to improve the coding of injury intent within their emergency care data, particularly of the ‘chief complaint’
-
that suitable geographical areas are decided upon between Redthread and UCLH, making it feasible to test an area-level approach (option 3).
-
Introduction
When we were scoping the project, it was unclear as to the extent to which we were going to be able to quantitatively evaluate the impact of the Redthread service. We therefore planned phase 1 as an investigation into the feasibility of such an evaluation: exploring the available data, how they could be used and assessing different evaluation methodologies. If a quantitative evaluation appeared feasible over the remaining time of the project, then this would be included in phase 2.
There are several potential benefits of hospital-based violence reduction services. For example, a report by NHS London recommends the following metrics:18
-
hospital reattendance rates
-
the number of people who receive an intervention or are offered support compared to the total number of young people attending hospital due to extra-familial harm
-
the number of young people completing goals within their personalised support plan
-
psychosocial or health and well-being questionnaires presented before and after a support programme.
For our evaluation, we focused on the impact on the use of hospital services, as there was potential for these to be more measurable over the duration of the project, and the data were more likely to be available. However, this does need to be balanced against the fact that a positive consequence of engaging with Redthread may be an increase in their engagement with health-care services and hence their likelihood to reattend hospital, even for harm-related incidents. Also, the influence of Redthread may not be limited to subsequent hospital attendance for just those who engage with the service, since any reduction in their likelihood of causing harm to others could reduce hospital attendances among the wider community.
In the rest of this chapter, we describe the options we proposed for analysis within phase 1, how each of them was assessed and our findings as to their relative feasibility. Although none of the options could be taken forward into phase 2, we conclude this chapter with recommendations for capture and processing of information that would allow the service to be evaluable in the future.
Methods
We considered three options for evaluating impact each reflecting a different perspective:
-
The impact on future use of hospital services for people:
-
engaging with the Redthread programme
-
referred to the programme
-
potentially eligible for the programme.
-
-
The impact on the use of emergency services at UCLH.
-
The impact on the use of hospital services among broader communities within which people engaging with Redthread live.
We assessed the feasibility of these options by:
-
presenting them to Redthread, UCLH and our expert advisers to gain their feedback as to which better matched their own expectations of impact
-
performing our own investigation into each option’s data requirements, including any access to individual person-level data, the linking of their records, the identification of comparators and the likelihood of detecting an impact
-
identifying the possible barriers to accessing the necessary data such as patient consent, information governance approvals and time.
Our measure of the future use of hospital services was attendance at ED and emergency admissions, where patients present with conditions or diagnoses that relate to activity that may be reduced as a consequence of the Redthread intervention, (e.g. violence-related injury, self-harm, substance abuse). Our reasons for choosing this measure were because we anticipated that data would be easier to obtain within the rapid context of the study, some of which we might already hold and have permission to use, and it has been used more widely in studies of similar services.
Since different young people have different levels of engagement with Redthread, it is important to establish which level of intervention is to be evaluated. For this report, we focus on assessments of the impact on individuals who were engaged in the longer-term programme rather than shorter-term crisis support. The reason for this is that it is likely to reveal greater benefits and is a more consistent intervention. Other evaluations have also taken this approach. 93 However, the options described in this section and our assessments of each one would also be relevant to evaluations using a wider definition of intervention.
General findings affecting the feasibility of an evaluation
Period of evaluation
The first year of data collection coincided with the COVID-19 lockdown and the service provided by Redthread was different in nature to the service that was implemented from April 2021 (see Chapter 1), and not one that they considered to be a model for an ongoing service. From an evaluation perspective, if we chose to focus on the more consistent service from April 2021, the numbers would be too few to observe any impact. If we included data from the previous year, there would be a question about the consistency of the service being evaluated.
Limitations of the emergency care dataset
The HES and ECDS to which we had access over the evaluation period could not be linked because the ECDS had no individual patient identifiers. This also meant that multiple attendances at ED for the same individual could not be identified.
Defining an appropriate measure of hospital attendance
Whichever option is chosen, identifying appropriate hospital attendances from the routine data is important, whether for measuring outcomes, past attendance histories or, in some options, selecting cases and controls. Ideally, relevant attendances would include those that are related to a person’s eligibility for YVIPs and which are potentially avoidable. 109 Although we can establish a list of codes for identifying relevant activity from routine hospital data, this can only be an approximation and, historically, UCLH has not coded ‘injury intent’ within the ‘chief complaint’ field in their ECDS. This indicates that an injury was sustained from an adverse event (as opposed to an accident) and is important for young people who are more likely to be exposed to violence and abuse. The completeness of this field is being addressed within the hospital.
One UK study of routine hospital inpatient data found that recurrent admissions were more common in young people with adversity-related injury than those with accidental injuries. 110 While it would be possible to identify these injuries in many cases within the admitted patient HES data, the available information in ECDS would make it harder for this distinction to be made. Also, the chances of detecting an impact will depend on adequate specificity (i.e. the chances that unavoidable reattendances are not selected). Possible codes that can be used to identify such activity within HES inpatient data and ECDS are shown in Appendix 3, Table 12.
Option 1a: targeted follow-up of patients engaged with the Redthread service
The aim of option 1a would be to assess the impact of engagement with Redthread on future hospital attendance (Figure 9). People engaging with the service (the ‘cases’) would be matched to a comparator cohort of patients (‘controls’) attending other hospitals without a similar youth violence prevention programme. Relevant future attendances would be those that corresponded to a specified range of conditions or reasons for attendance that could be potentially influenced by the service.
FIGURE 9.
Overview of option 1a.
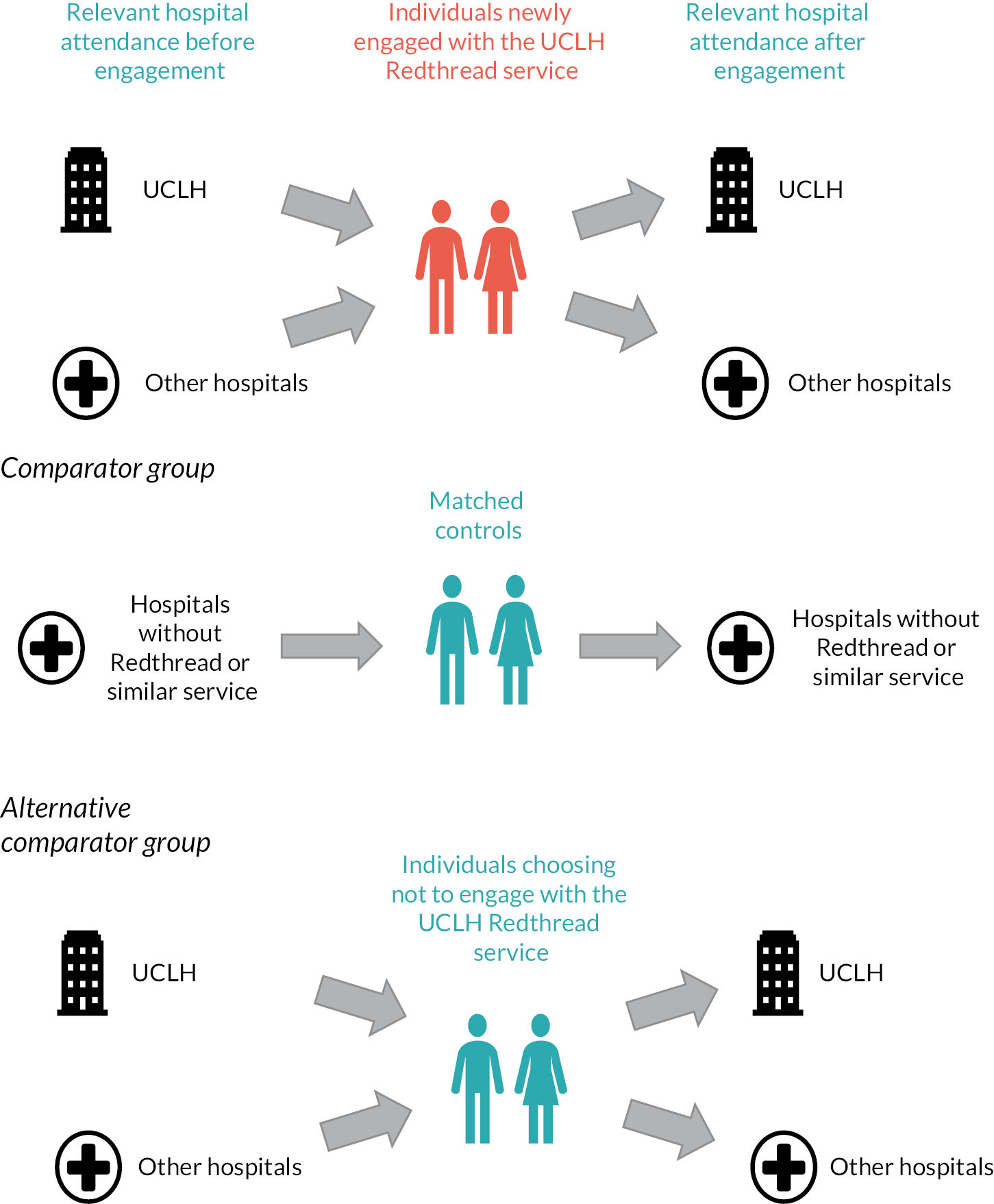
Data requirements
Cases would be identified from Redthread’s database and their records linked to routine hospital data. Reattendances would be extracted from links to national inpatient and emergency care data sets, namely HES and the ECDS for the ED. Identifying reattendances at other hospitals would be particularly important for UCLH services, where we estimate that of people aged 11–24 years who attend their ED, nearly half (47%) of their subsequent visits to ED (where they have one) will be at another hospital (see Appendix 2 and Figure 12). A link to national hospital data would also be important to enable us to assess past attendance histories, which, again, could be at other hospitals, and is likely to be an important matching variable. Linkage to HES and ECDS would need to be approved and carried out by NHS Digital.
FIGURE 12.
Proportion of subsequent ED reattendances by English acute trust between April 2018 and March 2020 following an initial ED visit to UCLH over the same period. Only the first reattendance for each individual is included.
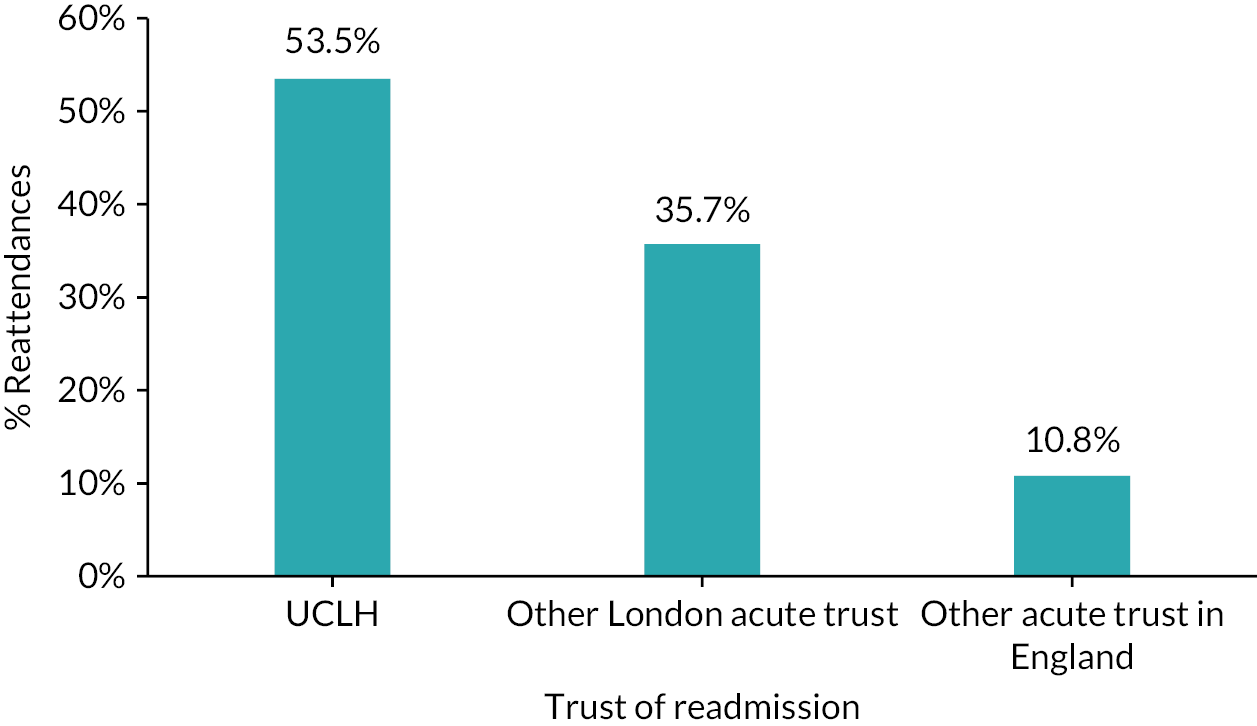
Redthread does collect its own data on reattendances up to two years after someone starts engaging with the programme. Staff gather these data retrospectively each month by identifying anyone who became engaged with Redthread in the same month one or two years previously and then searching the hospital records for any reattendances since. These reattendances are classified by Redthread as adversity or nonadversity related but are only picked up if they occur at UCLH.
An alternative means of collecting data might be to ask consenting individuals to report their own data, although this would rely on sufficient numbers consenting and maintaining reliable data returns.
Consent
Redthread’s typical consent process with the service user does not include sharing personal information beyond their own organisation (even if it is anonymised or pseudonymised). Therefore, sharing of individual user records from Redthread would not be possible, unless Redthread collect retrospective consent from young people, which is unlikely to get a high response rate, or we apply to use Section 251 of the NHS Act 2006. Section 251 involves the use of confidential patient information without the need for patient consent, subject to the approval of the confidentiality advisory group, and this would take several months. In addition, Redthread do not hold NHS numbers on their records, and this is a required identifier used by NHS Digital to carry out linkage.
Controls or comparators
The comparator group could be a cohort of patients attending hospitals in London without a similar violence prevention scheme, whose characteristics suggest that they might be eligible for, and likely to engage with, Redthread services. These patients would need to be identified from routine administrative hospital data. Although we could match on patient characteristics and reasons for hospital attendance, there are several noncoded features that could be highly relevant to the reason why the young person has been considered eligible for Redthread, which would make it difficult to establish the accuracy of any matching.
An alternative control group could be people who are referred to the Redthread service but do not engage with it. Again, there could be key differences in person characteristics that are not identifiable in the data and may introduce important biases, but if referrals are coded within the routine hospital data this may be a more achievable option.
Chances of detecting an impact
Based on evidence of the potential impact of similar services, we estimate that 110 people who engaged with the service would need to have been followed for six months to have an 80% chance of detecting a 10% reduction in reattendance. With longer follow-up and a greater assumed impact, the sample size could be smaller. Further details of this analysis, including projected sample sizes under different assumptions, are shown in Appendix 4 and Figure 13. From February 2020 to December 2021, a total of 59 young people engaged with the full longer-term programme rather than shorter-term crisis support; with an engagement rate of about five per month, we estimated that a total of 110 would be reached by the end of October 2022. If the aim were to evaluate only the service that had been operating since April 2021, then it would take somewhat longer. These calculations were for measuring the impact on those engaged in the longer-term programme in terms of hospital reattendance. If we included people receiving shorter-term crisis support, then it might take a shorter time to reach the required cohort size, although the required cohort size could be larger if the assumed impact of such support is less.
FIGURE 13.
Estimated sample sizes required under different assumptions of baseline reattendance rates and the effect of the Redthread intervention to achieve 80% power.
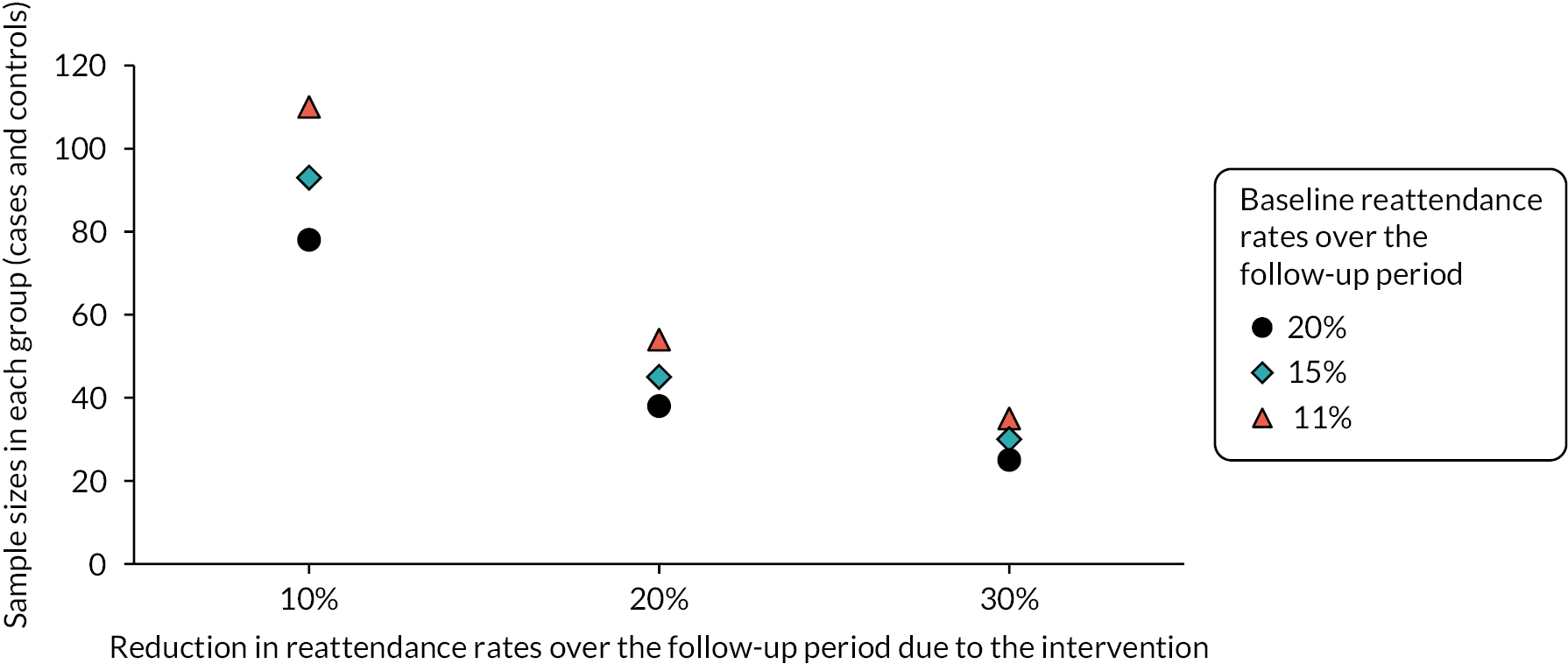
Summary of advantages and disadvantages of this option
This option is the only one that follows up cohorts of matched cases and controls and may be the most robust design of the options being considered, also offering most statistical power. However, being able to identify an appropriate control group remains an important barrier and the approach would have to accommodate the consenting process. Moreover, it does not account for the positive impact Redthread service users might have on others in the community. For example, by indirectly influencing a reduction in the numbers of hospital attendances of others.
Option 1b: targeted follow-up of patients referred to the Redthread service
The design of this analysis would be similar to option 1a (see Figure 9), where the cases include all patients who are referred to Redthread, not just those who engage with the programme. This is therefore more akin to an intention-to-treat approach.
Data requirements
Referrals cannot be reliably identified from the hospital’s own data unless referrals are better coded within the local hospital records, for example, by using a SNOMED code for violence reduction services, such as SCTID: 410236002, Violence control education (procedure), (see Chapter 5). There is a process for using such codes within UCLH but this was not applied in at least 85% of cases. If such codes were reported in the national ECDS there would be no need to link local to national records, an analysis could be carried out with ECDS and inpatient HES data. However, this relies on accurate clinical coding and may miss patients who are not referred through ED or are picked up through Redthread’s own data searches.
Consent
Once a referral is coded, all analysis would be based on routine hospital records, although the importance of consent is unclear, given that not all referrals will be engaging with the Redthread service. As a service evaluation conducted by UCLH with the intention of improving service delivery there may be no need for consent, although ethics approvals would still be required.
Controls or comparators
For this option, the control group would have to come from other hospitals, with associated challenges as described under option 1a.
Size of cohort
Since not all the cohort would be receiving the intervention, a larger sample would be needed to achieve appropriate statistical power. Also, if the referral code is only applied to ED records, people referred from departments other than ED may not be picked up.
Summary of advantages and disadvantages of this option
This option may circumvent the need to gain consent from people engaging with Redthread, since Redthread’s own data would not be used, but this is currently unclear. The other issues associated with option 1a around selecting appropriate controls and measuring benefits within a community remain. Also, people not referred through ED may be missed. Between February 2020 and December 2021, 43% of referrals were engaged with the service either in the longer-term programme of work (15%) or shorter-term crisis support (28%) so any impact of the intervention over that period would only be observed among a minority of cases and would therefore be harder to detect. However, since after the COVID-19 restrictions the service has been operating more as intended, engagement rates are expected to be higher which raises the power of this approach.
Option 1c: targeted follow-up of patients potentially eligible for the Redthread service
This analysis would have a similar matched case–control design as illustrated in Figure 9 (without the alternative comparator group), but cases would be identified from routine hospital records as individuals potentially eligible for the Redthread service. Therefore, this is essentially an evaluation of the impact of the Redthread intervention on eligible young people attending hospital as a whole group, rather than just on those who receive the service.
Data requirements
Data would all come from routine hospital records.
Selecting cases
There would be a major challenge in identifying who could be eligible for Redthread from the routine data. As mentioned above, when discussing the problems with identifying control groups under option 1a, there are several noncoded features that could be highly relevant to the reason why the young person has been considered eligible for Redthread. For example, it may not be obvious that a young person presenting at hospital is at risk, but a clinician may have reason to suspect they are a victim of an adverse event and would benefit from Redthread support.
Based on the list of clinical codes we identified within the ECDS, (see Appendix 3 and Table 12) we found 3275 patients aged 11–24 years who may have been eligible for Redthread attending ED between February 2020 and August 2021. As a comparison, over the same period, far fewer young people were referred to Redthread: 252 in all, of whom 43 became engaged in a longer-term programme with the service. There may be ways of improving the criteria for selecting potentially eligible people with more detailed analyses of hospital data but, as mentioned above, the data for UCLH are incomplete for some of the key fields that would help.
Consent
Since we would not know which of the cases actually engage with Redthread, the consenting issue for Redthread users would not be an issue.
Controls or comparators
Control groups derived from routine hospital data would be a better match than under options 1a and 1b, since the same fields would be used to identify both cases and controls. There would also be no data linkage required between information held on Redthread’s system and routine hospital data.
Size of cohort
Because a potentially eligible cohort derived in this way is so much larger than numbers referred to or engaging with Redthread, analysis of that cohort would be very likely to miss any direct impact of Redthread. This analysis is better viewed as an assessment of the service on the whole cohort of eligible young people attending UCLH.
Summary of advantages and disadvantages of this option
This option circumvents the need to gain consent from people engaging with Redthread, since Redthread’s own data would not be used. Also, it would be possible to obtain a better-matched control group. However, the issue associated with option 1a around selecting appropriate controls and measuring benefits within a community remains. Unless it becomes possible to identify eligible young people from the routine data with a reasonable degree of accuracy, any impact will only be observed among a minority of cases and therefore harder to detect.
Option 2: assessment of the impact of Redthread on emergency services at UCLH
The aim of this option would be to analyse the impact the Redthread service has on attendance at UCLH emergency services, particularly among individuals aged 11–24 years where the reasons for attendance may indicate that the young person was eligible for Redthread intervention or support (Figure 10). Differences in attendance before and after Redthread services were in operation would be compared with changes in attendance at other hospitals over the same period. Redthread (or other similar services) would not be operating at these other hospitals. To account for variable case mix, the populations would be directly standardised against a baseline national population. The ‘before’ period should probably predate the COVID-19 pandemic.
FIGURE 10.
Overview of option 2.
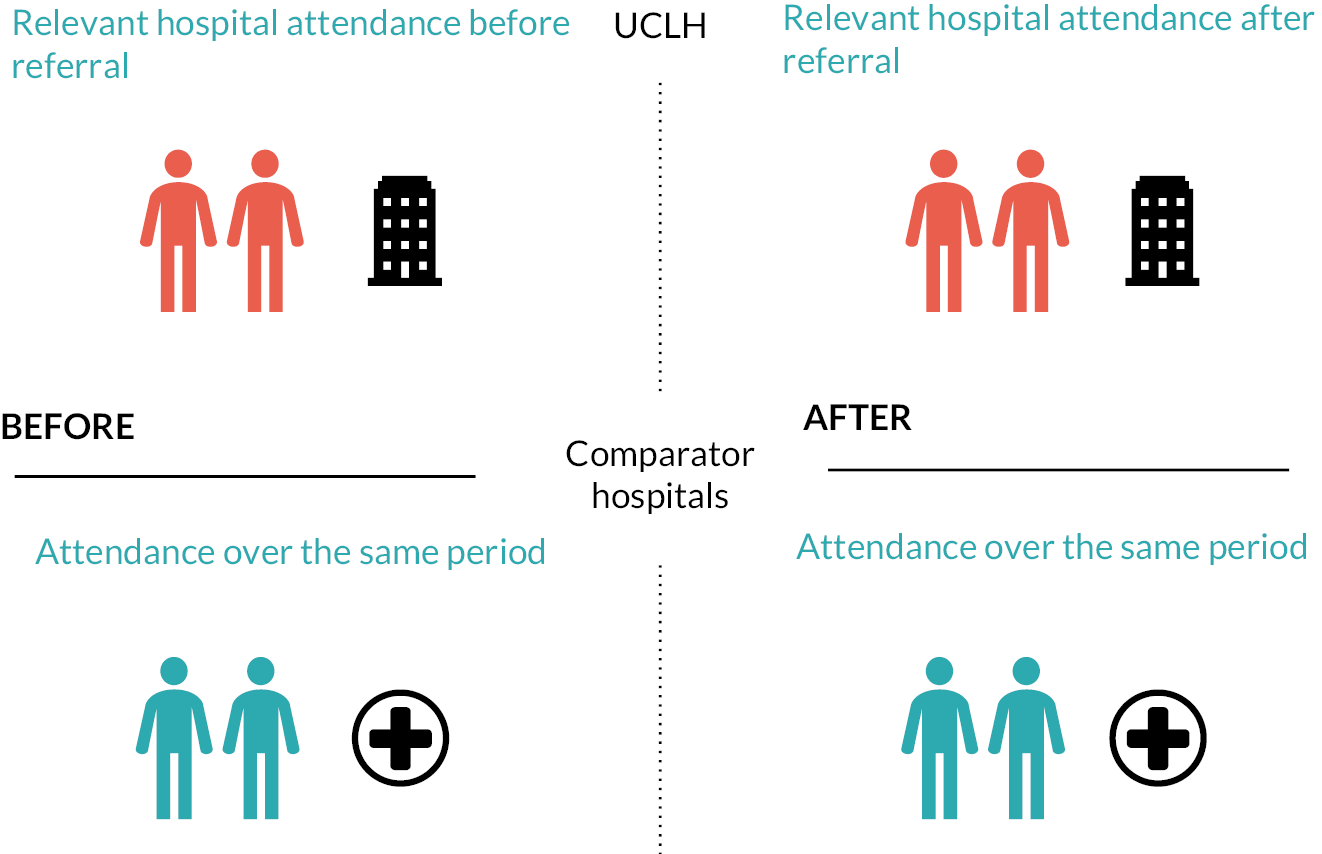
Data requirements
Data would all come from routine national datasets.
Consent
This analysis would only use routine data sets and would not be able to identify people engaging with Redthread, so no further consent would be needed.
Controls or comparators
Comparator hospitals would not be operating a YVIP over the same period. Ideally, these would be within London but, given the increasing prevalence of these programmes, it may be challenging to find such hospitals. However, since this is a before–after comparison, we could pick hospitals where they have such a service but where its use over the study period has remained stable.
Size of cohort
As mentioned under option 1c, we found 3275 patients aged 11–24 years who may have been eligible for Redthread attending the ED at UCLH between February 2020 and August 2021. However, this analysis relies on being able to identify groups of patients attending emergency services that would be specific enough for the evaluators to notice any impact Redthread might be having. This is unlikely to be achieved unless better eligibility criteria can be derived from the routine data.
Summary of advantages and disadvantages of this option
As with options 1a, 1b and 1c, if Redthread users become less likely to be involved with violence themselves, they would be indirectly influencing wider numbers of admissions, which would not be measured using this approach. Also, as with option 1c, unless it would be possible to identify eligible young people from the routine data with a reasonable degree of accuracy, any impact will only be observed among a minority of cases and therefore harder to detect.
As young people could be attending several different EDs in London, an analysis that only focuses on one hospital would lose any impact of Redthread services on attendances elsewhere. As mentioned above, just under half of reattendances to ED at English NHS hospitals following a visit to the UCLH department are at another hospital.
Option 3: assessment of the impact of Redthread on local communities
The aim of the third option would be to assess the impact a person’s engagement with Redthread might have on hospital attendances within the local neighbourhood in which the person lives (Figure 11). This would therefore also account for positive influences on others who may, themselves, become victims of violence or abuse and may be observable from patterns of area-level ED attendance and inpatient admission.
FIGURE 11.
Overview of option 3.
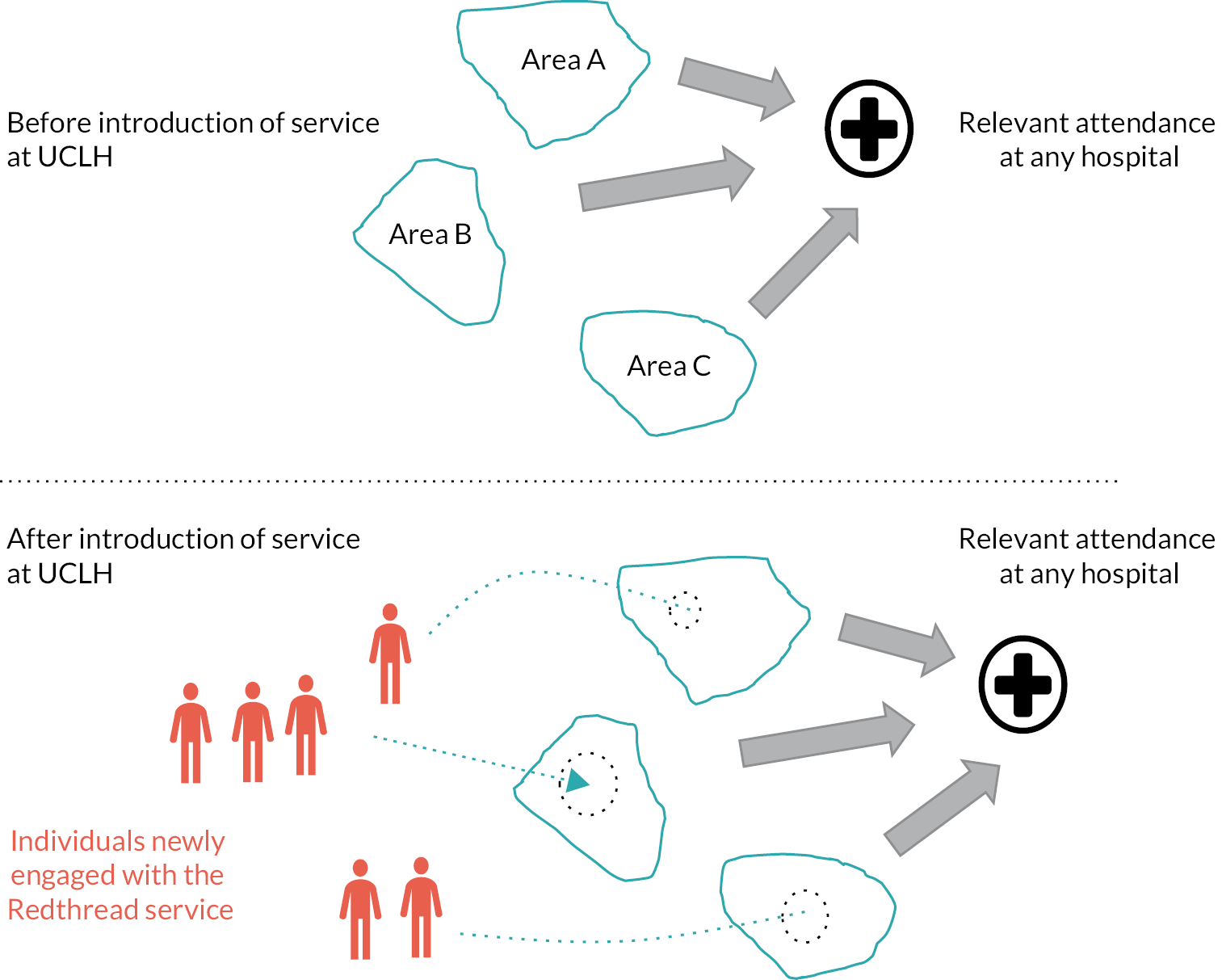
Analysis would investigate the relationship between the number of local people who have engaged with Redthread over time and changes in hospital attendance for residents of the same area. As with the previous options, criteria could be developed to allow a focus on attendances that are considered most relevant.
Supporting evidence for this approach
A previous literature review included the finding that violence in London is highly geographically concentrated, and a London-wide picture can mask significant variation between areas. 20 This report also confirms that many forms of violent crime are heavily clustered in a small proportion of lower super-output areas, so when responding to the problem of high instances of violence, a localised approach is valuable. If the Redthread intervention reaches individuals who are involved in gang-related violence, these areas may see an overall reduction in hospital presentations.
Data requirements
Areas where people engaging with Redthread live could be provided by Redthread themselves, thereby avoiding any need to link to hospital records. Other areas with similar characteristics where no one is engaging with Redthread should also be selected. Data on hospital attendance would come from HES and ECDS as before, although we would need to identify a suitable area of residence. Neighbourhoods could be defined as middle super-output areas (MSOA), census areas of mean population size of around 7200, which are recorded by Redthread. However, even though a MSOA field is available in ECDS, it is not currently populated. Other area fields are populated, however, such as electoral ward, but they would need to be used consistently across datasets.
Consent
Redthread would need to provide information about where their service users lived, which would be the only data required from them. Although there would be no explicit means to identify Redthread users in the hospital data, knowledge about UCLH attendance and area of residence might be enough to identify them in routine data. Where there were sufficiently high numbers within an area, aggregated numbers would be sufficient. Where there were small numbers, it might be possible to exclude those areas, given that the local impact might be small anyway, although the number of areas that are thus removed would need to be low in relation to those that are included.
Controls or comparators
Because this analysis is investigating relationships between levels of engagement in an area to outcomes there is no need for a comparator.
Likelihood of detecting any impact
Earlier in the project, we received data from Redthread that showed that of 28 people who were engaged in a longer-term programme, they were resident in a total of at least 16 MSOAs, and due to low numbers, some MSOAs had to be combined. This suggests that they may be too dispersed among different MSOAs and too low in number in comparison to relevant hospital attendance activity within the area, thus reducing the ability of such an analysis to detect Redthread’s impact. Since the MSOA field has not been populated in the national emergency care data, this is difficult to determine. However, we recommend improved coding or using areas that are recorded, such as electoral ward, so that the feasibility of an area-level option can be tested further.
Summary of advantages and disadvantages of this option
This option would not need to explicitly identify control groups and is the only option that takes account of any wider positive influence engagement that Redthread may have on local communities.
This approach assumes that any equivalent service at other hospitals remains stable for both before and after periods, so that any differences in hospital activity can mostly be attributed to the Redthread intervention at UCLH. To mitigate any problems, we could restrict to areas where this is more likely to be the case – so that the dominant change in service is that at UCLH.
Summary of options
Table 11 compares and summarises the requirements and issues associated with each option.
| Option | |||||
|---|---|---|---|---|---|
| 1a Matched case–control |
1b Intention to treat |
1c Evaluation of the eligible |
2 Before and after |
3 Geographical impact |
|
| Data requirements | Redthread data linked to routine national hospital ED and inpatient records | Routine national hospital ED and inpatient records with a referral code used by UCLH | Routine national hospital ED and inpatient records | Routine national hospital ED and inpatient records | Routine national hospital ED and inpatient records Redthread data for areas of residence |
| Cases | Patients identified from Redthread data | Patients identified as referrals in routine hospital records | Patients identified as ‘eligible’ from routine hospital records using diagnosis and reason for attendance codes | Relevant ED attendances and inpatient admissions from routine hospital records using diagnosis and reason for attendance codes | People aged 11–24 years resident in local geographical areas, many of which, but not necessarily all, are where there are people engaging with Redthread |
| Consent | Consent required from Redthread service users or Section 251 approval | Consent may still need to be required, but this is to be determined | No further consent required | No further consent required | Consent required from Redthread service users where numbers are small, but possible to work with aggregated data |
| Selecting relevant hospital attendances from routine data | Relevant ED attendances and admissions from routine hospital records using diagnosis and reason for attendance codes | Relevant ED attendances and admissions from routine hospital records using diagnosis and reason for attendance codes | Relevant ED attendances and admissions from routine hospital records using diagnosis and reason for attendance codes | Relevant ED attendances and admissions from routine hospital records using diagnosis and reason for attendance codes | Relevant ED attendances and admissions from routine hospital records using diagnosis and reason for attendance codes |
| Controls or comparators | Relevant ED attendances and admissions from hospitals without a YVIP using codes relating to diagnosis and chief complaint; alternatively, compare young people who choose to engage with the UCLH service with those who choose not to | Relevant ED attendances and admissions from hospitals without a YVIP using codes relating to diagnosis and chief complaint | Relevant ED attendances and admissions from hospitals without a YVIP using codes relating to diagnosis and chief complaint | Hospitals without a YVIP | Each area is compared against each other; no formal controls needed |
| Chances of detecting an impact | Approximately 110 cases required to observe a 10% reduction in attendance | A larger sample size needed as many referrals would not engage with the service | This depends on how well ‘eligible’ people can be identified from the data. Although many eligible people will not engage, and there is a risk some wrongly identified as ineligible will engage | There is a risk that the number of people who engage with Redthread is much smaller than the number of attendances or admissions that are counted as relevant | There is a risk that the number of relevant attendances or admissions from an area could be much greater than those that could be influenced by people engaging with Redthread |
| Other advantages | The most focused group of cases which is likely to have the best statistical power; the option that met with most approval by Redthread and UCLH | Can use routine hospital data exclusively, provided Redthread referrals are coded | Can use routine hospital data exclusively; a suitably matched control group would be easier to obtain | Can use routine hospital data exclusively; no need to link ECDS and HES records | Attempts to measure the impact of those engaging with Redthread on others in the community; no need to link ECDS and HES records |
| Disadvantages | No measure of the impact of those engaging with Redthread on others in the community; gaining consent from Redthread service users; an appropriate control group may be hard to establish from routine hospital data | Relies on coding of referrals; no measure of the impact of those engaging with Redthread on others in the community; an appropriate control group may be hard to establish from routine hospital data; harder to detect an impact that may exist; there may be issues with gaining consent | No measure of the impact of those engaging with Redthread on others in the community; harder to detect an impact that may exist; identifying eligible referrals from the routine hospital data | No measure of the impact of those engaging with Redthread on others in the community; no measure of the impact on attendances at other hospitals; may be hard to detect an impact that may exist | Statistical power currently unclear |
| Reasons why currently infeasible | Consenting process does not allow access to individual patient records from Redthread or linkage to national hospital records; Section 251 application was not feasible over the time period of the project; Nuffield Trust is currently not able to link HES with the ECDS | Referrals are only infrequently coded in the national data; Nuffield Trust is currently not able to link HES with the ECDS | Identification of eligible patients within the hospital data has not been sufficiently precise; Nuffield Trust is currently not able to link HES with the ECDS | Identification of relevant attendances and admissions in the hospital data has not been sufficiently precise | MSOAs of residence not reported in the national emergency care data which has hindered analysis using the area codes provided by Redthread |
Conclusions and recommendations
None of the options for analysis of impact has been feasible within the timescale for the project for the following reasons:
-
Gaining any consent to link data relating to people engaging with Redthread was not going to be possible.
-
The time it would take to gain further approvals to use linked data would put the completion of the project within the agreed timescale at risk and approvals would not be guaranteed.
-
The evaluation team did not have the facility to link emergency care and inpatient records.
-
COVID-19 had a major impact on the implementation of the service and corresponding recruitment numbers.
-
It was not possible to identify eligible groups of patients from routine hospital data with sufficient sensitivity and specificity.
Our options for assessment of impact have been limited to measuring reattendance, since this has been seen as the only feasible outcome that can be explored with the data available. However, this raises two important questions: first, how well one can identify from routine hospital records which reattendances would be potentially avoidable and, second, how well reattendance avoidance reflects all the advantages of using Redthread.
For this rapid evaluation, we have concluded that the best outcome would be to address the barriers and suggest ways forward to facilitate future evaluation of the Redthread service at UCLH and youth violence reduction services at other hospitals. The most effective options are likely to be either option 1a or option 3, although there is still some uncertainty about how well the impact of Redthread can be detected in area-level data.
Our recommendations are:
-
For Redthread to consider how to enable appropriate sharing of individual-level data on people who choose to engage and who choose not to engage with the service, along with the levels of engagement.
-
For analysts to maintain reattendance as one measure of impact and work with clinicians and Redthread to develop criteria from routine hospital records that can be used to identify which attendances are potentially avoidable.
-
Similarly, if option 1 is the preferred evaluation model, to develop criteria for identifying groups of patients attending other hospitals from which control groups can be selected. For clinicians to routinely record when a Redthread referral has been made by using the relevant code, rather than relying on free text.
-
For UCLH to improve the coding of injury intent within their emergency care data, particularly of the ‘chief complaint’.
-
That suitable geographical areas are decided upon between Redthread and UCLH, making it feasible to test an area-level approach (option 3).
Chapter 8 Discussions and conclusions
Overview
This study was a mixed-methods evaluation of the implementation and local impact of the Redthread YVIP service at UCLH.
We carried out searches for available evidence on hospital-based violent crime interventions for young people and reviewed existing and current evaluations of Redthread interventions (see Chapter 3). We also evaluated processes of implementation of the Redthread service at UCLH at different time points and developed an understanding of the programme theory (what Redthread call their ‘theory of change’) and factors that had enabled the service to be embedded in children, adolescent and young adults’ services at UCLH (see Chapter 4).
We reviewed the data being used and created by Redthread to manage the YVIP service at UCLH (see Chapter 5) and assessed the feasibility of using these data, in combination with other secondary datasets, undertake a cost analysis (see Chapter 6) and evaluate the impact of the service (see Chapter 7).
In this chapter, we provide a summary of our key findings. We also discuss the lessons learned in the context of the existing evidence, the strengths and limitations of our evaluation, recommendations for future research and conclusions.
Summary of key findings
Below, we describe our key findings.
Evidence reviews and current evaluation evidence (Chapter 3)
-
Available evidence indicates that young people who present in EDs from physical violent injury (e.g. arising from gun and knife crime) are at significant risk of repeat injury. Moreover, children and young people are vulnerable to a variety of risks in the community and can therefore re-present to EDs due to different forms of harm: physical assault interpersonal violence, substance misuse and severe mental health problems related to safeguarding issues.
-
To address young people’s exposure to risk and safeguarding harms, hospitals have introduced youth violence interventions within EDs and trauma centres that are focused on behavioural change. Hospital-based YVIPs are one approach and aim to reduce a young person’s overall risk of harm and reinjury. Most of the evidence base on these interventions comes from the United States. These programmes typically focus on gun injuries in the American health system context with injury recidivism tracked as a primary outcome, using hospital data.
-
Evidence suggests that YVIP can reduce reinjury. However, a problem with assessing the evidence base is the heterogeneity found across youth-based hospital interventions as a whole in terms of the nature of the intervention and how outcomes are reported. Some are brief behavioural interventions, some involve hospital social workers as opposed to youth workers, programmes can target different age ranges (e.g. young adults up to 30 years of age in some cases) and studies can include relatively small sample sizes.
-
In the context of high health treatment costs in the United States for gun injury, the evidence suggests youth violence interventions can be cost-effective where they help to prevent violent incidences.
-
The literature also highlights ongoing issues with data sharing across hospitals, meaning that measuring outcomes for repeat injury across different geographies and health providers, or systems, remains difficult.
-
Our review confirmed there is limited evidence from the UK health system, in particular about the impact of youth violence and youth worker hospital interventions focused on prevention.
Assessment of programme theory and implementation at UCLH (Chapter 4)
-
Within UCLH’s adolescent and paediatric services, the Redthread service is viewed positively and as filling a gap in service provision. Redthread’s status as an independent, non-statutory service was viewed as a factor which enabled vulnerable young people to share information with a youth worker. This information was often useful to clinicians and could help inform patient care. A youth worker could also advocate for young people within the hospital setting, and bridge services within the community (e.g. housing, specialist support services, social care and education). This underscores the importance to front-line clinicians of having stronger links with the community to support vulnerable young people following their discharge from hospital, especially those for whom child safeguarding protocols no longer apply (e.g. those aged over 18 years).
-
Paediatricians, child safeguarding experts and child and adolescent psychiatrists are particular champions of the Redthread service, perceiving that it not only fulfils a need for young people not met by standard clinical care, but that youth workers can help a young person to better engage in their medical care and treatment. The service is not viewed as duplicating other services or roles at UCLH (e.g. hospital social workers, playworkers or child safeguarding).
-
In practice, Redthread’s service goes beyond the ‘teachable moment’ (which provides an opportunity for dialogue with a young person about their health risk and personal motivation to introduce behavioural changes in their life). For example, Redthread has been engaged in a range of activities at UCLH, including:
-
long-term case management work (e.g. this could be up to six months, or more, engagement with a youth worker). This is intensive support for young people at highest risk of harm, commonly with complex social and family situations and who have experienced trauma
-
on-site short-term crisis support within the hospital (e.g. helping the person to get food, providing reassurance)
-
education and training for hospital and external staff (e.g. on contextual safeguarding); for example, with respect to safeguarding young people aged 11–24 years and how to engage positively with a young person in distress
-
awareness-raising and other communications within UCLH, for example attending safeguarding meetings, and activity to promote to staff how to make a referral.
-
-
The service was severely disrupted by the COVID-19 pandemic, and this impacted on the embedding of the Redthread service beyond paediatrics and adolescent services, affecting its influence within the adult ED in particular. Redthread is normally dependent on youth workers’ physical presence in EDs, however, youth workers were not on site at UCLH for some of the period, from March 2020 to April 2021. While the charity continued to provide case management support to young people virtually (which many young people were reported to like due to their habitual use of mobile devices), a lack of physical youth worker presence will have resulted in lower staff awareness of the service.
-
By winter 2021/22, Redthread was perceived to be well embedded in the paediatric ED and adolescent services (including wards), and there was increasing awareness of the service in outpatient departments which saw vulnerable young people with chronic illness. Redthread and clinical staff noted that more could be done to raise staff awareness of Redthread across the trust, especially among nurses, junior doctors and other staff working in adult ED. This is particularly important due to staff changes and turnover (e.g. rotations).
-
Identification of eligible young people was not solely dependent on youth workers being in ED, either paediatric or adult ED. Referral routes at UCLH were diverse and could come from other inpatient services. Changes had arisen due partly to the impact of COVID-19, therefore the identification of eligible referrals went beyond ED services.
-
Reasons for referral were by no means limited to young people with knife injuries or those who had been subject to sexual or physical assaults, but also included substance misuse, suicidal ideation and mental health crises. Staff observed a particular increase in young people presenting with severe mental health problems and distress on account of disruption caused by the COVID-19 pandemic (e.g. domestic violence and family instability). This raised questions about the most appropriate referral criteria for the service, given that Redthread is not a mental health crisis service.
-
The key implementation barriers faced were:
-
the impact of the COVID-19 pandemic, with paediatric and adolescent services being temporarily moved away from UCLH to neighbouring London trusts
-
UCLH staff changes and turnover during the implementation period which necessitates regular staff training to ensure all staff are aware of the service and how to refer
-
lack of physical space for Redthread (e.g. office space to ensure their presence and have confidential discussions with young people)
-
difficulties engaging young people aged over 18 years presenting in the adult ED, unless a clinician was aware of the Redthread service and had obtained consent prior to their discharge.
-
-
Staff suggested the following enablers were key to successful embedding of the service:
-
‘invested’ senior clinical and operational staff to champion the service locally and across departments (e.g. senior clinicians and ED managers)
-
integration of Redthread youth workers within hospital processes for identifying vulnerable young people and discussing their care (e.g. MDT inpatient reviews, safeguarding meetings, safety planning)
-
physical space near ED for engaging with young people (e.g. for confidential discussions)
-
electronic health-care record integration (e.g. Epic) which has been especially useful for enabling referrals to be made directly by clinicians when youth workers are off site; indeed, some staff even suggested a prompt might be helpful to remind clinicians they can refer an eligible young person to Redthread.
-
clear standard operating procedures have been agreed between the hospital and Redthread.
-
Description and review of data used to manage the Redthread service at UCLH (Chapter 5)
-
Redthread collect a wealth of data on individuals, particularly on those who engage longer term with the service. Data on engagement rates support the qualitative finding that a greater proportion of 11- to 17-year-olds referred to Redthread receive some form of support from the service (59%) compared with those aged 18–24 years (23%).
-
Describing the service users and measuring outcomes was challenging in the absence of linkage between Redthread data and routine health-care data. The main limitations to using Redthread data in isolation included:
-
Redthread’s consent model did not allow individual-level records to be shared beyond their organisation, and we could only analyse aggregated data
-
aggregated data could not be analysed with respect to multiple characteristics at the same time, so we could not establish whether there were inequalities in engagement levels within specific groups
-
data on hospital activity of service users were not regularly captured by Redthread and, when collected, only showed activity within UCLH. This is in the context of a hospital where nearly half of all 11- to 24-year-olds who reattended after an initial ED attendance did so at another hospital trust.
-
-
There were also limitations to only using data from UCLH’s patient administration system:
-
Redthread referrals were not consistently flagged, and where they had been recorded, there was no indication as to whether the individuals had accepted or declined support
-
UCLH did not systematically record information relating to the intent behind injuries, which would have helped us to understand whether an individual might have been eligible to receive Redthread services.
-
-
To improve identification of the eligible cohort, referrals to Redthread services should be recorded in a dedicated data field, and the injury intent emergency care data field should be completed, so that potentially relevant hospital attendances can be drawn out from the data more easily.
-
With respect to new hospital-based YVIPs, we recommend that prior to service roll-out, sufficient time is earmarked for setting out data requirements and to ascertain the feasibility of reasonable options for robust quantitative evaluation.
Costs of service at UCLH (Chapter 6)
-
We were unable to conduct a CEA due to a lack of good quality evidence describing the impacts of YVIPs on subsequent use of hospital services.
-
A CCA showed that there was a statistically significant decrease in assessed risks for young people engaged for longer-term YVIP support for the period April 2020 to November 2021 for the following risks:
-
‘experiencing further harm’
-
‘not maintaining positive relationships with family’.
-
-
The mean cost per person engaging with Redthread support, over a 21-month period was calculated to be £1865.
-
The mean cost for the emergency inpatient treatment of an artificially constructed group, similar to those likely to be referred to Redthread in UCLH, was estimated to be £5789 while the mean cost per attendance at the ED was £203.
-
Interpretation of these results should be made with caution due to our research being limited by the small sample of patients, lack of a control group, inability to evaluate effectiveness and the subjective assessment of risks based on Redthread personnel.
Feasibility of quantitative evaluation of service at UCLH (Chapter 7)
-
Redthread aims to have a positive impact across a wide range of aspects of young people’s lives, for example in education, crime, housing, benefits and employment, as well as reducing attendance at hospital. We focused on the latter as we considered it easier to quantify and monitor given the available data.
-
We considered a number of possible options for a rapid quantitative evaluation of the impact of the service but concluded that none of them would be currently feasible. The reasons for this are due to combinations of the following, some of which overlap with the data limitations described above:
-
relatively small numbers of young people have so far engaged in the longer-term programme with Redthread at UCLH, leading to likely insufficiently powered analyses of the impact of that particular programme over the period of the research project
-
lack of consent to enable access to individual person-level data for Redthread users to link to hospital administrative data
-
likely difficulty in being able to detect the impact of the service among wider cohorts (such as in people attending ED with potentially eligible presentations)
-
a lack of key information recorded in UCLH ED records; for example, information about the most likely human intent of the injury, and patient engagement with the violence intervention programme
-
our inability to link national hospital inpatient and emergency care records due to the lack of linkable patient identifiers across the datasets
-
the difficulty in identifying comparable control groups from routine hospital data.
-
-
We contend that, were data and governance barriers able to be resolved, the two most promising options for quantitative evaluation would be ones:
-
comparing the data of young people engaged with Redthread to a set of appropriately matched control individuals, and
-
studying the impact of Redthread at small area level.
-
-
We have therefore made recommendations to facilitate future evaluation:
-
For analysts to use reattendance as one measure of impact, and work with clinicians and Redthread to develop criteria from routine hospital records that can be used to identify which attendances are potentially avoidable.
-
Similarly, develop criteria for identifying groups of patients attending other hospitals from which control groups can be selected.
-
For Redthread and acute hospital partners to consider mechanisms by which information from the service, as to who chooses to engage with different levels of support, and who chooses not to engage, can be linked to the routine data for analysis purposes.
-
For clinicians to routinely record when a Redthread referral has been made by using the relevant code in the patient administration system, rather than only using free text. If a person is identified by Redthread themselves, then for this to be also flagged in the routine patient data.
-
That suitable geographical areas are decided upon between Redthread and UCLH, making it feasible to test an area-level approach.
-
How findings relate to previous research
In this section we present our findings in relation to previous research.
Service implementation
Several findings from this evaluation at UCLH align with observations from Redthread evaluations at other NHS trusts.
First, NHS staff are receptive to youth workers being on site and value Redthread as an independent, expert, professional service which fills a gap within current NHS provision and has potential to bridge secondary health-care and community services.
Second, the critical importance of timely consent of young people within emergency settings, given the ‘opt-in’ model that underpins the charity’s programme theory and ethos (i.e. young people must voluntarily engage with the service). However, compared with MTCs in London (e.g. St Mary’s Hospital, St George’s Hospital), it appears that young people referred to the service at UCLH comprise a different population profile going beyond the local geographical boundaries (because of transport links) and have different physical injuries to those commonly arising from assault and gang violence (e.g. gun shot and knife wounds, which are usually directed to London MTCs). Therefore, even if gang involvement is directly or indirectly suspected in a case, clinicians speak of complex presentations and treating young people who are victims of sexual abuse, domestic violence, have severe mental health problems or a long-term condition that has flared up due to social factors (e.g. peer intimidation, family conflict). A youth worker’s case load at UCLH might therefore extend beyond short-term crisis support work to providing longer-term support beyond six months, and to helping young people who are not from the local borough and who require advocacy across statutory services both inside and outside of London. This suggests that the Redthread service model for local hospitals (such as UCLH) requires adaptation to reflect differences from MTCs, for example, more diverse referral pathways beyond adult ED including outpatients and specialist paediatric and adolescent services.
Finally, this NIHR RSET evaluation concords with an evaluation in the Midlands that found that services such as Redthread rely on ‘highly motivated individuals to promote adoption by giving access to NHS organisations, leveraging personal and professional networks and internal lobbying’. 80
Quantitative impact
Consistent good-quality evidence on the impact of violence intervention schemes on subsequent health-care use and other related outcomes has been lacking (see Chapter 3). As discussed in Chapters 5 and 7, we have not been able to contribute our own quantitative assessment of impact but have made recommendations for future evaluations. However, our reflections are in accordance with observations made in a qualitative evaluation of Redthread’s YVIP expansion into sites in the Midlands,35 where one of several ‘potential threats and barriers’ was identified as being ‘A failure to value and integrate routine data to describe how YVIPs are supporting the work of NHS and other staff, ensuring safety after discharge and securing engagement with community-based services’.
Costs
The acute treatment costs of penetrating trauma injury in England and Wales vary by patient, cause and body region of injury and treatment characteristics. Our findings are consistent with other studies in England and Wales showing that health-care costs are considerable and much higher than the costs of YVIP interventions. The costs reported for England and Wales, in 2008 by a Trauma Audit Research Network study, which focused on more severely injured patients and also included cost of prehospital care were estimated at £7983. 106 Another study, reviewing the cost of 187 gunshot injuries treated at a teaching hospital in Manchester, reported a mean cost of £2698 for patients admitted for inpatient care. 107 In most of the studies, the ED costs are not identified separately from the total health-care costs. A study conducted in South Wales estimated that about 30.0% of assaults resulted in a visit to the ED at a cost of £200 per attendance in 2019. 105
Another important economic aspect related to programmes targeting youth violence is that some, and possibly the most significant part, of the costs and benefits materialise outside of health and social care. These generally refer to costs associated with the criminal justice system or incarceration, but also costs associated with disability or lost productivity (as opposed to the generation of income from employment and tax). Health-care services have been estimated to be only a small fraction of the total costs (especially in relation to lifetime effects of the physical and emotional harm) amounting to 0.03% of total costs for homicide or 3–6% for crimes with injuries, rape or sexual offences. 103
Global research on violence has identified the burden and costs that violence places on health and social prospects across the life course. 111 Violence affects not only health outcomes, quality of life and social choices that people make but also have wider consequences on families, communities and society. 105
Increased spending on violence prevention would help to reduce the economic burden on the health-care system, the huge burden that arises from the long-term health impacts of adverse childhood experiences and would also increase the savings that would accrue outside of the health-care system.
Strengths and limitations
Strengths
Our study was carried out as a rapid, mixed-methods evaluation, integrating qualitative and quantitative methods. Components included a review of the evidence, interviews, meeting observations, and analysis of national hospital and local service activity and costs datasets. We were aided throughout by close collaboration with a variety of stakeholders including Redthread and UCLH staff, and external advisers. These relationships helped us to gain access to key people, information and datasets.
Despite the challenging circumstances brought about by the COVID-19 pandemic for UCLH and Redthread, we were able to conduct confidential interviews with front-line staff, Redthread managers and youth workers, and a small number of meeting observations, largely on account of working in close collaboration with clinical leads at UCLH, and general staff enthusiasm for the service.
The approach we brought to our quantitative analysis was thorough and broad in its scope. In trying to determine the feasibility of evaluation of impact, we considered several different perspectives: that of the individual young person, the hospital, and the community. This work has led to recommendations to improve future efforts at evaluation which will be helpful beyond the service at UCLH.
This study provides valuable reflections on the main costs of, and potential risk reductions resulting from Redthread YVIP service. It also gives an indication of the success rate Redthread might need to achieve in terms of preventing readmission to recoup the costs of its intervention.
Limitations
The implementation of the service was significantly disrupted by the COVID-19 pandemic, and this had consequences for how the service embedded itself at UCLH. Just as this had an impact on the traction of the Redthread service outside of paediatric and adolescent services, it also had an impact on our ability to engage with staff outside of those services. In particular, it remained particularly difficult to gain traction with the evaluation from staff based in the adult ED at UCLH and those with lower awareness of the Redthread service. Future evaluations or research studies will need to engage with staff treating young people in different parts of the trust beyond paediatric and young people’s services.
The uniqueness of the implementation of the service at UCLH (due to its particular context) also meant that our study would have benefitted from direct comparison with another ED in London. We recommend that multisite case studies are conducted at trust level in future to allow for systematic comparisons across hospitals, at similar time points. In particular, multiple case studies could be used to generate knowledge about how Redthread implementation processes, and youth violence services more generally, should be adapted and tailored given the types of services a trust provides, the staff skill mix and types of clinical presentations most commonly seen within EDs.
The research team were not able to approach young people who had engaged with Redthread to ask directly about the impact of the service for practical and ethical reasons. In addition, because of the pandemic and the necessary shift to remote data collection, we were not able to carry out observations of clinician–patient interactions. We may have therefore missed out on important insights into how the service was received by young people and its wider impacts. While we attempted to mitigate this limitation by seeking to interview Redthread’s youth ambassadors, this latter route also ultimately proved impractical.
While in one respect (as noted above) our analysis of the feasibility of measuring quantitative impact covered a variety of perspectives, for the evaluation of a service whose aims encompass many aspects of a young person’s life and experience, our focus on measuring impact solely via subsequent reattendances or re-admissions was a limitation. Moreover, it is possible that a positive consequence of engaging with Redthread could be an increase in their engagement with health-care services and hence their likelihood to reattend hospital, even for harm-related incidents, but we have no evidence as to the extent to which this might happen.
It is understandable that Redthread has taken utmost care to prevent data of supported young people being shared via strong consent processes, but it must be acknowledged that this has also meant that possibly the strongest options for analysis were not possible. Other routes to analysis were also difficult to realise due to a lack of specific data being collected by the hospital, in addition to relatively small numbers of young people having been engaged for longer-term support over the evaluation period.
The lack of linkable Redthread and hospital data meant that our analysis of costs was not based on directly measured costs of service recipients; we instead had to rely on a constructed group of patients with broadly similar characteristics and diagnoses. However, our success in constructing Redthread-eligible or Redthread-like populations from national hospital data was difficult to appraise. In addition, the constructed group were based only on those admitted as emergencies, and the relatively high cost of treatment per admission reflects this fact.
The analysis of consequences was based on data from Redthread’s risk assessment process. While informative, and based on the professional judgement of youth workers, this process was subjective, and should be considered with appropriate caution. The analysis was carried out with data from a very small number of young people, and the scale from 1–3 used for measuring risk indicator may miss on granularities of the distribution of the individual risk continuum.
Equality, diversity and inclusion
Participant representation
Redthread’s service was concerned with providing support to potentially vulnerable or at-risk young people aged 11–24 years. The service’s setting was an inner-city London hospital, close to major national and regional transport links. Of those who received a longer-term service from Redthread and whose ethnicity was known, approximately two-thirds were from nonwhite ethnic groups.
As such, this study reflects on a service which aims to improve the care and prospects of potentially underserved groups of individuals.
While it was not possible to conduct interviews with young people who had experienced the Redthread service for ethical and practical reasons, we interviewed Redthread youth workers and clinical and other staff whose responsibilities and experiences covered the care of potentially vulnerable younger people.
Future research
This evaluation has contributed to the qualitative evidence available on the implementation of a YVIP in a large London acute trust, however there are a number of additional areas that would benefit from future research.
These include:
-
mixed-methods, multisite case studies that enable cross-case comparisons to be undertaken
-
studies focused on the perspectives of young people who have engaged with or are potentially eligible for Redthread support, exploring any differences across age cohorts (e.g. under and over 18 years) and those that receive short-, medium- and longer-term support
-
studies that can solve the data challenges identified to be able to estimate quantitative impacts and cost-effectiveness
-
studies that are able to look beyond hospital-based outcomes and quantify the impact on, for example, educational attainment, recidivism, mental health and the use of drugs and alcohol.
We made limited progress in adding to the evidence of quantitative impact of such schemes but have discussed how this might be improved to enable future evaluation. Although many previous studies have focused on the direct impact of engaging with youth violence reduction services, we also propose an area-based approach which aims to capture less direct impacts on others within local communities. However, further work would need to be undertaken to better assess its feasibility.
We note that the Youth Endowment Fund has funded a research team from the University of Birmingham to study Redthread services across 13 sites, beginning in 2022. 112 There is limited information available as to the design of the study, but information from Redthread suggests that this will use a quasi-experimental design using propensity scoring matching.
Conclusions
To conclude, our evaluation was not able to determine a feasible approach to measuring the quantitative impact of Redthread’s YVIP at UCLH in the time available, but we have been able to reflect on data describing the service, including costs, and make recommendations to support future evaluation. We have been able to contribute to the qualitative evidence on the implementation of the service. Redthread’s service was largely viewed positively as a necessary service for young people at risk of harm (beyond involvement in violence), and one which was complementary to clinical and other statutory services. The service became particularly well embedded in paediatric ED and adolescent services, but less so in adult EDs, possibly in part as a consequence of the impact of the COVID-19 pandemic. The diverse reasons behind individual referrals, the various routes by which young people were identified, and the mix of specific support interventions provided together emphasised the view that this was a complex intervention, with challenges in implementation. Guidance published in 2022 to support implementation of violence reduction services has emphasised the need for evaluation to be undertaken as a key improvement activity and touches on data that ought to be routinely collected. 18 There is a clear need for good-quality evidence of impact and our recommendations may help to improve future evaluation.
Acknowledgements
We are grateful to all the participants who took part in this study. Thank you to the following: our clinical collaborators Dr Joanne Begent and Dr Yasmin Baki (Children and Young People’s Services, UCLH) for facilitating and supporting the evaluation; the Redthread team (John Poyton, Tiffany Brown, Richard Collinson, Chris Wignall, Supriya Tamang, Jenny Lambert, Franklyn Addo) for facilitating the evaluation and provided documents; Dr Chris Laing (Emergency Services Divisional Clinical Director, UCLH) for supporting data collection; Tim Slattery (UCLH) for providing patient-level information and costing system costs; Nadine Pfeifer, Edward Dickson and Phil Miller for peer-reviewing our study protocol; our NIHR RSET public patient involvement members, Raj Mehta, Fola Tayo, Jenny Negus and Nathan Davies for providing feedback on the plain English summary in this report. Many thanks to our evaluation advisory group for providing insights and feedback throughout the project: Michael Carver (Trauma Research Fellow, Centre for Trauma Sciences at Queen Mary University of London, Clinical Lead for Hospital-based Violence Reduction Models, NHS London) and Nadine Pfeifer (Provider Policy Senior Manager, Provider Development, NHS England).
Ethical approval
The project was categorised as a service evaluation by the Health Research Authority decision tool and University College London/University College London Hospitals Joint Research Office.
Funding
This project was funded by the National Institute for Health and Care Research Health Services and Delivery Research programme (RSET: 16/138/17).
Contributions of authors
Professor John Appleby (https://orcid.org/0000-0003-3839-9662) (Director of Research and Chief Economist, Nuffield Trust) was the principal investigator and led the overall evaluation. He led on, and contributed to, conception, design, analysis, and write-up of all aspects of the study, and is lead author of this report.
Theo Georghiou (https://orcid.org/0000-0001-9532-876X) (Senior Fellow, Nuffield Trust) contributed to the conception and design of the study, the quantitative aspects of the study and the write-up of the study.
Dr Jean Ledger (https://orcid.org/0000-0003-2523-7971) (Senior Research Fellow, University College London) contributed to the conception and design of the study, the qualitative aspects of the evaluation, the evidence review and the write-up of the study.
Lucina Rolewicz (https://orcid.org/0000-0003-4308-2408) (Researcher, Nuffield Trust) contributed to the conception and design of the study, the quantitative aspects of the evaluation and the write-up of the study.
Chris Sherlaw-Johnson (https://orcid.org/0000-0002-4851-6060) (Senior Fellow, Nuffield Trust) contributed to the conception and design of the study, the quantitative aspects of the evaluation and the write-up of the study.
Dr Sonila M. Tomini (https://orcid.org/0000-0002-4241-2121) (Research Fellow, University College London) contributed to the conception and design of the study, the economic evaluation and write-up of that part of the work.
Dr Jason M. Frerich (https://orcid.org/0000-0001-7594-6894) (Harvard University) contributed to the evidence review and the write-up of the study.
Pei Li Ng (https://orcid.org/0000-0001-8411-220X) (Project Manager, University College London) managed the evaluation and supported with drafting of the final report.
All authors contributed to integrating the findings of the study. All authors made critical revisions to the report for important intellectual content and approved the final manuscript. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the article are appropriately investigated and resolved.
Data-sharing statement
The use of HES admitted patient care data and emergency care data was governed by a data sharing agreement with NHS Digital covering NIHR RSET analysis (DARS-NIC-194629-S4F9X). HES data are reused with permission of NHS Digital (Copyright © 2022, NHS Digital. All rights reserved). All data requests should be submitted to the corresponding author for consideration.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
Appendix 1 Final search strategies across two databases
MEDLINE
Ovid MEDLINE(R) ALL <1946 to 14 February 2022>
-
Domestic Violence/ or Violence/ or Intimate Partner Violence/ or Gun Violence/ 43545
-
assault.mp. 12686
-
‘Wounds and Injuries’/ 80409
-
human trafficking.mp. 819
-
domestic violence.mp. or Domestic Violence/ 11958
-
Crime Victims/ or knife crime.mp. 11703
-
Wounds, Penetrating/ or stabbing.mp. 13277
-
(gang violence or gang).mp. 1459
-
gang exploitation.mp. 1
-
sexual exploitation.mp. 650
-
Adolescent/ or adolescent.mp. 2194729
-
Young Adult/ 978523
-
children.mp. or Child/ 2225512
-
juvenile.mp. 90983
-
Emergency Service, Hospital/ 80576
-
urgent care.mp. 2766
-
(Major Trauma Centre or Major Trauma Center).mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] 634
-
emergency department.mp. 99941
-
Hospitalization/ 125139
-
Pediatrics/ 57154
-
youth worker.mp. 24
-
Adolescent Development/ 5155
-
teachable moment.mp. 593
-
youth services.mp. 183
-
hospital-based violence prevention.mp. 10
-
intervention.mp. 723390
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 156293
-
11 or 12 or 13 or 14 3898408
-
15 or 16 or 17 or 18 or 19 or 20 308825
-
21 or 22 or 23 or 24 or 25 or 26 728825
-
27 and 28 and 29 and 30 554
-
limit 31 to (english language and yr=‘2012 - 2022’) 283
Embase <1980 to 2022 Week 06>
-
Domestic Violence/ or Violence/ or Intimate Partner Violence/ or Gun Violence/ 66651
-
assault.mp. 20248
-
‘Wounds and Injuries’/ 119213
-
human trafficking.mp. 950
-
domestic violence.mp. or Domestic Violence/ 14920
-
Crime Victims/ or knife crime.mp. 4016
-
Wounds, Penetrating/ or stabbing.mp. 10183
-
(gang violence or gang).mp. 1786
-
gang exploitation.mp. 1
-
sexual exploitation.mp. 1004
-
Adolescent/ or adolescent.mp. 1640407
-
Young Adult/ 445356
-
children.mp. or Child/ 2235948
-
juvenile.mp. 147699
-
Emergency Service, Hospital/ 7609
-
urgent care.mp. 4413
-
(Major Trauma Centre or Major Trauma Center).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword heading word, floating subheading word, candidate term word] 1159
-
emergency department.mp. 153578
-
Hospitalization/ 439434
-
Pediatrics/ 80304
-
youth worker.mp. 62
-
Adolescent Development/ 4264
-
teachable moment.mp. 778
-
youth services.mp. 230
-
hospital-based violence prevention.mp. 9
-
intervention.mp. 1106006
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 215902
-
11 or 12 or 13 or 14 3415021
-
15 or 16 or 17 or 18 or 19 or 20 656973
-
21 or 22 or 23 or 24 or 25 or 26 1110762
-
27 and 28 and 29 and 30 497
-
limit 31 to (english language and yr=‘2012 - 2022’) 366
Appendix 2 Variation in place of emergency department reattendance after an initial visit to UCLH emergency department
Background
The aim of this analysis was to understand the extent to which young people who attend the ED at UCLH will also visit other EDs around the country. This would indicate the implications of focusing an analysis of reattendance by Redthread service users to just UCLH or whether it would need to be widened to a wider set of hospitals across the country.
Methods
From the HES ED records, we selected the first attendance of any patient to the UCLH department between 1 April 2018 and 31 March 2020. If one of these patients had a subsequent visit recorded over the same period at an English NHS acute trust, we recorded the hospital trust where this occurred.
Results
There were 12,047 individuals who presented at UCLH ED between 1 April 2018 and 31 March 2020 with a subsequent visit over the same period at an English NHS acute trust. These reattendances took place at a total of 128 different acute trusts and 6441 (53.5%) were at UCLH; 4303 (35.7%) were at other London trusts, with the next most frequent trust being the Royal Free London NHS Foundation Trust with 673 (5.6%) of reattendances (Figure 12).
Appendix 3 Identification of people potentially eligible for youth violence intervention programmes from routine hospital administrative data
Background
The aim of this analysis was to investigate how routine hospital inpatient data and emergency care data could be used to identify people who might be eligible for YVIPs. This would serve three purposes; to identify:
-
control groups for individual patient-level analysis
-
non-elective hospital admissions and attendances that may be avoided by a successful YVIP, and
-
a case cohort for analyses of the impact on people eligible for YVIP.
Methods
Redthread record the reasons why young people present to hospital and are referred to their programme, and we mapped these reasons to relevant diagnosis and presentations codes within hospital data. The hospital data we investigated were HES for non-elective inpatient visits and the ECDS for ED attendance. Patient records were limited to young people aged 11–24 years (inclusive). For patients attending UCLH, we counted numbers between February 2020 (when the Redthread service began) and August 2021. For inpatient visits we recorded diagnoses on admission (primary or secondary) and for ED attendance we recorded the chief complaint.
Results
The reasons for hospital attendance and for referral to Redthread, as recorded by Redthread, are shown in Table 12, together with ICD10 codes from the inpatient data and chief complaint codes in the ECDS data to which we matched them.
Between February 2020 and August 2021, 252 young people were referred to Redthread, of whom 43 engaged with the full longer-term programme. In comparison, over the same period, there were 161 young people aged 11–24 years admitted to UCLH with at least one of the matched inpatient diagnosis codes and 3275 with one of the chief complaint codes.
The size of the matched group from the ECDS data could be reduced if UCLH reported information for an ‘injury intent’ code, as this would rule out accidental injuries. A similar analysis at another London teaching hospital found that, where injury intent was recorded, 21% relate to physical assault or self-harm.
Many reasons for referral to Redthread are not covered by these ICD-10 or chief complaint codes, particularly those that relate to risks and exploitation. Also, these matches are not precise, even though we may match a reason for referral, in some cases there may be no physical signs that correspond to a clinical diagnosis or chief complaint. This may be especially so at UCLH which is not a MTC and where the Redthread service has more focus on prevention.
Appendix 4 Power calculations for analyses of the impact of Redthread on future hospital attendance of those engaging with the service using a matched case–control study
Background
The power calculations presented in this appendix are for option 1a, which is for evaluating the impact of the Redthread programme on the future hospital attendance of people who engage with it. This was the preferred option for Redthread and UCLH and likely to be the one where there would be a higher likelihood of detecting an effect.
Methods
We aimed to estimate a sample size required to achieve a power of 80%, testing with a 95% confidence interval. To obtain this we required estimates for:
-
the baseline reattendance rates for young people eligible for Redthread in the absence of the programme, and
-
the likely impact of the programme on these reattendance rates.
For both, we investigated the literature for previous studies of similar patients. We were not able to use the ECDS because it had no patient identifiers that could be used to track the attendance patterns of individuals: each identifier was unique to each visit rather than for each individual.
Research is limited on reattendance to EDs for younger people, but NPC Associates (2017)92 found that the project baseline reattendance rate over 12 months in patients aged 11–25 years was 21%. Dickson et al. (2021)93 reported similar baseline reattendance at 18%. For inpatient readmissions, Herbert et al. (2015)110 found that the rate for adolescents aged 10–19 years who were admitted for adversity-related problems was 10.4% over a nine-year period, which equates to a much lower rate of 1.2% per year, many of whom would be likely to have come through the ED first anyway.
In terms of the impact of YVIPs on reattendance, a previous evaluation of the Redthread programme at St Mary’s Hospital in London estimated that hospital reattendance rates for those engaged with Redthread significantly decreased within one year by 33% (from 21% to 14%). 92 This reduction is similar to that reported by the Redthread service at Nottingham University Hospitals. 93
To assess statistical power, we analysed a range of scenarios and preferred to be cautious with our recommendations in case effect sizes of 33% are not realised. Our more cautious baseline assumption was to assume an 11% baseline reattendance rate over six months and effect sizes from 10% reductions to 30%.
Results
Estimated sample sizes under other scenarios are illustrated in Figure 13. With an 11% baseline reattendance rate, we estimated that 110 cases and 110 controls would need to be followed up to observe a reduction of 10%. With greater reductions of 30% the required sample sizes would be far lower, yet there is no guarantee that such an impact would be seen and it is better to recruit samples of sufficient size to give a better chance of more moderate impacts to be detected.
Appendix 5 Redthread service user risk assessment results
| Risk assessment variables | Earlier score n (%) | Recent score n (%) |
|---|---|---|
| Risk of young person of experiencing further harm | ||
| 1 = Low score | 12 (33.3) | 22 (61.1) |
| 2 = Medium score | 19 (52.8) | 11 (30.6) |
| 3 = High score | 5 (13.9) | 3 (8.3) |
| Risk of young person participating in further harm | ||
| 1 = Low score | 26 (72.2) | 29 (80.6 |
| 2 = Medium score | 8 (22.2) | 5 (13.9) |
| 3 = High score | 2 (5.6) | 2 (5.6) |
| Risk of exploitation (criminal, sexual, grooming) | ||
| 1 = Low score | 26 (72.2 | 29 (80.6) |
| 2 = Medium score | 6 (16.7) | 6 (16.7) |
| 3 = High score | 4 (11.1) | 1 (2.8) |
| Risk of young person experiencing criminal behaviour | ||
| 1 = Low score | 25 (69.4) | 28 (77.8) |
| 2 = Medium score | 6 (16.7) | 7 (19.4) |
| 3 = High score | 5 (13.9) | 1 (2.8) |
| Risk of young person participating in further criminal behaviour | ||
| 1 = Low score | 30 (83.3) | 29 (80.6) |
| 2 = Medium score | 3 (8.3) | 6 (16.7) |
| 3 = High score | 3 (8.3) | 1 (2.8) |
| Risk of young person continuing a lifestyle that exposes them to further harm/injury | ||
| 1 = Low score | 20 (55.6) | 25 (69.4) |
| 2 = Medium score | 11 (30.6) | 6 (16.7) |
| 3 = High score | 5 (13.9) | 5 (13.9) |
| Risk of young person not engaging in education, training, or employment | ||
| 1 = Low score | 19 (52.8) | 26 (72.2) |
| 2 = Medium score | 10 (27.8) | 5 (13.9) |
| 3 = High score | 7 (19.4) | 5 (13.9) |
| Risk of young person not maintaining positive relationships with family | ||
| 1 = Low score | 15 (41.7) | 22 (61.1) |
| 2 = Medium score | 13 (36.1) | 10 (27.8) |
| 3 = High score | 8 (22.2) | 4 (11.1) |
| Risk of young person not willing to engage with other services | ||
| 1 = Low score | 28 (77.8) | 30 (83.3) |
| 2 = Medium score | 7 (19.4) | 4 (11.1) |
| 3 = High score | 1 (2.8) | 2 (5.6) |
| Risk of young person not being able to identify escalating problems | ||
| 1 = Low score | 24 (66.7) | 25 (69.4) |
| 2 = Medium score | 8 (22.2) | 9 (25.0) |
| 3 = High score | 4 (11.1) | 2 (5.6) |
| Overall scoring: risk of harm to others | ||
| 1 = Low score | 31 (86.1) | 31 (86.1) |
| 2 = Medium score | 5 (13.9) | 5 (13.9) |
| 3 = High score | – | – |
| Overall scoring: risk of harm from others | ||
| 1 = Low score | 17 (47.2) | 24 (66.7) |
| 2 = Medium score | 15 (41.7) | 9 (25.0) |
| 3 = High score | 4 (11.1) | 3 (8.3) |
| Overall scoring: risk of harm to self | ||
| 1 = Low score | 21 (58.3) | 27 (75.0) |
| 2 = Medium score | 11 (30.6) | 6 (16.7) |
| 3 = High score | 4 (11.1) | 3 (8.3) |
| How safe do you feel right now? (10-point Likert scale)a | 7.11 10th percentile = 3 90th percentile = 10 |
7.77 10th percentile = 5 90th percentile = 10 |
Appendix 6 Redthread’s theory of change (October 2022 version)
FIGURE 14.
Redthread’s theory of change (October 2022 version).
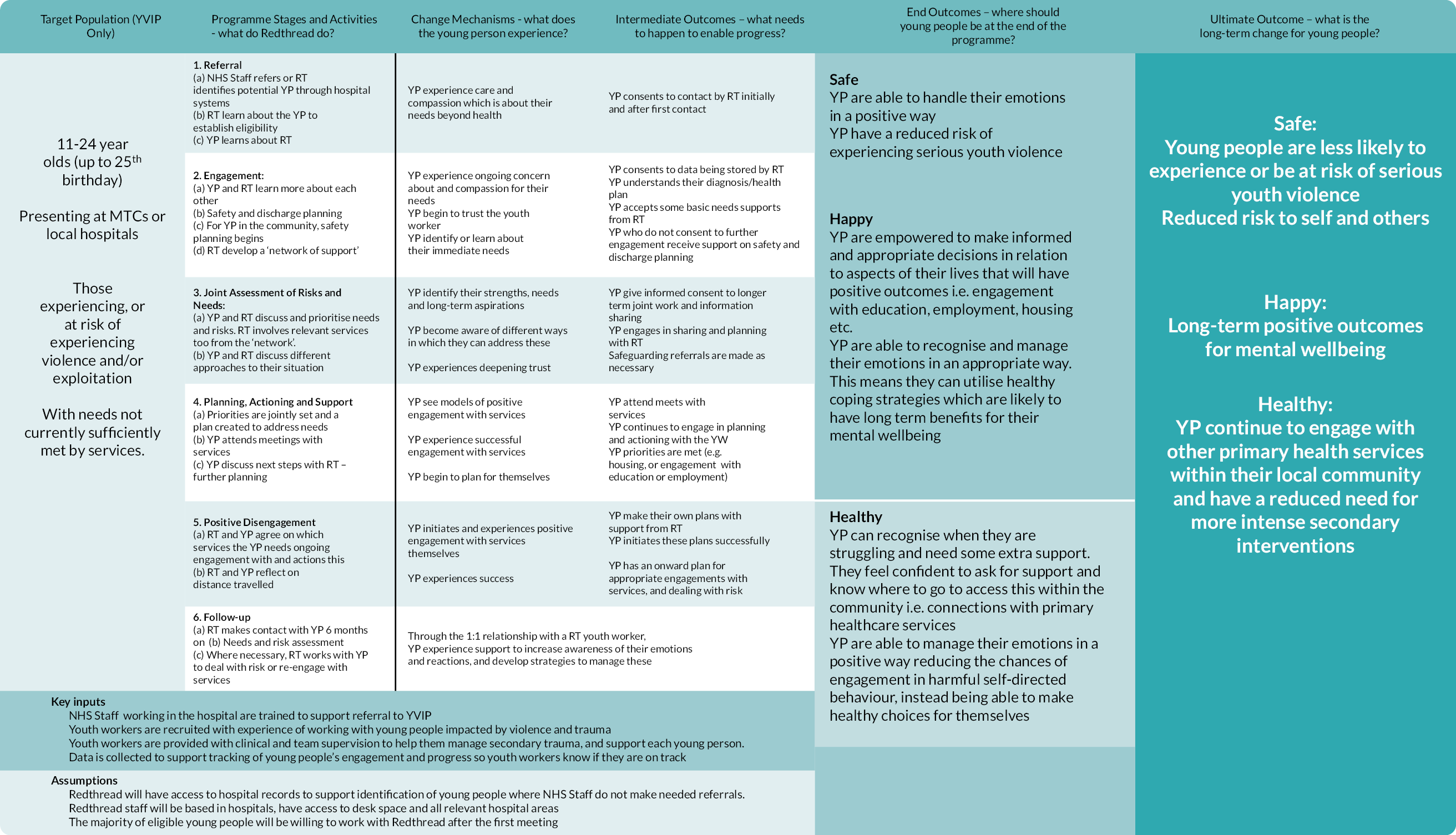
List of abbreviations
- CAMHS
- Child and Adolescent Mental Health Services
- CBA
- cost–benefit analysis
- CBI
- computer-based intervention
- CBT
- cognitive behavioural therapy
- CCA
- cost-consequence analysis
- CEA
- cost-effectiveness analysis
- ECDS
- Emergency Care Dataset
- ED
- emergency department
- HES
- Hospital Episode Statistics
- HRG
- Healthcare Resource Group
- HVIP
- hospital-based violence intervention programme
- MDT
- multidisciplinary team
- MSOA
- Middle Super Output Areas
- MTC
- major trauma centre
- NIHR
- National Institute for Health and Care Research
- PTSD
- post-traumatic stress disorder
- RCT
- randomised controlled trial
- RSET
- Rapid Service Evaluation Team
- TBI
- therapist-delivered intervention
- UCLH
- University College London Hospital
- YVIP
- youth violence intervention programme
