Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number NIHR129488. The contractual start date was in July 2020. The final report began editorial review in January 2022 and was accepted for publication in September 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the final manuscript document. However, they do not accept liability for damages or losses arising from material published in this manuscript.
Permissions
Copyright statement
Copyright © 2024 Randell et al. This work was produced by Randell et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Randell et al.
Chapter 1 Introduction
Overview
This study sought to understand what supports and constrains delivery of multifactorial falls risk assessment (MFRA) and tailored multifactorial falls prevention interventions in acute NHS Trusts in England. This was achieved through a realist review, a review of Trust falls prevention policies, and a multisite case study. The following chapter provides the background for the study, introducing the issue of inpatient falls and approaches to falls risk assessment and prevention, presents the study aims and objectives, and outlines the structure of the remainder of the report. Some text in this chapter has been reproduced from Randell et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Background
Inpatient falls
Falls are generally defined as ‘an unexpected event in which the participant comes to rest on the ground, floor, or lower level’. 2 They are the most common type of safety incident reported by acute hospitals. 3 More than 240,000 falls are reported in acute hospitals and mental health trusts in England and Wales each year,4 although under-reporting may mean the true incidence of falls is higher. 5,6 Falls are most common in patients aged 65 years or older, representing 77% of inpatient falls. 3 The majority of falls result from multiple interacting causes, most commonly age-related physiological changes, medical causes, medications and environmental hazards. 7
Overall, 28% of inpatient falls result in some level of harm and patients aged 65 years or older are more likely to be harmed. 3 The proportion of falls resulting in any fracture ranges from 1% to 3%, with reports of hip fracture ranging from 1.1% to 2.0%. 6 In 2015–6, inpatient falls in England resulted in 2500 hip fractures. 8 Outcomes for patients who acquire hip fractures in hospital are far worse than for those in the community who acquire hip fractures, with significant differences in mortality [relative risk (RR) = 3.00; 95% confidence intervals (CIs) 1.05 to 8.57], discharge to long-term high-level nursing care facilities (RR = 2.80; 95% CIs 1.10 to 7.09), and return to preadmission activity of daily living status (RR = 0.17; 95% CIs 0.06 to 0.44). 9
Even where no physical harm occurs, falls can lead to fear of falling and associated loss of confidence. 5,8 They can result in slower recovery,8 even when physical harm is minimal, and can have longer-term consequences for the patient’s health, as fear of falling may lead to restriction of activity and associated loss of muscle and balance function, increasing risk of falling. 5 Falls can also be a cause of significant distress for families and staff. 6,8 Falls in hospital are a common cause of complaints10 and can be a source of litigation. 11 They are also associated with increased length of stay and greater amounts of health resource use. 6 NHS Improvement (now part of NHS England) estimated inpatient falls cost the NHS and social care an estimated £630 million annually. 3 It is therefore a priority to reduce the number of patients who fall, and their risk of injury, in acute hospital settings.
Falls risk assessment
The traditional approach to managing falls in acute hospitals is to complete a falls risk prediction tool, sometimes referred to as falls risk screening tools or falls risk scores (such as STRATIFY12). Such tools typically provide a list of falls risk factors, assign a numerical value to the presence or absence of the risk factor, and then sum the numerical values together to represent the individual’s risk of falling (high, medium, low). 13 Interventions are then used to target individuals at high risk. 14 There are issues with the predictive validity of such tools; a systematic review of falls risk prediction tools found only moderate accuracy, comparable to the accuracy of nursing staff clinical judgement. 13 Consequently, such tools may either provide false reassurance about patients identified as low risk or result in most patients on a ward being identified as high risk. 14 Such tools are often completed only once, typically on admission, while a patient’s risk of falling can vary over time. There is also concern that their use gives false reassurance something is being done, even if no action to address falls risks has been taken. Additionally, with a tool of this kind, actions tend to be linked to the score and can lead to a ‘one size fits all’ approach even though the issues and needs of individual high-risk patients can be very different. 14 A stepped-wedge cluster randomised controlled trial (RCT) showed removing the risk score component from falls risk prediction tools does not negatively impact falls outcomes and can reduce time spent completing paperwork. 15
In light of the limitations of falls risk prediction tools, the NICE guideline on falls in older people states they should not be used and instead a MFRA should be undertaken. 16 The recently published World Falls Guidelines, for falls prevention and management for older adults, also recommend patients in hospital should receive a MFRA and advise against using falls risk prediction tools. 17 A multifactorial approach to falls risk assessment identifies individual risk factors for each patient, which may make them at risk of falling and that can be treated, improved, or managed during their stay (what tend to be referred to in the falls research literature as ‘modifiable’ risk factors). MFRAs, unlike risk prediction tools, do not include unmodifiable risk factors (i.e. cannot be treated, improved, or managed) such as age and sex. The NICE guideline includes the following modifiable risk factors: cognitive impairment; continence problems; falls history, including causes and consequences (e.g. injury and fear of falling); unsuitable or missing footwear; health problems that may increase a patient’s risk of falling; medications that increase the risk of falls; postural instability, mobility problems and/or balance problems; syncope syndrome; and visual impairment. The NICE guideline states that a MFRA should be undertaken for all inpatients 65 years or older and inpatients aged 50–64 years judged to be at higher risk of falling due to an underlying condition. Based on this assessment, a multifactorial intervention should be provided for the patient, tailored to their individual risk factors. For example, if visual impairment is identified, it might be decided that an optician visit should be arranged if the patient has lost their glasses or, if there is no known reason for poor eyesight, an ophthalmology referral is made. 18 In this way different patients, who have different risk profiles, will receive different interventions to reduce their risk of falls.
Preventing inpatient falls completely would only be possible with unacceptable restrictions to patients’ independence, dignity and privacy, such that some falls may be considered an inevitable consequence of promoting rehabilitation and autonomy. 6,10 Thus, there is a need to balance the risk of harm from falls and the risk of deconditioning. Nonetheless, it is estimated introduction of MFRA and tailored interventions, as recommended by the NICE guideline, could reduce the incidence of inpatient falls by 25–30% and the annual cost of falls by up to 25%. 3 Despite the NICE guideline being updated to include these recommendations in 2013, the 2022 National Audit of Inpatient Falls (NAIF) report noted that 34% of Trusts are still using falls risk prediction tools and, while there has been improvement in the proportion of patients receiving documented assessment for components of the MFRA included in the NICE guideline, there has been a reduction in the proportion of patients assessed for delirium. 19 Documented vision assessment (52%) and lying and standing blood pressure (LSBP, 39%) remain concerningly low. In interventions, a mobility care plan was in place for 90% of patients who required one, a continence care plan for 78% of patients who required one, and a delirium care plan for 61% of patients who required one. This suggests variation in the extent to which the NICE guideline is being followed and opportunities are being missed to reduce the likelihood of inpatient falls.
Given these findings, it is necessary to understand the contextual factors that support and constrain use of MFRA and tailored falls prevention interventions in acute hospitals, to improve practice.
Aims and objectives
The study aim was to determine how and in what contexts MFRA and tailored falls prevention interventions are used as intended on a routine basis in acute hospitals in the NHS in England. The objectives were as follows:
-
Use secondary data to develop a programme theory that explains what supports and constrains routine use of MFRA and tailored falls prevention interventions.
-
Refine the programme theory through mixed method data collection across three acute hospital Trusts.
-
Translate the programme theory into guidance to support MFRA and prevention and, in turn, adherence to the NICE guideline.
In addition, the study aimed to include the perspectives of patients and members of the public through involvement of lay people as members of the research team at all stages and through their regular evaluations of progress.
Structure of the remainder of the report
Chapter 2 describes the study design and research methods, including the methods used for public and patient involvement (PPI).
Chapter 3 presents findings of the theory construction phase of the realist review.
Chapter 4 presents the results of, and outputs of the steps we went through during, the prioritisation of theories for testing in later phases of the study.
Chapters 5 to 8 present findings of the theory testing phase of the realist review, a review of NHS Trust falls prevention policies, and the multisite case study, organised according to the four theories that were prioritised for testing. These four theories relate to leadership for falls prevention, shared responsibility for falls prevention among the multidisciplinary team, tools to facilitate falls risk assessment and care planning, and patient participation in falls prevention.
Chapter 9 concludes the report by reflecting on the implications of the study findings and outlining future research priorities.
Chapter 2 Design and methods
Public and patient involvement
Throughout the study, we were supported by DW, the lay member of the project management group, and a group of lay researchers recruited to the project (service users and carers who had either fallen themselves or cared for someone who fell in hospital); while we describe their involvement in the conduct of the research throughout the chapter, we conclude the chapter by providing a fuller account of our approach to PPI.
Overview
Realist evaluation provided an overall framework for this study. We conducted a realist review to develop programme theories, which were further refined through a multisite case study across three acute NHS Trusts. The study culminated with presentations to case sites to work with participants to determine implications of the study findings for practice. Below, we begin by describing realist evaluation before describing the three study phases. Some text in this chapter has been reproduced from Randell et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Realist evaluation
Falls risk assessment and prevention can be characterised as a complex intervention, aimed at producing change in the delivery and organisation of healthcare services and comprising several separate components that may act both independently and interdependently. 20 The study of complex interventions requires a strong theoretical foundation, to make explicit often implicit assumptions regarding how and why the intervention will provide the desired impact21 and how this is influenced by context. 22 Realist evaluation23 offers a framework for understanding for whom and in what circumstances complex interventions work. It involves building, testing, and refining the underlying assumptions or theories of how such interventions are supposed to work. It has been used for studying the implementation of a number of complex interventions in health care,24–26 including clinical guidelines. 27
From a realist perspective, interventions in and of themselves do not lead to outcomes. Rather, it is how recipients of the intervention choose to make use of, or not, the resources an intervention provides that determine outcomes, and such choices are highly dependent on context. For example, whether the introduction of a form for MFRA leads to the use of tailored falls prevention interventions and a subsequent reduction in falls depends on if, and how, nurses use that form. This choice may vary according to contextual factors, such as workload, confidence in their ability to undertake the assessment, and belief in the value of the assessment and associated interventions. Therefore, a realist approach is suitable when studying interventions where uptake and subsequent impacts have been found to be variable. Realist approaches are concerned with constructing programme theory that details how intervention components trigger responses in recipients (intervention mechanisms) within particular contexts to generate outcomes, described as context mechanism outcome configurations (CMOcs).
Realist review
Realist review represents a divergence from traditional systematic review methodology. 28 It starts by identifying programme theories and then uses empirical evidence from published studies to systematically evaluate these, allowing us to compare how an intervention is intended to work with how it actually works. Realist reviews are useful when considering the literature on interventions where there is limited primary research because, in contrast to systematic reviews, diverse sources of data can be considered as evidence, enabling reviews to make use of, for example, reports of local evaluations and quality improvement (QI) initiatives that have not been subject to peer review. 29
Realist approaches can be thought of as consisting of three phases: theory construction, theory testing and theory refinement, and we use this structure to describe the process of the realist review undertaken in this study.
Phase 1: theory construction
Search strategy
In July 2020, three sets of searches were undertaken by an information specialist with expertise in realist reviews (JW). Subject headings and free-text words were identified for use in the search concepts for all searches by the information specialist and project team members. The searches were also peer reviewed by another information specialist. The searches included words and synonyms for falls, risk assessment/accident prevention, and acute hospital settings (see Appendix 1 for full search strategies).
Practitioner theory search. Because stakeholders are likely to express how they think interventions work in informal contexts such as editorials, comments, letters and news articles,29 we searched the following databases for commentary-type articles and studies mentioning theories/conceptual models for falls risk assessment in acute hospital settings:
-
CINAHL (EBSCOhost)
-
HMIC Health Management Information Consortium (Ovid)
-
Ovid MEDLINE(R) and Epub Ahead of Print, In-process and Other Non-indexed Citations and Daily 1946 to 21 July 2020.
‘Key journal’ search of falls risk assessment articles. The project team identified the following key professional/trade journals and magazines: Nursing Times, Nursing Standard, Health Service Journal and Pharmaceutical Journal. These were searched using the following databases:
-
CINAHL (EBSCOhost)
-
EMBASE Classic + EMBASE (Ovid)
-
HMIC Health Management Information Consortium (Ovid)
-
Ovid MEDLINE(R) and Epub Ahead of Print, In-process and Other Non-indexed Citations and Daily 1946 to 21 July 2020.
Academic theory search. The discussion sections of systematic reviews often include authors’ theories about why interventions did or did not achieve the desired effect. 30 Therefore, we searched the following databases for systematic reviews of falls risk assessment:
-
CINAHL (EBSCOhost)
-
Cochrane Central Register of Controlled Trials (Wiley) Issue 7 of 12, July 2020
-
Epistemonikos www.epistemonikos.org/
-
HMIC Health Management Information Consortium (Ovid)
-
International HTA Database (INAHTA)
-
Ovid MEDLINE(R) and Epub Ahead of Print, In-process and Other Non-indexed Citations and Daily 1946 to 21 July 2020
-
PROSPERO www.crd.york.ac.uk/prospero/.
The results of these three sets of searches were stored and de-duplicated in an EndNote library. In addition, an advanced Google search was carried out, using the terms ‘falls prevention’ and ‘hospitals’.
Review strategy
Titles and abstracts were screened for relevance by three reviewers, NA, LM and HZ, guided by the following questions:
-
Is this about falls risk assessment and/or falls prevention interventions in the acute hospital setting?
-
Does it potentially contain ideas about how falls risk assessment and prevention work, for whom, and in what circumstances?
More specifically, the inclusion/exclusion criteria listed in Table 1 were applied.
| Inclusion | Exclusion |
|---|---|
|
|
Initially a liberal accelerated approach was to be used, where all abstracts and full texts are reviewed once and then those excluded are reviewed again by a different reviewer. 31 This approach is less time- and resource-intensive than having all records screened twice, while maximising inclusion, increasing the number retained in comparison to each record being reviewed once. 32 However, a large number of potentially relevant titles of papers were identified in the initial round of title/abstract screening. Given that the liberal accelerated approach would lead to inclusion of more citations for full-text retrieval from the second screen of excluded references, this number was considered unfeasible for the researchers to manage within the time frame allocated for theory construction. Ten randomly selected full texts from the included citations were found to be of limited relevance for theory construction. Therefore, the following inclusion criteria were added: (1) focus on risk assessment, rather than risk prediction and (2) use of multifactorial rather than single assessment tools. Longer-term settings were also excluded, explicitly. The refined criteria were used to rescreen the included citations, thus increasing the relevance of included literature for theory construction, while reducing numbers to a more manageable size. Use of the literature in theory construction allows flexibility as the aim is to capture ideas and assumptions, rather than perform an exhaustive search of the topic, and therefore this was considered a reasonable revision to our approach.
Full texts of potentially relevant texts were then retrieved and reviewed using the above criteria, but with emphasis on whether they contained ideas about how and why falls risk assessment and prevention strategies were implemented; the contextual factors that supported and constrained implementation; and/or the consequences or outcomes of these processes.
Data extraction and analysis
Initially, we had intended to analyse the data by importing papers into NVivo (QSR International, Warrington, UK) and coding them as contexts, mechanisms and outcomes, thereby drawing together coded data from multiple studies to configure a series of CMOcs. However, on trialling NVivo for this purpose, we found this approach resulted in coding large sections of text, which did not facilitate analysis. Therefore, data extraction forms were created in Microsoft Word (Microsoft Corporation, Redmond, WA, USA) with sections that enabled relevant discussions and data about the CMO concepts to be summarised. The form was also used to note any substantive theories referred to in the paper. To check consistency in use of data extraction forms, two researchers (NA, LM) used the forms to extract data from a systematic review and a practitioner theory paper and then met to discuss their experience and come to a shared understanding of the type of data to extract using the forms.
To summarise findings, data matrices (one line per citation, with columns capturing data on contexts, mechanisms and outcomes, drawn from summaries in the data extraction forms) were created. From these matrices, CMOcs were constructed, presented in tables with the first column providing details of the citation(s) that informed the CMOc. We did not assess the quality of papers in this phase, because the focus was to identify and catalogue ideas about how and why interventions work, rather than to assess the validity of those ideas. 33
Use of substantive theory
Drawing on substantive theory is recommended within realist methods. 23 In addition to noting substantive theories referred to in the included papers, we used Google Scholar to search for implementation theories. We first sought to identify mechanisms from the literature reviewed, with the intention of returning to the substantive theories, if necessary, to help address gaps in our CMOcs. Substantive theory supported organisation of the findings from Phase 1 of the review.
Prioritisation of theories for testing
Prioritising which CMOcs should be tested in later phases of the study was undertaken in collaboration with the Lay Research Group and Study Steering Committee (SSC). To facilitate this, the CMOcs were refined into a series of If–Then statements. CMOcs that were not feasible to test and/or did not have the potential to inform practice were removed. To prioritise this subset of CMOcs, the Lay Research Group and SSC were asked to rank the If–Then statements using an online form. Both groups were asked to give top rankings to the statements they believed were most likely to work in practice, and the Lay Research Group was asked, in addition, to give a high rank to statements likely to have most impact for patients and carers. Both groups then met, separately, in December 2020 to discuss their rankings. Members were offered an opportunity to rerank the statements following those meetings, if they had changed their minds. The SSC gave the Lay Research Group’s ideas precedence in determining the project’s next steps, in recognition of the importance of falls prevention for patients and carers.
Phase 2: theory testing
The CMOcs prioritised for testing encompassed similar mechanisms. To facilitate searches, we grouped mechanisms where appropriate, identifying six key concepts. The searches were conducted in two stages, based on the six concepts.
Stage 1: original EMBASE search
The first search took place in March 2021 using EMBASE (the most comprehensive health database) to gauge the size of the relevant literature in each concept and refine the search terms, before using them to search other databases.
Six searches were conducted to capture evidence for each concept. Subject headings and free-text words were identified for use in each search block (see Table 2 for concepts and search blocks; see Appendix 2 for full details of each search). For example, the ‘hospitals’ search block included the search words and headings: hospital, hospitalisation, nursing staff, medical staff, inpatient, acute patient, hospital patient, ward, hospital department, rehabilitation unit. No language or publication date limits were applied to the searches. Each concept was searched separately and downloaded into an EndNote library. Records were coded to record which concept search they derived from, and then the searches were combined in a single EndNote file, with separate groups for each of the six concepts. Duplicates were removed. There was a high degree of overlap between the records found by different searches. We tagged each EndNote record with the search or searches from which it had been generated so, even after duplicate removal, we could identify all the records retrieved for a particular concept.
| Concepts | Leadership | Staff empowerment | Facilitation | Patient-centred care | Shared responsibility | Expertise |
|---|---|---|---|---|---|---|
| Search blocks | Leadership, champions Implementation Falls risk assessment or prevention Hospitals | Staff training, empowerment Implementation Falls risk assessment or prevention Hospitals | Assessment tools or health information technology Implementation Falls risk assessment or prevention Hospitals | Patient-centred care Hospitals Falls reduction | Teams, shared responsibility Hospitals Falls reduction | Expertise Hospitals Falls reduction |
Two researchers (NA, LM) screened all citations and abstracts for relevance for theory testing using the following questions:
-
Is the study concerned with the context (acute hospitals) and the intervention (MFRA and/or falls prevention interventions) of interest in this study?
-
Does the study report the findings of an empirical investigation?
-
Does it include evidence to test the CMOcs?
While a clear theoretical divide can be made between traditional risk stratification and MFRA tools, hybrid approaches with the use of a risk stratification tool plus some tailoring may be seen in the literature and in practice and were included in the review. This approach enabled us to include studies such as those relating to the Fall Tailoring Interventions for Patient Safety (TIPS) study in the USA, which used the Morse Fall Scale to stratify patients according to risk, while leveraging health information technology (HIT) to select interventions tailored to identified risks. 34–38
The two researchers screened just over 10% of the citations to check consistency in decision-making. Conflicts were resolved between them. The number of relevant citations returned suggested the search strategy was identifying useful literature. To better understand their potential for theory testing, full texts were retrieved and reviewed for over 10% of included citations for the four concepts ranked highly by both the Lay Research Group and SSC: leadership, facilitation, patient participation and shared responsibility. Additionally, these concepts were prioritised because they included two that focused on implementation – leadership and facilitation – and two that focused on how implementation of practices might reduce patients’ falls risks – patient participation and shared responsibility. Based on full text review, and with consideration of the weight and volume of evidence and researcher time available, the decision was made to focus on these four CMOcs going forward and not test the CMOcs for staff empowerment and expertise.
Stage 2: additional database searches
Searches for the four CMOcs were designed following analysis of the original EMBASE search terms and scope of the CMOcs, using the following four search questions:
-
Leadership: search included terms for hospitals, falls prevention/assessment, implementation/adherence to guidelines and strategies, leadership and multifactorial risk assessment.
-
Facilitation: search included terms for hospitals, falls prevention/assessment, engagement/implementation, assessment tools/HIT and workflows.
-
Patient participation: search included terms for hospitals, falls prevention/assessment, multifactorial risk assessment, person-centred care and empowerment compassion.
-
Shared responsibility: search included terms for hospitals, falls prevention/assessment, multifactorial risk assessment, teamwork and shared responsibility.
Table 3 lists the information resources used in the initial search in May 2021. Within the project time frame, we were able to complete the synthesis for facilitation and patient participation. Searches for these two theory areas were rerun in August 2022 on all databases except NICE Evidence, which ceased in April 2022.
| Information resource | |
|---|---|
| Published literature | CINAHL (EBSCOhost) Ovid MEDLINE(R) ALL 1946 to 5 May 2021 Arts and Humanities Citation Index (Web of Science) 1975+ Science Citation Index-Expanded (Web of Science) 1900+ Social Sciences Citation Index (Web of Science) 1900+ Emerging Sources Citation Index (Web of Science) 2015+ |
| Grey literature | NICE Evidence Conference Proceedings Citation Index – Science (Web of Science) 1990+ Conference Proceedings Citation Index – Social Science and Humanities (Web of Science) 1990+ |
Subject headings and free-text words were identified for use in the search concepts for all searches by the Information Specialist and project team members (see Appendix 2 for full search strategies). The searches were peer reviewed by a second Information Specialist.
The results of the database searches were stored separately from the original EMBASE searches in an EndNote Library. Duplicate records were removed and titles and abstracts from the additional searches were screened using the same criteria as the original EMBASE search. Full texts of potentially relevant papers were reviewed using the same questions used in screening, with an emphasis on whether papers were considered useful for theory testing.
Phase 3: theory refinement
For theory refinement, NVivo was used to categorise sections of the manuscripts to support theory testing. For example, for facilitation, an overarching theme ‘Type of facilitation’ in NVivo had subthemes relating to alerts and reminders, and decision support. A sample of manuscripts was reviewed to identify additional themes, for example, in relation to study details (including intervention descriptions and study rationales) and influences on staff practices, with the development of subthemes, such as individual staff beliefs and attitudes. The themes were added to NVivo and tested for usability using a sample of manuscripts (n = 5) that varied in aims and methods and included qualitative and quantitative data. Researchers coded the manuscripts and met to discuss their experiences, suggest refinements, and develop a shared understanding of how to apply the themes to the texts. After refining the coding framework, manuscripts from the four concept searches were imported into NVivo and coded using the framework by NA and LM.
All manuscripts were coded using an overarching framework. Researchers began analysis of two CMOcs: one focused on implementation – facilitation – and one focused on falls risk reduction – patient participation. Details about the studies reported in these texts, including methods used, settings, samples, intervention description and comparator (if appropriate) were extracted into Excel.
Data from the concept-specific searches were collated. Analysis began by examining the interventions described by study authors, to understand the extent to which they reflected the resource component of the initial CMOc. The type and range of interventions were then described in narratives, prepared by the researchers. Following intervention description, manuscripts were reviewed to understand what the data suggested about the outcome of interest in the CMOcs. For example, for facilitation, the primary outcome of interest was whether recommended practices (e.g. MFRA) were implemented as intended, and for patient participation, the primary outcome of interest was the extent to which falls rates were reduced. Outcome data were recorded in tables to understand variation in intervention impact across studies.
After tabulating outcomes, researchers examined coded data and the original manuscripts to collate evidence to help explain variations in outcomes, and to assess the extent to which the mechanisms and context expressed in the original CMOc were evidenced by the literature. In doing so, they looked for data that supported and diverged from the CMOc logic. Narrative summaries were then written and were used to refine the initial CMOcs.
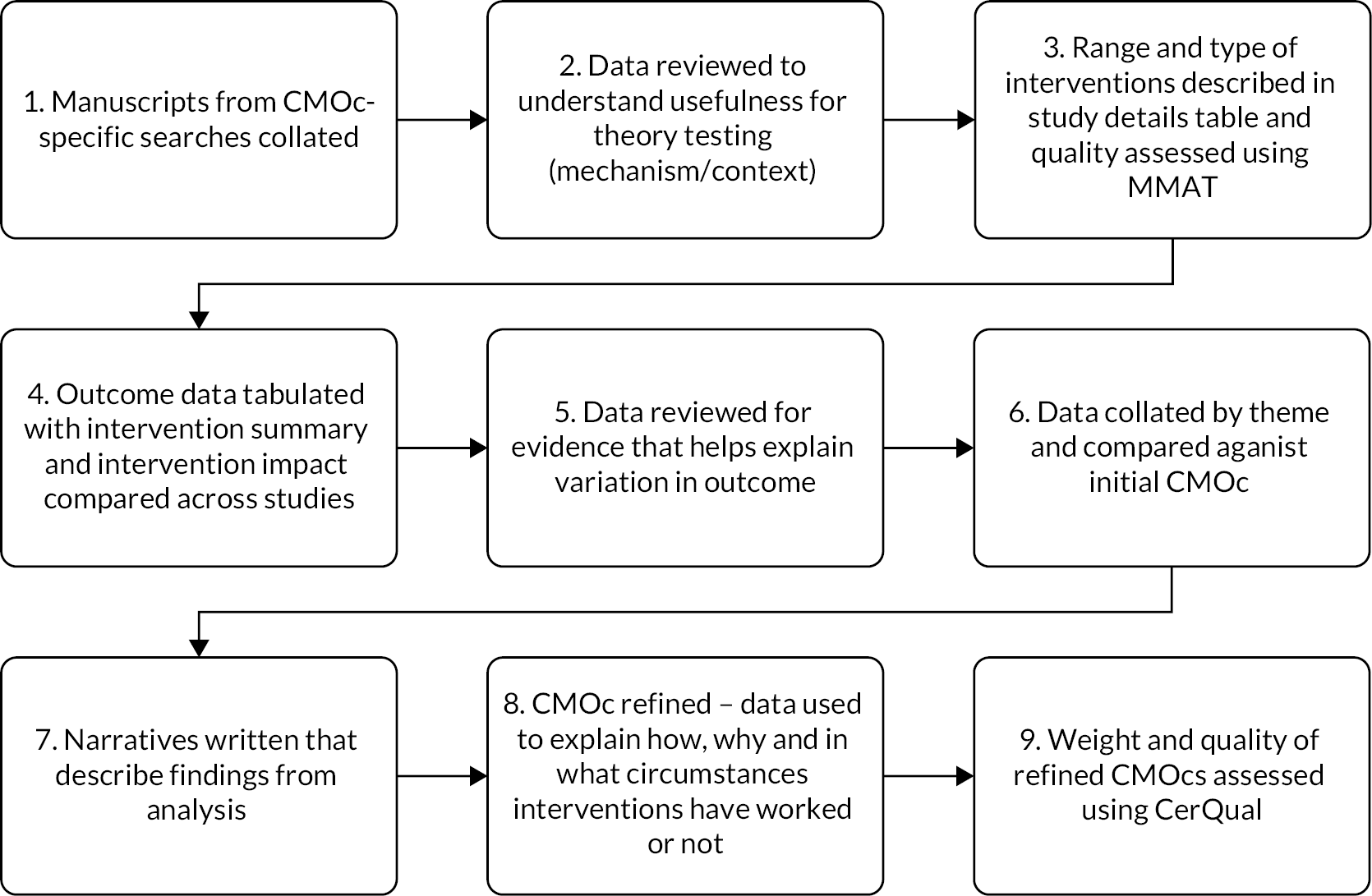
Following the steps of analysis depicted in Figure 1, the aim was to refine the first two CMOcs and then continue with the remaining two if time allowed. Although coded, time limitations meant we were not able to undertake theory refinement for leadership and shared responsibility, so the decision was made that data for testing the leadership CMOc would consist of the review of falls prevention policies (see Review of acute NHS Trust falls prevention policies) and data collected in the multisite case study, while data for testing the shared responsibility CMOc would consist of data gathered in the multisite case study only.
FIGURE 1.
Realist review analysis flowchart.
Quality assessment
The included texts for facilitation and patient participation were appraised using the mixed methods appraisal tool (MMAT),39 recorded in Excel, with the exception that such appraisals could not be undertaken for QI papers that did not contain sufficient information about methods.
To assess the strength of the body of evidence for the refined CMOcs, we used Grades of Recommendation, Assessment, Development and Evaluation-Confidence in the Evidence from Reviews of Qualitative research (GRADE-CERQual). 40 GRADE-CERQual has been used in previous realist reviews41,42 and fits well with the realist approach, involving consideration of the theoretical contributions of studies and encouraging reviewers to be sensitive to the importance of context. 43 It involves assessing each individual review finding based on the four components of methodological limitations, coherence, adequacy of data, and relevance. 40 Refinements to the facilitation and patient participation CMOcs were expressed as claims and linked to the specific studies that evidenced the claims. The evidence supporting each claim, and consequently the CMOc, was assessed for quality using GRADE-CERQual by NA, LM and RR. They undertook assessments separately and then came together to reach consensus, rating confidence in each claim as either high, moderate, low or very low.
Review of acute NHS Trust falls prevention policies
As a source of evidence for testing the leadership CMOc, we reviewed the policies of acute Trusts regarding falls risk assessment and prevention. The motivation was that this would provide insight into whether organisational-level policies support or constrain effective falls risk assessment and prevention. We aimed to collect and analyse falls policies from a random sample of around 10% of English Trusts (approximately 22 policies) but, if variation was found, we would increase the sample to around 15% (approximately 33 policies) to get a better sense of the variation. Policies were identified using the following sources:
-
a Google search using the following terms: ‘falls policy’ restricted to domain ‘nhs.uk’, ‘acute hospital falls policies’, ‘falls policy uk’, ‘inpatient falls hospitals uk’ (January 2021)
-
Freedom of Information sections of the websites of those Trusts for which we had a possibly outdated policy (February 2021)
-
the Falls and Fragility Fracture Audit Programme, who sent a request to a sample of Trusts that participate in the National Hip Facture Database (March 2021), including nine Trusts for which we already had policies but were unsure if they were up-to-date and to another 14 Trusts randomly selected from a list of English acute Trusts on the NHS website (www.england.nhs.uk/publication/nhs-provider-directory/) and
-
local collaborators in the three case study sites (see Multisite case study), who provided the most up-to-date falls policies for their Trusts.
Policies dated before 2013, when NICE multifactorial guidance was introduced, were excluded.
When reviewing these policies, we sought to assess adherence to the NICE guideline on falls in older people by checking whether a falls risk prediction tool was recommended; whether an approach was recommended that was tailored to the patient’s individual risk factors; and by looking for specific elements of the assessments undertaken (such as whether continence and cognitive impairment were assessed), as specified by NICE and captured also in the NAIF.
Multisite case study
Having completed the realist review, we continued refining our prioritised theories via a multisite case study with embedded units of analysis. 44 In line with a realist approach, we used a combination of qualitative and quantitative methods to gather data on the processes and contexts of falls risk assessment and prevention as well as the impacts. 29
Sampling of case sites
Data were collected across three NHS acute Trusts in England. This number was chosen to provide a balance between breadth and depth of investigation,45 enabling identification of organisational-level factors that impact on falls risk assessment and prevention while providing confidence in the generalisability of findings that are consistent across sites. Trusts were selected to ensure variation in key NAIF indicators at the time of writing the proposal,8 the HIT in place, and to include both teaching and district general hospitals (Table 4).
| Site | Per cent of eligible patients who received assessment/care plan | EHR | Hospital type | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Delirium | Continence CP | BP | Medication | Vision | Call-bell | Mobility aid | |||
| 1 | 10 | 82 | 39 | 43 | 56 | 80 | 69 | Locally developed | Teaching |
| 2 | 8 | 100 | 31 | 50 | 25 | 75 | 100 | Locally developed/AllScripts | Teaching |
| 3 | 67 | 67 | 8 | 7 | 13 | 50 | 17 | Cerner Millennium | District general |
We chose to sample across clinical areas in each site to enable us to be able to distinguish differences due to clinical area and Trust/unit-level factors. We decided that, in each Trust, we would undertake data collection in one older person/complex care ward and one orthopaedic ward. These areas were selected because they would provide different patient populations with different lengths of stay and different staff experience, with longer length of stay and staff having experience in managing older people at risk of falling on older person/complex care wards. Specific wards were identified through discussion with local collaborators at each site. An introduction to each ward is provided in Table 5. The two wards for Site 1 were located in different hospitals within the Trust; for Sites 2 and 3, the two wards were located within the same hospital.
| Site | Ward | Beds | Number of bays/side rooms | Nursing team organisation |
|---|---|---|---|---|
| 1 | Complex | 27 | Patients located either in single-bed side-rooms, including rooms in a separate side-ward (isolation unit), or on one of four, four-bed bays. | Nurses and HCAs were organised in three teams, each responsible for a number of beds: red group, blue group, and green group (in the isolation side ward). The ward board showed that ideally there should be four registered nurses (RNs) on each shift and five HCAs on the early and late shifts and three RNs and five HCAs on the night shift. |
| Orth | 23 | Patients located either in single-bed side-rooms or in one of five, four-bed bays. | Nurses and HCAs were organised in teams: sometimes three teams – blue, green, red and sometimes two teams only, blue and red. The ward board showed that ideally there should be three RNs on each shift and six HCAs on the early and late shifts and two RNs and six HCAs on the night shift. | |
| 2 | C | 28 | Patients located either in single-bed side-rooms of in one of five, four-bed bays. | Staff worked in three teams, responsible for groups of beds: the red team, blue team, and green team. The ward board showed that ideally there should be four RNs, four HCAs and one nursing associate on early and late shifts, and three RNs and three HCAs on the night shift. |
| O | 28 | Patients located either in single-bed side-rooms or in one of five, four-bed bays. | Staff worked in four teams, responsible for groups of beds: dark blue, pale blue, red, and yellow. The ward board showed that ideally there should be four (and sometimes five) RNs, six HCAs and one nursing associate on early and late shifts, and three RNs (sometimes four) and four HCAs on the night shift. | |
| 3 | C | 30 | Patients located on one of two sides to the ward. On each side, there was one large bay divided by a half-wall with 12 beds and other beds were in single side-rooms. | Staff worked on either the side of the ward that cared for up to 15 male patients, or the side that cared for up to 15 female patients. The ward board showed there should be five RNs and four HCAs on the early shift, four RNs and five HCAs on the late shift, and four RNs and four HCAs on the night shift. |
| O | 22 | Patients located either in single-bed side-rooms or in one of two–two-bed or two–three bed bays. | The ward was organised into three ‘pods’. Ideally there should be one RN and one healthcare worker per pod (referred to as a 3 : 3 ratio), amounting to four RNs and four HCAs on the early shift, four RNs and three HCAs on the late shift, and three RNs and three HCAs on the nightshift. |
Sampling within case sites
The intention had been to conduct two 4-hour periods of observation in each ward per month over 5 months. However, ward closures due to coronavirus disease 2019 (COVID-19) meant we needed to take a more flexible approach to data collection, undertaking data collection in those wards we could access, and spreading data collection over a longer period of time. Data collection was undertaken between November 2021 and June 2022. Observations were scheduled to ensure they took place at different times of day, including night shifts, and different days of the week, including weekends. In total, 251.25 hours of observations were undertaken. Table 6 provides a summary of the data collected.
| Site | Ward | Record review | Observations | Interviews | ||
|---|---|---|---|---|---|---|
| Patient/carer | Ward staff | Organisation | ||||
| 1 | Complex | 10 | 48.5 | 5 | 10 | 4 |
| Orth | 10 | 40.5 | 5 | 5 | ||
| 2 | C | 10 | 41 | 5 | 5 | 4 |
| O | 10 | 41.25 | 5 | 8 | ||
| 3 | C | 10 | 40 | 6 | 8 | 2 |
| O | 10 | 40 | 5 | 4 | ||
| Total | 60 | 251.25 | 31 | 40 | 10 | |
Sampling of interviews
Interviews were undertaken with a purposive sample of ward-level staff who had been observed, representing a range of professional groups, including doctors (three consultant geriatricians, one ortho-geriatrician and one trainee), nurses, healthcare assistants (HCAs) and physiotherapists (Table 7). Organisational staff with a remit for falls prevention beyond specific wards were identified and approached by the local collaborator in each site. Roles included Senior Nurse for Professional Practice Standards and Safety Team (Site 1), Deputy Chief Nurse (Site 2), Falls Specialist Nurses (Site 2) and Dementia Lead (Site 3). A total of 50 staff interviews were undertaken. Recruiting ward-level staff was challenging due to the pressures on the NHS at the time of undertaking data collection. Formal interviews were complemented by informal interviews, carried out while undertaking observations.
| Site | Ward | Ward manager/matron | Nurse-in-charge/senior nurse | Nurse | Doctor | Nurse associate/student nurse | HCA | Physiotherapist | OT | Pharmacist | Other |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Complex | 1 | 2 | 2 | 1 | 1 | 2 | 1 | 0 | 0 | 0 |
| Orth | 1 | 0 | 0 | 0 | 0 | 2 | 2 | 0 | 0 | 0 | |
| 2 | C | 2 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 |
| O | 2 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | |
| 3 | C | 0 | 2 | 2 | 2 | 0 | 1 | 0 | 0 | 0 | 1 |
| O | 1 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | |
| Total | 7 | 5 | 7 | 5 | 2 | 5 | 4 | 1 | 2 | 2 |
Interviews were undertaken with a purposive sample of patients/carers where the patient was either aged 65 or older or between 50 and 65 and judged to be at higher risk of falling and their care had been observed. Sampling sought to ensure variety in patients’ falls risk (based on staff advice) and to include both patients that staff deemed to be without cognitive impairment and carers of patients that staff deemed to have dementia. Twenty-eight patients were interviewed. The ability to recruit carers (to interview and provide consultee agreement for patients with cognitive impairment) was limited, owing to restrictions on visiting during much of the observation period; three family members and carers were interviewed. Therefore, in total 31 patients and carers were interviewed.
Sampling of patients for record review
On each ward, we reviewed the falls risk assessment and falls care plan for 10 patients (total = 60). This number was chosen on the basis it was a feasible amount of data to collect within the time frame of the study and would provide enough data for quantitative analysis to be undertaken.
Data collection
Ethnographic observations
Ethnographic methods, such as non-participant observation, have been used in previous realist evaluations as part of the process of theory testing and refinement,25,27 providing insight into the processes and contexts of care. The importance of observation for determining how and if guidelines are used in practice has been demonstrated. 27
In each case site, three researchers (NA, LM, RR) conducted observations independently in the same ward and at similar times. An observation protocol was developed, based on the CMOcs being tested and with input from the Lay Research Group and SSC, which defined what the researchers should pay attention to (see Appendix 3). Researchers recorded observations in fieldnotes. Following in the ethnographic tradition, in the early stage of study researchers kept the scope of the notes wide, on the basis that what previously seemed insignificant may come to take on new meaning in light of subsequent events. 45 In addition, the researchers recorded incidents of observer effects (e.g. participants asking ‘What are you writing?’) to allow analysis of whether participants’ awareness of the researchers’ presence changed over time. 46 The researchers regularly compared their notes to ensure they were capturing the necessary information at an appropriate level of detail and to reflect on what they were observing and identify necessary additions to the observation protocol. Fieldnotes were written up in detail as soon after data collection as possible, using a fieldnote template based on the observation protocol.
For the first two observation periods in each ward, the researchers undertook general observations, to become familiar with staff and the work of the ward. We sought to understand ward routines, including handovers, safety huddles, and multidisciplinary team meetings, and to capture wards’ physical layout. Attention was also paid to other artefacts that support falls prevention, such as electronic (or manual) whiteboards that indicate which patients are at risk of falling. Following this, the researcher selected a bay to observe where there was at least one patient aged 65 years or older or aged 50–64 years and judged to be at higher risk of falling due to an underlying condition. Ethnographic notes focused on patient care (for patients who had consented to be observed) or general staff activities, with attention to activities contributing to falls prevention. For example, whether walking aids were in reach of patients, whether and how call-bells were used. Visiting restrictions limited our ability to observe the contribution of carers to falls prevention, although these were eased towards the end of the observation period.
In each site, it was agreed the researcher would report inappropriate practice to the ward manager. The researcher would only intervene immediately if they witnessed dangerous or abusive behaviour.
Staff interviews
Semistructured interviews were conducted with staff to discuss our CMOcs. For this purpose, the interviews were conducted using the ‘teacher learner cycle’. 47 Here, the interviewer describes the theories to the interviewee, through their interview questions, and the interviewee is then invited to comment, expand on and discuss the theories, based on their experience. Through this process, the interviewer channels the interviewee’s responses to the task of developing and refining the theories. Staff interviews ranged between 10 and 90 minutes in duration, taking place at staff convenience on the ward or via Microsoft Teams. Interview topic guides were established for ward-level staff and organisational-level staff, based on the CMOcs. All interviews were audio-recorded and transcribed verbatim.
Interviews with patients and carers
Semistructured interviews were conducted with patients and/or their carers. Interview topic guides were established for patients and carers, based on the CMOcs and with input from the Lay Research Group. Interviews ranged between 5 and 50 minutes in duration. All interviews were audio-recorded and transcribed verbatim.
Record review
An Excel spreadsheet was developed for recording information from the patient record. The falls risk assessment and care planning documentation was situated within the electronic health record (EHR) in all sites. Data were extracted to assess whether (1) a falls risk assessment was completed for the patient on admission and within 6 hours (a policy at Site 1 and Site 2); (2) a care plan was documented for the patient and if this was completed on a day or night shift; and (3) the care plan was updated and if updates were completed on a day or night shift. In extraction, an assessment or care plan was documented as complete if all items included in the tool had a response documented. While we had hoped to undertake the record review prior to observing a patient’s care, so observations could be used to determine if the care plans were enacted, we were not granted EHR access at the sites in time for this to be possible.
Routinely collected data
Routinely collected data on reported number of falls and reported falls-related harms per ward per month was received from each Trust.
Analysis
Qualitative data analysis followed the steps of framework analysis. 48 The researchers began by familiarising themselves with the data by reading a selection of the observation and interview transcripts – a process facilitated by ongoing reading of transcripts throughout data collection. Researchers then met to discuss construction of a thematic framework to facilitate CMOc testing. Based on previous experience of indexing data for CMOcs, the decision was made to minimise the number of themes by keeping themes abstract to encompass explanation of mechanisms and contextual influences for example, for facilitation, ‘use of physical artefacts’ encompassed description of tools used, how they were used by staff and factors that appeared to support or constrain tool use. The thematic framework was then used to index the data. A series of matrix displays, based on the case dynamics matrices described by Miles and Huberman,49 were used as a next stage in analysis to facilitate cross-case analysis and obtain an overview of the data. One matrix display was produced for each site and for each CMOc being tested (12 in total). The matrix column headings summarised the content of the starting CMOc – clarifying the hypothesised contextual influences, resources offered, participant responses and impacts. In each matrix row, data were summarised, with reference to the indexed data, by Trust and ward, with rows representing organisational site interviews, orthopaedic ward staff interviews, orthopaedic ward observations, older person/complex care ward staff interviews, older person/complex care ward observations. The frameworks informed the site presentations, where findings were presented and discussed with participants, and then formed the basis of narrative summaries that described how the data supported or suggested a refinement or addition to the CMOc.
In addition, the Lay Research Group undertook an analysis of the qualitative data. After defining the task and what qualitative data analysis involved, the Lay Research Group members had about a month before the data analysis session to consider individually two sets of observation notes (one from an orthopaedic ward and one from an older person/complex care ward) and two interview transcripts (one from a patient and one from a carer). Following a general discussion about the materials and the effect of reading them on members, the Lay Research Group shared their thoughts on the individual observation notes and interviews. A number of patterns or themes were identified in the text, including themes about acknowledging patients as people and the impact staff attitudes had on falls prevention. Their analysis resulted in the recommendation of some approaches in falls care planning, such as using imagery (e.g. picture cards) in interactions with patients with communication difficulties such as people with dementia, or speak different languages. Their analysis was reported to the project management group and fed into the wider data analysis process described above. Because of this, their analysis is not reported separately in the following results chapters, but is, rather, incorporated within them (e.g. the importance of knowing patients as people is reflected in the analysis of case study data relating to patient participation in Chapter 8). Reflections on the results or outcomes of PPI itself on the study are reported in Chapter 9.
Analysis of quantitative data
Quantitative data consisted of, for each ward, the record review as described above. Descriptive statistics were produced in Excel, broken down by ward. While we also gathered routinely collected data on number of falls and falls-related harms, we did not undertake quantitative analysis of these data, because there may be differences in falls rates between wards that are unrelated to the effectiveness of their falls prevention practices; we present the data as line graphs purely as contextual information (see Appendix 4, Figures 9–11).
Development of guidance
In September 2022, we held online presentations at each case site, reporting our findings. These acted as a form of respondent validation, providing an opportunity for those we observed to say whether they recognised what we described. We also used these meetings to gather participants’ perspectives on the implications of the research for practice and how guidance should be disseminated, which we discuss in Chapter 9.
Study management
The study was undertaken by a multidisciplinary project management group, providing expertise in falls risk assessment and prevention, clinical decision-making, HIT and realist methods. Members brought different clinical expertise (nursing: DD, FH, AL; pharmacy: VL, HZ), while DW provided a patient perspective. Two researchers were employed on the project (NA, LM), both of whom had previously worked on projects using realist methods. In addition, both had received training in realist methods; NA has a PhD in realist evaluation, supervised by Ray Pawson, and LM had attended training at the Centre for Advancement in Realist Evaluation and Synthesis, University of Liverpool. A SSC was convened, which met with members of the project management group at three points over the course of the project.
The Lay Research Group
Rebecca Randell, the study Principal Investigator, and DW, the lay member of the project management group, met at an event organised by NIHR INVOLVE (a national advisory group that promotes public involvement in health and social care research). On preparing the outline application for this study, RR invited DW to join the project team. Following an initial meeting of RR, DW and NA to discuss the approach to PPI, DW drafted the PPI section of the submission. It was agreed we would recruit a team of ‘lay researchers’, rather than a more conventional lay advisory group; the term was chosen to reflect the active role we hoped to encourage in the project. Alongside this, NA met with DW to provide background information about realist methods. When the project was funded, RR and DW worked together to prepare an information sheet to send to lay people interested in joining. Four lay researchers were recruited from Leeds Older People’s Forum and from service user and carer contacts at Manchester University NHS Foundation Trust and, headed by DW, the Lay Research Group was formed. The Lay Research Group members were from diverse backgrounds (e.g. different ages, ethnicities and sex) who had either fallen themselves or who had cared for someone who had fallen in hospital. LM supported the group by setting up meetings, circulating papers, and taking notes, as well as offering advice and support throughout the project. LM and DW worked together to provide any necessary training for the Lay Research Group. Due to restrictions imposed by the COVID-19 pandemic, all Lay Research Group meetings took place online. An early activity, encouraged by DW, was for both Lay Research Group and project management group members to produce ‘mini-CVs’: short, informal, one-page documents describing background relevant to the project, relevant PPI or professional roles, and other interests; these provided a way for the project management group and Lay Research Group to get to know each other, while also emphasising everyone had something valuable to bring to the project. As described above, the lay researchers contributed to the prioritisation of theories for testing at the end of Stage 1 of the realist review, development of data collection tools for the multisite case study, and analysis of qualitative data collected within the multisite case study. DW regularly attended the project management group meetings, minutes of project management group meetings were shared with the Lay Research Group, and a joint Lay Research Group/project management group meeting was held as an opportunity for lay, clinical and academic colleagues to meet and consider the outputs of the study and its dissemination, and together agree on further work. Lay Research Group members also contributed to project dissemination, writing posts for the project blog (www.bradford.ac.uk/health/research/frames/blog/), presenting to a Commissioning Support Unit about the approach to PPI within the project, and participating in the site presentations. Further details of our approach to PPI are reported elsewhere, in a paper written jointly by lay and academic researchers. 50
In addition to meetings held for the activities described above, the Lay Research Group met three times over the course of the study to evaluate the PPI approach taken (discussed in Chapter 9). The evaluation method drew on the Guidance for Reporting Involvement of Patients and the Public (GRIPP2) short form reporting checklist,51 the UK standards for public involvement for better health- and social-care research. 52,53 and a scoring system developed by the NIHR Yorkshire and Humber Patient Safety Translational Research Centre on a scale of one to six, with a score of one reflecting poor adherence to the UK standards and a score of six reflecting excellent adherence. An evaluation sheet was developed to capture discussions. In the first evaluation in summer 2021, the Lay Research Group met to evaluate progress and allocate scores, then RR, NA and LM met separately to carry out their own review. Both groups decided on topics for discussion independently. Finally, they met together to review progress overall and a joint summary of progress against each standard was produced. For the second and third evaluations in February and October 2022, respectively, a ‘lighter touch’ was used, in which the Lay Research Group met to discuss whether anything had changed since the previous evaluation. In addition, the final evaluation also considered reflective statements written by lay and academic researchers as part of the process of co-authoring the PPI paper mentioned above,50 which focused on how it had felt to work together as partners on the project; what impact this had had on each person and/or the project; and what they felt had supported this.
Chapter 3 Theory construction
Introduction
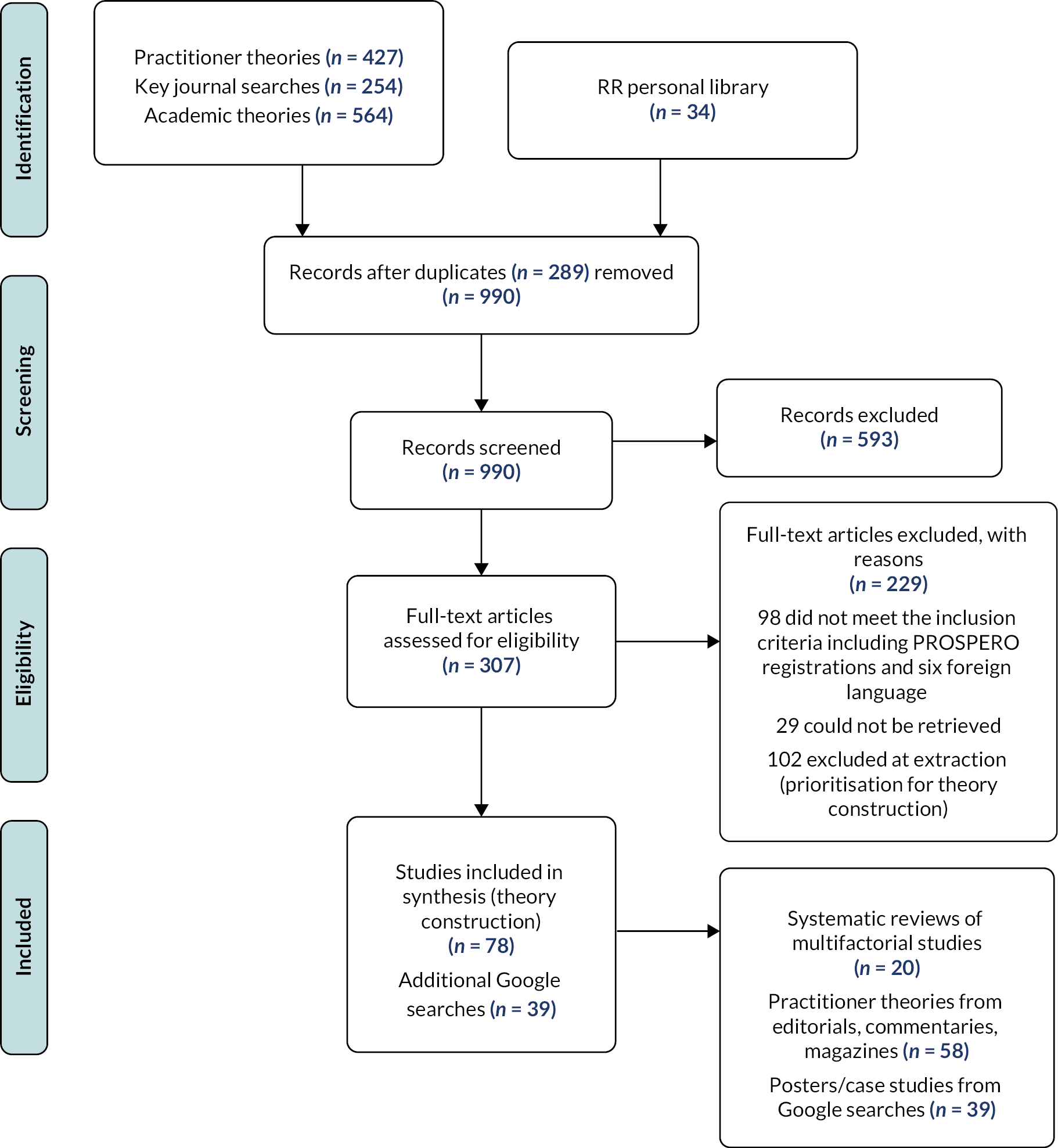
This chapter presents the findings of the theory construction phase of the realist review. The searches identified 1029 unique references to be screened, of which 117 were included in the synthesis [see the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram in Figure 2]. We first provide a summary of the included papers, including the interventions for preventing falls they describe, and the context of inpatient falls. We then use the Consolidated Framework for Implementation Research (CFIR)54 to organise the findings from the practitioner papers because it provides a comprehensive framework to categorise mechanisms, supports and constraints across multilevel contexts that is, at the micro (individual), meso (service/organisation) and macro levels (national).
FIGURE 2.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses diagram for theory construction searches.
Summary of included papers
The papers included in the analysis related to multifactorial risk assessment and prevention strategies specifically and falls prevention strategies more generally. While some papers talked about falls risk assessment and prevention being multidisciplinary, a limitation of the literature is that the majority focused specifically on it as an aspect of nursing practice.
Studies included in the reviews we identified took place in a range of countries with a similar healthcare system, including the USA, UK, Australia, Singapore, Sweden, France, Switzerland, the Netherlands and Germany. 55,56 Each covered multifactorial assessments and interventions in acute settings (sometimes compared with other settings and/or with single-factor interventions).
The term ‘multifactorial’ was interpreted in different ways, some authors emphasising interprofessional working,57 while others described the process of assessing risks and providing tailored combinations of interventions. 55,57 Assessment tools also varied, including comprehensive geriatric assessments58 and self-developed tools to assess patients’ multiple falls risks. 55,59 Some reviews included studies in which falls risk prediction tools were used, such as the Morse falls scale,55,60,61 TNH-STRATIFY,55 and the Hendrich II falls risk model. 55 While such tools are explicitly excluded from multifactorial approaches by NICE,62 we found the distinction between those tools and a multifactorial approach was often unclear: for example, a falls prevention toolkit in one study63 in the Avanecean et al. 55 review used HIT to generate interventions tailored closely to patient-specific areas of risk, identified via the Morse falls scale, including recent history of falling, gait characteristics and impaired mental status, all of which are recommended by NICE. Therefore, we included papers which incorporated the tailoring of interventions to individual risk factors, even where they were associated with the use of risk prediction tools.
The context of inpatient falls and falls prevention
Choi et al. 64 and others55,58 group risk factors as extrinsic (environmental) or intrinsic (patient-related) in nature, with each risk group comprising many different elements. Ward layout and medications given to patients were characterised as extrinsic factors, for example, while intrinsic factors include patient age, history of falls, and physical and cognitive health. The presence of both extrinsic and intrinsic risk factors can, in fact, make hospitals dangerous places for frail, older people, increasing their risk of falling. 64 A report from The National Patient Safety Agency on Slips, Trips and Falls in Hospital, discussed by Hairon,65 showed the most common time for falls is mid-morning, when patients are most likely to be moving around, and most falls are unwitnessed, sometimes owing to extrinsic factors associated with ward layout, which mean that a nurse caring for one patient behind closed doors or curtains cannot observe other at-risk patients at the same time.
Extrinsic and intrinsic risk factors require different interventions, tailored to manage the risks of individual patients. For example, it was noted above that many falls are unwitnessed and take place when patients are attempting to mobilise on their own, often to visit the toilet. Interventions that attempt to address these risks may include proactive nursing assistance with toileting, hydration and moving, such as hourly or intentional rounding; regular observation or moving beds closer to nursing stations; and use of special equipment, including height-adjustable beds and chairs, bed alarms and call-bells. 55,66,67 As well as these targeted interventions, Christy68 drew attention to basic, universal safety measures that should always be in place to address some extrinsic risk factors, such as ensuring patient rooms and hallways are free from trip hazards and flooring is dry.
Choi et al. 69 categorised these different types of interventions as environmental-related; care process and culture-related; and technology-related, with the latter two types being more frequently implemented than the first. According to this model, MFRA is an intervention categorised under ‘care process and culture’ that could trigger use of several other interventions to address individual risk factors for assessed patients and may be used alongside other universal interventions, for example, ward layout. However, this model did not explain what multifactorial practices involved, for example, which tools were used, how they were integrated into work routines, supports or constraints or links with reductions in falls risk. Therefore, we drew on practitioner ideas to develop our CMOcs.
Practitioner theories of implementation and impact
Intervention characteristics
Intervention characteristics in the CFIR cover how intervention features, such as complexity, strength of evidence, and adaptability, influence implementation. The included papers discussed implementation of national guidelines for falls prevention and the development of specific tools to assess and document falls risks and prevention strategies. They also considered interventions designed to support or improve implementation of guidelines and associated tools, such as the use of champions and falls education and training. In this section we focus on characteristics of national guidelines and the assessment tools themselves and discuss other types of intervention within the remaining domains.
Barker70 compared the 2004 and 2013 versions of NICE guideline on falls in older people, pointing out that a lack of integration between the two guidelines (the first focused on community care while the second was updated to incorporate inpatient falls) made the 2013 version difficult for clinicians to interpret, owing to visible differences in writing style and layout of the two elements. These differences were said to affect the quality of the guideline and make interpretation more difficult for clinicians, especially those who worked across care settings. Additionally, they noted that, to support clinicians, NICE had developed a falls in older people pathway, designed to be used interactively on the NICE website, although this might not be feasible for clinicians during their working day. There is a paper alternative, but it was 12 pages long, difficult to follow and not considered user friendly. This suggests ease of access to recommendations and their presentation may influence their use in practice. Furthermore, Glasper71 referenced a number of guidelines and resources, developed by NICE, the Royal College of Physicians, and the Care Quality Commission, available to support falls prevention in hospital but noted that ‘no matter how much advice bodies such as NICE produce it is often nurses who have to reconcile the reality of care delivery and the quest to reduce falls’ (p. 807), pointing to the practical day-to-day challenges of delivering recommendations, which are likely to vary between organisations depending on resources available.
Multifactorial falls risk assessment tools
A key component of the NICE guidelines is delivery of MFRA. A number of falls risk prediction tools were discussed in the literature, but Matarese and Ivziku72 noted that no single tool could identify all patients at risk of falls or accurately exclude all those who were not at risk of falling, a fact which underpins the NICE62 guidance. It was not clear in the literature reviewed (which included international studies and perspectives) if any standardised tools were used specifically for MFRA. Kelly and Dowling73 pointed out that there was no single, universally adopted assessment tool; institutions tended to develop their own. However, they described the most important characteristics of any tool were that it is easy to use, quick to complete, and reliably identifies at-risk patients. An assessment tool with a care plan was provided as an example of best practice, highlighting the importance of linking identified risks with actions to improve, manage or address risks. However, they also noted that the efficacy of the assessment depended on the skills of the healthcare professional undertaking it, indicating the influence of individual knowledge and experience on accurate risk identification. Christy supported this idea, commenting that nurses should not rely on assessment tools alone and that they should apply their clinical judgement to prevent falls. Characteristics of individuals that influence implementation and risk reduction are discussed further in Staff characteristics.
The idea that falls prevention practices should be easy to implement was echoed by Miake-Lye et al. 56 who noted that engagement of clinicians in design and development can help ensure an intervention will ‘mesh’ with existing clinical procedures, suggesting that to support implementation, falls prevention practices and tools should connect with and complement existing systems. Promoting this idea, Avanecean et al. 55 suggested that adherence to intervention protocols was supported where components were easily incorporated into existing practices and where it supported ongoing evaluation of falls prevention programmes. To this end, Sutton et al. 74 reflected on the use of a multifaceted care bundle to minimise patients’ falls risk and suggested that a rolling programme of auditing the care bundle elements could be incorporated into routine processes to support implementation by informing adaptations for example, by streamlining the documentation process. Analysing falls documentation and practice in this way has been argued to be an important part of falls prevention. 75
Health information technology
Health information technology can be used to capture and present data about falls to evaluate the causes of incidents and adherence to intervention components. 56 Hempel et al.,60 for example, note that integrating falls risk assessment into EHRs could support falls audit and feedback processes by providing ready access to data. A different function of HIT was discussed by Mashta,76 who described the use of an electronic alerting system, in which alerts generated by the hospital information system notified staff as soon as a new patient was admitted with a history of falls, while Barrett et al. 77 discussed use of HIT in their hospital’s falls prevention programme. Nurses used the EHR to record admission details and it acted as a prompt for the initial nursing assessments. A falls risk score was added as a mandatory screen in the EHR and nurses were required to enter a falls risk score directly into the patient’s electronic record on admission and to update it weekly until discharge. In their review of falls prevention strategies in the USA, Spoelstra et al. 75 reported on the use of an IT system to generate tailored falls prevention posters for individual patients and patient-specific alerts, in a study by Dykes et al. 63 Finally, Grant and McEnerney,78 in their article about one-to-one nursing, commented that nursing staff are often busy with routine clerical duties, which may constrain intervention delivery. They argued that EHRs make these clerical duties quicker to complete, giving nurses more time to spend with patients, and thereby reducing the likelihood of serious falls occurring.
Staff characteristics
The CFIR domain ‘characteristics of individuals’ refers to people’s knowledge and beliefs about the intervention. These factors may support the implementation of falls risk assessment and prevention practices, or they may constrain it, even if the intervention has features deemed supportive. For example, Miake-Lye et al. 56 discussed nurses’ ‘buy-in’ or commitment to falls prevention as an implementation support, but also noted the need to change the attitude that ‘nothing can be done’. Changing individual and group attitudes or motivation towards falls prevention programmes was discussed in many of the manuscripts reviewed,56,75,79 often with reference to the use of educational and training interventions to increase knowledge of falls risks and, consequently, attitude towards intervention delivery. For example, Glogovsky80 discussed how, when nurses understand falls prevention interventions, they are more engaged in preventing falls. A nurse supported this assertion; Johnson81 reported that reading a continuing professional development (CPD) article improved their knowledge of falls risk assessment tools, including the importance of completing an assessment for older inpatients both on admission and regularly during their hospital stay. They explained that this knowledge increased their confidence in undertaking the assessments and that they were more aware of the importance of taking a holistic approach, incorporating risk factors that they had not considered previously, such as oxygen tubing, which can present a trip hazard. The CPD article outlined the physical and psychological factors nurses should consider when undertaking assessments, and the effects that older people may experience because of a fall. The importance of engaging practitioners undertaking the assessment in this way was highlighted by Lindus,82 who described a nurse’s realisation of ‘going through the motions’ when undertaking a falls risk assessment. The nurse reflected that they were shown how to complete the falls prevention paperwork but had not made the association between the risk and the specific patient assessed.
Falls champions
The availability of staff dedicated to falls prevention was identified as a potential implementation support. Several authors described studies of staff – often nurses – who were dedicated to falls prevention activities, for example, in the role of falls ‘champions’. The amount of time and other resources available and the precise nature of the role varied. In one study included in the Avanecean et al. 55 review, for instance, two research nurses were made responsible for delivering a care planning intervention and received intensive training on delivery, implementation, and care plan development. While the intensive training may have generated the necessary ‘buy-in’ and engagement in risk identification, an additional support on delivery of the falls prevention strategy was that champions had ‘as much time as needed’ (p. 3022) to fulfil their responsibilities.
Authors described different functions of the champion role: for example, Duffin83 reported on the use of falls champions (often nurses) who met regularly to examine falls rates and evaluated care processes to support improvement. Sutton et al. 74 discussed spread of the FallSafe care bundle initiative in an acute hospital in the UK, providing the local perspective on a QI initiative that had involved multiple hospitals within the region. 10 This project relied on a network of falls champions – nurses or HCAs – who undertook e-learning to deliver the care bundle elements and attended training days. The champions had numerous responsibilities, but a key intention was that they would motivate and inspire ward colleagues and multidisciplinary teams to introduce and sustain the evidence-based initiative and ensure falls prevention was a priority on wards. To do this, the authors posited that champions needed a strong personality and leadership attributes. Furthermore, champions needed to recognise that several teaching and communication styles would be required to engage different staff in the implementation process.
Process of implementation
‘Process of implementation’ in CFIR refers to strategies or tactics that might influence implementation. These might include engaging appropriate individuals in implementation and reflecting on and evaluating progress. Some of the previous discussion has highlighted examples of such strategies, for example, the role of falls champions in the process of implementation, and the use of audit and feedback to evaluate the process of delivery and associated outcomes. QI frameworks were also used to support implementation of recommended falls practices, through a process of incremental improvement in the care processes under study. Approaches cited include the Define, Measure, Analyse, Improve, Control process80 and Plan, Do, Study, Act. 60 These types of improvement methods were also reported in posters from falls collaboratives in NHS Trusts and NHS Improvement falls collaborative case studies, retrieved from the Google searches, in which numerous interventions were used to improve process and outcome, often including use of champions and education and training.
Engaging ward staff in intervention delivery: shared responsibility
Health care is delivered by multidisciplinary teams. Although the literature reviewed as part of this study typically discussed falls incidents as a nurse-sensitive outcome, placing emphasis on the nursing team, the multidisciplinary nature of falls prevention was also acknowledged, for example, when pharmacists and physiotherapists receive referrals as part of the falls prevention strategy. 84 Communication has been identified as a key factor underpinning effective teamwork; Avanecean et al.,55 for example, commented that communication is essential in all falls prevention programmes because falls prevention is the responsibility of all staff. Despite its essential nature, communication between care teams was reported as variable. 85
Some papers discussed interventions that targeted communication between ward staff and how these may work to improve implementation of falls prevention practices and consequently reduce falls risks. For example, Avanecean et al. 55 discussed Fall TIPS, which generated a poster to facilitate communication about individual patient’s risk factors and interventions that were readily available at the bedside to help address them, and Lilley86 described the introduction of a ‘thorough safety briefing where we discuss patients at risk of falls’. This ward sister further discussed the use of postfall huddles that provided an opportunity for team reflection to inform simple changes to daily working patterns to prevent similar falls.
Engaging patients and carers in falls prevention practices: patient participation
Healey87 noted that ‘varying patients’ preferences, myriad combinations of risk factors, the need to maintain independence, and the rapidly changing condition of a patient in an acute hospital mean that an adaptive approach to falls prevention is usually needed’. The concept of patient-centred care potentially offers an adaptive approach to falls prevention. Avanecean et al. 55 defined patient-centred care as an approach that ‘takes into account that each patient is an individual with his or her own unique characteristics and risk factors that may contribute to the occurrence of falls’ and hypothesised that this approach may reduce falls incidents. Similarly, other authors discussed the importance of actively involving patients in participation of falls prevention strategies. For example, Jones and Whitaker88 argue that patients must understand what their falls risks are and agree to the prevention strategies suggested by professionals if they are to comply with their implementation.
The literature provided examples of how a patient-centred approach might be realised, for example, using particular questions during the assessment. Christy68 reported that ‘patients and families became involved with their own falls prevention interventions when asked what might cause their fear of falling, and what they thought would prevent a fall’. Both Christy68 and Pearce89 point to communication between ward staff and the patient as a significant factor underpinning patient empowerment and participation in falls prevention. However, potential constraints on patient participation were also discussed, for example, variation across organisations in the information communicated to patients in terms of the interventions implemented on their behalf, and measures they could take to reduce their risk of a fall. 90
Hemsley et al. 91 and Reznik92 examined the experiences of individuals with communication disability and cognitive deficits, respectively. Patients with aphasia may not understand instructional education programmes or may not be able to indicate their needs to ward staff, and patients with decreased awareness may require more management of extrinsic factors, all of which are likely to influence how and to what extent patients are able, and should be expected to, participate in strategies to prevent falls. Speaking to these challenges, Tingle93 argued that there needs to be a balancing of risks, encouraging patients to be independent but also being mindful of their safety interests.
Inner setting
‘Inner setting’ in the CFIR refers to features of organisations, such as implementation climate and leadership. Miake-Lye et al. 56 identified leadership support from hospital directors and unit directors or clinical champions on wards as a theme of effective implementation in their systematic review of falls prevention programmes. They commented that while leadership may be considered an implementation support for programmes in general, more specific to falls prevention is multidisciplinary development and guidance within falls prevention programmes and overcoming the idea that falls are inevitable. Supporting this idea, Sutton et al. 74 suggested that the positive impact of leadership included inspiring others and ensuring falls prevention was a priority on wards, while Spoelstra et al. 75 discussed that organisation-wide training to educate staff about falls prevention would help develop a culture of safety that may engage staff in the practices necessary to ensure a safe environment for patients. West et al. 90 assessed nursing interventions to reduce patient falls and suggested that implementation of existing falls policies might be constrained by a high rate of turnover in leadership roles on clinical units and at the middle-management level, which meant leaders lacked experience to address implementation challenges. They noted that auditing compliance with local falls policies provided an opportunity to ‘educate novice leaders’ about the importance of evaluating the clinical practice of their staff but acknowledged that the daily challenges of operations and staffing issues may get in the way.
The staffing levels of wards and units was also discussed as a potential support or constraint on implementation of MFRA and prevention strategies. Christy68 argued that adequate staffing not only gives nurses time to provide hourly rounds to meet patient needs, reducing the likelihood of patients mobilising unassisted, it also gives them sufficient time to think critically and intervene to prevent falls. In their systematic review, Choi et al. 69 reported that most included studies implemented a considerable number of care process-related interventions that may demand time and effort from nurses. Environment-related interventions, the authors noted, could help to reduce falls by supporting the work of nurses, but despite evidence about the importance of the physical environment only a few hospitals were identified as introducing such interventions as part of their multifaceted falls intervention strategies.
Outer setting
‘Outer setting’ in the CFIR encompasses external policies and incentives, as well as whether patient needs and resources are prioritised by organisations. The influence of external policies was discussed in several texts. For example, Barker70 considered the impact of the NICE guidance that instigated our study, indicating potential constraints such as lack of funding. They note that the costing statement for the guideline stated that implementation is unlikely to have a significant cost impact for the NHS, based on the possibly incorrect assumption that most parts of MFRA and prevention are already standard practice.
In the USA, Spoelstra et al. 75 speculated that a motivation for healthcare managers and staff to reduce falls rates was the decision by the Centre for Medicare and Medicaid Services in 2008 not to continue funding costs associated with inpatient falls. Other policy drivers highlighted in this paper included hospitals’ desire to attain Magnet status and the requirement by the Joint Commission for accredited hospitals to conduct falls risk assessments for their patients. Mashta76 reflected on how falls prevention became a top priority for many UK hospitals as one of the eight ‘high impact actions’ developed by nurses at the request of England’s Chief Nurse in 2010.
Programme theory and CMO configurations
Various factors were identified that may work to support or constrain implementation of MFRA and prevention strategies, within the different domains of the CFIR. Our analysis suggests that alongside tools that guide and facilitate delivery of recommended falls prevention practices, other factors that may support or constrain implementation include individual clinical knowledge; confidence and expertise; the extent to which the ward team and patient and carer participate in the strategy; falls leadership within different levels of the organisation; and prioritisation of resources for falls prevention, for example, in ring-fenced time to deliver the strategy.
Drawing on this analysis, we constructed a series of tentative CMOcs. Combining them with the CMOcs included in the proposal (see Appendix 5) resulted in a total of 25 CMOcs (Table 8).
| Reference | Context | Mechanism | Outcome | |
|---|---|---|---|---|
| Resource | Response | |||
| 1. Protocol + Healthcare Improvement Scotland: Falls Case Studies94 + Google search Posters related to NHS Improvement Initiative | Attention drawn to weaknesses in local falls prevention practices, for example, through local or national audits or an adverse event | QI initiative on falls | QI: QI initiatives are introduced and attention is focused on falls prevention | More complete falls risk assessments and adherence to protocols for falls prevention |
| Data on national performance in falls prevention National body support to providers to adopt improvement methodologies and create a learning community to discuss changes they are implementing and share findings |
QI: Trusts implement change and share experiences via posters | Reduce injurious falls and increase reporting of falls | ||
| 2. Protocol + Avanecean et al.55 | Nurses seen as key staff in preventing falls Resource-constrained setting |
Falls prevention emphasised as a priority by the ward manager and/or ward has dedicated trained falls prevention nurses | Leadership: activities such as safety huddles maintain nurses attention on falls prevention | More complete falls risk assessments and adherence to protocols for falls prevention |
| 3. Avanecean et al.;55 Lindus;82 Kelly and Dowling73 | Nurses seen as key staff in preventing falls Resource-constrained setting |
Prevention strategy accompanied by implementation framework to facilitate integration + assessment tool is user friendly and quick to complete | Facilitation/easy integration: nurses choose to integrate prevention strategies that can be easily incorporated into their normal workflow | Correct and timely implementation of falls prevention strategy |
| 4. Sutton et al.74 | Nurses seen as key staff in preventing falls Some nurses have limited education on falls prevention and typically charged with communicating with nursing team rather than leading improvement across professional boundaries |
FallSafe intervention
|
Expertise/leadership: FallSafe leads become knowledgeable about falls prevention, grow in confidence, and become falls ‘specialist’ Facilitation: ward staff find implementation of components manageable due to staged approach and equipment available for use as intended Learning culture: culture of learning rather than blame develops around implementation and impact of components Learning community: learning via shared experiences of implementing FallSafe bundles |
Delivery of ‘essentials’ of falls prevention including
|
| 5. Glasper,71 Glogovsky;80 Barrett et al.;77 Grant and McEnerney78 |
Resource-constrained setting | Digital support for falls risk assessment and recording falls interventions (e.g. prompts/checklists, use of hand-held devices at the bedside) | Workflow facilitation: nurses find it easier and quicker to complete assessments and record interventions using the digital support provided | More complete falls risk assessments and care plans |
| 6. Cunningham;95 Sutton et al.;74 Christy;68 Heaton;96 Hughes;97 NHS Improvement Falls Collaborative case studies, 2017; Nursing Standard: ‘Falls prevented by checking patients have what they need’;98 Ward et al.;99 East and North Hertfordshire NHS Trust falls poster 2, 2018; Healthcare Improvement Scotland: Falls Case Studies94 | Patient-centred culture, which focuses on care, compassion and learning rather blaming | Patient-centred support for staff and patients/carers, which is both institutional [e.g. senior member(s) of staff with a remit to prevent falls, falls committees, falls policies] and available to individuals (e.g. encouragement, time for staff, patients and carers to talk to and listen to each other training/mentorship, reward, caring and active listening) | Staff empowerment: staff feel valued and empowered to learn and to put patients’ needs first in falls prevention Staff feel it is acceptable to explore the tension between risk prevention and patient rehabilitation in ways that are tailored to each individual patient Staff engagement: staff feelings of empowerment have the potential to transform fatalistic views to proactive engagement Patient empowerment: patients and carers feel heard and empowered and feel they have been given necessary information to reduce their falls risk |
Multifactorial falls prevention strategy is implemented, with patients’ needs at its heart Patients (and their carers) are better able to understand their own risk factors for falling (because these are explained to them), more likely to follow guidance (because they understand it) and ask for help (because they do not feel like a nuisance) |
| 7. Falls Improvement Collaborative poster 2, Dartford and Gravesham NHS Trust, 2018C | Hospital/ward has policy on MFRA, which makes it clear that prediction tools are no longer to be used and trains/coaches staff in implementing this policy | MFRA policy and training programmes | Knowledge: staff understand they must no longer use prediction tools and why | Staff apply MFRA policy |
| 8. Protocol + West et al.90 | When staffing levels are low and/or workload is high/there is high turnover/high use of agency staff | MF risk assessments MF interventions Induction/training events and information |
Resource strained prioritisation: clinical staff select which risk assessments and interventions they will use with patients, based on their perceptions of the patient’s particular vulnerabilities Resource strained prioritisation: managers cannot find time to induct and train all new or agency staff fully in multifactorial approaches, so that new/agency staff are not aware of their responsibilities and/or do not understand how to apply these approaches properly |
Leading to certain patients not receiving a MFRA or falls prevention interventions tailored to their individual needs |
| 9. Protocol | When nursing staff are required to undertake many different risk assessments | MF risk assessments | This creates a cognitive burden so that nursing staff find it difficult to integrate the information from the different risk assessments to determine which interventions should be prioritised for the patient | Leading to a standard bundle of interventions being provided to all patients |
| 10. Protocol + Perdue100 West et al.;90 Barker70 |
If patients and/or carers do not adhere to falls prevention advice If falls prevention advice is not delivered in a way that takes patients’/carers’ needs and perspectives into account |
Falls prevention advice/programmes/info sheets | Staff motivation: nursing motivation decreases Patient motivation: patient/carer motivation to follow the advice and/or understanding of the advice decreases |
Leading to fewer falls risk assessments being undertaken, leading to patients and carers not following the advice, which may put patients at higher risk of falling |
| 11. Barker et al.70 | Lack of integration between 2004 and 2013 NICE guidelines makes the latter difficult for clinicians to interpret | NICE has developed a falls in older people pathway, which is designed to be used interactively on the website. The paper version is not user friendly and more difficult to follow as it prints on 12 pages | Interpretation challenges: inconsistency between guidelines affects quality and makes interpretation difficult for clinicians who work across different care settings + during their working day not all clinicians will have access to the internet | Same issue as was experienced regarding implementation of 2004 guidance – inconsistency in care provision across sectors Longer-term perspective needed – there are interventions to reduce immediate risk, for example, reviewing the environment, but in isolation these will be ineffective in reducing long-term falls risk. Prevention and maintenance key |
| 12. Nursing Standard: ‘Falls risk’ needs revisiting101 | Clinical unit and/or wider organisation has a culture that places more importance on avoiding falls than on applying multifactorial, tailored approaches specific to individual patient’s needs | MF risk assessments MF interventions |
Restriction: clinical staff focus on preventing falls by restricting patient mobility | Patients considered at risk of falls receive restrictive interventions rather than multifactorial interventions tailored to their individual needs, which may lead to deconditioning and, conversely, a higher risk of falling in the future |
| 13. Avanecean et al.;55 Manojlovich et al.;66 Jones and Whitaker;88 Perdue;100 Christy68 | Patients have different risk factors and preferences Patients may have a lack of awareness about their own falls risk Organisational strategies apply the same approach to all patients regardless of individual needs |
Patient-centred strategy – refers to interventions targeted towards individuals (e.g. person-centred education, posters that alert nurses to patient risk, physical therapy exercises Multifactorial refers to strategies that target individuals’ specific risk factors and which involve/engage patients in the risk assessment process Information/education is typically included in these strategies |
Patient engagement: providing care that is respectful and responsive to patient preferences, needs, and values engages patients in the falls prevention strategy – they participate in the interventions and are less likely to take actions that increase their risk of falling | Patient risk factors addressed/managed, and they are less likely to fall Patient anxiety about falls reduced and they continue activities of daily living |
| 14. Barker70 | Patients may have a lack of awareness about their falls risk or forget their falls risk during their inpatient stay, which then leads to attempts to mobilise, for example, to go to the toilet, which creates a falls risk | Visual cues about falls prevention, such as leaflets, posters, alert signs and stickers are used | Patient empowerment: cues reduce patient misunderstanding about their fall risk and provide a prompt/reminder/legitimise that it is ok to ask nurses for help rather than take risks | Patients understand their falls risk and ask nurses for help when they need to mobilise |
| 15. Avanecean et al.;55 Manojlovich et al.66 | Falls reduction is the responsibility of all staff, lack of communication and understanding of patient risk factors may contribute to falls | Poster of individual risk factors identified from risk assessment displayed at patient bedside and interventions for example, assistive technologies readily available | Shared responsibility: patient risk factors communicated to all staff Vigilance of patients at risk for falls increases because accountability for patient falls is distributed to all staff, not just direct patient care providers | Staff aware and ready to support patients so they do not engage in risky behaviour, helping to reduce falls |
| 16. Rimland et al.;57 Choi et al.69 | Reasons why patients fall are multifactorial, including intrinsic and extrinsic factors | Falls risk assessment tool incorporates three key domains – exercise, physical environment and assistive technologies | Structure for systematic approach: nurses use assessment tool as a prompt/reminder to assess each area, enabling them to capture risk factors specific to each patient | Risk factors identified and care plan to address/manage risk factors put in place for each patient |
| 17. Rimland et al.;57 Choi et al.;69 Johnson;81 Kelly and Dowling;73 Healthcare Improvement Scotland: Falls Case Studies94 | Reasons why patients fall are multifactorial, including intrinsic and extrinsic factors Assessing patient falls risk may be challenging as patients may not understand why they fall/or their risk factors |
Falls risk assessment tool + nurse experienced in assessing falls | Structure and expertise: nurses use tool as a guide (comprehensive and systematic approach) but they use experience and ‘holistic approach’ in the assessment, for example, engaging carers and colleagues to make judgments about patients’ falls risks | Patients’ falls risks are successfully identified – supports ‘anticipatory nursing’ |
| 18. Rimland et al.;57 Choi et al.;69 Lindus;82 Kelly and Dowling73 | Reasons why patients fall are multifactorial, including intrinsic and extrinsic factors 50% of fallers have a second fall Nurses may not understand why patients fall – they complete forms but are ‘going through the motions’ |
Falls education, for example, use of DAME (drugs, age-related concerns. medication use, environment) | Application of professional learning: nurses gain knowledge of fall risk factors and understand the importance of the assessment process Therefore, asking more in-depth questions to identify risk factors |
Patient risk factors identified + nurses champion patient safety |
| 19. Kelly and Dowling;73 Krishna and Van Cleave;102 Healey;87 Lilley86 | Reasons why patients fall are multifactorial, including intrinsic and extrinsic factors + they occur at different times of day in different locations, etc. | Falls incidence should be recorded, analysed and reflected on by ward team, for example, in postfall huddles. Provides insight into (ward-specific) how, when, why/who falls, etc. | Application of group learning: learning from huddles/reflection reveals ward/service-specific QI opportunities, for example, changing staffing levels at different times of day/small changes in work patterns, for example, moving high risk patients to nurse visible positions | Continuous falls improvement ethos Patients feel safer, knowing they can easily communicate with nurses, for example, if they want to mobilise with help |
| 20. Sutton et al.;74 Glogovsky;80 Grant and McEnerney;78 Perdue;100 Barker;70 Bellingham;84 Hairon;65 Dykes;103 George Elliot Hospital, Falls Improvement Collaborative poster 2, 2017 | Falls have multifactorial aetiologies and require a concerted, integrated, multidisciplinary response | Multidisciplinary team members are available at appropriate times to work on preventing falls | Teamwork/adaptation: opportunities are taken at multidisciplinary team meetings to review MF risk assessments and plan/refine tailored interventions (e.g. falls risk and MFRA compliance are standard items on multidisciplinary team meeting agendas) Teamwork: multidisciplinary team members understand/listen to each other’s as well as patients’/carers perspectives and act on these |
Multidisciplinary team works together effectively with the aim of preventing falls |
| 21. Avanecean et al.55 | Patients have different risk factors and preferences Organisational strategies apply the same approach to all patients regardless of individual needs |
Standardised assessment/risk prediction tool | Missed opportunities: nurses use a tool to guide and document assessment but may not identify risks specific to each patient, for example, current knowledge of falls, current functional level | Risk factors are not consistently or comprehensively identified |
| 22. Avanecean et al.55 Barker70 |
Patients have different risk factors and preferences Patients may have a lack of awareness about their falls risk Organisational strategies apply the same approach to all patients regardless of individual needs |
Standardised tools may not account for individual risk factors, for example, current knowledge, current functional level | Patient inactive in strategy: patient does not engage in risk prevention strategy because it is not tailored to their needs + continues to take risks | Risk factors are not addressed/managed to reduce falls |
| 23. Barker70 | Falls reduction is responsibility of all staff Lack of communication and understanding of patient risk factors may contribute to falls |
Multifactorial strategy that does not include information tools to communicate risk factors to staff | Confusion: patients may receive inconsistent messages about their falls risk from staff and become confused about their risk factors | Risk factors are not fully addressed/managed effectively and may lead to falls |
| 24. Avanecean et al.;55 Walmsley;104 Barker;70 Perdue;100 Choi et al.69 | Length of hospital stay may constrain the effectiveness of some interventions, for example, use of vitamin D and exercise interventions | Multifactorial strategy to identify and address individual risk factors | Intervention mechanism constrained: lack of vitamin D or exercise identified as a falls risk and patient referred for medication review and prescription or exercise intervention, but interventions do not take effect | Risk of falling not impacted during patient hospital stay – fall risk remains |
| 25. Hunt;105 Tingle93 | Tension between privacy and dignity, and observations of patient (physical layout of ward) | Multifactorial strategy to identify and address individual risk factors | Environmental influences: strategy may be implemented but depending on ward layout/nursing staff organisation, nurses may not be able to see/offer support to patients when needed. Patients may engage in risky behaviour | Preventable falls may occur |
Chapter 4 Prioritisation of theories for testing
Introduction
On completing the theory construction phase of the realist review, we had a total of 25 CMOcs. Prioritising which CMOcs should be tested in later phases of the study was a process completed in collaboration with the Lay Research Group and SSC, as described in Chapter 2. In this chapter, we present the outputs of the steps we went through and the final prioritised CMOcs.
Creation of If–Then statements
To facilitate the prioritisation process, the 25 CMOcs were refined into a series of 11 If–Then statements. We reviewed the CMOs to assess to what extent they were concerned with what works to support implementation and delivery of MFRA and tailored interventions. We also removed CMOcs that it was not feasible to test and/or did not have the potential to inform practice. The resulting If–Then statements are presented below.
Delivery of an MFRA and care plan
These If–Then statements relate to implementation, that is, what works to ensure that consistent, comprehensive, and ongoing MFRA and tailored interventions are delivered to eligible patients.
-
If there are nurses who are trained and dedicated to delivering falls prevention (e.g. falls leaders or champions), then they will lead implementation of the multifactorial falls prevention strategy on their ward, ensuring a consistent and co-ordinated effort to deliver the strategy across professional groups.
-
If assessment tools (including HIT) and processes are relatively quick and easy to use, and/or facilitate existing routines, then nurses will choose to integrate them into their work processes, helping to ensure that eligible patients receive a MFRA and appropriate interventions.
-
If ward staff receive feedback about their successes and challenges in delivering their multifactorial falls prevention strategy, which aims to promote learning rather than apportion blame, then they will feel supported and empowered to overcome implementation challenges.
-
If a community is in place across hospitals for falls leaders/champions to share experiences of delivering multifactorial falls prevention strategies, then they will learn from other hospitals and implement successful approaches to support delivery of such strategies.
-
If there is training and education for falls prevention available to ward staff, then they will understand the importance and benefits of multifactorial strategies for patients, carers, and the service, and feel empowered to, and/or accountable for, delivering ‘best practice’ in the form of patient-centred assessments and interventions to all eligible patients.
Delivery of interventions tailored to individual falls risk factors
These If–Then statements relate to falls prevention, that is, what works to prevent/reduce patient falls in an acute setting.
-
If a multifactorial, patient-centred strategy is delivered, then patients (and/or their carers) will understand their risk of falling and why particular preventative interventions are being used, and feel empowered to take part in those interventions, thereby reducing the risk of falling. For example, patients could use the call-bell/ask ward staff for help in getting up and moving about.
-
If multifactorial strategies include sharing information between ward staff (e.g. through posters/safety huddles/handovers), then they will develop a shared responsibility for falls prevention and become more vigilant of patients at risk from falls.
-
If falls training, education and tools are available to ward staff, then they will develop expertise in falls that they will apply in practice, for example, by asking patients more in-depth questions during multifactorial assessments to ascertain their risk of falling, leading to identification of risks relevant to each patient.
-
If falls incidences are recorded, analysed and discussed by ward staff, for example, in safety huddles, then they will learn about how, where and when falls are most likely to occur, enabling them to make changes to work patterns and routines to support multifactorial falls prevention strategies, for example, by locating high risk patients’ beds in visible locations.
-
If multidisciplinary team members are available at the right times, then they will participate in the falls risk assessment and care planning process, leading to team engagement and co-operation in delivering the multifactorial strategy.
-
If wards are adequately staffed, then nurses will have the time to think critically about the falls prevention strategy and work to ensure patients’ needs are met, for example, by providing enough for patients to drink, managing pain effectively, and helping patients to get up to visit the toilet; therefore patients who have difficulty walking safely on their own will be less likely to do so without assistance.
Results of prioritisation
Members of the Lay Research Group and SSC prioritised statements differently but with some common focus, for example, around communication; training and education; and the importance of an accountable, team-based culture rather than a blame culture.
On the advice of the SSC, the final choice of CMOcs for testing took account of the rankings and comments of both the Lay Research Group and SSC but prioritised the lay voice in the final choice. We converted the If–Then statements back into CMOcs and produced a shortlist of eight for testing. This included the six most highly ranked statements by the Lay Research Group; one statement highly ranked by SSC; and one statement that was relatively highly ranked by both the Lay Research Group and SSC. We identified that the eight CMOcs encompassed similar mechanisms, allowing us to combine certain CMOcs, reducing the number to six.
-
Leadership: where falls prevention is prioritised by organisations, for example, in organisational policy and provision of resources (C), falls leaders/champions (staff trained and dedicated to supporting delivery of multifactorial falls prevention strategies on their wards, for example, by offering training and education to new staff) inspire and support delivery of the strategy in a consistent and co-ordinated way (M), so that all patients eligible receive a MFRA and tailored intervention strategies (O).
-
Staff empowerment: where falls prevention is prioritised by organisations, for example, in organisational policy and provision of resources (C), and training and education about falls prevention is available to ward staff, then they will understand the importance and benefits of delivering multifactorial strategies for patients, carers, and the service, and feel empowered to, and/or accountable for (M) delivering ‘best practice’ in the form of patient-centred assessments and interventions to all eligible patients (O).
-
Facilitation: there is variation across services in how and the extent to which MFRAs are implemented. In contexts where nurses are educated about falls risks and prevention practices (C), if MFRA tools (including HIT) that reflect best practice recommendations are relatively quick and easy to use and are easily integrated into existing workflows, staff will complete them with patients because they facilitate implementation of recommended practice (M), helping to ensure that all patients eligible receive a comprehensive, MFRA and appropriate interventions (O).
-
Patient participation: where patients have the capacity to engage in the MFRA process (C), and a patient-centred approach is taken, for example, where staff involve patients and carers in the assessment and care planning process, taking into consideration their needs and preferences, and communicate the strategy effectively to them, then patients will understand their strategy and they will have the confidence/reassurance to participate in specific interventions, for example, using the call-bell to alert nurses rather than attempting to mobilise alone (M), thereby collaborating with ward staff in implementation of the strategy to reduce their risk of falling (where they are capable and able to do so) (O).
-
Shared responsibility: where there is a culture of learning, rather than apportioning blame, from errors (C), if information about patients’ falls risks is effectively communicated between ward staff (e.g. through posters/safety huddles/handovers), then staff will develop a sense of shared responsibility for falls prevention and become more vigilant of patients at risk from falls (M), thereby supporting implementation of multifactorial strategies to prevent falls (O).
-
Expertise: in contexts where falls incidences are recorded, analysed, and discussed by ward staff, (e.g. in safety huddles) (C), then they will learn more about MFRA and prevention (e.g. how, where, and when falls are most likely to occur and what works to prevent them) (M), enabling them to make appropriate changes to work patterns and routines, (e.g. by locating high-risk patients’ beds in visible locations) (O).
These six CMOcs are presented as an Initial Programme Theory (IPT) in Figure 3.
FIGURE 3.
Initial programme theory depicting mechanisms that support implementation of falls prevention practices.
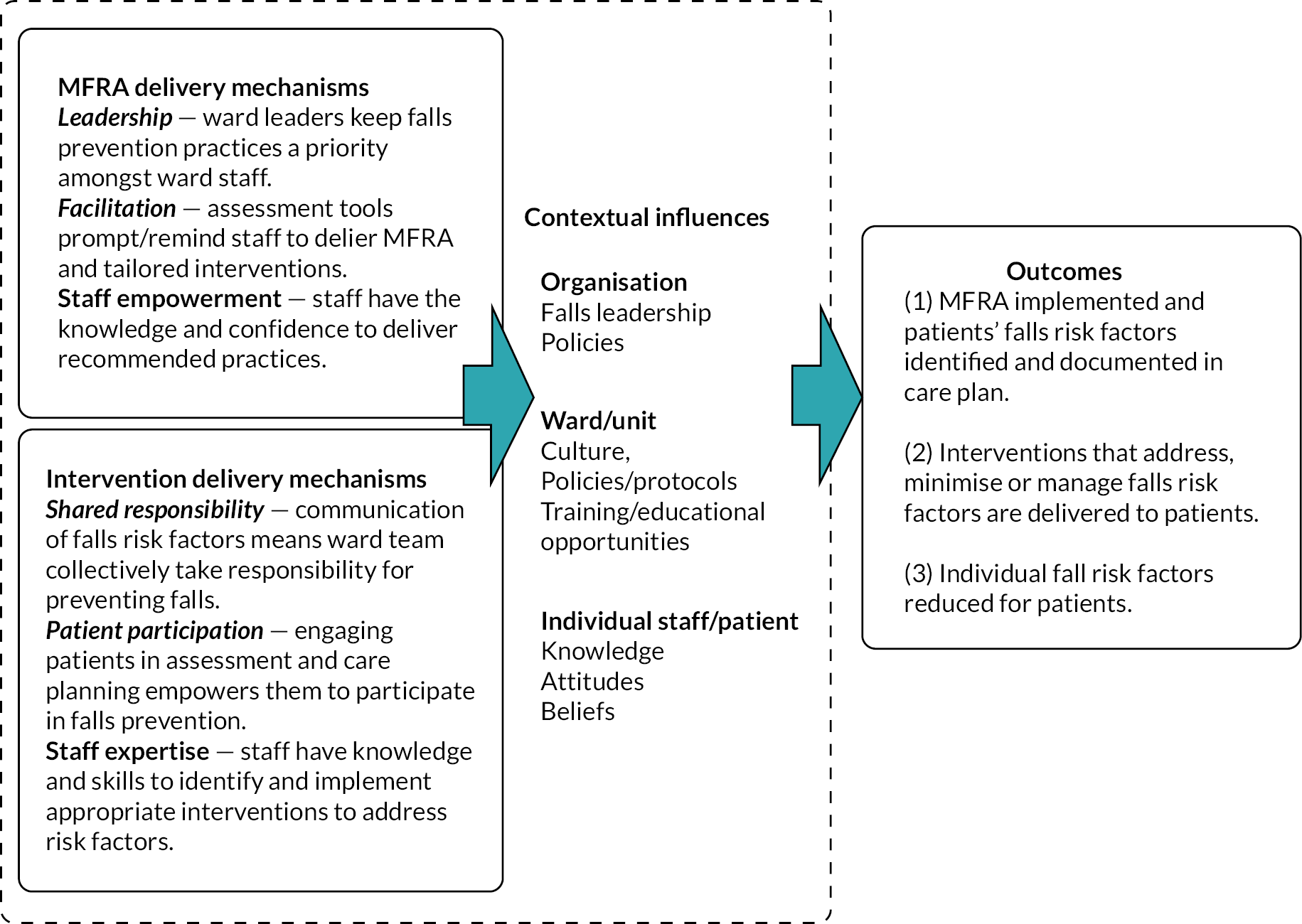
As described in Chapter 2, time limitations meant that we decided to focus on testing four CMOcs, selecting the four concepts that were ranked highly by both the Lay Research Group and SSC: leadership, facilitation, patient participation and shared responsibility. In the next four chapters, we present the findings from the testing of these CMOcs.
Chapter 5 Leadership
Introduction
This chapter describes testing and refinement of the leadership theory. The original CMOc was as follows:
Where falls prevention is prioritised by organisations, e.g. in organisational policy and provision of resources (C), falls leaders/champions – staff trained and dedicated to supporting delivery of multifactorial falls prevention strategies on their wards, e.g. by offering training and education to new staff – inspire and support delivery of the strategy in a consistent and co-ordinated way (M), so that all patients eligible receive a multifactorial falls risk assessment and tailored intervention strategies (O).
To test this theory, we first drew on Trust policies identified in undertaking the realist review and then the findings of the multisite case study.
Findings from the review of Trust policies
In total, 25 policies were obtained, 17 of which were clearly up to date, whereas we remained unsure if the remaining eight policies were the most recent.
Typically, many policies began with an introduction, in which they set out the scope and aims of the policy (some made explicit reference to NICE guidance at this point), defined what is meant by a fall, and stated who the policy applied to. Then, the bodies and individuals accountable for overseeing and implementing the policy were often outlined. Some policies also outlined assessment, intervention, and postfalls review processes (assessment forms were sometimes included as an appendix), whereas others gave little detail, providing instead digital links to online forms (to which we did not have access). This was particularly the case when assessment forms were embedded within EHRs and other digital systems. In several policies, it was noted that only online versions of forms were kept up to date, which may have discouraged authors from appending paper versions of the form. This variation in the level of detail within policies means that the following findings should be interpreted with caution: as can be seen from Table 9, wherever it was not clear whether a condition was met, this was because the relevant practice was not stated in the policy, rather than clearly not met.
| Number of Trust policies that showed adherence to NICE guidance | Condition met | Condition not met | Not stated whether condition is met or not |
|---|---|---|---|
| Risk prediction tool is not used? | 22 [NB includes one Trust where policy refers to the use of the Falls Risk Assessment Tool/FRAT – a tool that generates a risk score – in the Emergency Department (ED) only. Otherwise, policy states that it is a requirement that each individual patient has an adequate MFRA and an appropriate management plan initiated and implemented]. | 0 | 3 |
| Recommend tailored/MF approach? | 20 | 0 | 4 plus 1 where tailored approaches are mentioned only in relation to high-risk patients about whom ward staff are concerned or who fall despite standard measures, referred to the Falls Team. |
| Asst for over 65s and people aged 50–64 with an underlying condition | 24 | 0 | 1 |
| Cognitive impairment assessed | 20 | 0 | 5 |
| Continence assessed | 18 | 0 | 7 |
| Fall history assessed | 20 | 0 | 5 |
| Footwear assessed | 23 | 0 | 2 |
| Medication assessed | 21 | 0 | 3 plus 1 where policy is only stated in relation to patients admitted to ED for a fall. |
| Postural instability, mobility problems and/or balance problems assessed | 19 | 0 | 5 plus 1 where policy is only stated in relation to patients admitted to ED for a fall. |
| Syncope syndrome assessed | 18 | 0 | 6 plus 1 where policy is only stated in relation to patients admitted to ED for a fall. |
| Visual impairment assessed | 18 | 0 | 6 plus 1 where policy is only stated in relation to patients admitted to ED for a fall. |
With this caveat in mind, we found most policies appeared to adhere to most aspects of the NICE guidelines, and therefore our sample of just over 10% of English Trusts was regarded as sufficient. There appeared to be particularly high adherence (in 20 or more of the 25 policies reviewed) around offering some form of falls assessment to patient groups most at risk of falling (24/25); assessing footwear (23/25); not using a risk prediction tool (22/25); assessing medication taken by patients (21/25); recommending a tailored or multifactorial approach to falls risk assessment and management (20/25); assessing cognitive impairment (20/25); and assessing the patient’s history of falls (20/25).
A lower number of policies (19 or less of the 25 reviewed) demonstrated adherence to the following elements: assessing visual impairment (18/25 policies); assessing continence (18/25); assessing syncope syndrome (19/25 either explicitly mentioned this assessment and/or measured postural blood pressure as part of the falls assessment); and assessing postural, mobility problems and/or balance problems (19/25). As noted above, however, these levels may not represent actual lower adherence, but merely a lack of detail in the policy.
In summary, this suggests that failure to provide a MFRA and tailored falls prevention interventions is not because organisational-level policies do not, in the main, reflect NICE guidance, but, instead, appears to relate to how those policies are resourced and implemented at ward-level.
Findings from the multisite case study
Organisational-level leadership for falls prevention
In each site, the ultimate responsibility for falls prevention fell to Boards of Directors and Chief Executives, and this was delegated to various individuals and bodies, including Chief Nurses or Directors of Nursing at organisational-levels and matrons at clinical service unit or departmental-levels. Each Trust also had committees or groups to which Boards of Directors delegated responsibility for falls prevention, and some also linked to multiprovider Falls Collaboratives. At Site 2, for example, the Collaborative was a city-wide multidisciplinary group reporting to several committees including the Trust Professional Board, which aimed to provide strategic direction for falls prevention and to feed learning and good practice back to key stakeholders, including ward managers. Membership comprised clinical and academic experts in falls management, including matrons, falls, and improving quality leads and local commissioners. Sites 1 and 3 had similar Collaboratives. At Site 3, for example, a multidisciplinary Collaborative reported to several committees, including the Trust’s Clinical Outcomes Group, and its membership included matrons, falls champions or link practitioners, and representatives from therapy, data and moving and handling teams.
Each Trust also had organisational teams who supported implementation of falls policies. These teams typically had both organisation-facing, assurance elements to their work as well as ward-facing, supportive elements. In Site 1, for instance, an organisational team, working alongside several other quality and safety-focused teams, provided assurance on key nursing performance indicators and patient safety markers, such as completion of MFRAs and falls care plans. They reported outcomes to governance committees, the Board of Directors and the chief nurse. The team also offered falls prevention induction and refresher training to staff. At Site 2, a team of falls specialist nurses provided corporate reporting and support for wards, for example, training falls link practitioners (see Falls champions). At Site 3, a smaller Trust than Sites 1 and 2, the Dementia Lead was responsible for implementing interventions and strategies to reduce the risk of patients falling and providing staff education and guidance on falls prevention. They also oversaw an enhanced care team, which offered one-to-one support for people at increased risk of falling and maintained strong links with matrons. The role of matrons in falls leadership was also highlighted in interviews across sites.
Falls champions
The role of falls champions was identified in all three sites, although postholders were referred to as falls link practitioners. This role was allocated to nurses and HCAs, undertaken alongside their normal roles. In practice, however, there were active link practitioners in Sites 2 and 3 only. During observations, we observed them working on their wards, as this fieldnote extract from the Site 2 older person/complex care ward describes:
The falls link nurse is chatting with the patient in bed 5. They are trying to convince them to have an ECG but the patient is saying that they don’t want one. The link nurse is explaining it’s because of their fall this morning – they’ve done her blood pressure, her blood, and an X-ray of her hip.
Duties of falls link practitioners were outlined in organisational falls prevention policies in Sites 2 and 3, although staff acknowledged that pressures of work on wards, aggravated by COVID-19, meant it was not always possible to fulfil the duties described in the policies. Trusts aimed to appoint HCAs as well as nurses as falls link practitioners, because the former made a fundamental contribution to falls prevention and they believed staff were more likely to be inspired by someone in a similar role. Reflecting this, in Site 2, a role descriptor specified that link practitioners were expected, among other duties, to act as role models for falls reduction in their clinical areas, and to provide advice and education for the assessment, intervention, and management of patients who had fallen or were at risk of falling. They were also expected to facilitate regular audits of falls management practice on wards and raise patient safety concerns.
Falls link practitioners at Site 2 received training in quarterly 2- to 3-hour sessions where specialist nurses provided up-to-date information about falls prevention practices and procedures. However, it could be difficult for link practitioners to attend the training they were entitled to, owing to the pressure of work on the wards. On one of the wards we observed, the falls link practitioner showed us a falls file they maintained, which was kept in the staff room and accessible to all staff. Contents included a role descriptor for falls link practitioners and PowerPoint slides about enhanced observations of care (EOC), with information about calculating risk scores. These scores were used to identify patients in need of one-to-one care or being placed on a cohort bay (i.e. a bay where patients assessed as being at risk of falling were co-located). The file also included information about adult falls risk assessment and care planning, including how to create a falls care plan on the EHR; a section on postfalls actions; and copies of audits about falls process compliance (the last audit was dated around 8 months before).
In the orthopaedic ward in Site 2, a senior nurse explained that falls link practitioners updated and maintained a falls board. This board listed, under a heading of ‘Falls Prevention’, the following strategies: call-bell within reach, low rise bed if available, cohort bay if available, correct footwear, and risk assessment completed and updated. The board also displayed a note that EOC scores should be updated daily. The nurse explained that a recent increase in falls was thought to be due to staff scoring patients too low on the EOC scores, therefore work was being undertaken to ensure scores were completed accurately. There was also a link nurses’ board, which gave the names of postholders.
At Site 3, the falls link practitioner role was being reviewed and relaunched, given that it had not been possible to prioritise link practitioner work during COVID-19 and not all wards had them. Falls link practitioners at Site 3 were expected to support good practice in falls prevention and management in their wards by attending training and relevant meetings, including the Falls Collaborative, and by giving information and advice to colleagues, patients and carers. Visual displays about falls prevention, like those described in Site 2, were observed in Site 3. Whether updating this information was the role of the falls link practitioner was unclear, but the nurse allocated this role in the older person/complex care ward described reinforcing messages about falls prevention to colleagues. However, like Site 2, the Site 3 link practitioner described finding the role challenging because they were busy as a nurse. Efforts were made to address this issue, for example, by booking meeting and training dates well in advance, so that ward managers could take link practitioners’ absences into account in rotas, and by offering shorter training events, for which link practitioners received CPD points and certificates, to encourage attendance. Such training was intended to empower falls link practitioners to educate colleagues about falls prevention, and we saw some evidence of that in the falls boards on wards, which disseminated information about prevention practices.
We were not able to identify falls link practitioners on either ward at Site 1: on one ward, the post was vacant, and on the other ward, a member of staff explained that a more fluid approach was being taken, whereby a nurse or HCA was designated each day to lead on falls: ‘In the Safety Huddle on a morning the nursing staff would take it in turns. So they’ll identify someone each day to be a champion for falls risks, nutrition, skin care, toileting, etc.’ (Physiotherapist, Orthopaedic Ward, Site 1). However, in observing the safety huddle on this ward, we did not see this happening. The participant noted that, while the role of falls link practitioner might be useful, it would be difficult for one person to find time to do it. They felt the current model of ‘collective’ working, with multiple staff members sharing responsibility for falls prevention on the ward, was ‘fine as it is’. As in Site 2 and Site 3, falls prevention messaging directed to staff was displayed on wards.
Leadership of falls prevention practices on wards
Falls prevention practices of interest in this study focused on the implementation of MFRAs and interventions tailored to address individual risk factors. At Site 1 the organisational falls prevention policy stated that ward managers (rather than falls champions) should ensure all patients were assessed for their risk of falling according to the Trust’s guidelines. The Site 1 policy also stated that ward managers should make sure staff were aware of their falls assessment and prevention responsibilities, including undertaking falls refresher training every 3 years; investigate causes of all incidents and ensure actions and recommendations were acted on to prevent recurrence; and ensure falls prevention information was displayed in patient areas and provided to patients at risk of falling. A ward manager in the Site 1 older person/complex care ward explained how, as a manager, they identified areas for improvement via monthly review of metrics and, through shared learning with other wards, implemented changes that had improved compliance in completing risk assessments on their ward. The ward manager had introduced a handover board, which helped staff focus on improving practice in specific areas, such as carrying out falls risk assessments. Ultimately this messaging was directed at nursing staff because, across all sites and wards, nurses were responsible for completing falls risk assessments and care plan for patients, and sisters and nurses-in-charge of shifts supported delivery of certain falls prevention interventions. In other words, nurses with different levels of seniority on the ward had day-to-day responsibility for delivering key areas of falls prevention practice, including leading discussion about patients’ falls risks in safety huddles and multidisciplinary team meetings.
Staff told us that falls link practitioners’ authority was less well defined than ward managers or nurses-in-charge of shifts and reflected that falls link practitioners might feel ‘too scared’ to make decisions that involved significant changes such as bed moves or waiving an aspect of policy in the interests of patient safely ‘because that would be whoever’s in charge’ (Nurse-in-charge, Site 2), namely, the ward manager or nurse-in-charge. When observing events such as safety huddles and handovers, we did not see link practitioners taking a leading role. In addition, on one ward in which there had been an increase in falls, the falls link practitioner was not involved in a review to address the problem, and instead more senior nurses were involved.
Provision of training and support
Training and support for ward staff to implement falls prevention practices was provided in different ways. Most falls prevention training for new staff or refresher training for existing staff was not provided by link practitioners, but by organisational-level teams. For example, at Site 1, falls prevention training was provided as part of new staff induction by a central team and covered enhanced care, falls prevention, and medication. A senior nurse explained how recommendations from NAIF informed the development of their Trust’s falls training programme, which was mandatory for all new starters.
In comparison to Site 1, a ward manager at Site 3 pointed out that many experienced staff were assessors and supervisors for student nurses, providing on-the-job training themselves, and were therefore ‘very good at questioning why we do things’ (Ward manager, Site 3). At Site 2, compulsory training for new starters was also described, but the face-to-face version had been replaced by online training, as part of COVID-19 social distancing measures. Staff felt online training was less effective, especially for inexperienced staff or international staff new to UK health care. One ward had an influx of new staff who had not received face-to-face training and the ward manager believed this could have impacted delivery of falls prevention practices. Alongside formal training, a Site 2 falls specialist nurse described how informal discussion was used to support implementation of falls prevention practices; a lot of their work focused on EOC scores, ensuring they were accurate and prompting appropriate action, that is, that the right level of patient supervision was in place.
In terms of practical implementation of support at ward level, a key strategy discussed was messaging, for example, providing visual displays and reminders about expectations and policy on wards. A senior nurse at Site 1 explained that LSBP was included in their mandatory training programme in response to recommendations from NAIF, but added that ongoing communication and reminders to ward staff were needed to embed the practice in routine processes (and, in fact, we observed LSBP being taken at Site 1). However, a staff member at this site suggested an enthusiastic leader could, in fact, demotivate tired colleagues by encouraging them to do tasks they did not have time to do and what they needed, rather, was practical help. A ward manager emphasised this point: ‘I think, if you have a team that are frazzled, and the morale is low, the attitude isn’t there to want to engage and collaborate. People get a little bit, “Oh, this is pointless”’ (Ward manager, older person/complex care ward, Site 1). An organisational leader at Site 3 thought the best response was sensitivity to the demands staff faced, which meant taking incremental approaches to change. The need for sensitivity was echoed by a ward manager at Site 2, who prioritised staff well-being and offered practical support. In addition, a ward manager in Site 3 talked about the importance of ‘leading by example [ … ] So I do think my role is to hopefully teach a little bit, pass on my knowledge to the members of staff’ (Ward manager, orthopaedic ward, Site 3). However, a Site 2 matron discussed that, in the current NHS workforce, staff tended to move into leadership positions earlier than in the past and, therefore, did not have the same ‘exposure’ that supports decision-making and the ability to lead by example.
Consistent delivery of falls prevention practices
Record review indicated that falls risk assessments and care plans were documented quite consistently across sites (see Figures 4 and 5).
FIGURE 4.
Falls risk assessment documented on admission.
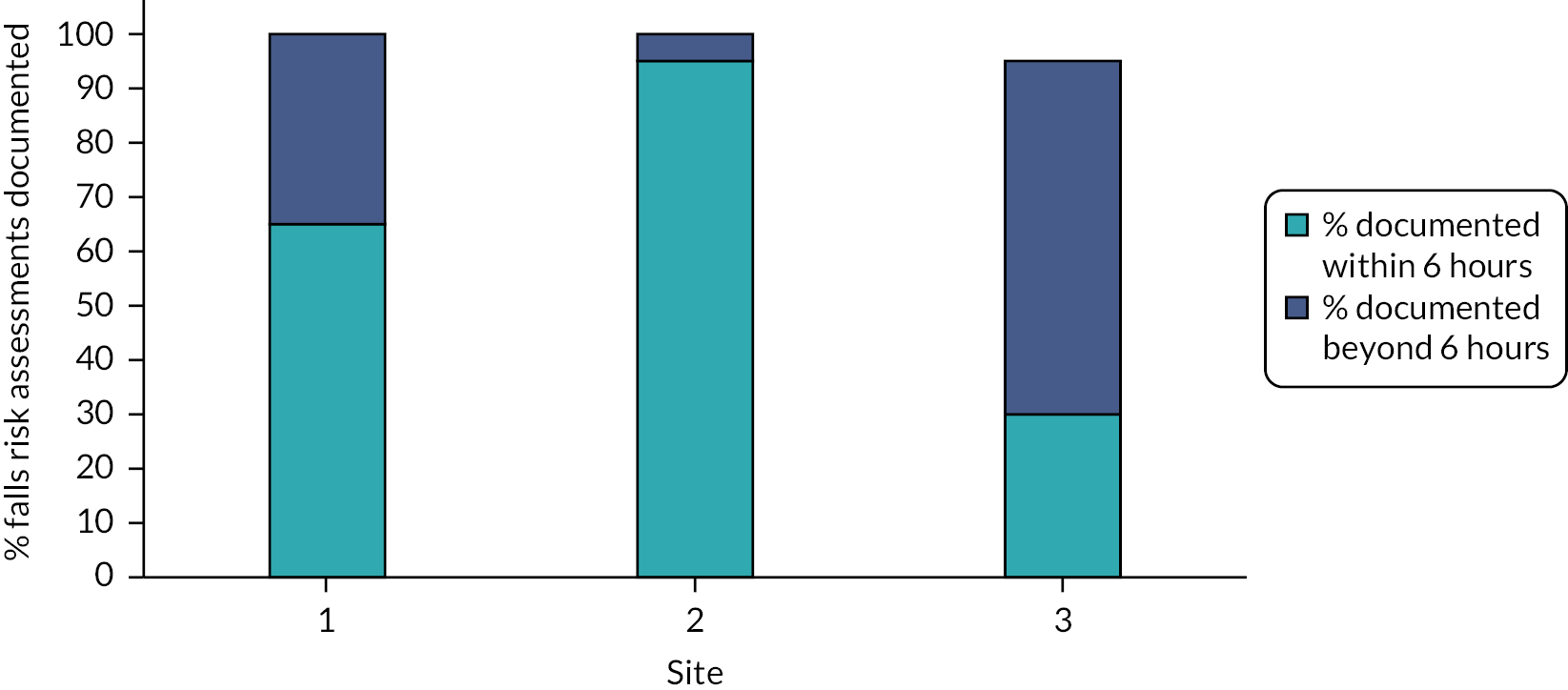
FIGURE 5.
Falls prevention care plan documented after first falls risk assessment.

There was variation in the number of falls per month and falls with injury (see Appendix 4, Figures 9–11). Although this was likely to be a natural variation rather than statistically significant, discussion with senior nurses at Site 1 provided some insight into why they believed falls and injury numbers varied from month to month. Falls incidents were attributed to not having staff to consistently provide one-to-one care to keep patients safe from falls. A ward manager in the Site 1 older person/complex care ward explained that their patient population fluctuated in terms of dependency, and patients could also be confused, agitated, delirious, or ‘wandersome’, which put them at risk of falls, so that ‘the biggest risk that we have when we’re delivering care is identifying those patients who require more intensive supervision’ (Ward Manager, older person/complex care ward, Site 1). Staff in other wards and sites described similar situations in terms of patient population and had attributed rises in falls incidents to similar issues.
Participants emphasised that staffing levels should consider not only patient numbers, but patient acuity. COVID-19 meant staff shortages were frequently observed during fieldwork, due to both staff sickness and staff being ‘pinched’ to work elsewhere in the hospital. While we did not capture data on staffing levels for all shifts observed, the data we captured suggested that the number of nurses and HCAs per shift averaged 80% of the numbers required for safe staffing, ranging from 50% to 100% for nurses and 40% to 100% for HCAs.
Some staff believed provision of resources was not solely a matter of prioritisation, but also a practical and logistical challenge. Pointing to the staffing crisis in the NHS, they explained that even where funds were made available by senior management to employ staff, it was often difficult to fill posts, especially for nurses and HCAs caring for older people, which were seen as particularly difficult jobs. The impact of experienced staff leaving the NHS was believed to add to this problem. However, a member of staff on the Site 3 older person/complex care ward talked about how, just as patients might have both modifiable and non-modifiable falls risk factors, so organisations had to work with factors that were modifiable and non-modifiable; while they might not be able to make more staff available, they could change the way staff were managed, and this could make a difference.
Theory refinement
Based on the data presented above, we were able to make refinements and additions to the leadership theory (Table 10), highlighting the importance of nursing leadership, the value of sensitive leadership, and the impact of resource constraints on falls prevention practices, in terms of staffing and training.
| Context | Mechanism | Outcome | |
|---|---|---|---|
| Resource | Response | ||
| Organisational policy states nurses complete a falls risk assessment and care plan, and senior nurses lead decision-making regarding allocation of resources for falls prevention practices on the ward. Lack of adequate staffing. |
Nursing staff allocated to role of falls link practitioner, where duties include educating ward staff, auditing practice, and updating visual displays on the ward. | Nursing leadership: falls link practitioners prioritise care delivery and the role focuses on dissemination of information. Ward staff approach senior nurses for practical support to deliver falls prevention practices. |
Authority to lead falls prevention practices resides with senior nurses rather than falls link practitioners. |
| Wards caring for patients with high levels of dependency and high levels of cognitive impairment. Reliance on supervision, for example, one-to-one care, as key falls prevention strategy. Lack of adequate nursing staff. |
Senior nurses monitor, remind, and support staff to deliver falls prevention practices in ways that are sensitive to their workload burden. | Intervention delivery constrained: nurses document falls risk assessment and care plan for patients in need. However, resources do not always support delivery of supervision for patients in need of enhanced observations. | Falls prevention practices are consistently documented but falls may result when patients do not receive the level of supervision required due to staff shortages. Senior nurses escalate concerns about patient safety to hospital managers. |
| Significant numbers of new staff. | Formal training about hospital falls prevention policy provided by organisational teams for new starters on induction and as refresher sessions for existing staff, delivered online. | Training constrained: information from online training may not be absorbed by staff in the same way as face-to-face training, impacting on their understanding and delivery of hospital falls prevention practices. | Nurses may not have knowledge to support consistent delivery of falls prevention practices, despite nursing leadership on the ward. |
| Organisations not able to prioritise falls prevention by providing sufficient resources. | Falls leaders sensitive to pressures faced by staff, introduce changes carefully and incrementally, and offer practical support to ward staff. | Sensitive leadership: nurses feel pressured but also respected/understood and continue to try to implement strategies. | Multifactorial strategies are implemented to an extent; gaps are identified and learnt from. |
Chapter 6 Shared responsibility
Introduction
This chapter describes the testing and refinement of the shared responsibility theory through the multisite case study. The original CMOc stated the following:
Where there is a culture of learning, rather than apportioning blame, from errors (C), if information about patients’ falls risks is effectively communicated between ward staff (e.g. through posters/safety huddles/handovers), then staff will develop a sense of shared responsibility for falls prevention and become more vigilant of patients at risk from falls (M), thereby supporting implementation of multifactorial strategies to prevent falls (O).
Communication within and between professional groups
When we interviewed doctors, physiotherapists, occupational therapists (OTs), pharmacists and HCAs, they explained that typically they do not access the falls risk assessment in the nursing documentation. These professionals documented their care input in different spaces on the EHR (not reviewed as part of this study) but noted there might be much overlap with the falls risk assessment. Staff explained that verbal communication was used to share information across different professional groups, with formal verbal communication, for example, in safety huddles, being standard practice. Different reasons were given for the priority placed on verbal communication, some staff mentioning the volume of written documentation, such that information can be missed, while others were concerned that not everything gets written down. During fieldwork we observed ward meetings including nursing handovers, multidisciplinary team meetings where representatives from different specialities meet to discuss patient care, and safety huddles. Nursing handovers took place at shift changes when nursing teams gathered to ‘hand over’ patients to nurses and HCAs on the next shift, typically referring to handover notes (documents printed from the EHR that provided a summary of each patient). Table 11 provides an example of handover comments documented in the EHR for three patients at Site 1, who consented to have their records reviewed.
| Patient 1 | Patient 2 | Patient 3 |
|---|---|---|
| Weight: to do LSBP: to do Physio: WBAT. Further physio needed as patient being transfused. SSKIN: vulnerable, 2 hourly Plan 2/3: on IVPAB, check YB following 2 units of blood. Discharge: has private carer, assess post CP |
VTE: ENOX ABX: IV Teic Weight: 13.2.22 LSBP: 14/1 Physio: WBAT left lower limb, independent with frame or supervision with crutches, 01/03/22 discharge from physio SSKN: 4 hourly turns Mattress: breeze – patient wants to keep OT: 22/02 awaiting conversation with daughter regarding key safe. 03.02.22 FSTF and a kitchen trolley to be delivered Plan 2/3: Monitor INR, MOFD from ortho, start warfarin bundle Discharge: please put on EDAN their GP is to chase up gynaecology. NHT on discharge antibiotics and diuretics (?), need prescribing on her EDAN. NHT OPAT, equipment key safe. |
Weight: to do LSBP: to do Physio: FWB W2F + ADI, transfer only (1 March 2022) Social: nothing noted Discharge: nothing noted Plan 2/3: continue bowel care, stop dihydrocodeine (delirium) can have pr oxycodone. Replace 6/2 first and then prescribed folic acid, vit D loading then FLS refer for Iv bisophos, add in ferritin, RPT FBC UEs LFTS TFS tomorrow, if H6 falling consider RBC, update NOK and gell collateral (?) |
Table 11 indicates that information documented for each patient varied in detail but interventions are not explicitly listed against a ‘falls risk factor’ item, as they are for pressure ulcers (SKKIN) for patients 1 and 2. Even so, some items relate to falls risk factors, for example, LSBP is listed and physiotherapist guidance about how to mobilise patients safely, such as weight bearing as tolerated (WBAT).
Observations of handovers revealed that nurses typically summarised the points noted on handover documents, patient by patient. Information shared verbally that was explicitly linked to falls prevention included identifying patients who had been admitted with a fall, patients with a fall alarm, and advice ‘to watch’ patients who were able to mobilise.
Handovers were attended by nurses and HCAs, so sharing information beyond nursing staff relied on other channels of communication. Safety huddles were held across all wards and were sometimes attended by multiple professional groups, especially when they were held in ‘office hours’, when staff other than nurses and HCAs were available. For example, in attendance at one safety huddle observed on the Site 1 older person/complex care ward were 17 staff including five junior doctors, one consultant (who led the meeting), the senior sister/nurse-in-charge, the ward clerk, the discharge co-ordinator, two nurses, and two HCAs. Safety huddles were typically used to highlight patients in categories of interest/concern to the ward for example, falls risk and discharges for the day. Those patients categorised at high risk of falling were discussed, typically noting interventions in place, such as cohorting and use of a falls sensor. Safety huddles followed a similar format across sites, although in Site 2 we observed a proforma being used that included safeguarding, consent, and deprivation of liberty safeguards (DoLS), falls, patients requiring heightened observations, infection prevention issues, pressure ulcers, special diets, fluid balance, patients with do not resuscitate (DNR), anybody with an Early Warning Score of three or higher, and current ward matters. At some safety huddles in the Site 2 older person/complex care ward, as all patients on the ward were considered at risk of falling, the patients discussed at the huddle were those considered ‘particularly high risk of falls’ based on the EOC score and requiring a level of supervision. Patients’ individual falls risk factors and interventions to modify those risks were not routinely shared between professional groups during safety huddles. Although patients discussed in safety huddles may be those prioritised as at high risk of falls, details provided about their falls risk factors could vary, depending on probing by attendees. Even so, individual falls risk factors were not discussed in detail.
In addition to safety huddles, communication between professional groups happened during multidisciplinary team meetings, which took place around midday. Patients were discussed in turn, covering issues, such as medications, discharge arrangements, and mobility.
Informal communication between professional groups
Information was also communicated informally between professional groups. We most frequently observed communication between nurses and HCAs, but communication involving physiotherapists, doctors, and pharmacists was also observed. Examples of informal communication observed included staff checking with each other if jobs such as skin rounds and taking blood pressure had been completed, staff requesting help from each other to help move/mobilise or monitor patients, and providing updates to colleagues about patients’ condition, for example, if a patient was in pain and required medication. A Site 3 nurse explained that updates from physiotherapists and OTs were provided verbally. Nurses shared these updates with HCAs (who often had primary responsibility for aiding patient mobilisation) and made a note of the information to later update the EHR. Additionally, non-nursing staff would proactively ask for information. For example, a Site 3 nutritional assistant, who had worked for the organisation for over 10 years (as a HCA and then nutritional assistant), was familiar with the roles of different professional groups, so knew who to ask for the required information. Furthermore, the nutritional assistant supported patients in mobilising even though it was not their role specifically. To work in cohesive ways, such as this, it was important to know the roles and responsibilities of different professional groups, to understand who to ask for advice and refer issues to.
Availability of professional groups on wards facilitated informal communication about patient care needs. For example, a Site 3 pharmacist described being able to talk to nursing staff about patients because the nurses were always there. Wards were staffed in different ways, which influenced how and the extent to which informal communication took place. For example, the pharmacist described how, on the orthopaedic ward, fractured neck of femur patients had orthogeriatric input on a daily basis, providing an opportunity for the pharmacist to discuss with them medications that could increase their risk of falling. As another example, the Site 2 orthopaedic ward, with 28 beds, had a dedicated physiotherapist team, whose office was next to the nurses’ station. A physiotherapist in this team explained they were constantly discussing patients’ mobility needs with other ward staff. The Site 2 older person/complex care ward was not resourced in the same way as orthopaedics. During an observation of this ward, a physiotherapist discussed that they worked across three wards, and on the day of observation there was one physiotherapist and a physiotherapy assistant for 60 patients. A senior support worker on this ward emphasised there could be conflicting priorities between physiotherapists and the nursing team, for example, physiotherapists sometimes transferred several patients from bed to chair. While the support worker acknowledged this might contribute to patient recovery, it could also create challenges for nursing teams (especially when short staffed) who later needed to put the patients back into bed with assistance.
Consistency of staffing was also discussed as an influence on communication. For example, a consultant at Site 3 described bank nurses, who worked on wards on a temporary basis, for example, to cover staff shortages, but did not know the patients as well as permanent staff, which could impact on information communicated to other professional groups. A matron in Site 1 also highlighted the importance of consistent staffing for cohesive team working.
Visual communication tools
Visual tools were also used to communicate information about patients to ward staff. Patient bed boards, placed on the walls above patient beds, were used across wards and sites. In Site 2, a red falling leaf symbol was displayed on bed boards to identify patients at risk of falling, as well as being displayed on electronic whiteboards. In Site 3, magnets that visualised information such as mobility needs, skin needs, and falls risk were attached to bed boards. In terms of falls risk, the magnet displayed items such as ‘high risk’ and ‘low risk’, with boxes that staff could tick to indicate the patient’s condition. Bed boards were typically used to communicate patient transfer (from bed to chair) and mobilisation needs. Table 12 provides examples of notes taken about bed boards within one ward.
| 1 December 2021 | 7 Apil 2022 |
|---|---|
| I notice that above P12’s bed, and above the bed of the patient who is sleeping, there is a laminated poster. It is divided into four squares. I look at P12’s. It gives the patient’s name and a date (30/11/21). One box says ‘Falls risk assessment’ and then below it says ‘At risk: Yes No’. The yes is circled. Another box says ‘How can I mobilise?’ Written below this it says ‘NWB Left Arm. Arjo + 2 people, must protect L arm when moving’. Another box is titled ‘L&S BP’ and then says ‘Is a L + S BP needed? Yes No’. Neither the yes or no is circled. I notice that neither of the patients on the other side of the ward have these posters. | There are physio notes the whiteboards behind beds 9, 10 and 11. Bed 12 doesn’t have notes as far as I can see. The notes are as follows: Bed 9 – NWB [non-weight bearing] Right UL [upper limb], transfer hold AO1, Collar and cuff Bed 10 – Arjo + 2 transfer. NWB LUL Bed 11 – W2F AO2 (Arjo if struggle) The patients in beds 10, 11 and 12 have bed rails up. |
Table 12 demonstrates that information to support mobilisation differed by patient. During observations, across sites, information displayed on bed boards was often noted as variable, incomplete, or not up to date. Mobilisation information needed to be available at a glance for staff members to have the necessary information to support them to mobilise, especially those who did not know patients, such as bank staff. On the Site 1 older person/complex care ward, we observed a patient walking with the assistance of two student nurses to the toilet when the patient said they could not see because they did not have their glasses on; that the patient needed glasses when mobilising was not information that was typically shared, either verbally or visually.
Falls prevention as a shared responsibility
The CMOc hypothesised that communication of falls risk factors would promote staff vigilance of patients at risk of falls and participation in falls prevention strategies in contexts where there was a culture of learning rather than blame from falls incidents. In a Site 1 organisational-level interview, it was stated that the emphasis was on learning from falls, rather than allocating blame. This site undertook root cause analysis for falls with injury that involved reviewing the falls risk assessment documentation. Across sites, completion of the falls risk assessment and falls care plan was seen as a nursing responsibility and was audited, a fact nurses were aware of. Interview data suggested experiences of institutional culture differed between organisational and ward staff. However, interviewees discussed that an emphasis on supervision as a falls prevention strategy was more influential on the extent to which they felt responsibility was or could be shared between the multidisciplinary team.
Analysis of ward communication revealed that patients classified at high risk of falls and in need of supervision were usually those prioritised for discussion in safety huddles, which sometimes brought together different professional groups. While different professional groups perceived some responsibility for falls prevention, it was largely seen as a nursing responsibility. For example, a physiotherapist in Site 1 described how anyone who had concerns about a patient in terms of their falls risk should discuss it with the ward sister, with a view to moving them to a cohort bay. This understanding of shared responsibility for falls prevention was expressed by a physiotherapist in Site 2, who noted that although physiotherapists led decision-making about how to safely mobilise patients and assisted patients to sit out, patient supervision was typically provided by nurses and HCAs (although in Site 1 we also observed security personnel providing patient supervision). A consultant in Site 2 echoed this, explaining that preventing falls was probably considered a supervision issue, predominantly ‘left with nursing staff’. In a similar vein, a falls specialist nurse in this site pointed to the fact that it is nursing staff who were with the patient throughout the day. However, the falls specialist nurse felt other members of staff should participate in these interventions, for example, when a falls sensor sounded, it should be treated as an emergency by all staff, but ‘we see students, we see [foundation year 1s], we see everybody walking straight past that because it’s not their problem and it totally defeats the purpose of it’. In the training they provided, the nurse said they emphasised that all staff should respond to alarms; ‘until you can tell me that it’s been turned off and everything is fine, it’s your problem if you hear that’. This seems to suggest an expectation for other professionals to intervene in the same way as nursing staff and, while supervision was seen predominantly as a nursing responsibility, other members of the ward team were observed, and described in interview, helping nursing teams with supervision. For example, a pharmacist in Site 3 described how they would respond to a falls alarm going off if they were the person nearest to the patient.
Other staff described their role in relation to specific risk factors. Four physiotherapists were interviewed, three of whom were based on orthopaedic wards, who explained that on those wards, physiotherapists would typically assess all patients as part of their rehabilitation, that is, the intervention was not reliant on mobility being identified as a falls risk factor in the nursing assessment. Two pharmacists were interviewed, one of whom explained that medication review in relation to falls risk might not be explicit in the documentation but was considered as part of the holistic care of the patient. Furthermore, the pharmacist explained complexities in modifying medications regarding falls prevention, for example, when considering reducing Benzodiazepines (sometimes used to treat delirium) ‘with a view to the GP weaning them off’ they must also consider the risk of withdrawal. The pharmacist noted that there could be differences in opinion with doctors. Additionally, the pharmacist commented that they experienced competing priorities, for example, in terms of caring for new patients coming in and being discharged, ‘so sometimes certain aspects of your work get stepped down on a particular day’, thereby delaying medication review.
On the Site 1 older person/complex care ward, we observed a consultant geriatrician undertaking a ward round of patients admitted overnight, while the junior doctors visited the other patients on the ward. Before going to see each patient, they reviewed their details on the EHR, including looking at lab results, X-rays and electrocardiograms (ECGs). This fieldnote extract describes the consultant’s review of two patients:
They say to me that they don’t specifically look at falls but will mention it if there has been a change. They go into the patient’s room. [ … ] They then ask the patient about where they live and to what extent they live independently. They live on the ground floor and did their own shopping. The consultant asks if they fall. They say they had three falls close together. [The patient] jokes, ‘think that’s to do with the whiskey’. The consultant explores this – how often do they drink? [ … ] We come out of the room and the consultant types up their notes. They tell me that the patient seems quite steady – they were able to move round to the commode on their own. [ … ] We go to see the second new patient who is in the first bay. The consultant says this patient has a high risk of falls (although the nurse thought they were ‘okay’). In the clinical notes, it says the patient’s mobility has deteriorated. [ … ] The patient has dementia. They need the toilet and are trying to get out of bed. [ … ] In the corridor, the consultant talks to one of the HCAs/nursing assistants about moving the patient to the falls bay because the patient who is just being discharged was in the falls bay. The HCA/nursing assistant says they were going to move another patient (the patient in bed 2) but that it is the doctor’s decision. The consultant says the new patient has had a lot of falls and has come in with a fall, but they don’t know the other patient. The CSW/NA says the patient in bed 2 gets up and they have been asked to watch them. The consultant says to see if they can get a sensor for that patient.
Interesting in this extract is that, while the consultant said they did not specifically look at falls, they did explore falls risk factors and influenced which falls prevention interventions two patients would receive.
On the Site 2 older person/complex care ward, we observed a junior doctor undertaking a ‘mobility audit’, although this seemed motivated by a desire to prevent deconditioning rather than prevent falls:
They say that are looking at things like if the patient is sat out, if they have a Zimmer frame in reach, physiotherapist notes. Things that would encourage mobility if present and constrain mobility if not present. They say that mobility is important in hospital as patients can get ‘deconditioned’ the less mobile they are.
Even so, the weight of responsibility for supervision was felt by nursing teams and, because wards were often understaffed, implementation of supervision could be stressful and demoralising. For example, a HCA at Site 1 described the work of staffing a cohort bay as ‘draining’ but, due to staffing numbers, they could not rotate roles with other HCAs to alleviate the work, as they used to do.
Theory refinement
Based on the data presented above, we were able to make refinements and additions to the shared responsibility theory (Table 13), highlighting how and where supervision is used as a key falls prevention strategy. Because patient dependency means that a large proportion of patients on the types of wards we observed require supervision, responsibility for falls prevention lies largely with nursing staff.
| Context | Mechanism | Outcome | |
|---|---|---|---|
| Intervention | Staff response | ||
| Supervision used as key falls prevention strategy. High dependency within patient population. |
Meetings that bring together different professional groups focus on discussion of patients stratified at a high risk of falls, receiving a level of supervision. | Responsibility not shared equally: professional groups work to modify individual risk factors through informal discussion but interventions to prevent falls focus on supervision of patients identified as high risk. | Nursing teams carry the weight of responsibility for preventing falls because they deliver supervision and are present on wards throughout shifts. Alongside responsibility, the work can be draining and demoralising due to insufficient staffing. |
| Professional groups are not able to work cohesively because staff other than nurses have limited time on the ward, and there are temporary or new staff who do not know patient conditions or colleagues’ roles. Supervision used as key falls prevention strategy. High dependency within patient population. |
Meetings that bring together different professional groups focus on discussion of patients stratified at high risk of falls, receiving a level of supervision. | Information sharing constrained: communication between professional groups constrained because staff are not available for informal discussion or may not be aware of information that needs to be communicated. | Nursing team deliver supervision but receive less support from other professional groups, exacerbating the draining and demoralising experience due to insufficient staffing. |
| Organisational expectation that nurses complete falls risk assessment and falls care plan. | Auditing completion of falls documentation and reliance on nursing documentation when looking at causes of falls. | Organisational messaging: nurses are aware that completion of falls documentation is audited, reinforcing message that nurses are responsible for falls prevention. | Nurses less likely to seek support from other professional groups in preventing falls. |
Chapter 7 Facilitation
Introduction
This chapter describes the testing and refinement of the facilitation theory, first using empirical studies identified through the realist review and then through the multisite case study. The original CMOc was as follows:
In contexts where nurses are educated about falls risks and prevention practices (C), if MFRA tools (including HIT) that reflect best practice recommendations are relatively quick and easy to use and are easily integrated into existing workflows, staff will complete them with patients because they facilitate implementation of recommended practice (M), helping to ensure that all eligible patients receive a comprehensive, multifactorial falls risk assessment and appropriate interventions (O).
Findings from the realist review
Number and range of included studies
Figure 6 presents the results of the theory testing searches for all four prioritised CMOcs. In total, 28 manuscripts were used to test the facilitation CMOc. The studies were conducted in a range of countries including the USA,34–38,106–116 Canada,116,117 Spain,118 Australia,119–121 Singapore,122,123 Brazil,124 Japan,125 Taiwan,126 Belgium127 and the UK18 (see Appendix 6, Table 24 for study details). Studies tended to focus on nursing practice, although several studies considered the multidisciplinary team in delivery of interventions. 18,106,113
FIGURE 6.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses diagram for theory testing searches.
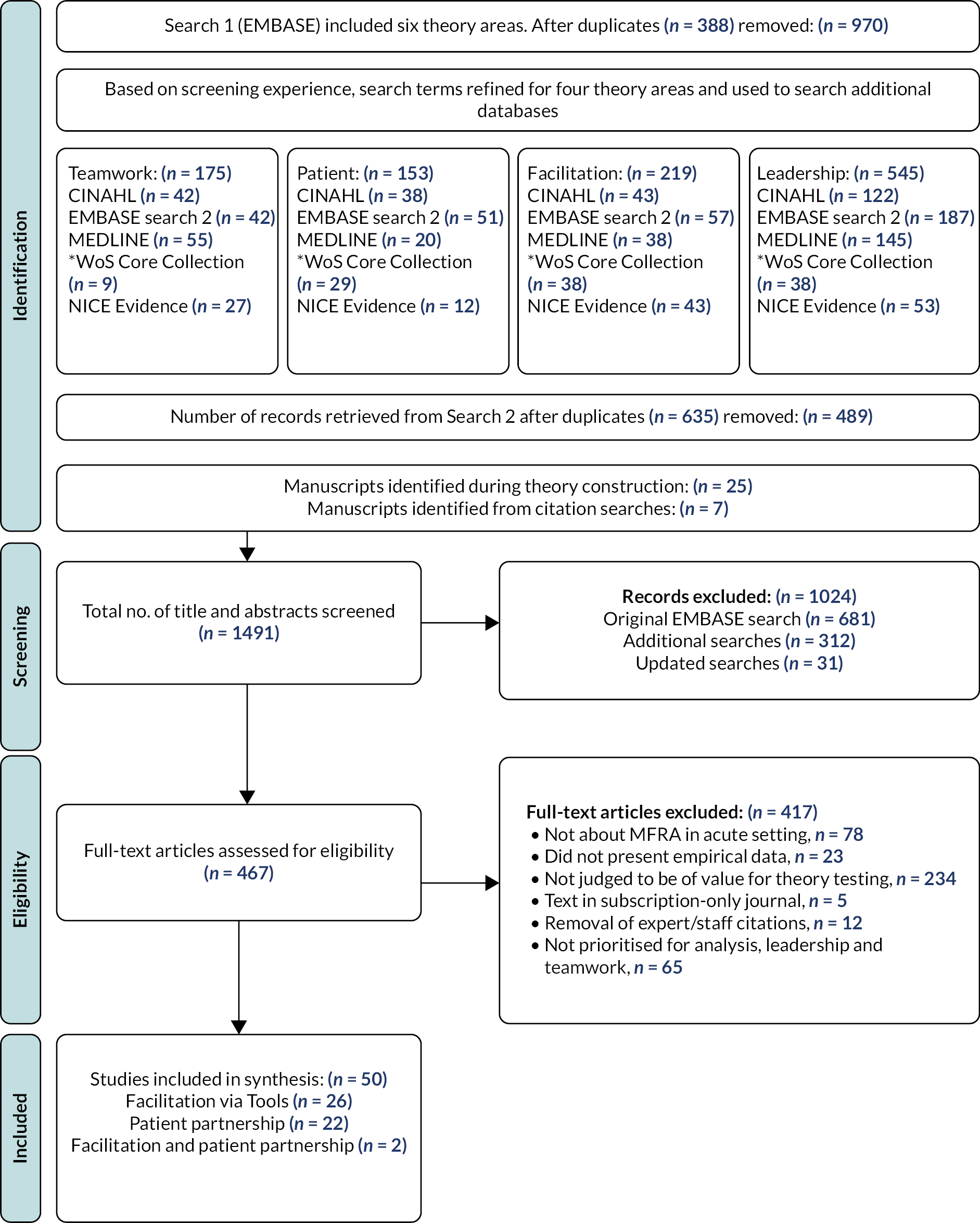
The studies encompassed a range of aims and objectives. Twelve studies were single-site QI projects that aimed to reduce falls incidence using interventions to promote adherence to existing falls prevention programmes or by developing, implementing and evaluating a novel falls prevention strategy. 106,107,109–112,114,117–119,124,125 Other studies shared similar aims to the QI projects, describing the implementation and impact of falls prevention programmes through a RCT, uncontrolled before and after survey, comparison of matched hospitals and survey. 18,113,122,127 The remaining studies examined HIT, exploring supports and constraints on implementation of HIT,36 the impact of the digitising the nursing process,37,108,115,126 auditing compliance with intervention protocol34,38,128 and clinicians’ attitudes towards using HIT for falls prevention. 120,121
The studies took place in a variety of settings: four in Emergency Departments (EDs),107,111,112,114 while others took place in acute medical and surgical units, older person evaluation units and acute wards, and intensive care units (ICUs). 18,34,35,109,110,113,117–124,127
Falls prevention tools
To understand the role of tools in facilitating implementation of falls prevention practices, we reviewed manuscripts to identify what tools were offered to staff; we grouped these as follows: (1) falls risk assessment tools; (2) care planning and intervention delivery tools; and (3) HIT tools.
Falls risk assessment tools
Falls risk assessment tools were described in the majority of manuscripts and included ten ‘validated’ or publicly available tools, such as the Morse Fall Scale,34–38,124 the Memorial Emergency Department Fall Risk Assessment Tool (MEDFRAT),111 the fall risk for older people (FROP) tool121 and KINDER 1. 107,114 Seven studies described locally developed tools, sometimes designed as part of the project concerned after reviewing the falls literature and/or in response to identifying common risk factors on the unit. 18,106,112,117,119,125,127 In nine studies, it was unclear from the description if they were using a published tool or had developed it locally. 108–110,113,115,118,121,122,126
The assessment tools provided items/domains to guide risk identification and manage individual falls risks in hospital. The NICE guideline recommends nine assessment items. The tools identified in this review varied in the number and type of assessment items provided. Examples, and how they compare to the NICE guideline, are presented in Table 14.
| Item | NICE (2013) | MORSE Fall Scale | KINDER 1 | Site specific106 |
|---|---|---|---|---|
| 1 | Cognitive impairment | Mental status | Altered mental state | Disorientated |
| 2 | Continence | N/A | N/A | Requires assistance toileting |
| 3 | Falls history | History of falling | Presented to ED due to fall | Two falls in the last 12 months |
| 4 | Footwear | N/A | N/A | N/A |
| 5 | Health problems | Secondary diagnosis (more than two medical diagnoses in the chart) | N/A | N/A |
| 6 | Medication | N/A | N/A | High-risk medication Patient taking more than four medications |
| 7 | Postural instability, Mobility/balance | Gait | Impaired mobility | Unsteady gait |
| 8 | Syncope syndrome | N/A | N/A | N/A |
| 9 | Visual impairment | N/A | N/A | N/A |
| Others (not in NICE) | N/A | Ambulatory aid IV/No IV |
Age 70 or older Nurse judgement |
At-risk behaviours |
Table 14 highlights variation in items included in assessment tools. Even where some items appear superficially similar, for example, falls history and history of falling, they are not the same; falls history within the NICE guidance refers to trying to understand how, where, when, and why falls occurred (which might identify syncope or other treatable causes), while the tools listed treat history of falling as a ‘yes/no’ question.
We reviewed manuscripts to identify rationales in choice of tools. Koh et al. 122 incorporated a mandatory five-item assessment tool in the nursing assessment notes to prompt nurses to complete a falls risk assessment on patient admission and shift changes. Other authors sought to standardise the content of the assessment process. For instance, Ohde et al. 125 noted that ‘assessments and intervention plans varied from ward to ward’ (p. 2). In response, a six-item assessment tool was developed and introduced to practice.
Maia et al. 124 explained that their audit showed no standardised and validated instrument was used by nursing staff for falls risk assessment. They suggested that absence of a tool may result in inappropriate decisions about degree of risk for patients and affect intervention choices. Therefore, they adopted the Morse Fall Scale, chosen because it had been translated and culturally adapted for their context of Brazil and because it was understood to be easy to apply.
The idea that tools should be easily used as part of the existing workflow was discussed by Dempsey119 who described use of an injury risk assessment form developed for the service, based on the falls literature and the collective experience of clinicians. The tool was designed because of the following:
It was believed that, to succeed, the programme must not place unrealistic demands on time, or require an extension of an already onerous workload. Existing assessment tools, such as the Morse Falls Scale, were considered complicated and time consuming. (p. 481)
Thus, although Maia et al. 124 selected the Morse Fall Scale for ease of use, others considered it complicated and time-consuming. Similarly, Ireland et al. 117 reported that a constraint on implementation of new guidelines within the organisation was competing priorities on staff time and limited resources. For this reason, a falls prevention strategy was developed to ‘facilitate timely clinical implementation’ (p. 199). In creating such a strategy, a Falls Working Group reviewed the literature on falls risks and available assessment tools and developed their own three-item screening tool, which considered the following: (1) altered cognition or confusion; (2) a recent fall; and (3) the judgment of the primary clinical nurse. Their aim was to encourage staff to adopt the basic screening tool and develop and test additional screening criteria in the patient populations over time, that is, to adapt the tool as necessary by adding items specific to unit/wards.
Capan et al. 106 described developing a ‘homegrown tool’ after profiling their patient falls population. In contrast to Ohde et al. 125 and Maia et al.,124 Capan et al. 106 explained their hospital had a falls risk assessment tool but it was not identifying those at high risk of falling. Therefore, they developed a tool better suited to the patient profile. Introducing assessment tools with items tailored to reflect the risks of specific patient populations was also described in the ED studies. For example, Pop et al. 112 noted that risk factors on inpatient tools, such as toileting ability, ‘are impractical to assess in triage’, and others are not applicable on arrival, for example, presence of IV or tethered equipment. They also pointed to falls risk factors unique to the ED, such as intoxication. A new ED falls risk screening tool was developed as part of this QI project and included the following: history of falls in the past 3 months; confusion/disorientation; intoxication/sedation; dizziness/weakness; history of neurological diagnosis; use of assistive gait device; and unsteady gait. The hospital was a centre for neurological care and diagnoses affecting comprehension and co-ordination were common site-specific risk factors, hence this was also included in the tool.
Townsend et al. 114 explained that their ED used the Hendrich II Fall Risk Model (HFRM), a risk prediction tool, to be consistent with the inpatient tool adopted by the wider hospital (completed by nursing staff on patient admission). However, a practice review established that the tool was not sufficiently completed in the ED to calculate a risk score. Therefore, KINDER 1, an ED-specific tool, was selected as part of their falls prevention strategy. The authors speculated that KINDER 1 might facilitate falls risk screening of patients at triage or initial interaction with emergency nurses because it was easier to use than the HFRM. To support consistency in tool use, given the number of nurses who were new to practice and/or new to the ED at the time of the project, they added additional prompts to each item to support risk assessment.
Care planning and intervention delivery tools
A care plan outlines how falls risk factors, identified during an assessment, will be addressed or managed on the ward/unit. Tools designed to support care planning and intervention varied across studies. Some studies described protocols that illustrated how the care planning process should work. 112,117,119 For example, with Ireland et al. ’s117 three-item, Yes/No falls risk screen, if the answer to an item was no, universal falls precautions were to be put in place, including assessing the environment for safety. If the answer to an item was yes, further assessment of at least nine items was to be undertaken. If and to what extent tools were used to link interventions with individual risks was not made explicit. This was also the case in two ED studies, where the KINDER 1 assessment tool was used,107,114 although in one a column had been added to the assessment tool where users could note which intervention(s) had been selected in response to specific risks, facilitating documentation of the plan. 114
Other texts included greater detail about how care planning was supported. Ohde et al. 125 provided examples of how the assessment items used in their tool had been linked with intervention plans so that information to support decision-making in the choice of intervention was available to staff. The tool developed by Capan et al. 106 provided guidance to identify high-risk patients and listed five general falls prevention interventions that must be used for patients considered at high risk of falling, including a written guide to preventing falls to be reviewed with the patient and their family and guidance to support decision-making regarding choice of interventions to address individual risks, such as gait and continence, providing tick-boxes to document which interventions were implemented or if patients refused interventions.
In contrast to the majority of studies described, Fall TIPS and an iPad-based study leveraged HIT to automatically link falls risk factors with interventions. 34–38,120,121 Use of HIT is discussed further below but Duckworth et al. 34 noted that, while the risks that contribute to inpatient falls are well defined, research is needed into protocols that link risks to evidence-based interventions. Similarly, Healey et al. 18 noted few studies had examined the effect of implementing evidence-based interventions to mitigate individual risks, especially in hospitals. In their study, a targeted risk factor reduction core care plan was introduced. The care plan was preprinted and included a brief falls risk factor screen (covering eyesight, medication, LSBP, urine test, difficulties with mobility, and environmental checks, such as reviewing bed height) and related interventions, for example, undertaking medical review of prescriptions, physiotherapy referral for mobility issues, and moving patients with a history of falls closer to the nurses’ station where possible. The reverse of the plan contained a brief summary of evidence, such as medications most likely to be implicated in falls and local advice, such as optical testing arrangements.
Titler et al. 113 designed a Targeted Risk Factor Fall Prevention Bundle to reduce or modify patient-specific falls risk factors. They used a taxonomy to classify falls prevention interventions as follows: (1) universal falls precautions, for example, reducing environmental risks for falls, such as keeping patient rooms and corridors free of clutter; (2) general falls prevention interventions, for example, bedside table, call-light, and other personal items within reach; and (3) targeted individual risk-specific interventions, for example, assistance with toileting when needed. Targeted interventions were grouped by categories of risk to address: (1) previous falls; (2) mobility limitations; (3) elimination; (4) medications; (5) factors that increase risk for serious injury from a fall (e.g. anticoagulants); and (6) cognitive and mental status. A set of six quick reference guides were created, organised by risk factor categories, with suggested fall prevention interventions to address each. Additionally, posters were developed about falls, patient-specific falls risk factors and falls prevention interventions to mitigate these risks. The posters were used in staff education and were posted in key areas, such as medication rooms and nurses’ stations.
Visual tools were described in several studies. 34,35,38,106,109,111–114,117,120–122,124,125 Typically these were designed to (1) make patients at risk of falls visible to staff, for example, Koh et al. 122 used pink name cards above beds, pink stickers on clinical/nursing notes, and pink identification bracelets for high-risk patients; and (2) alert or remind staff and carers of interventions in use for patients, for example, Hefner et al. 109 developed a Falls Wheel to be displayed on patients’ doors. It had two overlaying circles; the top circle instructed staff that universal falls precautions should be implemented for all patients and the bottom circle contained information about the additional safety measures put into place for individual patients, based on their assessed risk status.
Health information technology
Seventeen studies referred to use of HIT. 34–37,107,108,110–112,114,115,118,120,121,124–126 Seven studies described assessment and/or care planning processes within EHRs but did not focus on the impact of HIT as part of the study objectives. 107,111,112,114,118,124,125 The remaining 10 studies focused specifically on the role of HIT. For example, Lytle et al. 110 explored nurses’ use of computerised decision support (CDS) in falls prevention. They examined the impact of the following: (1) an ‘admission documentation incomplete’ falls risk assessment indicator; (2) a ‘shift documentation incomplete’ falls risk assessment indicator; and (3) a ‘rules-based alert’ for patients at high risk of falls and not on a falls care plan. These provided links to appropriate documentation sections within the EHR.
The Fall TIPS intervention, reported in five papers,34–38 leveraged HIT to promote use of evidence-based falls prevention practices. Nurses were expected to record the assessment online, from which the Fall TIPS software identified a core set of evidence-based interventions directly linked to patient-specific risk factors. Nurses could further tailor these interventions, based on their knowledge of patients. Three patient-specific outputs were automatically generated: a care plan, a bedside poster, and an educational handout for patients and carers. The posters featured icons, rather than text, to make information easier to understand for all members of the care team (including patients and carers), regardless of their literacy levels. 35 The studies focused on how different modalities of the intervention impacted on patient engagement and the impact of strategies used to promote adoption of Fall TIPS. In addition, Businger et al. 36 reported implementation challenges of a Patient Safety Learning Laboratory (PSLL), a suite of patient- and provider-facing tools to raise awareness of safety issues and prevention strategies, one element of which was Fall TIPS.
One study focused on an iPadTM-based tool that supported direct entry of clinicians’ assessments of patients’ falls risks. 120,121 Nursing staff in the hospital had reported that paper-based posters, which required nurses to place coloured adhesive dots on eight different parts of the poster to indicate falls risks, were time-consuming and difficult to use, and hence not completed consistently. With the new tool, clinicians entered on an iPadTM patients’ details (age, bed location, need for a mobility aid) and their own clinical judgment (yes/no responses) about the patient’s day- and night-time falls risk for 13 different movement and location types. The interface had buttons that indicate areas of risk when pressed and it took ˂5 minutes to use per patient. Like Fall TIPS, the tool automatically generated a tailored care plan poster. The study evaluated acceptability and clinical efficacy of the HIT tool compared to the paper-based tool previously used.
The remaining HIT studies looked at correlations between HIT use and outcomes, such as documentation of falls prevention practices in the EHR and falls rates/incidents. For example, Dowding et al. 108 assessed the impact of an integrated EHR on nurse-sensitive outcomes (including falls), using a controlled interrupted time series analysis. Wu et al. 126 reported on implementation of a standardised computerised nursing process documentation system (SCNPDS) and, later, the move from an assessment tool based on the Morse Fall Scale to a multifactorial hospital-specific scale, which included risk items relating to age; sex; gait; high-risk medication; dizziness; paraesthesia of foot; need for assistance with mobility; falls history; and presence of caregiver. On admission, nurses carried out the risk assessment and entered the data into the SCNPDS to run the nursing admission notes. They then entered the care planning data set to select a personal care plan for patients at risk of falling, outlining actions and teaching to be undertaken with the patient. These care plans were to be re-evaluated every shift to complete the nursing documentation process.
Outcomes
Implementation of recommended practices was the key outcome of interest in the CMOc. Typically, implementation was assessed using quantitative measures, such as number of patients receiving falls risk assessments on admission pre- and postintervention, or measures of fidelity, for example, displaying a visual tool as required by an intervention protocol. In Appendix 7, Table 25, we summarise outcome data, where provided, on the following: (1) delivery of a falls risk assessment; (2) documentation of a falls prevention care plan; (3) use of interventions targeted to individual falls risks, and (4) falls incidents and rates.
Delivery of falls risk assessments
Twelve studies assessed delivery of a MFRA as documented in the patient record, and 10 studies demonstrated an improvement. 37,108,110,115,117,118,122,124–126 However, Koh et al. 122 reported an improvement in compliance in completing a falls risk assessment in both the intervention and control hospital. Dowding et al. 108 explored the impact of digitising risk assessment of hospital-acquired pressure ulcers (HAPU) and falls and found a statistically significant increase in HAPU documentation rates but the increase for falls risk was not significant. Cook et al. 107 found compliance documenting a falls risk assessment did not improve following introduction of an ED-specific tool, although the tool supported more accurate identification of patients at risk of falls. Dempsey119 found documentation of an assessment (and other processes) initially improved and was associated with fewer falls, but compliance was inconsistent over the longer term and on a downward trend.
Care planning and intervention delivery
Seven studies assessed whether care plans were delivered,37,110,113,118,124–126 six of which also assessed compliance in documenting the care plan in the clinical record. 110,113,118,124–126 Ohde et al. 125 reported improvement in documentation of an appropriate intervention plan (and falls risk assessment). Maia et al. 124 studied two wards, the internal medicine unit (IMU) and ICU and found use of interventions according to risk factor improved in both wards, while Albornos-Munoz et al. 118 found documentation of targeted interventions declined in two out of three wards. Lytle et al. 110 reported documentation of care plans did not significantly improve after alerts were introduced into the EHR. Wu et al.,126 examining the impact of digitising nursing documentation, found nurses did not document care plans for all patients assessed as at risk of falls and that more patients who received a care plan fell than those who did not have a care plan documented. Carroll et al. 37 reported that documentation of an MFRA and care plan improved, while documentation of intervention delivery did not.
Titler et al. 113 reported significant improvements (p < 0.001) in implementation of interventions targeted to individual risks, including those associated with mobility, toileting, cognition, and injury risk reduction, but not for those targeting medications. Hefner et al. 109 found the Falls Wheel was correctly displayed 95% of the time and updated to match risk levels in the EHR 70% of the time. Fall TIPS posters were displayed 72% of the time in one study and 80% in the other. 34,35
Falls incidence and rates
Seventeen papers provide information about falls rates, incidents and injuries. Nine papers reported a decrease in recorded falls postimplementation,18,106,107,109,112,114,117,124,125 although few reported whether the change was significant. Only one took the form of a RCT, finding a significant reduction in recorded falls on wards that used a targeted risk factor reduction core care plan (RR 0.79, 95% CI 0.65 to 0.95) compared to control wards (RR 1.12, 95% CI 0.96 to 1.31). 18 There was a significant difference in the change between intervention and control wards (RR 0.71, 95% CI 0.55 to 0.90, p = 0.006), although there was no reduction in the incidence of falls-related injuries.
The remaining studies were observational studies without control groups and therefore with potential for factors other than the falls prevention initiatives to have confounded their results.
Ohde et al. 125 also found a significant decrease in reported falls, in their observational study of a new approach to falls prevention in a Japanese hospital, in which the overall organisation-wide falls rate decreased from 2.13 falls per 1000 patient in 2004 to 1.53 falls per 1000 patient days in 2010 (p = 0.039), postimplementation. Bone fracture rates due to falls among hospitalised patients also declined, though not significantly, from 0.04 fractures per 1000 patient days in 2004 to 0.02 fractures per 1000 patient days in 2010. Conversely, in their study about a falls prevention protocol in an ED, Cook et al. 107 reported a significant decrease in the falls with injury rate, from 0.09 per 1000 visits to 0.03 per 1000 visits, representing a 66% decrease in injuries postimplementation (p < 0.05), whereas the decrease in falls overall was not significant: 0.73 falls per 1000 visits preimplementation to 0.55 falls per 1000 visits postimplementation, representing a 25% decrease (p = 0.18). The remaining studies reporting declining rates of falls did not specify if the decreases were statistically significant. 106,109,112,114,117,124
Eight papers reported no significant change in falls rates postimplementation or varying falls rates. 108,110,113,118,119,121,122,126 Albornos-Munoz et al. 118 reported falls rates increasing in two of the three study wards after implementation of new approaches to falls risk assessment and prevention, although the study was underpowered to detect statistical significance. Dempsey119 reported that a new falls prevention programme at first achieved a significant decrease in the rate of falls from 3.63 to 2.29 per 1000 occupied bed-days (p = 0.05) but this was not sustained over time. After the project, the falls rate initially remained low but then began to rise, eventually exceeding preintervention levels at 6.8.
How, why and in what contexts do MFRA and care planning tools work?
Although most studies described MFRA tools and pointed to their role in the facilitation process, there was a paucity of data about how and why staff responded to these tools. A further challenge in the analysis was that, typically, MFRA tools were not used in isolation. Often, multiple interventions were used to address implementation barriers as part of QI strategies, for example, staff incentives, education, training, and feedback were introduced alongside the assessment and care planning tools of interest. Therefore, we focused on tools as the resource of interest and examined what shaped clinician use and impact as key contextual influences of interest (including additional interventions used).
Analysis suggests the tools can facilitate delivery of recommended practices by (1) prompting staff to complete recommended tasks and actions and (2) automating parts of the falls prevention process. Contextual influences that help explain variation in tool impact include the following: (1) staff knowledge, experience, and attitude (sometimes targeted by educational and training interventions used as part of the study); (2) the complexity of ward work, including patient condition and movement between wards; (3) application of clinical judgment; and (4) physical resources needed to deliver interventions and multidisciplinary teamwork.
Prompting delivery of recommended practices
Tools were often described as being integrated into staff workflow, either in paper-based formats,18,106,122 for example, in care co-ordination rounds, or in the EHR. 34,35,37,38,107,108,110,111,114,115,118,120,121,124–126 There was some evidence that physical presence of tools within staff workflow facilitated delivery by acting as a reminder to staff and drawing attention to required tasks. 18,110,119,122 To work in this way, tools needed to be clearly visible to staff, with authors discussing constraints on tool use where this was not the case. 110,111,118 For example, McCarty et al. 111 integrated MEDFRAT into their EHR, locating it in the triage tab, which staff rarely used. To address this, MEDFRAT was then made available in two locations in the EHR with indication of whether it had been completed or not. Compliance delivering the assessment was not captured as part of this study, but McCarty et al. discussed staff reaction being unanimously positive, due to it being tailored to the ED. Therefore, location and tool content supported use in practice.
Lytle et al. 110 investigated CDS within the EHR, which alerted staff to incomplete risk assessments and care plans. They reported a significant improvement in documentation of falls risk assessments but not documentation of care plans for high-risk patients. Through focus groups, they identified visibility of alerts as a potential explanation. Lytle et al. 110 also commented that the alerts were introduced as part of a hospital-wide EHR roll-out where 54 legacy applications were retired. Falls care planning was digitised, having previously been paper-based. They reasoned that the ‘process [was] different enough for the care plan to be overlooked’ (p. 535) and ‘the volume of changes with implementation of a hospital-wide EHR made it difficult to focus on a single aspect such as the available CDS tools’ (p. 536). Therefore, alongside location in the EHR, staff awareness was not focused on the care plan.
Albornos-Munoz et al. 118 also highlighted staff awareness as influential on tool use, describing how it was yet to become embedded in ward practice. Consequently, staff training was incorporated as part of the QI strategy. This led to improved compliance in delivering falls risk assessment on patient admission, although impact on the care planning process was variable.
Educational interventions were frequently used alongside tools to support knowledge acquisition, and implementation, of falls prevention practices. 106,107,109,111–114,117–119,122,124,125 Koh et al. 123 found nurses perceived lack of knowledge as a barrier to implementation of falls prevention practices. They explicitly sought to address this in their intervention study through education sessions, feedback, and change champions and found a significant increase in nurse knowledge (p < 0.01). Koh et al. 122 also integrated a simplified assessment tool ‘into the normal nursing outline’, where it was intended to prompt staff to complete assessment on admission and at every change of shift. They found compliance in delivering a falls risk assessment on admission improved in both the intervention and control hospital. The tool, therefore, acted as a prompt in a context of increased staff awareness and acceptance of the importance of the falls prevention programme. To explain improvement in the control group, Koh et al. pointed to national drivers of practice operating at the time of the study, specifically a new Clinical Practice Guideline that mandated falls risk assessment.
Healey et al. 18 considered no additional training in the care plan tool they described was necessary for staff because it was similar in format to those used for other conditions and it was made available within routinely used forms. The authors discussed that the single piece of documentation ‘could be seen as prompting and co-ordinating assessments and interventions that already commonly occur, if not consistently, on wards for older patients’ (p. 394). Compliance documenting the risk assessment or care plan was not reported as part of this study, but a significant reduction in RR of recorded falls on intervention wards was observed. The authors speculated that interventions with more immediate potential for risk reduction may have contributed to this outcome or the care plan may have been effective ‘in concentrating the minds of staff on the existence of fall risk factors and promoting action to remove or ameliorate them where possible’. 18 Dempsey119 discussed how education was provided as part of a falls prevention programme, but ‘much of the workforce was undergoing some form of internship that made consistency in care difficult’ (p. 482). Even so, a reduction in falls incidents was achieved using a simple tick system that linked risk factors and possible falls prevention strategies, leading Dempsey to argue the following:
It is the act of the assessment itself rather than the tool that provides the successful outcome. The completion of any assessment tool gave the task an emphasis that may not have been achieved otherwise and that may simply have provided a focus for the application of clinical judgement. (p. 481)
Automating assessment and care planning processes
Three interventions used HIT to automate delivery of falls prevention practices – Fall TIPS, an iPadTM-based system, and an automated fall risk assessment instrument integrated into three clinical information systems. 34–38,115,120,121 Fall TIPS and the iPad-based system involved staff completing a falls risk assessment electronically, from which care plans and posters were automatically generated. Duckworth et al. 34 shared insight into organisational factors that influenced staff use of Fall TIPS, highlighting ‘unsophisticated EHR platforms, lack of funds for the toolkit build, and lack of staff engagement to successfully support the roll out’ (p. 2). Fall TIPS was developed to respond to these kinds of barriers, by varying the level of automation offered; Duckworth et al. 34 examined three Fall TIPS modalities: (1) a tailored falls prevention poster generated by the EHR; (2) display of care plan on bedside monitors; and (3) a paper-based, laminated version of the toolkit. They found no difference in rates of adherence across modalities, but some wards took longer to reach 80% adherence. Dykes et al. 35 explained that, in three of four participating hospitals, the automatically generated care plan could be further tailored by nurses, based on their knowledge of patients, although this was not possible in one hospital due to constraints of the vendor software. Hence, like levels of automation, the customisation function was also dictated by the sophistication of hospital IT systems. Nonetheless, significant improvement was observed across hospitals in mean number of falls risk assessments completed by nurses using Fall TIPS per patient, per day (increased by 25% from the first month).
Hefner et al. 109 and Teh et al. 120 provided insight into staff experiences of using these types of tools, both paper-based and computer-based. For example, despite high levels of adherence displaying the Falls Wheel (95%), staff felt updating it was a competing priority, which they did not have time for. 109 Other issues reported included that its placement in some locations could lead to diminished visibility and inadvertent wheel changes by patients, families, and staff. Nurses also noted the limited involvement of other staff beyond direct patient care providers. Teh et al. 120 reported similar findings; alongside technical difficulties in using the iPadTM application, staff said it was difficult to ensure the automatically generated care plan posters were physically relocated when patients were moved into other beds.
Experience using HIT was reported as influential on uptake. Currie et al. 115 found that experience using the clinical information system predicted initial use of an automated tool. A survey conducted by Teh et al. 120 found that some staff perceived the principal barriers for the use of the iPad tool was lack of time (39.3% of post-trial survey respondents), while 21.4% of respondents mentioned lack of usability. The main recommendation for improvement was for more staff training (32.1% of respondents), especially from staff who had already used the tool, suggesting they felt a need for more support to use it effectively. Despite this, 75% of respondents to the post-trial survey wanted to continue using the tool and saw it as a useful snapshot of patients’ falls risks. Clinicians’ perceptions of tool acceptability trended higher on one ward, possibly due to a longer staff training period on that ward and greater senior nursing endorsement and involvement in the tool design. 121 Other contextual factors considered to have affected results were the level of clinician experience in implementing preventive strategies and patient-related factors, such as frailty.
Automating the falls prevention process more fully may help to address some of the challenges of manual work noted by Teh et al. and Hefner et al., with the Fall TIPS bedside display modality guaranteeing the information displayed is up-to-date (or at least as up-to-date as the EHR). 129 However, more comprehensive and iterative implementation strategies were used to support uptake and use of HIT. 35,36 For example, Dykes et al. 35 used the Institute for Healthcare Improvement’s Framework for Spread to structure adoption by promoting engagement among different stakeholders. Spread is underpinned by a number of factors, including leadership; set-up; ideas; communication; social system; knowledge management; and measurement and feedback. Dykes et al. 35 showed how they used each of these factors to facilitate spread of Fall TIPS, for example, in relation to set-up, they involved stakeholders in identifying toolkit requirements and in usability and pilot testing and offered ‘“just-in-time” round the clock training for professional and paraprofessional caregivers’ (p. 155) on toolkit use. Nevertheless, implementation can remain a challenge, as Dykes et al. 35 conceded:
Changing behaviour and practice is difficult, even when the rationale and methods for change are embraced by caregivers. Nurses and other caregivers in acute care hospitals are busy. The patients are sick and the workflows are complex. (p. 157)
This type of environment demands that if innovations are to be adopted, they must be thoughtfully introduced using a framework that provides the communication, peer support, feedback, and time needed to assure an effective transition to adoption, culture change and sustained improvement.
Influences on tool use and impact
A number of factors were identified that appeared to influence use of tools, in particular, for practices that followed an initial fall risk assessment, as documented in clinical records. For example, Maia et al. 124 reported low compliance with documentation of reassessments following a change in medical condition or a fall (50%) in the IMU. They explained that patients admitted to the IMU who became unstable or suffered significant clinical deterioration were transferred to the ICU. However, the same criterion in the ICU showed 86% compliance with best practice, which they attributed to patients being unstable and needing frequent assessment. Lytle et al. 110 noted occasions where falls risk assessment changed from positive to negative, and the care plan was discontinued, but if the assessment changed again to positive, the care plan was not always reinitiated on the system. Albornos-Munoz et al. 118 reported that two out of three wards studied did not demonstrate improvements in documenting a care plan (nor a reduction in falls) and commented that ‘the associated activities [that cause falls] are more complex and depend much more on other interventions, such as patient education, exercise and medication reviews’. Therefore, factors such as changes in patient condition, movement between wards, and involvement of multiple professionals may influence the extent to which tools facilitate and are used to document the care process as intended.
To help explain the subsequent downward trend in compliance with the falls prevention programme and increase in falls rates following initial success, Dempsey119 explored staffing levels (number of nurses) and skill mix (years of experience and casual staff); patient acuity (resource allocation); and patient activity (number of patients treated and occupied bed-days). Critical points were identified where the number of bed-days reached a certain level frequently (3500). These points disrupted care provision and were associated with an increase in adverse events. Dempsey discussed a tension between ‘must do’ task-based work that involved attending to patients’ immediate needs and caring or ‘being with’ patients, with ‘must do’ work taking priority. Dempsey saw this conflict as significant in the rising incidence of patient falls, as well as decreasing nurse satisfaction levels.
Some studies provided insight into what constrained delivery of interventions recommended in tool guidance. For example, McCarty et al. 111 reported some interventions were not available for staff to use, for example, nurses reported a lack of call-bells. Other authors pointed to the multidisciplinary nature of preventing falls. 113,118 Titler et al. 113 reported significantly increased use of interventions for mobility, toileting, cognition, and risk reduction for injury (p < 0.001) following implementation of their falls prevention bundle, although medication interventions, such as pharmacy review, avoiding use of medications that increase falls risk, and toileting prior to administration of analgesics did not show significant improvement. Furthermore, increased use of interventions related to mental status risk (such as physician consultation for mental status changes), and scheduled rounding were not demonstrated. Titler et al. 113 used a Translating Research Into Practice (TRIP) strategy to support uptake of the targeted interventions but it was not clear how this strategy effectively engaged non-nursing staff. In comparison, Capan and Lynch106 addressed teamwork from inception onwards in the development and implementation of their falls risk assessment and intervention tool, designed by a multidisciplinary falls prevention task force. Patients’ falls risks and interventions were discussed by nurses and care associates during change-of-shift reports, and care co-ordination rounds that took place daily. These involved a nurse, physician assistant, case manager, and nurse manager, with a pharmacist and dietician attending on certain days, to discuss the total plan of care for all patients on the unit. The authors noted the following:
This is an opportune time for the nurse and case manager to consult with the pharmacist about at-risk medications. It is also during this time that the fall risk assessment and interventions are discussed to ensure that an accurate assessment was made and that interventions are being followed. (p. 158)
Although data about use of targeted interventions were not reported, the number of falls decreased from 70 in 2004 to 37 in 2005, although this QI study does not state whether or not this is statistically significant.
Milisen et al. 127 surveyed 49 healthcare workers in 17 Belgian older person wards on their views about the feasibility of implementing a falls prevention practice guideline, which covered in-depth MFRA and targeted interventions. The guideline was regarded as useful by staff (69.4% judged in-depth MFRA to be useful and 70% believed individual interventions were useful), and a small majority (62.3%) believed it could be successfully integrated into their daily practices over a longer period. The most identified barrier for implementation was the large time investment (81.1%) – MFRA on average required 76.1 ± 34.8 minutes; initiating an individual treatment plan was only recorded by nine teams and estimated to take 30.6 ± 22.7 minutes. Issues around teamwork were also cited, namely lack of communication between different disciplines (35.8%) and lack of multidisciplinary teamwork (28.3%). The authors suggested that HIT could provide a solution to these problems, in place of the paper worksheets used by the hospitals concerned, and pointed to Fall TIPS findings about HIT improving multidisciplinary communication. They also reported respondents recommending that teamwork might be improved by giving specific members of staff a remit to co-ordinate assessments and interventions.
Theory refinement
Based on the literature presented above, we were able to make refinements and additions to the facilitation theory, moving from a single CMOc to four CMOcs concerned with facilitation (Table 15). The evidence supporting the claims of the CMOcs and GRADE-CERQual assessment of the evidence are presented in Appendix 8, Table 26.
| CMO | Context | Mechanism | Outcome | |
|---|---|---|---|---|
| Intervention | Staff response | |||
| F1 | Where staff understand (through experience, or education or feedback) how and why falls prevention practices reduce falls risk factors. | MFRA tools are located visibly and intuitively in the EHR or are embedded clearly within ward practice and offer a structure to guide identification of fall risk factors. However, assessment tools vary in type and number of assessment items. | Reminder: tool draws staff attention to the tasks required, for example, completing an assessment of individual falls risk factors and prompts action. | More consistent documentation and delivery of falls risk assessments but content of assessment may differ depending on tool used by service. |
| F2 | Ward conditions are complex – patients’ condition may change, they may swap beds or move wards, and they may require multiple interventions. | MFRA tools are located visibly and intuitively in the EHR or are embedded clearly within ward practice and offer a structure to guide identification of fall risk factors. However, tools vary in type and number of assessment items. | Prioritisation: staff attention is focused on care delivery rather than documenting care processes. | Documentation of care process may be less consistent, particularly after the initial assessment. |
| F3 | Staff who are educated and experienced in identifying and managing falls risk factors. | MFRA tools are visible to staff in their work routines and provide guidance for assessing risk and linking risk with interventions. | Clinical judgement: where tool guidance does not align with clinical judgement or resources available, staff apply care according to their own judgement. | Care may not be in line with tool recommendation, but action taken to manage risks using ward resources. |
| F4 | IT systems support HIT function and staff are trained and experienced with use of HIT. Where staff understand (through experience, or education or feedback) how and why falls prevention practices reduce falls risk factors. |
MFRA tools are located visibly and intuitively in the EHR or are embedded clearly within ward practice. Care plans, poster, and information leaflet automatically generated from software. | Automation: interventions to address falls risks automatically selected and documented in care plan and patient poster. Staff display poster at patient bedside and action care plan. | Reduced variation in development and documentation of care plan that links falls risks with appropriate interventions. Task load of clinical staff reduced. Falls prevention strategy more visible in poster at patient bedside. |
| Manual work: staff see manual work as competing priority with other responsibilities. | Display of poster may be disrupted by patient flow, for example, between beds and wards. | |||
Findings from the multisite case study
The refined facilitation theory highlighted that there is likely to be variation in practice because the contents of tools differ across sites, with some incorporating stratification of patients by risk. The CMOcs hypothesised that complex ward work and clinical judgement may influence the extent to which tools prompted desired practices, and that HIT was being introduced in some sites that automated practice.
Falls risk assessment and care planning tools
We explored whether the nine items recommended by NICE for a comprehensive MFRA were included explicitly in each site’s falls risk assessment, falls care plan or whether it could be identified in other nursing assessments (Table 16).
| NICE | Site 1 | Site 2 | Site 3 |
|---|---|---|---|
| Cognitive impairment | A/CP | A | A |
| Continence | CP | A | N |
| Fall history | A | A | A |
| Footwear | CP | ? | CP |
| Health problems | N | A | N |
| Medication | N | A | CP |
| Postural instability, mobility and/or balance problems | A/CP | A | A |
| Syncope syndrome | CP | N | ? |
| Visual impairment | CP | A | N |
Table 16 indicates that, typically, the nine items recommended by NICE were included as a prompt in at least one space within the nursing documentation. However, they were not always explicitly incorporated in the falls risk assessment tool and there was variation between sites in phrasing of questions/prompts and tool content. Site 2, for example, included seven items recommended by NICE within its falls risk assessment tool and additional items, such as ‘Patient anxious about falling’.
At Site 3, completing the three-item assessment automatically calculated a score that categorised patients as high, medium or low risk. There was awareness that categorising patients in this way did not reflect the principles of NICE or the spirit of the Trust’s own falls prevention policy, which stated that people at risk of falling would be offered a MFRA and, where assessed at increased risk of falling, an individualised multifactorial intervention. However, this site was in the process of updating its EHR and the assessment documentation was being adapted to be more inclusive of individual falls risk factors and provide a better guide for staff in delivery of falls prevention practices.
While Site 3 was the only organisation using a score to stratify patients by falls risk, on all wards studied, staff explained that they attempted to identify patients considered at high risk of falls. Site 2 used the EOC scores to identify high-risk patients. High-risk patients were typically understood as needing some level of supervision to maintain safety, for example, one-to-one care, being placed on a cohort bay, intentional rounding.
Based on falls risk assessment and care planning documentation alone, it was not always clear the extent to which individual risk factors were comprehensively addressed for each patient at different sites. For example, in Site 1, the first care plan documented was called the ‘Intervention Plan’ and prompted staff to document actions against 15 items (Table 17).
|
A ‘Daily Care Plan’, an abbreviated version of the intervention plan, was used for updates after the Intervention Plan. Similarly, the care planning documentation in Site 3 prompted staff to enter responses for individual risks but was not as comprehensive as that provided in Site 1.
In Site 2, while the assessment included more NICE items than in Sites 1 and 3, the care plan did not prompt staff to enter responses for individual risks. A Falls Specialist Nurse explained that the documentation allowed nurses to link interventions to risks, but questioned the extent to which this happened in practice. Observation revealed that the ward manager on the orthopaedic ward had worked with the IT department to code falls interventions into the EHR to facilitate documentation. This meant that if they typed in ‘falls0’ or ‘falls1’, standard text relating to actions was inserted automatically; ‘falls0’ generated text about appropriate footwear, whereas ‘falls1’ generates text about call-bell use.
Examining the falls prevention documentation alone suggests why there is variation in how, and the extent to which, individual falls risk factors are identified and modified for patients across sites. However, nursing documentation in its entirety includes assessments that contribute to falls prevention even if they are not explicitly labelled on the EHR as such. For example, in Site 1, the falls risk assessment was part of the Nursing Specialist Assessment (NSA), completed for all patients on admission to a ward. Alongside the falls risk assessment, documentation included sections titled Cognition and Mental Capacity, Mobility, Elimination – Bladder, and Elimination – Bowel.
Use of tools in falls prevention
An aim of data collection was to observe falls risk assessments taking place in real time, to better understand how tools were used by nurses to identify and modify patient falls risk factors. During fieldwork researchers explicitly requested to shadow nurses while completing falls risk assessments. However, few assessments were observed in real time. Care plan updates were observed but often as a demonstration for the researchers rather than as part of normal work. Ward staff explained that patients are assessed when they are admitted to the ward and admissions can happen at any time throughout the day. Furthermore, care plans are typically updated during quiet times, often on the night shift, as data from the clinical record review indicated.
While laptops on wheels were observed on all wards, these were not used for completing falls documentation at the bedside. Assessing patients’ care needs was described as a dynamic process, not necessarily reliant on direct use of tools. For example, a Falls Specialist Nurse in Site 2 explained how a nurse might assess a patient’s condition and potential needs based on direct observation and conversation, identifying potential falls risks, for example, use of glasses and walking aids, for incorporation into the assessment. Similarly, a nurse in Site 3 described this type of dynamic assessment of patients, explaining that they ‘know’ quickly if a patient will take risks, presumably by direct observation and early interactions, and that the assessment is an ongoing process because patients’ conditions change. Observations supported interviewees’ accounts, showing how information was collated in a dynamic way and was not reliant on use of EHR tools, with the relevant sections of the EHR being completed at a later point, typically at the nurses’ station. Observations also revealed challenges in collating information about risks, for example, patients may not be able to communicate effectively if they are confused or in pain, an issue we return to in Chapter 8.
Tools as practice prompts
Context mechanism outcome configuration 1 in the facilitation theory suggested tools may work simply by prompting staff to complete recommended practices, for example, assessing items necessary to comprehensively identify individual falls risk factors. If assessments are documented retrospectively on the EHR, as observed, it is only at this retrospective point that they can work as a prompt. However, across sites, nurses described finding the tools as useful prompts. For example, a nurse in the Site 3 older person/complex care ward described the items prompting assessment of risk factors that may not be remembered when nurses are addressing the immediate concerns and care needs of patients on admission to the ward.
Alongside prompting assessment of specific risks, a Site 1 nurse described that the assessment tool provided an opportunity to rethink how a patient’s condition and their care needs have changed over time. As described, the Site 1 falls care plan facilitated documentation of interventions to address individual falls risk factors. However, a matron on the orthopaedic ward commented that there are many interventions ‘that are blanket for everyone’ and she did not think nurses felt ‘empowered’ to deviate from these. She gave the example of the risk assessment suggesting a patient needed to be located in a cohort bay and explained that a nurse would not want to deviate from this for fear of consequences if they did and the patient fell.
As described in Chapter 6, supervision was seen as key in preventing falls. Allocating these types of interventions was typically based on classification of patients as high risk of falls, However, a ward manager in Site 2 described how the patient population meant that a large proportion of patients were categorised as in need of a high level of supervision. Even where fully staffed, participants explained that numbers may not be sufficient to support the levels of supervision thought necessary to maintain patient safety. Therefore, nurses used their clinical judgement, based on observation, to manage resources. Patients’ conditions fluctuate, so nurses can reallocate resources as patients improve and require less supervision. Senior nurses and ward managers explained that they escalated concerns to managers when staff shortages made it difficult to implement supervision as a strategy.
Tools as evidence of practice
Context mechanism outcome configuration 1 in the facilitation theory hypothesised that staff experience and knowledge of falls prevention practices would support implementation of the risk assessment and tailored interventions in response to tool prompts. As described in Chapter 5, falls prevention training was provided across sites but had been disrupted by COVID-19, potentially limiting the knowledge of new staff.
Nursing experience was described as influential on tool use, but with emphasis on documentation as evidence of practice:
If there’s a complaint, or there’s ever anything that somebody wants to question what you’ve done on that shift, for whatever reason, then that’s your evidence. Because the nurses, old chestnut: if it isn’t written down it hasn’t happened.
Ward Manager, Site 3 Orthopaedic Ward
The idea that tools should be completed as a record of care delivery was considered to be deeply ingrained in nursing practice to provide ‘evidence’ against complaints. As described in Chapter 6, Trusts audited falls documentation for compliance with hospital policy. Despite the dynamic, ongoing nature of risk assessment described by nurses, an organisational member of staff in Site 1 explained that, from an organisational perspective, if EHR documentation is incomplete then that information is assumed to be unknown, and presumably not acted on, by ward staff. In other words, knowing that the documentation was audited and fearing blame could sometimes motivate nurses to ensure documentation was completed.
Tools as a tick-box exercise
In interviews across sites, nurses felt that documentation consumed their time, due to the number of assessments and care plans that they were expected to complete. Contributing to the documentation burden was duplication, for example, a nurse at Site 3 explained that they repeated assessment information on the SBAR (situation, background, assessment, recommendation) documentation and commented: ‘we spend more time on this [documentation] than with patient care’ (Nurse-in-Charge, older person/complex care ward, Site 3). The tension between care delivery and documentation was exacerbated by the staff/patient ratio, patient dependency, and the delivery of high levels of supervision. A Site 1 nurse described how, in this context, completing the documentation can become a ‘tick-box exercise’. When nurses have competing priorities and are working under pressure, they may look to complete the EHR documentation as quickly as possible rather than using it as prompt or an opportunity to consider how care needs have changed. Another consequence is that documentation may not be fully completed, a point which nurses spoke to in interviews and which we saw in observations.
In Site 2, the EHR enabled responses from one care plan to be copied-and-pasted to another during care plan updates. While this can speed up document completion, the information does not necessarily reflect changes in patient condition or the care delivered. Similarly, a nurse in Site 3 explained that nurses often prioritise care delivery over documentation. Therefore, what they document from memory may only reflect 80% of care provided. We also observed care plans being updated during the night shift, and not by the nurse who had cared for the patient through the day. Data from the record review suggested that this was a common practice (see Figure 7).
FIGURE 7.
Time of care plan update.

In Site 3, a nurse-in-charge explained that they may prioritise the assessment of certain patients, for example, those that they considered at high risk of falls. While they prompted staff to complete documentation for all patients (partly because it contributes to falls investigation and learning), they said that staff–patient ratios may mean that care delivery was prioritised over completing documentation for patients that they observed to be a lower falls risk, providing bed-bound patients as an example.
Theory refinement
Through the multisite case study, we were able to make a series of refinements and additions to the facilitation CMOcs (Table 18). Specifically, CMOc F1 becomes two CMOcs, reflecting what happens when tools are completed retrospectively; CMOc F2 is revised to reflect the dynamic nature of falls risk assessment and the potential for completion of documentation to become a tick-box exercise; and CMOc F5 is added to reflect the consequences of supervision being a key falls prevention strategy. We were unable to test automation of practice via HIT, as described in CMOc F4, because this technology was not available at sites, although our findings regarding information on bed boards being variable or incomplete reported in Chapter 6 does support the theory that updating such displays is a competing priority with other responsibilities.
| CMO | Context | Mechanism | Outcome | |
|---|---|---|---|---|
| Intervention | Staff response | |||
| F1a | Where staff understand (through experience, education or feedback) how and why falls prevention practices reduce falls risk and incidents. | MFRA tools are located visibly and intuitively in the EHR or are embedded clearly within ward practice and offer a structure to guide identification of fall risk factors. However, assessment tools vary in type and number of assessment items. | Reminder: tool draws staff attention to the tasks required, for example, completing an assessment of individual falls risk factors and prompts action. | More consistent documentation and delivery of falls risk assessments but content of assessment may differ depending on tool used by service. |
| F1b | Experienced nurses assess patients immediate care needs on admission to the ward and undertake a dynamic and ongoing assessment throughout their stay but also have time to use the EHR during their shift, when wards are staffed sufficiently. |
MFRA tools are located visibly and intuitively in the EHR or are embedded clearly within ward practice and offer a structure to guide identification of fall risk factors. However, assessment tools vary in type and number of assessment items. | Reminder: tools are completed retrospectively where they draw staff attention to risk items that they may have forgotten in the immediate patient assessment. | Patients receive falls risk assessment that covers the risk factors included in the tool. |
| F2 | Documentation is deeply ingrained in nursing practice, but nurses have multiple assessments to complete that are a competing priority with direct patient care, particularly where staff numbers are not sufficient to address dependency levels on the ward. | MFRA tools are located visibly and intuitively in the EHR or are embedded within ward practice. Items/prompts in assessment vary across organisations. | Prioritisation: nurses prioritise care delivery and undertake dynamic, ongoing assessment of patient risk factors to support allocation of limited resources. Documentation completed retrospectively. | Nurses work to deliver care and provide safety for patients. EHR tools can be reduced to a tick-box exercise that is, they do not provide an accurate reflection of the care delivered and do not act as a practice prompt, but fulfil the documentation requirements of the organisation. |
| F3 | Staff who are educated and experienced in identifying and managing falls risks. | MFRA tools are visible to staff in their work routines and provide guidance for assessing risk and linking risk with interventions. | Clinical judgement: where tool guidance does not align with clinical judgement or resources available, staff provide care according to their own judgement. | Care may not be in line with tool recommendation, but action is taken to manage risks using ward resources. |
| F4 | IT systems support HIT function and staff are trained and experienced with use of HIT. Where staff understand (through experience, or education or feedback) how and why falls prevention practices reduce falls risk factors. |
MFRA tools are located visibly and intuitively in the EHR or are embedded clearly within ward practice. Care plans, poster and information leaflet automatically generated from software. | Automation: interventions to address falls risks automatically selected and documented in care plan and patient poster. Staff display poster at patient bedside and action care plan. | Reduced variation in development and documentation of care plan that links falls risks with appropriate interventions. Task load of clinical staff reduced. Falls prevention strategy more visible in poster at patient bedside. |
| Manual work: staff see manual work as competing priority with other responsibilities. | Display of poster may be disrupted by patient flow, for example, between beds and wards. | |||
| F5 | Supervision is a key part of ward falls prevention strategy. However, wards are often not staffed to capacity and a high proportion of ward population have cognitive impairment and/or require assistance to mobilise safely. | MFRA tools are located visibly and intuitively in the EHR or are embedded within ward practice and are used alongside tools that support decision-making regarding use of supervision. | Stratification: nurses assess individual risk factors but also categorise patients as high risk to allocate supervision as a key strategy to prevent falls in the ward population. | Staff numbers are not always sufficient to deliver the level of supervision required. Technologies, such as falls sensors used to alert staff to high-risk patients, do not always work effectively. Creates an environment of high pressure for nurses with competing priorities. |
Chapter 8 Patient participation
Introduction
This chapter describes the testing and refinement of the patient participation theory, first using empirical studies identified through the realist review and then through the multisite case study. The original CMOc was as follows:
Where patients have the capacity to engage in the MFRA process (C), and a patient-centred approach is taken, e.g. where staff involve patients and carers in the assessment and care planning process, taking into consideration their needs and preferences, and communicate the strategy effectively to them, then patients will understand their strategy and have the confidence/reassurance to participate in specific interventions (M), thereby reducing their risk of falling (O).
Findings from the realist review
Number and range of included studies
Twenty-four manuscripts were included in CMOc testing34,38,63,129–149 (see Appendix 9, Table 27 for study details). Ten studies34,38,63,129,130,134,135,138,139,142 examined interventions that sought to engage patients in the assessment and/or care planning process to encourage their participation in falls prevention interventions. Five studies examined Fall TIPS. 34,38,63,129,146 Studies were conducted in the USA,34,38,63,129,130,132,133,135,136,139–142,144–146,149 Australia,131,134,147,148 the UK,143 Sweden137 and New Zealand. 138 As with testing the facilitation CMO, it was found that most empirical literature related to patient participation focused on nursing practice. Several studies describe interventions to involve carers, as well as patients, in falls prevention. 38,130,134
Eight studies were QI projects,38,130,131,133,135,139,142 which aimed to reduce falls incidences in single sites with interventions that promoted adherence to existing or novel falls prevention programmes. Nine studies used quantitative methods,34,63,129,134,136,137,144–146 three of which evaluated falls prevention practices, using randomised and non-randomised control trial designs. 63,129,134 Seven studies used qualitative methods to explore patient and professional experiences of falls prevention practices132,140,141,143,147,148 and Martin et al. 138 evaluated an intervention that promoted patient participation in falls prevention using realist (mixed) methods.
All studies except for Martin et al. 138 took place in acute hospitals, in a range of clinical areas such as medical-surgical units130,136 and oncology units,38,133,137,139 among others. The study by Martin et al. 138 took place within an older person’s health rehabilitation hospital; we included this study, despite its non-acute setting, because of its relevance to this CMOc, given that many of its findings about tailoring communication for patients with specific characteristics are transferable to acute settings (and pertinent to the implementation of MFRA and tailored interventions). Few studies explicitly discussed working with patients with cognitive differences, such as dementia and delirium, or of patients whose ability to communicate with staff was constrained by language differences. 130,131,133,135,145 Only Haines et al. 134 explicitly included both groups. The Fall TIPS intervention explicitly included patients with different languages, and implicitly included patients with cognitive impairment, given that the intervention was offered to all adult inpatients in participating units. 34,38,63,129,146 Patients with cognitive impairment or who did not speak the language of the country in which the intervention took place were specifically excluded from two intervention studies. 139,142 Martin et al. 138 excluded patients with moderate to severe cognitive impairment [defined as Montreal Cognitive Assessment (MoCA)16 > 23/30] or delirium (screened using 4AT17 and then MoCA) but included mildly cognitively impaired patients and those who were hard of hearing, and specifically addressed their capacity to engage in falls assessment and prevention, thereby providing valuable evidence. Studies reporting patient perspectives excluded patients with severe and moderate cognitive impairment or who could not communicate in the language of the country in which the research took place,132,136,137,140,143,144 but two136,143 included patients with mild cognitive impairment.
Interventions to promote patient participation in falls prevention
In the CMOc, we think of resources as what healthcare professionals offered to patients through their interactions, specifically that they (1) provided an opportunity for patients’ needs and preferences to be incorporated in decision-making about their care and (2) communicated their individual care plan effectively to patients. The interventions varied in content and form; they can be conceived, broadly, on a continuum from staff-directed initiatives, with patients taking a somewhat passive role, to practices in which patients take a more active role as partners in the falls prevention team, illustrated in Figure 8. Drawing on the patient-centred framework described by Kullberg et al.,137 the continuum moves from one-way information transfer to more or less passive patients, to two-way information exchange, in which patients and healthcare professionals contribute in partnership. In the studies reviewed, we identified interventions that incorporated approaches along the continuum and for different purposes. Below we describe these interventions, beginning with those that most closely reflect the CMOc.
FIGURE 8.
Patient involvement continuum.

Patient participation in assessment and care planning
Nine papers described interventions that explicitly sought to engage patients as active participants in the assessment, care planning, or care delivery process, including three which reported findings from the Fall TIPS study. 38,63,129,130,134,135,138,139,142 Authors explained that a reason for using this approach was that they had identified a mismatch between patients’ and professionals’ perspectives on falls risks. Radecki et al. 139 explained that the falls literature has consistently identified a discrepancy between professionals’ assessments and patients’ perceptions of falls risk, with patients’ values, beliefs and personal identities influencing their intention to participate in falls prevention strategies. Sitzer142 noted the following:
Although older patients may not perceive themselves to be at risk for falling while in the hospital, patients who sustained a fall while hospitalized wanted to know they were at risk, why they were at risk, and what they could do to prevent falling. (p. 46)
However, the author explained that falls prevention strategies rarely actively involve patients and that information provision ‘can be inconsistent and performed within silos’. 142 To engage patients as active participants in falls prevention, both Radecki et al. 139 and Sitzer142 implemented tools that enabled patients to self-assess their falls risks. In the latter study, for example, a computer-based, interactive patient care system (IPCS) was used, with the ability to administer an automated patient self-assessment of falls risk (SAFR). Patients could use this tool to answer questions about whether they possessed characteristics known to be associated with falling, for example, whether they had fallen in the past 12 months and whether they felt unsteady or used a cane or walker to walk, and to access falls prevention education. Nurses helped patients use the SAFR and assessed their responses. Similarly, Radecki et al. 139 used an intervention designed to engage patients as experts in their own care as ‘safety collaborators’ (p. 220); patients co-produced falls risk assessments and falls prevention plans with staff using a patient fall assessment tool (PFAT) administered within 24 hours of admission. The precise form of the tool was not specified, except to state that its design was informed by ‘a review of the literature for similar tools, processes, and education [and] an evaluation of the institution’s falls and contributing risk factors [ … ] to ensure local trends and needs were addressed’ (p. 221). Following assessment, nurses transcribed risk factors and the mutually agreed falls prevention plan onto a laminated board, which included an area to record patient-specific falls and injury risk factors, activity status, level of assistance needed for mobilisation, as well as safety equipment to be used during patient mobilisation. Through self-assessment, therefore, patients were provided with an opportunity to communicate their perspectives about their falls risk to ward staff, and to collaborate with staff to develop a care plan, which was then reinforced with a visual tool, the laminated board.
Martin et al. 138 reported a realist evaluation of the Safe Recovery Programme (SRP), which involved dedicated staff (a physiotherapist and a nurse, 1.4 FTE) and four retired nurse volunteers working with patients on one or more occasions to develop personalised goals to prevent falls. The study was undertaken to understand how the intervention, which had previously been implemented in Australia, worked as part of a pilot in four older persons’ rehabilitation wards in New Zealand. Rather than focusing on changing staff behaviours and ward risk-minimisation practices, the SRP incorporated patient-directed education and individualised goal setting, using a combination of video and written resources, alongside dyadic goal-setting discussions. It was hypothesised that the interventions would motivate patient participation in risk mitigation through enactment of personally determined falls prevention strategies. Patients were also encouraged to proactively seek help from staff, who received training to provide positive reinforcement. These ideas closely mirror the CMOc – that patient participation is achieved by personalising the assessment and care planning process through consideration of individual needs and preferences.
Other studies described different ways in which patients were encouraged to participate. Bargmann and Brundrett,130 for example, described a multicomponent falls prevention programme that took place after an analysis of falls suggested patients lacked understanding of their falls risk and corresponding prevention measures. A novel falls prevention strategy was introduced that included daily patient education on factors contributing to patients’ falls risks; an educational handout on falls risk factors, which included the patient’s John Hopkins Falls Assessment Tool (JHFAT) and key falls safety education points; and a patient falls safety agreement. The falls safety agreement stated that the patient had been educated on falls risk prevention strategies, acknowledged falling could cause serious injuries, and agreed to ask for help to prevent falls. Staff were encouraged to educate family members, especially if patients were unable to receive education on arrival. Rather than an explicit emphasis on patients’ preferences, the focus was on educating patients so they understood their falls risks and interventions and confirmed their agreement to actively participate in the strategy.
Haines et al. 134 also used education to involve patients and carers in falls prevention practices. They reported a RCT of a falls education programme for older patients in acute and subacute wards in two Australian hospitals. A motivation in conducting the trial was to examine whether the intervention was effective for patients with a cognitive impairment. The intervention used written and video-based materials to communicate falls prevention strategies to patients, covering information such as cause, frequency, and outcomes of falls and encouraging self-reflection on individual risk, problem area identification, development of preventive strategies and behaviours, goal setting, and goal review. Two approaches were tested in the trial: one in which patients were provided only with the educational materials to work through on their own, while in the other, complete programme, materials were supplemented by one or more follow-ups with a physiotherapist at the patient’s bedside.
Fall TIPS, described in Chapter 7, was developed, over time, to be more patient-centred. 38 For example, the tool was revised when a case-control study suggested the reason some patients still fell was their non-adherence to their falls prevention plan. As a result, patients in the revised scheme were not only informed about their plan through the posters and handouts generated as part of the intervention, but were involved from the outset, with their families and carers, as partners with staff in all three steps of falls prevention: (1) conducting falls risk assessments; (2) developing a tailored falls prevention plan; and (3) implementing the falls prevention plan consistently. The Fall TIPS studies did not describe how patients and carers interacted with staff during these processes to share their needs and preferences, but Dykes et al. 129 explained their rationale that patients’ involvement would make them more likely to believe they were at risk of falling and therefore more likely to follow their prevention plan. This approach to inclusion was found to be particularly important for younger patients, who often did not believe they were at risk of falling, especially if they were independent at home. Therefore, involving patients in the falls risk assessment and care planning process was intended to support their understanding and acceptance of their own falls risks, which their participation in the prevention strategy aimed to reduce.
Interacting with patients in care delivery
Three studies discussed how patients’ needs were elicited as part of care delivery. 131,133,145 Cann and Gardner131 sought to change models of practice from ‘patient allocation’, where each nurse had an individual case load of patients and provided exclusive care to that group with little collaboration from other nursing staff, to a ‘practice partnership’ model that included four main components: working in partnership; clinical handover at the bedside; comfort rounds; and environmental modifications. The comfort round element of the model was particularly relevant to the CMOc. Such rounds, also known as intentional, purposeful, or hourly rounding, involve healthcare staff (often nurses and HCAs) intentionally checking on patients at regular intervals to ensure their needs are being met. Cann and Gardner131 noted they enabled patients to participate more fully in their own care, giving them a greater sense of control and enhanced satisfaction.
Similarly, in the QI study by Goldsack et al.,133 hourly rounding was undertaken on an adult medical stroke unit and a haematology/oncology unit. The intention was to decrease call-bell usage, by ‘engaging patients as active partners in fall prevention where possible’ and ‘establishing a culture of accountability to the strategy and staff buy-in’ (p. 26). Rounding was to be conducted every hour between 600 and 2200 hours and every 2 hours between 2200 and 600 hours. It was performed by nurses and patient care technicians in the stroke unit, and nurses only in the oncology unit. The protocol for rounding included specific questions that offered opportunities to elicit patient needs and preferences in the care process, especially the question ‘What else can I do for you before I leave? I have time’ (p. 27).
In addition to Cann and Gardner131 and Goldsack et al.,133 a descriptive, cross-sectional survey by Zadvinskis et al. 145 explored three areas: (1) work engagement, which they defined as the ‘dedicated, absorbing, vigorous nursing practice that emerges from settings of autonomy and trust and results in safer, cost-effective patient outcomes’; (2) intentional rounding; and (3) bedside shift reporting, which involved face-to-face interaction between nurses to transfer information, authority, and responsibility during transitions in care at the patient bedside. However, the paper included no information about what form rounding took, how (and whether) nurses interacted with patients during rounds, and whether they asked about their needs and preferences.
Visual communication and reinforcement
Five studies described use of visual tools to communicate and reinforce individual falls risks and prevention strategies. 38,63,129,138,139 For example, alongside dyadic goal setting as part of the SRP, Martin et al. 138 described use of posters that highlighted key SRP messages (i.e. know when you need help, ask for help, and wait for help) as well as recording individual goals. Posters were a key component of Fall TIPS, used to reinforce communication of individualised falls prevention strategies and goals. 38 Colour-coded ‘patient-friendly’38 icons were used, together with plain-text language (English and Spanish, the main languages in this context) at a basic, consumer level of literacy. These features were designed to make the outputs as accessible as possible to a wide range of patients, such as those with mild cognitive impairments, who may find it easier to understand icons, and non-English speaking patients.
Similarly, the PFAT tool reported by Radecki et al. 139 had a simple, easy-to-read format (Microsoft Word Flesch Reading Ease 84.7/100 and Flesch Kincaid Grade Level 3.7). The authors theorised that (as in Fall TIPS) the presence of a clearly visible, icon-based wall poster and other environmental cues – for example, call-bell in place – would remind patients to ask for help and to stop and think before moving.
Outcomes
Falls rates
There is some evidence that falls rates declined following implementation of the interventions described38,63,112,129,130,133–135,139 (see Appendix 10, Table 28 for a summary of study outcomes). This was the case in three randomised trials,63,129,134 although falls rates only declined among cognitively intact patients who received the complete programme in the trial reported by Haines et al. 134 Likewise, Dykes et al. 38 reported rates declining in only one of the two participating hospitals; rates declined in one unit only in the studies reported by Goldsack et al.;133 in Radecki et al. 139 falls rates declined only in units that had a higher baseline rate of falls. In other studies, the rate of falls did not change significantly overall,131 and in some it increased postimplementation145 or increased in certain contexts. For example, Dykes et al. 38 reported an increase in the rate of falls in one participating hospital (but not whether this was significant); Radecki et al. 139 reported an increase in a unit that had a lower baseline rate of falls; and Haines et al. 134 reported an increase in falls rates among cognitively impaired patients who received the complete programme.
Patient knowledge and participation
Nine studies38,63,129,130,134,135,138,139,142 examined interventions that sought to engage patients in the assessment and/or care planning process and communicate falls prevention strategies to them via posters, boards and signs;38,63,129,135,138,139 educational handouts;130 educational videos and multimedia materials;134,142 and patient education sessions. 134,138 However, studies varied in the amount and type of data presented to evidence patient knowledge and participation (see Appendix 10, Table 28). Dykes et al. 129 provided some evidence that patient understanding improved postintervention of Fall TIPS. They undertook a three-question audit including the following: (1) Is the Fall TIPS poster updated with the correct patient information? (2) Can the patient/family express their fall risk factors? and (3) Can the patient/family express their fall-prevention plan? A mean rate of compliance with the audit was reported as 86% in one site and 95% in the remaining two sites but no further detail was provided.
In the study by Radecki et al.,139 patients completed a knowledge-in-action survey at baseline and postintervention in which they reported if they (1) knew they were a falls risk; (2) knew their own risk factors; (3) were involved in plan development; (4) knew how to prevent falls; and (5) always followed the falls prevention plan. Responses to question (3) (involvement in care planning) showed statistically significant improvements between baseline and intervention groups (p = 0.0007). However, there was no significant difference pre- to postintervention in any of the other questions. These findings suggest that even when patients perceive themselves as being involved as a partner in the care planning process, a disconnect may remain between falls prevention planning and patients identifying themselves as at risk of falling and going on to participate in falls prevention strategies. Martin et al. 138 conducted patient surveys to explore beliefs about falls risk and prevention strategies and experiences of intervention implementation. Survey results showed that, despite the goal setting process and patient-directed education, patients had variable awareness of their own risk of falling while in hospital: 56% disagreed to some extent that they were at risk of falling and 57% tended to not be concerned about their risk of falling while in hospital.
Haines et al. 134 did not measure patient knowledge or participation, but they did report the type of goals documented by patients to help prevent falls. In the complete programme group (the intervention most closely aligned with the CMOc), in which educational materials and one-to-one follow-up with a physiotherapist were provided, significant reductions in falls incidents were reported among cognitively intact patients. The most common goal related to asking for help, followed by identifying environmental hazards, using walking aids or other aids, waiting for help after it had been asked for, wearing safe footwear or clothing, and doing more exercise to get stronger and better balance. These goals were grouped as working more effectively with healthcare staff, identifying environmental hazards, and using appropriate aids and equipment. The realist evaluation by Martin et al.,138 in which patients participated in dyadic goal setting, also provided details about patient goals, which were similar to those set by patients in the study by Haines et al. 134 The most common goals set by patients in Martin et al. 138 were using call-bells (19%); planning out tasks (10%); and not rushing (10%).
How, why and in what contexts does patient participation work?
From interview and focus group data collected as part of Martin et al. ’s138 realist evaluation, they elucidated four mechanisms underpinning why patients may participate in interventions:
-
Gaining permission: where ward staff explained ward systems to patients and made it clear that they could call for help and assistance when needed.
-
Increased awareness of risk: if staff made patients aware of the risk of falling via personalised conversations, patients were more likely to draw on relevant strategies to keep themselves safe.
-
Empowerment to act: where goals were aligned with patient values, they were more likely to act in their own interests to keep themselves safe.
-
Reminders: environmental cues prompted patients to ask for help and plan activities.
The findings from this study provide insight into how messaging works, for example, in discussion of increased awareness of risk, Martin et al. noted the importance of creating an ‘interactional space in which patients could integrate new knowledge into their existing beliefs’ (p. 266). The educators and volunteers involved in intervention delivery emphasised that creating such a space required time to establish rapport, to engage with and motivate patients, and personalise interactions. ‘Taking time’ was said to promote learning and changes in beliefs around falls risk and the authors reported that the goals developed in these conversations appeared to be most effective at creating behavioural change. A fifth mechanism was also reported by Martin et al.: the continuous prioritisation of falls prevention messaging by ward staff. This was where feedback from the educators and visual reminders, such as posters, reinforced the amount and consistency of messaging provided to patients by staff.
Martin et al. 138 reported that the volunteers in their study, as well as being retired nurses, were a similar age to some patients and, using their skills of listening, teaching and reflecting, created ‘engaging, personalised and safe interactional spaces’. Through this, they were able to ‘draw out’ patients to talk about some issues in more depth. Therefore, to provide the type of interaction that engages patients in conversations that lead to participation in falls prevention may be dependent on the skills of the assessor and their ability to create interactional rather than task-focused spaces. Radecki et al. 139 pointed to similar qualities. They explained that units that demonstrated improvement in falls rates had a higher percentage of experienced nurses (defined as more than 2 years’ experience) and discussed that this may have influenced the outcome (although there was a ceiling effect in one unit under study that had a baseline measure of no falls incidents). Radecki et al. 139 elaborated that nurses with less experience may be in ‘task mode’ meaning that they view the intervention as a task rather than a process through which communication and partnership with the patient is enhanced.
Bargmann and Brundrett130 reported a reduced falls rate following implementation of their falls prevention bundle and patient safety agreement. A key component of the intervention was education for professionals to support implementation of the intervention as intended. Compliance in using the intervention was measured and, after the initial audit, staff incentives (contributions to purchase snacks) were introduced to increase compliance towards a target of 90%. Following the incentive programme, adherence with bed alarms and the fall safety agreement rose to 89% after 3 months. The programme was said to have improved the culture of safety on the unit, which in turn supported an increase to 95% of patients correctly stating their fall risk.
Patient perceptions, attitudes, beliefs and capabilities
In Martin et al. ’s138 study, the content of messaging (and how mechanisms worked) was influenced by patient circumstances that can be grouped broadly as follows: (1) patients new to the ward; (2) patients without a history of falls incidents; (3) patient negotiating a new or changing self-concept; and (4) patients with mild memory impairment or who were cognitively overwhelmed. Data presented in other studies supported findings from Martin et al. suggesting patients’ perception of their falls risk do not always align with their assessed risk. 136,140,143,144,147,148 For example, in an interview study conducted by Radecki et al.,140 patients who believed they were at risk of falling had physical limitations that clearly put them at risk. In comparison, falls risk factors such as medication changes or post-ICU weakness ‘may not be tangible or “real” for the patient’ (p. 117) and consequently not be accepted or acted upon. The challenge here, then, is not just communicating non-physical risk factors to patients but doing so in a way that leads to patient acceptance of those risk factors and subsequent behavioural change to help avoid falls, as described by Martin et al. 138 in the ‘increased awareness of risk’ mechanism.
A recent fall or fear of falling were reported to influence patient acceptance and participation in falls prevention. For example, Kiyoshi-Teo et al. 136 noted that a fall within the past 3 months and an injurious fall within the past year were associated with increased falls prevention action by patients but less confidence in their ability to prevent a fall. Martin et al. 138 noted patients who had experienced a fall recently explicitly linked ‘keeping yourself safe’ messages to this experience.
In Turner et al.’s143 interview study, loss of balance during functional activities, such as walking, standing up from the toilet, or washing/dressing, was reported as the main reason why participants fell. Participants who fell had performed these activities alone as they felt safe enough to do so – four out of the five participants were independently mobile (with aids) prior to admission and before falling, so requiring assistance represented a substantial change in their needs. Rush et al. 141 discussed ‘a tension between safety and risk taking’ related to a desire for independence, which clouded patients’ perception of their falls risk and the need to communicate for help. Similarly, Twibell et al. 144 surveyed 158 patients to understand their intention to follow falls prevention advice. They identified a link between self-efficacy and incentive to act and suggested intention to engage in a behaviour does not necessarily lead to actual engagement in falls prevention plans. For example, patients may report an intention to ask for help but, if help is not quickly available, patients who are confident and unafraid may perform high-risk behaviours. Turner et al. 143 found some patients had in fact requested assistance from staff but did not – or could not (out of an urgent need for the toilet) – wait for help to arrive.
This was discussed in other studies also. 132,140 For example, needing the toilet combined with loss of balance or unexpected weakness was the main cause of falls reported in the interview study by Carroll et al. 132 They described patients encountering emotional and physical obstacles to using strategies to address this cause of falls, such as using the call-bell, for example, patients might feel they were burdening busy staff by calling for help. Carroll et al. 132 supported clear messaging that nurses do not mind being disturbed by call-bells even if they appear busy and that they want to help. This is like the messaging described by Martin et al. 138 that triggered the mechanism, ‘gaining permission’. Martin et al. 138 suggested that spoken and unspoken ‘rules’ within ward systems need to be made explicit to patients new to wards or feeling overwhelmed so they feel they have permission to request assistance when needed. The physical obstacles reported by Carroll et al. 132 related to things such as positioning and access to call-bells. They explained: ‘one participant was provided her call light but on the side where she had weakness, so she was unable to put her call light on when she needed assistance’ (p. 4).
Patients with cognitive impairment
Older inpatients with cognitive impairments are more likely to sustain serious injury after a fall. 150,151 However, only seven studies explicitly included patients with cognitive impairment, three of which reported the inclusion of patients with mild impairment. 38,63,129,134,136,138,143 Some detail was provided about how interventions were designed to support comprehension for patients with differing cognitive abilities, such as colour-coded ‘patient-friendly’ (p. 404) icons used in Fall TIPS. 37 The fourth patient mechanism described by Martin et al. 138 is reminders, that is, where posters are displayed for patients, call-bells are in place, and coloured tags are used on frames, patients will remember to participate in strategies to keep themselves safe from falls. These visual cues are likely to be useful for all patients, but the above authors note that reminders may be particularly useful for patients with mild cognitive impairment or those feeling cognitively overwhelmed.
In terms of impact, in the RCT by Haines et al.,136 patients with cognitive impairment who received multimedia falls prevention education experienced a significantly higher rate of injurious falls per 1000 patient-days than those in the control group (7.49 vs. 2.89) when they were supported by staff to review the educational materials and set their own falls prevention goals. The authors stated that cognitive impairment may have constrained patients’ ability to adhere to safety plans, as well as making them more willing to report injuries from falls. They did not specify how cognitively impaired patients were supported by staff to understand and follow safety plans.
Knowing the patient as safe
Rush et al. 141 conducted focus groups with nurses to understand their experiences with inpatient falls. Their findings demonstrated that nurses use strategies to gather information themselves or through colleagues or carers to achieve a sense of ‘knowing the patient as safe’ (p. 359): an ‘ongoing affirmation’141 that the patient was free from harm. The key strategies described by nurses in the study were as follows: (1) risk assessment within routine practice; (2) monitoring, in which nurses checked on patients and their environments; and (3) communicating, examples of which emphasised the individualising of messages for patients as previously discussed.
The success of these strategies was variable. Assessment tools were not perceived as providing an accurate judgement of falls risk consistently for nurses to rely on, and monitoring was influenced by a combination of patients’ distance from nurses’ stations and staffing levels. For example, patient proximity enabled nurses to better see and hear patients and know they were safe, while low staffing levels constrained nurse vigilance when making rounds and the direct contact needed to know patients were safe. Two-way communication was important. Therefore, alongside staff communicating information to patients, patients and families communicating a need for help to nurses was also emphasised. The success of communication could be constrained by patients who desired independence or did not want to disturb nurses and timing of communication. When a patient called for help but nurses could not be reached or were unavailable, patients did not have information to make decisions about their course of action and nurses were also unaware of changes in their status. When strategies failed to provide nurses with knowledge of their patients as safe and patients fell, this created considerable stress for nurses and prompted them to use a range of coping strategies, one of which was denial: nurses could not accept ownership for a fall when they perceived it was the result of a patient’s omission or action.
Rush et al. 141 concluded that ‘the critical, often taken for granted, activities used by nurses’ in knowing the patient as safe had the potential to resolve the tension between patient safety and independence. However, this knowing must be expanded to include the meaning falls have for patients and attend to factors beyond nurses’ control such as environmental redesign and staffing.
Theory refinement
The mechanism in the original CMOc, taking patients’ needs and preferences into account in care plan development and communicating the prevention plan to the patient triggered their participation in the plan and reduced their risk of falling, in contexts where patients had capacity to engage in assessment and care planning. The studies provided greater detail about how and why this type of intervention may work and the contexts that influence impact.
Thinking about outcomes, in the first instance, the studies helped us build explanations in two areas: (1) how and why patients participate in falls prevention activities as an end-point; and (2) how patient participation may contribute to reducing incidents of falls as the overall aim of falls prevention strategies. For example, patients may participate in falls prevention by using call-bells (an impact in itself) in response to interventions, but if staff do not respond to their requests for help, they may attempt to mobilise on their own, particularly where there is a sense of urgency (e.g. for the toilet), creating a falls risk and potentially leading to falls.
In terms of mechanisms of patient participation, we focused on patient responses and what influences these responses. In summary, patients can experience emotional and physical barriers to participation. For example, they may be reluctant to use call-bells for fear of disturbing busy nurses or may not accept they are at risk of falling if they are not obviously limited physically. For these reasons, rather than staff simply considering needs and preferences in general, as stated in the original CMOc, the studies suggest that messages in the assessment, care planning, and intervention process need to be individualised to the emotional barriers experienced by patients to trigger mechanisms, such as gaining permission and acceptance of falls risk. We grouped these as empowering patients, for example, generating knowledge or confidence to participate in strategies to keep them safe. The idea that these types of interventions are more likely to be successful with patients without severe cognitive impairment was supported to a certain extent, with the question remaining of how can falls prevention strategies be delivered to patients with differing levels of cognitive impairment in a patient-centred way? A further influence on patient participation suggested in the studies was the type or quality of interaction between professional and patient, with risk assessment and care planning being seen not as a ‘task’ but as a vehicle to enhance communication, an attitude that may come with experience as staff become familiar with the process.
Finally, partnerships between professionals and patients/carers have the potential to impact on falls risks. Given sufficient resources, staff can be responsive to patients’ requests for help and can keep patients informed about any changes to their care plans or falls risks, ensuring that patients are not forced to engage in risky behaviour, thereby reducing their likelihood of falling.
Based on the data, Table 19 presents refinements to the initial CMOc, with the addition of new CMOcs. The evidence supporting the claims of the CMOcs and GRADE-CERQual assessment of the evidence are presented in Appendix 8, Table 26.
| CMO | Context | Mechanism | Outcome | |
|---|---|---|---|---|
| Resource | Response | |||
| P1 | Patients with capacity have different perspectives and circumstances that may influence if/how they participate in falls prevention strategies in hospital. Staff have the time and skills to create interactional rather than task-focused spaces for assessment and care planning. |
Staff individualise falls prevention messages for patients, that is, that account for their circumstances and perspectives. | Patient empowerment: patients are empowered (increased confidence to ask for help, knowledge about their falls prevention strategy, acceptance of their falls risks) to participate in appropriate strategies. | Patients participate in interventions such as using the call-bell and avoid taking risks. |
| P2 | If staff are not responsive to patients’ requests for help mobilising or performing functional tasks, for example, due to task load/awareness. | Staff individualise goal setting and falls prevention messages to the patient, that is, that account for their circumstances and perspectives. | Taking risks: patients are confident they can, or feel urgency to, mobilise by themselves, for example, to get to the toilet. | Patient at risk of falling, particularly if hurrying. |
| P3 | Patients with cognitive impairment have falls risk factors like other patients but additionally may have problems with memory, attention and confusion. | Staff individualise falls prevention messages to patient that is, that address their emotional barriers to participation. | Taking risks: patients may struggle to understand or retain information and are unable to communicate needs unambiguously to staff, despite messaging. | Patients take actions that may lead to a fall. |
| P4 | Patients with cognitive impairment have falls risk factors like other patients but additionally may have problems with memory, attention and confusion. | Staff undertake ongoing assessment of risk and monitoring of patient. | Knowing the patient is safe: staff collate the information necessary to understand if the patient is safe from harm. | Staff intervene in behaviour that may lead to a fall. |
Findings from the multisite case study
Interventions in which patients were encouraged to participate
Within the case sites, the interventions in which we observed patients participating included using the call-bell to ask for help when mobilising; wearing non-slip socks; wearing the correct glasses or hearing aids (if needed) and using mobility devices, such as walking sticks or frames; engaging in physiotherapy and rehabilitation; and taking time to get up/walking carefully (especially important for patients with postural hypotension). Other interventions, such as bed and chair alarms and sensors that alerted when a patient got up, did not require active patient participation.
Use of interventions differed across wards, depending on patient need and condition. For example, bed-bound patients recovering from surgery on orthopaedic wards might at first be unable to undertake physiotherapy and might rely heavily on using call-bells to obtain assistance from staff.
Interactions to encourage patient participation
Context mechanism outcome configuration P1 hypothesised that patient participation would be realised where ward staff created ‘interactional spaces’ that enabled falls prevention messages to be tailored to patient circumstances, addressing constraints to their participation. Although, as noted in Chapter 7, nurses’ capacity to create such spaces to share falls prevention messages was limited by the dynamic and implicit nature of falls risk assessments and care planning and by competing priorities on their time, staff emphasised the importance of ‘getting to know’ patients so that they could communicate and frame information in ways more likely to be accepted by and, perhaps, acted on by patients.
On the wards studied, large proportions of patients experienced some level of cognitive impairment, and some of these patients could struggle to understand or retain the meaning of direct or explicit messaging, such as instructions to wait for assistance before mobilising (the situation was complex, as cognitive impairments are experienced differently by different people at different times). However, staff told us that even acutely impaired patients might be able to understand the implicit dimensions of messages, such as whether a staff member really wanted to help them, and might respond to such messaging in ways that supported their safe care. In other words, the quality of the communication could constitute a form of messaging that triggered a degree of participation. For example, a cognitively impaired patient who could not understand they needed to wait for assistance before walking might be soothed when being supported to walk by a staff member they trusted, and potentially less likely to fall owing to agitated behaviour. We observed these kinds of interaction many times on the wards between patients, nurses, HCAs, and other staff, even though nurses were not always resourced to spend time with patients in the way the CMOc suggests.
Notwithstanding the importance of implicit messaging, many cognitively impaired patients were perceived by staff to be unable to participate fully in keeping themselves safe and thus required supervision to prevent them from falling. To support them in this, staff explained it was important to understand their behaviour. Wandering, for example, where patients became restless and walked the corridors, was also referred to as ‘walking with purpose’ because it tended to have underlying meaning for the person. If staff understood such behaviour, it could inform their care, for example, if they knew that a patient tended to be particularly active in the morning, they would provide supervision at that time, but perhaps not at other times. In other words, getting to know patients, understanding their perspectives and behaviours was recognised as a mechanism to inform messaging (where appropriate) and care delivery.
In comparison to messaging about patient-specific, tailored interventions, all patients in all sites were supposed to have access to call-bells to request assistance if needed. A nurse in Site 3 explained that patients were able to discern whether staff were sincere when they encouraged them to use call-bells and alert to conflicting messages, which might be conveyed implicitly through facial expression or tone of voice, reflecting the point made above about the impact of implicit messaging, this time for all patients and not only those with a cognitive impairment. Therefore, to generate patient assurance (or permission), this nurse emphasised to colleagues the need to convey an attitude of wanting to help to all patients on a shift-by-shift basis.
Nurses often explained they had limited time to get to know patients. For this reason, they sometimes relied on other staff to pass on information that could inform messaging and care delivery, such as HCAs. Some wards, namely the orthopaedic and older person/complex care wards at Site 3 and the orthopaedic ward at Site 2, employed staff with a specific remit for patient engagement, known as engagement support staff (Site 3) or activity co-ordinators (Site 2), who spent time with patients, chatting, reading to them, playing games, or encouraging them to engage in crafts. A nurse at Site 2 explained that the activity co-ordinator could encourage patients to participate in keeping themselves safe and could also pass information to the nursing team. Such information was shared either verbally or by completing documentation about patients’ individual needs (e.g. safe mobilisation needs). All three Trusts had such documentation, which was called ‘This is Me’ at Site 1, ‘Getting to Know Me’ at Site 2 and ‘See Who I Am’ at Site 3. Similar support from engagement support workers was observed at Site 3.
Physiotherapists and OTs also had time to interact with patients during therapy sessions and emphasised the need for two-way communication: ‘Making sure that [patients] understand what we’re doing and why and try and get someone on board with that and look at different ways around it’ (Physiotherapist, orthopaedic ward, Site 1). During fieldwork we observed physiotherapists attempting to encourage patients to participate in therapy (and thereby decrease their risk of falling), using different strategies if patients were not inclined to engage, for example, offering the patient a cup of tea and biscuit after the session. A pharmacist also highlighted the importance of ‘having patients [as] part of the conversation’, exploring medication options with them to find the best solutions to their needs and concluding: ‘I think it makes for a better, longer lasting position with patients and it gets them bought into what you’re trying to do’ (Pharmacist, orthopaedic ward, Site 3).
‘Knowing the patient is safe’
For patients with a cognitive impairment, CMOc P4 hypothesised that the nursing practice of knowing the patient is safe, rather than tailored messaging, would work to modify falls risk factors. The practice of knowing the patient is safe consisted of collating information via formal assessment, monitoring, and communication. These practices were enacted for all patients but, for some patients with cognitive impairments, could be done in a way that negated the need for their active participation in response to explicit messaging, for example, in relation to using the call-bell to ask for support.
Patients with cognitive impairment were often placed in cohort bays in Sites 1 and 2 or received one-to-one care. At Site 3, the layout of both wards made it difficult to establish a cohort bay as such, but staff told us they tried to group at-risk patients in more visible beds near to nurses’ stations, and sometimes patients were seated in the doorways to their rooms, with a tray-table in front of them, so that staff could monitor them more easily. Even where bays were conducive for cohorting, staff described challenges of using this strategy to know patients were safe. For example, other patients on a cohort bay might be at risk while the staff member on the bay was busy with one patient behind the curtains, and there were insufficient resources to provide more staff to monitor patients while this work was being done. Staff also talked about how monitoring patients on a cohort bay could be both stressful and boring, leading to staff ‘tuning out’ to a degree if they were there for a long time, and therefore becoming less vigilant. Similarly, they reported being tempted, sometimes, to leave the bay briefly to help colleagues, especially when patients appeared to be settled, or if they were asked directly to help others.
Intentional rounding (sometimes called comfort rounds or care and communication rounding), where staff checked on patients at regular intervals, was also used. A care worker on the Site 1 orthopaedic ward explained that during these 2- or 4-hourly rounds, they asked patients how they were, if they needed any help going to the toilet and checked call-bells were in reach, thereby helping them to participate in call-bell and toileting-related interventions. Staff talked about how a proactive approach can prevent patients from getting up without the required assistance, although the tension between preventing patients from falling and preventing deconditioning was acknowledged, as this quote from a Site 1 organisational-level interviewee describes:
One of the things we’ve done in the past year or so is to bring about a continence promotion team because we know that good management of continence will prevent falls. This is about some of this proactive questioning as part of rounding about do you need the toilet? Is there anything else that you need that I can get for you? So we’re pre-empting patient’s care needs before they almost even know that they need it. So you lessen their demand for needing to get up and about. Conversely, we should be encouraging our patients to get up and about and mobilise because we don’t want them to decondition, we don’t want them to if they’re a bit of a falls risk. It’s a bit of a dichotomy really in terms of what we can promote and how strong we can promote it without adversely affecting other harms.
The role of families and carers
During observations, the support provided by families and carers was disrupted due to COVID-19 because visiting was restricted and families and carers experienced difficulties contacting busy staff by telephone. However, data collection revealed that families, carers and visitors could play an important role in encouraging loved ones to participate and passing information to staff that could help them understand patients’ circumstances and behaviour. This was particularly important for those patients with cognitive impairments, who were unable to give staff such information themselves. A nurse in the Site 2 orthopaedic ward provided an example of speaking with family members about a patient with cognitive impairment who told the nurse the patient drank coffee every morning and not tea, enabling staff to understand why the patient was trying to get up (to find another drink). Speaking to family members to understand patient behaviour enabled ward staff to reduce the likelihood of patients taking actions that would increase their risk of falling, without the need for patient-directed messaging.
Additionally, carers could be a valuable source of support and information for patients with capacity, when, for example, they did not feel well enough to talk or when a personal or emotional issue made them reluctant to talk. For example, a carer in Site 1, whose mother experienced a fall in a toilet on the ward, thought that she had fallen while trying to remove her incontinence pants alone. The carer explained ‘my mum would never say to anybody: “I need help getting my incontinence pants off”’ through embarrassment, which suggests that, where staff are not able to create interactional spaces to enable patients to reveal sensitive issues, this may put them at risk due to embarrassment or other factors. In the above example, the carer also explained that her mother had difficulty understanding what staff were saying to her when they spoke with an accent, but she did not want to say this for fear of appearing critical. However, the carer said that, if asked, she would have been able to correct any misconceptions that had arisen between staff and her mother.
Carers also provided additional supervision for patients, supporting ward staff, watching out not just for their own loved ones, but also others on the same bay. For example, at a weekend observation on a falls cohort bay on the orthopaedic ward at Site 2, visitors were present for two of the three patients, all of whom had cognitive impairments. The visitors interacted with their loved ones in various ways: one visitor gave her relative a shave and helped him to eat, another showed her relative some photographs and joked with him. Put simply, alongside aiding staff in supervision, they took on jobs that would otherwise fall to staff, such as personal care. The visitors also interacted with the patient with no visitors, which he seemed to appreciate. The patient sat calmly in his chair while they were there, whistling and chatting, and did not attempt to mobilise unsafely.
In terms of the impact of restricted visiting during the COVID-19 pandemic, staff discussed the demotivating effect on patients of not having visitors, as well as the loss of information to themselves and added logistical challenges of contacting relatives and carers by telephone. They told us they missed this additional help, although some also said visitors caused extra work and felt that visiting restrictions had, in fact, taken some pressure off them. Towards the end of the observation period, however, visiting restrictions were eased.
Visual cues and reminders to patients
In addition to interactions to inform patient messaging and care delivery, the wards displayed a number of visual reminders of the main falls prevention messages to patients. For example, all wards had some variant of a ‘Call, Don’t Fall’ poster, displayed on bays, corridors, and in toilets and some had reminders about appropriate footwear. All sites had leaflets or videos with falls prevention advice for patients and their families, covering matters like using call-bells and appropriate walking aids, although patient awareness of their falls risks (see Patients as participants in falls prevention practices) raises questions about to what extent these were given to patients. We saw falls prevention display boards on wards, although it was not always clear to us whether these were directed at staff or patients (some may have been directed at both).
Visual aids were also used to remind patients who might struggle to understand written labels or instructions in English (e.g. icons to identify toilets or showers). Some wards used red-coloured Zimmer frames, which we were told were easier for patients with cognitive impairments to locate.
Patients as participants in falls prevention practices
To understand the extent to which patients participated in falls prevention interventions in response to staff interactions, we asked the patients we interviewed (all of whom had capacity) what they remembered about their falls risk assessment and falls prevention messages on admission to the ward. Across the three Trusts, 72% of patients/carers interviewed said they were not aware of having had a falls risk assessment, even though the record review of Trust EHR systems showed that such assessments were indeed taking place. Patient awareness of assessment varied between Trusts and wards, as did patient understanding of their own falls risks: some were very aware (often because they had fallen before or had a pre-existing condition that made falling more likely and had learnt through experience), while others appeared less well informed, making vague statements about feeling shaky or simply that they fell because they were ‘old’.
Patients frequently remembered being encouraged to use the call-bell and talked about seeing ward posters that reinforced this message to them. Some also remembered being encouraged to mobilise with appropriate footwear and walking aids, and recalled individualised messaging from physiotherapists, such as how to use a Zimmer frame, given their physical limitations or gait.
Patients talked about circumstances and perspectives likely to shape how they responded to, and acted on, the messaging directed at them by ward staff. They acknowledged receiving much information when they were admitted to hospital, which could be overwhelming, calling for clarity and conciseness, but on the other hand, they needed to feel respected: ‘You’ve got to be able to put it so that the person listening to you doesn’t think, “Oh for God’s sake. Obviously I know that”’ (Patient, orthopaedic ward, Site 2). Some also expressed the desire not to bother busy nurses.
Finally, we also saw patients helping each other to participate (e.g. telling staff a fellow patient needed help or comforting each other) or, sometimes, inhibiting participation by upsetting or agitating each other.
Patient experiences of participation
All patients were provided with, and advised to use, call-bells to request assistance when needed. CMOc P2 hypothesised that, where staff were not responsive to patients’ use of call-bells, they may take actions that increase their risk of falling, for example, trying to mobilise without the required assistance. Patients in all three sites described this experience and the wait time was especially distressing for those who needed the toilet urgently. A patient in Site 2 explained they did not want to take actions that increased their risk of falling, but sometimes felt they had to, to avoid making ‘a mess’. Another patient from Site 2 explained they had gone to the toilet by themself twice in the night before the interview, despite being aware that two people were supposed to accompany them, partly because they believed it would be difficult to obtain assistance from two busy staff members. Our observations captured similar experiences, for example, a bed-bound patient was observed repeatedly pressing the call-bell for help to go to the toilet on the Site 1 orthopaedic ward. This patient could not get out of bed unassisted, so was unable to risk mobilising on their own, but during the same observation another more mobile patient, who had earlier been assisted to the toilet by staff, took that risk. On this occasion, there was only a few moments’ delay between pressing the call-bell and a staff member arriving to help, but the patient had already rushed to the toilet alone, which illustrates the level of responsiveness sometimes needed to avoid patients taking actions that increase their risk of falling. Delayed staff responses to patients were observed on cohort bays also, when the staff member on the bay was busy with one patient at the same time as another needed help. Therefore, patients receive messaging about using call-bells (although nursing attitude in delivery may vary) but a key constraint on acting on this messaging is staff response time. Several patients commented that they thought staff ability to respond quickly to call-bells or to support other forms of participation was related to workload and short-staffing. Certainly, we saw occasions where a single HCA was trying to respond to the requests of several different patients on a bay, resulting in some patients having to wait.
However, when staff did have the time necessary to support patients, the impact of this was observed. For example, on the Site 1 older person/complex care ward, we observed a HCA supporting a patient to walk down the corridor with a Zimmer frame. The support worker asked the patient what they needed (whether they would like a wheelchair) and responded in a way that was attuned to their needs, both physically (i.e. walking behind the patient so they could support them if they started to fall) and emotionally (reassuring them that they had time). Similar examples of staff interacting in ways that encouraged patients to accept help were also captured. For example, a patient at Site 1, who had been ashamed to experience diarrhoea while bed-bound, described the ‘kindness’ and ‘consideration’ they experienced from the nurses, which helped them to feel more acceptable, which, in turn, involved accepting help.
Patients with cognitive impairment
Context mechanism outcome configuration P4 hypothesised that, where patients had difficulty understanding or retaining information or were unable to communicate their needs to staff, staff needed to perform practices not reliant on patient participation to help prevent falls. Patients with cognitive impairment could transition between periods of calm to agitation quickly and behaviours such as ‘walking with purpose’, or trying to leave the ward, were also observed and falls incidents were attributed to this. Staff told us that their behaviour could be affected by other contextual factors, too, such as length of stay, the extent to which they were able to spend time with familiar people, and the number of times they moved wards or beds.
Even where wards were staffed to provide supervision to all patients in need, other skills were needed to help calm cognitively impaired patients in moments of distress or agitation, such as speaking calmly, responding to them at their own level of understanding, and not contradicting them. For example, on the Site 2 orthopaedic ward, we observed a HCA talking to a patient who had stood up abruptly, saying they wanted to go home. Rather than telling the patient they could not go home, the HCA negotiated a better time to go there, repeating the conversation as needed. As a result, the patient was able to walk safely when they wanted but also accepted support from the staff members present. The need to remind patients, perhaps repeatedly, without becoming bored or irritated was observed as an important trait in caring for cognitively impaired patients. These findings reflect the importance of targeted, implicit messaging outlined in Interactions to encourage patient participation.
Theory refinement
The data collected in staff, patient and carer interviews and ethnographic observations enabled further refinements to be made to the patient participation CMOcs, outlined in Table 20. Specifically, CMOcs P1 and P2 have been refined to capture the specific contextual factors we observed – multiple patients requiring assistance and staffing levels; a strategy we observed nursing staff using, namely advising patients to use the call-bell; and the consequences of this. CMOc P3 is revised to show how sensitive communication can support patients to avoid taking risks of the kind described in the literature-based version of this CMOc. CMOc P4 is revised to reflect the strategy we observed of receiving information about patients from other staff, family and carers, supplementing assessment and monitoring. It becomes two CMOcs, reflecting the fact that this was a strategy used with both patients with cognitive impairments and patients without. CMOc P5 is added to capture the strategy of normalising patients’ experiences, generating more willingness to accept help.
| CMO | Context | Mechanism | Outcome | |
|---|---|---|---|---|
| Resource | Response | |||
| P1 | Patient population has high levels of dependency, with patients requiring assistance mobilising and to use the toilet. Ward is staffed sufficiently to be responsive to patients’ needs. | Staff advise all patients to use the call-bell each shift and consistently convey the attitude that they want the patient to call for help when needed and that they are happy to help. | Gaining permission: patients are reassured that staff want them to use the call-bell to request assistance and are attended in a timely way by staff when they do so. | Patients wait for assistance and do not attempt to move unassisted, reducing risk of falling. |
| P2 | Patient population has high levels of dependency, with patients requiring assistance mobilising and to use the toilet. Ward is not staffed sufficiently to deliver supervision. | Staff advise all patients to use the call-bell each shift and consistently convey the attitude that they want the patient to call for help when needed and they are happy to help. | Taking risks: patients are confident they can, or feel an urgency to, mobilise by themselves for example, to get to the toilet. | Patients at risk of falling, particularly if hurrying. |
| P3 | Patients with cognitive impairment may have problems with memory, attention, confusion, and may not be able to communicate effectively with ward staff. Furthermore, patients may become agitated quickly after periods of calm. | Staff with interactional skills, such as patience to repeat advice, engage with patients’ experience (even if not rooted in the reality of the situation) through authentic (and often implicit) communication, and do not contradict them. | Risk avoidance: patients can be reassured, distracted, and accept help if skills are used appropriately. | Patient does not take, or reduces, actions that increase their risk of falling or is supported/supervised when mobilising, reducing the risk of falls. |
| P4a | Patients with cognitive impairment may have problems with memory, attention, confusion, and may not be able to communicate effectively with ward staff. | Information about patient circumstances and perspective are collated from staff with remit to spend time ‘getting to know patients’ and from family and carers. | Tailoring of care delivery: ward staff understand patients’ behaviour and put measures in place to account for these circumstances, for example, making sure patients are supervised when they are likely to be restless. | Behaviours that increase the chance of falling are modified or patients are more closely observed so staff can intervene to mitigate such behaviours. |
| P4b | Patients may not feel comfortable disclosing sensitive information to unfamiliar ward staff. | Information about patient circumstances and perspectives are collated from staff with remit to spend time ‘getting to know patients’ and from family and carers. | Tailoring of care delivery: staff involved in direct care delivery are more fully informed of patients’ falls risk factors and can better support care needs to prevent falls. | Individual falls risk factors more comprehensively addressed in care delivery. |
| P5 | Patients require assistance in hospital for sensitive issues, such as toileting, that may not have been an issue at home. | Staff normalise patient condition through caring interactions, for example, showing patience and kindness. | Acceptance: patients feel comfortable and accept assistance provided. | Patients assisted as needed to reduce falls risk factors. |
Chapter 9 Discussion and conclusions
Revisiting the objectives
The study objectives were as follows:
-
to use secondary data to develop a programme theory that explains what supports and constrains routine use of MFRA and falls prevention interventions
-
to refine the programme theory through mixed method data collection across three acute hospital Trusts and
-
to translate the programme theory into guidance to support MFRA and prevention and, in turn, adherence to the NICE guideline.
Additionally, the study aimed to include the perspectives of patients and members of the public through involvement of lay people within the research team at all stages and through their regular evaluations of progress. We discuss these objectives below, summarising our findings and considering the strengths, limitations, and implications of our work. We also reflect on issues of ethnicity, diversity, and inclusion in our work. We conclude with implications for practice and recommendations for future research.
Using secondary data to develop a programme theory
Through our realist review, we developed an initial programme theory that explains what supports and constrains routine use of MFRA and falls prevention interventions, as presented in Chapter 4. Within the study, we were able to use secondary data to test two of the CMOcs that made up that programme theory, concerned with facilitation of MFRA and patient participation.
Analysis suggested that if tools are visible in staff workflow, they may facilitate implementation of MFRAs and tailored interventions by prompting completion of required tasks. 18,110,111,118,122 The literature also pointed to the complexity of care delivery, for example, in terms of patient acuity and limited resources, that may disrupt use of tool guidance and documentation of care processes. Automating practices via HIT appears a promising implementation support34,38,115 but may introduce additional training requirements to support technology use and additional manual tasks that may be seen as a competing priority on staff time. 109,120
The literature suggested patients’ circumstances should inform the messaging directed to them to enable them to participate in falls prevention interventions. 138,146–148 The quality of interaction between patients and professionals appeared to underpin successful messaging,138,139 but creating such interactions relied on staff experience, skills, and time, resources that may be constrained outside the context of an intervention study. 138,139 Furthermore, some patients are not able to remember or understand messaging due to cognitive impairment, with one study indicating potential harm to these patients. 134 Therefore, other strategies are needed to support falls prevention in these populations. The review also revealed a lack of research involving those with cognitive impairment or who do not speak English.
Theory development was achieved via iterative literature searches, building on practitioner ideas with evidence from empirical studies, and allowed for inclusion of different types of data. Including different methodologies can be considered a study strength, providing examples from clinical practice, but proved challenging to synthesise because there was much variation, for example, in outcomes assessed, description of methods, and data reported. Use of GRADE-CERQual to assess the strength of evidence associated with the CMOcs can also be considered a review strength; it supported team discussion about key findings, often leading to further CMOc refinements. We would recommend use of GRADE-CERQual in future realist reviews.
Realist review limitations
A limitation of the review is that, with the time available, we were only able to complete data synthesis for two CMOcs, despite having screened and indexed manuscripts for four CMOcs. There has been discussion in the literature about how much time should be spent in developing the initial programme theory in realist studies;152,153 we recommend researchers reduce time spent in this phase, allowing greater time in the theory testing and refinement phases. To achieve this, lessons may be learnt from rapid realist reviews. 154 For example, while we undertook three different searches across multiple databases and a Google search, we could have narrowed our search by focusing on reviews and studies mentioning theories/conceptual models and searching just one or two key databases. Additional limitations result from limitations in the literature: the literature focused on nursing practice and was dominated by QI studies with weak research designs.
Refining the programme theory through a multisite case study
In our multisite case study, we used multiple methods of data collection – ethnographic observations, interviews with staff, patients and carers, and review of patient records – to test the four prioritised CMOcs from our initial programme theory. This combination of methods provides rich description and fresh insights regarding the realities of MFRA and prevention in acute hospitals in England, addressing a previous gap in the literature and strengthening the knowledge base.
Leadership
We found falls link practitioners were expected to provide advice and education around assessment, intervention, and management of patients who had fallen or were at risk of falling and undertake audits of falls management practice on wards, but pressures of work, aggravated by COVID-19, meant it was not always possible to fulfil such duties. Nonetheless, we found fairly consistent documentation of MFRAs and care plans across sites. This was supported by senior nurses who monitored, reminded, and helped staff to deliver falls prevention practices while also being sensitive to the pressures staff were under.
Shared responsibility
We explored communication as a mechanism for multidisciplinary engagement in falls prevention, observing formal and informal communication of falls risks. While at the organisational-level there were multidisciplinary groups with responsibility for falls prevention, at ward-level responsibility for falls prevention largely fell to nursing staff. Rather than communication, this was linked to completion of MFRAs being a nursing responsibility and the emphasis on patient supervision as a key falls prevention strategy; while staff understood falls prevention as multidisciplinary, sharing responsibility was constrained because it was nursing staff who were responsible for patient supervision.
Facilitation
The realist review revealed a paucity of literature regarding how and why staff responded to MFRA and care planning tools, a gap the case study was able to address. The literature suggested such tools could act as practice prompts and nurses we spoke to agreed that they could be useful reminders to assess certain items. However, predominantly we found documentation was completed retrospectively and competing priorities on nurse time could reduce the process to a tick-box exercise, potentially compromising documentation quality.
We found variation across case sites in number and type of assessment items included in falls risk assessment tools within EHRs. All tools identified individual patient risk factors, but categorisation of patients as high or low risk was used to determine which patients should receive supervision. This finding provides insight into why falls risk prediction tools continue to be used – to help allocate, often scarce, staff resource to supervise patients identified as at ‘high risk’ of falling. Many patients on the wards observed had some level of cognitive impairment or needed assistance mobilising, meaning that many were stratified as at high risk of falling using the risk prediction tools available. These circumstances placed a greater emphasis on nursing teams for preventing falls on the ward as they were responsible for delivering supervision, constraining shared responsibility as discussed above.
Patient participation
National Institute of Health and Care Excellence recommends that healthcare professionals involved in assessment and prevention of falls should discuss with patients changes they themselves will make to prevent falls, promoting patient participation in falls prevention programmes. 16 The guideline also states that patients and their carers should be provided with information orally and in writing that explains patients’ individual risk factors for falling in hospital. However, workload pressures meant nursing staff had little time to talk with patients about why they were at risk of falling or to provide explicit advice about what they could do to prevent themselves from falling (although patients were advised to use the call-bell). The costing statement for the NICE guideline stated that implementation was unlikely to have a significant cost impact for the NHS70 but this fails to recognise the resource of staff time needed to engage meaningfully with patients to explain their falls risk.
Helping patients understand their falls risks and how they can prevent falls is important and non-nursing staff, such as engagement support workers, were able to have such conversations. While several studies in the realist review described providing information and education to family members and carers regarding falls risks, the case study also revealed that family members and carers can act as an important source of information about patients’ falls risks.
The realist review highlighted a lack of involvement of patients with cognitive impairment in previous studies. Through our observations we were able to provide some insight into the experiences of such patients. While these patients were constrained in the extent to which they could participate in interventions, such as using call-bells, staff could use relational skills such as speaking calmly, responding to the patient at their own level of understanding, and not contradicting them to help calm them in moments of distress or agitation and reduce behaviours that may result in falls. More generally, the quality of the interaction between staff and patients could reduce the likelihood of them taking actions that increase their risk of falling, although wards were often not staffed sufficiently for staff to be able to respond to patient needs, leading to patients mobilising alone. This finding about the centrality of the relationship between staff and patients reflects person-centred theory. 155 For example, Kitson et al. describe the importance of meeting patients’ relational needs to manage the fundamentals of care in ways that maintain patient dignity. 156 In dementia care, positive person work involves processes such as recognising the individuality of the person and negotiating with them about their needs and preferences. 157 These processes were observed on the wards in our study, encouraging patients (with and without cognitive impairments) to participate in keeping themselves safe. Other studies report similar findings about engaging patients in their own care through person-centred approaches, for example, when encouraging patient participation in delirium prevention strategies in acute hospitals. 158
Nurse staffing
A theme across the CMOcs, especially in relation to facilitation and patient participation, is that of nurse time. While our observations took place during a time of staff shortages due to COVID-19, nursing staff suggested that documentation burden is a persistent issue, as is finding time to talk to patients about their falls risks and how to prevent themselves from falling. There is substantial evidence from studies across many countries that nurse staffing levels [i.e. ratio of registered nurses (RNs): patients] are associated with patient outcomes, including patient safety and mortality; an increase of one patient per nurse in terms of workload has been associated with increased odds of mortality of between 7% and 16%. 159,160 The substitution of RNs with nursing assistants to compensate for lack of staff is also associated with poorer patient outcomes. A study across six European countries found that substituting one nurse assistant for a professional nurse for every 25 patients is associated with a 21% increase in the odds of a patient dying. 161 Nurses are more likely to leave nursing care undone in hospitals where staffing levels are poor and the work environment is also considered poor. 162,163 A European study found the types of care this can affect include ‘comfort/talk with patients’ (53%), ‘developing nursing care plans/care pathways’ (42%) and ‘educating patients and families’ (41%),162 processes we have shown to be important in engaging patients in falls prevention. Where hospitals had more favourable work environments, lower nurse:patient ratios, and lower proportions of nurses carrying out non-nursing tasks, fewer nurses reported leaving nursing care undone. What does all this mean for our research? Given that nurses in our study were probably working in less-than-optimal conditions regarding staffing and work environment, it is not surprising that some of the care activities the NICE guideline recommends for preventing inpatient falls, such as talking to and educating patients, were left undone. From this evidence, potential solutions, such as substituting professional nurses with HCAs, will not improve outcomes for patients. However, what we do not have is evidence about what difference additional resource (e.g. engagement support workers) on top of the staffing complement might make to outcomes, suggesting an area for future research.
Commonly used falls prevention strategies
Observation also revealed strategies commonly used for falls prevention – patient supervision, bed and chair alarms, and non-slip socks – despite lack of research evidence to recommend their use. 17,164 This suggests the need for guidance that clearly links particular falls risks to evidence-based interventions, which the current NICE guideline does not provide. Of particular concern is the use of patient supervision as a key falls prevention strategy, given its resource-intensive nature. There is a lack of high-quality research on patient supervision; in fact, reduction in its use has been found to be associated with a reduction in inpatient falls. 165 Previous research on patient supervision points to how it can be caring and therapeutic or passive and/or custodial, both of which we observed. 164 As a restrictive intervention,165,166 patient supervision may lead to deconditioning while also negatively impacting a patient’s autonomy, privacy, and dignity. 6,7 Interestingly, studies of cohort bays, undertaken in the USA, reveal a greater level of staffing – for example, one nurse and two nurses’ aides for an eight-bed bay167 or one nurse and one clinical technician for a four-bed bay;168 while this may allow for a more caring and therapeutic approach where patients have greater autonomy, even these studies fail to show a positive impact on fall rates.
Observer effects
A frequent concern regarding ethnographic data collection is that the presence of researchers changes the behaviour of those they seek to observe. We did not witness behaviours that required us to intervene or inform ward managers. We emphasised to staff that we were not there to assess their practice and the 8-month period of data collection enabled staff to become familiar with our presence. Analysis of fieldnotes we made regarding observer effects suggests staff were too busy and under pressure to be concerned about our presence. Staff talked openly, for example, telling us about falls that had happened on the ward, and appeared pleased to have an opportunity to talk about the challenges of their work. Where we did occasionally experience reluctance to be observed was when we asked staff if we could observe them completing falls risk assessments and care plans.
Case study limitations
A case study limitation was that we were unable to access patient records prior to observations, preventing assessment of whether care plans were enacted. Additionally, our observations focused on nursing staff, as they were most present on the wards, although we observed other professional groups and captured their perspectives in interviews. COVID-19 visiting restrictions limited our ability to observe the contribution of carers to falls prevention, although these were eased later in the observation period.
Developing guidance
When we presented our findings to case sites, participants agreed with our analysis. In discussing their implications, two key themes emerged: (1) the need for lessons learnt to be disseminated to all professional groups through leaflets and training materials; and (2) the need for leaflets for patients and carers, individualised to patients, providing them with information about their falls risks and how to reduce their risk of falling. Participants said stories and vignettes from our fieldnotes would be a good way to disseminate information because they are ‘real-life’ examples and some sites asked for permission to use our materials within their own falls prevention training.
In response, we produced a draft guidance leaflet based on our findings (see Implications for practice for implications of our findings for practice), which includes one vignette. We produced a set of PowerPoint slides that provide additional vignettes and discussion prompts that can be accessed by individuals or incorporated into training. We sought feedback on our draft guidance leaflet via a NAIF webinar to falls leads (June 2023) and a symposium at the Royal College of Nursing International Research Conference (September 2023). We have revised the guidance leaflet considering the feedback.
Providing individualised leaflets for patients and carers could be high-tech or low-tech; the Fall TIPS software generates leaflets for patients,63 but an alternative is a leaflet where the relevant options can be ticked. We have produced a draft paper-based patient leaflet that allows for this. Our patient leaflet has been revised based on feedback from our Lay Research Group. We will further develop it through a workshop with a wider group of service users and carers, including people living with dementia, and intend to incorporate appropriate icons or images, as well as text. Using existing patient leaflets for falls prevention as examples, such as those developed by the Royal College of Physicians,169 key questions to explore are as follows: (1) Given patients’ request for conciseness, what additional information should be included? For example, should more information be given about actions that multidisciplinary teams can take (e.g. reviewing medications)? (2) Which icons are most easily understandable by a wide range of audiences? (3) What else is needed to ensure the leaflet is understandable, useful and acceptable?
Once these activities are complete, we will send the guidance leaflet and patient leaflet for professional typesetting and layout design before dissemination. In addition to sharing the materials with our case sites and via social media, the Royal College of Nursing Professional Lead for Older People and Dementia will work with us to seek Royal College of Nursing endorsement of the materials and disseminate them more widely. We have been invited to write a practically focused article for the practitioner journal Nursing Older People and will use this to promote our guidance materials, providing links to the materials on our website. We have also agreed with the British Geriatrics Society that, after their conference, we will write a blog for the British Geriatrics Society website, which will also provide links to the materials. We are in conversation, too, with NAIF about how they can support wider dissemination.
Public and patient involvement
In Chapter 1, we explained that the research aimed to consider the perspectives of patients and members of the public through involvement of lay people at all stages and their regular evaluations of progress against this aim. In Chapter 2, we described the approach to PPI and how the Lay Research Group was involved in the conduct of the study. The outcomes of their work on prioritising theories for refinement and analysing findings from the case studies are embedded within Chapters 4–8. Here, we report the results of PPI in the study overall and reflect critically on the extent to which it influenced the research, drawing particularly on the evaluations carried out by the Lay Research Group.
The Lay Research Group gave excellent evaluation scores to the project. Fundamentally, they attributed this success to the caring, respectful, and honest relationships built and maintained between lay and academic researchers throughout the study. They highlighted the inclusive, non-hierarchical attitude to leadership and power-sharing established by RR and DW and the complementary roles of DW, as Lay Research Group lead, and LM, the academic researcher who supported the Lay Research Group. Consistent, ongoing communication throughout the project was also important, not only in Lay Research Group meetings, but also between meetings (e.g. through social e-mails and by sharing project management group minutes with Lay Research Group members). Practical arrangements facilitated lay researchers’ work, such as embedding invitations to online meetings within the body of e-mails so they could be opened by members who did not have electronic diaries, thereby avoiding delays at the beginning of meetings.
Overall, these factors created an environment in which lay researchers felt enabled, listened to and valued, and therefore empowered to offer their experiences, which were often personal and painful, to generate insight and change. This had a strong positive impact on the research, which PPI changed and strengthened. Examples include the Lay Research Group’s prioritisation of theories for testing (approved without amendment by Study Steering Group), which determined the focus of the study, and the changes they made to data collection tools, which helped academic researchers ask meaningful questions in patient and carer interviews and look out for things on wards they might otherwise have missed. Lay researchers also contributed to the presentation of findings to the participating Trusts in September 2022. With at least one lay person present at every presentation, they took part in the discussions with researchers, clinicians, and managers about impacts and how findings could be disseminated most effectively. Positive impact was also felt at a personal level. Lay researchers said involvement helped them to make something positive from their own or family members’ difficult experiences of falling.
Deep lay involvement of this kind can generate challenges as well as positive impacts, and these were also experienced on this project. 170,171 One lay researcher, for example, was upset during data analysis, when reading vivid ethnographic accounts and interview transcripts and reflected on how, for a while, this caused her to step back from some of her work as a public contributor, because she felt overwhelmed by the scale of the pressures on hospitals and their staff and patients (team members supported her and made it clear she could take as much time as she needed, which she said helped her to process her feelings and return refreshed, later). In their final evaluation, the Lay Research Group recommended, for future projects, that such potential impacts should be included in role descriptors given to prospective lay contributors before projects begin and be discussed with them. They also suggested providing contact details for organisations like the Samaritans and reflected that it had been helpful to discuss feelings in the group and to prepare the reflective statements that were used in their co-authored journal article and in the final evaluation, which had helped them to identify, share, and work through personal responses.
Overall, PPI greatly strengthened the research. That we are able to evidence this is thanks to the innovative evaluation approach developed by the Lay Research Group and shared by them through their co-authored journal article. 50
Equality, diversity and inclusion
We included as participants in the study people with cognitive impairment. This decision was made when preparing the ethics application and the dearth of the literature about falls risk assessment and prevention for people with a cognitive impairment emphasised its importance. We also sought to include patient participants who did not speak English; this was highlighted as an important issue by the Lay Research Group and is another gap in the literature. We had information sheets translated into the three most spoken non-English languages across the case sites (Urdu, Arabic and Polish). However, all patients we encountered could speak English and, while we did not specifically collect data on this, we would say the patients in the wards we observed were predominantly white British, despite the case study hospitals being located in cities and towns that are more ethnically diverse than the UK average. We did not consider ethnicity when selecting case sites, instead focusing on characteristics of sites in terms of falls prevention, HIT, and whether or not they were a teaching hospital. However, we would recommend that future studies include sites where they are more likely to be able to recruit non-English speakers and that they include funding for resources to support this, for example, translators. While we did not collect data on the ethnicity of the healthcare professionals included in the study, our anecdotal observation is that they were more diverse.
The research team is gender-balanced and diverse in terms of range of disciplines; academic, NHS and lay members; and members of different professional groups. However, it is predominantly white, with only three members from ethnic minorities. In future studies, we will consider how we can provide development opportunities for researchers from under-represented groups through involvement in the study.
In recruiting the Lay Research Group, we actively sought ethnic diversity. Their insights were valuable in terms of making us aware of how issues of language may impact falls prevention practices and encouraging us to translate our information sheets to support wider participation.
Implications for practice
Our findings have a number of implications for practice. We present these according to the four theory areas.
Leadership
Our findings emphasise the importance of experienced nursing leaders, the need for role clarity and the authority to target resources. For role clarity and to avoid duplication of effort, we suggest that managers should make sure there is a clear distinction and communication between ward manager/nurse-in-charge roles and falls link practitioners about falls prevention. If falls link practitioners are to fulfil their roles, adequate time to do so needs to be allocated and protected, including time for training.
Shared responsibility
There is a need to recognise that MFRA and prevention should not be, and cannot be, the responsibility of nursing staff alone; a comprehensive MFRA requires the input of other professional groups. Greater multidisciplinary team, and patient and carer, involvement in MFRA and selection and delivery of interventions is required. This message should be emphasised by Board members and managers. Additionally, we recommend the following actions:
-
Managers should ensure the ethos of the NICE guideline is understood by ward teams, that is, it is not just about documentation of MFRAs but multidisciplinary and patient and carer input to ensure modifiable risk factors are addressed.
-
Managers, front-line healthcare professionals, and support workers should work together to consider how systems and processes can be revised to better support multidisciplinary approaches to falls risk assessment and prevention.
-
Staff who lead and organise safety huddles should involve colleagues from different disciplines, clinical and non-clinical, wherever possible in huddles, for example, by holding them at times they can attend (normally between 9.00 and 17.00).
-
Managers should ensure that there are processes in place to update bed boards regularly and accurately, to ensure that all members of the multidisciplinary team have access to accurate information about the assistance a patient needs to mobilise.
-
Managers and IT teams should consider how EHRs can better support multidisciplinary working. This could include, for example, ensuring the falls risk assessment is fully integrated with and easily accessible by clinicians, such as doctors and allied health professionals and automatically triggering a request for a medication review when this is identified as a risk factor for a patient.
-
Managers, front-line healthcare professionals, and support workers should reflect together on how decisions about which patients require supervision are made and consider what alternatives there may be to supervision.
Facilitation
Documentation burden, combined with constraints on nursing time, potentially reduce the quality of falls documentation, while also requiring nurses to make a choice between ‘must do’ work and ‘being with’ patients. 119 While nurse staffing issues contribute to this, the current NHS workforce crisis combined with resource constraints mean we cannot address the problem by simply recruiting more nurses. Therefore, managers and IT teams should work with nursing staff to identify ways to reduce documentation burden. This could include removing duplication of information and autopopulating items where the information is already available in EHRs. Our findings related to facilitation also suggest the following:
-
Managers and IT teams should work together to ensure that items included in falls risk assessment tools align with NICE guidance. Thought should be given to ways in which items are phrased and how information is entered to avoid tick-box responses.
-
Board members and managers should emphasise to healthcare professionals that falls risk assessment tools and falls care plans are tools to support practice. This means moving away from a culture where documentation is seen as something to be audited and blame assigned when not completed to a culture of learning and continuous development.
Patient participation
Trusts should consider how they can ensure patients receive individualised information about their falls risks and how they can reduce their risk of falling. We have described how patient leaflets could be individualised but, whatever the solution, for successful implementation, it must not create an additional burden for nursing staff.
It is also important to recognise that providing patients with a leaflet is unlikely to be enough, with our findings emphasising the importance of interactions between staff and patients; it is interesting to note changes to the patient participation CMOcs following our observations, emphasising that, in the absence of formal interventions, patience and kindness may reduce behaviours that can lead to falls, a point that we have made clear in our guidance leaflet for staff. Trusts should consider providing staff with guidance on brief but sensitive ways to talk with patients about risks and preventing falls. Our research highlighted the role of engagement support workers in supporting people with dementia, to reduce their risk of falling; while there is some evidence of benefits of such roles,172 further research is required to evaluate their potential to support falls prevention.
Recommendations for future research
Our research has highlighted several challenges in delivering MFRA and prevention as anticipated by the NICE guideline, as well as use of interventions for which there is an inadequate evidence base. As noted above, a multidisciplinary approach to falls prevention is required; consequently there is a need for research to develop interventions that support multidisciplinary teams to undertake MFRAs and select evidence-based interventions that address patients’ individual falls risks. We have highlighted the use of patient supervision as a key falls prevention strategy despite the lack of evidence; thus, there is a need to determine the impacts and costs of this approach against alternatives. Nurses lack time to talk to patients about their falls risks and how to prevent themselves from falling. Some sites use engagement support workers to support falls prevention and the realist review provided qualitative evidence of the benefits of volunteers supporting patients to reduce their risk of falling,138 but further evidence is needed. At the time of our observations, the presence of visitors was limited, but families and carers may also be able to support this. In summary, we recommend future research addresses:
-
Development and mixed method and economic evaluation of interventions to support multidisciplinary teams to undertake, and involve patients in, MFRA and selection and delivery of tailored interventions.
-
Mixed method and economic evaluations of cohort bays and one-to-one care, comparing this to tailored alternatives.
-
Mixed method and economic evaluations of engagement support workers, volunteers, and/or carers to support falls prevention.
More generally, we recommend that future research on falls risk assessment and prevention includes those with cognitive impairment and patients who do not speak the main language of the country in which the research is taking place.
Acknowledgements
We would like to thank all of the NHS staff who participated in this research, for generously giving their time to be interviewed and for their willingness to have their work practice observed. We would also like to thank Heather Smith and Sue Ward, co-applicants who made important contributions to the study design and data analysis in the earlier phases of the study.
We are very grateful to the members of our Lay Research Group, Jamil Abdulkader, Eva Davison, Tina Frost and Basma Issa.
We thank our Study Steering Committee for the support and guidance given over the course of the project: Dr Tom Downes, Professor Joanne Greenhalgh, Manoj Mistry, Professor Catherine Pope, Professor Liz Sampson, Professor Nick Sevdalis, Professor Cath Taylor and Dr Julie Whitney.
Contributions of authors
Rebecca Randell (https://orcid.org/0000-0002-5856-4912) (Professor in Digital Innovations in Healthcare, Use of HIT and Realist evaluation) was the principal investigator, led the design of the study, contributed to data collection and analysis, and is lead author of this report.
Lynn McVey (https://orcid.org/0000-0003-2009-7682) (Research Fellow, Qualitative research) contributed to the realist review, undertook data collection, and was involved in the analysis and preparation of this report.
Judy Wright (https://orcid.org/0000-0002-5239-0173) (Senior Information Specialist, Literature searching) was co-applicant, designed and undertook the searches for the realist review, and was involved in study design and preparation of this report.
Hadar Zaman (https://orcid.org/0000-0002-4252-2822) (Head of School for Pharmacy and Medical Sciences, Pharmacy) contributed to the realist review and was involved in study design, analysis and preparation of this report.
V-Lin Cheong (https://orcid.org/0000-0001-9938-1592) (Consultant Pharmacist Elderly and Interfaces of Care, Pharmacy) contributed to data collection and was involved in study design, analysis and preparation of this report.
David M Woodcock (https://orcid.org/0000-0002-3781-3246) (Lay member, Public and Patient Involvement) was co-applicant, lead the Lay Research Group, and was involved in study design, analysis and preparation of this report.
Frances Healey (https://orcid.org/0000-0002-8266-3910) (Visiting Professor, Falls research) was co-applicant and was involved in study design, analysis and preparation of this report.
Dawn Dowding (https://orcid.org/0000-0001-5672-8605) (Professor in Clinical Decision Making, Clinical decision making) was co-applicant and was involved in study design, analysis and preparation of this report.
Peter Gardner (https://orcid.org/0000-0002-8799-0443) (Professor of Healthcare Quality and Safety, Human factors) was co-applicant and was involved in study design, analysis and preparation of this report.
Nicholas R Hardiker (https://orcid.org/0000-0002-7629-5664) (Dean, Nursing Informatics) was co-applicant and was involved in study design, analysis and preparation of this report.
Alison Lynch (https://orcid.org/0000-0002-8006-8341) (Group Deputy Chief Nurse, Falls risk assessment and prevention) was involved in study design, analysis and preparation of this report.
Chris Todd (https://orcid.org/0000-0001-6645-4505) (Professor of Primary Care and Community Health, Falls research) was co-applicant and was involved in study design, analysis and preparation of this report.
Christopher Davey (https://orcid.org/0000-0002-9050-379X) (Assistant Professor, Optometry) was involved in study design, analysis and preparation of this report.
Natasha Alvarado (https://orcid.org/0000-0001-9422-4483) (Senior Research Fellow, Theory driven evaluation) was co-applicant, responsible for day-to-day management of the project, led the realist review, undertook data collection, and was involved in the analysis and preparation of this report.
Patient data statement
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it is important that there are safeguards to make sure that they are stored and used responsibly. Everyone should be able to find out about how patient data is used. #datasaveslives You can find out more about the background to this citation here https://understandingpatientdata.org.uk/data-citation
Data-sharing statement
All data will be kept until December 2027 and can be accessed by other researchers during this time, subject to the necessary ethical approvals being obtained. Requests for access to this data should be addressed to the corresponding author.
Ethics statement
National Health Service ethics approval for this study was granted by the Yorkshire and The Humber – Bradford Leeds Research Ethics Committee on 17 September 2020 (ref: 20/YH/0221).
Information governance statement
The University of Bradford is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, the University of Bradford is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here www.bradford.ac.uk/data-protection/
Publications
Randell R, Wright J, Alvarado N, Healey F, Dowding D, Smith H, et al. What supports and constrains the implementation of multifactorial falls risk assessment and tailored multifactorial falls prevention interventions in acute hospitals? Protocol for a realist review. BMJ Open 2021;11:e049765. https://doi.org/10.1136/bmjopen-2021-049765
Randell R, McVey L, Zaman H, Wright J, Cheong VL, Dowding D, et al. Designing Health IT to Support Falls Prevention in Hospitals: Findings from a Realist Review. Proceedings of the AMIA 2022 Annual Symposium. 2022.
Alvarado N, McVey L, Wright J, Healey F, Dowding D, Cheong VL, et al. Exploring variation in implementation of multifactorial falls risk assessment and tailored interventions: a realist review. BMC Geriatr 2023;23(381).
McVey L, Frost T, Issa B, Davison E, Abdulkader J, Randell R, et al. Working together: reflections on how to make public involvement in research work. Res Involv Engag 2023;9(14).
Disclaimers
This manuscript presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Randell R, Wright JM, Alvarado N, Healey F, Dowding D, Smith H, et al. What supports and constrains the implementation of multifactorial falls risk assessment and tailored multifactorial falls prevention interventions in acute hospitals? Protocol for a realist review. BMJ Open 2021;11.
- Lamb SE, Jørstad-Stein EC, Hauer K, Becker C, Europe PFN, Group OC. Development of a common outcome data set for fall injury prevention trials: the prevention of falls network Europe consensus. J Am Geriatr Soc 2005;53:1618-22.
- NHS Improvement . The Incidence and Costs of Inpatient Falls in Hospitals 2017.
- Office for Health Improvement and Disparities . Falls: Applying All Our Health 2022. www.gov.uk/government/publications/falls-applying-all-our-health/falls-applying-all-our-health (accessed 22 January 2024).
- Becker C, Woo J, Todd C. Oxford Textbook for Geriatric Medicine. Oxford: Oxford University Press; 2017.
- Oliver D, Healey F, Haines TP. Preventing falls and fall-related injuries in hospitals. Clin Geriatr Med 2010;26:645-92.
- Oliver D. Preventing falls and fall injuries in hospital: a major risk management challenge. Clinical Risk 2007;13:173-8.
- Royal College of Physicians . National Audit of Inpatient Falls: Audit Report 2017 2017.
- Murray GR, Cameron ID, Cumming RG. The consequences of falls in acute and subacute hospitals in Australia that cause proximal femoral fractures. J Am Geriatr Soc 2007;55:577-82.
- The Health Foundation . Closing the Gap through Clinical Communities: The FallSafe Project 2012.
- Oliver D, Killick S, Even T, Willmott M. Do falls and falls-injuries in hospital indicate negligent care: and how big is the risk? A retrospective analysis of the NHS Litigation Authority Database of clinical negligence claims, resulting from falls in hospitals in England 1995 to 2006. Qual Saf Health Care 2008;17:431-6.
- Oliver D, Britton M, Seed P, Martin FC, Hopper AH. Development and evaluation of evidence based risk assessment tool (STRATIFY) to predict which elderly inpatients will fall: case–control and cohort studies. BMJ 1997;315:1049-53.
- Haines TP, Hill K, Walsh W, Osborne R. Design-related bias in hospital fall risk screening tool predictive accuracy evaluations: systematic review and meta-analysis. J Gerontol A Biol Sci Med Sci 2007;62:664-72.
- Oliver D. Falls risk-prediction tools for hospital inpatients time to put them to bed?. Age Ageing 2008;37:248-50.
- Jellett J, Williams C, Clayton D, Plummer V, Haines T. Falls risk score removal does not impact inpatient falls: a stepped‐wedge, cluster‐randomised trial. J Clin Nurs 2020;29:4505-13.
- National Institute for Health and Clinical Excellence . Falls in Older People: Assessing Risk and Prevention: Clinical Guideline 2013.
- Montero-Odasso M, van der Velde N, Martin F, Masud T, Ryg J, Pieruccini-Faria F, et al. World guidelines for falls prevention and management for older adults: a global initiative. Age Ageing 2022;51.
- Healey F, Monro A, Cockram A, Adams V, Heseltine D. Using targeted risk factor reduction to prevent falls in older in-patients: a randomised controlled trial. Age Ageing 2004;33:390-5.
- Royal College of Physicians . National Audit of Inpatient Falls (NAIF) Annual Report 2022 2022.
- Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ 2021;374.
- Medical Research Council . Developing and Evaluating Complex Interventions: New Guidance 2008.
- Campbell NC, Murray E, Darbyshire J, Emery J, Farmer A, Griffiths F, et al. Designing and evaluating complex interventions to improve health care. BMJ 2007;334:455-9.
- Pawson R, Tilley N, Tilley N. Realistic Evaluation. Thousand Oak, CA: SAGE Publications Ltd; 1997.
- Byng R, Norman I, Redfern S, Jones R. Exposing the key functions of a complex intervention for shared care in mental health: case study of a process evaluation. BMC Health Serv Res 2008;8.
- Greenhalgh T, Humphrey C, Hughes J, Macfarlane F, Butler C, Pawson R. How do you modernize a health service? A realist evaluation of whole-scale transformation in London. Milbank Q 2009;87:391-416.
- Ranmuthugala G, Cunningham FC, Plumb JJ, Long J, Georgiou A, Westbrook JI, et al. A realist evaluation of the role of communities of practice in changing healthcare practice. Implement Sci 2011;6.
- Rycroft-Malone J, Fontenla M, Bick D, Seers K. A realistic evaluation: the case of protocol-based care. Implement Sci 2010;5.
- Pawson R. Evidence-Based Policy: A Realist Perspective. London: SAGE Publications Ltd; 2006.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review: a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10:21-34.
- Randell R, Honey S, Alvarado N, Pearman A, Greenhalgh J, Long A, et al. Embedding robotic surgery into routine practice and impacts on communication and decision making: a review of the experience of surgical teams. Cogn Technol Work 2016;18:423-37.
- Khangura S, Konnyu K, Cushman R, Grimshaw J, Moher D. Evidence summaries: the evolution of a rapid review approach. Syst Rev 2012;1:1-9.
- Ganann R, Ciliska D, Thomas H. Expediting systematic reviews: methods and implications of rapid reviews. Implement Sci 2010;5:1-10.
- Wong G, Westhorp G, Pawson R, Greenhalgh T. Realist Synthesis: RAMESES Training Materials. London: The RAMESES Project; 2013.
- Duckworth M, Adelman J, Belategui K, Feliciano Z, Jackson E, Khasnabish S, et al. Assessing the effectiveness of engaging patients and their families in the three-step fall prevention process across modalities of an evidence-based fall prevention toolkit: an implementation science study. J Med Internet Res 2019;21.
- Dykes PC, Carroll DL, Hurley A, Gersh-Zaremski R, Kennedy A, Kurowski J, et al. Fall TIPS: Strategies to Promote Adoption and use of a Fall Prevention Toolkit 2009:153-7.
- Businger AC, Fuller TE, Schnipper JL, Rossetti SC, Schnock KO, Rozenblum R, et al. Lessons learned implementing a complex and innovative patient safety learning laboratory project in a large academic medical center. J Am Med Inform Assoc 2020;27:301-7.
- Carroll DL, Dykes PC, Hurley AC. An electronic fall prevention toolkit: effect on documentation quality. Nurs Res 2012;61:309-13.
- Dykes PC, Duckworth M, Cunningham S, Dubois S, Driscoll M, Feliciano Z, et al. Pilot testing fall TIPS (tailoring interventions for patient safety): a patient-centered fall prevention toolkit. Joint Commiss J Qual Patient Saf 2017;43:403-13.
- Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ Inf 2018;34:285-91.
- Lewin S, Booth A, Glenton C, Munthe-Kaas H, Rashidian A, Wainwright M, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. Implement Sci 2018;13.
- Charles JM, Rycroft-Malone J, Aslam R, Hendry M, Pasterfield D, Whitaker R. Reducing repeat pregnancies in adolescence: applying realist principles as part of a mixed-methods systematic review to explore what works, for whom, how and under what circumstances. BMC Pregn Childb 2016;16.
- Rivas C, Vigurs C, Cameron J, Yeo L. A realist review of which advocacy interventions work for which abused women under what circumstances. Cochr Datab Syst Rev 2019;2019. https://doi.org/10.1002/14651858.CD013135.pub2.
- Haines TP, Lee D-CA, O’Connell B, McDermott F, Hoffmann T. Why do hospitalized older adults take risks that may lead to falls?. Health Expect: Int J Publ Part Health Care Health Pol 2015;18:233-49.
- Yin R. Case Study Research. Design and Methods. Los Angeles, CA: SAGE; 2009.
- Hammersley M, Atkinson P. Ethnography: Principles in Practice. London: Routledge; 1995.
- McDonald S. Studying actions in context: a qualitative shadowing method for organizational research. Qual Res 2005;5:455-73.
- Pawson R. Theorizing the interview. Br J Sociol 1996;47:295-314.
- Ritchie J, Spencer L. Analyzing Qualitative Data. London: Routledge; 1994.
- Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. Thousand Oaks, CA: SAGE Publications Ltd; 1994.
- McVey L, Frost T, Issa B, Davidson E, Abdulkader J, Randell R, et al. Working together: reflections on how to make public involvement in research work. Res Invol Engag 2023;9.
- Staniszewska S, Brett J, Simera I, Seers K, Mockford C, Goodlad S, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. BMJ 2017;358.
- National Institute of Health and Care Research . National Standards for Public Involvement in Research 2018. www.invo.org.uk/wp-content/uploads/2019/11/UK-standards-for-public-involvement-v6.pdf (accessed 21 July 2022).
- UK_Public_Involvement_Standards_Development_Partnership . UK Standards for Public Involvement: Better Public Involvement for Better Health and Social Care Research 2019. https://sites.google.com/nihr.ac.uk/pi-standards/standards (accessed 21 July 2022).
- Breimaier HE, Heckemann B, Halfens RJ, Lohrmann C. The Consolidated Framework for Implementation Research (CFIR): a useful theoretical framework for guiding and evaluating a guideline implementation process in a hospital-based nursing practice. BMC Nurs 2015;14:1-9.
- Avanecean D, Calliste D, Contreras T, Lim Y, Fitzpatrick A. Effectiveness of patient-centered interventions on falls in the acute care setting compared to usual care: a systematic review. JBI Datab Syst Rev Implement Rep 2017;15:3006-48.
- Miake-Lye IM, Hempel S, Ganz DA, Shekelle PG. Inpatient fall prevention programs as a patient safety strategy: a systematic review. Ann Intern Med 2013;158:390-6.
- Rimland JM, Abraha I, Dell’Aquila G, Cruz-Jentoft A, Soiza R, Gudmusson A, et al. Effectiveness of non-pharmacological interventions to prevent falls in older people: a systematic overview the SENATOR project ONTOP series. PLOS ONE 2016;11.
- Tricco AC, Thomas SM, Veroniki AA, Hamid JS, Cogo E, Strifler L, et al. Comparisons of interventions for preventing falls in older adults: a systematic review and meta-analysis. JAMA 2017;318:1687-99.
- Evans D, Hodgkinson B, Lambert L, Wood J, Kowanka I. Falls in acute hospitals; a systematic review. JBI Libr Syst Rev 1998;1:1-56.
- Hempel S, Newberry S, Wang Z, Booth M, Shanman R, Johnsen B, et al. Hospital fall prevention: a systematic review of implementation, components, adherence, and effectiveness. J Am Geriatr Soc 2013;61:483-94.
- Coussement J, De Paepe L, Schwendimann R, Denhaerynck K, Dejaeger E, Milisen K. Interventions for preventing falls in acute- and chronic-care hospitals: a systematic review and meta-analysis. J Am Geriatr Soc 2008;56:29-36.
- National Institute of Health and Care Excellence (NICE) . Falls in Older People: Assessing Risk and Prevention 2013.
- Dykes PC, Carroll DL, Hurley A, Lipsitz S, Benoit A, Chang F, et al. Fall prevention in acute care hospitals: a randomized trial. JAMA 2010;304:1912-8.
- Kannus P, Khan KM, Lord SR. Preventing falls among elderly people in the hospital environment. Med J Aust 2006;184:372-3.
- Hairon N. Using a range of interventions to prevent falls in hospital. Nurs Times 2007;103:23-4.
- Manojlovich M, Lee S, Lauseng D. A systematic review of the unintended consequences of clinical interventions to reduce adverse outcomes. J Patient Saf 2016;12:173-9.
- Oliver D, Hopper A, Seed P. Do hospital fall prevention programs work? A systematic review. J Am Geriatr Soc 2000;48:1679-89.
- Christy R. Preventing falls in hospitalized older adults. Nursing 2017;47:1-3.
- Choi YS, Lawler E, Boenecke CA, Ponatoski ER, Zimring CM. Developing a multi-systemic fall prevention model, incorporating the physical environment, the care process and technology: a systematic review. J Adv Nurs 2011;67:2501-24.
- Barker W. Assessment and prevention of falls in older people. Nurs Older People 2014;26:18-24.
- Glasper A. Policies and strategies to prevent patient falls in hospital. Br J Nurs 2019;28:806-7.
- Matarese M, Ivziku D. Falls risk assessment in older patients in hospital. Nurs Stand 2016;30:53-6.
- Kelly A, Dowling M. Reducing the likelihood of falls in older people. Nurs Stand 2004;18:33-40.
- Sutton D, Windsor J, Husk J. A care bundle approach to falls prevention. Nurs Times 2014;110:21-3.
- Spoelstra SL, Given BA, Given CW. Fall prevention in hospitals: an integrative review [corrected] [published erratum appears in Clin Nurs Res 2012;21(2):243]. Clin Nurs Res 2012;21:92-112.
- Mashta O. Slow and steady wins. Nurs Stand 2010;25:18-9.
- Barrett JA, Bradshaw M, Hutchinson K, Akpan A, Reese A, Metcalfe L, et al. Reduction of falls-related injuries using a hospital inpatient falls prevention program. J Am Geriatr Soc 2004;52:1969-70.
- Grant L, McEnerney J, Proctor T. Making time for nurses to reduce patient falls. Nurs Times 2013;109:21-3.
- Nyman SR, Victor CR. Older people’s recruitment, sustained participation, and adherence to falls prevention interventions in institutional settings: a supplement to the Cochrane systematic review. Age Ageing 2011;40:430-6.
- Glogovsky D. Patient safety how can policy change guide nursing practice to reduce in-patient falls?. Nursing 2017;47:63-7.
- Johnson B. Falls risk assessment. Nurs Stand 2017;31:64-5.
- Lindus L. Preventing falls in older people: assessment and interventions. Nurs Stand 2012;26.
- Duffin C. Hospitals should do more to reduce incidence of falls, says RCP report. Nurs Stand 2015;30.
- Bellingham C. Pharmacists can play an important role in preventing falls in older people. Pharmaceut J 2001;267.
- Potera C. Preventing falls in acute care hospitals. Am J Nurs 2011;111.
- Lilley G. How do you achieve a 50% reduction in falls?. Nurs Times 2017;71.
- Healey F. Preventing falls in hospitals. BMJ 2016;532.
- Jones D, Whitaker T. Preventing falls in older people: assessment and interventions. Nurs Stand 2011;25:50-5; quiz 56.
- Pearce L. Preventing falls in hospital [including commentary by Dawne Garrett]. Nurs Manag: UK 2017;23.
- West GF, Rose T, Throop M. Assessing nursing interventions to reduce patient falls. Nursing 2018;48:59-60.
- Hemsley B, Steel J, Worrall L, Hill S, Bryant L, Johnston L, et al. A systematic review of falls in hospital for patients with communication disability: highlighting an invisible population. J Safety Res 2019;68:89-105.
- Reznik D. FALL PREVENTION Diane Goodman’s viewpoint, ‘an insider’s view on fall prevention’ (April). Am J Nurs 2013;113.
- Tingle J. Comment: preventing patient falls in hospital. Br J Nurs 2007;16.
- Healthcare Improvement Scotland . Falls Case Studies June 2018 2018.
- Cunningham M. Risk assessment crucial for prevention of falls ‘Assessment of vulnerable patients cuts hospital falls’, nursingtimesnet. Nurs Times 2012;108.
- Heaton C. Creating a protocol to reduce inpatient falls. Nurs Times 2012;108:16-8.
- Hughes R. Older people falling out of bed: restraint, risk and safety. Br J Occupat Therap 2008;71:389-92.
- Anonymous . Falls prevented by checking patients have what they need. Nurs Stand 2009;24.
- Ward L, Fenton K, Maher L. The high impact actions for nursing and midwifery 3: staying safe, preventing falls. Nurs Times 2010;106:12-3.
- Perdue C. Falls in older people: taking a multidisciplinary approach. Nurs Times 2003;99:28-30.
- ‘Falls risk’ needs revisiting. Nurs Stand 2017;31.
- Krishna KM, Van Cleave RJ. Decrease in the incidence of patient falls in a geriatric hospital after educational programs. J Am Geriatr Soc 1983;31.
- Dykes PC. Adding targeted multiple interventions to standard fall prevention interventions reduces falls in an acute care setting. Evid Based Nurs 2012;15:109-10.
- Walmsley A. Preventing falls among older people in hospital: results are not surprising. BMJ 2008;336.
- Hunt L. Accident or design. Health Serv J 2009;119:27-9.
- Capan K, Lynch B. A hospital fall assessment and intervention project. J Clin Outc Manag 2007;14:155-60.
- Cook NS, Komansky BJ, Urton MS. Do no harm: a multifactorial approach to preventing Emergency Department falls: a quality improvement project. J Emerg Nurs 2020;46:666-74.
- Dowding DW, Turley M, Garrido T. The impact of an electronic health record on nurse sensitive patient outcomes: an interrupted time series analysis. J Am Med Inform Assoc 2012;19:615-20.
- Hefner JL, McAlearney AS, Mansfield J, Knupp AM, Moffatt-Bruce SD. A falls wheel in a large academic medical center: an intervention to reduce patient falls with harm. J Healthc Qual: Off Publ Nat Assoc Healthc Qual 2015;37:374-80.
- Lytle KS, Short NM, Richesson RL, Horvath MM. Clinical decision support for nurses: a fall risk and prevention example. Comput Inform Nurs 2015;33:530-7.
- McCarty CA, Woehrle TA, Waring SC, Taran AM, Kitch LA. Implementation of the MEDFRAT to promote quality care and decrease falls in community hospital emergency rooms. J Emerg Nurs 2018;44:280-4.
- Pop H, Lamb K, Livesay S, Altman P, Sanchez A, Nora ME. Tailoring a comprehensive bundled intervention for ED fall prevention. J Emerg Nurs 2020;46:225-232.e3.
- Titler MG, Conlon P, Reynolds MA, Ripley R, Tsodikov A, Wilson DS, et al. The effect of a translating research into practice intervention to promote use of evidence-based fall prevention interventions in hospitalized adults: a prospective pre-post implementation study in the US. Appl Nurs Res 2016;31:52-9.
- Townsend AB, Valle-Ortiz M, Sansweet T. A successful ED fall risk program using the KINDER 1 fall risk assessment tool. J Emerg Nurs 2016;42:492-7.
- Currie LM, Bakken S, Bufe G, Mellino LV. Compliance with use of Automated Fall-injury Risk Assessment in Three Clinical Information Systems 2006.
- Thatphet P, Kayarian FB, Ouchi K, Hogan T, Schumacher JG, Kennedy M, et al. Lessons learned from Emergency Department fall assessment and prevention programs. Cureus 2021;13.
- Ireland S, Lazar T, Mavrak C, Morgan B, Pizzacalla A, Reis C, et al. Designing a falls prevention strategy that works. J Nurs Care Qual 2010;25:198-207.
- Albornos-Munoz L, Melian-Correa E, Acosta-Arrocha A, Gallo-Blanco C, Bejar-Bacas F, Alonso-Poncelas E, et al. Falls assessment and interventions among older patients in two medical and one surgical hospital wards in Spain: a best practice implementation project. JBI Datab Syst Rev Implement Rep 2018;16:247-57.
- Dempsey J. Falls prevention revisited: a call for a new approach. J Clin Nurs 2004;13:479-85.
- Teh RCA, Visvanathan R, Ranasinghe D, Wilson A. Evaluation and refinement of a handheld health information technology tool to support the timely update of bedside visual cues to prevent falls in hospitals. Int J Evid-Based Healthc 2018;16:90-100.
- Teh RC, Wilson A, Ranasinghe D, Visvanathan R. Use and clinical efficacy of standard and health information technology fall risk assessment tools. Austr J Age 2017;36:327-31.
- Koh SLS, Hafizah N, Lee JY, Loo YL, Muthu R. Impact of a fall prevention programme in acute hospital settings in Singapore. Singapore Med J 2009;50:425-32.
- Koh SS, Manias E, Hutchinson AM, Donath S, Johnston L. Nurses’ perceived barriers to the implementation of a Fall Prevention Clinical Practice Guideline in Singapore hospitals. BMC Health Serv Res 2008;8:1-10.
- Maia FDOM, Da Cruz DDALM, Shimoda GT, Sichieri K, Iida LIS. Falls prevention strategies for adult inpatients in a university hospital of Sao Paulo, Brazil: a best practice implementation project. JBI Datab Syst Rev Implement Rep 2018;16:1720-36.
- Ohde S, Terai M, Oizumi A, Takahashi O, Deshpande GA, Takekata M, et al. The effectiveness of a multidisciplinary QI activity for accidental fall prevention: staff compliance is critical. BMC Health Serv Res 2012;12.
- Wu MW, Lee TT, Lai SM, Huang CY, Chang TH. Evaluation of electronic health records on the nursing process and patient outcomes regarding fall and pressure injuries. Comput Inform Nurs 2019;37:573-82.
- Milisen K, Coussement J, Arnout H, Vanlerberghe V, De Paepe L, Schoevaerdts D, et al. Feasibility of implementing a practice guideline for fall prevention on geriatric wards: a multicentre study. Int J Nurs Stud 2013;50:495-507.
- Dykes PC, Carroll DL, Hurley AC, Benoit A, Middleton B. Why do patients in acute care hospitals fall? Can falls be prevented?. J Nurs Adm 2009;39:299-304.
- Dykes PC, Burns Z, Adelman J, Benneyan J, Bogaisky M, Carter E, et al. Evaluation of a patient-centered fall-prevention tool kit to reduce falls and injuries: a nonrandomized controlled trial. JAMA Netw Open 2020;3.
- Bargmann AL, Brundrett SM. Implementation of a multicomponent fall prevention program: contracting with patients for fall safety. Mil Med 2020;185:28-34.
- Cann T, Gardner A. Change for the better: an innovative model of care delivering positive patient and workforce outcomes. Collegian 2012;19:107-13.
- Carroll DL, Dykes PC, Hurley AC. Patients’ perspectives of falling while in an acute care hospital and suggestions for prevention. Appl Nurs Res 2010;23:238-41.
- Goldsack J, Bergey M, Mascioli S, Cunningham J. Hourly rounding and patient falls: what factors boost success?. Nursing 2015;45:25-30.
- Haines TP, Hill AM, Hill KD, McPhail S, Oliver D, Brauer S, et al. Patient education to prevent falls among older hospital inpatients: a randomized controlled trial. Arch Intern Med 2011;171:516-24.
- Johnson JE, Veneziano T, Green J, Howarth E, Malast T, Mastro K, et al. Breaking the fall. J Nurs Adm 2011;41:538-45.
- Kiyoshi-Teo H, Northrup-Snyder K, Cohen DJ, Dieckmann N, Stoyles S, Winters-Stone K, et al. Older hospital inpatients’ fall risk factors, perceptions, and daily activities to prevent falling. Geriatr Nurs 2019;40:290-5.
- Kullberg A, Sharp L, Johansson H, Bergenmar M. Information exchange in oncological inpatient care: patient satisfaction, participation, and safety. Eur J Oncol Nurs: Off J Eur Oncol Nurs Soc 2015;19:142-7.
- Martin RA, Dickie B, Skinner H, Hurring S, Marshall R, Hanger HC. Implementing a ‘safe recovery’ fall prevention program: refining intervention theory using realist methods. Austr J Age 2020;39:e259-70.
- Radecki B, Keen A, Miller J, McClure JK, Kara A. Innovating fall safety: engaging patients as experts. J Nurs Care Qual 2020;35:220-6.
- Radecki B, Reynolds S, Kara A. Inpatient fall prevention from the patient’s perspective: a qualitative study. Appl Nurs Res 2018;43:114-9.
- Rush KL, Robey-Williams C, Patton LM, Chamberlain D, Bendyk H, Sparks T. Patient falls: acute care nurses’ experiences. J Clin Nurs 2009;18:357-65.
- Sitzer V. Development of an automated self-assessment of Fall Risk Questionnaire for hospitalized patients. J Nurs Care Qual 2016;31:46-53.
- Turner N, Jones D, Dawson P, Tait B. The perceptions and rehabilitation experience of older people after falling in the hospital. Rehab Nurs: Off J Assoc Rehab Nurs 2019;44:141-50.
- Twibell RS, Siela D, Sproat T, Coers G. Perceptions related to falls and fall prevention among hospitalized adults. Am J Crit Care: Off Publ Am Assoc Crit-Care Nurs 2015;24:e78-85.
- Zadvinskis IM, Carr J, Schweitzer KE, Patil N, Clifton WD, Ebert KE. The impact of nursing work and engagement on patient falls. J Nurs Adm 2019;49:531-7.
- Christiansen TL, Lipsitz S, Scanlan M, Yu SP, Lindros ME, Leung WY, et al. Patient activation related to fall prevention: a multisite study. Joint Commiss J Qual Patient Saf 2020;46:129-35.
- Hill A-M, Francis-Coad J, Haines TP, Waldron N, Etherton-Beer C, Flicker L, et al. ‘My independent streak may get in the way’: how older adults respond to falls prevention education in hospital. BMJ Open 2016;6.
- Hill A-M, McPhail SM, Francis-Coad J, Waldron N, Etherton-Beer C, Flicker L, et al. Educators’ perspectives about how older hospital patients can engage in a falls prevention education programme: a qualitative process evaluation. BMJ Open 2015;5.
- Vonnes C, Wolf D. Fall risk and prevention agreement: engaging patients and families with a partnership for patient safety. BMJ Open Qual 2017;6.
- National Institute of Health and Care Excellence (NICE) . NICE Impact Dementia 2020.
- Royal College of Physicians . National Audit of Inpatient Falls (NAIF) Audit Report 2020 2020.
- Flynn R, Schick-Makaroff K, Levay A, Greenhalgh J. Developing an initial program theory to explain how patient-reported outcomes are used in health care settings: methodological process and lessons learned. Int J Qual Methods 2020;19.
- Francis-Auton E, Sarkies MN, Pomare C, Long JC, Hardwick R, Nguyen HM, et al. Real talk: a realist dialogic approach in a realist evaluation. Int J Qual Methods 2022;21.
- Saul J, Willis C, Bitz J, Best A. A time-responsive tool for informing policy making: rapid realist review. Implement Sci 2013;8.
- McCormack B, McCance T. Person-Centred Practice in Nursing and Health Care: Theory and Practice. London: John Wiley & Sons; 2016.
- Kitson AL, Dow C, Calabrese JD, Locock L, Athlin AM. Stroke survivors’ experiences of the fundamentals of care: a qualitative analysis. Int J Nurs Stud 2013;50:392-403.
- Kitwood T, Brooker D. Dementia Reconsidered Revisited: The Person Still Comes First. London: McGraw-Hill Education; 2019.
- Lee-Steere K, Liddle J, Mudge A, Bennett S, McRae P, Barrimore SE. ‘You’ve got to keep moving, keep going’: understanding older patients’ experiences and perceptions of delirium and nonpharmacological delirium prevention strategies in the acute hospital setting. J Clin Nurs 2020;29:2363-77.
- Ball JE, Bruyneel L, Aiken LH, Sermeus W, Sloane DM, Rafferty AM, et al. RN4Cast Consortium . Post-operative mortality, missed care and nurse staffing in nine countries: a cross-sectional study. Int J Nurs Stud 2018;78:10-5.
- Lasater KB, Aiken LH, Sloane D, French R, Martin B, Alexander M, et al. Patient outcomes and cost savings associated with hospital safe nurse staffing legislation: an observational study. BMJ Open 2021;11.
- Aiken LH, Sloane D, Griffiths P, Rafferty AM, Bruyneel L, McHugh M, et al. RN4CAST Consortium . Nursing skill mix in European hospitals: cross-sectional study of the association with mortality, patient ratings, and quality of care. BMJ Qual Saf 2017;26:559-68.
- Ausserhofer D, Zander B, Busse R, Schubert M, De Geest S, Rafferty AM, et al. RN4CAST Consortium . Prevalence, patterns and predictors of nursing care left undone in European hospitals: results from the multicountry cross-sectional RN4CAST study. BMJ Qual Saf 2014;23:126-35.
- Bruyneel L, Li B, Ausserhofer D, Lesaffre E, Dumitrescu I, Smith HL, et al. Organization of hospital nursing, provision of nursing care, and patient experiences with care in Europe. Med Care Res Rev 2015;72:643-64.
- Wood VJ, Vindrola-Padros C, Swart N, McIntosh M, Crowe S, Morris S, et al. One to one specialling and sitters in acute care hospitals: a scoping review. Int J Nurs Stud 2018;84:61-77.
- Greeley AD, Tanner EP, Mak S, Begashaw MM, Miake-Lye IM, Shekelle PG. Sitters as a patient safety strategy to reduce hospital falls. Ann Intern Med 2020;172:317-24.
- Brennan S, Sykes R, Meredith H, Brennan W. Making 1–1 support person centred and an effective therapeutic intervention. J Med Healthc SRC JMHC-269 2023;221:2-7. https://doi.org/1047363/JMHC/2023.
- McNicoll L, Cournoyer K, Roach R, Carroll D, Collins K, Riley B. Close observation medical unit: a successful model for nursing and geriatrics collaboration. J Am Geriat Soc 2013;61:S58-9.
- Skowronsky C, Bena JF, Albert NM. Close observation unit to prevent falls and minimize use of patient care companions. J Nurs Care Qual 2015;30:38-43.
- Royal College of Physicians . Falls Prevention in Hospital: A Guide for Patients, Their Families and Carers 2016. www.rcplondon.ac.uk/projects/outputs/falls-prevention-hospital-guide-patients-their-families-and-carers (accessed 6 June 2023).
- Maguire K, Britten N. ‘You’re there because you are unprofessional’: patient and public involvement as liminal knowledge spaces. Sociol Health Illness 2018;40:463-77.
- Lonbay S, Pearson A, Hamilton E, Higgins P, Foulkes E, Glascott M. Trauma informed participatory research: reflections on co-producing a research proposal. Gateways: Int J Commun Res Engag 2021;14:1-8.
- Lourida I, Gwernan-Jones R, Abbott R, Rogers M, Green C, Ball S, et al. Activity interventions to improve the experience of care in hospital for people living with dementia: a systematic review. BMC Geriatr 2020;20.
- Currie LM, Bakken S, Bufe G, Mellino LV. Compliance with Use of Automated Fall-injury Risk Assessment in Three Clinical Information Systems n.d.;900.
Appendix 1 Theory construction searches
This appendix reports the final search strategies used for all databases searched for stage 1 of the realist review. On 22 July 2020 we conducted three sets of searches, each comprising several database searches. The purpose of the search was to identify the literature describing assumptions and theories underlying fall risk assessments in acute hospital settings. Subject headings and free-text words were identified for use in the search concepts for all searches by the Information Specialist and project team members. The searches were peer reviewed by an Information Specialist.
Table 21 summarises the databases searched and the order of search strategies presented below the table.
| Search name | Databases searched | Type of publication or study |
|---|---|---|
| 1.1 Practitioner theory search | CINAHL (EBSCOhost) HMIC Health Management Information Consortium (Ovid) Ovid MEDLINE(R) and Epub Ahead of Print, In-process and Other Non-indexed Citations and Daily <1946 to 21 July 2020> |
Commentary pieces Policy documents Studies mentioning theories or theoretical concepts |
| 1.2 Key journal search | CINAHL (EBSCOhost) EMBASE Classic + EMBASE (Ovid) <1947 to 2020 July 21> HMIC Health Management Information Consortium (Ovid) Ovid MEDLINE(R) and Epub Ahead of Print, In-process and Other Non-indexed Citations and Daily <1946 to 21 July 2020> |
Trade journal article or news item |
| 1.3 Academic theory search | CINAHL (EBSCOhost) Cochrane Central Register of Controlled Trials (Wiley) Issue 7 of 12, July 2020 Epistemonikos www.epistemonikos.org/ HMIC Health Management Information Consortium (Ovid) International HTA Database (INAHTA) https://database.inahta.org/ Ovid MEDLINE(R) and Epub Ahead of Print, In-process and Other Non-indexed Citations and Daily <1946 to 21 July 2020> PROSPERO www.crd.york.ac.uk/prospero/ |
Systematic review |
Search 1.1: practitioner theory search
CINAHL (EBSCOhost) 1981–present
Date run: 22 July 2020
-
S29 S22 AND S28 220
-
S28 S23 OR S24 OR S25 OR S26 OR S27 443,776
-
S27 TI ((view or views)) OR TI editorial OR TI letter* 88,866
-
S26 TI “Comment on” OR TI commentary OR TI opinion* 60,866
-
S25 (MH “News”) 9948
-
S24 (MH “Policy and Procedure Manuals”) OR (MH “Hospital Policies”) OR (MH “Practice Guidelines”) OR (MH “Health Policy”) OR (MH “Public Policy”) 156,362
-
S23 TI ((policy or policies or guideline* or recommendation* or position)) OR TI ((theor* or concep* or logic)) OR AB ((theor* or concep* or logic) n1 (framework* or model* or analy* or evaluat*)) 183,949
-
S22 S12 AND S21 3341
-
S21 S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 588,974
-
S20 TI hospital* OR AB hospital* 443,811
-
S19 TI (inpatient or inpatients) OR AB (inpatient or inpatients) 50,179
-
S18 TI (((rehabilitation or geriatric) n1 (ward? or unit? or department?))) OR AB (((rehabilitation or geriatric) n1 (ward? or unit? or department?))) 4564
-
S17 TI (((acute or sub-acute or subacute) n3 (care or ward?))) OR AB (((acute or sub-acute or subacute) n3 (care or ward?))) 25,578
-
S16 (MH “Inpatients”) 81,879
-
S15 (MH “Hospital Units+”) 95,192
-
S14 (MH “Subacute Care”) OR (MH “Acute Care”) 9672
-
S13 (MH “Hospitalization”) 35,680
-
S12 S10 OR S11 11,240
-
S11 (MH “Morse Fall Scale”) OR (MH “Fall Risk Assessment Tool”) OR (MH “Fall Risk (Saba CCC)”) OR (MH “Fall Prevention (Iowa NIC)”) OR (MH “Hendrich Fall Risk Model”) OR (MH “Safety Behavior: Fall Prevention (Iowa NOC)”) 380
-
S10 S4 AND S9 11,097
-
S9 S5 OR S6 OR S7 OR S8 200,311
-
S8 (MH “Patient Safety”) 60,372
-
S7 TI ((fall* n3 (assess* or screen* or prevent* or predict*))) OR AB ((fall* n3 (assess* or screen* or prevent* or predict*))) 8089
-
S6 TI risk assess* OR AB risk assess* 47,861
-
S5 (MH “Risk Assessment”) 103,677
-
S4 S1 OR S2 OR S3 50,072
-
S3 TI (fall or falls or faller*) OR AB (fall or falls or faller*) 41,406
-
S2 (MH “Hip Fractures/PC”) 864
-
S1 (MH “Accidental Falls”) 22,724
HMIC Health Management Information Consortium (Ovid) <1983–present>
Date run: 22 July 2020
-
falling/ (563)
-
(fall or falls or faller*).tw. (2653)
-
1 or 2 (2745)
-
exp risk assessment/or risk management/or risks/ (5389)
-
risk assess*.tw. (1136)
-
(fall* adj3 (assess* or screen* or prevent* or predict*)).tw. (383)
-
accident prevention/or preventive measures/or safety measures/ (6726)
-
4 or 5 or 6 or 7 (12,379)
-
Commentaries/ (18)
-
Comment on”.ti. (29)
-
editorial.ti. (279)
-
letter.ti. (398)
-
Opinions/ (778)
-
opinion*.ti. (516)
-
Views/ (6902)
-
(view or views).ti. (3583)
-
(letter* adj3 editor*).ti. (1)
-
(evidence* adj8 (policy or policies)).tw. (1441)
-
policy/or health policy/or public policy/ (9125)
-
(policy or policies or guideline* or recommendation* or position).ti. (12,388)
-
(theor* or concep* or logic).ti. (2829)
-
((theor* or concep* or logic) adj (framework* or model* or analy* or evaluat*)).ab. (1897)
-
or/9-22 [Theories] (33,927)
-
3 and 8 and 23 [Falls AND Risks AND Theories] (30)
Ovid MEDLINE(R) and Epub Ahead of Print, In-process and Other Non-indexed Citations and Daily <1946 to 21 July 2020>
Date run: 22 July 2020
-
Accidental Falls/or exp Hip Fractures/pc (25,500)
-
(fall or falls or faller*).tw,kw. (147,448)
-
or/1-2 [falls] (156,010)
-
Risk Assessment/ (265,251)
-
risk assess*.tw,kw. (69,315)
-
(fall* adj3 (assess* or screen* or prevent* or predict*)).tw,kw. (10,733)
-
exp Accident Prevention/ (86,806)
-
or/4-7 [assessment or prevention] (391,875)
-
Hospitalization/ (107,412)
-
Subacute Care/ (1049)
-
Hospital Units/ (10,146)
-
exp Hospitals/ (274,581)
-
Rehabilitation Centers/ (8183)
-
Inpatients/ (21,949)
-
((acute or sub-acute or subacute) adj3 (care or ward?)).tw,kw. (31,737)
-
((rehabilitation or geriatric) adj (ward? or unit? or department?)).tw,kw. (6423)
-
inpatient?.tw,kw. (107,879)
-
hospital*.tw,kw. (1,294,309)
-
or/9-18 [hospital] (1,485,504)
-
3 and 8 and 19 [Fall assmt and prevention in hospitals] (3313)
-
(policy or policies or guideline* or recommendation* or position).ti. (209,315)
-
guideline/or practice guideline/ (34,299)
-
policy/or public policy/or exp health policy/ (138,961)
-
(theor* or concep* or logic).ti. (206,285)
-
((theor* or concep* or logic) adj (framework* or model* or analy* or evaluat*)).ab. (74,749)
-
or/21-25 [Policy, Guideline or overt Theory] (599,087)
-
Comment/ (861,900)
-
Letter/ (1,091,147)
-
Editorial/ (536,220)
-
news/or newspaper article/ (218,702)
-
“Comment on”.ti. (27,827)
-
(letter* adj3 editor*).ti. (17,425)
-
opinion*.ti. (15,543)
-
(view or views).ti. (54,684)
-
or/27-34 [Discussion papers Hidden Theory] (2,145,770)
-
26 or 35 [Theory Search] (2,683,132)
-
3 and 8 and 19 and 36 (177)
Search 1.2: key journal search
Relevant falls risk assessment articles and commentaries were searched for in the following key trade magazines or journals: Nursing Standard, Nursing Times, Pharmaceutical Journal, Health Service Journal. Databases covering these key journals were searched.
CINAHL (EBSCOhost) 1981–present
Date run: 22 July 2020
| # | Query | Results |
|---|---|---|
| S17 | S14 OR S16 | 168 |
| S16 | S12 AND S15 | 79 |
| S15 | JN nursing standard | 59,378 |
| S14 | S12 AND S13 | 89 |
| S13 | JN nursing times | 52,673 |
| S12 | S10 OR S11 | 11,240 |
| S11 | S4 AND S9 | 11,097 |
| S10 | (MH “Morse Fall Scale”) OR (MH “Fall Risk Assessment Tool”) OR (MH “Fall Risk (Saba CCC)”) OR (MH “Fall Prevention (Iowa NIC)”) OR (MH “Hendrich Fall Risk Model”) OR (MH “Safety Behavior: Fall Prevention (Iowa NOC)”) | 380 |
| S9 | S5 or S6 or S7 or S8 | 200,311 |
| S8 | (MH “Patient Safety”) | 60,372 |
| S7 | TI ((fall* n3 (assess* or screen* or prevent* or predict*))) OR AB ((fall* n3 (assess* or screen* or prevent* or predict*))) | 8089 |
| S6 | TI risk assess* OR AB risk assess* | 47,861 |
| S5 | (MH “Risk Assessment”) | 103,677 |
| S4 | S1 OR S2 or S3 | 50,072 |
| S3 | TI (fall or falls or faller*) OR AB (fall or falls or faller*) | 41,406 |
| S2 | (MH “Hip Fractures/PC”) | 864 |
| S1 | (MH “Accidental Falls”) | 22,724 |
EMBASE Classic + EMBASE (Ovid) <1947 to 21 July 2020>
Date run: 22 July 2020
-
(fall or falls or faller*).tw. (220,189)
-
falling/ (40,451)
-
1 or 2 (237,166)
-
risk assessment/ (567,038)
-
risk assess*.tw,kw. (97,678)
-
(fall* adj3 (assess* or screen* or prevent* or predict*)).tw,kw. (15,117)
-
accident prevention/ (17,289)
-
hip fracture/pc [Prevention] (2210)
-
4 or 5 or 6 or 7 or 8 (622,377)
-
3 and 9 (21,538)
-
pharmaceutical journal.jn. (21,130)
-
10 and 11 (10)
HMIC Health Management Information Consortium (Ovid) <1983–present>
Date run: 22 July 2020
-
falling/ (563)
-
(fall or falls or faller*).tw. (2653)
-
1 or 2 (2745)
-
exp risk assessment/or risk management/or risks/ (5389)
-
risk assess*.tw. (1136)
-
(fall* adj3 (assess* or screen* or prevent* or predict*)).tw. (383)
-
accident prevention/or preventive measures/or safety measures/ (6726)
-
4 or 5 or 6 or 7 (12,379)
-
health service* journal.jn. (13,050)
-
3 and 8 and 9 (10)
-
pharmaceutical journal.jn. (2407)
-
3 and 8 and 11 (4)
-
10 or 12 (14)
Ovid MEDLINE(R) and Epub Ahead of Print, In-process and Other Non-indexed Citations and Daily <1946 to 22 July 2020>
Date run: 22 July 2020
-
Accidental Falls/or exp Hip Fractures/pc (25,502)
-
(fall or falls or faller*).tw,kw. (147,405)
-
or/1-2 [falls] (155,967)
-
Risk Assessment/ (265,290)
-
risk assess*.tw,kw. (69,279)
-
(fall* adj3 (assess* or screen* or prevent* or predict*)).tw,kw. (10,727)
-
exp Accident Prevention/ (86,820)
-
or/4-7 [assessment or prevention] (391,878)
-
nursing time*.jn. (39,139)
-
3 and 8 and 9 (26)
-
nursing standard.jn. (35,276)
-
3 and 8 and 11 (33)
-
health service* journal.jn. (10,933)
-
3 and 8 and 13 (3)
-
10 or 12 or 14 (62)
Search 1.3: academic theory search
CINAHL (EBSCOhost) 1981–present
Date run: 22 July 2020
| # | Query | Results |
|---|---|---|
| S25 | S12 AND S21 AND S24 | 166 |
| S24 | S22 OR S23 | 188,189 |
| S23 | TI (Literature review* or systematic n2 review* or narrative n2 review* or critical n2 review* or scoping review* or synthesis or meta-analys* or “meta analysis” or realist n2 review*) OR AB (“Search filter*” or “search strateg*” or “literature search*”) | 149,311 |
| S22 | (MH “Systematic Review”) OR (MH “Literature Review”) OR (MH “Scoping Review”) OR (MH “Concept Analysis”) | 94,643 |
| S21 | S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 | 588,974 |
| S20 | (MH “Inpatients”) | 81,879 |
| S19 | (MH “Hospital Units+”) | 95,192 |
| S18 | (MH “Subacute Care”) OR (MH “Acute Care”) | 9672 |
| S17 | (MH “Hospitalization”) | 35,680 |
| S16 | TI hospital* OR AB hospital* | 443,811 |
| S15 | TI (inpatient or inpatients) OR AB (inpatient or inpatients) | 50,179 |
| S14 | TI (((rehabilitation or geriatric) n1 (ward? or unit? or department?))) OR AB (((rehabilitation or geriatric) n1 (ward? or unit? or department?))) | 4564 |
| S13 | TI (((acute or sub-acute or subacute) n3 (care or ward?))) OR AB (((acute or sub-acute or subacute) n3 (care or ward?))) | 25,578 |
| S12 | S10 OR S11 | 11,240 |
| S11 | (MH “Morse Fall Scale”) OR (MH “Fall Risk Assessment Tool”) OR (MH “Fall Risk (Saba CCC)”) OR (MH “Fall Prevention (Iowa NIC)”) OR (MH “Hendrich Fall Risk Model”) OR (MH “Safety Behavior: Fall Prevention (Iowa NOC)”) | 380 |
| S10 | S4 AND S9 | 11,097 |
| S9 | S5 OR S6 OR S7 OR S8 | 200,311 |
| S8 | (MH “Patient Safety”) | 60,372 |
| S7 | TI ((fall* n3 (assess* or screen* or prevent* or predict*))) OR AB ((fall* n3 (assess* or screen* or prevent* or predict*))) | 8089 |
| S6 | TI risk assess* OR AB risk assess* | 47,861 |
| S5 | (MH “Risk Assessment”) | 103,677 |
| S4 | S1 OR S2 OR S3 | 50,072 |
| S3 | TI (fall or falls or faller*) OR AB (fall or falls or faller*) | 41,406 |
| S2 | (MH “Hip Fractures/PC”) | 864 |
| S1 | (MH “Accidental Falls”) | 22,724 |
Cochrane Central Register of Controlled Trials (Wiley) Issue 7 of 12, July 2020
Date run: 22 July 2020
| ID | Search | Hits |
|---|---|---|
| #1 | MeSH descriptor: [Accidental Falls] this term only | 1447 |
| #2 | MeSH descriptor: [Hip Fractures] explode all trees and with qualifier(s): [prevention and control – PC] | 149 |
| #3 | (fall or falls or faller*):ti,ab,kw | 17,295 |
| #4 | #1 or #2 or #3 | 17,383 |
| #5 | MeSH descriptor: [Risk Assessment] this term only | 8650 |
| #6 | (risk assess*):ti,ab,kw | 100,689 |
| #7 | (fall* near/3 (assess* or screen* or prevent* or predict*)):ti,ab,kw | 2943 |
| #8 | MeSH descriptor: [Accident Prevention] explode all trees | 3928 |
| #9 | #5 or #6 or #7 or #8 | 106,001 |
| #10 | #4 and #9 | 4842 |
| #11 | MeSH descriptor: [Hospitalization] this term only | 5065 |
| #12 | MeSH descriptor: [Subacute Care] this term only | 16 |
| #13 | MeSH descriptor: [Hospital Units] this term only | 194 |
| #14 | MeSH descriptor: [Hospitals] explode all trees | 3555 |
| #15 | MeSH descriptor: [Rehabilitation Centers] this term only | 308 |
| #16 | MeSH descriptor: [Inpatients] this term only | 924 |
| #17 | ((acute or sub-acute or subacute) near/3 (care or ward?)):ti,ab,kw | 3091 |
| #18 | ((rehabilitation or geriatric) next (ward? or unit? or department?)):ti,ab,kw | 1226 |
| #19 | inpatient*:ti,ab,kw | 17,486 |
| #20 | hospital*:ti,ab,kw | 168,547 |
| #21 | 176-#20 | 177,578 |
| #22 | #4 and #9 and #21 | 1141 |
(CDSR = 114)
Epistemonikos (Epistemonikos Foundation) – all available dates
Date run: 22 July 2020
Title/Abstract: fall OR falls OR faller*
AND
Title/Abstract: “risk assessment” or “risk prevention” or “falls assessment” or “falls prevention”
AND
Title/Abstract: hospital* or inpatient* or ward or wards or acute
Limited: Systematic Reviews
49 hits
Database: HMIC Health Management Information Consortium (Ovid) <1983–present>
Date run: 22 July 2020
-
falling/ (563)
-
(fall or falls or faller*).tw. (2653)
-
1 or 2 (2745)
-
exp risk assessment/or risk management/or risks/ (5389)
-
risk assess*.tw. (1136)
-
(fall* adj3 (assess* or screen* or prevent* or predict*)).tw. (383)
-
accident prevention/or preventive measures/or safety measures/ (6726)
-
4 or 5 or 6 or 7 (12,379)
-
exp hospitals/ (15,398)
-
((acute or sub-acute or subacute) adj3 (care or ward?)).tw. (2677)
-
((rehabilitation or geriatric) adj (ward? or unit? or department?)).tw. (524)
-
inpatient?.tw. (3739)
-
hospital*.tw. (49,895)
-
or/9-13 [Acute Hosp Wards] (57,296)
-
3 and 8 and 14 (197)
-
systematic reviews/or literature reviews/or meta analysis/ (6695)
-
(Literature review* or (systematic adj2 review*) or (narrative adj2 review*) or (critical adj2 review*) or scoping review* or synthesis or meta-analys* or “meta analysis” or (realist adj2 review*)).ti. (4659)
-
(“Search filter*” or “search strateg*” or “literature search*”).ab. (1140)
-
or/16-18 [Systematic Reviews] (8438)
-
15 and 19 (13)
Ovid MEDLINE(R) and Epub Ahead of Print, In-process and Other Non-indexed
Citations and Daily <1946 to 21 July 2020>
Date run: 22 July 2020
-
Accidental Falls/or exp Hip Fractures/pc (25,500)
-
(fall or falls or faller*).tw,kw. (147,448)
-
or/1-2 [falls] (156,010)
-
Risk Assessment/ (265,251)
-
risk assess*.tw,kw. (69,315)
-
(fall* adj3 (assess* or screen* or prevent* or predict*)).tw,kw. (10,733)
-
exp Accident Prevention/ (86,806)
-
or/4-7 [assessment or prevention] (391,875)
-
Hospitalization/ (107,412)
-
Subacute Care/ (1049)
-
Hospital Units/ (10,146)
-
exp Hospitals/ (274,581)
-
Rehabilitation Centers/ (8183)
-
Inpatients/ (21,949)
-
((acute or sub-acute or subacute) adj3 (care or ward?)).tw,kw. (31,737)
-
((rehabilitation or geriatric) adj (ward? or unit? or department?)).tw,kw. (6423)
-
inpatient?.tw,kw. (107,879)
-
hospital*.tw,kw. (1,294,309)
-
or/9-18 [hospital] (1,485,504)
-
3 and 8 and 19 [Fall assmt and prevention in hospitals] (3313)
-
meta-analysis/ or “systematic review”/ (194,072)
-
(Literature review* or (systematic adj2 review*) or (narrative adj2 review*) or (critical adj2 review*) or scoping review* or synthesis or meta-analys* or “meta analysis” or (realist adj2 review*)).ti. (551,543)
-
(“Search filter*” or “search strateg*” or “literature search*”).ab. (66,610)
-
or/21-23 [Systematic reviews] (635,237)
-
20 and 24 (139)
PROSPERO International prospective register of systematic reviews (NIHR) – all available dates
Date run: 22 July 2020
Title only search: (falls or fall or faller*) and (risk or assess*)
62 hits
International HTA Database (INAHTA) – all available dates
Date run: 23 July 2020
| 17 | #16 AND #8 AND #7 | 21 |
| 16 | #15 OR #14 OR #13 OR #12 OR #11 OR #10 OR #9 | 1791 |
| 15 | (hospital* OR inpatient* or ward or wards or acute)[Title] OR (hospital* OR inpatient* or ward or wards or acute)[abs] | 1760 |
| 14 | “Inpatients”[mh] | 42 |
| 13 | “Rehabilitation Centers”[mh] | 10 |
| 12 | “Hospital Units”[mh] | 7 |
| 11 | “Subacute Care”[mh] | 0 |
| 10 | “Hospitals”[mhe] | 64 |
| 9 | “Hospitalization”[mh] | 28 |
| 8 | #6 OR #5 OR #4 OR #3 | 803 |
| 7 | #2 OR #1 | 103 |
| 6 | “Accident Prevention”[mhe] | 97 |
| 5 | (fall* AND (assess* or screen* or prevent* or predict*))[Title] OR (fall* AND (assess* or screen* or prevent* or predict*))[abs] | 72 |
| 4 | “Risk Assessment”[mh] | 102 |
| 3 | (risk assess*)[Title] OR (risk assess*)[abs] | 609 |
| 2 | (fall or falls or faller*)[Title] OR (fall or falls or faller*)[abs] | 102 |
| 1 | “Accidental Falls”[mh] | 18 |
Appendix 2 Theory testing searches
This appendix reports the final search strategies used for all databases searched for stage 2 of the realist review.
-
Search 2.1: EMBASE scoping search of six theories
-
Search 2.2: multiple database search of four theories
-
Search 2.3: update search of two prioritised theories.
The purpose of these searches was to identify the literature that could provide evidence to support, refute, or refine our chosen theories. The first search scoped six potential CMOcs identified by the project team. This search was conducted in EMBASE only to gauge the size of the relevant literature in each of the six proposed CMOcs and refine the search before translating into other databases.
The CMOc list was refined into four search questions for search 2.2 and run in multiple databases (Table 22). The final search (2.3) updated the two theories (CMOcs) that had been prioritised for full review.
| Search name and scope | Search date | Databases searched |
|---|---|---|
| 2.1 6 theories: Leadership Staff training/empowerment Assessment tools/health information technologies Patient-centred care Staff expertise Shared responsibility/teamwork |
2 March 2021 | EMBASE <1996 to 2021 Week 08> |
| 2.2 4 theories: Leadership Facilitation Patient partnership Shared responsibility |
6 May 2021 and 7 May 2021 | CINAHL (EBSCOhost) EMBASE Classic + EMBASE (Ovid) 1947 to 5 May 2021 Ovid MEDLINE(R) ALL 1946 to 5 May 2021 Arts and Humanities Citation Index (Web of Science) 1975+ Conference Proceedings Citation Index – Science (Web of Science) 1990+ Conference Proceedings Citation Index – Social Science and Humanities (Web of Science) 1990+ Science Citation Index-Expanded (Web of Science) 1900+ Social Sciences Citation Index (Web of Science) 1900+ Emerging Sources Citation Index (Web of Science) 2015+ NICE Evidence www.evidence.nhs.uk/ |
| 2.3 2 prioritised theories: Facilitation Patient partnership |
1 August 2022 | CINAHL (EBSCOhost) EMBASE Classic + EMBASE (Ovid) 1947 to 29 July 2022 Ovid MEDLINE(R) ALL 1946 to 29 July 2022 Arts and Humanities Citation Index (Web of Science) 1975+ Conference Proceedings Citation Index – Science (Web of Science) 1990+ Conference Proceedings Citation Index – Social Science and Humanities (Web of Science) 1990+ Science Citation Index-Expanded (Web of Science) 1900+ Social Sciences Citation Index (Web of Science) 1900+ Emerging Sources Citation Index (Web of Science) 2015+ |
Subject headings and free-text words were identified for use in the search concepts for all searches by the Information Specialist and project team members. The searches were peer reviewed by an Information Specialist.
Table 22 summarises the three searches and the order of searches.
Search 2.1: EMBASE scoping search of six theories
EMBASE (Ovid) 1996–2021 Week 8
Search date: 2 March 2021
Records found: 1358 in total from download of six search lines (lines 40, 53, 64, 76, 86, 96). These were deduplicated to leave 970 records in the EndNote Library
Search strategy:
---------------- --------------- ---------- ------------ ------------- --------------
-
hospitalization/ (380,692)
-
hospital department/or exp ward/ (394,030)
-
exp hospital/ (1,060,104)
-
medical staff/ (30,743)
-
nursing staff/ (53,204)
-
rehabilitation center/ (13,386)
-
subacute care/ (1105)
-
exp clinical handover/or collaborative care team/or exp rapid response team/ (10,875)
-
exp hospital patient/ (184,493)
-
((acute or sub-acute or subacute) adj3 (care or ward?)).tw,kw. (45,721)
-
((rehabilitation or geriatric) adj (ward? or unit? or department?)).tw,kw. (10,024)
-
inpatient?.tw,kw. (176,834)
-
(acute adj5 patient?).tw,kw. (302,957)
-
hospital*.tw,kw. (1,829,684)
-
or/1-14 [hospital] (2,688,257)
-
*falling/ (11,365)
-
falling/pc (2719)
-
(fall? adj2 (assess* or risk? or prevent* or reduc* or occur* or frequenc* or screen)).tw,kw. (22,530)
-
or/16-18 [Falls prevention or risk assessment] (28,603)
-
implement*.tw,kw. (672,165)
-
(sustain* adj4 (program* or practice* or intervention?)).tw,kw. (13,916)
-
Adopt*.tw,kw./freq=2 (44,117)
-
Adopt*.ti. (16,283)
-
deliver*.tw,kw./freq=2 (336,819)
-
(adher* or comply or complian*).tw,kw. (452,974)
-
fidelity.tw,kw. (32,350)
-
implementation science/ (1734)
-
exp protocol compliance/ (15,146)
-
*health care planning/ (21,195)
-
*practice guideline/ (77,969)
-
or/20-30 [Implementation or Adherence to Guidelines and strategies] (1,538,880)
-
15 and 19 and 31 [Implementation AND Falls Prevention AND Hospitals] (1542)
-
leadership/ (67,428)
-
total quality management/ (69,290)
-
leader*.tw,kw. (86,965)
-
champion*.tw,kw. (9647)
-
(organi#ation* adj3 (support* or strateg*)).tw,kw. (11,289)
-
exp *“organization and management”/ (410,957)
-
or/33-38 [Leadership] (558,040)
-
32 and 39 [Leadership Falls Implementation Hospitals] (371)
-
staff training/ (13,513)
-
continuing education/ (28,691)
-
*medical education/ (75,344)
-
*nursing education/ (29,715)
-
(training* adj3 (staff or professional? or nurs* or doctor? or clinical or medical or clinician?)).tw,kw. (56,356)
-
(educat* adj3 (staff or professional? or nurs* or doctor? or clinical or medical or clinician?)).tw,kw. (125,827)
-
(empower* adj3 (staff or professional? or nurs* or doctor? or clinician?)).tw,kw. (2807)
-
(accountab* adj3 (staff or professional? or nurs* or doctor? or clinician?)).tw,kw. (976)
-
(responsib* adj3 (staff or professional? or nurs* or doctor? or clinician?)).tw,kw. (9080)
-
((fedback* or feedback* or fed-back* or feed-back*) adj3 (staff or professional? or nurs* or doctor? or clinician?)).tw,kw. (3902)
-
empowerment/ (10,465)
-
or/41-51 [Staff training and empowerment] (289,563)
-
32 and 52 [Staff training Empowerment and Falls Implementation Hospitals] (182)
-
clinical assessment tool/ (24,623)
-
(assess* adj4 tool?).tw,kw. (89,900)
-
(electronic adj2 record?).tw,kw. (80,127)
-
*fall risk assessment/ (588)
-
medical informatics/ or nursing informatics/ (21,855)
-
exp hospital information system/ (20,817)
-
exp information technology device/ (133,716)
-
(information adj3 (technolog* or system or computeri* or electronic)).tw,kw. (62,537)
-
digital*.tw,kw. (169,019)
-
or/54-62 [Assessment tools or health info technology] (552,944)
-
32 and 63 [Assessment Tools or HIT and Falls Implementation Hospitals] (261)
-
(fall* adj6 (decreas* or declin* or reduc* or lower* or fewer or less*)).tw,kw. [REDUCTION in falls] (17,691)
-
patient care/ (282,843)
-
shared medical appointment/ (126)
-
(patient? adj2 (centred or centered)).tw,kw. (35,234)
-
(patient? adj5 perspective?).tw,kw. (31,276)
-
(patient? adj4 need?).tw,kw. (109,033)
-
patient participation/ (26,089)
-
(engag* adj3 (patient? or famil* or carer? or caregiver? or player*)).tw,kw. (18,827)
-
(multifacet* or multi-facet* or tailor*).tw,kw. (154,544)
-
or/66-73 [Patient Centred Care] (604,660)
-
15 and 19 and 74 [Patient Centred Care Falls Acute Hospital] (799)
-
15 and 19 and 65 and 74 [Patient Centred and Hospitals and Falls Reduction] (307)
-
medical expert/ (12,634)
-
expert nurse/ (198)
-
nursing expertise/ (179)
-
expert*.tw,kw. (278,203)
-
(experienced adj3 (staff or professional? or nurs* or doctor? or clinician? or physiotherapis? or pharmacist?)).tw,kw. (11,376)
-
champion?.tw,kw. (6814)
-
(specialist? adj2 (fall? or nurse)).tw,kw. (7782)
-
or/77-83 [Expertise] (306,887)
-
15 and 19 and 84 [Expertise and Falls Acute Hospital] (259)
-
15 and 19 and 65 and 84 [Expertise and Hospitals and Falls Reduction] (95)
-
multidisciplinary team/or collaborative care team/ (11,349)
-
((share* or sharing) adj3 (responsibility or responsible or accountability or accountable)).tw,kw. (2621)
-
collaborat*.tw,kw./freq=2 (46,785)
-
(team* adj3 (share* or sharing or communic*)).tw,kw. (7307)
-
(team* adj3 (multidisciplin* or interdisciplin* or multi-disciplin* or inter-disciplin* or interprofessional* or inter-professional*)).tw,kw. (58,028)
-
cooperation/or teamwork/ (58,992)
-
public relations/ (39,835)
-
or/87-93 [Team collaboration] (192,129)
-
15 and 19 and 94 [Teams and Falls Acute Hospital] (332)
-
15 and 19 and 65 and 94 [Teams and Hospitals and Falls Reduction] (142)
Search 2.2: multiple database search of four theories
Leadership
CINAHL (EBSCOhost)
Search date: 6 May 2021
Records found: 122
| # | Query | Results |
|---|---|---|
| S31 | S12 AND S15 AND S21 AND S25 AND S30 | 122 |
| S30 | S26 OR S27 OR S28 OR S29 | 245,878 |
| S29 | TI ((risk n2 (assess* or evaluat*)) or guideline* or protocol*) AND AB ((risk n2 (assess* or evaluat*)) or guideline* or protocol*) | 33,732 |
| S28 | (MH “Protocols+”) | 42,099 |
| S27 | (MH “Practice Guidelines”) | 81,201 |
| S26 | (MH “Risk Assessment”) | 114,437 |
| S25 | S22 OR S23 OR S24 | 686,998 |
| S24 | TI (leader* or champion* or facilitator* or (organi#ation* n3 (support* or strateg*)) or ((quality or safety or nurse* or matron) n3 lead*)) OR AB (leader* or champion* or facilitator* or (organi#ation* n3 (support* or strateg*)) or ((quality or safety or nurse* or matron*) n3 lead*)) | 96,386 |
| S23 | (MH “Quality Management, Organizational”) OR (MM “Management+”) | 603,390 |
| S22 | (MH “Leadership”) | 44,897 |
| S21 | S16 OR S17 OR S18 OR S19 OR S20 | 384,391 |
| S20 | (MH “Guideline Adherence”) | 15,898 |
| S19 | (MH “Systems Implementation”) OR (MH “Program Implementation”) OR (MH “Implementation Science”) | 30,900 |
| S18 | TI (engage* or “buy in” or (Cognitive n2 participat*)) OR AB (“buy in” or (Cognitive n2 participat*)) | 16,158 |
| S17 | TI (sustain* n4 (program* or practice or practices or intervention or interventions)) OR AB (sustain* n4 (program* or practice or practices or intervention or interventions)) 6822 | |
| S16 | TI (implement* or adopt* or deliver* or adher* or comply or complian* or fidelity) OR AB (implement* or adher* or comply or complian* or fidelity) | 344,120 |
| S15 | S13 OR S14 | 18,729 |
| S14 | TI (fall* n2 (assess* or risk* or prevent* or reduc* or occur* or frequen* or screen*)) OR AB (fall* n2 (assess* or risk* or prevent* or reduc* or occur* or frequen* or screen*)) 14,235 | |
| S13 | (MH “Accidental Falls/PC”) | 10,323 |
| S12 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 829,664 | |
| S11 | (MH “Multidisciplinary Care Team+”) | 46,811 |
| S10 | (MH “Medical Staff, Hospital+”) OR (MH “Nursing Staff, Hospital”) | 27,035 |
| S9 | (MH “Hospitals+”) | 121,072 |
| S8 | (MH “Hospital Units”) OR (MH “Rehabilitation Centers”) | 15,793 |
| S7 | (MH “Inpatients”) | 83,955 |
| S6 | (MH “Subacute Care”) OR (MH “Acute Care”) | 10,376 |
| S5 | (MH “Hospitalization”) | 38,763 |
| S4 | TI hospital* OR AB hospital* | 476,803 |
| S3 | TI (inpatient or inpatients) OR AB (inpatient or inpatients) | 54,348 |
| S2 | TI (((rehabilitation or geriatric) n1 (ward? or unit? or department?))) OR AB (((rehabilitation or geriatric) n1 (ward? or unit? or department?))) | 4834 |
| S1 | TI (((acute or sub-acute or subacute) n3 (care or ward?))) OR AB (((acute or sub-acute or subacute or patient*) n3 (care or ward? or patient*))) | 258,661 |
EMBASE Classic + EMBASE (Ovid) 1947 to 5 May 2021
Search date: 6 May 2021
Records found: 187
----------- ------------ -------------- ----------- ----------- -------- -------------
-
hospitalization/ (420,992)
-
hospital department/or exp ward/ (439,715)
-
exp hospital/ (1,302,934)
-
medical staff/ (40,310)
-
nursing staff/ (74,427)
-
rehabilitation center/ (17,387)
-
subacute care/ (1151)
-
exp clinical handover/ or collaborative care team/ or exp rapid response team/ (11,414)
-
exp hospital patient/ (199,241)
-
((acute or sub-acute or subacute) adj3 (care or ward?)).tw,kw. (51,102)
-
((rehabilitation or geriatric) adj (ward? or unit? or department?)).tw,kw. (12,324)
-
inpatient?.tw,kw. (199,814)
-
(acute adj5 patient?).tw,kw. (369,927)
-
hospital*.tw,kw. (2,200,719)
-
or/1-14 [hospital] (3,282,770)
-
*falling/ (12,578)
-
falling/pc (2954)
-
(fall? adj2 (assess* or risk? or prevent* or reduc* or occur* or frequen* or screen*)).tw,kw. (25,940)
-
or/16-18 [Falls prevention or risk assessment] (32,853)
-
implement*.tw,kw. (724,768)
-
(sustain* adj4 (program* or practice* or intervention?)).tw,kw. (14,660)
-
Adopt*.tw,kw./freq=2 (49,567)
-
Adopt*.ti. (20,665)
-
deliver*.tw,kw./freq=2 (374,349)
-
deliver*.ti. (176,933)
-
(adher* or comply or complian*).tw,kw. (526,988)
-
fidelity.tw,kw. (35,433)
-
implementation science/ (1982)
-
exp protocol compliance/ (15,723)
-
engage*.ti. (20,887)
-
engage*.tw,kw./freq=2 (52,149)
-
(intervention adj2 deliver*).tw,kw. (7304)
-
(Cognitive adj2 participat*).tw,kw. (729)
-
“buy in”.tw,kw. (2788)
-
or/20-34 [Implementation or Adherence to Guidelines and strategies] (1,730,025)
-
leadership/ (76,777)
-
total quality management/ (72,191)
-
leader*.tw,kw. (102,125)
-
champion*.tw,kw. (10,691)
-
(organi#ation* adj3 (support* or strateg*)).tw,kw. (12,500)
-
exp *“organization and management”/ (577,268)
-
facilitator*.ti. (6305)
-
facilitat*.tw,kw./freq=2 (94,889)
-
((quality or safety or nurse* or matron*) adj3 lead*).tw,kw. (13,991)
-
or/36-44 [Leaderships] (841,009)
-
risk assessment/ (618,392)
-
(risk adj2 (assess* or evaluat*)).tw,kw. (196,115)
-
exp practice guideline/ (601,575)
-
guideline*.tw,kw. (613,857)
-
exp clinical protocol/ (106,751)
-
protocol?.tw,kw./freq=2 (185,559)
-
protocol?.ti. (86,947)
-
or/46-52 [Multifactorial risk assessment] (1,767,880)
-
15 and 19 and 35 and 45 and 53 [Leadership CMO1 – final] (187)
Ovid MEDLINE(R) ALL 1946 to 5 May 2021
Search date: 6 May 2021
Records found: 145
-
Hospitalization/ (115,592)
-
Subacute Care/ (1169)
-
Hospital Units/ (10,319)
-
exp Hospitals/ (284,007)
-
medical staff, hospital/ or nursing staff, hospital/ (66,506)
-
exp Patient Care Team/ (70,042)
-
Rehabilitation Centers/ (8356)
-
Inpatients/ (23,637)
-
((acute or sub-acute or subacute) adj3 (care or ward?)).tw,kf. (34,662)
-
((rehabilitation or geriatric) adj (ward? or unit? or department?)).tw,kf. (6803)
-
(acute adj5 patient?).tw,kf. (227,174)
-
inpatient?.tw,kf. (116,838)
-
hospital*.tw,kf. (1,383,898)
-
or/1-13 [hospital] (1,835,443)
-
Accidental Falls/pc [Prevention and Control] (9549)
-
(fall? adj2 (assess* or risk? or prevent* or reduc* or occur* or frequen* or screen*)).tw,kf. (17,142)
-
15 or 16 [Falls] (21,139)
-
implement*.tw,kf. (545,160)
-
(sustain* adj4 (program* or practice* or intervention?)).tw,kf. (11,220)
-
Adopt*.tw,kf./freq=2 (37,248)
-
Adopt*.ti. (16,394)
-
deliver*.tw,kf./freq=2 (258,583)
-
deliver*.ti. (137,239)
-
(adher* or comply or complian*).tw,kf. (343,916)
-
fidelity.tw,kf. (30,445)
-
Health Plan Implementation/ (6379)
-
implementation science/ or technology transfer/ (2784)
-
Guideline Adherence/ (33,374)
-
engage*.tw,kf./freq=2 (39,474)
-
engage*.ti. (17,196)
-
(intervention adj2 deliver*).tw,kf. (5693)
-
(Cognitive adj2 participat*).tw,kf. (547)
-
“buy in”.tw,kf. (1792)
-
or/18-33 [Implementation or Adherence to Guidelines and strategies] (1,263,268)
-
Leadership/ (42,613)
-
Total Quality Management/ (12,588)
-
exp *“organization and administration”/ (729,180)
-
leader*.tw,kf. (83,493)
-
champion*.tw,kf. (7722)
-
(organi#ation* adj3 (support* or strateg*)).tw,kf. (10,007)
-
facilitator*.ti. (5290)
-
facilitat*.tw,kf./freq=2 (72,113)
-
((quality or safety or nurse* or matron*) adj3 lead*).tw,kf. (10,657)
-
35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 [Leadership] (899,951)
-
exp Risk Assessment/ (284,216)
-
(risk adj2 (assess* or evaluat*)).tw,kf. (137,873)
-
guideline/ or practice guideline/ (35,660)
-
guideline*.tw,kf. (386,469)
-
protocol?.tw,kf./freq=2 (126,031)
-
protocol?.ti. (69,596)
-
exp Clinical Protocols/ (174,448)
-
or/45-51 [Multifactorial risk assessment] (1,055,597)
-
14 and 17 and 34 and 44 and 52 [Leadership CMO1 final] (145)
NICE Evidence
Search date: 7 May 2021
Records found: 53
(“falls prevention” or “falls assessment” or “falls reduction”) and (hospital or inpatient or “acute care” or “acute ward” or “acute patient” or “rehabilitation unit” or “rehabilitation ward”) and (leadership or champions) and (“risk assessment” or “risk evaluation” or “evaluation of risk”)
Sorted by Relevance.| Sort by Date
Filters applied:
Evidence type: Evidence Summaries
Evidence type: Primary Research
Evidence type: Systematic Reviews
Evidence type: Audit and Inspection Reports
Evidence type: Health Technology Assessments
Web of Science Core Collection Databases available at the University of Leeds (searched simultaneously):
Arts and Humanities Citation Index (Web of Science) 1975–present
Conference Proceedings Citation Index- Science (Web of Science) 1990–present
Conference Proceedings Citation Index- Social Science and Humanities (Web of Science) 1990–present
Science Citation Index-Expanded (Web of Science) 1900–present
Social Sciences Citation Index (Web of Science) 1900–present
Emerging Sources Citation Index (Web of Science) 2015–present
Search date: 6 May 2021
Records found: 38
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, ESCI Timespan=1900–2021
| # 18 | 38 | #17 AND #14 AND #10 AND #6 AND #5 |
| # 17 | 1,540,383 | #16 OR #15 |
| # 16 | 1,297,929 | TOPIC: (guideline* or protocol*) |
| # 15 | 267,027 | TOPIC: (risk near/2 (assess* or evaluat*)) |
| # 14 | 327,496 | #13 OR #12 OR #11 |
| # 13 | 22,680 | TS=((quality or safety or nurse* or matron*) near/3 lead*) |
| # 12 | 37,727 | TOPIC: (organi?ation* near/3 (support* or strateg*)) |
| # 11 | 279,723 | TOPIC: (leader* or champion* or facilitator*) |
| # 10 | 2,790,544 | #9 OR #8 OR #7 |
| # 9 | 30,806 | TOPIC: (sustain* near/4 (program* or practice* or intervention$)) |
| # 8 | 296,045 | TI=(adopt* or deliver* or engage*) |
| # 7 | 2,495,757 | TS=(implement* or adher* or comply or complian* or fidelity or “buy in” or (Cognitive near/2 participat*)) |
| # 6 | 28,251 | TS=(fall$ near/2 (assess* or risk$ or prevent* or reduc* or occur* or frequen* or screen*)) |
| # 5 | 1,439,343 | #4 OR #3 OR #2 OR #1 |
| # 4 | 225,361 | TOPIC: (acute near/5 patient$) |
| # 3 | 7518 | TOPIC: ((rehabilitation or geriatric) near/1 (ward$ or unit$ or department$)) |
| # 2 | 35,941 | TOPIC: ((acute or sub-acute or subacute) near/3 (care or ward$)) |
| # 1 | 1,254,128 | TOPIC: (hospital* OR inpatient*) |
Facilitation
CINAHL (EBSCOhost)
Search date: 6 May 2021
Records found: 32
| S39 | S12 AND S15 AND S21 AND S34 AND S38 | 32 |
| S38 | S35 OR S36 OR S37 | 260,284 |
| S37 | TI ((facilitation or workflow* or work-flow* or embed* or integrat* or routine* or routini* or “system* fit*”)) OR AB ((facilitation or workflow* or work-flow* or embed* or integrat* or routine* or routini* or “system* fit*”)) | 252,176 |
| S36 | (MH “Health Care Delivery, Integrated”) | 12,531 |
| S35 | (MH “Systems Integration”) OR (MH “Workflow”) | 4610 |
| S34 | S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 | 423,968 |
| S33 | (MH “Information Technology+”) | 18,859 |
| S32 | (MH “Medical Informatics”) OR (MH “Nursing Informatics”) OR (MH “Health Informatics”) | 12,075 |
| S31 | (MH “Clinical Information Systems+”) OR (MH “Health Information Systems+”) OR (MH “Hospital Information Systems”) OR (MH “Nursing Information Systems+”) OR (MH “Patient Record Systems+”) OR (MH “Health Information Networks”) OR (MH “Decision Support Systems, Clinical”) | 59,097 |
| S30 | TI “clinic* decision* support system*” OR AB “clinic* decision* support system*” | 1098 |
| S29 | TI (electronic* n3 nurs* n3 document*) OR AB (electronic* n3 nurs* n3 document*) | 182 |
| S28 | TI (risk* n3 screen* n3 tool*) OR AB (risk* n3 screen* n3 tool*) | 674 |
| S27 | TI ((“risk assess*” n4 (bundle* or instrument* or care plan* or multi-factorial or multifactorial))) OR AB ((“risk assess*” n4 (bundle* or instrument* or care plan* or multi-factorial or multifactorial))) | 380 |
| S26 | TI ((information n3 (technolog* or system or computeri* or electronic))) OR AB ((information n3 (technolog* or system or computeri* or electronic))) | 29,460 |
| S25 | TI ((electronic n2 record*) or digital*) OR AB ((electronic n2 record*) or digital*) | 66,503 |
| S24 | (MH “Clinical Assessment Tools+”) | 252,835 |
| S23 | TI (assess* n4 tool*) OR AB (assess* n4 tool*) | 31,239 |
| S22 | (MH “Fall Risk Assessment Tool”) | 164 |
| S21 | S16 OR S17 OR S18 OR S19 OR S20 | 384,391 |
| S20 | (MH “Guideline Adherence”) | 15,898 |
| S19 | (MH “Systems Implementation”) OR (MH “Program Implementation”) OR (MH “Implementation Science”) | 30,900 |
| S18 | TI (engage* or “buy in” or (Cognitive n2 participat*)) OR AB (“buy in” or (Cognitive n2 participat*)) | 16,158 |
| S17 | TI (sustain* n4 (program* or practice or practices or intervention or interventions)) OR AB (sustain* n4 (program* or practice or practices or intervention or interventions)) | 6822 |
| S16 | TI (implement* or adopt* or deliver* or adher* or comply or complian* or fidelity) OR AB (implement* or adher* or comply or complian* or fidelity) | 344,120 |
| S15 | S13 OR S14 | 18,729 |
| S14 | TI (fall* n2 (assess* or risk* or prevent* or reduc* or occur* or frequen* or screen*)) OR AB (fall* n2 (assess* or risk* or prevent* or reduc* or occur* or frequen* or screen*)) | 14,235 |
| S13 | (MH “Accidental Falls/PC”) | 10,323 |
| S12 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 | 704,077 |
| S11 | (MH “Multidisciplinary Care Team+”) | 46,811 |
| S10 | (MH “Medical Staff, Hospital+”) OR (MH “Nursing Staff, Hospital”) | 27,035 |
| S9 | (MH “Hospitals+”) | 121,072 |
| S8 | (MH “Hospital Units”) OR (MH “Rehabilitation Centers”) | 15,793 |
| S7 | (MH “Inpatients”) | 83,955 |
| S6 | (MH “Subacute Care”) OR (MH “Acute Care”) | 10,376 |
| S5 | (MH “Hospitalization”) | 38,763 |
| S4 | TI hospital* OR AB hospital* | 476,803 |
| S3 | TI (inpatient or inpatients) OR AB (inpatient or inpatients) | 54,348 |
| S2 | TI (((rehabilitation or geriatric) n1 (ward? or unit? or department?))) OR AB (((rehabilitation or geriatric) n1 (ward? or unit? or department?))) | 4834 |
| S1 | TI (((acute or sub-acute or subacute) n3 (care or ward* or patient*))) OR AB (((acute or sub-acute or subacute) n3 (care or ward* or patient*))) | 73,897 |
EMBASE Classic + EMBASE (Ovid) 1947 to 5 May 2021
Search date: 6 May 2021
Records found: 45
EMBASE Classic + EMBASE <1947 to 5 May 2021>
Search strategy:
---------- ------------ ------------ ---------- -------------- ----------- -----------
-
hospitalization/ (420,992)
-
hospital department/ or exp ward/ (439,715)
-
exp hospital/ (1,302,934)
-
medical staff/ (40,310)
-
nursing staff/ (74,427)
-
rehabilitation center/ (17,387)
-
subacute care/ (1151)
-
exp clinical handover/ or collaborative care team/ or exp rapid response team/ (11,414)
-
exp hospital patient/ (199,241)
-
((acute or sub-acute or subacute) adj3 (care or ward?)).tw,kw. (51,102)
-
((rehabilitation or geriatric) adj (ward? or unit? or department?)).tw,kw. (12,324)
-
inpatient?.tw,kw. (199,814)
-
(acute adj5 patient?).tw,kw. (369,927)
-
hospital*.tw,kw. (2,200,719)
-
or/1-14 [hospital] (3,282,770)
-
*falling/ (12,578)
-
falling/pc (2954)
-
(fall? adj2 (assess* or risk? or prevent* or reduc* or occur* or frequen* or screen*)).tw,kw. (25,940)
-
or/16-18 [Falls prevention or risk assessment] (32,853)
-
implement*.tw,kw. (724,768)
-
(sustain* adj4 (program* or practice* or intervention?)).tw,kw. (14,660)
-
Adopt*.tw,kw./freq=2 (49,567)
-
Adopt*.ti. (20,665)
-
deliver*.tw,kw./freq=2 (374,349)
-
(adher* or comply or complian*).tw,kw. (526,988)
-
fidelity.tw,kw. (35,433)
-
implementation science/ (1982)
-
exp protocol compliance/ (15,723)
-
engagement.tw,kw. (97,441)
-
engage*.tw,kw./freq=2 (52,149)
-
(intervention adj2 deliver*).tw,kw. (7304)
-
(Cognitive adj2 participat*).tw,kw. (729)
-
“buy in”.tw,kw. (2788)
-
or/20-33 [Engagement or Implementation] (1,725,436)
-
clinical assessment tool/ (25,003)
-
(assess* adj4 tool?).tw,kw. (94,602)
-
(electronic adj2 record?).tw,kw. (83,628)
-
*fall risk assessment/ (605)
-
medical informatics/or nursing informatics/ (23,031)
-
exp hospital information system/ (25,135)
-
exp information technology device/ (201,010)
-
(information adj3 (technolog* or system or computeri* or electronic)).tw,kw. (70,350)
-
digital*.tw,kw. (211,640)
-
(“risk assess*” adj4 (bundle* or instrument* or care plan*)).tw,kw. (604)
-
((multi-factorial or multifactorial) adj4 risk assessment*).tw,kw. (130)
-
(risk* adj3 screen* adj3 tool*).tw,kw. (1181)
-
clinical decision support system/ (3800)
-
clinic* decision* support system*.tw,kw. (3087)
-
health information management.tw,kw. (909)
-
medical information system/or bedside information system/ (22,022)
-
(electronic* adj3 nurs* adj3 document*).tw,kw. (137)
-
or/35-51 [Assessment tools including health info technology] (692,085)
-
workflow/ (26,854)
-
integration/ (6459)
-
data integration/ (544)
-
facilitation.tw,kw. (39,629)
-
(workflow* or work-flow*).tw,kw. (43,560)
-
system? fit*.tw,kw. (459)
-
Embed*.tw,kw. (176,919)
-
integrat*.tw,kw. (705,509)
-
(routine* or routini*).tw,kw. (628,385)
-
or/53-61 [Workflows concept] (1,543,566)
-
15 and 19 and 34 and 52 and 62 [HIT tools CMO4 – final] (45)
Ovid MEDLINE(R) ALL 1946 to 5 May 2021
Search date: 6 May 2021
Records found: 30
Ovid MEDLINE(R) ALL <1946 to 5 May 2021>
Search strategy:
--------- ----------- ----------- ---------- ------------ ------------- --------------
-
Hospitalization/ (115,592)
-
Subacute Care/ (1169)
-
Hospital Units/ (10,319)
-
exp Hospitals/ (284,007)
-
medical staff, hospital/or nursing staff, hospital/ (66,506)
-
exp Patient Care Team/ (70,042)
-
Rehabilitation Centers/ (8356)
-
Inpatients/ (23,637)
-
((acute or sub-acute or subacute) adj3 (care or ward?)).tw,kf. (34,662)
-
((rehabilitation or geriatric) adj (ward? or unit? or department?)).tw,kf. (6803)
-
(acute adj5 patient?).tw,kf. (227,174)
-
inpatient?.tw,kf. (116,838)
-
hospital*.tw,kf. (1,383,898)
-
or/1-13 [hospital] (1,835,443)
-
Accidental Falls/pc [Prevention and Control] (9549)
-
(fall? adj2 (assess* or risk? or prevent* or reduc* or occur* or frequen* or screen*)).tw,kf. (17,142)
-
15 or 16 [Falls] (21,139)
-
implement*.tw,kf. (545,160)
-
(sustain* adj4 (program* or practice* or intervention?)).tw,kf. (11,220)
-
Adopt*.tw,kf./freq=2 (37,248)
-
Adopt*.ti. (16,394)
-
deliver*.tw,kf./freq=2 (258,583)
-
deliver*.ti. (137,239)
-
(adher* or comply or complian*).tw,kf. (343,916)
-
fidelity.tw,kf. (30,445)
-
Health Plan Implementation/ (6379)
-
implementation science/or technology transfer/ (2784)
-
Guideline Adherence/ (33,374)
-
engage*.tw,kf./freq=2 (39,474)
-
engage*.ti. (17,196)
-
(intervention adj2 deliver*).tw,kf. (5693)
-
(Cognitive adj2 participat*).tw,kf. (547)
-
“buy in”.tw,kf. (1792)
-
or/18-33 [Implementation or Adherence to Guidelines and strategies] (1,263,268)
-
Risk Assessment/mt [Methods] (34,919)
-
(assess* adj4 tool?).tw,kf. (64,154)
-
(electronic adj2 record?).tw,kf. (43,674)
-
medical informatics/or health information exchange/or exp medical informatics applications/or exp medical informatics computing/or nursing informatics/ (460,638)
-
exp Hospital Information Systems/ (28,271)
-
exp health information management/ (1788)
-
exp Medical Records Systems, Computerized/ (42,909)
-
(information adj3 (technolog* or system or computeri* or electronic)).tw,kf. (52,606)
-
digital*.tw,kf. (157,475)
-
(“risk assess*” adj4 (bundle* or instrument* or care plan*)).tw,kf. (487)
-
clinic* decision* support system*.tw,kf. (2415)
-
(electronic* adj3 nurs* adj3 document*).tw,kf. (118)
-
Decision Support Systems, Clinical/ (8422)
-
or/35-47 [Assessment tools including health IT] (787,014)
-
workflow/ (6346)
-
systems integration/ (9571)
-
facilitation.tw,kf. (30,997)
-
(workflow* or work-flow*).tw,kf. (29,615)
-
system? fit*.tw,kf. (333)
-
Embed*.tw,kf. (138,578)
-
integrat*.tw,kf. (568,134)
-
(routine* or routini*).tw,kf. (405,465)
-
or/49-56 [Workflows] (1,141,149)
-
14 and 17 and 34 and 48 and 57 [Facilitation Tools CMO 4] (30)
NICE Evidence
Search date: 7 May 2021
Records found: 43
(“falls prevention” or “falls assessment” or “falls reduction”) and (hospital or inpatient or “acute care” or “acute ward” or “acute patient” or “rehabilitation unit” or “rehabilitation ward”) and (“clinical decision support system” or “assessment tool”) and (workflow or routine or “system fit”)
Sorted by Relevance.| Sort by Date
Filters applied:
Evidence type: Evidence Summaries
Evidence type: Primary Research
Evidence type: Systematic Reviews
Evidence type: Audit and Inspection Reports
Evidence type: Health Technology Assessments
Web of Science Core Collection
Databases available at the University of Leeds (searched simultaneously): Arts and Humanities Citation Index (Web of Science) 1975–present
-
Conference Proceedings Citation Index – Science (Web of Science) 1990–present;
-
Conference Proceedings Citation Index – Social Science and Humanities (Web of Science) 1990–present;
-
Science Citation Index-Expanded (Web of Science) 1900–present;
-
Social Sciences Citation Index (Web of Science) 1900–present;
-
Emerging Sources Citation Index (Web of Science) 2015–present.
Search date: 6 May 2021
Records found: 25
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, ESCI Timespan=1900–2021
| # 24 | 25 | #23 AND #22 AND #10 AND #6 AND #5 |
| # 23 | 2,857,583 | TOPIC: (facilitation or workflow* or work-flow* or embed* or integrat* or routine* or routini* or “system* fit*”) |
| # 22 | 1,106,013 | #21 OR #20 OR #19 OR #18 OR #17 OR #16 OR #15 OR #14 OR #13 OR #12 OR #11 |
| # 21 | 151 | TOPIC: (electronic* near/3 nurs* near/3 document*) |
| # 20 | 606 | TOPIC: (“health information management”) |
| # 19 | 3188 | TOPIC: (“clinic* decision* support system*”) |
| # 18 | 1302 | TOPIC: (risk* near/3 screen* near/3 tool*) |
| # 17 | 1074 | TOPIC: ((multi-factorial or multifactorial) near/4 risk assessment*) |
| # 16 | 21 | TS=(“risk assess*” near/4 (“care plan*”)) |
| # 15 | 739 | TS=(“risk assess*” near/4 (bundle* or instrument*)) |
| # 14 | 656,213 | TOPIC: (digital*) |
| # 13 | 46,322 | TOPIC: (electronic near/2 record$) |
| # 12 | 337,953 | TOPIC: (information near/3 (technolog* or system or computeri* or electronic)) |
| # 11 | 99,734 | TOPIC: (assess* near/4 tool$) |
| # 10 | 2,791,484 | #9 OR #8 OR #7 |
| # 9 | 30,828 | TOPIC: (sustain* near/4 (program* or practice* or intervention$)) |
| # 8 | 296,145 | TI=(adopt* or deliver* or engage*) |
| # 7 | 2,496,599 | TS=(implement* or adher* or comply or complian* or fidelity or “buy in” or (Cognitive near/2 participat*)) |
| # 6 | 28,263 | TS=(fall$ near/2 (assess* or risk$ or prevent* or reduc* or occur* or frequen* or screen*)) |
| # 5 | 1,439,906 | #4 OR #3 OR #2 OR #1 |
| # 4 | 225,427 | TOPIC: (acute near/5 patient$) |
| # 3 | 7521 | TOPIC: ((rehabilitation or geriatric) near/1 (ward$ or unit$ or department$)) |
| # 2 | 35,952 | TOPIC: ((acute or sub-acute or subacute) near/3 (care or ward$)) |
| # 1 | 1,254,650 | TOPIC: (hospital* OR inpatient*) |
Shared responsibility
CINAHL (EBSCOhost)
Search date: 6 May 2021
Records found: 42
| S36 | S12 AND S15 AND S20 AND S28 AND S35 | 42 |
| S35 | S29 OR S30 OR S31 OR S32 OR S33 OR S34 | 439,642 |
| S34 | TI ((responsib* n3 (staff or professional or professionals or nurs* or doctor* or clinician*))) OR AB ((responsib* n3 (staff or professional or professionals or nurs* or doctor* or clinician*))) | 8563 |
| S33 | (MH “Social Responsibility+”) | 30,941 |
| S32 | (MH “Interpersonal Relations+”) | 293,747 |
| S31 | TI ((ownership or communicat* or vigilan*)) OR AB ((ownership or communicat* or vigilan*)) | 143,611 |
| S30 | TI ((joint* n3 (responsibility or responsible or accountability or accountable))) OR AB ((joint* n3 (responsibility or responsible or accountability or accountable))) | 227 |
| S29 | TI (((share* or sharing) n3 (responsibility or responsible or accountability or accountable))) OR AB (((share* or sharing) n3 (responsibility or responsible or accountability or accountable))) | 1788 |
| S28 | S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 134,358 | |
| S27 | TI ((team* n5 (huddle* or handover*)) or teamwork* or “team work*”) OR AB ((team* n5 (huddle* or handover*)) or teamwork* or “team work*”) | 9804 |
| S26 | (MH “Interdepartmental Relations”) OR (MH “Public Relations”) | 5253 |
| S25 | (MH “Teamwork”) | 16,113 |
| S24 | TI ((team* n3 (share* or sharing or communic* or multidisciplin* or interdisciplin* or multi-disciplin* or inter-disciplin* or interprofessional* or inter-professional*))) OR AB ((team* n3 (share* or sharing or communic* or multidisciplin* or interdisciplin* or multi-disciplin* or inter-disciplin* or interprofessional* or inter-professional*))) | 23,302 |
| S23 | TI collaborat* | 22,997 |
| S22 | (MH “Collaboration”) | 46,618 |
| S21 | (MH “Multidisciplinary Care Team+”) | 46,806 |
| S20 | S16 OR S17 OR S18 OR S19 | 245,854 |
| S19 | TI ((risk n2 (assess* or evaluat*)) or guideline* or protocol*) AND AB ((risk n2 (assess* or evaluat*)) or guideline* or protocol*) | 33,722 |
| S18 | (MH “Protocols+”) | 42,093 |
| S17 | (MH “Practice Guidelines”) | 81,196 |
| S16 | (MH “Risk Assessment”) | 114,426 |
| S15 | S13 OR S14 | 18,732 |
| S14 | TI (fall* n2 (assess* or risk* or prevent* or reduc* or occur* or frequen* or screen*)) OR AB (fall* n2 (assess* or risk* or prevent* or reduc* or occur* or frequen* or screen*)) | 14,238 |
| S13 | (MH “Accidental Falls/PC”) | 10,324 |
| S12 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 | 703,827 |
| S11 | (MH “Multidisciplinary Care Team+”) | 46,806 |
| S10 | (MH “Medical Staff, Hospital+”) OR (MH “Nursing Staff, Hospital”) | 27,034 |
| S9 | (MH “Hospitals+”) | 121,025 |
| S8 | (MH “Hospital Units”) OR (MH “Rehabilitation Centers”) | 15,791 |
| S7 | (MH “Inpatients”) | 83,940 |
| S6 | (MH “Subacute Care”) OR (MH “Acute Care”) | 10,379 |
| S5 | (MH “Hospitalization”) | 38,752 |
| S4 | TI hospital* OR AB hospital* | 476,571 |
| S3 | TI (inpatient or inpatients) OR AB (inpatient or inpatients) | 54,338 |
| S2 | TI (((rehabilitation or geriatric) n1 (ward? or unit? or department?))) OR AB (((rehabilitation or geriatric) n1 (ward? or unit? or department?))) | 4830 |
| S1 | TI (((acute or sub-acute or subacute) n3 (care or ward* or patient*))) OR AB (((acute or sub-acute or subacute) n3 (care or ward* or patient*))) | 73,873 |
EMBASE Classic + EMBASE (Ovid) 1947 to 2021 May 05
Search date: 6 May 2021
Records found: 42
EMBASE Classic + EMBASE <1947 to 5 May 2021>
Search strategy:
-------- ---------- ------------- ----------- ----------- ------------ ---------------
-
hospitalization/ (420,992)
-
hospital department/ or exp ward/ (439,715)
-
exp hospital/ (1,302,934)
-
medical staff/ (40,310)
-
nursing staff/ (74,427)
-
rehabilitation center/ (17,387)
-
subacute care/ (1151)
-
exp clinical handover/ or collaborative care team/ or exp rapid response team/ (11,414)
-
exp hospital patient/ (199,241)
-
((acute or sub-acute or subacute) adj3 (care or ward?)).tw,kw. (51,102)
-
((rehabilitation or geriatric) adj (ward? or unit? or department?)).tw,kw. (12,324)
-
inpatient?.tw,kw. (199,814)
-
(acute adj5 patient?).tw,kw. (369,927)
-
hospital*.tw,kw. (2,200,719)
-
or/1-14 [hospital] (3,282,770)
-
*falling/ (12,578)
-
falling/pc (2954)
-
(fall? adj2 (assess* or risk? or prevent* or reduc* or occur* or frequen* or screen*)).tw,kw. (25,940)
-
or/16-18 [Falls prevention or risk assessment] (32,853)
-
risk assessment/ (618,392)
-
(risk adj2 (assess* or evaluat*)).tw,kw. (196,115)
-
exp practice guideline/ (601,575)
-
guideline*.tw,kw. (613,857)
-
exp clinical protocol/ (106,751)
-
protocol?.tw,kw./freq=2 (185,559)
-
or/20-25 [Multifactorial risk assessment] (1,743,357)
-
multidisciplinary team/ or collaborative care team/ (12,645)
-
collaborat*.tw,kw./freq=2 (50,596)
-
collaborat*.ti. (40,601)
-
(team* adj3 (share* or sharing or communic*)).tw,kw. (7724)
-
(team* adj3 (multidisciplin* or interdisciplin* or multi-disciplin* or inter-disciplin* or interprofessional* or inter-professional*)).tw,kw. (61,882)
-
cooperation/ or teamwork/ (64,251)
-
public relations/ (62,742)
-
(team* adj5 huddle?).tw,kw. (337)
-
(team* adj5 handover?).tw,kw. (230)
-
(teamwork* or team-work*).tw,kw. (20,866)
-
or/27-36 [Teamwork] (247,513)
-
((share* or sharing) adj3 (responsibility or responsible or accountability or accountable)).tw,kw. (3181)
-
(joint adj3 (responsibility or responsible or accountability or accountable)).tw,kw. (586)
-
ownership.tw,kw. (17,297)
-
communicat*.tw,kw. (442,253)
-
exp interpersonal communication/ (717,292)
-
*“organization and management”/ (65,602)
-
alertness/ (19,538)
-
vigilan*.tw,kw. (32,155)
-
(responsib* adj3 (staff or professional? or nurs* or doctor? or clinician?)).tw,kw. (11,898)
-
or/38-46 [Shared Responsibility] (1,148,502)
-
15 and 19 and 26 and 37 and 47 [Falls in Hospital and Risk Assessment and Teamwork and Shared Responsibility] (42)
Ovid MEDLINE(R) ALL 1946 to 5 May 2021
Search date: 6 May 2021
Records found: 55
Search strategy:
-------- ---------- ------------ ------------ ------------ ------------ --------------
-
Hospitalization/ (115,592)
-
Subacute Care/ (1169)
-
Hospital Units/ (10,319)
-
exp Hospitals/ (284,007)
-
medical staff, hospital/or nursing staff, hospital/ (66,506)
-
exp Patient Care Team/ (70,042)
-
Rehabilitation Centers/ (8356)
-
Inpatients/ (23,637)
-
((acute or sub-acute or subacute) adj3 (care or ward?)).tw,kf. (34,662)
-
((rehabilitation or geriatric) adj (ward? or unit? or department?)).tw,kf. (6803)
-
inpatient?.tw,kf. (116,838)
-
(acute adj5 patient?).tw,kf. (227,174)
-
hospital*.tw,kf. (1,383,898)
-
or/1-13 [hospital] (1,835,443)
-
Accidental Falls/pc [Prevention and Control] (9549)
-
(fall? adj2 (assess* or risk? or prevent* or reduc* or occur* or frequen* or screen*)).tw,kf. (17,142)
-
15 or 16 [Falls] (21,139)
-
exp Risk Assessment/ (284,216)
-
(risk adj2 (assess* or evaluat*)).tw,kf. (137,873)
-
guideline/or practice guideline/ (35,660)
-
guideline*.tw,kf. (386,469)
-
protocol?.tw,kf./freq=2 (126,031)
-
protocol?.ti. (69,596)
-
exp Clinical Protocols/ (174,448)
-
or/18-24 [Multifactorial risk assessment] (1,055,597)
-
exp Patient Care Team/ (70,042)
-
Cooperative Behavior/ (44,475)
-
collaborat*.tw,kf./freq=2 (35,346)
-
collaborat*.ti. (32,563)
-
(team* adj3 (share* or sharing or communic*)).tw,kf. (4639)
-
(team* adj3 (multidisciplin* or interdisciplin* or multi-disciplin* or inter-disciplin* or interprofessional* or inter-professional*)).tw,kf. (34,335)
-
exp interprofessional relations/or physician-nurse relations/ (70,564)
-
(team* adj5 huddle?).tw,kf. (106)
-
(team* adj5 handover?).tw,kf. (115)
-
(teamwork* or team-work*).tw,kf. (14,050)
-
or/26-35 [Teamwork] (228,807)
-
((share* or sharing) adj3 (responsibility or responsible or accountability or accountable)).tw,kf. (2440)
-
(joint* adj3 (responsibility or responsible or accountability or accountable)).tw,kf. (604)
-
ownership.tw,kf. (13,717)
-
communicat*.tw,kf. (325,944)
-
exp Interpersonal Relations/ (334,498)
-
exp *“Organization and Administration”/ (729,180)
-
vigilan*.tw,kf. (22,242)
-
(responsib* adj3 (staff or professional? or nurs* or doctor? or clinician?)).tw,kf. (8985)
-
or/37-44 [Shared Responsibility] (1,323,953)
-
14 and 17 and 25 and 36 and 45 [Falls in Hospital and Risk Assessment and Teamwork and Shared Responsibility] (55)
NICE Evidence
Search date: 7 May 2021
Records found: 27
(“falls prevention” or “falls assessment” or “falls reduction”) and (hospital or inpatient or “acute care” or “acute ward” or “acute patient” or “rehabilitation unit” or “rehabilitation ward”) and (“team huddle” or “team handover” or “interdisciplinary team” or “team share” or teamwork or interprofessional or “care team”) and (communication or collaboration or responsibility or ownership or accountability) and (“risk assessment” or “risk evaluation” or “evaluation of risk”)
Sorted by Relevance.| Sort by Date
Filters applied:
Evidence type: Evidence Summaries
Evidence type: Primary Research
Evidence type: Systematic Reviews
Evidence type: Audit and Inspection Reports
Evidence type: Health Technology Assessments
Web of Science Core Collection
Databases available at the University of Leeds (searched simultaneously):
-
Arts and Humanities Citation Index (Web of Science) 1975–present
-
Conference Proceedings Citation Index- Science (Web of Science) 1990–present
-
Conference Proceedings Citation Index- Social Science and Humanities (Web of Science) 1990-present
-
Science Citation Index-Expanded (Web of Science) 1900–present
-
Social Sciences Citation Index (Web of Science) 1900–present
-
Emerging Sources Citation Index (Web of Science) 2015–present
Search date: 6 May 2021
Records found: 9
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, ESCI Timespan=1900–2021
| # 20 | 9 | #19 AND #14 AND #9 AND #6 AND #5 |
| # 19 | 1,273,025 | #18 OR #17 OR #16 OR #15 |
| # 18 | 9478 | TOPIC: ((responsib* near/3 (staff or professional$ or nurs* or doctor$ or clinician$))) |
| # 17 | 1,258,633 | TOPIC: (ownership or communicat* or vigilan*) |
| # 16 | 1068 | TS=(joint* near/3 (responsibility or responsible or accountability or accountable)) |
| # 15 | 6067 | TOPIC: (((share* or sharing) near/3 (responsibility or responsible or accountability or accountable))) |
| # 14 | 455,274 | #13 OR #12 OR #11 OR #10 |
| # 13 | 228 | TOPIC: ((team* near/5 (huddle$ or handover$))) |
| # 12 | 34,696 | TOPIC: ((team* near/3 (multidisciplin* or interdisciplin* or multi-disciplin* or inter-disciplin* or interprofessional* or inter-professional*))) |
| # 11 | 10,763 | TOPIC: ((team* near/3 (share* or sharing or communic*))) |
| # 10 | 422,965 | TS=(collaborat* or teamwork* or “team work*”) |
| # 9 | 1,540,975 | #8 OR #7 |
| # 8 | 1,298,433 | TOPIC: (guideline* or protocol*) |
| # 7 | 267,127 | TOPIC: (risk near/2 (assess* or evaluat*)) |
| # 6 | 28,265 | TS=(fall$ near/2 (assess* or risk$ or prevent* or reduc* or occur* or frequen* or screen*)) |
| # 5 | 1,439,877 | #4 OR #3 OR #2 OR #1 |
| # 4 | 225,435 | TOPIC: (acute near/5 patient$) |
| # 3 | 7521 | TOPIC: ((rehabilitation or geriatric) near/1 (ward$ or unit$ or department$)) |
| # 2 | 35,954 | TOPIC: ((acute or sub-acute or subacute) near/3 (care or ward$)) |
| # 1 | 1,254,611 | TOPIC: (hospital* OR inpatient*) |
Patient participation
CINAHL (EBSCOhost)
Search date: 6 May 2021
Records found: 35
| # | Query | Results |
|---|---|---|
| S37 | S12 AND S15 AND S20 AND S29 AND S36 | 35 |
| S36 | S30 OR S31 OR S32 OR S33 OR S34 OR S35 | 829,085 |
| S35 | TI ((compassion* or listen* or respect* or empower* or communicat*)) OR AB ((compassion* or listen* or respect* or empower* or communicat*)) | 569,095 |
| S34 | (MH “Empowerment”) | 14,502 |
| S33 | (MH “Empathy”) OR (MH “Respect”) | 14,446 |
| S32 | (MH “Interpersonal Relations+”) | 293,759 |
| S31 | (MH “Listening”) | 3900 |
| S30 | (MH “Compassion”) | 2156 |
| S29 | S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 | 189,301 |
| S28 | (MH “Patient Autonomy”) | 6773 |
| S27 | TI (((person-centred or person-centered or individuali* or personali*) n2 care)) OR AB (((person-centred or person-centered or individuali* or personali*) n2 care)) | 7646 |
| S26 | TI ((multifacet* or multi-facet* or tailor*)) OR AB ((multifacet* or multi-facet* or tailor*)) | 39,589 |
| S25 | TI ((engag* n3 (patient? or famil* or carer? or caregiver? or player*))) OR AB ((engag* n3 (patient? or famil* or carer? or caregiver? or player*))) | 9745 |
| S24 | (MH “Consumer Participation”) | 21,098 |
| S23 | TI ((patient or patients) n5 (need* or perspective* or autonom*)) OR AB ((patient or patients) n5 (need* or perspective* or autonom*)) | 81,650 |
| S22 | TI (((patient or patients) n2 (centred or centered))) OR AB (((patient or patients) n2 (centred or centered))) | 16,711 |
| S21 | (MH “Patient Centered Care”) OR (MH “Shared Medical Appointments”) | 31,822 |
| S20 | S16 OR S17 OR S18 OR S19 | 245,878 |
| S19 | TI ((risk n2 (assess* or evaluat*)) or guideline* or protocol*) AND AB ((risk n2 (assess* or evaluat*)) or guideline* or protocol*) | 33,732 |
| S18 | (MH “Protocols+”) | 42,099 |
| S17 | (MH “Practice Guidelines”) | 81,201 |
| S16 | (MH “Risk Assessment”) | 114,437 |
| S15 | S13 OR S14 | 18,729 |
| S14 | TI (fall* n2 (assess* or risk* or prevent* or reduc* or occur* or frequen* or screen*)) OR AB (fall* n2 (assess* or risk* or prevent* or reduc* or occur* or frequen* or screen*)) | 14,235 |
| S13 | (MH “Accidental Falls/PC”) | 10,323 |
| S12 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 | 704,077 |
| S11 | (MH “Multidisciplinary Care Team+”) | 46,811 |
| S10 | (MH “Medical Staff, Hospital+”) OR (MH “Nursing Staff, Hospital”) | 27,035 |
| S9 | (MH “Hospitals+”) | 121,072 |
| S8 | (MH “Hospital Units”) OR (MH “Rehabilitation Centers”) | 15,793 |
| S7 | (MH “Inpatients”) | 83,955 |
| S6 | (MH “Subacute Care”) OR (MH “Acute Care”) | 10,376 |
| S5 | (MH “Hospitalization”) | 38,763 |
| S4 | TI hospital* OR AB hospital* | 476,803 |
| S3 | TI (inpatient or inpatients) OR AB (inpatient or inpatients) | 54,348 |
| S2 | TI (((rehabilitation or geriatric) n1 (ward? or unit? or department?))) OR AB (((rehabilitation or geriatric) n1 (ward? or unit? or department?))) | 4834 |
| S1 | TI (((acute or sub-acute or subacute) n3 (care or ward* or patient*))) OR AB (((acute or sub-acute or subacute) n3 (care or ward* or patient*))) |
EMBASE Classic + EMBASE (Ovid) 1947 to 5 May 2021
Search date: 6 May 2021
Records found: 47
Search strategy:
--------- ----------- ----------- --------- ----------- ---------- ---------- ---------
-
hospitalization/ (420,992)
-
hospital department/or exp ward/ (439,715)
-
exp hospital/ (1,302,934)
-
medical staff/ (40,310)
-
nursing staff/ (74,427)
-
rehabilitation center/ (17,387)
-
subacute care/ (1151)
-
exp clinical handover/or collaborative care team/or exp rapid response team/ (11,414)
-
exp hospital patient/ (199,241)
-
((acute or sub-acute or subacute) adj3 (care or ward?)).tw,kw. (51,102)
-
((rehabilitation or geriatric) adj (ward? or unit? or department?)).tw,kw. (12,324)
-
inpatient?.tw,kw. (199,814)
-
(acute adj5 patient?).tw,kw. (369,927)
-
hospital*.tw,kw. (2,200,719)
-
or/1-14 [hospital] (3,282,770)
-
*falling/ (12,578)
-
falling/pc (2954)
-
(fall? adj2 (assess* or risk? or prevent* or reduc* or occur* or frequen* or screen*)).tw,kw. (25,940)
-
or/16-18 [Falls prevention or risk assessment] (32,853)
-
risk assessment/ (618,392)
-
(risk adj2 (assess* or evaluat*)).tw,kw. (196,115)
-
exp practice guideline/ (601,575)
-
guideline*.tw,kw. (613,857)
-
exp clinical protocol/ (106,751)
-
protocol?.tw,kw./freq=2 (185,559)
-
or/20-25 [Multifactorial risk assessment] (1,743,357)
-
patient care/ (317,371)
-
shared medical appointment/ (137)
-
(patient? adj2 (centred or centered)).tw,kw. (36,785)
-
(patient? adj5 perspective?).tw,kw. (33,299)
-
(patient? adj4 need?).tw,kw. (123,089)
-
patient participation/ (29,364)
-
(engag* adj3 (patient? or famil* or carer? or caregiver? or player*)).tw,kw. (20,011)
-
(multifacet* or multi-facet* or tailor*).tw,kw. (164,230)
-
((person-centred or person-centered) adj2 care).tw,kw. (3453)
-
patient autonomy/ (6173)
-
(patient? adj3 autonom*).tw,kw. (12,059)
-
((individuali* or personali*) adj2 care).tw,kw. (8927)
-
or/27-38 [New Patient Centred Care] (689,386)
-
empathy/ (28,635)
-
compassion*.tw,kw. (16,029)
-
exp interpersonal communication/ (717,292)
-
listen*.tw,kw. (42,836)
-
respect/ (1344)
-
(empower* adj3 (staff or professional? or nurs* or doctor? or clinician? or patient?)).tw,kw. (9706)
-
empowerment/ (10,858)
-
respect*.tw,kw./freq=2 (1,001,127)
-
respect*.ti. (14,093)
-
communicat*.tw,kw./freq=2 (122,590)
-
communicat*.ti. (83,765)
-
or/40-50 [Compassion Empowerment] (1,877,721)
-
15 and 19 and 26 and 39 and 51 [Falls in Hospital and Risk Assessment and Person-centred care and Empowerment Compassion] (47)
Ovid MEDLINE(R) ALL 1946 to 5 May 2021
Search date: 6 May 2021
Records found: 20
Search strategy:
--------- ---------- ---------- ------------ ------------ -------------- -------------
-
Hospitalization/ (115,592)
-
Subacute Care/ (1169)
-
Hospital Units/ (10,319)
-
exp Hospitals/ (284,007)
-
medical staff, hospital/or nursing staff, hospital/ (66,506)
-
exp Patient Care Team/ (70,042)
-
Rehabilitation Centers/ (8356)
-
Inpatients/ (23,637)
-
((acute or sub-acute or subacute) adj3 (care or ward?)).tw,kf. (34,662)
-
((rehabilitation or geriatric) adj (ward? or unit? or department?)).tw,kf. (6803)
-
(acute adj5 patient?).tw,kf. (227,174)
-
inpatient?.tw,kf. (116,838)
-
hospital*.tw,kf. (1,383,898)
-
or/1-13 [hospital] (1,835,443)
-
Accidental Falls/pc [Prevention and Control] (9549)
-
(fall? adj2 (assess* or risk? or prevent* or reduc* or occur* or frequen* or screen*)).tw,kf. (17,142)
-
15 or 16 [Falls] (21,139)
-
exp Risk Assessment/ (284,216)
-
(risk adj2 (assess* or evaluat*)).tw,kf. (137,873)
-
guideline/or practice guideline/ (35,660)
-
guideline*.tw,kf. (386,469)
-
protocol?.tw,kf./freq=2 (126,031)
-
protocol?.ti. (69,596)
-
exp Clinical Protocols/ (174,448)
-
or/18-24 [Multifactorial risk assessment] (1,055,597)
-
exp Patient-Centered Care/ (21,417)
-
Shared Medical Appointments/ (33)
-
(patient? adj2 (centred or centered)).tw,kf. (26,112)
-
(patient? adj5 perspective?).tw,kf. (22,183)
-
(patient? adj4 need?).tw,kf. (73,644)
-
Patient Participation/ (26,982)
-
(engag* adj3 (patient? or famil* or carer? or caregiver? or player*)).tw,kf. (13,206)
-
(multifacet* or multi-facet* or tailor*).tw,kf. (128,445)
-
(person adj2 (centred or centered)).tw,kf. (6622)
-
personal autonomy/ (17,428)
-
autonom*.tw,kf. (147,232)
-
((individuali* or personali*) adj2 care).tw,kf. (6083)
-
or/26-37 [Patient Centred Care] (446,228)
-
Empathy/ (19,888)
-
compassion*.tw,kf. (11,571)
-
listen*.tw,kf. (35,198)
-
exp Interpersonal Relations/ (334,498)
-
respect*.tw,kf./freq=2 (655,328)
-
respect*.ti. (11,346)
-
respect/ (443)
-
empower*.tw,kf. (29,195)
-
empowerment/ (409)
-
communicat*.tw,kf./freq=2 (90,369)
-
communicat*.ti. (68,439)
-
or/39-49 [Compassion Empowerment] (1,165,982)
-
14 and 17 and 25 and 38 and 50 [Falls in Hospital and Risk Assessment and Person-centred care and Empowerment Compassion] (20)
NICE Evidence
Search date: 7 May 2021
Records found: 12
(“falls prevention” or “falls assessment” or “falls reduction”) and (hospital or inpatient or “acute care” or “acute ward” or “acute patient” or “rehabilitation unit” or “rehabilitation ward”) and (“patient centered” or “patient centered” or patient centred or patient centered multifaceted or tailored or autonomy or “patient participation”) and (“risk assessment” or “risk evaluation” or “evaluation of risk”)
Sorted by Relevance.| Sort by Date
Filters applied:
Evidence type: Evidence Summaries
Evidence type: Primary Research
Evidence type: Systematic Reviews
Evidence type: Audit and Inspection Reports
Evidence type: Health Technology Assessments
Web of Science Core Collection
Databases available at the University of Leeds (searched simultaneously):
-
Arts and Humanities Citation Index (Web of Science) 1975–present;
-
Conference Proceedings Citation Index- Science (Web of Science) 1990–present;
-
Conference Proceedings Citation Index- Social Science and Humanities (Web of Science) 1990–present;
-
Science Citation Index-Expanded (Web of Science) 1900–present;
-
Social Sciences Citation Index (Web of Science) 1900–present;
-
Emerging Sources Citation Index (Web of Science) 2015–present.
Search date: 6 May 2021
Records found: 29
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, ESCI Timespan=1900–2021
| # 19 | 29 | #18 AND #17 AND #9 AND #6 AND #5 |
| # 18 | 5,738,974 | TOPIC: (compassion* or listen* or respect* or empower* or communicat*) |
| # 17 | 398,635 | #16 OR #15 OR #14 OR #13 OR #12 OR #11 OR #10 |
| # 16 | 9364 | TOPIC: (patient$ near/3 autonom*) |
| # 15 | 10,186 | TS=((person-centred or person-centered or individuali* or personali*) near/2 care) |
| # 14 | 227,277 | TOPIC: (multifacet* or multi-facet* or tailor*) |
| # 13 | 16,446 | TOPIC: (engag* near/3 (patient$ or famil* or carer$ or caregiver$ or player*)) |
| # 12 | 73,290 | TOPIC: (patient$ near/4 need$) |
| # 11 | 24,325 | TOPIC: (patient$ near/5 perspective$) |
| # 10 | 55,014 | TOPIC: (patient$ near/2 (centred or centered)) |
| # 9 | 1,541,009 | #8 OR #7 |
| # 8 | 1,298,454 | TOPIC: (guideline* or protocol*) |
| # 7 | 267,143 | TOPIC: (risk near/2 (assess* or evaluat*)) |
| # 6 | 27,330 | TOPIC: (fall$ near/2 (assess* or risk$ or prevent* or reduc* or occur* or frequenc* or screen)) |
| # 5 | 1,439,993 | #4 OR #3 OR #2 OR #1 |
| # 4 | 225,441 | TOPIC: (acute near/5 patient$) |
| # 3 | 7521 | TOPIC: ((rehabilitation or geriatric) near/1 (ward$ or unit$ or department$)) |
| # 2 | 35,955 | TOPIC: ((acute or sub-acute or subacute) near/3 (care or ward$)) |
| # 1 | 1,254,725 | TOPIC: (hospital* OR inpatient*) |
Search 2.3: update search of two prioritised theories
Facilitation
CINAHL (EBSCOhost)
Search date: 1 August 2022
Records found: 43
| # | Query | Results |
|---|---|---|
| S39 | S12 AND S15 AND S21 AND S34 AND S38 | 43 |
| S38 | S35 OR S36 OR S37 | 295,429 |
| S37 | TI ((facilitation or workflow* or work-flow* or embed* or integrat* or routine* or routini* or “system* fit*”)) OR AB ((facilitation or workflow* or work-flow* or embed* or integrat* or routine* or routini* or “system* fit*”)) | 286,828 |
| S36 | (MH “Health Care Delivery, Integrated”) | 13,765 |
| S35 | (MH “Systems Integration”) OR (MH “Workflow”) | 5346 |
| S34 | S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 | 469,656 |
| S33 | (MH “Information Technology+”) | 20,764 |
| S32 | (MH “Medical Informatics”) OR (MH “Nursing Informatics”) OR (MH “Health Informatics”) | 12,898 |
| S31 | (MH “Clinical Information Systems+”) OR (MH “Health Information Systems+”) OR (MH “Hospital Information Systems”) OR (MH “Nursing Information Systems+”) OR (MH “Patient Record Systems+”) OR (MH “Health Information Networks”) OR (MH “Decision Support Systems, Clinical”) | 62,889 |
| S30 | TI “clinic* decision* support system*” OR AB “clinic* decision* support system*” | 1303 |
| S29 | TI (electronic* n3 nurs* n3 document*) OR AB (electronic* n3 nurs* n3 document*) | 197 |
| S28 | TI (risk* n3 screen* n3 tool*) OR AB (risk* n3 screen* n3 tool*) | 781 |
| S27 | TI ((“risk assess*” n4 (bundle* or instrument* or care plan* or multi-factorial or multifactorial))) OR AB ((“risk assess*” n4 (bundle* or instrument* or care plan* or multi-factorial or multifactorial))) | 412 |
| S26 | TI ((information n3 (technolog* or system or computeri* or electronic))) OR AB ((information n3 (technolog* or system or computeri* or electronic))) | 33,802 |
| S25 | TI ((electronic n2 record*) or digital*) OR AB ((electronic n2 record*) or digital*) | 79,211 |
| S24 | (MH “Clinical Assessment Tools+”) | 276,801 |
| S23 | TI (assess* n4 tool*) OR AB (assess* n4 tool*) | 36,074 |
| S22 | (MH “Fall Risk Assessment Tool”) | 179 |
| S21 | S16 OR S17 OR S18 OR S19 OR S20 | 433,844 |
| S20 | (MH “Guideline Adherence”) | 16,876 |
| S19 | (MH “Systems Implementation”) OR (MH “Program Implementation”) OR (MH “Implementation Science”) | 34,426 |
| S18 | TI (engage* or “buy in” or (Cognitive n2 participat*)) OR AB (“buy in” or (Cognitive n2 participat*)) | 18,593 |
| S17 | TI (sustain* n4 (program* or practice or practices or intervention or interventions)) OR AB (sustain* n4 (program* or practice or practices or intervention or interventions)) | 7956 |
| S16 | TI (implement* or adopt* or deliver* or adher* or comply or complian* or fidelity) OR AB (implement* or adher* or comply or complian* or fidelity) | 390,241 |
| S15 | S13 OR S14 | 20,543 |
| S14 | TI (fall* n2 (assess* or risk* or prevent* or reduc* or occur* or frequen* or screen*)) OR AB (fall* n2 (assess* or risk* or prevent* or reduc* or occur* or frequen* or screen*)) | 15,922 |
| S13 | (MH “Accidental Falls/PC”) | 10,958 |
| S12 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 | 772,650 |
| S11 | (MH “Multidisciplinary Care Team+”) | 49,799 |
| S10 | (MH “Medical Staff, Hospital+”) OR (MH “Nursing Staff, Hospital”) | 29,619 |
| S9 | (MH “Hospitals+”) | 128,590 |
| S8 | (MH “Hospital Units”) OR (MH “Rehabilitation Centers”) | 16,781 |
| S7 | (MH “Inpatients”) | 85,946 |
| S6 | (MH “Subacute Care”) OR (MH “Acute Care”) | 11,259 |
| S5 | (MH “Hospitalization”) | 43,860 |
| S4 | TI hospital* OR AB hospital* | 532,701 |
| S3 | TI (inpatient or inpatients) OR AB (inpatient or inpatients) | 61,118 |
| S2 | TI (((rehabilitation or geriatric) n1 (ward? or unit? or department?))) OR AB (((rehabilitation or geriatric) n1 (ward? or unit? or department?))) | 5417 |
| S1 | TI (((acute or sub-acute or subacute) n3 (care or ward* or patient*))) OR AB (((acute or sub-acute or subacute) n3 (care or ward* or patient*))) | 81,585 |
EMBASE Classic + EMBASE <1947 to 29 July 2022>
Search date: 1 August 2022
Records found: 57
Search strategy:
-------- --------- --------- ---------- --------- ---------- ----------- --------------
-
hospitalization/ (478,011)
-
hospital department/or exp ward/ (500,590)
-
exp hospital/ (1,406,920)
-
medical staff/ (42,122)
-
nursing staff/ (76,712)
-
rehabilitation center/ (18,901)
-
subacute care/ (1508)
-
exp clinical handover/or collaborative care team/or exp rapid response team/ (13,877)
-
exp hospital patient/ (222,261)
-
((acute or sub-acute or subacute) adj3 (care or ward?)).tw,kw. (54,304)
-
((rehabilitation or geriatric) adj (ward? or unit? or department?)).tw,kw. (13,043)
-
inpatient?.tw,kw. (220,506)
-
(acute adj5 patient?).tw,kw. (397,349)
-
hospital*.tw,kw. (2,403,565)
-
or/1-14 [hospital] (3,569,217)
-
*falling/ (13,345)
-
falling/pc (2951)
-
(fall? adj2 (assess* or risk? or prevent* or reduc* or occur* or frequen* or screen*)).tw,kw. (28,030)
-
or/16-18 [Falls prevention or risk assessment] (35,283)
-
implement*.tw,kw. (817,689)
-
(sustain* adj4 (program* or practice* or intervention?)).tw,kw. (16,587)
-
Adopt*.tw,kw./freq=2 (53,825)
-
Adopt*.ti. (22,299)
-
deliver*.tw,kw./freq=2 (391,321)
-
(adher* or comply or complian*).tw,kw. (565,478)
-
fidelity.tw,kw. (39,034)
-
implementation science/ (2954)
-
exp protocol compliance/ (18,558)
-
engagement.tw,kw. (112,073)
-
engage*.tw,kw./freq=2 (59,254)
-
(intervention adj2 deliver*).tw,kw. (8426)
-
(Cognitive adj2 participat*).tw,kw. (805)
-
“buy in”.tw,kw. (3176)
-
or/20-33 [Engagement or Implementation] (1,883,705)
-
clinical assessment tool/ (26,509)
-
(assess* adj4 tool?).tw,kw. (106,630)
-
(electronic adj2 record?).tw,kw. (98,321)
-
*fall risk assessment/ (660)
-
medical informatics/or nursing informatics/ (23,891)
-
exp hospital information system/ (27,015)
-
exp information technology device/ (214,637)
-
(information adj3 (technolog* or system or computeri* or electronic)).tw,kw. (73,764)
-
digital*.tw,kw. (236,637)
-
(“risk assess*” adj4 (bundle* or instrument* or care plan*)).tw,kw. (663)
-
((multi-factorial or multifactorial) adj4 risk assessment*).tw,kw. (148)
-
(risk* adj3 screen* adj3 tool*).tw,kw. (1353)
-
clinical decision support system/ (4833)
-
clinic* decision* support system*.tw,kw. (3630)
-
health information management.tw,kw. (998)
-
medical information system/or bedside information system/ (22,768)
-
(electronic* adj3 nurs* adj3 document*).tw,kw. (155)
-
or/35-51 [Assessment tools including health info technology] (763,497)
-
workflow/ (33,077)
-
integration/ (6797)
-
data integration/ (1220)
-
facilitation.tw,kw. (40,639)
-
(workflow* or work-flow*).tw,kw. (53,221)
-
system? fit*.tw,kw. (493)
-
Embed*.tw,kw. (191,639)
-
integrat*.tw,kw. (778,087)
-
(routine* or routini*).tw,kw. (673,222)
-
or/53-61 [Workflows concept] (1,679,788)
-
15 and 19 and 34 and 52 and 62 [HIT tools CMO4 – final] (57) Medline
Ovid MEDLINE(R) ALL <1946 to 29 July 2022>
Search date: 1 August 2022
Records found: 38
Search strategy:
-------- -------- ---------- ------------ ----------- --------- ---------- ------------
-
Hospitalization/ (129,166)
-
Subacute Care/ (1351)
-
Hospital Units/ (10,446)
-
exp Hospitals/ (306,482)
-
medical staff, hospital/or nursing staff, hospital/ (68,147)
-
exp Patient Care Team/ (72,215)
-
Rehabilitation Centers/ (8576)
-
Inpatients/ (27,507)
-
((acute or sub-acute or subacute) adj3 (care or ward?)).tw,kf. (38,212)
-
((rehabilitation or geriatric) adj (ward? or unit? or department?)).tw,kf. (7341)
-
(acute adj5 patient?).tw,kf. (245,691)
-
inpatient?.tw,kf. (130,036)
-
hospital*.tw,kf. (1,525,967)
-
or/1-13 [hospital] (2,001,274)
-
Accidental Falls/pc [Prevention & Control] (10,342)
-
(fall? adj2 (assess* or risk? or prevent* or reduc* or occur* or frequen* or screen*)).tw,kf. (19,084)
-
15 or 16 [Falls] (23,286)
-
implement*.tw,kf. (628,881)
-
(sustain* adj4 (program* or practice* or intervention?)).tw,kf. (13,120)
-
Adopt*.tw,kf./freq=2 (42,809)
-
Adopt*.ti. (18,039)
-
deliver*.tw,kf./freq=2 (288,133)
-
deliver*.ti. (150,863)
-
(adher* or comply or complian*).tw,kf. (377,119)
-
fidelity.tw,kf. (34,472)
-
Health Plan Implementation/ (6629)
-
implementation science/or technology transfer/ (3267)
-
Guideline Adherence/ (34,788)
-
engage*.tw,kf./freq=2 (47,833)
-
engage*.ti. (20,598)
-
(intervention adj2 deliver*).tw,kf. (6761)
-
(Cognitive adj2 participat*).tw,kf. (627)
-
“buy in”.tw,kf. (2105)
-
or/18-33 [Implementation or Adherence to Guidelines and strategies] (1,419,513)
-
Risk Assessment/mt [Methods] (38,091)
-
(assess* adj4 tool?).tw,kf. (74,557)
-
(electronic adj2 record?).tw,kf. (53,541)
-
medical informatics/or health information exchange/or exp medical informatics applications/or exp medical informatics computing/or nursing informatics/ (490,892)
-
exp Hospital Information Systems/ (30,283)
-
exp health information management/ (1943)
-
exp Medical Records Systems, Computerized/ (46,872)
-
(information adj3 (technolog* or system or computeri* or electronic)).tw,kf. (59,321)
-
digital*.tw,kf. (181,775)
-
(“risk assess*” adj4 (bundle* or instrument* or care plan*)).tw,kf. (525)
-
clinic* decision* support system*.tw,kf. (2939)
-
(electronic* adj3 nurs* adj3 document*).tw,kf. (123)
-
Decision Support Systems, Clinical/ (9161)
-
or/35-47 [Assessment tools including health IT] (868,790)
-
workflow/ (8215)
-
systems integration/ (9627)
-
facilitation.tw,kf. (32,835)
-
(workflow* or work-flow*).tw,kf. (37,281)
-
system? fit*.tw,kf. (368)
-
Embed*.tw,kf. (153,897)
-
integrat*.tw,kf. (644,447)
-
(routine* or routini*).tw,kf. (440,520)
-
or/49-56 [Workflows] (1,271,193)
-
14 and 17 and 34 and 48 and 57 [Facilitation Tools CMO 4] (38)
Web of Science Core Collection
Databases available at the University of Leeds (searched simultaneously):
-
Arts and Humanities Citation Index (Web of Science) 1975–present;
-
Conference Proceedings Citation Index- Science (Web of Science) 1990–present;
-
Conference Proceedings Citation Index- Social Science and Humanities (Web of Science) 1990–present;
-
Science Citation Index-Expanded (Web of Science) 1900–present;
-
Social Sciences Citation Index (Web of Science) 1900–present;
-
Emerging Sources Citation Index (Web of Science) 2015–present.
Search date: 1 August 2022
Records found: 38
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, ESCI Timespan=1900–2021
-
# 24 #23 AND #22 AND #10 AND #6 AND #5
-
# 23 TOPIC: (facilitation or workflow* or work-flow* or embed* or integrat* or routine* or routini* or “system* fit*”)
-
# 22 #21 OR #20 OR #19 OR #18 OR #17 OR #16 OR #15 OR #14 OR #13 OR #12 OR #11
-
# 21 TOPIC: (electronic* near/3 nurs* near/3 document*)
-
# 20 TOPIC: (“health information management”)
-
# 19 TOPIC: (“clinic* decision* support system*”)
-
# 18 TOPIC: (risk* near/3 screen* near/3 tool*)
-
# 17 TOPIC: ((multi-factorial or multifactorial) near/4 risk assessment*)
-
# 16 TS=(“risk assess*” near/4 (“care plan*”))
-
# 15 TS=(“risk assess*” near/4 (bundle* or instrument*))
-
# 14 TOPIC: (digital*)
-
# 13 TOPIC: (electronic near/2 record$)
-
# 12 TOPIC: (information near/3 (technolog* or system or computeri* or electronic))
-
# 11 TOPIC: (assess* near/4 tool$)
-
# 10 #9 OR #8 OR #7
-
# 9 TOPIC: (sustain* near/4 (program* or practice* or intervention$))
-
# 8 TI=(adopt* or deliver* or engage*)
-
# 7 TS=(implement* or adher* or comply or complian* or fidelity or “buy in” or (Cognitive near/2 participat*))
-
# 6 TS=(fall$ near/2 (assess* or risk$ or prevent* or reduc* or occur* or frequen* or screen*))
-
# 5 #4 OR #3 OR #2 OR #1
-
# 4 TOPIC: (acute near/5 patient$)
-
# 3 TOPIC: ((rehabilitation or geriatric) near/1 (ward$ or unit$ or department$))
-
# 2 TOPIC: ((acute or sub-acute or subacute) near/3 (care or ward$))
-
# 1 TOPIC: (hospital* OR inpatient*)
Patient participation
CINAHL (EBSCOhost)
Search date: 1 August 2022
Records found: 38
| # | Query | Results |
|---|---|---|
| S37 | S12 AND S15 AND S20 AND S29 AND S36 | 38 |
| S36 | S30 OR S31 OR S32 OR S33 OR S34 OR S35 | 922,896 |
| S35 | TI ((compassion* or listen* or respect* or empower* or communicat*)) OR AB ((compassion* or listen* or respect* or empower* or communicat*)) | 647,264 |
| S34 | (MH “Empowerment”) | 15,895 |
| S33 | (MH “Empathy”) OR (MH “Respect”) | 15,919 |
| S32 | (MH “Interpersonal Relations+”) | 312,612 |
| S31 | (MH “Listening”) | 4156 |
| S30 | (MH “Compassion”) | 2855 |
| S29 | S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 | 209,365 |
| S28 | (MH “Patient Autonomy”) | 7103 |
| S27 | TI (((person-centred or person-centered) n2 care)) OR AB (((person-centred or person-centered) n2 care)) | 3506 |
| S26 | TI ((multifacet* or multi-facet* or tailor*)) OR AB ((multifacet* or multi-facet* or tailor*)) | 46,302 |
| S25 | TI ((engag* n3 (patient? or famil* or carer? or caregiver? or player*))) OR AB ((engag* n3 (patient? or famil* or carer? or caregiver? or player*))) | 11,834 |
| S24 | (MH “Consumer Participation”) | 23,040 |
| S23 | TI ((patient or patients) n5 (need* or perspective* or autonom*)) OR AB ((patient or patients) n5 (need* or perspective* or autonom*)) | 92,545 |
| S22 | TI (((patient or patients) n2 (centred or centered))) OR AB (((patient or patients) n2 (centred or centered))) | 19,014 |
| S21 | (MH “Patient Centered Care”) OR (MH “Shared Medical Appointments”) | 34,229 |
| S20 | S16 OR S17 OR S18 OR S19 | 273,020 |
| S19 | TI ((risk n2 (assess* or evaluat*)) or guideline* or protocol*) AND AB ((risk n2 (assess* or evaluat*)) or guideline* or protocol*) | 39,055 |
| S18 | (MH “Protocols+”) | 43,946 |
| S17 | (MH “Practice Guidelines”) | 84,876 |
| S16 | (MH “Risk Assessment”) | 133,363 |
| S15 | S13 OR S14 | 20,168 |
| S14 | TI (fall* n2 (assess* or risk* or prevent* or reduc* or occur* or frequenc* or screen)) OR AB (fall* n2 (assess* or risk* or prevent* or reduc* or occur* or frequenc* or screen)) | 15,519 |
| S13 | (MH “Accidental Falls/PC”) | 10,958 |
| S12 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 | 737,031 |
| S11 | (MH “Multidisciplinary Care Team+”) | 49,799 |
| S10 | (MH “Medical Staff, Hospital+”) OR (MH “Nursing Staff, Hospital”) | 29,619 |
| S9 | (MH “Hospitals+”) | 128,590 |
| S8 | (MH “Hospital Units”) OR (MH “Rehabilitation Centers”) | 16,781 |
| S7 | (MH “Inpatients”) | 85,946 |
| S6 | (MH “Subacute Care”) OR (MH “Acute Care”) | 11,259 |
| S5 | (MH “Hospitalization”) | 43,860 |
| S4 | TI hospital* OR AB hospital* | 532,701 |
| S3 | TI (inpatient or inpatients) OR AB (inpatient or inpatients) | 61,118 |
| S2 | TI (((rehabilitation or geriatric) n1 (ward? or unit? or department?))) OR AB (((rehabilitation or geriatric) n1 (ward? or unit? or department?))) | 5417 |
| S1 | TI (((acute or sub-acute or subacute) n3 (care or ward?))) OR AB (((acute or sub-acute or subacute) n3 (care or ward?))) | 29,494 |
EMBASE Classic + EMBASE <1947 to 29 July 2022>
Search date: 1 August 2022
Records found: 51
Search strategy:
--------------------------------------------------------------------------------
-
hospitalization/ (478,011)
-
hospital department/or exp ward/ (500,590)
-
exp hospital/ (1,406,920)
-
medical staff/ (42,122)
-
nursing staff/ (76,712)
-
rehabilitation center/ (18,901)
-
subacute care/ (1508)
-
exp clinical handover/or collaborative care team/or exp rapid response team/ (13,877)
-
exp hospital patient/ (222,261)
-
((acute or sub-acute or subacute) adj3 (care or ward?)).tw,kw. (54,304)
-
((rehabilitation or geriatric) adj (ward? or unit? or department?)).tw,kw. (13,043)
-
inpatient?.tw,kw. (220,506)
-
(acute adj5 patient?).tw,kw. (397,349)
-
hospital*.tw,kw. (2,403,565)
-
or/1-14 [hospital] (3,569,217)
-
*falling/ (13,345)
-
falling/pc (2951)
-
(fall? adj2 (assess* or risk? or prevent* or reduc* or occur* or frequen* or screen*)).tw,kw. (28,030)
-
or/16-18 [Falls prevention or risk assessment] (35,283)
-
risk assessment/ (676,072)
-
(risk adj2 (assess* or evaluat*)).tw,kw. (207,299)
-
exp practice guideline/ (654,361)
-
guideline*.tw,kw. (678,665)
-
exp clinical protocol/ (113,463)
-
protocol?.tw,kw./freq=2 (203,598)
-
or/20-25 [Multifactorial risk assessment] (1,900,128)
-
patient care/ (336,364)
-
shared medical appointment/ (223)
-
(patient? adj2 (centred or centered)).tw,kw. (38,317)
-
(patient? adj5 perspective?).tw,kw. (36,791)
-
(patient? adj4 need?).tw,kw. (134,309)
-
patient participation/ (32,642)
-
(engag* adj3 (patient? or famil* or carer? or caregiver? or player*)).tw,kw. (22,707)
-
(multifacet* or multi-facet* or tailor*).tw,kw. (186,436)
-
((person-centred or person-centered) adj2 care).tw,kw. (3687)
-
patient autonomy/ (6808)
-
(patient? adj3 autonom*).tw,kw. (12,599)
-
((individuali* or personali*) adj2 care).tw,kw. (10,122)
-
or/27-38 [New Patient Centred Care] (750,341)
-
empathy/ (30,690)
-
compassion*.tw,kw. (18,236)
-
exp interpersonal communication/ (767,566)
-
listen*.tw,kw. (45,751)
-
respect/ (1815)
-
(empower* adj3 (staff or professional? or nurs* or doctor? or clinician? or patient?)).tw,kw. (10,670)
-
empowerment/ (11,880)
-
respect*.tw,kw./freq=2 (1,083,331)
-
respect*.ti. (14,558)
-
communicat*.tw,kw./freq=2 (125,774)
-
communicat*.ti. (89,269)
-
or/40-50 [Compassion Empowerment] (2,018,728)
-
15 and 19 and 26 and 39 and 51 [Falls in Hospital and Risk Assessment and Person-centred care and Empowerment Compassion] (51)
Ovid MEDLINE(R) ALL <1946 to 29 July 2022>
Search date: 1 August 2022
Records found: 20
Search strategy:
--------------------------------------------------------------------------------
-
Hospitalization/ (129,166)
-
Subacute Care/ (1351)
-
Hospital Units/ (10,446)
-
exp Hospitals/ (306,482)
-
medical staff, hospital/or nursing staff, hospital/ (68,147)
-
exp Patient Care Team/ (72,215)
-
Rehabilitation Centers/ (8576)
-
Inpatients/ (27,507)
-
((acute or sub-acute or subacute) adj3 (care or ward?)).tw,kf. (38,212)
-
((rehabilitation or geriatric) adj (ward? or unit? or department?)).tw,kf. (7341)
-
(acute adj5 patient?).tw,kf. (245,691)
-
inpatient?.tw,kf. (130,036)
-
hospital*.tw,kf. (1,525,967)
-
or/1-13 [hospital] (2,001,274)
-
Accidental Falls/pc [Prevention and Control] (10,342)
-
(fall? adj2 (assess* or risk? or prevent* or reduc* or occur* or frequen* or screen*)).tw,kf. (19,084)
-
15 or 16 [Falls] (23,286)
-
exp Risk Assessment/ (304,882)
-
(risk adj2 (assess* or evaluat*)).tw,kf. (158,055)
-
guideline/or practice guideline/ (37,170)
-
guideline*.tw,kf. (436,990)
-
protocol?.tw,kf./freq=2 (144,789)
-
protocol?.ti. (82,808)
-
exp Clinical Protocols/ (185,718)
-
or/18-24 [Multifactorial risk assessment] (1,170,591)
-
exp Patient-Centered Care/ (23,405)
-
Shared Medical Appointments/ (69)
-
(patient? adj2 (centred or centered)).tw,kf. (30,442)
-
(patient? adj5 perspective?).tw,kf. (25,542)
-
(patient? adj4 need?).tw,kf. (81,555)
-
Patient Participation/ (28,786)
-
(engag* adj3 (patient? or famil* or carer? or caregiver? or player*)).tw,kf. (15,786)
-
(multifacet* or multi-facet* or tailor*).tw,kf. (149,582)
-
(person adj2 (centred or centered)).tw,kf. (8428)
-
personal autonomy/ (18,073)
-
autonom*.tw,kf. (160,104)
-
((individuali* or personali*) adj2 care).tw,kf. (7146)
-
or/26-37 [Patient Centred Care] (499,191)
-
Empathy/ (21,941)
-
compassion*.tw,kf. (13,607)
-
listen*.tw,kf. (38,347)
-
exp Interpersonal Relations/ (346,375)
-
respect*.tw,kf./freq=2 (718,155)
-
respect*.ti. (11,900)
-
respect/ (786)
-
empower*.tw,kf. (34,326)
-
empowerment/ (688)
-
communicat*.tw,kf./freq=2 (103,219)
-
communicat*.ti. (74,092)
-
or/39-49 [Compassion Empowerment] (1263366)
-
14 and 17 and 25 and 38 and 50 [Falls in Hospital and Risk Assessment and Person-centred care and Empowerment Compassion] (20)
Web of Science Core Collection
Databases available at the University of Leeds (searched simultaneously):
-
Arts and Humanities Citation Index (Web of Science) 1975–present;
-
Conference Proceedings Citation Index-Science (Web of Science) 1990–present;
-
Conference Proceedings Citation Index-Social Science and Humanities (Web of Science) 1990–present;
-
Science Citation Index-Expanded (Web of Science) 1900–present;
-
Social Sciences Citation Index (Web of Science) 1900–present;
-
Emerging Sources Citation Index (Web of Science) 2015–present.
Search date: 1 August 2022
Records found: 32
Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, ESCI Timespan=1900–2021
-
# 19 #18 AND #17 AND #9 AND #6 AND #5
-
# 18 TOPIC: (compassion* or listen* or respect* or empower* or communicat*)
-
# 17 #16 OR #15 OR #14 OR #13 OR #12 OR #11 OR #10
-
# 16 TOPIC: (patient$ near/3 autonom*)
-
# 15 TS=((person-centred or person-centered or individuali* or personali*) near/2 care)
-
# 14 TOPIC: (multifacet* or multi-facet* or tailor*)
-
# 13 TOPIC: (engag* near/3 (patient$ or famil* or carer$ or caregiver$ or player*))
-
# 12 TOPIC: (patient$ near/4 need$)
-
# 11 TOPIC: (patient$ near/5 perspective$)
-
# 10 TOPIC: (patient$ near/2 (centred or centered))
-
# 9 #8 OR #7
-
# 8 TOPIC: (guideline* or protocol*)
-
# 7 TOPIC: (risk near/2 (assess* or evaluat*))
-
# 6 TOPIC: (fall$ near/2 (assess* or risk$ or prevent* or reduc* or occur* or frequenc* or screen))
-
# 5 #4 OR #3 OR #2 OR #1
-
# 4 TOPIC: (acute near/5 patient$)
-
# 3 TOPIC: ((rehabilitation or geriatric) near/1 (ward$ or unit$ or department$))
-
# 2 TOPIC: ((acute or sub-acute or subacute) near/3 (care or ward$))
-
# 1 TOPIC: (hospital* OR inpatient*)
Appendix 3 Observation protocol
| Date: | Site ID: | Visit no: | Start time: | End time: | Total duration: |
Do not record personal-identifiable information.
Location and activity
-
Location may include ward, meeting room, etc. If it helps to illustrate extrinsic/environmental factors associated with falls prevention, draw a plan of the ward/bay.
-
Activity may include bay observation, handover, huddle, team meeting, intentional rounding, training session.
-
Are there any posters on ward walls/patients’ or carers’ information boards about falls prevention measures in place?
Open fieldnote record
Detailed notes and reflections of the researcher, completed during the period of observations, with focus on how and in what contexts multifactorial falls risk assessment (MFRA) and tailored falls prevention interventions are used as intended on a routine basis and what supports and constrains routine use of MFRA and falls prevention interventions, including the following:
-
context; description of conditions under which staff and patients/carers operate and interact, including constraints and pressures and the nature of the environment, including how noisy/busy it is (call-bells, monitors, conversations, movement of people and how many people are around)
-
who is participating in risk assessment and interventions
-
whether the actions of staff such as ancillary staff appear to have an impact on falls (e.g. by moving call-bells)
-
the nature, purpose and frequency of the activity/interaction (note times where relevant, e.g. timing of intentional rounding/length of time taken on huddles, etc.). Pay attention to issues around continence/toileting, as falls are often associated with these
-
how individuals and teams appear to respond to, participate in, feel about, describe, explain, and make sense of multifactorial risk assessment and prevention activities, as well as concerns and preoccupations (where verbalised, e.g. risk aversion)
-
think about what you’d expect to see staff doing to prevent falls; whether/how they do that; and how they balance the tension between ‘doing for’ patients and ‘doing with’ patients and supporting independence
-
the researcher’s perceptions of the relationship of the observed activity to the aims of the study
-
whether and how falls risk and prevention, and other types of risk (e.g. pressure ulcer), are discussed
-
if falls occur during the period of observations, is the incidence rate higher on a particular ward, particular time of the day, after a particular activity (e.g. during/after meals or tea round, after taking toxic medication, blood test, after a phone call)? Are the incident and the activities that led to it recorded?
Specific detail for context mechanism outcome configurations
Leadership
Is there a falls champion/leader visible on the ward? Or dedicated to the ward? If so, find out when they’re on shift and try to arrange some observations when they’re around. (Not all hospitals have champions, may be a falls team/committee, members of which we can interview.)
What activities/interactions are they involved in? For example, huddles, falls assessments, information provision, clinical governance meetings?
How do ward staff respond/interact with the lead?
Do they appear to be supporting/driving falls assessment and intervention delivery? How? For example, feedback of performance in falls prevention?
How do leaders respond to a fall incident? For example, lead postfall huddle? What is the discussion focused on? For example, does it indicate culture of learning as opposed to blaming?
Facilitation
What tools are used by the service to record the risk assessment and care plan, for example, paper-based, electronic, both?
If tools are electronic, how do staff access them? For example, what hardware is available on the ward: desktop PCs, iPads, Computers on Wheels, is there a desktop icon to access the tools?
What is offered via these tools – for example, what questions and prompts are provided in the assessment tool, are alerts/reminders built into electronic systems for assessment and intervention delivery, do they support decision-making about what interventions to use for an identified risk?
How do ward staff utilise the tools, for example, respond to alerts, use questions in assessment?
Is the act of doing the assessment separate from the act of recording it (e.g. do staff complete a paper assessment form at the bedside, and later transfer the information to an electronic system, or do they complete the assessment on a iPad or computer on wheels at the bedside?)
What appears to support/constrain assessment and care plan delivery, for example, number of staff on ward, type of patient?
Shared responsibility
What is the staff mix on the ward? Number and roles.
Which staff conduct falls risk assessment and develop the care plan?
How is information about patients’ individual falls risk and care plan communicated between ward staff? For example, poster/ward huddles, informally, where is the care plan accessible to staff and patients?
What information is communicated between staff in relation to falls between shifts? Is there evidence of communication about falls between different types of staff (e.g. nurses informing nursing assistants about patients at risk of falling)?
Who participates in fall prevention activities? For example, do you observe staff assisting patients when mobilising, responding to the call-bell promptly, advising/reminding them and carers about fall prevention activities? Do patients and carers appear to be part of the falls prevention ‘team’?
In general, which staff are available to support patients on the ward?
How does the team respond to a fall incident?
Patient participation
What sort of questions are patients/carers asked, if any, during the assessment? For example, open – that allow patients to respond in their own words – or closed?
Are interventions to address falls risk discussed, negotiated and agreed in partnership with patients and carers? Are their concerns and preferences discussed? Do staff check that patients and carers understand them (inc. if they can hear them properly on a noisy ward or if hard of hearing)?
How are falls risks and interventions communicated to patients and carers by ward staff? Are patients/carers informed clearly which interventions they need to take part in, and which are the responsibility of staff? For example, ringing the call-bell for help walking could be a patient’s responsibility, but reviewing medication would be clinicians’ responsibility.
What happens during the assessment and care planning process if a patient’s first language is not English and they struggle to understand the questions, or a patient has memory/cognitive impairments?
Do patients use call-bells/wait for ward staff to help them mobilise?
Are patients reassessed? How is the reassessment performed and communicated to patients and carers?
Observer effects
Record observer effects (e.g. participants asking ‘What are you writing?’) to allow analysis of whether participants’ awareness of researchers’ presence changes over time. Discuss observer effects directly with those being observed, such as asking participants to discuss how ‘normal’ a particular day is. Be confident to share what you’re writing with people if they want to see it.
Theory refinement
Record whether anything observed today is likely to require a refinement of the programme theory, and how.
Appendix 4 Routinely collected data
FIGURE 9.
Number of falls incidents by month, orthopaedic wards.
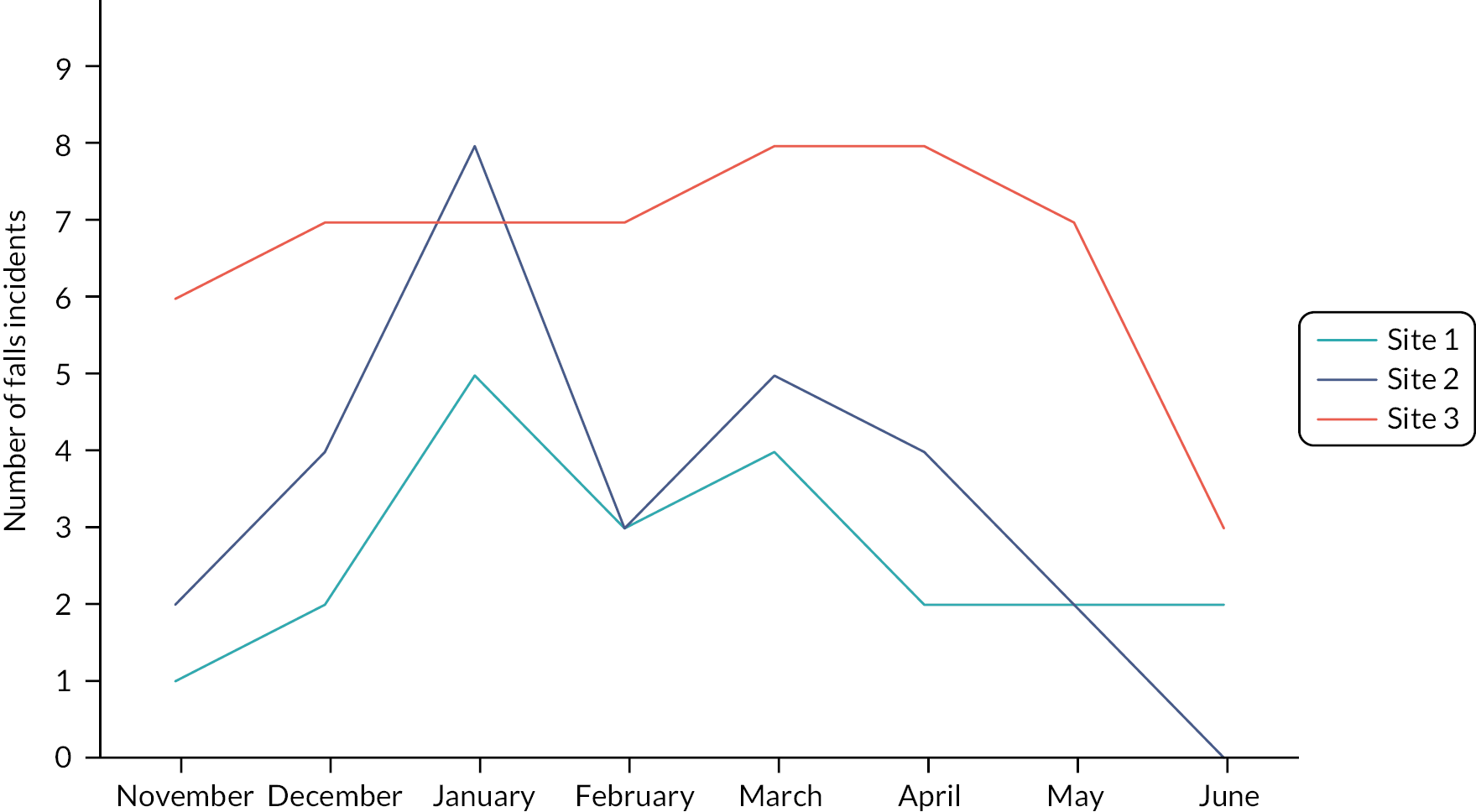
FIGURE 10.
Number of falls incidents per month, older person/complex care wards.
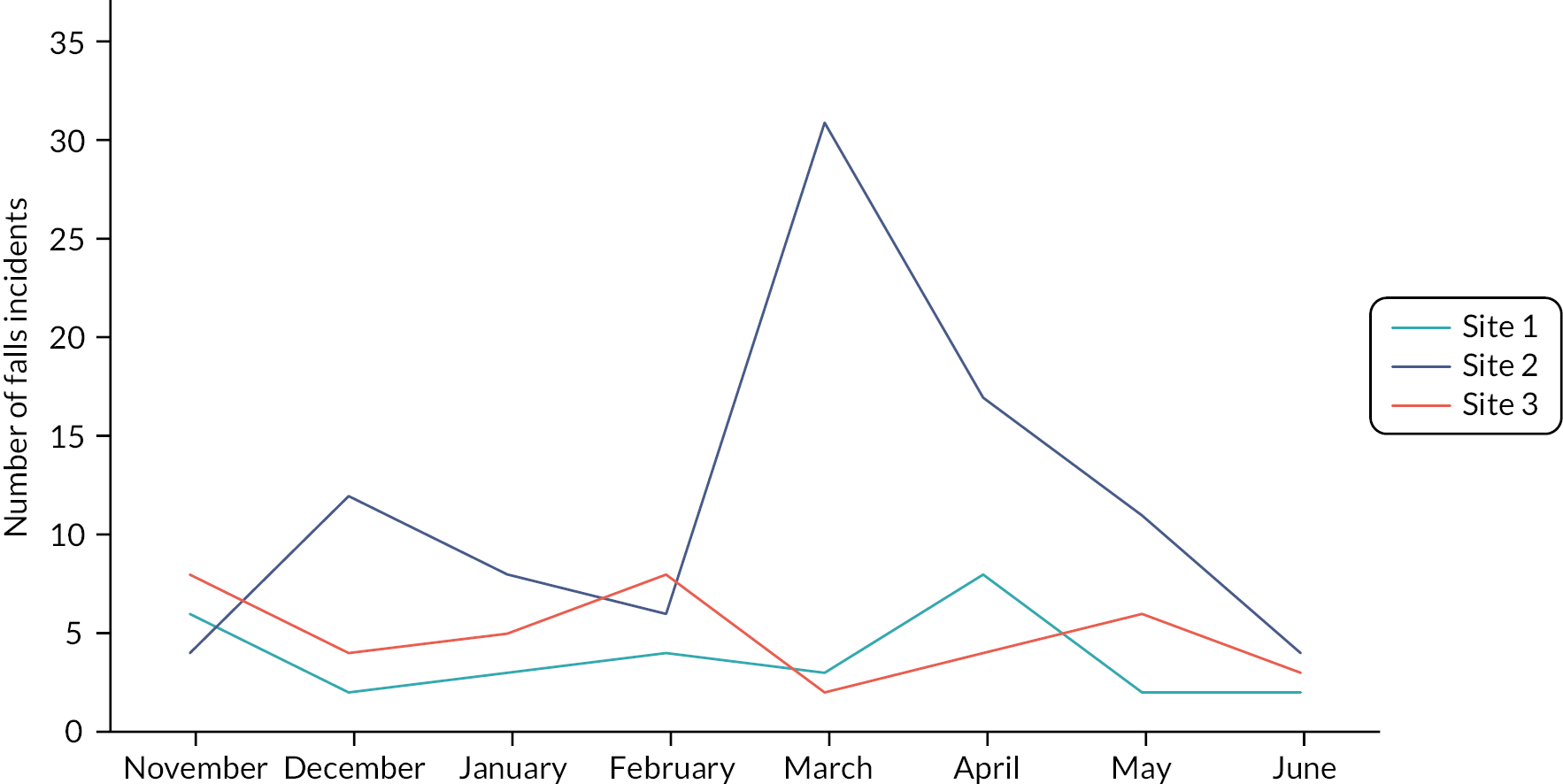
FIGURE 11.
Number of falls with injury per month.
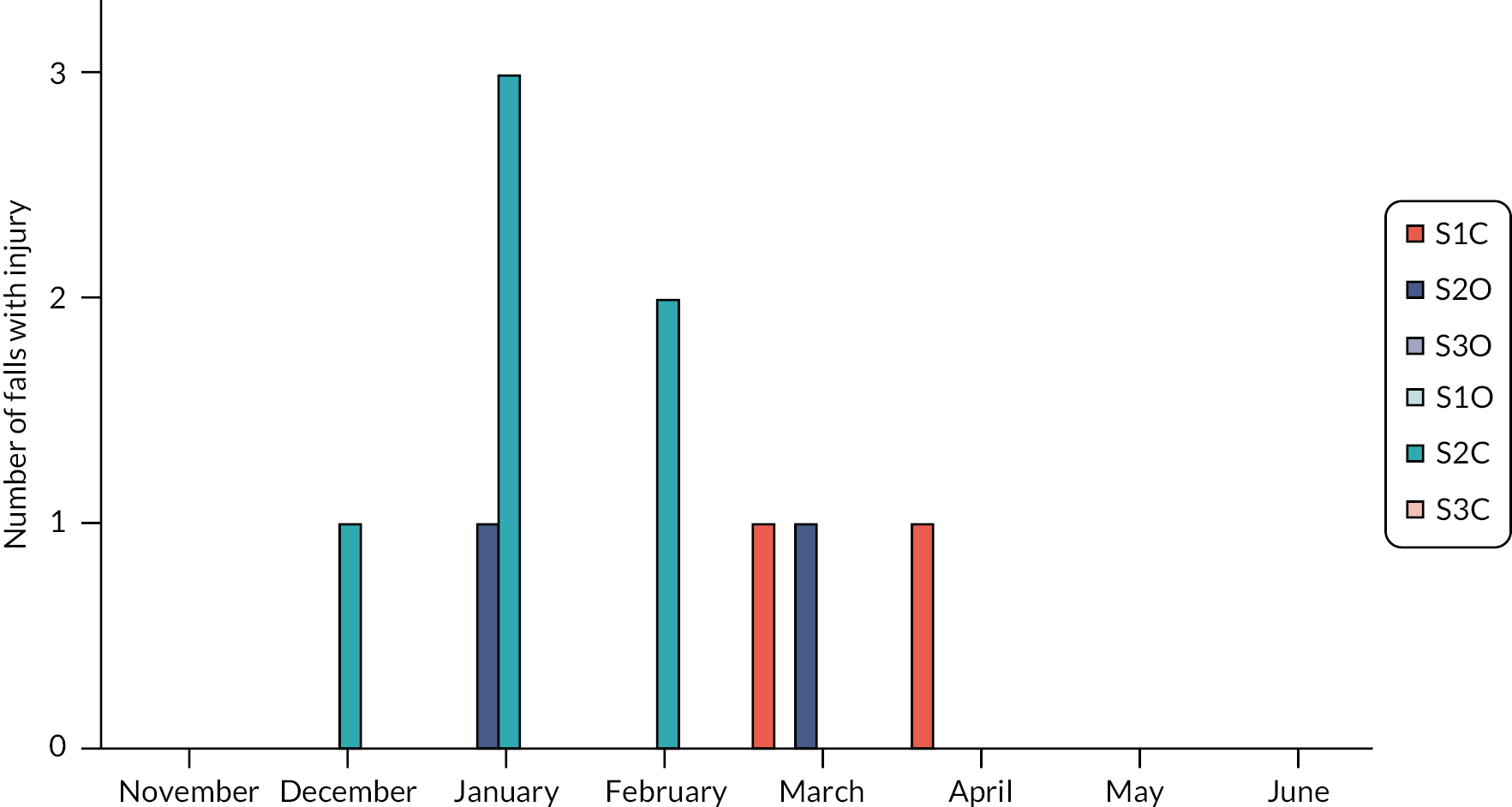
Appendix 5 Initial theories
| Context | Mechanism | Outcome | |
|---|---|---|---|
| Resource | Response | ||
| When staffing levels are low and/or workload is high | MF risk assessments | Nursing staff select which risk assessments they will undertake for patients, based on their perceptions of the patient’s particular vulnerabilities | Leading to certain patients not receiving a falls risk assessment |
| When nursing staff are required to undertake a large number of different risk assessments | MF risk assessments | This creates a cognitive burden so that nursing staff find it difficult to integrate the information from the different risk assessments to determine which interventions should be prioritised for the patient | Leading to a standard bundle of interventions being provided to all patients |
| When attention is drawn to weaknesses in local falls prevention practices, for example, through local or national audits or an adverse event | QI initiative on falls | Quality improvement (QI) initiatives are introduced and attention is focused on falls prevention | Leading to more complete falls risk assessments and adherence to protocols for falls prevention |
| If falls prevention is emphasised as a priority by the ward manager | Practices such as safety huddles and nursing handovers | Can be used as an opportunity to maintain nursing staff attention on falls prevention |
Leading to more complete falls risk assessments and adherence to protocols for falls prevention |
| If patients do not adhere to falls prevention advice | Falls prevention advice/programmes/info sheets | Nursing motivation decreases | Leading to fewer falls risk assessments being undertaken |
Appendix 6 Study details: facilitation CMOc
| Citation and country | Setting | Sample | Intervention description | Study design (inc. comparator if applicable) |
|---|---|---|---|---|
| 1. Albornos-Munoz et al. 2018,118 Spain | Two medical and one surgical ward in one hospital. | Patients of 65 years or over. | Multifaceted fall prevention strategy with patient-level, nurse-level and unit-level interventions used to overcome barriers to implementation. | QI project, clinical audit conducted pre–post intervention. |
| 2. Businger et al., 2020,36 USA | Twelve inpatient units in an acute care hospital. | Stakeholders including study personnel. Tools impacted 12,628 patient admissions. | The Patient Safety Learning Laboratory, a suite of health information technology (HIT) tools integrated within an Electronic Health Record (EHR) vendor system. | Observational study, to share challenges, recommendations and lessons learnt from implementation. No comparator. |
| 3. Capan and Lynch, 2007,106 USA | 357 bed acute hospital. | Patients admitted to the hospital. | Multifaceted fall prevention strategy with patient-level, nurse-level, and unit-level interventions, including site-specific fall risk assessment and intervention tool that underwent pilot testing. | QI project, compared rate of falls before and after introduction of strategy. |
| 4. Carroll et al., 2012,37 USA | Four hospitals (two academic medical centres and two community hospitals) within a single healthcare system. | Randomly selected medical records for patients on the eight study units (four intervention units; 5267 patients) and four usual care units (5116 patients) during three separate study visits. | Fall Tailoring Interventions for Patient Safety (TIPS) toolkit, integrated in EHRs. Staff entered risk data, and the software tailored fall prevention interventions to address specific determinants of falls risk. The toolkit generated bed posters comprising brief text with accompanying icons, patient education hand-outs, and plans of care. | Nursing documentation related to fall risk and prevention was reviewed to evaluate the effectiveness of the toolkit for promoting documentation of fall risk status and planned and completed fall prevention interventions. Comparator was documentation in the usual care units. |
| 5. Cook et al., 2020,107 USA | Trauma centre, Emergency Department in a tertiary care teaching hospital. | Adult patients. | Multifaceted fall prevention strategy with patient-level, nurse-level, and unit-level interventions including an ED-specific fall risk assessment tool. | QI project. Comparator: postintervention monthly unit data. |
| 6. Currie et al., 2006,173 USA | A large multisite academic medical centre. | 25% sample of patients in 52 nursing units at the three sites. | Fall-Injury Risk Assessment instrument integrated into three different platforms. | Bedside audits were performed every 5 weeks. Compliance with use of the instrument in units in which it was integrated into the daily shift assessment was compared with units that did not have complete electronic nursing documentation. |
| 7. Dempsey, 2004,119 Australia | Acute medical wards in a regional teaching hospital. | Patients admitted in two periods (pre–post intervention). | Multifaceted fall prevention strategy with patient-level, nurse-level and unit-level interventions, including a site-specific falls risk assessment tool and a choice of interventions. | QI project – practice review after 5 years of falls prevention programme to assess sustainability. Comparator: two cohorts of patients (pre–post intervention). |
| 8. Dowding et al., 2012,108 USA | Twenty-nine hospitals in a large integrated healthcare organisation. | Patient clinical records. | Integrated EHR including computerised physician order entry, nursing documentation, risk assessment tools, and documentation tools. | Interrupted time series analysis examining hospital-acquired pressure ulcers (HAPU) and falls. Comparator: per cent patients with completed risk assessments for HAPU/falls and rates of HAPU/falls compared pre- and post-EHR implementation. |
| 9. Duckworth et al., 2019,34 USA | Six neurology units and seven medical or medical-surgical units in three acute care centres. | Nurses submitted 1209 audits for the patient engagement measure and 1401 for the presence of the Fall TIPS poster at the bedside. | Fall TIPS in three modalities, including (1) laminated Fall TIPS poster; (2) electronic Fall TIPS poster; and (3) paperless patient safety e-bedside display. | Implementation science study auditing patient engagement and adherence with poster display. Compared modalities of intervention. |
| 10. Dykes et al., 2009,35 USA | Four acute care hospitals. | 685 patients on the units using the Fall TIPS toolkit. | Original Fall TIPS toolkit, which identified a core set of evidence-based interventions directly linked to the patient-specific risk factors and generated a bed poster, a plan of care and an educational handout. | Interim paper assessing impact of adoption strategies via audits. Compared mean number of fall risk assessments completed by nurses using Fall TIPS per patient, per day from first month after implementation to present. |
| 11. Dykes et al., 2017,38 USA | Two large medical centres. | 31 patients on the medical units answered the presurveys, and 33 patients answered the postsurveys. | Fall TIPS: Framework for Spread was used to support uptake and included four phases: (1) communicating ‘better ideas’; (2) planning and setup; (3) spread within the target population; and (4) continuous monitoring and feedback related to adoption and spread of the innovation. | QI project involving patient surveys and measuring protocol adherence, patient falls and falls-related injury rates. No comparator. |
| 12. Healey et al., 2004,18 UK | Care of older person wards and associated community units of a district general hospital. | Control (956 pre, 905 post) Intervention (776 pre, 749 post). | In the intervention wards, staff used a preprinted care plan for patients identified as at risk of falling and introduced appropriate remedial measures. | A group (ward) randomised trial evaluated impact on RR of falls. Comparator: usual care on control wards. |
| 13. Hefner, et al., 2015,109 USA | A large health system, comprising five hospitals. | 800 spot checks of patient rooms. | Falls Wheel (visual tool): the top circle instructed viewers that universal fall precautions should be implemented for all patients; information about the specific fall risk categories then guided which additional safety measures were to be put into place for each patient. | QI project, pre–post intervention audits. |
| 14. Ireland et al. 2010,117 Canada | 60 units in a RNs’ Association of Ontario (RNAO) healthcare organisation. | Random audits of 193 patient medical records on 15 medical-surgical units were undertaken. | Hospital-wide, multifaceted fall prevention strategy with patient-level, nurse-level and unit-level interventions strategy called ‘Don’t Fall for It’, comprising routine patient risk screening of all patients and universal and targeted interventions. | QI project, pre–post intervention audits. |
| 15. Koh et al., 2008,123 Singapore | Medical, surgical, geriatric units, at five acute care hospitals. | Nurses (n = 1830). | N/A | Survey to identify nurse perceptions of barriers to implementing a clinical practice guideline. The validated questionnaire, ‘Barriers and facilitators assessment instrument’, was administered. No comparator. |
| 16. Koh et al., 2009,122 Singapore | Two acute care hospitals with closely matched perceived barriers to implementation of innovation. | All nursing staff (n = 641) working in medical, surgical, and geriatric units. 193 patient records on 15 medical-surgical units. | Multifaceted fall prevention strategy with patient-level, nurse-level and unit-level interventions designed to address barriers to implementation and including use of a mandatory falls risk assessment tool. | Comparative study, preintervention, postintervention and 6-month follow-up, including knowledge assessment of nursing staff, and audits of fall rates and fall prevention practices. |
| 17. Lytle et al., 2015,110 USA | 16 adult units (general medicine and surgical) in an academic health centre. | One medical and one surgical unit were selected for retrospective chart review. | Falls prevention Computer Decision Support tools including reminders for (1) ‘admission documentation incomplete’; (2) ‘shift documentation incomplete’; and (3) a ‘rules-based alert’ for patients at high risk of falls and not on a fall prevention plan of care. | QI project, which used a pre/post quasi-experimental study design. |
| 18. Maia et al., 2018,124 Brazil | Two units in a University Hospital. | Adult and older adult inpatients (48 in one unit, 18 in the other). | Multifaceted fall prevention strategy with patient-level, nurse-level and unit-level interventions, to overcome barriers to implementation. Included introduction of standardised falls risk assessment tool. | QI project – clinical audit conducted pre–post intervention. |
| 19. McCarty et al., 2018,111 USA | Emergency Departments (12 sites) of an integrated healthcare delivery system | 11 of the 12 EDs were visited over a 4-month period; 60 nurses attended training sessions. | Multifaceted fall prevention strategy with patient-level, nurse-level and unit-level interventions, including introduction of the Emergency Department Fall-Risk Assessment Tool (MEDFRAT), programmed into the EHR. | QI project focused on implementation of strategy. No comparator. |
| 20. Milisen et al., 2013,127 Belgium | 17 geriatric wards, selected at random out of 40 hospitals. | 49 healthcare workers. | A practice guideline including four consecutive parts: (1) case finding, that is, identification of persons at risk for falling; (2) in-depth multifactorial assessment of risk factors; (3) targeted interventions; and (4) transfer of information at discharge. | Feasibility study using questionnaire. No comparator. |
| 21. Ohde et al., 2012,125 Tokyo | A 520-bed community-based, tertiary-level, teaching hospital. | All adult inpatients, except for maternity, preventative health screening and intensive care patients. | Multifaceted fall prevention strategy with patient-level, nurse-level and unit-level interventions, including introduction of a fall risk assessment tool and intervention protocol. | QI project. Within group pre–post intervention comparison. |
| 22. Pop et al., 2020,112 USA | Emergency Department academic medical centre. | Staff participating in education sessions. | Components of the intervention were selected on the basis of a review of fall prevention research and included fall risk assessment, safe ambulation, safe toileting, staff communication, early warning and patient education. | QI project. No comparator. |
| 23. Teh et al., 2017,121 Australia | Acute Medical Unit and Geriatric Evaluation and Management (GEM) unit at a tertiary teaching hospital. | All patients admitted to both wards during the trial period. (AMU n = 424, GEM n = 111). | iPadTM-based assessment tool. Black-and-white A4-sized bedside posters were automatically printed at assessment completion to be displayed at patient’s bedside. | Trial comparing the iPad-based tool with the traditional fall risk for older person (FROP) tool in fall risk screening. |
| 24. Teh et al., 2018,120 Australia | Acute Medical Unit and Geriatric Evaluation and Management (GEM) unit at a tertiary teaching hospital. | Ward staff – pretrial focus group n = 5, survey n = 48; post-trial focus group n = 5, survey n = 29. | iPadTM-based assessment tool for direct clinician entry of up to 13 common falls risk activities, with automatic generation of visual cues for bedside display. | Mixed methods pilot study with focus groups and surveys. Pre- and post-trial focus findings were compared. |
| 25. Thatphet et al., 2021,116 USAs and Canada | Five hospitals EDs located in the USA and Canada. | Three physicians, two ED nurses, and one programme co-ordinator (key informants). | N/A: describes the experiences of Emergency Departments with geriatric fall programmes. | Semistructured, open-ended telephone/skype interviews recruited from a purposeful sampling technique. No comparator. |
| 26. Titler et al., 2016,113 USA | 13 adult medical-surgical units from three community hospitals. | Licensed nurses (n = 157 pre; 140 post) and adult patients (n = 390 pre and post). | Targeted Risk Factor Fall Prevention Bundle, focusing on interventions that reduced or modified patient-specific fall risk factors. A Translating Research Into Practice (TRIP) multifaceted implementation intervention was used to promote uptake and use of the fall prevention bundle. | A prospective pre–post implementation cohort design using questionnaires (Stage of Adoption, and Use of Research Findings in Practice Scale). |
| 27. Townsend et al., 2016,114 USA | Emergency Department in one hospital. | Reviewed fall data for each quarter of 2013, including risk assessments scores, the total number of falls, and the circumstances of each fall. | Multifaceted fall prevention strategy with patient-level, nurse-level, and unit-level interventions, including introduction of an Emergency-Department-specific fall risk tool, the KINDER1. | QI project. Data were collected and compared retrospectively prior to the project launch and concurrently after project implementation. |
| 28. Wu et al., 2019,126 Taiwan | One medical centre. | Clinical records of 19,695 patients were analysed. | Standardised Computerised Nursing Process Documentation System, including electronic data entry, scores on the risk assessment template and health assessment and Nursing Care Plans. | Retrospective study to identify patients at high risk of falls and explore the relationship between Nursing Care Plans and falls and pressure injury incidences. A run chart of fall injury incidence rate from 2007 to 2017 is used to the determine effect of SCNPDS. |
Appendix 7 Summary of outcomes: facilitation CMOc
| Citation | Tools described in study (or study aim) | Delivery of a MFRA and care plan | Falls incidents and rates |
|---|---|---|---|
| 1. Albornos-Munoz et al., 2018118 | Standardised tool used by the institution. Nb in use 8 months prior to project. | Compliance Improved in falls risk assessment on admission: this improved on all wards. In the follow-up period, compliance improved by 11.9% (p > 0.05) in ward M1, by 12.1% (p > 0.05) in ward M2, and by 33.9% (p ¼ 0.06) in ward Q3. Compliance decreased in two out of three sites for targeted interventions implemented according to risk factors. In ward M1, compliance decreased from 100% at baseline to 60% at follow-up. In ward M2, compliance decreased from 11.1% at baseline to 9.1% at follow-up. In ward Q3, compliance improved from 25% at baseline to 40% at follow-up. |
Falls rates varied: the number of patients with registered falls increased postimplementation in ward M1, from 0% at baseline to 8.3% (n = 1, no injury incurred), as well as in ward M2, from 7.7% (n = 2, one fall with ‘no injury’ and one with mild injury) at baseline to 10% (n = 4, three falls with ‘no injury’ and one with ‘mild injury’). In ward Q3, the baseline figure was 10% (n = 1, no injury) and 0% at follow-up. Numbers were, however, small, and whether changes were significant is not stated. |
| 2. Businger et al., 202036 | Patient Safety Learning Laboratory (PSLL), a suite of HIT tools including Fall TIPS (uses Morse Fall Scale). | Not measured as part of study. | Not measured as part of study. |
| 3. Capan and Lynch, 2007106 | Site-specific, eight-item tool, developed through profiling patient falls population. |
Not measured as part of study.
|
Falls rates decreased: postimplementation, total falls rate dropped from 0.45 per 100 patient-days in 2003 to 0.32 per 100 patient-days in 2005 and 0.24 per 100 patient-days in the third quarter of 2006. Overall, the falls rate halved over 2 years. Severity of fall-related injuries also declined: since 2005, falls with no injury decreased by 50%, falls with minor injury by 52%, and falls with severe injury by 86%. No information was provided about whether results were statistically significant. |
| 4. Carroll et al., 201237 | Fall TIPS (Morse Fall Scale). | Patients on the intervention units were more likely to have fall risk documented (89% vs. 64%, p G.0001). Significantly more comprehensive plans of care were documented for the patients on the interventions, although no differences were found in documentation of completed interventions compared with usual care unit patient records. | Not measured as part of study. |
| 5. Cook et al., 2020107 | KINDER 1, five-item Emergency Department tool | No change in compliance with falls risk assessment: screening of patients was consistent at more than 95% compliance pre- and poststudy. | Only falls with injury rates decreased significantly: Postimplementation, falls rate decreased from 0.73 falls per 1000 visits (pre) to 0.55 falls per 1000 visits (post), representing a 25% decrease (p = 0.18). The injury rate decreased from 0.09 per 1000 visits (pre) to 0.03 per 1000 visits (post), a 66% decrease in injuries (p < 0.05). |
| 6. Currie et al., 2006115 | Fall-Injury Risk assessment instrument integrated into three clinical information systems. | Compliance improved in falls risk assessment: compliance with use of the automated instrument increased from 43% to 78% on units that did not have complete electronic nursing documentation. Units in which the instrument was integrated into the daily shift assessment, had 99–100% compliance. | Not measured as part of study. |
| 7. Dempsey, 2004119 | Site-specific tool. | Compliance not maintained over the longer term: routine audits were used to assess compliance with assessment of risk, identification of patients at risk, introduction of prevention strategies, and documentation of these. Compliance with the Falls Prevention Programme averaged 88% but was inconsistent (69–94%) and was on a downward trend and a practice review revealed that compliance deteriorated over the next 5 years. | Decrease in falls rates not sustained over time: following the original QI project in 1995–96, rate of falls decreased significantly from 3.63 to 2.29 1000 occupied bed-days (p = 0.05). The falls rate initially remained lower but continued to rise and by 2001 had exceeded preresearch levels at 6.8 per 1000 OBD. |
| 8. Dowding et al., 2012108 | Integrated EHRs, incorporating computerised physician order entry, nursing documentation, risk assessment tools, and documentation tools. | Compliance improved but not significantly: over the time period of the study, mean rates for risk assessment documentation for falls increased but EHR implementation was not significantly associated with an increase in documentation rates for falls risk (0.36; –3.58 to 4.30). | Falls rates did not decrease: EHR implementation was not associated with a significant decrease in fall rates (–0.091; –0.29 to 0.11). Irrespective of EHR implementation, falls rates did not decrease significantly over time (0.0052; –0.01 to 0.02). Hospital region was a significant predictor of variation for fall rates (0.57; 0.41 to 0.72). |
| 9. Duckworth et al., 201934 | Fall TIPS in three modalities: the original EHR version; a paper-based version; and an e-bedside display version. | Compliance improved: 1209 audits were submitted for the patient engagement measure and 1401 for presence of Fall TIPS poster at bedsides. All units reached 80% adherence for both measures. While some units maintained high levels of patient engagement and adherence (especially with the poster), others showed improvement over time, reaching clinically significant adherence (> 80%) by the final month of data collection. | Not measured as part of study. |
| 10. Dykes et al., 200935 | The original Fall TIPS toolkit, falls risk assessment tool in her, which produced bed posters and plans of care. | Compliance improved: outcomes included ‘Framework for Spread’ Toolkit adoption measures: adherence ranged from 72% (% patients with tailored Fall TIPS poster hanging above bed, Hospital B) to 97% (% patients for whom fall risk assessment completed within past 24 hours during weekly safety rounds, Hospital B). Significant improvement noted across hospitals in mean number of fall risk assessments completed by nurses using Fall TIPS per patient, per day: increased by 25% across sites from first month > implementation to current practice (from 1.7 pre to 2.0 the first month, p < 0.003). | Not measured as part of study. |
| 11. Dykes et al., 201738 | Fall TIPS low-tech modality, comprising laminated paper poster on which to record falls risk assessment and care plan in English and Spanish. | BWH unit compliance with using Fall TIPS averaged 82%, the mean fall rate decreased from 3.28 to 2.80 falls per 1000 patient-days from January through June 2015 versus 2016, and the mean fall with injury rate for these periods decreased from 1.00 to 0.54 per 1000 patient-days. At MMC, compliance averaged 91%. Patient knowledge survey results show improvement in knowledge of the risks for falls and the ways to prevent falls. | The mean fall rate increased marginally from 3.04 to 3.10, while the mean fall with injury rate decreased from 0.47 to 0.31 per 1000 patient-days. |
| 12. Healey et al., 200418 | Targeted risk factor reduction core care plan. | Not measured as part of study. | Falls risk measured: significant reduction in the RR of recorded falls on intervention wards (RR 0.79, 95% CI 0.65 to 0.95) but not on control wards (RR 1.12, 95% CI 0.96 to 1.31). The difference in change between the intervention wards and control wards was highly significant (RR 0.71, 95% CI 0.55 to 0.90, p = 0.006). |
| 13. Hefner et al., 2015109 | Falls Wheel, a visual communication tool of a patient’s falls risk and risk of injury. | Compliance improved: the process audit of one unit showed that the Falls Wheel was displayed correctly 95% of the time across the 4-month data collection period. This audit also found that the Falls Wheel matched the risk level in the EHR 70% of the time. The other fall prevention techniques such as ‘fall interventions consistent with risk’ and ‘risk assessment updated in the EHR’ were in place 98–99% of the time. | Falls rates decreased: across the health system from baseline in FY 2013 to FY 2014, falls with harm dropped from 33 to 17, a reduction of 48%. No information provided about whether this was a significant decrease. |
| 14. Ireland et al., 2010117 | Site-specific, three-item risk screen. | Compliance improved in documentation of falls risk: random audits conducted at baseline and at 6-month postimplementation on 193 patient medical records on 15 medical-surgical units indicated a 13% improvement in documentation of fall risk. | Falls rates decreased: falls rates per 1000 patient-days reduced by 20% for the implementation year 2008, compared with the 2007 baseline rate. No info about significance. No information was provided about whether results were statistically significant. |
| 15. Koh et al., 2008123 | Survey to assess nurse barriers to participation in falls prevention strategies. | An 80.2% response rate was achieved. The greatest barriers to implementation of clinical practice guidelines reported included knowledge and motivation, availability of support staff, access to facilities, health status of patients, and, education of staff and patients. | Not measured as part of study. |
| 16. Koh et al., 2009122 | Site-specific tool. | Compliance with falls risk assessment improved in the intervention and control hospital: measured by a completed fall risk assessment tool in the medical records, increased from 50.2% in 2004 to 99.3% in 2006 (p < 0.05). At the control hospital the use of the fall risk assessment tool increased from 60.6% in 2004 to 99.4% in 2006 (p < 0.05) for all the medical records audited. | Falls rates did not change: postimplementation, there was a non-significant reduction in fall rates from 1.44 to 1.09 per 1000 patient-days at the intervention hospital. No reduction in the fall rate was observed at the control hospital. |
| 17. Lytle et al., 2015110 | Computerised decision support (CDS) including indicators for incomplete documentation. | Compliance improved: documentation of fall risk assessments on the 16 units improved significantly according to quarterly audit data (p = 0.05), whereas documentation of the plans of care did not. | Falls rates did not change: mean falls per 1000 patient-days increased from 3.13 pre-CDS to 3.35 post-CDS (median, 2.53 to 2.97), which was not significant. Mean falls with injury per 1000 patient-days were 0.447 pre-CDS and 0.490 post-CDS (median, 0.0 to 0.0 post-CDS), which was not significant. |
| 18. Maia et al., 2018124 | Morse Fall Scale. | Compliance improved in falls risk assessment within 12 hours of admission. IMU – assessment 77% from 67%, ICU Assessment 72% from 55%, Compliance improved for targeted interventions used according to risk factors. IMU interventions 79% from 61% at baseline. ICU Interventions 73% from 56%. |
Falls rates decreased in one unit: preliminary rates were measured on the IMU only, from November 2016 to February 2017, where they decreased from 3.99 per 1000 bed-days in November 2016 to 0 falls per 1000 bed-days in February 2017. Patients who fell during this period suffered no further harm. |
| 19. McCarty et al., 2018111 | The Memorial Emergency Department Fall Risk Assessment Tool (MEDFRAT). | Not measured as part of study. | Not measured as part of study. |
| 20. Milisen et al., 2013127 | Survey to assess staff experiences implementing a Clinical Practice Guideline. | Not measured as part of study. | Not measured as part of study. |
| 21. Ohde et al., 2012125 | Site-specific tool. | Compliance improved for falls risk assessment: in the first 6 months, compliance with use of the falling risk assessment tool at admission was 91.5% in 2007 (3998/4368), increasing to 97.6% in 2010 (10,564/10,828). Compliance improved for implementing care plan: the staff compliance rate of implementing an appropriate intervention plan was 85.9% in 2007, increasing to 95.3% in 2010. |
Falls rates decreased: the overall hospital-wide fall rate was 2.13 falls per 1000 patient days in 2004 versus 1.53 falls per 1000 patient days in 2010, representing a significant decrease (p = 0.039). Bone fracture rates due to falls among hospitalised patients declined, though not significantly, from 0.04 fractures per 1000 patient-days in 2004 to 0.02 fractures per 1000 patient-days in 2010. |
| 22. Pop et al., 2020112 | Site-specific tool. | Not measured as part of study. | Falls rates started to decrease: preliminary results at end of 6 months of evaluation showed that the quarterly fall rate in the ED reduced to 0.27 falls per 1000 visits, with no fall-related injuries. Long-term outcomes not reported, nor whether decrease was statistically significant. |
| 23. Teh et al., 2017121 | HIT tool to support direct iPadTM entry of patients’ fall risks and automated production of black-and-white A4-sized bedside posters. | HIT tool and paper-based score completion rates were similar, and their values correlated marginally (Spearman’s correlation coefficient 0.33, p < 0.01). | Falls rates did not change. They trended towards reduction on AMU (4.20 vs. 6.96, p = 0.15) and increase on GEM (10.98 vs. 6.52, p = 0.54) with HIT tool implementation, but not significantly. |
| 24. Teh et al., 2018120 | HIT tool to support direct iPadTM entry of patients’ fall risks and automated production of black-and-white A4-sized bedside posters. | Not measured as part of study. | Not measured as part of study. |
| 25. Thatphet et al., 2021116 | Experiences of emergency departments (EDs) with geriatric fall programmes. | Not measured as part of study. | Not measured as part of study. |
| 26. Titler et al., 2016113 | Targeted Risk Factor Fall Prevention Bundle. | Compliance implementing some targeted interventions improved: use of fall prevention interventions improved significantly (p < 0.001) for mobility, toileting, cognition, and risk reduction for injury, but did not change for those targeting medications. Nurses’ mean adoption scores increased significantly for ambulation; postfall huddles; and Use of Research Findings in Practice scores. Adoption scores did not change significantly for medication review and delirium screening. |
Falls rates did not change although they demonstrated a trend towards significant decrease, declining by 22% (p = 0.09). There was a non-significant decline in fall injury rates (p = 0.73), with reductions in the severity of fall injury for major and moderate categories from 26% preimplementation to 11% postimplementation. |
| 27. Townsend et al., 2016114 | KINDER 1. | Not measured as part of study. | The total number of falls decreased; reported falls without injuries dropped from 0.21 to 0.07 per 1000 patients, and falls with injuries were reduced from 0.21 to 0.0 per 1000 patients. |
| 28. Wu et al., 2019126 | Standardised Computerised Nursing Process Documentation System (SCNPDS). | Compliance varied. Overall documentation compliance increased significantly from 93.04% to 94.42% (p = 0.039). Average scores for patient care, nursing efficiency, education/training, usability and usage benefits were 2.92, 2.78, 2.98, 2.61 and 2.87 (on a 4-point Likert scale), respectively. Data from the hospital’s EHR in 2015 were also analysed. Results showed that nursing staff did not implement care plans for all patients who received high-risk scores and the presence of a fall care plan correlated significantly with actual falls. In other words, significantly more patients who received NCPs fell than those without a nursing care plan (p < 0.001), yet 10-year run-chart data showed fall rates remained fairly stable from 2007 to 2017. |
Falls rates did not change: 10-year run-chart data showed fall rates remained fairly stable from 2007 to 2017. |
Appendix 8 GRADE-CERQual
| Summary of review finding | Studies contributing to the review finding | Methodological limitations | Coherence | Adequacy | Relevance | CERQual statement of confidence in the evidence | Explanation of CERQual assessment |
|---|---|---|---|---|---|---|---|
| Where MFRA tools are clearly visible to staff in their work routines, they can prompt delivery and documentation of a falls risk assessment. However, there is variation in practice because MFRA tools vary in number and type of assessment items and whether they stratify patients by risk. | 18,37,106–108,110–112,114,116–119,122,124–126 | Minor to Moderate concerns: 11 studies were QI projects that varied in levels of detail provided about methods. Five studies used quantitative methods (including a RCT and Interrupted Time Series analysis) had clearly described aims and methods, as did one semistructured interview study. | Minor to Moderate concerns: Three studies described tools as a practice reminder/prompt. Eleven studies measured compliance documenting MFRAs with ten demonstrating improvement and one no change pre–post tool. Three studies demonstrated that tool visibility can constrain use of tool. The 17 studies describe use of publicly available and locally developed tools that vary in assessment items and use of stratification. |
Moderate to Serious concerns: Data presented are largely quantitative, focusing on process measures such as compliance in documenting an assessment. Differences in assessment items can be distinguished where tools are clearly described. There is little data about staff experiences using tools but staff feedback and focus group data from two studies suggest visibility can constrain tool use. | Minor concerns: all studies were conducted in inpatient, acute settings with adults/older patients. Eight studies were undertaken in the USA. The remaining studies took place in the USA and Canada, Canada, the UK, Spain, Australia, Singapore, Brazil, Tokyo and Taiwan. | Moderate confidence – it is likely that the review finding is a reasonable representation of the phenomenon of interest. | Minor-moderate concerns regarding methodological limitations, coherence, and relevance. |
| Documentation and delivery of processes that follow a falls risk assessment, for example, use of targeted interventions, can be constrained by changes in patient condition, movement between wards, availability of interventions recommended in tools, and communication between different professional groups, leading to variation in practice as documented in the clinical record. | 37,107,110,111,113,118,119,124–127 | Minor to Moderate concerns: Seven studies were QI projects that varied in levels of detail provided about methods. Four studies clearly described methods that were appropriate to answer clear research questions. | Minor to Moderate concerns: Five papers show improvement in documentation of a falls risk assessment, but variation in documentation of follow-up processes. One paper reported that improvement was not sustained over the longer term. Eight papers discuss constraints on follow-up processes, but data to support these claims are variable. | Moderate to Serious concerns: Data are mostly quantitative and take the form of process measures, for example, use of targeted interventions as documented in the clinical record. Some focus group and survey data about user experience provided in two studies. | Minor concerns: All studies were conducted in inpatient settings with adults and included, or focused on, older patients. Five studies took place in the USA. The remaining studies took place in Australia, Belgium, Brazil, Spain, Taiwan and Tokyo. | Moderate confidence – it is likely that the review finding is a reasonable representation of the phenomenon of interest. | Minor-moderate concerns regarding methodological limitations, coherence and relevance. |
| Tool recommendation does not always align with staff clinical judgement and can constrain tool use where tools do not provide space to document clinical judgement. | 106,107,110,126 | Moderate to Serious concerns: three out of four studies are QI projects and vary in the amount of detail provided about methods. Some findings are anecdotal rather than linked to specific data collection methods. |
Minor concerns: three studies indicated that tools were not used as intended where tools did not align with clinical judgement. In one study, space to document clinical judgement was said to empower staff and support allocation of limited resources. | Moderate to Serious concerns: the amount and richness of data supporting explanation of clinical judgement is variable, with some limited to author accounts. | Minor concerns: all studies were conducted in inpatient setting, with adult/inpatient population. Three studies were conducted in the USA and one in Taiwan. | Low to Moderate confidence: it is possible/likely that the review finding is a reasonable representation of the phenomenon of interest. | Moderate/serious concerns in methods and adequacy. |
| HIT can facilitate delivery of falls prevention practices by automating processes, reducing clinician’s task-load. However, HIT introduces additional training needs and user tasks (e.g. poster display) that may be seen as competing priorities on staff time. | 34–36,38,109,115,120 | Minor to Moderate concerns: five studies audited intervention compliance (two of which were QI projects) that vary in level of detail provided about research methods. One study was an observational study. One study was mixed methods pilot with clearly described research aims and objectives. | Minor concerns: six studies examined technology that automated falls prevention practices, showing good levels of adherence. Three studies detailed staff experiences using the HIT and the impact of novel manual tasks, suggesting experience, training and competing priorities may influence use at the ward level. | Minor concerns: qualitive and quantitative data were reported detailing staff experiences of tool use and compliance using HIT. | Minor concerns: all studies were conducted in acute inpatient settings with adults and included older patients. Six studies took place in the USA and the remaining study took place in Australia. | High confidence: it is highly likely that the review finding is a reasonable representation of the phenomena of interest. | Minor concerns in coherence, adequacy and relevance. Minor/moderate concerns in methodological limitations. |
| In hospital, patient circumstances can constrain their participation in falls prevention strategies. These circumstances include not wanting to disturb busy nurses by requesting their help, not perceiving or believing they are at risk of falls, not understanding their falls risks. | 132,136,138,140,141,143,144,147 | Minor concerns: the eight papers included five qualitative studies, two quantitative studies and a mixed methods realist evaluation. Most studies clearly described research aims and methods. |
Minor concerns: seven studies discuss patient experiences with falls prevention, including reasons why patients might not participate in falls prevention activities. Three studies explored nurses’ experiences of falls and interactions with patients. | Minor concerns: the qualitative studies provide rich data from patient and nurses’ perspectives and one realist evaluation explained the links between these experiences and appropriate ‘messaging’. | Minor concerns: all studies were in acute settings except one rehab hospital. Five studies took place in the USA, one in Australia, one in New Zealand and one in the UK. | High confidence: it is highly likely that the review finding is a reasonable representation of the phenomena of interest. | Minor concerns in Coherence, Adequacy and Relevance. |
| Where hospital staff understand patients’ circumstances through meaningful and directed interactions, they can personalise falls prevention messages to improve patient knowledge, skills and confidence to participate in falls prevention strategies. | 34,38,129,134,137–139,146–148 | Minor concerns: two studies were QI, five were quantitative (including one randomised and one non-randomised trial), two were qualitative and one a mixed method realist evaluation. The majority clearly described research aims and methods. | Minor to Moderate concerns: two studies indicated improvement in patient knowledge and confidence, three studies indicated good levels of adherence to patient engagement measures, and one study indicated that the intervention helped reconcile differences in patient/staff perspectives. In one study, patient understanding of falls risks and participation in care plan implementation did not change and one study showed variable awareness of falls risks. | Minor concerns: six studies used quantitative measures to assess patient engagement or activation (knowledge, skills and confidence), or participation in care plan development. Two studies reported goals set as part of the intervention and three studies provided rich description using qualitative data of patient and professional perspectives. | Minor concerns: all studies were in acute settings except one rehab hospital. Five studies were conducted in the USA, three in Australia, one in Sweden and one in New Zealand. | High confidence: it is highly likely that the review finding is a reasonable representation of the phenomena of interest. | Minor concerns in Methods, Adequacy and Relevance. |
| Interventions that encourage cognitively intact patients to participate in falls prevention practices are associated with a reduction in falls. However, it is unclear whether this outcome is because the intervention has led to patient participation in tailored interventions/goals. | 38,63,129–131,133–135,139,145,149 | Minor to Moderate concerns: seven of the 11 papers were QI studies and differed in the level of detail about methods. Two studies were RCTs and one a non-RCT, one quantitative with clearly described research aims and methods. | Minor to Moderate concerns: five studies evaluated interventions that aimed to involve patients in the assessment and care planning process. Two studies showed a reduction in falls, one a reduction in cognitively intact patients only, one a reduction in units with a higher baseline rate of falls, in one study falls rates varied between hospitals studied. Three studies evaluated patient agreements and reported that fall rates declined. Three studies evaluated intentional rounding. One study reported a reduction in fall rates in one unit, in one study the fall rate did not change, and in one study fall rates increased where purposeful rounding was completed more frequently. |
Minor to Moderate concerns: seven studies report falls rates per 1000 bed-days, including two RCTs and one non-RCT that evaluated interventions to involve patients in assessment and care planning. A RCT and the non-RCT demonstrated a significant reduction in fall rates. The other RCT found that the intervention reduced falls among cognitively intact patients only. The RCTs and two other studies provide data about goals set and patient engagement (knowledge of falls risks) but not whether patients participated in falls prevention interventions. |
Minor concerns: all studies were conducted in inpatient settings with adults and included, or focused on, older patients. Nine studies took place the USA and two in Australia. |
High confidence: it is highly likely that the review finding is a reasonable representation of the phenomena of interest. | Minor concerns in Coherence, Adequacy and Relevance. |
| There is a paucity of literature examining the use of patient participation interventions with cognitively impaired patients. Where available, evidence suggests that, depending on severity of impairment, education, goal setting and follow-up may not lead to participation to support falls prevention. | 134,138 | Minor concerns: study aims and methods clearly described in both studies. One study was a three-group RCT and one was a mixed method realist evaluation. |
Minor concerns: two out of 24 studies reviewed explicitly examined intervention use or impact with patients with cognitive impairment. One study examined intervention use with mildly impaired patients suggesting reminders prompted participation but fall rates were not measured. One study found that cognitively impaired patients allocated education and physiotherapy follow-up with goal setting incurred a significantly higher rate of injurious falls than participants in the control group. |
Minor concerns: one study was a three-group randomised trial that found that cognitively impaired patients allocated education and follow-up incurred a significantly higher rate of injurious falls than participants in the control group. One study included qualitive interviews with patients with mild cognitive impairment. | Moderate to Minor concerns: studies were conducted in inpatient settings with adults and a rehabilitation hospital. One study took place in Australia and one in New Zealand. | High confidence: it is highly likely that the review statement is a reasonable representation of the phenomena of interest. | Minor concerns in methods, coherence, and adequacy. |
Appendix 9 Study details: patient participation CMOc
| Citation and country | Setting | Sample | Intervention description | Study design (inc. comparator if applicable) |
|---|---|---|---|---|
| 1. Bargmann and Brundrett, 2020,130 USA | A medical-surgical telemetry unit in a military trauma centre. | Initial postimplementation audit was undertaken with 17 patients and project began once 90% of staff received face-to-face training. | Multifaceted falls prevention bundle, including (1) daily patient education on what contributed to their falls risk during shift assessments; (2) patient educational hand-out on fall risk factors; and (3) a fall safety agreement, which patients were encouraged to sign. | QI project, compared baseline and postintervention falls rates per 1000 patient-days. |
| 2. Cann and Gardner, 2012,131 Australia | Acute surgical ward in a hospital. | All adult patients and ward nursing staff. 1115 patients admitted preimplementation and 1069 postimplementation. | Practice Partnership Model of Care with four components: (1) staff working in partnership with each other, rather than each nurse providing exclusive care for an individual caseload of patients; (2) clinical handover at the bedside; (3) comfort rounds every 1–2 hours; and (4) environmental modifications. | QI project: Pre-test–post-test. |
| 3. Carroll et al., 2010,132 USA | An acute care hospital. | Nine patients who had fallen while inpatients, within 48 hours of interviews. | N/A: patients were interviewed about their experiences of a fall and how further falls could be prevented. | Qualitative interviews, no comparator. |
| 4. Christiansen et al., 2020,146 USA | Medical units at three acute hospitals. | Patients (n = 343) | Fall TIPS (Tailoring Interventions for Patient Safety), available in three modalities: (1) laminated poster; (2) electronic poster; (3) patient safety e-bedside display. Authors stated that each unit selected the modality that worked best for that unit’s workflow, but did not report which units chose which modality, or report results per modality. | Patient survey. The short form Patient Activation Measure (PAM-13) adapted for fall prevention assessed patient’s knowledge, skill and confidence in managing his or her fall prevention. Comparator: patient activation measured before and after implementation of Fall TIPS in the three hospitals. |
| 5. Duckworth et al., 2019,34 USA | Six neurology units and seven medical or medical-surgical units in three acute care centres. | Nurses submitted 1209 audits for the patient engagement measure and 1401 for the presence of the Fall TIPS poster at the bedside. | Fall TIPS: study examined whether three modalities of Fall TIPS (original EHR version; a laminated poster version; and e-bedside display version) impacted on patient engagement in falls prevention process and thus on Fall TIPS efficacy. | Implementation science study auditing patient engagement and adherence with poster display. Compared modalities of intervention. |
| 6. Dykes et al., 2010,63 USA | Four acute hospitals in one healthcare system. | All patients admitted to the hospitals during study period. 5160 patients in intervention group and 5104 patients in control group. | Fall TIPS: original Fall TIPS toolkit, a tool within participating hospitals’ EHRs, which integrated existing communication and workflow patterns. Once staff entered risk data from patients, the software tailored fall prevention interventions to address specific determinants of falls risk. The toolkit produced bed posters composed of brief text with an accompanying icon, patient education handouts, and plans of care. | Quantitative stratified, cluster randomised trial. Comparator: four control units in the four participating hospitals, where patients received usual care. |
| 7. Dykes et al., 2017,38 USA | Two oncology, three neurology and two medical units at one hospital, and a large medical unit at a second hospital. | At the first hospital, 31 patients on the medical units answered presurveys and 33 patients answered postsurveys. At the second hospital 32 patients answered presurveys and 30 patients answered postsurveys. | Fall TIPS: a development of the Fall TIPS intervention, intended to enhance its patient-centred focus. In this iteration, a low-tech modality was added to the original EHR-based tool, in the form of a colour-coded, icon-based laminated paper poster in English and Spanish. | QI project involving patient surveys and measuring protocol adherence, patient falls and falls-related injury rates. No comparator. |
| 8. Dykes et al., 2020,129 USA | Fourteen adult medical units in three academic medical centres. | All patients admitted to participating units during study period, comprising: 17,948 preintervention and 19,283 postintervention. | Fall TIPS: three modalities of the Fall TIPS toolkit: (1) original EHR-based tool; (2) care plan displayed on laminated paper poster; and (3) care plan displayed on electronic e-bedside screen display. | Quantitative non-randomised control trial. Each unit served as its own control. |
| 9. Goldsack et al., 2015,133 USA | An adult medical stroke unit (Unit 1) and a haematology/oncology unit (Unit 2) in a hospital. | 56 patient flow sheets selected for review: 27 from Unit 1 and 29 from Unit 2. 108 staff were surveyed about the last round they completed. 20 staff in Unit 1 and 20 staff in Unit 2 also took part in a postimplementation survey. |
Patient-centred proactive hourly rounding, conducted every hour between 06.00 and 22.00 hours and every 2 hours between 22.00 and 06.00 hours. Rounding was performed by nurses and patient care technicians (Unit 1) or nurses only (Unit 2) based on differences in RN staffing between the two units. | QI project. Patient falls rates per 1000 patient-days were compared on the two participating units before and after implementation. |
| 10. Haines et al., 2011,134 Australia | Acute (orthopaedic, respiratory, and medical) and subacute (geriatric, neurorehabilitation) wards in two hospitals. | Older hospital patients (> 60 years), n = 1206: 401 patients in the complete programme group, 424 in the materials only group and 381 in the control group. | Multimedia patient education programme combined with trained health professional follow-up (complete program), multimedia patient education materials alone (materials only) and usual care (control). | Three group randomised control trial. Comparator: participants randomised to the control group, who received usual care. |
| 11. Hill et al., 2015,148 Australia | Eight aged care rehabilitation hospital units. | All physiotherapists (n = 10) trained as ‘educators’ in delivering the Safe Recovery Programme were invited to participate in the focus group. | Safe Recovery Programme: individualised education which involved providing patients with a multimedia package (a DVD to view and a written workbook to read) followed up by between one and three individualised sessions with a physiotherapist trained as an educator. Educators also trained multidisciplinary staff to facilitate their support of the programme. | A qualitative exploratory study including a focus group and an interview (n = 10 educators), and review of written educator notes and reflective researcher fieldnotes based on interactions with the educators during the primary study. No comparator. |
| 12. Hill et al., 2016,147 Australia | Eight aged care rehabilitation hospital wards in hospitals that provide acute and rehabilitation care. | Participants who responded (n = 473) Older patients (n = 757) who were eligible (mini-mental state examination score > 23/30) | Safe Recovery Programme: the education programme provided participants with a three-step message: (1) know if you need help; (2) ask for help; and (3) wait for help. The educator helped participants to develop a personalised action plan consisting of strategies that allowed them to engage safely in required mobility tasks on the ward and work co-operatively with staff, such as ringing the bell if they required help. | A prospective qualitative survey to understand patient response to the programme and their identified barriers to engaging in falls prevention strategies. No comparator. |
| 13. Johnson et al., 2011,135 USA | Nursing department in one hospital. | All patients admitted to the hospital in study period: 12,159 patients were assessed over 3 years (2231 in 2008; 4739 in 2009; and 5189 in 2010). | Multifaceted falls prevention programme, called ‘Helping Hands’, which including engaging patients and families in falls prevention and asking them to sign a fall safety agreement contract. | QI project, compared rate of falls pre- and postimplementation. |
| 14. Kiyoshi-Teo et al.,136 2019, USA | Three medical-surgical units at a Veterans Health Administration (VA) hospital. | Sixty-seven older inpatients (> 65 years). | N/A: reports older inpatients’ responses to surveys about the level of importance and confidence they felt for fall prevention in their current hospitalised state; their fears or concerns about falling; their levels of activation, willingness and ability to make independent actions to manage their health and care; daily activities they undertook to prevent themselves from falling; risk of falls due to medications; and cognitive status. | Quantitative surveys and chart reviews. No comparator. |
| 15. Kullberg et al., 2015,137 Sweden | Department of Oncology in one hospital. | One hundred and four cancer patients. | N/A: reports patients’ perceptions of information exchange about falls prevention with doctors and nurses and associations with patient satisfaction, participation and safety at inpatient oncology wards. | Quantitative questionnaires. No comparator. |
| 16. Martin et al., 2020,138 New Zealand | Four rehabilitation wards in an older person’s health rehabilitation hospital. | 72 patients took part in surveys. 49 staff took part in preintervention surveys and 44 in postintervention surveys. Patients took part in qualitative interviews (n = 11). Eight ward staff took part in focus groups, along with six SRP educators. |
SRP: used patient-directed education and individualised goal setting to educate patients about how to keep themselves safe in hospital. Two SRP educators (1.4 FTE), a physiotherapist and a nurse, were employed to implement the pilot. A3 wall posters were used to highlight key SRP messages as well as recording individual goals patients had identified to keep themselves safe. Four retired nurse volunteers delivered initial SRP education and goal-setting sessions to individual patients. | Realist evaluation, involving qualitative surveys, interviews and focus groups. No comparator. |
| 17. Radecki et al., 2018,140 USA | An academic health centre. | 12 patients. | N/A: reports patients’ perspectives of falls prevention in an acute care setting, to aid in the design of patient-centred strategies. | Qualitative interviews. No comparator. |
| 18. Radecki et al., 2020,139 USA | Four non-intensive care inpatient units in a trauma centre. | 203 patients (103 at baseline and 100 during the intervention) completed knowledge-in-action survey. 40 nurses completed a nurse usability survey. | Patient fall self-assessment tool (PFAT): a self-completed assessment tool to engage patients to coproduce the fall prevention plan. Within 24 hours of admission to the unit, nurses and patients identified risk factors and developed a fall prevention plan together. The nurse transcribed the risk factors and plan onto a laminated board in the patient’s room, which included areas to record activity status and level of assistance needed for mobilisation, and to select safety equipment. | QI project using patient and staff surveys. Compared rates of falls and falls with injury per 1000 patient-days during baseline (9 weeks before implementation) and implementation. |
| 19. Rush et al., 2009.141 Country not stated but appears to be USA | Cardiology, urogynaecology, general surgery and trauma units in a hospital. | 15 nurses. | N/A: reports acute care nurses’ experiences with patient falls. | Qualitative focus groups. No comparator. |
| 20. Sitzer et al., 2016,142 USA | Four acute care units, four progressive care units and one short-stay observation unit in an acute care community hospital. | 60 patients in the acute care units, 35 patients in the progressive care units and 25 patients in the short-stay observation unit. | Self-assessment for falls risk (SAFR) and fall prevention education. Patients performed their own fall risk assessment via a six-item questionnaire using a modified version of the Schmid fall risk assessment tool on an interactive device in their rooms. They were notified automatically of their falls risk status and provided with additional resources to prevent falls, such as a fall prevention video. | QI project. No comparator. |
| 21. Turner et al., 2019,143 UK | Two rehabilitation wards in a general hospital. | Five older patients (aged in 70s and 80s) who fell on the wards. | N/A: reports experiences of older patients who fell during their hospital stay. | Qualitative interviews and document review. No comparator. |
| 22. Twibell et al., 2015,144 USA | Acute teaching hospital. | 158 patients. | N/A: reports hospitalised adults’ perceptions related to risk for falling, fear of falling, expectations of outcomes of falling and intention to engage in behaviours to prevent falls. | Quantitative correlational study. Nurses’ assessments and patients’ perceptions of the risk for falling were compared. |
| 23. Vonnes et al., 2017,149 USA | Comprehensive Cancer Centre. | Patients from low to high risk were required to sign the Fall Prevention Agreement on admission. | To promote patient and family participation in the fall reduction and safety plan, the Fall Risk and Prevention Agreement was introduced upon admission. Using the Morse Fall Scoring system, patients’ risks of falling was communicated on the Fall Risk and Prevention Agreement. Besides admission, patients were reassessed based on change of status, transfer or after a fall occurred. | QI project. Compared falls and falls injuries rates two-quarters prior to implementation of the agreement and eight-quarters postimplementation. |
| 24. Zadvinskis et al.,145 2019, USA | 41 inpatient nursing units across seven healthcare facilities in a healthcare system. | 808 RNs surveyed about their falls practices and levels of engagement. | Purposeful rounds, during which staff intentionally checked on patients at regular intervals to ensure their needs were being met. | Quantitative descriptive analysis. Compared falls rates in the nursing units but not over time. |
Appendix 10 Summary of outcomes: patient participation CMOc
| Citation | Intervention (if applicable) | Patient goal setting/understanding or knowledge of falls risk factors and prevention strategies | Falls incidents and rates |
|---|---|---|---|
| 1. Bargmann and Brundrett, 2020130 | Fall Safety Agreement: patients encouraged to sign. | No evidence that patient participation/understanding improved: audits were undertaken to measure patient understanding by asking them if they knew what their falls risk was, but empirical data about this measure were not reported. | Rate of falls declined: following implementation, the unit’s falls rate decreased from 1.59 per 1000 patient bed-days for 2016 to 1.38 per 1000 patient-days for 2018. The lowest falls rate was during the second quarter of 2017, immediately after implementation of the bundle; the falls rate was 0.54 per 1000 bed-days. Additionally, the unit experienced two of the longest stretches of falls-free days since May 2015: 87 and 88 days. p-values not given. |
| 2. Cann and Gardner, 2012131 | Comfort rounds every 1–2 hours. | Patient participation/understanding not measured, although patients’ use of call-bell reduced significantly from 1277 uses per 100,000 patient hours to 523 uses (p = < 0.001). | Rate of falls did not change: patient falls per 100,000 patient hours decreased, but not significantly, from 13.9 to 10.9 (p = 0.500). |
| 3. Carroll et al., 2010132 | Patient perception study. | Patients discussed what constrained them from participating in falls prevention interventions, for example, pressing need to use the bathroom clouding their memory of physical limitations and preventing them from taking time to attain balance; staff not answering call-bell in time and patients mobilising on their own; not wanting to bother nurses, even when encouraged to ask for help; not being aware of their risk of falling; and receiving inconsistent messages about their falls risks from different nurses. Patients asked to be included in falls risk communication and to be part of falls prevention team. Nurses need to share a consistent and clear message that they are there for patient safety. | Rate of falls not measured. |
| 4. Christiansen et al., 2020146 | Fall TIPS (Tailoring Interventions for Patient Safety), available in three modalities: (1) laminated poster; (2) electronic poster; (3) patient safety e-bedside display. | Patient activation: researchers used the short form Patient Activation Measure (PAM-13) adapted for fall prevention. This 13-item survey assesses a patient’s knowledge, skill, and confidence in managing his or her fall prevention. Patient activation improved from preintervention to postintervention at all sites (BWH, p < 0.0001; NYP, p = 0.0373; MMC, p < 0.0001). Overall, the mean PAM score improved from 63.82 (standard deviation [SD] ± 17.35) to 80.88 (SD ± 17.48), p < 0.0001 | Rate of falls not measured. |
| 5. Duckworth et al., 201934 | Fall TIPS in three modalities: (1) laminated poster; (2) electronic poster; (3) patient safety e-bedside display. | To assess patient engagement in the three-step fall prevention process, random audits were conducted, asking: ‘Does the patient/family member know their fall prevention plan?’ In addition, audits were conducted to measure adherence, defined by the presence of the Fall TIPS poster at the bedside. Overall, 1209 audits were submitted for the patient engagement measure and 1401 for the presence of the Fall TIPS poster at the bedside. All units reached 80% adherence for both measures. While some units maintained high levels of patient engagement and adherence with the poster protocol, others showed improvement over time, reaching clinically significant adherence (> 80%) by the final month of data collection. | Rate of falls not measured. |
| 6. Dykes et al., 201063 | Fall TIPS original toolkit, falls risk assessment tool in her, which produced bed posters and plans of care. | Patient participation/understanding not measured: the trial did not measure patient participation or understanding, although they did examine whether the care plan poster was printed, which aimed to encourage patients to participate (the poster was printed for 93.2% of patients, with 89% adherence in placing the bed poster above the patient’s bed). | Rate of falls declined: during the 6-month intervention period, the number of patients with falls differed between control and intervention units (p = 0.02). Site-adjusted fall rates were significantly higher in control units per 1000 patient-days than in intervention units (3.15; p = 0.04). The intervention was found to be particularly effective with patients aged 65 years or older per 1000 patient-days (p = 0.003). No significant effect was noted on falls-related injuries. |
| 7. Dykes et al., 201738 | Fall TIPS low-tech modality, laminated poster on which to record falls risk assessment and care plan in English and Spanish. | Patients’ ability to identify own risks improved significantly in two hospitals (Brigham and Women’s Hospital/BWH, Boston and Montefiore Medical Centre/MMC, New York), but their ability to identify what to do to prevent falls improved in one hospital only. There were varying levels of improvement from the baseline to post Fall TIPS in patient surveys about their ability to identify own falls risks and what to do prevent themselves from falling, measured using five-point Likert scale at baseline and after implementation. Scores for perceived ability of patients to identify fall risk (pre mean 3.7; post 4.5, p = 0.031) and knowledge of how to prevent falls (pre mean 3.7; post 4.4, p = 0.264). At MMC, there was improvement from baseline to post Fall TIPS scores for perceived ability of patients to identify falls risk (pre mean 4.0; post 4.6, p = 0.023) and knowledge of how to prevent falls (pre mean 3.6; post 4.7, p = 0.001). Authors do not comment on whether patients participated actively in falls prevention. | Rate of falls varied: at BWH the mean fall rate decreased from 3.28 per 1000 patient-days from January to June 2015 to 2.80 per 1000 patient-days from January to June 2016. The mean falls-related injury rate for the same months decreased from 1.00 per 1000 patient-days in 2015 to 0.54 per 1000 patient-days in 2016. At MMC the mean falls rate slightly increased – from 3.04 per 1000 patient-days for January through June 2015 to 3.10 per 1000 patient-days for January through June 2016. The mean falls-related injury rate for the same months decreased from 0.47 per 1000 patient-days in 2015 to 0.31 per 1000 patient-days in 2016. p-values not given. |
| 8. Dykes et al., 2020129 | Fall TIPS in three modalities: (1) original EHR-based tool; (2) laminated poster; (3) electronic e-bedside display. | Some evidence that patient understanding improved: after implementation, Site 1 had a mean compliance rate of 86% on a three-question audit, which asked the following: (1) Is the Fall TIPS poster updated with the correct patient information? (2) Can the patient/family express their fall risk factors? and (3) Can the patient/family express their fall-prevention plan? Sites 2 and 3 had mean compliance rates > 95%, but no further detail is provided. Authors do not comment on whether patients participated actively in falls prevention. | Rate of falls declined: there was an overall adjusted 15% reduction in falls after implementation compared with before (2.92 vs. 2.49 falls per 1000 patient-days; p = 0.01) and an adjusted 34% reduction in injurious falls (0.73 vs. 0.48 injurious falls per 1000 patient-days; p = 0.003). The decrease in falls was largest for patients younger than 65 years; units achieved an 18% reduction in patient falls in this age group in the postintervention period (p = 0.02) versus a 10% reduction for patients aged 65 and older (p = 0.28), with the latter difference not being statistically significant. The decrease in injurious falls was largest for patients aged 65 years or older, among whom units achieved a 48% reduction in the postintervention period (p = 0.004) versus a 19% reduction for patients younger than 65 (p = 0.28), with the latter difference not being statistically significant. |
| 9. Goldsack et al., 2016133 | Proactive rounding every hour during the day and every 2 hours at night. | Patient participation/understanding not measured, but of the 108 rounds observed, 88% of the prescribed steps (which included asking patients about their needs) were completed on average. Attention to patients’ comfort needs (occurred in 98% of rounds) and access to the call-bell (occurred in 97% of rounds) were the most-often performed tasks in the rounds. Staff reported asking patients if they could do anything else for them most frequently (in 96% of completed rounds). | Rate of falls declined in one unit and did not change significantly in the other: on Unit 1, where staff and leadership were engaged in the project from the outset, the 1-year baseline mean fall rate was 3.9 falls/1000 patient days. The pilot period falls rate of 1.3 falls/1000 patient days was significantly lower than the baseline falls rate (p = 0.006). On Unit 2, where there was no run-in period, the 1-year baseline mean falls rate was 2.6 falls/1000 patient days, which fell, but not significantly, to 2.5 falls/1000 patient days during the pilot period (p = 0.799). |
| 10. Haines et al., 2011134 | Multimedia patient education programme combined with trained health professional follow-up (complete program); multimedia patient education materials alone (materials only); and usual care (control). | Patients identified ways they could participate in preventing themselves from falling, although whether they went onto achieve these goals was not measured: of the 280 patients allocated to the complete programme group at the Princess Alexandra Hospital site, 273 patients recorded a total of 700 goals in relation to behaviour modification in their education materials. The most common goal (142 patients) related to asking for help, followed by identifying environmental hazards (131 patients), using walking aids or other aids (97 patients), waiting for help after it has been asked for (71 patients), wearing safe footwear or clothing (38 patients), and doing more exercise to get stronger and better balance (34 patients). Of the 299 patients allocated to the materials-only intervention at the Princess Alexandra Hospital site, 31 patients recorded a total of 75 goals. The most common goals related to asking for help and waiting for help to arrive once it had been asked for (14 patients each), followed by identifying environmental hazards (9 patients) and using aids (8 patients). | Rate of falls declined for cognitively intact patients in the complete program only: rates of falls per 1000 patient-days did not differ significantly between groups but there was a significant interaction between the intervention and presence of cognitive impairment. Falls were less frequent among cognitively intact patients in the complete program group: 4.01 per 1000 patient-days, compared to 8.18 per 1000 patient-days in the cognitively intact materials-only group (p = 0.03) and 8.72 per 1000 patient-days in the cognitively intact control group (p = 0.006). The effect was reversed, however, among participants with impaired cognitive function in the complete programme, who incurred a significantly higher rate of injurious falls per 1000 patient-days than those in the control group (7.49 vs. 2.89, p = 0.02). |
| 11. Hill et al., 2015148 | SRP: focus groups with physiotherapists who delivered SRP falls prevention education to patients and staff. | Falls prevention education led to mutual understanding between staff and patients which assisted patients to engage in falls prevention behaviours. Mutual understanding was derived from the following observations: the educators perceived that they could facilitate an effective three-way interaction between staff actions, patient actions and the ward environment, which led to behaviour change on the wards. This included engaging with staff and patients and helping them to reconcile differing perspectives about falls prevention behaviours. | Rate of falls not measured. |
| 12. Hill et al., 2016147 | SRP: semistructured questionnaire for older patients in SRP, identifying barriers to engaging in falls prevention strategies. | Participants stated that the education provided within the SRP raised their awareness, knowledge and confidence to actively engage in falls prevention strategies, such as asking for assistance prior to mobilising. Participants’ thoughts and feelings about their recovery were the main barriers they identified to engaging in safe strategies, including feeling overconfident or desiring to be independent and thinking that staff would be delayed in providing assistance. The most common task identified as potentially leading to actions that increase the risk of falling was needing to use the toilet. | Rate of falls not measured. |
| 13. Johnson et al., 2011135 | ‘Helping Hands’ intervention including fall safety agreement between patients/carers and staff. | Patient participation/understanding not measured. | Rate of falls declined: From 2008 to 11 total falls per year decreased by 16.6% and the number of injuries from falls decreased by 9.4%. p-values not given. |
| 14. Kiyoshi-Teo et al., 2019136 | Patient perception study, identifying associations among patients’ falls risk factors, perceptions, and daily activities. | A fall within 3 months before hospitalisation was associated with patients according more importance to preventing falls and indicating that they engaged in more daily activities to prevent falling, but these patients also had decreased levels of confidence related to preventing falls (p < 0.05). Perception measures (concern: r = 0.52; patient activation: r = 0.46) were positively associated with measures of daily activities to prevent falls (p < 0.001). Authors conclude that addressing patient-centred measures such as perceptions of and daily activities for fall prevention could add value to existing fall prevention programmes. | Rate of falls not measured. |
| 15. Kullberg et al., 2015137 | Patient perception study, investigating patients’ perceptions of information exchange and associations with patient satisfaction, participation and safety. | Patients rated doctors’ and nurses’ information provision lower than their technical and interpersonal skills, with only 13% considering information exchange to have been ‘excellent’. Falls risk assessments using the Downton Fall Risk Index were registered for 73% of responding patients, but only 39% reported having discussed their risk of falling during the hospital stay. 30 patients had documented fall prevention actions, and of these, half (15) reported having discussed their falls risk. Only one of the four patients who fell as inpatients reported having discussed falls risk during the hospital stay. | Downton Fall Risk Index scores were not associated with actual falls or fall prevention actions. Four patients reported having experienced an inpatient fall: one with Downton score 4 (high fall risk), two with score 0 (no fall risk), and the final patient was not falls risk assessed. For two of these four patients, fall prevention actions were registered in the EHR. |
| 16. Martin et al., 2020138 | SRP: patient-directed education and individualised goal-setting to educate patients to keep themselves safe in hospital. A3 wall posters used to highlight key messages and individual goals. | Patients identified ways they could participate in preventing themselves from falling, although whether they went onto achieve these goals was not measured. The most common goals that patients identified and were written on the wall related to using their call-bell (19%); planning out tasks (10%); having their frame within reach (9%); and not rushing (10%). Patients set an average of 2.8 goals per person. However, patient surveys showed they had variable awareness of their own risk of falling while at hospital: 56% disagreed to some extent that they were at risk of falling and 57% tended to not to be concerned about their risk of falling while in hospital. | Rate of falls not measured. |
| 17. Radecki et al., 2018140 | Patient perception study, described patients’ perspectives of fall prevention in acute care. | Most patients were aware of being identified as a fall risk and more than half (all of whom had physical limitations that put them at risk) agreed they were a fall risk. Patients were able to describe actions they would take to prevent themselves falling, such as being careful or holding on to something, but whether they took such actions in practice was not measured. Ninety per cent of patients believed they shared the same fall prevention plan as nurses and when they felt interventions were useful, they did not describe any barriers to participating in the fall prevention plan. The most frequently mentioned constraint on the partnership between nurses and patients was time spent waiting. Developing truly patient-centred programmes may reduce over-reliance on bed alarms and allow for implementation of strategies aimed to mitigate modifiable risk factors leading to falls. | Rate of falls not measured. |
| 18. Radecki et al., 2020139 | Patient fall self-assessment tool (PFAT): self-completed assessment tool to engage patients in coproducing fall prevention plans. | Patient participation in care plan development increased but patient understanding of their own falls risks and participation in care plan implementation did not change. Patients took part in knowledge-in-action surveys at baseline and postintervention. The survey asked patients to indicate, whether they (1) knew they were a falls risk; (2) knew their own risk factors; (3) were involved in plan development; (4) knew how to prevent falls; and (5) always followed the fall prevention plan. Responses to question (3) showed statistically significant improvements between the baseline and intervention groups (p = 0.0007) but responses to the remaining questions was similar between baseline and intervention groups. | Rate of falls declined in units which had with higher baseline falls but remained the same or increased in units that performed better at baseline: both units with higher baseline falls and falls with injury rates (2.68 and 1.43 per 1000 patient-days for falls and 1.34 and 0.71 per 1000 patient-days for falls with injuries) showed improvements, with fall rates decreasing to 1.28 and 0 per 1000 patient-days, respectively, and the rates of falls with injuries falling to 1.28 and 0 per 1000 patient-days. The highest-performing unit at baseline (zero falls) sustained the trend in the postintervention period and experienced no falls, but the next best baseline performing unit showed an increase in fall rates from a baseline of 1.38 per 1000 patient-days to 2.86 per 1000 patient-days and a rate of zero for falls with injuries to 0.72 per 1000 patient-days. p-values not given. |
| 19. Rush et al., 2009141 | Staff perception study, reports acute care nurses’ experiences with patient falls. | Nurses described the importance of ‘knowing the patient as safe’: a continuous confirmation that patients were free from harm. Such knowing involved key strategies of assessment, monitoring and communicating. Variable conditions influenced whether these strategies were effective in giving nurses the knowledge they needed to keep patients safe. When strategies failed to provide nurses with knowledge of their patients as safe and patients fell, this created considerable stress for nurses and prompted them to use a range of coping strategies. | Rate of falls not measured. |
| 20. Sitzer, 2016142 | Self-assessment for falls risk (SAFR) and fall prevention education. Patients performed their own fall risk assessment on interactive devices. | Patient participation/understanding not measured (the study measured the reliability and validity of the SAFR patient questionnaire). | Rate of falls not measured. |
| 21. Turner et al., 2019143 | Patient perception study, reports experiences of older patients who fell during their hospital stay. | Patients understood they had fallen owing to a loss of balance, and all had been identified as unsteady in their falls risk assessment on admission. Falling while in hospital fall affected patients’ experiences of rehabilitation and resulted in changes to ways they believed they could participate in rehabilitation. For example, some patients reported being more likely to avoid daily activities they had previously carried out and/or acknowledged they needed more help from others than before they fell. For some patients there was a subtle shift in the locus of control from themselves to staff. | Rate of falls not measured. |
| 22. Twibell et al., 2015144 | Patient perception study, explored patients’ perceptions of risk of falling; fear of falling; expectations of outcomes of falling; and intention to engage in behaviours to prevent falls. | Patients’ intentions to engage in behaviours to prevent falls were correlated with increased confidence in their ability to perform high-risk behaviours without help and without falling (p < 0.001); decreased fear of falling (p < 0.001); and decreased perceived likelihood of adverse outcomes if they did fall (p < 0.001). Although nurses’ assessments indicated a risk for falls, 55.1% of patients did not perceive a high likelihood of falling while hospitalised. Whereas 75% of patients intended to ask for help before getting out of bed, 48% were confident that they could get out of bed without help and without falling. | Rate of falls not measured. |
| 23. Vonnes and Wolf, 2017149 | Fall Risk and Prevention Agreement, signed by patients and/or families acknowledging their understanding and reception of fall prevention education. | Patient participation/understanding not measured, although authors note that this patient population often overestimates their abilities and functional status and conclude that engagement with patients and families during the admission process communicated the need for a collaborative effort for fall prevention during the patient’s hospitalisation. | Fall and fall injuries rates were compared two-quarters prior to implementation of the fall agreement and eight-quarters postimplementation. Falls and fall injuries on the medical oncology unit had an overall reduction of 37% and 58.6%, respectively. p-values not given. |
| 24. Zadvinsksis et al., 2019145 | Purposeful rounds, during which staff intentionally checked on patients at regular intervals. | Patient participation/understanding not measured. | Rate of falls greater in units with more purposeful rounds: it was found, unexpectedly, that the nursing units that had more nurses performing frequent purposeful rounds experienced greater falls with injury, with a ratio of incidence in those units and incidence in the units with fewer nurses performing frequent purposeful rounds at 1.06 (p = 0.003). The incidence of falls with injury in the nursing units with more nurses performing frequent purposeful rounds was 1.06 times (or 6% higher) that of those units with fewer nurses performing frequent purposeful rounds. The study did not include a patient acuity measure, so not possible to determine if this affected results. |
Glossary
- Cohort bay
- Bay where patients considered to be at high risk of falling are placed, with a staff member (typically a healthcare assistant) always present. Also referred to as a falls bay.
- Engagement support workers
- Staff with a specific remit for patient engagement, who spend time with patients, chatting, reading to them, playing games, or encouraging them to engage in crafts. Also referred to as activity co-ordinators.
- Falls link practitioners
- A role allocated to nurses and healthcare assistants, which involves the following: acting as a role model for falls reduction; providing a resource for advice and education for the assessment, intervention and management of patients who have fallen or are at risk of falling; facilitating regular audits of falls management practice on wards; and raising patient safety concerns. This role is undertaken alongside practitioners’ normal roles, although some time may be protected for activities and training.
- Falls risk prediction tools
- Tools that provide a list of falls risk factors, assign a numerical value to the presence or absence of the risk factor, and sum the numerical values together to represent the individual’s risk of falling (high, medium, low). Also referred to as falls risk screening tools or falls risk scores.
- Intentional rounding
- A practice where staff check on patients at regular intervals, for example, every 2 or 4 hours, to ask how patients are, if they need help toileting, and check call-bells are in reach. Also referred to as comfort rounds or care and communication rounding.
- Lay researchers
- Service users and carers who contributed to carrying out this research.
- Multifactorial falls risk assessment
- An approach to falls risk assessment where the focus is on identifying a patient’s individual falls risk factors that can be treated, improved or managed during their stay. This approach is recommended by the NICE guideline on falls in older people and the World Falls Guidelines.
List of abbreviations
- CDS
- computerised decision support
- CERQual
- Confidence in the Evidence from Reviews of Qualitative research
- CFIR
- Consolidated Framework for Implementation Research
- CMOc
- context mechanism outcome configuration
- COVID-19
- coronavirus disease 2019
- CPD
- continuing professional development
- DNR
- do not resuscitate
- DoLS
- deprivation of liberty safeguards
- ECG
- electrocardiogram
- ED
- Emergency Department
- EHR
- electronic health record
- EOC
- enhanced observations of care
- FROP
- fall risk for older people
- GRADE
- Grades of Recommendation, Assessment, Development and Evaluation
- HAPU
- hospital-acquired pressure ulcers
- HCA
- healthcare assistant
- HFRM
- Hendrich II Fall Risk Model
- HIT
- health information technology
- ICU
- intensive care unit
- IMU
- internal medicine unit
- IPCS
- interactive patient care system
- JHFAT
- John Hopkins Falls Assessment Tool
- LSBP
- lying and standing blood pressure
- MEDFRAT
- Memorial Emergency Department Fall Risk Assessment Tool
- MFRA
- multifactorial falls risk assessment
- MMAT
- mixed methods appraisal tool
- MoCA
- Montreal Cognitive Assessment
- NAIF
- National Audit of Inpatient Falls
- OT
- occupational therapist
- PFAT
- patient fall assessment tool
- PPI
- public and patient involvement
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PSLL
- Patient Safety Learning Laboratory
- QI
- quality improvement
- RCT
- randomised controlled trial
- RN
- registered nurse
- RR
- relative risk
- SAFR
- self-assessment of falls risk
- SCNPDS
- standardised computerised nursing process documentation system
- SRP
- Safe Recovery Programme
- SSC
- Study Steering Committee
- WBAT
- weight bearing as tolerated
