Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number NIHR135589. The contractual start date was in April 2022. The draft manuscript began editorial review in April 2023 and was accepted for publication in November 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Daniel et al. This work was produced by Daniel et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Daniel et al.
Chapter 1 Introduction
Box 1 provides a summary of Chapter 1 of this report.
-
Historically, women’s health has been confined to a focus on reproductive health. However, there has been a call for broader conceptualisations.
-
Women’s sexual and reproductive health needs are complex and vary across the life course from menarche to post menopause. A range of organisations, venues and professionals are involved in service provision for women’s health. Services in England are often not well integrated across organisations and there are challenges in access, workforce and resources and fragmented commissioning.
-
Local teams across the UK established Women’s Health Hubs (WHHs) in response to these challenges to improve provision, experiences and outcomes. These emerging models have been highlighted as best practice and wider adoption has been recommended.
-
The government identified the opportunity to integrate women’s health services more effectively, with a more woman-centred, life-course approach, reflected in the Women’s Health Strategy for England. The strategy, published in July 2022, encouraged the expansion of WHHs across the country, with additional funding to support implementation announced in March 2023.
-
There was no agreed definition of a WHH. Hubs were not necessarily a ‘place’, but a ‘concept’, and the term had been applied differently across health and care services.
-
In response to WHHs being identified as an important policy topic, the National Institute for Health and Care Research (NIHR) asked the BRACE Rapid Evaluation Centre to undertake a rapid evaluation of current hub evidence and practice. This evaluation aimed to provide information on hub models, how they were being implemented and how successfully.
-
The evaluation was supported by Stakeholder and Women’s Advisory Groups.
What is women’s health?
Conceptualisations of women’s health
Women’s health has historically been confined to a focus on sexual and reproductive health, including childbearing and menstruation. However, there has been a call for broader conceptualisations:1,2
Women’s health involves women’s emotional, social, cultural, spiritual and physical wellbeing and is determined by the social, political and economic context of women’s lives as well as by biology. 2 (p. 118)
The focus on sexual and reproductive health may be linked to the role that contraception and abortion access has played in transforming women’s autonomy, to make choices about having a family. 3 Organisations such as the Faculty of Sexual and Reproductive Healthcare conceptualise women’s health as existing on a continuum, with experiences and needs throughout the life course. 2–4 This acknowledges that needs change alongside life events and with age and draws attention to both stages and points of transition (e.g. the start of menstruation through to menopause). 3,4 This enables a preventive, rather than just reactive, approach to women’s health and extends beyond a medical model to improve health and well-being across generations. 4
Service provision
Women’s health needs can be understood and grouped in a number of ways and include pregnancy-related (e.g. pregnancy planning, fertility), sexual health-related (e.g. sexual pleasure) and non-pregnancy-related (e.g. incontinence). 5,109 These are met by a range of providers, professionals and venues, which also varies locally, as described in Box 2.
Organisations:
-
As part of their core service, primary care practices provide advice and treatment, for example contraception [excluding fitting of long-acting reversible contraception (LARCs)], sexually transmitted infection (STI) testing, cervical screening, menopause management and treatment. They refer women as required, for example specialist Sexual and Reproductive Health or gynaecology clinics. They may fit LARCs as part of a Locally Enhanced Service contract.
-
Sexual and reproductive health services – are sometimes called sexual health, family planning or genitourinary medicine (GUM) clinics. They offer a full range of contraception and STI testing and advice. They may also offer sexual-assault support, hepatitis and human papillomavirus (HPV) vaccination, post-exposure prophylaxis for human immunodeficiency virus (HIV) and cervical screening.
-
Pharmacies – provide access to contraception, emergency contraception, advice and STI screening.
-
LARC hubs – in some areas, hubs have been established to improve access to and uptake of LARC for contraceptive and/or gynaecological reasons, for example at a designated GP practice.
-
Community gynaecology services – can provide enhanced-level gynaecological care beyond what is offered in primary care, for example ultrasound, hysteroscopy, biopsy, management of complex menopause and heavy menstrual bleeding. Some may offer complex contraception. This may be provided in community settings to avoid the need for hospital gynaecology referrals.
-
Hospital gynaecology services – provide a range of outpatient assessment, testing and treatment for more specialised or complex gynaecological conditions, including suspected cancer, in secondary care settings. Provide inpatient care including gynaecological surgery.
-
Maternity services – provide inpatient, outpatient and community care during pregnancy, antenatal, intrapartum, postnatal and neonatal care.
-
Abortion services – provide access to support and perform termination of pregnancies, for example in a hospital or clinic. Often provided by private-sector organisations.
-
Private clinics – provide access to any and all of the above on a fee basis, for example screening, menopause, sexual health and contraception provision and support.
-
Outreach and specialised services for particular communities – often provided by outreach teams, for example local sexual health services, and offer support such as access to contraception for homeless women.
Professionals:
-
GPs and GPs with special interest in women’s health or sexual health.
-
Practice nurses.
-
Advanced nurse practitioners.
-
Pharmacists.
-
Consultant gynaecologists – medical and surgical care for conditions that affect the female reproductive system, including cancer.
-
Consultants in community sexual and reproductive health care – trained to deliver specialist care with a focus on population health management, for example for contraception, medical gynaecology, menopause and pregnancy and unplanned pregnancies.
-
Genitourinary medicine consultants – diagnose and manage STIs, genital infections and conditions.
-
Specialty doctors and specialty trainee doctors in the specialties listed above, physician associates, nurses and healthcare assistants in the specialties listed above.
In England, these services are provided in a range of primary and secondary care settings, with a variety of funding and commissioning arrangements. The complexity of the landscape often means that provision is not well integrated, and artificial divisions between contraception and reproductive health have led to challenges in access to contraception in England. 6 Following the 2012 Health and Social Care Act, responsibility for the provision of contraception, sexual and reproductive health provision was split between different commissioning bodies, for example local authorities, NHS England, and Clinical Commissioning Groups (CCGs), which have now been replaced by Integrated Care Systems (ICSs). 6,7 Services have been described as ’shaped by the source, availability and amount of funding available, rather than by women’s needs’ (p. 12). 6 Local authorities have largely had responsibility for preventive and public health services, including sexual health and contraception services, whereas the NHS has responsibility for the assessment and treatment of disease in primary care (including prescribing) or via referral for specialist health services. This fragmented model of commissioning can result in services that are disjointed, which may not reflect local population needs, and may lead to unwarranted variation in spending by local organisations, and difficulties in comparing investment between localities. 7 A particular consideration is that long-acting reversible contraception (LARCs), specifically intrauterine devices/systems (coils), may be required for either contraceptive purposes or gynaecological reasons. Separate sexual health and gynaecology commissioning arrangements mean that services are often not funded to provide coils for both reasons in one setting. A case has been made for collaborative commissioning, with a clear mandate and resources, supported by strong public health leadership. 8
Several factors seem to be interacting to increase perceived pressure on women’s health services: NHS budgets are under pressure, and local government has experienced cuts to funding; there are workforce and training gaps, for example insufficient staff with the right skills and experience. The COVID-19 pandemic and waiting-list backlogs have impacted on access. 4,6,9 Suggested improvements have included more strategic leadership accountability, models of care that incorporate sexual and reproductive health needs, sustainable workforce models that provide care for those with complex needs and provision for all. 4
Women’s experiences
The challenges described above can result in negative experiences for women seeking care. Women may be moved between services due to gaps in care pathways, have difficulty accessing appointments (including long waiting), experience variation in interest and expertise at the first point of contact, and may be required to attend multiple appointments with different providers, wasting time and resources. 6 Women are ‘being left without clear direction of where to access the support and services they need’,10,11 as care is not structured around their needs. 10,11
The Better for Women report by the Royal College of Obstetricians and Gynaecologists emphasised the need to focus on and adopt a life-course approach to women’s health. 9 As part of the report, a UK-wide survey of women was commissioned, which highlighted poor access to basic women’s health services, barriers to care and a need for improvements to services. 9 To inform the first Women’s Health Strategy for England,12 the government collected evidence from women. Five topics were identified for prioritisation: gynaecological conditions; fertility, pregnancy loss and postnatal support; the menopause; menstrual health and mental health. 13
Areas in need of improvement included women not feeling heard and difficulties with service access. 14 Women reported that their symptoms were often dismissed and that obtaining a diagnosis was challenging. Most respondents relied on family or friends for information and identified a particular lack of information on menstrual well-being, menopause and gynaecological conditions. Being taken seriously and offered appropriate treatments for menopause were further areas where shortcomings were reported. The majority of women suggested that service access was not convenient regarding location or time. 14 Women suggested changes at system level, including hubs and drop-in centres, as well as greater diversity in provision. 14 The evidence collected supported the need for a more joined-up approach to women’s health care and the implementation of WHHs, including one-stop shops (discussed further later).
Geographical variation and inequalities
Across the country, there is also variation in the quality and availability of sexual and reproductive health services, with a lack of ownership and accountability in the system for women’s healthcare needs. 4,9,15–17 This has been shown to particularly affect women seeking support for fertility treatment and menopause4 and cervical screening. 18 It has been suggested that political prioritisation of women’s health services is required to drive improvements, particularly for women from disadvantaged backgrounds, who experience the worst outcomes. 18 There are significant inequalities in sexual and reproductive health, with young people and ethnic minority groups among those disproportionately impacted. 15,19 For example, unmet need in contraception access is suggested by higher abortion rates among people from socially disadvantaged and/or ethnic minority backgrounds, and under 25s. 4 Additionally, women with disabilities can face barriers in accessing cervical screening or contraception. 4 It is also important to consider lesbian, gay, bisexual, transgender, queer, questioning and other sexual and gender identities (LGBTQ + ) service users. There is a paucity of high-quality research in this area, and routine data are not often collected in a way that enables appropriate examination of health inequalities. 20 Long-standing inequalities in service access and provision for women from disadvantaged and minority groups have likely widened because of COVID-19. 18
Development of Women’s Health Hubs
In recognition of these issues, there have been increasing calls for a more collaborative, holistic and integrated approach to delivering women’s health care, designed around women’s needs. 6,9,15 Local teams across the UK responded to the challenges in delivering services by establishing WHHs to improve access, experience and outcomes for their population, to address inequalities, and reduce costs. Some known models were already well established, while others were set up and/or starting to function around the time of the COVID-19 pandemic. Hubs function to meet the integrated needs of women’s reproductive health care by providing access to a practitioner with appropriate skills, in a community setting (usually primary care, although not necessarily at their own practice or provided by their own practice team). Although still emerging, these early models were highlighted as best practice,11,21 with wider roll-out recommended. 9 There appeared to be an increasing expectation among women in the population that healthcare provision needed to change. For example, in the UK-wide Royal College of Obstetrics and Gynaecology women’s survey, almost half of participants supported the idea that one-stop women’s health clinics and/or drop-in facilities would improve access. 9
The Primary Care Women’s Health Forum has actively promoted and supported the development of new ‘hub’ models. It has drawn together the expertise of hub leaders across England, and launched a WHH toolkit, to support others to implement these models. 11,93 Their work is evidence of the significant learning available within the professional community from the early experience of hub development, but it also illustrates the ongoing diversity of models and local variation in provision.
Policy context in England
The opportunity to integrate women’s health services more effectively, with a more woman-centred, life-course approach, was reflected in the first Women’s Health Strategy for England (the Strategy), published in July 2022. To support implementation and raise the profile of women’s health, a Women’s Health Ambassador was also appointed. 12 The Strategy aimed to improve the health and well-being of women and girls in England, by taking a life-course approach and ‘embedding hybrid and wrap around services as best practice’ (p. 8). 12 The Strategy set out several immediate steps being taken to improve women’s experiences and outcomes, including ‘encouraging the expansion of women’s health hubs around the country and other models of one-stop clinics, bringing essential women’s services together to support women to maintain good health and create efficiencies for the NHS’ (p. 8). 12 It described how WHH models ‘provide integrated women’s health services at primary and community care level, where services are centred on women’s needs and reflect the life-course approach, rather than being organised by individual condition or issue’ (p. 8). 12 Reducing the LARC backlog for both gynaecological and contraceptive reasons was an impetus for the development and roll-out of WHHs, as stated in the Strategy: ‘A key aim of hub models is to improve women’s access to the full range of contraceptive methods, and in particular LARC’ (p. 8). 12
Local commissioners and providers were strongly encouraged to consider adopting these models of care. 12 In mid-March 2023, a £25 million investment to ‘accelerate the development of new women’s health hubs to benefit women’ was announced with the aim to see at least one hub in every ICS. 22 The Department of Health and Social Care (DHSC) was also working collaboratively with multidisciplinary stakeholders to develop resources to support the creation of WHHs, including a best-practice guide. 22
While WHHs are emerging, there are many examples of models of integrated care which provide more joined-up care closer to home. Integrated care first appeared in targets and legislation in 1972, with further developments in later years. For example, in 2006, the Department of Health launched ‘Care Closer to Home’ demonstration sites to define appropriate new models of care. The sites were in six specialties, one of which was gynaecology; all sites attempted to reduce repeated visits, improve access and address the need for integrated and/or one-stop services. 23 In 2008, Integrated Care Pilots were launched to explore different ways of integrating care, with an aim of providing care closer to service users. 24 Later developments were driven by major policy reforms: for example, commitments to integrated care in the 2014 Five Year Forward View,25 and the introduction of the New Care Model Vanguard sites, which aimed to pilot new models of care for the health and care system that could be rolled out more widely. 26 Specific ‘hub’ models are also increasingly mentioned in NHS policy and are outlined in Chapter 2.
Moves towards greater integration in commissioning and delivery of sexual and reproductive health services mirror a wider direction of travel in English policy with the government’s commitment to integration of care across a population footprint. 27–29 This was reflected in the development of primary care networks (PCNs), place-based partnerships and ICSs to integrate care across organisations and settings and improve population health. In addition, GP federations have been established in some areas. These are groups of primary care providers which form a single entity with shared systems and records. They work together to deliver services for women across multiple PCNs, and to bridge the gap between ICSs and PCNs. 30 Federations, PCNs and ICSs provide opportunities for supporting the development and implementation of WHHs across England. 6,9
What is a Women’s Health Hub?
When this evaluation commenced in 2022, WHHs were understood differently by stakeholders, and we did not identify a single agreed definition of a WHH. Hubs were referred to as not necessarily a ‘place’, but a ‘concept’, and the term was used differently across health and social care services.
The Primary Care Women’s Health Forum, described WHHs as follows:
At the core of any Women’s Health Hub framework is convenient access to a range of services for all women. Women’s Health Hubs bring existing healthcare services together to provide holistic, integrated care. This care is accessible, delivered by trained healthcare professionals, supported by specialists. This results in better outcomes for patients. A Women’s Health Hub is not a building, there is no need to invest in new physical space. It is not a major financial investment, it’s about efficiencies of scale. 31
In the Women’s Health Strategy, a vision for WHHs was described: ‘hub models can provide management of contraception and heavy bleeding in one visit, integrate cervical screening with other aspects of women’s health care, or manage menopause at the same time as contraception provision for women over 40’ (p. 26). 12
There was, however, an emerging consensus that WHHs were characterised by some core features which provided the basis for a working definition for the evaluation.
A working definition for the evaluation
Through work with experts and service users, it was evident that a detailed definition for the evaluation was needed to draw boundaries around what a WHH is, distinct from other specialist services, for example a community gynaecology service or LARC hub. We have sought to build on the definitions from the Primary Care Women’s Health Forum and in the Women’s Health Strategy. 12 The working definition which underpinned this evaluation was a set of common features which were widely recognised by the community of practitioners as typifying a hub approach, as follows:
-
Women’s Health Hubs are based in the community and work at the interface between primary and secondary care and/or the voluntary sector and wider.
-
Women’s Health Hubs offer more than a single service (and include the provision of both gynaecological services and contraception) or demonstrate plans to do so.
-
Women’s Health Hubs have more than one organisation involved in the process of service delivery, including in design, commissioning and/or provision of care, beyond simply referring in.
Our interim evaluation report included an additional criterion:
WHHs are co-commissioned or joint-commissioned, meaning two or more organisations are responsible for tasks such as awarding or reallocating contracts to providers32 (or moving towards this) and/or have evidence of integrated governance and leadership models. 33 (p. 12)
However, during the course of the evaluation we observed that a number of hubs were currently able to provide both contraception and gynaecology services without a formal joint-commissioning arrangement. While some were working towards more integrated commissioning, this was not always the case. Similarly, there were not consistent integrated formal governance and leadership approaches across WHH models. Rather than exclude these models from our definition and evaluation, we revised our definition to be more inclusive in the final evaluation report. We discuss the challenges and opportunities for integration further in the results and discussion sections.
Although there may be future lessons from private models of WHHs, in this evaluation we focus on WHHs funded and operating within the NHS only.
The evaluation
Women’s Health Hub models are largely new and emerging, with examples of hubs in planning or set-up, and wider roll-out of hubs recommended. However, there was a paucity of research on these models. Through our scoping work for the evaluation, we identified significant diversity in the existing landscape, and a need to define, map and understand the current approaches and produce learning, to inform future development and investment.
Evaluation aim
The overall aim of the evaluation was to explore the ‘current state of the art’, mapping the landscape, studying experiences of delivering and using hub services and defining key features and early markers of success to inform policy and practice. Specifically, the study evaluated why, where and how hubs have been implemented; why different approaches have been taken; how inequalities have been considered and experiences of implementation, delivery and receiving services. The evaluation explored the successes and challenges of hubs and potential improvements, including different stakeholder group perspectives of what hubs are intended to achieve, and whether hubs were making progress towards this. It also explored what is known about performance, outcomes and costs and how they are measured.
Evaluation questions
The study sought to answer the following evaluation questions:
-
What are WHHs, and is there variation in how stakeholders name and define them?
-
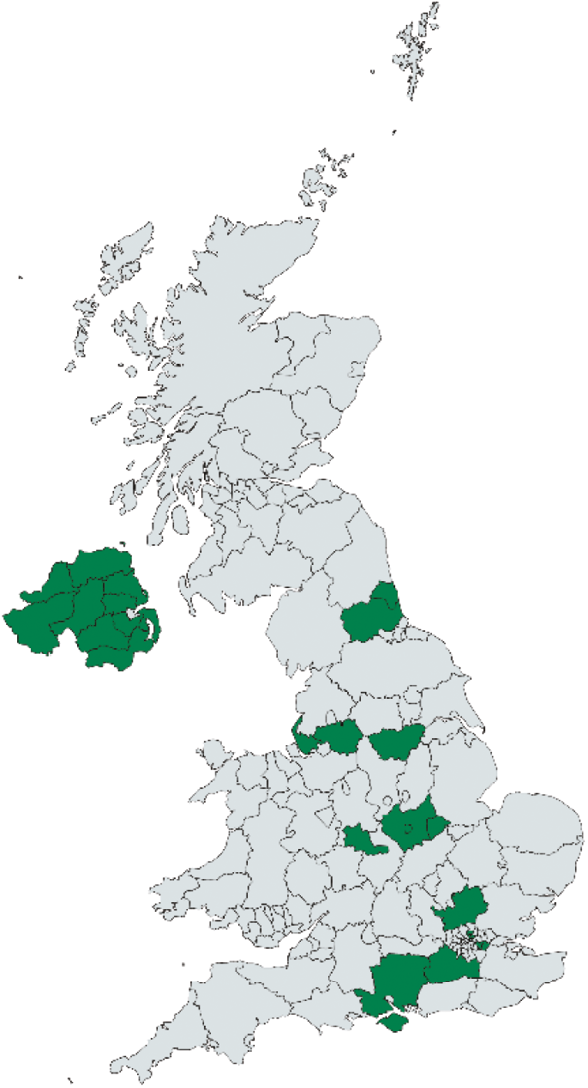
How many WHHs have been established or are in development across the UK, where are they, and what are their characteristics, including models of structure, commissioning and delivery?
-
Why have WHHs been implemented, and how are they intended to address health inequalities?
-
What have WHHs achieved to date? How do WHHs achieve this?
-
What are the experiences and perspectives of staff regarding WHH set-up, commissioning, funding, implementation and delivery?
-
What are the experiences and perspectives of women who have used hub services?
-
How are WHHs’ performance, outcomes and costs measured, and how might they be measured in future?
Development of the evaluation design
The protocol was developed after a detailed scoping phase in early 2022 which included:
-
Interviews with 10 key stakeholders to gather insights and experiences of WHHs and to define the evaluation scope (this included WHH leaders, national policy and practice leaders and representatives of key organisations including the Primary Care Women’s Health Forum, Faculty of Sexual and Reproductive Healthcare and Royal College of Obstetricians and Gynaecologists).
-
Identification and review of relevant published and grey literature to locate existing WHHs to understand the context and inform evaluation design and questions.
-
Establishment of a Stakeholder Advisory Group to support the evaluation.
-
A stakeholder workshop to refine the evaluation focus and questions.
-
A meeting with three women with lived experience of NHS women’s health services to discuss their views about what the evaluation should explore.
Wider input
Stakeholder Advisory Group
A multidisciplinary Stakeholder Advisory Group provided expertise and advice to support the study, meeting three times. The group discussed a range of topics related to women’s health, the Strategy and the evaluation. We also sought advice and guidance from the group on an ad hoc basis throughout. Details on the group’s specific input can be found in Chapter 3.
Women’s Advisory Group
The evaluation involved women with lived experience of NHS care for women’s health issues from the outset. Three women took part in the scoping work, and subsequently joined our Women’s Advisory Group. The Women’s Advisory Group provided input throughout the evaluation and used lived experiences to shape the project. This comprised a diverse group of seven women with varying experiences of NHS care for women’s health issues, including smear tests, endometriosis and menopause. The Group was chaired by a woman with experience of public involvement in research and evaluation. The team also met separately with an eighth member who was unable to join the main group meetings, who provided additional input including on terminology, the hub concept and delivery and inequalities. Our public contributors were drawn from across England and included different demographic backgrounds including age, ethnicity and sexual orientation.
Four virtual meetings were held with the group at key points in the evaluation. Meeting dates were agreed with the Group in advance, and any relevant documentation, for example topic guides, was shared before each meeting, along with meeting slides and an agenda. Where members were unable to attend, they could meet researchers separately later, or provide feedback via e-mail.
The Group helped to shape the study, provided advice and feedback, and contributed to framing and prioritisation of findings. Their input included:
-
Highlighting the need to include a more diverse group of women who may not access WHHs. As a result, we changed the methods to include focus groups with women in communities to hear about awareness and understanding of hubs, and any potential barriers to access.
-
Advising on appropriate ways to recruit women to participate, suggesting routes for data collection with patients using hub services and stressing the importance of flexibility and appropriateness, being mindful of women’s differing needs and preferences.
-
Providing guidance and perspectives regarding important criteria for selecting the hubs to be involved in in-depth evaluation.
-
Suggesting that we explore patient pathways in/out and back into WHHs, and how this is understood by and communicated to women.
-
Providing input into the design of evaluation tools, reviewing tools and providing feedback.
-
Reviewing the plain language summary for the protocol and report.
-
Reflecting and commenting on emerging findings and their relevance to women.
-
Providing advice about framing and disseminating the findings, particularly for the public.
-
Reflecting on the concept of WHHs as emerging models of care.
Working with policy-makers
We liaised closely with the Women’s Health Ambassador and Women’s Health Policy team at the DHSC in several ways, including:
-
discussing the interim report findings, and areas of evaluation focus
-
discussing priorities and work plans to ensure complementary approaches and avoid duplication
-
sharing copies of evaluation tools for example interview guides
-
sharing our working theory of change to inform policy discussions
-
sharing a working list of identified WHHs, which could be shared with ministers
-
meeting to discuss costs and benefits of women’s health models and potential considerations for economic analysis
-
connecting our stakeholders with the policy team to aid their work around understanding costs and benefits of models
-
reviewing a DHSC survey tool designed to collect information on hub costs
-
presenting at the policy team’s WHHs Expert Forum, held to initiate collaboration with stakeholders and support local areas to implement WHH models
-
meeting to discuss key conditions for funding of WHHs.
Structure of the report
In October 2022, an interim report was published, which focused on early findings from an online survey to map the current UK WHH landscape. 33 This report builds on the earlier output. Chapter 2 summarises relevant literature. Chapter 3 provides an overview of the methods utilised in the evaluation, and the findings are presented in Chapter 4. Chapter 5 presents insights from the Women’s Advisory Group and Chapter 6 summarises and discusses the study findings, exploring implications for research, policy and practice.
Chapter 2 Mapping of relevant literature
To locate this study within existing research and evidence on integrated care, specifically hub models, we undertook an initial pragmatic and rapid review of relevant academic and grey literature, revisiting our searches throughout the course of the evaluation. This included exploration of evidence for integrated care models outside the context of women’s health. A summary of the topics we reviewed can be found in Table 1. This section first explores what is known about WHHs, to demonstrate gaps in knowledge addressed in this evaluation. We then describe the literature on hub models, followed by relevant evidence and theory from the broader integrated care literature.
| Topic area | Relevance to the evaluation |
|---|---|
| WHHs | The grey literature describing WHHs provides a wide range of practice-based evidence to support hub implementation, though there is a lack of formal academic research on this topic. A review of what is known about WHHs provides a foundation on which the evaluation builds. |
| Hub models | Literature that describes hub models for women’s health is limited. We draw on the wider evidence exploring hub models in other health contexts to inform the evaluation. |
| Integrated care literature | The integrated care evidence base offers insights into the implementation, impact and dimensions of integrated care which can be applied to WHHs. Integrated care theory acts as a ’sensitising’ concept for the evaluation, supporting the interpretation of findings. |
What do we know about Women’s Health Hubs?
Although WHHs are a relatively new concept and we did not identify any published academic literature describing or evaluating their effectiveness, the grey literature offers important insights into these models and how they are intended to improve health services for women. The Primary Care Women’s Health Forum WHH webpages describe what a WHH is at a high level,11 and share early learning through case studies34 and a toolkit to support services with planning and implementation. 35–37 Key messages from the Primary Care Women’s Health Forum case studies are summarised in Table 2.
| Overarching aims | |
| Drivers | |
| Challenges | |
| Enablers | |
| Early benefits |
A number of models and ways of organising and providing women’s health services are described in the Primary Care Women’s Health Forum case studies and wider literature on WHHs. These include hub-and-spoke models,34 one-stop-shop models,39,43 PCN-based models,34 inter-practice referral models44 and community gynaecology models. 34 However, definitions of these terms are unclear. In our findings, we explore and, where possible, define models.
The case studies and resources provide valuable evidence to support hub implementation. Case studies were developed collaboratively with leaders and early implementers in WHHs. However, there has not been any comprehensive mapping of WHHs to date, and descriptions of models in the grey literature vary in detail and focus, with no in-depth exploration of the experiences of WHH staff and women using services. Our evaluation builds on and addresses the gaps in current evidence.
What is known about ‘hub’ models in health care?
Hub models are increasingly mentioned in NHS policy across a variety of contexts and are being implemented for different purposes across England. For example, NHS England recently set out plans to create health and well-being hubs, known as ‘Cavell Centres’, aiming to bring health and social care services together in one building. 45 Hub models in the literature focus on a number of different health conditions and services, such as child and family hubs, which include voluntary and community organisations pooling resources. 46 However, the evidence for hub models has not been synthesised, and there is no agreed definition of a hub, and terms are used inconsistently in policy and academic literature. Hubs and similar models can be adapted to a range of contexts, and a key message from the evidence is that one size does not fit all. 47–50
Hub-and-spoke models are described as providing complex services in a central ‘hub’ (typically a hospital), linked to a network of more local ’spokes’ (less specialised hospitals/community venues). 51 A model may have a single hub or multiple hubs; similarly, any number of spokes may feature in a hub model. 52 The activities within hubs and spokes may vary, along with the way they are managed. For example, different spokes may provide different services and there may be variation in the way women access them. 52 In hub-and-spoke models of maternity services, a hub may be a consultant-led ward in a hospital, surrounded by midwifery-led units. 53
Hub models can provide care as a one-stop shop, meaning a broad number of services are available under one roof,54 ideally in a single visit, reducing the need for numerous appointments. 55 There are a range of examples of one-stop shops, bringing together professionals and service providers to improve and integrate care. 56–58 These models have been described as user-focused, providing opportunities for staff development, and were recommended by the Royal College of Gynaecologists and Obstetricians during COVID-19 to reduce risk of exposure for staff and women. 59 One-stop-shop models in primary care have been associated with improved patient satisfaction, particularly with continuity of care and accessibility. 54 In an evaluation of a GP hub-and-spoke model of sexual and reproductive health services, a sexual health centre acted as a hub, with GP practices as spokes. The model was led by nurses, and hub staff provided training and education to upskill nurses in sexual and reproductive health care, so that the GPs and nurses could provide human immunodeficiency virus (HIV)/sexually transmitted infection (STI) testing and treatment, with more complex cases referred to the hub. 60 The model was found to be acceptable and feasible by women and by clinicians, integrating with usual practice well. 60 However, there are concerns that providing all services under one roof may have a negative impact on the sustainability of standalone services, and data on the cost-effectiveness of these models are inconclusive. 61
Bostock and colleagues describe a number of limitations in evaluations of hub-and-spoke models in health care, including a lack of clarity in the definition, the absence of service user voice in evaluations, and limited evaluation of the role of context. 52 Predictors of a ’successful spoke’ are also uncertain, specifically in the context of SRH services. 60 This evaluation adds to a limited body of literature on hub models in women’s health care.
Integrated health care
In this evaluation, integrated care is used as a ’sensitising concept’ to support our exploration of how WHHs are set up, structured, staffed and measured. Sensitising concepts act as a starting point for analysis and are ‘background ideas that inform the overall research problem’ (p. 2). 62 Integration is a key concept in descriptions of hub models, and a core aim of WHHs is to integrate services and care for women, but integration has many dimensions. Here, we provide an overview of integrated care definitions, theory and evidence and highlight key challenges to evaluating integrated care. The literature offers insights into the implementation, impact, and dimensions of integrated care which can be applied to WHHs. 47,63,64 It also provides a framework for understanding the examples of hub models identified in this evaluation, supports our interpretation of findings and shows the ways in which WHHs may function. Evaluations of integrated care for women’s health are sparse in the literature, and there is a lack of evidence for decision-makers to assess which care models work best for women’s health, are most effective and likely to be used by those with greatest need. 60 In the discussion of this report, we reflect on the extent to which our evaluation adds clarity for decision-makers.
Definitions
There is no widely accepted definition of integrated care, which has been described in the literature as ‘diverse’, ’synergistic’, ‘ambiguous’ and ‘dynamic’, evolving to meet the changing needs of a population. 65–67 Integrated care can be:
… best understood as an emergent set of practices intrinsically shaped by contextual factors, and not as a single intervention to achieve predetermined outcomes … [it] is a broad concept, used to describe a connected set of clinical, organizational, and policy changes aimed at improving service efficiency, patient experience, and outcomes. 67 (p. 446)
Integrated care is generally understood to be co-ordinated, be that through combining physical resources (e.g. rooms and buildings), by workforce, through bringing together professionals from different services, and by systems, for instance integrating patient record systems across sectors of care. 65 Integrated care involves the removal of boundaries within the health sector (such as those between primary and secondary care), between health and associated services (e.g. health and social care) or both (e.g. in bringing specialised teams together to address both mental and physical health aspects of a condition). 25 Integration can be vertical, with integration between organisations involved at different stages of the patient pathway (e.g. hospitals running GP practices) or horizontal, between organisations at similar stages of a patient pathway, such as GPs working within PCNs. 68
Aims of integrated care
Integrated care intends to achieve the NHS quadruple aim of improving patient experience, population health, the efficiency of healthcare systems (i.e. value for money) and workforce well-being. 69 Integrated care initiatives also often aim to address health inequalities,70 and evidence suggests that benefits of integration may be greater in deprived areas, by improving access to care for underserved populations. 70
Models often tend to be implemented by high-performing early adopters. 70 They are often run by passionate volunteers, by organisations with a strong history of integrated working, and where funding and guidance are provided from national bodies. 71,72
Aims of integrated care vary by stakeholder groups and are often contradictory, meaning positive outcomes for one stakeholder group may lead to negative outcomes for others. 73 Integrated care can require investments in space, specialist resources and staff, and time for patients to be heard, and this does not always align with organisational objectives to reduce costs. 67 A common feature of integrated care is patient-centredness,65,71,73–75 designing services around the needs, preferences and values of patients and families and the type of care they feel is required. 65,71 Our evaluation explores a range of stakeholder perspectives, including those of women using WHHs and others in the community who may find it more difficult to access services. A summary of aims of integrated care can be found in Box 3.
Theory and evaluations of integrated care programmes suggest that these models aim to:
-
Change the way in which health and social care services are delivered71
-
Improve the efficiency25 and cost-effectiveness of healthcare systems71
-
Manage demand82 in light of increasing chronic care expenditure83
-
Reduce hospital admissions71,83 and improve population health25
-
Improve patient experience,25 for instance, by ensuring patients feel heard71
-
Reduce the need for repeat appointments23
-
Produce better patient outcomes,25 including health65 and clinical effectiveness,71 particularly those with the most complex needs,73 such as those with multiple long-term conditions71
-
Provide person-centred care71 with patient and carer involvement in the services they receive74,75
-
Ensure professional adherence to disease-specific protocols and guidelines67,83
-
Share financial responsibility with other stakeholders, and in the long term83
Benefits of integrated care
Stated advantages and outcomes of models of integrated care are numerous and relate to healthcare resources and health system function (e.g. efficiencies in the workforce), improved quality of patient care (e.g. improvements in mortality and morbidity, a reduction in unnecessary harm) and outcomes for staff (e.g. staff work satisfaction). 47,65,73,76–79 For example, the NHS has advocated models of care which bring ‘care closer to home’ for many years. 47,76,77,80,81 Outcomes for integrated care models are often context-specific, meaning they may be unique to the demographics and needs of a local population and geography (e.g. due to variations in transport and proximity to a patient’s home of services). 66,71,72
The advantages of integrated care models may vary according to clinical severity and complexity. It has been suggested that integrated care has the potential to improve outcomes among patients with the most complex needs, particularly given the risk of increased costs of care in these groups. 73
Evidence
The relationship between greater care integration and outcomes is complex, and evidence of effectiveness of integrated care is mixed. 65,73 This is, in part, due to the methodological difficulty of evaluating integrated care initiatives. Programmes are heterogeneous in terms of interventions and outcomes,70 and existing evidence has been reported to be of variable quality and reliability, largely observational and small scale. 67,70 Nevertheless, there is evidence in the literature of improvements in patient experience, health outcomes, staff experience and cost savings following the implementation of integrated care models. 70–72 For example, stakeholders involved in an early evaluation of vertical integration describe the overall impact on health system costs as beneficial, with improvements in managing patient demand. 82 In children and young people’s services, a range of benefits have been described. These include better communication between clinicians and patients, care received closer to home and improvements to quality of life, staff experience and a reduction in unnecessary tests. 70
The evidence of cost-effectiveness of integrated care remains limited and mixed, with some studies identifying potential savings, but others reporting increases in costs. 67,70,71,73,84–87 This is somewhat paradoxical, in light of consistent strong support for integrated care among decision-makers. 67,73 Conclusions from evaluations and reviews of the evidence show a need for better understanding of which integration approaches work best, in which contexts, and what influences success. 71 Concerns have also been expressed about safety, affordability, balancing efficiency with choice, expectations about impact not being met and failure to integrate rather than simply co-locate services. 47,81,88
Integrated care theory
A variety of frameworks is available to describe and explore integrated care, and they can be used to inform evaluations of these models. 89,90 In this evaluation, we drew on integrated care frameworks to explore the different dimensions of integration in WHHs. 90
Available frameworks have been developed using systematic literature reviews and stakeholder and expert consultations. They explore how care is integrated (i.e. the specific integration activity or intervention implemented), and the level at which the integration takes place (e.g. meso/mico/macro levels). 65,91 There was no single framework of integrated care that was best suited for this evaluation. However, Table 3 summarises five key dimensions of integration we explored, underpinned by a framework from van der Klauw. 92 This was selected due to its comprehensiveness, clear presentation of integrated care and utility for the evaluation. This was supported by theory from two other frameworks: Singer et al. 65 and Hughes et al. 67
| Type of integration | Description | Examples |
|---|---|---|
| Functional/administrative | ‘Back office’ and support functions and the extent to which they are integrated and co-ordinated across organisations and/or sectors. This may include formal documentation and protocols that support decision-making and accountability. | Technologies to facilitate communication and information-sharing (e.g. shared electronic health records). |
| Structural/organisational | Formal connections (or physical, financial and operational ties) and relationships between organisations that can be used to ensure continuity in transitions between organisations and/or professionals. | Alliances, contractual arrangements, organisational change (e.g. mergers), MDTs/integrated care teams, and joint commissioning. |
| Interpersonal | Collaboration and teamwork between professionals within and between organisations. | Working together to overcome barriers to implementation. |
| Clinical | The co-ordination, streamlining and integration of care/services with the aim to maximise the value for patients. | Integrated care pathways, single point of entry for multiple services, service integration (e.g. gynaecology and contraception, inter-practice referrals, training clinics). |
| Systems and whole systems | Focuses on the whole healthcare system, and the systems within it, and may involve consideration of the extent to which these are supportive of integration, including from a regional and national perspective. | PCNs, place-based partnerships, ICSs/boards. A whole-system approach to integration seeks to implement multiple, often interrelated, changes or interventions. |
We used this table to assist in the exploration of forms of integration in the hub models in our evaluation, which is described in the relevant sections of the results and discussion. There is a need for further empirical research to assess the validity of integrated care frameworks.
Chapter 3 Methods
Box 4 provides a summary of Chapter 3 of this report.
-
The evaluation adopted a rapid mixed-methods design, combining quantitative and qualitative data collection at local, regional and national levels.
-
The evaluation comprised three work packages (WPs):
-
Work package 1: Mapping the current landscape and context for WHHs. This included analysis of pre-evaluation scoping interviews, desk research an online survey of leads from hubs across the UK, development of a database of UK WHHs and interviews with regional stakeholders in England.
-
Work package 2: Detailed research in four purposively selected exemplar hub sites in England, including interviews with staff and service users, focus groups in local communities and documentary analysis.
-
Work package 3: Interviews with national stakeholders, and consolidation of findings from all WPs to generate evidence on WHH models.
-
-
Participants included: 85 interviews (40 WHH and wider staff, 7 regional stakeholders, 6 national stakeholders and 32 patients); 4 focus groups with 48 women and 10 evaluation scoping interviews undertaken prior to commencing the study were included in analysis.
-
Analysis: qualitative data from interviews, focus groups and documents were analysed using a team-based rapid analysis approach; quantitative survey data were analysed descriptively. Different data sources were analysed separately, and collaboratively reviewed, refined and combined by the team, to develop findings and implications.
Study design
The evaluation aimed to be rapid and responsive, exploring a policy-relevant issue during its implementation, producing findings that are relevant and beneficial for policy and practice in real time employing rapid evaluation approaches. We set out to locate hubs and capture useful insights regarding how they were working and early learning that could improve understanding of these models. The exploratory evaluation was conducted with predominantly qualitative methods. Formal quantitative evaluation of impact was beyond scope, with many hubs at an early stage of implementation, and with limited availability of relevant quantitative data. Impact evaluations require adequate time for services to be implemented and embedded within a system, for individuals to use the service, for data owners to collect and curate data, and for researchers to obtain these data. 94
A mixed-methods approach was taken in order to explore the ‘current state of the art’ of WHHs, mapping the landscape, studying experiences of delivering and using hub services and defining key features and early markers of success to inform policy and practice (the aim and research questions are presented in detail in Chapter 1). The evaluation combines national mapping, in-depth work in purposively selected sites and interviews with regional and national leaders to generate evidence which balances breadth with depth to inform scale-up and spread of WHHs.
The evaluation comprised three WPs, summarised in Table 4.
| Work package | Methods overview | Description | Evaluation questions |
|---|---|---|---|
| WP1 |
|
Mapping of the current landscape and context for WHHs, providing a description of different hub characteristics and models in place | RQs 1–3, 7 |
| WP2 | In-depth work in four exemplar hub sites
|
In-depth work with four exemplar hub sites to understand more about why and how hubs have been funded, commissioned and implemented, experiences of hub delivery (including patient experiences), measurement of performance and outcomes and successes and challenges | RQs 1–7 |
| WP3 |
|
Bringing together and consolidating findings from WPs 1 and 2 to generate evidence on WHH models and provide implications for policy, practice and research | RQs 1, 7 |
Mixed methods were employed as follows:
-
Pre-evaluation scoping interviews (qualitative) informed the design of the hub database and mapping survey (quantitative), and the topic guides for all interviews and focus groups (qualitative).
-
The pre-evaluation scoping interviews (qualitative) and mapping survey findings (quantitative) informed the sampling of the exemplar hub sites (qualitative).
-
At the analysis and interpretation stage, we drew on quantitative and qualitative findings to answer the research questions and identify implications for policy, practice and research, integrating different data sources relevant to the questions explored. The role of quantitative and qualitative findings varied according to the questions and topics addressed. The triangulation of different data sources is described in further detail in Data analysis and triangulation across all work packages.
At scoping, in collaboration with policy and practice leaders, a decision was made to focus the in-depth evaluation in England to build contextual knowledge and enable a comparative approach that would not be possible if models from the devolved nations were included, as they differ in terms of health policy, structure and commissioning.
All data collection was undertaken between April 2022 and March 2023, before the recent announcement of funding to support WHH development. 22
The qualitative analysis framework can be found in Appendix 1. Design of the evaluation tools, including the survey and topic guides, and data analysis was undertaken by the evaluation team. This was underpinned by the study aims and evaluation questions, and informed by the scoping work (see Chapter 1), relevant literature (see Chapter 2), emerging findings from the mapping survey, and with input from our Stakeholder and Women’s Advisory Groups.
Protocol approval
The study topic was prioritised for rapid evaluation by NIHR after receiving a request from the DHSC in 2021, in respect of evaluating WHHs. An initial scoping note was prepared in October 2021, followed by the preparation of a full protocol in 2022. The protocol drew on scoping findings to better understand the context and landscape of WHHs. More details on the scoping methods are in Chapter 1. The protocol was revised in July and November 2022 to reflect feedback from the project’s Women’s Advisory Group and to make minor amendments, for example to the timelines for regional interviews following delays to the publication of the Women’s Health Strategy. 12 This was published on the NIHR HSDR webpage.
Ethical approval
The study was approved by the Research Ethics Committee at the University of Birmingham (ERN_22-0669). The project team completed the HRA Decision Tool and liaised with the Head of Research Ethics and Governance at the University of Birmingham, who confirmed that the study met the criteria for service evaluation. Approval by the Health Research Authority or an NHS Research Ethics Committee was therefore not required.
Participants, sampling and data collection
Work package 1 participants, sampling and data collection: mapping the current landscape and context
National scoping interview data (pre-evaluation work, January–February 2022)
The scoping work which informed the evaluation design included interviews with 10 key informants, which were conducted between January and February 2022. Participants included experts leading WHH policy and practice, with roles in commissioning, clinical care, leadership, policy-making, education and training. Stakeholders were from organisations including the DHSC, Primary Care Women’s Health Forum, Faculty of Sexual and Reproductive Healthcare, local authorities, NHS primary and community care and hospital trusts. Interviews followed a topic guide developed by the study team informed by discussions with policy stakeholders, which explored definitions, hub aims and contexts, existing locations and models, evidence, indicators of success and plans for scaling up.
Desk research to inform the database of Women’s Health Hubs (pre-evaluation work, updated throughout the study)
Scoping work included the interviews described above, and a review of relevant published and grey literature to locate existing WHHs and understand the context was undertaken. Scoping findings were used to develop a database of UK WHHs, which was refined throughout the evaluation. To identify models in addition to those located during the scoping work, the team conducted desk research. Requests for information about current and planned WHHs were disseminated via the Primary Care Women’s Health Forum, Faculty of Sexual and Reproductive Healthcare and the Stakeholder Advisory Group.
We built on the database throughout the evaluation, adding and refining information through methods including desk research, insights from the Stakeholder Advisory Group and the survey. Desk research identified documentary/video evidence which was reviewed to inform mapping and understanding of models, including service websites and materials produced for the Primary Care Women’s Health Forum as part of their WHH toolkit. For example, case studies, videos, webinars and guidance created to support the development of new WHHs. The focus of this work was on identifying models which met our working definition of a WHH, and LARC-only or community gynaecology models were not included in the database.
Survey of Women’s Health Hubs leads (May–December 2022)
An online survey of leaders of all known hubs across the UK was undertaken to gather descriptive information and map the current landscape (see Box 5 for topics covered). The survey participants were service leaders (e.g. lead commissioners, hub providers). In the survey, in recognition of the complex women’s health landscape and varied terminology in use services were referred to as ‘integrated community WHHs or services’. The questionnaire was informed by the evaluation questions and pre-evaluation scoping work, with additional input from a consultant in sexual and reproductive health and a health economist with expertise in sexual health and women’s reproductive health. The survey was piloted and refined with a consultant in sexual and reproductive health to ensure that the questions were appropriate, and to check for ease of comprehension and completion.
-
Respondent information.
-
Hub background (e.g. stage of development, year launched, populations served, organisations involved in design/delivery, rationale and aims).
-
Commissioning and funding (e.g. commissioning arrangements, contractual arrangements, additional funding, leadership/governance).
-
The service and pathways (e.g. delivery model, services provided, venues, out-of-hours provision, referral/triage processes).
-
Workforce (e.g. different roles involved, existing local sexual/reproductive health services, training, competency assessment).
-
Data/metrics used to measure hub activity or quality.
-
Additional information (e.g. how hub is reducing inequalities, patient/public involvement in design or delivery of hub).
-
Facilitators and barriers to hub implementation.
The survey was open from May until December 2022 to enable information on new and developing WHHs to be gathered and was administered using the online platform SmartSurvey.
The survey was distributed in several ways: by e-mail to a lead stakeholder in each known hub in the database; the Stakeholder Advisory Group who shared the survey link within their networks and throughout the course of the project provided iterative support to identify new hubs for inclusion; the survey was advertised via the Primary Care Women’s Health Forum, Faculty of Sexual and Reproductive Healthcare and social media. Known contacts were sent multiple reminders to complete the survey. Four hub leads participated in a call or provided e-mail correspondence to complete the survey with a member of the evaluation team. Seventeen survey responses are included in the analysis for this report (Table 5), from a range of respondents (Table 6). Due to the open recruitment approach, and unknown denominator (the number of hubs in the UK was not known), it was not possible to determine a response rate.
| Total | 39 |
|---|---|
| Included in analysis (see Chapter 4) | 17 |
| Excluded as the services did not meet our definition of a WHH (e.g. focused on providing gynaecological services only, with no plans to expand into contraception) | 9 |
| Excluded as respondents reported that there was no WHH in their area | 13 |
| Role | Respondents |
|---|---|
| GP with special interest in women’s health (England)/GP with enhanced skills in gynaecology (Northern Ireland) | 5 |
| GP | 5 |
| Consultant in community gynaecology and reproductive health care | 3 |
| Consultant in sexual and reproductive health | 1 |
| Other | 3 |
Interviews with regional stakeholders (October–November 2022)
To further understand the landscape in which WHHs are situated, following the publication of the Strategy12 we interviewed seven regional stakeholders across six NHS England and NHS Improvement regions. One interviewee provided both regional and national perspectives. We aimed to interview leaders with a regional perspective in each of the NHS England regions, but it was not possible to locate an appropriate contact in one region.
A purposive sampling approach was taken, identifying key informants using desk research with input from known contacts, including members of the Stakeholder Advisory Group. Potential interviewees were approached by e-mail, which included an information sheet and consent form. Reflecting the heterogeneity in women’s health services across England, we identified a variety of regional stakeholders for interview, for example a senior commissioning manager and a sexual and reproductive health consultant who offered regional insights.
Interviews were semistructured and followed a tailored topic guide developed by the study team, informed by the evaluation questions, scoping work (national interviews, review of relevant published and grey literature and scoping workshops) and other emerging findings. This included current context for development and early progress of WHHs, challenges in provision of women’s SRH and how hubs relate (or not) to other developments, such as ICSs.
Work package 2 participants, sampling and data (exemplar hub evaluation)
Sampling and recruitment of exemplar hub sites (July–October 2022)
The identification of WHH exemplar sites involved a series of steps to understand existing hubs, explore and define criteria for selection, and then finalise the case-study hubs. To select the WHH exemplar hub sites for in-depth evaluation, findings from the 11 WHH survey respondents received at the time of hub sampling (July 2022) were analysed, along with public health profiles from Public Health England’s Fingertips portal95 and rurality information from the Office for National Statistics. 96 A summary was produced of site characteristics, similarities and differences for all known WHHs. This included hub status, launch year, leadership, commissioning arrangements and information about deprivation, ethnicity and rurality. We then held an internal workshop to identify potential characteristics and factors to guide the selection process.
The early evaluation work helped to guide this process, for example:
-
Findings from the survey, in particular the heterogeneity of models, highlighted the need to maximise diversity in selection.
-
A review of integrated care literature showed the importance of contextual factors, such as whether hubs were located in urban or rural areas.
A list of over 10 dimensions of hub model/context variation was developed, including size/catchment area, workforce mix and local deprivation. To select the sites, we presented survey findings, alongside potential hub characteristics and dimensions, to our Stakeholder and Women’s groups to further develop and prioritise the list. Five priority criteria were used for the final site selection, the process for which took place over several team meetings. The criteria are presented below:
-
Stage of development of hub site: most sites were still in development as hubs were a relatively new initiative often characterised by incremental improvements and growth. Only WHHs actively offering services to women were selected for in-depth evaluation.
-
Location/geography: this was considered to encompass urban, rural and regional variation.
-
Clinical leadership (e.g. GP-led or consultant-led): early evaluation work suggested this may be an important dimension to explore.
-
Commissioner (e.g. commissioned by NHS or local authority commissioners, or joint-commissioned) and role of commissioning: as above, early work suggested this may be a key area of variation.
-
Type of hub model (e.g. hub and spoke, one-stop shop): an aim of the evaluation was to capture a variety of hub structures.
Other criteria from our ‘long list’ were also considered to ensure relevance of findings generated, for example deprivation. We selected the four sites to maximise diversity of the priority characteristics, though due to the number of sites and characteristics identified, and heterogeneity of hubs, it was not possible for the sample to include all of them. Sites in Northern Ireland were excluded from selection due to the evaluation’s focus on the English context.
A researcher was allocated to each site to act as their point of contact and to conduct data collection, which supported consistency and enabled relationship-building. All researchers had substantial experience of undertaking and analysing qualitative interviews. A lead stakeholder was also identified at each site, using our prior knowledge and information from the survey. Contact was made with each of the four lead stakeholders via e-mail, inviting them to participate and including an information sheet detailing the purpose of the in-depth evaluation and what was involved. The lead researcher for each site subsequently arranged a virtual meeting with lead stakeholders to discuss the evaluation process, obtain an overview of local context, hub plans and implementation and to identify key local stakeholders. All four sites approached agreed to participate in the evaluation.
Exemplar hub site interview and focus-group sampling, recruitment and data collection (October 2022 to March 2023)
Interviews with 72 participants were conducted in the sites (Table 7), and 4 focus groups were held with 48 people. Professional backgrounds of clinical staff participants included general practice (15), nursing (4), gynaecology (2) and sexual and reproductive health (5). Non-clinical participants were in management and administration (10) and commissioning (4) roles.
| Site | Directly involved in the hub services, for example sexual and reproductive consultants, administrators, nurses, GPs | Other stakeholders, for example referring GPs, hospital consultant | Women | Total |
|---|---|---|---|---|
| Site 1 | 6 | 4 | 8 | 18 |
| Site 2 | 8 | 3 | 7 | 18 |
| Site 3 | 8 | 1 | 8 | 17 |
| Site 4 | 7 | 3 | 9 | 19 |
| Total | 29 | 11 | 32 | 72 |
Staff interviews
In each site, researchers interviewed staff involved in the hub, and staff in the wider health system, based on their roles in relation to WHHs. Individuals were identified through discussions with the local hub leads to identify key roles, and by snowballing via other interview participants. Between September 2022 and January 2023, 40 staff were interviewed (Table 7). Lead hub stakeholders facilitated contact. Sampling focused on identifying a range of key informants in different roles and contexts. Participants included GPs, nurses, sexual and reproductive health consultants, commissioners, administrators and referring GPs. Potential interviewees were approached by e-mail, which included a consent form and information sheet. Interviews were conducted face to face, online or by telephone, with most conducted online. In two sites, researchers interviewed staff at the hub site. Written or verbal consent was obtained from all participants. Participants either returned a signed consent form (hard copy or electronically by e-mail), or, in instances where verbal consent was provided, interviewers read out consent statements at the beginning of interviews and asked participants to confirm their consent. This process was audio-recorded. Semistructured interviews followed two separate topic guides, developed by the study team and informed by the evaluation questions and emerging findings from other WPs. Topic guides were tailored for (1) WHH staff and (2) staff in the wider health system. Topics included hub aims, experiences of implementing a hub and delivering services, what worked well and less well, early impacts and links with local systems. The majority of interviews were 45 minutes to 1 hour in duration.
Interviews with service users
Interviews were conducted with 32 women who had used their local WHH in each of the 4 sites to explore their experiences (Table 7). The Women’s Advisory Group recommended a flexible approach to recruiting service users to participate, tailored to consider the context in each site. A convenience sampling approach working through clinical gatekeepers was taken, with two different approaches adopted in different sites, described below:
-
In three sites, hub professionals shared information about the evaluation with women during appointments. A ‘consent to contact’ approach was adopted, whereby those interested were asked to consent for their details to be shared with researchers who would contact them to arrange an interview. Interviews were undertaken either by telephone or by videoconferencing [Zoom (Zoom Video Communications, San Jose, CA, USA) or MS Teams], depending on interviewee’s preference.
-
In one site, six of the seven women who took part were interviewed face to face, by a researcher visiting two different hub clinic locations on that day in order to recruit women from different geographical areas and hub settings (a seventh woman also took part online). The health professional running the clinic shared information about the evaluation with all women attending the clinic, and those who were willing to be interviewed met with the researcher in a separate area following their appointment.
Information about the study, including background details and study purpose, was provided to participants via information sheets and verbally, with participants able to speak with researchers should they have had any questions. Verbal or written consent was obtained as described earlier. Women interviewed face to face provided written consent in person. Interviewees received a £10 shopping voucher as compensation for their time. The topic guide was informed by the evaluation questions, emerging findings from other evaluation work, and insights from the Women’s Advisory Group. It was also reviewed and refined by the study Women’s Group. It included questions exploring awareness of women’s health services, experiences of services including accessibility and satisfaction, and what could be improved. Women were also asked to complete a demographics form, though it was not possible to collect this from all participants (Table 8). Of those for whom it was possible to collect this information, most of the sample were White British, all described their sex as female and over two-thirds left education at or before 18.
| Demographic variable | Category | Service user interview participants | ||
|---|---|---|---|---|
| Frequency | % all (n = 32) | % providing data (n = 23) | ||
| Age | 18–19 | 1 | 3 | 4 |
| 20–29 | 3 | 9 | 13 | |
| 30–39 | 4 | 13 | 17 | |
| 40–49 | 5 | 16 | 22 | |
| 50–59 | 9 | 28 | 39 | |
| 60–69 | 1 | 3 | 4 | |
| 70–79 | 0 | 0 | 0 | |
| Missing data | 9 | 28 | – | |
| Sex | Female | 23 | 72 | 100 |
| Missing data | 9 | 28 | – | |
| Gender identity | Yes (same as at birth) | 21 | 66 | 91 |
| No, non-binary | 1 | 3 | 4 | |
| Missing data | 10 | 31 | – | |
| Sexual orientation | Heterosexual | 18 | 56 | 78 |
| Bisexual | 2 | 6 | 9 | |
| Gay or lesbian | 1 | 3 | 4 | |
| Other | 1 | 3 | 4 | |
| Prefer not to say | 1 | 3 | 4 | |
| Missing data | 9 | 28 | – | |
| Age when completed full-time education | 16 years | 3 | 9 | 13 |
| 18 years | 7 | 22 | 30 | |
| 19 years | 2 | 6 | 9 | |
| 21 years | 1 | 3 | 4 | |
| 22 years | 5 | 16 | 22 | |
| Other | 5 | 16 | 22 | |
| Missing data | 10 | 31 | – | |
| Ethnic group | White: English, Welsh, Scottish, Northern Irish or British | 18 | 56 | 78 |
| White: Irish | 1 | 3 | 4 | |
| White: any other white background | 1 | 3 | 4 | |
| Mixed or multiple ethnic groups | 2 | 6 | 9 | |
| Black, Black British, Caribbean or African | 1 | 3 | 4 | |
| Missing data | 9 | 28 | – | |
| Long-term health conditions | Yes | 7 | 22 | 30 |
| No | 16 | 50 | 70 | |
| Missing data | 9 | 28 | – | |
Focus groups with women in local communities
Following input from the Women’s Advisory Group (see Chapter 5), the evaluation plan was extended, to add focus groups with women in communities perceived by hub leaders/stakeholders to be less likely to access a hub. The aim was to capture the experiences of women who may find it harder to access WHH services.
One focus group was undertaken in each site (Table 9), two were face to face in local community venues and two were online (to suit availability and preferences of the women taking part). Demographic information is presented in Table 10. A purposive sampling approach was used to identify community groups to host focus groups, in populations where WHH site leads/stakeholders reported barriers to access to women’s health services or those who were less likely to engage with services. In three sites, a community group was identified to host a focus group via the lead hub stakeholder, who helped the team broker access and facilitated recruitment. In the fourth site, where the hub lead did not have an existing link, the team identified and contacted a suitable community group through one of the other interview participants. Overall, a convenience sampling approach was taken for participants, where a researcher attended existing group events, and group members were invited to join a group discussion during/after their usual session. However, for one of the virtual focus groups, a separate meeting was arranged at the request of the participants.
| Focus group | Group information (type of group and participants) | Participants |
|---|---|---|
| 1 | Women’s group with women from African backgrounds | 10 |
| 2 | Women’s exercise group serving a deprived community | 16 |
| 3 | Women’s health group serving those who live in a more rural community | 5 |
| 4 | Women’s group based in an ethnically diverse community | 17 |
| Demographic variable | Category | Women’s focus-group participants | ||
|---|---|---|---|---|
| Frequency | % all (n = 48) | % providing data (n = 17) | ||
| Age | 18–19 | 0 | 0 | 0 |
| 20–29 | 0 | 0 | 0 | |
| 30–39 | 1 | 2 | 6 | |
| 40–49 | 4 | 8 | 24 | |
| 50–59 | 1 | 2 | 6 | |
| 60–69 | 5 | 10 | 29 | |
| 70–79 | 6 | 13 | 35 | |
| Missing data | 31 | 65 | – | |
| Sex | Female | 17 | 35 | 100 |
| Missing data | 31 | 65 | – | |
| Gender identity | Yes (same as at birth) | 15 | 31 | 88 |
| No, non-binary | 0 | 0 | 0 | |
| Missing data | 33 | 69 | – | |
| Sexual orientation | Heterosexual | 17 | 35 | 100 |
| Bisexual | 0 | 0 | 0 | |
| Gay or lesbian | 0 | 0 | 0 | |
| Other | 0 | 0 | 0 | |
| Prefer not to say | 0 | 0 | 0 | |
| Missing data | 31 | 65 | – | |
| Age when completed full-time education | 16 years | 8 | 17 | 47 |
| 18 years | 3 | 6 | 18 | |
| 19 years | 3 | 6 | 18 | |
| 21 years | 1 | 2 | 6 | |
| 22 years | 1 | 2 | 6 | |
| Other | 1 | 2 | 6 | |
| Missing data | 31 | 65 | – | |
| Ethnic group | White: English, Welsh, Scottish, Northern Irish or British | 17 | 35 | 100 |
| White: Irish | 0 | 0 | 0 | |
| White: any other white background | 0 | 0 | 0 | |
| Mixed or multiple ethnic groups | 0 | 0 | 0 | |
| Black, Black British, Caribbean or African | 0 | 0 | 0 | |
| Missing data | 31 | 65 | – | |
| Long-term health conditions | Yes | 5 | 10 | 29 |
| No | 12 | 25 | 71 | |
| Missing data | 31 | 65 | – | |
Materials were provided to the group by the group’s leader in advance, to ensure members were aware that a researcher would be attending and understand what may be involved, including that participation was voluntary. The Women’s Advisory Group advised on content and members reviewed drafts of topic guides and information sheets for women service users and focus groups. The group discussion guide included questions exploring awareness and use of women’s health services, awareness and understanding of WHHs and potential barriers and facilitators to using hubs and improvements to local services. The researchers explicitly asked participants about their awareness and use of their local hub model, and none had received care from a WHH. For three focus groups, consent was obtained from participants via signed consent forms returned via e-mail or in person, and in the fourth verbal consent was recorded. Focus-group participants received a £10 voucher as thanks, and community groups were also reimbursed for their time and/or premises use.
For most interviews, there was no prior relationship between the evaluator and participants, with the exception of interviews with the hub leader at each exemplar site, where more frequent contact and meetings to discuss the evaluation had occurred. Participants were provided with an information sheet which detailed reasons for the evaluation being conducted. Researchers’ personal goals or reasons for being involved in the evaluation were not disclosed.
Exemplar hub documents (WP2)
Participants and site contacts were asked to share documents that could illustrate the local context, and the approach to hub set-up, implementation, commissioning and decision-making, costs and outcomes. Documents included business cases, service specifications and anonymised patient feedback.
Work package 3 sampling, participants and data collection
Interviews with national stakeholders
In January–March 2023, we interviewed six key national stakeholders, including leaders from organisations including the DHSC, Faculty of Sexual and Reproductive Healthcare, Primary Care Women’s Health Forum and the Royal College of Obstetrics and Gynaecologists and Royal College of General Practice. Three of these individuals had also participated in the project scoping interviews in early 2022. One interviewee covered both regional and national perspectives.
Semistructured interviews followed a tailored topic guide, with questions exploring how WHHs align with wider policy and developments, for example PCNs and ICSs, workforce and training, and reflections on the strategy and WHHs and intended hub aims and impacts. Verbal consent was recorded for all participants.
Qualitative interview and focus-group recording and transcription across all work packages
All interviews were audio-recorded with permission, transcribed verbatim by a professional transcription service, checked for accuracy (with researchers returning to the original voice recording if they needed to address any transcription gaps or errors) and anonymised. Three exemplar hub focus groups were audio-recorded, transcribed verbatim and anonymised. In a fourth, it was not possible to record and field notes were taken by the researcher. Focus-group transcripts were checked alongside recordings to ensure accuracy, which supported familiarisation with interview data. Transcripts were not returned to participants for comment.
Data analysis and triangulation across all work packages
Between November 2021 and March 2022, data from the survey, interviews, focus groups and documents were analysed. The team held weekly meetings for the duration of the project (April 2022 to March 2023) to share and discuss the approach to analysis, insights and emerging findings. On the following pages, the separate analysis of survey, interview, focus group and documentary data is described, followed by the approach to triangulation across data sources.
Survey analysis
Initial survey analysis was undertaken in July 2022 with 11 respondents, to aid selection of the 4 hubs for in-depth evaluation [see Work package 2 participants, sampling and data (exemplar hub evaluation)]. Analysis was updated in September 2022 (for the interim report) and January 2023 (for the final report). Survey data were exported into Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) for analysis. Descriptive statistics were computed for quantitative data, and free-text responses thematically analysed for reporting.
Analysis of interviews, focus groups and documents
Qualitative data from all interviews, focus groups and documents were analysed using a team-based rapid analysis approach, to deliver timely findings with methodological rigour. 97 Researchers reviewed each data item and summarised the main issues in the data into a ’summary template’ matrix in Microsoft Excel, with no formal coding of data. An initial summary template matrix was developed by the team following a review of the first four interview transcripts alongside the evaluation questions, with separate rows in the matrix to summarise different questions and findings. Each researcher summarised data they collected in a separate matrix (including data from their in-depth evaluation site, regional and national interviews). The research team systematically summarised each data item into the relevant summary template matrix, referencing the location of findings in the raw data and highlighting exemplar quotes and any key reflections and interpretation. Exemplar hub data were summarised by the lead researcher for each site. The summary template matrix structure was refined during the course of analysis, with regular discussion and reflection by the team (see Appendix 1). Analysis of summary template content was undertaken alongside analysis of other data sources and is described in the following section.
Triangulation across data sources
Triangulation of different methods can be conducted to ensure comprehensiveness and completeness of data collected, to explore convergences and discrepancies in different data sources and to check the credibility of findings. 98 Different sections of analysis were allocated to individual team members, informed by the evaluation questions and planned outputs. This was undertaken by four team members, all of whom were involved in data collection. Each researcher reviewed and summarised relevant data and analysis from across WPs, identifying and exploring similarities and differences between sources, participants and contexts. Summary reports were then reviewed, refined and combined by all five members of the research team. Participant validation of findings was not undertaken.
The relative importance of data sources varied according to the evaluation topic explored, and this is explained below. In order to consolidate the presentation of the approach to triangulation, topic areas and outputs are presented in a different order to the results sections of the main report.
Description, map and summary profiles of Women’s Health Hubs
Analysis drew predominantly on the descriptive data in the survey and desk research. Analysis was underpinned by the development of the WHH database, led by one of the evaluation team. All known hubs were entered into the database, and more were added as they were identified throughout the evaluation. Database fields related to hub characteristics and the evaluation and survey questions. The database was populated using quantitative and qualitative data gathered throughout the evaluation. The database was continuously reviewed to inform mapping and understanding of models, addressing gaps in information and adding detail where available. Hub leads were contacted directly to clarify details where possible. A map and description of WHHs were produced for an interim report in October 2022 and updated for the final report in early 2023. Mapping software was used to present the distribution of WHHs across the UK. 99 Tables, figures and narrative descriptions were produced to summarise the key features of models. Profiles of all identified hubs were produced at the end of the evaluation. Outputs were reviewed and refined by the whole evaluation team. Where possible, hub leaders also reviewed the profile of their service for accuracy and completeness.
Definitions and vision, models and approaches, influences on set-up, implementation and sustainability, advice for others, what is next for Women’s Health Hubs
Analysis drew predominantly on interview sources to develop detailed descriptions of experiences and perspectives. Scoping and national and regional interviews offered perspectives regarding the wider WHH policy and practice context, while exemplar hub sites provided more granular insights into the development of models in practice. The survey and desk research informed the more descriptive elements, and enabled interpretation of the representativeness of the exemplar hubs compared with the national picture.
Achievements, outcomes which are (or could be) used to assess impact and inequalities
Identification of current measures, outcomes and impacts and approaches to tackling inequalities drew predominantly on survey, desk research and documentary sources from WHH sites. Exploration of potential future measures, considerations and challenges was drawn from interview data, particularly from exemplar hubs.
Experiences and perspectives of women
Analysis was predominantly informed by data and analytical summaries of interviews and focus groups with women in the exemplar hub sites. Documents from desk research and exemplar hubs (e.g. patient feedback reports) and interviews with hub staff also provided some insights into women’s experience.
Development of the theory of change
A theory of change provides a framework to describe and illustrate the logic, assumptions and principles that link what a service or programme does, why and how it does it, with its intended outcomes and results. 100 Theories of change can be important in replicability and understanding what works and why, which is particularly important for initiatives and programmes which wish to scale up or expand, as is the case with WHHs. 101 They can take various forms, and Ghate100 describes how they usually include needs, inputs, activities, outcomes along with implementation outcomes and mechanisms of change.
We developed a theory of change for WHHs drawing on a framework from Ghate100 using Braithwaite et al.’s102 non-linear model, to begin to capture the complex processes that typify implementation. This was deemed appropriate given the emergent and heterogeneous nature of WHHs. The theory of change was developed across a series of evaluation team meetings and a workshop. Theories of change were sketched for each of the four in-depth evaluation sites by the lead researcher for each site, using the summary template matrix for the site to populate a Theory of Change template based on the Ghate framework. They were then reviewed collaboratively by the research team and consolidated into a single theory of change, also drawing on the wider evaluation data and analysis. At this stage, the theory of change is an initial iteration, which is evolving and can act as a tool to guide further implementation and evaluation.
Development of implications for policy, practice and research
Bringing together the findings, implications for policy and practice were identified, to support the commissioning, implementation and delivery of WHHs. Implications for future evaluation, particularly key areas of focus and considerations for any later work, were produced. The team held internal workshops in which findings were considered and implications suggested, which were also discussed with the Stakeholder Advisory Group prior to final refinement and development.
Involvement of the Stakeholder Advisory Group
As mentioned in Chapter 1, a Stakeholder Advisory Group provided expertise and advice to support the study; their input included
-
Connecting the evaluation team with existing hub model leads to support the WHH mapping survey.
-
Developing our understanding of the women’s healthcare context.
-
Advising on criteria for exemplar hub site selection, and site selection.
-
Refining a working definition of WHHs.
-
Supporting the identification of outcome measures.
-
Identifying key stakeholders for regional and national interviews.
-
Sense-checking early findings and interpretations.
How the study differs from the protocol
There were two variations to the approach described in the initial protocol (Version 1.4, 8 November):
-
The team proposed using a team-based approach to analyse qualitative data guided by the principles of the framework method. 103 Instead, as described above, a team-based rapid analysis approach based on Taylor et al. 97 was adopted, as it was felt this offered both methodological rigour as well as a rapid approach to analysis to deliver timely findings.
-
We proposed that a typology of WHHs would be produced if feasible. This was not practicable for several reasons. The development of a typology was to be informed by the mapping survey, which gathered information about WHH models and context, but often this information was incomplete in survey responses. For some, this was because the stage of hub development was too early to provide details. The smaller than expected number of hubs identified also limited our ability to develop a typology with limited data. In addition, through desk research and stakeholder networks, we identified multiple areas where hubs may have existed, but did not receive a response to requests to complete the survey, resulting in further information gaps. While there were multiple examples of specific models of interest, for example one-stop shops, findings suggested that labels were applied differently, and there was variation in how they were understood. As a result, clear distinctions between model types could not be drawn reliably. Developing a meaningful typology was not possible due to the limited data, and the substantial heterogeneity in WHHs.
-
However, as described in the site selection criteria, it was possible to provide a categorisation of hub types with the information used to guide selection. Hubs varied in several dimensions, including:
-
Leadership model: for example GP-led; sexual and reproductive health consultant-led
-
Services offered: LARC-focused; wider provision, for example including gynaecological care
-
Hub venue: based at a GP practice; other venue, for example community hospital.
-
Chapter 4 Results
Box 6 provides a summary of Chapter 4 of this report.
-
This chapter outlines the findings from the evaluation. It is structured as the following:
-
Stakeholder perspectives on the definition of a WHH.
-
A descriptive summary of the identified hubs.
-
Description of hub models used and approaches/strategies to implementation.
-
Factors influencing hub set-up, implementation, sustainability, scale and spread.
-
What hubs have achieved to date and how hub performance can be measured/monitored.
-
The impact of hubs on reducing inequalities and unmet need.
-
Women’s perspectives and experiences of hubs and wider women’s health services.
-
Advice for those considering implementing a hub.
-
What next for WHHs?
-
-
This chapter presents analysis which triangulates findings from across different WPs and data sources in the evaluation (see Chapter 3). Where data are from one source (e.g. the survey), this is highlighted in the text.
-
One aspect to note is the use of CCG and/or ICS. In 2022, Integrated Care Board (ICBs) replaced CCGs, which for some hubs was after (or during) the set-up of the service. Therefore, we primarily refer to CCGs unless an activity was specifically conducted at an ICS level or by an ICB.
Stakeholder perspectives of definitions of and vision for Women’s Health Hubs
This section describes interviewee accounts of what hubs could or should aim to be, including whether there was a shared vision, and whether different groups of people define WHHs differently. Some interviewees answered with a specific hub in mind, whereas others provided regional and national perspectives. Women using hub services were not asked to define a WHH, but they were asked about what women’s health services should offer, and their insights are included where relevant.
How do stakeholders define hubs?
Hubs were often described as a network of community services, where staff working within hubs work with other services in the local community (e.g. voluntary sector, non-healthcare statutory services, acute and community trusts). Interviewees described how WHHs may come from an existing primary care, sexual and reproductive and/or community gynae service by the addition or ‘bolting on’ of new treatments, or an adjustment of a way of working (e.g. bringing different staff together). Hubs were described as ‘a natural extension’ of existing services (EH3, internal interview) and a ‘refinement of the community gynae service’ (EH1, external interview).
Many interviewees indicated that WHHs should provide semi-specialised care beyond what primary care could usually be expected to deliver, but at a less specialised or complex level than secondary care provision. Hubs were therefore perceived as a middle ground between the GP and hospital service. In line with this, clinicians working across two sites defined hubs through their focus on non-surgical management and interventions.
I only found out about it through going to the doctor with an issue to do with the gynae area and then sort of got the vibe that it was something that was kind of like a middle-man between seeing a doctor [GP] and having to go to the hospital to the gynaecology clinic there.
EH1, patient interview
Most interviewees suggested that a hub was not necessarily a physical place, but a concept. Overall, they advocated a flexible approach to the physical setting, informed by pragmatism and a need to align with existing services and resources. To some, the defining feature of WHHs was the way care was integrated and provided (e.g. bringing different expertise together) rather than the physical building where care was provided. This aligns with the idea that WHHs may provide care virtually (i.e. using video conferencing or telephone appointments).
… So it doesn’t have to be that services and clinics are at one designated address or site within that PCN and that that has to be the set location, it’s more the concept of sharing skills within a patient population and improving that access, and hopefully less distance for patients to travel and not always needing to go to secondary care, but it’s not necessarily just one static venue in one location in a city nearby practices and PCNs, but it’s more the concept of sharing clinics, skills, resources amongst a patient population.
National interview
A common view was that hubs should take a broad and holistic approach to women’s care, and interviewees described an ambition to provide care in a way that minimises the need for multiple appointments, reducing fragmented care.
… whatever their concerns and issues are they could be sorted at one point exactly at the same visit, whatever we can … we try to cover everything for that woman, rather than separate appointments for heavy bleeding, separate for coil fitting, separate for smear.
EH4, internal interview
The intention for women to get the right care at the right time, from the most appropriate clinician(s), was shared, to avoid women being sent back and forth between different professionals and services. This approach to care was reflected in the frequent use of the term one-stop shop by different stakeholder groups (i.e. women using services, commissioners, staff working in hubs and surrounding services). For instance, women hoped for a one-stop shop to access expertise, advice or the opportunity for a ‘full MOT’ covering general health issues in addition to SRH.
… rather than a patient having to go to multiple places, multiple clinicians, it should be a one-stop shop. And the reality is across a life course, all of these things overlap and interreact, so it makes sense to put them all together.
EH4, external interview
Interviewees tended to use the term one-stop shop to describe the experience of using a service, rather than to define a particular model or draw boundaries around what a WHH should be. Other terms relating to models (e.g. hub and spoke) did not feature in interviews.
Interviewees suggested that WHHs should be comprehensive in their offer. For instance, that they should provide ‘… everything related to women’s health’ or a ‘complete package of care’ including menopause care, contraception, scans, heavy menstrual bleeding, pelvic pain and fertility.
What I feel a Women’s Health Hub is, is that whatever the problem if it is women’s health-related they can deal with it, whether it be the menopause clinic that they very kindly offer, which they can always self-refer, whether it be contraception, whether it be menstrual problems and irregularities, it’s a central point where all of these services can be accessed ….
EH4, external interview
Some women interviewed suggested that hubs should include maternity services, and a commissioner with a regional perspective described there being a ‘maternity corridor’ that does not link up well with other services. The scope of services that some interviewees felt should be included was very broad, spanning services beyond gynaecology and sexual health, such as services for mental health, bone health and cardiovascular risks. This was framed under the perspective that women are ‘… more than just their reproductive organs, but that is a good start’, as stated by a woman using hub services (EH4, internal interview). However, many interviewees suggested that WHHs should focus on core areas of women’s health such as LARC, at least in the early stages of hub development, and expand once the service is functioning well. Interviewees felt the care provided should be appropriate for women of all ages, with the phrases ‘cradle to the grave’ and ‘life-course approach’ arising in interviews. It was noted that some services may be on their way to being a WHH and that services may be on a continuum of a ‘hub way of working’, rather than this being binary status (hub/not a hub).
… I think that lots of people don’t think of that [WHH as on a continuum] because the ‘hub’ suggests that it’s everything, particularly in sexual and reproductive health … I would say three of those things [you need in order to be a hub] means you’re maybe bronze. Five, six, known as silver. Ten might be gold or you know ten plus two might then put you into a platinum.
Regional interview
Compared to women we interviewed, stakeholders working in the area of women’s health were more likely to draw boundaries around the type of care that should be provided by WHHs. It was acknowledged that there is, in practice, a limit to the number of services a hub can provide and that what is needed is strong integration with surrounding services and clear integrated pathways.
But you can’t have every service there … it [what is needed] may be education and advice and then a really good-quality referral so that they’re actually confident you’re referring to somebody who is going to be able to meet that need, where the waiting list is not, you know, two years/three years, etc., so that there’s a real understanding … you need really to make sure that it is well integrated and that the pathways do work, because otherwise you just end up pushing a problem somewhere else, you know, and everyone gets dissatisfied.
EH1, external interview
The key characteristics of WHHs described in this section are summarised by the following quote from a hub leader:
Women’s Health Hub is a concept. It’s about using what resources you’ve got. It’s about working in an existing infrastructure and sort of trying to reduce health inequalities, to improve access, and to link up a more holistic approach to women’s healthcare so that women aren’t having to go, for example, one place for contraception, another place for other services, but linking it up. It doesn’t have to be a new, purpose-built building. It doesn’t have to be a whole new infrastructure with a new manager and new lead.
EH2, internal interview
Variation in stakeholder definitions of Women’s Health Hubs
Most participants who discussed the topic described defining WHHs as a challenge. Definitions were described to be emerging conceptually.
… what is a women’s health hub? What does it absolutely precisely look like? I don’t think we’ve actually defined that yet. I think we bandy around that kind of term and it means, as many terms do, different things to different people.
Regional interview
A number of national stakeholders stated that through their discussions with colleagues and healthcare professionals, it was evident that there is a lack of a shared, clear understanding of what WHHs are and that people interpret the term hub differently and that consensus was needed.
… I was really concerned that people were looking, this is healthcare professionals, looking at this idea of a Women’s Health Hub very, very differently, you know, and there wasn’t a national understanding of what it was, which is why I think we’ve got to get a very easy to understand baseline offering out there that people can build on ….
National interview
This interviewee described confusion regarding whether WHHs are a ‘whole new commissioned piece’. National interviewees suggested that some services may determine that they are implementing a hub when in reality the care is not joined up or integrated. There was also concern that sites may be implementing a model that can be defined as a hub without realising it, and that women will not understand what a hub is, while the aim is for hubs to be a recognisable part of the NHS landscape in the future.
Many suggested that what a WHH means or looks like will be different for different people and will vary based on local resources and needs. The idea that there is no one-size-fits-all for WHHs was emphasised: for example, that WHHs will ‘… be slightly different in every PCN’ (EH1, internal interview). Consequently, a flexible definition was suggested to be required to fit models with local needs and resources.
I think there’s not always one size fits all, I think necessity is the mother of invention and people will, where there’s a bit of tenacity and passion, enthusiasm and skill and determination, I think services will crop up looking slightly different in different regions.
National interview
Despite the apparent acceptance of variation, some national stakeholders suggested that in practice most people working in this field had a shared vision. These interviewees described how differences manifested themselves in the way hubs are designed and deliver care.
A number of other defining hub characteristics were described by participants, but they were given less priority. They were that WHHs should:
-
Be women-centred and provide non-judgemental and friendly support.
-
Be co-produced, so it is not assumed what would work for local women.
-
Consider offering support with social issues (e.g. money and housing) to prevent health issues occurring and worsening.
-
Sit within a wider movement to improve and raise awareness on women’s health.
Some participants discussed how hubs align with ongoing policies and priorities, including the establishment of ICSs, the NHS Long-Term Plan, multidisciplinary working, moving care closer to home and tackling inequalities. Participants did not report any current links between WHHs and other hub models in the NHS, for example maternity, mental health and family hubs.
There was broad consensus across interviewees on the following:
-
There is no one-size-fits all and that WHHs will vary based on local needs and resources with a need for flexibility in definitions.
-
Women’s Health Hubs sit within a network of services and should aim to link with and integrate across organisations and sectors.
-
Women’s Health Hubs are ’semi-specialised’, providing care that sits between primary and secondary services.
-
Women’s Health Hubs should be comprehensive in the services they offer and minimise the need for multiple appointments, providing ‘holistic’ care.
-
Women’s Health Hubs do not have to be a completely new service.
Interviewees highlighted that there are confusion and variation in definitions. Perspectives shared here were broadly in alignment with our working definition (see Introduction, ‘a working definition for the evaluation’).
Why have Women’s Health Hubs been implemented?
A wide range of reasons were described as driving hub implementation. The most commonly cited was to bridge the gap between primary and secondary care. WHHs were set up to improve access to appropriate and timely care in the community in a way that reduces inequalities, waiting times, inappropriate referrals and overall pressure on primary and secondary care.
… I was just really, really passionate that all women should have a choice about accessing LARC in primary care … and that all women should have that choice, not just the women who happened to have a LARC fitter in their own practice.
EH2, internal interview
Some interviewees described additional drivers that were not specific to WHHs, including COVID-19 care backlogs and an NHS agenda to design services so that existing resources are utilised more effectively to cope with increasing demand and budget pressures. Others described a wider movement towards integrated care as a justification for WHHs, for instance to provide more joined-up care pathways and bring people with skills and ideas together for collaborative working.
The impetus for the implementation of a WHH in some sites was an observation of unmet need, postcode lotteries, or service gaps and inequalities in access and quality of care. For example, the need to ensure that young women, women living in deprived areas and women with specific cultural needs are appropriately represented and served. This includes the observation of unwarranted variations, for example in referral rates and triage processes across PCNs and practices, such as GP referral rates to community and secondary care services.
In all exemplar sites, implementation was driven by individuals with a passion for and expertise in women’s health. For example, in one hub the lead was keen to utilise LARC training she had undertaken, and to offer this service to neighbouring practices without LARC fitters. Hub implementation was also influenced ‘top down’, by local, regional or national programmes and initiatives: for example, CCG programmes to transform outpatient services and reduce secondary care waiting lists, ICB agendas to provide joined-up, patient-centred care, and PCNs prioritising sexual health. In one site, the clinical lead was directly approached by their CCG and asked to develop a hub in line with aspirations to increase availability of community-based care. Participants also cited wider societal and professional influences on implementation, including an increase in female GPs (and thus awareness and motivation to improve women’s health), and a recent rise in demand by women seeking menopause support following media campaigns.
What do current Women’s Health Hubs models aim to achieve?
Hubs were described as aiming to achieve a broad range of outcomes simultaneously and it was often not clear which aims were the priority. However, in the survey, all hubs (n = 14) selected the following aims: to improve choice for women, reduce waiting times, reduce the number of appointments needed for a problem and/or reduce use of secondary care.
Overall, aims that were described in the survey and interviews were often about improvements in the following:
-
The type of services available so that care feels holistic (e.g. to enable women to have multiple SRH needs met in a single visit, and bring together a range of services).
-
The way services are organised, and the location/venue in which care is provided (e.g. to reduce inappropriate referrals to secondary care, provide appropriate expertise and care more locally, and provide more joined-up/integrated care across services and sectors).
-
Access to care (e.g. to decrease barriers and waiting times, expand the reach and scope of services, maximise access and convenience).
-
Reducing inequalities (e.g. ensure fairer access to care, reduce variation in access and quality across GP practices and regions).
-
Quality of care (e.g. standardisation and consistency of care, improve patient outcomes, improve referral processes, early intervention, better resolution of symptoms).
-
Women’s experience (e.g. improved listening to and empowering of women to have a voice in their care, enable more proactivity and self-management of symptoms, ensure women receive help earlier, have fewer appointments and examinations, a reduction in travel time and more choice, e.g. over venues and times).
The interviews in the exemplar hubs highlighted the differences in specificity of hub aims. While some had very specific and targeted objectives (e.g. to support the delivery of the 18-week waiting time target for secondary care), others were broader and more high level. Overall, hub objectives appeared to be more high level: for instance, stating the aim of reducing referrals to secondary care without specifying a target. The broad aims of WHHs were summarised succinctly by a survey respondent:
To bridge the gap between primary and secondary care and allow collaborative working and learning between GPs and gynaecology consultants. To allow women to receive the right treatment in the right place at the right time using our triage model and utilise community clinics outside of [gynaecology service] by using a single point of access. Help reduce backlog in secondary care.
Survey respondent
Descriptive summary of active Women’s Health Hubs
We identified 17 services across the UK that meet our definition of a WHH (see Chapter 1) and were active (i.e. seeing women at the time of the evaluation). Most were located in England (N = 13), with four in Northern Ireland (Figure 1). No hubs were identified in Wales or Scotland. As described in Chapter 3, we used multiple methods to identify active hubs. Profiles of all identified hubs can be found in Appendix 2.
In addition to the 17 active hubs, we identified areas which are at some point along the journey to setting up a hub (from early discussions to having secured funding) but were not yet seeing women. These were:
-
Cornwall
-
South Durham
-
Somerset
-
South-west London
-
Tower Hamlets.
Stakeholders mentioned a further eight areas where they had heard that a WHH may be in place, but we were unable to obtain information on these services (e.g. no response to the survey, or no contact details for hub leads were found). These areas were Blackpool, Cumbria, Edinburgh, Leeds, Norfolk, Nottingham, South Wigan and York/North Yorkshire.
We also identified areas which had integrated community gynaecology or LARC services in place which did not meet our working definition of a WHH. These were:
-
Oxford: community gynaecology service only, with no plans to expand into LARCs
-
Rochdale: community gynaecology service only, with no plans to expand into LARCs
-
South-east London: separate community gynaecology service and LARC hub without integration of these two services (and no current plans for integration)
-
Kingston-upon-Thames: women’s hub focused on other needs (e.g. women fleeing domestic violence), not gynaecology or sexual health
-
Lambeth and Southwark: LARC hub only
-
Aberdeen: privately run (non-NHS) service.
It is important to note that the community gynaecology and LARC hub services listed do not reflect the total number of these models in the UK, only those which were identified opportunistically via stakeholders, or through our survey.
Key features of women’s health hubs
Table 11 summarises the key features of the 17 hubs. The majority were described by respondents as currently operational with plans to expand. This is also reflected by launch dates, with some having only launched in the past 3 years, with some hubs relatively new and in set-up and/or starting to function at the time of the COVID-19 pandemic.
| Code | Location | Year set-up | Status | Hub local name | Clinical leadership | Commissioning model | Delivery model | Venues | LARC offered Contraception, gynaecological reasons, both | Other services offered | Population served |
|---|---|---|---|---|---|---|---|---|---|---|---|
| A | Bexley and Greenwich, England | 2022 | Operational, no plans to expand | Market street clinic | SRH consultant- | Multiple commissioners involved | Hub-and-spoke, one-stop shop | Two community practices | ✓ both | ✓ | – |
| B | Birmingham, England | 2016 | Operational, plans to expand | Modality gynaecology | GP | NHS trust | Hub-and-spoke | Four sites (three GP, one pharmacy) | ✓ both | ✓ | 100,000+ |
| C | Durham North, England | Early 2000s | Operational, plans to expand | Durham gynae | GP | CCG/ICB only | One-stop shop | Two GP practices | ✓ both | ✓ | – |
| D | Eastern Region, Northern Ireland | 2017 | Operational, no plans to expand | Southern Federation Gynaecology Service | GP | Multiple commissioners involved | One-stop shop | Nine GP practices | ✓ both | ✓ | 100,000+ |
| E | Guildford and Waverley, England | 2014 | Operational, plans to expand | Guildford and Waverley Community Gynaecology Service | GP | CCG/ICB only | One-stop shop | One GP practice | ✓ both | ✓ | 100,000+ |
| F | Hackney, England | 2021 | Operational, plans to expand | Community gynae PCN hub | SRH consultant | CCG/ICB only | Hub-and-spoke and virtual | Three GP practices and community gynae | ✓ gynaecology (plans to add contraception) | ✓ | 50,000–99,999 |
| G | Hampshire and Isle of Wight, England | 2022 | Operational, plans to expand | WHH | GP | No formal commissioning arrangements | Virtual | GP practices (number not known) | ✓ both | ✓ | 50,000–99,999 |
| H | Haringey and Islington, England | 2017 | Operational, plans to expand | The Gynaecology Collaborative | GP | CCG/ICB only | One-stop shop | Three community gynaecology venues, two secondary care sites | ✓ gynaecology | ✓ | 100,000+ |
| I | Hertfordshire, England | – | – | Enhanced Community Gynaecology Service/community gynae clinics | Gynaecology consultant- | CCG/ICB only | – | Four GP practices | – | – | – |
| J | Leicester, England | 2020 | Operational, plans to expand | Women’s health clinic | GP | No formal commissioning arrangements | Clinician travelling to GP practices | Two GP practices | ✓ both | ✓ | 100,000+ |
| K | Liverpool, England | 2019 | Operational, plans to expand | Liverpool WHHs | GP | Local authority only | Multiple PCN hubs, separate hub-and-spoke models | Multiple GP clinic venues across city | ✓ both | ✓ not part of core offer | 100,000+ |
| L | Manchester, England | 2006 | Operational, plans to expand | Manchester Community Gynae Service and Level 3 Contraception service | SRH consultant | Multiple commissioners involved | One-stop shop | Community hospital primarily, with other sites | ✓ both | ✓ | 100,000+ |
| M | Newcastle, England | 2001 | Operational, no plans to expand | Newcastle upon Tyne Community Gynaecology Service | SRH consultant | Multiple commissioners involved | One-stop shop, virtual | Central clinic plus GP practices, pharmacies | ✓ both | ✓ | – |
| N | Northern Region, Northern Ireland | 2019 | Operational, plans to expand | Northern Gynaecology GPES service | GP | Multiple commissioners involved | Hub-and-spoke | Four GP practices | ✓ both | ✓ | 100,000+ |
| O | Sheffield, England | 2019 | Operational, plans to expand | Sexual Health Sheffield Hub | GP-led | Multiple commissioners involved | Hub-and-spoke | Six GP practices | ✓ both | ✓ | 100,000+ |
| P | Southern Region, Northern Ireland | 2019 | Operational, plans to expand | – | GP-led | – | One-stop shop, hub-and-spoke | Four venues | ✓ both | ✓ | 100,000+ |
| Q | Western Region, Northern Ireland | 2019 | Operational, plans to expand | Western Federation | GP-led | Multiple commissioners involved | One-stop shop | Two GP practices | ✓ both | ✓ | 100,000+ |
The table highlights the varied nomenclature for local hubs. Despite meeting our definition of a WHH, most hubs did not refer to themselves as a WHH, or only did so informally (e.g. not in any documentation). Other terms used instead of ‘hub’ included ‘community gynaecology service’ or ‘clinics’. Only three locally referred to the service as a ‘hub’.
Respondents providing information on the population served by their hub (N = 12) offered services to all women in the area, not just to specific groups of women. However, women usually had to be registered with a GP in a specific location to access hub services. Some hubs aspired to expand the geographical area the hub covered.
Models and approaches used across Women’s Health Hubs
This section describes the models implemented across the 17 active WHHs. It focuses on delivery models, leadership, organisations involved in design/delivery, commissioning/funding, service venues, implementation approaches, workforce and training. We also outline a theory of change for hub development. A brief summary of the findings presented in this section is provided in Box 7.
Most hubs were defined by leaders as one-stop shops or hub-and-spoke models. However, these terms are not standardised and are open to different interpretations. Hubs offered a range of services to patients, particularly LARCs (for gynaecological and contraceptive reasons), heavy menstrual bleeding and menopause, and many hubs planned to expand the services offered. They were often seen as an intermediary service between primary and secondary care. While hubs aimed to improve access to care, most were not offering appointments out-of-hours or in online/group video consultations yet (although most offered telephone consultations).
Hubs were most often led by GPs, reflecting the primary care-focused nature of many hub models (e.g. most hub venues were based in GP practices, and GPs deliver services in most hubs). A range of organisations were involved in hub design and delivery in addition to GPs (e.g. local authorities, secondary care, CCGs/ICBs). Commissioning mechanisms varied in type and formality, with some hubs combining different approaches for different services due to existing commissioning silos. All hubs offered some form of training to staff working in the service, which ranged in formality. Many also offered education opportunities to local clinicians, particularly GPs.
Implementation approaches were similar across hubs, informed by initial mapping of existing services (and gaps), scoping and designing the hub and securing funding/buy-in, before moving onto implementation activities (often starting as a small-scale pilot and building on this over time). The implementation approaches involved different forms of integration, most often including professional integration.
Hub delivery models
Specific hub delivery models
Table 12 provides an overview of the types of hub models as described by respondents. Most were defined as one-stop shops and/or a hub-and-spoke models. A further two hubs provided some virtual care alongside face to face. Virtual activities include consultations (e.g. online/video) and engagement and education sessions for women and local clinicians.
| Delivery model | Hubs reporting this modela (hub reference) |
|---|---|
| One-stop shop | 9 (hubs A, C–E, H, L, M, P, Q) |
| Hub-and-spoke | 6 (hubs A, B, F, N, O, P) |
| Virtual | 3 (hubs F, G and M) |
| Pop up | 0 |
| Other | 2b |
When exploring hub model labels further and interrogating the data, it became clear that there were different interpretations of one-stop shop and hub-and-spoke models across individuals and hub sites. Examples of variation are provided in Box 8. There was also no agreed definition to describe these hub models in the NHS, which may have contributed to the variation in usage. Given the ambiguity in how these delivery model terms appeared to be understood, it was difficult to reach a meaningful assessment of which hubs had adopted specific models. This is explored further in the discussion.
-
The types and/or number of services that need to be offered to be considered a one-stop shop (e.g. if a hub offers LARC services only or a wider spectrum of services).
-
Whether the hub aspect of a hub-and-spoke model is a physical location offering services to patients, or a non-physical aspect (e.g. central triage/co-ordination point).
-
Whether the spoke aspects of a hub-and-spoke model are physical locations offering services (either as a one-stop shop or a more limited offer) or virtual support (e.g. online education events).
-
The extent to which different aspects of a hub are linked, for example via cross-referrals or operating as discrete services.
-
Whether patients can see more than one healthcare professional in one appointment (this may be expected in a one-stop-shop model, but only two of the self-defined one-stop-shop hubs in the survey reported offering this).
Clinical offer
Figure 2 summarises the services offered by hubs. All 17 hubs responding to the survey question reported that LARCs were offered for gynaecological reasons. Other frequently reported services include LARCs for contraception (N = 15, all except hubs F and H), and 16 hubs offered heavy menstrual bleeding consultation (all except hub N) and treatment and menopause care (all except hub K). No hub reported offering pelvic physiotherapy or termination of pregnancy services. While seven hubs reported offering women’s health counselling/psychology, this was often limited to psychosexual counselling rather than broader mental health support. As mentioned earlier, most respondents reported launching their hub with a limited range of services before expanding the offer, or reported aspirations to expand in this way. The initial service offer in part depended on the skills and interests of those leading hub development (e.g. leaders with expertise and interest in LARC may initially focus the hub offer on this).
FIGURE 2.
Services offered (N = 17).
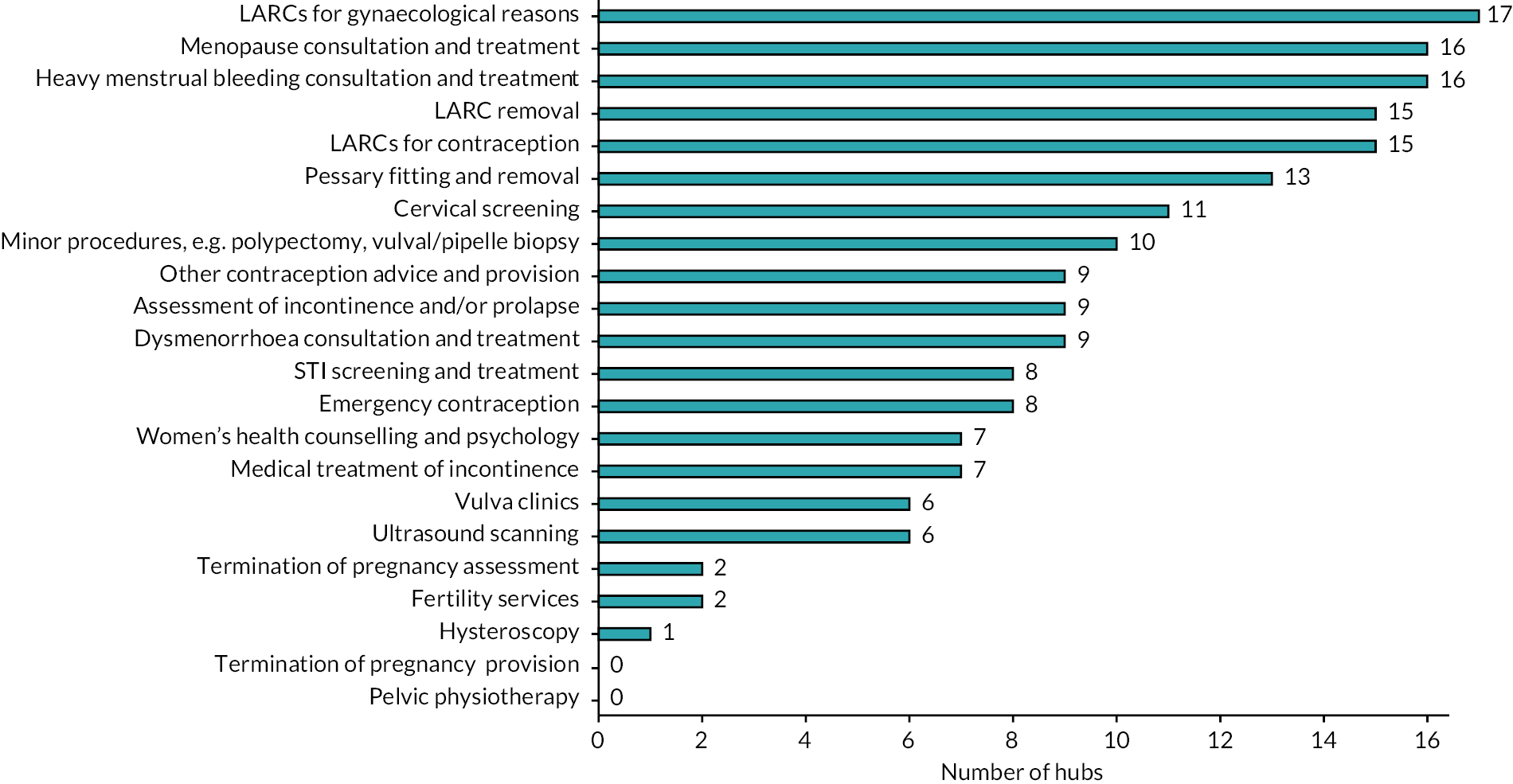
Four hubs offered services in the evening and four at weekends (Table 13). While one of the main objectives was to improve access to care, most hubs only offered services during core hours, though some respondents reported aspirations to offer out-of-hours services in the future. A range of appointment formats were offered (Table 13), with 15 hubs offering appointments face to face and by telephone, with 2 hubs also offering online/video appointments. Only one offered online group consultations.
| Out-of-hours provision | Number of hubs (N = 17) |
|---|---|
| Appointment format | Number of hubs (N = 15) |
| Evenings | 5 (hubs A, D, J, L, O) |
| Weekends | 5 (hubs A, B, J, L, O) |
| None | 11 (hubs C, E–I, K, M, N, P, Q) |
| Face to face | 15 (hubs A–F, H, J–Q) |
| Telephone | 15 (hubs A–F, H, J–Q) |
| Online/video | 2 (hubs E, M) |
| Group video consultations | 1 (hub F) |
Hubs were often seen as offering services that were more complex than a regular GP could support, but not as complex as specialist secondary care services are trained and equipped to manage. Participants described how upskilling hub staff could widen the offer and manage more patient care outside of secondary care. However, some reported situations where hubs may offer the same services as ’standard’ primary care for a particular reason, to meet local needs or due to local context. For example, women who prefer to see a female clinician may visit a hub where this is not available in primary care.
… it’s [ultrasound scanning] something I’d really love to upskill in and it would enable us to, for example, do more with our core clinic, so we could deal with lost [coil] threads and more complex/deeper procedures where we’d normally refer to secondary care service, but hopefully with those skills under our belt and the right support, and agreed competencies, oversight and pathways and dialogue with our secondary care consultants, there is arguably some more things that we can begin to take on in primary care.
Scoping interview
While most services were offered as one-to-one consultations with a clinician, some hubs also offered support via online or in-person engagement and education events with women or clinicians. These may be focused on, for example, menopause, contraception and fertility, or reaching out to specific vulnerable groups. This was described as of equal importance to one-to-one consultations, as educational events can support women to self-manage, reducing the number of appointments in primary care.
Many interviewees highlighted the importance of avoiding an overly prescriptive, top-down specification of the service offer in hubs, to allow flexibility to tailor to local needs.
It depends on their population needs …. With a very old population maybe you want to start concentrating on pessary care, a younger population you might be wanting to sort of look at early menopause care. I think people have got to tailor make it to their population, for their particular needs ….
Scoping interview
However, others noted some degree of standardised, baseline service offer is still needed in addition to tailoring the service to support sharing of learning, avoid reinvention of the wheel and ensure equitable provision (discussed further in Influences on hub set-up, implementation and sustainability).
What I’m quite concerned about is that we’ve done it in the past, we’ve gone off and done lots of different things, said every area’s got to sort out what they need, but actually you need a baseline offer, so that it is similar across the county, even if you can tweak it, because otherwise everybody’s trying to embed this in every corner of the UK and it’s such a waste of energy.
Scoping interview
While a frequently stated objective for many hubs was to provide holistic care, in reality the focus was on core sexual and reproductive health needs. There was minimal discussion of wider issues, such as mental health (beyond psychosexual health), non-gynaecological conditions (e.g. heart disease) or social well-being. However, many stakeholders suggested that hubs should adopt a wider holistic view of care and there was one account of a hub currently in set-up which had included weight-management services in its design.
Leadership models
Throughout the evaluation, we explored leadership roles, and perspectives of who should be involved in leadership. While we recognise that there are multiple types of formal leadership (e.g. clinical, operational, commissioning), as well as differences between leadership and management, most participants did not make this distinction in the interviews. In many cases, leadership and management roles were blended. There was also a focus on expert leadership (i.e. the ability to lead as the individual(s) have valuable knowledge, expertise and/or qualifications) by individuals with a specific interest and passion for women’s health (see Influences on hub set-up, implementation and sustainability). Interviewees described roles and organisations involved in hub leadership, although this often involved collaborative partnership working, and did not necessarily involve formalised leadership roles, responsibilities or accountability. Participants also described different functions of leadership, for example leadership of hub implementation, or day-to-day clinical leadership of hub teams.
Survey respondents were asked to state which role(s) were driving the establishment of the hub (Table 14). In most cases, a single individual was reported to be performing this role, usually GPs with a special interest in women’s health, with SRH consultants, secondary care gynaecologists, local authority commissioners and CCG representatives also cited. In four hubs, multiple roles were involved in driving hub establishment (hubs A, H, K, M).
| Role driving hub establishmenta | Number of hubs (hub reference) |
|---|---|
| Role clinically leading hub | Number of hubs (hub reference number) |
| GPs with a special interest in women’s health | 12 (hubs B–E, G, H, J, K, M, N, P, Q) |
| SRH consultants | 3 (hubs A, L, M) |
| Secondary care gynaecologists | 3 (hubs F, H, I) |
| Local authority commissioners | 3 (hubs A, K, O) |
| CCG representatives | 2 (hubs A, H) |
| GPs | 12 (hubs B–E, G, H, J, K, N–Q) |
| SRH consultants | 4 (hubs A, F, L, M) |
| Secondary care gynaecologists | 1 (hub I) |
All hubs were clinically led by doctors, over half by GPs (Table 14), with SRH and gynaecology consultants in the remainder. Only one hub reported a difference in the role that was driving establishment of the hub and who was clinically leading it (hub N, driven by local authority commissioner and clinically led by a GP). Many hubs described a governance structure in place to oversee the hub implementation, activity and budget, to whom the clinical lead was accountable (see Implementation approaches for further detail).
There were various roles and responsibilities held by hub clinical leads, which included:
-
Responsibility for hub governance and management (reporting and accountable to a governance board).
-
Designing patient pathways.
-
Developing and maintaining relationships with other stakeholders, for example secondary care, PCN leads
-
Quality assurance, overseeing of staff training, ensuring appropriate guidelines/standard operating procedures were in place.
-
Identifying issues and areas for improvement.
Interviewees shared opinions regarding the advantages and disadvantages of hubs being clinically led by secondary care consultants and GPs (Box 9), and there was some discordance among participants, with a tendency to favour their local model. Some suggested that hubs could be clinically led by GPs alongside, or with clinical support/oversight from, secondary care or community gynaecology consultants. Others expressed concerns about GP-led models (see Box 9), preferring consultant gynaecology or SRH consultant clinical leadership due to their specialist training to manage more complex issues.
-
✓ Greater access to specialist resources and flexibility than primary care in terms of, for example, number of clinics, staff to draw on and staff training offer.
-
✓ Reported to have specific knowledge of governance/management aspects relevant to clinically leading a hub.
-
✓ Are trained to deal with more complex issues.
-
✓ Have a specific system-networking remit (spanning primary care, secondary care and public health).
-
✓ Important to have a primary care perspective as a key focus of hub design.
-
✓ Have a more holistic approach due to the generalist and life-course approach in primary care.
-
✗ Have fewer specialist resources available than secondary care.
-
✗ Have competing priorities leading to a lack of capacity.
-
✗ Have more limited training/qualifications to manage more complex, cross-disciplinary patients (leading to safety concerns with a GP-led model).
-
✗ May face more challenges in developing relationships across the system which stakeholders may already have – while these relationships can be created, this takes time and resource.
Note: these statements are based on participant accounts and are not statements of fact.
Having consultant input I think is really important though because there are some GPs who can do a lot, but what we want is to be able to manage the patients as much as possible within that place. If you want to do that, that’s where you need SRH consultant leadership, but you don’t need them to be delivering a lot of the work, because a lot of GPs are really well placed to do some of it.
EH4, internal interview
Others reported that non-GP primary care roles such as nurses could offer some aspects of clinical leadership in hubs:
It [hub leadership] is primary care as in the bigger multidisciplinary team. And in one area it might be led by a nurse to start with or even a pharmacist or a paramedic or a GP, but then … it should grow from there to get a bigger team.
EH3, internal interview
In addition to clinical leadership roles, interviewees also commented on the importance of having commissioner involvement in hub strategic leadership to establish models and unlock resource. Local authority representation in the collaborative hub commissioning and leadership arrangements was cited often, as councils are pivotal organisations as leads for sexual health commissioning. However, it was suggested that hubs should not be solely local authority-led as the NHS was a key stakeholder.
… I would really question the extent to which local authorities are both best placed to and really responsible for taking some of the lead for contraception in primary care, I think the NHS has always been slightly missing on this agenda ….
Regional interview
Organisations involved in hub design and delivery
Varied organisations were involved in designing and delivering hubs, indicating the varied population footprints a hub can adopt. For example, some hubs served women across one or more ICS/CCG footprints (e.g. hub E). Others served one or more PCN areas (e.g. hubs I and N) or GP Federations (e.g. all Northern Ireland hubs). Most often survey respondents described the involvement of GP practices in both providing hub services and/or referring women to the hub (mentioned by all 14 responding hubs) (Table 15). Involved in over half of hubs were local authorities, NHS acute trusts, PCNs and CCGs/ICBs.
| Organisation involved | Number of hubs (N = 14) |
|---|---|
| GP practices | 15 |
| Local authorities | 10 |
| NHS acute trusts | 10 |
| PCNs | 8 |
| CCGs/ICBs | 7 |
| NHS community trusts | 4 |
| Voluntary sector | 3 |
| Women’s groups | 2 |
| Private sector | 1 |
Interviews explored how organisations were involved in hub design and delivery. CCGs and local authorities had been involved in the commissioning and designing of the hubs, including by supporting identification of gaps in existing services, and mapping pathways. Secondary care providers often (but not always) accepted referrals from hubs and supported hubs in other ways, for example hub staff attending hospital gynaecology meetings, gynaecologists providing clinical advice for complex women and contributing to communication materials and guidelines.
… so when there is a little bit of an overlap in terms of when does something have to go to secondary care, when can it be handled in primary care, I think that relationship is very precious to ask for help when needed, to check we’re all being careful to abide by the right levels of competencies and qualifications, and if we are looking to upskill that we’ve got the support of secondary care with that.
Scoping interview
Pharmaceutical companies providing LARC devices had also provided input. They provided resource and expertise to support the set-up of hubs, including modelling costs and outcomes for LARC services, designing guidance, tools and pathways, and training clinical staff.
Funding, commissioning and contracting models
Funding and commissioning models
As described in the introduction, commissioning and funding for women’s health in England is complex, with different organisations having responsibility for relevant areas of provision. In addition, at the time of data collection, there was no dedicated national funding stream for WHH implementation and delivery. There were a range of commissioning arrangements in place for hubs (Table 16). Some involved multiple commissioners (local authorities and CCGs/ICBs), for example, LARC services commissioned by local authority, and gynaecology services commissioned by the CCG/ICB. Others were commissioned by a single commissioner (e.g. CCG/ICB or local authority only).
| Commissioning arrangement | N hubs (hub reference) |
|---|---|
| Multiple commissioners involved (CCG and local authority) | 7 (hubs A, D, L, M, N, O, Q) |
| Commissioned by CCG (or equivalent) only | 5 (hubs C, E, F, H, I) |
| Commissioned by local authority only | 1 (hub K) |
| There are no formal commissioning arrangements in place | 2 (hubs G, J) |
| NHS trust commissioned | 1 (hub B) |
Interviewees also discussed the challenge of commissioning barriers (particularly that contraception is funded by local authority and gynaecology services by ICBs). Some interviewees noted the potential benefit of pooled budgets or collaborative commissioning arrangements across local authorities and CCGs to overcome these silos. This is discussed in further detail in Influences on hub set-up, implementation and sustainability.
Some hubs reported utilising funding sources that were not directly related to gynaecology/SRH but that aligned with certain objectives of the hub, for example COVID-19 recovery programmes to reduce secondary care waiting lists, extended access funding or funding for the Additional Roles Reimbursement Scheme (which provides funding for additional roles to create multidisciplinary teams (MDTs) according to the needs of local services). 104–106
Contractual arrangements
The hubs had various contracting arrangements in place, as identified in the survey (Table 17), with the most frequently reported arrangement being a locally enhanced service. This is funding for services supplementary to those that are already offered in the core GP practice contract. Other contracting arrangements included subcontracting by secondary care providers, direct contracts with primary care, block contracts with pooled budgets (with CCG/ICB) and a direct contract with the ICB and local authority. Three hubs had a combination of contracting arrangements for different aspects of their services.
| Contracting arrangement | N hubs (hub reference) |
|---|---|
| Locally Enhanced Servicea | 5 (hubs I, K, N, P, Q) |
| Contract with secondary care provider | 3 (hubs B, E, F) |
| Combination of contracting arrangements for different aspects of hub services | 3 (hubs J, L, O) |
| Block contract with pooled budgetb | 1 (hub H) |
| Direct contract with primary care | 1 (hub M) |
| Direct contract with ICB and local authority | 1 (hub A) |
Some participants reflected on the advantages and disadvantages of using a locally enhanced service arrangement. It had been used successfully to overcome the commissioning silos, enabling LARCs to be commissioned for both contraceptive and gynaecology reasons. It was described as ensuring that provider reimbursement aligned with the actual service costs, to account for all activity and ensure financial viability. However, it was suggested that there may be variable sign-up to the offer by GP practices, leaving some areas without provision.
Interviewees also described strengths and limitations associated with block contracts (i.e. a set payment is offered to a provider to deliver a defined service) and activity or performance-based contracts (i.e. providers are paid for the volume of activity, which may fluctuate over time) (Box 10).
-
✓ Income can be more predictable.
-
✓ Reduced administrative burden.
-
✗ Less flexible.
-
✗ Fluctuations in patient demand can be difficult to manage (particularly for small services run by GP practices, like most hubs).
… we have always said we cannot be on a block contract, we’re too small a set up to work, especially whilst there’s still such clear growth … these sorts of novel services are much more … vulnerable and put on a block contract just would make them very difficult to accommodate fluctuations of activity and particularly growth and changes to referral patterns ….
EH3, internal interview
Activity-based contracts
-
✓ Potentially allow for greater flexibility.
-
✗ Unless there is a specified requirement to review the tariffs at regular intervals, they may not increase to match increases in costs over time (e.g. to expand hub vision/goals, salary/rent increases). Building in regular tariff reviews can be beneficial in ensuring the hub is reimbursed an appropriate amount for the procedures it performs and so can be sustainable.
-
✗ Some activities do not have a dedicated tariff attached, for example payment for procedure but not patient counselling, which can make re-negotiations difficult. Hub leaders working with commissioners to ensure that payments reflect costs may help to ensure the service remains financially viable.
… we have to set up a service in a way that allows you to make sure it remains viable from a funding perspective as costs and vision change and that might include costs of rent, energy, costs of people and so you’ve almost got to factor in and we didn’t have anything factored in to our initial contract around the annual incremental increase but yet your staff expect incremental pay rises….
EH3, internal interview
Venue of hub services
From the survey and interviews, there was wide variation in the number of venues provided by individual hubs, ranging between 1 and 9. Most were offered in GP practices, with some also delivering services in a hospital setting, sexual health clinic, community NHS trust or pharmacy-based clinic (Table 18). Activities such as engagement and education events were held online, usually delivered by primary care hub staff. From the survey, six hubs provided information on the number of clinics offered, which varied substantially (between 8 and 56 clinics per month).
| Hub venue | Number of hubs (hub reference) |
|---|---|
| GP practices | 13 (hubs A–F, I–K, M–Q) |
| Hospital setting | 3 (hubs F, H, L) |
| Sexual health clinic | 2 (hubs A, M) |
| Community NHS trust | 1 (hub H) |
| Pharmacy-based clinic | 1 (hub B) |
Challenges were described in co-ordinating and standardising hub services offered across multiple PCNs and/or GP practices, as each had their own set of standard practices. While this can offer advantages (e.g. access to a broader range of clinical roles in different GP practices/PCNs), it does require separate discussions and solutions to manage. GP federations may also offer support by acting as an interface between GPs and secondary care and subcontracting with PCN GP leads.
… all the GPs are independent and PCNs hopefully bring them together and it makes some joint decisions, but largely they work independently and so the advantage of having an overview is that you can kind of try and bring all those things together and have a sort of bird’s eye view ….
EH1, internal interview
Implementation approaches
Implementation processes
Participants reported that hub implementation occurred in stages, beginning with mapping existing services and gaps, designing a hub model to address these gaps, securing funding/buy-in and setting up the hub. These stages will be briefly outlined and they are summarised in Figure 3. Where data were available on implementation processes, the stages outlined below occur in most hubs in some form.
FIGURE 3.
Summary of WHH implementation processes.
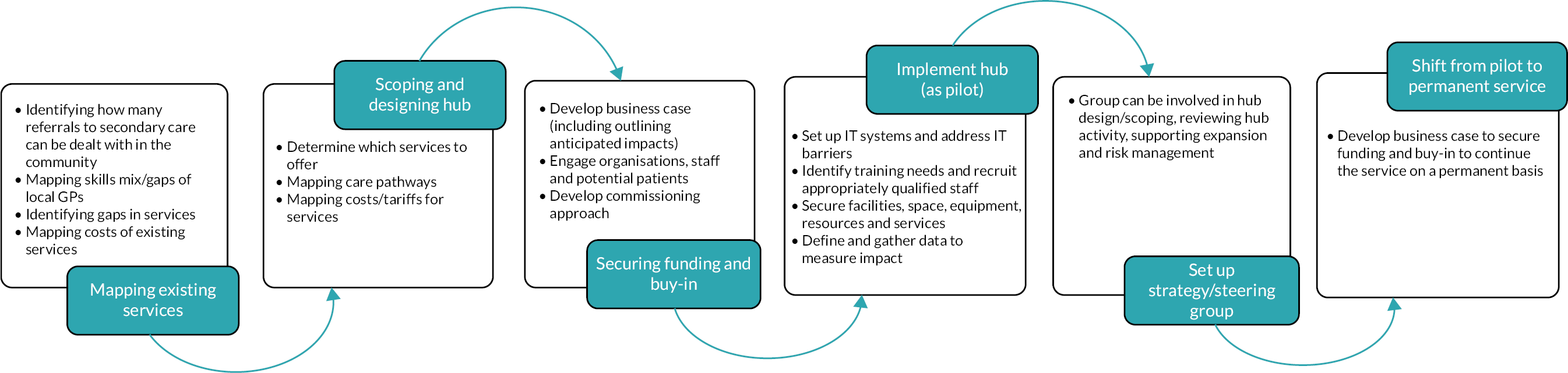
Existing services and gaps were mapped in some hubs to inform the design and scope of the hub model. This included, for example, reviewing referral numbers and reasons for referral to secondary care to identify how much could be moved into the community, mapping skills mix/gaps of local GPs, identifying gaps in services (e.g. low LARC uptake) and mapping costs of existing services. These activities were often performed in collaboration across organisations (e.g. GPs, commissioners, secondary care), which was reported to support the development of a shared hub vision and strategy.
And so an audit was done to see, out of all the GP referrals in the [area name], how many could have been managed outside the hospital, if you had the right kind of skill, to manage it. That’s where it started. Stakeholders were involved. I was involved because I was a community gynaecology consultant. Hospital consultants were involved and GPs were involved.
EH4, internal interview
After mapping existing services and gaps, sites then moved on to scoping and designing their hub model: for example, deciding which services to offer, mapping care/referral pathways and modelling costs and tariffs for potential hub services. Again, this process often involved a range of stakeholders and organisations (e.g. GPs, secondary care, commissioners, pharmaceutical companies). This planning was then used to develop a business case to secure funding and outline anticipated impacts of the hub (e.g. cost savings, reduced waiting lists) to support buy-in from commissioners and potential providers (e.g. GPs). Often this was initial funding to develop a proof-of-concept pilot hub, with additional buy-in and identification of funding required at a later stage to move to an established service (see next section).
The next thing that was done was a business case, to look at … basically two things; saving money and reducing waiting times. And then the appropriateness of what should be seen. And then the business case included … what would they cost? How would you set that up? What was the administrative structure?
EH4, internal interview
Once the early design phase was completed and funding and buy-in had been secured, hubs could then move towards implementation activities, which included:
-
Setting up IT systems and addressing IT barriers where they existed, for example sharing of data/systems.
-
Identifying training needs and recruiting staff with required expertise/qualifications.
-
Identifying facilities, physical space, necessary resources/services (e.g. testing services, implants/coils) and equipment (e.g. gynaecology couches).
-
Defining and gathering intelligence to measure impacts.
Some hubs set up a steering or strategy group to oversee the implementation and delivery of the hub. As with the early design phase, this often involved stakeholders across multiple organisations (e.g. primary care staff, secondary care staff, commissioners, public/patients). These groups undertook varied activities, including reviewing hub activity, discussing plans for hub growth, inputting into patient pathway design and risk management.
Respondents from only six hubs in the survey reported having patient/public involvement in hub design and delivery (hubs B, F, H, L, M, O). This took the form of, for example, members of the public on the hub steering/strategy group, hosting women’s engagement events/public consultations and incorporating patient feedback into hub service design. In nine hubs, respondents reported that there had been no involvement of patients/public in hub design and delivery. Involvement of women in the design and delivery of WHHs was not frequently discussed. Two exemplar sites reported activities, including exploring local transport, accessibility and inequalities with a patient committee, past consultation about potential hub changes, a patient engagement subgroup chaired by Healthwatch with user representatives, and user involvement in developing hub information. One interviewee described the importance of working bottom-up and involving women:
You could impose something very top-down, you could say ‘this is what we’re going to do’, … but then I think we will lose that kind of population neighbourhood everybody onboard everybody – including women …. So I really believe that it has to be a much more bottom-up thing.
EH1, internal interview
The survey also provided other examples of involvement across different UK hub sites, with six hubs providing further information, including:
-
A local group commissioned by the Public Health Team to undertake both online and face-to-face consultations with local women, with a reference group being supported.
-
A patient engagement event, supported by local charities with an interest in women’s health.
-
The involvement of Healthwatch, in terms of both gathering feedback and their inclusion on a hub steering group.
Some sites also reported collecting patient feedback, which one interviewee described was used to improve services via a ‘You said, we did’ approach, with changes made in response to patient comments, keeping women involved in service development. Respondents from nine other hubs reported that there had been no involvement of women in hub design and delivery.
Implementation strategies
As with the implementation process, implementation strategy was similar across hubs (where data were available). Most models were initially small scale (in scope of services and/or geographical reach) and expanded and evolved over time. However, the exemplar hubs evidenced variation in whether hubs are created as new entities or built from existing provision: two were set up from scratch as a brand-new service (while building on existing staff knowledge and qualifications), and two were developed from existing services.
As described previously, hubs may begin as commissioned pilots to test ways of working before becoming a core service which can then be expanded and additional services added. All exemplar hubs were initially implemented as a pilot of some form. Overall, starting the hub as a small service and expanding over time was reported to be an effective approach to developing in a sustainable way.
… the CCG then said they would commission a small pilot. We developed a kind of proposal and it was tiny and I think the key was not to be too all-singing, all-dancing, at that point to say, you know, ‘we can give this a go’ …. And then that sort of gave some traction and then we’ve built on that and it’s grown and I think unless there’s a proof of concept, unless there’s a proper evaluation, getting an organisation to commit to a model is not going to happen ….
EH1, internal interview
However, findings from our exemplar hubs highlighted some of the challenges of starting as a pilot. The short-term, limited nature of pilot funding means there are concerns of funding not continuing following the pilot and the service being discontinued. This uncertainty was linked to challenges in establishing networks and relationships with other local services. Pilots also required services to be agile and set up with the limited time and resources available. The need for financial workarounds to implement pilots was discussed, along with a need to rely on the goodwill of others (e.g. to offer physical space), which created challenges for sustainability and scale-up.
Most hubs we identified had evolved over time, changing and expanding their offer as the service became more established. This was demonstrated in all four exemplar hub sites and in most hubs completing the survey. Expansion included:
-
Offering additional services.
-
Seeing a greater number of women/offering more clinics.
-
Hiring more staff.
-
Covering a greater geographical area (e.g. covering more PCNs, allowing cross-PCN referrals).
-
Involving additional organisations.
This service was initially developed as a LARC (implant & coil) service …. The service also included some basic STI screening & cervical cytology …. The hope is that eventually these hubs will include additional services such as menopause, urogynaecology (pessary changes), vulval medicine etc.
Survey respondent
Many of the hubs had already launched before the onset of the COVID-19 pandemic. While this caused disruption at the time (e.g. reducing or stopping non-urgent services), participants did not perceive the pandemic to have caused long-lasting effects on hub implementation, and COVID-19 disruption was not a key theme arising from the research. In some areas, COVID-19 was described as facilitating hub implementation where the local health system was focused on tackling substantial increases in secondary gynaecology waiting lists (e.g. utilising COVID-19 recovery funding programmes to grow hubs).
Approaches to integration
As outlined in Chapter 2, there are different dimensions of integration. We identified multiple integration frameworks and have used concepts from three frameworks to describe five types of integration. We did not include specific questions about integration in the survey. However, some questions did provide insights on aspects of integrated care planning and provision, such as commissioning arrangements between organisations and sectors, organisations/structures (e.g. leadership and organisations that form the hub) and services offered, all described earlier in this chapter.
In Table 19, we provide examples from the four exemplar hubs of how they have implemented different aspects of integrated care.
| Integration type | Examples |
|---|---|
| Structural/organisational |
|
| Functional/administrative |
|
| Clinical/coordination and integration of care |
|
| Interpersonal |
|
| Normative |
|
| Systems/whole systems |
|
Integration activities overlap in places with the implementation strategies described in Figure 4 (e.g. setting up a steering committee and developing a business case). This is because when these activities are undertaken in collaboration between organisations and sectors, they can be perceived as examples of integrated care planning and provision. Many of the examples of integration relate to the set-up and planning of hubs under ’structural/organisational’ integration. Understanding this stage was a key aim of the evaluation. Examples include MDTs (EH1, EH4) and steering committees, which facilitated collaboration and cooperation in the design, development and oversight of hubs (interpersonal).
FIGURE 4.
Theory of change: how WHHs might work – cyclical, incremental growth. LES, Locally Enhanced Service; PH, Public Health.
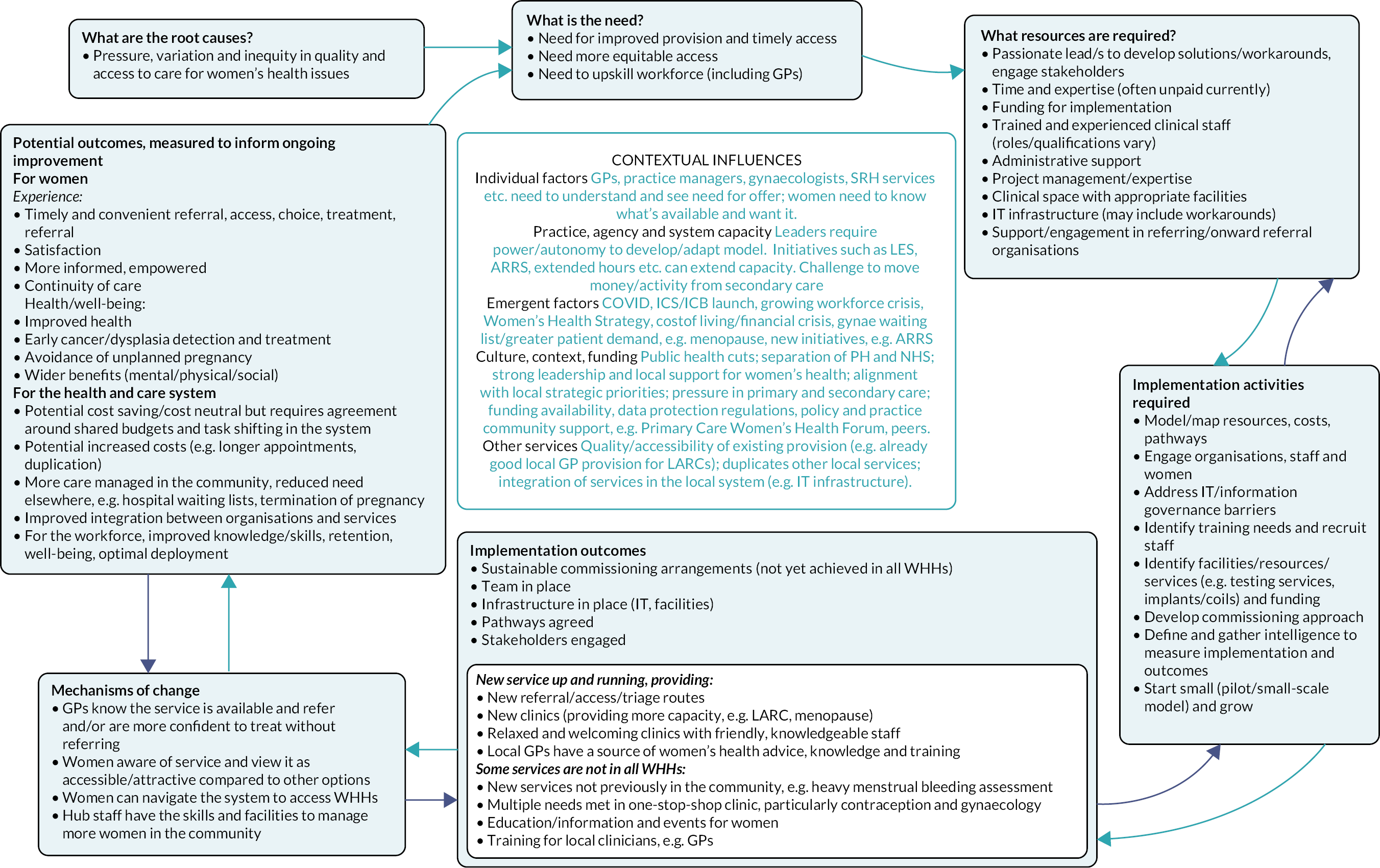
As WHHs were often conceived from the motivation of passionate local leaders, normative integration was common, in the form of shared values developed through the skilled communication and networks of hub leads. Another common type of integration was the integration of back-office or administrative functions to enable the successful day-to-day functioning of a hub (e.g. for booking/referring, testing and prescribing) and the ability to provide a wider clinical offer. Challenges to integrated working were common, as were proposed solutions. These are described in the Influences on hub set-up, implementation and sustainability section.
Workforce models and approaches
Workforce varied across models. The most frequently reported roles were GPs with special interest in women’s health and administrators (Table 20).
| Role | Hubs (N = 16) | Role | Hubs (N = 16) |
|---|---|---|---|
| GP with special interest | 13 | Nursing assistants | 1 |
| Administrators | 11 | Data analysts | 1 |
| Healthcare assistant | 7 | Hospital gynaecology associate specialists | 0 |
| Hospital gynaecology consultants | 5 | Hospital gynaecology trainees | 0 |
| Practice nurses | 5 | GUM consultants | 0 |
| GPs | 3 | GUM associate specialists | 0 |
| Community SRH consultants | 3 | GUM trainees | 0 |
| Specialist nurses | 2 | Physiotherapists | 0 |
| Community SRH trainees | 2 | Physician assistants/associates | 0 |
| GP trainees | 2 | Care assistants | 0 |
| Counsellors | 1 | Ultrasonographers | 0 |
| Community SRH specialists | 1 | Pharmacists | 0 |
| Advanced nurse practitioners | 1 | Othera | 1 |
Some interviewees suggested that there are opportunities for greater involvement of other staff roles, particularly related to offering a more holistic service that takes into account the wider aspects of women’s health (Box 11).
Nurses:
-
Could have greater responsibility in hub delivery, for example be a first point of contact for the hub, with GPs able to provide more specialist support if needed. For example, in one hub, nurses were trained to fit LARCs and in others, nurses supported the triage of hub referrals.
-
Advanced nurse practitioners in particular were highlighted as being very experienced and requiring little support from GPs to see patients.
So I think that it [WHHs] needs a much more nurse-led approach. I think that nurses are probably better placed to deal with a lot of those issues and be the first point of contact. And then obviously consultants, GPs and special interests are there to deal with their specialty interests, if you like, so you need to be able to call on the right person to do the right thing, but I think that’s a triage model and initial point of contact could be nurse-led.
National interview
Pharmacists:
-
Role in patient education and disease prevention (e.g. smoking cessation).
-
Already involved in emergency and routine oral contraception provision.
-
Can be trained in LARC fitting (which may be more cost-effective than GP fitters).
Physiotherapists: support for pelvic floor care and mobility.
Physicians’ associates: some early work had been undertaken in one hub to explore training in LARC fitting.
Nursing associates: some early work had been undertaken in one hub to explore potential role.
Other groups mentioned but not currently involved included midwives, third-sector women’s groups, social prescribers and well-being psychologists.
Some exemplar site interviewees discussed the advantage of having GPs with special interest in women’s health delivering hub services (direct care, distinct from leading the hubs). First, they offer more specific expertise than a GP without special interest, enabling the hub to offer services that are more advanced than a routine GP appointment. Some also reported that primary care staff are better able to provide care in a more holistic manner (e.g. longer appointment times to allow time for discussion with the woman and considering the woman as a whole), where secondary care may be more focused on episodic care.
Because it’s run by GPs, I think that we offer a very holistic service to our patients. So we give them time and we’re familiar with looking at the whole because whilst a woman might present with a gynae problem it’s influenced by a lot of things including mental health, abdominal problems as well as just the gynae presenting problem.
EH3, internal interview
It was also suggested that GPs with special interest may offer different expertise than some secondary care professionals who may be involved in women’s care, as they straddle both generalist primary care and specialist women’s health practice. Respondents in one exemplar hub site suggested that primary care was a more acceptable environment and that pathways were more flexible than hospital, for example psychosexual counselling can be offered on a long-term basis over multiple sessions, which would not be possible for a hospital waiting-list-based service. In addition, primary care-based hub staff suggested that hospital consultants would find it more difficult to slot women in if they need to be seen or rearrange appointments themselves, which was possible in primary care.
But I think it’s [psychosexual counselling] much more amenable or much more to be in the intimate environment of a GP surgery where you can see people. And they might need to be seen over several years, and that doesn’t really fit into a hospital waiting list follow-up type service. Because [a primary care clinician] can say ‘I need to see this lady in six weeks’ and then she can jiggle things around to fit that in.
EH3, external interview
Training, education and competency requirements
Training and education provided by Women’s Health Hubs
All 17 hubs participating in the survey reported offering training to healthcare professionals working in the hub. This varied from informal support to formal training for qualifications. Informal support included discussing complex cases and offering advice. Formal training for GPs was provided in all exemplar hubs, for example LARC fitting and menopause care, including contribution to formal Faculty of Sexual and Reproductive Healthcare training/qualifications. This was usually provided by experienced and qualified hub clinicians, with one hub also having pharmaceutical company support in LARC training.
… it’s so amazing to learn from everyone’s clinical experience because everyone is so experienced within women’s health but also from a GP perspective, which is such a different tilt on gynaecology than from a secondary care perspective.
EH3, internal interview
Other staff were offered training, for example nurses trained in referral triage, and cervical smear clinic practice, and trainee nurse associates trained to work as chaperones. Some hubs were also exploring training physician’s associates and pharmacists to fit LARCs.
Training less expensive hub staff to perform procedures, for example LARC fitting, was put forward as an approach to reduce costs and reduce GP workforce pressures. Training was stated to improve clinician confidence in performing procedures and to support recruitment and retention of staff by offering professional development opportunities.
… When I first started, I would be with another healthcare assistant or with a nurse and we would train for like a good month, month and a half until you feel confident into doing a clinic. I mean, gynae is quite a specialised clinic and there’s a lot of things that need to be done, but if you’re not getting the training then they don’t feel confident in doing that.
EH4, internal interview
Participants also described offering training and support to local clinicians outside of the hub. While there was some offer of formal training in hub clinics, this tended to focus more on informal opportunistic advice and training. Training was reported to be predominantly for local GPs, with fewer offering this to other primary care staff. Types of education for non-hub staff are outlined in Box 12.
-
GPs and student doctor shadowing in clinics.
-
Advice and feedback to local GPs on their gynaecology referrals, for example noting where a patient could be treated in primary care instead of referring to the hub or secondary care.
We look at all GP [gynaecology] referrals … if the patient perhaps doesn’t need a referral if they’ve had a little bit of advice then we go back to the GP to give advice and so there’s learning there. And then in addition it helps us support the GPs follow the pathways correctly, so we might go back and suggest that they do something differently, so there’s an educational element in our role in triaging.
EH3, internal interview
-
Answering questions/discussing patients with GPs.
-
Forums and educational events for GPs, for example on LARC fitting, menopause.
-
Supporting set-up of local support and education networks.
-
Formal LARC fitter training for primary care staff.
-
Supporting implementation of other LARC services/hubs.
-
Supporting undergraduate and postgraduate training.
Competency assessments and review
Most hubs reported requiring staff to be up to date on relevant qualifications and standards (e.g. Faculty of Sexual and Reproductive Healthcare modules, letters of competence, menopause care) and to engage in annual appraisals. One hub had implemented a competency pathway for healthcare assistants.
Participants noted the importance of training being obtained from an accredited body to deliver hub services, where relevant (e.g. the Institute of Psychosexual Medicine or the British Menopause Society). This was reported by one scoping interviewee to be useful in supporting the credibility of clinicians working in hubs and to support in any litigation claims. One national interviewee reported that GPs would need secondary care supervision to sign off their competencies. Some exemplar hubs noted the importance of monitoring staff performance and confidence in undertaking a certain procedure and, if needed, putting more support, training or supervision in place. One participant suggested that the training and qualification requirements were a risk to scaling-up services and should be less prescriptive given the time and cost implications of formal training (see Influences on hub set-up, implementation and sustainability).
I am very nervous that people will expect training and qualifications that A, won’t be appropriate, B will take a long time and C just will be too costly and people won’t do them.
National interview
Theory of change for hub implementation
As described in Chapter 3, we developed a theory of change (Figure 4) for WHH implementation based on the structure outlined in the paper by Ghate et al. 100 It is important to highlight that visual representations cannot fully illustrate the complexity of health system change, and we do not intend to suggest that the implementation process for WHHs is linear. The theory of change uses the findings from the evaluation to illustrate broadly how WHH implementation could work, rather than aligning with any specific model we explored, and no model demonstrated every characteristic in the theory. The outcomes listed represent the aims of WHHs, rather than what we currently have strong evidence to show. The unintended consequences (including any additional costs) and assumptions regarding what hubs can achieve have not yet been measured or tested. This theory also does not capture wider societal or long-term impacts, for example societal benefits from reduced unplanned pregnancies. The theory focuses on women’s health only in terms of reproductive and sexual health as this is the current focus of the hubs identified in the evaluation.
Influences on hub set-up, implementation and sustainability
This section explores influences on hub set-up, implementation, as well as scale-up and spread of WHHs, which is an explicit aim of the Women’s Health Strategy for England. 12 It is also crucial that models are sustainable, to become an embedded part of local health systems and pathways. We therefore also describe what interviewees reported as the biggest challenges for sustainability, and what could support this. First, we describe how national and local context may impact on WHH implementation. Many of the influences on implementation of WHHs also describe influences on integration, as WHHs are integrated care models. For example, where hubs bring together professionals across disciplines, organisations and sectors, this can bring challenges to the successful implementation of a service (e.g. by increasing the need for effective communication processes), as well as benefits to the experiences of women using them (e.g. by a wider offer of treatments).
Survey respondents were asked to identify their top three barriers and facilitators to implementation (Table 21) to highlight the relative importance of the many challenges experienced. Overall, these align with the themes from the interview data that are presented in this section. We approached the triangulation of multiple data sources on influences with the aim of being comprehensive in the data we collected, rather than to compare or check for accuracy. However, it is worth noting that the functionality and interoperability of IT infrastructure and systems were described as important by interviewees but did not appear in the top three from survey respondents.
| Survey respondent’s ‘top three’ implementation issues | Frequency (n = 17) | |
|---|---|---|
| Implementation barriers | Funding and commissioning issues | 10 |
| Staff recruitment and/or capacity | 8 | |
| Challenges with collaborating | 7 | |
| Implementation facilitators | Committed and experienced GPs | 7 |
| Supportive leadership | 6 | |
| Collaborations/relationships across services and organisations | 5 | |
National policy and practice context
Many national-level challenges were described, including change in government and policy teams, the COVID-19 backlog and competing health service priorities, rising demand for SRH services (particularly menopause care), and the availability and cost of devices such as IUDs. However, some hubs reported how some apparent challenges were in fact drivers of hub implementation (Box 13). For instance, the need to innovate and reduce COVID-19 backlogs and secondary care pressures helped to make the case for WHHs.
Key messages regarding the national policy and practice context:
-
National-level changes and pressures have created challenges for hub implementation, but have also provided impetus for service development and innovation.
-
To date, hub implementation has been developed by local leaders from the bottom up, with no national structures or standardisation.
-
Stakeholders highlighted a need for national, regional and system-level leadership and support for WHH implementation and welcomed the publication of the Women’s Health Strategy and appointment of the Women’s Health Ambassador.
-
Leaders identified a need for balance between top-down standardisation and bottom-up development of WHH approaches, to provide support while enabling the flexibility to design services according to local needs and context.
-
Solutions to commissioning challenges may be context-specific and locally determined, with variations appearing across regions, PCNs, local authorities and GP practices.
A lack of clarity about where the overall responsibility lies for WHHs was described, with specific designated leadership for women’s health having been absent from national, regional and ICS portfolios, which has since been addressed at the national level with the appointment of the Women’s Health Ambassador and team. A regional interviewee described how currently ‘… it’s sort of everybody’s responsibility and nobody’s to get it going’. WHHs explored in this evaluation have been designed and implemented before the Women’s Health Strategy was published. They have been developed from the ‘bottom up’ by local leaders in a small proportion of health systems in England, rather than ‘top down’ and nationally directed and mandated. Interviewees described this local, bottom-up approach as having enabled innovation, rapidity and responsiveness to local needs and priorities. However, there was tension between standardisation and flexibility in hub implementation, with stakeholders also reporting a lack of standardisation and a desire for greater national support and direction. For example, an interviewee commented that conversations were needed around shifting resources across budgets with ‘the people that matter’ (EH2, internal interview).
Several interviewees highlighted that support at a national policy level was helpful in driving change and developing and embedding WHHs. Overall, however, participants reported a lack of associated national funding or guidance for the policy (at the time of fieldwork) and many participants described the need for a regional and national, cohesive programme for women’s health beyond maternity care, which included oversight, drive, infrastructure and support. This was described as hindering progress, particularly in terms of overcoming commissioning barriers. A need was also reported for regional and national champions, including in NHS England, to expedite hub implementation.
… and it’s always struck me that NHS England, they don’t have a lead for contraception … without sort of leadership at a national level sort of filtering down, it’s always going to be a struggle getting buy in on some of these things.
Regional interview
The publication of the Women’s Health Strategy in 202212 had started to address the gaps in national guidance by recommending the setting up of hubs, and participants welcomed the new focus and prioritisation of women’s health and the newly appointed role of a Women’s Health Ambassador. While the importance of a national drive and, to varying extents, standardisation of approach was described by participants, many expressed concerns about this jeopardising the ability of hubs to develop out of, and respond to, local priorities, needs and resources.
I’d love it if there was more infrastructure there and I think it just slowly grows over time. But I think the completely alternative option is your top-down model, and most of the time, particularly – I think it still works better to build bottom up, because you know you’re working with what you’ve got. You know you’ve got your providers actually saying ‘This is the real-life challenges. This is what we can and what we can’t do. This is the capacity we’ve got’. ‘Oh well that IT idea won’t work because this system won’t speak to this system’.
EH2, internal interview
Local context and variation
Problems and solutions to commissioning challenges are often context-specific and locally determined. Variations in how different commissioners and providers work, the needs of local populations and local capacity for implementing WHHs were described as impacting hub implementation (Box 14). These variations can appear across regions, PCNs, local authorities and GP practices, and one participant commented that implementing a hub model across a large area with a greater number of organisations meant that there would be more variation to contend with. Variations in existing service provision, access and quality were also described and this lack of standardisation was said to hinder hub implementation, integration and widespread improvements across a whole area. It was also highlighted that the strength of existing women’s health services in an area may determine the need for a WHH.
Key messages regarding the role of local context:
-
Problems and solutions to commissioning challenges are often context-specific and locally determined.
-
Variations can appear across regions, PCNs, local authorities and GP practices.
-
These variations can include how different commissioners and providers work, the needs of local populations, and local capacity for implementing WHHs, and the strength of existing women’s health services (and thus need for a WHH).
-
Implementing a WHH in an area formed of many organisations and stakeholders can be challenging and requires effective collaboration and relationship-building.
Within our network there are four surgeries and within the four surgeries, three of them were already providing coils and implants so just from our perspective … we didn’t feel like it was worth doing all that extra admin and you know trying to get funding and everything for something that we’re already doing … it just so happens there’s a lot of female GPs who are interested in contraception so the need wasn’t as big in our area for the hub model.
EH2, external interview
Interviewees and survey respondents frequently described the importance of building relationships with ‘key people in each part of [the] system’ (EH4, external interview), particularly primary and secondary care, and between GPs and consultants. However, some experiences of difficulties working with individuals across the healthcare system were described. At the stage of setting up a hub, some interviewees described apprehension from local stakeholders regarding the changing approach to women’s health, and how this would impact on their own services. In models where hubs were providing services usually delivered in primary care, fear was expressed that GPs would be de-skilled, or that work and funds would be diverted away from the GP. In hub models undertaking procedures usually delivered in secondary care, concerns were raised about a potential loss of resources from secondary care, and about the clinical safety and quality of care outside hospital settings.
However, such issues were not reported to have persisted following hub set-up. For example, one site reported that clear communication and demonstration of the hub team’s qualifications had improved perceptions in the local area. Multidisciplinary engagement meetings were described as beneficial in advertising hubs and attracting interest as well as reassuring staff in surrounding services who may be concerned about the impact of WHHs on their service. This may be difficult where a hub is aiming to provide care across a large number of PCNs or local authorities.
… the consultants at the Royal [name of place] were rather apprehensive about the service and worried about how much work we would take over and they were suspicious or were concerned about what our role would be and how they would work with us, but over the years we’ve managed to forge really good relationships with the clinical team ….
EH3, internal interview
External stakeholder characteristics and behaviours were described as influencing hub implementation. For example, staff from different organisations who were willing to work together to resolve issues, and open to learning about ways to do things better (e.g. by improving the appropriateness of referral pathways), were said to be crucial in making progress. Motivation and an interest in women’s health were also acknowledged as key.
… they need to want to do it, you know, the nurse, the doctor needs to be interested enough in sexual health to want to be a sexual health specialist, there are so many calls from doctors to be specialists in other things ….
EH1, external interview
Funding and commissioning for Women’s Health Hubs
A range of costs were associated with setting up and implementing hubs, and sites reported that considerable work was needed to identify and access funding in their areas. Although sites had been able to access funds for some activities, there were often constraints around how funding could be used, and additional funds for increased activity could be difficult to access. Commissioning challenges were prolific, and participants across all exemplar sites described funding as a barrier to WHHs to varying degrees and described pressures on funding, with reduced spending in areas such as public health, and resources not matching increasing demand in other areas (Box 15).
Key messages regarding funding and commissioning:
-
Funding and commissioning barriers were reported frequently.
-
Innovative and motivated leaders and workarounds to overcome commissioning barriers were common across exemplar sites. There were concerns that all health systems may not have the capacity for similar leadership and creativity, which may impact on equity of scale-up, spread and sustainability of WHHs.
-
Teams implementing hubs have benefited from support from commissioners and ICBs.
-
A number of examples of ICB involvement and support were provided; yet, overall, interviewees expressed a desire for increased ICB involvement.
Public Health has had such phenomenal cuts and the NHS has had budget increases that are not even kept in line with inflation and/or growth. The whole sector has been in a prolonged period of efficiency savings, cuts, whatever you want, however you want to describe it ….
Regional interview
Lack of new funding or cuts and the wider climate of austerity were identified as hindering delivery across hub sites. Impacts of funding constraints included reductions in the range of services offered, reduced training offered to external staff, less community engagement, threats to financial viability, gaps in staffing (e.g. for planning and coordination of implementation) and less opportunity to grow the service (e.g. increasing the volume of clinics and venues). In interviews conducted before the announcement of national funding to support hub development,22 a few interviewees noted that funding would be needed for nation-wide WHH roll-out and provided examples of how the funds could be spent.
If [the strategy] came with some money, that would enable me to be able to get that £30 uplift for the coil fitting that’s going to make it doable, that would then start the process rolling.
Regional interview
Examples were shared across sites of motivated leaders utilising existing resources and being innovative in the absence of dedicated funding. However, it was suggested that it is unlikely that everyone will have the motivation or resources to do this.
Some people haven’t got the capacity, and I think that’s going to be a big player, big factor, as to whether people have got the time to really devote to it to get it properly sorted.
EH2, internal interview
Fragmented commissioning
Siloed commissioning presented a challenge to providing LARC services for both gynaecology and contraception reasons, and to moving funding and activity into the community from secondary care. A stakeholder currently developing a hub reflected on the difficulties linked to where funding was allocated in the health and social care system.
Because one of the problems we’ve got is our local secondary care provider has got a block contract. So they’re not working on tariffs, so we can’t suck money out on a tariff basis. We’re going to have to argue waiting lists and access and desirability and Government vision strategy, and wouldn’t it be nice to be able to offer this ….
Regional interview
A key aim of WHHs is to address this fragmentation, a theme which appeared repeatedly in the data. Within most exemplar sites, fragmented commissioning was both a driver (i.e. a motivator of change) and barrier, for instance, by preventing some of the exemplar sites from providing comprehensive contraception and gynaecology services together.
Interviewees described a willingness and motivation to address commissioning challenges and develop solutions. They described working collaboratively with local stakeholders to develop appropriate and flexible commissioning and funding arrangements. This involved discussing risks and costs, and how best to utilise local partnerships and agreements. For example, some interviewees described collaborative commissioning arrangements between local authorities and CCGs to share costs (e.g. for the provision and fitting of coils) so that commissioning structures do not restrict whether a woman can have a coil fitted based on the reason this is needed (i.e. contraception or gynaecological reasons).
Where formal commissioning arrangements had not been implemented, a range of creative workarounds were described to overcome problems faced by staff working in WHHs or surrounding services. For example, some hubs provide the care that a woman requires even if they are not paid to do it.
Workarounds are examples of innovation and problem-solving to manage challenges in the commissioning of services. However, concerns were raised around the impact of workarounds on the standardisation, scale-up and spread of WHHs. For example, an interviewee described how WHH services were being provided by drawing on capacity and funding for extended-hours appointments (i.e. appointments outside 9 a.m. to 5 p.m.). However, it was acknowledged that not everyone would want or be able to use their enhanced access hours in this way.
… some PCNs just wouldn’t want to do a Women’s Health Hub in their extended hours because they might want to do something else in their extended hours or they might want to just do general GP work in that extended hours. – I don’t think it’s a long-term solution – it’s an innovative solution but not necessarily like a long-term sustainable ….
EH2, internal interview
Engagement and support from commissioners
Commissioners worked with hubs to make the case for and support the implementation of hubs, for example by modelling the financial viability of plans, developing business cases and setting priorities. Having a dedicated commissioner with time, capacity, enthusiasm for and understanding of women’s health was a facilitator to hub set-up in some sites. It was noted that many health systems may not have this kind of support available. Engaging commissioners with evidence about the costs and benefits of WHHs was mentioned as a facilitator to obtaining funding. Gathering and sharing evidence with commissioners had supported hub initiation, continuation and expansion and had been used to reassure partner organisations about the impact on their services.
… this [WHH] is a really important exciting development that we’re very keen to understand quickly what this means [via results of the pilot evaluation] so that we can then write that into our strategy and then within probably the next year look to change what we’re going to be commissioning ….
EH1, external interview
Clinical Commissioning Group/Integrated Care Board and primary care network engagement and support
Clinical Commissioning Groups/ICBs, PCNs (and to a lesser extent, GP federations) were mentioned as key stakeholders required for hubs to work well. A number of examples were provided of how CCG involvement had facilitated hub implementation in some sites. This includes collaboration and engagement with CCGs to identify funding and facilities and most often to overcome IT challenges. In one site, a commissioner described support from CCG IT staff to enable data-sharing across organisations, and to create guidance for other organisations, which was crucial to hub set-up. In another site, CCGs provided support with ‘tricky’ negotiations around contracts and agreements between primary and secondary care, drawing on the expertise and knowledge from CCG colleagues. Collaboration appeared to work well when a CCG was involved and supportive in designing and setting up the hub while providing hub leaders with sufficient flexibility and freedom to design care using their knowledge of the needs of local women.
And really, they [the CCG] gave us a very broad brief and a lot of freedom to develop it [the WHH] in the way that we wanted to. And they basically said do as much as you possibly can within the confines of your expertise. So really it was down to us to define what we thought would be helpful and what would help women’s health services in the community ….
EH3, internal interview
Participants reported some challenges following the launch of ICBs in 2022, including their early status, tensions or difficulties in partnership working, competing priorities across health and social care and varying population needs in different parts of place-based partnerships. The move to ICBs was described as creating uncertainty and additional work to sustain stakeholder engagement.
Everybody in the ICB is new to their role … everybody in the hospital is new because the clinical directors change every couple of years and the specialty managers and associate directors change every couple of years … they’ve got to be physically brought on board with the journey, with the concept, with the relationships, with the way it works from a funding perspective.
EH3, internal interview
Overall, interviewees described a need for more ICB input: for instance, by helping navigate commissioning barriers and by providing a population health perspective over a larger area. It was suggested that there should be a designated women’s health lead in each ICB (separate from maternity), to take ownership and accountability and champion WHHs, as well as share learning and demonstrate impact.
Resources
A range of resources were seen as essential in setting up, running and improving WHHs. These include clinical and administrative spaces, equipment and IT infrastructure and systems. Identifying resources created organisational and logistical challenges and involved considerable work, which was described as time-consuming, including arranging meetings, acquiring space, booking rooms, ordering equipment and communicating with administrators (Box 16). A practice manager commented on the need for strong infrastructure to support hub implementation.
-
Securing required resources for WHHs can be challenging, including identifying clinical and administrative spaces, equipment, and IT infrastructure and systems.
-
The potential barriers due to IT system incompatibilities across primary, secondary and community sectors are key, and careful early planning may reduce the impact of this on the implementation process.
-
Eliciting the support of experts working to improve digital infrastructure across health systems may facilitate hub set-up and solutions to IT barriers.
If you try and deliver that service on a faulty or on a fragile infrastructure, you know what’s going to happen. It is going to fail. Now with the best will in the world, even if you’ve got the most committed people, if you don’t give them the tools to do the job, they will do their best but that will not be good enough.
EH1, external interview
Clinical and administrative spaces
Although WHHs are not necessarily a physical space, clinic space is required. Across several sites, identifying clinic space, waiting areas and administrative offices was a challenge. This limited service capacity and expansion. In one site, this resulted in the closure of a rural hub venue and reduced service provision across the area. A lack of space also meant one site could not run concurrent clinics, limiting opportunities for shared learning between staff working in the hub, and training and shadowing of hub staff. Interviewees noted the importance of ICS support to navigate this issue.
Equipment
As WHHs are providing intermediate-level services, participants described requiring investment in specialist equipment. In one site, staff implementing hubs in GP practices described challenges in sourcing a gynaecology couch and suitable lighting. Delayed delivery of a bed had prevented a clinic opening as planned. A range of costs were associated with the ongoing operation and enhancement of WHHs: for example, ongoing provision and easy access to laboratory services, treatment and equipment costs.
IT infrastructure and systems
IT issues were a common barrier in relation to both initiation and ongoing operation of WHHs and substantial challenges in setting up and/or using IT systems were described across most exemplar sites. This was particularly related to the lack of interoperability between different IT systems within the NHS (e.g. between GPs within a PCN and between PCNs), and across primary, community and secondary care. This was described as the ‘biggest challenge’ (EH2, internal interview) and a ‘a massive, massive, tricky, tricky area’ (EH2, internal interview). This impacted on the management of hubs, patient data and the alignment of referral pathways across organisations. For example, in one site, a consultant running a clinic in a GP practice brought her hospital laptop to clinics due to frustrations with the primary care IT systems. However, she could not connect to the GP practice Wi-Fi and was unable to print sample forms without going back to the hospital.
System incompatibility was a particular issue in PCN-level interpractice referral models, where it was challenging to prescribe electronically, book appointments, order and process tests (e.g. difficulties with access to cervical cytology and microbiology laboratory systems) and claim costs for equipment or testing. The lack of statutory status for PCNs meant that prescriptions had to be requested and claims processed via the patient’s own GP practice systems. Receptionists in GP practices hosting hub clinics could not access the clinic booking lists to manage women arriving on the day. Hub staff had worked extensively to develop successful workarounds, but they were described as time-consuming and inefficient, taking up valuable time for women and staff. They may also present risk, for instance, by increasing the likelihood of error where information must be manually transferred between systems.
It was reported that the impact of system incompatibility could be addressed to some extent by local agreements, ensuring compliance with data-protection legislation. Substantial work to develop a common shared record at PCN level made set-up easier at one site, and there was better interoperability which was widely welcomed, but challenges still remained, for example in referrals between PCNs.
… there were so many different obstacles to unravel and I think that this is where the PCN model has really, really, really helped move this forward, because one of the major obstacles was IT, but the PCN model enabled that cross refer-[ral], patients to be able to be seen, into practice, as it were, so they solved a lot of the IT issues.
EH2, external interview
Workforce
Human resources, specifically, strong leadership and a clinical and administrative hub team were described as key. In this section, we explore accounts of workforce requirements and the main challenges to obtaining and retaining a hub with adequate capacity and the right skills (Box 17).
-
Strong leadership and a team with adequate capacity and skills were a key requirement in hub sites we explored, and a need for funding to support staffing was highlighted.
-
A number of challenges to obtaining and retaining adequate staff to implement and run hubs were described, including national staffing issues, costly qualifications and limited time for training.
-
NHS schemes for new roles and ways of funding extended-hours services may improve issues around staffing.
Leadership: characteristics and commitments
Strong leadership was identified as critical in the implementation and success of WHHs, with examples shown of knowledgeable, passionate and motivated clinicians and commissioners with a positive attitude to innovation and service integration. Leaders demonstrated advanced clinical, leadership and management expertise, local service and workforce knowledge (e.g. referring patterns, training needs), and an ability to engage effectively with decision-makers and wider stakeholders.
Women’s Health Hub leaders often performed this role with limited or no financial reimbursement, in addition to existing roles and responsibilities. It was highlighted that many areas may not have sufficient leadership capacity to implement a hub. The reliance on passionate and motivated leadership was described as potentially creating issues in terms of financial viability, resilience and sustainability of hubs, with issues arising when leaders move on (e.g. retirement) or take long-term leave (e.g. maternity or sickness).
If anything happens to [hub lead], or if [hub lead] changes her mind about it or decides to do something else, then I think the service would collapse, because I’ve got too many other things … I’m not in a position where I could take over running the service in the same ways that she does, and she has lots of skills.
EH3, internal interview
It was suggested that clinical leaders require support and that collaboration with regional and national ‘key players’ or ‘champions’ can play a key role. By connecting with and building on the work already under way across England, leaders can be supported to advocate for women and mobilise and drive forward the agenda of WHHs via a shared understanding of the need and value of hubs.
The hub team: strong, diverse and with sufficient capacity
Strong, diverse teams with adequate capacity were perceived as supporting the implementation of WHHs. While committed and experienced GPs with a special interest, sexual and reproductive health consultants and GPs were central to many WHH models, building a MDT (including administrators, specialty doctors, nurses and healthcare assistants) drawn from different organisations and sectors, and at different stages of their career, was described as supporting service resilience and sustainability. In one area, success in increasing workforce capacity was described as the reason why a PCN-based hub had ‘charged ahead’ and was offering a service to out-of-area women, where neighbouring hubs had struggled to expand in this way (EH2, external interview).
And you can run a fantastic service for women if you’ve got the right staff mix. And your staff will be happy, they’ll be well supervised, they’ll be working efficiently. But if you just try and bodge it together, with two or three people, in some little professional cul-de-sac, and to try and turn that around is a real challenge ….
Regional interview
However, access to an adequate pool of staff was experienced as a barrier by all sites at various points and extents, impacting the number of clinics that could be delivered. Participants also highlighted the importance of identifying implementation leaders and teams, alongside the clinical and administrative team delivering clinical care. A national interviewee commented that the role of most staff working in women’s health services is to deliver care, stating that primary care is overwhelmed, and it is too much to ask them to implement WHHs without additional dedicated roles to support this.
Challenges in recruiting and maintaining a strong team
A number of challenges to obtaining a strong and diverse team were discussed. These include a national shortage of trained staff, high staff turnover and limitations in access and feasibility of training for women’s health.
National workforce challenges
Several participants commented on workforce issues with shortages of and difficulties recruiting skilled, interested or experienced staff. This was reported as impacting implementation and scale-up of WHHs in an already stretched system by increasing hub leaders’ workloads, decreasing the breadth of services offered and the number of women seen, and limiting the growth and expansion of hubs.
I mean, we’ve got a workforce problem in primary care and I think that is going to be the thing that stops us developing services that are widely commissioned because we don’t have sufficient staff …. We’re aware that all it takes is a nurse to go on maternity leave or a nurse to go on sick and you simply can’t find a replacement, so you have no service, you have no nurse for two weeks, if you’re running a service and you don’t have anybody to do your smears and your wound dressings and so on for two weeks, that’s a serious problem.
EH1, external interview
Interviewees explained that in order for hubs to be adequately staffed, people need to be hired into or re-directed into the hub from other services, with a finite pool of available staff. For instance, a newly trained GP may be expected to run a clinic in a different practice. This was described as a deterrent to some commissioners and GP managers approached by hubs as they felt they could not afford to release clinicians away from providing general medical services. This also raised questions regarding how to back-fill GP time spent working in hubs, unless GPs were doing this at times outside their existing commitments. There were also fears that GPs may prefer to work in women’s health, and choose to reduce their general primary care commitments in order to work in a hub, further hollowing out the GP workforce. In addition, high staff turnover in local services, including among administrators, was described as creating uncertainty, and additional work, for example by requiring constant re-introductions to the hub team, ways of working, services and referral pathways.
Access to and feasibility of training for women’s health in Women’s Health Hubs
Having accredited qualifications was suggested to be useful in supporting the credibility of clinicians working in hubs and to support in any litigation claims. Training to ensure and maintain a throughput of skilled staff was important for resilience and a ‘continued supply of trained individuals’ (Scoping interview), reducing reliance on a small number of individuals. This was viewed as particularly important for sustainability, as models tend to have been set up or facilitated by passionate individuals, who invested personal time and resource into hubs, which may not be possible elsewhere.
So, the gynae service in [place], it works because [name] has been absolutely dedicated and gone above and beyond what normally healthcare professionals and GPs do in terms of setting up and keeping the gynae service going. So, that’s all, that’s due to her and, to a certain extent, [name] as well, but that [name] has always been the driving force.
EH3, internal interview
However, challenges in training and education reduced opportunities for staff within hubs and staff in surrounding services to expand their knowledge and expertise. This was identified as a potential barrier to the recruitment of hub staff. Interviewees identified the issues of a lack of funding and high cost of qualifications as a barrier. Interviewees reported that primary care pressures limit GPs’ availability to attend training across the board, not just in relation to women’s health, which may also create a potential barrier to training hub staff based in primary care. Contractual issues can also be present, with one site noting honorary contracts used to be needed for external sexual health staff to offer training to hub staff. This issue was overcome by having a service-level agreement with PCNs so individual contacts are not needed.
Local history and context
A final challenge reported by participants was the local history and culture of a service, which can make changes in skill mix difficult. For instance, what is ‘inherited’ can hinder change.
Our workforce is quite patchy because it’s what was inherited. And if you inherit a nurse-run service, and you say well actually we would like to have a different staffing set-up, in that place, you can’t have it, because it’s almost impossible to argue for it because the argument will come back ‘We’ve never had a consultant there. Why do you need one?’
Regional interview
Addressing staffing issues
Wider funding opportunities were suggested as a solution to staffing issues, such as the NHS’s Additional Roles for Reimbursement Scheme (ARRS), which provides additional NHS funding for new roles to support multidisciplinary working across PCNs. This scheme had been used to reimburse PCN-level staffing in support administration and clinical care in one of our exemplar sites. The ARRS roles could also be used for task-shifting and upskilling other health professionals such as physician associates to undertake procedures such as coil fitting, but this was still evolving in practice, with some participants raising concerns that the safety and feasibility of these changes needed to be explored. Primary care Extended Hours and Enhanced Access schemes were also suggested as an approach to resourcing out-of-hours clinics, but examples of this in practice had not been identified. Additional suggestions to improve staffing issues were more general (e.g. treating staff well, collegiate team working, good management and supervision and providing opportunities for networking). It was also suggested that WHHs may improve staff retention by offering new roles, opportunities for professional development and diversification of clinicians’ portfolios, at a time when many staff were struggling with low morale, and many were considering leaving.
Examples were provided of ways in which WHHs may support staff retention to women’s health services. Overall, staff working hubs were positive about their experiences and some expressed pride in what they had achieved and an enjoyment of working with others with a shared goal and passion for women’s health. Some hubs were able to offer women longer appointments than they would receive in other services, which was described as having a positive impact on some staff on satisfaction. One site gathered data that suggested their hub employees had positive outcomes in happiness and job satisfaction and associated this with higher levels of retention. In two sites, examples were provided of hubs providing training opportunities and allocating protected time for staff to achieve their qualifications. In another site, a GP undertaking additional training in the hub said if it was not for the hub and the supervision from the hub lead, she would not have been able to embark on further training for women’s health.
I’m doing a postgraduate diploma for GPs … practitioners with a special interest in gynaecology and she’s kindly been my mentor. And I wouldn’t have had the opportunity to even do the diploma let alone have her as my mentor if I hadn’t been part of this clinic but obviously that comes with a bit of paperwork as well.
EH3, internal interview
Advice for others
Throughout interviews, participants shared potential lessons for others who may wish to build their own.
Advice offered by several stakeholders was to learn from elsewhere, through engagement and learning with teams leading WHHs in other areas of the country. There was acknowledgement that local areas and needs differ and so it was necessary to take this information and identify how to make it work locally.
So yes, my advice to anybody wanting to set it up would be go and speak to somebody who’s doing it, who’s doing it very well, who’s had it recognised nationally that they’re doing it very well.
EH4, internal interview
There was also recognition of the wider resources that could be drawn on, including toolkits from the Primary Care Women’s Health Forum and a pharmaceutical company, which could help others to develop models.
… the work at the Primary Care Women’s Health Forum is a real support to GPs out there across the country … a nice little area for resources, a go to for people in other areas who want to get something going but they just don’t know how to start.
EH2, internal interview
The role of the Primary Care Women’s Forum in bringing people together and providing support for those wanting to move forward with hubs was also mentioned by a small number of stakeholders.
I think from a concept to delivery point of view, there’s a lot that needs to be done in terms of being able to engage with commissioners with the appropriate information and a lot of the work with Primary Care Women’s Health Forum is around supporting people how you put a business case forward outlining those summary points.
Scoping interview
Piloting a service was suggested as a useful strategy before any potential wider roll-out for proof of concept, acceptability and financial viability.
I think my message would be, it takes a lot of hard early work to get that moving, and …. But it can be quite easily done. Map out the clinical directors across your PCNs. Target where you want to be. Maybe pilot one, go for it, and then start to roll it out. Get your fees right. If the IT lined up ….
EH2, internal interview
Hubs could build on the work that other areas have already begun, rather than start from scratch, and utilise their resources, highlighting that WHHs do not need to be a brand-new building or service. A small number of interviewees advised to map and draw on the resources and workforce that already exist when developing WHHs and, for example, design a hub service around the skills of clinicians involved.
And then ultimately you’d have to sort of design a service around the people that you have, or at least the people that you think you can get!
EH3, internal interview
More widely, the importance of considering infrastructure and resource at the outset was emphasised: for example, ensuring physical space and equipment, such as gynaecology couches, are in place and that there is creativity in how resources are used. IT challenges were reported across most sites and so trying to get functioning systems in place early on to support hub delivery was something else for other potential sites to consider.
If you want a truly integrated service … they need to have access to our IT. But there are various GDPR barriers to overcome. You need a special portal. So again, that’s a wider service consideration before you create a hub. What infrastructure do you need to deliver it.
EH3, external interview
The IT perspective, I think the learn bit would be to try and engage the …. Whoever’s got the contracts, I’m guessing it’s the ICB …. For us it’s informatics [name of place], with …. If you get them on it as early as possible, to look at the possible functionalities and how to get round stuff, that’s worth its weight in gold.
EH2, internal interview
Some highlighted how having managerial expertise and administrative and project management support in place was necessary to overcome challenges to setting up a hub.
You have to have somebody, or more than one person, to come and work within the team and, indeed, have a leadership or management role …. They have to work within it, and to have worked in it, they have to have had a certain amount of experience and qualification in order to start, and that all takes time.
EH3, internal interview
The pre-existence or development of relationships with relevant stakeholders, including those with decision-making powers, was another important consideration when building a WHH model. Building effective relationships and collaborating with partners were highlighted as important to success.
But I think if I was giving somebody advice on how to reproduce it, ideally you’d have a good working relationship already with the trust.
EH3, internal interview
Identifying someone to take the lead for an area or PCN was advised by a small number of interviewees, who could, for example, lead on discussions around logistics and drive work forward.
Nominating hub ‘champions’ was also suggested as something to consider. This could include professionals, for example local GPs or PCN leads to champion the service, or women who have received care through the hub. Securing support from local stakeholders, raising awareness, getting people engaged, and cultivating a passion for the hub were all suggested by interviewees.
Let them see your passion. Let them share your passion and support you. Go to your ICB and get patient champions.
EH4, internal interview
Other advice included:
-
Ensuring hub leaders are given time to focus on hub set up and development.
-
Collecting appropriate data and being clear about the goals of a hub.
-
Working with others and involving everyone (e.g. primary and secondary care, public health, women) in discussions, including around commissioning.
-
Choosing what is most important to focus on and doing things slowly.
-
Starting with core women’s health services and building upon these (which may be contraception, or gynaecology care depending on local resources and expertise of staff implementing a hub).
What has been achieved, and how performance is measured
While it was beyond scope for the evaluation to collect and analyse primary data to determine the success of WHHs across England, we have identified early insights into hub success through analysis of reports of aggregated data from hub leaders and accounts of performance from the survey, interviews and documents (presentations and performance and monitoring reports). The overarching achievement described by participants across the country was the successful set-up of local hub models, often with limited or no additional funding, and alongside service pressures, and more recently the COVID-19 pandemic.
What is measured, and what has been achieved
Through the survey, fieldwork and documentary analysis the evaluation team identified summary statistics from sites across the country (not restricted to in-depth evaluation sites), usually in the form of frequency data. These data evidenced how hubs were providing access and care for hundreds of women in their local health systems. Variation in measures and numerators and unknown denominators in the minimal available data prevent meaningful comparison and evaluation of the relative benefits of different models, so this is not presented in this report. Accurate and consistent reporting will be important to enable in-depth evaluation and understanding of relative performance and costs of models in future. However, some selected meaningful summary statistics were available, in particular:
-
Onward referral rates to secondary care gynaecology ranged from 5% to 14% (Birmingham, Guildford and Waverley, Manchester), highlighting achievements in treating women in hubs the community and reducing gynaecology waiting lists. Variations may reflect differences in the women accessing services in these areas, or in the services offered.
-
Triage times and waiting times varied but were short (Birmingham, Guildford and Waverley, Leicester), with triage within days and appointments within a few weeks or less, evidencing how models are improving access in a context where gynaecology waiting lists are high.
-
One site (Hackney) reported a 14% reduction in secondary care gynaecology referrals by local PCN GPs following hub implementation, which may indicate a shift in referral patterns towards the hub, and/or increasing routine management of women’s health issues in primary care without onward referral, due to increased knowledge and confidence in local GPs.
-
One site (Liverpool) reported an 8.5% increase in LARC fitting rates in the local population following hub implementation, evidencing a real population-level impact on local women in a context where access to LARCs was a key local challenge.
While current measures prevented meaningful comparison, through interviews and documentary analysis we identified diverse performance measures for WHHs, reflecting the locally driven design and implementation of these models. Appendix 3 lists a comprehensive and detailed summary of both current and potential measures identified through the evaluation. This has been consolidated in Table 22, which summarises the key measures that could be used to evaluate hub performance consistently, guided by evaluation participants’ priorities, and with the expert opinion of the evaluation team.
| Potential hub performance measures |
|---|
Inputs/resources
|
Activities/processes
|
Outcomes
|
Many sites reported high levels of satisfaction among women who used their services in local measurement exercises, aligning with the accounts of women we interviewed (see Chapter 5 for further detail). There were also accounts of high levels of satisfaction among staff working in WHHs, and possible links to staff retention (as discussed in the workforce findings).
Considerations for measurement and comparison of Women’s Health Hub achievements
Timing: Often hub models were new and emerging, and while local data can provide insights into what has been achieved, participants highlighted that longer-term measurement is required to measure activity, outcomes and impact in a meaningful way.
We need to have a look at that when it’s been running for a much longer time and look at the impact it’s had on the existing [services].
EH1, internal interview
Purpose/vision and local context: Most measures adopted varied according to the aims, model and services offered by the hub, which was informed by local service and population needs, and therefore were not consistent across all models and populations. Some participants with a broad view of WHHs suggested that general health outcomes, for example cardiovascular disease rates or smoking cessation, could be included, though the models we identified focused on reproductive health outcomes and were not addressing these outcomes directly at the current time.
Population/service boundaries, and proportion versus frequency: Currently hub performance is predominantly reported in the form of frequency data, and at hub level, for example referrals received per month, number of LARCs fitted in the hub. While this is a good indicator of activity and processes, it does not illustrate the population-level impact. Hubs may have different footprints/catchment areas, including PCNs and local authority areas. Measuring outcomes at population rather than service level and reporting rates is important to measure health impact and costs in the system and to enable comparison between different areas, populations and models. System-wide rather than organisation-specific performance indicators can also encourage different stakeholders to collaborate to achieve common goals.
Comparing hubs: While there is overlap in some measures used by hubs, these have been locally developed, and there are no shared standard indicators used for reporting. Some measures are consistent, for example referrals, DNAs. The information shared by participants and in documents for this evaluation was insufficient to enable meaningful direct comparison of different hubs and models.
Benchmarking and targets: While some hubs have targets in place, others do not, and it is not clear what an appropriate target would be. Where targets exist, they are not consistent between hubs.
We haven’t done anything formal. Honestly it’s all how many numbers can we get, how many women can we actually get an implant or a coil in, how many can we get covered really. But, yeah, so one of the … managers was actually saying maybe we should have a target each year and I’m like what?! But, yeah, we will.
EH2, internal interview
Comparing sites within a hub: Within some hub models, it may be relevant to compare between sites, for example compare referral rates between GP practices, or compare uptake/activity between different hub locations/clinics or other services offering the same procedures, such as reasons for referral or LARCs fitted at different locations including sexual health clinics. Some hubs are doing this currently.
Trends: For all measures, measuring trend can identify improving/declining uptake and performance. In the evaluation, we identified hubs monitoring trends in different outcomes over time by month, quarter and year, but this would need to be consistent for comparison.
Transfer or increase in activity: For some measures, it may be possible to monitor whether the hub is moving existing activity from primary or secondary care or delivering additional capacity and activity. For example, comparing numbers and rates of LARC fitting in GP practices, in hubs, in SRH and in secondary care gynae. While LARC prescribing in primary care and SRH can be compared using prescribing data, the way in which LARCs are prescribed for use in hubs varies, and this may be more challenging. We did not identify evidence of hubs routinely measuring this, but it will be important to assess value for money and impact on other services in the health system.
Long-term impact measurement: There are many ‘downstream’ impacts of hubs across the life course. For example, there are health, social and economic benefits for women, families and wider society in avoiding unplanned pregnancy, or addressing debilitating menstrual bleeding and pain. We have not identified any evidence of longer-term impact measurement for hub models currently in place.
Measuring costs: Assessing the costs and benefits of WHHs is challenging in such a mixed landscape with different models, in different populations, and with limited availability of data to interrogate economic costs and benefits in a meaningful way. Some hub leaders have reported that their models are cost-effective or cost-saving, but there needs to be further exploration of what this means in this context, given the variety of hub models and services developed. For example, the scope of these existing analyses might be limited to focus on whether the costs associated with WHH service provision are within the limits of the funding available locally, or generate income for the particular GP practice or network. There are potentially a range of cost savings associated with shifting care from secondary care to the community setting. There might also be efficiencies associated with appropriate services being delivered by a multidisciplinary workforce, for example utilising the skills of nursing assistants or advanced nurse practitioners, alongside GPs with special interests. There are also a wide range of benefits that hubs could deliver, through improved health outcomes by providing more ‘joined-up’ care, for example reduced unplanned pregnancy, earlier cancer detection. There are a wide range of scenarios whereby hub models may reduce costs in the health system, but assumptions require further modelling and testing, particularly over the longer term. There is also a range of potential unintended consequences which may impact on any costs, for example, there may be unintended duplication of services within the local healthcare system, particularly in the early stages. A number of potentially ‘hidden’ costs were identified in our evaluation, including the time and skills invested by hub leaders, particularly in setting up the hubs, and in relation to the inefficiencies created by needing to adopt ‘workarounds’ to deal with the challenges associated with fragmented commissioning arrangements.
Unintended consequences: With any complex service intervention, it is important to consider unintended consequences elsewhere in the health system, which can be measured as the approach is scaled up. Our participants highlighted a number of areas where this may occur. For example, there is a risk of widening inequalities if the new hub service is easier to access for already advantaged women (measurement of inequalities is discussed further in the following section). An important concern for some was the risk of deskilling primary care staff or destabilising GP practices due to care moving from primary care to the hub, although many of our participants were keen to stress that models were intended to strengthen and complement primary care. A related worry for some interviewees was that GPs receiving additional training in women’s health may leave general practice to work in hubs or the private sector, depleting an already stretched workforce, with at least one account of this occurring. It is also possible that WHHs will increase costs to the system, and this requires careful evaluation. Increased costs could result from a more expensive model, by unlocking unmet need and increasing volumes of care delivered or by duplicating existing provision in other services.
Challenges in measurement: In addition to the challenges described above, the work of collecting data and measuring activity and outcomes required staff capacity and expertise. In one site, an expert from the pharmaceutical industry provided implementation support which included designing a template for the GP record to enable hub leaders to extract data from systems more easily. Some hubs had specific individuals whose role it was to assemble and report data. Further challenges described included knowing what to collect, difficulty interpreting data, and the fact that primary care does not routinely report women’s health activity in a way that could be easily compared. It was also suggested that some of the more measurable outcomes at system level were downstream, for example prevention of termination of pregnancy, meaning it would be more difficult to demonstrate a causal link with hub activity.
Women’s Health Hubs’ impact on inequalities and unmet need
While interview participants described an objective to address socioeconomic and demographic inequalities, the key issues were predominantly described as geographical (i.e. a ‘postcode lottery’ of local GP women’s health expertise), clinical (e.g. poor access to menopause care due to increased demand), or due to commissioning/service boundaries (e.g. women who need LARC for contraception can access it rapidly via SRH but women who need it for gynaecological reasons may wait for more than a year for secondary care appointments).
The approach to tackling inequalities
A range of approaches were described by hub leaders to address local inequalities:
-
Providing clinics in areas of greatest need/deprivation, for example rural areas.
-
Providing materials and outreach for specific communities.
-
Mapping inequalities, monitoring uptake of hub services in different groups/areas and planning to address gaps, for example in trained LARC fitters.
-
Providing choice of telephone and video consultations to enable women with commitments to attend.
-
Providing phone access in addition to online, though some services are only providing digital.
-
Working with third-sector organisations, patient engagement events.
-
Engagement focused on specific groups.
-
Ensuring that clinic locations have adequate transport links.
-
Providing out-of-hours access.
-
Providing GP education focused on needs of underserved groups.
Participants also suggested strategies not yet in place, including using a mobile WHH bus to visit different areas, self-referral to minimise barriers to booking and colocating the hub with other services used by women, for example children’s health services.
In terms of health inequalities, I suppose by being an open access clinic it means you’re removing the barriers to care of going via the GP who they have also referral who then does it for somebody else and signpost and that can be quite disruptive to ladies, especially busy ladies so I suppose one of the things is direct access because that’s one phone call, one referral form, that would certainly mean that you would contact instead of putting off that and especially because the GP lines are so busy with all the other problems, so I think that would probably decrease your health inequalities.
EH4, internal interview
Potential challenges in tackling inequalities through WHHs were also identified, including the stigma and taboo surrounding women’s health issues for some communities, and awareness and access issues. Overall, out-of-hours provision was rare. Where there were few venues, it was suggested that they may be difficult for some women to reach. Women with more complex lives and fewer resources may be particularly affected, and there were concerns that demand for services was so high that it would be more disadvantaged women who struggled to gain access.
We cannot create the capacity to meet the demand and it is always, when things like that happen, it’s the ones who aren’t articulate or intelligent or – not intelligent, that’s the wrong word, but who lead, some people lead a chaotic lifestyle. Some people have young kids. Some people who aren’t able to, they can’t speak the language, they aren’t able to navigate the system are the ones who get left out and that’s a big, big concern for us. And it isn’t because we are not trying, because we are.
EH4, internal interview
Participants also highlighted the importance of women knowing about the service and that their problems could be addressed:
I mean, people put up with stuff for years and years and you just think if they don’t know about it or it’s not promoted then how are they going to know what the treatment is to get better.
EH4, internal interview
What is measured?
Systematic measurement of the impact on inequalities was still emerging in the sites we explored. Information on outcomes gathered through this evaluation and accounts from local leaders indicate that further work is needed to understand how hubs address inequalities quantitatively. Currently local performance measurement tends to focus on activity. Uptake and impact of hub services for different population groups, for example minorities or socially excluded women, are not routinely assessed. There was one account of comparing demographics of women accessing the hub with the local population and discussing with commissioners and working with communities to address gaps, but more recently funding pressures made this more challenging.
Hub leaders stated that they were committed to addressing inequalities, and it is often a specific aim of the models, and this is reflected in approaches which provide services in underserved or deprived geographical areas, though it is not clear what proportion of women accessing the services are in the target groups (e.g. affluent women may travel to access hub services located in a low-income area).
What could be measured to understand hub impacts on inequalities?
Comparison of general measures of uptake, activity and outcomes by different groups of women, and how this compares with the general local population served, will be key to understanding inequalities impacts and unmet needs. It is likely that patterns of use of different services in the local health system may vary between groups, so measuring access and outcomes for different services in the local health system beyond the hub is important. Measures that could be used to explore inequalities may vary according to local population needs and system priorities, but could include:
-
Deprivation (e.g. Index of Multiple Deprivation decile of woman’s postcode)
-
Ethnicity
-
English-language needs
-
Age
-
Specific socially excluded groups (e.g. homeless women, asylum-seeking women)
-
Diagnosis (e.g. women with specific issues such as endometriosis)
-
Disability.
Comparing Women’s Health Hub success in addressing inequalities
Comparing hub models’ achievements in this area will be challenging, due to the variation in local populations, needs and service landscape. Success in access/outcomes for key demographic groups can be compared between hubs, for example measuring LARC access by demographic group. However, it will also be important to understand how hubs are meeting the needs of their specific local population, what the local priorities are and how they have tailored their local provision, to avoid inappropriate comparisons of performance on inequalities. Where hubs have similar models and populations, this will allow for appropriate comparisons and benchmarking. Where hubs have particular priorities internal comparisons of trends may be more appropriate, for example how referral rates to the hub for women from deprived postcode areas change over time. Here a local leader describes the need for local tailoring and for population intelligence.
You can learn from other models, that’s great, but the key thing is very much tailor the needs of your local population and fully understanding what women need locally … there’s so many variations that you just can’t, you know, treat things [the same] because they’re different women, they’re different demographics that you will find that they tend to approach services differently, access services differently.
EH1, internal interview
Women’s Health Hubs’ impact on system-level inequalities
Some participants highlighted the challenges in tackling inequalities where the hub was not accessible to all women in the local area.
I think the big inequalities for that service is that it’s just one part of [name of place] … how do we level up, because we definitely, I wouldn’t want to see anything levelled down, but then how will everyone have, you know, do we – ideally you’d want a hub in every locality wouldn’t you?EH4, external interview
There was a sense among several staff that accessing WHHs could help tackle stigma around women’s health, offer women more choice and meet their needs. Hubs being based in GP practices were seen by a small number of interviewees to help ensure women can access services, due to their familiarity, location in local communities, and a more acceptable environment and reduced stigma, particularly compared with attending a sexual health clinic.
And so I think a general clinic [in a GP practice] with a safe space inside it could be a really good place, because no one’s going to bat an eyelid if someone sees them going there. But if they’re going to a dedicated STI clinic it’s got a big fat label on it.
EH2, internal interview
Accessibility of WHHs was another consideration for several, including parking and public transport requirements, and local venues to facilitate access. In one site particularly, rurality and available travel routes to the hub were considered potential barriers to access.
A few interviewees mentioned provision for those for whom English is not their first language, explaining what interpreting support was in place, though there was a sense that this could be improved.
… we use Language Line and all of that. So that side of things I think probably needs to be better but … because lots of patients have somebody helping them, either a sister, people that don’t speak the language, or a partner or whatever, but then we involve Language Line ….
EG2, internal interview
It was noted that digital access to hub services may lead to the exclusion of some, for example older women, and so offering alternative ways to access and receive services was important.
… people who are lost will be the people who cannot use computers, people who do not use English as their first language.
EH4, internal interview
The potential for hubs to exacerbate health inequalities was flagged in a small number of interviews. Reflections centred on geographical variation in provision across areas with WHHs, resulting in inequalities in access. In one site, funding cuts and reorganisation was reported to have reduced capacity to undertake inequalities-focused quality-improvement work.
And at the moment there is an element of that [postcode lottery] because it’s not up and running in all the PCNs.
EH2, external interview
It was suggested that there were challenges in accessing services via a GP referral model, and that some women would find it harder to get an appointment; therefore the difficulties in accessing primary care at the current time would need to be considered.
A small number of participants suggested that GP referral could equate to easier/universal access, for example removing the need for women to have to find the service themselves. Additional approaches to addressing inequalities were highlighted through the survey, including:
-
Engaging with particular ethnic minority communities, for example through engagement events.
-
Launching services in areas of particular high needs, for example an area of high social deprivation.
-
Services in easy-to-access locations with adequate transportation links.
-
Offering evening and weekend appointments.
-
Consideration of domestic violence at initial consultations, for example screening questions.
-
Use of interpreters.
What is next for Women’s Health Hubs?
Stakeholders expressed various hopes, suggestions and plans for the future development of WHHs, locally and nationally. Locally, these primarily focused upon expansion and improvement of existing hubs, with expansion being grouped in three main ways: in terms of geography, workforce/capacity and of services offered. Ambitions to expand the coverage of existing WHHs in local sites were articulated, for example opening new venues and improving access in parts of an area that may not be, or were less well, served currently.
We have clinics running in two PCNs. So those PCNs have five practices each, so covers quite a large population within that area. The plan is that we broaden and provide clinics right across all eight.
EH1, internal interview
Plans to increase current staffing and capacity in hubs were also described, with a number of sites sharing ideas to train or recruit new staff, increase the number of clinics or consider widening availability, for example to include weekends or evenings.
We’ve just gone to the Board yesterday to see whether we can recruit another 16-hour ANP [advanced nurse practitioner] … that’s what we’d really like, but to do more sort of a Saturday clinic, an evening clinic.
EH2, internal interview
Improving the range of services offered at WHHs was frequently mentioned. Examples of services that hubs would like to provide included: pelvic physiotherapy, pessary fitting and removal and menopause care, though there were several reflections around the balance of what to offer in a hub compared to via a ‘normal’ GP.
I think that there are a number of emergent models out there and I think before we can really decide what a Women’s Health Hub does, we need to get the primary care piece right. So we need to agree are women going to continue to go to primary care for their normal sort of treatment and be referred then to the hub for additional expertise ….
National interview
Other suggestions for improvement included, for example enhancing current IT systems, increasing local engagement and advertising of hubs, working to identify issues and impact on the local population, and clarifying or improving funding/commissioning routes.
Linked to this, looking at other access routes, for example self-referral, was also mentioned several times, though this could bring challenges around demand.
I think we would all really like there to be a self-referral element, but I don’t think that will happen straight away, just because it’s complicated and you’ve got to start somewhere otherwise you never start.
Scoping interview
Several shared aspirations for the development of hubs across the country, with hopes of scale-up and spread. A small number of views were reported around the footprint hubs should operate at, for example one stakeholder wanted to see hubs set up in every PCN in England, while others stated that PCN level might be too small a footprint and working at a GP federation, ‘place’ or ICS level could be more appropriate.
I do believe that we want to pay for a national spread, so that there is the same, no postcode lottery … I think our aspiration should be to have one in every PCN, sort of focus on women’s health, to what extent that is depends on what their needs are.
Scoping interview
Ideas of how to support plans to scale and spread the model were proposed. For example, national interviewees suggested sharing learning and best practice (which could be done via a hub network), using quality-improvement methodologies to set up hubs with plans at the outset to scale and spread, and mapping local areas to understand population need and current offer so that hubs could be developed to fill local gaps and encourage uptake.
There was also a suggestion about linking or dovetailing with other hub models, such as community diagnostic centres, to synergise and support the spread of WHHs.
I’m hoping that we can dovetail with that. Why have two centres – why have a Women’s Health Hub in a place where they’ve got really good clinical diagnostic centres because we could synergise with them.
National interview
Chapter 5 Women’s experiences and perspectives
Box 18 provides a summary of Chapter 5 of this report.
-
Across the exemplar hubs, we interviewed 32 patients who attended an appointment at a WHH and held 4 focus groups in local communities with 48 women with lower uptake of hub services (see Chapter 3 for methods).
-
Most participants were unaware of the term WHHs, and there was some lack of awareness about what they were or offered.
-
Patients reported attending hubs for a range of reasons, and across all exemplar sites, experiences were largely positive, including when care at a WHH was compared to other services.
-
Though there were a few examples where things had gone less well, for example communication about what would be involved.
-
In focus groups, some women raised concerns about whether hub services would be accessible to all, and often went to GPs for support.
-
Facilitators and barriers to uptake included awareness, waiting times and accessibility.
-
The Women’s Advisory Group also provided insights regarding hubs, including how the concept may be perceived by women in the community.
Women’s perspectives were drawn from interviews with individuals who had used hub services in each of our exemplar sites, and one focus group in each site with women from populations at risk of exclusion that local leaders reported were less likely to access services (Tables 8 and 10). Demographic data were not available in almost a third of interviews and two-thirds of focus groups, which limited assessment and interpretation of the diversity of our sample. However, available data suggested the following perspectives were represented:
-
At least a fifth of service user interviewees were from ethnic minority backgrounds; Asian and Asian British women were not represented. Focus-group participants with known ethnicity were all White British. However, focus groups were held in specific group settings where members belonged to communities at risk of exclusion, and two of these groups included participants from ethnic or religious minority communities (demographic information was not available for these 27 women, over half of all focus-group participants).
-
Most left education at or before 18.
-
A range of age groups were interviewed, though service users were younger and focus-group participants were older.
-
A fifth of interview participants reported lesbian, gay, bisexual or other sexual orientation, though only heterosexual orientation was reported in focus groups.
-
All focus-group participants who shared gender-identity information described their sex as female and other gender identities were not represented.
Hub patients’ perspectives and experiences
Awareness of Women’s Health Hubs and services
Most women interviewed who had received care in a hub were not aware of the term ‘Women’s Health Hub’, or that it was the name of the service they had attended. Interviewees referred to the services by different names, for example community gynaecology.
I had no idea these hubs existed. So, just having information out there that they are there would be great. More information about them, the sort of services you can have, and what you can even access.
EH4, patient interview
Some had not known that the service existed or was offered in a particular venue until they were referred or signposted there, or had enquired locally.
If it wasn’t for the nurse at my doctor’s surgery referring me, I wouldn’t know anything about it. Didn’t even know that [venue] … I’ve lived here for about 14 years but didn’t even know that existed.
EH1, patient interview
There was also some lack of awareness regarding who organised hubs and what services they offered. Some described only knowing that the hub offered a service particular to their need. Similarly, in the focus groups many women were unaware that WHHs existed, what or where they were or what they offered.
I think women need to know that these services are there because from this little meeting, it looks like a lot of women are not even aware that the service is there.
EH1, group interview
In one group, a woman shared an example of searching the internet for community gynaecology and menopause support, but their local hub did not appear in the results.
Accessing and receiving care at a hub
Services
Women reported attending WHHs for a range of reasons. This included LARC fittings and removals for contraceptive or gynaecological reasons, cervical smears, investigations/scans and accessing support for example with the menopause. Women were able to access hub services via different routes, including through GP referral and self-referral online or by telephone. In some instances, women had received a telephone triage call prior to an in-person appointment. In one site, an interviewee described how this covered a wide range of issues:
I did have quite an extensive consultation … they took me through a whole list of things, so going through my health history, like mental health, sexual health. They asked about what we were talking about as it being a safe space. They asked … if I’d ever experienced any domestic or sexual abuse and wanted to chat to me if that was the case effectively. So they did quite a thorough check beforehand.
EH4, patient interview
Digital communication, for example text messages or e-mail, was mostly preferred by interviewees and they appreciated receiving appointment reminders. Some reported receiving letters or action plans following an appointment, explaining details such as general information, results or appointment summaries, which they valued.
A few women, in one hub, explained how the ability to contact the hub directly again if there were any problems or they wanted follow-up support was valued. As one described, they felt that the help provided was prompt, useful and meant that she did not have to go back through a GP to access support.
Experiences of Women’s Hubs and wider services
What was good about hubs and what difference did they make?
Across all exemplar sites, experiences were largely positive.
It’s quite good that I’ve actually been seen today via another doctor in another surgery, that’s not even my own … if your GP can’t give you that help then I think it’s a really positive thing, that it does spread worldwide.
EH2, patient interview
Women interviewed often commented on how friendly, caring and pleasant hub staff were and how staff put them at ease.
The two of them are such a good team … I just feel so comfortable and if I have a problem I now feel I can ring them.
EH3, patient interview
The demographics of hub staff were also mentioned by a small number of interviewees, including from ethnic minority groups, for example their ethnic diversity, which could provide a sense of inclusivity and preferences to be seen by female doctors with whom women may feel more comfortable or who understood their concerns more.
So it was really nice that it was a woman there, because that really makes me feel at ease.
EH4, patient interview
Several interviewees also commented on the value of having continuity in who was providing their care:
Well I think because she’s specialised so she knows exactly what she’s talking about. You didn’t feel like you had to explain it all again and again and again and, you know, she was the same lady that put my coil in so I don’t know if she’s the only doctor that does it, but she was so knowledgeable about stuff.
EH3, patient interview
The location of WHHs, availability of parking and public transport were other features that some appreciated, for example hubs being close by or offering more choice locally.
Some of these findings align with written patient feedback collected by the hub sites and reviewed by the evaluation team. Feedback included satisfaction with waiting times, access to clinicians, friendly staff and a willingness to recommend the service to friends and family.
Women we interviewed reported receiving treatment or care they needed, for example a prescription for hormone replacement therapy, which helped to resolve their problem. One woman described how she finally got a solution to cycle-related symptoms of severe depression and suicidality:
… obviously getting the right treatment. It hasn’t fixed things, and obviously there’s a lot of difficulties. But in terms of the intensity of things, and like feeling like I want to do something – it’s stopped many admissions, it’s stopped a lot of A&E visits. I may function a bit better now. Also, just being heard and listened, and to trial and let’s see if this works, and it’s changed like, given me the options to choose things.
EH1, patient interview
There were a few examples of how interviewees reported that care was holistic, or that they received care for multiple issues at once, though this often appeared to be opportunistic rather than an explicit service offer that women knew about before attending. Being able to receive different services at the same time was described as reducing the need for multiple appointments, and making access easier for those with other commitments:
… so I’m working different hours every week, so it was really helpful that I could get the ultrasound and the appointment at the same time rather than having to schedule two different appointments around work.
EH3, patient interview
Some described feeling listened to, and having time to talk things through. Examples of how staff reassured women and took time to explain processes and procedures were given. There was a sense that women were being seen by committed professionals with expertise and knowledge.
I’ve always come out feeling really reassured and that I’ve got an action plan to sort of move forward with, like it felt like people were actually understanding, listening and explaining things to me!
EH1, patient interview
Several interviewees emphasised how their appointments had helped them feel more in control, for example by discussing treatment options. One woman reported that this was particularly important when receiving more intimate care.
I got listened to even when I had slightly different choices. I didn’t get ‘Well you should do this’. That gives me that agency and that kind of feeling of control which I think is really important in these kinds of scenarios.
EH4, patient interview
Two people using WHHs commented that they felt they were an inclusive and safe space for all people who need to use these services. In the first example, the interviewee said that the reception was used for multiple clinics; therefore, the waiting room was a mixed-gender space. The interviewee described this as being reassuring for people who are transgender or non-binary. In the second example, the participant reported that they were aware that the service was for women and non-binary people prior to their appointment, which gave them confidence going into their appointment and that the service met their expectations well. This was supported by documentation from the site that explained that trans men and non-binary individuals assigned female at birth are included in the service and that it aims to provide care that is appropriate, inclusive and sensitive.
Comparing hubs to other services
When women reflected on how receiving care at a WHH compared to other services, for example at their local GP surgery or hospital gynaecology department, the feedback was positive. Several reported that the care was more personal, private or that they felt more comfortable. Specific examples of how women had been treated at other services were provided, with the hub comparing favourably:
And I think when you’ve spent years not being listened to, whether it be professionals or family, whatever, it’s just nice to have someone listen, take it on board, have a conversation, and just see what works. And no rush like, whereas other departments in hospitals or specialities, it’s like you’re discharged, that’s it. Even if they haven’t found a cause, they’re like well that test was clear, so we can’t see anything.
EH1, patient interview
A few women reported that the hub offered them more flexibility in the way that appointments were arranged or gave the opportunity to go away and return to see someone later, which was across hub models delivered both in GP practices and in community locations. Several commented on how appointments were longer than at, for example, their GP practice.
It felt personal. I didn’t feel like I was just being rushed through, as you do in the doctor’s now. I felt that that person was taking proper time to sit down with me, ask me lots of questions and allowed me to ask lots of questions back ….
EH4, patient interview
Several women described how there had been explanation and discussion that had not occurred, or to the same extent, in other settings.
My first appointment was in the hospital and it was so much different from going to the hub and it didn’t feel as comfortable and as friendly. The gynaecologist who, you know, did the investigations on me, he wasn’t very forthcoming with what he’d found, and it was kind of like I went in and then walked out not knowing much about what was going on …. But when I went to the hub, you know, they were very thorough, they talked through everything with me and then talked through different routes and avenues and treatments etc. so they were so much more thorough.
EH3, patient interview
Similarly, another interviewee said they felt they were treated humanely and respectfully. They said that the clinician used a trauma-informed approach to ensure the consultation and procedure felt safe and comfortable, and this had not happened in other parts of the health system (e.g. in accident and emergency).
There was also a suggestion that women were accessing specialists in women’s health, who were experienced and knew how to provide support or treat their issues.
I’ve been on HRT for 18 months or so through my GP, but I haven’t been satisfied with the level of understanding of menopause through my GP practice and I wanted to speak with a specialist.
EH4, patient interview
There were a small number of examples given of difficulties women had experienced in interactions with their regular GPs, for example, reluctance to prescribe hormone replacement therapy. One woman described how her GP had refused to treat her condition, which had been considered manageable in primary care, and so she asked to be referred back to the hub.
… so I said ‘You’re going to have to refer me back because if you can’t do this, if you can’t even talk to me about this stuff then this isn’t good enough’. So he did refer me back.
EH4, patient interview
Overall, among a number of women, there were perceptions that primary care experiences were rushed, less expert and there was a sense that they weren’t always listened to about their women’s health issues. Further, when hubs were compared to secondary care, it was perceived that hubs were more woman-centred and flexible about appointments, though there were also reports of good experiences in both.
I really don’t blame my old GP, he was an elderly gentleman, he looked after me for the other things but this bit it was almost like ‘oh, you’ve got to learn with it’.
EH1, patient interview
What went less well or could be improved in Women’s Health Hubs?
While women’s accounts were overwhelmingly positive, there were a few examples where things had gone less well, or that could be improved. Perceptions of waiting times to access hub services were mixed but some women would have liked to access hub services more quickly. There were also several examples of women waiting longer for a more flexible appointment time. Some suggested ways for WHHs to increase awareness or improve in future. This included changes to what the hubs are, what they offer and how they are accessed. Interviewees also recommended that WHHs should do more to raise awareness of their services in local communities, including via social media and providing information in local GP practices, such as detailing what hubs offer and how they could be accessed. For a few interviewees and focus-group participants, a reliance on healthcare professional referral was not always perceived to work well. Several mentioned potential problems with this approach, for example one person reported how her GP had not been aware of the service, which delayed her access to the hub.
My GP didn’t even know that was there, the service because obviously when they have discussions in multi-disciplinary meetings, someone raised something …, that there’s a service in [name of place], she said she wasn’t aware of it.
EH1, patient interview
In another example, a woman reported that, when she asked, there had been some reluctance from her GP to refer her into the hub.
I said they was aware of these specialists [in the hub], and they [GP] almost were a bit reluctant to let me know, and that’s how it started. It probably wasn’t but that’s how it felt.
EH3, patient interview
Across interviews and focus groups, women said that it could be difficult to get through to their GP practices to get appointments, or may sometimes be reluctant to access their GP; other access routes, for example self-referral, therefore could be helpful.
It takes you a month, yeah, it can take you weeks even now to access a GP. No appointments at GPs, nothing. It’s been two months now. I’m crying to get a GP and this is something really, really worrying because by the time you go and the GP tells you ‘oh, it’s too late’, imagine?
EH1, group interview
Examples of how initial communication could have been better were reported by a few women, which included needing more clarity about booking, clinic location and what would be involved.
… like I didn’t really realise that it wasn’t through my GP, it was through – this wasn’t my usual doctors … so it was all a bit confusing
EH2, patient interview
A small number of women had also been confused about whether they had been referred to, or accepted by, the hub and expected timelines.
You sometimes want to know is it weeks, is it months, are they working towards a particular timeline to get back to me? Because I did actually call my GP I think twice to say, ‘has the referral been made and how long do you think it will be?’
EH3, patient interview
A desire for more information regarding follow-up or next steps after an appointment was also expressed by a few interviewees. There was a small number of instances where problems weren’t yet resolved, though these women still reported wider satisfaction with the staff and service.
So I wanted further clarification from her about that because it’s not what I want to do and I’d like to know why and that kind of thing. But I don’t know how to access this doctor. She’s not my GP … I’m not sure if I am one of her patients so I’m not really sure where I stand with that …. And whether I should be going to my GP again …. So I’m a little bit confused as to who’s leading me with this.
EH1, patient interview
One interviewee raised concerns about a GP taking on responsibility for aftercare:
… a consideration is about the aftercare of patients which is a little bit of a shame really because they may give some great advice and whatever, but can the GP maintain it safely? I don’t know.
EH1, patient interview
Issues around follow-up link to a wider point raised by a few interviewees, about the communication or information continuity within organisations, and between different parts of the healthcare system. There was a sense that different professionals or organisations may not communicate effectively, and this could impact on the care that a woman received.
… the reason that I went to [hub] is because my GP couldn’t work out why I was on an oestrogen-only HRT when I should have been on perhaps a mixed one. But the reason I was because I’d had a Mirena coil fitted, but he didn’t have that on my records because I had it done at [hub]. That’s not very joined up to me. Everyone should know what’s going on here
EH4, patient interview
One interviewee also shared a concern that the name ‘Women’s health hub’ could give the impression that some people who should be able to use the service (e.g. non-binary or transgender people) were not welcome or able to access the service.
… I would feel quite strongly against the use of the term Women’s Health Hubs, because it just excludes so many people, you know, there are lots of people in society who menstruate or have a uterus who might need to access all of these services, but they don’t identify as women.
EH4, Patient interview
The interviewee acknowledged that finding inclusive alternative names for services can be challenging but highlighted the importance of providing a service that is not only gender-inclusive, but is clearly advertised as such. This concern was also raised by a member of the evaluation Women’s Group (Box 20). Another interviewee recommended that hubs have groups that can bring together and support people who are transgender or non-binary.
Using health services for women’s health needs
During focus groups, women who had not used hubs reflected on the services they currently used for support with women’s health-related issues. Women often described going to their GP first, though they reported challenges in accessing the GP, with some expressing preferences for female doctors, who were not always available.
I would love for it to be a woman, you know? So all those things they have to take into consideration. That’s why cultural issues. That is not something that we do in our culture so for certain things like that it has to be a woman.
EH1, group interview
Some mentioned that there wasn’t much support available for their women’s health needs, that it had reduced compared with times past, with one woman describing it as ‘non-existent’.
It must be about 10 years ago they shut them [community contraception clinics] down because then you had to start going to the doctor’s, but then you’re taking an appointment off someone to get your pill.
EH2, group interview
Consequently, a few women had sought alternative methods of support, including accessing community groups or paying for alternative therapies or private health care. For information around women’s health issues, women primarily described either talking to their friends or accessing information online. However, this was not possible for all, for example some who did not use the internet described relying on family or friends to help.
Two groups, including one in a more deprived community, also raised concerns around ‘postcode lotteries’ and whether hub services might not be accessible for all women. Some questioned whether women in more affluent areas might find it easier to access help.
When they are open I am at work, so I think if this hub here it can also be in [name of place] – it’s supposed to be everywhere, not only in [name of place].
EH1, group interview
A need for women to self-advocate to access/navigate services and receive support was also raised by another group in a more rural community, who suggested that accessing provision relied on women speaking up for themselves. Some described how women from certain communities may have needs that were not being met; two groups of women from ethnic minority backgrounds expressed preferences for describing symptoms in their first language and being able to speak with someone who understands them. One group also mentioned the importance of being able to have written information translated to aid understanding, while in another some mentioned wanting to see a healthcare professional who understands their culture or background. Both groups also expressed preferences for seeing female doctors.
… people who can speak the languages so they can express themselves because what we’re finding is when you’ve got an illness, when you try to translate it into English, first of all it’s explaining yourself, then secondly you might not get it correct in English and the other person can’t understand so they don’t put down the severity of the illness
EH4, group interview
Yeah, to understand the women – culture, background and their language because some people will speak English as their second language. Sometimes we can’t express what is going on, you know, because we can’t say it in English.
EH1, group interview
What do women think Women’s Health Hubs should look like?
Participants were invited to reflect on what they would like women’s health services/hubs to look like. They gave examples of services they would like to see, including contraception, cervical smears, fertility, breast care, screening, maternity and postnatal services and support, sexual health and menopause care. Mental health support was also sometimes mentioned. Hubs could offer education, advice and information for women in local areas, and several expressed a desire to be able to see female doctors in hubs. While many focused specifically on women’s health services, a few stated that they would like a hub to be somewhere where women could receive advice and checks for any health problem, for example blood pressure. There were suggestions that WHHs could include support groups or be a ’safe space’ offering women a private, trusted place to go, for example for women who had experienced abuse.
I would like to see consultation, advice, like people come to you to ask say about like contraception or sex or any health problems really that they’ve been thinking about. And also somewhere where someone is a victim of domestic violence or sexual abuse or anything like that, that they could come and it would be a safe space.
EH4, patient interview
Several participants described how WHHs could be somewhere you could get everything you need in one place, without referral elsewhere, offering support holistically across the life course. When discussed, interviewees and focus-group participants described the idea of WHHs in positive terms, saying that they could be good for women:
I do think it’s a great idea to bring everything together because there can be so many anxieties about accessing support …, to know that you’re going to a space that has really good knowledge and is confident in offering support to women who menstruate I think would be really valuable.
EH4, patient interview
However, there were a small number of concerns raised about the sustainability of any new services:
… the hub to be there, to continue, because maybe it could reach up to 2 or 3 years and then close down, you know? So it’s to leave it, to continue this service to grow, not to be closed down.
EH1, group interview
In two focus groups, women suggested WHHs could be mobile, with clinic facilities in buses that can go to where they are needed in local communities, for example a local supermarket car park or mosque.
… there should be a mobile unit that has everything to do with health on it that goes and stands in different car parks across [place], like a mobile that can be moved, and people can go in and have a screening done, have everything done ….
EH4, group interview
The importance of accessibility, and the potential for services being more community-based, was also emphasised:
… accessibility is important. The hub has to be near the people so they can reach it with transport. And also access for those women who have disabilities. So there has to be more accessibility and also the time, like what I said before, is also important. So the location of it is also important, it has to be local. Also the transport is accessible.
EH1, group interview
Further, as mentioned previously, the opportunity to access support in a woman’s first language would be welcomed.
Facilitators and barriers to women’s uptake of services
Across sites, facilitators and barriers could be identified or inferred from interviews with women and staff, and in focus groups. Factors included an awareness of hub services, a convenient or familiar location and stigma associated with accessing sexual and reproductive health services (Box 19).
Facilitators
-
Awareness of hub services among women and healthcare professionals, and buy-in.
-
A convenient or familiar location.
-
Accessibility of public transport links and/or parking.
-
Flexibility and choice in appointment dates and times, including offers of video or phone consultations where required/desired.
-
Doing community outreach – going to where women are in communities and engaging with them about services.
-
Understanding of culture and/or religion and opportunities to speak in first languages.
-
Opportunities to be seen by a female doctor.
Barriers
-
Rurality of service – difficulty accessing via public transport/car or long travel times.
-
Long waiting times to access a hub.
-
Reliance on particular routes of access:
-
GP referral, for example, difficulties getting through to surgeries for appointments, or requirements to tell receptionists the reason behind calling.
-
Use of digital/online systems to book appointments, linked to issues of digital exclusion.
-
-
Stigma associated with accessing sexual and reproductive health services.
-
Delays seeking help among women, for example reluctance to bother a doctor or think their issues are serious enough to do so.
-
Potential reliance on self-advocacy.
-
Needing child care support.
Staff views of women’s experiences
Professionals working in and outside the WHHs were positive about patients’ experiences. They mentioned a range of benefits, including easy and convenient access, a more intimate or relaxing experience, and opportunities for some continuity of care. Some reported that women were more able to ask questions, were more informed and empowered, listened to, and able to take their time in appointments.
… we have more time, more used to dealing with people and so communicating with patients and that’s really appreciated, so people are very thankful for the time and thought that goes into their care, they feel heard and that their problem is addressed and they understand how to manage it ….
EH3, internal interview
There were also comparisons made to care provided elsewhere in the system: for example, the value of shorter wait times compared to other services and a sense that a hub could offer a more comfortable experience.
… the wait time for [place] at the minute … it’s brilliant compared to what they would have been expecting, which is a three month wait to go to [different place]. So at the minute, very well received.
EH1, internal interview
In one site, several professionals highlighted the value of patients being able to directly re-contact the service following treatment completion, should they experience any issues or need further help, providing reassurance for women. One interviewee described how this differed from other services, such as in secondary care, where a patient would be discharged and require a new referral to access further support.
Across all exemplar sites, receiving positive patient feedback was mentioned by professionals. In one site, interviewees remarked how women liked the hub so much they wanted to remain a hub patient, while in another staff talked about receiving few complaints, which they stated reflected their service quality.
I do feel that what, the care that they’re actually receiving is just so humungous to them and life changing, they’re telling their friends and we do get a lot of that.
EH3, internal interview
Insights from our Women’s Advisory Group
As noted in Chapter 1, a Women’s Advisory Group was established to provide input throughout the evaluation. The Group provided valuable insights regarding WHHs, including how the concept may be perceived by women. A summary of the key messages from the Group, including those from the interim report, is presented in Box 20, categorised in themes.
-
The terminology of ‘hubs’ was described as confusing, implying a physical location with a range of services under one roof. It was mentioned that this should be carefully considered to ensure clarity when communicating with women. Focusing on key principles, for example putting women first, may be a way of putting boundaries around what hubs are.
-
Women asked questions about the inclusivity of the term ‘women’ in ‘Women’s Health Hubs’, though it was also acknowledged that using ‘women’ helps to distinguish the hub service.
-
Hubs should consider how to reach all communities, including ethnic minority groups, those who are disadvantaged and/or underserved by existing services. There were concerns about what the outcomes might be for women who do not or cannot engage with hubs, and therefore that hubs could potentially worsen inequalities and/or require self-advocacy to access or navigate systems.
-
Hubs should carefully consider how they communicate with women. Clarity around the hub offer is key to ensure awareness and understanding about what they offer and how they link with other health and care services for women.
-
The group highlighted that there was a bigger message linked to this work – that women’s health matters and this is heightening awareness across the system and the country. This was valued by the Women’s Advisory Group.
-
It was stated that there are some assumptions linked to WHH development and roll-out, which would be important to unpack: for example, that women will engage with local hub services, or that service access will necessarily be improved compared to what currently exists.
-
Religious and cultural factors should be considered by hubs: for example, language barriers and how to reach women in different communities, stigma in ethnic minority groups around accessing support for women’s health and a preference for seeing female doctors. Doing outreach with groups (e.g. carers, queer communities, ethnic minority groups) could be helpful to ensure their needs are being considered.
-
It was described that there was a lack of clarity around what WHHs are aiming to do, which services are ‘in’ and ‘out’ and where the boundaries between hubs and other services lie, and what is considered to be ‘women’s health’. Concerns were raised around whether mental health services would be included, and there was confusion regarding how maternity pathways fitted with hubs, as maternity care was viewed as a central part of women’s health care.
-
They reported that there was a focus on service integration in this work, but that it was vital that this is thought about in relation to being responsive to women, their needs and improving communication between teams – not simply the physical relocation of staff and services.
-
Choice was considered important – could WHHs offer another route for women to access care rather than replace existing services?
-
Hubs should ensure that there is flexibility in appointments. This was perceived to be a benefit of attending appointments with GPs as women can ensure the appointment is convenient for their needs and amend as needed. Such details were considered important for encouraging women to engage with WHHs, particularly for those with responsibilities such as child care.
-
There were concerns that a focus on economic recovery and reducing the NHS backlog may take precedence over ambitions to improve women’s health, and encouraging the expansion of WHHs across the country. Further, there were queries around whether a (perceived) lack of finances was likely to delay any development and roll-out of hubs.
-
It was mentioned that WHHs could represent a shift in working in the healthcare system and so it would be important for hubs to consider how to ensure that healthcare professionals were on board with changes, and that these processes were sensitively handled. This was also considered important considering current system pressures.
-
There was also apprehension about whether the development of WHHs would mean that local GP surgeries would no longer offer services such as smear tests or contraception support. It was suggested that this could create additional challenges, for example in rural areas, where transportation and travel times may be issues, and this in turn could reduce women’s engagement with their health. Points were raised about whether there was a risk that providing more integrated services could be at the cost of convenient access for those who need it and the deskilling of current healthcare professionals.
Chapter 6 Discussion and conclusions
Summary of key findings
This rapid evaluation included a mapping exercise to identify all WHHs, descriptions of the models in use, and the exploration of experiences of national leaders, WHH staff, and women using hub services and living in areas served by WHHs. Findings presented in the report add to the sparse literature on integrated care for women’s health.
Definitions, aims and models
-
Women’s Health Hub models across the UK were diverse, with different perspectives regarding the role and definition of a ‘hub’, and varied service offers, catchment areas and nomenclature. It was rare for hubs to offer and advertise multiple services at the same time, and the terms one-stop shop and hub-and-spoke were applied differently. Most hubs were evolving with plans to expand their offer and/or reach. The majority of hubs were multivenue, and there was a mix of GP and community clinic venues, with most GP-based.
-
Some participants reported that there was a shared vision across stakeholders about what a WHH is and should achieve, and WHHs broadly aimed to improve local women’s health access, quality and experience. The hubs we identified inhabited an ‘intermediate space’ between standard primary care and specialist secondary care. The boundaries varied in different hub sites.
-
Some professionals and women wanted to see a wider range of services impacting on women’s health, for example maternity, cardiovascular, mental health, though the focus of hub implementation was on reproductive health and gynaecology services.
-
All hubs used a GP referral pathway, and while some expressed a desire for self-referral, concerns were raised regarding the ability to manage demand without a primary care referral model.
-
Hubs were clinically led by doctors, usually GPs with special interest. There was a mix of formal and informal leadership and oversight. There were a range of perspectives about leadership, and it was not possible to determine an optimum leadership model from the available data. There was no common approach to staffing, and while GPs were usually key, there were examples of diverse multidisciplinary delivery models, and there were different opinions on the clinical benefits and costs associated with delivery by different health professionals.
-
Commissioning models were diverse, and there were many examples of formal and informal creative approaches to identify and access resources to set up and run WHHs and, in some cases, share costs across different parts of the health and social care system. No clear optimum commissioning model was identified as it was dependent on local context and interest, and existing systems/processes.
-
Many WHHs supported women’s health training, education and capacity-building in health systems, although the scale and scope of these activities varied.
-
We found no evidence of WHHs integrating with other hub models currently, for example community diagnostic hubs, perinatal mental health hubs, though these models are also still emerging.
Service aims and outcomes
-
Most parts of the UK did not have a WHH. We identified 17 active hubs, and 5 areas setting up a service. There were also many other services providing women’s health care in the community which did not meet our definition of a WHH.
-
Hubs across the UK have provided care for many hundreds of women. Measurement of processes and outcomes was evolving, and outcomes measured and data sources varied, making comprehensive assessment and comparison difficult.
-
In part due to hubs often being in their infancy and some only recently starting to see women, data on outcomes were limited, but where they were reported by WHHs they indicated that WHHs have the potential to deliver shorter waiting times, increased LARC fitting rates, and reductions in secondary care gynaecology referral rates and waiting lists.
-
Some participants expressed concerns about potential unintended consequences of WHHs such as widening inequalities (if women in already more advantaged groups find it easier to access hub services), destabilising existing services and workforce, or increasing costs (either through service duplication or unlocking of unmet need).
-
While hub leaders aimed for models to reduce disparities, and were implementing strategies to do so, evidence was still emerging regarding whether this is achieved in practice. Data limitations meant that the impact of WHHs on inequalities could not be assessed.
-
Women reported a positive experience of hub access and care. Generally, women using hubs and women in the community were not aware of the term ‘women’s health hub’ but welcomed the concept. Our Women’s Group suggested that the ‘hub’ term may be confusing as it indicated that hubs were a place.
Implementation facilitators and barriers
-
Interviewees described successes in hub implementation, suggesting ‘good practice’ and providing learning for others developing hub models.
-
Committed, collaborative clinical and non-clinical leaders working across boundaries, with sufficient workforce capacity and enthusiasm, appear to be important to success. Hubs were often implemented incrementally, with piloting, evaluation and evolution of models, and relied on leaders devoting time, resources and goodwill ‘beyond the day job’.
-
Additional expertise to support implementation was key for some hubs, for example NHS, local authority, pharmaceutical company provision of strategic/clinical/project management capacity. Leaders described using local intelligence to measure and model population need and to estimate hub costs and benefits to inform implementation.
-
There were examples of established hubs sharing policies, advice and tools to support colleagues implementing new hubs elsewhere without ‘reinventing the wheel’.
-
While ICBs were viewed as a potential route to expedite hub scale-up, participants noted that there were no designated system leaders with responsibility for women’s health, and this area was competing for attention with acute health and social care priorities.
-
While some hubs had involved women in service development, this was not extensive.
-
Participants highlighted the need for flexibility in hub models to meet the local context, balanced with some standardisation to understand and compare hubs and outcomes across the NHS.
-
A number of the challenges described are common to health and service improvement work, including access to funding, facilities and equipment, workforce, stakeholder engagement, and wider system competing priorities and pressures, further exacerbated by COVID-19. 66,67,70,71,110
-
Many of the challenges were familiar in integrated care. Commissioning and funding barriers were often cited, along with workforce challenges, lack of interoperability of IT systems and data-sharing, identifying physical space, ensuring smooth patient pathways, and allaying concerns about loss of activity and funding in other parts of the system. There were examples of overcoming these barriers to achieve different forms of integration.
-
While hubs had frequently adopted creative approaches to identifying funding and overcoming commissioning barriers, often they constituted ‘workarounds’ rather than long-term solutions. Some hubs had reached an impasse in expanding their offer due to commissioning barriers, for example identifying what funding and activity could move from secondary care gynaecology to the hub, or identifying a long-term solution to enable offer of LARC for both gynaecological and contraceptive reasons in the hub. Finding solutions to the challenge of transferring money or resources between organisations has been identified as critical in the success of integrated care models. 70,73
-
We found evidence that in some models information-sharing, IT and interoperability issues had impacted on WHH referral, prescribing, testing, follow-up, record-keeping and communication across care interfaces, which are challenges facing many working to integrate care. 111 Strategic-level action is already under way in ICSs to address these challenges, and the barriers are not unique to WHHs. However, WHHs are often at the ’sharp end’ of cross-boundary working.
Discussion of the findings in the context of the wider literature
The diversity of WHH approaches in place across England means that this is a complex policy and practice area. There is no standardisation of models, and no common language or application of the term ‘Women’s Health Hub’. With our evaluation stakeholder group, we have worked to articulate a clear working definition of a WHH. Flexible, context-dependent hub design is likely to be required to meet local needs and resources. 60,66 We therefore have not specified in our definition which model in particular implementation teams should use, which professionals should lead it, or finer details about how hubs are resourced. However, we acknowledge that this diversity in models risks creating confusion for women, professionals and policy-makers which may impact on engagement, implementation, uptake and evaluation/monitoring. Our working definition provides a foundation that can be refined as evidence and experience in implementing WHHs grows, to support decision-makers to assess which care models work best for women’s health, are most effective, and likely to be used by those most at need, which is currently lacking in the literature. 60
While both top-down and bottom-up drivers of system change can be effective, top-down standardisation of the approach to WHH models and implementation may limit adaptation to fit local needs, context, leadership, workforce and resources. 102,112 While a key ambition of hubs was to reduce health inequalities, variation in hub design and implementation and services offered may exacerbate inequalities by increasing variation in services between geographical areas. Some uniformity would enable understanding and knowledge transfer, and fair and appropriate performance measurement and evaluation of models. The learning is still ongoing regarding the relative benefits and limitations of different models, including alternative models of women’s health service provision that were not explored in this evaluation. The evidence suggests that due to the complexity of integrated care models and the systems in which they function, adapting approaches to local context (including financial, geographical, professional and organisational factors) is necessary, and a ‘cookie cutter’ approach to WHH implementation is unlikely to be successful. 47–49,76,80,113 It is likely that a balance is necessary between standardisation and locally defined models, involving agreement on the desirability of standardisation versus adaptability of different WHH components. 114 Clear definitions of what a hub is will also help to avoid simple rebadging of local services as WHHs in response to policy initiatives, without meaningful transformation of care pathways.
The current small number of hubs and early stage of development for many indicate that it will take some time to scale-up and spread WHHs across the NHS, for existing models to reach their full potential and to offer women multiple services in the same place/visit. Health systems across England are at different starting points and have different existing assets, which can help or hinder implementation. 115 The early stage of scale-up presents an opportunity to develop guidance, agree core components, align approaches (where appropriate), capture the learning and test assumptions regarding different ways of working. This includes identifying any unintended consequences, which are a common feature of complex system change. 102 Harmonising approaches to describing the key components of WHHs and measuring activity, impact and cost will facilitate evaluation and comparison of models, including measuring the anticipated impact on inequalities. It will help to build the evidence feedback loops to inform ongoing adaptation and adoption of WHH models, and ultimately show whether WHHs are achieving their intended goals. 102
There are some core elements of hub models that would benefit from clearer definition. First, hub model terminology was applied in different ways, with concepts such as one-stop shop and hub-and-spoke used in a variety of ways, a challenge that has been observed in other integrated care initiatives. 10 Agreed model definitions would improve understanding, evaluation and replication. For example, what range of services would need to be available at the same hub visit for it to be considered a one-stop shop (and does this need to include both gynaecological care and contraception)? And where referral and triage functions are virtual or remote, is this the ‘hub’, with linked satellite clinics the ’spokes’?
Regarding one-stop-shop approaches, for some women it may not be meaningful or timely to combine all of their women’s health care in the same appointment, and some may prefer to visit their GP for some elements of care, for example for a smear test with a practice nurse they know and trust. Similarly, some women may not want all of their care needs resolved in one visit and may prefer time to make choices and receive further treatment, all of which could be possible in a hub model. The high levels of patient satisfaction observed in WHHs are welcome and linked to the fact that they provide specialist expertise in the community that most GPs cannot, and are more accessible than secondary care. One-stop-shop models may bring a risk of overcentralisation of services and destabilising primary care. 61 While women may prefer WHHs and have high levels of satisfaction, it is possible that in an efficient health system some women may never need to use hub services if their needs can be met within primary care without additional resource. It has been suggested that integrated care models have the potential to improve outcomes among women with the most complex needs,73 and where some needs can be met efficiently in primary care, WHHs may be better targeted for women with specific needs requiring expert input. While the evaluation has offered insights into women’s views and needs, and some sites had involved women in their service development, there is scope for further research and involvement as these models are scaled up, to coproduce and deliver consistently woman-centred models. 65,74 For example, LARC provision was dominant in existing WHHs. LARCs have clear benefits and there is a need to improve access. 6 Leaders have described beginning their WHH implementation with LARCs with plans to expand the offer. However, women and professionals have called for more holistic models of care that address women’s needs across the life course, and there are concerns that some women, particularly from more marginalised groups, may feel pressure to accept LARCs. 12 Involving women in developing WHH models can ensure that they are designed around their needs and the inequalities they face.
Women’s Health Hub stakeholders described how resources to support implementation had been essential to establishing their model. The announcement in March 2023 of £25 million to support expansion could be transformative for areas that face challenges in identifying resources to support hub implementation. The hubs we identified were led by motivated, passionate experts, and it is also likely that local health systems will find hub implementation more challenging where they do not have enthusiastic, designated leaders to drive things forward,66,71,72 or a history of successful integrated working. 70,71,82,116 Therefore, identification and support of local champions in the system is important. Engagement of the wider workforce was also important to gain buy-in and establish pathways in the sites we explored. 60 Our study participants described pre-existing strong networks across and within organisations, and work to build multidisciplinary relationships in their localities, which can facilitate collaborative working to support implementation. 82,116 In areas where there is low enthusiasm or workforce capacity in women’s health care, it may be unrealistic to expect a hub to be implemented in the short term. However, the Women’s Health Strategy and work of the Primary Care Women’s Health Forum and others were helping to make the case and build this enthusiasm and support among leaders across England.
Successful approaches and teams could inform learning for other areas. Some hubs were developing commissioning models involving joint arrangements between local authorities and the NHS, overcoming a major barrier to women’s care to provide LARC for both contraception and gynaecological reasons. However, challenges remain, and difficulties moving funding or resource between organisations in a system can hinder integration. 70,73 Hubs were often using ‘workarounds’ or undertaking some procedures on a ‘goodwill’ basis, without appropriate full reimbursement. While local and national leaders were working to find solutions (e.g. Faculty of Sexual and Reproductive Healthcare, Primary Care Women’s Health Forum and English HIV & Sexual Health Commissioners Group), further attention and support at regional and national level may assist in overcoming these challenges, for example, how to effectively move appropriate gynaecology services (and associated funding) from secondary care settings into community-based hubs. The systems approach to health care in England continues to mature, but overcoming organisational barriers is challenging. 117,118 With hospital gynaecology clinic waiting lists at an all-time high, WHHs can play a key role in addressing current pressures, while at the same time evidencing their potential role in the health system.
The evidence shows that integrated care models often require investment in workforce and facilities66,67 and, where this is required, WHHs may be challenging to deliver at scale unless resource can be identified from within or outside health systems. While additional funding was announced to support WHH implementation, plans for allocation were still in development. While early evidence has suggested that hubs can improve care and are deemed financially viable by providers, there is mixed evidence from other health areas on whether integrated care models can reduce system-level costs. 67,71,73,84 While hubs may be viewed as an approach to manage demand in a health system,82 and self-referral may be a solution, some stakeholders expressed concerns about meeting the demand that a direct-access model might unlock, and this has not been tested at scale.
Workforce gaps also threatened scale-up, spread and sustainability, with a finite pool of doctors, nurses and allied health professionals to staff new services. Through workforce mapping, education and engagement, and with robust pathways and guidance, WHHs can upskill the local general primary care workforce to provide more and better women’s health care without onward referral, rather than deskilling GPs. They can also provide opportunities for GPs, nurses and other professionals with an interest in this area, and some suggested that it could be a route to GP retention, which aligns with evidence that subspecialisation and portfolio careers can keep GPs in the workforce. 119 Integrated care models can have unintended impacts and destabilise other areas78 and a continuous system-wide approach to building and retaining the workforce is important to avoid loss of capacity elsewhere.
Examples of professional, service, functional and organisational integration were found across exemplar sites. Professional integration, such as MDT meetings and case management, was particularly common, as has been found in other evaluations of integrated care initiatives. 67,84 No examples of system or whole-system integration were found, which in an NHS context can be interpreted as integration across an entire ICS. Instead, there was a bottom-up approach to developing models within smaller footprints in the models we explored.
There is a need for further exploration to identify the optimum approaches to integration in different contexts. 71 This is true for integration in general, and specifically in the context of women’s health, with most evidence on integrated care arising from research with older adults. 73 This evaluation did not include an in-depth analysis of the appropriateness and efficacy of different approaches to integration in WHHs. However, we have set the foundation for further investigation by describing the types of integration identified, which types may be more straightforward to implement (e.g. professional), and which may require more resources and support (e.g. system and whole system).
There is a growing recognition of the need for integration that constitutes large-scale reform and whole-system reconfiguration rather than new models at a service level. 67 The likely benefits of whole-system integration in the context of women’s health care warrant further exploration, and WHHs may play a central role, spanning organisational boundaries.
Recommendations for decision-makers
Implementing at pace and scale nationally
-
Hubs were small scale and rare, and the evidence of effective approaches to implementation was emerging. Further scale-up of WHHs is likely to take time and resources, and different health systems will be at different stages of readiness. Sustainable national scale-up and spread are likely to require an incremental approach, and resource to support implementation and share learning, with concurrent, consistent monitoring and evaluation.
-
Diversity and local autonomy to develop context-specific solutions need to be balanced with a degree of standardisation. While services vary between hubs, it may be beneficial to develop a ‘core’ offer that all WHHs should aim to provide. This should be developed through collaborative, multidisciplinary prioritisation, which includes women with different experiences and backgrounds.
-
A collaboratively agreed national set of definitions for key terms would support clear communication among stakeholders, including ‘Women’s Health Hub’, one-stop shop, ‘holistic’ and ‘hub-and-spoke’. Defining the types and levels of integration being adopted beyond these labels would facilitate clear understanding and comparison of models. A clear definition of criteria to be met for a WHH to be considered ’set up’ rather than ‘in development’ would support monitoring of implementation across the NHS.
-
Many areas lack the local champions and contexts that support WHH establishment. Implementation may be expedited by introducing designated roles at regional and ICS level to raise the profile of women’s health.
-
There is a substantial community of practice and expertise in women’s health driving the hubs agenda forward, including national organisations and leaders from across disciplines and geographical areas. Continued national engagement and support for these groups can aid expansion of this community and share learning. While the focus of the Women’s Health Strategy and most of our evaluation was England, there is further learning to be gained from other areas, particularly Northern Ireland, where WHHs have been established to serve the whole population.
-
The commissioning challenges in English women’s health care are a major barrier to providing a comprehensive WHH offer. Existing WHHs had developed a range of creative ‘workarounds’ to overcome barriers, but these generally were not long-term solutions, and the underlying challenges remained. Local partners need to develop joined-up, co-ordinated and collaborative commissioning approaches for WHHs, focused on achieving better outcomes for women, reducing inequalities and ensuring the efficient use of resources across the health and care system. ICBs, with their responsibilities to plan and deliver joined-up services focused on population need, would seem well placed to play a role in such developments. Since the evaluation, Women’s Health Champions have been appointed in each ICB to drive this agenda. 120 There may be scope for national-level guidance to further support local commissioning approaches around WHHs (acknowledging the need to account for local contexts), drawing on the existing evidence and evolving processes.
-
Ongoing WHH implementation can draw on the extensive evidence base regarding ‘what works’ in implementing integrated care and hub-based models.
Embedding Women’s Health Hubs in local health systems
-
Leadership was key in establishing WHHs at the local level, and identifying, resourcing and supporting designated leaders will be crucial to establishing hubs in new locations. While hubs were all led by doctors, other members of the MDT also made a substantial contribution, and there may be opportunity to develop nursing and other professional leadership roles as hubs evolve.
-
Context-specific, system-level assessment of needs, resources (particularly workforce), opportunities and priorities involving women and other local stakeholders will be necessary to identify gaps, opportunities, and what is possible, including avoiding duplicating existing provision that is working well. WHHs can play an important part in a local women’s health landscape, aligning with other initiatives and services, such as access to contraception through community pharmacies.
-
Our evaluation focuses on areas where WHHs had been successfully implemented. Some areas may face significant barriers to WHH establishment, which require further exploration and support. It is possible that on assessment some areas may deem that a WHH is not the best approach to improve women’s health in their population at the current time.
-
Clarity regarding where hubs sit in local pathways is crucial, and their focus and specialist input are likely to vary based on local needs, assets and challenges. For example, a hub model may deliver one or more of the following: (1) elements of what is ’standard’ GP care because it has not been possible to deliver locally (e.g. menopause care), or (2) a more specialist level of input already provided by some GPs (e.g. LARC fitting) to address local access issues, or (3) services that are traditionally available in secondary care (e.g. hysteroscopy, ultrasound) to reduce the need for secondary care, tackle waiting lists and bring care closer to home.
-
For WHHs to be sustainable in the longer term, local partners will need to work together to develop integrated commissioning and delivery of hub models, clearly identifying the types and levels of integration being adopted, and with ICBs playing a key role in overcoming current barriers. As outlined above, this will depend on a detailed understanding of local needs and systems, and effective partnership working to identifying optimal approaches for addressing local challenges. To avoid confusion and ensure safe care, joined-up pathways and feedback loops are needed across care interfaces, including test results, follow-up planning and information-sharing. Work to address challenges and establish ways of working in the wider system can facilitate integration, including electronic record interoperability and information transfer, prescribing and ordering tests between services.
-
Hub design and implementation approaches need to explicitly identify and measure the forms of inequality being addressed, and consider intersectionality between multiple dimensions of inequality. Leaders may wish to consider focusing hub implementation in or for specific underserved communities to tackle inequalities head on.
-
It will be important to identify and mitigate potential unintended consequences of hub implementation, for example duplication of existing services, widening inequalities if less disadvantaged women find it easier to access services, and detrimental impacts on other services.
-
Many hubs aspired to deliver a wider range of services than they were able to offer, with LARCs a common focus. Participants also highlighted other areas which they would like to see more integrated, for example maternity services. While leaders have worked tirelessly to develop and implement hub models, their work was often focused on specific aspects of women’s health rather than encompassing the whole life course. There may be benefit and learning to be gained by closer collaboration and identification of interdependencies with colleagues and service users working on other community integration and hub models, for example family hubs, sexual-assault referral centres, integrated community dermatology.
Ensuring a woman-centred approach
-
While women were involved in the development of some WHH models, there is scope for much more national and local involvement of women with a range of lived experiences to ensure that approaches align with their needs and priorities across the life course, including consideration of women’s wider needs beyond their reproductive health. Involvement of women whose health needs have historically been underserved is particularly important.
-
It is essential that women know how to access the care they need if the service landscape becomes more complex. A ‘hub’ could mean a venue or a place, but where it incorporates multiple venues and virtual support it may be a challenging concept for the public to understand. We heard mixed views regarding whether it is important that women know that they are accessing a WHH, and whether WHHs should be a recognisable entity in the local health system, and this would benefit from further exploration with professionals and women with diverse backgrounds and experiences.
-
It is also important that women are able to access care, and the GP is often the first port of call to navigate the health system. Many women describe challenges in accessing primary care at the current time, which may be a barrier to WHH access. If alternative referral routes are introduced, it will be important to ensure that they are understood and accessible to all women.
Recommendations for further research
-
While the evaluation offered some insights into the potential impact of WHHs, the diversity of hub models, the relatively small number of active hubs and limitations in available data mean that we do not yet have clear and definitive evidence that they will improve outcomes and address inequalities across health systems if implemented at scale.
-
There is a need to build the evidence base, with consistent and comparable approaches to description and measurement. Given the heterogeneity in hub models, detailed descriptions of the leadership, commissioning, contracting, provider and delivery models will be essential to understand and compare approaches, including describing the levels and types of integration.
-
Future evaluation would need to consider both hub-level and system-level impact and costs across services and the population and explore potential unintended consequences of WHHs. Many hubs are in their infancy, and many more will be implemented in the near future. Further evaluation should only be undertaken once models have become sufficiently operational and data are available to enable measurement of impact.
-
To understand the impact on inequalities, future work should apply an intersectional lens to take account of the complex barriers faced by different women, and compare the perspectives, experiences, access and outcomes for different groups of women living in areas served by hubs across the life course. Along with impact evaluation, there is also a need for further work to understand implementation, the resources required, optimum approaches and why WHHs have been difficult to implement in some areas.
-
There are some exciting innovations being delivered via WHHs which could be explored through further work, such as virtual group consultations.
-
There are some key assumptions which would benefit from additional exploration, including: what kind of care women want and prefer; the relative benefits of different women’s health service models (including services not meeting our definition of a WHH), clinical leadership approaches (including the role of nurses and allied health professionals), different hub sizes/footprints and workforce models; the cost-effectiveness of different hub models and comparison with other types of service provision; the impact on workforce challenges and retention; and whether hub models can provide a genuine one-stop shop.
Box 21 provides a summary of key messages from the evaluation.
-
Only 17 active WHHs were identified in the UK, and most were at an early stage of implementation.
-
Most women in the UK did not have access to hubs at the time of writing.
-
Women’s Health Hubs are diverse and evolving.
-
There was no agreed definition of a WHH. We developed a new working definition.
-
There was no standard or ‘typical’ model.
-
Hubs aimed to improve healthcare access, quality and experience. Leaders were committed to reducing inequalities but approaches and evidence were still evolving.
-
Women’s Health Hubs focused on reproductive health and gynaecological care, with LARCs offered most frequently.
-
Models were integrated into patient pathways between usual primary care and secondary care services.
-
Services were mostly clinically led by GPs.
-
While often described as one-stop shops, hubs rarely offered multiple services at the same visit.
-
Most operated out of multiple venues, often primary care or community venues.
-
Workforce approaches varied considerably.
-
Implementation was helped by passionate and committed leadership working collaboratively across boundaries, sufficient workforce capacity, funding, and policy and strategic support.
-
A range of commissioning approaches were observed, often involving workarounds to overcome barriers.
-
Few hubs had involved women in the design and development of the service.
-
Challenges included IT issues, competing priorities and pressures in the system and identification of funding and other resources.
-
A balance between top-down standardisation and bottom-up needs-based development of WHH approaches appears to be important.
-
Hubs tended to ’start small’ and expand services and/or reach incrementally.
-
Women reported positive experiences of hub access and care, though they were not familiar with the term ‘women’s health hub’.
-
Development of metrics and the measurement of hub outcomes vary, making assessment and comparison difficult.
-
Available data indicate that hubs have provided care for hundreds of women to date.
-
In 2023, a £25 million investment to ‘accelerate the development of new women’s health hubs to benefit women’ was announced with the aim to see at least one hub in every ICS.
-
Scale-up should focus on meeting women’s needs through the life course and addressing inequalities in access and outcomes.
-
Scale-up is likely to take time, resource and collaborative working, with localities at different stages of readiness, and substantial commissioning barriers remain. Engagement of leaders and involvement of women and multidisciplinary stakeholders will be necessary.
-
Definitive evidence of the impact and costs of WHHs and the relative benefits of different approaches is lacking: consistent population-level data collection and analysis will be key to understand models and measure impact at system level to ensure that WHHs provide sustainable provision, complement existing services, and avoid duplication.
Strengths and limitations of the study
This was an early evaluation of WHHs, which aimed to explore the ‘current state of the art’ of WHHs and experiences of delivering and using services and define key features and early markers of success. To our knowledge, it is the only national academic evaluation of integrated women’s health service models. The evaluation combined breadth and depth in data collection, utilising a range of methods via a two-stage process, which allowed for exploratory work to map the landscape and understand the wider context followed by in-depth evaluation in four exemplar hub sites. The evaluation had strong stakeholder engagement, which included both a Women’s Advisory Group and a Stakeholder Advisory Group. The groups were involved throughout the evaluation from shaping its design and conduct to analysis and emerging findings. We have also liaised closely with the Women’s Health Ambassador and Women’s Health Policy team at the DHSC throughout, and supported their work on WHHs.
Many WHHs were identified through the work presented in this report. However, there was no comprehensive list/database of hubs, and they are understood differently by stakeholders with no agreed definition. The term ‘hub’ may be unclear to some, particularly whether it implies a physical location, and the term was being used differently across health and social care services. This variation meant that it was challenging to identify WHH models across the UK, particularly as stakeholders in local areas may not recognise their service as a hub. It is therefore possible that examples exist that were not uncovered.
While there were some well-established hubs, many were at an early stage of development and/or have plans to expand in both scope and reach, for example adding additional services, with new areas planning to implement hubs all the time. The hub landscape is ever evolving and so the findings presented represent a snapshot in time and each hub’s development and progress at the time the evaluation was completed.
The hub mapping work was UK-wide, and while we made efforts to secure participation in the survey from WHHs across the UK, we found that identified models were concentrated in England and Northern Ireland. We sought to compile information about as many local models as possible, though this was challenging as some survey respondents may not have been familiar with all the details of their WHHs, and some sites only submitted partial responses. It was also not possible to review some documentation from sites due to sensitivity and confidentiality. Consequently, we were not able to gather sufficiently recent and granular-level detail with which to accurately develop a WHHs typology. Data availability also limited understanding of hub processes and outcomes; for example, it was not possible to explore access rates of hub services for different demographic groups within the populations served.
As part of the evaluation, we aimed to interview a regional stakeholder in each NHS England region, but it was not possible to locate an appropriate contact in one region, which aligns with our participants’ accounts highlighting the lack of regional strategic oversight for women’s health.
It is important to acknowledge that this early rapid evaluation predominantly reflects the perspectives of stakeholders in areas where enthusiastic leaders have established WHH models, which is not the norm across England, and therefore may provide a particularly positive and supportive assessment of their role and value in health systems. The evaluation also presents more provider-led rather than user-focused insights. This can be explained by the relative volume and richness of staff interview, documentary and survey data, and the complexity of policy, commissioning and provider issues surfaced. A substantial number of women took part in interviews or focus groups, representing users and non-users of hubs (sampling limitations are discussed shortly). However, most women were not familiar with the hub concept and insights into the role of WHHs in the care system were limited. Women’s experiences of service access and care in areas served by hubs and involvement in hub development require further exploration as the concept and nomenclature become more embedded.
A convenience sampling approach via clinical gatekeepers was taken for interviews with hub service users. In this rapid early evaluation, it was not possible for researchers to sample and recruit women directly, for example by screening clinic lists to recruit key demographic groups, and it is possible that interview participants were not representative of all service user views and experiences. Sites were not asked to report the characteristics of all women approached, or who declined to participate. A lack of service-level demographic data meant that it was not possible to determine the representativeness of the women who took part compared with all service users. It was not possible to determine whether the limited diversity of the service users interviewed reflects (1) low attendance at WHH for women in minority groups or (2) low recruitment of these groups from services which were being accessed by women from minority backgrounds. While women from a range of backgrounds were involved in the study, some groups were not well represented. For example, few participants with known ethnicity were from minority groups, and there were few LGBTQ + individuals. However, missing demographic data limited assessment of diversity. For example, as a result of the focus-group sampling approach involving groups for women in specific communities, women from ethnic minority backgrounds will have been present in the focus groups, though this was not captured in the demographic data (Table 10). Overall, the context of rapid recruitment and data collection employing convenience sampling meant that it was not possible to interrogate WHH user or local population perspectives in a way that accounted for the intersectionality in lived experience across the population and the life course. Evidence suggests that rapid evaluation may have limitations related to the ability to access a wider range of perspectives and experiences. As Smith et al. describe, it may take time to engage groups that are seldom heard in research, which is a challenge for rapid evaluations. 94
The in-depth evaluation focused on England, as there are features unique to the current English context, including commissioning challenges and the establishment of PCNs and ICSs, which were identified as important to explore. Further, given the current diversity in the landscape, it was deemed important to focus efforts on one nation to build contextual knowledge, enabling a more comparative approach that would not be possible if devolved nations were included.
This timescale for this rapid, early evaluation required a pragmatic approach to balancing breadth and depth of evaluation to deliver findings in a short study duration. However, it was still possible to explore a wide range of perspectives and contexts and gather a substantial dataset. We employed rapid analysis methods to enable the team to interrogate these data and collaboratively develop findings in a relatively short time frame. While it is possible that some finer detail was missed due to this approach, this method has been shown to deliver valid findings compared to more traditional approaches. 97
Equality, diversity and inclusion
Equality, diversity and inclusion were addressed in this study in several ways.
Site and participant characteristics:
-
Desk research and a mapping survey were undertaken to aid work to build a database of developing and existing WHHs. This was used to support the development of criteria for the selection of hubs for in-depth evaluation to encourage diversity in relation to elements including hub models and services provided, levels of deprivation, population ethnicity and geography (including areas with more and less rurality).
-
We recruited four exemplar hub sites from different regions in England, with some variation in population diversity and deprivation, and rurality.
-
The in-depth hub sites were asked to identify a wide range of stakeholders working in and linked to their hubs to participate in the evaluation. Hub sites were encouraged to include GPs, nurses, sexual and reproductive health consultants, commissioners, administrators and staff in the wider health system. Interviews were also conducted with key national and regional stakeholders to ensure reflections were gathered at every level.
-
One element was the focus groups with women in communities to understand more about local women’s health services and factors that help or hinder women from accessing services such as hubs. We worked with local community leaders and groups to hold the focus groups, with the aim of reaching a diverse group of women, including those who may not typically take part in research. There was some diversity noted in the focus groups across the four sites, in two sites the participants were from ethnic minority groups, in a third site participants were from a group serving a more deprived community and in the fourth were from a rural area.
-
Across interviews with women and focus groups, demographic information was collected for 40 participants in total. The diversity and representativeness of this sample and limitations resulting from missing data are discussed in Chapter 5 and above in the limitations section.
-
Data relating to staff personal demographics, for example ethnicity, age, were not collected as we focused on their roles and professional characteristics.
Evaluation topics related to equality, diversity and inclusion:
-
One study aim was to explore if and how inequalities have been considered in the development and implementation of WHHs. We were keen to understand existing inequalities in women’s health services and how hubs intended to, and were, impacting on these. Many of the evaluation tools included questions relating to equality, diversity and inclusion. In the mapping survey and in interviews, we explored the extent to which inequalities were a consideration for hubs and the progress made to address these, which is reported in Chapter 4.
-
Further, following feedback from the Women’s Advisory Group (please see below) highlighting the need to include women who are not accessing the hub services, we added focus groups with women in communities with lower uptake of WHH services to the evaluation.
Wider involvement:
-
From the outset, the design and delivery of the study were underpinned by a deep commitment to stakeholder involvement. This includes the establishment of a Stakeholder Advisory Group, composed of members with considerable experience in the field of women’s health, including clinicians, policy stakeholders and a woman with lived experience, and a Women’s Advisory Group – a public involvement group formed to use their experiences of NHS women’s health care to support the evaluation.
-
The Stakeholder Advisory Group was formed during the project scoping stage and has informed and supported study design and delivery throughout via three workshops and ad hoc regular e-mail and online contact. The group helped to shape the study, for example developing our understanding of the women’s healthcare context, working with us to develop and refine a definition of hubs, and sense-checking early findings and interpretations.
-
The Women’s Advisory Group was made up of seven women of diverse backgrounds, ethnicities, ages and experiences of NHS care for women’s health issues. The group had a lay chair, with one group member chairing all meetings that took place. We worked with the group from the beginning of the project and their input included: advising on effective ways to reach women to take part in interviews or focus groups (including ethnic minority groups and those who are disadvantaged and the seldom heard); sharing reflections on topics to focus on during interviews with women with experience of hub services and reviewing guides; commenting on criteria for selecting hub sites for in-depth evaluation and discussing which outcomes could or should be measured in future to assess impact, and reflecting on emerging findings. During the scoping work to inform the study design, we also undertook rapid consultation with three women with experience of NHS care for women’s health issues. An example of the direct influence of the group can be found in Chapter 5, in the addition of focus groups with women in communities. The team also met with a woman with lived experience outside of the group meetings.
Evaluation team:
-
The evaluation team consisted of researchers from two organisations (University of Birmingham and RAND Europe) incorporating interests and expertise such as applied health research and evaluation, maternity and women’s health, qualitative research, participatory research, public health and health economics. Though the team was composed of all women, there was a mix of backgrounds in relation to age, research experience and, to a lesser degree, ethnicity. The qualifications of the evaluation team ranged from MSc to PhD.
-
All members of the evaluation team are women with direct experience of accessing women’s health services in the NHS in England. All have an interest in women’s health and two of the team had prior considerable experience in evaluating maternity and women’s health topics. One member of the team (BT) is a public health physician with previous experience of working in sexual health services. The evaluation team acknowledged that their experiences and positionality around women’s health and gender inequalities influenced the design and conduct of the evaluation and interpretation of findings. For example, prior knowledge and personal and professional experiences of challenges and priorities in women’s health may have influenced the development of the topic guide, or interpretation and prioritisation of findings. The team adopted a reflexive approach, meeting regularly and surfacing and questioning assumptions throughout the evaluation process. The team also sought alternative perspectives and challenge through involvement of a multidisciplinary Stakeholder Group and diverse Women’s Group to guide evaluation design, conduct, interpretation and dissemination.
-
From the start of the project, the study lead sought to work inclusively, with all team members invited to be involved in all elements of the study, including data collection, analysis, reporting and dissemination. We held weekly team meetings and had a series of half day meetings throughout the study to encourage and support a sense of team working and to ensure that they were well supported to plan and conduct the evaluation.
-
We also drew on a specialist advisor throughout who gave advice and guidance about the evaluation design and focus, key findings, and the wider context of women’s health.
Conclusions
At the start of this evaluation, WHHs were a set of innovative service models spread across the UK, and at the end of the evaluation, they were an explicitly stated policy objective for the DHSC. Our findings identified that the few existing WHHs are diverse, and continuously evolving, with many at an early stage of development or delivery, with some employing innovative approaches such as virtual group consultations. The launch of the Women’s Health Strategy, and the associated funding to support hub implementation announced in March 2023, provides an opportunity to expedite the spread of these models, and to provide the implementation resource that our stakeholders suggest is often key to success. However, the heterogeneity in models and contexts, and the complexity of women’s health care, means that rapid scale-up may be challenging, and substantial commissioning barriers must be overcome. Our findings suggest that implementing models informed by local needs and resources will be necessary, and requires input from women, particularly those who are least well served by current services. We do not yet have clear evidence for the system-level impact or costs of WHHs, and the gathering of consistent data to test assumptions, and measure and learn from WHH achievements, including impacts on inequalities, will enable evaluation of further scale-up. WHHs have the potential to transform women’s access to care, and the there is a large community of experts striving to improve women’s health care. The Strategy provides a further catalyst to national-level change, alongside the emerging system-level approaches to health improvement driven by ICBs, and wider population interest in women’s health.
Additional information
Acknowledgements
We would sincerely like to thank all the participants in this study and leads at exemplar hub sites who helped to co-ordinate interactions with interviewees. We would also like to thank everyone who gave their time to support the project, share the survey or to connect us with potential stakeholders involved in hub-type models. This includes all the members of the Women’s Advisory Group and the Stakeholder Advisory Group for their support, advice and feedback from the evaluation design to shaping the findings. We are grateful to the policy team at the Department of Health and Social Care and Dame Lesley Regan for their support with the evaluation and promotion of the mapping survey and to colleagues from the Faculty of Sexual and Reproductive Healthcare and Primary Care Women’s Health Forum. We recognise that the point during which the study was conducted was a time of pressure in healthcare services; therefore, we are incredibly grateful that, despite this, staff still found time to support and contribute to the study. We would also like to thank BRACE colleagues and members of the BRACE Steering Group, for their constructive feedback and input throughout the study; Dr Jo Ellins, Professor Iestyn Williams and Sophia Christie for undertaking critical review of the draft of the report; Ann Evans, Cathy Dakin and Chloe Skillan (BRACE Centre senior/research administrators) for providing varied and valued support throughout; and members of the Women’s Advisory Group for reviewing the ‘plain language summary of the report.
Contributions of authors
Kelly Daniel (née Singh) (https://orcid.org/0000-0002-4513-1026) (Evaluation Fellow, University of Birmingham) was the project manager of the study. She co-led the conception and design of the study, conducting scoping research and leading the writing of the protocol, and led data collection and analysis at one exemplar hub site, as well as supporting analysis for a second site. She contributed to the design of the survey and qualitative research. She also led the University of Birmingham ethical approval processes. She undertook regional and national interviews, overall data analysis and interpretation and is a co-author of the final report.
Jennifer Bousfield (https://orcid.org/0000-0002-5671-2336) (Senior Analyst, RAND Europe) led data collection and analysis at one exemplar hub site. She led the review of literature and development of a definition, contributed to regional and national interviews, overall data analysis and interpretation and is a co-author of the final report.
Lucy Hocking (https://orcid.org/0000-0002-8319-962X) (Senior Analyst, RAND Europe) led data collection and analysis at one exemplar hub site. She led the distribution and analysis of the mapping survey, contributed to regional and national interviews, overall data analysis and interpretation and is a co-author of the final report.
Louise Jackson (https://orcid.org/0000-0001-8492-0020) (Senior Lecturer, University of Birmingham) contributed to the design of the study, overall data analysis and interpretation and is a co-author of the final report.
Beck Taylor (https://orcid.org/0000-0002-3559-7922) (Clinical Associate Professor, University of Warwick) was the principal investigator for the study. She co-led the conception and design of the study, conducting scoping research and supporting the writing and development of the protocol, and led data collection at one exemplar hub site, along with analysis. She contributed to the design of the qualitative research, leading the development of the mapping survey. She undertook regional and national interviews, overall data analysis and interpretation and is a co-author of the final report. She provided critical review of the final report and is the guarantor and corresponding author.
All authors contributed to integrating the findings of the study. BT made critical revisions to the report for important intellectual content and approved the final manuscript. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the article are appropriately investigated and resolved.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/JYFT5036.
Primary conflicts of interest: The authors declare no competing interests.
Patient data statement
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it is important that there are safeguards to make sure that they are stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Data-sharing statement
Due to the consent process for data collection, the qualitative and survey data gathered for this study cannot be shared. Sources of data that are already publicly available are provided either in the text or in references. All other enquiries should be sent to the corresponding author.
Ethics statement
Ethical approval was from the University of Birmingham Humanities and Social Sciences Research Ethics Committee (April/May 2022, ERN_22-0669).
Information governance statement
BRACE and the University of Birmingham is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation the University of Birmingham is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details of our Data Protection Officer here.
Publications
Daniel K, Hocking L, Bousfield J, Taylor, B. Early evaluation of WHHs Interim summary report. October 2022. URL: www.birmingham.ac.uk/documents/college-social-sciences/social-policy/brace/whh-interim-summary-paper-final.pdf
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Hallam L, Vassallo A, Pinho-Gomes A-C, Carcel C, Woodward M. Does journal content in the field of women’s health represent women’s burden of disease? A review of publications in 2010 and 2020. J Women Health 2022;31:611-9. https://doi.org/10.1089/jwh.2021.0425.
- Cohen M. Towards a framework for women’s health. Patient Educ Couns 1998;33:187-96. https://doi.org/10.1016/S0738-3991(98)00018-4.
- Faculty of Sexual and Reproductive Healthcare . Better Care, a Better Future: A New Vision for Sexual and Reproductive Health Care in the UK 2015. www.fsrh.org/documents/fsrh-vision/ (accessed 24 October 2023).
- Department of Health and Social Care . Our Vision for the Women’s Health Strategy for England. Policy Paper 2021. www.gov.uk/government/publications/our-vision-for-the-womens-health-strategy-for-england (accessed 24 October 2023).
- Burgess T, Eastham R, Limmer M, Murphy C, Raymond-Wlliams R, Sowemimo A. Long Acting Reversible Contraception in the UK. British Pregnancy Advisory Service; 2021.
- All-Party Parliamentary Group on Sexual and Reproductive Health . Women’s Lives, Women’s Rights: Strengthening Access to Contraception Beyond the Covid-19 Pandemic 2020. www.fsrh.org/documents/womens-lives-womens-rights-full-report/ (accessed 24 October 2023).
- The King’s Fund . Sexual Health Inquiry: Written Submission to the Health and Social Care Committee 2019. www.kingsfund.org.uk/publications/sexual-health-inquiry (accessed 24 October 2023).
- Lowbury R. Sexual Health Commissioning in Local Government, Collaborating for Better Sexual and Reproductive Health and Wellbeing: Local Government Association 2019. www.local.gov.uk/publications/sexual-health-commissioning-local-government-0 (accessed 24 October 2023).
- Royal College of Obstetricians and Gynaecologists . Better for Women: Improving the Health and Wellbeing of Girls and Women 2019. www.rcog.org.uk/better-for-women (accessed 24 October 2023).
- NIHR Evidence: Women’s Health: Why do women feel unheard? 2022. https://doi.org/10.3310/nihrevidence_54676.
- Primary Care Women’s Health Forum . Women’s Health Hubs 2021. https://whh.pcwhf.co.uk/ (accessed 24 October 2023).
- Department of Health and Social Care . Women’s Health Strategy for England 2022. www.gov.uk/government/publications/womens-health-strategy-for-england (accessed 24 October 2023).
- Department of Health and Social Care . Women’s Health Strategy: Call for Evidence 2021. www.gov.uk/government/consultations/womens-health-strategy-call-for-evidence/womens-health-strategy-call-for-evidence (accessed 24 October 2023).
- Department of Health and Social Care . Consultation Outcome: Results of the ‘Women’s Health – Let’s Talk about It’ Survey 2022. www.gov.uk/government/consultations/womens-health-strategy-call-for-evidence/outcome/results-of-the-womens-health-lets-talk-about-it-survey (accessed 24 October 2023).
- House of Commons Health and Social Care Committee . Sexual Health Fourteenth Report of Session 2017–2019 (HC 1419) 2019. https://publications.parliament.uk/pa/cm201719/cmselect/cmhealth/1419/1419.pdf (accessed 24 October 2023).
- Public Health England . Sexual Health, Reproductive Health and HIV: A Review of Commissioning 2017. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/640578/Sexual_health_reproductive_health_and_HIV_a_survey_of_commissioning.pdf (accessed 24 October 2023).
- Ismail M, Wylde L. Workforce Needs Assessment to Deliver Patient Access, Provision and Sustainability of Long-Acting Reversible Contraception (LARC) in Primary Care 2021. https://pcwhf.co.uk/resources/access-provision-and-sustainability-of-larc-in-primary-care/ (accessed 24 October 2023).
- Jefferies D. The Women’s Health Strategy: Ensuring No Women Are Left Behind. The King’s Fund; 2021.
- Public Health England . Women’s Reproductive Health Programme: Progress, Products and Next Steps 2021. www.gov.uk/government/publications/phe-womens-reproductive-health-programme-2020-to-2021/womens-reproductive-health-programme-progress-products-and-next-steps (accessed 24 October 2023).
- McGowan VJ, Lowther HJ, Meads C. Life under COVID-19 for LGBT+ people in the UK: systematic review of UK research on the impact of COVID-19 on sexual and gender minority populations. BMJ Open 2021;11. https://doi.org/10.1136/bmjopen-2021-050092.
- Faculty of Sexual and Reproductive Healthcare . Opportunities to Embed Sexual and Reproductive Healthcare Services into New Models of Care: A Practical Guide for Commissioners and Service Providers 2019. www.fsrh.org/documents/fsrh-report-2019-new-models-of-care-sexual-reproductive-health/ (accessed 24 October 2023).
- UK Gov . Press Release £25 Million for Women’s Health Hub Expansion 2023. www.gov.uk/government/news/25-million-for-womens-health-hub-expansion (accessed 24 October 2023).
- Department of Health and Social Care . Shifting Care Closer to Home Care Closer to Home Demonstration Sites: Report of the Specialty Subgroups 2007. www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_079728 (accessed 24 October 2023).
- RAND Europe and Ernst and Young . Ernst &Amp; Young LLP National Evaluation of the Departments of Health’s Integrated Care Pilots: Final Report 2012. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/215103/dh_133127.pdf (accessed 24 October 2023).
- NHS England . NHS Five Year Forward View 2014. www.england.nhs.uk/publication/nhs-five-year-forward-view/ (accessed 24 October 2023).
- NHS England . New Care Models: Vanguards – Developing a Blueprint for the Future of NHS and Care Services 2016. www.england.nhs.uk/wp-content/uploads/2015/11/new_care_models.pdf (accessed 24 October 2023).
- NHS England . NHS Long Term Plan 2019. www.longtermplan.nhs.uk/ (accessed 24 October 2023).
- Department of Health and Social Care . Integration and Innovation: Working Together to Improve Health and Social Care for All 2021. www.gov.uk/government/publications/working-together-to-improve-health-and-social-care-for-all/integration-and-innovation-working-together-to-improve-health-and-social-care-for-all-html-version (accessed 24 October 2023).
- Department of Health and Social Care . Health and Social Care Integration: Joining up Care for People, Places and Populations 2022. www.gov.uk/government/publications/health-and-social-care-integration-joining-up-care-for-people-places-and-populations (accessed 24 October 2023).
- NHS Confederation . New Network for GP Federations Launched in England 2021. www.nhsconfed.org/news/new-network-gp-federations-launched-england (accessed 24 October 2023).
- Primary Care Women’s Health Forum . Developing a Women’s Health Hub 2021. https://whh.pcwhf.co.uk/resources/developing-a-womens-health-hub/ (accessed 24 October 2023).
- Bennett L. Co-Commissioning: A New Relationship Between GPs and Their CCG 2015. www.kingsfund.org.uk/blog/2015/03/co-commissioning-new-relationship-between-gps-and-their-ccg (accessed 24 October 2023).
- Daniel K, Hocking L, Bousfield J, Taylor B. Early Evaluation of Women’s Health Hubs 2022. www.birmingham.ac.uk/research/brace/projects/womens-health-hubs.aspx (accessed 24 October 2023).
- Primary Care Women’s Health Forum . The Women’s Health Hub Toolkit: Case Studies 2021. https://whh.pcwhf.co.uk/ (accessed 24 October 2023).
- Primary care Women’s Health Forum . The Women’s Health Toolkit: Financial Planning 2021. https://whh.pcwhf.co.uk/ (accessed 24 October 2023).
- Primary Care Women’s Health Forum . The Women’s Health Hub Toolkit: How to Measure Success 2021. https://whh.pcwhf.co.uk/ (accessed 24 October 2023).
- Primary Care Women’s Health Forum . The Women’s Health Hub Toolkit: Training Plan 2021. https://whh.pcwhf.co.uk/ (accessed 24 October 2023).
- Faculty of Sexual and Reproductive Healthcare . Opportunities to Embed Sexual and Reproductive Healthcare Services into New Models of Care: A Practical Guide for Commissioners and Service Providers 2019. http://allcatsrgrey.org.uk/wp/wpfb-file/1fsrh-report-srh-in-new-models-of-care-november-2019-pdf/?utm_source=rss&utm_medium=rss&utm_campaign=1fsrh-report-srh-in-new-models-of-care-november-2019-pdf (accessed 24 October 2023).
- Primary Care Women’s Health Forum . Setting up a Women’s Health Hub in Durham: A Case Study 2021. https://whh.pcwhf.co.uk/ (accessed 24 October 2023).
- Primary Care Women’s Health Forum . Setting up a Women’s Health Hub in Hackney: A Case Study 2021. https://whh.pcwhf.co.uk/wp-content/uploads/2022/05/Setting-up-a-Womens-Health-Hub-in-Hackney-a-case-study.pdf (accessed 24 October 2023).
- Primary Care Women’s Health Forum . Video Resources 2021. https://whh.pcwhf.co.uk/resources/developing-a-womens-health-hub (accessed 24 October 2023).
- Primary Care Women’s Health Forum . An Example of Success from Liverpool 2021. https://whh.pcwhf.co.uk/wp-content/uploads/2022/04/An-Example-of-Success-from-Liverpool.pdf (accessed 24 October 2023).
- Local Government Authority . Collaboration and Cooperation: Sexual and Reproductive Health Commissioning 2019. www.local.gov.uk/publications/collaboration-and-cooperation-sexual-and-reproductive-health-commissioning (accessed 24 October 2023).
- Local Government Association . Liverpool Council: Setting up a Network of Women’s Health Hubs 2022. www.local.gov.uk/case-studies/liverpool-council-setting-network-womens-health-hubs (accessed 5 January 2024).
- Jenkins R. NHS England to Pilot Six Super Hubs Including GPs and Other Health Services 2022. www.pulsetoday.co.uk/news/premises/nhs-england-to-pilot-six-super-hubs-including-gps-and-other-health-services/ (accessed 24 October 2023).
- Erens B, Wistow G, Mounier-Jack S, Douglas N, Jones L, Manacorda T, et al. Early Evaluation of the Integrated Care and Support Pioneers Programme: Interim Report 2015. https://piru.ac.uk/assets/files/Early_evaluation_of_IC_Pioneers_Final_Report.pdf (accessed 24 October 2023).
- Imison C, Naylor C, Maybin J. Under One Roof: Will Polyclinics Deliver Integrated Care?. King’s Fund; 2008.
- Moynihan B, Davis D, Pereira A, Cloud G, Markus HS. Delivering regional thrombolysis via a hub-and-spoke model. J R Soc Med 2010;103:363-9. https://doi.org/10.1258/jrsm.2010.090434.
- Hawkes N. Hospitals without walls. BMJ 2013;347. https://doi.org/10.1136/bmj.f5479.
- Khakwani A, Rich AL, Powell HA, Tata LJ, Stanley RA, Baldwin DR, et al. The impact of the ‘hub and spoke’ model of care for lung cancer and equitable access to surgery. Thorax 2015;70:146-51. https://doi.org/10.1136/thoraxjnl-2014-205841.
- Elrod JK, Fortenberry JL. The hub-and-spoke organization design: an avenue for serving patients well. BMC Health Serv Res 2017;17. www.ncbi.nlm.nih.gov/pmc/articles/PMC5516840/.
- Bostock L, Britt R. Effective Approaches to Hub and Spoke Provision: A Rapid Review of the Literature. Social Care Research Associates; 2014.
- Independent Maternity Review . Ockenden Report – Final: Findings, Conclusions, and Essential Actions from the Independent Review of Maternity Services at the Shrewsbury and Telford Hospital NHS Trust (HC 1219) 2022. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1064302/Final-Ockenden-Report-web-accessible.pdf (accessed 24 October 2023).
- Schäfer WL, Boerma WG, Schellevis FG, Groenewegen PP. GP practices as a one‐stop shop: how do patients perceive the quality of care? A cross‐sectional study in thirty‐four countries. Health Services Res 2018;53:2047-63. https://doi.org/10.1111/1475-6773.12754.
- Dawson S, Callander N, Roche C, Kingsland T, Desmond N. Integrated sexual healthcare: the development and review of one model of service delivery. J Integr Care 2000;4:73-80. https://doi.org/10.1177/146245670000400201.
- UK Gov . Our Health, Our Care, Our Say: A New Direction for Community Services 2006. www.gov.uk/government/publications/our-health-our-care-our-say-a-new-direction-for-community-services (accessed 24 October 2023).
- Hall J, Eisenstadt N, Sylva K, Smith T, Sammons P, Smith G, et al. A review of the services offered by English Sure Start Children’s Centres in 2011 and 2012. Oxford Rev Educ 2015;41:89-104. https://doi.org/10.1080/03054985.2014.1001731.
- Sheaff R, Halliday J, Ovretveit J, Byng R, Exworthy M, Peckham S, et al. Integration and Continuity of Primary Care: Polyclinics and Alternatives: A Patient-Centred Analysis of How Organisation Constrains Care Co-ordination. Southampton: NIHR Journals Library; 2015.
- Tolu LB, Feyissa GT, Jeldu WG. Guidelines and best practice recommendations on reproductive health services provision amid COVID-19 pandemic: scoping review. BMC Publ Health 2021;21:1-10. https://doi.org/10.1186/s12889-021-10346-2.
- Ong JJ, Fairley CK, Fortune R, Bissessor M, Maloney C, Williams H, et al. Improving access to sexual health services in general practice using a hub-and-spoke model: a mixed-methods evaluation. Int J Environ Res Public Health 2022;19.
- French R, Coope C, Graham A, Gerressu M, Salisbury C, Stephenson J. One stop shop versus collaborative integration: what is the best way of delivering sexual health services?. Sex Transm Infect 2006;82:202-6. https://doi.org/10.1136/sti.2005.018093.
- Bowen GA. Sensitizing Concepts. Thousand Oaks, CA: SAGE; 2020.
- Wolfe I, Lemer C, Cass H. Integrated care: a solution for improving children’s health?. Arch Dis Child 2016;101:992-7. https://doi.org/10.1136/archdischild-2013-304442.
- González-Ortiz LG, Calciolari S, Goodwin N, Stein V. The core dimensions of integrated care: a literature review to support the development of a comprehensive framework for implementing integrated care. Int J Integr Care 2018;18. https://doi.org/10.5334/ijic.4198.
- Singer SJ, Kerrissey M, Friedberg M, Phillips R. A comprehensive theory of integration. Med Care Res Rev 2018;77:196-207. https://doi.org/10.1177/1077558718767000.
- Malachowski C, Skopyk S, Toth K, MacEachen E. The Integrated Health Hub (IHH) model: the evolution of a community based primary care and mental health centre. Commun Ment Health J 2019;55:578-88. https://doi.org/10.1007/s10597-018-0339-4.
- Hughes G, Shaw E, Greenhalgh T. Rethinking integrated care: a systematic hermeneutic review of the literature on integrated care strategies and concepts. Milbank Q 2020;98:446-92. https://doi.org/10.1111/1468-0009.12459.
- Heeringa J, Mutti A, Furukawa MF, Lechner A, Maurer KA, Rich E. Horizontal and vertical integration of health care providers: a framework for understanding various provider organizational structures. Int J Integr Care 2020;20. https://doi.org/10.5334/ijic.4635.
- Arnetz BB, Goetz CM, Arnetz JE, Sudan S, vanSchagen J, Piersma K, et al. Enhancing healthcare efficiency to achieve the quadruple aim: an exploratory study. BMC Res Notes 2020;13:1-6. https://doi.org/10.1186/s13104-020-05199-8.
- Maile EJ, Singh R, Black GB, Blair M, Hargreaves DS. Back to the future? Lessons from the history of integrated child health services in England. Future Healthc J 2022;9:183-7. www.rcpjournals.org/content/futurehosp/early/2022/04/14/fhj.2021-0093.full.pdf (accessed 24 October 2023).
- Lewis RQ, Ling T. Integrated care pilots in England revisited. J Integr Care 2019;28:7-13. https://doi.org/10.1108/JICA-05-2019-0016.
- Mantler T, Jackson KT, Ford-Gilboe M. The CENTRAL hub model: strategies and innovations used by rural women’s shelters in Canada to strengthen service delivery and support women. J Rural Commun Dev 2018;13:115-32. https://journals.brandonu.ca/jrcd/article/view/1572/358 (accessed 24 October 2023).
- Baxter S, Johnson M, Chambers D, Sutton A, Goyder E, Booth A. Understanding new models of integrated care in developed countries: a systematic review. Health Serv Delivery Res 2018;6. https://eprints.whiterose.ac.uk/136498/ (accessed 24 October 2023).
- Struckmann V, Leijten FR, van Ginneken E, Kraus M, Reiss M, Spranger A, et al. Relevant models and elements of integrated care for multi-morbidity: results of a scoping review. Health Policy 2018;122:23-35. https://doi.org/10.1016/j.healthpol.2017.08.008.
- Roughead EE, Vitry AI, Caughey GE, Gilbert AL. Multimorbidity, care complexity and prescribing for the elderly. Aging Health 2011;7:695-70. https://doi.org/10.2217/ahe.11.64.
- Pitchforth E, Nolte E, Corbett J, Miani C, Winpenny E, van Teijlingen E, et al. Community hospitals and their services in the NHS: identifying transferable learning from international developments–scoping review, systematic review, country reports and case studies. Health Serv Deliv Res 2017;5:1-220. https://doi.org/10.3310/hsdr05190.
- Salisbury C, Purdy S. Providing care closer to home. BMJ 2007;335. https://doi.org/10.1136/bmj.39371.523171.80.
- Lawrence PR, Lorsch JW. Differentiation and integration in complex organizations. Admin Sci Quart 1967;12:1-47. https://doi.org/10.2307/2391211.
- Stein K, Rieder A. Integrated care at the crossroads: defining the way forward. Int J Integr Care 2009;9. https://pubmed.ncbi.nlm.nih.gov/19513179/ (accessed 24 October 2023).
- Imison C, Naylor C, Maybin J. Under One Roof: Will Polyclinics Deliver Integrated Care?. London: King’s Fund; 2008.
- Imison C, Curry N, Holder H, Castle-Clarke S, Nimmons D, Appleby J. Shifting the Balance of Care: Great Expectations. London: Nuffield Trust; 2017.
- Sidhu M, Pollard J, Sussex J. Vertical Integration of GP Practices with Acute Hospitals in England and Wales: Rapid Evaluation. Southampton: NIHR Health Services and Delivery Research Topic Report; 2020.
- Tsiachristas A, Dikkers C, Boland MR, Rutten-van Mölken MP. Exploring payment schemes used to promote integrated chronic care in Europe. Health Pol 2013;113:296-304. https://doi.org/10.1016/j.healthpol.2013.07.007.
- Stokes J, Checkland K, Kristensen SR. Integrated care: theory to practice. J Health Serv Res Pol 2016;21:282-5. https://doi.org/10.1177/1355819616660581.
- Rocks S, Berntson D, Gil-Salmerón A, Kadu M, Ehrenberg N, Stein V, et al. Cost and effects of integrated care: a systematic literature review and meta-analysis. Eur J Health Econ 2020;21:1211-21. https://doi.org/10.1007/s10198-020-01217-5.
- Looman WM, Huijsman R, Fabbricotti IN. The (cost‐) effectiveness of preventive, integrated care for community‐dwelling frail older people: a systematic review. Health Soc Care Commun 2019;27:1-30. https://doi.org/10.1111/hsc.12571.
- Amado GC, Ferreira DC, Nunes AM. Vertical integration in healthcare: what does literature say about improvements on quality, access, efficiency, and costs containment?. Int J Health Plann Manage 2022;37:1252-98. https://doi.org/10.1002/hpm.3407.
- Sibbald B, McDonald R, Roland M. Shifting care from hospitals to the community: a review of the evidence on quality and efficiency. J Health Serv Res Pol 2007;12:110-7. https://doi.org/10.1258/135581907780279611.
- Peterson K, Anderson J, Bourne D, Charns MP, Gorin SS, Hynes DM, et al. Health care coordination theoretical frameworks: a systematic scoping review to increase their understanding and use in practice. J Gen Intern Med 2019;34:90-8. https://doi.org/10.1007/s11606-019-04966-z.
- Honisett S, Loftus H, Hall T, Sahle B, Hiscock H, Goldfeld S. Do integrated hub models of care improve mental health outcomes for children experiencing adversity? A systematic review. Int J Integr Care 2022;22. https://doi.org/10.5334/ijic.6425.
- Leijten FR, Struckmann V, van Ginneken E, Czypionka T, Kraus M, Reiss M, et al. The SELFIE framework for integrated care for multi-morbidity: development and description. Health Pol 2018;122:12-2. https://doi.org/10.1016/j.healthpol.2017.06.002.
- Van der Klauw D, Molema H, Grooten L, Vrijhoef H. Identification of mechanisms enabling integrated care for patients with chronic diseases: a literature review. Int J Integr Care 2014;14. https://doi.org/10.5334/ijic.1127.
- Primary Care Women’s Health Forum 2023. https://pcwhf.co.uk/ (accessed 24 October 2023).
- Smith J, Ellins J, Sherlaw-Johnson C, Vindrola-Padros C, Appleby J, Morris S, et al. Rapid evaluation of service innovations in health and social care: key considerations. Health Soc Care Deliv Res 2023;11:1-47. https://discovery.ucl.ac.uk/id/eprint/10175896/1/3042650.pdf (accessed 30 October 2023).
- Office for Health Improvements and Disparities n.d. https://fingertips.phe.org.uk/ (accessed 24 October 2023).
- Office for National Statistics . Rural Urban Classification (2011) of Local Authority Districts in England n.d. www.ons.gov.uk/methodology/geography/geographicalproducts/ruralurbanclassifications/2011ruralurbanclassification (accessed 24 October 2023).
- Taylor B, Henshall C, Kenyon S, Litchfield I, Greenfield S. Can rapid approaches to qualitative analysis deliver timely, valid findings to clinical leaders? A mixed methods study comparing rapid and thematic analysis. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-019993.
- O’Cathain A, Murphy E, Nicholl J. Three techniques for integrating data in mixed methods studies. BMJ 2010;341. www.bmj.com/content/341/bmj.c4587.full (accessed 30 October 2023).
- Map Chart n.d. www.mapchart.net/ (accessed 24 October 2023).
- Ghate D. Developing theories of change for social programmes: co-producing evidence-supported quality improvement. Palgrave Commun 2018;4:1-13. https://doi.org/10.1057/s41599-018-0139-z.
- Bradach JL. Going to scale: the challenge of replicating social programs. Stanf Soc Innov Rev 2003:19-25. https://cir.nii.ac.jp/crid/1571135650732253184 (accessed 24 October 2023).
- Braithwaite J, Churruca K, Long JC, Ellis LA, Herkes J. When complexity science meets implementation science: a theoretical and empirical analysis of systems change. BMC Med 2018;16:1-14. https://doi.org/10.1186/s12916-018-1057-z.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13:1-8. https://doi.org/10.1186/1471-2288-13-117.
- Department of Health and Social Care . £7 Billion for NHS and Social Care for COVID-19 Response and Recovery. Press Release 2021. www.gov.uk/government/news/7billion-for-nhs-and-social-care-for-covid-19-response-and-recovery#:~:text=The%20government%20is%20continuing%20to,billion%20to%20%C2%A3136%20billion (accessed 30 October 2023).
- NHS England . Enhanced Access to General Practice Services through the Network Contract DES – Frequently Asked Questions n.d. www.england.nhs.uk/gp/investment/gp-contract/network-contract-directed-enhanced-service-des/enhanced-access-faqs/ (accessed 30 October 2023).
- NHS England . Network Contract Directed Enhanced Service: Additional Roles Reimbursement Scheme Guidance. Guidance 2019. www.england.nhs.uk/publication/network-contract-directed-enhanced-service-additional-roles-reimbursement-scheme-guidance/ (accessed 30 October 2023).
- British Medical Association . Enhanced Services GP Practices Can Seek Funding For. 2021. www.bma.org.uk/advice-and-support/gp-practices/gp-service-provision/enhanced-services-gp-practices-can-seek-funding-for (accessed 30 October 2023).
- Goddard M, Mannion R, Ferguson B. Contracting in the UK NHS: Purpose, Process and Policy. York: University of York; 1997.
- Mann S, Stephenson J. Reproductive Health and Wellbeing: Addressing Unmet Needs. British Medical Association; 2018.
- Wakida EK, Talib ZM, Akena D, Okello ES, Kinengyere A, Mindra A, et al. Barriers and facilitators to the integration of mental health services into primary health care: a systematic review. Syst Rev 2018;7:1-13. https://doi.org/10.1186/s13643-018-0882-7.
- Steele Gray C, Gagnon D, Guldemond N, Kenealy T. Handbook Integrated Care. Cham: Springer; 2021.
- Lanham HJ, Leykum LK, Taylor BS, McCannon CJ, Lindberg C, Lester RT. How complexity science can inform scale-up and spread in health care: understanding the role of self-organization in variation across local contexts. Soc Sci Med 2013;93:194-202. https://doi.org/10.1016/j.socscimed.2012.05.040.
- Greenhalgh T, Papoutsi C. Spreading and scaling up innovation and improvement. BMJ 2019;365. https://doi.org/10.1136/bmj.l2068.
- Baker GR, Shaw J, Steele-Gray C, Commisso E, Rayner J, Wodchis W. Adaptation and standardization of integrated care practices to facilitate scale-up and spread: insights from Ontario case studies. Int J Integr Care 2018;18. https://doi.org/10.5334/ijic.s2170.
- Pavlickova A. Capacity-building assets for integrated care: how to use the existing evidence to accelerate the adoption and scaling-up of integrated care?. Int J Integr Care 2021;21:347-8. https://doi.org/10.5334/ijic.ICIC20207.
- Starling A. Some Assembly Required: Implementing New Models of Care, Lessons from the New Care Models Programme 2017. www.health.org.uk/publications/some-assembly-required-implementing-new-models-of-care (accessed 24 October 2023).
- Hammond J, Lorne C, Coleman A, Allen P, Mays N, Dam R, et al. The spatial politics of place and health policy: exploring sustainability and transformation plans in the English NHS. Soc Sci Med 2017;190:217-26. https://doi.org/10.1016/j.socscimed.2017.08.007.
- Taylor B, Hewison A, Cross-Sudworth F, Morrell K. Transformational change in maternity services in England: a longitudinal qualitative study of a national transformation programme ‘Early Adopter’. BMC Health Serv Res 2022;22. https://doi.org/10.1186/s12913-021-07375-3.
- Marchand C, Peckham S. Addressing the crisis of GP recruitment and retention: a systematic review. Br J Gener Pract: J Royal Coll Gener Pract 2017;67:e227-37. https://doi.org/10.3399/bjgp17X689929.
- Department of Health and Social Care and Maria Caulfield MP . Boost for Women and Girls As Women’s Health Strategy Turns One 2023. www.gov.uk/government/news/boost-for-women-and-girls-as-womens-health-strategy-turns-one (accessed 30 October 2023).
Appendix 1 Qualitative analysis matrix
| Research questions | Domains |
|---|---|
| N/A | Interviewee background |
| 1, 2 | Any description of relevant local context |
| N/A | Regional context |
| N/A | National context |
| 1 | Definition of a WHH |
| 2, 3 | Rationale for WHH set-up, including any local contextual factors |
| 2, 3, 4 | Aim of women’s health hub |
| 2, 3 | How WHHs differ from existing services and fit into the existing landscape |
| 2, 4 | Description of WHH model |
| 2, 4 | General description and implementation story |
| 2, 4 | Population served (all women/subgroups, size, population) |
| 2, 4 | Leadership model |
| 2, 4 | Commissioning approach, funding and resources |
| 2, 4 | Staffing, training, experience needed |
| 2, 4 | The clinic offer (e.g. clinic location, settings, number of sessions, frequency, services offered) |
| 2, 4 | Sectors/services involved in delivery |
| 2, 4 | Typical patient journey (referral, triage, communication, appointment, follow-up) |
| 2, 4 | Links to other parts of the system, links to other hubs or integrated/place-based approaches |
| 2, 5 | Training/development provided for staff working in and outside of hub |
| 3, 5, 6 | How the hub addresses local need/inequalities (planned and in practice, according to women and others) |
| 4, 5 | What is going well/facilitators to set-up and delivery |
| 4, 5 | What is going less well/barriers to set-up and delivery |
| 4, 7 | Intended and actual impact of hub (including referral numbers, costs, outcomes, inequalities) –what has been achieved/what hasn’t? |
| 4, 7 | How intended and actual impact is measured now and in the future (including referral numbers, costs, outcomes, inequalities) |
| 4, 6 | Women’s description of what services accessed, referral and communication processes, follow-up |
| 4, 5, 6 | Experiences of using the hub – what was good and what difference did it make |
| 4, 5, 6 | Facilitators and barriers to using hub services |
| 4, 5, 6 | What could be improved about hubs, what services are/could be offered and any reflections on wider education/information. |
| 4, 6 | Women’s awareness and perceptions of hubs and the hub model |
| 4, 6 | What women think women’s services should offer |
| 4, 5 | Hub staff experiences and perceptions of working in the hub, including service delivery (e.g. referral, services offered), what is good/could be improved |
| 4, 5 | Non-hub staff awareness, experiences and perceptions of the hub/working with the hub, including what services are/could be offered, how referral works and what is good/could be improved |
| 1, 2, 3 | The role of policy, key organisations (e.g. Primary Care Women’s Health Forum, RCOG, FSRH) evidence in driving hub implementation, and alignment of practice with policy. |
| 2, 4, 5 | The future and sustainability of hubs |
| N/A | Integrating care (reflections and practical examples) |
| 5, 7 | Advice to others |
| N/A | Other points |
Research questions:
-
What are WHHs, and is there variation in how stakeholders name and define them?
-
How many WHHs have been established or are in development across the UK, where are they and what are their characteristics, including models of structure, commissioning and delivery?
-
Why have WHHs been implemented, and how are they intended to address health inequalities?
-
What have WHHs achieved to date? How do WHHs achieve this?
-
What are the experiences and perspectives of staff regarding WHH set-up, commissioning, funding, implementation and delivery?
-
What are the experiences and perspectives of women who have used hub services?
-
How are WHH performance, outcomes and costs measured, and how might they be measured in future?
Appendix 2 Hub summaries
Bexley and Greenwich
Launch year: 2022. The service was built on existing gynaecology/SRH services in the area.
Rationale for launching hub and objectives: Need for services to be provided in one location, reduced delays in accessing care, reduced referrals to secondary care.
Population covered: All women in the area.
Services offered: Hub services offered in two Community practices in community NHS Trust. Services include LARCs (for contraception and gynaecology), emergency contraception, other contraception advice/provision, cervical screening, heavy menstrual bleeding consultation and treatment, dysmenorrhoea consultation and treatment, menopause consultation and treatment, STI screening and treatment, women’s health counselling and psychology, ultrasound scanning, assessment of incontinence and/or prolapse, medical treatment of incontinence, pessary fitting and removal, termination of pregnancy assessment, vulva clinics, minor procedures. Women are able to see more than one healthcare professional in the same visit. Appointments can be in person or by phone and are offered in evenings and weekends.
Organisations involved: All practices in the area refer into the hub, two Community practices provide hub services, one CCG/ICS, two local authorities, one NHS acute trust, one NHS community trust.
Model: Hub-and-spoke, one-stop shop.
Leadership structure: SRH consultant-led.
Commissioning arrangements: Multiple commissioners involved (local authority and CCG).
Contracting arrangements: Direct contract with ICS and local authority.
Patient pathway: Referrals to the hub come from GPs. Complex referrals are triaged by a senior clinician.
Workforce: One community SRH consultant (1 FTE), one community gynaecologist (0.6 FTE), four GP trainees (2 FTE), one integrated sexual health specialty doctor (1 FTE), nine specialist nurses (FTE not provided), three healthcare assistants (3 FTE), one counsellor (0.5 FTE), eight administrators (8 FTE), one data analyst (1 FTE).
Staff training: Yes, for example a general training programme for FSRH/BASHH and BMS (topics not specified).
Performance and monitoring: Currently in place: number of clinics delivered, number of women attending, LARC fitting rates, patient experience feedback and budget/spend. Future aspiration: waiting times between referral and appointment, number of referrals to secondary care, hub staff experience/feedback, local non-hub staff experience/feedback and GP training/upskilling numbers.
How inequalities are addressed: Taking part in public health listening exercises.
Birmingham
Launch year: 2016.
Rationale for launching hub and objectives: Initially the hub was set up as a pilot as part of the NHS 5-year forward view. The aim was to reduce unnecessary secondary care referrals, provide care closer to home and integrate primary and secondary care.
Population covered: > 100,000, no restrictions and accept referrals from across the city and surrounding areas.
Services offered: Hub services offered in four sites (GP practice and pharmacy). Offering 800–100 appointments per month. Services include LARC fitting/removal for contraception, gynaecological reasons, emergency contraception, contraception advice, provision of cervical screening, heavy menstrual bleeding consultation and treatment, dysmenorrhoea consultation and treatment, menopause consultation and treatment, STI screening and treatment, women’s health counselling and psychology, ultrasound scanning, hysteroscopy, assessment and treatment of incontinence and/or prolapse, pessary fitting and removal, vulva clinics, minor procedures, for example polypectomy, vulval/pipelle biopsy. Women are not able to see more than one healthcare professional in the same visit. Appointments can be by phone or in person. Appointments are offered at the weekend.
Organisations involved: Large GP Partnership (Modality) and local NHS trusts (Sandwell and West Birmingham and UHB) contracting organisation.
Model: ‘Hub-and-spoke’. Central referral and triage system, with ’spoke’ clinics in four locations.
Leadership structure: Clinical lead for the service is a GPwSI in Women’s Health, accountable to a Medical Director and Governance Team within Modality. Modality community services has an Executive team as well as a Board team. Clinical oversight from consultant gynaecologist.
Commissioning arrangements: Commissioned by NHS Trust.
Contracting arrangements: Service is subcontracted by Sandwell and West Birmingham NHS Foundation Trust and University Hospital Trust Birmingham (secondary care).
Patient pathway: Women are referred by GP through electronic records system. GP or nurse triages within 5 days. Direct subspecialty appointments for menopause, urogynaecology and endometriosis.
Workforce: GP clinical lead. Team of 4 GPSIs, 2 nurses, 10 consultants and a GP trainee, administrators (6 WTE). Pool of HCAs dedicated to supporting all outpatient services including Gynaecology and Contraception. Shared resources across all services that Modality Gynaecology and contraception team use: Administration Team Leads, ICP Nurse, Estates compliance officer, data analysts, IT and also directors – managing, finance, commercial, medical.
Staff training: Support primary care professionals training to become GPSIs/nurses with specialist interest. Staff complete external postgraduate diploma in women’s health plus in-house training, competency framework and sign-off.
Performance and monitoring: Currently in place: attendance figures, waiting times, LARC fitting rates, secondary care referral rate, patient and staff experience, financial performance.
How inequalities are addressed: Service delivered from sites that are easy to reach with good transport links, changed in response to demand, DNA rates and feedback of patients. The team is exploring delivering information in different languages/formats.
Durham North
Launch year: The hub was a provider-initiated service set up in the early 2000s as the lead GP had the passion, expertise and desire to offer more women’s health services locally. A broad range of services are offered, although much of the current demand is focused on menopause. Due to a loss of GP skills from retirement, since the pandemic many local GP practices have opted not to offer LARCs for contraception, which created additional pressure on the hub. Therefore, in 2022, another local GP with special interest in women’s health set up satellite LARC clinics for contraception only to reduce pressure on the hub, allowing the hub to focus on the more complex cases it is intended to support (this LARC-only service is not included in this summary or wider analysis).
Rationale for launching hub: Passionate and experienced local GP who wanted to set up additional women’s health services in the area.
Population covered: All women in the footprint of what was North Durham CCG.
Services offered: Services include LARCs for gynaecological and contraception reasons, heavy menstrual bleeding consultation and treatment, menopause consultation and treatment, pessary fitting and removal, assessment of incontinence and/or prolapse, minor procedures (e.g. polypectomy). Much of the demand is currently focused on menopause. Women are not able to see more than one healthcare professional in the same visit (as there is only one healthcare professional working in the hub). Appointments are mostly in person with some phone appointments also possible. Appointments are not offered out-of-hours.
Organisations involved: two GP practices providing hub services (lead GP rents a room to offer services out of these practices), one CCG/ICS.
Model: One-stop shop.
Leadership structure: GP-led.
Commissioning arrangements: Commissioned by CCG only.
Contracting arrangements: Contract direct with CCG.
Patient pathway: GP practices across the area refer patients to one of the two GP practices the lead GP operates out of (the patient chooses which practice to attend). Admin team have a booking system to book patients in directly to see the hub GP.
Workforce: one GP with special interest in women’s health, one nurse, three admin staff.
Staff training: Yes, for example training for nurse staff, GP and nursing students observe hub clinics.
Performance and monitoring: Report key performance indicators to CCG, including service user feedback, waiting times, DNA rates, types of clinical conditions seen in clinic.
How inequalities are addressed: The two practices the services are offered in are located in deprived areas (outside of the city centre). One of the practices used to be based in a more affluent area but uptake was low due to difficulty accessing the practice, so it was moved to a practice in a more deprived area. Staff can arrange for an interpreter to be present if needed.
Eastern Region Northern Ireland
This response covers the Eastern Federation area – Belfast and South East.
Launch year: 2017; the hubs are regional across Northern Ireland and have been rolled out in different trusts at different time points.
Rationale for launching hub and objectives: To improve access to services and primary care management for women, reduce secondary care referrals and offer training.
Population covered: All women in the area (specific focus on vulnerable groups). Covers Eastern Federation.
Services offered: Services are offered in nine GP practices. Services include LARCs for contraception and gynaecology, heavy menstrual bleeding consultation and treatment, menopause consultation and treatment and pessary fitting/removal. Women are not able to see more than one healthcare professional in the same visit. Appointments can be face to face or by phone. Appointments are offered in evenings.
Organisations involved: GP practices across the federations refer in; nine practices provide hub services across eight GP federations.
Model: One-stop shop.
Leadership structure: GP-led.
Commissioning arrangements: Commissioning arrangement between the Strategic Planning and Partnership Group (SPPG) (previously the Health and Social Care Board) and Federation Support Unit.
Contracting arrangements: Referring practices are contracted through a Local Enhanced service to fund the GP federations to deliver.
Patient pathway: Patients referred by their GP. All referrals are triaged by GPs with enhanced skills working in the hubs.
Workforce: Nineteen GPs with special interests in women’s health, one or two healthcare assistants per hub, at least one administrator per hub.
Staff training: Yes, for example pessary training, training for letters of competence in intrauterine techniques or subdermal contraceptive implants.
Performance and monitoring: Currently in place: number of clinics delivered; number of women attending; waiting times between referral and appointment; LARC fitting rates; number of referrals to secondary care; patient experience feedback; GP training/upskilling numbers; budget/spend.
How inequalities are addressed: Vulnerable groups of women are prioritised in provision of LARC (e.g. non-English speakers, sex workers, homeless and other vulnerable women). They also provide rapid access for women who wish to discontinue a LARC if planning a pregnancy.
Guildford and Waverley
Launch year: Launched in pilot in 2014 and moved to a core service in 2017.
Rationale for launching hub and objectives: Knowledge that many gynaecology referrals to secondary care can be effectively treated in the community or primary care by a GP with special interest.
Population covered: All women in the area, covering a population of over 100,000.
Services offered: Hub services offered in one GP surgery. Started as a focus on irregular bleeding before expanding to other services. Services now include LARCs for contraception and gynaecology, heavy menstrual bleeding consultation and treatment, dysmenorrhoea consultation and treatment, menopause consultation and treatment, women’s health counselling and psychology (psychosexual counselling), ultrasound scanning, pessary fitting/removal, vulva clinics and minor procedures. Women are not able to see more than one healthcare professional in the same visit. Appointments can be face to face, by phone and by video. Appointments are offered slightly outside of usual hours (8.30 a.m. to 6.30 p.m.).
Organisations involved: Twenty GP practices referring in, one GP practice offering hub services, four PCNs, one CCG/ICS, one local authority, one NHS acute trust.
Model: One-stop shop.
Leadership structure: GP-led.
Commissioning arrangements: Commissioned by CCG only.
Contracting arrangements: Contract via secondary care provider.
Patient pathway: Patients referred by their GP into the central referral system. All gynaecology referrals are triaged by a nurse and/or GP in the hub to determine if the patient can be seen in the hub or referred on to the hospital.
Workforce: Three GPs (0.8 FTE), one practice nurse (0.2 FTE), one healthcare assistant (0.5 FTE), three admin staff (0.6 FTE).
Staff training: Yes, for example newly qualified GP as part of an external training scheme to become a GP with special interest; local GPs, hospital trainees and GP trainees can observe hub clinics; coil training for GPs who have formal qualifications but would like to develop their confidence or to train in offering cervical blocks.
Performance and monitoring: Currently in place: number of clinics delivered; number of women attending; waiting times between referral and appointment; number of referrals to secondary care; patient experience feedback; budget/spend.
How inequalities are addressed: Offering gynaecology care to patients in more rural areas and by offering a more holistic service.
Hackney
Launch year: In 2021, the community gynaecology services expanded to provide hub services across a PCN, and via online engagement events and consultations, on a pilot basis. The following year, a second PCN was brought into the model and a hotline was set up for clinicians to have a direct line to guidance and support for women’s health by speaking with a specialist in the hub.
Rationale for launching hub and objectives: Key drivers were an increasing demand, new technology and patient expectations, the need to reduce inequalities in outcomes and experience and the need to reduce hospital-based care. The hub aims to implement more equitable care, closer to home. It intends to reduce geographical and socioeconomic variation. This includes variation in GP referral rates to community gynaecology services and variations in GP skills and expertise in women’ health across practices and PCNs.
Population covered: City and Hackney (population approx. 270,000), with a population size serviced by each PCN hub of approx. 30,000–50,000.
Services offered: The tripartite model approach offers direct service provision to patients, virtual group consultations and engagement events, and delivers practitioner support and education. A range of gynaecological services are offered, including LARC, cervical screening, menopause, STI screening, pessary fitting and a vulval clinic. There are plans for contraception to be formally added to the hub offer. The hub has procedures clinics for more specialist, intermediate care (including LARC fitting).
Organisations involved: Community gynaecology service and two PCNs, with three GP practices providing PCN hub services.
Model: Hub-and-spoke, and virtual.
Leadership structure: Women’s health/SRH consultant-led.
Commissioning arrangements: Commissioned by ICB (then CCG) on an annual basis (as a rolling pilot).
Contracting arrangements: None that are formal, but there are plans to joint-commission with the local authority.
Patient pathway: Referrals to the hub come from GPs, but patients can ’self-refer’ to online engagement events (on receiving a text from their GP with a link to join) and online group consultations.
Workforce: Two community SRH Consultant/public health consultants (1 FTE), one community SRH associate specialist (0.4 FTE), one community SRH trainee (0.2 FTE), one GP with special interest in women’s health (0.5 FTE), one healthcare assistant (0.5 FTE), one project manager (0.5 FTE).
Staff training: Yes; the hub has a developed a set of local competency-based standards and facilitates the training of individual GPs and practice nurses outside of the hub.
Performance and monitoring: A large number of KPIs are being collected, which include data on clinics, referrals and appointments (e.g. inward and onward referrals into the hub), proximity of home address to the clinic or time to get to the clinic and change in rate of GP visits. Outcomes are also collected specifically on the virtual group consultations, such as number in attendance, satisfaction and resulting behaviour change, patient well-being. They are also collected for the clinician outcomes from education and include measures of change in competence and satisfaction.
How inequalities are addressed: The focus of hub activities is to improve access to expertise for women across a footprint, and to provide options to women as to where and how they engage, learn and receive care for women’s health (face to face, online and in a number of venues). The PCN model aims to reduce the barrier of travel by making clinics more accessible (reducing need to travel to a single centre). There is an ‘inequalities lead’ for the site, and a project manager, who support the hub to collect appropriate data to measure inequalities and design projects to address them.
Hampshire and Isle of Wight
Launch year: Initial 7-month pilot in a PCN, started in 2022. Service has since expanded to be offered in 5 of the 10 Hampshire PCNs. Working group meeting in April 2023 will further develop future plans for the hub with ICB input.
Rationale for launching hub and objectives: A review of a local educational programme highlighted the benefit of collaborative working across services. Desire to upskill local GPs.
Population covered: All women in the area, covering a population of 50,000–99,999.
Services offered: Currently at the early stage of development where the hub is currently offering MDT discussion of cases which are then referred to specialist GPs. Services offered are LARCs (for contraception and gynaecological reasons), emergency contraception, other contraception advice and provision, cervical screening, heavy menstrual bleeding consultation and treatment, dysmenorrhoea consultation and treatment, menopause consultation and treatment, STI screening and treatment, women’s health counselling and psychology, fertility services, assessment of incontinence and/or prolapse, medical treatment of incontinence, pessary fitting and removal, termination of pregnancy assessment.
Organisations involved: Organisations involved are GP practices providing hub services, PCNs, NHS acute trusts and NHS community trusts.
Model: Virtual (at the current early stages of development).
Leadership structure: GP-led.
Commissioning arrangements: There are no formal commissioning arrangements in place.
Patient pathway: GPs collate cases for discussion at hub multidisciplinary team meetings, after which women are referred to specialist GPs (with input from acute or community trust staff) for ongoing care. Referrals to the hub are not triaged.
Workforce: Two hospital gynaecology consultants, two community SRH consultants and four GPs with special interest in women’s health.
Staff training: Yes, for example SRH and menopause training. One of the key aims of the hub is to upskill local GPs.
Performance and monitoring: Metrics to collect were being decided on at the time of data collection. During the pilot, treatment and care outcomes were compared to before the pilot was introduced.
Haringey and Islington
NB: This summary has not been reviewed by the site lead.
Launch year: Launched hub services in different venues in stages, starting in 2017, with the most recent being summer 2021 to add another secondary care venue.
Rationale for launching hub and objectives: Greater collaboration, connection and learning between primary and secondary care, support women to access the right care at the right time and place, greater utilisation of non-gynaecology community clinics, reduce backlog in secondary care.
Population covered: All women in the area, covering a population of 100,000+.
Services offered: Hub services offered in three community gynaecology service venues and two secondary care sites. Services include LARCs for gynaecology, other contraception advice/provision, cervical screening, heavy menstrual bleeding consultation and treatment, dysmenorrhoea consultation and treatment, menopause consultation and treatment, women’s health counselling and psychology, ultrasound scanning, assessment of incontinence and/or prolapse, medical treatment of incontinence, pessary fitting and removal, vulva clinics, minor procedures. Women are not able to see more than one healthcare professional in the same visit. Appointments can be in person or by phone.
Organisations involved: Eighty-five GP practices refer into the hub, eight PCNs, one CCG/ICS, two local authorities, three NHS acute trusts, one NHS community trust.
Model: One-stop shop.
Leadership structure: GP-led.
Commissioning arrangements: Commissioned by CCG only.
Contracting arrangements: Block contract with pooled budget.
Patient pathway: GP practices refer all gynaecology referrals to central system. Patients are triaged by GPs with special interest in women’s health and accepted to the hub, referred to secondary care or referred to another community clinic.
Workforce: Three hospital gynaecology consultants (40%), 1 community SRH consultant (12.5%), 12 GPs with special interest in women’s health (2.5 FTE) and 3 healthcare assistants (1.5 FTE).
Staff training: Yes, for example menopause further education, vulval clinic training.
Performance and monitoring: Currently in place: number of clinics delivered, number of women attending, waiting times between referral and appointment, LARC fitting rates, termination of pregnancy rates, number of referrals to secondary care, patient experience feedback, local non-hub staff experience/feedback, budget/spend. Future aspiration: hub staff experience/feedback.
How inequalities are addressed: Use of language interpreters, incorporating feedback from patients, lay individuals attending clinical governance meetings.
Hertfordshire
NB: This summary has not been reviewed by the site lead.
Launch year: Not provided.
Rationale for launching hub: A review of a local educational programme highlighted the benefit of collaborative working across services.
Population covered: Not provided.
Services offered: Not provided.
Organisations involved: four GP practices (not stated if referring or providing practices), one CCG/ICS, one local authority.
Model: Not provided.
Leadership structure: Gynaecology consultant-led.
Commissioning arrangements: Commissioned by CCG only.
Contracting arrangements: Locally Enhanced Service.
Patient pathway: Not provided.
Workforce: Seventeen hospital gynaecology consultants, three GPs with special interest, one admin staff. FTEs not provided.
Staff training: Yes, for example information and support for local GPs (particularly for complex HRT).
Performance and monitoring: Not provided.
How inequalities are addressed: Not provided.
Timeline of hub set-up and development: Not provided.
Leicester
Launch year: Initially one clinician offering LARC and gynaecology services to local GPs, with a second GP added to offer additional LARC services. Initially covered one PCN area and now expanding into a second. Hub started as a pilot in 2020 which was due to come to an end in Spring 2023 (work was under way to secure continuity of the service).
Rationale for launching hub and objectives: Waiting lists were very long to access secondary care gynaecology and menopause care (putting pressure on primary care). Primary care provision of menopause/HRT was limited and sexual health services were struggling to provide adequate LARC services. Lack of co-ordination of women’s health provision across the area or services out of regular working hours. Clinicians lacked knowledge about menopause care (at a time when many women were seeking support for this).
Population covered: All women in the area (Leicester, Leicestershire and Rutland), covering a population of < 50,000 patients.
Services offered: Hub services are offered out of two GP practices (one LARC services only, the other LARC and non-LARC services). Services include LARCs for contraception and gynaecology, ultrasound scanning, pessary fitting, cervical screening, heavy menstrual bleeding consultation and treatment, dysmenorrhoea consultation and treatment, menopause consultation and treatment, assessment of incontinence and/or prolapse, medical treatment of incontinence, pessary fitting and removal and minor procedures, for example polypectomy, vulval/pipelle biopsy. Women are not able to see more than one healthcare professional in the same visit. Appointments can be face to face and by phone. Appointments are offered in evenings and weekends.
Organisations involved: Eighteen GP practices referring to the hub, two PCNs, two local authorities, one CCG/ICS, one private-sector organisation.
Model: Two clinicians travelling out to GP practices.
Leadership structure: (Former) GP-led.
Commissioning arrangements: No formal commissioning arrangements in place.
Contracting arrangements: Contract with local authority to provide LARC services. No contracts in place for other services.
Patient pathway: GPs and physician associates can book in a patient for hub consultations themselves. Women are also able to self-refer. Patients are not triaged before booking an appointment.
Workforce: Two GPs, one admin staff, one advanced nurse practitioner.
Staff training: Yes, for example coil-fitting training, ultrasound scanning training.
Performance and monitoring: Currently in place: number of clinics delivered; number of women attending; waiting times between referral and appointment; LARC fitting rates; number of referrals to secondary care; budget/spend.
How inequalities are addressed: Referrals via GP practice supports more equal access as the onus is not on the patient to find the service themselves. High numbers of students in the area who are a vulnerable group, support offered by, for example, talks on abnormal bleeding and highlight of low LARC rates for staff at practice with high proportion of students. Hub covers a deprived area of Leicester city, with local women who face language and cultural barriers to accessing care. The hub actively reaches out to these women (and books hub appointments) via over-40s health checks.
Liverpool
Launch year: Pilot in 2019, formal launch in 2020 in first Primary Care Network (PCN) (gradual expansion).
Rationale for launching hub and objectives: Improve access and uptake of LARC, increase equity across the city, provide services to women who couldn’t access in their own GP practice, provide and reimburse LARC for any reason.
Population covered: All women in the city can access as one PCN hub offers citywide service. Hubs and clinics currently located in six of nine PCNs in the city.
Services offered: Hub clinics in GP practices in each PCN. Services include mostly LARCs (coils/implants) for both contraceptive and gynaecological reasons such as heavy menstrual bleeding, endometrial protection for HRT and painful periods. Some opportunistic smear tests, STI screening, menopause advice and pessary fitting (not part of the core offer but commissioning arrangements). Plans to expand the offer. Appointments include telephone and in-person clinics. Appointments are not offered in evenings or weekends.
Organisations involved: PCN-level model, delivered in primary care. LARC clinics in GP practices in each PCN. Other organisations involved local SRH service (refers women, trains LARC fitters, provides STI testing pre-LARC fitting); local authority (commissioning lead); local Women’s Hospital (provides training and advice to hub clinicians).
Model: Hub-and-spoke PCN-level inter-practice referral model (GP practices refer to their PCN hub). One hub offers citywide referral. PCN hubs operate independently (no formal citywide structure).
Leadership structure: Each PCN model manages its own service with GP hub lead in each PCN. Citywide GP lead who provides support and oversight (currently not a formal governance arrangement of funded post).
Commissioning arrangements: Commissioned through local authority Locally Enhanced Service.
Contracting arrangements: Locally Enhanced Service for LARCs, recent agreement to set up additional arrangement for pessaries.
Patient pathway: Most women are referred by their GP. Some referred by SRH service, as an alternative choice for LARC. One PCN accepts online self-referrals from anywhere in the city, but others offer to women in their own PCN.
Workforce: North Liverpool PCN, two GPs, two nurse associates; SWAGGA PCN, three GPs, one care co-ordinator/HCA; iGPC PCN, four GPs, one care co-ordinator; Central PCN, four GPs, one care co-ordinator; Picton, one pharmacist, one physician’s associate; Childwall/Wavertree PCN, three GPs, one care co-ordinator.
Staff training: Some clinicians working in hubs train other professionals. Women’s Health Forum and a separate Fitter Forum, regular newsletter, resources/tools, events and communications. LARC fitting training pathway streamlined and shared widely. Lapsed/current fitters have been mapped to identify and address gaps.
Performance and monitoring: Currently in place: Claims for LARC procedures (implants, IUD/IUS) in hubs, and citywide. Future aspiration: measurement of impact on inequalities, termination rates.
How inequalities are addressed: Clinic venues focus on higher-need/deprived locations. Working with ICB Inequalities Lead and Gynae Network to plan work to expand model.
Manchester
There are two services provided seamlessly at the hub – a community gynaecology service and a Level 3 (L3) contraception service.
Launch year: The L3 contraception service has been provided for decades; the community gynaecology service was launched in 2006. The two services were brought together by moving into a new building, the Withington Community Hospital.
Rationale for launching hub and objectives: To provide gynaecological care closer to home for patients and to help with reducing pressures on secondary care waiting lists. To provide, support and manage women with contraception and complex contraception needs.
Population covered: For community gynaecology, women in south and central Manchester PCNs, covering a population of 353,666 (persons), 179,526 (females). The service will see women from the north of Manchester, as/if appropriate/needed. Women from Manchester and Trafford are able to access the L3 contraception service [786,933 (population footprint), 398,520 (females)]; in addition, 20% of activity is generated from women in Greater Manchester.
Services offered: Hub services offered in Withington Community Hospital, with nine sites for contraception/sexual health services as well as clinical and educational outreach. Services include LARCs for contraception and gynaecology, emergency contraception, other contraception advice and provision, complex contraception and complex LARC procedures, cervical screening, heavy menstrual bleeding consultation and treatment, menopause consultation and treatment, STI screening and treatment, women’s health counselling and psychology (psychosexual), pregnancy advice and referral, pre-conception counselling, ultrasound scanning, assessment of incontinence and/or prolapse, medical treatment of incontinence, pessary fitting/removal, vulval dermatology clinics, medical management of polycystic ovary syndrome. Appointments can be face to face or by phone.
Organisations involved: For community gynaecology – all south and central Manchester GP practices referring in, one NHS trust, one local authority, one ICS. For the L3 service – nine sites offering services, one NHS trust, referring organisations (e.g. GP practices), one ICS. This service includes Greater Manchester so covers local authorities across this area.
Model: One-stop shop primarily based in Withington for community gynaecology. For the L3 service, there are multiple sites (5 hubs open 5–6 days a week, 10 sites in total).
Leadership structure: SRH consultant-led, providing governance, training including for primary care and CSRH and managing complex work including referrals from primary and secondary care.
Commissioning arrangements: Mixed commissioning. Parts of the service separately commissioned: community gynaecology is commissioned by CCG/ICB commissioners and L3 contraception is commissioned by local authority commissioners, though all came under Manchester Health and Care Commissioning, now ‘Greater Manchester Integrated Care Partnership’ (Greater Manchester ICP).
Contracting arrangements: Two block contracts (one for each service)
Patient pathway: For community gynaecology, patients are referred by their GP, which goes into the care gateway system. All referrals are triaged by either GPs with special interest in gynaecology or the lead clinician. New to follow-up ratio is high; most patients are seen and managed at their first visit. Patient-initiated follow-up is in place. For L3 contraception, patients can refer themselves, but GPs and other healthcare professionals, for example pharmacists, obstetric consultants, can also refer, for example, urgent cases and routine complex cases.
Out of hours: Some specialist procedures, for example coil procedures and implant clinics offered on a Saturday, as well as routine contraception. Most L3 locations have evening opening.
Workforce: Consultants, specialty doctors, GPs, nurses, nursing/healthcare assistants, administrative staff as well as trainees (e.g. specialities in CSRH, GUM as well as GP trainees).
Staff training: Yes, for example in-house staff and medical student training, LARC fitter forums, updates provided around the menopause and contraception, FSRH training including specialty training programme, medical students and GPs can observe clinics, essentials course for primary care colleagues and GP and nurse training around menopause and LARC.
Performance and monitoring: Currently in place for community gynaecology include number of clinics delivered; number of women attending; waiting times between referral and appointment; number of referrals to secondary care; patient experience feedback; hub staff and local non-hub staff experience feedback; budget/spend.
Similar metrics in place for L3 contraception include number of attendances; number of face-to-face and phone consultations; LARC fitting rates; LARC waiting times; LARC and specialist clinic waiting times; patient experience feedback; budget/spend.
How inequalities are addressed: Offering gynaecology care to patients in south and central Manchester and plans to expand. Use of interpreters when required. Screening for domestic violence. The L3 contraception service work in the community with outreach teams, and self-referral is accepted. Access versus population profile (e.g. postcode and demographics) is monitored. They also work with, and support, organisations such as My Body Back.
Websites:
Newcastle
Launch year: 2001 but with major changes in 2012 with changes in commissioning.
Rationale for launching hub and objectives: There was a local health need, with long waits to be seen in gynaecology and local interest from GPs and SRH consultants.
Population covered: All women in the area (no population size provided) across Newcastle upon Tyne, North Tyneside and Northumberland until 2012. Since then via Choose and Book across the region.
Services offered: Currently services are offered in a contraception and sexual health clinic central base, and Newcastle GP practices and pharmacies provide emergency contraception, implants and intrauterine contraception and DIY STI kit distribution. Hub services include LARCs for contraception, emergency contraception, other complex contraception advice and provision, cervical screening, STI screening and treatment, management of HIV, women’s health counselling and psychosexual counselling. LARCS for gynaecological indications, medical gynaecology consultation and treatment including heavy menstrual bleeding, PMS and menopause including ultrasound scanning on site and minor procedures with referral via Choose and Book. Deep implant removal service for the NE region referral via Choose and Book for those living outside Newcastle. All appointments can be face to face, by phone or by online. Appointments are not offered in evenings or weekends.
Organisations involved: Regional GP practices refer in the contraception and sexual health central clinic. Newcastle GP practices have inter-practice referral pathways plus refer to the contraception and sexual health central clinic and pharmacies providing elements of care, one local authority, one acute trust.
Model: One-stop shop, virtual.
Leadership structure: SRH consultant-led.
Commissioning arrangements: Contraception and sexual health service is currently commissioned by local authority only. There are plans for a move to co-commissioning with the ICB from 2023 to extend services into primary care, initially for contraception/sexual health and LARCs for all indications. The CCG/ICB commissions the community gynaecology service, via gynaecology in the hospital trust.
Contracting arrangements: Contraception and sexual health service holds a contract with the local authority for contraception and sexual health. Service going out to contract in 2023. Direct contract with primary care. Newcastle GP practices and pharmacies are subcontracted to provide elements of service (emergency contraception, intrauterine contraception, implants and DIY STI kit distribution). The CCG/ICB contracts the community gynaecology service.
Patient pathway: Patients are referred by primary, secondary and tertiary services for specialist clinics (community gynaecology) via Choose and Book. Patients can self-refer for STIs and contraception. Referrals are triaged daily by two SRH consultants and a CSRH registrar.
Workforce: One community gynaecologist (0.6 WTE), one sexual and reproductive heath consultant (0.8 WTE) one CSRH trainee (0.8 WTE), GPs, practice nurses in practices.
Staff training: Yes, for example FSRH training including LARCS, menopause training, BASSH STI training.
Performance and monitoring: Currently in place: number of clinics delivered; number of women attending; waiting times between referral and appointment; LARC fitting rates; termination of pregnancy rates.
How inequalities are addressed: Face-to-face interpreters provided including signing for the deaf. Learning disabilities nurse supporting referred patients to the contraception and sexual health central clinic. Outreach nurse service to hostels.
Northern region, Northern Ireland
Launch year: 2019; the hubs are regional across Northern Ireland and have been rolled out in different trusts at different time points.
Rationale for launching hub and objectives: A scoping exercise was undertaken to understand the need. There was less access to family planning clinics, fewer GPs were providing services in-house and there were long waiting times for secondary care.
Population covered: All women in the area, covering a population of over 100,000. Covers Northern Trust area.
Services offered: Hub services offered in four GP practices. Services include LARCs for contraception and gynaecology, assessment of incontinence and/or prolapse, menopause consultation and treatment and pessary fitting/removal. Women are not able to see more than one healthcare professional in the same visit. Appointments can be face to face or by phone. Appointments are not offered in evenings or weekends.
Organisations involved: GP practices across the federations refer in; four GP practices provide hub services across four GP Federations and BSO Board. There are 17 GP federations and 18 hubs across Northern Ireland.
Model: Hub-and-spoke.
Leadership structure: GP-led.
Commissioning arrangements: Multiple commissioners involved (local authority and local commissioning group).
Contracting arrangements: Locally enhanced service contract.
Patient pathway: Patients referred by their GP using an electronic referral to the host practice. All referrals are triaged by GPs with enhanced skills in host practices.
Workforce: Eight GPs with special interests in women’s health, one practice nurse, four healthcare assistants, four administrators and four practice managers.
Staff training: Yes, for example training for GPs with enhanced skills for pessaries, GP, trainee and nurse training in letters of competence in intrauterine techniques or subdermal contraceptive implants.
All GPs have opportunities to attend educational events paid for by the FSU. During the past year they have attended the Primary Care Women’s Health Forum conferences, Faculty of Sexual and Reproductive Health and British Association for Sexual Health and HIV conferences, the British Menopause Society menopause café Hot Topics, and own in-house educational meetings on the menopause, Significant Event Analysis and clinical governance. Across Northern Ireland, a series of treatment guidelines were developed for practices alongside a series of webinars, which contribute to CPD, to upskill and support primary care in diagnosing and managing common conditions. The service also focuses on continued professional development.
Performance and monitoring: Currently in place: number of clinics delivered; number of women attending; waiting times between referral and appointment; LARC fitting rates; number of referrals to secondary care; patient experience feedback; GP training/upskilling numbers; budget/spend. All practices have received updated SOPs and have undergone or are undergoing clinical governance visits.
How inequalities are addressed: Answer not provided.
Sheffield
Launch year: Sheffield County Council ceased contracting with provider of integrated health services, GPs and community pharmacies in 2019 in favour of setting up a new service based on population health needs assessment. The new model consisted of two aspects: specialist integrated SRH services, and community SRH and gynaecology services. The contract was awarded in 2019 for 5 years with the opportunity to extend to 10.
Rationale for launching hub: Need for better access to care, low LARC uptake, lack of pathway for emergency IUD fitting, need for more integrated community gynaecology and SRH services, high referrals to secondary care, need for greater resilience in SRH workforce, changing demographics (higher student and migrant population), reduction in specialist SRH clinics and budget and long travel needed to access care.
Population covered: All women in the area, covering a population of over 100,000.
Services offered: Services are offered in six community hubs delivered via GP practices. Services include: LARC for contraception and gynaecology, emergency contraception, other contraception advice/provision, heavy menstrual bleeding consultation and treatment, menopause consultation and treatment, STI screening and treatment, pessary fitting/removal and minor procedures. Women are able to see more than one healthcare professional in the same visit. Appointments can be face to face and by phone.
Organisations involved: Approximately 88 GP practices referring into the 6 hubs, 15 PCNs, 1 ICB, a local authority, 1 NHS acute trust, 2 voluntary sector organisations.
Model: Hub-and-spoke.
Leadership structure: GP-led.
Commissioning arrangements: Multiple commissioners involved (local authority and ICB).
Contracting arrangements: Local authority is associate commissioner to ICB contract with provider, budgets are separate. Local authority funding is via a block contract and ICB uses a cost and volume tariff.
Patient pathway: A single point of access telephone number is available for patients and professionals. Patients are then triaged by a nurse and booked into the hub if appropriate.
Staff training: Yes, for example LARC fitting training for nurses. Staff working in integrated sexual health service and the community service spend time in both services to gain broader experience and share knowledge.
Performance and monitoring: Currently in place: number of clinics delivered; number of women attending; waiting times between referral and appointment; LARC fitting rates; termination of pregnancy rates; number of referrals to secondary care; patient experience feedback; hub staff experience/feedback; GP training/upskilling numbers; budget/spend.
How inequalities are addressed: Hub venues located in areas that are easy to access and to support equal access across the area. Evening and weekend services are offered.
Southern region, Northern Ireland
NB: This summary has not been reviewed by the site lead.
Launch year: 2019; the hubs are regional across Northern Ireland and have been rolled out in different trusts at different time points.
Rationale for launching hub and objectives: To improve access and primary care management of women with common gynaecological conditions.
Population covered: All women in the area, covering a population of over 100,000. Covers Southern Federation area.
Services offered: Services are offered in four locations across the region. Services include LARCs for contraception and gynaecology, heavy menstrual bleeding consultation and treatment and menopause consultation and treatment. Women are not able to see more than one healthcare professional in the same visit. Appointments can be face to face or by phone. Appointments are not offered in evenings or weekends.
Organisations involved: GP practices across the federations refer in; four locations provide hub services across three GP Federations (Southern Federation).
Model: Hub-and-spoke, one-stop shop.
Leadership structure: GP-led.
Commissioning arrangements: Commissioned by local authority only.
Contracting arrangements: Locally enhanced service contract.
Patient pathway: Patients referred by their GP. All referrals are triaged by GPs with enhanced skills.
Workforce: Five GPs, nursing team support, admin team support.
Staff training: Yes, no particular details provided.
Performance and monitoring: Currently in place: number of clinics delivered; number of women attending; waiting times between referral and appointment; LARC fitting rates; patient experience feedback.
How inequalities are addressed: Answer not provided.
Website: No.
Western Region Northern Ireland
NB: This summary has not been reviewed by the site lead.
Launch year: 2019.
Rationale for launching hub and objectives: Regionally – locating GPs with interest and host practices. To improve access and primary care management of women with common gynaecological conditions.
Population covered: All women in the area, covering a population of over 100,000. Covers Western Trust area.
Services offered: Hub services offered in two GP practices. Services include LARCs for contraception and gynaecology, contraceptive advice, cervical screening, heavy menstrual bleeding consultation and treatment, menopause consultation and treatment and pessary fitting/removal. Women are not able to see more than one healthcare professional in the same visit. Appointments can be face to face or by phone. Appointments are not offered in evenings or weekends.
Organisations involved: Thirty-two GP practices refer in; two GP practices provide hub services across two GP Federations.
Model: One-stop shop.
Leadership structure: GP-led.
Commissioning arrangements: Multiple commissioners involved (local authority and local commissioning group).
Contracting arrangements: Locally enhanced service contract.
Patient pathway: Patients referred by their GP (through commissioning group). Referrals are triaged by GPs with interest.
Workforce: Two GPs, two GPs with special interests in women’s health, two practice nurses, admin team support
Staff training: Yes, for example LARC training.
Performance and monitoring: Currently in place: number of clinics delivered; number of women attending; waiting times between referral and appointment; LARC fitting rates; number of referrals to secondary care; patient experience feedback; hub staff experience feedback; GP training/upskilling numbers; budget/spend.
Appendix 3 Potential measures to monitor and evaluate Women’s Health Hubs
| Measures of inputs/resources | Value/purposea |
|---|---|
| Measures of process/activity/outputs | Value/purposea |
| Measures of Outcome/impact | Value/purposea |
| Number and location of sites, type of venues | Indicator of the scale and distribution of provision, enables comparison with local needs |
| Number of clinic sessions offered per month/population served | Indicator of scale of provision |
| Appointment duration offered (e.g. 30 minutes, 20 minutes) | Key measure to compare with other services, e.g. providing more time than other services may deliver better experience and quality of care. Appointment duration will impact service costs. |
Number and whole-time-equivalent staff/population served:
|
Indicator of scale of provision, diversity of expertise and workforce, may indicate risks to sustainability, e.g. where there is a small team delivering the service. Can enable comparisons of skill mix and workforce costs between models. |
| Availability of equipment in hub venues (e.g. gynaecology beds, ultrasound and hysteroscopy equipment) | Indicator of resources required to deliver service, can enable comparison of different models and resource requirements. |
| IT infrastructure measures, e.g. electronic referral pathways, shared records access possible between referrer and hub, facilities for electronic prescribing, ordering tests. | Indicator of maturity of digital infrastructure supporting the hub. |
| Service budget/costs. | Can inform cost and cost–benefit comparisons between hub models, and comparisons with other women’s health services, e.g. primary care, secondary care. |
| Clinical care | |
| Referrals: number, rate, source and reason for referrals and bookings [self (online/phone)/GP/other e.g. secondary care, including breakdown by GP practice]. Inappropriate referrals. |
Indicator of uptake/referral by GPs/women. Rates would need to be interpreted with caution as increases may indicate better detection and appropriate referral, or an increase in referral where care could have been delivered by the practice. Referral reason may also be of value. Inappropriate referrals may be useful to (1) draw boundaries around the different parts of the service and monitor any drift, e.g. women being referred for care usually provided within GP global sum, or (2) monitor reduction in referrals where GPs are becoming more confident to manage within the practice due to education/support from hub experts. The definition of inappropriate referral may vary and would need to be defined. |
| Appointments completed [phone, face to face, which professionals, where, what type (first, follow-up)] | Indicator of activity, including trends over time, and to identify where additional capacity may be required. Mode of contact, professional and location can help to inform modelling of resource, workforce and training needs/opportunities and costs for different models. Could consider monitoring unused clinic slots to indicate uptake/efficiency. |
| DNAs and cancellations by provider and reason. | Useful as standard in any service, to compare over time, and with secondary care and other hub models. |
| Outcome of appointment: number and proportion of women for onward referral, follow-up appointment, discharge from the service. New to follow-up ratio. | This measure can illustrate variation between models and clinicians in addressing problems efficiently, but can also illustrate clinical complexity of women being seen who may need multiple appointments. |
| Women seen (in different venues, virtually, times, e.g. out of hours). | Useful to explore uptake/access of different service offers, to flex service model and compare and contrast different approaches. |
| Waiting times to triage and appointment (average, maximum). Size of waiting list. | Key measure and indicator of quality in terms of improving access to care. |
| Reason for attending (distinct from reason for referral, captures self-referrals). | Important measure given the variation in service offer between different hub models. Can also indicate local women’s needs, where provision/uptake does not align with expected needs, and variation between populations. |
| Number of issues addressed at each appointment (average/mean). | This measure could be used to illustrate efficiency and whether a ‘one-stop shop’ approach is needed and/or offered, e.g. smear tests and coil fittings at the same visit. |
| Education sessions delivered to women, mode of delivery (e.g. online/face to face) and number and characteristics of women attending each session. | These measures can evaluate the offer and uptake of these sessions to extend reach to more women than could be seen 1 : 1, including indicating demand and need for different topics, timings/venues and delivery methods. Demographic information can indicate whether services are reaching all women. |
| Referrals to secondary care from the hub (% of women visiting the hub referred), including 2-week wait, and referrals for reasons that could be expected to be managed in primary care. | It is not clear what the ‘right’ rate of referral to secondary care from the hubs should be, and this is likely to vary depending on the population needs, GP referral patterns, and which services and expertise the hub can offer. Measuring this will enable comparison of similar models for benchmarking, and different models to understand how they impact on secondary care referral rates in the local system. |
| Time to referral and sharing test reports with secondary care for suspected cancer. Time to treatment for suspected cancer. | Indicator of safe, timely pathways. |
| Staff training and education | |
| Compliance with statutory training and supervision requirements for hub staff. | Monitoring of these measures should be routine, and is likely to be less useful to measure and compare models. |
| Number of staff attending training in hub clinics (whether working in the hub or not), number of staff completing training/qualifications. | Indicator of scale of training and education activity provided and success in upskilling the workforce. |
| Number of educational tools/events/guidelines developed (e.g. webinars), and number of professionals, e.g. GPs reached, e.g. event attendance. Separate activity to clinical training in hub clinics. | Indicator of educational activity to upskill wider system workforce. |
| Feedback calls/letters to referrers. | Indicator of effective communication and follow-up to improve practice and efficiency of referral pathways. |
| Number of advice and guidance requests from GPs, and timeliness of response. | Indicator of hub role in supporting primary care practice and learning. |
| Access to care/treatment outcomes (can be calculated at individual practice, hub, PCN, LA and ICS level) | |
| Proximity of hub to address of women visiting (or travel time to hub). | Indicator of impact on access to care, whether model is bringing care closer to women. |
| Number/rate of new referrals to secondary care gynae in the health system (from any source). | Indicator of impact on access to care across the health system, movement of care into the community, and upskilling of local GPs. |
| Waiting lists for key conditions and procedures (e.g. LARC), and for secondary care gynaecology (number and proportion of women waiting, for how long, reason for referral, 18-week target, 2-week waits for cancer). | |
| Number of and reason for women’s health appointments in other parts of the health system (e.g. primary care, SRH service, gynae outpatients). | Useful to identify whether impact on service capacity, and whether activity in the hub is additional (new women accessing care) or reflects a shift from another part of the system (e.g. if menopause care appointments in primary care reduce). |
| LARCs (implants, IUS, IUD) | Important to distinguish between LARC for contraception and gynaecological reasons, to identify that hubs are able to deliver both. |
fitted/removed/replaced/failed:
|
|
| LARC choice at population (practice/PCN/LA/ICS) level: | Indicator of reach and uptake of LARC offer. |
Number and % women
|
|
| Procedures completed, e.g. pessary fit, polyp removal, cervical cautery. | Indicators of type and volume of care provided to women. |
| Tests including screening (e.g. blood, ultrasound, smear test, hysteroscopy, STI screening). | |
| Treatments (prescriptions for HRT, bleeding, STIs etc.). | |
| Health and well-being outcomes/impacts at hub and local population level | |
Satisfaction with care:
|
Indicators of service quality and impact. Standardisation of questions/tools with other services/models is ideal. It is important to report coverage and response rate of surveys/tools. |
| Self-reported improvement in symptoms (e.g. pain, bleeding). | |
| Impact of education interventions for example events on women’s knowledge/well-being/behaviour change. | |
| Complications/safety issues/serious incidents. | Indicators of potential quality and safety issues. |
| Complaints. | |
| Teenage pregnancy rates. | Key indicators of sexual and reproductive health in local systems, though it may be challenging to identify direct links between hub services and changes for some of these outcomes. |
| Termination of pregnancy rates. | |
| STI rates. | |
| Screening rates (cervical, breast if provided). | |
| HPV vaccination rates. | |
| Staff/workforce outcomes | |
| LARC fitters per 1000 women age 16–49 in the local health system. | Indicator of provision (whether based in the hub or not) and training/recruitment needs. It may be useful to include lapsed fitters and waiting lists for LARC training to indicate attrition/training needs. |
| GPs and nurses with additional training in women’s health per 1000 women in the local health system. | Indicator of provision (whether based in the hub or not) and training/recruitment needs. |
| GPs/nurses and others working in specialist level women’s health per 1000 women in the local health system. | |
| Local system GP/nurse confidence/knowledge/competence in managing routine conditions e.g. menopause. | Indicator of upskilling of workforce in wider health system, standardised measure would enable comparison. |
| Satisfaction with the hub services from staff across the system, e.g. GPs, SRH professionals, secondary care gynaecologists. | Indicator of service quality and successful integration with existing pathways and services. |
| Satisfaction, sickness and staff turnover in the hub against national benchmarks, time to fill vacancies. | Indicator of sustainability and workforce issues. |
List of abbreviations
- ARRS
- Additional Roles for Reimbursement Scheme
- BRACE
- Birmingham, RAND and Cambridge Evaluation Centre
- CCG
- Clinical Commissioning Group
- DHSC
- Department of Health and Social Care
- GP
- general practitioner
- GUM
- genitourinary medicine
- HIV
- human immunodeficiency virus
- HPV
- human papillomavirus
- ICB
- Integrated Care Board
- ICS
- integrated care system
- IT
- information technology
- LARC
- long-acting reversible contraception
- LGBTQ+
- lesbian, gay, bisexual, transgender, queer, questioning and other sexual and gender identities
- PCN
- Primary Care Network
- PMS
- premenstrual syndrome
- SRH
- sexual and reproductive health care
- STI
- sexually transmitted infections
- WHH(s)
- Women’s Health Hub(s)
- WP
- work package
Note: During the course of the evaluation, CCGs were abolished and replaced with Integrated Care Boards. However, the report refers to CCGs, which were the commissioning bodies when identified hubs were established.
Notes
Labelling of quotes from interviews and focus groups
The interview coding used throughout the report is provided in the table below.
| Interview label | Description |
|---|---|
| EH1 | Exemplar hub site 1 |
| EH2 | Exemplar hub site 2 |
| EH3 | Exemplar hub site 3 |
| EH4 | Exemplar hub site 4 |
| Patient | Patient of an exemplar hub |
| Group | Exemplar hub focus group with local women |
| Internal | Staff member working within the hub to design and/or deliver the service |
| External | Staff member working outside of the hub to design and/or deliver the service |
| Scoping | Scoping interviewee |
| National | National-level stakeholder |
| Regional | Regional-level stakeholder |
A note on terminology
Defining Women’s Health Hubs
At the time the evaluation was undertaken, stakeholders highlighted that the ‘Women’s Health Hub’ (WHH) label did not have a clear and consistent definition, and not all organisations providing women’s health services in the community would refer to themselves as WHHs. WHHs are not necessarily a ‘place’ but a ‘concept’ and are distinct from other hubs which may support women’s health, for example mental health and family hubs, though inevitably there are links. We have explored the diversity in terminology in use, and perspectives regarding nomenclature, as part of our evaluation.
Using the term ‘women’
While we refer to women throughout this document, we recognise that WHHs may also serve people who are transgender, non-binary, with variations in sex characteristics (VSC) or who are intersex. The evaluation considered the needs of all people who are in need of services provided by hubs and was not limited to cisgender women. We have reported on issues of inclusivity around gender that were found in our data.
The primary focus of this study is WHHs in England, with the request for the evaluation initially coming from Public Health England/Office for Health Improvement and Disparities with strong support from policy teams in the Department of Health and Social Care. However, the hub mapping research was conducted across the UK to try to offer a comprehensive overview of the current landscape, gain wider insights and maximise learning, as there is limited evidence on WHHs to date.