Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number NIHR127920. The contractual start date was in February 2020. The draft manuscript began editorial review in January 2023 and was accepted for publication in November 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Siriwardena et al. This work was produced by Siriwardena et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Siriwardena et al.
Chapter 1 Introduction and objectives
Overview
In this chapter, we set out the background, context, gaps in evidence and aims of the Community First Responder (CFR) role in the current and future rural health and care workforce. We describe the rationale for and development of CFR schemes in the UK in response to the need to provide timely emergency care to rural communities, discuss what we know about CFR schemes and CFRs, and set out the gaps in evidence, before describing the composition and expertise of the study team, the aims and objectives of the research and the structure of the report.
Background
Development of Community First Responder schemes
Community First Responder schemes have supported ambulance services to provide emergency care to rural communities since the 1990s, when the UK government encouraged the use of volunteers to get help more quickly to people with emergencies in rural areas. 1,2 CFR schemes organise volunteers to support Emergency Medical Services (EMS) working with ambulance services who dispatch them to provide urgent care to patients in both rural and urban areas. 3 CFRs are members of the public or off-duty medical, nursing or allied health professionals who volunteer to reach a potential life-threatening emergency, primarily in their local community, in the first vital minutes and who provide appropriate care until more highly skilled ambulance staff arrive. 3
Volunteering has been defined as ‘any activity in which time is given freely to benefit person, group, or organization’. 4 Theories about why people volunteer have been extensively explored, and these are based on individuals’ characteristics and their relationships with others, and the community context in which they live or work. 4 From an individual motivational perspective, functionalist theory describes the importance of values (acting on values such as humanitarianism), understanding (seeking to exercise or learn skills), enhancement (the potential to grow and develop psychologically), career (access to current or future career-related experience), social (strengthening social relationships and networks) and protective functions (reducing negative feelings, e.g. guilt, or addressing personal problems) served through volunteering. 5 The first three are considered more common reasons for and more important motivators of volunteering than the last three. 5
Community First Responders need to be distinguished from First Responders, a term used widely in the USA primarily to refer to EMS staff, including paramedics and emergency medical technicians (EMTs) and also other emergency services staff such as fire service and police staff, who are trained and equipped to respond to emergencies to complement EMS in rural areas, but this term has been loosely expanded more recently to include lay people, including sports centre staff, teachers, lifeguards or workplace first aiders, who respond to an emergency. 6,7 CFRs have operated in a number of countries other than the UK, including the USA (for over four decades),8 Ireland,9 Sweden,10 Norway,11 Japan,12 Thailand,13 India,14 Uganda,15 Iraq16 and South Africa,17 but evidence for their role and activity has been obtained largely using case study, qualitative or survey methods. 3,18 Their role in different countries has varied from dealing primarily with out-of-hospital cardiac arrest (OHCA),9–13 road traffic accidents and traumatic injury14–16 to more general first aid for a wider variety of incidents. 8,17
The number of CFR schemes has grown to the current number of around 2431, using over 12,000 volunteers, in the UK. 19 A decade ago CFRs responded to around 2% of calls,1 but the literature suggests that this figure may have increased,20 particularly in the context of pressure on healthcare budgets, centralisation of health resources and workforce shortages. 21 CFRs are considered an increasingly important part of the pre-EMS care workforce both in the UK and elsewhere, especially in rural areas where it is more difficult to provide or access emergency care within a reasonable time. 1,21 Although they do not replace ambulance clinicians, CFRs are thought to add capacity and capability to an ambulance service’s response. 1
Community First Responders have been considered important particularly for providing emergency care, and particularly in rural areas,12,22 where health services are less accessible and outcomes from OHCA and trauma are worse. This is due to various factors affecting rural areas, including an older population, difficulties recruiting skilled health personnel, the centralisation of healthcare services towards larger urban communities, and longer intervention or transport times. 23,24
Another driver of CFRs in rural areas has been poorer access to EMS and the worse health outcomes that result from this. A systematic review of 31 studies from the USA, Australia, Europe and Asia found that EMS in urban areas were more likely to have shorter response, on-scene and transport times than EMS operating in rural areas and that patients in urban areas attended by EMS had greater rates of survival from OHCA or trauma. 24 In this review, rurality was defined differently in different countries because ‘the distinction between the urban and the rural population is not yet amenable to a single definition that would be applicable to all countries or, for the most part, even to the countries within a region’. 25
A number of CFR schemes in England operate as independent charities (funded by public donations) working with ambulance services or as volunteer groups overseen by ambulance services. These include specific charities such as Lincolnshire Integrated Voluntary Emergency Service (LIVES) in Lincolnshire and Hatzola (https://hatzola.org/) in London and Manchester (and metropolitan areas in other countries),26 and CFR schemes involving medical students, linked to medical schools in England. 27 CFRs are often but not always trained, equipped and managed by ambulance services, but they sometimes use marked response vehicles and may be dispatched to a variety of emergencies. 3,27,28
Community First Responders complement the work of ambulance services,22 improving a patient’s condition by arriving quickly, recording vital signs (e.g. pulse, blood pressure or temperature) and performing basic clinical techniques, such as cardiopulmonary resuscitation (CPR)9 of people whose heart has stopped (cardiac arrest), before handing care over to ambulance staff. 1,19
Organisation of Community First Responder schemes
Community First Responders are usually organised and dispatched based on their geographical location and level of training and experience, ranging, for example, from level 1 (basic) to level 4 (enhanced) depending on work experience (e.g. qualified paramedic, nurse or doctor) and training, but the number of and criteria for different levels may vary from one service to another. The training of CFRs generally consists of first-person on-scene first aid administered prior to the arrival of an ambulance,22 and covers medical topics such as emergency first aid, basic life support, airway management, CPR, oxygen therapy, defibrillator use, recognition and initial management of cardiac conditions, choking, strokes, significant bleeds and breathing difficulties. Although CFRs were developed primarily to respond quickly to life-threatening emergencies such as OHCA, their role has expanded so that they respond to different types of emergencies such as falls or patients with chronic conditions. 1,18
In participating ambulance trusts, there is a dedicated procedure whereby all incoming 999 calls are assessed for signs of critical illness or injury before the decision is made to dispatch a CFR or an ambulance clinician. The decision to dispatch a CFR is generally based on a combination of fixed dispatch criteria, clinical decision-making of the dispatcher and availability of a CFR. CFRs vary in the types of emergencies they respond to, what they are trained to do and the equipment they carry; they are classified by ambulance services according to these skills [e.g. in East Midlands Ambulance Service (EMAS) CFRs are classed from level 1 to level 6]. 1
Community First Responders can be dispatched during the day or night to a broad range of patients depending on availability and skill levels. They are not usually sent to children, pregnant women, those in labour or with acute abdominal pain or to incidents deemed unsafe because they involve violence or firearms. Ambulance clinicians are usually dispatched when a CFR is sent unless they are not available, in which case the CFR is required to seek advice from a clinician or refer the patient to other services (D Skarratts, personal communication, 22 March 2022; J Costerd, personal communication, 13 April 2022).
Effectiveness of Community First Responders
When considering the effectiveness of CFRs, attention has been focused largely on OHCA. OHCA affects around 60,000 people each year in England alone, for whom resuscitation is commenced or continued by ambulance staff. Early recognition by relatives or bystanders, accessing EMS and providing rapid CPR and defibrillation using an automated external defibrillator (AED) significantly increase the chance of resuscitation, survival and a good neurological recovery but only 55% of cases not witnessed by EMS receive CPR and only around 2% defibrillation with 25.8% being admitted to hospital alive and 7.9% surviving to hospital discharge. 29
Community-level initiatives to increase lay responders and CFRs, for example in the Heart Safe programme in Minnesota, USA, have led to greater use of CPR and AEDs by bystanders and first responders before the ambulance arrives,30 but the effect on OHCA outcomes is less clear. Another community initiative in Piacenza, Italy, ‘Progetto Vita’, has led to survival to hospital discharge of 41.4% (39 of 95) patients treated under the scheme compared with 5.9% (193 of 3271) of EMS patients.
A systematic review of observational studies of public access defibrillation (PAD) showed a high median overall survival of 40% for patients with OHCA treated with PAD, but this compared non-dispatched lay first responders with dispatched professional (fire or police officer) first responders and found higher survival to hospital discharge with the former (53.0%, range 26.0–72.0%) than with the latter (28.6%, range 9.0–76.0%). 31
In a Cochrane review of randomised controlled trials (RCTs) and quasi-randomised control studies investigating the effect of CFRs dispatched to OHCA in adults and children (older than 4 weeks of age), comparing a combination of CFRs and EMS with EMS alone for outcomes of survival and neurological function, two completed studies met the inclusion criteria, and although one noted higher rates of CPR and the other greater AED use before the ambulance arrived, neither found improvements in survival beyond admission to hospital, which was recorded in only one of the studies. 32
An evaluation of a rural CFR scheme, LIVES in England in 2003, found that around 10% of ambulance calls were attended by CFRs, and when CFRs attended they arrived first in 60% of incidents, with benefits in speed of response and high rates of patient satisfaction, but no clear advantage in return of spontaneous circulation (ROSC) from OHCA. 33
Gaps in the evidence base for Community First Responders
Evidence for CFRs’ role and activity is largely derived from qualitative or survey studies,3,18 but, despite this limitation, CFRs are broadly perceived as positive by ambulance services and communities. 1,18,22 This has led to general support for their incorporation in EMS in the UK. A Delphi study of UK ambulance service chief executives, operational leads and medical directors on future EMS design found high agreement that CFRs, including lay and health professional members of local communities, should be trained and fully integrated into the EMS. 34
A systematic review of the international literature on CFRs found that volunteers were motivated to become CFRs for altruistic reasons, wanted more feedback on their contribution to patient care and were often confused in the public mind with ambulance staff. 3 A previous interview study of CFRs’ experiences with patients and ambulance staff broadly supported these findings. 18 Whereas this latter study explored experiences and insights of CFRs themselves, the views of other key stakeholders, including service users (patients and others involved in contacting the ambulance service) and ambulance staff, were lacking from this and previous studies.
Despite considerable investment in schemes from the volunteers themselves, donations and contributions from health services, a recent scoping review identified key unanswered questions: how effective are CFR schemes, how do they achieve anticipated benefits, what do they cost, how are they perceived by service users and healthcare providers, and how might they develop and be improved in future for rural and other communities?3
The evidence for effectiveness of CFRs is unclear, even for OHCA,32 the condition for which CFRs were first introduced in rural areas. There have been few, if any, studies looking into the costs or other outcomes of care of CFR schemes. 3
Innovations and developments currently fall into two main categories: first, innovation from expanding the CFR workforce (e.g. fire and rescue services providing CFR capability), and, second, innovation in the types of emergencies CFRs attend; for example, in some regions CFRs attend older people who fall but are at low risk of injury.
As a result, further evidence is needed on how CFRs contribute to rural services in terms where they operate (i.e. rural or urban areas) and the type of calls and the demographics of the people they attend, as well as what they do, how this is perceived by various interested stakeholders, the cost of provision, what effect this has on service users and outcomes and how this could be improved or expanded. 3
This study sought to provide evidence on the contribution and costs of CFR schemes to rural health as well as how these services can be optimised or developed further to benefit rural communities.
Study team
We brought together an interdisciplinary team, including patient representatives (AB, PM), members of the healthier ageing patient and public involvement (HAPPI) group and a patient panel (see below), research clinicians from relevant clinical backgrounds (AS, IT, RØ), and those with expertise in health services research and mixed methods (AS), statistics (ZA, VB), economics and econometrics (MS, CR, MH), sociology [(general practice (GP)], qualitative methods (AS, GP, VP, JP, IT, RØ) and trauma psychology (RØ). Several members of the team had worked together on a systematic scoping review,3 an exploratory qualitative study18 and an evaluation of a CFR falls service (the falls response partnership) in Lincolnshire,35 which laid the groundwork for the study. This core team was augmented by scientific, clinical and lay experts who contributed to the study steering and oversight committees.
Study aim
We aimed to investigate the current activities, costs of provision and outcomes of CFR schemes, and explore views of patients, public, CFRs, CFR leads and primary care commissioners on CFRs, working with our stakeholders to develop recommendations for future innovations in rural CFR provision.
Our research questions were:
-
How are CFRs contributing to rural health care?
-
Do they provide value for money?
-
How are they perceived by patients and other providers?
-
How can CFR schemes develop to support future rural health and care services?
Study objectives
Our objectives were to:
-
1. Describe the contribution of CFRs to rural healthcare provision in terms of the numbers and timing of calls attended, together with the types of conditions and the characteristics of people attended.
-
2. Evaluate the costs, funding sources and consequences of CFR schemes.
-
3a. Explore ambulance policies, guidelines and protocols for CFRs.
-
3b. Explore stakeholder (patients, relatives, ambulance staff, primary care, commissioners, CFRs and CFR scheme organisers) experiences and perceptions of CFRs’ current role and potential for future developments and innovations. We also aimed to ask CFRs and CFR scheme organisers about the challenges in and solutions to recruiting, training and retaining CFRs in rural areas and how to ensure governance and accountability for safe, high-quality care.
-
4. Assimilate and integrate data derived from objectives 1–3, synthesising these to develop a list of recommendations for future innovations.
-
5. Prioritise recommendations for future developments/innovations in rural CFR provision through a consensus stakeholder workshop.
Report structure
The study objectives related closely to the work packages and the mixed methods used. We used a cross-sectional design to investigate CFR activity, a questionnaire to collect data on workforce and costs, econometric methods to estimate outcomes, a documentary content analysis of policies, protocols and guidelines and a qualitative interview study to explore CFR, patient–public, ambulance service and wider stakeholder experiences and perceptions of CFRs’ current role and potential for future development. We integrated the data from these earlier work packages to inform a stakeholder consensus workshop at which a modified nominal group technique (mNGT) was used to agree recommendations for potential future innovations for the CFR workforce.
The methods and methodology are described in Chapter 2, including the design, setting, theoretical basis, ethics and details of the component studies. The results are presented in Chapter 3 for each of the component studies addressing the different objectives above, including the integration of results and details of patient and public and stakeholder involvement. The study fundings are discussed in Chapter 4 and the conclusions are presented in Chapter 5.
Chapter 2 Methods
Overview
This chapter sets out our research methods, including the overall design of the study, our theoretical approach, ethics and governance approvals and details of the methods of the component studies, including cross-sectional studies describing calls attended by CFRs, the resource survey summarising cost information, and the studies detailing the outcomes of CFR attendance, including the effect of CFR presence on time of attendance, on the outcomes of OHCA, and on a CFR service responding to calls for people who had fallen at home. We also describe the qualitative methods used in the documentary analysis of CFR policies, guidelines and protocols and an interview study of stakeholders involved in CFR schemes including patients, their relatives, CFRs themselves and CFR leads as well as ambulance staff and ambulance commissioners. Finally, we describe the methods used to integrate the quantitative and qualitative findings and how these informed the consensus study that sought to prioritise potential innovations for CFRs, particularly those working in rural communities.
Overall study design and setting
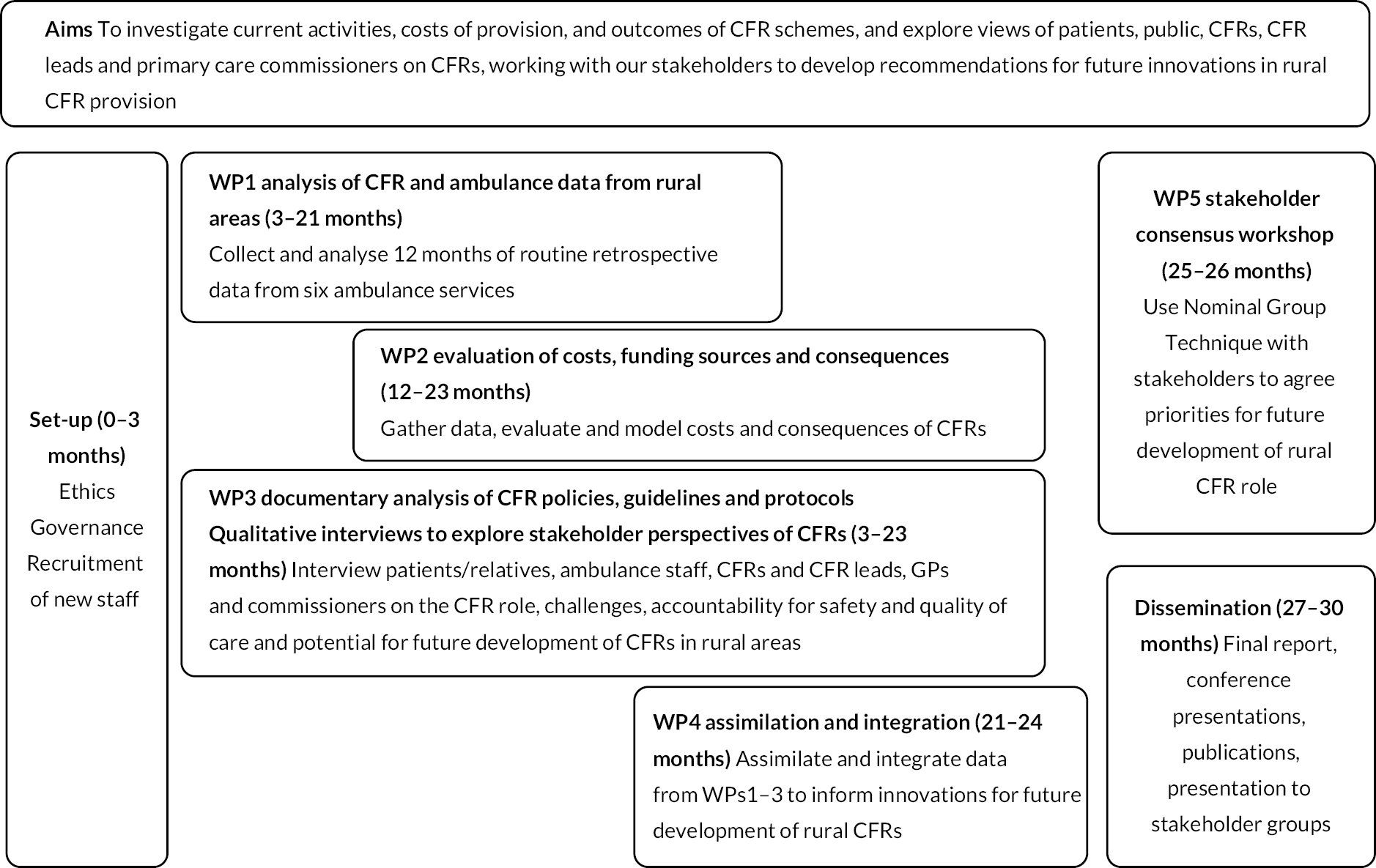
We used a complex, convergent, mixed-methods design36 to guide our approach, working with expert and lay stakeholders throughout the research to increase the validity of our findings, add weight to the recommendations and increase the chance of their future adoption. The flow chart of study activities is shown in Figure 1.
FIGURE 1.
Community First Responders’ role in the current and future rural health and care workforce: study flow chart.
We analysed quantitative data (ambulance and CFR data and costs) and qualitative data (ambulance CFR policies, guidelines and protocols together with interviews exploring stakeholder experiences and perceptions) from six regional ambulance services providing care to a large part of rural England. The services were EMAS, South East Coast Ambulance (SECAmb), South Central Ambulance Service (SCAS), West Midlands Ambulance Service (WMAS), Yorkshire Ambulance Service (YAS) and South Western Ambulance Service Foundation Trust (SWASFT) NHS Trusts.
We assimilated and integrated the findings and presented these to a stakeholder consensus event involving all these trusts and including members of our patient and public involvement (PPI) panel and a wider stakeholder group, using a mNGT to prioritise areas for future development and innovation in CFR schemes.
Theory
We used a lens of pragmatism,37 which enabled us to combine qualitative and quantitative methods focusing on outcomes. Our aim, to develop recommendations for future developments and innovations in rural CFR provision, required a broad theoretical approach that acknowledged three key aspects: multiple ‘actors’ in a complex system, ‘behaviour change’ and ‘causal pathways’. The ‘actor’, ‘behaviour change’ and ‘causal pathway’ (ABC) framework38 incorporates these to increase the likelihood that recommendations for change are implemented.
Community First Responders work in a complex system of multiple ‘actors’ (health and social care providers and staff) and environments (health and social care organisations and contexts) that interact with and adapt to each other at macro (interorganisational), meso (intraorganisational) and micro (healthcare worker–patient) levels. We integrated quantitative and qualitative findings using the method of triangulation described as ‘following a thread’, developed by Moran-Ellis et al.,39 and described by O’Cathain et al.,40 to explore hypotheses generated using one method with another, to gain a fuller understanding of the different phenomena identified. This allowed us to describe an ‘actor-based system map’, defining the problems to be addressed, depicting the main actors currently involved in solving these and examining the relationships between them. This also helped us to articulate the structural and behavioural changes needed to address the problems identified in a sustainable way. Through the integration of data we sought to develop possible causal impact pathways, theories of action (pathways and interventions promoting actor-level change) and a theory of change (i.e. the ways in which actor-level changes could lead to systems changes and impacts). 38 The approach to integration was to some extent dependent on findings from the different components of the study and is described in Chapter 3, Integration. 40
This approach also took heed of the theory of co-production, with problems and solutions focused on the main outcome of producing recommendations for future CFR scheme development in rural areas, explored in collaboration with both lay public and professional stakeholders. 41
Ethics and governance
Ethics approval was obtained from the NHS Research Ethics Committee (IRAS project ID 277205, registration reference NCT04279262). The necessary research permissions were approved by the NHS Health Research Authority, and the study was conducted in accordance with the principles of the Research Governance Framework for Health and Social Care. Research governance permissions were granted by the participating ambulance NHS trusts. The general monitoring of the study was performed by a combination of ethics and NHS governance review and monitoring by quality assurance staff from the University of Lincoln as the sponsor.
Cross-sectional study describing calls attended by Community First Responders
Design
We used a retrospective observational study design. Routine data were collected for analysis from electronic clinical records accessed from 6 of 10 ambulance services in England between 1 January 2019 and 31 December 2019. 42
Data collection and processing
Routine anonymised individual patient data sets, assigned a unique (non-personally identifiable) number from the six ambulance services, were collected and analysed. These included resource type, call category, clinical condition (chief complaint and impression group), date and time, geographical location (incident postcode), demographic information (age, sex, ethnicity) and whether they were conveyed by ambulance to hospital. The data sets were standardised and cleaned to derive the same variables for all of them. Rurality was defined according to the following categories under current UK government definitions: major conurbation (A1), minor conurbation (B1), city and town (C1), city and town in sparse setting (C2), town and fringe (D1), town and fringe in sparse setting (D2), village (E1), village in sparse setting (E2), hamlets and isolated dwellings (F1), hamlets and isolated dwellings in a sparse setting (F2). 43 Rural areas were identified based on the incident postcode and a new standardised binary variable representing rurality was created with 1 assigned to rural categories (D1, D2, E1, E2, F1, F2) and 0 to the urban categories (A1, B1, C1, C2). According to the Office for National Statistics (ONS), all rural settlements have a population of under 10,000 people. Postcode records allowed linkage with Index of Multiple Deprivation (IMD) decile, ranging from 1, highest deprivation level, to 10, lowest deprivation level, which was included as another variable.
The data set obtained from the six ambulance services consisted of routinely collected clinical dispatch records from two triage systems, the Advanced Medical Priority Dispatch System (AMPDS)44 or NHS pathways. 45 The AMPDS was used by EMAS, SWASFT and YAS and the NHS pathways were used by WMAS, SECAmb and SCAS. Due to the heterogeneity and the multitude of dispatch records, the chief complaints were divided by a clinician (NS) into the following main categories: injury/trauma, cardiorespiratory, gastrointestinal/urinary, obstetric/gynaecological, neurological/endocrine, infections/allergies and psychosocial/palliative. The conditions without a specific label (e.g. other medical condition) were grouped in a category labelled as ‘other’. Examples of the most common chief complaints in each category can be seen in Appendix 1, Table 22. Thus, the dispatch data were standardised for all ambulance services. There were five call categories from category 1, the most urgent category representing an immediate response to a life-threatening condition, to category 5, a non-urgent category representing stable cases that require hospital transport. Patient age was separated into five categories: ≤ 19 years, 20–39 years, 40–59 years, 60–79 years and ≥ 80 years. Time taken to arrive, computed as the difference between arrival and dispatch time, was divided into nine categories: < 3 minutes, 3 to < 5 minutes, 5 to < 7 minutes, 7 to < 10 minutes, 10 to < 15 minutes, 15 to < 20 minutes, 20 to < 30 minutes, 30 to < 60 minutes and ≥ 60 minutes.
Statistical analysis
Descriptive statistical analyses presented numbers and percentages of call categories, condition categories, conveyance and patient demographics attended first in rural or urban areas by CFRs or other ambulance staff. Proportion tests were used to directly compare the differences between CFR and ambulance attendances in both rural and urban areas. Univariable logistic regression models were used to identify independent predictors of CFRs’ first presence on scene. To account for possible confounding effects, a multivariable logistic regression model was computed to establish which factors predicted the presence of a CFR first on scene. Due to the limited previous evidence on the role of CFRs, the multivariable logistic model used was exploratory and thus the selection of the predictor variables was not based on variables defined a priori. The only hypothesis formulated based on previous evidence was that CFRs would attend more cases in rural areas and more urgent cases given that their initial role was to attend OHCA, and this was confirmed by our descriptive analysis and multivariable logistic model.
The variables rurality, call category, condition category, age, gender, ethnicity, deprivation index, conveyance and arrival time were used as predictors and the assumptions of multicollinearity, and no outliers were checked. The assumptions of independence of observations and no multicollinearity] [Variance Inflation Factor (VIF) < 1.5] were met, and the maximum likelihood estimation method was used. The assumption of the linear relationship between continuous predictors and the logit transformation of the outcome was not checked as all predictors were binary or categorical. The predictor variables chosen were based on the descriptive statistics reported in this paper and their suitability was confirmed using DAGitty software,46 which facilitates the construction of causal diagrams and confirmed that no further adjustments were needed to estimate the effects of the predictors on the outcome.
The mathematical model representing the logistic regression given the selected predictors was:
The analysis of the multivariable logistic model was run in Stata version 16 (StataCorp LP, College Station, TX, USA) using the following line of code:
Survey of Community First Responder costs and resource use
Background
There has been a lack of attention to the cost of providing CFRs. Although CFRs are volunteers, there will be inevitable costs of workforce management as well as of providing training and equipment, and possibly other expenses.
Design
We used a self-administered cross-sectional survey design to assess workforce and resources used for CFRs in the ambulance services. A bespoke questionnaire was designed for issue to ambulance trusts, asking for information on the trust workforce of volunteer CFRs, the budget allocated to CFRs and the actual expenditure incurred in managing their CFRs; data were sought for the financial years 2017–8, 2018–9 and 2019–20. The questionnaire was sent by e-mail to trust directors of research and heads of research.
The first version of the questionnaire (v1.0) was piloted with EMAS. After minor amendments arising from responses received to the pilot, a second version of the questionnaire (v2.0) was drafted and issued (see Report Supplementary Material 1) to the other ambulance trusts. The second version was not reissued to EMAS.
The questionnaire was separated into three parts: (1) human resources, (2) financial resources and (3) detailed financial breakdown. In total there were 17 questions, all but one of which asked for entry of a data value.
Counterfactual analysis of effect of Community First Responders attendance on response time
Background
An important aspect of the EMS response is the time taken to respond and attend, with a short wait for help contributing to patients’ experiences of care and their sense of feeling reassured that services had attended to help. 47 Response time has been used for many years to measure service quality in terms of timeliness and this is supported by extensive studies, involving a wide range of stakeholders including patients and the public as well as service providers and commissioners, into important measures of the quality and impact of ambulance service care. 48
Ambulance services are required to attend patients within a target timeframe that depends on the triaged category of the emergency. 49 The attendance targets are among the list of key performance indicators set by NHS England that ambulance services are required to meet. The attendance targets, six in total, are expressed as minimum time thresholds, applying to the following measures: the average of the time taken to attend patients by emergency severity categories 1 and 2; and the (90th) percentile in the distribution of those attendance times, again varying by emergency severity, categories 1–4. The target thresholds are listed in Table 1 (most severe = category 1 to least severe = category 4).
| Call severity category | Mean target (minutes) | 90th percentile target (minutes) |
|---|---|---|
| 1: life-threatening/very serious injuries | 7 | 15 |
| 2: emergency calls | 18 | 40 |
| 3: urgent calls | – | 120 |
| 4 and 5: moderately urgent or less urgent calls | – | 180 |
Design
We used a counterfactual analysis based on a geography local to the scene of the incident to estimate the timing benefit that may be attributable to CFRs’ presence compared with their absence. The counterfactual episodes are assumed to represent what the ambulance response would be without the presence of CFRs. We compared, by severity category and urban–rural classification, the travel time distributions of the CFR episodes to counterfactual episodes as well as the attendance times of both to the target thresholds.
The important reference time points for attendance targets are the time when the emergency (999) call is received by the ambulance emergency operations centre (EOC) and the time when an emergency vehicle (EV) first attends the patient. Evidence has shown that ambulance services have increasingly struggled to meet attendance targets since these were introduced in 2017. 49
Dispatching a CFR to an emergency stops the target clock if the CFR is first to arrive at the scene and attend the patient. Accordingly, first-on-scene attendance is one aspect where a workforce of volunteer CFRs may contribute value.
A second comparison focuses on travel time, from when the EV first departs to the incident until its arrival at scene. The calculation of travel time modifies the attendance time by removing from its calculation the period prior to dispatch that is due to the EOC organising the response to the emergency. The shorter the travel time, the sooner the CFR or ambulance clinician reaches the patient.
Data collection and processing
Episode data for the calendar year 2019 were supplied by EMAS in two tranches: (1) episodes of dispatch for EVs that arrived at scene, and (2) episodes involving EVs stood down pre arrival. To avoid underestimation of attendance time, it was necessary to include data from the second tranche for the circumstance in which a dispatched EV was stood down prior to arrival at scene but was later re-engaged by the EOC to the original call and did eventually attend at scene. EV attendance time calculations were constructed by including the sum of repeated durations of periods of dispatch to stood down, to which was added the time of final dispatch up to attendance at scene, which was obtained using the first tranche of data.
Key time points and data variables in the progression from the beginning of the emergency until emergency services attended at scene are displayed in Figure 2. The blue labels are variable names either taken directly from the episode data or constructed.
FIGURE 2.
Engagement of emergency services units up to attendance.

A single call number was generated for each incident and either one or many EV resources identified by call sign were allocated to each call number. Concatenating the call sign to the call number ensured that each EV involved was represented by a single unique identifier. Whether or not the assigned EV arrived was indicated using resource stood down and time resource arrived at scene. The latter was also utilised to establish order of arrival when multiple EV resources attended the same incident.
Resource type was used to designate CFR involvement, indicated in particular by ‘Community First Responder’, ‘First Responder Intermediate’, ‘Lives Responder Scheme’, ‘Medical First Responder’, ‘Mountain Rescue’, ‘RAF CAR’ and ‘Volunteer Aid Society Vehicle’. For purposes of assigning episode comparators, the following EVs were included: ‘dual-crewed ambulance’, ‘solo responder (car)’, ‘private ambulance service’ and ‘urgent vehicle’.
Urban–rural indicators were assigned to each episode according to its postcode location linked to ONS-NSPL (National Statistics Postcode Lookup) data, where the rural–urban classification is dated to the 2011 census.
Counterfactual episodes over a localised geography
The counterfactuals to CFR episodes were constructed using those episodes that did not involve CFRs occurring either at or in the neighbourhood of the same postcode as the location of the incident, ensuring a like-for-like comparison. We define this neighbourhood – the localised geography – as the next highest geography beyond postcode level in the ONS hierarchy, the ‘lower super output area’ (LSOA11). The ONS-NSPL data contain linked pairings of postcode-level and LSOA11 geographies.
Descriptive statistics were used to compare the distributions of attendance times for CFR episodes with counterfactual episodes as well as both with the target thresholds. The key assumption underlying the following comparisons was that the counterfactual episodes represented what the ambulance response would be without dispatch of CFRs.
Comparison of achievement of target thresholds
The first comparison concerned success at achieving NHS target thresholds. We computed two statistics – mean and 90th percentile – on data constructed as time resource arrived at scene less time call taken when, for CFR dispatches, the CFR was the first to attend on-scene, and for counterfactual dispatches not involving CFRs when we used the first ambulance to attend on-scene to locations within the localised geography.
Comparison of travel time to attend
The second comparison used data constructed as time resource arrived at scene less time resource mobile. This was formed across all CFR dispatches provided they attended at scene. Each CFR dispatch was matched with a counterfactual set of ambulance-only dispatches to its localised geography. From the mean of travel times of the latter, we subtracted the travel time of the CFR dispatch and term this quantity Δ where, should Δ > 0, the CFR takes less time to travel to the emergency than the ambulance. Descriptive statistics are used to describe Δ.
Cross-sectional study of Community First Responder response to out-of-hospital cardiac arrest outcomes
Design
We used a cross-sectional design linking data from EMAS and LIVES on OHCA to investigate the effect of CFRs attending on outcomes.
Data collection and processing
We were provided with routinely collected data from EMAS and LIVES for OHCA between the 999 calls to hospital transportation from electronic patient report forms (ePRFs) and data related to survival status at hospital discharge. EMAS screened their electronic clinical database of patient records for OHCA case records, dispatch codes and related clinical or treatment terms. Incidents of OHCA cases were entered into a cardiac arrest database, cleaned and verified by trained members of the EMAS clinical audit team. Outcome data on admission to hospital and survival at hospital discharge were gathered from regional hospitals for those patients conveyed to hospital under data-sharing protocols.
Data submitted included the following information:
Inputs and outcomes – whether occurrence witnessed, initial cardiac rhythm, ROSC at any time, ROSC at hospital handover, survival to hospital discharge.
Demographic information – patient age and sex, date/time of event, event location, aetiology, receiving hospital.
Interventions – bystander CPR, PAD use, other interventions, airway management.
Timing – call time, time to arrive, on-scene time, time to convey to hospital.
By examining timings provided by EMAS and LIVES, we were able to differentiate between episodes where a CFR arrived before or after EMS.
Analysis
We derived Utstein-style50 templates for OHCA incidents presenting to EMAS attended by both CFRs (LIVES) and ambulance staff. We compared outcomes for ROSC and 30-day survival using multivariable regressions models comparing CFR arrival before EMS with EMS alone for both.
Evaluation of a Community First Responder response to adults who had fallen
Background
The falls response partnership combines the EMAS NHS Trust and LIVES Lincolnshire First Responders to form an innovative approach ensuring a safe health and social care response to people in Lincolnshire who fall. Its aims were foremost to recover the patient from their fall and then conduct a follow-up in which patient needs could be identified and appropriate service referrals made so that future falls could be prevented. In addition, the design aimed to reduce pressures on the ambulance service and emergency departments and to help retain staff at LIVES.
Lincolnshire Integrated Voluntary Emergency Service CFRs are trained and supported with two-staffed, lifting-equipped vehicles [bariatric service vehicles (BSVs)] that, when on-call, may be despatched by EMAS to attend adults who fall. Remote management of the incident from the EMAS EOC is provided by the EMAS clinical assessment team (CAT) in real time. Following treatment, the patient may either be discharged at-scene or ambulance backup may be despatched for further at-scene paramedic support and treatment with the further possibility of conveying the patient to hospital. While the service was initially designed for patients assessed by computer-aided dispatch (CAD) to have had a (least severe) category 4 fall, after approximately 2 months of operations this was upgraded to include falls assessed to be category 3 and category 2 (Box 1).
Category 1: life-threatening/very serious injuries.
Category 2: emergency calls.
Category 3: urgent calls.
Category 4: less urgent calls.
The FRP commissioned LIVES to provide an immediate patient assessment on arrival, treating the individual in their own home with basic first aid if required, assisting them back to their feet and, if the patient was then discharged, ensuring that they were in a comfortable and safe environment, with a follow-up assessment conducted within 24 hours to ensure an appropriate referral to prevent further falls. The follow-up assessment (including a standardised falls risk assessment tool) was done by LIVES and an onward referral for additional support made where appropriate. The options for further action included referral to the Lincolnshire Wellbeing Service for further assessment, support or equipment; a GP referral for assessment of frailty, dizziness, hyper-/hypotension, other medical problems or medication review; services providing strength and balance training; or to an occupational therapist working in the community falls team based at Lincolnshire Community Health Services NHS Trust for more complex needs.
The FRP was initiated in December 2018 with operating hours of 8 a.m. to 8 p.m. It began with just one EMAS-owned BSV loaned to LIVES (call sign BSV5), and a second BSV was soon added (call sign BSV4). By the end of June 2019, a total of 445 episodes of care involving FRP had been recorded. By vehicle, BSV5 responded to falls in West and South Lincolnshire and operated within the City of Lincoln, North Kesteven, West Lindsey, South Kesteven and South Holland; BSV4 responded to falls in East Lincolnshire and Boston and operated within the borough of Boston and East Lindsey.
Pilot economic evaluation
Smith et al. 35 reported on a model-based economic evaluation of the FRP during the pilot period December 2018 to June 2019 (see Report Supplementary Material 3). Their main finding was that improvement in effectiveness and cost-effectiveness of FRP compared with standard care was inversely related to ambulance backup and conveyance rates following FRP attendance, for as those rates increase so do costs and FRP patient referral rates decrease. Patient benefit, that is mitigation of the risk of recurrent falls, depended on attendance to referred clinicians, whether that be to the patient’s GP or to a community falls services or to occupational therapists at Lincolnshire Community Health Services NHS Trust. Their baseline modelling, for a hypothetical cohort of size 1000 falls patients, is given in Table 2, where the incremental cost-effectiveness ratio (ICER) by at-risk time horizon, hereafter ‘horizon-ICER’, can be selected from 1 month up to 5 months beyond the initial fall. The perspective of the analysis was the NHS, and all prices were expressed in 2019–20 values.
| Month | Per-patient cost (£) | Cost increment (£) (1) | Total cohort falls | Benefit increment (2) | aICER:(1)/(2)/1000 | ||
|---|---|---|---|---|---|---|---|
| FRP | Standard care | FRP | Standard care | ||||
| 1 | 1316.14 | 1113.49 | 202.66 | 1398 | 1448 | −50 | £4544.17 |
| 2 | 1839.67 | 1612.15 | 227.52 | 1556 | 1648 | −92 | £2298.97 |
| 3 | 2047.92 | 1835.48 | 212.44 | 1619 | 1738 | −119 | £1636.86 |
| 4 | 2130.76 | 1935.49 | 195.26 | 1644 | 1778 | −134 | £1363.92 |
| 5 | 2163.71 | 1980.28 | 183.42 | 1654 | 1796 | −143 | £1238.05 |
These results can be explained as follows. For the FRP, the model begins with 1000 falls costing the NHS in the first month £1316 per fall. Under standard care the corresponding figure is £1113; thus the incremental per-patient cost of the FRP compared with standard care is £203. During the first month, 1398 falls were predicted under the FRP, implying 398 patients with repeat falls by the end of the first month. The corresponding figures under standard care were 1448 and 448. During the first month, the baseline model predicted 50 fewer repeat falls under the FRP than with standard care for a cohort size of 1000, yielding a 1-month at-risk horizon-ICER of £4544; that is, the additional cost to the NHS of using the FRP rather than standard care to prevent one fall was £4544 for an at-risk period of 1 month beyond the initial fall. However, on extending the at-risk horizon to 5 months, the horizon-ICER reduced to £1238 per fall avoided.
A key driver of the baseline case is the differential between the rates of conveyance to hospital for falls patients; for the FRP, the observed rate over the pilot period was 68%, while for standard care the observed rate was 62.7%, a difference of 5.3% compared with the FRP. Under the FRP, a substantial cost is added when patient circumstances dictate that ambulance backup is required; in particular, estimates of the average intervention cost are £195 without backup but £440 when backup is required. 35
A scenario analysis that examined variation in FRP backup rates (set between 62% and 68%) resulted in Figure 3, which displays the horizon-ICERs against a continuum of conveyance rates. Improvement occurs as conveyance rates fall (i.e. moving from right to left on the graph) and is uniform at any selected at-risk time horizon.
FIGURE 3.
Horizon-ICER by FRP conveyance rate.
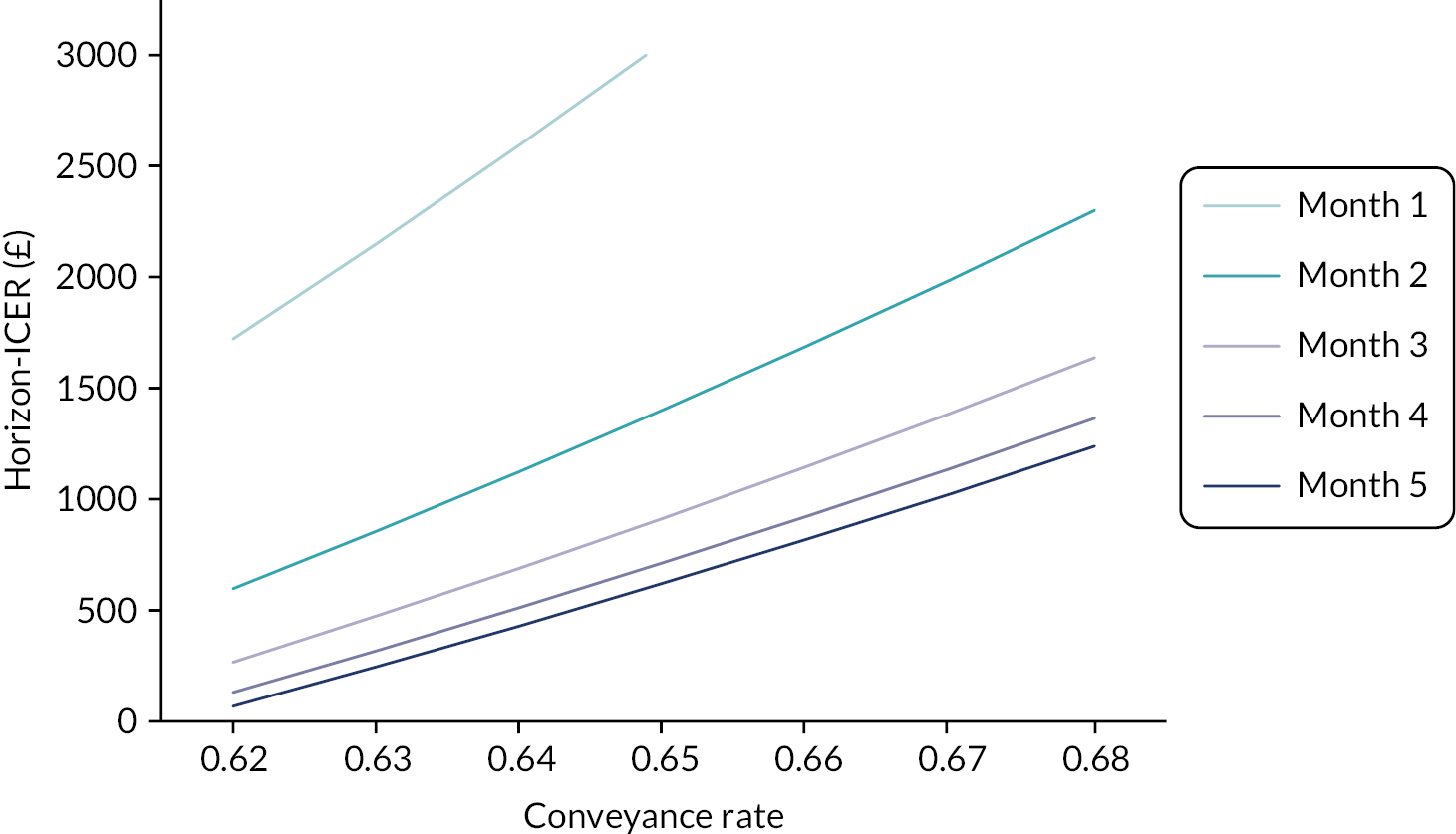
For example, matching the FRP backup rate to that observed in standard care (62.7%), with all other factors held constant, the value of the 5-month horizon-ICER dropped to £192 per fall avoided. Indeed, further extrapolation beyond that depicted in the graph to the FRP backup rate of 56.3% finds FRP dominating standard care at every time at-risk horizon, and FRP becomes cost saving at this point.
The LIVES-EMAS FRP was recommissioned by Lincolnshire County Council in February 2020. In this study we revisit the FRP and examine its operation using descriptive statistics over the period April 2020 to December 2021 using a cross-sectional design that linked FRP episode data from EMAS and LIVES.
Documentary analysis of Community First Responder policies, guidelines and protocols
Background
The documentary analysis addressed the research objective of understanding CFR structures (e.g. guidelines, protocols, personnel, equipment, training) in participating ambulance services.
NHS England’s Five Year Forward View51 emphasises community engagement in decision-making as a means of strengthening future health and care services. The CFR schemes have been in line with the community engagement initiative, and over 2500 CFR schemes have been operationalised in the UK. Keeping the diverse range of CFR schemes in mind, we aimed to conduct an inquiry into policies, protocols and guidelines developed for the regulation of CFRs.
Design
We conducted an analysis of ambulance/CFR policy, guideline and protocol documents in participating ambulance services using content and discourse analysis to understand current structures for CFR involvement. 52
Collection of documents
We requested CFR leads and managers in the ambulance trusts to provide documents developed as policies, guidelines and protocols for CFR roles. We analysed the documents using a comparative method by employing an institutionalist approach to policy analysis. 53 In establishing and developing public policy, the institutionalist perspective outlines the roles of the state or a government body in developing procedures and relationships between policy-makers and those that are subject to policy and how the latter are affected. Our analysis used two prominent document-analysis methods, namely content analysis and discourse analysis. 53,54
Content and discourse analysis
Content analysis was used to quantify the occurrence of certain key words, phrases, topics and concepts in the policies, guidelines and protocols retrieved. The discourse analysis developed themes that were identified from the content analysis and focused on how the CFRs were discussed in the policy documents, including how CFR roles were structured, the governance mechanism, support services, training and equipment.
Qualitative study of Community First Responder roles, governance of Community First Responder schemes, innovations and future developments
Background
The aim of the qualitative study was to explore the experiences and perceptions of CFR stakeholders on the current roles of CFRs, governance of CFR schemes, challenges, solutions and future opportunities. The objectives of this aspect were:
-
to explore patients’ and relatives’ experiences and perceptions of care provided by CFRs
-
to explore the experiences and/or perceptions of ambulance staff, CFRs, CFR scheme organisers, primary care staff and commissioners on the CFR role, the governance of CFR schemes, and the potential for further development of and innovation in the CFR role
-
to explore the views of CFRs and CFR scheme organisers about challenges and solutions to recruiting, training and retaining CFRs in rural areas.
This section addresses the study objectives by analysing primary qualitative data from a range of stakeholders involved in the operation of CFR schemes, that is CFRs, CFR leads and managers, ambulance staff, commissioners, and patients and relatives of the patients.
Design
Qualitative methods seek to elaborate the views and beliefs of participants to understand complex social phenomena,55 and it was appropriate to address the research questions, which required an exploration of the operation of CFR schemes, particularly the experiences, perceptions and actions of stakeholders involved in the CFR processes. Therefore, we adopted an interpretivist paradigm of research and conducted this qualitative study in six rural ambulance services and regions in England, UK. The six research sites were rural ambulance services, which enabled us to explore and understand the functions of CFR schemes in rural health care, where CFR services are crucial.
Recruitment
The selection of participants was informed by the concept of purposive sampling56 to include a diverse range of stakeholders and their perceptions, experiences, practices and innovations until data saturation was achieved. 57,58
We purposively sampled patients, relatives and ambulance staff identified from records of patients who had been attended by a CFR in a rural location in the previous 6 months using the quantitative data from ambulance services in the cross-sectional study above. For each ambulance service, from the data set provided, a random sample was generated of 100 incidents where a CFR had attended a rural emergency in the latter half of 2019. The data set included details of patient age group, sex and ethnicity, together with chief complaint, clinical impression, incident rurality, IMD, call category, AMPDS code and outcome (see and treat at scene or see and convey to hospital). To recruit participants, the ambulance services were asked to contact the patient, CFR and ambulance staff members for tranches of 10–20 incidents, ideally with all three involved in the same incident.
Although we sought to interview patients, relatives, CFRs and ambulance staff attending the same event, this was only achieved for one set of interviews. Ambulance staff were also recruited through ambulance service research leads. CFRs were also recruited through ambulance CFR leads and we sought to recruit CFRs, patients and relatives through social media (X, San Francisco, CA, USA). Primary care commissioners were recruited through the National Ambulance Commissioner’s Forum.
We sought to recruit a maximum variation sample of patients (according to age, sex, condition and ethnicity), ambulance staff (sex, experience, ethnicity and role), CFR (sex, ethnicity, length of experience, skill level) and CFR scheme leads (independent charity and ambulance trust oversight schemes). We also advertised the study and recruited via internal advertisements, e-mails and social media at the ambulance services involved in the study and their associated CFR schemes.
Data collection
Three researchers (VHP, JP and IT) conducted the interviews using separate interview schedules for each participant category (see Report Supplementary Material 2). These were developed based on the participants’ roles and responsibilities to discuss and explore a wide range of experiences and practices in the CFR functions. The interviews took place between April 2020 and December 2021, which was in the midst of the COVID-19 pandemic and frequent nationwide lockdowns and led us to conduct the in-depth interviews online. 59 The interviews were audio-recorded with the participants’ written consent and subsequently transcribed. The length of the interviews ranged from 30 to 60 minutes.
Data analysis
We familiarised ourselves with the interviews and the emergent data through reading the transcripts. A thematic analysis approach guided the data analysis. 60 The thematic analysis consisted of several steps in which we (GP, VHP, JP and NS) organised and synthesised data by constructing short-codes, grouping the short-codes and synthesising meaning based on more broadly identified themes. Three researchers (GP, VHP and JP) used NVivo12 (QSR International, Warrington, UK) to inductively code the transcripts, periodically compiled to produce a comprehensive list of codes as they were identified from the data. The codebooks were combined to create a coding framework, and the framework was then amended following a series of discussions within the research team (GP, VHP, JP, IT and NS). NVivo12 supported the production of data outputs for each code. GP and VHP extracted the data outputs and documented the variations in practices, governance and experiences of CFR operations within each ambulance service. They further collapsed the similar themes and organised them under higher-level themes. The data outputs were read, reviewed and re-read to identify overarching themes.
Data debriefing with PPI and information validation for improved methodological rigour are discussed later in this chapter.
Stakeholder consensus workshop prioritising Community First Responder innovations
Background
A consensus workshop of stakeholders was convened to present and discuss recommendations developed from the earlier studies and to prioritise recommendations for development and innovation in CFR schemes. We applied nominal group technique (NGT) methods to innovations relevant to the current and future roles of CFRs.
Design
We used a mNGT as a consensus method to introduce, generate, discuss and prioritise actual and potential innovations for CFRs and CFR schemes, particularly focusing on those in rural areas. The mNGT, also termed expert panel method, is a structured, facilitated, face-to-face meeting of key informants designed to generate ideas, agree a list of those most relevant through discussion and rank them through two or more rounds of voting to reach a consensus, if possible, on the priorities for innovation. 61,62 The modifications of the original NGT introduced in this study included use of a hybrid meeting format, allowing in-person and online participation, together with introduction of learning from previous quantitative and qualitative components of the wider study. Important to NGT is a combination of qualitative (discussion) and quantitative (voting or ranking) methods to understand why certain innovations are prioritised more than others.
Recruitment
We invited stakeholders and representatives from seven rural regional ambulance services in England to the consensus meeting. We ensured that experts from different disciplines were invited, including patient representatives, CFRs, ambulance clinicians and leads. Although the consensus meeting took place in 2022 after the majority of the adult population had been vaccinated against the SARS-Cov-2 virus, cases of COVID-19 were still high in England, travel was affected and some individuals were still at risk and therefore avoiding meetings, so we organised this as a hybrid face-to-face and online meeting. We checked participants’ availability and preference for mode of participation, either face to face at the University of Lincoln campus or online via Microsoft Teams (Microsoft Corporation, Redmond, WA, USA). A list of participants was finalised based on their consent to participate.
Structure
The consensus meeting was structured in four stages or sessions: (1) presentation of information to all participants; (2) silent generation of ideas, and discussion in small groups; followed by (3) voting on ideas, feedback and discussion by all; and (4) a final vote, discussion and summary by all participants. Each session was facilitated by the chief investigator, with members of the research team facilitating small-group discussions to ensure that all participants’ opinions and ideas were included and discussed throughout the consensus process. Participants were allocated in advance to small groups to ensure that each group represented a diverse range of stakeholders, ambulance services and regions.
Session 1
The presentation session comprised a series of three presentations by members of the research team to provide insight into the empirical study’s key findings. The purpose of these presentations was to expand participants’ knowledge and understanding of the CFR schemes and research findings in order to foster meaningful engagement from all stakeholders, irrespective of their experience with the CFR schemes or research.
The quantitative section analyses data from ambulance services that identified how many people CFRs attended, the proportion of ambulance calls attended, the characteristics of people (age, sex, condition) attended, how quickly CFRs attended and what happened to patients when the ambulance arrived.
The econometrics section discussed the costs of CFR scheme provision and the funding sources and provided information on their value to ambulance services.
The qualitative section presented an overview of perceptions, experiences, challenges and governance of CFRs, CFR organisers, ambulance staff and commissioners.
Each presentation included a brief question-and-answer session, and a discussion among participants to elicit reflections on the study findings.
Session 2
The second session built on the discussion from session 1 to supplement ideas for innovations and change. Participants were organised into three groups, one face to face and two online via Microsoft Teams. Each group was assigned facilitators to help guide the generation of ideas, as well as (in a non-participatory way) observing and documenting the discussion in their groups. At the end of this session, the ideas were collated and summarised in advance of an initial process of voting to rank innovations.
Session 3
Participants reconvened in the main group. A member of the research group presented the synthesised version of the innovations, and these were discussed again in the main group. Participants (excluding research team members) voted on all the innovations presented. This was followed by feedback on the ranking and a discussion of the votes. The content of the discussion was informed by the minutes or observation notes from session 2, as well as the results of the vote.
Session 4
The concluding session consisted of a further vote to rank and a final discussion among the participants.
Data analysis
The ranking or prioritisation of innovations was achieved using a joint information systems committee (JISC) online survey (www.jisc.ac.uk/online-surveys) circulated to participants so that they could vote anonymously during the consensus meeting. All the innovations presented, suggested through the generation of ideas, and discussed were collated and entered into the JISC survey. These were rated individually by participants (excluding research team members) using a Likert scale of 1 to 5, with 1 representing ‘not a priority’ and 5 representing an ‘essential priority’. The first survey was administered during session 3, followed by a discussion and a further survey during session 4. The results at the end of each round were exported to Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) and these were ranked using median scores and interquartile ranges.
The discussion (qualitative component) during the consensus meeting was important for understanding why certain innovations were ranked (quantitative component) above or below others. The consensus meeting was audio-recorded and transcribed verbatim for later analysis. We used inductive and deductive thematic analysis60 to explore the varying viewpoints on the innovations presented and discussed. This involved reading and re-reading transcripts and inductive coding using NVivo 12. Later, a deductive analysis was performed, based on the attributes of innovations framework. 63
Patient, public and wider stakeholder involvement
Background
The importance of PPI in health and social care research has been widely accepted in the UK and supported by funding bodies such as the National Institute for Health and Care Research (NIHR) and patient organisations such as Involve (https://involve.org.uk/). In the last decade, public engagement in research has shifted from the passive provision of data as research participants to a much more active role working alongside researchers to design, develop, conduct and disseminate research. 64 In this study, we included two public contributors as co-applicants and research team members, both members of the HAPPI group, a wider PPI panel recruited for this study and a public member of the oversight committee. In the following section we describe how the partnership between researchers and PPI members informed and facilitated the research activities.
The patient and public involvement panel
On the advice of the oversight group, we expanded our public contributors on the study. A group of seven patient and public representatives were selected from a pool of expressions of interest received from open recruitment through the NIHR Applied Research Collaboration East Midlands to other Applied Research Collaborations and related organisations. We selected members to ensure a wide geographical representation to include the regions of participating ambulance services and to ensure wider representation of people of different sex, ethnic minority status and disabilities. 65
Professional advisory groups as stakeholders
We engaged with a number of key professional stakeholder groups during the study. The National Ambulance Research Steering Group (NARSG), which was composed of research leads from ambulance services in the UK, was involved in the initial design of the study and recruitment of participating sites. This group reports to the National Ambulance Services Medical Directors’ group, which itself reports to the Association of Ambulance Chief Executives. We also engaged with the College of Paramedics Research and Audit Committee through its chairperson, also a member of NARSG, and with the National Ambulance Service First Responder Managers’ Forum. We invited members of these groups, and they attended the consensus workshop.
Summary
The PPI panel members in this study were recruited to increase geographical and demographic representation. The public contributors and professional advisory groups contributed throughout the various aspects of the study, providing input on study design, advising on recruitment, reviewing findings, and contributing to the study steering and oversight groups and the consensus workshop.
Chapter 3 Results
Text in this section is reproduced from Botan V, Asghar Z, Rowan E, et al. What Is the Contribution of Community First Responders to Rural Emergency Medical Service Provision in the UK? Paper presented at: Society for Academic Primary Care Annual Scientific Meeting: Recovery and Innovation; 4–6 July 2022; University of Central Lancashire, Preston, England, which is an open access article distributed under the terms of the Creative Commons CC BY-NC licence, which permits unrestricted use, distribution, and reproduction in any medium, for non-commercial use, provided the original work is properly cited. See http://creativecommons.org/licenses/by-nc/4.0/.
Overview
This chapter sets out our findings from each of the work packages and substudies that relate to the objectives. This includes a detailed description of CFR activities in the cross-sectional study. We presented data on resource use, workforce and costs from the survey designed to investigate this. The outcomes of CFR attendance are described in terms of timeliness of response, response to falls and outcomes for OHCA. The documentary analysis of CFR policies, guidelines and protocols explores the structures in ambulance services supporting CFRs’ roles and responsibilities. The qualitative interviews describe CFR recruitment training and retention, their role, governance and innovations, and their activities providing care for patients. The findings from each of these are integrated to develop an actor-based system map. Finally, the results of the consensus meeting summarise the priorities given to different innovations that had or could be introduced into rural CFR schemes.
Cross-sectional study findings
Rural versus urban
We found 4,501,274 separate ambulance attendances to individual patients in the sample from the six participating ambulance services (see Appendix 1, Figure 16). Missing data varied for the variables used, from no missing data for deprivation or rurality to high rates for ethnicity (see Appendix 1, Table 20).
Of these ambulance attendances, 3,671,512 (82.8%) were in urban areas and 763,553 (17.2%) were in rural areas. CFRs were present overall in 136,438 (3.0%) and arrived first in 86,880 (1.9%) of these calls.
Community First Responders were present on scene first for 3.9% of all rural attendances and for 1.5% of urban attendances (Table 3). Proportion tests indicated that CFRs attended first on scene for a statistically significant higher proportion of the calls in rural than in urban areas.
| CFR | Rural, n (%) | Urban, n (%) |
|---|---|---|
| Present first* | 29,741 (3.9) | 54,207 (1.5) |
| Present after ambulance* | 17,645 (2.3) | 34,845 (1.0) |
| Not present** | 716,167 (93.8) | 3,582,460 (97.5) |
| Total | 763,553 (100.0) | 3,671,512 (100.0) |
Call urgency
Community First Responders attended more than 9% of the total number of category 1 calls and almost 5% of category 2 calls, with a statistically significant higher proportion of more urgent call categories 1 and 2 in both rural and urban settings. While 14.4% of CFR first attendances in rural areas were for category 1 calls, only 5.8% of ambulance staff attendances in rural areas were for category 1 calls. Similarly, 14.2% of CFR first attendances and only 7.4% of ambulance staff attendances in urban areas were for category 1 calls. When looking at category 2 calls, these represented 67.3% of CFR first attendances in rural areas and only 56.4% of ambulance staff first attendances. The results were similar for urban areas, with 70.8% of CFR first attendances for category 2 calls and only 55.8% of ambulance attendances for category 2 calls. Compared with ambulance staff, CFRs also attended a statistically significantly lower proportion of category 3 calls in both rural and urban settings and of category 4 calls only in rural settings. Detailed results can be seen in Table 4.
| Call category | Rural: CFR on scene | Urban: CFR on scene | Overall: CFR on scene | |||
|---|---|---|---|---|---|---|
| No, n (%) | Yes, n (%) | No, n (%) | Yes, n (%) | No, n (%) | Yes, n (%) | |
| 1** | 42,714 (5.8) | 4274 (14.4) | 267,066 (7.4) | 7706 (14.2) | 313,035 (7.4) | 12,434 (14.3) |
| 2** | 413,924 (56.4) | 20,013 (67.3) | 2,017,328 (55.8) | 38,375 (70.8) | 2,467,140 (58.2) | 60,174 (69.4) |
| 3** | 209,436 (28.5) | 4631 (15.6) | 1,027,743 (28.4) | 6937 (12.8) | 1,249,389 (29.5) | 12,120 (14.0) |
| 4* (only rural) | 36,639 (3.4) | 430 (1.5) | 98,762 (2.7) | 637 (1.2) | 127,536 (3.0) | 1118 (1.3) |
| 5 | 12,247 (1.7) | 337 (1.1) | 68,814 (1.9) | 499 (0.9) | 82,345 (1.9) | 922 (1.1) |
Clinical conditions
Community First Responders attended a statistically significant higher proportion of people with cardiorespiratory and neurological/endocrine conditions. The most common cardiorespiratory conditions were breathing difficulties, chest pain and stroke, whereas the commonest neuroendocrine conditions were loss of consciousness or fainting, convulsions and hypo- or hyperglycaemia (see Appendix 1, Table 22).
In the overall sample, 30.2% of CFR attendances were for cardiorespiratory conditions while only 19.2% of ambulance staff attendances were for this condition category, and 13.4% of CFR attendances were for neurological/endocrine conditions compared with 8.8% of ambulance staff attendances. Detailed results with differences between rural and urban areas can be seen in Table 3 (and differences by ambulance service are shown in Appendix 1, Table 21). An important proportion of CFR attendances was for injury/trauma conditions (20.1%), but this was lower than for ambulance staff attendances (23.2%). CFRs also attended a lower proportion of gastrointestinal/urinary and psychosocial/palliative conditions than ambulance staff, as seen in Table 5.
| Chief complaint category | Rural: CFR on scene | Urban: CFR on scene | Overall: CFR on scene | |||
|---|---|---|---|---|---|---|
| No, n (%) | Yes, n (%) | No, n (%) | Yes, n (%) | No, n (%) | Yes, n (%) | |
| Cardiorespiratory** | 142,330 (20.3) | 8912 (31.1) | 654,448 (18.9) | 15,318 (29.5) | 807,533 (19.2) | 25,229 (30.2) |
| Gastrointestinal/urinary* | 42,491 (6.1) | 1279 (4.5) | 211,081 (96.1) | 2443 (4.7) | 256,904 (6.1) | 3925 (4.7) |
| Infections/allergy/ENT/ophthalmology | 10,593 (1.5) | 563 (2.0) | 54,778 (1.6) | 1022 (2.0) | 65,914 (1.6) | 1639 (2.0) |
| Injury/trauma** | 164,227 (23.4) | 5925 (20.7) | 800,349 (23.1) | 10,347 (19.9) | 975,405 (23.2) | 16,798 (20.1) |
| Neurological/endocrine** | 56,504 (8.1) | 3925 (13.7) | 310,450 (9.0) | 6975 (13.4) | 370,430 (8.8) | 11,210 (13.4) |
| Obstetric/gynaecological | 3337 (0.5) | 40 (0.1) | 21,606 (0.6) | 79 (0.2) | 25,241 (0.6) | 125 (0.2) |
| Psychosocial/palliative* | 29,137 (4.2) | 567 (2.0) | 220,408 (6.4) | 1579 (3.0) | 252,927 (6.0) | 2224 (2.7) |
| Other** | 251,891 (36.0) | 7475 (26.1) | 1,186,880 (34.3) | 14,175 (27.3) | 1,450,916 (34.5) | 22,272 (26.7) |
Comparison across ambulance services
Community First Responders first attendances compared with ambulance staff first attendances across all ambulance services presented a series of common characteristics, including the higher percentage of attendances in rural areas (see Appendix 1, Table 21), a higher percentage of attendances for the most urgent call categories 1 and 2 (see Appendix 1, Table 23) and for cardiorespiratory and neurological/endocrine conditions (see Appendix 1, Table 24).
Conveyance to hospital
On average, the percentage of patients conveyed to hospital by ambulance services when CFRs were on scene was slightly lower in both rural and urban settings. The difference was small (about 2%) but statistically significant (Table 6). The demographic characteristics of patients are represented in Table 7.
| Outcome | Rural: CFR on scene | Urban: CFR on scene | Overall: CFR on scene | |||
|---|---|---|---|---|---|---|
| No, n (%) | Yes, n (%) | No, n (%) | Yes, n (%) | No, n (%) | Yes, n (%) | |
| Conveyed** | 451,058 (68.4) | 18,841 (65.9) | 2,138,626 (67.8) | 34,522 (65.8) | 2,616,985 (67.9) | 55,098 (65.6) |
| See and treat** | 208,858 (31.7) | 9771 (34.2) | 1,016,235 (32.2) | 17,966 (34.2) | 1,240,296 (32.2) | 28,882 (34.4) |
| Variable | Rural: CFR on scene | Urban: CFR on scene | Overall: CFR on scene | |||
|---|---|---|---|---|---|---|
| No, n (%) | Yes, n (%) | No, n (%) | Yes, n (%) | No, n (%) | Yes, n (%) | |
| Age group (years) | ||||||
| < 19 | 56,929 (8.7) | 2558 (9.4) | 335,455 (10.4) | 4811 (9.9) | 396,904 (10.1) | 7685 (9.8) |
| 20–39 | 77,172 (11.8) | 2760 (10.2) | 586,212 (18.2) | 6894 (14.1) | 670,131 (17.1) | 9972 (12.7) |
| 40–59 | 96,814 (14.8) | 4082 (15.1) | 580,166 (18.0) | 8484 (17.4) | 684,484 (17.4) | 13,017 (16.5) |
| 60–79 | 191,112 (29.3) | 8473 (31.3) | 817,666 (25.3) | 13,583 (27.9) | 1,021,359 (26.0)* | 22,974 (29.2) |
| ≥ 80 | 230,320 (35.3) | 9233 (34.1) | 909,794 (28.2) | 15,001 (30.8) | 1,153,170 (19.4)** | 25,069 (31.9) |
| Sex | ||||||
| Female | 351,996 (52.8) | 14,634 (52.4) | 1,781,189 (53.2) | 27,101 (53.3) | 2,156,036 (53.1) | 43,158 (52.9) |
| Male | 315,110 (47.2) | 13,285 (47.6) | 1,565,606 (46.8) | 23,739 (46.7) | 1,902,169 (46.9) | 38,501 (47.5) |
| Ethnicity | ||||||
| Ethnic minority | 3632 (1.1) | 132 (1.0) | 88,395 (5.9) | 1012 (4.1) | 92,361 (5.0)* | 1150 (2.9)* |
| Mixed ethnicity | 1331 (0.4) | 60 (0.4) | 12,552 (0.8) | 187 (0.8) | 13,973 (0.8) | 251 (0.6) |
| White | 320,850 (98.5) | 13,523 (98.6) | 1,398,953 (93.3) | 23,725 (95.2) | 1,739,903 (94.2)** | 38,346 (96.5)** |
| Deprivation | ||||||
| Low income (IMD ≤ 5)** | 213,812 (29.1)* | 9310 (31.3)* | 2,244,710 (62.0) | 27,195 (50.2) | 2,485,155 (56.4) | 38,743 (44.6) |
| High income (IMD > 5)** | 520,000 (70.9)* | 20,431 (68.7)* | 1,372,595 (38.0) | 27,012 (49.8) | 1,923,105 (43.6) | 48,137 (55.4) |
Predictors of Community First Responder attendance
Univariable and multivariable logistic regression models determined the factors predicting CFRs presence on scene (Table 8). For the multivariable model, the assumption of no multicollinearity (Spearman’s rho < 0.7, the highest value being 0.28) was met, and the model showed a good fit to the data [χ²(25) = 12,887.51, p < 0.001]. The main predictors of CFR presence were rurality [odds ratio (OR) 2.05, 95% confidence interval (CI) 1.99 to 2.11; p < 0.001], conditions including cardiorespiratory (OR 9.20, 95% CI 5.08 to 16.64; p < 0.001) and neurological/endocrine (OR 9.26, 95% CI 5.12 to 16.77; p < 0.001) and call categories 1 (OR 5.19, 95% CI 3.86 to 6.99; p < 0.001) and 2 (OR 4.44, 95% CI 3.31 to 5.96; p < 0.001), with the narrow CIs indicating that their estimates were extremely precise. CFRs were also less likely to attend patients from minority ethnic backgrounds, those from more deprived areas and those aged < 39 years.
| Predictor of CFR presence on scene | Univariable model, OR (95% CI) | Multivariable model, OR (95% CI) |
|---|---|---|
| Rurality (urban) | 1 (–) | 1 (–) |
| Rural | 2.70 (2.67 to 2.74) | 2.05 (1.99 to 2.11) |
| Chief complaint category (obstetric/gynaecological) | 1 (–) | 1 (–) |
| Cardiorespiratory | 6.31 (5.29 to 7.52) | 9.20 (5.08 to 16.64) |
| Gastrointestinal/urinary | 3.09 (2.58 to 3.69) | 5.13 (2.83 to 9.33) |
| Infections/allergies/ENT | 5.02 (4.18 to 6.03) | 6.10 (3.34 to 11.13) |
| Injury/trauma | 3.48 (2.92 to 4.15) | 5.36 (2.96 to 9.71) |
| Neurological/endocrine | 6.11 (5.12 to 7.29) | 9.26 (5.12 to 16.77) |
| Psychosocial | 1.78 (1.48 to 2.13) | 4.20 (2.31 to 7.64) |
| Other impressions | 3.10 (2.60 to 3.70) | 6.20 (3.43 to 11.22) |
| Call category (5) | 1 (–) | 1 (–) |
| 1 | 3.55 (3.32 to 3.79) | 5.19 (3.86 to 6.99) |
| 2 | 2.18 (2.04 to 2.33) | 4.44 (3.31 to 5.96) |
| 3 | 0.87 (0.81 to 0.93) | 1.12 (0.83 to 1.50) |
| 4 | 0.78 (0.72 to 0.85) | 0.77 (0.54 to 1.11) |
| Arrival time categories in minutes (15–20 minutes) | 1 (–) | 1 (–) |
| < 3 | 1.11 (1.06 to 1.16) | 1.14 (1.06 to 1.23) |
| 3 to < 5 | 1.23 (1.19 to 1.28) | 1.27 (1.20 to 1.34) |
| 5 to < 7 | 1.33 (1.29 to 1.38) | 1.35 (1.28 to 1.42) |
| 7 to < 10 | 1.33 (1.29 to 1.38) | 1.40 (1.33 to 1.47) |
| 10 to < 15 | 1.24 (1.20 to 1.27) | 1.23 (1.17 to 1.29) |
| 20 to < 30 | 0.92 (0.89 to 0.96) | 1.12 (1.06 to 1.19) |
| 30 to < 60 | 1.27 (1.21 to 1.33) | 2.39 (2.23 to 2.55) |
| 60 to > 60 | 4.32 (3.98 to 4.69) | 7.03 (6.35 to 7.79) |
| Conveyance (see and treat) | 1 (–) | 1 (–) |
| See and convey | 0.90 (0.89 to 0.92) | 0.89 (0.86 to 0.91) |
| Age group in years (< 19 years) | 1 (–) | 1 (–) |
| 20–39 | 0.77 (0.75 to 0.79) | 1.00 (0.94 to 1.06) |
| 40–59 | 0.98 (0.95 to 1.01) | 1.18 (0.94 to 1.06) |
| 60–79 | 1.16 (1.13 to 1.19) | 1.26 (1.19 to 1.32) |
| ≥ 80 | 1.22 (1.09 to 1.15) | 1.27 (1.20 to 1.33) |
| Gender (male) | 1 (–) | 1 (–) |
| Female | 0.99 (0.98 to 1.00) | 1.04 (1.01 to 1.07) |
| Ethnicity (white) | 1 (–) | 1 (–) |
| Ethnic minorities | 0.56 (0.53 to 0.60) | 0.78 (0.72 to 0.82) |
| Mixed | 0.82 (0.72 to 0.92) | 0.91 (0.78 to 0.82) |
| Deprivation (low income) | 1 (–) | 1 (–) |
| High income (IMD > 5) | 1.61 (1.58 to 1.63) | 1.28 (1.25 to 1.32) |
Summary
We analysed 4.5 million incidents from six English regional ambulance services during 2019, before the COVID-19 pandemic. CFRs attended first a higher proportion of calls in rural areas (almost 4% of calls) than in urban areas (around 1.5% of calls). They were significantly more likely to attend rural (vs. urban) areas and higher-priority emergency or urgent (category 1 and 2 compared with category 3, 4 or 5) calls for cardiorespiratory and neurological and endocrine (vs. other emergency) conditions but also attended lower-category calls for conditions such as falls. They were also significantly more likely to attend older (vs. younger), white (vs. minority ethnic) people in more affluent (vs. deprived) areas, even after taking rurality into consideration.
Resource and workforce survey findings
Survey responses
Of the six trusts sent the questionnaire, responses were obtained from the following: EMAS NHS Trust, SCAS NHS Foundation Trust, SECAmb Service NHS Foundation Trust, WMAS University NHS Foundation Trust and YAS NHS Trust.
Some trusts provided incomplete data because resource data were either not collected or not available, and where costs data were incomplete, this was because CFR operations were not separately disaggregated from the wider operations of the trust.
Community First Responder workforce
Yorkshire Ambulance Service supported the largest number of CFRs in each financial year and SECAmb the smallest (Table 9). Among the four trusts supplying counts across each financial year, CFR numbers increased over time at just one, SCAS, averaging approximately + 30% year-on-year, while at the other trusts numbers declined, averaging approximately −10% year-on-year.
| Service | Financial year | ||
|---|---|---|---|
| 2017–8 | 2018–9 | 2019–20 | |
| Total number of volunteer CFRs | |||
| EMAS | – | – | 636 |
| SCAS | 505 | 623 | 863 |
| SECAmb | 618 | 496 | 411 |
| WMAS | 520 | 512 | 442 |
| YAS | 948 | 945 | 900 |
| Active number of volunteer CFRs (on-call at least once) | |||
| EMAS | – | – | – |
| SCAS | 505 | 623 | 863 |
| SECAmb | 391 | 403 | 399 |
| WMAS | – | – | – |
| YAS | – | – | 900 |
| Number of new volunteer CFRs recruited | |||
| EMAS | – | – | – |
| SCAS | 161 | 60 | 239 |
| SECAmb | – | 86 | 131 |
| WMAS | 44 | 22 | 0 |
| YAS | – | – | 200 |
| Number of volunteer CFRs leaving the service | |||
| EMAS | – | – | – |
| SCAS | – | – | 94 |
| SECAmb | 188 | 144 | 139 |
| WMAS | – | – | 18 |
| YAS | – | – | 250 |
South East Coast Ambulance was the only trust to record that its complement of CFRs was less than fully active (‘active’ defined here as CFRs being available on-call at least once during the financial year, which is less stringent than the minimum 20 hours per month of volunteering sought by trusts); in particular, 63% was the least proportion active, occurring in 2017–8.
In 2019–20, a total of 570 new volunteers were recruited across the four trusts reporting counts, while 501 volunteers left their role as CFRs.
South Central Ambulance Service was the only trust to record the age-sex distribution of CFRs, with between just under two and up to three times more male CFRs than female CFRs, and an age distribution that saw on average 17% of CFRs aged > 65 years while 22% on average were aged 18–35 years; in the other two age ranges, 36–50 years and 51–65 years, both averages being just over 30%. Across all three financial years, WMAS reported a male-to-female ratio of 60 : 40.
Community First Responder work patterns
South Central Ambulance Service and YAS recorded the on-call working pattern in 2019–20 of their typical CFR as follows:
-
average duration on-call: 7 hours
-
average number of on-calls per week: 0.94
-
percentage solo operating: SCAS – 100%, YAS – 95%, SECAmb – 96%, WMAS – 60%.
Community First Responder work location
Table 10 records the geographical distribution (rural, urban or both) of CFRs’ area of operation. Only SECAmb had a roughly equal urban–rural split between location of operations of their CFRs workforce. EMAS and YAS showed CFRs operating more often in urban locations, whereas for SCAS and WMAS operations conducted in rural areas were more frequent.
| Service | Financial year | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 2017–8 | 2018–9 | 2019–20 | |||||||
| Urban | Rural | Both | Urban | Rural | Both | Urban | Rural | Both | |
| EMAS | – | – | – | – | – | – | 60 | 30 | 10 |
| SCAS | – | – | – | – | – | – | 22 | 54 | 24 |
| SECAmb | 38 | 57 | 5 | 42 | 53 | 5 | 44 | 48 | 8 |
| WMAS | 30 | 70 | 0 | 30 | 70 | 0 | 30 | 70 | 0 |
| YAS | – | – | – | – | – | – | 75 | 25 | 0 |
Community First Responder training
Community First Responders across all trusts were reported to have undertaken at least one training course per year. A variety of courses were undertaken ranging from those provided internally by trusts through to external certificate courses. SCAS, SECAmb and YAS all ran internal courses, the last exclusively so for its 900 CFRs in 2019–20. The in-house training taken in 2019–20 by 719 SCAS CFRs was supplemented by a higher-ranked level 3 CFR course taken by 114 CFRs. SECAmb’s internally governed CFR course was taken by 86 CFRs in 2018–9 and then replaced in 2019–20 by courses from FutureQuals® [Future (Awards and Qualifications Ltd), Coalville, UK] suite of level 3 First Responder on Scene, taken by 131 CFRs. CFRs at EMAS received training courses from the BTEC (Business and Technology Education Council) ‘first person on scene’ suite; in 2019–20 numbers were level 4 Enhanced 15, level 3 Intermediate 357 and level 2 Basic 264. However, in 2022–3, these BTEC courses were no longer offered, having been replaced with new regulated versions. WMAS also used courses from FutureQuals® Level 3 for its lower-level training and for higher levels of training courses from the Institute of Health Care Development® (Edexcel, London, UK) ‘first person on scene’ suite.
Financial resources
Aggregate costs for CFR budget and expenditure are summarised in Table 11.
| Service | Financial year | |||||
|---|---|---|---|---|---|---|
| 2017–8 (£) | 2018–9 (£) | 2019–20 (£) | ||||
| Budget | Expenditure | Budget | Expenditure | Budget | Expenditure | |
| SCASb | 869,044 | 868,349 | 827,678 | 870,014 | 838,341 | 870,119 |
| SCACc | 250,000 | 288,568 | 230,000 | 224,833 | 314,000 | 218,454 |
| Totald | 735,044 | 772,917 | 673,678 | 710,847 | 768,341 | 704,573 |
| SECAmb | 849,244 | 564,904 | 666,852 | 677,808 | 426,551 | 401,841 |
| WMAS | – | 54,082 | – | 34,890 | – | 40,347 |
| YAS | – | – | 873,200 | 856,340 | 811,210 | 703,632 |
The South Central Ambulance Charity (SCAC) supplemented financing provided by the SCAS trust and fully supported CFR operations. Combining SCAS and SCAC, net of estimated provisions due to co-responders, the 3-year grand averages were just over £725,000 for both budget and expenditure. When expressed per CFR, budget and expenditure average £1142 per year and £1163 per year, respectively. This average does, however, mask the large, per-CFR, drop in budget and expenditure resulting from the upswing in CFR numbers, from, respectively, £1456 and £1531 in 2017–8 to £890 and £816 in 2019–20.
The large disparity between the SECAmb CFR budget for 2017–8 and SECAmb CFR expenditure in that year, over £284,000, was largely due to an underspend in equipment and maintenance amounting to £187,000. This is consistent with a possibly lower than expected active CFR rate, 63%, experienced in that year. In the next two financial years that gap had largely disappeared, with a slight overspend in 2018–9 followed by an underspend in 2019–20, and activity rates had started to climb back towards 100%. The budget provision per CFR averages £1252 per year, while incurred expenditure per active CFR averages £1378 per year.
West Midlands Ambulance Service does not determine an annual budget provision for CFR operations. Unlike the other trusts, large cost items such as CFR support staff are not attributed to CFR operations at WMAS. The magnitude of expenditure on CFR operations reported by WMAS if compared with, for example, SECAmb, which has had similar numbers of CFRs to WMAS, totals approximately 10% of that spent at SECAmb. Mileage reimbursement for the use of personal cars accounts for over 60% of expenditure at WMAS. This was followed by equipment, at least in 2017–8, when AED batteries and pads were replaced in large numbers (since then these items have been provided through local community efforts until 2022–3, when funding by NHS Charities Together commenced), added to which consumable equipment was provided to CFRs at local hubs. From 2018to 2019 replenishment practice for CFRs changed to replacements taken from stocks held by ambulances on scene, the cost of which is attributed elsewhere by the trust.
Yorkshire Ambulance Service provided financial figures for two of the three financial years sampled, 2018–9 and 2019–20. There was underspend of budget in both years, substantially so in 2019–20 by over £100,000. The wages of CFR trainers were by many times over the largest item at YAS, amounting to almost 70% of the total expenditure in 2018–19 and increasing to almost 80% in 2019–20. The CFR budget averages £913 per CFR per year, while expenditure in 2018–9 was £906 per CFR, dropping to £782 per CFR in 2019–20.
Community First Responder support staff
Staff numbers were reported by SECAmb and YAS, totalling under 10 full-time each year at SECAmb and under 20 full-time each year at YAS. Most CFR support staff at YAS were trainers, who were required in large numbers as, unlike at the other trusts, all CFR training at YAS was internal, numbering 16 trainers in 2018–9 and 15 trainers in 2019–20. At SECAmb there were two CFR trainers in each year. Including other staff (CFR team managers, co-ordinators and administrators), the total cost of CFR support staff at YAS averaged £690,000 per year had and £338,000 per year at SECAmb. The wage bill per support staff member at YAS averaged £36,000 and at SECAmb averaged £44,000.
Equipment
A detailed breakdown of equipment was given by SCAS, when purchases were funded by SCAC. The item of largest expenditure reported was Mangar Lifting Cushions: £50,000 in 2018–9 and £21,000 in 2019–20. This was followed by CFR Observation Kit and Bag, £9000 in 2018–9 and £2000 in 2019–20. Other equipment provided by SCAC for CFRs included pulse oximeters, defibrillator batteries, Terrafix (Stoke-on-Trent, UK) devices and tympanic thermometers.
Mileage
Mileage reimbursements were recorded by two trusts, SECAmb and WMAS, at per-mile rates of £0.45 and £0.56, respectively. CFRs at these trusts were reimbursed for travel totalling 294,838 miles across the three financial years, yielding an average (the SECAmb calculation uses counts of active CFRs) of claimed travel per CFR of 111 miles per year. A third trust, SCAS, recorded claims for mileage for January–March 2020 totalling £890.78 for 1978 miles travelled. The claims, attributable to personal vehicle use by CFRs, were reimbursed through SCAC.
In contrast to WMAS, where CFRs use personal cars when on despatch, SCAC provided CFRs with a fleet of cars, 35 in 2018–9 and 38 in 2019–20 (see fleet pictured at www.scas.nhs.uk/what-we-do/community-first-responders/). Each car was restricted by corporate agreement to not exceed 5000 miles per year, which resulted in rotations in the allocation of vehicles to keep under that limit. The combined costs of purchase and maintenance of the fleet averaged £307,000 per year.
Summary
Community First Responders varied in number between 400 and 900 across ambulance services, but substantial numbers were active and available for duty. They were distributed in both rural and urban areas to different extents across different service regions. In the two trusts providing this information, the average duration on-call was 7 hours, with on average one shift per week provided and CFRs mostly operating alone, although one trust had two-fifths of CFRs operating in pairs. The costs of providing CFR schemes varied approximately 20-fold between ambulance services from £40,000 to over £800,000 per year. Costs were incompletely recorded and reported, which may have partly accounted for this. True costs, because of under-reporting, may have been at the upper end of or even higher than these figures. Costs were attributed to staff providing management and training, together with reimbursement of out-of-pocket costs of volunteering including fuel and vehicle use.
Timing of Community First Responder attendance findings
Comparison of achievement of target thresholds
When CFRs were dispatched, all but one of the eight 90th percentile thresholds were attained, whereas the ambulance response alone failed to meet the target in every instance but one. For mean attendance time, the targets were universally missed whether or not CFRs were dispatched (Table 12).
| Call category for rural/urban calls with or without CFR | Sample size | Time to attend | |
|---|---|---|---|
| Mean (minutes) | 90th percentile (minutes) | ||
| Rural emergency with CFR | |||
| 1 | 455 | 11.19 | 17.20 |
| 2 | 9031 | 20.82 | 34.32 |
| 3 | 961 | – | 91.48 |
| 4 | 66 | – | 126.05 |
| Urban emergency with CFR | |||
| 1 | 557 | 9.17 | 14.95 |
| 2 | 16,418 | 21.45 | 37.90 |
| 3 | 1510 | – | 111.43 |
| 4 | 85 | – | 144.72 |
| Rural counterfactual | |||
| 1 | 3846 | 12.25 | 19.90 |
| 2 | 87,956 | 40.80 | 77.97 |
| 3 | 30,550 | – | 227.00 |
| 4 | 1744 | – | 196.97 |
| Urban counterfactual | |||
| 1 | 19198 | 8.04 | 13.02 |
| 2 | 32,8882 | 35.03 | 70.62 |
| 3 | 102,222 | – | 235.15 |
| 4 | 6180 | – | 192.75 |
Comparison of travel time to attend
The results comparing estimated travel times for CFRs with ambulance vehicles are shown in Table 13. Apart from life-threatening category 1 emergencies occurring in urban areas when an ambulance EV took less time on average to travel to the scene than a CFR (8.04 vs. 9.17 minutes), the results for all other combinations of severity and urban–rural location show a time advantage in favour of CFRs. This was further accentuated in rural emergencies, when the gap in travel times becomes uniformly larger relative to urban emergencies. This is further evidenced by the smoothed estimate of the distribution of differences given in Figure 4, where the bulk of the area underneath the smoothed distributions lies to the right of zero in all but one case.
| Emergency severity category | Sample size | Δ | |
|---|---|---|---|
| Mean (minutes) | Median (minutes) | ||
| Rural emergency | |||
| 1 | 790 | 0.37 | 0.99 |
| 2 | 10,327 | 5.92 | 6.64 |
| 3 | 1135 | 6.34 | 8.20 |
| 4 | 62 | 7.26 | 9.23 |
| Urban emergency | |||
| 1 | 1351 | −1.73 | −1.36 |
| 2 | 19,641 | 1.67 | 2.13 |
| 3 | 1737 | 2.63 | 3.86 |
| 4 | 88 | 0.41 | 2.30 |
FIGURE 4.
Smoothed distributions of differences (ambulance-CFR) in travel times Δ by emergency severity and urban–rural classification. (a) Category 1, urban (kernel = epanechnikov, bandwidth = 1.0071); (b) category 1, rural (kernel = epanechnikov, bandwidth = 1.3756); (c) category 2, urban (kernel = epanechnikov, bandwidth = 0.8443); (d) category 2, rural (kernel = epanechnikov, bandwidth = 0.9802); (e) category 3, urban (kernel = epanechnikov, bandwidth = 1.4396); (f) category 3, rural (kernel = epanechnikov, bandwidth = 1.9948); (g) category 4, urban (kernel = epanechnikov, bandwidth = 4.5208); and (h) category 4, rural (kernel = epanechnikov, bandwidth = 3.4505).
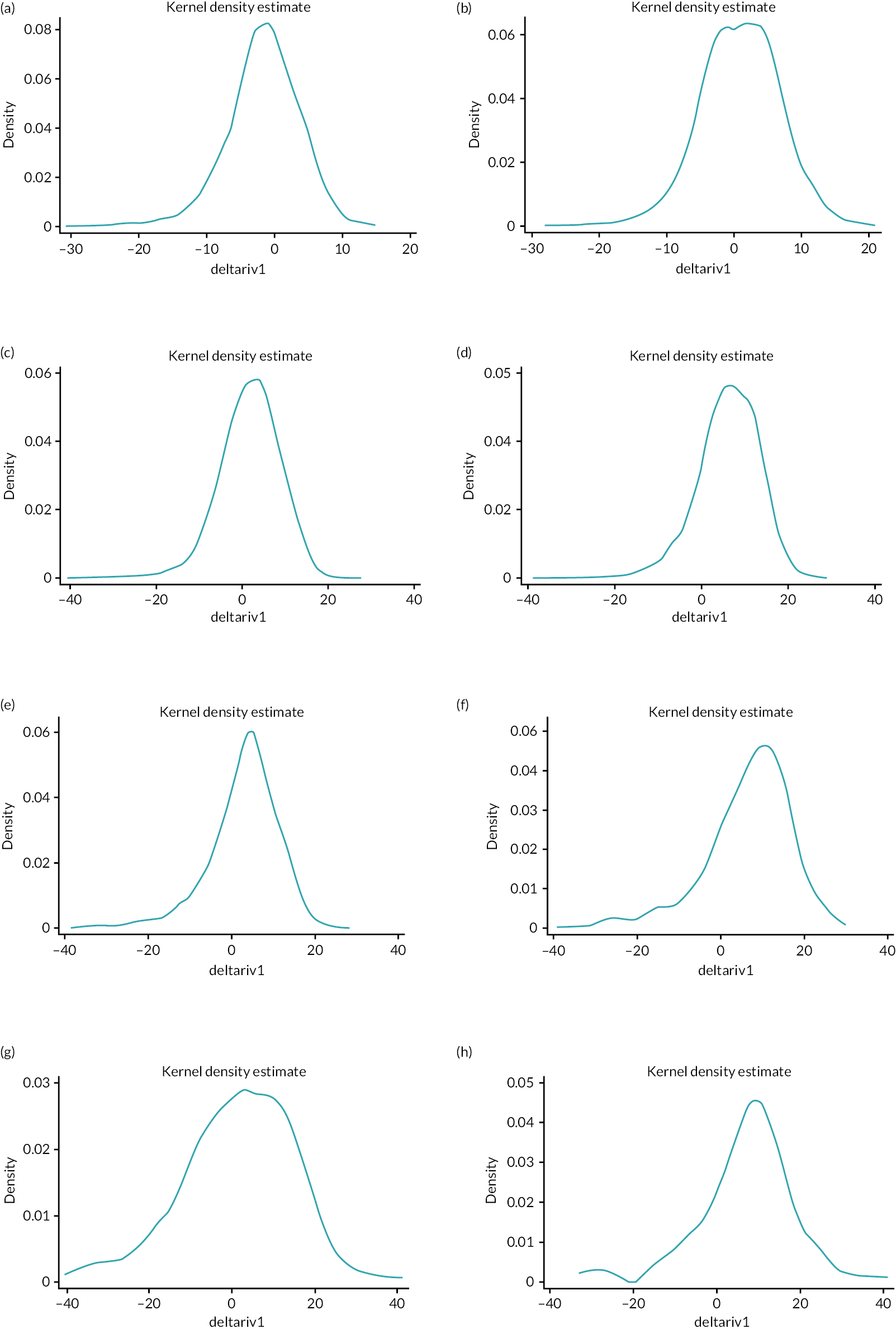
Summary
There was a clear advantage in terms of shorter response time when CFRs attended than for an ambulance response alone, and this was amplified when the incident occurred in a rural area.
Effect of Community First Responder attendance at out-of-hospital cardiac arrest
Utstein templates
We present data in the internationally recommended Utstein style50 for OHCA incidents presenting to EMAS attended by both CFRs (LIVES) and ambulance staff (Figure 5), by ambulance staff only (Figure 6) and when a CFR attended before ambulance arrival (Figure 7).
FIGURE 5.
Cardiac arrest incidents linking LIVES and EMAS data. VF, ventricular fibrillation; VT, ventricular tachycardia.
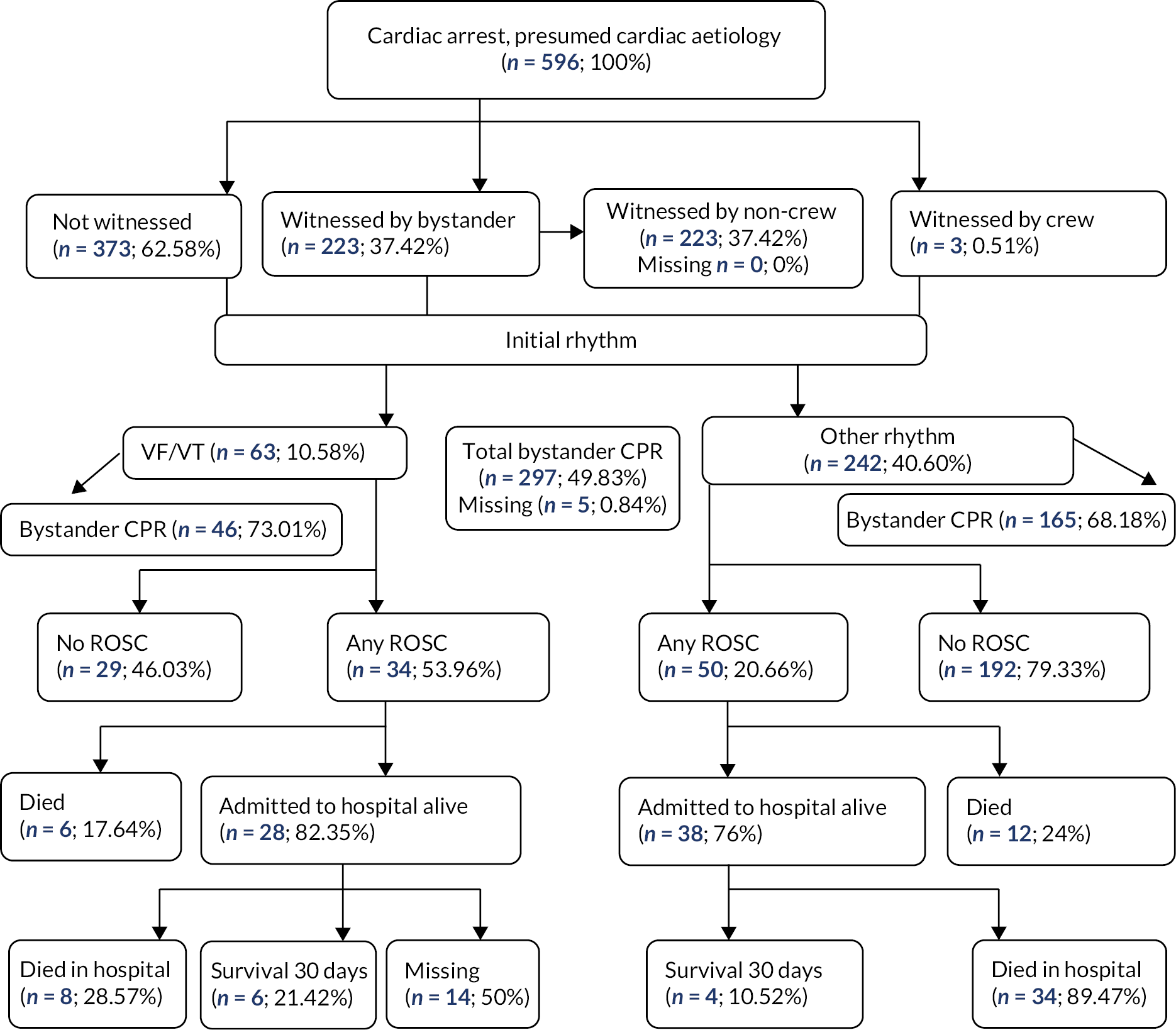
FIGURE 6.
Cardiac arrest incidents for EMAS. VF, ventricular fibrillation; VT, ventricular tachycardia.
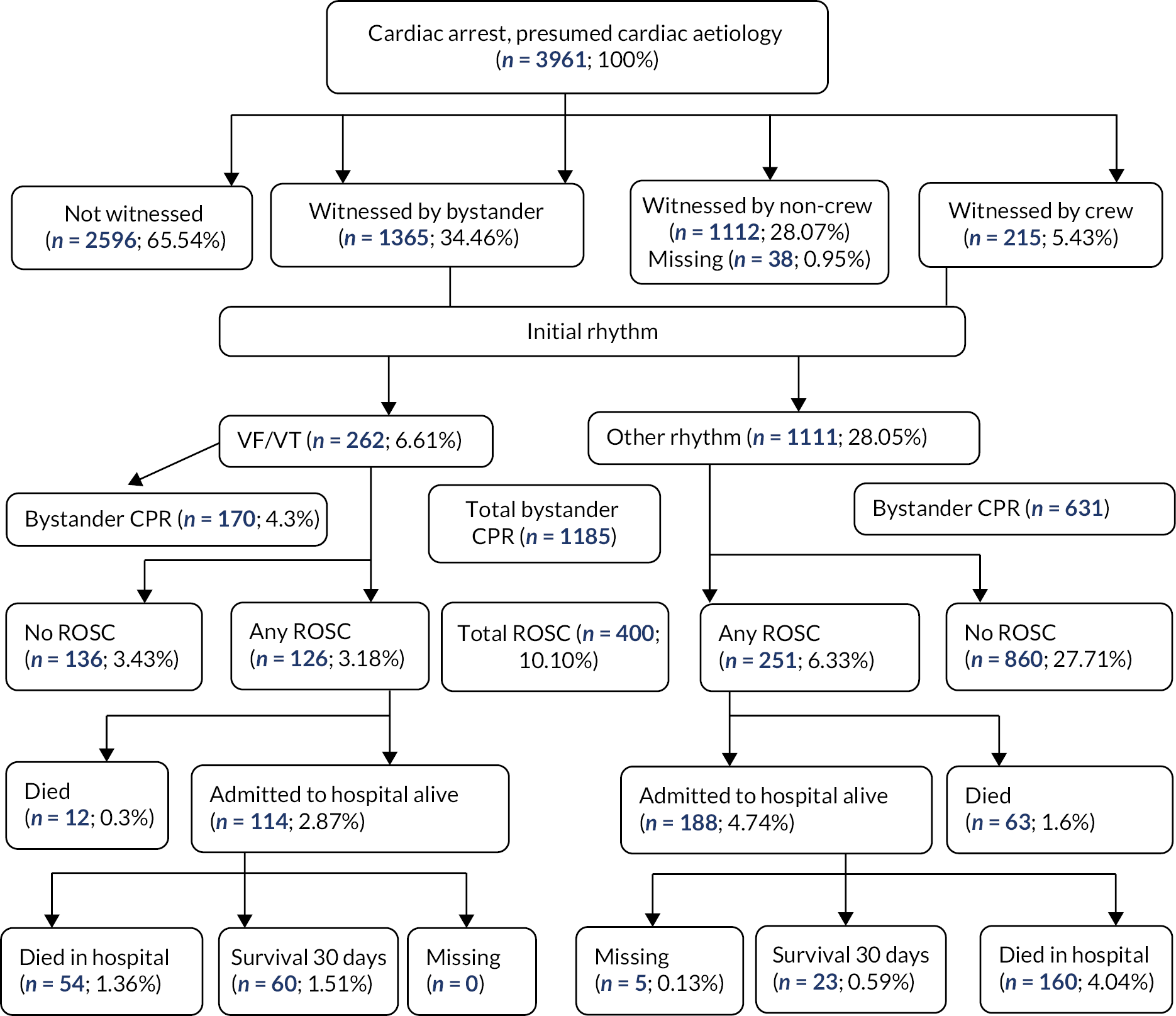
FIGURE 7.
Cardiac arrest incidents where a CFR arrived on scene before EMS. VF, ventricular fibrillation; VT, ventricular tachycardia.
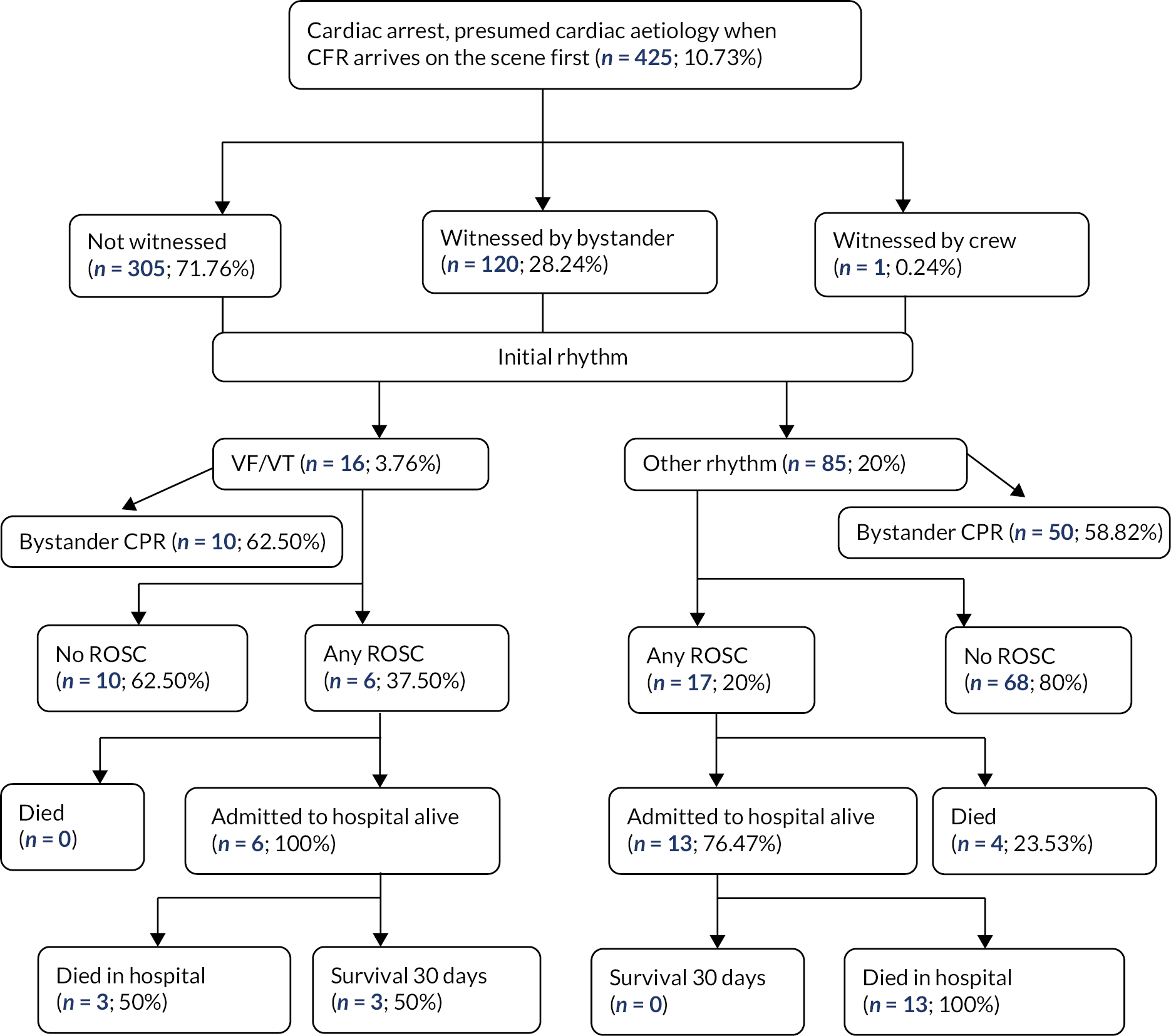
Comparison of Community First Responder and ambulance outcomes
We compared outcomes for ROSC (Table 14) and 30-day survival (Table 15) using multivariable regressions models comparing CFR arrival before EMS with EMS alone for both using multivariable regression models. CFR attendance was not associated with higher ROSC or 30-day survival from OHCA.
| OR | Coefficient | 95% CI | p-value | Significance | |
|---|---|---|---|---|---|
| CFR arrived before EMS | 0.834 | −0.182 | −0.741 to 0.378 | 0.525 | |
| Witnessed arrest | 2.883 | 1.059 | 0.768 to 1.35 | < 0.01 | *** |
| Bystander CPR | 1.044 | 0.043 | −0.227 to 0.314 | 0.753 | |
| VF/VT | 54.369 | 3.996 | 3.444 to 4.548 | < 0.001 | *** |
| Asystole | 18.932 | 2.941 | 2.441 to 3.441 | < 0.001 | *** |
| PEA | 31.419 | 3.447 | 2.899 to 3.995 | < 0.001 | *** |
| First responder resuscitation | 1.137 | 0.129 | −0.945 to 1.202 | 0.814 | |
| CFR resuscitation | 1.253 | 0.226 | −0.235 to 0.687 | 0.337 | |
| IMD decile | 1.019 | 0.019 | −0.043 to 0.081 | 0.548 | |
| Rural area | 0.647 | −0.435 | −0.739 to −0.131 | 0.005 | *** |
| Male | 0.765 | −0.268 | −0.525 to −0.01 | 0.042 | * |
| Ethnicity: Asian or Asian British | 1.068 | 0.066 | −0.638 to 0.77 | 0.854 | |
| Ethnicity: White British | 1.312 | 0.271 | −0.199 to 0.742 | 0.259 | |
| Age | 0.99 | −0.01 | −0.017 to −0.004 | 0.001 | *** |
| Constant | 0.014 | −4.278 | −4.879 to −3.677 | < 0.001 | *** |
| Survival to discharge 30 days | OR | Coefficient | 95% CI | p-value | Significance |
|---|---|---|---|---|---|
| CFR arrived before EMS | 0.954 | −0.048 | −1.191 to 1.096 | 0.935 | |
| Witnessed arrest | 2.837 | 1.043 | 0.417 to 1.669 | 0.001 | *** |
| Bystander CPR | 1.029 | .028 | −0.536 to 0.593 | 0.922 | |
| VF/VT | 32.12 | 3.469 | 2.586 to 4.353 | < 0.001 | *** |
| Asystole | 2.232 | .803 | −0.137 to 1.743 | 0.094 | |
| PEA | 5.086 | 1.626 | 0.628 to 2.624 | 0.001 | *** |
| First responder resuscitation | 0.743 | −0.297 | −2.946 to 2.353 | 0.826 | |
| CFR resuscitation | 0.581 | −0.544 | −1.627 to 0.54 | 0.326 | |
| IMD decile | 0.974 | −0.026 | −0.155 to 0.102 | 0.688 | |
| Rural area | 0.709 | −0.344 | −0.948 to 0.261 | 0.265 | |
| Male | 1.343 | 0.295 | −0.252 to 0.842 | 0.291 | |
| Ethnicity: Asian or Asian British | 0.945 | −0.057 | −1.148 to 1.034 | 0.918 | |
| Ethnicity: White British | 0.638 | −0.45 | −1.219 to 0.319 | 0.252 | |
| Age | 0.968 | −0.033 | −0.044 to −0.021 | < 0.001 | *** |
| Constant | 0.04 | −3.22 | −4.229 to −2.212 | < 0.001 | *** |
Summary
Community First Responder attendance before the ambulance arrived was not associated with improved ROSC or 30-day survival outcomes from OHCA.
Falls response partnership evaluation findings
Descriptive analysis
As a result of the recommissioning of the falls response programme (FRP), an important change in operation from the pilot stage was the replacement of the EMAS-owned BSVs with three similarly equipped LIVES-owned vehicles, their call signs being FRP1, FRP2 and FRP3. Operating with more vehicles had the effect of increasing in size the area that the FRP covered. In Figure 8, a heat density mapping of the incidents attended by each FRP vehicle is shown. FRP1 responded to emergencies mostly in and around Bourne and Spalding, occasionally attending as far afield as Louth and Mablethorpe. FRP2 responded mostly in and around Skegness, occasionally attending emergencies as far afield as Spalding and Long Sutton. FRP3 responded mostly in and around Lincoln but also attended calls in Gainsborough and Grantham.
FIGURE 8.
Heat density map of attendance by FRP vehicle. (a) FRP1; (b) FRP2; and (c) FRP3.
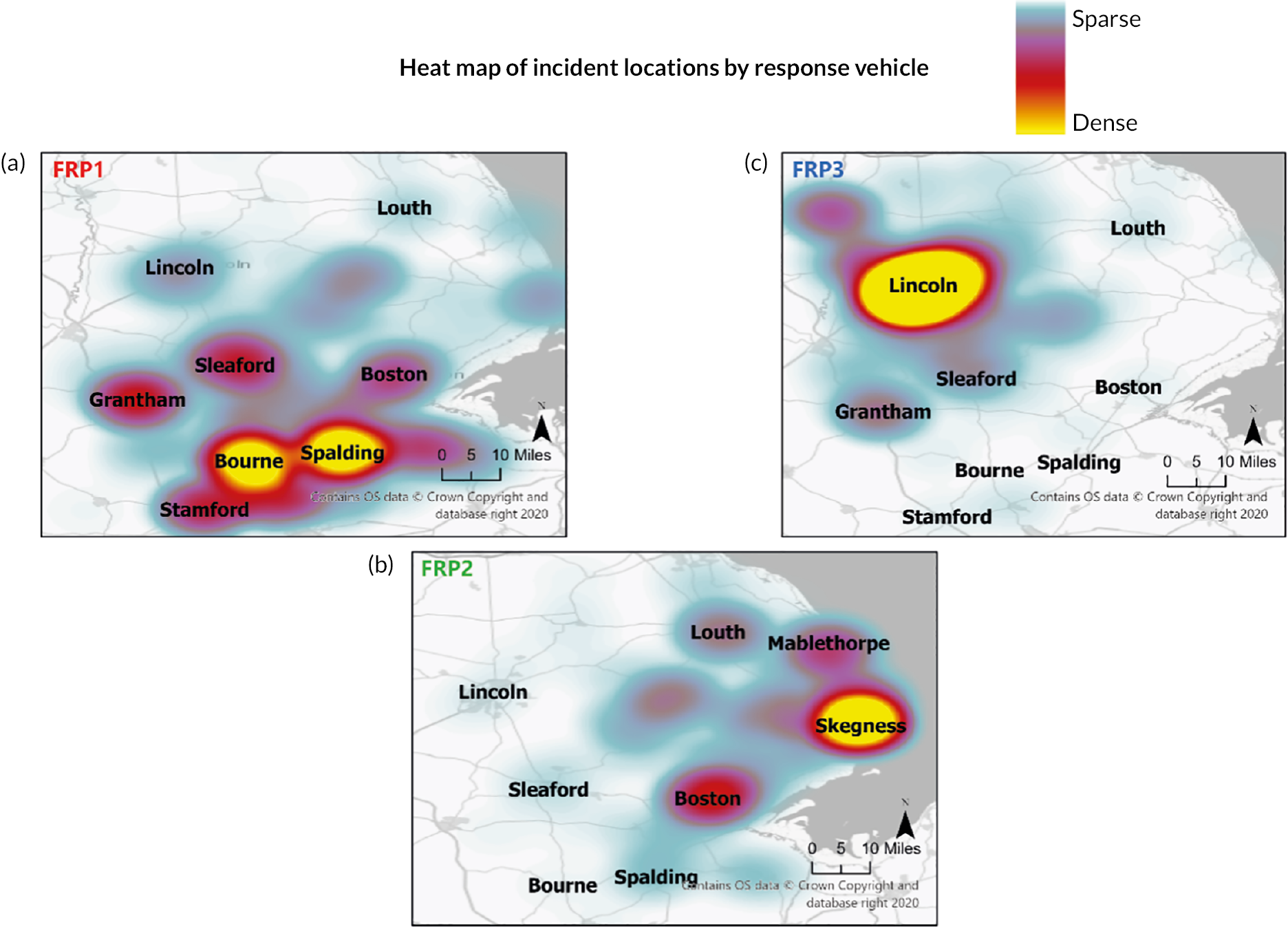
The heat map was derived from a total of 2090 incident attendances over the 21-month sample frame (April 2019 to December 2021), thus averaging 33.2 attendances per month by each LIVES CFR team. Further separation by urban–rural classification reveals totals of 1221 (58.4%) incidents in urban areas and 869 (41.6%) incidents in rural areas.
Using postcode data, Figure 9 gives the location of FRP attendances as well as indicating whether the patient had suffered a fall or had another type of emergency. Most incidents attended by the FRP, 1793 (85.8%) in total, were to falls patients, with the remainder to other types of emergencies, classified as non-falls. Among falls patients, the urban–rural split of incident location was urban (57.2%) and rural (42.8%).
FIGURE 9.
Falls response programme incident attendance by falls and non-falls.
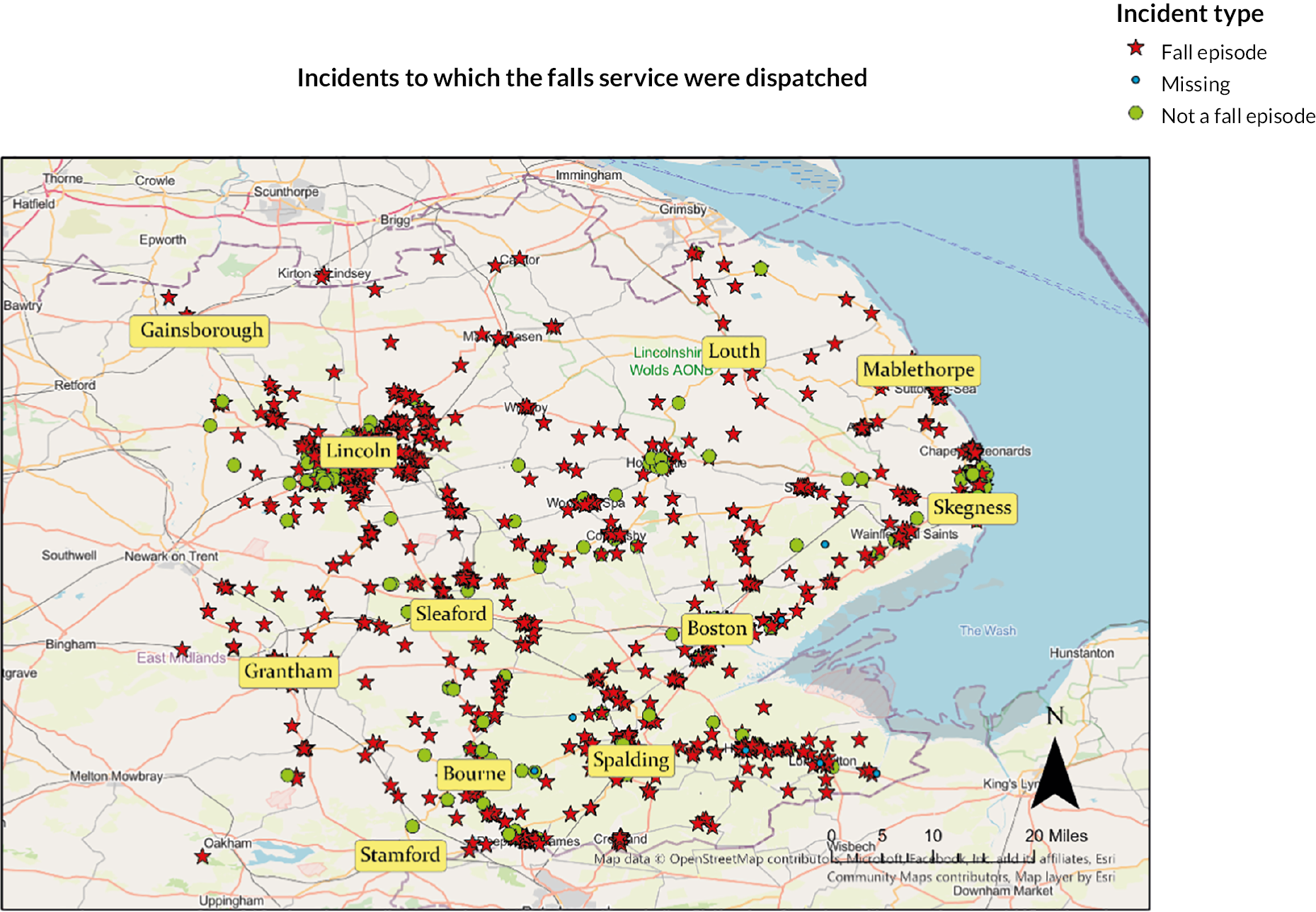
In addition to emergency type, call category was another determinant of whether a falls patient could receive treatment in accordance with the FRP protocols. In Figure 10, attendances to falls patients by the FRP service are displayed by severity and separated by whether FRP protocols were followed (left panel) or not (right panel).
FIGURE 10.
Call severity of falls incidents. (a) Protocol followed; and (b) protocol not followed.

Category 1 life-threatening falls were ineligible for FRP treatment, but this did not exclude EMAS dispatching the FRP to an incident of this severity. The FRP vehicles were dispatched to attend 44 category 1 falls, locations of which are shown in Figure 10b. On the other hand, FRP treatment could be administered to falls patients classified category 2 or lower, but the right panel shows that many (n = 227) were not treated in accordance with FRP protocols.
The FRP protocol was followed in 1517 episodes of care (72.6% of all incidents attended; 84.6% of all falls incidences attended), where incident locations factored by severity call category are given in Figure 10a. Of these episodes, 812 (53.5%) were to calls located in urban areas and 705 (46.5%) in rural areas.
The locations of the 1517 incidents depicted in Figure 10a – those incidents in which FRP treatment was administered as per the FRP protocol – are replotted in Figure 11 classified by whether or not the FRP service was backed up by an EMAS ambulance unit(s).
FIGURE 11.
Ambulance unit backup.
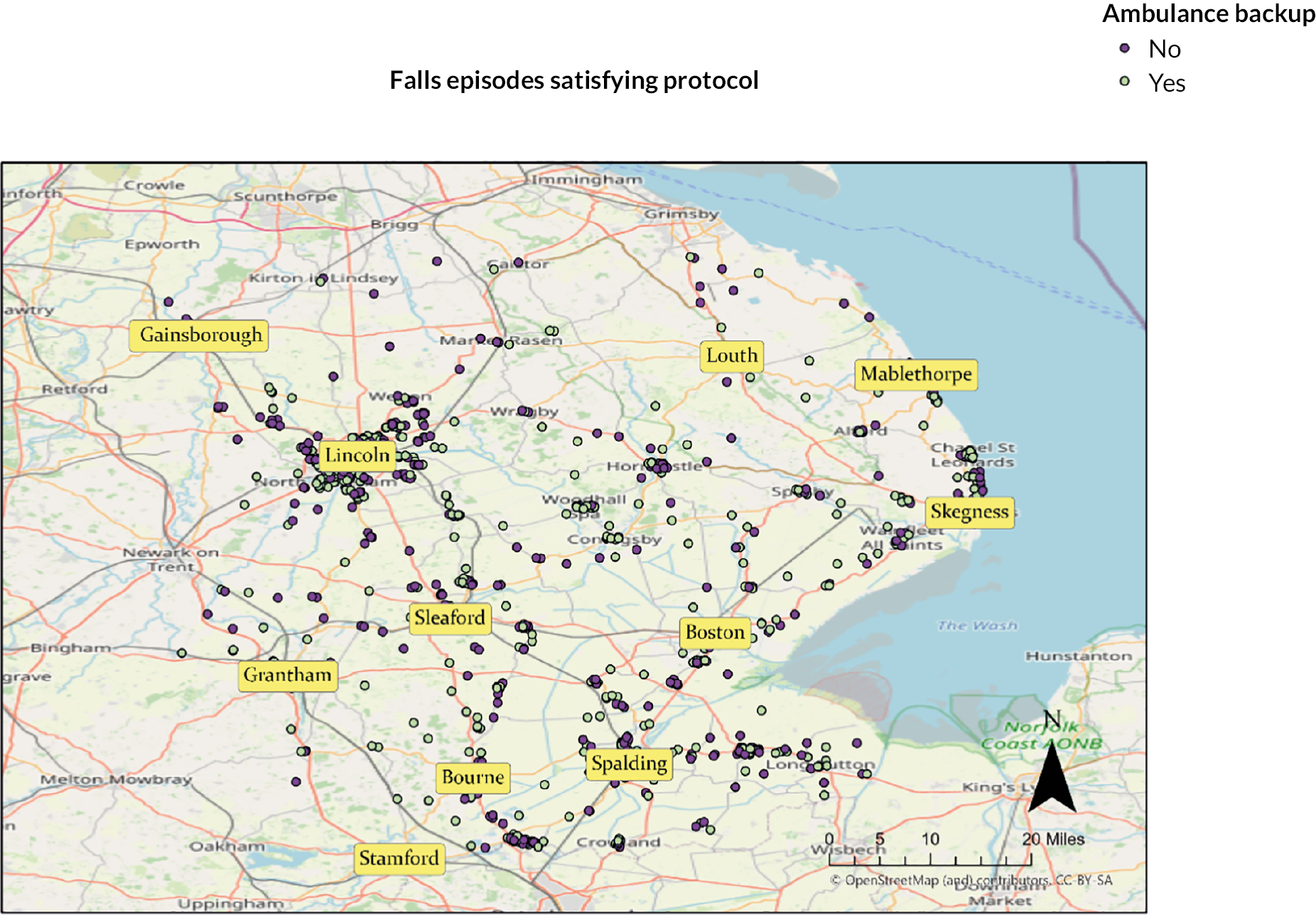
The observed ambulance backup rate was 51.9% when patients were treated as per the FRP protocol. Of this group, 60.2% of incidents were located in urban areas and 39.8% in rural areas. In addition, for the group sent backup, 75.4% of patients were conveyed to hospital, while 24.6% were subsequently discharged at-scene.
Comparing the recommissioned with the piloted Falls Response Programme
For the pilot period of 7 months, 445 falls patients were treated as per FRP protocol by LIVES CFRs using a fleet of two BSVs, averaging 31.8 patients per month per CFR team. For the recommissioned FRP service, over 21 months 1517 falls patients were treated per protocol using a fleet of three vehicles, the average reducing to 24.1 patients per month per CFR team. The ‘gap’ between these averages was due to the use of FRP as auxiliary to the regular emergency services, involving dispatch and attendance at non-fall emergencies as well as life-threatening category 1 falls. Auxiliary use of the FRP was negligible over the pilot period but not so the recommissioned FRP, which was used in this capacity to the extent of, on average, 9.1 calls per month per CFR team.
Results from the pilot showed that the key driver of cost-effectiveness of the FRP over standard care given to category 2 or less falls patients was the rate of backup support required by the FRP. The backup rate observed during the pilot was 68% and for the recommissioned FRP it fell considerably to 51.9%. Our pilot economic modelling suggests that in this circumstance the recommissioned FRP may have the further advantage of being cost saving to the NHS (see Report Supplementary Material 3). 35
Summary
The falls response introduced as an innovation in one county enabled CFRs to attend people who had fallen, reduced ambulance attendance because only around half required an ambulance backup, and was potentially cost saving.
Documentary analysis findings
Seven ambulance trusts responded with a total of 10 documents: seven CFR policies, one COVID-19 guideline for CFRs and two protocols for specialist CFR roles.
Content analysis
The content analysis involved examining keywords, phrases, topics and concepts in the policies and developed a coding manual using keywords from previously published studies of CFRs,3,18 expertise within the research team (GP, VHP, IT, NS) and an inductive approach to identify new keywords. We identified and analysed the frequency distribution of 37 keywords in 10 documents, ensuring that terms ending in -ance, -ed, -es, -ies, -ing, -s and -ship were included in the analysis (Table 16).
| Key words/phrases (variables) | Document 1 | Document 2 | Document 3 | Document 4 | Document 5 | Document 6 | Document 7 | Document 8 | Document 9 | Document 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Level(s): pathways to volunteering | 39 | 1 | 1 | 3 | 4 | 18 | 31 | 12 | 7 | 3 |
| Responsibility(ies) | 29 | 22 | 24 | 18 | 0 | 16 | 53 | 40 | 7 | 7 |
| Training/train | 53 | 20 | 43 | 7 | 1 | 43 | 23 | 41 | 11 | 10 |
| Equipment | 25 | 15 | 28 | 1 | 3 | 15 | 15 | 31 | 3 | 7 |
| Device | 9 | 12 | 2 | 0 | 0 | 2 | 29 | 10 | 0 | 0 |
| Procedure(s) | 21 | 16 | 25 | 7 | 3 | 20 | 16 | 18 | 8 | 17 |
| Support | 15 | 18 | 13 | 12 | 0 | 25 | 35 | 35 | 1 | 5 |
| Checks(ing) | 33 | 8 | 55 | 8 | 0 | 12 | 8 | 10 | 2 | 3 |
| Monitor(ing) | 14 | 4 | 10 | 5 | 1 | 5 | 9 | 12 | 6 | 3 |
| Governance | 29 | 7 | 18 | 1 | 0 | 5 | 46 | 17 | 16 | 12 |
| Suspension or termination | 8 | 2 | 0 | 0 | 0 | 18 | 2 | 1 | 2 | 0 |
| Rewards or benefits | 1 | 3 | 5 | 6 | 0 | 5 | 1 | 1 | 0 | 0 |
| Learn* | 2 | 1 | 3 | 0 | 0 | 3 | 5 | 2 | 0 | 0 |
| Safe*(ty) | 8 | 10 | 12 | 5 | 1 | 22 | 28 | 46 | 9 | 15 |
| Risk* | 10 | 2 | 12 | 1 | 20 | 4 | 23 | 30 | 0 | 1 |
| Value | 1 | 0 | 3 | 9 | 0 | 16 | 3 | 5 | 0 | 0 |
| Patient | 28 | 13 | 25 | 21 | 3 | 55 | 43 | 49 | 16 | 23 |
| *care | 12 | 5 | 8 | 3 | 0 | 18 | 21 | 30 | 1 | 6 |
| Treatment | 6 | 9 | 5 | 0 | 0 | 17 | 2 | 4 | 3 | 1 |
| Operat* | 33 | 7 | 21 | 1 | 0 | 42 | 40 | 19 | 10 | 21 |
| Security | 2 | 2 | 6 | 0 | 0 | 5 | 2 | 5 | 4 | 1 |
| Public | 4 | 10 | 4 | 3 | 0 | 8 | 13 | 50 | 6 | 1 |
| Assessment* | 15 | 6 | 20 | 0 | 5 | 21 | 21 | 35 | 3 | 11 |
| Ethics | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| autonomy | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| equit* y | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| welfare | 2 | 5 | 5 | 0 | 0 | 5 | 5 | 4 | 0 | 1 |
| selection | 25 | 3 | 9 | 6 | 0 | 1 | 5 | 4 | 0 | 0 |
| equality | 3 | 2 | 2 | 3 | 0 | 2 | 7 | 4 | 1 | 1 |
| diversity | 1 | 1 | 0 | 2 | 0 | 1 | 0 | 4 | 1 | 0 |
| rural | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 |
| practice | 16 | 17 | 15 | 3 | 0 | 13 | 21 | 18 | 6 | 6 |
| role | 5 | 13 | 35 | 11 | 0 | 35 | 10 | 36 | 0 | 0 |
| relation* | 3 | 1 | 8 | 5 | 1 | 27 | 7 | 26 | 2 | 1 |
| document* | 22 | 6 | 18 | 2 | 1 | 19 | 2 | 16 | 4 | 18 |
| deliver* | 11 | 2 | 2 | 3 | 0 | 4 | 11 | 2 | 1 | 1 |
| grade | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
Our findings identified which and how often the keywords were used and distributed across included documents. Keywords such as ‘patient’ and ‘care’ were evenly distributed across the documents. The relative infrequency of phrases such as ‘rural’ indicated that rurality was not a focus of attention in the policy objectives. Understanding that certain keywords were more common in some documents than others and the changing of the dominating keyword across documents was the most significant finding.
The content analysis revealed the occurrence of keywords in the policy documents, but an understanding of the context was not established. Hence, we used discourse analysis to understand the contexts in which the keywords were used to relate to each other to form a discourse, as noted in the next section.
Findings
The overall discourse that emerged from the texts highlighted the objectives of CFR policies, which were to ensure benefits to the NHS and discussions on the usefulness of to the ambulance services. The governance mechanisms of the trusts were in accordance with legislation and the directives of the Care Quality Commission, the healthcare regulator. It was implicit in the documents that monitoring and compliance with government standards were essential for quality assurance. The findings revealed that the fundamental objective of the policies was to guide the CFRs in delivering high-quality care and facilitate trusts to provide quality assurance and demonstrate clinical governance, as demonstrated by the following excerpts:
The Care Quality Commission is an independent regulator of all health and adult social care services in England, to ensure that care provided meets government standards of quality and safety. The purpose of this framework supports the CFR contribution to meeting the aspects of care to ensure compliancy under the Health and Social Care Act 2012.
WMAS CFR Governance Framework v4.2 2018
CFRs play an integral role within SCAS, when attending emergency incidents within your local communities you will be providing emergency care and support prior to the arrival of our ambulance clinicians. The support you will be providing to your community is something that can’t be underestimated and subsequently, you will have been trained and given all the information you require to carry out this role. Thank you for joining us and we hope you enjoy responding with us.
SCAS CFR Handbook 2020
The Trust Board acknowledges the positive effect on patient outcomes achievable by a well-managed and effectively governed Community First Responder network, and is committed to providing support for this group of volunteers.
SECAMB Community First Responder Policy v0.2 2018
Discourse on Community First Responder roles and responsibilities
Community First Responders were specifically described as volunteers, regardless of whether they worked directly for the trust or indirectly under a local scheme, and throughout the documents a difference was maintained between trust employees and volunteers. Possible explanations include the contrast between paid and unpaid labour. In general, CFRs were seen as complementary and/or supplementary to the trust’s and NHS’s services and sometimes as volunteers who participate in the trust’s community involvement and outreach activities. Thus, CFRs were designed to bolster the NHS overall:
Volunteers provide a service to patients and their relatives. Their role is intended to complement NHS services and it is not intended that they will be used as a direct replacement for paid employment opportunities.
NWAS Volunteer Policy December 2019 v2.0
The Trust utilises Responders to supplement core ambulance resources. Responders are volunteers who have been trained to attend medical emergencies and deliver basic life support, oxygen therapy and defibrillation using an AED.
SWASFT Responder Governance Policy v9 2019
The role of the volunteer is to complement paid staff to enhance patient experience by undertaking specific tasks within clear role descriptions and guidelines. The role of the volunteer is limited so that it does not constitute paid work, and the time a volunteer is engaged in volunteering varies from an hour to several hours per week. Therefore, induction and refresher training should be at a level relevant to the CFR role.
WMAS CFR Governance Framework v4.2 2018
The CFR role in rural areas was not made explicit, although rurality was mentioned. Some documents acknowledged that it was essential to seek the assistance of CFRs to meet healthcare objectives in rural areas set by the government:
In line with the organisation’s mission statement: ‘To respond to patients, emergency and urgent care needs quickly and safety to save lives, relieve anxiety, pain and suffering’, South West Ambulance Service NHS Foundation Trust (the Trust) is committed to providing the population of the South West with the highest standard of out-of-hospital care. The Trust provides emergency care to around 2,500 people every day. All UK Ambulance Trusts have to respond to 75% of incidents triaged as potentially life-threatening, within 8 minutes. The enlarged organisation covers the largest rural area of the UK, providing ambulance services to a population which serves a resident population of over 5.3 million people, plus an estimated annual influx of more than 17.5 million tourists and covers almost 10,000 square miles, which is approximately 20% of the English mainland.
SWASFT Responder Governance Policy v9 2019
The CFRs’ responsibilities were set out in the various documents and included:
-
Complete a patient report form.
-
Familiarise themselves with the NHS Constitution and the trust’s core values.
-
Ensure that their behaviours reflect trust’s core values when they are undertaking voluntary activity and representing the trust.
-
Adhere to responsibilities set out in trust’s code of conduct.
-
Raise concerns.
-
Take account of the Working Time Directives.
-
Follow guidelines in policies relevant to the CFR.
-
Ensure that equipment is clean and in a serviceable condition when handing over.
-
Keep equipment and consumables safe and ensure the equipment is serviceable.
-
Inform the community and engagement training officer (CETO) through their co-ordinator when levels of medications are running low.
-
Use online communication networks sensibly and responsibly and consider the wider implications of using social networking sites.
-
Not to breach any confidentiality.
-
Ensure that they do not fall outside requalification period or be asked to stand down.
-
Report criminal charge or conviction immediately.
-
Be aware of their responsibilities towards consumption of alcohol and ensure that their alcohol level is zero.
-
Report any changes or endorsements to their driving licence.
-
Maintain their vehicle in a safe and roadworthy condition and ensure that it is sufficiently covered by suitable motor insurance and MOT (Ministry of Transport test).
-
Ensure that they produce their driving licence, MOT certificate and insurance certificate for ongoing checks.
-
Inform their insurer that their private vehicle is being used for a responding purpose and is liable for any claims when using the vehicle for responding.
-
Always adhere to the trust’s infection prevention and control policy and help ensure continued compliance of the trust with the Health and Social Care Act (2008).
-
Be responsible for providing their own defence at their own expense.
-
Comply with health and safety standards as set by the trust.
-
Not assess and leave patients on-scene without the clinical responsibility being taken by a responding clinician or a clinical supervisor.
-
Report if they are pregnant at the earliest opportunity.
-
Highlight any items requiring servicing prior to the expiry date.
-
Report any actual or potential incident using the trust’s incident reporting procedure.
-
Take sufficient rest and where relevant manage their normal employment commitments and their CFR voluntary time.
-
Follow the guidelines on attire for responding to minimise the risk of injury to themselves.
-
Raise with their local manager any perceived deficiencies or lack of contemporary experience in any practice area.
-
Ensure that the scope of practice is maintained.
-
Maintain sufficient fitness for their duties.
Discourse on Community First Responder structures
This section highlights the keywords examined in the documents and how CFR roles and responsibilities are structured and governed to meet the quality standard.
Recruitment and selection
The documents described how CFRs were identified and recruited in accordance with trust and other regulations, who was responsible for recruitment, and what happened to unsuccessful applicants. For example:
The Trust commits to implementing a robust recruitment procedure for all of its patient facing volunteers… Recruitment and selection compliance must be received prior to confirming a training place for a CFR. Compliance comprises: Application Form, Interview with two panellists, one of whom must be Trust staff, Proof of identity with photographic identity and address, Two references to the satisfaction of the Trust. National Insurance Number. Full driving licence, with access to a class B vehicle which is road worthy and have adequate insurance on this vehicle, which must be taxed and have an MOT if applicable, Disclosure and Barring Service check, Occupational health clearance to carry out the volunteer role.
SECAMB Community First Responder Policy v0.2 2018
Equality and diversity
The phrases ‘equality and diversity’ noted in the policies primarily referred to the trust’s stance on equality and diversity matters, particularly on being inclusive in the recruitment of CFRs and guiding them to treat patients and their relatives with respect and dignity:
This policy embraces diversity, dignity and inclusion in line with Human Rights guidance. We recognise, acknowledge and value difference across all people. We will treat everyone with respect, courtesy and with consideration for their individual backgrounds. We will ensure that everyone is treated fairly and that we convey equality of opportunity in service delivery and employment practice.
EMAS Responder Policy v7.1 2018
Benefits and rewards
There was no clear discourse on benefits or rewards, but instead a few sentences clarifying that CFRs were not eligible for any benefits and were not obliged to report to His Majesty’s Revenue and Customs. CFRs were advised to consult existing employers or job centres prior to volunteering to ensure that their benefits arrangements would still be maintained. Moreover, the issue of CFRs using trust names for their personal benefits and the repercussions of this were highlighted:
Volunteers are not employees and are not obliged to commit their time to NWAS. At the same time NWAS is not obliged to provide opportunities for voluntary activities when a volunteer is available. This means that any agreement with a volunteer is binding in honour only and is not intended to form a contract. For clarity this means that there is no entitlement to benefits such as pay or annual leave.
NWAS Volunteer Policy December 2019 v2.0
CFRs are reminded that it is appropriate to consult their employers/Job Centre Plus and gain approval to undertake their role as a CFR as this may have an impact on their employment/benefits.
WMAS CFR Governance Framework v4.2 2018
Governance
The discourse on governance explained who and what was governed by CFR policies, which included individual CFRs, external schemes operating under their own governance arrangements and equipment purchased by charitable funds. The governance discourse also highlighted the committees and groups that oversaw all monitoring efforts and had the power to ultimately make decisions in all governance processes, ranging from recruitment to termination of CFRs
This policy acknowledges that there are schemes that exist which operate under their own governance arrangements; however, this policy offers guidance to the minimum levels of assurance required by EMAS for such schemes.
EMAS Responder Policy v7.1 2018
Operations
The discourse around the term ‘operation’ highlighted the chain of command that governed operations. For example, although the third-party CFR schemes operated under their own governance structure, they were required to report to a trust to receive quality assurance. Individual responders needed to strictly adhere to regulations and abide by the rules about who to approach for activities such as using a trust vehicle, fitting blue lights, raising concerns and reporting health changes. The chain of command was formed of a hierarchy of individuals in committees, hubs and teams that govern all aspects of CFR activities, ranging from chief executives, directors of operations, strategic operations director, head of operations, head of community response managers, operational unit managers, responder managers, tactical commanders, operational bronze commanders, CETO, community responder officers and duty managers:
If you have a complaint or an issue that is causing you concern or information that you may want to request regarding wider SCAS or Charity issues you should follow the recognised chain of command. In the vast majority of cases, issues can be dealt with at an appropriate level without the need to escalate to Director, Non-Executive Director or Board level. If it is necessary to further escalate any issue above the level of Head of Operations or SCAS Charity Chief Executive, we will inform you of that decision.
SCAS CFR Handbook 2020
Procedure and process
The keywords ‘procedure’ and ‘process’ followed a clear discourse in the documents. First, there was a list of procedures in the documents, including procedures for incident reporting and safeguarding, procedures for medicines management, procedures for shadowing ambulance crew, procedures for staff who are also CFRs, procedures for booking on/off duty and procedures for claiming mileage. The second segment of the discourse focused on the implementation and staff awareness of these procedures. A focus was placed on ensuring that these procedural documents were available in both physical and digital formats. Third, the discourse moved on to compliance with the procedures. Compliance discourse dominated the policy discussions, which centred primarily on monitoring the effectiveness of procedures, annual reviews and keeping the procedures up to date. The final segment of the discourse focused on the investigative, problem-solving and termination processes in the event that compliance with the procedures failed:
You are only authorised to act within the agreed procedures and protocols of CFRs as defined during the CFR induction course training, within this document, your scope of practice and any clinical updates issued by the CET Department. Please note: criminal proceedings may also be brought against a CFR by any injured party. Reported instances that may lead to an investigation by the Trust may include, but are not limited to: Breach of the applicable Trusts’ policies and procedures, especially those concerning clinical protocols, confidentiality and health and safety.
SCAS CFR Handbook 2020
Checking
The discourse of ‘checking’ included policy statements in relation to assessing CFRs’ eligibility for the CFR role and providing regulatory agencies with confidence that institutions (trusts) were complying with quality standard frameworks. Various types of checks were discussed in the categories of pre-selection checks (ID, driver, DBS); training checks to ensure proficiency and competency; pre-activation checks to provide assurance that all suitability checks had been successfully performed and approved; pre-shift (daily) checks performed on vehicles, medicines pouches and other devices to ensure serviceability; ongoing checks biannually, annually and triannually (depending on the level of the CFR); assurances on disclosure, driving licences, proficiency and identity; and compliance checks to ensure that individuals and third-party schemes were complying with organisational policy standards:
Activation of New CFRs. The CRM is responsible for updating CRA on the active status of a CFR. This will only be undertaken when there is assurance of the following: • The recruitment documentation is complete (including DBS, references and self-health questionnaire). • Evidence of a valid MOT (if applicable), driving licence and motor insurance has been provided. • Evidence of successful completion of the required level of education, training and familiarisation shifts. • Receipt of a signed CFR Agreement.
WMAS CFR Governance Framework v4.2 2018
Monitoring
The monitoring discourse centred on the organisational monitoring of policy documents for compliance with quality assurance frameworks and the minimum requirements of regulatory bodies. This was accomplished by establishing formal agendas or using compliance schedules to locally monitor various CFR activities. Examples of responder activities monitored were minimum hours for proficiency standards (hours of responding per month in some trusts), monitoring performance in training, monitoring equipment use (and equipment return for ex-CFRs), monitoring records of patients who decline treatment by CFRs, monitoring medicines managements (storage, temperature, etc.) and monitoring CFR behaviour:
It is suggested that to further support clinical effectiveness a CFR is expected to: • Complete a monthly skills audit forms (enhanced CFRs only until EPR available) • Complete reflective practice through case reviews • Complete audits related to clinical outcome. In addition, monitoring clinical effectiveness the following is available: • Familiarisation shift for CFRs • Attendance at study sessions to refresh skills • Annual Post Qualification Updates • Implement support and ongoing learning from identified development areas • One to one meeting annually to discuss clinical activity Both internal and external verification are carried out annually to ensure compliance and quality assurance.
WMAS CFR Governance Framework v4.2 2018
Support
We found four discourses about ‘support’. First, CFR training and the capacity to deliver basic life support were expected to boost prehospital survival from OHCA. Second, this addressed the welfare and support of CFRs in situations of distress following an incident, such as giving statements to the police, raising concerns, monitoring changes in health status, providing support for responder networks and meetings, and providing additional support to responders whose behaviour had prompted concerns. Third, support from the trust assisted individuals and schemes to generate charity funds at promotional events. Fourth, emphasis was placed on supporting staff to efficiently implement policies within localities. The following excerpt demonstrates the discourse of support:
It is acknowledged that CFRs will become involved in situations that are new, unusual and in some cases very distressing for those involved. You can be assured that structured and effective welfare arrangements are readily available to any CFR that requires them. Current arrangements within the Trust include: • Informal discussion • Formal debrief • Trauma Risk Management (TRiM) assessment • Employee Assistance support (online and telephone support) • Formal counselling referral • All of which can be accessed directly via the Clinical Coordination Centre (CCC), CETO and/or the CET department. Asking for and receiving support is not a sign of weakness; it is a natural part of the role.
SCAS CFR Handbook 2020
Patients
Phrases pertaining to ‘patients’ tended to focus on CFRs’ competence, appropriateness and fitness to deliver high-quality service to patients, standardising patient care throughout the trust for optimal outcomes, and increasing patient survival in prehospital settings through a number of activities. Such activities included assessing the patient’s condition and communicating the assessment to clinicians, performing any required treatment within the scope of practice at the CFR level, treating patients with dignity and their personal information with confidentiality, and adhering to protocols such as the prohibition against transporting patients in CFR vehicles, and handing over patients to clinicians and then documenting the care and any adverse events. The documentation of patient care was substantially emphasised in the discourse, as documentation could be audited and used to provide assurance to regulatory bodies:
South Central Ambulance Service NHS Foundation Trust has both legal and moral obligation to uphold a duty of care to its patients, staff and volunteers. Therefore, all information contained within this handbook will be reviewed bi-annually or sooner as circumstances dictate.
SCAS CFR Handbook 2020
Treatment
The discourse of treatment was mostly about rules for administering treatment to patients on-scene, following protocols for ensuring patients’ safety and comfort, and treating patient information as confidential. The protocols consisted of various rules from arrival to handover and documentation. There were protocols for arrival on the scene, which usually included staying in touch with the clinical hub or a responsible officer and performing a dynamic risk assessment. Moreover, there were protocols for the CFRs treating the patients, their relatives and carers with dignity and respect; protocols for assessing the patient condition and treatment, which might consist of conducting basic life support and defibrillation; protocols for accepting gifts in appreciation of treatment; and protocols for documenting patient treatment using variety of reporting forms: SBAR documentation when no treatment was given, and patient report forms, which are later transferred to ePRFs:
CFRs must complete a specific CFR PCR for every incident where they have patient contact. Form meets data protection by being a document with no reference to individual patients. CFRs must record any and all decisions and observations made, and treatment given, or the reasons why treatment was not given, on the PCR. This is a legal document which may need to be referred to in the future for an investigation or by a Coroner. Process: Yellow copy to go with crew, White copy is given to CDO/CDT and passed to Clinical Audit for scanning, storage and audit. CFR PCR can be cross referenced to crew PCR by incident number and date. NB: Currently pending review the CFR PCR is still called a Patient Report Form.
YAS Volunteer Procedure CFR Policy v7.0 2020
Care
The discourse of care centred on providing high-quality care and being responsible for the care provided in accordance with the standards established by regulatory authorities. Topics covered on care included the CFR handing over care to the ambulance team, third-party schemes showing evidence of documenting care, patient safety during care, and providing care with compassion, safeguarding and accountability:
The Trust will ensure that the governance framework remains fit for purpose and complies with the wider framework of regulations and best practice defined by authorities such as the NHS Litigation Authority, Health & Safety Executive, the Care Quality Commission and our commissioning partners.
SWASFT Responder Governance Policy v9 2019
Practice
‘Practice’ was another discourse that evolved, and the discourse was usually about CFRs strictly practising within their defined scope so that they remained covered by Public Liability insurance cover. This distinct discourse centred on establishing consistent standards of good practice across trust and within policy documents, as well as ensuring the successful implementation of the policy documents in real-world practice. The regulation committees would subsequently obtain assurance of the effective implementation of the standards outlined in the documents through meetings and annual reports:
Public Liability cover awarded to Community First Responders includes acting within scope of practice, promoting their role in the wider community, and demonstrating Cardio-Pulmonary Resuscitation and Automated External Defibrillator use. Voluntary Services must be notified of public events being attended by Community First Responders to activate the cover. The following activities negate the public liability cover for Community First Responders and must not take place in any circumstances at a public event: Providing first aid event cover, Accepting donations of cash or cheques, Finance, Fundraising [individual]
SECAMB Community First Responder Policy v0.2 2018
Safety
The discourse on safety was around CFR compliance with organisational health and safety procedures such as safeguarding patients, working within the scope of practice, safe moving and handling of patients, hygiene and infection prevention control, CFR health, observing safe driving regulations, use of personal protective equipment (PPE) and incident scene safety. The subject of safety-related discussions also included consequences of non-compliance, which could be either an internal investigation or a stand-down:
The CFR Activation Policy details the criteria and process for the activation of volunteer CFRs. In particular it includes the specific incidents which CFRs can be sent to and the restrictions intended to keep volunteers safe. It also includes provision for CFR welfare and support and out of hours arrangements for this also. CFRs must follow the direction of the EOC staff for their own safety and the Trust reserves the right to dismiss any CFR who, following an investigation, is shown to have gone against the direct instructions of the EOC.
YAS Volunteer Procedure CFR Policy v7.0 2020
Risk
The identification of risk and its elimination or reduction was the key discourse on risk. CFRs’ mental and physical health, adverse events and near misses, responder personal hygiene and cleanliness when attending patients, working beyond the scope of defined practices, theft of equipment, misuse of personal information, and lone working were recognised as risks. Both trusts and CFRs were responsible for identifying and mitigating risks. Despite the fact that trusts had many templates for reporting various risks, CFRs were expected to participate in dynamic risk assessment. Internal inquiry or immediate stand-down was the consequence of non-compliance:
The Trust Board holds overall responsibility for the management of risks with the Trust and for determining the level of risk that is acceptable and accountable for ensuring that there are effective arrangements in place to manage the risks associated with Responders.
EMAS Responder Policy v7.1 2018 20.1.1
Whilst Responders are expected to operate in accordance with the arrangements described in this policy, they must also engage in a process of continual risk assessment, better known as a dynamic risk assessment. If unacceptable levels of risk are perceived, the Responder must take steps to mitigate the risk/s to the best of their ability.
SWASFT Responder Governance Policy v9 2019
Documentation and records
The discourse on documentation emphasised that all activities related to CFR were documented for auditing and quality assurance purposes. Three types of documentation were identified. (1) Patient care documentation was centred on documenting any CFR actions pertaining to patient care using the following templates: patient report form or patient clinical record form, adverse event form, incident report form, no treatment (SBAR) form, and patients’ refusal of CFR’s help report. (2) Trust policy documentation centred on documenting adherence and compliance concerns, document storage and access, annual reviews and revisions. (3) Maintaining records of responder activities on databases included training and education records, disclosure checks, other evidence of suitability, record on CFR activities and incident reports, and responders’ equipment:
All Responders are required to complete a patient report form … SBAR documentation is permitted only when there’s NO treatment or drugs administered to the patient by the Responder in order to capture initial information. More importantly, when Responders attend patients, the SBAR information is to be transferred to a paper PRF form at the earliest opportunity prior to the Responder booking clear. Both of these documents will then be passed to the back-up DCA/FRV to complete and secure (or transfer to the EEPRF system).
EMAS Responder Policy v7.1 2018
These forms are specifically designed to provide the completing CFR with structured guidance to ensure that the Trust’s CFR treatment protocols are followed completely and correctly. In the interests of data protection and security, these forms have been designed to remain anonymous ensuring that only authorised personnel may obtain access to specific patient identifiable information. To ensure both patient safety and your protection, all CFRs are required to complete a CAS 130, a patient report form (PRF) or patient clinical record (PCR) (See SharePoint) for every allocated incident, either during the incident, or if not appropriate for whatever reason, immediately following the incident, recording the results of any assessment undertaken and/or treatment(s) provided.
SCAS CFR Handbook 2020
Welfare
Welfare was about CFR welfare and the support provided when CFRs found themselves affected by a health issue such as pregnancy or inability to drive, or after attending distressing incidents, and providing CFRs with access to non-denominational chaplaincy, Trauma Risk Management practitioners, and counselling services:
The Clinical Hub are responsible for informing the relevant Community Responder Officer (or Responder Manager in their absence) in the first instance of any incident that may have caused distress to a Responder. If the Community Responder Officer cannot be contacted, a text or pager message must be sent to the Officer with details of the incident. In the absence of a response from the Community Responder Officer, the appropriate Duty Clinical Support Officer or Duty Officer must be informed. A Responder Welfare form must be completed in all instances by the Clinical Hub and forward to the relevant Community Responder Officer.
SWASFT Responder Governance Policy v9 2019
Suspension and termination
The suspension and termination discourse was about three types of disciplinary procedures: (1) automatic termination, (2) immediate termination after investigation and (3) suspension during investigation. Automatic termination is actioned if a CFR is determined to have committed egregious misconduct: he or she will be terminated immediately. Refusal to comply with regulations, failure to report criminal convictions, violation of driving standards and it being deemed that additional training was unsuitable all result in immediate termination. Suspension (i.e. withdrawing the CFR from responding) appeared to be employed in cases when patient safety, the reputation of the trust and the safety of the CFR were at stake. Actions that might result in suspension were concerns about a CFR’s behaviour, allegations that might bring the trust into disrepute, and failure to submit medical devices for inspection and assessment. Some trusts explored learning from missed opportunities if a CFR decided to terminate their agreement with them:
A CFR may elect to cease volunteering with the Trust at any time; there is no requirement for a formal period of notice. On leaving the Trust, an interview will take place between a representative of the Trust and the CFR to discuss the reason for leaving. During this interview the return of ID badge, equipment and uniform is expected.
WMAS CFR Governance Framework v4.2 2018
Equipment and devices
Equipment and devices, including that owned by external schemes, were managed in line with trust policies. Equipment was managed using a checklist of approved devices, and the statuses of devices were tracked in databases for audit purposes to ensure management, maintenance and servicing in accordance with standards. The management of equipment included storage, replenishment, maintenance, procedures for missing or damaged equipment, annual inspections, adherence to manufacturers’ manuals and completing forms for auditing:
The location and service schedule of all medical devices will be maintained through the Medical Devices Database … No other medical device or consumable may be used, unless stated in the Responder Bag Checklist. All equipment will be issued by the appropriate Community Responder Officer or Responder Manager.
SWASFT Responder Governance Policy v9 2019
Training
The discourse on training was in relation to the following: achieving minimum training requirements, external schemes’ own training requirements and assurance to the trust, ongoing training requirements for assurance checks, the content of training delivered, training required for different types and levels of CFRs, practicing within trained scope, accessing training documentation and trainer requirements. Training criteria, standards and content varied widely between trusts, but the ability of the CFRs to administer basic life support was common in all documents. There was a ‘weak’ discourse around documenting responder training records for auditing and quality assurance purposes:
Voluntary Services will conduct a quarterly audit of the central repository of training records for the following assurances: Clinical training including re-qualifications, have been completed by each Community First Responder and is up to date Statutory and mandatory training recorded has been completed by Community First Responders
SECAMB Community First Responder Policy v0.2 2018
Summary
The NHS recognises the importance of CFRs to their local communities, and it was apparent from the documents that ambulance services invested substantial efforts to ensure that CFR programmes were effective, with procedures for recruitment, selection, training, support and monitoring. However, there are risks involved with the roles that CFRs perform, as they are individuals with (often) little clinical expertise who provide care to fellow community members voluntarily. Risks involved in CFR work include risks to CFR themselves, to patients and the public, and to the NHS ambulance trust that they represented. Ambulance trusts had established governance frameworks for checking compliance with frameworks such as rules, standards and procedures in order to mitigate risk. Variations in the frameworks create confusion that could interfere with regulatory body auditing programmes and the public’s perception of CFRs roles, and possibly discourage recruitment and retention of CFRs.
Qualitative findings
Participants
We conducted semistructured interviews with 47 different stakeholders engaged in the functions of CFR schemes, including CFRs, CFR leads, ambulance staff, commissioners of ambulance services and patients or relatives of patients who had received care from a CFR (Table 17). Most CFR leads were also ambulance clinicians. We recruited fewer patients and relatives (5/15) or commissioners (2/5) than we initially set out to, and the reasons for this are discussed below.
| Ambulance services | CFRs | CFR leadsa | Ambulance cliniciansa | Commissioners | Patients and relatives |
|---|---|---|---|---|---|
| EMAS | 6 | 2 | 0 | 1 | 1 |
| SCAS | 3 | 3 | 0 | 0 | 2 |
| SECAMB | 3 | 7 | 1 | 0 | 0 |
| SWASFT | 0 | 1 | 0 | 0 | 0 |
| WMAS | 3 | 2 | 3 | 1 | 0 |
| YAS | 6 | 0 | 0 | 0 | 2 |
| Total (N = 47) | 21 | 15 | 4 | 2 | 5 |
Themes
Findings arising from the empirical analysis are presented in the following three sections. The analysis identified different spheres of (A) varied experiences and determinants of CFR recruitment, training and retention; (B) CFR roles, governance, innovations and future opportunities; and the importance attributed to the notion that (C) patients are the reason for CFR schemes within the health system.
A. Varied experiences and determinants of Community First Responder recruitment, training and retention
The process of CFR recruitment was asked about and identified as a key theme in the analysis. The next section elaborates on the rudiments of CFR enrolment and addresses the study objective of eliciting the views of CFRs and CFR scheme organisers about the challenges in and solutions to recruiting, training and retaining CFRs in rural areas.
Altruistic and personal motivations for community engagement and becoming a Community First Responder
Caring for and helping their local community was found to be an important motivation and inspiration for becoming and being a CFR. CFRs were principally motivated by the philanthropy of giving back to the community and serving their own localities. Almost all CFRs participating in the study depicted their decision to take on the CFR role as a proactive and positive choice:
I wanted to put something back into the community; that was it basically.
CFR_BL_07102021
The motivation for becoming a CFR was often attributed to prior experiences of community engagement and leadership, as well as first-hand observations of care provided by a CFR to someone in their locality. In general, they saw the role of CFR as a crucial opportunity to contribute back to society and their local community.
I was president of the local Lions club when my tenure as the president finished. I wanted to put something into the community …
CFR_AA_20092021
I retired from work at a very young age (38 [years]); after retirement, I was feeling there wasn’t enough goals in my life, and I stumbled across the CFR role. A neighbour called me in, she had a very nasty head injury, and I called 999, and it was actually a CFR that came out first; and at the end of the day when the neighbour was treated, I talked to the CFR, and I knew at once that was the role for me. I knew it would be rewarding and fulfilling; being able to care for people … That is how I came into it.
CFR_BL_07102021
Some participants who were retired emergency care and health practitioners such as firefighters, nurses and paramedics mentioned their prior experiences of practising first aid and other emergency medical care before becoming a CFR and that being a CFR was simply an extension of or transition from professional practice to the voluntary CFR role. These transitions represented an additional way of demonstrating compassion and contributing to the local community by delivering emergency and prehospital care:
I was a nurse and came off the register, and because I wasn’t working, so I had lots of skills, and I thought I could be useful in the local community. I don’t work. I’m at home … I have medical knowledge, and I quite enjoy getting out and helping the community really.
CFR_FW_21092021
In addition to the motivator of serving the community, some participants reported other benefits of becoming a CFR, such as it being a means of gaining crucial first-aid training, practice and experience. This training and experience as a volunteer CFR along with the relevant university degree was to lead them to a paramedic career in ambulance services:
I’ve only been doing this [CFR role] since 2019. I think others have been here a long time and they love it. Me personally, I’m looking to join the ambulance service.
CFR_MM_22072021
He’s at the start of their potential career pathway, and perhaps have an aspiration to become a paramedic, some [CFR] experience can assist them with their onward journey … to become a paramedic.
CFR_TK_04112021
Processes for advertising, recruiting and selecting Community First Responders
Community First Responder recruitment was often promoted via publicity including through community events, where current CFRs and other stakeholders set up kiosks to raise public knowledge of ongoing CFR services and recruitment opportunities through ambulance services. Periodically, posters or radio advertisements were used to publicise opportunities to volunteer as a CFR. Ambulance services also published volunteer placement advertisements for online applications, sometimes via the NHS employment forum:
We advertise the volunteer placement … We do that through an ‘NHS jobs’ [advert]. Additionally to that we will then do some form of campaigning in the community. So whether that’s putting posters up or visiting groups, or doing something on the radio etc. That’s how we find people.
CFRLead_RH_19112020
The selection of applicants for the CFR role depended on a range of factors and was often based on their potential contribution and benefit to the ambulance service. Study participants noted that preference was given to rural candidates who submitted a full application form. Applicants with previous medical and/or emergency response professional experiences were given priority throughout the recruitment process. The recruitment process also involved interviews with potential applicants, when recruiters considered four important aspects for selection: motivation, time commitment, training commitment and quality service delivery:
In the pre-assessment, we ask them questions essentially when they come for interview … it’s things like – What motivates you to want to do it with us and not any other voluntary aid society? What is your time and commitment? So – What can you give us? So we know whether to invest early on.
CFRLead_ND_17062020
The process of recruiting CFRs was similar to the checking and self-declaration involved in the recruitment of employees to the ambulance services. The various aspects of the recruitment of CFRs included checks of personal ID and driving records, DBS (Disclosure and Barring Service) check, occupational and health screening, and sometimes reference checks. The study findings showed that the policies in relation to checking discussed in Documentary analysis findings were followed to ensure quality assurance in the recruitment process:
Once you’ve been successful at interview, we’ll start the recruitment process. So we’ll do a disclosure and check, we’ll do occupational health screening, as well as then reference checks.
CFRLead_RH_19112020
Challenges to recruitment
Public policy implementations in health are often challenged by social realities and contextual factors. The challenges to the recruitment of CFR processes involved a prolonged recruitment period, governance, geographical factors and the age group of CFRs.
We found that the lengthy recruitment time for several CFRs resulted in dissatisfaction with the recruitment process, as well as the attrition of prospective applicants. The period of recruitment that caused dissatisfaction among CFRs varied from 6 to 18 months. Delays in the recruitment process seemed to be incidental to some trusts/ambulance services, with participants from ambulance services correlating recruitment delays with recurrent policy changes in the training curriculum for CFRs. Changes in training governance were introduced at the institution level, rendering recruitment delays inevitable:
We’ve had quite a few CFR that were really keen. Started the recruitment process, and it took so long that they gave up. One of them got pregnant just after she qualified, it took them so long. She would have been a really good responder. Obviously, she can’t respond now … if you’ve an interview, 6 months later you get offered a place, 3 months later you’re on a course, then 4 months before you can get your buddying done, and before you know it’s a year and sometimes longer …
CFR_LF_11102021
A CFR lead rationalised the delays by providing an institutional account of changes in governance policies:
So we’ve had a pause on recruitment the last 6 months or so, because we’ve just been reviewing the level 2 course and it’s just been going through re-accreditation. So rather than continue training people through on that, we wanted to pause it, make sure the course was right, and then we carry on again.
CFRLead_CC_12062020
Geography was another factor that posed a challenge to CFR recruitment. Participants in the study emphasised the continued difficulty of finding qualified candidates who met the requirements of the recruitment processes. In sparsely populated rural areas, there was a continuing migration to metropolitan areas, leaving the rural area with fewer potential residents to take up CFR roles. It was also suggested that someone becoming a CFR in order to pursue employment as a paramedic was advantageous for specific geographic locations as those CFRs eventually became paramedics and remained in the region, supporting healthcare delivery there:
The whole health-care sector in L always struggles to recruit because of the geography… We were counting off our hands how many of our CFRs have gone on the become ambulance technicians, paramedics, nurses, doctors, medical students; that sort of stuff … And we are quite proud, I’m an example. I came in as a CFR, we’ve got quite a lot of joiners, become a CFR, and then become a health-care professional, and stay.
CFRLead_CC_12062020
The older age group of many CFRs was identified as a key obstacle to recruitment and retention. The overwhelming majority of CFRs were older, with some aged > 70 years, which was connected to the nature of the CFR as a volunteer workforce. The commitment necessary for the role was more practical for retired individuals with fewer family or other obligations who were committed to contributing to society. Recruiters were aware that older age was a problem in CFR recruitment and retention and were interested in the possibilities of recruiting a younger population for CFR roles:
So in some areas, we’ve lost the whole CFR group ... why are we not encouraging younger people; even different genders, is two particular areas to focus on. In some of our areas we already know most of the group are over 70, we are already recruiting, but obviously we are not engaging in some way … There is a weakness in the process really.
CFRLead_RH_19112020
An awareness of the challenges in CFR recruitment was evident in the perceptions and experiences of those concerned with governance, such as CFR leads and managers, and various amendments were put in place to solve the recruitment and retention issues. For example, a CFR lead explained their next 5-year plan for CFR recruitment and noted:
We’ve actually got a recruitment strategy for the next [coming] year, irrelevant of COVID, of about 100 responders a year [will be recruited]. And that’s based on them spread over basically coming into the organisation with almost like a 3-month induction and support package for each individual, spread across all the districts. So that’s to start to sort of spread them out over the year. So a hundred a year, and there’s always natural wasters [dropouts] … So we probably expect that for a hundred coming in each year, we may lose 20–30 out of that. So we’d hope to have a gain of about 70 responders a year over the next sort of 4 or 5 years.
CFRLead_CC_12062020
Community First Responder initial and ongoing training
The study findings revealed the importance of CFR training modules and mode of delivery, and the implications for CFR training experiences. Training covered aspects such as basic life support, trauma management, falls case management, dementia awareness and training in the use of specific equipment, including education on gloves, Entonox, personal protective equipment, blood pressure measurement equipment, defibrillator, oxygen administration, bandages and plasters, and foil blankets. The categories of training, supply of equipment and training in operating the equipment were not universal and varied throughout the six ambulance services. The differences in CFR training can be traced to the differences in CFR policies and governance mechanisms, noted above.
There were two types of training: initial training and refresher courses or periodic (biannual and annual) requalification. Typically, the induction training consisted of a 5-day course encompassing the technical aspects of CFR roles and patient care, as well as 1 day on the documentation process and values and goals of the ambulance service. The refresher training typically lasted 1 day, depending on the nature of the training and the introduction of new devices or CFR responsibilities. The CFRs recognised the buddying process as an important component of the CFR training, providing them with real-world experiences of volunteering and patient care:
What we used to have when we first started, the training will come to us and we would meet up in the village hall, and we do some scenario training and updates. At the moment, we go into training, every 6 months we go and requalify. So we got sent an electronic exam paper, with 30 questions on it. We do online and return. Then we go in and do a practical session, and it always be CPR, and it might be something different like choking scenarios.
CFRLead_GR_29092021
We identified that some participants appreciated the structured and organised approach to delivery of CFR training, while others wanted more local flexibility and more bespoke training. The experiential challenges of CFR training often related to the additional time commitment required. The brief approach to delivering some training modules posed another challenge for a group of CFRs during the training, especially refresher training. The numerous ways in which CFRs diverged, such as by education, career and skills, indicated that CFRs were capable of absorbing the training modules to varying degrees. Delivering training courses to all CFRs in the same format had the desired impact for some CFRs while causing difficulties for others:
It was [a training for a] new equipment … If I’m really honest, it was those add on upskilling sessions that I was probably least impressed with. It felt really rushed … I just felt like the trainer couldn’t really be bothered and also, when they were going through, and I’m not a stupid person, I’ve got a master’s degree … but I just felt overwhelmed by what they were trying to say because they were rushing through. They made loads of assumptions that people knew acronyms, knew what tools were, when actually, we don’t. I think the training is for those that are comfortable with it, but they forget that it’s not the same as the other people.
CFR_NM_22072021
In addition to the complications of delivery of training modules, the (re)training process and inflexible approach caused a discrepancy between the interests of the CFRs and those of the ambulance services; consequently, substantial attrition of CFRs was found, which was attributed to inflexible retraining:
We had a wobble about 2 years ago when they got a bit efficient over people having to retrain, and teaching old dogs new tricks. Some people got pretty fed up with that, and we lost quite a few good people then, which was a shame but other than that. If you look after people, particularly in a volunteering role, they will stay, because they’re not doing it for the money. If you start then getting a bit [curse word] with them because they haven’t done recerts for online tests, and there is a genuine reason for it … you have to give people a bit of flexibility.
CFR_LF_11102021
Community First Responder lead participants emphasised the availability of free training, the obligation to reappear for regular requalification, and the implementation of safety and management mechanisms for monitoring CFR training requirements.
So that’s with the 6-monthly re-course. If their care is brought into question, we ask them to be open and honest, but at the same time if needed, it will get reported. So we will get informed of it anyway, and we will look at it case by case and decide if we’re going to go down a potential training route, or whether it is just an informal chat that is needed but we see them every 6 months … So we do keep a close eye on them.
CFRLead_BC_06102021
Moreover, we also found that the lack of availability of freely accessible accredited training courses was a crucial challenge. The training programme was an attraction for some individuals as it could be accessed free from the ambulance service via the CFR schemes as a gateway to paid employment elsewhere. This phenomenon of potential CFRs having accredited training resulted in high recruitment and high attrition. The governance team had concerns and requested audits of the continuing implementation to determine if CFRs were volunteering:
Yes, an in-house training course. They moved away from that … they moved away from the accreditors, because there seems to be a high turnover of CFRs. People would come; get the qualifications, and leave.
CFRLead_MW_09072020
Retention of Community First Responder workforce
The factors that led to CFRs discontinuing their voluntary roles were rooted at both the individual level and the institutional EMS level. Changes in personal circumstances and an inability to spend sufficient time were the most often cited reasons for attrition among CFRs. CFR participants reported that their original expectations of responsibilities before entering the CFR workforce and their anticipated level of commitment often did not match the actual work, which was sometimes also impacted by changes in their personal lives. As a consequence, some CFRs undertook little or no activity after training, and this was identified as a major cause of CFR dropout:
We have got a bit of a flow in, but retention can be a bit of a problem, because stuff happens in people’s lives. They will start off with all good intentions, and something happens, and they get out of the habit of logging on.
CFR_MR_27092021
Some CFRs who were unable to adapt to their new or altered roles were disappointed by changes in policy and role. For instance, eliminating a CFR’s ability to use an EV (blue) light was seen as undesirable by some, and a number of CFRs withdrew as a result:
The role is changed quite a lot. So I have joined with the new role. Whereas lots of people stop responding a few years ago when they took away the lights and things, because they said they weren’t doing it if they didn’t have that.
CFR_MM_30092021
Prolonged recruitment and inactivity after training were acknowledged by CFR leads and ambulance services as a cause of attrition. Some applicants for the CFR role quit schemes before training commenced:
I think the number of people who show interest and are willing drop out of the process because it takes aeons for people to get to be responders; you have to attend the course and the course is run once in a blue moon. and they are very difficult to get onto because the location is 100 miles away from where you are. Nothing about it is particularly friendly or encouraging.
CFRLead_ML_05052021
Given the voluntary nature of the CFR role, some research participants concluded that a key approach to strengthening retention was to make the recruitment process more rigorous to (re)ensure the motivation and commitment of prospective CFRs.
The COVID-19 pandemic introduced new impediments to CFR operations, with discontinuation of CFR recruitment and training, and trained CFRs sometimes being deprived of their roles, leading to additional dropouts.
I think at the moment retention is an issue, purely because we were stood down for a significant amount of last year … I think it’s giving them pause to reflect on whether they want to come back because there are still risks with COVID, and is that something that they want to put themselves into … I think there is just over 100 haven’t returned. You’re probably going to lose 10 to 15% of those.
CFRLead_SV_29042021
B. Community First Responder roles, governance, innovations and future opportunities
This section addresses the study objective of exploring the experiences and perceptions of stakeholders involved in the CFR schemes implementation on the CFR role, governance of CFR schemes, and the potential for further development and innovation of the CFR roles. The stakeholders were ambulance staff, CFRs, CFR scheme managers and commissioners.
Community First Responder roles in patient care versus administration and management
We identified two key categories of CFR role: patient care and administration and management. The patient care roles included a number of steps when responding to patients, including assessing patient signs and symptoms, exchanging information, providing rapid emergency response, and co-ordinating with ambulance crews regarding patient care and support.
Identifying a patient’s condition
The typical response to a call from the control room of an ambulance service began with the deployment of the CFR. Generally, the control room shared information on a patient’s condition with the CFR, but often on arrival the CFR identified a different set of patient symptoms.
The CFRs compared patient information that they documented through their own measurements and assessments with the information provided by the control room. The assessment process included body posture, breathing pattern, possible bleeding, pulse and heart rate. These data were then recorded in the patient record form (PRF). The CFR participants highlighted the frequent mismatch between the patient information received from the control room and their first-hand observations recorded on the scene:
It immensely varies on what sort of cases I attend. A lot of times things [patient information] will come through and it [control room] will say unconscious, not breathing or whatever, and I walk in the room and they’re [patients] sat at the kitchen table conscious and breathing. But in some cases, patients’ conditions are severe than what they [control room] said.
CFR_MM_30092021
Information sharing with control room and ambulance staff
The precise patient information collected and checked by CFRs was communicated with the control room and the ambulance en route. The electronic PRF, or ePRF, was identified as an essential instrument in the process of information sharing, which facilitated the sharing of patient information among the stakeholders engaged in patient care. The ePRF was not, however, uniformly accessible across all ambulance services:
Most of us have paper PRFs, whereas the [ambulance service] CFRs have tablets. So when we are on-scene, observing blood pressure, temperature, respiration rates, oxygen saturation, we document them on our paper PRF, and hand that over to ambulance crew then they arrive.
CFR_MM_18102021
The information-sharing practices of CFRs also emphasised interprofessional collaboration between the CFRs and the ambulance crews. Moreover, the provision by CFRs of precise patient information also helped ambulance clinicians attending or en route to recognise the severity of the patient’s condition and formulate their treatment strategies in a timely manner:
Once we reach, we do a proper assessment and take observations, patient history. If they [patient] are sick enough, we get back in touch with the desk [control room], and tell them the severity of the patient, we need help quicker, when is help coming? We also ring up to the clinical team if we need more help and support from what we have found.
CFR_FW_92021
Similarly, an ambulance clinician noted:
When we respond to emergency calls, generally we see a CFR already on scene and have started patient assessment and sometimes treatment too. We listen to what they have to say first before handover.
Ambulance_JK_11102021
Intervention response
The patient care activities or practices of CFRs depended on the type of patient they attended and their scope of practice. The most common categories of patients reported as being attended by CFRs were people with breathing difficulties, chest pain, heart attack, stroke, epilepsy, cardiac arrest, burns, trauma, asthma, diabetes, unconsciousness and falls. In response, CFRs were able to provide treatments such as oxygen, clear airway obstruction, provide CPR and defibrillation, and lift older patients who had fallen:
If there’s anything we can do for them in terms of what we carry, we do the best possible. For example, if somebody has got difficulty breathing, and need oxygen or salbutamol, then we administer the oxygen on and give them salbutamol.
CFR_TW_11102021
It was found that CFRs’ intervention response was limited when patient care required a response outside the scope of CFR practice, and in these instances, they were required to adhere to CFR policies to call for professional assistance. The types of emergencies not usually attended by CFRs were maternity cases of women in labour, road traffic collisions, patients with mental health disorders and children:
Sometimes you can’t do a lot, but you have to reassure them [patients and relatives]. The biggest skills is communication. I say this to any new CFRs. There are two sides that you have to develop as a CFR, one is the communication side, and the others.
CFR_AA_20092021
Collaboration with ambulance clinicians
The relationship between the CFRs and the ambulance clinicians was complex, showing tension between collaboration and dominance. When a collaborative relationship was established, the CFRs not only handed over the PRF to the ambulance crews but also engaged closely with ambulance clinicians to provide operational assistance on scene in order to stabilise a patient’s condition and facilitate their transfer to the nearest facility. However, when a collaborative relationship was not established, the CFRs handed over their PRF and departed from the scene:
I was staying and helped because I am on duty. Sometimes I help them to take the stretcher out, prepare other ambulance process to load the patient. They [ambulance crew] also appreciate it.
CFR_DC_18072021
Similarly, an ambulance clinician noted:
I attended a cardiac arrest patient. A CFR was already there, doing CPR and giving oxygen. That was a busy day, and no other ambulance and support available. So we used CFR as our second resource, and it turned out to work. The patient was in bad shape, and the CFR knew what to do.
Ambulance_WM_07112021
By contrast, another ambulance clinician stated:
I don’t know whether it’s more of an ego thing, with some paramedics, that cause the issue rather than a lack of engaging with CFRs, it might be a case some of the people I know have issues with them that they are quiet – I like to do things my way, and that’s it.
Ambulance_SM_26072021
In addition to providing direct patient care, other aspects of CFR responsibilities included:
-
wearing a CFR uniform
-
the maintenance of equipment by CFR leads
-
using equipment
-
logging on to a shift using a mobile phone application
-
carefully and properly using the CFR vehicle
-
undertaking periodic training
-
raising awareness about the CFR schemes
-
fundraising
-
mentoring newly recruited CFRs.
Contingencies of Community First Responder governance
Understanding governance enables us to reflect on the underlying principles and values, institutional structures, and layers of competing stakeholders engaged in governance practices. Although the principles of governance are also ingrained in the previously discussed themes, this section focuses on the institutional governance mechanisms of workforce management, policy implementation, communication, and administrative roles.
Psychological support for Community First Responders
The role of CFRs, especially in attending critically ill patients, exposed them to experiences of encountering fatal or end-of-life situations. These, sometimes traumatic, experiences could potentially negatively affect the psychological well-being of CFRs. The management of traumatic experiences can become difficult among lay CFRs who do not have prior professional experience in medical or emergency care. The possible mental hardship attributed to the CFR role was recognised by participating ambulance services, and counselling units had been established to support CFRs in managing potentially traumatic experiences:
There is a system in place where if a CFR attends an unsuccessful cardiac arrest, or cardiac arrest that is traumatic, the team leader for their local area should be told, and their leader, and first call will be made to that CFR to make sure they are OK … There is also a well-being hub.
CFRLead_SV_29042021
Yes, because they are working for [ambulance service], they fall under our occupational health, and they have full access to all our health and well-being services. So as part of our process, if it’s a file attends a traumatic job, it will get noted in the shift report. These shift reports are looked at every day, by us managers, and we will always follow up with a welfare call and we can refer our CFRs on to things like occupational health, we have lots of different services that can use.
CFRLead_BC_06102021
Workforce management
The participants accountable for managing CFRs reported producing work plans and rosters for the CFRs, ensuring that the minimum time necessary for the CFRs to operate and retain their skills was taken. These processes were routinely monitored to assess the contribution of CFRs to the ambulance services from an institutional standpoint. The participants leading CFRs identified maintaining their time commitment as a crucial challenge for CFR schemes:
Yeah, the challenge is to maintain their commitment …
CFRLead_ND_17062020
The other important aspect of workforce management was retention, which was discussed in the earlier sections.
Communication
Communication with CFRs was deemed critical for successfully implementing CFR schemes. In the functioning of the CFR schemes, communication in several dimensions was rooted as systematic but occasionally inefficient. Communications in most CFR scheme were governed by a centralised policy directive. The ambulance services e-mailed any policy amendments pertaining to CFRs. We also found that the head of operations typically directed communications to the operational manager, who then instructed the CFR lead or CFR lead manager and, ultimately, the CFRs. In the context of these centralised communication mechanisms, confrontations sometimes arose when initiatives or CFR roles were modified without the awareness of the CFRs:
The communication is poor. So they said … A falls vehicle was promised for years. Eventually had the training, and now it’s gone completely silent. Nobody is even telling us that it’s not running anymore … there is a lack of communication, which leads to a lack of engagement and confidence.
CFRLead_TP_11052021
When I found out that we were doing Entonox, [later] I found that out through a paramedic. So, the communication could be better …
CFR_BN_13092021
Usually, communication between the CFRs and the ambulance clinicians proved beneficial, as stated in the section on Information sharing with control room and ambulance staff. However, when there was little or no communication between CFRs and other stakeholders, the patient-care situation became challenging. The repeated incidences of ‘oh, I didn’t know you were going to be here’ resulted in contradictory teamwork on site, as neither the CFRs nor the ambulance clinicians were aware of the other’s presence.
Adherence to policies
The primary function of the governance structure was to ensure that the CFR performed and maintained institutional quality assurance for ambulance services. CFR leads rigorously monitored CFR practices, and continually evaluated these to maintain the standardisation of processes. The adherence to CFR regulations and scope of practices was also assured through mandatory training in those areas:
Exactly, so it’s about setting guidelines and boundaries, to give them an element of autonomy, but that actually they are representing an organisation, and we need to know what you are doing.
CFRLead_ND_17062020
Another CFR noted:
So in the CFR group we’ve got our own drug policy, and membership policy, our own skills policy …
Interviewer: So who’s responsible for these policies and protocols then?
Res: So it is our co-ordinator.
CFR_BN_13092021
The ambulance services sought to rigorously govern the process of shaping CFR practices by adherence to policies. As indicated in the documentary analysis, non-compliance with policies or protocols would often result in an instant stand-down or even dismissal. In addition, we identified practices of stringent policy implementation, with non-compliance leading to the termination of a CFR’s role:
I’ve said that it utterly does not make sense. I was challenging a couple months ago on CFRs still have to wear flimsy plastic aprons to every job. I am happy to do that indoors, but outdoors in a field on a windy day, they are a liability; so I challenged that recently – I got the answer that if I don’t want to conform to PPE, then quit.
CFR_BL_07102021
The process of enacting CFR policies and adhering to the legitimate scope of CFR practice contained therein caused a contradiction between the CFRs’ purpose in serving the community and the governance of CFR schemes. Ambulance clinicians who witnessed these instances of tension characterised recurring restrictions on the CFRs’ role, leading to disengagement over time, as a challenge for the future development of CFR schemes:
I feel like there’s always a us and them mentality between the CFRs and the ambulance service, and I think that’s probably a big barrier, is the fact that CFRs will often be – could we [not] do this? And the ambulance service will be like – no, you cannot do that because of X, Y and Z, because we have policies in place and that is not your role. I think that can just create an element of disinterest. It can stop people wanting to be better or do more in that job because they think – what’s the point?
Ambulance_I_07092021
Fundraising
Fundraising was an integral part of CFR schemes and individual roles that augmented resources for CFR activities. The funding sources identified were ambulance services and charity funding. Most charitable funding stemmed from donations made at public events, which also served to raise public awareness of the CFR schemes. The revenues earned from different sources were used for training, equipment and car insurance, among other things:
Our responders are amazing: they do all sorts of weird and wacky fundraising and charitable bits and pieces. We do a lot of CPR training in school ... community groups. And sort of try and support and spread the word and the importance of CPR, and the use of defibs, etc. … they are very active as responders go in that sort of area.
CFRLead_CC_12062020
Although fundraising seemed to be an integral aspect of the governance of CFR schemes, some CFR lead manager participants were dissatisfied with the mechanism through which charitable funds were dispersed. The charity funds were accumulated and added to a central fund held by ambulance services, and accessing this fund was characterised as a complex and bureaucratic procedure requiring authorisation from many administrative staff at different hierarchical levels of the ambulance service:
It is quite a big corporate machine now. The funds will go into a central pot. For instance if we wanted to buy [something] … We have two managers in our scheme now. So we applied to them … which are £1000 each, and they talked to the ambulance, and they say what do you think, and if they say they will support it, then the money comes to us.
CFRLead_GR_29092021
Fundraising was a crucial aspect of CFR scheme activities, and although CFRs were urged to undertake them, these responsibilities were not obligatory. As a result, non-compliance with the guidelines promoting fundraising activities was not considered a reason for termination from the CFR role:
It’s a really fine balance. Because I don’t want to lose them for their commitment to the patients, but equally I don’t want to turn them away because – you won’t raise money.
CFRLead_ND_17062020
Innovations already adopted by some Community First Responder schemes
Our findings revealed a number of innovations that had been developed and brought into CFR operations. These innovations originated at participating services, varied by ambulance service region, and were adopted by CFRs to various extents. In this section, we discuss the categories of the innovations and their attributes. The innovations included in CFR schemes were classified into two categories and five attributes (Figure 12).
FIGURE 12.
Attributes of innovations.
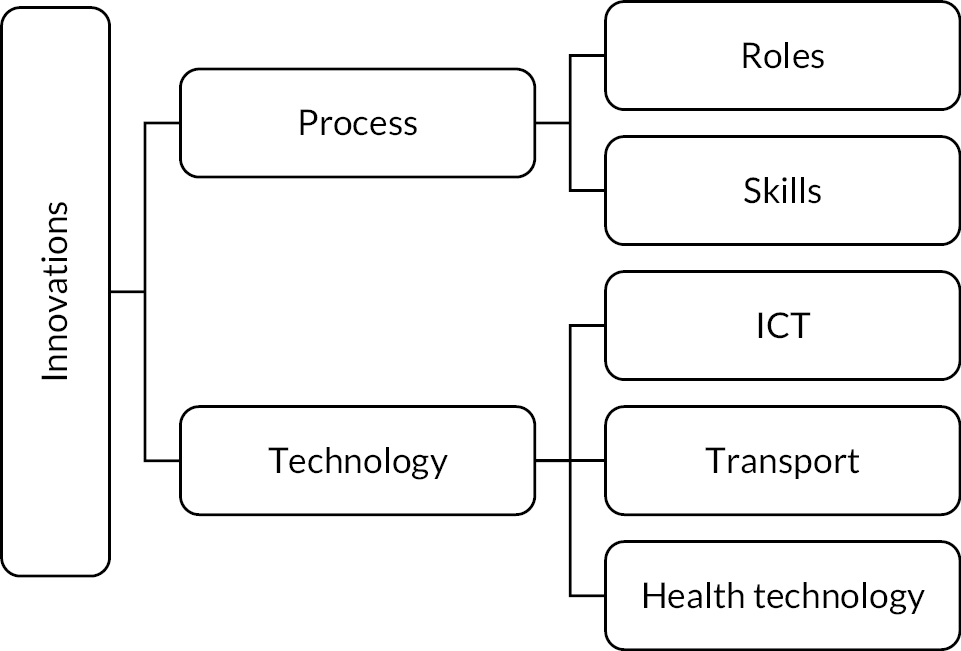
Role and skills innovation
The role innovation included the extension of CFRs’ scope of practice, for example the use of risers for lifting fall patients. Elsewhere, as part of the expansion of the CFR role, a group of CFRs with previous firefighter and police experience were granted permission to attend accident cases. Moreover, during the pandemic, the idea of modifying CFR responsibilities around social care was also put forward by commissioners:
Yes, we’ve got a couple in N, and they have been issued with a riser chair, and it’s basically a lifting device which can used by CFRs. Our conditions in the control room will look at the fall, patient stood on the floor unable to get up, they will follow a flow chart to see if CFR’s suitable to be sent … they can test the patient’s blood pressure, heart rate, etc., so that is a really good scheme.
CFR_BA_10032021
I think again in the P, just looking at the rural area, there have been trials of sending certain responders to road traffic collisions, again just because if it’s a nasty road traffic collision, these CFRs had to have some kind of previous knowledge … they previously worked for the fire service or the police, and that allowed them to be eligible to respond to these emergencies …
CFR_BA_10032021
The skills innovation primarily referred to the development and delivery of specialised training to CFRs so that they could undertake a specific set of roles and tasks. Some CFRs, for instance, had received specialised training to attend falls patients who had a low likelihood of sustaining an injury. New training for CFRs increased their ability to respond to these falls incidents, which fitted into the fundamental concept of CFR programmes, in which trained volunteers help those needing urgent care. CFRs also received specialised training in the use of risers when attending falls patients:
Patients will sit on floors for quite a number of hours, and they obviously tend to be older generation … and actually there’s potentially a CFR around the corner, that could go and help. Well, at the moment they were not allowed to move patients. So we are doing a trial in N … to improve that fall service, and education amongst our CFRs, so that they can go and assess non-injury falls, so that we can get some of these patients moved off the floor.
CFR_MW_09072020
Technology innovations
The ICT (information and communication technology) innovations referred to various innovations that were technological in nature. For example, CFRs used Google Maps to navigate to patients’ locations or houses, but the majority of dwellings in rural regions have names instead of numbers, making it difficult for CFRs to identify patients’ homes as Google Maps does not offer house names. In response to this issue, the ambulance service developed an application for use by the ambulance crew. Later, the same technology was also supplied to CFRs travelling to rural areas, and this innovation enabled CFRs to reach patients more efficiently. Elsewhere, another ambulance service used a similar communication device with live tracking, enabling the CFRs to determine the distance and arrival time.
Similarly, an electronic handover form was designed and implemented so that CFRs could share information with ambulance clinicians. Another ICT innovation was a radio with a panic button, which was issued to some CFRs to assure their safety and security for the challenging circumstances under which they often operated. The panic button was designed to be used in ‘hostile’ situations to alert the control room of a potential threat, and the control room would subsequently notify the police to ensure the CFR’s safety:
I would love to see CFRs issued with these radios because they have a panic button; so if you press the top it immediately alerts the control room to say there’s an emergency; and I’ve had a couple of risky situations before where a patient has turned volatile quite quickly, and it’s a bit rubbish trying to fumble through your pockets to try and get your phone out discreetly during the control room.
CFR_BA_10032021
The idea of the ambulance service assigning a specialised CFR vehicle for response purposes was an innovation in the transport attribute. The dedicated CFR vehicles increased the motivation of CFRs to engage by eliminating the burden of fundraising for the personal car insurance needed when using their own transport for the CFR role. Moreover, the dedicated car was believed to promote community recognition and identity, in the same way that ambulances are recognised:
We have a scheme car, like a marked ambulance car, that we use on our own shift, So I have a scheme car, I go on shift …
CFR_MM_30092021
The use of Entonox was a contentious topic in the scope of CFR practice, with some areas allowing Entonox to be used by CFRs and others excluding it from their scope of practice. As a result, the supply, training and use of Entonox was recognised as a health technology innovation:
So we are looking at … a business case has gone in, just before COVID around supporting CFRs having Entonox. An [ambulance service] leased or owned car, trying the use of Entonox. So we are at the point where we’ve got a train-the-trainer package being rolled out to our training officers, to deliver to those people it would hit as a trial. So it would be about 30 CFRs that will be getting Entonox before the end of the year. So if that’s successful then we can roll it out, and that will make a massive difference in the rural areas.
CFRLead_MW_09072020
Future opportunities
The potential future development of CFR schemes and practices emerged in two broad categories: CFR role development and CFR scheme governance development.
Community First Responder role development
We found that the experiences and possibilities of expanding the CFR role in the future were key areas of discussion. The CFR role was limited, with its scope of practice differing from one ambulance service to the next. However, study participants rationalised vital elements of the expansion of the role by alluding to the complications of emergency care delivery in distant locations, which was the ultimate goal of CFR schemes. For example, a clinician from an ambulance service suggested equipping CFRs with electrocardiogram (ECG) devices to use in rural areas or areas with a high prevalence of cardiac illness. It was suggested that the CFR would take an ECG and record the results in the ePRF, which would be linked to a server and shared with ambulance clinicians for interpretation and prioritisation according to the reading:
I think being able to do an ECG. In those rural environments, chest pain becomes increasingly common when people are elderly, in those rural areas, a lot of farmers and people that are elderly … they don’t even have to recognise a systemic, nowadays the CFRs have tablets [ePRF] like we do, and it’s all connected … they could send that ECG off to a paramedic that could recognise a rhythm, and they could be like that is an MI, we will prioritise an ambulance to get to you; even though they should be doing that anyway, that would be nice.
Ambulance_I_07092021
The expansion of the CFR role to attending patients who had fallen was also emphasised and recognised as important. The incorporation of more specialised training in the future development of the role was also reiterated:
So there is some aspect of a supplementary training package. With the enhanced role, with a non-injury fall call … they can go to an assessment with the patient, but sometimes having an additional understanding of that patient ECG … These are the things that are being considered for this enhanced role that they could be feeding back into the control room.
CFR_TK_04112021
A further role expansion for the future development of CFR schemes was social care. This entailed social care roles for CFRs in their communities, particularly in rural areas of socioeconomic deprivation where people lacked access to health and care services. It was felt that these marginalised populations might benefit most from the involvement of CFRs in social care, broadening the CFR role beyond healthcare delivery:
They live in a small community … I think things like the loneliness services and picking up medications and things like that, I think that can only be positive, in a way that I think we missed out a lot of the soft touches, that would reduce demand on the health-care services; and it’s soft touches like that, identifying people that are slightly ill, see them on a regular basis along with the ambulance service … I think they have something to offer in that respect.
Ambulance_MH_29072021
Future development of Community First Responder governance
In addition to the future evolution of CFR roles, an important theme was the further development of governance mechanisms. Participants suggested structural modifications to optimise CFR operations. National standards were suggested for operational and performance assessment. The purpose of a national standard was also to determine the minimal requirements for standards in different CFR schemes, allowing schemes to be compared and benchmarked, and informing the design of an interscheme learning programme. The objective of this programme was to facilitate communication between ambulance services about the initiatives or components of initiatives that functioned well in specific contexts and how implementation challenges were addressed in different schemes. These future developments in governance were recognised for their potential to strengthen CFR schemes:
I think a national endorsement of the work, and some minimum standards, perhaps some benchmarking, who is doing it better than others. What would improve rural response particularly if they knew they were utilising the best model possible …
Commissioner_JE_05082021
The need for CFR schemes to engage with socially marginalised groups was acknowledged, which would add value to the diversity and inclusion policy of ambulance services:
I mentioned before, the R, stuff like that. But they’ve got the visibility and the structure to it … but I think it could be a much bigger impact and make a bigger difference to not just the rural aspect of things, but particularly … hard to reach groups, ethnic groups, and deprived communities.
Commissioner_SL_10072020
The continuing requirement for CFRs and the need to recruit and retain them were important in the continuation of CFR schemes and resulted in the need to further develop the governance of schemes. It was emphasised that the CFR governance framework should incorporate professional support, high-quality training, and safety and security mechanisms. Leadership at the highest levels of ambulance services desired continuation of the CFR programmes and an expansion of the role in rural emergency care:
I would like to hear that they feel professionally supported; the training is of the highest quality, that they feel safe and comfortable doing the work that they do.
Commissioner_JE_05082021
C. Patients are the reason for Community First Responder schemes in the health system
Improved patient and family experience
The operation of CFR schemes from patients’ perspectives provided insights into the important features and characteristics of CFR schemes as well as the care delivered by CFRs. This section addresses the objective of exploring patients’ and relatives’ experiences and perceptions of the care provided by CFRs.
The most common conditions reported by participants for which an ambulance was called were falls, heart palpitations, asthma and stroke. Patients and their family members were naturally alarmed by these emergencies. CFRs arriving first at a patient’s location to provide emergency care was considered helpful, although in some instances an ambulance arrived on scene before the CFR. Many patients and relatives were unable to provide details of the care provided by CFRs, but they reported that the care provided by a CFR while waiting for an ambulance was essential:
I’d probably be sitting on the side of the road, not knowing quite what to do, and obviously wouldn’t be able to give him the medical help that he needed … and when you are on your own in the middle of the street, it’s hard. So getting a first responder though straight away, you do know you’ve got somebody with medical experience, and it takes the pressure off me for a bit.
PatientsRelative_BA_002
Patients and family members remarked that although it could be difficult to locate homes in remote places, CFRs had no trouble doing so because of their familiarity with the area. The difficulties were eased by family members keeping lights on to allow CFRs and ambulance crews to readily identify the location.
Patients and relatives of patients who participated in interviews felt that the provision of CFRs and the system of care prior to the ambulance arriving was efficient, and they emphasised their positive experiences with both CFRs and ambulance clinicians. The rapid response by a CFR before the ambulance and the actions of CFRs offered patients and family members reassurance that they were being treated in a timely way, which increased their expectation of a positive outcome:
Very efficient, while waiting for the ambulance to get me to hospital. I was in a terraced house then, they had to bring the stretchers down the back alley, across the garden … They got me out through the back doors and out into the ambulance, and straight off to hospital.
PatientsRelative_JD_12052021
And I’ve always been quite impressed actually that they can get there that bit quicker than an ambulance sometimes, and it does save precious time, you know, waiting for an ambulance.
PatientsRelative_BA_002
Patients and their families noted negative experiences with ambulance services when there were significant delays in an ambulance arriving, particularly when they were not informed that there would be a delay:
I had to phone up several times because I can’t lift him back. I can’t get him up. He was just lying there on the floor, and he must have been there about an hour and a half.
PatientsRelative_BAR
The problem of community awareness
Patients and family members who participated in the study were largely unaware of CFR schemes and who CFRs were. Community awareness was a crucial factor in the operation of CFR schemes, as service users were often not informed that a CFR had been allocated or would arrive before the ambulance. Despite this, patients and family members observed that people often called an ambulance in a panic because of acute symptoms, and the arrival of a CFR reassured family members that the ambulance service would deliver care to them:
I’ve never really thought about the first responders. I’ve never really thought is it something that happens before an ambulance; and it’s about who gets there first.
PatientsRelative_AB_12052021
I was just told that one has been dispatched to you, but that never arrived, and then I found again – oh well, we are very busy, as soon as there is one, we will come. Nobody actually mentioned the first responder coming out.
PatientsRelative_BA_002
The CFR uniform increased confusion among patients and family members, as one relative noted:
They might have come in a different car, and it might be confusing, because they do look like ambulance staff, because they wear all the things, but they have like L on the uniform or something.
PatientsRelative_BA_002
Summary
Overall, CFRs and the CFR schemes were regarded as integral to prehospital care delivery by ambulance services. The CFRs were limited to their legitimate scope of practice, but stakeholders who participated in the study noted possibilities for role expansion. Ambulance services continually experimented with innovations and implemented them in the CFR operation through trials. The majority of innovations improved the coherence of CFR practice and the safety of patients and CFRs themselves. Moreover, ambulance services have long been involved in the recruitment and training of CFRs and have encountered challenges of workforce attrition.
Beneficiaries of CFR services, including patients, relatives and ambulance services, viewed the provision of CFRs as a safe, effective strategy while waiting for an ambulance. The assessment of patients’ conditions and the initiation of prehospital care were valued and reassuring to both patients and their family members:
None of [our] … CFRs have ever caused any harm to patients. We have had different things over the years with them but nothing that would cause harm to any patients.
CFRLead_CM_16112020
A landscape view of the CFR schemes might be interpreted as a top-down policy implementation of prehospital care delivery utilising trained community volunteers, in contrast to a bottom-up approach with community engagement in health services.
Integration
The complex mixed methods involved the integration of quantitative and qualitative findings, which was achieved through the study design, during the analysis and through the development of recommendations for future practice and innovations in CFR provision. The ABC framework,38 incorporating the notions of multiple ‘actors’ operating in a complex system, ‘behaviour change’ and ‘causal pathways’, helped us to think about our approach to integration (Figure 13). Using the method of triangulation described as ‘following a thread’,39,40 we explored hypotheses generated using one method with others to gain a fuller understanding of the different phenomena identified.
FIGURE 13.
The ABC theory applied to CFRs’ role in the current and future rural health and care workforce.

Integration through design
The study design required the collection and analysis of quantitative and qualitative data together, which allowed multiple points of integration throughout the study.
For example, quantitative data on incidents at the six ambulance services provided data for the cross-sectional studies, but the initial data analysis allowed us to identify a random sample of 100 patients, CFRs and ambulance staff for incidents in rural locations together with demographic information on patients attended and other details of the incident, which enabled us to contact participants for interview through the ambulance services. Unfortunately, we were able to identify only one triad of patient/relative, CFR and ambulance staff member using this method because of a lack of response.
The cross-sectional studies largely preceded the qualitative interviews, which allowed further integration. For example, the quantitative analysis showed that CFRs had a higher rate of attendance at incidents in rural areas, and were less likely to attend patients from minority ethnic backgrounds or from more deprived areas, or younger people (aged < 39 years), allowing us to explore possible explanations for these differences in the interview study.
The results of the earlier cross-sectional and qualitative studies were presented at the consensus workshop and informed the list of CFR innovations and subsequent discussion and voting.
Integration through analysis
The organisational context in which CFRs functioned was described in the documentary analysis. This showed how participating ambulance trusts sought to ensure that CFRs maintained high-quality, safe, effective, efficient and equitable practice that was closely incorporated into the wider operations of EMS.
The quantitative analysis provided additional context, showing that CFRs attended a greater proportion of incidents in rural areas. The quantitative analysis also showed the benefits of CFRs attending in terms of a more rapid response to incidents, particularly in rural areas, the earlier response being welcomed by the patients and their relatives interviewed as providing reassurance and enhancing their experience of care. The innovative CFR response to falls in one county, which often did not require ambulance backup, provided a possible explanation for the reduced conveyance rate associated with CFR attendance. The finding from the quantitative analysis that CFRs attended people with cardiorespiratory and neurological and endocrine conditions but that they also attended those with a wide variety of other conditions matched the wide variation and type of incidents that CFRs in interviews reported being dispatched to, including lower-acuity problems such as falls.
We interviewed the main actors involved, including patients, relatives, the public, CFRs, CFR leads in ambulance services and charities, ambulance staff and commissioners. Although these stakeholders were identified at the outset, their perceptions of CFRs, learned through the interviews, the relationships between them and the similarities and differences of their views on the current and future role of CFRs and how this should be developed were assimilated with the quantitative findings to inform an actor-based system map (Figure 14).
FIGURE 14.
Actor-based system map for CFRs’ role in the current and future rural health and care workforce.

Participant interviews revealed the trajectory or course by which volunteers joined and continued (or left) their role as CFRs, describing their delivery of services to patients and the perceptions and recognition of their identity as members of the rural health care workforce by community members and health professionals. Different actors were also able to provide insights, from interviews, into areas that had been explored in other aspects of this study, such as CFR policies and governance (in the documentary analysis), workforce and training, and recruitment and retention (in the resource and workforce survey). They were also able to describe a wide range of innovations that had already been introduced in some areas, as well as others that were being considered, for discussion and ranking in the consensus workshop. The interviews also provided information on the changes to processes and structures needed to address the barriers to CFRs operating in a rural community context as displayed in the actor-based system map (Figure 14). The relationship between quantitative and qualitative findings described above is summarised in Table 18.
| Quantitative findings | Qualitative findings | Meta-inference |
|---|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
The interviews and consensus meeting also allowed us to consider the causal impact pathway by which behavioural change could be brought about, the theories of action (pathways and interventions promoting actor-level change) and the theory of change (i.e. the ways in which actor-level changes could lead to systems changes and impacts). 38 This included engaging with stakeholders to engender greater ownership of change, understanding innovations from the perspective of different stakeholders and involving a wide range of actors in a consensus meeting to prioritise innovations.
Summary
The integration of quantitative and qualitative data was achieved through both research design and data analysis, allowing us to triangulate findings and develop an actor-based system map of the CFR role, function and meaning and a classification of future innovations.
Consensus meeting findings
Participants
A total of 26 participants participated in the consensus workshop. This comprised 11 ambulance services representatives from all 6 participating ambulance services and one other, 6 patient panel members and 9 researchers from the research team.
Innovations
The list of ideas and innovations identified from the empirical findings and introduced at the consensus workshop is noted in Box 2.
-
Dedicated car for CFRs.
-
Navigation and communication gadget with live tracking.
-
Radio with panic button.
-
Handover e-form.
-
Entonox use.
-
CFRs attending accident cases.
-
CFRs attending falls patients (using riser).
-
CFRs’ social care and public welfare role.
-
CFRs’ access to blue light.
-
Blood glucose meter.
-
Glucogel use.
-
Transferring patients to hospital.
-
Termination of resuscitation guidelines.
-
Better communication from/with control room.
-
Creating awareness of CFRs through NHS.
-
Creating awareness and promoting CFRs in community.
-
More funding support from ambulance service.
-
Decentralisation in developing CFR policies.
-
Retain the CFR role as it is now (no change).
In session 2, consensus participants were divided into two online groups and one face-to-face group. During the session they generated and discussed additional round-robin ideas on innovations. In Box 3 we list the innovations discussed in the three groups.
-
National minimum standards (for governance, etc.).
-
Standard call sets.
-
Standardised training.
-
National volunteer certificate training.
-
Education of the community members by CFRs, for example CPR.
-
Reward and recognition.
-
Increase equality, diversity and inclusion in CFR schemes.
-
Specific mandatory and relevant training for CFRs.
-
Support to leave at home.
-
Dual CFR crew.
-
Ongoing training and mentorship.
-
Clearer job description.
-
Increased number of volunteers.
-
Differentiation and specialisation of CFR roles.
-
Opportunities for different levels of contribution of CFRs.
-
Insurance for the CFRs (older ages).
-
Portability of training.
-
Providing help with hospital transport.
-
Counselling and support for CFRs.
-
Better documentation and data for quality assessment.
-
The distinction between types of CFRs (lay, fire, etc.)
-
Peer support/hot debriefs.
When the session finished, all the innovations presented, generated and discussed were collated and entered into the JISC online survey. Innovations were prioritised using a Likert scale of 1 to 5, with 1 representing ‘not a priority’ and 5 representing an ‘essential priority’. One survey was administered during session 3 of the consensus workshop, followed by a discussion of its findings. The survey was administered for a second time, at the beginning of session 4, after which there was further discussion.
Qualitative results
The qualitative results provide important context for understanding why some innovations were prioritised over others.
For example, the importance of counselling particularly following difficult or traumatic incidents in the isolation of working as a CFR was emphasised:
The need for counselling [is important]. We are lone people, and believe you and me, as a community responder, I’ve now dealt with three people that I knew who’ve died of a cardiac arrest. Yes, [being a] CFR can be lonely, and I think that, in fact, it should be standard practice that after any CFR has dealt with a cardiac arrest where the outcome has been death, there should be an automatic phone call to that responder to help support them. Crews can support each other, CFRs can’t.
In addition, the notion of peer support as distinct from professional counselling for CFRs was debated and discussed:
The consensus around debriefs after critical incidents and trauma is that the most important thing is actually the peer support that is available for emergency services. So, I think the emphasis should be on peer support, and that has the advantage – which is linked to the community – of being non-professional and it’s provided by others who know intimately through their own experience what it’s like to deal with these critical incidents and to live in certain communities, and so it de-professionalises it …
Information technology to help CFRs locate incidents, communicate with ambulance services and ensure their safety was highlighted as being important:
A contemporary navigation map helps CFRs to find the location of patients easily, especially in remote and rural areas. The navigation map highlights the name of the house, as well as automatically navigate the CFRs to reach the patients.
A radio with a panic button, is a significant innovation for ensuring safety of the CFRs, which would be used in hostile situation. For example, there was an incident where a CFR was held hostage and in that situation the CFR tried to call the control room asking for help, but the call was missed. So, having a radio with a panic button will help to improve the security of the CFRs in such situations.
Training relevant to the CFR role was another area that was considered essential for maintaining high-quality care:
As a responder, I’m being given training in child abuse. I don’t think that giving me an hour’s course on child abuse gives me the right to make those kinds of judgements. So, I think we need to make sure that training is very, very relevant. To give a CFR fire training on evacuating patients from hospital is totally irrelevant, but I had to do it to stay as a CFR. So, we really do need to consider that.
National standards for training were felt to be helpful for ensuring quality of care:
There should be national standardisation so people can move around, and so the public knows that when a CFR attends, they’ve had some sort of training. But the roles should be defined, because there are a lot of CFRs that do only want to operate in their own community, and there are some that are looking at it as a progression to another career.
The national standards would also increase the transferability of training from one region to another:
In terms of portability within services, in-house training courses mean nothing to anyone else. When you move an internal certificate to another organisation, it doesn’t mean anything. Actually, that portability level helps with some of our recruitment and retention.
Creating greater awareness of and promoting CFRs in the community was offered as a way of address the general public’s lack of knowledge about CFRs, but it could also improve CFR recruitment and retention:
You need to be reaching out to the community … There’s a lot of willingness, I think, in the community to help out, but somebody has to be set up to actually help us as community members get involved, get trained and start doing things that are useful.
Although there was some support for activities such as CFRs transferring patients to hospital, this was seen as giving rise to potential risks for patients and CFRs:
The CFRs should be able to transfer the patients to nearby hospital particularly in remote areas where ambulance arrival time is more than 30 minutes. And that would also reduce the cost of patient transfer as compared to allocation of an ambulance.
After discussion, some innovations, such as emergency ‘blue’ lights for CFR vehicles, were considered less important:
Data suggests that the CFRs should be able to use a blue light, which will enable CFRs to reach patients early, while getting around traffic and delays. On the other hand, some suggest blue light access for all CFRs might pose a risk for the CFR themselves as well as others on the road since it requires a high level of driving skills.
Another aspect of the discussion was the need expressed by one participant for greater clarity of the CFR role:
There becomes a point where we actually need to go back to basics and ask ourselves what the role is about and what we’re wanting them to achieve. Do we want our CFRs to go to category 1 calls? Do we want them to go to category 3 and category 4 calls? Do we want them to go out and man welfare stations? What is it that we’re wanting from our four or five hours a week?
This was also expressed as a tension between the desire among some stakeholders to innovate and the feeling, particularly among some CFRs, that they wanted the role to remain focused on prehospital emergency care, which is why they had joined as volunteers:
There is an ongoing persistent concern about expanding the CFR role, and [recommended that] the CFR role should be maintained in its current form.
Survey results
A total of 17 consensus participants (i.e. excluding research team participants) took part in the first survey, and the results of the prioritisation revealed that the requirement for communication gadgets with live tracking, national minimum standards, standardised training, an increased number of volunteers, counselling support for CFRs and peer support were prioritised as essential. All these innovations had a median score of 5, indicating that all respondents classed them as being ‘essential priority’. By contrast, innovations such as CFRs attending road accident cases, CFRs’ access to blue lights and patient transfer to hospitals were given the lowest priority, all having a median of 1, which indicated that all respondents regarded them as ‘not a priority’.
Sixteen consensus participants participated in the second survey, and the results indicated that the innovations considered to be essential priority were communication gadgets with live tracking, better communication with the control room, creating awareness and promoting CFR in communities, standardised training, mandated and specific training for CFR, counselling support for CFRs and peer support. The innovations categorised as not a priority were the same after both rounds, and these included CFRs’ access to blue lights and patient transfer to hospital by CFRs.
The comparison of the priorities in round 1 and round 2 showed that the following innovations increased in priority: having a dedicated car for CFRs, a requirement of electronic handover form, the future roles of CFRs attending road accident cases, the future roles of CFRs attending falls patients using risers, use of GlucoGel (Venture Life Group PLC, Bracknell, Berkshire, UK), a system of creating awareness and promoting CFRs within the communities, the requirement of national volunteer certificate training to specify a few. There were also innovations that decreased in priority after discussion, such as CFRs having a social and public care role, CFRs working as a dual crew, termination of resuscitation guidelines and receiving more funding support from ambulance services. Table 19 shows score differences and priority of innovations comparing rounds 1 and 2.
| Innovations | Round 2, median (IQR) | Round 1, median (IQR) |
|---|---|---|
| Counselling and support for CFRs | 5 (5–5) | 5 (4–5) |
| Peer support/hot debriefs | 5 (4–5) | 5 (4–5) |
| Better communication from/with control room | 5 (4–5) | 5 (4–5) |
| Navigation and communication gadget with live tracking | 5 (4–5) | 5 (4–5) |
| Specific mandatory and relevant training for CFRs | 5 (4–5) | 5 (4–5) |
| Standardised training | 5 (4–5) | 4 (4–5) |
| Creating awareness and promoting CFRs in community | 5 (4–5) | 4 (4–5) |
| National minimum standards (for governance, etc.) | 4.5 (4–5) | 5 (4–5) |
| Increase equality, diversity and inclusion in CFR schemes | 4.5 (2.75–5) | 4 (2–5) |
| Increased numbers of volunteers | 4 (4–5) | 5 (4–5) |
| Radio with panic button | 4 (3–5) | 4 (3–5) |
| Blood glucose meter | 4 (3–5) | 4 (3–5) |
| Education of community members by CFRs, for example CPR | 4 (3–5) | 4 (3–5) |
| Ongoing training and mentorship | 4 (3–5) | 4 (4–5) |
| Clearer job description | 4 (3–5) | 4 (3–5) |
| Better documentation and data for quality assessment | 4 (3–5) | 4 (4–5) |
| Creating awareness of CFRs through NHS | 4 (3–4) | 4 (3–4) |
| Distinction between types of CFRs (lay, fire, etc.) | 4 (3–4) | 4 (3–4) |
| Standard call sets | 4 (2.75–5) | 4 (3–5) |
| Reward and recognition | 4 (2.75–5) | 4 (2–5) |
| Insurance for the CFRs (older ages) | 4 (2.75–5) | 4 (3–5) |
| Opportunities for different levels of contribution of CFRs | 4 (2–5) | 4 (3–4) |
| Differentiation and specialisation of CFR roles | 4 (2–5) | 3 (3–4) |
| Glucogel use | 4 (2–4.5) | 4 (2–4) |
| Handover e-form | 3.5 (3–5) | 4 (2–5) |
| Portability of training | 3.5 (2.75–4) | 3 (2–4) |
| National volunteer certificate training | 3.5 (2–4) | 3 (2–4) |
| Support to leave at home | 3.5 (1–4) | 3 (2–4) |
| More funding support from ambulance service | 3 (3–4.25) | 4 (3–4) |
| Dedicated car for CFRs | 3 (2–4.25) | 2 (2–3) |
| CFRs attending falls patients (using riser) | 3 (2–3.25) | 2 (2–3) |
| Retain CFR role as it is now (no change) | 3 (1–4) | 2 (1–3) |
| Termination of resuscitation guidelines | 2.5 (1.75–4) | 3 (3–4) |
| Entonox use | 2 (1–4) | 2 (2–3) |
| Decentralisation in developing CFR policies | 2 (1–3) | 2 (1–3) |
| Providing help with hospital transport | 2 (1–3) | 1 (1–2) |
| CFRs’ social care and public welfare role | 2 (1–3.25) | 3 (2–4) |
| CFRs attending accident cases | 2 (1–2.25) | 2 (1–3) |
| Dual CFR crew | 1.5 (1–3) | 2 (1–3) |
| Transferring patients to hospital | 1 (1–2) | 1 (1–2) |
| CFR access to blue light | 1 (1–1.5) | 1 (1–2) |
Summary
The consensus process led to a prioritised set of innovations for future roles of CFRs in rural emergency care provision. The prioritisation of innovations reflected the prospects for the future development of CFR schemes based on the experiences of patients and the public, CFRs, ambulance clinicians and ambulance service leaders.
Chapter 4 Discussion
Overview
In this chapter, we summarise our research findings, interpret these in relation to previous research, describe the strengths and limitations of our approach, and summarise the implications for practice and recommendations for future research.
Main findings
Emergency calls attended by Community First Responders
The cross-sectional study was the first to our knowledge to provide an exhaustive, quantitative analysis of the number, rate, dispatch conditions, urgency, location and characteristics of patients attended by CFRs. 42 This offered a widescale analysis investigating the contribution of CFRs to EMS, and showed that CFRs attended first a higher proportion of calls in rural areas (almost 4% of total calls) than in urban areas (around 1.5%) in six English regional ambulance services in 2019, before the COVID-19 pandemic.
Community First Responders attended all call categories but mainly the most urgent categories (categories 1 and 2), which included 83.7% of all CFR first attendances. CFRs attended patients with a range of dispatch conditions, but the most common categories were cardiorespiratory (30.2% of CFR attendances), injury and trauma (20.1%), and neurological and endocrine (13.4%). Compared with attendance by ambulance service staff, CFRs were more likely to attend cardiorespiratory and neurological and endocrine conditions and less likely to attend injury and trauma, gastrointestinal, urinary, psychosocial or palliative conditions. Conveyance to hospital was around 2% lower when CFRs were present on scene.
The multivariable logistic regression model confirmed that CFRs were more likely to be called out to rural (compared with urban) areas. The calls where CFRs were in attendance were more likely to involve older, white people in more affluent areas with cardiorespiratory and neurological conditions as emergency or urgent calls.
Resource use and allocation
To the best of our knowledge, the survey and analysis of resources used, how these were allocated and the CFR workforce in five of the six participating ambulance services was the first of its kind. Although CFRs are largely unpaid volunteers, they incur costs for the ambulance services and charities that support them. Resource data were incomplete because they were neither collected nor available in some cases because CFR costs were not disaggregated from other ambulance service costs. Costs varied widely (around 20-fold) between ambulance trusts, partly because they were incomplete, ranging from £40,000 per year to over £800,000. The costs were attributed to staff providing management, organisation and training together with non-pay costs such as equipment and reimbursement of out-of-pocket (fuel and vehicle use) expenses.
Where recorded, CFRs worked on average around one shift per week for around 7 hours, and they were distributed in both rural and urban areas, varying according to ambulance service, with CFRs in some ambulance services predominantly rurally located and others mainly operating in urban settings.
Outcomes of Community First Responder attendance
We investigated CFR outcomes for timing of attendance, and OHCA as well as the CFR falls intervention in Lincolnshire. CFRs provided a clear time benefit in terms of achieving response time targets and earlier attendance at incidents, particularly in rural locations. CFRs were also able to respond to people who fell, particularly when those people were not injured or unwell, and no ambulance backup was required in around half of the falls incidents attended. Economic modelling suggested that this was likely to be cost saving to the NHS. 35 Finally, we did not find any clear benefit or disbenefit to OHCA outcomes when CFRs arrived before ambulance staff.
Discourse analysis of Community First Responder policies and protocols
The analysis of CFR policies and protocols, to our knowledge the first on this subject, revealed the extent to which ambulance services invested efforts to ensure that CFR programmes were integrated into ambulance service structures, enabling them to operate effectively and safely. 52 This also revealed risks associated with volunteer roles and how these were mitigated. The risks, which included risks to CFR themselves, to patients and the public, and to the ambulance service, were addressed through policies that enacted governance frameworks to ensure compliance with rules, standards and procedures. These operated from selection and recruitment through to training and operation to termination of the role. The variation in these frameworks across services, which could create confusion for commissioning, regulatory oversight and public understanding of the CFR roles, could also affect the recruitment and retention of volunteers.
Stakeholder perspectives
Interviews with patients, relatives, CFRs, CFR leads, ambulance staff and commissioners across five ambulance service regions ensured that perspectives from a wide range of stakeholders were considered, providing the largest study of its kind. 66 We recruited fewer patients and relatives or commissioners than we initially set out to, which means that findings from these groups need to be interpreted with caution, and the reasons for this are discussed below. The original contribution of this study is the identification of a set of inter-related CFR practices in facilitating timely prehospital care delivery and patient transfer. This study also contributes to the understanding of different CFR roles and the rural context in which they operate. From a focus on disease-specific CFR roles,9 this study expands the CFR discourse to include the CFR functions in broader prehospital and social care provision.
Community First Responders were motivated by their interest in engaging with their local community to provide urgent care, particularly in more remote areas where ambulance services were less easily accessed. This posed problems for recruitment in sparsely populated areas, which was exacerbated by the availability of mostly retirees and an older volunteer workforce compared with urban locations. Recruitment, support and training were often lengthy processes but needed to develop an effective volunteer workforce. There were many factors, such as conflicting pressures or priorities, mismatch between expectations and the reality of the CFR role and changes in the role and the effect of the pandemic, which affected retention.
Community First Responders’ actions were important in bridging the gap between the emergency call and the arrival of ambulance clinicians by providing early assessment and intervention (Figure 15). Receiving an alert from the ambulance control and obtaining initial patient information paved the way for the next stage of reaching patients. The CFRs’ response started with the acquisition of further patient information and validation of the information from the control room. The CFRs exchanged complete and precise patient information with the control room for triaging and to update the responding ambulance clinicians so that they were more prepared on arrival. The CFRs provided a rapid emergency response, including CPR and defibrillation, and the final step was to engage with ambulance crews to expedite patient transfer and minimise transfer time. Thus, CFRs performed vital emergency healthcare practices, particularly for life-threatening conditions, by delivering direct or indirect care interventions. These actions were especially important when the ambulance’s arrival was delayed.
FIGURE 15.
Conceptual map of CFR practices.

Innovations included changes in processes and structures (Figure 14), for example expansion in the CFR role and scope of practice, skill development for attending new types of emergencies such as falls or road traffic collisions, ICT applications for communication with ambulance call centres and staff or navigation to incidents, specialised vehicles and the availability of new treatments, including for pain management.
Other aspects raised included the importance of psychological support, good workforce management and communication to ensure adherence to policies, and the need for volunteers to raise funds for equipment and running costs.
The scope of practice of CFRs differed from one ambulance service to another, but there were indications that the role had already developed significantly into new areas, such as attending people who had fallen or road traffic collisions, and suggestions by some, but not all, stakeholders that new roles, for example in social care, should be considered.
Finally, patients and their relatives who had been attended by CFRs were overwhelmingly positive about the response and care they received, and the reassurance of a timely response from someone with expertise arriving in advance of an ambulance clinician, but this contrasted with a perceived lack of awareness about CFRs and their role among the general population.
Priorities for innovation in the rural Community First Responder workforce
The mNGT, used as part of a consensus workshop, allowed us to reflect on the research findings, introduce new areas for improvement and discuss these ideas for innovation with a wide and informed stakeholder group, which included public contributors, CFRs, ambulance leaders and staff from all six ambulance services and regions.
The areas that were most highly rated after two rounds of voting were counselling and support for CFRs, peer support and hot debriefs, better communication from and with the ambulance control room (or EOC), together with navigation and communication equipment, specific mandatory and standardised training for CFRs, and creating awareness and promoting CFRs in the community and among the general public.
Equality, diversity and inclusion
Research team
Our research team was interdisciplinary due to the complex nature of the work and the importance of public contributors and wide expertise including knowledge of ambulance services, primary care, data management, statistics, sociology, econometrics, health economics and mixed methods. The chief investigator and 7 other co-authors were from a minority ethnic group, and 5 of the 15 were women. One member of the team went on maternity leave and returned before the completion of the report after having her baby. We included team members with disabilities. We had five early career researchers in the team, all of whom played an important role in the study, leading on key areas of the work and on authoring publications arising from them, while being supported by senior members of the team.
Public contributors
We successfully expanded our public contributors on the study, as described above (Patient, public and wider stakeholder involvement), from our two lay co-applicants and steering group members to a panel of seven patient and public representatives, through which we were able to ensure geographical representation from all participating ambulance regions, covering most of England, with lay members of different sexes, ethnic minority statuses and with and without disabilities. 65 Their contributions were essential and are described in detail below.
Data
We used routine data sets from six regional ambulance services, which included details of patients’ clinical conditions, age group, sex, region, ethnic minority status and socioeconomic deprivation, as a result of which we were able to include a wide range of participants in our analysis, reflecting people attended by ambulance services and CFRs. 65 The statistical models were also able to take these factors, where relevant, into account in our analyses.
Interviews
We sought to recruit widely for the interviews of patients, relatives and ambulance staff, using different methods including ambulance records, ambulance service CFR and research leads and their teams, and social media. To ensure inclusivity in interviews, we identified a random sample of 100 records of patients attended by CFRs in a rural setting in the previous 6 months using the quantitative data provided by all six ambulance service regions. Patient data included age group, sex, ethnicity67 and socioeconomic status, allowing us to sample across all these demographic characteristics using maximum variation sampling. Ambulance staff were also recruited for differences in sex, experience, ethnicity and role, and CFRs for differences in sex, ethnicity, length of experience and skill level. 68
Contributions of patients and the public
Public contributors
Public contributors included two co-applicants who were members of the study steering committee, and another who was a member of the study oversight group and a PPI panel. The panel included two male (and five female) participants, three participants from minority ethnic groups and one participant with a disability. It also included one member who was a CFR. The lived experiences of this group were instrumental at various stages of the study. The panel members met on two occasions to provide views at the initial design stage and on the findings. Members were also invited to the consensus meeting, and six attended.
The public members provided advice on and input to the overall study design, development of study materials, analysis and interpretation of the findings in each work package, through membership of the study steering groups, oversight group and patient panel. The panel helped formulate recommendations and advised on the content and mode of delivery of study outcomes to lay audiences. Their role in shaping the overall direction of and output from the research was critical in ensuring that our approach was sensitive to and grounded in the needs of the wider community that the research may influence.
Validity and methodological rigour
Members of the PPI panel were presented with emerging findings from the study on the activities, operations and practices of CFRs. We found that these meetings supported the research process through discussions about the social reality of CFR functions from members or their relatives who had received or provided care (one member was a CFR). These meetings with PPI members were important for validating the data and the subsequent interpretation.
Patient and public involvement member P asked how the CFRs and ambulance can communicate better because local (CFRs) would know how to get past a road closure, and ambulance arrival could be faster. PPI member M mentioned a sophisticated communication system using mobile phone/satellite navigation, which logs the call as it happens and navigates to the patient’s location while avoiding road closures. A researcher then confirmed that these types of equipment were not universal and that they differed between ambulance services. The research team agreed that the differences in innovations between the ambulance services would be explicitly noted and explored further.
Thus, the PPI helped the establishment of internal validity in the CFR study. The contributions of the PPI participants were not limited to the qualitative methods but also included the quantitative component. For example, PPI member M commented on the number of trauma calls, as this was larger than they had expected. A researcher explained that, for the purposes of the study, this category was very broad and included falls of different types as well as injuries other than serious trauma. They agreed that these different types of injury could be separated out.
The understanding of public contributors helped to achieve validity and methodological rigour.
Roles in achieving consensus
The PPI panel members participated in the consensus workshop and actively contributed to the production of ideas and innovations, as well as their prioritisation. An important contribution to the discussion of innovations was around the challenges for CFRs in navigating remote locations and the safety of CFRs. The conclusion of the consensus workshop emphasised the requirement for an improved navigation system and the development of national standards.
For example, during the consensus meeting a public contributor stated:
It’s important that there are national standards across the ambulance trusts to make sure CFRs have all got the same opportunities, i.e. best practices. So, in areas that have best practices, they ought to be rolled out to other areas. There need to be national standards, not only in terms of the CFR role and all the role’s different variations but also as far as recording things and making sure of that in future monitoring.
AB_05052022
The public contributors fully engaged in the research process and represented a range of public perspectives.
Comparison with previous research
Proportion of Emergency Medical Services calls attended by Community First Responders
Previous research emphasised the positive role and potential for CFRs in complementing the work of ambulance services, particularly for rural emergencies, but their contribution has not been well described before. 3 A finding from the previous study in 2007, suggesting that CFRs attended around 2% of all calls,1 was confirmed in this study, but we also found that the proportion was double this in rural areas.
Types of clinical conditions attended by Community First Responders
We found that CFRs were sent to people with a wide variety of conditions, but they predominantly attended the most urgent call categories 1 and 2. CFRs in all six services in this study were dispatched to people with illnesses other than cardiovascular disease and trauma, including neurological, endocrine, gastrointestinal, urinary, psychosocial and end-of life conditions, which suggests that they are being dispatched by UK ambulance services to people with a wide range of conditions. This suggests that CFRs were not restricted to responding to calls from patients with chest pain and cardiac arrest, as was the case in some services over a decade ago. 1 However, they do attend, in larger proportions than ambulance staff, calls from people with cardiorespiratory (breathing problems, chest pain, stroke) and neurological (loss of consciousness, convulsions, collapse) or endocrine (hypo- or hyperglycaemia) conditions.
Equity of Community First Responder care to different population groups
Community First Responder attendance was less likely for younger people, those from ethnic minority groups or those living in more deprived areas than for older, White British people living in more affluent areas. Although this partly reflects the rural population, which overall is older, less deprived and less ethnically diverse,69,70 the results remained the same even after controlling for rurality in the multivariable logistic regression model. People attended by CFRs are likely to be characterised by complex inter-relationships between patterns of population morbidity, help-seeking behaviour, access to services, and the location, availability and dispatch of CFRs, which may be different in rural areas. 71 These differences area likely to vary by country, region and CFR scheme. In one study of CFRs attending OHCA in Ireland, CFR schemes were more likely to be centred in areas of higher deprivation, but beyond a catchment of 4 minutes there were no differences in area-level deprivation of incidents attended by CFRs. 72 Some CFR schemes, for example medical student responder schemes, run through a number of English medical schools and operating under the auspices of ambulance services in England, are largely based in urban areas and because of this are more likely to attend patients of white ethnicity than other CFRs and ambulance staff alone, and more likely to attend incidents in areas of higher compared with lower socioeconomic deprivation. 73
Costs, resource use and outcomes
Costs varied widely between ambulance services, as did the numbers in the CFR workforce and what resources were used for, including CFR management, training, equipment and fuel, but the analysis was hampered by incomplete data.
Previous research has identified that the commitment of resources to support volunteers is key to ensuring volunteer goodwill, engagement and retention and that strong management support, communication, training, equipment and out-of-pocket expenses are essential human and physical resource requirements for maintaining a CFR workforce integrated with ambulance services. 74
Previous studies have documented perceptions among experts that a CFR response could improve outcomes but also highlighted the need for more evidence on outcomes of the CFR response, whether from the perspective of the patient, CFR, ambulance service, commissioner or researcher. 3,75 Although studies have investigated the impact of lay responders on OHCA (see Out-of-hospital cardiac arrest survival)10 or trauma,16 this study documents the wider benefits of CFRs attending.
Response times
Community First Responder attendance was associated with a shorter response time and greater likelihood of achieving response time targets than ambulance response alone, a difference in response times that was greater for incidents in rural areas. CFRs were more likely to arrive more quickly than 15 minutes (compared with 15–20 minutes), which was expected given the more urgent nature of the conditions that they attended, but they were also more likely to arrive at incidents later than 20 minutes, which indicated that they were also being directed to less urgent cases when ambulance crews might have been delayed attending, such as falls. In one previous small-scale study of an inner-city medical student CFR scheme in which 89 emergency calls were attended alongside West Midlands Ambulance Service, the mean CFR response time across all calls was on average 3 minutes and 8 seconds faster than ambulance crew response times, with the greatest difference in response time (12 minutes) for calls related to falls. 28
Out-of-hospital cardiac arrest survival
Community First Responder attendance was not associated with improved ROSC or 30-day survival outcomes from OHCA in our analysis. This is in line with previous rigorous studies but at odds with evidence from other observational studies.
In a Cochrane review of RCTs and quasi-randomised control studies investigating the effect of CFRs dispatched to OHCA in adults and children (older than 4 weeks of age), comparing CFRs combined with EMS versus EMS alone, in terms of survival and neurological function, there were two completed studies meeting inclusion criteria comprising a total of 1136 participants. 32 One, a cluster RCT of 469 adults with a witnessed OHCA, conducted in Amsterdam, Netherlands, during 2000 and 2002 and investigating police and fire service first responders equipped with AEDs, found no difference in survival at hospital discharge (OR 1.3, 95% CI 0.8 to 2.2), despite all 72 incidences of defibrillation performed before EMS arrival occurring in the intervention group and even though the study reported increased survival to hospital admission in the intervention group (OR 1.5, 95% CI 1.1 to 2.0). 76 The other was an RCT conducted in Stockholm, Sweden, between 2012 and 2013 investigating the dispatch of nearby lay volunteers to witnessed and unwitnessed OHCA in adults and children aged ≥ 8 years in addition to EMS responders including ambulance, police and fire services, which found no difference in 30-day survival (OR 1.34, 95% CI 0.79 to 2.29; 1 RCT; 612 participants) despite a significant increase in CPR performed before EMS arrival (OR 1.49, 95% CI 1.09 to 2.03). 10 Neither study assessed neurological function or health-related quality of life at hospital discharge or at 30 days. The overall certainty of evidence for the outcomes of included studies was low to moderate. The review authors concluded that there was moderate-certainty evidence that CFR interventions resulted in increased rates of CPR or defibrillation before EMS arrival but no evidence that this translated into improved survival. 32
One explanation could be related to timing and rates of defibrillation. When comparing CFRs carrying mobile AEDs and fixed PADs, more shocks were delivered by fixed PADs and outcomes were better than with mobile AEDS carried by CFRs. Most (over 85%) OHCAs occur at home,29 and people the affected tended to be older and with unwitnessed arrests, who therefore receive fewer shocks and experienced greater delays in starting CPR and attaching an AED. 77
The lack of evidence from improved OHCA contrasts with the finding using registry data that European regions that dispatched lay and professional first responders showed higher ROSC and survival rates than regions without. 78 Technological innovations for CFRs such as text messages79 or Global Positioning System applications have been found to be associated with earlier response times80 and defibrillation, with a small study on a rural island even showing good survival outcomes. 81
Reduced conveyance to hospital
Community First Responder attendance was associated with a small (around 2%) but still significantly lower conveyance rate, a finding at odds with their attendance at people with more urgent conditions who were more likely to be transported to hospital. Possible explanations include CFRs also attending low-risk incidents such as falls where an ambulance response, following advice from a health professional, is not always deemed necessary, as found in the FRP, or that the most urgent cases were associated with higher death rates and therefore those people who died were not conveyed to hospital. However, this result should be interpreted with caution as only qualified ambulance staff convey patients, and the differences in rates were small.
Patient and family experience
Community First Responder schemes and the role of CFRs contributing to the delivery of emergency care in rural regions were linked to patients and their family members reporting feeling reassured by the presence of CFRs, despite a lack of awareness of CFRs in their communities. Positive patient and family experiences accorded with expert opinion that community first response can be an important source of support and comfort for patients’ relatives. 75 The reassurance of a CFR arriving quickly and providing initial assessment and treatment before handing over to a clinician was an important outcome, and was similar to that provided by ambulance staff, where a short wait for help, good communication, professionalism and continuity provided confidence to patients and their relatives. 47
Personal and community engagement and resilience
The findings from this study were consistent with those of other studies demonstrating that a key determinant of becoming a CFR was the desire to provide a service to and engage with the community, but that other factors including previous experience observing a CFR attending an emergency or cardiac arrest, experience as a healthcare worker or the potential for learning and future work in EMS were also motivators for some. 3,9,82 These motivations aligned with the first four motivations of functional theory developed by Clary et al. 5 which include individual values, seeking understanding through learning or skills development, enhancement though psychological growth and career progression.
In a mixed-methods study, a questionnaire survey to emergency response volunteers in China found that participants were more willing to volunteer if they resided in rural areas, had stronger community bonds and felt responsible to contribute, but interviews revealed that they were less likely to volunteer in the context of a poor policy environment (lack of funding, regulation or co-ordination) or programme management (recruitment and training). 83
Motivations were assessed during recruitment and previous experience during training and allocation of roles, while management support was seen as important to ensure that functions were carried out safely and effectively and that CFRs could be maintained in their role. These aspects have been found in previous studies to be vital to successful volunteer programmes. 84 We found that changes in personal life and circumstances, as well as the challenge of committing time alongside concurrent employment or conflicting priorities, were the primary reasons trained CFRs left the workforce.
The psychological impact of being a CFR and the need for psychological support has been identified as being important in other studies,75 with CFRs shown to be affected by stress through frustration at not being able to help more, struggles with emotional or mental health demands, or the loneliness of the CFR role. 20 By contrast, the relative resilience of lay responders, even in high-stress situations such as cardiac arrest85 or mass terror incidents,86 has been observed. A phenomenological study87 found that a realistic understanding of limitations, confidence in skills, the ability to handle positive and negative outcomes, and a degree of emotional detachment enabled CFRs to function in stressful situations without experiencing negative psychological consequences, and these attributes might be considered when recruiting volunteers to this role. A questionnaire study85 comparing volunteers who had been exposed to stressful mass terror incidents with those who had not found higher but subclinical rates of post-traumatic symptoms and positive effects on self-efficacy among the former.
The operations of CFR schemes and the practices of CFRs within rural communities were aligned with the concept of community resilience,88 whereby it can be argued that CFR schemes, as an effort to include communities in rural health care, were framed as enhancing a community’s ability to cope with and respond to the requirement of rapid care for patients who seek EMS. 75,89 The CFRs played an important bridging role in ensuring the resilience of the community. 22
Relationship between ambulance staff and volunteers
Although we found many examples of positive and collaborative relationships between CFRs and ambulance services, this and previous research has also found ambivalence in the relationship. In this study, we found that ambivalence arose from perceptions of communication, role, accountability trust and of CFRs being valued (or not) by ambulance staff. 3,18 A focus group study exploring conflicts between volunteers and paid staff in a non-profit organisation in Madrid, Spain, found tension arose because conflicts in tasks, processes and relationships were more important than differences in status, with greater levels of conflict in paid staff than volunteers. 90 A survey study exploring the differences between paid employees and volunteers found that while fair task division and minimising role overlap reduced tension in both groups, staff focused on task- and process-related approaches to managing interactions whereas volunteers valued relationships and feeling appreciated. 91 This finding provides insights into ways of improving the relationship between these groups.
Governance of Community First Responder schemes
Governance structures including policies, guidelines, protocols and systems for recruitment, management and training together with the need to ensure compliance with rules, standards and procedures provided the means to integrate CFRs into ambulance service structures and to ensure their effective and safe operation, while mitigating risks to patients and the public, to CFRs, and to the ambulance service. These structures aligned with best practices for public sector volunteering92 and to varying degrees aligned or were at odds with factors that aided integration with ambulance services, as discussed below. 74
Factors encouraging the integration of CFRs into ambulance services were investigated in a study involving surveys and interviews of senior managers responsible for ambulance volunteers and first responders from Australia and New Zealand, which found that commitment to a volunteer model, leadership, good communication, shared protocols, appropriate resources and rewards, and relative autonomy of CFR schemes were considered important. 74 The relative autonomy of CFR schemes is realised by some large charitable and independent schemes such as LIVES, but this is less apparent in many schemes run by ambulance service.
Community First Responder schemes in themselves are relatively innovative aspects of the healthcare system and EMS. There is a perception among managers and experts, at least in the Antipodean context, that many innovations have taken place in CFR schemes but remain unevaluated or unpublished. 74
Strengths and limitations
Our study was conducted during and in the context of the COVID-19 pandemic, but we were mainly interested in CFR activities and operations outside the pandemic. We used quantitative data prior to the pandemic and, although qualitative data were gathered during the pandemic, the effect of COVID-19 was outside the scope of this study.
The cross-sectional study benefitted from a very large data set (about 4.5 million observations) covering most of rural England over a period of 1 year. It is also the first study to evaluate the resource costs, workforce distributions and benefits of CFRs in terms of time to attend and response to falls incidents. This study was also the first to use large-scale qualitative methods across most rural regions of England to explore the perspectives and experiences of a diverse group of stakeholders involved in the operations of CFR schemes.
The multivariable logistic regression model was exploratory, and the suitability of the predictors was carefully interpreted due to the limitations of DAGitty software. These included problems with the program in accurately assessing and accommodating models with highly intricate relationships among variables and its limited capability to handle categorical variables. 46
The observational design, using routinely collected data rather than data purposefully collected for research, had inherent limitations. Postcode records indicated where the incidents happened but may not have corresponded to the patient’s home address. Ethnicity data were missing in around 20% of cases. The number of missing data points for each variable is listed in Appendix 1, Table 20. Time to arrive calculated as arrival time minus dispatch time could have also been contaminated as dispatch records do not always reflect the initial time the first resource was dispatched. However, the arrival times were carefully cleaned, negative times were excluded from the analysis and their distributions were checked for each ambulance service, all showing normal distributions, slightly skewed towards lower times, as expected, and within the same range across all six ambulance services. We did not apply imputation methods because some variables had high rates of missing data, such as ethnicity (58%) or arrival time (24%), which would have precluded the application of such techniques, whereas other variables, including call category (3.9%) and condition category (4.7%), had low rates of missingness, so the results would be unlikely to change.
The resource and workforce data were limited by incomplete responses to the survey from most of the ambulance services. The counterfactual analysis of CFR response times compared with the response times of regular ambulance services was restricted to a single ambulance service. This was also the case for the analysis of OHCA outcomes. The evaluation of the FRP, which was active in a single county, was restricted to its area of operation. We were able to access CFR data from LIVES, the CFR scheme operating in Lincolnshire, for the OHCA and FRP analysis, but missing data and discrepancies between CFR and ambulance data were limiting factors in the analysis. Improved CFR data recording would be valuable for more robust evaluation of outcomes, as well as providing information for improvement. 93
The qualitative study benefited from a large number of interviews from a wide range of participants, although we were unable to recruit as initially intended, and smaller numbers of patients, relatives and commissioners were interviewed than we had planned. This means that it is more difficult to draw conclusions about the views of these stakeholders on CFRs from our analysis. Although we could not find evidence of poor service delivery or risks to patient safety, we recognise that these issues may have manifested without being revealed through the interviews.
Implications for service delivery
Community First Responders in England contribute a small proportion but large absolute numbers of emergency responses on behalf of ambulance services, particularly in rural areas and for the most serious incidents,42 suggesting that the CFR role should be continued and supported. The decision to take up CFR-related innovations needs to be considered in the light of evidence of the role’s effectiveness and safety, and balanced with other priorities, while supporting implementation with training, equipment and other resources. An example is the implementation of the inhaled analgesic methoxyflurane in some CFR schemes. 94
The range of incident types that CFRs are dispatched to has increased beyond their original remit to attend cardiac arrests, and this extension of their role requires alignment of training, resources, protocols and governance. 3 Previous studies have shown variation in clinical interventions provided by CFRs, reflected in differences in training and the drugs they are allowed to administer. 1 CFRs perceived their role to be changing, but some in this study and others remain concerned about expanding the scope of their responsibilities. 18
The finding that CFRs attend the most urgent calls more quickly, particularly in rural areas where access to health care may be worse, is of interest for the UK, but also for many other countries where CFRs operate. It is relevant for high-, low- and middle-income countries where healthcare systems are under strain or where access to medical facilities is more difficult because of a variety of factors including pressure from pandemics, lack of resources, infrastructure problems or military conflict. 95
To develop and extend the CFR role in the future, ambulance services need to understand and appreciate their contribution and to foster their relationship with CFR schemes. They need to carefully consider potential facilitators such as management decentralisation, volunteer input into decision-making, appropriate resourcing including accurately identifying costs and integration of volunteers into EMS, while addressing potential barriers such as communication, funding, training, health and information technology and maintaining robust systems of governance and safety. 34,74
Implications for future research
Further research is required using rigorous methods to evaluate the effectiveness and cost-effectiveness of CFR and CFR-related interventions and innovations for patients, particularly when innovations are being introduced and modified rapidly. One framework that has been used for evaluation of innovations, the IDEAL (Idea, Development, Exploration, Assessment, Long-term monitoring) framework, may be useful here. 96 This involves an initial report focusing on an explanation and a description of the idea, which may have been planned, accidental or forced. This is followed by a focus on the technical details and feasibility of the innovation as it is developed through rapid iterative modification of the innovation, usually at a smaller scale at one or more centres. Next is to explore potential benefits and adverse effects and to consider replication by others. As the innovation gains wider acceptance and is considered against current treatment or ways of working, it requires assessment using more formal evaluation techniques, comparing outcomes against current standards or best practice. Finally, long-term monitoring involves surveillance for late or rarer problems or changes in use. 96
Research is also needed to understand the impact of the role on a CFR's well-being, their effects on the communities in which they live, and how positive effects can be enhanced and negative effects ameliorated. Educational benefits may derive from working as a medical student first responder,73 and the wider literature on volunteering suggests positive effects on contributions to society, behaviour, physical and mental health, work and occupational achievement for those of working age, but these effects are complicated by volunteer bias (i.e. volunteers tend to be healthier) and tend to have been studied in less stressful voluntary activities,97,98 and less is known about the impact of volunteering on CFRs.
Given the benefits of including CFRs in the EMS response shown in this study, further studies to understand how to enhance motivation to join CFR schemes, how CFRs should be selected, trained and supported, and the personal attributes and organisational culture that will enable them to continue in their role are needed. To understand ambulance clinicians’ perspectives of current and future CFR roles and innovations, further research exploring ambulance service perspectives would be useful.
There were changes in the operation of European first responder schemes as a result of the COVID-19 pandemic, including restricted activation of CFRs in some countries including regions of England and changes to CPR (omission of rescue breaths and administration of compression-only CPR),99 and these changes should be explored in anticipation of future pandemics.
Summary
Community First Responders contribute to EMS delivery particularly in rural areas and especially for more urgent calls. The work of CFRs has expanded from its original purpose to attend OHCA. There are benefits to CFRs providing a prehospital response in terms of response times and patient experience and the potential for CFRs to attend and manage low-acuity incidents without an ambulance response, which could be cost saving for some interventions. The findings have implications for the continuing role of CFRs working with ambulance services, accurate identification of costs, the relationship between ambulance services and CFR schemes and the introduction of innovations. Further research is needed to identify innovations that are eventually taken up by CFR schemes and the reasons for adoption, and these need to be evaluated for effectiveness and cost-effectiveness before sustained or wider implementation. Further research is also needed to explore the impact of the CFR role on volunteers themselves and the communities in which they live. Future research should also seek to understand how to increase volunteering to CFR schemes, and how CFRs should be selected, trained and supported in their role.
Chapter 5 Conclusion
We set out to investigate the activities, costs of provision, and outcomes of CFR schemes, and to explore the views of patients, the public, CFRs, CFR leads and primary care commissioners on the role of CFRs in the current and future rural health and care workforce in order to develop recommendations for future innovations in rural CFR provision.
Community First Responders attended 1.92% of attendances (86,880 of 4.5 million) in six ambulance services during the year 2019, attending first on scene in a significantly higher proportion of rural (3.9%) compared with urban (1.5%) attendances overall, although the urban–rural distribution of CFRs varied across services.
Community First Responders were significantly more likely than ambulance crews to attend higher category (category 1 and 2) calls. They also attended patients with a wide variety of clinical conditions, attending significantly more calls for cardiorespiratory (e.g. breathing problems, chest pain, stroke), neurological (e.g. loss of consciousness, convulsions, collapse) and endocrine (e.g. hypo- or hyperglycaemia) conditions than ambulance staff. The calls attended included a high proportion of injury and trauma calls, although this was significantly lower than for ambulance staff. The wide range of clinical conditions attended, including less acute conditions such as falls, was also reported in interviews with CFRs.
Costs of CFRs varied from £40,000 to over £800,000 per year (i.e. around 20-fold) across participating ambulance trusts, but because costs were incompletely recorded and reported, the true costs may have been higher. Costs were attributed to staff providing management support, organisation and training of CFRs, together with the reimbursement of out-of-pocket volunteering costs, including fuel and vehicle use. CFRs were distributed in both rural and urban areas to different extents across different ambulance service regions. In trusts providing this information, the average duration on-call was 7 hours, with on average one shift per week provided, and CFRs mostly operated alone.
Community First Responder attendance was associated with a shorter response time and higher likelihood of meeting response time targets than for ambulance staff attending without CFRs. Conveyance was slightly lower when CFRs attended, which may have been due to patients who died as a result of cardiac arrest or CFR attendance at lower category calls such as low-risk falls where conveyance may not have been needed. An innovative CFR falls service in one county was shown to be effective and likely to be cost-effective, with high levels of CFR attendance and only around half that required an ambulance attendance. CFR attendance was not associated with improved OHCA outcomes. One less positive aspect of care quality was equity, with CFRs significantly less likely to attend younger people, those from ethnic minority groups or those living in more deprived areas than older, White British people living in more affluent areas, even after correcting for rurality.
Community First Responder policies, guidelines and protocols were designed to ensure that there were procedures for recruitment and that CFRs operated effectively and safely. Interviews with patients, relatives, ambulance staff, CFRs, CFR scheme leads and primary care commissioners explored experiences and perceptions of CFR recruitment, the current role and the future potential for developments and innovations. This revealed details of what motivated CFRs to enlist as volunteers, how CFRs performed their role, what helped or hindered them, and how they achieved positive outcomes. Am important outcome reported by patients and relatives was a positive experience of CFR attendance and care.
A number of actual and potential innovations were put forward by interviewees and through the mNGT, in the consensus workshop, and these were rated through two rounds of voting and discussion, with the highest ranked being counselling and support for CFRs, peer support and hot debriefs, better communication from and with the ambulance control room, together with navigation and communication equipment, specific mandatory and standardised training for CFRs, and creating awareness and promoting CFRs in the community and among the general public.
The findings have implications for the continuation of CFRs schemes, their relationship with ambulance services, the need to accurately identify costs, and the decision to introduce innovations while also ensuring that they are acceptable to CFR volunteers and supporting their implementation with training, equipment and other resources.
Further research is required to identify which innovations are taken up by CFR schemes, to evaluate the effectiveness and cost-effectiveness of CFR and CFR-related interventions and innovations, to explore the impact of the CFR role on individuals and communities, to understand how to motivate people to volunteer for CFR schemes, how CFRs should be selected, trained and supported, and how they can be effectively used during pandemics.
Additional information
Acknowledgements
We thank the patients, relatives, CFRs, ambulance staff and GP commissioners who participated in the interviews. We are grateful to research leads at the ambulance services (EMAS, SCAS, SECAmb, SWASFT, WMAS and YAS) and LIVES who provided data for this study, and helped with recruitment to the interviews, to members of the study steering committee, members of the patient reference group (Ruby Bhatti, Nick Filer, Sumaria Naseem, Mike Sheil and Solveig Warren) and to the chairperson (Professor Jeremy Dale) and members (Dr Tomás Barry, Dr Nicholas Taub, Lissie Wilkins and Professor Guiqing Lily Yao) of the scientific oversight committee for their valuable advice and support. Our thanks to Sam Lewis for advice on behalf of the sponsor. We thank Dr Jasmine Harvey for her work on the documentary analysis and initial interviews, Jordan Engel Stevens for his work on the pilot evaluation of the Falls Response Programme and Bronwyn ET Smith for constructing the maps displayed. Finally, thanks to Sue Bowler, who provided excellent administrative support for the whole study.
Contributions of authors
Aloysius Niroshan Siriwardena (https://orcid.org/0000-0003-2484-8201) (Chief Investigator) led the study conception and design, took responsibility for all aspects of the study, assisted with data collection, ensured data integrity and accuracy of analysis, interpreted the data, and drafted and critically revised this manuscript. He is guarantor for the study.
Gupteswar Patel (https://orcid.org/0000-0002-6989-5848) (Qualitative Researcher) was involved in the qualitative data collection, analysis and interpretation, and drafted and critically revised this manuscript.
Vanessa Botan (https://orcid.org/0000-0003-1583-3913) (Statistician) was involved in the statistical analysis and interpretation, and drafted and critically revised this manuscript.
Murray D Smith (https://orcid.org/0000-0002-5363-4184) (Health Economist and Econometrician) was involved in the study conception and design, supervised and conducted econometric analysis and interpretation, and drafted and critically revised this manuscript.
Viet-Hai Phung (https://orcid.org/0000-0002-5827-590X) (Qualitative Researcher) was involved in the qualitative data collection, analysis and interpretation, and critically revised this manuscript.
Julie Pattinson (https://orcid.org/0000-0002-9824-3400) (Qualitative Researcher) was involved in the qualitative data collection, analysis and interpretation, and critically revised this manuscript.
Ian Trueman (https://orcid.org/0000-0002-5875-8979) (Qualitative Researcher) was involved in the qualitative data collection, analysis and interpretation, and critically revised this manuscript.
Colin Ridyard (https://orcid.org/0000-0003-4346-1221) (Health Economist and Econometrician) was involved in econometric and health economic data collection, analysis and interpretation, and drafted and critically revised this manuscript.
Mehrshad Parvin Hosseini (https://orcid.org/0000-0002-4366-7919) (Health Economist and Econometrician) was involved in econometric analysis and interpretation, and drafted and critically revised this manuscript.
Zahid Asghar (https://orcid.org/0000-0003-2564-2096) (Statistician) was involved in the study conception and design, supervised statistical data analysis and interpretation, and critically revised this manuscript.
Roderick Orner (https://orcid.org/0000-0002-3181-7238) (Clinical Psychologist) was involved in the qualitative data interpretation and critically revised this manuscript.
Amanda Brewster (https://orcid.org/0000-0001-8987-0368) (Public Contributor) was involved in the data interpretation and critically revised this manuscript.
Pauline Mountain (https://orcid.org/0000-0002-6442-0448) (Public Contributor) was involved in the data interpretation and critically revised this manuscript.
Elise Rowan (https://orcid.org/0000-0003-4509-9828) (Database Manager) was involved in the ethical approvals, data interpretation and critically revised this manuscript.
Robert Spaight (https://orcid.org/0000-0003-4361-5876) (Ambulance Research Lead) was involved in the data collection, interpretation and critically revised this manuscript.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/JYRT8674.
Primary conflicts of interest: Aloysius Niroshan Siriwardena reports National Institute for Health and Care Research (NIHR) funding for the following projects: NIHR132744, NIHRDH-PB-PG-0815-20012, NIHRDH-HSDR/17/99/34, NIHRDH-HSDR/15/145/04, NIHRDH-PB-PG-1216-20034, NIHRDH-HSDR/14/47/22, NIHRDH-HTA/16/84/01 and NIHRDH-HSDR/13/54/75.
Patient data statement
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that they are stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Ethics statement
Ethical approval was obtained from the NHS Research Ethics Committee (IRAS project ID: 277205, registration reference: NCT04279262).
Information governance statement
The University of Lincoln is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679.
Under the Data Protection legislation, the University of Lincoln is the Data Processor; EMAS, SECAmb, SCAS, SWASFT, WMAS and YAS were the Data Controller and we processed personal data in accordance with their instructions. You can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for the University of Lincoln Data Protection Officer here (compliance@lincoln.ac.uk) and for participating NHS trusts as follows: EMAS (www.emas.nhs.uk/your-service/your-information), SECAmb (www.secamb.nhs.uk/privacy-statement/), SCAS (www.scas.nhs.uk/privacy-statement/), SWASFT (www.swast.nhs.uk/welcome/foi-key-documents/subject-access-request), WMAS (wmas.nhs.uk/privacy-notice/) and YAS (www.yas.nhs.uk/tc/privacy-policy/).
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the HSDR programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Publications
Botan V, Asghar Z, Rowan E, Smith MD, Patel G, Phung VH, et al. EP10 Community first responders’ contribution to rural emergency medical service provision in the UK. Emerg Med J 2022;39:e5.
Patel G, Phung VH, Pattinson J, Trueman I, Ørner R, Botan V, et al. PP21 Factors affecting community first responders’ role in rural emergencies: a qualitative interview study. Emerg Med J 2022;39:e5.
Botan V, Asghar Z, Rowan E, Smith M, Patel G, Phung V, et al. Community First Responders’ contribution to emergency medical service provision in the UK. Ann Emerg Med 2023;81:176–83.
Hosseini SMP, Smith MD, Patel G, Smith BET, Siriwardena AN. PP47 Effectiveness of falls response partnership in emergency medical services in Lincolnshire, UK: an economic evaluation. Emerg Med J 2023;40:A19–20.
Patel G, Botan V, Phung VH, Trueman I, Pattinson J, Hosseini SMP, et al. PP44 Consensus on innovations and future change agenda in community first responder schemes in England: a national nominal group technique study. Emerg Med J 2023;40:A18.
Patel G, Phung VH, Trueman I, Ørner R, Siriwardena AN. Common hierarchies, varied rules – the problem of governing community first responders in prehospital care for quality standards: documentary discourse analysis. BMC Health Serv Res 2023;23.
Patel G, Phung V, Trueman I, Pattinson J, Botan V, Hosseini SMP, et al. “It’s like a swan, all nice and serene on top, and paddling like hell underneath”; Community First Responders’ practices in attending patients and contributions to rapid emergency response in rural England, United Kingdom: a qualitative interview study. Scand J Trauma Resusc Emerg Med 2023;31:7.
Phung VH, Patel G, Pattinson J, Trueman I, Siriwardena AN. PP13 Community first responders – their identity and relationship with patients and the ambulance service: a qualitative interview study. Emerg Med J 2023;40:A6.
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Healthcare Commission . The Role and Management of Community First Responders: Findings from a National Survey of NHS Ambulance Services in England 2007.
- Turner J, Coleman P, Sampson FC. A Review of Emergency Medical Responses in Lincolnshire. Sheffield: University of Sheffield; 2010.
- Phung VH, Trueman I, Togher F, Orner R, Siriwardena AN. Community first responders and responder schemes in the United Kingdom: systematic scoping review. Scand J Trauma Resusc Emerg Med 2017;25.
- Wilson J. Volunteering. Annu Rev Sociol 2000;26:215-40.
- Clary EG, Snyder M, Ridge RD, Copeland J, Stukas AA, Haugen J, et al. Understanding and assessing the motivations of volunteers: a functional approach. J Pers Soc Psychol 1998;74:1516-30.
- Harris C, McCarthy K, Liu EL, Klein K, Swienton R, Prins P, et al. Expanding understanding of response roles: an examination of immediate and first responders in the United States. Int J Environ Res Public Health 2018;15.
- Ko SY, Ro YS, Shin SD, Song KJ, Hong KJ, Kong SY. Effect of a first responder on survival outcomes after out-of-hospital cardiac arrest occurs during a period of exercise in a public place. PLOS ONE 2018;13.
- Kay BJ. ‘Barefoot doctors’ in rural Georgia: the effect of peer selection on the performance of trained volunteers. Soc Sci Med 1984;19:873-8.
- Barry T, Guerin S, Bury G. Motivation, challenges and realities of volunteer community cardiac arrest response: a qualitative study of ‘lay’ community first responders. BMJ Open 2019;9.
- Ringh M, Jonsson M, Nordberg P, Fredman D, Hasselqvist-Ax I, Håkansson F, et al. Survival after public access defibrillation in Stockholm, Sweden – a striking success. Resuscitation 2015;91:1-7.
- Rortveit S, Meland E. First responder resuscitation teams in a rural Norwegian community: sustainability and self-reports of meaningfulness, stress and mastering. Scand J Trauma Resusc Emerg Med 2010;18.
- Toyokuni Y, Suzukawa M, Yamashita K, Yonekawa C, Kubota K, Yasuda Y, et al. Introduction of the Community First Responder system into Japan: is that possible?. Int J Emerg Med 2013;6.
- Pattanarattanamolee R, Sanglun RY, Nakahara S. Community-based first tesponder network in rural Thailand: a case study of out-of-hospital cardiac arrest. Prehosp Disaster Med 2021;36:234-6.
- Pallavisarji U, Gururaj G, Girish RN. Practice and perception of first aid among lay first responders in a southern district of India. Arch Trauma Res 2013;1:155-60.
- Jayaraman S, Mabweijano JR, Lipnick MS, Caldwell N, Miyamoto J, Wangoda R, et al. First things first: effectiveness and scalability of a basic prehospital trauma care program for lay first-responders in Kampala, Uganda. PLOS ONE 2009;4.
- Murad MK, Issa DB, Mustafa FM, Hassan HO, Husum H. Prehospital trauma system reduces mortality in severe trauma: a controlled study of road traffic casualties in Iraq. Prehosp Disaster Med 2012;27:36-41.
- Slingers M, De Vos S, Sun JH. Ten years of the community-based emergency first aid responder (EFAR) system in the Western Cape of South Africa: what has happened, what has changed, and what has been learned. Afr J Emerg Med 2022;12:299-306.
- Phung VH, Trueman I, Togher F, Orner R, Siriwardena AN. Perceptions and experiences of Community First Responders on their role and relationships: qualitative interview study. Scand J Trauma Resusc Emerg Med 2018;26.
- Mort AJ, Fitzpatrick D, Schneider A, Wilson P, Mellish C. Pre-hospital technology research: reflecting on a collaborative project between ambulance service and academia. J Paramed Pract 2015;7:184-91.
- Kindness P, Fitzpatrick D, Mellish C, Masthoff J, O’Meara P, McEwan M. An insight into the demands and stressors experienced by Community First Responders. J Paramed Pract 2014;6:362-9.
- Matinrad N, Reuter-Oppermann M. A review on initiatives for the management of daily medical emergencies prior to the arrival of Emergency Medical Services. Cent Eur J Oper Res 2022;30:251-302.
- Roberts A, Nimegeer A, Farmer J, Heaney DJ. The experience of Community First Responders in co-producing rural health care: in the liminal gap between citizen and professional. BMC Health Serv Res 2014;14.
- Elden OE, Uleberg O, Lysne M, Haugdahl HS. Community paramedicine–cost–benefit analysis and safety with paramedical emergency services in rural areas: scoping review protocol. BMJ Open 2020;10.
- Alanazy ARM, Wark S, Fraser J, Nagle A. Factors impacting patient outcomes associated with use of Emergency Medical Services operating in urban versus rural areas: a systematic review. Int J Environ Res Public Health 2019;16.
- United Nations Statistical Division . Population Density and Urbanization 2017. http://unstats.un.org/unsd/Demographic/sconcerns/densurb/densurbmethods.htm (accessed 2 January 2023).
- Chan T, Braitberg G, Elbaum D, Taylor DM. Hatzolah emergency medical responder service: to save a life. Med J Aust 2007;186:639-42.
- Seligman WH, Ganatra S, England D, Black JJ. Initial experience in setting up a medical student first responder scheme in South Central England. Emerg Med J 2016;33:155-8.
- Campbell A, Ellington M. Reducing time to first on scene: an ambulance–Community First Responder scheme. Emerg Med Int 2016;2016.
- Hawkes C, Booth S, Ji C, Brace-McDonnell SJ, Whittington A, Mapstone J, et al. OHCAO collaborators . Epidemiology and outcomes from out-of-hospital cardiac arrests in England. Resuscitation 2017;110:133-40.
- Boland LL, Formanek MB, Harkins KK, Frazee CL, Kamrud JW, Stevens AC, et al. Minnesota Heart Safe Communities: are community-based initiatives increasing pre-ambulance CPR and AED use?. Resuscitation 2017;119:33-6.
- Baekgaard JS, Viereck S, Moller TP, Ersboll AK, Lippert F, Folke F. The effects of public access defibrillation on survival after out-of-hospital cardiac arrest: a systematic review of observational studies. Circulation 2017;136:954-65.
- Barry T, Doheny MC, Masterson S, Conroy N, Klimas J, Segurado R, et al. Community first responders for out-of-hospital cardiac arrest in adults and children. Cochrane Database Syst Rev 2019;7.
- Turner J. Evaluation of the Clinical and Ambulance Service Operational Impact of the Lincolnshire Integrated Voluntary Emergency Service (LIVES). Sheffield; 2004.
- Hassan TB, Barnett DB. Delphi type methodology to develop consensus on the future design of EMS systems in the United Kingdom. Emerg Med J 2002;19:155-9.
- Smith MD, Stevens JE, Siriwardena AN. Evaluation of the Falls Response Partnership’s Community First Responder Response to Adults Who Have Fallen in Lincolnshire. Unpublished Report for Lincolnshire County Council Public Health Department. Lincoln: University of Lincoln; 2020.
- Teddlie C, Tashakkori A. Foundations of Mixed Methods Research: Integrating Quantitative and Qualitative Techniques in the Social and Behavioral Sciences. London: SAGE Publications Ltd; 2009.
- Tashakkori A, Teddlie C. Sage Handbook of Mixed Methods in Social and Behavioral Research. Los Angeles, CA: SAGE Publications Ltd; 2010.
- Koleros A, Mulkerne S, Oldenbeuving M, Stein D. The actor-based change framework: a pragmatic approach to developing program theory for interventions in complex systems. Am J Eval 2018;41:34-53.
- Moran-Ellis J, Alexander VD, Cronin A, Dickinson M, Fielding J, Sleney J, et al. Triangulation and integration: processes, claims and implications. Qual Res Psychol 2006;6:45-59.
- O’Cathain A, Murphy E, Nicholl J. Three techniques for integrating data in mixed methods studies. BMJ 2010;341.
- Boyle D, Harris MD. The Challenge of Co-production: How Equal Partnerships Between Professionals and the Public are Crucial to Improving Public Services. London: NESTA; 2009.
- Botan V, Asghar Z, Rowan E, Smith MD, Patel G, Phung V-H, et al. Community First Responders’ contribution to emergency medical service provision in the United Kingdom. Ann Emerg Med 2023;81:176-83.
- DEFRA . Definition of Rural Areas Using the Rural Urban Classification 2016. www.gov.uk/government/collections/rural-urban-classification (accessed 1 September 2018).
- Clawson JJ, Dernocoeur KB. Principles of Emergency Medical Dispatch. Englewood Cliffs, NJ: Prentice-Hall; 1988.
- NHS Digital . NHS Pathways 2021.
- Textor J, Hardt J, Knuppel S. DAGitty: a graphical tool for analyzing causal diagrams. Epidemiology 2011;22.
- Togher FJ, O’Cathain A, Phung VH, Turner J, Siriwardena AN. Reassurance as a key outcome valued by emergency ambulance service users: a qualitative interview study. Health Expect 2015;18:2951-61.
- Turner J, Siriwardena AN, Coster J, Jacques R, Irving A, Crum A, et al. Developing new ways of measuring the quality and impact of ambulance service care: the PhOEBE mixed-methods research programme. Programme Grants Appl Res 2019;7.
- Turner J, Jacques R, Crum A, Coster JE, Stone T, Nicholl J. Ambulance Response Programme: Evaluation of Phase 1 and Phase 2 Final Report. Sheffield: University of Sheffield; 2017.
- Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, et al. International Liaison Committee on Resuscitation . Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation 2004;110:3385-97.
- NHS England . The Five Year Forward View 2014.
- Patel G, Phung VH, Trueman I, Orner R, Siriwardena AN. Common hierarchies, varied rules – the problem of governing community first responders in prehospital care for quality standards: documentary discourse analysis. BMC Health Serv Res 2023;23.
- Gormley WT. Institutional policy analysis: a critical review. J Policy Anal Manage 1987;6:153-69.
- Parsons DW. Public Policy: An Introduction to the Theory and Practice of Policy Analysis. Aldershot: Edward Elgar; 1995.
- Abdullah Kamal SSLB. Research paradigm and the philosophical foundations of a qualitative study. PEOPLE Int J Soc Sci 2019;4:1386-94.
- Campbell S, Greenwood M, Prior S, Shearer T, Walkem K, Young S, et al. Purposive sampling: complex or simple? Research case examples. J Res Nurs 2020;25:652-61.
- Bryman A. How Many Qualitative Interviews Is Enough? Expert Voices and Early Career Reflections on Sampling and Cases in Qualitative Research. Southampton: National Centre for Research Methods, University of Southampton; 2012.
- Grady MP. Qualitative and Action Research: A Practitioner Handbook. Bloomington, IN: Phi Delta Kappa Educational Foundation; 1998.
- Gray LM, Wong-Wylie G, Rempel GR, Cook K. Expanding qualitative research interviewing strategies: Zoom video communications. Qual Rep 2020;25:1292-301.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101.
- Van de Ven AH, Delbecq AL. The nominal group as a research instrument for exploratory health studies. Am J Public Health 1972;62:337-42.
- Siriwardena AN, Whitley GA. Prehospital Research Methods and Practice. Bridgwater: Class Professional Publishing; 2022.
- Adams R, Tranfield D, Denyer D. A taxonomy of innovation: configurations of attributes in healthcare innovations. Int J Innov Manag 2011;15:359-92.
- Domecq JP, Prutsky G, Elraiyah T, Wang Z, Nabhan M, Shippee N, et al. Patient engagement in research: a systematic review. BMC Health Serv Res 2014;14.
- National Institute for Health and Care Research (NIHR). INCLUDE . Better Healthcare Through More Inclusive Research 2022. https://sites.google.com/nihr.ac.uk/include/home (accessed 2 January 2023).
- Patel G, Phung VH, Trueman I, Pattinson J, Botan V, Parvin Hosseini SM, et al. ‘It’s like a swan, all nice and serene on top, and paddling like hell underneath’: community first responders’ practices in attending patients and contributions to rapid emergency response in rural England, United Kingdom – a qualitative interview study. Scand J Trauma Resusc Emerg Med 2023;31.
- National Institute for Health and Care Research . Improving Inclusion of under-Served Groups in Clinical Research: Guidance from INCLUDE Project 2022. www.nihr.ac.uk/documents/improving-inclusion-of-under-served-groups-in-clinical-research-guidance-from-include-project/25435 (accessed 2 January 2023).
- Witham MD, Anderson E, Carroll C, Dark PM, Down K, Hall AS, et al. INCLUDE writing group . Developing a roadmap to improve trial delivery for under-served groups: results from a UK multi-stakeholder process. Trials 2020;21.
- DEFRA . Statistical Digest of Rural England 2021.
- DEFRA . Rural Population and Migration 2021.
- Local Government Association, Public Health England . Health and Wellbeing in Rural Areas 2017.
- Masterson S, Teljeur C, Cullinan J. Are there socioeconomic disparities in geographic accessibility to community first responders to out-of-hospital cardiac arrest in Ireland?. SSM Popul Health 2022;19.
- Orsi A, Watson A, Wijegoonewardene N, Botan V, Lloyd D, Dunbar N, et al. Perceptions and experiences of medical student first responders: a mixed methods study. BMC Med Educ 2022;22.
- O’Meara P, Tourle V, Rae J. Factors influencing the successful integration of ambulance volunteers and first responders into ambulance services. Health Soc Care Community 2012;20:488-96.
- Heffernan E, McSharry J, Murphy A, Barry T, Deasy C, Menzies D, et al. Community first response and out-of-hospital cardiac arrest: a qualitative study of the views and experiences of international experts. BMJ Open 2021;11.
- van Alem AP, Vrenken RH, de Vos R, Tijssen JG, Koster RW. Use of automated external defibrillator by first responders in out of hospital cardiac arrest: prospective controlled trial. BMJ 2003;327.
- Colquhoun MC, Chamberlain DA, Newcombe RG, Harris R, Harris S, Peel K, et al. A national scheme for public access defibrillation in England and Wales: early results. Resuscitation 2008;78:275-80.
- Oving I, de Graaf C, Masterson S, Koster RW, Zwinderman AH, Stieglis R, et al. ESCAPE-NET Investigators . European first responder systems and differences in return of spontaneous circulation and survival after out-of-hospital cardiac arrest: a study of registry cohorts. Lancet Reg Health Eur 2021;1.
- Zijlstra JA, Stieglis R, Riedijk F, Smeekes M, van der Worp WE, Koster RW. Local lay rescuers with AEDs, alerted by text messages, contribute to early defibrillation in a Dutch out-of-hospital cardiac arrest dispatch system. Resuscitation 2014;85:1444-9.
- Caputo ML, Muschietti S, Burkart R, Benvenuti C, Conte G, Regoli F, et al. Lay persons alerted by mobile application system initiate earlier cardio-pulmonary resuscitation: a comparison with SMS-based system notification. Resuscitation 2017;114:73-8.
- Sarkisian L, Mickley H, Schakow H, Gerke O, Jørgensen G, Larsen ML, et al. Global positioning system alerted volunteer first responders arrive before emergency medical services in more than four out of five emergency calls. Resuscitation 2020;152:170-6.
- Timmons S, Vernon-Evans A. Why do people volunteer for community first responder groups?. Emerg Med J 2013;30.
- Shi M, Xu W, Gao L, Kang Z, Ning N, Liu C, et al. Emergency volunteering willingness and participation: a cross-sectional survey of residents in northern China. BMJ Open 2018;8.
- Grossman JB, Furano K. Making the most of volunteers. Law Contemp Prob 1999;62:199-218.
- Berglund E, Olsson E, Jonsson M, Svensson L, Hollenberg J, Claesson A, et al. Wellbeing, emotional response and stress among lay responders dispatched to suspected out-of-hospital cardiac arrests. Resuscitation 2022;170:352-60.
- Roditi E, Bodas M, Jaffe E, Knobler HY, Adini B. Impact of stressful events on motivations, self-efficacy, and development of post-traumatic symptoms among youth volunteers in emergency medical services. Int J Environ Res Public Health 2019;16.
- Davies E, Maybury B, Colquhoun M, Whitfield R, Rossetti T, Vetter N. Public access defibrillation: psychological consequences in responders. Resuscitation 2008;77:201-6.
- Skerratt S. Enhancing the analysis of rural community resilience: evidence from community land ownership. J Rural Stud 2013;31:36-4.
- Wyche KF, Pfefferbaum RL, Pfefferbaum B, Norris FH, Wisnieski D, Younger H. Exploring community resilience in workforce communities of first responders serving Katrina survivors. Am J Orthopsychiatry 2011;81:18-30.
- Lopez-Cabrera R, Arenas A, Medina FJ, Euwema M, Munduate L. Inside ‘Pandora’s Box’ of solidarity: conflicts between paid staff and volunteers in the non-profit sector. Front Psychol 2020;11.
- von Schnurbein G, Hollenstein E, Arnold N, Liberatore F. Together yet apart: remedies for tensions between volunteers and health care professionals in inter-professional collaboration. Voluntas 2023;34:1-13.
- Brudney JL. The effective use of volunteers: best practices for the public sector. Law Contemp Prob 1999;62:219-55.
- Heffernan E, Keegan D, Mc Sharry J, Barry T, Tugwell P, Murphy AW, et al. Community first response and out-of-hospital cardiac arrest: identifying priorities for data collection, analysis, and use via the nominal group technique. Resusc Plus 2022;9.
- Welsh Ambulance Services NHS Trust . Welsh Ambulance Service Introduces Fast-Acting New Pain Relief 2023. https://ambulance.nhs.wales/news/nhs/2023/welsh-ambulance-service-introduces-fast-acting-new-pain-relief/ (accessed 3 July 2023).
- Kobusingye OC, Hyder AA, Bishai D, Hicks ER, Mock C, Joshipura M. Emergency medical systems in low- and middle-income countries: recommendations for action. Bull World Health Organ 2005;83:626-31.
- Wilson PM, Boaden R, Harvey G. Plans to accelerate innovation in health systems are less than IDEAL. BMJ Qual Saf 2016;25:572-6.
- Wilson J, Musick M. The effects of volunteering on the volunteer. Law Contemp Prob 1999;62:141-68.
- Thoits PA, Hewitt LN. Volunteer work and well-being. J Health Soc Behav 2001;42:115-31.
- Andelius L, Oving I, Folke F, de Graaf C, Stieglis R, Kjoelbye JS, et al. ESCAPE-NET investigators . Management of first responder programmes for out-of-hospital cardiac arrest during the COVID-19 pandemic in Europe. Resusc Plus 2021;5.
Appendix 1 Supplementary figure and tables from cross-sectional study
FIGURE 16.
Flow chart showing data inclusion from each ambulance service.
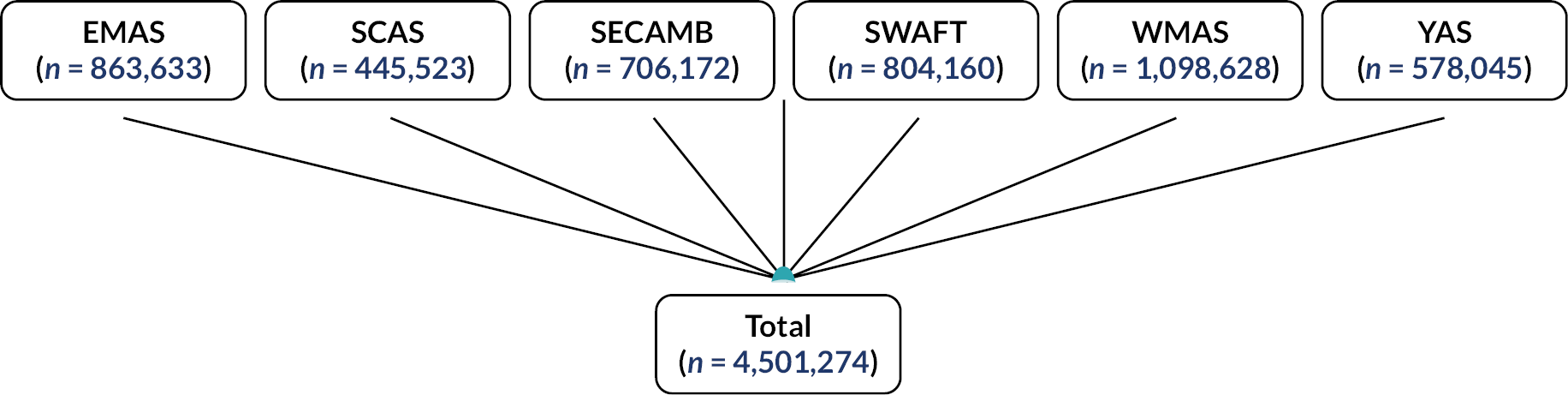
| Variable | Number | Percentage |
|---|---|---|
| Call category | 175,061 | 3.9 |
| Condition category | 211,735 | 4.7 |
| Conveyance | 553,895 | 12.3 |
| Deprivation | 0 | 0 |
| Gender | 360,451 | 8.0 |
| Age group | 495,597 | 11.0 |
| Ethnicity | 2,612,555 | 58.0 |
| Arrival time | 1,105,471 | 24.6 |
| Ambulance service | First resource | Rural, n (%) | Urban, n (%) |
|---|---|---|---|
| EMAS | CFR | 6768 (4.4) | 13,071 (2.3) |
| Ambulance staff | 146,873 (95.6) | 544,587 (97.7) | |
| SCAS | CFR | 3699 (4.9) | 9310 (2.5) |
| Ambulance staff | 71,612 (95.1) | 359,087 (97.5) | |
| SECAMB | CFR | 3323 (2.7) | 7997 (1.4) |
| Ambulance staff | 118,277 (97.3) | 576,549 (98.6) | |
| SWASFT | CFR | 12,101 (6.2) | 14,401 (2.7) |
| Ambulance staff | 183,256 (93.8) | 561,999 (97.3) | |
| WMAS | CFR | 2692 (2.1) | 4077 (0.4) |
| Ambulance staff | 124,492 (97.9) | 959,037 (99.6) | |
| YAS | CFR | 1258 (2.0) | 5351 (1.1) |
| Ambulance staff | 61,980 (98.0) | 502,444 (98.9) |
| Cardiorespiratory | Gastrointestinal | Allergies/ENT/Infections | Injury/trauma | Neurological/endocrine | Obstetric/gynaecological | Psychosocial/palliative |
|---|---|---|---|---|---|---|
| Breathing problems (25.8%) | Abdominal pain (20.3%) | Allergic reaction (27.8%) | Back injury (19.6%) | Unconscious fainting (21.2%) | Maternity (18.5%) | Psychiatric problem (5.4%) |
| Chest pain (20.9%) | Acute abdomen (12.4%) | Sepsis (19.8%) | Fall injury (14.8%) | Convulsions/fitting (17.3%) | Pregnancy/miscarriage (14.7%) | Overdose/poisoning (5.3%) |
| Stroke (5.8%) | Vomiting (6.1%) | Febrile illness (10.2%) | Fracture (7.4%) | Hypo- or hyperglycaemia (11.1%) | Labour and childbirth (6.4%) | Alcohol intoxication/alcohol related (4.8%) |
| Chest infection (4.6%) | Diarrhoea (4.6%) | Epistaxis (4.2%) | Limb injury (5.8%) | Collapse (3.8%) | Labour (non-delivery) (6.0%) | Anxiety/depression (3.1%) |
| Bleeding (4.6%) | Urinary tract infection (UTI) (2.08%) | Rash (2.0%) | Head/neck injury (2.2%) | Dizziness/vertigo (2.2%) | Vaginal bleeding (4.9%) | Panic attack (2.6%) |
| Ambulance service | First resource | Category 1 | Category 2 | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| EMAS | CFR | 2523 | 12.7* | 15,724 | 79.3* |
| Ambulance staff | 77,544 | 9.7 | 482,077 | 60.3 | |
| SCAS | CFR | 1426 | 11.0* | 9899 | 76.0* |
| Ambulance staff | 24,737 | 6.2 | 224,847 | 56.0 | |
| SECAMB | CFR | 2294 | 20.3* | 7964 | 70.4* |
| Ambulance staff | 43,222 | 6.5 | 394,551 | 59.0 | |
| SWASFT | CFR | 4548 | 15.6* | 17,308 | 59.3 |
| Ambulance staff | 46,637 | 6.1 | 461,493 | 60.4 | |
| WMAS | CFR | 918 | 13.6* | 3375 | 50.0 |
| Ambulance staff | 67.554 | 6.5 | 535,015 | 51.7 | |
| YAS | CFR | 725 | 10.8* | 5904 | 88.3* |
| Ambulance staff | 53,341 | 9.3 | 369,157 | 64.6 | |
| Ambulance service | First resource | Cardiorespiratory | Neurological/endocrine | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| EMAS | CFR | 6761 | 34.1 | 3143 | 15.9 |
| Ambulance staff | 159,280 | 19.5 | 77,297 | 9.4 | |
| SCAS | CFR | 4372 | 34.7 | 2591 | 20.6 |
| Ambulance staff | 103,167 | 24.9 | 55,481 | 13.4 | |
| SECAMB | CFR | 1000 | 20.1 | 280 | 12.8 |
| Ambulance staff | 41,903 | 17.1 | 15,586 | 12.6 | |
| SWASFT | CFR | 9773 | 35.3 | 3436 | 12.4 |
| Ambulance staff | 211,473 | 29.0 | 55,126 | 7.6 | |
| WMAS | CFR | 1480 | 21.7 | 1301 | 19.1 |
| Ambulance staff | 188,693 | 17.3 | 137,025 | 12.6 | |
| YAS | CFR | 1843 | 28.1 | 459 | 7.0 |
| Ambulance staff | 103,017 | 18.5 | 29,915 | 5.4 | |
List of abbreviations
- ABC
- ‘actor’, ‘behaviour change’ and ‘causal pathway’
- AED
- automated external defibrillator
- AMPDS
- Advanced Medical Priority Dispatch System
- BSV
- bariatric service vehicle
- CETO
- community and engagement training officer
- CFR
- Community First Responder
- CI
- confidence interval
- CPR
- cardiopulmonary resuscitation
- EMAS
- East Midlands Ambulance Service
- EMS
- Emergency Medical Services
- EOC
- emergency operations centre
- ePRF
- electronic patient report form
- EV
- emergency vehicle
- FRP
- falls response programme
- GP
- general practice
- HAPPI
- healthier ageing patient and public involvement
- ICER
- incremental cost-effectiveness ratio
- ICT
- information and communication technology
- IMD
- Index of Multiple Deprivation
- JISC
- joint information systems committee
- LIVES
- Lincolnshire Integrated Voluntary Emergency Service
- mNGT
- modified nominal group technique
- NARSG
- National Ambulance Research Steering Group
- NGT
- nominal group technique
- NIHR
- National Institute for Health and Care Research
- NSPL
- National Statistics Postcode Lookup
- OHCA
- out-of-hospital cardiac arrest
- ONS
- Office for National Statistics
- OR
- odds ratio
- PAD
- public access defibrillation
- PPE
- personal protective equipment
- PPI
- patient and public involvement
- PRF
- patient record form
- RCT
- randomised controlled trial
- ROSC
- return of spontaneous circulation
- SCAC
- South Central Ambulance Charity
- SCAS
- South Central Ambulance Service
- SECAmb
- South East Coast Ambulance
- SWASFT
- South Western Ambulance Service Foundation Trust
- WMAS
- West Midlands Ambulance Service
- YAS
- Yorkshire Ambulance Service
Notes
-
Community First Responder Study Human & Financial Resources Questionnaire for Ambulance Trusts
-
Evaluation of the Falls Response Partnership’s community first responder response to adults who have fallen in Lincolnshire
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/JYRT8674).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
