Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number 17/42/42. The contractual start date was in February 2019. The draft manuscript began editorial review in March 2022 and was accepted for publication in May 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Adams et al. This work was produced by Adams et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Adams et al.
Chapter 1 Introduction
Background: scientific background and explanation of rationale
Burden and impact of staff sickness absenteeism and presenteeism on the National Health Service and patients
The NHS in the UK is one of the top 10 employers in the world, with 1.3 million employees. 1 However, sickness absenteeism costs the NHS approximately £2.4 billion per year2 (£1 in every £40 of total NHS budget), with an annual average of just under 10 absence days per employee. 3 In 2016, this was 46% higher than other UK industries and 27% higher than the average in the public sector4,5 and is associated with worse patient outcomes, such as increased inpatient mortality, hospital acquired infections, longer bed stays, reduced completion of patient-care tasks and reduced patient satisfaction. 6–10 There is a well-established association between mental ill health among staff, reduced patient satisfaction and increased medication errors. 7–10 Since the start of the COVID-19 pandemic, rates of absenteeism have risen and reports of stress and mental ill health have increased. 1,11,12
A greater potential cost is that of presenteeism (attending work while unwell),13–15 with 44% of NHS staff in 2020 reporting pressure to attend work when feeling unwell,11 with associated reduction in ability to work effectively and negative impact on patients. 8
With greater than ever pressure within the NHS, interventions to tackle the main determinants of work productivity (absenteeism and presenteeism) are increasingly important for staff well-being, improving patient care and for the economy. Estimates suggest that reducing staff absence levels by a third could save 3.4 million working days a year. 16
The health of National Health Service staff
Among NHS hospital staff overall, 44% reported feeling unwell as a result of work-related stress and 29% experienced musculoskeletal problems (MSK) as a result of work activities in the last 12 months. 11 Local surveys indicate that nearly half of hospital staff are overweight or obese, staff generally have low levels of exercise and 10–12% smoke (unpublished local NHS data). 17,18 While the prevalence of cardiovascular disease (CVD) is up to five times greater amongst those over 50 years old, MSK and mental health problems are common across all age groups of NHS staff (unpublished local NHS data). 19
Determinants of absenteeism and presenteeism among National Health Service staff
The main cause of sickness absenteeism in the NHS is mental ill health at 25.4% of all recorded days lost in 2019, nearly double that of 201020 and peaking at 32.4% during the first wave of the COVID-19 pandemic. 21 This is followed by MSK complaints affecting 16%. 22 Poor lifestyle (smoking, lack of physical activity) and overweight/obesity are also important independent determinants of absenteeism and presenteeism,23–27 with CVD being up to five times greater amongst staff over 50 years old (unpublished local NHS data). 19 Absenteeism varies by occupational group, being highest in the lowest-paid (healthcare assistants), professions allied to medicine and infrastructure support staff,28 those working unsocial hours,4,16 and among older workers (unpublished local NHS data). 29 Presenteeism rates follow similar patterns. 30
National Health Service health and well-being policy
In response to the high levels of staff ill health and sickness absenteeism, NHS England created a ‘Healthy Workforce Programme’, supported by the Royal College of Physicians,31 with a £450 million financial incentive for Trusts to improve staff health and well-being and thereby patient care. 32 Key actions included making the NHS CVD health check (for those aged 40–74 years without pre-existing diabetes or CVD)33 more accessible for staff in the workplace and improving access to physiotherapy, mental health, weight management and smoking cessation services. 34 In most hospitals, occupational health services, which are often outsourced, do not have a preventive or well-being role and therefore new initiatives are required. Since then, mainly in response to staff need during the pandemic, NHS hospitals have implemented a variety of health and well-being initiatives, although most are focused on mental well-being, are likely to be short term and have yet to be thoroughly evaluated. 35,36
Recommended interventions for identification and management of mental health, musculoskeletal health and cardiovascular disease in the general population
Mental health complaints
Screening for anxiety/depression improves outcomes when followed by clinical assessment and treatment for screen positives. 37 National Institute for Health and Care Excellence (NICE) recommends using validated screening tools for common mental disorders, for example, Patient Health Questionnaire-9 items (PHQ-9),38 Generalised Anxiety Disorder-7 (GAD-7)39 questionnaire to assess, stratify and guide effective evidence-based stepped care,40 according to three categories of severity.
Musculoskeletal complaints
National Institute for Health and Care Excellence recommends using risk tools for assessing MSK pain (e.g. STarT Back41) to guide treatment. 42–45 STarT Back is a simple prognostic questionnaire that helps clinicians identify modifiable risk factors (biomedical, psychological and social) for back pain disability. The resulting score stratifies patients into three risk categories which are matched to a treatment package [self-management, physiotherapy and physiotherapy with cognitive–behavioural therapy (CBT)]. This approach has been shown to reduce disability and to be cost-effective. A similar tool has been developed for other MSK disorders (STarT MSK). 46 For NHS staff with MSK disorders, NHS England recommends rapid access to rehabilitation. 47
Cardiovascular risk
Public Health England recommends a national risk assessment and management programme for 40- to 74-year-olds without pre-existing diabetes or CVD (the NHS health check). 48 The NHS health check includes CVD risk stratification (e.g. using the QRISK2 tool), with behavioural change support and treatment (e.g. with statins or antihypertensives) of newly identified risk factors, with appropriate management based on relevant NICE guidance. Evaluations of the NHS health check suggests that the programme has benefits in identification and management of those at high risk of CVD, and in impacting on risk factors, such as reduction in body mass index (BMI). 49 However, uptake and proper implementation of health checks are relatively low, particularly among those of working age,33,50 and their long-term effectiveness is controversial. 51
Workplace interventions to address absenteeism and presenteeism
There are several systematic reviews and many individual studies which evaluate the effectiveness of workplace health promotion or return-to-work programmes,24,52–54 but few are conducted among healthcare staff, and they rarely consider impact on absenteeism or presenteeism, or include a control group. Most interventions for healthcare staff are aimed at promoting mental health and well-being. 55
Of most relevance, an evaluation of health screening specifically targeted to 635 low-paid government workers aged 40 and over using the NHS health check with referral to appropriate interventions56 showed improvement in most markers of cardiovascular health after 9 months, although attendance rates were relatively low (20%).
In another feasibility study, 253 hospital employees attended a workplace CVD health check in three NHS hospital sites, received tailored advice, signposting to health-related information, relevant free services and advice to visit their general practitioner (GP) where appropriate. 52 Forty-seven per cent were overweight/obese and many reported existing health problems. Participants perceived the clinic to be convenient, informative and useful for raising awareness of health issues. After 5 weeks, they reported dietary changes (41%); increase in physical activity (30%); smokers reported quitting/cutting down (44%) and those exceeding alcohol limits reported cutting consumption (48%). Fifty-three per cent of those advised to visit their GP complied.
No studies have, however, evaluated the cost effectiveness of interventions targeted at screening for and early management of the main causes of sickness absenteeism in healthcare settings – essential evidence before Trusts will invest limited healthcare resources. The evidence available reinforces the need to focus on high-risk groups, provide interventions of sufficient intensity and optimise attendance to maximise the chances of interventions being effective. 57,58 The most effective model is likely to be a combination of health screening and health/wellness programmes with targeted interventions. 59
Based on learning from a recent pilot staff health screening clinic (SHSC) set up at Queen Elizabeth Hospital Birmingham (QEHB), we have developed a health screening service, including pathways for direct invitation, assessment for MSK, mental health and CVD problems (the three major causes of staff absenteeism) and onward referral, for hospital employees.
We present the results of a pilot randomised controlled trial (RCT) to assess the feasibility of conducting a full RCT to evaluate the effectiveness and cost effectiveness of this service in reducing absenteeism and presenteeism within NHS hospitals.
Chapter 2 Methods
Aims and objectives
The aim of this pilot trial was to assess the feasibility of a definitive RCT evaluating the clinical and cost effectiveness of a health screening clinic compared to usual care, in reducing sickness absenteeism and presenteeism amongst NHS staff.
The key objectives were to:
-
describe recruitment rates
-
describe participant characteristics and assess generalisability compared to the hospital workforce
-
describe intervention screening assessment results
-
describe recommended referrals and attendance at those referrals
-
assess the feasibility of measuring the outcomes relating to the definitive trial, and obtain an estimate of the standard deviation (SD) of the proposed primary outcomes for a full RCT
-
assess levels of contamination between intervention and usual care arms to inform RCT design (individual vs. cluster RCT)
-
describe and explain the fidelity to the intervention and evaluate the barriers and enablers to participation
-
describe the views, experiences and satisfaction of participants and those delivering the health checks
-
explore feasibility of the trial/service in other NHS and non-NHS settings
-
quantify the costs of undertaking the screening service and its consequences.
Trial design
A multicentre, two-arm, parallel group, open-label, 1 : 1 individually randomised pilot RCT of a complex intervention comparing a SHSC with usual care.
Participants
Setting
The trial was conducted in three large urban hospitals and one rural district general hospital within three NHS Hospital Trusts in the West Midlands (see Table 1), allowing the testing of practical aspects in a range of sites.
| Hospital | Staff | Setting |
|---|---|---|
| QEHB (University Hospitals Birmingham NHS Foundation Trust) | 9000 | The largest single-site hospital in the country. Regional centre for cancer, largest solid organ transplantation programme in Europe, a regional Neuroscience and Major Trauma Centre. Ethnically diverse staff recruited locally |
| Heartlands Hospital (University Hospitals Birmingham NHS Foundation Trust) | 11,000 | Includes four secondary care city-based hospital sites (Heartlands, Good Hope, Solihull and the Chest Clinic); one of the top five employers in the West Midlands |
| Birmingham Children’s Hospital (Birmingham Women’s and Children’s NHS Foundation Trust) | 6000 | Secondary and Tertiary care hospital serving 384,000 women and children annually |
| Hereford Hospital (Wye Valley NHS Trust) | 3000 | One of the smallest rural District General Hospitals in England, serving a population of 180,000 |
Eligibility criteria
All employees in the participating hospitals who were able to provide informed consent were eligible to participate except those who had previously attended a pilot health screening clinic at QEHB or who were currently taking part in another drug trial (with the exception of COVID-related drugs/vaccines) or health and well-being trial.
Recruitment
Recruitment occurred in several phases, aiming to reflect the workforce characteristics of each hospital. Anonymous human resources (HR) data providing sociodemographic and occupational characteristics were obtained to choose wards which reflected the characteristics of the whole hospital population. Posters advertising the trial were displayed in departments/wards for a minimum of 2 weeks (or more if local arrangements required) before invitations were sent out, during which time staff could request not to receive an invitation. In order to be accessible to the full workforce, participants were informed of the trial through staff meetings, noticeboards and ward champions, and invited through multiple approaches including e-mail and personal invitation. Reminder letters were sent to non-responders after 2 weeks, with up to two further reminders if necessary. Local staff were engaged to raise trial awareness and arrange cover to allow attendance at the health screening clinic.
Consent
Potential participants joined the trial via a weblink to a custom-designed electronic trial data collection platform hosted by the Birmingham Clinical Trials Unit (BCTU). Those with limited access to the internet could complete a paper-based expression of interest through the internal mail system, then attend the clinic to complete consent and other forms online. Consent was obtained through the trial platform, via participants’ own electronic devices or using tablets provided to the health screening clinic staff, and ongoing consent was confirmed at each follow-up point. The participant information sheet (was provided with the initial invitation and was also available on the trial platform). Participants could contact the research team by telephone or request contact from the research team via the trial platform to ask any questions.
Randomisation and blinding
On completion of the baseline questionnaire, clinic staff received an alert to check eligibility criteria and consent, and participants were then randomised to intervention or usual care using an integrated randomisation module on the trial platform. Randomisation was at the level of the individual in a 1 : 1 ratio, using a minimisation algorithm (with random element) to ensure balance on the following variables:
-
age (< 40, ≥ 40 years)
-
sex (male, female, prefer not to say)
-
job category (categories as self-reported)
-
nightshift work (yes/no)
-
hospital.
Given the nature of the intervention, blinding of participants and nurses conducting the screening clinic was not possible.
Interventions
Intervention arm
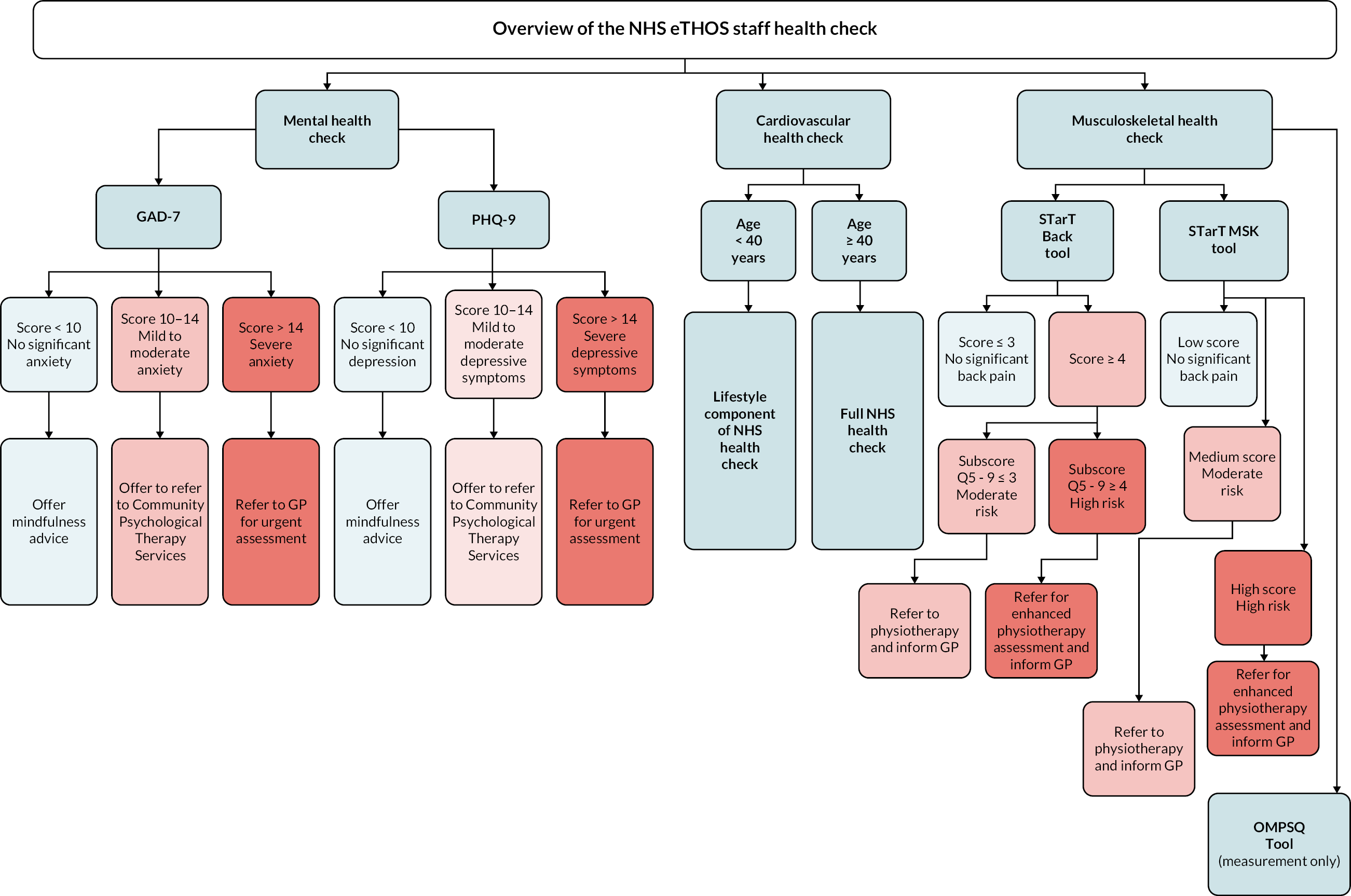
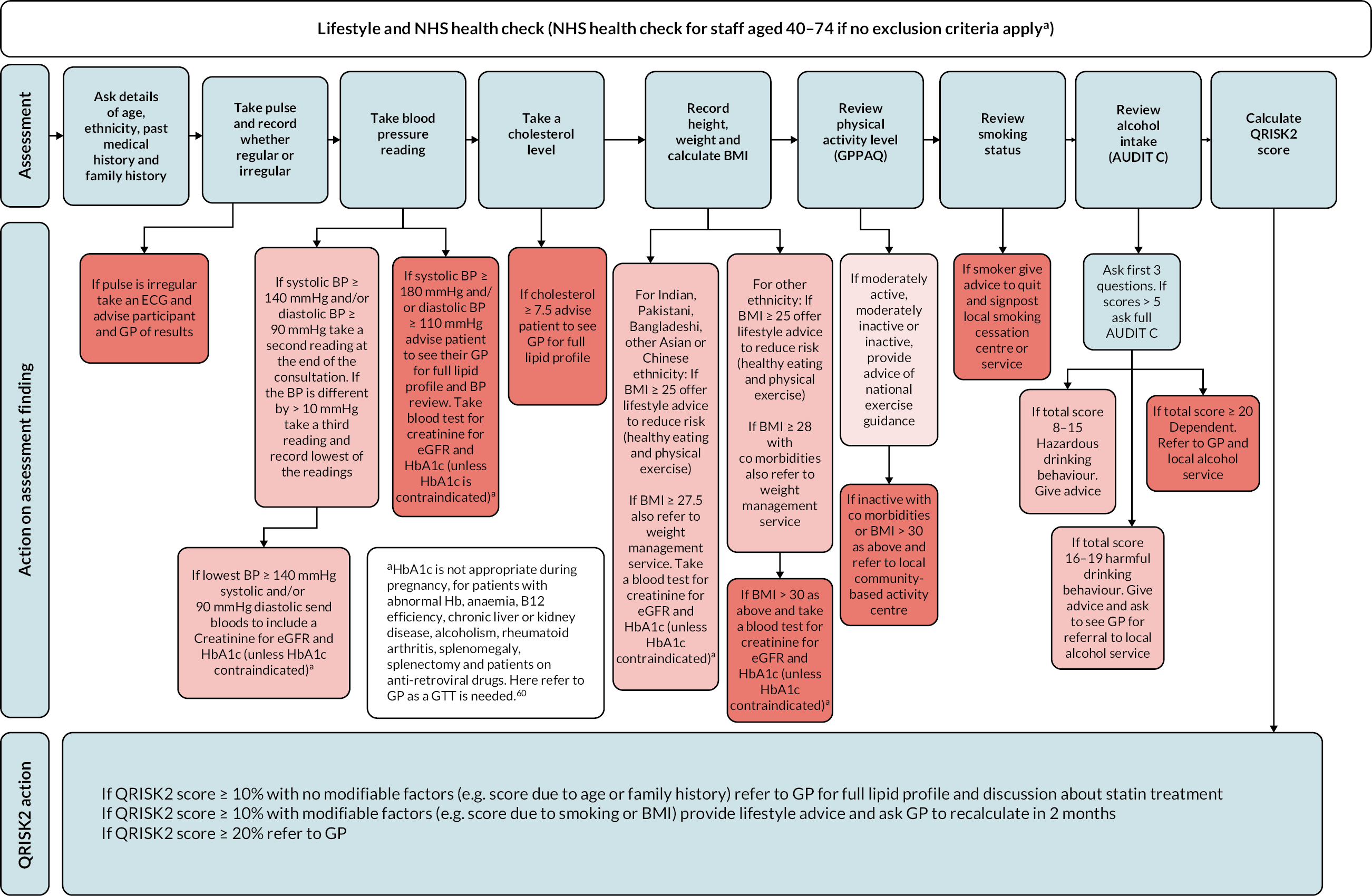
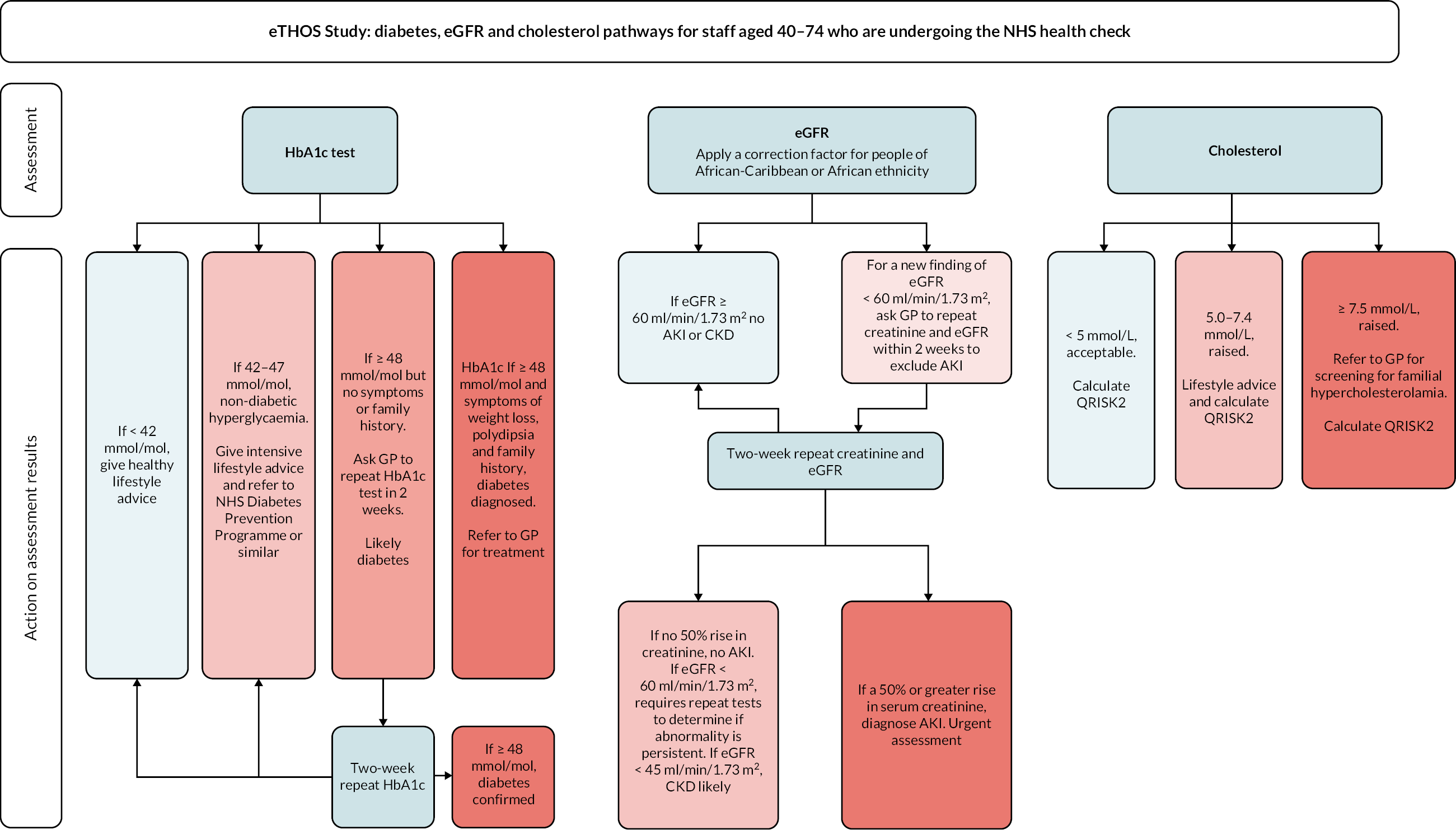
Participants received an invitation to a SHSC, available during or outside work time (generally 7 a.m.–5 p.m., Monday–Friday), administered by trained clinic nurses [hereafter known as enhancing the Health of NHS Staff (eTHOS) nurses]. A maximum of three attempts was made to contact participants to arrange an appointment. The screening appointment consisted of two stages: (1) screening assessment for three components: mental health, MSK health and finally cardiovascular health, followed by (2) advice and/or referral, according to level of risk, to appropriate services for management according to NHS/NICE recommendations (see Figure 2). The screening assessment was delivered by nurses, with consultant physician oversight at each centre, supported by a standardised protocol and prompts from the electronic data platform. All data from participants were entered directly onto the electronic platform in a paperless system.
FIGURE 1.
Overview of staff health screening intervention. From National Institute for Health and Care Excellence 2016. 60
The eTHOS nurses explained the screening scores to participants and, where applicable, any recommended actions. Local pathways were used; these included self-referral to the staff physiotherapy service, local mental health support (e.g. healthy minds, Frontline19), lifestyle changes as directed in appropriate leaflets and websites, advice to visit their GP, recommendations to the GP that a direct referral be made for the participant and/or a request that the GP arrange a follow-up appointment with the participant. Where there were concerns regarding safety, the eTHOS nurse would immediately inform the local site principal investigator (PI) who would then contact the GP.
Participants reporting relevant diagnosed conditions currently being treated did not receive the referral element of that component. A results letter detailing findings and recommendations was sent to participants and their GPs for appropriate action.
Mental health check
Participants self-completed the GAD-739,40 (anxiety) and PHQ-938,40 (depression) screening questionnaires to assess mental health and were categorised into three levels of risk (see Figure 1). Participants without significant anxiety/depressive symptoms were offered online mindfulness advice. 61 Those who were moderately affected were advised to seek support from local counselling services such as Birmingham Healthy Minds,62 and those severely affected were referred to their GP for immediate treatment.
Musculoskeletal health check
The Keele STarT Back Screening Tool41 was self-completed to categorise risk of future disability of low back pain into three levels (low, moderate and high risk). The STarT MSK tool (also three levels) was used for non-back complaints,46 and the Orebro musculoskeletal pain screening questionnaire (OMPSQ) score63 was also calculated to enable comparison with international studies. Based on a model of stratified care, those with moderate or high scores on the STarT Back or STarT MSK tools were referred to physiotherapy teams according to NICE guidance,42–45 either directly or via their GP. Those with high scores were recommended to receive enhanced physiotherapy including CBT to address associated psychological problems. In practice, in part, due to pressures of the COVID-19 pandemic, direct referrals and CBT were largely unavailable.
Cardiovascular health check
Participants aged 40 years and over received the NHS health check, delivered face to face by the eTHOS nurses. 48 This included lifestyle checks with self-completed questionnaires and clinical measures: BMI, exercise level [general practice physical activity questionnaire (GPPAQ) questionnaire],64 smoking status, alcohol intake (AUDIT C questionnaire);65 QRISK2 score66 and clinical measures [pulse, blood pressure, electrocardiogram (ECG), cholesterol, glycated haemoglobin (HbA1c), estimated glomerular filtration rate (eGFR) and creatinine tests if appropriate]. Actions included referral to GP, weight management, smoking cessation and alcohol reduction services, as well as brief advice on exercise and diet according to UK recommendations (see Figure 1). The dementia awareness component for those over 65 years was excluded as there were known to be few employees in this category. Participants aged under 40 years were assessed for lifestyle components of the NHS health check only: BMI, exercise level, smoking status and alcohol intake, with the same advice applied and referrals to appropriate services. Clinical measures and associated blood samples were not collected from participants aged under 40 years.
Occupational health
All participants with an identified health condition were also asked whether they perceived that their condition was affected by/or affected their ability to work and what adjustments at work might improve their workability. If affected, they were offered an additional optional referral to occupational health.
Usual care
Participants randomised to receive usual care did not attend the health screening clinic. Usual care consisted of standard access to medical services for management of any presenting condition (either through occupational health or their GP) and any health promotion/counselling initiatives provided for staff during the pandemic. They remained eligible for the NHS health check via their GP as usual if they were aged 40 years or older.
Outcomes
This pilot trial was originally planned to have a 52-week follow-up to fully test the processes for a definitive trial but was reduced to 26 weeks due to the pandemic-related delays.
Primary outcomes and stop/go criteria
Three coprimary outcomes were originally planned to inform criteria to progress to the definitive trial:
-
Recruitment (consented) as a proportion of those invited.
-
Referral to any recommended services as a result of the three screening components (usually GP, local physiotherapy/community psychological services) – intervention arm only.
-
Attendance at any recommended services at 26 weeks (self-report) – intervention arm only.
We defined ‘referral’ as anyone who was eligible for a referral, that is, they recorded a suitable risk value and were not already being treated for that condition.
Due to additional pandemic-related delays, following discussions with the funder, it was agreed not to extend the duration of the trial in order to complete follow-up of all participants to 6 months. This meant that only a small number of participants reached the 26-week follow-up assessment, leaving limited data available to reliably assess the third coprimary outcome on attendance. After discussion with the Trial Oversight Committee (TOC), it was agreed that acceptance of the referral (signifying intention) which was collected during the screening assessment, should be used as a proxy for attendance.
The decision to continue to a full trial was informed by progression criteria using a traffic light system as guidance (see Table 2), with flexibility built in to allow for uncertainty in cost effectiveness despite either low participation, referral or attendance rates. The three coprimary outcomes formed stop/go criteria when considered together. If any of these values fell into the ‘amber’ zone, then the trial would require modifications to proceed to full trial. If all were ‘red’, then the trial would be considered unfeasible.
| Criteria | Description | Progression criteria | ||
|---|---|---|---|---|
| Green (go), % | Amber (pause), % | Red (stop), % | ||
| Recruitmenta | % of invited employees consenting to take part | > 25 | 15–25 | < 15 |
| Referred to a serviceb (defined as eligible for a referral) | % of participants randomised to intervention arm referred to specified services | > 30 | 10–30 | < 10 |
| Attendance at referralsc (defined as accepting a referral) | % of referrals which resulted in self-reported attendance at the service at least once. Measured at 26 weeksd | > 50 | 30–50 | < 30 |
| ACTION | If ALL criteria are GREEN, proceed to full trial with protocol unchanged | If ANY of these criteria are AMBER, adapt protocol appropriately using information from the process evaluation before proceeding to full trial | If ALL of these criteria are RED, consider whether current protocol is not feasible. If ONE OR TWO of these criteria are RED, consider whether adaptations are needed | |
Secondary outcomes were collected to inform the design of the definitive RCT and any modifications required:
Secondary outcomes
-
Comparison of baseline characteristics of included participants and hospital population for assessing generalisability.
-
Description of the results of the intervention screening assessments.
-
Number and type of referrals to recommended services (intervention arm only).
-
Attendance at each individual recommended service (acceptance of referral during screening assessment, self-report at 26 weeks; intervention arm only).
-
Lifestyle relevant to screening intervention advice and referrals (self-report at 26 weeks compared with baseline) including Physical Activity Index measuring exercise levels (GPPAQ),64 smoking status, weight (kg).
-
Acceptability of intervention to participants and health screening clinic staff (interviews within the Process Evaluation).
-
Feasibility of trial processes (completeness of relevant data items, interviews).
-
Indication of contamination (comparing pre/post data for health behaviours and health care/other service utilisation in control arm).
Outcomes related to the definitive trial
-
Sickness absenteeism at 26 weeks with reasons, measured by days and spells:
-
self-report absolute absenteeism, relative absenteeism and relative hours of work – for last 7 days and last 28 days [World Health Organization Health and Work Performance Questionnaire (WHO-HPQ)]69
-
self-report absenteeism using 6-month recall period
-
employee records of absenteeism, which will be the primary outcome of the definitive trial. Routinely collected data from the NHS Electronic Staff Record Programme, linked to employee ID.
-
-
Presenteeism at 26 weeks [self-report absolute presenteeism and relative presenteeism for last 28 days (WHO-HPQ)]. 69
-
Attendance at occupational health service at 26 weeks (self-report).
-
Healthcare utilisation at 26 weeks (self-report) including GP consultations and hospital admissions.
-
EuroQol-5 Dimensions, five-level version (EQ-5D-5L) index value measuring health-related quality of life (HRQoL) (EuroQol EQ-5D 5-level)70 at 26 weeks.
-
Resource use and costs collected by self-report questionnaire to participants on health service utilisation and information from the screening assessment regarding duration and resources used.
Data collection and management
Data were collected at several points during the trial: eligibility screening, baseline, during the screening clinic and at the 26-week follow-up (see Table 3). Study data were entered into a custom-designed REDCap (Research Electronic Data Capture) database hosted by the University of Birmingham, either directly by participants or by clinic staff. 71,72
| Visit | Eligibility screening, consent and randomisation | Baseline | Intervention screening visit | 26-week follow-up data collection (± 4 weeks) |
|---|---|---|---|---|
| Trial registration | X | |||
| Consent to eligibility screening | X | |||
| Eligibility screening | X | |||
| Participant information and contact details | X | |||
| Valid informed consent | X | |||
| Staff payroll number | X | |||
| NHS number (optional) | X | |||
| Demographics (DOB, gender, education, marital status) | x | |||
| Smoking status | x | x | ||
| Exercise level (GPPAQ questionnaire) | x | x | x | |
| Ethnicity | x | |||
| Diagnosed medical conditions | x | |||
| Current medications | x | |||
| Health status (EQ-5D questionnaire) | x | x | ||
| Height | x | |||
| Weight | x | x | ||
| Health service utilisation | x | x | ||
| Current employment | x | X | ||
| Absenteeism and presenteeism (WHO-HPQ questionnaire) | x | x | ||
| Occupational Health Resource Utilisation | x | x | ||
| Randomisation | X | |||
| Health screening (intervention group only) | ||||
| MSK health (if applicable) | ||||
| STarT Back screening tool (participant completion) | x | |||
| STarT Back screening tool (review) | x | |||
| STarT MSK screening tool (participant completion) | x | |||
| STarT MSK screening tool (review) | x | |||
| OMPSQ tool (participant completion) | x | |||
| OMPSQ tool (review) | x | |||
| Impact on work questions: MSK health | x | |||
| Mental health (if applicable) | ||||
| GAD-7 questionnaire (participant completion) | x | |||
| GAD-7 questionnaire (review) | x | |||
| PHQ-9 questionnaire (participant completion) | x | |||
| Impact on work questions: Mental health | x | |||
| Cardiovascular health (if applicable) | ||||
| Personal details checked from baseline (age, ethnicity) | ||||
| BMI | x | |||
| Smoking status (review from baseline questionnaire) | x | |||
| Alcohol intake (review of AUDIT C questionnaire) | x | |||
| Exercise level (review of GPPAQ questionnaire) | x | |||
| Cardiovascular risk calculator (QRISK2 score) | x | |||
| Clinical measures (if age ≥ 40 years) | ||||
| ECG | x | |||
| Pulse | x | |||
| Blood pressure | Up to three readings | |||
| Blood tests (criteria for taking blood must be met) | x | |||
| Cholesterol | x | |||
| HbA1c (if indicated as per NHS health check) | x | |||
| eGFR (if indicated as per NHS health check) (calculated using creatinine or U&Es, according to Trust policy) | x | |||
| Recommendations from the health screening clinic (intervention group only) | x | |||
| Recently diagnosed health conditions | x | |||
| Trust staff characteristics | X | |||
| Trust absenteeism rates | X | |||
| Participant absenteeism data | X | x |
Self-reported data were collected on all participants prior to randomisation. All respondents were provided with the option to provide reasons for taking/not taking part in the study. For those who consented to take part, we collected contact details and NHS number, where available (this was optional), to assess the feasibility of future linkage to routine data such as hospital admissions, GP records, other healthcare utilisation and mortality data. In the baseline questionnaire, we collected information on demography, employment details, selected diagnosed medical conditions and current medications, absenteeism (WHO-HPQ),69 presenteeism (WHO-HPQ),69 HRQoL (EQ-5D-5L),70 smoking status, height, weight, exercise levels (GPPAQ),64 receipt of NHS health check and health service utilisation. Where the baseline remained incomplete, prompts were sent after 24 hours, 2 and 7 days, and then a final reminder giving participants the option to complete it at a later date.
At 26 weeks, participants were sent a follow-up questionnaire for online completion to report attendance at any recommended services (intervention arm only), and other outcomes as detailed above. Where follow-up questionnaires remained incomplete, one reminder was sent.
Consent was obtained from trial participants to collect the following additional linked data from HR records:
-
participant age, sex, ethnicity, staff group and staff grade
-
number of hours contracted to work
-
hours worked – full-time equivalent
-
sickness absenteeism and non-sickness absences relating to COVID-19 only, for the previous 24 months and from randomisation to 26 weeks follow-up (start/end dates, duration in days, recorded reason)
-
leaving date (should participant leave employment of the Trust during trial participation).
Additional anonymised data were collected at the time of site set-up from hospital HR records, at whole hospital level and for those invited, on age, sex, ethnicity, job role and number of days absent in order to assess the generalisability of the included participants.
Key data collection forms and questionnaires are available on the National Institute for Health and Care Research (NIHR) Funding and Awards website https://fundingawards.nihr.ac.uk/award/17/42/42.
Sample size
As the eTHOS trial was a pilot study, no formal sample size calculations were undertaken. The study was not designed or powered to detect a statistically significant difference in efficacy between the two trial arms. However, preliminary sample size calculations were computed for the definitive RCT. To detect a clinically important effect size for days of sickness absence of 0.1 of a SD would require 4200 participants for an individually randomised trial.
A relatively large number of participants were required for this pilot trial in order to achieve reliable estimates of the referral and attendance rates downstream along the screening pathway and to allow assessment of the intervention in different hospitals, better precision in determining the SD of the primary outcome and provision of health economic information required to persuade other hospitals to consider investing in participating in the definitive trial. We aimed to recruit 480 participants (20 per week) in 24 weeks. The target recruitment for each site differed depending on their total staff number and capacity to deliver the intervention: 170 each for QEHB and Heartlands Hospital, 93 for Birmingham Children’s Hospital and 47 for Hereford Hospital. With this sample size, the 95% confidence interval (CI) for the proportion of staff recruited could be estimated to be 4% either side of the estimate (e.g. for a 25% recruitment rate, the 95% CI would lie between 21% and 29%).
Statistical methods
The primary comparison groups were composed of those randomised to the health screening (intervention) arm and those randomised to the usual care (control) arm. All analyses used the intention-to-treat principle, that is, all participants were analysed in the treatment group to which they were randomised, irrespective of adherence or other protocol deviation. Analyses used available data only, although the number of missing data is reported in order to inform decisions regarding data collection for the definitive trial.
Primary outcomes
Recruitment rate was calculated in two ways:
-
percentage of invited employees that consented to take part in the trial with 95% CI
-
percentage of invited employees who were randomised into the trial with 95% CIs.
Referral to a service was calculated as the percentage (with 95% CI) of participants randomised to the intervention arm that were eligible for a referral to any of the specified services (GP, physiotherapy, community psychological services). Participants were eligible for a referral if they met the score requirement for any of the mental health, MSK or cardiovascular health check assessments and were not already being treated for the referring concern.
As there were few follow-up data on self-reported attendance at referrals (because of resources restrictions forcing early trial closure), attendance at any recommended service was estimated by self-reported ‘intention’ (as agreed with the TOC). During the intervention screening, participants were given the option to accept or reject a referral to any service. The estimate of attendance at any recommended service was then determined by the proportion of participants in the intervention arm eligible for a referral that accepted that referral and presented as a percentage with 95% CI. Data from the 26-week follow-up questionnaires are provided in Appendix 2.
Secondary outcomes
Analyses were mainly descriptive, summarising binary outcomes using number of responses with percentages, and continuous outcomes with means and SDs, or medians and interquartile ranges as appropriate. No statistical modelling was undertaken, and no p-values are reported. No subgroup analyses were planned for this feasibility study.
Process evaluation
A mixed-methods process evaluation explored programme reach, fidelity of screening delivery, attendance at referrals and participants’ views of the intervention to support any modifications required for the design of the definitive trial.
Quantitative data collection and analysis
Quantitative data to support the process evaluation were obtained from:
-
Recruitment and intervention data, for example, response rate; proportions of those invited consenting, being randomised and attending the screening.
-
Baseline questionnaire to assess characteristics, for example, age, ethnicity, marital status, Index of Multiple Deprivation, educational attainment and employment role of the employees recruited to study (programme reach). We also obtained hospital-level HR data to compare the characteristics of those invited and those consenting with the whole hospital populations.
-
Logs kept by the staff health screening programme recording attendance, trial database records of screening tests undertaken and duration of contacts (fidelity).
-
Healthcare issues identified at the employee screening, and referrals made to GP and other services (fidelity).
-
Self-report of attendance, and intention to attend at recommended services from intervention screening and 26-week follow-up questionnaire (uptake).
-
Brief questionnaire at eligibility stage to staff not taking up the offer of the study to ascertain reasons for not participating (reach).
Findings were presented with descriptive statistics.
Qualitative data collection and analysis
Aims
The overall aim of the qualitative process evaluation was to obtain the views of relevant stakeholders on the feasibility and acceptability of the staff health screening intervention and trial and inform any protocol adaptations needed for a full trial. This was done by interviewing: NHS staff who received the trial intervention (trial participants); the eTHOS nurses who were delivering the intervention; providers of follow-on services, for example, GPs and ‘Healthy minds’; and outside agencies who could potentially benefit from the intervention, for example, other NHS organisations who might be willing to run the trial such as ambulance services and GP groups, and non-healthcare organisations who might be interested in delivering and evaluating such a service for their setting.
Objectives
Specific objectives of the interviews were to obtain:
-
trial participants’ views and experiences:
-
views and experiences of the health screening – the concept of health screening and their experiences of it
-
views about being offered the screening and whether or not it has enabled them to access health screening that they may not otherwise have accessed
-
views and experiences of the trial processes
-
evidence of contamination amongst the usual care arm
-
acceptability of being randomised to usual care
-
barriers and facilitators to accessing/attending the screening intervention
-
views and experiences of booking the appointment
-
views and experiences of screening location
-
reasons for not attending
-
views on confidentiality in relation to the screening and the potential for findings to be used by an employer
-
views on the role of occupational health services
-
response to referral recommendations.
-
-
research staff views and experiences:
-
any contextual differences in delivery of the intervention
-
satisfaction in relation to the training received
-
acceptability of the intervention in theory/practice and experiences of delivering the intervention.
-
-
providers of follow-on services:
-
acceptability of health checks
-
experience of receiving referrals, the acceptability of the process and impact of referrals on capacity
-
availability of appropriate referral pathways.
-
-
outside agencies’ views of potential feasibility of service:
-
reflections on feasibility and acceptability of the intervention and trial and conducting it in other local contexts.
-
Participants and recruitment
Due to the COVID-19 pandemic-related delays and forced truncation of the trial, recruitment for the process evaluation took place over 4 months (July–October 2021), instead of the planned 14-month period. All trial participants were eligible for interviews if they had agreed to be approached for the qualitative study. Those eligible were invited using their preferred methods of contact and the study information sheet either e-mailed or posted to them. Where recruitment targets had not been reached, one reminder was sent to those who had not yet responded.
We contacted representatives from providers of follow-on services (e.g. GPs or physiotherapists) to whom trial participants had been referred either directly or using contacts known to the trial team.
We also contacted a range of relevant outside agencies where staff health screening might be of interest in the future. This included those providing services for the hospitals involved in the trial, non-hospital-based NHS organisations, organisations independent of the NHS concerned with health care and local large businesses completely unrelated to health care as suggested by the trial team. Study information sheets were e-mailed to potential interviewees once an appropriate person within the organisation had been identified.
Participants were given the option to complete their consent form online or on paper (and post it back to the substudy team). When completing their consent, trial participants could also agree to the qualitative team contacting their GP, declining did not exclude them from participating in the 1 : 1 interview. Participants were permitted to withdraw up to 2 weeks after the interview.
Sampling
We aimed, where possible, to recruit a purposive, maximum variation sample of trial participants with a broad representation of age, gender, ethnicity, occupation, site, shift pattern and department who had had different experiences of the trial (see Table 4). The other interview groups were chosen pragmatically. Table 4 also includes details of our target numbers for recruitment, and the time frame for recruiting from the different groups as originally planned, with reasons. Regarding site, we also aimed to match the distribution of the target recruitment numbers using the ratio outlined in Table 5.
| Participant group | Target numbers | Time frame post randomisation | Reason |
|---|---|---|---|
| Trial participants | Total = 48 | ||
| Intervention arm | |||
|
8 | After 3 months | Allow time to book appointment |
|
10 | Within 3 months | Get immediate feedback on trial experience |
|
25 | 3–4 months | Give participants chance to arrange referrals |
|
5 | 3 months | Allow time for contamination to occur |
| From start of recruitment | |||
| eTHOS nurses | 10 | 3 months | Allow time to get experience of intervention delivery |
| Providers of follow-on services | 12 | 3 months | Allow time to ascertain impact of trial on service provision |
| Outside agencies | 10 | No delay | Get immediate feedback on views relating to the trial |
| Ratio | |
|---|---|
| QEHB | 4 |
| Heartlands Hospital | 3 |
| Birmingham Children’s Hospital | 2 |
| Hereford Hospital | 1 |
However, due to COVID-19, this plan could not be adhered to and a pragmatic approach was taken instead. All eligible participants in the intervention arm were invited to participate, and invitations were sent to all controls until the target number of participants had been reached.
Data collection
Trial participants were invited to 1 : 1 focused qualitative interviews lasting approximately 30 minutes, with a choice of either zoom, telephone or face-to-face interviews if COVID-19 restrictions allowed. Other participants were offered the choice of 1 : 1 interview or a group interview with their colleagues if they preferred. Participants who did not attend screening (see Table 4) were also invited to respond to written questions via e-mail or post (see NIHR Funding and Awards website https://fundingawards.nihr.ac.uk/award/17/42/42). Semistructured topic guides (see NIHR Funding and Awards website https://fundingawards.nihr.ac.uk/award/17/42/42) guided interview conduct and were refined iteratively following initial interviews.
Data were recorded either on Zoom or an encrypted recorder and transferred via secure file transfer to an external company for transcription. Interviews were transcribed intelligent/clean verbatim and anonymised. All video files were destroyed as soon as transcription was complete.
Analysis
A thematic analysis of content was informed by the framework analytical approach. 73 Analysis and discussion included the experienced qualitative team: RR, a qualitative researcher; KJ, a GP and public health consultant with experience of mixed-methods research; KR, a nurse and epidemiologist with experience of mixed-methods research; RLA, a nurse and qualitative researcher in primary care and public health; CP, a non-clinical qualitative researcher in primary care; CH, a physiotherapist postgraduate with experience of mixed-methods research; RJ, an epidemiologist with experience of mixed-methods research; PA, a public health consultant with experience of mixed-methods research; with input from the patient and public involvement (PPI) and trial oversight and collaborator’s groups to provide multiple perspectives on the data. Data collection and analysis ran concurrently so that emergent analytical themes could inform further data collection.
As soon as two trial participants’ interviews had been completed from groups B–D (see Table 4), the data collection team (RLA, CH and CP) each independently coded the transcripts using NVivo 12 (QSR International, Warrington, UK). The team then met to discuss and compare codes and agree a combined, draft coding index. The revised draft was shared with the wider qualitative team (RR, KJ, KR, RJ, PA) and further refined. The data collection team then selected two new transcripts on which to independently test the revised index; the index was further refined and the rest of the transcripts coded.
Transcripts from the other participant groups were coded using the same index with minor modifications. RLA (a nurse) collected the data for and coded the eTHOS nurses’ transcripts. CH (a physiotherapist) collected the data for and coded the physiotherapist transcripts with support from RLA. PB (non-clinical) collected the data for and coded the transcripts from the outside agencies with support from RLA. RLA collected the data for and coded the single GP transcript.
The codes were then exported to a single framework file and the data were summarised by the participant group by RLA and CP. Emergent themes were discussed with the wider qualitative team throughout.
Health economic analysis
Data collection focused on estimating the NHS resources required for screening and resulting costs and measuring the baseline quality of life of all participants using EQ-5D-5L. A descriptive analysis was then undertaken presenting information on the average costs of screening per participant and quality-of-life outcomes.
Resource use
All participating centres were contacted to collect information on their estimated time taken for each screening clinic task, the grade of the member of staff responsible and the cost of the individual blood tests. Responses were collated and a typical duration for each task was agreed upon by the study team. The amount of staff time required for each screening task was then multiplied by the relevant unit costs obtained from standard sources74 (see Table 6). Unit costs are shown in Tables 6 and 7.
| Job title | Pay band or specialty training years | Cost per working hour (£) |
|---|---|---|
| Registrar | ST3 | 50.00 |
| Nurse specialist/team leader | Band 6 | 50.00 |
| Nurse | Band 5 | 40.00 |
| Healthcare assistant | Band 3 | 27.00 |
| Healthcare assistant | Band 2 | 25.00 |
| Blood tests | Unit cost (£) |
|---|---|
| Cholesterol | 1.35 |
| eGFR | 3.18 |
| HbA1c | 8.00 |
Costs
The cost of screening included the cost of staff time to undertake all tasks and the cost of blood tests. The total cost of blood tests per participant was weighted taking into account the proportion who received each type of blood test. Those tasks that were directly related to processing and reporting blood tests were only applied to the proportion who had at least one blood test. Costs were only applied to those who actually attended screening.
Certain tasks could be performed by healthcare professionals of different pay bands (e.g. a nurse, band 5; a nurse specialist, band 6; or a healthcare assistant, band 2 or 3). Analysis was undertaken so that the cost of screening per participant could be presented for all possible combinations, including the highest possible cost (where all tasks are carried out by the higher potential pay bands) and the lowest possible cost (for the lower pay bands).
Quality of life
The EQ-5D-5L questionnaire, containing five dimensions (mobility, self-care, usual activities, pain and discomfort, anxiety and depression), was given to participants to complete at baseline and responses were valued using the cross-walk algorithm. 75 Descriptive analysis was undertaken to calculate the mean, SD and range of the overall EQ-5D-5L score, and also the frequency of responses within each dimension.
Patient and public involvement
We recruited a participant advisory group (PAG) consisting of four to six clinical, administrative and retired NHS staff who could provide us with their insights on how the eTHOS trial might be received by NHS staff. They met on a regular basis throughout the project to provide advice. The group was led by Margaret O’Hara (PPI expert coinvestigator) who assisted in recruiting members to the PAG and facilitating communication with the eTHOS team. There was also a hospital staff member of the TOC.
The general contribution of the PAG included: version testing the eTHOS database to ensure it was user-friendly, discussions on how to keep participants engaged during delays due to the COVID-19 pandemic and reviewing study documents. They were specifically asked how the eTHOS team could encourage ethnic diversity; the PAG recommended staff networks to reach out to, including ethnic minorities, faith centres and chaplaincies. It was also suggested that managers be asked to actively encourage all staff to participate. If eTHOS proceeds to full trial, the PAG recommended that funding for dedicated community engagement should be included to encourage grass root communication.
We also recruited a stakeholder advisory group representing a wider body of professionals, for example, GPs relevant to the trial. They provided advice at regular intervals; one GP highlighted that referral for certain high-risk conditions, for example, severe depression would be most effective if by direct telephone call.
Overall, the PAG and the stakeholder group were very supportive of the trial and its potential impact on the health and well-being of the NHS staff.
Data storage and confidentiality
Participants’ personal data were held securely and treated as strictly confidential, in line with the General Data Protection Regulation 2018. Electronic records were held on a secure, password protected, web-enabled customised database hosted by BCTU or on secure, password-protected University of Birmingham servers (including audio recordings). Paper records were transferred from the participating study centres to the trial office at BCTU and kept in a locked cabinet in a locked room. Any data processed outside BCTU were anonymised. Data will be stored for at least 10 years according to the University of Birmingham policy.
Monitoring
Birmingham Clinical Trials Unit, a UK Clinical Research Collaboration (UKCRC) registered trials unit, was the co-ordinating centre and was involved in the development, design and conduct of the trial since conception. A Trial Management Group oversaw research methodology, clinical trial coordination, data management, statistical analysis, compliance with Good Clinical Practice and all regulatory requirements, in conjunction with the sponsor. A TOC (combining the function of trial steering and data management committees) with an independent chair and lay representative oversaw, advised on and monitored the trial.
Impact of COVID-19 pandemic on trial delivery and summary of changes
Although ethical approval for the trial was obtained in March 2020, it was not able to commence due to the COVID-19 pandemic. Two hospital sites granted permission to commence the trial in December 2020, but after a short period, in February 2021, recruitment was paused again due to a spike in COVID-19 cases. The trial recommenced in May 2021 in all four sites. A 6-month extension to the trial was awarded from the funder until October 2021. The original trial was planned to include a 52-week follow-up; however, due to the delays, a 26-week follow-up was then agreed instead, but only a few people reached this time point before trial closure. Changes therefore were:
-
shortened total recruitment period and reduced number of participants recruited
-
limited 26-week follow-up data (both self-report and hospital personnel data)
-
no 52-week follow-up data (including no information to inform likely effect size)
-
modification to definition of attendance at referrals
-
modification to data collection documents to include reference to COVID-19 illness and adjusted working arrangements
-
reduced number of qualitative interviews, with adjusted time frame and sampling
-
health economic analysis reduced in scope
-
modifications to trial delivery (inability to promote the trial during face-to-face staff meetings, part of the screening intervention carried out online in some cases, all qualitative interviews carried out online)
-
reduced scope for consulting PPI and stakeholder groups.
A list of protocol amendments is found in Appendix 1.
Chapter 3 Results of the trial
Recruitment, participant flow and impact of the COVID-19 pandemic
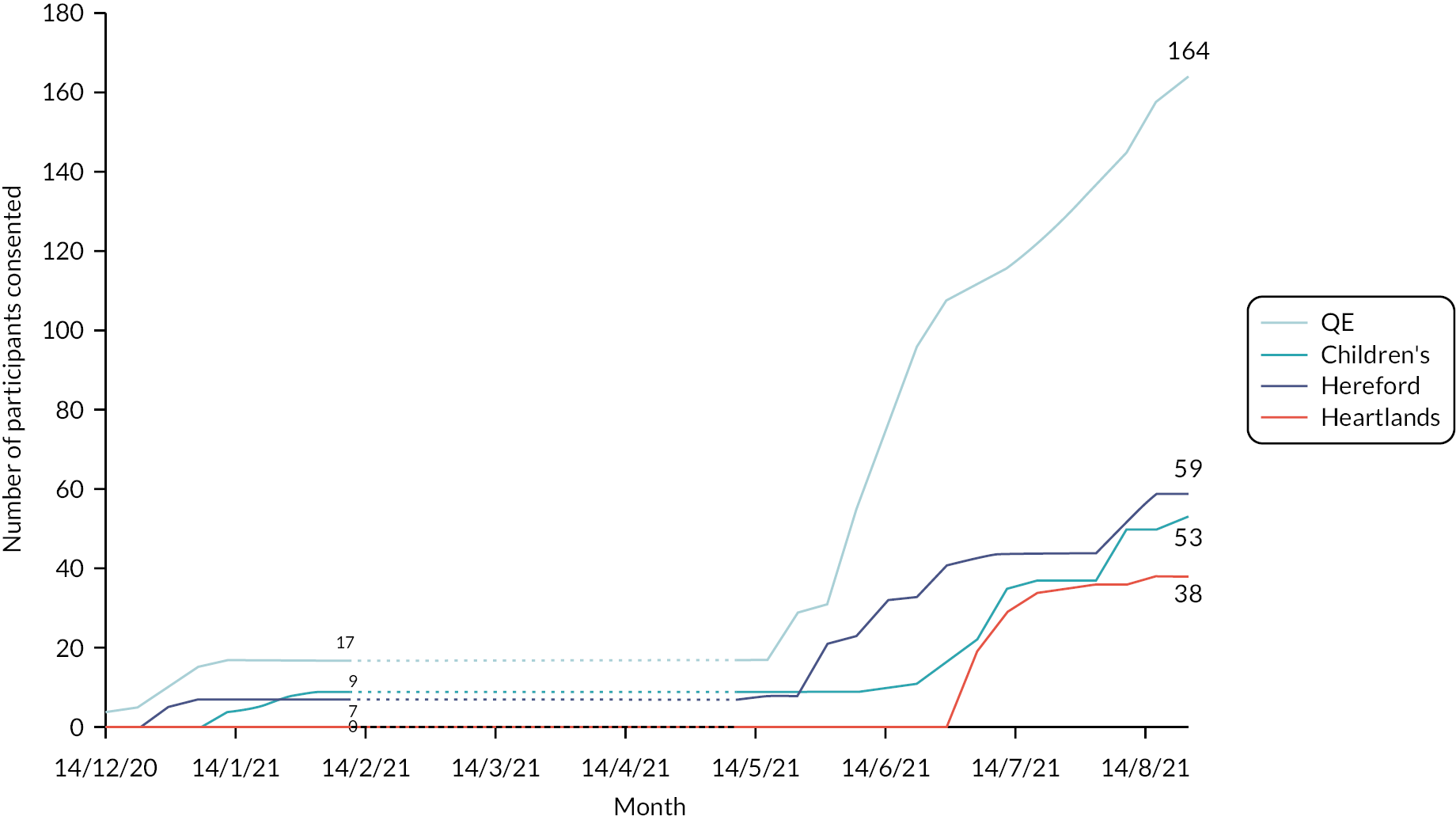
The eTHOS trial was initially due to commence recruitment in March 2020 but was delayed due to a pause in non-essential hospital research during the early phases of the COVID-19 pandemic. After a 2-week opt-out period, recruitment commenced in the first site on 16 December 2020, followed by a second and third site in early mid-January 2021. Shortly afterwards, the trial was paused to recruitment due to an increase in COVID-related hospital admissions and was then restarted on 21 May 2021 when a 6-month extension was granted. Recruitment continued until 27 August 2021 when the trial closed to recruitment to allow the data to be analysed before the end of the funding extension (see Figure 2). Therefore, recruitment and follow-up did not follow the original plans.
FIGURE 2.
Cumulative recruitment by site; dashed line indicates when the trial was paused.
Overall, 3788 from a total of 24,344 NHS staff across the four sites were invited to take part (see Figure 3). Of the 490 staff who provided a response, 422 (86.1%) expressed interest in taking part. Three hundred and nine (73.6%) stated that they were most prompted to take part because of receiving an e-mail about the study. Thirty-five (8.3%) had seen the posters about the trial, 25 (6.0%) were prompted by an invitation pack through the Trust postal system and 22 (5.2%) had heard about the trial from a colleague (see Table 8). Sixty-one staff gave reasons for not taking part in the trial. Reasons given included: not being interested in taking part in research (24.6%), too busy (21.3%), worried about confidentiality (13.1%) and felt they were unable to take time out of work (9.8%). Other reasons (44.3%) were also given, the majority of these being that they were leaving/retiring/going on maternity leave.
FIGURE 3.
Participant flow through the eTHOS pilot trial. AKI, acute kidney injury; CKD, chronic kidney disease; UHB, University Hospitals Birmingham. a26-week follow-up was only collected in those participants recruited prior to the study pausing to recruitment.

| Total (N = 490) (%) | |
|---|---|
| Are you interested in taking part in the eTHOS trial? | |
| Yes | 422 (87.4) |
| No | 61 (12.6) |
| Missing | 7 |
| If no, why are you not interested in taking part?a | |
| I’m not interested in taking part in research | 15 (24.6) |
| I’m too busy | 13 (21.3) |
| I’m worried about confidentiality | 8 (13.1) |
| I can’t take time out of work | 6 (9.8) |
| I have already had a health check | 5 (8.2) |
| I have concerns relating to the COVID-19 pandemic | 1 (1.6) |
| Other | 27 (44.3) |
| If yes, what most prompted you to take part in the eTHOS trial? | |
| I received an invitation pack through the Trust’s postal system | 25 (6.0) |
| I received an invitation by e-mail | 309 (73.6) |
| I heard about the trial from a colleague | 22 (5.2) |
| I heard about the trial at my team/department meeting | 11 (2.6) |
| My location of work has displayed posters/cards about the trial | 35 (8.3) |
| My location of work has been visited by ward champions/research team | 13 (3.1) |
| Other | 5 (1.2) |
| Missing | 2 |
Of the 353 eligible to take part, 314 consented (8.3% of those invited and 65.4% of our planned target of n = 480). Consent rates varied by site (see Table 9). In total, 236 were randomised into the study; n = 118 to the intervention screening arm and 118 to usual care. Seventy-eight participants were not randomised as they did not complete the baseline questionnaires or forms or were ineligible. Of the 118 randomised to the intervention, 101 (85.6%) attended and completed the screening clinic. Very few participants [26/236 (11.0%)] had reached the 26-week follow-up data collection time point by trial closure.
| Centre | Date opened | Trial pause date | Trial restart date | Trial end date | Weeks opena | Number invited | Number consented | Percentage consented of those invited (%) | Mean no. consented per week |
|---|---|---|---|---|---|---|---|---|---|
| QEHB | 2 December 2020 | 13 January 2021 | 25 May 2021 | 27 August 2021 | 20 | 1811 | 164 | 9.1 | 8.2 |
| Heartlands Hospital | 16 June 2021 | – | – | 27 August 2021 | 11 | 654 | 38 | 5.8 | 3.5 |
| Birmingham Children’s Hospital | 18 December 2020 | 7 February 2021 | 7 June 2021 | 27 August 2021 | 19 | 844 | 53 | 6.3 | 2.8 |
| Hereford Hospital | 8 December 2020 | 11 January 2021 | 25 May 2021 | 27 August 2021 | 19 | 479 | 59 | 12.3 | 3.1 |
| Total | 2 December 2020 | 7 February 2021 | 25 May 2021 | 27 August 2021 | 27 | 3788 | 314 | 8.3 | 11.6 |
Baseline characteristics of participants
Table 10 provides baseline characteristics for each of the treatment groups and overall. The mean (SD) age of participants was 42.5 (10.4) years and included staff between the ages of 22 and 68 years. The majority were female [188/236 (79.7%)] and of white British ethnic origin [n = 192/236 (82.1%)], and 107 (45.7%) lived in areas within the poorest two quintiles of deprivation. Seventy-six (32.2%) were allied health professionals, scientists or technical staff and 63 (26.7%) were registered nurses or midwives. Half of participants (50.4%) were recruited from the QEHB hospital, with the remainder spread across the other three sites.
| SHSC (N = 118) (%) | Control (N = 118) (%) | Total (N = 236) (%) | |
|---|---|---|---|
| Minimisation variables | |||
| Age (years) | |||
| < 40 | 45 (38.1) | 44 (37.3) | 89 (37.7) |
| ≥ 40 | 73 (61.9) | 74 (62.7) | 147 (62.3) |
| Mean (SD) | 42.4 (10.1) | 42.6 (10.7) | 42.5 (10.4) |
| Median (IQR) | 42.0 (34.0–51.0) | 43.5 (33.0–51.0) | 43.0 (34.0–51.0) |
| Range | 23.0–65.0 | 22.0–68.0 | 22.0–68.0 |
| Sex | |||
| Male | 24 (20.3) | 24 (20.3) | 48 (20.3) |
| Female | 94 (79.7) | 94 (79.7) | 188 (79.7) |
| Prefer not to say | 0 (–) | 0 (–) | 0 (–) |
| Job category | |||
| Allied health professionals/healthcare scientists/scientific and technical | 39 (33.1) | 37 (31.4) | 76 (32.2) |
| Medical and dental | 5 (4.2) | 8 (6.8) | 13 (5.5) |
| Registered nurses and midwives | 31 (26.3) | 32 (27.1) | 63 (26.7) |
| Nursing or healthcare assistants | 9 (7.6) | 11 (9.3) | 20 (8.5) |
| Wider healthcare team | 15 (12.7) | 12 (10.2) | 27 (11.4) |
| General management | 3 (2.5) | 4 (3.4) | 7 (3.0) |
| Other occupational group | 16 (13.6) | 14 (11.9) | 30 (12.7) |
| Nightshift worker | |||
| Yes | 5 (4.2) | 2 (1.7) | 7 (3.0) |
| No | 113 (95.8) | 116 (98.3) | 229 (97.0) |
| Hospital | |||
| QEHB | 61 (51.7) | 58 (49.2) | 119 (50.4) |
| Heartlands Hospital | 14 (11.9) | 17 (14.4) | 31 (13.1) |
| Birmingham Children’s Hospital | 18 (15.3) | 19 (16.1) | 37 (15.7) |
| Hereford Hospital | 25 (21.2) | 24 (20.3) | 49 (20.8) |
| Sociodemographic variables | |||
| Highest level of qualification | |||
| No formal qualifications | 1 (0.9) | 2 (1.7) | 3 (1.3) |
| GCSE, CSE, O level or equivalent | 12 (10.2) | 13 (11.0) | 25 (10.6) |
| A-level/AS level or equivalent | 18 (15.3) | 17 (14.4) | 35 (14.8) |
| Degree level or higher | 79 (67.0) | 78 (66.1) | 157 (66.5) |
| Other | 8 (6.8) | 8 (6.8) | 16 (6.8) |
| Marital status | |||
| Single, never married | 23 (19.5) | 25 (21.2) | 48 (20.3) |
| Married or domestic partnership | 78 (66.1) | 82 (69.5) | 160 (67.8) |
| Widowed | 2 (1.7) | 0 (–) | 2 (0.9) |
| Divorced | 11 (9.3) | 9 (7.6) | 20 (8.5) |
| Separated | 4 (3.4) | 2 (1.7) | 6 (2.5) |
| Live alone | |||
| Yes | 7 (5.9) | 11 (9.3) | 18 (7.6) |
| No | 111 (94.1) | 107 (90.7) | 218 (92.4) |
| Ethnic group | |||
| White/white British | 101 (86.3) | 91 (77.8) | 192 (82.1) |
| Mixed/multiple ethnic groups | 4 (3.4) | 5 (4.3) | 9 (3.9) |
| Asian/Asian British | 9 (7.7) | 11 (9.4) | 20 (8.6) |
| Black/African/Caribbean/Black British | 2 (1.7) | 3 (2.6) | 5 (2.1) |
| Other ethnic group | 1 (0.9) | 5 (4.3) | 6 (2.6) |
| Prefer not to say | 0 (–) | 2 (1.7) | 2 (0.9) |
| Missing | 1 | 1 | 2 |
| Index of Multiple Deprivation (quintile)a | |||
| 1 (most deprived) | 27 (22.9) | 26 (22.4) | 53 (22.7) |
| 2 | 26 (22.0) | 28 (24.1) | 54 (23.1) |
| 3 | 29 (24.6) | 31 (26.7) | 60 (25.6) |
| 4 | 24 (20.3) | 16 (23.8) | 40 (17.1) |
| 5 (least deprived) | 12 (10.2) | 15 (12.9) | 27 (11.5) |
| Missing | 0 | 2 | 2 |
Seventeen (7.6%) reported being a current smoker, while 48 (21.5%) were ex-smokers (see Table 11). From self-reported weight, only 68 (30.6%) were classified as of healthy weight, whereas 38.7% were overweight and 30.2% obese. Seventy-two (30.9%) were either inactive or moderately inactive, and 155 (65.7%) reported being in good or very good health. Forty-three (18.5%) reported a previous clinical diagnosis of asthma, 71 (30.7%) anxiety, 67 (28.5%) depression, 25 (10.7%) hypertension, 24 (10.3%) hypercholesterolaemia and 12 (5.2%) diabetes.
| SHSC (N = 118) (%) | Control (N = 118) (%) | Total (N = 236) (%) | |
|---|---|---|---|
| Demographic and baseline variables | |||
| Smoking status | |||
| Never smoked | 73 (66.4) | 85 (75.2) | 158 (70.9) |
| Ex-smoker | 26 (23.6) | 22 (19.5) | 48 (21.5) |
| Current smoker | 11 (10.0) | 6 (5.3) | 17 (7.6) |
| Missing | 8 | 5 | 13 |
| If current or ex-smoker, pack yearsa | n = 24 | n = 18 | n = 41 |
| Mean (SD) | 10.0 (8.1) | 13.7 (10.6) | 11.5 (9.3) |
| Median (IQR) | 11.0 (2.8–15.8) | 9.5 (6.0–18.0) | 9.5 (4.0–16.0) |
| Range | 0.3–27.8 | 3.0–39.0 | 0.3–39.0 |
| Missing | 0 | 1 | 1 |
| BMI (kg/m2)b | |||
| Underweight | 1 (0.9) | 0 (-) | 1 (0.5) |
| Healthy weight | 38 (33.9) | 30 (27.3) | 68 (30.6) |
| Overweight | 43 (38.4) | 43 (39.1) | 86 (38.7) |
| Obese | 30 (26.8) | 37 (33.6) | 67 (30.2) |
| Missing | 6 | 8 | 14 |
| GPPAQ | |||
| Inactive | 16 (13.8) | 14 (12.0) | 30 (12.9) |
| Moderately inactive | 22 (19.0) | 20 (17.1) | 42 (18.0) |
| Moderately active | 31 (26.7) | 38 (32.5) | 69 (29.6) |
| Active | 47 (40.5) | 45 (38.5) | 92 (39.5) |
| Missing | 2 | 1 | 3 |
| General health | |||
| Very good | 27 (22.9) | 23 (19.5) | 50 (21.2) |
| Good | 53 (44.9) | 52 (44.1) | 105 (44.5) |
| Fair | 36 (30.5) | 40 (33.9) | 76 (32.2) |
| Bad | 2 (1.7) | 3 (2.5) | 5 (2.1) |
| Very bad | 0 (-) | 0 (-) | 0 (-) |
| EQ-5D-5L c | |||
| Mean (SD) | 0.799 (0.171) | 0.789 (0.165) | 0.793 (0.168) |
| Median (IQR) | 0.812 (0.740–0.879) | 0.768 (0.696–0.879) | 0.795 (0.711–0.879) |
| Range | 0.0140–1.000 | 0.255–1.000 | 0.0140–1.000 |
| Missing | 2 | 1 | 3 |
| Diagnosed medical conditions (self-reported) | |||
| Asthma | 21/117 (18.0) | 22/116 (19.0) | 43/233 (18.5) |
| COPD/chronic bronchitis/emphysema | 0/115 (–) | 2/117 (1.7) | 2/232 (0.9) |
| Cancer | 1/117 (0.9) | 4/117 (3.4) | 5/234 (2.1) |
| Heart failure | 0/117 (–) | 2/115 (1.7) | 2/232 (0.9) |
| Hypercholesterolaemia (high cholesterol) | 14/117 (12.0) | 10/117 (8.6) | 24/234 (10.3) |
| Anxiety | 38/117 (32.5) | 33/114 (29.0) | 71/231 (30.7) |
| Depression | 35/118 (29.7) | 32/117 (27.4) | 67/235 (28.5) |
| Rheumatoid arthritis | 5/116 (4.3) | 1/116 (0.9) | 6/232 (2.6) |
| High blood pressure | 11/117 (9.4) | 14/117 (12.0) | 25/234 (10.7) |
| Stroke/TIA (mini stroke) | 1/116 (0.9) | 0/116 (–) | 1/232 (0.4) |
| Heart disease | 3/117 (2.6) | 0/116 (–) | 3/233 (1.3) |
| Atrial fibrillation | 2/115 (1.7) | 3/116 (2.6) | 5/231 (2.2) |
| Diabetes | 7/117 (6.0) | 5/116 (4.3) | 12/233 (5.2) |
| Chronic kidney disease | 0/116 (–) | 0/117 (–) | 0/233 (–) |
| Peripheral arterial disease | 0/117 (–) | 0/115 (–) | 0/232 (–) |
| Other medical condition(s) | 48/117 (41.0) | 47/117 (40.2) | 95/234 (40.6) |
Overall, 56 (24.1% of all respondents and 38.6% of 145 eligible participants over 40 years) reported ever having received an NHS health check to assess CVD risk (see Table 12). One hundred and nineteen (50.6%) had consulted a healthcare professional previously for a mental health problem and 150 (63.6%) for a MSK problem. Thirty-two (13.6%) had attended a weight management programme in the past and 13 (5.5%) a smoking cessation programme.
| SHSC (N = 118) (%) | Control (N = 118) (%) | Total (N = 236) (%) | |
|---|---|---|---|
| Over 40s NHS health check | |||
| Ever received over 40s NHS health check? | |||
| Yes | 23 (19.7) | 33 (28.7) | 56 (24.1) |
| No | 94 (80.3) | 82 (71.3) | 176 (75.9) |
| Missing | 1 | 3 | 4 |
| If yes, when? | n = 23 | n = 33 | n = 56 |
| < 1 year ago | 2 (8.7) | 1 (3.0) | 3 (5.4) |
| 1–5 years ago | 15 (65.2) | 18 (54.6) | 33 (58.9) |
| > 5 years ago | 6 (26.1) | 14 (42.4) | 20 (35.7) |
| If no, why not? | n = 94 | n = 82 | n = 176 |
| I am under 40 years old | 43 (45.7) | 42 (51.9) | 85 (48.6) |
| I have been invited, but I’m not interested | 0 (–) | 0 (–) | 0 (–) |
| I have been invited, but didn’t have time to attend | 3 (3.2) | 3 (3.7) | 6 (3.4) |
| I have been invited, but I forgot to attend | 1 (1.1) | 1 (1.2) | 2 (1.1) |
| I have not been invited to receive the health check | 46 (48.9) | 34 (42.0) | 80 (45.7) |
| Other | 1 (1.1) | 1 (1.2) | 2 (1.1) |
| Missing | 0 | 1 | 1 |
| Number of times consulted a GP during past 14 days | |||
| 0 | 96 (82.1) | 102 (87.2) | 198 (84.6) |
| 1 | 18 (15.4) | 12 (10.3) | 30 (12.8) |
| 2 | 3 (2.6) | 3 (2.6) | 6 (2.6) |
| Missing | 1 | 1 | 2 |
| Number of times consulted a practice nurse during past 14 days | |||
| 0 | 110 (93.2) | 116 (98.3) | 226 (95.8) |
| 1 | 7 (5.9) | 2 (1.7) | 9 (3.8) |
| 2 + | 1 (0.9) | 0 (-) | 1 (0.4) |
| Number of times consulted a pharmacist during past 14 days | |||
| 0 | 114 (96.6) | 113 (96.6) | 227 (96.6) |
| 1 | 4 (3.4) | 3 (2.6) | 7 (3.0) |
| 2 | 0 (–) | 1 (0.9) | 1 (0.4) |
| Missing | 0 | 1 | 1 |
| Ever consulted a healthcare professional (or equivalent) for mental health problems? | |||
| Yes – in the last year | 33 (28.0) | 16 (13.7) | 49 (20.9) |
| Yes – more than 1 year ago | 30 (25.4) | 40 (34.2) | 70 (29.8) |
| No | 55 (46.6) | 61 (52.1) | 116 (49.4) |
| Missing | 0 | 1 | 1 |
| Ever consulted a healthcare professional (or equivalent) for MSK problems? | |||
| Yes – in the last year | 35 (29.7) | 39 (33.0) | 74 (31.4) |
| Yes – more than 1 year ago | 43 (36.4) | 33 (28.0) | 76 (32.2) |
| No | 40 (33.9) | 46 (39.0) | 86 (36.4) |
| Ever attended a smoking cessation programme? | |||
| Yes – in the last year | 0 (–) | 0 (–) | 0 (–) |
| Yes – more than 1 year ago | 7 (6.0) | 6 (5.1) | 13 (5.5) |
| No | 110 (94.0) | 112 (94.9) | 222 (94.5) |
| Missing | 1 | 0 | 1 |
| Ever attended a weight management programme? | |||
| Yes – in the last year | 5 (4.3) | 7 (5.9) | 12 (5.1) |
| Yes – more than 1 year ago | 8 (6.8) | 12 (10.2) | 20 (8.5) |
| No | 104 (88.9) | 99 (83.9) | 203 (86.4) |
| Missing | 1 | 0 | 1 |
| Admitted to hospital for any unplanned reason in last 12 months | |||
| Yes | 8 (6.8) | 4 (3.4) | 12 (5.1) |
| No | 110 (93.2) | 114 (96.6) | 224 (94.9) |
| If yes, number of times | n = 8 | n = 4 | n = 12 |
| 1 | 6 (75.0) | 4 (100.0) | 10 (83.3) |
| 2 | 2 (25.0) | 0 (-) | 2 (16.7) |
| If yes, total nights | |||
| 0 | 0 (-) | 1 (25.0) | 1 (8.3) |
| 1 | 3 (37.5) | 2 (50.0) | 5 (41.7) |
| 2 + | 5 (62.5) | 1 (25.0) | 6 (50.0) |
| Admitted to hospital for any planned reason in last 12 months | |||
| Yes | 5 (4.3) | 4 (3.5) | 9 (3.9) |
| No | 112 (95.7) | 111 (96.5) | 223 (96.1) |
| Missing | 1 | 3 | 4 |
| If yes, number of times | n = 5 | n = 4 | n = 9 |
| 1 | 3 (75.0) | 4 (100.0) | 7 (87.5) |
| 2 | 1 (25.0) | 0 (-) | 1 (12.5) |
| Missing | 1 | 0 | 1 |
| If yes, total nights | |||
| 0 | 0 (-) | 0 (-) | 0 (-) |
| 1 | 1 (25.0) | 4 (100.0) | 5 (62.5) |
| 2 + | 3 (75.0) | 0 (-) | 3 (12.5) |
| Missing | 1 | 0 | 1 |
There was an even spread of duration of employment and most people (94.5%) had permanent contracts with a median working week of 4.0 days (see Table 13). Fifty-nine (25.0%) worked rotating shifts, while the majority (69.9%) worked daytime only. One hundred and forty-one (60.0%) reported being absent from work in the last year for reasons of ill health, where the mean (SD) number of days was 10.5 (29.9) and the maximum was 185 days. Conversely, data from HR records indicated a mean of 13.2 (27.3) days absent. There was no clear correlation (r = 0.52) or systematic error between self-reported absenteeism and HR absenteeism data (see Figure 4). As measured by the WHO-HPQ, participants report a mean (SD) of 77.2% (SD 18.5) absolute presenteeism which indicates that participants actual performance at work is 77.2% that of their best possible performance, over the previous 4 weeks. Reasons for sickness absesnteeism before randomisation are provided in Table 14. One hundred and thirty-four out of the 314 (42.7%) consenting participants provided an NHS number.
| SHSC (N = 118) (%) | Control (N = 118) (%) | Total (N = 236) (%) | |
|---|---|---|---|
| Employment details | |||
| Years at current workplace | |||
| < 1 year | 10 (8.5) | 9 (7.6) | 19 (8.1) |
| 1–2 years | 14 (11.9) | 19 (16.1) | 33 (14.0) |
| 3–5 years | 22 (18.6) | 21 (17.8) | 43 (18.2) |
| 6–10 years | 16 (13.6) | 20 (17.0) | 36 (15.3) |
| 11–15 years | 19 (16.1) | 21 (17.8) | 40 (17.0) |
| > 15 years | 37 (31.4) | 28 (23.7) | 65 (27.5) |
| Contract type | |||
| Permanent | 114 (96.6) | 109 (92.4) | 223 (94.5) |
| Temporary – with no agreed end date | 1 (0.9) | 1 (0.9) | 2 (0.9) |
| Fixed period – with an agreed end date | 3 (2.5) | 8 (6.8) | 11 (4.7) |
| Shift pattern | |||
| Regular daytime | 87 (73.7) | 78 (66.1) | 165 (69.9) |
| Regular night | 5 (4.2) | 2 (1.7) | 7 (3.0) |
| Rotating | 24 (20.3) | 35 (29.7) | 59 (25.0) |
| Other | 2 (1.7) | 3 (2.5) | 5 (2.1) |
| Usual shift length (hours) | |||
| Mean (SD) | 9.0 (1.9) | 9.5 (2.0) | 9.3 (2.0) |
| Median (IQR) | 8.0 (7.5–10.0) | 8.8 (7.8–11.8) | 8.4 (7.5–11.5) |
| Range | 5.5–13.0 | 5.8–13.0 | 5.5–13.0 |
| Missing | 4 | 2 | 6 |
| Number of days worked a week, including overtime/extra hours | |||
| Mean (SD) | 4.3 (0.9) | 4.2 (1.0) | 4.2 (0.9) |
| Median (IQR) | 4.0 (4.0–5.0) | 4.0 (3.0–5.0) | 4.0 (3.5–5.0) |
| Range | 2.0–7.0 | 2.0–6.0 | 2.0–7.0 |
| Absenteeism/presenteeism | |||
| Absenteeism up to 12 months before randomisation (HR records) | |||
| Absenteeism (WTE days) | |||
| Mean (SD) | 13.6 (27.4) | 12.8 (27.3) | 13.2 (27.3) |
| Median (IQR) | 1.6 (0.0–10.0) | 2.0 (0.0–11.4) | 2.0 (0.0–10.7) |
| Range | 0.0–137.0 | 0.0–136.8 | 0.0–137.0 |
| 0 | 50 (42.7) | 46 (40.0) | 96 (41.4) |
| 1–2 | 18 (15.4) | 16 (13.9) | 34 (14.7) |
| 3–5 | 11 (9.4) | 12 (10.4) | 23 (9.9) |
| 6–9 | 6 (5.1) | 8 (7.0) | 14 (6.0) |
| 10–19 | 8 (6.8) | 13 (11.3) | 21 (9.1) |
| 20 + | 24 (20.5) | 20 (17.4) | 44 (19.0) |
| Missing | 1 | 3 | 4 |
| Absenteeism (spellsa) | |||
| Mean (SD) | 1.2 (1.5) | 1.5 (1.9) | 1.3 (1.7) |
| Median (IQR) | 1.0 (0.0–2.0) | 1.0 (0.0–2.0) | 1.0 (0.0–2.0) |
| Range | 0.0–7.0 | 0.0–10.0 | 0.0–10.0 |
| Missing | 1 | 3 | 4 |
| Absenteeism 12–24 months before randomisation (HR records) | |||
| Absenteeism (WTE days) | |||
| Mean (SD) | 12.0 (25.1) | 16.5 (31.9) | 14.2 (28.7) |
| Median (IQR) | 1.8 (0.0–11.0) | 3.7 (0.0–16.0) | 2.7 (0.0–12.1) |
| Range | 0.0–164.7 | 0.0–186.0 | 0.0–186.0 |
| 0 | 48 (41.0) | 39 (33.9) | 87 (37.5) |
| 1–2 | 15 (12.8) | 12 (10.4) | 27 (11.6) |
| 3–5 | 12 (10.3) | 16 (13.9) | 28 (12.1) |
| 6–9 | 10 (8.6) | 10 (8.7) | 20 (8.6) |
| 10–19 | 14 (12.0) | 15 (13.0) | 29 (12.5) |
| 20 + | 18 (15.4) | 23 (20.0) | 41 (17.7) |
| Missing | 1 | 3 | 4 |
| Absenteeism (spellsa) | |||
| Mean (SD) | 1.4 (1.7) | 1.5 (1.6) | 1.5 (1.6) |
| Median (IQR) | 1.0 (0.0–2.0) | 1.0 (0.0–2.0) | 1.0 (0.0–2.0) |
| Range | 0.0–10.0 | 0.0–8.0 | 0.0–10.0 |
| Missing | 1 | 3 | 4 |
| Absenteeism (self-reported) | |||
| Taken time off work during the last 12 months due to ill health or otherwise? | |||
| Yes | 69 (58.5) | 72 (61.5) | 141 (60.0) |
| No | 49 (41.5) | 45 (38.5) | 94 (40.0) |
| Missing | 0 | 1 | 1 |
| Number of days off work in the last 12 months (0 days for those who have not taken any time off) | |||
| Mean (SD) | 7.1 (19.0) | 13.7 (37.2) | 10.5 (29.9) |
| Median (IQR) | 0.0 (0.0–3.0) | 0.0 (0.0–4.0) | 0.0 (0.0–4.0) |
| Range | 0–130.0 | 0.0–185.0 | 0.0–185.0 |
| 0 | 58 (56.8) | 59 (54.6) | 117 (55.7) |
| 1–2 | 11 (10.8) | 12 (11.1) | 23 (11.0) |
| 3–5 | 15 (14.7) | 14 (13.0) | 29 (13.8) |
| 6–9 | 2 (2.0) | 5 (4.6) | 7 (3.3) |
| 10–19 | 6 (5.9) | 4 (3.7) | 10 (4.8) |
| 20 + | 10 (9.8) | 14 (13.0) | 24 (11.4) |
| Missing | 16 | 10 | 26 |
| Absenteeism (WHO-HPQ) | |||
| Absolute absenteeismb (using 7-day estimate) (hours lost per month) | |||
| Mean (SD) | −4.3 (38.2) | −11.7 (50.7) | −8.0 (45.0) |
| Median (IQR) | 0 (−19.0–0) | 0 (−30.0–0) | 0 (−22.0–0.0) |
| Range | −130.0–146.0 | −212.0–150.0 | −212.0–150.0 |
| Missing | 2 | 1 | 3 |
| Absolute absenteeismb (using 28-day estimate) (hours lost per month) | |||
| Mean (SD) | 11.6 (43.6) | 5.5 (43.2) | 8.6 (43.4) |
| Median (IQR) | 0 (−10.0–20.0) | 0 (−10.0–15.0) | 0 (−10.0–17.0) |
| Range | −130.0–160.0 | −132.0–150.0 | −132.0–160.0 |
| Missing | 3 | 3 | 6 |
| Relative absenteeismb (using 7-day estimate) | |||
| Mean (SD) | −0.06 (0.49) | −0.14 (0.63) | −0.10 (0.57) |
| Median (IQR) | 0.0 (−0.14–0.0) | 0.0 (−0.20 0.0) | 0.0 (−0.16–0.0) |
| Range | −4.3–1.0 | −4.4–1.0 | −4.4–1.0 |
| Missing | 2 | 1 | 3 |
| Relative absenteeismc (using 28-day estimate) | |||
| Mean (SD) | 0.05 (0.51) | −0.02 (0.64) | 0.02 (0.58) |
| Median (IQR) | 0.0 (−0.07–0.17) | 0.0 (−0.07–0.11) | 0.0 (−0.07–0.13) |
| Range | −4.3–1.0 | −4.7–1.0 | −4.7–1.0 |
| Missing | 3 | 3 | 6 |
| Relative hours of workd (using 7-day estimate) | |||
| Mean (SD) | 1.1 (0.5) | 1.1 (0.6) | 1.1 (0.6) |
| Median (IQR) | 1.0 (1.0–1.1) | 1.0 (1.0–1.2) | 1.0 (1.0–1.2) |
| Range | 0.0–5.3 | 0–5.4 | 0–5.4 |
| Missing | 2 | 1 | 3 |
| Relative hours of workd (using 28-day estimate) | |||
| Mean (SD) | 0.9 (0.5) | 1.0 (0.6) | 1.0 (0.6) |
| Median (IQR) | 1.0 (0.8–1.1) | 1.0 (0.9–1.1) | 1.0 (0.9–1.1) |
| Range | 0.0–5.3 | 0.0–5.7 | 0.0–5.7 |
| Missing | 3 | 3 | 6 |
| Presenteeism (WHO-HPQ) | |||
| Absolute presenteeisme | |||
| Mean (SD) | 78.1 (17.3) | 76.3 (19.6) | 77.2 (18.5) |
| Median (IQR) | 80.0 (70.0–90.0) | 80.0 (70.0–90.0) | 80.0 (70.0–90.0) |
| Range | 0.0–100.0 | 0.0–100.0 | 0.0–100.0 |
| Missing | 4 | 1 | 5 |
| Relative presenteeismf | |||
| Mean (SD) | 1.0 (0.2) | 1.0 (0.3) | 1.0 (0.3) |
| Median (IQR) | 1.0 (0.9–1.1) | 1.0 (0.9–1.1) | 1.0 (0.9–1.1) |
| Range | 0.25–1.7 | 0.25–2.0 | 0.25–2.0 |
| Missing | 6 | 2 | 8 |
| SHSC (N = 118) (%) |
Control (N = 118) (%) |
Total (N = 236) (%) |
|
|---|---|---|---|
| Level 1 reason for absenteeism up to 12 months before randomisation (HR records)a | |||
| Total spells of absence | 142 | 170 | 312 |
| Coronavirus (COVID-19) | 18 (12.7) | 29 (17.1) | 47 (15.1) |
| Anxiety/stress/depression/other psychiatric illnesses | 17 (12.0) | 15 (8.8) | 32 (10.3) |
| Back problems | 3 (2.1) | 5 (3.0) | 8 (2.6) |
| Other MSK problems | 11 (7.8) | 14 (8.2) | 25 (8.0) |
| Cold, cough, flu – influenza | 7 (4.9) | 16 (9.4) | 23 (7.4) |
| Asthma | 0 (–) | 1 (0.6) | 1 (0.3) |
| Chest and respiratory problems | 4 (2.8) | 4 (2.4) | 8 (2.6) |
| Headache/migraine | 15 (10.6) | 6 (3.5) | 21 (6.7) |
| Blood disorders | 1 (0.7) | 2 (1.2) | 3 (1.0) |
| Heart, cardiac and circulatory problems | 1 (0.7) | 1 (0.6) | 2 (0.6) |
| Ear, nose, throat | 1 (0.7) | 4 (2.4) | 5 (1.6) |
| Dental and oral problems | 2 (1.4) | 1 (0.6) | 3 (1.0) |
| Eye problems | 1 (0.7) | 1 (0.6) | 2 (0.6) |
| Endocrine/glandular problems | 0 (–) | 1 (0.6) | 1 (0.3) |
| Gastrointestinal problems | 14 (9.9) | 22 (12.9) | 36 (11.5) |
| Genitourinary and gynaecological disorders | 5 (3.5) | 6 (3.5) | 11 (3.5) |
| Infectious diseases | 13 (9.2) | 12 (7.1) | 25 (8.0) |
| Injury, fracture | 2 (1.4) | 5 (3.0) | 7 (2.2) |
| Nervous system disorders | 4 (2.8) | 0 (–) | 4 (1.3) |
| Pregnancy-related disorders | 1 (0.7) | 0 (–) | 1 (0.3) |
| Emergency leave | 2 (1.4) | 2 (1.2) | 4 (1.3) |
| Other known causes – not elsewhere classified | 12 (8.5) | 13 (7.7) | 25 (8.0) |
| Unknown causes/not specified | 8 (5.6) | 10 (5.9) | 18 (5.8) |
| No sickness absence | 50 | 46 | 96 |
| Missing | 1 | 3 | 4 |
| Level 1 reason for absenteeism 12–24 months before randomisation (HR records)a | |||
| Total spells of absence | 161 | 176 | 337 |
| Coronavirus (COVID-19) | 5 (3.1) | 11 (6.3) | 16 (4.8) |
| Anxiety/stress/depression/other psychiatric illnesses | 6 (3.7) | 13 (7.4) | 19 (5.6) |
| Back problems | 6 (3.7) | 6 (3.4) | 12 (3.6) |
| Other MSK problems | 9 (5.6) | 13 (7.4) | 22 (6.5) |
| Cold, cough, flu – influenza | 35 (21.7) | 24 (13.6) | 59 (17.5) |
| Asthma | 1 (0.6) | 1 (0.6) | 2 (0.6) |
| Chest and respiratory problems | 7 (4.4) | 7 (4.0) | 14 (4.2) |
| Headache/migraine | 12 (7.5) | 8 (4.6) | 20 (5.9) |
| Benign and malignant tumours, cancers | 0 (–) | 2 (1.1) | 2 (0.6) |
| Heart, cardiac and circulatory problems | 1 (0.6) | 3 (1.7) | 4 (1.2) |
| Burns, poisoning, frostbite, hypothermia | 0 (–) | 1 (0.6) | 1 (0.3) |
| Ear, nose, throat | 8 (5.0) | 3 (1.7) | 11 (3.3) |
| Dental and oral problems | 3 (1.9) | 2 (1.1) | 5 (1.5) |
| Eye problems | 1 (0.6) | 3 (1.7) | 4 (1.2) |
| Endocrine/glandular problems | 0 (–) | 2 (1.1) | 2 (0.6) |
| Gastrointestinal problems | 17 (10.6) | 23 (13.1) | 40 (11.9) |
| Genitourinary and gynaecological disorders | 5 (3.1) | 4 (2.3) | 9 (2.7) |
| Infectious diseases | 5 (3.1) | 7 (4.0) | 12 (3.6) |
| Injury, fracture | 5 (3.1) | 6 (3.4) | 11 (3.3) |
| Nervous system disorders | 2 (1.2) | 0 (–) | 2 (0.6) |
| Pregnancy-related disorders | 11 (6.8) | 9 (5.1) | 20 (5.9) |
| Skin disorders | 1 (0.6) | 2 (1.1) | 3 (0.9) |
| Emergency leave | 0 (–) | 3 (1.7) | 3 (0.9) |
| Other known causes – not elsewhere classified | 14 (8.7) | 15 (8.5) | 29 (8.6) |
| Unknown causes/not specified | 7 (4.4) | 8 (4.6) | 15 (4.5) |
| No sickness absence | 48 | 39 | 87 |
| Missing | 1 | 3 | 4 |
FIGURE 4.
Bland–Altman plot comparing self-reported and HR-reported absenteeism.
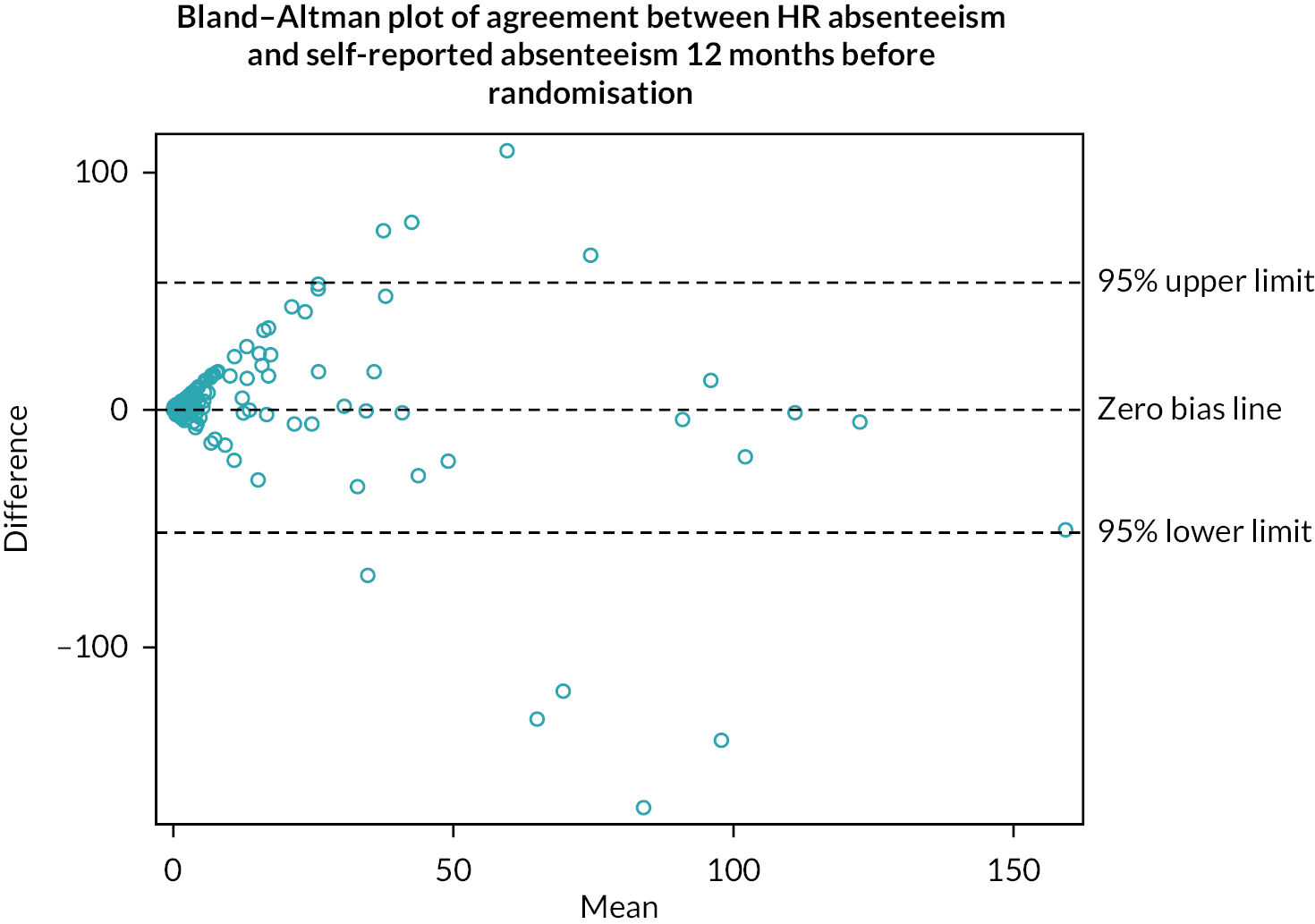
Primary outcomes and stop/go criteria
Recruitment
Three hundred and fourteen of the 3788 invited staff gave their consent to take part in the trial, which equated to 8.3% (95% CI 7.4% to 9.2%) of those invited, which met the red stop/go criterion for this outcome (see Table 15). Of the 314, 236 were randomised, which equated to 6.2% (95% CI 5.5% to 7.0%) of those invited.
| Criteria | Description | Progression criteria | ||
|---|---|---|---|---|
| Green (go) | Amber (pause) | Red (stop) | ||
| Recruitment (uptake) | Percentage of invited employees consenting to take part. | > 25% | 15–25% | < 15% 314 (8.3%) 95% CI (7.4% to 9.2%) |
| Referred to a service (defined as eligible for a referral) | Percentage of participants randomised to the intervention arm requiring referral to a service (GP, local psychological services, physiotherapy). | > 30% 57 (48.3%) 95% CI (39.0% to 57.7%) |
10–30% | < 10% |
| Attendance of referralsa (defined as accepting a referral) | Percentage of those referred who self-report attending the service at least once – measured at 26 weeks. | > 50% | 30–50% 18 (31.6%) 95% CI (19.9% to 45.2%) |
< 30% |
| Action | If ALL criteria are GREEN, proceed to full trial with protocol unchanged. | If ANY of these criteria are AMBER, adapt protocol appropriately using information from process evaluation before proceeding to full trial. |
If ALL of these criteria are RED, consider current protocol not feasible and do not progress to a full trial.
If ONE OR TWO of these criteria are RED, consider whether adaptations are needed. |
|
Referral
Fifty-seven of 118 [48.3% (95%CI 39.0% to 57.7%)] participants randomised to the intervention arm were eligible for referral to at least one service (GP, local psychological or physiotherapy services), which met the green stop/go criterion.
Attendance at referrals
Attendance data for this outcome are presented here as the agreed proxy outcome (intention to attend). During the intervention, 18 of the 57 participants accepted a referral to at least one service. This equated to 31.6% (95% CI 19.9% to 45.2%) of those eligible for referral and met the amber stop–go progression criterion, although the CIs are wide, spanning both the red and green criteria.
Due to the database structure, we were unable to determine whether five of those eligible for a psychological referral confirmed attendance. In the above estimates, we have used a conservative approach and assumed all five participants did not accept a referral. Similarly, six participants eligible for a GP referral from HbA1c, cholesterol, eGFR and QRISK2 components were not offered a referral and all six were assumed not to have accepted. However, if we assume all 10 accepted a referral (as one participant already accepts a referral from another component), then 28/57 participants accepted a referral in total, which equates to 49.1% (95% CI 35.6% to 62.7%) (still in the amber category).
Overall, the stop/go criteria were in the red, green and amber zones (Table 15); therefore, the TOC recommended that a full-scale trial should proceed, but with modifications drawn from the findings of the secondary outcomes and process evaluation (see later).
Secondary outcomes
Assessing generalisability (programme reach)
Table 16 compares the demographics of the hospital, invited and randomised populations. The selected invited population was similar to the hospital population, reflecting the full range of characteristics. However, the participants who responded and eventually took part in the trial were slightly more likely to be female, but more likely to be white British (78.0% compared to 59.7%), allied health professionals (14.0% compared to 6.9%) and healthcare scientists (11.9% compared to 5.0%). They were less likely to be from estates and ancillary (2.5% compared to 4.7%), medical and dental (5.5% compared to 11.9%) and nursing and midwifery registered staff groups (26.7% compared to 33.4%). Generalisability could be improved.
| Population | |||
|---|---|---|---|
| Hospital (N = 24,344) (%) | Invited (N = 3788) (%) | Randomised (N = 236) (%) | |
| Sex | |||
| Male | 23.6 | 22.8 | 20.3 |
| Female | 76.4 | 77.2 | 79.7 |
| Age | |||
| Mean (SD) | 42.7a | 41.9a | 42.5 (10.4) |
| Ethnicity | |||
| White British | 59.1 | 59.7 | 78.0 |
| White other | 5.7 | 5.4 | 3.4 |
| Mixed | 2.5 | 2.3 | 3.8 |
| Asian/Asian British | 16.6 | 16.5 | 8.5 |
| Black/Black British | 7.8 | 7.3 | 2.1 |
| Other ethnic groups | 3.6 | 4.1 | 2.5 |
| Unknown/missing | 4.8 | 4.8 | 1.7 |
| Part-time | |||
| Yes | 37.1 | 35.6 | 35.3 |
| No | 62.9 | 64.4 | 64.7 |
| Missing | 0 | 0 | 2 |
| Staff group | |||
| Add Prof Scientific and Technic | 4.1 | 3.1 | 5.5 |
| Additional clinical services | 16.7 | 18.3 | 11.9 |
| Administrative and clerical | 21.2 | 16.9 | 20.3 |
| Allied health professionals | 6.0 | 6.9 | 14.0 |
| Estates and ancillary | 6.8 | 4.7 | 2.5 |
| Healthcare scientists | 3.6 | 5.0 | 11.9 |
| Medical and dental | 12.6 | 11.9 | 5.5 |
| Nursing and midwifery registered | 28.9 | 33.4 | 26.7 |
| Other (no specified) | – | 1.7 | |
Results of intervention screening assessments
Mental health screen
Of the 101 participants who completed the screening clinic, the median score on the GAD-7 questionnaire for anxiety was 5.0 [interquartile range (IQR) 2.0–7.0], out of a possible score of 21. Eighty-five (84.2%) reported minimal or mild anxiety, but 11 (10.9%) were classified as having moderate anxiety and 5 (5.0%) severe anxiety (see Table 17). On the PHQ-9 score for depression, out of a possible score of 27, the median (IQR) was 4.0 (2.0–8.0). Most people reported minimal or mild depression, but 13 (12.9%) reported moderate or moderately severe depression and 4 (4.0%) severe depression.
| SHSC (N = 101) (%) | |
|---|---|
| Receiving mental health check | 101 |
| GAD-7a | |
| Mean (SD) | 5.3 (4.5) |
| Median (IQR) | 5.0 (2.0–7.0) |
| Range | 0.0, 20.0 |
| Minimal anxiety (score < 5) | 49 (48.5) |
| Mild anxiety (score 5–9) | 36 (35.6) |
| Moderate anxiety (score 10–14)b | 11 (10.9) |
| Severe anxiety (score 15 +)c | 5 (5.0) |
| PHQ-9d | |
| Mean (SD) | 5.7 (5.1) |
| Median (IQR) | 4.0 (2.0–8.0) |
| Range | 0.0, (21.0) |
| Minimal depression (score < 5) | 53 (52.5) |
| Mild depression (score 5–9) | 31 (30.7) |
| Moderate depression (score 10–14)b | 9 (8.9) |
| Moderately severe depression (score 15–19)c | 4 (4.0) |
| Severe depression (score 20 +)c | 4 (4.0) |
Musculoskeletal health screen
The vast majority of participants had no significant back pain, although eight (7.9%) were at moderate risk of poor clinical outcome and two (2.0%) at high risk on the StarT Back tool (see Table 18). Twenty-seven (27.0%) scored with moderate risk on the StarT MSK tool for other types of pain, and five (5.0%) high risk. The mean score on the short OMPSQ was 35.2 (SD = 13.3). Nine (12.5%) participants scored over 50, indicating higher risk for future work disability. There were moderate–strong correlations between the OMPSQ and the StarT Back tool (r = 0.65) and the StarT MSK tool (r = 0.79) among the 72 participants completing the OMPSQ score.
| SHSC (N = 101) (%) | |
|---|---|
| Receiving MSK health check | 101 |
| StarT Back tool a | |
| Mean (SD) | 1.2 (1.7) |
| Median (IQR) | 0.0 (0.0–2.0) |
| Range | 0.0–8.0 |
| Low risk (overall score < 4) | 91 (90.1) |
| Moderate risk (overall score 4 + and subscore < 4)b | 8 (7.9) |
| High risk (overall score 4 + and subscore 4 +)b | 2 (2.0) |
| STarT MSK toolc | |
| Mean (SD) | 2.8 (3.1) |
| Median (IQR) | 2.0 (0.0–5.0) |
| Range | 0.0–10.0 |
| Low risk (score < 5) | 68 (68.0) |
| Moderate risk (score 5–8)b | 27 (27.0) |
| High risk (score 9 +)b | 5 (5.0) |
| Missing | 1 |
| OMPSQ (Short)d | n = 72 |
| Mean (SD) | 35.2 (13.3) |
| Median (IQR) | 36.0 (24.5–42.5) |
| Range | 11.0–85.0 |
| Score ≤ 50 (not indicating higher estimated risk for future work disability) | 63 (87.5) |
| Score > 50 (indicating higher estimated risk for future work disability) | 9 (12.5) |
| Missing | 7 |
Cardiovascular disease screen
According to the BMI results, 38 (38.0%) and 32 (32.0%) participants were classified as overweight and obese, respectively (see Table 19). For physical activity, 46 (46.0%) self-reported as being active. Twelve (11.9%) reported increasing or higher risk on the AUDIT C alcohol dependence tool and 10 (9.9%) were current smokers. Forty-six (45.5%) received additional CVD health checks and of the remaining 55 excluded, 39 (70.9%) were under 40 years of age and 26 (29.1%) were already diagnosed or being treated with relevant conditions. Results of the blood pressure and blood tests are presented in Table 19. Twenty-eight (27.7%) participants were eligible for additional blood tests as they were 40 and over, had raised blood pressure and a BMI in the obese category. Three (13.0%) had results indicative of diabetes, and three (10.7%) indicative of kidney disease. Of those eligible for the QRISK2 score, nine (14.5%) had medium risk and two (3.2%) had high risk of developing CVD in the next 10 years.
| SHSC (N = 101) (%) |
|
|---|---|
| BMI (kg/m2)a | |
| Mean (SD) | 28.3 (6.4) |
| Median (IQR) | 27.2 (23.8–31.8) |
| Range | 16.8–50.3 |
| Underweight | 1 (1.0) |
| Healthy weight | 29 (29.0) |
| Overweight | 38 (38.0) |
| Obese | 32 (32.0) |
| Missing | 1 |
| GPPAQ | |
| Inactive | 9 (9.0) |
| Moderately inactive | 18 (18.0) |
| Moderately active | 27 (27.0) |
| Active | 46 (46.0) |
| Missing | 1 |
| AUDIT Cb | |
| Mean (SD) | 3.9 (3.8) |
| Median (IQR) | 3.0 (1.0–5.0) |
| Range | 0.0–23.0 |
| Lower risk (score < 8) | 89 (88.1) |
| Increasing risk (score 8–15) | 10 (9.9) |
| Higher risk (score 16–19) | 1 (1.0) |
| Possible dependence (score 20 +) | 1 (1.0) |
| Current smoker | |
| Current smoker who wants to quit | 8 (7.9) |
| Current smoker who does not want to quit | 2 (2.0) |
| Non-smoker/ex-smoker | 91 (90.1) |
| Additional cardiovascular health checks | |
| Excluded from additional cardiovascular health checks | 55 |
| Excluded due to being aged under 40 years | 39 (70.9) |
| Excluded due to being on cholesterol-lowering medication or previously diagnosed conditionsc | 16 (29.1) |
| Receiving additional cardiovascular health checks | 46 |
| Pulse | |
| Regular | 46 (100.0) |
| Irregular | 0 (–) |
| Blood pressure (mmHg)d | |
| Eligible for blood pressure treatment | 1 (2.2) |
| No blood pressure treatment required | 45 (97.8) |
| Cholesterol (mmol/l) | |
| No referral (< 7.5) | 46 (100) |
| Required referral (7.5 +) | 0 (–) |
| Additional blood tests | |
| Excluded from additional blood tests | 73 |
| Receiving additional blood tests e | 28 |
| HbA1c (mmol/mol)f | |
| Indication of diabetes (≥ 48) | 3 (13.0) |
| Pre-diabetic (42–47.99) | 3 (13.0) |
| Normal (< 42) | 17 (73.9) |
| Missing | 5 |
| U&E/eGFR (ml/minute/1.73 m2)g | |
| Indication of kidney disease (< 60) | 3 (10.7) |
| Normal (≥ 60) | 25 (89.3) |
| QRISK2 score | |
| Excluded from QRISK2 h | 39 |
| Receiving QRISK2 | 62 |
| QRISK2i | |
| Low risk (< 10%) | 51 (82.3) |
| Medium risk (10–19.9%) | 9 (14.5) |
| High risk (20% +) | 2 (3.2) |
Details of subsequent referrals needed
Many (n = 62; 61.4%) of the 101 intervention participants who completed the intervention met criteria for referral to at least one service (see Table 20). Five participants were already being treated for all components requiring a referral, meaning 57 (56.4%) were eligible for referral to at least one service; 46 (45.5%) participants were eligible for referral to their GP (14 accepted), 10 (9.9%) to local psychological services (1 accepted) and 17 (16.8%) to physiotherapy (4 accepted).
| SHSC (completed intervention) (N = 101) |
SHSC (randomised to intervention) (N = 118) |
|
|---|---|---|
| Required referrala to at least one serviceb | 62 (61.4%) | 62 (52.5%) |
| Total number of required referrals | 98 | 98 |
| Referred to GP | 46 | 46 |
| Referred to local psychological services | 15 | 15 |
| Referred to physiotherapy | 37 | 37 |
| Eligible for referral to at least one service b , c | 57 (56.4%) | 57 (48.3%) |
| Total number of eligible referrals | 73 | 73 |
| Referred to GP | 46 | 46 |
| Referred to local psychological services | 10 | 10 |
| Referred to physiotherapy | 17 | 17 |
| Accepted referral to at least one service b | 18/57 (31.6%) | 18/57 (31.6%) |
| Total number of accepted referrals | 19 | 19 |
| Referred to GP | 14 | 14 |
| Referred to local psychological services | 1 | 1 |
| Referred to physiotherapy | 4 | 4 |
Outcomes at 26 weeks
Very limited data were collected at the 26-week follow-up as only 26 people had reached that time point (after three withdrawals). However, only four completed the questionnaires in the intervention arm and three in the usual care arm. This precluded meaningful analyses of attendance at referred services, changes in lifestyle, quality of life, healthcare utilisation, absenteeism, presenteeism, assessment of contamination and any indication of effect size (SD) for the definitive trial; however, data tables are presented in Appendix 2 for completeness. HR sickness absence records 26 weeks after randomisation were available for all 26 participants.
Completeness of data items and attendance at screening clinic (fidelity)
One hundred and eighteen participants in each arm completed the baseline questionnaire and were randomised, 101 participants completed the initial self-completion screening questionnaires prior to the screening clinic and of those, 102 nurse-intervention forms were completed. Individual data items were generally well completed with few missing data, especially for the intervention screening data. A sample of clinic logs indicated low deoxyribonucleic acid (DNA) rates. Duration of screening sessions is presented in the health economics section below.
Resource use and costs of the intervention
Resource use
The base-case times for each screening task, grades of staff responsible for each task and disaggregated costs per task are presented in Table 21. Tasks were related to contacting the participant to book the appointment, clinic tasks for all participants (paperwork, greeting the participant and completing the screening), tasks relevant for those who required blood tests, and production of GP results/referral letters.
| Task | Base-case time (minutes) | Pay band/speciality training years | Task cost (£ per task) |
|---|---|---|---|
| Contact participant to book clinic appointment | 10.00 | 2 | 4.17 |
| Complete any relevant paperwork | 10.00 | 3 | 4.50 |
| 2 | 4.17 | ||
| Greet participant into clinic | 5.00 | 2 | 2.08 |
| Set up participant with Participant Intervention Screening form to complete | 5.00 | 3 | 2.25 |
| Complete nurse intervention screening and review available results/recommended actions with participant | 45.00 | 6 | 37.50 |
| 5 | 30.00 | ||
| Prepare blood samples and sent to laboratory for processing (where relevant) | 15.00 | 3 | 6.75 |
| Obtain blood results (where relevant) |
5.00 | 3 | 2.25 |
| Review blood results (where relevant) |
10.00 | ST3 | 8.33 |
| 6 | 8.33 | ||
| Inform participant of blood test results (where relevant) |
10.00 | 6 | 8.33 |
| Edit/review GP/participant letters from trial team | 45.00 | 6 | 37.50 |
| Send GP/participant letters | 5.00 | 2 | 2.08 |
Out of 118 intervention arm participants, 101 actually attended screening and 56 (55.4%) received at least one blood test. Using the cost of each blood test and the proportion receiving each test, the average cost of blood tests per participant was calculated as £3.29 (Table 22).
| Blood tests | Cholesterol | eGFR | HbA1c | Total cost (£) |
|---|---|---|---|---|
| Unit cost (£) | 1.35 | 3.18 | 8.00 | – |
| Number (%) receiving each blood test | 46 (45.5) | 27 (26.7) | 23 (22.8) | – |
| Average cost of blood test per participant (£) | 0.61 | 0.85 | 1.82 | 3.29 |
As previously calculated, 55.4% of participants received at least one blood test. Therefore, any costs associated with tasks for blood tests were only included for this proportion of the participants. Table 23 shows the weighted cost of each task for each combination of staff grade.
| Task | Proportion of participants requiring task | Total pay band of staff | Cost of task per participant (£) |
|---|---|---|---|
| Contact participant to book clinic appointment (maximum three attempts) | 1.00 | 2 | 4.17 |
| Complete any relevant paperwork | 1.00 | 2 | 4.17 |
| 1.00 | 3 | 4.50 | |
| Greet participant into clinic | 1.00 | 2 | 2.08 |
| Set up participant with Participant Intervention Screening form to complete | 1.00 | 3 | 2.25 |
| Complete Nurse Intervention Screening and review available results/recommended actions with participant | 1.00 | 6 | 37.50 |
| 1.00 | 5 | 30.00 | |
| Prepare blood samples and sent to laboratory for processing (where relevant) | 0.55 | 3 | 3.71 |
| Obtain blood results (where relevant) | 0.55 | 3 | 1.24 |
| Review blood results (where relevant) | 0.55 | ST3 | 4.58 |
| 0.55 | 6 | 4.58 | |
| Inform participant of blood test results (where relevant) | 0.55 | 6 | 4.58 |
| Edit/review GP/participant letters from trial team | 1.00 | 6 | 37.50 |
| Send GP/participant letters | 1.00 | 2 | 2.08 |
The overall maximum screening cost per participant (including blood tests) was £107.48 if the highest band staff were used and £99.98 if the lowest band staff ran the clinic (Table 24).
| Salary band of healthcare professionals performing tasks | Total cost of salaries for tasks (£) | Total cost including: salaries and cost of blood tests (£) |
|---|---|---|
| Highest possible cost, with all highest possible band staff | 104.19 | 107.48 |
| Intermediate cost, with bands 6 and 2 | 103.86 | 99.65 |
| Intermediate cost, with bands 5 and 3 | 96.69 | 107.15 |
| Lowest possible cost, with all lowest possible band staff | 96.36 | 99.98 |
Quality of life
Complete EQ-5D-5L data were available for 233/236 participants randomised (response rate 98.7%). The mean score was 0.793 (SD 0.168) with a range from 0.0140 to 1.000 (see Table 11). The responses for each dimension can be found in Figure 5. This shows that participants reported few problems with mobility, self-care or usual activities. However, 22.8% reported at least moderate pain or discomfort and 18.9% were at least moderately anxious or depressed.
FIGURE 5.
Distribution of scores by EQ-5D domains.

Chapter 4 Process evaluation
Quantitative evaluation
Quantitative data relating to recruitment, programme reach, intervention fidelity, referrals, attendance at the screening, intention to attend referrals and resource use/costs have been presented in the previous chapter.
Qualitative evaluation
Participant recruitment
Recruitment to the qualitative part of the process evaluation occurred during the second wave of trial recruitment, between July and October 2021. We conducted 51 (63.8%) out of the 80 interviews originally planned (see Table 25).
| Trial participants | eTHOS nurses | Providers | Outside agencies | |
|---|---|---|---|---|
| Target (n) | 48 | 10 | 12 | 10 |
| Contacted (n) | 93 | 12 | 6 | 13 organisations |
| Interviewed (n) | Needed referral to other services = 16 Did not need referral = 5 Usual care = 8 Did not attend screening = 2 |
8 | 3 physios 1 GP |
13 |
| Total interviewed (n) | 31 | 8 | 4 | 13 |
| Organisations represented (n) | 4 | 4 | 3 | 8 |
Participant characteristics
The largest planned group was the trial participants. Ninety-three participants were invited to participate, of whom 31 responded and were interviewed. The length of interviews varied from 10 to 40 minutes depending on their category. All interviews (and consent) were conducted online.
Demographic characteristics of the trial participants included in the interviews (age, sex, ethnicity, usual hours) broadly matched those of the distribution within the trial (see Table 26). However, the sample was not distributed across the four sites as originally intended and our interview sample contains proportionately more registered nurses and midwives. We did not have the opportunity to purposively sample interviewees as intended because of a low response rate, marked reduction of the recruitment period (4 months instead of 18 months), sites commencing the study at different times and the need to allow sufficient time between consenting to the main trial and invitation to participate in the qualitative substudy.
| n (%) | n (%) | |||
|---|---|---|---|---|
| Job category | ||||
| Age, mean (range) | 39.6 (23–54) | Registered nurses and midwives | 13 (42) | |
| Female | 26 (84) | Allied/scientists/technical | 3 (10) | |
| White British | 25 (81) | Other occupational group | 3 (10) | |
| Medical and dental | 2 (6) | |||
| Site | Healthcare assistants | 2 (6) | ||
| QEHB | 15 (48) | Wider healthcare team | 1 (3) | |
| BWC | 7 (23) | General management | 1 (3) | |
| WVT | 7 (23) | |||
| BHH | 2 (6) | Usual hours | ||
| Day shift | 21 (68) | |||
| Rotating shifts | 9 (29) | |||
| Night | 1 (3) | |||
Although we were able to interview the full complement of nurses delivering the intervention, due to the compressed time frame and service restrictions during the pandemic, we were limited in recruitment of providers receiving referrals, finally interviewing three physios and one GP. Table 27 provides a summary of the type and size of outside agencies spoken with.
| Characteristic | Healthcare or NHS-relateda | Unrelated to health care or the NHS | |
|---|---|---|---|
| NHSa | Non-NHS | ||
| Number of participants | 4 | 2 | 7 |
| Number of organisations | 4 | 1 | 3 |
| Number of employees | |||
| Small (1–400) | 1 | ||
| Medium (401–999) | |||
| Large (> 999) | 4 | 0 | 3 |
| Interviewee’s primary roles | |||
| Managerial | 1 | 1 | |
| Senior leadership | 4 | 1 | 1 |
| HR/well-being | 1 | 1 | |
| Occupational health | 1 | 2 | |
| Secondary rolesb | |||
| Clinical (secondary role) | 4 | 1 | 1 |
| Mental health first aid (secondary role) | 1 | ||
The remainder of this chapter presents the data from the qualitative interviews supported by interviewee quotes (see Box 1 for key to participant identifiers). The data are organised under participant type (trial participant, eTHOS nurse, service provider and outside agencies).
Table 28 lists the topics covered in each section and summarises the key findings within the data. A summary of the cross-cutting themes arising from these data can be found in ‘Cross-cutting themes’.
| Topic | Summary |
|---|---|
| Trial participants | |
|
There was much gratitude regarding the opportunity to participate in the intervention, particularly in the light of COVID-19, the experiences of which prompted a demand for mental health screening tools addressing work-related stress. However, some participants also had expectations that went beyond the scope of what screening tools can offer |
|
Key motivators for participation were the hope that the research would lead to positive changes in the workplace, and as an alternative to attending a GP appointment – particularly given the increased access issues within the pandemic |
|
The recruitment processes were largely visible (although this may have been skewed by COVID-19) and accessible and, although questionnaires were long, manageable. Suggestions were made about changing the content and delivery of the tool itself |
|
There was no evidence of contamination A future trial might consider a wait-list control |
|
Some staff from off-site locations were not able to attend the screening. A mobile service and flexible clinic times could help. The ability to attend during work time was harder for ward-based staff. There is tension between preventing future absenteeism and service delivery |
|
Remote options might be considered to increase the convenience of attending screening |
|
Those unconcerned about confidentiality gave clear reasoning as to why this had not been a concern to them |
|
There was a perception that occupational health was limited to established health problems, particularly those arising from a work-related injury, rather than screening, preventing, supporting or enabling staff. Some participants declined referral to occupational health where it was indicated due to their line manager being notified |
|
Participants had, in the main, responded well to the recommendations. However, some concerns about referral pathways were raised, and barriers to lifestyle changes identified |
| eTHOS nurses | |
|
While pauses due to COVID-19 had affected the eTHOS nurses, they were generally satisfied with the training, although they made suggestions for improvement to the training, support protocols and the database |
|
The eTHOS nurses agreed that there was a need for support with staff well-being; however, there were expectations from participants that went beyond the scope of what screening tools can offer in terms of staff referrals and addressing the root causes of staff ill health |
|
Some differences in the way the intervention was delivered across the sites suggests acceptability of several options including mobile delivery and within an occupational health department. Some database changes were suggested. Challenges with recruitment arose from the pandemic context |
| Follow-on service providers | |
|
As with the previous groups of participants, the service providers agreed that the intervention was important in meeting staff well-being needs; however, they too recognised the need for change not only across the NHS, but also within their own service areas in order to be able to support staff needs |
|
Findings were limited by a very small number of staff interviewed, but there was no evidence of detrimental impact on their service through a large number of referrals |
|
The data highlight the fluidity of referral pathways and therefore the need to maintain close links with providers |
| Outside agencies | |
|
Outside agencies largely echoed the findings from the preceding participants in relation to the importance of such an intervention, as well as the need to address the tension between staff well-being and service delivery and the potential limitations in referral pathways |
|
There was interest in supporting the trial, with the pandemic context making the trial more appealing to one non-healthcare setting. Issues for other organisations included capacity and, for those with staff working across multiple sites, delivery issues |
Trial participant (P)
eTHOS nurse (eN)
Physiotherapist (PT)
GP
Interviewee from an outside agency (OA)
Trial participants
Intervention acceptability
We present this topic within the trial participant feedback first as it sets the context for all other aspects of the evaluation. Furthermore, it was very difficult to disentangle participants’ views of the concept of health screening from their evaluation of the screening programme (intervention) itself.
Satisfaction with the content and concept
The word cloud (see Figure 6) was generated with the qualitative analysis software NVivo. It captured key words used in the positive feedback regarding the intervention; the font sizes used depict the frequency of use (the larger the word, the more frequently it was used).
FIGURE 6.
Trial participants’ evaluation of the intervention.

As can be seen, it was well received, participants could see its long-term value in improving sickness absence and staff retention:
good that we’re now looking at reasons why, and different factors that might affect someone … a lot of people … tend to ignore their own health … until they’re forced to pay attention to it. So trialling something like a health check is beneficial.
P10
The intervention provided NHS staff with an opportunity to access health care that they could not otherwise obtain; this opportunity was highly valued and is explained further below. In addition, one trial participant explained how important it was to have a space where staff, who are focused on other people’s needs, can actually talk about their own needs, and reflect on their own lifestyles: ‘nice to have a chat with somebody about your health, about you … in a healthcare setting it’s sometimes all about other people’ (P8).
It was recognised that while findings from the intervention might, in the short term, increase time away from work for conditions that people had not previously been aware of, the benefits of having these conditions treated early was more important: ‘if anything was picked up nice and early then it’s obviously going to help the NHS isn’t it?’ (P16).
The intervention was seen as a good vehicle for improving health, and this in turn could boost staff morale: ‘I think it’s likely to improve morale, I think it’s likely to improve the fitness of the workforce and therefore their happiness’ (P18).
The pandemic had heightened the need for this: ‘Especially with COVID the sense of the stress on the wards that’s quite sad to see’ (eN8).
The non-judgemental delivery of the findings and subsequent recommendations was also valued: ‘the face-to-face thing isn’t somebody telling you off or judging you, or giving you set goals’ (P16).
This quote summarises the positive feedback well: ‘I felt like it was exactly what I needed at that time, and I am thankful that I did partake in it’ (P11).
Dissatisfaction with the content
A number of participants did, however, describe the intervention as being like a staff audit, rather than a tool for improving health:
I think the main reason was that we’re in this pandemic and we wanted to get out of it, and I think the main point was that what can we do to get ourselves out of this situation quickly, or what can we do to help.
P15
It was basically more of a data input.
P22
A number also expressed disappointment that they had not been entitled to a blood test. This appeared to have been exacerbated by the fact that the well-being clinic run prior to the COVID-19 pandemic at this site had offered the same blood tests to all attendees, regardless of age or risk factors: ‘My dad is diabetic, so I thought maybe they would screen me for that’ (P13).
Some also felt that the mental health screening did not reflect their perception of their own mental health and had expected to be able to freely share their work-related concerns in the appointment, rather than being restricted to a computerised questionnaire:
I did a questionnaire with regards to my mood, with regards to my depression and things, that came back okay, which I was quite surprised about because during that time I was really struggling … So I was quite surprised by those results.
P20
Another said: ‘I can’t say it told me anything I didn’t know’ (P16).
One trial participant also pointed out that it would be useful to include substance misuse in the screening.
Concern was expressed by some, that despite eTHOS revealing health conditions, the underlying issues such as workload may not be addressed:
There’s not enough staff on the ground level doing the job, and people make choices like you’re going to have more coffee or more sugary drinks to stay awake to keep going, to push through, because it’s quick, it’s easy, it gives you a boost … I stress eat when I get to work, so as soon as I sit down … and start checking my e-mails, that’s when I open a packet of crisps.
P21
The problem is there’s things you can’t control, things you can control it’s fine, the stress is fine you can go a way round and you can do that, but unfortunately the ship is sinking and you are bailing it out.
P22
Concern was also expressed that knowledge of health issues could exacerbate anxieties: ‘It can also be a bit of a burden as well and possibly pull up things that you don’t necessarily need or want to know about, could be coincidental findings’ (P5).
Interestingly, very few of the trial participants actually expressed dissatisfaction with their experience of the intervention tool itself, and only one stated that they would not recommend it.
Summary: intervention acceptability
There was much gratitude regarding the opportunity to participate in the intervention, particularly in the light of COVID-19, the experiences of which prompted a demand for mental health screening tools addressing work-related stress. However, some participants also had expectations that went beyond the scope of what screening tools can offer.
Motivation to participate
When participants were asked why they had signed up for the study, there was repeated reference to the barriers they faced when trying to get appointments with their GP. Trial participants explained how difficult it was trying to contact and arrange GP appointments around their shifts. The intervention was therefore seen as a welcome alternative to contacting the GP:
One morning I was coming out of work I decide to phone [for a GP appt] as soon as I leave the building, and I walk home, which is half an hour, and maybe two minutes after reaching [home] then somebody was there, I was 90 something in queue … to speak to a practice nurse, and you couldn’t get appointment … so that’s exactly why I don’t really go to the doctor very often.
P2
It seemed that some trial participants also signed up for the study because they expected to be able to access support more quickly through this route: ‘They think they come in here because they are going to get some sort of fast track treatment’ (RN5).
For some, there was also a reluctance to see their GP unless it was really urgent.
I am not a GP person, I tend not to go to GPs. I fully appreciate how busy they are and the importance of the work they do so I do tend to self-remedy if there is anything problematic, I certainly haven’t been to my GP with neck, shoulder and back pain because I know exactly what they are going to tell me to do anyway, go to a physio, so I haven’t bothered them.
P11
However, these obstacles to attending the GP may have resulted in some participants having unrealistic expectations about what the screening involved. Some viewed it as equivalent to a GP appointment expecting to be examined or invited to set their own agenda for discussion: ‘There was no, “So what brought you here, what were you hoping to get out of this, what issues have you been having that prompted you to come?”’ (P10).
And some gave the impression that they viewed the intervention as an assessment of all aspects of their health, rather than one that was limited to the three specific components screened for:
I suffer with an underactive thyroid … and I thought well it would probably be a good thing to just have an update really and see what’s going on, and see if you guys, I don’t know, pick up anything that hadn’t been picked up.
P20
The irony of not having time to attend the GP was also highlighted: ‘Staff that say they’re too busy to go to the GP … but they call in sick’ (P14).
Finally, participants hoped that the data would be harnessed to justify elements of positive changes in the workplace:
To help the big managers realise it’s not just people moaning, that there is actual health things … some evidence behind it … You just feel like work is so busy nobody has got time to listen to your problems, you’ve just got to get on and do the job.
P27
Summary: motivation to participate
Key motivators for participation were the hope that the research would lead to positive changes in the workplace, and as an alternative to attending a GP appointment – particularly given the increased access issues within the pandemic.
Trial processes
Advertising/recruitment
The process of ward visits, posters, e-mails, reminders and for at least one site advertising on their disability network seems to have worked well: ‘It was everywhere at the time, and then it’s appealing to you’ (P28).
However, as one person pointed out, the visits made by the eTHOS nurses may have been more visible because of the general lack of visitors during COVID-19.
Trial participants raised the importance of getting recruitment material right, and that the e-mail subject line was critical. It was suggested that explaining that the meeting with the eTHOS Nurse would be non-judgemental: ‘Might be helpful to get some people on-board’ (P16).
Also, to emphasise that ALL are eligible as one member of staff who was new had initially assumed they would not be eligible.
Trial documentation and questionnaires
While the processes were considered to be: ‘Easy … very straightforward … explained well’ (P18).
They were also described as: ‘Long [but] doable’ (P15).
And staff seemed to be able to walk away and come back without being timed out. Participants were able to complete the documentation at their convenience during their working day, break time or time off.
While some felt they had probably not interpreted the questions correctly, others felt that they were not ambiguous:
Different people might answer the questions differently I believe, so there’s no benchmark … it seems to be that … the noisier ones are probably going to be … stressed, and the people that might actually be more stressed might not necessarily say they are.
P22
There was no questions that were ambiguous.
P24
A couple of participants were disappointed that the intervention’s audit-type nature, combined with being asked to complete it alone, made the experience feel quite impersonal:
Then you go and sit at a computer and then [the eTHOS nurse] leaves the room … maybe it’s a little bit impersonal, maybe it would be better if the person was to ask, but then it would turn into a longer appointment.
P29
Summary: trial processes
The recruitment processes were largely visible (although this may have been skewed by COVID-19) and accessible, and questionnaires, although long, were manageable. Suggestions were made about changing the content and delivery of the tool itself.
Usual care arm
Contamination
We explored whether or not participants in the usual care group had been prompted to make any lifestyle changes, perhaps as a result of participants in the intervention arm sharing information with them. None of the control participants interviewed reported having made any lifestyle changes or booked any medical appointments following their randomisation.
Knowing that we would not be able to complete the planned follow-up, we also asked intervention arm participants if they had discussed the intervention with colleagues. No one reported any such discussions going beyond a recommendation to sign up for the trial.
Acceptability
There was disappointment amongst the control arm participants about not having been offered the intervention: ‘I am a bit concerned I didn’t go [to the intervention]’ (P1).
And a number of intervention participants expressed relief at not being randomised to the control: ‘I would have been gutted if I had been randomised to non-intervention, because I would have missed out on this’ (P13).
Wait-list control
After discussion with the qualitative oversight group, we asked participants about the acceptability of being offered the intervention once their trial follow-up had been completed. This was well received: ‘Really good idea’ (P19).
Although other respondents were more ambivalent about whether or not they would attend: ‘I think [I would attend]’ (P27).
Such an offer would obviously have an impact on the capacity of the eTHOS nurses, but this was not viewed by them as a problem.
Summary: usual care arm
There was no evidence of contamination. A future trial might consider a wait-list control.
Barriers and facilitators to attendance
Non-responders
A number of trial participants shared experiences demonstrating a lack of will to participate amongst other colleagues: ‘She didn’t want to be told what she already knew, whereas myself and my other colleague found it’s a positive … you will just get the group of people that you probably want to get not taking part’ (P12).
Clearly there is a need to explore ways in which the messaging around the screening could encourage engagement in this group of people. To further illustrate this, one participant explained the difficulty they have getting staff to complete the Trust annual feedback survey, even though staff have negative things they want to say:
The surveys, they send out paper copies if it’s not completed, and we find them in the staffroom six months down the line still not completed. So … no matter what you do you are never going to get everybody to look at it.
P30
One incentivisation suggested was remuneration or other similar reward.
Booking appointment
Feedback about the booking process was very positive; trial participants were pleased with the ‘ease’ and ‘speed’ of the process, they found it ‘flexible’ and the eTHOS nurses ‘accommodating’. While no complaints were expressed about line managers not supporting attendance, we found that minimising the impact the appointment had on the workplace was a common concern: ‘It was great having a seven o’clock in the morning appointment, I could just do it before I officially start’ (P5).
How this was achieved varied according to the trial participant’s role and the degree of control they had over their workload. Some diarised the appointment and were able to do so at the beginning of their working day, others were able to do so during their working day. Some attended before the beginning of their shift, for example, 7 a.m., others during their shifts with the agreement of their line manager. All participants selected appointments in the morning or early afternoon. There were reports of some line managers making shift adjustments to enable staff to attend: ‘I was lucky my manager said, “You can go, go and take half an hour off the ward,” … we’ll put you in an area where you don’t have to’ (P11).
However, eTHOS nurses from one of the sites had experience of one particular line manager requiring them to provide written confirmation that the trial participant had actually attended their appointment. In addition, one ward manager that we spoke to felt they would have to limit the release of staff to shift changeover times.
On a pragmatic note, when signing up, participants were asked to choose their preferred method of contact. Participants could not always remember which methods they had selected, one got confused by receiving e-mails to their personal and work accounts and others reported missing e-mails. If going to full trial, it may be of benefit to encourage participants to allow eTHOS nurses to use all methods of contact to make the appointment.
Release from duties – culture of attendance
The line managers who participated in the qualitative interviews were, not surprisingly, very proactive and viewed the need to release staff from the workplace as one of their responsibilities and that the impact on workload was inconsequential given the potential gains in terms of productivity from the reduction in absences, and happier staff. However, it was clear that this ethos was part of a mixed narrative. There was a clash between a culture oriented around having sufficient staff on duty for service delivery versus the theoretical knowledge that facilitating time off to prevent ill health was the best way to achieve this. One trial participant explained that there was no point having staff: ‘drag themselves in … and then not be any use’ (P16).
But in the same narrative, relating to presenteeism, explained that it was: ‘[a] nightmare [when they had a member of staff who was off sick] all the time … you always end up talking about the ones that really take the Mick and will be off for anything at all’ (P16).
We saw experiences of managers finding the dual role of staff care and workplace efficiency as a burden:
I am busy, I don’t check in with my staff as often as I should … you almost don’t want to ask them because you are scared because they are going to then be off sick, because then that’s more stress that’s piled onto you.
P8
Furthermore, the perception that sickness was a bad thing was reinforced by the organisation through actions like: ‘Being sent a letter by the chief exec congratulating me on my 100% attendance, which amused me greatly’ (P16).
Mental health, at times, appeared to be undervalued: ‘I have always felt that mental health is something that’s been quite undervalued and under looked with the NHS, there’s been a mentality of just, “Get on with it”’ (P23).
Interestingly, it was noted that we should be: ‘[t]alking about people’s well-being rather than their sickness’ (P16).
Another trial participant felt that if people were unable to attend during worktime that this may well be an indicator of problems in the workplace.
I would wonder why someone would want to come in on their day off … I wonder if that’s an indicator of them thinking well my manager said I can go, but I have to do it in my breaktime, so I would be looking into why would they want to come in and do it on their day off.
P10
An example of such a concern can be seen in P13’s quote on p. 63.
eTHOS nurses at one of the sites noted that ward staff were more likely to come in their own time and that busy, off-site staff, working office hours were unable to attend. eTHOS nurses at two of the other sites felt that most chose to come during working time, whereas at the fourth site, not all staff were allowed to do this.
The pandemic was described as putting more pressure than normal on staff and management to reduce waiting lists and attend work, even if sick, contributing to poorer mental health outcomes for NHS workers:
It’s hard with COVID but you just feel like if you’re not well you have still got to go to work because they need you, everybody is needed, everybody every minute, every extra hour, minute that you can give is just helpful. So just pressure from that really.
P27
Screening location
Although some trial participants said they would have been willing to travel, overall they said that being on-site made it easier to attend, that less travel time meant less time off work:
I have about an hour’s drive to get to work and so if I need a GP appointment then I need to be away from work for quite a period of time … and I’ve got friends and colleagues around that travel a long way … it’s [eTHOS] more convenient.
P19
Another important factor regarding location was familiarity: ‘It’s familiar surroundings, which can be comforting rather than being sent to some random primary care centre’ (P10).
One person particularly valued the fact that it was run by Trust nurses: ‘It’s okay having your GP and stuff, but having somebody that understands, that nurses as well, that work at the same Trust, that know what’s going on’ (P28).
Another said that with an initiative run by the Trust/NHS: ‘You ha[ve] got that expectation of trust if it’s something that’s done through the hospital rather than an external company’ (P30).
Echoing this, a number said that an offsite location would make it harder for some to fit into their day, especially if they were using public transport.
However, there were requests for more flexibility around site location. eTHOS Nurses at one of the sites reported that they had been asked if they might be able to take the clinic to a particular department. The nurses were happy to do so; however, the participants subsequently attended the clinic in its usual location. These eTHOS nurses also said that in theory they would have been happy to take the clinic to off-site participants too, but it would have potentially raised practical issues around insurance for using a car for work and transporting sharps, access to a quiet room and also mobile devices to use the screening tool along with access to the internet.
The eTHOS nurses also explained that not all off-site facilities have access to Trust transport to the main site, that staff would be unlikely to find parking at the main site and leaving their own place of work would probably mean losing that parking space. Review of the recruitment records completed by the eTHOS nurses revealed that one off-site location felt unable to participate in the trial because of ‘having to attend appointment through worktime’.
Suggestions about alternative locations are also reported in Reasons for not attending.
Summary: barriers and facilitators to attendance
Some staff from off-site locations were not able to attend the screening. A mobile service and flexible clinic times could help. The ability to attend during work time was harder for ward-based staff. There is tension between preventing future absenteeism and service delivery.
Reasons for not attending
No written feedback was received for those who did not attend their screening appointment. The two participants who agreed to be interviewed explained that multiple factors had prevented them from attending. One had been unable to attend their appointment or reschedule it because of sick leave. The other was unable to get away from work on the day of the scheduled appointment and could not reschedule due to annual leave followed by sick leave. Both would have liked to reschedule if the trial had not closed.
These participants did not live locally and the location of the clinic was a further barrier to them rescheduling. For one, an alternative place of their choosing would have been more acceptable. In addition, both made the unprompted suggestion that a virtual appointment (phone call or online) would have made attending easier: ‘Or like I say whether it could all be completed online or something like that, because that just gives another option to let people get involved with it’ (P30).
However, another participant recognised that, although some would not like this option, it potentially had additional advantages for some:
Everything is online. It’s easier to talk to someone online … some people find it easier to talk to a randomer on the computer about their life, then other people … might find it less caring if there’s not a human in the room with them. So I reckon that works both ways … It’s not like you’re telling someone they have got cancer or anything.
P21
Telehealth was also brought up by the service providers (physios and GPs). While the COVID-19 pandemic had provided an opportunity for people to recognise the benefits of telehealth, it had, at times, increased staff workload. And there are some things that are understandably very hard to assess virtually. At least one Trust had been unable to make sufficient investments in technology to facilitate telehealth.
Summary: reasons for not attending
Remote options might be considered to increase the convenience of attending screening.
Confidentiality
Trial participants on the whole expressed little concern about confidentiality in relation to screening. For some, there was a cultural expectation that confidentiality would be upheld by healthcare professionals during appointments, putting them at ease: ‘You’re dealing with people who have to have privacy at their heart all the time because they are dealing with patients and parents, so actually I didn’t even give that a second thought, no’ (P8).
Knowledge of research processes was also reported as reassurance that confidentiality will be upheld (a number of interviewees participated because they had previous experience of working in research):
Not really because I’ve done some research stuff before, like learning about research, so I knew that it wasn’t going to, they can’t just disclose stuff to my employer, and it was run by the university rather than my work, so I didn’t feel like there was going to be any repercussions or anything, like it was going to go in my file or anything like that.
P11
Good relationships with line managers were cited when rationalising a lack of concern about confidentiality:
But I have a really good relationship with my line manager and my team anyway, so we’re only a really small unit, so I don’t know if that makes a difference, there’s only 16 of us, so for me personally no, it wouldn’t.
P14
Line manager knowledge was not a requirement of eTHOS, something which appealed to a minority of employees, and was reported to be a positive of the intervention:
I think it’s very confidential, I think it’s the best way, because through occupational health, I got referral through occupational health, but my manager knew all about that, so she had the letter about it and what I told occupational health, so I don’t like that aspect of it. So I think I feel that this trial is very confidential, and you feel safe there.
P13
However, some participants felt that line manager knowledge and support for staff screening was key if changes to working conditions are to be made, to help resolve any health issues contributed to by the workplace:
I think your employer should know if there’s certain things that have been found in a health check. I think that working for someone like the NHS is they are very hot on that stuff so if you do have even mental or physical issues I think there’s a lot in place that can help people.
P10
eTHOS nurses reported that in specific cases staff may be concerned or may feel uncomfortable with screening, if, for example, the screening nurse was managed by them:
We’ve got a proportion of people that are in that situation that they have half changed their mind because they have realised that it would be potential discussing with colleagues. My line manager, for example, half completed and then has stopped, so it may be that they don’t feel that it’s clinically appropriate or professionally appropriate.
eN6
Of the staff who decided to attend screening in their own time, only one reported doing so out of concerns for their privacy: ‘In intensive care I would also have had to have probably tell somebody where I am going and I didn’t want to have to explain I had an appointment, and it was easier to just do on my day off’ (P13).
Summary: confidentiality
Those unconcerned about confidentiality gave clear reasoning as to why this had not been a concern to them.
Role of occupational health
The role of occupational health tended to be summarised in contrast to the eTHOS intervention, as a service designed to tackle pre-existing issues:
Occupational health is there, but that’s more if you have issues, once the issue has actually arisen, as opposed to looking at preventative care in a screening and potentially getting you to change your lifestyle before things become problematic.
P12
Employee participants felt there were question marks over whether occupational health services would have the capacity to host health screening. Services were already perceived to be stretched: ‘Well I suppose I know from referring staff for occupational health appointments they are inundated and swamped, and whether they would be able to do that I don’t know’ (P16).
The current pandemic was seen to be exacerbating pressures on occupational health capacity:
Because of COVID there was a triage going on so getting seen by occupational health has been a job and a half, which COVID has had a lot to answer for left, right and centre hasn’t it? But it was a lot more difficult to get seen than it was previously, and they haven’t done a lot of referring to other places.
P19
A minority of staff reported dissatisfaction with previous occupational health engagement, with one interviewee reporting the workplace changes as being minimal, and another that they were obstructive:
They seem to moan and not want to turn up to stuff. I don’t know, I used to work at a different hospital and their occupational health seemed to be quite good, whereas the one at this Trust, I just think it’s, ‘Stay away,’ they don’t see very caring towards staff … they are just obstructive sometimes.
P21
The lack of need to be referred by a line manager was seen by some interviewees as a benefit to eTHOS, concerns were raised with regard to personal health issues being shared by others in the workplace (P13 on p 62) and negatively impacting future job applications:
One of the things would be depends who it [the screening] was run by and their perception of the confidentiality and whether it would then go against them say if they were going to apply for another job later down the line [e.g. because of] back pain.
P11
However, interviewees did not specifically raise a lack of confidentiality as a reason to avoid occupational health referral. The majority of interviewees reported a good relationship with their line manager and had no concerns about personal health data being shared with them specifically: ‘No, I don’t think so. I am quite open with my manager anyway’ (P27).
The eTHOS nurses at one of the sites felt that staff were fully aware of and how to get an occupational health referral. However, this was not necessarily the case: ‘I wouldn’t know how to contact them to be honest. I tried to contact them to rearrange an appointment or something and I couldn’t find the number, and it’s really difficult’ (P28).
Those at the other sites did not comment and were not directly asked. eTHOS nurses (in contrast to trial participants) reported that some participants did not want occupational health referrals in the context of explaining that line managers would be informed of such a referral:
I have had a couple of the questions have been, ‘Do you want me to refer you to occupational health?’ And then there’s this spiel about if we refer you to occupational health your manager will be informed and can access what is said, and they haven’t wanted to.
eN1
Summary: role of occupational health
There was a perception that occupational health was limited to established health problems, particularly those arising from a work-related injury, rather than screening, preventing, supporting or enabling staff. Some participants declined referral to occupational health where it was indicated due to their line manager being notified.
Response to referral recommendations
The types of referrals and recommendations that participants might have received are described in Intervention arm. As we were unable to collect 6-month follow-up data to assess uptake of referral recommendations, we explored this in depth in the qualitative interviews.
Positive feedback
Results were reported to be received in a timely fashion, and were in a clear and accessible format, for the majority of trial participants in the intervention arm:
Yes. So they were really good … my cholesterol results came later and then they put that in the report that got sent home. So I got that very quickly really, I think it was within a week to ten days I got that report, so it was really good.
P3
Referrals were largely well received by participants. The majority of those recommended to seek a referral, or signposted towards resources (services or information), reported actively following these up: ‘She give me the healthy eating and stuff, then she asked me to follow that, and that she gave me the link as well … I have tried to cut down the few stuff’ (P26).
Trial participants agreed that well-being resources had improved in response to the pandemic, thus aiding the ability to action screening recommendations:
And the pandemic, I mean … there was quite a big shift really in how management were treating the staff in terms of all of a sudden there was all this talk about resources and, ‘You can share your concerns,’ and things, and share, you know … health issues if you’re stressed etc.
P12
In one case, screening tool results were perceived as the validation needed to gain the confidence to access GP services:
I was scoring quite high on the anxiety and depression scales, so they did advise me to go to my GP, which gave me the confidence that okay maybe I actually do feel this … it gave me a reason to access.
P11
While there were some systems and initiatives in place to support staff, there was limited awareness of them. Staff reported being signposted to resources they previously had no awareness of: ‘I was given lots of information about things that I can access that I wouldn’t have known about before’ (P29).
This perspective was mirrored by eTHOS nurse feedback: ‘Nobody had ever heard of the Live Well app previously, so they seem to have gone away with something useful’ (eN1).
Raising staff awareness of internal initiatives and services, therefore, was an additional benefit for those randomised to the intervention arm of eTHOS. However, despite some leaflets being provided by the trials’ unit, eNs also obtained their own leaflets, for example, details about local services. Therefore, it should be noted that the services available to participants will have varied from site to site.
The screening process itself was perceived to act as an impetus or incentive to improve the healthiness of one’s lifestyle. A typical response was to frame conversations at screening as ‘getting the alarm bells ringing’:
After having the blood results … it made me think … I sat down and I spoke to my husband about it, and my husband said, ‘Look, this is a bit of an alarm, it does ring alarm bells, and I would quite like to have you here for the next 40 years not the next 20 or 30,’ and I thought I need to do this for me.
P20
Some respondents discussed the pandemic negatively influencing their health, reporting stress at work as impacting their lifestyle:
Monday to Thursday I would never have alcohol at home, but during the pandemic I slipped into a habit of if it had been a particularly stressful day or whatever that sitting in the garden at home and having a G&T, and it was because you couldn’t go and do anything else when we were in full lockdown. So I slipped into that habit, and I’ve stopped doing that again now.
P7
Receiving the health screening intervention was reported to act as a motivator to go back to pre-pandemic lifestyles. In the case of P7, the act of open conversation itself was of therapeutic value, and was perceived as helping them process their raised alcohol consumption:
So I think going to speak to someone, although I knew that I had got into a habit of doing that, I think saying it out loud to someone and then them saying back about what units are and stuff was really helpful, because it just makes it feel a bit real then. So that definitely helped prompt me to say right okay I don’t feel the need to do that anymore.
P7
eTHOS nurses similarly reported feeling the intervention helped trial participants get back on track with healthy lifestyle choices: ‘Most people seem to know what they should be doing and will join things like Weight Watchers, so it’s just hoping that this will give them a bit of a nudge in the right direction’ (eN8).
A number of interviewees disclosed concerns about their mental health. A minority of these interviewees received a referral to a specific service designed to enable fast access to counselling for patient-facing clinical staff: ‘Frontline19’. The experience of referral to Frontline19 was reported in glowing terms by interviewees. It was reported as reducing the waiting time for an appointment, and critically, as preventing mental health from reaching a crisis point, as a result of this reduction:
It [Frontline19] was great, amazing, anything was better than waiting nine months for an NHS referral … come September when I have got the actual NHS one … I think I probably would have spiralled out of control probably by this appointment.
P13
At least one site found themselves having to ask the PI to contact participants’ GPs because of their suicide risk but no one needed to take any of the participants to the accident and emergency department for immediate treatment:
I think the twice that we have done it [contacted the GP directly] was in that severe depression. The one girl had actually stated some suicidal thoughts so that was really quite important I think. Then the other one I think was at a level where she hadn’t got the motivation, she was so depressed, to do anything. So I think in some circumstances it is necessary. But on the whole I think it’s like the referrals for physio, I think it’s good for people to self-care and do it themselves, and it is them that’s going to make the appointment.
eN8
Finally, an important point to note is that just because someone has declined a GP appointment does not mean that they are ignoring the issues identified; their preferred mode of treatment may simply differ from options listed in the screening tool:
I haven’t gone to see my GP, my GP hasn’t contacted me. [I’ve] put … my own coping strategies in place … when I go to bed I use things like lavender spray, I use things like meditation things on my phone … when I go to sleep … I actively think of good memories to push [the bad memories] away, … doing Joe Wicks body app thing, … eating healthier … I don’t want to be someone that’s on the medication long term.
P29
Negative feedback
Despite the majority of participants suggesting that results were explained clearly, in two cases, participants demonstrated a lack of understanding regarding the outcome of screening: ‘I think it’s basically it would have been to go to maybe occupational health I would imagine, so a referral maybe for that, but I don’t think there was anything else’ (P22).
A minority of trial participants in the qualitative substudy who received a referral suggested they were yet to take up the advice given or utilise the resources they were signposted to. Barriers to lifestyle changes were perceived. These included a busy working life, parental responsibilities and a lack of motivation:
Personally having children and a really busy work life, and I work fulltime, it’s almost impossible to join a gym or to find time … I know I can do something about it, and I do when I feel like it.
P21
Constraints were also perceived to exist preventing coping strategies recommended within the workplace from being implemented:
A lot of the things are not possible, like in the bulletin it says go for a walk on your lunchbreak and things like that, but we often just have time to eat and that’s it, so in an ideal world it’s lovely, but practicalities is a bit difficult isn’t it?
P24
Interviewees tended to report not following up on an issue if they felt it was minor, they could manage their issues without further advice or they did not feel their issue was a cause for concern:
I don’t feel like I need any input. It was the first time that I had experienced anything like that, but managed it myself really, and as things have progressed naturally with the pandemic that has subsided … it’s very mild anxiety, and it was definitely triggered from things like death rates and changes in the hospital and things like that.
P7
Some participants reported dissatisfaction with the range of resources offered at screening, suggesting support with the implementation of lifestyle changes was what was needed, rather than advice or educational materials:
I am just wondering if anything else could be offered. I am not sure in what form, but the more the better really … I was given the sheet on healthy eating and balanced diet … perhaps are there any support groups or local … because I think being in healthcare … we’re aware of what we should do, it’s actually doing it that’s the problem.
P24
Indeed, a common concern was that there was: ‘No service provision … just a recommendation’ (P9).
There was confusion with one of the GP referrals where locally the phrase ‘local weight reduction management services’ used in the GP letter equates to: ‘Weight management service, which is the referral pathway for people who are considering bariatric surgery’ (GP1).
The GP therefore interpreted the results letter as a request to refer the patient for bariatric surgery, but this was not what the patient wanted. However, the GP confirmed that it was probably not necessary to change the wording as this was a local issue only.
This was reflected by one eTHOS nurse who suggested that some participants were difficult to refer, either due to multiple health issues or due to a refusal to engage in with GP services:
One was difficult last week because she didn’t want antidepressants, she didn’t want us to refer to the GP, so I was trying to talk through that with her. I am actually going to email my PI just to double check that I did the right things for her.
eN8
One participant expressed concern, not for themselves, but hypothetically, that access to in-house physio might be delayed by a line manager’s lack of time to complete the occupational health referral. This highlighted the range of different referral routes within the trial. At two of the sites, staff could contact their physio department directly, whereas at another site, physio was accessed through the occupational health department. Similarly, some eTHOS nurses reported a level of cynicism from trial participants around GP and occupational health referral, suggesting that some staff felt it was not worth attending, in part, due to waiting times for services:
I think I have had a few people talk about eTHOS and I’ve had a slight roll of the eyes of, ‘Oh yeah, I know about that. … What’s the point of going to occupational health, or whatever? There’s no point going to your GP because you are just going to get fobbed off, you’re going to wait a year for some physio’.
eN6
Summary: response to referral recommendations
Participants had, in the main, responded well to the recommendations. However, some concerns about referral pathways were raised, and barriers to lifestyle changes identified.
Enhancing the Health of National Health Service Staff nurses
The four sites are described in Table 1; one used a room in a different part of the hospital from the clinical research facility (CRF) and had difficulty with the internet connection there. Another site ran the clinic from the occupational health department – those in the qualitative study who attended the screening here had no concerns about its location and felt that it was logical. All locations entailed a walk away from participants’ workplaces. None of the attendees expressed any concerns about this.
In order to facilitate employee participation, one site agreed that participants could complete the screening tool prior to attending their appointment. Another gave them the option to complete it in a private room, without the nurse being present.
The eTHOS nurses seemed to be aware of participants’ job roles, no contextual differences in delivery of the intervention to different cadres of staff (e.g. healthcare professionals vs. ancillary staff) were mentioned.
Training
The training was described as ‘good’ (eN8) ‘fine’ (eN3), ‘great’ (eN2) and the eTHOS nurses had felt well supported throughout.
There were, however, things that might have made the delivery easier from the outset and which would be needed if going to full trial and being rolled out to new sites. The opportunity to practise on a ‘dummy’ participant as part of the training would have been highly valued. The importance of experience in delivering the intervention was also evidenced by the fact that support from colleagues who had been running the ‘Staff Well’ clinic was found by one site to have been ‘[v]ery useful’ (eN1).
These two sites seemed to have had less concerns than the two who had not been able to access such support. Training needs were exacerbated by the fact that the trial was paused shortly after training, during which time there were a lot of staff changes.
What was most needed was better preparation for communicating and managing high scores in the screening tools. This was most evident when communicating results relating to mental health, obesity and alcohol: ‘I didn’t find it difficult to explain, more [it was] … the emotive side … [that was] difficult to deliver rather than the explanation’ (eN5).
As eN5 trailed off, eN6 joined in saying:
Explaining that your cholesterol is potentially high because … your BMI is obese … and all of that it’s just an uncomfortable type of situation … It could be somebody a lot more senior than you, or a close colleague.
eN6
And from another site: ‘Some things I just didn’t know … especially when it’s all the mental health side of things I felt a bit out of my depth really’ (eN4).
It was suggested that a clear standard operating procedure might have been of benefit.
Equally important though was the need for a distress pathway to support the eTHOS nurses with the management of participants’ mental health concerns which were at times distressing, not just for the trial participants, but for the nurses delivering the intervention too:
‘The care for my team as well. This is an emotive topic, and they’re going to take on some of this’ (eN6).
Summary: training
While pauses due to COVID-19 had affected the eTHOS nurses, they were generally satisfied with the training, although making suggestions for improvement both to the training, support protocols and the database.
Acceptability of concept
Absenteeism was recognised as an important issue, and the intervention’s attempt to address this perceived as being a step in the right direction:
It is needed, there are massive issues even within small departments, and the impact it has, sickness rates, is phenomenal. We can see that in our own department, so if you take that on as the whole NHS it’s a massive problem.
eN6
Staff participating in the trial had reported to the eTHOS nurses that the intervention made them feel appreciated, seeing it as a way of the Trust demonstrating that they valued their staff: ‘They appreciate that the employer is doing something for them, so they can be able to get an assessment of their well-being at work’ [eN2 (from a different site to P18 p. 52)].
One of the eTHOS nurses also highlighted the irony that some private companies offer their staff annual health checks whereas the NHS does not, despite the need. It was also mentioned that for some employees, discussing their own health within their workplace was perceived as ‘taboo’; therefore, providing a staff space for them to do so was seen as a positive: ‘Some of these subjects are quite taboo … so if it’s raised with them and it’s there, they feel more comfortable to do that’ (eN5).
However, despite these positives, eTHOS nurses from some of the sites had important concerns about the intervention – that it fell short of what staff were expecting. These eTHOS nurses were concerned that they were not able to offer the information or services needed to truly help people:
I felt slightly embarrassed … that they have come with GAD scores of X amount and they are telling us that they have had suicidal thoughts for 20 years, and there’s still nothing that anybody can do, and I go, ‘Here’s a leaflet, thanks for your time.’ … we just feel like we’re just scratching the surface, and we’re putting another sticky plaster over a situation.
eN6
I could only offer what she already knew and what already didn’t meet her needs.
eN4 (from a different site)
We felt that these sentiments were crucial and have used the term ‘sticking plaster’ in our cross-cutting themes.
To further elaborate, examples of participant feedback were given and additional concern expressed that over time, this could result in a decline in staff interest in the intervention:
We’ve had participants say, ‘No I won’t take the leaflets because I’ve had all them ten times.’ … I think it just needs a lot of input … [or people will say], ‘Actually it’s not achieving anything, I wouldn’t bother going now we know that. What’s the point of going to occupational health, or whatever? There’s no point going to your GP because you are just going to get fobbed off, you’re going to wait a year for some physio.’
eN6
It was suggested that a more cost-effective way of achieving the intervention’s goals would be to: ‘Just [run] a good Well-being campaign within each Trust? … people could probably Google mental health services within your local area and find Healthy Minds for example’ (eN6).
In addition, when asked, the eTHOS nurses confirmed that there were also examples of workplace culture being behind health concerns:
I saw a woman this morning and she’s working 60 hours a week being paid 37½, … it’s not good for your health … it’s what’s expected, or her words were, ‘They don’t understand what we do, the executive level don’t understand how people are working, and what needs to be done.’
eN8
Summary: acceptability of concept
The eTHOS nurses agreed that there was a need for support with staff well-being; however, there were expectations from participants that went beyond the scope of what screening tools can offer in terms of staff referrals and addressing the root causes of staff ill health.
Intervention delivery experience
The eTHOS nurses talked favourably about the departmental visits, commenting on the importance of making pre-arranged appointments. However, sometimes it had been difficult to identify who was the most appropriate contact for each department; therefore, visits had been easier with those departments known to them. Wards had been less receptive than other departments due to the nature of their work making it difficult to leave the patients in their care.
On the other hand, the eTHOS nurses also described how the pandemic had complicated the study or made it more challenging. Changes to staff working patterns rendered recruitment problematic:
The recruitment I think is quite difficult going out and trying to encourage people to come in, been a bit, and whether that’s more to do with actually the time that we’re trying to do that with lockdowns and the staff redeployment, and then units reopening and then having a huge workload that they are trying to get people back in whilst also having staff shortages it has been quite difficult.
eN4
The forced postponement of eTHOS due to the pandemic was also reported to have reduced the momentum of the research:
The stopping and starting that we had because of COVID didn’t help, we half got going and then you would stop for a few months, and then we had to pick it back up again. So it’s going back to day one again, so that was also a challenge.
eN6
On a more positive note, eTHOS nurses from one site felt the pandemic had normalised research on wards due to the large amount of rapid response COVID-19 research being conducted, encouraging eTHOS participation:
I think research in general at the moment is very much in the news, and it’s very, they have been so used to seeing research nurses on the wards that we did go for COVID trials or whatever, had we done it pre-COVID.
eN1
The eTHOS nurses described the trial participants as ‘[f]orthcoming’ (eN2).
And they ‘[l]ove[d] the online consenting’ (eN1).
When it came to the actual delivery of the intervention, some of the eTHOS nurses considered it to be ‘[b]read and butter’ (eN6).
Whereas others found that as time went on and they obtained more experience it ‘[g]ot better’ (eN3).
For some there was a sense that the appointments sometimes needed ‘[p]ad[ding] out’ (eN1).
A varying, wide range of information and services were available at the different sites. The eTHOS nurses found that it was most useful to have gone through the information in advance so that they were familiar with their content and could then go through them with the participant.
While, on the one hand, having all the required responses available to read out from the database meant they could ‘[j]ust follow REDCap’ (eN4).
On the other hand, they also found it useful to paraphrase the text in the database: ‘You can just read it off the computer, off the database if you want, but that never feels particularly comfortable for me’ (eN8).
There were also occasions when the eTHOS nurses found the need to use clinical judgement which the database did not facilitate, that is, if there was an explanation for a participant’s high results negating the need for further intervention, for example, recent bereavement or bradycardia in a triathlete.
Finally, one site also had concerns about difficult disclosures relating to colleagues:
One of the nurses … was put in quite an uncomfortable situation, because they were talking about bullying and harassment that’s been going on in the workplace, and the participant was giving names of staff that the nurse works with, it’s not in [our unit], but … if you work here long enough there’s a good chance that you know quite a few people. So the nurse felt uncomfortable in that situation.
eN6
The eTHOS nurses also made a number of practical recommendations regarding changes that could be made to the study design, for example, database flow, process for signing off normal blood results details of which have been collated and filed for future reference.
Summary: intervention delivery experience
Some differences in the way the intervention was delivered across the sites suggests acceptability of several options including mobile delivery and within an occupational health department. Some database changes were suggested. Challenges with recruitment arose from the pandemic context.
Follow-on service providers
We made a number of attempts to contact Healthy Minds but were unable to identify anyone with whom we could discuss the trial. We did not contact smoking cessation services as the tight time frame within which we recruited gave little opportunity for participants to contact the service and it was still very unclear what services were available within the COVID-19 pandemic restrictions.
Instead, for pragmatic reasons, we asked trial participants interviewed in the qualitative substudy if they were happy for us to contact any provider that they had made direct contact with. Both the participants who had attended referral appointments with their GPs at the time of interview gave us the name of the GP that they had seen. One of these GPs responded to our subsequent request to arrange an interview.
In addition, we approached specific physiotherapists from each of the adult sites. Physiotherapists from two of the adult sites consented to participate in the qualitative substudy.
Acceptability of concept
The providers were, to varying degrees, supportive of the concept but it was recognised that its effectiveness would be limited by the extent to which staff engaged with it. But it was seen as a positive starting point: ‘Starts the conversation about lifestyle, and the majority of … staff … I see … are deconditioned’ (PT3).
It was pointed out that the intervention’s impact would depend on what exactly providers could offer: ‘So what I would say is there’s massive benefits if the screen tool is picking things up, that is then the availability of the services to provide that’ (PT2).
The need for physiotherapy with CBT is an example of potential issues around availability as not every site could offer such a service and where it was available, the capacity for referrals was limited. Limitations were also reported in relation to infrastructure, with gyms having been reassigned as ward space due the pandemic and with no imminent plans to restore them to their original use.
There was also concern about the intervention’s limitations. Although the physiotherapy departments had an in-house self-referral system for staff, the physiotherapists reported that they did not feel that there had been any extra service provision to support it.
As I said occ health, just seems, the referrals we get seems to grow and grow anyway without really any extra staff, and I think, I’m sure as everywhere in the NHS, we’re just being asked to do more with less people all the time.
PT1
In relation to organisational culture, one physiotherapist talked about the benefits of creating an environment where staff left the ward, ideally for a walk, for at least 15 minutes during their working day. This physiotherapist also viewed exercise prescriptions as being just as important as physiotherapy. In addition, it was pointed out that other organisations have dedicated physios for their staff.
Finally, there have been negative experiences in primary care of non-NHS screening programmes which have brought up ‘[i]ncidentalomas’ (GP1).
The GP explained that alarmed patients had presented with findings from private screening programmes such as a raised prostate-specific antigen (PSA) test or osteoarthritis which the GPs then had difficulty explaining to the patients as being not clinically relevant. This echoed concerns also expressed by participants.
Summary: acceptability of concept
As with the previous groups of participants, the service providers agreed that the intervention was important in meeting staff well-being needs; however, they too recognised the need for change not only across the NHS, but also within their own service areas in order to be able to support staff needs.
Impact on service
Each of the physiotherapy departments represented had self-referral systems in place for staff. Trial participants requiring physiotherapy accessed treatment using this system, that is, using the same referral route as staff not involved in the study. Therefore, the physiotherapists had no way of identifying which members of staff had been referred as a result of eTHOS’s screening process. However, neither reported any noticeable increase in referral rates. This is useful as one of the physio departments had previously expressed concern that they would not have capacity for any additional staff referrals and had suggested that referrals should be picked up by another site within the Trust.
We identified that the impact on GPs would vary depending on how many practices there were serving the local site, the size of such practices and the extent to which staff lived locally or commuted from surrounding areas. Another important factor was whether or not the hospital sites offered in-house or subcontracted services such as physiotherapy or mental health support. Therefore, the impacts would be greater on large practices in small communities where staff tended to live locally and the site had no in-house services.
The GP interviewed was from a practice that served a number of the interviewed trial participants. They had only become aware of the study because of confusion over a referral arising from eTHOS. None of the staff in the practice had remarked on an increase in referral rates from eTHOS or staff at the local hospital.
Summary: impact on service
Findings were limited by a very small number of staff interviewed, but there was no evidence of detrimental impact on their usual service through a large number of additional referrals from the trial.
Referral pathways
A challenge faced by both eTHOS nurses and GPs was that local services for weight management and smoking cessation change over time. Services, if available, are commissioned by the local authority that frequently contract the delivery and management to outside agencies. This means that providers change according to who has won the contract in the most recent round of bids. Other services (e.g. some slimming groups) are entirely private and may not have any links with statutory authorities; they may change time and location of sessions depending on availability of local representatives to run them. These factors were all compounded by the COVID-19 pandemic and staff not knowing what services were running within the current constraints, constraints which themselves were frequently changing:
We have … no access to dietician support for weight management locally … there are other referral pathways … like the health lifestyle trainers, which is through [names local leisure centre] which is the local council run gym, swimming pool etc., there has been historically. I don’t know how active it’s now, certainly back then, years ago, it was a very popular option, but I have heard very little, and whether that’s because things shutdown over COVID and haven’t got going again, or whether it’s just not been as well promoted recently I don’t know.
GP1
In addition, one of the sites was unaware that the in-house physiotherapy referral process had changed. During the physio interviews, we discovered that each site seemed to have a physiotherapist dedicated to staff referral. If the intervention went to full trial, actively involving these physiotherapists in setup would improve lines of communication between the staff delivering the intervention and the physiotherapy department.
Summary: referral pathways
The data highlight the fluidity of referral pathways and therefore the need to maintain close links with providers.
Outside agencies
We interviewed other NHS organisations, agencies providing services for the hospitals involved in the trial and healthcare and non-healthcare organisations unrelated to the NHS. Details of these agencies are summarised in Table 27.
Acceptability of concept
Outside agency respondents tended to report feeling that health screening would be a positive step to take that tackled absenteeism:
I thought the tool was good, and it’s much better than what happens with nurses at the minute, which is really just crisis management, once they go off sick then there’s some sort effort made to try and deal with it.
OA3
The health and well-being of staff were recognised as important to service quality in industries as diverse as health care and manufacturing:
If we don’t have a workforce that is healthy coming to work and are in a good place to do their work then none of the other stuff happens. So yes I think it’s hugely important. It’s a key direction of travel for us as a team … if we don’t get that bit right then the rest of it suffers.
OA10
The intervention was perceived to be particularly important in light of the pandemic:
I think with what’s going on in the world right now people need as many interventions as possible, and I think people overlook their general health, their musculoskeletal issues because they are dealing with dodging COVID or dealing with grief or stress. So I think it’s a fantastic idea.
OA11
Health screening was seen as an innovation to more traditional approaches to staff well-being, often characterised as ‘firefighting’:
We know that if we put more money into prevention we would spend less overall, as in do you know what I mean? But it’s a chicken and egg situation where we would describe ourselves I used the term this week we’re firefighting again at the moment.
OA9
Despite support for the screening intervention, screening was also perceived by some to place too much emphasis on the individual employee to enact change, when they may be powerless to establish a responsibility for workplace environmental adaptations or cultural change; something seen as a key causal mechanism of mental and physical health decline:
I believe that part of the mental health issues that nurses suffer in a hospital environment is due to the way that they are managed, but I thought the tools reflected that all of these issues were intrinsic rather than some of them being extrinsic … it felt a little bit like it was blaming the nurse for the position that they have got in, whereas the reality is that the nurses quite often will say there’s job pressure, there’s time pressures, but I am not always respected or treated very well, I feel that I have to work without supervision or above the level that I feel competent. But that wasn’t really reflected in the process … it seemed like somebody would present with a problem and the tool said to them it’s your problem, go away and sort it out, we’ll give you some help. It didn’t feel like there was that top down view where it says maybe we are causing part of that problem, what can we do to prevent it in the first place, rather than dealing with it once it manifested itself.
OA3
Referral pathways were also problematised. Instead of the onus being on GPs, it was felt internal NHS services should be accessible: ‘It really should flag straight to in-house, if hospitals have in-house referrals for physiotherapy or in-house counselling services rather than it being sent to a GP and GP then saying please can you sort this out’ (OA13).
Summary: acceptability of concept
Outside agencies largely echoed the findings from the preceding participants in relation to the importance of such an intervention, as well as the need to address the tension between staff well-being and service delivery and the potential limitations in referral pathways.
Feasibility of intervention delivery
Widespread, strong interest was reported in trial participation by outside agency respondents with respondents making offers to obtain support from key stakeholders:
Practice wise I would just need to run it past the practice manager, get her to be happy … if you want me to do that I am happy to. CCG wise I would have to take it to the chief exec of the CCG and probably HR, again happy to do that.
OA13
One outside agency offered data for comparison in way of support for the study:
One of the things that I might note is that whilst we might not be that useful for the trial, we do gather a lot of data about this sort of stuff … it might be that we can offer some useful contrasts or some comparisons, so we might add some value there where if you ask us for metrics we could perhaps give you equivalence from the private sector.
OA3
The vaccination roll-out was perceived to have demonstrated the feasibility of delivering healthcare provision on site at some outside agencies. One organisation was keen to build upon the momentum of the vaccine programme, feeling eTHOS represented a good opportunity to be ‘the next something’:
We have shown that we can put 4000 through a programme in a day, we can do some amazing things, so we know we can do it if we get the design right and if we hit that sweet spot the business is willing to release them from the line … we have a lot of goodwill with our trade union colleagues, they want to work with us, so we have got an engaged trade union and workforce ready to do something, we just need to present them with the next something, and I think we’ll get good engagement on that.
OA8
Challenges to trial success were reported to be largely practical, that is having to travel for screening appointments due to not being on site, or ensuring the study is visible to staff when they are rarely in a work building. This was particularly the case for agencies where staff perform a lot of remote working, such as community nursing and paramedics:
They [staff] don’t spend huge amounts of time on the hub. So we have got ways of dealing with that, but that is definitely a challenge, because we are not highly visible because they are not there if that makes sense?
OA10
People then have to travel because it’s not actually going to be based at their own base. So that then, so the model needs to be thought through in a dispersed organisation geographically, because face to face works really well in the big sites so that you could go to the dental hospital, you could go to [hospital], you could go to [hospital], there’s staff here at headquarters, there are a number of big sites, but there are lots of teams who have got the same needs who are based in very small health centres, and some of them may prefer this type of engagement.
OA1
The primary barrier was funding nurse time to deliver the intervention. Those employing clinical staff did not have capacity to run a trial without such funding:
We do have nurses doing occupational health work. The challenge is they are flat-out. I think what we learnt from some of these initiatives that we have already run is we can provide the facilities, we can provide the patient, what we really struggled to deliver was the actual clinicians.
OA8
Participants working in the provision of occupational health were concerned about short-term increases in demand for their services due to manager concerns around staff health and contamination:
Managers will become aware of something they weren’t before, and then might go right I need to know the advice, yes I am sure they are doing this research screening programme but I need to know how I manage them now, what are the impacts for how they are working. The only other thing is the expectation staff … who hear about it later will go, ‘I wish I had known about that, I will speak to occupational health, I will see what they are doing now.’
OA9
We explored with the one interviewed GP whether or not they would be interested in delivering the screening tool to NHS staff either as part of a RCT or as a funded service. The GP felt that their practice would be unlikely to have capacity for either, regardless of funding.
Summary: feasibility of intervention delivery
There was interest in supporting the trial, with the pandemic context making the trial more appealing to one non-healthcare setting. Issues for other organisations included capacity and, for those with staff working across multiple sites, delivery issues.
Cross-cutting themes
Through conducting interviews with a diverse range of participants and describing the data by the original objectives, we have identified four recurring cross-cutting themes arising from the data. These are summarised in Figure 7 and expanded upon below.
FIGURE 7.
Cross-cutting themes in the process evaluation.
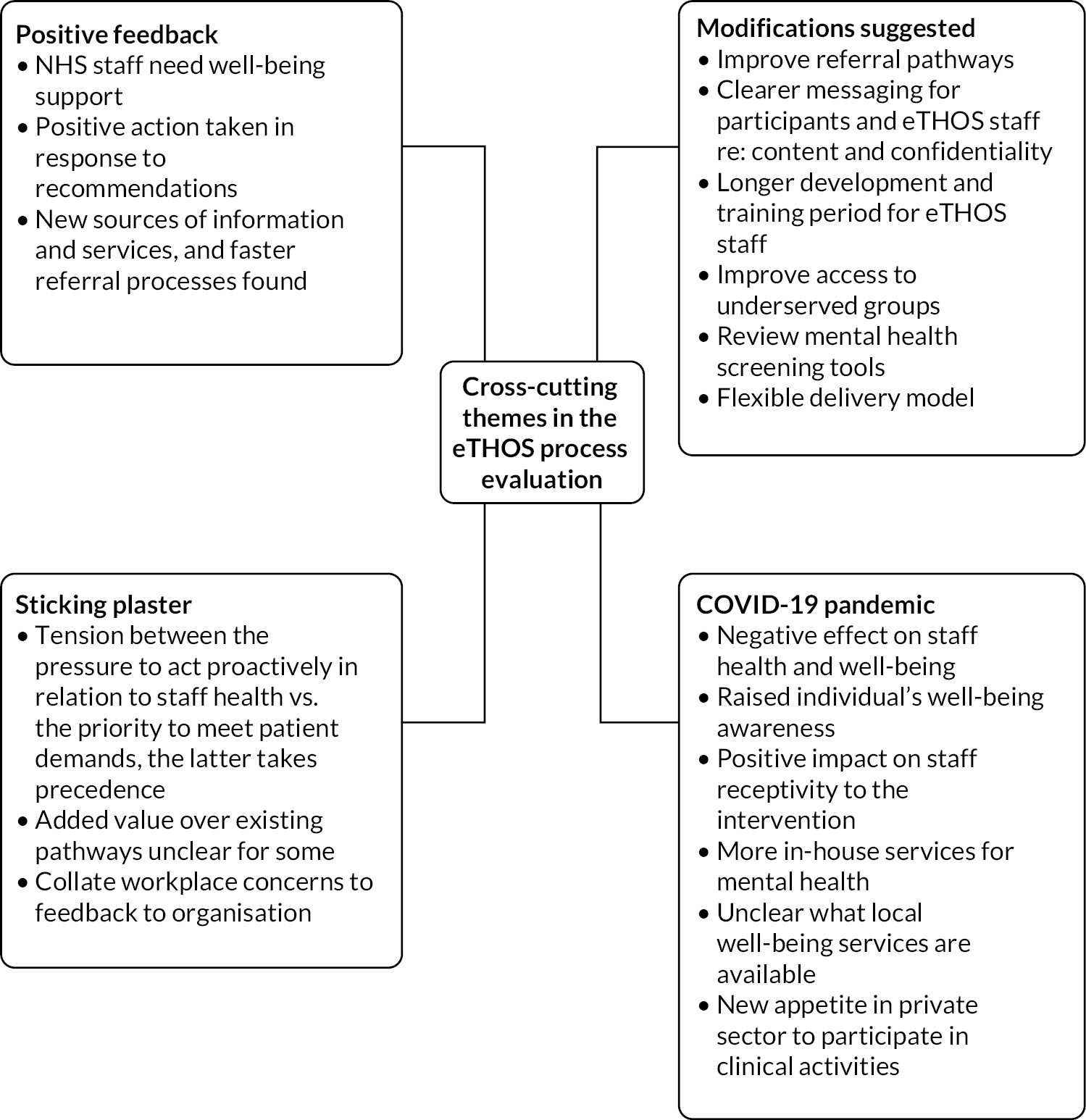
-
Positive feedback:
-
The findings overwhelmingly confirm that NHS staff need well-being support.
-
In principle, the intervention was welcomed.
-
There was evidence of participants taking positive action in response to the recommendations they had received.
-
Some found new sources of information and services which they had not been previously aware of. Faster referral processes were also found.
-
-
Modifications suggested:
-
There are a number of ways in which the study design and processes could be modified to:
-
- improve participant experience
-
- manage expectations
-
- offer more choice.
-
-
We may be reaching the self-aware and not the staff groups most in need.
-
-
Sticking plaster:
-
Well-being within the NHS is an increasingly important issue. The intervention being trialled here cannot resolve this by itself. Its limitations are comparable with those of other, similar tools, these limitations include:
-
- not providing direct referrals
-
- questions about the appropriateness of the measures being used
-
- recommendations not being suitable for people’s complex lives and workplace pressures.
-
-
There is discord within the NHS between the pressure to act proactively in relation to staff health versus the priority to meet service delivery demands, with the latter taking precedence. Without attempts to resolve these cultural issues the tool being trialled here could be accused of merely acting as a ‘sticking plaster’.
-
-
COVID-19 pandemic:
-
While the pandemic has had a substantial, negative effect on staff health and well-being, it has also served to raise individual’s awareness of their own well-being:
-
- These two factors have had a positive impact on staff receptiveness to the intervention – with this in mind consideration may be needed on how to maintain uptake of such a service should it be rolled out in the longer-term future.
-
-
The pandemic has also had a mixed effect on services – on the one hand, there were more services available to staff in relation to mental health, but, on the other, it was unclear what was currently available for things like smoking cessation and weight management.
-
Finally, we found a new appetite within non-healthcare-related organisations for delivering large-scale health interventions that would not previously have been considered achievable.
-
Chapter 5 Discussion and conclusions
Discussion
Key findings
Primary outcomes
Despite significant disruption and delays (and early trial closure) due to the COVID-19 pandemic, we have shown that it is feasible to recruit participants to and deliver a RCT of an NHS hospital SHSC. We have shown that there is both a clinical need (as evidenced by 48% screened attendees requiring referrals) and an enthusiasm for such a service (findings from the qualitative data), which has heightened since the start of the pandemic. While recruitment rates of 8.3% of those invited were lower than anticipated, this is offset by the fact that 48.3% of those randomised to the screening intervention group were eligible for a follow-up appointment for further diagnostic tests and appropriate management with either their GP (81%), mental health (18%) or physiotherapy services (30%). Unfortunately, due to early trial closure, it was not possible to determine whether those referred onward attended their appointments, but we ascertained that 31.6% intended to do so. Collectively, the three stop/go criteria were red, green and amber; therefore, the TOC recommended that a full-scale trial should proceed, but with modifications (see below) to adapt to local context and adopt processes to engage better with underserved communities, to improve both reach and effectiveness for the full-scale trial.
Recruitment and generalisability
We were able to recruit quickly to the trial, achieving two-thirds of our original target recruitment of n = 480 largely within less than 4 months, by applying flexible strategies to increase invitations where needed, while maintaining a representative sampling frame. The vast majority of participants were recruited using e-mail, with online consent and data collection using their own devices. Although multiple approaches were used to engage with all groups of staff, representation of ethnic minority and lower paid staff needs addressing for the full trial in order to fully reach the most underserved groups.
Intervention delivery, acceptability and satisfaction
Four different hospital sites utilised a nurse-led electronic screening intervention with prompts and electronic data collection which was efficient and promoted good fidelity, although this was viewed as difficult to personalise at times by a few staff. This needs to be addressed with more training and guidance for the full trial. Participants appreciated the convenience of the onsite service and valued the time to focus on their own needs. However, some felt that it did not reflect or address their stress levels appropriately or meet their expectations in providing faster access to additional services, for example, physiotherapy or as an alternative to a standard GP appointment. There were also concerns that it would not address the wider determinants of ill health and problems in the workplace, that it was just a ‘sticking plaster’. eTHOS staff delivering the intervention generally found the delivery of the study feasible, although there were a number of suggestions from staff both delivering and receiving the intervention to adapt the approach for a full trial (see below).
Comparison with existing literature
While current smoking rates in our staff participants were slightly lower than other studies (8% vs. 10–12%),17,18 many more were overweight or obese – 69% compared with just over half found in other surveys of NHS staff. 17,18 Sixty-nine per cent were active or moderately active; this compares reasonably with the Public Health England data. 76 Sixteen per cent and 17% reported current symptoms of anxiety and depression with the screening tools, reflecting the impact of the COVID-19 pandemic observed in other published studies. 77 Just under 40% of those eligible reported ever having received an NHS health check, which is a little lower than the national average of 43.8% in 2019–20. 78
Our participants reported being absent for a mean of 10.5 days in the previous 12 months, although the HR records indicated this was higher at 13.2 days, more than previously reported literature and therefore reflecting increased rates during the pandemic. 79
Recruitment rates to our trial were less than expected, with 8% of those invited consenting to take part (6% finally randomised). These were lower than comparable studies pre pandemic,56 and may be reflective of the pressures of healthcare staff during the pandemic. However, it is well established that recruitment to trials of healthy adults is generally lower than that of participants with particular diseases and therefore our projections were probably optimistic. Consistent with other studies, recruitment rates were generally lower among those of minority ethnic groups, lower paid staff and those working nightshifts, a feature which requires addressing in a future full trial, but which should be easier post pandemic as more face-to-face opportunities will arise for recruitment.
Among those randomised to the screening intervention, there was a high need (i.e. those eligible) for onward referrals (48.3%), particularly to the GP (38.9%) and physiotherapist (14.4%). These are conservative figures as 14% of those randomised did not receive the intervention. Provisional acceptance of referrals was around one-third of those eligible.
Strengths and limitations
A major strength of our trial was the use of electronic data capture throughout the recruitment process, intervention delivery and outcome data collection. While more complex to develop, it minimised the need for face-to-face contact during the pandemic, reducing staff pressures for delivery and data entry and minimising risk of infection. Most participants entered the study directly through the trial website after receiving an e-mail from Trust systems. The electronic system also allowed for flexibility, as staff could participate during or outside work hours, and/or on their own devices if they wished. It is possible that a few staff would have been excluded from participating if we had not also had the option to complete consent and baseline data collection at the screening clinic, and optimisation of this method of recruitment needs to be considered for the full trial to ensure underserved groups with less access to Trust e-mails have the opportunity to participate.
Our electronically driven intervention also promoted high fidelity to the assessments and processes within the protocol, although some viewed this as being impersonal and lacking flexibility at times when there was clinical need. Despite the prompts, eTHOS nurses did not always feel it appropriate to state that they had referred (e.g. when they had encouraged self-referral), leading to some potential misclassification. Questionnaires were quite long, but they were thought to be largely manageable and completed well and used standard self-report questionnaire instruments.
While most people were prompted to join the trial via their work e-mail, our multifaceted trial promotion strategy improved recruitment as some were prompted through the posters, postal invitations and by word of mouth. Unfortunately, we found that recruitment was less successful within ethnic minority groups and lower paid workers, and this may have led to response bias affecting the assessment of health need or referrals required. Many of the face-to-face opportunities planned to promote the trial (daily briefings and staff rooms) were unavailable during the pandemic which may have impacted both on overall recruitment and participant demography. Our phased approach to sampling allowed us to invite participants in a way which was representative of the hospital population, but further work needs to be done to optimise engagement in those groups.
Because of the pressures of the pandemic, we were delayed in starting the trial, and therefore the majority of the recruitment and intervention delivery was compressed into a 6-month period, allowing little room for reflection and adaptation of methods. Despite this, recruitment was rapid and a large pool of available staff and flexible deployment of our phased plan meant that we could recruit two-thirds of our target in only 3 months. The time constraints and reduced availability of service staff and space available meant that both internal and external referrals to physiotherapy and mental health services, in particular, were more limited; smoking cessation and weight management services were already disrupted and GPs under pressure. As a consequence, referral pathways were not always clear. This situation is already improving and we will be able to recruit sites with good pathways in place for the full trial.
Due to early closure of the trial in response to the pandemic and funder timelines, we were unable to complete our planned follow-up in all participants and unable to fulfil the planned number of qualitative interviews, although the data retrieved were rich. Time frames and sampling for the interviews were suboptimal, and although broadly generalisable of trial participants, included more nurses than other groups. Limited follow-up also precluded assessment of some secondary outcomes including definitive trial effectiveness outcomes and likely data completeness. The final process of generation of referral letters could not be automated in the time frame but this will be addressed in future iterations of the database.
Aside from the practical problems, the COVID-19 pandemic completely altered the health, health service and research context. It is not clear how recruitment and clinical need might have been impacted; the pandemic raised the profile and culture of research amongst the healthcare staff population, but conversely may have contributed to research fatigue. The results of this feasibility study may not be fully generalisable to non-pandemic times but gives a good indicator about what can be achieved even under enormous pressure.
Generalisability
We conducted this feasibility trial in four different hospitals, but three were large teaching hospitals in central Birmingham, two of which were part of the same Trust. One of these (QEHB) had already run a similar pilot clinic and therefore there will be some lack of generalisability; performance of new Trusts in a larger trial might differ. However, the small rural hospital outperformed their recruitment targets and delivered the intervention similarly to the large urban hospitals.
Implications for research
Justification for full trial
Of the three interlinked stop–go criteria informing the decision to proceed to full trial, the first (recruitment) was in the red zone. The second (referrals required) was firmly in the green zone, reflecting the strong clinical need in the NHS staff population for health assessment, intervention and improvement. The third criterion (attendance at referrals) was in the amber zone, suggesting the need for modifications to optimise attendance at referral services. The TOC considered the balance of all three together, and in line with the pre-agreed criteria (if one or two of these criteria are red, consider whether adaptations are needed) recommended to proceed to full trial, but with modifications, paying attention to areas of the protocol which could boost recruitment overall and especially from the more underserved groups. Recruitment rates are likely to have been affected by the pandemic, but nonetheless, from speaking to staff, there was demonstrable enthusiasm and from the high referral rates, clear clinical need to provide a service to improve NHS staff health, which supports evaluation within a definitive RCT.
Implications/potential modifications for full-trial design
There was no evidence of contamination from discussions within the qualitative interviews; therefore, an individual RCT would remain the design of choice (compared to a cluster RCT), which will enable an achievable sample size for the definitive trial.
We conducted the trial in a range of different types of hospitals, including a large urban hospital with experience of a similar intervention, another without experience, a children’s hospital with different systems and services in place and a small rural hospital. This experience suggests that a range of other sites could be recruited for the definitive trial, and interviews with other healthcare and non-healthcare organisations indicated their interest too, where resources would allow. More flexible clinic times, and the provision of alternative options, could be explored for the full trial such as a mobile service and a greater range of out-of-hours appointments to improve inclusion.
It was also clear from interviews that many participants were wary of being involved with occupational health services, as they were viewed as lacking confidentiality (line managers are frequently informed) and a service for the benefit of the employer rather than the employee. While their role should perhaps be more preventive and provide health and well-being services such as eTHOS, a large cultural shift would be required for staff members to engage with a trial run by the occupational health department and therefore the definitive trial should not involve occupational health staff and run the risk of adversely impacting recruitment.
While our approach to recruitment was successful for many (most people responded to an e-mail), additional strategies would be needed to recruit the underserved groups, and specific minority staff network groups and leaders could be engaged in order to do so.
Messaging to potential participants needs to be clearer in order to reduce concerns about confidentiality, optimise recruitment and manage expectations. Those unconcerned about confidentiality gave clear reasoning as to why this had not been a concern to them; this information could be considered in the communication strategy for the definitive trial. Wait-list controls might also be a potential option to encourage people to participate. This could also aid trial retention.
Electronic data capture was considered convenient, but extra training and practice (e.g. role play) could be provided to ensure sufficient familiarity with the questions, improve the personalisation of how the assessment was delivered, address points of difficulty and gain an understanding of how best to deal with unforeseen issues (such as NHS staff members asking screening nurses medical questions or for additional information about lifestyle and risk), while maintaining fidelity to the intervention. Intervention delivery could be enhanced in general by more time for initial and refresher training to practice the screening intervention.
Consideration (on a site-by-site basis) of clearer referral pathways is important for the full trial, in order to optimise attendance at referrals and realise health outcomes. This could include exploring the possibility of direct referrals to in-house services such has physiotherapy or mental health support, or smoking cessation services where available, and ensuring sufficient capacity. Hospital physiotherapists interviewed suggested the potential for exercise prescriptions and the need to maintain close links internally and with outside authorities to keep abreast of changing referral pathways. For the full trial, we will ensure that we recruit sites with well-established and functioning referral pathways and local service availability, and work with staff in the Trusts to ensure visibility and buy-in of the trial by all relevant services.
Acknowledging the 25% dropout between consent and randomisation, the amount of data collected and length of questionnaires should be reviewed prior to a full trial. Further consideration should also be given to the mental health screening tools used, as qualitative interviews with staff revealed their concerns that occupational stress and burnout may not be adequately identified and treated.
There was no evidence from this study that self-reported absenteeism data could replace HR data as the potential primary outcome as correlation between the two was poor. While HR data are not always straightforward to obtain, it would be likely to be more accurate than self-report. There is also insufficient information to judge the feasibility of determining presenteeism outcomes, although the baseline presenteeism questionnaire showed good completion rates.
The resource use and cost data were relatively straightforward to collect using data from both the trial database and surveys/discussions with the eTHOS nurses at each site. These provided initial estimates of the cost of screening, although a more detailed site-by-site data collection would be required in a full trial, to allow presentation of the full range of clinic organisation scenarios.
Table 29 provides a summary of pros and cons of proceeding to a full trial.
| Domain | Pros | Cons |
|---|---|---|
| Setting |
|
|
| Recruitment and data collection |
|
|
| Clinical need/demand |
|
|
| Screening clinics and data collection |
|
|
| Generalisability |
|
|
Implications for other trials in similar settings and during a pandemic
The key finding of relevance to other trials in similar settings is the benefit of an electronically driven recruitment, intervention and data capture system, which is possible in such a large, well-organised occupational setting. It allowed us to recruit and collect data flexibly and easily under rapidly changing circumstances.
Additional research recommendations
Given the findings, in particular within the qualitative analyses, and the ongoing pressures within the NHS post COVID, the following are potential areas for further research:
-
better ways to engage and include underserved occupational groups in research and health promotion services
-
better methods to capture and measure workplace stress
-
exploration of the impact of working in the NHS on staff mental health and well-being
-
the interplay between workplace culture and sickness absenteeism/presenteeism, and development and evaluation of interventions to improve workplace culture
-
the prevalence and nature of presenteeism and the impact of presenteeism on NHS costs and patient care
-
the value of occupational health services and their role in health promotion and prevention of sickness absenteeism/presenteeism
-
effectiveness and cost effectiveness of onsite mental health and well-being services for NHS staff
-
development and evaluation of health screening interventions in non-healthcare settings.
Implications for practice
Enhancing the Health of NHS Staff was a feasibility trial and therefore there are no direct implications for practice until the full trial has been conducted. However, there are a number of observations which can be drawn from the data and the experience gained through this pilot.
First, that the health of NHS staff warrants attention, with nationally validated/supported screening tools identifying a high burden of previously undiagnosed poor health. Without intervention, this could have significant impact for the future NHS workforce, and therefore patient care.
Second, that NHS staff welcomed and valued the staff screening clinic. Although staff highlighted that the clinic could not address all of their concerns or the workplace challenges or cultures which might be exacerbating ill health, most agreed that the clinic focused on important aspects of ill health.
Third, it is possible to deliver a staff health clinic even within highly challenging clinical environments, such as during waves of a pandemic. This supports the deliverability of the clinic across diverse healthcare settings in more normal times.
Fourth, this trial had widespread support from NHS Trusts at executive board level, enabling its delivery when the NHS was faced with competing priorities and highlighting the value health organisations placed on our endeavour to improve NHS staff health. All three Trusts have asked to be part of the definitive study and others have expressed a strong interest. This also highlights the likelihood that a definitive study would be supported by national healthcare organisations and that any effective services adopted nationally.
Fifth, for the staff health clinic to be most effective, there must be clearly identified pathways for onward referrals, within a reasonable time frame. During the COVID-19 pandemic, there was a disconnect to community services such as counselling, physiotherapy, smoking cessation and weight management, although this situation is now improving. Rapid access to in-house services outside of our trial could potentially be considered by hospitals to address the clear needs identified within their staff population, supplemented by close relationships with community provision. A centrally funded service could potentially have a number of models, including a hub and spoke from larger hospitals.
Conclusions
Despite significant delays and amendments required due to the COVID-19 pandemic, we were able to assess the most important aspects of the feasibility of a RCT to evaluate the clinical and cost effectiveness of a novel hospital-based SHSC in reducing absenteeism and presenteeism. Recruitment was feasible in a short space of time, and delivery of the intervention was feasible, efficient and acceptable. Although a lower proportion of staff took part than anticipated, the screening assessments revealed significant health needs of NHS staff and thus collectively the findings support proceeding to full trial but with modifications to the study protocol. The pandemic has disproportionately impacted the health of healthcare workers, and this study has highlighted the enthusiasm and clinical need for such a service. With some suggested practical modifications, the reach and effectiveness of the intervention could be optimised.
Additional information
Acknowledgements
We would like to thank the patient advisory and stakeholder groups for their useful advice on study design, conduct and materials. Also, Antony Cobley who led the development of the Trust’s Well-being agenda and has provided HR support for the present study, and Sara Wood for her advice on occupational health procedures. The trial oversight committee, in addition to Rachel Jordan, are: Rod Taylor (University of Glasgow and University of Exeter), David Fishwick (University of Sheffield), Kate Dunn (Keele University), Chris Hyde (University of Exeter) and Alex Blackwell (Worcestershire Royal Hospital). We are also most grateful to Jonathan Hill and Paul Campbell from the School of Primary, Community and Social Care, Keele University for allowing us to use the STarT tools and their contributions to early discussions.
This study was delivered and supported by the NIHR Birmingham Clinical Research Facility (both the Adult and Children’s CRFs).
We are very grateful to all the individuals who consented to participate in our research: the NHS staff who participated in the trial itself, the eTHOS nurses, service providers, outside agencies and trial participants who contributed to the process evaluation. We are also grateful to the eTHOS nurses at each of the sites who facilitated and undertook data collection, and the HR business partners, workforce and health informatics staff at each of the sites who painstakingly supplied us with invitation lists, department summary data and anonymised sickness and absence data.
We also wish to thank members of our PPI and stakeholder groups, who provided thoughtful advice and discussion of findings, which helped us to better reflect service user perspectives in our work.
Contributions of authors
Rachel Adams (https://orcid.org/0000-0002-1798-3854) (Qualitative Research fellow) contributed to design of qualitative data collection, led and contributed to all aspects of qualitative data collection and analysis, managed outputs and led the write-up of the qualitative research.
Rachel E Jordan (https://orcid.org/0000-0002-0747-6883) (Professor of Epidemiology and Primary Care) is cochief investigator with particular interest in trial design and epidemiology. She conceived and designed the project, cowrote the application to secure the research funds from the NIHR, oversaw day-to-day work on design, set-up, data collection and analysis, and cowrote and co-ordinated write-up and other outputs.
Alisha Maher (https://orcid.org/0000-0002-9738-2935) (Medical Statistician) contributed to the running of the pilot trial, undertook the statistical analysis and contributed to the writing of Chapter 3.
Peymane Adab (https://orcid.org/0000-0001-9087-3945) (Professor of Chronic Disease Epidemiology and Public Health) supported co-PIs with trials’ design and epidemiology, contributing to the application, study design, overall analysis and write-up and oversight of the qualitative study.
Timothy Barrett (https://orcid.org/0000-0002-6873-0750) (Leonard Parsons Professor of Paediatrics and Child Health) is the subinvestigator for Birmingham Women’s and Children’s Hospital, contributed to the application, study design and progress reviews at collaborators’ meetings with particular attention to clinical aspects including application to a site concerned with Children’s Health.
Sheriden Bevan (https://orcid.org/0000-0002-0389-4412) (Senior Trial Manager) was the trial manager, leading set-up, day-to-day trial management and collection of trial data.
Lucy Cooper (https://orcid.org/0000-0003-2184-7908) (Clinical Research Advanced Nurse Practitioner) is the PI for Birmingham Women’s and Children’s Hospital, contributed to the application, study design and progress reviews at collaborators’ meetings with particular attention to clinical aspects including application to a site concerned with Children’s Health.
Ingrid DuRand (https://orcid.org/0000-0002-1146-2687) (Respiratory Consultant) is the PI at Hereford Hospital, contributed to the application, study design and progress reviews at collaborators’ meetings with particular attention to clinical aspects including application to a rural site.
Florence Edwards (https://orcid.org/0000-0002-3330-1972) (Intern) conducted economic evaluation, drafting its write-up.
Pollyanna Hardy (https://orcid.org/0000-0003-2937-8368) (Senior Statistician) provided oversight of all initial statistical aspects, contributing to the application, study design, set-up and running of the trial.
Ciara Harris (https://orcid.org/0000-0002-8985-1359) (Chartered Physiotherapist and Qualitative Research Assistant) contributed to setup, data collection and analysis for the qualitative study with particular attention to the contribution of physiotherapists.
Nicola R Heneghan (https://orcid.org/0000-0001-7599-3674) (Senior Lecturer in Musculoskeletal Rehabilitation Sciences) contributed to the application, advised on design, progress reviews at collaborators’ meetings with particular attention to musculoskeletal screening and involvement of physiotherapists.
Kate Jolly (https://orcid.org/0000-0002-6224-2115) (Professor of Public Health and Primary Care) led the process evaluation, contributing to the application, study design, overall analysis and write-up and oversight of the qualitative study, also advising on trial design and epidemiology.
Sue Jowett (https://orcid.org/0000-0001-8936-3745) (Professor of Health Economics) led and oversaw all aspects of the economic evaluation contributing to the application, study design, overall analysis and write-up.
Tom Marshall (https://orcid.org/0000-0001-9277-5214) (Professor of Public Health and Primary Care) advised on health checks, contributing to the application, study design and progress reviews at collaborators’ meetings.
Margaret O’Hara (https://orcid.org/0000-0001-9812-5183) (Patient and Public Involvement and Engagement in Research Lead) advised on public and patient involvement and engagement (PPI), contributing to the application, study design and organisation of PPI meetings.
Christopher Poyner (https://orcid.org/0000-0001-6271-2626) (Qualitative Research Fellow) contributed to qualitative study data collection, analysis and write-up.
Kiran Rai (https://orcid.org/0000-0002-3250-0275) (Honorary Research Fellow) initially led qualitative study, contributed to oversight of the qualitative study.
Hugh Rickards (https://orcid.org/0000-0002-8678-5827) (Consultant in Neuropsychiatry, Honorary Reader in Neuropsychiatry) advised on mental health aspects, contributing to the application, study design and progress reviews at collaborators’ meetings.
Ruth Riley (https://orcid.org/0000-0001-8774-5344) (Lecturer in Applied Health Research) advised on the qualitative study, contributing to the application, qualitative study design and its oversight.
Natalie Ives (https://orcid.org/0000-0002-1664-7541) (Reader in Clinical Trials, Senior Statistician) contributed to the running of the pilot trial, provided oversight for the statistical analysis and contributed to the writing of Chapter 3.
Steven Sadhra (https://orcid.org/0000-0001-8829-0986) (Honorary Professor in Occupational Health) advised on workplace impact, workplace interventions for risk reduction, study design and progress reviews at collaborators’ meetings.
Sarah Tearne (https://orcid.org/0000-0001-7944-2917) (Trials Management Team Leader) provided oversight for trial management in the design stage.
Gareth Walters (https://orcid.org/0000-0002-7436-2261) (Consultant in Occupational Respiratory Medicine) is the PI for University Hospitals Birmingham NHS Foundation Trust with primary responsibility for Heartlands Hospital and contributed to the application, study design and progress reviews at collaborators’ meetings with particular attention to clinical aspects including application to a city-based site.
Elizabeth Sapey (https://orcid.org/0000-0003-3454-5482) (Professor, Consultant in Respiratory Medicine and General Internal Medicine) is cochief investigator with particular interest in clinical aspects and application to the primary adult site. She conceived and designed the project, cowrote the application to secure the research funds from the NIHR, oversaw study design, setup, data collection, analysis and write-up. Also acted as PI at QEHB.
All authors contributed to the study, revising the manuscript and approving the final version before submission.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/KDST3869.
Primary conflicts of interest: Peymane Adab has received research grants with payment made to the institute from NIHR, MRC, Yong Ning Pharmaceuticals Ltd Co. COLT Foundation and NIHR for grants awarded to RP-PG-0109-10061, RP-DG-1215-10002, 14/185/13, NIHR132630, 16/137/95, 17/128/04, 17/92/39 and NIHR129593. She has received travel and accommodation costs to attend NIHR Funding Committee and related meetings and travel, accommodation and honorarium to attend Irish Health Research Board Funding Committee. She is the Chair of TSC for NIHR Funded MapMe trial (2020–), Chair of TSC for NIHR funded Action 3:30 feasibility study (completed 2019), Chair of NIHR Funded Fellowship to evaluate HENRY (completed 2019) and a member of MRC-funded Natural Experiments Evaluations Project Oversight Group (ongoing) with no funding attached. She is a member of the Obesity Health Alliance Independent Obesity Strategy Working Group (2019–21) (unfunded), the Chair of NIHR Public Health Research Funding Committee (Institution payment), Deputy Director of NIHR School for Public Health Research (Institution payment), an output assessor for Panel A, subpanel 2 (Public Health, Health Services and Primary Care) in 2021 Research Excellence Framework (Personal payment) and a member of Wellcome Trust Early Career Advisory Group in Population and Public Health (Personal honorarium), a member of NIHR Palliative and End of Life Care Research Partnerships call panel, a member of NIHR/UKRI ‘Long COVID’ funding call panel (Research into the longer-term effects of COVID-19 in non-hospitalised individuals) and a member of NIHR COVID-19 Recovery and Learning Funding Committee. Timothy Barrett has received grants from the NIHR for grant awarded PGfAR NIHR 202358, MRC and LifeArc in the last 36 months. He has received honoraria as a member of the Novo Nordisk Global Expert Panel for childhood type 2 diabetes. Ingrid DuRand is an Associate Editor of Thorax. Pollyanna Hardy is a member of NIHR HTA Commissioning Board. Kate Jolly was a subcommittee chair of NIHR Programme Grants for Applied Health Research during the period of the grant. Rachel E Jordan has received research grants with payment made to the institute from NIHR and MRC. Sue Jowett has been a member of HTA Funding Committee Policy Group (formerly CSG) and HTA Evaluation and Trials Committee. Tom Marshall has been a member of Expert Panel for the Review of the NHS Health Check Programme 20 December–21 July with no payments received. Hugh Rickards has received consulting fees from Roche and Novartis for Advisory Boards and donated the fee to the Huntington’s Disease Association (England and Wales). He is the Physio for FND DMEC Chair, Commend (ACT in MND) DMEC Chair, the Chair of Huntington’s Disease Association board of trustees and the Chair of Chair of the UK Huntington’s disease network. Ruth Riley has received funding from the NIHR for grants awarded HSDR NIHR129341 and NIHR RfPB PB-PG-0418. Elizabeth Sapey has received grants from the Wellcome Trust, MRC, NIHR EME, NIHR HTA, HDR-UK, BLF, EPSRC and Alpha 1 Foundation in the last 36 months. She has been awarded honoraria for a lecture about COVID treatments (GSK), attended virtual conference at ERS 2020 (AstraZeneca), and participated advisory board for COPD (Boehringer Ingelheim).
BCTU staff contributing to the trial
Sheriden Bevan, Pollyanna Hardy, Nicholas Hilken, Natalie Ives, Alisha Maher, Catherine Moakes, William McKinnon, Gurmail Rai, Caroline Rick, Sarah Tearne, Kamila Ziomek.
Data-sharing statement
Data are available upon reasonable request. All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Ethics statement
The study has received ethical and research governance approval on 13 January 2020 through the IRAS process. Ref: IRAS261855.
Information governance statement
The University of Birmingham is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, the University of Birmingham is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here: https://www.birmingham.ac.uk/privacy.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the HSDR programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- NHS Digital . NHS Workforce Statistics, February 2021 England and Organisation 2021. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-workforce-statistics/february-2021 (accessed July 2021).
- NHS Employers . NHS Workforce Health and Wellbeing Framework 2019. www.nhsemployers.org/sites/default/files/media/NHS-Workforce-HWB%20Framework-updated-July-18_0.pdf (accessed February 2022).
- NHS Digital . NHS Sickness Absence Rates April 2009–March 2019 Annual Tables 2019. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-sickness-absence-rates/january-2019-to-march-2019-and-annual-summary-2010-11-to-2018-19 (accessed July 2021).
- NHS England . NHS Sickness Absence Rates October 2016 to December 2016 2017. www.content.digital.nhs.uk/catalogue/PUB23900 (accessed July 2018).
- Chartered Institute of Personnel and Development . Absence Management 2016 2016. www.cipd.co.uk/Images/absence-management_2016_tcm18-16360.pdf (accessed 12 September 2022).
- The Work Foundation, Aston Business School, RAND Europe . Health and Wellbeing of NHS Staff – A Benefit Evaluation Model 2009. https://rand.org/content/dam/rand/pubs/technical_reports/2009/RAND_TR758.pdf (accessed January 2023).
- Aiken LH, Clarke SP, Sloane DM, Lake ET, Cheney T. Effects of hospital care environment on patient mortality and nurse outcomes. J Nurs Adm 2008;38:223-9. https://doi.org/10.1097/01.NNA.0000312773.42352.d7.
- Pilette PC. Presenteeism in nursing: a clear and present danger to productivity. J Nurs Adm 2005;35:300-3. https://doi.org/10.1097/00005110-200506000-00006.
- Powell M, Dawson J, Topakas A, Durose J, Fewtrell C. Staff satisfaction and organisational performance: evidence from a longitudinal secondary analysis of the NHS staff survey and outcome data. Health Serv Deliv Res 2014;2:1-306. https://doi.org/10.3310/hsdr02500.
- Taunton RL, Kleinbeck SV, Stafford R, Woods CQ, Bott MJ. Patient outcomes: are they linked to registered nurse absenteeism, separation, or work load?. J Nurs Adm 1994;24:48-55.
- NHS . NHS Staff Survey National Results 2020. www.nhsstaffsurveys.com/results/national-results/ (accessed January 2022).
- van der Plaat DA, Edge R, Coggon D, van Tongeren M, Muiry R, Parsons V, et al. Impact of COVID-19 pandemic on sickness absence for mental ill health in National Health Service staff. BMJ Open 2021;11. https://doi.org/10.1136/bmjopen-2021-054533.
- Dew K. Pressure to work through periods of short term sickness. Br Med J 2011;342.
- Goetzel RZ, Long SR, Ozminkowski RJ, Hawkins K, Wang S, Lynch W. Health, absence, disability, and presenteeism cost estimates of certain physical and mental health conditions affecting US employers. J Occup Environ Med 2004;46:398-412.
- Rantanen I, Tuominen R. Relative magnitude of presenteeism and absenteeism and work-related factors affecting them among health care professionals. Int Arch Occup Environ Health 2011;84:225-30.
- Boorman S. NHS Health and Well-being. Final Report, November 2009. Leeds; 2009.
- Blake H, Mo PK, Lee S, Batt ME. Health in the NHS: lifestyle behaviours of hospital employees. Perspect Public Health 2012;132:213-5. https://doi.org/10.1177/1757913912457309.
- Mittal TK, Cleghorn CL, Cade JE, Barr S, Grove T, Bassett P, et al. A cross-sectional survey of cardiovascular health and lifestyle habits of hospital staff in the UK: do we look after ourselves?. Eur J Prev Cardiol 2018;25:543-50.
- Demou E, Smith S, Bhaskar A, Mackay DF, Brown J, Hunt K, et al. Evaluating sickness absence duration by musculoskeletal and mental health issues: a retrospective cohort study of Scottish healthcare workers. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-018085.
- NHS Digital . Sickness Absence Due to Mental Health Reasons 2010 and 2019 pq43100 2020. https://digital.nhs.uk/data-and-information/supplementary-information/2020/sickness-absence-due-to-mental-health-reasons-2010-and-2019_pq43100 (accessed July 2021).
- NHS Digital . NHS Sickness Absence by Reason 2020. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-sickness-absence-rates/july-2020 (accessed July 2018).
- NHS Digital . Reasons for Sickness Absence by Organisation Type April 2019 ah2935 2019. https://digital.nhs.uk/data-and-information/find-data-and-publications/supplementary-information/2019-supplementary-information-files/nhs-sickness-absence-rates-in-england-by-reason-and-organisation (accessed July 2021).
- Bielecky A, Chen C, Ibrahim S, Beaton DE, Mustard CA, Smith PM. The impact of co-morbid mental and physical disorders on presenteeism. Scand J Work Environ Health 2015;41:554-64. https://doi.org/10.5271/sjweh.3524.
- Cancelliere C, Cassidy JD, Ammendolia C, Côté P. Are workplace health promotion programs effective at improving presenteeism in workers? A systematic review and best evidence synthesis of the literature. BMC Public Health 2011;11:1-11.
- Christensen JR, Kongstad MB, Sjøgaard G, Søgaard K. Sickness presenteeism among health care workers and the effect of BMI, cardiorespiratory fitness, and muscle strength. J Occup Environ Med 2015;57:e146-52.
- Schultz AB, Edington DW. Employee health and presenteeism: a systematic review. J Occup Rehabil 2007;17:547-79. https://doi.org/10.1007/s10926-007-9096-x.
- Pit WS, Hansen V. The relationship between lifestyle, occupational health, and work-related factors with presenteeism amongst general practitioners. Arch Environ Occup Health 2016;71:49-56.
- NHS Digital . NHS Sickness Absence Rates January 2019 to March 2019 and Annual Summary 2010–11 to 2018–19 2019. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-sickness-absence-rates/january-2019-to-march-2019-and-annual-summary-2010-11-to-2018-19 (accessed July 2021).
- Office for National Statistics . Sickness Absence in the Labour Market: 2016. Analysis Describing Sickness Absence Rates of Workers in the UK Labour Market 2016. www.ons.gov.uk/employmentandlabourmarket/peopleinwork/labourproductivity/articles/sicknessabsenceinthelabourmarket/2016 (accessed July 2018).
- Admasachew L, Dawson J. The association between presenteeism and engagement of National Health Service staff. J Health Serv Res Policy 2011;16:29-33.
- Royal College of Physicians . Work and Wellbeing in the NHS: Why Staff Health Matters to Patient Care 2015.
- NHS England . Commissioning for Quality and Innovation (CQUIN). Guidance for 2016 17 2017. www.england.nhs.uk/wp-content/uploads/2016/03/cquin-guidance-16-17-v3.pdf (accessed July 2018).
- NHS . Online Display of NHS Health Check Official Statistics 2019. www.healthcheck.nhs.uk/commissioners_and_providers/data/ (accessed July 2021).
- NHS . £5 Million Plan to Improve the Health of NHS Staff 2015. https://www.england.nhs.uk/2015/09/improving-staff-health/ (accessed July 2018).
- Blake H, Gupta A, Javed M, Wood B, Knowles S, Coyne E, et al. COVID-well study: qualitative evaluation of supported wellbeing centres and psychological first aid for healthcare workers during the COVID-19 pandemic. Int J Environ Res Public Health 2021;18.
- Clarissa C, Quinn S, Stenhouse R. ‘Fix the issues at the coalface and mental wellbeing will be improved’: a framework analysis of frontline NHS staff experiences and use of health and wellbeing resources in a Scottish health board area during the COVID-19 pandemic. BMC Health Serv Res 2021;21:1-11.
- O’Connor EA, Whitlock EP, Beil TL, Gaynes BN. Screening for depression in adult patients in primary care settings: a systematic evidence review. Ann Intern Med 2009;151:793-80. https://doi.org/10.7326/0003-4819-151-11-200912010-00007.
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606-13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x.
- Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092-7. https://doi.org/10.1001/archinte.166.10.1092.
- National Institute for Health and Care Excellence . Common Mental Health Problems: Identification and Pathways to Care 2011. www.nice.org.uk/guidance/cg123 (accessed July 2018).
- Hill JC, Whitehurst DG, Lewis M, Bryan S, Dunn KM, Foster NE, et al. Comparison of stratified primary care management for low back pain with current best practice (STarT Back): a randomised controlled trial. Lancet 2011;378:1560-71. https://doi.org/10.1016/S0140-6736(11)60937-9.
- National Institute for Health and Care Excellence . Low Back Pain and Sciatica in Over 16s: Assessment and Management. 2020. www.nice.org.uk/guidance/ng59 (accessed July 2018).
- National Institute for Health and Care Excellence . Neck Pain – Cervical Radiculopathy 2018. https://cks.nice.org.uk/neck-pain-cervical-radiculopathy (accessed July 2018).
- National Institute for Health and Care Excellence . Neck Pain – Non-Specific 2018. https://cks.nice.org.uk/neck-pain-non-specific (accessed July 2018).
- National Institute for Health and Care Excellence . Shoulder Pain 2017. https://cks.nice.org.uk/topics/shoulder-pain/#!management (accessed July 2021).
- Dunn KM, Campbell P, Lewis M, Hill JC, van der Windt DA, Afolabi E, et al. Refinement and validation of a tool for stratifying patients with musculoskeletal pain. Eur J Pain 2021;25:2081-93.
- NHS Employers . Rapid Access to Treatment and Rehabilitation for NHS Staff 2016. www.nhsemployers.org/~/media/Employers/Documents/Retain%20and%20improve/Rapid%20access%20to%20treatment%20and%20rehabilitation%20for%20NHS%20staff%20v5.pdf (accessed July 2018).
- Public Health England . NHS Health Check Programme Standards 2014. www.healthcheck.nhs.uk/latest-news/nhs-health-check-programme-standards-launched/ (accessed July 2018).
- Hinde S, Bojke L, Richardson G, Retat L, Webber L. The cost-effectiveness of population Health Checks: have the NHS Health Checks been unfairly maligned?. J Public Health 2017;25:425-31.
- Robson J, Dostal I, Sheikh A, Eldridge S, Madurasinghe V, Griffiths C, et al. The NHS Health Check in England: an evaluation of the first 4 years. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-008840.
- Krogsbøll LT, Jørgensen KJ, Larsen CG, Gøtzsche PC. General health checks in adults for reducing morbidity and mortality from disease. Cochrane Database Syst Rev 2012;10.
- Blake H, Bennett E, Batt ME. Evaluation of occupational health checks for hospital employees. Int J Workplace Health Manag 2014;7:247-66. https://doi.org/10.1108/IJWHM-07-2013-0027.
- Bolier L, Ketelaar SM, Nieuwenhuijsen K, Smeets O, Gärtner FR, Sluiter JK. Workplace mental health promotion online to enhance well-being of nurses and allied health professionals: a cluster-randomized controlled trial. Internet Interv 2014;1:196-204.
- Dugdill L, Brettle A, Hulme C, McCluskey S, Long A. Workplace physical activity interventions: a systematic review. Int J Workplace Health Manag 2008;1:20-4. https://doi.org/10.1108/17538350810865578.
- Raine GA, Thomas S, Rodgers M, Wright K, Eastwood AJ. Workplace-based interventions to promote healthy lifestyles in the NHS workforce: a rapid scoping and evidence map. Health Serv Deliv Res 2020;8:1-82.
- Abbas SZ, Pollard TM, Wynn P, Learmonth A, Joyce K, Bambra C. The effectiveness of using the workplace to identify and address modifiable health risk factors in deprived populations. Occup Environ Med 2015;72:664-9.
- Groeneveld IF, Proper KI, van der Beek AJ, Hildebrandt VH, van Mechelen W. Lifestyle-focused interventions at the workplace to reduce the risk of cardiovascular disease – a systematic review. Scand J Work Environ Health 2010;36:202-15. https://doi.org/10.5271/sjweh.2891.
- Pereira MJ, Coombes BK, Comans TA, Johnston V. The impact of onsite workplace health-enhancing physical activity interventions on worker productivity: a systematic review. Occup Environ Med 2015;72:401-12. https://doi.org/10.1136/oemed-2014-102678.
- Arena R, Arnett DK, Terry PE, Li S, Isaac F, Mosca L, et al. The role of worksite health screening: a policy statement from the American Heart Association. Circulation 2014;130:719-34. https://doi.org/10.1161/CIR.0000000000000079.
- National Institute for Health and Care Excellence . Cardiovascular Disease: Risk Assessment and Reduction, Including Lipid Modification n.d. www.nice.org.uk/guidance/cg181 (accessed July 2018).
- NHS . Mindfulness n.d. www.nhs.uk/mental-health/self-help/tips-and-support/mindfulness/ (accessed July 2018).
- NHS Birmingham and Solihull Mental Health . Birmingham Healthy Minds – A Free IAPT Service for Depression and Anxiety n.d. www.bsmhft.nhs.uk/our-services/birmingham-healthy-minds/ (accessed July 2018).
- Linton SJ, Boersma K. Early identification of patients at risk of developing a persistent back problem: the predictive validity of the Örebro Musculoskeletal Pain Questionnaire. Clin J Pain 2003;19:80-6.
- Ahmad S, Harris T, Limb E, Kerry S, Victor C, Ekelund U, et al. Evaluation of reliability and validity of the General Practice Physical Activity Questionnaire (GPPAQ) in 60–74 year old primary care patients. BMC Fam Pract 2015;16. https://doi.org/10.1186/s12875-015-0324-8.
- Public Health England . Alcohol Use Disorders Identification Test Consumption (AUDIT C) n.d. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/684826/Alcohol_use_disorders_identification_test_for_consumption__AUDIT_C_.pdf (accessed July 2018).
- Hippisley-Cox J, Coupland C, Vinogradova Y, Robson J, Minhas R, Sheikh A, et al. Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ 2008;336:1475-82. https://doi.org/10.1136/bmj.39609.449676.25.
- Jordan RE, Adab P, Sitch A, Enocson A, Blissett D, Jowett S, et al. Targeted case finding for chronic obstructive pulmonary disease versus routine practice in primary care (TargetCOPD): a cluster-randomised controlled trial. Lancet Respir Med 2016;4:720-30. https://doi.org/10.1016/S2213-2600(16)30149-7.
- Adab P, Fitzmaurice DA, Dickens AP, Ayres JG, Buni H, Cooper BG, et al. Cohort profile: the Birmingham Chronic Obstructive Pulmonary Disease (COPD) cohort study. Int J Epidemiol 2017;46. https://doi.org/10.1093/ije/dyv350.
- Kessler R, McInnes K. World Health Organization Health and Work Performance Questionnaire (HPQ). HPQ Short Form (Absenteeism and Presenteeism Questions and Scoring Rules) Harvard Medical School 2007. www.hcp.med.harvard.edu/hpq/index.php (accessed July 2018).
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. https://doi.org/10.1007/s11136-011-9903-x.
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377-81. https://doi.org/10.1016/j.jbi.2008.08.010.
- Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. REDCap Consortium . The REDCap consortium: building an international community of software platform partners. J Biomed Inform 2019;95. https://doi.org/10.1016/j.jbi.2019.103208.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13:1-8.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2020. Canterbury: Personal Social Services Research Unit, University of Kent; 2020.
- van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 2012;15:708-15. https://doi.org/10.1016/j.jval.2012.02.008.
- Public Health England . Physical Activity: England 2020. https://fingertips.phe.org.uk/profile/physical-activity/data (accessed February 2022).
- De Kock JH, Latham HA, Leslie SJ, Grindle M, Munoz S-A, Ellis L, et al. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Public Health 2021;21:1-18.
- Public Health England . NHS Health Check: England 2020. https://fingertips.phe.org.uk/profile/nhs-health-check-detailed/data#page/4/gid/1938132726/pat/159/par/K02000001/ati/15/are/E92000001/iid/91735/age/219/sex/4/cat/-1/ctp/-1/yrr/1/cid/4/tbm/1 (accessed February 2022).
- NHS . NHS Sickness Absence Rates January to March 2021, and Annual Summary 2009 to 2021, Provisional Statistics 2021. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-sickness-absence-rates/march-2021-annual-summary-2009-to-2020 (accessed February 2022).
Appendix 1 List of protocol amendments
| Protocol amendments | ||||
|---|---|---|---|---|
| Amendment number | Date of amendment | Protocol version number | Type of amendment | Summary of amendment |
| The following amendments and/or administrative changes have been made to this protocol since the implementation of the first approved version. | ||||
| AM04 | 15 July 2020 | 2.0 | Substantial |
|
| AM08 | 21 April 2021 | 3.0 | Non-substantial |
|
| AM09 | 28 May 2021 | 4.0 | Non-substantial |
|
| AM11 | 25 October 2021 | 5.0 | Substantial |
|
Appendix 2 Outcome data at 26 weeks
| SHSC (N = 118) (%) | Control (N = 118) (%) | |
|---|---|---|
| Attended SHSC | 102 (86.4) | 0 (–) |
| Didn’t attend SHSC | 16 (13.6) | 118 (100.0) |
| SHSC arm | ||
| If attended SHSC, completed screening in full? | ||
| Yes (in full) | 101 (99.0) | – |
| No (partly completed) | 1 (1.0) | – |
| Completed screening in full by site | n = 101 | |
| QEHB | 48/61 (78.7) | – |
| Heartlands Hospital | 14/14 (100.0) | – |
| Birmingham Children’s Hospital | 16/18 (88.9) | – |
| Hereford Hospital | 23/25 (92.0) | – |
| SHSC (completed 26-week follow-up) (N = 4) | |
|---|---|
| Total referrals made (self-reported) | N = 2 (50%) |
| Referred to GP | 2 |
| Referred to local psychological services | 0 |
| Referred to physiotherapy | 0 |
| Of those referred, attended at least one service by 26 weeksa | 1 |
| Total appointments attended as a consequence of referral | N = 1/2 (50%) |
| Attended appointment with GP | 1 |
| Attended appointment with local psychological services | 0 |
| Attended appointment with physiotherapy | 0 |
| Baseline | 26 weeks | |||
|---|---|---|---|---|
| SHSC (N = 4) (%) | Control (N = 3) (%) | SHSC (N = 4) (%) | Control (N = 3) (%) | |
| GPPAQ | ||||
| Inactive | 1 (25.0) | 0 (–) | 0 (–) | 0 (–) |
| Moderately inactive | 0 (–) | 2 (66.7) | 1 (25.0) | 2 (66.7) |
| Moderately active | 2 (50.0) | 1 (33.3) | 2 (50.0) | 1 (33.3) |
| Active | 1 (25.0) | 0 (–) | 1 (25.0) | 0 (–) |
| Smoking status | ||||
| Never smoked | 4 (100.0) | 3 (100.0) | 4 (100.0) | 3 (100.0) |
| Ex-smoker | 0 (–) | 0 (–) | 0 (–) | 0 (–) |
| Current smoker | 0 (–) | 0 (–) | 0 (–) | 0 (–) |
| Weight (kg) | ||||
| Mean (SD) | 69.5 (13.1) | 72.5 (11.5) | 71.9 (16.1) | 73.7 (12.7) |
| Median (IQR) | 67.0 (59.0–80.0) | 75.0 (60.0–82.6) | 67.5 (59.5–84.2) | 76.0 (60.0–85.0) |
| Range | 58.0–86.0 | 82.6–60.0 | 59.0–93.4 | 60.0–85.0 |
| SHSC N = 4 (%) | Control N = 3 (%) | |||
|---|---|---|---|---|
| Baseline | 26 weeks | Baseline | 26 weeks | |
| Have you ever received the over 40s NHS health check from your GP? | ||||
| Yes | 0 (–) | 0 (–) | 1 (33.3) | 2 (100.0) |
| No | 4 (100.0) | 3 (100.0) | 2 (66.6) | 0 (–) |
| Missing | 0 | 1 | 0 | 1 |
| If yes, when did you receive the over 40s NHS health check from your GP? | ||||
| < 1 year ago | – | – | 0 (–) | 1 (50.0) |
| 1–5 years ago | – | – | 0 (–) | 0 (–) |
| > 5 years ago | – | – | 1 (100.0) | 1 (50.0) |
| If no, why have you never received the over 40s NHS health check from your GP? | ||||
| I am under 40 years old | 2 (50.0) | 1 (33.3) | 0 (–) | – |
| I have been invited but I’m not interested | 0 (–) | 0 (–) | 0 (–) | – |
| I have been invited but I didn’t have time to attend | 0 (–) | 0 (–) | 1 (50.0) | – |
| I have been invited but I forgot to attend | 0 (–) | 0 (–) | 0 (–) | – |
| I have not been invited to receive the health check | 2 (50.0) | 2 (66.6) | 1 (50.0) | – |
| Other | 0 (–) | 0 (–) | 0 (–) | – |
| Missing | 0 | 0 | 0 | – |
| How many times have you consulted a GP regarding your health during the past 14 days? | ||||
| 0 | 4 (100.0) | 3 (100.0) | 3 (100.0) | 3 (100.0) |
| Missing | 0 | 1 | 0 | 0 |
| How many times have you consulted a practice nurse regarding your health during the past 14 days? | ||||
| 0 | 4 (100.0) | 3 (100.0) | 3 (100.0) | 3 (100.0) |
| Missing | 0 | 1 | 0 | 0 |
| How many times have you consulted a pharmacist regarding your health during the past 14 days? | ||||
| 0 | 4 (100.0) | 3 (100.0) | 2 (100.0) | 3 (100.0) |
| Missing | 0 | 1 | 1 | 0 |
| Have you ever consulted a healthcare professional or equivalent practitioner for mental health problems such as stress, anxiety, or depression (or within the last 6 months at 26-week follow-up)? | ||||
| Yes | 4 (100.0) | 1 (25.0) | 0 (–) | 0 (–) |
| No | 0 (–) | 3 (75.0) | 3 (100.0) | 3 (100.0) |
| Have you ever consulted a healthcare professional or equivalent practitioner for musculoskeletal problems (or within the last 6 months at 26-week follow-up)? | ||||
| Yes | 2 (50.0) | 0 (–) | 1 (33.3) | 0 (–) |
| No | 2 (50.0) | 4 (100.0) | 2 (66.6) | 3 (100.0) |
| Have you ever attended a smoking cessation programme (or within the last 6 months at 26-week follow-up)? | ||||
| Yes | 0 (–) | 0 (–) | 0 (–) | 0 (–) |
| No | 4 (100.0) | 4 (100.0) | 3 (100.0) | 3 (100.0) |
| Have you ever attended a weight management programme (or within the last 6 months at 26-week follow-up)? | ||||
| Yes | 0 (–) | 1 (25.0) | 0 (–) | 0 (–) |
| No | 4 (100.0) | 3 (75.0) | 3 (100.0) | 3 (100.0) |
| In the last 12 months, have you been admitted to hospital (spent at least one night) for any planned reason (excluding giving birth) (or within the last 6 months at 26-week follow-up)? | ||||
| Yes | 0 (–) | 0 (–) | 0 (–) | 0 (–) |
| No | 4 (100.0) | 4 (100.0) | 3 (100.0) | 3 (100.0) |
| In the last 6 months, have you been admitted to hospital (spent at least one night) for any unplanned reason (i.e. emergency) (or within the last 6 months at 26-week follow-up)? | ||||
| Yes | 0 (–) | 0 (–) | 0 (–) | 0 (–) |
| No | 4 (100.0) | 4 (100.0) | 3 (100.0) | 3 (100.0) |
| SHSC (N = 12) | Control (N = 14) | |
|---|---|---|
| HR records | ||
| Sickness absenteeism 26 weeks after randomisation (WTE days) | ||
| Mean (SD) | 6.2 (10.0) | 6.3 (9.6) |
| Median (IQR) | 1.3 (0.0–7.8) | 2.6 (0.0–8.0) |
| Range | 0.0–29.4 | 0.0–35.0 |
| Sickness absenteeism 26 weeks after randomisation (spellsa) | ||
| Mean (SD) | 1.3 (1.2) | 1.4 (1.4) |
| Median (IQR) | 1.0 (0.0–2.5) | 1.0 (0.0–2.0) |
| Range | 0.0–3.0 | 0.0–4.0 |
| SHSC (N = 4) | Control ( N = 3) | |
| Self-reported | ||
| Taken time off work during the last 6 months due to ill health or otherwise? | ||
| Yes | 2 (50.0%) | 0 (–) |
| No | 2 (50.0%) | 3 (100.0%) |
| If yes, number of days off work in the last 6 months for the following reasons: | ||
| Total | ||
| Mean (SD) | 4.5 (3.5) | – |
| Median (IQR) | 4.5 (2.0–7.0) | – |
| Range | 2.0–7.0 | – |
| Mental health issues (e.g. stress, anxiety, depression) | ||
| 0 | 2 (100.0%) | – |
| Cardiovascular health | ||
| 0 | 2 (100.0%) | – |
| Musculoskeletal health (i.e. joint or muscle pain or problems) | ||
| 0 | 1 (50.0%) | – |
| 2 | 1 (50.0%) | – |
| Diarrhoea and vomiting | ||
| 0 | 2 (100.0%) | – |
| Respiratory infections | ||
| 0 | 2 (100.0%) | – |
| Other reasons | ||
| 0 | 1 (50.0%) | – |
| 7 | 1 (50.0%) | – |
| WHO-HPQ | ||
| Absolute absenteeismb (using 7-day estimate) (hours) | ||
| Mean (SD) | −11.5 (13.3) | 4.0 (6.9) |
| Median (IQR) | −8.0 (−21.0, −2.0) | 0.0 (0.0–12.0) |
| Range | −30.0–0.0 | 0.0–12.0 |
| Absolute absenteeismb (using 28-day estimate) (hours) | ||
| Mean (SD) | 22.3 (41.3) | −8.0 (21.6) |
| Median (IQR) | 0.0 (−3.0–70.0) | −2.0 (−32.0–10.0) |
| Range | −3.0–70.0 | −32.0–10.0 |
| Missing | 1 | 0 |
| Relative absenteeismc (using 7-day estimate) | ||
| Mean (SD) | −0.08 (0.09) | 0.03 (0.05) |
| Median (IQR) | −0.06 (−0.1, −0.01) | 0.0 (0.0–0.08) |
| Range | −0.2–0.0 | 0–0.08 |
| Relative absenteeismc (using 28-day estimate) | ||
| Mean (SD) | 0.1 (0.3) | −0.05 (0.1) |
| Median (IQR) | 0.0 (−0.02–0.5) | −0.01 (−0.2–0.1) |
| Range | −0.02–0.5 | −0.2–0.1 |
| Missing | 1 | 0 |
| Relative hours of workd (using 7-day estimate) | ||
| Mean (SD) | 1.1 (0.09) | 0.97 (0.05) |
| Median (IQR) | 1.06 (1.0–1.1) | 1.0 (0.9–1.0) |
| Range | 1.0–1.2 | 0.92–1.0 |
| Relative hours of workd (using 28-day estimate) | ||
| Mean (SD) | 0.9 (0.3) | 1.1 (0.1) |
| Median (IQR) | 1.0 (0.5–1.0) | 1.0 (0.9–1.2) |
| Range | 0.5–1.0 | 0.9–1.2 |
| Missing | 1 | 0 |
| Level 1 reason | SHSC (N = 12) (%) | Control (N = 14) (%) |
|---|---|---|
| Total number of spells of absence | n = 15 spells in 8 people | n = 20 spells in 10 people |
| COVID-19 | 1 (6.7) | 3 (15.0) |
| Back problems | 2 (13.3) | 1 (5.0) |
| Other musculoskeletal problems | 2 (13.3) | 1 (5.0) |
| Cold, cough, flu – influenza | 1 (6.7) | 5 (25.0) |
| Headache/migraine | 0 (–) | 1 (5.0) |
| ENT | 0 (–) | 4 (20.0) |
| Gastrointestinal problems | 4 (26.7) | 2 (10.0) |
| Genitourinary and gynaecological disorders | 1 (6.7) | 1 (5.0) |
| Infectious diseases | 1 (6.7) | 0 (–) |
| Injury, fracture | 1 (6.7) | 0 (–) |
| Pregnancy-related disorders | 1 (6.7) | 0 (–) |
| Other known causes – not elsewhere classified | 1 (6.7) | 1 (5.0) |
| Unknown causes/not specified | 0 (–) | 1 (5.0) |
| No sickness absence | 4 | 4 |
| SHSC (N = 4) | Control (N = 3) | |
|---|---|---|
| WHO-HPQ | ||
| Absolute presenteeisma | ||
| Mean (SD) | 77.5 (9.6) | 83.3 (11.5) |
| Median (IQR) | 75.0 (70.0–85.0) | 90.0 (70.0–90.0) |
| Range | 70.0–90.0 | 70.0–90.0 |
| Relative presenteeismb | ||
| Mean (SD) | 1.0 (0.2) | 1.1 (0.2) |
| Median (IQR) | 1.0 (0.9–1.1) | 1.0 (1.0–1.3) |
| Range | 0.9–1.3 | 1.0–1.3 |
| SHSC (N = 4) (%) | Control (N = 3) (%) | |
|---|---|---|
| In the last 6 months, have you attended occupational health for any of the following? | ||
| Total | ||
| Yes to any | 1 (25.0) | 0 (–) |
| No to all | 3 (75.0) | 2 (100.0) |
| Missing | 0 | 1 |
| Cardiovascular health | ||
| Yes | 0 (–) | 0 (–) |
| No | 4 (100.0) | 3 (100.0) |
| Missing | 0 | 0 |
| Mental health well-being | ||
| Yes | 0 (–) | 0 (–) |
| No | 4 (100.0) | 2 (100.0) |
| Missing | 0 | 1 |
| Musculoskeletal health | ||
| Yes | 1 (25.0) | 0 (–) |
| No | 3 (75.0) | 3 (100.0) |
| Missing | 0 | 1 |
| Other health problems | ||
| Yes | 0 (–) | 0 (–) |
| No | 4 (100.0) | 2 (100.0) |
| Missing | 0 | 1 |
| SHSC (N = 4) (%) | Control (N = 3) (%) | |
|---|---|---|
| In the last 6 months have you received the over 40s NHS health check from your GP? | ||
| Yes, less than 6 months ago | 0 (–) | 1 (50.0) |
| Yes, over 6 months ago | 0 (–) | 1 (50.0) |
| No, I’ve never been asked | 2 (66.6) | 0 (–) |
| No, I am under 40 years old | 1 (33.3) | 0 (–) |
| Missing | 1 | 1 |
| How many times have you consulted a GP regarding your health during the past 14 days? | ||
| 0 | 3 (100.0) | 3 (100.0) |
| Missing | 1 | 0 |
| How many times have you consulted a practice nurse regarding your health during the past 14 days? | ||
| 0 | 3 (100.0) | 3 (100.0) |
| Missing | 1 | 0 |
| How many times have you consulted a pharmacist regarding your health during the past 14 days? | ||
| 0 | 3 (100.0) | 3 (100.0) |
| Missing | 1 | 0 |
| In the last 6 months, have you consulted a healthcare professional or equivalent practitioner for mental health problems such as stress, anxiety or depression? | ||
| Yes | 1 (25.0) | 0 (–) |
| No | 3 (75.0) | 3 (100.0) |
| If yes, please tell us as best you can how many times you have seen each type of healthcare professional for your mental health in the last 6 months: | ||
| GP – NHS visit | ||
| 1 | 1 (100.0) | – |
| GP – Non-NHS visit | ||
| 0 | 1 (100.0) | – |
| Practice nurse – NHS visit | ||
| 0 | 1 (100.0) | – |
| Practice nurse – Non-NHS visit | ||
| 0 | 1 (100.0) | – |
| Psychologist – NHS visit | ||
| 0 | 1 (100.0) | – |
| Psychologist – Non-NHS visit | ||
| 0 | 1 (100.0) | – |
| Psychiatrist – NHS visit | ||
| 0 | 1 (100.0) | – |
| Psychiatrist – Non-NHS visit | ||
| 0 | 1 (100.0) | – |
| Counsellor – NHS visit | ||
| 0 | 1 (100.0) | – |
| Counsellor – Non-NHS visit | ||
| 0 | 1 (100.0) | – |
| Hospital consultant – NHS visit | ||
| 0 | 1 (100.0) | – |
| Hospital consultant – Non-NHS visit | ||
| 0 | 1 (100.0) | – |
| Accident and Emergency – NHS visit | ||
| 0 | 1 (100.0) | – |
| Accident and Emergency – Non-NHS visit | ||
| 0 | 1 (100.0) | – |
| Have you seen any other types of healthcare professional for mental health problems such as stress, anxiety or depression in the last 6 months? | ||
| Yes | 1 (100.0) | – |
| In the last 6 months, have you consulted a healthcare professional or equivalent practitioner for musculoskeletal problems, i.e. joint or muscle pain or problems? | ||
| No | 4 (100.0) | 3 (100.0) |
| In the last 6 months, have you had any NHS investigations (e.g. X-ray)? | ||
| Yes | 1 (25.0) | 1 (33.3) |
| No | 3 (75.0) | 2 (66.6) |
| In the last 6 months, have you attended a smoking cessation programme? | ||
| No | 4 (100.0) | 3 (100.0) |
| In the last 6 months, have you attended a weight management programme? | ||
| Yes | 1 (25.0) | 0 (–) |
| No | 3 (75.0) | 3 (100.0) |
| In the last 6 months, have you been admitted to hospital (spent at least one night) for any planned reason (e.g. planned surgery)? (exclude giving birth) | ||
| No | 4 (100.0) | 3 (100.0) |
| In the last 6 months, have you been admitted to hospital (spent at least one night) for any unplanned reason (i.e. emergency)? | ||
| No | 4 (100.0) | 3 (100.0) |
| SHSC (N = 4) | Control (N = 3) | |
|---|---|---|
| EQ-5D-5La | ||
| Mean (SD) | 0.728 (0.206) | 0.946 (0.0941) |
| Median (IQR) | 0.803 (0.598–0.858) | 1.000 (0.837–1.000) |
| Range | 0.427–0.879 | 0.837–1.000 |
List of abbreviations
- BCTU
- Birmingham Clinical Trials Unit
- BMI
- body mass index
- CRF
- clinical research facility
- CVD
- cardiovascular disease
- eGFR
- estimated glomerular filtration rate
- eTHOS
- enhancing the Health of NHS Staff
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- GAD-7
- Generalised Anxiety Disorder-7 questionnaire
- GP
- general practitioner
- GPPAQ
- general practice physical activity questionnaire
- HbA1c
- glycated haemoglobin
- HR
- human resources
- HRQoL
- health-related quality of life
- MSK
- musculoskeletal
- NIHR
- National Institute for Health and Care Research
- OA
- interviewee from an outside agency
- OMPSQ
- Orebro musculoskeletal pain screening questionnaire
- P
- trial participant
- PAG
- participant advisory group
- PHQ-9
- Patient Health Questionnaire-9 items
- PI
- principal investigator
- PPI
- patient and public involvement
- PT
- physiotherapist
- QEHB
- Queen Elizabeth Hospital Birmingham
- RCT
- randomised controlled trial
- REDCap
- Research Electronic Data Capture
- SHSC
- Staff Health Screening Clinic
- TOC
- Trial Oversight Committee
- WHO-HPQ
- World Health Organization Health and Work Performance Questionnaire
- WTE
- whole time equivalent
