Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number NIHR127430. The contractual start date was in October 2019. The final report began editorial review in October 2021 and was accepted for publication in June 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Millar et al. This work was produced by Millar et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Millar et al.
Chapter 1 Introduction
Improving the collaboration and integration of services has become a mantra for health-care systems around the globe. The need to work across organisational boundaries is promoted as a solution for achieving the necessary innovation, coordination, efficiency and relationships to meet the financial, demographic, workforce and quality challenges currently being faced. 1 The COVID-19 pandemic has sharpened the policy focus on interorganisational collaborations (IOCs) and partnership working as a response to the pressures brought on by the pandemic. 2
Interorganisational collaboration includes the formation of alliances, groups, associations, networks and mergers. 3–7 Such arrangements have been closely linked to policy contexts where governments have mandated collaboration or have sought to create conditions for ‘co-opetition’ between providers to expand the market position of high-performing organisations. 1
A variety of factors have been attributed to achieving success within such initiatives, including the importance of organisational capacity, having a shared vision with realistic aims, building trust, the availability of robust governance structures and collaborative leadership. 8–13 However, realising the advantages of collaboration is far from straightforward. 14 Notable barriers to IOCs are include the geographical distance between partners, the influence of historical events, competitive behaviour, the regulatory environment, a lack of organisational resources and coordination, power imbalances, and incompatible organisational structures and cultures. 8,15–17
Historical developments
England, UK, has seen no shortage of attempts to promote IOC. The apparent need for improved partnership working can be traced back at least as far as the introduction of ‘national planning systems’ in the 1960s. Subsequent policy developments include the 1974 NHS reorganisation and the National Health Service and Community Care Act 1990. 300 Both policy developments encouraged improved collaboration between the NHS and local authorities. 18 The New Labour government, during its early years of government, espoused a shift away from competition to collaboration with a raft of policy initiatives, including joint commissioning arrangements, pooled budgets, health improvement programmes, health action zones and a duty of partnership for NHS bodies and local authorities. 8,19,20 Nevertheless, these initiatives struggled to achieve their desired goals and outcomes,19,21 with the ambiguity surrounding collaborative arrangements, such as joint commissioning, posing further practical and technical challenges to attributing any performance improvements being made. 22 The challenging policy logics of hierarchical control and market competition that characterised New Labour’s term of office are also noted as challenges for developing collaboration across NHS providers. 23,24
The Five Year Forward View
Although the Health and Social Care Act 2012301 promoted competition, the Five Year Forward View3 gave emphasis to developing and piloting new care models to encourage interorganisational and cross-sectoral partnership working. 25,26 In response to significant variations in quality across the NHS provider sector, the Care Quality Commission (CQC)27 also promoted a range of partnership options for ‘challenged’ organisations and organisations assessed as requiring ‘special measures’. 6 The options included options for mandated support, with the appointment of one or more partner (or ‘buddy’) organisations to provide support, with-longer term options including merger and acquisition. To improve coordination and standardisation of services across the provider sector, the 2014 Dalton review4 outlined a menu of collaborative approaches, including the voluntary pooling of resources by multiple organisations (e.g. joint ventures and federations) and consolidation arrangements (e.g. integrated care organisations and mergers), as well as buddying arrangements between lower- and better-performing organisations to facilitate the sharing of best practices.
A stream of research has sought to evaluate the collaborative approaches introduced by the Five Year Forward View. 10,12,25,28 Studies provide evidence of how new care models have helped to stimulate organisational innovation and promote system-wide collaboration. 25 Billings et al. 10 note a set of facilitative factors, including the development of relationships and alliances, effective local and national leadership, the availability of expert knowledge and skills, and additional tranches of funding. Challenges have also been highlighted with regard to overly ambitious policy expectations and the collection and use of performance information, as well as difficulties in developing ongoing relationships with regulators. Furthermore, questions remain about whether or not the agenda has had sufficient time and support to develop approaches responsive to population need. 26 In addition, questions remain about the limited effect of the vanguard programme on reducing hospital activity. 29
Mergers and acquisitions between under- and well-performing providers have received much attention, with concerns raised regarding the time, cost and complexity for stakeholders involved, and the variable financial and clinical quality improvements being achieved. 30 The impact of ‘buddy’ hospitals providing support to struggling organisations or those in special measures appears to have aided organisational improvement and turnaround, as measured by the CQC performance ratings. 6,31 Despite the Health and Social Care Act 2012301 promoting competition, Allen et al. 32 note how commissioners chose mainly to use collaborative strategies to affect major service reconfigurations, and this was also endorsed as a suitable approach by providers.
The NHS Long Term Plan and beyond
The policy focus on collaboration continued with the publication of the NHS Long Term Plan. 33,34 Building on Sustainability and Transformation Partnerships (STPs), integrated care systems (ICSs) have been introduced, which bring together mental health, social and acute care, specialist services, primary care and local government, with the aim of promoting greater regional coordination and more of a population health focus. 33,35 Primary care networks (PCNs) hold shared budgets, with the aim of developing new services to enhance integration, improve sustainability, secure additional funding and improve economies of scale. 36,37 NHS provider collaboratives also contribute towards the ICS agenda with the development of specialist mental health-care pathways. 38
Within the current context of the pandemic,39 new Health and Care Bill aims to accelerate the shift towards greater collaboration with the accompanying legislation to accomplish much of what was put forward in the NHS Long Term Plan. 40 Proposals include a duty for the NHS and local authorities to collaborate with ICSs, which are now statutory bodies, comprising ICS Health and Care Partnerships (bringing systems together to support integration) and an ICS NHS body (responsible for day-to-day running of the ICS), and include commissioning functions. The arrangements will allow NHS providers and Clinical Commissioning Groups (now ICS NHS bodies) to make joint decisions via joint committees and committees-in-common arrangements, as well as bring in other partners. Competition law [through the Competition and Markets Authority (London, UK)] and regulatory functions promoting competition are removed, along with the need for competitive tendering if not providing value. The introduction of provider collaboration reviews by the CQC to encourage learning about health and social care collaboration provides a further statement of intent with regard to how regulation can facilitate collaboration and partnership working in the delivery of services. 41
The formation of a mandated ICS agenda raises questions about the potential of ICSs to undermine existing collaborative relationships and their susceptibility to enacting hierarchy-based governance and behaviours, rather than ‘place-based collaboration’. 42 Emerging findings from ICS so far point to challenges ahead in developing the relationships, trust, accountability and authority for successful joint working. 43 A similar picture is painted with regard to PCNs, with limited progress being reported. 37 Concerns have also been raised about the regulatory implications of the policy proposals. For example, with the current inspection regime focused on individual organisations,44 it is not at all clear how ICSs will be scrutinised and performance rated. 45 Sanderson et al. 46 note that, although the intention of STPs was to create conditions for common pool resources at a ‘system’ level, local actors often struggle to agree local rules, citing conflicts with the continued regulatory focus on the financial sustainability of individual organisations.
Research rationale
Despite the burgeoning evidence base and increased policy emphasis on collaborative working, notable gaps in knowledge persist. 17,47,48 Criticisms have been lodged at the limited number of actionable insights generated from integrated care policies,49 and the failure to demonstrate successful outcomes for staff, users, financial sponsors or other stakeholders. 21 Collaboration often falls short of expectations, so much so that its continued appeal to policy-makers has been likened to ‘an expression of faith’, rather than driven by tangible evidence. 50
The ambiguities and uncertainties surrounding the nature and effect of collaboration mean that achieving ex ante objectives is unlikely, given that ‘the act of collaborating with others often results in the interactive adaptation of perceptions and performance goals’ over time. 51 The term collaboration is also deemed problematic in the way it potentially glosses over the diverse array of mechanisms that can be used to describe how organisations work together and the relative appropriateness of these mechanisms for different tasks and contexts. 52
As a result, our understanding of the mechanisms and processes for spreading and sustaining evidence about successful relationships is limited. Many questions remain about how interorganisational arrangements, such as mergers, alliances, joint ventures and buddying collaborations, work, for whom and in what circumstances. Indeed, appeals have been made to further identify the elements of successful collaboration, particularly the assessment of effectiveness for horizontal collaborations between health-care providers. 1 There is also a need for further empirical research to better understand the interplay of barriers and their context dependence, as well as their underlying causes and visible symptoms. 15
The literature in this area calls for more robust theoretical frameworks and more sustained empirical research to explore which types of partnership approaches work (or not) in particular circumstances, why and for whom. 13 Although general theories of how IOCs work have been proposed, establishing the causal links between issues such as culture, leadership and governance in strengthening or weakening collaborations requires further development. Auschra,15 for example, calls for greater understanding of the barriers to the integration of care in interorganisational settings, with the need for more attention devoted to using existing organisation and network theories that address such barriers. Auschra15 notes that ‘while reviewing existing literature, it became clear that the notion of “barriers” lacks theoretical underpinning’. 15
Given the complexities of collaborative arrangements, Guarneros-Meza et al. 53 advocate ‘theories of change’ approaches to assess how collaboration synergies and coordination are shaped by contexts, behaviours and structures, and this is achieved by asking ‘how’ and ‘why’ partnership practices are carried out in different contexts. Applications of realist methodology in relation to partnership working are also advocated as an approach well suited for studying multiple interventions implemented in diverse contexts with a range of stakeholders. 54 However, applications of realist approaches to understanding IOCs within health-care settings has hitherto remained an underdeveloped area.
Research aims and objectives
The aim of our research is to provide useful intelligence regarding how, why and in what circumstances different approaches to IOC are effective in improving the performance of NHS provider organisations. To do this, a realist synthesis of evidence was carried out with the following inter-related supporting objectives:
-
To explore the main strands of the literature about IOC and identify the main theoretical and conceptual frameworks that can be used to shed light on the conditions and antecedents for effective partnering across sectors and stakeholders.
-
To assess the empirical evidence with regard to how different interorganisational practices may (or may not) lead to improved performance and outcomes.
-
To understand and learn from NHS evidence users and other stakeholders about how and where IOC can best be used as a mechanism to support turnaround processes.
-
To develop a typology of IOC that considers different types and scales of collaborative ventures that are appropriate for particular NHS provider contexts.
-
To generate evidence-informed practical guidance for NHS providers, policy-makers and others with responsibility for implementing and assessing IOC arrangements in the NHS.
Our research provides practical guidance and learning to support NHS leaders with assessments of the different candidate partnering approaches available. Our research has important implications and learning, regarding the principles and methods that are required if collaborative approaches are to work successfully across boundaries and to engage the workforce and wider population within these collaborative efforts, for those engaged in leadership.
Chapter outline
This report is structured into eight chapters and arranged as follows. Chapter 2 provides the context for this work, with a review of typologies, drivers and dynamics associated with the life cycle of collaboration. Chapter 3 presents the methodology employed, providing an overview of the realist synthesis approach and our stakeholder analysis. Chapter 4 presents the results of the realist synthesis, drawing on 86 items of literature and analysing how, why and for whom do IOCs in health-care work in particular circumstances. Chapter 5 refines understanding of collaborative functioning with the presentation of findings based on primary data collected from a range of stakeholders, including policy-makers, practitioners and patient representatives. Chapter 6 presents findings from the stakeholder interviews and develops a novel theory of collaborative performance that aims to further explicate the mechanisms underlying collaboration that drive performance improvement. Chapter 7 assesses the implication of the findings, with an outline of the final version of our realist theory of how and why IOC works. Chapter 7 also presents options for the translation of our research into practice, with the development and piloting of tools designed to assess the readiness for collaboration. The report concludes (see Chapter 8) with a summary of how the project has fulfilled its objectives and with recommendations for developing future research, policy and practice in this important area of policy and practice.
Chapter 2 Background
The purpose of this chapter is to start the process of gaining a better understanding of IOCs. Given the large, multifaceted and complex nature of IOCs, the aim here is to provide an essential first step of theory-building in articulating ‘what the programme is’, ‘who is the supposed target’ and ‘what is the supposed outcome’. 55,56 To this end, we combine a review of grey literature (e.g. policy and organisational strategy documents within the NHS) and narrative and systematic reviews of evidence to capture key definitions, typologies, ingredients and outcomes associated with IOCs (see Appendix 1 for methods). Excerpts of this chapter have been reproduced with permission from Aunger et al. 61 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Definitions and terminology
A variety of terms have been used to describe joint working, including integration, collaboration, partnering and partnership working. Partnership working is a widely used to describe the joint development of organisational structures or working across boundaries by the sharing of resources, authority and accountability. The following definitions capture these arrangements:
. . . a mutually beneficial process by which stakeholders or organizations work together towards a common goal. 57
. . . a negotiation between people from different organisations with a commitment to working together over more than the short term to secure improvements which could not have been achieved by acting alone. 17
. . . a series of events in the history of a system, leading to the evolution of new structures of interaction and new shared meanings. 54
‘Partnering’ is another term that is commonly used in the literature. Miller and Millar13 suggest that partnering is useful term for understanding various joint working arrangements. Crowley and Karim58 define partnering as:
. . . a cooperative strategy [that an organization implements] by modifying and supplementing the traditional boundaries that separate organizations in a competitive climate. In this way, partnering can be used to create a cohesive atmosphere [in which] all project team members openly interact and perform. 58
Interorganisational collaboration is a similar term and has been defined as follows:
. . . interorganizational collaboration is the set of communicative processes in which individuals representing multiple organizations or stakeholders engage when working interdependently to address problems outside the spheres of individuals or organizations working in isolation. The outcomes of these processes have the potential to benefit or harm the parties to the collaboration, as well as others. 59
[Interorganizational collaboration] the belief that more valuable knowledge can be created than if each organization were to work alone as complementary resources and competencies from partners can create interorganizational synergies. 60
Although defined differently by different authors, common to many definitions of partnership working, partnering and collaborating is the notion of working together to achieve benefits that would otherwise not be attainable by working alone. The core notion of ‘working together’ is a commonality across these terms. We will primarily be using the term IOC in this report, but the terms partnership working and partnering may also be used in particular instances of joint working.
Types of partnering
A range of scales and types of partnership working can be identified, and these different types of partnering have been presented as existing along a continuum by various authors. 8,61,62 Glasby et al.,8 for example, distinguish between ‘depth and breadth’ of partnership arrangements. Similarly, Sullivan and Skelcher62 categorise several different collaborative relationships, ranging from networks (i.e. informal ad hoc relationships) through to formal partnerships, federations and mergers (see Table 1).
| Form of collaboration | Loose network | Merger into single organisation |
| Rules of governance | Self-government | Hierarchy and overarching constitution |
| Organisational and policy terminology | Network | Integration |
With a particular focus on NHS providers, Miller and Millar13 identify a variety of partnering practices linking NHS providers, ranging from structural partnering, such as organisational mergers and acquisitions, through to individual partnering arrangements, such as buddying between executives and clinicians across provider organisations to provide mentoring support and guidance. 13 Miller and Millar13 also suggest that partnering can sit along a continuum, from a voluntary intrinsic act to work together through to partnerships that are mandated by government regulators (see Figure 1).
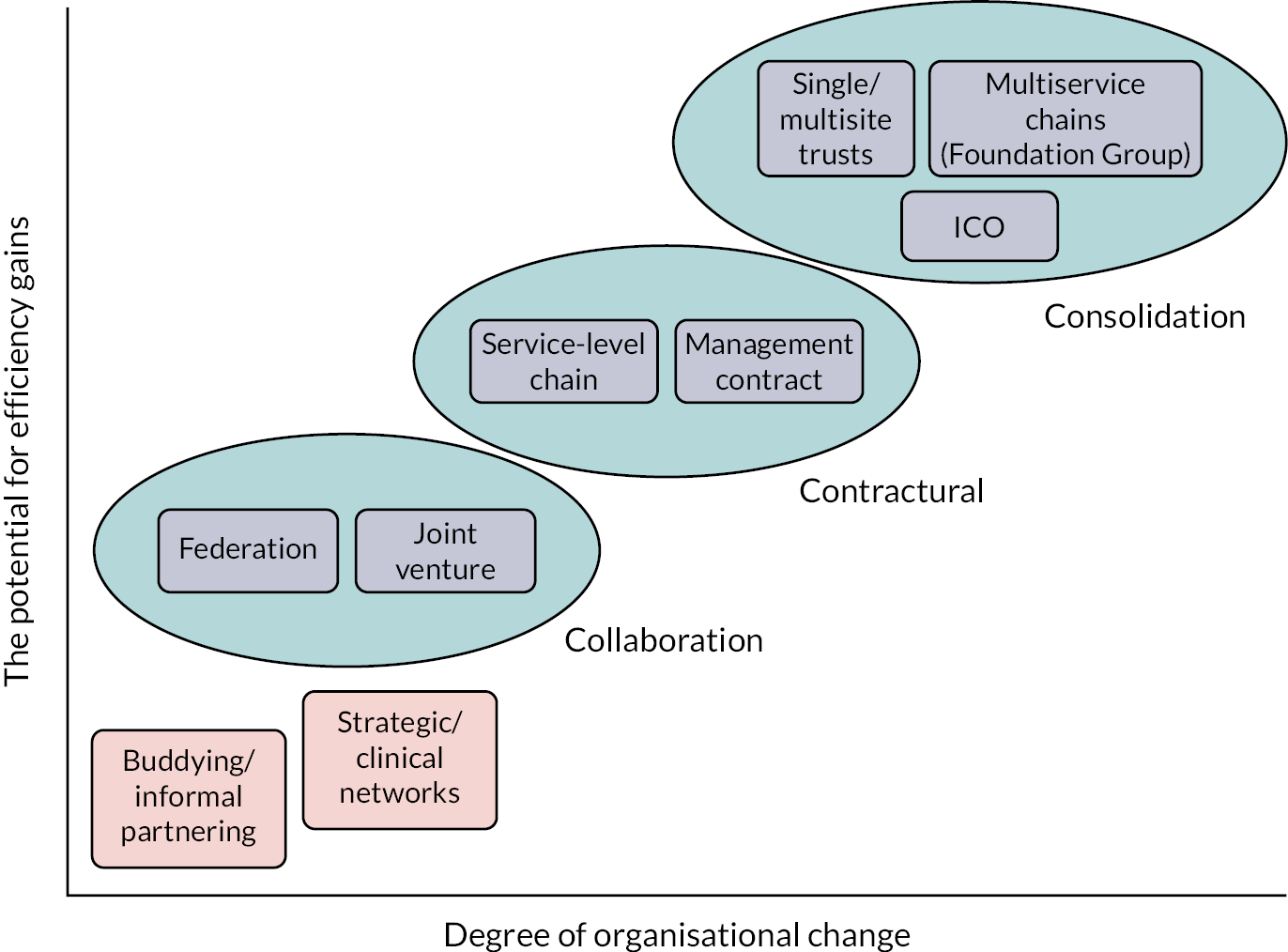
The 2014 Dalton review4 outlined a range of provider models of care. The Dalton review distinguished between different interorganisational forms, including collaborative arrangements (i.e. a voluntary pooling of resources, which involves two parties creating a third to provide a particular service to both initiators), contractual arrangements (i.e. more formalised agreements) and consolidatory arrangements (i.e. a change of ownership, encompassing mergers and acquisitions)4 (see Figure 2).
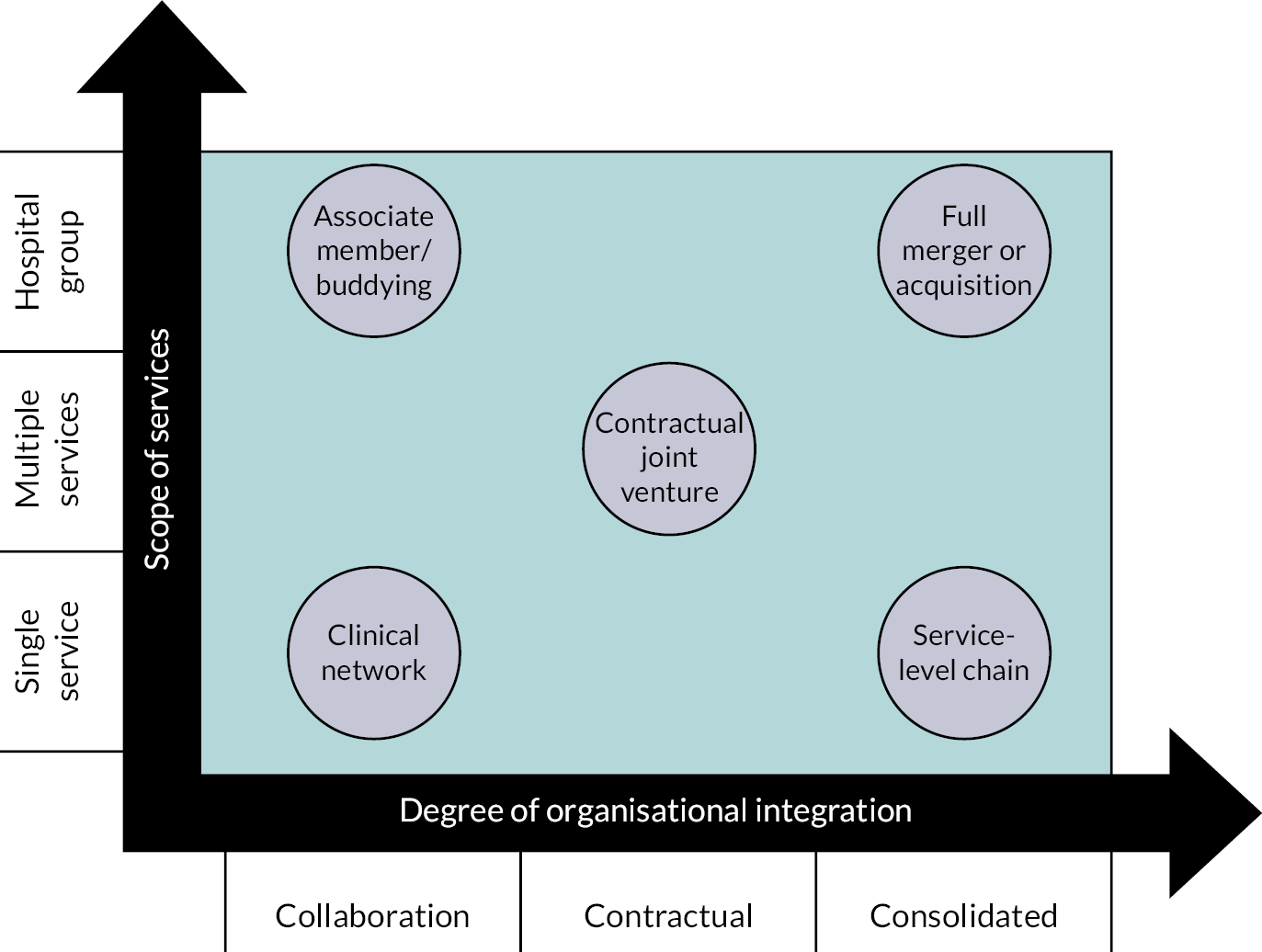
The NHS England publication ‘No Hospital is an Island’64 built on the Dalton review typology by developing a framework for acute care collaboration models. The NHS England publication64 depicted organisational forms by their degree of organisational integration, as well as by the scope of services they intend to deliver (see Figure 3).
FIGURE 3.
A framework of acute care collaboration models, depicting organisational forms by their degree of organisational integration, as well as the scope of services they intend to deliver (contains public sector information licensed under the Open Government Licence v3.0). 64
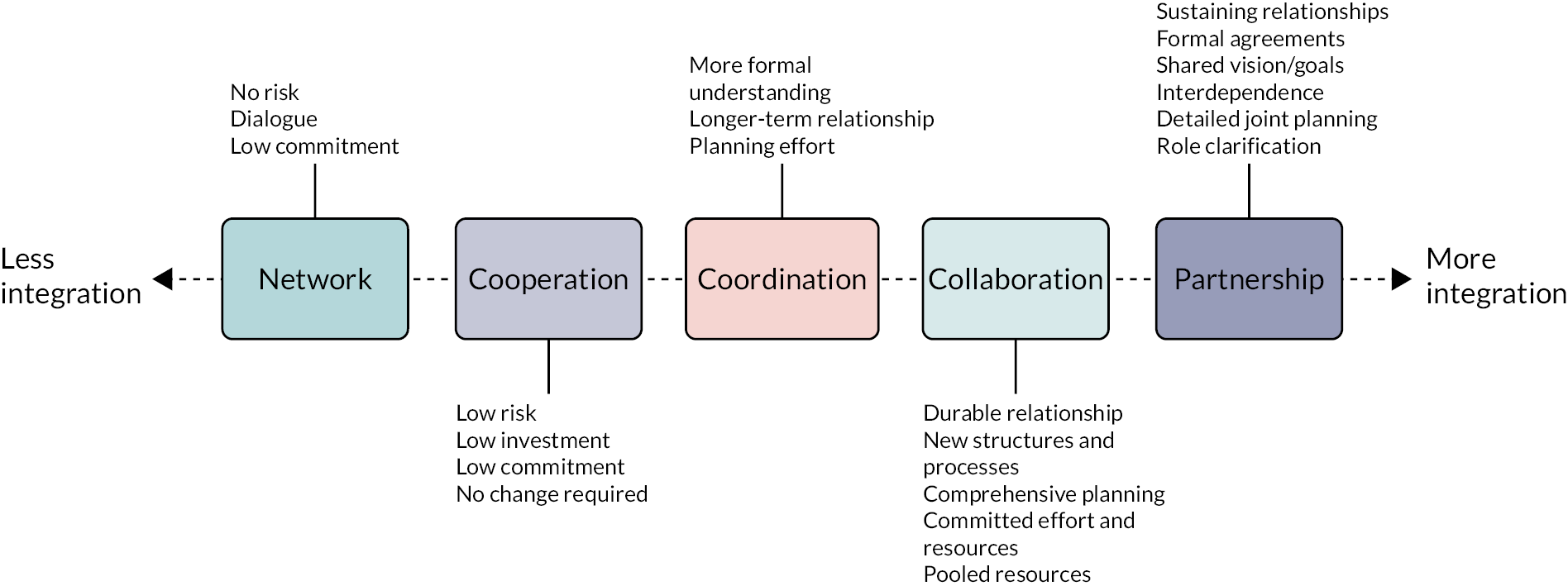
Another example comes from the Northern Ireland Audit Office (Belfast, UK). 65 The Northern Ireland Audit Office arranges different partnering arrangements by their degree of integration, from networks characterised by low commitment at the bottom of the spectrum, through cooperation, coordination and collaboration, to fully fledged partnerships, which require formal agreements and detailed joint planning (see Figure 4). 65
Across these various typologies, the key characteristics at play are the degrees of integration, whether a collaboration is mandated or voluntary, and whether the collaboration is cross-sector or within specific services. Although the terminologies used to describe such arrangements (i.e. alliances vs. hospital groups) can be fluid and are not universally agreed on,61 the typologies use a range of partnering types (see Table 2).
| Type | Definition |
|---|---|
| Informal partnering | Voluntary arrangements characterised by flexible small-scale collaborations focused on sharing organisational learning |
| Buddying | A form of mandated collaboration to encourage organisational turnaround. Buddying often involves organisations with more experience being asked to mentor, advise or train other organisations of lesser performance |
| Federation | A relatively informal agreement whereby several organisations collaborate on delivery of a service or administrative provision. Legal agreement is not required but a memorandum of understanding is required |
| Clinical network | A network that intends to reduce unwarranted variation in particular subtypes of care by fostering collaboration to optimise these particular care pathways |
| Joint venture | Creation of a new legal entity by multiple other entities that serves to deliver a service for, and on behalf of, the multiple originator entities |
| Provider collaborative | Partnerships of providers with new responsibilities for pathway and budget management for specialised services (e.g. mental health) |
| PCN | General practices and community, mental health, social care and pharmacy services collaborating to deliver primary care |
| Service-level chain | A provider that is contracted to provide services for another |
| Multiservice chain, group or alliance | A separate ‘group’ that sets governance, standards, protocols and procedures, often with procurement and back office functions. Each site has delegated decision-making within the parameters set by the designated board |
| Management contract | When control of a set of operations is handed to another organisation to manage for an agreed duration |
| ICS | Multiple organisations from primary, community, acute, mental and public health, and social care get brought together to manage patients across defined care pathways |
| Merger | The combination of two organisations to form a new organisation |
| Acquisition | The subsumption of one organisation by another |
What are collaborations intending to achieve?
Despite emphasis being placed on collaboration and integration across health-care systems, questions continue to be raised about the lack of robust evidence regarding whether or not such relationships lead to desired outcomes. 48 This has largely been explained by the ‘wicked problems’ collaboration is often looking to solve and the resulting challenges and dilemmas regarding how to measure collaborative effectiveness and success. 53,66 Guarneros-Meza et al. 53 review a range of measures and frameworks to demonstrate how collaborative performance can include several measures, comprising the quantity and quality of service outputs, consumer satisfaction, service objectives, expenditure data, equity in the allocation of resources and service outcomes. 67 The measures and frameworks can encompass common models of assessing performance, relating to goal attainment (outcomes), performance targets (outputs) and cultural efficacy-measuring factors, such as changes in rhetoric, emotions and symbols. 48 Silvia,51 drawing on Mandell and Keast,68 shows how effectiveness can be measured at three inter-related levels of network operations:
-
The operating level: the extent to which participants have developed a better understanding of each other, and whether or not they have developed a shared language and culture, new ways of communication and the ability to find common ground.
-
The organisational level: activating, framing, mobilising and synthesising activities, as measured by the creation of a shared vision, the establishment of member commitment to the network’s mission and the inclusion of all network members in the collaborative process.
-
The environmental level: the ability to successfully meet the needs of external stakeholders and constituencies (e.g. citizen awareness and the outcome proxies).
A review of partnering outcomes by Aunger et al. 61 found that evidence from NHS policy documents, such as the Dalton review4 and NHS Five Year Forward View,3 advocates different collaborative arrangements to provide a range of potential benefits to population health by improving care, quality and efficiency. A review of NHS provider mergers by NHS Improvement (2017b) claims that merged organisations have the potential to help the local health economy by standardising care and quality, increasing market share in clinical services, improving financial sustainability, avoiding market share erosion and improving reputation to aid in staff recruitment (see also Aldwych Partners30). Aunger’s et al.’s review of strategic plans from 26 NHS providers demonstrated how intended outcomes can be arranged into the four broad categories of ‘delivering consistent high quality care’, ‘developing our people’, ‘leveraging scarce resources’ and ‘embracing innovation’. 69 Within these larger categories, long-term and multiple medium-term objectives can also be identified. For example, within delivering consistent high-quality care, an objective is to ‘provide members (i.e. clinicians) with access to world-leading specialists from within the Healthcare Alliance’, by ‘enabling clinician-to-clinician relationships, facilitating knowledge share and access to specialist opinion’. 69
Drivers for interorganisational collaboration
Alongside outcomes, a range of perspectives and empirical research has been put forward to understand the stated and unstated drivers for IOCs. Table 3 summarises the results of the systematic search, which identified the following domains and organisation theories associated with the formation of IOCs in health care.
| Domain | Driver for IOCs | Underlying theories of organisation |
|---|---|---|
| Expansion | Seeking competitive advantage | Strategic choice: organisations pursue IOCs to increase competitiveness or market power Agency: individuals pursue IOCs to benefit primarily themselves rather than organisations |
| Consolidation | Efficiencies and economies of scale | Transaction cost economics: organisations should organise boundary-spanning activities to minimise production and transaction costs |
| Participation | Increasing responsiveness and alignment to needs | Stakeholder: organisations require greater alignment with stakeholder groups who can affect or are affected by the achievement of objectives |
| Learning | Enhancing position through superior knowledge | Absorptive capacity: IOCs are driven by value, assimilation and application of new knowledge Normative isomorphism: IOCs are driven by professions and interorganisational network pressures regarding best practice |
| Sustenance | Fulfil resource needs and manage scarce resources | Resource dependency: organisations must engage in exchanges with their environment to obtain resources to survive or prosper Common pool resource: IOCs are driven by self-management of limited resources in a way that benefits all |
| Mimicry | Obtain legitimacy or conformance to prevailing social norms | Mimetic isomorphism: IOCs are driven by intentionally and unintentionally copying to prove legitimacy |
| Coercion | Mandated pressures to conform | Coercive isomorphism: IOCs pursue activities in agreement with prevailing government rules, requirements and norms |
These dynamics can be summarised as follows.
Expansion
Drivers for IOC draw attention to the organisational expansion within market environments where collaboration is sought for competitive advantage and strategic position. 70 Forming an IOC for market expansion can be linked with strategic choice theory, which proposes that an organisation will enter into a collaboration if the benefits exceed the costs and if the collaboration will increase the ability of the firm to deliver superior products, improve service efficiency or increase market power. 71
The perspective of expansion is captured by Postma and Roos,78 who draw attention to how the formation of health-care mergers can represent a strategic attempt by organisations to gain market power by merging with a competitor. 72–75 Angeli and Maarse76 investigate the evolution of mergers and acquisitions across Western European health-care providers. Angeli and Maarse76 chart the rise of financial service organisations acting as acquirers in mergers and acquisitions, which have been driven by the introduction of market elements in health-care financing and provision, the broadening of private practice and for-profit medicine, the retrenchment of public financing arrangements and the closure of public hospitals or the conversion of public hospitals into more private-like entities. Expansion of market power can also be attributed to the self-interests and personal ambition of managers as a potential motive for collaboration. 77,78 Such a perspective resonates with agency theory, which suggests that managers act as utility maximisers,79 where the architects of IOCs may seek to have their organisations partner with others to increase their reputation in the marketplace or to increase their benefits by managing a larger organisation. 78
Consolidation
The formation of IOCs is driven by the need to consolidate services within a market environment. Connections are made here with transaction cost economics and theories of interfirm collaboration,80,81 which focus on how organisations organise their boundary-spanning activities to minimise production and transaction costs.
Various collaborative efforts37,70 highlight the economic drivers for overall and unit cost savings through improved economies of scale. Much of the coverage related to transaction cost economics underpins the rationale for mergers. 76,82,83 A literature review and secondary data analysis by Gaynor et al. 84 traced the hospital ‘merger mania’ in England between 1997 and 2006. The review84 highlights how the drivers for these mergers included facilitating hospital or service closures to release capacity in the short term, secure financial viability of smaller organisations and enlarge the hospital to provide better services for the buyers of services. Fulop et al. 85,86 outline similar economic drivers for trust mergers as an opportunity to take advantage of economies of scale and scope (especially regarding management costs) to rationalise the provision of services by reducing excess capacity to treat patients. Resulting efficiencies can lead to improved clinical quality, as usage of specialised unit increases, quality of medical training increases, and staff recruitment and staff retention become more effective.
Participation
Drivers for IOC draw attention to how such forms can increase participation of stakeholders to reduce environmental uncertainty. Such assumptions connect with a stakeholder theory of organisations at the centre of an independent web of stakeholders with a responsibility to consider their needs with making decisions/transactions. 87,88 In a health-care context, these stakeholders are typically patients, members of the public, staff, board members and government. 78,89,90
Increased participation is aligned to multi-hospital arrangements that are better able to improve quality by ensuring community needs are identified, assessed and assigned priority for service, with comprehensive services reaching those most in need. 70 Greater alignment with patients and public interests is connected to the ethos of integrated care in ‘meeting the needs of people with chronic diseases’91 and the drivers for joint commissioning as a way to overcome fragmentation by achieving ‘a seamless service’ where ‘assessment of need is unhindered by organisational boundaries’. 302 Reflecting on partnership working in mental health, Glasby and Lester92 and others have identified the importance of a service with a single point of contact as beneficial for service users and their carers who can often experience fragmented services, a lack of continuity and conflicting information in situations where local agencies fail to collaborate effectively. 92,93 Smith et al. 37 document how improvements to patient care and service provision featured as reasons to form collaborations in primary care. Collaborating between practices can help fill gaps in service provision where single practices are not able to provide all services, where patients need better coordinated care and where improved planning and provision of services at a population level is needed. Hunter and Perkins’ study94,95 of local strategic partnerships and local area agreements found that providing a coordinated approach to tackling public health issues was a prerequisite of effectively resolving such issues.
Learning
Drivers for IOCs often arise from a desire for greater organisational learning and to improve the ability of organisations to absorb knowledge from partners. 96,97 Absorptive capacity is central to such an approach, with a firm’s ability to recognise the value of new knowledge, assimilate it and apply it in a business setting. 98 A rationale for IOC formation is that firms form partnerships to capitalise on opportunities to learn or enhance their competitive position through superior knowledge. 99
Within IOCs, such conditions for learning have the potential to increase capability and innovation through education and skills development. 70 Studies of mergers of health-care providers identified organisational learning and shared practice as stated drivers for merging. 86 Sharing of knowledge fosters coordination of care, as best practices become shared between organisations,90 including learning from different perspectives. 92,94,95,100 Van Raak et al.,90 in their study of integrated care in the Netherlands, finds motivations to collaborate based on opportunities for learning about other providers whom they had never encountered before, and generating new concepts for care delivery to improve performance. Westra et al. 101 examine how health-care organisations balance competition and cooperation in a situation of ‘coopetition’, where knowledge-sharing and interorganisational learning are considered the primary motives to cooperate with competitors. Leach et al. 102 present a case study of a buddying agreement to help teams undertake change and develop a medical pathway where ‘improved learning’ underpins the aim to promote close working partnerships, compassionate leadership and improve quality and safety.
Sustenance
Drivers for IOC resonate with the desire for sustainability and the need to fill a perceived resource need or to exert power or control over organisations that possess scarce resources. The sustainability of IOCs draws attention to systems and how organisations must engage in exchanges with their environment to obtain resources. Resource dependence theory posits that organisations require resources from their environment and, therefore, cooperative interorganisational relationships will be formed as a managerial response to the need for critical resources controlled by others in the environment. 90,103,104
In their review of multi-hospital systems in the USA, Provan103 documents drivers to establish such forms as the need to access critical resources, with Markham and Thomas noting the development of ‘lateral’ or ‘service alliances’, in which similar types of organisations with similar needs and dependences come together to achieve benefits, such as economies of scale, enhanced access to scarce resources and increased collectives. 78 Van Raak et al. 90 also capture how access to resources was an important reason for becoming involved, where participants benefited from cooperation to exert power over organisations that possessed desired means. Smith et al. 37 note how issues of sustainability, both in terms of finances and the primary care workforce, emerged as significant across their evaluation of PCNs, and were identified as key reasons to enter into collaborations in primary care.
Mimicry
Drivers for IOCs in health care draw attention to the institutional environments shaping how organisations collaborate to obtain legitimacy or to succumb to isomorphic pressures by mimicking or copying others. Such a viewpoint aligns with institutional theory, which posits that environments impose pressures on organisations to appear legitimate and to conform to prevailing social norms. 71,105 Legitimacy can gain access to critical resources and expertise, as well as enhance reputation and gain visibility.
Dickinson and Glasby17 note that, through interorganisational partnerships, smaller organisations can gain legitimacy by increasing their recognisability, image and standing. Collaborations can also be perceived as socially desirable because of the positive outlook that partnership working inspires. Field and Peck77 outline how ‘the modus operandi of the perceived market leaders is likely to be copied by other organisations in the belief that this is the most effective way of operating’, with merger motives connected to examples of ‘mimicking’ (i.e. uncritically copying business practices from the private sector). 78 In their study of joint commissioning, Dickinson and Glasby22 document how joint commissioning can be understood as producing efficiencies, empowerment and productivity, but also with other potential meanings as inherently a ‘good thing’. Connections to institutional theory can also be found in Dickinson and Glasby’s17 analysis of a mental health partnership. Dickinson and Glasby17 found that a large number of staff members found it hard to identify what their partnership had been set up to achieve. Although some previous internal policy documents set out process-based aspirations (e.g. a single point of access for service users), these process-based aspirations were often very unspecific and often focused on processes and outputs, rather than on outcomes.
Coercion
Contributions draw attention to the interlinkages between mimetic pressures to conform and wider institutional and systemic pressures mandating collaboration. 78,86,90 What Works Scotland198 notes that many partnerships that claim to operate through collective governance are, in reality, also shaped by mandates from central government. The presence of such hierarchical mechanisms leads to less powerful partners feeling disenfranchised and lost within the partnership106 and, in turn, less likely to engage. 107
Fulop et al. 86 note that the unstated drivers for mergers include facilitating hospital or service closures and securing financial viability of smaller organisations. 108 In the research by Fulop et al.,86 common to all mergers was the need to maintain quality and level of service in the context of external policy drivers, with reconfigurations informed by pressures for improvements to services and closer cooperation with local government and partnership agencies. Dickinson and Glasby17 also find that, although staff often claim that mental health partnerships provide better services for users, the majority of the potential benefits cited by staff are to do with responding to national and local politics to make more efficient use of scarce organisational resources. Central government produced coercive isomorphism by both explicit techniques (e.g. a legal duty for health and social care agencies to work together) and more subtle techniques (e.g. making partnership a necessary feature for some sources of funding).
Although the stated goals of PCNs in the United Kingdom (UK) are to improve population health, share staff and improve personalisation of care,109 Smith et al. 37 also found that the reasons to enter PCNs appear to be more tightly focused on policy and financial incentives, with practices obligated to form PCNs and accept the financial incentives associated with networks for fear that they would be ‘left behind’. 37 In their study of STPs, Sanderson et al. 46 argue that, although the intention of STPs was to create conditions at a ‘system’ level for purchasers and providers to act as a self-governed common pool, local actors were not able to agree local rules, citing the conflict with the continued regulatory focus on the financial sustainability of individual organisations.
These various drivers draw attention to the often paradoxical and multifaceted nature of a collaborative endeavour (see Figure 5). The drivers also show how individual theories and perspectives are in themselves insufficient for capturing the complexities, norms and traditions involved in relationship formation. 63,71
FIGURE 5.
Depicting the drivers for IOC.

Initial ‘ingredients’ for success
A range of ingredients for success have been outlined to determine the key shaping factors affecting collaboration. In an exploratory empirical study of mergers, buddying and contracting across NHS providers, Miller and Millar13 identified the ‘ingredients’ for successful partnering, which included effective senior and clinical leadership, the importance of trust between partners, acquiring meaningful data, and regulatory approaches that combine both quality improvement and assurance approaches. In addition, Hudson and Hardy110 depict how the determinants of a successful partnership include having an existing local history of partnership working, effective monitoring and reviewing of organisational learning, having a shared vision, and development and maintenance of trust through behaviours and attitudes, such as ‘fairness’, openness and honesty, sacrifice and accountability.
Likewise, a recent systematic review of reviews12 sought to determine ‘shaping factors’ of how cross-sector health-care collaborations work, and identified resources and capabilities (e.g. organisational capacity), motivation and purpose (e.g. shared vision, unrealistic aims, competing aims, national policies, commitment), relationships and cultures (e.g. trust, historic relationships, communication), governance and leadership (e.g. decision-making, accountability, leadership support) and external factors (e.g. geography, social/economic context) as key ‘shaping factors’.
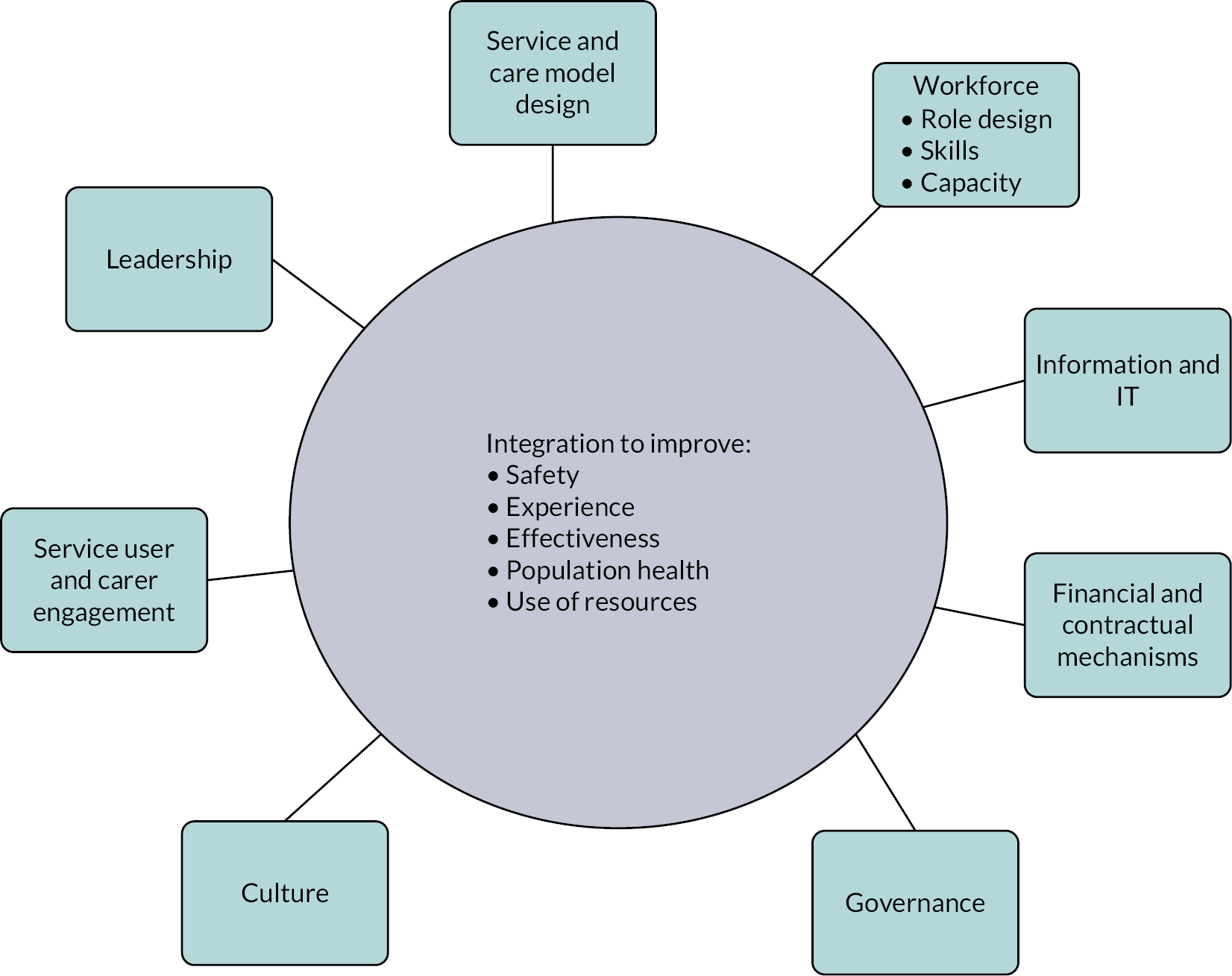
In addition, Aunger et al. 61 developed a typology of shaping factors for successful collaboration that incorporated a typology by the Advancing Quality Alliance111 (see Figure 6) and was supplemented with other emerging evidence from the review. 17,65,112–114
Aunger et al. 61 argue that the examination of organisational perspectives and theories surrounding the integration of these elements leads to the understanding that different partnering types are likely to interact with some elements more than others (see Table 4). For example, a partnership synergy theory suggests that certain characteristics are intrinsic to partnerships, namely leadership, administration and management, governance and efficiency. 115 As such, one could argue that partnering interventions largely exert their forces of change through changes to service and care model design, leadership, governance, and financial and contractual mechanisms, and that subsequent changes to information technology (IT) systems, culture and workforce occur as knock-on effects.
| Domain | Definition | Emerging evidence regarding factors affecting partnering success |
|---|---|---|
| Culture | The values and common behaviours of the workforce | Organisations have cultures that provide staff with a sense of autonomy Mutual agreement to work together A proper cultural integration plan is put into place in cases where high integration is required |
| Leadership | The senior management at the organisation(s) | Leadership style, which involves all levels of workforce in partnership arrangements Building networks and shared vision Leaders with charismatic and inspirational leadership styles Approaching the partnership with a strong belief in partnership Performance of due diligence (i.e. robust cultural integration plans, team-building across sites, role modelling, realistic expectations and plans, and utilising employee input) |
| Governance | The systems and processes concerned with ensuring the direction, effectiveness, supervision and accountability of the organisation(s) | Ability to align internal and external resources, activities and demands The ability to share power between partners Proper establishment of shared accountability between partners |
| IT systems | The IT infrastructure in place to support the organisation(s) | Enablement of information-sharing across partners The degree to which resources are dedicated to this aspect of integration Understanding of data requirements across partners |
| Workforce | The collective staff that work at each organisation | How well workforce practices and procedures are aligned Coordination to reduce variation in quality of care Having performed appropriate due diligence in the lead up to any workforce changes Engagement of staff at all levels of the organisation in the partnership process Understanding of workforce capability and capacity Group accountability and shared values |
| Service user engagement | Involving stakeholders in the partnership process | Engagement and involvement of a range of perspectives with those affected by changes to services Feedback mechanisms throughout partnering process Patients and users have ability and power to influence the partnership process in a manner that improves outcomes for them |
| Service and care model design | The way in which health care is delivered | Mutual agreement between partners on the new care model, arising from partnership Agreement between partners on desired outcomes of partnership |
| Financial and contractual mechanisms | How organisation(s) are supported by finances and a legal framework | Performance of appropriate due diligence and cost–benefit analyses to determine ideal partnership type for organisations involved (e.g. in strategic outline cases) Agreement on shared outcomes and joint performance measures |
Stages of the collaboration life cycle
A variety of contributions have sought to capture how organisations may go through multiple collaborative arrangements throughout their lifetime. We conducted a systematic review and ‘best-fit’ framework synthesis116 to identify key literature regarding the life cycle of collaborations in a health-care setting, and this resulted in the formation of several key stages, including contemplating, connecting, planning, implementation and maintenance or dissolution (see Figure 7). The full methodology can be seen in Appendix 2.
FIGURE 7.
A life cycle model of IOC conclusion.
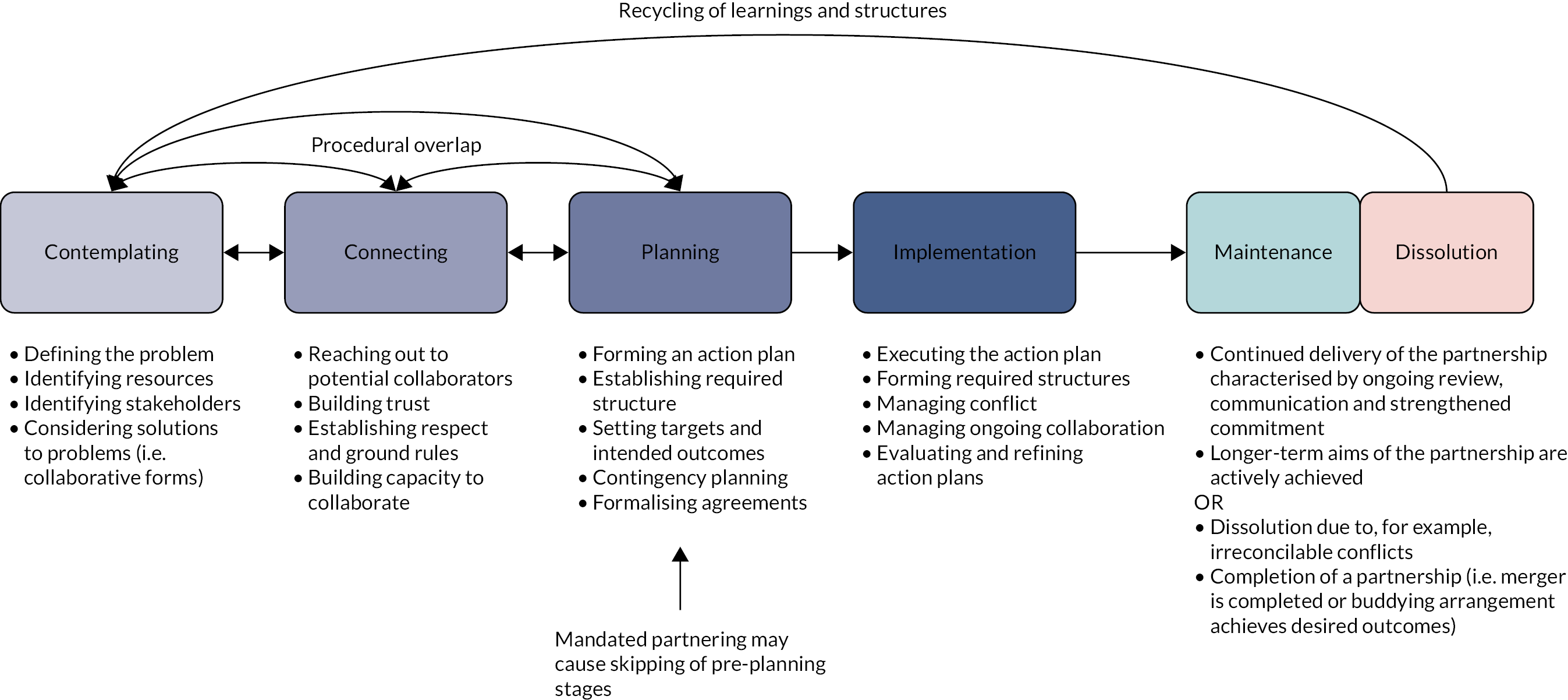
The contemplation aspect of collaborating incorporates behaviours analogous to ‘thinking about’ collaborating before it actually begins. 117,118 For example, the paper by Hudson et al. 119 puts forward behaviours such as ‘recognizing the need to collaborate’ and ‘identification of a legitimate basis for collaboration’. These behaviours and others have been integrated into the model as ‘defining the problem’, ‘identifying resources’, ‘identifying stakeholders’ and ‘considering solutions to problems, i.e. collaborative forms’. 119
The connecting phase revolves around behaviours that establish the initial processes of relationship-building between actors. For example, Lowndes and Skelcher89 put forward ‘informality, trust and cooperation, willingness to work together’ as key features of connecting. Likewise, ourpartnership.org.uk121 establish that, in this stage, ‘partners get to know each other and plan future activities’ and undergo ‘realistic self-appraisal and appraisal of partners’. 89,120,121
The planning phase includes behaviours such as ‘setting targets, establishing management teams’,122 ‘fostering partnership working values and engagement’123 and ‘developing basic agreement’. 120
The implementation phase includes behaviours such as ‘managing inevitable conflict between partners’,121 ‘experience of difficulties in new relationship’120 and ‘evaluating and refining action plan’,122 and is characterised by the beginning and middle phases of putting the collaboration into action, undergoing problem-solving as conflicts arise.
The maintenance phase refers to ‘building mechanisms to overcome barriers’120 and ‘sustaining trust between members’. 124,125 In this phase, the ultimate outcomes of partnerships are most likely to be achieved, as the focus moves from the functioning of the partnership to the achievement of goals.
Dissolution-type behaviours, such as ‘letting partnership die, or keeping certain aspects but not others’89 and ‘ending one or more partners’ involvements’121 can also feature at this phase due to either irreconcilable conflicts or the aims of the collaboration being achieved.
Figure 7 depicts the full life cycle model, which includes the behaviours and processes identified that are intrinsic to various stages of a collaborative life cycle.
The aim of this chapter has been to provide insights into the principles, characteristics and outcomes associated with health-care IOCs. Given the complex and multifaceted nature of IOCs, the next stage is to develop these findings with a methodological approach able to grasp these underlying contexts, dynamics and outcomes over time. In the next chapter, we outline how a realist synthesis approach is employed to better understand how IOCs work, why and for whom do they benefit.
Chapter 3 Methodology
This chapter will present the design and methods for the realist review and evaluation aspects of the project. Excerpts of the chapter have been reproduced from Aunger et al. 137,138 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Taking a realist perspective
A variety of theoretical contributions have sought to improve understanding of IOCs in health care. 14,48,110,126,127 These authors have generated valuable insights as to ‘what’ leads to successful partnering, but less so to how and why particular features enable collaborations to be successful. In this sense, IOCs can be seen as interventions that frequently fall into the trap of what Dixon-Woods and Martin128 term ‘magical thinking’, that is, the assumption that ‘doing X’ will lead to outcome Y without any articulation of how and why this change will occur, and this means that, often, the assumptions underlying how collaboration is intended to work are left implicit.
Any collaborative effort is likely to have a long and complex process of implementation, from initial discussions between stakeholders to the realisation of the intended benefits and/or failure. However, until now, few have used a realist lens to shed light on this phenomenon. Using a realist methodology to identify when, how and in what circumstances the causal links during implementation break or hold, as well as why collaboration may lead to better performance. A realist methodology also enables synthesis of all literature types in acknowledging the complexity of the interventions that constitute an area such as IOC.
Realist methods are built on the epistemological approach of critical realism, which is based on the concept of generative causation, where mechanisms generate outcomes that are context sensitive. 129,130 In realist terms, contexts refer to the situations into which interventions are introduced that affect the operation of the intervention mechanisms. 129 An intervention may work through one mechanism in one set of contextual features, but work through a different mechanism, producing a different outcome, in another. As a result, context and mechanism are keenly interlinked and cannot be separated. 129 Mechanisms, in realist terms, are the interactions between programme resources and the changes in reasoning by programme actors that occur as a result. 131 Mostly, these mechanisms are not directly observable but, nonetheless, can be explanations of why particular outcomes come to be. 129
Those who have used a realist perspective to understand IOCs have focused on particular subtypes and contexts of collaboration. 127,132,133 However, to the best of our knowledge, none have yet attempted to address the wider topic of IOCs between health-care providers. In this project, we have drawn on realist methodology in both synthesis and evaluation types to test and refine a robust theory of how IOCs in health-care work, to what extent, why and in what circumstances.
A starting point of realist evaluation is identifying the ideas and assumptions underlying how programmes or interventions work, known as programme theories. Realists also work with the premise that programmes are never universally successful, rather how they work (i.e. their mechanisms) to produce outcomes is shaped by contextual features. The goal of realist evaluation is to explain how contextual features shape the mechanisms through which a programme works, and this is achieved through testing and refining programme theories, expressed as context–mechanism–outcome configurations (CMOCs). Initially, CMOCs are tentative ideas, and as the project progresses these ideas are brought into conversation with evidence (i.e. tested in relation to the evidence) and are then refined to produce a more detailed explanation of how context shapes mechanisms. 129,130 A refined theory can support the process of adapting the intervention to local circumstances. The aim of this project is to produce a fully refined and actionable theory for practitioners and those implementing such arrangements.
Methods: realist synthesis
Details of search strategies
Theory gleaning
Searching processes in realist reviews tend to be evolutionary in nature, and that was the case here. 134 Initially, systematic searches were conducted to gather evidence about how IOC works and the contextual factors that shape across a range of entities, such as alliances, buddying, mergers, acquisitions and hospital groups. Searches were run between 20 February 2020 and 4 March 2020 on databases including the Healthcare Management Information Consortium (HMIC), MEDLINE, Social Policy and Practice and PsycINFO (see Appendix 3 for search strategies). The HMIC commentary search (see Appendix 3) was run on 12 January 2021. The searches were limited to 1990 onwards to provide the most up-to-date literature. In addition, a Google Scholar (Google Inc., Mountain View, CA, USA) search was conducted on 11 March 2020 to identify any grey literature or papers missed. The Google Scholar search used the terms ‘theory organisational collaboration’ to identify theoretical papers and ‘interorganisational collaboration healthcare’. Reference-scanning and citation-tracking was also employed to ensure as many papers were identified as possible (see Appendix 3 for the full systematic search strategy).
After data synthesis, we realised that we lacked elucidation on some of the mechanisms underlying how leadership, among other elements, may be key to understanding the process of collaboration. Therefore, a non-systematic purposive search was used to identify middle-range theories (MRTs), which would allow us to gain further insight into mechanisms uncovered through our analysis of papers identified in our initial searches. MRTs were identified using terms and combinations of terms such as ‘inter-organisational conflict’, ‘inter-organisational communication’, ‘inter-organizational trust’, ‘organisational capacity’, ‘collaborative leadership’, ‘organizational flexibility and effectiveness’, ‘collaborative accountability and governance’ and ‘collaborative regulatory environment’. The searches were conducted in Google Scholar in May 2020. Finally, we conducted an additional Google Scholar search in December 2020 using the terms ‘confidence’ and ‘trust’, ‘formalisation’, ‘contract’ and ‘contractualization’, combined with ‘inter-organisational collaboration’ or ‘partnership’ or ‘network’, for further MRT papers.
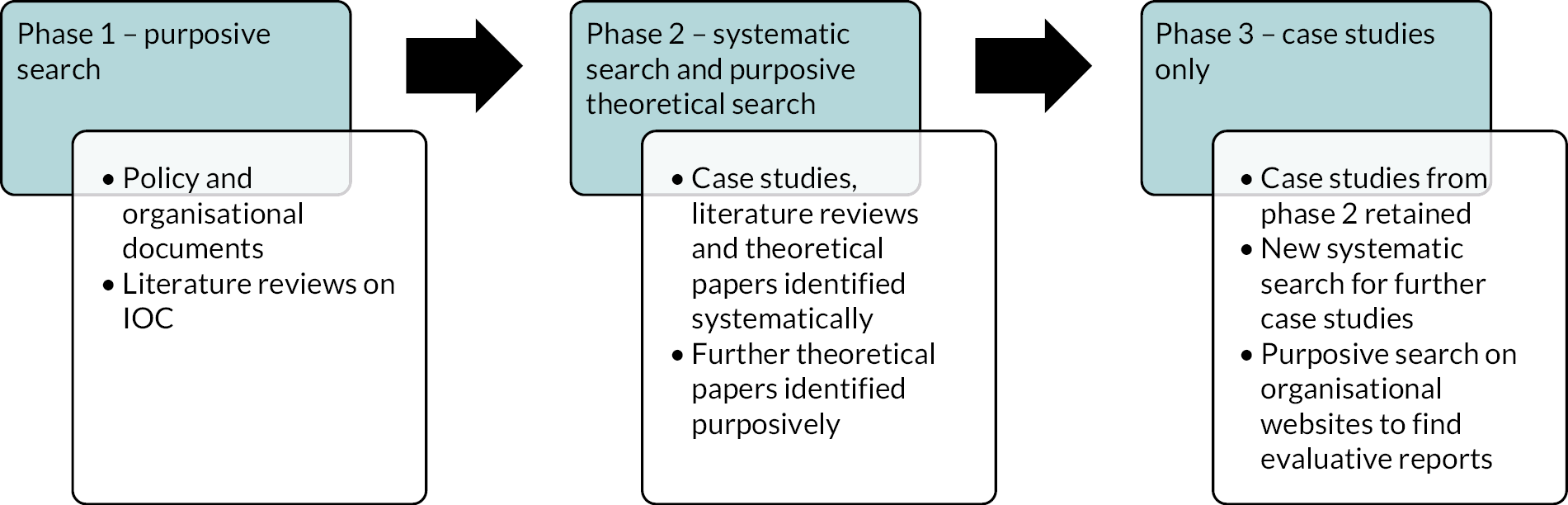
Theory refinement
Literature for this refinement stage of our realist synthesis was identified through a combination of existing literature from prior stages (systematically searched), novel (to this stage) systematic searches intended to locate case study literature explicitly and grey literature sources (for identifying organisational reports and evaluations), as is typical of a realist synthesis. 134 Case studies from the existing search were included here, with these case studies being brought over into this refinement stage of the synthesis. In addition, a novel systematic search was conducted on 10 June 2020 on the Social Policy and Practice database to identify additional case studies. Further searches for grey literature were conducted on 7 October 2020 and 8 October 2020 on UK-specific websites for evaluations of collaboration types, including The King’s Fund (London, UK), the National Institute for Health and Care Excellence (NICE) (London, UK), the Nuffield Trust (London, UK), The Health Foundation (London, UK) and NHS Employers (London, UK). The searches were on the publication sections of each website, with a focus on identifying evaluative reports. The searches used the terms ‘collaboration’, ‘partnership’ and ‘integration’ and were limited to 2012 onwards to maximise relevance to contemporary developments in collaborative arrangements. Figure 8 depicts the full methodology of this realist project.
FIGURE 8.
Depiction of phases in developing realist theory. Adapted with permission from Aunger et al. 135 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original text.

Inclusion criteria
Theory gleaning
Selection of documents was performed on the basis of relevance to the realist synthesis, as is typical of a realist review. 130 The systematic review used the following inclusion criteria for the title and abstract stage: ‘the paper clearly relates to collaborations between one or more public sector organisations on either a structural or individual level’ and ‘the paper is a case study, evaluation, opinion, or review’. In the full-text screening, as well as that for relevance, the paper had to include ‘propositions about the success or failure of collaboration in the public sector, mechanisms underlying how collaboration works, or include information about “entry points” (i.e. drivers of collaboration)’. Exclusion criteria for all stages included papers that ‘relate to collaborations or partnerships between staff and patients rather than between organisations’. Titles and abstracts were screened by Justin Avery Aunger, with a subset of 10% screened by Ross Millar in accordance with other systematic reviews. 12 Agreement was reached for all selected papers.
Theory refinement
For the refinement stage, we included only papers that (1) were case studies or evaluations (defined as reporting results of arrangements using descriptive methods), (2) report on an IOC between health care-providing organisations and (3) were in English (because of resource limitations of the study). Some papers had both literature review and case study portions, and these papers were also included, but data extraction was performed on the case study parts only. Selected studies were then subject to rigour and relevance checks in line with realist synthesis methodology.
Rigour and relevance screening
In line with guidance from Wong,136 the screening for rigour was ongoing during the analysis process and aimed primarily to increase the trustworthiness of the findings. This process involved including a CMOC only when supported by (1) clear data in included studies and (2) multiple sources. 136 For theoretical sources of evidence, only theories that had seen significant use in the literature since publication were used in the building of our MRTs and CMOCs. If documents were excluded on the basis of trustworthiness, then the reasons for doing so were to be recorded; however, no studies or extracts were excluded on this basis.
Data extraction
Data extraction was carried out by one reviewer (JAA), which involved combing the included papers for information relating to mechanisms underlying collaboration, programme theories and contextual factors (often termed ‘success factors’ or barriers). As is typical of a realist review,134 identified passages in the documents were highlighted for relevance, before being extracted into separate documents according to realist logic and how they aided in understanding the intervention. This was performed using custom data extraction forms (available on request).
For the refinement stage, another custom data extraction form was created, which recorded the study, collaboration type, primary driver (as best deduced from the study), CMOCs that fit into prior theory and novel CMOCs (which could be novel in context, mechanism or outcome) that did not fit wholesale into the prior theory. This type of custom form is typical in a realist synthesis and is available in Report Supplementary Material 1. In addition, we attempted to extract information on whether studies were reporting on externally mandated forms of partnering or voluntary forms, but it was not always possible to determine this information, unfortunately, because of inconsistent reporting by authors.
Realist synthesis methods
Theory gleaning
The highlighted passages from the included documents were coded according to whether the passage sheds light on entry points into collaboration, contextual factors, mechanisms or other elements relating to collaborations that helped elucidate the underlying ideas and assumptions regarding how collaboration was intended to work and the sorts of contextual features that might shape the different mechanisms underpinning these. Most successful factors and barriers were typically identified to be the inverse of one another, and so these factors/barriers were amalgamated into becoming contextual factors at a later stage of the synthesis. As more papers were extracted, categories that were found to be thematically similar were merged to result in the final categories seen in this review. Contextual factors, mechanisms, outcomes and entry points into collaboration were coded separately, but contextual factors had their posited underlying mechanisms recorded alongside them, as well as any potential outcomes. The sources that supported the existence of these contextual factors were also recorded. Synthesis results were regularly discussed by Justin Avery Aunger and Ross Millar to maintain validity and consistency.
In some cases, mechanisms were explicit in papers identified in the systematic review and in other cases the evidence was missing. Therefore, in cases where analysis was completed and mechanisms were missing, a purposive search was used to locate MRTs that could elucidate mechanisms that were triggered by these contextual features inherent to collaborations. Contextual factors were then clustered according to their underlying mechanisms and the case study and review literature, and MRT evidence synthesised. The theoretical clarity of mechanisms and the evidence underpinning them were discussed by two authors (JAA and RM), and CMOCs were then formed. Included documents then underwent a second pass, using specific search terms relating to mechanisms, and identified contextual factors to ensure all sources of relevant information were included.
Theory refinement
Using the existing realist programme theories from step 2 of this realist synthesis process as a base, we aimed to test our existing CMOCs against case studies and improve our understanding of how CMOCs are situated temporally and causally to improve our theory of collaboration in health care, and this constituted phase 3 of our overall analysis (see Figure 9). Literature was identified through systematic searches of databases and searches of organisational websites. The literature was then categorised by collaboration type, as well as whether the collaboration was a mandated or voluntary arrangement (as could best be identified), and the literature was then rigorously searched to identify CMOCs. Testing of existing CMOCs then occurred against the newly identified literature from this stage’s searches, and this comprised identifying whether CMOCs were identical to the existing CMOCs from the theory gleaning phase, or could be considered novel in terms of context, mechanism or outcome content or novel in terms of the relationship of one CMOC to another. Although we did not intend for the focus here to be on theory gleaning, novel CMOCs were still included when identified with sufficient evidence to support them. Both CMOCs from the existing theory that had support as well as novel CMOCs not present in the existing theory were recorded. Any conflicting information about the configuration of existing CMOCs was also recorded.
FIGURE 9.
Evolution of literature synthesis by phase of review. 61,138 Adapted with permission from Aunger et al. 135 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original text.
The process resulted in significantly more overall CMOCs than were present in our prior realist phase, and this allowed us to gain a greater understanding of how the outcomes of certain CMOCs can become a context for another further down the chain. To identify these relationships, these CMOCs were deductively coded in NVivo 12 into categories according to their mechanism to better investigate the literature for presence of demiregularities, which, in realist terms, are patterns of how outcomes generally come to occur. 137 The data were then used to refine the MRT and programme theories to provide a better understanding of the links between these elements. This chapter was written according to the RAMESES (Realist And Meta-narrative Evidence Syntheses: Evolving Standards) II reporting standards. 134 All data requests can be submitted to the corresponding author for consideration.
Methods: realist evaluation
Objectives
We conducted a realist evaluation to further test our refined programme theory by exploring the experiences of a range of stakeholders across several examples of IOCs in England. Our primary objective was to test the mechanisms of collaborative functioning and CMOC derived from literature against the stakeholders’ views to explore whether previously identified mechanisms and CMOCs, and causal links between them, were affirmed, refuted or revised, and to refine our understanding of how IOCs work, in which circumstances and why. In addition, we sought to elucidate the part of the causal chain that links collaborative behaviour to collaborative performance to identify how and why performance benefits may arise from the process of collaborating. We intended to produce a refined realist programme theory rooted in both literature and practice, with a view towards practical use in the future.
In the realist evaluation, for collaborative functioning, our prior programme theory135 was adopted as a MRT, against which interview data were ‘tested’, based on the realist synthesis, and this means that we explored if and how interview findings affirmed prior CMOCs, proposed refinements to existing CMOCs or, and to what degree, identified CMOCs that were novel. This theory, which we adopted as the MRT, will be outlined in the following realist synthesis chapter.
For understanding collaborative performance, Dickinson and Sullivan’s48 framework (adapted from McKenzie216) was adopted as a MRT to inform our analysis. Dickinson and Sullivan’s48 framework was selected as a MRT for three main reasons: (1) the framework focuses on performance rather than the functioning aspect of the causal chain; (2) the framework provides three criteria against which realist mechanisms can be categorised and (3) the framework captures cultural efficacy, which neatly complements the concept of programme mechanisms as changes in participant reasoning within realist theory. Thereby, we assume that frameworks relying purely on the ‘techno-bureaucratic’ aspects of performance would likely neglect key social components of the causal chain. Enabling a greater understanding of collaborative performance forms an essential part of the overall programme theory.
Therefore, the final aim of our realist evaluation was to produce a refined MRT, seeking to answer ‘what works in IOCs, for whom, under what circumstances, why and how?’, as well as ‘how do performance improvements in IOCs in health care arise, why, and what underpins them?’. This chapter was written in accordance with the RAMESES II reporting standards for realist evaluations. 139
Details on programmes evaluated
The ‘programmes’ evaluated comprised a range of IOCs, as outlined in our initial realist theory paper. 61 The programmes included arrangements of relatively low integration (i.e. buddying) through to highly integrative types, such as mergers. Our interviewees had direct experience of four different types of IOC and comprised five examples of hospital groups, two alliances, three ICSs and two mergers. The IOCs reflect a range of drivers and contextual differences. Although mergers result in formation of a singular organisation, we consider mergers to be collaborative entities during the merger process until the fully merged organisation begins operating38 (see Table 2 for full details on the types of IOCs and regulatory organisations included in this evaluation).
Data collection methods
The realist evaluation drew on interviews conducted with an ‘issue network’140 of stakeholders, comprising the leaders or architects of collaborative programmes, regulators, policy-makers, professional bodies, front-line staff and patient representatives. We defined these stakeholders as ‘a broad collection of individuals possessing knowledge about the issue in question with some influence on policy outcomes’.
Recruitment process and sampling strategy
Participants were identified through contacts via our Study Advisory Group and from direct contact with potential individual and organisations identified through scoping work. Phase 1 interviews were conducted, which had a particular focus on ‘theory gleaning’ and explored current programme theories being used to develop partnering approaches across NHS providers. Recruitment to phase 1 used a purposive sampling approach, with further snowball sampling employed to identify relevant stakeholders within this ‘issue network’. Phase 2 participants were also recruited, drawing on a selection of key informants from NHS provider organisations currently engaged in a range of partnering activities. Here, particular attention was paid to testing and refining programme theories identified in from the literature and the theory gleaning interviews to produce refined theory.
Participants were chosen based on their likelihood of being able to provide rich information about various aspects of the programme theory, from being engaged in implementing such arrangements themselves to delivering the policy and regulatory agendas.
Participants were approached to participate via e-mail. Patient representatives were recruited from patient representative bodies and were intended to be greater experts on outcomes rather than ‘mechanisms’. 141
Sample
The final sample comprised 37 interviews with 34 participants and one focus group with 8 patient representatives. The interviews and focus group were conducted across England between January 2020 and May 2021. Table 5 outlines the characteristics of the participants.
| Case studies of IOC programmes | Role (interview code) |
|---|---|
| Hospital group 1 (South) | Director (2) × 2 |
| Hospital group 2 (South) | Director (3) × 2 |
| Hospital group 3 (South) | CEO (18) |
| Hospital group 4 (South) | Lead (29) Director of improvement (35) |
| Alliance 1 (North) | Executive nurse (10) Former CEO (12) Director (20) CEO (22) Medical director (23) Workforce director (26) |
| Alliance 2 (North) | CEO (17) Director (19) |
| ICS 1 (North) | CEO (13) |
| ICS 2 (South) | Lead (14) |
| ICS 3 (South) | Lead (25) |
| Integrated care provider (North) | Manager (16) |
| Merger (South) | Director (21) |
| Wider stakeholder perspectives | Academic and non-executive (1) |
| Provider policy lead (4) | |
| Provider policy inspectorate lead (5) | |
| NHS provider association [6 (× 2) and 11] | |
| Professional regulator (7) | |
| Regional inspectorate lead (8) | |
| Policy transformation lead (9) | |
| Patient representative lead (15) | |
| Third sector representative (24) | |
| Local government representative (28) | |
| Private sector representative (27) | |
| Patient representatives (30–34; focus group) |
Interviews and setting
Semistructured interviews were conducted by experienced qualitative interviewers (JAA, RM, AMR and DF). The interviews drew on realist interview methodology, with the focus on gleaning and refining theory. 141 Questions were posed that would both directly and indirectly work towards these aims. Earlier phase 1 interviews were more focused on theory gleaning and were conducted alongside construction of the programme theory in our earlier realist review. 138 Later phase 2 interviews incorporated direct questions, in which the programme theory was explained to the participant and the participant was asked about particular elements, with the intention of refining and consolidating theory directly in a manner in line with the teacher–leaner cycle. 141 This strategy was used particularly with the participants with whom we were able to conduct follow-up interviews. The interview guide was refined and developed as our interviews progressed. Owing to the emergence of the COVID-19 pandemic shortly after the start of the research, interviews were conducted virtually over Zoom (Zoom Video Communications, San Jose, CA, USA) or Microsoft Teams (Microsoft Corporation, Redmond, WA, USA) and recorded on an external dedicated encrypted audio-recorder. Interviews lasted between 30 and 90 minutes, but were typically closer to 60 minutes in length. Files were sent for verbatim transcription at a third-party transcription service.
Data analysis
Analysis was performed in NVivo 12 software by one coder (JAA). Coding logic was independently verified by a second coder (RM). Coding was performed retroductively. 142 Retroduction uses both inductive and deductive logic. 143 Retroduction involves thinking through what causal powers might be at work in producing observed patterns or changes in patterns. Retroduction is underpinned by a belief that an understanding of causation cannot be achieved using only observable evidence. Use of retroduction meant that analysis was carried out in a deductive manner for features relating to our existing realist theory; however, for better sorting and understanding of themes, codes within higher-order codes were created inductively where commonalities were identified. 144
For the collaborative performance analysis, the framework of cultural efficacy, technological effectiveness and organisational efficiency was used as broad codes in the interpretation of the results and the mechanisms identified. Therefore, higher-order codes for excerpts relating to cultural efficacy, technological effectiveness and organisational efficiency were created prior to the start of coding. However, within these higher-order categories, we inductively created subcodes for excerpts that supported various concepts, such as ‘communication’ and ‘improved reputation’, as demiregularities (or semi-predictable CMOC patterns) were identified in the transcripts. Within the codes for these concepts, we then analysed the excerpts for identifiable connections and outcomes to formulate the explicit CMOCs. Transcripts themselves were not anonymised, as the coders were also the interviewers, rather any information that would identify participants was withheld from this final report.
Chapter 4 How do interorganisational collaborations in health care work, why and whom do they benefit?
A realist synthesis
The purpose of this chapter is to present findings from the second and third stage of this realist synthesis (see Figure 1). Drawing on reviews, MRTs and case studies and organisational evaluation literature, we aim to glean initial CMOCs and test these CMOCs against case study literature. In doing so, the chapter seeks to better understand how CMOC configurations of IOC are chained together causally and how differences between contexts affect their implementation. The chapter will present a refined programme theory, explaining how, why and for whom IOCs in health care work.
Excerpts of the chapter have been reproduced with permission from two sources. First, Aunger et al. 135 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text. Second, Aunger et al. 138 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Paper selection
Theory gleaning searches
From the systematic search, a total of 2769 titles and abstracts were screened, which were filtered down to 117 full texts. The Google Scholar searches conducted on 11 March 2020 produced 426,000 results on this specific day, and the first 40 pages of results were screened, resulting in four further papers. At this stage, 52 papers were included (see Figure 10). The 52 papers were then screened for relevance (i.e. whether the papers included sufficient descriptive depth regarding contextual factors, mechanisms and outcomes underlying IOC), which resulted in 35 included papers. Reference-scanning and citation-tracking resulted in a further four papers, giving a total of 39 papers included in the theory gleaning analysis (see Figure 10).
FIGURE 10.
A PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) diagram reflecting all papers included in this realist synthesis. NT, Nuffield Trust; THF, The Health Foundation.

Agreement between independent reviewers was 100%. Fourteen purposively identified papers were also drawn on, which outlined the MRTs used to elucidate the workings of mechanisms, bringing the total number of papers included in the gleaning phase to 53.
Theory refinement searches
For the new systematic search, the Social Policy and Practice database search identified 2144 papers. After deduplication against our existing literature library for this project (please see additional file 1 for the full details of this search strategy) there were 1092 papers. Abstracts were then screened for relevance and 104 papers remained. At this point, papers were most frequently excluded because of not being related to IOCs or for not being case studies. After full-text screening, 48 papers were considered eligible for the review; however, after screening for relevance and rigour, only 13 papers were included. Papers were removed for being insufficiently descriptive (i.e. lacking relevance). The searches on the websites of The King’s Fund, the NICE, the Nuffield Trust, The Health Foundation and NHS Employers resulted in an additional 15 papers. Thirteen of these papers were included, but two were removed for lack of relevance. Two further studies were identified through citation-tracking and a final paper was identified in a department newsletter after the search was completed. Four other papers were also brought over on rescreening of studies from the gleaning phase. As a result, 33 total unique papers were included in this theory refinement portion of this realist synthesis.
Literature characteristics
There was a total of 86 studies when n the theory gleaning and refinement stages were combined (see Figure 10). Papers in the literature covered a wide range of IOC types (see Table 6), including 55 case studies, evaluative reports or case–control studies, 16 reviews and 1 briefing. 15,17,21,22,32,37,44,47,60,84,85,94,100,102,113,119,145–200
| Study | Country | Partnership type | Sector | Methods and sample (where applicable) | Phase of use in synthesis |
|---|---|---|---|---|---|
| Adedoyin et al.145 | USA | Merger | Social work programmes | Journaling to report personal experiences and retrospective descriptions of the merger process | Gleaning and refinement |
| Auschra15 | N/A | Partnerships (mixed) | Health care | Review | Gleaning |
| Allen et al.32 | England | Joint commissioning | Health care | Case study with 42 interviews and documentary analysis | Refinement |
| Ball et al.47 | Scotland | Community health partnership/integrated care | Health and social care | More than 30 interviews with professionals, public and voluntary sector. Use of the partnership assessment tool211 | Gleaning and refinement |
| Billings and De Weger146 | England | Contracting | Health and social care | Review | Gleaning |
| Cameron et al.146 | England | Joint working | Health and social care | Review | Gleaning |
| Casey60 | Mixed | Partnerships (mixed) | Health and social care | Review | Gleaning |
| CQC148 | England | STP/accountable care organisation | Health and social care | Evaluation, based on inspection reports based on visits to 25 independent-sector adult social care providers and a 4-day visit to the organisation | Refinement |
| Cereste et al.149 | UK | Merger | Hospitals and mental health/community trusts | Focus group, and questionnaire answered by 457 trusts (mostly chief executives, finance directors, etc.) | Refinement |
| Community Network153 | England | Provider alliance/Integrated care | Health and social care | Summary report from a wider project – case studies (methods unknown) | Refinement |
| Community Network154 | England | Provider alliance/Integrated care | Health and social care | Summary report from a wider project – case studies (methods unknown) | Refinement |
| Community Network151 | England | Provider alliance/Integrated care | Health and social care | Summary report from a wider project – case studies (methods unknown) | Refinement |
| Community Network150 | England | Provider alliance/Integrated care | Health and social care | Summary report from a wider project – case studies (methods unknown) | Refinement |
| Community Network152 | England | Provider alliance/Integrated care | Health and social care | Summary report from a wider project – case studies (methods unknown) | Refinement |
| Cortvriend155 | England | Primary care trust | Acute care, primary care | Focus groups, with 31 participants taking part across five such groups, each containing four to eight participants | Refinement |
| Crump and Edwards156 | England | Provider chains | Acute care | Interviews (non-NHS, n = 11; NHS, n = 5) | Refinement |
| Das-Thompson et al.157 | England | Integrated care | Health and social care | Briefing | Gleaning |
| Dickinson and Glasby17 | England | Partnerships (mixed) | Health and social care | Review | Gleaning |
| Dickinson and Glasby22 | England | Integrated care | Health and social care | Five case study sites, using documentary analysis, interviews and focus groups | Refinement |
| Dickinson et al.158 | England | Merger | Health and social care | Case study, 23 semistructured interviews with range of people (from service users to CEOs) | Gleaning and refinement |
| Douglas159 | England | Alliances | Health and social care | Review | Gleaning |
| Dowling et al.21 | England | Partnerships (mixed) | Health and social care | Review | Gleaning |
| Erens et al.160 | England | Integrated care | Health and social care | Case studies of 25 integrated care pioneers, involving documentary analysis, qualitative interviews and surveys | Refinement |
| Evans and Kiloran161 | England | Partnerships (mixed) | Health and social care | Case study, a realist evaluation, including semistructured interviews with key stakeholders (unknown quantity) | Gleaning |
| Ferrier and Valdmanis162 | USA | Mergers | Acute care | Case control study of hospital mergers | Gleaning |
| Findlay et al.163 | Scotland | Health boards | Health and social care | Literature, documentary analysis, non-participant observation and semistructured interviews with 44 participants | Refinement |
| Forbes et al.164 | England and Scotland | Integrated care | Health and social care | Four case studies, two in England and two in Scotland; semistructured interviews (n = 16) were used | Refinement |
| Foundation Trust Network165 | England | Buddying | Acute care | Twelve trusts as case studies, involved in buddying; using surveys, desk research, structured interviews and documentary analysis | Refinement |
| Fowler Davis et al.166 | England | NHS vanguards | Health and social care | Service evaluation with embedded team; qualitative in-depth interviews | Refinement |
| Fulop et al.85 | England | Merger | Health and social care | Nine trusts (cross-sectional) and four trusts (case studies), using in-depth interviews and documentary analysis | Gleaning and refinement |
| Gannon-Leary et al.167 | England | Partnerships (mixed) | Health and social care and voluntary sector | Evaluation and literature review; narrative ‘experiential’ methodology | Gleaning and refinement |
| Gaynor et al.84 | England | Mergers | Acute care | Case–control study | Gleaning |
| Glasby and Dickinson168 | England | Partnerships (mixed) | Health and social care | Review | Gleaning |
| Gulliver169 | England | Joint commissioning, mental health | Health and social care | Evaluation; narrative ‘experiential’ methodology | Refinement |
| Gulliver et al.170 | England | Joint commissioning, mental health | Health and social care | Evaluation of a mental health service; utilising interviews with service users and staff, postal surveys, focus groups, observations and documentary analyses | Refinement |
| Hearld et al.171 | USA | Alliances | Health and social care | Case study of 16 alliances; quantitative data from surveys and qualitative interviews | Gleaning and refinement |
| Henderson et al.172 | USA | PCN | Health and social care | Evaluations of six primary care clinics and community-based organisations; qualitative methods comprising 54 interviews and 10 focus groups, with a review of 80 documents | Refinement |
| Hudson et al.119 | Mixed | Partnerships (mixed) | Public sector | Review | Gleaning |
| Hunter and Perkins94 | England | Partnerships (mixed) | Public health | Case study; 3-year study of public health partnerships (2007–10) in nine localities across England, involving semistructured interviews at strategic and operational levels | Gleaning |
| Huxham113 | Mixed | Partnerships (mixed) | Public sector | Theoretical review | Gleaning |
| Idel et al.173 | Israel | Merger | Acute care | Prospective study with quantitative methods; using a questionnaire (n = 128 participants) | Gleaning and refinement |
| Jones174 | England | PCN | Primary care | Report of experiences; narrative ‘experiential’ methodology | Refinement |
| Kendall et al.175 | England | Community health partnerships | Community health | Review | Gleaning |
| Kershaw et al.176 | England | STP | Health and social care | Case study of five STPs in London; phase 1 (small scale interviews with leaders), phase 2 (26 semistructured interviews with leaders and stakeholders) and groups discussions | Gleaning and refinement |
| Lalani et al.177 | England | Quality improvement collaborative | Acute care | Evaluation with researcher-in-residence model, based on two sites and comprising 15 semistructured interviews | Refinement |
| Leach et al.102 | England | Buddying | Health and social care | Evaluation, using quantitative performance data and a mixed-methods staff survey | Gleaning and refinement |
| Lewis178 | Australia | Primary care partnership | Primary care | Case study of two PCPs; using a network research methodology including both surveys and interviews with 37 people | Refinement |
| Lim179 | UK | Merger | Health and social care | Quantitative analysis of merger data from nine hospitals relating to staff job satisfaction | Gleaning and refinement |
| Mandell and Steelman180 | Mixed | Partnerships (mixed) | Public sector | Review | Gleaning |
| Maniatopoulos et al.181 | UK | Vanguards (11 different cases) | Health and social care | Comparative case studies, including 66 semistructured qualitative interviews across nine vanguards, as well as documentary analysis of included | Refinement |
| Mervyn et al.182 | England | Network | Health and social care | Exploratory case study, employing 12 initial semistructured interviews, a literature review and then an additional 21 interviews with another sample | Refinement |
| Murray et al.100 | USA | Accountable care organisation | Health and social care | Longitudinal case studies from 2012 to 2017 with two accountable care organisations, including 115 semistructured interviews and observational data based on seven site visits | Gleaning and refinement |
| Naylor et al.183 | England | Integrated care | Health and social care | Five case study sites with acute hospital providers that have moved towards integrated care, utilising 39 in-depth interviews and site visits | Refinement |
| NHS Employers44 | England | Vanguards | Health and social care | In-depth case studies on three vanguards, including semistructured interviews (n = 13), focus groups (n = 3) and documentary evidence | Refinement |
| NHS Professionals184 | England | Partnerships (mixed) | Health and social care | Review | Gleaning |
| NHS Providers185 | England | Integrated care | Health and social care | A briefing by a policy organisation that uses interviews (unknown number) | Refinement |
| NHS Providers186 | England | Integrated care | Health and social care | Case studies from three health and social care partnerships in England, in the format of a series of organisational reports | Refinement |
| NHS Providers and NHS Clinical Commissioners187 | England | Joint commissioning | Health and social care | Policy report drawing on a literature review and in-depth semistructured interviews with clinical commissioning (n = 9), national thought (n = 5) and provider leaders (n = 10) | Refinement |
| Peck et al.188 | England | Joint commissioning | Health and social care | Case study of a combined trust, using annual semistructured interviews with managers, postal surveys with (n = 169 in 1999 and n = 143 in 2000) and exploratory workgroups | Gleaning and refinement |
| Pickup189 | England | Integrated care/joint commissioning, mental health | Adult services | Case study in the format of an ‘experiential report’ | Refinement |
| Round et al.190 | England | Integrated care | Primary, acute, community, mental health and social care | Programme evaluation design, using documentary analysis, 31 stakeholder semistructured interviews, focus groups and observational data | Gleaning and refinement |
| Shaw191 | England | Mergers | Health and social care, integrated trust | Case study of merger of two trusts, using qualitative methods and semistructured interviews with 42 people. Documentary analysis was also used | Gleaning and refinement |
| Smith et al.37 | England | PCNs | Primary care | Qualitative cross-comparative case study across four sites, using rapid evidence assessment, a workshop with academics and policy experts, interviews with stakeholders, observations, survey and documentary analysis | Refinement |
| Southby and Gamsu192 | England | Integrated care, PCNs | Primary care and voluntary and community sectors | Case study design comprising four cases, each with a GP and voluntary and community sector organisation, using 18 semistructured interviews with GPs, practice managers, practice nurses and senior managers, and a focus group of 14 participants | Refinement |
| Southwark and Lambeth Integrated Care193 | England | Integrated care | Health and social care | Report regarding organisational experience of an integrated care programme, using evaluative as well as anecdotal evidence | Refinement |
| Starling and The Health Foundation194 | England | Vanguards | Health and social care | Case studies, interviewing 45 middle-to-senior clinical and non-clinical leaders and evaluators across eight vanguard sites | Gleaning and refinement |
| Steininger et al.195 | Austria | Hospital merger | Acute care | Qualitative case study of the merge of IT systems, involving interviews with 40 stakeholders | Refinement |
| The King’s Fund196 | England | Joint commissioning | Community care | Report as part of an evaluation. Observations and interviews were used (unclear quantities) | Gleaning and refinement |
| Timmins197 | England | Integrated care | Health and social care | Analysis of leaders’ experiences with integrated care and collaboration in a report format. Based on interviews with 16 chairs and leads | Refinement |
| What Works Scotland198 | UK | Public services | Public sector | Review | Gleaning |
| Wildridge et al.199 | UK | Partnerships (mixed) | Public sector | Review | Gleaning |
| Zuckerman et al.200 | USA | Alliances | Health care | Review | Gleaning |
In addition, 14 theoretical papers were included. The 14 papers comprised one paper on partnership synergy,115 one paper on trust,14 two papers on conflict,201,202 one paper on power,203 one paper on coordination,125 one paper on leadership,204 two papers on organisational flexibility,203,205 one paper on task complexity,206 two papers on confidence and formalisation207,208 and two papers on proximity theory. 209,210
Theory gleaning
Partnership synergy as a middle range theory
Frequently mentioned in seven of the systematically reviewed studies15,47,60,113,158,167,168,175 was the concept of partnership synergy, which was first coined by Lasker et al. 115 as a means for explaining how partnerships achieve advantage over independent, competitive working. Therefore, this theory was adopted as a MRT, which explains how there are ‘partnership functioning’ (hereby collaborative functioning) mechanisms essential to explaining the processes of working together, as well as ‘partnership performance’ (hereby collaborative performance) mechanisms that underpin the improvements that collaborating seek to attain. Lasker et al. 115 put forward partnership synergy as an intermediate outcome that comes after the functioning of the partnership, but precedes the effectiveness of it (see Figure 11). 115 This means that, when working well together, a combination of resources and skills of the partners is what enables achievement above and beyond what would have been possible individually.
FIGURE 11.
Simplified depiction of our MRT and the essential roles of trust, confidence and faith. This figure has been adapted with permission from two sources. First, Aunger et al. 138 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original text. Second, Lasker et al. 115
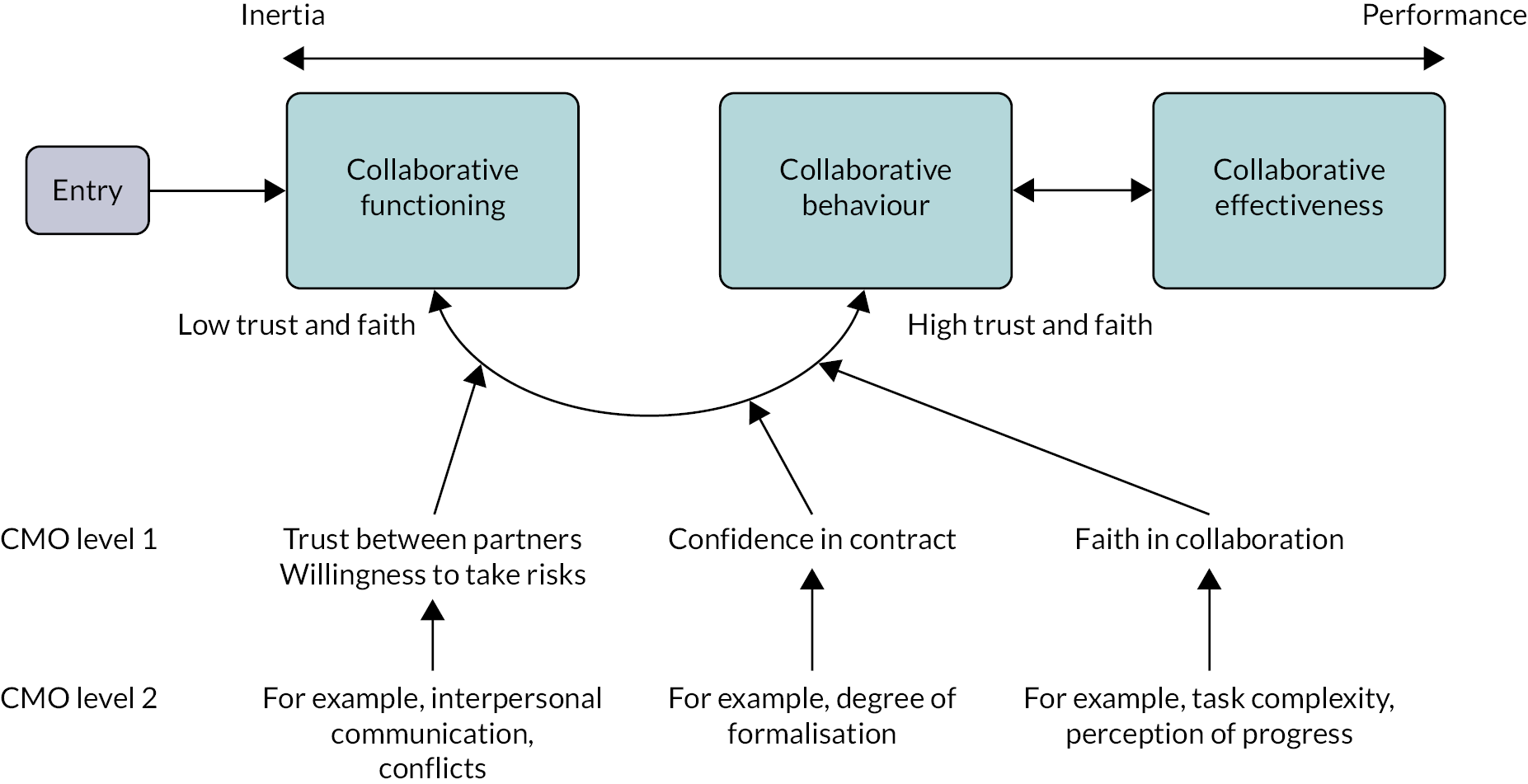
Partnership synergy can be considered a mechanism whereby a context of high collaborative functioning leads to greater collaborative synergy and, therefore, improved collaborative performance. Improved collaborative performance is likely to be an outcome in itself, which results from mechanisms involved with an improved ability to achieve health care-related outcomes, such as reduced duplication of effort, economies of scale and competitive advantage. 115 However, these performance-related mechanisms will depend on the aims and structure of each individual collaboration. We also add to the MRT the concept of collaborative inertia, which was put forward by Huxham,113 one of the systematically identified studies.
Collaborative inertia occurs when organisations and actors get ‘bogged down’ in the day-to-day functioning of the partnership. 113 While trying to optimise the daily functioning, achievement of the actual aims of the collaboration fall by the wayside, as significant resource and time is devoted to collaborative functioning rather than accomplishment of outcomes. It is possible that a collaboration will engage in a period of inertia in its earlier stages of formation, before synergy is later achieved. This concept of inertia was also put forward by a number of the included studies60,113,119,158,184 and is defined as when ‘the output from collaborative arrangements often appears to be negligible or the rate of output to be extremely slow’,13 and this is also depicted in Figure 12.
FIGURE 12.
Depiction of key aspects of refined programme theory. Adapted with permission from Aunger et al. 138 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original text.

This MRT theory, taken together, proposes that the mechanisms comprising ‘partnership functioning’ need to have their context configured very favourably before ‘synergy’ and, therefore, enhanced performance can be achieved. However, we have reframed the concept of partnership synergy as ‘collaborative behaviour’ to make it a more well-defined and testable concept. As partnership functioning relies on many other contextual factors and the mechanisms that enable collaboration, these will be explored in the following section as elements that enable synergy (or collaborative behaviour) and, therefore, partnership effectiveness and accomplishment of its aims.
Gleaning initial context–mechanism–outcome configurations
Our gleaning phase identified that several mechanisms are essential to how collaborations function. The mechanisms included trust, risk tolerance, faith, confidence, conflict, power, interpersonal communication, leadership, cultural integration, perception of progress and perception of task complexity. Our MRT incorporated the trust-building loop by Vangen and Huxham14 and its focus on risk-taking as a driver of collaborative, rather than competitive, attitudes and behaviours. Within the trust-building loop, trust acts as an enabler for organisations to enhance their risk tolerance. Furthermore, we identified a role for ‘faith’,138 where, both individually and collectively, actors have belief that the collaborative endeavour (i.e. the intervention) is a virtuous and beneficial undertaking, thereby worthy of working on. Faith is, therefore, likely to drive actors to dedicate time and effort to engaging in collaborative behaviour, but will change over time in response to other mechanisms and contextual factors.
Therefore, we posited that trust and faith serve as dual drivers for actors to begin behaving collaboratively. In addition, trust and faith also serve as mechanisms in realist terms. In our theory, at the gleaning phase, building trust and faith were key processes that constitute the ‘collaborative functioning’ stage of collaborations. Achievement of a high level of trust and faith across the organisation allows for a synergistic state in which partners achieve maximal collaborative behaviour. Our prior work also indicated that in more integrative types of collaboration (e.g. a merger) or collaborations that are mandated, trust may be progressively replaced by ‘confidence’ in contractual mechanisms as a means for driving collaborative behaviour. 138 This is because much of the risk of engaging in collaborative behaviour is enshrined in contractual obligation rather than the building of trusting, robust interpersonal relationships.
Our theory identified that, at least initially, collaboration requires daily efforts to maintain interpersonal ties and build relationships for ‘collaborative functioning’ to occur. Mechanisms found to be key to collaborative functioning identified in the review were trust and faith, with conflict, interpersonal communication, leadership and cultural integration being within different CMOCs (see Figure 11). 138 As is evident in this applied example, these CMOCs operate through one another, forming chains that are situated in temporal stages as the collaboration develops over time (see Figure 12). Our theory posited that once trust and faith reach a certain threshold, then a novel state is entered, termed ‘collaborative synergy’, in which the benefits of collaboration can be attained. Since our refined version of the theory, this has been reframed as ‘collaborative behaviour’ to make ‘synergy’ a more tangible concept. 138 Driven by the integration of skills, knowledge and resources of partners, performance benefits may include innovations brought about by sharing of expertise, cost savings from better bargaining power and reduced duplication of effort across health systems.
For this section of the chapter, we adopt our theory from the gleaning phase as the MRT for understanding in this refinement phase. A full description of the CMOCs identified in this literature can be viewed in Box 1. These CMOCs were taken as a foundation for the refinement phase of the realist synthesis and the refined theory will be explored in more detail in the following section. Further details of the theory gleaning stage can be found in Aunger et al. 138
High partnership functioning characterised by high trust and faith (context) will enable collaborative behaviour to occur (mechanism), leading to greater task achievement (outcome).
Low partnership functioning characterised by low trust and faith (context) will lead to collaborative inertia (mechanism) and reduced task achievement (outcome).
High confidence and faith (context) will lead to collaborative behaviour (mechanism), which will lead to greater task achievement (outcome).
Perception of progress and performanceA high degree of intraorganisational conflict (context) will lead to a lessened perception of progress (mechanism), causing reduced faith (outcome).
Having unambitious aims for the collaboration (context) will lead to a lessened perception of progress (mechanism), causing reduced faith (outcome).
Having absent key actors (context) will lead to a lessened perception of progress (mechanism), causing reduced faith (outcome).
Having workforce instability (context) will lead to a lessened perception of progress (mechanism), causing reduced faith (outcome).
Greater organisational flexibility (context) will lead to an enhanced perception of progress (mechanism), causing increased faith (outcome).
Continuous evaluation (context) will lead to an enhanced perception of progress (mechanism), causing increased faith (outcome).
Having clarity of roles (context) will lead to an enhanced perception of progress (mechanism), causing increased faith (outcome).
Partnership functioning ConflictHaving appropriate accountability arrangements (context) can reduce conflict (mechanism), improving trust (outcome).
Having greater cultural compatibility (context) can reduce conflict (mechanism), improving trust (outcome).
Having a vision shared between partners (context) can reduce conflict (mechanism), improving trust (outcome).
A slow pace of development (context) can increase conflict (mechanism), reducing trust (outcome).
Failing to achieve a collaborative task (context) can increase conflict (mechanism), reducing trust (outcome).
Stopping a collaboration inappropriately (context) can increase conflict (mechanism), reducing trust (outcome).
TrustA destructive conflict resolution strategy (context) can reduce trust (mechanism) leading to reduced perception of progress and faith (outcome)
A constructive conflict resolution strategy (context) can improve trust (mechanism), leading to improved perception of progress and faith (outcome).
Having existing successful collaborations (context) can improve initial trust (mechanism), causing improved aims and objectives and greater collaborative behaviour (outcomes).
Having appropriate legal agreements in place that do not take away the perception of altruism (context) can improve trust (mechanism), leading to greater collaborative behaviour (outcome).
Overambition in the aims of the collaboration (context) can reduce perception of progress (mechanism), leading to reduced trust and faith (outcome).
Significant conflict (context) can reduce trust (mechanism), reducing collaborative behaviour (outcome).
ConfidenceGreater formalisation in a mandated or more integrative collaboration type (context) can increase confidence (mechanism), leading to greater collaborative behaviour (outcome).
PowerLarger-size discrepancies of involved organisations (context) can lead to domination by a single partner and a significant power imbalance (mechanism), thereby reducing trust (outcome).
Unequal resource distribution in the collaboration (context) can lead to domination by a single partner and a significant power imbalance (mechanism), thereby reducing trust (outcome).
Mandated collaboration where one organisation is usually told to collaborate with a ‘better-performing’ one (context) can lead to domination by a single partner and a significant power imbalance (mechanism), thereby reducing trust (outcome).
FaithInvolvement of stakeholders in planning the collaboration (context) can improve the perceived authenticity of the collaboration (mechanism), thereby improving faith (outcome).
An inauthentic partnership in which no one respects or believes that it can achieve its stated aims (context) leads to reduced faith in the partnership (mechanism), which can lead to reduced collaborative behaviour (outcome).
When perception of progress stalls (context) then the faith can be significantly reduced (mechanism), leading to partnership dissolution (outcome).
Interpersonal communication/coordinationIncompatible organisational cultures (context) combined with a high level of communication (mechanism) can lead to conflict (outcome).
Greater geographical proximity of partners (context) can lead to increased interpersonal communication (mechanism), which can increase or decrease trust, depending on whether or not conflict is occurring (outcome).
Leadership (context)A collaborative leadership style (context) can improve trust (mechanism), which increases collaborative behaviour (outcome).
Mandated collaboration with low initial trust (context) enables leaders to push out those with a conflicting vision (mechanism), which can improve how shared the vision for the collaboration is (outcome).
A voluntary collaboration (context) combined with a combative leadership approach (mechanism) can lead to an imbalance in power (outcome).
Cultural integrationHaving an inclusive leadership style (context) can lead to better cultural integration (mechanism) and, therefore, greater trust (outcome).
Perception of task complexityHaving interoperable IT systems (context) can lead to a reduction in perceived task complexity (mechanism), which enhances faith (outcome).
A larger organisation size (context) leads to a greater perceived task complexity (mechanism), thereby reducing faith and increasing initial trust requirements (outcomes).
Having simpler aims for the collaboration (context) leads to a reduced perception of task complexity (mechanism), which can lower initial faith requirements (outcome).
A favourable regulatory environment for collaboration (context) can lower perception of complexity (mechanism) and thereby improve initial faith (outcome).
Theory refinement
Refining the context–mechanism–outcome configurations of collaborative functioning
This refinement of our realist synthesis gave greater insight into how CMOCs are situated in the timeline of development of collaborations, which is how we have structured this section of the chapter. In addition, refinement of our realist synthesis has given further insight into atemporal mechanisms (i.e. mechanisms that can activate at any time) and how these affect the process of collaborating. This section will explain the various mechanisms of the refined theory, when they activate and in response to which contextual factors.
Context–mechanism–outcome configuration coding and establishment of context–mechanism–outcome configuration chains: refinement of mechanisms
Extraction of CMOCs from included studies resulted in 338 CMOCs being identified, many of which were functionally identical and analogous to demiregularities. The majority of the CMOCs were explored in the prior section. 138 As previously mentioned, coding of CMOCs was performed according to which mechanism a context activates. The below ‘initial mechanisms’ were used as preliminary deductive codes; however, these were updated as CMOCs when other mechanisms were identified in the literature (see Table 7). By the end of the process, novel CMOCs were not being identified, as they were all analogous to demiregularities that had been already found. In terms of frequency, the CMOCs most identified were CMOCs with trust or confidence as the mechanism, then ‘perception of progress’, faith, interpersonal communication and information-sharing, task complexity, cultural assimilation, conflict, and clarity and sharedness of vision. For the sake of brevity and because of the complexity of IOC, every CMOC and their contextual factors will not be explored here; however, further details of the CMOCs are provided in Report Supplementary Material 1, along with the full table of CMOCs identified in each respective paper. In the refinement stage, some mechanisms from the gleaning phase were redesignated as parts of the contextual environment, including leadership and power, which now form aspects of the contextual environment, rather than being mechanisms in themselves.
| Refined mechanism and its type | Explanation | Most frequent outcome |
|---|---|---|
| Effectiveness through collaboration, enabling innovation, reduced duplication of effort, sharing of best practices, increased access to resource, reduced gaps in services and increased influence over others (i.e. changes to resources, behaviours and mental processes) | The ‘ultimate outcomes’ that usually underlie actual improvements to key metrics of organisational performance | N/A |
| Changes towards collaborative behaviour from competitive behaviour (behaviour) | A move from competitive organisational behaviours to collaborative ones | Collaborative effectiveness |
| Risk threshold (cognitive process) | How much risk an organisation is willing to take on with a collaborator | Collaborative behaviour |
| Faith (cognitive process) | A belief in the collaborative endeavour as a positive force and, therefore, a motivation to work on its goals | Collaborative behaviour |
| Perception of progress (cognitive process) | Whether or not actors perceive advancement towards the goals of the collaboration | Faith |
| Conflict (cognitive process) | The perception by organisational actors that they are in opposition to collaborators in some way | Trust |
| Approach to conflict resolution and accountability (cognitive processes) | Processes and attitudes in place that lessen the severity of conflict | Conflict |
| Trust (cognitive process) | A psychological state comprising the intention to accept vulnerability based upon positive expectations of the intentions or behaviour of another 212 | Risk threshold |
| Confidence (cognitive process) | A belief that a collaborator will behave collaboratively because of contractual or other obligations | Risk threshold |
| Initial trust (cognitive process) | Trust that manifests as a result of pre-existing contextual factors | Trust |
| Cultural assimilation (cognitive process) | How well actors between organisations are aligning in terms of attitudes and behaviours | Trust |
| Interpersonal communication and information-sharing (behaviour) | The behaviour of communicating and sharing information | Trust |
| Perception of task complexity/initial faith (cognitive process) | How complex actors perceive the collaborative endeavour to be | Faith |
| Clarity and sharedness of vision (cognitive process) | How well defined and to what extent the vision between partners is agreed on | Trust |
| Perceived legitimacy of collaboration (cognitive process) | How actors perceive the collaboration in terms of its authenticity | Initial faith |
Mechanisms specific to early stages of collaboration
Our initial CMOCs138 identified that essential to establishing ‘initial faith’ (i.e. whether or not engaging in collaboration is feasible and worth the risk and effort) are factors such as financial constraints, the regulatory environment and its favourability to collaboration and organisational size (which may affect the perceived difficulty of the task). A further contextual factor identified in this refinement stage was the reputation of the specific form of collaboration being considered. For example, some papers176 referred to negative perceptions due to collaborations being associated with privatisation of the NHS, and this lowered actors’ desire to engage with this form of collaboration in the first place (i.e. their initial faith in the endeavour). Also tied into faith as a precursor mechanism is the perceived legitimacy of collaboration, which often affects a collaboration from the outset. Impacting this mechanism is stakeholder involvement, which can serve to increase its legitimacy in the eyes of staff, whether or not a partnership is voluntary and whether or not staff perceive the collaboration as a threat professionally. 173
Related to the level of initial faith is that of initial trust. Initial trust was put forward during the theory gleaning phase of our realist synthesis as likely to come into play in the ‘connecting’ phase of collaboration, during which organisations seek partners and establish initial relationships. 213 Contextual elements identified as essential to determining this initial level of trust are the history of collaborating or competing between the organisations,37,176,181,191 organisational reputations44 and, at a later stage, the strength of legal agreements. 186 These factors have been found to enhance or undermine trust. For example, legal agreements can act as an initial reassurance when relying on a partner, but can also undermine collaborations if the legal agreements do not allow for attribution of collaborative behaviours to altruistic intent. 22,44 Furthermore, this refinement stage also identified that a context of historical health system failures can lower initial trust,187 as evidenced by NHS Providers, which put forward that ‘a legacy of challenges, can lead to a break-down in trust and dialogue and an entrenchment of organisational ‘fortress mentalities’. 187 As trust and risk are intricately linked, then this level of initial trust is essential to setting the degree of risk an organisation is willing to take on with its partner, which can affect the aims and outcomes a partnership seeks to accomplish. 44,100
Middle stage of collaboration
During the ‘mid-life’ of a collaboration, a multitude of factors come into play that can help rapidly increase the level of trust, buffering against potential conflicts that may occur. Chief among these factors are ‘quick wins’ with a partner, which also help to increase faith. 44,166 These small successes serve to rapidly bolster trust and can be increased further through factors such as seconding staff188,189 and having open, honest, stable and empathetic leadership. 187,197 Alongside these quick wins are longer-term battles, such as the need to ensure effective interpersonal communication between key organisational actors, managing conflict100,163,167,183 and either creating a new culture or helping build bridges between existing ones. 37,145,153
With respect to ensuring appropriate communication between collaborators, a number of contextual elements are key. Geographical proximity is one element that is difficult to mitigate, as a greater geographical distance between collaborators increases time spent building relationships significantly by allowing for ease of arranging meetings and enabling informal interaction. 165 Greater geographical proximity was most often cited as improving communication, but can also be unhelpful if conflict is already occurring. 172,192 In addition, having a larger size and/or quantity of organisations involved can make communicating more difficult because of the increased number of involved actors and moving parts. 85 Compatibility of IT systems,37,160 joint staff appointments183 and having regular collaboration-wide meetings can also work to increase trust as an outcome through the mechanism of interpersonal communication. 102,158 When cultures are mismatched or not mutually understood, conflict can occur, which thereby reduces trust. 188 Improving cultural assimilation by configuring the context is also possible, which can also go on to enhance trust. A mutual cultural understanding can be fostered by ensuring that a shared vision of the collaboration is in place153 by having a cross-organisational ‘inspirational leader’ who also engages in role-modelling behaviours158 and by supporting staff through the transition. 173 It mutual cultural understanding also be improved by having joint teams of staff to work on shared goals, which can improve a sense of collegiality. 150,154 It was evident in the literature that certain passive elements, such as the pre-existing degree of cultural distance and whether or not the collaboration is perceived as forced on staff, can also significantly change the difficulty of cultural assimilation. 197
Atemporal elements impacting collaboration
Conflicts between organisations can occur as a result of deteriorations in trust, as a result of ‘acute events’, such as failures on specific tasks, or from accumulating tensions caused by cultural distance. 100,138 Conflicts directly cause a loss of faith in the collaboration and trust between partners. 138 Therefore, there is a reciprocal relationship between conflict and trust, and conflict and faith (see Figure 2), and this is supported by excerpts such as ‘Conflict, for example due to competition between partners, increases the difficulty in predicting the partner’s behaviour and increases the uncertainty in the decision to trust’. 44 Reductions in faith can also lead to intraorganisational conflict. 138 We also found that conflict can be modulated when it occurs by the approach to conflict resolution. Conflict resolution is now a mechanism in itself in this refined theory, which can dampen the impact of conflict on trust or faith. 183
This refinement stage further identifies that use of external, impartial deal brokers and committees can lessen the impact of conflict on trust by moving the locus of that trust to the third party rather than the partner,167 along with having robust governance structures that are not imbalanced in either direction in terms of power. 183 Likewise, conflict itself can be mitigated by leaders bringing a constructive approach to conflicts, by proactively attempting to reduce power imbalances and by avoiding or managing any senses of takeovers in the case of mergers or other more integrative collaboration types. 44 Although conflict interacts with both trust and faith, so too does the degree to which the collaborative vision is shared and its clarity. The clarity of vision is more keenly interlinked with faith, which is supported by quotes such as ‘most sources concur that a clear vision and/or mission statement should include attainable goals and that lack of clarity about vision can be a serious barrier to engagement’. 167 Here, engagement can be considered similar to our concept of faith. However, the sharedness of the vision works through the mechanism of trust, as sharedness relates directly to the interorganisational perception of each organisation. The clarity and sharedness of vision are affected by patient and public engagement, which helps keep the focus on improving care quality (rather than secondary objectives), having inclusive decision-making processes and stable leadership. In many cases, significant leadership turnover meant starting over with trust-building exercises due to large changes in vision occurring. 155,171
As a final look into the role of faith, a key mechanism that links into faith as an outcome is ‘the perception of progress’. The perception of progress is interwoven with faith, but is not entirely the same concept (as one can have faith without much perception of progress). The perception of progress is essential for ensuring that momentum is maintained and that there is no stall into what is termed ‘collaborative inertia’, a situation in which there is insufficient faith to maximise work on the collaboration. 158 Having an increased perception of progress increases faith and a lesser perception of forward momentum reduces it, and this is supported by quotes from health-care leaders, such as:
So it is harder and less dynamic at the start, until you get a drumbeat going. Then it becomes easier because the peer group start doing it for you. 197
Affecting this perception of progress are contextual factors, such as appropriate degrees of ambition (as overambition can lead to disappointment),190,193 implementation of ‘quick wins’, having effective planning (which ensures that staff are working on the most appropriate projects at the right time156) and, importantly, having effective evaluation and dissemination processes (which ensure that staff are aware of the progress being made25,193).
These various review findings suggest a web of contextual elements, operating through many mechanisms to produce many outcomes and forming causal chains (see Figure 13). Some of these elements can be altered to be more beneficial to implementers (e.g. keeping ambitions realistic) and some cannot (e.g. geographical proximity). Although these elements discussed are those that underlie the functioning of the partnership, the review also identifies mechanisms that underlie material improvements to organisational performance.
FIGURE 13.
Example of how contextual elements and mechanisms may operate over time to drive a voluntary-type partnership into collaborative synergy. The lines represent how levels of trust and faith may change independently over time in response to the various numbered events. Adapted with permission from Aunger et al. 138 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original text.
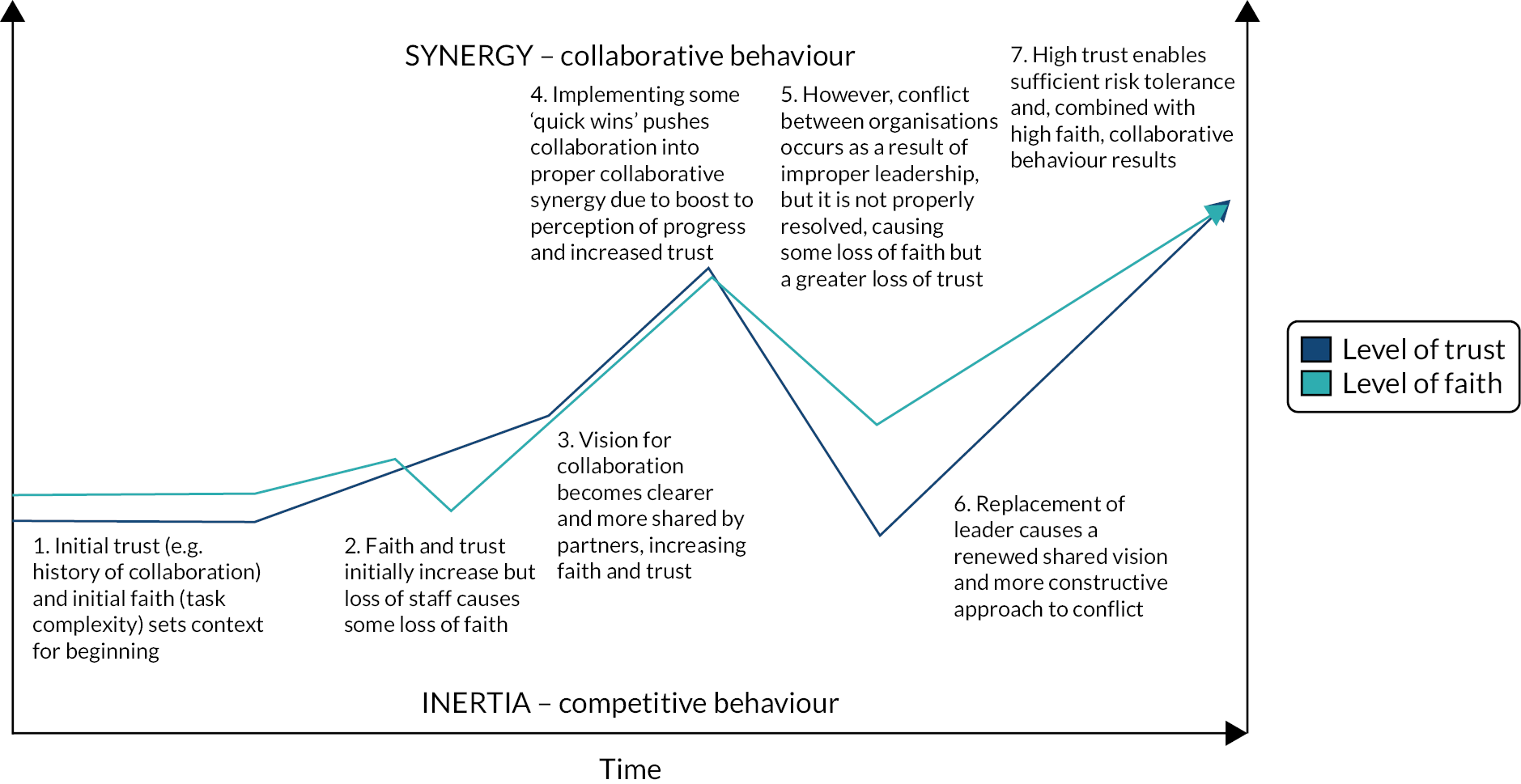
Refining context–mechanism–outcome configurations driving partnership performance
As trust and faith are maximised, work on managing conflicts, building collaborative structures and establishing relationships decreases. As a result, time and effort are freed up to create the conditions for collaborative ‘synergy’, which in our refined theory refers to a willingness to engage in collaborative, rather than competitive, behaviour (see Figure 3). Once risk tolerance and faith are maximised, then partners can strike out to work on risky innovations together, share best practices, pool resources, bid for contracts together, increase influence in the local health economy, reduce duplication of effort and better focus on inequalities in the health system, and these may be the mechanisms through which ‘ultimate outcomes’ of collaboration (i.e. performance improvements) are realised, occurring because of an accumulation of skill, knowledge and resources being brought to bear against problems encountered by the partnership. However, these benefits seldom come to fruition because of the sheer amount of work and goodwill that is required to rise above the quagmire of the daily functioning of the partnership, explaining why many collaborations are not successful. Studies capture contexts where ‘too much was being expected too soon . . . as they were still working out how to function operationally before they could accomplish goals such as decreasing workload and improving care’. 37
Achievement of this synergistic state is extremely difficult, as many collaborative endeavours are ‘set up for failure’ because of initial contextual conditions being configured in such an unfavourable manner that it becomes insurmountably difficult to build the relationships required. 214 These difficult contextual conditions can include a regulatory environment that still revolves around competition rather than collaboration,183 mandated partnerships and integrated care initiatives that do not allow for building of relationships, brought into place in conditions of pre-existing histories of competition and ‘bad blood’187 and a lack of financial support or consideration provided for collaborative endeavours to be implemented properly. 176 As outlined by our theory, these common contextual factors serve to undermine initial trust in partners and initial faith in the process and increase task complexity to a degree that makes them very difficult to overcome. One quote from an included study of buddying arrangements in the UK reflected this clearly:
Interviewees repeatedly said how difficult it would have been if their buddying arrangement had been imposed, and indeed those arrangements seen to be imposed by regulatory bodies appear to be have been the least successful. 165
This information provides implications for cross-sector initiatives, such as ICS or accountable care organisations taking place in the UK, as it demonstrates that context can be configured very unfavourably in these mandated arrangements, making it difficult to build trust and faith. In addition to many of these arrangements being mandated, cross-sector working brings additional challenges by requiring working between workforces of differing professional backgrounds. These professional differences manifest in a greater degree of cultural divide (a barrier that was referenced by many of the included case studies44,100). Likewise, in cross-sector arrangements, the number of partners and size of the involved organisations is likely to be greater, which further increases the difficulty of communicating effectively and clearly, and results in much higher task complexity. These are all concerns that require great tact to mitigate. Collaborative performance will be explored further in a later chapter by drawing on our empirical findings.
Refinements by collaboration type and collaborative functioning
Our initial rough realist theory suggested that partnerships can be characterised along a spectrum of integration, from full integration (i.e. mergers) to more informal endeavours involving fewer people (i.e. buddying, clinical networks). 61 Such differences between collaborative types (e.g. buddying vs. alliances) are also reflected in our findings as changes to contextual elements (i.e. whether or not they are mandated), and these changes can affect the task complexity, perceived legitimacy, faith and initial trust. Our review identifies how it is possible to trace how these changes affect implementation. For example, a voluntary buddying arrangement is likely to be relatively simple to implement, as it is unlikely to be perceived as threatening by staff, does not involve many organisations and, although perhaps not supported by formal legal agreements, is likely to involve partner self-selection. This arrangement is likely to start with a high degree of initial trust between partners and initial faith in the process. On the other hand, ICSs, which are now mandated to come into force in 2021, involve a significant number of large organisations coming together in a cross-sector manner, including local councils, primary and social care, and acute care,33 and this drastically increases task complexity by being cross-sector and having many involved organisations. Additional challenges include that it is likely such a move may be perceived as a threat by staff, reducing faith by reducing its legitimacy in their eyes. An ICS is also likely to increase difficulty of effective communication by having both great breadth and depth of organisations involved, making trust building more difficult, and there may be reduced initial trust from outset by being set in a local context of pre-existing competitive attitudes. In addition to that, being given a rapid timeline while having to overcome prior differences and conflicts poses an additional challenge, which requires a strict patient-centred focus shared across the system to overcome.
Our programme theory suggests that formalisation through contracts may be one means of enabling collaborative behaviour in such a situation where initial trust is likely to be low or complexity very high. The following section explores further how trust and its relationship to risk threshold may be replaced by confidence as a primary driver for collaborative behaviour in mandated or integrative collaboration types.
Trust versus confidence in integrative and mandated partnership types
In the gleaning phase of our realist synthesis, we identified a common CMOC that suggested that the formalisation of an arrangement through contracting facilitated trust relationships by having potential to act as a buffer where trust may otherwise be lacking. 138 Inversely, trust may also be undermined if too much collaborative behaviour is mandated through contract, as organisations assume that the partner will act collaboratively as a result of contractual obligation. We also found evidence that, with either mandated or otherwise more integrative types of partnerships (e.g. mergers), trust may not be the primary determinant of collaborative behaviour, as that role would instead shift to confidence. 138
Our updated review sought to further understand the relationship between confidence, formalisation, risk tolerance and trust. Although it was difficult to identify relevant information, our included literature identifies an inherent mistrust taking place in organisations involved in mandated partnerships, with perceptions of ‘taken over’, atmospheres of ‘them and us’ and domination of powerful partners resulting in a lack of trust and partnership strength. 164 Next to this lack of trust in mandated collaborations, formalisation was seen by sources as a means for risk management. Use of controls and contracts ‘to minimise uncertainties of behaviour by partners’ had value in instances where trust was low. 44 Another source put forward the notion that formalisation through contract is ‘primarily about managing risk, trying to situate the risk with the organisation/s most able to mitigate it, and giving them the power to do so’. 187 Therefore, we have added the concept of confidence, built through formalisation, to our programme theory diagram as a determinant of risk tolerance (see Figure 12). Greater confidence (context) will thereby increase risk tolerance (mechanism) for engaging in collaborative behaviour (outcome) (see Figures 12 and 14).
FIGURE 14.
Depiction of ‘causal web’ formed by CMOC chains of how and why health-care collaborations work. Light blue and dark blue elements relate to collaborative functioning. Adapted with permission from Aunger et al. 138 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original text.

However, while some sources were espousing formalisation as a means for improving trust, it was evident that other sources were warning that overformalisation could undermine the trust-building process:
[The] contribution [of contracts] is less in subsequent phases once trust grows, not least because early contracts cannot anticipate every eventuality. 44
This sentiment is echoed by the following quote from Dickinson and Glasby:22
. . . although a lot of the joint commissioning processes described to us were formalised and structural, people often recognised that joint working is essentially relational (based on informal conversations and interactions). 22
These findings indicate that voluntary collaborations should be careful not to overly rely on structural means of obligating collaborative behaviour where they should be focused on building relationships. Memoranda of understanding, although generally non-binding, increase trust between collaborators and thereby reduce perception of the risk taken on when engaging in collaborative behaviour. 178 We hypothesise that these non-binding contracts, such as memoranda of understanding, may be most appropriate as a tool to increase risk tolerance for less integrative or voluntary arrangements, where there is a risk of misattribution to obligation rather than genuine collaboration with the use of binding contracts, as Casey puts forward ‘there is a need for a balance between power-sharing and control, between processes and results, between continuity and change and between interpersonal trust and formalized procedures’. 60
A novel means of depicting context–mechanism–outcome configuration chains: ‘causal webs’
Our review findings suggest that CMOCs formed chains of generative causality as a result of the outcome of one CMOC becoming the context for another. For example, a larger organisational size (context) leads to greater task complexity (mechanism), which affects people’s faith in the process (outcome). 160 However, further down the chain, faith is a context in which collaborative behaviour (mechanism) occurs, leading to improved synergy (outcome) and, therefore, the ‘chains of causality’ emerged naturally from the linkages between CMOCs. As there is no common diagrammatical standard for how to depict CMOC chains in realist syntheses, we found that it was appropriate to depict our findings in the ‘causal web’ shown in Figure 14. In Figure 14, it should be simple to follow the aforementioned example of CMOC chain in the figure from organisational size (context 1) through to collaborative behaviour (outcome 2). This mode of representation draws similarities with the concept of a ‘context map’ put forward by Renger et al. 215 for use with realistic evaluations; however, our approach expands a context map by including both mechanism and outcome in the web with their own means of representation. Yet, it is important to note that the diagram does not depict how specific contexts alter the mechanisms, only which mechanisms are attached to which contextual factors, and which outcomes are attached to which mechanisms. 215 For specific dynamics, Figure 12, updated from our version in the theory gleaning phase based on the present refinements, depicts the key mechanisms and dynamics underlying the how of the workings of the CMOCs we identified.
Conclusion
Although many existing theories have delved into what underlies the process of IOCs in health care, this chapter builds on our knowledge of not only what but also how and why these elements work, and this was achieved by gleaning and refining CMOCs based on 86 papers to produce a refined realist theory. The theory has surfaced the inter-related roles of trust and risk tolerance, faith, task complexity, interpersonal communication, cultural integration and perception of progress, and how these elements drive collaborative behaviour. Likewise, the theory demonstrates that, in mandated or highly integrative collaborations, the locus may be shifted from trust towards contractual obligation and a sense of confidence that the partner will act collaboratively. The theory also builds on similar existing findings in the literature from other authors by linking contexts, mechanisms and outcomes together into a long causal chain, as this allows an understanding of how initial environmental and interorganisational conditions set levels of trust, faith and task complexity, and how these mechanisms can be managed later in the process of collaborating. These chains of CMOCs were situated within a ‘web of causality’, which allowed us to depict how distant contextual items and their mechanisms work to affect more long-term outcomes, including collaborative behaviour. This version of our programme theory will be tested further in the following chapter, which is based on findings from the empirical side of the project.
Chapter 5 How do stakeholders understand the ‘functioning’ of interorganisational collaboration?
The purpose of this chapter is to present the findings from interviews undertaken with a range of policy, practitioner and patient representative perspectives regarding how they understand and experience the mechanisms of collaborative functioning. The chapter organises these findings around the mechanisms central in the realist review (i.e. trust, faith, risk tolerance and confidence). Other supporting mechanisms are also captured along with the contexts influencing these interactions.
Building and sustaining trust in collaboration
Interviews provided a range of insights into how building trust was deemed essential to maintaining and building collaborative efforts. To nurture trusting relationships, leaders described the need for experience, with a demonstrable track record of involvement in collaboration and delivery in improvement. Authenticity was also connected to leaders’ understanding and visibility within local systems:
I think clinical leaders don’t move around as much as career managers, so I think that also means it is personal and because I know, you know, I know all of the GPs [general practitioners] . . . I’ve come across an awful lot of people and when you can just pick up the phone to people it’s a different conversation than if you’ve got to carefully craft a three page email isn’t it?
14; leader; ICS 2
If you have been around for as long as I have, you can draw on that work because the work I was doing in world-class commissioning 15 years ago was about how do you reduce health and equality as a managed care variation and use your resources to deliver the best outcomes that you can? . . . And, then I could point to the vanguards following the publication of the NHS plan, which was about the same sort of stuff. So, by harnessing all of that work, what I did straightaway was deposit this as a continuation of existing work, and what we really were about was by working together, how do we add value to that landscape? And, really setting out some firm principles which are the founding stones of what we do every day, really.
13
Recognition that collaborative leadership differed from ‘traditional NHS leadership learned behaviour’ was depicted as an approach that transcended boundaries, with a focus on people and place. Interviewees described the approaches used to build trust, with empathetic leadership characterised by enabling people to be supported to enter into a collaborative mindset. Alliance 2, for example, reflected on the challenges associated with the configuration of vascular services from three sites to two. A lengthy process of engaging with clinicians ‘to give it up’ without being forced to was depicted. Other examples also featured within interview accounts:
I think it’s to do with the strength of relationships, but also the skill of the facilitation and the use of the data and the evidence, and the involvement of all of the clinicians, who ultimately see the value for patients in adopting that approach. And that’s what came out. So I think if you take those sorts of approaches, you usually do get to the right outcome. The ones where you don’t do that, and I’ve experienced this before, is the ones where you’ve got just a very strong kind of political agenda running with one or two high profile leaders that just want your railroad stuff through, and it’s bad news when you’re in those situations.
17; chief executive officer; alliance 2
The importance of leadership in setting the tone and culture translated into demonstrating authenticity, visibility, empathy and openness:
I did become much more visible, spending time, with the rest of the executive team, visiting wards and departments, working alongside people, not just visiting and say hello, but actually acting in the role, whether that was as a porter or a nursing assistant or working in pathology, or whatever it might have been, and understanding, in a very small way, you know, what it was like to look through their lens.
12; former chief executive officer; alliance 1
Project management and boundary-spanning governance arrangements provided an important role in ensuring collaborations made progress and promoted consensus through understanding different organisational viewpoints, and this facilitated trusting relationships:
. . . a lot of what I do is understanding what each of the different organisations are thinking and what the people in it are thinking or what their concerns and worries are, and trying to sort of unpick those and find that consensus, find that area where everybody can agree and sort of . . . A lot of it is a bit of shuttle diplomacy in a way; you sort of go between people persuading these people to move this way and them to move a bit that way so you get them all into a place where they’re close enough together that they can work together.
19; director; alliance 2
Interpersonal communication
The ability to listen attentively and engage people in identifying areas for improvement was connected to building trust. In setting up alliance 2, interviewees described responding to cynicism to the proposed collaboration through getting a better understanding and appreciation of different perspectives. The power of informal interactions to build relationships was deemed a key mechanism for improving trust relationships:
[It] came from not waking up one morning and saying, ‘We’ve got to have an association and all get together’; it came from just going out for dinner and getting to know each other better, because there’s a group of colleagues that actually, I wanted to get to know, and they were really important to us.
17; chief executive officer; alliance 2
Creating conditions where people felt open to talk about their experiences was important for creating an environment to facilitate trust-building:
Alongside that are the issues about openness and transparency, where I think you can’t just say something; people have to see it and feel it, and they have to know that you’re interested in the good, the bad, the indifferent, and that you will report it, that you’re creating a culture whereby you want people to talk about the things that they struggle with as well as the things that they do exceptionally well.
12; former chief executive officer; alliance 1
The challenge of communicating across larger-scale groups required greater attention being paid to governance. Focused programmes of work were required within such contexts to bring people together to share common issues and develop common approaches:
. . . we’re running about 9 or 10 programmes of work across different parts of hospital and hospital services. We bring together all the different functional directors groups, so the finance directors meet, the medical directors, the nurses, the estates people; so, they all meet to sort of . . . they sort of share common issues and try and come up with common approaches to things.
19; director; alliance 2
Cultural integration
A range of interview responses stressed the importance of cultural integration in building trust and faith in collaboration. Developing cultures of improvement was seen as essential, particularly in the translation of learning from higher-performing organisations to more challenging contexts. Underlying a culture of improvement was recognition of ‘toxic’ cultures exemplified by bullying and imposing management. Organisations finding themselves in positions of ‘learned helplessness’ unable to reflect on progress and generate improvements also featured, along with silo thinking of organisations fixing their ‘own problems’ rather than proactively seeking help from partners:
I do think that there is a kind of mindset issue about institutions . . . [that] becomes a barrier to collaboration because actually people like to think they can fix their own problems, can’t they? Or seeking help for whatever reason is not done proactively.
20; director; alliance 1
Cultures of ‘telling and doing to’ needed to be replaced with empowering, listening and enabling cultures. To do so, an honest and reflexive approach to problem-solving and progression was called for, where successful cultures of improvement were those able to reflect and understand achievements but also be open about difficulties:
So I think that, you know, that there is the risk that you can come at it in a sort of nicey, nicey way, and pretending everything’s okay, when actually you don’t either don’t believe or don’t trust or don’t agree with what someone else is saying. And I think having a safe environment where you’ve got relationships to a stage where you can challenge and be upfront about that, you know, and speak truth about it. But then move on, and, you know, and carry on doing the work together.
26; head of workforce; alliance 1
Challenges were met when trying to work across different professional backgrounds and ways of working. Cultural divides were encountered with those working in hospitals, across systems, and those in primary care. Difficulties were encountered with the associated power dynamics of organisations leading innovative models being associated with the ‘the big players’ at the expense of innovations being done in smaller scale providers:
It’s kind of, ‘size matters’, isn’t it? We get to this thing of actually, ‘How big is my organisation?’ So, it becomes inquisitory doesn’t it? Sometimes it perhaps gets in the way of collaboration so, ‘How do we view success?’ . . . we set up these kinds of quasi-groups that are a bit self-serving in some ways that are about themselves and their own importance. And, yeah, if you go to some smaller organisations and think, ‘Actually I’m doing some really brilliant stuff in my population’ . . . it’s kind of punching above its weight, really punching above its weight, and I think that’s amazing. So, it has nothing to do with size. It won’t ever sit in the [local] group. It certainly will never feature as a big integrated care system.
20; director; alliance 1
Challenges of generating a cultural of collaboration was raised in relation to ICSs. To support such efforts, having an awareness of local issues and ‘the geography of place’ was needed with regard to interacting with local area issues. Regulators also had a potential role in supporting cultural integration, with the ability of CQC to work across boundaries and feedback to organisations and the public about what worked well and what needed to be different was mentioned in this regard:
. . . how decisions get made as the ICS becomes a statutory body. All of that will have to change how we work. And it might need all providers to rethink what it is they’re doing and how they’re doing it, to make sure that ultimately, we’re doing the right thing for patients across [locale].
26; head of workforce; alliance 1
The limits of trust and risk tolerance
Building trust was synonymous with the risk tolerance required to support collaborative behaviour:
. . . let’s take the risk, let’s work on it together, and let’s share the risk . . . It’s about sharing it, and not letting it come down to the money, because if you put money into everything, it either goes really political, or you just don’t get anywhere.
24; director of care quality; range
An NHS context historically poor at exchanging information was raised as a barrier to such dynamics, with a lack of openness about failure and limited risk-taking being raised. Reluctance to share people and expertise across boundaries was also connected to a workforce institutionally focused in ‘wearing the organisation’s badge’. Such risk intolerance meant that the NHS often turned to management consultants to fill the information gaps:
We bring in management consultants who try and deliver something, they’re not really bought into it, they don’t have any prior experience in the NHS normally, it’s a weird thing to do. If they do have other experience in the NHS they then use that jack up the prices, which is absolutely preposterous, and we never have that round conversation.
29; leader; hospital group 4
Risk tolerance was also connected to the importance of organisational sovereignty and striking a balance that ensured workforce had some security and autonomy preserved:
. . . the way things are run within [the group], we attempt to give autonomy to each of the care organisations that constitute our group. Yeah, that has a standard oversight framework if matters are not being delivered to the appropriate standard or where there may be some concern about performance or trajectories . . . Yet generally the preference being each of the places to an autonomy yet working to the principles of big group.
23; medical director; alliance 1
Well-documented challenges of integrating professional groups with different risk appetites featured within the interviews. The context of COVID-19 was cited as ‘instrumental’ in galvanising clinical engagement in collaboration, but there was work to be done to engage clinicians outside ‘the COVID-19 agenda’. The context of COVID-19 was also attributed with creating conditions of diminished trust where there was less ability to have face-to-face connections and build genuine relationships. Working virtually across boundaries was fragmenting communication, although others did raise the equalising qualities:
. . . since the COVID-19 interruption, no, I think there is less ability to have that connection with people and that authenticity of what the reason you’re making the changes are.
21; director of clinical service; merger
Risk tolerance was connected to patient interactions and local service provision. Although those leading IOCs expressed receiving patient support for proposed changes in recognition that increased travel times would be accepted for higher-quality care, concerns about meeting the needs of communities within designated systems was also raised.
Building and sustaining faith in collaboration
Leaders of collaborations provided a range of insights into their approaches for instilling faith in collaboration. To work through any complexities and challenges required a delicate balancing act to ensure that the collaboration was feasible and realistic. Overpromising and overambition had the potential to reduce faith. Therefore, strategies to enhance faith needed to be focused on deliverables to maintain engagement and momentum. To generate focus and priorities, strategies included the use of diagnostics to assess whether or not to progress with an idea. In addition, due diligence work was carried out by consultancies to look at the benefits of collaboration in terms of reducing unwarranted variation, increasing quality and increasing efficiency to identify particular projects to bring services closer together. The following quote outlines the importance of building and keeping faith in the collaboration:
. . . you’ve got to pick some bits within [the collaboration] that you can actually deliver on because that’s the sort of thing which is too big, too contentious, is going to take you too long, and you’re going to be 5 or 6 years into this not really feeling like it’s actually delivered anything and that’s when people are going to go, ‘Why are we . . .? We’ve not seen any outcome from this so what are we doing?’.
19; director; alliance 2
Consistency of approach in leadership improved faith where stability, consistency of message, priorities and approach were attributed with success. For example, to break down the complexity of ICSs, hospital group 3 described the need to carry out a ‘True North’ exercise, focusing on breakthrough objectives and corporate projects that could be shared across organisations. Increasing faith was also characterised by the leadership behaviours of visibility, communication of benefits, and listening and reacting appropriately:
[It’s] leadership that listens because very often what you see is the kind of knight in shining armour vision of leadership which is one organisation is swooping in to help the other and everything’s going to be fantastic afterwards, well, if that person who’s coming in doesn’t listen to what’s good in the other organisation as well as what needs to be put right . . . that’s not going to work because people will resent it.
07; professional body
To build faith, leaders described how developing collaborative endeavours required going ‘where the energy is’ to establish momentum. Focused efforts with engaged stakeholders had the potential to reduce anxieties about task complexity as well as build trust:
Myron’s Maxims? . . . you start where the energy is and build out from that, that you have to do real work to make these things happen, talking about theoretical things doesn’t really work, you have to actually identify some real things because real change happens in real work.
19
Involving appropriate stakeholders within the collaborative process was supported. For example, if the goal of the collaboration was population health, then the governance and messaging needed to reflect this by involving councils, public health, police, fire services, the third sector and the NHS. Embedding such approaches needed to engage a mixture of provider and commissioner leaders to facilitate efforts in extolling the benefits of system working. The role of an ICS was cited as a case in point, with leaders needing to frame the ICS agenda landscape as being part of the organisational fabric as opposed to ‘an administrative construct or bureaucratic burden’:
I do think we have to continue to push those boundaries about, ‘What is it in our hospital institutions?’ – because that’s really what we’re talking about . . . I think that the more that we can really think about what can we shift out of the hospital institutions and place as care in our localities that for me is where we need to put our efforts and attention. And I include in that some of the big diagnostic pieces . . . Shift it out and put it as an interface between the hospital institutions and primary care.
20; director; alliance 1
The perils of maintaining faith in collaboration were raised where the energy needed for collaboration and the requirement of leaders to ‘go the extra mile’ created conditions of fatigue and burnout:
. . . we have tried to protect the organisation from the transaction as best we can, and just keep running great services for our populations, while we’ve dealt with burning the midnight oil on trying to get the business case and the transaction going as fast as possible.
10; executive nurse; alliance 1
Wider questions about the rhetoric and reality of system working also needed to be addressed. Well-publicised examples of system-wide collaboration approaches that had not achieved the demonstrable impact it aspired to at the outset were mentioned:
I already arrive at the table with a degree of cynicism, 30 years, ‘God, I’ve been here before’, and, ‘We’ll play this game; we can play this game, it’s easy, we know the rules’. So, I don’t think people have a lot of faith actually at a big system level that it can work. I’m trying to think of at a really big STP level what . . . So, there are examples, aren’t there? We shifted the dial in X on some things around some population health metrics, which was kind of the core purpose of the 5-year plan. Actually did we do as much as we should’ve done and we could’ve done? I think that’s a different question. And actually did that happen because we collaborated at a system level or was it because actually everybody in their local bit was just doing a bit and when you add it all up it looks good? I don’t know.
20; director; alliance 1
Capacity constraints
Faith in the collaboration was connected to the capacity available to support collaboration. Maintaining motivation and commitment for collaboration required the navigation of resource constraints and limited finances that could potentially weaken the resilience and energy to change. Chronic issues in parts of the country required structural responses rather than partnerships to generate improvement in recognition of the problems facing some of the worst-performing organisations:
. . . they will improve by just being given special treatment rather than partnering with another organisation because nothing’s going to overcome that, they actually just need more injection of cash to help them because it’s more expensive to run their services. And I think that policy, central policy is slightly allergic to making special cases even though special cases need to be made.
11; policy executive
Similar points were raised about workforce shortages where the skill mix required for vertical integration and specialist care interdependences was not currently available. Organisational development teams, identified as crucial in collaboration efforts, were described as ‘bursting at the seams’ with demand in supporting existing change processes. The functions, such as analytical capability and project management capability, needed to maintain and improve services had been ‘stripped out’. The ‘partnership bandwidth’ for organisations to sustain multiple types of partnerships on different fronts simultaneously was brought into question:
I remember talking to someone from [trust], actually, so that I think they’re, you know, seen as an ICS, that has made particularly good progress. But they spent 18 months building relationships and didn’t do anything other than spend time together, talking about the challenges their organisations face, getting to know each other. And they spent 18 months doing that before they even tried to change anything about how they were running as an ICS. And that investment in time in building relationships, building trust, is hugely important. I think the challenge the NHS has got at the moment is it hasn’t got that luxury. So, you know, they’re going to have to do it, like as a mid-air refuel.
26; head of workforce; alliance 1
Within current capacity constraints, the development of ICS relationships was raised both as a challenge but also as an opportunity to have system-wide discussions about priority-setting and sustainability:
. . . through COVID, I think what we found is, a lot of providers have realised that it’s just not worth the risk of trying to pretend that you can deliver certain services, if you can’t. And actually saying, ‘Look, it’s fine. You do, you know, you deliver that because you’ve got the skills and ability to mobilise it now, we haven’t’. Whether they would have done that otherwise, when contracts are at stake . . . I don’t know”
02; director; hospital group 1
Limits to faith and capacity were encapsulated in hospital group 4’s experience of the vanguard initiative. Hospital group 4 developed three clinical programmes across an alliance as ‘fully funded, focused and structured’. Yet, following the completion of the vanguard, hospital group 4’s funding, energy and passion to go develop and co-fund initiatives was lost, as the clarity and impetus needed for sustainability was removed:
We kind of had a lot of momentum coming out but I think we didn’t recognise the difficulty that would happen when we no longer had that. And it’s not just the money, it’s also the focus that comes with it, it’s the political cover. When you don’t have that suddenly people are a lot more cautious, also they’re a lot less focused on it and they think about other things.
29; leader; hospital group 4
Task complexity
Our interviews identified how instilling faith in collaboration was connected to the perception of task complexity. The scale of the collaboration was raised, where increasing the number of organisations involved increased participants’ perception of task complexity. Challenges were singled out in relation to vertical integration of functions along a care continuum, where collaborations involving the relinquishment of specialist services were susceptible to being a ‘battleground for money or kudos’:
I sometimes wonder if some of the kind of vertical integration and cross sector integration has been a bit more challenged because the challenges aren’t always the same or the incentives aren’t always the same and the finance works differently, the contracts are different and I think, you know, where trusts can kind of come together in a slightly more streamlined kind of way sometimes so reflecting on that workforce piece I think there’s quite a range of different initiatives that we covered but a lot of them are trust to trust.
6b; provider association
Horizontal collaboration was facilitated when collaborations were located within coterminous boundaries (16). Such contexts proved problematic for alliance 1, where challenges were raised in connection with working across multiple local government and political constituency boundaries:
. . . the politics locally have been incredibly difficult, incredibly difficult, because the local politicians were adamant that X was to go into X, and not X. And that’s why it’s become so complex, that we’re disaggregating, we’re not just acquiring an organisation, we’re disaggregating it whilst acquiring it.
10; exec nurse; alliance 1
Integrated care system success was attributed to their maturity in terms of how far such contexts had progressed with vertical integration. Where alliance 1 cited continuing conflicts working within the ICS landscape where those with ‘the greatest powerbase’ continued to prevail (10), power dynamics were also connected to the formation of ICSs where the depleted resources of primary care, local government and social care meant that a greater need for acute sector experience was required:
So a lot of the capability to make the change happen to make the ICS successful, I think, sits in the acutes because they’re very good at mobilising things. Very good at making savings in efficiencies and have those hierarchies in infrastructure in that they can almost just ignore some elements, because it will happen by default, and should be putting energy into other things.
02; director; hospital group 1
Getting the ‘right geographical footprint’ to meet the population size featured as an enduring issue across the interviews. Collaborations considered over a larger footprint were both supported in gaining a more strategic focus in relation to population health; however, these collaboration were also limited in the ability to build faith and trust in collaborative endeavours. The nature of local population characteristics would also influence efforts, where having a smaller population or a more affluent and well-educated sociodemographic could lower task complexity in terms of issues the collaboration needed to tackle. Conversely, having a larger geographical distance between providers had the potential to increase complexity and make it harder to build trust because of difficulties in forming personal relationships.
Legitimacy
Connections between faith and the legitimacy of collaboration were made by a number of interviewees. The perceived legitimacy of a collaboration was connected to different types of partnership working. The drive for a ‘system-wide’ agenda underpinned by ICSs was supported in recognition that collaboration required a more strategic focus to improve population health and sustainable services. The ICS agenda provided a vehicle for achieving such endeavours:
. . . we’ve had quite a bit of feedback around the kind of helpful role that an ICS could play in facilitating or convening partners rather than kind of seeking to be a unit of delivery.
6; provider association
Although still emerging across health economies, concerns were also raised about the legitimacy of the ICS agenda in draining energy and momentum out of other collaborative activities. The mandating of ICS structures had the potential to stifle existing efforts:
. . . you spend so much time developing something and then halfway through ICSs come in and you’re kind of cut off at the knees.
29; leader; hospital group 4
. . . it’s almost like the bit about working in a system that we need to do but we don’t want to squash those that have gone first . . . we just want to help them along that way and get them to sort of get to local agreement.
09; policy transformation lead
Other risks were raised in relation to ICSs ‘recreating a SHA [Strategic Health Authority] provider structure’ in resorting to a centralised, hierarchical approach rather than acting as a ‘servant of the organisations in the system’. Provider collaboratives were raised in a similar vein as having potential as a facilitator for instilling collaboration, but potentially problematic in being defined by organisational structure rather than relationships:
As soon as you create an organisation which has responsibilities and accountabilities and holds budgets and people work for that particular organisation behaviours and things . . . there’s a risk that behaviours and things change understandably because of those responsibilities and accountabilities and things, and we’ve got to try and find a way of taking the good bits – that will bring some benefits that new organisation for us – but not losing the sense of being a real partnership and not recreating a sort of SHA [Strategic Health Authority] provider structure.
19; director; alliance 2
Group models were deemed attractive for the running and delivery of secondary care based on their ability to provide a mix of options to accommodate different needs and interests. For example, alliance 2 described how such an approach was preferable based on its ability to retain identity and sovereignty as an organisation, as opposed to being ‘thrown into merger’. Group models had the advantage of being able to demonstrate benefits without having to spend ‘2 years on a disruptive merger process’ (17). Alliance and group ways of working were, therefore, conducive to building faith and trust, as, often, organisational sovereignty for money, buildings and infrastructure or workforce would be retained:
Group models seem like an attractive model for the running and delivery of secondary care certainly services and I think that’s partly because it does have a reasonable mix but it’s reasonably loosely defined by me . . . so it probably means different things to different people but it also allows within it because of the sort of hierarchy it actually is making some of those decisions.
04; provider policy leader; range
Buddying, also referred to as a ‘management support agreement’ or ‘mutual aid’, was associated with a recognition that lighter-touch, time-limited collaborations to improve poor-performing organisations had benefits in sharing expertise and learning. However, in contrast with the mandated nature of special measures buddying arrangements, care was needed in having an appropriate cultural and organisational fit to create the conditions for collaboration. Financial support for the mentor within the buddy arrangements was also connected to facilitating collaboration:
So and I think it ended up being actually a relatively successful arrangement in terms of impact at [trust]. And I think from [trust’s] perspective it was pretty successful in terms of delivering a significant amount of cash into their organisation . . . but it was always viewed as a kind of time limited kind of fairly focused collaboration of doing some things which I think it did.
03; director of improvement; hospital group 2
Mergers were deemed a legitimate option in contexts that required building economies of scale and reducing the number of providers and consolidation as far as possible. Yet, such forms of mergers required being treated with caution in taking ‘people’s eye off the main ball’, as valuable time and energy was lost to merger processes rather than focus on the improvement of workforce, structures and governance. To overcome issues, pre-merger activities were encouraged, with integration efforts focusing on clinical pathways and back office consolidation to start delivering benefits early.
Stakeholder involvement was identified as serving to increase legitimacy. Leaders often found it helpful to have service users involved to keep the focus of the collaboration on outcomes. Local system reviews led by CQC in 2017 were highlighted as an attempt to look at local systems ‘through the lens of a local citizen’ to encourage better joint working (7, 5). The reputation of specific forms of collaboration also influenced the willingness to engage in forms of collaboration. Fears were expressed by public representatives that greater collaboration would lead to privatisation, which undermined the legitimacy of collaboration. The label of privatisation was also present elsewhere, with leaders being driven to collaborate in ways that could manage public anxieties about privatisation:
. . . the public really feared privatisation I’ve got to say, and they really just wanted integrated services. The alliance with providers, our local providers, and their preferred option would be an alliance approach as well as a step towards.
16; senior commissioning manager; merger 1
Demonstrating progress
Our interviews provided a number of insights into how the perception of progress was important for ensuring that momentum was maintained. Evidence that progress was being made increased faith by serving as a motivator to continue with the collaboration. Getting feedback and ‘positive reinforcement’ was deemed important to ensure buy-in. To do so, focusing on practical ‘quick wins’ to expose organisations to the goal of the collaboration and ensure staff remain engaged was suggested:
I think part of the problems sometimes mergers in particular suffer from it’s almost they’re sort of too big and theoretical to achieve anything, whereas, get a couple of teams working together on a specific problem, like, ‘how do you redesign this service?’ and suddenly everyone sees the point of collaboration and what it really means. So I guess focusing on the practical and sort of some quick wins, probably the same sorts of things that are important for projects more generally.
04; provider policy leader
That said, the promotion of quick wins was also susceptible to problems when tangible progress did not materialise in the longer term, which reduced faith and momentum:
I think that people are getting fatigued and wanting to see more outputs for it and if they don’t see that, if people don’t see things getting any different then it just becomes a talking shop and people start drifting away and I think that’s what we saw in some of the earlier integrated care models that people just thought we’ve just wasted a whole load of money like the Integrated Care Fund . . . 150 initiatives that all sound great but didn’t deliver very much and then it’s, well, should we put so much money into it next year or not because we can do a lot of the stuff ourselves.
02; director; hospital group 1
A perception of peer pressure was also connected to driving progress where organisations or teams want to avoid the perception of ‘falling behind’ or looking bad in front of others. The use of assessment and accreditation systems was cited as an example of being open and transparent in showing good, bad or indifferent progress was being made:
. . . so we took the [assessment and accreditation system] over and showed it to them and said, ‘We really want to deploy this, but we want to deploy it in a way that you’re with us on it’ . . . so we brought them all together and we showed them the outcomes . . . so they recognised for themselves the fact that they’d normalised such poor standards, and that if they continued to do that, patients would suffer, and their reputation would suffer. And so they very quickly got on board with the improvement journey.
10; executive nurse; alliance 1
Clarity of vision
Clarity of vision served to increase faith by reducing the possibility for miscommunication. Being able to articulate and construct a leadership narrative about the aims, goals and solutions that collaboration would achieve and the problems it would solve was connected to increased workforce engagement. Communicating a narrative of how the collaboration will be beneficial to staff through better alignment and ‘bringing parts together’ could also mitigate the potential exposure of collaboration being met with feelings of loss or being imposed on:
So it’s almost from a point of view of a member of staff is kind of what’s in it for me? Well, what’s in it for me as a member of staff, you know, what’s worked out? We’ve been able to make things better for patients but actually we’ve been able to grow our staff as well. And I think as a set of organisations in the NHS I think we’re for telling that story. And if we force ourselves to tell that story I think it would force us to change the reality of that in a more meaningful way as well . . .
03; director of improvement; hospital group 2
To generate a clear sense of purpose, key actors used a methodology embedded within organisations to work through problems. As with the nurturing of interpersonal communication, leaders describe customising quality improvement approaches. Inspired by Virginia Mason, hospital group 3 described ‘a eureka moment’ in translating the Virginia Mason approach into a local improvement programme to lead, manage and set objectives to support staff:
. . . they’re all versions, you know, of basic improvement methodology, if you stripe them back, you will see that they share common components to them . . . I think the most important thing is that you select the one that feels right for you, and you stick to that methodology and it becomes the discipline, it becomes the rhythm, you know, the beating heart of the organisation, and that people get familiar with it, they get trained in it, you know, it is the only method that they then use, and it’s applied in all sorts of situations, and then just becomes the way of doing things.
12; chief executive officer; alliance 1
Being ‘deliberate and visible’ about opportunities for partnership working was also connected to the need for inclusion of stakeholders. Involving patients and the public to help shape pathways and ‘cut out things not adding value’ was encouraged. To facilitate inclusion, having a communications strategy highlighting key issues and celebrating success was important. Dedicated programme leads also played a role in communicating the progress being through face-to-face relationships and meetings:
Having a communications strategy aligning with that vision to be delivered and supported by those leaders that is constant, reflected upon and respond to the different ways that people want to and need to hear those messages and that responds to their different concerns not to spoon feed because, you know; we’re all adults and we should be kind of empowered and enabled to operate as adults but in a way that actually relieves them of the anxiety that they might have about the situation that they are in.
07; professional body; range
Environmental influences on faith
Interviews supported our review findings that establishing ‘initial faith’ (i.e. if engaging in collaboration is feasible or, indeed, worth the risk and effort) was primarily shaped by factors related to the regulatory and policy environment. Owing to the timing of the fieldwork, it also identified the role of COVID-19 in shaping the perceived difficulty of the collaborative tasks at hand.
A shift in thinking was observed over recent years in the motivation and effort attributed to collaboration. The recent policy agenda in England emphasising collaboration was brought into view, where interviewees described a ‘movement’ from 2012 onwards as a reaction to the limits of competition within the Lansley reforms as a means to driving performance improvement. Mindsets around competition and ‘carving out a particular niche’ had increasingly changed, which had been driven by the Five Year Forward View3 agenda in incentivising people ‘to pay more interest in other parts of the system’:
. . . the realisation that you can’t necessarily specify and procure for healthcare became quite obvious so I think Simon Stevens came in he realised that and having come from a background of accountable care organisations internationally he’d got this view, the kind of blurring the edges a little bit about who was actually responsible for which bit of activity . . . But also thinking about quality at more macro level and also obviously some of the most powerful parts of the system with the ability to destabilise the NHS are the very large providers, so how do we rebalance that and bring those providers to the table with an incentive to population health long term?
02; director; hospital group 1
The vanguard programme was cited as providing investment and energy to develop leadership ideas and initiatives, as well as enabling opportunities to learn from organisations elsewhere. The learning from new care models was also connected to current thinking regarding ‘systems transformation’ and the NHS Long Term Plan’s33 objectives for ICSs:
. . . the vanguard programme was the first way that we came together and started collaborating and I think that was great that there was a bit of investment to do that and there was real energy for trying to drive on with that.
21; director of clinical service; merger
The COVID-19 pandemic was significant at the time of doing fieldwork, and was identified as being important in driving shared purpose and the spirit of collaboration. The COVID-19 pandemic had facilitated collaboration where established ‘bureaucratic burdens’ and ‘discussions about money and capital’ had been removed from the agenda. The COVID-19 pandemic had brokered discussions that ‘dispelled myths’ about other stakeholders and enabled people ‘to get on and do other things and think longer term’. Patient representatives also documented the COVID-19 pandemic as driving a significant increase in collaboration between their providers (34, focus group):
. . . [during COVID-19] so many people have just been in favour of the removal of bureaucracy so removing a ton of barriers to partnership working and to relationships has just been so helpful so whether that’s DTOC [delayed transfer of care] fines or continuing health care. I haven’t heard anybody sort of raise any concern or any anxiety about all of those bureaucratic burdens which were lifted and seem to have really accelerated kind of partnership working.
06; provider association
The COVID-19 experience was attributed with driving the formalisation of the ICS agenda in ‘facilitating or convening partners’ with provider collaborative models interpreted as a way to deliver on the priorities of ICSs:
. . . with wave one COVID-19, we saw a lot of people saying, ‘We’ll work together to do something’. And then it didn’t quite get bad enough in our area to compel that. So things went very quickly back to the way they were. The second wave of COVID-19, things were much more extreme where we were. So we did manage to change the models of care. And then the legislation is trying to, I think, put walls around some of those things. They wouldn’t necessarily had been there in normal time. So there’ll be some difficulties in trying to mainstream that.
02; director; hospital group 1
The formalisation of ICS structures created a recognition that contexts for collaboration were arguably now ‘stronger than ever’. However, the conversion of motivation and interest towards collaboration was by no means straightforward, with ongoing conflict with local partners stifling momentum. The move towards collaborative behaviour and away from competitive behaviour could be a turbulent one. Local competition ‘to be the best’ remained a challenge, as was the importance of organisational sovereignty and acknowledging existing boundaries. The power of professional status also featured where encroachment on professional standing could lead to resistance towards collaborative efforts:
. . . actually there is still very much that people want to hold onto their professional status, their standing, and where they’re at, and that it isn’t easy to maintain that vision of why you’re doing something because we’ve all got our own personal motivations for why we’re in work.
21; director of clinical service; merger
The present regulatory regimes promoting competition also featured, with documented challenges associated with working with regulators to support collaboration. Distrust of regulators built on experiences of broken promises about financial investment. The lasting effects and experiences of trying to collaborate within competitive environments was also raised, with the role of the Competition and Markets Authority ‘fresh in our minds’ as a detrimental impact on collaboration:
. . . the reward element, I believed then, and I still do now, could be, or could have been a sufficient element to reignite interest amongst organisations and to send the, you know, a huge signal that improvement is what the centre of the NHS attach importance to, and those organisations who step forward with competence and credibility would be rewarded to take on organisations that were in difficulty. That was the proposal that I put forward, and, in the end, we weren’t supported financially in the way that I was led to believe we were going to be . . .
12; former chief executive officer; alliance 1
Concerns were raised that as the COVID-19 pandemic recedes, the regulatory barriers that were previously lifted would be put back in place, stifling momentum:
. . . so the worry I suppose post COVID-19 is some of that coming back and those barriers going up again really.
06; NHS Providers; range
Regulatory perspectives reflected on the role inspections had in helping organisations ‘keep focused’ and to provide a benchmark for progress in the turnaround of organisational performance. However, it remained unclear what the CQC role would be within the ICS landscape in holding organisations and systems to account for performance. Although moving to ‘system by default’ was being encouraged by the centre, concerns were raised about whether or not CQC had the systems and processes in place to oversee the agenda:
I think that’s an area where we would encourage regulators to kind of take a slightly different view of, you know, ‘what is performance in a system and how do you measure that?’ And then, there’s a wider question of, you know, ‘does CQC have their remit to performance manage a system, regulate a system?’ Not really, and does NHSEI [NHS England and NHS Improvement] have a framework in place to performance manage a system? Maybe not quite yet, so I think there’s quite a lot of work still to be done there.
06b; provider association
One of the challenges for us is to be able to get enough information of good quality data upfront to try and make a targeted assessment. If we’re looking at a risk based assessment. you need good-quality data. At the moment the systems are not designed so that we can access that in a sort of real-time manner.
8; regional inspectorate lead
Improved collaboration between CQC and NHS England/NHS Improvement was called for:
I think COVID-19 has shown that actually lots of communities have benefitted from the systems that are in place and the mutual aid that’s happened. The provider collaborations that have actually sprung up from COVID-19 in particular have been legion and really interesting actually but at the moment there is a massive mismatch and I think, I think there has been a lack of desire from NHS England mainly and NHS Improvement and others to have a real conversation about what we want, they’ve just wanted to push through an approach and basically without, you know, we’ve got real incremental policy change without understanding the cumulative impact of all of these changes.
11; policy executive
That said, positives regarding collaboration were mentioned within the trajectories for performance improvement. The removal of contracting mechanisms across NHS contracts could lead to more innovative models of care, with an increased focus on social value, as could the moves to global budgeting. Recent changes to performance risk ratings, with a move away from waiting time performance standards to prioritising equal needs, also presented opportunities for more creative solutions to engage the workforce across boundaries.
The presence of conflict
Conflict had the potential to reduce trust and faith by sapping the energy and momentum needed for collaboration:
. . . everybody sits around a table in partnership, you don’t recognise the conflict in the room if you’re not familiar with the players in the room. But the conflict then gets played outside of the room, in corridor conversations and email conversations, etc.
10; executive nurse; alliance 1
The formation of ICSs and its enforced changes to existing ways of working were predicted to lead to conflict. Although early formations of ICSs were locally generated, the latest ICS incarnations moving to greater formalisation raised concerns as a centralised approach. Conflicts in the potential for ICS structures to be NHS hospital provider focused at the expense of other providers also featured:
I think providers are kind of getting themselves in . . . I guess, aligned, to various degrees, to kind of deliver on these agendas, even in some of the most difficult places . . . I think in terms of the more fragmented providers – mental health, primary care, that’s going to be a more difficult journey in terms of jockeying for position and influence, because the table is still not big enough for everybody. That’s where the tensions arise.
27; private sector representative
Conflicts were raised in response to the demands placed on providers as a result of COVID-19. The role of the private sector was described as being helpful during the initial COVID-19 response, yet different interests and motivations between the public and private sector continued to be played out:
You have to work with the private sector in a completely different kind of financial system, and there’s no question that it would . . . I mean, why would it come in with the NHS on that? It can help the NHS kind of, I guess, deal with some of its backlog, but only through using our resource, what I would call NHS staff to do those procedures.
27; private sector representative; range
Building confidence
Formalisation and the fostering of collaborative behaviour through contracts and regulatory requirements was highlighted. Interviewees were largely sceptical of the notion of mandated collaboration. To avoid bureaucratic burden and to also maintain assurance processes, an alliance approach that encouraged compact ways of working with organising principles and supporting contracts was being encouraged. Memoranda of understanding were typically used to operationalise group and alliances as a means to support collaborative working. Memoranda of understanding set out decisions, approved business cases and created committees in common, where required, as an option to build in governance and give confidence that structures were in place for different eventualities:
. . . the way the MOU [memorandum of understanding] set it out is the decisions are still the preserve of the trust boards but I suppose what the committee in common does is it allows us to get to the point where you’ve got the chairs and chief executives all recommending the same course of action or the same decision to the [partnership] boards, and so in practice unless we make a real hash of it the committee in common recommends something then it tends to get agreed, so they sort of do make some decisions.
19; director; alliance 2
The formalisation and mandated nature of the current ICS agenda raised a number of implications regarding the confidence surrounding collaboration. At one level, the ICS agenda was seen as driving leader behaviours to ‘get real collaboration’ going. However, limits to the mandated nature of collaboration were also raised:
. . . we’re only really starting to see some of that changing now system regulation so the leaders probably weren’t strong enough to get real collaboration going until fairly recently I think and even in some cases people are doing that because they kind of have to and not necessarily because they want to . . .
02; director; hospital group 1
Lack of clarity regarding the accountabilities associated with the ICS framework was creating ‘quite a bit of anxiety’ regarding what the eventual landscape would look like. Although the emphasis and energy was in place to promote collaboration and system working, the arrangements had no statutory underpinning, which lowered confidence between partners:
. . . we are asking organisations to works in systems, we’ve set the systems up and we’ve got ICSs and STPs across the country, they have no statutory underpinning whatsoever, they have office holders who have no formal role in law, they carry no liabilities.
11; policy executive; range
Concluding summary
Our interviews provide a range of insights into how the stakeholders understand the functioning of IOC between NHS providers. To build and sustain trust was connected to the leadership skills and behaviours of authenticity, empathy, visibility and generosity. A commitment to place-based approaches also features, along with the importance of stakeholder engagement, data analysis and project management.
Our findings show how a delicate balance is required for building faith in any IOC. The presence of energising leadership that engages receptive groups and inspires and builds momentum is tempered by an awareness of the stark capacity issues facing current NHS contexts. To navigate challenging contexts, and a potentially overwhelming agenda, the findings draw attention to the importance of priority-setting, where perceptions of progress characterised by quick wins or the use of visual data can build faith; however, increasing task complexity is likely to reduce faith when multiple professional, financial, local government and political constituency boundaries are affected. The findings raise important implications for ICSs where place-based approaches to population health are supported but increasing formalisation has the potential to reduce faith, as energy and momentum is taken out of other collaborative activities and placed into potentially hierarchical performance management structures. Finally, our findings also show how a delicate balance is needed in relation conflicts arising within collaborations. In support of our review, interviews also stress the need for confidence, particularly measures that encourage compact ways of working and memoranda of understanding raising important implications about the mandated requirements of ICS arrangements.
Chapter 6 How do interorganisational collaborations drive performance improvements?
The purpose of this chapter is to generate new insights into the nature of collaborative performance. Few contributions, to date, have delved deeply into how the benefits of collaboration are realised. To do so, the chapter analyses stakeholder interview and focus group data to better understand collaborative performance mechanisms as they occur, and their outcomes. A theory gleaning approach is employed where the collaborative performance framework put forward by Dickinson and Sullivan48 is combined with a realist methodology. The chapter concludes by arguing that, through the analysis and application of collaborative performance, a series of interlinked, testable mechanisms can be identified, with the potential for further refinement by future research.
Background
The literature on collaboration and networks highlights notable ambiguities and uncertainties about what collaborative arrangements achieve. Guarneros-Meza et al.,53 for example, note how interpretations of what constitutes a desirable public service outcome, and the dimensions that make up its performance, is likely to be shaped by pragmatic, political and social factors that can differ between contexts and among actors. The performance of collaboration can involve contextual, functional and behavioural variables, including:
-
a focus on management styles and their relationship with outputs and process outcomes
-
a focus on how structure and context encompass resource opportunities and constraints [i.e. the external environment (climate and turbulence) and previous legacies of hierarchical governmental arrangements]
-
the role of cultural efficacy within the external environment and context, defined as the overarching discourses and rituals.
Given the multifactorial nature of any collaborative endeavour, Salignac et al. 66 note that caution is, therefore, needed in making claims about performance improvement. The development standards and goals ‘may not reflect what the collaborative ultimately intends to or actually does achieve’. 51 A more realistic view of collaboration is required that better depicts ‘the interactive adaptation of perceptions and performance goals’ over time. 51
This chapter argues that through adopting a realist understanding of collaborative performance we may help to address some of these challenges. A realist understanding of mechanisms helps us to break down the various elements that generate improved performance. By mechanisms, we mean changes to people’s attitudes and behaviours, and/or changes to availability or allocation of resources introduced by collaboration, that can drive benefits to more long-term outcomes, such as improvements in care quality, safety, productivity and experience. 131
Up to now, our approach has been to incorporate partnership synergy theory as a high-level MRT to help us understand how collaborative behaviour (or ‘synergy’) links in to the ‘black box’ of collaborative performance. To further understand and generate a greater depth of understanding in relation to collaborative performance, the chapter will draw on a framework by Dickinson and Sullivan48 to act as a MRT to better understand the dimensions of collaborative performance mechanisms. Dickinson and Sullivan48 argue that much of how we understand collaborative performance in health and social care has been couched in ‘techno-bureaucratic’ understandings of collaboration, where a focus on efficiency and effectiveness arising from collaboration has been at the expense of analysing the performative and sociocultural dimensions that guide collaborative efforts.
Dickinson and Sullivan48 adapt McKenzie’s216 dimensions of performance into the domains of organisational efficiency, technological effectiveness and cultural efficacy (see Table 8), which are defined in the following ways:
| Organisational efficiency | Technological effectiveness | Cultural efficacy |
|---|---|---|
| What different forms of collaboration exist and how do their features differ from one another? Does collaboration lead to improved services? What measures demonstrate this? If collaboration does improve services and outcomes, which features of these collaborations produce these impacts? Is collaboration cost-effective compared with other forms of arrangements? |
What types of technology are being used? To what degree do technologies manage to execute their prescribed tasks? What negotiations and compromises are made between possible technology performances? |
What discourses of collaboration are present and what performative work do discourses do? How is the performance of collaboration designed/structured? How do actors perform a collaborative self? What are the affective dimensions of discourses and performances? What kinds of metaphors and symbols are present? |
-
Cultural efficacy refers to ‘an expression of staged or ritualized representations or enactments of particular social and cultural traditions’.
-
Technological effectiveness relates to how ‘technological advancements can enhance the performance of everyday objects’.
-
Organisational efficiency focuses on common understandings of organisational performance, ‘achieving more for less by employing tools of performance improvement’.
The following sections will present how the domains of cultural efficacy, technological effectiveness and organisational efficiency were reflected in the accounts of the stakeholders involved in our research. Although Dickinson and Sullivan48 outline several areas within their framework (see Table 9), our particular interest here is in those characteristics that could most suitably align with mechanisms that are realist in nature. In our reframing, cultural efficacy becomes ‘an understanding of how actors’ cultural efficacy (i.e. behaviours, attitudes, symbols, practices, identity and emotions) may change in a manner that could feasibly drive improvements in safety and quality of care further down the causal chain. Cultural efficacy also refers to changes in ‘values, ideas, and practices that may become challenged by collaboration’, as well as signposting that ‘how [actors] feel about collaboration in general, or collaboration with different institutions, has implications for what we do in practice and how we might go about this’.
| Domain of collaborative performance | Mechanism identified | Performance improvement identified |
|---|---|---|
| Cultural efficacy | Improved communication | Greater communication occurring between organisations in local health system |
| Enhanced awareness in local system | As a consequence of increased communication, actors have greater awareness of issues and what areas require work in the local system | |
| Learning and implementing improvement strategies | To what extent an improvement strategy is being implemented as a core component of the intervention (to collaborate) | |
| Improved organisational culture | A move from a less-productive set of attitudes and behaviours to a more-productive set | |
| Improving reputation in local system | An improved organisational reputation in the health system allows for access to novel resource and feeds into influence in the health system | |
| Sharing of clinical techniques | Sharing of knowledge that can improve care quality or attitudes and behaviours, which can improve culture | |
| Technological effectiveness | Ability to implement cross-organisational clinical pathways | Ability to work better with other organisations allows for improvements to clinical pathways for patients |
| Ability to access novel clinical technologies and expertise | Ability to access greater resource, which can enable innovation | |
| Improved economies of scale | Enablement of greater purchasing power and attainment of better pricing and recruitment to the workforce | |
| Organisational efficiency | Improved resource access | Ability to access greater resource |
| Improved influence in local health economy | Ability to affect the local and wider health economy, and increase patient volume and a more skilled workforce | |
| Improved coordination | Building on an enhanced awareness of the local system, improved coordination enables collaborators to work together on various endeavours | |
| Reduced duplication of effort | Greater awareness of system and coordination allows duplicated efforts to be prevented | |
| Improved resource distribution | Greater coordination allows for resources within a health system to be reallocated towards areas of greater need | |
| Consolidation of services to most clinically appropriate provider | Allows those in the collaboration to stop delivering certain services and for those services to be delivered where they are delivered at highest quality | |
| Improved coverage of patients | Collaboration enables coordination to identify and serve previously missed patients | |
| Loss of geographical proximity | An unintended mechanism of collaboration and consolidation, whereby patient access to services can be reduced because of geographical distance |
Our understanding of organisational efficiency draws particularly on the question ‘If collaboration does improve services and outcomes, which features of these collaborations produce these impacts?’. For technological effectiveness, we add to the concept by Dickinson and Sullivan48 by drawing on the definition of technology by the Oxford Dictionary as ‘the application of scientific knowledge for practical purposes’. This expands the notion of technology from machines and IT to include aspects, such as the sharing of knowledge, experience, evidence or expertise, that were previously unbeknownst from one organisation to another, and this relates directly to knowledge mobilisation across boundaries attained from research and development efforts. 217,218
Analysing intermediate performance mechanisms and outcomes
Cultural efficacy
The mechanisms identified within the collaborative performance domain of cultural efficacy included improved communication, improved coordination, the translation of improvement strategies, the improvement of organisational reputation and the ability to work across sectors.
Enhanced communication channels within local systems were identified in focus group discussions. Patient representatives captured how improved communication had the ability to improve patient flow and enable sharing of knowledge between organisations:
On one occasion my X-ray results were not available at [provider] because the communication between where I had the scan done and the main hospital didn’t exist. So, it is about communication and that’s the nub I think of partnerships.
31, focus group
Those leading collaborations described how improved communication enabled the translation and diffusion of improvement approaches between collaborative partners. Some key benefits of collaboration were based on ability to create the conditions to learn from other organisations and professions about how to improve services. Collaboration created conditions ‘to get to know each other and work together’, with the sharing of results and learning from each other creating conditions conducive to ‘quality improvement for everyone’:
. . . collaboration as opposed to like shaming everybody into improving . . . has been about if you all sit down and look at what you’re doing with patients of certain conditions on a regular basis you’ll level up, because you’ll start to learn from each other.
02; director; hospital group 1
Collaborating across boundaries made it possible to leverage new connections to drive greater delivery of services. For example, collaboration in response to COVID-19 was attributed with facilitating the vaccine rollout within localities:
. . . we have been hugely successful in getting to the marginalised communities. It’s been because of the relationships that we’ve had with those social value organisations, you know, CVS as the umbrella organisation, we’ve been able to vaccinate people who, you know, who many other localities have found it really, really difficult.
22; chief executive officer; alliance 1
The knowledge translation underpinning approaches to the turnaround of challenged organisations was also raised. Interviews reflected on the ability of collaboration to support the translation of best practice:
. . . [if it was possible] to codify what the good organisations were able to achieve, then it ought to be possible to move that into an organisation that was struggling and show them the sort of ingredients that could be mixed to make things better.
12; chief executive officer; alliance 1
Established methods and learning from academia were connected to having a wide range of benefits in relation to better care and financial sustainability, and improvements in staff well-being, morale and engagement. Leaders described the improvement strategy that they were sharing through their collaboration as rooted in organisational development:
So, we use in our trust the Athena team journey approach of Professor Michael West . . . one of the things that he’s promoted was these Athena team journeys . . . which is basically understanding the basics of what are people’s roles, what’s the vision of the team, how do you work together, how do you debate together, and how do you continue changing, and establishing a team within a team.
21; director of clinical service; merger 2
Other leaders turned to different sources for their improvement strategy. Therefore, private sector consultancies also featured in shaping the leadership approaches being undertaken to achieve organisational turnaround:
And it was about a £2.5M investment with [consultancy firm] and that launched what we call our patient first improvement programme and that’s been our absolute . . . our navigation tool since then and it’ has changed the way that we lead, manage, set our objectives.
18; chief executive officer; hospital group 3
A faith in quality improvement methodologies was highlighted as a case in point, where established tools and techniques could demonstrate and communicate improvements being made to different audiences, exemplifying how a change in cultural efficacy could take place through collaboration:
. . . we took . . . the breakthrough series model for improvement out into that organisation, and it is thriving, . . . And what we were saying was, ‘Tell us how you’d like to do this’, and then showing them the outcomes from that. So PDSAs [Plan-Do-Study-Act], tests of change, it’s just their language now, it’s just the way they do things.
10; executive nurse; alliance 1
Alongside the communication and translation of methods and information, interviewees connected collaborative performance with the competitive advantages for organisations involved. There were both reputational and financial advances for engaging with collaboration:
. . . two organisations . . . You know, they recognised that there was something in it for them as it were. So [provider] were, ‘Well, if we pull this off it’s good reputationally and we get a load of cash . . .’
03; director of improvement; hospital group 2
Collaboration brought competitive advantages, with measures of esteem associated with the visibility and recognition gained from the wider health system, and this was particularly the case for mergers, where the increase organisational size could enhance the organisation’s status as measured by league tables:
. . . because I think we do have a particular view about, ‘What’s the size of your organisation? Are you in the top 10 or the top 15? Where are you ranking in this?’ We rank everything, don’t we? There’s a league table for everything.
20; director; merger 2
Increases in organisational size enabled improved reputations and the potential to increase influence over the local health economy, and this was particularly reflected by interviewees from larger types of collaboration:
So, in the NHS we’ve got groups and they are big and a bit like us, and now we’ve developed an association of groups because actually, ‘we’re big and important and we want to influence’.
20; director; merger 2
This mechanism of improved reputation had the potential to drive workforce improvements by attracting better staff. The reputation attached to being a poor-performing organisation was also considered as important in driving the need to collaborate within contexts of organisational turnaround:
. . . so they [the partner] recognised for themselves the fact that they’d normalised such poor standards, and that if they continued to do that, patients would suffer, and their reputation would suffer. And so they very quickly got on board with the improvement journey.
10; executive nurse; alliance 1
Demonstrable improvements in CQC ratings had a reputational impact on those leading collaboration in providing reassurances regarding their approach to performance improvement:
So you know, it’s . . . it just feels good to me that . . . by the time I left the organisation, for whatever you might judge the CQC for, it was able to report that services were now ‘Good’ across X. And you know, for me that was just a reassurance that we had done the right thing.
12; chief executive officer; alliance 1
Collaborative performance also had symbolic qualities in delivering assurances that health and social care systems were working as intended. Seeking out IOCs provided a means of avoiding other forms of enforced collaboration that could undermine continuation of services from the organisation’s perspective:
. . . the consultation document says it’s going to be loads better for patients and staff that may or may not have been true or it may not be delivered. But, actually, the real outcome was to improve confidence in the child protection system in this struggling trust. And to carry on as a champion for children by making sure we don’t get merged in the specialist trust.
01; non-executive director; range
Organisational efficiency
Organisational efficiency was captured in a range of accounts recounting cost savings and resource constraints driving collaborative behaviour. Stabilising financial performance enabled cost savings and workforce changes, and were deemed to improve outcomes by concentrating services in different places. Achieving economies of scale across a geographical area, as well as standardisation occurring across boundaries to a specification and scale, with respect to human resources, clinical pathways and corporate functions, also featured as performance improvements.
Collaboration brought opportunities to improve workforce coordination and configuration of services through reducing duplication of effort and reallocating resources more appropriately:
. . . [it’s] much easier where we have a shared critical care service that gives opportunities for colleagues to work in different places and gives us the opportunity to use our assets differently.
23; chief executive officer; alliance 2
. . . collaborating together makes it more possible for your patients to access that service at the specification it needs to be delivered even if it’s not necessarily in your unit, you know, down the road or whatever. And then that will open up obviously access to more specialised or better facilities for patients but also kind of help to sustain the quality at a higher level.
02; director; hospital group 1
The ability to move staff around more easily when collaborating was also noted as enabling access to additional workforce capacity. Examples of ‘redirecting resources’ enabled by greater coordination were widely noted by those leadings IOCs:
. . . when we were trying to seek solutions to some of the thorny issues, so, workforce being one, we took a paper to boards across [local area] and said, ‘We can seed some medical leadership from [trust 1] for example into the emergency department at [trust 2] but we need others to work with us on actually where we can across the system get workforce support’, because the gap was too big for one organisation to suddenly dip in its back pocket and, hey presto, fill some of those gaps.
20; director; merger 2
The reduction in duplication of effort was extended to reduced costs, as centralisation and process redesign efforts were connected to demonstrable savings. Achieving economies of scale across a geographical area, as well as standardisation occurring across boundaries with respect to human resources, clinical pathways and corporate functions, all featured in driving collaborative performance:
We have one recruitment team. We have one medical staffing team . . . when the two trusts came together, a number of those functions were centralised, which does give you some economies of scale. So from a cost point of view, it has some benefits.
26; head of workforce; alliance 2
. . . the procurement work stream saves the trusts I presume £1M and £2M a year based on the joint procurements that they do that reduce the costs of things, which broadly pays for the cost of running [the collaboration].
19; director; hospital group 4
Wider perspectives regarding improved economies of scale were noted in relation to talent management of the workforce:
. . . we believe that the NHS in particular in this country is suffering from fragmentation that leads to a reduction in the opportunity to grab economies of scale. So, whether that’s the traditional economies of scale, you know, that would be procurement, but just as importantly, it’s really about talent, it’s clinical talent as well as technical talent, and being able to grab as much of that as possible.
22; chief executive officer; alliance 2
This ability for organisations in a collaboration to pool resources also enabled spending on projects that were not previously possible when operating alone, as a director of an alliance stated:
. . . we’ve brought in about £35M of capital funding through collaborative proposals for radiology systems, single laboratory information management system in pathology which will underpin all the pathology services working together.
19; director; alliance 2
The pooled resources that enabled purchasing of more expensive equipment or contracts had the ability to further enhance care quality. Collaborating enabled services to be contracted out to partners who were able to deliver those services better. Likewise, interviewees reported that working cross-sector in their collaboration enabled resources to be redirected to enable improved service coverage for patients:
And that is the partnering if you like, because we have got the third sector which allows us to reach people who find it difficult to engage with services. And that means we might actually make things better.
13; chief executive officer; ICS 1
However, although collaboration enabled expanding outwards, collaboration also allowed for consolidating services to a smaller number of providers where patients could be more easily referred within the collaboration. Service consolidation was connected with improved sustainability of service delivery:
. . . it’s a big town, had a district general hospital that at one stage provided the full range of treatments as you’d expect from something in the 1970s, 1980s. Yet now has been repurposed specifically around acute medicine.
23; medical director; alliance 2
However, in contrast, the interviews with patients also identified that consolidation of services had, in some cases, led to them having to travel further, which could have potential to reduce access for some. A patient representative recounted their experience as follows:
. . . instead of sending people to [hospital 1] to have their scan and then having them transferred to [hospital 2], it was better to actually take them straight to [hospital 2] which is another 15-minute drive in an ambulance.
Patient
Those involved in implementing collaborations also reflected such experiences:
Over time, it could mean that patients potentially have to go further for their treatment, rather than getting it locally. And, you know, sometimes regardless of how well their local hospital is rated, people want to go to their local hospital.
26; head of workforce; alliance 2
However, it was also apparent that caution was needed when considering the potential of organisational efficiency to simultaneously improve care and save money. Some scenarios were recalled of integration increasing costs as community services ran alongside acute services, and this may be the case when collaborative functioning is not optimised and also for particularly complex collaborations:
Most projects have struggled to do both, to improve care and to save money . . . the classic example was [trust] that seemed to be doing quite a good job early on at keeping people – more people in the community and then reducing admissions to hospital. But we never got to the stage of actually closing the beds that were we were previously admitting people to. We just filled them with somebody else . . . So, the people that were paying for care were paying for all this community service over here and they were still paying for the previous acute beds that are now just filled with other people.
01; non-executive director; range
Technological effectiveness
Technological effectiveness featured in interview accounts where the learning had been accumulated across organisations about how to re-design care pathways:
. . . we frequently will have visits from other hospitals and we will share where we are with our stroke service and share anything . . . why reinvent stuff that someone has already done?
21; director of clinical service; merger 2
Connections with organisational efficiencies were also made, with technological effectiveness also connected to reduced duplication of effort:
. . . the big programmes like the radiology, which was obviously very, very successful in terms of having joint reporting and having some joint policies, joint guidance, to us doing some joint clinical leadership training. And that’s all been really, again, that’s successful that we could do that.
35; director of improvement; hospital group 4
Within these arrangements, the enhanced communication fostered by collaboration allowed for the delivery of more integrated cross-organisational clinical pathways by enhancing data-sharing. Implementation of such pathways was found to give patients a more seamless experience when moving between providers both within and between sectors:
. . . so can we try and take out some of that cost and improve patient experience by joining some of that up? And that doesn’t necessarily mean a sort of integrated provider but it certainly does mean that all those different parts need to be working much more closely and effectively together.
04; provider policy leader; range
Technological effectiveness also encompassed enhancing access to technology, with the sharing of clinical innovations that organisations previously could not use:
. . . you know, if you look at [provider 1] and [provider 2] for example, you know, they’ve got robotic surgery in [provider 1] that [provider 2] patients can access more easily now.
15; chief of patient rep. body; range
The overall expansion of research and development was also enabled by enhanced access to resources:
. . . since we’ve become a group, research has exploded because we now have a footprint of 1.2 million patients and the electronic patient record in [locale] moving forward with a pace and purpose to get that in our North West sector care organisations.
23; medical director; alliance 1
Enhanced research and development could, in the longer term, further improve the kind of clinical quality that could be delivered in the providers involved in the collaboration.
Depicting the relationships between collaborative performance mechanisms
Figure 15 depicts how, within each of the collaborative performance domains, a range of mechanisms can be identified with associated performance improvements. Figure 15 shows that cultural efficacy can encompass mechanisms that underlie improvements to efficiency. For example, an enhanced awareness of the local system brought about by cultural efficacy can enable improved coordination, which thereby enables several other improvements, including redirection of resources and consolidation of services to more efficient or effective providers. Figure 15 also shows how increasing communication between providers within the local health system can enable many other mechanisms further down the causal chain, including the sharing of clinical practices in the technological effectiveness category.
FIGURE 15.
Depiction of mechanisms underlying collaborative performance.
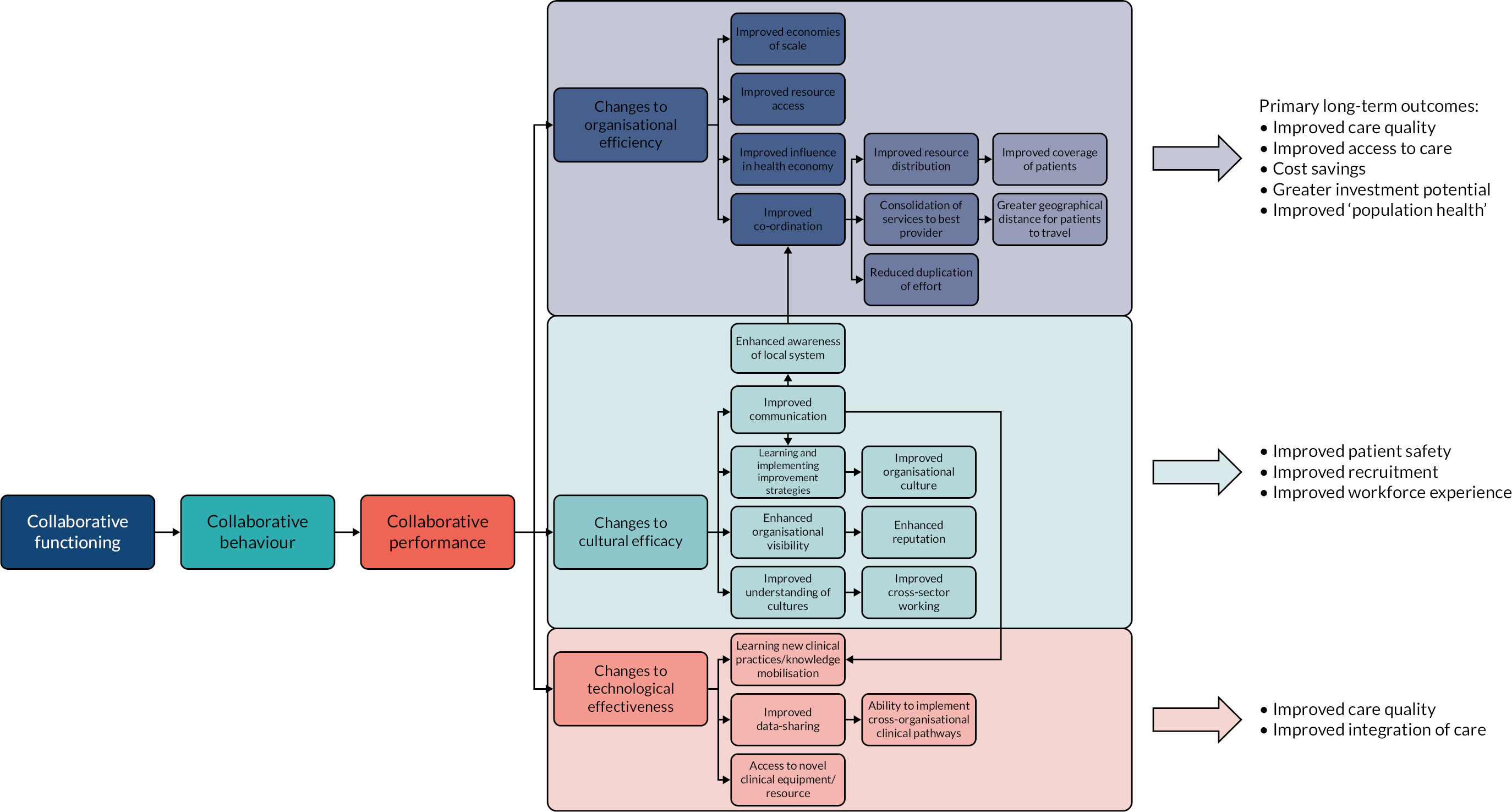
We have also connected the performance mechanisms to what we define as ‘long-term outcomes’, denoting the outer areas affected by collaborative activity. Some of these long-term outcomes will be explored in the following section. However, it is important to note that these links between mechanisms and outcomes require further research, and, accordingly, provide an important basis for further inquiry rather than definitive evidence. Table 9 outlines the intermediate mechanisms identified and how the mechanisms relate to performance improvements.
Long-term outcomes
Connections were made by the interviewees between the mechanisms underlying collaborative performance and the end points of improvements sought from collaborations. Outcomes arising from collaboration were particularly important:
. . . so for me the outcomes that are important are patient related outcomes, staff related outcomes, and what I would call efficiency related outcomes.
03; director of improvement; hospital group 2
A focus on improving population health as a desired outcome was particularly pronounced within accounts regarding the drivers of current collaborative activity. A range of contributions set out visions and goals to ‘bring together partners with a focus on health inequalities, deprivation, economic improvement and promote health and wellbeing as a shared purpose . . . ’ (17; chief executive officer; alliance 2). The focus on population health and reducing health inequalities was connected to the current ICS agenda as a driver for collaborative performance:
. . . if you look at what affects people’s health, it is have they got somewhere to live, have they got something to do, have they got someone to love? And, the economic recovery plans are going to be driven by city regions, getting to the heart of some of that issue, so who is going to have jobs, which sector has got jobs? We have, the care sector. Who is going to have jobs? We are. What about our supply chain? Well, the fact we can’t get PPE [personal protective equipment] reliably means we should make it ourselves locally . . . So, let’s put that together. And, then at the innovative end of the scale, this city region has 22% health-maintained jobs anyway, which has gone through a digital revolution. We have got the conditions locally to make that a reality, so let’s make it a reality. So, there is a really – and, then the other bit for us is the green agenda.
13; chief executive officer; ICS 1
The leadership challenge was framed as one of enabling collaboration towards a greater recognition of social outcomes and social value. The challenge translated into identifying the most vulnerable communities using broader measures (e.g. educational attainment of children, the uptake of free school meals or employment levels). Collaborating with the third sector and faith groups was also identified within such efforts:
. . . so we’ve been doing hypertension clinics in the mosque so working with the faith sectors, starting conversations about going and doing things at the foodbanks.
14; leader; ICS 2
Leaders attributed economic benefits to the place-based approaches already under way. One ICS leader illustrated the high level of cost savings they had achieved from collaborating:
So in 4 years, we had a £400M deficit gap in 2016. We’re breakeven now as a system. We had four organisations in requires improvement or special measures, now they’re all good or outstanding. We had the lowest investment profile into primary care 4 years ago in the country, we’re now in the in the in the mid-range. We’ve still got further work to do.
25; leader; ICS 3
The focus from ICS-based interviewees was on how they were able to do more to engage with communities, run employment programmes and employ a large number of staff from that, including some of the most deprived communities:
The last 2 years, you know, we’ve moved £20M-worth of procurement out of national procurement into local SMEs [small and medium-sized enterprises], local companies within [local area] alone, that’s where we’ve tried it first, and we’ve got some good success in [locale]. So that’s an ambition of recruiting 1000 people every year into pre-employment programmes, with an expectation that 85% of them will lead to permanent, good-quality jobs in health and care, and that we’re targeting those wards that are the most deprived or have the most challenges.
22; chief executive officer; alliance 1
To achieve the population health agenda required further development in creating a shift in understanding regarding provider collaboration. It was evident from the interviews that different systems were at different stages of development towards the ICS agenda:
. . . people might be at very different points in their journey so it’s not certain that you’re all terrible or you’re all good, it’s just about really trying to help them so that the outcomes we want around improving population health get there.
09; regulator
Wider challenges regarding outcomes were connected to ‘fundamental issues’ associated with the historical separation of health and social care systems ‘where integrated services have not been in policy-makers thinking’. Collaboration also surfaced contractual issues surrounding workforce development. Deeper considerations were needed regarding existing salary structures and funding arrangements:
. . . social care has come right up the agenda especially since COVID-19 and the integration across health and social care but we still have a different funding system which causes huge problems for people that want to collaborate across the two and so there is a sort of environmental point that I’d obviously apply across the country but there’ll be some that just apply locally as well.
04; provider policy leader; range
Patient perspectives on outcomes
Patient representatives were also able to shed light on outcomes they had seen from collaborative efforts in their local areas. Overall, these reflections presented diverse reactions to collaboration. Patient representatives raised concerns regarding the translation of collaborative intentions into practice. Scepticism was associated of the aspirations for implementing large-scale change:
. . . it seems generally that across the STPs in the three areas that there’s still lots of planning but nothing concrete is happening in terms of improvements or changes for patients and the public.
. . . one of my ex-colleagues who was a chief exec[utive] in an acute trust said, trying to get a trust to change is like trying to get dinosaurs to dance.
However, with respect to PCNs, patient representatives had seen improvements, with experiences of joined-up care:
They’ve rolled [PCNs] all out now so we’re in the final stages of it really and it has been successful. If you can’t get treatment in one of the GP [general practitioner] surgeries, as long as it’s within the cluster, they’ll refer you to another. Patient transport had been an issue but they’ve done a lot of consultation around that too.
Joined-up care had a positive impact on outcomes, with one patient representative highlighting the improvement to ‘technological effectiveness’ they had enjoyed:
. . . our local primary care network pharmacist contacted me and through that discussion with her she changed my medication. That was brilliant, that really worked. Because prior to that our [local general practice] did not have a resident pharmacist.
Several longer-term outcomes had also been noted, with one notable example in the staff-related outcomes:
[NHS trust] were having massive problems with recruitment of radiologists and consultant medical staff at [trust]. Since they’ve become part of a large university hospitals teaching trust they have succeeded in recruiting to the areas that [they’ve] had problems with.
Focus group
Another patient representative also had very positive experiences in their local system after a large merger took place:
I had to go in and have a little op[eration] and you couldn’t fault it, I got there at 7 o’clock in the morning, they gave me a side room to myself, I had it all day until I went home at 5 o’clock, it was brilliant and I’m excited for [the hospital] for the developments that they’re going to have.
Conclusion
This chapter presents the first comprehensive realist evaluation of how well-functioning IOCs can drive performance improvements. The chapter finds that cultural efficacy mechanisms prove to be particularly important for driving performance improvements from collaboration in other areas through improved communication, better coordination, shared improvement strategies and the enhancement of reputation. Organisational efficiency mechanisms are also identified, with the causal links between collaboration and improving financial and workforce resource allocation, and an increasing responsiveness and reduced duplication in service delivery. Technological effectiveness also connects with such areas and sheds light on the benefits collaboration can bring for research and development and working across clinical pathways. The full CMOC configurations identified in this chapter are depicted in Box 2.
Collaborative behaviour (context) drives improved communication in the local health system (mechanism), which enables actors to have an improved understanding of that health system (outcome).
An improved understanding of the local health system (context) leads to an improved ability to coordinate (mechanism), which can lead to improved coverage of patients and better population health (outcome).
Collaborative behaviour (context) can lead to the ability to learn and implement improvement strategies obtained from partners (mechanism), which can lead to a more productive organisational culture (outcome).
Collaborative behaviour (context) enables organisations to have a larger reach and impact in their local health system (mechanism), leading to a greater reputation (outcome).
Greater reputation (context) can lead to more skilled staff wanting to work in the local health system (mechanism), driving improved recruitment (outcome).
Working across organisational boundaries/collaborative behaviour (context) can lead to a better understanding of other organisational cultures (mechanism) and, thereby, an enhanced ability to work across sectors (outcome).
Organisational efficiencyCollaborative behaviour (context) can lead to cost savings in procurement (mechanism) and improved economies of scale (outcome).
Collaborative behaviour (context) can lead to improved economies of scale (mechanism) and an enhanced ability to acquire workforce talent (outcome).
Collaborative behaviour (context) can lead to improved influence in the local health system (mechanism), which can enable enhanced resource access and better attraction of patients (outcome).
Improved coordination (context) can enable consolidation of services to the most performant provider in the health system (mechanism) and, therefore, better quality of care (outcome).
Consolidation of services (context) can lead to a greater distance for patients to travel for the service they previously enjoyed (mechanism), which could reduce patient coverage (outcome).
Improved coordination (context) can also enable improved coverage of patients (mechanism), which can improve population health (outcome).
Improved coordination (context) enables reduced duplication of effort (mechanism) and, therefore, cost savings (outcome).
Technological effectivenessImproved communication (context) can lead to learning and implementation of novel clinical techniques from collaborators (mechanism) and, therefore, improved care quality and safety (outcome).
Improved communication (context) can lead to improved data-sharing (mechanism), which can enable improved ability to implement cross-organisational clinical pathways (outcome).
Improved coordination (context) can lead to the ability to implement cross-organisational clinical pathways (mechanism) and, therefore, improved care quality and safety (outcome).
Collaborative behaviour (context) can enable access to novel clinically useful equipment (mechanism), which can drive improved care quality and safety (outcome).
Chapter 7 Discussion and implications for translating realist theory into practice
This chapter draws together the key contributions made by the research. The chapter begins with an overview of our final refined theory and goes on to assess the theoretical, methodological and empirical implications of the study. The final section extends the discussion into the assessment of the different ways in which the research can support current policy and practice. The review findings are translated into actionable insights and practical tools to support those implementing health-care collaborations. In this regard, the chapter presents the results of a pilot of a practice-based diagnostic survey and a maturity matrix. Finally, we acknowledge the limitations of the study.
Developing a refined realist theory of interorganisational collaboration
Through analysis of theoretical, empirical and stakeholder evidence, this study has synthesised several MRTs and CMOCs to better understand how, why and in what circumstances IOCs are effective for NHS providers (see Figure 16).
FIGURE 16.
Achieving IOC: a synthesis of causal links between collaborative functioning and performance.
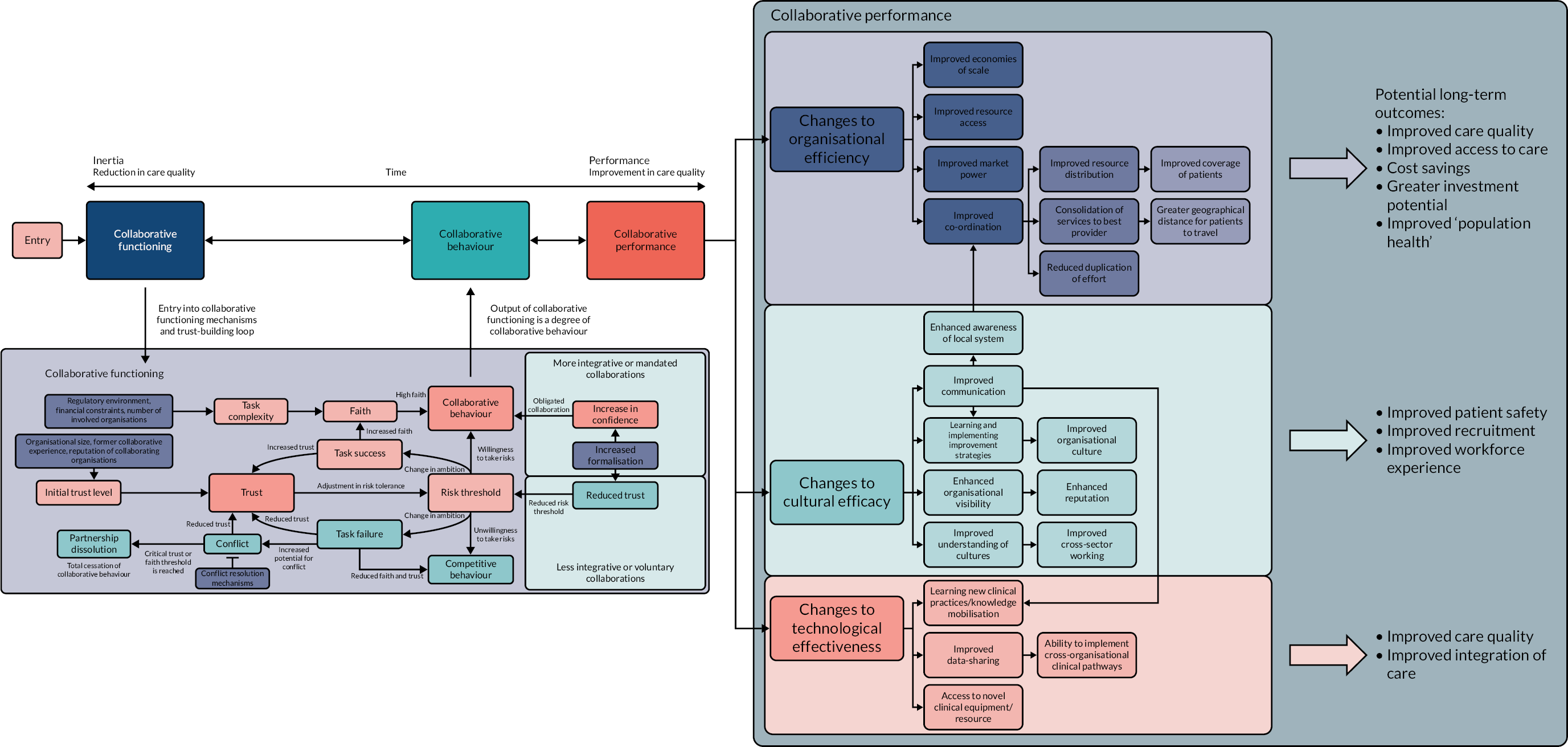
This research provides important insights into how the contexts and mechanisms of collaborative functioning may lead to successful collaborative behaviour. The research finds that the core mechanisms at play within collaborative functioning relate to the development of interorganisational relations linked to trust, faith and confidence. Crucially, the extent to which task success and task failure is achieved appear to be mediated by supporting mechanisms related to capacity, legitimacy, complexity, conflict and risk tolerance. The research breaks new ground in understanding the extent to which collaborative behaviours lead to performance improvement. The research finds that performance improvement can be achieved when the mechanisms of organisational efficiency, cultural efficacy and technological effectiveness are triggered, which, in turn, can drive improvements across a range of dimensions, including care quality, safety, efficiency and experience.
These findings have important implications regarding realist understandings of IOC. Our refined theory extends existing realist contributions to understanding collaborative synergy,132 with the development of CMOCs surrounding health-care IOCs. 135 The further articulation of partnership functioning mechanisms as essential precursors to collaborative behaviour and the accomplishment of collaborative performance is able to provide new insights into the potential of IOCs in driving ‘purposeful collective action’. 127
Theoretical implications
Our findings add to the small but growing evidence base regarding what works in relation to IOCs. The mechanisms identified by this research lends support to those identified in previous studies regarding the ‘shaping factors’ for IOCs and cross-sectoral collaborations. The factors include organisational factors, such as capacity, creating a shared vision, unrealistic aims, trust, communication, governance and leadership. 12,13
In addition, through its use of realist methods our contribution is also able to articulate how, where and why such factors resonate and for whom. For instance, our synthesis of theoretical, empirical and stakeholder evidence highlights how building trust and faith, particularly in the early phases of IOCs, helps to buffer against potential conflicts, particularly during the later stages of implementation. Our findings support other research that suggests that trust is closely linked with the concept of collaborative synergy (framed here as ‘collaborative behaviour’) and mutual successes. 54 The findings introduce new insights regarding the relationship between trust and risk tolerance to explain how trust is a necessary factor for engaging in collaborative behaviour. The concept of faith, although relatively intuitive, has often been under-represented in existing theories of IOC. 44 Our findings, therefore, provide new insights into how the ‘motivation to engage’ in the collaborative process. 127
Where realist evaluations have focused predominantly on collaborative functioning within the dynamics of IOCs,54,127,219,220 our extension of understanding collaborative performance48 provides an additional insight to realist contributions. Studies of IOC note the role of performance, highlighting the importance of alignment or ‘things coming together’ across involved organisations in the potential for generating synergy. 127 Our review findings explain why benefits are attained and also how they are achieved, with the articulation of casual links identified between collaborative functioning and performance.
Our research provides important insights into whom some of these changes benefit. For example, although consolidation of services may benefit patients with more mobility and transport access, stakeholder accounts also draw attention to how changes might also disadvantage patients who already struggle to access services. Those leading collaborations provide rich accounts of the challenges, conflict and energy required for joint working to function. The benefits and drivers for doing so were reflected in their desire to support population health, generate efficiencies and economies of scale, and promote shared learning and knowledge transfer, and also in furthering reputations and generating competitive advantage.
As this analysis is qualitative and realist in nature, it is not possible to identify to what degree performance improvements were realised within the case study examples. However, the research provides further valuable contribution in emphasising the importance of non-traditional outcomes outside conventional measures of efficiency and effectiveness, when evaluating collaborative relationships. 48,221 The articulation of the mechanisms of collaborative performance highlighted in this study lays the foundations for future development of a realist framework for assessing relationships between high-functioning IOCs and their performance against long-term outcomes.
Empirical implications
Our research has synthesised a range of evidence and, in doing so, provides a valuable contribution to the ongoing study of collaboration and integration of health services. Against the background of the current ICS policy agenda, the empirical findings of our research raise important implications for the prospects of a shift towards place-based collaboration. Defined as ‘the geographical level below an ICS at which most of the work to join up budgets, planning and service delivery for routine health and care services (particularly community-based services) will happen’,222 the implementation of place-based collaborations are likely to be essential for the overall functioning of ICSs. The King’s Fund have provided several principles to guide these efforts, including starting with a shared local vision, building a new relationship with communities, investing in multiagency partnerships, building up from what already exists locally, embedding effective place-based leadership and nurturing joined-up resource management. 222 There is potential for the theory arising from this project to feed into current discussions around place-based relationship-building and the role of anchor institutions. The role of faith, trust and other mechanisms signpost what is required in the development of place-based partnerships.
The issue of organisational failure and turnaround is central to both function and performance of IOCs. Failure and turnaround in health-care organisations has been the subject of a number of evidence reviews,223–225 but significant knowledge gaps have remained in relation to identifying the effective methods for turning around and achieving performance improvement in NHS provider organisations. Our findings assemble a range of insights into the mechanisms and outcomes of turnaround approaches. In doing so, the findings disentangle what Jas and Skelcher226 refer to as the ‘excellence theory’ underpinning the features associated with high-performing organisations.
The findings in relation to collaborative performance and cultural efficacy supports the suggestion that ‘absorptive capacity’ theory can provide useful insights into the causes and facilitators of organisational failure and turnaround. 224,227 The implications of our research suggest that the success of IOC can be explained, in part, by organisational learning and the extent to which internal knowledge processes are realigned with changing external environmental conditions.
Our empirical contributions also provide insights into alternative perspectives for understanding IOC, including the role of reputation and impression management in the establishment of collaborative functioning (i.e. building trust) and performance measurement (i.e. cultural efficiency). The contributions also identify how quality improvement and organisational development approaches give focus and method to collaborative functioning and shape the long-term outcomes of improved quality, safety and experience. The implications further capture how ‘techno bureaucratic’ approaches to collaborative performance loom large over the proceedings, with efficiency savings and economies of scale being sought after, and the role of consultancy and other third-party evidence informing such decision-making processes.
Policy implications
A central theme running throughout the empirical and stakeholder evidence identified by our review is the care needed when introducing mandated forms of collaboration. Mandated forms of collaboration are typically used with ICSs, provider collaboratives and PCNs now operating across England. 33 Yet, mandated collaboration is open to criticism regarding the extent to which this approach is able to foster the collaborative mechanisms required for performance improvement. 12,228–230
Our evidence, therefore, raises important concerns regarding the potential for the newly mandated ICS arrangements to impact negatively on existing collaborations that have already been built in well-established ICSs. 231 Our findings suggest that mandating collaboration is likely to make some of the central mechanisms, such as building trust and faith, more difficult, particularly within severe resource-constrained contexts and limited workforce capacity. However, these findings also draw attention to how the current agenda has the potential to kick start collaboration in many local systems where there previously was little relationship-building. A range of practical implications arise from the findings to support the translation of policy proposals, including the importance of focused activities, the implementation of improvement methodologies, the need for shared purpose and having clarity of vision. Attending to these mechanisms provide a crucial platform for any IOC and require consideration when embarking on or sustaining any collaborative venture.
These findings also raise important implications for policy regarding the types of regulation required to support collaborative working. The balance between individual and system accountability remains a contentious issue, and our findings suggest that accountabilities weighted towards the former are likely to limit the risk tolerance for collaborative behaviour to occur. The development of regulatory approaches to performance ratings and accountability is required to ensure that collaborative rather than competitive motivations prevail.
Translating context–mechanism–outcome configurations into practice
Figure 15 shows that to achieve a flourishing IOC requires attention to be paid to the connections between collaborative functioning and performance. For those wishing to develop an IOC, Table 10 sets out a range of practical steps that organisations and those in leadership positions can take in the development of IOCs. 127 Building on other contributions that have sought to translate realist reviews into practical guidance, Table 10 presents a series of ‘if . . . then . . . because’ action statements that can act as a guide for those tasked with developing IOCs that can facilitate performance improvement. 232,233
| IOC task | If (context) . . . then (outcome) . . . because (mechanism) ‘action’ statement |
|---|---|
| Leadership behaviours and attributes | If positive leadership traits and behaviours, including empathetic leadership, visibility, showing vulnerability, espousing local benefit, learning from others, persuasiveness, demonstrating commitment, generosity, consistency of approach and fostering a positive culture, are in place, then these can increase collaborative behaviour by enhancing trust and faith If negative leadership traits and behaviours, such as being ‘missing in action’, not being held accountable and being overly resistant to change, are in place, then these can significantly decrease faith and willingness to collaborate If a ‘culture of improvement’ for organisations is fostered through performing cultural due diligence and this can promote engagement in collaboration by improving faith If the collaboration works towards sharing improvement programmes and strategies across organisations, then this can drive organisational performance improvements by improving collaborative behaviour |
| Enhancing trust and interpersonal ties | If organisations work on understanding the impact of negative prior experiences in collaborations, then they can improve initial trust which can reduce conflict If organisations can foster a mutual understanding by formulating and instilling a shared vision, then they can reduce conflict through generating a cooperative atmosphere If the collaboration can deliver ‘quick wins’ at the beginning of the life cycle, then they can improve trust and faith because they avoid inertia and maintain momentum and ‘energy’ If collaborations can understand and mitigate the impact of the regulatory environment, then they can improve faith because it lowers the workforce’s perception of complexity If the collaboration can prioritise interpersonal communication between organisational actors, via face to face where possible, then they can improve trust because this helps to build interpersonal relationships If there is significant geographical distance between partners, then this can act as a barrier to trust formation because it can undermine the ability to have informal interactions If flexibility and a degree of autonomy within the IOC can occur, then it helps build trust because it avoids feelings of a loss of organisational autonomy (conflict) |
| Risk tolerance | If the collaboration implements an appropriate degree of formalisation, then it can enable the appropriate environment in which collaborative behaviour can occur, which improves trust and/or confidence |
| Faith and initial faith | If organisations include service users and front-line staff in its design, then this will improve faith because this helps keep the vision clearly focused on key outcomes If a clear vision is maintained from the outset, with clear outcomes and a logical path for achievement, then this improves trust because it helps to avoid conflict If the collaborations keep an appropriate level of ambition, then it improves faith because ambition prevents feelings of failure when ambitious goals are not achieved If collaborations involve very large organisations, or many partners, then this can reduce faith because it causes an increase in the perception of complexity If organisations can ensure that there is a perception of progress (i.e. forward momentum), then this will contribute to faith being maintained because there is ongoing evaluation and implementation of milestones If organisations implement ‘champions’ in the IOC, then this can help to spread the faith in the collaboration because ‘champions’ help share the vision within the workforce If collaborations can prevent a high degree of staff turnover, then they can prevent a loss of faith because every staff member that leaves needs to re-learn the vision of the collaboration If organisations can understand the reputation that the chosen IOC form has in the public (e.g. privatisation), then they can improve faith because they may be able to better understand the impact on the workforce |
| Managing mandated collaborations | If those involved can acknowledge that mandated IOCs usually manifest in unequal power structures, then they can reduce the negative impact of this on trust because they pre-emptively understand that additional conflicts may arise If mandated collaborations understand that building relationships and a truly cooperative environment cannot be forced, then this may aid collaborative behaviour in leveraging contractual and ‘confidence’ mechanisms to reduce perceptions of risk If the collaboration is mandated, then efforts should still be undertaken to build working interpersonal relationships because this improves trust and, thereby, collaborative behaviour |
| Confidence and formalisation | If organisations can ensure an appropriate level of formalisation of contract is in place, then they can increase collaborative behaviour because, for more complex, integrative or mandated collaborations, greater formalisation mitigates risk between partners when engaging in collaborative partners If collaborators can perform due diligence around potential areas of disagreement, and enshrining accountability mechanisms in contract, then this can improve trust because it can help to amicably resolve conflicts later on |
| Managing and resolving conflict | If shared and clear accountability is in place, then IOC conflict can be avoided because of these improved conflict resolution mechanisms If the IOC has clear dispute mechanisms in place, with adjudication by an unbiased third party, then trust can be improved because conflicts are more easily resolved If there is a clear and shared vision in place, then this improves trust because it helps to avoid conflicts occurring |
| Ensuring capacity for implementing the collaboration | If organisations recognise that implementing a collaboration requires significant time, effort and financial input, then they will have improved faith because their perception of progress will not be negatively affected If IOCs understand that initial performance drops may occur while resources are redirected towards the implementation of the collaboration, then collaborative behaviour will be enhanced because losses of faith will not take place If organisations begin a collaboration without first ensuring there is adequate capacity, then this can undermine faith and trust between partners because their perception of progress will be negatively affected. In addition, if funding to implement collaborations is sourced externally and it is not forthcoming, then faith and trust can be critically affected because capacity is no longer in place |
| Cultural integration | If a shared culture can be fostered between organisations, then trust can be improved because it helps to avoid cultural conflicts If the IOC is cross-sector or cross-service, then it may have a greater cultural divide because of differing professional backgrounds, which makes cultural integration more difficult If IOCs perform cultural due diligence prior to implementing the collaboration and implement a plan for cultural integration, then they can improve trust because it avoids unforeseen conflicts occurring later in the process |
A consideration of ‘if . . . then . . . because’ action statements can provide valuable support and guidance for anyone wishing to understand and develop an IOC.
Diagnosing the readiness and progress of a collaboration: a developmental survey
Based on the development of our action statements, our findings have enabled the creation of a survey to help organisations assess their readiness for collaboration or assess the progress being made by a particular collaboration.
The readiness for collaboration survey has been piloted with a mental health provider collaborative (see Appendix 4), with a subsequent workshop to discuss the findings taking place on 13 September 2021. For the 21 respondents who completed the survey, the results raised concerns about the time and resource capacity for implementing the collaboration, as well as a challenging landscape associated with significant history of competition with their partners (see Figure 17). That said, the respondents agreed that there was a shared vision for collaboration with their partners.
FIGURE 17.
Example question response.
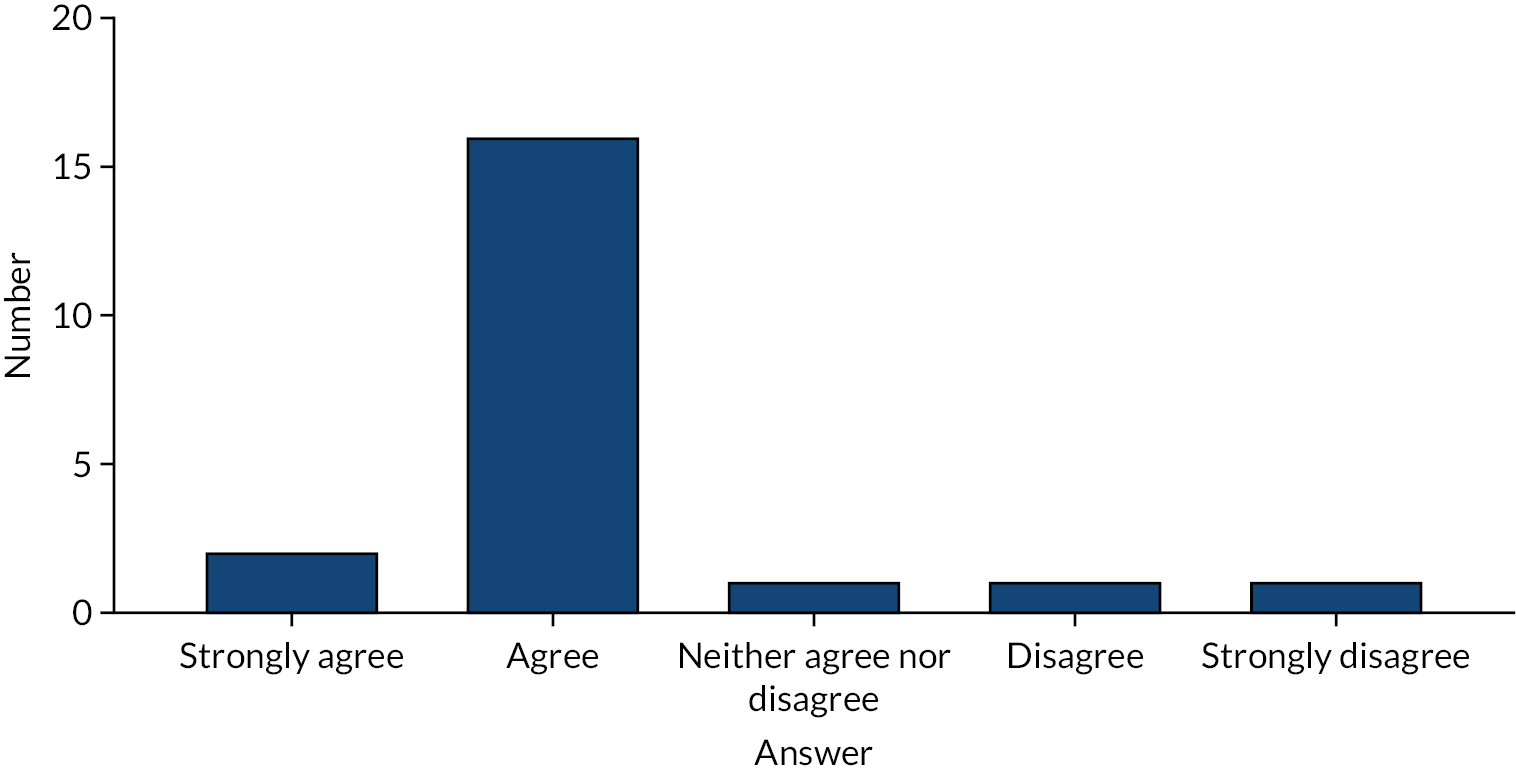
Feedback from piloting of the survey indicated that the survey provided a valuable means for stimulating discussion regarding the perceived readiness for collaboration. However, feedback also suggested that refinements were required to enhance the clarity of specific question items. Given the potential range of organisations and individuals involved in the collaboration, a larger sample may be needed from each organisation to be able to compare answers from different perspectives or stratified sampling to gain more in-depth insights into particular groups.
Designing a maturity index for collaboration
Alongside an understanding of collaborative readiness and progression through a survey, our findings can also provide a range of insights into the ‘maturity’ of an IOC. Building on the notable contribution of Westrum234 in understanding maturity is the idea of creating a climate that provides ‘good information flow’ that is able to ‘support and encourage other kinds of cooperative and mission enhancing behaviour, such as problem solving, innovation, and interdepartmental bridging’. 234 Westrum234 characterises different levels of maturity by different types of culture:
-
A pathological culture characterised by low cooperation, shirking of responsibilities and not open to change.
-
A bureaucratic culture characterised by modest cooperation and focused responsibilities.
-
A generative culture characterised by high degrees of cooperation and sharing of risks.
Westrum’s234 development of a maturity matrix aims to translate such ideas into reflective tools for discussion and reflection. Table 11 outlines our translation of Westrum234 into a maturity matrix that depicts different cultures of collaboration. Further testing is needed to ensure applicability to different collaborative types. Nonetheless, the matrix presents a good starting point for adaptation by other practitioners and researchers alike.
| Key element | Level of maturity | ||
|---|---|---|---|
| Pathological for collaboration | Bureaucratic for collaboration | Generative for collaboration | |
| Trust (i.e. ‘a psychological state comprising the intention to accept vulnerability based upon positive expectations of the intentions or behaviour of another’) | There is a low level of perceived trust between partners, and this may be due to a history of competition with the partner, poor history of collaboration or conflicts. There may be an unequal sense of power structure where one partner may receive more benefits of the collaboration than the other | There is a medium level of perceived trust between partners. There may be a history of competition, but the reputation of the partner is strong, few conflicts have occurred and the conflicts have been resolved amicably. There may be an unequal perception of power structure, but the partner seems unlikely to take advantage of it | There is a high level of perceived trust between partners. Conflicts, when they seldom occur, are solved amicably. Any history of competition is forgotten. There is no perception of any risk when it comes to relying on the collaborator to act altruistically. Any issues with the power structure in the collaboration do not present any barrier and are not perceived to be likely to be taken advantage of |
| Faith (i.e. a motivation or ‘energy’ to work on the collaboration) | There is a low level of perceived faith in the collaboration, and this is likely because members of the workforce perceive it to be not worth working on or otherwise extremely difficult to achieve properly. This is because collaboration could be far too ambitious and overly complex. Likewise, there is a perception that there is not enough resource to implement the collaboration properly. There may also be little sense of progress towards achieving the aims of the collaboration. Leadership may also not be sufficiently supportive in a manner that enables implementing the collaboration | There is a medium level of perceived faith in the collaboration. The workforce may perceive the collaboration as tentatively worth working on, but progress overall may be slow. Workers may feel that the collaboration will be difficult to achieve, but not entirely impossible. Workers feel that there is adequate resource available to implement the collaboration, but that it will be an uphill battle. Leadership is on board with the collaboration, but may not be properly focused on implementing it | There is a high level of faith in your organisation. The workforce is enthusiastic to work on the collaboration and morale is high. Sense of progression towards the aims and objectives of the collaboration is strong |
| Confidence [i.e. the belief that your partner(s) will behave collaboratively because they are obligated to] | Your collaboration is mandated or is very integrative (i.e. a merger), but does not have appropriate legal frameworks in place to enable collaborative behaviour. Or, it is a voluntary or non-integrative type of partnership (i.e. an informal arrangement), but has an overabundance of legal frameworks in place that are undermining the ability to build trust. Both partners feel that it is too risky to engage in any kind of altruistic behaviour | There are mutually agreed-on legal frameworks in place, which enables both partner(s) to feel confident that they can behave altruistically without negative consequences. However, the existence of these contractual obligations are making it difficult to build trust outside of the contract | The legal frameworks are perfectly suitable for the type of collaboration that is in place. Neither partner feels that there is a risk to engaging in collaborative behaviour, and that the legal frameworks in place also do not undermine the ability to engage in altruistic behaviour to build trust |
| Ease of cultural integration | You perceive your chances of being able to culturally integrate with the partner(s) as low, or otherwise there is currently no perceived progress towards neither an integrated culture nor a mutual understanding of cultures | You perceive there being some chance of being able to culturally integrate with the partner(s), but it is/will be an uphill battle | The organisations already have very similar cultures, or there is significant progress towards either having an integrated culture or mutual understanding and way of working between cultures |
| Perceived legitimacy (i.e. whether or not the collaboration is perceived as being a legitimate means to the advertised end) | The collaboration is not perceived as a legitimate effort, and this may be due to it being undermined by mandated forms of collaboration or due to a lack of stakeholder and workforce involvement in the arrangement | The collaboration is perceived somewhat as a legitimate effort. The collaboration may be mandated, but it involves stakeholders and the workforce in the planning and implementation of the arrangement | The collaboration is largely perceived as a legitimate undertaking. There is strong ownership among the workforce and patients and the public are involved |
| Interpersonal communication | There is little communication ongoing between partners. When communication does take place, there is a sense of uncomfortableness. There is an unwillingness to share information across organisations | There is some communication between partners and sometimes it can be uncomfortable. Your organisation is opening up to the idea of sharing information with the partner(s) | You feel no reservations about communicating and sharing information with your partners. There is frequent communication between partners and it feels second nature to do so. Both partners are receptive and communicative in a way that facilitates the building of positive interpersonal relationships. Information required for delivering patient care is also moving smoothly between organisations where required |
| Clarity of vision (i.e. how clear the aims and objectives of the collaboration are, as well as how to get there) | What the collaboration is hoping to achieve is unclear. Everyone you ask has a different concept of what it is hoping to achieve, and the road to achieving those outcomes is equally unclear. Even senior management seems to be lacking agreement on what is hoping to be achieved | Many members of the organisation are largely in agreement on what the collaboration is seeking to achieve, particularly in senior management and those who are architects of the collaboration. Some members at a lower level of the workforce are still lacking agreement, however. There is some clarity on how collaboration is seeking to deliver performance improvements | Most people you talk to agree on what the collaboration is seeking to achieve, and this even is the case across partners. There is a clear logic with respect to how the collaboration is going to lead to the desired performance improvements. There is a clear timeline of milestones along the way |
| Sharedness of vision (i.e. the degree to which the aims, objectives and plan for the collaboration is shared across partners) | Neither your organisation nor the partners in the collaboration have agreement on what is hoping to be achieved. When discussed, there is active disagreement on even what you are hoping to accomplish | Partners agree on the ultimate outcomes for the collaboration, but perhaps not on the best route for how to get there. There are occasionally disagreements, but these are resolved amicably for the most part | There is total agreement on the aims and objectives of the collaboration and how to get there. Both partners have formally signed off on a plan for how to reach the desired outcomes of the collaboration, and this agreement extends to the way people interact, with few or no conflicts on even small details of the plan |
| Risk tolerance (i.e. to what extent an organisation is willing to engage in behaviour a partner could take advantage of) | Your organisation is not willing to engage in altruistic behaviour, as you feel that your partner might not reciprocate or may even take advantage of the situation in a competitive manner to your organisation’s disadvantage | Your organisation is willing to engage in altruistic behaviour in some areas, but not in others, as your level of trust and confidence in your partner is not high enough and you have concerns that your partner will not behave in a competitive manner in certain areas | There are no barriers to engaging in behaviour that your partner could take advantage of if they wanted to. The concern that this may happen no longer exists and there is sufficient trust and confidence to allow you to work on the aims of the collaboration with the partner. You experience the partner behaving altruistically to your organisation’s benefit, and vice versa |
Limitations of the project
Literature component
Although every effort was made to be as exhaustive as possible in our search of the literature, including multiple waves of systematic searching, as well as searching the grey literature sources, it is possible we inadvertently omitted literature that would have been informative to the present review. A particular challenge was covering all the partnership types because of the myriad of overlapping terms used to refer to collaborations. In addition, although some included papers did document cases of collaborations that in dissolution (e.g. Murray et al. 100), these papers were under-represented. This is perhaps due to the biased under-reporting of failed collaborations arising from publication bias. Inclusion of more examples of unsuccessful collaborations would have provided further evidence to supplement our review. The study was predominantly focused on the UK; however, we did include several studies from abroad (e.g. Austria195 and the USA172) and we did not purposely remove any papers based on country-specific metrics. Indeed, additional information from other regulatory contexts would have been more informative. Nonetheless, owing to the scope of our project, it is likely that we missed important literature emanating from the experience of other countries and health systems.
Empirical component
Our sample was exclusively drawn from the English health system and it is not clear whether or not our findings would apply to other contexts. Our interview sample included senior staff members and executives. Such purposive sampling was driven by the need to gain a breadth of different arrangements we did not have the resource to identify a wide range of opinions and perspectives. Time and resource limitations were further hampered by the difficulties of carrying out fieldwork during the COVID-19 pandemic.
In addition, patient representatives were drawn from well-informed local Healthwatch volunteers, board members or employees, which meant the representatives could have had different perspectives from the general patient population. Furthermore, use of our prior theory in constructing the retroductive coding framework could have biased the analysis in favour of identifying excerpts that would support our theory. However, we attempted to mitigate this by being actively aware of this possibility during analysis.
Although the present research sought to generate insights into what is considered a collaborative ‘outcome’ in both a realist and pragmatic sense (i.e. what outcomes do stakeholders desire from collaborating), it was, nonetheless, difficult to draw out causal connections between what was happening in local health systems and national system long-term effects on patient safety, quality, etc. This is perhaps due to the inherent complexity present in health systems and the significant length of the causal chain. 235 There is also significant overlap, which is difficult to overcome, in terms of what people expect from partnerships (i.e. drivers and motivators) and what actually results from them (i.e. outcomes), and it is not always clear to which patients or the literature are referring. We have attempted to mitigate this by analysing the mechanisms within ‘collaborative these often overlap, they are not necessarily the same.
Theoretical limitations
Finally, depending on the level of analysis, it is possible to criticise the theory for not providing sufficient in-depth analysis. As previously mentioned, the analysis required a relatively elevated level of abstraction to embrace multiple types of IOC. This level of abstraction was required to keep the analysis process manageable and in many cases we did not have evidence for the range of collaborative types at this level of depth. Although novel in its contribution, our development of a realist theory for collaborative performance also requires development with further application. Nonetheless, we have signposted what and where future research on this topic is needed. Furthermore, our refinement of existing realist theory in relation to IOCs provides researchers with further opportunities to interrogate different types of collaboration across different contexts.
Chapter 8 Conclusion and recommendations
This chapter concludes the report with an overview of how the project has accomplished its objectives. This chapter also sets out recommendations for future research to support the development of IOCs between health-care providers.
Achieving the research objectives
Objective 1: to explore the main strands of the literature about interorganisational collaboration and to identify the main theoretical and conceptual frameworks that can be used to shed light on the conditions and antecedents for effective partnering across sectors and stakeholders
This project has incorporated key conceptual frameworks and theoretical perspectives that can be used to structure understanding and empirical investigation of IOC. Partnership synergy theory115 and collaborative performance48 informed the development of the MRTs used in the realist synthesis of evidence. The development of the initial rough theory identified a range of theoretical frameworks for understanding the formation and dynamics of IOCs over time, as detailed in Chapter 2. Our realist review and refined theory has gathered some of the foremost literature on IOCs in shedding light on the barriers, facilitators and other contextual elements affecting the process of collaboration.
Objective 2: to assess the empirical evidence with regard to how different interorganisational collaboration practices may (or may not) lead to improved performance and outcomes
Taken together, the review of the literature and empirical work in this area has helped to answer this question by providing valuable insights into the ‘black box’ of health-care IOCs. Through an iterative process of gleaning and refining the causal chain IOCs, we have been able to generate novel insights into how day-to-day operations translate into more causal elements, which, in turn, influence how performance improvements area realised. These insights included the core mechanisms driving collaborative behaviour, such as trust and confidence, and their link to risk tolerance, as well as faith, and the contextual factors and occurrences that can undermine success. Likewise, our analysis of the collaborative behaviour to collaborative performance component of the causal chain gives rise to new insights into how performance benefits are achieved.
Objective 3: to understand and learn from NHS evidence users and other stakeholders about how and where interorganisational collaboration can best be used as a mechanism to support turnaround processes
Our stakeholder analysis incorporated a variety of perspectives, from those with responsibility for leading IOCs, patient representatives, policy-makers, regulators and professional bodies, about how and where IOCs can best be used as a mechanism to support performance improvement. The important role performed by our Advisory Group should also be noted in terms of contributing valuable insights throughout the project, including ‘sense-checking’ the results and ensuring that the theory was understandable to end users.
These contributions have further refined our understanding of what works, for whom and in what circumstances in relation to IOC. The contributions draw attention to the various leadership qualities required, the capacity constraints and challenges being faced by NHS providers, the role of improvement methodologies and the importance of legitimacy and task complexity, as well as the significance of building confidence through contractual and compact ways of working.
Objective 4: develop a typology of interorganisational collaboration that considers different types and scales of collaborative ventures that are appropriate for particular NHS provider contexts
Our research identified how typologies of collaboration, and the extent to which the conditions and antecedents for effective partnering are influenced, can be shaped by the degree of integration associated with the collaborative endeavour. Other factors were equally important in terms of whether the IOC entered into was voluntary or mandated. These key characteristics informed the rest of our theoretical development and the key mechanisms we identified, such as the conception of the confidence versus trust spectrum, the degree of integration associated with different types of collaboration and whether or not the collaboration is mandated.
Given the shifting policy agenda during the lifetime of the project, as well as the onset of COVID-19, our stakeholder analysis made sense of these different types and scales of collaboration within the context of the ICS landscape and the role of IOCs in improving population health.
Objective 5: to develop evidence-informed practical guidance for NHS providers, policy-makers and others with responsibility for implementing and assessing interorganisational collaboration arrangements in the NHS
Our review has sought to translate our findings into practical guidance. This included the development of ‘if . . . then . . . because’ statements, the development of a collaboration maturity matrix and a diagnostic survey to understand collaboration readiness and progression. These tools translate our review findings into applications in practice. The initial pilot of our collaboration diagnostic survey with a mental health provider collaborative provided valuable results and is informing how this collaborative is being developed. Further testing and refining of the survey are needed to ensure applicability across a variety of interorganisational collaborative settings and to improve internal validity.
Future research directions
A range of theoretical, empirical and policy implications arise from this research. Specific issues that warrant further consideration and investigation include the following:
-
We call for a more inclusive sampling strategy to further refine our theory and better articulate what is working ‘for whom’ in relation to IOCs. Where much of the analysis of IOCs has captured the experiences, processes and outcomes from the perspective of those leading programmes and initiatives, further research is needed to gather workforce perspectives regarding how new processes are understood and operationalised, and how IOCs shape patient and user interactions.
-
Our research breaks new ground with the inclusion of patient representatives. Yet, further research is required to better grasp how IOCs can engage and improve population health, drawing on principles of co-design and co-production.
-
The COVID-19 pandemic raises a number of implications for the future of IOCs. Our research identifies how the pandemic has been a driver for activity where a central feature has been the use of digital platforms for communication. These digital communication methods have proved invaluable, yet clear limits to ‘interpersonal communication’ can be identified. Learning from our review suggested that contexts are likely to have a negative affect on the ability to build trust and generate the informal relationships and, therefore, further research is needed into digital platforms and their role in facilitating collaboration.
-
Further research is needed to investigate the applicability and adaptability of several elements raised by this project, such as the roles of faith, trust and other mechanisms in the formation and maintenance of place-based partnerships. Learning from other national contexts could facilitate such efforts, with further comparative studies of IOCs from across the UK and beyond.
-
Building on our realist theory of collaborative performance, further research is needed to disentangle the motivators and drivers from the ‘outcomes’ associated with IOCs. Such research resonates with a policy landscape placing greater emphasis on measuring the outcomes and social value generated from collaborative working.
-
Where our review has focused on the perspectives and implications of IOCs for NHS providers in England, further research is needed to critically engage with alternative partnership activities taking place within current policy agendas. Greater attention to the role of public/private partnerships is called for, and more analysis of the role of the private sector more specifically, within collaboration and integration initiatives. The place and positioning of social care within the IOC agenda also require further development, as does the role of the third sector and how these organisations intersect within the IOC landscape.
-
The role of regulation is crucial to developing different types and scales of IOCs. Yet, our understanding of regulatory functions and levers is relatively underdeveloped. A review of regulatory models and perspectives is, therefore, needed for overseeing and promoting collaborative ventures. Learning from other sectors and health-care contexts can provide a valuable contribution to supporting the IOC agenda.
These issues, along with many others, represent key lines of inquiry for any future research in this area. Given the significance and importance of IOCs to policy-makers, practitioners, patients and communities, our review has the potential to support the development of knowledge, skills and behaviours across a range of stakeholder groups. Following the recent government announcement of a leadership review to ‘improve processes and strengthen the leadership of health and social care in England’, our research can provide valuable insights into the leadership actions and behaviours that enable high-performing collaboration and integration across organisational boundaries. 236
Acknowledgements
We would like to acknowledge the following members of our Advisory Group who supported the research project:
Sarah Morgan (chairperson) (Director of the South East London ICS Workforce Programme and Director of Organisational Development Guys and St Thomas’ NHS Foundation Trust)
Ron Agble (Director of Partnerships and Transactions, Royal Free London NHS Foundation Trust)
Steve Beales (Assistant Director, North East London Health and Care Partnership)
Andrew Corbett-Nolan (Chief Executive, Good Governance Institute)
Sonia Dalkin (Associate Professor, Northumbria University)
Miriam Deakin (NHS Providers)
Tim Gardner (The Health Foundation)
Josie Harding (Head of Insight and Evaluation, Mid and South Essex Hospitals Group)
Sandra Haynes (Lead Governor, University Hospitals Birmingham)
Tom Howell (Head of Mental Health Provider Collaborative Development, NHS Birmingham and Solihull Clinical Commissioning Group)
Chris Smith (Good Governance Institute)
Mark Stafford (Partner, The Berkeley Partnership)
Leanora Volpe (NHS Providers)
Charlotte Williams (Chief Strategy and Improvement Officer, Mid and South Essex NHS Foundation Trust).
Contributions of authors
Ross Millar (https://orcid.org/0000-0001-5790-7947) (Reader, Health Organisation) was the principal investigator responsible for managing the project, supported the realist synthesis, conducted qualitative data collection and analysis, supported the development of practice-based tools and led the final report write-up.
Justin Avery Aunger (https://orcid.org/0000-0001-6975-4570) (Research Fellow) led the realist synthesis, prepared results for publication, conducted qualitative data collection and analysis, supported the development of practice-based tools and drafted chapters of the final report.
Anne Marie Rafferty (https://orcid.org/0000-0003-1010-6581) (Professor, Nursing Policy) conducted qualitative data collection and analysis, and contributed to editing the final report.
Joanne Greenhalgh (https://orcid.org/0000-0003-2189-8879) (Professor, Applied Social Research Methodology) conducted realist synthesis development and analysis, and contributed to editing the final report.
Russell Mannion (https://orcid.org/0000-0002-0680-8049) (Professor, Health Systems) provided analytical support and contributed to editing the final report.
Hugh McLeod (https://orcid.org/0000-0002-2266-7303) (Senior Lecturer, Health Economics) provided analytical support and contributed to editing the final report.
Deborah Faulks (https://orcid.org/0000-0002-2825-7268) (Engaging Communities Solutions) conducted data collection with patient representatives.
Publications
Aunger JA, Millar R, Greenhalgh J. When trust, confidence, and faith collide: refining a realist theory of how and why inter-organisational collaborations in healthcare work. BMC Health Serv Res 2021;21:602.
Aunger JA, Millar R, Greenhalgh J, Mannion R, Rafferty AM, McLeod H. Why do some inter-organisational collaborations in healthcare work when others do not? A realist review. Syst Rev 2021;10:82.
Aunger JA, Millar R, Rafferty AM, Mannion R. Collaboration over competition? Regulatory reform and inter-organisational relations in the NHS amidst the COVID-19 pandemic: a qualitative study. BMC Health Serv Res 2022;22:640.
Aunger JA, Millar R, Rafferty AM, Mannion R, Greenhalgh J, Faulks D, et al. How, when, and why do inter-organisational collaborations in healthcare work? A realist evaluation [published online ahead of print April 11 2022]. PLOS ONE 2022.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
Appendix 1 Initial rough theory methodology
A realist synthesis involves identifying and then testing and refining theories that explain how context shapes the mechanisms through which partnering interventions work to produce outcomes. Mechanisms are defined as the ‘underlying entities, processes, or [social] structures which operate in particular contexts to generate outcomes of interest’. 130 Dalkin et al. 131 go further in disaggregating the concept of a mechanism into its constituent parts, that is, as either a resource that the intervention introduces to the environment or the resulting reasoning that this incurs in the actors of the intervention. Contexts are defined as ‘relatively enduring and are what social programs aim to transform (rather than reproduce) by activating various structural, cultural, agential and relational mechanisms to produce various outcomes’,129 and outcomes are the outputs that the interventions or programmes are intended to generate. At the end of a realist synthesis, it is best practice to have produced a set of refined CMOCs that provide an explanation of how contexts shape mechanisms through which the intervention leads to particular outcomes, and why this is the case. 130 It is key to understand how interventions work, and why interventions do or do not work given the presence of different contextual factors.
Shearn et al. 237 propose that it is necessary to form an IRT to ‘become the object of the inquiry and the structure and framework for examining and synthesizing diverse evidence’. Therefore, the IRT that is being formulated here constitutes our initial groundwork for a fully encompassing theory that will explain ‘what is supposed to happen’, as well as ‘why it is supposed to work’. A rough initial theory ‘may or may not be constructed in realist terms’. 130 In the case of partnerships, the intervention can take many forms, have multiple entry points and can operate through hundreds or thousands of actors within organisations, encompassing individual and group behavioural dynamics. Therefore, with messy, complex interventions, such as ‘partnering’, the means through which the intervention is expected to work are often ambiguous or too heterogeneous to easily characterise. 54
In this case, to construct our IRT, policy and organisational documents were reviewed, as well as various ‘tacit theories’ present in similar topics in the literature. 237 A review of grey literature (i.e. policy and organisational strategy documents within the NHS) and academic literature was carried out from November 2019 to January 2020 to gain an understanding of existing typologies of partnering, the expected outcomes of partnering and the ‘active ingredients’ at work therein. This review utilised searching of Google, Google Scholar and NHS websites in an unstructured but purposive manner that was typical of a narrative literature review. 238 For searches of review papers around partnering, papers were included when they were clearly related to IOCs in the public sector. For organisational documents, Google searches were conducted using terms such as ‘NHS Foundation partnership strategic document’ and for other specific partnership types such as ‘alliance’ (see Tables 12–14), and the results trawled for strategic organisational documents. These strategic organisational documents involving partnerships were scoured for intended outcomes and the outcomes were extracted into a table. Once the included papers were reviewed and an appropriate categorisation was identified, thematic analysis was then performed in a deductive manner to identify appropriate classifications for these outcomes.
| Category of search term | Terms |
|---|---|
| Types of partnership | Associate member, buddying, clinical network, contractual joint venture, merger, acquisition, service-level chain, joint management, co-ordinating, consolidation, integrated care system, accountable care system, organisational franchises, hospital chains, management contract, federation, mutual, joint working, partnership working, alliance |
| Field | Healthcare, hospitals, acute care, primary care, community, general practice, public sector |
| Document type | Review, guide, model, framework |
| Category of search term | Terms |
|---|---|
| Types of organisation | NHS foundation, trust, provider, hospital, healthcare |
| Collaboration type | Partnership, alliance, collaboration, coordination, franchise, joint working, federation, network, joint venture, buddying, merger, acquisition |
| Document type | Strategic case, strategy, evaluation, proposed, agreement, memorandum of understanding, contract |
| Category of search term | Terms |
|---|---|
| Types of organisation | NHS England, NHS Improvement, The King’s Fund, UK Parliament, NHS Digital, NHS Employers |
| Collaboration type | Partnership, alliance, collaboration, coordination, franchise, joint working, federation, network, joint venture, buddying, mergers, acquisitions |
| Document type | Review, recommendations, lessons, success, failure, factors, guide |
Policy documents were identified in a similar fashion, with keywords such as ‘NHS England’, ‘Partnership’, ‘Collaboration’, etc., with multiple policy-maker organisations (e.g. NHS Providers, NHS Improvement) searched for. NHS Foundation, NHS England, NHS Providers and other organisational sites were also trawled for such documents. Once an initial draft of this paper and theory was developed, it was then presented to and deliberated by a panel of 11 experts from a range of organisations with an interest in partnering policies, including NHS Improvement, the Good Governance Institute (London, UK), The Health Foundation and NHS Providers, for review and refinement of its theoretical content, during the course of a 2-hour workshop.
Appendix 2 Life cycle methodology
‘Best fit’ framework synthesis methodology
This ‘best fit’ framework synthesis methodology was chosen for this study. 116 Frequently used in improvement studies in health care,239,240 the ‘best fit’ framework synthesis method was chosen for its flexible and rigorous approach to synthesising existing frameworks (in this case, process models) with novel data, enabling key gaps in existing understanding to be covered with the formation of a new ‘meta-framework’ (termed here as a ‘composite model’). This new composite model would be purpose-built from many sources of evidence for the public sector. 116 The ‘best fit’ method for framework synthesis for improvement science116,241,242 involves seven systematic steps. However, as the best fit methodology is not completely rigid and has a number of permutations for various intended objectives, we selected the ‘meta-framework’ strategy proposed by Booth and Carroll,116 which uses an a priori framework as a base, against which stages and behaviours from other frameworks/models are coded to build a novel framework/model.
Given this approach, our method was as follows: (1) conduct a systematic search to identify models in the literature, (2) extract models and key behaviours from identified studies, (3) select an a priori framework from stages of included models using thematic analysis and separating key behaviours from stages of models, (4) code stages from other models against the a priori framework, (5) create new themes for any stages that cannot be coded against the a priori framework, (6) code previously separated behaviours against the new framework, adding stages if required, and (7) draw on additional evidence to add relationships between stages in the model. This method differs from a traditional systematic review by adding a method for synthesising theories and frameworks, rather than focusing on efficacy or findings of the included studies.
Systematic search
Search
Systematic searches were conducted around the areas of collaboration in a health-care setting, encompassing a wide range of partnership types, such as alliances, buddying, mergers, acquisitions and hospital groups. Google Scholar searches, citation-tracking and reference-scanning were used to identify wider public sector literature.
Search strategy
Searches were run between 20 February 2020 and 4 March 2020 on databases, including HMIC, MEDLINE, Social Policy and Practice and PsycINFO. The databases were chosen for their relevance to the health-care sector. In addition, a more informal Google Scholar search was conducted on 11 March 2020 to identify any grey literature or elements missed, as well as reference-scanning and citation-tracking. This search combined terms including ‘public sector’, ‘inter-organisational collaboration’, ‘life cycle’ and ‘model’ or ‘framework’.
Study selection
Inclusion criteria were the paper had to (1) clearly relate to collaborations between one or more organisations on either a structural or individual level and (2) be a case study, evaluation, opinion or review. Therefore, papers outlining public–private partnerships would be included at this stage. To reach the final stage of inclusion, the paper had to be relevant to the procedural aspects of partnership by either (1) presenting a model developed for, or explicitly applied to, collaborations in the public sector or (2) relating to behaviours required for planning or implementing partnerships in the public sector. Exclusion criteria for all stages included papers that relate to collaborations or partnerships between staff and patients rather than between organisations. Titles and abstracts were screened by one main reviewer, with a subset of 10% of the total titles and abstracts screened by an independent party.
Data extraction
Data extraction was carried out by one reviewer, which involved combing the included papers for models of the stages that partnerships go through and the behaviours key to these stages. This information was then extracted into separate documents before being categorised and tabulated for relevance to the review.
Appendix 3 Search strategy
Text in this appendix has been reproduced with permission from Aunger et al. 138 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Theory gleaning
Healthcare Management Information Consortium: commentary
Date of search:
Date range searched:
Search strategy
-
buddying.mp.
-
(clinical adj1 network).mp. [mp = title, other title, abstract, heading words]
-
merger.mp.
-
acquisition.mp.
-
(joint adj1 management).mp. [mp = title, other title, abstract, heading words]
-
consolidation.mp.
-
(coordinating or co-ordinating or coordination or co-ordination).mp. [mp = title, other title, abstract, heading words]
-
(hospital adj1 chain$).mp. [mp = title, other title, abstract, heading words]
-
federation.mp.
-
(joint adj1 working).mp. [mp = title, other title, abstract, heading words]
-
(partnership adj1 working).mp. [mp = title, other title, abstract, heading words]
-
alliance.mp.
-
(joint adj1 commissioning).mp. [mp = title, other title, abstract, heading words]
-
vanguard.mp.
-
exp Integration/
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15
-
health care/or acute care/or medical care/or primary care/or public sector/
-
16 and 17
-
opinion*.ti.
-
(view or views).ti.
-
editorial.mp.
-
note.mp.
-
comment.mp.
-
letter.mp.
-
or/19–24
-
18 and 25
-
limit 26 to yr = “1990”
Healthcare Management Information Consortium: review, framework, theory, evaluation
Date of search:
Date range searched:
Search strategy
-
buddying.mp.
-
(clinical adj1 network).mp. [mp = title, other title, abstract, heading words]
-
merger.mp.
-
acquisition.mp.
-
(joint adj1 management).mp. [mp = title, other title, abstract, heading words]
-
consolidation.mp.
-
(coordinating or co-ordinating or coordination or co-ordination).mp. [mp = title, other title, abstract, heading words]
-
(hospital adj1 chain$).mp. [mp = title, other title, abstract, heading words]
-
federation.mp.
-
(joint adj1 working).mp. [mp = title, other title, abstract, heading words]
-
(partnership adj1 working).mp. [mp = title, other title, abstract, heading words]
-
alliance.mp.
-
(joint adj1 commissioning).mp. [mp = title, other title, abstract, heading words]
-
vanguard.mp.
-
exp Integration/
-
health care/or acute care/or medical care/or primary care/
-
administration/or organisational structure/or organisational theory/or organisations/
-
15 or 16 or 17
-
7 or 10
-
18 and 19
-
1 or 2 or 3 or 4 or 5 or 6 or 8 or 9 or 11 or 12 or 13 or 14 or 20
-
evaluat$.mp.
-
interven$.mp. [mp = title, other title, abstract, heading words]
-
assess$.mp. [mp = title, other title, abstract, heading words]
-
trial.mp. [mp = title, other title, abstract, heading words]
-
model.mp. [mp = title, other title, abstract, heading words]
-
review.mp. [mp = title, other title, abstract, heading words]
-
(case adj1 study).mp. [mp = title, other title, abstract, heading words]
-
theory.mp. [mp = title, other title, abstract, heading words]
-
22 or 23 or 24 or 25 or 26 or 27 or 28 or 29
-
21 and 30
-
limit 31 to yr = “1990 -Current”
OVID: MEDLINE and PsycINFO
Date of search:
Date range searched:
Search strategy
-
buddying.mp.
-
(clinical adj1 network).mp.
-
merger.ti.
-
acquisition.ti.
-
(joint adj1 management).mp.
-
consolidation.ti.
-
(coordinating or co-ordinating or coordination or co-ordination).ti.
-
(hospital adj1 chain$).ti.
-
federation.ti.
-
(joint adj1 working).ti.
-
(partnership adj1 working).mp.
-
alliance.ti.
-
(joint adj1 commissioning).ti.
-
vanguard.mp.
-
systems integration/or “health care facilities, manpower, and services”/or “health care economics and organizations”/or health services administration/or “health care quality, access, and evaluation”/
-
partnership.mp.
-
partnering.mp.
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 16 or 17
-
15 and 18
-
limit 19 to yr = “1990 -Current”
Social Policy and Practice database
Date of search:
Date range searched:
Search strategy
-
partnering.mp. [mp = abstract, title, publication type, heading word, accession number]
-
partnership.mp. [mp = abstract, title, publication type, heading word, accession number]
-
“joint working”.mp. [mp = abstract, title, publication type, heading word, accession number]
-
merger.mp. [mp = abstract, title, publication type, heading word, accession number]
-
acquisition.mp. [mp = abstract, title, publication type, heading word, accession number]
-
alliance?.mp. [mp = abstract, title, publication type, heading word, accession number]
-
“partnership working”.mp. [mp = abstract, title, publication type, heading word, accession number]
-
buddying.mp. [mp = abstract, title, publication type, heading word, accession number]
-
(clinical adj1 network).mp. [mp = abstract, title, publication type, heading word, accession number]
-
(coordinating or co-ordinating or coordination or co-ordination).mp. [mp = abstract, title, publication type, heading word, accession number]
-
(joint adj1 commissioning).mp. [mp = abstract, title, publication type, heading word, accession number]
-
vanguard.mp. [mp = abstract, title, publication type, heading word, accession number]
-
integration.mp. [mp = abstract, title, publication type, heading word, accession number]
-
healthcare.mp. [mp = abstract, title, publication type, heading word, accession number]
-
hospital?.mp. [mp = abstract, title, publication type, heading word, accession number]
-
evaluat*.mp. [mp = abstract, title, publication type, heading word, accession number]
-
intervention.mp. [mp = abstract, title, publication type, heading word, accession number]
-
model.mp. [mp = abstract, title, publication type, heading word, accession number]
-
review.mp. [mp = abstract, title, publication type, heading word, accession number]
-
(case adj1 study).mp. [mp = abstract, title, publication type, heading word, accession number]
-
theory.mp. [mp = abstract, title, publication type, heading word, accession number]
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13
-
14 or 15
-
16 or 17 or 18 or 19 or 20 or 21
-
22 and 23 and 24
Theory refining
Social Policy and Practice database
Date of search: 10 June 2020.
Results: 2144.
Results after deduplication: 1092.
Search strategy
-
partnering.mp. [mp = abstract, title, publication type, heading word, accession number]
-
partnership.mp. [mp = abstract, title, publication type, heading word, accession number]
-
“joint working”.mp. [mp = abstract, title, publication type, heading word, accession number]
-
merger.mp. [mp = abstract, title, publication type, heading word, accession number]
-
acquisition.mp. [mp = abstract, title, publication type, heading word, accession number]
-
alliance?.mp. [mp = abstract, title, publication type, heading word, accession number]
-
“partnership working”.mp. [mp = abstract, title, publication type, heading word, accession number]
-
buddying.mp. [mp = abstract, title, publication type, heading word, accession number]
-
(clinical adj1 network).mp. [mp = abstract, title, publication type, heading word, accession number]
-
(coordinating or co-ordinating or coordination or co-ordination).mp. [mp = abstract, title, publication type, heading word, accession number]
-
“joint commissioning”.mp. [mp = abstract, title, publication type, heading word, accession number]
-
vanguard.mp. [mp = abstract, title, publication type, heading word, accession number]
-
healthcare.mp. [mp = abstract, title, publication type, heading word, accession number]
-
hospital?.mp. [mp = abstract, title, publication type, heading word, accession number]
-
public health.mp. [mp = abstract, title, publication type, heading word, accession number]
-
mental health.mp. [mp = abstract, title, publication type, heading word, accession number]
-
primary care.mp. [mp = abstract, title, publication type, heading word, accession number]
-
(case adj1 (study or studies)).mp. [mp = abstract, title, publication type, heading word, accession number]
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12
-
13 or 14 or 15 or 16 or 17
-
evaluation.mp. [mp = abstract, title, publication type, heading word, accession number]
-
18 or 21
-
19 and 20 and 22
Appendix 4 Readiness for collaboration survey
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/KPLT1423).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
List of abbreviations
- CMOC
- context–mechanism–outcome configuration
- CQC
- Care Quality Commission
- HMIC
- Healthcare Management Information Consortium
- ICS
- integrated care system
- IOC
- interorganisational collaboration
- IT
- information technology
- MRT
- middle-range theory
- NICE
- National Institute for Health and Care Excellence
- PCN
- primary care network
- PRISMA
- Preferred Reporting Items for Systematic reviews and Meta-Analyses
- RAMESES
- Realist And Meta-narrative Evidence Syntheses: Evolving Standards
- STP
- Sustainability and Transformation Partnership