Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number NIHR128068. The contractual start date was in September 2019. The final report began editorial review in December 2021 and was accepted for publication in October 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the final manuscript document. However, they do not accept liability for damages or losses arising from material published in this manuscript.
Permissions
Copyright statement
Copyright © 2024 Webb et al. This work was produced by Webb et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Webb et al.
Chapter 1 Background
Background research
Perinatal mental health (PMH) difficulties can occur during pregnancy or after birth. They affect up to one in five women and the cost to the UK is estimated to be £8.1 billion for every annual cohort of women, with 72% of this cost attributable to the long-term impact on the child. 1 PMH difficulties commonly consist of anxiety disorders, depression, post-traumatic stress disorder (PTSD) and stress-related conditions such as adjustment disorder. Many disorders are comorbid2,3 and severe postnatal mental illness is one of the leading causes of maternal death. 2
Perinatal mental health difficulties are particularly important because of the potential negative impact on women, their partners, children and families. This impact varies according to the type of mental illness, severity and timing (e.g. whether pre- or postnatal; acute or chronic; pre-existing or new onset) but, overall, the evidence shows a severe and enduring impact. For example, perinatal mental illness (PMI) is associated with a range of adverse outcomes for women, such as an increased risk of stillbirth4–6 as well as an increased risk of maternal suicide. 2,7–9 PMH difficulties are also associated with a decline in relationship satisfaction and an increased risk of relationship breakdown. 10–12 In terms of infant and childhood outcomes, PMH difficulties are associated with an increased risk of pre-term birth,13,14 and longer-term impacts on children’s cognitive15–18 and behavioural development,17,19,20 as well as being associated with an increased risk of children developing mental health difficulties themselves. 21–23
It is therefore important to identify and assess PMH difficulties quickly so that women who need treatment are able to access it. However, a survey of 200 women living in the UK found that 23% had not sought professional help for their symptoms. 24 It is also estimated that only 30–50% of women with PMH difficulties are identified and less than 10% are referred to specialist care. 25,26 This is likely due to a range of factors at individual, health professional (HP), interpersonal, organisational political and societal levels. For example, HPs not asking about mental health, lack of effective assessment, barriers to women seeking help or attending treatment, clinician barriers to diagnosis and treatment, lack of services to refer on to or limited understanding of effective treatments.
Recognising the barriers and facilitators to identification, assessment, referral and treatment for PMH difficulties is therefore important for health and social care services working with perinatal women. The need for this is evident in calls for research,27 UK strategy and policy,28,29 and clinical guidelines. 30,31 For example, in 2014, the National Health Service (NHS) set out plans for £365 million to be spent on PMH services from 2016–2128 as part of the Five Year Forward View. These services were to ensure 30,000 more women each year would access evidence-based specialist mental health care during the perinatal period. Similarly, the Scottish Mental Health Strategy aimed to improve the recognition and treatment of PMH difficulties. 31 The full implementation of these plans would mean women being asked about their mental health and well-being during antenatal booking visits, being screened for mental health difficulties, assessment within two weeks of referral and being provided with evidence-based psychological interventions within one month of initial assessment. 30–32 Furthermore, in 2019 NHS England set out a Long Term Plan for PMH, pledging an additional £2.3 billion a year and stating that by 2023/24, 66,000 women with moderate to severe mental health difficulties should have access to specialist care from pre-conception to 24 months postnatal. 33 Identifying barriers to women accessing treatment, as well as barriers to implementing PMH assessment and treatment in NHS services, is therefore important to inform these initiatives.
This evidence synthesis therefore aims to identify potential barriers and facilitators to identification, assessment, referral and treatment of PMH difficulties across the care pathway, both in terms of women accessing care or treatment, as well as in terms of NHS services implementing new assessment and treatment initiatives. This will be used to inform a conceptual framework of barriers and facilitators to PMH care that will inform health care services and practice, care pathways, and highlight where further research is needed.
Evidence explaining why this research is needed now
Perinatal mental health is a priority for UK strategy and policy,28,29 clinical guidelines,30,31 HP organisations26,34,35 and third-sector organisations. 36,37 While there have been large improvements in PMH service provision since the publication of the Five Year Forward View,28 in a progress review carried out in 2017 by the All-Party Parliamentary Group on Mental Health, The Royal College of Psychiatrists stated that teenage pregnancies, care beyond the baby’s first year and comorbid substance abuse remained areas lacking in focus and investment. The King’s Fund also reported that in some local areas, recommendations for expanding PMH services were being achieved by retraining existing staff without employing more, an approach that is not sustainable in the long term. 38 Furthermore, in 2020 the Maternal Mental Health Alliance identified that 20% of clinical commissioning groups (CCGs) in England still did not have specialist PMH services. These gaps in specialist PMH service provision are even higher in Wales (71.4%) and Scotland (85.7%). 39 These treatment gaps may mean women are not accessing the care that they need. 26 Given the recent provision of £2.3 billion a year to PMH services,33 this is a crucial time to understand what barriers exist and how they can be overcome.
Reasons why women are not identified and treated for PMH difficulties are complex and multifaceted and likely due to two broad factors: (1) lack of availability of services, which in the current context is possibly due to difficulties implementing services; and (2) difficulties accessing services from women’s perspectives. These difficulties are likely to occur at multiple levels (e.g. individual level factors, HP factors, organisational and wider political-social factors40) and across the care pathway. 41 The care pathway has been defined by Goldberg and Huxley (1992)41 who provided a framework for understanding how a person reaches mental health services. Their Pathways to Care Model shows how, as a person moves through the care pathway, certain factors act as filters that prevent people from accessing mental health care. The first filter is ‘illness behaviour’, where a person needs to pay attention to their symptoms and then make the decision to seek help. If this is not done, this is the first ‘filter’ out of the care pathway. The second filter is the HP’s ability to recognise mental illness, the third is referral on to mental health services and the last filter is admission to hospital beds.
Difficulties in implementing services and accessing services from women’s perspectives are also likely to be impacted by an environment where health care services are highly heterogenous, with variation both within and between services. In some cases, care pathways and treatments are based on organisational factors or assumptions that are not evidence-based. For example, prior to 2016 some CCGs had never commissioned a PMH service and women in these areas were referred to mainstream adult psychiatry services. 42
Guidelines for implementing PMH services have been developed by both NHS England in 201643 and the National Collaborating Centre for Mental Health in 2018. 44 These state the need for multi-agency working across all levels of care and services, expansion of workforce capacity, working with providers and those with a lived experience, and evidence-based service plans. Despite this guidance, large treatment gaps are still reported. 45 The lack of consistent implementation and the development of future implementation plans suggests it is both timely and important to understand what factors may affect implementation of PMH care and at present there are no reviews on barriers and facilitators to implementing PMH care in the NHS or other health care services.
Several systematic reviews of qualitative literature have identified potential barriers to women seeking help for PMH difficulties. Barriers include a reluctance to acknowledge symptoms and lack of support from partners and family members; a lack of ability for women to talk about their feelings openly due to perceived social pressures and stigma; fear of losing custody of their child; and a lack of knowledge of PMH difficulties among mothers. 46–48 Women also cite practical factors influencing their decision to seek help, such as the cost of treatment, finding childcare, lack of health insurance and transport issues. 49
Other factors that may influence whether women access care or treatment include HP factors. For example, in a survey of general practitioners (GPs) and midwives, just under a third reported having had no training in PMH. 34,50 This lack of training may be particularly critical given the importance of interpersonal factors in whether women seek help and access treatment. For example, qualitative studies of women’s experiences of PMH care suggest having a trusting relationship with a HP and being helped to discuss feelings in an unrushed, conversational manner are associated with increased acceptability and disclosure. 51–53
In terms of organisational factors, research suggests that lack of referral pathways, lack of specialised services and inadequate assessment influence whether women receive treatment or not. 46,49
Social and cultural factors are also important. Different cultural norms and health care systems will influence women and HPs understanding of PMH as well as the availability of assessment and treatment. Attitudes towards mental health, such as stigma, may affect women’s willingness to disclose their symptoms and seek help. 46–48
Over 20 published systematic reviews have explored women’s barriers and facilitators to accessing PMH care. However, each systematic review varies slightly in relation to its aim, inclusion criteria and analysis and no evidence synthesis has been carried out to combine the results into a single body of evidence. This would make it easier for health care providers and policy makers to access the information and use it to inform their decisions. 54,55
Conceptual framework
The above evidence highlights that many factors may influence whether or not women are identified, assessed, referred, and receive treatment for PMH difficulties. These are likely to operate at different levels, and across the care pathway. They may be due to barriers in implementing services, or barriers from women’s perspectives in accessing services.
Critically, there are no reviews on barriers and facilitators to implementing PMH care in NHS or other health care services. In addition, no evidence synthesis has been carried out to combine the evidence of multiple reviews about barriers from women’s perspectives in accessing services into a single body of evidence. Lastly, no reviews have combined information from both implementation literature and barriers and facilitators to accessing PMH care from women’s perspectives. Synthesising this literature coherently would make it easier for health care providers and policy makers to access the information and use it to inform their decisions about PMH services and care. One way to do this is through the use of a conceptual framework. A conceptual framework can be defined as a ‘network, or a plane, of interlinked concepts that together provide a comprehensive understanding of a phenomenon or a phenomena’. 56 The development of a conceptual framework can highlight areas for improvement and provide an empirical basis for recommendations for future practice and research.
Definitions and scope
The literature on PMH, identification, assessment and treatment is complex so it is important to define the key terms and scope of this synthesis.
Perinatal mental health difficulties include common affective disorders experienced during pregnancy or the first year after birth, such as depression and anxiety (e.g. generalised anxiety disorder, phobias, panic, obsessive compulsive disorder), stress-related disorders (e.g. acute stress disorder, PTSD), adjustment disorders, and other psychiatric disorders (e.g. psychosis, personality disorders). Symptoms can be mild, moderate or severe. All PMH difficulties were included. We excluded substance misuse disorders because they raise unique challenges in terms of assessment and treatment that may not be generalisable to other disorders.
We define PMH care as identification, assessment, referral and treatment for PMH difficulties.
How assessment of PMH is conceptualised is important. In particular, the distinction between assessment and case identification is important because they have different implications in terms of barriers and facilitators to accessing treatment. PMH assessment refers to identifying women who may be at risk for PMH difficulties, or who have PMH difficulties. Case identification uses psychiatric definitions of disorders, such as the American Psychiatric Association’s Diagnostic and Statistical Manual57 to identify women who fulfil diagnostic criteria for a disorder. Women who meet criteria (i.e. cases) are more likely to reach the threshold for onward referral and treatment. In this project we include both assessment and case identification to examine their implications in terms of barriers and facilitators to accessing care or treatment.
Perinatal mental health treatment refers to any treatment or prevention strategy to reduce PMH symptoms. Services offering treatment vary widely. In primary care or maternity care GPs, midwives and health visitors may offer supportive care for women with mild or moderate PMH difficulties. Evidence suggests primary care is the main provider, with 90% of common mental disorders being managed in primary care. 41 Specialist mental health services vary. For example, the NHS England specialist PMH services target the top 5% of women, that is, those with the most severe difficulties. These are likely to be women with severe postpartum depression, psychosis or other complex disorders, many of whom may require inpatient psychiatric treatment. In contrast, NHS Talking Therapies (formerly known as Improving Access to Psychological Therapies, IAPT) is a community-based outpatient service that predominantly treats moderate affective disorders such as anxiety, depression, PTSD and adjustment disorders. Increasing numbers of NHS Talking Therapies services now have a PMH specialist. In addition, there are increasing community services provided by third-sector organisations, such as peer support services for women with moderate PMH difficulties. These different settings (primary care, maternity care, psychiatric and specialist PMH services) will have different barriers in terms of implementing services and women accessing treatment. In this project we aimed to consider different health and social care settings throughout.
Some services provide interventions focused on outcomes associated with poor PMH. These include parent-infant, couple or family interventions. In this project we focus on interventions for maternal mental health and exclude literature that focuses on mother-infant, couple or family interventions because these are aimed at associated outcomes rather than PMH per se and raise different issues in terms of accessing services.
The scope of this project is also on PMH of women and those who identify as women, rather than partners or those who identify as men. Partner’s and men’s PMH is important but is an area that requires research and evidence synthesis in its own right. Current research into partner’s and men’s PMH is sparse compared to research on women, and there are likely to be differences in barriers and facilitators to PMH care for men compared to women.
Chapter 2 Research questions and overview
Based on the literature summarised above, our research question was: what are the barriers and facilitators to PMH assessment, care and treatment at individual, interpersonal, organisational, political and societal levels? How can these be used to inform and improve PMH care in different health and social care settings?
Primary research objective
Our primary research objective was to develop a conceptual framework of barriers and facilitators to PMH care (defined as identification, assessment, care and treatment) to inform PMH services, and highlight where further research is needed.
Secondary objectives
Our secondary research objectives were to:
-
determine the barriers and facilitators to implementing PMH assessment, care and treatment in health and social care services;
-
identify differences in barriers and facilitators across different health and social care settings;
-
evaluate the quality of this evidence;
-
extract recommendations for implementation, practice and research based on the barriers and facilitators identified;
-
determine the barriers and facilitators to women accessing PMH care or treatment;
-
evaluate the quality of these reviews;
-
map the geographical distribution of the evidence to establish generalisability and gaps in the evidence;
-
map the findings on to a conceptual framework;
-
conduct a consultation of the conceptual framework and recommendations with a panel of expert stakeholders (e.g. women, GPs, commissioners, third-sector organisations, etc.);
-
make recommendations for practice and future research for PMH assessment, care and treatment.
Research overview
This research used a focused systematic review [Review 1 (R1)], a meta-review of reviews [Review 2 (R2)], conceptual framework and expert stakeholder panel to answer the research questions. It was carried out in three phases: Phase 1 was a focused systematic review of research into implementing PMH care into health and social care services (R1). Phase 2 was a meta-review of reviews into the range of barriers and facilitators to women accessing PMH care (R2). Phase 3 mapped the findings from phases 1 and 2 on to a conceptual framework and refined it through consultations with three expert panels of stakeholders (see Figure 1).
FIGURE 1.
MATRIx study overview.
Patient public involvement
This project was developed with patient public involvement (PPI) representatives from the National Childbirth Trust (NCT) in England (Jennifer Holly and Sarah McMullen) and the Maternal Mental Health Change Agents (MMHCA), a group of women with lived experience of PMH difficulties in Scotland (collaborators). These organisations ensured that we had PPI input from perinatal women generally as well as those affected by PMH problems. Representatives from the NCT and MMHCA co-ordinated PPI input throughout the research and were involved in the dissemination of the project.
Chapter 3 Review methods
This chapter outlines the methods for the two systematic reviews: R1 barriers to implementing assessment, care and treatment for PMH difficulties into health and social care settings, at individual, HP, organisational and wider levels; and R2 barriers and facilitators to women deciding to seek help, accessing help and engaging in PMH care using a systematic review of reviews.
Protocol and registration
Both reviews were registered on PROSPERO: R1 PROSPERO (CRD42019142854); R2 PROSPERO (CRD42020193107).
Ethical review
Ethical permission is not required for systematic reviews of available literature.
Search strategy
Literature searches and study selection are reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. 58
Search terms were identified through hand searches of PMH literature, scoping searches and in consultation with a specialised librarian at the University of Oxford Bodleian Health Care Libraries, Nia Roberts.
To identify papers for R1 we used a mixture of the PICO (Population, Intervention, Comparison, Outcome)59 and SPIDER (Sample, Phenomenon of Interest, Design, Evaluation, Research type)60 research question format to identify four clusters of search terms (see Table 1) relating to:
-
Population: NHS and other health or social care services for women in the perinatal period treating women with mental health difficulties.
-
Phenomenon of interest: implementing assessment, supportive care or treatment interventions, programmes or protocols for PMH into health or social care services.
-
Outcome: qualitative implementation outcomes (e.g. acceptability, feasibility).
-
Evaluation: barriers/facilitators.
| Search terms for R1 (barriers and facilitators to implementation) | ||||
|---|---|---|---|---|
| Population | Screening/intervention | Implementation | Barriers/facilitators | |
| Perinatal period | Mental health difficulties | |||
| Search terms for R2 (barriers and facilitators from women’s perspective) | ||||
| Population | Screening/intervention | Barriers/facilitators | Study design | |
| Perinatal period | Mental health difficulties | |||
| Prenatal care/; perinatal care/; postnatal care/; pregnancy/; pregnant women/ pregnancy; pregnant; pre-nat*; prenat*; prepart*; prepart*; ante-nat*; antenat*; ante-part*; antepart*; peri-nat*; perinat*; peri-part*; peripart*; puerper*; post-nat*; postnat*; post-part*; postpart*; parent?; mother*; maternal; father*; paternal; infan*; newb;n?; neonat*; baby; babies |
mental disorders/; exp anxiety disorders/; exp mood disorders/; exp ‘trauma and stressor related disorders’/; Adaptation/; Psychological/ mental*; psych*; anxiety; anxious; depress*; mood?; affect*; distress*; stress; trauma*; posttrauma*; post-trauma*; adjustment disorder*; phobia*; phobic; obsessive compulsive; wellbeing; well-being |
Mass screening/; diagnosis/; early diagnosis/; psychotherapy/; behavior therapy/; exp cognitive behavioral therapy/; counseling/exp directive counseling/; antidepressive agents/exp anti-anxiety agents/ screen*; detect*; diagnos*; assess*; identifi*; prevent*; prophyla*; intervention?; counsel*; therap*; healing; listen*; supp;t*; care; healthcare; service; medication*; drug?; antidepress*; anti-depress*; antianxiety; anti-anxiety; improving access to psychological therap*; iapt |
Implementation Science/; Health Plan Implementation/; Program Evaluation/; Implement*; impact*; feasibl*; acceptab*; process; project*; system*; evaluat* |
barrier?; challenge?; obstacle?; facilitat*; enabl*; opportunit* |
| Prenatal care/; perinatal care/; postnatal care/; pregnancy/; pregnant women/ prenancy; pregnant; pre-nat*; prenat*; prepart*; prepart*; ante-nat*; antenat*; ante-part*; antepart*; peri-nat*; perinat*; peri-part*; peripart*; puerper*; post-nat*; postnat*; post-part*; postpart*; parent?; mother*; maternal; father*; paternal; infan*; newb;n?; neonat*; baby; babies |
mental disorders/; exp anxiety disorders/; exp mood disorders/; exp ‘trauma and stressor related disorders’/; Adaptation/; Psychological/ mental*; psych*; anxiety; anxious; depress*; mood?; affect*; distress*; stress; trauma*; posttrauma*; post-trauma*; adjustment disorder*; phobia*; phobic; obsessive compulsive; wellbeing; well-being |
Mass screening/; diagnosis/; early diagnosis/; psychotherapy/; behavior therapy/; exp cognitive behavioral therapy/; counseling/exp directive counseling/; antidepressive agents/exp anti-anxiety agents/ screen*; detect*; diagnos*; assess*; identifi*; prevent*; prophyla*; intervention?; counsel*; therap*; healing; listen*; supp;t*; care; healthcare; service; medication*; drug?; antidepress*; anti-depress*; antianxiety; anti-anxiety; improving access to psychological therap*; iapt |
barrier?; challenge?; obstacle?; hurdle?; obstruct*; drawback?; issue?; difficult?; promot*; supp;t; encourag*; fact;?; facilitat*; enabl*; opp;tunit*; engage*; assist* | Systematic review; meta-analysis; evidence synthesis; realist synthesis; realist review; qualitative synthesis; meta-synthesis*; meta synthesis*; metasynthesis; meta-ethnograph*; metaethnograph*; meta ethnograph*; meta-study; metastudy; meta study |
Pre-planned searches were carried out by a specialist librarian, Nia Roberts, on MEDLINE (1946–present), EMBASE (1974–present), PsychInfo (1806–present) and CINAHL (1982–present). Full search syntax and databases searched can be found in the supporting information of the published review61 and Supplementary material S1.
To identify papers for R2 we used the SPIDER research question60 to identify four clusters of search terms relating to:
-
Sample: women in the perinatal period (conception to one year postpartum).
-
Phenomenon of interest: assessment, care or treatment for PMH.
-
Design: systematic review papers.
-
Evaluation: women’s barriers and facilitators.
Pre-planned searches were carried out by a specialist librarian, Nia Roberts, on MEDLINE (1946–present); EMBASE (1974–present); PsychInfo (1806–present); CINAHL (1982–present), Scopus; and Cochrane Database of Systematic Reviews (Issue 8 of 12, August 2021). Full search syntax and databases searched can be found in Supplementary material S2.
Search process
Medical subject heading (MeSH) terms and search terms described above were used to query the databases for literature published from inception to 11 December 2019 for R1 and to 4 August 2021 for R2. Forward and backward searches of included studies were carried out by Rebecca Webb and were completed by 31 March 2020 for R1 and 8 September 2021 for R2.
Eligibility criteria
For R1, the following parameters were used for inclusion in the review:
-
Population: NHS and other international health or social care services for women in the perinatal period.
-
Intervention: implementing assessment, care, referral pathways or treatment interventions, programmes or protocols for PMH into health or social care services.
-
Outcome: implementation outcomes (i.e. barriers, facilitators).
Studies were included if they made statements about factors that either facilitated or impeded implementation of PMH assessment, care, referral or treatment. These statements could be from qualitative interviews with HPs or women; or from studies describing the implementation of PMH care.
For R2, studies with the following characteristics were eligible for inclusion in the review:
-
Population: women in the perinatal period (conception to 12 months after birth) experiencing mental health difficulties, who may or may not have decided to seek help, accessed help or engaged in PMH care (defined as assessment, referrals and/or treatment/intervention programmes) from health or social care services.
-
Outcome: barriers and facilitators (defined as any individual, HP, interpersonal, organisational, political or societal factors that women believed impeded (barriers) or aided (facilitators) them to seeking, accessing or engaging in help for PMH difficulties).
-
Design: systematic reviews that used a PRISMA search strategy.
Studies were included if they made descriptive statements about barriers and facilitators to women deciding to seek help, accessing help and engaging in PMH care. These descriptions had to be drawn from perinatal women’s experiences. Only systematic reviews were included. Reviews that did not use a clearly reported PRISMA58 search strategy were excluded. Reviews were also excluded if they were not conducted on the target population (e.g. focused on men/partners, HPs); focused on substance misuse (which has unique challenges in terms of assessment and treatment); did not focus on the mental health of perinatal women; did not examine any barriers/facilitators regarding seeking help, accessing help and engaging in PMH care; and were non-English publications.
Study selection
For both reviews, search results were initially imported into Endnote and duplicates were removed by a specialist librarian, Nia Roberts.
For R1 animal studies, case reports and book reviews were also removed. Remaining studies were imported into Eppi-Reviewer 4, where results were screened by title and abstract by Nazihah Uddin, the research assistant on the project. A proportion (10%) of the results were double screened by Rebecca Webb, the research fellow on the project. Decisions to include or exclude were concordant between reviewers in 88.11% of cases. Following abstract and title screening, full text screening was carried out by Rebecca Webb. A proportion of full texts (10%) were double screened by Nazihah Uddin and decisions to include or exclude were concordant between reviewers in 90.90% of cases. Disagreements for both title and abstract and full text screening were discussed and resolved by both researchers.
For R2, once duplicates were removed, the specialist librarian also removed papers relating to fetal distress, oxidative distress and those not published in English. Remaining studies were imported into Eppi-Reviewer 4, where results were double screened by title and abstract by Rebecca Webb and Georgina Constantinou, a research assistant in maternal and child health research. An additional proportion (n = 166, approximately 7%) of titles and abstracts were triple screened by Nazihah Uddin. Decisions to include or exclude were concordant between Rebecca Webb and Georgina Constantinou in 94.2% of cases and between Rebecca Webb and Nazihah Uddin in 99.4% of cases. Disagreements were discussed and resolved by all reviewers by applying the relevant inclusion criteria. Once title and abstract screening was complete, full text screening was carried out by Rebecca Webb and Georgina Constantinou. An additional proportion (n = 9, approximately 10%) were triple screened by Nazihah Uddin. Decisions to include or exclude were concordant between Rebecca Webb and Georgina Constantinou in 91.4% of cases and between Rebecca Webb and Nazihah Uddin in 100% of cases.
Data extraction
For R1, data extraction was carried out by Rebecca Webb using Eppi-Reviewer 4 which allows for line-by-line coding. A new ‘codeset’ labelled ‘data extraction’ was created and contained every item to be extracted from the data (e.g. year of publication, country of study). Each paper was read in full, and relevant parts of the text highlighted (e.g. the country of the study) and applied to the relevant code.
For R2, data extraction was carried out using Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) by Rebecca Webb. Each paper was read in full, and relevant parts of the text inputted into the relevant part of the spreadsheet. Methodology of included reviews was copied on to one sheet, and results on to another to aid analysis. Double coding of extracted data was carried out for a proportion of included reviews (n = 3, 10%) by Georgina Constantinou. Data extraction matched in 85% of cases.
The data that were extracted was guided by the Cochrane Systematic Review for Intervention Data Collection form62 for both reviews, and the AMSTAR 263 critical appraisal tool for R2 (see Table 2 for extracted data).
| R1 | |||
|---|---|---|---|
| Study characteristics | Sample | Assessment/care/treatment characteristics | Implementation outcomes |
| R2 | |||
| Review characteristics | Characteristics of included studies | Characteristics of included participants | Outcomes |
| Year | Size | Type (intervention, assessment, support) | Barriers |
| Country | Age | Name | Facilitators |
| Setting | Ethnicity | Year started | |
| Design | Employment | Year ended | |
| Aim | Education | Description | |
| Children | Who care is aimed at | ||
| Socio-economic status | Theoretical model of care | ||
| Mental health difficulties | Medium of care (e.g. face to face) | ||
| Measurement of mental health difficulties | Person providing care | ||
| Obstetric details | Training of people providing care | ||
| Gender/sex | |||
| Other demographic details | |||
| Recruitment | |||
| Year | Number of studies included | Mental health difficulty examined | Barriers |
| Aim | Year of each study’s publication | Number of participants | Facilitators |
| Design | Country of each of the studies | Age of participants | |
| Search strategy | Perinatal period | ||
| Inclusion/exclusion criteria | Ethnicity of participants | ||
| Screening/study selection | Socio-economic status of participants | ||
| Data extraction | Other demographic details of participants | ||
| Quality assessment | |||
| Data analysis | |||
Assessing the robustness of results
For R1, the methodology sections of included studies were assessed for quality with the Joanna Briggs Critical Appraisal Tools for qualitative research,64 cross-sectional studies65 and text and opinion. 66 Each point on the checklists can be coded as either yes, no, unclear or not applicable. Each tool was separated into domains that reflected the question of interest (see Box 1). Where most questions within a domain were answered with yes, this domain was rated as having high quality; where the majority were answered with no, this domain was rated as having low quality. Medium quality was when there was a mixture of yes and no answers.
-
Is there congruity between the stated philosophical perspective and the research methodology?
-
Is there congruity between the research methodology and the research question or objectives?
-
Is there congruity between the research methodology and the methods used to collect data?
-
Is there congruity between the research methodology and the representation and analysis of data?
-
Is there congruity between the research methodology and the interpretation of results?
-
Is there a statement locating the researcher culturally or theoretically?
-
Is the influence of the researcher on the research, and vice versa, addressed?
-
Are participants, and their voices, adequately represented?
-
Is the research ethical according to current criteria or, for recent studies, is there evidence of ethical approval by an appropriate body?
-
Do the conclusions drawn in the research report flow from the analysis, or interpretation, of the data?
-
Is the source of the opinion clearly identified?
-
Does the source of opinion have standing in the field of expertise?
-
Are the interests of the relevant population the central focus of the opinion?
-
Is the stated position the result of an analytical process, and is there logic in the opinion expressed?
-
Is there reference to the extant literature?
-
Is any incongruence with the literature/sources logically defended?
-
Were the criteria for inclusion in the sample clearly defined?
-
Were the study subjects and the setting described in detail?
-
Was the exposure measured in a valid and reliable way?
-
Were objective, standard criteria used for measurement of the condition?
-
Were confounding factors identified?
-
Were strategies to deal with confounding factors stated?
-
Were the outcomes measured in a valid and reliable way?
-
Was appropriate statistical analysis used?
Adapted with permission from the Joanna Briggs Institute (JBI), the JBI Critical Appraisal tools for use in JBI Systematic Reviews 2017. 64–66 Permission granted 28 November 2021.
Rebecca Webb completed the methodological quality assessments for the included papers, and dual critical appraisal of 16 (35%) papers was done by Nazihah Uddin. Nazihah Uddin initially screened nine papers, which were discussed, and conflicts were resolved. Following this screening, the final seven papers were screened by Nazihah Uddin. Coders assigned the same score to 13 (81%) of the 16 papers. All disagreements were discussed and resolved by both researchers, and the final appraisal for these 16 papers is based on agreed answers.
For R2, methodology sections of included reviews were appraised using the AMSTAR 263 criteria (see Box 2). Critical domains in the appraisal of systematic reviews according to AMSTAR 2 include protocol registration, adequacy of literature search, justification of study exclusion, risk of bias, appropriateness of meta-analytic methods, consideration of risk of bias when interpreting results and assessment of publication bias. If more than one critical domain is not met (critical flaw), a systematic review should be evaluated as having critically low confidence in the results of the review. One critical flaw means reviews should be evaluated as low confidence. More than one non-critical flaw means reviews should be evaluated as moderate confidence and no or one non-critical flaw means reviews should be evaluated as high confidence. 63
-
Did the research questions and inclusion criteria for the review include the components of PICO?
-
Did the report of the review contain an explicit statement that the review methods were established prior to the conduct of the review and did the report justify any significant deviations from the protocol?a
-
Did the review authors explain their selection of the study designs for inclusion in the review?
-
Did the review authors use a comprehensive literature search strategy?a
-
Did the review authors perform study selection in duplicate?
-
Did the review authors perform data extraction in duplicate?
-
Did the review authors provide a list of excluded studies and justify the exclusions?a
-
Did the review authors describe the included studies in adequate detail?
-
Did the review authors use a satisfactory technique for assessing the risk of bias (RoB) in individual studies that were included in the review?
-
Did the review authors report on the sources of funding for the studies included in the review?
-
If meta-analysis was performed, did the review authors use appropriate methods for statistical combination of results? (Not applicable.)
-
If meta-analysis was performed, did the review authors assess the potential impact of RoB in individual studies on the results of the meta-analysis or other evidence synthesis? (Not applicable.)
-
Did the review authors account for RoB in primary studies when interpreting/discussing the results of the review?
-
Did the review authors provide a satisfactory explanation for, and discussion of, any heterogeneity observed in the results of the review?
-
If they performed quantitative synthesis did the review authors carry out an adequate investigation of publication bias (small study bias) and discuss its likely impact on the results of the review? (Not applicable.)
-
Did the review authors report any potential sources of conflict of interest, including any funding they received for conducting the review?*
a Critical domain for this review.
Shea BJ, Reeves BC, Wells GA, Thuku M, Hamel C, Moran J, et al. 63 AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017;21:358.
Given that all studies in this review were qualitative, the AMSTAR 263 items related to meta-analysis were not relevant and were removed. Further, given the debate in the literature regarding the appropriateness of conducting risk of bias assessments on qualitative research, we downgraded the items relating to risk of bias from being a critical flaw, to just a flaw. Quality appraisal of all studies was carried out by Nazihah Uddin and Rebecca Webb. Ratings were concordant in 90% of cases.
A large proportion of the reviews were rated as having low and critically low confidence in the evidence (see Chapter 4). A decision was made to include reviews where confidence in results was evaluated as low and critically low because some of these reviews focused more on marginalised women, such as refugees, migrant women, women with a low income and women living in lower middle income countries (LMIC). Including these reviews ensured that the experiences of these seldom heard women were captured. To improve validity of results, a qualitative sensitivity analysis was carried out to assess whether themes remained consistent across all reviews, regardless of their quality rating. The methods proposed by Harden (2007)67 and Carroll et al. (2012)68 were followed, so sensitivity analysis was carried out in two ways: (1) synthesis contribution; and (2) evidence of adequate description of themes.
To examine whether higher quality reviews contributed more to the themes, a measure of ‘synthesis contribution’ was calculated for each review (as outlined by Harden, 200767). This involved dividing the number of barriers and facilitators identified by the specific review in question (see ‘Number of themes’ column in Table 3) by the total number of barriers and facilitators identified in R2 (n = 62 themes). For example, the findings from Bina (2020)69 contributed to 31 out of 62 themes, giving this review a synthesis contribution score of 50% (see Table 3).
| Study | Number of themes | Overall synthesis contribution % (all themes) |
|---|---|---|
| Bina, 202069 | 31 | 50.00 |
| Brealey et al., 201074 | 13 | 20.97 |
| Button et al., 201746 | 26 | 41.94 |
| Dennis and Chung-Lee, 200647 | 28 | 45.16 |
| Evans et al., 202075 | 8 | 12.90 |
| Giscombe et al., 202076 | 6 | 9.68 |
| Hadfield and Wittkowski, 201772 | 25 | 40.32 |
| Hansotte et al., 201770 | 19 | 30.65 |
| Hewitt et al., 200977 | 13 | 20.97 |
| Holopainen and Hakulinen, 201978 | 6 | 9.68 |
| Jones et al., 201479 | 10 | 16.13 |
| Jones, 201980 | 19 | 30.65 |
| Kassam, 201981 | 8 | 12.90 |
| Lucas et al., 201982 | 9 | 14.52 |
| Megnin-Viggars et al., 201548 | 26 | 41.93 |
| Mollard et al., 201683 | 5 | 8.06 |
| Morrell et al., 201684 | 16 | 25.81 |
| Newman et al., 201985 | 13 | 20.97 |
| Nilaweera et al., 201486 | 6 | 9.68 |
| Praetorius et al., 202087 | 3 | 4.84 |
| Randall and Briscoe, 201888 | 2 | 3.23 |
| Sambrook Smith et al., 201989 | 19 | 30.65 |
| Schmied et al., 201790 | 27 | 43.55 |
| Scope et al., 201791 | 13 | 20.97 |
| Slade et al., 202092 | 15 | 24.19 |
| Sorsa et al., 202193 | 19 | 30.65 |
| Staneva et al., 201594 | 11 | 17.74 |
| Tobin et al., 201895 | 19 | 30.65 |
| Viveiros and Darling, 201849 | 16 | 25.81 |
| Watson et al., 201996 | 28 | 45.16 |
| Wittkowski et al., 201497 | 2 | 3.23 |
Each study’s synthesis contribution scores were plotted against the number of quality criteria the study met (see Figure 4). Statistical analysis (Pearson’s correlation) was used to help interpret the plots. To examine whether removing lower quality reviews influenced the number of themes, themes that were only supported by lower quality reviews were identified.
To examine whether removing lower quality reviews influenced the description of themes, data were assessed for ‘thickness’ or ‘thinness’ (as done by Carroll et al., 201268). A ‘thin’ description refers to a set of statements, such as this quote about HPs dismissing women’s symptoms:
[The study authors] found that women also felt that providers were downplaying the symptoms they were experiencing. 70 (p12)
A ‘thick’ description provides the context of experience and circumstances71 such as this description of HPs minimising symptoms:
Having symptoms dismissed or attributed to factors other than [postpartum depression] PPD by HPs led to women ‘remaining silent’. Some women perceived that their difficulties would only be taken seriously when there were concerns about risk of harm to themselves or the infant. One woman said, ‘I kept going to this doctor and he used to give me a pep talk and send me home …’. 72(p738)
It is argued that the extent to which a text provides a thick description shows evidence of the authenticity of the results. 73
Data analysis
Review 1 results were analysed by Rebecca Webb using thematic synthesis;98 line-by-line data extraction of statements referring to facilitators or barriers to implementing PMH assessment, care and treatment was carried out in Eppi-Reviewer. Next, codes were re-read and assigned a descriptive theme based on their meaning and content. Themes were developed and revised as each study was re-read. Once all codes had been assigned into themes, these themes were mapped on to a systems level model adapted from Ferlie and Shortell’s (2001) Levels of Change framework40 (e.g. individual level factors, HP factors, organisational factors and larger system factors) and then grouped to reflect different stages of the care pathway adapted from Goldberg and Huxley’s (1992) Pathways to Care model41 (e.g. deciding to disclose, assessment of PMH and access to care and treatment). Mapping of descriptive themes was developed deductively from the initial theoretical framework and then inductively revised as new themes emerged. The mapping of descriptive themes aided the development of the analytical themes. Here, inferred barriers and facilitators were generated. Following this, recommendations for implementing PMH care were drawn from a dictionary of implementation strategy terms and definitions. 99,100
Review 2 results were also analysed by Rebecca Webb using a thematic synthesis98 in NVivo (QSR International, Warrington, UK) and Microsoft Excel. First, line-by-line data coding of statements referring to facilitators or barriers to accessing PMH care from the results section of each paper was carried out. Next, codes were revisited and assigned a descriptive theme based on their meaning and content. Themes were developed and revised as each review was re-read. Once all codes had been assigned into themes, these themes were mapped on to a multi-level framework adapted from Ferlie and Shortell’s (2001) Levels of Change framework40 and the findings from R1. 61 Mapping of descriptive themes was developed deductively from the initial theoretical framework and then inductively revised as new themes emerged. The mapping of descriptive themes was discussed by the project research team before being finalised.
Chapter 4 Studies included in the reviews
Study selection
Both reviews were reported in accordance with PRISMA guidelines. 58 Enhancing Transparency in Reporting the Synthesis of Qualitative (ENTREQ) research guidelines101 were also followed.
Results of searches are shown in Figures 2 and 3. For R1, database searching identified a total of 21,535 citations. After screening by title and abstract, 10,130 records were excluded, leaving 931 papers to be screened by full text. Screening of full texts left 43 studies to be included in the review. Forward and backward searches identified a further three papers. Therefore, 46 qualitative studies were included in the qualitative synthesis (see Figure 2). Excluded texts are given in Supplementary material S3.
FIGURE 2.
PRISMA flow diagram for R1.

FIGURE 3.
PRISMA flow diagram for R2.
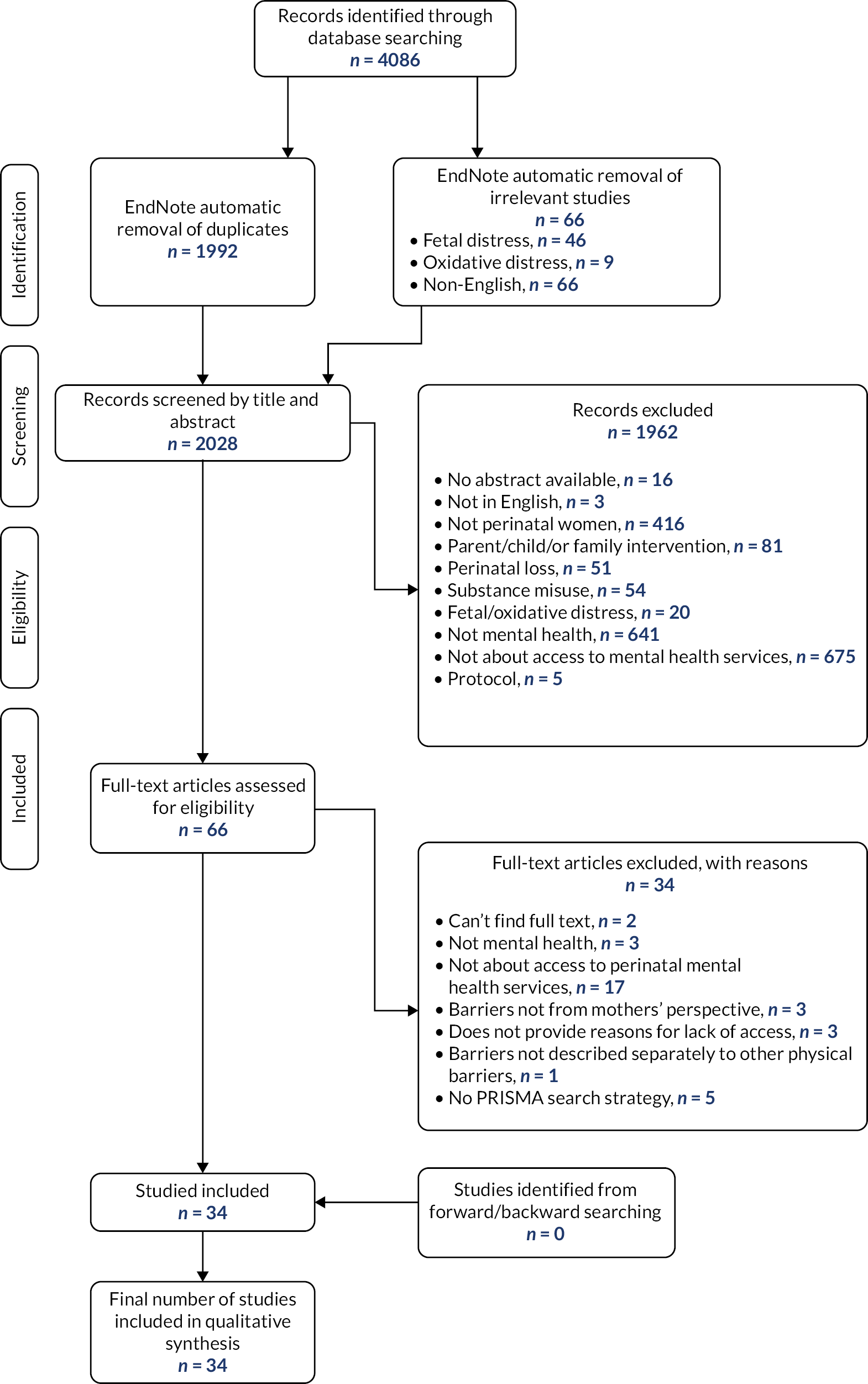
For R2, database searching identified a total of 4086 citations. After duplicates, and studies not meeting inclusion criteria were removed, 2028 articles were left to be screened. Screening by title and abstract led to 1962 records being excluded, leaving 66 papers to be screened by full text. Screening of full texts identified 32 reviews, all of which were qualitative, to be included in the meta-review (see Figure 3). Excluded texts are given in Supplementary material S4.
Characteristics of included studies
For R1, studies were mainly (n = 39) carried out in higher income countries (HICs)102 with well-established highly ranked health care systems. 103 The majority were carried out in the USA (n = 16). Implementation occurred in a wide range of settings including hospitals (n = 14); primary care (n = 12); community-based care, such as community clinics or home visiting (n = 12); online or remote (n = 3); maternity care (n = 3) and specialist PMH care (n = 2). No studies examined implementation in social care settings. Most of the studies (n = 22) looked at the implementation of care services (including screening, referral and treatment); 18 studies were about the implementation of interventions and 6 were about screening only. For the intervention studies most were implementing cognitive behavioural therapy (n = 7) or another type of talking therapy (n = 8). For the screening studies, most were implementing the Edinburgh Postnatal Depression Scale (EPDS)104 (n = 5).
Ten of the studies were descriptive papers, describing the implementation of PMH care. The remaining were qualitative papers, interviewing key stakeholders about their views and experiences on the implementation of the care. Twenty studies interviewed only HPs, nine interviewed only perinatal women and seven interviewed both. Sample sizes ranged from 6 to 809 with a mean of 46.81; median = 24; interquartile range (IQR) = 16.25–33.35 (see Appendix 1 for more details).
For R2, reviews were published between 2006 and 2021 (M = 2017, Mdn = 2018; IQR = 2016–2019). The number of studies included in each review varied from 4 to 40 (M = 16, Mdn = 13, IQR = 9–19) with a total of 344 papers included across all systematic reviews. The number of women included in each review varied from 95–85,190 (M = 5080; Mdn = 463; IQR = 226–1715). The reviews included studies carried out in 24 different countries, the majority of which were HICs, mostly the USA and UK. One review included studies that were carried out only in sub-Saharan Africa. 97 Most reviews (n = 23) focused on perinatal depression, followed by a mixture of perinatal mood disorders (e.g. depression, anxiety, distress; n = 5). Only one study focused on postnatal psychosis105 and one on birth trauma. 92 Included studies were carried out across the perinatal period. Twenty-four of the reviews included studies that reported recruiting ethnic minority women. Six reviews included studies on the experiences of migrant women and/or ethnic minority women (see Appendix 2 for more details).
Analysis of the robustness of the results (sensitivity analyses)
For R1, most studies (n = 44) had a quality rating above 70% suggesting that studies were well-conducted with a low risk of bias. Seven studies were assigned a 100% quality rating (see Appendix 3).
For R2, the majority of reviews were evaluated as having low (n = 14) or critically low (n = 5) confidence with their results. The remainder had moderate (n = 8) or high (n = 5) confidence (see Appendix 4).
As described above, a sensitivity analysis was carried out for R2. In terms of synthesis contribution, there was no correlation between synthesis contribution and the number of criteria each review met (r = 0.142, p = 0.437) (see Figure 4). Furthermore, only four themes (cultural/spiritual causes of mental illness, age, previous diagnoses and appropriateness of care) were only identified by lower quality studies showing that the majority of themes (58 out of 62; 93.55%) were supported by both higher quality and lower quality papers.
FIGURE 4.
Synthesis contribution vs. quality appraisal criteria met for papers in R2.

In terms of richness of data, removing lower quality papers meant that the identified theme Language barriers lost some of its richness. For example, it led to the removal of quotes expressing frustration from women whose first language was not English:
… you don’t know where to go, what to do, who to trust, especially when you are coming by yourself … you believe that you speak English, but when you get here you realize that you don’t … 90(p18)
Sometimes when you have a baby, a woman comes from the hospital. Bengali girls don’t come with the midwife, we don’t understand what they say, we just sit there staring at their faces. 46(p695)
The removal of lower quality papers from the sub-theme Fear of being seen as a bad mum also led to the loss of richness of data, such as the removal of quotes from women who had migrated from their country of birth:
Back home, if someone has this problem, everyone gossips, you get this feeling that people are not dealing with you normally or as if you are abnormal almost …90(p12)
Lastly, the removal of lower quality studies meant important information was removed from the Characteristics of service sub-theme, such as women feeling services prioritised physical needs (n = 2), lack information about screening guidelines (n = 2) and the logistics of care (e.g. location, time of appointments) (n = 3).
Overall, the qualitative sensitivity analysis found that the majority of themes were supported by both the higher quality and lower quality reviews. Including all reviews meant there was more richness in the data and greater inclusion of marginalised women, such as refugees, migrants and women living in sub-Saharan Africa. This sensitivity analysis suggests that the results from R2 can be interpreted with reasonable confidence.
Chapter 5 Results of the reviews
This chapter outlines the theoretically informed care pathway structure and multi-level framework used to summarise areas in which barriers to PMH care may arise. The most commonly cited barriers and facilitators are then described at each stage of the care pathway, and for each level of the multi-level framework. This section includes results from both reviews combined.
Frameworks for presenting the results
Care pathway
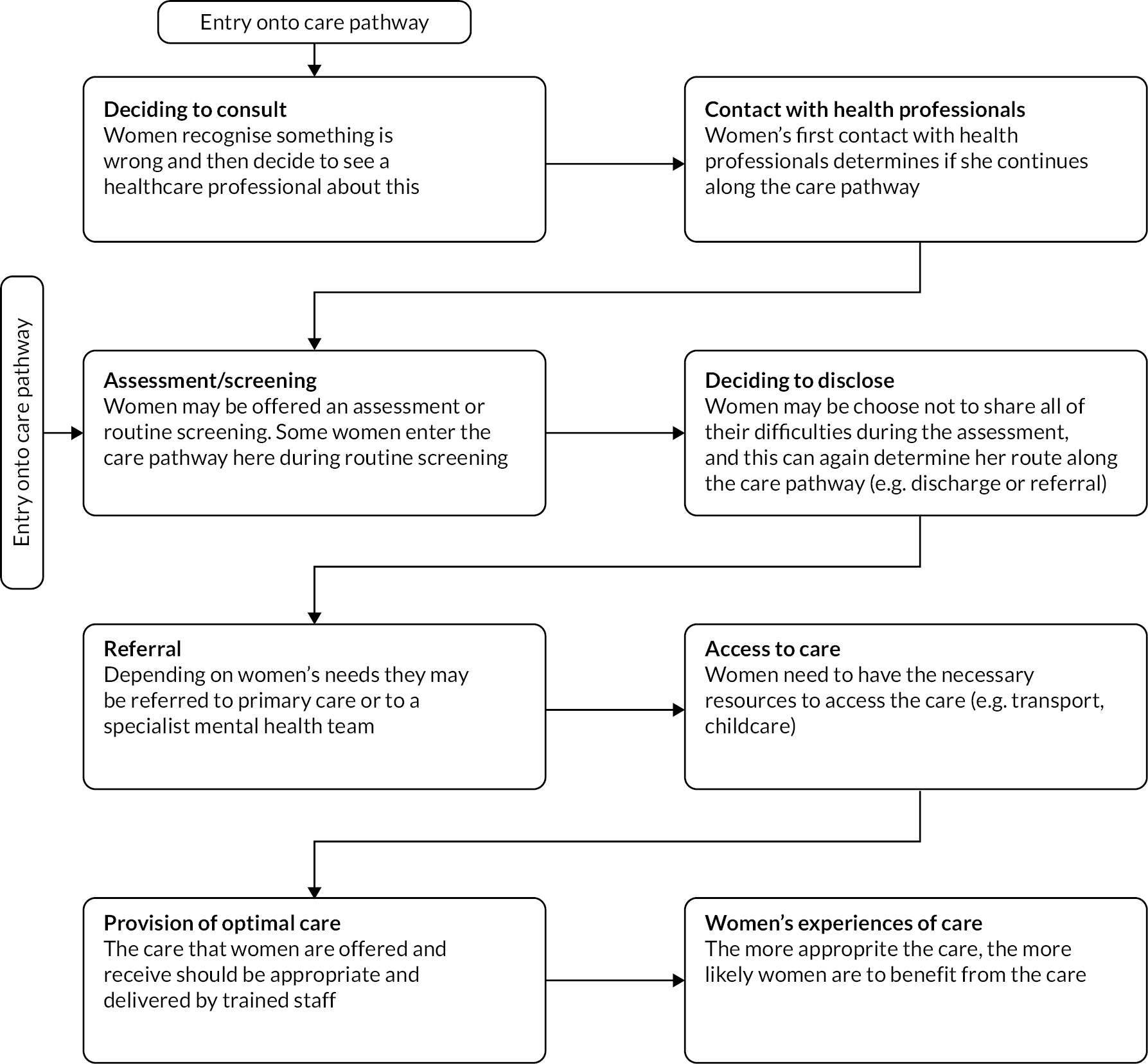
We used a care pathway based on Goldberg and Huxley’s (1992)41 Pathways to Care model to understand how a woman may access mental health services. In Goldberg and Huxley’s model, as a person moves through the care pathway, there are certain factors that act as filters, which prevent people from accessing mental health care. The first filter is illness behaviour, where a person needs to pay attention to their symptoms and then make the decision to seek help. If this is not done, this is the first filter out of the care pathway. The second is the HP’s ability to recognise mental illness; the third is referral on to mental health services and the last filter is admission to hospital beds.
Our care pathway is more detailed and includes the following eight stages: (1) deciding to consult for PMH difficulties; (2) first contact with HPs; (3) assessment/screening for PMH; (4) deciding to disclose PMH difficulties; (5) referral on to appropriate services; (6) access to treatment; (7) provision of optimal care and treatment; and (8) a woman’s experience of treatment (see Figure 5). It is possible that at each stage in the care pathway, a woman may fall through the gaps and ultimately not receive the care that she needs. The decision to disclose has been included after assessment because women have a choice about whether they complete an assessment honestly and thus disclose their symptoms. However, women may also decide whether to disclose their symptoms on first contact with a HP, especially if they are seeking help from their GP. Therefore, it is important to note that a woman may enter the care pathway either stages 1 or 3, and that some parts of the pathway are redundant in health care systems where the woman can contact mental health services directly (e.g. via NHS Talking Therapies services in the UK). Further, the process is not always linear, and some women might jump over certain stages or repeat certain stages.
FIGURE 5.
The MATRIx care pathway.
Multi-level framework
Ferlie and Shortell’s Levels of Change framework40 was adapted to describe the seven different levels at which barriers and facilitators to PMH care may occur: (1) individual level factors (e.g. beliefs about mental illness, inability to attend care); (2) HP level factors (e.g. knowledge about PMI, confidence in addressing PMI); (3) interpersonal factors (e.g. the relationship between women and HPs); (4) organisational level factors (e.g. service integration, continuity of carer, choice of assessment tools); (5) commissioner level factors (e.g. referral pathways); (6) political factors (e.g. women’s immigration status); and (7) societal factors (e.g. stigma).
Determining the barriers and facilitators to perinatal mental health care
System level barriers and facilitators will be described at each step of the care pathway and include results from both reviews (R1 and R2). Please note that in the process of merging results from both reviews a new multi-level factor was added (commissioner level) therefore the levels and themes described may differ slightly to the published papers.
The most commonly cited barriers and facilitators will now be described at each stage of the care pathway, and for each level of the multi-level framework. The stage of the care pathway will be blue, bold and italicised; the level of the multi-level framework being described will be in italic font. For information on all of the multi-level factors at each stage of the care pathway (see Appendix 5).
Deciding to consult
At the individual level some women believed there was no point in seeing a HP because they would only be offered medication:46,48,69,80,83,84,86,90
I knew she would just write a prescription and send me away … that wasn’t what I wanted. 46(p695)
Other factors that acted as barriers to women’s decision to consult were not understanding HPs roles,46,48,83,84,86,90 or not understanding what PMI is:46,47,69,70,72,80,82,84,85,89–91,95,96
I don’t really know what their job is. Nobody gave me, like, the parameters of this role of the health visitor and, so, I think if that happened then you’d … be able to use them better. 46(p695)
Nobody has ever told me what it is really [postpartum depression]…I just sit here sometimes and I am crying for no reason, but I could have detected it earlier if someone had explained to me what your first symptoms were, but nobody told me. 82(p11)
Linked to this, if women believed their symptoms were caused by spiritual factors,46,90,97,106–108 external causes such as life stressors,46,47,69,82,90,94–96 physical causes such as hormones46,69,79,85,89,90,94,96,105 or were a normal part of motherhood,47,49,76,79,89,90,92,93 deciding to consult could be hindered by women seeking out spiritual guidance before seeking professional help,70,81,90,96 or ignoring symptoms:69,72,80,85,90,92
They say that she (mother) is being possessed, so instead of medicines they go for talisman (spiritual treatment). 106(p6)
I thought it was just lack of sleep and this heavy cold. I thought that after a good night’s sleep it would get better, and I would be able to manage. 46(p696)
Not knowing where to go to seek help,47,48,69,70,90,93,95,109 fear of social services involvement47,80,96,105,110 and a lack of support from friends and family46,47,69,78,80,82,86,89,90,93,105 were also barriers to women consulting.
The largest individual level facilitators to women deciding to seek help were recognising that something was wrong:46,49,69,72,92,93,94,105
That’s when I thought, you know: ‘Something is really wrong here, I need to go to the doctors if I’m thinking about killing myself’. 46(p694)
At the organisational, commissioner and political levels, a lack of culturally sensitive care,47,69,80,90,96 no appropriate or timely services48,49,80,85 and a woman’s economic status69,70,80,82,95 prevented help-seeking:
That is probably why a lot of Black women don’t bother going to the system … the majority have had nightmares. So you’re thinking, ‘What’s the point in going back?’96(p9)
… if she has no money, how is she going to find help [with PPD]?70(p12)
At the societal level, stigma,46,47,49,69,70,72,80,81,83,86,93,95,96,108 culture46,47,76,80,81,87,89,90,94–97,106–108 and maternal norms of being a strong woman and a good mother46,69,70,72,78,81–83,86,90,93,94,111 all prevented women from deciding to consult:
There’s a huge stigma about feeling depressed, particularly postnatal. 46(p696)
The pressure to cope alone was also part of the social imperative to be ‘a strong Black woman’.
(author quote)95(p97)
Contact with health professionals
Women’s first contact with HPs was important and mostly impacted by factors at the HP level. The most frequent reasons for women dropping out of the care pathway at first contact with HPs was due to them being dismissive about mental illness, or normalising women’s symptoms,46,47,70,72,85,93,96,105 not recognising women’s attempts at help-seeking48,49,95,96 or appearing too busy and not making enough time to address PMH concerns:77,96,112
I did ask for support, but I didn’t really get any. And the health visitor’s response – ‘Well you seem like you’re doing all right’ – which kind of closes it off, doesn’t it. 46(p696)
I kept going to this doctor and he used to give me a pep talk and send me home […] those years were horrible because virtually he said to me … that I would just have to put up and shut up!72(p732)
Assessment/screening
Multiple factors affected assessment of PMI. At the individual level, the most cited barrier was the presence in the consultation of family and friends with negative beliefs about mental illness:113–119
I think they were actually stifled in being able to speak and talk and get it out because their partner was always sitting beside her. 116(p5)
At the HP level, a lack of knowledge about PMI47–49,69,92,107,115,120 and assessment-specific behaviours such as carrying it out in a tick box way49,74,89,90,92,96,114,118,119,121–123 were barriers to assessment. On the other hand, carrying out an assessment in an individualised way, taking women’s individual differences into account was a facilitator:
I try and tie it in with pain. We have certain protocols that we ask for pain levels and things like that. So, you know, when I ask them, ‘How’s your pain? Have you had a chance to take care of your postpartum depression screening? No, okay that’s fine. I’ll just stop back later’. I incorporate it into other things, so it doesn’t seem to be such a nagging thing. 123(p451)
At the interpersonal level, women and HPs being able to speak open and honestly about assessment was the most cited facilitator:74,77,114,124,125
And I was so grateful, and then I just talked to her, and it was so nice to be able to talk freely with her [about the EPDS] at the time. 124(p617)
At the organisational level, facilitators were having enough staff in order for assessment to take place,49,107–109,115,116,118,122,125,128 HPs who had received training in assessment,69,74,107,109,113,116,119,122,125,127–131 and a clear assessment and referral process within the organisation. 109,119,122,123,128 Where this was not the case, these factors acted as barriers to assessment:
How much extra time do you need to allocate when you get a high positive? You need to have the capacity within your system to manage it if you’ve got someone who’s suicidal. 122(p6)
I’ve never received any formal training in this area. I do not feel adequately trained to detect postpartum depression. 128(p170)
Other organisational level factors impacting assessment were the wording of the assessment tools,46,74,77,114,119,123 for example whether the questions made sense, and the acceptability of assessment or screening for both HPs and women:48,49,74,75,77,83,89,109,113,114,118,122–125,127,128
I have some moms [who] ask questions about it, like, ‘What does it mean where things are getting on top of me? What do you mean?’ You know, so they, they don’t always understand the questions114(p532)
No. I didn’t mind doing that. I mean it was quick, and simple and … it was nice. 124(p616)
Deciding to disclose
Women deciding to disclose their PMH symptoms was also affected by multiple factors. At the individual level, fear of being judged as a bad mother46,49,74,79,82,92,93 and fear of social services involvement69,74,75,85,124,127 were the most cited barriers:
I even went in at 3 months and I talked to a health nurse, and I just lied through my teeth because I thought, what are they going to do if they find out I can’t be a good mom?72(p732)
Because of the fear of postnatal depression and the taboo of social services and having your children taking [sic] away from you, I wasn’t going to admit anything to anyone …46(p696)
At the HP level, appearing too busy was the most cited barrier to disclosure:46–48,92,127
The health visitor said something like: ‘You know, in this community we have to look after a thousand and something babies’. And that instilled in me the feeling, like: ‘Oh, they are very busy these people, and I don’t have to be bothering them all the time’. 46(p696)
The most cited facilitator was HPs appearing genuinely interested in women’s well-being:46,85,92,96,119,127
Women were more likely to discuss their concerns with professionals who appeared caring and genuinely interested in their well-being: ‘She asked how I was. As soon as she said it, you know, “How are you feeling?”, I just cried’. 46(p696)
At the interpersonal level, a lack of a trusting relationship between women and HPs74,77,95,109,116,119,124,125,127,130 was the most cited barrier to disclosure:
I didn’t trust them I suppose so I didn’t tell the health visitors how I was feeling. 124(p618)
I: What are your views about the midwife asking these type of screening questions about mental health at the booking visit? P: If I didn’t know the midwives and they hadn’t known my history I think I probably wouldn’t have been honest with them. 119(p44)
At the organisational level, a lack of continuity of carer48,72,74,89,96,122,125,132 was the most cited barrier:
All CRs [community representatives] and some HPs [health professionals] regarded continuity of carers as critical to build trust, improve symptom monitoring and encourage disclosure: ‘everyday my doctor was changed I couldn’t make a relationship with … my doctor’. 122(p7)
At the societal level, stigma,46,48,76–78,84,93,96,116,119,122,124,127,130,134 culture47,48,74,76–78,87,89,90,95,96,116,127 and maternal norms46,47,72,74,77,79,89,92,119,124 were all barriers preventing the disclosure of PMH symptoms:
Oh well, I think there’s plenty, I mean I think there’s a huge stigma about feeling depressed particularly postnatal depression and people want to be, not to be thought of as a, you know, not being good mothers. 124(p618)
… in a context where suicide is still seen as a sign of weakness, a character flaw, it is difficult for individuals to ‘confess’ suicidal states and suicidal feelings. 87(p440)
I didn’t just … open up totally … to them. I wouldn’t want to … You know, it’s like an African community, and I felt, you know … If one person knows about it, 2 people know about … 3 people know about it … so I just cut off, um … I know it’s just the stigma … It’s just, you know, oh … look at the girl … I think it’s just, it’s just that I don’t want the stigma to just keep following me around. 78(p1742)
Referral
The most commonly cited factors affecting referral were HP and organisational level barriers. At the HP level, their knowledge about services and referral pathways49,70,109,120 was the most cited barrier. At the organisational level, lack of collaborative working across services69,112,113,116,120,127,129 and confusing organisational referral procedures116,120,122,127,129,130,134 were barriers.
The HPs interviewed in both Trusts were not always aware of the services available in other areas of the health service and recommended the provision and circulation of named links to support more joined up working.
Links with mental health are not the best, it is difficult to refer women unless they need to be admitted. (author quote)120(p103) If they are stable the mental health team are not so interested. Sometimes there is a lack of information from the key worker and information being shared. 120(p103)
At the commissioner level, confusing referral pathways was a barrier. 113,116,120,122,125,126 Participants spoke about the complexity of negotiating referrals:
We have to send the form; the patient has to ring to say did you get the form and I am now confirming that I am going to go and then they get an appointment, for someone who is very distressed and you are asking them to jump through hoops. 116(p5)
Access to treatment
Multiple factors influenced access to treatment. At the individual level, the most cited barriers to accessing care were logistical issues such as not having childcare,46,47,69,70,84,85,89,91,95,96,113,114,134,135 the location of the care and difficulties travelling there69,70,83–85,95,96,108,114,134–137 and the timing of appointments. 47,69,85,91,96,133,135 In some cases, these barriers could be exacerbated by a lack of support from family and friends:86,96,108–110,122,133,137
… they cannot take their child with them to their session … (and) a lot of times they cannot afford day care. 113(p4)
Yes, there was the issue of travelling. I cannot drive and my husband was admitted to the hospital …137(p4)
I can’t share my issues with my family. They don’t care about me, they don’t help me with the activities or remind me to do them or are willing to accompany me to the hospital. 133(p9)
Additional personal difficulties such as a lack of employment70,106,120,130,138 or women’s symptoms of their mental illness49,93,110,135 were also individual barriers to care:
My husband’s business is not doing well, financially we are struggling, we have children to look after, we have the responsibility to marry them off and give them dowry etc., all these worries are pulling me down. Talking to [the peer volunteer] can’t help me. 106(p6)
When I was experiencing mental health issues, it was harder for me to get out, sort of on a schedule and be punctual. 93(p15)
At the interpersonal level, language barriers were the biggest barrier to women accessing care48,70,89,96 and, related to this, a lack of culturally sensitive care was the most cited organisational level barrier to access:46,49,70,76,89,90,96
Hispanic women reported feeling ‘shuttled from service to service’ because no one knew how to take care of their culture. (author quote)90(p18)
Similarly, women reported that services did not recognise their cultural needs:
You need someone who’s on the same wavelength as you, who shares the same cultural experiences as you, which sometimes isn’t available. 46(p695)
Where logistical support was provided this was a facilitator to access, but when it was not provided it was a barrier:46,72,83,85,91,96,108,109,122,137,139
And we were offered a crèche facility; I used to take him there; otherwise it would have been really difficult for me. 137(p4)
At the commissioner level, the most cited barrier to access was a lack of appropriate or timely services for women:46,48,49,69,85,89,95,109,112,113,130
You shouldn’t have to press that danger button of ‘I’m gonna self-harm’ or ‘I’m gonna hurt my children’ for someone to help you. 48(p756)
At the political level, refugee or immigrant women fearing deportation70,81,90,95,109,134 and a lack of financial resources to pay for health care49,69,70,81,82,95,106,108,109,113,114,134,139,140 were barriers to access. These were often interlinked and exacerbated by each other:
… as Hispanics we do not have insurance and money is what really counts. 70(p12)
Because when you’re legal you can take the child to the day care and look for a job … if you don’t work, it’s like you’re dead, being alive. We want our papers so we can progress; not so we can leave or be a load to anyone, but just to work – to buy a home and give our kids a good life … I get depressed because I can’t live like normal people because I’m always thinking if I leave or if I stay …90(p13)
At the societal level, stigma,47,70,72,91,95,96,110,134 culture49,70,76,89,106 and maternal norms49,96 were also barriers for women choosing to access care:
It was difficult for me to accept that [I should see a psychiatrist] because, in our country, those who go to a psychiatrist are crazy. And I thought, ‘I’m not crazy. I don’t need it.’ And [the social worker] told me, ‘Not only crazy people need a psychiatrist, necessarily. In your case, you need it’. 110(p938)
Provision of optimal care
HP, interpersonal and organisational level factors were most likely to impact provision of optimal care. At the HP level, a lack of knowledge about PMH and treatment options,48,109,116,129,141–143 and low confidence in addressing PMH133,138,139,143,144 were barriers to the provision of optimal care:
[Women report] ‘Oh I was seeing so and so but when they found out I was pregnant they discontinued my medication’. That … happens frequently. Very frequently … their provider won’t [prescribe] because of their pregnancy. 142(p171)
Look, I feel insecure at the moment, as I have not yet had the chance to try IPT [interpersonal therapy], and I have to practice, and along with that get ready to try this method with a client and feel comfortable with it. 144(p79)
On the other hand, HPs possessing valued characteristics,94,105,106,114,130,138,145,146 such as being trustworthy and caring, were facilitators to the provision of optimal care:
… She was always there if I have a question or something and she always gets back to me no matter what. 114(p530)
At the interpersonal level, a lack of trusting relationship was a barrier to optimal care provision:69,72,91,146,147
Sometimes, I don’t feel very connected to the person that I call … so, sometimes, it gets awkward during the phone conversation. 146(p8)
At the organisational level, facilitators were collaborative working between106,109,116,120,122,129,131,142 and within organisations:122,126,129,130,134,136,138,139,148
[A patient] was discontinued off her lithium … [when she] found out she was pregnant … she wanted to hang herself … the OB [obstetrician] attending was saying, ‘She’s this far along in her pregnancy; the lithium isn’t going to hurt … and what’s worse for this woman? To expose her baby to lithium or to hang herself?’ … we were able to facilitate a conversation between the OB doctor and the patient’s psychiatrist and she did a great job … (and) put the woman back on lithium …142(p172)
A lack of training related to PMI and interventions was the most cited organisational level barrier74,106,109,114,120,126,132,138,141,143,146–149 to the provision of optimal care:
Midwives are not well equipped with mental health knowledge and skills. If midwives were trained on mental health they could do a better job …108(p6)
Organisational level facilitators to the provision of optimal care included providing culturally sensitive care47,81,95,96,109,116,146 that is individualised,48,49,114,116,123,132,137,145,146,148,150 appropriate to the women’s needs,116,132,133,138,139,143–149 flexible,93,109,129,133,138,144,146 delivered at home72,126,138,141,147 and provides information about PMI:47,48,72,80,84
… the online course, it was tailored to my needs at the time and I think that’s how it helped so much. 151(p26)
Flexibility in length of appointments was identified as a facilitator of effective assessment and support of immigrant women.
(author quote)109(p194)
Finally, another commonly valued aspect of support was receiving information from the HP. While the women found it helpful to learn about mental health and PPD [postpartum depression], they also valued the inclusion of information or feedback about parenting.
(author quote)72(p731)
At the commissioner level, a lack of appropriate and timely services79,108,113,116,120,138,147 and complexities around funding services were the most cited barriers to providing optimal care:109,120,128,134,135,139,140
Someone with PMH issues really does not belong in the general psychiatric outpatient clinic. 116(p6)
We are unable to serve every woman in need of ongoing care. We are therefore working on additional funds, both internally and externally, to secure long-term physical and behavioral health care for our patients. 140(p7)
At the political level, immigration status, such as being dependent on one’s partner,76,81,90,95,96 was a barrier to care:
Because we make argument, sometimes he hit me. I was alone and nobody to help me. Sometimes I was very nervous. I felt I’m his slave not his wife. He wanted everything to his hand and make control for everything in my life. I don’t think this is life. 90(p14)
At the societal level, stigma47,48,82,106,130,132,138,150 and culture81,95,109,113,135,144 were also barriers to optimal care:
She got upset when I told her that the assessment indicated that she has depression. She said that she is not mad and stopped me from coming in when I went for my next visit. 106(p6)
We deal with a lot of undocumented immigrants (and) a lot of people with different cultural diversities … (allowing) … strangers … into their home or even discussing certain things over the telephone is difficult and sometimes just taboo for some cultures … So that is a roadblock that we constantly come upon. 113(p4)
Women’s experience of treatment/care
Multiple factors impacted women’s experience of treatment or care. At the individual level, social isolation70,76,79,81,82,95,96 was a barrier to women’s experience of care as it exacerbated their mental health difficulties further:
My husband just don’t understand how I feel, everybody just keep saying Dimaak kharaab hai [mind is not working properly]. 96(p9)
It’s really awful being with other women that look as if they are coping, that’s just as bad as being with nobody. 79(p494)
At the HP level, those who provided hope to mothers, were caring, supportive, empathetic and went above and beyond meant women had a positive care experience:47,48,72,74,77,84,90,94,138
So she was like supportive and kept in contact quite a lot, ringing me to see I was ok and if I needed to talk, she was there sort of thing. 72(p733)
They (staff at a francophone settlement support centre) helped me by trying to find places (to live) where it would be least expensive for me, which I appreciated a lot90(p16)
Related to this, development of a trusting relationship and rapport at the interpersonal level47,48,72,84,106,110 and continuity of carer46–48,72,92 at the organisational level were also associated with a positive care experience:
It was the not having to start explaining again to someone new which was so great. 46(p695)
Other facilitators at the organisational level were culturally sensitive care47,72,81,90,95,96 that was individualised and person-centred,48,49,72,75,84,90,91,92,96,137,148 and that provided women with an opportunity to talk:47,72,75,81,84,87
I appreciated the visit from the nurse who came to see me. She was the only person who talked to me about my feelings at that time, and my depression. I found it interesting because she came and talked to me … it was nice to be able to talk to someone about it. 87(p444)
Where support was facilitated by someone from the same ethnic background, women felt that the sessions were culturally specific and sensitive. ‘Because she (the group support facilitator) understood what we go through, how our culture is, and how our belief systems are. She could understand us better than anyone else.’
(Pakistani mother)96(p10)
Lastly, most women valued group support48,72,75,78,79,84,90,92,95,96,108,137,152 despite hesitance at first:
I was a bit intimidated – intimidated’s [sic] the wrong word I was a bit hesitant at first because I thought oh my God I’ve gotta sit in front of a bunch of other people and talk about the problems I was having, you know what are they gonna think of me, but it actually ended up being better for me being in a group. 152(p3523)
[when you start going to the group] you know that you are not alone. So many mothers are going through what you are going through. And some are even MORE than yourself …78(p1751)
Barriers and facilitators to perinatal mental health care in different health and social care settings
The most commonly cited barriers and facilitators in different health and social care settings will now be described.
Hospitals
Within hospitals the most cited barriers influencing implementation were HP level barriers, such as HP’s negative perception of the care being provided122,123,128,133,139,143,146,148 and organisational level barriers, such as lack of time or a heavy workload,107,121,122,128,130,146,148 lack of training for HPs107,122,128,130,133,143,146 and unclear workflow procedures:121–123,128,139,148
The one thing I can think of within our system is [that we need] more consistent [reporting of EPDS scores]. We are doing it, but not consistently. In our nursing [shift-change] reports [we could] say where we are with it … they sometimes say, ‘Oh the postpartum was a 4 and 0 [on item 10 which assesses suicidal thought]’ and then they move on. Or they could say, ‘I gave them the EPDS, or I’ve asked them to do it.’ You know, it’s nice to know where they are at with it.
(Nurse)123(p449)
At the societal level, stigma was the most cited barrier. 107,121,122,130,133,134,148
Primary care
In primary care, the most cited individual level barrier was family presence in the consultation. 106,108,110,115–117,124,137 Organisational level barriers such as heavy workload or lack of time108,115,116,118,144,149 were frequently cited.
Can I be honest with you sometimes I wonder if you really want to open this can of worms and it’s so much easier just to jolly along and check the BP, check the urine, check this and that and have them out the door and see the next patient.
(GP)117(p4)
At the societal level, stigma106,108,110,115,116,118,124,144 and culture106,108,115,116,137,144 negatively affected implementation.
Community settings
In community settings or community-based delivery, HP level factors such as the characteristics of the person providing the care109,114,132,138,141,147 was an important factor in implementation:
My experience … she liked to hear, she wanted to hear about that, and what stuff was normal.
(Mother about a peer mentor)147(p31)
Training was the most cited organisational level factor. 109,114,126,127,131,132,136,138
Maternity services
Within maternity services, organisational level factors were important for implementation, including training119,120,125 and continuity of carer:119,120,125
… If I didn’t know the midwives and they hadn’t known my history I think I probably wouldn’t have been honest with them.
(Mother about a midwife)119(p44)
Remote or online care
Organisational level factors were the most important, in terms of the design and delivery of the care. Most cited facilitators were flexibility,145,151 techniques used,145,151 privacy and confidentiality,145,153 ability to fit in with the women’s schedule145,151 and relevance to women:145,151
I loved that I could access the program anytime. It fit into my schedule in a way that traditional therapy could not have, as my baby is demanding and my husband works out of town.
(Mother)145(p213)
Low- and high-income countries
Across LMICs the most cited organisational level barrier was lack of training106–108,133 and the most cited societal level barrier was stigma. 106–108,133
Similarly, where health services were carried out in higher income countries, but with women from a refugee or different cultural backgrounds, the most cited organisational level barriers were lack of HP training,109,122,125,127,130 along with HPs’ heavy workloads. 109,122,125,127,130 The most cited societal level barrier was stigma:110,122,125,127,130,141
It was difficult for me to accept that [I should see a psychiatrist] because, in our country, those who go to a psychiatrist are crazy. And I thought, ‘I’m not crazy. I don’t need it’.
(Mother who had moved to the USA)110(p938)
Geographical distribution of evidence and mental health condition examined
Studies in R1 were mainly carried out in Western HICs. Geographical distribution of evidence is shown in Figure 6 and studies listed in Appendix 7. The majority of studies were carried out in the USA (n = 18), followed by the UK (n = 7); Australia (n = 6); Canada (n = 3), Norway (n = 2); and Ireland (n = 2). Remaining studies were carried out in LMICs, including Pakistan (n = 2); Israel (n = 1); Peru (n = 1); Ghana (n = 1); South Africa (n = 1); Uganda (n = 1) and Singapore (n = 1).
FIGURE 6.
Geographical distribution of studies from R1.
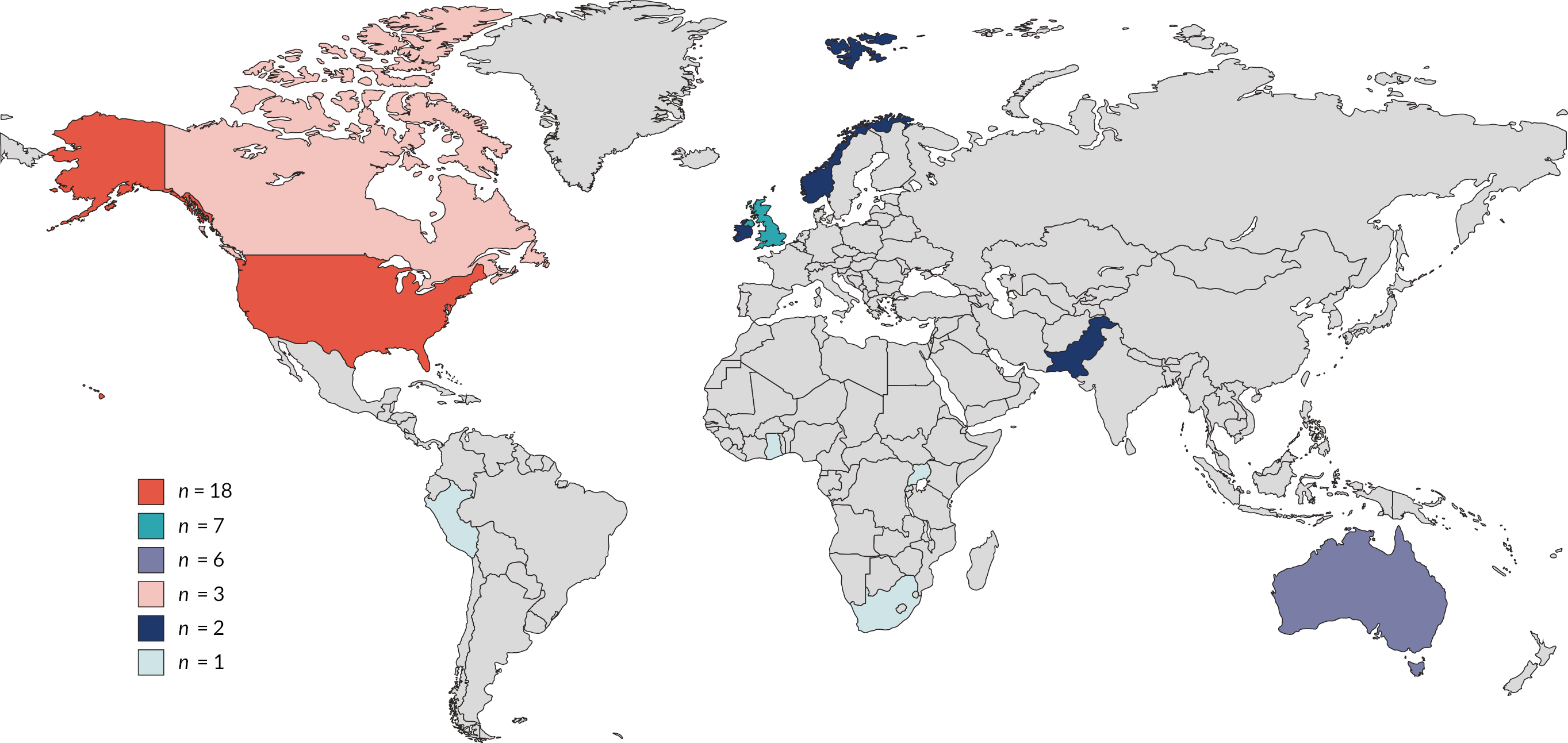
In R2 the country that individual studies in each review were carried out in was noted. Where over 50% of the studies in a review were from the same country or area, reviews were assigned the status of mainly: carried out in the UK (n = 9); Western HICs (n = 19); or LMICs (n = 1). Four of the reviews did not provide enough details of individual studies to be able to determine their geographical distribution.
Evidence in both reviews predominantly focused on perinatal depression. In R1 most of the studies (n = 32) focused on perinatal depression. The rest focused on unspecified PMH difficulties (n = 7), followed by anxiety (n = 1) and birth trauma (n = 1). Three studies did not specify which mental health difficulty they were targeting (n = 3). In R2 most reviews (n = 23) focused on perinatal depression, followed by a mixture of perinatal mood disorders (e.g. depression, anxiety, distress; n = 5). Only one review focused on postnatal psychosis105 and one on birth trauma. 92
Chapter 6 Development of the MATRIx conceptual framework
This chapter details the development of the MATRIx conceptual framework. Eight stages, outlined by Jabareen (2009),56 were carried out to develop the conceptual framework. These will be described in more detail below and in Figure 7.
FIGURE 7.
Conceptual framework process.
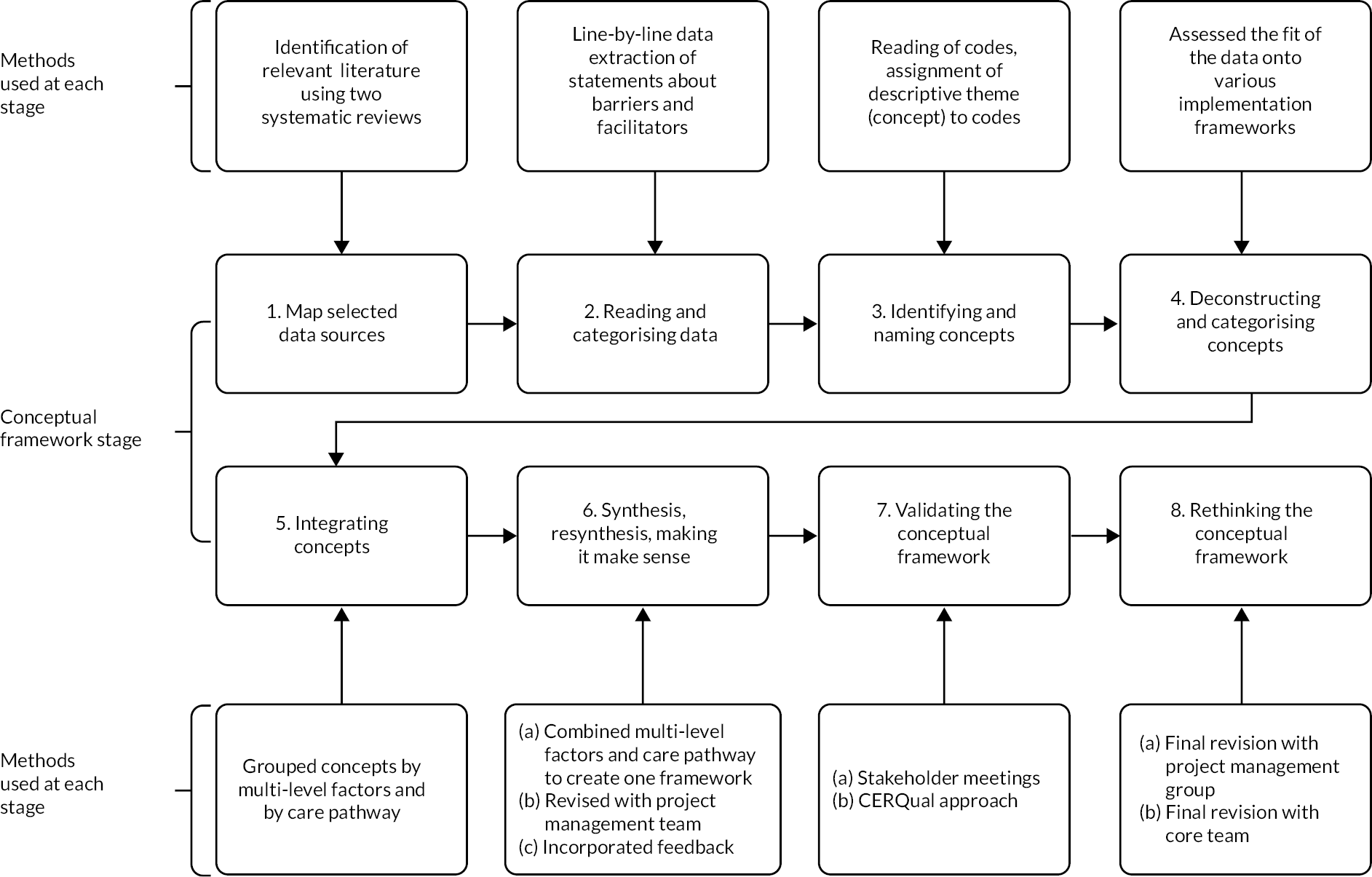
What is a conceptual framework?
A concept relates to knowledge or an idea about a certain topic. 154 We will use the themes identified in the systematic reviews described above to refer to our concepts.
A conceptual framework can be defined as a ‘network, or a plane, of interlinked concepts that together provide a comprehensive understanding of a phenomenon or phenomena’. A conceptual framework can highlight areas for improvement and provide an empirical basis for recommendations for future practice and research. 56
Why is a conceptual framework needed?
Our primary research objective was to develop a conceptual framework of barriers and facilitators to PMH care to inform PMH services and practice, care pathways, and highlight where further research is needed.
The results from both reviews presented above provide an understanding of barriers and facilitators to implementing PMH care and to women deciding to seek help, accessing help and engaging in PMH care. However, in order to provide evidence-based recommendations for policy and practice related to PMH service provision, it is important that the results of both reviews are synthesised. A conceptual framework is one way of doing this.
Development of the conceptual framework
The method described by Jabareen (2009)56 involves eight stages. We describe how we conducted these stages below.
Mapping the selected data sources
This process includes identifying relevant literature regarding the phenomenon in question. In order to do this, the two systematic reviews described in Chapter 3 were conducted.
Reading and categorising selected data
The aim of stage 2 is to read the selected data and categorise it by discipline. As described in Chapter 3 line by line data extraction of statements referring to facilitators or barriers to PMH assessment, care and treatment was carried out for both reviews. Therefore, data was categorised by barriers and facilitators.
Identifying and naming concepts
The third stage is to read and re-read the selected data and ‘discover’ concepts. This was done by re-reading the extracted data and assigning a descriptive theme/concept based on its meaning and content. Themes/concepts were developed and revised as each study was re-read.
Deconstructing and categorising the concepts
The aim of stage 4 is to deconstruct each concept and to organise and categorise the concepts. 56 This stage was completed by assessing the fit of the data on to various implementation frameworks (Consolidated Framework for Implementation,155 Reach Effectiveness Adoption Implementation Maintenance156 and Ferlie and Shortell’s Levels of Change framework)40 for Review 1 and then mapping the concepts for Review 2 on to the same framework (see above).
Integrating concepts
The aim of stage 5 is to integrate and group together concepts that have similarities to one new concept. 56 Concepts were grouped by multi-level factors of barriers and facilitators (see Figures 8 and 9) and the care pathway (see Figures 10 and 11).
FIGURE 8.
Multi-level model of barriers and facilitators to implementing perinatal mental health care (R1).
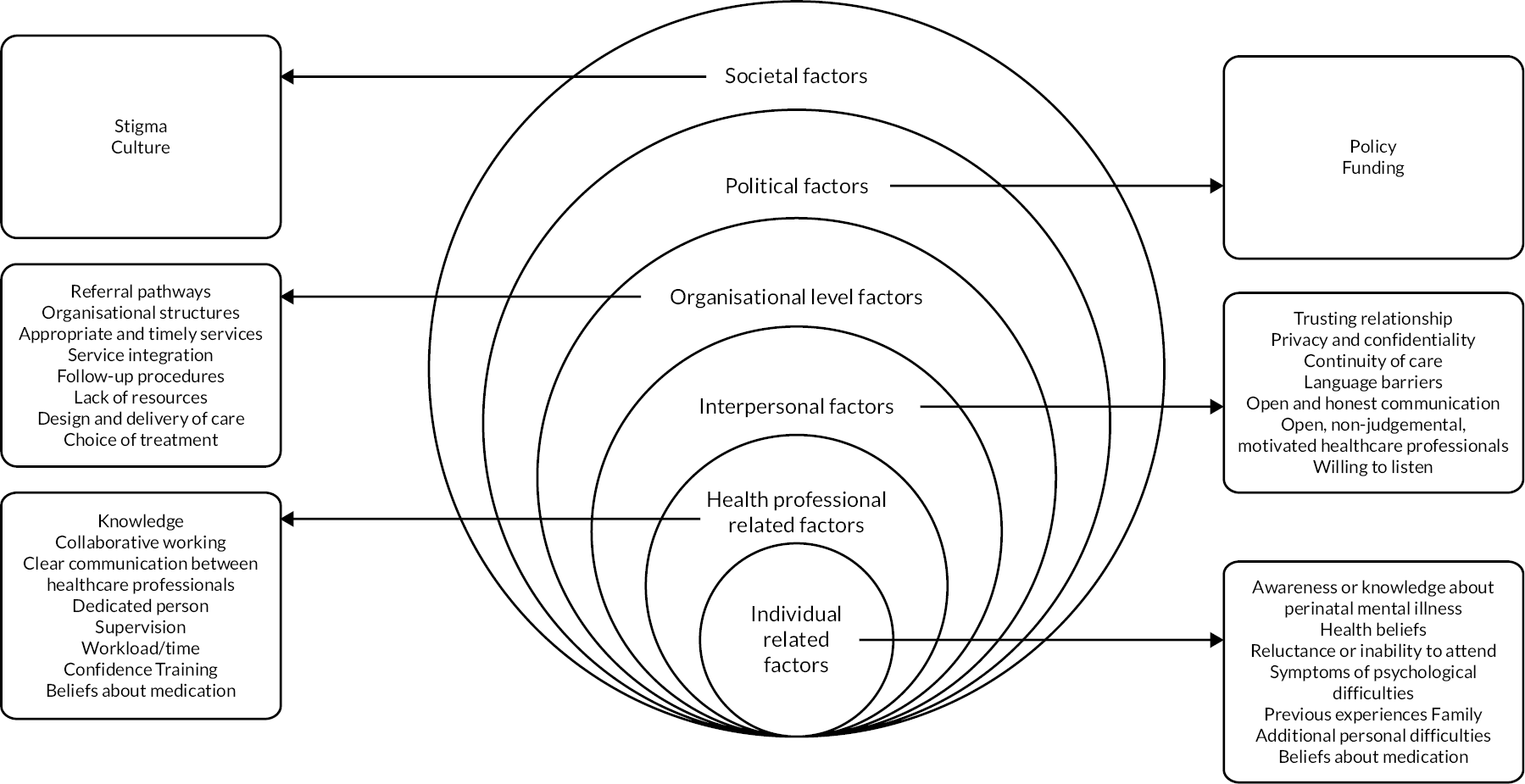
FIGURE 9.
Multi-level model of barriers and facilitators to women accessing perinatal mental health care (R2).

FIGURE 10.
Multi-level barriers and facilitators to implementation mapped on to the care pathway (R1).
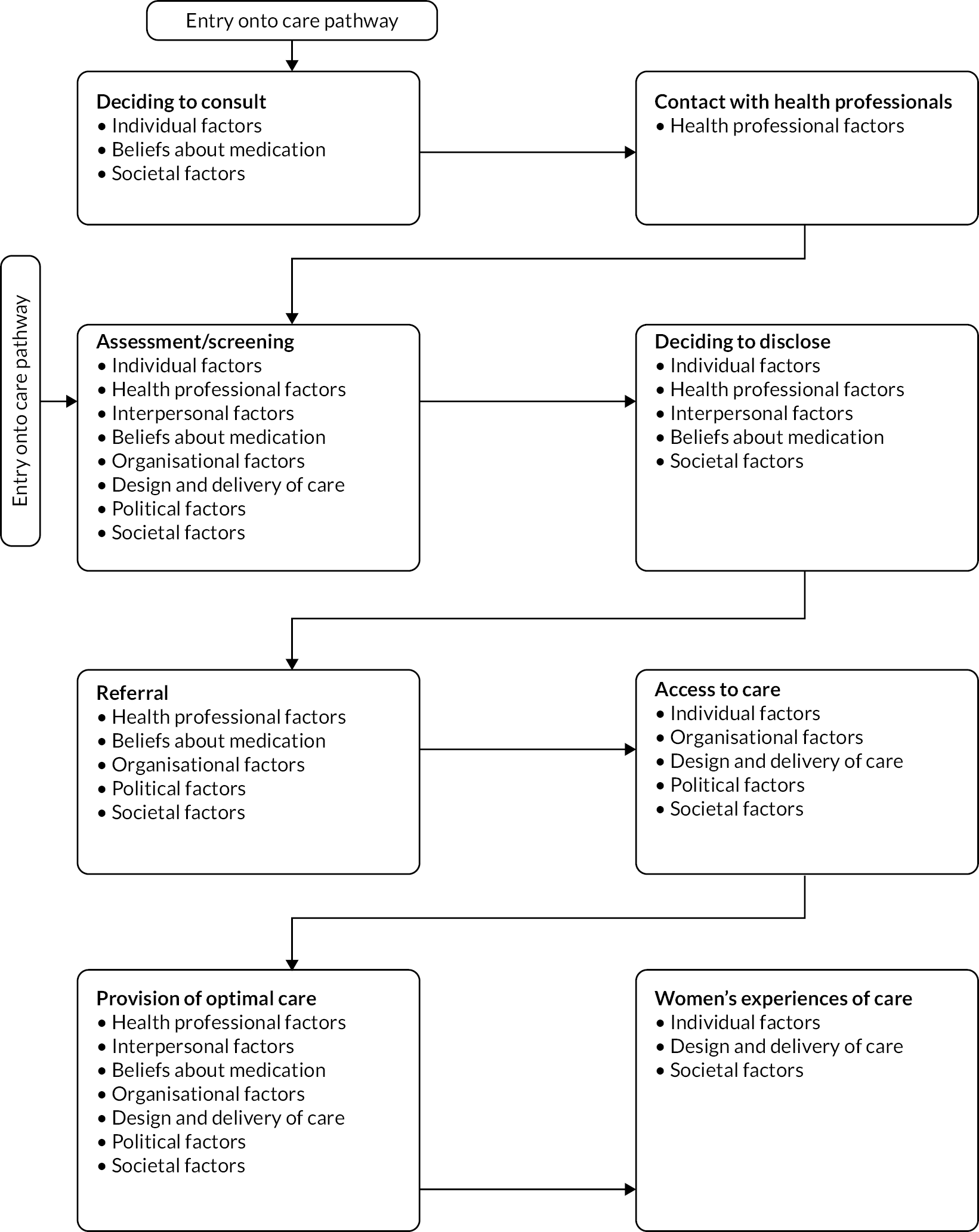
FIGURE 11.
Multi-level barriers and facilitators to women accessing perinatal mental health care mapped on to the care pathway (R2).
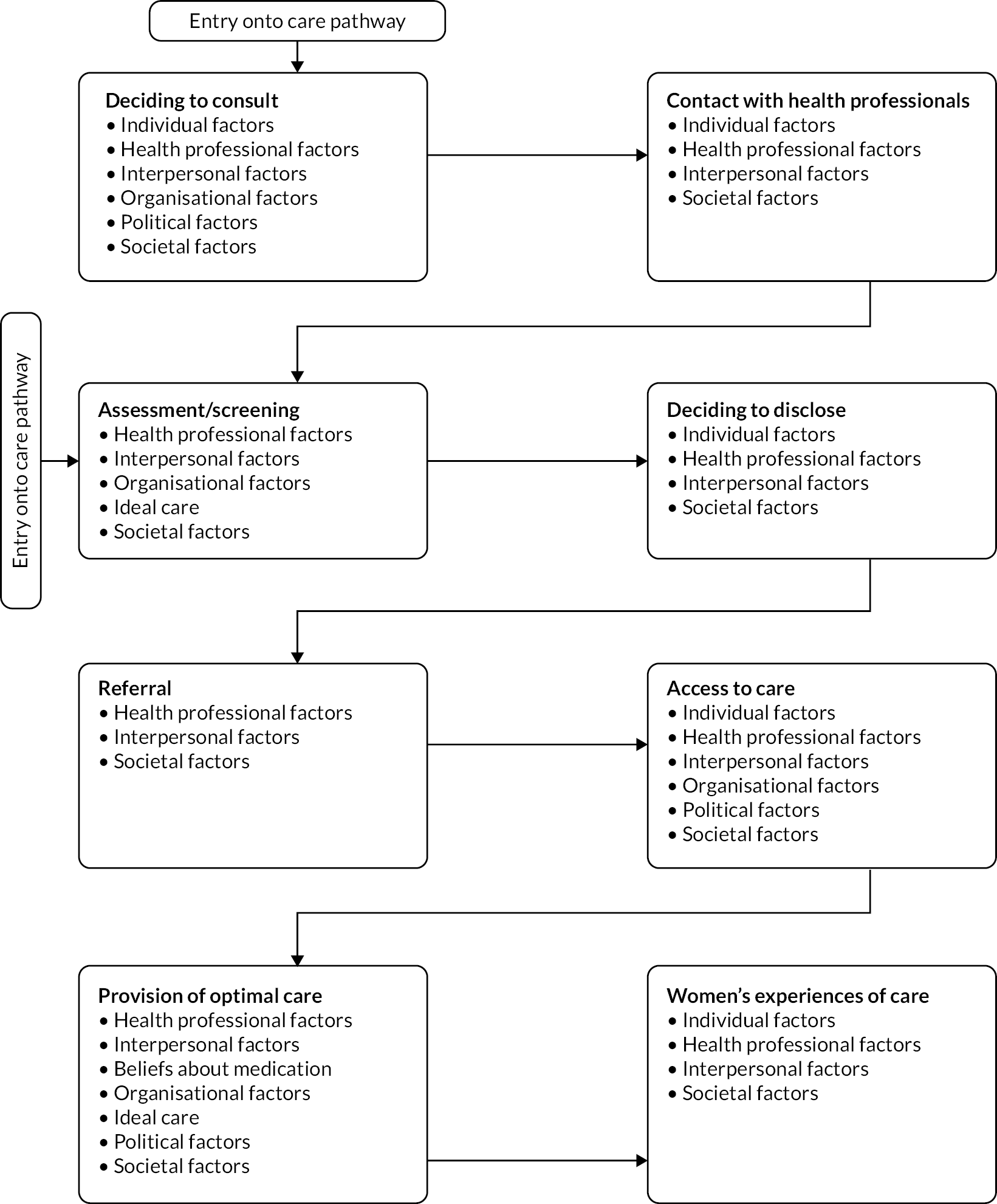
Synthesis, resynthesis and making it all make sense
The aim in this phase is to synthesise concepts into a theoretical framework, using an iterative process of repetitive synthesis and resynthesis. 56 This was done in multiple stages:
-
Combining multi-level factors and care pathway. Figures 8–11 were combined together to create a draft framework (see Appendix 8, version 1). At this stage, all factors identified from both reviews were included.
-
Revision with project management group. Feedback on the draft framework was obtained from members of the project management group (Rebecca Webb, Abigail Easter, Camilla Rosan, Agnes Hann, Elizabeth Ford, Fiona Alderdice, Judy Shakespeare and Susan Ayers). This included researchers and clinicians with expertise in maternal and child health, perinatal health and well-being, PMH care, strategy and transformation and clinical psychology. Suggestions made by members of the project management group included considering the importance of outcome measurements; integration of different services; logistical issues such as co-location; and inclusion of a step between organisational and political structure, for example, middle management.
-
Incorporating feedback. Another version of the draft framework was developed after incorporating the feedback from the previous step (see Appendix 8, version 2).
Validating the conceptual framework
The aim in this phase was to validate the framework. This was done using two steps: (1) stakeholder meetings to ascertain whether the proposed framework and its concepts made sense to practitioners and other stakeholders;56 (2) assessing the confidence with the evidence. This step is in line with the development of National Institute for Health and Care Excellence (NICE) guidelines,157 where evidence is rated using the Grading of Recommendations Assessment, Development and Evaluation (GRADE)158 to assess the certainty of evidence before recommendations are made.
-
Stakeholder meetings. Following the approach of Leamy (2011),159 three panels of stakeholders were consulted about the draft conceptual framework (see Appendix 8, version 2). Panels were held online via Microsoft Teams. The first panel comprised women, their partners and third-sector organisations that represent perinatal women (e.g. NCT, Maternal Mental Health Change Agents). The second panel comprised HPs from different disciplines working for relevant NHS services. The third panel comprised commissioners and policy makers. Characteristics of stakeholders are shown in Table 4.
| Stakeholder group | N | Role |
|---|---|---|
| Women and families | 10 | Lived experience of PMI (n = 8) Fathers (n = 2) Mothers (n = 7) Not reported (n = 1) |
| HPs | 11 | Specialist PMH midwives (n = 4) Specialist midwife in homelessness and substance misuse (n = 1) Specialist nurse (n = 1) GP (n = 2) Team manager PMH (n = 1) Health visitor (n = 1) Academic in health research (n = 1) |
| Commissioners and policy makers | 5 | Implementation lead (n = 1) Project manager (n = 1) Training and workforce lead (n = 1) Clinical lead (n = 1) Local specialist PMH service lead (n = 1) |
During the stakeholder meetings, attendees were asked to review the conceptual framework and consider questions such as:
-
How does the framework fit with your experience of implementing/accessing PMH services?
-
Does the framework include everything? Have we missed anything? What?
-
In your view, what are the most important facilitators/barriers to implementing/accessing PMH services?
-
In your view, what are the top recommendations for clinical practice?
-
How can we disseminate this for most impact?
Conversations were recorded, analysed and suggestions and recommendations were noted. These are summarised in Table 5
| Women and families | HPs | Policy makers and commissioners |
|---|---|---|
|
|
|
-
Using the CERQual approach to assess confidence with the evidence. The CERQUAL approach was used to assess the confidence of the results for each of the concepts in the framework. 160 To do this, each multi-level concept identified from reviews and feedback from stakeholders was assessed on methodological limitations,161 coherence,162 adequacy of data163 and relevance of data164 pertaining to that item. Specific rules were followed to rate the confidence of the evidence for each concept (see Table 6).
| High confidence | Medium confidence | Low confidence | Very low confidence | |
|---|---|---|---|---|
| Methodology | R1: all domains were rated as high quality R2: high confidence – no or one non-critical flaw |
R1: most domains were rated as high quality R2: moderate confidence – more than one non-critical flaw |
R1: most domains were rated as low quality R2: low confidence – one critical flaw |
R1: all domains were rated as low quality R2: critically low confidence – more than one critical flaw |
| Coherence | All summaries were consistent in their content | Over half of the summaries were consistent in their content | Summary contents had a mix of two different concepts | No consistency across summary contents |
| Adequacy | 21+ papers and more than half of the papers had thick data descriptions | 10–20 papers and more than half of the papers had thick data descriptions | 5–9 papers and/or less than half of the papers had thick data descriptions | < 5 papers and/or less than half of the papers had thick data descriptions |
| Relevance | R1: studies carried out in UK/NHS R2: reviews where more than 50% of included studies were carried out in the UK/NHS |
R1: studies carried out in Western countries, or countries with universally government-funded health care (e.g. Canada) R2: reviews where more than 50% of included studies met the above stipulation |
R1: lower middle-income countries, or countries with universal health insurance coverage R2: reviews where more than 50% of included studies met the above stipulation |
R1: countries without universal health insurance coverage (e.g. USA) R2: reviews where more than 50% of included studies met the above stipulation |
| Overall rating | Three or all aspects (methodology, coherence, adequacy, relevance) of a concept rated as high confidence | Three or all aspects of a concept was rated as moderate confidence | Three or all aspects of a concept was rated as low confidence | Three or all aspects of a concept was rated as very low confidence |
Methodological limitations were based on the methodological assessments described in Chapter 3.
Coherence was assessed by looking at the evidence assigned to that concept and identifying any outliers or ambiguous elements in the data. To do this, a summary from each of the papers that contributed to a concept was written out. Coherence ratings were based on whether the summaries all had similar content.
Adequacy was assessed by looking at both the quantity and richness of the data for each concept. Where over half of the studies had thin data descriptions (see above), a concept could not score above low confidence.
Relevance was assessed by identifying the country and health system of each study within a concept. Given that PMH is a priority for UK strategy and policy,28,29 and research organisations,27 we defined direct relevance as studies carried out in the UK/NHS (or for R2, where more than 50% of studies included in a review were carried out in the UK/NHS, see Appendix 7). Partial relevance was studies carried out in Western Countries, or in countries with universally government-funded health care (e.g. Canada). Indirect relevance was studies carried out in LMIC, or countries with non-universal insurance or health care coverage (e.g. USA).
The confidence of each of these four aspects can be rated as: high confidence, moderate confidence, low confidence and very low confidence. This meant that each concept was left with four confidence ratings. All four confidence ratings were then taken to give an overall confidence rating for each concept. Where a concept had an even split of ratings and the ratings were next to each other in quality (e.g. high, medium, low, very low; or high, high, medium, medium) the rating assigned to the ‘relevance’ of a concept was given a higher weighting. This was on the basis of the importance of recommendations being relevant to the NHS context. Where a concept had an even split of ratings, but the ratings were apart from each other in terms of quality (e.g. high, high, low low), the rating in the middle of these was given (e.g. medium). A decision was made to not assign any higher than ‘low confidence’ to concepts where adequacy was given a ‘very low’ rating. This was to avoid putting too much emphasis on concepts where more research is needed.
Rethinking the conceptual framework
This step involved finalising the conceptual framework. This was done in two steps:
-
Final revision with the project management group. The most recent draft of the conceptual framework was discussed by members of the project management group (Rebecca Webb, Abigail Easter, Elizabeth Ford, Fiona Alderdice, Helen Cheyne, Jennifer Holly, Judy Shakespeare, Rose Coates, Sally Hogg and Susan Ayers). Feedback consisted of two main points. The first related to whether concepts with very low/low confidence ratings should be removed. As the majority of these concepts related to under-researched populations, removing them from the framework would continue the cycle of under-representation of these groups. It was therefore decided to include all concepts in the framework but provide an indication of the confidence rating scale. Recommendations for practice should be based on concepts with high/moderate confidence ratings, and recommendations for research based on concepts with low/very low confidence ratings. The second point was related to the language used. The framework presented was a framework of barriers, and it was decided that the negative language may act as a barrier itself. It was suggested that a framework of facilitators might also be appropriate and useful.
-
Final revision with the core team. For final revisions members of the core team met for a one-day workshop to consider all the feedback given (Rebecca Webb, Judy Shakespeare and Susan Ayers). It was agreed that the following changes should be made:
-
The decision to use two conceptual frameworks was made. One specifically related to barriers to PMH care, and the second related to facilitators to PMH care. The data were reassessed, and barriers and facilitators were separated.
-
The language of both frameworks was scrutinised to remove or reduce any blaming or negative language.
-
Some of the HP level barriers and facilitators (e.g. training and heavy workloads) were moved to the service manager level. This is because it is the service’s responsibility to provide this rather than the HPs.
-
Based on the funding structures in the UK, funding complexities was moved to commissioner level, rather than government level. Although the government provides a set amount of money for PMH services, the complexities of sourcing funding appeared to be more at the commissioner level.
-
The framework was reviewed to ensure graphics and icons were representative and inclusive.
-
Chapter 7 The MATRIx conceptual frameworks
Description of the conceptual frameworks
The MATRIx conceptual frameworks aim to understand key barriers and facilitators to PMH identification, assessment, care and treatment in order to improve PMH services. Syntheses of the reviews identified 78 key factors that can impact on PMH care. These are summarised in two conceptual frameworks which provide pictorial representations of 66 barriers (see Figure 12) and 39 facilitators (see Figure 13) across the care pathway and at multiple levels (note: there is overlap with 27 of the barriers and facilitators; see Appendix 9).
FIGURE 12.
The MATRIx barriers to perinatal mental health care conceptual framework.
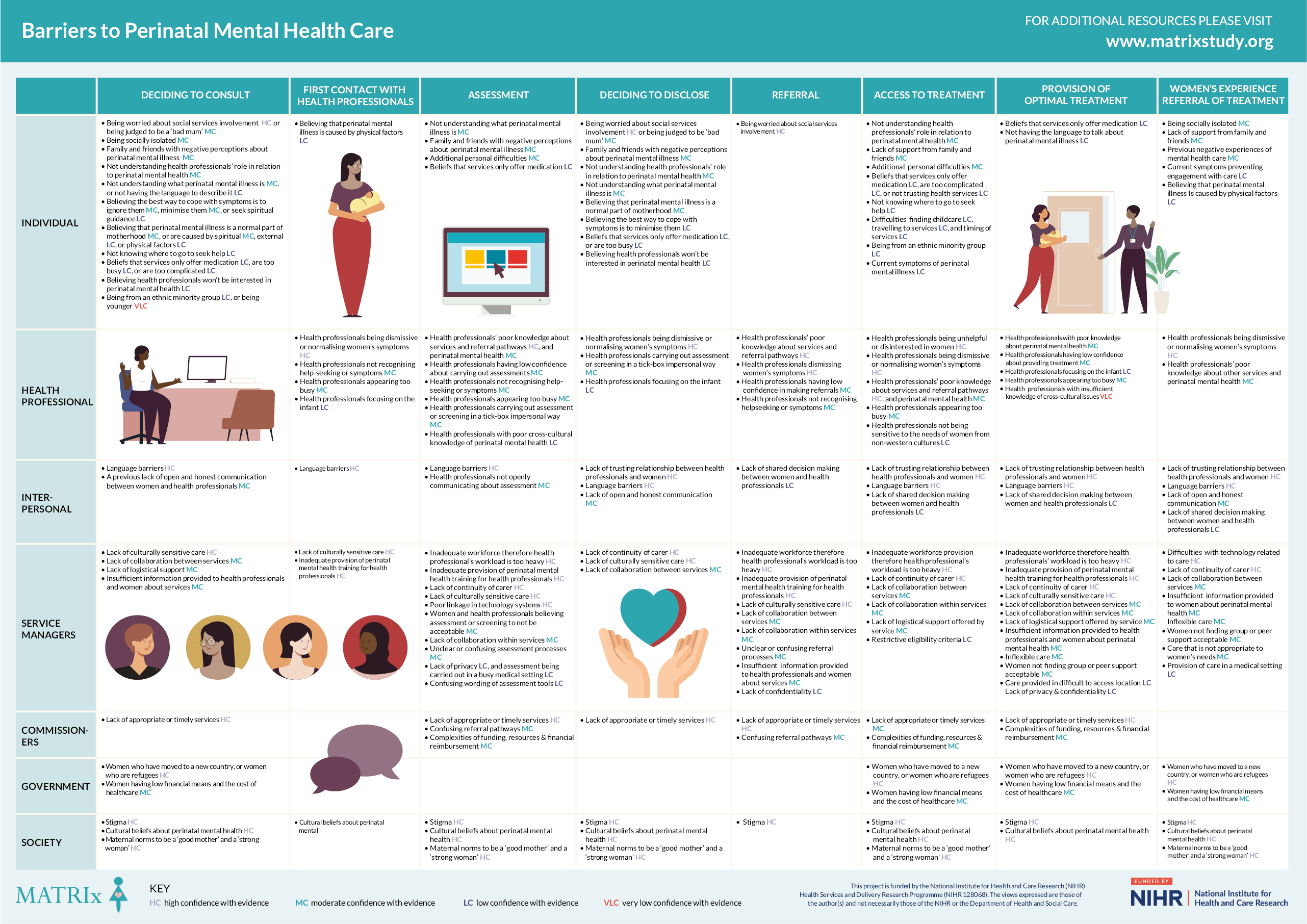
FIGURE 13.
The MATRIx facilitators to perinatal mental health care conceptual framework.
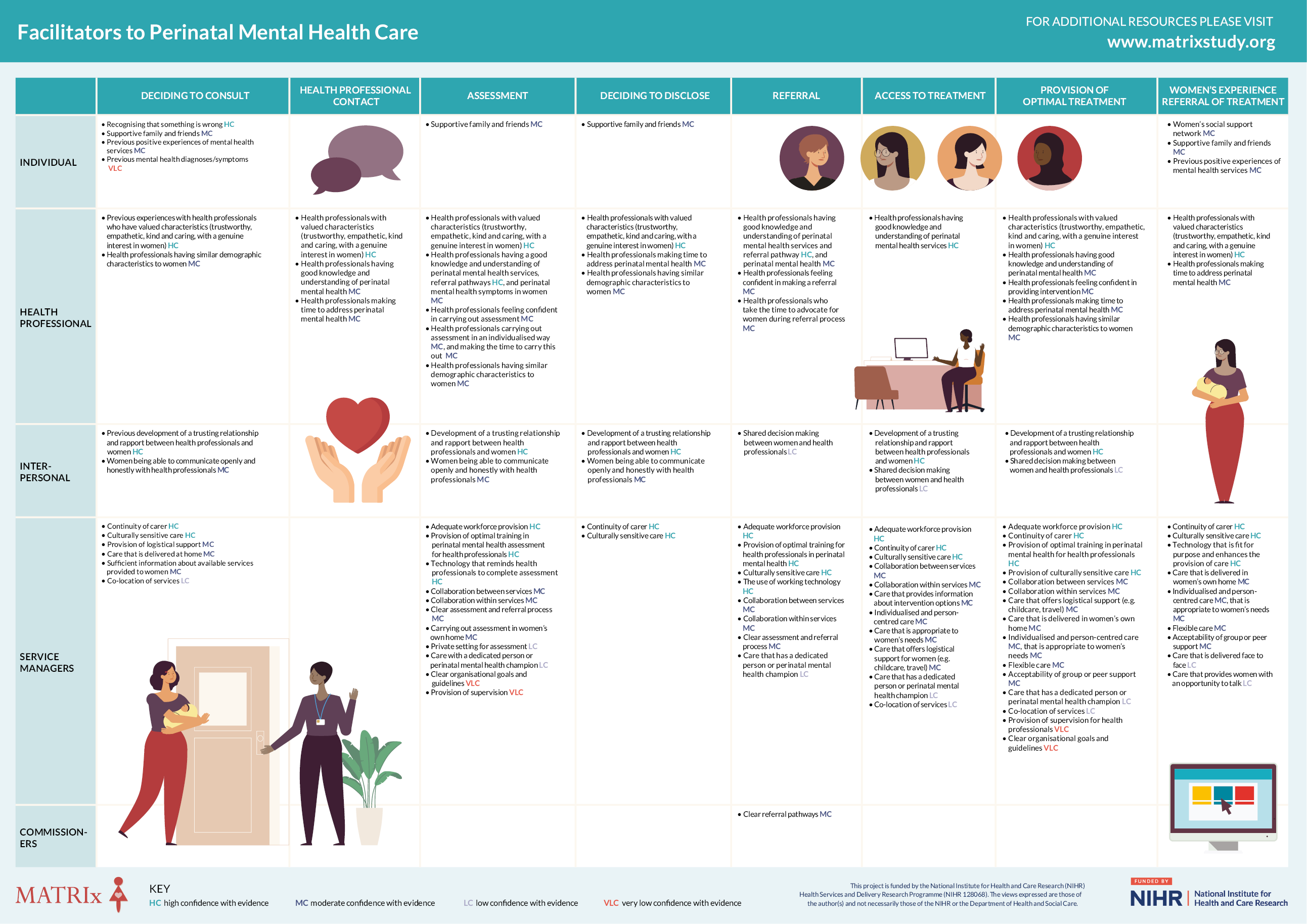
These conceptual frameworks were used to inform the development of evidence-based recommendations which aim to address these barriers and ensure that all women are able to access the support they need. Recommendations were made for policy, practice and researchers.
Confidence in results
The confidence in the results will now be discussed, based on the results from the CERQual ratings (see Appendix 6). It should be noted that all papers were included in the CERQual ratings and were not split by stage of the care pathway.
Of the 78 concepts identified, 14 were assigned a rating of high confidence with the evidence. These included women’s fear of social services involvement or their child/children being removed from their care; HPs knowledge about PMH services and referral pathways; HPs being dismissive or normalising women’s symptoms; HPs valued characteristics (e.g. warm, genuinely interested, kind, empathetic); trusting relationship between women and HPs; language barriers; adequate workforce provision; high-quality training for all HPs; continuity of carer; culturally sensitive care; lack of appropriate or timely services to refer women on to; and stigma, culture and maternal norms.
Just under half of concepts (n = 33) received a rating of moderate confidence. These concepts included being judged as a bad mum, support (or lack of support) from family and friends; HPs confidence in addressing PMH; HPs not recognising help-seeking or PMI; HPs carrying out assessment in a person-centred way with open and honest communication between women and HPs; collaboration within and between services; clear assessment and referral procedures; services that offer logistical support for women; individualised and appropriate care provision; a lack of clear referral pathways; and the economic status of women.
Slightly fewer (n = 25) concepts received a rating of low confidence, suggesting more research is needed. These concepts included women’s knowledge and understanding of the causes of mental illness, and where to go to seek help; demographic factors such as the woman’s ethnicity or current symptoms/diagnoses; HPs focusing too much on the infant; shared decision-making between women and HPs; co-location of buildings; care with a dedicated mental health champion; and care that offers an opportunity to talk.
Only four concepts received a very low confidence rating, suggesting more research is needed into women’s age or previous diagnoses/symptoms impacting help-seeking and access; the provision of supervision within organisations; and organisational guidelines.
MATRIx framework of barriers to perinatal mental health care
The MATRIx conceptual framework of barriers to PMH care is made up of factors that prevent the implementation of, or women accessing, PMH care. The MATRIx conceptual framework of barriers is shown in Figure 12.
Individual level barriers with moderate and high confidence in the evidence included (in order of evidence confidence): being scared of social services involvement or being judged to be a ‘bad’ mum; having a lack of support from family and friends or them having negative perceptions about PMI; being socially isolated; not understanding HPs’ roles in relation to PMH; not understanding what PMI is, or believing PMI symptoms are due to physical causes, or are a normal part of motherhood; believing the best way to cope with symptoms is to ignore them, or minimise them; and lastly, previous negative experiences of mental health care.
HP level barriers with moderate and high confidence included: HPs being dismissive or normalising women’s symptoms or not recognising help-seeking or symptoms; appearing too busy; having poor knowledge about services, referral pathways and PMH in general; HPs having low confidence about addressing PMH; and lastly HPs carrying out assessment or screening in a tick box or impersonal way.
Interpersonal level barriers with moderate and high confidence were: no trusting relationship between HPs and women; language barriers; and a lack of open and honest communication.
At the organisational/service manager level, barriers with moderate and high confidence in the evidence were: inadequate workforce therefore HP’s workload is too heavy; inadequate provision of PMH training for HPs; lack of continuity of carer; lack of culturally sensitive care; difficulties with technology related to care; lack of collaboration within and between services; lack of logistical support offered by a service; insufficient information provided about the care; inflexible care; care that is not appropriate to women’s needs; confusing wording of assessment tools; assessment of screening viewed as unacceptable; and lastly, unclear or confusing assessment and referral processes within an organisation.
At the commissioner level, all three barriers had high or moderate confidence with evidence, and these were: lack of appropriate or timely services; complexities of funding, resources and financial reimbursement; and lastly, confusing referral pathways.
Political level barriers rated as having moderate confidence with the evidence were: women being a refugee or immigrant, and a woman’s economic status tied in with the cost of health care.
At the societal level, stigma, culture and maternal norms were all rated as having high confidence with the evidence.
MATRIx framework of facilitators to perinatal mental health care
The MATRIx conceptual framework of facilitators to PMH care is made up of factors that aid the implementation of, or women accessing, PMH care. The conceptual framework for facilitators to PMH care is shown in Figure 13. Fewer facilitators to PMH care were identified which suggests more research is needed.
Individual level facilitators with high or moderate confidence in the evidence were women recognising that something is wrong, having supportive family and friends and a strong support network. Previous positive experiences of mental health services were also a facilitator.
At the HP level, facilitators with high confidence ratings were: HPs possessing valued characteristics, such as being trustworthy, empathetic, kind, caring with a genuine interest; going above and beyond to meet women’s needs; and having knowledge of other services and referral pathways. Facilitators with moderate confidence were HPs having similar demographics to women; having good knowledge and understanding of PMH; feeling confident in addressing PMH; making time to address PMH; and carrying out assessment in an individualised way.
Interpersonal level facilitators were the direct opposite to the barriers. Development of a trusting relationship and rapport between HPs and women; and women being able to communicate open and honestly with HPs.
At the organisational/service manager level, facilitators with a high level of confidence were the provision of continuity of carer and culturally sensitive care for women; adequate workforce provision; and provision of optimal training in PMH. Furthermore, technology that worked well and was fit for purpose was a facilitator to PMH care. Facilitators with moderate confidence were individualised, person-centred, flexible care that is appropriate to women’s needs and delivered face to face; the provision of logistical support for women; or care that is delivered at home; group or peer support; sufficient information about available services; collaboration within and between services; and clear organisational assessment and referral processes.
At the commissioner level, one facilitator with moderate confidence was clear referral pathways.
Outputs from the MATRIx conceptual frameworks
The MATRIx conceptual frameworks were used as the basis to develop multiple outputs. The aim of these outputs was ensuring recommendations are disseminated and implemented. These outputs include:
-
an animation aimed at HPs and service managers to show what ‘best practice’ services look like;
-
an animation aimed at policy makers to show how PMH services should be designed;
-
infographics for HPs, service managers, commissioners and policy makers with recommendations on the best ways to design and deliver PMH care;
-
an infographic for women and families about ways to navigate an imperfect system;
-
a summary report with more detailed information about the MATRIx study, the conceptual framework and recommendations;
-
a website with clickable links, quotes and information about each part of the conceptual frameworks;
-
dissemination events during Maternal Mental Health Awareness Week (May 2022) where the conceptual frameworks and recommendations were presented to large audiences, and a Question and Answer session was held.
Chapter 8 Recommendations for policy and practice
International recommendations for implementing perinatal mental health care
The barriers to implementation identified in R1 were formulated into recommendations. Where consistent barriers were identified (e.g. lack of training), a recommendation to overcome this barrier was made (e.g. provide health care professionals with training). Where consistent facilitators were identified, a recommendation to utilise this facilitator was made. Finally, implementation strategies that matched the recommendations were drawn from a dictionary of implementation strategy terms and definitions. 99,100 These recommendations were made from an international perspective and are summarised in Table 7 and are discussed briefly below.
| Consistent barriers or facilitators identified by the review | Recommendation | Implementation strategies (ERIC implementation strategies) |
|---|---|---|
| Design of the care | ||
| Appropriateness of care Choice Clear delivery |
Women to have choice in the care they receive so that it is relevant, acceptable and fits in with their lifestyle. | Conduct local consensus discussions with providers and stakeholders (including women) so service design is relevant. |
| Continuity of carer Delivery in healthcare setting Delivery in home setting |
Women to be offered care that is appropriate to their individual needs. | If not in place, create new clinical teams by adding new disciplines which allows women choice in the care they receive. |
| Family Fitting in with women life style Flexibility |
Women to be given the choice about their family being involved in care. | Develop strategies with women to problem solve around uptake and adherence. |
| Language barriers Medication Open inclusion criteria |
Care should be woman centred, one to-one with continuity of carer. | Involve women and their family members in design of care and implementation efforts to ensure service delivery is acceptable to women and their families. |
| Patient centred Practical support Privacy and confidentiality |
Care should be delivered clearly and honestly, and each aspect of care should be clearly explained. | Obtain and use women and her families feedback to ensure service design is relevant. |
| Relevance to women Service integration Symptoms of psychological difficulties Technology |
Care needs to be easily accessible (e.g., open inclusion criteria, central location, ways women can access care to be well advertised in healthcare settings or the community). | Form partnerships with other agencies that can provide additional support (e.g., citizens advice, translation services). |
| Techniques women found useful Timing Trusting relationship Women’s additional personal difficulties |
Care to be flexible in terms of times of appointments and where they are offered (e.g., offering support during an infant health check, at home). | Where possible, locate main building in a central location with good transport links, use accessible sites with access for pushchairs, co-plan locations of appointments with women or consider home visits to increase access. |
| Women’s perception of the care Women’s reluctance or inability to attend Wording of assessment tools |
Additional practical support to be offered including childcare, travel expenses, links with citizens advice or social work. | Conduct local needs assessment to identify what is needed within the community. |
| A private space for women and HP feelings and care. Provision of interpreters or translations of assessment materials/therapy tools. Technology enabled care for both women and HPs, for example virtual consultations via only platforms (e.g., NearMe, Livi, Skype). |
Develop resource sharing agreements to enhance available space for service provision. Promote identification and building of working relationships and networks which will promote collaborative problem solving, pooled resources and shared goals. |
|
| Conduct local needs assessment to identify what are the most common languages spoken within the community. Recruit and train multilingual staff. Use data experts, through hiring or consultations to inform the management and use of data. |
||
| Use data warehousing techniques to integrate clinical records across facilities and organisations. Encourage co-production or user experience testing of technology to ensure ease of usability and integration into the workflow. |
||
| Characteristics of HPs providing the care | ||
| Communication between HPs Confidence of healthcare providers HPs’ perception Knowledge of healthcare providers Open and honest communication Previous experiences Training Trusting relationship |
HPs providing the care should be open, non-judgmental, willing to listen, motivated, sensitive to verbal cues and interested in women. Provision of a dedicated person to act as advocate Knowledgeable and confident healthcare providers who have had relevant training, including training in communication skills. HPs should feel positively about the care they are providing. |
HPs to receive accreditation for participating in training about, and providing high quality care, team working, and clear communication. Multidisciplinary working, and development of engagement across disciplines. Conduct ongoing training to ensure those providing the care are knowledgeable about PMH and the service provided. Create a learning collaborative to encourage learning of all providers, and therefore aid implementation. Identify and prepare champions to act as women’s advocatesMake training dynamic to ensure engagement with training. |
| Organisational factors | ||
| Clear workflow procedures Collaborative working Dedicated person Supervision |
A healthcare system that supports HPs through supervision, collaborative working and a clear point of contact. Clear workflow procedures so that each individual involved in the care understands their role. |
Conduct local consensus discussions with those providing the care, to ensure they feel the strategy is relevant for addressing women’s needs Involve key stakeholders from all levels in pathway mapping exercises to identify and solve blocks and barriers. Involve executive boards in the implementation effort to ensure they provide relevant resources needed. Organise implementation team meetings with HPs to ensure those in charge are given protected time to reflect on the implementation effort. Provide clinical supervision. |
| Political factors | ||
| Clear referral pathways | Global recommendations | Global implementation strategies |
| Funding Lack of appropriate or timely services Lack of resources |
Free healthcare or clear and easily accessible insurance policies where free healthcare is unavailable. | Access funding through charities, insurance policy income and other means. |
| Organisational structure Policy Women’s reluctance or inability to attend |
Adequate funding to ensure each PMH care has the practical resources it needs to function (e.g., support staff, staff development, online resources, medication). | Alter patient/consumer fees where free healthcare is not available, such as in the USA, create fee structures where women pay less for preferred treatments. |
| Ensuring there are clear pathways to refer to timely appropriate services. Ensuring healthcare policy is supportive of PMH services. |
Build a coalition of health visitors, midwives, primary care practitioners, psychologists and psychiatrists or international equivalents to encourage referral and reduce risk of women falling through care pathway gaps. | |
| Recruitment of more staff to ensure adequate resources for service delivery. UK recommendations Adequate funding to ensure there are appropriate services that women can be referred to within and across catchment areas (e.g., across NHS trusts). |
Promote identification and relationship building with other services such as social care, citizens advice, drug and alcohol services and charities to form partnerships whereby resources (including physical space for treatment) are shared ensuring women are provided with holistic support. Involve executive boards to ensure communication between desired innovation and funders. |
|
| Use other payment schemes to ensure service providers are rewarded for their work. Create or review a workforce development strategy to understand workforce needs and put actions in place to meet these needs. |
||
| UK implementation strategies Access new funding such as through application to the PMH Community Services Development Fund to facilitate service delivery. |
||
| Utilise commissioning guidance produced by National Collaborating Centre for Mental Health31 on service development. This includes multi agency working across health services and the care pathway; developing an understanding of local need; building a case for the new service model; creating staff recruitment and training plans and monitoring the impact of the new service. | ||
| Wider societal factors | ||
| Culture Family Health beliefs Medication Stigma |
Research suggests public mental health campaigns can increase knowledge about mental illness and improve attitudes about people with mental illness175–179. Therefore, increasing women’s families and public mental health literacy through education within the community, during childbirth classes and at healthcare appointments should be carried out. | Conduct local consensus discussions with providers and stakeholders (including women) to understand what is needed in terms of mental health literacy. Involve women and their family members in design of care and implementation efforts to ensure mental health literacy delivery is relevant, appropriate and delivered in the correct settings. |
R1 found that for successful implementation and delivery to occur, PMH care had to meet women’s needs. Therefore, the evidence suggests that service design may benefit from co-production. One potential way this could be done is illustrated by a UK based co-production service (Croydon Service User Network) where both the design and delivery of care is carried out by professionals and service users. This is a network where members participate in the running of the service, feedback their views and work alongside staff to help run group care programmes. 165 In addition, services could utilise toolkits such as The Co-Production Star which ‘enables organisations … to map how much co-production is already taking place, improve existing co-production approaches, identify the potential for new approaches and scale out co-production across services and communities’. 166
R1 found that choice of care and personalised care was key to implementation and delivery. Therefore, the evidence suggests that in services where this is not already implemented, multidisciplinary teams should be created to facilitate choice and personalised care and ensure an adequate workforce to meet women’s needs. The building of a coalition of health visitors, midwives, GPs, therapists, psychologists and psychiatrists is needed to encourage referral and reduce the risk of women falling out of the care pathway. Collaboration between services is also needed with a focus on the identification and building of working relationships and networks with other services (e.g. Citizens Advice).
Many individual level barriers to implementation and delivery of PMH care identified in R1 related to logistical issues. Women could not always attend appointments because of the inflexibility of services. The evidence suggests that increasing the flexibility and accessibility of services could be done through offering home visits. Where this is not possible, providing out-of-hours appointments in a location with good transport links and an accessible building to allow for pushchairs or provision of virtual consultations using web-based platforms such as NearMe (approved for use by the Scottish Government)167 or Livi (an accredited NHS supplier)168 is recommended.
R1 found that technology can be a facilitator to implementation, for example through reminders to assess women’s mental health,116 online referral systems127 and online interventions. 114,146 However, where technology was not fit for purpose, this was a barrier. This evidence suggests that technology should be co-produced with HPs and women, to ensure ease of usability and integration into the workflow. Evidence outside of the review suggests it is also important that in-person consultations are offered where possible because of the challenges of using virtual consultations in areas of high deprivation and with those for whom English is not their first language,169 as there is a risk of increasing health inequalities. 170,171
R1 found that a lack of training was a significant barrier to implementing PMH care. The evidence suggests that HPs should be provided with necessary training in PMH in order to provide a high-quality, evidence-based service. Ensuring HPs provide innovative care can be encouraged through creating accreditation or membership requirements and a learning collaborative. It is also important that HPs work in an organisation that supports their efforts to provide high-quality PMH care. Involving executive boards and ensuring HP implementation team meetings will encourage managerial understanding and should therefore promote effective implementation.
The evidence from R1 suggests that funding complexities and difficulties are a barrier to implementation. Funding is required to ensure high-quality care provision. This suggests that funding needs to be available, easily accessible and ring-fenced at a local level in order to prevent essential PMH funds being diverted to other local services. 172 Funding structures may need to be revised depending on the needs of the community in which the service is delivered (e.g. affordable health insurance where free health care is not available). 173,174
International recommendations for perinatal mental health care
The barriers identified from women’s perspectives in R2 about help-seeking and accessing PMH care were used to develop recommendations about the optimal characteristics of PMH care. These are made from an international perspective and are summarised in Table 8.
| System level factor | Theme | Recommendation |
|---|---|---|
| Societal | Stigma Culture Maternal norms |
International, culturally sensitive public mental health campaigns to increase knowledge about mental illness and improve attitudes about people with mental illness. The continuation of international policies to promote gender equality. |
| Political | Immigration and economic status Healthcare costs |
Equal rights to healthcare. Free health care. Laws to protect those with immigration status. |
| Organisational | Lack of services/overstretched services Characteristics of the service Collaboration across services |
Individualised and culturally appropriate care co-designed with women. Improved funding for PMH services. Improved guidance for implementing PMH care.a |
| Interpersonal | Continuity of carer Relationship and rapport Language barriers Shared decision-making Communication Information provision |
Training in communication skills. Training in PMH to reduce stigma. Training in cross-cultural presentations of mental health difficulties. |
| HPs | Characteristics Time Training and knowledge |
Training in communication skills. Training in PMH to reduce stigma. Training in cross-cultural presentations of mental health difficulties. |
| Individual | Beliefs about health services Beliefs about HPs Beliefs about mental illness Fear of judgment Logistics |
Improvement of mental health literacy. Free access to health care. Woman-centred care. |
R2 highlighted a complex interplay of multi-level factors that influence women’s help-seeking and access to PMH care. Societal factors such as stigma, maternal norms and culture play a large role in women accessing care and the effects can be seen in all system levels. Research suggests that public mental health campaigns can increase knowledge about mental illness and improve attitudes about people with mental illness. 175–179 This evidence therefore suggests public health efforts need to be made to increase women’s, families’ and the public’s mental health literacy through public health campaigns, education within the community, such as antenatal education, and at health care appointments.
R2 found that maternal norms were associated with women believing that they needed to be strong and show they could cope. Maternal norms were a barrier to women accessing PMH care. Research suggests that there may be some potential to change societal beliefs around maternal norms through increasing societal expectations about fathers’ roles in the family through more equal parental leave and rights. For example, in countries where parental leave is more equal (e.g. Finland), the uptake of paid paternity leave is higher. 180 Changing society’s maternal norms could also be achieved through increasing women’s equality. For example, research suggests that stereotypes of what a mother or a woman should look like are beginning to change in countries where women have gained more participation in the labour force181–183 and have the right to access contraception and abortion. 184–186 However, research is needed to corroborate these findings.
At the political level, R2 identified that immigration and economic status and health care costs were barriers to women accessing PMH care. The results also show how race and gender interact to influence women’s experiences of the health care system (intersectionality). 187 This finding is supported by research in general health care that has found ethnic minority and migrant women are disproportionately affected by existing barriers to accessing health care. 188,189 R2 found that these barriers include language and communication barriers, stigma, the cost of health care190 and the inability to access culturally appropriate services. 191 The evidence shows the need for equal rights to health care, regardless of immigration or economic status. The evidence also suggests that changes at the legislative level are needed to protect those who have migrated to a different country from being penalised for accessing health care. 190,192
At the organisational level, R2 identified a range of factors that women viewed as ideal care. Women appreciated the opportunity to discuss screening results with HPs and for it not to be filled out as a tick box exercise. 89 In terms of treatment, women wanted the opportunity to talk to someone (a HP or a peer) about their difficulties. 72,75,81,84,94,193 They found peer support offered them a sense of validation which they appreciated. 79 Further, the evidence suggests that the length of treatment should be flexible and based on women’s needs. Women did not want a one-size-fits-all approach but wanted personalised care that was culturally appropriate. 46,48,49,72,75,84,90,91,95,96,193
At the interpersonal and HP level, the characteristics of the HPs were important, as was their communication with women. Women reported that some HPs normalised their symptoms or were dismissive of their attempts to seek help at first contact, or assessment. This could be a reflection of inadequate training. 194–197 Another key training need is cultural sensitivity and cross-cultural understanding of PMH. Some reviews in R2 identified that women were treated in a culturally insensitive way by HPs, and that ethnic minority women were less likely to be offered treatment or be asked about their mental health. 198–206 The evidence suggests that it is therefore crucial that communication, cultural sensitivity and cross-cultural mental health training are provided to HPs.
In terms of individual level factors, many of these barriers can be improved through the recommendations suggested above. For example, improvement of knowledge around mental health is likely to reduce a woman’s fear of judgment, self-stigma and increase her awareness of the symptoms she is experiencing which may encourage help-seeking. 207,208
UK recommendations for policy and practice
Recommendations for UK practice and policy were developed from recommendations provided by the stakeholder consultations and the conceptual framework. During the stakeholder consultations, attendees were asked ‘In your view, what are the top recommendations for clinical practice?’ Answers to this question can be found in Table 9. In terms of the conceptual frameworks, where the confidence with the evidence was low or moderately low, recommendations for future research were made (see Chapter 9). Where a concept had high or moderate confidence in the evidence, a recommendation to enact this concept in practice was made. This was firstly done by reframing the barriers into answers to the question ‘What would help to improve PMH identification, assessment and treatment?’, and by looking at the guidance provided by stakeholder groups in relation to recommendations. Examples of good practice were also taken from the stakeholder consultation events, and from the NHS Future Platform (see Table 10). Each recommendation has a number next to it which relates to the audience the recommendation is aimed at. Additional information related to the recommendations can be found in Box 3. Recommendations are for third-party organisations, HPs, service managers, government and commissioners and the four devolved NHS oversight organisations (e.g. NHS England).
| Women and families | HPs | Policy makers and commissioners |
|---|---|---|
Training
|
Training
|
Training
|
Service provision
|
Service structure
|
Service structure
|
Stakeholder specific recommendations – silos
|
Stakeholder specific recommendations – commissioning
|
|
|
|
|
Stakeholder specific recommendations – IT
|
| Evidence | Recommendations | |
|---|---|---|
| Women |
|
1Development of information aimed at increasing awareness of PMI such as (1) infographics/leaflets disseminated through maternity services, primary care, third sector organisations (e.g. NCT), and antenatal classes (2) short animations and videos disseminated via social media on:
|
|
2–4Provision of care that meets women’s needs is flexible, easy to access and provides childcare | |
|
4A fair welfare and economic system that ensures that no one is living in poverty or in financial hardship | |
| HPs |
|
2–4Provision of an adequate number of workers to meets women’s needs (see below) |
|
2Multidisciplinary meetings, co-location, encouragement of a culture of team working, joint working, sharing knowledge, and approachability a(see Box 3) | |
|
2&4Implementation of PMH good practice guides209 which cover: | |
|
|
|
|
5Participates in CPD activities related to PMH including participating in high quality training (see below). Consider HPs receiving accreditation for participating in training100 | |
|
2&4Recruitment of staff positive interest and attitude towards providing high quality care to women. Consider HP receiving accreditation for providing high quality care, team working, and clear communication100 | |
| Interpersonal |
|
2Recruit translators or form partnerships with other agencies that can provide additional support (e.g., translation services, interpreters100) to translate infographics/leaflets into local languagesb and to act as an interpreter at appointments if women feel comfortable. 2Investment in live translation tools or telephone interpreting such as Language Line. |
|
2–4Provision of continuity of carer across the care pathwayc | |
| Service managers |
|
2–4Ensure an adequate workshop to meet needs by utilising a workforce planning tool210 and considering if there are a sufficient number of people in each of the key roles (psychiatrist, pharmacist, nurse, psychologist, occupational therapist, support staff, admin, peer support). Ensure a diverse workforce211 |
|
2–4Clear & easily accessible guidelines on where to refer women to depending on their need. Development of one referral form that can be uploaded and amended, discussed at multidisciplinary team meetingsd. Encouragement of a workspace that involves co-location, a culture of team working, sharing knowledge, approachability | |
|
2&4Provision of training for all people working in a health service. Consider the use of simulation traininge. Training should:
|
|
Training should cover:
|
||
|
2Encourage co-production or user experience testing of technology to ensure ease of usability and integration into the workflow. Employment of a liaison person who has access to all systems to bridge the gap between different services. 6Using compatible IT systems for easy access to information. |
|
|
2&4Encourage co-production of caref. Collaborate with organisations such as The Motherhood Group to ensure care is culturally appropriate. Provide peer support to women who feel it would benefit them. Consider provision of home visits for care and deliver care face-to-face. If home delivery is not possible, ensure practical support is available such as childcare. | |
|
2&4Use easy to understand assessment tools. Collaborate with organisations such as The Motherhood Group to ensure cultural appropriateness. Design or update assessment tools that use pictures alongside words for use with women whose English speaking and understanding is limitedh. Ensure HPs have enough time to carry out assessment by creating an adequate workforce (see above) 5Provide assessment in a woman-centred way. Explain questions or wording that women are not clear about. Clearly discuss results with women and explain next steps. |
|
| Commissioners |
|
4&6To provide services that meet the needs of the population, commissioners must212:
|
|
4&7Continued policy support from NHS England, and NHS related to PMH care, such as the publication of the Five Year Forward View28 and Long Term Plan33, NHS England, and Delivering Effective Services214 report for NHS Scotland. | |
| Government and regulatory bodies |
|
4Free health care for all at the point of accessj Suspension of NHS charging regulations until a full independent review of their impact on individual and public health, simplification of charging criteria and exemptions and safeguards to protect vulnerable patients and ensure they are not denied the care they are entitled to, is carried outk 4A fair welfare and economic system that ensures that no one is living in poverty or in financial hardshipl |
|
4The provision of a comprehensively researched and adequate budget provided to the Department of Health and Social Care, Health and Social Care Directorates and so all healthcare needs for that financial year can be met 4Where possible, reduction of in-year funding changes in England so local areas know exactly how much they can spend at the start of the year215. |
|
| Society |
|
4&7NHS Mental Health Campaign focused on stigma reductionm |
-
The Greater Manchester Perinatal Parent Infant Mental Health Model of care works within an integrated system, making sure all services work together, preventing silo style working216
-
ACACIA Family support provide pre and postnatal depression support services. They have translated patient information into multiple languages (Arabic, Bengali, Chinese, French, Hindu, Polish, Punjabi, Romanian, Samoan and Urdu). 217
-
The Tower Team based in the Tower Hamlets, London is a high-risk caseload midwifery team that works closely with the perinatal mental health team and the consultant obstetrician for mental health at St. Thomas hospital. The tower teams offer continuity of care for women with severe mental illness from their maternity booking appointment throughout the pregnancy, intrapartum and for up to 28 days postpartum. 218
-
Perinatal Mental Health Service at South West London and St Georges Mental Health NHS Trust.
-
Brighton and Sussex University Hospitals NHS Trust provide Perinatal Mental Health Simulation Training on the identification and management of common perinatal mental health problems using actors and real life settings.
-
The Motherhood Group provide training related to engaging with black women. 219
-
One example of a successful co-produced service is the co-production of perinatal mental health services in Ealing, Hammersmith, Fulham & Hounslow. There was strong engagement with lived experience experts from the start. 218
-
For example, How are you feeling screening tools by Abi Sobowale (Sheffield South West NHS Trust)
-
A guide for commissioning services is available for London. However, this was published in 2017 and needs updating in line with this conceptual framework. 218
-
Despite the NHS being free for UK residents, there are NHS charging regulations in place for those who are not residents of the United Kingdom. NHS charging regulations have a large negative impact on pregnant and postnatal women, in terms of their mental health220 increasing stress and anxiety, their vulnerability to domestic violence221 and maternal deaths that may have been prevented through access to antenatal care. 222,223 Furthermore, Public Health England has identified NHS charging for maternity care as one of the key issues that exacerbates poorer health outcomes for women and babies of colour. 224
-
This recommendation is in line with: (a) a joint statement set out by the Royal College of Physicians, the Royal College of Paediatrics and Child Health, the Royal College of Obstetricians and Gynaecologists and the Faculty of Public Health in 2018, calling for a suspension of NHS Charging;225 (b) a statement from the Academy of Medical Royal Colleges in 2019 released a statement calling for the suspension of the NHS charging regulations until a full independent review on individual and public health is carried out;226 (c) a statement from the Royal College of Paediatrics and Child Health calling for an end to NHS charging due to its adverse effects on child health and wider public health;227 (d) a report from Maternity Action calling for the immediate suspension of charging for NHS maternity care given the different effect on women access to maternity care. 228
-
Everyone has the right to a standard of living adequate for the health and well-being of [them]self and of [their] family, including food, clothing, housing and medical care and necessary social services, and the right to security in the event of unemployment, sickness, disability, widowhood, old age or other lack of livelihood in circumstances beyond [their] control and to ensure “motherhood and childhood are entitled to special care and assistance. All children, whether born in or out of wedlock, shall enjoy the same social protection.
-
Based on research suggests public mental health campaigns can increase knowledge about mental illness and improve attitudes about people with mental illness. 175,177,179
-
The Future NHS Platform for National Perinatal Mental Health provides examples of pathways and system delivery models: Maternal mental health services-> MMHS Resources-> 3. Pathways and system delivery models
It is important to note that these recommendations were developed during the COVID-19 pandemic, which had a large impact on the delivery of health services. In terms of PMH care, level of demand for PMH services increased, whereas staff capacity decreased due to illness, school closures and staff being redeployed to COVID-19 health care. There was a significant increase in digital service provision and a reduction in face-to-face services. These changes posed challenges for both services and women. The impact of these changes is still being felt now, and the Maternal Mental Health Alliance has called on the UK government to future-proof PMH services against future pandemics and public health crises. They recommend that this is done by the UK government guaranteeing a minimum high standard of mental health care for pregnant women and mothers of young infants. Thus, although the recommendations of the MATRIx conceptual frameworks may be difficult to achieve in the current climate, the recommendations can be used alongside the Maternal Mental Health Alliance’s recommendations to design and deliver best practice, and future-proof care. 229 While recovery from COVID-19 and capacity issues may still be being resolved, it is still important to look towards the future in the design and delivery of services.
Recommendations for third-party organisations
The results from both reviews, stakeholder discussions and the development of the conceptual frameworks indicate that women may not always have a clear understanding of PMH and the services available. This suggests that the development of information aimed at increasing awareness of PMH would be beneficial. Therefore, recommendations for third-party organisations, such as the National Institute for Health and Care Research Applied Research Collaboration (NIHR ARC) Maternity, Mental Health and Perinatal Mental Health Themes, and the Royal Colleges include: (1) collaborating to develop infographics, leaflets, short videos and animations to increase women’s awareness of PMI; and (2) the recommissioning of public mental health campaigns aimed at reducing stigma related to mental illness. The evidence reviewed, stakeholder discussions and the structure of NHS funding show that commissioners are important in ensuring that PMH is funded appropriately, and referral pathways are developed. This suggests that third-party organisations should also develop guidelines on commissioning PMH care and referral pathways for commissioners.
Recommendations for health professionals
The research identified found that HPs may lack time, confidence and knowledge to address women’s PMH concerns. Therefore, it is recommended that HPs participate in continuing professional development (CPD) activities related to PMH, including participating in high-quality training.
Recommendations for service managers
The evidence reviewed and feedback from stakeholders suggest that PMH care needs to be appropriate to women’s needs. This could be by offering women choice in the type of care they receive, ensuring care is culturally appropriate and inclusive, and offering continuity of carer when possible. The evidence therefore suggests that service managers should provide care that: (1) meets women’s needs. This may include peer or group support, as well as logistical help. It is recommended that, where possible, care is co-designed with women and organisations such as The Motherhood Group to ensure care is culturally appropriate; (2) uses easy to understand assessment tools, including pictorial aids; (3) ensures the recruitment of translators or formation of partnerships with other agencies that can provide additional support (e.g. translation services, interpreters);100 (4) where possible, provides continuity of carer across the care pathway, for example, relationship-based GP practice care, where the same GP sees the mother each time she consults. 230
To provide high-quality care, the evidence reviewed and stakeholder meetings suggest that services managers should: (5) ensure an adequate workforce to meet women’s needs by utilising a workforce planning tool;210 (6) recruit staff with a positive interest and attitude towards providing high-quality care to women; (7) provide training for all people working in a health service, including receptionists and administrative staff, and consider the use of simulation training. Training must be time-protected; (8) encourage a culture of multidisciplinary team working, joint working and knowledge sharing; (9) design clear and easily accessible guidelines about referral and assessment pathways within the organisation; and (10) encourage co-production or user experience testing of technology to ensure ease of usability and integration into the workflow. Use the same IT systems across all NHS trusts/health services. Where this is not possible, consider the employment of a liaison person who has access to all systems to bridge the gap between different services.
Recommendations for policy makers
Many elements of the conceptual frameworks can be modified by policy makers and government activity, for example, workforce provision, health care capacity, training, etc. Therefore, we recommend that policy makers review the MATRIx frameworks and use them to inform development of comprehensive, strategic and evidence-based services to ensure effective PMH care.
At a more specific level, the evidence reviewed and feedback from the stakeholder groups suggest that policy makers and commissioners should: (1) provide adequate financial resources to ensure that service managers are able to meet the recommendations given above; and (2) design clear referral pathways and ensure a clear and easy to access funding structure. Furthermore, guidelines for commissioners suggest that commissioners should have a good knowledge212 about PMH, and that people with lived experience are consulted prior to decisions regarding the commissioning of services being made. 213
At the governmental level, the research identified suggests that immigration and economic status and health care costs were barriers to women accessing PMH care. The results also show how race and gender interact to influence women’s experiences of the health care system (intersectionality). 187 The evidence shows the need for equal rights to health care regardless of immigration or economic status. The evidence also suggests that changes at the legislative level are needed to protect those who have migrated to a different country from being penalised for accessing health care. 190,192 To reduce these health inequalities identified by the reviews further, we recommend free health care for all at the point of access for everyone. A recent report by Maternity Action has highlighted the impact that NHS Charging has had on refugee and immigrant women in deterring help-seeking and access. 228 We thus also recommend suspension of NHS charging regulations until a full independent review of their impact on individual and public health is carried out, a recommendation in line with multiple organisations. 225–228 To further reduce health inequalities in access to PMH care, we recommend the development of a fair welfare and economic system that ensures that no one is living in poverty or in financial hardship.
Furthermore, evidence from the reviews and stakeholder discussions (see Table 9) suggest that the current funding structures for health care are complex and adequate funding can be difficult to access. NHS England is also subject to funding changes throughout the financial year,215 making it difficult for commissioners and service managers to plan services. We therefore recommend the development of a clear and easy to access funding structure for commissioners and service managers, equality of funding distribution and adequate funding provision to ensure service needs are met. This recommendation is reliant on the provision of a comprehensively researched and adequate budget provided to the Department of Health and Social Care and Health and Social Care Directorates, and a reduction of in-year funding changes in England so local areas know exactly how much they can spend at the start of the year.
Chapter 9 Discussion
Summary of results
The research detailed in this report reviewed the evidence on barriers and facilitators to implementing PMH care, and to women seeking help and accessing PMH care and treatment. Results from reviews were then synthesised and two conceptual frameworks of key barriers and facilitators to PMH identification, assessment, care and treatment were developed. The conceptual frameworks (see Figures 12 and 13) were developed using an eight-stage approach set out by Jabareen (2009)56 and are based on evidence from 46 primary research papers on implementing PMH care (R1), and 32 systematic reviews on women’s barriers and facilitators to accessing care (R2).
These frameworks were used to provide evidence-based recommendations for international and NHS policy, practice and future research. The MATRIx frameworks led to the identification of 22 evidence-based recommendations for practice and commissioning. Despite being aimed at different stakeholder groups, these recommendations are all highly intertwined and the uptake of one would be likely to have positive effects on others. For example, the continuation of prioritising funding for PMH services by the government231 and NHS England33 will impact on the amount commissioners can allocate to PMH services, thus impacting on the workforce, increasing opportunities for continuity of carer models, staff training and other resources such as translators and logistical support.
Relevance to the wider literature on perinatal mental health
At the individual level, barriers identified included no family support for mental health difficulties, lack of awareness or knowledge about PMH, beliefs about medication, reluctance or inability to attend mental health services, previous experiences of mental health services and additional personal difficulties. It is important to note that these individual level factors do not develop in isolation but often compound one another. For example, women’s beliefs about health services and HPs are likely to come from their previous experiences of health services. This is supported by research carried out with other populations such as young people,232 suicidal people207 and refugees233 that found previous experiences of health care influences help-seeking behaviour.
Societal factors, such as stigma, maternal norms and culture, are likely to play a role in women’s fear of judgment about acknowledging PMH difficulties. The systematic reviews showed a clear overlap between feeling judged as a bad mother, maternal norms to be strong and able to cope, and stigma. Further, some cultural understandings of PMI increase this fear and stigma. R2 found that women from black, Asian and Hispanic backgrounds living in Western countries were more likely to believe symptoms of mental illness were seen as a sign of weakness, or failure, and such symptoms were highly stigmatised in their culture. 46,47,89,90,95 This finding is supported by previous research that has found stigma is one of the leading barriers to help-seeking234–236 and that certain cultural beliefs may amplify the effects of stigma. 237–239
Women also faced logistical challenges such as lack of childcare and lack of transport facilities to access care. These factors were linked to political factors such as economic status. For example, where women had low or no income, other factors such as unstable housing took priority. 82 Women who had migrated into a country had additional barriers such as fear of deportation for accessing health care, or an inability to obtain healthcare insurance. 70
At the HP level, a facilitator to implementation was HPs having a positive perception of the care provided. For example, where HPs internalised the value and importance of assessment, they would be more likely to assess women. This is in line with several implementation theories, such as the internalisation aspect of the Normalization Process Theory,240,241 the Diffusion of Innovation Theory and the Technology Acceptance Model, all of which suggest that users’ perceptions of an innovation are important for their decision to use an innovation. 242–244
Other facilitators to implementation were HPs who were genuinely interested in women, took time to listen and were kind and caring. This genuine interest in women suggests that intrinsic motivation, which is where individuals perform a certain action or behaviour for personal satisfaction without any external reward (e.g. praise or money),245 may play an important role in the implementation of PMH care. Health care providers are increasingly utilising payment for performance models,246,247 such as the payment by results system used within the NHS to improve implementation. These models are based on performance improving with extrinsic motivation and, while there is some evidence that this method works,247 the results from this evidence synthesis did not reflect this. Furthermore, for HPs to act on intrinsic motivation to be kind and to care for people, they need to be working in a well-resourced setting and not experiencing burnout. Burnout is associated with compassion fatigue,248 which is a term used to describe HPs becoming disconnected from or desensitised to patients and patients’ families. 249 Both burnout and compassion fatigue are associated with negative outcomes for patients, such as HPs being less engaged with patients, as well as negative outcomes for HPs themselves. 250 Therefore, it is important service providers ensure that they have an adequate workforce and have support in place to ensure staff well-being.
Another HP level barrier was normalising women’s symptoms or not recognising their attempts to seek help, particularly at first contact. This is probably partly due to a lack of time and training. For example, one of the most cited barriers identified across both reviews was HPs’ heavy workloads, meaning they do not have the time to address PMH. For example, research suggests that consultations where mental health problems are discussed take longer, and HPs feel there is not enough time to address concerns fully. 251,252 Research also suggests that inadequate training in mental health is associated with feelings of anxiety and fear around patients with mental illness, a desire to avoid them, and less effective treatment. 194 This may mean HPs close down conversations about PMI prematurely. Women’s decision to disclose is related to HPs getting it right the first time. Therefore, it is important there is adequate time and training for HPs to feel confident addressing PMH, so every woman gets the response she needs the first time, whomever she sees.
At the interpersonal level good communication, allowing for clear information provision and shared decision-making between women and HPs facilitated women continuing along the care pathway. The systematic reviews in R2 suggested that women were not always included in decision-making regarding medication48 or referral72 and this impacted on their experience of care. Poor communication was further exacerbated by language barriers and women experienced culturally insensitive care from HPs. 89,96 Previous research also supports these findings, showing that communication with HPs influences individuals’ experiences of care. 253,254 Good communication between women and HPs is more likely to develop where there is continuity of carer. A real-life example of this is the lack of relationship-based care carried out in general practice. In a survey of 43 GPs, less than a quarter had responsibility for ongoing contact with the same patients, meaning it impacted their ability to see women in the perinatal period on a regular basis. 34 As identified in this work, lack of contact on a regular basis limits opportunities to develop trusting relationships.
At the organisational level, lack of services, the characteristics of the services (i.e. prioritisation of physical health, no language support services, difficult to access location, the need to attend appointments without the baby) and poor collaboration across services were barriers. These barriers have also been identified in other systematic reviews of help-seeking and health care access. 232,255,256 Poor collaboration across and within services is often due to working in ‘silos’. Organisations are often made up of multiple teams, divisions or departments. These can act as physical silos which prevent certain groups of individuals from working with one another. However, silos are not always physically present within an organisation, they may also be based on employees’ beliefs257 (e.g. we are the midwives, they are the doctors). It is argued that silos provide a feeling of safety by keeping ‘those who are not like us’ out. 258 However, this can create an ‘us-and-them’ mentality which can fragment organisations. 259
Furthermore, working in silos promotes groups achieving their own goals, rather than everyone working together to meet an overall goal. 260 It is therefore not surprising that research suggests that silo working within the NHS can have a negative impact on care. For example, one study found that silo working led to increased length of hospital stay. 261 The NHS has published multiple documents on breaking down silo working, both within the NHS and in terms of links with outside organisations. For example, in the Five Year Forward View28 one of the aims was to ensure better integration between health and social care through multidisciplinary working and providing more holistic care. 262 Furthermore, the NHS Long Term Plan33 sees the future of the NHS as investing in and working with the local community to improve the health of those living within that community. 263 Therefore, it is important that these plans are implemented successfully to improve the care provided to these individuals.
Limitations and recommendations for future research
For both reviews, a decision was made to only synthesise literature carried out with perinatal women. This means that the results from this review may not be generalisable to fathers, partners and families. Fathers’ and partners’ PMH is important so this is an area that requires research and evidence synthesis in its own right. Given that the NHS Long Term Plan has set aside money for the delivery of mental health checks for fathers/co-parents of women receiving specialist community PMH care,33 it is important to conduct research to understand the barriers and facilitators of PMH care for fathers, birth partners and co-parents.
These reviews also excluded services for substance misuse because these disorders raise unique challenges in terms of assessment and treatment that may not be generalisable to other disorders. Future research is therefore needed to understand the needs of women who suffer from substance misuse disorders. Furthermore, for both reviews a limitation of the methodology is that only reviews published in academic journals and written in English language were included. Relevant reviews from health services, charities, third-sector organisations and other grey literature may have been missed.
For R1 the large number of citations meant a decision was made to double screen 10% of abstracts so some papers may potentially have been missed. However, the high concordance of the double screening conducted makes this unlikely. Similarly, only 10% of papers included in R1 had dual critical appraisal of methodological quality which may have influenced the results of this appraisal. However, no papers were rejected on the basis of quality making this less problematic. Similarly, in R2 only 10% of studies had duplicate data extraction. However, concordance was high, so it is unlikely that any key themes were missed.
In terms of the development of the conceptual frameworks, the use of CERQual to evaluate confidence in the findings is a strength, but ratings were done by one researcher (Rebecca Webb) which may mean they are slightly less valid. However, the CERQual approach is described thoroughly and specific rules for each of the assessments were discussed and agreed with the research team to ensure ratings were standardised (see Appendix 6).
There are also some limitations in terms of the evidence included in the reviews. For example, there was a lack of research carried out in specialist services or for women with severe PMI. None of the implementation papers in R1 examined these. Only two reviews in R2 included studies of women with postnatal psychosis or postnatal PTSD, and only three included studies directly related to specialist PMH services. There may be different barriers for other PMH difficulties difficulties therefore future research should focus on researching the barriers and facilitators to women with disorders other than depression (anxiety, PTSD, OCD) as well as more severe PMH difficulties, and issues for neurodivergent women (such as those with autism who are at high risk for anxiety and depression). 264,265 Linked to this, only three studies from one review were directly related to admission to hospital beds, which is the fourth filter of the Goldberg and Huxley (1992)41 model. Given the large gaps in inpatient PMH service provision across the UK and globally,266–268 future research is needed that focuses on the implementation of mother-baby psychiatric units, or international equivalents. Furthermore, more research is needed that focuses on the provision of PMH care for women in universal services. UK evidence suggests primary care is the main provider for PMH care, with 90% of common mental disorders being managed in primary care services. 41 Therefore, we need to understand what changes are needed to improve care provision in universal services.
Most research included in R1 and R2 only looked at barriers to PMH care. This can be seen from the conceptual frameworks, where far fewer concepts are included in the framework of facilitators (see Figure 13) compared to barriers (see Figure 12). Furthermore, most of the research identified was carried out in HICs, meaning we still are not able to have a full cross-cultural picture of barriers and facilitators to PMH care. There was some evidence that beliefs that mental health difficulties being caused by spiritual factors were a barrier to women accessing help, because it was believed the best person to help would be a spiritual leader. However, studies carried out with ethnic minority women and those living in non-western countries or cultures were sparse and we were unable to draw conclusions about this. More research is therefore needed to understand barriers relating to more diverse populations and to include women who migrate from LMICs to HICs. Furthermore, research carried out in a variety of different countries may further our understanding of different barriers and facilitators based on health care systems across the world (e.g. free vs. paid health care).
Lastly, no identified studies or reviews focused on the experiences of the lesbian, gay, bisexual, transgender and queer (LGBTQ) community. Carrying out research with the LGBTQ community is a research priority. 269 Furthermore, this project did not assess the needs of fathers/birth partners and therefore it is unclear if the frameworks are applicable for anyone other than women in the perinatal period.
Other individual level factors that were identified by the conceptual frameworks that need further research are women’s beliefs about health services, such as whether they are approaching the correct HP/service, whether the service will have the capacity to help and whether the service offers more than medication. Furthermore, there was some emerging evidence of other individual level barriers such as certain demographics, and women not feeling psychologically ready to receive treatment, or whose symptoms prevented them for engaging with treatment.
At the HP level, one factor that may warrant further research is whether the impact of good supervision is a facilitator to implementing and delivering high-quality PMH care. Furthermore, one barrier to treatment may be HPs not having a good understanding of medication use during the perinatal period, and this should be researched further. At the interpersonal level shared decision-making with women about their future care options may also act as a facilitator, but more research is needed.
The importance of incorporating outcome measures into the conceptual frameworks was based on feedback from members of the research programme management group. This was not identified from the literature and may reflect the nature of service commissioning in the NHS, where services need to show that they are working in order to be recommissioned. Thus, outcome measures to evaluate services need further attention. It is important that outcome measures used are adequately measuring what the services aim to treat (such as a reduction in symptoms and increased quality of life) but that they are also culturally appropriate and sensitive to women’s needs so as not to discourage women for accessing further care due to the completion of inappropriately chosen measures. Previous research has examined this but implementation of it has been poor and may need updating given the findings of this research programme (e.g. culturally appropriate measures). 270 Further research at the organisational level should focus on ideal timing and length of care and whether more open inclusion criteria and clear organisational structures are facilitators to care.
Recommendations for further work
It is important that results from this work are disseminated as widely as possible to ensure positive changes can be made to PMH health policy and practice. Ideas for dissemination were identified during the stakeholder group meetings and are summarised in Table 11.
| Stakeholder group | Dissemination suggestions |
|---|---|
| Women and families | Families
|
HPs
Third party
|
|
| HPs |
|
| Commissioners and policy makers |
|
Based on these stakeholder recommendations, results from both systematic reviews, the conceptual frameworks and evidence-based recommendations we propose a series of possible dissemination strategies shown in Table 12. A knowledge translation framework was applied to these dissemination strategies – the interaction-focused framework. 280 This framework highlights the need to identify the most appropriate mode of interaction and the level of detail that should be provided. Therefore, research was identified about where each stakeholder obtains their information from, and the type of information they find the most helpful.
| Who | Information sources | Type of information | What | How? |
|---|---|---|---|---|
| Women and families and third-party organisations | Internet, health professionals, television, family and friends, magazines271 | Information about a specific medical condition or new/experimental treatments. Reliable, credible information271 |
|
|
| HPs | Medical reference sources (e.g. medical dictionaries); Health care pamphlets; Supervisors; Colleagues; Managers;272 PubMed; MEDLINE; Google; Centers for Disease Control and Prevention (or national alternatives)273 | Summarised information that can be provided to patients if appropriate274 Short courses, webinars1 |
|
|
| Service managers | PubMed; MEDLINE; Google; Centers for Disease Control and Prevention (or national alternatives)273 | Practical knowledge, guidelines and programme planning273,275 Local information276 |
|
|
| Policy makers and commissioners | Research suggests policy makers’ interests are guided by party priorities and emphasised by ‘real-world’ stories from constituents276,277 Policy makers likely rely on staff to help them identify priority information, so colleagues or employees of policy makers should be a key target audience for dissemination efforts278,279 |
Information needs to be understandable, concise and unbiased Brief summary of research, infographics, briefs. Messages should be focused and professional (not academic)276 |
|
|
| Societal barriers | Reports, infographics and animations about stigma, psychoeducation about mental illness and a public mental health campaign such as Time to Change Campaign |
|
For example, results suggest that mothers’ beliefs about PMH (e.g. the causes and where to seek help) and fear of judgement and social services involvement may prevent women from seeking or accessing help. It is therefore recommended that infographics, reports and animations for women and their families, similar to those reported above, are developed, which aim to inform families about PMH and break down cross-cultural barriers. These should be disseminated through universal health services, such as GP surgeries and maternity services; via social media and online, for example, websites such as Netmums, Tommy’s and Mumsnet.
Results from the reviews also identified that HPs’ knowledge about PMH can either be a barrier or facilitator to women accessing care and continuing along the care pathway. We therefore recommend the development of good practice guide(s) which cover the different symptoms and appropriate responses, as well as further training opportunities. This could be disseminated via multiple organisations such as the clinical networks for PMH, local maternity system, PMH workstreams, service managers, webinars, social media, unions, professional journals (e.g. Practice Midwife, BMJ, British Journal of General Practice) and training courses (e.g. Readwell and Health Education England Training hubs).
There were many barriers to women accessing and receiving optimal care in the design and the delivery of services. It is therefore recommended that a document for service managers is designed which utilises the results from the reviews to design a good practice guide. This guide could include examples of good practice and ways to overcome barriers such as language barriers, workforce, training and technology issues. Dissemination should be via networks such as the Perinatal Quality Network; Maternity Networks for NHS improvement; NHS Talking Therapies Clinical Networks; PMH Clinical Networks; Academic Health Science Network; Health Education England Training Hubs and the Community Mental Health Transformation work.
The conceptual frameworks (see Figures 12 and 13) and reviews identified commissioning and political barriers that also prevent women from seeking help, accessing care and experiencing optimal care. It is therefore recommended that a policy and commissioning guide is developed which covers topics such as ‘what is PMH and why is it important?’, ‘what should PMH care look like?’ and ‘how can this be commissioned?’, as well as how to break down postcode lottery in service provision. This guide could be disseminated to local commissioning groups and disseminated via PMH clinical networks in England, Wales, Scotland and Northern Ireland.
Finally, results suggest that stigma is still entrenched within societies and is a barrier across the care pathway. It is therefore recommended that future work focuses on the development of reports, infographics and animations, such as those mentioned above, that aim to break down this stigma. This could be through psychoeducation about mental illness and/or public mental health campaigns. This could be developed in collaboration with charitable and third-sector organisations such as Mind, The Maternal Mental Health Alliance and the 1001 Critical Days All-Party Parliamentary Group.
Future work should be carried out to build on the dissemination strategy in Table 12. Research suggests that active, targeted and multifaceted dissemination strategies are more effective in encouraging behaviour change,281,282 therefore this should be taken into account. Given the range of findings identified by this research programme, to ensure effective and impactful dissemination, a priority setting strategy of what should be disseminated would be useful. Future work could use a similar method to Barber et al. 283 to identify important findings to be disseminated. Barber et al. 283 propose a three-stage method to identify key priorities: (1) stakeholder meetings to identify key priorities; (2) literature reviews to ensure priorities are in line with best practice and existing measures; (3) modified Delphi panel. Once dissemination priorities are identified, dissemination strategies can be put in place to ensure impactful dissemination. A dissemination planning tool, such as the one proposed by Carpenter et al.,284 can be used to help with this. This tool involves identifying exactly who you want to share your results with, working with dissemination partners, ensuring the message is communicated effectively and lastly, evaluating success.
Chapter 10 Conclusion
Overall, the findings from the reviews point to a complex interplay of individual and system level factors across different stages of the care pathway that can influence effective implementation and women accessing PMH care. The identified barriers and facilitators point to the need for women-centred, flexible care, delivered by well-trained, knowledgeable and empathetic HPs working within an organisational and political structure that enables them to deliver continuity of carer. They also suggest a need for an international effort to reduce stigma for PMH.
The findings from both reviews led to the development of the MATRIx conceptual frameworks. These provide pictorial representations of 39 facilitators and 66 barriers that intersect across the care pathway at different levels. The conceptual frameworks led to the development of evidence-based recommendations which aim to break down these barriers to ensure that all women are able to access the support they need during this critical vulnerable period. Recommendations are made for health care policy and practice and for researchers and third-party organisations.
While recommendations are based on the evidence, they may be more or less achievable, depending on the local and national context and pressures on services. Furthermore, it is recognised that the recommendations of the MATRIx conceptual frameworks may be difficult to achieve given the impact that COVID-19 had on health services. 229 However, it is still important to design and where possible deliver best practice and future-proofed services.
Recommendations for policy
Many elements of the conceptual frameworks can be modified by policy makers and government activity (e.g. workforce provision, health care capacity, training, etc.). Therefore, we recommend that policy makers review the frameworks and take comprehensive, strategic and evidence-based efforts to ensure that there is an effective system of PMH care.
The evidence suggests that funding is required to ensure high-quality care provision. This is particularly important given the impact of the COVID-19 pandemic on PMH services. 229 Therefore, the provision of a comprehensively researched and adequate budget is needed so that all health care needs for that financial year can be met. Funding needs to be adequate for service needs and easily accessible. Funding structures may need to be revised depending on the needs of the community in which the service is delivered (e.g. affordable health insurance where free health care is not available).
The evidence suggests health inequalities are a barrier to PMH care. It is therefore advisable that policy is put in place: (1) to improve equality between the sexes/genders by ensuring equal rights for women and men; (2) in terms of ethnicity, for example, changes at the legislative level are needed to protect those who have migrated to a different country from being penalised for accessing health care; and (3) in terms of income, a fair and easily accessible welfare system is needed to prevent health inequalities based on deprivation.
Recommendations for practice
The evidence suggests that women want choice in the care they receive, and that care is appropriate to their needs. Therefore, it is recommended that care is co-produced with women and is personalised and culturally appropriate. Increasing the flexibility and accessibility of services should be done through offering home visits and, where this is not possible, providing out-of-hours appointments located in an area with good transport links and an accessible building to allow for pushchairs. In addition, service managers could consider the provision of virtual consultations using web-based platforms, but women should be given the choice about whether virtual consultations are the right choice for them.
Culturally sensitive care and increased accessibility of care is required for women who are unable to speak, or have difficulty speaking, the country’s official language. This can be done via pictorial aids, the purchase of products such as Language Line or through collaboration with translation agencies.
The evidence suggests that technology can be a facilitator to PMH services in terms of assessment, referral and intervention. However, where technology is not fit for purpose, this is a barrier. It is therefore recommended that technology systems should be co-produced with HPs and women to ensure ease of usability and integration into the workflow.
The evidence shows that a lack of collaborative working within and between services was a barrier to PMH care. It is therefore recommended that multidisciplinary teams should be created which facilitate choice and personalised care and ensure an adequate workforce to meet women’s needs. We need to break down silo working and encourage collaborative and joint working within and across services. Collaboration between services is needed with a focus on the identification and building of working relationships and networks with other services (e.g. Citizens Advice). Furthermore, the building of a coalition of health visitors, midwives, GPs NHS Talking Therapies practitioners, psychologists and psychiatrists is needed to encourage referral and reduce the risk of women falling out of the care pathway.
The evidence shows that HPs who lack knowledge and confidence related to PMH can be a barrier to care. Therefore, HPs should be provided with high-quality training that is delivered face to face and incorporates role-play simulators where appropriate. This should include training in cultural sensitivity and cross-cultural mental health needs. Training time for HPs should be built into workloads and time protected.
Recommendations for research and third-party organisations
Future research should focus on addressing the gaps identified by this project such as: father/birth partners, severe PMH disorders, specialist and primary care services, diverse samples, outcome measures and facilitators to implementation of and access to PMH care.
Further work and dissemination based on the results of the MATRIx project include the development of infographics, reports and animations for women and their families, the use of public health campaigns to break down stigma, and the development of guidelines for HPs, service managers and commissioners. Furthermore, future work should look at designing a strategic dissemination plan to ensure that the results from the MATRIx study are disseminated as impactfully as possible.
Acknowledgements
We would like to acknowledge our collaborators Agnes Hann, Camilla Rosan, Andrea Sinesi and Clare Thompson for their input throughout the project. Thanks are also due to Nia Roberts who conducted the literature searches for both evidence reviews, and to Nazihah Uddin and Georgina Constantinou who assisted with screening, methodological quality appraisals and data extraction for the reviews.
We are very grateful for the advice and oversight of the Study Steering Committee: Professor Jenny Billings (Chair), Dame Professor Cathy Warwick, Kathryn Grant, Dr Fiona Campbell and Dr Sarah Taha. Finally, many thanks to the health professionals, managers, commissioners, parents and other stakeholders who gave us their valuable feedback on the frameworks.
Contributions of authors
Rebecca Webb (https://orcid.org/0000-0002-8862-6491) conducted the research as research fellow and was supported and supervised by the core management team and PPI respresentatives. She wrote the report.
Elizabeth Ford (https://orcid.org/0000-0001-5613-8509) was part of the the MATRIx Programme Management Group who oversaw and developed the MATRIx research programme and part of the core management team who supported and supervised the research.
Judy Shakespeare (https://orcid.org/0000-0003-0770-8098) was part of the the MATRIx Programme Management Group who oversaw and developed the MATRIx research programme and part of the core management team who supported and supervised the research.
Abigail Easter (https://orcid.org/0000-0002-4462-6537) was part of the the MATRIx Programme Management Group who oversaw and developed the MATRIx research programme and part of the core management team who supported and supervised the research.
Fiona Alderdice (https://orcid.org/0000-0003-2404-5644) was part of the the MATRIx Programme Management Group who oversaw and developed the MATRIx research programme.
Jennifer Holly (https://orcid.org/0000-0003-2492-1552) supported and supervised the research as PPI representative.
Rose Coates (https://orcid.org/0000-0002-6944-6428) provided specialist expertise and input.
Sally Hogg (https://orcid.org/0000-0003-1796-0369) provided specialist expertise and input.
Helen Cheyne (https://orcid.org/0000-0001-5738-8390) was part of the the MATRIx Programme Management Group who oversaw and developed the MATRIx research programme.
Sarah McMullen (https://orcid.org/0000-0001-5325-0458) was part of the the MATRIx Programme Management Group who oversaw and developed the MATRIx research programme and supported and supervised the research as PPI representative.
Simon Gilbody (https://orcid.org/0000-0002-8236-6983) was part of the the MATRIx Programme Management Group who oversaw and developed the MATRIx research programme.
Debra Salmon (https://orcid.org/0000-0003-2562-2116) was part of the the MATRIx Programme Management Group who oversaw and developed the MATRIx research programme.
Susan Ayers (https://orcid.org/0000-0002-6153-2460) was part of the the MATRIx Programme Management Group who oversaw and developed the MATRIx research programme and part of the core management team who supported and supervised the research.
All authors were involved in the design of the research, and oversaw and provided input into the conduct of the research and development of the frameworks. All authors read and contributed to the report.
Ethics statement
Ethical permission is not required for systematic reviews of available literature.
Data-sharing statement
Access to data extraction forms, data analysis tables and NVivo analysis documents are available on request to the corresponding author.
Disclaimers
This manuscript presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Bauer A, Parsonage M, Knapp M, Lemmi V, Adelaja B. Costs of Perinatal Mental Health Problems. London: Centre for Mental Health; 2014.
- Saving Lives, Improving Mothers’ Care: Lessons Learned to Inform Maternity Care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2016–18. Oxford: National Perinatal Epidemiology Unit, University of Oxford; 2020.
- Saving Lives, Improving Mothers’ Care: Lessons Learned to Inform Maternity Care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2017–19. Oxford: National Perinatal Epidemiology Unit, University of Oxford; 2021.
- McAllister-Williams RH, Baldwin DS, Cantwell R, Easter A, Gilvarry E, Glover V, et al. British Association for Psychopharmacology consensus guidance on the use of psychotropic medication preconception, in pregnancy and postpartum 2017. J Psychopharmacol 2017;31:519-52.
- Rusner M, Berg M, Begley C. Bipolar disorder in pregnancy and childbirth: a systematic review of outcomes. BMC Pregn Childb 2016;16:1-18.
- Vigod SN, Kurdyak PA, Dennis CL, . Maternal and newborn outcomes among women with schizophrenia: a retrospective population-based cohort study. BJOG: Int J Obstet Gynaecol 2014;121:566-74.
- Fuhr DC, Calvert C, Ronsmans C, Chandra PS, Sikander S, De Silva MJ, et al. Contribution of suicide and injuries to pregnancy-related mortality in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Psychiat 2014;1:213-25.
- Grigoriadis S, Wilton AS, Kurdyak PA, Rhodes AE, VonderPorten EH, Levitt A, et al. Perinatal suicide in Ontario, Canada: a 15-year population-based study. CMAJ 2017;189:E1085-92.
- Palladino CL, Singh V, Campbell J, Flynn HA, Gold K. Homicide and suicide during the perinatal period: findings from the National Violent Death Reporting System. Obstet Gynecol 2011;118:1056-63.
- Bower D, Jia R, Schoppe-Sullivan SJ, Mangelsdorf SC, Brown GL. Trajectories of couple relationship satisfaction in families with infants: the roles of parent gender, personality, and depression in first-time and experienced parents. J Soc Pers Relatsh 2013;30:389-40.
- Garthus-Niegel S, Horsch A, Handtke E, von Soest T, Ayers S, Weidner K, et al. The impact of postpartum posttraumatic stress and depression symptoms on couples’ relationship satisfaction: a population-based prospective study. Front Psychol 2018;19. https://doi.org/10.3389/fpsyg.2018.01728.
- Hinton L, Locock L, Knight M. Support for mothers and their families after life-threatening illness in pregnancy and childbirth: a qualitative study in primary care. Br J Gen Pract 2015;65:e563-9. https://doi.org/10.3399/bjgp15X686461.
- Ding X-X, Wu Y-L, Xu S-J, Zhu R-P, Jia X-M, Zhang S-F, et al. Maternal anxiety during pregnancy and adverse birth outcomes: a systematic review and meta-analysis of prospective cohort studies. J Affect Disord 2014;159:103-10. https://doi.org/10.1016/j.jad.2014.02.027.
- Glover V. The Oxford Handbook of Perinatal Psychology. Oxford: Oxford University Press; 2016.
- Liu Y, Kaaya S, Chai J, McCoy DC, Surkan PJ, Black MM, et al. Maternal depressive symptoms and early childhood cognitive development: A meta-analysis. Psychol Med 2017;47:680-9. https://doi.org/10.1017/S003329171600283X.
- Murray L, Cooper P. The impact of postpartum depression on child development. Int Rev Psychiatry 1996;8:55-63. https://doi.org/10.3109/09540269609037817.
- Netsi E, Pearson RM, Murray L, Cooper P, Craske M, Stein A. Association of persistent and severe postnatal depression with child outcomes. JAMA Psychiatry 2018;75:247-53. https://doi.org/10.1001/jamapsychiatry.2017.4363.
- Oyetunji A, Chandra P. Postpartum stress and infant outcome: a review of current literature. Psychiatry Res 2020;284. https://doi.org/10.1016/j.psychres.2020.112769.
- Letourneau N, Dennis CL, Cosic N, Linder J. The effect of perinatal depression treatment for mothers on parenting and child development: a systematic review. Depress Anxiety 2017;34:928-66. https://doi.org/10.1002/da.22687.
- Prenoveau JM, Craske M, West V, Giannakakis A, Zioga M, Lehtonen A, et al. Maternal postnatal depression and anxiety and their association with child emotional negativity and behavior problems at two years. Dev Psychol 2017;53:50-62. https://doi.org/10.1037/dev0000221.
- Glasheen C, Richardson GA, Fabio A. A systematic review of the effects of postnatal maternal anxiety on children. Arch Womens Ment Health 2010;13:61-74. https://doi.org/10.1007/s00737-009-0109-y.
- O’Donnell KJ, Glover V, Barker ED, O’Connor TG. The persisting effect of maternal mood in pregnancy on childhood psychopathology. Dev Psychopathol 2014;26:393-40. https://doi.org/10.1017/S0954579414000029.
- Rees S, Channon S, Waters CS. The impact of maternal prenatal and postnatal anxiety on children’s emotional problems: a systematic review. Eur Child Adolesc Psychiatry 2019;28:257-80. https://doi.org/10.1007/s00787-018-1173-5.
- Moore D, Drey N, Ayers S. Use of online forums for perinatal mental illness, stigma, and disclosure: an exploratory model. JMIR Ment Health 2017;4. https://doi.org/10.2196/mental.5926.
- Gavin NI, Meltzer-Brody S, Glover V, Gaynes BN. Identifying Perinatal Depression and Anxiety: Evidence-Based Practice in Screening, Psychosocial Assessment, and Management. New York, NY: Wiley-Blackwell; 2015.
- Royal College of Obstetricians and Gynaecologists . Maternal Mental Health: Women’s Voices 2017. https://doi.org/10.1145/1518701.1518861.
- National Institute for Health Research . Commissioning Brief: 17 105 Perinatal Mental Health Services 2017. www.researchgate.net/profile/Sheetal-Bhurke/publication/320264531_17_105_Supporting_Information1_Perinatal_MH_services_Final/links/59d89e200f7e9b12b36833eb/17-105-Supporting-Information1-Perinatal-MH-services-Final (accessed 30 November 2021).
- NHS England . NHS England: The NHS Five Year Forward View 2014.
- Scottish Government . Mental Health Strategy: 2017–2027 2017.
- National Institute for Health and Care Excellence (NICE) . Antenatal and Postnatal Mental Health: Clinical Management and Service Guidance 2014.
- Scottish Intercollegiate Guidelines Network (SIGN) . SIGN 127: Management of Perinatal Mood Disorders 2012.
- NHS England . The Perinatal Mental Health Care Pathways 2018.
- NHS England . The NHS Long Term Plan 2019.
- Khan L. Falling through the Gaps: Perinatal Mental Health and General Practice. Wales: Centre for Mental Health; 2015.
- Public Health Agency . Regional Perinatal Mental Health Care Pathway 2017.
- Boots Family Trust Alliance . Perinatal Mental Health: Experiences of Women and Health Professionals 2013. https://maternalmentalhealthalliance.org/wp-content/uploads/Boots-Family-Trust-Alliance-report.pdf (accessed 30 November 2021).
- Maternal Mental Health Alliance . The Everyone’s Business Campaign 2015. https://maternalmentalhealthalliance.org/campaign/ (accessed 30 November 2021).
- All-Party Parliamentary Group on Mental Health . Progress of the Five Year Forward View for Mental Health: On the Road to Parity 2017.
- Maternal Mental Health Alliance . Women in a Quarter of the UK Still Can’t Access Vital Maternal Mental Health Services: Press Release 2018. https://maternalmentalhealthalliance.org/news/women-in-a-quarter-of-the-uk-still-cant-access-vital-maternal-mental-health-services/ (accessed 5 August 2021).
- Ferlie EB, Shortell SM. Improving the quality of health care in the United Kingdom and the United States: a framework for change. Milbank Q 2001;79:281-315. https://doi.org/10.1111/1468-0009.00206.
- Goldberg D, Huxley P. Common Mental Disorders: A Bio-Social Model. New York, NY: Tavistock/Routledge; 1992.
- NHS Clinical Commissioners . Support from the Start: Commissioning Early Intervention Services for Mental Ill Health 2016.
- NHS England . Implementing the Five Year Forward View for Mental Health 2016.
- National Collaborating Centre for Mental Health . The Perinatal Mental Health Care Pathways: Full Implementation Guidance 2018.
- Maternal Mental Health Alliance . Map of Specialist Community Perinatal Mental Health Teams (UK) 2020.
- Button S, Thornton A, Lee S, Ayers S, Shakespeare J. Seeking help for perinatal psychological distress: a meta-synthesis of women’s experiences. Br J Gen Pract 2017;67:e692-9. https://doi.org/10.3399/bjgp17X692549.
- Dennis CL, Chung-Lee L. Postpartum depression help-seeking barriers and maternal treatment preferences: a qualitative systematic review. Birth 2006;33:323-31. https://doi.org/10.1111/j.1523-536X.2006.00130.x.
- Megnin-Viggars O, Symington I, Howard LM, Pilling S. Experience of care for mental health problems in the antenatal or postnatal period for women in the UK: a systematic review and meta-synthesis of qualitative research. Arch Womens Ment Health 2015;18:745-59. https://doi.org/10.1007/s00737-015-0548-6.
- Viveiros CJ, Darling EK. Barriers and facilitators of accessing perinatal mental health services: The perspectives of women receiving continuity of care midwifery. Midwifery 2018;65:8-15. https://doi.org/10.1016/j.midw.2018.06.018.
- Hogg S. Prevention in Mind: All Babies Count: Spotlight on Perinatal Mental Health. Falling through the Cracks. London: Maternal Mental Health Alliance; 2018.
- Armstrong SJ, Small RE. The paradox of screening: rural women’s views on screening for postnatal depression. BMC Publ Health 2010;10. https://doi.org/10.1186/1471-2458-10-744.
- Coates R, Ayers S, de Visser R. Women’s experiences of postnatal distress: A qualitative study. BMC Pregn Childb 2014;14:1-14. https://doi.org/10.1186/1471-2393-14-359.
- Coates R, de Visser R, Ayers S. Not identifying with postnatal depression: a qualitative study of women’s postnatal symptoms of distress and need for support. J Psychosom Obstet Gynecol 2015;36:114-21.
- Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Inf Libr J. 2009;26:91-108. https://doi.org/10.1111/j.1471-1842.2009.00848.x.
- Samnani SS, Vaska M, Ahmed S, Turin TC. Review typology: the basic types of reviews for synthesizing evidence for the purpose of knowledge translation. J Coll Physicians Surg Pak 2017;27:635-41.
- Jabareen Y. Building a conceptual framework: philosophy, definitions, and procedure. Int J Qual Methods 2009;8:49-62.
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders: DSM-5 2014;5.
- Moher D, Liberati A, Tetzlaff JM, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med 2009;6. https://doi.org/10.1016/j.jclinepi.2009.06.005.
- Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S. PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res 2014;14:1-10.
- Cooke A, Smith D, Booth A. Beyond PICO: the SPIDER tool for qualitative evidence synthesis. Qual Health Res 2012;22:1435-43.
- Webb R, Uddin N, Ford E, Easter A, Shakespeare J, Roberts N, et al. MATRIx Study Team . Barriers and facilitators to implementing perinatal mental health care in the NHS and other health and social care settings: a systematic review. Lancet Psychiatry 2021;8:521-34. https://doi.org/0.1016/S2215-0366(20)30467-3.
- Cochrane . Data Collection Form for Intervention Review: RCTs and Non-RCTs 2014. https://view.officeapps.live.com/op/view.aspx?src=https%3A%2F%2Fcommunity.cochrane.org%2Fsites%2Fdefault%2Ffiles%2Fuploads%2Finline-files%2FERC%2520data%2520collection%2520form%2520for%2520intervention%2520reviews%2520for%2520RCTs%2520and%2520non-RCTs.doc&wdOrigin=BROWSELINK (accessed 1 May 2020).
- Shea BJ, Reeves BC, Wells GA, . AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017;21. https://doi.org/10.1136/bmj.j4008.
- The Joanna Briggs Institute . The Joanna Briggs Institute Critical Appraisal Tools for Use in JBI Systematic Reviews: Checklist for Qualitative Research 2017.
- The Joanna Briggs Institute . The Joanna Briggs Institute Critical Appraisal Tools for Use in JBI Systematic Reviews: Checklist for Analytical Cross Sectional Studies 2017.
- The Joanna Briggs Institute . The Joanna Briggs Institute Critical Appraisal Tools for Use in JBI Systematic Reviews: Checklist for Text and Opinion 2017.
- Harden A. ‘Qualitative’ Research, Systematic Reviews, and Evidence-Informed Policy and Practice. London: University of London; 2007.
- Carroll C, Booth A, Lloyd-Jones M. Should we exclude inadequately reported studies from qualitative systematic reviews? An evaluation of sensitivity analyses in two case study reviews. Qual Health Res 2012;22:1425-34.
- Bina R. Predictors of postpartum depression service use: a theory-informed, integrative systematic review. Women Birth 2020;33:e24-32. https://doi.org/10.1016/j.wombi.2019.01.006.
- Hansotte E, Payne SI, Babich SM. Positive postpartum depression screening practices and subsequent mental health treatment for low-income women in Western countries: a systematic literature review. Publ Health Rev 2017;38:1-17. https://doi.org/10.1186/s40985-017-0050-y.
- Geertz C. The Interpretation of Cultures: Selected Essays. New York, NY: Basic Books; 1973.
- Hadfield H, Wittkowski A. Women’s experiences of seeking and receiving psychological and psychosocial interventions for postpartum depression: a systematic review and thematic synthesis of the qualitative literature. J Midwifery Womens Health 2017;62:723-36. https://doi.org/10.1111/jmwh.12669.
- Popay J, Rogers A, Williams G. Rationale and standards for the systematic review of qualitative literature in health services research. Qual Health Res 1998;8:341-51. https://doi.org/10.1177/104973239800800305.
- Brealey SD, Hewitt C, Green JM, Morrell J, Gilbody S. Screening for postnatal depression: is it acceptable to women and healthcare professionals? A systematic review and meta-synthesis. J Reprod Infant Psychol 2010;28:328-44. https://doi.org/10.1080/02646838.2010.513045.
- Evans K, Spiby H, Morrell J. Non-pharmacological interventions to reduce the symptoms of mild to moderate anxiety in pregnant women: a systematic review and narrative synthesis of women’s views on the acceptability of and satisfaction with interventions. Arch Womens Ment Health 2020;23:11-28. https://doi.org/10.1007/s00737-018-0936-9.
- Giscombe T, Hui A, Stickley T. Perinatal mental health amongst refugee and asylum-seeking women in the UK. Ment Health Rev J. 2020;25:241-53.
- Hewitt CE, Gilbody S, Brealey SD, Paulden M, Palmer S, Mann R, et al. Methods to identify postnatal depression in primary care: an integrated evidence synthesis and value of information analysis. Health Technol Assess 2009;13:1-145. https://doi.org/10.3310/hta13360.
- Holopainen A, Hakulinen T. New parents’ experiences of postpartum depression: a systematic review of qualitative evidence. JBI Database Syst Rev Implement Rep 2019;17:1731-69. https://doi.org/10.11124/JBISRIR-2017-003909.
- Jones CCG, Jomeen J, Hayter M. The impact of peer support in the context of perinatal mental illness: a meta-ethnography. Midwifery 2014;30:491-8. https://doi.org/10.1016/j.midw.2013.08.003.
- Jones A. Help seeking in the perinatal period: a review of barriers and facilitators. Soc Work Public Health 2019;34:596-605.
- Kassam S. Understanding experiences of social support as coping resources among immigrant and refugee women with postpartum depression: an integrative literature review. Issues Ment Health Nurs 2019;40:999-1011. https://doi.org/10.1080/01612840.2019.1585493.
- Lucas G, Olander EK, Ayers S, Salmon D. No straight lines – young women’s perceptions of their mental health and wellbeing during and after pregnancy: a systematic review and meta-ethnography. BMC Womens Health 2019;19:1-17. https://doi.org/10.1186/s12905-019-0848-5.
- Mollard E, Hudson DB, Ford A, Pullen C. An integrative review of postpartum depression in rural US communities. Arch Psychiatr Nurs 2016;30:418-24. https://doi.org/10.1016/j.apnu.2015.12.003.
- Morrell J, Sutcliffe P, Booth A, Stevens J, Scope A, Stevenson M, et al. A systematic review, evidence synthesis and meta-analysis of quantitative and qualitative studies evaluating the clinical effectiveness, the cost-effectiveness, safety and acceptability of interventions to prevent postnatal depression. Health Technol Assess 2016;20:1-414. https://doi.org/10.3310/hta20370.
- Newman TC, Hirst J, Darwin Z. What enables or prevents women with depressive symptoms seeking help in the postnatal period?. Br J Midwifery 2019;27:219-27. https://doi.org/10.12968/bjom.2019.27.4.219.
- Nilaweera I, Doran F, Fisher J. Prevalence, nature and determinants of postpartum mental health problems among women who have migrated from South Asian to high-income countries: a systematic review of the evidence. J Affect Disord 2014;166:213-26. https://doi.org/10.1016/j.jad.2014.05.021.
- Praetorius R, Maxwell D, Alam K. Wearing a happy mask: mother’s expressions of suicidality with postpartum depression. Soc Work Ment Health 2020;18:429-59.
- Randall L, Briscoe L. Are women empowered to make decisions about the use of antidepressants in pregnancy?. Br J Midwifery 2018;26:329-35. https://doi.org/10.12968/bjom.2018.26.5.329.
- Sambrook Smith M, Lawrence V, Sadler E, Easter A. Barriers to accessing mental health services for women with perinatal mental illness: systematic review and meta-synthesis of qualitative studies in the UK. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-024803.
- Schmied V, Black E, Naidoo N, Dahlen HG, Liamputtong P. Migrant women’s experiences, meanings and ways of dealing with postnatal depression: a meta-ethnographic study. PLOS ONE 2017;12. https://doi.org/10.1371/journal.pone.0172385.
- Scope A, Booth A, Morrell J, Sutcliffe P, Cantrell A. Perceptions and experiences of interventions to prevent postnatal depression: a systematic review and qualitative evidence synthesis. J Affect Disord 2017;210:100-10. https://doi.org/10.1016/j.jad.2016.12.017.
- Slade PP, Molyneux DR, Watt DA. A systematic review of clinical effectiveness of psychological interventions to reduce post traumatic stress symptoms following childbirth and a meta-synthesis of facilitators and barriers to uptake of psychological care. J Affect Disord 2021;281:678-94. https://doi.org/10.1016/j.jad.2020.11.092.
- Sorsa MA, Kylmä J, Bondas TE. Contemplating help-seeking in perinatal psychological distress: a meta-ethnography. Int J Environ Res Public Health 2021;18.
- Staneva AA, Bogossian F, Wittkowski A. The experience of psychological distress, depression, and anxiety during pregnancy: a meta-synthesis of qualitative research. Midwifery 2015;31:563-73. https://doi.org/10.1016/j.midw.2015.03.015.
- Tobin CL, Di Napoli P, Beck CT. Refugee and immigrant women’s experience of postpartum depression: a meta-synthesis. J Transcult Nurs: Off J Transcult Nurs Soc. 2018;29:84-100. https://doi.org/10.1177/1043659616686167.
- Watson H, Harrop D, Walton E, Young A, Soltani H. A systematic review of ethnic minority women’s experiences of perinatal mental health conditions and services in Europe. PLOS ONE 2019;14. https://doi.org/10.1371/journal.pone.0210587.
- Wittkowski A, Gardner PL, Bunton P, Edge D. Culturally determined risk factors for postnatal depression in sub-Saharan Africa: a mixed method systematic review. J Affect Disord 2014;163:115-24. https://doi.org/10.1016/j.jad.2013.12.028.
- Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008;8:1-10. https://doi.org/10.1186/1471-2288-8-45.
- Powell BJ, McMillen JC, Proctor EK, Carpenter CR, Griffey RT, Bunger AC, et al. A compilation of strategies for implementing clinical innovations in health and mental health. Med Care Res Rev 2012;69:123-57. https://doi.org/10.1177/1077558711430690.
- Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0209-1.
- Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol 2012;12. https://doi.org/10.1186/1471-2288-12-181.
- The World Bank . World Bank Country and Lending Groups n.d. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed 30 November 2021).
- Tandon A, Murray C, Lauer J, Evans D. Measuring Overall Health System Performance for 191 Countries. Geneva: World Health Organization; 2000.
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 1987;150:782-6. https://doi.org/10.1192/bjp.150.6.782.
- Forde R, Peters S, Wittkowski A. Recovery from postpartum psychosis: a systematic review and metasynthesis of women’s and families’ experiences. Arch Womens Ment Health 2020;23:597-612. https://doi.org/10.1007/s00737-020-01025-z.
- Atif N, Lovell K, Husain N, Sikander S, Patel V, Rahman A. Barefoot therapists: barriers and facilitators to delivering maternal mental health care through peer volunteers in Pakistan: a qualitative study. Int J Ment Health Syst 2016;10:1-12. https://doi.org/10.1186/s13033-016-0055-9.
- McCauley M, Abigail B, Bernice O, Van Den Broek N. ‘I just wish it becomes part of routine care’: healthcare providers’ knowledge, attitudes and perceptions of screening for maternal mental health during and after pregnancy: a qualitative study. BMC Psychiatry 2019;19.
- Nakku J, Okello ES, Kizza D, . Perinatal mental health care in a rural African district, Uganda: a qualitative study of barriers, facilitators and needs. BMC Health Serv Res 2016;16. https://doi.org/10.1186/s12913-016-1547-7.
- Ganann R, Sword W, Newbold KB, Thabane L, Armour L, Kint B. Provider perspectives on facilitators and barriers to accessible service provision for immigrant women with postpartum depression: a qualitative study. Can J Nurs Res Rev Can Rech En Sci Infirm 2019;51:191-20. https://doi.org/10.1177/0844562119852868.
- Young CA, Burnett H, Ballinger A, Castro G, Steinberg S, Nau M, et al. Embedded maternal mental health care in a pediatric primary care clinic: a qualitative exploration of mothers’ experiences. Acad Pediatr 2019;19:934-41. https://doi.org/10.1016/j.acap.2019.08.004.
- Johnson S, Adam S, McIntosh M. The lived experience of postpartum depression: a review of the literature. Issues Ment Health Nurs 2020;41:584-91. https://doi.org/10.1080/01612840.2019.1688437.
- Myors KA, Johnson M, Cleary M, Schmied V. Engaging women at risk for poor perinatal mental health outcomes: a mixed-methods study. Int J Ment Health Nurs 2015;24:241-52. https://doi.org/10.1111/inm.12109.
- Boyd RC, Mogul M, Newman D, Coyne JC. Screening and referral for postpartum depression among low-income women: a qualitative perspective from community health workers. Depress Res Treat 2011;2011:1-7. https://doi.org/10.1155/2011/320605.
- Doering JJ, Maletta K, Laszewski A, Wichman CL, Hammel J. Needs and challenges of home visitors conducting perinatal depression screening. Infant Ment Health J 2017;38:523-35.
- Higgins A, Downes C, Monahan M, Gill A, Lamb SA, Carroll M. Barriers to midwives and nurses addressing mental health issues with women during the perinatal period: the Mind Mothers study. J Clin Nurs 2018;27:1872-83. https://doi.org/10.1111/jocn.14252.
- Noonan M, Doody O, O’Regan A, Jomeen J, Galvin R. Irish general practitioners’ view of perinatal mental health in general practice: a qualitative study. BMC Fam Pract 2018;19:1-10. https://doi.org/10.1186/s12875-018-0884-5.
- Pineros-Leano M, Tabb KM, Sears H, Meline B, Huang H. Clinic staff attitudes towards the use of mhealth technology to conduct perinatal depression screenings: a qualitative study. Fam Pract 2015;32:211-5. https://doi.org/10.1093/fampra/cmu083.
- Vik K, Aass IM, Willumsen AB, Hafting M. ‘It’s about focusing on the mother’s mental health’: screening for postnatal depression seen from the health visitors’ perspective – a qualitative study. Scand J Public Health 2009;37:239-45. https://doi.org/10.1177/1403494808100275.
- Williams CJ, Turner KM, Burns A, Evans J, Bennert K. Midwives and women’s views on using UK recommended depression case finding questions in antenatal care. Midwifery 2016;35:39-46. https://doi.org/10.1016/j.midw.2016.01.015.
- Rowan C, McCourt C, Bick D. Provision of perinatal mental health services in two English strategic health authorities: views and perspectives of the multi-professional team. Evid Based Midwifery 2010;8:98-106.
- Fernandez y Garcia E, Lacaze C, Ratanasen M. Continuous quality improvement for postpartum depression screening and referral. Pediatr Int 2011;53:277-9. https://doi.org/10.1111/j.1442-200X.2011.03342.x.
- Nithianandan N, Gibson-Helm M, McBride J, Binny A, Gray KM, East C, et al. Factors affecting implementation of perinatal mental health screening in women of refugee background. Implement Sci 2016;11.
- Segre LS, Pollack LO, Brock RL, Andrew JR, O’Hara MW. Depression screening on a maternity unit: a mixed-methods evaluation of nurses’ views and implementation strategies. Issues Ment Health Nurs 2014;35:444-54. https://doi.org/10.3109/01612840.2013.879358.
- Shakespeare J, Blake F, Garcia J. A qualitative study of the acceptability of routine screening of postnatal women using the Edinburgh Postnatal Depression Scale. Br J Gen Pract J R Coll Gen Pract 2003;53:614-9.
- Willey S, Gibson-Helm M, Finch T, East C, Khan N, Boyd L, et al. Implementing innovative evidence-based perinatal mental health screening for refugee women. Women Birth 2018;31. https://doi.org/10.1016/j.wombi.2018.08.033.
- Ammerman RT, Putnam FW, Teeters AR, Van Ginkel JB. Moving beyond depression: a collaborative approach to treating depressed mothers in home visiting programs. Zero Three 2014;34:20-7.
- Feinberg E, Smith MV, Morales MJ, Claussen AH, Smith DC, Perou R. Improving women’s health during internatal periods: developing an evidenced-based approach to addressing maternal depression in pediatric settings. J Womens Health 2006;15:692-703. https://doi.org/10.1089/jwh.2006.15.692.
- Kim JJ, La Porte LM, Adams MG, Gordon TEJ, Kuendig JM, Silver RK. Obstetric care provider engagement in a perinatal depression screening program. Arch Womens Ment Health 2009;12:167-72. https://doi.org/10.1007/s00737-009-0057-6.
- Judd F, Stafford L, Gibson P, Ahrens J. The early motherhood service: an acceptable and accessible perinatal mental health service. Australas Psychiatry 2011;19:240-6. https://doi.org/10.3109/10398562.2011.562294.
- Kerker BD, Greene JA, Gerson R, Pollock M, Hoagwood KE, Horwitz SM. Screening for and preventing perinatal depression. J Child Fam Stud 2018;27:3169-75. https://doi.org/10.1007/s10826-018-1157-6.
- Lind A, Richter S, Craft C, Shapiro AC. Implementation of routine postpartum depression screening and care initiation across a multispecialty health care organization: an 18-month retrospective analysis. Matern Child Health J 2017;21:1234-9. https://doi.org/10.1007/s10995-017-2264-5.
- Chartier MJ, Attawar D, Volk JS, Cooper M, Quddus F, McCarthy JA. Postpartum mental health promotion: perspectives from mothers and home visitors. Public Health Nurs 2015;32:671-9. https://doi.org/10.1111/phn.12205.
- Atif N, Nazir H, Zafar S, Chaudhri R, Atiq M, Mullany Luke C, et al. Development of a psychological intervention to address anxiety during pregnancy in a low-income country. Front Psychiatry 2019;10.
- Cox EQ, Raines C, Kimmel M, Richardson E, Stuebe A, Meltzer-Brody S. Comprehensive integrated care model to improve maternal mental health. JOGNN: J Obstet Gynecol Neonatal Nurs 2017;46:923-30. https://doi.org/10.1016/j.jogn.2017.08.003.
- Friedman SH, Kaplan RS, Rosenthal MB, Console P. Music therapy in perinatal psychiatry: use of lullabies for pregnant and postpartum women with mental illness. Music Med 2010;2:219-25.
- Eappen BS, Aguilar M, Ramos K, Contreras C, Prom MC, Scorza P, et al. Preparing to launch the ‘Thinking Healthy Programme’ perinatal depression intervention in Urban Lima, Peru: experiences from the field. Glob Ment Health 2018;5. https://doi.org/10.1017/gmh.2018.32.
- Masood Y, Lovell K, Lunat F, Atif N, Waheed W, Rahman A, et al. Group psychological intervention for postnatal depression: a nested qualitative study with British South Asian women. BMC Womens Health 2015;15. https://doi.org/10.1186/s12905-015-0263-5.
- Munodawafa M, Lund C, Schneider M. A process evaluation exploring the lay counsellor experience of delivering a task shared psycho-social intervention for perinatal depression in Khayelitsha, South Africa. BMC Psychiatry 2017;17:1-12. https://doi.org/10.1186/s12888-017-1397-9.
- Ormsby SM, Dahlen HG, Ee CC, Keedle H, Smith CA. ‘Acupuncture for antenatal depression: It’s worth giving it a go’: a qualitative study. Women Birth 2018;31:166-76. https://doi.org/10.1016/j.wombi.2017.09.018.
- Lomonaco-Haycraft KC, Hyer J, Tibbits B, Grote J, Stainback-Tracy K, Ulrickson C, et al. Integrated perinatal mental health care: a national model of perinatal primary care in vulnerable populations. Prim Health Care Res Dev 2018;20. https://doi.org/10.1017/S1463423618000348.
- Beeber LS, Lewis VS, Cooper C, Maxwell L, Sandelowski M. Meeting the ‘now’ need: PMH-APRN-interpreter teams provide in-home mental health intervention for depressed Latina mothers with limited English proficiency. J Am Psychiatr Nurses Assoc 2009;15:249-59. https://doi.org/10.1177/1078390309344742.
- Byatt N, Biebel K, Debordes-Jackson G, Lundquist RS, Moore Simas TA, Weinreb L, et al. Community mental health provider reluctance to provide pharmacotherapy may be a barrier to addressing perinatal depression: a preliminary study. Psychiatr Q 2013;84:169-74. https://doi.org/10.1007/s11126-012-9236-0.
- Reed M, Fenwick J, Hauck Y, Gamble J, Creedy DK. Australian midwives’ experience of delivering a counselling intervention for women reporting a traumatic birth. Midwifery 2014;30:269-75. https://doi.org/10.1016/j.midw.2013.07.009.
- Bina R, Barak A, Posmontier B, Glasser S, Cinamon T. Social workers’ perceptions of barriers to interpersonal therapy implementation for treating postpartum depression in a primary care setting in Israel. Health Soc Care Community 2018;26:e75-84.
- Pugh NE, Hadjistavropoulos HD, Hampton AJD, Bowen A, Williams J. Client experiences of guided internet cognitive behavior therapy for postpartum depression: a qualitative study. Arch Womens Ment Health 2015;18:209-19. https://doi.org/10.1007/s00737-014-0449-0.
- Shorey S, Ng ED. Evaluation of a technology-based peer-support intervention program for preventing postnatal depression (Part 2): qualitative study. J Med Internet Res 2019;21. https://doi.org/10.2196/12915.
- Leger J, Letourneau N, Weaver K. Gaining perspective: peer mentors’ experiences with an intervention project for mothers with postpartum depression. Clin Nurs Stud 2015;3:29-36.
- McKenzie-McHarg K, Crockett M, Olander EK, Ayers S. Think pink! A sticker alert system for psychological distress or vulnerability during pregnancy. Br J Midwifery 2014;22:590-5. https://doi.org/10.12968/bjom.2014.22.8.590.
- Drozd F, Haga SM, Lisøy C, Slinning K. Evaluation of the implementation of an internet intervention in well-baby clinics: a pilot study. Internet Interv 2018;13:1-7. https://doi.org/10.1016/j.invent.2018.04.003.
- O’Mahen H, Flynn HA. Preferences and perceived barriers to treatment for depression during the perinatal period. J Womens Health 2008;17:1301-9. https://doi.org/10.1089/jwh.2007.0631.
- O’Mahen H, Grieve H, Jones J, McGinley J, Woodford J, Wilkinson EL. Women’s experiences of factors affecting treatment engagement and adherence in internet delivered behavioural activation for postnatal depression. Internet Interv 2015;2:84-90. https://doi.org/10.1016/j.invent.2014.11.003.
- Hadfield H, Glendenning S, Bee P, Wittkowski A. Psychological therapy for postnatal depression in UK primary care mental health services: a qualitative investigation using framework analysis. J Child Fam Stud 2019;28:3519-32. https://doi.org/10.1007/s10826-019-01535-0.
- Jallo N, Salyer J, Ruiz RJ, French E. Perceptions of guided imagery for stress management in pregnant African American women. Arch Psychiatr Nurs 2015;29:249-54. https://doi.org/10.1016/j.apnu.2015.04.004.
- Deleuze G, Guattari F, Tomlinson H, Burchell G. What Is Philosophy?. New York, NY: Columbia University Press; 1994.
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-50.
- Glasgow RE, Harden SM, Gaglio B, Rabin B, Smith ML, Porter Gwenndolyn C, et al. RE-AIM planning and evaluation framework: adapting to new science and practice with a 20-year review. Front Public Health 2019;7. https://doi.org/10.3389/fpubh.2019.00064.
- National Institute for Health and Care Excellence (NICE) . Appendix H: Appraisal Checklists, Evidence Tables, GRADE and Economic Profiles | Tools and Resources | Developing NICE Guidelines: The Manual | Guidance n.d. www.nice.org.uk/process/pmg20/resources/developing-nice-guidelines-the-manual-appendices-2549710189/chapter/appendix-h-appraisal-checklists-evidence-tables-grade-and-economic-profiles (accessed 6 July 2022).
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE Working Group . GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924-6. https://doi.org/10.1136/BMJ.39489.470347.AD.
- Leamy M, Bird V, Le Boutillier C, Williams J, Slade M. Conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. Br J Psychiatry 2011;199:445-52.
- Lewin S, Bohren MA, Rashidian A, Munthe-Kaas H, Glenton C, Colvin CJ, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings – paper 2: how to make an overall CERQual assessment of confidence and create a summary of qualitative findings table. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0689-2.
- Munthe-Kaas H, Bohren MA, Glenton C, Lewin S, Noyes J, Tunçalp Ö, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings – paper 3: how to assess methodological limitations. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0690-9.
- Colvin CJ, Garside R, Wainwright M, Munthe-Kaas H, Glenton C, Bohren MA, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings – paper 4: how to assess coherence. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0691-8.
- Glenton C, Carlsen B, Lewin S, Munthe-Kaas H, Colvin CJ, Tunçalp Ö, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings – paper 5: how to assess adequacy of data. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0692-7.
- Noyes J, Booth A, Lewin S, Carlsen B, Glenton C, Colvin CJ, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings – paper 6: how to assess relevance of the data. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0693-6.
- Slay J, Stephens L. Co-Production in Mental Health: A Literature Review 2013. https://neweconomics.org/uploads/files/ca0975b7cd88125c3e_ywm6bp3l1.pdfs.org) (accessed 1 May 2020).
- Scottish Co-production Network . An Introduction to the Co-Production Star 2015. https://www.coproductionscotland.org.uk/resources/an-introduction-to-the-co-production-starroduction Network (coproductionscotland.org.uk) (accessed 1 May 2020).
- NHS Lanarkshire . Near Me. Services n.d. www.nhslanarkshire.scot.nhs.uk/services/nearme/ (accessed 29 November 2021).
- Livi . Livi n.d. www.livi.co.uk/ (accessed 29 November 2021).
- Bakhai M, Croney L, Waller O, Henshall N, Felstead C. Using Online Consultations in Primary Care. London: NHS; 2020.
- Latulippe K, Hamel C, Giroux D. Social health inequalities and eHealth: a literature review with qualitative synthesis of theoretical and empirical studies. J Med Internet Res 2017;19.
- Parker RF, Figures EL, Paddison CAM, Matheson JIDM, Blane DN, Ford JA. Inequalities in general practice remote consultations: a systematic review. BJGP Open 2021;5.
- Tubb A. NHS England Announce Specialist Mental Health Support for New Mums Now Available across England. London: Maternal Mental Health Alliance; n.d.
- NHS Quality Improvement Scotland . Standards for Integrated Care Pathways for Mental Health 2007. www.wdhscp.org.uk/media/1070/standards-for-integrated-care-pathways-for-mh_dec07-1.pdf (accessed 19 June 2023).
- National Institute for Health and Care Excellence (NICE) . Developing Local Care Pathways for Common Mental Health Disorders 2021.
- Dietrich S, Mergl R, Freudenberg P, Althaus D, Hegerl U. Impact of a campaign on the public’s attitudes towards depression. Health Educ Res 2010;25:135-50. https://doi.org/10.1093/her/cyp050.
- Evans-Lacko S, Malcolm E, West K, Rose D, London J, Rüsch N, et al. Influence of Time to Change’s social marketing interventions on stigma in England 2009–2011. Br J Psychiatry 2013;202:s77-88. https://doi.org/10.1192/bjp.bp.113.126672.
- Jorm AF, Christensen H, Griffiths KM. The impact of beyondblue: the national depression initiative on the Australian public’s recognition of depression and beliefs about treatments. Aust NZ J Psychiatry 2005;39:248-54. https://doi.org/10.1111/j.1440-1614.2005.01561.x.
- Makowski AC, Mnich EE, Ludwig J, Daubmann A, Bock T, Lambert M, et al. Changes in beliefs and attitudes toward people with depression and schizophrenia: results of a public campaign in Germany. Psychiatry Res 2016;237:271-8. https://doi.org/10.1016/j.psychres.2016.01.029.
- Sampogna G, Bakolis I, Evans-Lacko S, Robinson E, Thornicroft G, Henderson C. The impact of social marketing campaigns on reducing mental health stigma: results from the 2009–2014 Time to Change programme. Eur Psychiatry 2017;40:116-22. https://doi.org/10.1016/j.eurpsy.2016.08.008.
- OECD, Social Policy Division . Parents’ Use of Childbirth-Related Leave 2019.
- Eagly AH, Nater C, Miller DI, Kaufmann M, Sczesny S. Gender stereotypes have changed: a cross-temporal meta-analysis of U.S. public opinion polls from 1946 to 2018. Am Psychol 2020;75:301-15. https://doi.org/10.1037/amp0000494.
- Lopez-Zafra E, Garcia-Retamero R. Do gender stereotypes change? The dynamic of gender stereotypes in Spain. J Gend Stud 2012;21:169-83. https://doi.org/10.1080/09589236.2012.661580.
- Valiquette-Tessier SC, Gosselin J, Young M, Thomassin K. A literature review of cultural stereotypes associated with motherhood and datherhood. Marriage Fam Rev 2019;55:299-32. https://doi.org/10.1080/01494929.2018.1469567.
- Centre for Reproductive Rights . The World’s Abortion Laws. Resources 2021. https://reproductiverights.org/worldabortionlaws (accessed 29 November 2021).
- Finlay JE, Canning D, Po JYT. Reproductive Health Laws around the World. Cambridge, MA: Harvard University; 2012.
- Haddad LB, Nour NM. Unsafe abortion: unnecessary maternal mortality. Rev Obstet Gynecol 2009;2:122-6.
- Crenshaw K. Mapping the margins: intersectionality, identity politics, and violence against women of color. Stanford Law Rev 1991;43:1241-99. https://doi.org/10.2307/1229039.
- Jayaweera H. Access to healthcare for vulnerable migrant women in England: a human security approach. Curr Sociol 2018;66:273-85. https://doi.org/10.1177/0011392117736307.
- Mirza HS, Sheridan AM. Multiple Identity and Access to Health: The Experience of Black and Minority Ethnic Women. London: Centre for Racial Equality Studies, Middlesex University; 2003.
- Germain S, Yong A. COVID-19 highlighting inequalities in access to healthcare in England: a case study of ethnic minority and migrant women. Fem Leg Stud 2020;28:301-10. https://doi.org/10.1007/s10691-020-09437-z.
- Grey T, Sewell H, Shapiro G, Ashraf F. Mental health inequalities facing UK minority ethnic populations. J Psychol Issues Organ Cult. 2013;3:146-57. https://doi.org/10.1002/jpoc.21080.
- Potter JL, Milner A. Tuberculosis: Looking Beyond ‘Migrant’ As a Category to Understand Experience 2018.
- Falah-Hassani K, Shiri R, Dennis CL. The prevalence of antenatal and postnatal co-morbid anxiety and depression: a meta-analysis. Psychol Med 2017;47:2041-53. https://doi.org/10.1017/S0033291717000617.
- Knaak S, Mantler E, Szeto A. Mental illness-related stigma in healthcare: barriers to access and care and evidence-based solutions. Healthc Manage Forum 2017;30:111-6. https://doi.org/10.1177/0840470416679413.
- Health Education England . Specialist Health Visitors in Perinatal and Infant Mental Health: What They Do and Why They Matter 2016.
- Royal College of Midwives . Specialist Mental Health Midwives: What They Do and Why They Matter 2018.
- Coates D, Foureur M. The role and competence of midwives in supporting women with mental health concerns during the perinatal period: a scoping review. Health Soc Care Community 2019;27:e389-405. https://doi.org/10.1111/hsc.12740.
- Choi H, Yamashita T, Wada Y, Narumoto J, Nanri H, Fujimori A, et al. Factors associated with postpartum depression and abusive behavior in mothers with infants. Psychiatry Clin Neurosci 2010;18:218-39. https://doi.org/10.1111/j.1440-1819.2010.02063.x.
- Crear-Perry J, Maybank A, Keeys MR, Mitchell N, Godbolt D. Moving towards anti-racist praxis in medicine. Lancet 2020;396:451-3. https://doi.org/10.1016/S0140-6736(20)31543-9.
- Iheduru-Anderson KC, Wahi MM. Rejecting the myth of equal opportunity: an agenda to eliminate racism in nursing education in the United States. BMC Nurs 2021;20. https://doi.org/10.1186/s12912-021-00548-9.
- Khan S, Mian A. Racism and medical education. Lancet Infect Dis 2020;20. https://doi.org/10.1016/S1473-3099(20)30639-3.
- Petty J, Metzl JM, Keeys MR. Developing and evaluating an innovative structural competency curriculum for pre-health students. J Med Humanit 2017;38:459-71. https://doi.org/10.1007/s10912-017-9449-1.
- Watters E. Crazy Like Us: The Globalization of the American Psyche. New York, NY: Free Press; 2010.
- López SR, Guarnaccia PJ. Cultural psychopathology: uncovering the social world of mental illness. Annu Rev Psychol 2000;51:571-98. https://doi.org/10.1146/annurev.psych.51.1.571.
- Ventevogel P, Jordans M, Reis R, De Jong J. Madness or sadness? Local concepts of mental illness in four conflict-affected African communities. Confl Health 2013;7:1-16. https://doi.org/10.1186/1752-1505-7-3.
- Yap PM. Koro: a culture-bound depersonalization syndrome. Br J Psychiatry 1965;111:43-50. https://doi.org/10.1192/bjp.111.470.43.
- Hom MA, Stanley IH, Joiner TE. Evaluating factors and interventions that influence help-seeking and mental health service utilization among suicidal individuals: a review of the literature. Clin Psychol Rev 2015;40:28-39. https://doi.org/10.1016/j.cpr.2015.05.006.
- Kelly CM, Jorm AF, Wright A. Improving mental health literacy as a strategy to facilitate early intervention for mental disorders. Med J Aust 2007;187:s26-30. https://doi.org/10.5694/j.1326-5377.2007.tb01332.x.
- University of Liverpool . Supporting Mental Healthcare in a Maternity and Neonatal Setting: Good Practice Guide and Case Studies 2021.
- Future NHS . Mental Health Long Term Plan Analytical Tool 2021. https://future.nhs.uk/system/login?nextURL=%2Fconnect.ti%2FMHLTPat%2Fgrouphome (accessed 29 November 2022).
- NHS North Region . Suggested PMH Workforce Planning KLOEs Developed by North Region 2021. https://future.nhs.uk/PMHSCN/grouphome (accessed 22 October 2021).
- Moreton R, Collinson B, Sandhu J. Working With Commissioners and Policy-Makers: Workforce Development and Multiple Disadvantage 2021. www.tnlcommunityfund.org.uk/media/insights/documents/Working-with-commissioners-and-policy-makers-2020.pdf?mtime=20210224184031&focal=none (accessed 11 November 2021).
- Woodall J, Davison E, Parnaby J, Hall AM. A Meeting of Minds: How Co-Production Benefits People, Professionals and Organisations 2019. www.tnlcommunityfund.org.uk/media/A-Meeting-of-Minds_How-co-production-benefits-people-professionals-and-organisations.pdf (accessed 11 November 2021).
- NHS Scotland . Delivering Effective Services: Needs Assessment and Service Recommendations for Specialist and Universal Perinatal Mental Health Services 2019. www.pmhn.scot.nhs.uk/wp-content/uploads/2019/03/PMHN-Needs-Assessment-Report.pdf (accessed 29 November 2021).
- The King’s Fund . How Funding Flows in the NHS 2020.
- Greater Manchester Combined Authority . Greater Manchester Perinatal and Parent Infant Mental Health Service: Championing 1001 Critical Days 2020.
- Acacia Family Support . Help for Black, Asian and Minority Ethnic Mums Dads and People of Colour 2021. www.acacia.org.uk/bame/mums-dads/# (accessed 29 November 2021).
- NHS London Clinical Networks . Perinatal Mental Health Services for London: Guide for Commissioners 2017.
- The Motherhood Group . Understanding Diverse Motherhood: Workshop and Training 2021. https://themotherhoodgroup.org/training/ (accessed 29 November 2021).
- Feldman R. What Price Safe Motherhood? Charging for NHS Maternity Care in England and Its Impact on Migrant Women. London: Maternity Action; 2018.
- Harris S, Hardwick J. A Vicious Circle: The Relationship between NHS Charges for Maternity Care, Destitution, and Violence Against Women and Girls. London: Maternity Action; 2019.
- Nullums LB, Rustage K, Hargreaves S, Friedland JS, Miller A, Hiam L. Access to Healthcare for People Seeking and Refused Asylum in Great Britain: A Review of Evidence. Cardiff: Equality and Human Rights Commission; 2018.
- Knight M, Bunch K, Tuffnell D, . Saving Lives, Improving Mothers’ Care: Lessons Learned to Inform Maternity Care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2015–17. Oxford: MBRRACE-UK; 2019.
- Public Health England . Maternity High Impact Area: Reducing the Inequality of Outcomes for Women from Black, Asian and Minority Ethnic (BAME) Communities and Their Babies 2020.
- Royal Colleges . Royal Colleges Support Suspension of NHS Overseas Visitor Charges Pending Review 2018. www.rcplondon.ac.uk/news/royal-colleges-support-suspension-nhs-overseas-visitor-charges-pending-review (accessed 11 November 2021).
- Academy of Medical Royal Colleges . NHS Charges to Overseas Visitors Regulations: A Statement from the Academy of Medical Royal Colleges 2019.
- Royal College of Paediatrics and Child Health . Access to Healthcare for Migrant and Undocumented Children: Position Statement 2021.
- Maternity Action . Breach of Trust: A Review of Implementation of the NHS Charging Programme in Maternity Services in England 2021.
- Papworth R, Harris A, Durcan G, Wilton J, Sinclair C. Maternal Mental Health During a Pandemic: A Rapid Review of COVID-19’s Impact. Wales: Centre for Mental Health; 2021.
- Royal College of General Practitioners . The Power of Relationships: What Is Relationship Based Care and Why Is It Important? General Practice COVID-19 Recovery 2021. www.rcgp.org.uk/policy/general-practice-covid-19-power-of-relationships.aspx#:~:text=In%20this%20initial%20report%2C%20we,why%20it%20needs%20to%20be (accessed 12 July 2022).
- Frazer L. Autumn Budget and Spending Review: A Stronger Economy for the British People 2021. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1043688/Budget_AB2021_Print.pdf (accessed 29 November 2021).
- Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry 2010;10. https://doi.org/10.1186/1471-244X-10-113.
- Byrow Y, Pajak R, Specker P, Nickerson A. Perceptions of mental health and perceived barriers to mental health help-seeking amongst refugees: a systematic review. Clin Psychol Rev 2020;75. https://doi.org/10.1016/j.cpr.2019.101812.
- Clement S, Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, et al. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med 2015;45:11-27. https://doi.org/10.1017/S0033291714000129.
- Coleman SJ, Stevelink SAM, Hatch SL, Denny JA, Greenberg N. Stigma-related barriers and facilitators to help-seeking for mental health issues in the armed forces: a systematic review and thematic synthesis of qualitative literature. Psychol Med 2017;47:1880-92. https://doi.org/10.1017/S0033291717000356.
- Schnyder N, Panczak R, Groth N, Schultze-Lutter F. Association between mental health-related stigma and active help-seeking: systematic review and meta-analysis. Br J Psychiatry 2017;210:261-8. https://doi.org/10.1192/bjp.bp.116.189464.
- Mantovani N, Pizzolati M, Edge D. Exploring the relationship between stigma and help-seeking for mental illness in African-descended faith communities in the UK. Health Expect 2017;20:373-84. https://doi.org/10.1111/hex.12464.
- Marwaha S, Livingston G. Stigma, racism or choice: why do depressed ethnic elders avoid psychiatrists?. J Affect Disord 2002;72:257-65. https://doi.org/10.1016/S0165-0327(01)00470-0.
- Zolezzi M, Alamri M, Shaar S, Rainkie D. Stigma associated with mental illness and its treatment in the Arab culture: a systematic review. Int J Soc Psychiatry 2018;64:597-609. https://doi.org/10.1177/0020764018789200.
- May C, Finch T, Mair F, Ballini L, Dowrick C, Eccles M, et al. Understanding the implementation of complex interventions in health care: the normalization process model. BMC Health Serv Res 2007;7:1-7. https://doi.org/10.1186/1472-6963-7-148.
- May C, Mair F, Finch T, . Development of a theory of implementation and integration: normalization Process Theory. Implement Sci 2009;4:1-9. https://doi.org/10.1186/1748-5908-4-29.
- Chiu HH. Employees’ intrinsic and extrinsic motivations in innovation implementation: the moderation role of managers’ persuasive and assertive strategies. J Change Manag 2018;18:218-39. https://doi.org/10.1080/14697017.2017.1407353.
- Rogers EM. Diffiusion of Innovations. New York: Free Press; 2003.
- Venkatesh V, Morris MG, Davis GB, Davis FD. User acceptance of information technology: toward a unified view. MIS Q Manag Inf Syst. 2003;1:425-78. https://doi.org/10.2307/30036540.
- Ryan RM, Deci EL. Intrinsic and extrinsic motivations: classic definitions and new directions. Contemp Educ Psychol 2000;25:54-67. https://doi.org/10.1006/ceps.1999.1020.
- Battye F. Payment by results in the UK: progress to date and future directions for evaluation. Evaluation 2015;21:189-203. https://doi.org/10.1177/1356389015577464.
- Lindenauer PK, Remus D, Roman S, Rothberg MB, Benjamin EM, Ma A, et al. Public reporting and pay for performance in hospital quality improvement. N Engl J Med 2007;356:486-96. https://doi.org/10.1056/NEJMsa064964.
- Henson JS. Burnout or compassion fatigue: a comparison of concepts. Medsurg Nurs 2020;29:77-95.
- Joinson C. Coping with compassion fatigue. Nursing (Lond) 1992;22:116-8.
- Kelly L. Burnout, compassion fatigue, and secondary trauma in nurses: recognizing the occupational phenomenon and personal consequences of caregiving. Crit Care Nurs Q 2020;43:73-80.
- Parker D, Byng R, Dickens C, Kinsey D, McCabe R. Barriers and facilitators to GP–patient communication about emotional concerns in UK primary care: a systematic review. Fam Pract 2020;37:434-44.
- Zantinge EM, Verhaak PFM, Kerssens JJ, Bensing JM. The workload of GPs: consultations of patients with psychological and somatic problems compared. Br J Gen Pract 2005;55:609-14.
- Brondani MA, Alan R, Donnelly L. Stigma of addiction and mental illness in healthcare: the case of patients’ experiences in dental settings. PLOS ONE 2017;12. https://doi.org/10.1371/journal.pone.0177388.
- Timmermann C, Uhrenfeldt L, Birkelund R. Ethics in the communicative encounter: seriously ill patients’ experiences of health professionals’ nonverbal communication. Scand J Caring Sci 2017;31:63-71. https://doi.org/10.1111/scs.12316.
- Anderson ML, Wolf Craig KS, Ziedonis DM. Deaf people’s help-seeking following trauma: experiences with and recommendations for the Massachusetts behavioral health care system. Psychol Trauma Theory Res Pract Policy 2017;9:239-48.
- Satinsky E, Fuhr DC, Woodward A, Sondorp E, Roberts B. Mental health care utilisation and access among refugees and asylum seekers in Europe: a systematic review. Health Policy 2019;123:851-63. https://doi.org/10.1016/j.healthpol.2019.02.007.
- Diamond M, Allcorn S, Stein H. The surface of organizational boundaries: a view from psychoanalytic object relations theory. Hum Relat 2004;57:31-53.
- Forsten-Astikainen R, Hurmelinna-Laukkanen P, Lämsä T, Heilmann P, Hyrkäs E. Dealing with organizational silos with communities of practice and human resource management. J Workplace Learn 2017;29.
- McNeil KA, Mitchell RJ, Parker V. Interprofessional practice and professional identity threat. Health Sociol Rev 2013;22:291-307.
- Dell RK. Breaking organizational silos: removing barriers to exceptional performance. J Am Water Works Assoc 2005;97:34-6.
- Batchelor G. How Silo Working Is Leading to Longer Length of Stay. and What to Do about It. Edge Health; 2017.
- Bennett S. Integrated Personal Commissioning: Emerging Framework 2016. www.england.nhs.uk/wp-content/uploads/2017/06/ipc-emerging-framework.pdf (accessed 30 November 2021).
- Reed S, Gopfert A, Wood S, Allwood D, Warburton W. Building Healthier Communities: The Role of the NHS As an Anchor Insitution 2019. https://reader.health.org.uk/building-healthier-communities (accessed 29 November 2021).
- Gotham K, Brunwasser SM, Lord C. Depressive and anxiety symptom trajectories from school age through young adulthood in samples with autism spectrum disorder and developmental delay. J Am Acad Child Adolesc Psychiatry 2015;54:369.e-76.e3.
- Lever AG, Geurts HM. Psychiatric co-occurring symptoms and disorders in young, middle-aged, and older adults with autism spectrum disorder. J Autism Dev Disord 2016;46:1916-30.
- Meltzer-Brody S, Brandon AR, Pearson B, Burns L, Raines C, Bullard E, et al. Evaluating the clinical effectiveness of a specialized perinatal psychiatry inpatient unit. Arch Womens Ment Health 2014;17:107-13. https://doi.org/10.1007/s00737-013-0390-7.
- The Royal Australian and New Zealand College of Psychiatrists . Mothers, Babies and Psychiatric Inpatient Treatment 2021.
- Wisner KL, Austin MP, Bowen A, Cantwell R, Glangeaud-Freudenthal NMC. Identifying Perinatal Depression and Anxiety: Evidence-Based Practice in Screening, Psychosocial Assessment, and Management. New York, NY: John Wiley & Sons; 2014.
- Greenfield M, Darwin Z. Trans and non-binary pregnancy, traumatic birth, and perinatal mental health: a scoping review. Int J Transgender Health 2020;22:203-16.
- Gray R, Savage-McGlynn E. Developing a Perinatal Mental Health Indicator in England (PMHI) 2018. www.npeu.ox.ac.uk/research/projects/154-perinatal-mental-health-indicator (accessed 29 November 2021).
- Clarke MA, Moore JL, Steege LM, Koopman RJ, Belden Jeffery L, Canfield SM, et al. Health information needs, sources, and barriers of primary care patients to achieve patient-centered care: a literature review. Health Informatics J 2016;22:992-1016. https://doi.org/110.1177/1460458215602939.
- Majid S, Foo S, Luyt B, . Adopting evidence-based practice in clinical decision making: nurses’ perceptions, knowledge, and barriers. J Med Libr Assoc JMLA 2011;99. https://doi.org/110.3163/1536-5050.99.3.010.
- Evidence-based information needs of public health workers: a systematized review. J Medi Libr Assoc n.d. https://jmla.pitt.edu/ojs/jmla/article/view/109/289 (accessed 17 June 2022).
- Understanding the Information Needs of Health Professionals – Toxicology and Environmental Health Information Resources: NCBI Bookshelf n.d. www.ncbi.nlm.nih.gov/books/NBK45472/ (accessed 17 June 2022).
- Kapadia-Kundu N, Sullivan TM, Safi B, Trivedi G, Velu S. Understanding health information needs and gaps in the health care system in Uttar Pradesh, India. J Health Commun 2012;17:30-45. https://doi.org/10.1080/10810730.2012.666625.
- Brownson RC, Jones E. Bridging the gap: translating research into policy and practice. Prev Med 2009;49:313-5. https://doi.org/10.1016/J.YPMED.2009.06.008.
- Brownson RC, Eyler AA, Harris JK, Moore JB, Tabak RG. Getting the word out: new approaches for disseminating public health science. J Public Health Manag Pract 2018;24:102-11. https://doi.org/10.1097/PHH.0000000000000673.
- Morgan MG. Risk Communication: A Mental Models Approach. Cambridge: Cambridge University Press; 2002.
- Tabak RG, Reis RS, Wilson P, Brownson RC. Dissemination of health-related research among scientists in three countries: access to resources and current practices. Biomed Res Int 2015;2015:1-9. https://doi.org/10.1155/2015/179156.
- Jacobson N, Butterill D, Goering P. Development of a framework for knowledge translation: understanding user context. J Health Serv Res Policy 2003;8:94-9. https://doi.org/10.1258/135581903321466067.
- Changing Provider Behavior: An Overview of Systematic Reviews of Interventions on JSTOR n.d. www.jstor.org/stable/3767642?pq-origsite=summon&saml_data=eyJzYW1sVG9rZW4iOiIyYjdiNjVkYi1lOWFkLTRkYTAtOWQyZS0yOTNjYTI5Nzg5ZWUiLCJpbnN0aXR1dGlvbklkcyI6WyI0OGU3NDQ3YS1lOGM2LTRiZDQtYjQwOC1jMzVkZmY4ZjZiYTMiXX0&seq=1 (accessed 17 June 2022).
- Evidence-Based Practice Center Systematic Review Protocol Project Title: Communication and Dissemination Strategies To Facilitate the Use of Health and Health Care Evidence I: Background and Objectives for the Systematic Review 2012. www.effectivehealthcare.ahrq.gov (accessed 17 June 2022).
- Barber CE, Patel JN, Woodhouse L, Smith C, Weiss S, Homik J, et al. Development of key performance indicators to evaluate centralized intake for patients with osteoarthritis and rheumatoid arthritis. Arthritis Res Ther 2015;17. https://doi.org/10.1186/s13075-015-0843-7.
- Agency for Healthcare Research and Quality . Dissemination Planning Tool: Exhibit A from Volume 4 n.d. www.ahrq.gov/patient-safety/reports/advances/planning.html (accessed 17 June 2022).
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983;67:361-70. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x.
- Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl Psychol Meas 1977;1:385-401. https://doi.org/10.1177/014662167700100306.
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606-13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x.
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Patient Edition (SCID-I/P, 11/2002 Revision). New York, NY: New York State Psychiatric Institute; 2002.
- Whooley MA, Avins AL, Miranda J, Browner WS. Case-finding instruments for depression: two questions are as good as many. J Gen Intern Med 1997;12:439-45. https://doi.org/10.1046/j.1525-1497.1997.00076.x.
Appendix 1
| 1. Author, year, country, 2. Quality rating | 1. Design, 2. Healthcare setting |
Description of care | 1. Recipient of care, 2. Provider of care |
Training of providers | 1. Sample interviewed, 2. N |
Interview sample demographics |
|---|---|---|---|---|---|---|
|
|
Moving Beyond Depression Programme using In-Home Cognitive Behavioural Therapy (IH-CBT). 15-weekly sessions, 60 minutes each plus booster sessions at 1 month post-treatment. |
|
2 days to learn IH-CBT, workshops on CBT, learning from pilot cases, audiotapes of treatment sessions. | N/A | N/A |
|
|
CBT based on THP. Adapted in Pakistan to make it deliverable through peers. |
|
Trained and supervised by non-specialist THP facilitators. 4-day classroom and 2-day field training. Fortnightly group and field supervisions. |
|
Mothers: Mean age = 28 100% married Number of children: Mean = 3 Education: Mean = 6.6 years 81% in joint family structure Peer volunteers: Age M = 33 75% married Children M = 2 Education: M = 11 years 75% in a joint family structure |
|
|
Happy Mother Healthy Baby – based on cognitive behaviour therapy principles. Involved development of an empathetic relationship, challenging thoughts, behaviour activation, difficulties solving and involving family members. |
|
5-day workshop followed by two practice cases of perinatal anxiety. |
|
Mean age of women = 26 years and 42% were primigravida. Years of schooling mean was 4 years. Majority of HCPs interviewed had over 10 years of experience. |
|
|
Short-term in-home psychotherapy intervention. Mothers in the intervention group received 16 contacts over a 22-week period. |
|
6-hour course in Spanish/English. | N/A | N/A |
|
|
Eight sessions of IPT that aims to reduce depressive symptoms and improve interpersonal functioning. |
|
2-day 16-hour IPT training led by an experienced IPT trainer. |
|
All female. Mean age = 47.7 years. 13 had a Master of Social Work degree, 7 a BSW degree plus a master’s degree, four had only a BSW degree. Average of 19 years experience including 11 years employment in the Health Maintenance Organizations. |
|
|
Academic-community partnership focusing on screening and barriers to mental health utilisation. Home visits which include screening for postnatal depression and assistance in referral to mental health services. |
|
NR |
|
All female. Mean of 2.3 years of employment at agency. Most only have a college a degree (31.2%) Most of African American ethnicity (50%). |
|
|
Pharmacotherapy for perinatal depression |
|
NR |
|
Education levels ranged from postgraduate year 1 to 4. Faculty and staff participants had 1–23 and 4–27 years of clinical experience respectively. |
|
|
Towards Flourishing Mental Health Promotion Strategy – a demonstration project added to an existing home visiting programme aimed at preventing mental health difficulties. |
|
Training to enhance knowledge of mental health promotion and to implement strategy. |
|
NR |
|
|
Universal screening and a perinatal psychiatry programme. All mothers screened at 1, 3 and 6-month well-baby clinic visits and 6-week postnatal visits and referred as needed based on EPDSc cut-off scores. The NICU clinic met 1 day/week with 5–8 women. Nurse-practitioners met with mothers and families at the NICU bedside. |
|
Education about psychiatric issues, education for obstetric and paediatric providers about signs and symptoms, risk factors and treatment options. | N/A | N/A |
|
|
Home visitation – utilised either the Parents as Teachers or the Healthy Families home-visiting models. Frequency of visits range from weekly to monthly or less frequent dependent on needs. Actual length of programme varies but may serve families with children up to 5 years old. |
|
Training to learn depression screening process. |
|
Majority spent less than 5 or 10+ years in home visiting. Home-visiting supervisors spent 15 years in home visiting. Majority of clients received home visiting for 5–12 or 25+ months. |
|
|
Women screened at 6 time points. Offered a free, universal online preventative intervention called Mamma Mia – 44 online sessions. |
|
2-days pre-service delivery training, written educational materials, information brochure for pregnant women, pamphlets to aid in their programme delivery, coaching sessions, and a 2-day maintenance seminar. |
|
Either completed bachelor’s degree and education in public health or psychiatric nursing, a master’s degree in midwifery, or a 6-year professional degree in clinical psychology. More than a third had education in the EPDSc Mean age was 52.6 years. Majority were female. |
|
|
Thinking Healthy Programme – non-pharmacological cognitive behavioural intervention, 16 one-hour sessions grouped into five modules. | Four days training by Socios En Salud in maternal-child health, providing accompaniment to mothers invited to participate. | N/A | N/A | |
|
|
Paediatric-based maternal depression detection and management system – structured, standardised and validated screening tool and guidance to assess and manage depression. |
|
NR | N/A | N/A |
|
|
The Lullaby 101 Program – hour-long weekly lullaby group |
|
NR | N/A | N/A |
|
|
Patient Health Questionnaire4-2 – screening with verbal administration and a yes or no answer format. Converted to a written format. |
|
NR | N/A | N/A |
|
|
Accessible services for immigrant women with postnatal depression. Services defined as first contact services for women experiencing postnatal depression (e.g. family physicians, public health nurses), other services supportive of women experiencing postnatal depression, and specialty services such as psychiatrists. |
|
NR |
|
Job roles included nurses, social workers, perinatal psychiatrists, community health workers, and administrators. Some were immigrant women themselves. |
|
|
Group therapy interventions – 6 sessions, 2 hours long each. 12 individuals in each session. |
|
NR |
|
Average age was 32, most married, had 1 or 2 children, all White British ethnicity. Either completed therapy in the last 6 months or 2 years. All had received therapy focusing on postnatal depression. Either received CBT based therapy or Eye Movement Desensitisation and Reprocessing. |
|
|
Screening and discussing perinatal mental health difficulties with women in the perinatal period. |
|
Perinatal mental health training. |
|
54.1% midwives and 45.9% nurses. Majority female 99.8%. Aged 50 years and over 34%. Most had a postgraduate diploma/master/PhD as their highest academic qualification 45.5%. Majority were in their role for 11 years or more. |
|
|
12 weeks guided imagery intervention – mind creates mental images that connect to emotions leading to changes in feeling and physiologic states. 4 tracks with each track lasting 20 minutes. Participants listened to one track once a day, first in a sequenced order from week 1–4 and then in their own order from week 5–12. |
|
N/A |
|
Mean 24.75 years. Mean gestational age was 15.53 weeks. 25% participants were primigravida’s. 28% – second pregnancy. 22% – third pregnancy. Majority were not married, had a high school degree or higher education, they were not employed, income less than $15,000. |
|
|
The Early Motherhood Service (EMS) – Monday to Friday 9 a.m. to 5 p.m. or referrals directed to the triage service. Assessments occur antenatally on maternity ward or during the postnatal period on site at the hospital, the EMS office or woman’s home. |
|
Specialist training in perinatal mental health, family therapy, cognitive behaviour therapy, and grief counselling. |
|
N/A |
|
|
On-site depression prevention intervention – individual format, sessions offered in either English or Spanish at time of their prenatal appointments. |
|
10 hours of classroom and didactic sessions. | N/A | N/A |
|
|
EPDSc in the context of a programme that facilitates screening, provides behavioural health follow up, educates providers and maintains a 24/7 hotline for crisis intervention. EPDSc screening conducted at 24–28 weeks of gestation, positive screens passed on to internal team of mental HCPs. It is then documented and communicated to obstetric provider. |
|
NR |
|
Job roles were obstetricians (n = 19) or nurse-midwives (n = 3). Participants represented both hospital-employed and private practice groups in geographically and socio-economically diverse suburban communities of a major metropolitan area. |
|
|
Mothers Offering Mentorship and Support (MOMS) – home based peer support, in-home weekly visits for 12 weeks, duration of 1 hour to 1.5 hours. |
|
NR |
|
NR |
|
|
Postnatal depression screening programme using EPDSc and treatment initiation process. EPDS forms given at 1-, 2- and 4-month routine well-child visits, reviewed and sent to a centralised screening location for further review. If patient within health care system, EPDS entered into medical record. High scores to be discussed with woman and offered referrals. |
|
Electronic learning module included as part of routine mandatory annual education process of clinicians that explained the new process of screening. | N/A | N/A |
|
|
Integrated Perinatal Mental Health program – screening is done initially at the obstetric intake visit using EPDS. Negative score –> provide education and anticipatory guidance. Positive score –> acknowledge, assess and refer. An EPDS is administered twice during pregnancy. All screened at 6-week postnatal, 2-, 4- and 6-month well-child visits. |
|
NR | N/A | N/A |
|
|
Positive Health Programme – psychosocial intervention, 23 women put into 4 groups using the cognitive behavioural model. 12 weekly group sessions over 3 months, manual organised into 9 sessions. Adapted for and offered to British South Asian women. |
|
NR |
|
Interview participants – aged 20–45 years. Most married, one divorced. Majority Pakistani ethnicity. |
|
|
Routine screening for maternal mental health during and after pregnancy. |
|
NR |
|
20 doctors, and 4 nurse midwives. Majority female (n = 13). Aged between 25 and 50 years Most were junior doctors and have between 1 and 5 years of experience providing routine maternity care. |
|
|
Pink sticker communication system – alerts midwifery and obstetric staff ensuring identified women receive appropriate tailored, and emotionally intelligent care. |
|
4 hours of specific training in perinatal psychology, information on the pink sticker system, combining info about psychological presentations and education on how midwives could support women with difficulties through pregnancy and labour. |
|
Midwives ranged across seniority from at least 2 years qualified to very senior, had all cared for a number of women who had presented with a pink sticker within the last year. All women participants had delivered within the previous year. |
|
|
Task sharing counselling intervention – 6 to 8 sessions. The sessions were structured manual-based psychosocial individual face-to-face counselling sessions either at participant homes or at the clinic. |
|
5-day workshop on how to implement the manual-based intervention. 2–3 hours weekly group supervision and ongoing training in addition to 30 minutes of individual supervision monthly. |
|
Education levels ranged from grade 9 to grade 12 and had at least 2.5 years of previous experience in the community doing health promotion. Mean age of 37.2 years. |
| Based on CBT, IPT and problem-solving therapy principles. Sessions were in the antenatal phase and could continue to postnatal phase. Referrals were made if participants showed any suicidal ideation and if assistance needed was beyond the scope of the workers’ intervention. | ||||||
|
|
Perinatal and infant mental health (PIMH) services – ‘Supporting Families Early’ policy which provides a framework of promotion, prevention, early intervention and treatment for mothers, infants and their families. Psychosocial assessment and depression screening in the antenatal and early postnatal periods aims to identify women at risk for poor perinatal mental health. The needs of women identified with risk factors are discussed at multidisciplinary case review meetings and, if necessary, referral to specialised services is initiated. The risk factors are categorised into three levels: (1) level 1: no risks identified; (2) level 2: social issues, such as poor support networks; and (3) level 3: complex issues, such as maternal mental illness. |
|
NR |
|
Clinicians’ job roles included nurses, social workers and psychologists and had been working between 2 and 8 years. Managers and stakeholders had been involved in the PIMH service for 2–12 years. Mean age of women was 28 years. Majority (77.5%) were born in an English-speaking country and were partnered (73.4%). 57.3% had more than 1 child, 47.5% had experienced a pregnancy or infant loss. Majority (84.8%) were referred via the midwives in antenatal clinic. |
|
|
Volunteers from within the community are nominated by members of the community to form Village Health Teams (VHTs). These VHTs are entrusted with taking care of health matters of the village where they live, and they mobilise people for health programmes as well as identify and refer individuals who need care. There is no built structure at this level and there are no qualified health staff. The Kamuli district has only one psychiatric clinical officer (equivalent of a nurse practitioner or nurse prescriber) and a handful of psychiatric nurses. These are all based at the only public hospital and largely work in non-mental health clinics, leaving most of the district with no access to psychiatry personnel. Perinatal women with mental illness are only identified if they are severe enough to be psychotic or suicidal, in which case they are not treated but immediately referred to the regional hospital in the neighbouring district of Jinja, 60 km away. Depression and other common mental disorders normally remain undetected and untreated at the primary care level. |
|
NR |
|
Age range from 18 to 47. Majority female participants (84%). Majority of pregnant and postnatal women only had primary education (n = 36). All Village Health Teams had secondary education. All key informants had up to tertiary education. Majority of participants were from Christian religion. |
|
|
Perinatal mental health screening – Edinburgh Postnatal Depression Scalec |
|
NR |
|
Roles of HCPs included midwives, obstetricians, nurses, psychiatrist, mental health expert, maternity general practice liaison officer, community mental health team leader, refugee health experts, bicultural worker, interpreters. Majority of women were from an Afghan ethnicity. |
|
|
Perinatal mental health care in Ireland – booking appointment with midwife where midwives ask about emotional issues, but this is not always done. Postnatal care is primarily provided by Public Health Nurses who screen for PND and anxiety using the Whooleyf questions and EPDSc and refer to the GP for diagnosis and treatment interventions. |
|
NR |
|
Majority had 5–10 years of experience. Majority were from Urban practice type. There were equal numbers of males and females. |
|
|
Online treatment –11-sessions of Behavioural Activation for Postnatal Depression |
|
N/A |
|
Mean age was 31.3 years. 30% had an £40,000 to £49000 income. 40% had an income of £80,000+ Work status was either homemaker, full or part time employment, a student or volunteer. Majority (80%) were in a relationship. 40% had up to post-16 qualification. Majority (56%) had 1 child. |
|
|
Referral on to acupuncture – a new treatment within the hospital, which is individually tailored low-risk Chinese medical treatment as a supplementary therapeutic option for antenatal depression. |
|
NR |
|
Majority of participants were female. Two professionals had spent less than 5 years in their area of expertise. However, most had worked for more than 30 years in their current roles. |
|
|
Mobile health technology – use of mobile electronic devices to assist in healthcare provisions and management. |
|
NR |
|
Sample included nutritionists, nurses, case managers, administrative assistants, intake specialists and programme coordinators. |
|
|
Specialised internet therapy programme adapted from a Therapist-Assisted Internet Cognitive Behavioural Therapy (TAICBT) programme for major depression. Programme consisted of 7 modules. Following completion, weekly offline homework activities were assigned, and clients received one email a week from their assigned internet therapist. |
|
Trained in and supervised in the provision of TAICBT. |
|
Majority (92%) from Caucasian ethnicity. Majority (96%) were married/common law/engaged. Majority (87%) had a college, some university or undergraduate degree. Most (46%) had given birth once. |
|
|
Promoting resilience in mothers’ emotions’ (PRIME) – counselling. Women were offered this antenatally and 6 weeks postnatal. |
|
Workshops, written manuals, digitally recorded counselling vignettes. |
|
All were female, aged 26–59 years, with a mean of 13 years clinical midwifery experience. 7 were educated in the tertiary sector and 11 in a hospital-based midwifery programme. |
|
|
NHS perinatal mental health services offered by two different NHS Trusts. |
|
NR |
|
NR |
|
|
Train the Trainer Maternal Depression screening programme (TTT) – incorporated the use of the EPDSc tool. |
|
Lectures and activities to train to administer the screening tool. |
|
Most nurses were white/non-Hispanic and ranged from 36 to 55 years of age. Majority had a bachelor’s degree and approximately 1/3 were employed full-time. |
|
|
Oxford City Postnatal Depression Strategy – routine screening with EPDSc at 8 weeks and 8 months after birth. Subsequent actions such as non-directive counselling is based on screening score and health visitor assessment. |
|
4–6 half-day sessions followed by 2-monthly supervision. 6–8 hours of personal study using a resource pack entitled ‘The emotional effects of childbirth’ and 1 day of basic training and subsequent mentoring. |
|
The mean of the women was 34 years; range=19 to 42 years. Majority (n = 37) were white. Most (n = 24) were upper or middle class. |
|
|
Technology-based peer support intervention programme (PIP) – support from peer volunteers for at least one month after birth including a minimum of once a week correspondence through any technology-based means. Frequency and duration were tailored to maternal needs. |
|
Training session by a psychiatrist. |
|
Mothers: 25–40 years of age 50% were Chinese; 45% Malay; 5% Indian 95% married 80% university undergraduates 50% monthly household income of over 5000 S$ Peer volunteers: 25–54 years 90% were Chinese; 90% married’ 68% university graduates; 47% monthly household income of over 5000 S$ |
|
|
EPDSc screening by health visitors. |
|
NR |
|
Six of the participants were experienced health visitors with a three-year bachelor’s degree and 1 year of specialising in a community health service. |
|
|
Perinatal mental health screening programme – routine use of the mental health psychosocial questionnaire and use of EPDSc. Undertook screening using iPad and the I-cope system (generates immediate screening score and report with recommendation). Following assessment, women referred to counselling or other services. |
|
NR |
|
Employed across all areas of implementation and included midwives, midwifery managers, bicultural workers and administrators, the Refugee Health Nurse Liaison, and counsellors. |
|
|
Women were asked the Whooleyf questions by midwives during their booking appointment. |
|
NR |
|
Most midwives were aged 50+. All White-British ethnicity. Most been practicing for over 20 years and over since completing midwifery training. Most had no mental health qualification. Most women were aged 30–39 years. Majority of White-British ethnicity. Majority had previous experience of depression. |
|
|
All women complete the EPDSc at each well child visit, provided by medical assistants, filled out via self-report and reviewed by paediatrician or social worker. Multidisciplinary team work together to create an individualised plan for each parent-child dyad. Appointments (2–45 minutes) scheduled so they are seen on the same day as their child’s paediatric visit. Women can be offered follow-up for an unlimited number of appointments at a frequency mutually agreeable. Women could be prescribed medication or referred for therapy or other services. |
|
NR |
|
Six participants were monolingual Spanish speakers, age ranged from 25 to 49 years. Nearly half were active patients at time of interview whilst other half had ceased receiving care for various reasons. Majority (60%) were Hispanic-white ethnicity. Majority (80%) had a primary diagnosis of a major depressive disorder. |
Appendix 2
| Review details | Participant details | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| N studies about women (Total N), Years (range) | Inclusion criteria | Country of studies | N, M (SD) | Age | Perinatal period | Ethnicity | Mental illness | Socio-economic status | |
| Bina (2020)69 | 31 (35) 1993–2018 |
Service use for postpartum depression or ‘distress’ from women (and HCP) perspectives | 11 countries (4 LMIC) | 7219 232.9 (414.7) |
NR | 2 weeks – up to 3 years postnatal | Six studies specified recruitment of migrant women or ethnic minority women r(EA; H; Ar) | Depressive symptoms, emotional difficulties or current/past diagnosis of mood disorder | Two studies recruited women with low income. One study recruited women using Medicaid |
| Brealey et al. (2010)74 | 13 (16) 1997–2007 |
Acceptability to women (and HCP) of screening to identify women with increased risk of postnatal depression | Five countries (all HIC) | 1715 131.9 (253.06) |
24–34 M (n = 8) = 29.63 |
First antenatal appointment – 12 months after birth | Two studies recruited ethnic minority women (B; EA; Ar) | Women at risk of postnatal depression | One study reported marriage (29/30 women were married) |
| Button et al. (2017)46 | 24 (24) 1993–2016 |
Help-seeking for postnatal depression | Nine studies carried out in UK; no other countries reported | NR | NR | Postnatal | Nine studies recruited ethnic minority women Three studies had mixed samples | Postnatal depression | NR |
| Dennis and Chung-Lee (2006)47 | 40 (40) NR |
Maternal help-seeking barriers and facilitators and treatment preferences for postnatal depression | 3 were explicitly stated (all HIC) | NR | NR | Up to 1 year after birth | Three studies recruited ethnic minority women(SA; EA; B; Ar) | Postnatal depression | NR |
| Evans et al. (2017)75 | 14 (14) 2009–15 |
Acceptability of non-pharmacological interventions for antenatal anxiety | Six countries (all HIC) | 235 16.8 (9.6) |
NR | Between 6 and 40 weeks gestation | NR | Eight studies recruited women with a history of mood concerns/anxiety or depression | Two studies recruited women with ‘social risk factors’ |
| Forde et al. (2020)105 | 13 (15) 2003–18 |
Published empirical studies exploring women’s or family members' experiences of PP and/or recovery using a qualitative methodology | Four countries (all HIC) | 103 7.92 (2.96) |
Range: 23–62 | All postnatal, ranging from 4 months to 26 years after onset of postnatal psychosis | One woman was an Orthodox Jewish woman | All women had recovered from, or were currently experiencing postnatal psychosis | NR |
| Giscombe et al. (2020)76 | 8 (8) 2008–17 |
Refugee or asylum-seeking women, with mental health complications during perinatal period | Three countries (all HIC) | NR | NR | NR | Syrian refugees, Eritrean refugees | Six studies recruited women with depression; 3 with PTSD (1 study recruited both depression and PTSD) | All women were refugees or asylum seekers |
| Hadfield and Wittkowski (2017)72 | 17 (17) 2004–15 |
Mothers with postnatal depression and their experiences about help-seeking for psychosocial support | Four countries (all HIC) | 532 31.3 (25.97) |
Range 18–45 M (n = 2) = 30.2 |
Postnatal | Three studies recruited women who weren’t born in the UK(B; EA) | Postnatal depression | NR |
| Hansotte et al. (2017)70 | 18 (18) 2004–15 |
Screening for postnatal depression and barriers to accessing treatment in low-income women in Western countries | Two countries (all HIC) | 85190 5011 (11613) |
M (n = 11) = 25.11 | Postnatal | All studies recruited a diverse sample of migrant women or ethnic minority women (B; L; W; As; NI) | Self-report depression symptoms or depression diagnosis | All women were low-income living in high-income Western countries |
| Hewitt et al. (2009)77 | 13 (16) 1997–2007 |
Acceptability to women (and HCP) about methods to identify postnatal depression | Five countries (all HIC) | 1715 131.9 (253.06) |
M (n = 8) = 29.63 | Postnatal: 1–12 months Antenatal: all trimesters |
Four studies recruited ethnic minority women (Ar; EA; B; NI; NS) | Perinatal depression | Two studies looked at marriage. The majority of women were married (87–97%) |
| Holopainen and Hakulinen (2019)78 | 13 (15) 2005–15 |
Mothers (and fathers) experiences of postnatal depression symptoms | Seven countries (all HIC) | 199 15.31 (8.21) |
Ages ranged from 16 to 45 | 1–12 months after birth | Five studies recruited ethnic minority women (B; L; H; SA; EA) | Most studies looked at symptoms of depression, two looked at diagnoses | One study recruited low-income women, one recruited adolescent mothers. Most women were married (n = 3; 59–66%). Most women had more than 9 years of education (n = 2; 87–100%) |
| Jones et al. (2014)79 | 5 (5) 1995–2012 |
Women’s experiences of peer support for any degree of perinatal mental illness | Three countries (all HIC) | 95 19 (18.93) |
NR | 6 weeks to 2 years after birth | NR | Postnatal depression diagnosis or symptoms | NR |
| Jones (2019)80 | 19 (19) 2008–17 |
Help-seeking in women with perinatal depression | All USA | 6089 358.90 (1226.22) |
NR | Pregnancy to 6 months after birth | Six studies were ethnic minority women (B; L; SA; EA; NS) | All had perinatal depression identified through screening measures, or self-reported | All women had pregnancy complications. Three studies recruited women on a low income |
| Kassam (2009)81 | 11 separate populations 1999–2013 |
Voices of immigrant and refugee women with postnatal depression in terms of social support as a coping resource | Three countries stated (HIC and UMIC countries) | 191 23.88 (10.89) |
All aged over 17 | Screened high on a postnatal depression scale within 2 weeks – 5 years after birth | All studies recruited migrant women or ethnic minority women (NS; As; Ar; SA; H) | Most had postnatal depressive symptoms, identified through screening. One study reported depression diagnosis | One study looked at risk profile of women (e.g. low income, experienced violence, experienced war, previous mental health difficulty). All women in two studies were married or in a relationship. One study recruited low-income women |
| Lucas et al. (2019)82 | 19 (19) 1999–2017 |
Young women’s perception of their mental health and well-being | Three countries (all HIC) | 356 18.74 (10.02) |
Ages ranged from 13–25. M (n = 2) = 18.75 |
11 studies recruited were parents (3 months – 2 years postnatal). 2 studies recruited pregnant women. Remaining studies recruited both pregnant and postnatal women |
Majority of studies (15) recruited ethnically diverse (L; B; H; SA; M; As) samples. Four studies did not report ethnicity | Depressive symptoms, depression diagnosis, other diagnoses (bipolar, panic disorder, mood disorder) | All women were young (maximum age 25) |
| Megnin-Viggars et al. (2015)48 | 39 (39) 2001–13 |
Women with, or at risk of developing postnatal mental health difficulties and their views on factors that improve or diminish access to perinatal mental health services | Only reported for 3 studies (all UK) | 955 24.49 (43.77) |
One study recruited teenage mother. No other ages reported | Antenatal and postnatal | Five studies recruited ethnically diverse samples (B; NS; SA) | Most studies recruited women with depression (n = 14) or women at risk (n = 18) of perinatal mental health difficulties | One study recruited teenage mothers |
| Mollard et al. (2016)83 | 11 (11) 1995–2014 |
Women living in rural areas of the USA with PPD. Looking at screening uptake, intervention acceptability, lived experience, help-seeking | All USA | 1610 146.36 (159.57) |
NR | Postnatal | 5 studies recruited ethnically diverse samples (NI; B; NS; H) | Postnatal depression symptoms, most used EPDSa (n = 6) screen | All women lived in rural locations, three studies recruited low-income women |
| Morrell et al. (2016)84 | 38 individual samples of women in the qualitative review 1987–2013 |
Pregnant and postnatal women, views on preventative or targeted services for PND | Eight countries (1 LMIC – India) | 1673 (34 studies reported sample size) 49.21 (98.49) |
Ages ranged from 15–54 M (n = 12) = 28.62 |
Pregnancy and postnatal | 10 recruited ethnically diverse samples (SA; EA, B; H; NI; L; M; NS) | Depression – both symptoms and diagnoses | 25 studies reported sociodemographic characteristics. 16 studies reported marital status, in all but 1 study the majority of women were married/cohabiting/in a relationship. 8 studies reported education status: most had completed high school or above. 4 studies recruited low-income women or those living in an impoverished/deprived area |
| Newman et al. (2019)85 | 4 (4) 2008–16 |
Women with depression during the postnatal period sharing views on help-seeking | Three countries (all HIC) | 118 29.5 (9) |
M (n = 3) = 31.97 | Postnatal | NR | Depressive symptoms, measured by EPDSa | NR |
| Nilaweera et al. (2014)86 | 9 (15) | Women who have migrated from South Asian countries to live in high-income countries, barriers and enablers to health care access | Four countries (all HIC) | 20,788 2309.78 (3926.13) |
NR | 2 weeks to 5 years postnatal | All studies recruited women born in South Asia | Most (n = 5) used EPDSa to assess postnatal depression symptoms | NR |
| Praetorius et al. (2020)87 | 8 (8) 1999–2016 |
Mothers with depression and suicidality | Five countries (3 HIC, 1 UMIC, 1LMIC) | 199 24.88 (12.52) |
Ages range from 17 to 44 | Pregnancy and postnatal | All studies recruited diverse samples (B; L; M; SA; EA; Ar; W) | All women had depression and suicidality | NR |
| Randall and Briscoe (2018)88 | 4 (4) 2005–14 |
Women’s decision-making process around antidepressant use during pregnancy | Two countries (all HIC) | 368 92 (37.09) |
Ages ranged from 25–34 M (n = 2) = 31 |
Pregnancy | 3 studies reported ethnicity. The majority of women were white (77.5–95%) | Depression – 1 study used the CES-Db to identify depressive symptoms | Three studies report education, the majority (82.5–100%) were educated to above high school level. Three studies reported relationship status, the majority (80–98%) were married/living with partner |
| Slade, Molyneux and Watt (2021)92 | 13 (13 – qualitative papers only) 2007–19 |
Help-seeking for birth trauma/postnatal PTSD | Seven countries (1 UMIC; 6 HIC) | 394 30.31 (32.85) |
Ages range from 2–45 M (n = 4) = 32 |
Up to 18 months after birth | Eight studies reported ethnicity. One study reported recruiting ethnic minority women r(B; H) | All PTSD after birth | One study recruited low-income women. Two studies reported marital status, over 58% were married. Two studies reported higher education, at least 50% of women had completed this |
| Sambrook Smith et al. (2019)89 | 24 (35) 2007–18 |
Barriers to accessing perinatal mental health care from the perspective of women (families and HCP) | All UK | 384 16 (8.80) |
NR | Postnatal | Nine recruited ethnic minority women (B; SA; EA) | Most looked at depressive symptoms (n = 12). Studies also recruited women with antenatal anxiety (n = 1), postnatal psychosis (n = 5), PTSD (n = 1) and substance misuse (n = 1) | NR |
| Sorsa, Kylmä and Bondas (2021)93 | 14 (14) 2002–18 |
Help-seeking in women with perinatal distress | Five countries (all HIC) | 345 24.65 (11.99) |
Ages ranged from 18 to 55 M (n = 7) = 30.21 |
Antenatal and postnatal | NR | Postnatal depression (n = 8); Prenatal depression (n = 2); Perinatal mental health needs (n = 2); Postpartum mood disorder (n = 1); Bipolar disorder (n = 1) | NR |
| Schmied et al. (2017)90 | Twelve individual samples 1999–2015 |
Migrant women living in high-income countries | Four countries (all HIC) | 250 20.83 (12.52) |
M (n = 5) = 29.4 | Postnatal | All studies recruited migrant women or ethnic minority women (SA; EA; H; B; Ar; L) | Depressive symptoms or formal diagnosis | One study recruited low-income women |
| Scope et al. (2017)91 | Twelve individual samples 1987–2014 |
Service user views on uptake, acceptability of preventative interventions for PND | Seven countries (all HIC) | 982 (reported by author) | 13–45 years | Antenatal and postnatal | NR | NR | NR |
| Staneva et al. (2015)94 | 8 (8) 2006–12 |
Women’s experience of antenatal mental health difficulties | Five countries (1 LMIC – Cambodia) | 1094 14 (6.26) |
Ages ranged from 16 to 47 | Antenatal | Most studies (n = 6) recruited ethnically diverse samples (B; M) | Self-report distress, depression (n = 5); diagnoses depression/anxiety (n = 2); FOC = 1 | 50–100% of women were in a relationship |
| Tobin et al. (2018)95 | 8 (individual samples) 2004–13 |
Refugee or immigrant women’s experiences of postpartum depression | Three countries (all HIC) | 139 17.38 (7.98) |
Age ranges between 17 and 54 years | Postnatal | All studies recruited migrant women and ethnic minority women (L; H; SA;EA;B) | Postnatal depression | Six studies reported relationship status 50–85% of women were married/in a relationship |
| Viveiros and Darling (2019)49 | 7 (26) 2009–18 |
To explore women’s (and midwives’) perceptions on factors that impede access to perinatal mental health care in high resource settings | Two countries (both HIC) | 301 43 (66.30) |
One study reported age range from 23 to 40 | Antenatal and postnatal | Two studies recruited ethnic minority women, one recruited all black women | PTSD symptoms (n = 1); mental health difficultiess (n = 2); mental illness diagnosis (n = 1) | NR |
| Watson et al. (2019)96 | 15 (15) 1994–2015 |
Ethnic minority women’s experience of perinatal mental ill health, help-seeking and perinatal mental health services in Europe | All UK | 4970 331.33 (1173.09) |
NR | Antenatal and postnatal | All studies recruited ethnic minority women (SA; NS; N; EA; M) | Distress, depression, mood and mental health, well-being | NR |
| Wittkowski et al. (2014)97 | 12 (12) 1983–2009 |
Culturally determined risk factors of PND in sub-Saharan Africa | Three countries – all sub-Saharan Africa | 3642 404.67 (343.16) |
NR | Postnatal | NR | All used self-report measures of depression | NR |
Appendix 3
| Domain 1: Design and methodology | Domain 2: Researcher influence | Domain 3: Participants | Domain 4: Interpretation of results | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Qualitative | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Rating/risk of bias |
| Qualitative | Domain 1: Design and methodology | Domain 2: Researcher influence | Domain 3: Participants | Domain 4: Interpretation of results | |||||||
| Domain 1: Author credentials | Domain 2: Opinion development | Domain 3: Literature support | Rating/risk of bias | ||||||||
| Text and opinion | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Rating/risk of bias | ||||
| Domain 1: Participants | Domain 2: Methodology | Domain 3: Analysis | Rating/risk of bias | ||||||||
| Cross-sectional | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | |||
| Ammerman et al. (2014)126 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | No | Yes | Moderate |
| Atif et al. (2016)106 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Minor |
| Atif et al. (2019)133 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Minor |
| Bina et al. (2018)144 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Minor |
| Boyd et al. (2011)113 | Unclear | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Minor |
| Byatt et al. (2013)142 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | No | Yes | Moderate |
| Chartier et al. (2015)132 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Minor |
| Doering et al. (2017)114 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | No/limited |
| Drozd et al. (2018)149 | Unclear | Yes | Yes | Yes | Yes | No | No | No | Yes | Yes | Moderate |
| Friedman et al. (2010)135 | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | No | Yes | Moderate |
| Ganann et al. (2019)109 | Unclear | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Minor |
| Hadfield et al. (2019)152 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | No/limited |
| Jallo et al. (2015)153 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Minor |
| Kerker et al. (2018)130 | Yes | Yes | Yes | Yes | Yes | No | No | No | Yes | Yes | Moderate |
| Kim et al. (2009)128 | Yes | Yes | Yes | Yes | Yes | No | No | No | Yes | Yes | Moderate |
| Leger et al. (2015)147 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Minor |
| Masood et al. (2015)137 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Minor |
| McCauley et al. (2019)107 | Unclear | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | No/limited |
| McKenzie-McHarg et al. (2014)148 | Unclear | Yes | Yes | Unclear | Unclear | No | No | No | Yes | Yes | Serious |
| Munodawafa et al. (2017)138 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No methodological concerns |
| Myors et al. (2015)112 | Unclear | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Minor |
| Nakku et al. (2016)108 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Minor |
| Nithianandan et al. (2016)122 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | No/limited |
| Noonan et al. (2018)116 | Unclear | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Minor |
| O’Mahen et al. (2015)151 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No |
| Ormsby et al. (2018)139 | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | No/limited |
| Pineros-Leano et al. (2015)117 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No |
| Pugh et al. (2015)145 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No |
| Reed et al. (2014)143 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Minor |
| Rowan et al. (2010)120 | Yes | Yes | Yes | Yes | Yes | No | No | No | Yes | Yes | Moderate |
| Segre et al. (2014)123 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Minor |
| Shakespeare et al. (2003)124 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Minor |
| Shorey et al. (2019)146 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Minor |
| Vik et al. (2019)118 | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | No | Yes | Moderate |
| Willey et al. (2019)125 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Minor |
| Williams et al. (2016)119 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Minor |
| Young et al. (2019)110 | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | No/limited |
| Beeber et al. (2009)141 | Yes | Yes | Yes | Yes | Yes | N/A | Minor | ||||
| Cox et al. (2017)134 | Yes | Yes | Yes | Yes | Yes | N/A | Minor | ||||
| Eappen et al. (2018)136 | Yes | Yes | Yes | Yes | Yes | N/A | Minor | ||||
| Feinberg et al. (2006)127 | Yes | Yes | Yes | Yes | Yes | N/A | Minor | ||||
| Garcia Fernandez et al. (2011)121 | Yes | Yes | Yes | Yes | Yes | N/A | Minor | ||||
| Judd et al. (2011)129 | Yes | Yes | Yes | Yes | Yes | N/A | Minor | ||||
| Lind et al. (2017)130 | Yes | Yes | Yes | Yes | Yes | N/A | Minor | ||||
| Lomonaco-Haycraft et al. (2018)140 | Yes | Yes | Yes | Yes | Yes | N/A | Minor | ||||
| Higgins et al. (2018)115 | Yes | No | Yes | N/A | N/A | N/A | Yes | Yes | Minor | ||
Appendix 4
| Author, year | Q1. PICO | Q2. Protocol* | Q3. Study design | Q4. Literature search* | Q5. Study selection | Q6. Data extraction | Q7. Excluded studies* | Q8. Included studies | Q9. ROB | Q.10 Funding | Q13. ROB interpretation | Q14. Heterogeneity | Q16. Conflict of interest* | Rating |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bina, 202069 | Yes | Yes | No | Partial yes | Yes | No | Partial yes | Yes | No | No | No | Yes | No | LOW |
| Brealey et al., 201074 | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Partial yes | No | Yes | Yes | No | CRITICALLY LOW |
| Button et al., 201746 | Yes | No | Yes | Yes | No | No | Partial yes | Partial yes | Yes | No | Yes | Yes | Yes | LOW |
| Dennis and Chung-Lee, 200647 | Yes | No | Yes | Yes | No | Yes | No | Partial yes | No | No | No | No | No | CRITICALLY LOW |
| Evans et al., 202075 | Yes | Yes | Yes | Yes | Yes | Yes | Partial yes | Yes | Yes | No | Yes | Yes | Yes | HIGH |
| Forde et al., 2020105 | Yes | Yes | Yes | Partial yes | Yes | No | Partial yes | Ys | Yes | No | Yes | Yes | Yes | MODERATE |
| Giscombe et al., 202076 | Yes | No | Yes | Partial yes | No | No | Partial yes | Yes | Yes | No | No | Yes | No | CRITICALLY LOW |
| Hadfield and Wittkowski, 201772 | Yes | Yes | Yes | Yes | No | No | Partial yes | Yes | Yes | No | Yes | Yes | Yes | MODERATE |
| Hansotte et al., 201770 | Yes | No | Yes | Yes | Yes | Yes | Partial yes | Yes | No | No | No | Yes | Yes | LOW |
| Hewitt et al., 200977 | Yes | Yes | Yes | Yes | Yes | Yes | Partial yes | Yes | Yes | No | Yes | Yes | Yes | HIGH |
| Holopainen and Hakulinen, 201978 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | HIGH |
| Jones et al., 201479 | Yes | No | Yes | Yes | No | Yes | No | Partial yes | Yes | No | Yes | Yes | Yes | CRITICALLY LOW |
| Jones, 201980 | Yes | No | Yes | Partial yes | Yes | No | Partial yes | Yes | No | No | Yes | Yes | Yes | LOW |
| Kassam, 201981 | Yes | Yes | Yes | Partial yes | No | No | Partial yes | Yes | Yes | No | Yes | Yes | Yes | MODERATE |
| Lucas et al., 201982 | Yes | Yes | Yes | Yes | Yes | Yes | Partial yes | Yes | Yes | No | Yes | Yes | Yes | HIGH |
| Megnin-Viggars et al., 201548 | Yes | Yes | Yes | Partial yes | No | Yes | Partial yes | Yes | Yes | No | Yes | Yes | No | LOW |
| Mollard et al., 201683 | Yes | No | Yes | Partial yes | No | No | Partial yes | Partial yes | No | No | No | Yes | Yes | LOW |
| Morell et al. 201684 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Ye | No | Yes | Yes | Yes | HIGH |
| Newman et al., 201985 | Yes | No | Yes | Yes | No | No | Partial yes | Yes | Yes | No | No | No | Yes | LOW |
| Nilaweera et al., 201486 | Yes | No | No | Partial yes | No | No | Partial yes | Yes | Yes | No | Yes | Yes | Yes | LOW |
| Praetorius et al., 202087 | No | No | Yes | Yes | No | Yes | Partial yes | Partial yes | No | No | No | No | Yes | LOW |
| Randall and Briscoe, 201888 | Yes | No | No | Partial yes | Yes | No | Partial yes | Partial yes | Yes | No | No | Yes | Yes | LOW |
| Sambrook Smith et al., 201989 | Yes | Yes | Yes | Partial yes | Yes | No | Partial yes | Yes | Yes | No | Yes | Yes | Yes | MODERATE |
| Schmied et al., 201790 | Yes | No | Yes | Partial yes | Yes | No | Partial yes | Yes | Yes | No | Yes | Yes | Yes | LOW |
| Scope et al., 201791 | Yes | Yes | Yes | Partial yes | Yes | Yes | Partial yes | Yes | Yes | No | Yes | Yes | No | LOW |
| Staneva et al., 201594 | Yes | Yes | Yes | Partial yes | Yes | No | Partial yes | Yes | Yes | No | Yes | Yes | Yes | MODERATE |
| Slade et al., 202092 | Yes | Yes | Yes | Yes | No | No | Partial yes | Yes | Yes | No | Yes | Yes | Yes | MODERATE |
| Sorsa et al., 202193 | Yes | No | Yes | Partial yes | Partial yes | Yes | Partial yes | Yes | Yes | No | Yes | Yes | Yes | LOW |
| Tobin et al., 201895 | Yes | Yes | Yes | Yes | No | No | No | Yes | Yes | No | No | Yes | Yes | MODERATE |
| Viveiros and Darling, 201849 | Yes | No | No | Yes | Yes | No | Partial yes | Yes | No | No | No | Yes | Yes | LOW |
| Watson et al., 201996 | Yes | Yes | Yes | Partial yes | Yes | No | Partial yes | Yes | Yes | No | Yes | Yes | Yes | MODERATE |
| Wittkowski et al., 201497 | Yes | No | Yes | Partial yes | No | No | Partial yes | Yes | Yes | No | Yes | Yes | No | CRITICALLY LOW |
Appendix 5
Papers supporting the multi-level themes at different stages of the care pathway
| Theme | Total number of papers that contribute to this theme | Number of papers that contribute to this theme within this stage of the care pathway | Studies |
|---|---|---|---|
| 1 Women | |||
| 1.1 Beliefs about health services | |||
| 1.1.1 Services only offer medication | 14 | 5 | Bina, 202069; Button et al., 201746; Jones, 201980; Megnin-Viggars et al., 201548; Nilaweera et al., 201486 |
| 1.1.2 Services are stretched | 2 | 1 | Hadfield and Wittkowski, 201772 |
| 1.1.3 Services are too complicated | 2 | 1 | Ganann et al., 2019 109 |
| 1.2 Beliefs about healthcare professionals | |||
| 1.2.1 Not understanding healthcare professionals’ role | 12 | 6 | Button et al., 201746; Megnin-Viggars et al., 201548; Mollard et al., 201683; Morrell et al., 2016184; Nilaweera et al., 201486; Schmied et al., 201790 |
| 1.2.2 Believing healthcare professionals won’t be interested | 2 | 1 | Bina, 202069 |
| 1.3 Beliefs about perinatal mental illness | |||
| 1.3.1 What is it? | |||
| 1.3.1.1 What is perinatal mental illness? | 18 | 14 | Bina, 202069; Button et al., 201746; Dennis and Chung-Lee, 200647; Hadfield and Wittkowski, 201772; Hansotte et al., 201770; Jones, 201980; Lucas et al., 201982; Morrell et al., 201684; Newman et al., 201985; Sambrook Smith et al., 201989; Schmied et al., 201790; Scope et al., 201791; Tobin et al., 201895; Watson et al., 201996 |
| 1.3.1.2 No language to describe perinatal mental illness | 5 | 4 | Brealey et al., 201074; Staneva et al., 201594; Tobin et al., 201895; Watson et al., 201996 |
| 1.3.2 Causes of perinatal mental illness | |||
| 1.3.2.1 Spiritual/cultural causes | 6 | 6 | Atif et al., 2016106; McCauley et al., 2019107; Nakku et al., 2016108, Button et al., 201746; Schmied et al., 201790; Wittkowski et al., 201497 |
| 1.3.2.2 External causes | 8 | 8 | Bina, 202069; Button et al., 201746; Dennis and Chung-Lee, 200647; Lucas et al., 201982; Schmied et al., 201790; Staneva et al., 201594; Tobin et al., 201895; Watson et al., 201996 |
| 1.3.2.3 Physical causes | 13 | 9 | Bina, 202069; Button et al., 201746; Forde et al., 2020105; Jones et al., 201479; Newman et al., 201985; Sambrook Smith et al., 201989; Schmied et al., 201790; Staneva et al., 201594; Watson et al., 201996 |
| 1.3.2.4 A normal response to motherhood? | 9 | 8 | Dennis and Chung-Lee, 200647; Giscombe et al., 202076; Jones et al., 201479; Sambrook Smith et al., 201989; Schmied et al., 201790; Slade et al., 202092; Sorsa et al., 202193; Viveiros and Darling, 201949 |
| 1.3.3 How to cope with symptoms | |||
| 1.3.3.1 Ignore them | 6 | 6 | Bina, 202069; Hadfield and Wittkowski, 201772; Jones, 201980; Newman et al., 201985; Schmied et al., 201790; Slade et al., 202092 |
| 1.3.3.2 Seek spiritual guidance | 4 | 4 | Hansotte et al., 201770; Kassam, 2013981; Schmied et al., 201790; Watson et al., 201996 |
| 1.3.3.3 Minimise them | 14 | 2 | Staneva et al., 201594; Watson et al., 201996 |
| 1.4 Deciding to seek help | |||
| 1.4.1 Recognising something is wrong | 8 | 8 | Bina, 202069; Button et al., 201746; Forde et al., 2020105; Hadfield and Wittkowski, 201772; Slade et al., 202092; Sorsa et al., 202193; Staneva et al., 201594; Viveiros and Darling, 201949 |
| 1.4.2 Where do I go to seek help? | 9 | 8 | Ganann et al., 2019109; Bina, 202069; Dennis and Chung-Lee, 200647; Hansotte et al., 201770; Megnin-Viggars et al., 201548; Schmied et al., 201790; Sorsa et al., 202193; Tobin et al., 201895 |
| 1.5 Fear of judgement | |||
| 1.5.1 Fear of being seen as a bad mum | 9 | 2 | Bina, 202069; Forde et al., 2020105 |
| 1.5.2 Social services/removal of child | 17 | 5 | Young et al., 2019110 Dennis and Chung-Lee, 200647; Forde et al., 2020105; Jones, 201980; Watson et al., 201996 |
| 1.7 Social and family life | |||
| 1.7.1 Social isolation or support | 9 | 2 | Jones et al., 201479; Viveiros and Darling, 201949 |
| 1.7.2 Family and friends’ beliefs | 30 | 11 | Bina, 202069; Button et al., 201746; Dennis and Chung-Lee, 200647; Forde et al., 2020105; Holopainen and Hakulinen, 201978; Jones, 201980; Lucas et al., 201982; Nilaweera et al., 201486; Sambrook Smith et al., 201989; Schmied et al., 201790; Sorsa et al., 202193 |
| 1.8 Sociodemographic factors | |||
| 1.8.1 Ethnicity | 2 | 2 | Bina, 202069; Dennis and Chung-Lee, 200647 |
| 1.8.2 Age | 2 | 2 | Bina, 202069; Hansotte et al., 201770 |
| 1.9 Mental health factors | |||
| 1.9.1 Previous experiences of mental health care | 6 | 4 | Button et al., 201746; Hadfield and Wittkowski, 201772; Hansotte et al., 201770; Watson et al., 201996 |
| 1.9.2 Previous diagnoses or symptoms | 2 | 2 | Bina, 202069; Sorsa et al., 202193 |
| 1.9.3 Current diagnoses or symptoms | 6 | 1 | Sorsa et al., 202193 |
| 2.3 Healthcare professional’s attributes | |||
| 2.3.1 Similar demographic characteristics | 6 | 2 | Dennis and Chung-Lee, 200647; Watson et al., 201996 |
| 2.3.3 Valued characteristics | 25 | 1 | Jones, 201980 |
| 3 Interpersonal | |||
| 3.1 Trusting relationship and rapport | 23 | 1 | Dennis and Chung-Lee, 200647 |
| 3.2 Language barriers | 16 | 2 | Dennis and Chung-Lee, 200647; Schmied et al., 201790 |
| 3.4 Open and honest communication | 9 | 2 | Schmied et al., 201790; Watson et al., 201996 |
| 4 Organisational | |||
| 4.1 Overall organisational aspects | |||
| 4.1.1 Co location and buildings | 7 | 1 | Bina, 202069 |
| 4.1.2 Service integration and collaborative working | 17 | 1 | Newman et al., 201985 |
| 4.2 Characteristics of PMH care | |||
| 4.2.1 Across the care pathway | |||
| 4.2.1.1 Continuity of carer | 17 | 1 | Button et al., 201746 |
| 4.2.1.2 Culturally sensitive care | 19 | 5 | Bina, 202069; Dennis and Chung-Lee, 200647; Jones, 201980; Schmied et al., 201790; Watson et al., 201996 |
| 4.2.1.5 Logistical support | 13 | 1 | Jones, 201980 |
| 4.2.1.6 Home delivery | 10 | 1 | Jones 201980 |
| 4.2.1.8 Provision of information | 7 | 1 | Schmied et al., 201790 |
| 5 Commissioners | |||
| 5.2 Lack of appropriate or timely services | 22 | 4 | Jones, 201980; Megnin-Viggars et al., 201548; Newman et al., 201985; Viveiros and Darling, 201949 |
| 6 Political | |||
| 6.1 Immigration status | 9 | 3 | Bina, 202069; Hansotte et al., 201770; Schmied et al., 201790 |
| 6.2 Economic status and healthcare costs | 16 | 5 | Bina, 202069; Hansotte et al., 201770; Jones, 201980; Lucas et al., 201982; Tobin et al., 201895 |
| 7 Societal | |||
| 7.1 Stigma | 43 | 14 | Nakku et al., 2016108 Bina, 202069; Button et al., 201746; Dennis and Chung-Lee, 200647; Hadfield and Wittkowski, 201772; Hansotte et al., 201770; Jones, 201980; Kassam, 201981; Mollard et al., 201683; Nilaweera et al., 201486; Sorsa et al., 202193; Tobin et al., 201895; Viveiros and Darling, 201949; Watson et al., 201996 |
| 7.2 Culture | 30 | 15 | Atif et al., 2016106; McCauley et al., 2019107; Nakku et al., 2016108 Button et al., 201746; Dennis and Chung-Lee, 200647; Giscombe et al., 202076; Jones, 201980; Kassam, 201981; Praetorius et al., 202087; Sambrook Smith et al., 201989; Schmied et al., 201790; Staneva et al., 201594; Tobin et al., 201895; Watson et al., 201996; Wittkowski et al., 201497 |
| 7.3 Maternal norms | 27 | 13 | Bina, 202069; Button et al., 201746; Hadfield and Wittkowski, 201772; Hansotte et al., 201770; Holopainen and Hakulinen, 201978; Johnson et al., 2020112; Kassam, 201981; Lucas et al., 201982; Mollard et al., 201683; Nilaweera et al., 201486; Schmied et al., 201790; Sorsa et al., 20219; Staneva et al., 201594 |
| Theme | Total number of papers that contribute to this theme | Number of papers that contribute to this theme within this stage of the care pathway | Studies citing this theme |
|---|---|---|---|
| 1 Women | |||
| 1.3.2 Causes of perinatal mental illness | |||
| 1.3.2.1 Spiritual/cultural causes | 6 | 2 | Dennis and Chung-Lee, 200647; Schmied et al., 201790 |
| 2 Healthcare professional | |||
| 2.1 Healthcare professionals knowledge about PMH | |||
| 2.1.1 Healthcare professionals knowledge about PMI | 17 | 1 | McKenzie-McHarg et al., 2014 148 |
| 2.2 Getting it right the first time | |||
| 2.2.1 Being dismissive or normalising symptoms | 11 | 8 | Button et al., 201746; Dennis and Chung-Lee, 200647; Forde et al., 2020105; Hadfield and Wittkowski, 201772; Hansotte et al., 201770; Newman et al., 201985; Sorsa et al., 202193; Watson et al., 201996 |
| 2.2.2 Not recognising help seeking or PMI | 5 | 4 | Megnin-Viggars et al., 201548; Tobin et al., 201895; Viveiros and Darling, 201949; Watson et al., 201996 |
| 2.2.3 Focussing on infant | 2 | 1 | Megnin-Viggars et al., 201548 |
| 2.2.4 Making time | 11 | 3 | Myors et al., 2015112 Hewitt et al., 200977; Watson et al., 201996 |
| 2.3 Healthcare professional’s attributes | |||
| 2.3.3 Valued characteristics | 25 | 2 | Myors et al., 2015112 Newman et al., 201985 |
| 3 Interpersonal | |||
| 3.2 Language barriers | 16 | 2 | Button et al., 201746; Sambrook Smith et al., 201989 |
| 4 Organisational | |||
| 4.1 Overall organisational aspects | |||
| 4.1.7 Training | 28 | 1 | Nakku et al., 2016 108 |
| 4.2 Characteristics of PMH care | |||
| 4.2.1 Across the care pathway | |||
| 4.2.1.2 Culturally sensitive care | 19 | 2 | Dennis and Chung-Lee, 200647; Sambrook Smith et al., 201989 |
| 7 Societal | |||
| 7.2 Culture | 30 | 3 | Dennis and Chung-Lee, 200647; Nilaweera et al., 201486; Sambrook Smith et al., 201989 |
| Theme | Total number of papers that contribute to this theme | Number of papers that contribute to this theme within this stage of the care pathway | Studies citing this theme |
|---|---|---|---|
| 1 Women | |||
| 1.1 Beliefs about health services | |||
| 1.1.1 Services only offer medication | 14 | 2 | Doering et al., 2017 114 ; Williams et al., 2016 119 |
| 1.3 Beliefs about perinatal mental illness | |||
| 1.3.1 What is it? | |||
| 1.3.1.1 What is perinatal mental illness? | 18 | 1 | Kerker et al., 2018 130 |
| 1.7 Social and family life | |||
| 1.7.2 Family and friends’ beliefs | 30 | 7 | Boyd et al., 2011 113 ; Doering et al., 2017 114 ; Higgins et al., 2018 115 ; Noonan et al., 2018 116 ; Pineros-Leano et al., 2015 117 ; Vik et al., 2009 118 ; Williams et al., 2016 119 |
| 1.7.3 Additional personal difficulties | 7 | 2 | Boyd et al., 2011 113 ; Williams et al., 2016 119 |
| 2 Healthcare professional | |||
| 2.1 Healthcare professionals knowledge about PMH | |||
| 2.1.1 Healthcare professionals knowledge about PMI | 17 | 7 | Higgins et al., 2018115; McCauley et al., 2019108; Rowan et al., 2010120 Bina, 202069; Dennis and Chung-Lee, 200647; Megnin-Viggars et al., 201548; Slade et al., 202092; Viveiros and Darling, 201949 |
| 2.1.2 Healthcare professional’s knowledge about services/referral pathways | 8 | 1 | Higgins et al., 2018 115 |
| 2.1.3 Healthcare professionals confidence | 9 | 3 | Cox et al., 2017 134 ; Fernandez y Garcia et al., 2011 121 ; Higgins et al., 2018 116 |
| 2.2 Getting it right the first time | |||
| 2.2.2 Not recognising help seeking or PMI | 5 | 2 | Bina, 202069; Watson et al., 201996 |
| 2.2.4 Making time | 11 | 1 | Bina, 202069 |
| 2.2.5 Assessment specific behaviours | 12 | 12 | Doering et al., 2017114; Fernandez y Garcia et al., 2011121; Nithianandan et al., 2016122; Segre et al., 2014123; Vik et al., 2009118; Williams et al., 2016119 Brealey et al., 201074; Sambrook Smith et al., 201989; Schmied et al., 201790; Slade et al., 202092; Viveiros and Darling, 201949; Watson et al., 201996 |
| 2.3 Healthcare professional’s attributes | |||
| 2.3.1 Similar demographic characteristics | 6 | 1 | Nithianandan et al., 2016 122 |
| 2.3.2 Culturally sensitive | 4 | 2 | Kassam, 201981; Nilaweera et al., 201486 |
| 2.3.3 Valued characteristics | 25 | 4 | Boyd et al., 2011113; Doering et al., 2017114; Kim et al., 2009129 Hewitt et al., 200977 |
| 3 Interpersonal | |||
| 3.1 Trusting relationship and rapport | 23 | 3 | Doering et al., 2017114; Higgins et al., 2018116 Bina, 202069 |
| 3.2 Language barriers | 16 | 3 | Doering et al., 2017 114 ; Ganann et al., 2019 109 ; Nithianandan et al., 2016 122 ; Pineros-Leano et al., 2015 117 ; Segre et al., 2014 123 ; Willey et al., 2018 126 ; Williams et al., 2016 119 |
| 3.4 Open and honest communication | 9 | 5 | Doering et al., 2017114; Shakespeare et al., 2003124, Brealey et al., 201074; Hewitt et al., 200977; Willey et al., 2018125 |
| 4 Organisational | |||
| 4.1 Overall organisational aspects | |||
| 4.1.2 Service integration and collaborative working | 17 | 1 | Lomonaco-Haycraft et al., 2018 140 |
| 4.1.3 Collaboration within services | 14 | 3 | Higgins et al., 2018 115 ; Nithianandan et al., 2016 122 ; Segre et al., 2014 123 |
| 4.1.4 Adequate workforce provision/healthcare professionals workload | 17 | 11 | Ammerman et al., 2014126; Feinberg et al., 2006127; Ganann et al., 2019109; Higgins et al., 2018115; Kim et al., 2009128; McCauley, et al., 2019107; Nakku et al., 2016108; Nithianandan et al., 2016122; Noonan et al., 2018116; Vik et al., 2009118; Willey et al., 2018125 Viveiros and Darling, 201849 |
| 4.1.5 Clear assessment and referral process | 11 | 6 | Ganann et al., 2019109; Kim et al., 2009128; Nithianandan et al., 2016122; Segre et al., 2014123; Williams et al., 2016119 Bina, 202069 |
| 4.1.6 Provision of supervision | 3 | 1 | Vik et al., 2009 118 |
| 4.1.7 Training | 28 | 14 | Boyd et al., 2011113; Feinberg et al., 2006127; Ganann et al., 2019109; Judd et al., 2011129; Kerker et al., 2018130; Kim et al., 2009128; Lind et al., 2017131; McCauley et al., 2019107; Nithianandan et al., 2016122; Noonan et al., 2018116; Willey et al., 2018125; Williams et al., 2016119 Bina, 202069; Brealey et al., 201074 |
| 4.1.9 Organisational goals/guidelines | 2 | 1 | Ammerman et al., 2014 127 |
| 4.2 Characteristics of PMH care | |||
| 4.2.1 Across the care pathway | |||
| 4.2.1.1 Continuity of carer | 17 | 1 | Higgins et al., 2018 115 |
| 4.2.1.2 Culturally sensitive care | 19 | 3 | Brealey et al., 201074; Hewitt et al., 200977; Watson et al., 201996 |
| 4.2.1.3 Privacy and confidentiality | 7 | 3 | Higgins et al., 2018115; Nithianandan et al., 2016122, Giscombe et al., 202076 |
| 4.2.1.4 Dedicated person/PMH Champion | 9 | 2 | Kim et al., 2009 128 ; Lomonaco-Haycraft et al., 2018 140 |
| 4.2.1.6 Home delivery | 10 | 2 | Myors et al., 2015113 Brealey et al., 201074 |
| 4.2.1.7 Hospital delivery | 5 | 1 | Shakespeare et al., 2003 124 |
| 4.2.1.9 Technology | 11 | 7 | Fernandez y Garcia et al., 2011 121 ; Kim et al., 2009 128 ; Lind et al., 2017 131 ; Noonan et al., 2018 116 ; Pineros-Leano et al., 2015 117 ; Willey et al., 2018 125 ; Williams et al., 2016 119 |
| 4.2.2 Assessment specific characteristics | |||
| 4.2.2.1 Wording of assessment tools | 6 | 6 | Doering et al., 2017114; Segre et al., 2014123; Williams et al., 2016119 Brealey et al., 201074; Button et al., 201746; Hewitt et al., 200977 |
| 4.2.2.2 Acceptability of assessment/screening | 17 | 17 | Boyd et al., 2011113; Doering et al., 2017114; Feinberg et al., 2006127; Ganann et al., 2019109; Kim et al., 2009; Nithianandan et al., 2016; Segre et al., 2014128; Shakespeare et al., 2003124; Vik et al., 2009118; Willey et al., 2018125, Brealey et al., 201074; Evans et al., 202075; Hewitt et al., 200977; Megnin-Viggars et al., 201548; Mollard et al., 201683; Sambrook Smith et al., 201989; Viveiros and Darling, 201949 |
| 5 Commissioners | |||
| 5.1 Referral pathways | 6 | 1 | Higgins et al., 2018 115 |
| 5.2 Lack of appropriate or timely services | 22 | 5 | Doering et al., 2017 114 ; Higgins et al., 2018 115 ; Kerker et al., 2018 131 ; Noonan et al., 2018 116 ; Williams et al., 2016 119 |
| 5.3 Financial complexities | 8 | 2 | Feinberg et al., 2006 127 ; Ganann et al., 2019 109 |
| 7 Societal | |||
| 7.1 Stigma | 43 | 6 | Atif et al., 2016 106 ; Chartier et al., 2015 132 ; Higgins et al., 2018 115 ; McCauley et al., 2019 107 ; Shakespeare et al., 2003 124 ; Vik et al., 2009 118 |
| 7.2 Culture | 30 | 7 | Boyd et al., 2011113; Ganann et al., 2019109; Higgins et al., 2018115; Segre et al., 2014128 Brealey et al., 201074; Hewitt et al., 200977; Tobin et al., 201895 |
| 7.3 Maternal norms | 27 | 1 | Sorsa et al., 202193 |
| Theme | Total number of papers that contribute to this theme | Number of papers that contribute to this theme within this stage of the care pathway | Studies citing this theme |
|---|---|---|---|
| 1 Women | |||
| 1.1 Beliefs about health services | |||
| 1.1.1 Services only offer medication | 14 | 2 | Sorsa et al., 202193; Tobin et al., 201895 |
| 1.1.2 Services are stretched | 2 | 1 | Dennis and Chung-Lee, 200647 |
| 1.2 Beliefs about healthcare professionals | |||
| 1.2.1 Not understanding healthcare professionals’ role | 12 | 5 | Brealey et al., 201074; Hadfield and Wittkowski, 201772; Hewitt et al., 200977; Sambrook Smith et al., 201989; Scope et al., 201791 |
| 1.2.2 Believing healthcare professionals won’t be interested | 2 | 1 | Hadfield and Wittkowski, 201772 |
| 1.3 Beliefs about perinatal mental illness | |||
| 1.3.1 What is it? | |||
| 1.3.1.1 What is perinatal mental illness? | 18 | 3 | Atif et al., 2019133 Megnin-Viggars et al., 201548; Staneva et al., 201594 |
| 1.3.2 Causes of perinatal mental illness | |||
| 1.3.2.4 A normal response to motherhood? | 9 | 1 | Williams et al., 2016 119 |
| 1.3.3 How to cope with symptoms | |||
| 1.3.3.3 Minimise them | 14 | 2 | Shakespeare et al., 2003124 Slade et al., 202092 |
| 1.5 Fear of judgement | |||
| 1.5.1 Fear of being seen as a bad mum | 9 | 7 | Brealey et al., 201074; Button et al., 201746; Jones et al., 201479; Lucas et al., 201982; Slade et al., 202092; Sorsa et al., 202193; Viveiros and Darling, 201949 |
| 1.5.2 Social services/removal of child | 17 | 6 | Feinberg et al., 2006127; Shakespeare et al., 2003124 Bina, 202069; Brealey et al., 201074; Evans et al., 202075; Newman et al., 201985 |
| 1.7 Social and family life | |||
| 1.7.2 Family and friends’ beliefs | 30 | 2 | Nilaweera et al., 201486; Viveiros and Darling, 201949 |
| 2 Healthcare professional | |||
| 2.2 Getting it right the first time | |||
| 2.2.1 Being dismissive or normalising symptoms | 11 | 4 | Ganann et al., 2019109 Dennis and Chung-Lee, 200647; Hadfield and Wittkowski, 201772; Megnin-Viggars et al., 201548 |
| 2.2.3 Focussing on infant | 2 | 1 | Megnin-Viggars et al., 201548 |
| 2.2.4 Making time | 11 | 5 | Feinberg et al., 2006127 Button et al., 201746; Dennis and Chung-Lee, 200647; Megnin-Viggars et al., 201548; Slade et al., 202092 |
| 2.2.5 Assessment specific behaviours | 12 | 1 | Slade et al., 202092 |
| 2.3 Healthcare professional’s attributes | |||
| 2.3.3 Valued characteristics | 25 | 6 | Feinberg et al., 2006127; Williams et al., 2016119 Button et al., 201746; Newman et al., 201985; Slade et al., 202092; Watson et al., 201996 |
| 3 Interpersonal | |||
| 3.1 Trusting relationship and rapport | 23 | 10 | Feinberg et al., 2006127; Ganann et al., 2019109; Kerker et al., 2018130; Noonan et al., 2018116; Shakespeare et al., 2003124; Willey et al., 2018125; Williams et al., 2016119 Brealey et al., 201074; Hewitt et al., 200977; Tobin et al., 201895 |
| 3.2 Language barriers | 16 | 1 | Ganann et al., 2019 109 |
| 3.4 Open and honest communication | 9 | 1 | Vik et al., 2009 118 |
| 4 Organisational | |||
| 4.1 Overall organisational aspects | |||
| 4.1.2 Service integration and collaborative working | 17 | 1 | Hadfield et al., 2019 152 |
| 4.2 Characteristics of PMH care | |||
| 4.2.1 Across the care pathway | |||
| 4.2.1.1 Continuity of carer | 17 | 8 | Chartier et al., 2015132; Nithianandan et al., 2016122; Willey et al., 2018125 Brealey et al., 201074; Hadfield and Wittkowski, 201772; Megnin-Viggars et al., 201548; Sambrook Smith et al., 201989; Watson et al., 201996 |
| 5 Commissioners | |||
| 5.2 Lack of appropriate or timely services | 22 | 1 | Williams et al., 2016 119 |
| 7 Societal | |||
| 7.1 Stigma | 43 | 18 | Atif et al., 2019133; Feinberg et al., 2006127; Kerker et al., 2018130; Nithianandan et al., 2016122; Noonan et al., 2018116; Shakespeare et al., 2003124; Williams et al., 2016119 Button et al., 201746; Giscombe et al., 202076; Hewitt et al., 200977; Holopainen and Hakulinen, 201978; Megnin-Viggars et al., 201548; Morrell et al., 201684; Sambrook Smith et al., 201989; Schmied et al., 201790; Scope et al., 201791; Sorsa et al., 202193; Watson et al., 201996 |
| 7.2 Culture | 30 | 13 | Feinberg et al., 2006127; Noonan et al., 2018116 Brealey et al., 201074; Dennis and Chung-Lee, 200647; Giscombe et al., 202076; Hewitt et al., 200977; Holopainen and Hakulinen, 201978; Megnin-Viggars et al., 201548; Praetorius et al., 202087; Sambrook Smith et al., 201989; Schmied et al., 201790; Tobin et al., 201895; Watson et al., 201996 |
| 7.3 Maternal norms | 27 | 14 | Shakespeare et al., 2003124; Williams et al., 2016119 Brealey et al., 201074; Button et al., 201746; Dennis and Chung-Lee, 200647; Hadfield and Wittkowski, 201772; Hewitt et al., 200977; Jones et al., 201479; Megnin-Viggars et al., 201548; Newman et al., 201985; Nilaweera et al., 201486; Praetorius et al., 202087; Sambrook Smith et al., 201989; Scope et al., 201791; Slade et al., 202092 |
| Theme | Total number of papers that contribute to this theme | Number of papers that contribute to this theme within this stage of the care pathway | Studies citing this theme |
|---|---|---|---|
| 1.5 Fear of judgement | |||
| 1.5.2 Social services/removal of child | 17 | 1 | Boyd et al., 2011 113 |
| 2 Healthcare professional | |||
| 2.1 Healthcare professionals knowledge about PMH | |||
| 2.1.2 Healthcare professional’s knowledge about services/referral pathways | 8 | 4 | Ganann et al., 2019109; Rowan et al., 2010121 Hansotte et al., 201770; Viveiros and Darling, 201949 |
| 2.1.3 Healthcare professionals confidence | 9 | 2 | Cox et al., 2017 134 ; Nithianandan et al., 2016 122 |
| 2.2 Getting it right the first time | |||
| 2.2.1 Being dismissive or normalising symptoms | 11 | 1 | Dennis and Chung-Lee, 200647 |
| 2.2.2 Not recognising help seeking or PMI | 5 | 1 | Button et al., 201746 |
| 2.2.4 Making time | 11 | 1 | Ganann et al., 2019 109 |
| 3 Interpersonal | |||
| 3.3 Shared decision making | 4 | 1 | Hadfield and Wittkowski, 201772 |
| 4 Organisational | |||
| 4.1 Overall organisational aspects | |||
| 4.1.2 Service integration and collaborative working | 17 | 7 | Bina et al., 2018 144 ; Boyd et al., 2011 113 ; Feinberg et al., 2006 127 ; Judd et al., 2011 129 ; Myors et al., 2015 112 ; Noonan et al., 2018 116 ; Rowan et al., 2010 121 |
| 4.1.3 Collaboration within services | 14 | 2 | Lind et al., 2017 131 ; Willey et al., 2018 125 |
| 4.1.4 Adequate workforce provision | 17 | 1 | Ammerman et al., 2014 126 |
| 4.1.5 Clear assessment and referral process | 11 | 7 | Cox et al., 2017 134 ; Feinberg et al., 2006 127 ; Judd et al., 2011 129 ; Kerker et al., 2018 130 ; Nithianandan et al., 2016 122 ; Noonan et al., 2018 116 ; Rowan et al., 2010 121 |
| 4.1.7 Training | 28 | 2 | Bina et al., 2018 144 ; Judd et al., 2011 129 |
| 4.2 Characteristics of PMH care | |||
| 4.2.1 Across the care pathway | |||
| 4.2.1.2 Culturally sensitive care | 19 | 1 | Nithianandan et al., 2016 122 |
| 4.2.1.3 Privacy and confidentiality | 7 | 1 | Feinberg et al., 2006 127 |
| 4.2.1.4 Dedicated person/PMH Champion | 9 | 1 | Nithianandan et al., 2016 122 |
| 4.2.1.8 Provision of information | 7 | 2 | Jones, 201980; Megnin-Viggars et al., 201548 |
| 4.2.1.9 Technology | 11 | 1 | Feinberg et al., 2006 127 |
| 4.2.3 Intervention characteristics | |||
| 4.2.3.2 Individualised and person centred | 19 | 1 | Doering et al., 2017 114 |
| 5 Commissioners | |||
| 5.1 Referral pathways | 6 | 5 | Ammerman et al., 2014 126 ; Boyd et al., 2011 113 ; Nithianandan et al., 2016 122 ; Rowan et al., 2010 121 ; Willey et al., 2018 125 |
| 5.2 Lack of appropriate or timely services | 22 | 1 | Lomonaco-Haycraft et al., 2018 140 |
| 7 Societal | |||
| 7.1 Stigma | 43 | 3 | Boyd et al., 2011113; Myors et al., 2015112 Morrell et al., 201684 |
| Theme | Total number of papers that contribute to this theme | Number of papers that contribute to this theme within this stage of the care pathway | Studies citing this theme |
|---|---|---|---|
| 1 Women | |||
| 1.1 Beliefs about health services | |||
| 1.1.1 Services only offer medication | 14 | 2 | Ganann et al., 2019 109 ; Young et al., 2019 110 |
| 1.1.3 Services are too complicated | 2 | 1 | Tobin et al., 201895 |
| 1.1.4 Women’s mistrust and fear of services | 2 | 2 | Boyd et al., 2011113 Jones, 201980 |
| 1.2 Beliefs about healthcare professionals | |||
| 1.2.1 Not understanding healthcare professionals’ role | 12 | 3 | Dennis and Chung-Lee, 200647; Hadfield and Wittkowski, 201772; Sambrook Smith et al., 201989 |
| 1.4 Deciding to seek help | |||
| 1.4.2 Where do I go to seek help? | 9 | 1 | Hansotte et al., 201770 |
| 1.6 Logistics of accessing perinatal mental healthcare | |||
| 1.6.1 Childcare | 14 | 14 | Boyd et al., 2011113; Cox et al., 2017134; Doering et al., 2017114; Friedman et al., 2010135 Bina, 202069; Button et al., 201746; Dennis and Chung-Lee, 200647; Hansotte et al., 201770; Morrell et al., 201684; Newman et al., 201985; Sambrook Smith et al., 201989; Scope et al., 201791; Tobin et al., 201895; Watson et al., 201996 |
| 1.6.2 Timing of care | 7 | 7 | Atif et al., 2019133; Friedman et al., 2010135 Bina, 202069; Dennis and Chung-Lee, 200647; Newman et al., 201985; Scope et al., 201791; Watson et al., 201996 |
| 1.6.3 Location/travel | 13 | 13 | Cox et al., 2017134; Doering et al., 2017114; Eappen et al., 2018136; Friedman et al., 2010135; Masood et al., 2015137; Nakku et al., 2016108 Bina, 202069; Hansotte et al., 201770; Mollard et al., 201683; Morrell et al., 201684; Newman et al., 201985; Tobin et al., 201895; Watson et al., 201996 |
| 1.7 Social and family life | |||
| 1.7.2 Family and friends’ beliefs | 30 | 8 | Atif et al., 2019133; Ganann et al., 2019109; Masood et al., 2015137; Nakku et al., 2016108; Nithianandan et al., 2016122; Young et al., 2019110 Nilaweera et al., 201486; Watson et al., 201996 |
| 1.7.3 Additional personal difficulties | 7 | 5 | Atif et al., 2016106; Kerker et al., 2018130; Munodawafa et al., 2017138; Rowan et al., 2010120 Hansotte et al., 201770 |
| 1.8 Sociodemographic factors | |||
| 1.8.1 Ethnicity | 4 | 2 | Hansotte et al., 201770; Watson et al., 201996 |
| 1.9 Mental health factors | |||
| 1.9.3 Current diagnoses or symptoms | 6 | 4 | Friedman et al., 2010135; Young et al., 2019110 Sorsa et al., 202193; Viveiros and Darling, 201949 |
| 2 Healthcare professional | |||
| 2.1 Healthcare professionals knowledge about PMH | |||
| 2.1.1 Healthcare professionals knowledge about PMI | 17 | 1 | Megnin-Viggars et al., 201548 |
| 2.1.2 Healthcare professional’s knowledge about services/referral pathways | 8 | 2 | Sambrook Smith et al., 201989; Slade et al., 202092 |
| 2.2 Getting it right the first time | |||
| 2.2.1 Being dismissive or normalising symptoms | 11 | 1 | Watson et al., 201996 |
| 2.2.4 Making time | 11 | 1 | Watson et al., 201996 |
| 2.3 Healthcare professional’s attributes | |||
| 2.3.2 Culturally sensitive | 4 | 1 | Watson et al., 201996 |
| 2.3.3 Valued characteristics | 25 | 3 | Morrell et al., 201684; Newman et al., 201985; Schmied et al., 201790 |
| 3 Interpersonal | |||
| 3.1 Trusting relationship and rapport | 23 | 1 | Dennis and Chung-Lee, 200647 |
| 3.2 Language barriers | 16 | 4 | Hansotte et al., 201770; Megnin-Viggars et al., 201548; Sambrook Smith et al., 201989; Watson et al., 201996 |
| 3.3 Shared decision making | 4 | 1 | Bina, 202069 |
| 4 Organisational | |||
| 4.1 Overall organisational aspects | |||
| 4.1.1 Co location and buildings | 7 | 2 | Boyd et al., 2011 113 ; Judd et al., 2011 129 |
| 4.1.2 Service integration and collaborative working | 17 | 3 | Rowan et al., 2010120 Sambrook Smith et al., 201989; Watson et al., 201996 |
| 4.1.3 Collaboration within services | 14 | 1 | Sambrook Smith et al., 201989 |
| 4.1.4 Adequate workforce provision/healthcare professionals workload | 17 | 2 | Rowan et al., 2010120 Bina, 202069 |
| 4.2 Characteristics of PMH care | |||
| 4.2.1 Across the care pathway | |||
| 4.2.1.1 Continuity of carer | 17 | 1 | Tobin et al., 201895 |
| 4.2.1.2 Culturally sensitive care | 19 | 7 | Button et al., 201746; Giscombe et al., 202076; Hansotte et al., 201770; Sambrook Smith et al., 201989; Schmied et al., 201790; Viveiros and Darling, 201949; Watson et al., 201996 |
| 4.2.1.4 Dedicated person/PMH Champion | 9 | 3 | Ganann et al., 2019109 Bina, 202069; Megnin-Viggars et al., 201548 |
| 4.2.1.5 Logistical support | 13 | 11 | Ganann et al., 2019109; Hadfield et al., 2019152; Masood et al., 2015137; Nakku et al., 2016108; Nithianandan et al., 2016122; Ormsby et al., 2018139 Button et al., 201746; Mollard et al., 201683; Newman et al., 201985; Scope et al., 201791; Watson et al., 201996 |
| 4.2.1.8 Provision of information | 7 | 1 | Randall and Briscoe, 201888 |
| 4.2.1.10 Service inclusion criteria | 3 | 3 | Boyd et al., 2011113; Ganann et al., 2019109 Viveiros and Darling, 201949 |
| 4.2.3 Intervention characteristics | |||
| 4.2.3.2 Individualised and person centred | 19 | 2 | Ganann et al., 2019109 Watson et al., 201996 |
| 4.2.3.3 Appropriateness | 15 | 1 | Pugh et al., 2015 145 |
| 5 Commissioners | |||
| 5.2 Lack of appropriate or timely services | 22 | 11 | Boyd et al., 2011113; Ganann et al., 2019109; Kerker et al., 2018130; Myors et al., 2015112 Bina, 202069; Button et al., 201746; Megnin-Viggars et al., 201548; Newman et al., 201985; Sambrook Smith et al., 201989; Tobin et al., 201895; Viveiros and Darling, 201949 |
| 5.3 Financial complexities | 8 | 1 | Rowan et al., 2010 120 |
| 6 Political | |||
| 6.1 Immigration status | 9 | 6 | Cox et al., 2017134; Ganann et al., 2019109 Hansotte et al., 201770; Kassam, 201981; Schmied et al., 201790; Tobin et al., 201895 |
| 6.2 Economic status and healthcare costs | 16 | 14 | Atif et al., 2016106; Boyd et al., 2011113; Cox et al., 2017134; Doering et al., 2017114; Ganann et al., 2019109; Lomonaco-Haycraft et al., 2018140; Nakku et al., 2016108; Ormsby et al., 2018139 Bina, 202069; Hansotte et al., 201770; Kassam, 201981; Lucas et al., 201982; Tobin et al., 201895; Viveiros and Darling, 201949 |
| 7 Societal | |||
| 7.1 Stigma | 43 | 8 | Cox et al., 2017134; Young et al., 2019110 Dennis and Chung-Lee, 200647; Hadfield and Wittkowski, 201772; Hansotte et al., 201770; Scope et al., 201791; Tobin et al., 201895; Watson et al., 201996 |
| 7.2 Culture | 30 | 5 | Atif et al., 2016106 Giscombe et al., 202076; Hansotte et al., 201770; Sambrook Smith et al., 201989; Viveiros and Darling, 201949 |
| 7.3 Maternal norms | 27 | 2 | Viveiros and Darling, 201949; Watson et al., 201996 |
| Theme | Total number of papers that contribute to this theme | Number of papers that contribute to this theme within this stage of the care pathway | Studies citing this theme |
|---|---|---|---|
| 1 Women | |||
| 1.1 Beliefs about health services | |||
| 1.1.1 Services only offer medication | 14 | 4 | Dennis and Chung-Lee, 200647; Hadfield and Wittkowski, 201772; Megnin-Viggars et al., 201548; Tobin et al., 201895 |
| 1.3 Beliefs about perinatal mental illness | |||
| 1.3.1 What is it? | |||
| 1.3.1.2 No language to describe perinatal mental illness | 5 | 1 | Bina et al., 2018 144 |
| 2 Healthcare professional | |||
| 2.1 Healthcare professionals knowledge about PMH | |||
| 2.1.1 Healthcare professionals knowledge about PMI | 17 | 7 | Beeber et al., 2009141; Byatt et al., 2013142; Ganann et al., 2019110; Judd et al., 2011129; Noonan et al., 2018116; Reed et al., 2014143 Megnin-Viggars et al., 201548 |
| 2.1.3 Healthcare professionals confidence | 9 | 5 | Atif et al., 2019 133 ; Bina et al., 2018 144 ; Munodawafa et al., 2017 138 ; Ormsby et al., 2018 139 ; Reed et al., 2014 143 |
| 2.2 Getting it right the first time | |||
| 2.2.3 Focussing on infant | 2 | 1 | Button et al., 201746 |
| 2.2.4 Making time | 11 | 3 | Noonan et al., 2018116 Dennis and Chung-Lee, 200647; Viveiros and Darling, 201949 |
| 2.3 Healthcare professional’s attributes | |||
| 2.3.1 Similar demographic characteristics | 6 | 3 | Leger et al., 2015 147 ; Masood et al., 2015 137 ; Shorey and Ng, 2019 146 |
| 2.3.2 Culturally sensitive | 4 | 1 | Viveiros and Darling, 201949 |
| 2.3.3 Valued characteristics | 25 | 9 | Atif et al., 2016106, 2019133; Doering et al., 2017114; Kerker et al., 2018130; Munodawafa et al., 2017138; Pugh et al., 2015145; Shorey and Ng, 2019146 Forde et al., 2020105; Staneva et al., 201594 |
| 3 Interpersonal | |||
| 3.1 Trusting relationship and rapport | 23 | 5 | Hadfield et al., 2019152; Leger et al., 2015147; Shorey and Ng, 2019146 Bina, 202069; Scope et al., 201790 |
| 3.2 Language barriers | 16 | 3 | Beeber et al., 2009 141 ; Munodawafa et al., 2017 138 ; Pineros-Leano et al., 2015 117 |
| 3.3 Shared decision making | 4 | 2 | Megnin-Viggars et al., 201548; Randall and Briscoe, 201888 |
| 4 Organisational | |||
| 4.1 Overall organisational aspects | |||
| 4.1.1 Co location and buildings | 7 | 5 | Cox et al., 2017 134 ; Judd et al., 2011 129 ; Munodawafa et al., 2017 138 ; Ormsby et al., 2018 139 ; Young et al., 2019 110 |
| 4.1.2 Service integration and collaborative working | 17 | 8 | Atif et al., 2016 106 ; Byatt et al., 2013 142 ; Ganann et al., 2019 110 ; Judd et al., 2011 129 ; Lind et al., 2017 131 ; Nithianandan et al., 2016 122 ; Noonan et al., 2018 116 ; Rowan et al., 2010 120 |
| 4.1.3 Collaboration within services | 14 | 9 | Ammerman et al., 2014 126 ; Cox et al., 2017 134 ; Eappen et al., 2018 136 ; Judd et al., 2011 129 ; Kerker et al., 2018 130 ; McKenzie-McHarg et al., 2014 148 ; Munodawafa et al., 2017 138 ; Nithianandan et al., 2016 122 ; Ormsby et al., 2018 139 |
| 4.1.4 Adequate workforce provision/healthcare professionals workload | 17 | 4 | Bina et al., 2018 144 ; Drozd et al., 2018 149 ; Kerker et al., 2018 130 ; Nakku et al., 2016 108 |
| 4.1.6 Provision of supervision | 3 | 2 | Atif et al., 2019 133 ; Munodawafa et al., 2017 138 |
| 4.1.7 Training | 28 | 15 | Ammerman et al., 2014136; Atif et al., 2016106, 2019133; Beeber et al., 2009141; Chartier et al., 2015132; Doering et al., 2017114; Drozd et al., 2018149; Ganann et al., 2019109; Leger et al., 2015147; McKenzie-McHarg et al., 2014148; Munodawafa et al., 2017138; Reed et al., 2014143; Rowan et al., 2010120; Shorey and Ng, 2019146 Brealey et al., 201074 |
| 4.1.9 Organisational goals/guidelines | 2 | 1 | Willey et al., 2018 125 |
| 4.2 Characteristics of PMH care | |||
| 4.2.1 Across the care pathway | |||
| 4.2.1.1 Continuity of carer | 17 | 4 | O’Mahen and Flynn, 2008150; Rowan et al., 2010120 Megnin-Viggars et al., 201548; Viveiros and Darling, 201949 |
| 4.2.1.2 Culturally sensitive care | 19 | 7 | Ganann et al., 2019109; Noonan et al., 2018116; Shorey and Ng, 2019146 Dennis and Chung-Lee, 200647; Kassam, 201981; Tobin et al., 201895; Watson et al., 201996 |
| 4.2.1.3 Privacy and confidentiality | 7 | 3 | Atif et al., 2019 133 ; Jallo et al., 2015 153 ; O’Mahen and Flynn, 2008 150 |
| 4.2.1.4 Dedicated person/PMH Champion | 9 | 3 | Chartier et al., 2015 132 ; Rowan et al., 2010 120 ; Willey et al., 2018 125 |
| 4.2.1.5 Logistical support | 13 | 1 | Leger et al., 2015 147 |
| 4.2.1.6 Home delivery | 10 | 5 | Ammerman et al., 2014126; Beeber et al., 2009141; Leger et al., 2015147; Munodawafa et al., 2017139 Hadfield and Wittkowski, 201772 |
| 4.2.1.7 Hospital delivery | 5 | 1 | Dennis and Chung-Lee, 200647 |
| 4.2.1.8 Provision of information | 7 | 5 | Dennis and Chung-Lee, 200647; Hadfield and Wittkowski, 201772; Jones, 201980; Megnin-Viggars et al., 201548; Morrell et al., 201684 |
| 4.2.3 Intervention characteristics | |||
| 4.2.3.1 Opportunity to talk | 7 | 2 | Hadfield and Wittkowski, 201772; Jones et al., 201479 |
| 4.2.3.2 Individualised and person centred | 19 | 11 | Chartier et al., 2015133; Doering et al., 2017114; Masood et al., 2015137; McKenzie-McHarg et al., 2014148; Noonan et al., 2018116; O’Mahen and Flynn, 2008150; Pugh et al., 2015145; Segre et al., 2014123; Shorey and Ng, 2019146 Megnin-Viggars et al., 201548; Viveiros and Darling, 201849 |
| 4.2.3.3 Appropriateness | 15 | 12 | Atif et al., 2019 133 ; Bina et al., 2018 144 ; Chartier et al., 2015 133 ; Drozd et al., 2018 149 ; Leger et al., 2015 147 ; McKenzie-McHarg et al., 2014 148 ; Munodawafa et al., 2017 139 ; Noonan et al., 2018 116 ; Ormsby et al., 2018 139 ; Pugh et al., 2015 145 ; Reed et al., 2014 143 ; Shorey and Ng, 2019 146 |
| 4.2.3.4 Flexible | 11 | 7 | Atif et al., 2019133; Bina et al., 2018144; Ganann et al., 2019109; Judd et al., 2011130; Munodawafa et al., 2017139; Shorey and Ng, 2019146 Sorsa et al., 202193 |
| 4.2.3.5 Group support | 14 | 3 | Masood et al., 2015137 Dennis and Chung-Lee, 200647; Scope et al., 201791 |
| 5 Commissioners | |||
| 5.2 Lack of appropriate or timely services | 22 | 7 | Boyd et al., 2011113; Leger et al., 2015147; Munodawafa et al., 2017138; Nakku et al., 2016108; Noonan et al., 2018116; Rowan et al., 2010120 Jones et al., 201479 |
| 5.3 Financial complexities | 8 | 7 | Cox et al., 2017 134 ; Friedman et al., 2010 135 ; Ganann et al., 2019 109 ; Kim et al., 2009 128 ; Lomonaco-Haycraft et al., 2018 140 ; Ormsby et al., 2018 139 ; Rowan et al., 2010 120 |
| 6 Political | |||
| 6.1 Immigration status | 9 | 5 | Giscombe et al., 202076; Kassam, 201981; Schmied et al., 201790; Tobin et al., 201895; Watson et al., 201996 |
| 6.2 Economic status and healthcare costs | 16 | 3 | Hansotte et al., 201770; Kassam, 201981; Lucas et al., 201982 |
| 7 Societal | |||
| 7.1 Stigma | 43 | 8 | Atif et al., 2016106; Chartier et al., 2015132; Kerker et al., 2018130; Munodawafa et al., 2017138; O’Mahen and Flynn, 2008150 Dennis and Chung-Lee, 200647; Lucas et al., 201982; Megnin-Viggars et al., 201548 |
| 7.2 Culture | 30 | 6 | Bina et al., 2018144; Boyd et al., 2011113; Friedman et al., 2010135; Ganann et al., 2019109 Kassam, 201980; Tobin et al., 201895 |
| Theme | Total number of papers that contribute to this theme | Number of papers that contribute to this theme within this stage of the care pathway | Studies citing this theme |
|---|---|---|---|
| 1 Women | |||
| 1.3.2 Causes of perinatal mental illness | |||
| 1.3.2.3 Physical causes | 13 | 1 | O’Mahen and Flynn, 2008 150 |
| 1.7 Social and family life | |||
| 1.7.1 Social isolation or support | 9 | 7 | Giscombe et al., 202076; Hansotte et al., 201770; Jones et al., 201479; Kassam, 201981; Lucas et al., 201982; Tobin et al., 201895; Watson et al., 201996 |
| 1.7.2 Family and friends’ beliefs | 30 | 3 | Atif et al., 2016106; O’Mahen and Flynn, 2008150 Hadfield and Wittkowski, 201772 |
| 1.9 Mental health factors | |||
| 1.9.1 Previous experiences of mental health care | 6 | 2 | O’Mahen and Flynn, 2008150 Evans et al., 202075 |
| 1.9.3 Current diagnoses or symptoms | 6 | 2 | Chartier et al., 2015 132 ; Hadfield et al., 2019 152 |
| 2 Healthcare professional | |||
| 2.1 Healthcare professionals knowledge about PMH | |||
| 2.1.1 Healthcare professionals knowledge about PMI | 17 | 2 | Dennis and Chung-Lee, 200647; Morrell et al., 201684 |
| 2.1.2 Healthcare professional’s knowledge about services/referral pathways | 8 | 1 | Dennis and Chung-Lee, 200647 |
| 2.2 Getting it right the first time | |||
| 2.2.1 Being dismissive or normalising symptoms | 11 | 1 | Megnin-Viggars et al., 201548 |
| 2.2.4 Making time | 11 | 1 | Dennis and Chung-Lee, 200647 |
| 2.3 Healthcare professional’s attributes | |||
| 2.3.3 Valued characteristics | 25 | 9 | Munodawafa et al., 2017138 Brealey et al., 201074; Dennis and Chung-Lee, 200647; Hadfield and Wittkowski, 201772; Hewitt et al., 200977; Megnin-Viggars et al., 201548; Morrell et al., 201684; Schmied et al., 201790; Staneva et al., 201594 |
| 3 Interpersonal | |||
| 3.1 Trusting relationship and rapport | 23 | 6 | Atif et al., 2016106; Young et al., 2019110 Dennis and Chung-Lee, 200647; Hadfield and Wittkowski, 201772; Megnin-Viggars et al., 201548; Morrell et al., 201684 |
| 3.2 Language barriers | 16 | 1 | Masood et al., 2015 137 |
| 3.3 Shared decision making | 4 | 2 | Hadfield and Wittkowski, 201772; Scope et al., 201791 |
| 3.4 Open and honest communication | 9 | 1 | Hadfield and Wittkowski, 201772 |
| 4 Organisational | |||
| 4.1 Overall organisational aspects | |||
| 4.1.2 Service integration and collaborative working | 17 | 1 | Noonan et al., 2018 116 |
| 4.2 Characteristics of PMH care | |||
| 4.2.1 Across the care pathway | |||
| 4.2.1.1 Continuity of carer | 17 | 5 | Button et al., 201746; Dennis and Chung-Lee, 200647; Hadfield and Wittkowski, 201772; Megnin-Viggars et al., 201548; Slade et al., 202092 |
| 4.2.1.2 Culturally sensitive care | 19 | 6 | Dennis and Chung-Lee, 200647; Hadfield and Wittkowski, 201772; Kassam, 201981; Schmied et al., 201790; Tobin et al., 201895; Watson et al., 201996 |
| 4.2.1.6 Home delivery | 10 | 3 | Ammerman et al., 2014127; Judd et al., 2011129 Hansotte et al., 201770 |
| 4.2.1.7 Hospital delivery | 5 | 3 | Atif et al., 2019 133 ; Boyd et al., 2011 113 ; Kerker et al., 2018 130 |
| 4.2.1.8 Provision of information | 7 | 1 | Scope et al., 201791 |
| 4.2.1.9 Technology | 11 | 3 | Jallo et al., 2015 153 ; Shorey and Ng, 2019 146 , Doering et al., 2017 115 |
| 4.2.3 Intervention characteristics | |||
| 4.2.3.1 Opportunity to talk | 7 | 6 | Dennis and Chung-Lee, 200647; Evans et al., 202075; Hadfield and Wittkowski, 201772; Kassam, 201981; Morrell et al., 201684; Praetorius et al., 202087 |
| 4.2.3.2 Individualised and person centred | 19 | 11 | Masood et al., 2015137; McKenzie-McHarg et al., 2014148 Evans et al., 202075; Hadfield and Wittkowski, 201772; Megnin-Viggars et al., 201548; Morrell et al., 201684; Schmied et al., 201790; Scope et al., 201791; Slade et al., 202092; Viveiros and Darling, 201949; Watson et al., 201996 |
| 4.2.3.3 Appropriateness | 15 | 4 | Pugh et al., 2015145 Evans et al., 202075; Megnin-Viggars et al., 201548; Scope et al., 201791 |
| 4.2.3.4 Flexible | 11 | 4 | Hadfield et al., 2019152; O’Mahen and Flynn, 2008150; Pugh et al., 2015145 Watson et al., 201996 |
| 4.2.3.5 Group support | 14 | 13 | Hadfield et al., 2019152; Masood et al., 2015137; Nakku et al., 2016108 Evans et al., 202075; Hadfield and Wittkowski, 201772; Holopainen and Hakulinen, 201978; Jones et al., 201479; Megnin-Viggars et al., 201548; Morrell et al., 201684; Schmied et al., 201790; Slade et al., 202092; Tobin et al., 201895; Watson et al., 201996 |
| 4.2.3.7 Face to face delivery | 4 | 4 | O’Mahen and Flynn, 2008150; Pugh et al., 2015145; Shorey and Ng, 2019147 Schmied et al., 201790 |
| 6 Political | |||
| 6.1 Immigration status | 9 | 1 | Ganann et al., 2019 109 |
| 6.2 Economic status and healthcare costs | 16 | 2 | Munodawafa et al., 2017 138 ; Nakku et al., 2016 108 |
| 7 Societal | |||
| 7.1 Stigma | 43 | 2 | McKenzie-McHarg et al., 2014148 Hadfield and Wittkowski, 201772 |
| 7.2 Culture | 30 | 4 | Masood et al., 2015137 Kassam, 201981; Schmied et al., 201790; Watson et al., 201996 |
| 7.3 Maternal norms | 27 | 1 | Jones et al., 201479 |
Appendix 6
| 1 Women | ||||||||
| 1.1 Beliefs about health services | ||||||||
| 1.1.1 Services only offer medication | The belief that health services will only offer medication to treat PMH concerns | Doering et al., 2017; Ganann et al., 2019; Williams et al., 2016; Young et al., 2019;110,111,115,120 Bina, 2020; Button et al., 2017; Dennis and Chung-Lee, 2006; Hadfield and Wittkowski, 2017; Jones, 2019; Megnin-Viggars et al., 2015; Nilaweera et al., 2014; Sorsa et al., 2021; Tobin et al., 201846-48,69,72,80,86,93,95 |
14 | Moderate confidence | Low confidence | High confidence | Low confidence | Low confidence |
| 1.1.2 Services are stretched | The belief that PMH services are too stretched and will therefore be unable to help women | Dennis and Chung-Lee, 2006; Hadfield and Wittkowski, 201747,72 | 2 | Low confidence | Very low confidence | Low confidence | Moderate confidence | Low confidence |
| 1.1.3 Services are too complicated | Services being too complex or complicated | Ganann et al., 2019110 Tobin et al., 201895 SH |
2 | Moderate confidence | Very low confidence | High confidence | Moderate confidence | Low confidence |
| 1.1.4 Women’s mistrust and fear of services | Having little trust in health services | Boyd et al., 2011114 Jones, 201980 |
2 | Moderate confidence | Very low confidence | High confidence | Low confidence | Low confidence |
| 1.2 Beliefs about HCPs | ||||||||
| 1.2.1 Not understanding HCPs’ roles | Not understanding the roles of HCPs and how their roles related to PMH | Brealey et al., 2010; Button et al., 2017; Dennis and Chung-Lee, 2006; Hadfield and Wittkowski, 2017; Hewitt et al., 2009; Megnin-Viggars et al., 2015; Mollard et al., 2016; Morrell et al., 2016; Nilaweera et al., 2014; Sambrook Smith et al., 2019; Schmied et al., 2017; Scope et al., 201746–48,72,74,77,83,84,86,89–91 | 12 | Low confidence | Low confidence | Moderate confidence | Moderate confidence | Moderate confidence |
| 1.2.2 Believing HCPs won’t be interested | Believing HCPs won’t be interested in PMH | Bina, 2020; Hadfield and Wittkowski, 201769,72 | 2 | Moderate confidence | Very low confidence | Low confidence | Moderate confidence | Low confidence |
| 1.3 Beliefs about perinatal mental illness | ||||||||
| 1.3.1 What is it? | ||||||||
| 1.3.1.1 What is perinatal mental illness? | Having poor or no knowledge about PMI | Atif et al., 2019; Kerker et al., 2018131,134 Bina, 2020; Button et al., 2017; Dennis and Chung-Lee, 2006; Hadfield and Wittkowski, 2017; Hansotte et al., 2017; A. Jones, 2019; Lucas et al., 2019; Megnin-Viggars et al., 2015; Morrell et al., 2016; Newman et al., 2019; Sambrook Smith et al., 2019; Schmied et al., 2017; Scope et al., 2017; Staneva et al., 2015; Tobin et al., 2018; Watson et al., 201946–48,69,72,80,82,84,85,89–91,94–96 |
18 | Moderate confidence | Moderate confidence | High confidence | Moderate confidence | Moderate confidence |
| 1.3.1.2 No language to describe perinatal mental illness | Not having the language to describe PMI | Bina et al., 2018145 Brealey et al., 2010; Staneva et al., 2015; Tobin et al., 2018; Watson et al., 201974,94–96 |
5 | Moderate confidence | Very low confidence | Moderate confidence | Moderate confidence | Low confidence |
| 1.3.2 Causes of perinatal mental illness | ||||||||
| 1.3.2.1 Spiritual/cultural causes | Believing that symptoms are caused by cultural or spiritual factors | Atif et al., 2016; McCauley et al., 2019; Nakku et al., 2016107–109 Button et al., 2017; Schmied et al., 2017; Wittkowski et al., 201446,90,97 |
6 | Moderate confidence | Low confidence | Moderate confidence | Moderate confidence | Moderate confidence |
| 1.3.2.2 External causes | Believing that symptoms are caused by external factors such as jobs, being a migrant | Bina, 2020; Button et al., 2017; Dennis and Chung-Lee, 2006; Lucas et al., 2019; Schmied et al., 2017; Staneva et al., 2015; Tobin et al., 2018; Watson et al., 201946,47,69,82,90,94–96 | 8 | Moderate confidence | Low confidence | Moderate confidence | Low confidence | Low confidence |
| 1.3.2.3 Physical causes | Believing that symptoms are caused by physical factors such as tiredness and hormones | O’Mahen and Flynn, 2008151 Bina, 2020; Button et al., 2017; Dennis and Chung-Lee, 2006; Forde et al., 2020; C. C. G. Jones et al., 2014; Newman et al., 2019; Sambrook Smith et al., 2019; Schmied et al., 2017; Staneva et al., 2015; Watson et al., 201946,47,69,79,85,89,90,94,96,105 |
13 | Low confidence | Low confidence | High confidence | Moderate confidence | Low confidence |
| 1.3.2.4 A normal response to motherhood? | Believing symptoms are just a normal response to motherhood | Williams et al., 2016120 Dennis and Chung-Lee, 2006; Giscombe et al., 2020; Jones et al., 2014; Sambrook Smith et al., 2019; Schmied et al., 2017; Slade et al., 2020; Sorsa et al., 2021; Viveiros and Darling, 201847,49,76,79,89,90,92,93 |
9 | Low confidence | Low confidence | Moderate confidence | Moderate confidence | Moderate confidence |
| 1.3.3 How to cope with symptoms | ||||||||
| 1.3.3.1 Ignore them | Women may deal with symptoms by ignoring them and assuming they will go away on their own | Bina, 2020; Hadfield and Wittkowski, 2017; Jones et al., 2014; Newman et al., 2019; Schmied et al., 2017; Slade et al., 202069,72,79,85,90,92 | 6 | Low confidence | Low confidence | Moderate confidence | Moderate confidence | Moderate confidence |
| 1.3.3.2 Seek spiritual guidance | Women may cope with symptoms by seeking spiritual guidance | Hansotte et al., 2017; Kassam, 2019; Schmied et al., 2017; Watson et al., 201970,81,90,96 | 4 | Moderate confidence | Very low confidence | High confidence | Moderate confidence | Low confidence |
| 1.3.3.3 Minimise them | Women may minimise or deny their symptoms | Shakespeare et al., 2003125 Bina, 2020; Dennis and Chung-Lee, 2006; Forde et al., 2020; Hewitt et al., 2009; Holopainen and Hakulinen, 2019; Jones et al., 2014; Kassam, 2019; Megnin-Viggars et al., 2015; Schmied et al., 2017; Slade et al., 2020; Staneva et al., 2015; Tobin et al., 2018; Watson et al., 201947,48,69,77–79,81,90,92,94–96,105 |
14 | Moderate confidence | Low confidence | High confidence | Moderate confidence | Moderate confidence |
| 1.4 Deciding to seek help | ||||||||
| 1.4.1 Recognising something is wrong | The first step to seeking help for many women, was recognising that something was ‘wrong’ | Bina, 2020; Button et al., 2017; Forde et al., 2020; Hadfield and Wittkowski, 2017; Slade et al., 2020; Staneva et al., 2015; Viveiros and Darling, 201846,49,69,72,92,94,105 | 8 | Moderate confidence | Low confidence | High confidence | Moderate confidence | Moderate confidence |
| 1.4.2 Where do I go to seek help? | The next step to help-seeking is then understanding where to go in order to seek help | Ganann et al., 2019110 Bina, 2020; Dennis and Chung-Lee, 2006; Hansotte et al., 2017; Megnin-Viggars et al., 2015; Schmied et al., 2017; Sorsa et al., 2021; Tobin et al., 201847,48,69,70,90,93,95 |
9 | Low confidence | Very low confidence | High confidence | Low confidence | Low confidence |
| 1.5 Fear of judgment | ||||||||
| 1.5.1 Fear of being seen as a bad mum | Fear of being judged and being seen as a bad mother | Bina, 2020; Brealey et al., 2010; Button et al., 2017; Forde et al., 2020; Jones et al., 2014; Lucas et al., 2019; Slade et al., 2020; Sorsa et al., 2021; Viveiros and Darling, 201846,49,69,74,79,82,92,93,105 | 9 | Low confidence | Low confidence | High confidence | High confidence | Moderate confidence |
| 1.5.2 Social services/removal of child | Fear of social services involvement or their child being removed from their care | Boyd et al., 2011; Feinberg et al., 2006; Shakespeare et al., 2003; Young et al., 2019111,114,125,128 Bina, 2020; Brealey et al., 2010; Button et al., 2017; Dennis and Chung-Lee, 2006; Evans et al., 2020; Forde et al., 2020; Hadfield and Wittkowski, 2017; Hewitt et al., 2009; A. Jones, 2019; Megnin-Viggars et al., 2015; Newman et al., 2019; Tobin et al., 2018; Watson et al., 201946–48,69,72,74,75,77,80,85,95,96,105 SH |
17 | Moderate confidence | Moderate confidence | High confidence | High confidence | High confidence |
| 1.6 Logistics of accessing perinatal mental health care | ||||||||
| 1.6.1 Childcare | Lack of childcare as a barrier to PMH care | Boyd et al., 2011; Cox et al., 2017; Doering et al., 2017; Friedman et al., 2010114,115,135,136 Bina, 2020; Button et al., 2017; Dennis and Chung-Lee, 2006; Hansotte et al., 2017; Morrell et al., 2016; Newman et al., 2019; Sambrook Smith et al., 2019; Scope et al., 2017; Watson et al., 201946,47,69,70,84,85,89,91,96 |
14 | Moderate confidence | Low confidence | High confidence | Low confidence | Low confidence |
| 1.6.2 Timing of care | Timing of appointments and services offered | Atif et al., 2019; Friedman et al., 2010134,136 Bina, 2020; Dennis and Chung-Lee, 2006; Newman et al., 2019; Scope et al., 2017; Watson et al., 201947,69,85,91,96 |
7 | Moderate confidence | Low confidence | Moderate confidence | Low confidence | Low confidence |
| 1.6.3 Location/travel | Location of services or travel costs to get to services | Cox et al., 2017; Doering et al., 2017; Eappen et al., 2018; Friedman et al., 2010; Masood et al., 2015; Nakku et al., 2016109,115,135–138 Bina, 2020; Hansotte et al., 2017; Mollard et al., 2016; Morrell et al., 2016; Newman et al., 2019; Tobin et al., 2018; Watson et al., 201947,69,85,91,96 |
13 | Moderate confidence | Low confidence | High confidence | Low confidence | Low confidence |
| 1.7 Social and family life | ||||||||
| 1.7.1 Social isolation or support | Women’s experiences of social support or social isolation | Giscombe et al., 2020; Hansotte et al., 2017; A. Jones, 2019; Jones et al., 2014; Kassam, 2019; Lucas et al., 2019; Tobin et al., 2018; Viveiros and Darling, 2018; Watson et al., 201949,70,76,80–82,95,96 | 9 | Low confidence | Low confidence | Moderate confidence | Moderate confidence | Moderate confidence |
| 1.7.2 Family and friends’ beliefs | Women’s family and friends’ beliefs about mental illness | Atif et al., 2016, 2019; Boyd et al., 2011; Doering et al., 2017; Ganann et al., 2019; Higgins et al., 2018; Masood et al., 2015; Nakku et al., 2016; Nithianandan et al., 2016; Noonan et al., 2018; O’Mahen and Flynn, 2008; Pineros-Leano et al., 2015; Vik et al., 2009; Williams et al., 2016; Young et al., 2019107,109–111,114–120,123,134,138,151 Bina, 2020; Button et al., 2017; Dennis and Chung-Lee, 2006; Forde et al., 2020; Hadfield and Wittkowski, 2017; Holopainen and Hakulinen, 2019; A. Jones, 2019; Lucas et al., 2019; Nilaweera et al., 2014; Sambrook Smith et al., 2019; Schmied et al., 2017; Sorsa et al., 2021; Viveiros and Darling, 2018; Watson et al., 201946,47,49,69,72,78,80,82,86,89,93,96,105 |
30 | Moderate confidence | High confidence | Moderate confidence | Moderate confidence | Moderate confidence |
| 1.7.3 Additional personal difficulties | Personal difficulties outside of PMH such as unemployment | Atif et al., 2016; Boyd et al., 2011; Kerker et al., 2018; Munodawafa et al., 2017; Rowan et al., 2010; Williams et al., 2016107,114,120,121,131,139 Hansotte et al., 201770 |
7 | Moderate confidence | Low confidence | Moderate confidence | Moderate confidence | Moderate confidence |
| 1.8 Sociodemographic factors | ||||||||
| 1.8.1 Ethnicity | Women’s ethnicity | Bina, 2020; Dennis and Chung-Lee, 2006; Hansotte et al., 2017; Watson et al., 201947,69,70,96 | 4 | Low confidence | Very low confidence | High confidence | Moderate confidence | Low confidence |
| 1.8.2 Age | Women’s age | Bina, 2020; Hansotte et al., 201769,70 | 2 | Low confidence | Very low confidence | High confidence | Very low confidence | Very low confidence |
| 1.9 Mental health factors | ||||||||
| 1.9.1 Previous experiences of mental health care | Previous experiences of mental health care | O’Mahen and Flynn, 2008151 Button et al., 2017; Evans et al., 2020; Hadfield and Wittkowski, 2017; Hansotte et al., 2017; Watson et al., 201946,70,72,75,96 |
6 | Moderate confidence | Low confidence | High confidence | Moderate confidence | Moderate confidence |
| 1.9.2 Previous diagnoses or symptoms | Previous experiences of mental health symptoms or diagnoses | Bina, 2020; Sorsa et al., 202169,93 | 2 | Low confidence | Very low confidence | High confidence | Very low confidence | Very low confidence |
| 1.9.3 Current diagnoses or symptoms | Current experiences of mental health symptoms or diagnoses | Chartier et al., 2015; Friedman et al., 2010; Hadfield et al., 2019; Young et al., 2019111,133,136,153 Sorsa et al., 2021; Viveiros and Darling, 201849,93 |
6 | Low confidence | Low confidence | High confidence | Moderate confidence | Low confidence |
| 2. HCP | ||||||||
| 2.1 HCP’s knowledge about PMH | ||||||||
| 2.1.1 HCP’s knowledge about PMI | HCP’s knowledge about PMH actual and perceived by women | Beeber et al., 2009; Byatt et al., 2013; Ganann et al., 2019; Higgins et al., 2018; Judd et al., 2011; McCauley et al., 2019; McKenzie-McHarg et al., 2014; Noonan et al., 2018; Reed et al., 2014; Rowan et al., 2010108,110,116,117,121,130,142–144,149 Bina, 2020; Dennis and Chung-Lee, 2006; Megnin-Viggars et al., 2015; Morrell et al., 2016; Slade et al., 2020; Viveiros and Darling, 201847–49,69,84,92 SH |
17 | Moderate confidence | Moderate confidence | High confidence | Moderate confidence | Moderate confidence |
| 2.1.2 HCP’s knowledge about services/referral pathways | HCP’s knowledge about PMH services and referral pathways actual and perceived by women | Ganann et al., 2019; Higgins et al., 2018; Rowan et al., 2010110,116,121 Dennis and Chung-Lee, 2006; Hansotte et al., 2017; Sambrook Smith et al., 2019; Slade et al., 2020; Viveiros and Darling, 201847,49,70,89,92 |
8 | Moderate confidence | Low confidence | High confidence | High confidence | High confidence |
| 2.1.3 HCP’s confidence | HCP’s confidence in addressing PMH | Atif et al., 2019; Bina et al., 2018; Cox et al., 2017; Fernandez y Garcia et al., 2011; Higgins et al., 2018; Munodawafa et al., 2017; Nithianandan et al., 2016; Ormsby et al., 2018; Reed et al., 2014116,122,123,134,135,139,140,144,145 SH |
9 | Moderate confidence confidence | Low confidence | High confidence | Moderate confidence | Moderate confidence |
| 2.2 Getting it right the first time | ||||||||
| 2.2.1 Being dismissive or normalising symptoms | HCP dismissing or normalising symptoms | Ganann et al., 2019110 Button et al., 2017; Dennis and Chung-Lee, 2006; Forde et al., 2020; Hadfield and Wittkowski, 2017; Hansotte et al., 2017; Megnin-Viggars et al., 2015; Newman et al., 2019; Sorsa et al., 2021; Watson et al., 201946–48,70,72,85,93,96,105 SH |
11 | Low confidence | Low confidence | High confidence | High confidence | High confidence |
| 2.2.2 Not recognising help-seeking or PMI | HCP not recognising help-seeking or PMI | Bina, 2020; Button et al., 2017; Megnin-Viggars et al., 2015; Tobin et al., 2018; Watson et al., 201946,48,69,95,96 | 5 | Moderate confidence | Very low confidence | High confidence | Moderate confidence | Moderate confidence |
| 2.2.3 Focusing on infant | HCP focusing mainly on the infant | Button et al., 2017; Megnin-Viggars et al., 201546,48 | 2 | Low confidence | Very low confidence | High confidence | Moderate confidence | Low confidence |
| 2.2.4 Making time | A HCP who makes time to address PMH concerns | Feinberg et al., 2006; Myors et al., 2015; Noonan et al., 2018113,117,128 Bina, 2020; Button et al., 2017; Dennis and Chung-Lee, 2006; Hewitt et al., 2009; Megnin-Viggars et al., 2015; Slade et al., 2020; Viveiros and Darling, 2018; Watson et al., 201946–49,69,77,92,96 |
11 | Low confidence | Low confidence | Moderate confidence | High confidence | Moderate confidence |
| 2.2.5 Assessment specific behaviours | HCP’s assessment specific behaviours, such as asking about PMH, carrying out in a tick box way or in a personalised way | Doering et al., 2017; Fernandez y Garcia et al., 2011; Nithianandan et al., 2016; Segre et al., 2014; Vik et al., 2009; Williams et al., 2016115,119,120,122–124 Brealey et al., 2010; Sambrook Smith et al., 2019; Schmied et al., 2017; Slade et al., 2020; Viveiros and Darling, 2018; Watson et al., 201949,74,89,90,92,96 |
12 | Moderate confidence | Low confidence | Moderate confidence | Moderate confidence | Moderate confidence |
| 2.3 HCPs’ attributes | ||||||||
| 2.3.1 Similar demographic characteristics | HCP having similar demographics to women | Leger et al., 2015; Masood et al., 2015; Nithianandan et al., 2016; Shorey and Ng, 2019123,138,147,148 Dennis and Chung-Lee, 2006; Watson et al., 201947,96 |
6 | Moderate confidence | Low confidence | High confidence | Moderate confidence | Moderate confidence |
| 2.3.2 Culturally sensitive | HCP being sensitive to women from all cultures | Kassam, 2019; Nilaweera et al., 2014; Viveiros and Darling, 2018; Watson et al., 201949,81,86,96 | 4 | Moderate confidence | Very low confidence | Moderate confidence | Moderate confidence | Low confidence |
| 2.3.3 Valued characteristics | HCP possessing valued characteristics Trustworthy, empathetic, kind, caring with a genuinine interest, and going above and beyond | Atif et al., 2016, 2019; Boyd et al., 2011; Doering et al., 2017; Kerker et al., 2018; Kim et al., 2009; Munodawafa et al., 2017; Myors et al., 2015; Pugh et al., 2015; Shorey and Ng, 2019107,113–115,129,131,134,139,146,147 Brealey et al., 2010; Button et al., 2017; Dennis and Chung-Lee, 2006; Forde et al., 2020; Hadfield and Wittkowski, 2017; Hewitt et al., 2009; Jones, 2019; Megnin-Viggars et al., 2015; Morrell et al., 2016; Newman et al., 2019; Schmied et al., 2017; Slade et al., 2020; Staneva et al., 2015; Watson et al., 201946–48,72,74,77,80,84,85,90,92,94,96,105 SH |
25 | Moderate confidence | High confidence | High confidence | High confidence | High confidence |
| 3. Interpersonal | ||||||||
| 3.1 Trusting relationship and rapport | The development of a trusting relationship and rapport between HCP and women | Atif et al., 2016; Doering et al., 2017; Feinberg et al., 2006; Ganann et al., 2019; Hadfield et al., 2019; Higgins et al., 2018; Kerker et al., 2018; Leger et al., 2015; Noonan et al., 2018; Shakespeare et al., 2003; Shorey and Ng, 2019; Willey et al., 2018; Williams et al., 2016; Young et al., 2019107,110,111,115–117,120,125,126,128,131,147,148,153 Bina, 2020; Brealey et al., 2010; Dennis and Chung-Lee, 2006; Hadfield and Wittkowski, 2017; Hewitt et al., 2009; Megnin-Viggars et al., 2015; Morrell et al., 2016; Scope et al., 2017; Tobin et al., 201847,48,69,72,74,77,84,91,95 |
23 | Moderate confidence | High confidence | Moderate confidence | High confidence | High confidence |
| 3.2 Language barriers | Difficulties in communicating due to language barriers | Beeber et al., 2009; Doering et al., 2017; Ganann et al., 2019; Masood et al., 2015; Munodawafa et al., 2017; Nithianandan et al., 2016; Pineros-Leano et al., 2015; Segre et al., 2014; Willey et al., 2018; Williams et al., 2016110,115,118,120,123,124,126,138,139,142 Dennis and Chung-Lee, 2006; Hansotte et al., 2017; Megnin-Viggars et al., 2015; Sambrook Smith et al., 2019; Schmied et al., 2017; Watson et al., 201947,48,70,89,90,96 SH |
16 | Moderate confidence | Moderate confidence | High confidence | High confidence | High confidence |
| 3.3 Shared decision-making | Shared decision-making between HCP and women | Hadfield and Wittkowski, 2017; Megnin-Viggars et al., 2015; Randall and Briscoe, 2018; Scope et al., 201748,72,88,91 | 4 | Low confidence | Very low confidence | Moderate confidence | Moderate confidence | Low confidence |
| 3.4 Open and honest communication | Open and honest communication between HCP and women | Doering et al., 2017; Shakespeare et al., 2003; Vik et al., 2009; Willey et al., 2018115,119,125,126 Brealey et al., 2010; Hadfield and Wittkowski, 2017; Hewitt et al., 2009; Schmied et al., 2017; Watson et al., 201972,74,77,90,96 SH |
9 | Moderate confidence | Low confidence | Moderate confidence | High confidence | Moderate confidence |
| 4. Organisational | ||||||||
| 4.1 Overall organisational aspects | ||||||||
| 4.1.1 Co-location and buildings | Location of the service including co-location of different services within the same building | Boyd et al., 2011; Cox et al., 2017; Judd et al., 2011; Munodawafa et al., 2017; Ormsby et al., 2018; Young et al., 2019111,114,130,135,139,140 Bina, 202069 SH |
7 | Moderate confidence | Low confidence | Moderate confidence | Low confidence | Low confidence |
| 4.1.2 Service integration and collaborative working | Collaborative working across services SH |
Atif et al., 2016; Bina et al., 2018; Boyd et al., 2011; Byatt et al., 2013; Feinberg et al., 2006; Ganann et al., 2019; Hadfield et al., 2019; Judd et al., 2011; Lind et al., 2017; Lomonaco-Haycraft et al., 2018; Myors et al., 2015; Nithianandan et al., 2016; Noonan et al., 2018; Rowan et al., 2010107,110,113,114,117,121,123,128,130,132,141,143,145,153 Newman et al., 2019; Sambrook Smith et al., 2019; Watson et al., 201985,89,96 |
17 | Moderate confidence | Moderate confidence | Moderate confidence | Moderate confidence | Moderate confidence |
| 4.1.3 Collaboration within services | Collaborative working within services SH |
Ammerman et al., 2014; Cox et al., 2017; Eappen et al., 2018; Higgins et al., 2018; Judd et al., 2011; Kerker et al., 2018; Lind et al., 2017; McKenzie-McHarg et al., 2014; Munodawafa et al., 2017; Nithianandan et al., 2016; Ormsby et al., 2018; Segre et al., 2014; Willey et al., 2018116,123,124,126,127,130–132,135,137,139,140,149 Sambrook Smith et al., 201989 |
14 | Moderate confidence | Moderate confidence | Moderate confidence | Moderate confidence | Moderate confidence |
| 4.1.4 Adequate workforce provision/HCP’s workload | Ensuring an adequate workforce provision so PMH can be addressed | Ammerman et al., 2014; Bina et al., 2018; Drozd et al., 2018; Feinberg et al., 2006; Ganann et al., 2019; Higgins et al., 2018; Kerker et al., 2018; Kim et al., 2009; McCauley et al., 2019; Nakku et al., 2016; Nithianandan et al., 2016; Noonan et al., 2018; Rowan et al., 2010; Vik et al., 2009; Willey et al., 2018108–110,116,117,119,121,123,126–129,131,145,150 Bina, 2020; Viveiros and Darling, 201849,69 SH |
17 | Low confidence | Moderate confidence | High confidence | High confidence | High confidence |
| 4.1.5 Clear assessment and referral process | Clear assessment and referral processes within the organisation | Cox et al., 2017; Feinberg et al., 2006; Ganann et al., 2019; Judd et al., 2011; Kerker et al., 2018; Kim et al., 2009; Nithianandan et al., 2016; Rowan et al., 2010; Segre et al., 2014; Williams et al., 2016110,120,121,123,124,128–131,135 Bina, 202069 SH |
11 | Moderate confidence | Low confidence | Moderate confidence | Moderate confidence | Moderate confidence |
| 4.1.6 Provision of supervision | Supervision for HCPs | Atif et al., 2019; Munodawafa et al., 2017; Vik et al., 2009119,134,139 | 3 | Moderate confidence | Very low confidence | High confidence | Very low confidence | Very low confidence |
| 4.1.7 Training | Provision of training for all HCPs working with perinatal women | Ammerman et al., 2014; Atif et al., 2016, 2019; Beeber et al., 2009; Bina et al., 2018; Boyd et al., 2011; Chartier et al., 2015; Doering et al., 2017; Drozd et al., 2018; Feinberg et al., 2006; Ganann et al., 2019; Judd et al., 2011; Kerker et al., 2018; Kim et al., 2009; Leger et al., 2015; Lind et al., 2017; McKenzie-McHarg et al., 2014; Munodawafa et al., 2017; Nakku et al., 2016; Nithianandan et al., 2016; Noonan et al., 2018; Reed et al., 2014; Rowan et al., 2010; Shorey and Ng, 2019; Willey et al., 2018; Williams et al., 2016107,109,110,114,115,117,120,121,123,126–134,139,142,144,145,147–150 Bina, 2020; Brealey et al., 201069,74 SH |
28 | Moderate confidence | High confidence | High confidence | High confidence | High confidence |
| 4.1.9 Organisational goals/guidelines | Clear organisational goals and guidelines | Ammerman et al., 2014; Willey et al., 2018126,127 | 2 | Low confidence | Very low confidence | Very low confidence | Very low confidence | Very low confidence |
| 4.2 Characteristics of PMH Care | ||||||||
| 4.2.1 Across the care pathway | ||||||||
| 4.2.1.1 Continuity of carer | Care that provides the same HCP along the care pathway | Chartier et al., 2015; Higgins et al., 2018; Nithianandan et al., 2016; O’Mahen and Flynn, 2008; Rowan et al., 2010; Willey et al., 2018116,121,123,126,133,151 Brealey et al., 2010; Button et al., 2017; Dennis and Chung-Lee, 2006; Hadfield and Wittkowski, 2017; Megnin-Viggars et al., 2015; Sambrook Smith et al., 2019; Slade et al., 2020; Tobin et al., 2018; Viveiros and Darling, 2018; Watson et al., 201946–49,72,74,89,92,95,96 SH |
17 | Moderate confidence | Moderate confidence | High confidence | High confidence | High confidence |
| 4.2.1.2 Culturally sensitive care | Care that is culturally sensitive to women’s needs | Ganann et al., 2019; Nithianandan et al., 2016; Noonan et al., 2018; Shorey and Ng, 2019110,117,123,147 Bina, 2020; Brealey et al., 2010; Button et al., 2017; Dennis and Chung-Lee, 2006; Giscombe et al., 2020; Hadfield and Wittkowski, 2017; Hansotte et al., 2017; Hewitt et al., 2009; Jones, 2019; Kassam, 2019; Sambrook Smith et al., 2019; Schmied et al., 2017; Tobin et al., 2018; Viveiros and Darling, 2018; Watson et al., 201946,47,49,69,70,72,74,76,77,80,81,89,90,95,96 |
19 | Moderate confidence | Moderate confidence | High confidence | High confidence | High confidence |
| 4.2.1.3 Privacy and confidentiality | Care that is private and maintains women’s confidentiality | Atif et al., 2019; Feinberg et al., 2006; Higgins et al., 2018; Jallo et al., 2015; Nithianandan et al., 2016; O’Mahen and Flynn, 2008116,123,128,134,151,154 Giscombe et al., 202076 |
7 | Moderate confidence | Low confidence | Moderate confidence | Low confidence | Low confidence |
| 4.2.1.4 Dedicated person/PMH Champion | Care that has a dedicated person or PMH Champion | Chartier et al., 2015; Ganann et al., 2019; Kim et al., 2009; Lomonaco-Haycraft et al., 2018; Nithianandan et al., 2016; Rowan et al., 2010; Willey et al., 2018110,121,123,126,129,133,141 Bina, 2020; Megnin-Viggars et al., 201548,69 |
9 | Moderate confidence | Low confidence | Moderate confidence | Low confidence | Low confidence |
| 4.2.1.5 Logistical support | Logistical support for women including easily accessible location, childcare, travel costs | Ganann et al., 2019; Hadfield and Wittkowski, 2017; Leger et al., 2015; Masood et al., 2015; Nakku et al., 2016; Nithianandan et al., 2016; Ormsby et al., 201872,109,110,123,138,140,148 Button et al., 2017; Jones, 2019; Mollard et al., 2016; Newman et al., 2019; Scope et al., 2017; Watson et al., 201946,80,83,85,91,96 |
13 | Moderate confidence | Low confidence | High confidence | Moderate confidence | Moderate confidence |
| 4.2.1.6 Home delivery | Care that is delivered at home | Ammerman et al., 2014; Beeber et al., 2009; Judd et al., 2011; Leger et al., 2015; Munodawafa et al., 2017; Myors et al., 2015113,127,130,139,142,148 Brealey et al., 2010; Hadfield and Wittkowski, 2017; Hansotte et al., 2017; Jones, 201970,72,74,80 |
10 | Moderate confidence | Low confidence | High confidence | Moderate confidence | Moderate confidence |
| 4.2.1.7 Hospital delivery | Care that is delivered in hopsital/medical setting | Atif et al., 2019; Boyd et al., 2011; Kerker et al., 2018; Shakespeare et al., 2003114,125,131,134 Dennis and Chung-Lee, 200647 |
5 | Low confidence | Very low confidence | Low confidence | Low confidence | Low confidence |
| 4.2.1.8 Provision of information | Whether care provides information | Dennis and Chung-Lee, 2006; Hadfield and Wittkowski, 2017; Jones, 2019; Megnin-Viggars et al., 2015; Morrell et al., 2016; Randall and Briscoe, 2018; Schmied et al., 201747,48,72,80,84,88,90 | 7 | Low confidence | Low confidence | Moderate confidence | Moderate confidence | Moderate confidence |
| 4.2.1.9 Technology | The use of technology in care | Doering et al., 2017; Feinberg et al., 2006; Fernandez y Garcia et al., 2011; Jallo et al., 2015; Kim et al., 2009; Lind et al., 2017; Noonan et al., 2018; Pineros-Leano et al., 2015; Shorey and Ng, 2019; Willey et al., 2018; Williams et al., 2016115,117,118,120,122,126,128,129,132,147,154 SH |
11 | Moderate confidence | Low confidence | High confidence | High confidence | High confidence |
| 4.2.1.10 Service inclusion criteria | Inclusion criteria of services | Boyd et al., 2011; Ganann et al., 2019110,114 Viveiros and Darling, 201849 |
3 | Low confidence | Very low confidence | Moderate confidence | Low confidence | Low confidence |
| 4.2.2 Assessment specific characteristics | ||||||||
| 4.2.2.1 Wording of assessment tools | How assessment tools are worded | Doering et al., 2017; Segre et al., 2014; Williams et al., 2016115,120,124 Brealey et al., 2010; Button et al., 2017; Hewitt et al., 200946,74,77 |
6 | Low confidence | Low confidence | High confidence | High confidence | Moderate confidence |
| 4.2.2.2 Acceptability of assessment/screening | Whether assessment tools and assessment/screening in general are acceptable to women and HCPs | Boyd et al., 2011; Doering et al., 2017; Feinberg et al., 2006; Ganann et al., 2019; Kim et al., 2009; Nithianandan et al., 2016; Segre et al., 2014; Shakespeare et al., 2003; Vik et al., 2009; Willey et al., 2018110,114,115,119,123–126,128,129 Brealey et al., 2010; Evans et al., 2020; Hewitt et al., 2009; Megnin-Viggars et al., 2015; Mollard et al., 2016; Sambrook Smith et al., 2019; Viveiros and Darling, 201848,49,74,75,77,83,89 |
17 | Low confidence | Moderate confidence | Moderate confidence | Moderate confidence | Moderate confidence |
| 4.2.3 Intervention characteristics | ||||||||
| 4.2.3.1 Opportunity to talk | Interventions that provide an opportunity to talk | Dennis and Chung-Lee, 2006; Evans et al., 2020; Hadfield and Wittkowski, 2017; Jones et al., 2014; Kassam, 2019; Morrell et al., 2016; Praetorius et al., 202047,72,75,79,81,84,87 | 7 | Low confidence | Low confidence | High confidence | Low confidence | Low confidence |
| 4.2.3.2 Individualised and person centred | Individualised and person-centred interventions/care | Chartier et al., 2015; Doering et al., 2017; Ganann et al., 2019; Masood et al., 2015; McKenzie-McHarg et al., 2014; Noonan et al., 2018; O’Mahen and and Flynn, 2008; Pugh et al., 2015; Segre et al., 2014; Shorey and Ng, 2019110,115,117,124,133,138,146,147,149,151 Evans et al., 2020; Hadfield and Wittkowski, 2017; Megnin-Viggars et al., 2015; Morrell et al., 2016; Schmied et al., 2017; Scope et al., 2017; Slade et al., 2020; Watson et al., 201948,72,75,84,90–92,96 SH |
19 | Moderate confidence | Moderate confidence | Moderate confidence | High confidence | Moderate confidence |
| 4.2.3.3 Appropriateness | Appropriateness of intervention being offered, from women’s and HCPs’ point of view | Atif et al., 2019; Bina et al., 2018; Chartier et al., 2015; Drozd et al., 2018; Leger et al., 2015; McKenzie-McHarg et al., 2014; Munodawafa et al., 2017; Noonan et al., 2018; Ormsby et al., 2018; Pugh et al., 2015; Reed et al., 2014; Shorey and Ng, 2019117,133,134,139,140,144–150 Evans et al., 2020; Megnin-Viggars et al., 2015; Scope et al., 201748,75,91 |
15 | Moderate confidence | Moderate confidence | High confidence | Low confidence | Moderate confidence |
| 4.2.3.4 Flexible | Flexibility of intervention | Atif et al., 2019; Bina et al., 2018; Ganann et al., 2019; Hadfield et al., 2019; Judd et al., 2011; Munodawafa et al., 2017; O’Mahen and Flynn, 2008; Pugh et al., 2015; Shorey and Ng, 2019110,130,134,139,145–147,151,153 Sorsa et al., 2021; Watson et al., 201993,96 |
11 | Moderate confidence | Low confidence | High confidence | Moderate confidence | Moderate confidence |
| 4.2.3.5 Group support | Group/peer support as an intervention | Hadfield et al., 2019; Masood et al., 2015; Nakku et al., 2016109,138,153 Dennis and Chung-Lee, 2006; Evans et al., 2020; Hadfield and Wittkowski, 2017; Holopainen and Hakulinen, 2019; Jones et al., 2014; Megnin-Viggars et al., 2015; Schmied et al., 2017; Scope et al., 2017; Slade et al., 2020; Tobin et al., 2018; Watson et al., 201947,48,72,75,78,79,90–92,95,96 SH |
14 | Moderate confidence | Low confidence | Moderate confidence | High confidence | Moderate confidence |
| 4.2.3.7 Face-to-face delivery | Face-to-face delivery of intervention | O’Mahen and Flynn, 2008; Pugh et al., 2015; Shorey and Ng, 2019146,147,151 Schmied et al., 201790 SH |
4 | Moderate confidence | Very low confidence | High confidence | High confidence | Low confidence |
| 5. Commissioners | ||||||||
| 5.1 Referral pathways | Clear referral pathways | Ammerman et al., 2014; Boyd et al., 2011; Higgins et al., 2018; Nithianandan et al., 2016; Rowan et al., 2010; Willey et al., 2018114,116,121,123,126,127 SH |
6 | Moderate confidence | Low confidence | Moderate confidence | High confidence | Moderate confidence |
| 5.2 Lack of appropriate or timely services | Lack of appropriate and timely services to refer women on to | Boyd et al., 2011; Doering et al., 2017; Ganann et al., 2019; Higgins et al., 2018; Kerker et al., 2018; Leger et al., 2015; Lomonaco-Haycraft et al., 2018; Munodawafa et al., 2017; Myors et al., 2015; Nakku et al., 2016; Noonan et al., 2018; Rowan et al., 2010; Williams et al., 2016109,110,113–117,120,121,131,139,141,148 Bina, 2020; Button et al., 2017; Jones, 2019; Jones et al., 2014; Megnin-Viggars et al., 2015; Newman et al., 2019; Sambrook Smith et al., 2019; Tobin et al., 2018; Viveiros and Darling, 201846,48,49,69,79,80,85,89,95 SH |
22 | Low confidence | High confidence | High confidence | High confidence | High confidence |
| 5.3 Financial complexities | Financial complexities including funding, and sourcing money and resources for services and financial reimbursement | Cox et al., 2017; Feinberg et al., 2006; Friedman et al., 2010; Ganann et al., 2019; Kim et al., 2009; Lomonaco-Haycraft et al., 2018; Ormsby et al., 2018; Rowan et al., 2010110,121,128,129,135,136,140,141 SH |
8 | Moderate confidence | Low confidence | Moderate confidence | Moderate confidence | Moderate confidence |
| 6. Political | ||||||||
| 6.1 Immigration status | How the immigration status of women may impact their PMH care journey | Cox et al., 2017; Ganann et al., 2019110,135 Bina, 2020; Giscombe et al., 2020; Hansotte et al., 2017; Kassam, 2019; Schmied et al., 2017; Tobin et al., 2018; Watson et al., 201969,70,76,81,90,95,96 SH |
9 | Moderate confidence | Low confidence | High confidence | High confidence | High confidence |
| 5.2 Economic status and healthc are costs | How the cost of health care, and women’s economic status may impact their PMH care journey | Atif et al., 2016; Boyd et al., 2011; Cox et al., 2017; Doering et al., 2017; Ganann et al., 2019; Lomonaco-Haycraft et al., 2018; Munodawafa et al., 2017; Nakku et al., 2016; Ormsby et al., 2018107,109,110,114,115,135,139–141 Bina, 2020; Hansotte et al., 2017; Jones, 2019; Kassam, 2019; Lucas et al., 2019; Tobin et al., 2018; Viveiros and Darling, 201849,69,70,80–82,95 SH |
16 | Moderate confidence | Moderate confidence | High confidence | Low confidence | Moderate confidence |
| 7. Societal | ||||||||
| 7.1 Stigma | Stigma related to mental illness | Atif et al., 2016, 2019; Boyd et al., 2011; Chartier et al., 2015; Cox et al., 2017; Feinberg et al., 2006; Higgins et al., 2018; Kerker et al., 2018; McCauley et al., 2019; McKenzie-McHarg et al., 2014; Munodawafa et al., 2017; Myors et al., 2015; Nakku et al., 2016; Nithianandan et al., 2016; Noonan et al., 2018; O’Mahen and Flynn, 2008; Shakespeare et al., 2003; Vik et al., 2009; Williams et al., 2016; Young et al., 2019107–109,111,113,114,116,117,119,120,123,125,128,131,133–135,139,149,151 Bina et al., 2018; Button et al., 2017; Dennis and Chung-Lee, 2006; Giscombe et al., 2020; Hadfield and Wittkowski, 2017; Hansotte et al., 2017; Hewitt et al., 2009; Holopainen and Hakulinen, 2019; A. Jones, 2019; Kassam, 2019; Lucas et al., 2019; Megnin-Viggars et al., 2015; Mollard et al., 2016; Morrell et al., 2016; Nilaweera et al., 2014; Sambrook Smith et al., 2019; Schmied et al., 2017; Scope et al., 2017; Sorsa et al., 2021; Tobin et al., 2018; Viveiros and Darling, 2018; Watson et al., 201946–49,69,70,72,76–78,80–84,86,89–91,93,95,96 SH |
43 | Moderate confidence | High confidence | High confidence | High confidence | High confidence |
| 7.2 Culture | Cultural beliefs about mental illness and seeking and accessing help | Atif et al., 2016; Bina et al., 2018; Boyd et al., 2011; Feinberg et al., 2006; Friedman et al., 2010; Ganann et al., 2019; Higgins et al., 2018; Masood et al., 2015; McCauley et al., 2019; Nakku et al., 2016; Noonan et al., 2018; Segre et al., 2014107–110,114,116,117,124,128,136,138,145 Brealey et al., 2010; Button et al., 2017; Dennis and Chung-Lee, 2006; Giscombe et al., 2020; Hansotte et al., 2017; Hewitt et al., 2009; Holopainen and Hakulinen, 2019; Jones, 2019; Kassam, 2019; Megnin-Viggars et al., 2015; Praetorius et al., 2020; Sambrook Smith et al., 2019; Schmied et al., 2017; Staneva et al., 2015; Tobin et al., 2018; Viveiros and Darling, 2018; Watson et al., 2019; Wittkowski et al., 201446–49,70,74,76–78,80,81,87,89,90,94–97 SH |
30 | Moderate confidence | High confidence | High confidence | High confidence | High confidence |
| 7.3 Maternal norms | Maternal norms of being a ‘good mother’ and a ‘strong woman’ | Shakespeare et al., 2003; Williams et al., 2016120,125 Bina, 2020; Brealey et al., 2010; Button et al., 2017; Dennis and Chung-Lee, 2006; Hadfield and Wittkowski, 2017; Hansotte et al., 2017; Hewitt et al., 2009; Holopainen and Hakulinen, 2019; Johnson et al., 2020; Jones et al., 2014; Kassam, 2019; Lucas et al., 2019; Megnin-Viggars et al., 2015; Mollard et al., 2016; Newman et al., 2019; Nilaweera et al., 2014; Praetorius et al., 2020; Sambrook Smith et al., 2019; Schmied et al., 2017; Slade et al., 2020; Sorsa et al., 2021; Staneva et al., 2015; Viveiros and Darling, 2018; Watson et al., 201946–49,69,70,72,74,77–79,81–83,85–87,89,90,92–94,96,112 SH |
27 | Moderate confidence | High confidence | High confidence | High confidence | High confidence |
Appendix 7
| 1–7Review | UK | HIC/Western | LMIC/Eastern | Don’t know |
|---|---|---|---|---|
| 1 | Hadfield et al., 2019; Masood et al., 2015; McKenzie-McHarg et al., 2014; O’Mahen and Flynn, 2008; Rowan et al., 2010; Shakespeare et al., 2003; Williams et al., 2016 120,121,125,138,149,151,153 |
Australia: Judd et al., 2011; Myors et al., 2015; Nithianandan et al., 2016; Ormsby et al., 2018; Reed et al., 2014; Willey et al., 2018113,123,126,130,140,144 Canada: Chartier et al., 2015; Leger et al., 2015; Pugh et al., 2015133,146,148 |
Ghana: Munodawafa et al., 2017139 Israel: Bina et al., 2018145 Pakistan: Atif et al., 2016, 2019107,134 |
|
| Ireland: Higgins et al., 2018; Noonan et al., 2018116,117 Norway: Drozd et al., 2018; Vik et al., 2009119,150 USA: Ammerman et al., 2014; Beeber et al., 2009; Boyd et al., 2011; Byatt et al., 2013; Cox et al., 2017; Doering et al., 2017; Feinberg et al., 2006; Fernandez y Garcia et al., 2011; Friedman et al., 2010; Ganann et al., 2019; Jallo et al., 2015; Kerker et al., 2018; Kim et al., 2009; Lind et al., 2017; Lomonaco-Haycraft et al., 2018; Pineros-Leano et al., 2015; Segre et al., 2014; Young et al., 2019110,111,114,115,118,122,124,127–129,131,132,135,136,141–143,154 |
Peru: Eappen et al., 2018137 Singapore: Shorey and Ng, 2019147 South Africa: McCauley et al., 2019108 Uganda: Nakku et al., 2016109 |
|||
| 2 | Brealey et al., 201074 – 53% Button et al., 201746 – 100% Forde et al., 2020105 – 66% Hadfield and Wittkowski, 201772 – 53% |
Bina, 202069 – 83% Evans et al., 202075 – 100% Giscombe et al., 202076– 88% Hansotte et al., 201770 – 100% Holopainen and Hakulinen, 201978 – 77% Jones et al., 201479 – 100% Kassam, 201981– 88% |
Wittkowski et al., 201497 – 100% (sub-Saharan Africa) | Dennis and Chung-Lee, 2006; Jones, 2019; Megnin-Viggars et al., 201547,48,80 |
| Hewitt et al., 200977– 53% Sambrook Smith et al., 201989– 100% Slade et al., 202092– 53% Viveiros and Darling, 201849 – 71% Watson et al., 201996 – 100% |
Lucas et al., 201982 – 100% Mollard et al., 201683 – 100% Morrell et al., 201684– 92% Newman et al., 201985– 100% Nilaweera et al., 201486 – 100% Praetorius et al., 202087– 75% Randall and Briscoe, 201888– 100% Schmied et al., 201790 – 100% Scope et al., 201791 – 95% Sorsa et al., 202193 – 100% Staneva et al., 201594– 88% Tobin et al., 201895– 100% |
Appendix 8
Development of the MATRIx conceptual framework
FIGURE 14.
Version one of the MATRIx conceptual framework (May 2021).
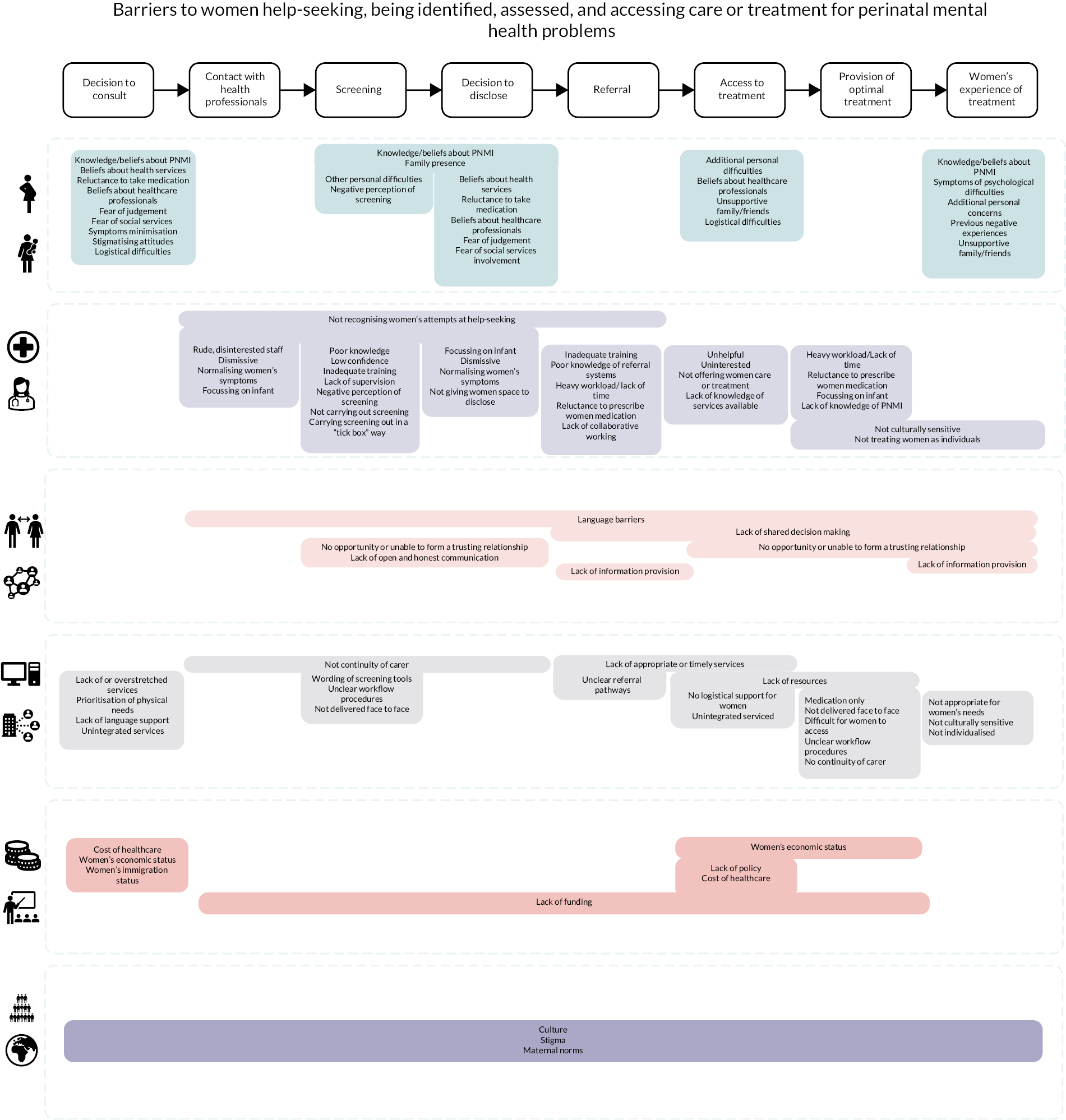
FIGURE 15.
Version two of the MATRIx conceptual framework (July 2021).

Appendix 9
| # | Barriers | Facilitators | |
|---|---|---|---|
| 1 | Assessment viewed as not acceptable by women and HCPs | 1 | Assessment viewed as acceptable by women and HCPs |
| 2 | Care provision lacks privacy and confidentiality | 2 | Care offeres privacy |
| 3 | Care that does not provide logistical support | 3 | Care that provides logistical support |
| 4 | Care that is not appropriate to women’s needs | 4 | Care that is appropriate to women’s needs |
| 5 | Care that is not delivered in a home setting | 5 | Home delivery of care |
| 6 | Care that lacks cultural sensitivity | 6 | Culturally sensitive care |
| 7 | Confusing organisational referral and assessment processes | 7 | Clear organisational assessment and referral processes |
| 8 | HCP not making time to address PMH difficulties | 8 | HCPs making time to address PMH |
| 9 | HCP carrying out assessment in an impersonal way (e.g. tick box exercise) | 9 | HCP carrying out assessment in a personalised way |
| 10 | HCPs having a poor knowledge about PMI | 10 | HCP having a good knowledge of PMH |
| 11 | HCP having a poor knowledge about services | 11 | HCP having a good knowledge of services and pathways |
| 12 | HCP having low confidence about addressing PMH | 12 | HCP having high confidence about addressing PMH |
| 13 | HCP not having received adequate PMH training | 13 | HCP having received adequate PMH training |
| 14 | HCP’s workload too heavy due to inadequate workforce provision | 14 | Adequate workforce provision to meet women’s needs |
| 15 | Inflexible care | 15 | Flexible care |
| 16 | Issues with technology | 16 | Working technology |
| 17 | Lack of collaboration between services | 17 | Collaboration between services |
| 18 | Lack of information provision about care and PMI | 18 | Care provides information about PMI and available services |
| 19 | Lack of support from family and friends | 19 | Supportive family and friends |
| 20 | No continuity of carer | 20 | Continuity of carer |
| 21 | No open honest communication between women and HCP | 21 | Open and honest communication |
| 22 | No relationship and rapport between women and HCP | 22 | Trusting relationship between women and HCP |
| 23 | No shared decision-making between women and HCP | 23 | Shared decision-making between women and HCP |
| 24 | Staff within services not working together | 24 | Collaboration within services |
| 25 | Women being socially isolated | 25 | Women’s social support network |
| 26 | Women viewing peer support as not an acceptable intervention | 26 | Women finding group support acceptable |
| 27 | Women’s previous negative experiences of mental health services | 27 | Women’s previous positive experiences of mental health services |
| 28 | Being an immigrant or a refugee woman | 28 | Care that offers an opportunity to talk |
| 29 | Care that is carried out in medical setting | 29 | Champion/dedicated PMH person |
| 30 | Complicated or confusing wording of assessment tools | 30 | Clear goals and guidelines |
| 31 | Complicated services | 31 | Clear referral pathways |
| 32 | Cultural barriers | 32 | Co-location of services |
| 33 | Current symptoms getting in the way of treatment | 33 | Face-to-face care |
| 34 | Funding complexities | 34 | HCP receiving supervision |
| 35 | HCP dismissive or normalising symptoms | 35 | Individualised person-centred care |
| 36 | HCP focusing only on infant | 36 | Previous mental health diagnoses/symptoms |
| 37 | HCP lacking cross-cultural knowledge of PMH | 37 | Recognising something is wrong |
| 38 | HCP not being interested in PMI | 38 | Valued characteristics of HCP |
| 39 | HCP not recognising help-seeking | 39 | Women and HCP having similar demographics |
| 40 | Lack of appropriate services | ||
| 41 | Lack of childcare | ||
| 42 | Language barriers | ||
| 43 | Maternal norms of being a ‘good mother’ and a ‘strong’ woman | ||
| 44 | Mother’s worries about being judged as a ‘bad mum’ | ||
| 45 | Restrictive eligibility criteria of care | ||
| 46 | Stigma | ||
| 47 | Stretched services | ||
| 48 | The belief that services only offer medication | ||
| 49 | Timing of services not suitable to women’s needs | ||
| 50 | Travel costs | ||
| 51 | Women’s additional personal difficulties | ||
| 52 | Women being from an ethnic minority | ||
| 53 | Women being on a low income | ||
| 54 | Women being worried about social services involvement | ||
| 55 | Women being younger | ||
| 56 | Women believing PMH symptoms are a normal part of motherhood | ||
| 57 | Women believing PMH symptoms are due to physical causes | ||
| 58 | Women coping with symptoms by ignoring them | ||
| 59 | Women coping with symptoms by seeking spiritual guidance | ||
| 60 | Women coping with PMI by minimising symptoms | ||
| 61 | Women not having the language to describe PMI | ||
| 62 | Women not knowing what PMI is | ||
| 63 | Women not knowing where to go to seek help | ||
| 64 | Women not understanding the role of HCPs | ||
| 65 | Women’s belief that PMI is caused by spiritual factors | ||
| 66 | Women’s belief that PMI is due to external causes |
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/KQFE0107).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
List of abbreviations
- AMSTAR
- A MeaSurement Tool to Assess systematic Reviews
- CCGs
- Clinical Commissioning Groups
- EPDS
- Edinburgh Postnatal Depression Scale
- GP
- general practitioner
- HIC
- higher income country
- HP
- health professional
- IQR
- interquartile range
- LGBTQ
- lesbian, gay, bisexual, transgender or queer
- LMIC
- lower middle income countries
- MATRIx
- Perinatal Mental Health Assessment and TReatment: an evidence synthesis and conceptual framework of barriers and facilitators to implementation
- NHS
- National Health Service
- PMH
- perinatal mental health
- PMI
- perinatal mental illness
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-analyses
- PTSD
- post-traumatic stress disorder
- R1
- Review 1
- R2
- Review 2
