Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number NIHR130588. The contractual start date was in November 2022. The draft manuscript began editorial review in January 2023 and was accepted for publication in January 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Cantrell et al. This work was produced by Cantrell et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Cantrell et al.
Chapter 1 Introduction
Background
The term ‘winter pressures’ refers to ‘how hospitals cope with the challenges of maintaining regular service over the winter period’. 1 Although attention typically focuses on additional demands on accident and emergency (A&E) services, pressures are exerted in terms of increased demand across the entire health and social care system. Increased prevalence of respiratory and cardiovascular illnesses during the winter places severe demands upon systems that already face difficulties in matching service provision to demand. Better or earlier planning and/or increasing service provision across integrated care (IC) systems and related sectors, such as housing, constitute just two of the possible responses to increased demand.
The COVID-19 pandemic response illustrates many issues that need to be addressed in planning for hospital discharge when the health system faces specific expected or unexpected system pressure. While very large numbers were rapidly discharged to care home beds in the early months of the pandemic, the discharge process generated significant concerns about whether the associated risks to both the discharged patients and the care homes had been sufficiently considered in the discharge planning process. 2
Winter pressures are a familiar phenomenon within the National Health Service (NHS) and represent the most extreme of many regular demands placed on health service provision. The impact of winter pressures is pervasive and operates along a continuum from public health, in mitigation via immunisation campaigns, through to discharge into social care and the community. Interventions target multiple points along this continuum, as well as whole-system approaches.
This mapping review focuses on one stage of the pathway, considered particularly problematic, namely the discharge process from hospital. Studies of discharge interventions and transfers of care are plentiful and international initiatives are reviewed in a recent scoping review. 3 However, a considerable challenge lies in identifying interventions that specifically are articulated as an explicit response to ‘winter pressures’. There is strong rationale for focusing on the subgroup of winter pressure interventions because these may represent interventions implemented in response to particularly acute and severe system pressure. This contrasts to interventions that seek to improve discharge within a system in ‘steady state’. While commentators on the current context articulate that the system experiences ‘winter’ pressures all year round, until recently, responses have targeted the context of winter pressures. Potentially, this set of studies therefore represents a highly relevant evidence base on discharge related interventions to inform current NHS planning.
This mapping review aims to chart and document the evidence in relation to winter pressures in the United Kingdom, together with either discharge planning to increase discharge (both a reduction in patients waiting to be discharged and patients being discharged to the most appropriate place) and/or IC. For the purposes of this review, ‘integrated care’ involves partnerships of organisations that come together to plan and deliver joined-up health and care services in NHS England.
Objective of the review
The primary objective of the mapping review is to address the question:
-
Which interventions in relation to discharge planning/IC have been suggested, tried or evaluated in seeking to address winter pressures in the United Kingdom?
The secondary review question is:
-
Which research or evaluation gaps exist in relation to service- or system-level interventions as a response to discharge planning/IC in the context of winter pressures?
In addressing this question the mapping review will seek:
-
to identify a potential winter pressures research agenda in relation to discharge planning/IC to inform commissioning of future research.
Chapter 2 Methods
We undertook a systematic mapping review to map the winter pressure literature, specifically in relation to discharge planning and IC, and to help to determine opportunities for further research. The mapping review explores the volume and characteristics of the available evidence in relation to discharge planning or IC in response to winter pressures.
The systematic mapping review closely adhered to published methods for a mapping review. The methodology described by James et al. 4 was used to guide the five stages of the review: setting the scope and inclusion criteria, searching for evidence, screening evidence, coding and database production, describing and visualising the findings.
Setting the scope and inclusion criteria
This mapping review focuses on interventions designed to reduce clinically unnecessary occupancy of hospital beds and demand on health services through discharge and transfer to social care or the community (e.g. ‘hospital at home’). Such interventions typically require improved linkages and communication between various health and social care services, captured in the concept of IC. Integrated care systems seek to capitalise on the benefits of such ‘joined-up’ systems.
Key to feasibility is the requirement for study authors to have linked their research or data explicitly to winter pressures. Numerous interventions have been proposed to handle discharge planning but not all have been explored within the context of a pressurised health or social care system. Insisting on this requirement helped in identifying interventions or mechanisms that offer promise within other pressurised care environments. Specifically, we based eligibility on the following aspects – population, exposure, comparative, outcome(s), study types:
-
users of UK health and/or social care systems (population)
-
winter pressures impacting on discharge, to social care and the community and IC (exposure)
-
other foreseeable, unusual or exceptional periods of demand (if appropriate) (comparison – may or may not be present)
-
increased smart discharge (both a reduction in patients waiting to be discharged and patients being discharged to the most appropriate place), system effects, health and health service outcomes, effects on patients, carers and staff (outcomes)
-
eligible types of study design: primary research study, evidence synthesis or research report (study types).
Searching for evidence
The mapping review took a two-pronged approach to identifying the evidence for this review. The first-stage search identified the interventions through explicit references to winter pressures. The second stage of further searching was undertaken of named interventions extending beyond winter pressures on Google Scholar (Google Inc., Mountain View, CA, USA) to find systematic reviews and guidance. More detail is provided below.
First-stage search
For the first stage, the literature search employed two separate methods according to the type of source being used. We searched databases that offer title and abstract search facilities using terminology relating to winter pressures. We examined retrieved items identified as initially relevant at full text to establish whether they contained data within the context of discharge planning or IC. We searched data sources that enabled full-text searching (e.g. Google Scholar) and other web searches by combining the winter pressure terms with the twin concepts of discharge planning and/or IC.
Search terms and languages
The literature search covered the period 2018–22 and was restricted to English only. This search cut-off date was determined by the need to optimise the relevance to the current context and ways of working. However, we have documented UK studies published before 2018 referenced in evidence syntheses or research reports as still being of contemporary relevance. International intervention in systematic reviews as mapped. We extracted findings from these studies for completeness.
-
Concept 1: winter pressure(s); winter plan(s)/planning; winter resilience; winter protection plan.
-
Concept 2: discharge plan(s)/planning; delayed transfer of care; discharge to assess (D2A); better care fund, increased smart discharge (both a reduction in patients waiting to be discharged and patients being discharged to the most appropriate place).
-
Concept 3: integrated care.
An initial search was conducted in October on MEDLINE and then translated to the other databases. The MEDLINE search strategy is provided in Appendix 1. The search used free-text terms for winter pressures and winter planning. We were unable to identify specific relevant thesaurus terms for winter pressures. To optimise sensitivity of the search, we did not use specific discharge/IC terminology in the search strategy but decided that judgements on discharge planning/IC context would be operationalised during title/abstract and full-text screening stages rather than relying on uneven application of database indexing.
Databases searched
-
MEDLINE Ovid Database: Ovid MEDLINE(R) and Epub Ahead of Print, In-Process, In-Data-Review & Other Non-Indexed Citations, Daily and Versions, 1946 to 11 October 2022.
-
HMIC Ovid: Health Management Information Consortium, 1979 to July 2022.
-
Social Care Online.
-
SSCI: Social Sciences Citation Index, 1900 to present.
-
King’s Fund Library.
Google Scholar was also searched through Harzing’s Publish or Perish software (www.harzing.com).
The following organisation websites were also searched to identify report about initiatives to improve discharge planning or IC process:
-
British Medical Association
-
Department of Health and Social Care
-
Health Foundation
-
King’s Fund digital archive
-
Nuffield Trust.
Searches on Google were also undertaken for winter pressures and discharge OR integrated care limited to .NHS, .GOV or .org sites.
Second-stage search
The second stage involved searches of Google Scholar for named candidate interventions from the literature and current practice. The searches were on Google Scholar for evidence broader than winter pressures. These searches were intended to retrieve reviews, ideally systematic reviews, and were limited to research published from 2012 to 2022. These searches helped with completing the intervention tables and identifying the evidence gaps.
Screening evidence
Study screening and selection was undertaken in Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA). A team of three reviewers independently screened the titles and abstracts of the 723 references from the searches. Articles meeting the inclusion criteria for titles and abstracts or items with insufficient detail on content relating to discharge planning or IC were reviewed at full text.
Study validity assessment
The primary purpose of the mapping review was to create a profile of the available evidence base and this was then used to identify potential evidence and synthesis gaps. We assessed individual studies at a study design level and not through individual critical appraisal. Initially identified items were categorised as primary research, evidence synthesis or research report. The last of these identified reports from organisations such as the Nuffield Trust, King’s Fund and Health Foundation that combine critical commentary, usually with primary data. Outputs from governmental or professional organisations were processed in a similar way. We identified research gaps from the distribution of primary studies and their research questions, summaries from evidence syntheses and recommendations from research reports. We then evaluated the authority and credibility of the research gaps accordingly.
Coding and database production
Metadata extraction and coding for studies were undertaken using Microsoft Excel. For mapping purposes, references were categorised at title and abstract stage according to study design, characteristics and broad thematic content. A data coding spreadsheet was used to code data for study type, population, intervention (if present), outcomes or findings and conclusion. Following granular coding, we then classified related studies within broader thematic categories that were be used to present study characteristics and to structure an accompanying narrative. Due to the time and resource constraints of the proposed work, missing or unclear information was not solicited from authors.
Describing and visualising the findings
Development of taxonomy
To classify into the broader thematic groups of interventions, we developed a taxonomy (see the Excel spreadsheet) documenting the candidate interventions together with other relevant supporting literature. Our team started from categories developed by the Cochrane Effective Practice and Organisation of Care Group for their systematic reviews of discharge planning cited by Parker et al. 2002. 5 These were further expanded using categories from a rapid review produced by the Centre for Clinical Effectiveness, Monash University. 6
This process resulted in the following broad groupings: structural (S), changing staff behaviour (CSB), changing community provision (CCP), IC, and targeting carers (TC). The draft taxonomy was reviewed for parsimony (to minimise duplication of concepts) and comprehensiveness (to include all named interventions identified to date). However, published commentary has documented the non-exclusivity and lack of precision of existing labels. Following the production of the draft map using the taxonomy, we decided that it would be useful to split the taxonomy headings into the following categories: hospital avoidance, alternate delivery site, facilitated discharge and cross-cutting.
Producing the map
Once the taxonomy was developed, tested and agreed, we mapped candidate interventions to the taxonomy of intervention types to produce the draft map. Following changes to the taxonomy, we updated the draft map to produce the final map.
Stakeholder involvement
During the mapping review, we consulted with stakeholders at the Department of Health and Social Care and the National Institute for Health and Care Research, as well as with a standing advisory group of patients and carers. This ensured that the review of winter pressures was informed by the views and experiences of stakeholders. The aim of this consultation was to:
-
conceptualise the scope of the review
-
illuminate the practical and personal challenges experienced by those planning or using health services during times of exceptional demand
-
inform the second phase of our search strategies by identifying specific strategies, initiatives and interventions that target discharge planning and IC in the context of winter pressures
-
identify gaps in the literature with a view to compiling a future research agenda.
Patient and public involvement
A patient and public involvement (PPI) meeting with members of the Evidence Synthesis Centre standing public advisory group was conducted on 30 November 2022 to discuss the mapping review. The meeting aimed to ascertain the group’s thoughts and experiences around discharge planning and IC interventions to minimise winter pressures. To help bring out their thoughts and opinions, we developed five scenarios around interventions found in the literature and asked what they liked about each approach and what were the drawbacks or what might have been overlooked. The five interventions used in developing the scenarios were D2A, same-day emergency care (SDEC), hospital avoidance response team, Care & Repair and telecare. The scenarios are provided in Appendix 2.
The PPI group met on 30 November online and five members attended. The group’s thoughts and experiences about the different scenarios were helpful and are provided in more detail in Appendix 2. At the end of the meeting, the group voted on which intervention they thought it would be most useful to fund future research into. Three members of the group voted for telecare, believing that the delivery of healthcare is moving in this direction and that it is important to have research to ensure it can be used effectively and to determine what works for different people and in which circumstances. One group member voted for hospital avoidance response team, emphasising their belief in the importance of paramedics in helping to mitigate winter pressures. Within this member’s local area, paramedics have been specially trained and with the long waiting times for an ambulance to arrive or with patients at A&E departments waiting to be seen, the role of paramedics is becoming more important. The final group member chose not to vote.
Chapter 3 Results
The initial ‘winter pressures’ search identified 723 items, of which 117 were judged to be relevant and used for the draft map. Subsequent targeted searches identified a further 62 items related to the different taxonomy headings, together with references to guidance and websites (see tables below). A modified Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram reflecting the searches and selection process in this review is provided in Appendix 3, Figure 2.
Findings: taxonomy
The final taxonomy is presented in Table 1. The taxonomy reflects the focus of the review on supporting early discharge where safe and appropriate, but also includes interventions aimed at avoiding hospital admission through rapid response or delivering care in other settings. The ‘cross-cutting’ category groups interventions that could be delivered at different stages of the patient pathway and/or different applications of a particular technology (e.g. digital and data).
| Hospital avoidance | Alternative delivery site | Facilitated discharge | Cross-cutting |
|---|---|---|---|
| Structural | Structural | Structural | Structural |
| S – same day services | S – specialist units | S – bed management | S – communication and teamwork |
| S – extra service delivery | S – same day services (see ‘hospital avoidance’) | S – discharge co-ordinators | S – digital and data |
| S – discharge to assess | S – extra service delivery (see ‘hospital avoidance’) | ||
| Changing community provision | Changing community provision | S – monitoring and review | S – prioritisation and triage |
| CCP – rapid response/see and treat | CCP – care homes | S – patient flow | S – governance |
| CCP – single point response | CCP – community teams | S – managed care approaches | |
| CCP – step-up facilities | CCP – home care | Changing community provision | S – policies |
| CCP – telecare | CCP – rehabilitation, recovery and reablement | S – seven-day services | |
| CCP – step-down beds | S – staff redeployment | ||
| CCP – other agencies | S – volunteers | ||
| CCP – private sector | |||
| CCP – social care | Changing staff behaviour | ||
| CCP – voluntary services | CSB – clinical audit | ||
| CSB – education of staff | |||
| CSB – protocols/guidelines | |||
| CSB – quality improvement programmes | |||
| CSB – quality management systems |
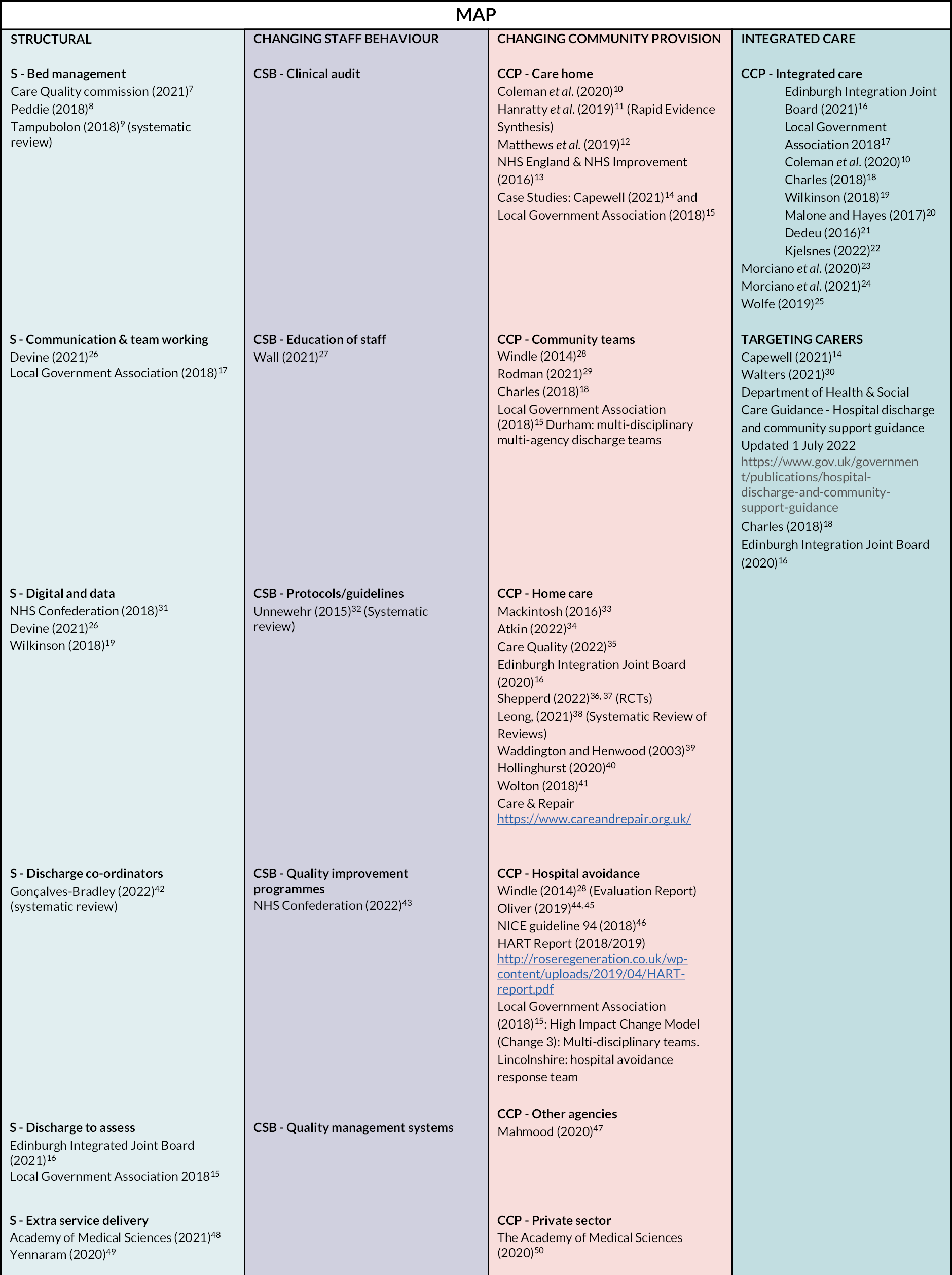
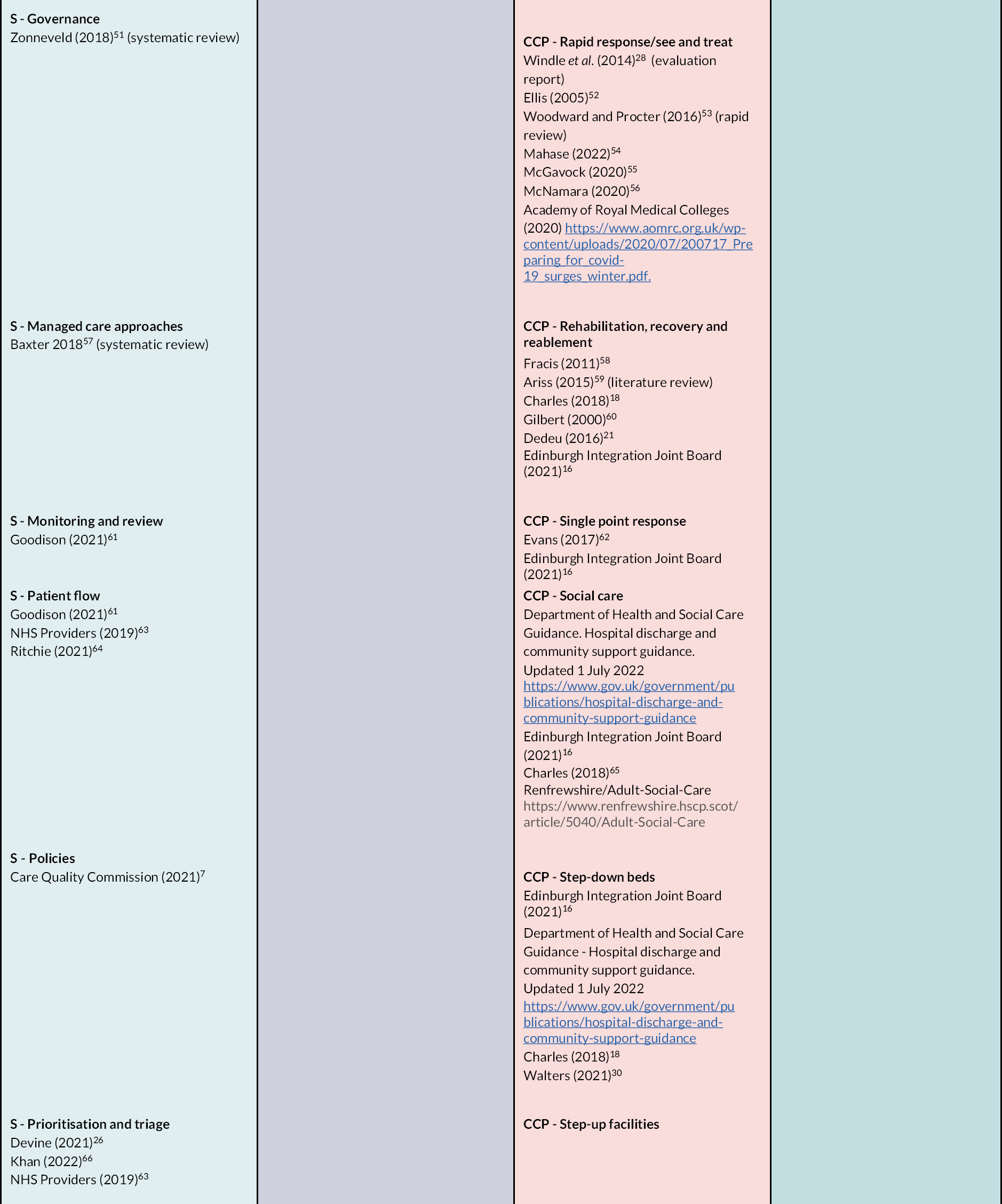
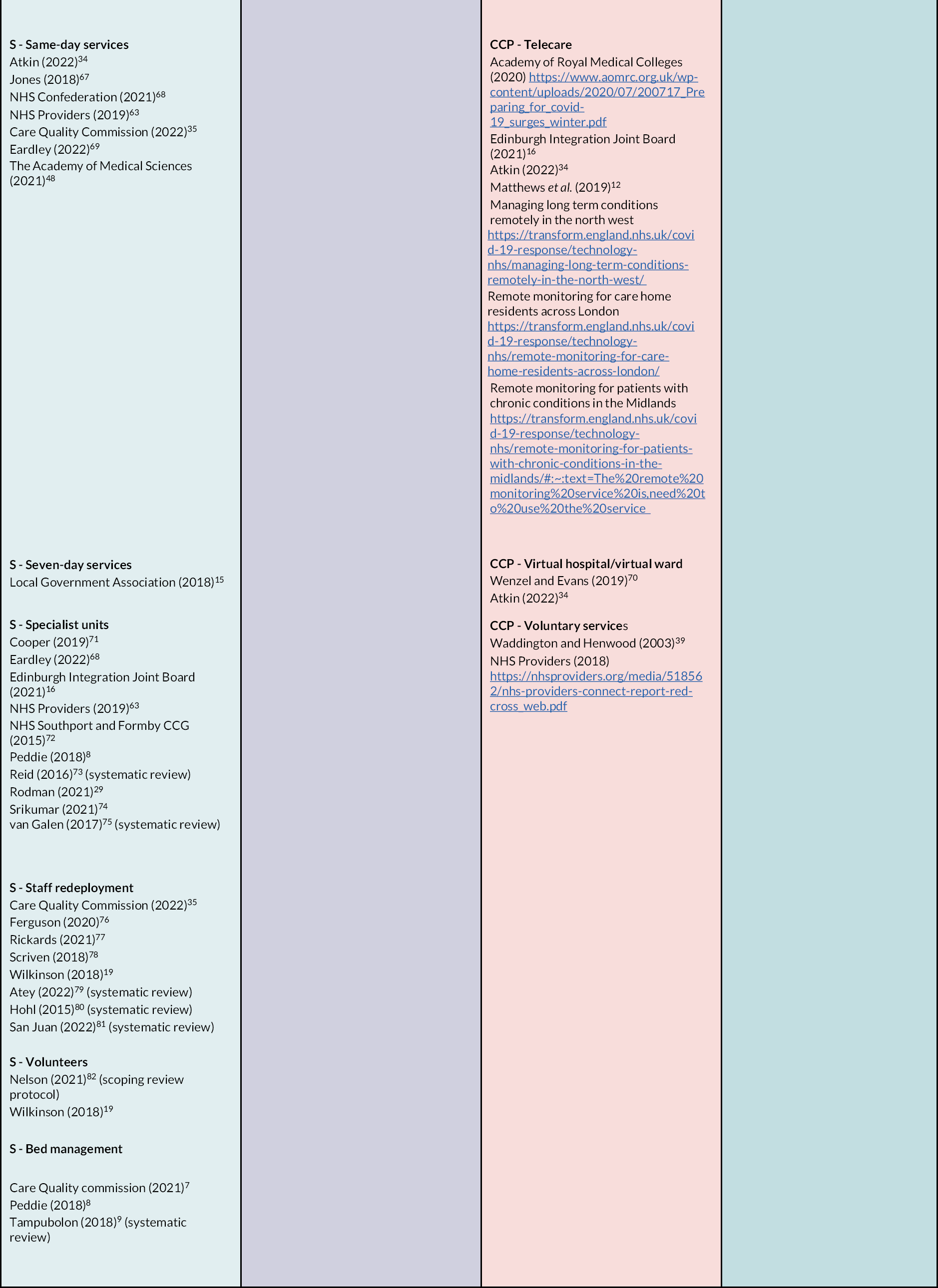
Findings: map
The final map (Figure 1) is provided below and is also available as an accompanying PDF. The map lists key evidence sources for candidate interventions and is colour coded under the headings of the taxonomy S, CSB, CCP, IC, and TC. Modelling and workforce planning were excluded from the scope. Interventions delivered at different stages of the patient pathway are not differentiated in the map but are identified in Table 1.
FIGURE 1.
Map of winter pressures research organised by taxonomy headings. Note: a list of references for the report is available in the supplementary material (see Report Supplementary Material 1).
Findings: taxonomy headings/interventions
Findings are presented in the following tables following the order of the taxonomy presented in Table 1. Definitions and sample interventions are presented first, followed by a separate table of supporting evidence and identified research gaps under each taxonomy heading. For brevity within the report, the tables for the taxonomy headings with limited evidence are provided in the appendices.
Structural interventions
Findings for taxonomy headings classified as structural are summarised in the tables below. The tables are organised by the different stages of the patient pathway and first cover hospital avoidance then alternative delivery sites, followed by facilitated discharge and then Tables 18–34 cover cross-cutting headings. Detailed information can be found in the tables, with brief overviews before and after each group.
Hospital avoidance
The main taxonomy headings for hospital avoidance are same-day services (Tables 2 and 3); extra service delivery (see Appendix 4, Tables 53 and 54); see also 7-day services (see Appendix 4, Tables 61 and 62).
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| S – same-day services | Services provided the on the same day without need for hospital admission | Same-day services could help with winter pressures by reducing admissions |
| Example interventions: same-day emergency care (SDEC)/ambulatory emergency care/ambulatory care unit surgical hubs/elective surgical hubs/high-volume low-complexity surgical hubs | SDEC – provision of same-day emergency care for patients otherwise admitted to hospital. Patients that present with relevant conditions can be rapidly assessed, diagnosed and treated without needing to be admitted to a ward and if a clinician deems clinically safe they can go home the same day | SDEC aims to benefit patients and the healthcare system by reducing waiting times and hospital admissions where appropriate. Winter 2018/19 witnessed an increased use of ambulatory care units |
| Surgical hubs – located at existing hospital sites and provide common procedures performed relatively quickly and effectively in one place, with patients able to return home the same-day | Surgical hubs help to deal with the rise in healthcare provision needed over the winter by enabling surgeons to continue to treat patients for routine operations preventing waiting list backlogs |
| Supporting evidence | Results/findings/recommendations (from abstracts) |
|---|---|
| SDEC | We have identified four published evaluations since 2018 of SDEC. A short research article describes the moving the ambulatory care service to a new purpose-built ambulatory emergency care unit.88 Increased numbers of ambulatory care patients were seen in 2018 compared with same period in 2016/17 and in the number of same day discharges |
| Winter pressure specific | |
| Atkin et al. 202234 | |
| Care Quality Commission 202235 | |
| Jones 201867 | |
| NHS Confederation 202126 | |
| NHS Providers 201963 | New challenges are faced with the moving of the unit but changes have enabled patients to access ambulatory care and be seen in a more appropriate care setting. Another short research article describes a hospital running a 2-week pilot of an ambulatory care unit in December 2017. During the pilot calls attended by ambulatory care unit middle grade ranged from 12 to 20 each day. Phone advice to the referring general practitioner (GP) was required in approximately 25% of these calls, which potentially avoided attendance. Of about four patients seen each day by the unit there was a < 25% conversion rate to admission with most discharged directly or re-attended later that week. Patients admitted to ambulatory care unit were seen within 30 minutes of their arrival and had a management plan within 2–3 hours. Following the promising results of the pilot, a permanent unit was approved89 |
| Guidance | |
| NHS England 202182 | |
| NHS England 202183 | |
| Royal College of Emergency Medicine 201984 | |
| Royal College of Physicians of Edinburgh 201985 | |
| NHS England 201886 | |
| Published evaluations | A poster abstract describes the introduction of an ambulatory care service which helped increase the percentage of 0-day discharges to 15% and an improvement in A&E 4-hour target, exceeded to 5%90 |
| Pincombe et al. 202287 | |
| Ash 201988 | An economic evaluation from Australia of a medical ambulatory care service found that it was cost-effective for GPs and patients referred from wards but the impact for patients referred from the emergency department (ED) was less clear |
| Varrier 201989 | |
| Ali and Karmani 201890 | |
| Case studies | Evidence reveals multiple knowledge gaps in how best to structure SDEC services and identify appropriate patients, to gain maximum benefit for patients and for healthcare services. Additional services could help the delivery of SDEC (e.g. virtual wards) but the effect of running the additional services on current service delivery needs to be considered |
| Ambulatory Emergency Care Network 201991 | |
| Ambulatory Emergency Care. n.d.91 | |
| NHS Improving Quality n.d.65 | |
| Surgical hubs | No published evaluation on surgical hubs, NHS guidance on design and layout of elective hubs |
| Winter pressure specific | |
| Eardley 202268 | |
| Academy of Medical Sciences 202148 | The Royal College of Surgeons report on the case for surgical hubs gives the impact of winter and COVID-19 pressures as important drivers in developing surgical hubs. Three case studies demonstrating promising findings are provided in the case for surgical hubs report |
| Guidance | |
| Getting It Right First Time 202292 | |
| Published evaluations | |
| No published evaluations, NIHR call in February 2022. 22/26 HSDR Evaluating the high volume low complexity surgical hubs model: Commissioning brief. URL: www.nihr.ac.uk/documents/2226-hsdr-evaluating-the-high-volume-low-complexity-hvlc-surgical-hubs-model-commissioning-brief/29940 (accessed 23 November 2022) | |
| Case studies | |
| Royal College of Surgeons of England 202293 (includes case studies) | |
| Research gaps | |
| For SDEC: only small, low methodological quality evaluations and case studies. Guidance available from the NHS and relevant professional bodies. Need to further research the effectiveness of SDEC | |
| For surgical hubs: guidance on planning effective surgical hubs. No published evaluations; NIHR published a call to evaluate the surgical hubs model in February 2022, indicating a need for research in this area, which is in the process of being commissioned. The Royal College of Surgeons report on the case for surgical hubs includes three case studies | |
| Research priority | |
| Few UK initiatives (implementation and research gap) | |
Same-day services
Extra service delivery
The tables for the taxonomy heading extra service delivery are provided in Appendix 4. This heading includes a broad category of interventions, making it difficult to identify general research priorities.
Same-day services fall into two broad categories: SDEC followed by discharge without hospital admission, and routine surgery performed on a day-case basis, with patients returning home on the day of surgery. Both have been widely adopted and are supported by relevant guidance. However, a clear need remains for further research and evaluation (see Table 3).
Extra service delivery takes a variety of forms and some successes have been reported in both emergency and elective care (see Appendix 4, Table 54) but the evidence base remains limited.
Alternate delivery site
The heading ‘alternative delivery site’ covers a variety of specialist units delivering services outside general hospitals or in demarcated areas within them. Examples are acute medical units and short-stay units. More information and the evidence is provided in Tables 4 and 5.
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| S – specialist units | Specialists units are units to deliver a particular service | Specialist units can provide services, separately from hospitals, which reduce admissions, reduce infection by keeping patient groups separate, and enable patients to receive the care they require |
| Surgical hubs/elective surgical hubs/high-volume, low-complexity surgical hubs | Surgical hubs are located at existing hospital sites and provide common procedures that can be performed relatively quickly and effectively in one place or high-volume, low-complexity surgeries. They will bring together staff with the required skills and expertise in one place | Surgical hubs help to deal with the rise in healthcare provision needed over the winter by enabling surgeons to continue to treat patients for routine operations preventing waiting list backlogs. They improve infection control by keeping these patients separate from the ED and other wards in the acute hospital. Reduce number of operation being cancellations at short notice when hospitals are full |
| Acute medicine urgent access clinic/acute medicine clinic | The clinic allows early outpatient review of symptoms and outstanding investigations. This means that clinicians can discharge patients sooner with an appointment to attend the clinic | Help doctors to discharge patients earlier from ED, acute medical units expedite discharge from post-take ward round and help to manage the increased healthcare usage during the winter months |
| Acute medical unit/acute assessment unit/medical assessment unit | Acute medical units provide rapid assessment investigating and treatment for acutely ill medical patients through referral by the ED, their GP or outpatient services. Patient can receive acute medical assessment in one unit staffed by specialist medical and nursing personnel with equipment required for the assessment. Patients can be admitted for a short hospital stay for ongoing assessment or discharged home the same-day | Reduces number of patients going to the ED during this busy time of year, which helps with patient flow throughout the hospital |
| CRT + and long-COVID-19 single point of access | To provide a triage point to allied health professional rehabilitation services for people recovering from COVID-19 | Provide triage for people recovering from COVID-19 without them disrupting flow within health and social care |
| Frail elderly short-stay unit | Short-stay unit that assesses frail older people as soon as they come into hospital to ensure that they get the best possible care and treatment when they are in hospital and are supported (e.g. through comprehensive geriatric assessment) to recover when they leave | Help with flow of frail older people through health and social care services, useful in winter when their healthcare usage could increase |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Acute medicine urgent access clinic | A recent survey of medical doctors at Warrington Hospital on the introduction of new acute medicine urgent access clinic found promising experiences. 93% of doctors believed that the introduction of the clinic allowed them to discharge patients earlier from the acute take, 77% believed that the clinic enabled quicker discharge from the ED, 79% of the doctors believed the clinic had sped up discharge from post-take ward round and 87% that it had sped up discharge from the acute medical unit. Further details of the introduction of the clinic at Warrington and Halton Hospitals NHS Foundation Trust are provided in a case study in the RCP Chief Registrar Scheme 2017/18 year book. |
| Winter pressure specific | |
| Cooper 201970 | |
| Additional evidence | |
| Royal College of Physicians (RCP) 201894 | |
| Acute medical unit | Two reviews published after 2012 were retrieved on acute medical units. A literature review from van Galen et al.75 concluded that current literature demonstrates an overall beneficial effect after implementation. The systematic review by Reid et al.72 concluded that acute medical units were associated with reductions in hospital length of stay and less convincingly mortality when implemented in European and Australasian settings. |
| Winter pressure specific | |
| Peddie and Gordon 20188 | |
| Additional evidence | |
| Systematic reviews: | |
| van Galen et al. 201774 | |
| Reid et al. 201672 | A prospective cohort study8 found results that suggest the median length of stay for the patients moved ‘out of hours’ was significantly less than that of the patients moved ‘within’ hours group. This could be due to the higher number of ‘boarders’ in the ‘out of hours’ group (36/57 patients = 63.2%) when compared to the ‘within hours’ group (32/162 patients = 19.8%). Boarding while unacceptable still exists and it is not only related to winter months. |
| Guidance | |
| NICE 201895 | |
| Community resource team (CRT) + and long-COVID SPOA/post-COVID-19 assessment services | The Edinburgh Integration Joint Board’s evaluation of winter planning 2020/21 provides brief outcomes of funding project which includes the CRT+ and SPOA service. The CRT+ service received 23 referrals, of which 16 (70%) were considered at risk of hospital admission. The service was able to support 100% admission avoidance at 48 hours and 83% at 7 days. The SPOA service acted as a triage point to allied health professional rehabilitation services and 290 referrals were received during the period November 2020 to end of March 2021; 314 onward referrals were made, demonstrating the success of SPOA to rehabilitation services. |
| Winter pressure specific | No further evidence was found on these services. |
| Edinburgh Integration Joint Board 202116 | |
| Additional evidence | |
| None | |
| Frail elderly short-stay unit | Additional ‘winter funding’ from central government in September 2013 enabled the establishment of a frail elderly short-stay unit in November 2013, as part of NHS Southport and Formby CCG service developments to reduce admissions and length of stay for frail older people. |
| Winter pressure specific | |
| NHS Southport and Formby Clinical Commissioning Group (CCG) 201572 | |
| Published evaluations | A conference abstract from 201496 details the outcomes of a 12-week pilot of a frail elderly short-stay unit. The average length of stay in the unit was 4.7 days and total length of stay (including subsequent inpatient care) was 6.5 days, which had a positive impact on the care of the elderly wards. |
| Michael and Ijaola 201496 (conference abstract) | |
| Ring-fenced arthroplasty unit | A conference abstract detailed the assessment of a ring-fenced arthroplasty unit performance during winter pressures and the pandemic (December–March 2018–9 and 2019–20).73 The unit performed 280 total hip and knee replacements in 2019–20 and the patients had a mean length of stay of 43 hours. This showed a reduction when compared with the length of stay in 2018–9 of 69 hours when 288 total hip and knee replacements were performed. Early discharge, defined as within 36 hours of surgery, occurred for 74% of patients in 2019–20 vs. 24% in 2018–9, which add up to 333 inpatient days saved. |
| Winter pressure specific | No further evidence was found on ring-fenced arthroplasty units. |
| Srikumar et al. 202173 (conference abstract) | |
| Additional evidence | |
| None | |
| Speciality review at rapid access clinics | The Edinburgh Integration Joint Board’s evaluation of winter planning 2020/21 details how NHS Lothian intended to use the additional funding for winter 2020/21, which including avoiding admission with services developed to provide certain initiatives including speciality review at rapid access clinics. |
| Winter pressure specific | No further evidence was found on speciality review at rapid access clinics. |
| Edinburgh Integration Joint Board 202116 | |
| Additional evidence | |
| None | |
| Research gaps | |
| Research in specialist units other than acute medical units could be helpful. | |
| Research priority | |
| Acute medical units, low – good-quality systematic review(s) and plentiful UK research studies (no gap). | |
| Other: high – few UK initiatives (implementation and research gap). | |
Specialist units
In summary, acute medical units have a good evidence base overall, with some research specific to winter pressure conditions. Frail elderly short-stay units have been supported by winter pressure funding but we found limited research on these and other types of specialist unit.
Facilitated discharge
Facilitated discharge is a key area for health and care services dealing with winter pressures. It includes interventions to optimise use of resources and minimise length of stay for patients in hospital, planning for discharge and discharge with support in place prior to a full assessment of health and care needs (D2A).
Bed management
There was limited evidence for bed management to reduce winter pressures (see Appendix 4, Tables 50 and 51). By ensuring optimum use of inpatient bed capacity, it could potentially reduce the number of patients occupying an inpatient bed that could be discharged safely. The lack of UK initiatives make bed management a high research priority.
Discharge co-ordinators
Discharge co-ordinators have responsibility for discharge planning and can contribute to facilitated/supported discharge and reduce delayed transfers of care freeing up beds for new patients. More information about discharge co-ordinators and the evidence base is provided in Tables 6 and 7.
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| S – discharge co-ordinators | Individual with designated responsibility for discharge planning. Early discharge requires robust systems to be in place to develop plans for management and discharge, and to allow an expected date of discharge to be set within 48 hours (LGA 2018)17 | Contributes to various forms of facilitated/supported discharge. Could be a temporary role or given extra support to cover winter pressures |
| Example interventions: often part of complex multidisciplinary team (MDT) interventions (e.g. hospital at home; cited in Williams 202297), Oxfordshire Integrated Liaison Hub (LGA 2018)17 | Integrated liaison hub staffed by MDT including qualified nurses and therapists with expertise in discharge planning, discharge planners, administrators and staff from adult social care (in-reaching) | Reduces delayed transfers of care and hence frees up hospital beds for new patients |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific | |
| Initiative: | |
| Oxfordshire Integrated Liaison Hub (LGA 2018)17 | The liaison hub has delivered a fully integrated service, which has resulted in a reduction in delays and the release of acute beds. Service users are cared for in a more appropriate environment and for some patients rehabilitation occurs earlier in their pathway |
| Systematic reviews (in reverse chronological order) | A structured discharge plan that is tailored to the individual probably brings about a small reduction in hospital length of stay and unscheduled readmission for older people with a medical condition. Discharge planning at an appropriate time in a hospital admission can facilitate the organisation and timely discharge of a patient from hospital and the organisation of post‐discharge services. Even a small reduction in length of stay can be important in freeing up capacity for subsequent admissions in a system during a shortage of acute hospital beds |
| Gonçalves-Bradley et al. 202242 | |
| Dimla et al. 202298 | Reviews role of social workers in discharge planning for older people. The most common support measures were assessment, education, care co-ordination, liaison and engagement with families and providers, conflict resolution, counselling and post-discharge follow-up. Barriers included medical complexity, lack of communication, time constraints, limited family support, availability of resources and patient safety |
| Doshmangir et al. 202299 | General review of interventions to manage use of hospital services. Discharge planning was found effective in reducing hospital length of stay |
| Williams et al. 202297 | Review found that providing early supported discharge (ESD) intervention for older adults admitted to hospital for acute medical reasons can significantly reduce the length of their acute hospital stay, without adversely affecting their mortality, function, health-related quality of life, hospital readmissions, long-term care admissions and cognition |
| Guidance | |
| National Institute for Health and Care Excellence (NICE): transition between inpatient hospital settings and community or care home settings for adults with social care needs. 2016100 Age UK recommends appointment of a discharge co-ordinator when discharge is likely to be complex101 |
Recommends a designated discharge co-ordinator for all patients with care needs |
| Research gaps | |
| Focusing on discharging older adults from the acute hospital setting to home, Harris (2005)102 noted that further research was required to assess the cost-effectiveness of community-based interventions. Similarly, NICE recommended extending research to assess the effectiveness of home interventions post discharge.97,100 Impact of ESD interventions on stakeholders including patients, family carers and professionals97 | |
| Research priority | |
| Moderate – few UK research studies but plentiful UK initiatives and recent systematic reviews (research gap) | |
Discharge to assess
Discharge to assess aims to minimise unnecessary delays in hospital discharge. More information and the evidence base are provided in Tables 8 and 9.
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| S – D2A | People who do not require an acute hospital bed but may still require care services are provided with short-term funded support to be discharged to their own home or another community setting, with subsequent assessment for longer-term care and support needs. No set model for D2A; it may work alongside time for recuperation and recovery, ongoing rehabilitation or reablement (Department of Health, Directors of Adult Social Services, NHS England. Quick Guide: Discharge to assess. London: NHS England; 2016. www.england.nhs.uk/blog/martin-vernon-3) | Minimises unnecessary delays in hospital discharge. Not specific to winter but frequently mentioned in winter planning documents |
| Example interventions: D2A, home first; safely home; step-down | D2A and home first (see above). Step-down beds provide short-term accommodation to bridge the gap between hospital and home (LGA 2018)17 | See above |
| Supporting evidence | Results/findings/recommendations (from abstracts) |
|---|---|
| Winter pressure specific | |
| Edinburgh Integrated Joint Board 2021 (Assistant Practitioners; Occupational therapy; Home First therapists)16 | Increased referrals in 2020/21 compared with previous winter. Assistant practitioners and Home First therapists contributed to skill mix |
| Local Government Association 201817 (D2A) | Five successful local initiatives described |
| Published evaluations | |
| Does a D2Aprogramme introduced in England meet the quadruple aim of service improvement? Jeffery et al. 2022103 | Aims appeared to be me |
| Gadsby et al. 2022104 | Service was difficult to implement and desired outcomes elusive |
| Offord et al. 2017105 | Reduction in length of stay from 5.5 to 1.2 days |
| Initiatives/case studies | |
| Pilarska J. Discharge to assess: an East Lothian experience. Physiotherapy 105(Suppl 1):E64–E64. https://doi.org/10.1016/j.physio.2018.11.025 (accessed 23 November 2022) | Full text not available |
| NHS England. Discharge to assess: South Gloucestershire and Bristol. URL: https://bnssghealthiertogether.org.uk/staff-and-partners/discharge-to-assess/#:~:text=Discharge%20to%20Assess%20is%20our,can%20be%20supported%20to%20recover (accessed 23 November 2022) | Early pilot reported reduction in bed days and financial savings but also ongoing operational issues |
| Discharge to Assess with HomeLink Healthcare. Retaining the Positive Improvements from the Pandemic. URL: https://www.ihpn.org.uk/wp-content/uploads/2021/06/Discharge-to-Assess-Case-Study-HomeLink-Healthcare.pdf (accessed 23 November 2022) | No outcome data |
| NICE Shared learning database: Supporting best patient outcomes through a joint Discharge to Assess, Home First service. URL: https://www.nice.org.uk/sharedlearning/supporting-best-patient-outcomes-through-a-joint-discharge-to-access-home-first-service (accessed 23 November 2022) | Bristol/Gloucester/Somerset. No outcome data but detailed description of implementation |
| Edwards and Anwer 2019106 | Reports significant benefits on a Discharge to Assess process on improving patient flow and improving hospital performance in managing unscheduled care |
| Lawlor et al. 2019107 | Reports that rapid discharges can be facilitated which reduced length of stay and increased patient and family’s satisfaction with the discharge process |
| Bath: Home First/D2A. URL: https://www.local.gov.uk/case-studies/bath-home-firstd2a (accessed 23 November 2022) | Step-down apartments for people discharged but unable to return home. A previous review of the service found that the six units saved £561,762 for the NHS by enabling discharge of patients, and the Social Return on Investment was £6.21 for every £1 invested (where no reablement care package is required) |
| Orkney Health and Care. 2021. Integration Joint Board: Progress of Home First Service Pilot. URL: www.orkney.gov.uk/Files/Committees-and-Agendas/IJB/IJB2021/IJB30-06-2021/I17_Home_First_Service_Pilot-original.pdf (accessed 23 November 2022) | Evaluation of pilot recommended that winter planning funding be used to sustain the service |
| Other evidence | |
| Healthcare Improvement Scotland. 2021. Discharge to Assess. URL: https://www.healthcareimprovementscotland.org/evidence/rapid_response/rapid_response_02-21.aspx (accessed 23 November 2022) | Rapid review finds very limited evidence for D2A |
| Healthwatch Staffordshire. 2019. Report on Discharge to Assess (D2A) at Staffordshire Hospitals. URL: https://healthwatchstaffordshire.co.uk/wp-content/uploads/2020/01/Discharge-to-Assess-D2A-Healthwatch-Staffordshire-report-October-2019.pdf (accessed 23 November 2022) | Healthwatch reports provide ‘real-world’ data on patient experience |
| Health and Social Care Moray. Discharge to Assess. URL: https://hscmoray.co.uk/discharge-to-assess.html (accessed 23 November 2022) | |
| Healthwatch Coventry. 2019. Experiences of D2A pathways in Coventry summary report. URL: www.healthwatchcoventry.co.uk/sites/healthwatchcoventry.co.uk/files/HW_Coventry_Summary_Report_Discharge_to_assess_JUNE2019.pdf (accessed 23 November 2022) | |
| Healthwatch Suffolk. 2019. Discharge to Assess (D2A): a qualitative evaluation of patient experience (Ipswich Hospital) – Executive summary. URL: https://healthwatchsuffolk.co.uk/wp-content/uploads/2021/11/D2A-2019-Executive-Summary.pdf (accessed 23 November 2022) | |
| Systematic reviews (in reverse chronological order) | |
| Conneely et al. 2022108 | Umbrella review of ED-based discharge interventions. Review found that the evidence base for the effectiveness of ED interventions in reducing adverse outcomes is limited, due to the poor quality of the randomised controlled trials (RCTs). Higher quality intervention RCTs as well as a focus on intervention development with the engagement of stakeholders are required |
| Platzer et al. 2020109 | Based on nine studies, this review found that inter-professional or multi-professional interventions had no impact on mortality rate but either positive or neutral effects on physical health, psychosocial wellbeing and utilisation of healthcare services |
| Guidance | |
| Department of Health, Directors of Adult Social Services and NHS England. Quick Guide: Discharge to Assess. Transforming urgent and emergency care services in England. n.d. URL: www.nhs.uk/NHSEngland/keogh-review/Documents/quick-guides/Quick-Guide-discharge-to-access.pdf (accessed 23 November 2022) | |
| Welsh Government. 2021. Home First: The Discharge to Recover then Assess model (Wales) | |
| Department of Health and Social Care. 2022. Hospital discharge and community support guidance. URL: www.gov.uk/government/publications/hospital-discharge-and-community-support-guidance/hospital-discharge-and-community-support-guidance#how-nhs-and-local-authorities-can-work-together-to-plan-and-implement-hospital-discharge-recovery-and-reablement-in-the-community (accessed 23 November 2022) | |
| NHS England. Act Now – Getting People ‘Home First’. n.d. URL: www.england.nhs.uk/wp-content/uploads/2018/12/3-grab-guide-getting-people-home-first-v2.pdf (accessed 23 November 2022) | |
| NHS England. Principle 5: Encourage a supported ‘home first’ approach. n.d. URL: www.england.nhs.uk/urgent-emergency-care/reducing-length-of-stay/reducing-long-term-stays/home-first (accessed 23 November 2022) | |
| Research gaps | |
| The evidence base comprises plentiful UK initiatives and case studies but few peer-reviewed research studies. The case studies vary in depth of reporting and the interventions described as D2A or Home First are highly diverse. Evaluations almost use a before/after approach to assess effectiveness, with no control group. However, given that D2A and Home First are already in wide use, it would seem appropriate for research to focus on how best to implement interventions and obtain optimum value for money. We identified no systematic reviews of D2A, although some broad reviews focus on related areas (see above). We identified a synthesis gap with available evidence suggesting that a review based on realist principles may be appropriate to support ongoing implementation of D2A/Home First | |
| Research priority | |
| Moderate – few UK research studies but many UK initiatives (research gap) | |
Monitoring and review
Monitoring and review are interventions to quickly identify patients suitable for discharge or transfer. There was limited evidence for monitoring and review; the tables can be found in Appendix 4, Tables 55 and 56.
Patient flow
Patient flow is a broad heading that covers a range of interventions to ensure that patients move through the health and care system as quickly and efficiently as possible while maintaining safety and patient focus. More information is provided in Tables 10 and 11.
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| S – patient flow | Covers a range of interventions to ensure patients move through the health and care system as quickly and efficiently as possible while maintaining safety and patient focus | At periods of high demand, it is particularly important to minimise unnecessary contacts and use telephone or video appointments if appropriate to avoid patients choosing to attend the ED. Closely related to ‘monitoring and review’ and ‘prioritisation and triage’ |
| Example interventions: patient flow bundle; flow navigation centres | Flow navigation centres (hubs) receive referrals directly from NHS24 (Scotland). They offer rapid access to a senior clinical decision maker within the multidisciplinary team, via a telephone or video consultation where possible64 | Optimising patient flow at the point of entry into the system (prehospital) |
| The SAFER patient flow bundle is applicable to inpatient wards (excluding maternity). In highly specialist settings, daily review can identify patients who would benefit from transfer to a lower-intensity community setting63 | Optimising patient flow within hospitals |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific | |
| NHS Providers 2019 (SAFER patient flow bundle)63 | Rolled out by NHS during winter 2018/19 |
| Ritchie 2021. Flow navigation centres64 | The additional step of seeking immediate help for urgent problems via NHS24 (111 service) diverted to local flow navigation centres may add to the complexity and length of the care journey for some patients |
| Case studies/evaluations | |
| Yeovil District Hospital (Sethi 2020)110 | Interventions to improve inpatient flow also improved ED clinical quality indicators |
| Kent acute hospitals optimisation programme (LGA 2018)17 | 59% reduction in long-term residential placements and a 54% reduction in short-term beds |
| Kent Single Health Resilience Early Warning Database (SHREWD) (LGA 2018)17 | SHREWD indicators vital to identifying areas of pressure as they arise |
| Systematic review | |
| Åhlin et al. 2022111 | Review of barriers to patient flow in hospitals. Long lead times, inefficient capacity co-ordination and inefficient patient process transfer were identified as the main barriers. Barriers were caused by inadequate staffing, lack of standards and routines, insufficient operational planning and a lack in information technology functions. Review includes a framework for policy makers |
| Guidance | |
| NHS Improvement. Rapid improvement guide: the safer patient flow bundle. 2022 | |
| NHS Improvement. Good practice guide: focus on improving patient flow. 2017 | |
| URL: https://improvement.nhs.uk/uploads/documents/Patient_Flow_Guidance_Case_studies_13_July.pdf (accessed 23 November 2022) | |
| Research gaps | |
| We identified one UK research paper and a small number of initiatives related to patient flow as well as a recent systematic review. This relatively small body of evidence may overstate the size of the research gap as patient flow is difficult to disentangle from related areas such as bed management, discharge planning, monitoring and review, and prioritisation and triage | |
| Research priority | |
| Moderate – few UK initiatives (implementation and research gap) but one UK research study and a recent systematic review | |
We found that some aspects of facilitated discharge are relatively well researched, particularly D2A and similar interventions (e.g. Home First). Interventions with little UK evidence were sometimes supported by systematic reviews, although the quality of these reviews varied. Some taxonomy headings (e.g. ‘bed management’ and ‘discharge co-ordinators’) were often evaluated as part of a broader process of ‘discharge planning’.
Cross-cutting
The cross-cutting section of the taxonomy covers a diverse group of structural changes with broad applicability, including multidisciplinary and multiagency teams, use of digital technology and data, monitoring and accountability in the healthcare system, national and local policies, staff redeployment and the role of volunteers.
Communication and teamwork
Detailed information on communication and teamwork interventions is provided in Tables 12 and 13.
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| S – communication and teamwork | Tackles barriers at the interface between disciplines and or agencies (e.g. NHS and local government, hospitals and care homes) | Such barriers may become more pronounced as a defensive reaction to periods of exceptional demand/pressure on staff |
| Example interventions: use of advice and guidance; MDTs/multiagency discharge teams | Generalists and specialists working together to avoid admission. Co-ordinated discharge planning based on joint assessment processes and protocols and on shared and agreed responsibilities | Unnecessary hospital admissions are avoided. More efficient discharge process |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific | |
| Devine 2021 (better use of advice and guidance)26 | Identified as a key initiative but no further details provided |
| Local Government Association 2018 (MDTs/multiagency discharge teams)17 | Three local initiatives (Lincolnshire, Durham and Kent) described. Lincolnshire hospital avoidance response team supported 1553 people between December 2015 and August 2017; 303 admissions were avoided and indicative savings of between £1,094,000 and £1,362,000 were achieved |
| Systematic review | |
| Coffey et al. 2019112 | The most effective interventions to avoid inappropriate readmission to hospital and promote early discharge included integrated systems between hospital and community care, multidisciplinary service provision, individualisation of services, discharge planning initiated in hospital and specialist follow-up |
| Guidance | |
| NHS England. MDT Development: Working toward an effective multidisciplinary/multiagency team 2014. URL: https://diabetes-resources-production.s3-eu-west-1.amazonaws.com/diabetes-storage/migration/pdf/NHS%2520England%2520-%2520MDT%2520development%2520%28January%25202014%29.pdf (accessed 23 November 2022) | |
| Research gaps | |
| From the systematic review (high-quality but broad in scope): key elements for which evidence was identified and which merit further study include integrated systems spanning acute and home-based services; multidisciplinary care provision; person-centred services; and discharge initiated in acute care predischarge initiated with specialist follow-up | |
| Research priority | |
| Unclear – UK initiatives and good-quality broad systematic review but UK research studies unclear | |
Digital and data
Detailed information on digital and data interventions for discharge planning is provided in Tables 14 and 15.
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| S – digital and data | Optimal use of digital technology and sharing of patient data to support decision-making | Data sharing potentially facilitates quicker and safer discharge (e.g. supplying all required prescriptions). Digital technology can enable monitoring of a patient’s condition at home or in a community setting after discharge |
| Example interventions: digital health centre; data sharing; prescription tracking | Digital health centre (Tameside and Glossop Integrated Care NHS Foundation Trust): community and care home teams provided with observation equipment. Hospital-based team of nurses provide clinical advice and, where appropriate, patient can be treated remotely.31 Effective management of treatment lists by sharing patient data (no further details supplied).26 Pharmacy prescription tracker (Luton and Dunstable University Hospital), including electronic prescribing during ward rounds19 | Aims to reduce ED attendances and associated admissions. Improves treatment pathway and saves time in treatment and discharge. Service can be quickly stepped up in response to demand, including extra prescribing pharmacists and a 7-day 12-hour service |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific | |
| Digital health centre31 | Between March 2017 and May 2018, 46/47 local care homes signed up. Outcomes included 1263 ED attendances prevented; 400 GP interactions avoided; and 725 prescriptions issued without need for a face to face appointment |
| Management of treatment lists by data sharing19 | No data provided |
| Prescription tracking19 | No data provided |
| Systematic reviews | |
| Kattel et al. 2020113 | Delayed or insufficient transfer of discharge information between hospital-based providers and primary care remains common. Creation of electronic discharge summaries seems to improve timeliness and availability but does not consistently improve quality |
| Mehta et al. 2018114 | This review found a paucity of information on evidence of real-world use of big data analytics in health care |
| Guidance | |
| NHS England and NHS Improvement. Pharmacy and Medicines Optimisation: A Toolkit for Winter 2018 URL: www.sps.nhs.uk/articles/pharmacy-and-medicines-optimisation-a-toolkit-for-winter-2018-19 (accessed 23 November 2022) | |
| Research gaps | |
| Systematic review identifies few examples of real-world impact using big data analytics Many initiatives in this and related sections but few comparative research studies |
|
| Research priority | |
| Moderate – few UK research studies but plentiful UK initiatives (research gap) | |
Governance
No UK research studies or initiatives were identified related to governance. The tables for this taxonomy heading are provided in Appendix 4, Tables 57 and 58.
Managed care approaches
Managed care is primarily a feature of insurance-funded health systems (particularly the United States) and evidence of its use to address winter pressures is unlikely to be relevant to the UK setting. Further details about this taxonomy heading can be found in Appendix 4, Table 52.
Policies
The tables for the policies taxonomy heading are provided in Appendix 4, Tables 59 and 60. No evidence was identified for this heading specifically. Most policies would cover one or more headings from elsewhere in the taxonomy.
Structural: seven-day services
The tables for the seven-day services taxonomy heading are provided in Appendix 4, Tables 61 and 62. Limited evidence was identified for this heading indicating a need to further research the effectiveness of seven-day services.
Prioritisation and triage
Information about prioritisation and triage interventions to avoid admissions is provided in Tables 16 and 17.
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| S – prioritisation and triage | Prioritisation and triage (assigning patients to care based on the urgency of their needs) can take place at different levels of the healthcare system. In addition to triage in urgent and emergency care settings, times and/or sites can be allocated to more or less urgent procedures | Can help to avoid hospital admission when safe and appropriate. Reducing variation where possible for routine procedures may represent a more efficient use of resources at times of high demand. Closely related to ‘Patient flow’ (e.g. green/red day system linked to SAFER patient flow bundle) |
| Example interventions: green/red days; ‘hot’ (trauma) and ‘cold’ (elective) sites for orthopaedics; rapid assessment areas | Examples of separation by time (red days indicate when a patient is awaiting an intervention); degree of urgency; and prioritisation in the ED | See above |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific | |
| Green/red days (NHS Providers 2019)63 | Widely recommended and implemented |
| Hot (trauma) and cold (elective) sites for orthopaedics (Khan 2022)66 | See case study case studies below |
| Nurse triage models in rapid assessment areas (Devine 2021)26 | No data presented |
| Case studies/evaluations | |
| Analysis of data from National Joint Registry for hospitals with different service structures (Khan et al. 2022)66 | Supports need to separate hot and cold sites |
| NHS England. United Lincolnshire Hospitals sees hot and cold orthopaedic success. 2019. URL: https://gettingitrightfirsttime.co.uk/united-lincolnshire-hospitals-see-hot-and-cold-orthopaedic-success (accessed 23 November 2022) | Since launching the pilot in August 2018, United Lincolnshire Hospitals NHS Trust has seen on-the-day cancellation rates drop by more than one-third. Length of stay has also improved, with the average for orthopaedic procedures falling from 2.9 to 2.4 days |
| The Royal Berkshire NHS Foundation Trust outpatient services transformation programme115 | Referrals to outpatient services are now triaged and streamed. The number of patients reviewed virtually on patient-initiated follow-up and seen closer to home has increased |
| Research gaps | |
| Prioritisation and triage is a broad area covering a wide range of possible interventions. Designation of green and red days for in-patients assists patient flow, which is relatively well researched (see above). Separation of different types of orthopaedic surgery on different sites (hot and cold) has some supportive evidence and is recommended as part of the Getting it Right First Time programme. Triage (primarily in emergency and urgent care settings) has an extensive evidence base but the intervention mentioned by Devine (2021)26 was not identified in a search of Google Scholar, suggesting a paucity of research in this area | |
| Research priority | |
| Moderate – few UK research studies but plentiful UK initiatives (research gap) | |
Staff redeployment
Staff redeployment can help improve patient flow by deployment of specialist staff to support other settings, which gives patients easy access to specialist staff. Systematic reviews exist for certain staff redeployment initiatives, the use of pharmacists in the ED and redeployment of staff to the intensive care unit. However, research gaps remain in other areas where the only evidence is unevaluated UK initiatives. Further information is provided in Appendix 4, Tables 63 and 64.
Volunteers
Volunteers can be used to support paid staff in times of high demand, which can help to increase access to advice or services. The detailed information is provided in Tables 18 and 19.
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| S – volunteers | Use of volunteers to improve patient flow through the health and social care system | Help with patient flow through health and social care services; useful in winter when healthcare usage increases |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific | |
| Wilkinson 201819 | Protocol for scoping review demonstrates the need for review of the evidence for volunteers supporting hospital to home transfers.81 The feature by Wilkinson on how pharmacists are helping to relieve winter pressures includes an initiative in the Wye valley, called Pharmacy Volunteers.19 Volunteers help the pharmacy team to deliver urgent medicines to ward and department in the County Hospital and volunteers have supported the pharmacy team to deliver 18,000 urgent medicines over 18 months and the scheme has won an award. Service analysis demonstrates that the average delivery time for urgent medicine is 5.4 minutes, meaning that per week, an estimated 35 hours has been saved. Volunteers deliver urgent medicines to mainly (40%), day-case surgery (10%) and the discharge lounge (8%) |
| Additional evidence | |
| Nelson et al. 202181 | A broad evidence review commissioned by the HelpForce fund in 2017 identified three areas of volunteering with roles to play and that can be effective: commissioned services, organisation (provider)-based services and social action.117 If well supported and enabled, volunteers can be effective in all these roles |
| Guidance | |
| NHS England. Recruiting and Managing Volunteers in NHS Providers 2017116 | |
| Published evaluations | |
| Boyle et al. 2017117 | |
| Ross et al. 2018118 | |
| Research gaps | |
| Evaluations of specific volunteer roles | |
| Research priority | |
| Few UK initiatives (implementation and research gap) | |
In summary, evidence support for initiatives in this group varied widely. The winter pressure search identified UK initiatives to support improved teamwork, together with associated guidance (see Table 19). Various initiatives have applied data sharing and digital technology, but we found a relative lack of research studies. Actions at the organisational level, (e.g. involving changes in governance or formulation and implementation of policy) play an important part in responding to winter pressures, but we found that this was not reflected in research. Further research studies are needed in the area of seven-day services, although promising case studies do exist. Staff redeployment has achieved successes within the pharmacy profession. Further research into staff redeployment would be useful. Volunteers have been used within the NHS in many different areas but there needs to be further evaluation of these initiatives in relation to winter pressures.
Changing staff behaviour
Findings for taxonomy headings classified as CSB are summarised in Appendix 5, Tables 65–74. The taxonomy headings were clinical audit, education of staff, protocols/guidelines, quality improvement programmes and quality management systems. Within this taxonomy section, we identified limited initiatives or research studies. CSB can take time and initiatives to minimise winter pressures are generally implemented rapidly without the time for thorough evaluation or to measure all potential outcomes. Initiatives to minimise winter pressures could potentially be too short to make changes to staff behaviour and they might not measure staff behaviour as an outcome. Further research studies could plan evaluations that consider a variety of outcomes including changes in staff behaviour, although it can be difficult to measure.
Changing community provision
In the first version of the taxonomy, as employed during the initial winter pressures mapping process, all CCP entries were subsumed under a single overarching heading. Subsequently, as we sought evidence on the specific intervention types, the review team decided to differentiate community provision within three subcategories. We believe that this is the first and most important step towards starting to think how different types of intervention attempt to respond to winter pressures in advance of a realistic focus on mechanisms. The three subcategories are therefore labelled as CCP – hospital avoidance, CCP – alternate delivery site, and CCP – facilitated discharge. Each is considered, together with specific interventions under each subcategory in the tables below.
Hospital avoidance
Findings for taxonomy headings classified as CCP are summarised in Tables 20–23 and Appendix 6, Tables 75–78. The taxonomy headings were rapid response/see and treat, single point response and step-up facilities.
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| CCP – hospital avoidance | Provides active treatment by healthcare professionals outside hospital for a condition that otherwise would require admission | Offers treatment outside hospital as alternative to acute hospital inpatient admission |
| Example interventions: ‘Community Connect’ (Somerset) | Works alongside Home First discharge model using mix of voluntary, community and social enterprise and microprovider provision to provide rapid response away from hospital setting. Drew upon robust community infrastructure including village agents (people who link their local communities to services/information they need and at times deliver it themselves) countywide | Harnesses community resilience to allow people to receive care closer to their home, support admission avoidance and link to D2A model (home with therapy support and reablement beds) |
| Hospital avoidance response team | Provided to either prevent an avoidable A&E attendance or admission, or to speed up discharge from secondary care. Facilitates supported discharge and provides up to 72 hours of care and support to resettle a person at home offering ‘bridging the gap service’ for 72-hour period offering telecare unit, enabling access to responders 24/7 – assurance of support through the night if required and wellbeing service assessment with onward referral as appropriate | 72-hour period gives other domiciliary or reablement services opportunity to commence later in the pathway supporting the clinical assessment service to avoid hospital admission and/or attendance at A&E |
| Example interventions: Lincolnshire Independent Living Partnership: hospital avoidance response team. URL: www.local.gov.uk/case-studies/lincolnshire-independent-living-partnership-hospital-avoidance-response-team (accessed 23 November 2022) | Service delivered by Lincolnshire Independent Living Partnership, which takes referrals from secondary care discharge hubs, A&E in-reach teams, the ambulance service, primary care and community health providers | Provides appropriate support and referral bypassing formal presentation to hospital services |
| Example interventions: Talking Cafes (Somerset) | Village agents run talking cafes (face to face or online) to offer a point of contact and reassurance. Village agent service works with local authority and GPs to support the vulnerable, setting up food and equipment networks, and harnessing support from within communities | Increase community resilience by offering local events where people can get information, advice, support or even company |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific | |
| Windle et al. 201428 [evaluation] | No demonstrable changes in monthly emergency admissions. Emergency bed days fell from (mean) 6.55 to 6.28 days. Significant increase in zero bed-nights. Short-term evaluation did not enable full cost-effectiveness evaluation; each intervention seemed to demonstrate value for money against cost of an acute admission |
| Systematic reviews | |
| Huntley et al. 2017119 | Concludes many available options are safe and appear to reduce resource use. However, cost analyses and patient preference data lacking |
| Gravelholt et al. 2014120 | Several interventions reduced hospital admissions and may represent important aspects of nursing home care to reduce hospital admissions. Quality of evidence low |
| Commentary on systematic reviews | |
| Oliver 2019a44 Oliver 2019b45 | Systematic reviews, &‘found no consistent evidence for interventions to reduce hospital attendance or admissions. Systematic review focusing on people over 65 with predicted high risk of admission also found no compelling evidence’. Cochrane reviews on Ha H, even for selected patient groups, showed mixed results |
| Published evaluations | |
| Rose Regeneration. Hospital Avoidance Response Team: Evaluation report 2019. URL: http://roseregeneration.co.uk/category/reports/page/3 (accessed 23 November 2022) | Service filled ‘distinctive gap in service provision and has made materially important contribution to the quality of life of its beneficiaries.’ Individuals supported by service almost universally positive. Supported around 120 hospital discharges and 25 admission avoidances per month. Review suggests that hospital avoidance response team contributed to supporting almost 25% of all individuals (2018/19). Over 6 months, 967 individuals accepted by service. £565,100 of savings (£245,100 net) delivered to NHS. In social value has delivered £8.43 per £1 invested |
| Local Government Association. High Impact Change Model (Change 3): Multidisciplinary teams. Lincolnshire: hospital avoidance response team 201815 | |
| Additional evidence | |
| NICE Guideline NG94 201846 | Covers organising/delivering emergency/acute medical care for people aged over 16 in community and in hospital. Aims to reduce need for hospital admissions by giving advanced training to paramedics and providing community alternatives to hospital care. Also promotes good-quality care in hospital and joint working between health and social services |
| Oliver 2019a44 Oliver 2019b45 | NHS plan ‘aims to reduce acute hospital bed use through roll-out of NHS 111 advice line/web service, GP-led urgent treatment centres, community multidisciplinary rapid response teams, and enhanced support for care home residents’. Problems: ‘exit block’ in patients who could technically leave, potential risks from admission, and patients whose problems might have been dealt with upstream/closer to home. Case mix of acute hospitals has grown older, more medically complex, and more acute despite success in sending more patients home within 24 hours or to ambulatory care. Patients often choose to attend hospital – often for reassurance |
| Research gaps | |
| Plentiful systematic reviews on hospital avoidance/hospital at home (see separate entry). However, included studies generally poor quality and overall results inconclusive | |
| Research priority | |
| Low – good-quality systematic review(s) and plentiful UK research studies (no gap) | |
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| CCP – rapid response/see and treat | Aim to support user by providing urgent response in their own home or other location either to prevent admission or to facilitate discharge from the acute hospital sector. Usually led by nurse/allied health professional; cover diverse interventions including administration of intravenous therapies, peg tube and catheter replacement, crisis psychiatric care and provide enhanced care to palliative care patients (NICE Guideline NG94) | Aims to treat potential hospital admissions in situ thereby reducing admission and potential utilisation of hospital services and beds |
| Example interventions | ||
| Falls specialist response car | Provided by ambulance service under call sign K466, staffed with community treatment team nurse and paramedic. London Ambulance Service Control Centre identifies patients on criteria including the patient being over 65 years. Service operates 7 days a week from 07:00 to 19:00 | Aims to keep 20 patients at home per week to reduce attendance, admissions and ambulance conveyances to the ED |
| Community-based falls response service | Seek to improve response times and enable ambulance services to prioritise higher acuity patients. Service handles level one and two falls (no known illness or injury, or minor injury/illness) for adults over 18 years in people’s own homes or in care homes. All people who fall and are unable to get up receive appropriate clinical assessment to determine level of response. Co-ordinated by appropriate level clinicians (e.g. advanced practitioners within ambulance emergency control room) with clinical follow-up to assess fall reason and risk assess where appropriate | Part of winter resilience plans. Aims to reduce pressures on general practice and social care, and reduce admissions to hospital |
| Community urgent care schemes | Collective name for services that improve quality/capacity of care for people through delivery of urgent, crisis response care within 2 hours and/or reablement care responses within 2 days. Some providers offer a single, integrated service that covers all these types of care from crisis response to reablement. This is preferred service delivery model | Seeks to avoid demands on hospital care by providing a community-based service that targets urgent needs |
| Hull Fall First | Falls pick up/wellbeing response service within Hull. Involves Hull CCG, Humberside Fire and Rescue, Yorkshire Ambulance Service, Hull City Council and City Health Care Partnership. Healthcare experts provided clinical training to a team of firefighters | Aims to ensure an appropriate level of clinical response according to causes and severity of falls ensuring only most critical cases are transported to hospital |
| Rapid response vehicle with wireless point-of-care testing (Oxford) (Novak et al. 2022)121 |
Rapid response vehicle, staffed by specialist paramedic and equipped with wireless point-of-care testing platform to transmit results to hospital electronic patient record systems, dispatched to frail, non-injured patients. Results obtained on scene and transmitted to Oxford University Hospitals electronic patient record system. Patients discussed over telephone with a senior acute medical assessment physician at trust for advice/decision support and to co-ordinate referral to other services | Relieves pressure on physical attendance and increases availability of senior clinician |
Rapid response/see and treat
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific | |
| Windle et al. 201428 – evaluation report | No demonstrable changes in monthly emergency admissions. Emergency bed days fell from (mean) 6.55 to 6.28 days. Significant increase in zero bed-nights. Short-term evaluation did not enable full cost-effectiveness evaluation; each intervention seemed to demonstrate value for money against cost of an acute admission |
| Academy of Royal Medical Colleges. Preparing for COVID-19 Surges and Winter. 2020. URL: www.aomrc.org.uk/statements/academy-statement-preparing-for-covid-19-surges-and-winter (accessed 23 November 2022) | Community urgent care schemes |
| Systematic reviews | See rapid review below |
| Rapid review | |
| Woodward and Procter. 201653 (rapid review). URL: www.healthylondon.org/wp-content/uploads/2017/11/Rapid-review-Rapid-response-teams-and-see-and-treat-models.pdf (accessed 23 November 2022) | Reviews literature on rapid response teams/see and treat models that support non-conveyance to A&E/admission avoidance. Key characteristics: response times are short, usually assessment within 2 hours. Social care often included, especially for frail, vulnerable patients and older falls patients. Usually single point of access (SPOA). Most initiatives allow any health provider/social care to refer. Services usually offered to patients for set time after which patients are referred. Many initiatives had direct links to other health/social services for onward referral. Common focus on frail, vulnerable patients/older falls patients. Most referral pathways reduce admissions, improve patient outcomes and are popular with patients |
| Other major studies | |
| Published evaluations | |
| Point-of-care testing by ambulance services: Novak et al. 2022121 – service evaluation | 3 month evaluation included 56 patients (21 M, 35 W; median age of 86 years). 17 patients with non-standard blood test results transferred to hospital, plus 10 without such results; 27 admitted in total. 29 patients remained in their usual environment; of these, 4 presented to hospital within next 30 days. No deaths or adverse events reported. Intervention feasible and, when combined with telephone advice and decision support from secondary care physicians, may be effective in reducing hospital admission for frail patients in supportive care environments |
| Community-based falls response service (FRS). Case studies. McGavock 202055 | FRS attended 479 falls (2016–17). 79% of FRS patients remained at home vs. 35% of falls attended by non-FRS crews. Only 37% of patients who remained at home attended hospital within a month. 483 referrals made to community services through pathways not available to core emergency vehicles. Overall referrals from ambulance services to community falls service reduced by 44%. Qualitative evaluation indicates high patient satisfaction. Collaboration between paramedics/physiotherapists provides significant benefits to patient, providing alternatives to ED (e.g. equipment, falls prevention advice and onward referral). More patients treated at home. Work needed to establish best practice guidelines |
| Paramedic in hospice team (Mountbatten Isle of Wight). Singer 2021122 | Conducts assessments, using experience of visiting patients within community and decides on course of action/referral or input required. Two paramedics integrated within community palliative care team. Paramedics give intravenous infusions to patients within their homes to help avoid clinical environments. Paramedics have extensive patient assessment and diagnostic skillsets added to by in-house training on catheterisation/advance care planning and end-of-life care supplementing care provided by nursing staff within the community team. Role remains in its infancy; hospice services work differently and therefore no set rules for paramedic scope of practice |
| Case study: Hull Fall First | Quantitative impact difficult to quantify because of how falls are recorded in health datasets |
| NHS England. Going Further for Winter: Community-based falls response. 2022. URL: www.england.nhs.uk/long-read/going-further-for-winter-community-based-falls-response (accessed 23 November 2022) | The following outcomes were observed locally: reduced number of people requiring A&E attendance because of a fall; reduced number of admissions due to rapid response meaning patients were not experiencing a long lie; increased follow-up from therapy falls team; better patient experience for patients that experienced a fall |
| Case study: Community frailty response service. McNamara 2020.56 CCP: rapid response/see and treat | Describes expansion/adaptation of frailty response team to assess older people in their usual place of residence. Team had commenced weekend service to a limited area in February 2020. Following demand related to COVID-19 pandemic, service expanded and model of care adapted to offer 7-day service to entire catchment area. 592 patient reviews completed in first 105 days of operation with 43 patients transferred to hospital for further investigation/management following assessment |
| Case study: Falls specialist response car. Woodward and Procter. 201653 (rapid review). URL: www.healthylondon.org/wp-content/uploads/2017/11/Rapid-review-Rapid-response-teams-and-see-and-treat-models.pdf (accessed 23 November 2022) | In 2015/2016 team visited 1821 patients and managed to keep 66.5% at home avoiding need for emergency ambulance, A&E attendance/admission. Demonstrated safe, economic and desirable intervention from perspective of patient/service so elderly frail fallers stay in their homes. Also wider impact on organisations, teams and individuals. Continuous measurement essential to developing service. Having data readily available helps to understand what makes a successful referral. Key to keeping referral number up is relationship with ambulance control room. Working on sustaining increase in referrals, aiming for average of 20/week kept at home. Engaging with similar schemes to spread model across LAS services |
| Additional evidence | |
| Mahase 202254 | NHS England to create a ‘community-based falls response service’ in all systems for people who have fallen at home, including in care homes, and will reduce ‘unwarranted variation in ambulance conveyance rates’ |
| Research gaps | |
| Larger systematic evaluations warranted to establish utility and cost-effectiveness of point-of-care testing by ambulance services (Novak et al. 2022).121 Potential need to review rapid response/see and treat services/initiatives in update to Woodward and Procter 201653 (rapid review) | |
| Research priority | |
| Moderate – no/poor systematic review but plentiful UK research studies (synthesis gap) | |
Single point response
Single point response is where co-ordination centres provide a single point access to health and/or social care services. Limited evidence was found for single point response; there were UK initiatives but limited UK research studies, making it a research gap. There is a need for robust evaluations of SPOA services. Tables with further information about this taxonomy heading are provided in Appendix 6, Tables 75 and 76.
Step-up facilities
There was limited evidence for step-up facilities. The tables are provided in Appendix 6, Tables 77 and 78. Discussion around community beds generally focuses on step-down rehabilitative care with little attention on step-up services, which can limit the demand for emergency care. Step-up facilities are a high research priorities, there are few UK initiatives making it an implementation and research gap.
Alternate delivery site
Findings for alternative delivery suites are presented in detail in Tables 24–33 and associated summary paragraphs.
Care homes
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| CCP – care homes | Discharge from hospital to care home may be necessary to meet health and care needs that cannot be addressed adequately in the community. Care homes provide care for people with complex comorbidities and high levels of physical frailty and cognitive impairment | Discharge from hospital to care home benefits health services by releasing beds for alternative occupants. High levels of dependency place heavy load on hospital care. However, admission to care home may incur significant costs for the individual and society. Premature discharge to care home may also result in readmission |
| Example interventions: enhancing health in care homes | Offering people joined-up, co-ordinated health and care services, for example by aligning community nurse teams and GP practices with care homes | Helps to reduce unnecessary admissions to hospital as well as improve hospital discharge |
| Example interventions: Information sharing from social care in Herefordshire and Worcestershire. Care Quality Commission35 | People’s vulnerabilities included on care home residents’ care plans – shared with ambulance crews, as well as visiting clinicians and hospital staff | To facilitate speedy and efficient assessment of needs and appropriate identification of services |
| Example interventions: St Catherine’s (Preston, Chorley and South Ribble, Lancashire) ‘winter pressures’ care homes project | Free education programme offered to all care homes for 6 months commencing in November 2020. Complemented by input from clinical nurse specialist | To improve care home contribution to system resilience during winter |
| Example interventions: trusted assessors | Using trusted assessors to carry out a holistic assessment of need. Carries out assessments of hospital patients on behalf of care homes, who need to consider what the patient’s needs are and whether they would be able to meet those needs | Avoids duplication and speeds up response times so that people are discharged in a safe and timely way |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific | No evidence |
| Systematic reviews | |
| Kobewka 2020123 | High-quality evidence that age, impaired physical function, disabilities in performing activities of daily living, absence of informal caregiver and frailty predict need for supportive services after discharge. Stroke only unique diagnosis with moderate evidence of independent effect on outcome. All models at moderate/higher risk of bias |
| Richardson et al. 2019124 (qualitative) | Four themes: preparing for transition; quality of communication; quality of care; family engagement and roles. Need for robust evidence to guide best practice. Evidence suggests transition is challenging for all stakeholders. People with dementia have specific needs that require attention |
| Rapid evidence synthesis | |
| Enhancing health in care homes: Hanratty et al. 201911 | Synthesis across four key areas: technology, communication/engagement, workforce and evaluation. Few large, high-quality research studies, particularly from UK. Key findings: (1) Technology: promising interventions include games to promote physical activity/mental health/wellbeing. (2) Communication/engagement: structured communication tools enhance communication. No robust evidence on engagement with communities. (3) Evaluation: 6/65 measurement tools validated for UK care homes. Methodological quality poor. (4) Workforce: joint working within/beyond care home and initiatives where staff taking on new but specific care tasks associated with enhanced outcomes. Evidence for staff taking on traditional nursing tasks limited. Provides limited support for innovations in NHS vanguards |
| Other major studies | |
| Primary care network enhanced health in care homes service specification: Coleman et al. 202010 | Using published evidence/official documentation compared/contrasted original enhanced health in care homes model/framework, subsequent draft specifications and final proposals, ahead of implementation. Problems related to GP contracts/COVID-19 means initial variability over who is responsible for delivery. Unknown whether service, delivered at pace within current circumstances, will achieve/affect outcomes envisaged by pilots. Interpretation of developing policy for enhanced health in care homes requires further follow-up research. Evaluations of policy success/failure should consider context/differing power relations that may impact subsequent take-up and roll-out. Recommends longitudinal approach to enable holistic view of policy implementation |
| Emergency admissions from nursing and residential homes: practice-based audit: Evans 2011125 | Audit achieved 43% reduction in emergency admissions and 45% reduction in deaths in hospital but at expense of a 12% increase in visits. Improved anticipatory planning and increased medical/nursing support for patients/staff in residential homes may help to further reduce emergency admissions/deaths in hospital in future |
| Published evaluations | |
| Kandiah 2022126 | Service description and analysis of a two-site pilot involving pharmacists supporting care home residents with medications post discharge. Service data (March 2020 to June 2021) analysed to identify what was delivered to residents. 103 residents received medicines reconciliation. 29 received additional structured medication review. Latter cohort significantly more likely to receive medicines and illness-related information and have medicines stopped. Further evaluation required for value of medicines review alongside medicines reconciliation |
| St Catherine’s (Lancashire) ‘winter pressures’ care homes project Additional Evidence Case Studies Capewell 202114 P119 Solidarity, skills and support: St Catherine’s (Lancashire) ‘winter pressures’ care homes project [poster] |
56 patients referred, 69% from hospital palliative care team; 4 patients died before assessment, 68% of patients seen within 7 days of referral. 29 patients died during project timescale, 93% of deaths in a care home. Single hospital admission precipitated by acute event. Documentation of advance care planning and escalation of treatment plans improved by intervention. Potential hospital admissions avoided in 14 cases due to advance care plans. Challenges for carers in attending education. Education well-received. Further work required to improve accessibility and to assess longevity of benefit. Responded more timely compared with ‘normal care’. Identified inadequate and inconsistent documentation |
| Trusted assessors | |
| Case studies | |
| Local Government Association. Trusted assessors. URL: www.local.gov.uk/our-support/our-improvement-offer/care-and-health-improvement/systems-resilience/overall-approach/trusted-assessors (accessed 22 November 2022). Examples of local initiatives: Newcastle Gateshead CCG: trusted assessment; Lincolnshire: care home trusted assessor; Blackburn with Darwen Home First with trusted assessment | Newcastle Gateshead CCG: trusted assessment: 66% of patients transferred same day, 28% next day and 3% at later date. Issues identified related to mobility, communication and discharge planning Lincolnshire: care home trusted assessor: In April 2016, coverage extended to all hospital sites in Lincolnshire and Peterborough and 7 day working began in late 2017. Over first full year, 439 referrals made, 340 assessments completed and 304 discharges supported, leading to estimated saving of 735 bed days |
| Local Government Association 201815 | Blackburn with Darwen Home First with trusted assessment: Approach worked successfully over winter months; evaluated after 12 months. Approach focuses on ‘home first’. Ward staff undertake partial assessment on ward. Person discharged to their home, with full assessment on day 3. Wraparound care offered for up to 5 days, with multidisciplinary staff enabling individual as much as possible. Approach rolled out in partnership with county council, hospital trust and care foundation trust. Key to success are inter-professional relationships and time taken to co-design trusted assessment document. Training/communication have helped to embed approach. Co-located teams key to resolving issues |
| Additional evidence | |
| Oliver 2019b45 | ‘Small-scale pockets of innovation have modestly cut hospital attendance or admissions – shown in recent reports on primary care home projects or NHS England’s “enhanced health in care homes” vanguards’ |
| NHS England and NHS Improvement 201613 | |
| Local Government Association 201815 | |
| Research gaps | |
| Hanratty et al. 201911 identifies key issues/gaps for future research and evaluation. Future work requires high-quality experimental studies, economic evaluations and research sensitive to UK context | |
| Research priority | |
| Moderate – few UK research studies but plentiful UK initiatives (research gap) | |
Community teams
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| CCP – community teams | Provide holistic care to patients, carers and families within community setting. Multidisciplinary teams (e.g. team leader, clinical leads, nurses, physiotherapists, occupational therapists, care co-ordinators, support workers, administrators). Support housebound or those whose condition requires nursing or therapy at home. Also provide clinician-led clinics in community | Offers alternative venue to some hospital care |
| Example interventions: Multidisciplinary community teams | Co-ordinated discharge planning based on joint assessment processes and protocols and on shared/agreed responsibilities | Promotes effective discharge and positive outcomes for patients |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific | |
| Enhanced community teams: Windle et al. 201428 (evaluation report) | No demonstrable changes in monthly emergency admissions. Emergency bed days fell from (mean) 6.55 to 6.28 days. Significant increase in zero bed-nights. Short-term evaluation did not enable full cost-effectiveness evaluation; each intervention seemed to demonstrate value for money against cost of acute admission |
| Multidisciplinary community chronic obstructive pulmonary disease (COPD) teams | |
| Rodman 202129 | |
| Wilkinson et al. 2014127 | Multidisciplinary community COPD teams for frequent acute exacerbations of COPD. Team functions range from admission avoidance/ESD for COPD only, through to ongoing management support and oxygen assessment services or pulmonary rehabilitation. Support during acute exacerbation of COPD from MDT can have significant impact on admission rates, especially for ‘frequent flyers’127 |
| Systematic reviews | |
| O’Connell Francischetto et al. 2022128 (systematic review of systematic reviews) | 66 moderate or high-quality reviews. Statistically significant positive impact on mortality, readmissions, length of hospital stay, patient health status and costs found for interventions providing ‘rehabilitation, therapy or care at home (or in the community) around the time of discharge’ reducing length of stay; ‘primary care interventions’, ‘discharge planning/co-ordination or case management’ and ‘patient education’. Different types/configurations of discharge interventions benefit older patients when compared to usual care. Highlights which intervention types make no difference or have negative impacts |
| Lowthian et al. 2015129 (systematic review – meta-analysis) | Five experimental/four observational studies. Emergency department community transition strategies (ED-CTS) included geriatric assessment with referral for post-discharge community-based assistance, with different components and delivery methods. Four studies included in meta-analysis. Compared with usual care, no appreciable benefit for ED-CTS for unplanned reattendance up to 30 days, unplanned hospital admission up to 30 days or mortality up to 18 months. Variability between studies precluded analysis of impact of ED-CTS on functional decline and nursing-care home admission. Limited high-quality data exist to guide optimal ED community transition |
| Other major studies | |
| Published evaluations | |
| Case study: Durham: multidisciplinary multi-agency discharge teams: Local Government Association15 | Proactive case management focuses on standardisation of care and risk management, and development of emergency care plans. MDT meetings involve GP practice teams, district nurses, social workers, therapists etc. and voluntary sector. In cases of deterioration in condition, specialist assessment/support offered through rapid access clinics. These aim to maintain patient in community or arrange a planned admission; linking in with intermediate care, domiciliary care and reablement. Integrated discharge management team focuses on home first principles. System-wide approach includes: reablement as default; D2A arrangements with care sector/community health providers; work with care homes; and assessment by ‘other’ professionals |
| Reactive Emergency Assessment Community Team (Ipswich and East Suffolk). Social Care Institute for Excellence. Hospital discharge and preventing unnecessary hospital admissions (COVID-19). URL: www.scie.org.uk/care-providers/coronavirus-covid-19/commissioning/hospital-discharge-admissions (accessed 23 November 2022) | Has resulted in better patient outcomes, smoother pathways, care closer to home, reduced hospital stays (and associated decline), and lower overall costs |
| Additional evidence | |
| Charles 201818 | |
| Wilkinson et al. 2014127 | |
| Research gaps | |
| There is a need to better integrate researchers and clinicians in the design and evaluation process, and for increased reporting, including appropriate robust evaluation of efficacy and effectiveness (Lowthian et al. 2019)129 | |
| Research priority | |
| Moderate – few UK research studies but plentiful UK initiatives (research gap) | |
Home care
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| CCP – home care | Home care is health or supportive care in a patient’s own home from a professional caregiver. It may also be referred to as domiciliary care, social care or in-home care. Home care comprises diverse activities including nurses providing paramedical care and daily living help for ill, disabled or elderly people | Offers alternative venue to some hospital care. Clients receiving home healthcare may incur lower costs, receive equal to better care, and have increased satisfaction in contrast to other settings |
| Example interventions: multidisciplinary community teams | Co-ordinated discharge planning based on joint assessment processes and protocols and on shared and agreed responsibilities | Promotes effective discharge and positive outcomes for patients |
| Ambulance service home visits; collaboration in urgent and emergency care; Care Quality Commission 2022;35 Halliwell 2021130 | GPs at Northamptonshire practice had regular calls with ambulance service and worked together on patient cases to avoid unnecessary ED attendance. Ambulance service carried out visits to people’s homes for GP practice, in liaison with GPs, helping people to avoid going into hospital | Potential to reduce hospital admissions, ambulance calls and ED self-referrals |
| Example interventions: Dolphin Home from Hospital service | Aims to provide short-term post-discharge care at a more intensive level than normally provided by professionals such as district nursing. Generally delivered in user’s own home and led by nursing staff, sometimes with input from medical/allied health professionals (NICE Guideline NG9495) | Transfers care from hospital setting to home setting |
| Example interventions: Follow-up via home visits | Early assessment identifies patients for discharge with increased outpatient support, with follow-up via home visits, telephone consultation or remote monitoring | Transfers ongoing follow-up and monitoring from hospital setting to home setting |
| Example interventions: home visiting services | Visits undertaken by paramedics or qualified advanced nurse practitioners scheduled through the day rather than saving them for lunch and evening slots | Potential to reduce hospital admissions, ambulance calls and ED self-referrals |
| Example interventions: hospital to a healthier home | Aims to support vulnerable older people by making their homes safe, warm and more accessible | Aims for older people to be safely and more quickly discharged from hospitals to their homes and to prevent them being readmitted |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific | None specified |
| Systematic reviews | |
| O’Connell Francischetto et al. 2022128 (systematic review of systematic reviews) |
Statistically significant positive impact on mortality, readmissions, length of hospital stay, patient health status and costs found for: Interventions providing ‘rehabilitation, therapy or care at home (or in the community) around the time of discharge’ reducing length of stay; ‘primary care interventions’, ‘Discharge planning/co-ordination or case management’ and ‘patient education’ |
| Home-based intervention (HBI), education and support, for heart failure vs. usual care: Malik et al. 2019131 (meta-analysis) | 17 articles (3214 patients). HBI associated with reduced readmission rates and mortality (22 and 16% respectively; p < 0.05). Benefit of HBI increases significantly with longer follow-up. HBI in form of education and support significantly reduces readmission rates and improves survival of patients with heart failure. HBI to be considered in discharge planning of patients with heart failure |
| Hamline et al. 2018132 (paediatric population) | The review includes 71 articles. Most interventions improved satisfaction but interventions variably reduced use. Reduced use across patient groups was associated with interventions that focused on follow-up care, discharge planning, teachback-based parental education and contingency planning. Bundled care co-ordination/family engagement interventions associated with lower use in patients with chronic illnesses and neonates. The variability limits findings and reduces generalizability. Highlights utility of paediatric discharge bundle in reducing healthcare use |
| Allen et al. 2018133 (qualitative meta-synthesis) | Users’ experience of discharge and transitional care is the social process of ‘negotiation and navigation of independence (older people/carers), or dependence (health providers).’ Users’ strategies of questioning, discussion, information provision, information seeking, assessment and translation engaged them in negotiation and navigation. Themes reflected care integration that facilitated/lack of care integration that constrained the users’ experiences of negotiation and navigation of independence/dependence |
| Van Spall et al. 2017134 (systematic review and network meta-analysis) | Nurse home visits/disease management clinics decrease all-cause mortality after hospitalisation for heart failure. Along with nurse case management, they reduce all-cause readmissions. No significant difference in comparative effectiveness. Services reduce healthcare system costs to varying degrees |
| Feltner et al. 2014135 (systematic review and meta-analysis) | Home visit programmes and multidisciplinary care/heart failure clinics reduced all-cause readmission and mortality. These interventions should receive greatest consideration by systems or providers seeking to implement transitional care interventions for persons with heart failure |
| Other major studies | |
| Published evaluations | |
| Dolphin Home from Hospital service: Mackintosh 201633 | Most cases create savings in health professional time, even disregarding hospital bed costs. Cost of care at home excluded from evaluation together with potentially high cost of clients entering long-term residential care when unable to return home |
| Hollinghurst 202040 | |
| Wolton 201841 | Wolton used mixed methods to examine interactions between caseworkers across Care & Repair Cymru, their professional links and relationships with clients. Context in which caseworkers operate (agency location/issues encountered when delivering services) influences how they link with others |
| Care & Repair Cymru. URL: www.careandrepair.org.uk (accessed 13 November 2022) | Intervention group had increased risk of care home admission at 1, 3 and 5 years for those classified as fit and mildly frail, but reduced risk of care home admission for moderately and severely frail individuals. Service helped to prevent care home admissions for moderately/severely frail individuals |
| @home team St Thomas’s or King’s College Hospitals: Pickstone and Lee 2019136 | 1084 patients were referred to the @home team in a 3-month period with 755 (72%) referrals accepted. 387 local ED attendances were prevented (King’s College Hospital – 298 and St Thomas’s Hospital ED – 89). During the same time period, King’s College Hospital −71,688 ED attendances and St Thomas’s ED −48,030 attendances. The @home team did reduce ED attendances by a small number each month (1 in 300) the number although not enough to make significant impact on local ED average performance against 4-hour target |
| Additional evidence | |
| Follow-up home visits: Karlsson et al. 2019137 | Follow-up home visits by nurses can relieve patient anxiety, as patients are often unsure of next steps for medication/care. According to nurses, visits created trust in the nurse–patient relationship and ensured patient safety. Follow-up visits soon after discharge from hospital should become routine nursing, especially for older people with multi-morbidity |
| Oliver 2019b45 | ‘Small-scale pockets of innovation have modestly cut hospital attendance or admissions – shown in recent reports on primary care home projects’ |
| Research gaps | |
In paediatric population, co-ordinating follow-up, discharge planning, teach back-based parental education, and contingency planning are potential foci for future efforts to improve hospital to home transitions (Hamline et al. 2018132). Understanding, defining and measuring the components of homecare and homecare outcomes. Requires research to: (1) identify and define the components, or active ingredients, of homecare associated with user outcomes and experiences; and (2) identify and agree on outcomes which evaluative research should include (i.e. core outcomes set). O’Rourke and Beresford 2022138 have identified comprehensive research priorities for home care including:
|
|
| Research priority | |
| Moderate – few UK research studies but plentiful UK initiatives (research gap) | |
Hospital at home
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| CCP – hospital at home | Provides intensive, hospital-level care for acute conditions that normally require an acute hospital bed, in patient’s home for short episode through multidisciplinary healthcare teams | Offers alternative location for hospital-level care by managing those who would otherwise present to hospital safely in the community |
| Example interventions: hospital at home | Patients with chronic disease sent home to recover as part of a hospital at home programme. Signs of deteriorating health picked up after patient discharge from hospital. Connected real-time monitoring means less time spent on in-person visits and can help to improve clinical documentation | Offers alternative to hospital admission, by managing those who would otherwise remain in hospital safely in the community |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific | No studies |
| Systematic reviews | |
| ESD hospital at home (HaH) vs. admission avoidance HaH; Leong et al. 202138 (systematic review of systematic reviews) | 10 systematic reviews (4 high, 5 moderate and 1 low quality). ESD reviews generally revealed comparable mortality (RR 0.92–1.03) and readmissions (RR 1.09–1.25) to inpatient care, shorter hospital Admission avoidance reviews observed trend towards lower mortality and costs, and comparable or lower readmissions. Among reviews including both programme types, COPD reviews revealed lower mortality (RR 0.65–0.68) and post-HaH readmissions but unclear findings for resource use. For suitable patients, HaH generally results in similar/improved clinical outcomes vs. inpatient treatment |
| Echevarria et al. 2016139 (systematic review and meta-analysis) |
8 RCTs identified; 7 reported mortality and readmissions. Structure of ESD HaH schemes, particularly selection criteria applied and level of support provided, varied considerably. Compared with usual care, ESD HaH showed trend towards lower mortality (RRMH 0.66, 95% CI 0.40 to 1.09; p = 0.10). If return to hospital during acute period not considered readmission, ESD HaH associated with fewer readmissions (RRMH 0.74, 95% CI 0.60 to 0.90; p = 0.003), but if readmission considered, benefit was lost (RRMH 0.84, 95% CI 0.69 to 1.01; p = 0.07). Costs lower for ESD HaH than usual care. ESD HaH is safe in selected patients with acute exacerbation of COPD |
| Qaddoura et al. 2015140 | Limited number of modest-quality studies. HaH appears to increase time to readmission, reduce index costs, and improve health-related quality of life among patients requiring hospital-level care for heart failure |
| Other major studies | |
| HaH (geriatrician-led admission avoidance HaH with comprehensive geriatric assessment): Shepperd et al. 2021,36 202237 | Randomised trial evaluating a HaH scheme found it had the same clinical outcomes and was cheaper than hospitalisation. For older people with multimorbidity, admission to residential care may be avoided. Increased risk of transfer to hospital at 1 month, but not at 6 months. Patient satisfaction favoured HaH. At 6 months, mean difference in NHS, personal social care and informal care costs (−£3017, 95% CI −£5765 to −£269). Older people and caregivers played crucial role in supporting delivery of health care. Findings most applicable to patients referred from acute hospital assessment unit |
| Published evaluations | |
| Case study: evidence-based guideline and treatment bundle (dexamethasone, oxygen, intravenous fluids and thromboprophylaxis) for managing severe COVID-19: Schiff et al. 2022141 | Data retrospectively extracted from patient notes (December 2020 to February 202). Service users contacted for feedback. 125 adults with COVID-19 treated by @Home; 42 severe (34%) and 83 non-severe (66%) infections; average length of stay was 7 days (interquartile range 4–8). 875 hospital-occupied bed days saved. Service users emphasised importance of being with loved ones and value of respecting peoples’ wishes to be at home. @Home gave people with COVID-19 choice of active treatment at home, thereby extending available healthcare capacity beyond acute hospital setting |
| Additional evidence | |
| NHS England. Supporting Information for ICS Leads: Enablers for success: virtual wards including hospital at home. London: NHS England and NHS Improvement; 2022. URL: www.england.nhs.uk/wp-content/uploads/2022/04/B1382_supporting-information-for-integrated-care-system-leads_enablers-for-success_virtual-wards-including-hos.pdf (accessed 30 November 2022) – includes 6 case studies | Integrated care systems asked to deliver virtual ward capacity equivalent to 40/50 virtual ward ‘beds’ per 100,000 population (equivalent to up to 24,000 virtual ward beds) by December 2023. Outlined in 2022/23 priorities/operational planning guidance. Additional ‘bed’ capacity from efficient/productive use of resource/patient management. Each system expected to implement virtual wards for at least two pathways (acute respiratory infection, frailty) with other pathways being optional. Virtual wards to be developed across systems/provider collaborative. Virtual wards including HaH to be tech-enabled managing patients via digital platform managed remotely by clinical team |
| Winter pressure specific additional evidence | |
| Edinburgh Integration Joint Board 202016 | |
| Research gaps | |
| Future research should clarify costs of HaH programmes given current low-quality evidence on costs and address evidence gaps in caregiver outcomes/adverse events under HaH care.38 Future RCTs should clearly define readmission and provide data on patients who return to hospital during HaH and whether same patients are readmitted during the follow-up period (Echevarria et al. 2016).139 Larger RCTs necessary to assess effect of HaH on readmissions, mortality, and long-term costs.140 Further research that includes stronger carer support might generate evidence for health outcomes (Shepperd et al. 2021, 2022)36,37 | |
| Research priority | |
| Moderate – few UK research studies but plentiful UK initiatives (research gap) | |
Telecare
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| CCP – telecare | Telecare services use personal alarm and other monitored devices such as fall detectors or home sensors to call the monitoring centre in an emergency. Telecare offer alternative to moving into a care home or having a live-in carer | Transfer demands on physical premises and resources to remote delivery. Also may substitute for home visits |
| Example interventions | ||
| Remote consultations | Appointment takes place between a patient and a clinician over the telephone or using video, as opposed to face to face | Aims to reduce pressure on secondary care staff – allows for distributed service across multiple sites |
| Paediatric symptom smartphone application (app): Care Quality Commission 202235 | In Cornwall and Isles of Scilly, parents encouraged to download a paediatric app – parents and carers could input symptoms and be advised whether to provide care at home or seek medical attention. Newsletters developed to inform families | Reduces numbers of patients presenting to ED by targeting and prioritising symptoms |
| Remote consultations (Herefordshire and Worcestershire). Care Quality Commission 202235 | Care homes provided with computer tablets to enable remote consultations with frail/vulnerable residents – allowed virtual ward rounds from primary care and timely access to clinical advice. Care home staff supported with training. 30 care homes included in social media pilot to enable greater connectivity with family and friends | Allows more timely access to clinical advice and allows ongoing monitoring of frail and vulnerable patients |
| Remote monitoring | Allows clinical teams to keep track of patients with chronic conditions safely in the comfort of their own home. Forms part of broader plan to improve digital health services for people with chronic diseases | Aims to reduce pressure on hospital services and improve patient outcomes by noticing and dealing with early signs of deteriorating health in patients recently discharged from hospital and patients with long-term conditions |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific | |
| Atkin et al. 202234 | Telecare |
| Edinburgh Integration Joint Board 202016 | |
| Academy of Royal Medical Colleges. Preparing for COVID-19 surges and winter. 2020. URL: www.aomrc.org.uk/wp-content/uploads/2020/07/200717_Preparing_for_covid-19_surges_winter.pdf (accessed 23 November 2022) | Remote consultations |
| Edinburgh Integration Joint Board 202016 | |
| Collaboration in urgent and emergency care. Care Quality Commission35 | |
| Systematic reviews | |
| Feltner et al. 2014135 | Structured telephone support reduced heart failure-specific readmission and mortality. Interventions should receive greatest consideration by systems or providers seeking to implement transitional care interventions for persons with heart failure |
| Pandor et al. 2013142 | Structured telephone support human to machine and telephone monitoring with medical support provided during office hours showed beneficial trends, particularly in reducing all-cause mortality for recently discharged patients with heart failure. Where ‘usual’ care is worse, likely impact of telephone monitoring is greater |
| Other major studies | |
| Al Rajeh et al. 2019143 (UK survey) | 65 participants completed survey from 52 NHS trusts. 46% of trusts had used telehealth for COPD and 31% still provided telehealth services to patients with COPD. Telehealth most commonly used for baseline monitoring and to allow early detection of exacerbations, with 54% believing it to be effective. Various methods were used for setting alarm limits. The majority of respondents believe that at least 40% of alarms were false. Of the community COPD services that responded, about one-third are using telehealth. Services are believed it to be effective without robust evidence A variety of variables were monitored, there was a variety of hardware and varying techniques to set alarm limits |
| Cook et al. 2016144 | Qualitative interviews to explore views of ‘users/non-users’. ‘Users’ [patients who used service (N = 28)] and ‘non-users’ (either referred patients who declined service or had withdrawn after using the service). Having positive attitude and perceived need met by equipment influential in decision to adopt/engage in using service. Engagement with service centred on ‘usability’, ‘usefulness of equipment’ and ‘threat to identity and independence’. Reveals influential role of referrers in decision making. Need to engage with agencies on strategic level. Reassurance critical to continued engagement, particularly in older patients. Need for continued product development/innovation to increase usability/functionality of equipment |
| Published evaluations | |
| Case study: NHS England. Remote monitoring for patients with chronic conditions in the Midlands. URL: https://transform.england.nhs.uk/covid-19-response/technology-nhs/remote-monitoring-for-patients-with-chronic-conditions-in-the-midlands (accessed 22 November 2022) | Technology helps patients to self-manage their conditions at home while giving support and reassurance. Patients capture relevant clinical data and upload data using computer/tablet/smartphone connected to web-based remote monitoring platform (CliniTouch Vie, Spirit Healthcare, Belfast, UK). From the data, health professionals can spot long-term trends in patient’s condition and notice any deterioration before there is a need for hospital admission. Patients can also use the technology to have video assessment/consultation with health professionals as required. Clinicians can send direct messages to patients. All suitable patients are offered remote monitoring service. A tablet is provided to patients who need one. All changes to patient care/condition are documented in electronic patient records |
| Case study: Docobo® (Leatherhead, UK) – digital remote monitoring system and case management. Health Innovation Network. Innovation Collaborative: Rapid review of current remote monitoring in care homes across the UK. URL: https://healthinnovationnetwork.com/wp-content/uploads/2021/11/Innovation-Collaborative_Rapid-Review_Health-Innovation-Network.pdf (accessed 22 November 2022) | Docobo, digital remote monitoring system and case management solution for patients under care at home or care homes. Docobo or DOC@HOME deployed across UK (Bexley, Newham, West Yorkshire, Liverpool, Kent, Lancashire). 8-month pilot in Sussex Community Trust showed 75% reduction in admissions compared to same period in the previous year |
| Case study: care navigators for telecare: MacInnes et al. 2020145 | Training for care navigators focused on functioning/technical aspects of equipment. Training needs were also identified around supporting decision-making (e.g. assessing mental capacity). Care navigators valued the peer support networks and they developed good relationships with social care/telecare provider staff. Professionals making referrals to care navigators for telecare often did not understand the role of care navigators or funding eligibility. Care navigators have appropriate knowledge/decision-making skills for prescribing telecare. Comprehensive training is necessary to support decision making. Additionally, advocates peer support/education of professionals referring for telecare |
| Case study: managing long-term conditions remotely in the north west. NHS England Transformation Directorate. Managing long term conditions remotely in the North West. URL: https://transform.england.nhs.uk/covid-19-response/technology-nhs/managing-long-term-conditions-remotely-in-the-north-west (accessed 22 November 2022) | Liverpool telehealth hub model forms basis of digitally enabled COVID Oximetry @ Home (CO@H) services. In Lancashire and South Cumbria, plans urgently redeployed to deliver home oximetry monitoring, supported by technology. Over 3200 patients have been supported by digitally enabled CO@H services across two sites. Up to 200 patients safely monitored by a single nurse working in Cheshire and Merseyside telehealth hub. 81% of patients with oxygen saturation levels below 92% were safely managed by telehealth hub, resulting in patients not requiring hospital treatment. Only 3% of 819 patients needed referral to a GP, saving 787 referrals into primary care |
| Case study: rapid response and telecare service north-east England: Watson et al. 2020146 | Examined impact on service users/other stakeholders of services for elderly/vulnerable residents in social housing. Housing provider has rapid response team; includes 24/7 emergency response service combined with telecare service, funded by local authority for vulnerable clients with complex needs (self-funded by others). Service users reported feeling safer/more confident. Family carers reported improved health and wellbeing. No. of requests for ambulances responding to falls reduced. Vulnerable people with electronic monitoring/telecare support able to remain in own homes. Rapid response/telecare resulted in older people remaining independent in their homes for longer, improving quality of life and relieving stress on carers |
| Case study: NHS England. Remote monitoring for care home residents across London. URL: https://transform.england.nhs.uk/covid-19-response/technology-nhs/remote-monitoring-for-care-home-residents-across-london/#:~:text=Inhealthcare%20is%20the%20remote%20monitoring,uploaded%20to%20the%20secure%20portal (accessed 22 November 2022) | Project expands use of remote monitoring into care homes. In healthcare, remote monitoring systems were used in 48 care homes in project. Staff used portable devices to measure residents’ vital signs which were then uploaded to secure portal. Local GPs received alerts prompting them to take action when a resident’s health deteriorates. Care home staff also receive updates and guidance from GP via the system. The platform helps clinicians monitor residents’ health and care. Monitoring is via virtual ward rounds/virtual MDT meetings and through data integrated into NHS primary care clinical systems (EMIS Web and TPP SystmOne) used by GP practices |
| Case study: NHS England. Remote monitoring for patients with chronic conditions in the Midlands. URL: https://transform.england.nhs.uk/covid-19-response/technology-nhs/remote-monitoring-for-patients-with-chronic-conditions-in-the-midlands (accessed 22 November 2022) | Over 1000 patients supported across 4 pathways. Over 725 patients with heart failure and COPD supported (April 2020 to May 2021). 288 hospital bed days saved (January–April 2021). 218 patients with COVID-19 discharged after hospital admission with remote monitoring at home (November 2020 to May 2021). Only 10 readmissions to hospital within 14-day monitoring period. 50% reduction in readmissions among patients supported by COVID virtual ward |
| Research gaps | |
| Technology: meeting care needs. Use of technology to meet care needs or augment hands-on care. Includes evaluating current technologies and horizon scanning for promising technologies, including existing technologies with potential to translate to homecare (topic areas suggested by one stakeholder group only) | |
| Research priority | |
| Moderate – few UK research studies but plentiful UK initiatives (research gap) | |
Facilitated discharge
Findings on facilitated discharge are presented in detail in Tables 34–43, Appendix 6, Tables 79–82 and associated summary paragraphs.
Rehabilitation, recovery and reablement
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| CCP – rehabilitation, recovery and reablement | Usually provide time limited therapy for patients who require ongoing physiotherapy or occupational therapy to regain maximum independence. Users of rehabilitation schemes have often sustained a fracture and may have undergone surgery. Rehabilitation schemes delivered by multidisciplinary team, often led by physiotherapists/occupational therapists. ‘Doing with’ model vs. home care which is a ‘doing for’ model. Reablement services help people to retain or regain their skills and confidence so they can learn to manage again after a period of illness. Service usually provided in person’s own home by team of social care professionals | Minimises unnecessary delays in hospital discharge. Not specific to winter but frequently mentioned in winter planning documents. Reablement generally designed to help people learn or relearn skills necessary for daily living which may have been lost through deterioration in health and/or increased support needs. Central focus on regaining physical ability and active reassessment |
| Example interventions | ||
| Frontline occupational therapists: Social Care Institute for Excellence. Hospital discharge and preventing unnecessary hospital admissions (COVID-19). URL: www.scie.org.uk/care-providers/coronavirus-covid-19/commissioning/hospital-discharge-admissions (accessed 22 November 2022) | Occupational therapists moved to frontline calls to provide/advise on reablement, home equipment and adaptations so people did not lose skills and independence | |
| Advanced clinical practitioner roles: Hove 2022147 | Registered practitioner with expert knowledge base, complex decision-making skills and clinical competencies for expanded autonomous scope of practice. Characteristics shaped by context in which individual practices | |
| Reablement assistants | Reablement assistants work within the community, usually in peoples’ homes. They promote independence and choice for people through helping them work towards the reablement goals set out in their support plan. The assistants work closely with carers and other health professionals to meet each person’s needs | Reablement supports people to do things for themselves to try to prevent unnecessary admission to hospital or residential care |
| Reablement co-ordinators | Deliver outward facing service to co-ordinate services for people accessing community reablement. Work within support team, receiving referrals into the service via electronic systems, planning and co-ordinating resources to facilitate delivery of services | Reablement supports people to do things for themselves |
| Intermediate care beds – rehabilitation and reablement | Involves temporary stay in a care home, community hospital, or standalone intermediate care facility. Patient receives support similar to home-based intermediate care to help reach their goals. The sooner bed-based intermediate care starts, ideally within 2 days of referral, the better the chance of success | Intermediate care that aims to avoid unnecessary hospital admission involves rehabilitation to help patients continue to live at home when facing increasing difficulty with daily life due to illness or disability, or prevent a premature, permanent move into residential care |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific | |
| Edinburgh Integration Joint Board 202016 | Intermediate care beds – rehabilitation and reablement |
| Charles 201818 | |
| Edinburgh Integration Joint Board 202016 | Reablement coordinators and reablement assistants |
| Systematic reviews | |
| Van der Laag 2020148 | The review included 9 studies assessed as good to moderate quality. 18 factors were extracted and for 13 extracted factors, limited (n = 3), moderate (n = 5) and conflicting (n = 5) evidence found a significant association. The following factors are related to successful rehabilitation; caregiver, comorbidities, motor function, nutritional status and time from onset. These factors could support healthcare professionals to indicate successful rehabilitation at admission and help with deployment of early discharge planning and developing personalised rehabilitation trajectories |
| O’Connell Francischetto et al. 2022128 (systematic review of systematic reviews) | Statistically significant positive impact on mortality, readmissions, length of hospital stay, patient health status and costs found for: Interventions providing ‘rehabilitation, therapy or care at home (or in the community) around the time of discharge’ reducing length of stay; ‘primary care interventions’, ‘Discharge planning/co-ordination or case management’ and ‘patient education’ |
| Petterson et al. 2017149 | Specific roles of various professional and staff groups often insufficiently described, as are interventions. Lack of attention to person-centred aspects such as the meaningfulness of the specific activities |
| Tessier et al. 2016150 | Considering effectiveness and positive impact observed in several countries, implementation of reablement offers a promising avenue for policy makers |
| Boniface et al. 2013151 | Overall, occupational therapy in social care perceived as effective in improving quality of life for older people and their carers and cost-effective in making savings for other social and healthcare services. However, complex nature of social care services makes it difficult to disaggregate effectiveness of occupational therapy from other services |
| Dawson et al. (systematic review of systematic reviews)152 | Rehabilitation and post-rehabilitation support for patients with COPD is evaluated in three effectiveness systematic reviews with a complementary systematic review of qualitative data |
| Francis et al. 201158 | People using reablement welcome emphasis on regaining independence/better functioning. Reablement improves outcomes, particularly in restoring people’s ability to perform usual activities and improving their perceived quality of life. Reablement achieves cost savings through reducing/removing need for ongoing support via home care. Managers/care workers value flexibility and responsiveness of reablement. Delivery of reablement depends on suitably trained care workers who require specific training. Requirements for training, closer supervision of care workers and longer, more responsive and flexible visits all contribute to greater costs of reablement vs. home care. Higher cost likely offset by long-term savings from reduced social care needs |
| Other major studies | |
| Ariss et al. 201559 (secondary data analysis) | Provision of intermediate care is highly variable with different referral routes, team structures, skill mix and cost-effectiveness; in recent years, patients referred to intermediate care have complex needs associated with severe impairments; high percentage of patients referred do not require service; and teams including clinical support staff/domiciliary staff associated with small relative improvement. Interdisciplinary team working may be associated with better outcomes. Results viewed with caution. Measures used are reliable, valid and practical and suitable for benchmarking |
| Prospective cohort study of individuals referred to 3 English social care reablement services: Beresford et al. 2019153 | Outcomes included healthcare and social care related quality of life, functioning, mental health and resource use (service costs, informal carer time, and out‐of‐pocket costs). Positive changes were observed across all outcome domains. Improvements observed at discharge were, for most, retained at 6 months follow‐up. Patterns of change in functional ability point to the importance of assessing basic and extended activities of daily living. Findings from economic evaluation highlight importance of collecting data on informal carer time. Study demonstrates challenges/value, of including self‐report outcome and resource use in evaluations of reablement |
| Research gaps | |
| Integrating an enabling approach into homecare – whether an enabling approach (or reablement) should be integral to homecare practice.138 Evidence on user and carer views needs to be strengthened.58 High-quality research needed to strengthen evidence-base regarding reablement149 | |
| Research priority | |
| Moderate – few UK research studies but plentiful UK initiatives (research gap) | |
Step-down beds
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| CCP – step-down beds | Aim to provide community bed for patients following acute inpatient episode, not yet ready to go home, needing period of recuperation/recovery. Includes people requiring residential long-term placement who need further recovery period before being able to engage in active rehabilitation; they may need additional rehabilitation therapy before being able to return home: or may be yet to complete continuing healthcare or social care assessments for their long-term care needs prior to discharge home or long-term placement | Helps to relieve pressure on NHS beds and to flex capacity at times of especially high demand. Acute trusts need to plan effectively for sufficient acute beds as well as access to community beds to improve patient flow. Minimises unnecessary delays in hospital discharge. Not specific to winter but frequently mentioned in winter planning documents |
| Example interventions: step-down beds for discharge from stroke unit | Provide high level of support for patients who have had a cerebrovascular accident and to provide high-level rehabilitation to assist in gaining increased independence. Stroke schemes delivered by MDT (medical, nursing, allied health and social work, with assistance of generic rehabilitation assistants, covering physiotherapy and occupational therapy). Schemes often longer term than other schemes | Usually provide care in alternative setting to acute hospital |
| Step-down facilities (care and reablement centre): Social Care Institute for Excellence. Hospital discharge and preventing unnecessary hospital admissions (COVID-19). URL: www.scie.org.uk/care-providers/coronavirus-covid-19/commissioning/hospital-discharge-admissions (accessed 23 November 2022) | Buckinghamshire Council made up to 240 beds available as care and reablement centre within just 3 weeks, staffed by care workers and a team of volunteers | These facilities support people leaving hospital but unable to return home and those who live at home in need of short-term support |
| Example interventions: ‘D2A’ facility (see Discharge to Assess section): Social Care Institute for Excellence. Hospital discharge and preventing unnecessary hospital admissions (COVID-19). URL: www.scie.org.uk/care-providers/coronavirus-covid-19/commissioning/hospital-discharge-admissions (accessed 23 November 2022) | Reading Borough Council paid for use of hotel rooms at a local Holiday Inn. Others stayed in the hotel to protect shielding relatives, or self-isolated with COVID-19 symptoms | Operated ‘D2A’ facility, allowing time to arrange care packages and equipment for people due to go home |
| D2A facility (see Discharge to Assess section): Social Care Institute for Excellence. Hospital discharge and preventing unnecessary hospital admissions (COVID-19). URL: www.scie.org.uk/care-providers/coronavirus-covid-19/commissioning/hospital-discharge-admissions (accessed 23 November 2022); Pidd, H. Care room with a view: UK hotels offer respite to non-Covid patients. Guardian 3 May 2020. URL: www.theguardian.com/society/2020/may/03/care-room-with-a-view-uk-hotels-offer-respite-to-non-covid-patients (accessed 23 November 2022) | Hammersmith and Fulham made similar arrangements to Reading Borough Council (above) with Novotel but stood down when capacity not needed. Astute commissioning enabled good ongoing relationships with business while avoiding expensive contractual commitments | See above |
| Supporting evidence | Results/findings/recommendations (from abstracts) |
|---|---|
| Winter pressure specific | |
| Edinburgh Integration Joint Board 202016 | |
| Case study: step-down beds for discharge from stroke unit; Walters et al. 202130: CCP – step-down beds, TC – carer education | Of 82 patients referred for transfer, 80 were accepted. Mean length of stay was 19 days for patients with social complexity limiting discharge, and 11 days without (p < 0.001). The main needs making discharge difficult related to housing (21%), risk between calls/night needs (13%), hoarding (9%), self-neglect (5%), intensity required for family/carer education/training (11%) and no recourse to public finding 4%. 57 (75%) patients were discharged home; remainder required further rehabilitation, step-down care or placement. Social complexity significantly impacts on the stroke pathway flow independent of physical impairments |
| Systematic reviews | |
| Lowthian et al. 2015129 (meta-analysis) | Limited high-quality data exist to guide confident recommendations about optimal ED community transition strategies. Need for better integration of researchers and clinicians in design/evaluation process, and increased reporting |
| Other major studies | |
| Levin and Crighton 2019.154 Interrupted time series analysis | Step-down immediate care and the 72-hour discharge target associated with reduction in days delayed. Rate of days delayed continued to increase over time, although at a slower rate than if immediate care had not been implemented |
| Tinelli et al. 2022155 (cost-effectiveness analysis) | Investigates service and patient delivery costs, as well as health benefits gained, of healthcare provided after patients experience homelessness are discharged from hospital into step-down care vs. usual care vs. clinical and housing in-reach services. Three configurations compared vs. ‘standard care’ (control, defined as one visit by homelessness health nurse before discharge with receipt of information leaflet on local services). Promising evidence suggesting that, with delivery costs similar to bed-based intermediate care, step-down care secured better health outcomes and improved cost-effectiveness (vs. usual care) within NICE cost-effectiveness recommendations |
| Published evaluations: case studies | |
| Step-down beds: Charles 201818 | Birmingham Community Healthcare NHS Foundation Trust works with local authority to tackle delayed transfers of care. Common discharge policies/pathways agreed/adopted across health/social care. Social workers embedded within some teams at intermediate care facilities. Some overlap in service provision between social care/community health care, particularly around respite care, step-down beds and reablement. Beds commissioned by both CCG and local authority, and mixed pattern of provision by the trust and multiple nursing home providers |
| Additional evidence | |
| House of Commons Health Committee. Winter pressure in A&E: third report of session 2016–17156 | ‘Investment in new rehabilitative “step-down” beds, where patients can recover outside hospital, could deliver substantial gains’ |
| Research gaps | |
| Needs appropriate robust evaluation of efficacy/effectiveness of innovative models of care129 | |
| Research priority | |
| Moderate – few UK research studies but plentiful UK initiatives (research gap) | |
Virtual hospitals/wards
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| CCP – virtual hospitals/wards | Full-scale hospital with no physical location, meaning a patient cannot submit analyses or have surgery. Offers range of online consultations, helping patients to avoid travel and queues | Can help streamline emergency care delivery adding home-based telemedicine consultations with medical specialists. Paramedics can prevent health deterioration in timely fashion. Can mitigate shortage of physicians and other specialists. Patients may choose not to travel to a location for a consultation, but receive it without leaving their home |
| Example interventions: virtual ward | Support people (e.g. with frailty or acute respiratory infections at ‘home’, including care homes). Support includes remote monitoring using apps, technology platforms, wearables and medical devices (e.g. pulse oximeters). May also involve face to face care from multidisciplinary teams in community (sometimes called hospital at home) | Offer alternative location for safe and convenient care rather than be treated in a hospital |
| Example interventions: same-day emergency care virtual follow-up clinics. Care Quality Commission 202235 | In Herefordshire and Worcestershire, same-day emergency care virtual follow-up clinics, set up for patients who were too vulnerable to return to an ED | Reduce reattendance at ED by offering alternative venue for follow-up in patient’s own home |
| Example interventions: virtual clinics: Tower Hamlets chronic kidney disease e-clinic (Wenzel and Evans 201969) | Allows GPs to consult directly with consultants. E-clinic uses information‑sharing and digital communications to support single pathway from primary to secondary care | NHS long‑term plan highlights potential to redesign outpatient services to reduce visits, partly using digital solutions such as virtual clinics that allow follow-up for outpatients in primary care. Such services may be able to reduce waiting times and hospital appointments (NHS England 2019157) |
| Supporting evidence | Results/findings/recommendations (from abstracts) |
|---|---|
| Winter pressure specific | |
| Virtual wards: Atkin et al. 202234 | |
| Other major studies | |
| Vindrola-Padros et al. 2021158 (multisite mixed methods study July–August 2020 combining qualitative and quantitative approaches) | Analysed implementation and impact of remote home monitoring models from first wave of COVID-19 pandemic. Combined interviews with staff delivering models across 8 sites in England with data on staffing models/resource allocation. Models varied by healthcare setting and mechanisms for patient triage, monitoring and escalation. Implementation embedded in existing staff workloads/budgets. Good communication within clinical teams, culturally appropriate information for patients/carers and multiple approaches for patient monitoring (app/paper-based) facilitated implementation. Mean cost/monitored patient from £400 to £553, depending on model |
| Virtual outpatient clinic: Healy et al. 2019159 (RCT) | Virtual clinics can be effective and receive high levels of satisfaction from patients. Only six patients in outpatient clinic (OPC) group and 10 in virtual outpatient clinic (VOPC) group reported ongoing issues. Further follow-up indicated 78/82 (95%) VOPC patients very happy with their overall experience vs. 34/61 (56%) in actual OPC group (p < 0.001). Significant proportion of both cohorts preferred VOPC appointment as future follow-up of choice. Majority of patients discharged from surgical service could be better followed up by VOPC with significant proportion of patients reporting preference for/greater satisfaction with service |
| Additional evidence | |
| NHS England. Supporting Information for ICS leads: Enablers for success: virtual wards including hospital at home. 2022. URL: www.england.nhs.uk/wp-content/uploads/2022/04/B1382_supporting-information-for-integrated-care-system-leads_enablers-for-success_virtual-wards-including-hos.pdf (accessed 23 November 2022) – includes 6 case studies | ICSs to deliver virtual ward capacity equivalent to 40/50 virtual ward ‘beds’ per 100,000 population (equivalent to delivery of up to 24,000 virtual ward beds), by December 2023. Additional ‘bed’ capacity from efficient use of resource/patient management. Each system expected to implement virtual wards for at least two pathways with other pathways being optional. Virtual wards to be developed across collaboratives and based on partnership between secondary, community, primary, social care and mental health services and with independent sector. Virtual wards including hospital at home should be tech-enabled to maximise opportunities for patients, carers, and staff |
| Virtual hospitals: Wenzel et al. 201969 | Future changes in technology could lead to estate that is better for patients/staff, smarter and integrated. Technology likely to result in different NHS estate, with space used/configured in different ways. Technology/estate should be brought together within overarching vision for how health/care will be delivered in the future. Factors affecting optimal use of technology/estate include availability of skills, engagement with staff/patients and access to investment. Local systems will play key role through collaboration across organisations beyond NHS, and harnessing opportunities from working at scale. Clear role for national NHS bodies in supporting common data/technology standards and facilitating shared learning |
| Research gaps | |
| Need to evaluate effectiveness of models (e.g. using comparator data).158 Future research to focus on sustainability of models and patient experience (considering how models exacerbate existing inequalities in access to care)158 | |
| Research priority | |
| Moderate – few UK research studies but plentiful UK initiatives (research gap) | |
Other agencies
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| CCP – other agencies | Offers alternative to use of hospital services (e.g. by using housing services to ensure that patient is discharged home to safe, warm environment). Typically excludes social care services as an agency (see separate entry) given lower involvement of other agencies | Alleviates communication and co-ordination workload from hospital-based services especially in relation to safe discharge. Currently, one of biggest constraints for successful discharge is timely availability of community resources, such as housing160 |
| Example interventions | ||
| Healthy homes on prescription service; housing surgeries in primary care: Azam et al. 2019161 | Housing/health worked with GP practices to identify patients vulnerable to cold or damp housing. in addition to GP being prompted to ask about flu vaccinations, prompted to ask patients about housing conditions | Uses broad population health approach through integrated care organisations |
| Safe and Well Evaluation (Kent): Lakoma and Murphy162 | Safe & Well visits offered to households including anyone 70 years and above or with long-term health conditions | Shifts workload in hospital admission prevention to other agencies when they have additional capacity. ‘Safe and well’ checks aim to reduce health risks such as falls, loneliness and isolation and therefore reduce visits to A&E, broken hips and depression |
| NHS England. NHS and fire service sign new consensus to help vulnerable and reduce winter pressures. 2015. URL: www.england.nhs.uk/2015/10/nhs-and-fire-service (accessed 23 November 2022) | NHS sought help of fire service in partnership aimed at tackling health/social problems and reducing winter pressures. Fire service conducts 670,000 home safety checks each year, assessing homes of vulnerable and offering advice on safety. Enables firefighters to carry out ‘safe and well’ checks when visiting homes | |
| Safe and well visits: Azam et al. 2019161 | ||
| Gloucestershire Fire and Rescue Service 2015. URL: https://shorturl.at/lqxy5 (accessed 23 November 2022) | Working in collaboration with fire and rescue services to extend fire safety visits into safety and wellbeing visits – offering brief interventions and signposting to relevant services | Serves preventive or early warning system for potential risk and improves navigation of care services reducing more crisis-based demands |
| Supporting evidence | Results/findings/recommendations (from abstracts) |
|---|---|
| Winter pressure specific | None identified |
| Systematic reviews | |
| Farmanova et al. 2019163 | Scoping review included 15 examples of integrated care organisations in Organisation for Economic Co-operation and Development (OECD) countries from 57 reports. 7 key redesign strategies were identified: focusing on health/wellness, intersectoral action/partnerships, addressing health in vulnerable groups, and addressing wider determinants of health, including health service improvements. The redesign interventions had innovative ways for dealing with clinical/non-clinical problems. Examples include establishing housing surgeries in primary care, setting up social and provider networks for supporting patients with complex needs and expanding services scope of and workforce redesign. Broader use of these strategies/interventions has the potential reduce care needs and costs. Integrated population health-oriented care requires service redesign and changes in how organisations/care systems operate |
| Other major studies | |
| Tinelli et al. 2022155 (cost-effectiveness analysis) | Investigates cost-effectiveness of three ‘inpatient care co-ordination and discharge planning’ configurations: (1) clinical and housing in-reach service with no ‘step-down’ care. (2) clinical and housing in-reach, discharge co-ordination and ‘step-down’ intermediate care. (3) housing support workers providing in-reach and discharge co-ordination as well as step-down care. Each configuration compared with ‘standard care’. Collated service delivery costs, economic consequences for public services (e.g. NHS, social care, criminal justice, housing) and health utilities (quality-adjusted life years). With delivery costs similar to bed-based intermediate care, step-down care secured better health outcomes and improved cost-effectiveness within NICE cost-effectiveness recommendations |
| Published evaluations | |
| Safe and well evaluation: Mahmood et al. 202047 | Focus on fire safety but also at risk populations (e.g. evidence of hoarding could indicate obsessive–compulsive disorders or autism). Cites systematic review on fire safety (Senthilkimaran et al. 2019): Identified 10 studies (8 RCTs and 2 prospective cohort). Two RCTs assessed effects of home fire safety interventions on home fire safety knowledge at 4 months in school children. Demonstrated significant difference between groups (very low quality). One RCT examined computer-based vs. instructor-led interventions on home fire safety knowledge/behaviour immediately post intervention in adults and displayed no significant difference (very low quality). No evaluation of wider (collateral) safety/welfare benefits |
| Additional evidence | |
| Consensus statement on improving health and wellbeing between NHS England, Public Health England, Local Government Association Chief Fire Officers Association and Age UK. URL: www.england.nhs.uk/wp-content/uploads/2015/09/joint-consens-statmnt.pdf (accessed 23 November 2022) | NHS England, Public Health England, Fire and Rescue Service, Age UK and Local Government Association consensus on working together to prevent/minimise service demand, and improve quality of life of people with long-term conditions |
| Research gaps | |
| Requires evaluation of benefits, particularly added value over opportunistic visits. Evidence base linked to that for home care (see separate entry) | |
| Research priority | |
| Moderate – few UK research studies but plentiful UK initiatives (research gap) | |
Private sector
There was limited evidence on UK initiatives working with the private sector. The tables are provided in Appendix 6, Tables 79 and 80.
Social care
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| CCP – social care | Individuals, typically older patients and those with special needs often await defined care packages from social services before being discharged. Delays in providing these care packages often indicate suboptimal health/social care communication and integration | Well-documented winter increases in A&E waiting times, hospital length of stay, and demand for winter pressures wards is not explained simply by increased attendance. Factors that contribute include sicker patients requiring longer admissions and a lack of social care beds which causes lengthy delays to patient discharge with resultant impact on patient flow in A&E |
| Example interventions | ||
| Accelerated home first approach: Social Care Institute for Excellence. Hospital discharge and preventing unnecessary hospital admissions (COVID-19). 2022. URL: www.scie.org.uk/care-providers/coronavirus-covid-19/commissioning/hospital-discharge-admissions (accessed 13 November 2022) | Improved flow by accelerating home first approach. Hospital social work staff deployed into community to assess people within 24 hours of discharge. Central hub deals with step-up and step-down referrals with ‘hotlines’ for hospital and community in-reach teams | Accelerated assessment to identify any barriers to timely discharge and co-ordinated approach to addressing these |
| SPOA for social care – see also adult services response team (ASeRT) | SPOA for social care services including adult protection. Care at Home, community care and occupational therapy (ASeRT team) | Ensures social care delivered for whole population to single set of standards, processes and procedures |
| ASeRT: Renfrewshire Health and Social Care Partnershi. Adult social care. URL: www.renfrewshire.hscp.scot/article/5040/Adult-Social-Care (accessed 22 November 2023) | SPOA for service has moved responsibility for reassessment to SPOA | Ensures social care delivered for whole population to single set of standards, processes and procedures |
| Hub social worker enhancement | Enable assessments to be carried out earlier in hospital pathway to facilitate discharge home, or in the community to avoid admission | Minimises unnecessary delays in hospital discharge and unnecessary admissions. Funded as winter pressure response |
| Supporting evidence | Results/findings/recommendations (from abstracts) |
|---|---|
| Winter pressure specific | |
| Hub social worker enhancement: Edinburgh Integration Joint Board 202016 | Additional social workers based across community hub/cluster and acute hospital social work teams to prevent hospital admissions and to reduce delayed discharges. The hospital-based social work team provide a responsive service to any adult support and protection concern raised in acute care. The team aim to reduce delayed discharges by processing referrals/completing assessment within target timescales to reduce length of stay. Social workers were also able to facilitate discharge to person’s home with package of care or to a care home as an interim measure or a permanent placement |
| Systematic reviews | |
| Dimla et al. 202298 (systematic review) | Six studies from Canada/United States. Most common support measures employed by hospital social workers in discharge planning for older patients: assessment, education, care co-ordination, liaison and engagement with families and providers, conflict resolution, counselling and post-discharge follow-up. Medical complexity, lack of communication, time constraints, limited family support and availability of resources and patient safety were barriers to effective discharge planning. The included studies were from 1993 to 2014 not within UK context |
| Dawson et al. 2020152 (meta-review) | Nineteen reviews concerned with social care interventions. Summarises evidence and evidence gaps of nine broad types of health and social care interventions. Research recommendations generated both primary and secondary research. Ongoing research recommendations could be delivered if meta-reviews are conducted as living systematic reviews. Highlights lack of evidence for impact of social care interventions on healthcare outcomes. No meta-analysis level evidence for any social care intervention in any population supporting benefit for timely discharge |
| Spiers et al. 2019164 (systematic review and meta-analysis of observational studies from high income countries) | Investigates impact of availability/supply of social care on healthcare use by adults > 60 years. 12 studies, 10 in meta-analysis. 7/12 studies from UK. Seven good quality, 1 fair and 4 poor. Higher social care expenditure and greater availability of nursing/residential care associated with fewer hospital readmissions, fewer delayed discharges, reduced length of stay and expenditure on secondary healthcare services. Overall direction of evidence consistent, but effect sizes not confidently quantified. Little evidence on home-based social care. No data on primary care use. Adequate availability of social care holds potential to reduce demand on secondary health services |
| Dickson et al. 2017165 (meta-review of systematic reviews) | Most evidence relates to physical activity: physical activity interventions can be effective for people with long-term conditions/non-frail older people and may address quality of life and prevention outcomes. Physical activity interventions not typically within remit of social care but relatively cheap, easy to implement, and worth considering. More complex and recognisably social care interventions need evaluation, review and synthesis. Need to recognise influence of contextual factors on success of social care interventions. Particular need for safety measures when implementing social care interventions with vulnerable groups |
| De Sao Jose et al. 2016166 (systematic review of qualitative literature) | Positive and negative experiences of receiving social care relate, mostly, to relational dimension of care. Receiving social care per se does not automatically imply negative or positive experience. Attitudes and behaviour of carers primarily determines whether care experienced as positive or negative.’ Research on older persons’ experiences and perspectives of receiving social care, although important, is still limited. Identifies questions requiring attention in future studies |
| Published evaluations | |
| Accelerated home first approach: Social Care Institute for Excellence. Hospital discharge and preventing unnecessary hospital admissions (COVID-19). URL: www.scie.org.uk/care-providers/coronavirus-covid-19/commissioning/hospital-discharge-admissions (accessed 23 November 2022) | Portsmouth improved flow by accelerating home first approach. Length of stay reduced from 4 or 5 days to < 1 day |
| Additional evidence | |
| Department of Health and Social Care. Hospital discharge and community support guidance. Updated 1 July 2022. URL: www.gov.uk/government/publications/hospital-discharge-and-community-support-guidance (accessed 23 November 2022) | From April 2022, local areas should adopt discharge processes to meet needs of local population. Systems to work across health/social care to jointly commission and deliver discharge services. Identifies D2A, home first; multidisciplinary hospital discharge teams and transfer of care hubs, with professionals from across health, social care, housing and voluntary sectors. Everyone should have opportunity to recover/rehabilitate at home before long-term needs are assessed. This reduces hospital-acquired infections, falls and loss of physical/cognitive function by reducing time in hospital, and enables people to regain/achieve maximum independence. It supports hospital flow, maximising availability of hospital beds |
| Preston-Shoot 2019167 | Social care contribution often excluded from discharge planning and absent from significant discharge decisions: ‘Social care and housing needs were relegated behind medical needs when considering discharge’ |
| Research gaps | |
| Timely discharge only measured in discharge care intervention reviews (2/14). Not present in social care reviews (0/19).152 Social care and synthetic social support evidence152 focuses on subjective outcomes. Could be valuable for social care research to measure objective outcomes (e.g. use of care services). Reviews of social care interventions predominantly include older population with few studies including younger populations. Fewer reviews of social care than health care, and within these reviews, fewer RCTs than in healthcare reviews.152 Quality of life outcomes present in both health/social care systematic reviews; no meta-analysis evidence in social care or synthetic social support interventions reviews. Social care data comprised few RCTs in combination with less rigorous study types of a heterogeneous group of interventions152 | |
| Research priority | |
| Low – good-quality systematic review(s) and plentiful UK research studies (no gap) | |
Voluntary services
There was a shortage of research and of documented initiatives within the voluntary sector (see Appendix 6, Tables 81 and 82).
Within the CCP taxonomy section, which comprises three subsections and numerous interventions, we identified variable numbers of initiatives or research studies. Some areas, such as hospital at home, are well explored. Other approaches such as virtual wards are already stimulating their own initiatives and research agenda, motivated in part by significant growth in these remote initiatives during the pandemic. Other sectors such as the voluntary agencies and private sector are less frequently reported and even less frequently researched. Initiatives reported in this section are reported and evaluated in the short-term with little consideration of longer-term sustainment or rigorous evaluation. The Community sector has always been a ‘poor relation’ compared with the acute sector and has neither the resources nor infrastructure to tackle the complete research agenda required by such a whole system wicked problem. Further research studies could seek to undertake cross-cutting research along clinical pathways (e.g. primary care, acute care, social care) but this may require an integration of research strategies and research funding to mirror the integration of care taking place in the health sector itself.
Integrated care
Findings for the IC heading are presented in detail in Tables 44 and 45 and Appendix 7, Tables 83 and 84 and the associated summary paragraphs. Probably even more than any other section of the taxonomy, we found considerable overlap between IC interventions and other interventions. As mentioned above, a focus on ‘delivery site’ elsewhere in the taxonomy has meant that the section on IC tends to focus on initiatives that are distinctively branded as ‘integrated’. Furthermore, this particular category within the taxonomy, a specific focus identified during the commissioning of the review, is distinctive in that it operates across multiple levels; from integration at an organisation level, through shared pathways of care to frontline integration of health, social care and voluntary services staff within individual teams. As a consequence, coverage of this category is notably heterogeneous. As a combined front for research activity it would particularly benefit from exploration of mechanisms to establish whether these operate at multiple levels as a feature of integration or whether they operate exclusively within a single level or strata of the organisation.
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| IC – integrated care | Involves partnerships of organisations that come together to plan and deliver joined-up health/care services, and improve lives of people who live/work in their area | Improved communication between health and care services to speed up admission/discharge and to effect hospital avoidance |
| Example interventions | ||
| Comprehensive systems approach (Somerset): Social Care Institute for Excellence. Hospital discharge and preventing unnecessary hospital admissions (COVID-19). 2022. URL: www.scie.org.uk/care-providers/coronavirus-covid-19/commissioning/hospital-discharge-admissions (accessed 23 November 2022) | Comprehensive systems approach links hospital discharge and avoidance with Community Connect to maximise local support and connections | Outcomes through rapid response enhanced by locality neighbourhood approach and innovative microproviders delivering flexible support |
| Social Care Institute for Excellence. Hospital discharge and preventing unnecessary hospital admissions (COVID-19). 2022. URL: www.scie.org.uk/care-providers/coronavirus-covid-19/commissioning/hospital-discharge-admissions (accessed 23 November 2022) | Shares learning from seven health/care communities (July 2020 to June 2021). Challenges (1) bringing together health and social care data to understand demand and pressures on commissioned services, (2) availability and supply of domiciliary care. Workshops organised to explore challenges and inform local action plans | Demonstrated that better-staffed community hospitals can help get older people back to their own homes; and support for care homes by therapists and nurses can increase percentage of older people then returning home |
| Local Government Association. Developing a Capacity and Demand Model for Out of Hospital Care. London: LGA; 2021. URL: https://www.local.gov.uk/publications/developing-capacity-and-demand-model-out-hospital-care (accessed 23 November 2022) | ||
| High-impact user group; Bristol Royal Infirmary; Care Quality Commission | Multidisciplinary group works with ED frequent/‘high impact’ attenders (e.g. violence and aggression). High-impact user group aims to manage top 100 frequent attenders. Team of ED matron, consultant, psychiatry liaison nurse, homeless health team, drug/alcohol nurse, and primary care, with input from police, ambulance and other specialties | Creates individualised support plans and behavioural contracts and signposts people to other services to support them |
| Hull Integrated Care Centre (Charles 2018)18 | Facility to support integrated out-of-hospital care across health, social care, social housing, voluntary sector and other organisations. Hub initially to focus on supporting frail individuals identified through screening in primary care | Uses integrated single response model to facilitate appropriate navigation of health/care system |
| Opera Beds. Are integrated care centres the future? URL: https://operabeds.com/blogs/news/hull-integrated-care-centre (accessed 23 November 2022) | ||
| Integrated Care Across Northamptonshire (iCAN): Care Quality Commission35 | Programme of transformation work driven by Northamptonshire Health and Care Partnership to improve quality of care and achieve best possible health/wellbeing outcomes for older people across the county | Three key areas make up iCAN programme: community resilience: fully supported to live independently within community as older person. Frailty escalation and front door: assessed swiftly and treated effectively so older person remains independent. Flow and grip: fully aware of when they will leave hospital and available support once they are home |
| Example interventions: integrated primary and secondary care pharmacy team: NHS Improvement and NHS England 2018;168 Wilkinson 201819 | In 2018, NHS England published guidance outlining steps hospitals should take to use pharmacists in tackling winter pressures. Recommendations from the guidance included putting pharmacy professionals on wards for medicines management and to help discharge patients; placing pharmacists in ED to prescribe medicines before patients even reach wards; and extending pharmacy services hours to support hospital teams | Facilitating speed of discharge by removing barriers in making medicines available prior to discharge |
| Trusted assessors: Charles et al. 201818 | Local health economies use ‘trusted assessor models’: University Hospital Coventry and Warwickshire NHS Trust’s integrated discharge team is a trusted assessor for all residential and housing with care units in Coventry. The team can also restart packages of social care, if no change in people’s needs. Medway Community Healthcare staff can restart packages of care if care requirements unchanged | Enables one person to be the single point of contact for multiple teams to co-ordinate and make appropriate discharge suggestions to suit each patient’s needs |
| Supporting evidence | Results/findings/recommendations (from abstracts) |
|---|---|
| Winter pressure specific | None specific |
| Systematic reviews | |
| Dawson et al. 2020152 (systematic review of systematic reviews) | Seventy-one systematic reviews included: 62 quantitative, 7 qualitative and 2 mixed methods reviews. Fifty-two reviews of healthcare interventions and 19 reviews of social care interventions. Scrutinises existing evidence and evidence gaps of 9 broad types of health/social care interventions. Proposes that evidence for older person health/social care interventions can be systematically defined, filtered and organised by meta-reviews. Proposes structured research agenda for summarising evidence of health/social care interventions, indicating those suitable for co-provision |
| Combined health and social care poorly described in included systematic reviews. All 13 definitions came from healthcare systematic reviews with eight describing care in the community interventions and five describing discharge/transitional interventions. Combined health/social activity implied [as opposed to specific integrated working (with only two exceptions)]. Discharge and transitional interventions defined as ‘interventions that could be implemented in any health or social care setting (primary, secondary or community care), if they cross boundary between two or more settings.’ | |
| Farmanova et al. 2019163 | Fifteen examples of integrated care organisations in OECD countries from 57 articles/reports. Key redesign strategies included focusing on health/wellness, intersectoral action/partnerships, addressing health in vulnerable groups and wider determinants of health, including health service improvements. Redesign interventions included addressing clinical/non-clinical issues (e.g. establishing housing surgeries in primary care, establishing social and provider networks to support patients with complex needs and broadening of scope of services, workforce redesign). Potential reduced use of care/costs from wider adoption of strategies/interventions. Integrated care requires service redesign, supported by cohesive strategies to prevent disease, address social determinants and improve health equity |
| Sadler et al. 2019169 (systematic review and narrative synthesis) | Integrated care was negatively affected by poor relationships between service users and health/social care professionals. In two studies, some service users experienced limited involvement in discharge planning and conflicting information from providers. One UK study reports that recipients of integrated health/social care service highlighted lack of perceived interest from their social care provider in establishing a genuine rapport the between two services. Positive outcomes achieved for some user groups/individuals but not others. Lack of changed outcomes in social care, and service users’ low level of satisfaction with social care services appears to be associated with impact of agency work and social work prioritising of maintenance/prevention outcomes |
| Baxter et al. 201857 | One hundred and sixty-seven studies included. Evidence for perceived improved quality of care, increased patient satisfaction, and improved access to care. Evidence rated as inconsistent/limited regarding other reported outcomes. This includes the system-wide impacts on primary and secondary care, and healthcare costs. Limited differences between outcomes reported by UK and international studies. Overall, there was limited consideration of effects on service users in the literature. The models of integrated care may enhance patient satisfaction, increase perceived quality of care, and enable access to services. There is unclear evidence for other outcomes. Indications of improved access could have potentially important implications for services unable or struggling to cope with increasing demand for services |
| Damery et al. 2016170 | All outcomes showed significant reductions. Several potentially effective interventions. Interventions rarely demonstrated unequivocally positive effects. Questions remain about whether magnitude of potentially achievable gains from integrated care is enough to satisfy national targets for reductions in hospital activity |
| Gonzalez et al. 2014171 | Beneficial effects of integration of care on several outcomes, including reduced mortality, reduced hospital admissions and readmissions, improved adherence to treatment guidelines and quality of life |
| Philp et al. 2013172 | Reducing unnecessary use of acute hospital beds by older people requires integrated approach across hospital/community settings. Stronger evidence base has emerged in recent years about diverse interventions which may be effective. Local agencies need to work together to implement interventions to create a sustainable healthcare system for older people |
| Other reviews | |
| Stephenson et al. 2019173 (rapid review of systematic reviews and meta-analyses) | Integrated care may reduce risk of hospitalisation. Reviews including patients with diverse chronic conditions showed 19% reduction. Evidence from ED presentations indicates that integrated care has no effect overall but may reduce ED visits for patients aged 65 years or more. For patients with chronic obstructive pulmonary disease, integrated care was associated with reduced length of stay (2.5–4 days). Studies with shorter follow-up (3–12 months) appeared to show greater impact than studies with follow-up of 18 months plus. Generally, integrated care reduces use of hospital services. Some instances demonstrated no differences but no reviews reported increased use |
| Pearson et al. 2015174 (realist review) | At an organisational level, integrated working can facilitate delivery of intermediate care, but there is not a straightforward relationship between integrated organisational processes and integrated professional practice |
| European Observatory on Health Systems and Policies and Dedeu 201621 | Scottish government is integrating health and social services to improve quality/consistency and improve health outcomes in Scotland. A clear vision, strong political commitment, extensive partnerships, and health systems approach to integrating services enable strong accountability arrangements, transparent joint planning, and a clear outcomes framework. Government has provided funds to facilitate reform and has established clear communication mechanisms for managing transformational change |
| Other major studies | |
| Difference-in-differences analysis: Morciano et al. 202023 | In the preintervention period, vanguard sites had higher hospital use than non-vanguard sites. Post intervention, there was clear evidence of a substantial increase in emergency admissions among non-vanguard sites. The rise in emergency admissions was slowed by the vanguard integrated care programme, especially in care homes and during the third and final year. No significant reduction was found in bed days. In the short-term integrated care policies not sufficient to make large reductions in hospital activity, especially for population-based models |
| Difference-in-differences analysis: Alonso and Andrews 2022175 | Investigated impact of creation of integration authorities in Scotland – statutory bodies responsible for planning and resourcing adult social care, primary care, community health and unscheduled hospital care at local level. Employing a difference-in-difference style analysis compared delayed discharges in Scottish integration authorities with those for local authority areas in North of England for period 2013–19. Results suggest that health and social care integration led to improved performance on delayed discharges in Scotland (point estimate −0.236, 95% confidence interval −0.443 to −0.029). Findings suggest that vertical integration may enhance organisational efficiency and patient experience |
| Published evaluations | |
| Colclough et al. 2021176 | ESD: In quarter 1 2020, 29 patients were referred to ESD out of 161 patients admitted with COPD. Concludes ESD is safe and effective using trusted assessor model supported by digital technology and consultant virtual supervision to screen into this service |
| Collins 2018177 | Trusted assessor pilot: Care home staff report communications have improved with hospital because of intervention of trusted assessor which keeps all parties in discharge/admission loop. Hospital monitors potential reductions in bed days. Positive outcomes of pilot have helped build trust/co-operation |
| Case study: high impact user group (Bristol Royal Infirmary). Care Quality Commission | High Impact User Group showed 80% reduction in ED attendances and hospital admissions in ‘super-user’ group. Team leads regional network for frequent attenders to support other EDs. Many sites have set up similar model. Bristol Royal Infirmary has produced online toolkit with Academic Health Science Network to support other sites |
| Additional evidence | |
| Oliver 201945 | Nuffield Trust 2013178 reviewed models of integrated care out of hospital. Found ‘no consistent evidence that acute admission or bed use could be prevented or that this would save money’. Nuffield Trust 2019179 evaluation of integrated care models reached similar conclusions. |
| Research gaps | |
| Very little review evidence for combined health/social care for older person. Reflects practice and research mindsets in UK and elsewhere.152 13 reviews focused on combined/integrated health and social care interventions. One systematic review had clear, integrated health/social care definition for included studies. Despite how healthcare works with social care within many interventions (e.g. ED, discharge and transitional care), little mention of social care involvement. Reinforces persistence of healthcare and social care research as separate entities – not acknowledging combined activities. Pragmatic evaluation of local health/social care may address this better152 | |
| Research priority | |
| Low – good-quality systematic review(s) and plentiful UK research studies (no gap) | |
Winter improvement collaborative
The winter improvement collaborative was introduced on 1 November 2022, so there are no evaluations. Extra detail is provided in Appendix 7, Table 85.
Integrated care discharge ‘huddles’
There was limited evidence for huddles (see Appendix 7, Tables 83 and 84). Anecdotal evidence for huddles appears generally favourable but evaluation of huddles, especially at the hospital-wide level, is at its earliest stages. There needs to be further rigorous research that particularly focuses on the design of huddle programmes and implementation fidelity.
Within this taxonomy section, we identified numerous but varied approaches to integration and, as mentioned elsewhere, a focus on interventions that are formally labelled as ‘integrated care’ provides a potentially misleading picture of a landscape where integration is present to so many different degrees and at different levels. Indeed, the sheer heterogeneity of initiatives makes it challenging to take stock of current activity.
Integrated care organisations constitute one of the development areas for both health and care services and for research, and it seems that this research agenda will need a little supplementary stimulation. However, a particular focus on the contribution to hospital avoidance and prevention of delayed discharge would potentially harness the benefits of being able to track pathways throughout IC organisations rather than stop at the artificial borders between sectors, as may previously have been the case for more siloed research. Further research studies could therefore potentially capitalise on the new models of care to develop a more contemporary and forward-looking research agenda.
Targeting carers
Findings from the targeting carers initiatives are presented in detail in Tables 46 and 47 and associated summary paragraphs. Four overall approaches were classified as targeting carers, carer education, carer preparation, carer respite and carer support. As with other sections of the taxonomy, we found considerable overlap both within carer interventions and between other interventions and carer provision.
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| TC – carer education | Carer education, typically during periods of low demand when the carer can attend without compromising their care provision, helps a carer to build up their own capacity and resources. Attendance at carer education opportunities may require short-term respite (see below) with the expectation that this will offset longer unmanaged periods of demand that occur at times of high demand | Carer education increases knowledge and resources of individual carers and their capacity to anticipate and respond to crises. By handling individual demand using informal care resources the carer offers an alternative to unplanned presentation to acute services and/or admissions |
| TC – carer preparation | Carer preparation helps to anticipate certain types of need and demand thereby increasing the carer’s capacity to manage such individual demands as and when they arise | Carer preparation increases capacity of informal care to anticipate and respond to potential individual demands, preventing some crises and handling other demands using informal care resources as an alternative to unplanned presentation to acute services and/or admissions |
| TC – carer respite | Regular demands of caring can lead to physical and emotional exhaustion. Carer respite offers the opportunity for the carer to take a break from their caring responsibility. Carer respite may involve multiple different options (e.g. an hour each week, an occasional day, a week or two for a holiday, or a combination of all of these options) | Carer respite reduces occurrence of crises leading to unplanned demands upon acute services. Increases capacity of informal care to manage individual demand over an extended period and uses respite resources to handle demands as an alternative to unplanned presentation to acute services and/or admissions |
| TC – carer support | Carers often share similar needs and can act as self-help resource to one another. Providing opportunities to meet and support one another increases individual and collective carer resources and the capacity to manage demands. Attendance at carer support opportunities may require short-term respite (see above) | Carer support increases capacity of carer and thus of informal care to manage individual demand thereby providing an alternative to unplanned presentation to acute services and/or admissions |
| Supporting evidence | Results/findings/recommendations (from abstracts) |
|---|---|
| Winter pressure specific | None specified |
| Systematic reviews | |
| Collins et al. 2022180 (qualitative evidence synthesis) | Four synthesised findings from 69 findings in 16 papers. Patients/carers generally unprepared to manage at home post discharge after major trauma injury. Need identified for better information delivery and preparation of patients. Proposes a systematic approach to empowering patients/family caregivers through their recovery and rehabilitation. Adoption of patient centred principles may improve patient/carer experiences of discharge planning. Discharge planning that is organised, prepared and collaborative leads to a positive patient experience. Discharge information should be individualised and in an easily accessible format for patients/carers |
| Rodakowski et al. 2017181 (meta-analysis) | Fifteen included studies, 11 with readmission rates. Discharge planning interventions with caregiver integration associated with 25% fewer readmissions at 90 days (RR 0.75, 95% CI 0.62 to 0.91) and at 180 days 24% fewer (RR 0.76, 95% CI 0.64 to 0.90). Most studies reported statistically significant shorter time to readmission, shorter rehospitalisation, and lower costs of post-discharge care. Integration of caregivers into discharge planning for older adults, reduces the risk of hospital readmission |
| Mockford et al. 2015182 | Little evidence documents carer and patient perspectives of health and social care services during and after hospital discharge. Little published evidence to guide best practice for people with dementia who leave hospital and return home. Little evidence that discharge planning meets best practice. Absence of evidence on good outcomes for carers of people with dementia at hospital discharge |
| Other reviews | |
| Stockwell-Smith et al. 2018183 (integrated literature review) | For people with dementia, significant role of family carers in healthcare/social care decision-making has been reinforced via UK clinical guidelines (NICE) |
| Pearson et al. 2015174 (realist review) | Involving service users/carers in collaborative decision making is very important. It relies on health practitioners, service managers and commissioners awareness of the impact that organisational structures at the local level have on enabling/inhibiting collaborative decision making and care co-ordination. Health/social care professionals in their interactions with service users and care networks, should establish how different service users understand alternative care environments. This ensures that decisions made about the best place of care can be better informed and provides service users with increased involvement in these decisions which then should support patients in achieving their functional goals and help them to feel in control |
| Other major studies | |
| Ewing et al. 2018184 (qualitative) | Three NHS trusts in England: focus groups and interviews on experiences of carer support during hospital discharge. Barriers to supporting carers at hospital discharge were an organisational focus on patients’ needs, what practitioners perceived as carers’ often ‘unrealistic expectations’ of end-of-life caregiving at home and lack of awareness of patients’ end-of-life situation. Enhanced carer support requires assessment and support (hospital with community follow-up) using a carer-held record to manage transition. Expanding discharge planning to include assessment of carers’ support needs at transition, potentially prevents breakdown of care at home and patient readmissions to hospital |
| Davis et al. 2019185 | Priorities for discharge included remaining independent despite often feeling lonely at home; to remain in hospital if needed; and for services to ensure effective communication with families. The main research priority was facilitating independence, while establishing a permanent PPI panel involving older adults was viewed favourably |
| Research gaps | |
| Evidence base overwhelmingly qualitative. More information required on carer-centred outcomes | |
| Research priority | |
| Moderate – few UK research studies but plentiful UK initiatives (research gap) | |
The sheer breadth and scope of this taxonomy section made a comprehensive survey of research prohibitive. The heading is included in the taxonomy for completeness, as mentioned in the discussion targeting carers sustains its own research agenda. Nevertheless, we have identified the four key areas required within the targeting carers topic and have identified limited initiatives or research studies. The role of carers has not only been identified as pivotal but also represents a hidden cost alongside formal systems of care, often compensating for pressures within the overall health system. However, reliance on carers exerts its own impact on the carers themselves. ‘Winter pressures and the implications on carers’ would seem to constitute a promising area for further exploration. It remains to be seen whether benefits of, for example, carer respite during less-pressured times can produce a dividend during subsequent pressure points in terms of carer resilience and community support. Because of its often invisible nature, carer contributions can prove very challenging to measure.
Chapter 4 Discussion
Overview of discussion
The discussion starts with an overall summary of common findings over all intervention types. It then proceeds to brief summaries of the five overarching types of interventions: (1) structural interventions, (2) CSB, (3) CCP, (4) IC, and (5) targeting carers. Finally, the discussion summarises the research priorities and the potential for a realist review.
Overall summary
Undoubtedly the foremost limitation of this review is the absolute shortage of studies that describe and evaluate winter pressures in a specific way. As mentioned above, there is no shortage of studies that describe achievements against a backdrop of winter pressures or that describe quality improvements with multiple collateral benefits including an impact against winter demands. However, as a review team, we agreed that this is substantively different from interventions that specifically target winter pressures. Even following winter funding to identify specific targets for development could not guarantee that each intervention was conceived against the specific requirements particular to winter pressures as opposed to relieving capacity pressures more broadly. As a team, we found ourselves asking should ‘winter’ simply privilege the time when initiatives take place, conventionally ‘winter pressures’ have been attributed to a specific time period or even a specific date, or are we looking for something related to specific pressures on the system as characterised by the pressures observed at winter. This discussion is particularly relevant, given recent acknowledgement that in recent years winter pressures seem to be taking place ‘all the year round’. 186 This realisation had a considerable bearing on our decision, following the preliminary mapping specific to winter pressures, to expand to the evidence base on wider responses to health and social care system pressures.
Overall, the evidence base is characterised by large numbers of case studies, often published online or presented at conferences, and relatively few peer-reviewed journal articles. Case studies are often accompanied by guidance to support implementation of changes to services. This distribution of evidence probably reflects the urgent need to develop and implement solutions to the ever increasing winter (and increasingly year round) pressures on the health and care system. The majority of evaluations report positive effects on important outcomes, such as length of hospital stay, but many are uncontrolled or based on small samples, meaning that they need to be interpreted with caution.
A further interpretation of the evidence base, fuelled by the expansion of winter pressures to other times of the year, acknowledges that ‘winter pressures’, although undoubtedly real, tend to assume extra narrative significance by presenting a continuous systemic challenge in binary form. Politically, ‘winter pressures’ may become a device used to spotlight specific attention on health system under-resourcing so that these issues assume special significance over and above general awareness as highlighted by politicians, the popular media and public campaigns.
Summary of structural interventions
Structural responses to winter pressures were classified as ‘hospital avoidance’, ‘alternative delivery site’, ‘facilitated discharge’ and ‘cross-cutting’. In line with the review’s emphasis on timely hospital discharge and IC post discharge, most taxonomy headings fell into the latter two categories. Nevertheless, it is clear that avoiding admission in the first place (where clinically appropriate and feasible) and exploring care delivery in different settings both play important roles in the overall response.
In the area of hospital avoidance, we identified many UK initiatives around SDEC, mostly reported as case studies or evaluations of low methodological quality, suggesting a research gap. Surgical hubs are a more recent development and we have identified research and implementation gaps in this area. Extra service delivery takes a variety of forms and some successes have been reported in both emergency and elective care but the evidence base remains limited.
In terms of alternative delivery sites, acute medical units were defined by the Royal College of Physicians of London as long ago as 2007. 187 Recent systematic reviews have demonstrated their effectiveness. Other initiatives have involved developing specialist units using winter funding but these remain to be fully evaluated.
Some aspects of facilitated discharge are relatively well researched, particularly models based on D2A (also ‘Home First’ and others). In addition to case studies and guidance, we identified a range of Healthwatch reports providing a patient/carer perspective on how D2A services operate in real-life clinical practice. Interventions with little UK evidence were sometimes supported by systematic reviews, although the quality of these varied. Some taxonomy headings (e.g. ‘bed management’ and ‘discharge co-ordinators’) were often evaluated as part of a broader process of ‘discharge planning’. ‘Patient flow’ is another broad heading with some overlap with both ‘bed management’ and discharge planning. The concept of ‘patient flow’ is also broader than facilitated discharge, although its ultimate goal is ensuring safe discharge as soon as is clinically appropriate. This highlights an issue we found with the taxonomy of the overlap within the taxonomy headings.
Evidence support for initiatives defined as ‘cross-cutting’ varied widely. The winter pressure search identified UK initiatives to support improved teamwork, together with associated guidance (see Table 19). Various initiatives have applied data sharing and digital technology, but we found a relative lack of research studies. Actions at the organisational level (e.g. involving changes in governance or formulation and implementation of policy) play an important part in responding to winter pressures but this was not reflected in research. Further research studies are needed in the area of seven-day services, although promising case studies exist. Staff redeployment has achieved successes within the pharmacy profession and research involving other staff groups would be useful. Volunteers have been used within the NHS in many different areas but there needs to be further evaluation of these initiatives in relation to winter pressures.
We identified significant numbers of recent systematic reviews relevant to, but not targeted at, responses to winter pressures. These are potentially valuable but the review questions rarely overlap completely with the needs of addressing winter pressures, suggesting that further targeted evidence synthesis (perhaps using realist approaches to focus on the UK context) could be valuable. The diverse range of literature identified by this mapping review suggest that such an approach would be feasible for at least some approaches (e.g. D2A, reablement, virtual wards and optimising patient flow).
Summary of changing staff behaviour
Changing staff behaviour responses to winter pressures were all classified as ‘cross-cutting’.
There was recent guidance available for documenting local clinical audit from the Healthcare Quality Improvement Partnership. A case study from Shrewsbury and Telford Hospital used clinical audit to investigate compliance with the discharge process. The study found that, in 2019, patients were still being kept waiting for the same reasons in the discharge lounge and few patients were transferred to the discharge lounge.
Within the education of staff heading, there was one small research study on teaching staff about patient flow, which found that multimodal teaching approaches were the most successful at the ward level to make it relevant to staff. 27 Patient flow is one of the headings within structural interventions. The interventions introduced could also include education of staff, which again highlights the overlap within the taxonomy headings. Education of staff could be part of larger initiatives with multiple components but might not be the outcome that is been measured, more likely that the number of patients discharged or patient length of stay would be main outcomes measured. The importance of looking after the workforce and creating the best possible conditions for staff to do their best for patients was highlighted in a recent poster of a rapid review. 198
There was no evidence for the use of protocols or guidelines specifically to mitigate winter pressures. A systematic review from 2015 researching how to improve the quality of discharge summaries found that guidelines were useful for providing the key components of discharge summaries. 32
The lack of evidence for the use of quality improvement programmes to mitigate winter pressures could be due to the nature of winter pressures, with a need for implementation of rapid solutions without the time for thorough evaluation. However, the NHS Confederation has drawn six lessons from the pandemic experiences of the Q Community that would be useful to apply as winter pressures increase. Quality improvement programmes could be useful for introducing initiatives to mitigate winter pressures and would allow for more thorough planning and evaluation.
There was no evidence of the use of quality management systems to mitigate winter pressures. Within Scotland, there is a move from the use of quality improvement to the use of quality management to support better quality health and social care, indicating that quality management could become more important.
Changing staff behaviour can take time and initiatives to minimise winter pressures may need to be implemented rapidly without the time for thorough evaluation or to measure all potential outcomes. Initiatives could potentially be too short to make changes to staff behaviour and they might not measure staff behaviour as an outcome. Further research studies could plan evaluations that consider a variety of outcomes including changes in staff behaviour, although it can be difficult to measure.
Summary: changing community provision
Numerous approaches were classified as CCP. Community responses either seek to keep those who need not be admitted to a hospital within the community, whether through preventive or early warning measures or through substituting community for acute services as the point of delivery, or they seek to facilitate and accelerate hospital discharge. In the latter case, two overall approaches can be observed, either by co-ordinating the patient’s needs to remove obstacles to discharge or, again, by offering services traditionally delivered within acute care from a community setting. ‘Hospital avoidance’ from the community has been artificially separated from hospital avoidance within the structural category, simply on the basis of the setting from which avoidance is enacted. We considered that attributing initiatives and evidence to the setting is more helpful than aggregating all hospital avoidance schemes together. So, for example, a scheme that seeks to avoid hospital admission by meeting patient needs as an outpatient within acute services is distinguished from a scheme that seeks to avoid placing any demand on acute services.
Findings are presented in detail in Tables 20–23 and Appendix 6, Tables 75–78 and associated summary paragraphs. As with structural interventions, we found considerable overlap between definitions and interventions. In some cases, we found ourselves placing artificial demarcations between interventions; for example, in focusing telecare on ‘non-health’ care needs and in distinguishing ‘virtual wards’ where a single set of related functions (e.g. rehabilitation) takes place from a ‘virtual hospital’ that seeks to replicate the full range of functions offered by a physical hospital. Equally common are packages that can be coded for multiple components.
As with the King’s Fund report Reimagining Community Services: Making the most of our assets (2018),18 we have found that many areas are trying to improve co-ordination through introducing single points of access or trusted assessor arrangements. The intention is to reduce duplication in referral and assessment processes. Sometimes these changes are associated with creation of new roles with a specific care co‑ordination function (care navigators or care co-ordinators). The King’s Fund report highlights how these roles are intended to act as a ‘workaround’ to help people navigate complex and unco-ordinated services and highlights how ‘a better solution would be to make services less fragmented, so that this additional layer of complexity is not needed’. 18
Similarly, we identified commonality in interventions that seek to better co-ordinate care by bringing professionals together in integrated community teams. We discuss team-based approaches in the community under ‘community teams’ while whole system approaches are explored under a separate integrated care section. These multidisciplinary community teams typically assemble diverse community health and social care professionals working alongside groups of GPs. The teams often target older people or other groups that have relatively high health and care needs. 188 Teams are usually based within a local area and can involve multiple professionals.
The core teams can link into a wide network of local services to meet the full range of people’s needs. By working together in one team, staff across different disciplines can communicate regularly, share knowledge and expertise and co-ordinate care planning and delivery
p. 6018
Some aspects of CCP are comparatively well researched, particularly hospital at home services for a variety of healthcare needs, where several systematic reviews exist. Other less-researched initiatives, particularly trusted assessors, step-down facilities and SPOA for social care, are well represented by UK initiatives. Indeed, so many local constituencies are experimenting with such models that it is questionable whether it is meaningful to single specific initiatives for particular attention. Clearly, it could be valuable to explore variations across different models of the same initiative and to undertake robust evaluations.
Almost all of the initiatives are not specifically ‘winter pressures’ approaches. However, we have identified their use as winter pressure measures or as recipients for winter funding. This fact has been used to identify the candidacy of initiatives in this report for which we have subsequently sought more substantive and plentiful evidence. A key evaluation issue relates to whether to undertake evaluation specifically of initiatives within a winter pressures context or whether to evaluate them more widely on the understanding that they may be particularly beneficial when the health system is under particular strain as is exemplified by winter pressures.
As with structural interventions, the evidence base is characterised by large numbers of case studies, often published online or presented at conferences, and relatively few peer-reviewed journal articles. The imperative to tackle urgent issues and to adopt initiatives that have proved promising elsewhere can be detected across the evidence base. We have identified a need for extensive and robust evaluation, which could then be targeted for consolidated learning through reviews of case studies or even systematic reviews. Again, there is methodological cause for concern in the likely presence of multiple biases such as early adopter bias, hero innovator bias and reporting bias. A further possibility relates to the fact that organisations that are encountering particularly severe problems may adopt multiple responses, meaning that the strength of the effect is not replicated across more uniform sites or that positive impact may be achieved by a ‘kitchen sink effect’ of multiple indistinguishable interventions that are introduced simultaneously.
As with the D2A literature within structural interventions, the hospital at home literature is associated with significant numbers of recent systematic reviews. Their value is again dissipated by the lack of a specific focus on addressing winter pressures, suggesting that further targeted evidence synthesis (perhaps using realist approaches to focus on the UK context) could be valuable. Certainly, the plethora of different initiatives with diverse labels suggests that a focus on common mechanisms would prove more useful than a diffuse investigation based on interventions.
Summary: integrated care
Approaches to IC operate at multiple organisational levels. Evidence from Scotland allows exploration of vertical integration between health and social care services and its impact on delayed discharges. Early experience from the vanguards also allows comparison of system-wide integration. Less transformative experiences of integration are seen when health and social care agencies seek to deliver approaches to discharge planning in a joint approach that works across the respective organisational boundaries. Finally, frontline instances of IC can be achieved when health and social care agencies are represented in joint operations. This final approach is exemplified by, for example, social care and voluntary agencies being represented at a local level in discharge ‘huddles’. Other approaches involve placing staff within a different organisational environment; for example by placing social workers within a hospital or by providing community access to acute hospital expertise. These types of initiative have tended to be discussed under the delivery site for the initiative, whether an acute hospital (covered under structural) or community provision.
Integrated care poses challenges in both achieving and measuring an impact. The complexity of interventions that work across organisational boundaries means that it can take some time to organise new pathways of lasting permanence. Alternatively, short-term initiatives may be able to achieve short wins but this impact is either not sustained or, more typically, is not reported over longer periods, making evaluation problematic. Generally, evaluation of organisational approaches to improved discharge planning is neither as wide-ranging nor as sustained as it needs to be to provide reliable evidence. Measurement of long-term outcomes is therefore required.
Positive reporting bias is particularly likely to occur within new initiatives for IC. Where multiple measures are reported, accounts focus on those indicators that have achieved a positive outcome. Where initiatives are able to report less demonstrable achievements, they may focus on qualitative aspects of the integration, in terms of both structure and outcome. In particular, reports of IC initiatives focus little attention on the hidden costs in terms of staff time in setting up initiatives and in managing organisational change.
Notwithstanding such caveats, the pursuit of IC is supported by several studies that have demonstrated positive results and by a wealth of anecdotal experience of the breakdown of health and social care communications between separate agencies. Simplifying communications and procedures carries an implicit driver towards improvement, whether or not achieved in the short term or sustained over a longer period.
The specific challenge in relation to IC once more lies in the difficulty in attributing the impact of IC interventions and initiatives specifically to benefits to acute care use during times of winter pressure. By implication, care has to be integrated as a permanent feature across all seasons and patterns of demand. Commentators have observed that the health and social care systems now face ‘winter pressures’ all year round, making IC interventions more apposite as a response to endemic health service challenges. The other implication relates to the scale of change often required for change to take place, particularly involving multiple stakeholders and organisations. While any attempts at improving information flow and communication and operation of shared processes are to be welcomed, the capacity of organisations to be able to invest time and effort in organisational change at a time of systemic overload has to be questioned. A form of ‘natural selection’ may therefore take place whereby the more easily achieved small-scale adaptation of existing systems may be privileged over more radical system-wide transformation.
A more detailed analytical review could analyse initiatives against a tightly defined and recognised classification of integration. More significantly, a realist synthesis could focus on shared mechanisms by which different levels of integration achieve improvements in outcomes relating to admission avoidance or reduction in delayed discharge.
Summary: targeting carers
Approaches to targeting carers tend to fall within two main types of response: reducing either demand per se or inappropriate demand by improving carer navigation across the community/acute margins or increasing carer resource and resilience by equipping them to handle demands that might otherwise draw upon hospital-based resources. One of the challenges of the latter approach lies in the fact that carers themselves have their own health and care needs. Placing extra demands on those who are already finding it challenging to cope may represent a short-term solution that reaps later negative dividends (e.g. in the carer requiring extra support at another time). At best, this may simply spread demands upon the health and social care system more evenly across the year – for example when the carer requires respite services at other times of the year. Whether such a ‘transferred need’ presents acutely or is managed and planned exerts a considerable difference in the success of such measures. Of more concern is when placing an extra burden on a carer results in an immediate breakdown of informal support, meaning that both patient and their carer make demands on the system at a time of winter crisis and perhaps for an extended period in contrast to an otherwise brief episode.
Carer education and carer preparation are generally targeted at the carer in advance of any challenging situation. Education may involve knowledge of what to do when faced with a particular crisis, thereby increasing carer resilience and reducing demand upon acute services, or it may involve increasing carer capacity to navigate the care system appropriately, leading to better targeting of need. Preparation may involve practical skills or competencies that reduce demand on formal carers; for example, in being able to change dressings, administer medication. In both cases, education and preparation typically take place at a time of ‘normal’ demand on the health and care system and needs can be planned and anticipated.
Carer respite may occur in response to an acute need or crisis or may form part of a planned or managed response. Respite can take place on a very short-term basis; for example, allowing carers an hour or two away from the demands of their informal care, or it can take place over an extended period, as with accommodating an annual one- or two-week holiday. Again, the assumption behind such interventions is that a planned and managed period of time will not only place less demand on the system than an acute crisis but that its overall duration will typically be shorter than otherwise accumulated. Carer support may either be episodic or ongoing. Carers may offer mutual and reciprocal support developing their own resources to relieve demands on formal care, or carer support may be provided by health professionals, with the assumption that these may have more capacity (e.g. if located within the community) than is available within the acute care system.
The challenge in relation to targeting carers lies in the difficulty in attributing the impact of interventions specifically to benefits to acute care during times of winter pressure. The value of informal care in general to the health and social care system is well recognised and has been quantified. However, this contribution is typically conceived as relating to the whole year around, not specifically to times of system pressure. Carer interventions can be attributed to winter pressures where specific winter pressure funding is targeted at carers as beneficiaries. The challenge for evaluation may lie in the reverse direction with benefits from specific winter pressure interventions for carers delivering benefits that persist beyond the critical winter pressure period. The artificial separation of budgets, both across purposes and across organisations makes attribution of benefit to carer interventions particularly challenging.
Targeting carers has its own separate research agenda aside from winter pressure responses. Almost all the initiatives are not specific ‘winter pressures’ approaches. However, we have identified their use as winter pressure measures or as recipients for winter funding. This fact has been used to identify the candidacy of initiatives in this report for which we have subsequently sought more substantive and plentiful evidence. As for other initiatives, a key evaluation issue relates to whether to undertake evaluation specifically of carer initiatives within a winter pressures context or whether to evaluate them more widely on the understanding that they may be particularly beneficial when the health system is under particular strain as exemplified by winter pressures.
Research priorities: an overarching research agenda
As suspected from the outset, we identified few initiatives specifically identified as a response to winter pressures. Conversely, many initiatives tackling admission avoidance or reduction of length of stay and delayed discharge attributed the response to numerous factors which included ‘winter pressures’ alongside multiple contextual factors, including an increasingly ageing population and increased demands on health services. The lack of specificity of these responses suggests that an exploration of underpinning mechanisms and how these might contribute to tackling winter pressures, and indeed, other peaks of demand, as with a realist synthesis may be particularly useful. Methodologically, one of the most effective ways of identifying interventions or initiatives in response to winter pressures was in ‘following the money’ (i.e. looking at reports of how health organisations allocated funds directly attributed as winter funding). We then worked from a list of cursorily identified initiatives and interventions to match to the underpinning evidence base of systematic reviews and major studies. Even here, though, it was challenging to separate interventions targeted at winter pressures from more opportunistic approaches to allocating extra monies. We also observed that evidence coverage was very uneven and variable, with some heavily used interventions being well frequently supported (e.g. hospital at home) and yet other, equally used responses being based on hardly any evidence.
Taken as a whole, the evidence base, as briefly reviewed under different intervention types in relation to discharge planning and IC more generally, confirms the research priorities identified in a recent scoping review. 3 Across the range of interventions and initiatives we found a dearth of studies that explored patient, family and provider needs and experiences, particularly during the development and implementation of initiatives aimed at improving delayed discharges. This lack has similarly been highlighted in a review of patient and caregiver experience of delayed discharge. 189 These perspectives are typically gathered in relation to experiencing the issues rather than gauging the response to specific interventions. The exploration of D2A is a notable exception to this. 185 As a consequence of this omission, the patient and carer perspective is often excluded from the development and documentation of best practice.
We also observed a shortage of studies that measured impact of initiatives and interventions over the long term. The evidence base performs more strongly in terms of promising ‘candidate’ interventions than it does in terms of tried and tested approaches. As a consequence, short-term results may appear promising, while the drivers are apparent and the staff committed to change. However, little evidence is available on longer-term sustainability. Not only is the evaluation period short but the evaluation frame is narrow, with a focus on more readily observable targeted change rather than on the wider impact across other sectors such as primary and community care. In this connection, our evidence synthesis extends the exclusive hospital focus of the scoping review3 to include primary and community care, voluntary agencies, social care and, specifically, IC. However, in relation to IC, as mentioned previously, our review had to effect an artificial separation between initiatives that harnessed some degree of integration at any of a number of levels (grouped by setting) and those explicitly badged under ‘integrated care’. The value of the research priorities identified for each intervention derives more from the collective picture rather than any one set of recommendations.
The evidence base sees increasing recognition that hospital avoidance and reduction in delayed discharge is a ‘wicked’ whole-system problem and therefore any lens of evaluation benefits from being targeted at interventions that are implemented and integrated across sectors. However our evidence summaries extend beyond the relatively well-trodden sectors of hospital, primary care, and home and community care, to include other parties including voluntary agencies, the private sector and agencies such as housing and the fire brigade. Such an approach is essential if one is to ‘get at the root of the problem and ensure the implementation of an initiative in one setting does not simply shift the problem to another’ (p. 25). 3
Similarly, our evidence summaries seeks to address the suggestion to include ‘initiatives that are more upstream in nature (e.g. hospital admission avoidance, ED diversion and delivery models that proactively address the health and social care needs of individuals in community settings)’ (p. 25). 3
Stratified evidence priorities
Specific research gaps are identified under each intervention category in the taxonomy. For convenience these are listed in categories and the main priorities are documented in Table 48.
| High priorities | Research priorities |
|---|---|
| CCP – private sector | High – few UK initiatives (implementation and research gap) |
| CCP – step-up facilities | |
| CSB – clinical audit | |
| CSB – protocols/guidelines | |
| CSB – quality improvement programmes | |
| CSB – quality management systems | |
| Integrated care discharge huddle | |
| S – bed management | High – few UK initiatives (implementation and research gap) with caveat that interventions may be described as discharge planning/co-ordination |
| S – extra service delivery | High – few UK initiatives (implementation and research gap) |
| S – governance | |
| S – monitoring and review | |
| S – same-day services | SDEC: high – few UK initiatives (implementation and research gap) Surgical hubs: high – few UK initiatives (implementation and research gap) |
| S – specialist units | Acute medical units: low. Other: high – few UK initiatives (implementation and research gap) |
| S – volunteers | High – few UK initiatives (implementation and research gap) |
Other priorities are documented in Table 49.
| Moderate priorities | Research gap |
|---|---|
| CCP – care homes | Moderate – few UK research studies but plentiful UK initiatives (research gap) |
| CCP – community teams | |
| CCP – home care | |
| CCP – hospital at home | |
| CCP – other agencies | |
| CCP – rehabilitation, recovery and reablement | |
| CCP – single point response | |
| CCP – step-down beds | |
| CCP – telecare | |
| CCP – virtual hospital/virtual ward | |
| CCP – voluntary services | Moderate – few UK research studies but plentiful UK initiatives (research gap) |
| CSB – education of staff | |
| S – digital and data | |
| S – discharge co-ordinators | |
| S – D2A | |
| S – patient flow | Moderate – few UK initiatives (implementation and research gap) but one UK research study and a recent systematic review |
| S – prioritisation and triage | Moderate – few UK research studies but plentiful UK initiatives (research gap, synthesis gap) |
| S – seven-day services | |
| CCP – rapid response/see and treat | Moderate – no/poor systematic review but plentiful international research studies (synthesis gap) |
Recommendations for further research
The scoping review, published in 2021, concludes by identifying a potential need for ‘future research to consider a realist review of the literature on delayed hospital discharge to understand the context, mechanisms of impact, outcomes and theories of change, given that addressing a delayed discharge is a complex problem’ (p. 25). 3 Our own exploration has confirmed both this need and its potential contribution. In providing brief summaries of how the individual interventions and initiatives might contribute to relieving winter pressures, we have identified certain common underpinning mechanisms such as reassurance of the older person, establishment of clinical need, provision of a second/specialist opinion, transfer of venue and so on, which could be operationalised well within a realist review.
We would add that rather than focus on a ‘single sector and reactive approach to addressing delayed discharge’ (p. 26),3 our evidence summaries provide initial justification for including upstream anticipatory approaches viewed holistically across the widest possible array of sectors as they contribute within a whole system evaluation frame. However, it must be noted that, to remain both feasible and productive, the holistic lens required will necessitate a clear targeting and prioritisation of a focus for synthesis. The potential contribution of a realist approach is further attested to by identification of an existing realist synthesis in the specific area of intermediate care. 174 Another option discussed with the stakeholder is an implementation review of discharge interventions at the hospital/social care interface. The implementation review would focus on the factors that facilitate the implementation of the discharge interventions and their transferability, spread and sustainability using implementation studies where available or implementation data from other studies.
Strengths and limitations
This review benefitted from ongoing stakeholder involvement throughout the project to ensure that the deliverable is closely targeted to the requirements of the commissioner. Winter pressures is a broad topic that runs the full gamut of public health and health service provision from upstream public health approaches through to delayed discharge and overwhelmed capacity of social care provision. Detailed consultation helped to focus on the specific issues that have been found to be of strategic importance, as blockages to the entire system, that relate to health services reconfiguration and that command ongoing press and public interest and concern. Therefore, a strength of this report is its specific focus on discharge arrangements and on IC.
It soon became apparent, however, that health service and social care use takes place within a complex whole system. Focusing attention only a model that assumes admission as an inpatient as a default fails to capitalise on developments such as same-day services that seek to bypass any form of overnight stay. Furthermore, assuming presentation to an emergency department (ED) fails to take into account use of other points of access, particularly those that aim at community-based hospital avoidance. A strength of this review is its facility to extend beyond hospital-based interventions, a limitation openly acknowledged for previous scoping reviews. Indeed, inclusion of a significant body of community and voluntary service initiatives moves much closer to the concept of IC, although not necessarily badged as such. Broadening the coverage of the taxonomy, even given exclusion of any workforce or modelling interventions, necessarily holds consequences in the inevitable trade-off between breadth and depth. The review team was only able to focus on indicative items of evidence, namely systematic reviews and major UK studies. Between these items of evidence, privileged for rigour and relevance respectively, and the many identified case studies, privileged for currency and creativity, lies an extensive unacknowledged supply of studies exploring various aspects of admission avoidance, hospital discharge and IC provision. To this extent, the picture afforded by the individual intervention summaries is more a guide to evidence availability rather than a comprehensive snapshot of research activity. We encourage any research team that follows up any individual intervention summary to invest significant time in developing a more comprehensive picture of that topic. Nevertheless, the purpose of this report is to indicate promising areas for further research activity and so does not require a comparably comprehensive approach to a review that identifies effective interventions.
This review was conducted by three experienced reviewers with a collective portfolio across multiple health services and delivery review topics. This expertise was particularly important in this context because of the premium that the methodology placed on rapid identification and summary of indicative items – a particular strength of all three individuals. The three reviewers possessed the skillset to evaluate and appraise individual reviews and studies as identified but the rapid timescale and broad coverage of the review meant that this could not be performed formally and comprehensively for all retrieved items and could only be carried out opportunistically as reading of specific individual studies took place. The short timescale also meant that the team had to identify a collective point at which to draw a line under identification of further initiatives and to move on to taking stock of items already found and documenting their characteristics. In addition, time spent on each intervention type could not be standardised and so variability in coverage and depth reflects both different levels of research activity and different degrees of ease of study identification.
Finally, we must acknowledge the limitations of the taxonomy. In seeking to characterise each intervention within at least one place within the taxonomy, we have often simplified their characteristics. Interventions are frequently multicomponent and therefore typically include multiple headings from the taxonomy. In a few cases, where interventions possessed multiple defining characteristics or where discrete evidence on the intervention was less plentiful, we would duplicate entries across the taxonomy. However, our general intention was to try to make the intervention categories self-defining and discrete. A notable exception was the cross-boundary work on hospital avoidance, which necessarily appears in both structural interventions and community provision – in the former instance having the principal interpretation of admission avoidance and in the latter having the broader interpretation of acute hospital avoidance (both EDs and inpatient admission). In pursuing the further application of the taxonomy, we would encourage indexing interventions exhaustively across multiple taxonomy headings, potentially as a prequel to further work unpacking the mechanisms that underpin multiple intervention types attesting to the likely value of a planned realist approach.
Conclusions
We conducted a mapping review of evidence specifically related to winter pressures. It was challenging to attribute initiatives as a specific response to the winter pressures agenda, given both the lack of specificity and the artificiality of winter pressures as a binary, time-defined construct. This conception becomes progressively less useful as system pressures become a perennial issue, not a seasonal one. Few initiatives identified were specifically implemented as a response to winter pressures.
In seeking an evidence base, we extended a process of evidence summaries to general initiatives used to relieve pressures on admission and discharge. Hospital at home and D2A were well-supported initiatives but other responses, while also heavily used, were based on limited evidence. Across all intervention groups, we confirmed the lack of studies considering patient, family and provider needs when developing interventions aimed at improving delayed discharge; identified from previous reviews of discharge and of patient and care involvement. This is a particularly important omission, given the heavy dependence of formal healthcare systems on the contribution of informal caregivers, whether when in hospital or in the community.
Additionally, few studies measure the impact of interventions over a long time. Short-term results can appear promising, but evidence for longer-term sustainability is notably absent. Hospital avoidance and delayed discharge requires a whole-system approach. We conclude, alongside a previous scoping review, that it is imperative to consider the whole system to ensure that implementing an initiative in one setting does not simply move the problem to another setting.
Patient and public involvement
Stakeholder involvement was undertaken to ensure that the review was informed by the views and experiences of stakeholders at the Department of Health and Social Care and NICE, as well as with a standing advisory group of patients and cares.
The consultation aimed to:
-
highlight the practical and personal challenges experienced by those planning or using health services during times of exceptional demand
-
inform the second phase of our searches by identifying specific strategies, initiatives and interventions that target discharge planning and IC in the context of winter pressures
-
identify gaps in the literature with a view to compiling a future research agenda.
In the review proposal, we aimed to consult with stakeholders from the Department of Health and Social Care and NICE and a standing advisory group of patient and carers. The key stakeholders were involved in the proposal for review and commented on a draft map when they asked for findings to be included from research.
A standing advisory group of patients and carers met once during the project to discuss the group’s knowledge about different interventions that could be used to mitigate winter pressures and the research team found it especially interesting to elicit group opinions on which interventions might require research funding. The rapid nature of the project meant that discussions with the standing advisory group had to be concentrated within a single meeting. For a long project, we would include the standing advisory group earlier, enabling them to input into the scope of the review and discuss review findings, in particular through discussing the research gaps identified.
Equality, diversity and inclusion
As a secondary data study, our review did not include any research participants. We were, however, inclusive in the studies we selected.
Additional information
Contribution of authors
Anna Cantrell (https://orcid.org/0000-0003-0040-9853) (Research Fellow) was the lead reviewer and was involved in protocol development, information retrieval, study selection, data extraction and report writing.
Duncan Chambers (https://orcid.org/0000-0002-0154-0469) (Research Fellow) was involved in study selection, data extraction and report writing.
Andrew Booth (https://orcid.org/0000-0003-4808-3880) (Professor in Evidence Synthesis) was the methodological adviser and lead protocol developer, was involved in study selection, data extraction and report writing, and was the guarantor of the review.
All authors commented on drafts of the protocol and report.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/KRWH4301.
Primary conflicts of interest: Andrew Booth is a former member of the NIHR HS&DR Funding Committee and the NIHR Systematic Reviews Advisory Group, and Convenor of the Cochrane Qualitative and Implementation Methods Group.
Data-sharing statement
Any additional data not included in this report and its appendices are available on request. All queries should be submitted to the corresponding author.
Ethics statement
This review did not involve the collection or analysis of any data that were not included in previously published research in the public domain. It was therefore exempt from formal ethical review by the University of Sheffield Ethics Committee.
Information governance statement
NIHR is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under Data Protection legislation NIHR is the Data Processor; the Department for Health and Social Care (DHSC) is the Data Controller, and we process personal data in accordance with their instructions. You can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for DHSC’s Data Protection Officer here.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the HSDR programme or the Department of Health and Social Care. This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Fisher E, Dorning H. Winter Pressures: What’s Going on Behind the Scenes. London: Nuffield Trust; 2016.
- Iacobucci G. COVID-19: Lack of testing led to patients being discharged to care homes with virus, say auditors. Br Med J Publishing Group 2020;369.
- Cadel L, Guilcher SJ, Kokorelias KM, Sutherland J, Glasby J, Kiran T, et al. Initiatives for improving delayed discharge from a hospital setting: a scoping review. BMJ Open 2021;11.
- James KL, Randall NP, Haddaway NR. A methodology for systematic mapping in environmental sciences. Environ Evid 2016;5:1-13.
- Parker SG, Peet SM, McPherson A, Cannaby AM, Abrams K, Baker R, et al. A systematic review of discharge arrangements for older people. Health Technol Assess 2002;6:1-183.
- Yap G, Melder A. Hospital Winter Strategies: A Rapid Literature Review. Melbourne, Australia: Centre for Clinical Effectiveness, Monash Health; 2015.
- Care Quality Commission . COVID-19 Insight. Winter Pressures for Urgent and Emergency Care 2021.
- Peddie GJ, Gordon C. investigating immediate and intermediate patient outcomes following transfer from the acute medicine unit at the Western General Hospital, Edinburgh: a prospective cohort study. J Acute Med 2018;8:109-18.
- Tampubolon L. Bed management strategy for overcrowding at the emergency department: a systematic review. KnE Life Sci 2018;4:50-9. https://doi.org/10.18502/kls.v4i9.3557.
- Coleman A, Croke S, Checkland K. Improving care in care homes: what can Primary Care Networks learn from the Vanguards?. J Integr Care 2020;29:85-96. https://doi.org/10.1108/jica-06-2020-0037.
- Hanratty B, Craig D, Brittain K, Spilsbury K, Vines J, Wilson P. Innovation to enhance health in care homes and evaluation of tools for measuring outcomes of care: rapid evidence synthesis. Health Serv Deliv Res 2019;7:1-178. https://doi.org/10.3310/hsdr07270.
- Matthews PM, Block VJ, Leocani L. E-health and multiple sclerosis. Curr Opin Neurol 2020;33:271-6. https://doi.org/10.1097/wco.0000000000000823.
- NHS England, NHS Improvement . The Framework for Enhanced Health in Care Homes 2016.
- Capewell C, Bolton D, Wilkinson K, Hargreaves V. P-119 Solidarity, skills and support- St Catherine’s (Lancashire) ‘winter pressures’ care homes project. BMJ Support Palliat Care n.d.;11:A51-2. https://doi.org/10.1136/spcare-2021-hospice.136.
- Local Government Association . Managing Transfers of Care – A High-Impact Change Model: Changes 1–10 2018. www.local.gov.uk/our-support/partners-care-and-health/care-and-health-improvement/working-hospitals/managing-transfers-of-care/about (accessed 20 February 2024).
- Edinburgh Integration Joint Board . Evaluation of Winter Planning 2020 21 2021.
- Local Government Association . High Impact Change Model: Managing Transfers of Care 2018.
- Charles A, Ham C, Baird B, Alderwick H, Bennett L. Reimagining Community Services: Making the most of our assets. King’s Fund; 2018.
- Wilkinson E. NHS looks to pharmacy as it faces a tough winter. Pharmaceutical J 2018;301. https://doi.org/10.1211/PJ.2018.20205839.
- Malone S, Hayes M. Integrated care partnerships Northern Ireland: leading integration; delivering better outcomes. Int J Integr Care 2017;17. https://doi.org/10.5334/ijic.3544.
- Dedeu T. Developing integrated health and social care models in Scotland. Eurohealth 2016;22:11-5.
- Kjelsnes A, Feiring E. Models of integrated care for older people with frailty: a horizon scanning review. BMJ Open 2022;12:e0601-42. https://doi.org/10.1136/bmjopen-2021-060142.
- Morciano M, Checkland K, Billings J, Coleman A, Stokes J, Tallack C, et al. New integrated care models in England associated with small reduction in hospital admissions in longer-term: a difference-in-differences analysis. Health Policy 2020;124:826-33. https://doi.org/10.1016/j.healthpol.2020.06.004.
- Morciano M, Checkland K, Durand MA, Sutton M, Mays N. Comparison of the impact of two national health and social care integration programmes on emergency hospital admissions. BMC Health Serv Res 2021;21. https://doi.org/10.1186/s12913-021-06692-x.
- Wolfe I, Satherley RM, Scotney E, Newham J, Lingam R. Integrated care models and child health: a meta-analysis. Pediatrics 2020;145. https://doi.org/10.1542/peds.2018-3747.
- Devine J. A System Approach to the Demand Crunch. London: NHS Confederation; 2021.
- Wall O, O’Sullivan E. Teaching acute hospital staff and students about patient flow. Br J Nurs 2021;30:812-19. https://doi.org/10.12968/bjon.2021.30.13.812.
- Windle K, Essam N, Vos J, Godoy Caballero AL, Phung V-H, Sirdifield C, et al. Admission Avoidance Programme: Final report. Lincoln: University of Lincoln, Community and Health Research Unit; 2014.
- Rodman A. Identifying and managing seasonal exacerbations of COPD. Independent Nurse 2021;2021:14-8. https://doi.org/10.12968/indn.2021.11.14.
- Walters C, Youl M, Okin R, Christofi G, Warwick H, Nathan M, et al. The burden of under recognised social complexity in the hyperacute phase of the stroke pathway. experience on an acute step-down rehabilitation unit during winter pressures/COVID-19. Eur Stroke J 2022;7:1-41.
- NHS Confederation . System Under Strain: Why Demand Pressures Are More Than a Winter Phenomenon 2019. www.nhsconfed.org/publications/system-under-strain (accessed 22 February 2024).
- Unnewehr M, Schaaf B, Marev R, Fitch J, Friederichs H. Optimizing the quality of hospital discharge summaries–a systematic review and practical tools. Postgrad Med 2015;127:630-9.
- Mackintosh S. An Evaluation of the Dolphin Society Funded WE Care & Repair (Bristol) Home From Hospital Service. Bristol: West of England Care & Repair; 2016.
- Atkin C, Riley B, Sapey E. How do we identify acute medical admissions that are suitable for same day emergency care?. Clin Med J 2022;22:131-9.
- Care Quality Commission . Collaboration in Urgent and Emergency Care 2022. www.cqc.org.uk/publications/themes-care/collaboration-urgent-emergency-care (accessed 21 February 2024).
- Shepperd S, Butler C, Cradduck-Bamford A, Ellis G, Gray A, Hemsley A, et al. Is comprehensive geriatric assessment admission avoidance hospital at home an alternative to hospital admission for older persons? A randomized trial. Ann Intern Med 2021;174:889-98. https://doi.org/10.7326/M20-5688.
- Shepperd S, Cradduck-Bamford A, Butler C, Ellis G, Godfrey M, Gray A, et al. Hospital at Home admission avoidance with comprehensive geriatric assessment to maintain living at home for people aged 65 years and over: a RCT. Health Soc Care Del Res 2022;10:1-124. https://doi.org/10.3310/htaf1569.
- Leong MQ, Lim CW, Lai YF. Comparison of Hospital-at-Home models: a systematic review of reviews. BMJ Open 2021;11:e043285-85. https://doi.org/10.1136/bmjopen-2020-043285.
- Waddington E, Henwood M. Home and away: home from hospital, progress and prospects. J Integr Care 2003;11:40-2. https://doi.org/10.1108/14769018200300057.
- Hollinghurst J, Fry R, Akbari A, Watkins A, Williams N, Hillcoat-Nallétamby S, et al. Do home modifications reduce care home admissions for older people? A matched control evaluation of the Care & Repair Cymru service in Wales. Age Ageing 2020;49:1056-61. https://doi.org/10.1093/ageing/afaa158.
- Wolton JL. ‘We Are Probably Wales’ Best Kept secret’: An Exploration of the Role of Care &Amp; Repair Cymru Caseworkers in Facilitating Independent Living for Older People in Wales 2018. https://doi.org/10.23889/suthesis.49017.
- Goncalves-Bradley DC, Lannin NA, Clemson L, Cameron ID, Shepperd S. Discharge planning from hospital. Cochrane Database Syst Rev 2022;2. https://doi.org/10.1002/14651858.CD000313.pub6.
- Pereira P, Shah A. London: NHS Confederation; 2022.
- Oliver D. David Oliver: is hospital avoidance an elusive holy grail?. BMJ 2019;364. https://doi.org/10.1136/bmj.l746.
- Oliver D. David Oliver: avoiding hospital admission—are we really falling short?. BMJ 2019;364. https://doi.org/10.1136/bmj.l747.
- National Institute for Heath and Care Excellence . Emergency and Acute Medical Care in Over 16s: Service Delivery and Organisation 2018. www.nice.org.uk/guidance/ng94 (accessed 22 February 2024).
- Mahmood L, Morris S, Stanford-Beale R. Evaluation of Safe & Well Visits 2019/20. Maidstone: Kent Fire and Rescue Service; 2020.
- Academy of Medical Sciences . COVID-19: Preparing for the Future: Looking Ahead to Winter 2021 22 and Beyond 2021.
- Yennaram M, Ranachan H, Dyer R, Mohan V. Impact of late shift rapid response team (RRT) input on length of stay and discharge destination in emergency care. Med Health 2020;15:215-23.
- Academy of Medical Sciences . Academy of Medical Sciences Report: Preparing for a Challenging Winter 2020 21: Preparing for a Challenging Winter 2020 21 2020.
- Zonneveld N, Driessen N, Stussgen RAJ, Minkman MMN. Values of integrated care: a systematic review. Int J Integr Care 2018;18. https://doi.org/10.5334/ijic.4172.
- Ellis G, Langhorne P. Comprehensive geriatric assessment for older hospital patients. Br Med Bull 2005;71:45-59. https://doi.org/10.1093/bmb/ldh033.
- Woodward M, Proctor N. Avoiding A&E Through Rapid Response Teams and See and Treat Models: A Rapid Review of Existing Evidence. London: NHS England; 2016.
- Mahase E. NHS England announces ‘data driven war rooms’ to tackle winter pressures. BMJ 2022;379. https://doi.org/10.1136/bmj.o2515.
- McGavock R. Falls response service: a multidisciplinary response to 999 falls. Physiotherapy 2020;107. https://doi.org/10.1016/j.physio.2020.03.240.
- McNamara R, Donnelly K, Boyle N, Menzies D, Hollywood R, Little E, et al. Community frailty response service: the ED at your front door. Emerg Med J 2020;37:714-6. https://doi.org/10.1136/emermed-2020-210005.
- Baxter S, Johnson M, Chambers D, Sutton A, Goyder E, Booth A. The effects of integrated care: a systematic review of UK and international evidence. BMC Health Serv Res 2018;18:1-13.
- Francis J, Fisher M, Rutter D. Reablement: A cost-effective route to better outcomes. London: Social Care Institute for Excellence; 2011.
- Ariss SM, Enderby PM, Smith T, Nancarrow SA, Bradburn MJ, Harrop D, et al. Secondary analysis and literature review of community rehabilitation and intermediate care: an information resource. Health Serv Deliv Res 2015;3:1-180. https://doi.org/10.3310/hsdr03010.
- Gilbert P. Coming home: making reablement and rehabilitation happen in Worcestershire. J Integr Care 2000;8:40-4. https://doi.org/10.1108/14769018200000043.
- Goodison W, Lakra C, Okin R, Christofi G, Stevenson V, Farrell R, et al. Improving stroke patient flow during the COVID-19 pandemic using daily multidisciplinary neuronavigation: a novel north central London winter pressures project. Eur Stroke J 2021;6:3-568.
- Evans N. Preparation for winter pressures is ‘not enough’, warns NHS Providers. Ment Health Pract 2017;21:8-9. https://doi.org/10.7748/mhp.21.2.8.s8.
- NHS Providers . NHS Providers Briefing: The Real Story of Winter 2018 19 2019.
- Ritchie L. NHS Scotland Redesign of Urgent Care Second National Staging Report: April–September 2021 2021. www.gov.scot/publications/nhs-scotland-redesign-urgent-care-second-national-staging-report/documents (accessed 22 February 2024).
- NHS Improving Quality . Pennine Acute Hospitals NHS Trust: Nurse Led Triage, Assessment and Treatment of Ambulatory Patients Referred from Emergency Department and GPs 2017. www.southportandformbyccg.nhs.uk/media/1119/governing-body-march-2015-part-b.pdf (accessed 28 February 2024).
- Khan M, Khawar H, Perkins R, Pardiwala A. The Positive Impact of GIRFT (getting It Right First Time) on Arthroplasty Services in Times of COVID-19. Ann Med Surg (Lond) 2022;77.
- Jones E. Winter is Coming. HealthTech is Here. New York: Demos; 2018.
- Eardley I. Tackling the backlog. Bull R Coll Surg Engl 2022;104:224-7. https://doi.org/10.1308/rcsbull.2022.92.
- Wenzel L, Evans H. Clicks and Mortar: Technology and the NHS Estate. London: King’s Fund; 2019.
- Cooper M. Acute medicine clinics: the pathway to earlier discharge?. Clin Med J (Lond) 2019;19:S88-9. https://doi.org/10.7861/clinmedicine.19-2-s88.
- Southport and Formby Clinical Commissioning Group . Governing Body March 2015 Part B 2015. www.southportandformbyccg.nhs.uk/media/1119/governing-body-march-2015-part-b.pdf (accessed 28 February 2024).
- Reid LE, Dinesen LC, Jones MC, Morrison ZJ, Weir CJ, Lone NI. The effectiveness and variation of acute medical units: a systematic review. Int J Qual Health Care 2016;28:433-46.
- Srikumar B, Perianayagam GR, Narayan P, Pawar R, Antapur P. 1159 ring-fenced arthroplasty unit: the need of the hour during winter and a pandemic crisis. Br J Surg 2021;108. https://doi.org/10.1093/bjs/znab259.767.
- van Galen LS, Lammers EM, Schoonmade LJ, Alam N, Kramer MH, Nanayakkara PW. Acute medical units: the way to go? A literature review. Eur J Intern Med 2017;39:24-31. https://doi.org/10.1016/j.ejim.2016.11.001.
- Ferguson F. Physiotherapists in ED: a city wide service supporting board performance, government targets, professional growth and most importantly patient care. Physiotherapy 2020;107.
- Rickards E, Ascough L, Sibley S, Hampson O, Gossage E. The SWISS Nurse; respiratory nursing care without any borders. An admission avoidance winter pressure initiative. Eur Respiratory Soc 2021;58.
- Scriven N. Capacity issues need to be tackled by looking at all of acute provision. Br J Hosp Med (Lond) 2018;79:304-5. https://doi.org/10.12968/hmed.2018.79.6.304.
- Atey TM, Peterson GM, Salahudeen MS, Bereznicki LR, Wimmer BC. Impact of pharmacist interventions provided in the emergency department on quality use of medicines: a systematic review and meta-analysis. Emerg Med J 2022;40:120-7.
- Hohl CM, Wickham ME, Sobolev B, Perry JJ, Sivilotti ML, Garrison S, et al. The effect of early in-hospital medication review on health outcomes: a systematic review. Br J Clin Pharmacol 2015;80:51-6. https://doi.org/10.1111/bcp.12585.
- Vera San Juan N, Clark SE, Camilleri M, Jeans JP, Monkhouse A, Chisnall G, et al. Training and redeployment of healthcare workers to intensive care units (ICUs) during the COVID-19 pandemic: a systematic review. BMJ Open 2022;12. https://doi.org/10.1136/bmjopen-2021-050038.
- Nelson M, Armas A, Thombs R, Singh H, Fulton J, Cunningham HV, et al. Synthesising evidence regarding hospital to home transitions supported by volunteers of third sector organisations: a scoping review protocol. BMJ Open 2021;11. https://doi.org/10.1136/bmjopen-2021-050479.
- NHS England 2021.
- NHS England . Standard Guidance: Ambulance Clinician (on Scene) Referral to Same Day Emergency Care 2021.
- Royal College of Emergency Medicine . The RCEM Ambulatory Emergency Care Toolkit: Delivering Same Day Emergency Care from the ED 2019.
- Royal College of Physicians of Edinburgh, Society for Acute Medicine . Standards for Ambulatory Emergency Care: Report of a Working Group for Royal College of Physicians of Edinburgh and Society for Acute Medicine 2019. www.acutemedicine.org.uk/download/standards-for-ambulatory-emergency-care (accessed 22 February 2024).
- NHS Improvement . Ambulatory Emergency Care Guide. Same Day Emergency Care: Clinical Definition, Patient Selection and Metrics 2018.
- Pincombe A, Schultz TJ, Hofmann D, Karnon J. Economic evaluation of a medical ambulatory care service using a single group interrupted time‐series design. J Eval Clin Pract 2022;29:329-40.
- Ash A. Ambulatory care: to bed, or not to bed. Future Healthc J 2019;6:54-5.
- Varrier S. Introducing a medical ambulatory care service. Future Healthc J 2019;6.
- Ali A, Karmani J. 13 Audit of a newly developed ambulatory care service at Diana Princess of Wales Hospital Grimsby UK. Postgrad Med J 2018;94. https://doi.org/10.1136/postgradmedj-2018-fpm.24.
- Ambulatory Emergency Care Network . AECAP Case Studies 2019. www.ambulatoryemergencycare.org.uk/Programmes/AEC-Accelerator-Programme/AECAP-Case-Studies (accessed 22 February 2024).
- Getting It Right First Time . Design and Layout of Elective Surgical Hubs: A Guide for NHS Systems and Regions to Support Planning of Effective Surgical Hubs 2022.
- Royal College of Surgeons of England, Strategy Unit . The Case for Surgical Hubs 2022.
- Royal College of Physicians 2018.
- National Institute for Health and Care Excellence . Chapter 24: Assessment Through Acute Medical Units. Emergency and Acute Medical Care in Over 16s: Service Delivery and Organisation 2018. www.nice.org.uk/guidance/ng94/evidence/24.assessment-through-acute-medical-units-pdf-172397464637 (accessed 22 February 2024).
- Michael A, Ijaola F. P406: frail elderly short stay unit; a model of emergency care for older people. Eur Geriatr Med 2014;5.
- Williams S, Morrissey AM, Steed F, Leahy A, Shanahan E, Peters C, et al. Early supported discharge for older adults admitted to hospital with medical complaints: a systematic review and meta-analysis. BMC Geriatr 2022;22. https://doi.org/10.1186/s12877-022-02967-y.
- Dimla B, Parkinson L, Wood D, Powell Z. Hospital discharge planning: a systematic literature review on the support measures that social workers undertake to facilitate older patients’ transition from hospital admission back to the community. Australas J Ageing 2022;42:20-33. https://doi.org/10.1111/ajag.13138.
- Doshmangir L, Khabiri R, Jabbari H, Arab-Zozani M, Kakemam E, Gordeev VS. Strategies for utilisation management of hospital services: a systematic review of interventions. Glob Health 2022;18:1-39.
- National Institute for Health and Care Excellence . Transition Between Inpatient Hospital Settings and Community or Care Home Settings for Adults With Social Care Needs 2015. www.nice.org.uk/guidance/ng27 (accessed 22 February 2024).
- Glasper A. Ensuring smooth transition of frail elderly patients from hospital to community. Br J Nurs 2019;28:1338-9. https://doi.org/10.12968/bjon.2019.28.20.1338.
- Harris R, Ashton T, Broad J, Connolly G, Richmond D. The effectiveness, acceptability and costs of a hospital-at-home service compared with acute hospital care: a randomized controlled trial. J Health Serv Res Policy 2005;10:158-66. https://doi.org/10.1258/1355819054338988.
- Jeffery S, MacInnes J, Bertini L, Walker S. Does a discharge to assess programme introduced in England meet the quadruple aim of service improvement?. J Integr Care 2023;31:16-25. https://doi.org/10.1108/JICA-02-2022-0018.
- Gadsby EW, Wistow G, Billings J. A critical systems evaluation of the introduction of a ‘discharge to assess’ service in Kent. Crit Soc Policy 2022;42:671-94. https://doi.org/10.1177/02610183211065028.
- Offord N, Harriman P, Downes T. Discharge to assess: transforming the discharge process of frail older patients. Future Hosp J 2017;4:30-2. https://doi.org/10.7861/futurehosp.4-1-30.
- Edwards P, Anwer S. The affect of a pilot discharge to assess process on unscheduled care performance. Int J Integr Care 2019;19. https://doi.org/10.5334/ijic.s3334.
- Lawlor L, O’Reilly C, Platts A, Myler L. 32 exploring the efficacy of a discharge to assess model using a combined approach involving FITT, OPAT and CIT. Age Ageing 2019;48:iii17-65.
- Conneely M, Leahy S, Dore L, Trepel D, Robinson K, Jordan F, et al. The effectiveness of interventions to reduce adverse outcomes among older adults following Emergency Department discharge: umbrella review. BMC Geriatr 2022;22. https://doi.org/10.1186/s12877-022-03007-5.
- Platzer E, Singler K, Dovjak P, Wirnsberger G, Perl A, Lindner S, et al. Evidence of inter-professional and multi-professional interventions for geriatric patients: a systematic review. Int J Integr Care 2020;20. https://doi.org/10.5334/ijic.4683.
- Sethi S, Boulind C, Reeve J, Carney A, Bruijns S. Effect of hospital interventions to improve patient flow on emergency department clinical quality indicators. Emerg Med J 2020;37:787-92.
- Ahlin P, Almstrom P, Wanstrom C. When patients get stuck: a systematic literature review on throughput barriers in hospital-wide patient processes. Health Policy 2022;126:87-98. https://doi.org/10.1016/j.healthpol.2021.12.002.
- Coffey A, Leahy-Warren P, Savage E, Hegarty J, Cornally N, Day MR, et al. Interventions to promote early discharge and avoid inappropriate hospital (re)admission: a systematic review. Int J Environ Res Public Health 2019;16. https://doi.org/10.3390/ijerph16142457.
- Kattel S, Manning DM, Erwin PJ, Wood H, Kashiwagi DT, Murad MH. Information transfer at hospital discharge: a systematic review. J Patient Saf 2020;16:e25-33. https://doi.org/10.1097/PTS.0000000000000248.
- Mehta N, Pandit A. Concurrence of big data analytics and healthcare: a systematic review. Int J Med Inform 2018;114:57-65. https://doi.org/10.1016/j.ijmedinf.2018.03.013.
- Chan A, Green K, Kontra K, Chapman T, Wewerka C, Statham A. The Royal Berkshire NHS Foundation Trust outpatient services transformation programme to improve quality and effectiveness of patient care. Future Healthc J 2022;9:255-61. https://doi.org/10.7861/fhj.2021-0150.
- NHS England . Recruiting and Managing Volunteers in NHS Providers, A Practical Guide 2017. www.england.nhs.uk/publication/recruiting-and-managing-volunteers-in-nhs-providers-a-practical-guide (accessed 20 February 2024).
- Boyle D, Crilly T, Malby R. Can Volunteering Help Create Better Health and Care: An evidence review. London: South Bank University; 2017.
- Ross S, Fenney D, Ward D, Buck D. The Role of Volunteers in the NHS. London: King’s Fund; 2018.
- Huntley AL, Chalder M, Shaw ARG, Hollingworth W, Metcalfe C, Benger JR, et al. A systematic review to identify and assess the effectiveness of alternatives for people over the age of 65 who are at risk of potentially avoidable hospital admission. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-016236.
- Graverholt B, Forsetlund L, Jamtvedt G. Reducing hospital admissions from nursing homes: a systematic review. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-36.
- Novak A, Cherry J, Ali N, Smith I, Bowen J, Ray J, et al. Point-of-care blood testing with secondary care decision support for frail patients. J Paramed Pract 2022;14:54-62. https://doi.org/10.12968/jpar.2022.14.2.54.
- Singer M. P-123 The role of a paramedic in a community hospice/palliative/end-of-life care team. BMJ Supportive Palliat Care 2021;11. https://doi.org/10.1136/spcare-2021-Hospice.140.
- Kobewka D, Mulpuru S, Chassé M, Thavorn K, Lavallée L, English S, et al. Predicting the need for supportive services after discharged from hospital: a systematic review. BMC Health Res Serv 2020;20. https://doi.org/10.1186/s12913-020-4972-6.
- Richardson A, Blenkinsopp A, Downs M, Lord K. Stakeholder perspectives of care for people living with dementia moving from hospital to care facilities in the community: a systematic review. BMC Geriatr 2019;19. https://doi.org/10.1186/s12877-019-1220-1.
- Evans G. Factors influencing emergency hospital admissions from nursing and residential homes: positive results from a practice-based audit. J Eval Clin Pract 2011;17:1045-9. https://doi.org/10.1111/j.1365-2753.2010.01471.x.
- Kandiah J, Nazar H, Wright D. Formative service evaluation of transfer of care service for care home residents after hospital discharge. Int J Pharm Pract 2022;30:394-7. https://doi.org/10.1093/ijpp/riac045.
- Wilkinson T, North M, Bourne SC. Reducing hospital admissions and improving the diagnosis of COPD in Southampton City: methods and results of a 12-month service improvement project. NPJ Prim Care Respir Med 2014;24. https://doi.org/10.1038/npjpcrm.2014.35.
- O’Connell Francischetto E, Jones J, Davies S, Allen K, Combes G, Damery S. 682 impact of discharge interventions for older patients leaving hospital: a systematic review of reviews. Age Ageing 2022;51. https://doi.org/10.1093/ageing/afac036.682.
- Lowthian JA, McGinnes RA, Brand CA, Barker AL, Cameron PA. Discharging older patients from the emergency department effectively: a systematic review and meta-analysis. Age Ageing 2015;44:761-70. https://doi.org/10.1093/ageing/afv102.
- Halliwell A. COVID-19 insight: winter pressures on urgent and emergency care. Nurs Resident Care 2021;23:1-4. https://doi.org/10.12968/nrec.2021.23.4.10.
- Malik AH, Malik SS, Aronow WS. MAGIC (Meta-analysis And oriGinal Investigation in Cardiology) investigators . Effect of home-based follow-up intervention on readmissions and mortality in heart failure patients: a meta-analysis. Future Cardiol 2019;15:377-86. https://doi.org/10.2217/fca-2018-0061.
- Hamline MY, Speier RL, Vu PD, Tancredi D, Broman AR, Rasmussen LN, et al. Hospital-to-Home interventions, use, and satisfaction: a meta-analysis. Pediatrics 2018;142. https://doi.org/10.1542/peds.2018-0442.
- Allen J, Hutchinson AM, Brown R, Livingston PM. User experience and care for older people transitioning from hospital to home: patients’ and carers’ perspectives. Health Expect 2018;21:518-27. https://doi.org/10.1111/hex.12646.
- Van Spall HGC, Rahman T, Mytton O, Ramasundarahettige C, Ibrahim Q, Kabali C, et al. Comparative effectiveness of transitional care services in patients discharged from the hospital with heart failure: a systematic review and network meta-analysis. Eur J Heart Fail 2017;19:1427-43. https://doi.org/10.1002/ejhf.765.
- Feltner C, Jones CD, Cené CW, Zheng Z-J, Sueta CA, Coker-Schwimmer EJL, et al. Transitional care interventions to prevent readmissions for persons with heart failure. Ann Intern Med 2014;160:774-84. https://doi.org/10.7326/m14-0083.
- Pickstone N, Lee GA. Does the @home team reduce local Emergency Department attendances? The experience of one London service. Int Emerg Nurs 2019;46. https://doi.org/10.1016/j.ienj.2019.04.003.
- Karlsson M, Karlsson I. Follow-up visits to older patients after a hospital stay: nurses’ perspectives. Br J Community Nurs 2019;24:80-6. https://doi.org/10.12968/bjcn.2019.24.2.80.
- O’Rourke G, Beresford B. Research priorities for homecare for older people: a UK multi‐stakeholder consultation. Health Soc Care Community 2022;30:e5647-60. https://doi.org/10.1111/hsc.13991.
- Echevarria C, Brewin K, Horobin H, Bryant A, Corbett S, Steer J, et al. Early supported discharge/hospital at home for acute exacerbation of chronic obstructive pulmonary disease: a review and meta-analysis. COPD 2016;13:523-33. https://doi.org/10.3109/15412555.2015.1067885.
- Qaddoura A, Yazdan-Ashoori P, Kabali C, Thabane L, Haynes RB, Connolly SJ, et al. Efficacy of hospital at home in patients with heart failure: a systematic review and meta-analysis. PLOS ONE 2015;10:e0129282-82. https://doi.org/10.1371/journal.pone.0129282.
- Schiff R, Oyston M, Quinn M, Walters S, McEnhill P, Collins M. Hospital at home: another piece of the armoury against COVID-19. Future Healthc J 2022;9:90-5. https://doi.org/10.7861/fhj.2021-0137.
- Pandor A, Thokala P, Gomersall T, Baalbaki H, Stevens JW, Wang J, et al. Home telemonitoring or structured telephone support programmes after recent discharge in patients with heart failure: systematic review and economic evaluation. Health Technol Assess 2013;17:1-207.
- Al Rajeh A, Steiner MC, Aldabayan Y, Aldhahir A, Pickett E, Quaderi S, et al. Use, utility and methods of telehealth for patients with COPD in England and Wales: a healthcare provider survey. BMJ Open Respir Res 2019;6:e000345-45. https://doi.org/10.1136/bmjresp-2018-000345.
- Cook EJ, Randhawa G, Sharp C, Ali N, Guppy A, Barton G, et al. Exploring the factors that influence the decision to adopt and engage with an integrated assistive telehealth and telecare service in Cambridgeshire, UK: a nested qualitative study of patient ‘users’ and ‘non-users’. BMC Health Serv Res 2016;16. https://doi.org/10.1186/s12913-016-1379-5.
- MacInnes J. Care navigators decision‐making in prescribing Telecare for older people. Health Soc Care Community 2020;28:2431-40. https://doi.org/10.1111/hsc.13066.
- Watson P, Bearpark T, Ling J. The impact of rapid response and telecare services on elderly and vulnerable residents. Health Soc Care Community 2020;29:897-904. https://doi.org/10.1111/hsc.13123.
- Hove R. Health education England advanced clinical practitioner credential to build the workforce, that empowers people to live well with their LTCs. Physiotherapy 2022;114:e181-2. https://doi.org/10.1016/j.physio.2021.12.156.
- van der Laag PJ, Arends SAM, Bosma MS, van den Hoogen A. Factors associated with successful rehabilitation in older adults: a systematic review and best evidence synthesis. Geriatr Nurs 2021;42:83-9. https://doi.org/10.1016/j.gerinurse.2020.11.010.
- Pettersson C, Iwarsson S. Evidence-based interventions involving occupational therapists are needed in re-ablement for older community-living people: a systematic review. Br J Occup Ther 2017;80:273-85.
- Tessier A, Beaulieu M-D, Mcginn CA, Latulippe R. Effectiveness of reablement: a systematic review. Healthcare Policy 2016;11:49-5.
- Boniface G, Mason M, Macintyre J, Synan C, Riley J. The effectiveness of local authority social services’ occupational therapy for older people in Great Britain: a critical literature review. Br J Occup Ther 2013;76:538-47.
- Dawson S, Kunonga P, Beyer F, Spiers G, Booker M, McDonald R, et al. Does health and social care provision for the community dwelling older population help to reduce unplanned secondary care, support timely discharge and improve patient well-being? A mixed method meta-review of systematic reviews. F1000Res 2020;9. https://doi.org/10.12688/f1000research.25277.1.
- Beresford B, Mayhew E, Duarte A, Faria R, Weatherly H, Mann R, et al. Outcomes of reablement and their measurement: findings from an evaluation of English reablement services. Health Soc Care Community 2019;27:1438-50. https://doi.org/10.1111/hsc.12814.
- Levin KA, Crighton E. Measuring the impact of step down intermediate care on delayed discharge: an interrupted time series analysis. J Epidemiol Community Health 2019;73:674-9.
- Tinelli M, Wittenberg R, Cornes M, Aldridge RW, Clark M, Byng R, et al. The economic case for hospital discharge services for people experiencing homelessness in England: an in‐depth analysis with different service configurations providing specialist care. Health Soc Care Community 2022;30:e6194-205. https://doi.org/10.1111/hsc.14057.
- House of Commons Health Committee . Winter Pressure in Accident and Emergency Departments: Third Report of Session 2016–17 2016.
- NHS England . The NHS Long Term Plan 2021. www.longtermplan.nhs.uk/publication/nhs-long-term-plan (accessed 22 February 2024).
- Vindrola-Padros C, Singh KE, Sidhu MS, Georghiou T, Sherlaw-Johnson C, Tomini SM, et al. Remote home monitoring (virtual wards) for confirmed or suspected COVID-19 patients: a rapid systematic review. EClinicalMedicine 2021;37. https://doi.org/10.1016/j.eclinm.2021.100965.
- Healy P, McCrone L, Tully R, Flannery E, Flynn A, Cahir C, et al. Virtual outpatient clinic as an alternative to an actual clinic visit after surgical discharge: a randomised controlled trial. BMJ Qual Safety 2018;28:24-31. https://doi.org/10.1136/bmjqs-2018-008171.
- Xiao S, Tourangeau A, Widger K, Berta W. Discharge planning in mental healthcare settings: a review and concept analysis. Int J Ment Health Nurs 2019;28:816-32. https://doi.org/10.1111/inm.12599.
- Azam S, Jones T, Wood S, Bebbington E, Woodfine L, Bellis M. Improving Winter Health and Well-being and Reducing Winter Pressures. A Preventative Approach. Cardiff: Public Health Wales NHS Trust; 2019.
- Lakoma K, Murphy P. The evaluation of safe and well visits as part of the prevention activities of fire and rescue services in England. Int J Emerg Serv 2023;12:271-82. https://doi.org/10.1108/IJES-09-2022-0053.
- Farmanova E, Baker GR, Cohen D. Combining integration of care and a population health approach: a scoping review of redesign strategies and interventions, and their impact. Int J Integr Care 2019;19. https://doi.org/10.5334/ijic.4197.
- Spiers G, Matthews FE, Moffatt S, Barker RO, Jarvis H, Stow D, et al. Impact of social care supply on healthcare utilisation by older adults: a systematic review and meta-analysis. Age Ageing 2018;48:57-66. https://doi.org/10.1093/ageing/afy147.
- Dickson K, Sutcliffe K, Rees R, Thomas J. Gaps in the evidence on improving social care outcomes: findings from a meta-review of systematic reviews. Health Soc Care Community 2017;25:1287-303. https://doi.org/10.1111/hsc.12300.
- de São José J, Barros R, Samitca S, Teixeira A. Older persons’ experiences and perspectives of receiving social care: a systematic review of the qualitative literature. Health Soc Care Community 2016;24:1-11. https://doi.org/10.1111/hsc.12186.
- Preston-Shoot M. Self-neglect and safeguarding adult reviews: towards a model of understanding facilitators and barriers to best practice. J Adult Protect 2019;21:219-34. https://doi.org/10.1108/jap-02-2019-0008.
- NHS England, NHS Improvement . Pharmacy and Medicines Optimisation: A Toolkit for Winter 2018 19 2018.
- Sadler E, Potterton V, Anderson R, Khadjesari Z, Sheehan K, Butt F, et al. Service user, carer and provider perspectives on integrated care for older people with frailty, and factors perceived to facilitate and hinder implementation: a systematic review and narrative synthesis. PLOS ONE 2019;14:e0216488-88. https://doi.org/10.1371/journal.pone.0216488.
- Damery S, Flanagan S, Combes G. Does integrated care reduce hospital activity for patients with chronic diseases? An umbrella review of systematic reviews. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-011952.
- Martínez-González NA, Berchtold P, Ullman K, Busato A, Egger M. Integrated care programmes for adults with chronic conditions: a meta-review. Int J Qual Health Care 2014;26:561-70. https://doi.org/10.1093/intqhc/mzu071.
- Philp I, Mills KA, Thanvi B, Ghosh K, Long JF. Reducing hospital bed use by frail older people: results from a systematic review of the literature. Int J Integr Care 2013;13:e0-48. https://doi.org/10.5334/ijic.1148.
- Stephenson MD, Lisy K, Stern CJ, Feyer A-M, Fisher L, Aromataris EC. The impact of integrated care for people with chronic conditions on hospital and emergency department utilization: a rapid review. Int J Evid-Based Healthc 2019;17:14-26.
- Pearson M, Hunt H, Cooper C, Shepperd S, Pawson R, Anderson R. Providing effective and preferred care closer to home: a realist review of intermediate care. Health Soc Care Community 2015;23:577-93.
- Alonso JM, Andrews R. Does vertical integration of health and social care organizations work? Evidence from Scotland. Soc Sci Med 2022;307.
- Colclough R, Wagstaff R, Rees S, Breese K, Nicholls C, Porter S, et al. P129 Getting it right in a digital age – robust patient selection to an early supported discharge service. paper presented at: improving care pathways in adults and children 2021/11. Thorax n.d.;76. https://doi.org/10.1136/thorax-2021-btsabstracts.238.
- Collins B. P-210 Trusted assessor pilot – making sure that patients are where they need to be!. BMJ Support Palliat Care 2018;8. https://doi.org/10.1136/bmjspcare-2018-hospiceabs.235.
- Bardsley M, Steventon A, Smith J, Dixon J. Evaluating Integrated and Community-Based Care. London: Nuffield Trust; 2013.
- Kumpunen S, Edwards N, Georghiou T, Hughes G. London: Nuffield Trust; 2019.
- Collins J, Lizarondo L, Taylor S, Porritt K. Adult patient and carer experiences of planning for hospital discharge after a major trauma event: a qualitative systematic review. Disabil Rehabil 2023;45:3435-55. https://doi.org/10.1080/09638288.2022.2133180.
- Rodakowski J, Rocco PB, Ortiz M, Folb B, Schulz R, Morton SC, et al. Caregiver integration during discharge planning for older adults to reduce resource use: a metaanalysis. J Am Geriatr Soc 2017;65:1748-55. https://doi.org/10.1111/jgs.14873.
- Mockford C. A review of family carers’ experiences of hospital discharge for people with dementia, and the rationale for involving service users in health research. J Healthc Leadersh 2015;7:21-8. https://doi.org/10.2147/JHL.S70020.
- Stockwell-Smith G, Moyle W, Marshall AP, Argo A, Brown L, Howe S, et al. Hospital discharge processes involving older adults living with dementia: an integrated literature review. J Clin Nurs 2018;27:e712-25. https://doi.org/10.1111/jocn.14144.
- Ewing G, Austin L, Jones D, Grande G. Who cares for the carers at hospital discharge at the end of life? A qualitative study of current practice in discharge planning and the potential value of using The Carer Support Needs Assessment Tool (CSNAT) approach. Palliat Med 2018;32:939-49. https://doi.org/10.1177/0269216318756259.
- Davis SF, Silvester A, Barnett D, Farndon L, Ismail M. Hearing the voices of older adult patients: processes and findings to inform health services research. Res Involv Engagem 2019;5. https://doi.org/10.1186/s40900-019-0143-5.
- Iacobucci G. NHS ‘winter’ pressure could become norm in summer, experts warn. BMJ 2016;352. https://doi.org/10.1136/bmj.i905.
- Royal College of Physicians . Acute Medicine Task Force. Acute Medical Care: The Right Person, in the Right Setting-First Time 2007.
- Naylor C, Taggart H, Charles A. Mental Health and New Models of Care: Lessons From the Vanguards. King’s Fund; 2017.
- Everall AC, Guilcher SJT, Cadel L, Asif M, Li J, Kuluski K. Patient and caregiver experience with delayed discharge from a hospital setting: a scoping review. Health Expect 2019;22:863-73. https://doi.org/10.1111/hex.12916.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372. https://doi.org/10.1136/bmj.n71.
- Nicholson C, Jackson C, Marley J. A governance model for integrated primary/secondary care for the health-reforming first world – results of a systematic review. BMC Health Serv Res 2013;13. https://doi.org/10.1186/1472-6963-13-528.
- NHS Improving Quality; NHS England . NHS Services–open Seven Days a Week: Every Day Counts 2013.
- NHS England . Seven Day Hospital Services: The Clinical Case 2013.
- NHS England . Seven Day Hospital Services Resources n.d. www.england.nhs.uk/get-involved/resources (accessed 28 February 2024).
- Healthcare Quality Improvement Partnership 2020. www.hqip.org.uk/resource/documenting-local-clinical-audit-a-guide-to-reporting-and-recording (accessed 22 February 2024).
- Shrewsbury and Telford Hospital NHS Trust . An Audit of Compliance With SaTH Discharge Policy from the Patient Perspective 2014.
- Shrewsbury and Telford Hospital NHS Trust . A Re-Audit of Compliance With SaTH Discharge Policy from the Patient Perspective 2015.
- Shrewsbury and Telford Hospital NHS Trust . Third Re-Audit of Compliance With SaTH Discharge Policy from the Patient Perspective 2019.
- Miller CJ, Hall R, McFeeters M, Evans A, Orrock E, Day M. 91 systems leadership lessons from planning for winter pressures. BMJ Lead 2019;3. https://doi.org/10.1136/leader-2019-fmlm.91.
- Jones B, Kwong E, Warburton W. Quality Improvement Made Simple: What Everyone Should Know about Healthcare Quality Improvement. London: Health Foundation; 2021.
- Care Quality Commission . Driving Improvement: Case Studies from Eight NHS Trusts 2017. www.cqc.org.uk/publications/evaluation/driving-improvement-case-studies-nhs-trusts (accessed 22 February 2024).
- Health Improvement Scotland . Moving from Quality Improvement to Quality Management: Supporting Better Quality Health and Social Care for Everyone in Scotland 2022.
- Ross L. Glasgow city HSCP complex needs service - personalised and person-centred health and care. Int J Integr Care 2022;22. https://doi.org/10.5334/ijic.icic22204.
- Sezgin D, O’Caoimh R, Liew A, O’Donovan MR, Illario M, Salem MA, et al. all EU ADVANTAGE Joint Action Work Package 7 partners . The effectiveness of intermediate care including transitional care interventions on function, healthcare utilisation and costs: a scoping review. Eur Geriatr Med 2020;11:961-74. https://doi.org/10.1007/s41999-020-00365-4.
- Turner G, Clegg A. British Geriatrics Society . Best practice guidelines for the management of frailty: a British geriatrics society, age UK and royal college of general practitioners report. Age Ageing 2014;43:744-7. https://doi.org/10.1093/ageing/afu138.
- Mayo A, Allen A. Reducing admissions with social enterprises. Emerg Nurse 2010;18:14-7. https://doi.org/10.7748/en2010.07.18.4.14.c7901.
- Bynner C, McBride M, Weakley S. The COVID-19 pandemic: the essential role of the voluntary sector in emergency response and resilience planning. Volunt Sect Rev 2022;13:167-75. https://doi.org/10.1332/204080521x16220328777643.
- Randles M, Hickey S, Cotter S, Walsh C, O’Connor K, O’Sullivan C, et al. 144 the use of a multidisciplinary team discharge ‘huddle’ to improve patient flow and planning. Age Ageing 2019;48:iii1-16. https://doi.org/10.1093/ageing/afz102.30.
- Wilson F. West Lothian health and social care partnership integrated daily discharge flow huddle. Int J Integr Care 2022;22. https://doi.org/10.5334/ijic.icic22220.
- Franklin BJ, Gandhi TK, Bates DW, Huancahuari N, Morris CA, Pearson M, et al. Impact of multidisciplinary team huddles on patient safety: a systematic review and proposed taxonomy. BMJ Qual Saf 2020;29:1-2. https://doi.org/10.1136/bmjqs-2019-009911.
Appendix 1 MEDLINE search strategy
Database: Ovid MEDLINE(R) and Epub Ahead of Print, In-Process, In-Data-Review & Other Non-Indexed Citations, Daily and Versions <1946 to October 11, 2022>
Search strategy:
---------- ------------ ------------ ------------- ------------ ------------ ---------
-
(“winter plan” or “winter planning”).tw. (7)
-
“winter pressure*”.tw. (90)
-
“winter pressures”.kw. (4)
-
“winter resilience”.tw. (1)
-
“winter surge*”.tw. (27)
-
“winter demand*”.tw. (4)
-
or/1-6 (130)
-
limit 7 to yr=“2018 - 2022” (54)
-
limit 8 to english language (54)
Note: to optimise sensitivity, our experienced methodologist advised that judgements on discharge planning/integrated care context be operationalised during title/abstract and full-text screening stages rather than rely on uneven application of database indexing. Therefore, we did not use specific discharge/integrated care terminology in the search strategy.
Appendix 2 Patient and public involvement scenarios
-
Discharge to assess
-
Susie has recently suffered a fall and was admitted to her local general hospital for a couple of days. Her hospital has identified funding to support people to leave hospital as quickly as possible, when safe and appropriate to do so. Susie’s ongoing care and assessment will now take place out of hospital. Instead of getting a ‘snapshot’ of her long-term needs while Susie is in hospital she will be assessed over the next 6 weeks while she is back in her own home.
-
-
Same-day emergency care
-
Asif’s GP is concerned about his dizzy spells, sometimes leading to falls. He arranges for Asif to be transported to a same-day emergency care unit located in his local hospital. Asif is assessed within a short time of his arrival at the unit and undergoes a series of tests. At the end of the same day, Asif returns to his own home with some new medication. He will be contacted for follow-up if required. Also see video ‘What is Same Day Emergency Care (SDEC)?’ by NHS England at: https://youtu.be/rokhVD_1XSE.
-
-
Hospital avoidance response team
-
Dave phones 999 after a serious attack of acute bronchitis. He is put in contact with a specialist hub for severe breathing difficulties. Instead of an ambulance being sent to him, he receives a visit from a paramedic. The paramedic listens to what Dave has to say about his condition. After brief contact with the specialist hub the paramedic arranges for a change in medication and a follow-up visit.
-
-
Care and repair
-
Rosie wants to leave hospital as soon as possible. However, her health and social care workers are concerned that her home is currently neither warm enough nor safe enough for her to return home. They contact a local charity called Care & Repair, which arranges for volunteers to visit her house and prepare it for Rosie’s return.
-
-
Telecare
-
Jawinta has been discharged from hospital to her care home. Her ongoing heart condition will be monitored by the hospital from a portable transmitter beside her bed. She will also have a consultation over Skype or Zoom with a diabetic nurse who will contact her online every 3–4 weeks.
-
Patient and public involvement group input
The PPI group’s knowledge and thoughts about each scenario are provided below.
Discharge to assess
-
Good to free-up bed space so not delaying planning operations because of shortage of beds.
-
Concern about whether patients are properly assessed before discharge.
-
Positive for patient to be out of hospital but there needs to be a care plan in place; they are time consuming and should not be rushed.
-
Important to ensure that the patient will be safe in their own home or a care home.
Same-day emergency care
-
Concerned about discharge home with new medication; who will follow-up? Do GPs have time?
-
If a patient is living alone who can chase for follow-up?
-
Patients could need support in addition to care.
-
Care plans needed different if patient lives alone or has support.
-
OK if GP proactive response but usually need to keep asking due to pressure they are under.
-
Potential adverse effects of new medication.
-
Concerns that the availability of services differs so much from area to area, and we have to think about people living in rural areas.
Hospital avoidance response team
-
Rapid response good if reduces pressures on ambulances.
-
Outcomes could depend upon paramedic training and expertise.
-
Would paramedics be liaising with consultants from appropriate specialties?
-
Would paramedics understand medications and how they can interact other medications?
-
One group member discussed how paramedics were specially trained in their own area; paramedics are very good, and have extra skills and knowledge. Issue of continuity of care after paramedic; carers need reliable ongoing support.
Care and repair
-
One group member discussed how a family member in Bristol had used the service 10 years ago for alterations after knee replacement.
-
Not available everywhere, particularly in rural areas.
-
Repairs can take time, particularly given a shortage of workmen; typically, work needs to be completed promptly.
-
A real worry is cold homes and excess winter deaths. Energy bills and cost of living.
-
Third sector – great if reliable but services in different areas are very variable.
Telecare
-
Monitors, wearables useful, good to involve patients in reading and good to use and assurances reduce usage of services.
-
Good opportunity.
-
Care home staff sending to A&E as not properly trained.
-
Good idea but practicality staff not trained to use tech, staff need training in new equipment, depends on care homes and staffing.
-
Shortage of care home staff.
-
Staff training and turnover.
-
Big role for telecare moving forward; unavoidable and important to embrace technology.
-
Would assessment by diabetic nurse by Zoom or Skype be enough? Could need to be in person. Can patient express herself thoroughly online? Issue of communication.
-
Wearables/patient apps good; maybe not for all conditions; sometimes need face to face.
-
Who would be monitoring in care home?
-
Rising elderly population, more demands; technology needed but should not be fully dependent.
-
Technology needs to be supported.
Appendix 3 Modified PRISMA diagram
FIGURE 2.
Modified PRISMA 2020 flow diagram. aConsider, if feasible to do so, reporting the number of records identified from each database or register searched (rather than the total number across all databases/registers). bIf automation tools were used, indicate how many records were excluded by a human and how many were excluded by automation tools. Source: Page et al. 190 This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. The figure includes minor additions and formatting changes to the original figure. For more information, visit: www.prisma-statement.org.
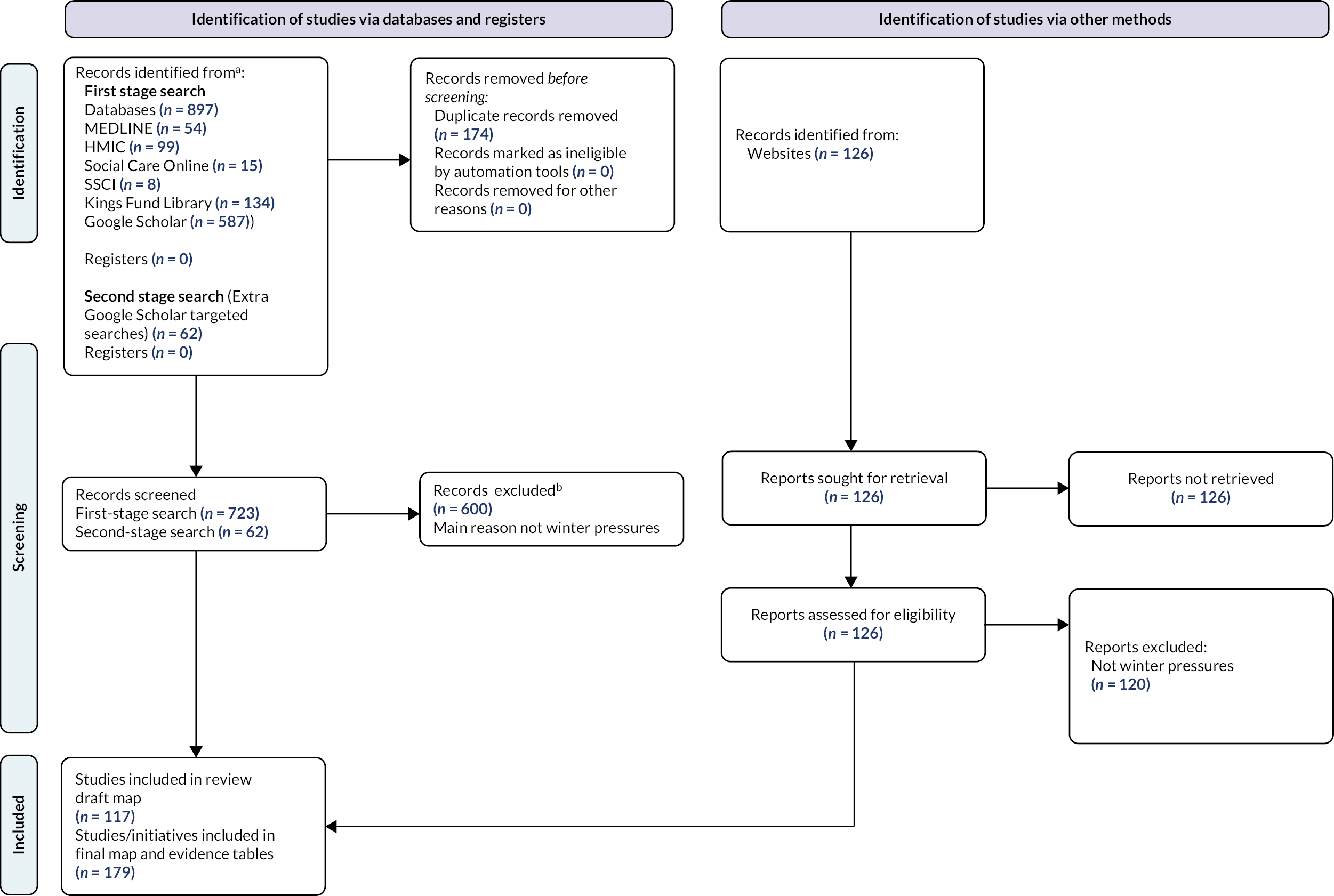
Appendix 4 Structural tables
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| S – bed management | Ensuring optimum use of inpatient bed capacity | Reduces number of patients occupying inpatient beds who could be safely discharged or placed elsewhere |
| Example interventions | Designated beds; patient ‘boarding’ (accommodation in inappropriate wards) | Designated beds: Allow safe discharge during winter COVID-19 waves ‘Boarding’: Placing patients in appropriate wards increases safety during stay and may allow faster discharge |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific | |
| Care Quality Commission 2021 (designated beds)7 | February 2021: Over 150 ‘designated settings’ within 100 local authorities |
| Peddie 2018 (patient ‘boarding’)8 | ‘Boarded’ patients had shorter length of stay (perhaps selected because short stay expected) but care perceived to be of lower standard Authors note that ‘NHS Greater Glasgow and Clyde have reduced boarding by 70% since 2007 through focused discharge planning’ [Beckett Daniel. Winter pressures in NHS Scotland 2008–2009: report for the Emergency Access Delivery team, Scottish Government Daniel Beckett. (20 March 2017). URL: www.shiftingthebalance.scot.nhs.uk/downloads/1251120568-Winter%20Pressures%20Report%20-%20final%20-%20rich%20text%20format.pdf] |
| Systematic review Tampubolon 20189 |
Changing policies for hospital bed management are worth exploring to improve hospital patient flow and length of stay. Downstream bed management is only one of the factors for potentially improving the overall organisation function. Other factors include the need to reorganise channels upstream and strengthen the internal organisation of EDs |
| Research gaps | |
| Systematic review included only five studies and poor quality (no quality/risk of bias assessment). Additional body of research based on mathematical modelling approaches | |
| Research priority: High – Few UK initiatives (implementation and research gap) with caveat that interventions may be described as discharge planning/co-ordination | |
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| S – managed care approaches | Managed care involves purchasers of health care (e.g. insurance companies) using their bargaining power to control prices and influence how health and care services are provided. Managed care is primarily a feature of insurance-funded health systems (particularly the USA) and evidence of its use to address winter pressures is unlikely to be relevant to the UK setting |
The rationale for managed care approaches is based on the role of financial incentives in improving quality of care, for example, financial penalties for readmissions would be expected to encourage providers to ensure that patients were discharged when medically fit and adequately supported after discharge |
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| S – extra service delivery | Provision of extra resources to support service delivery at times of increased demand (as distinct from changing the time/place of service delivery) | Given the availability of staff, extra services can be planned, implemented and discontinued at relatively short notice in response to (expected) peaks/troughs in demand |
| Example interventions | ‘Super Saturday’ clinics (extra sessions to tackle elective treatment waiting lists; also used for COVID-19 and influenza vaccination); Rapid response team (late shift team to support same-day discharge from emergency care) | Reduction of elective waiting lists may prevent patients’ conditions worsening and reduce future demand. Extra resources in emergency care can allow earlier discharge and reduce demand for inpatient beds |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific | |
| ‘Super Saturday’ clinics (Academy of Medical Sciences 2020)48 | No data reported but evidence of ‘super Saturday clinics’ being repeated (www.leedsth.nhs.uk/about-us/news-and-media/2022/03/04/leeds-childrens-hospital-delivers-hundreds-of-extra-appointments-and-trials-new-technology-on-super-) (accessed 23 November 2022) |
| Rapid response team49 | A total of 131 patients were assessed during 2016–17. Out of 131, 72 patients were discharged on the day of treatment. Out of 138 patients referred during 2017–18, 79 patients were discharged on the day of assessment. Service estimated to have saved 151 hospital bed days |
| Case studies/evaluations See above |
|
| Systematic reviews None found |
|
| Guidance Not applicable |
|
| Research gaps | |
| This is a broad category of interventions, making it difficult to identify general research priorities. Research and implementation are likely to be determined by the availability of staff and financial resources | |
| Research priority: High – Few UK initiatives (implementation and research gap) | |
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| S – monitoring and review | Monitoring and review interventions aim to identify patients suitable for discharge or transfer from more to less intensive levels of support. Involvement of professionals from different disciplines supports a holistic assessment of the patient’s needs | Early review (e.g. 7 days/week) can identify patients who would benefit from transfer to a less intensive community setting and reduce pressure on the most specialist services. Closely related to ‘patient flow’ and ‘prioritisation and triage’. Monitoring outside hospital is covered under ‘telecare’ |
| Example interventions: Daily multidisciplinary review | See Goodison 202161 for application in a hyper-acute stroke unit | See above |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific | |
| Goodison 2021 (‘neuronavigation’ for stroke unit patients)61 | Daily in-reaching neuronavigation on hyper-acute stroke unit identified stroke patients who benefitted from rapid transfer to community neurorehabilitation. The majority of patients were diverted away from the normal stroke pathway, reducing pressure on services not operating because of COVID-19 |
| Case studies/evaluations | |
| Systematic reviews Coffey et al. 2019112 Guidance |
Interventions exclusively delivered in the acute hospital pre-discharge and those involving education were most common but their effectiveness was limited in avoiding (re)admission. Successful pre- and post-discharge interventions focused on multidisciplinary approaches |
| Research gaps | |
| We identified only one piece of research related to monitoring and review in hospital in the context of winter pressures. This suggests substantial research gaps but the topic should be considered alongside related headings such as ‘patient flow’ and ‘prioritisation and triage’ | |
| Research priority: High – Few UK initiatives (implementation and research gap) | |
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| S – governance | NHS England defines clinical governance as ‘a system through which NHS organisations are accountable for continuously improving the quality of their services and safeguarding high standards of care by creating an environment in which excellence in clinical care will flourish’. Monitoring systems and processes for patient safety and care quality are elements of clinical governances. URL: www.england.nhs.uk/mat-transformation/matrons-handbook/governance-patient-safety-and-quality/ (accessed 23 November 2022) | Monitoring systems help to identify rising pressure on services and governance seeks to ensure that appropriate processes are followed, with named individuals held accountable and feedback (i.e. audit and administrative data) on outcomes |
| Example interventions | Any changes to governance systems, normally at the hospital level |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific | No supporting evidence identified |
| Case studies/evaluations | |
| Systematic reviews | |
| Zonneveld et al. 201851 Values of integrated care |
This review identified 23 underlying values that may drive behaviour, decision-making, collaboration and governance processes in integrated care networks. The most frequently identified values were ‘collaborative’, ‘co-ordinated’, ‘transparent’, ‘empowering’, ‘comprehensive’, ‘co-produced’ and ‘shared responsibility and accountability’. Authors suggest that values could serve as governance principles for the alignment between organisations in integrated care initiatives and partnerships, for example by influencing decision-making processes or leadership behaviour |
| Nicholson et al. 2013191 Guidance |
This review identified ten elements needed for integrated primary/secondary healthcare governance across a regional setting including: joint planning; integrated information communication technology; change management; shared clinical priorities; incentives; population focus; measurement – using data as a quality improvement tool; continuing professional development supporting joint working; patient/community engagement; and, innovation. All included studies (n = 21) evaluated the process of integrated governance and service delivery structures, rather than the effectiveness of services. Authors concluded that the elements listed above provide a focus for setting up integration initiatives, which need to be flexible for adapting to local conditions and settings |
| Research gaps | |
| We identified no UK research studies or initiatives related to governance. It is possible that the nature of the topic requires a more detailed and focused search to identify any relevant evidence | |
| Research priority: High – Few UK initiatives (implementation and research gap) | |
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| S – policies | Policies represent recommended or mandated actions and may be developed at a variety of levels, for example, national (devolved in UK); regional; local (e.g. local government, integrated care systems/boards); and institutional. See also CSB – Protocols and Guidelines | Policies can be developed in advance of expected winter pressures and/or enacted rapidly in response to changing circumstances. Their source may confer authority and they may be associated with monitoring and evaluation of implementation/effectiveness |
| Example interventions: Patient FIRST; NHS England winter resilience plans |
Patient FIRST is a Care Quality Commission policy for EDs in the wake of the COVID-19 pandemic. NHS England outlines required/recommended actions for Integrated Care Boards, NHS Trusts, GP practices and other organisations |
Increased efficiency and safety in the ED incorporating learning from the pandemic Prompts organisations to consider readiness for winter pressures and take appropriate actions |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific Project reset in emergency medicine: Patient FIRST URL: www.cqc.org.uk/publications/themes-care/project-reset-emergency-medicine-patient-first (accessed 23 November 2022) NHS England: Going further on our winter resilience plans (October 2022) URL: www.england.nhs.uk/wp-content/uploads/2022/10/BW2090-going-further-on-our-winter-resilience-plans-letter-oct-22.pdf (accessed 23 November 2022) Case studies/evaluations Systematic reviews Guidance Patient FIRST ED good practice toolkit (see URL above) |
|
| Research gaps | |
| Policies can support action to mitigate winter pressures at various levels but will generally cover one or more of the more specific headings within this taxonomy. This makes it difficult to identify evaluations and research gaps relating to policies per se. Policies are likely to be effective when they are supported by evidence and where resources are available to implement them | |
| Research priority: Unclear: most policies will cover one or more headings from elsewhere in the taxonomy | |
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| S – seven-day services (7DS) |
Provide high-quality safe care every day of the week from 8 a.m. to 8 p.m. to improve patient flow through the system and across the interface between health and social care | Minimise delays to patient flow through the system and across the interface between health and social care at the weekends to help manage increased healthcare usage during the winter months |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific Local Government Association. 201815 Additional evidence Guidance NHS Improving Quality; NHS England, 2013192 Published evaluations NHS England. 2013193 Seven Day Hospital Services: The Clinical Case. Case studies NHS England. n.d.194 |
Surrey, 7-day eight to eight social care led to reduction in length of stay for patients and hospital beds being freed up sooner. By locating adult social care staff in A&E and medical assessment units at weekends and weekday evening has helped reduce number of avoidable admissions. Social care information and advice was available 7 days a week helping patients, families, carers and health professional with effective decision-making. DTOC days have reduced by 17% in Surrey while increasing by 62% across England. The clinical case includes promising case studies |
| Research gaps | |
| Only small low methodological quality evaluations and case studies. Guidance available from the NHS. Need to further research the effectiveness of seven-day services | |
| Research priority: Moderate – Few UK research studies but plentiful UK initiatives (research gap) | |
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| S – staff redeployment | Redeployment of staff to improve patient flow through the health and social care system | Help with patient flow through health and social care services, useful in winter when healthcare usage increases |
| Examples of initiatives: Early Senior Review/Pharmacist on paediatric ward/Physiotherapists in ED/Respiratory nurse specialist in ED/Surgeons focus on day cases/Surgeons could support acute wards/Sharing staff between trusts |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific Care Quality Commission 202235 Ferguson 202075 (conference abstract) Rickards et al. 202176 (conference abstract) Scriven 201877 Wilkinson 201819 Additional evidence Guidance Published evaluations Systematic reviews Atey et al. 202278 Hohl et al. 201579 San Juan et al. 202280 Case studies |
The recent systematic review on the impact of pharmacist interventions in the ED78 found good evidence for improved quality use of medicines when pharmacists are included in the ED care teams. The number of medication errors reduced by a mean of 0.33 per patient. Patients had more complete and accurate medication histories, increased appropriateness of prescribed medications by 58% and time-critical medications initiation was quicker. However, no clear impact was observed on length of time spent in the ED or in hospital, and in-hospital mortality similar findings to the 2015 review.79 The feature by Wilkinson on how pharmacists are being reallocated to offer ward-based prescribing and 7-day pharmacy services to relieve winter pressures includes examples of relevant initiatives.19 Luton and Dunstable University Hospital has The pharmacy prescription tracker, part of the ‘control centre’ suite of tools and once the trust hits a specific level of pressure, a member of the senior pharmacy team attends the bed meetings that are held four times per day. The carefully managed system allows the pharmacy team to be actively aware throughout the day of wider hospital pressures and able to meet anticipated changes in demand. |
| A recent systematic review reviewed the evidence on the training and redeployment of healthcare workers to intensive care units (ICUs) during the pandemic.80 The review found that medical students experienced anxiety around treating critically ill patients and intubation procedures, they was also miscommunication with other healthcare workers and challenges from the tension between textbook medicine and complex social situation. The review findings could be helpful in informing future practice for redeployment and training in ICU settings for future pandemics and similar approaches could be introduced to mitigate the challenges of workforce shortage crisis affecting many countries and to mitigate winter pressures in UK. | |
| A conference abstract details how ED physiotherapist practitioner (EDPP) posts were introduced to 3 EDs in Scotland. Across the 3 sites (28 January 2019 to 7 April 2019) the EDPP managed 1045 patients, freeing up doctors and nurses to see other more medically complex patients.75 Another conference abstract details the introduction a respiratory nurse specialist within the ED to provide care for patients presenting with a respiratory condition.76 The nurse specialist prevented 240 admissions during a 5-month period and enabled discharges from ED to all community respiratory services. This initiative improved connections with community respiratory teams and standardisation of care for shared services. Examples of initiatives related to Winter pressures:35 Northamptonshire – shared strategy for workforce planning into the winter months was in place. Originally developed in response to the pandemic the workforce cell looked at national and local staffing drives as well as staff skills to determine where to move staff and where upskilling of staff would be helpful An example of this is the passporting of staff between NHS trusts in West Yorkshire and Harrogate, Suffolk and North East Essex, and Cornwall and the Isles of Scilly. Staff’s NHS competencies passport enabled their movement between providers within easily reduce staff gaps and improve patient care. |
|
| Research gaps | |
| Systematic reviews exist for certain staff redeployment initiatives, the use of pharmacists in ED and redeployment of staff to ICU. However, research gaps remain where only UK initiatives exist | |
| Research priority: Low – Good quality systematic review(s) and plentiful UK research studies (no gap) Moderate – Few UK research studies but plentiful UK initiatives (research gap) |
|
Appendix 5 Changing staff behaviour tables
CSB – Clinical audit
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| CSB – clinical audit | Clinical audit is a method to find out if healthcare delivery meets relevant standards and it allows patients and care providers to understand what their service is doing well and potential areas for improvement | A clinic audit could be used to assess different healthcare policies and procedures for example compliance with discharge policy which could they suggested areas for improvement which could help to improve patient flow |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific Clinical audit has been used for benchmarking to mitigate winter pressures. The Winter Society for Acute Medicine Benchmarking Audit provides a comparison of performance within acute medicine against clinical quality indicators during winter. Additional evidence Guidance Healthcare Quality Improvement Partnership 2020195 Published evaluations Case studies Shrewsbury and Telford Hospital 2014196 Shrewsbury and Telford Hospital 2015197 Shrewsbury and Telford Hospital 2019198 |
No evidence of the use of clinical audit to mitigate winter pressures Recent guidance from the Healthcare Quality Improvement Partnership on documenting local clinical audit195 A case study of the use of clinical audit to investigate compliance with discharge policy at Shrewsbury and Telford Hospital. The initial audit in 2014 evaluated compliance with the discharge policy and suggested changes to address identified problems.196 In 2015 re-audit sought to determine if recommendations from 2014 audit had been implemented, compliance with the 2015 discharge policy and any changes to improve the discharge experience for patients.196 In 2019, after changes from the previous audit had had time to be embedded in practice, a re-audit checked if recommendations from previous audits had been implemented.197 The 2019 audit found that patients were kept waiting for the same reasons in the discharge lounge, that transferral to the discharge lounge only happened for a small number of patients |
| Research gaps | |
| Clinical audit could be used at a local level as a methodology to investigate the effectiveness of initiatives to mitigate winter pressures. Clinical audits typically target local and national priorities, areas of clinical variability and adverse events and so are well aligned to the needs of exploring winter pressures. However, a tension exists between clinical demand and resources required for audit making most candidate approaches likely to be retrospective. The Winter Society for Acute Medicine Benchmarking Audit indicates the potential for national approaches relying on uniform national datasets. The recently announced Winter Improvement Collaborative (see separate entry) also relies on audit and benchmarking principles in targeting a narrow and specific range of indicators | |
| Research priority: Few UK initiatives (implementation and research gap) | |
Changing staff behaviour: education of staff
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| CSB – education of staff | Education of staff | Staff education is important to ensure that they can fulfil their roles and provide safe effective care making it an important part of new initiatives |
| Staff education about patient flow | Good patient flow in an acute hospital helps ensure patients experience minimal delays throughout their hospital journey. Effective processes, staff buy-in and staff education are needed for good flow |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific Wall and O’Sullivan 202127 Additional evidence Guidance Published evaluations Case studies |
Patient flow is especially important during winter pressures making it important to teach to acute hospital staff and students. This cross –sectional qualitative study considered the teaching of patient flow in one hospital group in Ireland.27 Study participants thought that is should be taught at undergraduate level possible as part of inter-professional education. Multimodal teaching approaches were highlighted as most effective. Teaching at the ward level would allow for it to be closest to employees at a time and place that would suit. The use of a teaching and learning framework for examples the TFU or Universal Design for Learning framework could be used to help plan teaching and materials that could adapted locally. To enable healthcare staff to fulfil their job requirement sufficient training and education is required. Educating staff in new initiatives designed to help mitigate winter pressures will be a key aspect |
| Miller et al. 2019199 (poster summarising rapid review) | Importance of looking after workforce and creating the best possible conditions for staff to do their best for patients was highlighted |
| Research gaps | |
| Education of staff could usefully be part of many initiatives to minimise winter pressures | |
| Research priority: Moderate – Few UK research studies but plentiful UK initiatives (research gap) | |
CSB – Protocols/guidelines
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| CSB – protocols/guidelines | Guidelines and protocols help to guide staff through a process or task | When introducing a new initiatives to minimise winter pressures having clear guidelines and protocols would help staff with implementation |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific Additional evidence Systematic review Unnewehr et al. 201532 Guidance Published evaluations Case studies |
No evidence for the use of protocols/guidelines to mitigate winter pressures A systematic review from 2015 aimed to consider how the quality of discharge summaries could be improved by (1) intervention, (2) reviews and guidelines of regulatory bodies; and (3) other practical recommendations.32 Guidelines were helpful for providing the key components of discharge summaries |
| Research gaps | |
| Protocols/guidelines are important when introducing new initiatives and thus could be an important part of new initiatives to mitigate winter pressures | |
| Research priority: Few UK initiatives (implementation and research gap) | |
CSB – Quality improvement programmes
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| CSB – quality improvement programmes | A systematic approach to improve quality in a specific area. The programme involves the people delivering the service in introducing initiative to improve their service | Quality improvement programmes are useful for implementing new initiatives and thus could be useful when introducing initiative to mitigate winter pressures |
| Healthcare quality improvement programmes have generated large numbers of healthcare quality improvement initiatives |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific Additional evidence Guidance NHS Confederation 202243 Jones et al. 2021200 Published evaluations Case studies Care Quality Commission 2017201 |
No evidence of the use of quality improvement programmes to mitigate winter pressures A recent publication from NHS Confederation presents six lessons from quality improvement to apply as winter pressures increase. The six lessons are drawn from the pandemic experiences of the Q community.43 A quick recent guide from the Health Foundation covers what everyone should know about healthcare quality improvement.200 The Care Quality Commission Driving Improvement includes case studies from eight NHS trusts201 A quality improvement programme could be used to introduce initiatives to minimise winter pressures |
| Research gaps | |
| The introduction of initiatives to minimise winter pressures could form part of quality improvement programmes and could use the six lessons in recent NHS Confederation publication and the quick guide from the Health Foundation. A quality improvement programme could be used to introduce initiatives to minimise winter pressures. The emphasis needs to be on initiatives that can be integrated within existing programmes and not on adding an additional burden at times of system pressure. Reflection after action, that is once pressures are relieved and after action review may offer a route to evaluation | |
| Research priority: Few UK initiatives (implementation and research gap) | |
CSB – Quality management systems
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| CSB – quality management systems | Quality management systems support the delivery of reliable and high-quality care | Quality management systems can help services to continue to deliver reliable and high-quality care while experiencing winter pressures |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific Additional evidence Guidance Healthcare Improvement Scotland 2022202 Moving from quality improvement to quality management: supporting better quality health and social care for everyone in Scotland. URL: https://ihub.scot/media/9012/qitoqms-vfinal.pdf (accessed 7 November 2022) Published evaluations Case studies |
No evidence of the use of quality management systems to mitigate winter pressures Healthcare Improvement Scotland is moving from quality improvement to quality management indicating quality management systems will become more important202 A quality management system could be used to introduce initiatives to minimise winter pressures |
| Research gaps | |
| The introduction of a quality management system could help with introducing initiatives to minimise winter pressures. Such systems will need evaluation and lessons learned will need to be disseminated not only within the organisation but across sectors and collaboratives. One challenge for quality improvement programmes lies in the fact that they are typically owned by a single organisation whereas approaches to mitigating winter pressures are by their very nature multi-organisational, multi-sectoral and multidisciplinary | |
| Research priority: Few UK initiatives (implementation and research gap) | |
Appendix 6 Changing community provision tables
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| CCP – single point response | Co-ordination centres that seek to provide a SPOA to health and/or social care services and therefore speed up interactions with services | Improved co-ordination of discharge planning and speedier discharge |
| Example interventions: Glasgow City HSCP Complex Needs Service | Operates SPOA to vulnerable, transient, and high-risk population, providing diverse medical, health and social care interventions for individuals with multiple and complex health and social care needs | Uses assertive outreach model to ensure appropriate assessment and level of response is in place relative to level of individual risk with aim of actively engaging ‘hard to reach’ individuals with a focus on women and young people |
| Example interventions: Home, But Not Alone Care Quality Commission (2022). Collaboration in urgent and emergency care35 |
Suffolk/North East Essex phone line open 9 a.m. – 5 p.m., 7 days/week, to help on topics including food, medication, loneliness and isolation. Provided practical support to vulnerable people, particularly regarding medicines, food supplies and transport to health and care services, and for other urgent/non-urgent needs. Health/council services created a SPOA – food, prescriptions, transport or support, and all linked into medical services | Offers SPOA with co-ordination of needs and faster response |
| Example interventions: Hull SPOA (Charles 2018)18 | Referrals for CHCP services were through a SPOA. Professionals, service users and carers could do referrals. A training support worker processed referrals, triaging them according to urgency/complexity decided what assessments were required and could connect them with services. Social care services had a separate SPO | Co-ordinated response with prioritisation according to need |
| Example interventions: Open House | Open House community café to provide support for carers and others needing support | Improved carer resilience and less dependence upon emergency medical services |
| Example interventions: SPOA for social care | Offers first point of contact for all social care services | Improved co-ordination and easier navigation of social care services |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific | |
| Systematic reviews | |
| Other major studies | |
| Published evaluations Case study: Glasgow City HSCP Complex Needs Service (Ross 2022)203 |
Multidisciplinary approach of service achieved positive/sustainable outcomes:
|
| Increased collaborative working across statutory, commissioned and third sector agencies. Outcomes/key findings confirm need for service model. Still developmental, but significant benefits from fully integrated, dynamic and highly performing team with rapid response to most vulnerable |
|
| Additional evidence | SPOA for social care Edinburgh Integration Joint Board 202016 Preparation for winter pressures is ‘not enough’, warns NHS Providers. Evans 201762 |
| Research gaps | |
| Need for robust evaluations of SPOA services. However benefits may be self-evident? | |
| Research priority: Moderate – Few UK research studies but plentiful UK initiatives (research gap) | |
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| CCP – step-up facilities | Typically provide care in a setting other than acute hospital. Time limited in nature, schemes aim to prevent admission to hospital, only advancing to hospital in cases of observed deterioration. Step-up schemes can target similar patients to rapid response. However, normally users require more intensive care than could be provided in their own home | Investment in ‘step-up’ community rehabilitation beds helps to relieve pressure on NHS beds and to flex capacity at times of especially high demand. Acute trusts need to plan effectively for sufficient acute beds as well as access to community beds to improve patient flow |
| Example interventions: Step-up facilities based in primary care ‘Bridging the Care Gap’ |
Closely aligned to step-down facilities, services that step-up from primary care, prior to acute care admission: ‘Two innovative-minded GPs have set up pharmacy, dentist and training centre within the practice. . .so that people don’t have to travel everywhere to do something. . .’ Focus on creating step-up facility on surgery land and using this to improve care for elderly. Housing recognised as a principal factor that leads to delayed discharges: ‘Resources in housing sector could be better used to support health and wellbeing’ | Enlarging the primary care offer to encompass step-up facilities means thinking more widely about environments in which people live and how partnership working with different agencies and sectors can support this. Innovative approaches to housing/health assist with workforce issues, for example including key-worker accommodation in housing development plans for healthier environments, and live-in carers and support workers |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific | |
| Systematic reviews | See Scoping reviews below |
| Scoping reviews Sezgin et al. 2020204 |
Examined intermediate care including transitional care interventions for middle-aged and older adults. Outcomes considered were patient function, healthcare utilisation and costs. Many studies reported positive outcomes for reducing hospital utilisation but results were mixed. Evidence on the interventions effectiveness on ED attendances, institutionalisation, function, and cost-effectiveness was limited. An association was found between intermediate care including transitional care interventions and reduced hospital stay but this finding was not across all studies |
| Other major studies | |
| Published evaluations | |
| Additional evidence Turner and Clegg 2014205 |
Decision about whether to send frail adult to hospital or to manage at home/in a step-up community facility often made by non-specialist health/social care staff, working in relative isolation in community settings, without backup of geriatrician or other specialist |
| Research gaps | |
| Often discussion around community beds focuses on ‘step-down’ rehabilitative care with little attention paid to ‘step-up’ services which can limit demand for emergency care156 | |
| Research priority: High – Few UK initiatives (implementation and research gap) | |
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| CCP – private sector | Offers alternative response to use of hospital services by using commercial services. Typically involves use of alternative premises and workforce. Although sometimes an expensive option it has been shown to be attractive when compared with hospital utilisation | Expedites hospital discharge and thereby releases hospital beds for other demand. Often in context of step-down services |
| Example interventions: Technological solutions Jones 201867 |
Potential technological solutions include rapid diagnostics, genetically-tailored medicine, AI-assisted analysis, and new models of remote/self-administered care. Highlights challenge of adopting innovation across current care system | Offers alternative venues, including home care, to acute NHS services and alternatives to NHS facilities. Also suggests potential for improved efficiencies |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific | Technological solutions Jones 201867 |
| Systematic reviews | |
| Other major studies | |
| Published evaluations (Mayo and Allen 2010206) |
Social enterprise rapid response teams can prevent unnecessary hospital admissions by helping patients to manage their conditions at home |
| Additional evidence The Academy of Medical Sciences 202050 |
Additional capacity can be provided through continued use of private or independent sector settings, to ensure sufficient flexibility to accommodate further spacing for lower risk COVID-19 areas throughout the winter. (King’s Fund 2020; National Audit Office 2020) |
| Additional evidence https://institute.global/policy/three-months-save-nhs (accessed 11 December 2022) |
The Telegraph reported in May 2022 that a poll of independent sector providers (representing 150 locations across England) revealed that one-in-four had not been involved in any discussions to make use of private-sector capacity to support the NHS for 2022–3 |
| Additional evidence NHS systems ‘making it harder for patients to go private’, say independent providers. URL: www.hsj.co.uk/quality-and-performance/nhs-systems-making-it-harder-for-patients-to-go-private-say-independent-providers/7032669.article (accessed 23 November 2022) |
Amount of NHS elective procedures carried out by the private sector in early 2022 was lower in eight of 10 largest specialties than in a comparable period before the pandemic, a Health Service Journal analysis reveals |
| Research gaps | |
| Shortage of research and of documented initiatives | |
| Research priority: High – Few UK initiatives (implementation and research gap) | |
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| CCP – voluntary services | Voluntary, Community and Social Enterprise organisations are well-placed to identify and respond to local needs. Involving them as full partners and ensuring they have the funding and autonomy to work closely with communities can increase community capacity, help build resilience and sustainability, and empower communities to design services and support that work for local people | Harness local awareness of needs and resilience to increase community capacity to support those who might otherwise require hospital admission |
| Example interventions: Somerset Community Connect www.scie.org.uk/care-providers/coronavirus-covid-19/commissioning/hospital-discharge-admissions (accessed 11 November 2022) |
Strong community partnerships in response to pandemic. People shielding contacted by village agents, social prescribers and district officers. Alongside voluntary community and social enterprise (VCSE), co-ordinate practical support and supplies – 1300 volunteers signed up as helpers. People linked with community groups such as neighbours helping neighbours. Activities included 16 online talking cafes | Building on existing platforms, adopted strengths-based and community-led approach to support those at risk during the crisis |
| Example interventions: Micro-providers (Somerset County Council) www.scie.org.uk/care-providers/coronavirus-covid-19/commissioning/hospital-discharge-admissions (accessed 23 November 2022) |
Somerset County Council recognised micro-providers as key workers despite being non-regulated provision and enabled its teams to support them to support each other. Micro-provider networks – small groups supporting each other in local area – moved online. Existing infrastructure meant transition was seamless and quick to co-ordinate | Offer people in remote areas access to home care – coming out to where they live to offer support they want at times they choose. Local, individual, tailored support at home prevented risk of infection and continued to support people within their community |
| Example intervention: Focus On Choice CCP: voluntary services |
Early engagement with patients, families and carers using robust protocol, underpinned by transparent escalation process enables people to consider their options. Voluntary/community sector can help to support patients to explore their choices and reach decisions about future care | Helps patients to receive care appropriate to their needs and achieve satisfaction |
| Example intervention: Home, But Not Alone (Suffolk and North East Essex) Care Quality Commission 2021. Collaboration in urgent and emergency care35 |
Phone line open 9 a.m. to 5 p.m., seven days/week, to help with food, medication, loneliness and isolation. Service provided practical support particularly regarding medicines, food, and transport and for other needs. Voluntary sector integral in support. Collaboration was key feature in tackling health inequalities. A SPOA was created by health/council services and the voluntary sector helped with pharmacy collection and transport. The community response was described as ‘phenomenal’ | Offers support to people in their own home. Helps identify when people might need treatment, to support quicker intervention |
| Example intervention: Assisted discharge services (e.g. British Red Cross) |
Some individuals may decline social care support if they think they do not need it, do not want to increase pressure on health/social care system, or do not want to pay for specific social care services if not at desired level. Support may be available from voluntary sector organisations (e.g. British Red Cross assisted discharge services). Many clinical staff and some social care staff not aware of voluntary care services. They may miss opportunities to signpost to other services or not know how to do so, so that people end up relying on sometimes inadequate informal care | Offers alternative services to relieve pressure on health/social care system |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific | Focus On Choice Local Government Association. 2018. High Impact Change Model.15 URL: www.local.gov.uk/sites/default/files/documents/25.1%20High%20Impact%20Change%20model%20CHIP_05_1.pdf Assisted discharge services (e.g. British Red Cross) NHS Providers connect (2018). URL: https://nhsproviders.org/media/518562/nhs-providers-connect-report-red-cross_web.pdf (accessed 23 November 2022) |
| Systematic reviews | |
| Published evaluations | |
| Additional evidence British Red Cross report – Nowhere else to turn: Exploring high intensity use of accident and emergency services (November 2021). URL: www.redcross.org.uk/nowhere-to-turn (accessed 23 November 2022) |
Shows that people from most deprived areas of UK and people with mental health issues most likely to attend A&E frequently. Calls for better support for people who frequently attend A&E with ‘nowhere else to turn’. Recommends:
|
| Highlights need to commission national cross-government strategy to reduce health inequalities | |
| Bynner et al. 2022207 | Indirect evidence from COVID pandemic: Iterative crisis requires relational skills of the voluntary sector to supplement the local state and provide sustainable response to the needs of vulnerable populations. Need for a new strategic and complementary relationship, one that fully engages locally embedded voluntary organisations at all stages of emergency response and resilience planning |
| Research gaps | |
| Shortage of research and of documented initiatives. | |
| Research priority: Moderate – Few UK research studies but plentiful UK initiatives (research gap) | |
Appendix 7 Integrated care tables
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| Integrated care discharge huddle | Hospital-wide, multidisciplinary team-based, patient discharge meeting often including social care staff and other agencies | To improve flow and discharge planning through multidisciplinary communication and problem solving |
| Example interventions: Multidisciplinary Team Discharge ‘Huddle’ Randles et al. 2019208 |
Introduces hospital-wide multidisciplinary team based huddles (HUDDLE) in a city centre hospital to improve flow and discharge planning | Rather than negative view of ‘bed blockers’, allows proactive approach to management and re-enablement of patients with complex care and discharge needs. Early identification of patients with complex needs allows greater focus on appropriate planning earlier in patient journey |
| Example interventions: West Lothian Health and Social Care Partnership Integrated Daily Discharge Flow Huddle Wilson 2022209 |
Introduces ‘Integrated Discharge Hub’ approach to hospital discharge planning where acute care staff work with social care professionals and local carers centre to solve community placement problems for patients awaiting placements | Seeks to improve patient flow through health and social care system, reduce delayed discharges and improve patient journey |
| Supporting evidence | Results/findings/recommendations (from abstract) |
|---|---|
| Winter pressure specific | None identified |
| Systematic reviews Franklin et al. 2020210 [systematic review – looks at safety only] |
Of 24 included articles, uncontrolled pre–post comparison was prevailing study design; we identified only two controlled studies. Among 12 unit-based studies that provided complete measures of statistical significance for reported outcomes, 11 reported statistically significant improvement among some/all outcomes. Objectives of huddle programmes and language used to describe them varied widely across studies |
| Other major studies | |
| Published evaluations Integrated daily flow huddle Wilson 2022209 |
West Lothian has:
|
| Strong, effective leadership, integrated daily flow huddle and patient tracker, achieved improved discharge management. Pandemic allowed testing of different discharge approach. Revised management structure introduced to ensure sustainability and enable further development of partnership’s Home First approach | |
| Randles et al. 2019208 Multidisciplinary Team Discharge ‘Huddle’ |
In 2018 there were 3918 ED presentations by adults over 75 and 2113 admissions (3704, 2081 respectively in 2017). The accuracy of discharge within 1 day of predicted discharge date ranged from 52.5% (January) to 72.6 % (November) and the average length of stay was 6.2days (SD 0.47). 172 patients (84 female, 88 male) admitted for slow stream rehabilitation which has a median length of stay of 30 days |
| Additional evidence | |
| Research gaps | |
| Anecdotal accounts of successful huddle programmes are abundant and the evidence appears to be favourable overall. High-quality peer-reviewed evidence on the effectiveness of huddles, especially at the hospital-wide level, is in its earliest stages. Further rigorous research is needed particularly focusing on the design of huddle programmes and implementation fidelity which would enhance the collective understanding on how huddles impact patient safety and other targeted outcomes | |
| Research priority: High – Few UK initiatives (implementation and research gap) | |
| Taxonomy heading | Brief description/definition | Mechanism for minimising winter pressures |
|---|---|---|
| IC – Winter Improvement Collaborative Mahase 202254 IC – Winter Improvement Collaborative |
Launched on 1st November 2022 to focus on ambulance handover/response times. Main objectives: to improve key performance metrics, including hours lost to ambulance handover delays, to improve ambulance service Category 2 response times and to learn from collaborative approach between national/regional systems/providers to further reduce clinical risk associated with handover delays. Three priority themes, each including initiatives for collaborative to test, deliver and evaluate with national, regional, regulatory/professional body support | To facilitate identification and uptake of good practice |
| Example interventions: Risk-based flow management models | For example, standardised escalation models to optimise flow | |
| Example interventions: Streaming and direct access | For example, direct access to most appropriate care pathway | |
| Example interventions: Ways of working/standardisation | For example, standardisation of pathways and capacity management |
List of abbreviations
- A&E
- accident and emergency
- CCP
- changing community provision
- CHCP
- City Health Care Partnership
- CSB
- changing staff behaviour
- D2A
- discharge to assess
- ED
- emergency department
- HSCP
- Health and Social Care Partnership
- IC
- integrated care
- ICS
- Integrated Care System
- PPI
- patient and public involvement
- S
- structural
- SDEC
- same-day emergency care
- TC
- targeting carers
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/KRWH4301).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
